Notes
Article history
This issue of Health Technology Assessment contains a project originally commissioned by the MRC but managed by the Efficacy and Mechanism Evaluation Programme. The EME programme was created as part of the National Institute for Health Research (NIHR) and the Medical Research Council (MRC) coordinated strategy for clinical trials. The EME programme is funded by the MRC and NIHR, with contributions from the CSO in Scotland and NISCHR in Wales and the HSC R&D, Public Health Agency in Northern Ireland. It is managed by the NIHR Evaluation, Trials and Studies Coordinating Centre (NETSCC) based at the University of Southampton
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Salisbury et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Structure of this report
This study was based on a randomised controlled trial (RCT) of PhysioDirect compared with usual care, incorporating an economic evaluation and nested qualitative research.
The report begins with a summary of the background to the problem of access to physiotherapy and a review of research on new approaches to improving access to physiotherapy and the use of telephone-based services in other relevant contexts. The first chapter concludes with a description of the research objectives.
The report then describes the methods and results from the RCT, followed by the methods and results from the economic analysis and then the methods and results from the qualitative research. Slightly unusually, the findings about the variables relating to the process of care are described before the results about the primary and secondary outcomes, because that makes it easier to interpret these outcomes.
The final chapter summarises and synthesises the findings from all three components of the study, providing interpretation in the light of previous studies. It also discusses the strengths and limitations of the research and its generalisability to the NHS and to other health-care systems. The conclusions are followed by recommendations for future research.
Background and objectives
Musculoskeletal problems and access to physiotherapy
Musculoskeletal (MSK) pain problems are one of the most common causes of disability. Over one-quarter of all patients registered in general practice will consult at least once for a MSK problem each year.1,2 Women consult with MSK problems more often than men, irrespective of age group.1–3 The high prevalence and persistent nature of many MSK problems makes MSK pain a major health problem.4 The most common types of chronic MSK pain are back pain and joint pain related to osteoarthritis,5 including knee pain and hand pain. For example, lifetime prevalence rates for low back pain as high as 84% have been reported.6
This high prevalence of MSK problems results in large direct and indirect health-care costs. 7 In 1998 alone, treatment for low back pain in the UK cost in the region of £10,668M,8 and recent reports suggest that these costs are likely to have risen by a further third in the last decade. 9 In the UK, low back pain is the fourth most common reason for consulting a general practitioner (GP) and is the most common MSK reason for consultation. Estimates suggest that between 6% and 9% of people registered with a GP consult annually with low back pain,10,11 which equates to approximately 5 million people each year in the UK. 8 In total, MSK pain accounts for around 15% of all GP consultations. 12 Most patients are managed with advice and analgesia, but many of these patients are also referred to physiotherapists, with 4.4 million new referrals to physiotherapy being made each year, of which 1.23 million are made by GPs. 13 The number of referrals to NHS physiotherapy increased by 37% in the 15 years between 1990 and 2005. 13 Guidelines for practice for common MSK conditions are increasingly recommending physical therapies, with recent guidelines for persistent low back pain recommending key treatments of exercise, manual therapy and acupuncture,9 and core treatments for the management of osteoarthritis of the knee including advice, education, exercise and weight loss. 14
Ensuring timely access to physiotherapy has long been an issue within the NHS, with waiting times of > 4 months in some areas. This is a problem for patients, because MSK conditions cause pain and disability, and for the economy, because these conditions are second only to mental health problems as a cause of days lost from work. In particular, back pain accounts for some 120 million days of certified absence from work each year and half of all patients with back pain who are off work for more than 6 months never return to employment. 8 Delayed access to physiotherapy is also a problem for the NHS because when patients are finally offered a physiotherapy appointment many fail to attend, and in other cases patients wait a long time for a physiotherapy consultation when it is unlikely that this will offer benefit, so it could be argued that much of the current physiotherapy resource is used inefficiently and ineffectively. While patients are waiting for physiotherapy they may repeatedly visit their GP and request medication, and the delay in access to physiotherapy may lead to unnecessary referrals to MSK interface services and outpatient orthopaedic specialists.
New service models: physiotherapy-led telephone assessment and advice services for musculoskeletal pain
In response to the problems described above, new service models have been developed that involve physiotherapy-led telephone assessment and advice as a way of managing patient demand and providing early access to physiotherapy advice. Physiotherapists in two areas of England, Huntingdon and Cheltenham, developed the concept and coined the term PhysioDirect at about the same time. The Huntingdon system was devised with the primary care lead for the primary care trust (PCT) and two local GP practices in 2001. By 2004, the whole of the population covered by Huntingdonshire PCT had access to the service, covering 155,000 people. A number of other PCTs have also since developed PhysioDirect services. Further details of the current service in Huntingdonshire are summarised in Box 1.
-
A computer program with templates containing dropdown boxes and free text designed for each region of the body records clinical data to assist the physiotherapist in making a diagnosis.
-
A section for advice about over-the-counter medication (if applicable), designed in conjunction with pharmacists.
-
The patient receives verbal and written advice on self-management, and is given a time frame for expected improvement and clear instructions to call back after a set period of time if their condition has not resolved as anticipated.
-
The GP receives a report on the outcome of the assessment.
-
The physiotherapist may also request a prescription or sickness certificate from the GP.
-
Clear pathways exist to move patients to tier II (or interface services) or on to secondary care.
Although there are several variations of PhysioDirect services, they all tend to involve patients being invited to telephone a physiotherapist for initial assessment and advice, following which many patients are posted information on self-management and exercise. Physiotherapists determine the priority of need, or ‘triage’, and provide rapid advice to the patient so that recommended self-management activities, such as postural improvements and exercise, can commence. Patients are advised to ring back if their condition does not improve and a time frame for the repeat call may be recommended. Some patients are invited for a face-to-face consultation if the initial telephone assessment establishes that this is necessary. Alternatively, they may be referred back to the GP or other health professional if that is appropriate. Within integrated services, patients may be referred to an interface service (where these exist) or on to secondary care following agreed local pathways. Thus PhysioDirect can form part of a streamlined patient management system that aims to ensure patient needs are met by the most appropriate clinician in a timely fashion. Some services are predominantly operated as call-back services, in which telephone assessments are pre-booked into physiotherapists’ diaries, and they make the call at a time of convenience for the patient. Additionally, patient assessments within PhysioDirect may be supported by computerised or paper-based templates.
Some services offer PhysioDirect in conjunction with self-referral to physiotherapy as a way of managing direct contacts from patients. Increasingly, the boundaries between telephone assessment and advice and self-referral services are blurring, given the impetus from recent Department of Health reports on MSK services,15 community services16 and the evidence about self-referral. 17,18
Summary of evidence about physiotherapy-led telephone assessment and advice services for musculoskeletal pain
The available evidence about physiotherapy-led telephone assessment and advice schemes for MSK pain, or PhysioDirect, was identified using searches on MEDLINE, EMBASE, The Cochrane Library, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Current Controlled Trials (CCT) database and the internet. These searches used terms and/or text words for ‘triage’, ‘PhysioDirect’, ‘telephone’ or ‘advice’ in combination with terms relating to physiotherapy [‘Physical Therapy Modalities’, ‘Exercise Therapy’, ‘Physical Therapy (Specialty)’, ‘physiotherapy.mp’]. We also specifically sought randomised trials of physiotherapy interventions using the Cochrane highly sensitive search strategy in combination with terms for physiotherapy. The search was originally conducted in August 2007 but the saved search in MEDLINE was conducted regularly throughout the research periods (2007–11) to identify any relevant new publications. A further comprehensive search to identify relevant literature since the protocol was written has been conducted in the following databases: NHS Evidence, Health Information Resources [Bandolier; UK Database of Uncertainties about the Effects of Treatments (DUETS); National Library of Guidelines, including National Institute for Health and Clinical Excellence (NICE) guidance, International Guidelines, Clinical Knowledge Summaries, NHS Evidence Specialist Collections (Musculoskeletal)]; TRIP database; Centre for Reviews and Dissemination [Database of Abstracts of Reviews of Effects (DARE), NHS Economic Evaluation Database (NHS EED) and Health Technology Assessment (HTA)]; Cochrane Database of Systematic Reviews (CDSR); EMBASE; MEDLINE; Physiotherapy Evidence Database (PEDro); Allied and Complementary Medicine Database (AMED); Cumulative Index to Nursing and Allied Health Literature (CINAHL); OTseeker; ISRCTN (International Standard Randomised Controlled Trial Number) Register; Medical Research Centre: Clinical Trials Unit; UK Clinical Research Network Study Portfolio; NIH records on ClinicalTrials.gov; Nederlands Trial Register; German Clinical Trials Register; and the Australian New Zealand Clinical Trials Registry. Citation tracking was also used to locate relevant articles.
We did not identify any published randomised trial that directly addressed the effectiveness or cost-effectiveness of PhysioDirect or similar schemes. There was, however, literature pertaining to the effectiveness of physiotherapy interventions for MSK problems, and about the benefits of early treatment with physiotherapy for MSK problems, which is relevant to the argument in favour of developing new services to provide earlier access to a physiotherapist. In addition, there have been several local audits and evaluations of physiotherapy-led telephone assessment and advice services, as well as studies and trials of telephone care by other health professionals for other conditions, which are relevant to this trial.
Physiotherapy interventions for patients with musculoskeletal problems
The most common problems leading to physiotherapy referral relate to the back, shoulder, neck or knee. With regard to back pain, most studies have concluded that manual therapy provided by physiotherapists offers little benefit over simple advice for acute low back pain. 19,20 The UK Beam Trial included patients with pain of variable duration and suggested that manual therapy has a modest effect,21 and some studies have suggested that it is possible to identify subgroups of patients more likely to benefit from this type of treatment,22,23 but a recent review concludes that manual therapy is no more effective than other common therapeutic approaches. 24 Although systematic reviews about the effectiveness of manual therapy have reached inconsistent conclusions, in subacute and chronic back pain there is evidence for the effectiveness of physiotherapy interventions based on promoting exercise. 25–28 Importantly, recent trials have shown that a single session of advice from a physiotherapist is as effective as a course of routine physiotherapy for patients with mild to moderate back problems. 29,30 With regard to neck pain, there is evidence from two Cochrane reviews that combined exercise and manual therapy is effective. 31,32 For shoulder pain, a review found evidence of benefit from a range of physiotherapy interventions. Exercise advice appears to be of benefit in rotator cuff disease and manual therapy provided additional benefit in one trial. 33 Exercise has been shown to be effective for knee pain related to osteoarthritis, with recent trials showing the effectiveness of physiotherapy-led advice and exercise. 34–36
In summary, there is evidence that patients with MSK pain problems can benefit from interventions offered by physiotherapists, while for some patients it is more cost-effective to provide brief advice, and for others, treatments from physiotherapists have little to offer. Therefore, a service that provides assessment, triage and advice initially and reserves more intensive (and expensive) treatments for those who do not improve may be the most cost-effective strategy. This is analogous to the ‘stepped-care’ approach, which is increasingly advocated in a range of conditions, for example mental health, where there is a high level of demand and a need to target resources. 37 In the context of physiotherapy, this approach should reduce costs for patients and for the NHS, provide earlier advice for all patients and effective treatments more quickly for those who may benefit from them (by screening out those unlikely to benefit), and be more convenient and accessible for patients as a whole.
Earlier compared with delayed physiotherapy treatment
Providing prompt and convenient access to health care is one of the major aims of the policy drive to make the NHS more responsive to patients' needs, with fast access for health care being seen as a benefit in itself, irrespective of the effects in terms of clinical outcomes. However there is evidence from several studies that early physiotherapy intervention provides faster symptom relief, improves quality of life, reduces absenteeism, leads to a reduction in physician consultations, and is more cost-effective. 38–42 This approach is supported by the guidance from the Clinical Standards Advisory Group (CSAG) on the management of back pain. Following a review of evidence and expert advice, the CSAG advised that patients with new episodes of back pain should have prompt access to physical therapy, with the aim of reducing the risk of symptoms and disability becoming entrenched. 43 More recently, specific guidelines for the management of patients with back pain persisting for > 6 weeks recommend early referral to a range of physical therapies. 9
Telephone advice services in health care generally, and in physiotherapy
PhysioDirect is based on a practitioner supported by computerised templates to assess the patient in a structured way, and to offer tailored, personalised advice. This reflects a wider trend to explore the use of this type of new technology in health care, for example in NHS Direct. Research in relation to the use of similar telephone triage systems in clinical settings other than physiotherapy has shown that it is safe, clinically accurate, cost-effective, acceptable to patients, and reduces the workload of clinicians,44–47 although some health practitioners have some concerns in using telephone triage in patients presenting with acute health problems. 48
Within physiotherapy, local evaluations and small studies suggest that services based on telephone advice given by physiotherapists are likely to be popular with patients,49–51 although there is no evidence about costs or outcomes, or the important issue of safety. Audits in the pioneering physiotherapy services in Cheltenham and Huntingdonshire in England suggest that 40–60% of patients referred by GPs to physiotherapy can be managed by telephone alone without a face-to-face consultation, telephone consultations take approximately half as long as face-to-face consultations, waiting times for a face-to-face appointment have been reduced from 4 weeks to 10 days and did-not-attend (DNA) appointment rates have been reduced from 15% to 1%. Patients appear to be very satisfied with the service, with 80% rating it as good or excellent. 52
Diagnoses made by physiotherapists or MSK triage services have been shown to be comparable with diagnoses made in face-to-face assessments and are not influenced by experience of the therapist. 53–55 In addition, therapists from different allied health professions agree on the prioritisation of patient care using telephone assessment systems. 56 There are some suggestions, however, that management of patients with MSK conditions over the telephone compares less favourably when conducted by less experienced physiotherapists in comparison with more experienced colleagues. 53,57
Related new developments in access to physiotherapy services
The Department of Health has recently published a report of the evaluation of self-referral to physiotherapy pilot sites. 17 Although the evaluation was not based on a randomised trial, the report is broadly supportive of the concept of self-referral, as are other non-randomised evaluations. 18,58–60 A small number of studies evaluating self-referral to physiotherapy services highlight potential patient benefits of direct access. 61–63 Many physiotherapy service leads will consider using PhysioDirect telephone systems to help them manage self-referral, which increases the salience of our study.
Rationale for a randomised trial of PhysioDirect for patients with musculoskeletal problems
PhysioDirect services have been established in a number of areas, notably in Huntingdonshire and Cheltenham in England. These have been commended by the Commission for Health Improvement and the NHS Working in Partnership Programme as examples of good practice and have won awards for innovation. Several other areas have established, or considered, similar services. The NHS White Paper ‘Our Health, Our Care, Our Say’16 highlighted the need to test new models of physiotherapy to overcome current deficiencies. Without a high-quality randomised trial testing the clinical effectiveness and cost-effectiveness of PhysioDirect, it is unclear whether or not such services should be more widely implemented.
This study is a RCT of PhysioDirect, an approach to improving access to physiotherapy services based on initial telephone assessment and written advice sent by post, followed by face-to-face care only when appropriate. This type of service is being introduced in different parts of the UK, but there is currently no evidence about the effectiveness or cost-effectiveness of PhysioDirect compared with usual care (based on a waiting list and eventual face-to-face care).
Summary of rationale for PhysioDirect
In summary, the rationale for PhysioDirect is to:
-
Provide equivalent outcomes for patients compared with usual care based on a waiting list for face-to-face treatment.
-
Provide faster access to advice, which would result in more rapid improvement in symptoms and may allow patients to return more quickly to work and usual activities.
-
Provide equivalent outcomes at lower cost, meaning that the PhysioDirect service is more cost-effective from an NHS perspective. The lower cost of PhysioDirect would be achieved by better tailoring the use of physiotherapy time in relation to need and capacity to benefit, using telephone consultations which were presumed to be less costly than face-to-face consultations, and by better use of resources through lower DNA rates.
-
Increase patient satisfaction because of easier access to advice from a physiotherapist.
Research objectives
-
To assess whether or not PhysioDirect is equally as effective as the usual models of physiotherapy based on patients going on to a waiting list and eventually receiving face-to-face care.
-
To investigate the cost-effectiveness of PhysioDirect compared with usual care.
-
To explore the experiences and views of patients, physiotherapists and their managers.
-
To investigate the health outcomes and experiences of different groups of patients (those in different age groups and with different types of problems) when referred to PhysioDirect rather than usual care.
Chapter 2 Randomised controlled trial: methods
Study design
The study is a pragmatic RCT, with participants randomised individually to one of two parallel groups, incorporating economic evaluation and nested qualitative research. The comparison is between patients randomised either to be offered a service based on initial telephone assessment and advice from PhysioDirect, followed by face-to-face treatment when necessary, or to be offered usual care consisting of allocation of patients to a waiting list for face-to-face care.
The study was designed to assess equivalence between the two treatment groups in the primary clinical outcome. If equivalence in clinical outcomes is established, differences in the costs of providing care and in the secondary outcomes (particularly waiting times for treatment, time lost from work and usual activities, patient satisfaction, patient preference) become particularly important and relevant to future provision of services.
The equivalence design was chosen over a conventional superiority design because there was no hypothetical justification to suggest that the PhysioDirect service would produce better clinical outcomes than usual care by the main follow-up time point of 6 months. However, because it was anticipated that patients randomised to PhysioDirect would receive advice more quickly than those randomised to usual care it was conceivable that they would achieve improved outcomes at the first time point of 6 weeks, but this was a secondary outcome. Furthermore, although we wanted to test a hypothesis of equivalence in the primary outcome we also wanted to test for difference in some of the secondary outcomes. For these reasons the study was designed as an equivalence study rather than a non-inferiority study, as the former would require a larger sample size and would provide power to establish differences in the secondary outcomes.
It is arguable that the most important outcome for this study would be improved cost-effectiveness – for example, the PhysioDirect service might be slightly less effective but substantially less costly and therefore might be cost-effective. However, the different sources of uncertainty in cost-effectiveness analyses make it very difficult to design a study with cost-effectiveness as the primary outcome and in particular to estimate the appropriate sample size for such a study. Furthermore, the interpretation of findings that a service is less effective and less costly than usual care is contentious. 64
Setting
PhysioDirect services were newly established for the purposes of the trial in four areas of England. Each physiotherapy service provided care for patients from a defined group of general practices within one of the following PCTs: Bristol, Somerset, Stoke-on-Trent, and Central and Eastern Cheshire. The total population covered across all four PCTs was approximately 625,000 people.
Patients from 94 general practices participated in this study. Participating GP practices were typical of NHS general practices in England, representing a broad mix of practice sizes, the smallest serving a population of 2121 and the largest 28,599 people. These practices covered a wide range of types of area, including inner-city, suburban, market towns and rural areas. Although detailed information about the population of each participating practice was not collected, between them the practices provide care for patients of all age groups. The areas differed in terms of their ethnic mix, but none had a high proportion of patients from non-white ethnic backgrounds. Although 12% of the population of Bristol is from black and minority ethnic (BME) groups, the BME population in the city is concentrated in particular inner-city wards. By contrast, only 1.2% of the population of Somerset is from BME groups. About 5% of the population of Stoke is from BME groups (predominantly Pakistani and Bangladeshi). About 3% of the Cheshire population is from a range of different minority ethnic communities.
Between them, in 2008 the existing physiotherapy services in these PCTs received approximately 18,300 referrals from primary care professionals in the general practices participating in the trial. This equates to 29.3 referrals per 1000 patients per annum, which is slightly higher than the rate of 24.4 reported in the most recent available figures for England. 13 However, these national data were last reported in 2004–5 and it was noted then that referral rates were rising by about 4% per annum. 13
The physiotherapy services that participated in the trial were typical of NHS primary care-based physiotherapy in the UK. NHS physiotherapists in the UK accept referrals from primary and secondary care physicians, other health-care practitioners (such as nurse practitioners and allied health professionals) and, in some cases, offer direct access or self-referral pathways to physiotherapy. Treatment is delivered following a clinical assessment of the patient by the physiotherapist, and common interventions for MSK conditions include advice and education, specific and general exercise, manual therapy and pain-relieving modalities, such as electrotherapy and acupuncture.
Participants
The inclusion criteria were deliberately as broad as possible in order to maximise generalisability and to reflect the ‘real-world’ operation of PhysioDirect services. Inclusion criteria were adults (aged ≥ 18 years) who were referred by GPs or other members of the primary health care team or who referred themselves (self referred) for physiotherapy for a MSK problem.
Exclusion criteria were children (< 18 years); patients referred to physiotherapy by a hospital consultant, emergency department or primary/secondary care interface service; those needing domiciliary physiotherapy; those needing postoperative physiotherapy; those needing physiotherapy for non-MSK problems; very urgent referrals; those who did not confirm that they wanted physiotherapy; second or subsequent referrals for physiotherapy for an individual during the trial period; people unable to communicate by telephone in English; and those with hearing difficulties who may have had difficulty communicating by telephone.
It was necessary to exclude participants who had problems that were so urgent that it was not safe to delay assessment for the length of time it would take to gain consent to the trial. Frequently, referrals were designated as urgent by the referring clinician. It was important not to exclude most of these referrals, as one of the potential advantages of a PhysioDirect service is that it allows an early telephone assessment by a physiotherapist to prioritise those who need urgent care. Therefore, all referrals to each participating service were screened by a senior physiotherapist on receipt (see below) and only those which were deemed very urgent were excluded from the study (regardless of whether or not the referring clinician had marked the referral as urgent). The excluded patients were contacted and offered physiotherapy in the usual way for urgent cases.
Recruitment of participants
General practitioners or health-care professionals in the relevant practices referred patients to physiotherapy in the usual way, although patients could refer themselves in some areas of Stoke, as that service already had developed a self-referral pathway for patients for some GP practices. Referrals to each physiotherapy service were screened by a senior physiotherapist within one working day of receipt to confirm that the patient appeared to be eligible for the study. These potentially eligible patients were sent information about the trial by post from participating physiotherapy centres, along with a consent form and a baseline questionnaire.
The consent form asked potential participants to choose from one of three options: to consent to participation in the trial; to state that they wanted physiotherapy but did not want to participate in the trial; or to state that they no longer wanted physiotherapy.
Those who agreed to participate were randomised into the trial; those who declined participation but wanted physiotherapy were put on the waiting list for usual care; and those who did not want physiotherapy were discharged. All referrals were logged in order of when the referral form was originally received, so the process of gaining consent did not affect the patient's position on the waiting list for face-to-face physiotherapy if they ultimately received usual care.
If people did not reply to the information letter, they were sent a reminder mailing after 2 weeks to encourage them to respond. The reminder informed them that if they did not respond in any way within 2 weeks of the date the reminder letter was sent then they would be discharged and taken off the physiotherapy waiting list. This is standard practice, in that most physiotherapy services and many hospital outpatient services send patients a ‘partial booking’ letter inviting them to respond to request an appointment, and patients who do not respond are discharged and removed from the waiting list.
Randomisation
Patients who gave consent to participate and had completed the baseline questionnaire were randomised in a 2 : 1 ratio to PhysioDirect or usual care. This allocation ratio was chosen to ensure that sufficient patients were randomised to PhysioDirect to make this new service viable, given that all non-consenting and excluded patients continued to receive usual care, as well as those randomised to usual care. Randomisation was undertaken using web or telephone access to a secure remote automated allocation system maintained by the UK Clinical Research Collaboration (UKCRC)-registered Bristol Randomised Trials Collaboration. Allocation was made at the level of the individual, stratifying by physiotherapy site and minimising by sex, patient age group, and site of the presenting MSK complaint. Allocation was therefore fully concealed. Periodic checks were made during the study of the allocation ratios according to the minimisation factors, to ensure that the randomisation schedule was performing as intended.
Following randomisation, patients were sent a letter either inviting them to contact PhysioDirect and explaining how to do so (intervention arm), or explaining that they were on a waiting list for a face-to-face physiotherapy appointment and would be contacted by the service when the next appointment became available (control arm).
The number of patients excluded from or not participating in the trial for different reasons was recorded. The age, sex and postcode of all patients were also recorded in anonymised form, to make it possible to compare participating and non-participating populations.
Description of intervention and control arms
Intervention: ‘PhysioDirect’
The intervention is defined as the patient being offered treatment within the PhysioDirect treatment pathway. PhysioDirect is the provision of an easily accessible telephone assessment and advice service from an experienced physiotherapist, supported by a computerised assessment algorithm. Following the telephone assessment, patients are usually given exercise advice and then invited to telephone back to report progress. They can then be invited for a face-to-face appointment if necessary, or this can be offered following the initial assessment if appropriate.
The rationale for PhysioDirect is that all patients will have access to earlier assessment and advice about their problem from a physiotherapist. Furthermore, those patients most likely to benefit from face-to-face physiotherapy should be able to receive it more quickly (by filtering out the patients who do not need face-to-face care), hopefully leading to a faster clinical improvement and a quicker return to work and/or usual activities.
The term ‘PhysioDirect’ is used variably by different services in the UK, but the model used in this trial was modelled closely on the system developed by the Huntingdonshire PCT in 2001. This service was runner-up in the 2003 Health and Social Care Awards. Currently, 350,000 people in Cambridgeshire are served by this PhysioDirect system. The established nature of the service, the structured format of the system and the experience of the Huntingdon physiotherapy staff both in using and training other physiotherapists to use this system all made the system particularly suitable for use in the PhysioDirect trial.
Setting up the service
In order to establish a PhysioDirect service, each participating site needed to train sufficient physiotherapists to provide telephone assessments using the assessment software and to provide a suitable office. Apart from the training and set-up costs, no extra physiotherapist resources were used within the study – the time of the existing staff was reallocated within existing resources.
Training the physiotherapists
All physiotherapists operating the PhysioDirect telephone services undertook a structured training programme led by the physiotherapy service in Huntingdon which involved attending a 2-day course of teaching, demonstrations and observation of live calls. Each PCT trained about eight physiotherapists in order to provide sufficient capacity across the week (with some contingency in case of absence) and without any one physiotherapist having to spend more than half of their time working on the PhysioDirect service.
The PhysioDirect software (see below) was installed at each of the PCTs in the PhysioDirect trial prior to the trial physiotherapists attending the Huntingdon training so that following the training session the physiotherapists could practise and hone their skills. The Huntingdon PhysioDirect trainers were available by telephone throughout this period to provide advice if problems were encountered.
A visit to each participating PCT was undertaken by a PhysioDirect trainer approximately 2 weeks after completion of the training programme. The trainer observed calls and facilitated a problem-solving session. The trainer then listened to individual calls and, using a structured format, assessed each physiotherapist's competency to utilise the system safely and effectively. If physiotherapists did not reach the required competency at the first site visit a further visit to recheck competency was carried out approximately 6 weeks after the initial training. The competency check consisted of the trainer assessing 53 aspects of the telephone assessment process and completing a checklist indicating whether or not each aspect was performed to a satisfactory level. Each section was evaluated on a yes/no basis, with overall comments about performance, issues to be addressed and an agreed action plan if required. All physiotherapists had to be certified as competent to undertake PhysioDirect before they assessed patients in the trial.
Office facilities
Each site required a quiet office with at least two computers with installed software, and a telephone system with headsets for the physiotherapists, a fax machine and an answering machine. Ideally (but not necessarily), the receptionist would work close by in an adjacent office.
The PhysioDirect software
Shortly after its inception, the Huntingdon PhysioDirect system was translated into a computer-based system to assist the safe, efficient and effective delivery of the telephone assessment and advice service. The challenge during the development of the computerised system was to maintain sufficient structure to guide an effective and efficient assessment by prompting physiotherapists to cover all key aspects of the patient assessment, while being flexible enough to be responsive to presentations of individual patients and taking account of the lack of visual clues provided by a patient during a face-to-face consultation. The system had to be as simple as possible as physiotherapists undertaking telephone assessment are required to perform a number of skills simultaneously, including asking questions, visualising the patient and their presentation, analysing the patient's responses, formulating the next question and typing responses into the system. The solution was to include mandatory fields with dropdown menus and tick boxes for key aspects of the assessment, with text boxes provided to allow the physiotherapists to record responses to supplementary questions eliciting further information or clarification from the patient.
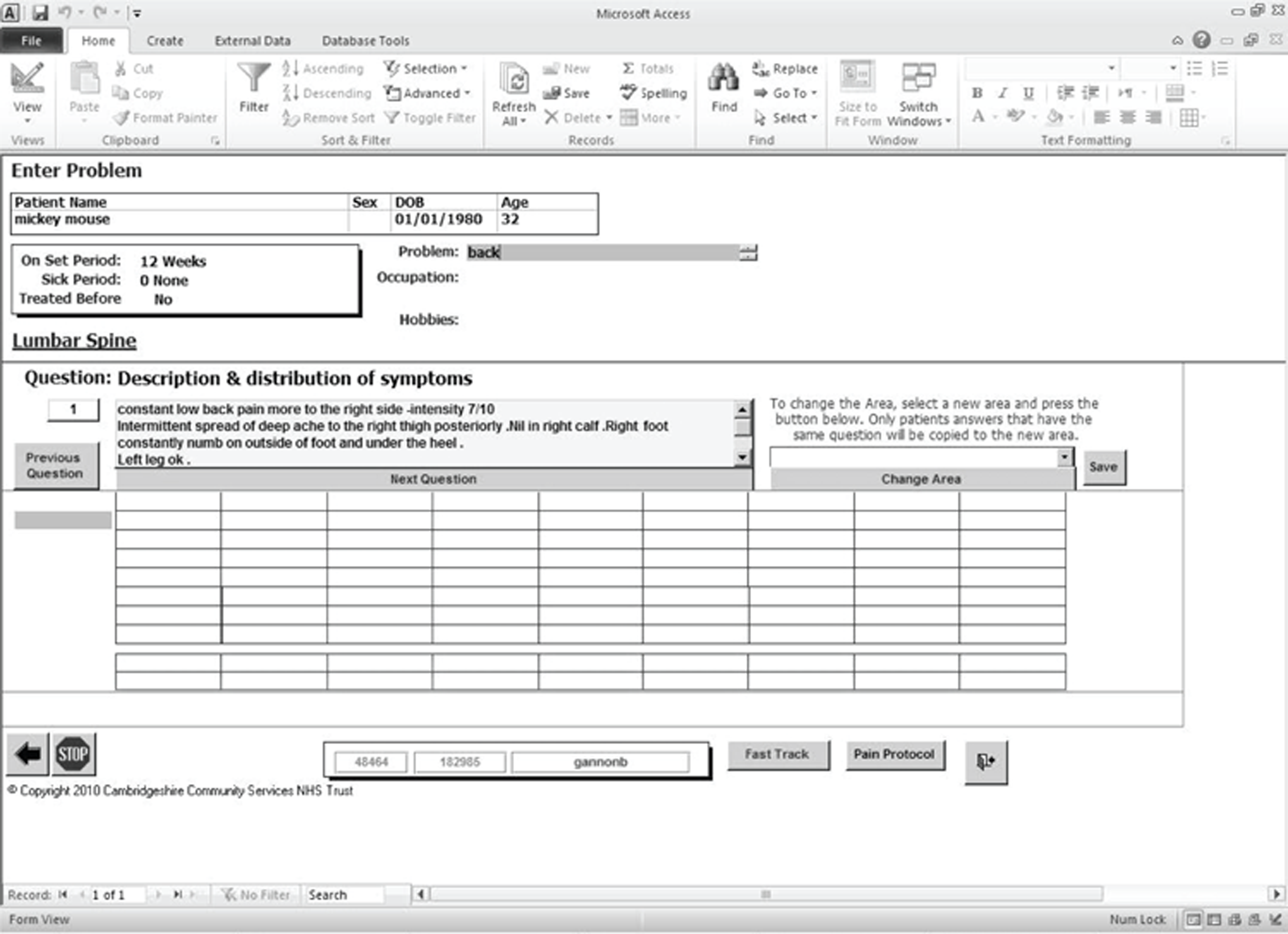
The software is a based on a program developed using Microsoft Access 2003 (Microsoft Corporation, Redmond, WA, USA), which first allows the patient's demographic details to be checked, then brief details regarding the patient's occupation, hobbies/activities and main problem for which they have been referred. When using the software the physiotherapist selects an appropriate assessment framework, depending on the area of the body affected. This ensures any relevant ‘special questions’ are asked that relate to that area. For example, if the patient is complaining of low back pain, questions regarding symptoms suggestive of cauda equina compression are included by the computer software in the assessment algorithm. This assessment, prompted by the software, includes the investigation and recording of the patient's presenting, medical and drug history, details of aggravating, easing and diurnal patterns and assists the physiotherapist in reaching a clinical diagnosis. An example screen from the system is shown overleaf.
Further information about the PhysioDirect software used in this trial can be obtained from Mrs Jill Gamlin, Physiotherapy Department, Hinchingbrooke Hospital, Hinchingbrooke Park, Huntingdon PE29 6NT, UK (e-mail: jill.gamlin@nhs.net).
Standardisation of PhysioDirect across the sites
All four physiotherapy services participating in this trial set up a PhysioDirect service following the same model of organisation and using the same assessment software as developed in Huntingdonshire (Figure 1).
FIGURE 1.
Example screen shot from PhysioDirect assessment software. Reproduced with permission from Cambridgeshire Community Services NHS Trust.
As far as possible, the PhysioDirect service was implemented in the same way in each of the four sites. The physiotherapists received the same training and were accredited in the same way, they used the same PhysioDirect software, and they used the same suite of advice and exercise leaflets. Furthermore, all recruitment and other research procedures were standardised in all sites. In this way, a high degree of consistency in how the intervention was delivered in each local service was ensured.
After the physiotherapists had been trained and assessed as competent to assess and advise patients via PhysioDirect, each physiotherapy site carried out a run-in period of at least 1 month to ensure smooth running of the service before patients to be included in the main trial were recruited. During this run-in period, all trial procedures of recruitment and randomisation were followed, making it possible to fully pilot the research procedures in parallel with the physiotherapy services gaining experience of the new way of working. Follow-up data collection for most outcome measures was also undertaken, although with less intensive use of reminders than in the subsequent main trial because of resource limitations.
Staffing the service
Based on advice from Huntingdon, it was decided that only experienced physiotherapists would be involved in providing the PhysioDirect telephone advice. Each service therefore trained several of their more senior staff who were on Agenda for Change Band 6 or above to conduct the PhysioDirect sessions. Details of the training and experience of these physiotherapists were collected at the training sessions. These are described in Table 1.
| Characteristic | No. | % |
|---|---|---|
| Sex (n = 32) | ||
| Male | 7 | 22 |
| Female | 25 | 78 |
| Age (years) | ||
| Mean (SD) | 12 | (8) |
| Seniority: Agenda for Change band (n = 31) | ||
| 6 | 13 | 42 |
| 7 | 17 | 55 |
| 8 | 1 | 3 |
| Any previous specific postgraduate training in telephone assessment or advice services? (n = 31) | ||
| Yes | 4 | 13 |
| No | 27 | 87 |
| Previous experience of using PhysioDirect or other telephone assessment system to advise patients? (n = 31) | ||
| Yes | 11 | 35 |
| No | 20 | 65 |
Because (in the context of a trial) only a minority of patients were randomised to PhysioDirect, the number of patients did not justify having a physiotherapist available to answer the telephone at all times in the week. Each site was asked to provide telephone sessions spread across a range of days of the week and at different times of day, to allow patients some choice about when to telephone. These opening times were included in the letter inviting patients to telephone the service. If patients telephoned at other times, an answerphone message asked them to telephone again when the service was open.
Process of the encounter
As soon as possible after consent to participate in the trial was received, patients were sent a letter inviting them to telephone an experienced physiotherapist for initial assessment and advice and explaining the times during which the PhysioDirect service was available each week. When a patient called the service, if a physiotherapist was not engaged in a call, they would be the first person the patient spoke to and the assessment would start immediately. If the staff were all engaged with other calls then the first person they would speak to would be a receptionist. The receptionist would take the patient's details and place them on a ‘call-back’ list along with information regarding when would be most convenient for this to happen. The physiotherapists would either field any calls arriving if they were free, or consult the call-back list for available patients.
The physiotherapist responding to the telephone call followed the computer-assisted assessment system to assess the patient and record the findings.
Process of care following the encounter
There were several possible outcomes following the initial telephone call:
-
In some cases, at the end of the call the physiotherapist posted a relevant advice leaflet about self-management and exercises to the patient, inviting them to telephone back to report progress after about 2–4 weeks, if appropriate. If the patient telephoned back they could be given further advice or be booked for a face-to-face consultation if necessary.
-
In some cases, the initial telephone call established that face-to-face assessment and/or care was needed, in which case this was arranged either by putting the patient on the PhysioDirect waiting list for face-to-face care or by arranging an urgent appointment if necessary.
-
In other cases, the initial assessment established that physiotherapy was unlikely to be effective and the patient was given appropriate advice or referred to another service, and discharged from physiotherapy.
-
In a few cases the initial assessment revealed that urgent medical intervention was required and these patients were sent to accident and emergency (A&E) with an accompanying fax detailing the need for attendance. If the medical intervention was not considered ‘an emergency’ then patients were asked to attend their GP, for example to obtain a radiograph.
The assessment process allocates patients to one of five categories. These categories and the subsequent management pathways are summarised in Table 2.
| Patient category | Management pathway |
|---|---|
Specific MSK problem and the assessment indicate that the patient can be given a sound explanation of the MSK problem:
|
Patient is given clear verbal explanation and advice. Information sent in the post to facilitate self-management
|
| The presenting problem is MSK but there are indications of serious pathology present | Specific pathway followed for presentation, e.g. cauda equina |
| Specific MSK condition but face-to-face assessment is required, for example neurological status assessment for patients with radiculopathy | Patient booked into clinic for face-to-face appointment for further examination and assessment |
| Not possible to make a sound diagnosis with telephone assessment | Patient booked for face-to-face appointment to clarify the diagnosis and commence appropriate management |
| The primary presenting problem is not MSK | Patient referred back to GP |
Providing PhysioDirect in the context of a randomised controlled trial
Separate waiting lists were held for patients randomised to PhysioDirect and to usual care, so that any impact of the PhysioDirect pathway on how long people waited for a face-to-face appointment could be detected. For the same reason, we sought to allocate physiotherapist time in proportion to the number of people who were randomised to the PhysioDirect arm of the trial. Based on experience in the pilot study it was possible to estimate the proportion of patients referred for physiotherapy who would be eligible for the trial and the proportion of those who would consent to take part. Using these data, and also taking into account that one in three of the eligible, consenting patients would be randomised to usual care, it was possible to estimate that approximately 20% of all patients would be allocated to PhysioDirect rather than usual care. Each site was therefore asked to allocate 20% of their total physiotherapist staff resources to patients allocated to the PhysioDirect arm of the trial, and within this proportion to allocate about half the time to telephone sessions and the remainder to face-to-face care for people in the PhysioDirect arm.
Patients randomised to the PhysioDirect arm could state at any time that they did not want to discuss their problem on the telephone but instead wanted to wait for a face-to-face appointment. This was allowed within the PhysioDirect pathway and did not mean that the patient needed to withdraw from the trial. It is important to note that the PhysioDirect ‘intervention’ was based on offering patients an initial telephone assessment with a physiotherapist, with face-to-face care available if necessary. The ‘intervention’ is not the telephone call, and a face-to-face consultation should not be equated with ‘usual care’. The PhysioDirect intervention is the care pathway, which can encompass both telephone advice and face-to-face care.
Control: usual care
The control arm is defined as the patient being offered treatment within the usual MSK physiotherapy care pathway.
Usual care involved patients being referred to a physiotherapist by a GP or other member of the primary health care team. In some areas in Stoke, PCT patients could also refer themselves directly. As is usual physiotherapy practice, patients were put on to a waiting list for an initial face-to-face physiotherapy assessment and then, if appropriate, had a series of follow-up treatment appointments. The waiting time differed considerably in the four participating physiotherapy services, at different sites providing physiotherapy within each service, and at different times of year. This reflects usual care in physiotherapy services more widely.
Outcome assessment
Outcomes were assessed at baseline, and at 6 weeks and 6 months after randomisation.
The primary outcome was clinical outcome at 6 months, assessed using the Physical Component Score (PCS) measure from the Short Form questionnaire-36 items, version 2 (SF-36v2) questionnaire. 65 The SF-36v2 PCS is a well-recognised generic measure of health status. It was particularly suitable for this trial because, unlike disease-specific measures, it is applicable to the wide range of MSK problems referred to physiotherapy.
Although there could be a concern that generic measures may be less responsive than disease-specific measures, the physical functioning and bodily pain scales of the SF-36 (which contribute most of the variation in the PCS summary measure) compare reasonably well with disease-specific measures in patients with MSK problems. 66–70
Several further measures of clinical outcome were also used. The first was the Measure Yourself Medical Outcomes Profile (MYMOP)71 questionnaire (version 2), which is a patient-generated measure. It allowed patients to specify up to two symptoms and one functional limitation for which they had been referred to physiotherapy, then follow-up questionnaires assessed change in those specific symptoms/limitations. This individualised and validated measure has also been used to assess patients with a wide range of problems. 71 The MYMOP was included as, by focusing on the patient's main problem, it might be more sensitive to change than the PCS. The MYMOP was designated an important secondary outcome.
Second, a single question was included as a global measure of individual rating of overall change, based on a seven-point Likert scale from ‘very much worse’ to ‘very much better’.
Third, we created a composite measure of response to treatment using the approach recommended by the Outcomes Measures in Rheumatology Clinical Trials – Osteoarthritis Research Society International (OMERACT-OARSI) initiative. 72 This combined measures of physical function (the SF-36 physical function scale), pain (SF-36v2 bodily pain scale) and overall perception of the main problem (question 1 from the MYMOP questionnaire).
Other secondary outcomes were:
-
costs (described in more detail later)
-
quality of life [measured using the EQ-5D measure73 (European Quality of Life-5 Dimensions; EuroQol health utility measure)]
-
the individual scales and the mental component summary measure from the SF-36
-
waiting times for treatment, based on data collected from routine physiotherapy records
-
time lost from work and usual activities, based on patient questionnaires
-
satisfaction with care provided (development of the measure is described in Appendix 2)
-
preference for physiotherapy or usual care if they needed physiotherapy in future, based on a single question in the patient questionnaire.
Process evaluation
Measures of the process of care were particularly important in this study. Data about the services provided included:
-
the number, type and duration of consultations with physiotherapists
-
time to first physiotherapy assessment (telephone or face to face) and to first face-to-face appointment, where applicable
-
rates of non-attended appointments with physiotherapists
-
the clinical grade or banding under Agenda for Change of all physiotherapists who provided care, and further details of the qualifications of the 32 physiotherapists who provided telephone advice in the PhysioDirect arm, as previously described.
In addition, it was important to collect data about the use of other health services in relation to the referral problem, particularly consultations in general practice, referrals to hospital outpatient services, hospital admissions, use of private physiotherapy and other private sector treatments. These are relevant to the economic evaluation but also to a full understanding of the impact of the different models of physiotherapy service on other health-care providers.
A system was established to collect, record and investigate details of any suspected adverse events (AEs) encountered by the trial participants.
Collection of data
Baseline data about patient characteristics, and the nature of the problem for which patients were referred to physiotherapy, were collected from the referral forms at each participating physiotherapy centre.
Outcome and process data were collected from questionnaires administered to patients at baseline, 6 weeks and 6 months after randomisation, from electronic data downloaded from the PhysioDirect software, from routine records of consultations collected by each physiotherapy service, and from general practice records.
The baseline patient questionnaire collected data about patient characteristics and about the outcome measures. Data about outcomes at follow-up were collected from similar questionnaires sent by post at 6 weeks and 6 months after randomisation. Non-responding patients were sent a first reminder questionnaire by post after 2 weeks, and a second after a further 2 weeks, if needed. If patients did not respond to this second reminder within 2 weeks, attempts were made for up to a further 2 weeks to collect outcome data by telephone. In this situation, priority was given to obtaining data about the primary outcome (the SF-36v2 PCS). Similarly, if patients did complete postal questionnaires but key questions were omitted then telephone contact was attempted in order to collect missing question items that were necessary to calculate the primary outcome.
Some ‘screening’ questions were included to identify patients who had accessed rarely used but potentially expensive resources (e.g. hospital admissions) because of the problem for which they were referred for physiotherapy. Patients who responded positively to these questions were then telephoned to obtain more detailed information.
Data about telephone consultations with the PhysioDirect service were collected by download from the assessment software used in this service. Data about face-to-face consultations were obtained from routine records maintained by each physiotherapy service. Data about primary care consultations were obtained from general practice notes, extracted by research staff. Details of consultations with NHS walk-in centres, emergency departments, hospital outpatient appointments and admissions were obtained from the patient questionnaire, as were details of non-NHS consultations.
Details of the physiotherapists participating in the PhysioDirect service were obtained from questionnaires administered before these physiotherapists undertook training to use the PhysioDirect software. Details of the grades of the other physiotherapists providing face-to-face consultations were obtained from the managers of each service.
Table 3 lists the various outcome measures, the timing of data collection and the source of the data.
| Measure | Timing | Source |
|---|---|---|
| Patient identifers, type of problem, age and sex | Pre-consent | Referral letter. Recorded (anonymised) in research database |
| Demographic details | Baseline | Baseline patient questionnaire, data from research database |
| SF-36v2 | Baseline, 6 weeks, 6 months | Patient questionnaires |
| MYMOP | Baseline, 6 weeks, 6 months | Patient questionnaires |
| EQ-5D | Baseline, 6 weeks, 6 months | Patient questionnaires |
| Overall rating of change | 6 weeks, 6 months | Patient questionnaires |
| Time lost from work and usual activities | Baseline, 6 weeks, 6 months | Patient questionnaires |
| Satisfaction with care provided | 6 weeks, 6 months | Patient questionnaire |
| Preference for PhysioDirect or usual care | Baseline, 6 months | Patient questionnaires |
| Waiting time for first assessment by a physiotherapist | Collected at end of study | Physiotherapy service records, from date of randomisation (and also from date the referral was originally received) to date of first telephone or face-to-face consultation |
| Patient and companion costs | 6 weeks, 6 months | Patient questionnaires |
| Cost of lost production associated with time off work and usual activities | 6 weeks, 6 months | Estimated from information in patient questionnaires |
| Costs of providing physiotherapy | Set up costs: collected during the PhysioDirect service set-up phase and once the service was operating | Set-up: data from PCTs about resources involved in setting up the PhysioDirect service; treatment: physiotherapy records, data collected within the trial about lengths of consultations, staff use of time, staff grades, etc. |
| Treatment over 6 months: collected at end of study | ||
| Costs in general practice (consultations, treatments, investigations) | Collected at end of study, from randomisation to 6 months' follow-up | Patient GP records – consultations costed using Netten and Curtis and NHS reference costs for other costs |
| Costs of prescriptions | Collected at end of study, from randomisation to 6 months' follow-up | Patient GP records, costed using the BNF |
| NHS secondary care costs (outpatients, inpatients, admissions) | 6 weeks, 6 months | Patient questionnaires for resource use, costed using NHS tariffs |
| Process evaluation: number, type and duration of consultations with physiotherapists; non-attended appointments with physiotherapists | Collected at end of study, from randomisation to 6 months' follow-up | Physiotherapy records |
| Qualifications and experience of physiotherapists | Collected at the beginning of the study | Online questionnaire completed by physiotherapists |
| Suspected adverse events and adverse events | Collected throughout study from randomisation to 6 months' follow-up | To be notified by patients, physiotherapy services, general practices or any other sources |
Data entry
All questionnaire data were entered into a bespoke database in Microsoft Access v2000. A 1-in-10 sample of each questionnaire type was independently checked to assess the accuracy of data entry. Of 58,615 fields checked, there were just 73 errors (0.125% error rate).
Blinding
In pragmatic trials of this type, as in the real world, it is not possible to blind participants or physiotherapists, whether they are in the intervention or control arm of the trial.
Most of the outcome data were obtained from patient questionnaires, which were therefore not blind to treatment allocation. However, all data entry from these questionnaires was conducted blind to allocation. The collection of data about PhysioDirect calls was by electronic download. The collection of data about face-to-face physiotherapy consultations from administrative records and from general practice records was conducted by research staff not involved in providing the intervention, as far as possible blind to allocation, although in some cases (7%; 160/2228) this was not possible because the allocation was recorded in the records.
Sample size and power
This study was powered to establish clinical equivalence using the PCS scale from the SF-36. At the time of planning the study, previous studies in a range of populations and conditions had suggested that a minimum clinically important difference on the SF-36v2 PCS was about 4 points [0.4 standard deviation (SD)],74–77 although the latest version of the SF-36v2 manual now suggests that ‘a minimum important difference of 2–3 points is reasonable’. 78
In this study, a difference of no greater than 2 points was conservatively specified as demonstrating equivalence. This is equivalent to an effect size of 0.2 SDs, which is considered a small effect size. 77 Sample sizes for analysis of 976 and 488 in the PhysioDirect and usual-care groups, respectively, would yield 95% power to reject a null hypothesis of non-equivalence (i.e. the difference in means, μPhysioDirect − μusual care, is not less than 0.2 SDs) with an overall two-sided alpha of 0.05 alpha if the observed difference in means is zero. The same sample size would yield 80% power to reject the null of non-equivalence if the observed difference between the groups is 0.046 SDs rather than zero.
The target sample size for patients completing the final 6-month follow-up questionnaire was 1000 patients in the PhysioDirect arm and 500 patients in the usual-care arm. Assuming 20% non-collection of the primary outcomes, it was necessary to recruit 1250 and 625 patients in the PhysioDirect and usual-care arms, respectively, or 1875 patients in total.
Statistical methods
The main hypotheses were that care via the PhysioDirect service would be clinically equivalent to usual care and more cost-effective at 6 months after randomisation.
Primary analysis
Analysis and presentation of data were conducted in accordance with CONSORT guidelines (Consolidated Standards of Reporting Trials), including the extensions relating to non-pharmacological trials, non-inferiority and equivalence trials and pragmatic trials. 79–83 The primary analysis employed multivariable regression to investigate between-group differences in SF-36 PCS score at 6 months' follow-up. The primary analysis was conducted on an intention-to-treat basis, with due emphasis placed on the confidence interval (CI) for the between-arm comparison when inferring equivalence (or otherwise) of the two groups. It was determined a priori that clinical equivalence between the arms would only be concluded if the 95% CI for the primary outcome lay wholly inside the range −2 to +2 points on the PCS. Analyses were adjusted for stratification variables (physiotherapy site), minimisation variables (age, sex, main referral problem) and baseline outcome variable scores.
Because the intervention is being offered either the ‘PhysioDirect’ or ‘usual care’ treatment pathway, all patients were analysed within their randomised groups and there is no difference between an ‘intention-to-treat’ and an ‘on-treatment’ analysis.
Secondary analysis
Sensitivity analysis
-
Repeating the primary analysis adjusting also for any variables exhibiting marked imbalance at baseline to check that this did not influence the findings.
-
Investigating the effect of missing primary outcome data using multiple imputation methods.
-
Investigating clustering of outcomes by (a) practice and (b) physiotherapy service.
Secondary outcomes
-
Assessing equivalence in clinical outcome using the MYMOP score at 6 months.
-
Examining clinical outcome at 6 weeks using the SF-36 PCS.
-
Comparison of the proportion of patients who ‘respond to treatment’ in each arm, in line with the OMERACT-OARSI recommendations,72 using the SF-36 physical function and bodily pain scales and the main problem score from the MYMOP.
-
Analyses of the other secondary outcomes using similar approaches as described for the primary outcome.
-
Investigation of process measures such as physiotherapy consultation rates, waiting times, physiotherapy DNA rates and consultation rates with other health-care services in the NHS and private sectors.
-
Repeated measures analysis using an interaction term for time to investigate any divergent/convergent pattern in the SF-36 PCS over 6 weeks' and 6 months' follow-up.
Subgroup analyses
Appropriate interaction terms were entered into the primary regression analysis for SF-36 in order to conduct pre-specified subgroup analyses according to site of presenting MSK problem, patient age group, socioeconomic status and PCT physiotherapy service. As the trial was powered to detect overall equivalence between the groups rather than interactions of this kind, these analyses were essentially exploratory and would need to be interpreted with due caution.
Economic analysis and qualitative research
The methods for the economic analysis and for the qualitative research are described in detail in subsequent chapters, after the main quantitative results from the trial.
Investigation of adverse events and serious adverse events
General practitioners from participating practices and physiotherapists treating trial patients were asked to report any death, hospitalisation, significant disability or incapacity, life-threatening circumstance or other medically significant occurrence that he/she considered may be potentially related to physiotherapy, or to the trial procedures, to the Chief Investigator within 5 days of occurrence. The Chief Investigator would investigate these using a predetermined set of criteria and report any related and unexpected serious adverse events (SAEs) to the Main Research Ethics Committee, within 15 days of becoming aware of the event, using the SAE report form for non-CTIMPs (Clinical Trial of an Investigational Medicinal Product) taken from the National Research Ethics Service website. A log would be kept of all AEs or SAEs reported to the Chief Investigator; his/her assessment of the intensity, causality, expectedness and seriousness of the AE; the reasons for those decisions; and (when appropriate) the dates on which the SAE was reported to the main Research Ethics Committee, Sponsor, and Data Monitoring and Ethics Committee.
Ethics and research governance approval
Multisite research ethics approval was obtained from Southmead Research Ethics Committee, Reference 08/H0102/95. All necessary research governance approvals were also obtained for each physiotherapy site.
Trial registration
Current Controlled Trials ISRCTN55666618.
UK Clinical Research Network (UKCRN) 4778.
The trial protocol has been published. 84
Summary of changes to the project protocol
The following changes were made to the original protocol after it was funded. The first five changes were all made before the trial started, the sixth was included a priori in the trial analysis plan, and the seventh was made during recruitment. All were approved by the Trial Steering Committee.
-
Patients who were referred by a primary care health professional or self-referred to physiotherapy were also included, rather than only those referred by a GP.
-
Needing physiotherapy for non-MSK problems was added as an exclusion criterion.
-
Sex was included as a minimisation factor in the randomisation procedure.
-
Analysis of health status in order to calculate quality-adjusted life-years (QALYs) was based on the EQ-5D measure rather than the Short Form questionnaire-6 Dimensions (SF-6D) measure derived from the SF-36v2.
-
The primary outcome was originally described as the clinical outcome assessed using two measures: the SF-36v2 PCS and the MYMOP. However, after discussion with the TSC it was agreed that having two primary outcomes could lead to problems in interpretation of findings. Therefore, the SF-36v2 (as the better established measure) was designated as the primary outcome and the MYMOP as an important secondary outcome. Wording was changed to clarify that the equivalence limit for the PCS was based on 2 points rather than 0.2 SDs.
-
The recruitment rate was defined as the percentage of patients consenting to participate from those responding to the initial letter to confirm that they did want physiotherapy. Patients who did not respond to the initial invitation or reminder letters from the physiotherapy service, despite reminders, were taken off the physiotherapy waiting lists and were defined as not eligible for the study.
-
Because of lower than anticipated follow-up rates at 6 months in patients recruited in the run-in phase it was agreed to continue inviting patients to the main trial until 2000 had given consent to participate, recognising that the final total recruited would be about 2143 patients because of the lag between invitation and consent. This sample size would provide the target sample size of 1500 patients completing questionnaires at 6 months, even if only 70% were followed up successfully.
Chapter 3 Randomised controlled trial: results
Generalisability
Patients were recruited between July 2009 and December 2009, and followed up until June 2010.
We considered several patient characteristics in order to evaluate the generalisability of this study: sex, age, deprivation (as measured in quintiles based on postcode), PCT and body region of MSK problem.
We compared the characteristics of patients in two groups: (a) those who were ineligible for the study on the basis of their referral letter (Table 4) or because they did not confirm that they wanted physiotherapy and (b) those who were eligible.
| Reason | No. (%) |
|---|---|
| < 18 years | 180 (13) |
| Hearing problems | 27 (2) |
| Non-English language | 27 (2) |
| Non-MSK problem | 166 (12) |
| Needs domiciliary physiotherapy | 197 (14) |
| Very urgent | 376 (26) |
| Postoperative | 105 (7) |
| In trial already | 178 (13) |
| Problem unsuitable for telephone consult | 135 (9) |
| Problem unsuitable for physiotherapy | 12 (1) |
| Patient unsuitable for telephone consult | 41 (3) |
| Other (reason stated) | 9 (1) |
| Other (reason not stated) | 89 (6) |
Among the eligible patients, we also compared those who did or did not consent to participate and were randomised to participate in the trial.
Obvious differences between those patients who were or were not eligible, reflecting the eligibility criteria, were observed for the site of MSK problem for which patients were referred to physiotherapy. A higher proportion of patients in Bristol and a lower proportion in Somerset were deemed eligible. More women were referred than men, and slightly fewer men were eligible. Patients who were eligible were slightly older than those whose who were ineligible (Table 5).
| Patient characteristics | Wanted physiotherapy and eligible: n = 6870 (100%) | Randomisation: n = 4523 (65.84%) | ||||
|---|---|---|---|---|---|---|
| No: n = 2347 (34.16%) | Yes:a n = 4523 (65.84%) | Test | Not randomised: n = 2267 (50.12%) | Randomised:a n = 2256 (49.88%) | Test | |
| Sex (%) | ||||||
| Female | 56.97 | 59.74 | x12 = 4.90, p = 0.03 | 59.91 | 59.44 | x12 = 0.10, p = 0.75 |
| Male | 43.03 | 40.26 | 40.09 | 40.56 | ||
| Median age (years) (IQR) | 46.0 (31.0 to 62.0) | 50.1 (37.3 to 63.0) | Rank-sum, z = −6.79, p < 0.001 | 52.00 (38.0 to 65.0) | 48.30 (36.5 to 61.3) | Rank-sum, z = 5.64, p < 0.001 |
| Deprivation quintile (5 = most deprived) (%) | ||||||
| 1 | 8.76 | 10.24 | x42 = 14.43, p = 0.01 | 10.31 | 10.32 | x42 = 7.16, p = 0.13 |
| 2 | 19.72 | 20.06 | 20.13 | 20.04 | ||
| 3 | 25.51 | 27.00 | 25.84 | 28.37 | ||
| 4 | 22.04 | 22.53 | 22.17 | 22.58 | ||
| 5 | 23.96 | 20.18 | 21.55 | 18.70 | ||
| PCT (%) | ||||||
| Bristol | 26.5 | 31.70 | x32 = 42.16, p < 0.001 | 30.14 | 21.55 | x32 = 5.29, p = 0.15 |
| Somerset | 29.19 | 23.17 | 23.79 | 33.29 | ||
| Cheshire | 21.39 | 23.86 | 24.39 | 23.36 | ||
| Stoke | 22.92 | 21.27 | 21.68 | 20.57 | ||
| Site of problem for which referred (%) | ||||||
| Cervica | 8.73 | 12.74 | x82 = 582.08, p < 0.001 | 13.06 | 12.15 | x72 = 3.78, p = 0.80 |
| Thoracic | 1.67 | 2.17 | 2.14 | 2.17 | ||
| Lumbar | 25.49 | 27.8 | 28.25 | 27.41 | ||
| Upper limb | 19.03 | 23.38 | 23.37 | 23.37 | ||
| Lower limb | 26.56 | 29.09 | 28.34 | 29.93 | ||
| Widespread pain | 0.68 | 0.58 | 0.47 | 0.67 | ||
| Multiple MSK | 4.32 | 3.76 | 3.90 | 3.64 | ||
| Other MSK | 6.46 | 0.49 | 0.47 | 0.67 | ||
| Non MSK | 7.06 | 0.00 | NA | NA | ||
Considering the eligible patients, those patients who were randomised were slightly younger, on average, than those who were not. Apart from this, there were few differences between those who were randomised and those who were not (Table 5).
Patients from the least deprived areas (quintile 1) were under-represented in this study in comparison with the national population. Patients who were from the most deprived areas were slightly less likely to be eligible or to consent to participate in the study and be randomised.
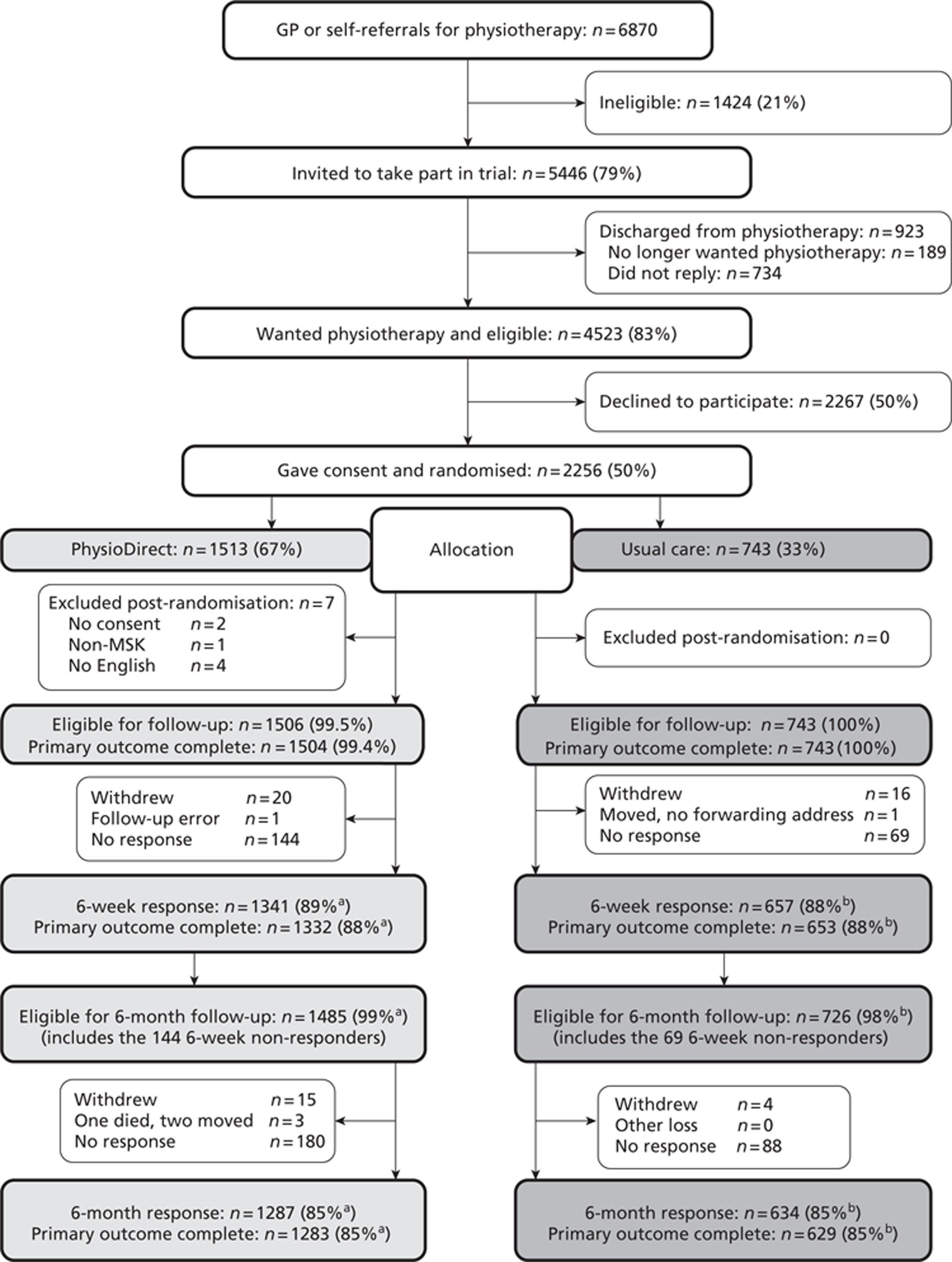
The recruitment rate, defined as the percentage of patients consenting to participate from those who were eligible (responding to the invitation letter confirming that they did want physiotherapy), was 2256/4523 or 50% (Figure 2).
FIGURE 2.
Consolidated Standards of Reporting Trials (CONSORT) diagram: flow of participants through the trial, a. Per cent is expressed as n/1506 × 100. b, Per cent is expressed as n/743 × 100.
Baseline comparability of randomised groups
No marked difference was observed between patients randomised to the two arms of the trial in terms of demographic, stratification/minimisation or outcome variables at baseline (Table 6). At baseline, 59% of participants in the trial were female, 96% were white, the majority were in employment, and patients from the least deprived areas were under-represented. Almost everyone had access to a telephone and the vast majority had access to a car (Table 7).
| Patient baseline characteristics | Randomised patients: n = 2249a (100%) | |
|---|---|---|
| Usual care: n = 743 (33.04%) | PhysioDirect: n = 1506 (66.96%) | |
| Sexb (%) | ||
| Female | 58.95 | 59.56 |
| Male | 41.05 | 40.44 |
| Median ageb (years) (IQR) | 48.18 (36.01 to 61.93) | 48.27 (36.72 to 61.01) |
| Ethnicity (%) | ||
| White | 95.79 | 96.71 |
| Black | 1.09 | 0.87 |
| Asian | 1.63 | 1.01 |
| Dual/mixed | 0.95 | 0.74 |
| Chinese | 0.14 | 0.13 |
| Other | 0.41 | 0.54 |
| Deprivation quintile (5 = most deprived) (%) | ||
| 1 | 9.92 | 10.57 |
| 2 | 20.95 | 19.61 |
| 3 | 29.33 | 27.96 |
| 4 | 21.79 | 22.88 |
| 5 | 18.02 | 18.98 |
| Employment status (%) | ||
| Employed | 57.05 | 62.08 |
| Unemployed | 6.16 | 4.70 |
| Student | 2.60 | 2.55 |
| Ill/disabled | 7.11 | 5.57 |
| Retired | 22.02 | 20.40 |
| Not working/other | 5.06 | 4.70 |
| Profession (%) | ||
| Administrative | 16.91 | 13.54 |
| Technical | 10.73 | 11.72 |
| Elementary | 8.78 | 10.21 |
| Manager | 10.57 | 9.34 |
| Personal services | 7.32 | 9.34 |
| Operatives | 5.53 | 5.62 |
| Professional | 17.56 | 17.97 |
| Customer services | 11.22 | 11.24 |
| Skilled trade | 11.38 | 11.01 |
| Patient baseline characteristics | Randomised patients: n = 2249a (100%) | |
|---|---|---|
| Usual care: n = 743 (33.04%) | PhysioDirect: n = 1506 (66.96%) | |
| Site of MSK problemb (%) | ||
| Cervical | 11.99 | 12.28 |
| Thoracic | 1.75 | 2.32 |
| Lumbar | 27.36 | 27.36 |
| Upper limb | 23.45 | 23.31 |
| Lower limb | 30.32 | 29.88 |
| Widespread pain | 0.94 | 0.53 |
| Multiple MSK | 3.64 | 3.65 |
| Other MSK | 0.54 | 0.66 |
| PCTb (%) | ||
| Bristol | 33.78 | 33.13 |
| Somerset | 22.21 | 23.11 |
| Cheshire | 23.42 | 23.44 |
| Stoke | 20.59 | 20.32 |
| Physiotherapy preference (%) | ||
| Usual care | 32.97 | 30.71 |
| PhysioDirect | 35.29 | 35.57 |
| No preference | 31.74 | 33.72 |
| Median time off work (days) (IQR) | 0 (0-5) | 0 (0-5) |
| English, native speaker (%) | ||
| No | 2.88 | 3.64 |
| Yes | 97.12 | 96.36 |
| Telephone (%) | ||
| No | 0.54 | 0.93 |
| Yes | 99.46 | 99.07 |
| Car (%) | ||
| No | 17.12 | 16.72 |
| Yes | 82.88 | 83.28 |
The most common reasons for referral were lower limb problems (including hip and knee problems), lumbar problems and upper limb problems (including shoulder). Participants from each of the PCTs were reasonably well represented, with Bristol contributing the highest proportion. People were fairly evenly split in their preference for future care between usual care, PhysioDirect and having no preference (see Table 7). There were no important differences in outcome measures assessed at baseline (Table 8).
| Patient outcome measures at baseline | Randomised patients: n = 2249a (100%) | |
|---|---|---|
| Usual care: n = 743 (33.04%) | PhysioDirect: n = 1506 (66.96%) | |
| SF-36v2 PCS | ||
| Mean (SD) | 37.72 (8.63) | 36.81 (8.88) |
| Median (IQR) | 37.59 (31.39 to 43.93) | 36.95 (30.44 to 43.16) |
| SF-36v2 MCS | ||
| Mean (SD) | 45.66 (13.29) | 46.07 (12.65) |
| Median (IQR) | 47.86 (36.24 to 56.55) | 48.46 (36.51 to 56.52) |
| MYMOP | ||
| Mean (SD) | 3.80 (0.99) | 3.84 (0.99) |
| Median (IQR) | 3.75 (3.25 to 4.50) | 4.00 (3.25 to 4.50) |
| EQ-5D | ||
| Mean (SD) | 0.56 (0.29) | 0.53 (0.30) |
| Median (IQR) | 0.69 (0.43 to 0.76) | 0.69 (0.23 to 0.76) |
Loss to follow-up
Primary outcome data were collected for 88% (1985/2249) of patients at the 6 weeks' follow-up time point and 85% (1912/2249) of patients at the primary outcome time point of 6 months, with no difference between trial arms. Details of the relationship between loss to follow-up and patient characteristics are given in Appendix 1.
Several differences were observed between patients for whom the primary outcome measure (SF36v2 PCS at 6 months) was collected and those for whom it was missing, although these differences were similar for both trial arms (see Appendix 1, Tables 62 and 63). With regards to the demographic characteristics, patients with missing data tended to be younger, unemployed and to come from more deprived areas. There was also an association between job type and missing primary outcome data (see Appendix 1, Table 62).
As described in Chapter 1 (see Summary of changes to the project protocol), we obtained ethical permission for a protocol amendment to continue inviting patients to participate until 2000 patients had been recruited, in order to ensure that we reached our target of 1500 patients for analysis. Because of the lag time between initial approach to patients and recruitment, and because the final follow-up rate was higher than assumed, the total number of patients available for analysis (1912) was higher than originally planned (1500).
Process of care
In the context of this trial it is most helpful to describe the types of care received by participants in each arm of the trial, before describing the primary and secondary outcomes. This will aid interpretation of these outcomes.
Number of telephone and face-to-face consultations
Patients in the PhysioDirect arm were offered an initial telephone call to assess their need and priority for a face-to-face appointment. Of all patients in the PhysioDirect arm, 1281 (85%) contacted the service at least once, with 97% (1239/1281) of these having an initial telephone call and 3% (42) having an initial face-to-face appointment. Of those having an initial telephone assessment, 47% (586/1239) were managed entirely on the telephone with the remainder having at least one face-to-face consultation. Of all patients in the PhysioDirect arm, only 46% (695/1506) eventually had any face-to-face appointments (Table 9).
| Type of appointment and time point | No. of patients (%) with different types of consultation/appointment | |
|---|---|---|
| Usual care: n = 743 | PhysioDirect: n = 1506 | |
| No appointments of any type | ||
| 6 weeks | 371 (50) | 292 (19) |
| 6 months | 125 (17) | 225 (15) |
| Only face-to-face appointmentsa | ||
| 6 weeks | 341 (46) | 20 (1) |
| 6 months | 540 (73) | 35 (2) |
| Only telephone consultations | ||
| 6 weeks | 7 (1) | 767 (51) |
| 6 months | 4 (0.5) | 586 (39) |
| Telephone and face to face | ||
| 6 weeks | 23 (3) | 427 (28) |
| 6 months | 73 (10) | 660 (44) |
| Home visit only | ||
| 6 weeks | 1 (0.13) | 0 (0) |
| 6 months | 1 (0.1) | 0 (0) |
| Odds of having at least one appointment or consultation, irrespective of type, OR (95% CI)b | ||
| 6 weeks | 4.49 (3.68 to 5.49), p < 0.001 | |
| 6 months | 1.13 (0.89 to 1.45), p = 0.32 | |
By the time of the first follow-up time point at 6 weeks after randomisation, 81% of patients in the PhysioDirect arm had received some sort of assessment appointment or consultation, compared with only 50% of those in the usual-care arm.
There is strong evidence that PhysioDirect greatly increases the odds of having at least one appointment or consultation (of any type) by 6 weeks [adjusted odds ratio (OR) 4.49 (95% CI 3.68 to 5.49); p < 0.001].
The following table shows the number of consultations that patients received in each arm of the trial. Over the 6-month follow-up period, patients in the PhysioDirect arm had significantly fewer face-to-face consultations, and fewer consultations in total (including telephone and face-to-face consultations), compared with those in the usual-care arm (Table 10).
| Consultations | Period | Usual care: n = 743 | PhysioDirect: n = 1506 | IRRa | 95% CI | p-value |
|---|---|---|---|---|---|---|
| Face-to-face, no. arranged:b mean (SD); median (IQR) | 6 weeks | 0.89 (1.13); 0 (0 to 2) | 0.58 (1.08); 0 (0 to 1) | 0.64 | 0.56 to 0.73 | < 0.001 |
| 6 months | 3.11 (2.63); 3 (1 to 4) | 1.91 (2.72); 0 (0 to 3) | 0.59 | 0.53 to 0.65 | < 0.001 | |
| Telephone: mean (SD); median (IQR) | 6 weeks | 0.04 (0.22); 0 (0 to 0) | 0.87 (0.55); 1 (1 to 1) | 19.79 | 13.85 to 28.28 | < 0.001 |
| 6 months | 0.13 (0.44); 0 (0 to 0) | 0.96 (0.63); 1 (1 to 1) | 7.34 | 5.87 to 9.17 | < 0.001 | |
| Home visits: mean (SD); median (IQR) | 6 weeks | 0.001 (0.04); 0 (0 to 0) | 0.002 (0.04); 0 (0 to 0) | 1.48 | 0.15 to 14.25 | 0.73 |
| 6 months | 0.004 (0.06); 0 (0 to 0) | 0.003 (0.06); 0 (0 to 0) | 0.82 | 0.20 to 3.45 | 0.79 | |
| Total consultations: mean (SD); median (IQR) | 6 weeks | 0.94 (1.17); 1 (0 to 2) | 1.46 (1.29); 1 (1 to 2) | 1.53 | 1.37 to 1.70 | < 0.001 |
| 6 months | 3.25 (2.70); 3 (1 to 5) | 2.87 (2.94); 1 (1 to 5) | 0.87 | 0.80 to 0.94 | 0.001 |
Table 11 below details the distribution of the number of face-to-face consultations experienced by patients in each arm. This is further divided into all of those patients, or only those patients who had any face-to-face consultations. For those who did have any face-to-face consultations, a ‘course of treatment’ was a mean number of face-to-face consultations of 3.77 (95% CI 3.57 to 3.96) and 4.13 (95% CI 3.94 to 4.33) in the usual care and PhysioDirect arms, respectively. The number of appointments was skewed with a median number of face-to-face consultations of 3 [interquartile range (IQR) 2 to 5] and 4 (IQR 2 to 6) in the usual care and PhysioDirect arms, respectively.
| No. of appointments | No. of patients | |||||||
|---|---|---|---|---|---|---|---|---|
| Face-to-face appointments | Face-to-face appointments in those who had any face-to-face appointments | |||||||
| PhysioDirect | Usual care | PhysioDirect | Usual care | |||||
| n | % of patients | n | % of patients | n | % of patients | n | % of patients | |
| 0 | 811 | (53.9) | 130 | (17.5) | ||||
| 1 | 97 | (6.4) | 99 | (13.3) | 97 | (14) | 99 | (16.2) |
| 2 | 108 | (7.2) | 110 | (14.8) | 108 | (15.5) | 110 | (17.9) |
| 3 | 136 | (9) | 123 | (16.6) | 136 | (9.6) | 123 | (20.1) |
| 4 | 98 | (6.5) | 96 | (12.9) | 98 | (14.1) | 96 | (15.7) |
| 5 | 78 | (5.2) | 70 | (9.4) | 78 | (11.2) | 70 | (11.4) |
| 6 | 70 | (4.7) | 45 | (6.1) | 70 | (10.1) | 45 | (7.3) |
| 7 | 40 | (2.7) | 24 | (3.2) | 40 | (5.8) | 24 | (3.9) |
| 8 | 23 | (1.5) | 17 | (2.3) | 23 | (3.3) | 17 | (2.8) |
| 9 | 13 | (0.9) | 10 | (1.4) | 13 | (1.9) | 10 | (1.6) |
| 10 | 11 | (0.7) | 4 | (0.5) | 11 | (1.6) | 4 | (0.7) |
| 11 | 8 | (0.5) | 8 | (1.1) | 8 | (1.2) | 8 | (1.3) |
| 12 | 5 | (0.3) | 1 | (0.1) | 5 | (0.7) | 1 | (0.2) |
| 13 | 4 | (0.3) | 3 | (0.4) | 4 | (0.6) | 3 | (0.5) |
| 14 | 2 | (0.1) | 2 | (0.3) | 2 | (0.3) | 2 | (0.3) |
| 15 | 1 | (0.1) | 0 | (0) | 1 | (0.1) | 0 | (0) |
| 16 | 1 | (0.1) | 0 | (0) | 1 | (0.1) | 0 | (0) |
| 17 | 0 | (0) | 1 | (0.1) | 0 | (0) | 1 | (0.2) |
| Total | 1506 | (100) | 743 | (100) | 695 | (100) | 613 | (100) |
Length of consultations
The mean and median lengths of the face-to-face consultations in minutes were 34.1 (SD 11.3) and 30 (IQR 30 to 40), respectively. Telephone consultations had a mean and median length of 23.9 (SD 12.2) and 23 (IQR 17 to 30) minutes, respectively.
The mean length of telephone calls in the PhysioDirect service was monitored throughout the trial and it was observed that the mean duration of calls decreased during the study. This is illustrated by Figure 3. The figure shows the mean duration of telephone calls, from the first week of calls in each site. However, as the study progressed an increasing proportion of calls were follow-up calls, which tended to be shorter.
FIGURE 3.
Mean duration of first telephone calls over time: all calls.

Figure 4 shows the same analysis restricted to first calls only, and confirms that call duration became shorter over the period of the trial.
FIGURE 4.
Mean duration of first telephone calls over time: first calls only.
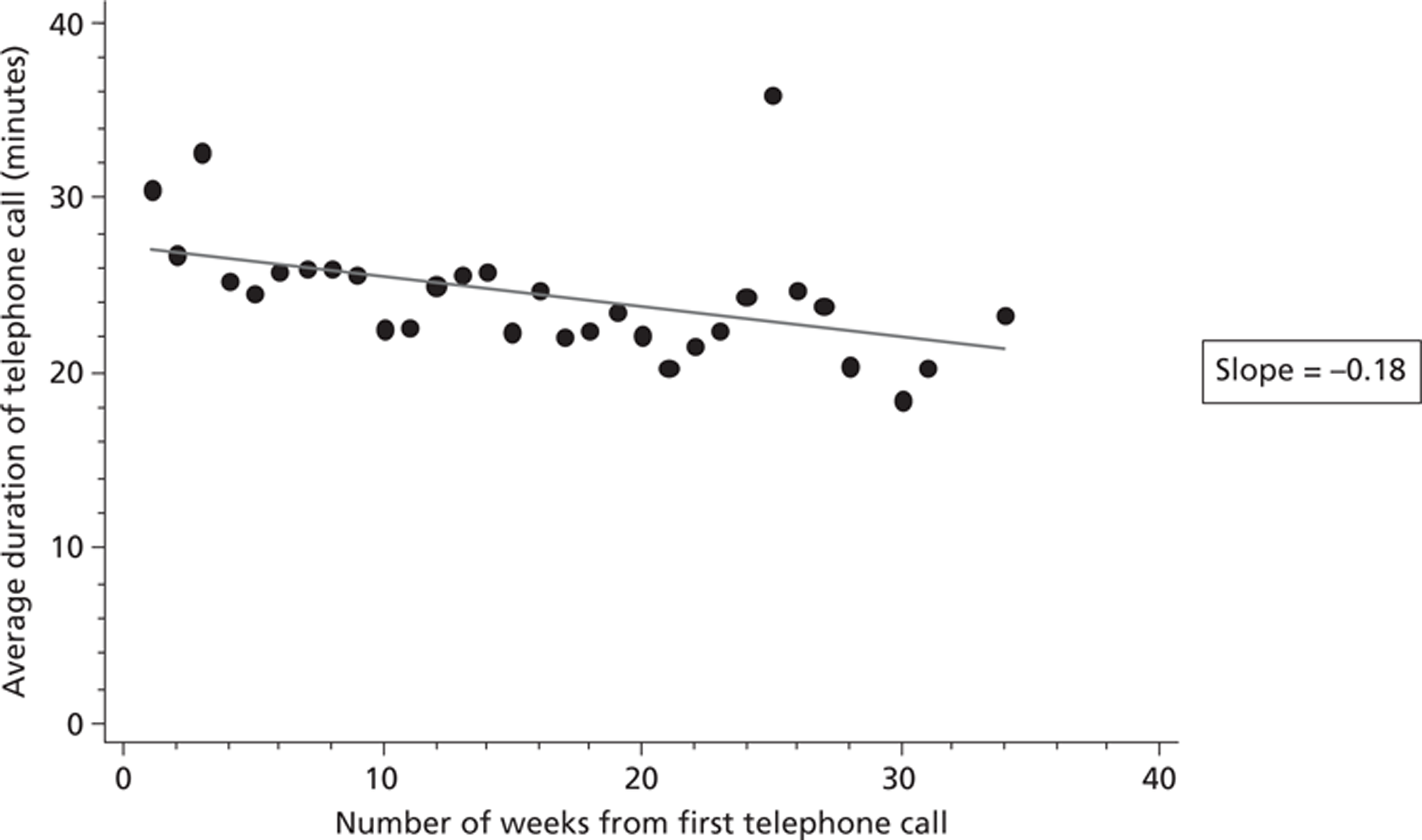
Did not attend rates
The rate of failed face-to-face appointments (DNA rate) at 6 months was measured in two different ways: (1) as an overall rate, namely the ratio of the number of unattended appointments over that of all appointments that had been scheduled; and (2) as an individual patient rate, with the DNA rate calculated for each patient as an incidence rate ratio (IRR) adjusted for age, sex and primary outcome at baseline and PCT.
The overall rate was substantially the same in the two trial arms, being 262/2310 (11%) for usual care and 279/2873 (10%) for PhysioDirect. The individual DNA rates had median 0 for both arms, with means of 0.12 for usual care and 0.09 for PhysioDirect. The effect estimated for PhysioDirect on the DNA rate (adjusting for age, sex, primary outcome at baseline and PCT) was 0.55 (95% CI 0.41 to 0.73) with p < 0.001. Therefore, there was strong evidence of PhysioDirect being associated with an average 45% reduction in individual patient DNA rate.
Waiting times
Waiting time to the first consultation, be it a telephone or face-to-face consultation, was calculated for each patient from both the referral date and the randomisation date (Table 12). The possible effect of PhysioDirect on each of those waiting times was estimated through Accelerated Failure Time analysis, adjusting for PCS at baseline, age, sex, main referral problem and PCT. Both in the referral and the randomisation case there was strong evidence (p < 0.001) of PhysioDirect substantially decreasing the waiting time, a reduction of up to 68%. This equates to a shorter wait of 7 days from randomisation. The median delay introduced by the need to obtain consent in the trial was 12 days (this is the difference between the date the referral was received and the date written patient consent was received).
| Date from | Waiting time (days): median (IQR) | Accelerated failure time analysisa | |||
|---|---|---|---|---|---|
| Usual care: n = 618 | PhysioDirect: n = 1281 | Arm–time ratio | 95% CI | p-value | |
| Referral | 48 (32 to 66) | 19 (13 to 32) | 0.43 | 0.41 to 0.46 | 0.001 |
| Randomisation | 34 (20 to 55) | 7 (4 to 15) | 0.32 | 0.29 to 0.35 | 0.001 |
One aim of PhysioDirect is to filter out people who will not benefit from face-to-face care, so that those who do need it can be seen more quickly. There was no evidence that the waiting time to first face-to-face appointment was different between the PhysioDirect and the usual-care arms (Table 13).
| Date from | Waiting time (days): median (IQR) | Accelerated failure time analysisa | |||
|---|---|---|---|---|---|
| Usual care: n = 613 | PhysioDirect: n = 695 | Arm–time ratio | 95% CI | p-value | |
| Randomisation | 35 (20 to 55) | 30 (17 to 55) | 0.95 | 0.88 to 1.03 | 0.25 |
Characteristics of patients seen in face-to-face appointments in the PhysioDirect arm
In an exploratory analysis, we compared the characteristics of patients in the PhysioDirect arm who were then seen in face-to-face appointments following initial telephone assessment with those who were managed entirely on the telephone (Table 14). There were no differences in terms of age or sex. However, there were slight differences according to site of MSK problem, and patients managed entirely on the telephone had slightly higher SF-36v2 PCS scores at baseline than those seen face to face [37.6 and 35.4, respectively, difference in means 2.36 (95% CI 1.38 to 3.33)].
| Patient baseline characteristics | Whether or not seen in face-to-face consultation: n = 1281a (100%) | |
|---|---|---|
| Telephone only: n = 586 (45.7%) | Telephone and face to face: n = 695 (54.3%) | |
| Referral problem, n (%) | ||
| Cervical | 64 (10.9) | 91 (13.1) |
| Thoracic | 11 (1.9) | 15 (2.2) |
| Lumbar | 165 (28.2) | 179 (25.8) |
| Upper limb | 131 (22.5) | 176 (25.3) |
| Lower limb | 195 (33.3) | 195 (28.0) |
| Widespread pain | 1 (0.2) | 6 (0.9) |
| Multiple MSK | 16 (2.7) | 31 (4.5) |
| Other MSK | 3 (0.5) | 2 (0.3) |
Primary outcome analysis
No evidence was found of a difference in the PCS of the SF-36v2 between the two trial arms at either the 6-week follow-up time point or the primary time point of 6 months, having adjusted for baseline outcome measure, sex, age, main referral problem and the patient's PCT (Table 15). The 95% confidence limits support the hypothesis of equivalence in terms of clinical outcome between the trial arms. Figure 5 illustrates the difference in means and confidence limits in relation to the observed variation in the primary outcome (SD) and the pre-specified equivalence limits of 2 points on the SF-36v2 PCS.
| Time point | SF-36v2 PCS | ||||||
|---|---|---|---|---|---|---|---|
| Usual care | PhysioDirect | Difference in meansa | 95% CI | p-value | |||
| Mean (SD) | n | Mean (SD) | n | ||||
| Baseline | 37.72 (8.63) | 743 | 36.81 (8.88) | 1504 | NA | NA | NA |
| 6 weeks | 41.81 (10.30) | 653 | 41.57 (10.26) | 1332 | 0.42 | −0.28 to 1.12 | 0.24 |
| 6 months | 44.18 (10.84) | 629 | 43.50 (10.94) | 1283 | −0.01 | −0.80 to 0.79 | 0.99 |
FIGURE 5.
Difference in means in relation to equivalence limits.
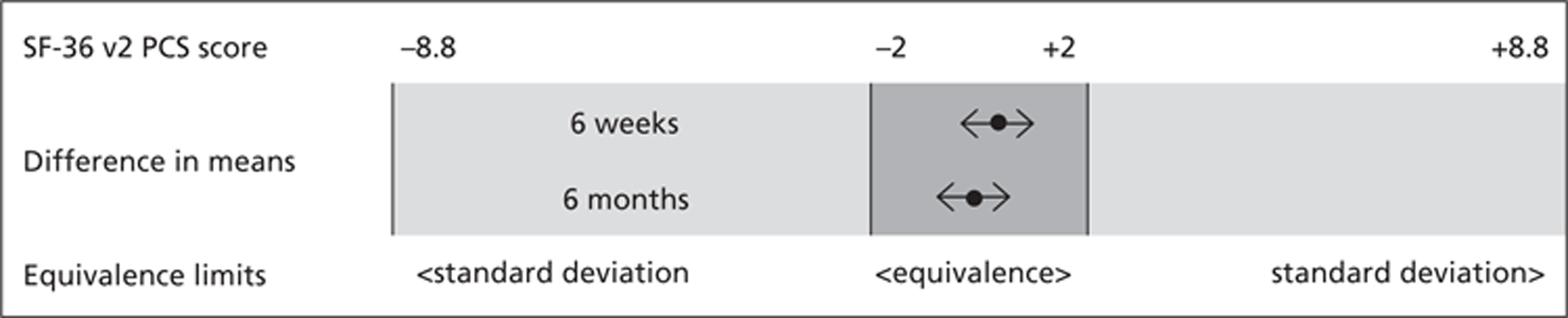
A repeated measure analysis was conducted to estimate possible variations in treatment effect on SF-36v2 PCS at different points in time, namely at 6 weeks and 6 months. The analysis showed no evidence of such variations, with an arm–time interaction for SF-36v2 PCS adjusted for outcome baseline, sex, age, referral problem and PCT of 0.001 (95% CI −0.0041 to 0.006; p = 0.76).
Secondary analyses
Sensitivity analyses
Adjustment for baseline imbalances
Some imbalance at baseline was observed for the employment status variable, but including it as a covariate in the ANCOVA did not change the conclusion of the original primary analysis, namely no evidence of any difference between PhysioDirect and usual care on SF-36v2 PCS at 6 months (Table 16).
| Additional adjustment | Arm difference: SF-36v2 PCS at 6 monthsa | 95% CI | p-value |
|---|---|---|---|
| None | −0.01 | −0.80 to 0.79 | 0.99 |
| Employment status | −0.24 | −1.01 to 0.54 | 0.55 |
Effect of missing primary outcome data
Although only about 15% of the primary outcome data were missing in each trial arm, multiple imputations were conducted to determine what effect those data might have had on the primary analysis. The conclusion that there was no evidence of difference between the trial arms was the same with or without multiple imputations of missing data (Table 17).
| Multiple imputations | Arm difference: SF-36v2 PCS at 6 monthsa | 95% CI | p-value |
|---|---|---|---|
| 0 | −0.01 | −0.80 to 0.79 | 0.99 |
| 20 | −0.03 | −0.76 to 0.82 | 0.94 |
Clustering effects
The possibility of clustering effects due to patients belonging to the same PCT or GP practice was explored through multilevel models with random effects attributed to those clusters. Each one of the models was compared with the original one (fixed effects) for its goodness of fit relative to the data by means of a log–likelihood ratio test or through its Akaike information criterion (AIC, lower value corresponding to a better fit), which accounts both for likelihood and parsimony of the model.
The only model for which there was some evidence of a better fit to the data than the one adopted for the primary analysis was a model accounting for a PCT clustering effect, but it maintained the conclusions of the original model (i.e. equivalence between PhysioDirect and usual care) and the clustering effect appeared to be very modest as indicated by an intracluster correlation (ICC) of 0.005 (Table 18).
| Model | Arm difference: SF-36v2 PCS at 6 monthsa | 95% CI | p-value | ICC | Likelihood ratio test vs linear (p-value) | AIC |
|---|---|---|---|---|---|---|
| FE | −0.01 | −0.80 to 0.79 | 0.99 | 0 | 1 | 13,528.62 |
| FE + RE intercept for: PCT | −0.003 | −0.80 to 0.79 | 0.99 | 0.005 | 0.01 | 13,533.55 |
| FE + RE intercept and slope for: PCT | −0.01 | −0.80 to 0.78 | 0.98 | Intercept: PCT < 0.001 Slope: baseline PCS < 0.001 Age < 0.001 | 0.11 | 13,534.29 |
| FE + RE intercept for: GP practice | −0.01 | −0.80 to 0.78 | 0.98 | 0.004 | 0.29 | 13,530.30 |
| FE + RE intercept and slope for: GP practice | −0.01 | −0.80 to 0.78 | 0.98 | Intercept: practice = 0.002 Slope: baseline PCS < 0.001 Age < 0.001 | 0.95 | 13,534.29 |
| FE + RE intercept for: PCT and GP practice | −0.01 | −0.80 to 0.78 | 0.98 | Intercept: PCT = 0.005 Practice = 0.005 | 0.07 | 13,535.00 |
| FE + RE intercept and slope for: PCT and GP practice | −0.01 | −0.80 to 0.78 | 0.97 | Intercept: PCT < 0.001 Practice = 0.002 Slope: baseline PCS < 0.001 Age < 0.001 | 0.35 | 13,541.72 |
Secondary outcomes
Clinical outcomes
A similar regression analysis as the primary one (same covariate adjustments) was conducted using a set of secondary outcomes, representing different ways of assessing health status. These were:
-
a patient-generated measure, focusing on specific symptoms (MYMOP)
-
a broad measure of health-related quality of life (EQ-5D) to be used in the economic analysis
-
a single question about the extent to which the main problem for which the person had been referred to physiotherapy had improved (global improvement score)
-
a measure of whether or not the individual had ‘responded to treatment’ using the OMERACT-OARSI criteria, based on a composite measure including physical function, pain and improvement in the main problem.
The results of the analysis of MYMOP showed a statistically significant difference between the trial arms at 6 weeks but this difference was very small and the CIs fell within the limits of equivalence that we specified for the MYMOP measure a priori (0.5 points). Both the global improvement score and the analysis according to the OMERACT-OARSI criteria also suggested that patients in the PhysioDirect arm were more likely to have improved to a greater extent by 6 weeks than those in the usual-care arm. The EQ-5D showed a slight trend towards benefit from PhysioDirect at 6 weeks but the difference was small and may well have been due to chance.
It is notable that all five measures of clinical outcome (the four secondary outcomes in Table 19 and the primary outcome SF-36v2 PCS) showed a similar pattern of slightly better scores from PhysioDirect at 6 weeks, with minimal difference after 6 months' follow-up.
| Outcome (higher value is better outcome except where specified) | Mean (SD) or percentage, sample size | Regression analysisa | |||||
|---|---|---|---|---|---|---|---|
| Usual care | PhysioDirect | Difference in means | |||||
| Mean (SD) | n | Mean (SD) | n | 95% CI | p-value | ||
| MYMOP (lower value is better outcome) | |||||||
| Baseline | 3.80 (0.99) | 743 | 3.84 (0.99) | 1504 | |||
| 6 Weeks | 2.92 (1.21) | 561 | 2.76 (1.28) | 1101 | −0.19 | −0.30 to −0.07 | 0.001 |
| 6 months | 2.40 (1.38) | 518 | 2.40 (1.43) | 1033 | −0.02 | −0.16 to 0.11 | 0.73 |
| EQ-5D | |||||||
| Baseline | 0.56 (0.29) | 731 | 0.53 (0.30) | 1480 | |||
| 6 weeks | 0.64 (0.26) | 554 | 0.64 (0.27) | 1080 | 0.01 | −0.01 to 0.03 | 0.29 |
| 6 months | 0.69 (0.27) | 508 | 0.69 (0.27) | 1020 | 0.01 | −0.02 to 0.03 | 0.61 |
| Global improvement score | |||||||
| Baseline | NA | NA | NA | NA | NA | ||
| 6 weeks | 3.54 (1.19) | 552 | 3.69 (1.28) | 1089 | 0.15 | 0.02 to 0.28 | 0.02 |
| 6 months | 4.07 (1.40) | 501 | 4.01 (1.44) | 1001 | −0.08 | −0.23 to 0.08 | 0.32 |
| OMERACT-OARSI | |||||||
| Baseline | NA | NA | NA | NA | NA | ||
| 6 weeks | 22.6% | 124/550 | 28.2% | 306/1085 | 1.37 | 1.08 to 1.75 | 0.01 |
| 6 months | 38.6% | 197/510 | 41.8% | 430/1029 | 1.14 | 0.92 to 1.43 | 0.24 |
It should be pointed out that there is some dependence between measures in that two of the elements in the OMERACT-OARSI ‘response to treatment’ measure were based on improvements in scores on the ‘physical function’ and ‘pain’ scales from the SF-36 questionnaire, and the questions that make up these scales also contribute to the SF-36 PCS score, which is the primary outcome.
The following table (Table 20) shows the scores for each of the individual scales from the SF-36v2 measure, at both 6 weeks and 6 months. There is no evidence of difference between the trial arms on any measure, at either time point. This table also demonstrates that all of the measures improved over time in both arms of the trial.
| Outcome | Baseline | 6 weeks | 6 months | Regression analysisa | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Usual care | PhysioDirect | Usual care | PhysioDirect | Usual care | PhysioDirect | ||||||||||
| Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Arm difference | 95% CI | p-value | |
| PCS | 37.7 (8.6) | 743 | 36.8 (8.9) | 1504 | 41.8 (10.3) | 653 | 41.6 (10.3) | 1332 | 44.2 (10.8) | 629 | 43.5 (10.9) | 1283 | 0.42 | −0.28 to 1.12 | 0.24 |
| −0.01 | −0.79 to 0.78 | 0.98 | |||||||||||||
| MCS | 45.7 (13.3) | 743 | 46.1 (12.6) | 1504 | 48.7 (12.2) | 653 | 48.7 (12) | 1332 | 48.7 (11.8) | 629 | 49 (11.9) | 1283 | −0.03 | −0.88 to 0.82 | 0.94 |
| 0.11 | −0.83 to 1.05 | 0.82 | |||||||||||||
| Physical functioning | 39.9 (10.2) | 743 | 39.3 (10.4) | 1506 | 43.0 (10.8) | 656 | 43.0 (10.9) | 1338 | 45.2 (10.8) | 632 | 44.7 (11.2) | 1284 | 0.52 | −0.19 to 1.23 | 0.14 |
| 0.00 | −0.75 to 0.75 | 1.00 | |||||||||||||
| Role-physical | 37.4 (11.2) | 743 | 36.7 (10.9) | 1502 | 43.2 (11.6) | 655 | 43.0 (11.3) | 1336 | 45.5 (11.5) | 630 | 45.0 (11.5) | 1284 | 0.27 | −0.60 to 1.15 | 0.52 |
| −0.08 | −1.00 to 0.84 | 0.86 | |||||||||||||
| Bodily pain | 34.9 (8.2) | 743 | 34.6 (8.2) | 1506 | 41.1 (9.6) | 657 | 40.9 (9.9) | 1338 | 43.2 (10.5) | 632 | 43.1 (10.6) | 1284 | 0.06 | −0.68 to 0.80 | 0.89 |
| 0.04 | −0.81 to 0.90 | 0.93 | |||||||||||||
| General health | 45.1 (10.5) | 743 | 44.6 (10.7) | 1506 | 45.9 (10.5) | 657 | 45.3 (10.8) | 1338 | 46.1 (10.6) | 634 | 45.7 (11.1) | 1284 | −0.07 | −0.66 to 0.51 | 0.81 |
| −0.14 | −0.79 to 0.51 | 0.66 | |||||||||||||
| Vitality | 43.7 (10.6) | 743 | 43.4 (10.7) | 1506 | 46.3 (10.8) | 655 | 46.3 (10.8) | 1334 | 47.4 (10.5) | 632 | 47.0 (11.1) | 1283 | 0.35 | −0.40 to 1.11 | 0.35 |
| −0.23 | −1.05 to 0.60 | 0.59 | |||||||||||||
| Social functioning | 40.4 (12.8) | 743 | 39.8 (12.6) | 1504 | 45.1 (12.2) | 657 | 45.0 (12.4) | 1338 | 46.1 (12.0) | 632 | 46.2 (12.2) | 1284 | 0.25 | −0.69 to 1.18 | 0.58 |
| 0.34 | −0.61 to 1.30 | 0.48 | |||||||||||||
| Role-emotional | 42.1 (14.6) | 743 | 42.3 (14.3) | 1498 | 46.6 (12.7) | 655 | 46.2 (12.9) | 1334 | 47.1 (12.2) | 630 | 47.1 (12.4) | 1283 | −0.32 | −1.24 to 0.59 | 0.51 |
| −0.06 | −1.07 to 0.95 | 0.92 | |||||||||||||
| Mental health | 45.4 (11.7) | 743 | 45.8 (11.4) | 1506 | 47.9 (11.4) | 655 | 48.2 (11.2) | 1334 | 48.3 (11.44) | 632 | 48.7 (11.3) | 1283 | 0.24 | −0.55 to 1.02 | 0.57 |
| 0.18 | −0.67 to 1.04 | 0.72 | |||||||||||||
Time lost from work
No evidence was found of a difference between the two trial arms in time lost from work due either to the medical condition or to physiotherapy-related treatment provided through the trial (Table 21). This analysis included only patients who were in work.
| Owing to | Time off work and arm-time ratio | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Baseline to 6 weeks | Baseline to 6 months | ||||||||||||||||
| Usual care | PhysioDirect | Arm-time ratio | p-value | Usual care | PhysioDirect | Arm-time ratio | p-value | Usual care | PhysioDirect | Arm-time ratio | p-value | |||||||
| Mean (SD), median (IQR) | n | Mean (SD), median (IQR) | n | Mean (SD), median (IQR) | n | Mean (SD), median (IQR) | n | Mean (SD), median (IQR) | n | Mean (SD), median (IQR) | n | |||||||
| Condition (days) | 3.10 (7.72), 0 (0 to 2) | 395 | 3.00 (7.53), 0 (0 to 2) | 866 | −0.2, (−1.12 to 0.63) | 0.64 | 5.35 (15.22), 0 (0 to 2) | 253 | 4.39 (11.44), 0 (0 to 2) | 511 | −0.95, (−3.02 to 1.05) | 0.27 | 7.14 (22.24), 0 (0 to 2), | 200 | 7.01 (18.03), 0 (0 to 3) | 390 | 0.08, (−3.21 to 3.35) | 0.94 |
| Physiotherapy (hours) | NA | NA | NA | 0.40 (1.21), 0 (0 to 0) | 656 | 0.40 (2.35), 0 (0 to 0) | 1340 | −0.01 (−0.14 to 0.18) | 0.94 | 0.98 (2.80), 0 (0 to 0), | 598 | 0.95 (4.73), 0 (0 to 0) | 1211 | −0.04 (−0.37 to 0.33) | 0.85 | |||
Preference for future care
Patients' preference for the type of care they would prefer (usual care, PhysioDirect or having no preference) was recorded both at baseline and at 6 months from randomisation. Although none of the categories was particularly favoured at baseline in either arm, after 6 months usual care was the preferred choice for those patients allocated to the usual-care arm, whereas patients allocated to the PhysioDirect arm appeared almost split in their preference between usual care and PhysioDirect. An analysis of the possible effect on preference by the PhysioDirect intervention by means of multinomial logistic regression provided evidence that it substantially increases the odds of preferring PhysioDirect to indifference (Table 22). So, although, normally, patients at 6 months would prefer usual care, PhysioDirect can reduce that tendency in its own favour. This is illustrated by Figure 6.
| Preference | Percentages and multinomial logistic analysisa | ||||
|---|---|---|---|---|---|
| Baseline | 6 months | Risk rate ratio | |||
| Usual care (n = 731) | PhysioDirect (n = 1462) | Usual care (n = 485) | PhysioDirect (n = 985) | ||
| None | 31.74 | 33.72 | 22.47 | 17.77 | Ref. |
| Usual care | 32.97 | 30.71 | 50.52 | 42.34 | 1.10 (95% CI 0.82 to 1.48); p = 0.53 |
| PhysioDirect | 35.29 | 35.57 | 27.01 | 39.90 | 1.98 (95% CI 1.43 to 2.74); p < 0.001 |
FIGURE 6.
Preference for PhysioDirect or usual care. (a) Baseline. (b) At 6 months.
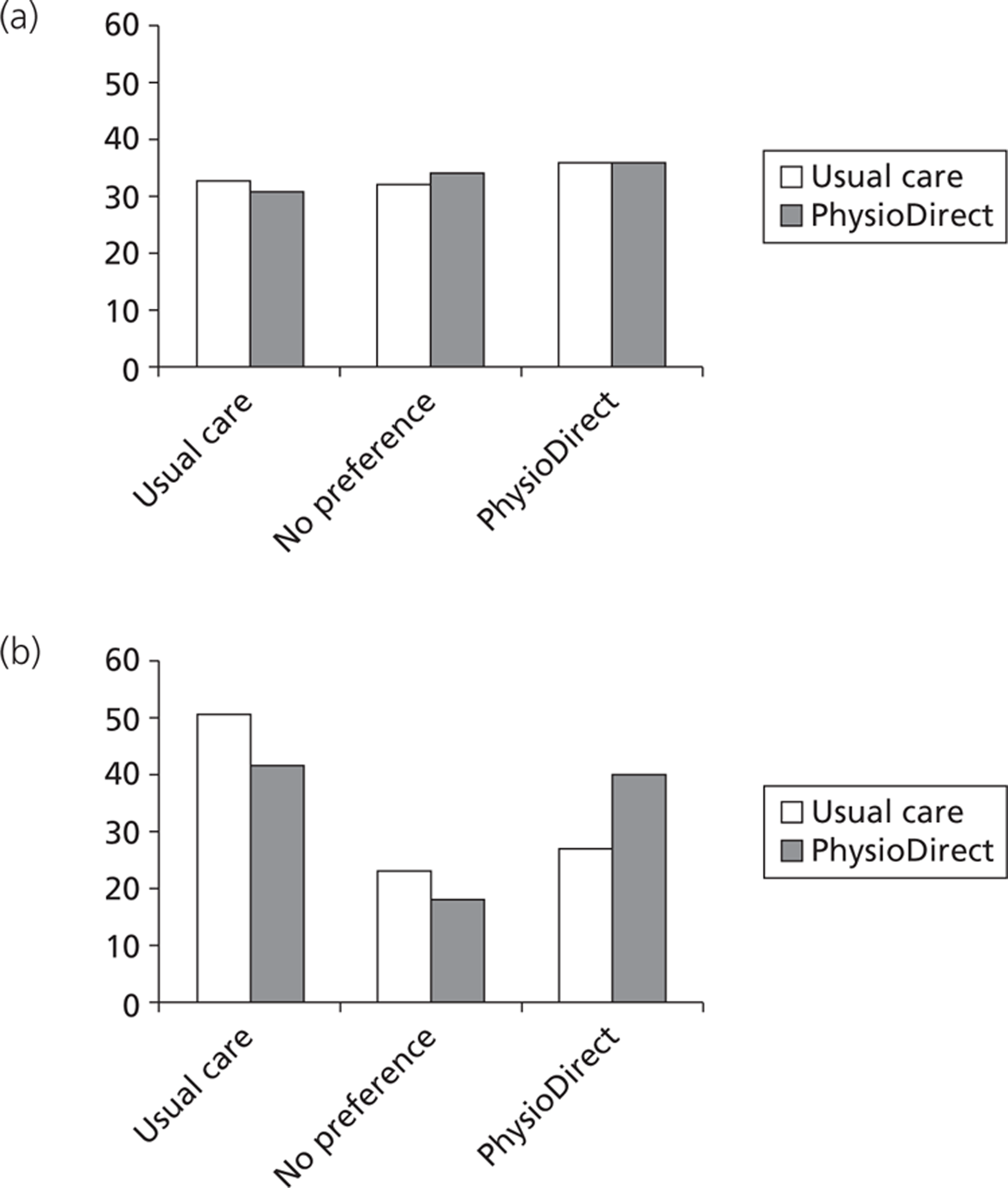
Patient satisfaction
Some evidence was found of slightly higher satisfaction for patients in usual care than for those in PhysioDirect with regards to both satisfaction with the quality of the consultation and overall satisfaction. No difference is evident with regards to satisfaction with access to the service (Table 23).
| Satisfaction | Time point | Arm | Regression analysisa | |||||
|---|---|---|---|---|---|---|---|---|
| Usual care | PhysioDirect | Arm difference | 95% CI | p-value | ||||
| Mean (SD) | n | Mean (SD) | n | |||||
| Consultationb | 6 weeks | 82.5 (17.6) | 378 | 77.6 (18.7) | 890 | −4.9 | −7.1 to −2.7 | < 0.001 |
| 6 months | 79.2 (19.2) | 368 | 75.7 (20.1) | 750 | −3.4 | −5.9 to 0.97 | 0.005 | |
| Accessa | 6 weeks | 71.4 (21.1) | 381 | 70.6 (22.3) | 869 | −0.8 | −3.4 to 1.7 | 0.502 |
| 6 months | 69.1 (20.8) | 367 | 69.2 (22.0) | 740 | 0.1 | −2.7 to 2.8 | 0.960 | |
| Overalla | 6 weeks | 83.7 (25.2) | 383 | 77.3 (27.4) | 885 | −6.5 | −9.6 to −3.4 | < 0.001 |
| 6 months | 79.7 (26.5) | 367 | 75.9 (28.3) | 739 | −3.8 | −7.3 to −0.3 | 0.031 | |
It is important to note that data presented in Table 23 are based on a comparison only of patients who had had any advice from a physiotherapist, either face to face or on the telephone. People who were still on the waiting list at 6 weeks following randomisation (predominantly in the usual-care group) did not complete the questionnaire, and satisfaction with access to care may be different among this group.
We explored whether or not there was an interaction between baseline patient preference and randomisation group in terms of satisfaction with the service, in other words, whether or not people's satisfaction with the service they received was related to their initial preference. We found no such interaction for any of the three components of satisfaction. We also explored whether or not there was an interaction between patient preference and randomisation group with respect to effectiveness (based on the primary outcome of SF-36v2 PCS). Again we found no such interaction.
Analysis of free-text comments from questionnaires to obtain the views of patients regarding waiting time from referral
We noted above that the people who may have been least satisfied with access were those who had not received any physiotherapy but they would not have completed the satisfaction questions. We observed that many people added free-text comments to the questionnaire. Therefore, in a post hoc analysis we undertook a quantitative analysis of these free-text comments.
In the final section of the 6-week and 6-month follow-up questionnaires, participants were invited to comment on ‘Things that were good about the service’ and ‘Things that could be improved’. These comments were entered in full as part of routine data entry. Content analysis was performed to assess:
-
Whether or not (from the comment) the patient had received physiotherapy (by telephone or face to face) at that point.
-
The patient's view of waiting time from referral, coded as positive, negative, both, or not stated. An example of when ‘both’ applied would be when the patient was appreciative of the prompt telephone contact but unhappy with the wait to be seen face to face.
The comments from all 6-week and 6-month questionnaires were coded by one researcher. Validation of the coding was carried out by a second researcher, independently coding a 1 in 10 sample. Where there were discrepancies, the coding was discussed and a final coding agreed. The resulting agreement for whether or not patients had had physiotherapy was 98% at 6 weeks and 97% at 6 months; the agreement for view of waiting time was 98% at 6 weeks and 95% at 6 months.
Results are shown comparing patients in the usual care and PhysioDirect arms of the trial (Tables 24 and 25).
| Item | Usual care, n/N (%) | PhysioDirect, n/N (%) |
|---|---|---|
| Those who made a free-text comment about things which were good, and/or things which could be improved | 374/743 (50%) | 777/1056 (74%) |
| Had received physiotherapy care (from comment) | 264/374 (70%) | 659/777 (85%) |
| Still waiting for physiotherapy care (from comment) | 73/374 (20%) | 45/777 (6%) |
| Uncertain (from comment) whether or not had had physiotherapy care | 37/374 (10%) | 73/777 (9%) |
| Those who commented specifically on waiting time | 117/374 (31%) | 215/777 (28%) |
| Positive about waiting time | 17/117 (15%) | 131/215 (61%) |
| Negative about waiting time | 99/117 (85%) | 80/215 (37%) |
| Positive and negative about waiting time | 1/117 (1%) | 4/215 (2%) |
| % of those commenting negatively about waiting time who were (from comment) still waiting for physiotherapy care | 40/99 (40%) | 19/80 (24%) |
| Item | Usual care, n/N (%) | PhysioDirect, n/N (%) |
|---|---|---|
| Those who made a free-text comment about things which were good, and/or things which could be improved | 348/743 (47%) | 670/1056 (63%) |
| Had received physiotherapy care (from comment) | 308/348 (89%) | 584/670 (87%) |
| Still waiting for physiotherapy care (from comment) | 12/348 (3%) | 12/670 (2%) |
| Uncertain (from comment) whether or not had had physiotherapy care | 28/348 (8%) | 74/670 (11%) |
| Those who commented specifically on waiting time | 98/348 (28%) | 157/670 (24%) |
| Positive about waiting time | 26/98(27%) | 109/157(69%) |
| Negative about waiting time | 70/98 (71%) | 44/157 (28%) |
| Positive and negative about waiting time | 2/98 (2%) | 4/157 (3%) |
| % of those commenting negatively about waiting time who were (from comment) still waiting for physiotherapy care | 3/70 (4%) | 2/44 (5%) |
It is clear from the results presented above that the free-text comments provide a different perspective, compared with the ‘access’ questions in the questionnaire, on respondents' views on waiting time for advice and treatment for physiotherapy. More positive comments were made in the PhysioDirect arm and more negative comments were made in the usual-care arm.
Adverse events
Despite requesting reports of AEs from physiotherapists and from GPs, and after reviewing the GP notes of all patients in the trial, no AEs were detected in either arm of the trial. In particular, no AEs were detected from 4323 consultations (1445 by telephone and 2878 face to face) over 6 months in 2249 patients allocated to PhysioDirect.
Subgroup analysis
Possible differences in the effect of PhysioDirect compared with usual care on the SF-36v2 PCS at 6 months between subgroups based on age, main referral problem, deprivation or PCT, were analysed by estimating the interaction term of those factors with assigned treatment. No evidence was found of subgroup differences for the primary outcome (Tables 26 and 27). However, potentially important differences cannot be excluded as the CIs are very wide, reflecting the limited power available for subgroup analyses.
| Subgroups at 6 months | SF-36v2 PCS | Randomisation– subgroup interactiona,b | 95% CI | p-value | |||
|---|---|---|---|---|---|---|---|
| Usual care | PhysioDirect | ||||||
| Mean | SD | Mean | SD | ||||
| Age (years) | |||||||
| 18 to < 25 | 47.6 | 10.8 | 47.3 | 9.1 | Ref. | 0.59 | |
| 25 to < 35 | 49.6 | 8.1 | 48.4 | 9.4 | −0.04 | −3.79 to 3.71 | |
| 35 to < 45 | 47.1 | 10.7 | 45.7 | 9.5 | −0.92 | −4.54 to 2.70 | |
| 45 to < 55 | 44.3 | 10.9 | 44.5 | 10.3 | 1.34 | −2.29 to 4.97 | |
| 55 to < 65 | 42.5 | 9.9 | 41.4 | 11.7 | 0.78 | −2.79 to 4.35 | |
| 65 to < 75 | 39.2 | 10.2 | 39.6 | 11.2 | 1.03 | −2.74 to 4.79 | |
| 75 to < 85 | 35.9 | 10.1 | 35.4 | 8.7 | 2.01 | −2.45 to 6.47 | |
| 85 to < 95 | 36.3 | 7.5 | 28.3 | 9.3 | −2.67 | −9.68 to 4.35 | |
| Site of problem | |||||||
| Cervical | 43.8 | 9.9 | 42.7 | 10.5 | Ref. | 0.28 | |
| Thoracic | 42.3 | 13.8 | 42.9 | 11.9 | 3.85 | −4.00 to 1.70 | |
| Lumbar | 44.1 | 10.9 | 42.2 | 10.5 | 1.35 | −1.27 to 3.96 | |
| Upper limb | 44.6 | 10.7 | 45.2 | 11.0 | 2.59 | 0.08 to 5.09 | |
| Lower limb | 45.0 | 10.9 | 44.2 | 10.8 | 0.14 | −2.32 to 2.59 | |
| Widespread pain | 33.8 | 11.5 | 37.7 | 12.4 | 4.76 | −3.88 to 3.40 | |
| Multiple MSK | 39.4 | 11.4 | 40.7 | 13.2 | 2.61 | −2.12 to 7.33 | |
| Other MSK | 42.8 | 14.9 | 41.1 | 14.2 | 3.39 | −5.29 to 12.07 | |
| Subgroups at 6 months | SF-36v2 PCS | Randomisation–subgroup interactiona | 95% CI | p-value | |||
|---|---|---|---|---|---|---|---|
| Usual care | PhysioDirect | ||||||
| Mean | SD | Mean | SD | ||||
| Deprivation quintile (5 = most deprived) | |||||||
| 1 | 46.7 | 10.0 | 45.0 | 10.7 | Ref. | 0.62 | |
| 2 | 44.2 | 11.7 | 44.9 | 10.4 | 0.76 | −2.44 to 3.97 | |
| 3 | 45.5 | 9.4 | 44.4 | 10.7 | −0.37 | −3.42 to 2.69 | |
| 4 | 43.6 | 11.2 | 42.5 | 11.1 | −1.20 | −4.41 to 2.00 | |
| 5 | 41.0 | 11.2 | 39.8 | 11.2 | −0.05 | −3.51 to 3.40 | |
| PCT | |||||||
| Bristol | 44.8 | 10.9 | 43.8 | 11.1 | Ref. | 0.78 | |
| Somerset | 45.0 | 10.6 | 44.8 | 10.5 | 0.57 | −1.46 to 2.59 | |
| Cheshire | 44.0 | 10.7 | 43.0 | 11.2 | 0.88 | −1.18 to 2.94 | |
| Stoke | 42.3 | 11.2 | 41.7 | 10.7 | 1.00 | −1.20 to 3.21 | |
Finally, we report descriptive data about the pattern of responses on the primary outcome for patients with different sites of MSK problem (Table 28). This demonstrates that different types of problem have different impacts on health status; most improve substantially over time (by up to 8 points, when the SD of the PCS in this population is 8.8 points at baseline); and that most of this improvement had occurred by 6 weeks following randomisation. Patients with thoracic or ‘other MSK’ problems improved the least over the 6 months' follow-up, whereas those with lumbar, limb or widespread pain problems improved the most. We have already demonstrated (see Table 15) that there is no evidence of difference overall between the trial arms in terms of improvement, or any evidence that some conditions benefited to a greater extent than others through a PhysioDirect service (see Table 26).
| Main referral problem | PCS at time | |||||
|---|---|---|---|---|---|---|
| Baseline | 6 weeks | 6 months | ||||
| Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | |
| Cervical | 38.87 (8.45) | 273 | 41.51 (10.64) | 240 | 43.07 (10.30) | 227 |
| Thoracic | 39.33 (8.98) | 48 | 42.69 (10.45) | 40 | 42.77 (12.18) | 38 |
| Lumbar | 34.62 (8.56) | 614 | 40.55 (10.27) | 540 | 42.81 (10.68) | 511 |
| Upper limb | 38.86 (8.43) | 525 | 42.59 (9.69) | 471 | 44.97 (10.87) | 451 |
| Lower limb | 37.47 (8.81) | 675 | 42.15 (10.34) | 600 | 44.47 (10.83) | 593 |
| Widespread pain | 30.21 (8.73) | 15 | 32.88 (10.90) | 14 | 36.18 (11.76) | 13 |
| Multiple MSK | 35.18 (8.79) | 82 | 40.29 (10.72) | 67 | 40.30 (12.54) | 67 |
| Other MSK | 38.55 (10.19) | 14 | 45.38 (10.33) | 12 | 41.71 (13.71) | 11 |
Chapter 4 Economic evaluation: methods
Aim
The aim of the economic evaluation was to compare the costs and benefits of a telephone advice and assessment service (referred to as ‘PhysioDirect’) with usual care in patients referred to the community physiotherapy service by primary care practitioners. Patients recruited to the study were randomly allocated to one of these two methods of service delivery. The primary analyses were from the perspectives of (1) the NHS and (2) patients and their families. Costs of lost productivity were also elicited and are presented separately.
The analysis was based on all costs incurred over the 6 months following randomisation to either PhysioDirect or usual care. Physical measures of resource use are presented separately from costs. The different viewpoints are separated throughout the analysis. For resource use, results are reported to two decimal places. For costs, results are reported to the nearest full penny. All costs are reported in 2009 prices.
The interventions
All patients were recruited following a GP referral to physiotherapy or patient self-referral.
Control Usual care involves an initial face-to-face assessment, which may be followed by one or more further appointments. Waiting times vary widely in different services and at different times but are typically between 4 and 8 weeks.
Intervention ‘PhysioDirect’ involves a telephone advice and computer-aided assessment, with written exercise and self-management information sent by post and face-to-face care if necessary.
The intervention and control arms of the trial are described in more detail in the previous chapter.
Form of analysis
Two forms of analysis were planned. The first used a cost consequences approach to compare the trial primary and secondary outcomes with cost from all three perspectives (NHS, patient and carer, and lost productivity). The second form of analysis planned was a cost-effectiveness (utility) analysis, with NHS costs being related to changes in QALYs. These were obtained using the EQ-5D measured at baseline, 6 weeks and 6 months, and valued using the tariff obtained from a UK general population survey to value the health states obtained using the EQ-5D measure. 85 QALYs were estimated using the area-under-the-curve approach, adjusted for differences in baseline utility. 86
Outcomes
The primary clinical outcome for the trial was the physical component summary (PCS) of the SF-36v2. Secondary outcomes included EQ-5D, SF-36v2 (MCS and individual scales), the MYMOP, personal perception of improvement, and patient satisfaction. Outcome data were collected by patient questionnaire at baseline, 6 weeks and 6 months.
Identification of relevant costs
The costs of the PhysioDirect service were compared with the costs of usual care from the point at which the patients were randomised to receive care in one of these two arms, until the 6-month follow-up. The analysis considered costs associated with the delivery of care from the perspective of the service provider, the patients and any carers, and the cost to society of lost production due to time off work by the patient and carers.
The scope of resource use identified as being relevant was identified in conjunction with physiotherapists and clinicians associated with the research and the provision of the two services. The analysis was confined to costs related to the reason for which the patient was referred to the physiotherapy service.
The costs identified as being of relevance in this analysis were as follows.
Direct costs to the health-care sector (NHS)
-
Cost of initial physiotherapy intervention, whether face-to-face or through PhysioDirect.
-
Cost of subsequent physiotherapy appointments, whether face-to-face or through PhysioDirect.
-
Primary and community care:
-
Face-to-face consultations GP, practice nurse, other health-care professionals.
-
Telephone consultations GP, practice nurse, other health-care professionals.
-
Out-of-hours contacts GP, practice nurse, other health-care professionals.
-
Home visits GP, community nursing teams.
-
Other primary care contacts NHS Direct, NHS walk-in centres.
-
-
Hospital care:
-
A&E visits.
-
Outpatient appointments/clinic visits.
-
Inpatient stays.
-
Prescribed medication.
-
Patients and their carers
-
Travel costs associated with health-care visits including to the physiotherapy service.
-
Over-the-counter medication.
-
Expenditure on prescriptions.
-
Out-of-pocket expenditure associated with the purchase of private or alternative treatments, for example private physiotherapy, complementary and alternative therapies.
-
Cost of telephone calls relating to physiotherapy consultations.
-
Loss of earnings associated with lost employment for those unable to obtain sick pay (including the self-employed and those not entitled to sick pay).
-
Disability payments received. Disability payments are a cost from the perspective of the Personal Social Services (Government) but from the perspective of society are a transfer payment and are therefore ignored in the analysis conducted from the societal perspective.
Costs associated with lost production
-
Time off work and usual activities by patient and carer associated with either attendance for treatment and/or the condition itself.
Measurement of resource use
Much of the measurement of resource use came from computerised systems including the PhysioDirect specific system, the various community systems in operation across the study sites, and the various GP systems. Here data were collected on a per-patient basis using computerised data collection forms.
Further information about resource use, particularly in relation to patient resource use, was derived from the questionnaires that patients were asked to complete at the time of their initial referral to physiotherapy and at 6 weeks and 6 months following randomisation. Only costs associated with the condition for which the patient was receiving physiotherapy were included.
One other source of resource-use data was also used. Time and motion studies of the PhysioDirect service were used to obtain information about activities undertaken during patient non-contact time, a vital element in understanding the costs associated with PhysioDirect.
In all cases, the aim was to measure the resources used for the 6 months between randomisation and the final 6-month follow-up.
Direct costs to the health-care sector (NHS)
PhysioDirect consultations
Patient-level data were collected for each appointment with PhysioDirect. These included the length of the telephone call and the grade of the physiotherapist making that call. Data about the length of the telephone call were obtained by download from the PhysioDirect assessment software, which recorded which physiotherapist conducted each telephone call, and the duration of each call, based on when the physiotherapist logged in to and out of the patient's electronic record.
A small time and motion study comprising observation of sessions at each site was conducted to determine how physiotherapists occupied themselves when assigned to PhysioDirect but not on the telephone to patients. Observation of this non-contact time was required to estimate the opportunity cost of that time. Time was categorised as consultation time, administrative time related to PhysioDirect appointments, administrative time related to face-to-face appointments, general administrative activity (e.g. dealing with e-mails) and work breaks. The aim was to undertake observational time and motion studies at points in the study when sites were expected to be fully operational, across a mix of day, time of day and location. Observations were undertaken over a 4-month period (September to December 2009) of four PhysioDirect sessions in Bristol, three in Somerset and two in each of Stoke and Cheshire, with physiotherapists ranging from Agenda for Change Bands 6 to 8a (representing the full range of grades of staff providing PhysioDirect sessions).
During the time and motion study it was noted that physiotherapists had to continue some administrative activities following each telephone call, such as collating information to send to the patient by post. The time spent on these activities was not captured within the times logged in to the PhysioDirect software. However, in Bristol (but not in the other three physiotherapy sites), physiotherapists recorded details of telephone calls in the same routine records as they recorded face-to-face consultations. Comparison of matched data about individual calls demonstrated that the mean duration of calls recorded in the routine record was 5 minutes longer than that recorded in the PhysioDirect software. It was therefore assumed that this represented the extra administrative time spent after each call, and furthermore that this could be applied to calls in the other three sites. Consequently, 5 minutes was added to the duration of call time for each call. In a small number of instances we noted that physiotherapists had logged in to patients records for a very short time, sometimes several times in quick succession on the same day. We assumed this was due to problems telephoning a patient, or physiotherapists accessing the records for administrative purposes. These short ‘calls’ were included in the costing, but 5 minutes was only added once for any given patient on any one day, even if more than one call from the patient was recorded on the same day.
Information about the capital requirements for PhysioDirect was obtained through dialogue with the study sites and research teams and relevant costs were obtained through these routes. The capital requirements for each site varied but in general the teams needed far less space than for treating patients face to face. Based on the data collected, capital requirements were allocated at 50% of the capital requirements for face-to-face physiotherapy sessions utilised by Curtis. 87
Face-to-face physiotherapy consultations
Data about face-to-face consultations were obtained from routine records maintained by physiotherapists at each site. These included the length of appointment, the grade of the physiotherapist seen and information about missed appointments. For most sites data were collected through the routine community databases. For Bristol and Somerset the ICS database was used; for Stoke the relevant database was Lorenzo. For Cheshire, where some sites did not use computerised systems, data were extracted from the patients' written notes.
Primary care consultations
Information was obtained from general practice records by researchers using a standard pro forma. Relevant consultations were identified as follows:
-
If the MSK condition for which the patient was referred was mentioned, the consultation was recorded, even if this was not the primary reason for the consultation.
-
If a patient had a MSK condition, but had a consultation about other problems and the MSK condition was not mentioned, these consultations were not recorded.
-
If a repeat prescription was issued on the same date as a consultation (i.e. was probably issued at the consultation) but there was no mention of the MSK condition at the consultation then the consultation was not recorded (but the prescription was recorded along with other repeat prescriptions for MSK problems).
Primary care consultations were recorded by type (e.g. face to face, telephone, out of hours, home) and by type of professional seen (e.g. GP, nurse).
Prescribed medication
Information was obtained from practice records by researchers using a standard pro forma. Relevant medication was defined as that prescribed for MSK conditions. It was not feasible to distinguish between medication prescribed for the condition for which the patient was referred for physiotherapy and any other MSK problem and so all MSK medication prescribed was included.
Any prescribed item that appeared in the chapters of the British National Formulary (BNF) detailed below was assumed to be a relevant prescription and details were recorded:
-
4.7.1–4.7.2 Analgesics
-
10.1.1 Non-steroidal anti-inflammatory drugs
-
10.1.2.2 Local corticosteroid injections
-
10.3 Drugs for the relief of soft-tissue inflammation.
Medication was recorded by name, route of administration, quantity and strength.
NHS Direct/walk-in centre consultations
Information about visits to NHS Direct or to walk-in centres related to the condition for which the patient was referred for physiotherapy was collected through the 6-week and 6-month questionnaires.
Visits to accident and emergency
Information about visits to A&E services was obtained from the questionnaires administered at 6 weeks and 6 months.
Secondary care outpatient consultations
Information about secondary care outpatient consultations related to the condition for which the patient was referred to the physiotherapy service was obtained from the questionnaires administered at 6 weeks and 6 months. This included information about the clinic name or department visited and the number of appointments. Where questionnaire data were ambiguous, for example with regard to the specialty, information about these consultations was obtained from GP records.
Secondary care inpatient stays
Information about secondary care inpatient stays related to the condition for which the patient was referred to the physiotherapy service was obtained from the questionnaires administered at 6 weeks and 6 months. Information obtained directly from this questionnaire was just whether or not the patient had received an inpatient stay. Any patient who answered ‘yes’ to this question was then telephoned to obtain further details about the location and length of stay.
Patients and their carers
Travel costs
Information about travel costs associated with health-care consultations for the condition being treated by physiotherapy was obtained from the patient questionnaires. Costs associated with travel to the GP and to the physiotherapy services were collected separately and then applied to all appropriate consultations.
Over-the-counter medication
Information about over-the-counter medication associated with the condition being treated by physiotherapy was obtained from the patient questionnaires. Individuals were asked to specify whether or not they had purchased over-the-counter medication and the total costs associated with any such purchases. They were not asked for details about the type of medication taken or the dosage.
Expenditure on prescriptions
Information about whether or not individuals paid for prescriptions was collected through the questionnaire. Individuals were asked to specify whether or not they paid for prescriptions, and if so, whether they paid on a per-item basis, or by purchasing a 3- or 12-month prepayment certificate.
Out-of-pocket expenditure
Information about out-of-pocket expenditure associated with the condition being treated by physiotherapy was obtained from the patient questionnaires. Individuals were asked to specify whether or not they had purchased any equipment or devices for the condition, or had had to pay for any extra help in the home (e.g. cleaning, gardening, ironing) or had paid for any form of private care (e.g. private physiotherapy, chiropractor, osteopath, other complementary and alternative therapies).
Loss of earnings
Information about whether or not the individual had experienced any loss of earnings associated with their condition was obtained directly from the individual through the patient questionnaires.
Disability payments
Information about disability payments received as a result of the condition for which the physiotherapy was provided was obtained from the questionnaires administered at 6 weeks and 6 months. This included information about the type(s) of benefit(s) received and the total amount paid over the previous 6 weeks (for the 6-week questionnaire) and since the previous questionnaire (for the 6-month questionnaire).
Costs associated with lost production
Information about whether the individual had experienced loss of productivity associated with their condition was obtained through the patient questionnaires. A number of questions were asked of each individual to facilitate the most accurate costing possible without asking questions that were excessively burdensome to respondents. Individuals were first asked whether or not they were in paid work. Individuals responding positively to this question were then asked whether or not their employment had been affected by their condition, specifically in terms of whether they had had to take sick leave, to work reduced hours or to take on restricted or altered activities. The total amount of time lost from work was asked. Similar information was also requested for time spent attending physiotherapy and general practice appointments, including telephone consultations with PhysioDirect.
Dealing with missing resource-use data
The extraction of computerised data from the physiotherapy records resulted in no missing data. Inevitably, however, some questionnaire and GP record data were missing. These missing data potentially affect all analyses, as elements of analysis from each perspective drew on questionnaire data for at least some aspects of resource use and on the questionnaire for analysis of outcomes in terms of QALYs gained.
Questionnaire data were missing for three reasons:
-
Patients withdrew from the study thus failing to complete questionnaires subsequent to their withdrawal.
-
Patients failed to complete entire questionnaires.
-
Patients failed to complete particular items within questionnaires.
General practitioner record data were missing for two reasons:
-
Patients moved practice during the trial period.
-
Patients records could not be identified at general practices.
For the baseline analysis, no attempt has been made to impute missing data arising from any of these causes. Within the sensitivity analyses, however (see below), missing data are imputed.
Valuation of resource use
Direct costs to the health-care sector (NHS)
PhysioDirect consultations
Methods used by Curtis87 in her estimation of a face-to-face physiotherapy appointment for a Band 5 member of staff were used in developing detailed costs for PhysioDirect appointments for each band of staff and in each location, based on median pay rates for each band from 1 April 2009 using the Agenda for Change. 88 Data on national insurance payments, overheads and capital overheads were taken from Curtis. 87 Capital overheads for telephone consultations were adjusted to 50% of the capital overheads for a face-to-face appointment to reflect the smaller amount of space required. Assumptions about the length of the working week and the number of weeks worked per year were also taken from Curtis. 87 More detailed information about salary and the associated superannuation costs was then utilised to obtain a cost for each band of staff from 3 to 8a.
In order to obtain a cost per hour of telephone contact, we combined the Curtis87 estimates of cost per hour with information from the computerised records of the PhysioDirect service once it had reached a steady state of operation. These records identified the proportion of time spent by physiotherapists actually dealing with PhysioDirect patients. To this was added data from the time and motion study, which identified activities undertaken during non-contact time, for example administration for face-to-face patients (rather than PhysioDirect patients) or general administration. All estimates were carried out on a site-specific basis.
Face-to-face physiotherapy consultations
Methods used by Curtis87 in her estimation of a face-to-face physiotherapy appointment for a Band 5 member of staff were used to develop more detailed costs for physiotherapy appointments for each band of staff and in each location, based on median pay rates for each band from 1 April 2009 using the Agenda for Change. 88 Data on national insurance payments, overheads and capital overheads were taken from Curtis. Assumptions about the length of the working week and the number of weeks worked per year were also taken from Curtis. 87 More detailed information about salary and the associated superannuation costs was then utilised to obtain a cost for each band of staff from 3 to 8a. Finally, information obtained from physiotherapy service managers about the level of non-contact time in each study site for each band of staff was used to obtain a site-specific cost for each band of staff.
Primary care consultations
Information about the costs associated with primary care consultations was primarily obtained from Unit Costs of Health and Social Care (Curtis87) on a per-surgery consultation or home visit basis as appropriate. Costs used are detailed in Table 29. Costs excluding qualification are used for all visits, as this service is not likely to have implications for the numbers or training of primary care staff. Costs for out-of-hours appointments with a GP were obtained using recent publications. 89
| Type of consultation | Cost per consultation (£) |
|---|---|
| GP | |
| Surgery consultationa | 27.00 |
| Home visita | 91.00 |
| Telephone consultationa | 16.00 |
| Out-of-hours consultation | 23.50 |
| Practice nurse | |
| Surgery consultation | 10.00 |
| Telephone consultationb | 5.93 |
| HCA/phlebotomist – surgery consultationb | 6.92 |
| District nurse home visitb | 24.00 |
Prescribed medication
The value of prescriptions issued in general practice (both when prescribed during a consultation or as a repeat prescription) was based on an estimate of the full cost to the NHS and was made up of four elements:
-
The basic price of the drug – from BNF90 – to cost the prescribed medication.
-
An average deduction for discount. This depends on the total value of prescriptions dispensed from the pharmacy in a month and varies from a 5.63% deduction to a 11.5% deduction (May 2010). A mid-point deduction of 8.56% was applied to all basic drug prices.
-
The professional fee: 90p per prescription (obtained from the Drug Tariff England and Wales: www.nhsbsa.nhs.uk/924.aspx).
-
The container allowance: 3.24p per prescription (obtained from the Drug Tariff England and Wales).
NHS walk-in-centre consultations
The national evaluation was used to value a consultation at a walk-in centre,91 with values adjusted to 2009 values using the pay and prices index. 87 The consultation value used was £31.99.
Visits to accident and emergency
Information about the costs of visits to A&E services was obtained from the National Schedule of Reference Costs for 2009–2010, using the value for A&E attendances that do not lead to subsequent admission. 92 The value used for an A&E consultation was £103.
Secondary care outpatient consultations and procedures
Information about the costs of visits to outpatient consultations in secondary care was largely obtained from the National Schedule of Reference Costs for 2009–2010,92 supplemented by direct information from the Bristol Homeopathic Hospital. Values used are shown in Table 30 for those specialties that were utilised by patients included in the trial.
| Type of consultation | Cost per first consultation (£) | Cost per follow-up consultation (£) | Cost per unknown consultation (£) |
|---|---|---|---|
| Cardiology | 171.00 | 113.00 | 124.00 |
| Dermatology | 112.00 | 86.00 | 92.00 |
| ENT | 106.00 | 74.00 | 85.00 |
| General medicine | 194.00 | 132.00 | 138.00 |
| Gynaecology | 139.00 | 97.00 | 112.00 |
| Haemophilia | 1070.00 | 793.00 | 785.00 |
| Neurology | 207.00 | 140.00 | 166.00 |
| Ophthalmology | 105.00 | 74.00 | 80.00 |
| Oral surgery | 128.00 | 95.00 | 111.00 |
| Orthopaedics | 121.00 | 83.00 | 96.00 |
| Pain management | 173.00 | 107.00 | 122.00 |
| Podiatry | 63.00 | 51.00 | 40.00 |
| Rheumatology | 213.00 | 125.00 | 135.00 |
| Thoracic surgery | 255.00 | 201.00 | 216.00 |
| Upper gastrointestinal surgery | 140.00 | 100.00 | 118.00 |
| Urology | 129.00 | 88.00 | 99.00 |
| Homeopathic hospital outpatient | 211.00 | 140.00 | 152.00 |
Information about the costs of procedures conducted in outpatient departments in secondary care was primarily obtained from the same source. 92 Values used are shown in Table 31 for those procedures that were utilised by patients included in the trial.
| Type of procedure | Cost per procedure (£) |
|---|---|
| Intermediate knee proceduresa | 1371 |
| Hydrotherapyb | 59 |
| MRI | 194 |
| Specialist MRI | 367 |
| DEXA | 78 |
| Ultrasonography | 63 |
| CT | 123 |
| Radiography | 26 |
| Minor hand proceduresa | 1021 |
Secondary care inpatient stays
Information about the costs of inpatient hospital stays was based upon the healthcare resource group (HRG) for the particular admission. HRGs were coded using an earlier version of HRGs than the current version, because of the fuller information available, and so cost data were used from 2007 to 2008 and inflated to 2009 prices. Costs were obtained from the National Schedule of Reference Costs 2007–2008 (www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_098945). Values used are shown in Table 32.
| Inpatient HRG | Cost (£) per FCE | |
|---|---|---|
| H04 | Primary knee replacement | 5613 |
| H08 | Joint replacements or revisions, site unspecified | 4023 |
| H17, H19 | Soft-tissue or other bone procedures – category 1 < 70 w/o cc and soft-tissue or other bone procedures – category 2 < 70 w/o cc | 1552 |
| H20, H21 | Muscle, tendon or ligament procedures – category 1 muscle, tendon or ligament procedures – category 2 | 1417 |
| H27 | Non-inflammatory bone or joint disorders > 69 or w cc | 997 |
| H28 | Non-inflammatory bone or joint disorders < 70 w/o cc | 954 |
| H30 | Infections of bones or joints | 19,715 |
| H37 | Closed pelvis or lower limb fractures < 70 w/o cc | 1685 |
| H45 | Minor fractures or dislocations | 1202 |
| H71 | Revisional procedures to hips | 7185 |
| H80 | Primary hip replacement cemented | 5305 |
| H85 | Intracapsular neck of femur fracture with fixation w/o cc | 4703 |
| R02 | Surgery for prolapsed intervertebral disc | 3192 |
| R03 | Decompression and effusion for degenerative spinal disorders | 5100 |
| R16 | Thoracic or lumbar spinal disorders < 70 w/o cc | 575 |
Patients and their carers
Cost of telephone calls to the physiotherapy service
The cost of telephone calls to the physiotherapy service was borne by patients. These were costed at the standard British Telecom rate prevailing at the time, i.e. 5.25p per minute plus 9p connection charge. Patients using the face-to-face service are required to call to make an appointment; in these cases a nominal charge relating to a 3-minute call was included.
It is recognised that patients may have used mobile phones on a ‘pay as you go’ basis, making calls more expensive, or may have had contract mobile phones or belonged to landline telephone contracts with included ‘free’ minutes. However, no information was available about these factors and so the standard British Telecom call rate was used.
Travel costs
Information about travel costs was obtained directly from the patient questionnaires except for the case of car mileage. Information about mileage costs was obtained from the Automobile Association schedule and a value of 46p per mile was used.
Over-the-counter medication
The total cost associated with over-the-counter medication was recorded by the individual in the questionnaire.
Expenditure on prescriptions
Information about the cost of prescription charges was obtained from the Department of Health.
Out-of-pocket expenditure
Information about the costs of out-of-pocket expenditure was obtained directly from the patient through either the initial questionnaire or the supplemental telephone interview.
Loss of earnings
Information about direct loss of earnings experienced by patients because of their condition was obtained through the questionnaire.
Disability payments
Costs associated with disability payments were obtained directly from the patient questionnaire.
Costs associated with lost production
It was assumed that all absence from work represented a loss in productivity and the human capital approach was therefore used to assign costs. Median hourly earnings (excluding overtime) by age and sex were obtained from the Office of National Statistics 2009 annual survey of hours and earnings,94 and applied to all estimates of time lost from work (Table 33).
| Age (years) | Men | Women |
|---|---|---|
| 16–17 | 175.20 | 189.20 |
| 18–21 | 285.50 | 268.30 |
| 22–29 | 421.60 | 392.90 |
| 30–39 | 571.10 | 497.50 |
| 40–49 | 605.90 | 457.70 |
| 50–59 | 569.70 | 434.10 |
| 60+ | 470.50 | 383.20 |
Discounting
Costs and outcomes were not discounted, as the study was limited to a period of 6 months.
Uncertainty
There were three elements involved in addressing uncertainty within the analysis.
Uncertainty resulting from patient variation
Uncertainty in the cost-effectiveness–utility ratios resulting from patient variation in resource use and effectiveness was captured by estimating CIs around the net benefit statistic and estimating cost-effectiveness acceptability curves (CEACs).
Uncertainty in specific estimates
In the trial, the same level of physiotherapist staffing was available to patients in the PhysioDirect and usual-care arms. The amount of staff time devoted to PhysioDirect telephone sessions was based on estimates of the likely proportions of patients being managed by telephone or face-to-face consultations. There is good reason to believe that because of the constraints of the randomised trial design, the PhysioDirect service did not operate at full capacity. Sensitivity analysis was therefore used to estimate relative cost-effectiveness assuming a more efficient PhysioDirect service. In two of the physiotherapy services participating in the trial the PhysioDirect service continued after the trial had ended and the physiotherapists' time was used more productively for several reasons. First, in the main trial only a minority of patients received PhysioDirect because of the combined effect of exclusions, non-participation in the trial or being randomised to usual care. Outside the trial the patient throughput to PhysioDirect was much higher and so the physiotherapists were busier. Second, staffing levels were adjusted in the light of experience to try to ensure that there were enough staff to operate the service but be working most of the time. Third, instead of trying to staff the service so that patients could be connected to a physiotherapist as soon as they phoned, after the trial the service mainly operated a call-back system in which patients telephoned and left their contact details and then the physiotherapists called them back at an agreed time. Data from one service (Bristol) on staffing levels and all call times from January to March 2011 were used as a basis for estimating the cost of running the service as if these conditions had prevailed during the trial. The data about staffing levels, number of calls and call durations were obtained in the same way as in the trial.
Sensitivity analysis was also carried out to test the effect of including or excluding hospital costs. Typically, in a primary care trial, few patients use secondary care but the cost, for those who do, is very high, and so small differences between trial arms in the number of people using secondary care may have a disproportionate effect.
Uncertainty resulting from missing data
The entire analysis was rerun following multiple imputation of missing data. The multiple imputation by chained equation procedure95 was used. This method uses regression techniques based on the values of available data to estimate missing values. Variables included in the regression model are those likely to predict most closely the missing values. The regression model used to impute missing cost data included age, sex, randomisation group, GP costs, practice nurse costs, cost of other primary care professionals, cost of prescribed medication and hospital costs. Missing EQ-5D scores were imputed using data on age, sex, randomisation group, PCT, referral problem, and SF-36v2 PCS and EQ-5D at each time point.
Chapter 5 Economic evaluation: results
Results are reported in UK sterling in 2009 prices. Despite most of the data being highly skewed, all data are reported as means because this is more relevant than medians for decision-makers using the information to plan services. All information is reported in terms of both resources used and costs. Information about resource use is reported correct to two decimal places and information about costs is reported correct to the nearest full penny. All SDs are reported correct to the same number of decimal places as the mean.
Resource use and cost per patient are provided, by item, for all those for whom data are available for that item. However, in order to estimate total per patient cost, the base-case analysis includes only those for whom complete data are available for all items of resource use. Base-case NHS costs use the participants for whom complete NHS cost and QALY data (n = 1272; 57%) were available; base-case personal costs use those for whom there were complete personal cost data (n = 995; 44%); complete cases for valuing lost productivity due to time off work are n = 1334 (59%). Numbers are included in all tables.
Each table of costs first presents the results using all of the data available and then, below, the costs for the 1272 participants with full data on all cost and QALYs (‘complete cases’) are presented.
NHS resource use
Consultations with physiotherapy services
Information about the total number of contacts with different aspects of the physiotherapy services is shown in Table 34. The associated costs are shown in Table 35. It is clear from these data that the total costs associated with provision of physiotherapy by PhysioDirect were slightly higher than the physiotherapy costs associated with usual care although the cost difference was not large.
| Physiotherapy services | n (patients) | Usual-care group: mean (SD) | n (patients) | PhysioDirect group: mean (SD) |
|---|---|---|---|---|
| Face-to-face appointments | ||||
| No. | 743 | 3.11 (2.63) | 1506 | 1.91 (2.72) |
| Total duration (minutes)a | 743 | 107.51 (88.92) | 1506 | 64.20 (89.31) |
| Telephone appointments | ||||
| No. | 743 | 0.13 (0.44) | 1506 | 0.96 (0.63) |
| Total duration (minutes)a | 743 | 4.21 (14.64) | 1506 | 27.37 (19.92) |
| Home visits | ||||
| No. | 743 | 0.00 (0.06) | 1506 | 0.00 (0.06) |
| Total duration (minutes)a | 743 | 0.14 (2.27) | 1506 | 0.12 (2.12) |
| All physiotherapy contacts | ||||
| No. | 743 | 3.25 (2.70) | 1506 | 2.87 (2.94) |
| Total duration (minutes)a | 743 | 111.86 (90.50) | 1506 | 91.70 (95.40) |
| Physiotherapy services | n | Usual-care group: mean £ (SD) | n | PhysioDirect group: mean £ (SD) |
|---|---|---|---|---|
| All available data | ||||
| Face-to-face appointments | 743 | 64.42 (53.00) | 1506 | 38.76 (53.92) |
| Telephone appointments | 743 | 5.22 (18.01) | 1506 | 35.17 (26.34) |
| Home visits | 743 | 0.08 (1.33) | 1506 | 0.08 (1.46) |
| Total physiotherapy cost | 743 | 69.73 (56.17) | 1506 | 74.01 (63.97) |
| Complete cases | ||||
| Face-to-face appointments | 432 | 73.26 (54.45) | 840 | 46.04 (58.15) |
| Telephone appointments | 432 | 5.47 (18.41) | 840 | 40.59 (25.19) |
| Home visits | 432 | 0.04 (0.85) | 840 | 0.12 (1.73) |
| Total physiotherapy cost | 432 | 78.77 (57.08) | 840 | 86.75 (65.47) |
Primary care and district nurse consultations
Information about the number of primary care consultations is shown in Table 36 and the cost of those consultations is shown in Table 37. There are few differences in cost but, again, overall the primary care costs for patients allocated to receive usual care were slightly smaller than those of patients allocated to receive PhysioDirect.
| Primary care services | n | Usual-care group: mean (SD) | n | PhysioDirect group: mean (SD) |
|---|---|---|---|---|
| GP consultations | 739 | 0.77(1.47) | 1484 | 0.87 (1.68) |
| Nurse consultations | 739 | 0.04 (0.22) | 1484 | 0.06 (0.32) |
| Other primary care consultations | 739 | 0.02 (0.14) | 1484 | 0.02 (0.17) |
| Total no. of primary care contacts | 739 | 0.83 (1.56) | 1484 | 0.96 (1.84) |
| Primary care services | n | Usual-care group: mean £ (SD) | n | PhysioDirect group: mean £ (SD) |
|---|---|---|---|---|
| All available data | ||||
| GP consultations | 739 | 19.21 (35.91) | 1484 | 21.69 (41.66) |
| Nurse consultations | 739 | 0.44 (2.37) | 1484 | 0.61 (3.17) |
| Other primary care consultations | 739 | 0.03 (0.57) | 1484 | 0.07 (1.31) |
| Total primary care cost | 739 | 19.68 (36.68) | 1484 | 22.37 (42.83) |
| Complete cases | ||||
| GP consultations | 432 | 18.34 (32.11) | 840 | 21.95 (41.86) |
| Nurse consultations | 432 | 0.50 (2.31) | 840 | 0.65 (3.38) |
| Other primary care consultations | 432 | 0.02 (0.33) | 840 | 0.06 (1.19) |
| Total primary care cost | 432 | 18.85 (32.69) | 840 | 22.66 (43.02) |
Prescribed medication
Information about the amount of prescribed medication in primary care, and the cost of that medication, is shown in Table 38. Medication provision through primary care was extremely similar across the two groups with mean medication costs for those allocated to PhysioDirect being very slightly lower than amongst those allocated to usual care.
| Medication | n | Usual-care group: mean (SD) | n | PhysioDirect group: mean (SD) |
|---|---|---|---|---|
| No. of prescriptions | 728 | 1.36 (2.73) | 1469 | 1.68 (3.72) |
| Medication cost (£) | ||||
| All available data | 728 | 11.04 (51.61) | 1469 | 10.33 (55.43) |
| Complete cases | 840 | 14.83 (65.53) | 840 | 10.25 (39.95) |
Hospital costs
Resource use associated with hospital visits, including visits to the A&E department, outpatient visits and associated procedures, and inpatient stays is shown in Table 39. Again, costs in the two groups are similar but the hospital costs associated with treatment in the PhysioDirect arm of the trials are slightly higher than those associated with usual care, as shown in Table 40.
| Hospital services | n | Usual-care group: mean (SD) | n | PhysioDirect group: mean (SD) |
|---|---|---|---|---|
| A&E (visits) | 467 | 0.02 (0.01) | 912 | 0.03 (0.01) |
| Outpatient (consultations) | 467 | 0.17 (0.83) | 910 | 0.35 (1.03) |
| Inpatient stays (FCEs) | 465 | 0.01 (0.10) | 910 | 0.01 (0.10) |
| Hospital services | n | Usual-care group: mean £ (SD) | n | PhysioDirect group: mean £ (SD) |
|---|---|---|---|---|
| All available data | ||||
| A&E | 467 | 1.99 (17.12) | 912 | 3.17 (20.84) |
| Outpatient | 467 | 30.74 (98.36) | 910 | 38.35 (126.05) |
| Inpatient | 465 | 51.02 (520.48) | 910 | 34.99 (399.62) |
| Total hospital cost | 459 | 83.04 (561.68) | 899 | 77.00 (446.24) |
| Complete cases | ||||
| A&E | 432 | 1.19 (11.05) | 840 | 3.32 (21.42) |
| Outpatient | 432 | 30.82 (98.72) | 840 | 39.34 (127.47) |
| Inpatient | 432 | 35.21 (448.00) | 840 | 36.65 (414.34) |
| Total hospital cost | 432 | 67.23 (489.66) | 840 | 79.32 (459.02) |
Table 41 summarises the three main elements of NHS costs other than physiotherapy. It shows that using all the data available the NHS costs are almost identical in the two arms. However, in the complete case analysis the NHS costs were higher in the PhysioDirect arm. Further examination of the data indicated that this was due to two patients in the usual care arm who had expensive hospital treatment but who had missing data on other variables and were therefore not included in the complete case analysis.
| NHS costs (other than physiotherapy) | n | Usual-care group: mean £ (SD) | n | PhysioDirect group: mean £ (SD) |
|---|---|---|---|---|
| All available data | ||||
| Primary care | 739 | 19.68 (36.68) | 1484 | 22.87 (42.83) |
| Medication | 728 | 11.04 (51.61) | 1469 | 10.33 (55.43) |
| Hospital costs | 459 | 83.04 (561.68) | 899 | 77.00 (446.24) |
| Total | 453 | 110.51 (110.51) | 888 | 110.25 (466.95) |
| Complete cases | ||||
| Primary care | 432 | 18.85 (32.69) | 840 | 22.66 (43.02) |
| Medication | 432 | 14.83 (65.53) | 840 | 10.25 (39.95) |
| Hospital costs | 432 | 67.23 (489.66) | 840 | 79.32 (459.02) |
| Total | 432 | 100.91 (502.02) | 840 | 112.23 (476.91) |
Costs to patients and their families
Cost of telephone calls related to physiotherapy
Table 42 gives the estimated costs to patients of telephoning the physiotherapy service. This includes calls to the PhysioDirect service for a consultation and calls to the face-to-face service to make an appointment. Costs to those in the PhysioDirect group are nearly twice as much as for the usual-care group, although absolute costs are relatively low.
| Telephone calls to the physiotherapy service | n | Usual-care group: mean (SD) | n | PhysioDirect group: mean (SD) |
|---|---|---|---|---|
| Cost of all calls to physiotherapy service | ||||
| All available data | 743 | 0.97 (0.99) | 1506 | 1.75 (1.29) |
| Complete cases | 303 | 1.09 (0.95) | 692 | 1.98 (1.21) |
Travel costs
Table 43 contains information about the proportions of patients reporting expenditure on travel to both physiotherapy services and primary care. For each, the associated cost is also included in Table 44. Unsurprisingly, travel costs for physiotherapy care were slightly higher for those who were allocated to receive usual care (because of the cost of travelling to the physiotherapy appointment).
| Patient travel | n | Usual-care group | n | PhysioDirect group |
|---|---|---|---|---|
| No. (%) reporting expenditure on travel to physiotherapy | 462 | 242 (52.4) | 1232 | 308 (25.8) |
| No. (%) reporting expenditure on travel to primary care | 669 | 116 (17.3) | 1337 | 237 (17.7) |
| Patient travel | n | Usual-care group: mean £ (SD) | n | PhysioDirect group: mean £ (SD) |
|---|---|---|---|---|
| All available data | ||||
| Travel cost for physiotherapy | 462 | 6.11 (11.48) | 1232 | 3.11 (8.51) |
| Travel cost for primary care | 669 | 0.65 (2.93) | 1337 | 0.75 (4.10) |
| Complete cases | ||||
| Travel cost for physiotherapy | 303 | 7.48 (12.18) | 692 | 4.15 (9.93) |
| Travel cost for primary care | 303 | 0.74 (2.06) | 692 | 0.65 (1.94) |
Out-of-pocket expenditures
The proportions of individuals reporting expenditure on over-the-counter medication, prescriptions and other out-of-pocket expenditure are given in Table 45. The costs in Table 46 are for those who provided detail of expenditure. The biggest area of difference in cost between the groups appears to be in the more costly use of private therapy among those allocated to receive PhysioDirect (although the proportion reporting expenditure on private care is similar and the variation in cost is very wide).
| Patient out-of-pocket expenses | n | Usual-care group | n | PhysioDirect group |
|---|---|---|---|---|
| No. (%) reporting expenditure on over-the-counter medication | 506 | 256 (50.6) | 1028 | 512 (49.8) |
| No. (%) reporting expenditure on prescriptions | 559 | 264 (47.2) | 1085 | 508 (46.8) |
| No. (%) reporting expenditure on private therapy | 484 | 89 (18.4) | 934 | 167 (17.9) |
| No. (%) reporting equipment purchase | 480 | 139 (29.0) | 939 | 233 (24.8) |
| No. (%) reporting payments for extra domestic help | 459 | 35 (7.6) | 928 | 76 (8.2) |
| Patient out-of-pocket expenses | n | Usual-care group: mean (SD) | n | PhysioDirect group: mean (SD) |
|---|---|---|---|---|
| All available data | ||||
| Cost of over-the-counter medication | 490 | 7.67 (14.09) | 987 | 8.61 (22.38) |
| Cost of prescriptions | 553 | 2.72 (8.95) | 1076 | 2.67 (8.33) |
| Cost of private therapy | 475 | 21.98 (70.34) | 915 | 39.34 (296.94) |
| Cost of equipment purchase | 473 | 17.16 (169.12) | 924 | 9.12 (56.42) |
| Cost of extra domestic help | 451 | 10.93 (64.31) | 905 | 13.68 (96.02) |
| Complete cases | ||||
| Cost of over-the-counter medication | 303 | 6.97 (13.30) | 692 | 7.53 (16.09) |
| Cost of prescriptions | 303 | 2.90 (9.46) | 692 | 2.63 (7.82) |
| Cost of private therapy | 303 | 18.87 (69.10) | 692 | 31.93 (175.52) |
| Cost of equipment purchase | 303 | 9.51 (44.50) | 692 | 6.25 (26.28) |
| Cost of extra domestic help | 303 | 10.00 (68.65) | 692 | 14.37 (104.25) |
Loss of earnings
A number of individuals reported that they had experienced a loss of earnings (Table 47) as a result of their physiotherapy condition.
| Loss of earnings | Usual-care group | PhysioDirect group | ||
|---|---|---|---|---|
| No. reporting loss of earnings | n | No. (%) | n | No. (%) |
| No. reporting | 598 | 30 (5.0) | 1209 | 64 (5.3) |
| Cost associated with loss of earnings | n | Mean (SD) | n | Mean (SD) |
| All available data | 598 | £46.69 (£409.72) | 1209 | £82.78 (£885.85) |
| Complete cases | 303 | £50.19 (£506.51) | 692 | £98.58 (£1026.85) |
Disability payments
The proportion of participants receiving disability payments due to their physiotherapy condition is shown in Table 48, along with mean amount received. The proportion of patients receiving these payments was similar in the two groups but patients in the usual-care group received, on average, considerably more than those in the PhysioDirect group though the variation among all participants is high as shown by the large SDs.
| Disability payments | n | Usual-care group | n | PhysioDirect group |
|---|---|---|---|---|
| No. reporting receipt of disability payments | No. (%) | No. (%) | ||
| No. reporting | 601 | 51 (8.5) | 1215 | 86 (7.1) |
| Value of disability payments received | Mean (SD) | Mean (SD) | ||
| All available data | 581 | £66.71 (£388.43) | 1180 | £49.15 (£314.78) |
| Complete cases | 303 | £74.38 (£439.65) | 692 | £55.74 (£324.15) |
Societal costs of lost production
Societal costs of lost production include the value of time off work to attend physiotherapy and time off work because of the condition. In Table 49 we show the proportion of participants who reported any time off work during the 6 months and the value of that lost productivity. Data on the total cost of lost productivity were available for 1334 (59%) participants.
| Time off work and associated costs | n | Usual-care group: mean (SD) | n | PhysioDirect group: mean (SD) |
|---|---|---|---|---|
| Lost productivity | ||||
| No. (%) taking any time off to attend physiotherapy consultation | 692 | 218 (31.5) | 1416 | 380 (26.8) |
| No. (%) for whom work has been affected because of condition | 477 | 141 (29.6) | 959 | 317 (33.1) |
| Cost | ||||
| Time off work (minutes) to attend physiotherapy consultation | 598 | 58.06 (167.81) | 1211 | 55.35 (276.90) |
| Time off work (days) because of the condition | 452 | 2.77 (13.97) | 884 | 2.30 (11.10) |
| All available data | ||||
| Value of time off work associated with physiotherapy | 598 | £12.90 (£38.99) | 1211 | £11.91 (£57.86) |
| Value of time off work associated with the condition | 452 | £265.92 (£1350.82) | 884 | £226.61(£1139.84) |
| Complete cases | ||||
| Value of time off work associated with physiotherapy | 451 | £14.28 (£42.32) | 883 | £14.05 (£65.49) |
| Value of time off work associated with the condition | 451 | £262.47 (£1350.32) | 883 | £226.69 (£1140.49) |
Quality-adjusted life-years
Table 50 gives the EQ-5D scores at baseline and the two follow-up points, along with QALYs over the 6-month period. We present results for all available patients, which vary according to the time period, and for complete cases (n = 1272). QALYs have been adjusted to allow for the difference in baseline EQ-5D between the two groups. Patients in both groups improved during the trial period. Patients in the PhysioDirect group had a slightly lower EQ-5D score at baseline and a slightly higher score at the end of the 6-month period than those in the usual-care group; QALYs in this group were therefore slightly higher.
| Quality of life and QALYs | n | Usual-care group: mean (SD) | n | PhysioDirect group: mean (SD) |
|---|---|---|---|---|
| EQ-5D at baseline | 731 | 0.555 (0.288) | 1480 | 0.530 (0.300) |
| 432 | 0.573 (0.281) | 840 | 0.556 (0.285) | |
| EQ-5D at 6 weeks | 554 | 0.643 (0.260) | 1080 | 0.643 (0.272) |
| 432 | 0.645 (0.254) | 840 | 0.656 (0.260) | |
| EQ-5D at 6 months | 508 | 0.688 (0.274) | 1020 | 0.691 (0.274) |
| 432 | 0.698 (0.265) | 840 | 0.699 (0.266) | |
| QALYs, adjusted for baseline difference | ||||
| All available data | 454 | 0.322 (0.079) | 881 | 0.331 (0.082) |
| Complete cases | 432 | 0.325 (0.077) | 840 | 0.332 (0.081) |
Summary of findings and conclusion
Cost consequences
Table 51 gives the cost–consequence matrix. Here, total cost per patient by category is given for all of the available data. Consequences are represented by each of the primary and secondary outcomes.
| Costs and consequences | n | Usual-care group: mean (SD) | n | PhysioDirect group: mean (SD) | Incremental difference (95% CI) |
|---|---|---|---|---|---|
| Costs (£) | |||||
| Total physiotherapy cost | 743 | 69.73 (56.17) | 1506 | 74.01 (63.97) | 4.28 (−1.12 to 9.69) |
| Cost of NHS services including physiotherapy | 453 | 189.19 (557.61) | 888 | 196.43 (472.02) | 7.24 (−49.68 to 64.10) |
| Total cost to patientsa | 303 | 33.36 (685.49) | 692 | 112.34 (1097.35) | 78.97 (−54.91 to 212.85) |
| Total value of all time off work | 451 | 276.75 (1355.00) | 883 | 240.74 (1147.20) | −36.01 (−174.69 to 102.66) |
| Consequencesb | |||||
| Difference (95% CI) c | |||||
| SF-36v2 PCS | 629 | 44.18 (10.84) | 1283 | 43.50 (10.94) | −0.01 (−0.80 to 0.79) |
| MYMOPd | 518 | 2.40 (1.38) | 1033 | 2.40 (1.43) | −0.02 (−0.16 to 0.11) |
| EQ-5D | 508 | 0.69 (0.27) | 1020 | 0.69 (0.27) | 0.01 (−0.02 to 0.03) |
| Global improvement score | 501 | 4.07 (1.40) | 1001 | 4.01 (1.44) | −0.23 to 0.08 |
| Response to treatment (OMERACT-OARSI) | 510 | 197 (38.6%) | 1029 | 430 (41.8%) | 1.14 (0.92 to 1.43) |
| Waiting time to first assessment and advice | 618 | 34 (20 to 55)e | 1281 | 7 (4 to 15)e | 0.32 (0.29 to 0.35)f |
| Patient overall satisfaction | 367 | 79.7 (26.5) | 739 | 75.9 (28.3) | −3.8 (−7.3 to −0.3) |
Cost-effectiveness analysis
Table 52 summarises the cost-effectiveness analysis using resource-use data from the NHS perspective. These data show that, although the costs to the NHS of the two services are remarkably similar, the cost of the PhysioDirect service is slightly higher overall than the cost associated with usual care. The incremental cost per QALY gained, obtained by dividing the difference in cost by the difference in QALYs, is £2889; the net monetary benefit (NMB) is £117 if society's willingness to pay for a QALY (λ) is valued at £20,000. Uncertainty around this value is illustrated in Figures 7 and 8. The cost-effectiveness plane shows the 5000 estimated incremental cost-effectiveness ratio (ICER) replicates produced using the bootstrapping technique. The CEAC shows the probability that the PhysioDirect service is cost-effective at different levels of willingness to pay for a QALY. At £20,000 per QALY gain the probability is 0.88 and at £30,000 it is 0.90.
| n | Mean among usual-care group | n | Mean among PhysioDirect group | Incremental difference (95% CI) | |
|---|---|---|---|---|---|
| Cost of physiotherapy (£) | 432 | 78.77 | 840 | 86.75 | 7.98 (0.69 to 15.27) |
| Cost of NHS services other than physiotherapy (£) | 432 | 100.91 | 840 | 112.23 | 11.32 (−45.08 to 67.72) |
| Total cost including physiotherapy (£) | 432 | 179.68 | 840 | 198.98 | 19.30 (−37.60 to 76.19) |
| QALYs | 432 | 0.325 | 840 | 0.332 | 0.007 (−0.003 to 0.016) |
| ICER (£) | 2889 | ||||
| Median NMB (95% CI) based on bootstrapped results (£) | |||||
| 20,000 | 117 (−86 to 310) | ||||
| 30,000 | 184 (−106 to 461) | ||||
FIGURE 7.
Cost-effectiveness plane for PhysioDirect (base-case analysis), showing 5000 bootstrapped replicates of the ICER: complete case data, adjusted QALYs.
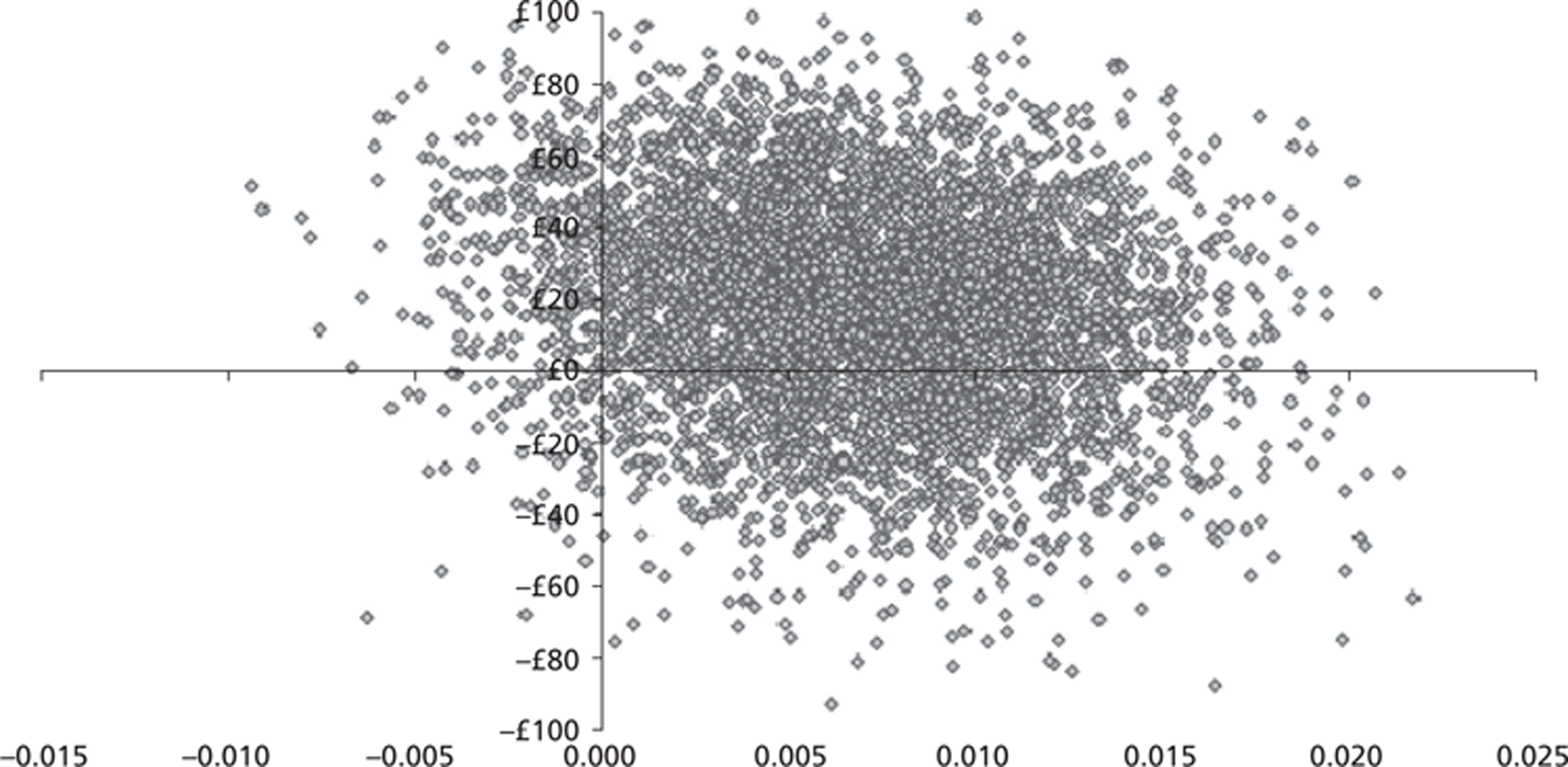
FIGURE 8.
Cost-effectiveness acceptability curve for the cost of PhysioDirect at different levels of willingness to pay, showing the probability that the intervention is cost-effective at different levels of willingness to pay: complete case data, adjusted QALYs.
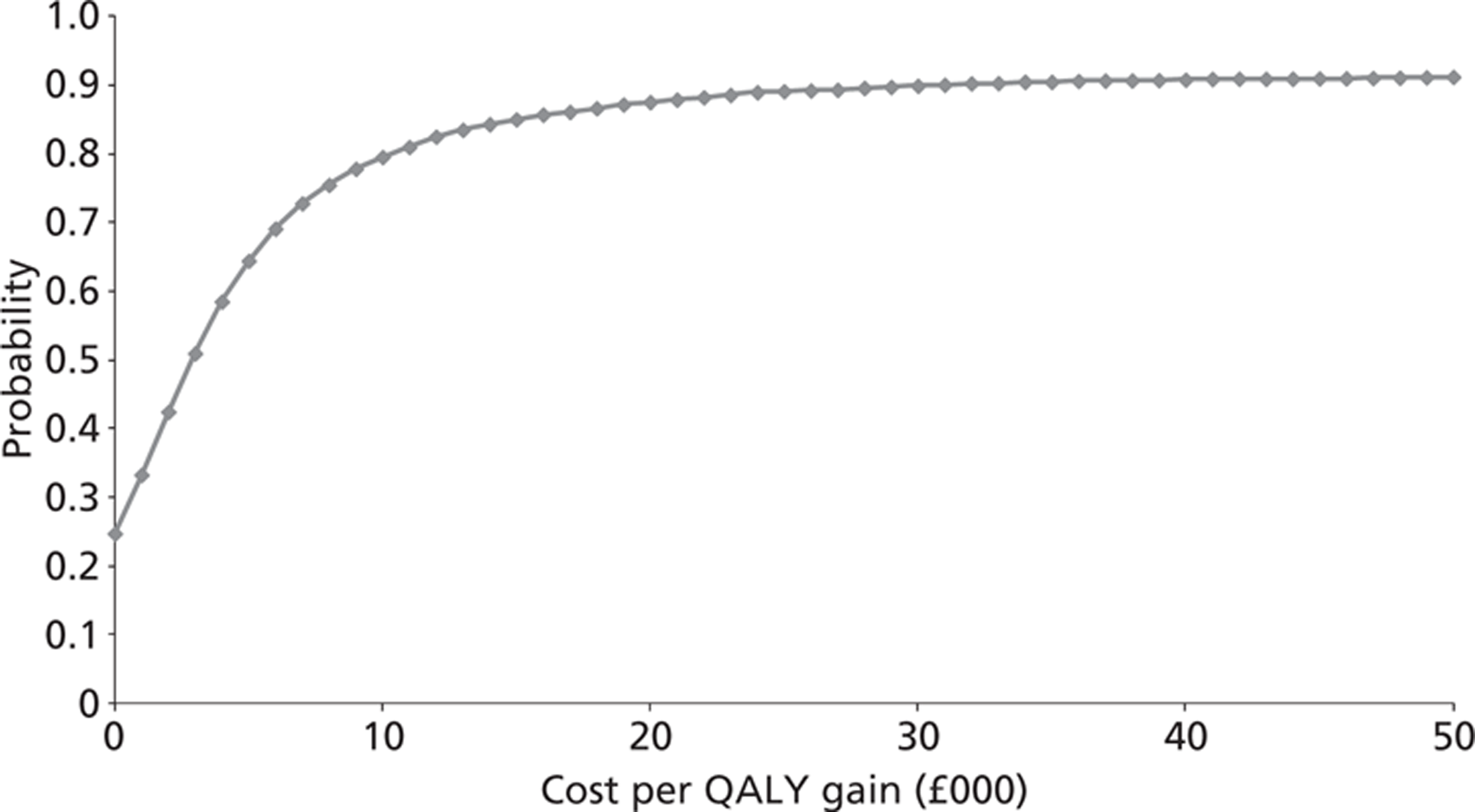
Sensitivity analysis
Impact of mimicking an efficient service
If the PhysioDirect services had run during the trial in the more efficient way as seen in Bristol following the trial, the amount of non-contact physiotherapist time would have been reduced in all four centres. During the trial, the physiotherapists spent about 35% of their time during PhysioDirect sessions on the telephone or dealing with directly related administration. In Bristol, after the trial, this was increased to 57%. The cost implications of this are shown in Table 53.
| n | Mean (SD) among usual-care group | n | Mean (SD) among PhysioDirect group | Incremental difference (95% CI) | |
|---|---|---|---|---|---|
| Cost of physiotherapy (£) | 432 | 76.56 | 840 | 72.22 | −4.34 (−11.25 to 2.57) |
| Cost of NHS services (£) | 432 | 100.91 | 840 | 112.23 | 11.32 (−45.08 to 67.72) |
| Total cost (£) | 432 | 177.46 | 840 | 184.44 | 6.98 (−49.89 to 63.85) |
| QALYs | 432 | 0.325 | 840 | 0.332 | 0.007 (−0.003 to 0.016) |
| ICER | 1045 | ||||
| Median NMB (95% CI) based on bootstrapped results (£) | |||||
| 20,000 | 127 (−74 to 319) | ||||
| 30,000 | 193 (−95 to 473) | ||||
Under this scenario, cost per patient in the PhysioDirect group is £14.53 less than under trial conditions and £2.11 less per patient in the usual-care group. The ICER is therefore lower, at £1045, and the NMB correspondingly higher at £127 (λ = £20,000). The probability of PhysioDirect being cost-effective at λ = £20,000 is 0.89; at £30,000 it is 0.90. This is illustrated in Figures 9 and 10.
FIGURE 9.
Cost-effectiveness plane for PhysioDirect (sensitivity analysis on cost of PhysioDirect mimicking an efficient service): complete case data, adjusted QALYs; showing 5000 bootstrapped replicates of the ICER.
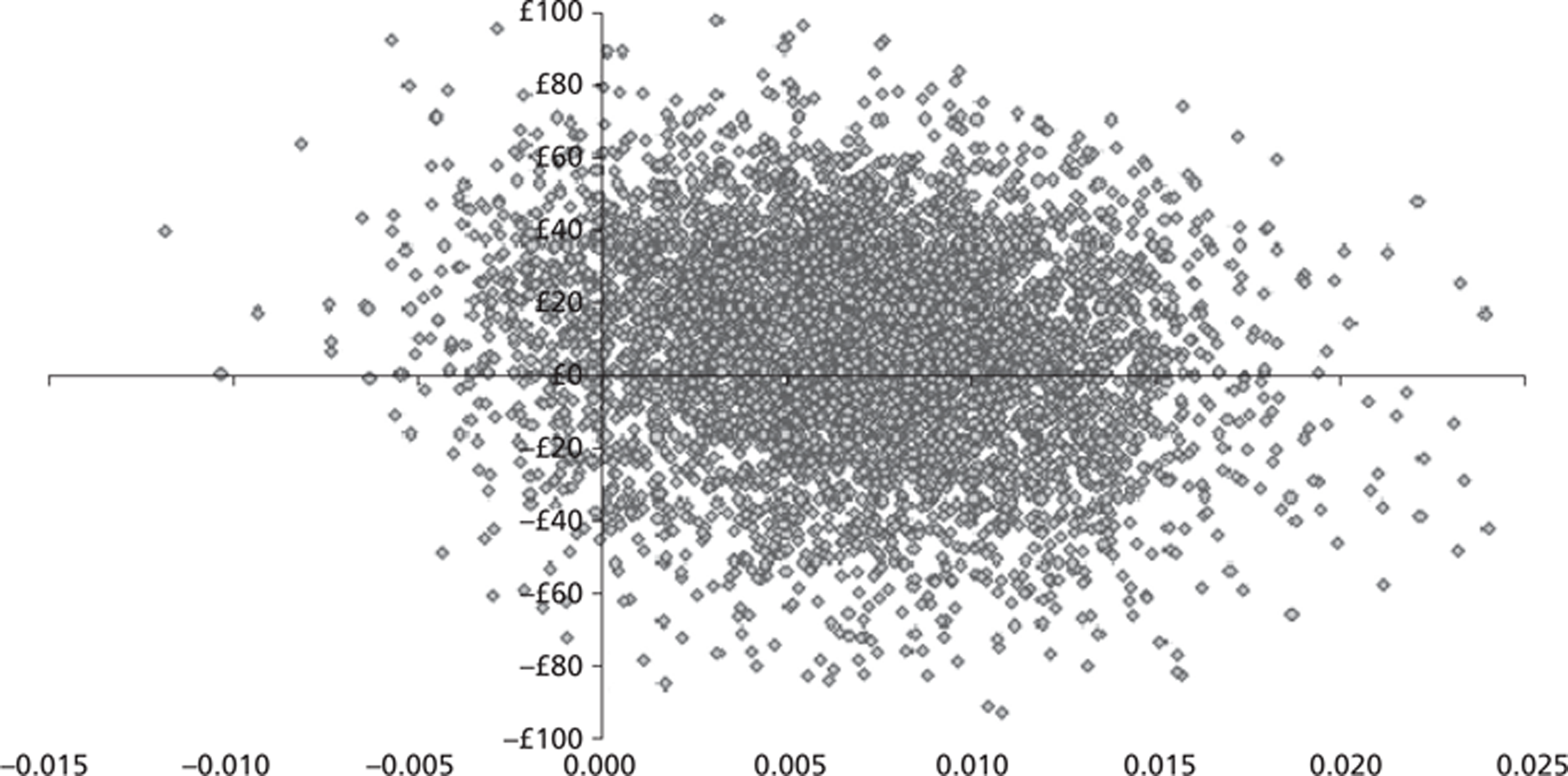
FIGURE 10.
Cost-effectiveness acceptability curve for PhysioDirect (sensitivity analysis on cost of PhysioDirect mimicking an efficient service), showing the probability that the intervention is cost-effective at different levels of willingness to pay; complete case data, adjusted QALYS.
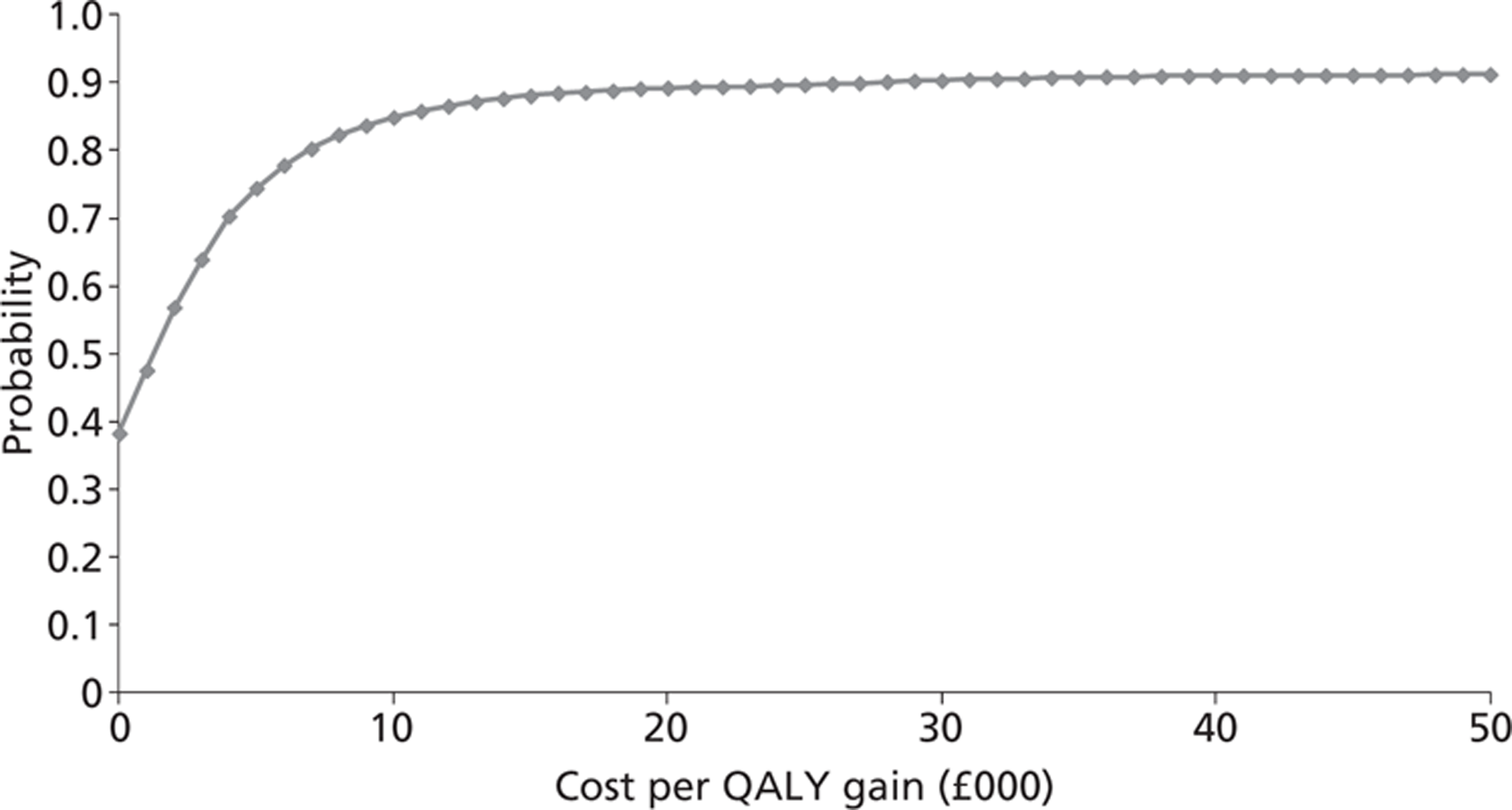
Impact of excluding hospital costs
Hospital costs accounted for 75% of all NHS costs yet only 19% participants reported using any secondary care. The main element of hospital costs was inpatient admissions but only 15 patients were admitted. The effect of removing hospital costs from the analysis is shown in Table 54 and Figures 11 and 12.
| n | Mean (SD) among usual-care group | n | Mean (SD) among PhysioDirect group | Incremental difference (95% CI) | |
|---|---|---|---|---|---|
| Cost of physiotherapy | 448 | 78.49 (572.14) | 869 | 86.84 (65.25) | 8.35 (1.21 to 15.50) |
| Cost of NHS services excluding secondary care | 448 | 33.75 (76.46) | 869 | 33.49 (63.76) | −0.25 (−8.05 to 7.54) |
| Total cost of NHS services including physiotherapy | 448 | 112.23 (99.62) | 869 | 120.33 (98.85) | 8.10 (−3.21 to 19.41) |
| QALYs | 448 | 0.323 (0.079) | 869 | 0.331 (0.082) | 0.007 (−0.002 to 0.017) |
| ICER (£) | 1084 | ||||
| Median NMB (95% CI) based on bootstrapped results (£) | |||||
| 20,000 | 142 (−41 to 324) | ||||
| 30,000 | 217 (−56 to 489) | ||||
FIGURE 11.
Cost-effectiveness plane for PhysioDirect (sensitivity analysis excluding hospital costs), showing 5000 bootstrapped replicates of the ICER.
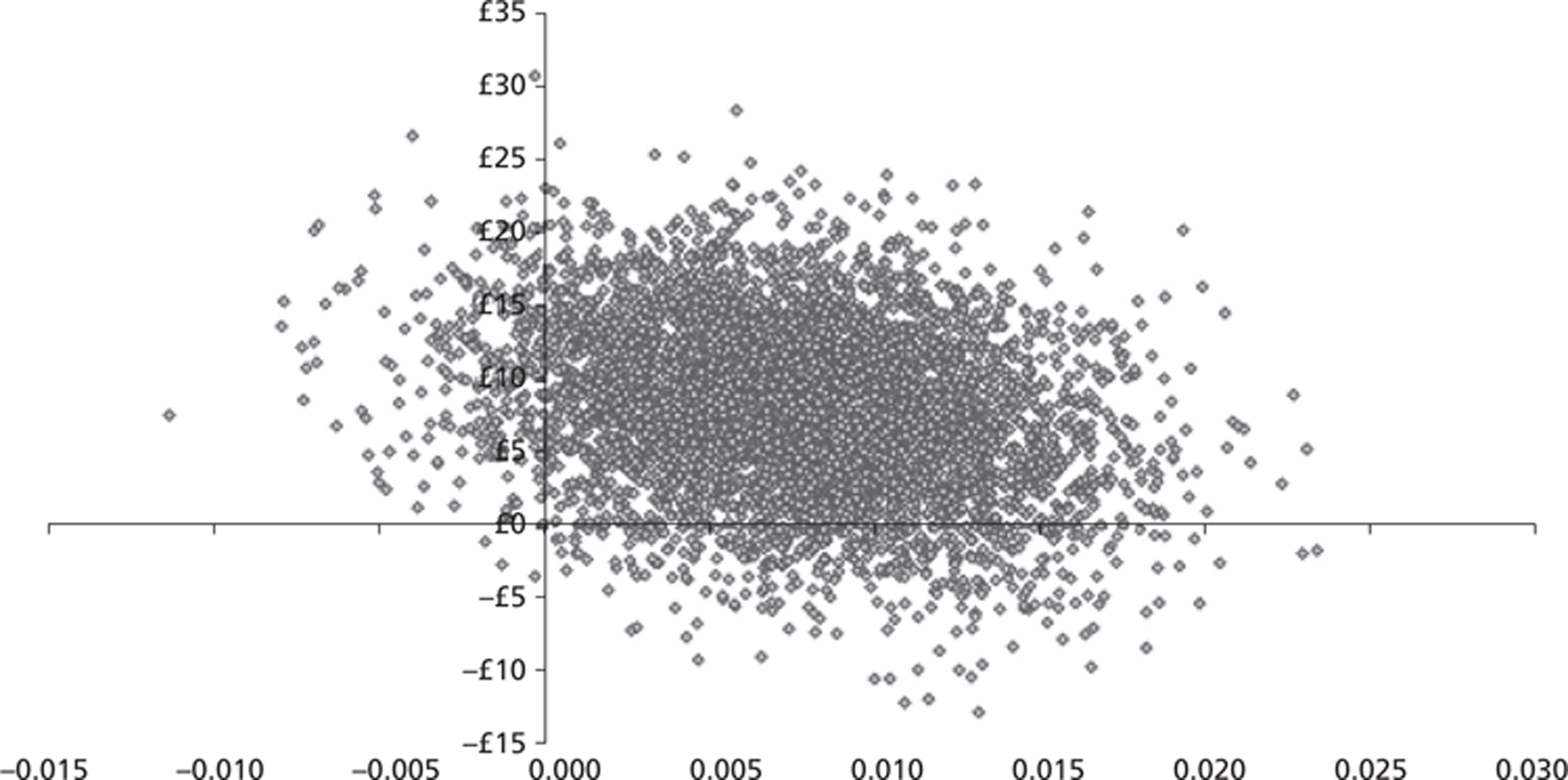
FIGURE 12.
Cost-effectiveness acceptability curve for PhysioDirect (sensitivity analysis excluding hospital costs) showing the probability that the intervention is cost-effective at different levels of willingness to pay.
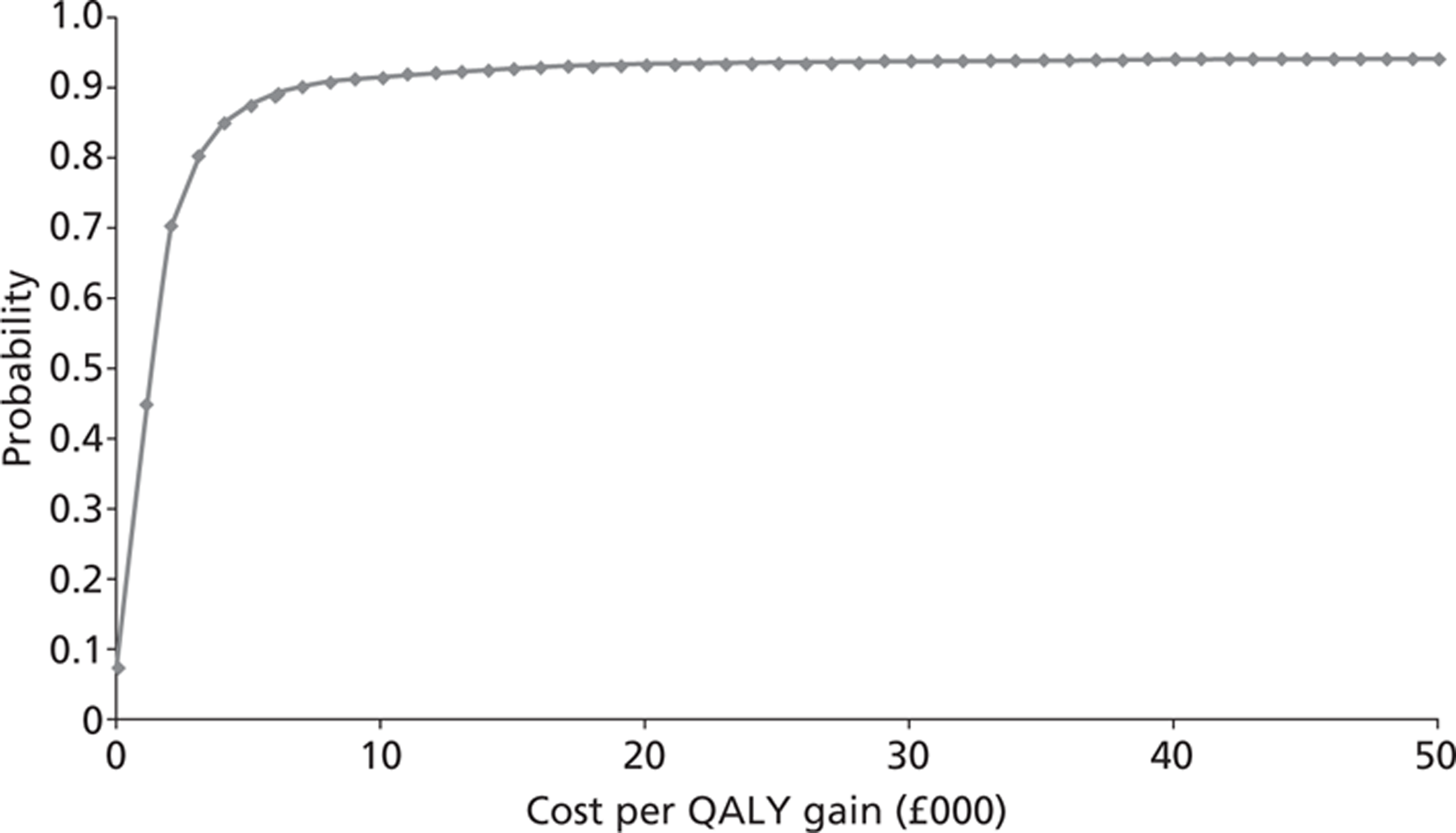
This analysis is based on all patients for whom we had primary care and medication costs and QALY data: n = 1317 (59%). There is almost no difference in NHS costs between the two groups; the cost difference is due entirely to the difference in the cost of physiotherapy. The ICER is therefore reduced (£1084) and the NMB higher at £142 (λ = £20,000) and £217 (λ = £30,000). The probability of PhysioDirect being cost-effective at λ = £20,000 is 0.93; at £30,000 it is 0.94.
Imputation of missing data
The results of imputing missing NHS cost and QALY data are shown in Table 55 and Figures 13–16. The mean cost of physiotherapy was lower for all patients after imputation than for those for whom we had complete data (overall mean £72.60 vs £84.04). This was true of patients in both groups, meaning that our base-case estimate of the cost of physiotherapy is conservative. Conversely, the imputed NHS cost data suggest that the complete case analysis may underestimate the true cost: the estimated cost in all patients after imputation was £131.48 compared with the base case of £108.38. The effect of imputing NHS costs is more marked in the usual-care group, which reduces the difference between the two groups. The overall effect is a reduction of the incremental cost of PhysioDirect compared with usual care from £19.30 (complete cases) to £4.46 (imputed cost data).
| n | Mean (SD) among usual-care group | n | Mean (SD) among PhysioDirect group | Incremental difference (95% CI) | |
|---|---|---|---|---|---|
| Cost of physiotherapy (£) | 743 | 69.73 (56.17) | 1506 | 74.01 (63.97) | 4.28 (−1.12 to 9.69) |
| Cost of NHS services (£) | 743 | 131.37 (465.49) | 1506 | 131.51 (384.36) | 0.17 (−36.13 to 36.48) |
| Total cost of NHS services including physiotherapy (£) | 743 | 201.09 (467.51) | 1506 | 205.55 (390.04) | 4.46 (−32.22 to 41.14) |
| QALYs | 743 | 0.320 (0.003) | 1506 | 0.322 (0.002) | 0.002 (−0.006 to 0.009) |
| ICER (£) | 2260 | ||||
| Median NMB (95% CI) based on bootstrapped results (£) | |||||
| 20,000 | 34 (−119 to 193) | ||||
| 30,000 | 52 (−172 to 285) | ||||
| Sensitivity analysis: more efficient service scenario | |||||
| Cost of physiotherapy (£) | 743 | 67.61 (54.19) | 1506 | 61.41 (59.13 | −6.20 (−11.26 to 1.14) |
| Cost of NHS services (£) | 743 | 131.37 (465.49) | 1506 | 131.54 (384.36) | −0.17 (−36.13 to 36.48) |
| Total cost of NHS services including physiotherapy (£) | 743 | 198.98 (467.48) | 1506 | 192.95 (389.52) | −6.02 (−42.68 to 30.63) |
| QALYs | 743 | 0.320 (0.003) | 1506 | 0.322 (0.002) | 0.002 (−0.006 to 0.009) |
| ICER (£) | −3054 | ||||
| Median NMB (95% CI) based on bootstrapped results (£) | |||||
| 20,000 | 47 (−113 to 202) | ||||
| 30,000 | 67 (−165 to 293) | ||||
FIGURE 13.
Cost-effectiveness plane for PhysioDirect (sensitivity analysis after imputing missing data, adjusted QALYs), showing 5000 bootstrapped replicates of the ICER.
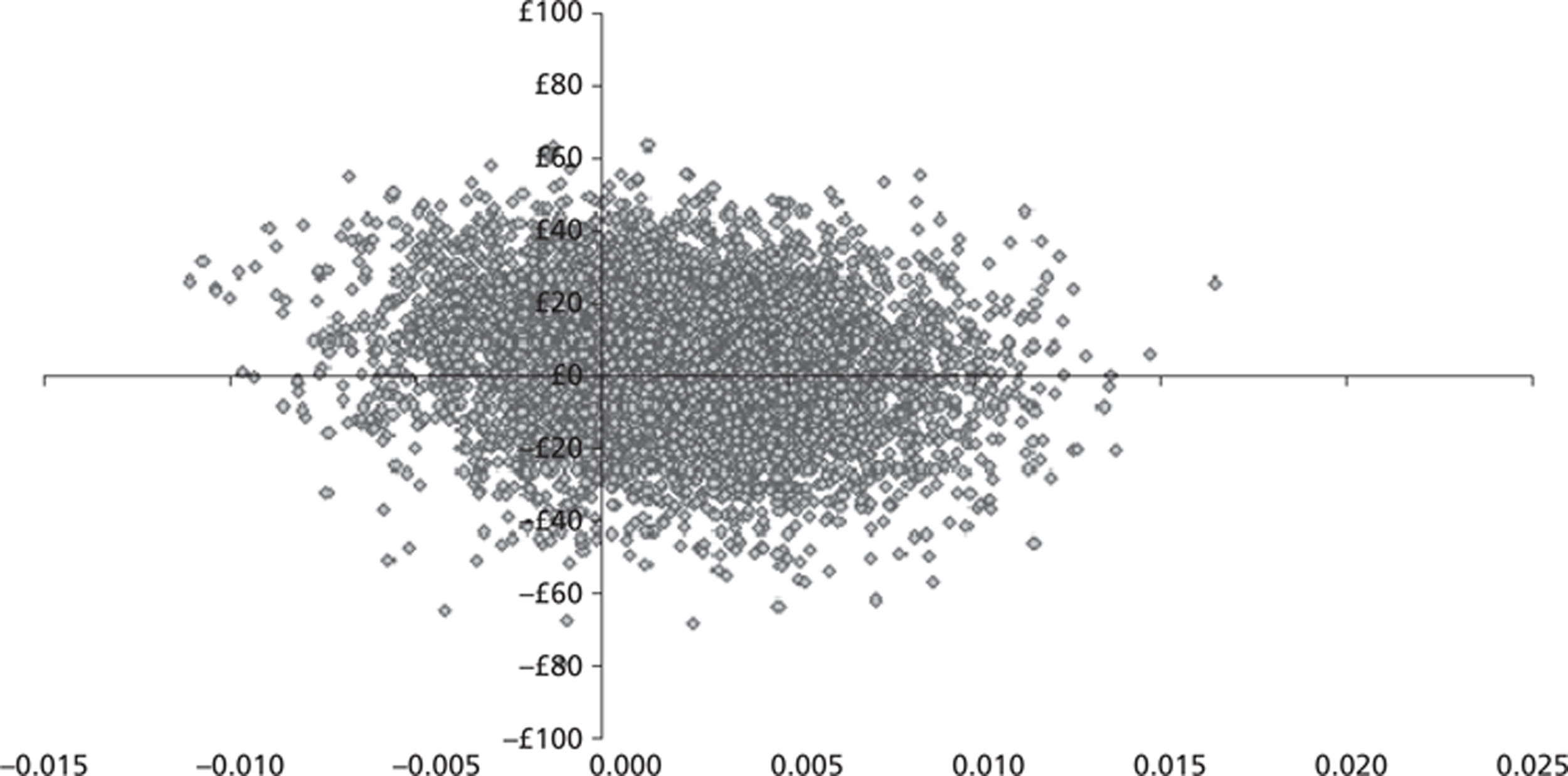
FIGURE 14.
Cost-effectiveness acceptability curve for PhysioDirect (sensitivity analysis after imputing missing data, adjusted QALYs), showing the probability that the intervention is cost-effective at different levels of willingness to pay.
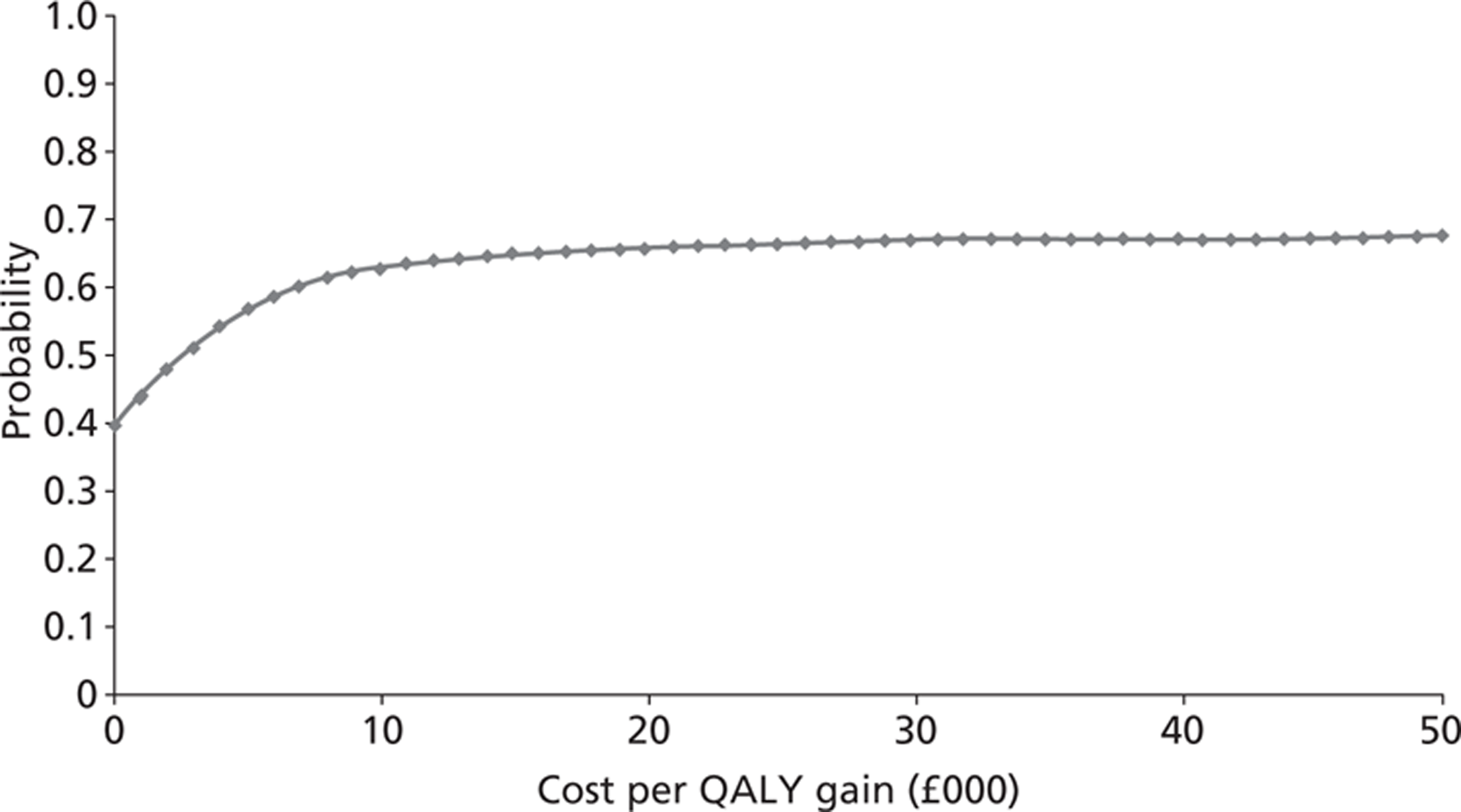
FIGURE 15.
Cost-effectiveness plane for PhysioDirect (sensitivity analysis after imputing missing data and with efficient service scenario, adjusted QALYs), showing 5000 bootstrapped replicates of the ICER.
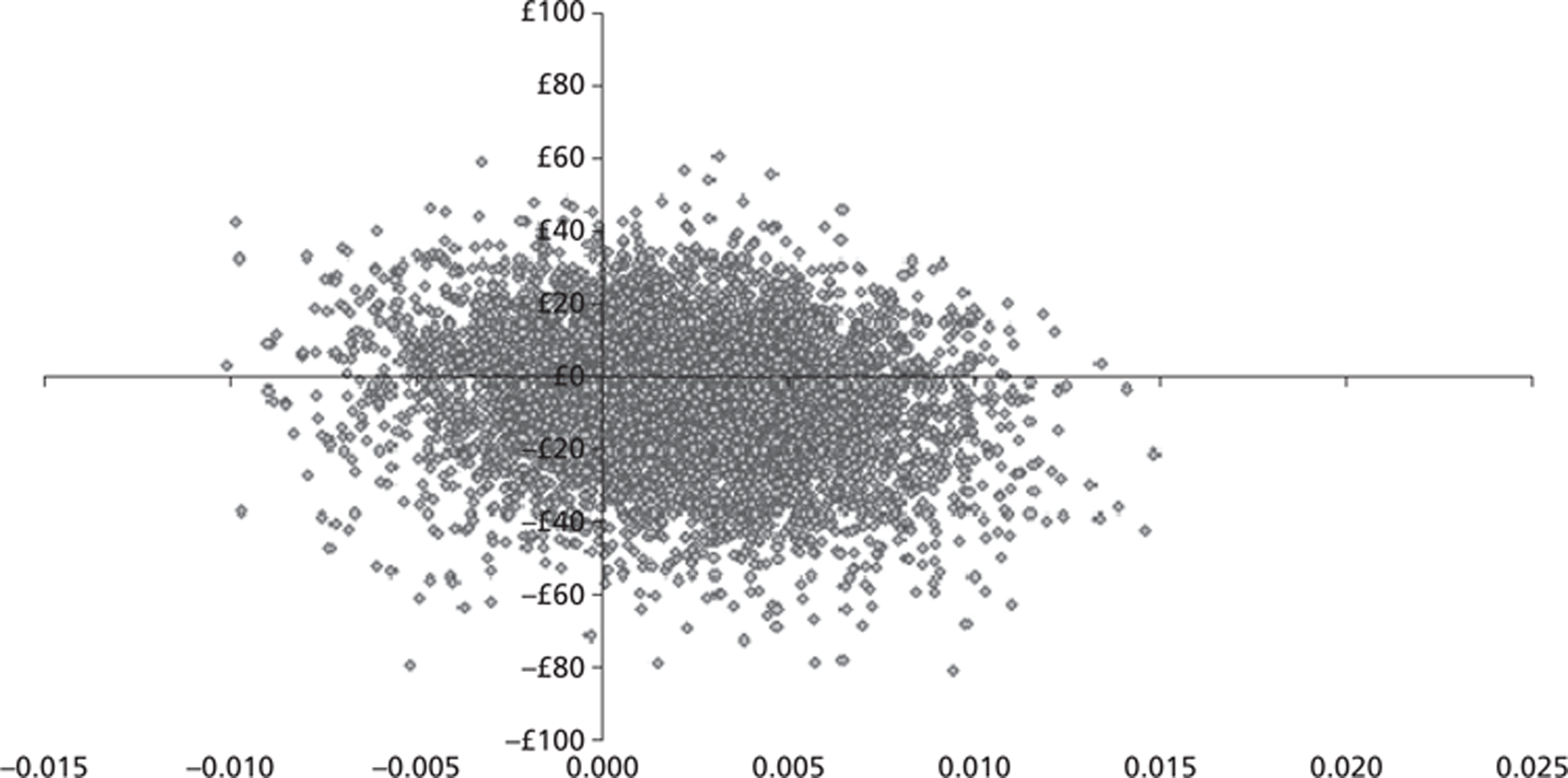
FIGURE 16.
Cost-effectiveness acceptability curve for PhysioDirect (sensitivity analysis after imputing missing data and with efficient service scenario, adjusted QALYs), showing the probability that the intervention is cost-effective at different levels of willingness to pay.
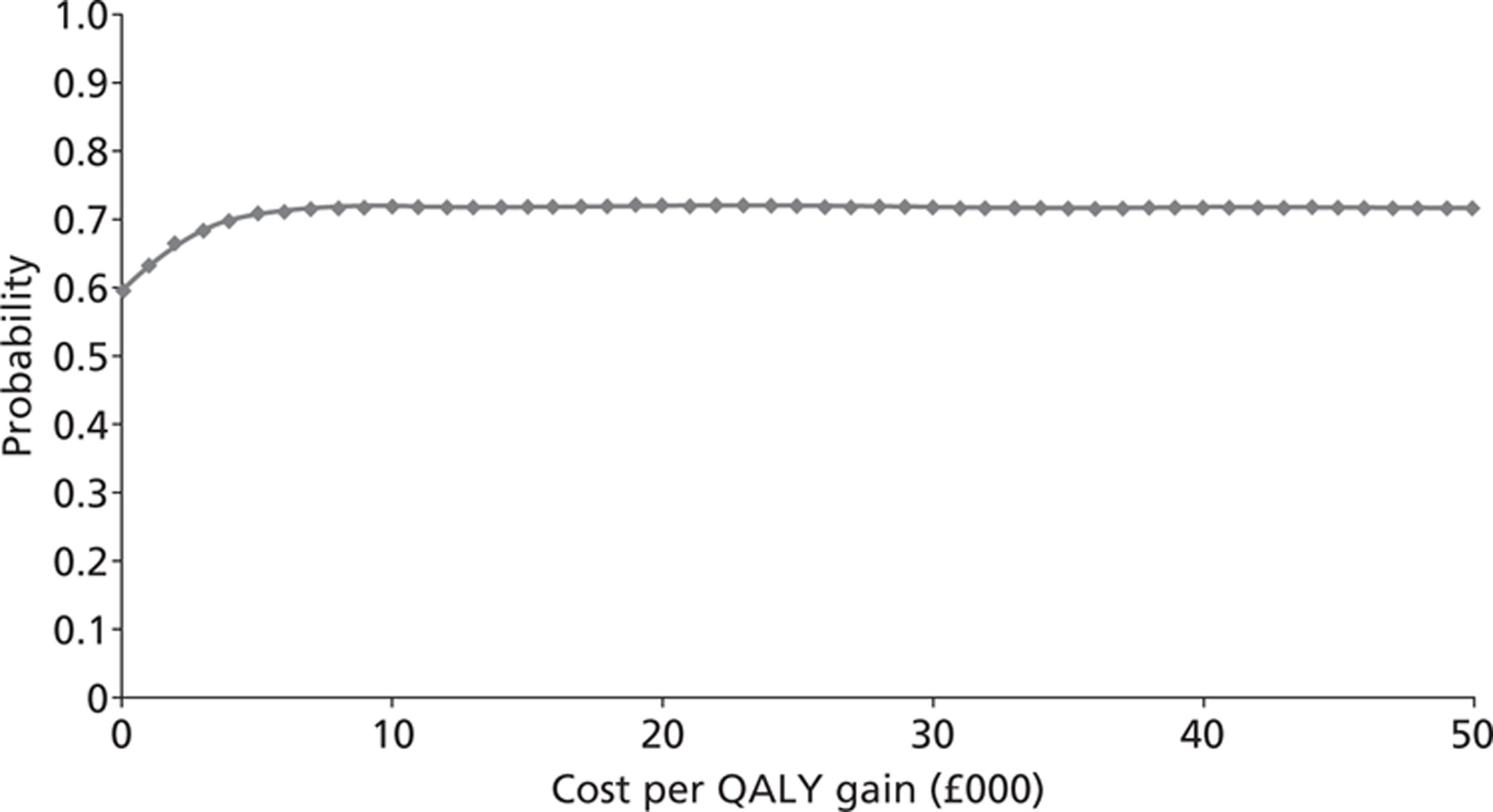
Sensitivity analysis using imputed cost data in the ‘more efficient service’ scenario suggests a possible cost saving of £6.02 per patient.
The effect of imputing missing EQ-5D data is to reduce QALYs gained from 0.3299 (complete cases) to 0.3216 (imputed data). The difference is greatest in the PhysioDirect group, giving a reduced incremental QALY gain of 0.0020 as against 0.0067.
Using imputed cost and QALY data the probability that the PhysioDirect service is cost-effective at £20,000 per QALY is 0.66 and at £30,000 it is 0.67. The probability under the ‘efficient service’ scenario of the sensitivity analysis is 0.72 at both £20,000 and £30,000 per QALY.
Use of Short Form questionnaire-6 Dimensions rather than European Quality of Life-5 Dimensions
It is possible to use the data from the SF-36 questionnaire to estimate QALYs using the SF-6D measure. 96 In a further sensitivity analysis (not prespecified a priori but in response to the request of a peer reviewer) we compared the findings using the SF-6D rather than the EQ-5D to generate QALYs. The results are shown in Tables 56 and 57 and Figure 17.
| n | Mean (SD) among usual-care group | n | Mean (SD) among PhysioDirect group | Incremental difference (95% CI) | |
|---|---|---|---|---|---|
| Sensitivity analysis: using EQ-5D (data set with complete EQ-5D, SF-6D and cost data) | |||||
| Total cost of NHS services including physiotherapy (£) | 386 | 186.44 (531.17) | 738 | 197.17 (462.32) | 10.73 (−49.29 to 70.76) |
| QALYs | 386 | 0.327 (0.077) | 738 | 0.332 (0.079) | 0.005 (−0.005 to 0.015) |
| ICER (£) | 2115 | ||||
| Median NMB (95% CI) based on bootstrapped results (£) | |||||
| 20,000 | 93 (−118 to 306) | ||||
| 30,000 | 146 (−159 to 448) | ||||
| Sensitivity analysis: using SF-6D (data set with complete EQ-5D, SF-6D and cost data) | |||||
| Total cost of NHS services including physiotherapy (£) | 386 | 186.44 (531.17) | 738 | 197.17 (462.32) | 10.73 (−49.29 to 70.76) |
| QALYs | 386 | 0.341 (0.045) | 738 | 0.344 (0.043) | 0.003 (−0.002 to 0.009) |
| ICER (£) | 3484 | ||||
| Median NMB (95% CI) based on bootstrapped results (£) | |||||
| 20,000 | 49 (−85 to 185) | ||||
| 30,000 | 80 (−107 to 265) | ||||
FIGURE 17.
Cost-effectiveness acceptability curves: sensitivity analyses comparing use of EQ-5D or SF-6D to generate QALYs, with or without imputation of missing data, showing the probability that the intervention is cost-effective at different levels of willingness to pay. (a) QALYs from EQ-5D, n = 1124. (b) QALYs from SF-6D, n = 1124. (c) QALYs from EQ-5D, imputed data. (d) QALYs from SF-6D, imputed data.
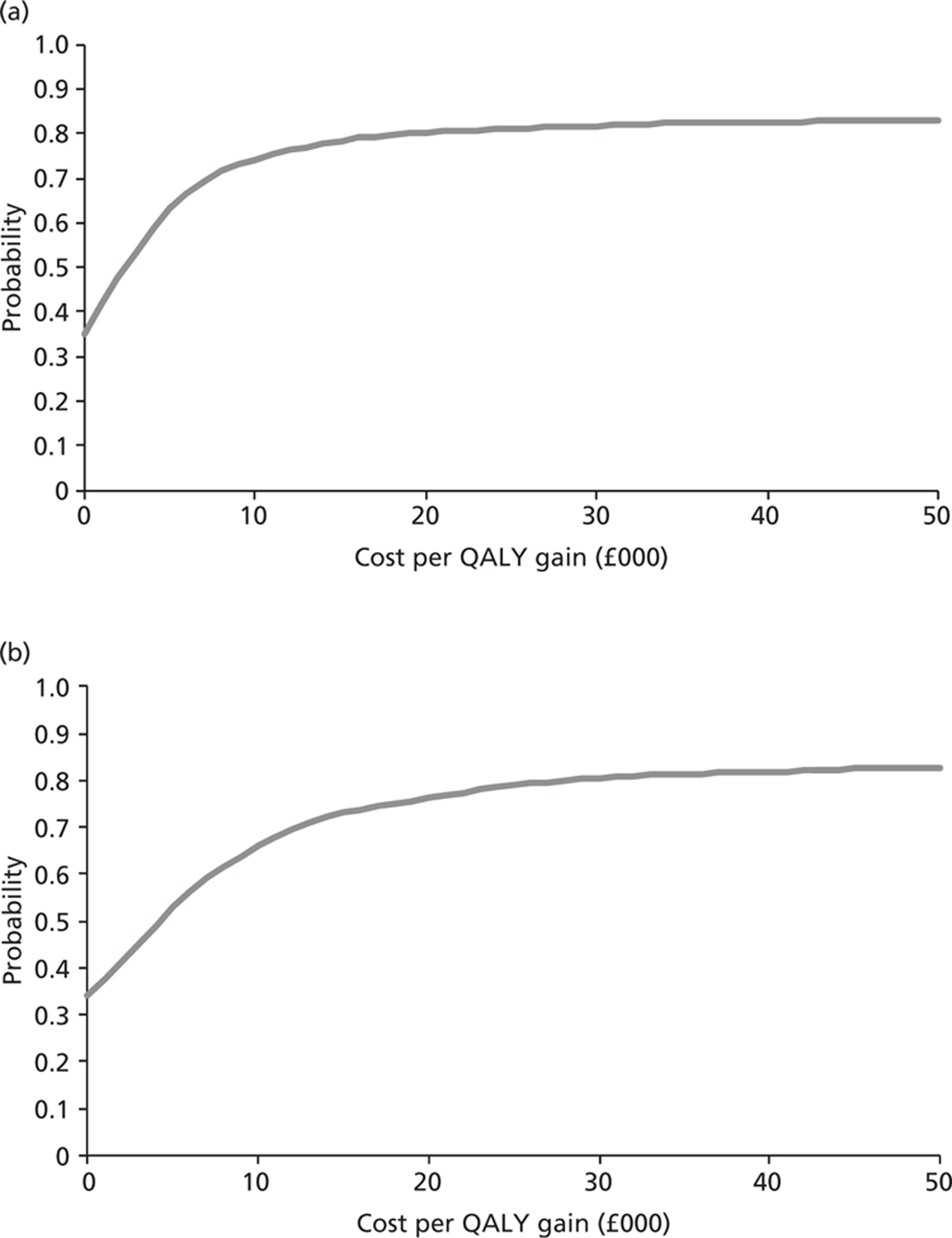
In order to compare the findings using the SF-6D or the EQ-5D it is necessary to include only patients who have data on both outcomes, as well as complete cost data. This reduced the denominator from 1272 patients to 1124 patients. In this group of patients, the cost-effectiveness of PhysioDirect assessed using the SF-6D was slightly lower than when assessed using the EQ-5D (see Table 56). The probabilities that PhysioDirect was cost-effective at the £20,000 and £30,000 willingness-to-pay thresholds were 76% and 80%, respectively.
After imputing missing data, PhysioDirect again appeared to be slightly less cost-effective when QALYs were assessed using SF-6D rather than EQ-5D. The probabilities that PhysioDirect was cost-effective at the £20,000 and £30,000 willingness-to-pay thresholds were 55% and 57%, respectively (see Table 57).
| n | Mean (SD) among usual-care group | n | Mean (SD) among PhysioDirect group | Incremental difference (95% CI) | |
|---|---|---|---|---|---|
| Sensitivity analysis: using EQ-5D (missing data imputed) | |||||
| Total cost of NHS services including physiotherapy (£) | 743 | 201.09 (467.51) | 1506 | 205.55 (390.04) | 4.46 (−32.22 to 41.14) |
| QALYs | 743 | 0.320 (0.003) | 1506 | 0.322 (0.002) | 0.002 (−0.006 to 0.009) |
| ICER (£) | 2260 | ||||
| Median NMB (95% CI) based on bootstrapped results (£) | |||||
| 20,000 | 34 (−119 to 193) | ||||
| 30,000 | 52 (−172 to 285) | ||||
| Sensitivity analysis: using SF-6D (missing data imputed) | |||||
| Total cost of NHS services including physiotherapy (£) | 743 | 201.09 (467.51) | 1506 | 205.55 (390.04) | 4.46 (−32.22 to 41.14) |
| QALYs | 743 | 0.339 (0.045) | 1506 | 0.340 (0.043) | 0.005 (−0.003 to 0.004) |
| ICER (£) | 8463 | ||||
| Median NMB (95% CI) based on bootstrapped results (£) | |||||
| 20,000 | 6 (−85 to 98) | ||||
| 30,000 | 11 (−117 to 140) | ||||
Summary of sensitivity analyses
Table 58 summarises the findings from the various sensitivity analyses that were conducted to assess the robustness of the conclusions under a range of different scenarios and assumptions.
Several trends are apparent from the above sensitivity analyses. The incremental cost per QALY (ICER) for the intervention is low. However, because the benefits in terms of QALYs and the costs are both very small, the NMB is also small (and the confidence estimates overlap zero). Under the most optimistic scenario (based on the more efficient service as observed outside the trial and after imputing missing data), the intervention is both more effective and less expensive. Under the least optimistic scenario (using the SF-6D to generate QALYs and imputing missing data), the NMB from PhysioDirect is negligible. It is notable that in all scenarios the probability that PhysioDirect is cost-effective is > 50%.
| No. | Scenario | n (% of all 2256 participants) | ICER (£) | NMB (95% CI) | Probability cost-effective at £20,000 per QALY threshold (%) |
|---|---|---|---|---|---|
| 1 | Complete case analysis | 1272 (56) | 2889 | 117 (−86 to 310) | 88 |
| 2 | More efficient service as observed after the trial | 1272 (56) | 1045 | 127 (−74 to 319) | 89 |
| 3 | Excluding hospital costs | 1317 (58) | 1084 | 142 (−41 to 324) | 93 |
| 4 | Imputation of missing data | 2256 (100) | 2260 | 34 (−119 to 193) | 66 |
| 5 | Imputation of missing data and more efficient service | 2256 (100) | −3054 | 47 (−113 to 202) | 72 |
| 6 | Using SF-6D rather than EQ-5D to generate QALYs | 1124 (50) | 3484 | 47 (−85 to 185) | 76 |
| 7 | Using EQ-5D in data set that also contains SF-6D, for comparison | 1124 (50) | 2115 | 93 (−118 to 306) | 80 |
| 8 | Using SF-6D rather than EQ-5D, imputed data | 2256 (100) | 8463 | 6 (−85 to 98) | 5 |
Chapter 6 Qualitative study: methods
Introduction
The aim of the qualitative study was to explore the acceptability and implementation of PhysioDirect from the point of view and experiences of the key stakeholders: the patients who took part in the randomised trial; the physiotherapists who provided the PhysioDirect service and their managers; and the GPs who referred patients for physiotherapy. Although there is little research evidence about the acceptability and implementation of PhysioDirect services, evidence from available qualitative studies in other areas of telemedicine informed the approach taken in this study.
One of the key concerns about telemedicine relates to diagnostic accuracy given that clinicians express worries about the loss of visual clues in telephone consultations, and that the lack of the visual component of patient assessment makes it difficult to establish whether or not patients may be seriously unwell. 48 The limited comparable data about PhysioDirect services also highlight that some physiotherapists express concern about the accuracy of patient diagnosis over the telephone. 53 A recent study, however, has shown concordance between patient diagnoses reached over the telephone and those resulting from traditional, face-to-face consultations. 53 A further potential concern about PhysioDirect services is that this new way of working might be viewed as undesirable by physiotherapists delivering the service. It appears that some physiotherapists have previously expressed concerns regarding their professional identity and the potential of telephone working to cause them to ‘de-skill’, in particular with respect to skills such as their physical assessment tests of painful body regions and joints as well as some types of treatment such as manual therapy. 53,97 Thus, the limited relevant research to date highlights some key concerns about physiotherapy telemedicine services that may affect their implementation and acceptability to health professionals.
No previous research studies could be found that specifically explored the views of patients about available PhysioDirect telephone services. This chapter summarises the evidence that emerged from the qualitative interview study that was nested within the PhysioDirect RCT.
Methodology: research design
The PhysioDirect service investigated in the randomised trial is an example of a complex intervention and, in line with MRC guidance,98 a qualitative study was nested alongside the main trial. The aims of the qualitative investigation were to explore the acceptability of PhysioDirect, to determine the key elements in how the service was perceived, and to understand the key barriers and facilitators to the successful implementation of the service. The perspectives of patients, physiotherapists, physiotherapy managers, GPs and PCT commissioners were sought through one-to-one, semistructured interviews in person or by telephone. Each of these interviews was directed by a topic guide informed by available literature. Appendix 3 shows an example of a topic guide. Patients, managers, GPs and commissioners were interviewed at one point in time, while longitudinal qualitative data were collected with a sample of physiotherapists (before and after the trial) to investigate if and how their views changed over time in the light of their experience of providing the PhysioDirect service. This chapter focuses on the beliefs and experiences of only patients and the physiotherapists who provided the PhysioDirect service and their managers.
Data collection and sampling
Patient interviews
Interviews were carried out after the patient's discharge from their physiotherapy episode of care in the trial. The aims were to explore the accessibility and acceptability of the physiotherapy service, the influence of PhysioDirect and usual physiotherapy care assessment and treatment on patients' perceptions of their care and its impact on their MSK problem, and to explore whether and how patients perceived that services could be improved.
Purposive sampling based on age, sex, presenting clinical problem and participating PCT was used to generate a diverse range of patient perceptions and experiences. In total, 388 patients were invited to take part in the qualitative interview study between August 2009 and April 2010, with 82 agreeing to be interviewed and 57 interviews being conducted. The reasons why the number agreeing to be interviewed and the final number of interviews were different were due to the difficulties in arranging convenient times for interviews and saturation of the data, i.e. no new themes emerged after the first 57 interviews.
Table 59 provides a summary of the characteristics of patients who took part in interviews, showing their key characteristics according to each of the sampling criteria. Slightly more women were interviewed than men, and although the average age was 58 years, there was a large range of ages, with the youngest person interviewed being 19 years and the oldest being 87 years. More patients were interviewed in the group that was randomised to the new PhysioDirect service than in the usual-care group, including those who received some or all of the components of the new service, as well as those who were randomised to the new service but who never telephoned or contacted the service. This was deliberate in order to fully explore patients' perceptions of the new service. To facilitate comparisons between the new PhysioDirect service and the usual physiotherapy service, nine interviews were conducted with patients randomised to usual care. Interviews were conducted with patients from each of the four participating PCTs, and patients were sampled to ensure a breadth of MSK problems affecting different bodily regions.
| Patient characteristics | No. | % |
|---|---|---|
| Sex | ||
| Male | 26 | 46 |
| Female | 31 | 54 |
| Age (years) | ||
| Mean (SD) | 58 (16.88) | |
| Range | 19–87 | |
| Trial group | ||
| PhysioDirect arm: telecare only | 25 | 44 |
| PhysioDirect arm: telecare + face-to-face care | 13 | 23 |
| PhysioDirect arm: did not ring the service | 10 | 17 |
| Usual physiotherapy care arm | 9 | 16 |
| PCT | ||
| PCT A | 17 | 30 |
| PCT B | 15 | 26 |
| PCT C | 13 | 23 |
| PCT D | 12 | 21 |
| Area of MSK complaint | ||
| Lower limb | 23 | 40 |
| Upper limb | 14 | 21 |
| Cervical spine | 5 | 25 |
| Lumbar spine | 12 | 9 |
| Multiple areas of pain | 3 | 5 |
Interviews with physiotherapists and their managers
The aim of the interviews with physiotherapists and their managers was to identify the salient issues involved with providing and managing the new PhysioDirect service and to explore its acceptability and implementability. A longitudinal design was used with the participating physiotherapists so that each was interviewed twice: once before treating patients in the PhysioDirect trial, and again when the trial had finished. The aim of the longitudinal design was to obtain insight into each physiotherapist's views, hopes and concerns prior to using the new service with patients and then in the second interviews to explore their experiences of using PhysioDirect with patients, following up on the key issues arising from the first interviews, while also exploring if there were any changes over time. The physiotherapy service managers were interviewed once after the trial had finished and these interviews explored the perceived impact of the PhysioDirect service, how it had been set up in each PCT, what it was like to manage the new service and other issues of importance to service managers which were perceived to facilitate or hinder its implementation or use.
From a total sample of 32 physiotherapists trained in the delivery of the PhysioDirect service, 16 physiotherapists were identified to be interviewed – four from each PCT. In each of the four PCTs, the key physiotherapy service manager overseeing the operational issues of the physiotherapy service was also invited for interview. The purposive sampling of physiotherapists was based on sex, clinical experience, whether they worked exclusively in the NHS or also in private practice, their experience of using telephone assessment systems previously and the circumstances under which they had became involved in the trial. All physiotherapists and managers who were invited for interview agreed and were interviewed.
Table 60 provides a summary of the physiotherapists and their managers who took part in the interviews, showing their key characteristics according to sampling criteria. Of the 16 physiotherapists interviewed across the four PCTs, 75% were female. They had a range of MSK outpatients experience ranging from 1 to 30 years, with an average MSK experience of 12 years. The majority (81%) worked exclusively in the NHS and 62.5% of the physiotherapists had previous experience of using telephone assessment within physiotherapy. Half of the physiotherapists reported that they had been invited to participate in the PhysioDirect trial by their managers, while the other half reported that they had volunteered to deliver the new PhysioDirect service in the trial. Of the four managers interviewed, 75% were female and had a range of experience of managing MSK services from 1 to 8 years, with an average of 4 years.
| Characteristics | Physiotherapists | Managers | ||
|---|---|---|---|---|
| Years of MSK experience | ||||
| Mean (SD) | 12 (9.3) | NA | ||
| Range, years | 1 to 30 | NA | ||
| Managing MSK services | ||||
| Mean (SD) | NA | 4 (3.16) | ||
| Range, years | NA | 1 to 8 | ||
| Sex | n | % | n | % |
| Male | 4 | 25 | 1 | 25 |
| Female | 12 | 75 | 3 | 75 |
| Agenda for Change pay band | ||||
| 6 | 9 | 56 | NA | NA |
| 7 | 7 | 44 | NA | NA |
| Exclusively working in the NHS | ||||
| Yes | 13 | 81 | NA | NA |
| No | 3 | 19 | NA | NA |
| Previously experience of using telephone assessment systems | ||||
| Yes | 6 | 37.5 | NA | NA |
| No | 10 | 62.5 | NA | NA |
| Involvement in the trial | ||||
| Invited | 8 | 50 | NA | NA |
| Volunteered | 8 | 50 | NA | NA |
Interviews with GPs and commissioners
The aim of the GP and commissioner interviews was to explore some of the key organisational and contextual issues that might influence the acceptability and implementation of the new PhysioDirect service. In each PCT, GPs and commissioners of MSK services were interviewed after the trial had finished but before the results of the trial were known. The sampling criterion for the commissioners was based upon whether they had a clinical or non-clinical background. A total of eight commissioners, two from each PCT, were identified and invited to take part in the interview study, of whom four (one from each PCT) responded and agreed to participate. GPs based in practices that had participated in the trial were invited to take part in the trial, based upon two key criteria: the PCT and their referral patterns to physiotherapy (high vs low referrers to physiotherapy). Eighty GPs were sent postal invites of whom 26 replied, 15 agreed to be interviewed and eight GPs in total were eventually interviewed (two from each PCT area). The GPs and commissioners were interviewed at their place of work.
Table 61 provides a summary of the GPs and commissioners who took part in the interviews, showing their key characteristics according to the sampling criteria. Of the eight GPs interviewed across the four PCTs, five were male. They had a range of general practice experience ranging from 10 to 30 years with an average experience of 20 years. Of the four commissioners interviewed, one was female, three had a non-clinical background and overall they had a range of experience of managing MSK services from 1 to 5 years with an average of 2 years.
| Characteristics | GPs | Commissioners | ||
|---|---|---|---|---|
| Years' experience as a GP | ||||
| Mean (SD) | 20 (6.31) | NA | ||
| Range, years | 10 to 30 | NA | ||
| Managing MSK services | ||||
| Mean (SD) | NA | 2 (1.9) | ||
| Range, years | NA | 1 to 5 | ||
| No. | % | No. | % | |
| Sex | ||||
| Male | 5 | 63 | 3 | 75 |
| Female | 3 | 37 | 1 | 25 |
| Clinical background | ||||
| Yes | 8 | 100 | 1 | 25 |
| No | 0 | 0 | 3 | 75 |
Recording and management of data
All of the interviews were digitally recorded. The audio recordings were stored on the researchers' password-protected drive and the audio files on the Dictaphone were then erased. The audio files were transcribed in full and saved in Microsoft Word (Microsoft Corporation, Redmond WA, USA) format and then anonymised. The transcripts were saved to both a password protected computer and the Framework software programme. Each case was given an identification number.
Analysis
A Framework approach was used to analyse the qualitative data from each of the three participant groups. 99 Framework is an analytical method that is pragmatic and is commonly used in health services research. 100 The Framework approach is a thematic, cross-sectional analysis that allows the researcher to simultaneously analyse across themes and cases. It enables qualitative findings and interpretations to build from the original data, allowing the analysis to maintain a clear auditable trail. The approach is a matrix-based method for analysing qualitative data that includes familiarisation with the data, the creation of a theoretical framework, indexing the data according to the Framework and the creation of summaries from the indexed data. These summaries are then finally mapped in charts and descriptive explanatory accounts are created. The audio files of the patients, the physiotherapists and their managers as informants were listened to several times and transcripts reread to identify key themes and concepts. The data were sorted and reduced to a manageable form, and a theoretical index was refined to summarise the essence of the transcripts. In order to ensure confirmability and trustworthiness, a sample of transcripts was double coded and the thematic framework was reviewed by the research team before it was applied to all of the data. A data summary was attached to each of the data labels on the index. Large charts of the index headings and attached summaries were created and descriptions that captured the essence of the summarised data across the cases were made with key themes identified. Finally, the themes were mapped and interpretation of those themes was reviewed by several study team members in order to construct overall explanations of the data.
Chapter 7 Qualitative study: results
Patients' perspectives: key themes
Analysis of the patient data highlighted the following five key themes: access to physiotherapy via PhysioDirect, reasons for not contacting the service, acceptable features of PhysioDirect, less acceptable features of PhysioDirect and the future of PhysioDirect services.
The first key theme presents details of access to physiotherapy and the second highlights the reasons that patients randomised to PhysioDirect chose not to contact the service. The third theme provides details of the acceptable features of PhysioDirect within which subthemes include a quick efficient service, PhysioDirect as ‘staged’ care, ‘helpful’ physiotherapists and trade-offs between acceptable and less acceptable features of PhysioDirect. Then, the theme of less acceptable features of PhysioDirect is presented, which consists of subthemes that include communication difficulties and PhysioDirect as an impersonal service. The final theme provides further information about of the future of PhysioDirect services within which subthemes include the role of the referring GP and future technologies. For each of these themes and subthemes, examples of patients' narratives are provided.
Access to physiotherapy via PhysioDirect
Musculoskeletal patients referred by their GP to physiotherapy in England generally have to wait for an outpatient appointment. There are no national guidelines or targets regarding an acceptable waiting time for physiotherapy; therefore, waiting times in England vary widely between services and range from < 1 week to > 52 weeks with the majority of patients waiting, on average, 4–5 weeks for treatment. 101 Improved access to physiotherapy is one of the key arguments for the use of PhysioDirect telephone advice and treatment services. 102 Most patients interviewed who were randomised to PhysioDirect and telephoned the service had little problem accessing it, finding it quick and easy.
I got through quite quickly. It was, I can't remember, it was answered almost immediately to be honest.
Patient 10,023 (telecare only)
I must have picked a convenient time because she just answered the phone.
Patient 40,022 (telecare only)
Others had some difficulties in getting through to the physiotherapist directly. Rather, they got through to the physiotherapy administrator who arranged for a physiotherapist to call them back at an arranged time convenient for the participant and physiotherapist. The participants for whom this was relevant perceived PhysioDirect as a call-back service and generally they found this method of access acceptable.
It was very easy to get through. I think I rang and the physio wasn't available but arranged to ring back at an agreed time.
Patient 10,104 (telecare only)
Some patients, however, complained about their inability to easily contact the PhysioDirect service, which caused some frustration. This mostly related to patients being unable to speak to someone directly, either a physiotherapist or administrator, and having to leave messages on telephone answering machines and then waiting to be contacted by the service.
It took quite a bit to get through. That was a bit annoying. It took several calls to get through. Kept leaving answer phone message, and nobody got back but eventually we, you know, we were playing telephone tag.
Patient 11,981 (telecare + face to face)
Reasons why patients randomised to PhysioDirect chose not to contact the service
Some patients who consented to participate in the randomised trial and who were randomised to the PhysioDirect service did not ring the service and did not receive physiotherapy care. The qualitative study sought to explore the reasons why these patients did not ring the service, given that these might be related to issues of acceptability of PhysioDirect telephone services. The data highlighted several reasons that included the cost of the telephone call, their decision to access private physiotherapy instead, their perception that their MSK problem had resolved and therefore they did not need to telephone PhysioDirect, their general belief that physiotherapy treatment would not be of benefit for their problem, the lack of face-to-face contact and patients' complicated lives or lifestyles, which meant that their MSK problem was viewed as less of a priority than other more pressing issues that they were currently facing.
Cost of the telephone call
The cost of the telephone call, or its perceived cost, was clearly an issue that some patients considered in deciding whether or not to use the PhysioDirect service and whether or not to telephone back after the initial telephone assessment and advice. The interviews revealed that some patients telephoned PhysioDirect from their mobile telephones. Other patients, when prompted on how they thought the service should be improved for the future, suggested that the telephone call should be free for patients. Patients had been told in the trial information leaflet that it was likely to take around 20 minutes to be assessed by the physiotherapists over the telephone. One clear recommendation for the future is that patient information should make it clearer that the physiotherapist can call the patient back at a convenient time, therefore transferring much of the cost of the telephone call to the PhysioDirect service.
I found it perfectly clear and they said this could take up to 20 minutes or a bit longer or whatever and it came down to funds again for phoning.
Patient 20,645 (randomised and did not ring)
Accessed private physiotherapy instead
A number of patients interviewed had access to private health care and some used their private health-care cover to provide physiotherapy instead of contacting the PhysioDirect service.
I was on holiday for three weeks and then I came back and got in contact with the firm and they said they'd pay and that's when I thought I don't need to bother with the national health if they're going to pay for it.
Patient 10,556 (randomised and did not ring)
Perceived lack of effectiveness of physiotherapy
Some patients' reasons for not contacting the PhysioDirect service were centred on the perceived lack of efficacy of physiotherapy for their MSK problem; therefore, they did not feel the need to contact the PhysioDirect service, as they did not believe that physiotherapy would aid their recovery. This is likely, however, to be a similar reason for non-attendance within usual physiotherapy care.
I ended up with the telephone thing, which, well, I would probably eventually have got around to ringing up and saying I didn't think physiotherapy was what I needed but I didn't get around to doing that.
Patient 20,469 (randomised and did not ring)
Lower perceived value of the PhysioDirect telephone call in comparison with face-to-face care
Some patients explained that although they did not contact the PhysioDirect service they would have made the effort to attend a face-to-face appointment if they had been randomised to receive usual care in the trial. This is important, as it appears there is a difference in how patients view physiotherapy face-to-face contact compared with telephone contact. Some patients felt that it was worth making an effort to obtain face-to-face physiotherapy but this was less true for a telephone contact. This seemed to suggest they placed lower value on the PhysioDirect telephone call as a method of accessing physiotherapy care.
So obviously, I can do things like that because they fitted in. Why did that one fit in? I was able to fit in it but I can't make the phone calls. Every time I phone them, sorry, they're not in.
Patient 40,770 (randomised and did not ring)
If you had a face-to-face appointment?
Interviewer
I would make the effort to do it.
Patient 40,770 (randomised and did not ring)
And:
You know that there's somebody sitting there waiting for you turn up and you don't or you're cancelling your appointment that somebody's gone to the trouble to make for you whereas a phone call's just a phone call and it can be any time and anywhere.
Patient 20,469 (randomised and did not ring)
Patients with other pressing priorities
Further reasons to explain why some patients did not ring the new PhysioDirect service were their other health problems or ‘busy and complicated’ lives. In these cases, patients did not prioritise contacting PhysioDirect to have their MSK problem assessed. Other more pressing issues in their lives, for example caring for disabled relatives or other health complaints, were of greater priority than the telephone call to the PhysioDirect service.
I got fed up and I just had so much to do and it was just another phone call, another, you know what I mean?
Patient 20,318 (randomised and did not ring)
I did fill them in and send them back and then my anxiety started to take over again really bad so, my, sort of, pain problems and stuff weren't so important.
Patient 11,465 (randomised and did not ring)
Acceptable features of PhysioDirect
A quick efficient service
Patients' narratives were full of descriptions of how the PhysioDirect telecare service was experienced as quick, efficient, convenient and preferable to the long waits for physiotherapy face-to-face care. In a previous study, Hills and Kitchen103 showed that waiting times are important with respect to patients' satisfaction with treatment. In the interview data, it was clear that the acceptable features of PhysioDirect centred on the service being perceived as quick, efficient and convenient.
Well, the thing I liked about it really, it didn't take long for them to get in touch with me.
Patient 10,552 (telecare only)
And:
It's a very good service, very quick, very prompt, very thorough.
Patient 30,196 (telecare only)
A good first step
Patients also described the PhysioDirect service as a good ‘first step’ to access physiotherapy services. The interviews provided an insight that PhysioDirect was perceived by patients to be the first stage in a physiotherapy ‘staged-care approach’, where levels of contact by the physiotherapist would increase depending on the complexity of the problem. Patients understood that there was another step or ‘stage’ if they needed it and saw PhysioDirect as a service within a larger, existing system.
It's a good first, yeah, I think it's a good starting point.
Patient 10,104 (telecare only)
I was fine because as I say, it's like anything. You've got to try something to see if you can resolve the problem and it's easier to resolve it in the simplest ways rather than go into the extreme ways, because maybe you don't need to go to the extreme, you can do the first stage first and that maybe resolves it. Or maybe you might have to go to the second stage and that resolves it.
Patient 20,353 (telecare only)
Helpful physiotherapist
From the patients' perspective, the attributes of the physiotherapist providing the PhysioDirect service were very important. Patients interviewed were very complimentary about the physiotherapists in the PhysioDirect service, describing them as thorough in their assessment, polite and helpful.
I found her very clear, thorough and very pleasant. She was very pleasant. She really was good.
Patient 10,290 (telecare only)
Other patients saw the physiotherapist as the ‘knowledge giver’, able to advise, provide information on the MSK condition and give time frames for the patient to phone back if things were not improving.
I did find the physiotherapist themselves very good and better able to explain to me what I needed to do and what they thought was causing the problems.
Patient 31,575 (telecare + face to face)
Trade-offs
Often, acceptable features of PhysioDirect were traded off by patients with some of the less acceptable features. Examples of such trade-offs that patients made in accessing the PhysioDirect service included quick access to the physiotherapy appointment, less waiting and a convenient time of appointment versus reduced continuity of care, the perceived impersonal nature of the service and the participant's ability to use the telephone. These findings are similar to those found in previous research about how patients decide to trade off certain issues, for example waiting time compared with access to a particular GP when accessing general practice. 104–106 The patient data highlighted that these trade-offs were an integral part of their PhysioDirect experience.
Not having somebody there seeing how far you can bend it or move it in a certain direction just takes a little bit of the personal side out of it. But, you know, on the flip side, it takes a lot of the time waiting to be able to see a physiotherapist.
Patient 30,196 (telecare only)
And:
I mean, you have to make the journey, you have to go, you have to sit there, you very rarely get in at the time of your appointment, you usually wait half an hour, or more, then you go in and you're in strange surroundings, whereas on the telephone, you're in your own home, it's immediate, you have no waiting time.
Patient 40,022 (telecare only)
Less acceptable features of PhysioDirect
Communication difficulty
Some patients found it difficult to describe their symptoms over the telephone, especially without the apparent benefit of physically pointing to and demonstrating their problems to the physiotherapist in person. It is acknowledged that describing pain is often challenging for patients. 107 However, the specific difficulty patients experienced appeared to relate to pinpointing and describing the exact anatomical areas of their MSK pain. Most patients also appeared to find it challenging to explain the movements they found painful or difficult to achieve, in order to respond to the physiotherapist's questioning during the telephone assessment of their MSK problem. Reliance upon their own descriptions and difficulties in their interpretation of what the physiotherapist meant in the assessment of their problem created areas of doubt for patients.
It's a bit difficult to physically explain what you're doing down the phone.
Patient 20,353 (telecare only)
And:
Yeah, I found it a bit, quite difficult, because it's hard to explain isn't it, even, not just on the phone but to anybody. I mean, the pain I was in was really, really bad, so, I would have preferred to have saw somebody, you know, because when you try and explain the areas or, you know, where the pain was, which it goes all the way down, down to there, it's a bit hard to describe on the phone, so, that's when I would have liked to have seen somebody.
Patient 10,253 (telecare only)
PhysioDirect as an impersonal service
PhysioDirect telephone care was seen by some patients who experienced it as impersonal. The words ‘not personal’ were used by patients in their narrative when describing the features they disliked about PhysioDirect. In comparison, none of the usual care patients described the service they received as impersonal. There was evidence that some patients felt they were unable to create a therapeutic relationship with the physiotherapist in PhysioDirect and felt that it inhibited any continuity of that relationship. Some also found that the telephone call was easily forgotten.
I just mean somebody who, you know, I just feel that this PhysioDirect, you are just a number on a piece of paper, but, like I say, if you rang me back in a month's time and actually had a conversation with me, I would feel that that was more personal than me having to ring and getting somebody completely different every time. That's all.
Patient 30,272 (telecare only)
And:
It didn't feel very real, a phone call is an odd, very easily dismissed from my day-to-day life, I've done the phone call and goodbye whereas if you have an ongoing relationship, an ongoing face to face, it becomes more part of your daily life.
Patient 20,081 (telecare only)
Patient perspectives of the future of PhysioDirect services
The role of the referring general practitioner
Looking to the future, patients expressed mixed views about the role of the GP in referral to physiotherapy. Some patients suggested that direct access to a physiotherapist without the referral from a GP would be more suitable for them. There was evidence in the patients' accounts that some would prefer not to involve the GP in the management of their MSK condition but this mostly centred on face-to-face care rather than the telephone-based care, and this was mostly from patients who had previous experience of physiotherapy.
In an ideal world, how would, how would you like to see a physio service?
Interviewer
Walk-in.
Patient 41,454 (usual care)
Other patients thought that the role of the GP was pivotal in the decision to have physiotherapy treatment, although this might be explained by patients' current experience where, in most services, patients must be referred to physiotherapy by their GP.
It's difficult because you can't, to access physio over the phone, you don't, you have to go through your GP first anyway, so, you need to have spoken to your GP first. Well, that's how I think you should do it.
Patient 20,053 (telecare only)
Future technologies
The uses of the internet and video or camera technologies were also mentioned in the patients' accounts when asked about services in future, with some patients clearly looking at health information online before and after the use of PhysioDirect.
I've printed off things, I've had information sent me, I've watched videos of chiropractors talking about whiplash.
Patient 10,253 (telecare only)
Patients also described how other technologies could work in future PhysioDirect services, creating innovative ways of amalgamating the process of providing treatment advice, along with the use of telemedicine and the internet. They could envisage integrated PhysioDirect services directing patients to approved websites where they might find helpful and evidence-based information about their condition and available treatments.
I suppose you could always have a website which contains the booklet information which people can download.
Patient 10,104 (telecare only)
And:
I suppose your service could be done on a one-to-one on broadband but that's only if everybody had the webcam, you know. The way things are going, I mean, these things come out with webcams on them.
Patient 20,353 (telecare only)
The use of technology and health highlighted by Wyatt and Sullivan108 suggests that the role of e-health for individual patients offers opportunities for prevention, choice, home-based care and chronic disease management, widening the access to health care for most patients. This view of an increased shift towards information for patients is also advocated by the Department of Health. 16,109
Physiotherapists' and their managers' perspectives
Analysis of the physiotherapists' and their managers' data highlighted six key themes related to the acceptability and implementation of PhysioDirect. The first theme relates to accuracy of diagnosis. The second theme is how physiotherapists adapted to work on the telephone within which subthemes include visualising a patient, joining in the assessment and enhanced communication skills. The third theme focuses on general information and generalised management within which subthemes are generalised rather than individualised treatment and promoting self-management. The fourth theme centres on communication concerns in relation to PhysioDirect, within which are subthemes of the impact on physiotherapist and patient relationships, PhysioDirect impairing continuity of care and PhysioDirect disengaging patients. The fifth theme highlights professional identity, which consists of the subthemes of professional identity and PhysioDirect skill set. The final theme is the operational features of PhysioDirect, within which subthemes include training, familiarisation, length of call times, computer literacy, the environment to provide the PhysioDirect service, managing a PhysioDirect service, implementation of PhysioDirect after the trial and the future of PhysioDirect services. For each of these themes and subthemes, examples of participants' narratives are provided.
Accurate diagnosis
The physiotherapists' main concern as reported in the first round of interviews was one of misdiagnosing the patient's problem over the telephone. The relatively little comparable evidence about PhysioDirect services highlights that some physiotherapists expressed concern about the accuracy of patient diagnosis. However, a recent study has shown agreement in patient diagnoses when reached over the telephone or through face-to-face consultations. 53
I think the main concerns are probably, from speaking to the other physios involved, is the, is it feels alien to not do the objective assessment, the way they normally work, so I think there's a lot of worry that that'll create misdiagnosis and then giving the wrong treatment, that's probably the main issue I've come across from the other physios.
Physiotherapist 22, time point 1
In the second round of interviews most physiotherapists seemed more confident about making a diagnosis over the telephone and felt that it could be done safely.
I think you can still get, if I was to talk to someone who'd sprained their ankle, I could still get the same diagnosis from talking to them. As if I just, if I looked at it as well.
Physiotherapist 22, time point 2
And:
So pretty much I would say that the diagnosis that the physios were making over the phone were pretty accurate really, so that was good.
Physiotherapist 13, time point 2
Adaptations physiotherapists made to working over the telephone
Patient visualization
The second round of interviews provided some insight as to how the physiotherapists adapted their way of working in order to deliver the PhysioDirect service. The majority of physiotherapists interviewed used techniques of visualisation in assessing patients in order to overcome the lack of visual feedback in the assessment process:
I think you've just – you've just got to totally switch off from everything else that's going on and put yourself in the – in the shoes of the patient, you've got to kind of imagine that they're at the end of the phone, they're, you know, sat on the bottom step or, you know, what's – what's going on and – and you're just trying to totally focus on what that patient is, you know, describing to you. And imagine almost as if you are in a cubicle with that patient. And chatting to them so that, you know, you're not doing anything different to, you know, you're still using the same skills that you would use if you were seeing somebody face to face. That's quite, quite difficult.
Physiotherapist 13, time point 2
As part of the PhysioDirect training package, physiotherapists received a published article,110 which described how NHS Direct nurses visualise their patients while triaging them over the telephone. It is clear from the data that the physiotherapists used similar techniques while assessing their patients over the telephone. However, it is less clear whether or not they would have visualised their patients in their assessments if they had not been trained to do so. On the one hand, this evidence may suggest that the training for the PhysioDirect system worked well, but, on the other hand, it could highlight that physiotherapists intrinsically also use these techniques. Nevertheless, there is evidence to suggest that some physiotherapists visualise patients while assessing them over the telephone.
Joining in the assessment
Physiotherapists described how they joined in with the assessment with the patient, moving their own arms and legs around to test if their explanations, questions and descriptions were accurate and comprehensible.
But you know, you've just got to try and switch off from, you know, if – if I'm moving my arm up and I know that a physio is laughing at me as I'm, you know, you've just got to shut everything else and just, you know, sort of stare into space and – and get on with it. And I think what you would do is try and sort of move your arm or move your leg because you're trying to think well how can I explain this to the patient so that they understand what I'm asking them to do? So it's almost like you've got to join in as well so that you know your instructions are clear.
Physiotherapist 13, time point 2
Enhanced communication skills
The physiotherapists described the need to enhance their communication skills in order to deliver the PhysioDirect service. This included the need to facilitate patients with their questioning in sufficiently lay language in order to ascertain the appropriate information from the patient:
I think it normally takes me quite a long time, because obviously that's really important for exactly you know, where you're talking about and obviously you know, different people have different perceptions of where their shoulder is, you know, is it up by the neck or is it kind of, down by the arm or you know, your exact and you know, you do need to know quite specific areas when you're kind of, talking about different pathological structures, so I think that is quite difficult over the phone.
Physiotherapist 10, time point 2
Other physiotherapists described focusing and listening attentively to the patient which they identified as a key component in the assessment in order to achieve a correct diagnosis:
From the patient and I think from that information, provided you're listening carefully and not just assuming answers, provided you do listen really carefully and that, you, you can I think our diagnoses were fairly good.
Physiotherapist 06, time point 2
Thus, physiotherapists' telephone assessments of patients combined a mixture of enhanced questioning, listening and visualisation techniques, as well as simultaneous participation in movements along with the patient.
General information and generalised management
Generalised rather than individualised treatment
The physiotherapists in their initial interviews expressed concerns that the PhysioDirect service might limit them to providing only rather generalised rather than individualised treatment to patients with MSK problems, given their inability to observe patient posture and specific movements.
The other ones that are involved on the phones, from the peer discussions that we've had, they seem to be feeling similar things to me, from what I can gather. One of them said to me that it's more of a generalised, analysis at the end because you can't look at which specific movements that are stiff or week, you're making a more general feeling that yes, this is probably a stiff knee or a weak knee and therefore, you're more likely to be giving them general exercises.
Physiotherapist 09, time point 1
And:
Yes, and I don't like the idea of being standardised practitioners because I don't think we are and I don't think we should be. I think we should have the scope to treat people differently, according to their individual, not just their, yes, their clinical needs but also their mental needs and the whole attitude of the patients, they'll all be slightly different. I just feel that we're, kind of, being squeezed into boxes and you're got to fit into the box where you're not going to get anywhere.
Physiotherapist 21, time point 1
There was some evidence in the second round of interviews that this concern remained and that the PhysioDirect service appeared to restrict their practice to the provision of generalised advice. Physiotherapists as a profession are autonomous practitioners, who have the knowledge to make clinical decisions and deliver the most appropriate intervention to individual patients. 111,112 Therapists felt that PhysioDirect standardised and protocolised care might limit their professional autonomy. This was, on the whole, in reference to the information leaflets provided within the PhysioDirect service in the trial, with some physiotherapists feeling restricted in what treatment they could advise.
It would have been better if I could, give, if there was flexibility for me to just give the exercises I wanted to do, so I'd find that, I get a leaflet, there is a couple of things I'd like to give to the patient, one was in one leaflet, one was in the other, which was obviously difficult, so there's things that I probably thought clinically, I want them to do this, but the leaflet that was more relevant to them did not contain that.
Physiotherapist 22, time point 2
PhysioDirect effective at providing self-management advice
Many of the physiotherapists felt that PhysioDirect was an effective medium through which to provide patients with advice about self-management, for example patients with osteoarthritis (OA).
I think the OA knees like those sort of situations. The osteoarthritic patients generally who need more range of movement and strengthening exercises just generally those patients and I think really what I said before, those patients who need more self management; those people that maybe are on the mend but just need that extra push to get better. Those sort of patients are ideal for, are ideal for PhysioDirect.
Physiotherapist 1, time point 1
The second round of interviews highlighted that physiotherapists felt that as patients were ‘only’ receiving PhysioDirect telecare, they felt obliged to spend longer on self-management advice during telephone calls than they would normally do in usual care:
The telephone assessment almost feels like it's more of, makes a bigger proportion of your treatment because you can't do any manual treatment perhaps. You're giving them advice and exercises and that's the package and so I think maybe I, I put a bit more emphasis on those sort of self treatment approaches then perhaps I would have done face to face. It feels that way. I'm not sure if that's accurate but I feel I gave good general self management advice.
Physiotherapist 29, time point 2
Communication concerns
Impact on the physiotherapist and patient relationship
In the initial interviews, physiotherapists expressed concerns regarding how they were going to communicate with the patients over the telephone, and they perceived that some aspects of physiotherapy treatment would not be easily communicated over the telephone. They felt that physiotherapy ‘is more than just words’, rather that the relationship with the patient is integral to effective physiotherapy.
I think it's more the rapport that you have to build up with a patient, to get them to comply with what's going on. You need to get some trust there and if you keep on talking to different people, it's hard to build up any trust.
Physiotherapist 22, time point 1
And:
I don't know whether it's just because of the ability to communicate with them, that I'm not sure they would understand just with the spoken word, whether they needed me to see or touch or do because that's what I find with physio, it's not so much what you do, it's the way in which you do it and you can't see it over the telephone.
Physiotherapist 11, time point 1
These concerns were realised. In the second round of interviews, physiotherapists felt that the PhysioDirect service tended to inhibit the normal therapeutic relationship that develops between the physiotherapist and patient. They perceived that there was an inability for patients to fully trust them and thus disclose information over the telephone. The lack of good rapport between the two parties may mean the physiotherapist might be less likely to identify what might be specifically causing the patient's problem.
But when you see a patient face to face, you build up a bit more of a rapport, you get to know them a little bit better, you know how to approach it better, and you can't do that on the phone, so part of your experience, your, what you're getting paid more to do, is lost, so.
Physiotherapist 22, time point 2
PhysioDirect impairs continuity of care
In PhysioDirect, patients often spoke to a different physiotherapist than the one that had initially assessed them over the telephone, when they called back to discuss progress several days or weeks later. The physiotherapists felt that this would negatively impact on their therapeutic relationship with the patient, and reduce the continuity of care with patients.
It's just nice, you can build up a really nice rapport with patients and I like that, whereas, you wouldn't necessarily get that over the phone because perhaps it would be more of a one-off, or, you wouldn't necessarily be the person taking the call off the same patient, if they phoned back. So, in terms of, maybe, kind of, consistency, I enjoy being there physically for my patients and being there in person.
Physiotherapist 07, time point 1
In the second round of interviews, there was some evidence that this reduction in continuity of care in the PhysioDirect service made developing a good rapport with patients more challenging:
They're loads and loads of things around this issue that might be influencing their physical problem. So that only comes out sometimes at first contact to a certain degree. If you then get that patient back in, they'll often tell you a little bit more and you can, you can get a better insight as to exactly what is going on and if you are treating that patient face to face, I think that is, is easier. On the telephone, you're a stranger; you're just a voice and they don't maybe want to give you things in as much detail. So you might be trying to delve but they're putting the anchors on and saying this is all I want to tell you at the moment.
Physiotherapist 04, time point 2
PhysioDirect disengages patients
Evidence from the first round of interviews with physiotherapists highlighted their concern that the PhysioDirect service might disengage patients. It appeared that some physiotherapists had concerns about patients not contacting the PhysioDirect service and not calling back if their MSK problem did not improve:
My concern is that sometimes patients, you speak to the general public about seeing the doctor and they say I spoke to the doctor and he said this, this and this but it hasn't really helped and I didn't go back. And you say why didn't you go back. Oh well, what he gave me for it, it didn't help. And, I think one of my concerns would be it empowers the patient, it puts the ball in the patient's court, but actually, if they think I tried those exercises, I had this assessment on the phone and we took half an hour, but it didn't really help, they might write off physio, they might say it didn't help and I'm not going down that route thank you, I want to go down a different route and we'll never know.
Physiotherapist 21, time point 1
This was also a concern in the second round of interviews and although many physiotherapists were surprised at how many patients they could successfully manage over the telephone, they were also surprised at how few patients seemed to recontact the service. The over-riding concern appeared to be that PhysioDirect might therefore disengage patients from physiotherapy through disappointment with the new service:
I've had two in a year. So no. They're not my own. But whether my patients call back on a different day and speak to someone else, there's no way of knowing that. So … but on the days that I work I've only had two people … we were only saying this the other day because I can't ever remember having to get into the right bit to write the comments when patients call back.
Physiotherapist 32, time point 2
And:
So I've been staggered so I'm taking from that that, that what we are giving them is actually proving to be quite helpful or they've been so disappointed in the advice given that they've decided not to bother coming back. I don't know. That's what's going to be really interesting.
And how would you feel if that was the case?
Interviewer
That they were so disappointed that they didn't? Very disappointed. Very disappointed.
Physiotherapist 29, time point 2
Professional identity
Evolving professional identity
Initially, one of the main concerns for the physiotherapists was that, if they were to spend the majority of their clinical time on the telephone assessing patients, they might become deskilled with respect to their physical and manual assessment and treatment techniques. They clearly saw these skills as key to their own professional identity.
I'd hate to be a physiotherapist who only talked to people on the phone, that would be terrible, you know, you'd really deskill and obviously, that wouldn't be good, but, I think it would be, if it is helpful, that's going to be good.
Physiotherapist 10, Time point 1
In the second interviews, they still expressed the desire not to spend the majority of their working week delivering the PhysioDirect service:
I can see the benefit of a mixture but for me, I wouldn't want to do more than say two sessions a week on the phone. I'd prefer my face-to-face contacts.
Physiotherapist 07, time point 2
And:
I wouldn't want to do any more than that, and I couldn't do more than half a day in any one stint, you couldn't do a day of that, it would be very difficult, I wouldn't do that as a job, I wouldn't be happy with that. If that was the way physio went, I'd go and get another job.
Physiotherapist 22, time point 2
Another reason as to why the physiotherapists did not want to spend the majority of their time on the telephone was that the PhysioDirect assessments were perceived to become rather monotonous and they felt they were repetitive if there were many patients to assess during the opening times of the PhysioDirect service:
By the end of the day, I'm sick of saying the same questions, you know, because you're kind of repeating the whole, this format of questions if you're kind of, you know, just repeating those continuously.
Physiotherapist 10, time point 2
Another more subtle issue related to the acceptability of PhysioDirect from the initial interviews was that some physiotherapists did not perceive that physiotherapy could be delivered over the telephone.
PhysioDirect is a different system I think you're doing it automatically, as a physio. You're making note of things automatically and it might be, you know, it might come out later on, but, you can't put that in a subjective assessment on a telephone consultation.
Physiotherapist 04, time point 1
Do you think there's any way you could get around that, other than bringing them in?
Interviewer
No. It's not, that's the problem, you can't compare it with like value to a face-to-face consultation.
Physiotherapist 04, time point 1
It appears that the professional identity of physiotherapists is not only influenced by the type of physiotherapy they deliver, but also there is evidence from the second round of interviews that it is linked to continuity of care. The physiotherapists reported that feedback from patients (whether their symptoms had improved or worsened) enabled the physiotherapist to reflect on their decisions and further develop themselves as a practitioner. PhysioDirect was viewed as limiting this feedback, as few patients seemed to call back to discuss how their problem was progressing.
You don't get the closure and the feedback loop and so it's difficult, more difficult to learn as a clinician using PhysioDirect about how your patients are doing 'cos you don't get the feedback loop whereas when we see them face to face and we say I want to see you again in a month to see how you're getting on, we get that feedback of how they're progressing and that helps us learn and develop.
Physiotherapist 21, time point 2
And:
I think the big concern is if all you did was assess on the phone, if that was what the whole profession did in the NHS, you know I think yes there'd be a real issue there with professional clinical development so it is very, potentially a very useful and effective service for managing resources and cost effectiveness and may have acceptable outcomes. If it was all you did, I think there would be real big shortfalls. Yes, long term it would be very damaging probably to yes, to the skill level within the profession.
Physiotherapist 21, time point 2
PhysioDirect physiotherapist skill set
In the first round of interviews, some physiotherapists recognised that there were certain additional skills they needed to assess patients well over the telephone. The additional development of these skills was suggested as a reason why some physiotherapists took part in the PhysioDirect trial (i.e. they hoped that their subjective assessment skills and communication skills would improve):
There's skill, obviously, in trying to get the information out of someone who struggles to relate and that's obviously part of the physio's ability to take that information. So, you know, for the patient, the experience is going to depend a lot on the person they're speaking to and how effective they are at getting that information and understanding what the patient's trying to tell them. So, there's a two-way thing, if the physio misses the point completely what the patient's trying to say, they're going to get the wrong diagnosis and the patient's going to feel that they've not really listened or understood.
Physiotherapist 23, time point 1
In the second round of interviews, they had clearer ideas as to what skills PhysioDirect physiotherapists should have. There was consensus from both the managers and the physiotherapists that the PhysioDirect service should be delivered by an experienced physiotherapist with at least Band 6 MSK experience (note: the Agenda for Change pay band is the tariff that NHS staff are allocated to on the basis of their knowledge, responsibility, skills and effort needed for the job). The skills that the PhysioDirect physiotherapist needed were perceived to centre on the ability to listen, visualise and make quick decisions.
A kind of an upgrade Band 6. So … but, but then saying that, I mean PERSON_H, who is in the study, he, he did very well and he's probably mid, mid kind of grade. I mean somebody with a lot of musculoskeletal experience. I mean we certainly wouldn't be looking at a Band 5 junior. They need to have had a good three, three years minimum.
Manager 3
Operational features of PhysioDirect
PhysioDirect training
The physiotherapists involved in the trial undertook a 2-day training package, which was held in Huntingdon, Cambridgeshire, before the start of the trial. The experience of the physiotherapists using the PhysioDirect software consists of two subthemes: training at Huntingdon and familiarisation with the PhysioDirect system. The physiotherapists interviewed were positive about their training at Huntingdon and thought that the training experience was beneficial, as it helped them to conceptualise how it might be operationalised within their own departments.
That was really good, really well delivered and really good to see the software in action and have a go. Yes, really, really helpful. I think without that, we'd be struggling a lot more to get our head around the software and stuff. It was essential, I would say.
Physiotherapist 21, time point 2
Familiarisation
This subtheme also explores how the physiotherapists became familiar with the computer software program and explores the difficulties that some physiotherapists had of becoming more confident to assess a patient over the telephone without the visual component of an traditional face-to-face assessment. Familiarisation with the computer software and being able to clinically reason over the telephone were other themes that emerged from the physiotherapists' views and experiences of the PhysioDirect training.
I think there's two sides to the practice; one is getting your head around operating the software whilst talking, which some people call multi-tasking, some people in this Trust suggest there are gender differences around that but, so one half of the challenge has been getting used to taking down the assessment in electronic form whilst doing your subjective examination and the second half has been actually the clinical challenge of working just on subjective information and not being able to do any clinical testing, not being able to see the patient, observe anything, and so trying to clinically reason and be, have a good level of certainty in your impression at the end, so, it's basically clinical reasoning in a different way, with less information.
Physiotherapist 21, time point 1
The second set of interviews with the physiotherapists suggested that they did get used to this way of assessing patients and reported that their confidence eventually improved with practice using the PhysioDirect service with patients:
So obviously that was challenging for a while, but we'd soon get into a routine and remember to ask it and, why you're asking it, to do it.
Physiotherapist 22, time point 2
And:
So … but yeah, you just get used to when to ask, when it best fits into the assessment. But that just comes with doing it. The more you do it, the more slick you become.
And when did you start to feel slick?
Interviewer
After about 6–8 weeks, probably.
Physiotherapist 32, time point 2
Length of telephone call times
A key physiotherapist concern was whether or not they would be able to complete a patient clinical assessment over the telephone within 20 minutes. This recommendation of a 20-minute telephone assessment time from the training team at Huntingdon caused some anxiety and unease amongst physiotherapists, as they felt it was too short to be able to glean all of the information from the patient required to make an accurate diagnosis. Some suggested that although this was the ‘target time’ for a telephone assessment, they would not let their clinical judgement be affected by a time frame:
If I can get all the clinical information out that I need to make an appropriate decision then yes. I haven't got to that stage yet, but, I may do, I don't know. I'm quite open-minded about it really. I'm not going to compromise my clinical judgement because of the time but I'm prepared to be not exactly proved wrong.
Physiotherapist 09, time point 1
Data from the PhysioDirect IT system and the qualitative interviews suggests that some physiotherapists achieved this guide of 20 minutes per telephone call during the trial while others did not. The average call time was 24 minutes overall. The second interviews also suggested that as physiotherapists became familiar with the process of assessing patients over the telephone, their call times decreased. Reasons as to why some did not were associated with not feeling sufficiently familiar with the PhysioDirect system owing to the relatively few patients telephoning the service while they were on duty and the perceived inadequacy of their own computer skills.
Computer literacy
Some of the older physiotherapists involved had reservations about their competence to use the IT systems within PhysioDirect and it was clear that they felt they were not sufficiently computer literate to assess the patient simultaneously with inputting assessment findings and information into the PhysioDirect software. The physiotherapists who had these concerns tended to be those who were older:
I didn't realise, when I initially signed up for it or said that I would be interested in doing it that it was going to be so computer based, because I'm an old lady and I tend to be handwriting based as opposed to screen and at the moment, I'm still finding, I mean, I've got used to it now but I'm finding it very hard to work on the screen instead of handwriting the notes, partly because I've used the same sort of assessment forms for donkey's years and I always ask my questions in a very set order so I know that I haven't missed anything out and it doesn't come up in that order on the screen and I find it hard to dodge backwards and forwards, because I'm just not competent with it yet, but, I'm sure it will come with practice.
Physiotherapist 2, time point 1
Concerns regarding how to navigate IT systems did not seem to affect the younger physiotherapists, as they were quite happy with the software and the computer.
Yeah, well, I've grown up with computers and I can touch type, so, typing and listening at the same time doesn't worry me.
Physiotherapist 16, time point 1
And:
Being quite young, I can quite easily work my way through a computer package, so, that's not a problem.
Physiotherapist 22, time point 1
Again, in the second round of interviews the physiotherapists who struggled with the IT aspects said that their typing skills did improve; however, there were others who did not have this experience:
Well, typing, I knew, would be a problem for me. I am quite slow and I tend to, I do quite like to have things written neatly rather than not having capitals or full stops, so, I do have to go over it a little bit, but, it's one thing I have done a lot more at home is do a lot more typing on the computer, so, I am a bit faster now.
Physiotherapist 06, time point 2
And:
And I knew I'd identified that you know, before I went into the study. As something that I, yes that, yes that I was concerned about because I don't sit and type and I haven't got the background of sitting and typing. I haven't done so I though right I'll probably improve as I go along and I did and my times came down so I was quite happy but again it was like lack of experience, lack of practice time so that was a bit of disappointment to me but I know that if, once you become more familiar with what's coming up on screen, then that would come.
Physiotherapist 04, time point 2
This was a problem for some physiotherapists as they generally worked only one or two PhysioDirect clinics per week (each of 3–4 hours) in the trial and felt that the PhysioDirect service did not have sufficient patients coming through in order for them to practice and feel sufficiently confident with the computer system.
Environment to provide PhysioDirect practice
The physiotherapists were concerned about the physical environment in which they delivered the PhysioDirect service, with the most common concern being the background noise in the offices in which they were working, as it made it difficult for the physiotherapists to assess patients with the PhysioDirect system. All used headsets as part of the trial, rather than relying on the handset of the telephone, as they needed their hands free to use the computer system in parallel with talking with the patient on the telephone:
I did dislike it when you were trying to assess and it was noisy, really annoying. ‘Cos you just, yes it's really annoying and people don't mean to be noisy but if you can't hear anything and then you can hear yourself talking, you can't concentrate, it's really off putting. You're kind of sitting there, finger in your ear, really trying to listen to the patient and there's a big conversation going on beside you.
Physiotherapist 25, time point 2
PhysioDirect as an inefficient use of PhysioDirect time
An initial concern for the physiotherapists prior to their use of the PhysioDirect service in the trial was that they might not be kept sufficiently busy during PhysioDirect clinics:
I don't mind that, I hope the phone goes just to keep busy.
Physiotherapist 22, time point 1
And:
That's not such an issue because although they're sitting on the telephone, they're still doing physio, they're still assessing a patient and giving them advice for a problem. It's not like they're sitting doing nothing, that'd be worse.
Physiotherapist 23, time point 2
This concern was realised as physiotherapists reported that the PhysioDirect service was not ‘busy enough’. This resulted in some therapists holding the opinion that the PhysioDirect service was an inefficient use of their time:
So that was a hard part of it actually because we were sitting feeling like we were wasting important clinical time so from that perspective, I have to just you know, mention that [laughing]. That was quite a large part of it. And that, I think influenced how we felt about things in general. So I think if we had, if I had been in a busier session I might feel a little bit more positive about it.
Physiotherapist 4, time point 2
Managing a PhysioDirect service
The interviews with physiotherapy managers highlighted that the unpredictable number of calls in each PhysioDirect clinic session made it difficult to manage the service. However, the physiotherapy managers did report, at the end of the trial, that they were overseeing this aspect of the service better:
Or when they got there the phone was absolutely mad. It seemed to be all or nothing. So I mean we had staff going there, I mean going there, sitting there, nothing to do, bored. A lot of them got a lot of CPD [continuing professional development] and discharges done, but other times they were going and then they were feeling under a lot of pressure because the phone was ringing.
Manager 3
And:
I think we'd have to – we would have to look it quite differently as to how we rolled it out because if from what we're scoping, if patients aren't going to use it we can't afford to have a physio in every hospital, sitting waiting for phone calls. Because that would be half my workforce, you know, it would – it just wouldn't be feasible. Not with 31,000 referrals.
Manager 2
The physical geography of the participating PCT and the population each served were perceived as important factors in managing the PhysioDirect service. It was felt unfeasible for physiotherapists to have to travel long distances to the PhysioDirect office to provide the PhysioDirect service. This was particularly an issue for the physiotherapy managers in charge of services serving largely rural areas:
There were quite a few logistical things which you wouldn't … if you were running it yourself out with the trial, you wouldn't have some element of that. So if you were working in an acute trust it would have been much more straightforward, because everybody would have been in one building, your call centre would have been in the building and it, it wouldn't have been … but we had to move staff, as I say, from one part of the patch to another part of the patch and be mindful of what was happening at their original base.
Manager 3
Implementation of PhysioDirect after the trial
Two of the physiotherapy services (out of the four that participated in the trial) carried on using the PhysioDirect service after the trial ended, but importantly both changed the way in which the service was offered and operationalised. The main difference was in how they managed patient referrals and calls into the service. In the amended services, GP referrals were screened by a physiotherapist and then, depending on the MSK problem and length of the local waiting list for physiotherapy, the patient was sent a letter inviting them to call the PhysioDirect service or they were put on a waiting list for face-to-face care. For example, patients with shoulder pain problems were viewed by physiotherapists as needing to be seen in traditional face-to-face consultations and so these patients were not given the choice of PhysioDirect but listed for face-to-face care, whereas those with back or lower limb problems were viewed as suitable for PhysioDirect and were automatically routed to physiotherapy via that pathway:
And we've obviously now in a way cherry picked what patients we think do best, so now when the patient referrals come into the department if they're shoulders we just straightaway put them on face-to-face waiting list and if they're kind of lower limb or backs that we think would do well then we put them to the – to the PhysioDirect method of working.
Manager 2
By essentially changing PhysioDirect to a call-back service only, the two sites that carried on using PhysioDirect did so in a way that enabled them to better predict the number of people ringing into the service. They did this through taking calls from patients and arranging convenient call-back times for the physiotherapist to contact the patient later, essentially using PhysioDirect only as a call-back service. Despite these changes, they still faced some challenges in predicting how many patients they could assess in 1 day.
And the other challenge was when we totally overloaded the system and had about 20 calls in one day and only one physio. Well, it wasn't that bad but it really overloaded the system and so, managing the right capacity and demand was quite difficult.
Physiotherapist 06, time point 2
The managers perceived PhysioDirect as a way to manage the long waiting lists in their services.
We used PhysioDirect very much to siphon off some of the bulge in referrals, so that some of the more urgent stuff could go through there, and that, you know, it was used as a sort of management tool really in that respect; worked quite well.
Manager 1
The reasons why the two other PCTs did not continue to provide the PhysioDirect service centred upon wishing to wait until the results of the randomised trial were known, as well as lack of support from service commissioners given current financial constraints.
The official reason they used was that; if you do a drug trial okay, for a drug you don't know its effectiveness, you wouldn't continue giving it to patients until you know, if it's really effective or not. So basically they [physiotherapy service commissioners] asked me to stop providing the service. If it's proven to be effective, to start again, but until then, they wouldn't pay for such a service.
Manager 4
Future of PhysioDirect services
Most of the physiotherapists could see PhysioDirect working within their PCT in the future and were not adverse to the idea of offering a future PhysioDirect-type service. They saw it as a tool to reduce waiting times or to help with the management of waiting lists. The majority of the physiotherapists mentioned the future of PhysioDirect working well within a service that offered self-referral to physiotherapy (direct access without the need for a referral from a GP) for patients, in order to promote patient choice in how to access the physiotherapy care they needed:
They could ring so I think on its own, it would be OK but it would be better in conjunction with other direct access systems because then you, it gives the patient more choice of how to have physio and also it wouldn't inundate the PhysioDirect system because they've got other options if they don't like the phone option.
Physiotherapist 23, time point 2
This was supported by physiotherapist managers, who suggested that PhysioDirect could be used to offer patient choice in how they access and receive physiotherapy. They envisaged that the choice would be given to the patient at the time of ringing the physiotherapy department of either a face-to-face appointment or a telephone assessment and advice session. This was thought to appropriately complement a self-referral system already in place within one of the participating PCTs.
Yeah, I don't know, that's my question and I wonder whether we could – I suppose our gold standard where we're always heading is if, if direct access is sustainable can we run the two side by side? So when a patient rings up for their same day, next day appointment we can ask them would you like this over the telephone or would you like it as a face to face?
Manager 2
Okay, so giving them a choice?
Interviewer
It is all about patients' choice isn't it, about giving them the options to access physiotherapy in whatever mode they want to.
Manager 2
And:
I believe it has a place in physio, okay, however, I don't think this will be the only way for patients to access a service, okay; there have been issues in their own economy that patients were not given a choice really so if it looked like a choice service.
Manager 4
It was evident that PhysioDirect was not seen as the only way to deliver physiotherapy services to patients but the managers clearly saw it as one option.
But I think, I think deep down I knew, ‘Well, it's not going to solve everything but it's definitely kind of got a, a kind of a role’.
Manager 3
General practitioners' perspectives: key themes
General ambivalence about PhysioDirect
In general, GPs tended to be ambivalent about the new PhysioDirect service in that they perceived it to be an issue for physiotherapists to decide upon and it had very little impact on their day-to-day work. This general ambivalence about PhysioDirect was due in part to their lack of knowledge about the details of the new service and receiving little direct feedback about it from patients. The only feedback they recalled receiving about the service was the information provided by physiotherapists on their discharge letters for individual patients.
I mean the only feedback I get really is at the end of their treatment, so when I get a discharge letter from the physios. But I didn't have any positive or negative feedback from the patients.
GP 6
One GP commented that his patients did feed back that they found it a little ‘unusual’ to be assessed over the telephone and that some patients seemed rather negative about PhysioDirect. Despite this patient feedback, however, this GP viewed the faster access to physiotherapy within the PhysioDirect service as a positive feature.
Yeah, I mean there were a few who were not really, you know, that, that happy. Said, you know, just had this discussion over the phone and they didn't, after that, you know, didn't, probably being a bit unusual made them more actually … negative I would say probably.
GP 34
Did you re-refer them then? Did you re-refer them for physio?
Interviewer
I don't think there, there was, there were any who, who, who, whom referred immediately. I don't think so. Because generally I think during that period the, my impression was what actually, they got access quicker and generally it worked quite well.
GP 34
Another reason for the general ambivalence among the GPs interviewed was that the trial did not impact on GPs' working practices when referring patients to physiotherapy. They continued to refer patients to physiotherapy in their usual ways, and patients were identified and invited to take part in the trial after the GP had referred them to the physiotherapy service.
Well we got the feedback, but I didn't even bother reading the pieces of paper; they said this patient was triaged this way or that way, and you know, as long as they were dealt with, I didn't really care [laughs], and so I knew it was happening, but I didn't really know what was happening, I didn't know how it worked or how well it was going.
GP 11
This lack of direct involvement of GPs with the new PhysioDirect service might account not only for the general ambivalence, but also for a lack of understanding among GPs about the service. The PhysioDirect service itself aimed not only to provider faster access to a physiotherapist who would assess the patient's MSK problem, but also to provide a treatment service to patients. For most, this treatment was initially commenced over the telephone but for some it also involved face-to-face care for those patients who needed it. The interviews highlighted that in general the GPs understood the service to be largely a triage service, to help sort patients by clinical need and to manage waiting lists rather than also to provide advice and treatment.
Well only that it seemed very easy to do, there wasn't a problem and the patients seemed to accept it, so we didn't have any resistance and they were quite happy to be contacted but I think they were contacted by phone and then it was kind of triaged what happened to them and that seemed all very straightforward.
GP 3
This misunderstanding about PhysioDirect being simply a triage service could be related to the GPs' previous experiences of practice nurse-led telephone triage systems for patients with other clinical conditions or their own experience of telephone consultations with patients. 113
Right, yes. I mean we are using triage more and more. I personally – I mean we're having to do more telephone consultations because we haven't got the manpower or the time to see everybody face to face.
GP 69
Perception of physiotherapy as a face-to-face service
Given the lack of knowledge among GPs about the new PhysioDirect service, an explanation of it was given during their interviews. Once the interviewer explained the PhysioDirect service, what it involved, and the implications for treatment of patients, GPs expressed some concerns about the relative lack of face-to-face physiotherapy care.
And I think, I think that would be my concern, is getting the proportion of phone time as opposed to seeing the patients. Cause there is only so much you can do on the phone. And if the purpose of the GP referring the patient is to get them treated, you know, to actually have hands-on treatment for the injury.
GP 6
It was clear that the GPs perceived physiotherapy to include ‘hands-on’ treatment and by removing the face-to-face component for many patients in the PhysioDirect service they felt that an essential and important aspect of physiotherapy care was lost. Although many patients randomised to the PhysioDirect arm of the trial had a telephone consultation and face-to-face care, approximately 40% were managed by telephone care alone and it was this telephone care alone that GPs expressed concern about. The reduction of face-to-face care in the PhysioDirect service appeared to shape its acceptability to GPs, as they believed that physiotherapy ‘over the telephone’ would be less effective than face-to-face care.
The reason we refer them is, and especially in our, you know, you want hands-on treatment, you want them to be seen. And a phone call's fine but, but that's not what people are expecting from a physio. You know, I can give them advice about ice and elevation and analgesia and that sort of thing. So if the purpose of the, the triage phone call is to assess urgency and like a function, fine, but not, but I don't think there's an awful lot … You know, I'm not a physio but my views, when you go see a physio you expect to be shown some exercises, you might have a bit of ultrasound, you will have, you might have some massage, that's the sort of thing you're gonna have. And you can't do that down the phone.
GP 6
In terms of the advice and self-management information provided through the PhysioDirect service, the GPs felt that they themselves could provide this type of simple advice and exercise information to patients with common MSK problems rather than directing them to a PhysioDirect service to provide similar information. In general, GPs interviewed were of the view that a physiotherapy service should provide patients with face-to-face ‘hands-on’ treatment that the GP recognised the patient needed from their own clinical assessment. Thus, overall although GPs felt that the PhysioDirect service provided faster access to physiotherapy and generally worked quite well, in that they received no complaints from their patients, it was clear that the GPs ultimately took the view that physiotherapy needs to be delivered in a face-to-face context in which therapists are able to use manual methods of treatment for MSK patients.
Commissioner perspectives: key themes
Importance of waiting time as a quality indicator
In order to ascertain information about how a service is performing commissioners discussed a number of quality indicators, including waiting times to access the service, patient DNA rates, patient complaints and feedback from GPs.
Well, one would be problematic performance against some of the key areas, key performance indicators, others are continual feedback (from) patients; complaints from patients through our [Patient Advice and Liaison service] PALS service. You know, regular feedback from other key partners like GPs that the service isn't you know, it's delayed or they're having problems engaging with the service or any other issues like that.
Commissioner 2
Waiting time was a key quality indicator, and varied across the four PCTs in a similar way to national variation, with one PCT having a very short wait of 2–3 weeks and others having waits of between 6 and 8 weeks and longer. Within the interviews a specific example was highlighted in which, previous to the trial, one of the PCTs had a waiting list to first physiotherapy appointment of 13 weeks and the service commissioners intervened in order to investigate this with a view to ensuring this long wait was reduced.
As far as our cluster goes we've been involved in some of the physiotherapy discussion because waiting lists went up through the roof, the service wasn't commissioned in time, a 13-week wait, so we wanted to get the physiotherapy rates waits down. So we were involved in saying was the capacity right, were we matching capacity? Were there enough physios? It was at that level we were involved.
Commissioner 4
This suggests that for commissioners, waiting times were an important indicator of the performance of physiotherapy services. The commissioners, however, did not indicate at what point waiting times became clearly unacceptable, although in the above example a wait of 13 weeks was certainly viewed as such.
Relative importance of physiotherapy
It appeared that physiotherapy services were generally not high on commissioners' agendas, unless one of several quality indicators such as waiting times or patient complaints alerted them to an underperforming service, or perhaps when the physiotherapy contract was due for renewal.
So unless somebody says, we haven't got enough physiotherapy, there's a problem with physiotherapy, our patients are complaining about physiotherapy, physiotherapy might not get looked at, because we can't look at everything, we have to align our health needs with our priorities and if it's ticking along, nobody's complaining about it.
Commissioner 3
It was clear that all of the commissioners interviewed felt that they had a good-quality physiotherapy service in their local area with good physiotherapy service leadership and that in general they took a reactive rather than a proactive approach to identifying services in need of their scrutiny as commissioners.
I know that we have a detailed specification that I was part of drafting, with the provider and I broadly know what we are commissioning, okay. I broadly know that the service is meeting its waiting time targets, it has few complaints, it has fairly limited DNA rates, I know it's got, had an influx of referrals, quite a hike in referrals in the last 1 or 2 years. I think it's a well managed service, I get a sense that, the Leads, the Service Leads, have their finger on the pulse, they really know the service well.
Commissioner 2
It appears that commissioners were often dominated by top-down policy and their views about health needs were particularly influenced by data related to the Quality and Outcomes Framework (QOF). Therefore, health areas such as mental health, cancer services and diabetes, which have QOF information, had a greater priority than the conditions that do not.
Now that we've got QOF, Quality and Outcome Framework, as part of the GP contract; they've got lots of registers, clinical domains across all the main disease groups and it is the main ones, it's about 10 or 12, so you've got heart disease, stroke, cancer, diabetes, blood pressure, chronic kidney disease, dementia; there's all sorts of things where they have registers. So if 90% of the population are registered and about the same amount will access their GP once or twice a year, your main source of live patient data is in primary care.
Commissioner 3
The relative lack of importance of physiotherapy services was also reflected in the commissioners' views that the PhysioDirect service per se was not included in their brief but that rather it would be up to the service providers to make a decision about whether or not they used PhysioDirect to help manage the demand for physiotherapy services.
Why do I need to commission PhysioDirect? I don't, for example, as a commissioner, I don't. As I have block contracts, I have, you know, I have a service in place that needs to meet the needs of my population, so should the provider be commissioning it? You know, is it the way – is PhysioDirect a mechanism by which the provider could manage the demand on their services? That's a, you know, another way of looking at it, why does it have to be me or the GP commissioner. You know, if we're not gonna mess around with the contracts and unpick them and all of what that entails, maybe the provider needs to be commissioning PhysioDirect as a way of managing demand.
Commissioner 1
PhysioDirect allocation of resources (implications for costs)
The context in which decisions about commissioning takes place was also reflected in the discussions about the costs of services, and there was a strong sense from all commissioners of the pressures they were under to deliver very substantial NHS cost savings within the financial year.
One of our biggest issues, you asked me what the biggest issues were, is that we are financially challenged. We and about 60% I think of all PCTs up and down the country are significantly financially challenged, we're all looking at being in deficit by the end of the year.
Commissioner 3
In relation to the perceived costs, the interviews highlighted commissioners' assumptions that the PhysioDirect service was likely to be cheaper than face-to-face care.
We're moving into very difficult times over the next three years where we've got to make … tens of millions of pounds of efficiency savings, so we are just not having a dialogue about more money, but if we can make better use of the pot that is allocated to physio, by having a PhysioDirect element, then that's very positive.
Commissioner 2
The commissioners, however, had concerns about whether or not having experienced physiotherapists deliver the PhysioDirect service was the most cost-effective approach. A commissioner suggested that highly skilled physiotherapists might not be the most appropriate people to deliver simple advice and self-management information to patients via the telephone and suggested this activity might be more appropriately carried out by less qualified staff.
The other opportunity around PhysioDirect though, is in using a different skill mix of staff. We've got to be careful that we use our experts wisely, exploit the specialisms, you know, and it; there would be opportunity to have a different mix of staff providing the information, I don't know, maybe skilled up assistant physios, for example, which means that you know, the pot of money could go further because you have, less costly staff being able to provide that basic advice and information and reassurance, which is something that patients always need.
Commissioner 2
The importance of trust between provider and commissioners
The importance of relationships between health-care providers and commissioners and of good knowledge about the services that are being commissioned was highlighted in the commissioners' interviews. Commissioners described these relationships as being crucially important for successful commissioning.
So an important part of the commissioning process is that you have well developed relationships, high levels of trust and that the Commissioner has a reasonable knowledge of the service being provided. If you take the example of a person who procures, why buys coffee for Waitrose or wine for Waitrose, for example, they will be intimate with the product, they will know the growers, they will know the context, they will actually have a good sense of what a good product, they have to know the product. In order to inform which is the grower they want to purchase off and why, you know, so, but they need to develop a relationship over a long period of time, often, and you need to foster trust and that involves compromise on both sides.
Commissioner 2
The interviews thus underlined the important role that effective personal relationships have in positively influencing whether or not a service is commissioned and implemented. Interestingly, all of the commissioners suggested they had positive working relationships with the providers of physiotherapy services in their PCTs.
Summary of qualitative findings
It appears that the PhysioDirect service was largely seen as acceptable by patients but many saw it as a first step to subsequent face-to-face contact. Access to the PhysioDirect service worked well for most patients contacting it, with patients valuing faster access to physiotherapy advice and care. Patients generally viewed the PhysioDirect service and the physiotherapists providing the service as acceptable and helpful. Patients' preferences and priorities for treatment defined the acceptable features of PhysioDirect but the acceptable features were traded off against the less acceptable features. Some patients, however, felt that the PhysioDirect service was impersonal and impaired their relationship with the physiotherapist, which made the service feel remote and, at least to some patients, less important.
The physiotherapists and their managers perceived the PhysioDirect service as broadly acceptable. They thought that physiotherapists could safely diagnose patients with MSK problems over the telephone, and found that it worked particularly well as a medium through which to provide self-management advice to patients. The physiotherapists along with their managers considered that the PhysioDirect service was helpful in improving access for patients to physiotherapy care and reducing physiotherapy waiting times. However, key concerns that made the new service less acceptable included the physiotherapists' perception that working within PhysioDirect meant that treatment tended to be more generalised rather than individualised. The physiotherapists also had concerns that continuity of care was impaired by PhysioDirect, suggesting that the telephone may impair the development of a good rapport with patients and that this might impair their ability to assess patients' broader psychosocial problems. Despite a period of ‘run-in’, during which the processes were tested prior to the main trial, physiotherapy managers found the unpredictable nature of the timing and volume of patient calls to the PhysioDirect service difficult to manage. Both the managers and the physiotherapists found this aspect of PhysioDirect unacceptable.
Another factor which may affect the implementation of the PhysioDirect service was the physiotherapists' reluctance to work more than two clinics (each lasting half a working day) per week in the PhysioDirect service. Although most physiotherapists interviewed were happy to provide a mixture of PhysioDirect and face-to-face care, universally they did not want to do work within PhysioDirect for the majority of their working week. These issues might make it difficult for physiotherapy managers, particularly of relatively small services, to implement a PhysioDirect service using their physiotherapy resource, although experience in other related services (such as the employment of nurses to staff NHS Direct) suggests that telephone-based services can tap into staff who have left the workforce but are attracted to the advantages of working on the telephone. Both the physiotherapists and their managers did foresee a PhysioDirect service working in the future to provide increased patient choice about how they would like to access and receive physiotherapy but recommended that PhysioDirect should not be the only way for patients to access physiotherapy care.
The evidence suggests that GPs were rather ambivalent about the PhysioDirect service although they felt that it could provide quicker access to physiotherapy. They appeared to accept PhysioDirect as long as patients did not complain about it and as long as it did not mean additional work for them as GPs. Their lack of direct involvement with the trial in some respects accounted for GPs' misconceptions of the PhysioDirect service as they tended to view it as a triage service rather than a ‘package of care’. However, once informed of the role and function of the PhysioDirect service GPs expressed concerns about the reduction of face-to-face, ‘hands-on’ treatment that both they and (they believed) their patients tended to expect from physiotherapists.
The data provided evidence that, at the time of interview, commissioners were acutely aware of the pressures to make cost savings in the NHS. Commissioners assumed that the PhysioDirect service would be a cheaper option in providing physiotherapy services. All of the commissioners felt that the physiotherapy service provided in their areas was of good quality. The interviews highlighted that physiotherapy services were generally not considered high priority unless there was evidence of problems such as patient complaints or unacceptably long waiting times. Waiting time was identified as a key quality indicator in commissioners' evaluations of physiotherapy services. The key to successful commissioning appeared to be the development of relationships with providers, which were characterised by mutual trust.
Strengths and weaknesses of the qualitative methods
The strengths of this qualitative study are that it was based on a large and diverse sample of patients that provided a rich qualitative data set collected across the four PCTs involved in the trial. The physiotherapist interviews conducted were longitudinal, and the strength of this approach was that the second round of interviews with the physiotherapists explored whether their views and opinions stayed the same or changed following completion of the trial. The weaknesses of the qualitative study are that although patients whose first language was not English were specifically sought and interviewed, none had such language barriers that they perceived this had caused problems with their access to or understanding of the PhysioDirect service. It is likely that patients with significant language barriers did not participate in the trial. Only two patients who were randomised to usual care and did not attend their physiotherapy appointment were interviewed. This makes it difficult to conclude that some of the reasons why patients randomised to the PhysioDirect service did not ring are not simply reasons to explain why patients fail to attend physiotherapy appointments generally.
Conclusions from qualitative study
The PhysioDirect service was broadly acceptable to patients, physiotherapists and their managers. Patients generally found it easy to access and perceived the advice given and the physiotherapists as helpful. PhysioDirect was not seen as a panacea to assess and treat patients but perceived by patients, physiotherapists and managers as one way to increase patient choice in accessing physiotherapy services, as a ‘good first step’, after which patients could be seen in face-to-face physiotherapy care if needed and to manage physiotherapy waiting lists. GPs and commissioners tended to take the view that the PhysioDirect service was acceptable as long as it was acceptable to patients and reduced waiting times. However, the difficulty in accurately predicting the number of telephone calls to the PhysioDirect service along with the reluctance of most physiotherapists to spend much of their time working in this new way are factors that need to be addressed if similar PhysioDirect services are to implemented more widely.
Chapter 8 Discussion
Summary of main results
The underlying rationale for PhysioDirect is reiterated in Box 2 and used as a framework to summarise the main results.
This study provides clear support for the hypothesis that PhysioDirect provides equivalent clinical outcomes to those of usual care by the end of the 6-month follow-up period. It also confirms that patients in the PhysioDirect arm received earlier advice and treatment from a physiotherapist.
There was limited evidence from several measures of health status that patients in the PhysioDirect arm had slightly better scores at 6 weeks than those in the usual-care arm, supporting the notion of earlier improvement. However, these differences were very small and may not have been clinically meaningful (e.g. the improvements in the SF-36v2 PCS score and the MYMOP score were less than the prespecified minimum clinically important difference).
Unlike the other measures of health status, the EQ-5D is used at three time points to generate QALYS that reflect the individual's quality of life over a period of time. Because the EQ-5D scores improved at an earlier point in the PhysioDirect arm than in the usual-care arm, and this improvement was sustained over 6 months, there was a slightly greater QALY gain in the PhysioDirect arm.
There was no clear evidence from data relating to the trial period that providing a PhysioDirect service was more or less costly to the NHS than usual care. The point estimate for the cost of providing physiotherapy was slightly greater than for usual care but the 95% CI included zero (no difference). The point estimate for the cost of all relevant NHS services was also slightly greater in the PhysioDirect arm, but the difference was very small within a wide CI that included zero.
However, sensitivity analyses demonstrated that PhysioDirect could be a less costly way of providing physiotherapy than usual care if the proportion of time that physiotherapists spend productively on the telephone was increased, as was achieved after the trial was completed.
The underlying assumption that a telephone consultation would be less expensive than a face-to-face consultation was found to be false. The reasons for this are discussed later.
To:
-
Provide equivalent clinical outcomes for patients compared with usual care based on a waiting list for face-to-face treatment.
-
Provide faster access to advice, which would result in more rapid improvement in symptoms and may allow patients to return more quickly to work and usual activities.
-
Provide equivalent outcomes at lower cost, meaning that the PhysioDirect service is more cost-effective from an NHS perspective. The lower cost of PhysioDirect would be achieved by better tailoring the use of physiotherapy time in relation to need and capacity to benefit, using telephone consultations which were presumed to be less costly than face-to-face consultations, and by better use of resources through lower DNA rates.
-
Increase patient satisfaction because of easier access to advice from a physiotherapist.
Patients in the PhysioDirect arm had a very small but earlier improvement in health status than those in the usual-care arm, which was achieved at a cost which was insignificantly greater. Combining these factors suggested that PhysioDirect is probably cost-effective, with an incremental cost per QALY gained of £2889. The NMB was £117 (95% CI –£86 to £310) if society's willingness to pay for a QALY was valued at £20,000 and the probability that PhysioDirect was cost-effective at this threshold was 88%.
Sensitivity analyses showed that the probability that PhysioDirect was cost-effective increased if we assumed that PhysioDirect could be provided more efficiently (as it was outside the trial) and decreased after imputing missing cost and outcome data, or using the SF-6D to estimate QALYs rather than the EQ-5D. However, in all scenarios PhysioDirect appeared to be cost-effective at a willingness-to-pay threshold of £20,000.
There was no evidence of a difference between PhysioDirect and usual care in cost to patients and their families, or to society through the costs of lost production. This reflects the fact that there was no evidence of difference in time lost from work or usual activities due to either the condition for which the patient was referred to physiotherapy or time needed to attend physiotherapy appointments.
There was no evidence that patients were more satisfied with access to care using PhysioDirect rather than usual care. Overall satisfaction, and satisfaction with the consultation, appeared to be slightly higher among those offered usual care.
PhysioDirect appeared to be safe, with no AEs being detected in 4323 consultations (1445 by telephone and 2878 face to face) over 6 months in 1506 patients allocated to PhysioDirect.
The qualitative research supported the notion that PhysioDirect is broadly acceptable to patients, although some patients saw it as a first stage in gaining treatment rather than an alternative to a face-to-face consultation. Many patients valued the faster access to advice and care provided by PhysioDirect and found the physiotherapists to be helpful during telephone consultations. However, some patients found the service to be impersonal and remote. The physiotherapists and their managers also felt PhysioDirect was an acceptable service, which was helpful in improving access and reducing waiting times. However, like the patients, some physiotherapists felt that the telephone nature of the service made it more difficult to establish rapport. They also found it difficult to manage the unpredictable nature of the timing and volume of calls. Almost universally, the physiotherapists were happy to provide PhysioDirect sessions for a small part of their working week but would not be happy to spend most of their time on that type of work. Both physiotherapists and their managers felt that PhysioDirect would have a useful role as one way rather than the only way for patients to access care in future.
Interpretation of results
This study finds clear evidence that providing care using PhysioDirect achieves equivalent clinical outcomes to those of system of usual care based on waiting for a face-to-face appointment. This finding is robust in that it is supported by evidence based on the use of a range of different measures addressing different aspects of clinical outcome, including generic health status, a patient-specified measure, overall patient perception of improvement and quality of life. This finding is also robust to secondary analyses to take account of baseline imbalance, imputation of missing data, and clustering by physiotherapy service and general practice.
This large study also provides reassurance that PhysioDirect is safe, in that no adverse events were detected among the 1506 people who were allocated this service despite active efforts to detect such adverse events by reviewing in detail every participant's medical records. Confidence in the safety of PhysioDirect needs to be qualified by noting that in this trial only experienced physiotherapists (Band 6 or higher under the NHS Agenda for Change) provided telephone assessments and advice, and that they had all undertaken brief further training and been assessed as competent in using PhysioDirect software to support their assessments. It cannot be assumed that PhysioDirect would be safe under other circumstances.
There was no evidence that PhysioDirect had different effects on clinical outcomes in patients with different demographic characteristics or different types of MSK problem for which they were referred to physiotherapy, although these analyses are exploratory as the study was not powered to detect these subgroup effects.
PhysioDirect provided much faster access to an initial assessment and advice from a physiotherapist, with patients in the PhysioDirect arm having an assessment after a median delay of 7 days compared with 34 days in the usual-care arm. For those patients who subsequently had a face-to-face appointment the improvement in waiting time was less impressive, with median waits of 30 and 35 days in PhysioDirect and usual-care arms, respectively. However, almost all of the patients in the PhysioDirect arm who eventually had a face-to-face appointment would have had at least one telephone consultation and had the opportunity to improve self-management and follow exercises on the advice of a physiotherapist while they were waiting for this appointment.
This improved access to care did not appear to be reflected in greater patient satisfaction with access to the service, although there are important limitations to this evidence as described below. Patients receiving care in the PhysioDirect arm were no more satisfied with access to physiotherapy than those in the usual-care arm and those patients receiving PhysioDirect reported a slightly lower level of overall satisfaction with the physiotherapy service than those receiving usual care. However, this difference is very small (3.8%, which equates to 0.19 points on a six-point scale from very poor to excellent) and may not be meaningful. The fact that patients in the PhysioDirect arm, almost half (47%) of whom were managed entirely on the telephone, were almost as satisfied with their consultations as patients in the usual-care arm (almost all of whom only had face-to-face consultations) may provide reassurance that physiotherapists are able to provide assessments and advice by telephone in a way that is acceptable to patients. By the end of the study, patients in the PhysioDirect arm were evenly split in terms of whether they would prefer PhysioDirect or usual care for a subsequent episode of care.
This study was conducted at a time when all physiotherapy departments were under pressure from their commissioners to increase patient throughput and reduce waiting times. It is notable that the course of treatment, for those patients who did receive face-to-face care, was short by international standards, with a median of 3 and 4 face-to-face appointments in the usual care and PhysioDirect arms, respectively. The counterintuitive finding that patients receiving face-to-face care in the PhysioDirect arm had more face-to-face appointments than those in the usual-care arm is explained by the fact that only 46% of PhysioDirect patients had any face-to-face consultations, and these were probably patients with more severe symptoms or more complex problems.
It is possible that longer courses of treatment might have led to greater benefits for patients in both arms of the trial, although this would also have increased costs. However, even with this limited number of treatment sessions, patients in the usual-care arm improved by a mean of 6.5 points on the SF-36v2 PCS over 6 months, which is equivalent to a large effect size of 0.75.
Not all of the claims which have been made by those advocating PhysioDirect were supported. One argument put forward in favour of PhysioDirect is that faster access to physiotherapy advice will allow people to lose less time from work, both because they do not need to take time off work for appointments and because they may recover more quickly. However we did not observe any impact of PhysioDirect on how many days patients lost from work. Furthermore, the qualitative study showed that for some people (particularly those at work), telephoning a physiotherapist to discuss their MSK problem was not always easy or convenient. A further claim has been that PhysioDirect leads to dramatic reductions in DNA rates, whereas we observed only a small reduction in the DNA rate for face-to-face appointments (10% PhysioDirect vs 11% usual care).
The qualitative research with patients provided greater insights into patients' attitudes towards PhysioDirect and helped to explain the quantitative findings. In general people found the PhysioDirect service acceptable, and they were very satisfied with the way the telephone consultation was conducted. Many found that PhysioDirect improved the accessibility of care and provided a quick and convenient service. However, some respondents clearly viewed the telephone call as less valuable than a face-to-face consultation. Some people found it difficult to describe their functional symptoms by telephone, while others were willing to trade off the limitations of the consultation against the benefits in terms of greater access and convenience. Overall, many participants felt that PhysioDirect provided a useful option or choice for people wanting early and more accessible advice, but saw it as a useful first stage in the assessment and advice process rather than as a replacement for face-to-face care.
The assumption that PhysioDirect would be more cost-effective than usual care is fundamental to the justification of a PhysioDirect service. We found evidence that PhysioDirect is probably cost-effective from the perspective of the NHS, although there are several factors that need to be considered in reaching this conclusion.
The finding that PhysioDirect is cost-effective is based on evidence that it provides very slightly greater benefits (QALYs) at very slightly greater cost. For both the benefits and the costs, the 95% CIs overlap zero, meaning that there is considerable uncertainty in the estimate of cost-effectiveness. This is reflected in the fact that the probability of it being cost-effective at a £20,000 willingness-to-pay threshold is 88%, and the NMB is only £127, with a 95% confidence from −£86 to £310.
The finding that providing physiotherapy via PhysioDirect was no less expensive than usual care within the trial can be explained by several factors. Although almost half of all patients who had any contact with physiotherapy in the PhysioDirect arm were managed entirely on the telephone, the cost of each telephone call was substantially greater than the cost of each face-to-face consultation. This counter-intuitive finding is partly because the physiotherapists providing telephone consultations were more experienced and on a higher salary band than the average physiotherapist but is mainly because only 35% of the time devoted to PhysioDirect sessions was spent on the telephone, with much unproductive time (the cost of which was attributed to the telephone consultations).
From the point of view of commissioners and managers of services, the cost of providing a physiotherapy service is probably more relevant than the overall cost of NHS services. There is good reason to believe that the proportion of time that the physiotherapists spent productively on the telephone could be increased outside the trial setting and once the service became more established and efficient. Indeed, we have provided evidence that this was observed in the service after the trial finished. This increased efficiency occurred because of a much greater throughput of patients to the PhysioDirect service, optimising the opening times and staffing levels, and operating a ‘call-back’ system in which patients leave a message with an administrator who pre-books the telephone call into the patient's and physiotherapist's diaries. Although this is not offering the immediate access to a physiotherapist that the initial service was aiming for, the qualitative interviews showed that this call-back approach, when it occurred, was acceptable to patients. The scenario used in the sensitivity analysis based on mimicking this type of more efficient service suggests that providing a physiotherapy service based on PhysioDirect would probably be less expensive than usual care, although the CI for the cost overlaps zero (difference in cost −£4.34, 95% CI −£11.25 to £2.57). Furthermore, there is evidence that average call durations for telephone consultations became shorter as the service became more established, which would further reduce the cost of delivering a PhysioDirect service.
The main cost-effectiveness analyses presented are based, as is conventional, on all relevant NHS costs. However, this does create difficulties in interpretation. Because the cost of physiotherapy is relatively low in comparison with the cost of secondary care (particularly inpatient stays), any difference between the trial arms in the cost of secondary care will overwhelm any difference in the cost of physiotherapy. In this study, the main factor leading to the greater NHS cost in the PhysioDirect arm was the greater cost of hospital care, largely due to the greater cost of inpatient stays. However this estimate is unstable as it is based on just 10 patients in the PhysioDirect arm and 5 patients in the usual-care arm, only 1% of the sample of patients in the trial. This is further illustrated by the finding that using all of the data available, the cost of hospital care is substantially lower for the PhysioDirect arm, but when only the cases with complete data on all cost and outcome variables are included (as in the primary cost-effectiveness analysis) the cost of hospital care is substantially greater in the PhysioDirect arm. These uncertainties are reflected in the wide CIs around the NMB.
Similar issues apply to the estimates of patient costs. The main factor driving the difference in patient costs was the difference between the trial arms in disability payments received. However, the proportion of patients receiving disability payments was very similar in each arm of the trial and the number of people receiving these payments was small (7% of respondents in the PhysioDirect arm and 8% in the usual-care arm). The difference between the arms was therefore due to a very small number of people in the usual-care arm receiving a higher level of benefit, and it is possible that these differences existed at baseline, rather than being related to the intervention.
Generalisability
Generalisability to other parts of the NHS
Generalisability is particularly important for pragmatic trials of this type, as they seek to establish the validity of the findings in real-life settings. It is important to consider how far our findings are applicable to patients and services in other settings.
This study was based on establishing a new PhysioDirect service within physiotherapy services in four different areas of England. Between them, these services are typical of outpatient services provided in the UK and in several other developed countries. The population of patients referred to the services was largely representative of the population of England, although it included a lower proportion of people from the most affluent areas. Among those referred for physiotherapy, a slightly lower proportion of patients from deprived areas were judged to be eligible and a smaller proportion of eligible patients from deprived areas agreed to participate. However, none of these selection effects was large.
The patients in the sample had a wide range of MSK problems as their main reason for referral. The most common reasons for referral related to back problems and upper and lower limb problems, which are typical of patients referred to physiotherapy clinics.
The provision of the intervention was largely based on the model developed over several years in Huntingdon. We were able to benefit from the experience gained in Huntingdon to inform the implementation of the PhysioDirect clinics in new areas. The use of the same PhysioDirect software provided a high degree of standardisation in the way in which the assessments were carried out and the use of a standard set of self-management and exercise leaflets helped to ensure standardisation in the advice that was delivered. Furthermore, the fact that the physiotherapists were all trained and accredited by the same small group of trainers from Huntingdon also helped to ensure that care of a consistent nature and quality was provided. It cannot be assumed that the findings from this trial would be similar in PhysioDirect services, which are not established on the Huntingdon model or did not use the same assessment software.
One threat to the generalisability of the findings to the UK is the proportion of patients who were eligible, and of those the proportion who agreed to participate. Of all physiotherapy referrals 21% were initially deemed ineligible. The most common reasons for ineligibility were related to the trial procedures rather than that people were ineligible for the service. These trial-related reasons were mainly that the patient's problem was too urgent to make it possible to conduct the consent process or that the patient was already in the trial. Apart from patients excluded for these two trial-related reasons, 87% of the remaining patients were deemed potentially eligible and sent information about the PhysioDirect service and the trial.
Of those invited to participate, 13% did not reply in any way and 3% replied to say that they no longer wanted physiotherapy. These figures are lower than we anticipated in the protocol and similar to those experienced outside a trial setting by physiotherapy services which ask patients to confirm that they want an appointment. As in normal practice, these patients were discharged from the service because they had not confirmed that they wanted physiotherapy. They were therefore treated in our analysis as ineligible rather than as declining consent for the trial.
Of all of those who wanted physiotherapy and were eligible, 50% consented to participate in the trial. Although this is a reasonably high recruitment rate for a community-based trial (and exactly the recruitment rate that was anticipated in the protocol), it still raises questions about the generalisability of the findings to the people who chose not to participate. It is unknown whether they declined participation because they did not want to undertake research procedures (e.g. to complete questionnaires) or because they did not want the possibility of being offered PhysioDirect. If the latter, this may reduce the generalisability of the study, as it would suggest that some people would be resistant to a service based entirely on PhysioDirect as the first point of contact. Services could offer PhysioDirect as an option, while also allowing people the alternative of waiting for a face-to-face appointment..
The importance of the justification for PhysioDirect
There are several factors which may need to be considered in relation to the generalisability of this research to other settings in the UK (e.g. to physiotherapy provided in occupational health services, by private health providers or via insurance companies) or to countries with different health-care systems. It is important to consider the main justification for introducing a PhysioDirect service and this may vary in different settings. Under the NHS in England, the main justification was to manage demand for physiotherapy, in the context of long delays for face-to-face physiotherapy. This desire to manage demand is linked to several other priorities, which may to some extent be mutually incompatible.
On one hand there is a desire to improve access to physiotherapy and to reduce user and GP dissatisfaction with long delays. One way of reducing delays within a given amount of resources is to use resources more efficiently. If telephone assessments could be provided at lower cost than face-to-face appointments, this could provide greater capacity within a limited resource, leading to shorter delays, assuming that the same number of people is referred to the service.
On the other hand, increasing the accessibility of services (due to shorter delays and/or more convenient provision) may well lead to an increase in demand, which may undermine any attempts to reduce treatment delays. In this scenario, greater efficiency could provide greater capacity to see more people within the same resources and this could justify the new service even if delays for treatment are not improved.
The introduction of PhysioDirect services may be motivated more by a desire to reduce costs and to increase cost-effectiveness, rather than to reduce delays. If this could be achieved by providing equivalent patient outcomes at lower cost (on the assumption that telephone calls are less expensive for the NHS than face-to-face consultations) then the total investment in physiotherapy could be reduced. Alternatively if PhysioDirect improves health gain by providing earlier treatment, even if at a slightly greater cost, this is justifiable if it achieves greater health benefits for a given investment than other competing claims for expenditure on health care.
A further priority for NHS policy is to make the service more responsive to consumer needs, and making a physiotherapist available by telephone may be convenient for many patients, as they may be able to telephone at a time that suits them and without taking time off work to attend an appointment.
In order to understand the implications of the findings of this trial, and the relevance to other countries, it is important to be explicit about the justification for PhysioDirect in a particular setting. Is it to manage existing demand and reduce delays, or to expand provision of services to meet greater demand within finite resources, or to reduce costs while providing the same volume of care, or to invest for improved health gain, or to improve the convenience and accessibility of care?
Our findings suggest that if the interest in introducing PhysioDirect is based on wishing to reduce waiting times and improve access to physiotherapy, this is supported by the evidence of this trial. If it is to reduce costs, or to manage demand by treating more patients within the same resource (which also implies reduced costs per case), then it cannot be assumed that PhysioDirect will reduce costs, although it could potentially do so as long as the PhysioDirect sessions are managed efficiently. If the justification is to achieve maximum health gain from an investment in health care then PhysioDirect is probably more cost-effective than usual care.
Generalisability to other countries
These considerations are particularly relevant in countries that, like the UK, have a health-care system that is free to patients at the point of use, with few effective rationing mechanisms other than delays for treatment. The waiting time for physiotherapy can be very long, leading to dissatisfaction on the part of the patient, the health professional who referred the patient and the physiotherapists themselves. A recent international survey does suggest that long waiting times for physiotherapy are common in many developed countries. 114 However, our findings may be less relevant to countries that do not have long waiting times. In these countries, PhysioDirect may still be justified if it reduces costs for patients or their insurers or if it provides a more convenient route to care.
Our findings suggest that whether or not PhysioDirect is a less costly and more cost-effective way of providing care is dependent on whether or not it can be provided efficiently, with physiotherapists using most of their time productively during sessions when they are available to answer the telephone. This is likely to be achieved by operating a call-back service and/or by operating the service on a large scale to even out fluctuations in demand. In terms of convenience to patients, there was evidence from the qualitative study that some patients valued the convenience offered by the PhysioDirect service. However, the quantitative results suggested that among those who had had contact with a physiotherapist, PhysioDirect might have been slightly less acceptable than usual care.
International comparisons suggest that the types of treatment provided by physiotherapists are similar in most developed countries but the typical length of a course of physiotherapy varies considerably. 58 In some countries, such as New Zealand, South Africa and Ireland, the number of treatment sessions is similar to that observed in this study. However, in other countries such as the Netherlands and the USA, a course of physiotherapy treatment typically includes between 7 and 9 sessions. 114 Our findings may therefore not be directly relevant to these countries. The number of treatment sessions often reflects the payment system in operation in each country and may change when these systems are revised (Lesley Holdsworth, Healthcare Improvement Scotland, 2011, personal observation).
Factors affecting implementation
A number of factors were observed which were of importance to the implementation of the PhysioDirect service. As previously described, it was possible to implement the service fairly rapidly because of the training and software provided by the experienced service in Huntingdon. In addition, the use of experienced physiotherapists, a substantial minority of whom had previous experience of conducting telephone consultations, also appeared to be an important factor in the successful introduction of the service. The fact that all four sites were set up as part of a research project may also have been a facilitating factor, as the research team helped to ensure consistency in how the new services were developed and to broker arrangements for example with regard to access to the software and the training.
The software was developed in Huntingdon over a number of years, and has been in daily use there, which meant that it was robust and relatively trouble-free during the study. However, it was developed in Microsoft Access on a limited budget for one particular physiotherapy service and so would benefit from further investment and development and would need stronger mechanisms for technical support if it were to be rolled out to more sites on a wider scale.
Investment in good telephone systems and provision of a suitable office is important to the smooth and efficient functioning of the PhysioDirect service. Because the trial involved implementation of PhysioDirect for a limited period and for only a small proportion of patients, this was achieved to a variable extent in our sites. Some sites had inadequate office facilities. It would be ideal if a receptionist could answer the telephone when all of the physiotherapists were busy on calls in order to make arrangements for the physiotherapist to telephone the patient back. Although this happened in our study, patients were also sometimes diverted to an answering machine instead, which reduced convenience and acceptability for patients.
Relationship of PhysioDirect to self-referral
In the UK, PhysioDirect services are increasingly being considered or implemented in conjunction with the introduction of allowing patient self-referral to physiotherapy, without the need for a referral from another health professional. In our trial, patients from a small number of GP practices in one of the four areas were able to refer themselves, but the vast majority of patients were referred by GPs [just 2% (49/2256) of patients in the trial were self-referred]. In theory, PhysioDirect may potentially have greater benefits in conjunction with self-referral as the demand for physiotherapy may increase, those requesting physiotherapy may have problems of shorter duration which are more likely to be managed by simple advice, and a higher proportion of requests may relate to problems which are inappropriate for physiotherapy. Therefore, an initial assessment and screening process provided by telephone may be advantageous (but only if it can be provided at lower cost than a face-to-face consultation). The evidence available from studies of self-referral pilot sites suggests that demand for physiotherapy does not necessarily increase from self-referral in itself if the area has a high level of provision, but self-referral may make ‘visible’ unmet demand if provision is not sufficient. The evidence also supports the notion that people who self-refer have less serious problems and consult a physiotherapist at an earlier stage of their illness than those accessing physiotherapy following a GP consultation. 17,58
Strengths and limitations
Strengths
Our trial has a number of strengths. As described above, the pragmatic nature of the trial based on PhysioDirect being implemented in a similar way in several different areas, and being offered to a range of patients who are typical of those referred by primary care practitioners to physiotherapy, maximises generalisability. This applies within the NHS and probably to countries with similar health-care systems.
Furthermore, this is a very large trial, and we recruited more than the original target number of patients. This provides precise estimates of effect sizes, and means that there is no ambiguity about the equivalence of the results relating to the primary outcome. This can be a problem for studies based on an equivalence design, as the point estimate may suggest equivalence but with one of the 95% CIs overlapping the prespecified equivalence limits.
This trial was conducted rigorously and in full conformity with CONSORT guidelines. It was conducted successfully without any major complications or the need for any important alterations to the original protocol. The recruitment rate for a large community-based trial in which recruitment was done by post is reasonably good, as is the retention rate with 89% and 85% of primary outcome data being available after 6 weeks' and 6 months' follow-up, respectively.
We used a number of different measures of clinical outcome because of a concern that a generic health measure such as the SF-36v2 PCS might be insufficiently sensitive to detect differences between the trial arms. If the measure was insensitive, we could fail to detect a difference that did in fact exist. Therefore, we combined the SF-36v2 with several other measures of health status: a patient-generated measure (MYMOP), a global question about improvement in the main problem for which the patient was referred to physiotherapy, and a measure of health-related quality of life (the EQ-5D). We also used the OMERACT-OARSI composite measure of response to treatment. There was clear evidence of equivalence using all five of these measures, which provides confidence about the conclusion that the two treatment arms provide equivalent clinical outcomes at 6 months' follow-up.
There are also indications that any concern about the sensitivity to change of the SF-36v2 was unfounded. First, the SF-36v2 PCS scores of patients in both arms improved by 0.75 of a SD over 6 months, which is a large effect size and demonstrates sensitivity to change. Second, there were large differences between the PCS scores of patients with different body regions affected by a MSK problem.
As well as different approaches to collecting data about clinical outcomes, we collected a range of data about other relevant outcomes which are important to patients, clinicians and commissioners of health services. This included data about the process of care, patient experience, time lost from work, use of other health services and patient preference. We collected data about the use of resources to allow us to estimate the economic effects of introducing PhysioDirect from a range of perspectives.
By combining these quantitative methods with qualitative research based on interviews with patients we were able to gain further insights into how people used the PhysioDirect service (in particular why they did or did not access it), their views about its place in the treatment and referral pathway, and ways in which it might be improved in future.
At the time this study was being planned, a small number of areas had instituted PhysioDirect services. During the course of this research the concept has become much more widespread and using an internet search we have identified 19 sites (excluding the four sites established for this study), which appear to be providing a service based on initial telephone assessment and advice for MSK problems. This internet search almost certainly provides an underestimate of the number of physiotherapy services working in this way. These developments confirm the relevance of this research to current developments in the provision of physiotherapy in the UK.
Limitations
As previously discussed there are some challenges to the generalisability of the trial, particularly the fact that only 50% of all eligible patients consented to take part. It is also important to reiterate that the findings reported here cannot necessarily be extrapolated to services that do not follow the Huntingdon model and do not involve experienced, trained physiotherapists using the Huntingdon PhysioDirect assessment software and an agreed set of advice and exercise leaflets.
Evaluation of new services
There is always a tension involved in evaluating newly established services. On one hand, it is important to conduct evaluation fairly early in the development of a new initiative. This makes it possible to identify and disseminate benefits from a new way of working, but also means that if there are disbenefits, wasted resources or safety concerns then these are identified quickly. On the other hand, services evolve and run more smoothly as they overcome initial teething problems, staff become more familiar with new procedures, and services are fine tuned in the light of experience. For these reasons, all of the new services in this trial had a run-in period of at least a month before they recruited patients to the main trial. During this period they practised providing PhysioDirect sessions and also piloted the research procedures.
However, several aspects of the service continued to evolve during the trial which will have had an impact on the cost-effectiveness of the service. For example, in some sites a high proportion of patients assessed by PhysioDirect were initially invited for face-to-face appointments. Through discussion with sites and by feeding back comparative performance data, this proportion reduced over time and became more similar between sites. It also became clear that the length of telephone assessments became shorter over several months, as the physiotherapists became more confident and more familiar with the software.
Conducting a randomised controlled trial in the context of a routine service
Conducting a RCT in the context of a routinely provided service inevitably has an effect on the way in which care is provided, which can have important implications for the results. The constraints which are inherent in a RCT, such as the need to standardise the intervention over a period of time (when in reality services constantly change in response to external events), to isolate and minimise contextual factors in multicentre studies (when in reality the service is appropriately adapted to the context) and to run different systems of care in parallel, tends to lead to compromises either in the service or in elements of the research design. For these reasons, some commentators have questioned the role of RCTs in the evaluation of new services,115 although others have argued that more pragmatic trials of this type are needed. 116
These considerations are very relevant to this study. First, only a small proportion of all patients referred for physiotherapy were offered PhysioDirect in this trial. Usual care continued to be provided for patients referred by hospital specialists, those referred from primary care or self-referred who were ineligible, those who declined to participate and those randomised to receive usual care. The overall effect of these factors meant that about 80% of all patients referred were still offered usual care, even although two out of three patients in the trial were allocated to PhysioDirect. Attempting to provide a PhysioDirect service on a small scale meant that it was not possible to provide a physiotherapist to answer telephone calls at all times in the week. Instead, sessions were conducted across a range of times on different days of the week, but for a substantial proportion of each week the service was not available. Outside the constraints of a trial, a local service is likely to make PhysioDirect the normal first point of contact for all patients referred from primary care or self-referred. A much higher call volume would mean that the service could be open at a wider range of times, making it more convenient for patients, and also more efficient for reasons described below.
The trial design also made it necessary to run separate waiting lists for face-to-face appointments for patients in the usual care and PhysioDirect arms. This reduced the flexibility for patients to obtain appointments at convenient times.
Allocation of physiotherapy resources in the context of the trial
From the outset of the study, we sought to ensure that the total physiotherapy resources in terms of the number of physiotherapist hours were distributed between the two arms of the trial in proportion to the number of patients we anticipated would be allocated to PhysioDirect or usual care. These estimates were based on routine data and the experience gained in a pilot study, and meant that 80% of resources were devoted to usual care. If resources had been allocated disproportionately, this would have been likely to have an impact on waiting times for treatment in the arm which was under-resourced, which may in turn have affected patient satisfaction and possibly clinical outcomes. Although one aim of PhysioDirect was to reduce waiting times, we wanted to ensure that any such effect was due to the effect of the intervention rather than an artefact created by uneven distribution of resources. However, because patients in the PhysioDirect arm of the main trial had fewer appointments in total, this meant that the physiotherapists' time allocated to PhysioDirect was not fully utilised. In the main analysis, and following conventional principles for economic analysis, this unproductive time was re-allocated to the PhysioDirect arm. The consequence of the decision to allocate physiotherapist time proportionately between usual care and PhysioDirect patients meant that the costs of physiotherapy for patients in the two arms were inevitably similar, using this approach to analysis.
In real life, outside the context of a trial, a physiotherapy service would reduce the numbers of physiotherapist hours provided for telephone sessions if the physiotherapists' time was not being used productively or would increase the number of patients having access to the service. Over time the managers of the service would ensure that the number of staff on the telephone matched demand for the service. They would also modify the operation of the service in the light of experience to ensure efficiency, for example by introducing a call-back system, as occurred in the two services that continued the PhysioDirect service after the trial. For this study it was important to conduct sensitivity analysis to model the costs of providing PhysioDirect under a realistic scenario using data about productivity from one of these continuing PhysioDirect services.
It is clear from this sensitivity analysis that PhysioDirect could be provided less expensively and be more cost-effective than it was in this trial, if the physiotherapists' time was used more productively when they are manning the telephone sessions. The proportion of productive time is never likely to approach 100%, even if the physiotherapists make outgoing telephone calls to patients rather than waiting for incoming calls, as this incurs wasted time phoning patients who are not available (as well as the additional costs of call charges). Another way to improve the efficiency of PhysioDirect would be to provide it on a larger scale. It would be feasible for one call centre to provide PhysioDirect for several areas, and providing the service on a larger scale would help to even out peaks and troughs in demand, as well as achieving other economies of scale (e.g. in terms of maximising the investment in telephone equipment). However, this change to a call-centre model may have other implications, for example for staff recruitment and turnover, as our qualitative research suggests that some physiotherapists would not want to spend most of their working time in this kind of environment.
Absence of a no-treatment arm
One limitation of pragmatic trials of this type, which compare a new treatment with usual care, is the absence of a ‘no-treatment’ or placebo/attention control group. The CONSORT guidance on reporting non-inferiority and equivalence trials emphasises the need to establish the efficacy of the reference ‘usual care’ treatment. 82 One limitation of this trial is that the inclusion of a broad range of patients makes it difficult to establish the efficacy of ‘usual care’, as most research about physiotherapy is based on patients with specific conditions. This trial replicates the way in which PhysioDirect services are implemented in real life, in that it is used to assess patients with a wide range of MSK problems. Current PhysioDirect services are not restricted to patients with, for example, knee pain. This study therefore maximises generalisability but at the expense of a good estimate of efficacy in the usual-care arm. In the most extreme sceptical position, one could argue that both treatment arms are equivalent because neither is effective. However, as a counter to this argument, there are a number of studies of the efficacy of physiotherapy for many of the conditions suffered by patients treated in this trial, as described in the introduction to this report. Furthermore, it would not be ethically justifiable or feasible to recruit patients to a study in which participants were offered the possibility of being randomised to a no-treatment arm, when physiotherapy is routinely available on the NHS. Finally, as it is very likely that physiotherapy is going to continue to be available on the NHS for the foreseeable future, a less costly service can be more cost-effective whether it is equally effective or equally ineffective.
Improvement in symptoms over time
It is notable that patients in both treatment arms improved similarly and considerably over the 6-month follow-up period (based on an improvement in SF-36v2 PCS scores of about 7 points) and that most of this improvement occurred by the time of the first follow-up questionnaire that was sent after 6 weeks. This finding may be interpreted as indicating that both types of treatment pathway were equally effective, or it could suggest that a large amount of natural resolution in symptoms occurs in the first few weeks after referral, or it could reflect a placebo or attention response. If, as seems likely, at least some of this improvement is due to natural resolution, the scale of this change makes it more difficult to detect small differences in the effectiveness of different treatment pathways.
Blinding
As is usual in pragmatic trials, it was not possible to blind participants to whether they were allocated to the PhysioDirect or usual-care arms of the trial. This may have led to bias if participants believed that one or other arm was more effective or preferable. Such bias may have been reduced if we had included an objective measure of clinical function rather than relying on self-reported measures. However, we did use a range of well-validated outcome measures, and patient-reported outcomes are more appropriate measures of the benefits of these different approaches to service delivery than objective measures of function. It is unlikely that patient attitudes to services would affect their responses to the SF-36v2 PCS, although they may have affected their responses on the patient satisfaction questionnaire.
As previously described, as far as possible all data were collected and entered blind to treatment allocation. The unequal allocation ratio made it impossible to maintain blinding during analysis.
Patient satisfaction
There is an important limitation to the analysis of patient satisfaction. Six of the nine questions in this questionnaire related to consultations with the physiotherapist. Of the remaining three questions, which formed the access scale, one referred to the hours the service was open, one to the convenience of the service and one to how long the patient had to wait to get advice from a physiotherapist. All but the last of these questions would not have been relevant to patients who had not received any physiotherapy. The questionnaire therefore instructed respondents to skip the questionnaire if they had not had any contact with a physiotherapist (including telephone advice or a face-to-face consultation).
It is likely that those people who were still waiting for physiotherapy by the time they were sent their first follow-up questionnaire after 6 weeks would have been most likely to be dissatisfied with access to the service but they did not have the opportunity to respond to the questionnaire. As people in the usual-care arm were much less likely to have had a consultation by 6 weeks, comparison between the PhysioDirect and usual-care arms in relation to the access questions at 6 weeks is not a randomised comparison and may be misleading.
For this reason, we explored in more depth the free-text comments in relation to access to care and waiting times for treatment that many patients made at the end of the questionnaire. These provided useful insights into the factors that determine patient satisfaction with the different services and ways in which they can be improved.
Limitations of routine data
Some of the data used to collect resource use for the economic evaluation came from routine records and may have been of limited reliability. Information about use of secondary care resources was based on patient questionnaires and we did not attempt to validate this against hospital records. Data about the duration of telephone calls in PhysioDirect came from electronic call records stored within the software, and these times may be unreliable if, for example, a physiotherapist did not log off the system when they finished a call. It became evident during time and motion studies that further time was incurred after many telephone calls, for example by collating leaflets to send to patients. We estimated the length of this ‘administrative time’ from the mean difference between the call times recorded by the PhysioDirect software and that recorded manually by physiotherapists in Bristol in routine records, but the latter may itself not have been a reliable gold standard, as the data exhibited clear digit preference for 5-minute intervals.
One advantage of using routine data is that it is almost complete, whereas there is considerable missing data in the variables obtained from patient questionnaires. This particularly affects the EQ-5D data and information about secondary costs, both of which are important in estimating cost-effectiveness. It is debatable whether or not the primary analysis should be based on complete case data, which omits a large number of cases and therefore has limited power due to the small sample size, or the imputed data, which has a larger sample but introduces a range of assumptions about the extent to which data are missing at random, and also the validity of the imputation model.
Relationship to previous studies
Studies of PhysioDirect
There are no similar studies of PhysioDirect with which to compare the findings of this trial, although there have been a number of local evaluations of services based on telephone advice given by physiotherapists. The only randomised trial was based on a comparison of telephone advice with no advice for people with back pain while they were waiting for a face-to-face appointment, and this (unsurprisingly) showed that those given telephone advice were more satisfied. 50 No evidence was collected about clinical or other outcomes. Local surveys have suggested that patients are very satisfied with PhysioDirect services, with 80% rating them as good or excellent, but these surveys have not included a control group. 52 Our study shows that patients' views are more nuanced. They do express satisfaction with telephone advice, but some patients view it as only a first step and some would prefer to wait for a face-to-face appointment.
No previous evaluations of PhysioDirect have assessed costs or outcomes, although they do provide information about the process of care. Our finding that about half of all patients can be managed with telephone advice alone is consistent with earlier audits in the pioneering services in Cheltenham and Huntingdonshire. 52 This supports the notion that our services were functioning in a similar way to these more established services. On the other hand, these same reports stated that DNA appointment rates were reduced from 15% to 1% following the introduction of PhysioDirect, and that telephone consultations take approximately half as long as face-to-face consultations. 52 Neither of these claims was supported by our data. We observed some reduction in DNA rates but not on the scale previously reported. Telephone consultations were shorter than face-to-face appointments, but after taking account of administration time following the telephone call (which is already included in the appointment slot for face-to-face appointments) the difference in call time was only 5 minutes.
Relationship to other studies of telephone-based triage services
Although there is little evidence about PhysioDirect services specifically, the findings of this trial resonate strongly with evaluation of other health service innovations which are designed to offer easier access to advice and/or triage to manage demand. These include telephone-based services such as NHS Direct and GP out-of-hours organisations, services providing easy face-to-face access such as NHS walk-in centres, and services designed to offer less expensive forms of care, such as making nurses rather than doctors the first point of contact in general practice. The findings of such studies demonstrate some consistent themes.
Telephone-based services can be designed that provide a safe assessment, and these services are often popular with the public, as they do make access easier and more convenient. 44,117 However, the idea that providing easier access to services will reduce pressure on other services does not appear to be sustained. With regard to both NHS Direct and NHS walk-in centres there is no evidence that they reduce demand on other providers and instead they largely appear to act as an additional rather than alternative source of help. 118,119
Furthermore, introducing a first-stage triage element in order to reduce pressure on other expensive resources does not necessarily appear to reduce costs. In some cases (examples include NHS Direct, NHS walk-in centres, General Practitioners with Special Interests), the new service can be more expensive than existing alternative services. 91,120 New services that appear to be efficient may not actually be so. For example, provision of an initial telephone assessment in general practice reduces the number of people who are seen face to face, but when account is also taken of the number of people who have both telephone and face-to-face consultations the overall costs appear to be similar (although further research to explore this is ongoing). 121
There are concerns that services designed to reduce pressure on existing providers can actually increase demand, owing to a combination of increased access untapping previously unexpressed demand for care and cautious triage algorithms, which means that patients are referred on to expensive services or for further investigations when previously they were not. For example, the substitution of nurses for doctors in general practice does not appear to reduce costs because, although nurses' salaries are lower, their consultation times are longer and they refer more people for investigations than doctors. 122
Whether or not a new triage and advice-based service is efficient depends on whether or not it causes any inflation in demand, the proportion of patients who contact the new service instead of (rather than as well as) another provider, and the proportion of patients who the new services refer on to other providers. Other key challenges for triage and advice services are whether or not the time of the staff providing advice can be used very productively and the overhead associated with managing an additional service. For a new service to be cost-effective it needs to provide equivalent or better care at a reduced or equivalent cost. The evidence from evaluations of a range of service innovations is that it is possible to provide equivalent care and improve access but very challenging to do so efficiently in a way that reduces costs.
Chapter 9 Conclusions
Implications for health care
This study demonstrates that physiotherapy services based on PhysioDirect are equally as effective as usual care based on a waiting list for face-to-face treatment. PhysioDirect provides faster access to assessment and advice. The care provided appears to be safe and broadly acceptable and convenient for patients, although there is no evidence that they are more satisfied with access to care using PhysioDirect.
PhysioDirect reduced the number of physiotherapy consultations in total but within the context of the trial the cost of physiotherapy using PhysioDirect was slightly more expensive than usual care. However, sensitivity analysis suggested that providing physiotherapy via PhysioDirect would be slightly cheaper than usual care when provided in a slightly modified way outside a trial. The implication for health services is that PhysioDirect could be a less expensive way to provide physiotherapy services than usual waiting list-based care but this cannot be assumed and depends on whether or not the time of physiotherapists is used productively.
PhysioDirect is probably cost-effective because the slightly greater total NHS costs are accompanied by slightly greater health gains, related to faster improvement in health status among those allocated to PhysioDirect. The level of certainty about increased cost-effectiveness is only moderate, because the differences between trial arms in both the costs and benefits are very small with wide CIs, but the overall finding about the cost-effectiveness of PhysioDirect is robust to a range of sensitivity analyses.
Providing a service based on PhysioDirect therefore appears to be justified in terms of benefits to patients, potentially lower costs for the provision of physiotherapy services and a level of cost-effectiveness that is well within the threshold usually used to justify services within the NHS.
In future, it is likely that PhysioDirect services will increasingly be provided in conjunction with direct access for patients (rather than following referral from another health-care professional) and may be offered as a choice for patients wanting quicker advice rather than as the only route to care. This is likely to increase the cost-effectiveness and acceptability of PhysioDirect because patients who self-refer are likely to contact the service with less severe problems of shorter duration, and such patients are particularly appropriate for the initial assessment and advice provided by a PhysioDirect service.
Recommendations for research
-
As services evolve, further research should explore the costs and benefits of PhysioDirect under different scenarios. In particular, it will be important to assess the costs and benefits of services once they are more established and provided on a wider scale and among patients who self-refer.
-
The PhysioDirect services in this study were all based on the assumption that it is necessary to use senior and experienced staff to undertake telephone assessment and advice, and these staff undertook further training in telephone consultation. Some recently established PhysioDirect services (and many triage services in other contexts) use less experienced staff. If services use less experienced staff it will be important to establish whether or not the clinical outcomes of the service are equally good (compared with more experienced staff and compared with face-to-face care) and particularly whether or not patient safety can be assured.
-
Similarly, some PhysioDirect services are not using computerised support in the assessment of patients. Further research is needed on the advantages and disadvantages of computer supported assessment, in physiotherapy specifically, but also in other fields of medicine where this is being used.
-
New technological developments are making possible other ways of assessing patients at a distance. These include the use of the internet combined with cameras (which allow better visualisation and thus may help address some of the concerns that patients and physiotherapists expressed about telephone assessment), and the use of mobile ‘smart telephone’ technology, where patients and physiotherapists could consult anywhere and at any time. This could be particularly relevant, for example, in assessing sports injuries.
-
There are advantages and disadvantages to evaluating new services soon after they have been established, and this is a recurring debate of relevance to many health service innovations. Further research should explore the extent to which the costs and outcomes of new services change over time and whether or not there is an optimum time at which to conduct evaluation of a new service.
-
Further research is needed to explore, in more depth, patients' perceptions, expectations and preferences with regard to services based on initial assessment and advice by telephone. Although this approach is designed to improve access to care, this research suggests that patients do not necessarily prefer this approach.
Acknowledgements
Contributions of authors
Chris Salisbury (Professor of Primary Health Care) Chief investigator – overall design of the study, supervised trial conduct, wrote first draft and undertook final editing of report.
Nadine E Foster (Professor of Musculoskeletal Health in Primary Care) Principal investigator for sites near Keele – supervised trial in these sites, contributed to design of trial and supervision of qualitative research.
Cherida Hopper (Trial manager) Managed all aspects of the conduct of the trial and supervised research staff.
Annette Bishop (Research Physiotherapist) Managed day-to-day conduct of the trial in sites near Keele, contributed to recruitment and collection of data. Wrote first draft of literature review chapter in report.
Sandra Hollinghurst (Senior Lecturer in Health Economics) Led the economic analysis, wrote first draft of economics chapter in report.
Jo Coast (Professor of Health Economics) Contributed to design and economic analysis.
Surinder Kaur (Research Associate) Managed day-to-day conduct of the trial in sites near Bristol, contributed to recruitment and collection of data.
Jennifer Pearson (PhD student) Designed and undertook qualitative research, wrote first draft of qualitative research chapter in report.
Angelo Franchini (NIHR Research Methods Training Fellow in Medical Statistics) Undertook the statistical analysis, wrote first draft of statistical results chapter.
Jeanette Hall (Operational lead for Outpatient Physiotherapy) Design and implementation of PhysioDirect services, advised about undertaking the trial in the NHS environment.
Sean Grove (Clinical Lead Physiotherapist) Design and implementation of PhysioDirect services and advised about training of physiotherapists.
Michael Calnan (Professor of Medical Sociology) Co-supervision of qualitative research.
John Busby (Research Assistant in Health Economics) Contributed to economic analysis by calculating primary care/physiotherapist resource use and prescription drug costs.
Alan A Montgomery (Reader in Health Services Research) Trial design, supervision of statistical analysis.
All authors contributed to the final report.
Disclaimers
The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from the material published in this report.
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the MRC, NETSCC, the HTA programme, the EME programme or the Department of Health.
Other acknowledgements
We are extremely grateful to the many other people who made this research possible:
-
The patients who agreed to participate in this research and gave their time in completing questionnaires.
-
The physiotherapists and physiotherapy reception staff in each site who took part in this research.
-
Research support staff: Debbie Johnson, Belinda Afford, Julia Carver (Bristol), Deborah D'Cruz, Shirley Caldwell, Jane Scharf, Catherine Warlow, Julie Young, Claire Calverley, Jo Bailey, Rhian Hughes (Keele).
-
PCT leads: Jeanette Hall, Sean Grove (Bristol), Alison Rossiter, Louise Benjamin (Somerset), Lucy Huckfield, Alan Naggington (Stoke), Jenny Dewsbury, Jonathan Kemp (Cheshire).
-
Heads of Community Physiotherapy: Claire Chapman (Bristol), Fiona Robinson (Somerset), Panagiotis Sarigiovannis (Stoke), Ruth Heaton (Cheshire).
-
Trial Steering Committee: Professor Martin Underwood (Chair), Professor Elaine Hay, Professor Jackie Oldham, Dr Lesley Holdsworth, Dr Mary Laynon, Jill Gamlin, Elaine Beck.
-
Data Monitoring Committee: Dr Richard McManus (Chair), Professor Lee Shepstone, Dr Simon Gates.
-
Bronwen Williams and Helen Thorp, who conducted the literature review and pilot study in preparation for this trial.
-
Jill Gamlin, who originally developed the concept of PhysioDirect in Huntingdon, and the senior physiotherapists from Huntingdon who provided training.
-
PhysioDirect software development: Nick Deane (Huntingdon PCT). Local IT staff in each PCT who facilitated network and software installation.
-
Support for analysis: John Busby (economic analysis), Trishna Rathod (changes in process of care over time).
-
Research database: Pete Shiarly (University of Bristol).
-
The Primary Care Research Network.
-
The GPs and practice managers from practices in Bristol, Somerset, Stoke and Cheshire, who referred patients for physiotherapy.
Publications
Foster NE, Williams B, Grove S, Gamlin J, Salisbury C. The evidence for and against ‘PhysioDirect’ telephone assessment and advice services. Physiotherapy 2011;97:78–82.
Salisbury C, Foster NE, Bishop A, Calnan M, Coast J, Hall J et al. ‘PhysioDirect’ telephone assessment and advice services for physiotherapy: protocol for a pragmatic randomised controlled trial. BMC Health Serv Res 2009;9:136.
Bishop A, Gamlin J, Hall J, Hopper C, Foster NE. PhysioDirect: Supporting physiotherapists to deliver telephone assessment and advice services within the context of a randomised trial. Physiotherapy 2013; in press. doi: 10.1016/j.physio.2012.08.002
Salisbury C, Montgomery AA, Hollinghurst S, Hopper C, Bishop A, Franchini A, et al. Effectiveness of PhysioDirect telephone assessment and advice services for patients with musculoskeletal problems: pragmatic randomised controlled trial. BMJ 2013;346:f43.
References
- Picavet HS, Schouten JS. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain 2003;102:167-78.
- Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord 2010;11.
- Bot SD, van der Waal JM, Terwee CB, van der Windt DA, Schellevis FG, Bouter LM, et al. Incidence and prevalence of complaints of the neck and upper extremity in general practice. Ann Rheum Dis 2005;64:118-23.
- White KP, Harth M. The occurrence and impact of generalized pain. Balliere's Best Practice & Research. Clin Rheumatol 1999;13:379-89.
- Brevick H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287-333.
- Walker BF. The prevalence of low back pain: systematic review of the literature from 1966 to 1998. J Spinal Disord 2000;13:205-17.
- Andersson GB. Epidemiological features of chronic low-back pain. Lancet 1999;354:581-5.
- Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000;84:95-103.
- London: NICE; 2009.
- Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ. Outcome of low back pain in general practice: a prospective study. BMJ 1998;316:1356-9.
- Dunn KM, Croft PR. Spine. 2005.
- McCormick A, Fleming D, Charlton J. Fourth national study 1991–1992. London: HMSO; 1995.
- National Statistics . NHS Physiotherapy services summary information for 2004–2005, England. Department of Health n.d. https://catalogue.ic.nhs.uk/publications/hospital/outpatients/nhs-phys-serv-summ-eng-2004-05/nhs-phys-serv-summ-eng-2004-05-rep.pdf (accessed 12 January 2013).
- The care and management of osteoarthritis in adults. London: NICE; 2008.
- The Musculoskeletal Services Framework – a joint responsibility: doing it differently. London: DoH; 2006.
- Our health, our care, our say: a new direction for community services. London: The Stationery Office; 2006.
- Self-referral pilots to musculoskeletal physiotherapy and the implications for improving access to other AHP services. London: DoH; 2008.
- Holdsworth LK, Webster VS, McFadyen AK. What are the costs to NHS Scotland of self-referral to physiotherapy? Results of a national trial. Physiotherapy 2007;93:3-11.
- Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. Cochrane Database Syst Rev 2004;1.
- Van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15:S169-91.
- UK Beam Trial Team . United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: cost effectiveness of physical treatments for back pain in primary care. BMJ 2004;329.
- Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute ‘nonspecific' low back pain: results of a randomized clinical trial. Spine 2006;31:623-31.
- Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med 2004;141:920-8.
- Rubinstein SM, van Middelkoop M, Assendelft WJJ, de Boer MR. Spinal manipulative therapy for chronic low-back pain. Cochrane Database Syst Rev 2011;2.
- Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev 2005;3.
- Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 2006;15:S192-300.
- van Tulder MW, Koes B, Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J 2006;15:S64-81.
- Smidt N. Effectiveness of exercise therapy: a best-evidence summary of systematic reviews. Aust J Physiother 2005;51:71-85.
- Frost H, Lamb SE, Doll HA, Carver PT, Stewart-Brown S. Randomised controlled trial of physiotherapy compared with advice for low back pain. BMJ 2004;329.
- Rivero-Arias O, Gray A, Frost H, Lamb SE, Stewart-Brown S. Cost-utility analysis of physiotherapy treatment compared with physiotherapy advice in low back pain. Spine 2006;31:1381-7.
- Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Bronfort G. Exercises for mechanical neck disorders. Cochrane Database Syst Rev 2005;3.
- Gross A, Miller J, D’Sylva J, Burnie SJ, Goldsmith CH, Graham N, et al. Manipulation or mobilisation for neck pain. Cochrane Database Syst Rev 2010;1.
- Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev 2003;2.
- Hay EM, Foster NE, Thomas E, Peat G, Phelan M, Yates HE, et al. Effectiveness of community physiotherapy and enhanced pharmacy review for knee pain in people aged over 55 presenting to primary care: pragmatic randomised trial. BMJ 2006;333.
- Foster NE, Thomas E, Barlas P, Hill JC, Young J, Mason E, et al. Acupuncture as an adjunct to exercise based physiotherapy for osteoarthritis of the knee: randomised controlled trial. BMJ 2007;335.
- Hurley MV, Walsh NE, Mitchell HL, Pimm TJ, Patel A, Williamson E, et al. Clinical effectiveness of a rehabilitation program integrating exercise, self-management, and active coping strategies for chronic knee pain: a cluster randomized trial. Arthritis Rheum 2007;57:1211-19.
- Bower P, Gilbody SM. Stepped care in psychological therapies: access, effectiveness and efficiency. Br J Psychiatry 2005;186:11-7.
- Nordeman L, Nilsson B, Moller M, Gunnarsson R. Early access to physical therapy treatment for subacute low back pain in primary health care: a prospective randomized clinical trial. Clin J Pain 2006;22:505-11.
- Wand B, Bird C, McAuley J, Dore C, MacDowell M, De Souza L. Early Intervention for the management of acute low back pain: a single-blind randomized controlled trial of biopsychosocial education, manual therapy, and exercise. Spine 2004;29:2350-6.
- Gatchel RJ, Polatin PB, Noe C, Gardea M, Pulliam C, Thompson J. Treatment- and cost-effectiveness of early intervention for acute low-back pain patients: a one-year prospective study. J Occup Rehabil 2003;13:1-9.
- Hagen EM, Eriksen HR, Ursin H. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain?. Spine 2000;25:1973-6.
- Zigenfus GC, Yin J, Giang GM, Fogarty WT. Effectiveness of early physical therapy in the treatment of acute low back musculoskeletal disorders. J Occup Environ Med 2000;42:35-9.
- Epidemiology review: the epidemiology and cost of back pain. London: HMSO; 1994.
- Lattimer V, George S, Thompson F, Thomas E, Mullee M, Turnbull J, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. BMJ 1998;317:1054-9.
- Lattimer V, Sassi F, George S, Moore M, Turnbull J, Mullee M, et al. Cost analysis of nurse telephone consultation in out of hours primary care: evidence from a randomised controlled trial. BMJ 2000;320:1053-7.
- Pinnock H, Bawden R, Proctor S, Wolfe S, Scullion J, Price D, et al. Accessibility, acceptability, and effectiveness in primary care of routine telephone review of asthma: pragmatic, randomised controlled trial. BMJ 2003;326.
- Bunn F, Byrne G, Kendall S. Telephone consultation and triage: effects on health care use and patient satisfaction. Cochrane Database Syst Rev 2004;4.
- McKinstry B, Watson P, Pinnock H, Heaney D, Sheikh A. Telephone consulting in primary care: a triangulated qualitative study of patients and providers. Br J Gen Pract 2009;59:e209-18.
- Hodgson K. Kidderminster helpline proves a success. Physiother Frontline 2001;7:22-3.
- Taylor S, Ellis I, Gallagher M. Patient Satisfaction with a New Physiotherapy Telephone Service for Back Pain Patients. Physiotherapy 2002;88:645-57.
- Clayson M, Woolvine M. Back Pain Direct Clinic: a collaboration between general practitioners and physiotherapists. Work Based Learning Prim Care 2004;2:38-43.
- NHS Working in Partnership Programme . Direct Access to Physiotherapy 2006. www.workloadmanagement.nhs.uk/uploads/gpdb/case_daphysio.pdf (accessed 16 December 2011).
- Turner D. An exploratory study of physiotherapy telephone assessment. Int J Ther Rehabil 2009;16:97-105.
- Russell T, Truter P, Blumke R, Richardson B. The diagnostic accuracy of telerehabilitation for nonarticular lower-limb musculoskeletal disorders. Telemed J E Health 2010;16:585-94.
- Patel S, Hossain FS, Colaco HB, El-Husseiny M, Lee MH. The accuracy of primary care teams in diagnosing disorders of the shoulder. J Eval Clin Pract 2011;17:118-22.
- Harding KE, Taylor NF, Leggat SG, Wise VL. Prioritizing patients for Community Rehabilitation Services: do clinicians agree on triage decisions?. Clin Rehabil 2010;24:928-34.
- Jette DU, Ardleigh K, Chandler K, McShea L. Decision-making ability of physical therapists: physical therapy intervention or medical referral. PhysTher 2006;86:1619-29.
- Leemrijse CJ, Swinkels IC, Veenhof C. Direct access to physical therapy in the Netherlands: results from the first year in community-based physical therapy. PhysTher 2008;88:936-46.
- Holdsworth LK, Webster VS, McFayden AK. Physiotherapists' and general practitioners' view of self-referral and physiotherapy scope of practice: results from a national trial. Physiotherapy 2008;94:236-44.
- Webster VS, Holdsworth LK, McFayden AK, Little H. Self-referral, access and physiotherapy: patients' knowledge and attitudes: results of a national trial. Physiotherapy 2008;94:141-50.
- Addley K, Burke C, McQuillan P. Impact of a direct access occupational physiotherapy treatment service. Occup Med (London) 2010;60:651-3.
- Williamson E, Williams M, Hansen Z, Joseph S, Lamb SE. Development and delivery of a physiotherapy intervention for the early management of whiplash injuries: the Managing Injuries of Neck Trial (MINT) Intervention. Physiotherapy 2009;95:15-23.
- Sephton R, Hough E, Roberts SA, Oldham J. Evaluation of a primary care musculoskeletal clinical assessment service: a preliminary study. Physiotherapy 2010;96:296-302.
- O’Brien BJ, Gertsen K, Willan AR, Faulkner LA. Is there a kink in consumers' threshold value for cost-effectiveness in health care?. Health Econ 2002;11:175-80.
- SF-36.org . A Community for Measuring Health Outcomes Using SF Tools n.d. www.sf-36.org/ (accessed 12 January 2013).
- Walsh TL, Hanscom B, Lurie JD, Weinstein JN. Is a condition-specific instrument for patients with low back pain/leg symptoms really necessary? The responsiveness of the Oswestry Disability Index, MODEMS, and the SF-36. Spine 2003;28:607-15.
- Kvien TK, Kaasa S, Smedstad LM. Performance of the Norwegian SF-36 Health Survey in patients with rheumatoid arthritis. II. A comparison of the SF-36 with disease-specific measures. J Clin Epidemiol 1998;51:1077-86.
- Angst F, Aeschlimann A, Steiner W, Stucki G. Responsiveness of the WOMAC osteoarthritis index as compared with the SF-36 in patients with osteoarthritis of the legs undergoing a comprehensive rehabilitation intervention. Ann Rheum Dis 2001;60:834-40.
- Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum 2001;45:384-91.
- Lurie J. A review of generic health status measures in patients with low back pain. Spine 2000;25:3125-29.
- Paterson C. Measuring outcomes in primary care: a patient generated measure, MYMOP, compared with the SF-36 survey. BMJ 1996;312:1016-20.
- Pham T, Van Der Heijde D, Lassere M, Altman RD, Anderson JJ, Bellamy N, et al. Outcome variables for osteoarthritis clinical trials: The OMERACT-OARSI set of responder criteria. J Rheumatol 2003;30:1648-54.
- Roberts C, Sarangi S. Theme-oriented discourse analysis of medical encounters. Med Educ 2005;39:632-40.
- Samsa G, Edleman D, Rothman ML, Williams GR, Lipscomb J, Matchar D. Determining clinically important differences in health status measures. Pharmaceconomics 1999;15:141-55.
- Kosinski M, Zhao SZ, Dedhiya S, Osterhaus JT, Ware JE. Determining minimally important changes in generic and disease-specific health-related quality of life questionnaires in clinical trials of rheumatoid arthritis. Arthritis Rheum 2000;43:1478-87.
- Wyrwich KW, Tierney WM, Babu AN, Kroenke K, Wolinsky FD. A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Health Serv Res 2005;40:577-91.
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003;41:582-92.
- Ware JE, Kosinski M, Bjorner JB, Turner-Bowker JM, Gandek B, Maruish ME. User's manual for the SF36v2 Health Survey. Lincoln, RI: Quality Metric Inc.; 2007.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340.
- Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340.
- Bourton I, Moher D, Altman DG, Schulz KF, Ravaud P. Extending the CONSORT Statement to Randomized Trials of Nonpharmcologic Treatment: Explanation and Elaboration. Ann Intern Med 2008;148:295-309.
- Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B, et al. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ 2008;337.
- Piaggio G, Elbourne DR, Altman DG, Pocock SJ, Evans SJ. Reporting of noninferiority and equivalence randomized trials: an extension of the CONSORT statement. JAMA 2006;295:1152-60.
- Salisbury C, Foster NE, Bishop A, Calnan M, Coast J, Hall J, et al. ‘PhysioDirect’ telephone assessment and advice services for physiotherapy: protocol for a pragmatic randomised controlled trial. BMC Health Serv Res 2009;9.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96.
- Curtis L. Unit Costs of Social and Health Care n.d. www.pssru.ac.uk (accessed 14 September 2010).
- Royal College of Nursing . Pay Rates 2009 10 n.d. www.rcn.org.uk/support/pay_and_conditions/pay_rates_2009_-_2010 (accessed 12 January 2013).
- Scott A, Simoens S, Heaney D, O’Donnell CA, Thomson H, Moffat KJ, et al. What does GP out of hours care cost? An analysis of different models of out of hours care in Scotland. Scott Med J 2004;49:61-6.
- British national formulary. London: BMA and RPS; 2009.
- Salisbury C, Chalder M, Manku-Scott T, Nicholas R, Deave T, Noble S, et al. The National Evaluation of NHS Walk-in Centres: Final Report 2002.
- Department of Health (DoH) . NHS Reference Costs 2009–2010 n.d. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_123459 (accessed 12 January 2013).
- Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al. Is hydroptherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis. Health Technol Assess 2005;9.
- Annual survey of hours and earnings. London: ONS; 2009.
- van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covarietes in survival analysis. StatMed 1999;18:681-94.
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002;21:271-92.
- Lyall J. Physiotherapy Direct worries. Frontline 2007;13:6-7.
- Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455-9.
- Ritchie J, Lewis J. Qualitative research practice: a guide for social science students and researchers. London: Sage Publications; 2003.
- Pope C, Ziebland S, Mays N. Qualitiative research in health care: analysing qualitative data. BMJ 2000;320.
- Jones R, Jenkins F. A survey of NHS physiotherapy waiting times and musculoskeletal workload and caseload in England 2009–10. Chartered Society of Physiotherapy 2011. www.csp.org.uk/sites/files/csp/secure/csp_pd090_waiting_times_survey.pdf (accessed 12 January 2013).
- Foster NE, Williams B, Grove S, Gamlin J, Salisbury C. The evidence for and against ‘PhysioDirect’ telephone assessment and advice services. Physiotherapy 2011;97:78-82.
- Hills R, Kitchen S. Satisfaction with outpatient physiotherapy: Focus groups to explore the views of patients with acute and chronic musculoskeletal conditions. Physiother Theor Pract 2007;23:1-20.
- Salisbury C, Goodall S, Montgomery AA, Pickin DM, Edwards S, Sampson F, et al. Does Advanced Access improve access to primary health care? Questionnaire survey of patients. Br J Gen Pract 2007;57:615-21.
- Gerard K, Salisbury C, Street D, Pope C, Baxter H. Is fast access to general practice all that should matter? A discrete choice experiment of patients' preferences. J Health Serv Res Policy 2008;13:3-10.
- Rubin G, Bate A, George A, Shackley P, Hall N. Preferences for access to the GP: a discrete choice experiment. Br J Gen Pract 2006;56:743-8.
- Morse JM. Researching illness and injury: methodological considerations. Qual Health Res 2000;10:538-46.
- Wyatt JC, Sullivan F. ABC of health informatics: eHealth and the future: promise or peril?. BMJ 2005;331:1391-3.
- King E, Rudat K, Andersen B, Grabarz A, Glendinning R, McHugh S, et al. Evaluation of Information Prescriptions. Final Report to the Department of Health London 2008.
- Edwards B. Seeing is believing: picture building: a key component of telephone triage. J Clin Nurs 1998;7:51-7.
- Chartered Society of Physiotherapy . Regulatory Requirements n.d. www.csp.org.uk/professional-union/professionalism/regulation/regulatory-requirements (accessed 12 January 2013).
- Hammond R, Wheeler JD, Porter S. Tidy's physiotherapy. London: Elsevier; 2008.
- Richards DA, Meakins J, Godfrey L, Tawfik J, Dutton E. Survey of the impact of nurse telephone triage on general practitioner activity. Br J Gen Pract 2004;54:207-10.
- Holdsworth LK, Webster V. An international Multi-centred Investigation of Patient Self-Referral and Physiotherapy Practice in Privately Funded Health Care Systems n.d. http://s3.amazonaws.com/zanran_storage/www.selfreferralphysioinfo.com/ContentPages/44216519.pdf (accessed 12 January 2013).
- Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ 1996;312:1215-18.
- Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA 2003;290:1624-32.
- O’Cathain A, Munro JF, Nicholl JP, Knowles E. How helpful is NHS direct? Postal survey of callers. BMJ 2000;320.
- Munro J, Sampson F, Nicholl J. The impact of NHS Direct on the demand for out-of-hours primary and emergency care. Br J Gen Pract 2005;55:790-2.
- Chalder M, Sharp D, Moore L, Salisbury C. Impact of NHS walk-in centres on the workload of other local healthcare providers: time series analysis. Br Med J 2003;326:532-4B.
- Coast J, Noble S, Noble A, Horrocks S, Asim O, Peters TJ, et al. Economic evaluation of a general practitioner with special interests led dermatology service in primary care. BMJ 2005;331:1444-9.
- Richards DA, Meakins J, Tawfik J, Godfrey L, Dutton E, Richardson G, et al. Nurse telephone triage for same day appointments in general practice: multiple interrupted time series trial of effect on workload and costs. BMJ 2002;325:1214-17.
- Hollinghurst S, Horrocks S, Anderson E, Salisbury C. Comparing the cost of nurse practitioners and GPs in primary care: modelling economic data from randomised trials. Br J Gen Pract 2006;56:530-5.
Appendix 1 Comparison of baseline characteristics between patients with or without missing primary outcome data
| Patient characteristics at baseline | Randomised: n = 2249a (100%) | |||||
|---|---|---|---|---|---|---|
| Usual care: n = 743 (33.04%) | PhysioDirect: n = 1506 (66.96%) | |||||
| Collected: n = 629 (84.66%) | Missing: n = 114 (15.34%) | Test | Collected: n = 1283 (85.19%) | Missing: n = 223 (14.81%) | Test | |
| Sex: % | ||||||
| Female | 59.46 | 56.14 | x12 = 0.44, p = 0.51 | 60.02 | 56.95 | x12 = 0.74, p = 0.39 |
| Male | 40.54 | 43.86 | 39.98 | 43.05 | ||
| Age: median (IQR) | ||||||
| Years | 50.12 (38.32 to 62.69) | 39.72 (29.07 to 51.66) | Rank-sum, z = 5.4, p < 0.001 | 50.01 (38.25 to 62.28) | 40.11 (29.22 to 51.69) | Rank-sum, z = 7.40, p < 0.001 |
| Ethnicity: % | ||||||
| White | 95.83 | 95.54 | x52 = 6.83, p = 0.23 | 97.07 | 94.59 | x52 = 8.72, p = 0.12 |
| Black | 1.12 | 0.89 | 0.79 | 1.35 | ||
| Asian | 1.76 | 0.89 | 0.71 | 2.70 | ||
| Dual/mixed | 0.96 | 0.89 | 0.71 | 0.90 | ||
| Chinese | 0.00 | 0.89 | 0.16 | 0.00 | ||
| Other | 0.32 | 0.89 | 0.55 | 0.45 | ||
| Deprivation: % | ||||||
| Quintile (5 = most deprived) | ||||||
| 1 | 9.85 | 10.28 | x42 = 14.97, p = 0.01 | 10.36 | 11.79 | x42 = 24.28, p < 0.001 |
| 2 | 22.50 | 12.15 | 20.31 | 15.57 | ||
| 3 | 29.89 | 26.17 | 28.96 | 22.17 | ||
| 4 | 21.84 | 21.50 | 23.41 | 19.81 | ||
| 5 | 15.93 | 29.91 | 16.97 | 30.66 | ||
| Employment status: % | ||||||
| Employed | 56.91 | 57.80 | x52 = 46.94, p < 0.001 | 61.15 | 67.42 | x52 = 40.39, p < 0.001 |
| Unemployed | 4.02 | 18.35 | 3.78 | 9.95 | ||
| Student | 2.73 | 1.83 | 2.36 | 3.62 | ||
| Ill/disabled | 6.91 | 8.26 | 5.36 | 6.79 | ||
| Retired | 24.76 | 6.42 | 22.70 | 7.24 | ||
| Not working/other | 4.66 | 7.34 | 4.65 | 4.98 | ||
| Profession: % | ||||||
| Administrative | 17.05 | 16.09 | x82 = 19.11, p = 0.01 | 14.70 | 6.91 | x82 = 31.06, p < 0.001 |
| Technical | 11.74 | 4.60 | 11.91 | 10.64 | ||
| Elementary | 8.71 | 9.20 | 9.40 | 14.89 | ||
| Manager | 9.47 | 17.24 | 8.74 | 12.77 | ||
| Personal services | 7.39 | 6.90 | 8.74 | 12.77 | ||
| Operatives | 4.55 | 11.49 | 5.77 | 4.79 | ||
| Professional | 18.75 | 10.34 | 19.44 | 9.57 | ||
| Customer services | 10.61 | 14.94 | 10.42 | 15.96 | ||
| Skilled trade | 11.74 | 9.20 | 10.88 | 11.70 | ||
| Patient characteristics at baseline | Randomised: n = 2249 (100%) | |||||
|---|---|---|---|---|---|---|
| Usual care: n = 743 (33.04%) | PhysioDirect: n = 1506 (66.96%) | |||||
| Collected: n = 629 (84.66%) | Missing: n = 114 (15.34%) | Test | Collected: n = 1283 (85.19%) | Missing: n = 223 (14.81%) | Test | |
| Referral problem (%) | ||||||
| Cervical | 11.62 | 14.04 | x72 = 8.83, p = 0.27 | 12.00 | 13.90 | x72 = 7.20, p = 0.41 |
| Thoracic | 1.43 | 3.51 | 2.26 | 2.69 | ||
| Lumbar | 26.43 | 32.46 | 26.89 | 30.04 | ||
| Upper limb | 23.89 | 21.05 | 23.46 | 22.42 | ||
| Lower limb | 31.69 | 22.81 | 30.71 | 25.11 | ||
| Widespread pain | 0.80 | 1.75 | 0.62 | 0.00 | ||
| Multiple MSK | 3.50 | 4.39 | 3.51 | 4.48 | ||
| Other MSK | 0.64 | 0.00 | 0.55 | 1.35 | ||
| PCT (%) | ||||||
| Bristol | 34.34 | 30.70 | x32 = 14.13, p < 0.01 | 34.29 | 26.46 | x32 = 35.17, p < 0.001 |
| Somerset | 24.17 | 11.40 | 24.94 | 12.56 | ||
| Cheshire | 21.62 | 33.33 | 21.43 | 34.98 | ||
| Stoke | 19.87 | 24.56 | 19.33 | 26.01 | ||
| Physiotherapy preference (%) | ||||||
| Usual care | 32.15 | 37.50 | x22 = 1.31, p = 0.52 | 29.66 | 36.70 | x22 = 35.17, p = 0.06 |
| PhysioDirect | 35.54 | 33.93 | 36.66 | 29.36 | ||
| No preference | 32.31 | 28.57 | 33.68 | 33.94 | ||
| Time off work: mean (SD), median (IRQ) | ||||||
| Days | 4.31 (9.10), 0 (0–4) | 5.08 (8.11), 0 (0–10) | Rank-sum, z = –1.17, p = 0.24 | 3.94 (8.42), 0 (0-4) | 5.14 (9.19), 0 (0-7) | Rank-sum, z = –1.34, p = 0.18 |
| English native speaker: % | ||||||
| No | 2.60 | 4.42 | x12 = 1.14, p = 0.29 | 3.49 | 4.50 | x12 = 0.55, p = 0.46 |
| Yes | 97.40 | 95.58 | 96.51 | 95.50 | ||
| Telephone: % | ||||||
| No | 0.16 | 2.65 | x12 = 11.11, p < 0.01 | 0.63 | 2.69 | x12 = 8.73, p < 0.01 |
| Yes | 99.84 | 97.35 | 99.37 | 97.31 | ||
| Car: % | ||||||
| No | 15.50 | 26.36 | x12 = 7.79, p < 0.01 | 15.96 | 21.08 | x12 = 3.57, p = 0.06 |
| Yes | 84.50 | 73.64 | 84.04 | 78.92 | ||
| Patient outcome measures at baseline | Randomised patients: n = 2249 (100%) | |||||
|---|---|---|---|---|---|---|
| Usual care: n = 743 (33.04%) | PhysioDirect: n = 1506 (66.96%) | |||||
| Collected: n = 629 (84.66%) | Missing: n = 114 (15.34%) | Test | Collected: n = 1283 (85.19%) | Missing: n = 223 (14.81%) | Test | |
| SF-36v2 PCS | ||||||
| Mean (SD) | 37.97 (8.66) | 36.31 (8.32) | Rank-sum, z = 2.11, p = 0.03 | 36.98 (8.92) | 35.81 (8.59) | Rank-sum, z = 1.93, p = 0.05 |
| Median (IQR) | 38.06 (31.85 to 44.38) | 36.09 (29.45 to 42.34) | 37.15 (30.55 to 43.38) | 35.47 (30.12 to 41.40) | ||
| SF-36v2 MCS | ||||||
| Mean (SD) | 46.42 (13.08) | 41.47 (13.69) | Rank-sum, z = 3.64, p < 0.001 | 46.76 (12.34) | 42.10 (13.68) | Rank-sum, z = 4.73, p < 0.001 |
| Median (IQR) | 49.38 (36.89 to 56.85) | 40.71 (33.01 to 53.83) | 49.39 (37.48 to 56.86) | 43.32 (31.75 to 53.63) | ||
| MYMOP | ||||||
| Mean (SD) | 3.76 (0.99) | 4.06 (0.94) | Rank-sum, z = –3.17, p < 0.01 | 3.79 (0.99) | 4.13 (0.95) | Rank-sum, z = –4.30, p < 0.001 |
| Median (IQR) | ||||||
| Lower better | 3.75 (3.25 to 4.33) | 4.00 (3.50 to 4.67) | 3.75 (3.25 to 4.50) | 4.00 (3.50 to 4.75) | ||
| EQ-5D | ||||||
| Mean (SD) | 0.57 (0.28) | 0.46 (0.32) | Rank-sum, z = 3.47, p < 0.001 | 0.54 (0.29) | 0.45 (0.32) | Rank-sum, z = 4.28, p < 0.001 |
| Median (IQR) | 0.69 (0.52 to 0.76) | 0.62 (0.16 to 0.69) | 0.69 (0.26 to 0.76) | 0.62 (0.12 to 0.69) | ||
Appendix 2 Development of patient satisfaction measure
The measures of satisfaction reported in Table 23 were derived from sets of questions given to patients at 6 weeks and 6 months. The questions items included:
-
six questions about satisfaction with the consultation, based on questions used in the doctor and nurse versions of the General Practice Assessment Questionnaire
-
three items about satisfaction with access (the hours the service was open, the length of time to wait for an appointment, and convenience of the service), which were issues identified through interviews with patients conducted for the pilot study for this trial, with the wording of the items also tested in that pilot study
-
a single question about overall satisfaction with the physiotherapy service.
The first two sets of question items had response options on a Likert scale with values of 1–6, with a higher value indicating greater satisfaction. The overall satisfaction question had response options from 1–5, with a lower value being higher satisfaction. The direction of this question was reversed in reported results for consistency.
Excluding the overall satisfaction question item, the remaining nine questions were analysed by factor analysis to ensure that they formed coherent and distinct components of satisfaction in the study population. As the responses were on an ordinal scale, the analysis was conducted on the polychoric correlation matrix estimated on the response values. As shown in Table 65, the first two factors appeared to account for all of the variance.
Table 66 shows how the questions of the second set can be grouped, with the first six associated with one factor relating to the consultation and the remaining three with another factor linked to satisfaction with access to the service.
| Factor analysis/correlation: method, principal factors; rotation, unrotated | No. of observations = 871; retained factors = 2; no. of parameters = 17 | |||
|---|---|---|---|---|
| Factor | Eigenvalue | Difference | Proportion | Cumulative |
| 1 | 6.27995 | 5.42285 | 0.8805 | 0.8805 |
| 2 | 0.85709 | 0.60661 | 0.1202 | 1.0006 |
| 3 | 0.25048 | 0.21186 | 0.0351 | 1.0358 |
| 4 | 0.03862 | 0.06268 | 0.0054 | 1.0412 |
| 5 | −0.02406 | 0.01527 | −0.0034 | 1.0378 |
| 6 | −0.03933 | 0.01549 | −0.0055 | 1.0323 |
| 7 | −0.05481 | 0.01337 | −0.0077 | 1.0246 |
| 8 | −0.06818 | 0.03913 | −0.0096 | 1.0150 |
| 9 | −0.10731 | – | −0.0150 | 1.0000 |
| How do you rate the following? | Factor 1 | Factor 2 | Uniqueness |
|---|---|---|---|
| a. How thoroughly the physiotherapist asked about your symptoms | 0.8768 | 0.2854 | 0.1498 |
| b. How well the physiotherapist listened to what you had to say | 0.8946 | 0.2663 | 0.1288 |
| c. How well the physiotherapist explained your problems or any treatment that you needed | 0.8962 | 0.2689 | 0.1244 |
| d. The information and advice you received | 0.8914 | 0.2981 | 0.1166 |
| e. The treatment you received from the physiotherapist | 0.8412 | 0.3612 | 0.1618 |
| f. How confident the physiotherapist made you feel about managing your problem | 0.8148 | 0.3618 | 0.2052 |
| g. How long you had to wait before you could get advice from a physiotherapist | 0.2583 | 0.6285 | 0.5383 |
| h. The hours that the physiotherapy service was open | 0.3262 | 0.8017 | 0.2508 |
| i. The convenience of the service you received | 0.4353 | 0.7895 | 0.1873 |
For each of the two identified factors, consultation and access satisfaction, a mean score was recalculated on a scale from 0 to 100, as a percentage of the maximum possible score (i.e. a score of ‘0’ represents extreme dissatisfaction on all question items and ‘100’ represents extreme satisfaction on all items). The overall satisfaction score was transformed to the same scale.
Appendix 3 Example topic guide: interviews with patients having PhysioDirect then face-to-face assessment
Aim and objectives: The overall aim of this study is to explore the acceptability of a new way of delivering physiotherapy services. Experiences of and views about how patients' experience physiotherapy are of particular interest and will explore musculoskeletal complaint, physiotherapy referral, decisions-making to consult, attitudes, beliefs and expectations of physiotherapy.
Background information: For the context of the interview it would be helpful to know some brief information about you. Can you give me some background information about yourself?
Prompts: Employment; spare time activities.
Problem: Can you tell me about the problem you were referred to physiotherapy for? How has it affected you in your day-to-day life?
Prompts: Length of time of the problem.
Process to physiotherapy: Can you tell me how you were referred to physiotherapy? What involvement did the GP have? Did the GP give you a diagnosis?
Physiotherapy expectations attitudes and beliefs: I would like to know what you think about physiotherapy. How you think physiotherapy would help your problem? I would like to know if you have ever had physiotherapy before. Can you tell me your experience of it?
Point of contact of PD: Can you tell me how you contacted the service? How many times did you contact the service?
Prompts: Opening time; ease of access.
Telephone call experience: I would like to know what your experience of talking to someone over the telephone was.
Prompts: Consultation and being assessed on the telephone first, physiotherapist information and advice on the telephone, what were you asked to do? What was the effectiveness of what you were asked to do? Call length; overall views of the value of the telephone service.
Face-to-face consultation and treatment experience: Can you tell me how you ended up seeing a physiotherapists face to face? Did you ring back into the service? Why did you end up being seen face to face?
Can you tell me about the consultation? How long did you wait for an appointment? What did the physiotherapist do? Can you tell me about the treatment you received? How many physiotherapy sessions did you have? What was your overall view of the face-to-face physiotherapy that you received?
Prompts: Consultation; information and exercises advice; treatment; physiotherapist.
Outcomes: I would like to know if the physiotherapy you received has helped your problem?
View of the service: I would like to know what you thought of the overall service [the telephone call(s) and the face-to-face physiotherapy] and what you liked and disliked about it? Is there anything you would change about any aspects of the service you received? Would you use it again? What impact has the service had on your problem?
Future suggestions: I would also like to get your views on accessing other services via the telephone.
Prompts: Do you telephone bank? Have you ever used NHS Direct or the GP out-of-hours services?
Appendix 4 Protocol
MRC PHYSIODIRECT TRIAL PROTOCOL: HISTORY OF VALIDATED VERSIONS
| Date | Version no. | Pages | Description of change |
|---|---|---|---|
| 21 November 2008 | 1.0 | ||
| 10 March 2009 | 1.1 | p. 5, section 3.5, second para: | … will telephone patients ‘about 48 hrs’ after … changed to … telephone patients ‘at two to three working days’ after … |
| p. 5, section 3.5, third para: | Addition of ‘gender’ to list of minimisation criteria (as second in list) | ||
| 27 July 2009 | 1.2 | p. 8, section 3.14, third para: | Additional criteria re. sample size. ‘1875 patients recruited and each PCT has recruited at least 300 patients’ |
| 18 January 2010 | 1.3 | p. 8, section 3.14, second para: | Changes in wording to clarify difference in primary outcome is based on points on SF36v2 PCS rather than SDs |
| p. 8, section 3.14, third para: | Increase in non-collection of primary outcomes from ‘20%’ to ‘30%’; increase in sample size from ‘1875’ to ‘2143’ patients recruited | ||
| p. 8, section 3.16, second para | … range –0.2 to 0.2 SDs … changed to … range –2 to +2 points … |
MRC PHYSIODIRECT TRIAL PROTOCOL
Title
Full title of trial
A pragmatic randomised controlled trial of ‘PhysioDirect’ telephone assessment and advice services for physiotherapy.
Brief title
The MRC PhysioDirect Trial.
Background
The problem to be addressed
Musculoskeletal problems are extremely common, accounting for 15% of all GP consultations. 1 Many 00of these patients are referred to physiotherapists, with 4.4 million new referrals to physiotherapy being made each year, of which 1.23 million are referred by GPs. 2 The number of referrals to NHS physiotherapy increased by 37% in the 15 years between 1990 and 2005. 2 Ensuring timely access to physiotherapy has long been an issue within the NHS, with waiting times of more than four months in some areas. This is a problem for patients, because musculoskeletal conditions cause pain and disability, and for the economy because these conditions are second only to mental health problems as a cause of days lost from work. In particular, back pain accounts for some 120 million days of certified absence from work each year and half of all patients with back pain who are off work for more than 6 months never return to employment. 3 Delayed access to physiotherapy is also a problem for the NHS because when patients are finally offered a physiotherapy appointment many fail to attend, and in other cases patients wait a long time for a physiotherapy consultation when it is unlikely that this will offer benefit, so much of the current physiotherapy resource is used inefficiently and ineffectively. While patients are waiting for physiotherapy they may repeatedly visit their GP and request medication, and the lack of access to physiotherapy may lead to unnecessary referrals to outpatient orthopaedic specialists.
This study is a randomised controlled trial of ‘PhysioDirect’, an approach to improving physiotherapy services based on initial telephone assessment and tailored written advice, followed by face-to-face care only when appropriate. This type of service is being introduced in different parts of the UK, but there is currently no evidence about the effectiveness or cost-effectiveness of PhysioDirect compared with usual care (based on a waiting list and eventual face-to-face care).
Principal research questions
-
Is PhysioDirect at least as effective as usual models of physiotherapy based on patients going on to a waiting list and eventually receiving face-to-face care?
-
What is the cost-effectiveness of PhysioDirect compared with usual care?
-
Do patients prefer PhysioDirect services rather than usual care; do they find PhysioDirect more convenient and does it address their perceived needs?
-
What are the health outcomes and experiences of different groups of patients (those in different age groups and with different types of problems) when referred to PhysioDirect rather than usual care?
Previous relevant research
We have reviewed the available evidence about telephone assessment and advice schemes for physiotherapy using searches on MEDLINE, EMBASE, The Cochrane Library, CINAHL, the Controlled Clinical Trials database and the Internet. These searches used terms and/or text words for ‘triage’, ‘PhysioDirect’, ‘telephone’ or ‘advice’ in combination with terms relating to physiotherapy (‘Physical Therapy Modalities’, ‘Exercise Therapy’, ‘Physical Therapy (Specialty)’, ‘physiotherapy.mp’). We also specifically sought randomised trials of physiotherapy interventions using the Cochrane highly sensitive search strategy in combination with terms for physiotherapy. We have not identified any published research which directly addresses the effectiveness or cost-effectiveness of PhysioDirect or similar schemes. There is, however, evidence about other key issues which are relevant to this trial.
For which conditions is physiotherapy effective, and what forms of treatment are effective?
The most common problems leading to physiotherapy referral relate to the back, shoulder, neck or knee. With regard to back pain, most studies have concluded that manual physiotherapy offers little benefit over simple advice for acute low back pain. 4 The UK Beam Trial included patients with pain of variable duration and suggested that manipulation may have a modest effect,5 and some studies have suggested that it is possible to identify sub-groups of patients more likely to benefit from manipulation. 6;7 In sub-acute and chronic back pain there is evidence for the effectiveness of physiotherapy interventions based on promoting exercise,8–11 while systematic reviews about the effectiveness of manipulation have reached inconsistent conclusions. 12;13 Importantly, recent trials have shown that a single session of advice from a physiotherapist is as effective as a course of routine physiotherapy for patients with mild to moderate back problems. 14;15 With regard to neck pain, there is evidence from two Cochrane reviews that combined exercise and manipulation are effective treatments for mechanical neck pain. 16;17 For shoulder pain, a review found evidence of benefit from a range of physiotherapy interventions. Exercise advice appears to be of benefit in rotator cuff disease and mobilisation provides additional benefit. 18 Exercise has been shown to be effective for knee pain linked to arthritis,11 and two recent trials from the Keele research centre have shown the effectiveness of physiotherapy-led advice and exercise, using exercise templates from a computer package. 19;20
In summary, it is becoming clear that for some conditions patients may benefit from physical treatment from a physiotherapist, for other conditions it is more cost-effective to provide brief advice, and in some situations physical treatments from physiotherapists have little to offer. Therefore the concept of an approach which provides assessment, advice and triage initially and reserves more intensive (and expensive) treatments for those who do not improve may be the most cost-effective strategy. This is analogous to the ‘stepped care’ approach which is increasingly advocated in a range of conditions, for example mental health, where there is a high level of demand and a need to target resources. In the context of physiotherapy, this approach should reduce costs for patients and for the NHS, provide earlier advice for all patients and physical treatment more quickly for those who may benefit from it (by screening out those unlikely to benefit), and be more convenient and accessible for patients as a whole.
Is there evidence that providing physiotherapy at an earlier stage is beneficial compared with delayed treatment?
Providing prompt and convenient access to health care is one of the major aims of the policy drive to make the NHS more responsive to patients’ needs, so fast access for healthcare is in itself seen as a benefit. There is also evidence from several studies that early physiotherapy intervention provides faster symptom relief, improves quality of life, reduces absenteeism, leads to a reduction in physician consultations, and is more cost-effective. 21–24 This approach is supported by the guidance from the Clinical Standards Advisory Group (CSAG) on the management of back pain. Following a review of evidence and expert advice, the CSAG advised that patients with new episodes of back pain should have prompt access to physical therapy, with the aim of reducing the risk of symptoms and disability becoming entrenched. 25
What evidence is available about the role of telephone advice services based on computerised algorithms in medicine generally, or physiotherapy specifically?
PhysioDirect is based on a practitioner following a computerised algorithm to assess the patient in a structured way, and to offer tailored, personalised advice. This reflects a wider trend to explore the use of this type of new technology in health care, for example in NHS Direct. Although there is little evidence about PhysioDirect, research in relation to the use of similar telephone triage systems in other clinical settings has shown that it is safe, clinically accurate, cost-effective, acceptable to patients, and reduces the workload of clinicians. 26–29 Within physiotherapy a number of small single-centre studies involving telephone advice for musculoskeletal problems have shown that it is popular with patients, although there is no evidence about costs or outcomes. 30–32
Why is a trial needed now?
PhysioDirect services have been established in a number of areas, notably in Huntingdonshire and Cheltenham. These have been commended by the Commission for Health Improvement and the NHS Working in Partnership Programme as examples of good practice and have won awards for innovation. Several other areas are considering establishing similar services. The recent NHS White Paper ‘Our Health, Our Care, Our Say’33 highlighted the need to test new models of physiotherapy to overcome current deficiencies. Unless a trial is undertaken soon, it is likely that PhysioDirect services will be widely implemented without any good evidence of effectiveness or cost-effectiveness.
Local evaluations and one small trial suggest that services based on telephone advice given by physiotherapists are likely to be popular with patients,31 although there is no evidence about costs or outcomes, or the important issue of safety. Audits in the pioneering services in Cheltenham and Huntingdonshire suggest that 40–60% of patients referred by GPs to physiotherapy can be managed by telephone alone without a face-to-face consultation, telephone consultations take approximately half as long as face-to-face consultations, waiting times for a face-to-face appointment have been reduced from four weeks to 10 days and ‘did-not-attend’ (DNA) appointment rates have been reduced from 15% to 1%. Patients are very satisfied with the service, with 80% rating it as good or excellent. 31;34;35
The trial
Study design
Individually randomised pragmatic randomised controlled trial with two parallel groups.
Description of intervention and control
Control: Usual care involves patients being referred by a GP or practice nurse to a physiotherapist. In some areas, patients may also refer themselves directly. Patients then wait for an initial face-to-face physiotherapy assessment and then usually have follow-up appointments for several weeks or months.
Intervention: ‘PhysioDirect’. As soon as a referral for physiotherapy is received the patient is invited to telephone a senior physiotherapist for initial assessment and advice. The physiotherapist will follow a computerised algorithm (as developed in Huntingdonshire) to assess the patient and record findings. In most cases, at the end of the consultation the physiotherapist will print a personalised tailored advice leaflet about exercises (based on ‘Physiotools’ software) and post it to the patient, inviting them to telephone back to report progress after 2 to 4 weeks. At that point they can be given further advice or be booked for a face-to-face consultation if necessary. Alternatively, the initial telephone call may establish that more urgent face-to-face care is needed, in which case this will be booked at the outset, or the assessment may establish that physiotherapy is unlikely to be effective and the patient can be given appropriate advice and discharged. In this way those patients most likely to benefit from face-to-face physiotherapy should be able to receive it much more quickly, hopefully leading to a faster improvement and a quicker return to work and usual activities.
There are several important points to note about the intervention, for clarification:
-
PhysioDirect is sometimes implemented in conjunction with direct patient access to physiotherapy (without referral from a GP). Currently, most areas still require patients to be referred by GPs, but current policy is to encourage physiotherapy services to allow self-referral. In this trial, we will include patients who are referred by GPs, refer themselves, or are referred by another member of the primary health care team. However, patients referred from secondary care (including emergency departments) or primary/secondary care interface services are excluded, as are requests for domiciliary physiotherapy, as these are likely to represent a different type of case mix.
-
At all four PCTs to be included in this trial, ‘usual care’ currently involves making face-to-face appointments from a waiting list. None of the PCTs currently has a PhysioDirect service. All four areas will set up a service following the same model of organisation and using the same software (that developed in Huntingdonshire), and the joint training will be arranged to ensure consistency in the way the intervention is developed. Each centre will have a three month run-in period to ensure smooth running of the service, and to pilot local administrative procedures for the trial, before we start recruiting patients for the main trial.
-
The comparison between PhysioDirect and usual care is not simply between a telephone consultation versus a face-to-face consultation, nor is it between an early telephone consultation versus a ‘waiting list control’ i.e. receiving no care. It is between two different care pathways, in one of which (PhysioDirect) patients will receive earlier and more easily accessible advice, mainly (but not entirely) by telephone, and in the other pathway (usual care) patients will wait longer on average for initial assessment which will always be face-to-face, but they may have had some care by the time of first outcome assessment. It is the use of telephone triage and assessment that makes the early provision of advice possible: the issues of telephone based care and the earlier provision of care are inextricably linked and cannot be separated in this pragmatic trial.
Setting
Four physiotherapy services in different areas, each providing a PhysioDirect service for practices within one primary care trust (PCT). These physiotherapy services will accept referrals from at least 100 general practices in total.
The PCTs which have agreed to host this trial are:
Bristol PCT, Somerset PCT, Stoke-on-Trent PCT and Central and Eastern Cheshire PCT.
Inclusion and exclusion criteria
Our intention is that the inclusion criteria should be as broad as possible to maximise generalisability and to reflect ‘real-world’ operation of PhysioDirect services.
Inclusion: Adults referred by General Practitioners (GPs), other members of the primary health care team, or self-referred for musculoskeletal physiotherapy.
Exclusion: Children (< 18 years); patients referred to physiotherapy by a hospital consultant, emergency department or primary/secondary care interface service; those needing domiciliary physiotherapy; those needing post-operative physiotherapy; those needing physiotherapy for non-musculoskeletal problems; those unable to communicate by telephone in English. (It would not be feasible to provide PhysioDirect services for people who cannot speak English. However, people who can speak English but cannot read and write English will be included, and their outcome data will be collected by telephone.)
Recruitment and allocation of participants
GPs or health care professionals in the relevant practices will refer patients to physiotherapy in their usual way, or patients may refer themselves (in which case a referral form will be completed by the physiotherapy receptionist). As soon as the referral is received at the physiotherapy site, a receptionist or a member of the research team (working for the PCT under an honorary contract or letter of access) will enter the patient's details on a database, the form will be screened by a senior physiotherapist to confirm that the patient is potentially eligible, and the patient will be sent information about the trial by post, along with a consent form and a baseline questionnaire. Patients will be offered three alternatives: to participate in the trial, to decline participation and to receive usual care (going on to a waiting list for a face-to-face appointment), or to indicate that they no longer need physiotherapy.
We intend that the trial will be adopted by the Comprehensive Research Network and we will engage the help of CRN nurses in promoting the trial and facilitating recruitment within local practices and physiotherapy sites. Since one of the purposes of PhysioDirect is to enable people to have speedy access to physiotherapy, it is important to minimise any delays introduced by the recruitment and allocation process. Where possible, study researchers or nurses from the comprehensive or primary care research networks will telephone patients at two to three working days after the information is sent by post to answer any questions about the study, and to encourage people to reply quickly so that their physiotherapy can be arranged, whether or not they choose to participate.
Consent forms and baseline questionnaires will be returned to the physiotherapy service administrative office. On receipt of a consent form, a research associate (working for the PCT under an honorary contract or letter of access) will enter this on the administrative database and will randomise the patient to PhysioDirect or usual care using web or telephone access to a remote allocation system maintained by the NCRI-accredited Bristol Randomised Trials Collaboration. Allocation will be made at the level of the individual, minimising by PCT, gender, patient age group and presenting complaint (back, neck, upper limb, lower limb, other). Patients will be randomised in a 2:1 ratio in favour of PhysioDirect. This is in order to ensure a sufficient number of cases going to PhysioDirect to allow an efficient service, given that patients declining to participate and those referred by hospital consultants will continue to receive usual care. Following randomisation, the research associate will use the database to mail-merge a letter to the patient, either inviting them to contact PhysioDirect and telling them how to do so (intervention arm), or telling them they are on a waiting list for a face-to-face appointment (control arm). No identifiable details of patients will leave the NHS Physiotherapy service and be taken to the research bases at Bristol and Keele Universities before patients have given their consent to the trial and for their information to be shared in this way.
Numbers of patients excluded for different reasons will be recorded. Age and sex of all patients will be recorded in anonymised form, to make it possible to compare participating and non-participating populations. Eligible patients who decline to participate will be asked if they are willing to indicate their reasons for non-participation from a range of options, and whether they would be willing to be sent a questionnaire in 6 months time (containing the primary outcome measures) even if they are not willing to take part in the research by being randomised.
Protection against sources of bias
It is not possible to blind participants to the type of care they will receive. Selection bias will be avoided by the system of remote allocation described earlier. Data about outcomes will be collected using self-completed questionnaires. These data will be entered by staff without knowledge of the allocation of the individual concerned.
Treatment period
This will vary for individual patients. In Bristol, the mean number of consultations per patient with traditional physiotherapy is 2.9, over several weeks.
Follow-up
Outcomes will be assessed at baseline, and at 6 weeks and 6 months after randomisation.
Outcome measures
Primary outcome
Clinical outcome at 6 months, assessed using the physical component summary (PCS) measure from the SF-36v2. The PCS is a well recognised generic measure of health status. It is particularly suitable for this trial because, unlike disease specific measures, it is applicable to the wide range of problems referred to physiotherapy. Although there is a concern that generic measures may be less responsive than disease specific measures, the physical functioning and bodily pain scales of the SF-36 (which contribute most of the variation in the PCS summary measure) compare reasonably well with disease specific measures in patients with musculoskeletal problems. 36–39
Secondary outcomes
We will also assess clinical outcome using the MYMOP40 questionnaire, and a global score for individual overall perception of improvement (seven point Likert scale from ‘very much worse’ to ‘very much better’). These will be important secondary outcomes. MYMOP is a patient generated measure. It allows patients to specify up to two symptoms and one functional limitation for which they have been referred to physiotherapy, and follow-up questionnaires assess change in those specific symptoms/limitations. This individualised and validated measure can also be used by patients with a wide range of problems. 40 The global improvement score is recommended by the Outcomes Measures in Rheumatology Clinical Trials- Osteoarthritis Research Society International (OMERACT-OARSI) meeting. 41
Other secondary outcomes: Costs; Quality of life (EQ5D); the individual scales and the mental component summary measure from SF-36; waiting times for treatment; time lost from work and usual activities; patients' perceptions of the accessibility of care (based on questions derived from the pilot study); satisfaction with care provided and preference for telephone or face-to-face assessment.
Cost-effectiveness
Incremental cost-effectiveness will be measured in terms of Quality Adjusted Life Years (QALYs), assessed using the EQ5D measure and costs as described in more detail below (see Analysis).
Collection of outcome measures
The baseline questionnaire will collect data about patient characteristics and about the outcome measures. Data about outcomes at follow-up will be collected from postal questionnaires sent to patients by the research associates at 6 weeks and 6 months. Data will be collected by telephone instead of post where patients do not respond to a postal questionnaire or a postal reminder, where patients express a preference for telephone administration, or where patients are unable to complete written questionnaires in English. The mode of administration will be recorded and accounted for in the analysis. Data about resource use will be extracted by research associates from physiotherapy service records and medical records, and details of use of other resources will come from the patient questionnaires.
Appendix A lists the various outcome measures and the source of the data.
Economic evaluation
The economic evaluation will be carried out from three perspectives. Costs to the NHS will include the cost of providing physiotherapy plus any other costs related to treating the condition for which the patient has been referred to the physiotherapy service. These include: primary care consultations, treatments and investigations, medication, secondary care consultations, and inpatient care. Set-up costs associated with the service will also be collected. Patient and companion costs will include travel, dependent carer costs, private treatment, over-the-counter medication, and loss of earnings. Societal costs will include use of social services, disability payments, and time off work.
Data will be obtained from four main sources: patient self-completion questionnaires at baseline, 6 weeks and 6 months after randomisation; primary care patient records; patient records at the physiotherapy services; and records kept as part of the trial detailing length of consultation, grade of staff, and amount of non-contact time. We will conduct a time and motion study to observe activities during non-contact time to estimate the opportunity cost of that time.
We will use Curtis and Netten42 to value primary and community care consultations. Primary care investigations will be valued at cost; the Department of Health tariff will be used for A&E visits, out-patient visits and investigations, and inpatient stays; and the British National Formulary will be used to cost prescribed medication. Most patient and carer costs will be directly reported; the AA schedule for valuing mileage will be used to cost car journeys. Time off work by patients and carers will be valued using the friction approach, which includes only the resources required to replace the employee. 43 There will be no need to discount costs or outcomes, as they will cover a period of less than one year.
Process evaluation
Process data about the physiotherapy services provided will include: the number, type and duration of consultations with physiotherapists; details of the types of advice and physiotherapy treatment given to patients; non-attended appointments with physiotherapists (DNA rates); and the qualifications and experience of all the physiotherapists involved at all four sites. Complaints and adverse events relating to the physiotherapy services will be systematically recorded and investigated.
Qualitative research
This is a ‘complex intervention’. In line with MRC guidance44 we will use qualitative research alongside the trial to study issues of implementation and to understand the key barriers and facilitators to the success of a PhysioDirect service. We will also examine the acceptability of the service and identify the factors (organisational, professional and patient related) which influence its successful implementation.
Patient interviews: Interviews will be carried out with a purposive sample of 40–60 patients to explore the accessibility of the service, the value, acceptability and influence of telephone and face-to-face care, and how the service could be improved. Invitation letters from the research teams based at Keele or Bristol, as appropriate, will be will be sent to selected patients from the main trial. Participants will be selected to ensure a diverse sample based on age, gender, ethnicity and presenting clinical problem in order to get the widest range of opinions and experiences. Patients may also be invited to attend a follow-up interview to further discuss their experience and views of the physiotherapy service received. Patients will be interviewed at a location convenient for them, e.g. home, GP surgery, physiotherapy site, or university site. Each interview will last approximately 45 min. The interviews will be digitally recorded and transcribed, and the interview transcripts will be anonymised.
Health Professional interviews: Interviews with key informants (physiotherapists, GPs and managers) will address contextual factors that act to facilitate or hinder the use and implementation of PhysioDirect or traditional physiotherapy services, or that influence outcomes, and the perceived value of the services. Participating physiotherapists will be interviewed both before receiving training in PhysioDirect and once they have gained experience of using PhysioDirect to treat patients. Invitation letters from the research teams based at Keele or Bristol, as appropriate, will be will be sent to all physiotherapists in the trial, and to selected GPs and service managers working within the local PCT. The total numbers to be recruited for interviews are:16–24 physiotherapists – before training in PhysioDirect and once they have gained experience in its use; 8–10 physiotherapy managers and commissioning managers;16–20 GPs (GPs will be recruited from different practice-based commissioning clusters within each PCT).
A researcher will contact the health professional by telephone to arrange a 30-min interview. Interviews will take place at the place of work, or by telephone in the case of GPs or commissioning managers. Telephone interviews may be shorter. The interviews will be digitally recorded and transcribed, and the interview transcripts will be anonymised.
Sample size and power calculations
This study is powered to establish clinical equivalence using the SF-36 PCS.
The PCS is transformed to scale from 0–100 with a mean of 50 and standard deviation (SD) of 10. The minimum clinically important difference in a range of populations and conditions has been estimated as being at least 4 points (0.4 SD). 45–48 However, we will specify a difference of no greater than 2 points as demonstrating equivalence, which is considered a small effect size. 48–Clinical equivalence between the arms will only be concluded if the 95% confidence interval for the difference between groups in the primary outcome lies wholly inside the range −2 to +2 points. In other words, non-equivalence occurs if the difference in means, μPhysioDirect – μUsual Care, is 2 points or farther from zero in either direction. Sample sizes for analysis of 488 and 976 in the Usual Care and PhysioDirect groups respectively will yield 95% power to reject a null hypothesis of non-equivalence with an overall alpha of 0.05 alpha, assuming that the observed difference in means is zero. The target sample size for patients completing the final six-month follow-up questionnaire is 1000 patients in the PhysioDirect arm and 500 patients in the Usual Care arm.
Assuming 30% non-collection of the primary outcomes, it will be necessary to recruit 1429 and 714 patients in the PhysioDirect and usual care arms, respectively, or 2143 patients in total. In order to ensure that all four PCTs contribute data to the study, patients will be recruited until 2143 patients have been recruited, and each PCT has recruited at least 300 patients.
Planned recruitment rate
All patients referred for NHS physiotherapy from participating practices will be entered on to a database, and recruitment will be organised as described previously. The national average GP referral rate to physiotherapy is 23 per 1000 p.a. 2 In our pilot study, 96% (267/277) of the patients referred were initially eligible for recruitment, 27% (72/267) of these did not respond to any correspondence from the physiotherapy service and were removed from the waiting list, 67% (131/195) of the remaining patients agreed to participate in the trial, and 82% (107/131) completed questionnaires at 3 months and 80% (105/131) at 6 months. We have made our recruitment estimates conservatively. Assuming 20 referrals/1000 population, 95% eligibility, 70% replying to correspondence, 50% consenting to participate and 80% retention at 6 months, it will be possible to recruit sufficient patients to achieve our sample size in 20 weeks. We anticipate recruiting 104 patients per physiotherapy site per month. As a contingency we have allowed 6 months per site for recruitment in the timetable.
Analysis
The main hypotheses are that PhysioDirect will be clinically equivalent to Usual Care and more cost-effective at 6 months after randomisation.
Analysis and presentation of data will be in accordance with CONSORT guidelines. The primary analysis will employ multivariable regression to investigate between-group differences in mean SF-36 PCS score at 6 months’ follow up. The primary analysis will be conducted on an intention-to-treat (ITT) basis, with due emphasis placed on the confidence interval for the between-arm comparison when inferring equivalence (or otherwise) of the two groups. Clinical equivalence between the arms will only be concluded if the 95% confidence interval for the difference between groups in the primary outcome lies wholly inside the range –2 to +2 points. Given the equivalence design and the generally conservative nature of ITT analysis, we will also investigate between-group differences using methods that model compliance with the allocated treatment arm, such as instrumental variable regression, to provide a per-protocol analysis. Descriptive practice-level and individual-level statistics will be used to ascertain any marked imbalance between the arms at baseline. Analyses will adjust for minimisation variables and baseline outcome variable scores, and will take appropriate account of the hierarchical nature of the data (practice and physiotherapy site). Sensitivity analyses making different assumptions will be conducted to investigate the potential impact of missing data.
In the economic analysis we will compare mean cost to the NHS per patient in each arm with mean QALY gain, using the EQ5D; thus we will estimate a cost–utility ratio of incremental cost per QALY gain. Secondary analysis will explore the QALY gain using the SF-6D,49–derived from the SF-36. We will also estimate a cost–consequences matrix presenting a comparison of cost per patient in each group from the patient and societal perspectives with a range of outcomes, for example personal perception of improvement and patient satisfaction. The effect of uncertainty in unit cost estimates or assumptions about resource use will be addressed in sensitivity analyses. Using a bootstrapping approach for data analysis, the results of the economic analysis will be presented using cost-effectiveness acceptability curves to reflect sampling variation and uncertainties in the appropriate threshold cost-effectiveness value. Special consideration will be given to costs associated with time off work and to service set-up costs.
Secondary analyses will include: (1) Assessing equivalence in clinical outcome using the MYMOP score. A difference of 0.5–1 points on a 7-point scale on the MYMOP profile score is considered clinically important. [http://www.pms.ac.uk/mymop/index.php?c = faqs]); (2) examining clinical outcome at 6 weeks using the SF-36 PCS; (3) comparing the proportion of patients who ‘respond to treatment’ in each arm, in line with the Outcomes Measures in Rheumatology Clinical Trials-Osteoarthritis Research Society International (OMERACT-OARSI) recommendations,41–using the SF-36 physical function and bodily pain scales and the global improvement score; (4) repeating the primary analysis adjusting also for any variables exhibiting marked imbalance at baseline to check that this does not influence the findings; (5) similar analyses for secondary outcomes (where p-values will be adjusted to account for multiple testing); (6) investigating the effectiveness and cost-effectiveness of PhysioDirect for patients of different age-groups or with different presenting problems; and (7) investigation of process measures such as physiotherapy consultation rates, physiotherapy DNA rates and consultation rates with other health care services in the NHS and private sectors.
Sub-group analyses: Appropriate interaction terms will be entered into the primary regression analysis for SF-36 in order to conduct pre-specified subgroup analyses according to presenting complaint, patient age-group and socio-economic status. Since the trial is powered to detect overall equivalence between the groups rather than interactions of this kind, the results of these essentially exploratory analyses will be presented using descriptive statistics and, where helpful, confidence intervals as well as p-values, and interpreted with due caution.
Although the study is powered in relation to patient level outcomes, some of our outcomes will be strongly clustered by physiotherapy site (particularly waiting times). The analysis of these outcomes will be descriptive only. Although the number of physiotherapy sites is small, we anticipate the impact of PhysioDirect on waiting times may be very large.
Qualitative analysis: Analysis of the qualitative data will use an inductive, thematic approach based on the method of constant comparison. Data collection and analysis will be carried out iteratively so that emerging themes in the analysis can be explored in depth in the interviews. Sampling will continue until no new themes emerge. A researcher will code the transcribed data, with a sample of interviews being independently coded by a second researcher to ensure transparency and agree emergent themes at successive stages of the data collection and analysis. Negative or deviant cases will be investigated closely.
Interim analysis: The quantitative data will be analysed at the end of the trial and there are no proposed interim analyses. The qualitative data will be analysed as data collection proceeds.
Trial management
The project will be led by Professor Salisbury (Chief Investigator), with Dr Foster having PI responsibility on the Keele Site. The trials manager will co-ordinate the research associates and project administrator and will monitor the trial continuously in line with the protocol and a written monitoring plan. Research associates will identify potential participants from referrals to physiotherapy sites, send information packs, administer recruitment, conduct randomisation, send follow-up questionnaires and reminders using telephone follow-up were needed, and collect resource-use data from physiotherapy services and GP practices. It is anticipated that these research associates will need to visit each physiotherapy site 2–3 times per week to facilitate this activity. Professor Salisbury and Dr Foster will meet the employed researchers in Bristol and Keele respectively each week. A Trial Management Committee, consisting of all the applicants and employed researchers, will meet regularly (initially monthly, then bimonthly) to oversee progress. The Trial Steering Committee will meet before the trial starts and then annually, or more frequently if necessary. The Data Monitoring Committee will also meet annually or more often if necessary.
Data preservation
We will share data in line with the four principles of the MRC data access policy. 50 All quantitative and qualitative data will be fully anonymised. This will involve creating data sets that anonymise or aggregate any variables which could in combination identify individuals, e.g. age, postcode, date of referral to physiotherapy. The practice, PCT and physiotherapy site will also be anonymised. After anonymisation, all datasets will be archived and stored for 20 years on a secure server at the University of Bristol, accompanied by study documentation and metadata. Professor Salisbury will be the data custodian. The availability of the datasets will be advertised on the UoB website, linked to a summary of the research project and its published outputs. The datasets will be made freely available on application to any bona-fide suitable qualified researcher upon submission of a protocol which provides a research question and research design which could be addressed by the data from this study, has been peer reviewed and received ethical and research governance approvals. Users of the data will also be subject to a written agreement which complies with the MRC guidance. 50 Data will be made available for sharing only after the publication of the final project report and the main papers in peer-reviewed journals.
System of monitoring and reporting adverse events
For this trial, adverse and serious adverse events include: death, hospitalisation, significant disability or incapacity, and any life-threatening circumstance, or any other medically significant occurrence. GPs will be notified of their patient’s participation in the PhysioDirect trial and asked to report any SAE or AE that they consider may possibly be related to either physiotherapy or the trial procedures to the Chief Investigator (CI) as soon as possible – and within no more than 5 working days of becoming aware of the event. The PhysioDirect site at each PCT is to report to the CI immediately any SAE or AE experienced by a study participant that may possibly be related to either physiotherapy or the trial procedures. The CI will assess whether the event was related to or resulted from any of the research procedures, according to the process laid out in PhysioDirect SAE SOP v1.0. [It is expected that events from the categories listed above will occur, but these are likely to be unrelated to the research procedures.] Any SAE considered to be related to the research procedures will be reported to the main Research Ethics Committee by the CI within 15 days of his/her becoming aware of the event. In addition, all such events will be reported to the trial sponsor and trial DMC.
Progress reporting
Progress reports will be submitted annually by the CI to the main Research Ethics Committee. Declaration of early termination will be made by the CI to the main Research Ethics Committee within 15 days of the termination. Declaration of the conclusion of the trial will be made by the CI to the main Research Ethics Committee within 90 days of the end of the trial. A summary of the final report will be submitted by the Chief Investigator to the main Research Ethics Committee within one year of the conclusion of the research.
The end of the trial is defined as the point at which the episode of treatment relating to the original referral or self-referral of every trial participant is complete; all participants have undergone to completion the administration procedures for the collection of the 6-month final follow-up data; all those selected for qualitative research have been interviewed, and data collection from medical records is complete.
Protocol references
- McCormick A, Fleming D, Charlton J. Morbidity statistics from general practice. London: HMSO; 1995.
- National Statistics DoH . NHS Physiotherapy Services Summary Information for 2004–2005, England 2005. URL: http://www ic nhs uk/statistics-and-data-collections/hospital-care/outpatients/nhs-physiotherapy-services:-summary-information-for-2004-–05-england.
- Maniadakis N, Grey A. The economic burden of back pain in the UK. Pain 2000;84:95-103.
- Van Tulder M, M BA, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;16:S169-191.
- UK BEAM Trial Team . United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary car. BMJ 2004;329.
- Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute ‘nonspecific’ low back pain: results of a randomised clinical trial. Spine 2006;31:623-31.
- Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med 2004;141:920-8.
- Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev 2005;3.
- Airaksinen O, Brox J-I, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 2006;15:S192-S300.
- van Tulder MW, Koes B, Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J 2006;15:64-81.
- Smidt N. Effectiveness of exercise therapy: a best-evidence summary of systematic reviews. Aust J Physiother 2005;51:71-85.
- Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. Cochrane Database Syst Rev 2004;1.
- van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain. A systematic review of randomised controlled trials of the most common interventions. Spine 1997;22:2128-56.
- Frost H, Lamb SE, Doll HA, Carver PT, Stewart-Brown S. Randomised controlled trial of physiotherapy compared with advice for low back pain. BMJ 2004;329.
- Rivero-Arias O, Grey A, Frost H, Lamb SE, Stewart-Brown S. Cost-utility analysis of physiotherapy treatment compared with physiotherapy advice in low back pain. Spine 2006;31:1381-7.
- Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Bronfort G, et al. Exercises for mechanical neck disorders [review] [148 refs]. Cochrane Database Syst Rev 2005;3.
- Gross AR, Hoving JL, Haines TA, Goldsmith CH, Kay T, Aker P, et al. Manipulation and mobilisation for mechanical neck disorders. Cochrane Database Syst Rev 2004;1.
- Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain [review] [87 refs]. Cochrane Database Syst Rev 2003;2.
- Hay EM, Foster NE, Thomas E, Peat G, Phelan M, Yates HE, et al. Effectiveness of community physiotherapy and enhanced pharmacy review for knee pain in people aged over 55 presenting to primary care: pragmatic randomised trial. BMJ 2006;333.
- Foster NE, Thomas E, Barlas P, Hill JC, Young J, Mason E, et al. Acupuncture as an adjunct to exercise based physiotherapy for osteoarthritis of the knee: randomised controlled trial. BMJ 2007;335.
- Wand BMB, Bird CM, McAuley JHB, Dore CJB, MacDowell MM, De Souza LH. Early Intervention for the Management of Acute Low Back Pain: A Single-Blind Randomised Controlled Trial of Biopsychosocial Education, Manual Therapy, and Exercise [miscellaneous article]. Spine 2004;29:2350-6.
- Gatchel RJ, Polatin PB, Noe C, Gardea M, Pulliam C, Thompson J. Treatment and cost-effectiveness of early intervention for acute low-back pain patients: a one-year prospective study. J Occup Rehabil 2003;13:1-9.
- Hagen EM, Eriksen HR, Ursin H. Does early intervention with a light mobilisation program reduce long-term sick leave for low back pain?. Spine 2000;25:1973-6.
- Zigenfus GC, Yin J, Giang GM, Fogarty WT. Effectiveness of early physical therapy in the treatment of acute low back musculoskeletal disorders. J Occup Environ Med 2000;42:35-9.
- Epidemiology review: the epidemiology and cost of back pain. HMSO; 1994.
- Lattimer V, George S, Thompson F, Thomas E, Mullee MA, Turnbull J, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. BMJ 1998;317:1054-9.
- Lattimer V, Sassi F, George S, Moore M, Turnbull J, Mullee M, et al. Cost analysis of nurse telephone consultation in out of hours primary care: evidence from a randomised controlled trial. BMJ 2000;320:1053-7.
- Pinnock H, Bawden R, Proctor S, Wolfe S, Scullion J, Price D, et al. Accessibility, acceptability, and effectiveness in primary care of routine telephone review of asthma: pragmatic, randomised controlled trial. BMJ 2003;326.
- Bunn F, Byrne G, Kendall S. Telephone consultation and triage: effects on health care use and patient satisfaction. Cochrane Database Syst Rev 2004;4.
- Hodgson K. Kidderminster helpline proves a success. Physiother Frontline 2001;7:22-3.
- Taylor S, Ellis I, Gallagher M. Patient satisfaction with a new physiotherapy telephone service for back pain patients. Physiotherapy 2002;88:645-57.
- Clayson M, Woolvine M. Back Pain Direct Clinic: a collaboration between general practitioners and physiotherapists. Work Based Learning Prim Care 2004;2:38-43.
- Department of Health . Our health, our care, our say: a new direction for community services. The Stationery Office 2006.
- NHS Working in Partnership Programme . Direct Access to Physiotherapy 2005. URL: http://www.workloadmanagement nhs uk/uploads/gpdb/case_daphysio.pdf.
- Physio Direct (East Gloucestershire) . East Gloucestershire PCT 2006.
- Walsh TL, Hanscom B, Lurie JD, Weinstein JN. Is a condition-specific instrument for patients with low back pain/leg symptoms really necessary? The responsiveness of the Oswestry Disability Index, MODEMS, and the SF-36. Spine 2003;28:607-15.
- Lurie J. A review of generic health status measures in patients with low back pain. Spine 2000;25:3125-9.
- Kvien TK, Kaasa S, Smedstad LM, Kvien TK, Kaasa S, Smedstad LM. Performance of the Norwegian SF-36 Health Survey in patients with rheumatoid arthritis. II. A comparison of the SF-36 with disease-specific measures. J Clin Epidemiol 1998;51:1077-86.
- Angst F, Aeschlimann A, Steiner W, Stucki G. Responsiveness of the WOMAC osteoarthritis index as compared with the SF-36 in patients with osteoarthritis of the legs undergoing a comprehensive rehabilitation intervention. Ann Rheum Dis 2001;60:834-40.
- Paterson C. Measuring outcomes in primary care: a patient generated measure, MYMOP, compared with the SF-36 survey. BMJ 1996;312:1016-20.
- Pham T, Van Der HD, Lassere M, Altman RD, Anderson JJ, Bellamy N, et al. Outcome variables for osteoarthritis clinical trials: The OMERACT-OARSI set of responder criteria [review] [12 refs]. J Rheumatol 2003;30:1648-54.
- Curtis L, Netten A. Unit Costs of Health and Social Care 2006 2006. URL: http://www pssru ac uk/uc/uc2006contents htm#contents.
- Ostelo RW, Goossens ME, de Vet HC, van den Brandt PA. Economic evaluation of a behavioural-graded activity program compared to physical therapy for patients following lumbar disc surgery. Spine 2004;29:615-22.
- Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455-9.
- Samsa G, Edleman D, Rothman ML, Williams GR, Lipscomb J, Matchar D. Determining clinically important differences in health status measures. Pharmaceconomics 1999;15:141-55.
- Kosinski M, Zhao SZ, Dedhiya S, Osterhaus JT, Ware JE. Determining minimally important changes in generic and disease-specific health-related quality of life questionnaires in clinical trials of rheumatoid arthritis. Arthritis Rheum 2000;43:1478-87.
- Wyrwich KW, Tierney WM, Babu AN, Kroenke K, Wolinsky FD. A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Health Serv Res 2005;40:577-91.
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003;41:582-9.
- Walters SJ, Brazier JE. What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health Qual Life Outcomes 2003;1.
- MRC . Principles for access to, and use of, MRC-funded research data n.d. URL: http://www mrc ac uk/Utilities/Documentrecord/index htm?d=MRC003759 2007.
Appendix A: data, outcome measures and source
| Measure | Timing | Source |
|---|---|---|
| Patient identifiers, type of problem, age and sex | Pre-consent | Referral letter. Recorded (anonymised) in research database |
| Demographic details | Baseline (BL) | BL patient questionnaire |
| SF36v2 | BL, 6 weeks, 6 months | Patient questionnaires |
| MYMOP | BL, 6 weeks, 6 months | Patient questionnaires |
| EQ5D | BL, 6 weeks, 6 months | Patient questionnaires |
| Overall perception of improvement | 6 weeks, 6 months | Patient questionnaires |
| Time lost from work and usual activities | BL, 6 weeks, 6 months | Patient questionnaires |
| Patients perceptions of accessibility of care | 6 weeks, 6 months | Patient questionnaires |
| Satisfaction with care provided | 6 weeks, 6 months | Patient questionnaire |
| Preference for PhysioDirect or usual care | BL, 6 months | Patient questionnaires |
| Waiting time for treatment | Collected at end of study | Physiotherapy service records, from date of referral received to date first telephone or face-to-face consultation |
| Patient and companion costs | 6 weeks, 6 months | Patient questionnaires |
| Cost of lost production associated with time off work and usual activities | 6 weeks, 6 months | Patient questionnaires |
| Costs of providing physiotherapy | Set-up costs: collected during set up phase and once the service is operating. | Set-up: data collected from PCTs about resources involved in setting up the service |
| Treatment over 6 months: collected at end of study. | Treatment: physiotherapy records, data collected within the trial about lengths of consultations, staff use of time, staff grades, etc. | |
| Costs in general practice (consultations, treatments, investigations) | Collected at end of study, from randomisation to 6 months | Patients GP records, consultations costed using Netten and Curtis and NHS reference costs for other costs |
| Costs of prescriptions | Collected at end of study, from randomisation to 6 months | Patients GP records, costed using BNF |
| NHS secondary care costs (outpatients, inpatients, admissions) | 6 weeks, 6 months | Patient questionnaires for resource use, costed using NHS tariffs |
| Process evaluation: number, type and duration of consultations with physiotherapists; types of advice and physiotherapy treatment given; non-attended appointments with physiotherapists (DNA rates) | Collected throughout study from randomisation to 6 months | Physiotherapy records |
| Qualifications and experience of physiotherapists | Collected throughout study from randomisation to 6 months | Obtained by research team from physiotherapy managers |
| Complaints and adverse events | Collected throughout study from randomisation to 6 months | Notified by patients, physiotherapy services, general practices or any other sources. See SAE SOP v1.0 |
List of abbreviations
- A&E
- accident and emergency
- AE
- adverse event
- AIC
- Akaike information criterion
- BME
- black and minority ethnic
- BNF
- British National Formulary
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CSAG
- Clinical Standards Advisory Group
- DNA
- did not attend
- DUETS
- Database of Uncertainties about the Effects of Treatments
- EQ-5D
- European Quality of Life-5 Dimensions (EuroQol health-utility measure)
- GP
- general practitioner
- HRG
- healthcare resource group
- HTA
- Health Technology Assessment
- ICC
- intracluster correlation coeefficient
- ICER
- incremental cost-effectiveness ratio
- IQR
- interquartile range
- ISRCTN
- International Standard Randomised Controlled Trial Number
- MCS
- Mental Component Score
- MSK
- musculoskeletal
- MYMOP
- Measure Yourself Medical Outcomes Profile
- NICE
- National Institute for Health and Clinical Excellence
- NMB
- net monetary benefit
- OMERACT-OARSI
- Outcomes Measures in Rheumatology Clinical Trials – Osteoarthritis Research Society International
- OR
- odds ratio
- PCS
- Physical Component Score
- PCT
- primary care trust
- RCT
- randomised controlled trial
- QALY
- quality-adjusted life-year
- QOF
- Quality and Outcomes Framework
- SAE
- serious adverse event
- SD
- standard deviation
- SF-36v2
- Short Form questionnaire-36 items, version 2
- SF-6D
- Short Form questionnaire-6 Dimensions
- UKCRC
- UK Clinical Research Collaboration
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices in which case the abbreviation is defined in the figure legend or at the end of the table.