Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 09/02/02. The contractual start date was in January 2011. The draft report began editorial review in February 2013 and was accepted for publication in May 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Mytton et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Commissioning brief
In autumn 2008 the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme published a research brief (reference 09/02) asking the question: are parenting interventions effective in the prevention of childhood injuries in children under 5 years? The brief specified that the technology, a parenting programme, should be developed by the researchers for delivery by a health professional to the families of children who had sustained a significant injury in the previous 12 months. The feasibility of testing the programme should be assessed against usual care, with a primary outcome being the number of injuries in the under-fives, together with a range of secondary measures including maternal and family outcomes (such as injury events in the siblings of the index child). The rationale for the research was the proposal that a range of positive outcomes of parenting interventions could also be effective in preventing unintentional injury in childhood, and that a randomised controlled trial (RCT) of a theoretically based intervention could test the causal pathway linking the intervention to the occurrence of childhood injury.
Outline of this report
This report describes our response to the commissioning brief. It documents how we developed and assessed the acceptability of a health promotion programme for the parents of young children that combined parenting support with injury prevention education. It also explores the feasibility of delivering and evaluating the programme through a cluster RCT.
In Chapter 1, we set the scene, describing the background to the issues, how we responded to the commissioning brief, the aims and objectives of the study, and the resulting component activities of the study. In Chapter 2 we summarise two systematic reviews: one of parenting interventions to prevent injuries and the second of the barriers and facilitators to parental engagement in parenting programmes. The findings of these reviews underpin the theoretical development of the parenting programme. Chapter 3 describes the development of the parenting programme, through collaboration with two voluntary sector organisations: Parenting UK (now known as Family Lives) and the Whoops! Child Safety Project. In Chapter 4 we describe the development of a tool to collect our primary outcome measure of parent-reported child injuries, and Chapter 5 describes a feasibility cluster RCT to assess the potential to evaluate the parenting programme in a main trial. Chapter 6 describes the parameters that would be necessary for a study of the cost-effectiveness of the parenting programme during a future trial. Following delivery of four courses of the parenting programme during the feasibility study, we evaluated the parenting programme from four perspectives and subsequently made changes to the intervention. These changes are described in Chapter 7. We draw our findings together in Chapter 8, where we discuss the strengths and weaknesses of our study, whether or not we have met our study objectives and the implications of our findings for a future trial. At the end of Chapters 2–7, learning points have been summarised and form the basis of the implications for a full trial detailed in Chapter 8. We report our conclusions in Chapter 9.
Background
Burden of disease from unintentional injury
Unintentional injury is a major cause of death and disability in children globally,1 and in the UK it is the leading cause of preventable death in children over the age of 1 year. In addition to those who die from injuries, many more suffer morbidity and possible long-term consequences. Half a million children aged 0–4 years attend UK hospitals every year because of a home injury, representing 78% of all injuries occurring to children in this age group. 2 The type and location of child injuries varies with age and developmental stage. Longitudinal cohort studies have shown that the majority of preschool injuries occur within the home, both in this country3,4 and in other high-income countries. 5 Injuries result from falls, hitting, being hit or crushed by objects, poisoning, and burns or scalds. 2
Risk factors for injury
A number of child, family and environmental factors are associated with increased risk of injury. Socioeconomic disadvantage is the risk factor most strongly associated with child mortality and morbidity. 6–12 Family structures such as single-parent families, step-families and large families, and factors that may relate to caregiver supervision such as very young parents, maternal life events, maternal depression and parental behaviours such as excessive use of alcohol, have all been associated with increased risk of child injury. 3,13–18 Male sex and difficult behaviour in childhood, particularly that relating to antisocial, aggressive or hyperactive behaviour, have been associated with increased incidence of unintentional injuries in the UK19,20 and in other high-income countries. 21
Parenting programmes
Parenting programmes are short-term interventions to promote changes in the behaviour of parents that support children. 22 They have been increasingly recognised as an intervention to improve the life chances of children owing to their effectiveness in reducing antisocial behaviour and conduct disorder, increasing educational attainment, and improving mental health and well-being outcomes in children and their parents. Consequently, they have become a core component of child and family policy in the UK. 23,24 Parenting programmes are usually delivered as face-to-face programmes, either individually or in groups. They have been developed on the basis of two main theoretical approaches, behavioural and relational, although some programmes combine elements of both. Behavioural approaches aim to develop parental understanding of the negative impact of attention to problem behaviour and lack of attention to positive behaviour, and to teach positive discipline practices including praise and time-out; relational programmes aim to improve interactions between parent and child, correcting inappropriate parental interpretations of child behaviour, increasing empathy and understanding of developmental phases.
Analyses of longitudinal studies have shown the influence of parents on child outcomes that are related to injury risk. Positive parenting behaviour and parent–child interaction, and a stimulating home environment have been associated with enhanced development by the age of 3 years25 and improved cognitive and behavioural outcomes in children by age 5 years26 or children who are well adjusted and developmentally competent. 27 The use of positive parenting practices, such as increased use of praise to encourage desirable behaviours, is associated with a reduction in injuries. 28 Supportive parent training can improve childcare practices for mothers with learning difficulties29 and enhanced carer supervision can reduce injury risk to children. 30,31 Parenting interventions have the potential to reduce poor maternal mental health and increase maternal self-efficacy,32,33 to improve maternal–child interactions,34 and to change child behaviour, especially behaviour that is challenging or could place the child at risk of injury. 32,35–37 Reductions in injury risk could also be mediated through information to enable parents to make realistic expectations of their child’s development and skills,38 enhanced parental knowledge of safety practices,39 improvement in the quality of the home environment,40 or through the use of home safety practices such as having a fitted and functioning smoke alarm, using stair gates or keeping sharp objects in a safe place. 41,42 Generic parenting support interventions delivered by health visitors, and which may or may not include a focus on injury prevention, have been shown to reduce injury rates in both prospective observational studies43 and RCTs. 44 Meta-analyses of RCTs measuring one-to-one parenting interventions that are delivered primarily through home visiting and primarily conducted with high-risk or disadvantaged families have demonstrated significantly lower risks of injury, as measured by parental self-report of either medically or non-medically attended injuries,45,46 but it is unclear if group-based programmes can achieve similar effects. Parental understanding of the relationship between injury risk and child behaviour and development is variable, and provision of educational anticipatory guidance has been recommended. 47
There is strong evidence that home safety education with the provision of safety equipment is effective in increasing a range of home safety practices. 42 The features of parenting interventions that are most effective are becoming clearer. A review of ‘what works?’ in parenting interventions has shown that interventions are more likely to be effective if they are delivered early in childhood, if intensity is proportional to need, if they include group activities where parents can benefit from the social aspect of working with peers, if they include formal programmes or manuals to maintain the consistency of the delivery of the intervention which should be delivered by trained staff, and if there is a focus on specific parenting skills and practical ‘take-home’ tips. 48 Parents value programmes that enable the acquisition of knowledge, skills and understanding, and facilitate acceptance and support from other parents. 49 The fear of being perceived as a bad parent may inhibit participation in programmes. Positive outcomes from programmes reduce feelings of guilt and social isolation, increase empathy with children, and give confidence to cope with challenging child behaviour. 50
Cost-effectiveness of parenting programmes
As well as being a health and well-being issue, child injury also has economic impacts. Scarce resources with competing uses in all health systems, and the need to decide between new, ‘efficacious’ primary prevention parenting programmes on the grounds of cost-effectiveness, have increased the significance of economic evaluation as a concept and methodology. 51,52 Recent guidance from the UK Medical Research Council for the development and evaluation of complex behavioural interventions suggests that efficacy and cost-effectiveness should be established before programmes are implemented at the population level. 53,54 However, the meaningful determination of these criteria is often problematic for complex interventions. It is therefore important to develop the conceptual and measurement process by which effectiveness and cost-effectiveness can be evaluated during a feasibility trial.
There are some studies to build upon. The cost-effectiveness of parenting programmes had not been widely studied55 at initiation of this study, but some evidence for modelling costs and longer-term savings56 and estimating the long-term return on investment57 has emerged during the time frame of this study. Previously, a systematic review of economic evaluations of child and adolescent mental health interventions demonstrated that most evaluations were small scale, had short time horizons for assessing outcomes and had limited reporting,58 a finding supported by a recent review of UK programmes to prevent child behaviour problems. 59 Some evidence of cost-effectiveness of parenting programmes has been published for group parenting programmes; a formal evaluation of one programme widely used in English Sure Start children’s centres demonstrated improved child behaviour outcomes for modest costs and considered the programme value for money. 60 This study has been used to produce a costing publication61 now widely used for this type of evaluation.
Aims of the study
The aims of this study were:
-
to develop a health professional-delivered programme for the parents of children aged 0–4 years that provides injury prevention education tailored to the stages of preschool child development, underpinned by the principles of parenting support
-
to assess the acceptability of the programme to parents and professionals
-
to assess the feasibility of delivering and evaluating the parenting programme through a cluster RCT, including the identification of appropriate parameters to determine cost-effectiveness in a future trial.
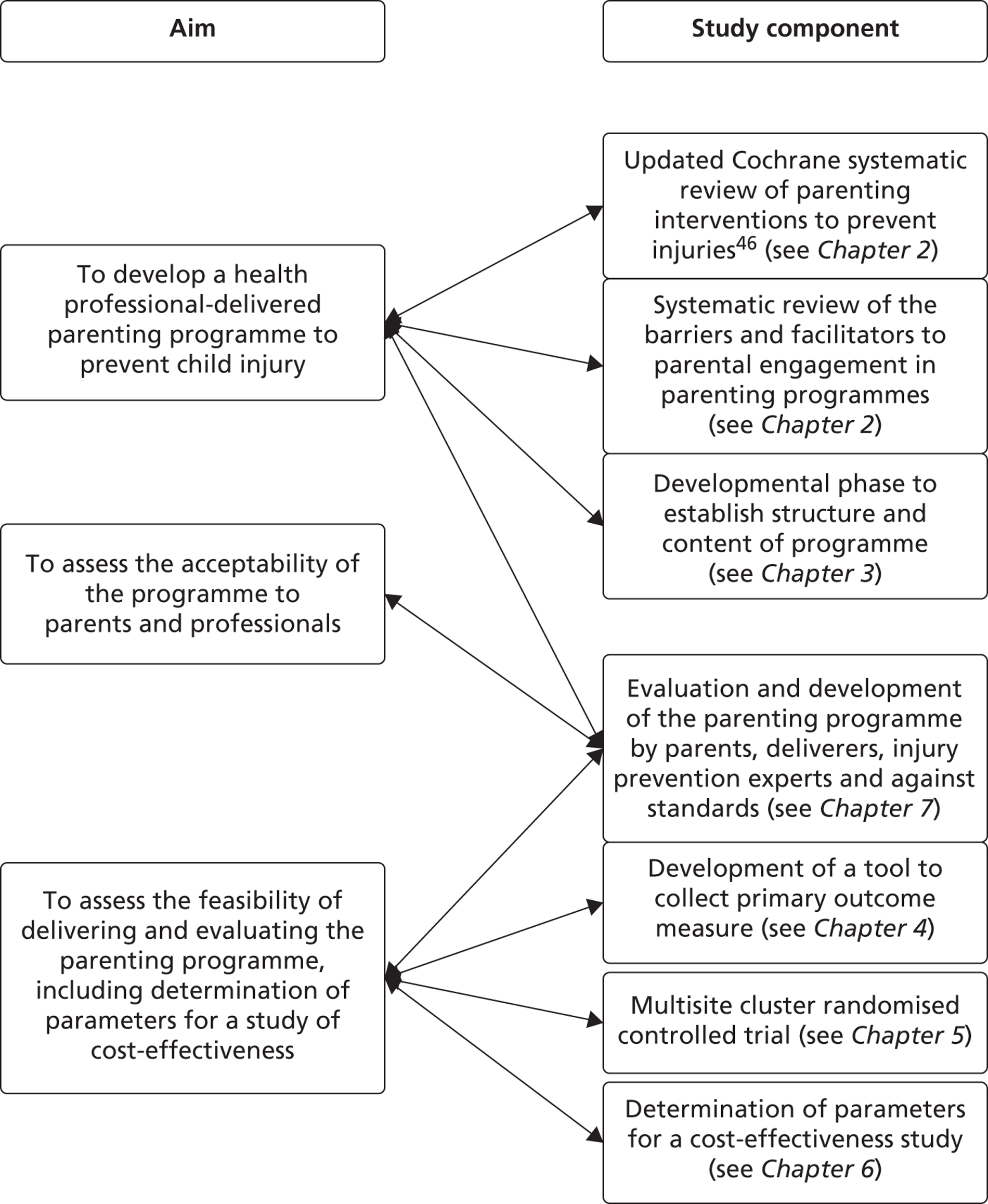
Component activities of the study, illustrates how the aims were addressed (see Figure 1). Specific objectives relating to the feasibility cluster RCT are detailed in Chapter 5.
How we responded to the brief
We decided to develop a programme in which parenting challenges and skills could be illustrated with injury risk and safety scenarios, providing the opportunity to concurrently deliver parenting skills development, effective communication, use of positive reinforcement, managing difficult behaviour, setting and maintaining appropriate boundaries, understanding how a child’s development influences their behaviour and injury risk, promoting self-assessment of home hazards and providing guidance on home safety practices and equipment. We chose to work with two voluntary sector organisations: Parenting UK, a parenting programme development organisation (now known as Family Lives), and the Whoops! Child Safety Project, which provides life-saving skills and first aid educational programmes for the public and professionals.
We interpreted a ‘significant’ injury (as specified in the commissioning brief) to be one where the parent sought medical attention following the injury event. The requirement to seek support can be considered a ‘teachable moment’ when parents may be receptive to information regarding injury risk in their children. 62 We were concerned from the outset that asking a parent to join a parenting programme after their child had sustained an injury could result in feelings of stigma, guilt or belief that they were perceived as an inadequate parent. In an attempt to destigmatise attendance to the programme, we chose to include a strong element of first aid and safety advice in our programme, as we knew that home safety education trials had successfully recruited parents of recently injured children63,64 and that parents are interested in learning first aid. 65
Support and information for the parents of young children in the UK is routinely provided in children’s centres; therefore, we decided to use the children’s centre as the setting to deliver our programme. As health visitors are the lead community health professional working with parents, they may be considered the most suitable to deliver the intervention. However, in recent years most areas have experienced a shortfall in the health visitor workforce. Consequently, many health visitors now work in teams, supervising other staff, including nursery or children’s nurses. Each children’s centre is linked to a health visiting team and most share a broadly similar catchment area. Therefore, we decided to identify pairs of health visitor teams and their associated children’s centre willing to participate in the study. The parenting programme would be delivered in the children’s centre, by the health visitor, cofacilitated by a member of her team.
The decision to deliver the parenting programme to groups of parents in children’s centre meant that there would be delays for some parents between recruitment and commencement of the group intervention. We anticipated that this, together with an intervention that was delivered over several weeks, could risk low retention rates.
Component activities of the study
The component activities of the study are mapped against the aims in Figure 1. The chapters relating to each of the component activities are specified to facilitate orientation through this report.
FIGURE 1.
Mapping of aims against the components of the study.
Parent advisory group
We wished to engage parents in all stages of the development and testing of the parenting programme, and so established a parent advisory group (PAG) at a children’s centre in Bristol that was not participating in the two arms of the feasibility trial. Parents who routinely attended the children’s centre were invited to participate in the advisory group. There were seven core members (all mothers) who attended most meetings, and two further mothers who attended once at the beginning. They were all approached by the community support manager and other community staff at the children’s centre and purposively sampled to include a range of socioeconomic backgrounds, education levels, experience of parent groups, number of children and involvement in activities at the children’s centre. The group was held in a small room at the children’s centre and crèche facilities were provided, if required. A community team staff member, who is also a local parent, attended the group as she knew some of the mothers and was a helpful facilitator.
The group met five times during the course of the study with an additional thank-you meeting just after the study had finished. Each meeting was facilitated by one or two of the researchers. Parents were asked to provide advice on the development of the intervention, identification of eligible families, recruitment and issues relevant for a future trial. Meetings with the PAG were timed, where possible, to allow feedback to the trial steering committee. Representatives of the group were invited to the trial steering committee, and attendance was supported by the researcher facilitator. When representatives of the group were unable to attend, comments from the group were fed back to the trial steering committee by the researcher facilitator.
Chapter 2 Development of a parenting intervention: theoretical phase
We conducted two evidence syntheses to underpin the development of the parenting intervention.
The first was an update of a systematic review published by Kendrick et al. 45 in the Cochrane Database of Systematic Reviews in 2007. This review synthesised evidence of the effectiveness of parenting interventions for preventing unintentional injuries in children, and on the possession and use of safety equipment and parental safety practices. The review included nine RCTs in the primary meta-analysis indicating that intervention families had a statistically significantly lower risk of injury [relative risk (RR) 0.82, 95% confidence interval (CI) 0.71 to 0.95], and that several studies reported greater use of home safety equipment and safety practices in intervention families. The authors noted that the majority of the interventions were multifaceted home-based interventions, and they were unable to determine if interventions delivered outside the home or delivered as group-based interventions were effective. An update of this systematic review was therefore required to identify if new evidence was available on these two issues specifically, in order to inform the development of the group-based, community-delivered parenting programme proposed.
The second evidence synthesis was conducted to explore the evidence explaining why parents do, or do not, engage and complete parenting programmes. Researchers have previously sought to identify the barriers and facilitators to parental engagement in such programmes but these have largely been taken from the perspective of providers, policy-makers or academics. 66,67 Studies have explored why parents believe that programmes may be helpful,50 but not parents’ beliefs on barriers and facilitators to engagement. A systematic review of the qualitative literature exploring the barriers and facilitators to parental engagement in parenting programmes was conducted to ensure that facilitators were utilised where possible and barriers were minimised in the proposed programme.
Systematic review 1: parenting interventions for the prevention of unintentional injuries in childhood
The full version of this Cochrane review can be found in The Cochrane Library (www.thecochranelibrary.com). 68 A summary of the findings from this review is reported below.
Objectives
The primary objective of the review was to update the evidence on the effectiveness of parenting programmes in preventing unintentional injury in childhood. The secondary objective was to evaluate the effectiveness of parenting programmes at increasing possession and use of home safety equipment and parental safety practices.
Methods
Studies for inclusion
We included RCTs, non-RCTs and controlled before-and-after (CBA) studies, which evaluated parenting interventions administered to parents of children aged 18 years and under. Included studies reported the primary outcome of self-reported or medically attended unintentional injury or injury of unspecified intent, or the secondary outcomes of possession and use of safety equipment or safety practices. This included the Home Observation for Measurement of the Environment (HOME) scale, which contains one subscale measuring organisation of the environment in relation to child development and safety. 69 Parenting interventions were defined as those with a specified protocol, manual or curriculum aimed at changing knowledge, attitudes or skills covering a range of parenting topics.
Search methods for identification of studies
A search strategy was devised for use in MEDLINE and adapted as necessary for other databases. We searched a range of bibliographic databases from the date of inception to January 2011, including Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews (CDSR), MEDLINE (Ovid SP), EMBASE (Ovid SP), PsycINFO, Social Science Citation Index, Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCOhost), ProQuest Dissertations and Theses, Education Resources Information Center (ERIC), Database of Abstracts of Reviews of Effectiveness (DARE), Applied Social Sciences Index and Abstracts (ASSIA) and ISI Web of Science: Social Sciences Citation Index. We also searched international and national websites including the Children’s Safety Network, the International Society for Child and Adolescent Injury Prevention, the Child Accident Prevention Trust, the Injury Control Resource Information Network, the National Injury Surveillance Unit, the Injury Prevention Web, SafetyLit, Barnardo’s Policy and Research Unit, National Children’s Bureau and Children in Wales. We hand-searched abstracts from the World Conferences on Injury Prevention and Control and the table of contents for the journal Injury Prevention from first publication to January 2011. There were no restrictions by language or publication status.
Selection of studies
A two-stage screening process was undertaken. Two reviewers independently scanned titles and abstracts of articles to identify articles to retrieve in full. The full articles were retrieved for those papers retained at this stage, which were independently assessed by two reviewers. At each stage where there was disagreement between reviewers, a decision was made by a third reviewer. Data extraction was undertaken independently by pairs of reviewers. We extracted data on study design, design of intervention, sociodemographic characteristics of participants and outcome data. If key data were not available in the published reports, we contacted study authors to obtain missing information.
Assessment of risk of bias in included studies
Critical appraisal of included studies was undertaken independently by two reviewers who assessed for risk of bias, including selection, performance, detection, attrition and reporting bias. Assessment was also made of the extent to which studies conformed to an intention-to-treat analysis.
Measures of treatment effect
Pooled RRs and 95% CIs were used for binary outcome measures and mean differences and 95% CIs for continuous outcome measures. The primary analysis included RCTs reporting injury rates and used random-effect models. We adjusted for clustering where necessary for cluster allocated studies. Statistical tests of homogeneity were undertaken using chi-squared tests and the I-squared statistic. Publication bias was assessed for the primary analysis using a funnel plot and Egger’s test. Sensitivity analyses were undertaken including only RCTs considered at low risk of selection, detection or attrition bias. For secondary analyses, where there were insufficient clinically homogenous studies to combine in a meta-analysis, their results were combined in a narrative review.
Results
Description of studies
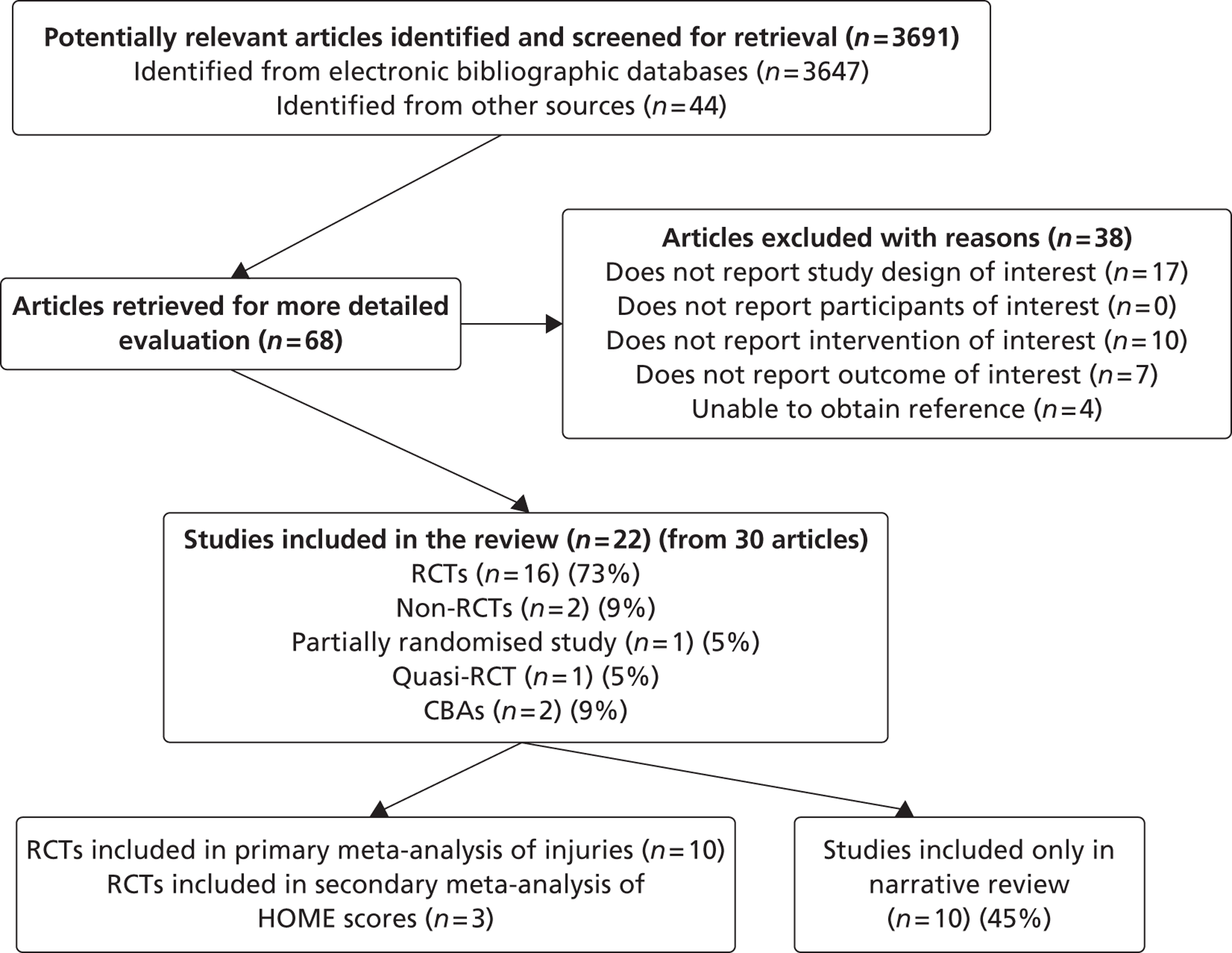
Twenty-two studies70–90 from 30 articles were included in the review (Figure 2 and see Appendix 1). Some authors reported results from the same study at different follow-up time points in separate papers and several authors reported results from the same study in more than one paper. Sixteen70–72,74,76–78,80,82–85,87,89,90 (73%) included studies were RCTs, two73,81 (9%) were non-RCTs, one86 (5%) was a partially randomised study with two randomised intervention arms and one non-randomised control arm, two75,88 (9%) were CBA studies and one79 (5%) was a quasi-RCT. Four studies73,75,81,88 used clustered allocation. Thirteen studies72–74,78–80,82,84,85,88–90 (59%) were from the USA, three from Australia70,83,87 (14%), two each from Canada76,86 (9%) and England71,75 (9%), and one each from Ireland81 (5%) and New Zealand77 (5%). Fifteen of the studies70–72,74,75,77–79,81,83–85,90 recruited socioeconomically disadvantaged participants. Two studies76,87 recruited participants with a learning disability, and three studies81,88 recruited consecutive newborns from a range of paediatric practices.
FIGURE 2.
Quorum flow chart detailing process of study selection for the review.
Seventeen studies70–75,77–81,83–86,89,90 evaluated multifaceted home visiting programmes aimed at improving a range of child, and often maternal, health outcomes. Three82,88 evaluated paediatric practice-based multifaceted interventions, aimed at improving a range of child health outcomes, all of which included some home visits. Two studies76,87 provided solely educational interventions in the home. None of the studies had injury prevention as a primary focus. All studies provided the intervention to individual parents. Four studies83,88,90 provided opportunities for peer support from other parents, one89 provided informal support from family and friends, and five studies78,80,82,85,90 provided parenting education to groups of parents which as a consequence would also provide opportunities for peer support.
Of 16 studies70,72–75,77–81,84–86,88,89 (73%) reporting medically attended or self-reported injury, two73,75 reported insufficient data to be included in the meta-analyses. Seven studies73,75,76,82,88,89 reported a range of safety outcomes such as use of socket covers and stair gates. Two studies87,89 reported home hazards using different tools, and one study82 reported scores from a home safety index. Ten studies70–72,74,83–86,89,90 measured the quality of the home environment using the HOME inventory. 69 One study73 measured the quality of the home environment using the Massachusetts Home Safety Questionnaire.
Risk of bias in included studies
In terms of selection bias, 1070,72,74,77,81,83–85,87,88 (63%) of the 16 RCTs had a low risk owing to adequate random sequence generation, and seven70,71,74,81,83,84,88 (44%) due to adequate allocation concealment. While 1571,72,74,76–78,80,81,83,85,87–90 (94%) of the 16 RCTs were judged to be at high risk of performance bias, only five77,78,80,81,83 (31%) were judged to be at high risk of detection bias. Six83,85,87–90 (38%) of the 16 RCTs had a high risk of attrition bias, and five78,83–85,89,90 (31%) were judged as being at high risk of selective reporting bias.
Effects of interventions
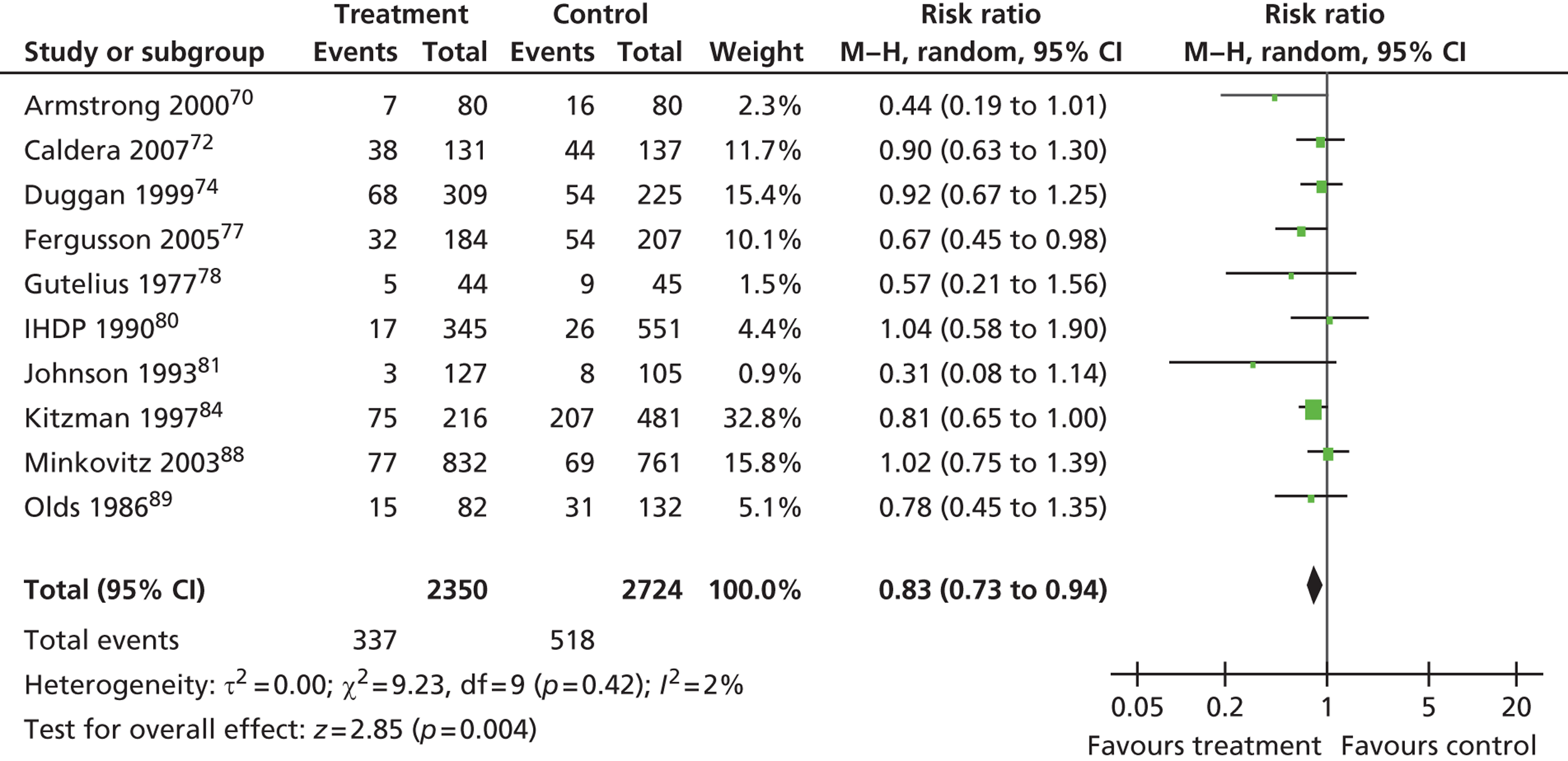
Medically attended or self-reported injury
Sixteen studies70,72–75,77–81,84–86,88,89 reported medically attended or self-reported injury; 10 of these70,72,74,77,78,80,81,84,88,89 reported results from RCTs and were included in the primary analysis which showed that intervention arm families had a statistically significant lower risk of injury than control arm families (RR 0.83, 95% CI 0.73 to 0.94) (Figure 3). There did not appear to be any evidence of publication bias among the 10 RCTs in the primary analysis {Egger’s test regression coefficient = –0.65 [standard error (SE) 0.49], p = 0.22}. Sensitivity analyses were undertaken for the primary analysis including only RCTs at low risk of various sources of bias. The findings were robust to including only those studies at low risk of detection and attrition bias but the effect size became statistically non-significant when analyses were restricted to studies at low risk of selection bias in terms of inadequate allocation concealment.
FIGURE 3.
Forest plot of medically attended or self-reported injury data – RCTs only. M–H, Mantel–Haenszel.
Home safety outcomes
Studies reported home safety practices and hazards using a variety of methods and scales. Data on total HOME scores at 12 months from three RCTs were included in a meta-analysis. The results showed that there was a non-statistically significant difference in pooled average total HOME scores between intervention and control arm families [mean difference 0.57, 95% CI –0.59 to 1.72; χ2 = 0.41, 2 degrees of freedom (df), p = 0.82; I2 = 0%], with intervention arm families scoring higher. Armstrong et al. 70 reported organisation of the home environment subscale scores and found a statistically significant difference favouring the intervention arm {mean score intervention arm 5.70 [standard deviation (SD) 0.77] vs. mean score control arm 5.11 (SD 1.16), p < 0.05}. Of the six studies72,83,84,86,89,90 not included in the meta-analysis owing to insufficient data but which reported total HOME scores or organisation of the environment subscale scores, two84,86 found statistically significant differences favouring intervention arm families, and four studies72,83,89,90 found no statistically significant difference between treatment arms, with one study83 finding statistically significant differences only among distressed mothers.
Seven studies73,75,76,81,88,89 reported a range of specific safety practices or use of items of safety equipment, such as use of electric sockets covers and stair gates, but each study measured different practices. Of the seven studies, five75,76,81,88,73 found effects favouring intervention arm families. Two studies87,89 reported measures of home hazards. Olds et al. 89 reported statistically significantly fewer observed hazards in the homes of intervention arm families than control arm families. Llewellyn et al. 87 found that intervention parents identified statistically significantly more dangers within the home and implemented a statistically significantly greater number of precautions to reduce the risk of injury than control arm parents. Three studies used composite home safety measures other than the HOME scale: two used the Home Safety Index82,91 and one used the Massachusetts Home Safety Questionnaire. 73 Families in the intervention arms of these three studies scored statistically significantly higher on safe practices and safer homes than the control group families.
Discussion
We found that parenting interventions, most commonly provided on a one-to-one basis in the home as part of multifaceted interventions to improve a range of child (and often maternal health) outcomes during the first 2 years of a child’s life, were effective in reducing self-reported or medically attended injury among young children. The finding was consistent across studies with little evidence of statistical heterogeneity between effect sizes and was robust to most aspects of study quality and study design. There was evidence that parenting interventions can have a positive effect on the use of home safety equipment and practices.
The strengths of the review include a comprehensive search strategy that included searching grey literature and hand-searching conference abstracts. The analysis adjusted for cluster allocated studies where necessary and a range of sensitivity analyses were undertaken to test assumptions regarding the potential for bias, uncertainty as to the extent to which the intervention was based on a protocol, manual or curriculum, follow-up period and injury type. The findings were robust to these assumptions. Limitations relate mainly to the generalisability of the findings, particularly the study populations which mainly comprised families considered to be ‘at risk’ of adverse child health outcomes. All studies provided the intervention to individual parents, and while several also included some parents’ groups, the findings may not be generalisable to group-based parenting interventions. Similarly, most studies provided the intervention mainly within the home, and so the findings may not be generalisable to parenting interventions provided outside the home.
Most studies used parental reports of injuries which may be subject to biased reporting, particularly as blinding participants to treatment arm allocation is not possible with interventions such as these. The quality of studies was variable, with either half or more of the RCTs included in the meta-analysis being susceptible to bias in terms of allocation concealment and/or outcome assessment. However, despite this, sensitivity analyses demonstrated little impact of excluding studies without blinded outcome assessment on the results. Only two studies included in the meta-analysis reported high attrition rates.
While our review suggests that parenting interventions are likely to improve home safety, there are other plausible explanations for why parenting interventions may reduce childhood injuries. All studies included in the primary and secondary meta-analyses were aimed at improving a range of child (and often maternal) health outcomes. Seven of these studies reported statistically significant improvements in child behaviour, four reported less punitive discipline practices among intervention group parents, six reported increased or improved mother–child interaction and two reported improvements in maternal psychological well-being. It is therefore possible that the reduction in childhood injuries may be mediated through improvements in child behaviour, more effective supervision or discipline practices or more positive interactions between mother and child, all of which may be associated with improved maternal psychological well-being.
Implications for this study
This systematic review supports the evidence that parenting interventions reduce parent-reported and medically attended child injuries and increase home safety practices and behaviour. The findings are stronger with regard to injury reduction than to home safety practices, suggesting that the mechanism may be a generic change in parenting. The review did not identify any group-based, community-delivered programmes such as that proposed for this study.
Learning points
-
Parenting interventions that include home-based, one-to-one, multifaceted components can reduce parent-reported and medically attended child injuries, and appear to improve home safety measures.
-
The mechanisms through which parenting programmes may reduce child injury are unclear but may include generic change in parenting.
-
There is no current evidence from RCTs of the effectiveness of solely group-based, community-delivered parenting programmes to reduce child injury.
Systematic review 2: barriers and facilitators to parental engagement in parenting programmes
To inform the development of the intervention we sought to identify the features of parenting programmes that enabled parents to join, and remain engaged with, programmes. Published evidence on this topic has largely been derived from surveys of those delivering or developing programmes. 48,66,67 We therefore conducted a systematic review of qualitative literature to identify studies where participants had provided evidence, for example through interview or focus groups, on the barriers and facilitators to their participation, and compared their perceptions with those delivering or researching programmes. We focused on evidence emerging from manualised group-based programmes that were more likely to be relevant to the proposed intervention.
The systematic review has been published online ahead of print in the journal Health Education and Behavior93 and the abstract is reproduced below, followed by a report of the implications of the findings for this study. Our search strategy identified 16,513 citations, from which we identified 26 for inclusion in the final review by using text-mining technology.
Abstract from manuscript accepted for publication
Parenting programmes have the potential to improve the health and well-being of parents and children. A challenge for providers is to recruit and retain parents in programmes. Studies researching engagement with programmes have largely focused on providers’, policy makers’ or researchers’ reflections of their experience of parents’ participation. We conducted a systematic review of qualitative studies where parents had been asked why they did or did not choose to commence, or complete programmes, and compared these perceptions with those of researchers and those delivering programmes. We used data-mining techniques to identify relevant studies and summarised findings using framework synthesis methods. Six facilitator and five barrier themes were identified as important influences on participation, with a total of 33 subthemes. Participants focused on the opportunity to learn new skills, working with trusted people, in a setting that was convenient in time and place. Researchers and deliverers focused on tailoring the programme to individuals and on the training of staff. Participants and researchers/deliverers therefore differ in their opinions of the most important features of programmes that act as facilitators and barriers to engagement and retention. Programme developers need to seek the views of both participants and deliverers when evaluating programmes.
Implications for this study
The review identified key features of programmes that enabled or hindered parental engagement and retention. Participants appeared to prioritise different issues compared with those delivering, or researching, programmes. However, on exploration, some of these issues were not entirely unrelated. For example, parents emphasised the need for trust in the person delivering the programme, while deliverer training appeared to emphasise the ability to deliver the manualised content of the programme rather than the ability to facilitate a group, including issues such as group cohesion. We have summarised the implications for the development of the parenting programme in this study in the learning points below.
Learning points
The key learning points from this review that are relevant to this study are detailed below.
-
Participants were interested in joining and completing parenting programmes if they believed that in doing so they would have the opportunity to learn new and specific skills, either for their own personal development or because they believed their skills would support their children.
-
The relationship between the participant, the deliverer and the other group members was very important. Participants needed to feel safe both with the deliverer and within the group. A known or trusted deliverer of the programme was helpful, but the deliverer needed to have the skills to present the programme in a non-judgemental, empathic and supportive manner. Participants needed to be able to relate to the other members of the group.
-
Practical issues such as the location, frequency and timing of the programme influenced parental engagement. Programmes needed to fit around existing commitments. Incentives such as childcare, travel expenses and refreshments were important.
-
Those delivering the programmes emphasised the need to be able to respond to the needs of the group, i.e. to be able to tailor the programme where necessary. This is in potential conflict with the production of manualised programmes that support fidelity of intervention delivery. Deliverer training needs to include group facilitation skills in addition to the ability to deliver the programme materials.
-
The potential difference in issues raised by participants and those delivering programmes indicate that both perspectives should be explored when evaluating programmes.
Theoretical model
We have developed a theoretical model through which positive outcomes from a parenting programme could lead to reductions in home injuries in preschool children (Figure 4).
FIGURE 4.
Theoretical model for the impact of a parenting programme on preschool home injuries.
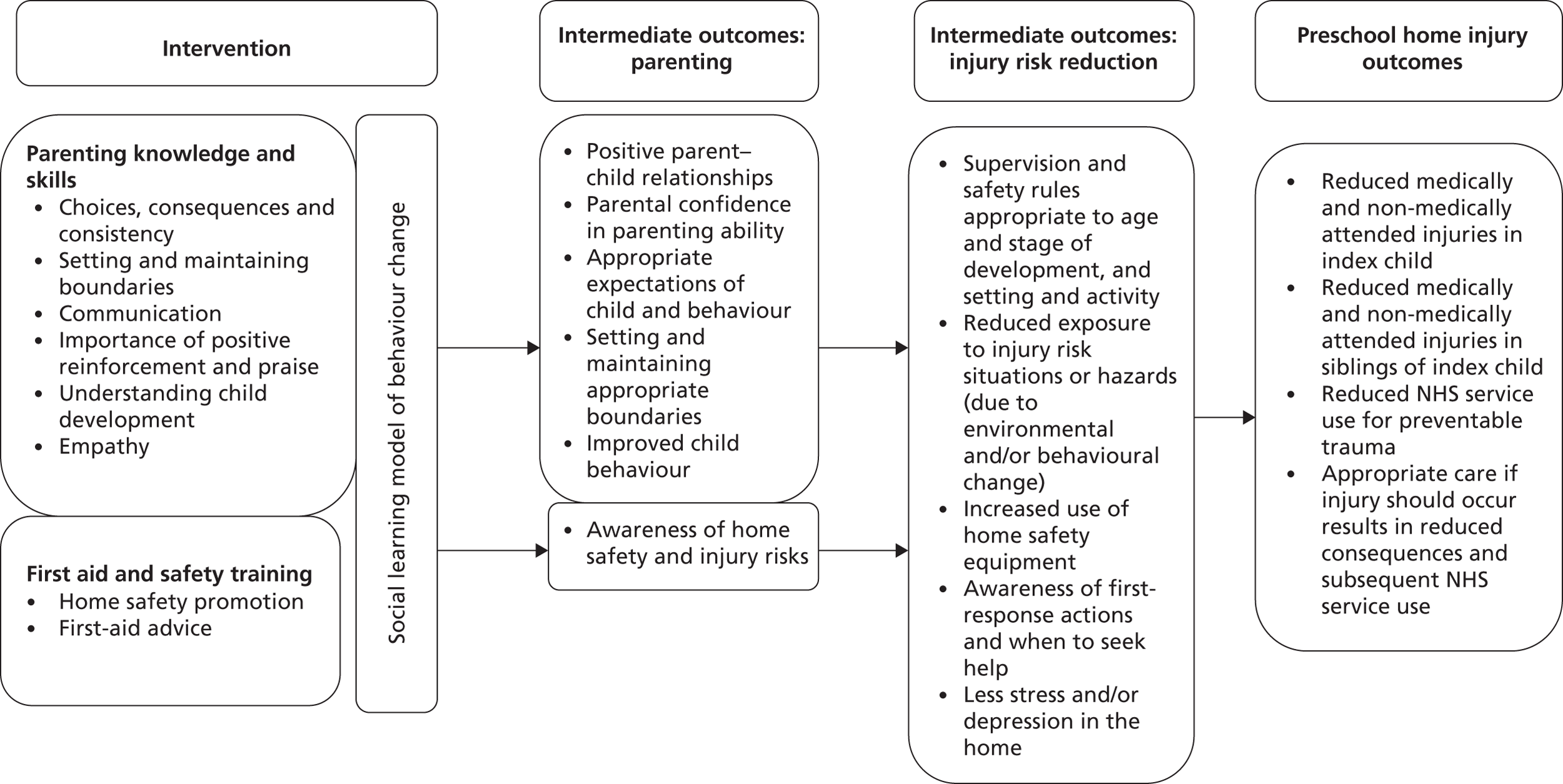
Effective parenting programmes have the potential to result in a range of outcomes that relate to how parents and children interact:
-
positive parent–child relationships and enhanced communication
-
parental confidence in parenting ability
-
appropriate expectations of child and behaviour
-
setting and maintaining appropriate boundaries
-
improved child behaviour.
We propose that a parenting programme that combines parenting skills and knowledge with first aid advice and home safety promotion has the potential to improve parental awareness of injury risks at different ages and stages. That in turn may lead to reduced home injuries in preschool children through a number of intermediate outcomes that reduce injury risk:
-
parental supervision and safety rules that are appropriate to the child’s age and stage of development, as well as the setting and activity
-
use of age-/developmental stage-appropriate safety rules
-
reduced exposure to home hazards as a result of environmental change (e.g. locked medicines cupboard, or removing or repairing tripping hazards)
-
increased use of home safety equipment
-
behavioural change that increases safe practices (e.g. handling hot beverages, storing medicines out of reach or not leaving child on a raised surface/alone in the bath)
-
reduction in stress, depression or anxiety in the home.
Should an injury occur, the consequences of that event may be reduced by:
-
parental awareness of immediate paediatric first aid actions
-
parental awareness of when to seek medical advice/when to treat injuries at home.
Reduced injury risk has the potential to result in fewer injury events taking place and fewer injuries sustained. It could be hypothesised that an effective parenting programme that incorporates a focus on injury prevention could result in fewer preschool home injuries presenting to emergency departments and other community NHS providers (e.g. NHS walk-in centres, or general practice). The reduction in injury risk may not eliminate injuries but may reduce the severity of the injury sustained. In these circumstances, a relative increase in the proportion of injuries that are minor or managed at home with first aid may be observed. Furthermore, if the parenting programme was successful in increasing parents’ knowledge of injuries and when to seek attention, this could result in increased health service use. For example, knowing that a bang to the head could lead to a potentially serious injury may encourage attendance at the emergency department. Providing information on when to seek help or advice will be required to encourage appropriate use of health-care services.
In Chapter 5 we have explored the feasibility of testing this model through a cluster RCT. A future trial would be required to determine if it is possible to reject the null hypothesis of no difference in injury outcomes for parents receiving or not receiving the parenting programme.
Chapter 3 Development of a parenting intervention: developmental phase
Objective
To develop a parenting programme to prevent recurrent unintentional home injuries in preschool children, together with the resources required to test the feasibility of evaluating the intervention.
Methods
Commissioning of Parenting UK to develop the programme
Parenting UK was commissioned to develop a group-based parenting programme. The commissioning brief specified that the programme should include:
-
parenting skills that have the potential to prevent injuries including, but not limited to:
-
relationship building
-
setting and maintaining boundaries
-
behaviour management
-
appropriate levels of supervision for the age and development of the child
-
-
first aid response to common injury scenarios occurring to children under the age of 5 years in the home, including but not limited to:
-
falls
-
burns and scalds
-
ingestions and poisonings
-
foreign bodies and choking
-
unconsciousness/recovery position
-
life-saving skills/cardiopulmonary resuscitation
-
cuts and wounds
-
broken bones
-
-
safety practices and equipment that, when used in an age-appropriate and/or development-appropriate way, can prevent injuries from occurring.
In addition, Parenting UK was requested to provide the materials, equipment and documentation to support the delivery of the programme during the testing of the intervention. This included the development of a programme manual for those delivering the programme to use as a reference aid. Six sets of materials were required to be produced for subsequent testing in a feasibility study.
Governance of the programme development
A programme development subgroup (PDS) was convened to oversee the development of the programme. Membership included three co-applicants: the chief investigator (JM), an academic with expertise in evaluating parenting programmes (S-SB) and a practising health visitor (BP), together with the Director of the Whoops! Child Safety Project, which provides first aid training for parents. This team communicated with the chief executive of Parenting UK and the manager employed by Parenting UK to carry out the development work. Communication between the manager and the PDS was by e-mail and teleconferences held every 3 weeks between February 2011 and July 2011. The emerging findings of the two systematic reviews conducted during the theoretical phase of this study were passed to the staff at Parenting UK to help inform development of the programme.
The Parenting UK manager was asked to keep a log to record the decisions and rationale for choices made during the development of the programme, to provide an interim report after 3 months, and to provide a final report. The manager from Parenting UK made a presentation to the research team at the end of 6 months (July 2011) to describe the course that had been produced, and seek final sign-off prior to production of the materials.
User involvement
The PAG was consulted prior to Parenting UK commencing work on the programme. During the PAG’s second meeting we asked the mothers what they had liked and disliked about any parent support courses that they had attended and what had been good or not so good about any first aid training or courses that they had attended. We then discussed the possible content and format of a course on first aid and home safety including resources and things they could do at home. They made some very helpful suggestions, which were passed onto the staff at Parenting UK.
At the next meeting of the PAG some of the resources developed by Parenting UK for use in the course were discussed. The outline of the course was described and members discussed some of the proposed activities. They were very positive about the content and resources, and this was fed back to the staff at Parenting UK.
Results
An 8-week programme, designed to be delivered in an acceptable, participant-friendly, incrementally progressive style, was produced and is summarised in Table 1, and described in more detail in Appendix 2. The content of each session, designed to be delivered over 90 minutes, was acknowledged to be challenging, particularly for a less skilled/experienced trainer. While acknowledging that some parenting programmes include sessions of 2 hours’ duration, the length of the sessions was chosen to be 90 minutes as a result of concerns that a longer session may reduce the likelihood of parents engaging with the programme owing to the perception of it being an onerous commitment. Each week started with a reflection on the previous week’s content and exploration of the application of knowledge or skills at home since the group last met. Each week ended with an opportunity to discuss and clarify details discussed that week together with suggestions of activities parents might wish to try at home.
| Week | Content |
|---|---|
| 1 |
Introduction to the course
|
| Discussion about the challenges parents face in keeping their children safe | |
| 2 |
Child development and injury risk. Illustrate with head
injury scenarios and advice
|
| Discussion of how home hazards link to injury and development | |
| 3 |
Communication between parents and children. Illustrate
with choking risk scenarios and advice
|
| Responding when your child is choking, preventing choking | |
| 4 |
Managing attention-seeking behaviour, using praise.
Illustrate with burn and scald scenarios
|
| Providing appropriate supervision for your child | |
| 5 |
Setting and maintaining boundaries. Illustrate with
ingestion and poisoning scenarios and advice
|
| Keeping children safe from poisons and ingestions/first response | |
| 6 |
Appropriate expectations of children. Illustrate with safe
play scenarios
|
| Safe toys and games at different ages | |
| 7 |
Attachment/how we react when upset or angry. Illustrate
with unconscious child scenarios
|
| What to do if your child were unconscious/recovery position and resuscitation | |
| 8 |
Drawing the course together
|
| Wrap up/thanks for participation/certificates of attendance |
The programme and trainer manual were developed through an iterative process informed through written comments on each draft version and three weekly teleconference discussions with the PDS. Some materials were identified from other programmes and resources and, where included, written permission was provided. The artwork was directly commissioned by Parenting UK for this programme. The decision log is summarised in Appendix 3.
The following outputs were delivered:
-
Twelve A4 trainer manuals – white polyvinyl chloride (PVC) ring binders, with a 4 × D-ring mechanism, clear pockets on the front cover and spine for colour inserts, and the contents divided into three sections: (1) general introduction to the programme and advice on running groups, (2) the contents of each of the 8 weeks of the programme, broken down into timed components and activities and (3) resources and materials used in each session.
-
Fifty A5 parent handbooks – white PVC ring binders with a 4 × D-ring mechanism and clear pockets on the front cover and spine for colour inserts – for the participants to store handouts provided during the weekly course sessions together with any notes that they chose to make.
-
Four sets of laminated pictures/tools for the delivery teams to use during session delivery.
-
Two resource kits (one for each study centre) were provided by the Whoops! Child Safety Project. Kits contained two burns dolls, doll for demonstration of resuscitation and choking response, choking tube, heat change colour mug, fire safety DVD, leaflets and an A3 poster tube with laminated drawings.
-
A ‘train the trainer’ package, designed as a 2-day course for delivery teams and described in detail in Appendix 4.
Support for those delivering the programme
The manager from Parenting UK made a number of recommendations regarding support for those delivering the programme. It was acknowledged that support to all the deliverers in a group face-to-face environment would enable shared learning and avoided duplication of information exchange. However, it was recognised that the courses were unlikely to be delivered concurrently across the study centres, resulting in deliverers having different support needs at different times. In addition, not all of the course deliverers would be available at the same time. Therefore, the manager at Parenting UK offered to be available to provide weekly telephone and e-mail support as required for those delivering the four courses planned during the feasibility study. The option of video conference contact was considered but rejected owing to the limited electronic access available to course deliverers in their usual work locations.
Discussion
The process of developing the 8-week programme, working with two voluntary sector organisations – Parenting UK to develop the programme, and the Whoops! Child Safety Project to advise on the first aid and safety content of the programme – proved to be a very constructive and positive experience for the organisations and researchers involved. The process of combining elements of parenting programmes with information on injury risk and injury prevention was acknowledged by all parties as challenging, but considered worthy of the effort on account of the perceived benefits of a programme with the potential to reduce unintentional injuries in the home for preschool children.
The programme was developed to provide a ‘spiral curriculum’ of parenting skills and knowledge, where issues were revisited several times during successive weeks of the course. This process encourages the participants to try the new skills themselves when at home, and then receive support and opportunities for discussion when the subject was revisited. The parenting skills and knowledge were introduced using injury risk and injury outcome scenarios to illustrate how parenting skills can help to keep children safe.
The challenge of intervention fidelity is well known among those developing and evaluating parenting programmes. The small-scale nature of the feasibility study of the programme meant that quite personalised support could be made available to those delivering the courses in the two study centres. It was acknowledged early on that any future trial or subsequent roll-out of the programme would need a different process to ensure fidelity of delivery and support for course facilitators. Recommendations made by Parenting UK are included in Chapter 8 (see Implications for a main trial).
Learning points
-
Voluntary sector organisations working with the participant group were informed and valued partners in the intervention development process.
-
The involvement of the voluntary sector organisations in the production of the 8-week parenting programme, informed by recommendations made by the PAG and a parents’ forum facilitated by Parenting UK resulted in an intervention more likely to meet the needs of the participant group than if developed from a theoretical perspective alone.
Chapter 4 Development of tool to collect primary outcome measure
Objective
The objective of this component was to develop a tool for parents to report unintentional home injuries occurring to their preschool children. This tool would be used during the study to test the feasibility of evaluating the parenting programme through a cluster randomised controlled design.
Elements required to be captured by the tool
The tool needed to capture the following features of each injury event:
-
the date of the event (to confirm occurrence was within the follow-up period)
-
the location of the injury event (to confirm that it was an injury occurring within the home, garden, drive or yard)
-
the type of injury sustained (e.g. cut, fracture, head injury, etc.)
-
the action that was taken [e.g. first aid, telephoned general practitioner (GP), took child to hospital, etc., to determine medically attended from non-medically attended injuries, and to enable the collection of data for any subsequent cost-effectiveness analysis]
-
whether the injury was sustained by the index child or by any preschool siblings in the household.
Development process
The follow-up period during which the tool would be tested was for 6 months. It was decided early on that a calendar-style record might be acceptable to parents. To develop the injury measure we planned to take designs to the PAG for discussion and feedback.
The initial two versions of the injury calendar were prepared on landscape A4 paper using a ‘month-to-a-view’ design with a box for each day of the month, in which the parent could indicate that an injury had been sustained. On the first version, the calendar filled one side, and space for adding detail about the injury event was made available on the reverse. On the second version, the calendar section was smaller, allowing details about the first two injury events that month to be included on the front and details of further injury events on the reverse. We anticipated that a parent might wish to stick the calendar on the door of the fridge, a kitchen cupboard or notice board for convenience. A series of tick boxes enabled the parent to record the location of the injury event, the type of injury and the action taken for up to six injury events that month. Tick boxes were used in an attempt to reduce the time taken to complete the record. The tool would have required six such pages, one for each month of the follow-up period. The PAG members did not like the initial designs, expressing concern about the appearance (too big for a fridge door) and the clarity of the instructions, and they were concerned that it would take too much time to complete. They felt that a 6-month collection period was lengthy and suggested they might give up completing it, or forget about it after a few weeks. The group discussed the value of incentives to continue and support their completion. Following this discussion, the study team agreed to redesign the tool based on the PAG’s feedback, and bring a revised tool back to them.
A new version of the diary was designed working with a graphic designer at the University of the West of England, Bristol. A month-to-a-view calendar design was retained but this time developed as a tall slimline calendar (A3 size, split lengthways, and spiral bound along the top short edge, suitable for hanging on the wall). A line for each day of the month provided space to record details of any injury events occurring on that day. The front page of the calendar was designed to provide instructions on how to complete the calendar, including a definition of ‘an injury’, and space to record the child’s name. For each month in the calendar, the first line was filled in with an example of how it could be completed. The unique identification number for each participant in the study could be recorded in the footer of each page. The text was reviewed to improve understanding and use language in common use; for example, ‘head injury’ was changed to ‘bang on the head’. This second design was presented to the PAG and was received very positively. They suggested having space to write additional comments on the reverse of each month, so that they would have space to explain what happened if they wished to.
Further minor amendments were made to the calendar, including adding space on the reverse of each month as recommended, and addition of a ‘don’t know’ option when recording the location of the injury. The final version of the tool is shown in Appendix 5.
Use of the injury calendar
The calendar was used for the feasibility study to collect parent-reported injuries in the preschool children of participants. The methodology and results (completion rates and data captured) are described in Chapter 5.
Discussion
The PAG was central to the development of the injury measure. They informed the appearance, content and utility of the design. Although the number of data items requested for each injury event was small, there was a risk of poor completion if either the format was too complicated or the instructions were not understandable. The familiarity of the slim spiral-bound calendar design was welcomed by the parents. The positive feedback from the second version of the tool increased our confidence that parents recruited to the feasibility study might complete the tool.
Originally we planned to call our primary outcome measure an injury diary. In July 2011 we decided to change the name from an injury diary to an injury calendar. A common understanding of a diary is that a certain amount of writing would be required and use of the word ‘calendar’ was felt helpful to promote the understanding that only brief notations were required. It was important to make the language used on the calendar easy to understand. While the early designs had tried to avoid medical terminology, comments from the PAG identified additional text suitable for amendment and made suggestions for ease of completion. The PAG suggested the option of text reminders for parents to encourage the completion and return of calendars.
The use of a professional graphic designer improved the appeal and familiarity of the calendar, which appeared to be particularly important in the acceptability of the final design when presented to the PAG. The designer was able to advise on the format to improve the likelihood that completion would be perceived as straightforward.
Learning points
-
The acceptability of a new parent-reported injury outcome measure was improved by the use of a graphic designer who recommended changes to simplify the information recording process and to increase the familiarity of the design.
-
The PAG provided feedback on designs, which increased the likelihood that the recording of potentially sensitive information would be completed.
Chapter 5 Feasibility study
Aim and objective
The aim of the feasibility study was to assess the ability to deliver and evaluate the parenting programme through a cluster RCT.
The objectives were:
-
to assess the recruitment and retention of parents
-
to assess compliance with delivery of the intervention
-
to determine the training, equipment and facilities needed for the delivery of the programme
-
to assess the collection of primary and secondary outcome measures
-
to clarify ‘normal care’
-
to assess the resource utilisation and costing data that would need to be collected in a main trial
-
to produce estimates of effect sizes to inform sample size estimation for a future trial.
The methods and results for objectives (a)–(e) and (g) are reported in this chapter. Objective (f) is reported in Chapter 6.
The protocol for this feasibility study has been published in the journal Injury Prevention. 94 The original study protocol (version 1) approved by NHS Ethics is presented in Appendix 6. The final protocol after amendments (version 4) is presented in Appendix 7.
Methods
Trial design, funding and approval
The feasibility study was a multicentre, cluster randomised, unblinded trial comparing the First-aid Advice and Safety Training (FAST) parent programme against usual care. The two study centres were Bristol and Nottingham.
The trial was funded by the NIHR HTA programme (reference number 09/02/02) and commenced in January 2011. It was approved by the South West Level 3 Research Ethics Committee (reference number 10/H0106/78) and was registered with the International Standard Randomised Controlled Trial Register (reference number 03605270).
Participants
Children’s centres
Inclusion criteria
In accordance with the original study protocol, children’s centres in both study centres were ranked according to the number of children aged 0–4 years who had attended the local children’s emergency department with an injury in the previous 12 months, and had a postcode that would have entitled them to access that children’s centre. Children’s centres with the highest rankings in each city (i.e. the centres with the largest numbers of young children attending with injuries) were invited to join the study until sufficient numbers of children’s centres had been recruited.
Exclusion criteria
Children’s centres were excluded from participating if they were already involved in other injury prevention research.
Parents
Inclusion criteria
Parents and carers (hereafter referred to as parents) were eligible for recruitment if they:
-
had a child under 5 years of age who sustained an unintentional physical injury in the home (or within the boundary of the home and garden/yard) for which they sought medical attention from a health professional at a NHS emergency department, minor injuries unit, or walk-in centre during the recruitment period or in the previous 12 months
-
were living at an address within the geographical catchment area of a children’s centre participating in the study.
Exclusion criteria
Parents were not eligible to join the study if:
-
they were unable to understand written and spoken English
-
the child suffered an injury suspected or confirmed to be intentional. Should an injury originally considered to be unintentional be later discovered to have been intentional then routine referral processes for safeguarding would be activated. The parent would not be asked to withdraw from the programme, but data for that child would not be included in the analysis.
If a parent already recruited to the study sought medical attention for an injury in a preschool sibling of the index child they would not be invited to join the study again.
Recruitment of children’s centres and health visitor teams
Recruitment of children’s centres and health visitor teams began in March 2011 and ended in January 2012. While it was feasible to rank children’s centres on the basis of rate of attendances of preschool children with injuries, it quickly became apparent that the factor most likely to influence the ability of a children’s centre to participate in the study was the engagement of the linked health visitor team. Each children’s centre is linked to a named health visitor team. The degree to which the children’s centre and the health visitor team are linked varies significantly from being based in a shared building and working closely together, to being linked in name only and working independently.
During the period between preparation of the original protocol and commencement of the study, organisational change combined with worsening health visitor capacity issues had resulted in:
-
change of the employer of health visitors in both study centres; neither of the new employers had been involved in initial discussions about the study prior to funding
-
new management structures within health visiting services in both cities in response to workforce capacity difficulties. Previously, health visitors were relatively autonomous professionals. The new structures placed managers as gatekeepers to health visitor teams, and required permission from the manager prior to engagement with the teams themselves. The identification and engagement of managers was difficult and slow in both centres.
In addition, another nationally funded injury prevention study based in children’s centres in both Bristol and Nottingham reduced the number of eligible children’s centres for this study.
The intended model of identification of paired children’s centres and health visitor teams was found not to capture the complex and variable ways in which children’s centres and their health visitor teams worked across the two study centres. In both cities, even though each children’s centre had a theoretical catchment area, parents attended the children’s centre that most appropriately met their needs rather than the one that was closest to them. In addition, children’s centres would not refuse a parent attending simply because they did not live locally. Children’s centres were found to have markedly variable facilities, with some not having the capacity to host both a programme and a crèche concurrently.
The identification of four pairs of linked children’s centres and health visitor teams in each centre was therefore achieved through a process of negotiation and an attempt to achieve a reasonable geographical distribution of participating children’s centres across each city.
Recruitment of parent participants
In our original protocol we anticipated identifying eligible parents through health visitor teams over 4 months. As a result of slower identification than anticipated, recruitment took place over 12 months (between May 2011 and April 2012) and during this period we added alternative strategies to identify the optimal methods for a future trial. Three further methods of identifying eligible families were assessed: emergency department identification using telephone contact, emergency department identification using postal contact, and identification via children’s centres (Table 2). At any one site several strategies ran concurrently. For three of the strategies (health visitor identification, emergency department identification via telephone contact, and children’s centre identification), the names and contact details of parents interested in finding out more about the study were passed to the research team who confirmed eligibility, provided further information and answered questions, and took consent. For the remaining strategy (emergency department identification via postal contact), potentially eligible participants contacted the researchers directly, who then confirmed eligibility and took consent.
| Study centre | Identification through health visitor teams | Identification via emergency department using telephone contact | Identification via emergency department using postal contact | Identification through children’s centres |
|---|---|---|---|---|
| Bristol | ✓ | ✓ | ✓ | |
| Nottingham | ✓ | ✓ | ✓ |
Identification of participants via health visitor teams
Recruitment via health visitor teams was the method specified in our original proposal and was used between May 2011 and March 2012. Health visitor teams are routinely faxed details of children who have sustained an injury and attended an emergency department, minor injuries unit or walk-in centre within their catchment area of responsibility. Upon receipt of a notification of attendance, a member of the health visiting team contacted the family to advise them that their local children’s centre was participating in a study to follow up preschool children who had an injury and that some children’s centres were providing a course for parents that included first aid advice and home safety information. To reduce the risk of stigmatisation, parents were not advised that the course was a parenting programme at this initial contact. Parents were asked if their details could be passed to the research team who would tell them more about the study. To facilitate the task, health visitor teams were provided with a guide to eligible families, a template to record eligible families and outcomes of contacts, a suggested script to guide the telephone discussion with families, and a parent information sheet. Health visitor teams were able to claim service support costs to cover the time taken for this additional work.
To reduce the workload for health visitors, we proposed that the health visitor clerk could undertake the task of contacting families. In practice, clerks did not feel confident to telephone parents and the task was undertaken by either a health visitor or a nurse in her team. We suggested that eligible families could be identified both prospectively and retrospectively (where a child had sustained an injury within the previous 12 months). The contact details of parents agreeing to have their contact details passed to the research team were sent to the research office via fax.
Identification of parent participants via emergency departments using telephone contact
This approach was used in the emergency department of the children’s hospital in Bristol. Ethical approval for the additional recruitment strategy was obtained in September 2011. Parents were not approached at the time of their presentation to the emergency department, but afterwards, by telephone. A research nurse and an administrator contacted the parents of children under the age of 5 years who had presented to the emergency department with an apparently unintentional injury where the hospital record suggested that the injury may have been sustained in the home or garden. The nurse advised the parent that there was a local study that aimed to support parents of young children to help keep them safe from injuries at home, and that parents who joined the study may be able to take part in a first aid advice and safety course. The parent was asked if their contact details could be passed to the research team who would contact them with more information.
Eligible parents were identified prospectively between October 2011 and March 2012, and retrospectively via a review of electronic attendance records between July 2011 and September 2011. To facilitate the task, the research nurse and administrator were provided with inclusion and exclusion criteria, a template to record eligible families and outcomes of telephone contacts, a suggested script to guide the telephone discussion with families, and a parent information sheet. The contact details of parents agreeing to have their information passed to the research team were sent to the research office via fax. The number of parents approached but declining to have their details passed to the research team was noted, together with the reason for refusal where provided.
Identification of parent participants via emergency departments using postal contact
This approach was used in the emergency department of the children’s hospital in Nottingham. Ethical approval for the additional recruitment strategy was obtained in September 2011. An emergency department research nurse performed a retrospective search of attendance records to identify potential eligible families with a general practice address that mapped to the catchment areas of children’s centres participating in the study. In November 2011, letters were sent to children who were identified as having attended the emergency department in the previous 6 months for treatment of an unintentional injury. Information sent to the parents included an introductory letter from the emergency department consultant, a parent information booklet, a reply slip and a freepost envelope. A reminder letter was sent out 2 weeks later to any parents who had not responded to the first letter. As a result of a low response rate, the time period of retrospective emergency department attendance was extended to from 6 months to 13 months (i.e. by a further 7 months). All potentially eligible parents identified in this second period were sent letters in January 2012.
Identification of parent participants via children’s centres
This approach was used in both study centres, Bristol and Nottingham, between December 2011 and April 2012. Approval from the ethics committee of the University of the West of England was obtained in November 2011. Following advice both from health visitors and from children’s centre staff, we established a fourth strategy to identify eligible families. In each of the four children’s centres in both Bristol and Nottingham members of the research team attended parent groups (such as ‘stay and play’ or ‘parent and toddler’ groups) to talk to parents about the study, hand out A5-sized flyers and answer questions. In addition, children’s centre staff were briefed on the study and encouraged to discuss the study with parents, hand out flyers and offer to ask the research team to contact the parent if they were interested. We provided the children’s centres with A3-sized posters and A5-sized flyers that contained information including the criterion of having a preschool child who had sustained a medically attended injury (see Appendix 8).
Parents who expressed an interest in the study could take home parent information sheets, consent forms and a stamped addressed envelope, or could complete them with the researcher at the children’s centre at that time if they wished. If consent was given at the children’s centre, parents could choose to complete the baseline questionnaires at the same time or take them home along with a stamped addressed envelope.
Randomisation and allocation
All parents recruited to the study consented to randomisation in the trial. The unit of randomisation was the children’s centre. The original proposal was to stratify the eight children’s centres by study centre (two strata) and randomly allocate within each centre to treatment arm using a remote automated system available through the Bristol Randomised Trials Collaboration based at the University of Bristol. Therefore, two children’s centres in each study centre would be randomly allocated to the intervention arm and two to the control arm. Allocation to intervention or control arms was delayed until after recruitment of families in each children’s centre had been completed to avoid the risk of post-randomisation recruitment bias. It was not be possible to blind parents, children’s centres, health visitor teams or researchers to intervention allocation.
Participation in the trial
In the original protocol we proposed that eligible families be identified by health visitor teams, followed by the researcher contacting the family by telephone to confirm eligibility and answer questions. If interested, families were sent the parent information booklet and consent form. A home visit was arranged to take written consent and collect baseline measures. The parent information booklet stated that the course provided in some children’s centres was a parenting programme containing first aid advice and safety information. While some families took up the offer of a home visit, others declined and we revised our procedure to one of negotiating with each participating family the method to complete the consent form and baseline measures that was most convenient for them: home visit, face-to-face meeting at an agreed location (e.g. the children’s centre), or by post with telephone support from the research team if required. On recruitment to the study, parents were asked to complete a questionnaire to record basic demographic details (e.g. age, sex, ethnic group, marital status, level of educational attainment, age and sex of children in their household). After commencement of the study, two additional questions were added to this initial questionnaire relating to whether or not they had ever previously attended a support course for parents or a first aid course. These questions were added because we recognised that previous participation in courses could influence their decision to participate in the study. A flow chart illustrating the proposed participant experience of the study is shown in Figure 5.
FIGURE 5.
Flow chart of parent participation as per original protocol.
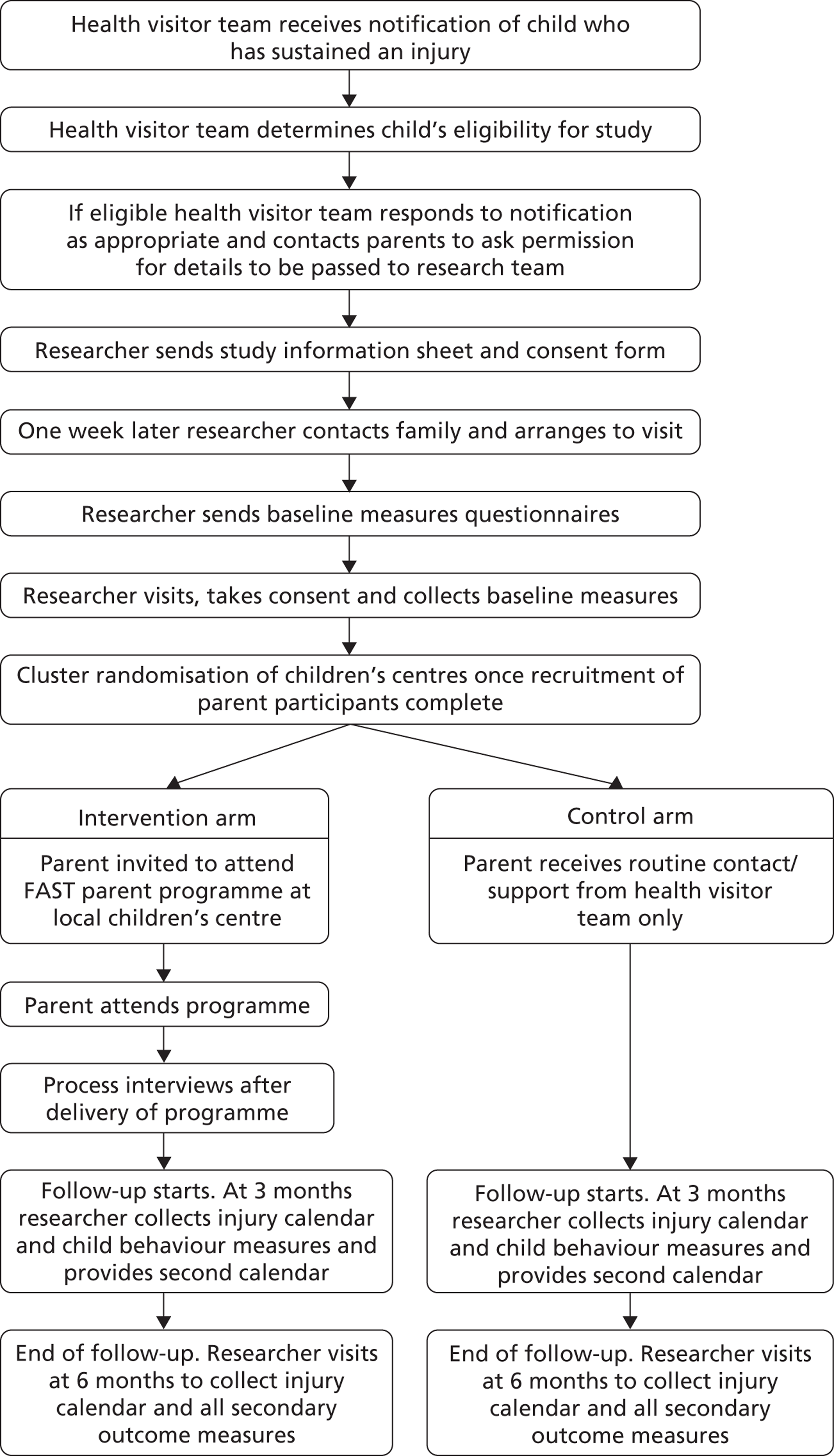
After completion of the baseline measures, parents’ allocation to intervention or control children’s centres was disclosed, and those families in the intervention arm were invited to join the parenting programme. After the parenting programme had completed, a period of 6 months’ follow-up commenced for both intervention and control families. We specified in the original study protocol that during this period parents in both arms of the trial would be asked to complete two 3-month injury calendars in which they could record home injuries occurring to both index children and their preschool siblings. We proposed that a home visit would be offered to all study participants after 3 months to collect the first injury record, to complete a short questionnaire and to give out the second 3-month injury calendar. A further home visit would be offered after 6 months to collect the second injury record and to complete the final study questionnaires. It was believed that home visits would be required to facilitate completion and return of the calendars. After commencing the trial, some parents declined home visits and, therefore, collection of the injury calendars and the interim and final questionnaires were negotiated individually with each participating parent: via home visit, face-to-face meeting at an agreed location, or return by post.
At all stages, parents were offered support to complete the injury records and questionnaires if required. Gift vouchers (£5 value) were given to parents upon completion and return of baseline, 3- and 6-month questionnaires and the injury calendars to thank participants for their time.
A final telephone contact with the families occurred after completion of the final study questionnaires. This telephone contact was from a researcher who the parents had not previously met, to conduct a short interview in order to understand their experiences of participating in the study as a whole.
Training of health visitors and cofacilitators to deliver the intervention
The original protocol stated that the parenting programme would be delivered by a health visitor and cofacilitator from the health visiting team linked to the participating children’s centre. A 2-day training event to enable the facilitators to deliver the programme was designed and provided by the manager from Parenting UK (see Appendix 4). Owing to slow recruitment and the first course starting later than planned, the training was delayed from September 2011 until November 2011 to ensure that the event was relatively close to the first occasion when the facilitators would deliver the programme. The training event took place in Nottingham. Attendees included a trainer from Parenting UK, two members of the research team from Bristol, two members of the research team from Nottingham, the two delivery teams (health visitor plus co–facilitator pair) from Nottingham, and the single delivery team from Bristol. Participants were provided with a training manual, a copy of the parents’ handbook, and had the opportunity to experience the resources available during the programme.
Delivery of intervention
Intervention arm children’s centres hosted the parenting programme and provided crèche facilities. Parents participating in the study who were within the catchment area of these children’s centres were invited to attend the programme and sent details of location, directions and timing of the programme sessions. In addition to the parenting programme, parents in the intervention arm received usual care from their health visitor team following the team’s receipt of the notification of attendance at the emergency centre, minor injuries unit or walk-in centre. Parent participants were given a certificate at the completion of the parenting programme. Details of the parenting programme are given in Chapter 3 and Appendix 2, where the 8-week programme is described.
Children’s centres in the control arm did not host the parenting programme. Parents recruited to the study and living within the catchment area of control arm children’s centres were sent a letter advising them that their local children’s centre was not running a first aid advice and safety course, but that we would like them to help us by completing an injury calendar and some further questionnaires. These families received usual care from their health visitor team. ‘Usual care’ by a health visitor team after receiving a notification of attendance for medical advice following an injury can be considered as one of four different actions: telephone contact, face-to-face contact, referral to services, or no action. The action taken by the health visitor team is determined by the circumstances of the event and the health visitor’s understanding of the needs of that family, and by the workforce capacity of the team.
Outcome measures
Primary outcomes
There was one primary outcome:
-
the rate of parent reported medically attended injuries to the index child or their preschool siblings occurring in a home setting.
In this study ‘an injury’ was defined as an event that resulted in a physical mark showing that something had happened (e.g. a bump, bruise, cut, burn, etc.) where the mark lasted for at least 1 hour after the event, or swallowing something that should not be swallowed.
The primary outcome was measured during a 6-month follow-up period commencing in both arms of the feasibility study after completion of the parenting programme. The outcome data were collected using the injury calendar designed for this purpose and described in Chapter 4. Calendars were sent to parents, with an explanation of how to complete the calendar, including a clear definition of what constituted ‘an injury’, together with a mobile telephone number to call in case of queries. In the original protocol parents were asked to complete the injury calendar for two consecutive 3-month periods. During the study parents were asked whether or not they would like to be contacted at the end of each month to remind them to move onto the next month of the calendar, and to provide support to complete the calendar if required. Contact was offered by telephone or text. In the original protocol it was proposed that home visits would be required to complete and collect the injury calendar. During the study, the collection of the injury calendar was discussed with each parent participant, and the method most convenient for the parent was used. In all cases, a stamped addressed envelope was sent to the parents for them to return an agreed number of pages from the calendar. Telephone calls and texts were used to remind parents to return calendar pages if necessary. Parents received a £5 gift voucher for returning each set of three calendar pages to thank them for their time.
Parent consent was obtained at recruitment to validate parent-reported injuries against emergency department, NHS walk-in centre and primary care records. A template was produced for each index child and any preschool siblings of participating families. Researchers in both study centres, blind to the content of the parent-completed injury calendars, worked with colleagues in emergency departments, walk-in centres and primary care, to screen electronic records for attendances for injury in these settings.
Secondary outcomes
Secondary outcomes specified in the original study protocol included:
-
parent-reported home injuries to the index child or their preschool siblings that did not require medical attention over the 6-month follow-up period (also recorded on the injury calendar described above)
-
child behaviour, using age-appropriate validated measures: the Strengths and Difficulties Questionnaire,95,96 the Battle of Wills questionnaire97 and the Infant Behavior Questionnaire98 at baseline, 3 months and 6 months
-
parental knowledge of how to respond to four common first aid scenarios, at baseline and 6 months, using a questionnaire previously developed by a member of the research team99
-
parent-reported home safety practices and use of home safety equipment, at baseline and 6 months, using a questionnaire previously developed by a member of the research team100
-
maternal well-being, using the Warwick–Edinburgh Mental Well-being Scale,101 at baseline and 6 months
-
parenting styles and practices, using the Parent Supervision Attributes Profile Questionnaire (PSAPQ),102 at baseline and 6 months.
Process measures
In the original study protocol we proposed the following process measures to quantify aspects of recruitment and delivery to inform any future main trial:
-
recorded by the health visitor team: the number of families eligible to participate, estimated from the number of notifications to the health visitor team
-
recorded by the research team: the number of families referred by the health visitor team to the researchers, and the number of families consenting to participate
-
recorded by the health visitors delivering the intervention: the number of intervention sessions delivered, the duration of each session and the number of attendees at each session.
Qualitative evaluation of the study
We used qualitative methods to explore the experience of receiving/delivering the intervention, and to explore a range of issues regarding the research methodology for scaling up to a future trial. Interviews, whether by telephone or face-to-face, used topic guides and were digitally recorded where consent was given to do so. An example topic guide is provided in Appendix 9. The content of topic guides was determined following team discussions and based upon previous experience of evaluating interventions with parents, the literature regarding barriers and facilitators to parental engagement in programmes, feedback on the programme from the PAG and the need to determine the strengths and areas for improvement of the programme. Digital recordings were transcribed and analysed thematically. Focus groups also used topic guides and were digitally recorded to validate the notes recorded on a flip chart. These notes were analysed thematically. Digital recordings from focus groups were not formally transcribed.
-
We interviewed a Nursery Nurse and Health Visitor Clerk in Bristol regarding their experience of recruiting to the study.
-
An interview was conducted with one of the research nurses in the Emergency Department in Bristol to determine the factors relating to the experience of attempting to recruit participants through this service.
-
Interviews were held in both study centres with the children’s centre managers regarding their participation in the study, both in recruitment and in hosting the parenting programme (for intervention arm centres). Interviews were either by telephone (Bristol) or face to face (Nottingham), conducted by the research team.
-
We conducted focus groups with parents in the intervention arm upon completion of the course to evaluate their perceptions of participation in the feasibility study and their views on the parenting programme. Focus groups were facilitated by two researchers, with one taking notes on a flip chart. In addition, at the end of each session of the parenting programme the parents participating were asked by the facilitators to record the components of that session that were the most and the least enjoyable and/or helpful for them. These paper records were available during analysis of the focus groups.
-
We held face-to-face interviews with the health visitors and nurses who had delivered the programme in Nottingham. In addition, a joint focus group across both study centres for all the trainers and cofacilitators after all the courses had been delivered was held in Bristol, facilitated by four of the researchers, with one taking notes on a flip chart. The interviews and focus group were used to explore issues regarding the content and delivery of the parenting programme, and to explore issues regarding recruitment and retention of participants for scaling up to a main trial.
At the end of the follow-up period, parents in the intervention and control arms were contacted, where possible, by telephone for a brief interview to collect information on their experience of participation in the study overall, on recruitment, completion of questionnaires and follow-up (including completion of the injury calendar). Telephone interviews were digitally recorded but not formally transcribed and points made by the participants were recorded in a chart to aid reporting using the principles of framework analysis.
Qualitative study outcomes relating to recruitment to, and participation in, the feasibility study are reported in the results section below. The outcomes relating to the parents and deliverers perceptions of the parenting programme are reported in Chapter 7.
Sample size
In both study centres an average of 60–100 children meeting the eligibility criteria for this study are notified to each health visitor team each year. We aimed to recruit a total of eight health visitor teams and up to 96 parents across the two study centres and both treatment arms. This equates to two health visitor teams and 24 parents per treatment arm in each study centre. We anticipated attrition of up to one-third of parent participants between recruitment and commencement of the intervention. As this was a feasibility study, a formal sample size calculation was not undertaken. We considered that collecting outcome data on approximately 32 families in each arm would be sufficient to address our objectives.
Statistical analyses
Data were analysed using Statistical Product and Service Solutions (SPSS; SPSS Inc., Chicago, IL, USA). Descriptive statistics (frequencies, proportions and means) were obtained to describe the characteristics of the participants, and the primary and secondary outcome measures. A rate of injury occurrence per unit period of follow-up in the index children and in their siblings was calculated. The focus of the analytical strategy was on recruitment and retention rates and any difference in the primary outcome to inform a future study. We evaluated the completion of secondary outcome measures by parent participants at each time point. We did not intend to conduct comparative analyses as the study was not powered to detect a difference between groups. Analyses were blind to treatment arm allocation.
User involvement
The PAG met five times during the course of the study with an additional thank-you meeting just after the study had finished. The introductory meeting was facilitated by the children’s centre manager and the mothers read and commented on our information leaflets for parents that were about to be submitted for approval by the Local Research Ethics Committee (SW3 Bristol). They were happy with the leaflets, did not suggest any changes and felt that they understood what people were being asked to take part in. All the mothers felt that the first aid course was a good idea, particularly for first-time mothers. Subsequent meetings discussed the development of the parenting programme, the design of the outcome measures booklet, the injury calendar, publicity materials for use in the children’s centres and the format and running of a main trial.
Telephone survey of children’s centres
During the course of the feasibility study it became apparent that ‘usual care’ for control arm participants may be an insufficient incentive to encourage parents to join the study, and that randomisation to receiving the parenting programme or accessing an alternative course may be more attractive. Through engagement with children’s centres in both study centres, it became apparent that the provision of first aid courses was very common. In order to determine the extent to which children’s centres routinely provided first aid courses for parents, delivered either by staff from the children’s centre or by an external agency, a telephone survey of children’s centres was undertaken in June 2012 in Nottingham and during July and August 2012 in Bristol.
A short telephone survey was designed. The contact details of children’s centres were found by searching websites of local authorities in Bristol, Nottingham City and Nottinghamshire County. A Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) spreadsheet was designed to record the contact details of each children’s centre, the job title of the responder and the survey responses.
Results
Recruitment
Recruitment of children’s centres and health visitor teams
Four children’s centres were recruited in Bristol (referred to as P, A, H and C) and four in Nottingham (referred to as B, F, D and L) through a process that required negotiation and agreement with linked health visitor teams.
In Bristol, one children’s centre (H) withdrew prior to any parents being recruited at that site. The reason for the withdrawal was that a senior manager at the centre had not approved the agreement to participate given by the junior manager, and a first aid course delivered by a private provider had been booked at the children’s centre for the same period in which we may have wanted to run our programme at that site. Owing to the risk of contamination from a concurrent independent first aid course, we accepted the withdrawal and identified a replacement children’s centre in a different location in the city (children’s centre O).
In Nottingham the health visitor teams attached to two children’s centres (D and L) requested to withdraw from the study as they did not have the capacity to contribute. They were therefore replaced with two alternative children’s centres (S and W, respectively.) Discussions indicated that children’s centre W was within walking distance of another centre (T) and that they worked closely together, sharing a catchment area and using each other’s facilities. Consequently, children’s centres W and T were treated as a single centre participating in the study (and hereafter referred to as children’s centre T).
In Bristol, none of the lead health visitors in the teams linked to participating children’s centres had the capacity to deliver the intervention or the capacity to provide a member of their skill mixed team to cofacilitate delivery. This decision taken by lead health visitors was supported by their line managers. One lead health visitor in the city, a co-applicant on the study, and working with a children’s centre not taking part in the study, agreed to deliver the programme in both intervention children’s centres. An advert was cascaded to all health visitor teams across the city to identify a cofacilitator to support delivery and a part-time children’s nurse working in another team unconnected to the study was identified to fulfil this role.
In Nottingham, a health visitor manager identified the health visitor teams that the researchers could approach regarding participation in the study. Senior health visitors in two of the teams expressed an interest in the study and therefore it was negotiated that these two health visitors, supported by a member of their skill mixed team, would be trained and deliver the programme in whichever of the children’s centres were randomised as intervention sites. One cofacilitator subsequently left her post before delivery of the programme commenced. It was intended that she would be replaced by one of her colleagues but a replacement was not identified. The senior health visitor in this pair delivered the programme alone. As she was very experienced in working with groups of parents, she felt comfortable with this arrangement.
Recruitment of parents
Across the two study centres we aimed to recruit 12 families from a total of eight children’s centre catchment areas (n = 96), with the expectation of attrition between recruitment and start of the intervention. We hoped that by the time of commencement of the parenting programme courses in those children’s centres in the intervention arm we would still retain approximately eight families from each children’s centre area (total number of retained participants n = 64). Using four methods to identify eligible participants, we recruited a total of 40 parents to the trial. The numbers of referred eligible and recruited parents, by method of identification and by children’s centre area, are summarised in Table 3.
| Methods of identification | Bristol children’s centres | Nottingham children’s centres | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| C | A | P | O | F | T | S | B | ||
| Referred parents: details of eligible families forwarded to study team | |||||||||
| Health visitors | 5 | 6 | 1 | NA | 3 | 1 | 1 | 0 | 17 |
| ED via telephone | 14 | 12 | 13 | 21 | NA | NA | NA | NA | 60 |
| ED via posta | NA | NA | NA | NA | 2 | 4 | 3 | 0 | 9 |
| Children’s centres | 1 | 5 | 3 | 4 | 1 | 1 | 0 | 0 | 15 |
| Total | 20 | 23 | 17 | 25 | 6 | 6 | 4 | 0 | 101 |
| Recruited parents | |||||||||
| Health visitors | 3 | 2 | 1 | NA | 3 | 1 | 0 | 0 | 10 |
| ED via telephone | 8 | 1 | 4 | 3 | NA | NA | NA | NA | 16 |
| ED via post | NA | NA | NA | NA | 1 | 2 | 2 | 0 | 5 |
| Children’s centres | 0 | 2 | 2 | 3 | 1 | 1 | 0 | 0 | 9 |
| Total | 11 | 5 | 7 | 6 | 5 | 4 | 2 | 0 | 40 |
If parents initially expressed an interest in the study but then declined to participate, they were asked if they were prepared to say why they did not want to take part. In Bristol, 14 parents provided a rationale (number = number of respondents): illness in the family (3), just had a baby/about to have a baby (2), not got the time (2), working (2), injury event still too upsetting (1), currently breastfeeding twins (1), moving house (1), too much of a commitment (1).
Identification of potentially eligible parents by health visitor teams was reported to be difficult for two reasons:
-
None of the health visitor teams routinely kept a dated log of faxed emergency department notifications. Unless action was required (e.g. family known to social services or child at risk) faxes were filed in paper records. Therefore, identification of potentially eligible families retrospectively required a trawl through paper records, which the teams did not have capacity to undertake.
-
Where teams attempted to telephone parents to ask if their contact details could be forwarded to the research team, the caller frequently had to make multiple attempts to contact the parent. This time commitment was perceived as onerous.
The identification of eligible parents via a postal mail-out from the emergency department was tried following a 30% response rate in an injury prevention study conducted by one of the co-applicants, where parents were asked to complete and return a questionnaire. Following a review of emergency department attendances of preschool children with injuries in the previous 6 months, 202 letters were sent out with a reminder letter sent 2 weeks later to those who had not responded (n = 200). A further review of attendances between 6 and 13 months previously led to an additional 149 letters being sent out, that is to say a total of 351 letters were posted. The response rate was very low with only nine families requesting further information (2.6%), one of which did not meet the inclusion criteria. In total, five parents were recruited via this strategy, a recruitment rate of 1.4% (5/351). Expressing interest in taking part in a trial is a greater commitment than completing a questionnaire and this may account for the poor outcome from this method of identification.
Identification of eligible parents via children’s centres involved either the researcher or children’s centre staff introducing the study to parents when they attended the centre for activities and support. Across the two study centres researchers attended 33 parenting groups (Nottingham children’s centres, n = 17; Bristol children’s centres, n = 16). While parents were generally interested in the issue of keeping their children safe from injuries, most stated that their child had not had an injury requiring medical attention. Attending the same groups over several weeks became increasingly less productive as a greater proportion of parents had already been approached to take part in the study.
Randomisation
In Bristol, two children’s centres were randomly allocated to intervention (n = 17 parents) and two to control (n = 12 parents). As recruitment to the study was slow, effort was directed at improving recruitment in two children’s centre areas first, allowing randomisation of this pair, with randomisation of the second pair of children’s centres 3 months later. As children’s centres had to book rooms for the course for 8 weeks, it was not possible to ask them repeatedly to delay the possible start date of the course because of the slow recruitment to the study. Therefore, a start date had to be agreed, and randomisation had to take place, before 12 families had been recruited in each children’s centre area.
In Nottingham, despite extensive efforts over 5 months, no parents were recruited from one children’s centre area (B), and only two parents from another children’s centre area (S). As it was not viable to randomise these two sites, they had to be withdrawn from the study. The two parents recruited at children’s centres were sent letters advising them that the study was no longer running in their area, but thanking them for their interest and participation to that point. As the primary interest of the study at this stage was to explore whether or not the intervention could be delivered rather than to determine intervention effect sizes, a decision was taken to non-randomly allocate both remaining children’s centres in Nottingham to the intervention arm. This decision allowed the parenting programme to run twice in Nottingham, maximising the opportunities for learning from delivery of two parenting programmes. The decision was taken with the agreement of the chairperson of the Trial Steering Committee. Neither the children’s centres nor parents were aware of their non-random allocation to the intervention arm.
Delivery of the intervention
In Bristol, because there was only one trainer and cofacilitator pair, the parenting programmes needed to run sequentially, as the health visitor and nurse could not be released from existing commitments twice in any one week. The first parenting programme course was run at children’s centre C on a Thursday afternoon, 13.30–15.00, between January and March 2012. Of the 11 mothers recruited at this site, two were not contactable by the time the course was due to start, four were not free on the afternoons when the course was running because of work or other regular commitments, and five stated that they would attend the course. The number of parents attending each session is shown in Table 4. The course was interrupted by two breaks, one when both the trainer and cofacilitator were unable to attend and one due to the half-term holiday.
| Week | No. of attendees (n = 11 recruited) |
|---|---|
| 1 | 2 |
| 2a | 4 |
| Staff absenceb | No course |
| 3 | 2 |
| Half-term holiday | No course |
| 4 | 1 |
| 5 | 2 |
| 6c | 3 |
| 7 | 2 |
| 8 | 1 |
Participants for the second parenting programme were recruited through children’s centre O. A total of six mothers were recruited prior to the start date of the course, which was held on Monday afternoons, 13.30–15.00 between April and June 2012. One parent worked on the day the course was running and another was not contactable after recruitment, leaving four potential attendees. One parent dropped out because she was getting married and would be spending time abroad during the course, and a second parent dropped out after week 1 of the course, possibly because her English was not strong enough to allow her to participate. The remaining two mothers attended regularly. This course was interrupted by two breaks, one for a bank holiday, the second for half term (Table 5). Two weeks before the course was due to commence the children’s centre manager disclosed that she had released one of the rooms that had been set aside for the crèche to another service provider. As we believed it important that the crèche and the course needed to be hosted in the same venue, the course was held in a nearby community hall already known to the parents attending the course. The health visitor and cofacilitator delivering course 2 had identified some issues with the order of activities during delivery of course 1. Therefore, and with the agreement of the chief investigator, the order of some activities was changed during course 2, while continuing to deliver the same material overall.
| Week | No. of attendees (n = 6 recruited) |
|---|---|
| 1 | 3 |
| 2 | 2 |
| 3a | 1 |
| Bank holiday | No course |
| 4 | 2 |
| 5 | 2 |
| 6 | 2 |
| Half-term holiday | No course |
| 7a | 1 |
| 8 | 2 |
Participants completing either course 1 or course 2 in Bristol were given certificates at the end of the programme. All parents in intervention and control arms (including intervention arm parents who had not been able to attend the programme) were sent injury calendars and asked to participate in the follow-up period.
In Nottingham, there were two delivery teams so that the parenting programmes could be delivered concurrently. A decision was taken to stagger the courses by 1 week to facilitate access to the shared box of programme resources. Course 1 was planned in children’s centre T on Tuesday lunchtimes, commencing 21 February 2012, and course 2 was planned in children’s centre C on Monday mornings, commencing 27 February 2012. Despite attempts by telephone, text message and letters to contact participants, none of the six parents recruited to attend course 1 at children’s centre T attended the first session on 21 February 2012, and none of the four parents recruited to attend course 2 at children’s centre C attended the first two sessions on 27 February or 5 March 2012. Of the six recruited parents in course 1, a reason for non-attendance was obtained for four: one had college commitments on the day of the course, one had a family commitment, one was moving house and one was unwell. Of the four parents due to attend course 2, a reason for non-attendance was obtained for one parent who had work commitments on that day.
The inability to deliver the courses to parents recruited to the study in Nottingham allowed the opportunity to explore alternative models of delivery of the intervention. Following discussions between study teams and children’s centres, and with the agreement of the chairperson of the Trial Steering Committee and the programme manager at the NIHR HTA, we attempted to identify new participants for the two courses by opening up the course to any parent attending either of the two children’s centres that were delivering the programme, irrespective of whether or not their child had sustained a medically attended injury in the previous 12 months. Posters were displayed in children’s centres and the children’s centre staff drew attention to the course. Researchers attended the children’s centres to promote the programme. Parents were told that a new course had been developed to help parents keep their child safe from injury and that we were looking for parents to test out the course and tell us what they thought of it. Parents were not formally recruited to the study at this stage but merely had to sign a list to register their interest to attend. Over the course of 1 week at children’s centre T, eight people registered to attend (seven parents plus the teenage son of a parent who was interested in child care), and over 2 weeks at children’s centre C, five people registered to attend (four parents plus the mother of a parent with learning difficulties, who attended with her daughter throughout the course). Hereafter, these parents are referred to as ‘open invite’ parents to distinguish them from those parents formally recruited to the study.
Course 1 at children’s centre T in Nottingham recommenced on 28 February 2012 and ran for 8 weeks until 1 May 2012, with a 2-week break for the Easter holiday. The course was delivered on Tuesday lunchtimes, 13.00–14.50 (90 minutes + 20-minute break). A sandwich lunch was offered from 12.30 to 13.00 to encourage attendance. The eight ‘open invite’ participants attended all eight sessions. One of the parents originally recruited to the study attended weeks 1 and 2 before dropping out of the course after she broke her arm (Table 6). Despite agreement to run the course at children’s centre T, this arrangement turned out not to be convenient for the children’s centre staff as they lost access to a room they normally used at lunchtime, and therefore after week 3 the venue was moved to a community centre a short walk away. This change of venue did not result in any loss of attendance by course participants. The health visitor delivering the course collected feedback from participants at the end of each week.
| Week | No. of attendees (n = 8 ‘open invite’ parents) |
|---|---|
| 1a | 9 |
| 2 | 9 |
| 3 | 8b |
| 4 | 8 |
| 5 | 8 |
| Easter | No course |
| Easter | No course |
| 6 | 8 |
| 7 | 8 |
| 8 | 8 |
Course 2 at children’s centre C in Nottingham recommenced on 12 March 2012. The health visitor and cofacilitator delivering this course could be released for a total of only 8 weeks, and as the first 2 weeks has been lost with no attendance, only 6 weeks remained available. Components of weeks 1 and 2 from the original course, and from weeks 7 and 8, were combined, and the sessions were extended from 90 minutes to 2 hours to try to deliver as many of the components in the original programme as possible. The course was delivered between 10.00 and 12.30 (120 minutes + 30-minute break). Participants were encouraged to attend from 09.30 to allow the programme to start by 10.00. The course was run between 12 March 2012 and 30 April 2012 with a 2-week break for Easter (Table 7). Two of the participants dropped out of the study after the 2-week break at Easter.
| Week | No. of attendees (n = 5 ‘open invite’ parents) |
|---|---|
| 1 + 2 | 5a |
| 3 | 5 |
| 4 | 5 |
| Easter | No course |
| Easter | No course |
| 5 | 3 |
| 6 | 3 |
| 7 + 8 | 3 |
At completion of the programmes for ‘open invite’ participants in Nottingham, participants were given certificates of attendance and a free first aid kit (provided at a discounted rate from a major pharmacy company). Ethical approval was obtained (University of the West of England, Bristol) to invite the ‘open invite’ participants who had completed the course to join the study at this point; specifically, to complete a form telling us details about themselves and their family, and to complete an injury calendar for a 3-month period. Of the eight participants completing the course at children’s centre T, seven parents consented to participate, and of the three participants completing the course at children’s centre C, two parents consented to participate.
In summary, our efforts resulted in three groups of participants: (1) those recruited via health visitor teams, via emergency departments or via children’s centres where parents were randomised to intervention or control arms, (2) those recruited via health visitor teams, via emergency departments or via children’s centres where parents were purposefully allocated to the intervention arm, and (3) participants attending the intervention following an open invitation to experience the programme. A diagram illustrating the flow of individual participants through the feasibility study is shown in Figure 6. A modified Consolidated Standards of Reporting Trials (CONSORT) flow chart including clusters and participants is shown in Figure 7.
FIGURE 6.
Flow diagram of individual participants through the feasibility study.
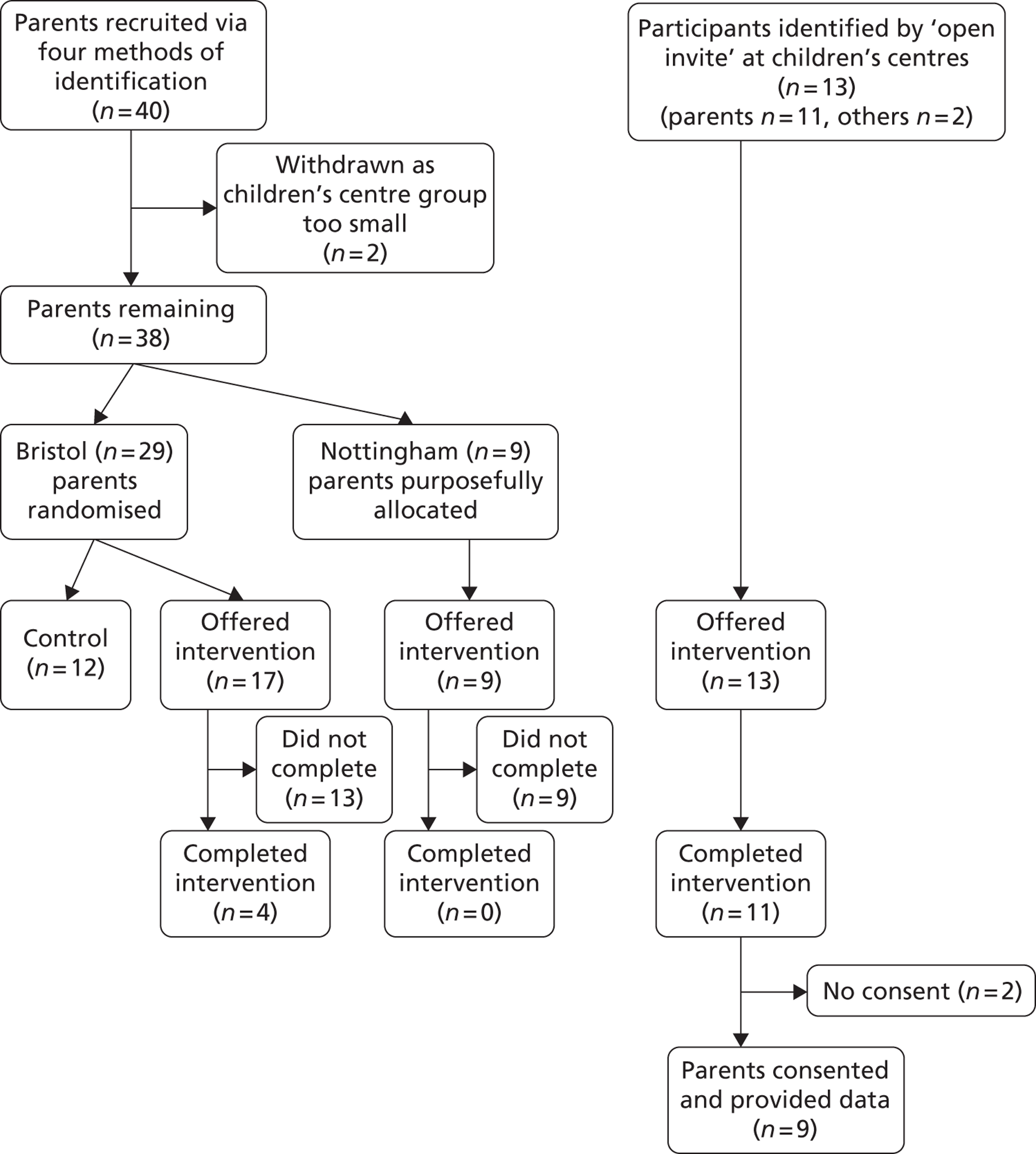
FIGURE 7.
Flow diagram of progress of clusters and individuals (modified CONSORT diagram to illustrate different recruitment strategies).
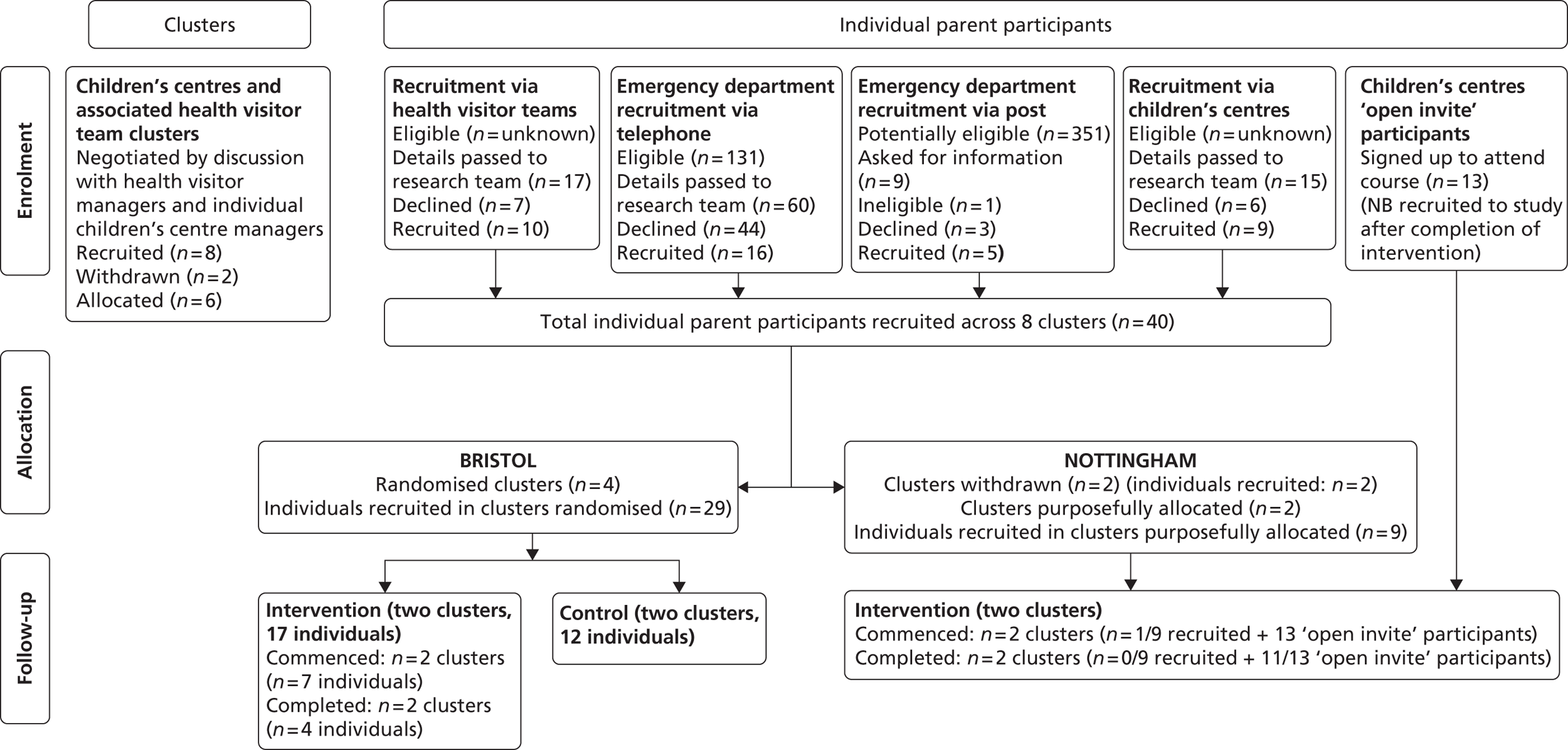
Retention and completion of measures
As identified in our protocol both recruitment and retention to the feasibility study were anticipated to be challenging. A summary of the retention and completion of measures for 51 participants is presented in Table 8. Data are shown for participants according to the three groups previously described: those randomised to intervention or control arms, those purposefully allocated to the intervention arm and those experiencing the intervention following an ‘open invite’.
| Randomised control arm participants (N = 12), n/N (%) | Randomised intervention arm participants (N = 17), n/N (%) | ‘Open invite’ participants (N = 13),a n/N (%) | Purposefully allocated participants (N = 9), n/N (%) | Total, n/N (%) | |
|---|---|---|---|---|---|
| Completed baseline questionnaire | 12/12 (100) | 17/17 (100) | 9/13 (69) | 9/9 (100) | 47/51 (92) |
| Commenced intervention | NA | 7/17 (41) | 13/13 (100) | 1/9 (11) | 21/39 (54) |
| Completed intervention | NA | 4/7 (57) | 11/13 (85) | 0/9 (0) | 15/21 (71) |
| Commenced follow-upb | 12/12 (100) | 16/17 (94) | 9/13 (69) | 7/9 (78) | 43/51 (84) |
| Returned 3-month follow-up questionnaireb | 6/12 (50) | 10/16 (63) | NA | 0/9 (0) | 16/37 (43) |
| Returned 6-month follow-up questionnaireb | 5/12 (42) | 9/16 (56) | NA | 1/9 (11) | 15/37 (41) |
| Returned all/partial injury calendar pagesc | 7/12 (58) | 10/16 (63) | 6/9 (67) | NA | 23/37 (62) |
| ED/WIC/GP data on injury attendance for validation available | 12/12 (100) | 16/16 (100) | 9/9 (100) | 7/7 (100) | 44/44 (100) |
Of 39 participants allocated to the intervention arm [randomised (n = 17), purposefully allocated (n = 9) and ‘open invite’ (n = 11)], only 15 completed the intervention, although completion was significantly higher (Fisher’s exact test, p = 0.002) among those recruited using the ‘open invite’ approach (85%) than using the other two approaches (31%).
Of the 17 parents randomised to the intervention arm, one withdrew from the study. Of the nine parents purposefully allocated to receive the intervention, two withdrew from the study after the first baseline visit. The remaining seven parents were sent 6-month follow-up questionnaires even though they had failed to attend the course. One of these returned their questionnaire. Reminder letters and a further questionnaire were sent but no further replies were received. These seven parents were not asked to complete injury calendars.
Of the 13 participants in the ‘open invite’ group, one was the mother of a parent with learning difficulties and one was the teenage son of a parent, who was interested in a career in child care. Of the 11 ‘open invite’ parent participants, nine subsequently consented to provide complete questionnaires and a 3-month injury diary.
The data show that approximately two-thirds of those sent injury calendars returned partial or complete calendar pages, suggesting that this new measure to record parent reported injuries in the home was relatively well received. Our early concern, that parents may be reluctant to report injuries occurring to their children for fear of being judged, does not appear to have been supported by this response rate. It was possible to obtain emergency department, NHS walk-in centre and general practice records to validate the parents’ reports of NHS service use for injuries for all of the participants who commenced follow-up.
Characteristics of participants in the study
Table 9 shows the characteristics of participants receiving the intervention and those in the control arm. The 26 parents either randomised or offered the intervention had 31 preschool children between them. The 12 parents randomised to the control arm had 18 preschool children between them. The data show that despite the problems with recruitment we were able to enlist parents, mostly mothers, across a range of ages, and with variable ethnicity, marital status and highest educational level. The index children of the parents recruited to the study were predominantly boys, reflecting the increased prevalence of home injuries in this group. None of the index children was below 3 months of age at the time the parents were recruited to the study.
| Variables | Values | Control arm, n/N (%) | Eligible to receive intervention [randomised (n = 17) + purposefully allocated (n = 9) + ‘open invite’ (n = 9)], n/N (%) |
|---|---|---|---|
| Parent/carer | |||
| Sex | Female | 11/12 (92%) | 34/35 (97%) |
| Male | 1/12 (8%) | 1/35 (3%) | |
| Age | Average (years) | 33.7 | 29.7 |
| Range (years) | 28–39 | 19–46 | |
| Ethnicity | White | 8/12 (67%) | 29/34 (85%) |
| Non-white | 4/12 (33%) | 5/34 (15%) | |
| Highest level education | At or before school-leaving age (UK = 16 years) | 3/12 (25%) | 15/34 (44%) |
| After school-leaving age (e.g. college, university) | 9/12 (75%) | 19/34 (56%) | |
| Marital status | Single/no partner | 2/12 (17%) | 15/34 (44%) |
| Married/partner | 10/12 (83%) | 19/34 (56%) | |
| Index child | |||
| Sex | Female | 4/12 (33%) | 15/35 (43%) |
| Male | 8/12 (67%) | 20/35 (57%) | |
| Age at entry to study | < 3 months | 0/12 (0%) | 0/34 (0%) |
| 3–12 months | 2/12 (17%) | 8/34 (24%) | |
| 13 months to < 2 years | 3/12 (25%) | 10/34 (27%) | |
| 2–5 years | 7/12 (58%) | 16/34 (48%) | |
| Other preschool siblings | Yes | 5/10 (50%) | 8/34 (24%) |
| No | 5/10 (50%) | 26/34 (76%) | |
| Average number of preschool siblings | 0.6 (6/10) | 0.3 (9/34) | |
After recruitment had commenced, we added two questions to our baseline questionnaire for participants: one asking whether or not the parent had previously attended a first aid course, and a second question asking whether or not the parent had previously attended a support course for parents. The rationale for adding these questions was that previous attendance at such courses could have influenced their decision to attend the FAST parent programme. Five parents recruited to the control arm, seven parents recruited to the intervention arm and all nine of the ‘open invite’ parents consenting to participate in the study were asked these questions. Attendance at first aid courses was common: four out of five parents in the control arm, five out of seven parents in the intervention arm and three out of nine parents in the ‘open invite’ arm. Previous attendance at a parent support programme was less common: none of five parents in the control arm, one of seven parents in intervention arm and three of nine parents in the ‘open invite’ arm.
Primary outcome
The primary outcome was the rate of parent-reported medically attended injuries to the index child or their preschool siblings occurring in a home setting. The injury calendar was used to collect this measure. The number of injury calendars sent to parents is summarised in Table 10. Six-month injury calendars for 16 index children and two preschool siblings were sent to 16 parents randomised to receive the intervention (108 child-months) and 3-month calendars were sent for nine index children and three preschool siblings of the nine ‘open invite’ parents (36 child-months). Injury calendars were not sent to the parents purposefully allocated to the intervention arm. Therefore, calendars covering 144 child-months were sent to parents offered the intervention. Six-month injury calendars were sent for 12 index children and six preschool siblings of 12 parents randomised to the control arm (108 child-months).
| Group | Parents sent calendars (n) | Children (index children + siblings) (n) | Months of calendars sent (n) | Child-months (n) |
|---|---|---|---|---|
| Randomised to intervention | 16 | 18 (16 + 2) | 6 | 108 |
| ‘Open invite’ parents receiving intervention | 9 | 12 (9 + 3) | 3 | 36 |
| Randomised to control | 12 | 18 (12 + 6) | 6 | 108 |
The number of injury calendars returned by parents, by study group, is summarised in Table 11. Calendars were returned for 60 child-months from 10 parents (10 index children + three siblings) randomised to intervention, and for 23 child-months from six ‘open invite’ parents (six index children + two siblings). Of these 83 child-months of observation from parents either randomised to intervention or in the ‘open invite’ group, 41 child-months were from parents who had completed the parenting programme. Calendars were returned for 62 child-months from six parents randomised to the control arm (six index children + five siblings). Parents who returned pages from the injury calendars did not always return all of the pages they had been sent.
| Group | Parents returning calendars (n) | Children (index children + siblings (n) | Calendar pages returned, actual/possible (%) | Proportion child months returned/total sent, n/N (%) |
|---|---|---|---|---|
| Randomised to intervention | 10 | 13 (10 + 3) | 60/78 (77) | 60/108 (56) |
| ‘Open invite’ parents receiving intervention | 6 | 8 (6 + 2) | 23/24 (96) | 23/36 (64) |
| Randomised to control | 6 | 11 (6 + 5) | 62/66 (94) | 62/108 (57) |
In total, 151 injuries were reported by the parents using the injury calendars. More injuries were reported by parents in the intervention arm of the study. Of the 25 parents eligible to receive the intervention (either randomised or ‘open invite’), who between them had 30 preschool children, 16 parents (64%) reported a total of 120 injuries in 21 index children or their preschool siblings. Of 12 parents randomised to the control arm, who between them had 18 children, seven parents (58%) reported a total of 31 injuries in 12 index children or their siblings. Participation in the intervention arm may have heightened awareness of injuries, which may have increased the risk of enhanced recall bias in this group.
This study was not powered to detect a difference in effect between groups and therefore we have not conducted an intention-to-treat analysis. An analysis of those receiving the intervention compared with the control group has been undertaken. The rate of any child injury reported by nine parents who completed the parenting programme and returned injury calendars (either randomised or ‘open invite’ parents) was 1.7 injuries per child-month (69 injuries over 41 child-months), compared with 0.5 injuries per child-month (31 injuries over 62 child-months) in the children of six parents in the control arm. We defined injuries as those causing a mark that lasted longer than 1 hour, or an ingestion event. However, visual analysis of the free text provided by parents describing the injuries suggests that parents who attended the parenting programme were more likely to report more minor injuries than those in the control arm. For example, one parent reported 24 injuries in her three preschool children over 3 months, while others reported injuries, such as ‘banged knee’ or ‘bumped head’, that required no action other than a ‘cuddle’. While this may illustrate an appropriate heightened awareness of injury following attendance at the parenting programme, it is possible that some injuries reported by parents on the injury calendars did not meet our definition of an injury. These findings suggest that amendments to the instructions on the calendar and the way the calendar is introduced to parents would be appropriate for a future trial to ensure that parents in both arms know when and when not to record an injury. It also suggests that a more objective outcome measure is needed rather than relying solely on parental report.
Heightened parental concern and major injuries were more likely to involve contact with NHS providers, and so these data were also captured in pursuit of an objective outcome. In the nine parents who completed the parenting programme (either randomised or ‘open invite’) and returned injury calendars, there was one injury reported that required NHS provider use over 41 child-months, that is to say a rate of 0.024 injuries per child-month or 0.024 episodes of NHS provider use per child-month. The single episode of NHS provider use was a telephone call to emergency services (‘phoned 999’) but the injury did not require any further NHS provider care. In comparison, in the seven parents randomised to the control arm who returned injury calendars, there was one injury reported that required four episodes of NHS provider use over 62 child-months, that is to say a rate of 0.016 injuries per child-month or 0.065 episodes of NHS provider use/child-month. These four episodes of NHS provider use were one episode each of ‘phoned NHS Direct’, ‘phoned GP’, ‘visited NHS walk-in centre’, and ‘visited emergency department’. One parent in the intervention arm who was unable to attend the parenting programme owing to work commitments but who did complete an injury diary for the 6-month follow-up period reported that her child broke their arm, requiring a visit to the hospital.
In order to illustrate the range of injuries reported by parents using the injury calendars, the number of injury events and the number of children injured in both intervention and control arms of the feasibility study are reported in Table 12. No comparisons between groups have been undertaken owing to the small samples in this feasibility study.
| Variable | Value | Index child | Any preschool siblings of index child | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (randomised and ‘open invite’ parents; n = 25) | Control (n = 12) | Intervention (randomised and ‘open invite’ parents; n = 5) | Control (n = 6) | ||||||
| No. of injury events | No. of children | No. of injury events | No. of children | No. of injury events | No. of children | No. of injury events | No. of children | ||
| Type of injury | Broken bone | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cut/graze/wound | 33 | 11 | 10 | 3 | 20 | 3 | 4 | 2 | |
| Burn/scald | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Sting/bite | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | |
| Bruise/swelling | 21 | 8 | 2 | 2 | 9 | 3 | 3 | 1 | |
| Swallowed something | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Bang on head | 15 | 8 | 6 | 3 | 4 | 2 | 2 | 2 | |
| Eye injury | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | |
| Tooth injury | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Other | 13 | 7 | 1 | 1 | 1 | 1 | 0 | 0 | |
| Location of injury | Kitchen | 5 | 3 | 0 | 0 | 5 | 2 | 2 | 1 |
| Bathroom | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | |
| Bedroom | 7 | 3 | 2 | 2 | 1 | 1 | 1 | 1 | |
| Stairs or steps | 4 | 3 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Living room | 21 | 8 | 2 | 1 | 9 | 2 | 4 | 2 | |
| Other room | 6 | 2 | 3 | 2 | 0 | 0 | 0 | 0 | |
| Garden/yard/drive | 37 | 11 | 9 | 4 | 16 | 3 | 0 | 0 | |
| Not known | 3 | 2 | 4 | 2 | 2 | 1 | 1 | 1 | |
| Action taken | First aid | 28 | 7 | 16 | 5 | 5 | 1 | 7 | 2 |
| Telephoned GP | 0 | 0 | 0 | 0 | 0 | 0 | 1a | 1 | |
| Telephoned hospital | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Telephoned dentist | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Telephoned NHS Direct | 0 | 0 | 0 | 0 | 0 | 0 | 1a | 1 | |
| Telephoned 999 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Visited GP | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Visited hospital | 1 | 1 | 0 | 0 | 0 | 0 | 1a | 1 | |
| Visited dentist | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Visited WIC | 0 | 0 | 0 | 0 | 0 | 0 | 1a | 1 | |
| Other | 53 | 11 | 4 | 3 | 29 | 4 | 2 | 1 | |
Parent-reported injury outcomes from the injury calendars were validated against emergency department, NHS walk-in centre and general practice records where available. The injury calendars for three children reported three injuries that resulted in NHS service use. Two of these were validated against emergency department, NHS walk-in centre or general practice records. The third was a report of dialling 999 after a child fell off his bike and banged his head. The parent did not report subsequent emergency department attendance. Our methods did not attempt to validate calls to the emergency services, but there was no emergency department record of an attendance for this child subsequent to the 999 call. A review of the records for index children and preschool siblings obtained from emergency departments (n = 61), NHS walk-in centres (n = 61) and general practices (n = 58) identified 12 episodes of NHS provider use. Two of these were for foreign bodies in the nose. As we had not asked parents to report objects up the nose or in the ears, these two have been excluded from further analysis. Of the remaining 10 events, two were reported by parents on injury calendars, four were not reported on injury calendars, and four were in children for whom no injury calendar pages were returned (one of these injuries was for a burn to the hand of a toddler on hair straighteners. The general practice record indicated that this injury had been treated in a burns unit, suggesting that this could have been an injury with significant consequences for the child). Table 13 summarises these data, indicating a sensitivity of the injury calendars of 20% and a specificity of 99%.
| Parent report of an injury event using NHS service use | ED/GP/WIC record of injury event having NHS service use | Total | |
|---|---|---|---|
| Yes | No | ||
| Yes | 2 | 1 | 3 |
| No | 8 | 146 | 154 |
| Total | 10 | 147 | 157 |
Secondary outcomes
The secondary outcomes reported by the parents randomised to intervention or control arms are reported in Table 14. Data have been reported as the proportion of questionnaires completed, frequency counts and scores at baseline and follow-up. Differences between groups should not be overinterpreted owing to the small numbers of participants for whom data are available, and statistical comparisons between groups have not been reported. These data have been included only to illustrate that the recording of this battery of secondary outcomes is feasible. Parental well-being was assessed using the Warwick–Edinburgh Mental Well-being Scale,101 and only one participant at follow-up invalidated the questionnaire by leaving one element unanswered. Mean scores fell slightly in both intervention and control groups at follow-up compared with baseline. Parenting supervision, assessed using the PSAPQ,102 was well completed by those returning questionnaires. Scores for the protectiveness and belief in fate subscales of the PSAPQ increased in a positive direction at the end of follow-up compared with baseline for parents in the intervention arm. Scores for supervision at follow-up were broadly static and those for risk tolerance increased compared with baseline for parents in the intervention arm.
| Questionnaire | Action/response | Intervention (N = 17), n/N (%) | Control (N = 12), n/N (%) |
|---|---|---|---|
| Parental well-being | |||
| Warwick–Edinburgh Mental Well-being Scale101 | Sent questionnaires | 17 | 12 |
| Completed at baseline | 17/17 (100%) | 12/12 (100%) | |
| Completed at 6-month follow-up | 9/17 (53%) | 5/12 (42%) | |
| Mean score at baseline | 51.8 | 53.9 | |
| Mean score at 6-month follow-up | 50.3 | 52.4 | |
| Child behaviour | |||
| aInfant Behaviour Questionnaire98 | Sent questionnaire | 3 | 3 |
| Completed at baseline | NA | NA | |
| Completed at 3-month follow-up | 2/3 (67%) | 3/3 (100%) | |
| Completed at 6-month follow-up | 2/3 (67%) | 3/3 (100%) | |
| Battle of Wills Questionnaire97 | Sent questionnaire | 6 | 4 |
| Completed at baseline | 6/6 (100%) | 3/4 (75%) | |
| Completed at 3-month follow-up | 2/6 (33%) | 0 (0%) | |
| Completed at 6-month follow-up | 2/6 (33%) | 0 (0%) | |
| Strengths and Difficulties Questionnaire95,96 | Sent questionnaire | 8 | 5 |
| Completed at baseline | 8/8 (100%) | 5/5 (100%) | |
| Completed at 3-month follow-up | 5/8 (63%) | 2/5 (40%) | |
| Completed at 6-month follow-up | 3/8 (38%) | 2/5 (40%) | |
| Parental supervision | |||
| Parental Supervision Attributes Profile Questionnaire102 | Sent questionnaire | 17 | 12 |
| Completed at baseline | 17/17 (100%) | 12/12 (100%) | |
| Completed at 6-month follow-up | 7/17 (41%) | 5/12 (42%) | |
| Protectiveness subscale score baseline | 35.5 | 36.8 | |
| Protectiveness subscale score follow-up | 37.6 | 33.2 | |
| Supervision subscale score baseline | 27.3 | 27.4 | |
| Supervision subscale score follow-up | 27.0 | 25.8 | |
| Risk tolerance subscale score baseline | 30.1 | 30.2 | |
| Risk tolerance subscale score follow-up | 31.9 | 32.0 | |
| Belief in fate subscale score baseline | 7.6 | 8.3 | |
| Belief in fate subscale score follow-up | 7.4 | 8.8 | |
| First aid knowledge | |||
| First aid knowledge | Sent questionnaires | 17 | 12 |
| Completed at baseline | 17/17 (100%) | 12/12 (100%) | |
| Completed at 6-month follow-up | 9/17 (53%) | 5/12 (42%) | |
| Scald | Confident/very confident to provide first aid at baseline | 12/17 (71%) | 12/12 (100%) |
| Confident/very confident to provide first aid at 6-month follow-up | 6/9 (67%) | 5/5 (100%) | |
| Correct answer at baseline | 11/17 (65%) | 8/12 (67%) | |
| Correct answer at 6-month follow-up | 7/9 (78%) | 5/5 (100%) | |
| Choking | Confident/very confident to provide first aid at baseline | 11/17 (65%) | 9/12 (75%) |
| Confident/very confident to provide first aid at 6-month follow-up | 3/9 (33%) | 5/5 (100%) | |
| Correct answer at baseline | 16/17 (94%) | 11/12 (92%) | |
| Correct answer at 6-month follow-up | 8/9 (89%) | 5/5 (100%) | |
| Cut leg on glass | Confident/very confident to provide first aid at baseline | 14/17 (82%) | 8/12 (67%) |
| Confident/very confident to provide first aid at 6-month follow-up | 5/9 (56%) | 5/5 (100%) | |
| Correct answer at baseline | 14/17 (82%) | 10/12 (83%) | |
| Correct answer at 6-month follow-up | 7/9 (78%) | 5/5 (100%) | |
| Swallowed bleach | Confident/very confident to provide first aid at baseline | 6/17 (35%) | 4/12 (33%) |
| Confident/very confident to provide first aid at 6-month follow-up | 5/9 (56%) | 3/5 (60%) | |
| Correct answer at baseline | 7/17 (41%) | 7/12 (58%) | |
| Correct answer at 6-month follow-up | 5/9 (56%) | 4/5 (80%) | |
| Home safety | |||
| Home safety equipment and practices | Sent questionnaires | 17 | 12 |
| Completed at baseline | 17/17 (100%) | 12/12 (100%) | |
| Completed at 6-month follow-up | 9/17 (53%) | 5/12 (42%) | |
| No unsafe rugs at baseline | 8/17 (47%) | 7/12 (58%) | |
| No unsafe rugs at 6 months | 3/9 (33%) | 1/5 (20%) | |
| Safe kettle at baseline | 13/17 (76%) | 9/12 (75%) | |
| Safe kettle at 6 months | 2/9 (11%) | 4/5 (80%) | |
| Have gas, electric or coal fire at baseline | 8/17 (47%) | 3/12 (25%) | |
| Have gas electric or coal fire at 6 months | 1/9 (11%) | 3/5 (60%) | |
| Fireguard on all fires at baseline | 7/8 (88%) | 2/3 (67%) | |
| Fireguard on all fires at 6 months | 1/9 (11%) | 3/3 (100%) | |
| Have stairs at baseline | 13/17 (76%) | 11/12 (92%) | |
| Have stairs at 6 months | 8/9 (89%) | 5/5 (100%) | |
| Top and bottom gates at baseline | 7/13 (54%) | 5/11 (45%) | |
| Top and bottom gates at 6 months | 3/8 (38%) | 1/5 (20%) | |
| Have window catches at baseline | 11/17 (65%) | 5/12 (42%) | |
| Have window catches at 6 months | 4/9 (44%) | 3/5 (60%) | |
| Usually/almost always use window catches at baseline | 10/11 (91%) | 5/5 (100%) | |
| Usually/almost always use window catches at 6 months | 4/4 (100%) | 3/3 (100%) | |
| Have smoke alarm(s) at baseline | 16/17 (94%) | 9/12 (75%) | |
| Have smoke alarm(s) at 6 months | 8/9 (89%) | 5/5 (100%) | |
| All smoke alarms working at baseline | 16/16 (100%) | 9/9 (100%) | |
| All smoke alarms working at 6 months | 5/8 (63%) | 5/5 (100%) | |
| All medicine cupboards have catches/locks at baseline | 3/17 (18%) | 1/12 (8%) | |
| All medicine cupboards have catches/locks at 6 months | 1/9 (11%) | 0 (0%) | |
| Never drink hot drinks while holding child at baseline | 13/17 (76%) | 8/12 (67%) | |
| Never drink hot drinks while holding child at 6 months | 7/9 (78%) | 3/5 (60%) | |
| Usually/almost always check toys for small parts at baseline | 8/17 (47%) | 3/12 (25%) | |
| Usually/almost always check toys for small parts at 6 months | 2/9 (22%) | 1/5 (20%) | |
The Strengths and Difficulties Questionnaire95,96 was used to assess child behaviour for children over 2 years; however, the use of different measures below the age of 2 years was problematic as parents reported developmental change between baseline and the end of follow-up, which meant that individual questions asked during infancy at baseline were no longer appropriate by the end of follow-up when the child was a toddler. The Strengths and Difficulties Questionnaire95,96 has not been validated for use in children below 2 years. For a future trial, it would be necessary to identify an alternative single measure that can assess child behaviour appropriate to the child’s developmental age between birth and 5 years, yet still provide a pre-test–post-test change score.
All of the participants returning questionnaires at baseline and follow-up were able to complete the questions relating to first aid knowledge and home safety practices and behaviours. Minor changes to wording and question structure for these questionnaires would be required for a future trial to avoid potential misinterpretation (though no evidence of misinterpretation was identified in questionnaires returned during the feasibility study).
Qualitative outcomes
This section describes the results of the qualitative interviews with parents regarding their recruitment to, and participation in, the feasibility study. Parents’ comments relating to their perception of the parenting programme, together with the perspectives of those delivering the course, are detailed in Chapter 7.
Recruitment to the study
The primary barrier to the identification of eligible families via the health visitor teams was the ability to identify someone who had the confidence and skills to telephone the parents, together with the capacity to undertake the task:
The only way that it was possible was because I was not full-time here, so I was able to do it because I had some extra hours given to me to do it.
Bristol nurse 4
Even though service support costs were made available to buy extra staff time, this did not always enable teams to participate:
. . . the additional support costs were of little value as there was no one to backfill with.
Nottingham manager 1
In two health visitor teams in Bristol, a member of staff (one nurse and one clerk) was interested in supporting the project, but even in these settings their limited capacity to contribute resulted in very small numbers of families contacted and referred to the research team despite co-operation with the study over several months.
In contrast, the identification of potentially eligible families by the research nurse in the emergency department was feasible. The telephoning of parents who had recently attended
. . . wasn’t a very onerous task.
Bristol research nurse
The task was considered
. . . straightforward and nice to know that we were being effective [. . . in identifying potential participants].
Bristol research nurse 1
She reported that the first aid advice component of the programme was attractive to parents, with one parent reported to have said:
I didn’t know what to do. We’ve been asking our children’s centres if we can have some first aid training.
Parent reported by Bristol research nurse 1
The confidence and enthusiasm of the research nurse was reflected in the number of potentially eligible families that she was able to refer to the research team (n = 60), 27% of whom were recruited to the study (n = 16).
Staff at children’s centres reported both facilitators and barriers to the identification of eligible families for the study. The posters (which had been designed with the PAG) were perceived as helpful to raise awareness of the study:
I thought the posters were fine. We took them around to all our groups and talked to people and always had them by the signing in sheets so that they could see it. That seemed to work all right.
Bristol children’s centre 2
But the inclusion of text relating to having had an injury was seen as unhelpful by two managers at one children’s centre:
I think they immediately then back off.
Bristol children’s centre 2
The managers suggested alternative text that could have been more appealing to parents using their centre:
You know, it could be very parent friendly and say, ‘Come and bring a friend’.
Bristol children’s centre 5
The main barrier to recruitment perceived by staff at children’s centres was the requirement that parents admit that their child had sustained an injury:
I think that put people off because they felt that they were being criticised . . . oh your child has had an accident and had to go to hospital and now you need to come on this course. It almost makes you into a bad parent – it’s that initial contact.
Nottingham children’s centre 1
I think . . . the hardest part was trying to get parents engaged in it because they wouldn’t necessarily want to tell us that their child had had an accident . . .’ it can make people think . . .’Ohh . . . what do they want to know that for . . .’ I think you would get a better response if it was a general, you know [i.e. a universal invitation].
Bristol children’s centre 2
Parents were reluctant to disclose injuries to children’s centre staff even if they had an existing relationship:
Families were concerned that if there had been an accident we were involved with social services.
Bristol children’s centre 1
These concerns were supported by the programme trainers and cofacilitators:
Inviting people because they have attended A&E was one of the reasons that they did not want to come along . . . I think that focus has been really, really unhelpful.
Bristol voice 1
One of the health visitor trainers from Nottingham commented that removal of the eligibility requirement that the child had to have sustained an injury was very helpful for engaging families when they made the invitation open to any parent at the children’s centre:
. . . making it available to anybody worked really well.
Nottingham voice 2
Children’s centre staff felt that the presence of the research team in the centre to promote the study was helpful:
Much better to have the information face to face – paperwork does not work for us . . . or have someone explaining the leaflet giving it out. A lot of parents don’t read it or they get so many leaflets it [just] goes in with something else.
Bristol children’s centre 1
In addition, having the researcher visit groups at the centre was beneficial in raising the awareness of injury prevention:
. . . the awareness that has been raised with [researcher] coming to the group, even if the parents didn’t sign up they still knew that this was happening and they think ‘Oh yeah . . . maybe I ought to think about the cupboard door.’ You know it just raises awareness even just discussing it.
Bristol children’s centre 5
Parents’ experience of taking part in the feasibility study
At the end of the 6-month follow-up period, we attempted to contact recruited parents in Bristol to explore their views of participating in the study overall. Fourteen of 29 randomised parents were contactable and agreed to be interviewed by telephone: seven from the control arm and seven from the intervention arm. They were geographically spread across the four participating children’s centre areas of the city.
Parents were asked about their experience of recruitment to the study. Three had been recruited after being approached by a member of their health visitor team. All had been happy to be approached via this route. One felt that, although it was a good idea to use the health visitor team to recruit to the study, the team said that they didn’t really have much time to do this.
Another mother was asked during a routine health visitor telephone call following a visit to the emergency department. She reported that finding time to answer a letter would be difficult, and so a telephone call was better.
Eight of those interviewed had been approached via a telephone call from the research nurse at the emergency department. Four parents remembered receiving a letter about the study before being telephoned by the research team; the other four remembered having a telephone call to ask if their details could be passed to the research team:
It was good to get a letter first to explain about the study a bit. If it had been a cold call I would have been more reluctant to take part, so it was nice to have the information sent first.
Others said that it was helpful to have a telephone call, as one needs time to answer a letter.
Another wondered why she had been chosen, asking if she was singled out because she had been to the emergency department with her child.
Overall, however, they felt that it was fine to recruit through the emergency department, as it was well explained by the caller (the research nurse).
The remaining three parents had been identified via their local children’s centre. All three felt that this was a good way of recruiting mothers to a study. It was reported to be nice to be asked to take part in person in a familiar group situation. Several agreed to take part in the study on the day after chatting to the researcher:
It is a good way to recruit people with someone there to talk to face to face rather than just leaflets advertising it.
All participants felt that the information provided about the study was easy to understand and gave them what they needed to be able to take part. However, one mentioned that she had not realised that the course would last 8 weeks and had thought it was just one session.
Parents were then asked specifically about their experience of completing the outcome measures and questionnaires. Most found the questions in the booklets not too difficult to answer but that they were time-consuming. Certain questions were specifically remarked upon, such as those referring to where sharp objects and medicines were kept in the house as these might be kept in multiple locations. Some of the behaviour questions were variable depending on when they were asked:
Those with a scale of 1–5 about how confident do you feel depends on which day you ask me.
Others found the format of some of the questions more difficult to answer:
It would have helped to have talked through the questionnaires on the phone to discuss the questions.
Some people might wonder why they are being asked the same questions at several time points and so maybe explain this in the letter?
Reinforcing the message that help was available to complete the questionnaires might have helped to overcome these concerns.
One parent felt that the child behaviour measure she was asked to complete was no longer relevant for her child who had progressed developmentally:
Some of the behaviour questions were difficult to answer as they were not relevant for my child at her age almost 1 year later.
Regarding the injury calendar, all the parents interviewed reported that the injury calendar was easy to understand and complete, self-explanatory and simple to follow. They found the monthly text reminders to turn over the page to the next month useful and a good idea as they helped them remember to fill the calendar in. One suggested that a mobile telephone application would be useful; this would make it easier to make note of an injury using her mobile telephone, as she always has it with her.
The calendar was really easy to fill in with all the options and extra space to write if needed. I kept it in the kitchen so it was handy if I needed it; it was a good size and not too big; self-explanatory and really simple to use.
All appreciated receiving the vouchers but they were happy to take part regardless. They thought that vouchers may be an incentive for some to take part and return their questionnaires, but they were not sure that vouchers would get more people to attend the course.
Telephone survey of first aid courses
Twenty-seven children’s centres were identified in Bristol and 84 in Nottingham City and County. In both Bristol and Nottingham some children’s centres worked in partnership with neighbouring centres, so that programmes and courses running at one centre were available to parents attending any of the centres in that cluster. During the telephone survey, if a respondent was responsible for more than one children’s centre, we ensured that their responses applied to all children’s centres under their responsibility. In Bristol, 34 children’s centres worked as 25 individual or clustered centres. We obtained information on 25/25 (100%) centres or clusters in Bristol and on 64/81 (73%) of centres across Nottingham City and Nottingham County areas.
Where information was available, 19/25 (76%) of children’s centres in Bristol and 39/64 (61%) in Nottingham were able to offer first aid courses to parents. Two of the six centres in Bristol not running courses had done so in the past and 21 of the 25 children’s centres in Nottingham (84%) that did not run courses said they would like to host them. The main barriers to hosting courses were lack of capacity in terms of staff or space, or lack of funding.
Across both study centres courses were most commonly run once or twice per year (range 1–6), typically comprising six sessions (range 1–7), with sessions most commonly lasting 2 hours (range 1.5 hours to ‘all day’). Providers varied but were most commonly from the local college or a local authority approved trainer. Voluntary sector providers such as St John’s Ambulance and the Red Cross provided the majority of the remaining courses. Courses were most commonly held during the daytime, with only three centres in Bristol and eight in Nottingham reporting evening or weekend sessions. Courses were most commonly able to host up to 12 parents but often ran with fewer participants and targeted groups of disadvantaged families, adults with few qualifications or parents of children under 1. Full details are provided in Table 15.
| Course element | Variable | Bristol (N = 19), n (%) | Nottingham City and County (N = 39), n (%) |
|---|---|---|---|
| Number of sessions per course | 1 | 5 (26) | 3 (8) |
| 2–5 | 2 (11) | 11 (28) | |
| ≥ 6 | 11 (58) | 25 (64) | |
| Not known | 1 (5) | 0 (0) | |
| Duration of each session | ≤ 2 hours | 15 (79) | 35 (90) |
| > 2 hours | 3 (16) | 4 (10) | |
| Not known | 1 (5) | 0 (0) | |
| Time to complete course | < 6 weeks | 7 (37) | 14 (36) |
| 6 weeks | 10 (53) | 23 (59) | |
| > 6 weeks | 1 (5) | 2 (5) | |
| Not known | 1 (5) | 0 (0) | |
| Course provider | Local college | 0 (0) | 27 (69) |
| Community learning team | 12 (63) | 2 (5) | |
| St John’s Ambulance/Red Cross | 3 (16) | 6 (15) | |
| Other | 2 (11) | 2 (5) | |
| Not known | 2 (11) | 2 (5) |
Discussion
Summary of findings
We conducted a feasibility trial of a new parenting programme designed to help reduce the occurrence of home injuries in preschool children. We sought to recruit 96 parent participants with a view to 64 participating in a two-arm trial of the FAST parent programme versus usual care. We tested five methods of parent participant identification and discovered the limitations of each. We were able to recruit 40 parents and, of these, 15 were retained through to the end of a 6-month follow-up period. We also engaged 11 ‘open invite’ parents, of whom nine were retained through to the end of a 3-month follow-up period. We delivered the parenting programme in four settings across the two study centres. We identified issues relating to study design, participant identification, recruitment, retention, intervention delivery and evaluation to inform a future trial. No serious or adverse events were reported.
Strengths and limitations of the feasibility study
Despite the challenges experienced during recruitment of both health visitor teams and parent participants to the feasibility study, we have been able to complete this project on time and within budget. Recruitment to the study took longer than anticipated and the sample originally proposed was not achieved. We carefully monitored recruitment and acted promptly when strategies appeared to be unsuccessful. Multiple strategies were used to determine the most appropriate method of identifying potentially eligible participants and recruiting them. This learning can inform the design of any future trial. The different strategies were implemented with appropriate ethical approval for each amendment to the study protocol, ensuring that the study was conducted with robust research governance. These changes were supported by an experienced trial steering committee that provided constructive advice and guidance. Despite the challenges with recruitment to the feasibility study we were able to run four courses of the parenting programme as proposed, and the evaluation of the delivery provided valuable lessons for the development of both the parenting programme and any future trial.
We used a mixed methods approach to evaluate the feasibility trial, including the development and testing of a new measure for recording parent reported injuries in the home. We also conducted a preliminary validation of the tool against emergency department, NHS walk-in centre and primary care records. Our feasibility trial showed that the proposed quantitative outcomes could be collected in a future trial; for example, 32 out of 48 (67%) partial or complete injury calendars for preschool children were returned by parents. We also used qualitative techniques to explore the experience of participation in the feasibility study, and capture the experience of the parenting programme from multiple perspectives. These outcomes of the feasibility study are able to support the rationale for the conduct of a future trial.
One notable strength of our feasibility study has been the involvement of parent advisors, who have significantly informed our decision-making. We established a PAG that provided guidance on new strategies for identification and recruitment of parents, on materials used during recruitment (e.g. posters), on documentation used in the trial (e.g. parent information sheets) and on the interpretation of outputs from the study. Parent advisors have attended the Trial Steering Committee meetings supported by the PAG facilitators. Our experience of user participation in this feasibility trial has become one of the case studies used in a NIHR study on Public Involvement in Research funded by the Health Services and Delivery Research Programme (reference: 10/2001/41).
The primary limitation of this feasibility study is the difficulty experienced in recruiting the planned number of parents to the study, despite the different identification strategies used. The main reason was the eligibility requirement to recruit parents with preschool children who had already sustained an injury where medical attention had been sought from an emergency department, NHS walk-in centre or minor injuries unit. We were concerned that this criterion would act as a barrier to recruitment and this appears to have been the case. Parents are naturally reluctant to admit that their child has sustained an injury for fear of being labelled as an inadequate parent. This fact compounds the issue that not all parents wish to attend parenting programmes. The health visitor teams and the children’s centre staff that we were working with advised that the need to admit that their child had sustained an injury was the primary reason that parents were reluctant to engage. The programme facilitators running the open access programme reported that they were pleased that the open access method had recruited the families they were seeking; several parents made comments such as ‘oh, that happened to [my child]’ during the course, suggesting that the programme had in fact recruited families where children had sustained injuries. The PAG recommended that the programme should be made available to all parents, ideally before a child has sustained any injuries.
A second limitation to the study has been the challenge of working with health visiting teams, both in asking them to help identify potentially eligible participants in the trial and also as a source of programme leaders to act as deliverers of the intervention. We had consulted extensively with health visitors before submitting our proposal, and one of our co-applicants is a practising health visitor. However, we could not have anticipated the extent to which NHS reorganisation, changes in health visitor managers and reduced workforce capacity would reduce the ability to identify teams that had the interest and capacity to work with us on the feasibility study. The challenge of recruiting parents to the study and the limited capacity of health visitor teams in Nottingham were key contributory factors to the necessity to withdraw two children’s centres where the research team had been unable to recruit sufficient parents to enable randomisation to intervention and control arms. For this reason, in Nottingham, both remaining children’s centres were purposefully allocated to the intervention arm to enable two courses of the parenting programme to run in that study centre.
Where parents had been recruited using the original eligibility criteria, the numbers of parents commencing the parenting programmes was small (two at one setting and three at a second setting). One of the main reasons for this was the long delay between recruitment and randomisation to intervention or control arms (up to 5 months) and to commencement of the course, due to our extended efforts to recruit up to 12 parents to each programme. During this delay some parents returned to work or took up other commitments at the same time as when the programme was due to run. A shorter duration between opening recruitment and commencing the programme would be required in any future trial. Of the five parents who were recruited to the original eligibility criteria and who commenced the programme, four (80%) completed the course. In Nottingham, where we tested the feasibility of ‘open invite’ access to the program, there was a very short delay between invitation and commencement of the programme (maximum 2 weeks) and much higher numbers of parents commenced the programmes (nine in one setting and five in a second setting). Of these 14 parents, 11 (79%) completed the course.
The implications of these strengths and limitations for future research have been described in Chapter 8.
Learning points
-
The need to admit that your child has sustained an injury is a significant barrier to recruitment. The faster rate of participant identification through the ‘open invite’ route [we engaged 11 parents (in two settings) over 2 weeks to attend the parenting programme when an ‘open invite’ policy was used, compared with 40 parents recruited over 10 months from four settings when using the criterion of having a child who had sustained a medically attended injury] suggests that rather than target families once an injury has occurred it would be better to target families before the injury event. Significantly more parents identified through the ‘open invite’ route completed the intervention compared with those recruited using the original criteria.
-
At this point in time health visitor teams do not have the capacity to support the identification of potential participants or the delivery of the parenting programme for any future trial.
-
Using children’s centres in deprived areas would be an appropriate method to identify families, and children’s centres would be supportive of this approach in a future trial.
-
The setting for delivery of the parenting programme should be flexible to respond to local capacity and facilities. The most important factors about the setting are that it is known to parents and easily accessible. Children’s centres may provide an appropriate setting but, where necessary, alternative community venues should be used.
-
A short period of time between identification/recruitment and the start of the programme appears to be important in avoiding attrition of participants before the programme commences.
-
Once parents commenced the programme, retention rates to the end of the course were good for both parents recruited against the original eligibility criteria (80%) and those identified through ‘open access’ (79%), suggesting that the programme was well received by those attending.
-
First aid courses are very commonly provided in children’s centre settings and can be considered to be part of usual care provided to users of these settings.
-
Approximately two-thirds of parents who were sent injury calendars returned them, and 151 injuries were recorded on the returned calendar pages, suggesting that the calendar was relatively well accepted as a measure and that parents appeared comfortable reporting injuries in their children as evidenced by the number of injuries reported.
-
Not all parents who were sent injury calendars returned them, and therefore checking the records of NHS providers is important in order to identify use of these services during the follow-up period.
-
Some of the parents did not report major injuries in the calendar. In a future trial the use of an objective measure of NHS provider use would be necessary, although it would not be possible to validate all NHS provider use: for example, following up telephone calls to NHS Direct or ‘999’ calls.
-
Many of the injuries reported by parents on the injury calendars appeared minor and may not have met the definition of an injury as provided. Support to complete the injury calendars correctly would be important in a future trial: for example, amendments to the instructions on the calendar and to the way the calendar is introduced to parents to help parents in both arms know when and when not to record an injury.
-
The list of injury types on the calendar should be reviewed (for example, the addition of objects getting stuck in the nose and ears).
-
An alternative measure for recording child behaviour needs to be identified that will allow a baseline post-test comparison even in young infants, in whom significant developmental change between baseline and completion of follow-up would be expected.
Chapter 6 Parameters for a cost-effectiveness study
This chapter describes the methods used to determine the parameters for a cost-effectiveness study in a future trial. We present the costs associated with developing the intervention, and indicative costs and savings that could be recorded in a future trial, together with a discussion of issues raised.
Objective
To assess the resource utilisation and costing data that would need to be collected in a main trial.
Methods
A resource use checklist was developed based on the approach taken by Edwards et al. 60 and amended in the light of formative monitoring and experience of programme development, training and delivery, so that costs could be identified, categorised and included in the final resource use tool. 103 Costs were monitored against a checklist of usual resource use or cost categories in economic evaluations, including costs associated with programme and ‘train the trainer’ development, recruitment, delivery (professional time, facilitator fees), overheads (room hire, refresh training), equipment (resources kit) and materials (booklets, posters and visual aids). We have categorised costs using distinct costing stages that are becoming more frequently applied in economic analyses of primary prevention interventions:104 set up or development of the intervention (stage 0), planning and preparation for delivery (stage 1), delivery (stage 2), and maintenance and reinforcement (stage 3).
A record of the programme development process was kept by the research team, alongside a decision log to record the rationale for the decisions made during development, including decisions relating to programme outputs and processes. These written records were examined to identify categories of resource use. Costs that would and would not recur once a programme is mainstreamed need to be distinguished for complex interventions such as this study. An economic evaluation of the delivery of a mainstreamed parenting programme in the UK would not include intervention planning and development costs, but these have been reported here as they illustrate the resource input required for high-quality programme development. Research costs associated with setting up the scientific study are similarly not recurring and are not reported here.
Cost estimates from a funder perspective were derived for the FAST parent programme based on the timing, quantity and frequency of resource use in 2011–12 prices across all cost items. Resource inputs identified were compared with those identified and estimated by Edwards et al. 60 and costed at 2011–12 prices. 61
The resources used during the first three stages (stage 0, development; stage 1, preparation; and stage 2, delivery) were recorded retrospectively by the project team and categorised. Expenses associated with stage 2 programme delivery, including crèche, postage and refreshments, were collected and costed using established sources,61 invoices and personal communications. Travel time was estimated for all trainer inputs at children’s centres. Space hire at the delivery venues is included because some children’s centres charge for use of their rooms and alternative community venues may need to be used, in addition to the resources connected with alternative use of space in children’s centres (the opportunity cost). Overhead and capital costs are not included. Costs that may be incurred during the roll out of a programme (stage 3, maintenance) are described below but have not been estimated.
The difficulty of identifying relevant measures of benefit or resource savings to the NHS to illustrate the cost-effectiveness of parenting programmes has been established previously. 55 These benefits tend to arise in the long term, and the short-term benefits are often difficult to capture. The injury calendar (see Chapter 4 and Appendix 5) was developed for this project and tested during the feasibility study for its potential to capture parent-reported injuries during the follow-up period and the actions of parents after their child sustained an injury that had resource implications for the NHS. The validity of parent-reported injuries and the acceptability of the measure are described elsewhere in this report.
Results
The resource use checklist for the development stage (stage 0) of the FAST parent programme is presented in Table 16 together with the total cost estimates of resource use and prices separately where possible. The FAST programme required at least 101 days of staff resource at the development stage, and there was a total cost £70,300. These are non-recurrent costs.
| Stage 0 resource use checklist | Non-recurrent initial training and programme development costs | ||
|---|---|---|---|
| Unit cost (£) | Number of units | Total cost (£) | |
| Programme development and development of the ‘train the trainer’ course | 600 | 70 days | 42,000 |
| Editorial project management | 546 | 11 days | 6005 |
| Project management | 750 | 7.5 days | 5625 |
| Parent focus group preparation and delivery, refreshments, travel costs and electronic contacts for feedback | NA | NA | 2400 |
| Travel costs to project team meetings | NA | 2 journeys | 150 |
| Design of resources (outsourced) | NA | NA | 5650 |
| Printing (outsourced) | NA | NA | 1851 |
| Other resources for kits, e.g. bandages, storage boxes for resources, plastic wallets, marker pens, etc. | NA | NA | 121 |
| Postage of manuals and resources to Nottingham and Bristol | NA | NA | 198 |
| Supervision/support, including report writing and additional ‘train the trainer’ supervision (owing to late start) | 600 | 10.5 days | 6300 |
| Stage 0 TOTAL | 70,300 | ||
The costs associated with preparation to deliver the programme (stage 1), including the 2-day ‘train the trainer’ event and the equipment and resources are presented in Table 17. It is difficult to separate research costs and identify the share of the total cost for venue, accommodation and travel items at stage one that apply to one programme delivery. The assumption for venue, accommodation and travel costs in Table 17 is that three units (i.e. the trainer and two health visitors) represent the share of the total cost for these items that applies at stage 1 of the programme. Overall, stage 1 of the programme has a total recurrent cost of £3702.
| Stage 1 resource use checklist | Recurrent programme running costs (i.e. mainstream cost) | ||
|---|---|---|---|
| Unit costs (£) | Number of units | Total (£) | |
| Kit from Whoops! Child Safety Project (burns dolls, colour-change heat mug, etc.) | 445.00 | 1 kit | 445.00 |
| ‘Train the trainer’ manual | 27.50 | 2 manuals | 55.00 |
| Parent handbook | 6.00 | 12 handbooks | 72.00 |
| Flashcard sets per course | 83.00 | 1 set | 82.50 |
| A3 posters | 1.85 | 2 posters | 3.70 |
| A4 posters | 1.93 | 3 posters | 5.79 |
| Certificates | 0.61 | 12 certificates | 7.39 |
| Group labels | 0.05 | 190 labels | 9.50 |
| Resources storage boxes and wallets | 20.00 | 1 box | 20.00 |
| Whoops! leaflet | 1.00 | 12 leaflets | 12.00 |
| ‘Train the trainer’ lead delivery | 600.00 | 2 days | 1220.00 |
| Practitioners’ ‘train the trainer’ time and backfill time (2 staff × 2 days)a | 334.00 | 4 days | 1338.00 |
| ‘Train the trainer’ venue hire, refreshment costs | 28.00 | 3 | 84.00 |
| Return rail travel to ‘train the trainer’ event | 46.77 | 3 | 140.30 |
| Accommodation | 69.00 | 3 | 207.00 |
| Stage 1 SUBTOTAL | 3702.18 | ||
The costs associated with the delivery of one programme (eight sessions) of the FAST parent programme are presented in Table 18. Staff costs have been estimated for 2 hours per session (90 minutes for delivery + 15 minutes for setting up + 15 minutes for packing away). The estimated total costs associated with delivery to eight parents were £3595.
| Stage 2 resource use checklist | Recurrent programme running costs | ||
|---|---|---|---|
| Unit costs (£) | Number of units | Total (£) | |
| Time for two group leaders running sessionsa | 44.00 | 32 hours | 1408.00 |
| Time for two group leaders outside sessions (e.g. preparation, follow-up with parents)b | 44.00 | 8 hours | 352.00 |
| Mileage to deliver sessionsc | 454.00 | 54p per mile | 245.16 |
| Children’s centre space rentald | 51.00 | 9 sessions | 459.00 |
| Crèchee | 90.75 | 9 × 2 hours 45 minutes | 816.75 |
| Refreshmentsf | 25.00 | 8 | 200.00 |
| Administration supportg | NA | NA | 99.00 |
| Telephone calls to parentsh | 0.08 | 192 minutes | 15.36 |
| Stage 2 SUBTOTAL | 3595.27 | ||
| FAST stages 1–2 | NA | NA | 7297.00 |
| Cost per child (n = 8) | NA | NA | 912.00 |
Overall, the average recurrent cost of one FAST programme at stages 1 (preparation) and 2 (delivery) was £7297 in 2011–12 prices. Feasibility costing indicates that the average cost of repeating the FAST programme in its mainstream form per child with eight parents participating would be £912 in 2011–12 prices.
There is one further category of resource use that is not pertinent to a feasibility study, but would need to be considered for a future trial: programme maintenance and replacement of the resources. Consideration of the final unit costs would need to include the trainer manuals, parent handbooks, ‘train the trainer’ events, costs associated with amendments to the programme content or activities (e.g. programme developer costs and running groups for parent advisors), ongoing supply of leaflets for future courses, replenishment of choking doll ‘lungs’, broken/lost resources, quality assurance assessment, administrative support, and telephone calls to parents. Parenting UK was paid £16,000 for further development work on the parenting programme in the light of the evaluation of the programme as part of this feasibility study.
The NHS service use costs during the follow-up period were monitored using the parent-completed injury calendar, validated against emergency department, NHS walk-in centre and GP records. Participants were able to complete the injury calendar successfully and enter codes to indicate the type of injury, location of the injury event and actions taken after the injury, for each injury event. Completion of injury calendars during the feasibility study indicates that parents found them acceptable as a recording tool. The data on NHS service use collected via this tool, together with validation data from NHS providers, can be costed using a range of assumptions, established sources and references in 2011–12 prices to determine the impact of the intervention on NHS service use for a future trial. Sources of prices are referenced in Table 19 together with frequencies of NHS service use as recorded on injury calendars as an illustration.
| Item | Action taken by parent after injury event during the follow-up period | Total number of events recorded by parents on injury calendar during feasibility study | Unit cost (£) |
|---|---|---|---|
| 1 | Telephoned GP practicea | 1 | 22.00 |
| 2 | Telephoned hospital A&Eb | 0 | 64.77 |
| 3 | Telephoned dentistc | 0 | 10.69 |
| 4 | Telephoned NHS Directd | 1 | 21.00 |
| 5 | Telephoned 999e | 1 | – |
| 6 | Visited GP practicef | 0 | 36.00 |
| 7 | Visited hospital A&Eg | 2 | 106.00 |
| 8 | Visited dentisth | 0 | 17.50 |
| 9 | Visited NHS WICi | 1 | 41.00 |
In Table 19 the following assumptions have been made. We had good sources of costs for item 1 (telephoning the GP, £22) and item 6 (visiting the GP, £36), so we have assumed that the ratio of these two costs is the same for item 2 (telephoning the hospital) and item 3 (telephoning the dentist). It has been assumed that when people telephone the GP, emergency department or the dentist, the outcome of triage completed by a receptionist is that a GP, a hospital doctor or a dentist might ring back to give advice. These assumptions may be less robust for the emergency department or the dentist, but in the absence of established sources for estimates unit costs have been derived using this method.
The injury calendar list of actions does not include emergency transfers to hospital by ambulance and this should be considered if the calendar were used in a future trial. During the study we also identified the need to amend this section of the calendar to encourage parents to record multiple actions taken following an injury if these occurred. For example, a parent could telephone NHS Direct and then take their child to the NHS walk-in centre, but then be referred to the emergency department. All of these actions could be recorded on the calendar.
Discussion
The economic evaluation completed during this feasibility study has attempted to provide conceptual, methodological and methods insights as well as findings from the feasibility study to enable the design of a future cost-effectiveness evaluation in a future trial. From a feasibility perspective it makes sense to emulate other successful approaches to economic evaluation for similar programmes. The learning from a recent rigorous economic evaluation of a similar programme,60 including the resource use checklist that enables non-recurrent and recurrent resources use to be identified and measured separately, was incorporated into this study. Furthermore, an injury calendar has been developed with a simple validation against NHS service use records. These tools now exist in prototype and can be used in a future trial.
This feasibility economic analysis has established the indicative non-recurrent development costs and recurrent programme preparation and running costs for a future trial. The costing is useful in highlighting the parameters for consideration and indicating the magnitude of recurrent programme costs once mainstreaming has taken place. These costs would need to be further estimated in a future trial with p-values and CIs to be considered accurate but indicative costs compare well with the costs in similar studies,60 where in a full trial the cost per child attending a parenting programme was £1595.46 (n = 8) in 2006 prices compared with £912 per child (n = 8) in 2011 prices for the FAST parent programme.
One very useful aspect of this feasibility study has been the chance to explore and understand some of the cost and outcome dimensions of complex parenting programmes in a community setting, as these dimensions are not well understood for full trial economic analysis. However, in a full trial other dimensions of cost and outcome would need to be considered. According to Wolfenstetter,107 the outcome dimensions of programmes could comprise ‘efficacy’, ‘reach’, ‘recruitment’, ‘response rate’, ‘maintenance compliance’, ‘social impact’ and ‘unintentional consequences’, such as adverse health effects. Cost dimensions include programme development, training and implementation incorporating recruitment to the programme, participant time costs and savings and ‘resource costs/savings to third party agencies’ resulting from the effect of the intervention. 107
Costs were estimated from a public sector perspective. However, we acknowledge that, in addition to these costs, the delivery of such programmes is dependent upon a substantial commitment from parents to make time to participate in the programme and travel to and from the venue. Recognition of this opportunity cost for parents supports the need for a social model of costing that reflects the cost of parents’ time. Ideally we would seek to estimate those costs in a future trial; however, methods and tools to capture these items are not yet fully established. 104
Intervention programmes in primary prevention, such as this, are front-loaded in terms of resources required to plan and develop the intervention. The resources deployed within parent programmes at the four stages described (development, preparation, delivery and maintenance) should be categorised separately in order for the mainstream delivery cost of the developed programme to be estimated and in recognition that development costs would not be incurred during mainstream implementation. In addition, identification of resources relevant to implementation of programmes ensures complete costing at the full trial stage. Feasibility studies need to identify the resources that would be used prospectively, both those not required during mainstream implementation (e.g. control group incentives) and those that would be required (e.g. trainer supervision to maintain intervention fidelity).
Learning points
-
It is possible to build a resource use checklist to determine the non-recurrent and recurrent costs associated with delivering this programme as part of a future trial.
-
The injury calendar is able to indicate the initial parent-reported NHS provider use costs in intervention and usual care arms of any future trial although amendments to the calendar are required in order to add the option of transfer by ambulance and allow the use of multiple NHS providers to be recorded.
-
Injury management is often associated with a range of NHS provider resources beyond the initial action, and this series of NHS savings relating to an injury event needs to be captured for full costing savings to be estimated in a future trial economic evaluation.
-
In a community setting effective parenting programmes depend upon parental participation in the programme, suggesting that a social perspective on costs that are outside the public sector should be developed to capture these resources.
Chapter 7 Evaluation and further development of the parenting programme
Objective
In our original proposal we intended to evaluate the parenting programme from two perspectives: firstly, the perspective of parents receiving the programme and, secondly, the views of the health visitors and cofacilitators delivering the programme. During the course of the study we identified the additional need to consider how well the programme met the criteria for an injury prevention initiative and, lastly, how well the programme met the criteria for a parenting programme. By understanding how the participants and facilitators experienced the programme, we were able to understand how that experience could potentially impact on the effectiveness of the intervention in a future trial, and suggest ways to develop the programme and the delivery mechanism prior to a future trial.
This chapter describes the methods and results of the four evaluations of the programme, the process of feeding back that information to Parenting UK and the subsequent further development of the intervention and concludes with a brief discussion and learning points.
Evaluation from the perspective of parents receiving the programme
This evaluation sought to answer the question ‘what was it like to participate in the programme?’ Feedback was collected from parents who had attended the FAST course through four focus groups: two in Bristol and two in Nottingham. Focus groups were led by two researchers in both study centres, using topic guides. Questions for the topic guides were derived from team discussions, ideas from the PAG and the need to determine the strengths and areas for development in the programme and the study. Feedback was collected on flipcharts and by notes taken during the discussion, and a digital recording was made to validate the flipchart record. Statements and issues raised during the focus groups were analysed thematically. The focus groups took place either immediately after the final session of the course or 1 week after the last session. Both focus groups in Nottingham and one of the focus groups in Bristol took place in the same venue as that where the course had been provided. The second focus group in Bristol took place in the home of one of the course participants as she was recovering from surgery and was unable to travel.
In Bristol, for each of the courses run, two parents had consistently attended. These parents took part in the two focus groups. In Nottingham, the parents participating in the focus group were those engaged through the ‘open invite’. Seven parents attended one focus group and two parents attended the second focus group.
The analysis resulted in four themes, detailed below.
Delivery of the programme
The format of the course as a regular commitment over a number of weeks was positively regarded by the majority of participants as it allowed time for information to be absorbed and gave them
. . . time to try things out.
Parent, Bristol course 1
The length of the sessions, at around 1.5 hours, was considered appropriate. A regular weekly format appeared preferable over a shorter more intense course:
You can’t take it all in in one day.
Parent, Nottingham course 2
A shorter, day-long course had previously been proposed by two Bristol parents who later withdrew after concerns over the time commitment. The status of the programme deliverer was important to the parents. The fact that the trainers had a health background provided the parents with confidence that they were not merely being delivered a pre-set content but that the trainers could add context and background. Participants appreciated a friendly, chatty style of delivery from the trainers. Four Bristol participants specifically mentioned locating the course in a local venue that was on a bus route, that was within walking distance for some and that had parking facilities, and reflected that this was all part of the thoughtfulness that had been a part of the course design. Parents who were not used to attending a children’s centre raised some concerns about using this as a venue; they did not know the staff there and were not confident in the crèche provision. Parents in Nottingham specifically raised the concern regarding children’s centres being perceived as locations where social services support families.
Course content and materials
Parents appeared comfortable with the combination of support for parenting, child development, first aid advice and safety. The majority of parents reflected that more first aid advice would have been helpful:
I thought it was all going to be first aid with a bit of parenting but it’s much more parenting with a bit of first aid.
Parent, Nottingham course 1
Several parents had previously attended courses for their jobs or for life skills, including courses on health and safety and a St John’s Ambulance Course. None had been offered this type of combined course previously. The parents who completed the course held it in positive regard:
. . . it was really interesting and very helpful.
Parent, Bristol course 2
[I] really enjoyed the course.
Parent, Nottingham course 2
The parenting guidance appeared to make sense with the safety advice. A small group of parents praised the quality and professionalism of the course materials:
. . . [it was] really well organised . . . felt really professional . . . very luxurious.
Parent, Bristol course 2
The parent handouts to take home each week were well received with a ‘nice folder’ (parent, Bristol course 2) which was ‘informative’ and ‘helpful (parent, Nottingham course 2).
I think it’s something I’ll refer to at other points, if something happens at least it’s something you can look back to.
Parent, Nottingham course 2
All groups commented that the activity cards caused confusion, especially if they were muddled up:
Every single time we had something with the cards, there was an awful lot of them.
Parent, Bristol course 1
The sessions with cards – there are some humungous amounts of cards.
Parent, Nottingham course 1
Three of the four groups identified that they would like a follow-on course which might support them as their children grew older; other requests for further information included advice about water hazards in the home, bandaging, what items they should have in a first aid box and checking expiry dates on their medicines and tablets, which suggested that they had considered home safety beyond the specific content of the parenting programme.
Group experience
A positive and shared group experience supported engagement with the programme. Development of group cohesion was facilitated by the social elements (e.g. provision of refreshments) and these were regarded as follows:
. . . a bit of a time out.
Parent, Bristol course 2
The chat made it what it is.
Parent, Nottingham course 2
Provision of a free crèche was regarded as
. . . incredible.
Parent, Nottingham course 1
Repeated attendance with the same people provided time for confidence to develop between group participants and the feeling that this was a group where it was safe and supportive. Parents responded to this commitment and felt able to
. . . talk freely [about their concerns].
Parent, Bristol course 1
Another felt that
. . . you can feel more comfortable with what you are saying.
Parent, Nottingham course 2
The programme became a social event with calls being made between participants in both Bristol and Nottingham to establish if other participants were attending. However, there was concern that too many people attending the course might have a negative impact:
. . . you would struggle to have the discussions.
Parent, Bristol course 1
Some parents felt that a group of up to eight parents would be appropriate. In Nottingham, one ‘open invite’ group had provided the option for participants to attend with a friend, an opportunity which was a boon for those who were less confident about attending alone.
Learning new knowledge and skills
Parents were enthusiastic about the opportunity to learn new skills and knowledge. They specified as particularly useful the parenting elements such as understanding the emotional arousal of the brain, how to communicate positively and appropriately with children (Bristol parents, both courses), and looking at a situation from a child’s point of view. Several parents talked of benefiting from the discussions on calm parenting, taking a more measured response to an event and positive praise. Parents also highlighted as important the first aid and safety knowledge, particularly watching the fire safety film, developing a fire escape route, wrapping a burn in cling film, and learning not to panic in an emergency. This last point was particularly important for one mother in Bristol; prior to the course she would have called her mother for help but now reported feeling more confident to manage situations herself. Generally, parents appeared to appreciate take-home messages about increased parental awareness and assessing potential dangers to their children:
I thought it useful in every sort of way . . . I thought it was really helpful.
Parent, Nottingham course 1
Parents reported taking specific actions to improve safety in the home as a result of participating in the course, including adding socket covers, putting locks on cupboards, putting hair straighteners away and installing baby-gates.
Evaluation from the perspective of those delivering the programme
In Bristol, two courses of the parenting programme were delivered by a single team of one health visitor and one community nurse as a cofacilitator. In Nottingham, one course was delivered by a senior health visitor without a cofacilitator, and a second course was delivered by a community nurse supported by a nursery nurse. Feedback was collected from health visitors and nurses via three routes: (1) recorded on weekly reflective notes, handwritten during delivery; (2) in interviews with researchers conducted after completion of the courses, and (3) during a focus group where all the deliverers met together, which was attended by four researchers. Questions for the interview topic guides were derived from team discussions, ideas from the PAG and the need to determine the strengths and areas for development in the programme and the study. During interviews, notes were taken by the researcher to record comments and issues. During the focus group, feedback was collected on flipcharts, notes were taken during the discussion and a digital recording was made to validate the flipchart record. Statements and issues raised on the reflective notes and during the interviews and focus groups were analysed thematically.
The health visitors and nurses were generally very enthusiastic about the course, its focus on injury prevention and the opportunities it presented. They confirmed the importance of first aid advice as a subject through which to engage parents:
. . . every parent wants to know first-aid, it’s a skill . . . first aid and a crèche pulls them in.
Bristol voice 1
The contents of the resource kit were perceived as helpful and well received by parents. Discussions with parents during course delivery were readily forthcoming, and those parents who were retained appeared to enjoy telling and hearing others’ stories. All the health visitors and nurses said that they would like to deliver further courses if opportunities arose.
The health visitors and nurses reflected on how the course could be developed further. These comments have been collated into the following themes.
Focus
Health visitors and nurses were concerned that the course was too heavily focused on parenting/behaviour change and not enough on safety awareness, anticipatory guidance and first aid advice. This echoed the perspective of some parents who had expressed concerns that the course was predominantly focused on parenting. The health visitors and nurses perceived the materials to be geared towards the assumption that the parents would be difficult to engage, and would have children who were exhibiting challenging behaviour (as has historically been the remit for parenting programmes). In reality, the parents engaging with the course had existing positive relationships with their children, were willing to learn and had healthy children without behavioural difficulties who had sustained injuries during the course of common play and daily life. One health visitor said:
. . . the starting point seems to be that parenting style is the main driver for accidents rather than developmental stage and environment.
Bristol voice 2
Health visitors were concerned that parents might feel ‘duped’ into having signed up to a first aid advice and safety training course, only to experience what was very obviously a parenting programme. They reported a greater need for ‘everyday parenting’ advice, such as how decisions should be made about what activities are safe for a child to try. Health visitors and nurses offered constructive suggestions for how the focus of the course could be better balanced by changing the order and volume of the content (see Content of each session, below).
Materials and resources
Once on the course, the families were engaged positively by the quality of the materials provided; two items specifically mentioned included the information video about how swiftly fire can take hold in a bedroom and the parents’ handbooks with weekly handouts. Some parents were reported to bring their handbooks regularly: some to write notes, some to show how they had undertaken tasks at home following the sessions. However, the materials that programme deliverers needed to take to and from the venues each week were heavy and bulky, particularly the parents’ handbooks and handouts. A wheeled case was suggested as an aid to transporting the materials and resources. Trainers reported that some safety/first aid advice materials appeared inconsistently provided; for example, there was no parent handout on the management of cuts and wounds but there were handouts for other injury types. The two courses in Bristol ran sequentially while the two in Nottingham ran concurrently, resulting in the single resources kit needing to be transported across the city each week for use by both delivery teams. The colour-change heat mug was broken twice in Nottingham. In future, each delivery team would need its own set of resources. The fire safety DVD was highly rated, though in each location it was a challenge to find a machine on which it could be played. Activities often involved picture cards – these all had the same colour border (lime green) on every pack. It was suggested that each pack could have a different coloured border to enable easy identification when cards become mixed together during activities.
Length of the course
The 8-week course was generally perceived as long, and health visitors and nurses were concerned that this may have been a barrier to recruitment. Each course had to have breaks in the middle owing to school holidays or bank holidays, and there was concern this could affect retention of parents (during one course in Nottingham two parents did not return after a 2-week break for Easter). It was suggested that a 6-week course would fit into one half of a school term. One delivery team in Nottingham had negotiated with their manager to have time out from normal activities in order to deliver the course over 8 weeks. When none of the original families turned up for the first week of the course, and they were forced to spend week two finding ‘new’ parents to attend, and there were only 6 weeks remaining. When they were able to restart the course, they were forced to condense the 8-week programme into 6 weeks. They were able to deliver all of the content by merging weeks 1 and 2 and weeks 7 and 8, and extending each session in between by 15–30 minutes. They managed to cover the content of the course in this manner and did not perceive the shorter duration to be detrimental to parent experience. There was a strong recommendation to deliver the course during the morning and not during afternoons, as parents are fresher then and not worried about collecting children from school.
Content of each session
The health visitors and nurses reported that the volume of material that needed to be covered in each session was very large. While they broadly tried to stick to the times recommended, they found there needed to be flexibility to respond to issues raised in discussion and some flexibility to adapt the materials to the educational level and needs of the participants. It was reported that some weeks felt very ‘top heavy’ with parenting and behaviour change instruction, with the injury prevention and first aid content seen as a disconnected ‘add-on’. Weeks 5 and 6 were highlighted as being particularly problematic in this way. Health visitors were concerned that the focus on parenting inadvertently risked stigmatising the attendees. They therefore suggested that the course could be made less stigmatising by reordering the content such that it was led by an injury topic. For example:
-
Injuries at different ages and stages – e.g. ‘today we are going to talk about burns and scalds’. Activity/discussion then explores different burns and scald risks at different ages/stages of development.
-
How to respond if your child has this injury – advice on appropriate first aid response to burns and scalds.
-
How to prevent this injury – discuss how to keep your child safe from burns and scalds at different ages.
-
Let the safety discussion lead into the parenting issues for that week, e.g. communication with your child, boundary setting, etc.
Each week could be titled with a different injury type, so that the parenting and behaviour change content is presented as supportive and complementary rather than the primary focus.
‘Train the trainer’
Health visitors and nurses reported that the 2-day ‘train the trainer’ event ‘felt amazing on the day’, but when they got round to delivering the course themselves for the first time they felt unprepared and had to undertake a lot of preparation in their own time to acquaint themselves with the materials and activities. There was an unintended long break (up to 4 months) between training and delivering the course owing to poor recruitment, which they reported added to their concerns about being prepared to deliver the sessions. They suggested that in future the ‘train the trainer’ event could allow greater opportunity to witness or attempt key activities or sessions themselves. All teams recognised the importance of trainers having the skills to manage, educate and respond to parents in order to facilitate their learning. Individual trainers perceived that they drew on their previous nursing experience to support parents. The trainers’ manual should be reordered so that everything for each week is in a single section, and that sections have different coloured borders for easy identification.
Location of course delivery
Health visitors and nurses recognised that children’s centres varied considerably, and suggested that community venues might on occasion be preferable to using children’s centres for delivery of the course. Rooms used in children’s centres were sometimes found to be small, hot, untidy or even unsafe. The managers of two children’s centres in Bristol reflected on the challenge of booking one room for the course and a second one for the crèche a long time in advance ahead, with the risk that neither would be used if that centre were randomised to the control arm of the study:
We said we can’t guarantee that as it was such a long way away . . . our programmes change quite quickly, so what we need to do is I think we need to make absolutely firm bookings . . . umm . . . nearer the time.
Bristol children’s centre 5
This issue led to one children’s centre having to give up a booked room owing to competing demands on space:
Our nursery provider needed to expand and increase their places and the only way we could do that was to give them our spare room . . . that was quite a priority for the most vulnerable families.
Bristol children’s centre 5
Therefore, a community venue had to be found at short notice that was able to host both the course and a crèche. In another location, the programme was asked to vacate the children’s centre mid-course and successfully relocated to a community venue. The amount of support offered by children’s centres to the teams during course delivery varied considerably. Two health visitor teams reported concerns that the children’s centre was perceived by parents to be a potentially stigmatising location.
Evaluation from the perspective of an injury prevention expert
Two injury prevention experts, Professor Elizabeth Towner (a co-applicant) and Dr Mariana Brussoni (an independent member of the Trial Steering Committee), agreed to evaluate the parenting programme against criteria for injury prevention interventions. Neither was directly involved in the development of the intervention.
Evaluation by Professor Elizabeth Towner
The parenting programme was evaluated against 16 health promotion criteria. The first 10 of these were adapted from McWhirter’s 10 principles of effective safety education. 108 These 10 principles were distilled from a literature review and are specifically targeted at the school setting and health promotion initiatives in school-aged children. The adaptations included more appropriate wording for the preschool setting; for example ‘Encourage the adoption of, or reinforce, a holistic approach within the wider community’ rather than ‘Encourage the adoption of, or reinforce, a whole school approach, within the wider community’; and ‘Involve parents in real decisions to help them keep their children safe’ rather than ‘Involve children and young people in real decisions to help them stay safe’.
The remaining six criteria were added by Elizabeth Towner, in consultation with Mariana Brussoni and Julie Mytton, to closely reflect the content of a preschool first aid training programme. For each of the 16 criteria, the trainers’ manual and participants’ handbook were examined to see whether or not the content was ‘limited or none’, ‘sufficient’ or ‘well addressed’.
The results of the evaluation are summarised in Appendix 10. Professor Towner concluded that, overall, the FAST parent programme was well structured and combined injury prevention and safety promotion messages with parenting advice. There was a strong emphasis on child development and injuries and this was illustrated using examples of different injury types. Safety was thus taught as part of anticipatory guidance and appropriate supervision was stressed. Particular attention was paid to psychosocial aspects of safety and parents were provided with both the confidence and the skills to anticipate and cope with injury events. The ethos of the programme was non-judgemental and parental contributions were encouraged and valued. There was a range of methods used: small and large groups and practical demonstrations, with an emphasis on practical examples of relevance to the context of the target audience. Professor Towner reported that it was not clear whether or not ‘working in partnership’ was sufficiently stressed, but acknowledged that this may be implicit, rather than explicit. It was also not clear whether or not parents had been involved in the development of the resource from the materials available. One additional concern was the inclusion of a parents’ handout from the resources used in the Solihull Approach parenting programme (www.solihullapproachparenting.com). This did not appear to be integrated into the rest of the package and the rationale for its inclusion was not clear.
Evaluation by Dr Mariana Brussoni
Dr Brussoni evaluated the parenting programme against the evidence statements contained in the Canadian Edition of the Child Safety Good Practice Guide. 109 The degree to which the evidence statement was addressed in programme was considered to be ‘limited or none’, ‘sufficient’, ‘well addressed’ or ‘not applicable’.
The results of the evaluation are summarised in a table in Appendix 11. Dr Brussoni concluded that the strengths of the programme included the curriculum’s language, which was simple, user friendly and engaging, and allowed for flexibility in adjusting for local parents’ interests and needs. In addition, the practical exercises that covered the safety topics were delivered in several different ways, helping to engage participants. Dr Brussoni made a number of specific recommendations:
-
The FAST parent programme curriculum included a question in the quiz on week 6 that touches on the importance of not carrying children in adults’ laps in the car, but there did not appear to be any other point in the curriculum where the importance of child safety seats or the need for children to ride in the back of the car were covered. Because the FAST curriculum was focused on home safety, it may not be appropriate to cover traffic safety. However, as this topic is introduced, it is important to cover it appropriately or consider removing mention of it altogether.
-
Consider discussing pool fencing. While most target parents will not have a pool in their home, there may be one in their housing block or in other venues they visit. It may be important to mention the need for pool fencing so that they are aware of the hazard that lack of pool fencing can be.
-
Mention the importance of supervision for drowning prevention for other bodies of water. It is discussed only in the context of baths. For the same reasons described above regarding pools, it may be important to include this.
-
Consider providing examples of the different types of window safety mechanisms available to prevent falls.
-
Consider providing information on obtaining and installing window safety mechanisms, stair gates and other home safety equipment.
-
Mention the importance of not using pressure-mounted stair gates at the top of stairs.
-
Provide information on fire safety products, such as child-resistant cigarette lighters, hearth gates and self-extinguishing cigarettes.
-
Mention the importance of storing poisons locked up and out of reach.
-
If applicable, provide numbers for poison control centres and inform parents of their purpose.
-
Mention the importance of not using baby walkers, bath seats and other injury hazard-producing equipment.
Evaluation against criteria for an effective parenting programme
The programme was evaluated by the chief investigator against the Children’s Workforce Development Council’s Parenting Programme Evaluation Tool. 110 This tool scores parenting programmes against a set of criteria based upon international standards of best practice in prevention and intervention services. It was designed for commissioners and service managers to make a quick assessment of the quality of a parenting programme and the extent to which it meets the needs of parents and children using their service. The tool evaluates four key elements of programmes:
-
specification of the target population
-
evidence-based content
-
well-developed training and implementation support
-
evidence that it works.
Each of these elements is made up of seven or eight questions, and is scored between 0 (lowest score) and 4 (highest score). Scores in different elements are not intended to be summed into an overall numerical score. For the purposes of this evaluation, the materials assessed included:
-
the commissioning brief provided to Parenting UK by the FAST study PDS
-
the decision log made by Parenting UK to record decisions made during development
-
the trainers’ manual, parents’ handbook and resources provided by Parenting UK and used during delivery of the programme.
Key element 1: a clearly specified target population
Results are shown in Table 20.
| Criteria: programmes should have defined eligibility criteria, including as a minimum the age range for children in the programme and processes including guidelines for collecting family-level demographic information, needs assessments and standardised measures for assessing child problems | |
|---|---|
| Item | Comment |
| 1. Does the programme clearly state who it is and is not designed for (parent and child characteristics)? | Yes, in commissioning brief provided to Parenting UK but not within the trainers’ manual |
| 2. Programmes should specify whether the content is suitable for parents with low, moderate, complex or high levels of need. Low need refers to parents seeking support for stresses and difficulties experienced by most families at some point in their child’s development | Category would be ‘low need’ as safety awareness and anticipatory guidance are suitable for every parent of a preschool child. Not appropriate to rate in this assessment as programme developed as part of research project. This is not specified in either the commissioning brief, decision log or manual |
| 3. Is the programmes content appropriately matched to the needs and characteristics of the target population? | Yes. Targeted to English-speaking parents of preschool children who have sustained a medically attended injury |
| 4. What is the classification of the programme (universal, targeted prevention, targeted, specialist or highly specialist) and how do parents access it? | Targeted prevention. Specified within commissioning brief. Not specified in manual |
| 5. What processes are in place for recruiting and enrolling parents? | Not applicable as recruitment determined by research trial |
| 6. What processes are in place for assessing and categorising parents’ and children’s needs? | Not applicable as participation and assessment of characteristics/risk factors determined by research trial |
| 7. What process is in place for ensuring that the programme is appropriate for the parents enrolled in it and assessing their progress? | Within the context of the research study the manual appropriately includes information on what to do if a child’s injury is identified as intentional. Suitability of parents to continue in a programme is not assessed mid-programme |
| 8. Are practitioner qualifications sufficient for the target population’s level of need? | Yes, health visitor or community nurses are suitably qualified to deliver the programme |
On basis of questions 1, 3, 4 and 8 (questions 2, 5–7 disregarded as research study), a rating of three was awarded. A score of four was not awarded because additional information should be added to the trainers’ manual where this is currently only included in the commissioning brief or decision log (e.g. eligibility criteria, classification as a targeted prevention programme, ability to match content to intended level of need, and practitioner qualifications).
Key element 2: what is the theory underpinning the programme and how is this reflected in its content and delivery?
Results are shown in Table 21.
| Criteria: programmes should be informed by sound theories of child development, evident in the design, content and activities and linked to parent and child outcomes. Content should be interesting and engaging so parents are motivated to participate and learn | |
|---|---|
| Item | Comment |
| 1. What is the theoretical basis of the programme? | Ingram and Luft (1969, 1970) Johari Window model of self-awareness, personal development, group development and understanding relationships111,112 |
| 2. Is there evidence that the theoretical basis is appropriate for the target population? | Builds on recommendations by NICE and SCIE 2006 for parenting programmes in preschool children.22 There is limited evidence that 1:1 injury prevention programmes with parents can reduce injuries (Kendrick45) |
| 3. Is the programme underpinned by a sound theory of change? | Kolb 1984113 – Experiential learning theory. NICE Behaviour Change guidance 2007 |
| 4. What are the programme’s short- and long-term outcomes? And are they linked to the theoretical basis and theory of change? | Not specified in the programme. Determined by the research project |
| 5. Are the programme’s theoretical basis, theory of change, and short and long-term outcomes accurately reflected in the content and activities? | Reflective learning based on personal experience + spiral curriculum. Short-term outcomes relate to mother’s self-esteem. Long-term outcomes relate to prevention of injuries |
| 6. How do parents learn during the course of the programme and is the content format and length sufficient for improving parent and child outcomes? | Currently 8 weeks, group based, facilitated content with activities and education drawing out parents’ experiences and beliefs, and introduction of new behaviours. Suggested ‘homeworks’. Use of different media – e.g. DVD, practical, flipchart, pictures |
| 7. Does the programme content include appropriate and sufficient methods for engaging and retaining parents? | Trainers’ manual does not include information on how to retain parents, though does have general guidance on group facilitation |
| 8. Are the programmes resources engaging and are the materials and activities appropriate for a variety of different learning styles? | Variety of resources and learning styles catered for. Resources newly developed |
An overall rating based on questions 1–8 is 3 for the parenting component of the intervention. Rationale: the programme is based on psychological theories although there is lack of clarity as to how the theories translate into activities. The materials are interesting and engaging but feedback from parents and deliverers suggests that there are minor problems hindering parents’ ability to engage with the programme. It should be noted that this evaluation has been based on the parenting component of the programme as the injury prevention component has been evaluated above using different standards. It should also be noted that this research study does not formally assess mothers’ confidence in preventing injuries, only mothers’ well-being.
Key element 3: training and implementation support
Results are shown in Table 22.
| Criteria: programmes are more likely to achieve their intended outcomes if they have developed systems for maintaining high-quality programme delivery across multiple settings, to include methods to ensure practitioners have necessary qualifications and support to deliver the programme with fidelity | |
|---|---|
| Item | Comment |
| 1. Are qualifications and experience necessary for practitioners to successfully deliver the programme? | Programme developed for delivery by health visitors or community nurses but this is not specified in trainers’ manual |
| 2. What training is available to instruct practitioners to deliver the programme? | Two-day ‘train the trainer’ event delivered by person developing the programme. Training not accredited |
| 3. What resources are available to enable practitioners to deliver the programme? Are they appropriate and adequate for practitioners to communicate the programmes content to participants? | Manual and resources provided to practitioners. Resources need to be available for each delivery team. Manuals need further development following deliverer feedback |
| 4. Has the programme developed processes for maintaining programme fidelity? | No. Fidelity of delivery a problem during feasibility study as practitioners identified need to adapt some activities to participants |
| 5. What mechanisms are available to support and supervise practitioners to deliver the programme? | Programme developer available by telephone on regular basis each week during delivery but only minimally accessed. Peer support between delivery teams available but barely used |
| 6. Has the programme developed a system for training trainers? | Two-day training event for current study. System not yet designed for any further trial or roll-out |
| 7. What mechanisms are available to support the implementation process, e.g. provision of checklists for ensuring agency readiness to implement a programme, a support service for managers and practitioners, booster training sessions to address agency-specific issues? | Processes for feasibility study included telephone support and peer support + researcher observation of delivery fidelity. System not yet designed for any further trial/roll-out |
Overall, the rating for this element, based on questions 1–5, would be 2, but is currently zero for questions 6 and 7. Further work would be required with regard to the ‘train the trainer’ programme and mechanisms to ensure intervention fidelity should the study progress to a main trial.
Key element 4: evidence that it works
The tool included seven questions relating to the evaluation of the effectiveness of the programme. These were not considered in this evaluation, as a formal trial of the effectiveness of the intervention has not yet been conducted.
In conclusion, the tool indicated that, from a parenting programme perspective, the eligibility criteria, the theoretical evidence underpinning the programme and the training support package are all reasonably robust, with areas for development acknowledged. It is recognised that the tool has been designed specifically to evaluate parenting programmes intended to support parents with difficulties, children with behavioural problems, or both. References throughout the tool relate to child behaviour being the underpinning reason for the parent engaging in the programme. For this reason, it is not directly applicable to the FAST parenting programme, which considers that neither parents participating in the programme nor their children have ‘problems’. The tool is also designed to evaluate programmes that are already published and available for commissioning. Element 4 of this tool could not be rated because the programme was at an early developmental stage.
Actions following evaluation
Further development of the intervention in response to the evaluation had not been included in the original project funding. However, approval was given to use underspent project funds for this purpose. Parenting UK was commissioned to undertake redesign of the parenting programme in response to evaluation outputs, specifically to:
-
address persisting concerns regarding perceived stigma associated with the occurrence of child injury and the ability to be a ‘good’ parent
-
add injury prevention and first aid advice content where gaps had been identified
-
reduce the duration to 6 weeks while building in further opportunities for flexibility to respond to parents’ concerns/issues raised in discussion
-
make some very pragmatic changes to the trainers’ manual, parents’ handbook and resources to facilitate ease of use, plus amending the trainers’ manual and parents’ handbook to reflect the changes made to the content.
The PDS was reconvened and the additional development work was completed between October 2012 and January 2013. One face-to-face meeting, three teleconference discussions and e-mail/telephone communication provided governance of the redevelopment process.
A revised 6-week programme was developed, designed to be delivered over six sessions of 2 hours each. It was designed to address different injury risks/first aid skills each week, and allow parenting skills to emerge from discussions about how to keep your child safe from the injuries being discussed that week. Each session now starts with an exploration of a particular type of injury and a discussion or activity to explore how that type of injury changes as the child develops from a baby to a preschool child. This component aims to give parents opportunities each week to understand child development and how their parenting needs to adapt as their child grows and learns new skills. This component is followed by advice on the first response required if an injury were to occur and when to know if parents need to seek further help. This section aims to enhance parents’ beliefs that they are capable and confident parents. Each session continues with parent skills on how to keep your child safe, using a ‘spiral curriculum’ where skills and knowledge are revisited several times during the course. Parenting skills and knowledge include, but are not limited to, effective parent–child communication, use of praise and positive reinforcement of positive behaviour, ability to set and maintain appropriate boundaries, and empathy. The session concludes with some suggestions of what the parent could try at home (both parenting skills and injury prevention activities) (Figure 8). The 6-week programme is described in detail in Appendix 12.
FIGURE 8.
Process and rationale of revised 6-week programme.
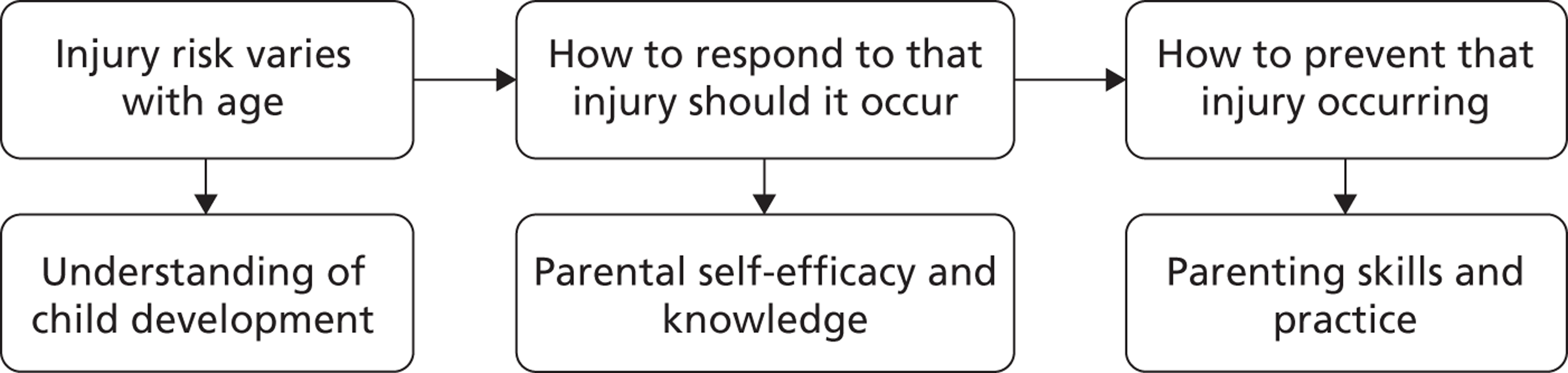
Discussion
The evaluation of the FAST parent programme from four perspectives showed that one of the main outputs from the feasibility study has been achieved, that is to say that it has been possible to develop a parenting programme which has the potential to be used to prevent home injuries in preschool children. While the programme was viewed favourably, opportunities were identified to change some of the content and format.
Injury, both actual and the risk of, has the potential to undermine parents’ confidence and make them feel like inadequate parents. The offer of any form of preventive programme, especially one with a focus on parenting, has the potential to make this situation worse. In a group of parents such as those who were the subject of this trial – parents whose children had recently experienced a medically attended injury – the link between ‘good’ parenting and injury occurrence needs to be particularly carefully managed and subtly introduced. For this reason, while parenting skills and knowledge underpin the revised course, they are intentionally not overemphasised throughout the programme. We emphasise that parents can ‘make their home safer’ and do encourage parents to consider the safety of their child’s physical home environment. However, our expectation is that any improved safety will more likely be secondary to changes in parental behaviour (improved parent–child communication, setting and maintaining of appropriate boundaries, supervision that anticipates child development) rather than secondary to physical changes made to the home environment.
The process of redeveloping the parenting programme identified the need for enhanced support for those delivering the programme, through guidance within the programme manual, through the ‘train the trainer’ programme and through trainer support during delivery. These aspects fell outside the additional funded and completed work to develop the parenting programme content.
Learning points
-
Practical issues such as the need for a wheeled case to transport programme materials and resources into and out of venues need to be addressed in any future trial.
-
Each programme delivery team should have its own set of resources in a future trial. A process to maintain and replace lost and broken equipment would need to be established.
-
In a future trial venues that host programme delivery should be encouraged to facilitate courses during the mornings when parents may be more engaged and less worried about collecting other children from school.
-
Future ‘train the trainer’ events need to be timed more closely to the first delivery of the programme for new trainers. At the ‘train the trainer’ event, there should be more time allocated to practicing delivery of some of the course materials. Training in group facilitation skills was acknowledged as very important, even for experienced health visitors.
-
Children’s centres need to be able to plan their programmes well in advance. Therefore, in a future trial, fixed periods when a course would run need to be agreed in advance and should not be repeatedly put back if numbers of participants available are too small to run the course.
Chapter 8 Final discussion
This chapter brings together the component sections of the study. In Summary of main findings of the study, the outcomes of the intervention development process and feasibility study are summarised and we have reflected on the key challenges faced during the feasibility trial. In Completion of study objectives and Criteria for success, we have returned to our original study objectives and pre-specified criteria for success and critically reviewed our achievements against those objectives. Lessons learnt collates all the bullet points previously reported in the ‘learning points’ boxes at the end of Chapters 2–6 of the report. We bring the findings from all four sections together in the final section, Implications for a future trial, where we consider the implications for a future trial under 10 different headings. For each of these, recommendations have been made on how a future trial should be conducted.
Summary of main findings of the study
The aim of the study was to develop and test the feasibility of delivering a children’s centre-based parenting programme to prevent recurrent unintentional home injuries in children aged 0–4 years, compared with normal care for such children. We developed a group-based parenting programme specifically designed to incorporate the principles of parenting support within the context of injury risk and response, and ran four courses of the programme. We tested five methods of recruiting parents to a cluster RCT of the parenting programme and discovered the limitations of each method. We developed a measure for collecting parent-reported injuries over a prolonged period and undertook a small-scale validation of that measure against health-care records. This output has the potential to be of value to other injury-prevention studies. We have determined the parameters for an evaluation of the cost-effectiveness of the programme if tested in a future trial.
In our original study protocol we highlighted two key challenges in conducting this study: engaging parents in a parenting programme following injury in their child and the risk of their feeling inadequate, stigmatised, guilty or concerned that the injury is believed to be intentional; and developing a research study in which health visitor teams could effectively contribute. Our concerns on both of these points turned out to be valid. The identification and recruitment of parents whose children had sustained a medically attended injury proved not to be feasible despite the multiple strategies attempted, and we ultimately did not achieve our intended sample size. Furthermore, despite a current reinvestment in health visitor training in England,114 the intended increase in numbers of health visitors has not yet translated into additional capacity within teams. Reorganisation fatigue, the challenge of negotiating access through managers attempting to limit the workload of their overstretched teams, and continuing capacity limitations within health visitor teams have led us to conclude that it is not feasible at the current time to design a study in which health visitors can recruit participants or deliver the intervention.
The existing evidence suggests that one-to-one generic parenting programmes that may or may not contain a specific focus on injury have been shown to reduce injury. 45 Group-based programmes would be more cost-effective and programmes that include safety and first aid advice should be more effective. An alternative view could be that holistic programmes work better than problem-specific programmes because parents respond better to programmes that appear to have been developed simply to support them than programmes that are developed to prevent a problem as defined by professionals. Most parenting programmes are designed to address some sort of problem, for example difficult child behaviour, but they may be effective if presented as holistic programmes. We know that parents are concerned about injury. This is evidenced by their interest and participation in first aid courses. Parents state that they would prefer to prevent the injury from happening in the first place rather than manage it after the event. We have demonstrated, however, that too much focus on children who have already been injured appears to have a negative impact on parents’ participation in programmes.
Each component of this study has provided learning points that have informed our understanding of the best way to approach research that attempts to reduce preschool injuries through the use of a parenting programme. The lessons learnt have been highlighted below and directly inform our understanding of the most appropriate methods to deliver a future trial. These are summarised in the Implications for a future trial, below.
Completion of study objectives
We describe below our success in completing the objectives specified in the study protocol:
-
To develop a health professional delivered parenting programme. An 8-week, group-based parenting programme designed to combine parenting skills and knowledge with first aid advice and safety training, and suitable for delivery in a children’s centre setting by a health professional, was developed according to our specification and delivered on time by our voluntary sector partner, Parenting UK.
-
To assess the acceptability of the parenting programme to parents and professionals. Our original proposal stated that we would evaluate the parenting programme from two perspectives: parent participants, and the perspective of the health professionals delivering the programme. In addition to these perspectives, we have also evaluated the programme from an injury prevention expert perspective, and against the Parenting Programme Evaluation Tool written by the Children’s Workforce Development Council. 110 Following these four evaluations we asked Parenting UK to undertake further development work on the programme to respond to the issues raised. A print-ready version of the revised 6-week programme has been produced.
-
To assess the feasibility of delivering the parenting programme against seven factors:
-
To assess recruitment and retention of parents within the trial. Using four strategies for recruitment we were able to recruit 40 of the planned 96 participants to the study using the eligibility criteria specified in the original study brief. We were also able to engage a further 11 parents using an ‘open invite’ approach where there was no requirement to have a preschool child who had sustained an injury. We found that the most significant barrier to recruitment was the requirement for parents to admit that their child had been injured. Of 39 participants offered the intervention [randomised (n = 17), purposefully allocated (n = 9) and ‘open invite’ (n = 11)] only 15 completed the intervention, although completion was significantly greater (Fisher’s exact test, p = 0.002) using the ‘open invite’ approach (85%) rather than the other two approaches (31%). Once parents started the programme retention rates were high (80% of those meeting the original eligibility criteria, and 79% of those in the ‘open invite’ group) suggesting that the programme itself was perceived as helpful by those attending.
-
To assess compliance with delivery of the intervention. We asked health visitor trainers and their cofacilitators about their ability to deliver the intervention as designed during qualitative interviews and focus groups. The primary challenge for trainers was the limited capacity within the 8-week programme to respond to issues raised by the course participants while still covering the content of the programme. This was a particular challenge for one of the ‘open access’ groups in Nottingham where the trainer needed to accommodate the learning and social needs of the group participants. These challenges were fed back to Parenting UK and used to inform the further development work during the revision to a 6-week programme. In a future trial a formal process to assess intervention fidelity would need to be implemented to document deviations from the programme.
-
To determine the training, equipment and facilities needed for delivery of the parenting programme. We provided a 2-day ‘train the trainer’ event for the trainers and their cofacilitators providing the parenting programme as part of the feasibility trial. The training event was evaluated positively afterwards. Trainers were encouraged to take advantage of e-mail and telephone support from the programme designer at Parenting UK after delivery of each session and to provide peer support to other teams. The delivery and evaluation of the parenting programme provided opportunities to reflect on how the ‘train the trainer’ event could be developed for any subsequent future trial, and week-by-week support from the developer or peers was not utilised as much as might have been anticipated. The materials and resources used during the delivery of the parenting programme were praised by the majority of users as being of high quality and engaging for parents. Each delivery team would need its own set of course resources for any subsequent trial. We anticipated delivering the four courses in children’s centres but, in practice, two courses were delivered (at least in part) in community centre venues. These venues proved equally successful, and any subsequent trial could utilise either venue according to facilities, local context and the parent participants’ needs.
-
To assess the collection of primary and secondary outcome measures. We developed and tested a tool (the injury calendar) for the collection of our primary outcome: parent-reported medically attended injuries in the index child and siblings of the index child. This proved to be acceptable to parents with 67% of parents returning calendar pages. Parents reported a large number of injuries using the tool (n = 151), both medically attended and non-medically attended, suggesting that for many of the participants the tool was not difficult to complete and that they were not concerned that they would be perceived badly by the researchers for returning a form reporting injuries in their children. Through a validation exercise we compared the parent reported medically attendances with emergency department (ED), NHS walk-in centre and GP records. We found one instance where a parent-reported NHS provider use was not found on the records searched, and four instances of NHS provider use not reported by parents returning calendar pages. These findings suggest that both methods are helpful to determine child injuries during any future trial. The sensitivity of the injury calendar for collecting medically attended injuries was only 20% although this should not be overinterpreted owing to the limited number of medically attended injuries identified and the small number of parents participating in the feasibility study. The study has identified the need for greater clarity of the information for parents on how to complete the injury calendar.
During the feasibility study we made amendments to only one of our five non-injury secondary outcome measures. We learned that the Strengths and Difficulties Questionnaire95,96 had become validated down to the age of 2 years and we therefore used this measure in preference for younger toddlers. We used the Infant Behaviour Scale – Revised-Short Form98 for children aged under 1 year.
Non-injury secondary outcome measures were collated into an A5-sized questionnaire booklets for parents, colour coded for the age of the child at entry to the study, for use at baseline and end of follow-up. These booklets were well completed by participating parents and we did not receive any feedback suggesting this format of presenting the questionnaires required amendment for any subsequent trial. We used the same child behaviour measure at follow-up as at baseline to enable a difference in scores to be estimated in both arms of the trial. However, some parents commented that infant behaviour questions used at baseline were no longer applicable at follow-up owing to the developmental progress of their child. In a future trial we would need to identify an alternative measure to assess behaviour change over periods of significant developmental change (e.g. in the first 2 years of life).
-
To determine what information to collect on ‘normal care’. In our original study protocol we proposed to compare the parenting programme intervention with ‘normal care’ where this was described as the actions taken by health visitor teams upon receipt of a notification of attendance at an emergency department or NHS walk-in centre for an injury. We discovered that health visitor teams have variable and locally determined ‘normal care’, and that most teams are using paper-based records with no central register of receipt of notifications of injuries or action taken. The challenge of collecting ‘normal care’ data in a main trial, even prospectively, and the inability to pool and interpret these data owing to locally determined factors means that we would not recommend this measure for any subsequent main trial. If the eligibility criteria for a future study were amended to any parent of a preschool child irrespective of a history of injury, then it would no longer be appropriate to use health visitor team response as ‘usual care’. We have therefore not attempted to meet this study objective as originally described. The implications for a subsequent main trial are further described below.
-
To assess which relevant resource utilisation/costing data need to be collected. We have collected detailed information on the non-recurrent costs associated with developing the parenting programme intervention and the recurrent costs that would need to be considered in a future trial. We believe that the injury calendar developed to collect our primary outcome measure would be suitable for recording NHS provider use as an economic outcome in any future trial.
-
To produce estimates of effect sizes to inform sample size estimation for a future trial. The low recruitment and completion rate meant that the number of medically attended injuries reported by parents was too small to make an estimate of the sample size required for a future trial. The implications of this outcome for a future trial are described below.
-
We have therefore met all the research objectives described in our original study proposal except the one relating to estimations of sample size for a future trial.
Criteria for success
In our original study proposal we set out eight criteria for success of the feasibility study. These criteria together with our experience and progress are summarised in Table 23.
| Number | Criterion specified in original study proposal | Outcome |
|---|---|---|
| 1 | Completion of the updated systematic review of parenting programmes for the prevention of injury and the qualitative review of barriers and facilitators for engagement of parents in programmes in a timely manner to allow opportunity to inform the development of the parenting programme | Completed |
| 2 | Development of an injury prevention parenting programme through collaboration with Parenting UK and its members, including the design and production of all materials for delivery and a training programme to enable training of lead health visitors and project managers | Completed. In addition, further development work on the parenting programme has been completed following our evaluation |
| 3 | Development of a recruitment process that can be undertaken by health visitor teams following notifications of medically attended injuries that enables the identification of a group of parents to whom the FAST parent programme can be delivered, including estimation of the recruitment rate for a main study | We have determined that recruitment of parents where a preschool child has been injured is not feasible for a future trial. Identification of parents at high risk of having a child who is injured, via children’s centres, is recommended rather than identification through health visitor teams |
| 4 | Identification of the reasons why parents may decline to participate in the study | The primary reason why parents declined to participate in this study was the stigma associated with disclosing that one’s child had sustained an injury |
| 5 | Estimation of retention rate for the main study and identification of the reasons why parents may fail to complete the study | Of 39 participants offered the intervention, only 15 completed the intervention, although completion was significantly greater using the ‘open invite’ approach (85%) rather than the other two approaches (31%). Once parents engaged with the programme retention rates were good (80%) |
| 6 | Identification of a method for collection of data on medically and non-medically attended injuries in the index child and their preschool siblings that are completed by parents participating in the feasibility study | Completed. We have developed an injury calendar to collect these data and have undertaken a small-scale validation against medical records that indicates that injuries are generally well reported by parents using this tool. The low sensitivity of the injury calendar (20%) may be a consequence of the small number of injuries requiring ED attendance and in a future trial may be improved with additional information for parents on how to complete the calendar |
| 7 | Assessment of a method of collecting outcome data from control children’s centre families that achieves engagement of families for the duration of the study | We were able to retain 7/12 (58%) parents randomised to the control arm and collect outcome data from them. Development of a control arm that avoids ‘no training’ may support engagement of control arm participants |
| 8 | Establishment of the number of children’s centres and the number of families that will need to participate in a future main trial | We have been unable to estimate the number of children’s centres and number of parents that will need to participate in a future trial owing to the small numbers of parents recruited. We propose estimating these numbers from published sources |
In our original proposal we suggested three criteria for continuation to a full trial:
-
A recruitment rate to the study of ≥ 25% of eligible families. We were unable to meet this criterion for recruitment through health visitor teams or via children’s centres because we were unable to determine the number of eligible families from these sources. We were able to recruit 26.7% of the eligible parents identified by emergency department attendance using telephone contact. The proposal that in a future trial all parents in the catchment area of a participating children’s centre would be eligible to attend the programme rather than only those whose child has sustained an injury means that this criterion would need to be revised for a future study.
-
Retention in the study of ≥ 70% of recruited families. Of 29 parents randomised to intervention (n = 17) or control (n = 12), 14 (48%) were retained through to the end of the 6-month period of follow-up and returned the final questionnaire booklets (nine parents in the intervention arm and five parents in the control arm). Of the nine ‘open invite’ parents who consented to provide information for the study, six (67%) returned injury calendars over a 3-month period of follow-up. These parents were not asked to complete final questionnaires.
-
Attendance at the programme sessions of 50%. In Bristol, of the seven parents in the intervention arm who commenced the programme, four (57.1%) attended at least 50% of the sessions. In Nottingham, of the 13 ‘open invite’ parents who commenced the programme, 11 (84.6%) attended at least 50% of the sessions.
Lessons learnt
For convenience we have reproduced below the lessons learnt from each of the component parts of this study.
Chapter 2, Theoretical basis for the intervention: lessons from two systematic reviews
-
Parenting interventions that include home-based, one-to-one, multifaceted components can reduce parent-reported and medically attended child injuries, and appear to improve home safety measures.
-
The mechanisms through which parenting programmes may reduce child injury are unclear but may include a generic change in parenting.
-
There is no current evidence from RCTs of the effectiveness of solely group-based community-delivered parenting programmes in reducing child injury.
-
Participants were interested in joining and completing parenting programmes if they believed that in doing so they would have the opportunity to learn new and specific skills, either for their own personal development or because they believed their skills would support their children.
-
The relationship between the participant, the deliverer and the other group members was very important. Participants needed to feel safe both with the deliverer and within the group. A known or trusted deliverer of the programme was helpful, but the deliverer needed to have the skills to present the programme in a non-judgemental, empathic and supportive manner. Participants needed to be able to relate to the other members of the group.
-
Practical issues such as the location, frequency and timing of the programme influenced parental engagement. Programmes needed to fit around existing commitments. Incentives such as childcare, travel expenses and refreshments were important.
-
Those delivering the programmes emphasised the need to be able to respond to the needs of the group, that is to say to be able to tailor the programme where necessary. This is in potential conflict with the production of manualised programmes that support fidelity of intervention delivery. Deliverer training needs to include group facilitation skills in addition to the ability to deliver the programme materials.
-
The potential difference in issues raised by participants and those delivering programmes indicate that both perspectives should be explored when evaluating programmes.
Chapter 3, Development of the parenting programme, and Chapter 7, Evaluation of the parenting programme
-
Voluntary sector organisations working with the participant group were informed and valued partners in the intervention development process.
-
The involvement of the voluntary sector organisations in the production of the 8-week parenting programme, informed by recommendations made by the PAG and a parents’ forum facilitated by Parenting UK, resulted in an intervention more likely to meet the needs of the participant group than if it had been developed from a theoretical perspective alone.
-
Practical issues, such as the need for a wheeled case to transport programme materials and resources into and out of venues, need to be addressed in any future trial.
-
Each programme delivery team should have its own set of resources in a future trial. A process to maintain and replace lost and broken equipment would need to be established.
-
In a future trial, venues that host programme delivery should be encouraged to facilitate courses during the mornings when parents may be more engaged and less worried about collecting other children from school.
-
Future ‘train the trainer’ events need to be timed more closely to the first delivery of the programme for new trainers. At the ‘train the trainer’ event, there should be more time allocated to practising delivery of some of the course materials. Training in group facilitation skills was acknowledged as very important, even for experienced health visitors.
-
Children’s centres need to be able to plan their programmes well ahead. Therefore, in a future trial, fixed periods when a course would run need to be agreed in advance and should not be repeatedly put back if numbers of participants available are too small to run the course.
Chapter 4, Development of the injury calendar
-
The acceptability of a new parent-reported injury outcome measure was improved by the use of a graphic designer who recommended changes to simplify the information recording process and to increase the familiarity of the design.
-
The PAG provided feedback on designs that increased the likelihood that the recording of potentially sensitive information would be completed.
Chapter 5, Feasibility of evaluating the parenting programme through a randomised controlled trial design
-
The need to admit that your child has sustained an injury is a significant barrier to recruitment. The faster rate of participant identification through the ‘open invite’ route [we engaged 11 parents (in two settings) over 2 weeks to attend the parenting programme when an ‘open invite’ policy was used, compared with 40 parents recruited over 10 months from four settings when using the criterion of having a child who had sustained a medically attended injury] suggests that rather than target families once an injury has occurred it would be better to target families before the injury event. Significantly more parents identified through the ‘open invite’ route completed the intervention compared with those recruited using the original criteria.
-
At this point in time, health visitor teams do not have the capacity to support the identification of potential participants or the delivery of the parenting programme for any future trial.
-
Using children’s centres in deprived areas would be an appropriate method to identify families, and children’s centres would be supportive of this approach in a future trial.
-
The setting for delivery of the parenting programme should be flexible to respond to local capacity and facilities. The most important factors about the setting are that it is known to parents and easily accessible. Children’s centres may provide an appropriate setting but where necessary alternative community venues should be used.
-
A short period of time between identification/recruitment and the start of the programme appeared to be important to avoid attrition of participants before the programme commences.
-
Once parents commenced the programme, retention rates to the end of the course were good both for parents recruited against the original eligibility criteria (80%) and for those identified through ‘open access’ (79%), suggesting that the programme was well received by those attending.
-
First aid courses are very commonly provided in children’s centre settings and can be considered to be part of usual care provided to users of these settings.
-
Approximately two-thirds of parents sent injury calendars returned them, and 151 injuries were recorded on the returned calendar pages, suggesting that the calendar was relatively well accepted as a measure and that parents appeared comfortable reporting injuries in their children as evidenced by the number of injuries reported.
-
Not all parents who were sent injury calendars returned them, and therefore checking the records of NHS providers is important in order to identify use of these services during the follow-up period.
-
Some of the parents did not report major injuries in the calendar. In a future trial the use of an objective measure of NHS provider use would be necessary, although it would not be possible to validate all NHS provider use such as, for example, following up telephone calls to NHS 111 or ‘999’ calls.
-
Many of the injuries reported by parents on the injury calendars appeared minor and may not have met the definition of an injury as provided. Support to complete the injury calendars correctly would be important in a future trial, for example amendments to the instructions on the calendar and to the way the calendar is introduced to parents to help parents in both arms know when and when not to record an injury.
-
The list of injury types on the calendar should be reviewed (e.g. the addition of objects getting stuck in the nose and ears).
-
An alternative measure for recording child behaviour needs to be identified that will allow a baseline post-test comparison even in young infants in whom significant developmental change between baseline and completion of follow-up would be expected.
Chapter 6, Determination of the parameters for a future cost-effectiveness evaluation of the programme
-
It is possible to build a resource use checklist to determine the non-recurrent and recurrent costs associated with delivering this programme as part of a future trial.
-
The injury calendar is able to indicate the initial parent-reported NHS provider use costs in intervention and usual care arms of any future trial although amendments to the calendar are required to add transfer by ambulance and allow the use of multiple NHS providers to be recorded.
-
Injury management is often associated with a range of NHS provider resources beyond the initial action, and this series of NHS savings relating to an injury event needs to be captured for full costing savings to be estimated in a future trial economic evaluation.
-
In a community setting, effective parenting programmes depend upon parental participation in the programme, suggesting that a social perspective on costs that are outside the public sector should be developed to capture these resources.
Implications for a future trial
Study eligibility
The targeted identification and recruitment of parents whose preschool child had sustained an injury resulted in considerable recruitment challenges and is the primary barrier to the success of a trial of the parenting programme intervention. The stigma associated with admitting that your child has sustained a medically attended injury appears to be even greater than we initially suspected. Parents who have attended courses during the feasibility study have reported feeling stigmatised by being invited to join the programme. Children’s centre managers and staff, and health visitor teams, have consistently advised us throughout the study that the best way to engage the families most at risk of child injury (e.g. families with chaotic lives, large families, or families with poor support) would be to provide a universally accessible programme. We therefore conclude that it is not feasible to run a future trial of the FAST parent programme using the existing eligibility criterion that specifies families where a child has sustained an injury.
Recommendation: In a future trial, we would recommend that targeting all parents from a high-risk population would be a more feasible strategy.
Recruitment
Identification of potential parent participants via health visitor teams has been shown not to be feasible owing to their current limited capacity. As we are recommending that a future trial should not target parents of children who have sustained an injury, identification and recruitment via emergency departments would not be appropriate. We have demonstrated through our experience in two children’s centres in Nottingham that making the programme universally accessible to parents was more effective in engaging parents in these two settings than targeting parents of injured children. These ‘open access’ parents were not formally recruited to the trial, but invited to attend a group that was starting the following week. While our experience suggests that the ‘open access’ route is less stigmatising, a future trial would need to evaluate recruitment to a group using these eligibility criteria. Personal contact with the researchers or informed children’s centre staff at the time of identification of eligible parents may help increase recruitment, rather than using posters and leaflets alone.
Recommendation: On the basis that a future trial should target all parents in a high-risk population, we suggest using children’s centres in deprived areas as venues for the identification of potential participants. The engagement of the senior managers of participating children’s centres would therefore be important to the success of the trial.
Randomisation
Recruitment through children’s centres would favour cluster randomisation in a future trial. Discussion with the manager of the children’s centre hosting our PAG confirmed our impression that individual randomisation of parents attending the same children’s centre would be unacceptable to both parents and children’s centre staff. On the basis of equity it would be preferable that all parents recruited at the same time should experience the same arm of the trial. The cluster would therefore be either at the level of the group or the level of the children’s centre. As during the feasibility study we would recommend that, in a multicentre future trial, clusters would be randomly allocated to intervention or control arm via a trials unit using a remote automated system.
Recommendation: Randomisation should be at the level of the children’s centre. Allocation to intervention or control arms would be delayed until after recruitment of parents to avoid post-randomisation recruitment bias.
Intervention delivery: recruitment of delivery teams
Our experience indicates that it is currently not feasible to ask health visitor teams to deliver the intervention alongside their existing workload. The current investment in England in health visitor training has not yet resulted in the capacity within teams to participate with intervention delivery in a future trial. It is possible that by the time of completion of a future trial the workload pressures on health visitor teams may have eased such that should the intervention be shown effective and cost-effective, the wider distribution of the programme could be considered through health visitor teams at that time. Parent participants in this feasibility study reported that they valued the knowledge and experience of the nurses delivering the programme. Therefore, for a future trial we would recommend that nurses be employed by the study to deliver the intervention in each locality. We acknowledge that the potential effectiveness of a programme in a future roll out may not be as great as the effect when evaluated in a trial using dedicated programme deliverers.
Children’s centres we have worked with have indicated an interest in supporting the further evaluation of this intervention. We propose that in a future trial each participating children’s centre would be encouraged to put forward a member of the children’s centre staff to be trained to be the cofacilitator for the nurse trainer. Discussion with the community support manager of the children’s centre hosting our PAG leads us to understand that this would be well received by children’s centre managers as an opportunity to develop skills in members of their staff, without additional cost to the children’s centre. We also anticipate this would encourage children’s centres to be committed to participation in a future trial, and may have the benefit of encouraging retention of parents during the delivery of the course as a familiar member of staff would be involved.
Recommendation: For a future trial, we would recommend that nurses be employed by the study to deliver the intervention in each locality, and each that participating children’s centre provide a staff member to be the cofacilitator for the nurse trainer.
Equipment and facilities
The resource kits (burns dolls, colour-change heat mug, choking tube, resuscitation dolls, fire safety DVD and images for group discussions) were well received by delivery teams and parent participants in the feasibility study.
Recommendation: In a future trial, each delivery team should be equipped with its own set of resources, a wheeled trolley/case to facilitate transport of the resource kit, and a process for replacing broken or lost items.
We recommend that a crèche facility be provided to enable parents to participate in the programme during a main trial, and, therefore, venues need to be identified that have the physical space to provide a room suitable for delivering the course to parents, as well as a nearby room available for a crèche. Where possible, the crèche or nursery facilities at the children’s centre would be used as we know that parents will feel more confident to use a crèche provider and venue known to them. If a children’s centre wished to participate in a main trial but was unable to provide such facilities, its participation would be dependent on the identification of a suitable alternative local community centre as a venue that would be acceptable to parents.
Recommendation: A crèche facility should be provided to enable parents to participate in the programme during a future trial.
Where children’s centres choose to host the programme in their own facilities, an agreement would need to be made to (i) protect the rooms for the programme and not release the rooms to alternative providers, should there be sufficient interest from parents in the course; and (ii) release the rooms for alternative providers should an inadequate number of parents have been recruited to the course by an agreed date.
Outcome measures
If the parenting programme is effective in helping parents to keep their preschool children safe from injuries we would expect a reduction in injury occurrence in all preschool children in that family. The intervention may be more likely to prevent the more serious injuries than minor ones, and may enable parents to feel more confident to manage minor injuries at home rather than seek medical attention. Alternatively, increased knowledge of when to seek medical attention could increase the use of health care. Therefore, it would be necessary to record both medically attended and non-medically attended injuries during a future trial to evaluate the full effects of the intervention. In order to record non-medically attended injuries, a measure to capture parent-reported injuries would be required. The injury calendar was shown in the feasibility study to be an acceptable tool for collecting parent-reported injuries. We have undertaken a limited validation of the tool and found it to be a good record of both health service use and self-care.
Recommendation: The injury calendar developed during this feasibility study should be used as the tool for collecting the injury outcomes in a future trial. Minor amendments to the calendar are required and further validation of the injury calendar against NHS provider records should take place. In addition, NHS provider records will need to be used as a method to collect injury outcomes in a future trial as this feasibility study has indicated that not all medically attended injuries will be recorded on injury calendars.
In order to establish the mechanism through which any injury risk reduction was achieved, it would be necessary to collect a range of measures as secondary outcomes. As established in this feasibility study, measures for parental well-being and parenting, parental knowledge of first aid and parentally reported home safety practices would be appropriate secondary outcomes in a future trial. Some parents reported that the child behaviour questions asked when their child was an infant at entry to the study were no longer appropriate when their child was a toddler at the end of the follow-up period almost 1 year later.
Recommendation: The parent well-being, parenting, first aid knowledge and parent reported home safety practices should be used in a future trial as secondary outcomes. A new measure for child behaviour that enables behaviour change to be recorded over periods of rapid developmental progress will need to be identified for use in any future trial.
Usual care
In our original study protocol we proposed to compare the parenting programme intervention with usual care where this was described as the actions taken by health visitor teams upon receipt of a notification of attendance at an emergency department or NHS walk-in centre for an injury. We discovered that health visitor teams have variable and locally determined usual care, and that most teams are using paper-based records with no central register of receipt of notifications or action taken. Importantly, the practice of usual care varies with time within teams, depending on the workforce capacity and the number of vacant positions in that team. At times teams are required to prioritise only the families in greatest need of support for direct contact.
Recommendation: It is no longer appropriate to record usual care as the action taken by a health visitor team following receipt of a notification of injury in a preschool child because in a future trial we would not recommend an eligible parent to be one whose child has sustained a medically attended injury.
We have identified that it is very common for children’s centres to provide first aid courses for parents in response to parents’ interests and also because children’s centres are encouraged to provide injury prevention as one of a range of health promotion topics. We propose that usual care should be the courses that the children’s centre would usually provide for parents. If the children’s centre were randomised to the intervention arm of a future trial then we would ask that the FAST parent programme be delivered instead of a first aid course if one were due to be given. We recognise that a no-training arm may be unattractive to parents being recruited to a future trial, and therefore where children’s centre would be randomised to the control arm and would not be routinely offering a first aid course, we would provide parents with a booklet of the first aid advice pages from the FAST programme parents’ handbook.
Recommendation: In a future trial, we would recommend that usual care should be the courses that a children’s centre would normally provide if the centre were not participating in a trial. Where a children’s centre would not usually provide a first aid course, we would provide a booklet of first aid advice to reduce the potential for parents to be reluctant to engage in a trial where one option is to receive no training.
Sample size
We were unable to achieve sufficient numbers in terms of recruitment and completion in the feasibility study owing to several difficulties, many of which were anticipated. An aim of this feasibility study was to investigate these problems and identify different approaches to overcome them. The low recruitment and completion rate has meant the number of medically attended injuries reported by parents was too small to make an estimate of the sample size required for a future trial.
Recommendation: A future trial needs to be cluster randomised, and powered around the primary outcome of injuries requiring NHS provider use, data for which should be drawn from published estimates. We recommend that a future trial should be two-staged with a pilot period to formally test the proposed new eligibility criteria and potential for recruitment via children’s centres, and during which it should be confirmed that early data are suggestive of an outcome in the desired direction of a reduction in NHS provider use.
‘Train the trainer’
We developed a 2-day ‘train the trainer’ event for trainers and cofacilitators delivering the programme. We encouraged trainers to seek peer support during delivery and offered telephone support from the programme developer at Parenting UK. The ‘train the trainer’ event was evaluated using feedback forms immediately after the training and through interviews and a focus group with trainers and cofacilitators after the courses had been delivered. In a future trial, regional trainers could be trained to both deliver and cascade training across a geographical area and be responsible for ensuring adequate intervention fidelity, validation of trainer skills, and that session content is always delivered with a sense of optimism and a non-judgemental approach. Consideration would need to be given to turnover of staff through natural change (for both regional trainers and local deliverers). The regional trainers could be responsible for ensuring the maintenance of programme resource kits and would know how to obtain replacement materials and equipment if required. Regional trainers’ ongoing learning needs would need to be supported, for example by refresh training, by teleconference support or by a moderated online forum.
Recommendation: A programme to meet the training and support needs of regional trainers and local deliverers would need to be developed for a future trial to reflect the changes to the intervention from an 8-week to a 6-week programme, to ensure high-quality training of a larger number of trainers and cofacilitators, and to support an intervention fidelity assessment process.
Name of the intervention
Since the funding of the feasibility study, there has been a rapid rise in the prominence and use of a parenting programme that also uses the acronym FAST: the Families And Schools Together parenting support programme.
Recommendation: The First-aid Advice and Safety Training parent programme should be renamed for a future trial to avoid any possible confusion for parents and practitioners with the Families and Schools Together programme.
In this chapter, we have summarised our main findings and reported on the completion of the study objectives and previously specified criteria for success. We have then summarised the lessons learnt from the component parts of the study and brought these together in the section on implications for a future trial.
Chapter 9 Conclusions
Implications for practice
We have successfully developed, and refined, a group-based parenting programme designed to prevent injuries in the home for preschool children. This programme, which combines injury prevention and first response advice underpinned by the principles of parenting, has the potential to prevent avoidable harm to children and reduce NHS provider use following trauma, subject to its being shown to be effective and cost-effective in a future trial. Were this to be demonstrated, the programme could be made widely available to community settings across the country.
Implications for research
We have developed, and undertaken early validation of, a tool to collect parentally reported home injuries in preschool children, and details of the care provided (including NHS provider use) following such injuries. This tool has the potential to be of use in further injury prevention research studies and could be adapted for other studies where participant use of NHS provider services is collected.
Appropriate data collection methods and tools for economic analyses of the intervention from a public sector perspective have been identified for use in a future study.
We have demonstrated the valuable contribution of a PAG to the development of the documentation, methodology and interpretation of findings in this study. The use of a group of advisors drawn from the setting of a group that routinely meets has been particularly successful and would appear to be a format that could be of value for other studies.
A future trial of the FAST parent programme appears justified. We recommend that any future trial should offer universal access to the programme. We have demonstrated a range of lessons learnt that would enable such a study to be conducted. We recommend that nurses should be recruited to be trained to deliver the programme outside of their existing contractual arrangements and children’s centre staff should be engaged as cofacilitators of the groups. A future trial should be cluster randomised at the level of the children’s centre, and powered around the primary outcome of medically attended injury. Secondary outcomes should include measures for child behaviour, parental well-being, parental supervision, parental knowledge of first aid and parentally reported home safety practices.
The comparator arm of the trial should be the usual programmes provided by the children’s centre in question, which may include a first aid course. Comparator arm participants should be provided with a booklet providing first aid advice.
Acknowledgements
We would like to acknowledge the contributions of the following people:
Mrs Jane Crane and the staff and parents at the Henbury Court children’s centre for providing a parent advisory group for this study.
Professor Rod Taylor (chairperson) and Dr Mariana Brussoni and Professor Andrea Gielan (independent members) of the trial steering committee.
Mrs Pamela Park and Mrs Vera Azuike from Parenting UK, and Mrs Carole Hewison from the Whoops! Child Safety Project for their support in developing the parenting programme.
The health visitors and community nurses in Bristol and Nottingham who delivered the programme.
Contributions of authors
Julie Mytton (Associate Professor in Child Health) was chief investigator, designed and led the study, and prepared the final report.
Jenny Ingram (Senior Research Fellow) conducted the qualitative systematic review, conducted qualitative evaluations and provided methodological support throughout the feasibility study.
Sarah Manns (Research Fellow) managed the feasibility study in the Bristol site, supported the qualitative systematic review and collected qualitative outcomes during the feasibility study.
Tony Stevens (Research Fellow) managed the feasibility study in the Nottingham site and collected quantitative and qualitative data during the feasibility study.
Caroline Mulvaney (Senior Research Fellow) conducted the update of the Cochrane systematic review and supported the conduct of the feasibility study in the Nottingham site.
Peter Blair (Senior Research Fellow, Statistician) provided methodological and statistical support, facilitated preparation of and interpreted the quantitative data.
Jane Powell (Professor of Public Health Economics) prepared the resource use checklist and costing data, and prepared the health economic parameters for publication.
Barbara Potter (Health Visitor) advised on the design and conduct of the feasibility study, was a member of the programme development subgroup, and delivered the programme in the Bristol site.
Elizabeth Towner (Professor of Child Health) member of the management group, evaluated the programme from an injury prevention perspective, and provided injury prevention expertise.
Alan Emond (Professor of Child Health) provided methodological and injury prevention expertise.
Toity Deave (Associate Professor in Child and Family Health) supported engagement with children’s centres in Bristol and provided methodological support.
James Thomas (Professor of Social Research and Policy) supported the systematic review of the barriers and facilitators to parental engagement in parenting programmes, providing technical and methodological advice.
Denise Kendrick (Professor of Primary Care Research) was principal investigator in the Nottingham site and supported delivery of the feasibility study and provided injury prevention expertise.
Sarah Stewart-Brown (Professor of Public Health) was a member of the programme development subgroup and provided parenting expertise.
All authors contributed to the preparation of the final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Peden M, Oyegbite K, Ozanne-Smith J, Hyder A, Branche C, Rahman F, et al. World Report on Child Injury Prevention. Geneva: World Health Organization; 2008.
- Royal Society for the Prevention of Accidents . Home and Leisure Accident Surveillance System 2011. www.hassandlass.org.uk/query (accessed 1 January 2011).
- O’Connor T, Davies L, Dunn J, Golding J. ALSPAC Study Team . Distribution of accidents, injuries and illness by family type. Pediatrics 2000;106. http://dx.doi.org/10.1542/peds.106.5.e68.
- Warrington S, Wright C. ALSPAC Study Team . Accidents and resulting injuries in premobile infants: data from the ALSPAC study. Arch Dis Child 2001;85:104-7. http://dx.doi.org/10.1136/adc.85.2.104.
- Langley J, Dodge J, Silva P. Accidents in the first five years of life. Aus Paediatr J 1979;15:255-9. http://dx.doi.org/10.1111/j.1440-1754.1979.tb01240.x.
- Reading R, Langford I, Haynes R, Lovett A. Accidents to preschool children: comparing family and neighbourhood risk factors. Soc Sci Med 1999;48:321-30. http://dx.doi.org/10.1016/S0277-9536(98)00311-6.
- Dowswell T, Towner E. Social deprivation and the prevention of unintentional injury in childhood. Health Edu Res 2002;17:221-37. http://dx.doi.org/10.1093/her/17.2.221.
- Edwards P, Green J, Lachowycz K, Grundy C, Roberts I. Serious injuries in children: variation by area deprivation and settlement type. Arch Dis Child 2008;93:485-9. http://dx.doi.org/10.1136/adc.2007.116541.
- Towner E, Dowswell T, Errington G, Burkes M, Towner J. Injuries in children aged 0–14 years and their inequalities. London: Health Development Agency; 2005.
- Edwards P, Green J, Roberts I, Lutchman S. Deaths from injury in children and employment status in family: analysis of trends in class specific death rates. BMJ 2006;333:119-21. http://dx.doi.org/10.1136/bmj.38875.757488.4F.
- Reading R, Jones A, Haynes R, Daras K, Emond A. Individual factors explain neighbourhood variations in accidents to children under 5 years of age. Soc Sci Med 2008;67:915-27. http://dx.doi.org/10.1016/j.socscimed.2008.05.018.
- Hippisley-Cox J, Groom L, Kendrick D, Coupland C, Webber E, Savelyich B. Cross sectional survey of socioeconomic variations in severity and mechanism of childhood injuries in Trent 1992–1997. BMJ 2002;324:1132-7.
- Bijur PE, Golding J, Kurzon M. Childhood accidents, family size and birth order. Soc Sci Med 1988;26:839-43. http://dx.doi.org/10.1016/0277-9536(88)90176-1.
- Orton E, Kendrick D, West J, Tata L. Independent risk factors for injury in pre-school children: three population-based nested case–control studies using routine primary care data. PLOSONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0035193.
- Bijur P, Kurzon M, Overpeck M, Scheidt P. Parental alcohol use, problem drinking, and children’s injuries. JAMA 1992;267:3166-71. http://dx.doi.org/10.1001/jama.267.23.3166.
- Rhodes K, Iwashyna T. Child injury risks are close to home: parental psychosocial factors associated with child safety. Matern Child Health J 2007;11:269-75. http://dx.doi.org/10.1007/s10995-006-0171-2.
- Morrongiello B, Corbett M, McCourt M, Johnston N. Understanding unintentional injury-risk in young children I: the nature and scope of caregiver supervision of children at home. J Pediatr Psychol 2006;31:529-39. http://dx.doi.org/10.1093/jpepsy/jsj045.
- Morrongiello B, Corbett M, McCourt M, Johnston N. Understanding unintentional injury risk in young children II: the contribution of caregiver supervision, child attributes, and parent attributes. J Pediatr Psychol 2006;31:540-51. http://dx.doi.org/10.1093/jpepsy/jsj073.
- Rowe R, Maughan B, Goodman R. Childhood psychiatric disorder and unintentional injury: findings from a national cohort study. J Pediatr Psychol 2004;29:119-30. http://dx.doi.org/10.1093/jpepsy/jsh015.
- Bijur P, Stewart-Brown S, Butler N. Child behavior and accidental injury in 11,966 preschool children. Am J Dis Child 1986;140:487-92. http://dx.doi.org/10.1001/archpedi.1986.02140190097036.
- Langley J, McGee R, Silva P, Williams S. Child behaviour and accidents. J Pediatr Psychol 1983;8:181-9. http://dx.doi.org/10.1111/j.1440-1754.1980.tb01307.x.
- Antisocial Behavior and Conduct Disorders in Children and Young People: Recognition, Intervention and Management. Clinical guideline 158. London: National Institute for Health and Care Excellence; 2013.
- No Health Without Mental Health. London: Department of Health; 2011.
- Lindsay G, Strand S, Davis H. A comparison of the effectiveness of three parenting programmes in improving parenting skills, parent mental well-being and children’s behaviour when implemented on a large scale in community settings in 18 English local authorities: the parenting early intervention pathfinder (PEIP). BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-962.
- Morrison Gutman L, Feinstein L. Parenting Behaviour and Children’s Development from Infancy to Early Childhood: Changes, Continuities and Contributions. London: Department for Education and Skills; 2007.
- Up to 7: Family Background and Child Development up to Age 7 in the Avon Longitudinal Study of Parents and Children (ALSPAC). London: Department for Education and Skills; 2006.
- Morrison Gutman L, Brown J, Akerman R. Nurturing Parenting Capability – The Early Years. London: Department for Children, Schools and Families; 2009.
- Schwebel D, Brezausek C, Ramey S, Ramey C. Interactions between child behavior patterns and parenting: implications for children’s unintentional injury risk. J Pediatr Psychol 2004;29:93-104. http://dx.doi.org/10.1093/jpepsy/jsh013.
- Feldman M, Case L, Sparks B. Effectiveness of a child-care training program for parents at risk for child neglect. Can J Behav Sci 1992;24:14-28. http://dx.doi.org/10.1037/h0078698.
- Morrongiello B, Corbett M, Brison R. Identifying predictors of medically-attended injuries to young children: do child or parent behavioural attributes matter?. Inj Prevent 2009;15:220-5. http://dx.doi.org/10.1136/ip.2008.019976.
- Schwebel D, Kendrick D. Caregiver supervision and injury risk for young children: time to re-examine the issue. Inj Prevent 2009;15:217-18. http://dx.doi.org/10.1136/ip.2009.022202.
- Stewart-Brown S, Patterson J, Mockford C, Barlow J, Klimes I, Pyper C. Impact of a general practice based group parenting programme: quantitative and qualitative results from a controlled trial at 12 months. Arch Dis Child 2004;89:519-25. http://dx.doi.org/10.1136/adc.2003.028365.
- Barlow J, Coren E, Stewart-Brown S. Parent-training programmes for improving maternal psychosocial health. Cochrane Database Syst Rev 2003;4. http://dx.doi.org/10.1002/14651858.CD002020.
- Coren E, Barlow J. Individual and group-based parenting programmes for improving psychosocial outcomes for teenage parents and their children. Cochrane Database Syst Rev 2001;3. http://dx.doi.org/10.1002/14651858.CD002964.
- Barlow J, Stewart-Brown S. Behaviour problems and group-based parent education programmes. J Develop Behav Pediatr 2000;21:356-70. http://dx.doi.org/10.1097/00004703-200010000-00007.
- Barlow J, Parsons J, Stewart-Brown S. Preventing emotional and behavioural problems: the effectiveness of parenting programmes with children less than 3 years of age. Child Care Health Develop 2005;31:33-42. http://dx.doi.org/10.1111/j.1365-2214.2005.00447.x.
- Petrie J, Bunn F, Byrne G. Parenting programmes for preventing tobacco, alcohol and drugs misuse in children < 18: a systematic review. Health Edu Res 2007;22:177-91. http://dx.doi.org/10.1093/her/cyl061.
- Sanders M, Markie-Dadds C, Turner K. Theoretical, Scientific and Clinical Foundations of the Triple P-Positive Parenting Programme: A Population Approach to the Promotion of Parenting Competence. Brisbane, QLD: The Parenting and Family Support Centre, University of Queensland; 2002.
- Gagnon A, Bryanton J. Postnatal parental education for optimizing infant general health and parent–infant relationships. Cochrane Database Syst Rev 2009;1. http://dx.doi.org/10.1002/14651858.CD004068.pub2.
- Kendrick D, Elkan R, Hewitt M, Dewey M, Blair M, Robinson J, et al. Does home visiting improve parenting and the quality of the home environment? A systematic review and meta-analysis. Arch Dis Child 2000;82:443-51. http://dx.doi.org/10.1136/adc.82.6.443.
- Kendrick D, Watson M, Mulvaney C, Burton P. How useful are home safety behaviours for predicting childhood injury?. Health Edu Res 2005;20:709-18. http://dx.doi.org/10.1093/her/cyh021.
- Kendrick D, Young B, Mason-Jones A, Ilyas N, Achana F, Cooper N, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev 2012;9. http://dx.doi.org/10.1002/14651858.CD005014.
- Emond A, Pollock J, Deave T, Bonnell S, Peters T, Harvey I. An evaluation of the First Parent Health Visitor Scheme. Arch Dis Child 2002;86:150-7. http://dx.doi.org/10.1136/adc.86.3.150.
- Roberts I, Kramer M, Suissa S. Does home visiting prevent childhood injury? A systematic review of randomised controlled trials. BMJ 1996;312:29-33. http://dx.doi.org/10.1136/bmj.312.7022.29.
- Kendrick D, Barlow J, Hampshire A, Polnay L, Stewart-Brown S. Parenting interventions for the prevention of unintentional injuries in childhood. Cochrane Database Syst Rev 2007;4. http://dx.doi.org/10.1002/14651858.CD006020.pub2.
- Kendrick D, Barlow J, Hampshire A, Stewart-Brown S, Polnay L. Parenting interventions and the prevention of unintentional injuries in childhood: systematic review and meta-analysis. Child Care Health Develop 2008;34:682-95. http://dx.doi.org/10.1111/j.1365-2214.2008.00849.x.
- Ingram J, Emond A. Parents’ perceptions of home injury risk and attitudes to supervision of preschool children: a qualitative study in economically deprived communities. Primary Health Care Res Develop 2009;10:98-108.
- Moran P, Ghate D, van der Merwe A. What Works in Parenting Support? A Review of the International Evidence. London: Department for Education and Skills; 2004.
- Bell M. Community based parenting programmes: an exploration of the interplay between environmental and organizational factors in a Webster Stratton project. Br J Soc Work 2007;37:55-72. http://dx.doi.org/10.1093/bjsw/bch283.
- Kane G, Wood V, Barlow J. Parenting programmes: a systematic review and synthesis of qualitative research. Child Care Health Develop 2007;33:784-93. http://dx.doi.org/10.1111/j.1365-2214.2007.00750.x.
- Sheill A, Hawe P, Gold L. Complex interventions or complex systems? Implications for health economic evaluation. BMJ 2008;336:1281-3. http://dx.doi.org/10.1136/bmj.39569.510521.AD.
- Weatherly H, Drummond M, Claxton K. Assessing the Challenges of Applying Standard Methods of Economic Evaluation to Public Health Interventions. York: Centre for Health Economics; 2009.
- Lancaster G, Dodd S, Williamson P. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Prac 2004;10:307-12. http://dx.doi.org/10.1111/j. 2002.384.doc.x.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1655.
- Cost Benefit Analysis of Interventions with Parents. London: Department for Children, Schools and Families; 2007.
- Bonin E, Stevens M, Beecham J, Byford S, Parsonage M. Costs and longer term savings of parenting programmes for the prevention of persistent conduct disorder: a modelling study. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-803.
- Knapp M, McDaid D, Parsonage M. Mental Health Promotion and Mental Illness Prevention: the Economic Case. London: London School of Economics; 2011.
- Romeo R, Byford S, Knapp M. Economic evaluations of child and adolescent mental health interventions: a systematic review. J Child Psychol Psychiatr 2005;46:919-30. http://dx.doi.org/10.1111/j.1469-7610.2005.00407.x.
- Stevens M. The cost-effectiveness of UK parenting programmes for preventing children’s behaviour problems – a review of the evidence [published online ahead of print 13 July 2012]. Child Fam Soc Work 2012. doi:10.1111/j.1365-2206.2012.00888.x.
- Edwards R, Ceilleachair A, Bywater T, Hughes D, Hutchings J. Parenting program for parents of children at risk of developing conduct disorder: cost effectiveness analysis. BMJ 2007;334:682-5. http://dx.doi.org/10.1136/bmj.39126.699421.55.
- Curtis L. Unit Costs of Health and Social Care 2011. Canterbury: PSSRU, University of Kent; 2011.
- Morrongiello B, Howard A, Rothman L, Sandomierski M. Once bitten, twice shy? Medically-attended injuries can sensitise parents to children’s risk of injuries on playgrounds. Inj Prevent 2009;15:50-4. http://dx.doi.org/10.1136/ip.2008.019398.
- Posner J, Hawkins L, Garcia-Espana F, Durbin D. A randomized, clinical trial of a home safety intervention based in an emergency department setting. Pediatrics 2004;113:1603-8. http://dx.doi.org/10.1542/peds.113.6.1603.
- King W, LeBlanc J, Barrowman N, Klassen T, Bernard-Bonnin A-C, Robitaille Y, et al. Long term effects of a home visit to prevent childhood injury: three year follow up of a randomized trial. Inj Prevent 2005;11:106-9. http://dx.doi.org/10.1136/ip.2004.006791.
- Potter B, Newell G. Accident Prevention in the Under 5s. Cheltenham: Severn NHS Trust and East Gloucestershire NHS Trust; 1997.
- Boddy J, Statham J, Smith M, Ghate D, Wigfall V, Hauari H. International Perspectives on Parenting Support. Non-English Language Sources. London: Department for Children, Schools and Families; 2009.
- Barrett H. Follow Up Work to Support the Implementation of the NICE/SCIE Guidance on Parenting Programmes. London: Social Care Institute for Excellence; 2009.
- Kendrick D, Mulvaney C, Ye L, Stevens T, Mytton J, Stewart-Brown S. Parenting interventions for the prevention of unintentional injuries in childhood. Cochrane Database Syst Rev 2013;3. http://dx.doi.org/10.1002/14651858.CD006020.pub2.
- Caldwell B, Bradley R. Home Observation for Measurement of the Environment: Administration Manual. Tempe, AZ: Family & Human Dynamics Research Institute, Arizona University; 2003.
- Armstrong K, Fraser J, Dadds M, Morris J. Promoting a secure attachment, maternal mood and child health in a vulnerable population: a randomized controlled trial. J Pediatr Child Health 2000;36:555-62. http://dx.doi.org/10.1046/j.1440-1754.2000.00591.x.
- Barlow J, Davis H, McIntosch E, Jarrett P, Mockford C, Stewart-Brown S. Role of home visiting in improving parenting and health in families at risk of abuse and neglect: results of a multicentre randomised controlled trial and economic evaluation. Arch Dis Child 2007;92:229-33. http://dx.doi.org/10.1136/adc.2006.095117.
- Caldera D, Burrell L, Rodriguez K, Crowne SS, Rodhe C, Duggan A. Impact of a state-wide home visiting program on parenting and on child health and development. Child Abuse Neglect 2007;31:829-52.
- Culp A, Culp R, Anderson J, Carter S. Health and safety intervention with first-time mothers. Health Edu Res 2007;22:285-94. http://dx.doi.org/10.1093/her/cyl079.
- Duggan AK, McFarlane EC, Windham AM, Rhode CA, Salkever DS, Fuddy L, et al. Evaluation of Hawaii’s Health Start Program. Future Children 1999;9:66-90. http://dx.doi.org/10.2307/1602722.
- Emond A, Pollock J, Deave T, Bonnell S, Peters TJ, Harvey I. An evaluation of the First Parent Health Visitor Scheme. Arch Dis Child 2002;86:150-7. http://dx.doi.org/10.1136/adc.86.3.150.
- Feldman MA, Case L, Sparks B. Effectiveness of a child-care training program for parents at risk for child neglect. Can J Behav Sci 1992;24:14-28. http://dx.doi.org/10.1037/h0078698.
- Fergusson DM, Grant H, Horwood LJ, Ridder EM. Randomized trial of the early start program of home visitation. Pediatrics 2005;116:803-9. http://dx.doi.org/10.1542/peds.2005-0948.
- Gutelius MF, Kirsch AD, McDonald S, Riddick Brooks M, McErlan T. Controlled study of child health supervision: behaviour results. Pediatrics 1977;60:294-30.
- Hardy JB, Streett R. Family support and parenting education in the home: an effective extension of clinic-based preventive health care services for poor children. J Pediatrics 1989;115:927-31. http://dx.doi.org/10.1016/S0022-3476(89)80744-9.
- The Infant Health and Development Program . Enhancing the outcomes of low-birth-weight, premature infants. A multisite, randomized trial. J Am Med Assoc 1990;263:3035-42.
- Johnson Z, Howell F, Molloy B. Community mothers’ programme: randomised controlled trial of non-professional intervention in parenting. Br Med J 1993;306:1449-52. http://dx.doi.org/10.1136/bmj.306.6890.1449.
- Johnston B, Huebner C, Tyll L, Barlow W, Thompson R. Expanding developmental and behavioural services for newborns in primary care: effects on parental well being, practice and satisfaction. Am J Prevent Med 2004;26:356-66.
- Kemp L, Harris E, McMahon C, Matthey S, Vimpani G, Anderson T, et al. Child and family outcomes of a long-term nurse home visitation programme: a randomised controlled trial. Arch Dis Child 2011;96:533-40. http://dx.doi.org/10.1136/adc.2010.196279.
- Kitzman H, Olds DL, Henderson CR, Hanks C, Cole R, Tatelbaum R, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomised controlled trial. J Am Med Assoc 1997;278:644-52.
- Koniak-Griffin D, Verzemnieks IL, Anderson NLR, Brecht M-L, Lesser J, Kim S, et al. Nurse visitation for adolescent mothers. Nurs Res 2003;52:127-36. http://dx.doi.org/10.1097/00006199-200303000-00009.
- Larson CP. Efficacy of prenatal and postpartum home visits on child health and development. Pediatrics 1980;66:191-7.
- Llewellyn G, McConnell D, Honey A, Mayes R, Russo D. Promoting health and home safety for children of parents with intellectual disability: a randomized controlled trial. Res Develop Disabil 2003;24:405-31. http://dx.doi.org/10.1016/j.ridd.2003.06.001.
- Minkovitz C, Hughart N, Strobino D, Scharfstein D, Grason H, Hou W, et al. A practice-based intervention to enhance quality of care in the first 3 years of life. J Am Med Assoc 2003;293:3081-91. http://dx.doi.org/10.1001/jama.290.23.3081.
- Olds DL, Henderson CR, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics 1986;78:65-78.
- St Pierre R, Layzer JI. Using home visits for multiple purposes: the Comprehensive Child Development Program. Future Children 1999;1:134-51. http://dx.doi.org/10.2307/1602725.
- Johnston B, Huebner C, Anderson M, Tyll L, Thomspon R. Healthy steps in an integrated delivery system. Child and parent outcomes at 30 months. Arch Pediatr Adolesc Med 2006;160:793-800. http://dx.doi.org/10.1001/archpedi.160.8.793.
- Massachusetts Home Safety Questionnaire. Boston, MA: Department of Public Health; 1996.
- Mytton J, Ingram J, Manns S, Thomas J. Facilitators and barriers to engagement in parenting programs: a qualitative systematic review. Health Educ Behav 2013. doi:10.1177/1090198113485755.
- Mytton J, Towner E, Kendrick D, Stewart-Brown S, Emond A, Ingram J, et al. The First-aid Advice and Safety Training (FAST) parent programme for the prevention of unintentional injuries in preschool children: a protocol. Inj Prevent 2013. http://doi:10.1136/injuryprev-2012-040689.
- Goodman R. The Strengths and Difficulties Questionnaire. London: Youth in Mind; 2012.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. http://dx.doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Toddler Questionnaire (Reference TQ, 18 months). Bristol: University of Bristol; 1992.
- Gartstein MA, Rothbart MK. Studying infant temperament via the Revised Infant Behavior Questionnaire. Infant Behav Dev 2003;26:64-86. http://dx.doi.org/10.1016/S0163-6383(02)00169-8.
- Kendrick D, Marsh P. Parents and first aid: I know what to do – but I’m not very confident. Health Edu J 1999;58:39-47. http://dx.doi.org/10.1177/001789699905800105.
- Watson M, Kendrick D, Coupland C. Validation of a home safety questionnaire used in a randomised controlled trial. Inj Prevent 2003;9:180-3. http://dx.doi.org/10.1136/ip.9.2.180.
- Tennant R, Hillier L, Fishwick R, Platt S, Stephen J, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. http://dx.doi.org/10.1186/1477-7525-5-63.
- Morrongiello B, Corbett M. The Parent Supervision Attributes Profile Questionnaire: a measure of supervision related to children’s risk of unintentional injury. Inj Prevent 2006;12:19-23.
- Manheim L. Health services research clinical trials: issues in the evaluation of economic costs and benefits. Control Clin Trials 2009;19:149-58. http://dx.doi.org/10.1016/S0197-2456(97)00146-3.
- Hollingworth W, Cohen D, Hawkins J. Reducing smoking in adolescents: cost effectiveness results from the cluster randomised ASSIST (A Stop Smoking in Schools Trial). Nicotine Tobacco Res 2011;14:161-8.
- GP Earnings and Expenses 2009/10. Leeds: The Information Centre; 2011.
- Munro J, Nicholl J, O’Cathian A, Knowles E, Morgan A. Evaluation of NHS Direct First Wave Sites: Final Report of the Phase 1 Research. Sheffield: Medical Care Research Unit, University of Sheffield; 2001.
- Wolfenstetter S. Conceptual framework for standard economic evaluation of physical activity programs in primary prevention. Prevent Sci 2011;12:435-51. http://dx.doi.org/10.1007/s11121-011-0235-4.
- McWhirter J, Francis C. Effective Safety Education Revisited. Principles of Effective Safety Education. London: Royal Society for the Prevention of Accidents; 2008.
- Mackay M, Vincenten J, Brussoni M, Towner E, Fuselli P. Child Safety Good Practice Guide. Good investment in unintentional child injury prevention and safety promotion – Canadian Edition. Toronto, ON: The Hospital For Sick Children; 2011.
- Parenting Programme Evaluation Tool (PPET). Leeds: Children’s Workforce Development Council; 2010.
- Luft J, Ingram H. Of Human Interaction. Palo Alto, CA: National Press Books; 1969.
- Luft J. Group Processes: An Introduction to Group Dynamics. Palo Alto, CA: National Press Books; 1970.
- Kolb DA. Experimental Learning: Experience as the Source of Learning and Development. Englewood Cliffs, NJ: Prentice Hall; 1984.
- Health Visitor Implementation Plan 2011–2015: A Call to Action. London: Department of Health; 2011.
- Fraser JA, Armstrong KL, Morris JP, Dadds MR. Home visiting intervention for vulnerable families with newborns: follow-up results of a randomized controlled trial. Child Abuse Negl 2000;24:1399-429.
- Duggan A, Caldera D, Rodriguez K, Burrell L, Rohde C, Crowne SS. Impact of a statewide home visiting program to prevent child abuse. Child Abuse Negl 2007;31:801-27.
- Duggan A, McFarlane E, Fuddy L, Burrell L, Higman SM, Windham A, et al. Randomized trial of a statewide home visiting program: impact in preventing child abuse and neglect. Child Abuse Negl 2004;28:597-622.
- Johnson Z, Molloy B, Scallan E, Fitzpatrick P, Rooney B, Keegan T, et al. Community Mothers programme – seven year follow-up of a randomized controlled trial of non-professional intervention in parenting. J Public Health Med 2000;22:337-42.
- Kemp L, Harris E, McMahon C, Matthey S, Vimpani G, Anderson T, et al. Miller Early Childhood Sustained Home-visiting (MESCH) trial: design, method and sample description. BMC Public Health 2008;8:424-35.
- Olds DL, Henderson CR, Kitzman H. Does prenatal and infancy nurse home visitation have enduring effects on qualities of parental caregiving and child health at 25 to 50 months of life?. Pediatrics 1994;93:89-98.
- Goodson BD, Layzer JI, St. Pierre RG, Bernstein L, Lopez M. Effectiveness of a comprehensive, five-year family support program for low-income children and their families: findings from the Comprehensive Child Development Program. Early Child Res Q 2000;15:5-39.
Appendix 1 Summary of included studies: participant and intervention characteristics
| Study | First author, year, study design | Study population | Age of child at start of programme | Intervention: key characteristics | Length of programme, months | Planned total contacts and plan of contacts | Delivery setting and mode |
|---|---|---|---|---|---|---|---|
| 1 | Armstrong 2000,70 Fraser 2000;115 RCT | EITHER one of physical domestic violence; childhood abuse of either parent; sole parenthood; ambivalence to the pregnancy. OR three of: maternal age < 18 years; unstable housing; financial stress; < 10 years’ maternal education; low family income; social isolation; history of mental health disorder; drug/alcohol abuse; domestic violence | Birth | Home visits comprised manualised programme aimed at enhancing parent’s relationship with the infant and positively influencing ability to provide a safer more nurturing and healthier environment for their child. Focus of home visits was to establish trust with family, enhancing parental self-esteem and confidence, providing anticipatory guidance for normal child development problems such as sleeping or crying behaviour problems, promoting preventive child health care and facilitating access to community services | 6 | Approximately 12 (weekly for 6 weeks, fortnightly until 3 months, monthly until 6 months) | Home; individual |
| 2 | Barlow 2007,71 Barlow 2008 (unpublished report); RCT | Vulnerable women using a range of criteria, e.g. mental health problems, domestic violence, drug/alcohol abuse | Prenatal | Visits from a health visitor trained in understanding the process of helping, skills of relating to parents effectively and methods of promoting parent–infant interaction using the Family Partnership Model | 18 | Approximately 72 (weekly visits) | Home; individual |
| 3 | Caldera 2007,72 Duggan 2007;116 RCT | ‘At-risk’ families: risks included maternal mental health, maternal substance abuse, partner violence | 50% prenatal, 50% birth | Home visitors to provide information, make referrals to community resources, help parents prepare for developmental milestones, screen and refer for developmental delay, and promote child environmental safety. They are to support positive parent–child interaction via role modelling and reinforcement of positive interaction and parental empathy. Use of parenting curricula is encouraged but no specific curriculum is required. They are encouraged to use the Individual Family Support Plan (IFSP) as a tool for teaching problem solving around family initiated goals | 24 | Approximately 32 (weekly for first 6–9 months) | Home; individual |
| 4 | Culp 2007;73 cluster non-RCT | First-time mothers living in rural community | Prenatal | Home visitors provided information, made referrals to community services, screened and referred for developmental delay and promoted child environmental safety. Home visiting used an individualised manualised curriculum. The three major foci were maternal health, child health and safety, and family functioning and parenting | 15 | Approximately 40 (weekly in first month, fortnightly for remainder of pregnancy, weekly for first 3 months postpartum, fortnightly from 3 to 12 months postpartum) | Home; individual |
| 5 | Duggan 1999,74 Duggan 2004;117 RCT | Families classified as at risk of child abuse and neglect | < 1 month | The ‘Healthy Start Programme’ is aimed at improving family functioning, preventing child abuse and promoting child health. Intervention included helping families to identify and build on strengths to improve family functioning, role modelling of problem solving skills, linking families with needed services, providing parenting education and modelling effective parent–child interaction | 24 | Approximately 45 (weekly visits decreasing to quarterly) | Home; individual |
| 6 | Emond 2002;75 cluster CBA study | First-time parents from deprived areas | Prenatal | Home visiting programme comprised part of the ‘Child Development Programme’ which is based on the principles of empowerment and is aimed at improving the health and development of young children by supporting and advising mothers during first phase of parenting using specially designed written materials [First Parent Health Visitor Scheme (FPHVS)] | 11 | Approximately eight (antenatal, birth, 3 weeks postnatal then every 5 weeks until 8 months) | Home; individual |
| 7 | Feldman 1992;76 RCT | ‘Mentally retarded mothers’ | 1–23 months | Parent training programme focusing on teaching basic child care skills (e.g. bottle feeding, crib safety, sleep safety and toilet training). Training consisted of verbal instruction, specially designed picture books depicting each stage of the child care task, modelling of each step by trainer, feedback on mothers performance, plus coupons for small gift items when mothers demonstrated 80% of trained skills correctly | 2 | As many as necessary for mother to learn skills (weekly) | Home; individual |
| 8 | Fergusson 2005;77 RCT | Two or more of the following risk factors: age of parents, social support, planning of pregnancy, parental substance abuse, financial situation, family violence | < 3 months | The ‘Early Start Program’ involved use of a social learning model approach which included assessment of family needs, development of positive partnership between family support worker and client, collaborative problem solving to devise solutions to family challenges, provision of support and mentoring and advice to assist families to mobilise their strengths and resources | 36 | Not reported | Home; individual |
| 9 | Gutelius 1977;78 RCT | Primigravid, unmarried, women aged 15–19 years, mothers to black babies, from deprived areas | Prenatal | Child health supervision with emphasis on counselling and anticipatory guidance plus well child care provided by paediatrician and nurse visiting child’s home. Cognitive stimulation programme provided by nurse home visits. Programme covered age appropriate forms of visual, auditory, tactile and motor types of stimulation with particular emphasis on language development. Group sessions for parents to discuss child rearing practices and other child and family problems | 36 | Approximately 64 routine visits (at least 9, 6 and 4 in years 1, 2 and 3 respectively); cognitive stimulation visits (at least 18,12 and 8 in years 1, 2 and 3 respectively) group sessions (16) | Home and elsewhere; individual and group |
| 10 | Hardy 1989;79 quasi-RCT | Inner city mothers of black babies, aged 18 years+ | Shortly after birth (< 10 days old) | Curriculum, plus pamphlets aimed at developing parenting and childcare skills, including topics such as well child care, sick child care, feeding, safety. Anticipatory guidance was given, developmental milestones discussed and suggestions made for enhancing development. Referral to social worker or educator for psychosocial issues | 24 | Approximately 10 (first at 7–10 days then 2–3 weeks prior to well child clinic appointments at 2, 4, 6, 9, 12, 15, 18, 21, 24 months) | Home; individual |
| 11 | IHDP 1990;80 RCT | Mothers of low-birth weight babies | Birth | Home visits focused on 2 curricula: (a) curriculum emphasising cognitive, linguistic and social development and (b) curriculum designed to provide a systematic approach to help parents manage self-identified problems. Attendance at child development centres and parent groups providing information on child rearing, health and safety as well as parent support (the Infant Health and Development Program) | 36 | Approximately 116 (weekly year 1, fortnightly years 2 and 3, bimonthly group meetings years 2 and 3) | Home and elsewhere; individual and group |
| 12 | Johnson 1993,81 Johnson 2000;118 RCT | First-time mothers living in deprived areas | Birth | Home visits by community mother to provide support and encouragement to first time parents in rearing children using the ‘Child Development Programme’, including modules on educational development, language development and cognitive development | 12 | Approximately 14 (once a month for first year + birth and 6-week visit) | Home; individual |
| 13 | Johnston 2004,82 Johnston 2006;91 cluster RCT | Pregnant women | Prenatal | Healthy Steps for Young Children programme (HS) beginning prenatally (PP + HS) or postnatally (HS). HS consists of risk reduction activities and universal components including developmental screening, anticipatory guidance and follow-up services offered to all families receiving care. HS participants received postnatal home visits, developmental advice and parent-initiated telephone support, developmental assessments conducted in tandem with scheduled well-child care, the Reach Out and Read literacy program and other risk-based screening services and parenting classes delivered by HS specialists. PP participants also received home visits to help parents create a safe, knowing and welcoming environment for their newborn, and screening and intervention for targeted risk factors such as smoking and domestic violence | 7 | Approximately seven (three prenatal home visits plus four postnatal home and office visits) | Home and elsewhere; individual and group |
| 14 | Kemp 2008,119 Kemp 2011;83 RCT | One or more of the following risk factors: aged < 19 years, current probable distress [assessed as an Edinburgh Depression Scale (EDS) score of 10+], lack of emotional and practical support, later antenatal care (20 weeks + gestation), major stressors in the past 12 months, current substance misuse, current or history of mental health problem or disorder, history of abuse in mother’s own childhood, history of domestic violence | Prenatal | Visits by a child health nurse commencing in addition to usual antenatal midwifery, obstetric and birthing services | 27 | Approximately 27 (antenatally: at least every second week; post natal: weekly until 6 weeks; fortnightly until 12 weeks; monthly to 6 months; bimonthly until 2 years) | Home; individual and group |
| 15 | Kitzman 1997;84 RCT | African-American women, no previous births, with at least two risk factors: unmarried, < 12 years education, unemployed | Prenatal | Intervention arm 1: free transportation to prenatal care
visits Intervention arm 2: intervention arm 1 + developmental screening and referral services for child Intervention arm 3: intervention arm 2 + prenatal home visits + 1 hospital + 1 home post-partum visit Intervention arm 4: intervention arm 3 + postnatal home visits from birth to 2 years of age Home visits comprised curriculum covering parental education on understanding infants’ communication signals, playing with children in ways that promote emotional and cognitive development and creating households that are safer for children. Help also provided to mothers to clarify goals and solve problems relating to completing education, finding work and planning future pregnancies |
27 | Average of seven (range, 0–18) home visits during pregnancy and 26 (range 0–71) visits from birth to child’s second birthday | Home; individual |
| 16 | Koniak-Griffin 2003;85 RCT | Pregnant women aged 14–19 years, first-time mothers | Prenatal | Early Intervention Program (IEP) provided to young mothers through home visits designed to influence maternal and child health | 15 | Maximum 17 (two prenatal and 15 postnatal) | Home; individual and group |
| 17 | Larson 1980;86 partial RCT | 18 –35 years, working class income, high school graduation or less | Prenatal | Group A: prenatal home visit, plus postnatal hospital visit,
plus postnatal home visits. Home visits followed protocol
consisting of counselling and advice relating to general
caretaking (e.g. feeding, sleeping, bathing, accident
prevention, encouragement to take part in well-child care),
mother–infant interaction (e.g. encouragement of
frequent reciprocal interaction), social status (reviewing
mother’s relationship with child’s father,
support systems and any areas of stress and concern) and child
development (e.g. reviewing child’s developmental
competence and suggesting activities to promote child’s
capabilities) Group B: postnatal home visits as for group A Group C: no home visits |
18 | Group A: one prenatal, one postpartum hospital visit, four
visits 1–6 weeks, five visits 6 weeks to 15
months Group B: seven visits 6 weeks to 6 months, three visits 6–15 months |
Home; individual |
| 18 | aLlewellyn 2003;87 RCT | Parents with intellectual disability | Under 5 years | Four groups with three intervention phases: Group 1: Home
Learning Programme (HLP) comprising 10 lessons with booklets
provided by parent educator at home covering understanding
sickness and health, when to call the doctor, how to take a
child’s temperature and check respiration, common
life-threatening emergencies, home safety. HLP delivered in
intervention phase 1 Group 2: home visits to discuss everyday experiences of raising children without educational input, delivered in intervention phase 1. HLP delivered in intervention phase 2 Group 3: usual care delivered in intervention phase 1. Mailed lesson booklets + telephone contact with parent educators to check progress with reading booklets and implementing information in booklets without any face-to-face education, delivered in intervention phase 2. HLP delivered in intervention phase 3 Group 4: standard community services delivered in intervention phase 1. HLP delivered in intervention phase 2 |
3 | 10 weekly | Home; individual |
| 19, 20 | Minkovitz 2003a,88 RCT; Minkovitz 2003b,88 cluster CBA study | Parents of newborns | Newborns < 4 weeks | Intervention arm: ‘Healthy Steps Programme’ which included well-child office visits to address questions and concerns about child development and behaviour and promotion of positive parent–child interactions, home visits to inform parents about fostering intellectual and emotional development, telephone line to answer questions about child development, parent groups to offer social support and interactive learning sessions and practice in problem solving, written information for parents emphasising importance of prevention and health promotion. Programme planned, implemented and process evaluated using the PRECEDE/PROCEED model | 36 | Six home visits in first 3 years plus parent groups | Home and elsewhere; individual and group |
| 21 | Olds 1986,89 Olds 1994;120 RCT | One of the following characteristics that predispose to infant health and developmental problems: age < 19 years; single parent; low socioeconomic status | Prenatal | Intervention arm 1: usual care + free transportation to prenatal and well child visits. Intervention arm 2: Intervention arm 1 + home visits during pregnancy. Intervention arm 3: Intervention arm 2 + postnatal home visits. Home visits comprised (a) detailed curriculum covering parental education regarding infant development aimed at improving parental behaviour that affects the child’s well-being (e.g. understanding infants temperament, need for responsive care-giving, physical health-care needs, managing common health problems), (b) enhancing informal support through encouraging family and friends to help with household responsibilities and child care, and (c) linking family with community health and social care services (e.g. well-child care, vocational training programmes, mental health counselling, etc.) | 27 | Intervention 1: free transport to prenatal and well child visits
(0 home visits) Intervention 2: free transport to prenatal and well-child visits + fortnightly home visits during pregnancy (six home visits) Intervention 3: free transport to prenatal and well-child visits + fortnightly home visits during pregnancy + postnatal weekly visits from birth to 6 weeks, every 2 weeks from 6 weeks to 4 months, every 3 weeks from 4 months to 14 months; every 4 weeks from 14 to 20 months; every 6 weeks from 20 to 24 months (39 home visits) |
Home and elsewhere; individual |
| 22 | St Pierre 1999,90 Goodson 2000;121 RCT | Women pregnant or had a baby < 1year and a family income at or below poverty guidelines | Child < 1 year | The Comprehensive Child Development Programme was not conceived as a home visiting program but it used home visits as the primary means for delivering case management and early childhood education. Short- and long-term program effects were expected for children and parents through the delivery of educational, health and social services tailored to each family. Case managers were expected to conduct home visits to each family. The model called for services to be provided to all families continuously from the time the family entered the program, before the child was 1 year old, until the child entered school | 60 | Approximately 78 home visits (fortnightly visits between ages birth and 3 years) | Home and elsewhere; individual and group |
Appendix 2 Detailed description of the content of 8-week FAST parent programme
| Week | Component (approximate duration of component in minutes) |
|---|---|
| 1 | Introduction to the course |
| Welcome and housekeeping (15) | |
| Icebreaker activity – collective parental experience in the group and introduction to course (15) | |
| Q&A: what do parents want for their children? (10) | |
| Activity: personal experience of having an injury, consequences and reflections (10); Q&A: difficulties parents may have in keeping their children safe (10) | |
| Wrap up, give out parents’ handbooks and suggest something for parents to try at home (10) | |
| 2 | Child development and injury risk. Illustrate with head injury scenarios |
| Welcome back: reflections on previous week. Icebreaker activity: how to put on a triangular bandage (15) | |
| Discussion: how children develop physically and socially. How development links to injury risk (15) | |
| Activity: what activities do children do at different ages? (10) then link accident risks to different activities (10). Head injury advice | |
| Activity (25): hunt the hazards picture quiz | |
| Wrap up: any questions, handouts to go in parents’ handbook, suggestions of what to try at home (spotting dangers at home), what we will cover next week (5) | |
| 3 | Communication between parents and children. Illustrate with choking risks scenarios |
| Welcome back: reflections on last session, experience of trying things at home. Introduction to this session (10–15) | |
| Q&A: how do we communicate with each other? (10) | |
| Activity: communication with and without active listening/interaction (15). Relate to communicating with your child (5) | |
| Discussion: what communication do children need? (10) | |
| Demonstration and discussion: choking risks. Choking tube activity (20) | |
| Wrap up, any questions, handouts to go in parents’ handbook, suggestions of what to try at home (practise communication tips), what we will cover next week (5) | |
| 4 | Managing attention-seeking behaviour, using praise. Illustrate with burn and scald scenarios |
| Welcome back: reflections on last session, experience of trying things at home. Introduction to this session (10–15) | |
| Activity: praise and how it makes us feel. How can we praise children? (20) | |
| Discussion: linking praise to communication skills from last week (10) | |
| Discussion: burns and scalds – what activities can cause burns and scalds? (10) | |
| Demonstration: colour-change heat mug (5) | |
| Activity: case scenarios with burns and scalds dolls and pictures. Check heat mug (10) | |
| What to do if child scalded (5) | |
| Activity: fire safety DVD (5) | |
| Discussion: reflection on DVD, risks of getting distracted, not knowing what your child is doing/where they are, etc. (5) | |
| Wrap up, any questions, handouts to go in parents’ handbook, suggestions of what to try at home (fire escape plan, try using praise), what we will cover next week (5) | |
| 5 | Setting and maintaining boundaries. Illustrate with ingestion and poisoning scenarios |
| Welcome back: reflections on last session, experience of trying things at home. Introduction to this session (10–15) | |
| Discussion: how our children’s behaviour reflects our behaviour. Setting boundaries. Introduction to the 3Cs: choices, consequences and consistency | |
| Activity: setting boundaries at different ages (activity cards) (15) | |
| Discussion on activity and what was learnt (10) | |
| Q&A: differences between discipline and punishment (5) | |
| Q&A: impact of what we call each other, reflect back to use of praise (5) | |
| Activity: identifying potential poisons (10) | |
| Discussion: how to keep children safe from poisons (10) | |
| Wrap up, any questions, handouts to go in parents’ handbook, suggestions of what to try at home (fire escape plan, try using praise), what we will cover next week (5) | |
| 6 | Appropriate expectations of children. Illustrate with safe play scenarios |
| Welcome back: reflections on last session, experience of trying things at home. Introduction to this session (10–15) | |
| Q&A: differences between mums and dads in how we teach and play with our children. Having realistic expectations of children (10) | |
| Q&A: what activities are appropriate for your child to try at different ages (15) | |
| Discussion: your child’s favourite toy (5) | |
| Activity: ‘choose well’ activity cards – games for children at different ages (20) | |
| Discussion and activity: recognising unsafe toys. Activity cards (10) | |
| Wrap up, any questions, handouts to go in parents’ handbook, suggestions of what to try at home (think about how much time you spend in activities with your child, look at your child’s toys for hazards), what we will cover next week (5) | |
| 7 | Attachment/how we react when upset or angry. Illustrate with unconscious child scenarios |
| Welcome back: reflections on last session, experience of trying things at home. Introduction to this session (10–15) | |
| Discussion: development of the baby’s brain. Attachment and link to need for good communication. How we don’t think rationally when our brain is full of emotions (e.g. if angry/upset/scared) both in children and adults (15) | |
| Activity: a child’s needs vs. a child’s wants (15), discussion (5) | |
| Q&A: how to manage emotions in ourselves and in our children (15) | |
| Demonstration: link to a very stressful situation – what would you do if your child were unconscious? Recovery position and cardiopulmonary resuscitation (25) | |
| Wrap up, any questions, handouts to go in parents’ handbook, suggestions of what to try at home (use of calming techniques if you or your child are upset), what we will cover next week (5) | |
| 8 | Drawing the course together |
| Welcome back: reflections on last session, experience of trying things at home. Introduction to this session (10–15) | |
| Activity: how safe is my home? (10) | |
| Q&A: what makes a good parent? (10) | |
| Activity: what pushes my buttons? (10) | |
| Q&A: how to respond if your child tests you (10) – reflect on the emotional brain, communication, etc. (10) | |
| Activity: I’m OK at… (parental self-confidence) (15) | |
| Wrap up, reflect on learning, any questions, thanks for participation. Give out certificates (5) |
Appendix 3 Decision log for the development of the 8-week FAST parent programme
The table shows extracts from the decision log kept by Parenting UK where the rationale for a decision relating to the parenting programme, the resources or the ‘train the trainer’ programme has been made on the basis of evidence or standards.
| Issue | Date | Comment and evidence supporting decision |
|---|---|---|
| ‘Train the trainer’ programme development | 16/5/11 | ‘Train the trainer’ programme to emphasise that each session has been designed to enable each parent on the course to receive unconditional positive regard from the trainer,a in keeping with the work outlined and identified as essential practice across a range of units by the Children’s Workforce Development Councilb |
| Trainers’ manual development | 30/6/11 | First aid advice and guidance that trainers will provide for participants will be adapted from Whoops! Child Safety Programme and confirmed by Carole Hewison |
| Guidance relating to the size of a burn that warrants hospital attention will be confirmed by a hospital burns unit before being finalised in the trainer manual | ||
| 8-week course structure | 16/5/11 | The programme responds to recommendations suggested in ‘National dissemination of effective parenting programmes to improve child outcomes’c as well as NICE guidanced |
Content
|
||
Delivery
|
||
| 15/7/11 | Following extensive research, it has been determined that there is no available DVD to show regarding how to perform CPR. Therefore, a demonstration of CPR will be given by trainers using the choking doll. Participants will be given website details to watch CPR and choking management videos as well as the information on where to access the nearest first aid training courses | |
| Disclaimer quotes have been approved by the University of West of England legal advisor. One quote will be provided for the trainers to convey prior to demonstration of choking and CPR management. The longer disclaimer quote will be included in the participant handbook | ||
| Programme timings | 16/5/11 | Eight sessions lasting no longer than 90 minutes of contentd |
| It would be desirable to also have refreshments available at the end of each session to enable trainers and any individual parents have availability for further discussion/clarification before leavinge | ||
| Where there is availability to a TV/video machine then the use of a home safety fire video will be used – an alternative is to have the video as a resource for loaning to parentse | ||
| Q&A activities have been used in various sessions to engage and encourage participation and uses the framework of Ingham and Luft’s Johari Window model for self-awareness, personal development, group development and understanding relationshipsf,g | ||
| Small group activities and the use of resources (cards and quizzes) will support the different learning styles of parents while also supporting participation and engagementb,e | ||
| Delivery components | 16/5/11 | As parent participants are not likely to know each other then the first session will aim to establish the group by spending time on introductions using a non-threatening icebreaker, establishing a working agreement and explanation of the course content – raising hope and expectations of learningh |
| Parents from minority ethnic groups may have extra burdens. Those who are well established may experience discrimination, while those who have arrived recently may additionally struggle with language difficulties and/or lack of information. Parenting styles that fit familiar circumstances in the country of origin may be challenged by and found unacceptable in the new settings in Britain. Equally, families from minorities may bring parenting styles that are advantageous in the new settings e.g. social cohesiveness and closer supervision of children that helps the well-being of the parents and protects children in higher-risk urban conditionsi | ||
| 8/7/11 | As the first session explores typical unintentional injuries of children, falls in particular, the participants will be provided with a handout out on head injury management adapted from Great Ormond Streetj and NICE guidelinesk | |
| 18/7/11 | Feedback from Parenting UK Parent Forum on the participant handouts has raised concern about the level of literacy required. However, the content was considered acceptable with one or two suggestions on two individual handouts, which will be taken into consideration at the meeting on 21 July for final PDS sign-offe | |
| Child development | 16/5/11 | The stages of development will be consistent with that identified in the Birth to 5 book and the Personal Child Health Record Bookl |
| The sessions will include theories of infant and child development taken from ‘Understanding babies’ communication from birth and from ‘The Social Baby’m and ‘The Social Toddler’n | ||
| Parenting components | 16/5/11 | Each session will incorporate an amalgamation of key elements
that any parenting programme should include:b,d
|
| Programme structure | 16/5/11 | The programme structure and organisation has taken into consideration the Parent Advisory Group comments regarding style and content of the programme. The skills and associated delivery style of content will be addressed in the ‘train the trainer’ programme to ensure that facilitators incorporate the various facets as identified in feedback from both the PAG and Parent Forum (May 2011) for a successful, engaging and meaningful programme |
| Parents will be able to reflect on their own experiences in childhood of being parented/having or being aware of injury – reflecting on that experience, what they learnt from it and how that results in action to change the situation and reduce the potential of future injuryo,p | ||
| Parents will be able to explore and understand the difference between discipline and punishment building on the notion of the importance of appropriate choices, consequences and the need for consistency particularly for behaviour management as identified across a range of different parenting programmesq,r,s | ||
| The sessions are developed to include Q&A segments and activities that build on normalising feelings and age appropriate development and behaviour and the concept of ‘good enough’ or ‘confident parenting’ that parents do, (though can be learnt) and identifying the factors of how families function and interactt |
Appendix 4 ‘Train the trainer’ event
| Day and time | Content | Resources needed |
|---|---|---|
| DAY 1 | ||
| 09.30 | Introduction – housekeeping; introduce self, programme background and 2-day training input | PPT |
| 09.45 | Participant intro | Flip chart |
| 10.00 | Working agreement | Flip chart |
| 10.15 | Group facilitation skills | |
| 10.30 | Facilitator role | Template forms |
| 10.35 | Managing difficult situations | |
| 10.50 | Kit bag | Kit bag and contents |
| 11.00 | COFFEE | |
| 11.20 | The trainer manual | Manual and Participant Handbook |
| 11.45 | Window on the world | |
| 11.50 | Group work and plenary | Window on the world |
| 12.00 | Diversity and values | |
| 12.20 | Understanding the emotional brain | |
| 12.45 | LUNCH | |
| 1.30 | Management of accidents (brainstorm) | Flipchart |
| 2.00 | Demonstration and practice of resources | Resources kit |
| 2.45 | Any questions? | |
| 3.00 | TEA | |
| 3.15 | Preventability of accidents | |
| 3.20 | Activity cards – all sets explanation | All flashcards |
| 3.50 | Homework | |
| 4.00 | End | |
| DAY 2 | ||
| 09.30 | Welcome and any questions. | PPT and handbook |
| 09.30 | Weekly sessions | |
| 9.40 | Groups – Tuckman theory | |
| 9.50 | Week 1 key messaging | Head injury advice |
| 10.10 | Week 2 key messaging | Two-part activity cards |
| 10.25 | Week 3 key messaging | Communication exercise; perspectives on feeding |
| 10.40 | First trainer activity – choking demo | Choking resources |
| 11.10 | COFFEE | |
| 11.30 | Week 4 key messaging | DVD – Praise flipchart; fire escape planner |
| 11.50 | Week 5 key messaging | Labelling of children; hazards/flashcards; choices/consequences |
| 12.15 | Week 6 key messaging | Choose well cards; perspectives on play; home safety quiz |
| 12.30 | Week 7 key messaging | |
| 12.35 | Second trainer activity – Emotional brain and needs and wants | |
| 1p.m. | LUNCH | |
| 1.45 | Third trainer activity – CPR and recovery position | |
| 2.15 | Week 8 key messaging | Participants’ topics; how safe is your home; I’m OK cards |
| 2.45 | Circle time evaluation | |
| 3p.m. | TEA | |
| 3.15 | Questions and clarification | Advise re: support |
| 4.00 | End | |
Appendix 5 Injury calendar for the collection of parent-reported home injuries
The front page and one month of the injury calendar have been reproduced to illustrate the format and content of the injury calendar. Calendars were printed to cover the six-month period of observation and spiral bound along the top edge, prior to sending to parents participating in the feasibility study.
Injury calendar for the collection of parent-reported home injuries (PDF download)
Appendix 6 Original study protocol
FAST Parent programme
Research Protocol (version 1, 25th October 2010)
1. Title
Long title: The FAST (First Aid & Safety Training) Parent programme for the prevention of recurrent unintentional home injuries in preschool children
Short title: The FAST Parent programme for the prevention of recurrent injuries in preschool children
2. Research Team
Principal investigator:
-
Dr Julie Mytton (JM), Senior Research Fellow, Faculty of Health and Life Sciences, University of the West of England, Bristol
Researchers
-
Two half time research fellows to be appointed (1× 0.5WTE, University of the West of England, Bristol and 1 × 0.5 WTE University of Nottingham)
Co-applicants
-
Professor Elizabeth Towner (ET), University of the West of England, Bristol
-
Professor Denise Kendrick (DK), University of Nottingham
-
Professor Sarah Stewart-Brown (SSB), University of Warwick
-
Professor Alan Emond (AE), University of Bristol
-
Dr Jenny Ingram (JI), University of Bristol
-
Dr Pete Blair (PB), University of Bristol
-
Dr Jane Powell (JP), University of the West of England, Bristol
-
Dr Toity Deave (TD), University of the West of England, Bristol
-
Dr Caroline Mulvaney (CM), University of Nottingham
-
Dr James Thomas (JT), Institute of Education, University of London
-
Mrs Barbara Potter (BP), Health Visitor, North Bristol NHS Trust
Collaborators
-
Mrs Carole Hewison, Project Director, WHOOPS! Child Safety Project, Gateshead
-
Mrs Pamela Park, Chief Executive, Parenting UK, London
2.1 Research team roles
Recruitment and quantitative data collection will be conducted by the research fellows (RF) appointed in Bristol and Nottingham, employed specifically for this project. JM will line manage and provide supervision for the RF in Bristol and CM will provide similar support for the RF employed in Nottingham. JM, CM and PB will analyse the quantitative data with the RFs. JI will facilitate the Parent Advisory Group and support the health visitors delivering the programme. JI will conduct the qualitative interviews in Bristol and CM will conduct those in Nottingham. JI will analyse the qualitative data supported by CM and TD. JP will collect and analyse the data for the economic analysis of the programme.
3. Background
Childhood injuries – the scale of the problem
Unintentional injury is the major cause of death in children over the age of 1 in the UK, and for each child that dies many more will suffer morbidity and possibly long term consequences. Over 2 million visits to accident and emergency departments and over 120000 admissions in children occurred in 2005 due to unintentional injury costing the NHS in the region of £146 million (1). Staying safe has been a fundamental component of child health policies such as Every Child Matters (2). The type and location of child injuries varies with age and the child’s stage of development. The majority of injuries occurring to preschool children occur in the home (3,4,5). Between 2000 and 2002 an average of 502,000 children aged 0–4 years attended hospital every year in the UK due to a home injury, representing 78% of all injuries occurring to children in this age group. The most frequent events leading to injuries in preschool children include, in order; falls, hitting/being hit/crushed by objects, poisoning, and burns/scalds (6). Inequalities in injury occurrence have been widely reported (7–12).
Risk factors for injury
A number of risk factors related to the family and the child have been associated with increased risk of injury. Single parents, step families and teenage parenthood, maternal life events and maternal depression were all associated with increased risk of medically attended child injury by age 2 in the Avon Longitudinal Study of Parents and Children (ALSPAC) (3). In a randomised controlled trial in Nottingham family factors including having a teenage mother or being in a single parent family were associated with increased risk of hospital attended injuries in preschool children (13). Family structure (14) and parental behaviours, such as excessive use of alcohol (15) have been associated with increased injury risk in children. Male sex and difficult behaviour in childhood, particularly that relating to antisocial, aggressive or overactive behaviour, have been associated with increased incidence of unintentional injuries in the UK (16, 17) and in other high income countries (18). Parental understanding of the relationship between injury risk and child behaviour and development is variable, and provision of educational anticipatory guidance has been recommended (19).
Parenting programmes
Parenting programmes are short term interventions to promote changes in the behaviour of parents and children that result in better health and wellbeing outcomes for both. They are usually delivered as face to face programmes, either individually or in groups. Parenting programmes have been increasingly recognised as an intervention to improve the life chances of children due to their effectiveness in reducing antisocial behaviour and improving educational and mental health outcomes in children, and the improved mental health and wellbeing of parents. Low socioeconomic status, unemployment, social exclusion or isolation, young or single parenthood and learning difficulties are known to adversely affect parenting. Consequently, parenting programmes have become a core component of child and family policy (20). Parenting programmes have been developed on the basis of two main theoretical approaches: behavioural and relational. Some programmes combine elements of both approaches. Behavioural approaches aim to develop parents understanding of the negative impact of attention to problem behaviour and lack of attention to positive behaviour, and teach positive discipline practices including praise and time out; relational programmes aim to improve interactions between parent and child, correcting misattributions and increasing understanding of developmental phases. Both have been developed to improve children’s mental health, the former with a particular emphasis on the prevention and treatment of antisocial behaviour and conduct disorder.
Analyses of longitudinal studies have shown the influence of parents on child outcomes that are related to injury risk. Research from the ALSPAC cohort has shown that positive parenting behaviour, parent–child interaction and a stimulating home environment were associated with enhanced development by the age of three (21) and improved cognitive and behavioural outcomes in children by age 5 (22). The ‘better’ the parenting, the more likely children are to be well adjusted and developmentally competent (23). Other studies, for mothers with learning difficulties, have shown that supportive parent training can improve childcare practices (24). Evidence suggests that enhanced carer supervision can help reduce injury risk to children (25,26). Parenting interventions have the potential to reduce poor maternal mental health and increase maternal self efficacy (27,28), to improve maternal–child interactions (29), and to change child behaviour, especially behaviour that is challenging or could place the child at risk of injury (27,30,31). Parenting interventions can reduce injury risk either through these mechanisms or through increased parental knowledge of safety practices (32), improvement in the quality of the home environment (33), or through the use of home safety practices such as having a fitted and functioning smoke alarm, using stair gates or keeping sharp objects safely (34,35). Parenting programmes have shown reductions in injury risk taking behaviour in primary school aged children (36). Health visitor interventions to support parents can reduce injury rates in both prospective studies (37) and meta-analysis of randomised controlled trials (38). Meta-analysis of parenting interventions, primarily conducted in high-risk or disadvantaged families, have demonstrated significantly lower risks of injury, as measured by parental self-report of either medically or non-medically attended injuries (39,40). Parents value programmes that enable the acquisition of knowledge, skills and understanding, and facilitate acceptance and support from other parents. Such outcomes reduce feelings of guilt and social isolation, increase empathy with children, and give confidence to cope with challenging child behaviour (41). A child’s medically attended injury represents a ‘teachable moment’ when parents are receptive to information regarding injury risk in their children (42).
The features of parenting interventions that are most effective are becoming clearer. There is strong evidence that home safety education and the provision of safety equipment are effective in increasing a range of home safety practices (35). A review of ‘what works?’ in parenting interventions has shown that interventions are more likely to be effective if they are delivered early in childhood, if intensity is proportional to need, if they include group activities where parents can benefit from the social aspect of working with peers, if they include formal programmes or manuals to maintain the consistency of the delivery of the intervention which should be delivered by trained staff, and if there is a focus on specific parenting skills and practical ‘take-home’ tips (43). A review of the effectiveness of parenting support programmes in European countries where universal early intervention approaches tend to be used, suggests that positive outcomes can also be achieved when the programme is delivered by non-health workers or agencies (44).
The cost effectiveness of parenting programmes has not been widely studied (45). A recent systematic review of economic evaluations of child and adolescent mental health interventions demonstrated that most evaluations were small scale, had short time horizons for assessing outcomes and had limited reporting (46). However, the cost effectiveness of parenting programmes has been established for group parenting programmes. A formal evaluation of Sure Start parenting programmes demonstrated improved child behaviour outcomes for modest cost and considered the programme value for money (47).
Justification for this proposal
Parenting interventions, usually delivered as part of a programme to improve a range of child and family outcomes, appear to be effective in reducing self-reported or medically attended injuries in young children (48). Due to the range of positive outcomes associated with the programmes, such as improved child behaviour, maternal self-efficacy or maternal–child interactions, it is unclear whether one of these outcomes is more effective in reducing child injury than another. We know that injury prevention education alone has not shown reduction in injury occurrence (35) but the hypothesis that injury prevention education in the context of a parenting programme may be effective remains to be tested. Furthermore, it is unclear whether group based programmes, delivered outside of the home can achieve reductions in injury occurrence similar to intensive one-to-one home based programmes. Evidence suggests that RCTs of home safety education can successfully recruit parents of recently injured children (49,50), and that parents are interested in learning first aid (51). We therefore propose to develop a parenting programme that provides injury prevention education through the delivery of first aid and safety training tailored to the stages of preschool child development and delivered to groups of parents in a community setting. We propose to test the feasibility of delivering that programme with a view to a future large scale randomised controlled trial.
4. Aims and objectives
4.1 Aim
To develop and test the feasibility of delivering a children’s centre based parenting programme to prevent recurrent unintentional home injuries in children aged 0–4 years; compared to normal care for such children.
4.2 Objectives
-
to develop a health professional delivered parenting programme
-
to assess the acceptability of the parenting programme to parents and professionals
-
to assess the feasibility of delivering the parenting programme
-
to assess recruitment and retention of parents within the trial
-
to assess compliance with the intervention during the follow up period
-
to determine the training, equipment and facilities needed for delivery of the parenting programme
-
to assess the collection of primary and secondary outcome measures
-
to determine which information to collect on ‘normal care’
-
to assess which relevant resource utilisation/costing data needs to be collected
-
to produce estimates of effect sizes to inform sample size estimation for the full trial
-
5. Study design
A multi-centre study using a cluster randomised controlled design will test the feasibility of delivering a parenting programme developed to prevent recurrent injuries occurring in the home for preschool children. The study will be based in Bristol and Nottingham.
5.1 Experimental group
The experimental arm of the trial will be ‘normal care’ plus a parenting programme. The parenting programme will be developed in collaboration with Parenting UK (a parenting programme development organisation). Engaging parents in a parenting programme following injury in their child may be difficult since the injury may result in feelings of stigmatisation, guilt or concern that the injury is believed to be intentional. Our programme will contain both home safety education (‘keeping your child safe’) and first aid training as methods of primary and tertiary injury prevention. Unpublished evidence from local injury prevention projects in Gateshead and Bristol suggest that parents are interested in learning first aid and willing to attend a group to do so. The emphasis on first aid and safety training is hoped to enhance acceptability and diffuse any negative feelings generated by being identified for participation in the programme. Interest in learning first aid is hoped to stimulate further interest in injury prevention and parenting to reduce injury risk. The programme will be delivered in children’s centres by Health Visitor teams, to groups of parents.
The parenting programme is likely to contain elements of existing parenting programmes that may reduce injury risk, for example, those intended to enhance parental self-efficacy and well being, improve parent/child communication, and improve child behaviour through the increased use of positive reinforcement, and the enablement of setting and maintaining boundaries (52). Evidence-based safety components are likely to include home safety education, assessment of home hazards, guidance on types, sources and fitting of home safety equipment and tailoring advice to both the home context and understanding how a child’s injury risks change as the child grows and develops (anticipatory guidance) (53).
Families in the experimental group will be invited to participate in 1 to 1 interviews after delivery of the parenting programme to explore parents’ views and experience of the programme.
5.2 Control Group
The control group will receive ‘normal care’. In both Bristol and Nottingham, Health Visitors are routinely sent details of children within their geographical area of responsibility that have sustained a medically attended injury, whether at A&E, or NHS Walk-in Centre. Usually the notification is sent by fax either on the same day as the injury or on the next working day. It is usual practice that following receipt of such notification the Health Visitor Team may take a range of actions determined by the circumstances of the event and the Health Visitor’s understanding of the needs of that family. Four different actions can be considered as part of ‘normal care’; telephone contact, face-to-face contact, referral to services, or no action. The use of each of these four possibilities will vary between locations and between Health Visitor Teams. For example, some Health Visitors may take every fax notification as an opportunity to make contact with a family, especially in deprived or multicultural communities, where parent initiated contact with Health Visitors is low. In other areas, workload or knowledge of families will mean that Health Visitors are much more selective of those families that they will contact.
5.3 Inclusion and exclusion criteria
Children’s centres
Inclusion criteria: In both Bristol and Nottingham children’s centres will be ranked according to the number of children aged 0–4 years who have attended the local Children’s Accident and Emergency department in the previous year, and had a postcode that would have entitled them to access that children’s centre. The four children’s centres with the highest rankings in each city (i.e. centres with largest number of injury notifications) will be invited to participate in the study. If one of these centres is unable to participate then the Centre with the next highest ranking will be invited.
Exclusion criteria: children’s centres will be excluded if they are already involved in other injury prevention initiatives.
Parents
Inclusion criteria: The parents/carers will be eligible for recruitment if they have a child under 5 years of age who has sustained an unintentional physical injury or ingestion in the home (or within the boundary of the home and garden/yard), that resulted in seeking medical attention from a health professional at an NHS Walk-In Centre, Minor Injuries Unit or in an Accident and Emergency department in secondary care during the recruitment period. Parents/carers must be living at an address within the geographical or general practice catchment area of a children’s centre participating in the study.
Exclusion criteria: Children suffering suspected or confirmed intentional injuries will be excluded. Should an injury originally considered to be unintentional be later discovered to have been intentional, then routine referral processes for safeguarding would be activated. That parent would not be asked to withdraw from the programme, but data from that child will not be included in the analysis. Parents/carers who are unable to understand written and spoken English will be excluded from the feasibility study.
5.4 Randomisation and allocation
The unit of randomisation will be the children’s centre . We will recruit a total of 8 children’s centres; four in Bristol and four in Nottingham. Those agreeing to participate will be stratified by study centre (two strata) and randomly allocated within strata to treatment arm using a remote automated system available through the Bristol Randomised Trials Collaboration (BRTC) based at the University of Bristol. Two children’s centres in each study centre will be randomly allocated to the intervention arm, and two children’s centres in each study centre will be allocated to the control or ‘normal care’ arm.
To reduce post-randomisation recruitment bias, informing the children’s centres and Health Visitor Teams of their allocation to intervention or control arms will be delayed until after recruitment of families in each children’s centre has been completed. If allocation to intervention or control arm is indicated to the Health Visitor Team/children’s centre at the time of randomisation, we anticipate two potential post randomisation recruitment biases; a) the Health Visitor Team could choose not to offer entry to the study if the team knew that the family were unlikely to participate or continue in the programme once commenced, and b) a family may be influenced in their decision to participate if they knew in advance that their children’s centre was, or was not, offering the FAST Parents programme. Therefore once recruitment has been completed Health Visiting Teams and children’s centres will be informed of their allocation. Health Visitors and Nursery Nurses from intervention children’s centres will be trained in delivery of the FAST Parents programme.
6. Ethical aspects
6.1 Ethics committee approval
Approval will be sought from a Type 3 committee; South West 3 REC (Bristol Central) based at University Hospitals Bristol.
6.2 Participant consent
Parents asked to participate in this research are entitled to choose whether or not to take part. Their decision will be voluntary and they will be competent to understand what is involved. Consent forms will be designed to assure the protection of their rights.
In the eight children’s centre areas participating in the study receipt of a notification of a medically attended injury by the Health Visitor Team will result in the team making a decision on ‘normal care’. The families will be contacted after completion of ‘normal care’ to advise them that their local children’s centre is participating in a study to follow up pre-school children who have had an injury and that some children’s centres will be offering first aid courses for parents. Parents will be asked if their details can be passed to the research team who will tell them more about the study. Refusal to participate in the programme will not prevent access to any other routinely available services, although will be recorded as an outcome of the feasibility study along with the reason for refusal where this is provided. The Health Visitor Teams will be given a list of the inclusion and exclusion criteria to enable them to determine eligibility of families for participating in the study.
Families that agree to be contacted by the research team will receive both written and verbal information. The research fellow will send a study information sheet and consent form to the family. One week later the researcher will contact the family and ask permission to visit. If the family agrees the researcher will send baseline measure questionnaires prior to the visit.
Parents living within the catchment areas of intervention children’s centres will be invited to participate in the FAST Parent programme. At the visit the researcher will verbally explain the study. The explanation will cover all the elements specified in the written information provided for the participant. The participants will be informed of the aims, methods and participation requirements of the study. They will be informed that the programme is intended to help reduce the risk of injuries in children, but because this is a new programme that has not previously been tested the likelihood of success is unclear. The researcher will explain that the programme will provide the opportunity to learn first aid and safety information in a ‘hands-on’ and interactive manner. Parents will be informed that we are interested in their experience of participating in the programme to help us understand how the programme could be improved. Parents will be advised that there are no anticipated risks to attending the programme.
Parents living within the catchment areas of control children’s centres will be invited to participate in an injury follow-up study, where the researchers are interested in children’s behaviour and whether a child who has had one injury has any further injuries. During the visit the researcher will verbally explain the study. The explanation will cover all the elements specified in the written information provided for the participant. The participants will be informed of the aims, methods and participation requirements of the study.
The participant will be given every opportunity to clarify any points they do not understand and if necessary ask for more information. At the end of the discussion the participant will be given time to reflect. The participant will be informed that they are at liberty to withdraw their consent to participate at any time, without prejudicing any future medical care.
The researcher will obtain the participants freely given written consent before participating in the study. The consent form will assure the participant of the confidentiality of the data collected. Participants attending children’s centres in the experimental arm of the study will be asked permission that the interviews conducted after the parenting programme can be audio recorded and to publish anonymised quotations from the study. With the agreement of the participants, the data will be anonymised and stored in accordance with data protection guidelines and University of the West of England, Bristol good practice. Both the researcher and the participants will retain copies of the signed consent forms.
Families who drop out after initially agreeing to participate will be asked about their decision and any information offered will be recorded as an outcome of the feasibility study.
7. Plan of investigation and scientific procedures
7.1 Delivery of the intervention
A local Health Visitor from Bristol and Nottingham will be recruited to deliver the FAST parent programme in the two study centres in each city during the feasibility study. They will be trained by Parenting UK to deliver the programme supported by the Nursery/Children’s Nurse or Health Visitor in the Health Visiting Team at that children’s centre . Crèche facilities will be provided to enable attendance at the parenting group and refreshments will be provided for parents.
To ensure fidelity in delivery of the programme the researcher in each study centre will attend the training in how to deliver the programme and will observe and record fidelity of programme delivery. In addition, Health Visitors delivering the programme will participate in teleconference discussions with each other and Parenting UK after the delivery of each session to raise issues, concerns and ensure the programme is delivered in as consistent a manner as possible.
Furthermore, the health economist (JP) will observe a selection of sessions to ensure that all resource costs are correctly included in the economic evaluation.
7.2 Post intervention data collection
7.2.1 Qualitative data collection – Part 1
After completion of the FAST Parent programme experienced qualitative researchers in the research team (JI and CM) will conduct interviews with parents in the experimental arm of the trial that agree to be interviewed to explore their experience of participating in the programme. Interviews will take place at their home or another convenient location. Interviews will also take place with members of the Health Visitor Teams, the children’s centres, and the Project Manager, and will aim to evaluate the process of the delivering the parenting programme and assess its feasibility for scaling up to a main trial. Interviews will be digitally recorded, transcribed, anonymised and analysed using thematic analysis techniques of coding the transcripts and developing themes and sub-themes. A qualitative analysis package, such as NVIVO8, will facilitate the analysis.
7.2.2 Quantitative data collection
Once the programme intervention has been delivered, a six month period of follow up of families in the experimental and control arms of the trial will commence. All families will be given a diary to record any injuries to the study child (and injuries to any siblings under the age of 5) in the following 3 months. A full explanation of how to complete the diary, including a clear definition of what constitutes ‘an injury’ will be given, together with a mobile telephone number to call in case of any queries.
At three months into the follow up period, parents will be contacted by the researcher to arrange a visit. A child behaviour questionnaire will be sent in advance of the visit. At the visit the researcher will collect the behaviour questionnaire, the first injury diary and provide a second diary to be completed as for the first diary, over the next 3 months.
At the end of the six months follow up period, the researcher will contact the family and ask permission to visit. Prior to the visit secondary outcome questionnaires will be sent to the family. At the visit the researcher will collect the last injury diary for the index child and will collect data for all the secondary outcome measures, offering support to complete the questionnaires if required.
The primary purpose of the home visits during the follow up period is to achieve high response rates for questionnaire outcome information during the feasibility study and home visits do not form part of the intervention.
7.2.3 Qualitative data collection – Part 2
After completion of the six month home visit, parents in the intervention and control arms of the study will be offered a telephone interview (conducted by JI and CM) to collect information on their experience of participation in the study from initial contact through to completion of follow up. Interviews will be digitally recorded, transcribed, anonymised and analysed using thematic analysis techniques as for the face to face interviews.
7.3 Interview conduct
Topic guides will be used in order to assist questioning during both face-to-face and telephone interviews. These guides are designed to direct but not dictate data collection and will incorporate considerable flexibility to allow participants to introduce new issues not anticipated by the researchers. The topic guides will be modified as necessary throughout the course of the study to reflect findings as they emerge. The researcher will use open-ended questioning techniques to elicit participants’ own experiences and views, and participants will be asked to provide examples. Face-to-face interviews for both parents and professionals are anticipated to last approximately 30 minutes. Telephone interviews may be briefer than 30 minutes.
7.4 Outcome measures
The outcome measures have been chosen to identify whether the parenting programme can reduce injury occurrence and the mechanism by which any change occurs.
7.4.1 Primary outcome measures
The number of injuries to the study child or preschool siblings occurring in a home setting, where ‘home’ includes any garden/yard (i.e. within the home boundary) during the period of follow up. Injuries occurring in the child’s own home will be recorded separately to those occurring in other people’s homes (e.g. relatives, friends or neighbours). Two measures will be collected:
-
parent-reported medically attended injuries to the study child
-
parent-reported medically attended injuries to the preschool siblings of the study child
Where ‘medically attended’ is defined as injuries that resulted in the parent/carer taking the child to A&E, to a Walk-In Centre, or to the GPs surgery
Validation of parent-reported medically attended injuries will be conducted by the researcher in Bristol and Nottingham, using A&E, Walk-in Centre and Primary Care records. The Health Visitors of all children attending an A&E in Bristol and Nottingham are routinely sent a notification of attendance for injury, and this will provide an additional method of validating parent-reported injuries requiring medical attention in A&E.
We will ensure that at recruitment to the study, parental consent will be requested to contact the General Practitioner of the index child and their siblings, and to search Walk-In Centre and A&E records for attendance.
7.4.2 Secondary outcome measures
Two further injury measures and five non-injury measures (to provide data on potential mechanisms of injury prevention) will be collected. Parents will be offered a voucher (Mothercare or similar) at both baseline and at the end of the six month follow up period to encourage completion of secondary outcome measures. Secondary outcome measures will include:
-
Parent-reported injuries to the study child that did not require medical attention (e.g. those treated at home or not requiring treatment).
-
Parent-reported injuries to the preschool siblings of the study child that did not require medical attention (e.g. those treated at home or not requiring treatment).
-
Child behaviour. We will use the Strengths and Difficulties Questionnaire (SDQ) for children over the age of 3 years and the Achenbach Child Behaviour Checklist (CBCL) for children between the ages of 18 months and 3 years.
-
First aid knowledge. The four-item Nottingham Safe at Home Project Questionnaire will be used to assess parental knowledge of how to respond to four common first aid scenarios (burns, cuts, choking and bleach ingestion).
-
Parent-reported safety practices and possession and use of safety equipment. We will use the home safety measure validated during a trial of the effectiveness of the provision of home safety equipment to prevent injuries conducted by one of the applicants (Denise Kendrick) (54,55).
-
Maternal wellbeing. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS) is a new well validated measure of mental wellbeing which has proved sensitive to change over the course of three different parenting programmes (56).
-
Parenting measure – The Parent Supervision Attributes Profile Questionnaire (57) – a 29 item measure assessing protectiveness, supervision, tolerance for children’s risk taking and belief in fate as a determinant of children’s safety.
7.4.3 Process outcome measures
-
Acceptability of the intervention will be assessed through feedback from parents at the end of each session of the parenting programme to identify features of that session that were most and least enjoyable and most and least helpful. Acceptability will be explored during the face-to-face and telephone qualitative interviews with parents and professionals
-
Feasibility of delivering the intervention will be assessed by the interviews with health professionals delivering the FAST Parent programme and also by documenting process measures including
-
the number of sessions delivered in each centre
-
the duration of each session
-
the number of attendees at each session
-
the extent to which each session followed the “curriculum” for that session
-
the number of sessions attended by parents
-
the completion of any home based activities for participating families, e.g. completion of a home safety assessment.
-
-
Recruitment to the feasibility study will be assessed by recording
-
the numbers of children’s centres and families eligible to participate
-
the numbers approached to participate and the numbers agreeing to participate.
-
Children’s centres and families choosing not to participate will be asked to complete a brief questionnaire to determine reasons for non-participation.
-
-
Retention in the feasibility study will be assessed for both children’s centres and families.
-
Collation of information on ‘normal care’ by Health Visitor Teams on receipt of an injury notification.
7.4.4 Economic evaluation measures
-
Resource use – costs. Programme delivery will be physically observed by the researcher conducting the economic analysis and monitored against a standard checklist of usual resource use or cost categories in economic evaluations (for example, programme development costs, recruitment costs, programme delivery, materials and overhead costs) (58). NHS costs relating to use of A&E, Minor Injuries Units or General practice visits due to an injury during the follow up period will be included using published cost-per-visit estimates.
-
Utility outcomes. Incremental cost per unit of change in score for outcome tool and confidence intervals will be calculated following the approach used by Tudor-Edwards and others in a recent rigorous economic evaluation of a similar programme. The resultant incremental cost effectiveness ratio (ICER) will be assessed for feasibility in measuring the cost-effectiveness of the parenting programme in the main study (59).
7.5 Data analysis
7.5.1 Quantitative analysis
Descriptive statistics (means, standard deviations and non-parametric measures where appropriate) will be used to describe the characteristics of the families, centres and children along with the primary and secondary outcome measures.
At recruitment to the trial, parents will be asked to report the number of siblings (both pre-school, and school age or older) in the index child’s household. If another pre-school sibling in the same family is injured during the recruitment period, the family will only be recruited to the study once. Through this data collection at recruitment, the research team will have a denominator for analysis of injuries in the siblings of the index child. The numerator for injuries in siblings will be identified through parental report and objective measures such as attendance at A&E and Walk-In Centres as detailed above. It will therefore be possible to calculate a rate of injury occurrence per unit period of follow up in the index children and in their siblings.
We know that the number of siblings a child has is associated with the risk of injury occurrence. The greater the number of siblings and having older siblings are both factors associated with increased risk of injuries in a child. Clustering of injuries within families is likely. The primary outcome measures of injuries requiring medical attention and those not requiring medical attention will therefore be analysed using hierarchical modelling, using the child as the unit of analysis, in recognition of the fact that these variables are not independent.
Outcome measures such as child behaviour or use of safety equipment will be assessed although the emphasis of the analytical strategy will be on point estimates of differences and their associated confidence intervals rather than p-values. Between-group comparisons will be conducted using multi-level modelling and will be used as an exploratory technique in preparation for a larger trial.
The 3 month injury diary and behaviour questionnaire data will not be used in any form of interim analysis. All injury data will be pooled for analysis at six months.
7.5.2 Qualitative analysis
All audio-recorded data will be fully transcribed, anonymised, checked for accuracy and then imported into a software package, NVivo8. Analysis will begin shortly after data collection starts, will be ongoing and iterative. Analysis will inform further data collection; for instance, analytic insights gathered in earlier interviews will shape the questions covered during later interviews.
Thematic analysis will be used to scrutinise the data in order to identify and analyse patterns and themes of particular salience for participants and across the dataset using constant comparison techniques. Firstly the transcripts will be read several times to gain familiarisation with the data and initial ideas noted. The transcripts will then be examined on a line-by-line basis with inductive codes being assigned to the segments of the data that provide insight in to the participants’ views and understanding of their experiences and assist in the development of an initial coding frame. New data will be compared initially to the previous data and then to the properties of emerging categories that contain the main themes. The process of constant comparison will allow for the generation of new themes, reclassify themes and incorporate themes within other themes. The coding frame will be modified, if needed as the analysis develops. The analysis will enable the research team to arrive initially at a descriptive account which will be developed into a theoretical account in the light of existing theoretical and applied literature.
Trial data and documentation will be retained securely by the principal investigator in Bristol according to local codes of research conduct (6 years in Bristol).
7.6 Researcher safety
The researchers will follow the University of the West of England’s Researcher Safety Guidance when conducting any field work away from university premises. This will involve undertaking an assessment of risk prior to arranging an interview, prior informing a designated person from the study team the details of an interview, and calling in when the interview has been completed at an agreed time. If the designated person is not contacted at the agreed time, the designated person will contact the researcher’s mobile telephone. If there is no answer, the designated person will phone the participant’s house. If contact has still not been made, the designated person will phone the police and ask them to visit the participant’s house.
7.7 Research governance
The sponsor for the research will be the University of the West of England, Bristol. A research fellow (Project Manager) will be appointed in both Bristol and Nottingham to oversee the day to day running of the project. The Project Manager will be supervised by Julie Mytton in Bristol and Caroline Mulvaney in Nottingham.
Governance of the feasibility study will be through a management group comprising the co-applicants and collaborators. The management group will meet monthly at the beginning and end of the study and bimonthly during the study. Meetings will be in person where possible and by teleconference were necessary. The management group will oversee the progress of the study and adherence to timescales and the project plan. Not all co-applicants will be required for every management group meeting. The principle investigator (JM) will report to a Trial Steering Committee (TSC) that will meet four times during the course of the study. The requirement for a Data monitoring and Ethics Committee (DMC) will be the decision of the Chairperson of the TSC. As this is a feasibility study, and there are no plans for interim data analysis that could potentially lead to early closure of the trial, we consider the trial to be low risk and do not anticipate the need for a DMC.
7.8 Writing up and dissemination
Findings of the study will be made available to the participating families. They will also be disseminated to the Parents Advisory Group (see below) and to Health Visiting teams and children’s centre managers at intervention and control sites. The findings of the feasibility study will be written in non-specialist language so that they may be accessible to families and a range of professionals. Any quotations from participant or professional’s interviews will be anonymised prior to inclusion in the study report.
We anticipate that a subsequent main trial would generate outcomes of interest to the health community, local authorities, the public and to academics. Care would be required not to disseminate the findings too widely after the feasibility study before a main trial; otherwise recruitment to the main trial may be compromised. We would however provide local feedback in Bristol and Nottingham and would prepare papers for publication and a UK conference presentation.
8.0 Service Users
The parent perspective on the development, implementation and management of this project are recognised as very important to the success of the research. The ability to engage parents in the programme in a non-stigmatising way is vital to the project’s success. The research team have therefore elected to work with a Parents Advisory Group rather than one or two named parents. We have identified a group of parents that currently regularly meet at a children’s centre in Bristol. One of these parents has worked with Dr Jenny Ingram on a previous project, and formally provided feedback during the development of this study. Dr Ingram would help facilitate the Parent Advisory Group to advise the research team, and will feedback on a regular basis to the management group and to the Trials Steering Committee. Feedback will either be by direct representation by a parent at the TSG meetings or through the facilitator (JI).We anticipate the group would meet at least four times during the course of the study. We believe that a Parent Advisory Group is a valuable resource which provides a critical mass and collective support to express parent’s perspectives.
The group have advised us on the preparation of the information sheets and consent forms. They will advise on the study process to help maximise acceptability, engagement, retention and compliance. We will ask them to help us prepare the final reports of the feasibility study in an accessible format for participating families.
There is a risk that lay advisors to research projects may lack confidence in their role and their ability to influence decision making. The University of the West of England, Bristol has an innovative new system to support the participation of lay research partners in projects. The system not only helps researchers identify lay partners where necessary, but can help fund expenses to enable lay partners attend meetings, and help them gain confidence in contributing their perspective by offering them formal status as a research partner by providing them with a staff card, access to the UWE library, ATHENS log in etc. We will be working closely with this group to enable successful parent inclusion in the research management and offer these benefits to the parents leading our advisory group.
Project timetable and milestones
Flow diagram
References
- Better safe than sorry; Preventing unintentional injury to children. London: Audit Commission; 2007.
- Every Child Matters: Change for Children. London: The Stationery Office; 2004.
- O’Connor T, Davies L, Dunn J, Golding J. Alspac Study Team . Distribution of accidents, injuries and illness by family type. Pediatrics 2000;106.
- Warrington S, Wright C. Alspac Study Team . Accidents and resulting injuries in premobile infants: data from the ALSPAC study. Arch Dis Child 2001;85:104-7.
- Langley J, Dodge J, Silva P. Accidents in the first five years of life. Aus Paediatr J 1979;15:255-9.
- Home and Leisure Accident Surveillance System [Internet] . ROSPA n.d. URL: www.hassandlass.org.uk/query/index.htm (accessed 28 August 2009).
- Reading R, Langford I, Haynes R, Lovett A. Accidents to preschool children: comparing family and neighbourhood risk factors. Soc Sci Med 1999;48:321-30.
- Dowswell T, Towner E. Social deprivation and the prevention of unintentional injury in childhood. Health Edu Res 2002;17:221-37.
- Edwards P, Green J, Lachowycz K, Grundy C, Roberts I. Serious injuries in children: variation by area deprivation and settlement type. Arch Dis Child 2004;93:485-9.
- Towner E, Dowswell T, Errington G, Burkes M, Towner J. Injuries in children aged 0–14 years and their inequalities. London: Health Development Agency; 2005.
- Edwards P, Roberts I, Green J, Lutchmun S. Deaths from injury in children and employment status in family: analysis of trends in class specific death rates. BMJ 2006;333.
- Reading R, Jones A, Haynes R, Daras K, Emond A. Individual factors explain neighbourhood variations in accidents to children under 5 years of age. Soc Sci Med 2008;67:915-27.
- Kendrick D, Mulvaney C, Burton P, Watson M. Relationships between child, family and neighbourhood characteristics and childhood injury: a cohort study. Soc Sci Med 2005;61:1905-15.
- Bijur PE, Golding J, Kurzon M. Childhood accidents, family size and birth order. Soc Sci Med 1988;26:839-43.
- Bijur P, Kurzon M, Overpeck M, Scheidt P. Parental alcohol use, problem drinking, and children’s injuries. JAMA 1992;267:3166-71.
- Rowe R, Maughan B, Goodman R. Childhood psychiatric disorder and unintentional injury: findings from a national cohort study. J Pediatr Psychol 2004;29:119-30.
- Bijur P, Stewart-Brown S, Butler N. Child behavior and accidental injury in 11,966 preschool children. Am J Dis Child 1986;140:487-92.
- Langley J, McGee R, Silva P, Willaims S. Child behaviour and accidents. J Pediatr Psychol 1983;8:181-9.
- Ingram J, Emond A. Parents’ perceptions of home injury risk and attitudes to supervision of preschool children: a qualitative study in economically deprived communities. Primary Health Care Res Develop 2009;10:98-108.
- Law J, Plunkett C, Taylor J, Gunning M. Developing policy in the provision of parenting programmes: integrating a review of reviews with the perspectives of both parents and professionals. Child Care Health Develop 2009;35:302-12.
- Morrison Gutman L, Feinstein L. Parenting behaviour and children’s development from infancy to early childhood: changes, continuities and contributions. Department for Education and Skills; 2007.
- Up to 7: Family background and child development up to age 7 in the Avon Longitudinal Study of Parents and Children (ALSPAC). Department for Education and Skills; 2006.
- Morrison Gutman L, Brown J, Akerman R. Nurturing parenting capability – the early years. Department for Children Schools and Families; 2009.
- Feldman M, Case L, Sparks B. Effectiveness of a child-care training program for parents at risk for child neglect. Can J Behav Sci 1992;24:14-28.
- Morrongiello B, Corbett M, Brison R. Identifying predictors of medically-attended injuries to young children: do child or parent behavioural attributes matter?. Inj Prevent 2009;15:220-5.
- Schwebel D, Kendrick D. Caregiver supervision and injury risk for young children: time to re-examine the issue. Inj Prevent 2009;15:217-8.
- Stewart-Brown S, Patterson J, Mockford C, Barlow J, Klimes I, Pyper C. Impact of a general practice based group parenting programme: quantitative and qualitative results from a controlled trial at 12 months. Arch Dis Child 2004;89:519-25.
- Barlow J, Coren E, Stewart-Brown S. Parent-training programmes for improving maternal psychosocial health. Cochrane Database Syst Rev 2003;4.
- Coren E, Barlow J. Individual and group-based parenting programmes for improving psychosocial outcomes for teenage parents and their children. Cochrane Database Syst Rev 2001;3.
- Barlow J, Stewart-Brown S. Behaviour problems and group-based parent education programmes. J Develop Behav Pediatr 2000;21:356-70.
- Barlow J, Parsons J, Stewart-Brown S. Preventing emotional and behavioural problems: the effectiveness of parenting programmes with children less than 3 years of age. Child Care Health Develop 2005;31:33-42.
- Gagnon A, Bryanton J. Postnatal parental education for optimizing infant general health and parent–infant relationships. Cochrane Database Syst Rev 2009;1.
- Kendrick D, Elkan R, Hewitt M, Dewey M, Blair M, Robinson J, et al. Does home visiting improve parenting and the quality of the home environment? A systematic review and meta-analysis. Arch Dis Child 2000;82:443-51.
- Kendrick D, Watson M, Mulvaney C, Burton P. How useful are home safety behaviours for predicting childhood injury?. Health Edu Res 2005;20:709-18.
- Kendrick D, Coupland C, Mulvaney C, Simpson J, Smith S, Sutton A, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev 2007;1.
- Petrie J, Bunn F, Byrne G. Parenting programmes for preventing tobacco, alcohol and drugs misuse in children <18: a systematic review. Health Edu Res 2007;22:177-91.
- Emond A, Pollock J, Deave T, Bonnell S, Peters T, Harvey I. An evaluation of the First Parent Health Visitor Scheme. Arch Dis Child 2002;86:150-7.
- Roberts I, Kramer M, Suissa S. Does home visiting prevent childhood injury? A systematic review of randomised controlled trials. BMJ 1996;312:29-33.
- Kendrick D, Barlow J, Hampshire A, Polnay L, Stewart-Brown S. Parenting interventions for the prevention of unintentional injuries in childhood. Cochrane Database Syst Rev 2007;4.
- Kendrick D, Barlow J, Hampshire A, Stewart-Brown S, Polnay L. Parenting interventions and the prevention of unintentional injuries in childhood: systematic review and meta-analysis. Child Care Health Develop 2008;34:682-95.
- Kane G, Wood V, Barlow J. Parenting programmes: a systematic review and synthesis of qualitative research. Child Care Health Develop 2007;33:784-93.
- Morrongiello B, Howard A, Rothman L, Sandomierski M. Once bitten, twice shy? Medically-attended injuries can sensitise parents to children’s risk of injuries on playgrounds. Inj Prevent 2009;15:50-4.
- Moran P, Ghate D, van der Merwe A. What works in parenting support? A review of the international evidence. London: Department for Education and Skills; 2004.
- Boddy J, Statham J, . International perspectives on parenting support. Non-English language sources. Department for Children Schools and Families; 2009.
- Cost Benefit Analysis of Interventions with Parents. Department for Children Schools and Families; 2007.
- Romeo R, Byford S, Knapp M. Economic evaluations of child and adolescent mental health interventions: a systematic review. J Child Psychol Psychiatr 2005;46:919-30.
- Edwards R, Ceilleachair A, Bywater T, Hughes D, Hutchings J. Parenting program for parents of children at risk of developing conduct disorder: cost effectiveness analysis. BMJ 2007;334.
- Kendrick D, Barlow J, Hampshire A, Stewart-Brown S, Polnay L. Parenting interventions and the prevention of unintentional injuries in childhood: systematic review and meta-analysis. Child Care Health Develop 2008;34:682-95.
- Posner J, Hawkins L, Garcia-Espana F, Durbin D. A randomized, clinical trial of a home safety intervention based in an emergency department setting. Pediatrics 2004;113:1603-8.
- King W, LeBlanc J, Barrowman N, Klassen T, Bernard-Bonnin A-C, Robitaille Y, et al. Long term effects of a home visit to prevent childhood injury: three year follow up of a randomized trial. Injury Prevention 2005;11:106-9.
- Potter B, Newell G. Accident Prevention in the under 5’s 1997.
- Stewart-Brown S. Improving parenting: the why and the how. Arch Dis Child 2008;93:102-4.
- Gielan A, Wilson M, McDonald E, Serwint J, Andrews J, Hwang W-T, et al. Randomized trial of enhanced anticipatory guidance for injury prevention. Arch Pediatr Adolesc Med 2001;155:42-9.
- Watson M, Kendrick D, Coupland C, Woods A, Futers D, Robinson J. Providing child safety equipment to prevent injuries: randomised controlled trial. BMJ 2005;330:178-83.
- Watson M, Kendrick D, Coupland C. Validation of a home safety questionnaire used in a randomised controlled trial. Inj Prevent 2003;9:180-3.
- Tennant R, Hillier L, Fishwick R, Platt S, Stephen J, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5.
- Morrongiello B, Corbett M. The Parent Supervision Attributes Profile Questionnaire: a measure of supervision related to children’s risk of unintentional injury. Inj Prevent 2006;12:19-23.
- Manheim L. Health Services Research Clinical Trials: Issues in the Evaluation of Economic Costs and Benefits. Control Clin Trials 2009;19:149-58.
- Campbell N, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F. Designing and evaluating complex interventions to improve healthcare. BMJ 2007;334:455-9.
Appendix 7 Final study protocol
Changes to the original study protocol are indicated by bold font
FAST Parent programme
Research Protocol (version 4, 14th February 2012)
1. Title
Long title: The FAST (First-aid Advice & Safety Training) Parent programme for the prevention of recurrent unintentional home injuries in preschool children
Short title: The FAST Parent programme for the prevention of recurrent injuries in preschool children
2. Research Team
Principal investigator:
-
Dr Julie Mytton (JM), Senior Research Fellow, Faculty of Health and Life Sciences, University of the West of England, Bristol
Researchers
-
Two half time research fellows to be appointed (1× 0.5WTE, University of the West of England, Bristol and 1 × 0.5 WTE University of Nottingham)
Co-applicants
-
Professor Elizabeth Towner (ET), University of the West of England, Bristol
-
Professor Denise Kendrick (DK),, University of Nottingham
-
Professor Sarah Stewart-Brown (SSB), University of Warwick
-
Professor Alan Emond (AE),, University of Bristol
-
Dr Jenny Ingram (JI), University of Bristol
-
Dr Pete Blair(PB), University of Bristol
-
Dr Jane Powell (JP), University of the West of England, Bristol
-
Dr Toity Deave (TD), University of the West of England, Bristol
-
Dr Caroline Mulvaney (CM), University of Nottingham
-
Dr James Thomas (JT), Institute of Education, University of London
-
Mrs Barbara Potter (BP), Health Visitor, North Bristol NHS Trust
Collaborators
-
Mrs Carole Hewison, Project Director, WHOOPS! Child Safety Project, Gateshead
-
Mrs Pamela Park, Chief Executive, Parenting UK, London
2.1 Research team roles
Recruitment and quantitative data collection will be conducted by the research fellows (RF) appointed in Bristol and Nottingham, employed specifically for this project. JM will line manage and provide supervision for the RF in Bristol and CM will provide similar support for the RF employed in Nottingham. JM, CM and PB will analyse the quantitative data with the RFs. JI will facilitate the Parent Advisory Group and support the health visitors delivering the programme. JI will conduct the qualitative interviews in Bristol and CM will conduct those in Nottingham. JI will analyse the qualitative data supported by CM and TD. JP will collect and analyse the data for the economic analysis of the programme.
3. Background
Childhood injuries – the scale of the problem
Unintentional injury is the major cause of death in children over the age of 1 in the UK, and for each child that dies many more will suffer morbidity and possibly long term consequences. Over 2 million visits to accident and emergency departments and over 120000 admissions in children occurred in 2005 due to unintentional injury costing the NHS in the region of £146 million (1). Staying safe has been a fundamental component of child health policies such as Every Child Matters (2). The type and location of child injuries varies with age and the child’s stage of development. The majority of injuries occurring to preschool children occur in the home (3,4,5). Between 2000 and 2002 an average of 502,000 children aged 0–4 years attended hospital every year in the UK due to a home injury, representing 78% of all injuries occurring to children in this age group. The most frequent events leading to injuries in preschool children include, in order; falls, hitting/being hit/crushed by objects, poisoning, and burns/scalds (6). Inequalities in injury occurrence have been widely reported (7–12).
Risk factors for injury
A number of risk factors related to the family and the child have been associated with increased risk of injury. Single parents, step families and teenage parenthood, maternal life events and maternal depression were all associated with increased risk of medically attended child injury by age 2 in the Avon Longitudinal Study of Parents and Children (ALSPAC) (3). In a randomised controlled trial in Nottingham family factors including having a teenage mother or being in a single parent family were associated with increased risk of hospital attended injuries in preschool children (13). Family structure (14) and parental behaviours, such as excessive use of alcohol (15) have been associated with increased injury risk in children. Male sex and difficult behaviour in childhood, particularly that relating to antisocial, aggressive or overactive behaviour, have been associated with increased incidence of unintentional injuries in the UK (16,17) and in other high income countries (18). Parental understanding of the relationship between injury risk and child behaviour and development is variable, and provision of educational anticipatory guidance has been recommended (19).
Parenting programmes
Parenting programmes are short term interventions to promote changes in the behaviour of parents and children that result in better health and wellbeing outcomes for both. They are usually delivered as face to face programmes, either individually or in groups. Parenting programmes have been increasingly recognised as an intervention to improve the life chances of children due to their effectiveness in reducing antisocial behaviour and improving educational and mental health outcomes in children, and the improved mental health and wellbeing of parents. Low socioeconomic status, unemployment, social exclusion or isolation, young or single parenthood and learning difficulties are known to adversely affect parenting. Consequently, parenting programmes have become a core component of child and family policy (20). Parenting programmes have been developed on the basis of two main theoretical approaches: behavioural and relational. Some programmes combine elements of both approaches. Behavioural approaches aim to develop parents understanding of the negative impact of attention to problem behaviour and lack of attention to positive behaviour, and teach positive discipline practices including praise and time out; relational programmes aim to improve interactions between parent and child, correcting misattributions and increasing understanding of developmental phases. Both have been developed to improve children’s mental health, the former with a particular emphasis on the prevention and treatment of antisocial behaviour and conduct disorder.
Analyses of longitudinal studies have shown the influence of parents on child outcomes that are related to injury risk. Research from the ALSPAC cohort has shown that positive parenting behaviour, parent–child interaction and a stimulating home environment were associated with enhanced development by the age of three (21) and improved cognitive and behavioural outcomes in children by age 5 (22). The ‘better’ the parenting, the more likely children are to be well adjusted and developmentally competent (23). Other studies, for mothers with learning difficulties, have shown that supportive parent training can improve childcare practices (24). Evidence suggests that enhanced carer supervision can help reduce injury risk to children (25,26). Parenting interventions have the potential to reduce poor maternal mental health and increase maternal self efficacy (27,28), to improve maternal–child interactions (29), and to change child behaviour, especially behaviour that is challenging or could place the child at risk of injury (27,30,31). Parenting interventions can reduce injury risk either through these mechanisms or through increased parental knowledge of safety practices (32), improvement in the quality of the home environment (33), or through the use of home safety practices such as having a fitted and functioning smoke alarm, using stair gates or keeping sharp objects safely (34,35). Parenting programmes have shown reductions in injury risk taking behaviour in primary school aged children (36). Health visitor interventions to support parents can reduce injury rates in both prospective studies (37) and meta-analysis of randomised controlled trials (38). Meta-analysis of parenting interventions, primarily conducted in high-risk or disadvantaged families, have demonstrated significantly lower risks of injury, as measured by parental self-report of either medically or non-medically attended injuries (39,40). Parents value programmes that enable the acquisition of knowledge, skills and understanding, and facilitate acceptance and support from other parents. Such outcomes reduce feelings of guilt and social isolation, increase empathy with children, and give confidence to cope with challenging child behaviour (41). A child’s medically attended injury represents a ‘teachable moment’ when parents are receptive to information regarding injury risk in their children (42).
The features of parenting interventions that are most effective are becoming clearer. There is strong evidence that home safety education and the provision of safety equipment are effective in increasing a range of home safety practices (35). A review of ‘what works?’ in parenting interventions has shown that interventions are more likely to be effective if they are delivered early in childhood, if intensity is proportional to need, if they include group activities where parents can benefit from the social aspect of working with peers, if they include formal programmes or manuals to maintain the consistency of the delivery of the intervention which should be delivered by trained staff, and if there is a focus on specific parenting skills and practical ‘take-home’ tips (43). A review of the effectiveness of parenting support programmes in European countries where universal early intervention approaches tend to be used, suggests that positive outcomes can also be achieved when the programme is delivered by non-health workers or agencies (44).
The cost effectiveness of parenting programmes has not been widely studied (45). A recent systematic review of economic evaluations of child and adolescent mental health interventions demonstrated that most evaluations were small scale, had short time horizons for assessing outcomes and had limited reporting (46). However, the cost effectiveness of parenting programmes has been established for group parenting programmes. A formal evaluation of Sure Start parenting programmes demonstrated improved child behaviour outcomes for modest cost and considered the programme value for money (47).
Justification for this proposal
Parenting interventions, usually delivered as part of a programme to improve a range of child and family outcomes, appear to be effective in reducing self-reported or medically attended injuries in young children (48). Due to the range of positive outcomes associated with the programmes, such as improved child behaviour, maternal self-efficacy or maternal–child interactions, it is unclear whether one of these outcomes is more effective in reducing child injury than another. We know that injury prevention education alone has not shown reduction in injury occurrence (35) but the hypothesis that injury prevention education in the context of a parenting programme may be effective remains to be tested. Furthermore, it is unclear whether group based programmes, delivered outside of the home can achieve reductions in injury occurrence similar to intensive one-to-one home based programmes. Evidence suggests that RCTs of home safety education can successfully recruit parents of recently injured children (49,50), and that parents are interested in learning first aid (51). We therefore propose to develop a parenting programme that provides injury prevention education through the delivery of first aid and safety training tailored to the stages of preschool child development and delivered to groups of parents in a community setting. We propose to test the feasibility of delivering that programme with a view to a future large scale randomised controlled trial.
4. Aims and objectives
4.1 Aim
To develop and test the feasibility of delivering a children’s centre based parenting programme to prevent recurrent unintentional home injuries in children aged 0–4 years; compared to normal care for such children.
4.2 Objectives
-
to develop a health professional delivered parenting programme
-
to assess the acceptability of the parenting programme to parents and professionals
-
to assess the feasibility of delivering the parenting programme
-
to assess recruitment and retention of parents within the trial
-
to assess compliance with the intervention during the follow up period
-
to determine the training, equipment and facilities needed for delivery of the parenting programme
-
to assess the collection of primary and secondary outcome measures
-
to determine which information to collect on ‘normal care’
-
to assess which relevant resource utilisation/costing data needs to be collected
-
to produce estimates of effect sizes to inform sample size estimation for the full trial
-
5. Study design
A multi-centre study using a cluster randomised controlled design will test the feasibility of delivering a parenting programme developed to prevent recurrent injuries occurring in the home for preschool children. The study will be based in Bristol and Nottingham.
5.1 Experimental group
The experimental arm of the trial will be ‘normal care’ plus a parenting programme. The parenting programme will be developed in collaboration with Parenting UK (a parenting programme development organisation). Engaging parents in a parenting programme following injury in their child may be difficult since the injury may result in feelings of stigmatisation, guilt or concern that the injury is believed to be intentional. Our programme will contain both home safety education (‘keeping your child safe’) and first aid advice as methods of primary and tertiary injury prevention. Unpublished evidence from local injury prevention projects in Gateshead and Bristol suggest that parents are interested in learning first aid and willing to attend a group to do so. The emphasis on first aid advice and safety training is hoped to enhance acceptability and diffuse any negative feelings generated by being identified for participation in the programme. Interest in learning first aid is hoped to stimulate further interest in injury prevention and parenting to reduce injury risk. The programme will be delivered in children’s centres by a Health Visitor and cofacilitator, to groups of parents.
The parenting programme is likely to contain elements of existing parenting programmes that may reduce injury risk, for example, those intended to enhance parental self-efficacy and well being, improve parent/child communication, and improve child behaviour through the increased use of positive reinforcement, and the enablement of setting and maintaining boundaries (52). Evidence-based safety components are likely to include home safety education, assessment of home hazards, guidance on types, sources and fitting of home safety equipment and tailoring advice to both the home context and understanding how a child’s injury risks change as the child grows and develops (anticipatory guidance) (53).
Families in the experimental group will be invited to participate in 1 to 1 interviews after delivery of the parenting programme to explore parents’ views and experience of the programme.
5.2 Control Group
The control group will receive ‘normal care’. In both Bristol and Nottingham, Health Visitors are routinely sent details of children within their geographical area of responsibility that have sustained a medically attended injury, whether at A&E, or NHS Walk-in Centre. Usually the notification is sent by fax either on the same day as the injury or on the next working day. It is usual practice that following receipt of such notification the Health Visitor Team may take a range of actions determined by the circumstances of the event and the Health Visitor’s understanding of the needs of that family. Four different actions can be considered as part of ‘normal care’; telephone contact, face-to-face contact, referral to services, or no action. The use of each of these four possibilities will vary between locations and between Health Visitor Teams. For example, some Health Visitors may take every fax notification as an opportunity to make contact with a family, especially in deprived or multicultural communities, where parent initiated contact with Health Visitors is low. In other areas, workload or knowledge of families will mean that Health Visitors are much more selective of those families that they will contact.
5.3 Inclusion and exclusion criteria
Children’s centres/Health Visitor teams
Inclusion criteria: In both Bristol and Nottingham children’s centres are linked to named Health Visitor teams. Children’s centres will be ranked according to the number of children aged 0–4 years who have attended the local Children’s Accident and Emergency department in the previous year, and had a postcode that would have entitled them to access that children’s centre. The four children’s centres with the highest rankings in each city (i.e. centres with largest number of injury notifications) where the Health Visitor team has the capacity to participate, will be invited to participate in the study. If one of these children’s centres is unable to participate then the children’s centre with the next highest ranking and their Health Visitor team will be invited.
Exclusion criteria: children’s centres and their linked Health Visitor team will be excluded if they are already involved in other injury prevention research studies.
Parents
Inclusion criteria: The parents/carers will be eligible for recruitment if they have a child under 5 years of age who has sustained an unintentional physical injury or ingestion in the home (or within the boundary of the home and garden/yard), that resulted in seeking medical attention from a health professional at an NHS Walk-In Centre, Minor Injuries Unit or in an Accident and Emergency department in secondary care during the recruitment period. Parents/carers must be living at an address within the geographical or general practice catchment area of a children’s centre participating in the study.
Exclusion criteria: Children suffering suspected or confirmed intentional injuries will be excluded. Should an injury originally considered to be unintentional be later discovered to have been intentional, then routine referral processes for safeguarding would be activated. That parent would not be asked to withdraw from the programme, but data from that child will not be included in the analysis. Parents/carers who are unable to understand written and spoken English will be excluded from the feasibility study.
5.4 Randomisation and allocation
The unit of randomisation will be the children’s centre . We will recruit a total of 8 children’s centres; four in Bristol and four in Nottingham. Those agreeing to participate will be stratified by study centre (two strata) and randomly allocated within strata to treatment arm using a remote automated system available through the Bristol Randomised Trials Collaboration (BRTC) based at the University of Bristol. Two children’s centres in each study centre will be randomly allocated to the intervention arm, and two children’s centres in each study centre will be allocated to the control or ‘normal care’ arm.
To reduce post-randomisation recruitment bias, informing the children’s centres and Health Visitor Teams of their allocation to intervention or control arms will be delayed until after recruitment of families has been completed. If allocation to intervention or control arm is indicated to the Health Visitor Team/children’s centre at the time of recruitment, we anticipate two potential post randomisation recruitment biases; a) the Health Visitor Team could choose not to offer entry to the study if the team knew that the family were unlikely to participate or continue in the programme once commenced, and b) a family may be influenced in their decision to participate if they knew in advance that their children’s centre was, or was not, offering the FAST Parents programme. Therefore once recruitment has been completed Health Visiting Teams and children’s centres will be informed of their allocation.
6. Ethical aspects
6.1 Ethics committee approval
Approval will be sought from a Type 3 committee; South West 3 REC (Bristol Central) based at University Hospitals Bristol.
6.2 Participant consent
Parents asked to participate in this research are entitled to choose whether or not to take part. Their decision will be voluntary and they will be competent to understand what is involved. Consent forms will be designed to assure the protection of their rights.
In the eight children’s centre areas participating in the study receipt of a notification of a medically attended injury by the Health Visitor Team will result in the team making a decision on ‘normal care’. The families will be contacted after completion of ‘normal care’ to advise them that their local children’s centre is participating in a study to follow up pre-school children who have had an injury and that some children’s centres will be offering first aid advice courses for parents. Parents will be asked if their details can be passed to the research team who will tell them more about the study. Refusal to participate in the programme will not prevent access to any other routinely available services, although will be recorded as an outcome of the feasibility study along with the reason for refusal where this is provided. The Health Visitor Teams will be given a list of the inclusion and exclusion criteria to enable them to determine eligibility of families for participating in the study.
Identification of eligible families may occur through alternative routes when it is inappropriate for Health Visitor teams to undertake recruitment themselves (e.g. reduced capacity within the team). Identification may occur via Emergency Departments (ED) where generation of the notification letter occurs. Eligible families will be contacted either by telephone by a member of the ED team and asked if their details can be passed to the research team who will tell them more about the study, or by letter sent by the ED team to the parents with a reply slip to the research team. Parents will not be approached during their ED visit, but afterwards. The number of parents approached but declining to have their details passed to the research team, or failing to return a reply slip, will be noted, together with the reason for refusal where this is provided. The member of the ED team will be given a list of the inclusion and exclusion criteria to enable them to determine eligibility of families for participating in the study.
Identification may also occur via primary care as the notification letter will routinely be sent to the child’s General Practitioner. Eligible families will be contacted by letter sent out by a member of the primary care team who will be provided with a list of the inclusion and exclusion criteria to enable them to determine eligible families. General Practices linked to the participating Health Visitor teams will be invited to support the study. A template letter will be provided for sending to eligible families that allows the surgery to add their own header/logo. The letter, sent from their General Practitioner, will introduce the FAST study, enclose the parent information sheet, and ask that if the parent is interested in participating they should telephone the local FAST Research Fellow (a mobile telephone number will be provided) or return a reply slip in a reply paid envelop. Parents will be able to choose whether or not to respond to the letter.
Families that agree to be contacted by the research team will receive both written and verbal information. The research fellow will send a study information sheet and consent form to the family. One week later the researcher will contact the family and ask permission to visit. If the family agrees the researcher will send baseline measure questionnaires prior to the visit.
Parents living within the catchment areas of intervention and control children’s centres will be invited to participate in the study. At the visit the researcher will verbally explain the study. The explanation will cover all the elements specified in the written information provided for the participant. The participants will be informed of the aims, methods and participation requirements of the study. They will be informed that the study is intended to help understand children’s behaviour after injuries and reduce the risk of further injuries. The researcher will explain that some families will have the opportunity to attend a programme will provide the opportunity to gain first aid advice and safety information in a ‘hands-on’ and interactive manner, but because this is a new programme that has not previously been tested the likelihood of success is unclear. Parents will be informed that we are interested in their experience of participating in the study and the programme to help us understand how they could be improved. Parents will be advised that there are no anticipated risks to participation.
The participant will be given every opportunity to clarify any points they do not understand and if necessary ask for more information. At the end of the discussion the participant will be given time to reflect. The participant will be informed that they are at liberty to withdraw their consent to participate at any time, without prejudicing any future medical care.
The researcher will obtain the participants freely given written consent before participating in the study. The consent form will assure the participant of the confidentiality of the data collected. Participants attending children’s centres in the experimental arm of the study will be asked permission that the interviews conducted after the parenting programme can be audio recorded and to publish anonymised quotations from the study. With the agreement of the participants, the data will be anonymised and stored in accordance with data protection guidelines and University of the West of England, Bristol good practice. Both the researcher and the participants will retain copies of the signed consent forms.
Families who drop out after initially agreeing to participate will be asked about their decision and any information offered will be recorded as an outcome of the feasibility study.
We aim to recruit 12 families from each of four children’s centre areas in Bristol (48 families) and from each of four Children’s centre areas in Nottingham (48 families). We expect that between recruitment and start of the intervention some families will drop-out of the study. We hope that about 8 families per children’s centre will remain in the study by the start of the intervention period (total = 64 families).
7. Plan of investigation and scientific procedures
7.1 Delivery of the intervention
Health Visitors from Bristol and Nottingham will be recruited to deliver the FAST parent programme in the two Children’s centres in each city during the feasibility study. They will be trained by Parenting UK to deliver the programme supported by a cofacilitator. The Nursery/Children’s Nurse or Health Visitor in the Health Visiting Team at that children’s centre will be invited to support delivery of the intervention, but if unable, a Health Visitor and cofacilitator independent of the Health Visitor teams participating in the study will be available to deliver the intervention. Crèche facilities will be provided to enable attendance at the parenting group and refreshments will be provided for parents.
To ensure fidelity in delivery of the programme the researcher in each study centre will attend the training in how to deliver the programme and will observe and record fidelity of programme delivery. In addition, Health Visitors delivering the programme will participate in teleconference discussions with each other and Parenting UK after the delivery of each session to raise issues, concerns and ensure the programme is delivered in as consistent a manner as possible.
Furthermore, the health economist (JP) will observe a selection of sessions to ensure that all resource costs are correctly included in the economic evaluation.
7.2 Post intervention data collection
7.2.1 Qualitative data collection – Part 1
After completion of the FAST Parent programme experienced qualitative researchers in the research team (JI and CM) will conduct interviews with parents in the experimental arm of the trial that agree to be interviewed to explore their experience of participating in the programme. Interviews will take place at their home or another convenient location. Interviews will also take place with members of the Health Visitor Teams, the children’s centres, and the Project Manager, and will aim to evaluate the process of the delivering the parenting programme and assess its feasibility for scaling up to a main trial. Interviews will be digitally recorded, transcribed, anonymised and analysed using thematic analysis techniques of coding the transcripts and developing themes and sub-themes. A qualitative analysis package, such as NVIVO8, will facilitate the analysis.
7.2.2 Quantitative data collection
Once the programme intervention has been delivered, a six month period of follow up of families in the experimental and control arms of the trial will commence. All families will be given a diary to record any injuries to the study child (and injuries to any siblings under the age of 5) in the following 3 months. A full explanation of how to complete the diary, including a clear definition of what constitutes ‘an injury’ will be given, together with a mobile telephone number to call in case of any queries.
At three months into the follow up period, parents will be contacted by the researcher to arrange a visit. A child behaviour questionnaire will be sent in advance of the visit. At the visit the researcher will collect the behaviour questionnaire, the first injury diary and provide a second diary to be completed as for the first diary, over the next 3 months.
At the end of the six months follow up period, the researcher will contact the family and ask permission to visit. Prior to the visit secondary outcome questionnaires will be sent to the family. At the visit the researcher will collect the last injury diary for the index child and will collect data for all the secondary outcome measures, offering support to complete the questionnaires if required.
The primary purpose of the home visits during the follow up period is to achieve high response rates for questionnaire outcome information during the feasibility study and home visits do not form part of the intervention.
7.2.3 Qualitative data collection – Part 2
After completion of the six month home visit, parents in the intervention and control arms of the study will be offered a telephone interview (conducted by JI and CM) to collect information on their experience of participation in the study from initial contact through to completion of follow up. Interviews will be digitally recorded, transcribed, anonymised and analysed using thematic analysis techniques as for the face to face interviews.
7.3 Interview conduct
Topic guides will be used in order to assist questioning during both face-to-face and telephone interviews. These guides are designed to direct but not dictate data collection and will incorporate considerable flexibility to allow participants to introduce new issues not anticipated by the researchers. The topic guides will be modified as necessary throughout the course of the study to reflect findings as they emerge. The researcher will use open-ended questioning techniques to elicit participants’ own experiences and views, and participants will be asked to provide examples. Face-to-face interviews for both parents and professionals are anticipated to last approximately 30 minutes. Telephone interviews may be briefer than 30 minutes.
7.4 Outcome measures
The outcome measures have been chosen to identify whether the parenting programme can reduce injury occurrence and the mechanism by which any change occurs.
7.4.1 Primary outcome measures
The number of injuries to the study child or preschool siblings occurring in a home setting, where ‘home’ includes any garden/yard (i.e. within the home boundary) during the period of follow up. Injuries occurring in the child’s own home will be recorded separately to those occurring in other people’s homes (e.g. relatives, friends or neighbours). Two measures will be collected:
-
parent-reported medically attended injuries to the study child
-
parent-reported medically attended injuries to the preschool siblings of the study child
Where ‘medically attended’ is defined as injuries that resulted in the parent/carer taking the child to A&E, to a Walk-In Centre, or to the GPs surgery.
Validation of parent-reported medically attended injuries will be conducted by the researcher in Bristol and Nottingham, using A&E, Walk-in Centre and Primary Care records. The Health Visitors of all children attending an A&E in Bristol and Nottingham are routinely sent a notification of attendance for injury, and this will provide an additional method of validating parent-reported injuries requiring medical attention in A&E.
We will ensure that at recruitment to the study, parental consent will be requested to contact the General Practitioner of the index child and their siblings, and to search Walk-In Centre and A&E records for attendance.
7.4.2 Secondary outcome measures
Two further injury measures and five non-injury measures (to provide data on potential mechanisms of injury prevention) will be collected. Parents will be offered a voucher (Mothercare or similar) at both baseline and at the end of the six month follow up period to encourage completion of secondary outcome measures. Secondary outcome measures will include:
-
parent-reported injuries to the study child that did not require medical attention (e.g. those treated at home or not requiring treatment).
-
parent-reported injuries to the preschool siblings of the study child that did not require medical attention (e.g. those treated at home or not requiring treatment).
-
Child behaviour. We will use the Strengths and Difficulties Questionnaire (SDQ) for children over the age of 2 years, and the Infant Behaviour Questionnaire – Revised, Very Short Form for children aged 3–12 months.
-
First aid knowledge. The four-item Nottingham Safe at Home Project Questionnaire will be used to assess parental knowledge of how to respond to four common first aid scenarios (burns, cuts, choking and bleach ingestion).
-
Parent-reported safety practices and possession and use of safety equipment. We will use the home safety measure validated during a trial of the effectiveness of the provision of home safety equipment to prevent injuries conducted by one of the applicants (Denise Kendrick) (54,55).
-
Maternal wellbeing. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS) is a new well validated measure of mental wellbeing which has proved sensitive to change over the course of three different parenting programmes (56).
-
Parenting measure – The Parent Supervision Attributes Profile Questionnaire (57) – a 29-item measure assessing protectiveness, supervision, tolerance for children’s risk taking and belief in fate as a determinant of children’s safety.
7.4.3 Process outcome measures
-
Acceptability of the intervention will be assessed through feedback from parents at the end of each session of the parenting programme to identify features of that session that were most and least enjoyable and most and least helpful. Acceptability will be explored during the face-to-face and telephone qualitative interviews with parents and professionals
-
Feasibility of delivering the intervention will be assessed by the interviews with health professionals delivering the FAST Parent programme and also by documenting process measures including
-
the number of sessions delivered in each centre
-
the duration of each session
-
the number of attendees at each session
-
the extent to which each session followed the “curriculum” for that session
-
the number of sessions attended by parents
-
the completion of any home based activities for participating families, e.g. completion of a home safety assessment.
-
-
Recruitment to the feasibility study will be assessed by recording
-
the numbers of children’s centres and families eligible to participate
-
the numbers approached to participate and the numbers agreeing to participate.
-
Children’s centres and families choosing not to participate will be asked to complete a brief questionnaire to determine reasons for non-participation.
-
-
Retention in the feasibility study will be assessed for both children’s centres and families.
-
Collation of information on ‘normal care’ by Health Visitor Teams on receipt of an injury notification.
7.4.4 Economic evaluation measures
-
Resource use – costs. Programme delivery will be physically observed by the researcher conducting the economic analysis and monitored against a standard checklist of usual resource use or cost categories in economic evaluations (for example, programme development costs, recruitment costs, programme delivery, materials and overhead costs) (58). NHS costs relating to use of A&E, Minor Injuries Units or General practice visits due to an injury during the follow up period will be included using published cost-per-visit estimates.
-
Utility outcomes. Incremental cost per unit of change in score for outcome tool and confidence intervals will be calculated following the approach used by Tudor-Edwards and others in a recent rigorous economic evaluation of a similar programme (47). The resultant incremental cost effectiveness ratio (ICER) will be assessed for feasibility in measuring the cost-effectiveness of the parenting programme in the main study (59).
7.5 Data analysis
7.5.1 Quantitative analysis
Descriptive statistics (means, standard deviations and non-parametric measures where appropriate) will be used to describe the characteristics of the families, centres and children along with the primary and secondary outcome measures.
At recruitment to the trial, parents will be asked to report the number of siblings (both pre-school, and school age or older) in the index child’s household. If another pre-school sibling in the same family is injured during the recruitment period, the family will only be recruited to the study once. Through this data collection at recruitment, the research team will have a denominator for analysis of injuries in the siblings of the index child. The numerator for injuries in siblings will be identified through parental report and objective measures such as attendance at A&E and Walk-In Centres as detailed above. It will therefore be possible to calculate a rate of injury occurrence per unit period of follow up in the index children and in their siblings.
We know that the number of siblings a child has is associated with the risk of injury occurrence. The greater the number of siblings and having older siblings are both factors associated with increased risk of injuries in a child. Clustering of injuries within families is likely. The primary outcome measures of injuries requiring medical attention and those not requiring medical attention will therefore be analysed using hierarchical modelling, using the child as the unit of analysis, in recognition of the fact that these variables are not independent.
Outcome measures such as child behaviour or use of safety equipment will be assessed although the emphasis of the analytical strategy will be on point estimates of differences and their associated confidence intervals rather than p-values. Between-group comparisons will be conducted using multi-level modelling and will be used as an exploratory technique in preparation for a larger trial.
The injury diaries and behaviour questionnaire data will not be used in any form of interim analysis. All injury data will be pooled for analysis at six months.
7.5.2 Qualitative analysis
All audio-recorded data will be fully transcribed, anonymised, checked for accuracy and then imported into a software package, NVivo8. Analysis will begin shortly after data collection starts, will be ongoing and iterative. Analysis will inform further data collection; for instance, analytic insights gathered in earlier interviews will shape the questions covered during later interviews.
Thematic analysis will be used to scrutinise the data in order to identify and analyse patterns and themes of particular salience for participants and across the dataset using constant comparison techniques. Firstly the transcripts will be read several times to gain familiarisation with the data and initial ideas noted. The transcripts will then be examined on a line-by-line basis with inductive codes being assigned to the segments of the data that provide insight in to the participants’ views and understanding of their experiences and assist in the development of an initial coding frame. New data will be compared initially to the previous data and then to the properties of emerging categories that contain the main themes. The process of constant comparison will allow for the generation of new themes, reclassify themes and incorporate themes within other themes. The coding frame will be modified, if needed as the analysis develops. The analysis will enable the research team to arrive initially at a descriptive account which will be developed into a theoretical account in the light of existing theoretical and applied literature.
Trial data and documentation will be retained securely by the principal investigator in Bristol according to local codes of research conduct (6 years in Bristol).
7.6 Researcher safety
The researchers will follow the University of the West of England’s Researcher Safety Guidance when conducting any field work away from university premises. This will involve undertaking an assessment of risk prior to arranging an interview, prior informing a designated person from the study team the details of an interview, and calling in when the interview has been completed at an agreed time. If the designated person is not contacted at the agreed time, the designated person will contact the researcher’s mobile telephone. If there is no answer, the designated person will telephone the participant’s house. If contact has still not been made, the designated person will telephone the police and ask them to visit the participant’s house.
7.7 Research governance
The sponsor for the research will be the University of the West of England, Bristol. A research fellow (Project Manager) will be appointed in both Bristol and Nottingham to oversee the day to day running of the project. The Project Manager will be supervised by Julie Mytton in Bristol and Caroline Mulvaney in Nottingham.
Governance of the feasibility study will be through a management group comprising the co-applicants and collaborators. The management group will meet monthly at the beginning and end of the study and bimonthly during the study. Meetings will be in person where possible and by teleconference were necessary. The management group will oversee the progress of the study and adherence to timescales and the project plan. Not all co-applicants will be required for every management group meeting. The principle investigator (JM) will report to a Trial Steering Committee (TSC) that will meet four times during the course of the study. The requirement for a Data monitoring and Ethics Committee (DMC) will be the decision of the Chairperson of the TSC. As this is a feasibility study, and there are no plans for interim data analysis that could potentially lead to early closure of the trial, we consider the trial to be low risk and do not anticipate the need for a DMC.
7.8 Writing up and dissemination
Findings of the study will be made available to the participating families. They will also be disseminated to the Parents Advisory Group (see below) and to Health Visiting teams and children’s centre managers at intervention and control sites. The findings of the feasibility study will be written in non-specialist language so that they may be accessible to families and a range of professionals. Any quotations from participant or professional’s interviews will be anonymised prior to inclusion in the study report.
We anticipate that a subsequent main trial would generate outcomes of interest to the health community, local authorities, the public and to academics. Care would be required not to disseminate the findings too widely after the feasibility study before a main trial; otherwise recruitment to the main trial may be compromised. We would however provide local feedback in Bristol and Nottingham and would prepare papers for publication and a UK conference presentation.
8.0 Service Users
The parent perspective on the development, implementation and management of this project are recognised as very important to the success of the research. The ability to engage parents in the programme in a non-stigmatising way is vital to the project’s success. The research team have therefore elected to work with a Parents Advisory Group rather than one or two named parents. We have identified a group of parents that currently regularly meet at a children’s centre in Bristol. One of these parents has worked with Dr Jenny Ingram on a previous project, and formally provided feedback during the development of this study. Dr Ingram would help facilitate the Parent Advisory Group to advise the research team, and will feedback on a regular basis to the management group and to the Trials Steering Committee. Feedback will either be by direct representation by a parent at the TSG meetings or through the facilitator (JI).We anticipate the group would meet at least four times during the course of the study. We believe that a Parent Advisory Group is a valuable resource which provides a critical mass and collective support to express parent’s perspectives.
The group have advised us on the preparation of the information sheets and consent forms. They will advise on the study process to help maximise acceptability, engagement, retention and compliance. We will ask them to help us prepare the final reports of the feasibility study in an accessible format for participating families.
There is a risk that lay advisors to research projects may lack confidence in their role and their ability to influence decision making. The University of the West of England, Bristol has an innovative new system to support the participation of lay research partners in projects. The system not only helps researchers identify lay partners where necessary, but can help fund expenses to enable lay partners attend meetings, and help them gain confidence in contributing their perspective by offering them formal status as a research partner by providing them with a staff card, access to the UWE library, ATHENS log in etc. We will be working closely with this group to enable successful parent inclusion in the research management and offer these benefits to the parents leading our advisory group.
Project timetable and milestones
Flow diagram
References
- Better safe than sorry; Preventing unintentional injury to children. London: Audit Commission; 2007.
- Every Child Matters: Change for Children. London: The Stationery Office; 2004.
- O’Connor T, Davies L, Dunn J, Golding J. Alspac Study Team . Distribution of accidents, injuries and illness by family type. Pediatrics 2000;106.
- Warrington S, Wright C. Alspac Study Team . Accidents and resulting injuries in premobile infants: data from the ALSPAC study. Arch Dis Child 2001;85:104-7.
- Langley J, Dodge J, Silva P. Accidents in the first five years of life. Aus Paediatr J 1979;15:255-9.
- Home and Leisure Accident Surveillance System [Internet] . ROSPA n.d. URL: www.hassandlass.org.uk/query/index.htm (accessed 28 August 2009).
- Reading R, Langford I, Haynes R, Lovett A. Accidents to preschool children: comparing family and neighbourhood risk factors. Soc Sci Med 1999;48:321-30.
- Dowswell T, Towner E. Social deprivation and the prevention of unintentional injury in childhood. Health Edu Res 2002;17:221-37.
- Edwards P, Green J, Lachowycz K, Grundy C, Roberts I. Serious injuries in children: variation by area deprivation and settlement type. Arch Dis Child 2004;93:485-9.
- Towner E, Dowswell T, Errington G, Burkes M, Towner J. Injuries in children aged 0–14 years and their inequalities. London: Health Development Agency; 2005.
- Edwards P, Roberts I, Green J, Lutchmun S. Deaths from injury in children and employment status in family: analysis of trends in class specific death rates. BMJ 2006;333.
- Reading R, Jones A, Haynes R, Daras K, Emond A. Individual factors explain neighbourhood variations in accidents to children under 5 years of age. Soc Sci Med 2008;67:915-27.
- Kendrick D, Mulvaney C, Burton P, Watson M. Relationships between child, family and neighbourhood characteristics and childhood injury: a cohort study. Soc Sci Med 2005;61:1905-15.
- Bijur PE, Golding J, Kurzon M. Childhood accidents, family size and birth order. Soc Sci Med 1988;26:839-43.
- Bijur P, Kurzon M, Overpeck M, Scheidt P. Parental alcohol use, problem drinking, and children’s injuries. JAMA 1992;267:3166-71.
- Rowe R, Maughan B, Goodman R. Childhood psychiatric disorder and unintentional injury: findings from a national cohort study. J Pediatr Psychol 2004;29:119-30.
- Bijur P, Stewart-Brown S, Butler N. Child behavior and accidental injury in 11,966 preschool children. Am J Dis Child 1986;140:487-92.
- Langley J, McGee R, Silva P, Willaims S. Child behaviour and accidents. J Pediatr Psychol 1983;8:181-9.
- Ingram J, Emond A. Parents’ perceptions of home injury risk and attitudes to supervision of preschool children: a qualitative study in economically deprived communities. Primary Health Care Res Develop 2009;10:98-108.
- Law J, Plunkett C, Taylor J, Gunning M. Developing policy in the provision of parenting programmes: integrating a review of reviews with the perspectives of both parents and professionals. Child Care Health Develop 2009;35:302-12.
- Morrison Gutman L, Feinstein L. Parenting behaviour and children’s development from infancy to early childhood: changes, continuities and contributions. Department for Education and Skills; 2007.
- Up to 7: Family background and child development up to age 7 in the Avon Longitudinal Study of Parents and Children (ALSPAC). Department for Education and Skills; 2006.
- Morrison Gutman L, Brown J, Akerman R. Nurturing parenting capability – the early years. Department for Children Schools and Families; 2009.
- Feldman M, Case L, Sparks B. Effectiveness of a child-care training program for parents at risk for child neglect. Can J Behav Sci 1992;24:14-28.
- Morrongiello B, Corbett M, Brison R. Identifying predictors of medically-attended injuries to young children: do child or parent behavioural attributes matter?. Inj Prevent 2009;15:220-5.
- Schwebel D, Kendrick D. Caregiver supervision and injury risk for young children: time to re-examine the issue. Inj Prevent 2009;15:217-8.
- Stewart-Brown S, Patterson J, Mockford C, Barlow J, Klimes I, Pyper C. Impact of a general practice based group parenting programme: quantitative and qualitative results from a controlled trial at 12 months. Arch Dis Child 2004;89:519-25.
- Barlow J, Coren E, Stewart-Brown S. Parent-training programmes for improving maternal psychosocial health. Cochrane Database Syst Rev 2003;4.
- Coren E, Barlow J. Individual and group-based parenting programmes for improving psychosocial outcomes for teenage parents and their children. Cochrane Database of Systematic Reviews 2001.
- Barlow J, Stewart-Brown S. Behaviour problems and group-based parent education programmes. J Develop Behav Pediatr 2000;21:356-70.
- Barlow J, Parsons J, Stewart-Brown S. Preventing emotional and behavioural problems: the effectiveness of parenting programmes with children less than 3 years of age. Child Care Health Develop 2005;31:33-42.
- Gagnon A, Bryanton J. Postnatal parental education for optimizing infant general health and parent–infant relationships. Cochrane Database Syst Rev 2009;1.
- Kendrick D, Elkan R, Hewitt M, Dewey M, Blair M, Robinson J, et al. Does home visiting improve parenting and the quality of the home environment? A systematic review and meta-analysis. Arch Dis Child 2000;82:443-51.
- Kendrick D, Watson M, Mulvaney C, Burton P. How useful are home safety behaviours for predicting childhood injury?. Health Edu Res 2005;20:709-18.
- Kendrick D, Coupland C, Mulvaney C, Simpson J, Smith S, Sutton A, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev 2007;1.
- Petrie J, Bunn F, Byrne G. Parenting programmes for preventing tobacco, alcohol and drugs misuse in children <18: a systematic review. Health Edu Res 2007;22:177-91.
- Emond A, Pollock J, Deave T, Bonnell S, Peters T, Harvey I. An evaluation of the First Parent Health Visitor Scheme. Arch Dis Child 2002;86:150-7.
- Roberts I, Kramer M, Suissa S. Does home visiting prevent childhood injury? A systematic review of randomised controlled trials. BMJ 1996;312:29-33.
- Kendrick D, Barlow J, Hampshire A, Polnay L, Stewart-Brown S. Parenting interventions for the prevention of unintentional injuries in childhood. Cochrane Database Syst Rev 2007;4.
- Kendrick D, Barlow J, Hampshire A, Stewart-Brown S, Polnay L. Parenting interventions and the prevention of unintentional injuries in childhood: systematic review and meta-analysis. Child Care Health Develop 2008;34:682-95.
- Kane G, Wood V, Barlow J. Parenting programmes: a systematic review and synthesis of qualitative research. Child Care Health Develop 2007;33:784-93.
- Morrongiello B, Howard A, Rothman L, Sandomierski M. Once bitten, twice shy? Medically-attended injuries can sensitise parents to children’s risk of injuries on playgrounds. Inj Prevent 2009;15:50-4.
- Moran P, Ghate D, van der Merwe A. What works in parenting support? A review of the international evidence. London: Department for Education and Skills; 2004.
- Boddy J, Statham J, . International perspectives on parenting support. Non-English language sources. Department for Children Schools and Families; 2009.
- Cost Benefit Analysis of Interventions with Parents. Department for Children Schools and Families; 2007.
- Romeo R, Byford S, Knapp M. Economic evaluations of child and adolescent mental health interventions: a systematic review. J Child Psychol Psychiatr 2005;46:919-30.
- Edwards R, Ceilleachair A, Bywater T, Hughes D, Hutchings J. Parenting program for parents of children at risk of developing conduct disorder: cost effectiveness analysis. BMJ 2007;334.
- Kendrick D, Barlow J, Hampshire A, Stewart-Brown S, Polnay L. Parenting interventions and the prevention of unintentional injuries in childhood: systematic review and meta-analysis. Child Care Health Develop 2008;34:682-95.
- Posner J, Hawkins L, Garcia-Espana F, Durbin D. A randomized, clinical trial of a home safety intervention based in an emergency department setting. Pediatrics 2004;113:1603-8.
- King W, LeBlanc J, Barrowman N, Klassen T, Bernard-Bonnin A-C, Robitaille Y, et al. Long term effects of a home visit to prevent childhood injury: three year follow up of a randomized trial. Inj Prevent 2005;11:106-9.
- Potter B, Newell G. Accident prevention in the under 5’s. Severn NHS Trust and East Gloucestershire NHS Trust; 1997.
- Stewart-Brown S. Improving parenting: the why and the how. Arch Dis Child 2008;93:102-4.
- Gielan A, Wilson M, McDonald E, Serwint J, Andrews J, Hwang W-T, et al. Randomized trial of enhanced anticipatory guidance for injury prevention. Arch Pediatr Adolesc Med 2001;155:42-9.
- Watson M, Kendrick D, Coupland C, Woods A, Futers D, Robinson J. Providing child safety equipment to prevent injuries: randomised controlled trial. BMJ 2005;330:178-83.
- Watson M, Kendrick D, Coupland C. Validation of a home safety questionnaire used in a randomised controlled trial. Inj Prevent 2003;9:180-3.
- Tennant R, Hillier L, Fishwick R, Platt S, Stephen J, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5.
- Morrongiello B, Corbett M. The Parent Supervision Attributes Profile Questionnaire: a measure of supervision related to children’s risk of unintentional injury. Inj Prevent 2006;12:19-23.
- Manheim L. Health Services Research Clinical Trials: Issues in the Evaluation of Economic Costs and Benefits. Control Clin Trials 2009;19:149-58.
- Campbell N, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F. Designing and evaluating complex interventions to improve healthcare. BMJ 2007;334:455-9.
Appendix 8 Poster used in children’s centres to support recruitment of parent participants in the feasibility study
Poster used in children’s centres to support recruitment of parent participants in the feasibility study (PDF download)
Appendix 9 Example topic guide used during the feasibility study
An example of a topic guide used in the feasibility study is shown below. Other topic guides and other supporting documentation (e.g. participant information sheets, questionnaire booklets, etc.) are available from the authors upon request.
Interview Topic Guide: children’s centre staff
After completion of FAST Parent Programme
Complete consent form
1. Introduction
Thanks. Introduce self. Re-state purpose of the interview and use of audio-recording
2. Background
Could you start by telling us your name, and the children’s centre that you work with/in?
3. Programme experience
Have you ever been involved with delivering/organising/hosting a programme for parents before? If so, what was it about? In what ways was it similar or different to this programme?
What was your experience of the FAST Parent Programme? (positive and negative features)
What were you hoping that parents would get out of the FAST Parent Programme? Do you think those expectations/needs were met? Why?
Were there features of the programme that you think were particularly enjoyed by the parents? Or were particularly helpful for the parents? What were they and why were they enjoyable/helpful?
Were there features of the programme that you think the parents did not enjoy or were not helpful? What were they and why do you think they did not work so well?
What did you think of the format of the programme? (number of sessions/frequency of sessions/duration of sessions?, the leadership required?, the materials used?)
What was your experience of having the course running in the children’s centre/Community Centre? (Positive and negative)
4. The future
Would you want to host/run another FAST Parent Programme in the future? Why?
5. Other issues
Any other issues that the participant would like to raise
Thank them for their time.
Appendix 10 Evaluation of the FAST parent programme using ten principles of effective safety education and six additional health promotion criteria
| Criteria | Limited or none | Sufficient | Well addressed | Notes |
|---|---|---|---|---|
| 1. Encourage the adoption of, or reinforce, a holistic approach within the wider community | Yes | Linked to good parenting advice | ||
| 2. Use active approaches to teaching and learning (including interactive and experiential learning) | Yes | Uses a variety of methods: question and answer, small group, whole group, DVDs, practical demonstrations. Trainers modelling good practice | ||
| 3. Involve parents in real decisions to help them keep their children safe | Yes | Safety tips provided for children of different ages | ||
| 4. Assess parents’ learning needs | Yes | Emphasis on child development and injuries | ||
| 5. Teach safety as part of a comprehensive spiral curriculum | Yes | Safety taught as part of child development and anticipatory guidance | ||
| 6. Use appropriate and practical examples | Yes | Meaningful analogies and anecdotes stressed – newspapers, TV news | ||
| 7. Work in partnership across wider community | Yes | Not clear if this is stressed, either in trainers’ manual or participants’ handbook | ||
| 8. Address known risk and protective factors | Yes | Enhancing supervision and linkage with ages and stages | ||
| 9. Address psychosocial aspects of safety, e.g. confidence, resilience, self esteem, self-efficacy | Yes | Ability for parents to recognize protective and resilience factors in families. Values participant contributions. Provides confidence to cope with injury events | ||
| 10. Adopt positive approaches which model and reward safe behaviour, within a safe, supportive environment | Yes | Promotes empowerment and independence. Promotion of praise for children. Be realistic about your child. How to cope with challenging behaviour | ||
| 11. Evidence-based content, both the injury prevention messages and the parenting content | Yes | Home-based injuries are well addressed – should concerns about baby walkers be included? | ||
| 12. Appropriate balance of parenting advice and injury prevention content | Yes | The programme is designed to combine these two elements but the parenting advice is more dominant in the package | ||
| 13. Suitability for preventing injuries in children between 0 and 5 years | Yes | Primary focus of programme | ||
| 14. Suitability for delivering in children’s centre settings by health visitor teams | Yes | Primary focus of programme | ||
| 15. Appropriateness of reading age of any materials produced | Yes | Participants’ handbook clearly written | ||
| 16. Involvement of parents in the development of the materials | Yes | Not clear whether this is stressed |
Appendix 11 Evaluation of the FAST parent programme against evidence standards of the Canadian edition of the Child Safety Good Practice Guide
| Evidence statement (from Child Safety Good Practice Guide – Canadian Edition, 2011) | Transfer and implementation points | Degree to which addressed in FAST curriculum | ||||
|---|---|---|---|---|---|---|
| Limited or none | Sufficient | Well addressed | NA | Notes | ||
| Child passenger safety | ||||||
| Child passenger restraints lead to decreases in death and injury | ✗ | FAST focus on home safety means road safety is not a central topic. Appears in week 6 quiz but does not seem to be presented as part of curriculum | ||||
| Keep children rear-facing as long as possible | ✗ | |||||
| Make parents aware of where available and how to use child passenger restraints | ✗ | |||||
| Rear seating position is the safest place location for child passengers regardless of whether or not there is a passenger-side air bag present | ✗ | |||||
| Address parents’ experiences of pressure to relax
seating rules and risk perception Provide strategies that support sound parental safety decisions |
✗ | Week 5 dedicated to strategies for parenting and setting rules | ||||
| Seat belts lead to decreases in death and injury | ✗ | |||||
| Increase parental awareness | ✗ | |||||
| Child cyclist safety | ||||||
| Use of bicycle helmets leads to reduction in injuries | ✗ | FAST focus on home safety means road safety is not a central topic | ||||
| Make parents aware of need for helmets and where they are readily available | ✗ | |||||
| Provide discounts or helmet give-away programs | ✗ | |||||
| Child water safety | ||||||
| Use of a personal floatation device for boating and other water recreational activities helps prevent drowning | ✗ | |||||
| Legislation requiring isolation fencing with secure, self-latching gates for all pools leads to a reduction in drowning when enforcement provisions are included | ✗ | |||||
| Make parents aware of need to fence private pools | ✗ | While pools can be part of home safety, the demographic target in this curriculum is unlikely to have backyard pools. However, may be relevant to mention in case there is a pool in the housing complex | ||||
| Strongly encourage parents to continue close supervision of their children around pools | ✗ | Supervision is discussed for baths, but not pools | ||||
| Water safety skills training (including swimming lessons) improves swimming performance | ✗ | |||||
| Strongly encourage parents to continue close supervision of their children around water; ability to swim does not replace the need for close parent supervision | ✗ | Supervision is discussed for baths, but not pools | ||||
| Encourage parents to enrol children in swimming lessons after 48 months (if not earlier) and continue with lessons. | ✗ | Focus on home safety may render this unnecessary to discuss | ||||
| Clarify that aquatic programs for infants and toddlers are not a way to decrease the risk of drowning | ✗ | |||||
| Falls prevention in children | ||||||
| Window safety mechanisms to prevent children from opening windows, such as bars and position locking devices, are an effective strategy to prevent falls | ✗ | Recommendation for use of window locks appears as safety tip for 1–3 years; however, types of locks are not discussed | ||||
| Provide information regarding purpose, availability and installation of window safety mechanisms | ✗ | Do not provide information on availability and installation | ||||
| Supply and install window safety mechanisms | ✗ | |||||
| Stair gates have shown to assist in the reduction of falls down stairs in young children when used at the top of stairs in households | ✗ | |||||
| Promote awareness of stair-gate use, availability and installation | ✗ | Need for stair-gates discussed though information on availability and installation is not provided | ||||
| Pressure gates should not be used at the top of stairs | ✗ | |||||
| Supply and install stair-gates | ✗ | |||||
| Educational programs encouraging use of fall prevention safety devices such as window safety mechanisms to prevent children from opening windows and down stairs increase use of equipment | ✗ | |||||
| Time education and develop materials and advice (style, language and examples) that suit target communities | ✗ | Developmental stage specific safety information Language is simple, examples are clear |
||||
| Adjust interventions according to practical limitations and parents’ cultural expectations. A particular barrier is parents’ inability to modify rented or shared accommodation | ✗ | Attempts made to keep language basic, but unclear how well would relate to other cultures | ||||
| Burn and scald prevention | ||||||
| Product modification, specifically child-resistant cigarette lighters, hearth gates and self-extinguishing cigarettes, are primary prevention strategies where the technologies have been developed, tested and found to be effective and which would prevent many fires from starting if adopted | ✗ | |||||
| Promote parental knowledge and modified product availability, accessibility, cost and ease of use | ✗ | No mention of products | ||||
| Legislation regulating the temperature of hot water from household taps is effective in reducing scald injuries | ✗ | |||||
| Ensure that hot water is set at safe temperatures by reducing temperature at the water heater or through the use of thermostatic mixing valves (TMVs) | ✗ | Recommend setting hot water thermostat to below 54 °C | ||||
| Smoke detector giveaway programs have proven successful when high-risk neighbourhoods are targeted and multifaceted community campaigns have the specific objective of installation of working smoke detectors | ✗ | |||||
| The distribution of smoke alarms alone is insufficient for improving installation rates; programs containing an education component showed more success | ✗ | |||||
| Timing of education and developing materials and advice (style, language and examples) that suit target communities (e.g., low-income, ethnic minority populations) are key to success | ✗ | |||||
| Uptake and success of interventions depends on adjusting interventions according to practical limitations and parents’ cultural expectations. A particular barrier is parents’ inability to modify rented or shared accommodation | ✗ | |||||
| Safety issues identified by a community are responded to show greater success in increasing smoke alarm installation rates | ✗ | |||||
| Fire safety skills training increases knowledge and behaviour of both children and parents. At this time there is no study directly linking training to injury reduction | Include mention of need for smoke alarms and guide through developing escape plan | |||||
| Programs using active participation by children in learning fire responses are more effective than those using passive methods | ✗ | Children are not target audience of programme | ||||
| When evaluating programs, actual demonstration of skills is likely a more reliable marker of children’s real response in fire situations than providing correct answers on a written test | ✗ | Children are not target audience of programme | ||||
| The addition of fear reduction techniques and teaching the rationale supporting the use of correct fire response behaviours may significantly improve skill retention | ✗ | Rationale provided. Not clear whether supplementary video helped reduce fear or provide further rationale | ||||
| Periodic repetition of material is required for maintenance of knowledge and skills | ✗ | Covered in week 4 and participants provided with fire escape route planner to take home. Follow-up on week 5 to see if planner completed and smoke alarms installed or checked | ||||
| The use of figures of authority in fire safety skills training (e.g. fire fighters) may increase knowledge gain | ✗ | Fire-fighters, etc. do not provide this component of training, but may be inappropriate to programme of this nature, where consistent facilitator and trust are needed | ||||
| Poisoning prevention in children | ||||||
| Secure storage for poisons removes a larger portion of poisoning risk than parental supervision and may be an effective means of preventing poisoning injury | ✗ | Mention to not store poisons in other containers but no mention of need to lock up out of reach | ||||
| Studies of how children access poisons suggest that the most vulnerable time is when the poisons are in use and that safe packaging alone cannot compensate for unsafe storage or use. This speaks to the need for improved safety of home storage of medications and improved home dispensing practice | ✗ | Mention child-safe packaging will only slow child down, not stop them altogether. No mention of storage needs | ||||
| Changes to the fixed environment need to be supported by regulation and education for industry and the community, with clear labelling (and clear administration instructions) on the package, parental education and improved supervision, ongoing paediatric counselling, and increased accessibility and affordability | ✗ | |||||
| Poison control centres result in considerable medical savings if the public is well informed regarding the use of their local poison control centre | ✗ | Provide NHS direct number and emergency number Are there poison control centres in England? |
||||
| Parental knowledge and availability, accessibility and ease of use of poison control centres will impact their use. Educational activities may assist in increasing parental knowledge | ✗ | |||||
| General child home safety | ||||||
| Home safety counselling (addressing issues such as using window bars, stair-gates, other home safety equipment and not using baby walkers, bath seats and other injury hazard producing equipment) can reduce the risk of child injury | ✗ | No mention of baby walkers and bath seats | ||||
| Availability, accessibility, cost, durability and ease of use of items recommended during home safety checks will impact their uptake | ✗ | |||||
| Providing free safety equipment increases use but evidence is less strong for discounted equipment | ✗ | |||||
| Effective provision of safety equipment involves ongoing support with installation and maintenance | ✗ | |||||
| Timing of education and developing materials and advice (style, language and examples) that suit target communities (e.g., low-income, ethnic minority populations) are key to success | ✗ | |||||
| Uptake and success of interventions depends on adjusting interventions according to practical limitations and parents’ cultural expectations. A particular barrier is parents’ inability to modify rented or shared accommodation | ✗ | Unclear to what extent this is addressed | ||||
| Home-based social support, such as home visiting programs for new mothers, has the potential to significantly reduce rates of child injury | ✗ | |||||
| Supportive home visiting for families with young children can provide education regarding issues such as using window bars, stair-gates, other home safety equipment and not using baby walkers, bath seats and other injury hazard-producing equipment | ✗ | |||||
| Availability, accessibility, cost, durability and ease of use of items recommended during home safety checks will impact their uptake | ✗ | |||||
| There is indirect evidence that individual-level education/counselling in the clinical setting are effective measures to reduce many childhood unintentional injuries | ✗ | |||||
| Availability, accessibility, cost, durability and ease of use of items recommended during home safety checks will impact their uptake | ✗ | |||||
| Those providing information also require initial and ongoing training to ensure content/material provided is up to date | ✗ | |||||
Appendix 12 Content of revised 6-week FAST parent programme
| Week | Injury theme for week | Component (duration in minutes) [parenting knowledge or skill] |
|---|---|---|
| 1 | Cuts and wounds (minor falls) | Welcome and introduction. Housekeeping. (10) Icebreaker activity – collective parental experience in the group (10) Discussion: we all know something about keeping children safe, but we know different things and have different concerns. We can learn from each other (15) Activity: cuts and wounds at different ages (10,) looking at the world from a child’s eye level [Empathy] First aid advice: what to do if your child has a cut, wound or nose bleed (10) [self-efficacy] Tea break (10) Question-and-answer session: children will want to try out the new skills they acquire and that this can be perceived by parents as being naughty, not listening or breaking the rules (15) [empathy, introduction to boundary setting and the 3Cs] Discussion: feeling safe and being safe (10) [introduction to attachment, introduction to positive reinforcement] Wrap up: any questions, handouts to go in parents’ handbook, suggestions of what to try at home (what activities/objects/places attract your child?), what we will cover next week (5) |
| 2 | Bumps, bruises and broken bones (more serious falls, includes head injuries) | Welcome back: reflections on last session, experience of trying
things at home. Icebreaker activity: how to put on a triangular
bandage (15) [self-efficacy] Discussion: how children’s development and skills can surprise us, physical skills develop before cognitive skills (10) [empathy]. Activity: risks of falls, broken bones and head injuries varies at different ages. Use ‘hunt the hazard’ picture cards. How siblings can influence a child’s injury risk (20) [empathy] First aid advice: head injuries, bruises and broken bones (15) [self-efficacy] Tea break (10) Discussion: what parents in group are already doing to keep their children safe from head injuries, bruises and broken bones (10) [self-efficacy] Discussion: how children learn and play. Introduction to concept of the ‘emotional brain’ and how this can affect both adults and children when we get upset or disappointed (20) [empathy, communication] Activity: effective communication. Reflect after activity on how non-verbal cues are important when communicating and what happens if we shout at each other (15) [communication]. Wrap up: any questions, handouts to go in parents’ handbook, suggestions of what to try at home (what boundaries might you want to try at home? Think about how they communicate with their child), what we will cover next week (5) |
| 3 | Burns and scalds | Welcome back: reflections on last session, experience of trying
things at home. Introduction to this session
(10–15) Activity: using praise and how it makes us feel (5) [positive reinforcement] Question-and-answer session: what do members of the group do already to keep their children safe from burns and scalds? What are the risks for burns and scalds at different ages? Reminder about physical development occurring before cognitive development (15) [self-efficacy, empathy] Activity: fill mug with boiling water to watch it change colour as it cools down (5) Discussion and group participation: experiencing or responding to a burn or scald is a distressing. Reminder about the emotional brain. How to use slow breathing to calm yourself or your child down if upset/distressed/angry (10) [empathy, self-efficacy] Activity: case studies using burns dolls and photographs. Check the heat mug (10) Tea break (10) First aid advice: what to do if your child has a burn or scald (10) [self-efficacy] Activity: fire safety DVD (5 minutes) plus discussion on having working smoke alarm and a fire escape plan (10) [self-efficacy] Check the heat mug (probably final time) Question-and-answer session: the difference between discipline and punishment. How to maintain a boundary. Remind about the 3Cs (15) [boundary setting and 3Cs] Discussion: the importance of praise to help reinforce the behaviour you want (10) [praise, communication, empathy] Check on the heat mug (if still hot on last occasion) Wrap up: any questions, handouts to go in parents’ handbook, suggestions of what to try at home (reflect on how often they praise their child. Try increasing the praise and see if it makes a difference. Check their smoke alarm, agree a fire escape plan with the family), what we will cover next week (5) |
| 4 | Drowning and safe play | Welcome back: reflections on last session, experience of trying
things at home. Introduction to this session
(10–15) Activity: where do we find water in the house and garden? Different risks at different ages, how might the drowning risk event happen? (15) Discussion: what would you do if you found your child under the water? (link to emotional brain, keeping calm) [self-efficacy] Demonstration: cardiopulmonary resuscitation and recovery position + discussion (25) Tea break (10) Discussion: how can you keep your child safe near water? Link to supervision, boundary setting, effective communication, home safety equipment (10) Q&A: differences between mums and dads in how they teach and play with their children. What is a safe toy? Link to child development, importance of praise and encouragement and supervision (20) Discussion: play from a child’s perspective – exploring something new may be part of learning and a child may be completely unaware of the risks associated with what they are doing. Contrast with ‘being naughty’ (5) [empathy] Activity: knowing what toys are safe – safety marks (10) [self efficacy] Wrap up: any questions, handouts to go in parents’ handbook, suggestions of what to try at home (effect of praise on encouraging appropriate play, reviewing their child’s toys for hazards), what we will cover next week (5) |
| 5 | Poisoning and ingestions | Welcome back: reflections on last session, experience of trying
things at home. Introduction to this session
(10–15) Discussion: poisoning and ingestion risks at different ages. Link to child development and learning (15) Activity: ingestion risk flashcards (10) First aid advice: what to do if you think your child has swallowed something they shouldn’t. Link to keeping calm (emotional brain) (10) Tea break (10) Discussion: what could you do to keep your child safe from poisoning and ingestions? Home safety equipment (e.g. cupboard locks) and link to local schemes. Link to parenting: supervision, boundary setting. (10) Q&A: children may demand attention when they are struggling with other things (10). Responding to different behaviours (10) [use of praise, effective communication] Discussion: rule making. Importance of consistency and appropriate boundary setting (10) [3Cs] Wrap up: any questions, handouts to go in parents’ handbook, suggestions of what to try at home (home safety quiz, discuss consistent boundary setting with partners/other household adults), what we will cover next week (5) |
| 6 | Unconscious or choking child | Welcome back: reflections on last session, experience of trying
things at home. Introduction to this session
(10–15) Activity + discussion: flipchart – choking risks at different ages (10) Demonstration: choking tube – show how objects can block the windpipe. Discuss how you would know if your child was choking. First aid advice: back slaps, chest thrusts, abdominal thrusts (25) Tea break (10) Discussion: how to keep your child from choking at home. Link to previous week’s discussion on choices, consequences and consistency in boundary setting, child development, supervision, 3Cs. (10) Activity: ‘how safe is your home’ checklist (10) Demonstration: cardiopulmonary resuscitation (10). Discussion Discussion: lifelong learning as a parent. Reflect on skills and knowledge learnt on course. What parents could do if they wanted to learn more (10) Wrap up: any questions, handouts to go in parents’ handbook, Thank you for coming, feedback on the course, give certificates of completion of course (5) |
List of abbreviations
- CBA
- controlled before-and-after (study)
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- df
- degree of freedom
- ED
- emergency department
- FAST
- First-aid Advice and Safety Training
- GP
- general practitioner
- HOME
- Home Observation for Measurement of the Environment
- HTA
- Health Technology Assessment
- NIHR
- National Institute for Health Research
- PAG
- parent advisory group
- PDS
- programme development subgroup
- PSAPQ
- Parent Supervision Attributes Profile Questionnaire
- PVC
- polyvinyl chloride
- RCT
- randomised controlled trial
- RR
- relative risk
- SD
- standard deviation
- SE
- standard error