Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/136/04. The contractual start date was in March 2013. The draft report began editorial review in March 2017 and was accepted for publication in November 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Matthew L Costa is a member of the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) General Board and reports grants from the trauma industry (Stryker Corporation, X-Bolt Orthopaedics, Onbone, Smith & Nephew plc, Heraeus Holding GmbH and DePuy Synthes Companies); grants from the AO Foundation; and grants from NIHR and the European Union outside the submitted work. Sarah E Lamb was a member of the NIHR HTA Additional Capacity Funding Board, NIHR HTA End of Life Care and Add-on Studies, NIHR HTA Prioritisation Group and NIHR HTA Trauma Board during this study.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Costa et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Adapted with permission from Achten et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Background
The tibia is the most commonly broken major bone in the leg. In younger patients, fractures of the tibia typically occur during sporting activity or road traffic accidents, but in older patients they can happen during simple falls. Injuries usually require hospital admission and surgery, resulting in prolonged periods (months) away from work and social activities.
The treatment of displaced, extra-articular fractures of the distal tibia (lower third) remains controversial. These injuries are difficult to manage because of the limited soft-tissue cover, poor vascularity of the area and proximity of the fracture to the ankle joint. Infections, non-union and malunion are well-recognised complications.
Non-operative treatment is one option and avoids the risks associated with surgery. Sarmiento et al. ,2 in 2003, reviewed 450 closed fractures of the distal tibia following functional bracing: 13.1% developed a malunion (defined as > 7° of angulation or 12 mm of shortening). Another study,3 using a more robust definition of 10 mm of shortening and 5° of angulation, found a higher rate of malunion (26.4%). In this study, Böstman et al. 3 treated patients using a long leg cast, and failure to maintain reduction led to surgical treatment with an intramedullary (IM) nail. Thirty-two out of 103 cases required nailing at a mean of 9 days following injury. Two patients in this group, and three in the non-operative group, went on to have a non-union. 3 Union rates were faster with IM nailing than with conservative treatment and median values were 12.5 and 14.5 weeks, respectively (p < 0.001). 3 Digby et al. 4 also found that non-operative treatment for tibial fractures in the metaphyseal region leads to unacceptable deformity and ankle stiffness. Therefore, operative treatment is now the treatment of choice for the majority of patients with a fracture of the distal tibia.
Surgical treatment options are expanding and include locked IM nails, plate and screw fixation, as well as external fixator systems, including the Ilizarov frame and hybrid fixators. External fixators may be beneficial in selected cases, particularly those involving severe soft-tissue injuries, but, in the UK, the IM nail and ‘locking’ plate options are most commonly used for extra-articular fractures. Mid-shaft fractures of the tibia are generally successfully treated with locked IM nails. However, in the more distal metaphyseal region of the tibia, the fixation may be less stable. 5 The bolts or screws that are inserted into the nail may break,6 malalignment may occur7 and there is a risk that the nail will penetrate into the ankle joint. 8,9
The development of locking plates, in which a thread on the head of the screws locks into the holes in the plate to create a ‘fixed-angle’ construct, has led to a recent increase in the use of locking plate fixation. However, locking plates are not without risks and they require greater soft tissue dissection, which carries a risk of infection, wound breakdown and damage to the surrounding structures. 10
In a retrospective study11 of 111 patients with extra-articular fractures of the distal tibia (4 to 11 cm proximal to the plafond), a comparison was made between IM nail and locking plate fixation. Seventy-six fractures were treated with an IM nail and 37 were treated with a medial plate. 11 Nine patients (12%) had a delayed union or non-union in the IM nail fixation group and one patient (2.7%) had a non-union after locking plate fixation (p = 0.10). Angular malalignment of ≥ 5° occurred in 22 patients with IM nails (29%) and two with locking plates (5.4%; p = 0.003). The authors concluded that fractures of the distal tibia may be treated successfully with locking plates or IM nails, but that delayed union, malunion and secondary procedures were more frequent after IM nailing. Janssen et al. 12 found similar results: delayed union was higher in the IM nail fixation group (25%) than in the locking plate fixation group (16.7%) and rotational malalignment was also higher in the IM nail fixation group (16.7%) than in the locking plate group (0%). However, this was not a randomised controlled trial (RCT) and the results do need to be interpreted with some caution. Randomised prospective assessment are necessary to further clarify these issues and provide information about costs associated with these fractures. 11
Only two prospective RCTs had been published when this trial began. 13,14 In the first,13 64 patients were randomised to either IM nail or plate fixation for the treatment of a closed extra-articular fracture. The time to union was found to be similar for the two groups and there was no difference in terms of Olerud–Molander Ankle Score (OMAS) at 2 years. However, a significant difference was observed in the number of wound complications: one in the IM nail fixation group versus seven in the plate group. This paper concluded that IM nailing is the treatment of choice for this injury. However, the method of randomisation was poorly described and so bias in group assignment may have occurred. The study used traditional (non-locking plates) rather than the newer fixed-angle devices. Furthermore, the study included patients with Tschene classification C2 soft-tissue injuries, which may have influenced the results. The second trial14 randomised 111 patients to either IM nail fixation or ‘locking’ plate fixation. This trial also showed no difference in the time to union but, 1 year after the injury, there was some evidence of improved American Orthopaedic Foot and Ankle Society functional scores in the IM nail fixation group. However, this was a single-centre investigation and > 20% of the patients in the trial were lost to follow-up.
In a meta-analysis, Zelle et al. 15 reviewed 1125 extra-articular fractures of the distal tibia. They reported that non-union, malunion and infection rates were similar for patients undergoing IM nailing and locking plate fixation. It must be noted that none of the studies in the review was a RCT.
Pre-pilot trial
We performed a pilot study involving 24 patients with extra-articular fractures of the distal tibia that were closed or Gustilo and Anderson grade 1. 16 The study was a RCT with clinical assessment, functional outcomes and radiological images performed at baseline and at 6 weeks, and 3, 6 and 12 months post surgery. The study was performed to obtain an estimate of the potential effect size to inform the sample size calculation for a larger definitive trial and to assess recruitment rates and study feasibility.
The study had 12 patients in each group. There was no statistically significant difference between the groups 6 months after the injury but there was a 10-point difference [standard deviation (SD) 20 points] in the Disability Rating Index (DRI)17 in favour of the IM nail group. More secondary procedures were required in the ‘locking’ plate fixation group. There was also a difference in the cost of the implants.
This pilot study, combined with the literature review, provided compelling evidence to support the development of a definitive RCT in multiple centres.
Null hypothesis
There was no difference in the DRI score between adults with a displaced fracture of the distal tibia treated with locking plate fixation versus IM nail fixation.
Objectives
The primary objective was to estimate the difference in the DRI scores between the trial treatment groups at 6 months after injury.
The secondary objectives were to:
-
estimate the difference in early functional status at 3 months and later functional status at 12 months
-
estimate the difference in health-related quality of life between the trial treatment groups in the first year after injury
-
determine the complication rate of IM nail fixation versus locking plate fixation in the first year after injury, including radiological complications – non-union and malunion
-
investigate, using appropriate statistical and economic analytical methods, the resource use, costs and comparative cost-effectiveness of IM nail fixation versus locking plate fixation.
Chapter 2 Methods
Adapted with permission from Achten et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Trial design
We conducted this project as a two-phased study. Phase 1 (internal pilot) determined the expected rate of recruitment in a large-scale multicentre RCT in this complicated area of trauma research. Phase 2 (main phase) was a RCT in 28 acute trauma centres across the UK.
Internal pilot summary
The pilot took place in six centres over a period of 6 months. Screening logs were kept at each site to determine the number of patients assessed for eligibility and reasons for any exclusion. In addition, the number of eligible and recruited patients, and the number of patients who declined consent/withdrew, were recorded.
Main randomised controlled trial summary
All adult patients presenting at the trial centres with an acute fracture of the distal tibia were potentially eligible to take part in the trial. The broad eligibility criteria ensured that the results of the study could readily be generalised to the wider patient population. A computer-generated randomisation sequence, stratified by centre and age, was produced and administered independently by a secure web-based service, Warwick Clinical Trials Unit (WCTU). Randomisation was on a 1 : 1 basis to either IM nail fixation or locking plate fixation. Both of these operations are widely used within the NHS and all of the surgeons in the chosen centres were familiar with both techniques.
Baseline demographic data, radiographs and pre-injury functional data using the DRI and the OMAS questionnaire were collected. The patients were also asked to fill out the EuroQol-5 Dimensions (EQ-5D) health-related quality-of-life questionnaire twice at baseline; once to indicate their typical pre-injury health status and a second time to indicate their current post-injury status.
In conjunction with the clinical team, a research associate performed a clinical assessment and recorded any early complications at 6 weeks, and a radiograph was taken. A further clinical assessment and radiograph was also taken at 12 months postoperatively to detect late complications. Functional outcome, health-related quality of life and resource use questionnaires were collected at 3, 6 and 12 months postoperatively.
Participants
Inclusion criteria
The inclusion criteria for this trial were that the patient:
-
was aged ≥ 16 years
-
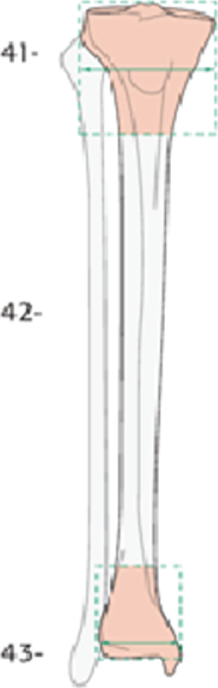
had any fracture that involves the distal tibial metaphysis, which was defined as a fracture extending within 2 Müller squares of the ankle joint18 (a Müller square is shown in Figure 1)
-
had a closed fracture
-
would, in the opinion of the attending surgeon, benefit from internal fixation of the fracture.
FIGURE 1.
Müller square. 18 Reproduced with permission. Copyright by AO Foundation, Biel, Switzerland.
Exclusion criteria
The exclusion criteria for this trial were that:
-
there is, in the opinion of the attending surgeon, a contraindication to IM nailing – the presence of total knee replacement OR the medullary canal is too narrow OR there is a pre-injury deformity of the medullary canal OR it is not possible to achieve fixation of four cortices with screws distal to the fracture
-
the fracture is open
-
there is a contraindication to anaesthesia
-
there is evidence that the patient would be unable to adhere to trial procedures or complete questionnaires
-
the fracture extends into the ankle joint (i.e. intra-articular fracture).
Screening and recruitment
All of the centres involved in the trial were UK NHS acute trauma centres. All of the centres provided definitive surgical fixation of this type of fracture in their hospital as part of routine clinical practice.
The internal pilot informed, and tested, the recruitment rate for the main trial. 16 Recruitment took place in six trial centres over a period of 6 months. The expected rate of recruitment was based on the pre-pilot study performed at the lead centre. The average recruitment rate for the pre-pilot study, during which 24 patients were recruited, was 1.3 patients per month. The other centres involved in the trial were all regional trauma units with similar catchment areas to the lead centre. However, a conservative recruitment rate of 0.75 patient per centre per month (pcpm) was estimated for the full trial based on our previous experience of multicentre trials, in which we found that recruitment outside the lead centre was at a lower rate. Our plan was to progress to the main phase if this recruitment rate could be achieved at the end of the internal pilot. Our intention was to recruit 320 participants, from a minimum of 18 centres in total (including the lead centre), over a 30-month period.
Screening logs were collected throughout the trial to assess the main reasons for patient exclusion as well as the number of patients unwilling to take part. Patients were screened by the research associates in the emergency department and trauma unit at the trial centres. The trial was carried out in accordance with the Mental Capacity Act 200519 and the procedures for undertaking trials in ‘emergency settings’ were followed as described in detail in Consent. The consent procedures were reviewed at the end of the pilot period.
Consent
Patients with a fracture of the distal tibia are admitted to hospital, through the emergency department, to a trauma ward. Patients are in pain and often treated with opiate-based painkillers during the initial treatment of their injury, so mental capacity may be impaired. However, although surgical treatment for a closed fracture of the tibia is urgent, it is not a time-critical intervention. In fact, traditionally, surgeons have deliberately waited a day or more before operating in order to let soft-tissue swelling settle. Once the leg is immobilised in a plaster cast, the pain is much better controlled, so mental capacity usually returns quite quickly following admission to the trauma ward.
During the internal pilot phase of the trial, we monitored the number of patients with impaired capacity and reviewed these data in conjunction with the Trial Steering Committee (TSC). In the context of this injury, by the time the patient was due to have surgery, none of the potentially eligible patients was judged to have reduced capacity according to the clinical team responsible for patient care. Therefore, informed consent from the patient was obtained by the local research associate before surgery. Patients were provided with verbal and written information about the study.
For those patients who withdraw from the trial after written consent had been obtained, data obtained up to the point of withdrawal have been included in the final analysis.
Randomisation
Following informed consent, the method of fixation was allocated using a secure, centralised, web-based randomisation service, delivered by an accredited clinical trials unit (WCTU). The randomisation service was available 24 hours each day to facilitate the inclusion of all eligible patients. The allocated treatment was reported to the research associate, who informed the treating surgeon. The surgeon then arranged the allocated surgery on the next available trauma operating list, as per standard practice at that institution; this ensured the integrity of the randomisation process. Allocation was implemented using a minimisation algorithm (sometimes referred to as adaptive randomisation) that attempts, at recruitment of each new patient, to balance the marginal totals for each level of the stratification factors. Experience indicates that, for studies in which some centres recruit only a relative small number of patients, this method tends to perform better than conventional stratification methods and may provide potential gains in efficiency. 20
Stratification by centre helped to ensure that any clustering effect related to the centre itself was equally distributed in the trial arms. The catchment area (the local population served by the hospital) was similar for all of the hospitals, each hospital being a trauma unit dealing with these fractures on a daily basis. Although it could have been possible that the surgeons at one centre may have been more expert in one or the other treatment than those at another centre, all of the recruiting hospitals were chosen on the basis that both techniques were routinely available at the centre, that is, theatre staff and surgeons were equally familiar with both forms of fixation. This did not eliminate the surgeon-specific effect of an individual at any one centre. 21 However, fixation of a fracture of the tibia is not an uncommon procedure and many surgeons will be involved in the management of this group of patients: between 10 and 30 surgeons at each centre, including consultants and trainees. Therefore, we expected that each individual surgeon would operate on only two or three patients enrolled in the trial – and indeed this was the case – greatly reducing the risk of a surgeon-specific effect on the outcome at any one centre.
Stratification on the basis of age was used to discriminate between younger patients with normal bone quality sustaining high-energy fractures and older patients with low-energy (fragility) fractures related to osteoporosis. The stratification would have helped to identify any effect related to the quality of the patients’ bone. The use of dual-energy X-ray absorptiometry is widely regarded as the gold standard for the assessment of bone density. However, such an investigation may be expensive and would not have been routinely available at all centres.
Therefore, we used age as a surrogate for bone density. In a large study in Norway, involving 7600 participants, it was demonstrated that bone mineral density remains stable up until the age of 50 years. After the age of 50 years, bone mineral density decreased steadily in males, while in females there was an initial decline between the ages of 50 and 65 years, with a further decline in both age groups thereafter. 22 Over 1000 patients with a fracture were recently assessed in a study by Court-Brown et al. 23 This study confirmed that there is a clear bimodal distribution according to the age of the patient. The crossover of the two peaks of incidence was around 50 years of age. These studies provide strong evidence that patients > 50 years of age become increasingly vulnerable to fragility fractures. Therefore, we chose an age of 50 years as the stratification cut-off point for this trial.
Sequence generation
A minimisation algorithm was used to allocate participants, so no random sequences were generated before the study. This is standard practice for trials conducted at WCTU.
Blinding
The type of fixation determines the site of clearly visible surgical scars. Specifically, the insertion of an IM tibial nail requires a surgical incision at the knee. Therefore, the patients could not be blind to their allocated treatment. In addition, the treating surgeons were also not blind to the treatment, but did not take part in the postoperative assessment of the patients. The functional outcome data were collected and entered into the trial central database via questionnaire administered by a research assistant/data clerk in the trial central office. The radiographs collected were reviewed by an independent assessor who was not involved in any other data collection or analysis.
Post-randomisation withdrawals
Participants could decline to continue to take part in the trial at any time and without prejudice. The participants were made aware that a decision to decline consent or withdraw would not affect the standard of care that they would receive.
Participants had two options for withdrawal:
-
Participants could withdraw from completing any further questionnaires but allow the trial team to continue to view and record any relevant hospital data that were recorded as part of normal standard of care, including radiographs and further surgery information.
-
Participants could withdrawal wholly from the study and only data obtained up to the point of withdrawal would be included in the final analysis of the study; thereafter, no further data were collected for that participant.
Once withdrawn, the patient continued under the care of their surgical team, as per normal clinical practice.
Interventions
All the hospitals involved in this trial used both methods of fixation as part of routine clinical care. Consultant orthopaedic trauma surgeons supervised the surgery, all of whom were familiar with both techniques. Operative fixation of fractures of the distal tibia usually takes place under a general anaesthetic, but this decision was made by the attending anaesthetist as per their usual clinical practice.
Each patient had the allocated surgery according to the preferred technique of the operating surgeon. Although the basic principles of IM nailing and locking plate fixation are inherent in the technique (see Intramedullary nail fixation and Locking plate fixation), there are several different implant systems and several different options for the positioning of the screws. Similarly, each surgeon would have made minor modifications to their surgical technique according to preference and the specific pattern of each fracture. In this trial, the details of the surgery were left entirely to the discretion of the surgeon, to ensure that the results of the trial could be generalised to as wide a group of patients as possible. A copy of the ‘operating record’ formed part of the trial data set.
Although all of the surgeons in the trial were familiar with both techniques, it is possible that an individual surgeon may have had more experience with one technique than the other. In general, the proficiency of an individual surgeon to perform the procedure may change over time, as the surgeon gains experience and expertise. The term ‘learning curve’ is often used to describe this process. It was important to be aware of this effect within the trial. Therefore, the operating time was recorded from the operative record for each surgery, as a proxy to measure the task ‘efficiency’ of the surgeons (quality assurance of the clinical process), and the number of complications (e.g. infections) at 6 weeks after surgery was also recorded as a patient-based outcome related to surgeon ‘expertise’. However, as there were a large number of centres and a large number of surgeons at each of these centres, no individual surgeon was expected to perform more than a handful of the procedures. Therefore, the effect of the surgeon and their learning curve would be minimal in this particular trial.
Intramedullary nail fixation
The IM nail is inserted at the proximal end of the tibia and passed down the hollow centre (medullary canal) of the bone in order to hold the fracture in the correct (anatomical) position. The reduction technique, the surgical approach, the type and size of the nail, the configuration of the proximal and distal interlocking screws and any supplementary device or technique were left at the discretion of the surgeon, as per standard clinical practice.
Locking plate fixation
A locking plate is inserted at the distal end of the tibia and passed under the skin onto the surface of the bone. Again, the details of the reduction technique, the surgical approach, the type and position of the plate, the number and configuration of fixed-angle screws and any supplementary device or technique were left to the discretion of the surgeon. The only stipulation was that fixed-angle screws must be used in at least some of the distal screw holes – this is standard practice with all distal tibia locking plates.
Rehabilitation
All patients randomised into the two groups received the same standardised, written physiotherapy advice detailing the exercises they needed to perform for rehabilitation following their injury. All of the patients in both groups were advised to move their toes, ankle and knee joints fully within the limits of their comfort. Weight-bearing status was recommended by the treating surgeon. In this pragmatic trial, any other rehabilitation input beyond the written physiotherapy advice (including a formal referral to physiotherapy) was left to the discretion of the treating clinicians. However, a record of any additional rehabilitation input (type of input and number of additional appointments) together with a record of any other investigations/interventions were requested as part of the 3-month, 6-month and 12-month follow-ups, which formed part of the trial data set.
Outcomes
The primary outcome measure for this study was the DRI. 17 The DRI is a validated questionnaire that is self-reported (i.e. filled out by the patient). 24 It consists of 12 items specifically related to function of the lower limb and provides an overall score from 0 to 100 points, in which 0 points represents no disability and 100 points represents complete disability. These data were collected at baseline, 3, 6 and 12 months postoperatively (Table 1). The DRI has been proven to be a robust and practical clinical and research instrument, with good responsiveness and acceptability for assessment of disability caused by impairment in the lower limb.
| Time point | Data collection |
|---|---|
| Baseline | DRI, OMAS questionnaire, pre-injury and current EQ-5D and radiographs |
| 6 weeks | DRI, OMAS questionnaire, EQ-5D, record of complications or other interventions and resource use questionnaire |
| 3 months | DRI, OMAS questionnaire, EQ-5D, record of complications or other interventions and resource use questionnaire |
| 6 months | DRI, OMAS questionnaire, EQ-5D, record of complications or other interventions and resource use questionnaire |
| 12 months | DRI, OMAS questionnaire, EQ-5D, radiographs, record of complications or other interventions and resource use questionnaire |
Existing guidance for the calculation of DRI scores is unclear as regards the appropriate way to calculate overall scores in the presence of missing items; the most common approach is to take an average of available item scores. Owing to the low number of missing items, all analyses presented used complete cases only, that is, 12 complete item responses out of 12.
The secondary outcome measures in this trial were as follows:
The OMAS questionnaire is a self-administered patient questionnaire designed to assess ankle pain and function. It is a good outcome tool for assessing symptoms after a fracture around the ankle joint. 25 The score is based on nine different items: (1) pain, (2) stiffness, (3) swelling, (4) stair climbing, (5) running, (6) jumping, (7) squatting, (8) supports and (9) work/activities of daily living. 16 The scoring system correlates well with parameters considered to summarise the results after this type of injury and, therefore, is recommended for use in scientific investigations.
The EQ-5D is a validated, generic health-related quality-of-life measure consisting of five questions regarding five dimensions of health. The answers can be converted into a health utility score. 26 It has good test–retest reliability, is simple for patients to use and gives a single preference-based index value for health status that can be used for broader cost-effectiveness comparative purposes.
All complications were recorded, including malunion, non-union, infection, wound complications, vascular and neurological injury and venous thromboembolism. A record was also kept of any other surgery required in relation to the index fracture, including removal of any surgical implant. The adverse events have been broken down into ‘local complications related to the fracture or its treatment’, ‘systemic complications potentially related to the fracture or its treatment’ and ‘unrelated adverse events’ during the 12 months after the injury.
For the radiographic evaluation of complications, standard anteroposterior and lateral radiographs of the tibia and fibula were taken at baseline, at 6 weeks and at 12 months after the injury, as described in Outcomes. The radiographs were viewed using OsiriX software version 7.5 (Pixmeo, Berne, Switzerland). The radiographs were reviewed by an independent trauma surgeon from University Hospitals Coventry & Warwickshire NHS Trust. An assessment was made on the alignment of the tibia in both the coronal (lateral) and sagittal (anteroposterior) views of the tibia, and there was also an assessment of any shortening present.
Threshold values were used to define ‘malunion’ as follows:3
-
coronal angulation of the distal tibia fixation of > 5°
-
sagittal angulation of the distal tibia fixation of > 10°
-
shortening of > 10 mm.
Threshold values have been shown to be more reliable than absolute measurements of deformity in the distal tibia (Thomas Wood, Department of Trauma and Orthopaedics, University Hospitals Coventry and Warwickshire NHS Trust, 2016, unpublished data).
We used techniques common in long-term cohort studies to ensure minimum loss to follow-up, such as collection of multiple contact addresses and telephone numbers, mobile phone numbers and e-mail addresses. Considerable efforts were made, by the trial team, to keep in touch with patients throughout the trial by means of newsletters, and so on.
Follow-up
Baseline, standardised radiographs were copied from the hospital picture archiving and communication system. Copies of the baseline clinical report forms and images were sent to the trial co-ordinating centre.
As part of routine clinical practice, patients were seen in the outpatient fracture clinic on a regular basis after this injury. For this trial, the sample size was based on the primary outcome measure at 6 months, when patients with an uncomplicated fracture may be expected to return to normal activities; but to ensure that all complications and secondary procedures were captured, we continued follow-up for 1 year. 14
The research associate performed a clinical assessment and made a record of any early complications at the 6-week routine follow-up appointment. Radiographs were taken at 6 weeks and 12 months (or before 12 months if the surgeon felt that the fracture was united). An uncomplicated fracture of the distal tibia would be expected to be clinically united at 6 months after the injury. However, radiographic union may lag behind the clinical picture. Therefore, the 12-month radiographs were used to assess if there are long-term complications, such as non-union and arthritis of the ankle joint.
The outcome and resource use data were collected using questionnaires at 3, 6 and 12 months postoperatively. Patients were asked to complete their 6-month and 12-month postoperative questionnaire during their routine follow-up appointments if they had one or to return them by post if they did not have an appointment at these time points. Text messages were sent to patients to inform them that a questionnaire was due or was on its way. Text messages were only sent to those patients who had given their prior consent to this by initialling the corresponding box on the consent form.
Adverse event management
Adverse events are defined as any untoward medical occurrences in a clinical trial participant that do not necessarily have a causal relationship with the treatment.
Serious adverse events (SAEs) are defined as any untoward and unexpected medical occurrence that:
-
results in death
-
is life-threatening
-
requires hospitalisation or prolongation of existing inpatients’ hospitalisation
-
results in persistent or significant disability or incapacity
-
is a congenital anomaly or birth defect
-
is any other important medical condition that, although not included in the above, may require medical or surgical intervention to prevent one of the outcomes listed.
All SAEs were entered onto the SAE reporting form and faxed to a dedicated fax machine at WCTU within 24 hours of the investigator becoming aware of them. Once received, causality and expectedness, as determined by the principal investigator at each centre, were confirmed by the chief investigator. SAEs that were deemed to be unexpected and related to the trial were notified to the Research Ethics Committee (REC) and sponsor within 15 days. All such events were reported to the TSC and Data Monitoring Committee (DMC) at their subsequent meetings.
Serious adverse events that may have been expected as part of the surgical interventions, and that did not need to be reported to the main REC, were complications of anaesthesia or surgery (e.g. wound complications, infection, damage to a nerve or blood vessel and thromboembolic events) and secondary operations for or to prevent infection, malunion or non-union or for symptoms related to the metalwork. All participants experiencing SAEs were followed up until the end of the trial, as described in the protocol.
Risks and benefits
The risks associated with this study were predominantly those associated with the surgery: infection, bleeding and damage to the adjacent structures such as nerves, blood vessels and tendons. Participants in both groups had surgery and were potentially at risk from any/all of these complications. We believed that the overall risk profile was similar for the two interventions, but assessment of the number of complications in each group was a secondary objective of this trial.
Statistical analysis
Sample size
The minimum clinically important difference (MCID) is 8 points on the primary outcome (DRI) measurement scale. The DRI is a 12-question, patient-reported, functional outcome measure (physical exercise or sports, running, heavy physical work, heavy lifting, carrying a bag, leaning over a wash-stand, making a bed, moderate physical work, walks, mounting stairs, sitting still more than briefly and dressing or undressing) converted to a 100-point scale in which 0 points represents normal function and 100 points represents complete disability. At an individual patient level, a difference of 8 points represents the ability to climb stairs or run, with ‘some difficulty’ versus with ‘great difficulty’. At a population level, 8 points represents the difference between a ‘healthy patient’ and a ‘patient with a minor disability’. In addition, 8 points corresponds approximately to the clinically worthwhile benefit identified in other studies24 and is slightly lower than the 10-point difference between treatment group means in our pre-pilot study.
The SD of DRI score in our pilot study was approximately 20 points; the sample size was also estimated for a larger and smaller SDs to obtain an indication of the sensitivity to changes in this parameter. Assuming the distribution of DRI score in the study populations to be approximately normal, which is consistent with assumptions made for other reported trials using DRI as the primary outcome measure, Table 2 shows the total trial sample size with two-sided significance set at 5% for various scenarios of power and sample SD.
| SD (points) | Power, sample size (n) | |
|---|---|---|
| 80% | 90% | |
| 15 | 112 | 150 |
| 20 | 198 | 264 |
| 25 | 308 | 412 |
In Table 2, the number of 264 patients, represented in bold, represented the most likely scenario, based on our current knowledge, for 90% power to detect the selected MCID. Allowing a margin of 20% loss during follow-up, this gives a value of 320 patients in total. Therefore, 160 patients randomised to each group would provide 90% power to detect a difference of 8 points in the DRI score at 6 months, with 90% power at the 5% significance level.
Standard statistical summaries (e.g. medians and ranges or means and variances, dependent on the assumed distribution of the outcome) and graphical plots are presented for the primary outcome measure and all secondary outcome measures. Baseline data are summarised to check comparability between treatment arms and to highlight any characteristic differences between those individuals in the study, those who were ineligible and those who were eligible but withheld consent.
Analysis plan
The detailed statistical analysis plan was created by the trial statisticians and agreed by the DMC at the start of the study, in line with standard operating procedures at WCTU. Any subsequent amendments to this initial statistical analysis plan were clearly stated and justified to the DMC.
Software
All routine data reporting and final analysis was conducted using Stata® version 14 (StataCorp LP, College Station, TX, USA). 27
Data validation
Prior to formal analysis, data were checked for outliers, missing values and validated using the defined score ranges for all outcome measures. Queries were reported to the trial co-ordinator and investigated with the relevant recruiting centre if appropriate. Any subsequent changes to the database were recorded in accordance with the relevant WCTU standard operating practice and the UK Fixation of Distal Tibia Fractures (FixDT) trial data management plan.
Missing data
Data may not be available as a result of withdrawal of patients, lack of completion of individual data items or loss to follow-up. Reasons for data ‘missingness’ were ascertained and reported as far as possible. Any patterns of missingness were carefully considered, including, in particular, whether or not data could be treated as missing completely at random. No formal statistical testing was planned to assess missingness, but model assumptions were checked and patterns of missingness explored. If judged appropriate, missing data in the primary outcome (DRI score) was imputed using the ice (imputation by chain equation) procedure in Stata version 14. Any imputed data were on an individual-item level, as opposed to an overall score level. Reasons for ineligibility, non-compliance, withdrawal or other protocol violations are stated and any patterns are summarised.
Interim analyses
There were no planned interim analyses for the UK FixDT study.
Final statistical analyses
Null hypothesis
The null hypothesis for the UK FixDT study was that there is no difference in the DRI score between adult patients with a fracture of the distal tibia treated with IM nail fixation versus locking plate fixation.
Multilevel model
The main analysis plan was to investigate differences in the primary outcome measure, the DRI score at 6 months after surgery, between the two treatment groups on an intention-to-treat basis. In addition, early functional status was also assessed and reported at 3 months and later functional status at 12 months. The unadjusted differences between treatment groups were assessed using a Student t-test, based on a normal approximation for the DRI score at 6 months, and at other occasions. Tests were two-sided and considered to provide evidence for a significant difference if p-values are < 0.05 (5% significance level). Estimates of treatment effects are presented with 95% confidence intervals (CIs).
In addition to the unadjusted analysis (t-tests), we planned to undertake regression analyses to adjust for any imbalance between test treatments groups in patient age group, baseline pre-injury score and sex. The fixed-effects analysis (linear regression model) was also generalised by adding a random effect for recruiting centre to allow for possible heterogeneity in patient outcomes because of, more generally, the recruiting centre. Outcome data were assumed to be normally distributed during modelling, but subsidiary analyses were also undertaken after appropriate variance-stabilising transformations. The primary focus was the comparison of the two treatment groups of patients and this was reflected in the analysis, which was conducted together with appropriate diagnostic plots to check the underlying model assumptions. Treatment effects are presented for both the unadjusted and adjusted analyses, with 95% CIs as appropriate.
Any interactions between age group or sex and the main treatment effect were not expected to be considerable, and the sample size calculations were not conducted with these potential analyses in mind. Analyses were, however, undertaken for each of these variables. Formal interaction tests were conducted and reported with appropriate 95% CIs.
Complications
The number of events were compared between treatment groups on an intention-to-treat basis, in line with the main outcome analyses. Complications profiles are presented in three sections: (1) local complications related to the fracture or its treatment, (2) systemic complications potentially related to the fracture or its treatment and (3) unrelated adverse events within the 12-month time frame of the trial. These include information from the 6-week follow-up appointment with the research associate, in conjunction with data from patient-reported questionnaires at 3, 6 and 12 months post randomisation, and any other reports of SAEs. The data were cross-referenced between multiple data sources and clinical judgement was used to classify events in to the presented categories.
Exploratory analysis
To complement the preplanned analysis, a post hoc exploratory analysis using DRI score at all four time points was conducted. This analysis simplified longitudinal data collected at four time points to a single value, namely the area under the curve (AUC), and facilitated comparisons of the AUCs between treatment groups. It is advisable, in the presence of missing data, to use summary statistics generated by mixed models, as estimates will not be biased under the assumption that data are missing at random or are missing completely at random. 28 Therefore, we fitted a repeated measures mixed model, with the same fixed-effect structure as used in the primary analyses (adjusted for sex and age group), but with a three-level random-effects structure, in which observations (time points) were nested within participants and participants nested within recruitment site. The mixed and margins commands in Stata version 14 were used to obtain parameter estimates and standard errors (SEs) and the lincom command used to calculate AUC for each group. 27 AUCs associated with the two treatment groups were tested using a t-test.
Health economic analysis plan
The following sections summarise the health economics analysis plan, with full details provided in Chapter 4.
Objectives
The economic evaluation was designed to estimate the costs of resource inputs and quality-adjusted life-year (QALY) profiles of each trial participant over the 12-month time horizon of the trial, allowing mean differences in costs and QALYs to be compared between the two arms of the trial. The primary objective was to evaluate the incremental cost-effectiveness of extra-articular distal tibia fractures treated with IM nail fixation versus locking plate fixation and to provide an estimate of the incremental net benefit.
Measurement of outcomes
Health-related quality of life was estimated using responses from the EQ-5D. This instrument facilitates the generation of a utility score from a person’s health-related quality of life. A health utility score refers to the preference that individuals have for any particular set of health outcomes. Patients completed the EQ-5D questionnaire at baseline and at 3, 6 and 12 months after randomisation, thus providing values of their health status at the time of questionnaire completion. Patients self-completed an additional EQ-5D at baseline, which assessed their pre-injury health-related quality of life. The standard UK (York A1) tariff values were applied to these responses at each time point to obtain utility scores. 29 The York A1 tariff set was derived from a survey of the UK general population (n = 3337), which used the time trade-off valuation method to estimate utility scores for a subset of 45 EQ-5D health states, with the remainder of the EQ-5D health states subsequently valued through the estimation of a multivariate model. 29 Resulting utility scores ranged from –0.59 to 1.0, with 0 representing death and 1.0 representing full health; values below 0 indicate health states worse than death. The second measurement component of the EQ-5D consists of a 20-cm vertical visual analogue scale (VAS) ranging from 100 (best imaginable health state) to 0 (worst imaginable health state), which provides an indication of the participant’s own assessment of their health status on the day of the survey. QALYs, which formed the main outcome of the economic analysis, were calculated using the AUC approach, assuming liner interpolation between the utility measurements. A five-level version of the EQ-5D (EuroQol-5 Dimensions, five-level version; EQ-5D-5L) was newly available at the start of the trial, but a UK tariff set for this version of the measure had not yet been published. Consequently, on advice from the TSC, it was decided to measure health-related quality-of-life outcomes using the EQ-5D.
Measurement of costs
Total costs for the two intervention arms were estimated by combining (1) resources used during the operation (implants and consumables), (2) total costs for the inpatient hospital stay and (3) patient-reported data on resource usage at 3, 6 and 12 months post randomisation. For the 3-month data, the recall period covered the period following hospital discharge; however, the recall period at subsequent time points covered the period since the last questionnaire was due to be completed. The trial participant questionnaires provided information on broader NHS and Personal Social Services (PSS) resource use as a result of the fracture. Specifically, the questionnaires captured the frequency of use of community-based health and social care services, number and duration of admissions to inpatient wards [classified as orthopaedics (your leg), orthopaedics (any bones), rehabilitation unit], number of diagnostic tests, use of outpatient services (classified as orthopaedics, physiotherapy, emergency department), medication use, and use of aids and adaptations. PSS included number of weeks of frozen/hot Meals on Wheels, laundry services and number of visits of carers and social workers. Total costs of resource usage were estimated by combining the unit cost data for each service with the resource usage data. In addition, the questionnaires captured private costs incurred by the patient as a result of the fracture, such as private physiotherapy. Productivity losses and lost income were also captured.
Cost-effectiveness analytical methods
An incremental cost-effectiveness analysis was performed, expressed in terms of incremental cost per QALY gained. Multiple imputation methods were used to impute missing data and avoid biases associated with complete-case analysis. The results of the economic evaluation were expressed in terms of incremental cost per QALY gained. A series of sensitivity analyses was undertaken to explore the implications of uncertainty on the incremental cost-effectiveness ratios (ICERs). Heterogeneity of cost-effectiveness results was addressed through the use of subgroup analysis. Further details are provided in Chapter 4.
Reporting
The reporting of the health economic evaluation is consistent with the Consolidated Health Economic Evaluation Reporting Standard statement. 30
Ethics approval and monitoring
Standard NHS cover for negligent harm was in place. There was no cover for non-negligent harm.
Ethics committee approval
The UK FixDT trial was approved by the Coventry and Warwickshire REC on 6 November 2012 (REC reference number 12/WM/0340) and by the research and development department of each participating centre. The final, approved, study protocol has been published. 1
Trial Management Group
The day-to-day management of the trial was the responsibility of the trial co-ordinator, who was based at WCTU and supported by the administrative staff. This management was overseen by the Trial Management Group (TMG), which met monthly to assess progress. It was also the responsibility of the trial co-ordinator to undertake training of the research associates at each of the trial centres. The trial statistician and health economist were closely involved in the setting up of data-capture systems and the design of databases and clinical reporting forms.
Trial Steering Committee
A TSC was responsible for monitoring and supervising the progress of the UK FixDT trial. The TSC consisted of independent experts, a lay member and the chief investigator on behalf of the TMG. Membership of the TSC is given in Acknowledgements.
Data Monitoring Committee
The DMC was independent of the trial and was tasked with monitoring ethics, safety and data integrity. The trial statistician provided the data and analyses requested by the DMC at each of the meetings. Membership of the DMC is given in Acknowledgements.
Patient and public involvement
Before the pilot study that led to the UK FixDT trial, an informal survey was conducted at a large university hospital trust to establish the opinion of patients and their carers with regard to research in orthopaedic trauma. We established that patients place great importance on research comparing different types of interventions in the area of trauma surgery. Furthermore, patients have demonstrated that they are willing to take part in such trials.
The opinions of patients regarding the interventions and the trial procedures were reviewed during the pilot study16 and informed the design of the UK FixDT trial and, specifically, the patient-facing materials.
Independent lay representation was present on the TSC. Members of the trauma patient and public involvement group also reviewed the progress of the UK FixDT trial at the annual National Institute for Health Research (NIHR) trauma trials meetings.
Chapter 3 Results
Screening and recruitment
Screening
Screening for potential participants began in April 2013. In total, 2118 patients with a tibial fracture were screened over 36 months. Screening data are presented to help assess the generalisability of the results to the overall population. Screening data are presented for all sites, with the exception of the Edinburgh site, which was closed to recruitment early in the main phase of the study.
There were significant differences in the total number of potential participants who were assessed between recruiting sites because of the varying practice at each site; for example, some sites screened children aged < 16 years but other sites were adult-only trauma centres. The wide variation in totals by centre indicates that some sites screened extensively and recorded any patient with a fracture involving the tibia; however, others appear to have only recorded fractures of the distal tibia on the screening logs.
The reasons why screened patients were not eligible (n = 1581) are detailed in Table 27, Appendix 1.
The most common reasons for participant ineligibility were that the fracture did not extend to within 2 Müller squares of the ankle joint (375/1581; 24%), the fracture was open (369/1581; 23%) and the fracture extended into the ankle joint (329/1581; 21%).
The total number of potentially eligible patients for the study was 537. The reasons why potentially eligible patients were not randomised (n = 216) are given in Table 28, Appendix 1.
Of the 537 eligible potential participants identified on screening logs, 40% (216/537) were not randomised. The conversion rate of eligible potential participants to randomised participants was therefore 60%. The most common reasons for non-participation were that there were no research staff available to consent the patient (n = 53; 25%) or that the surgeon had a preference to use an IM nail (n = 54; 25%). The other common reason was that the patient did not want to be part of a research study (n = 25; 12%). There were 18 potential participants for whom the reason for non-participation was ‘other’; these reasons included skin around ankle precluded plate fixation (n = 4), primary amputation (n = 3) and hind foot nail used (n = 2). The complete table of reasons why eligible potential participants were not randomised, by site, is given in Table 28, Appendix 1.
Data on sex and age were available for almost all of the patients screened (2003/2118; 95%). The largest subgroup of screened patients were men aged < 50 years, who accounted for 41% (819/2003) of the screened population.
Table 3 shows the age and sex of potentially eligible participants by randomised status (randomised or not randomised). The ages of both groups were similar and a t-test comparing the means of both groups showed no evidence of a difference in age (mean difference –0.9 years, 95% CI –4.1 to 2.3 years). Likewise, a two-sample test of proportions showed no evidence of a difference in sex distribution between the two groups (p = 0.818).
| Characteristics | Randomisation status | |
|---|---|---|
| Randomised | Not randomised | |
| Age (years) | ||
| n | 321 | 216 |
| Mean (SD) | 45.1 (16.3) | 46.0 (18.5) |
| Median (IQR) | 43.4 (31.6–57.5) | 44.8 (30.2–57.5) |
| Sex, n (%) | ||
| Female | 124 (39) | 80 (37) |
| Male | 197 (61) | 130 (60) |
| Missing | 0 (0) | 6 (3) |
Recruitment
The trial planned to recruit 320 participants in total. Formal recruitment began in April 2013, with the first participant being randomised on 22 April 2013 at the lead site, University Hospitals Coventry and Warwickshire NHS Trust. Recruitment was undertaken at 28 sites over 36 months, with the final participant being randomised on 3 May 2016. For reporting purposes, the final participant has been included in the April 2016 recruitment month for ease of presentation. Details of site names and their opening dates are listed in Table 4.
| Number | Full name | Opening date |
|---|---|---|
| 1 | University Hospitals Coventry & Warwickshire | 8 April 2013 |
| 2 | Addenbrookes Hospital | 2 May 2013 |
| 3 | Frenchay Hospital | 12 June 2013 |
| 4 | University Hospitals of Leicester | 16 July 2013 |
| 5 | Nottingham University Hospitals | 25 July 2013 |
| 6 | James Cook Hospital | 5 September 2013 |
| 7 | John Radcliffe Hospital | 20 December 2013 |
| 8 | Aberdeen Royal Infirmary | 14 January 2014 |
| 9 | Derriford Hospital | 15 January 2014 |
| 10 | Royal Stoke University Hospital | 31 January 2014 |
| 11 | Royal Sussex County Hospital | 30 January 2014 |
| 12 | Royal Infirmary of Edinburgh | 16 January 2014 |
| 13 | Royal Victoria Infirmary | 6 February 2014 |
| 14 | Glasgow Royal Infirmary | 11 March 2014 |
| 15 | Royal Berkshire Hospital | 8 May 2014 |
| 16 | Poole Hospital | 13 May 2014 |
| 17 | Queen Alexandra Hospital | 29 May 2014 |
| 18 | King’s College Hospital | 10 June 2014 |
| 19 | Aintree University Hospital | 15 July 2014 |
| 20 | Southampton General Hospital | 4 August 2014 |
| 21 | University Hospitals of Birmingham | 5 August 2014 |
| 22 | Leeds Teaching Hospital | 12 August 2014 |
| 23 | St George’s Hospital | 11 September 2014 |
| 24 | Hull Royal Infirmary | 13 October 2014 |
| 25 | North Tyneside General Hospital & Wansbeck General | 20 November 2014 |
| 26 | Heartlands Hospital | 3 February 2015 |
| 27 | Sunderland Royal Hospital | 26 February 2015 |
| 28 | Basingstoke & North Hampshire Hospital | 10 June 2015 |
The pilot phase was completed at the end of November 2013, with six sites open to recruitment. The planned recruitment rate was 0.75 participants pcpm. The recruitment rate averaged 0.6 participants pcpm during this phase, so the TSC recommended that the number of sites was increased from 18 to at least 24 to enable the trial to meet the target recruitment of 320 participants within the 30-month recruitment window. This resulted in a revised target of 0.6 participants pcpm.
Actual recruitment rates, by site, are shown in Table 29, Appendix 1. The overall observed recruitment rate for the main phase of the trial was 0.47 participants pcpm. This was somewhat lower than the revised target and so the number of trial sites was further increased to 28. One site was closed after just one patient was recruited, and screening data are not presented for this site.
Figure 2 illustrates the progression of recruitment over time, towards the required sample size target of 320. Recruitment slowed towards the end of the planned recruitment phase, so the recruitment window was extended, although this was still within the original timeline of the trial. Figure 3 shows the Consolidated Standards of Reporting Trials (CONSORT) flow diagram for the UK FixDT trial.
FIGURE 2.
Overall recruitment progression and target recruitment during the main phase (January 2014–April 2016) of the UK FixDT trial.
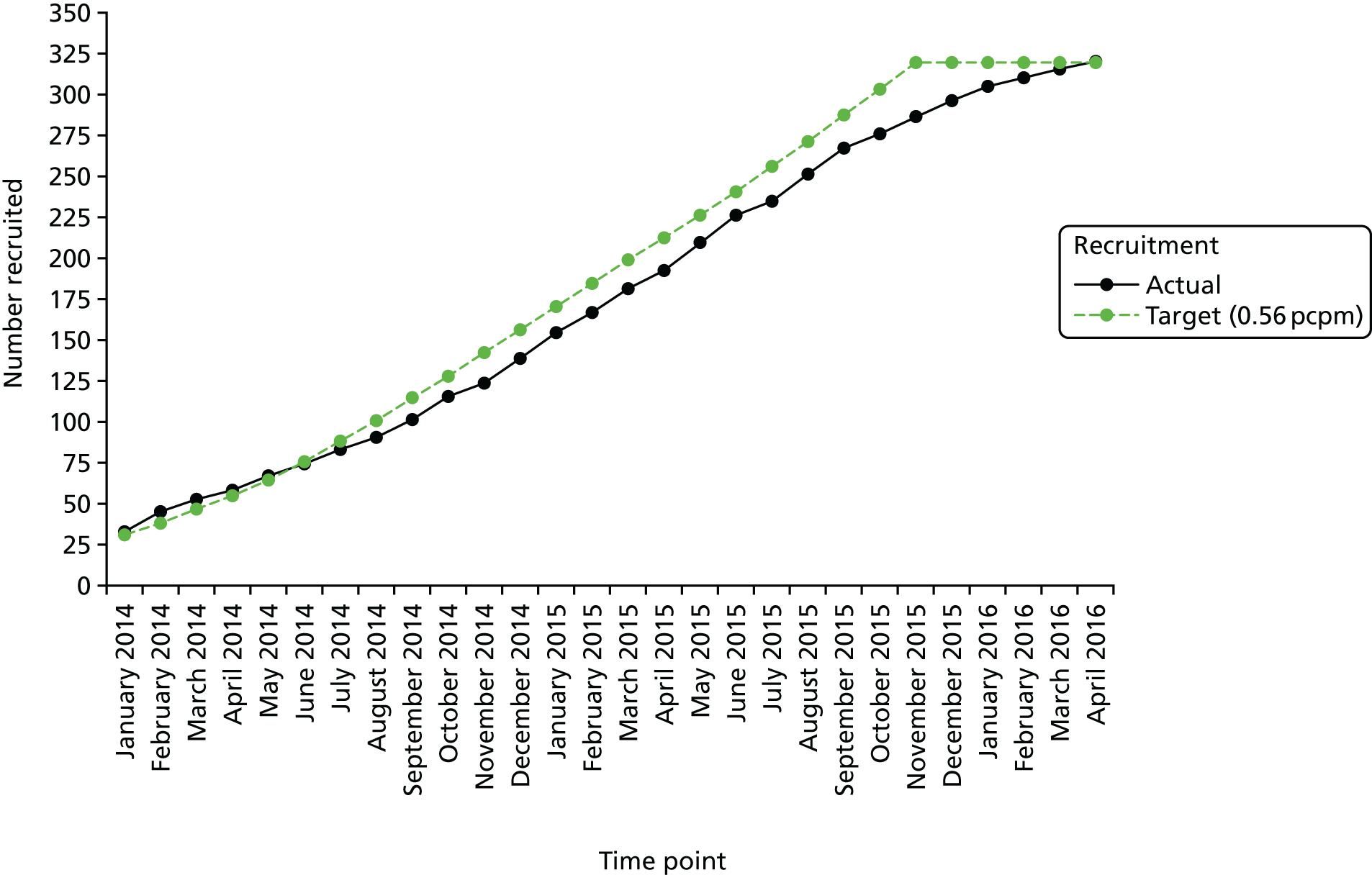
FIGURE 3.
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram.
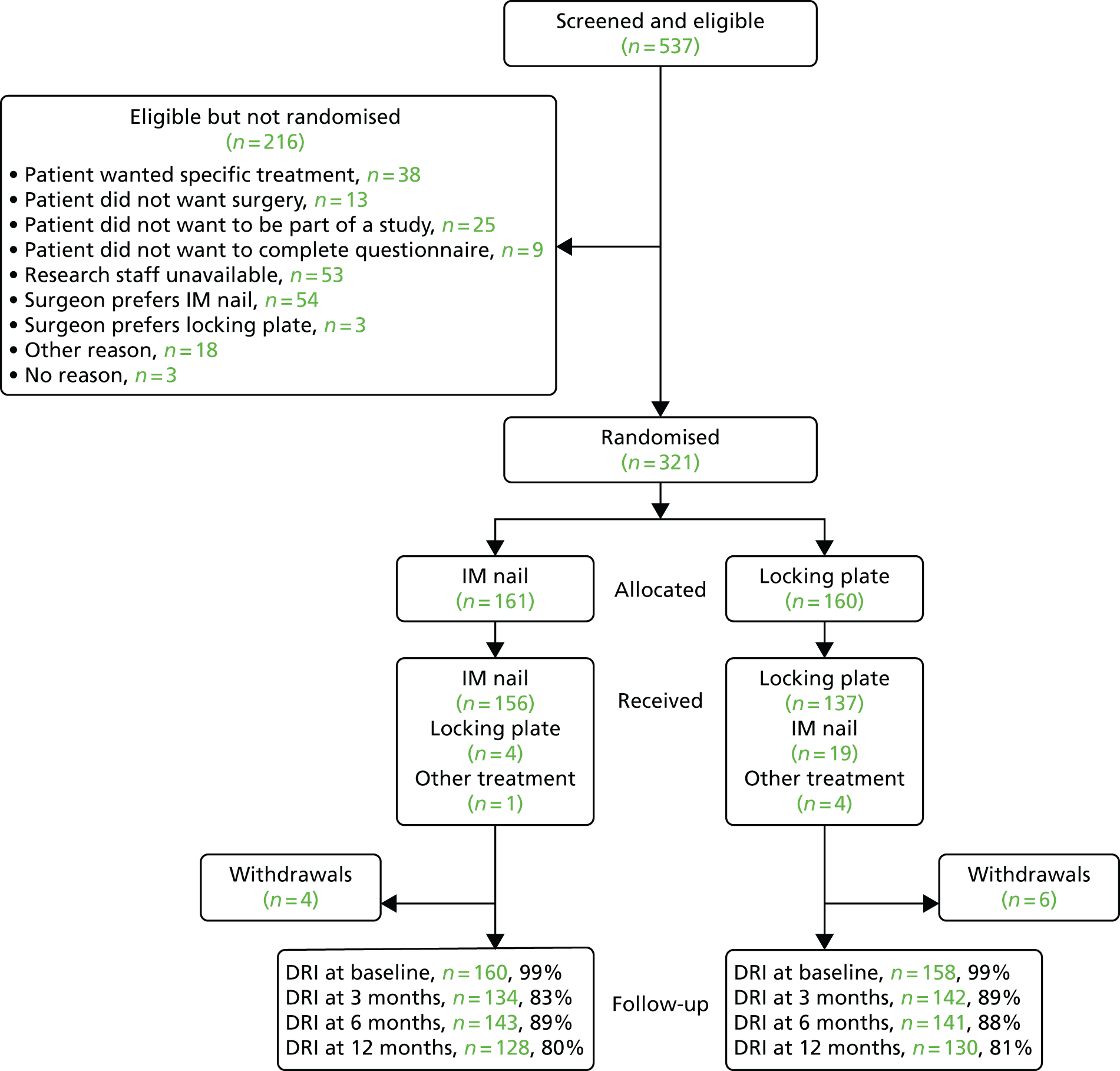
Table 5 describes the follow-up rates achieved during the trial. The expected follow-up rate used for sample size adjustment at 6 months was 80%. This was surpassed at the 6-month time point, with 88% of DRI assessments completed. Similar completion rates of 86% and 80% were achieved at the 3- and 12-month time points, respectively.
| Follow-up status | Time point, n (%) | |||
|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | |
| Returned questionnaire | 318 (99) | 276 (86) | 284 (88) | 258 (80) |
| Missed questionnaire | 3 (1) | 41 (13) | 29 (9) | 49 (15) |
| Consent withdrawn before time point | 0 (0) | 3 (1) | 6 (2) | 8 (3) |
| Died before time point | 0 (0) | 1 (< 1) | 2 (1) | 6 (2) |
Tables 30 and 31, Appendix 1 demonstrate recruitment by stratification variables, namely age group and centre. There is good balance with respect to each factor, indicating that the minimisation procedure used to allocate treatment was implemented successfully.
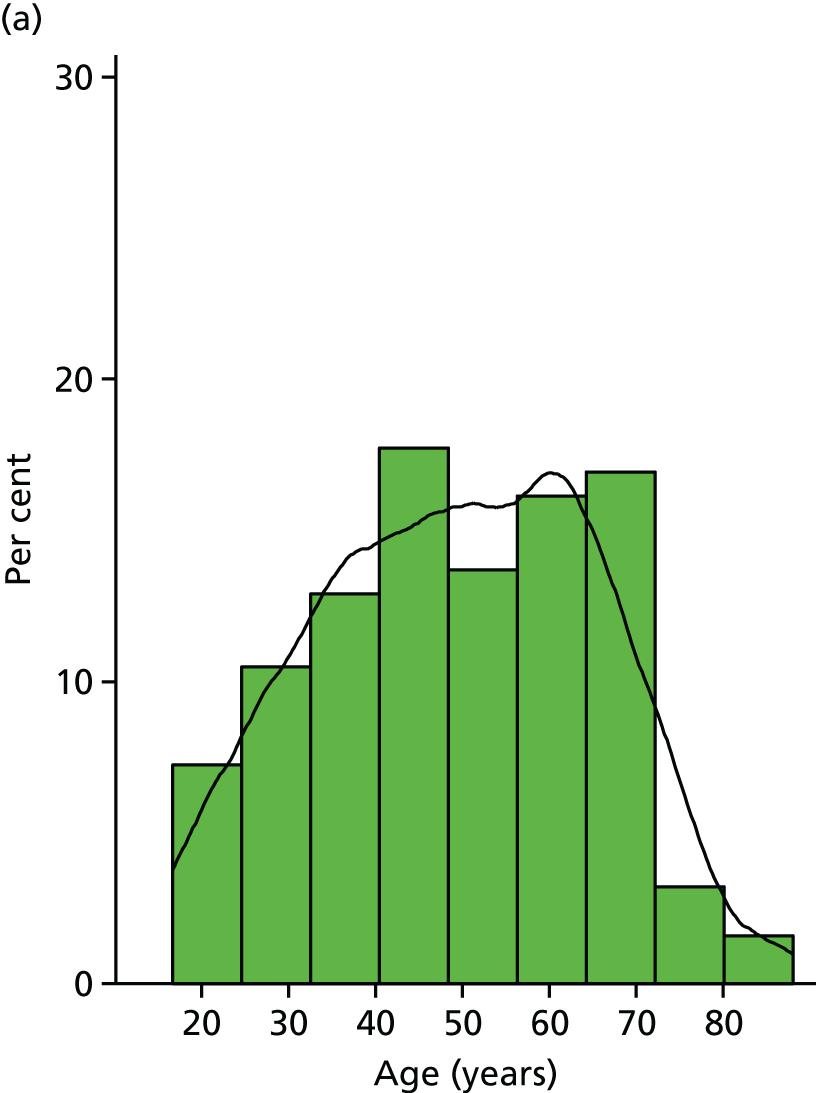
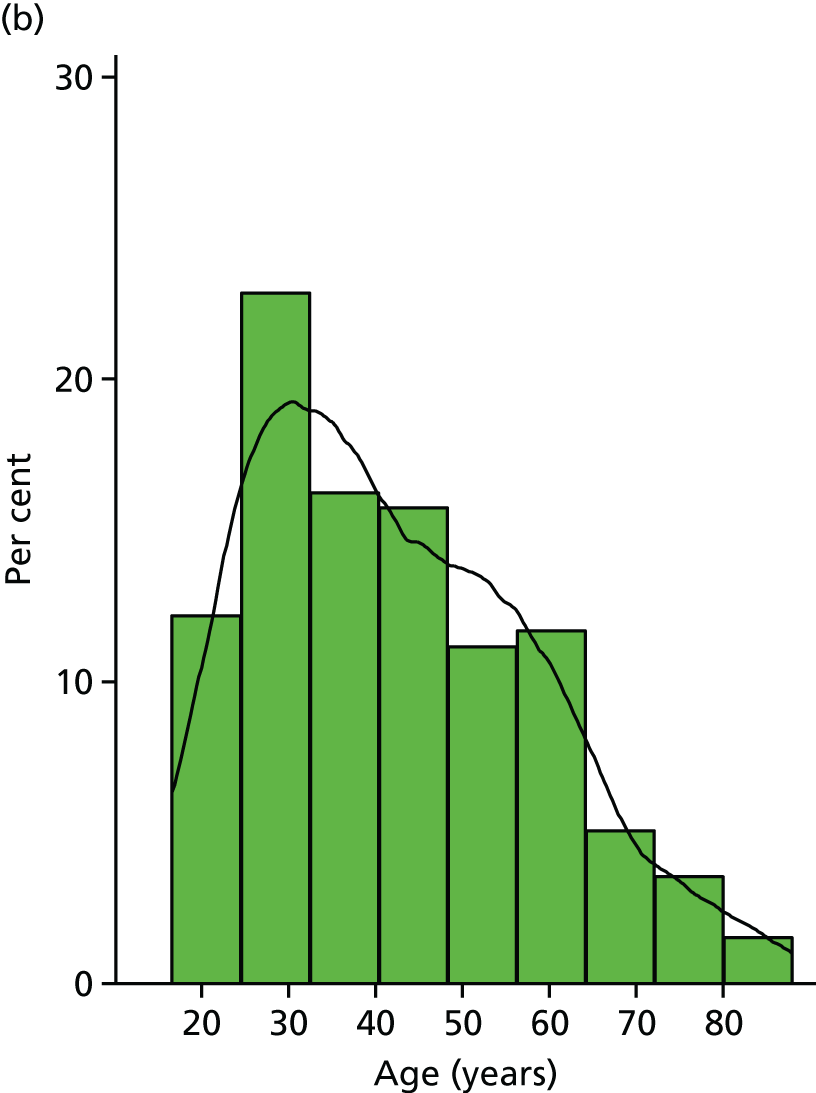
The histograms in Figure 4 show the distribution of age in years, separately by sex. The overlaid kernel density estimator (the kdensity option of the histogram function in Stata version 14) shows the smoothed distribution and highlights the differences between sexes, with a noticeable but expected peak in the number of young male patients randomised. The mean difference in age between men and women was 6.8 years, 95% CI 3.2 to 10.4 years.
FIGURE 4.
Age distribution of randomised participants by sex. (a) Female; and (b) male.
Participant characteristics
The baseline demographic and clinical data were collected directly from the participant at site as part of the baseline participant’s questionnaire. The baseline demographic and clinical characteristics of both treatment groups are well balanced, as shown by allocated treatment group in Table 6. Baseline patient-reported outcome measures also showed good balance with similar mean scores being seen across all four outcomes measures, as expected.
| Demographic and clinical characteristic | Treatment groupa | |
|---|---|---|
| IM nail fixation (N = 161) | Locking plate (N = 160) | |
| Age (years) | ||
| Mean (SD) | 44.3 (16.3) | 45.8 (16.3) |
| Median (IQR) | 41.3 (30–57) | 45.6 (32–58) |
| Sex, n (%) | ||
| Female | 65 (40) | 59 (37) |
| Male | 96 (60) | 101 (63) |
| Side of fracture, n (%) | ||
| Left | 67 (42) | 75 (47) |
| Right | 93 (58) | 84 (53) |
| Missing | 1 (1) | 1 (1) |
| Previous problems on the injured side, n (%) | ||
| Yes | 40 (25) | 36 (23) |
| No | 120 (74) | 123 (77) |
| Mechanism of injury, n (%) | ||
| Low-energy fall | 85 (53) | 87 (54) |
| High-energy fall | 27 (17) | 24 (15) |
| Road traffic accident | 15 (9) | 22 (14) |
| Crush injury | 8 (5) | 3 (2) |
| Contact sports injury | 14 (9) | 11 (7) |
| Other | 11 (7) | 12 (8) |
| Body mass index (kg/m2) | ||
| Mean (SD) | 27.7 (6.2) | 27.7 (6.9) |
| Median (IQR) | 26.5 (23–31) | 26.7 (23–30) |
| Current smoking status | ||
| Yes, n (%) | 53 (33) | 50 (31) |
| No, n (%) | 107 (66) | 108 (68) |
| If yes, for how many years smoking | ||
| n | 48 | 40 |
| Mean (SD) | 19 (12) | 26 (14) |
| Median (IQR) | 18 (10–28) | 28 (15–37) |
| Alcohol consumption (units per week), n (%) | ||
| 0–7 | 86 (53) | 87 (54) |
| 8–14 | 28 (17) | 24 (15) |
| 15–21 | 28 (17) | 22 (14) |
| > 21 | 18 (11) | 22 (14) |
| Diabetes, n (%) | ||
| Yes | 6 (4) | 7 (4) |
| No | 154 (95) | 152 (95) |
| DRI (pre-injury) | ||
| Mean (SD) | 9.9 (19.0) | 10.0 (18.4) |
| Median (IQR) | 1.1 (0–10.6) | 1.6 (0–11.5) |
| OMAS (pre-injury) | ||
| Mean (SD) | 91.4 (19.0) | 94.2 (14.0) |
| Median (IQR) | 100 (95–100) | 100 (95–100) |
| EQ-5D index score (pre-injury) | ||
| Mean (SD) | 0.860 (0.23) | 0.888 (0.21) |
| Median (IQR) | 1 (0.80–1.00) | 1 (0.85–1.00) |
| EQ-5D VAS score (pre-injury) | ||
| Mean (SD) | 81.5 (17.7) | 80.9 (17.5) |
| Median (IQR) | 85 (70–95) | 90 (74–90) |
At the baseline assessment, participants were also asked whether or not they had a strong treatment preference and, if so, for which treatment: 70% (222/321) had no preference; 16% (52/321) preferred IM nail fixation and 13% (43/321) locking plate fixation, with 1% (4/321) of participants not giving a response.
Interventions
Table 7 provides information on the surgical procedures performed. Table 8 provides further detail specific to those participants who received an IM nail or locking plate, respectively. Unless otherwise stated, all further analyses and tables in the remainder of the report will be described on an intention-to-treat basis.
| Operation details | Treatment groupa | |
|---|---|---|
| IM nail fixation (N = 161) | Locking plate (N = 160) | |
| Intraoperative problems, n (%) | ||
| Yes | 3 (2) | 3 (2) |
| No | 157 (98) | 156 (98) |
| Missing | 1 (1) | 1 (1) |
| If yes, what was the problem? (n) | ||
| Nerve injury | 0 | 0 |
| Vascular injury | 0 | 1 |
| Tendon injury | 0 | 0 |
| Extension of fracture | 3 | 2 |
| Intra-articular extension of the fracture, n (%) | ||
| Yes | 7 (4) | 3 (2) |
| No | 127 (79) | 128 (80) |
| Missing | 27 (17) | 29 (18) |
| Fixation of the fibula, n (%) | ||
| Yes | 10 (6) | 12 (8) |
| No | 150 (93) | 146 (91) |
| Missing | 1 (1) | 2 (1) |
| Any other surgery for additional injuries, n (%) | ||
| Yes | 8 (5) | 3 (2) |
| No | 152 (94) | 156 (97) |
| Missing | 1 (1) | 1 (1) |
| Lead surgeon grade, n (%) | ||
| Consultant | 90 (56) | 99 (62) |
| Staff grade/associate specialist | 13 (8) | 15 (9) |
| Specialist trainee | 50 (31) | 41 (26) |
| Other | 7 (4) | 4 (3) |
| Missing | 1 (1) | 1 (1) |
| Total number of surgeons present in theatre | ||
| Mean | 2.5 | 2.4 |
| n | 159 | 159 |
| Median | 2 | 2 |
| Missing | 2 | 1 |
| Operation total duration (minutes) | ||
| n | 158 | 158 |
| Mean (SD) | 124 (43) | 124 (44) |
| Median (IQR) | 120 (90–145) | 120 (96–151) |
| Treatment-specific operation detail | n (%) |
|---|---|
| IM nail fixation (n = 174) | |
| Number of bolts used in coronal plane | |
| 0 | 16 (9) |
| 1 | 50 (29) |
| 2 | 108 (62) |
| Missing | 0 (0) |
| Number of bolts used in sagittal plane | |
| 0 | 67 (39) |
| 1 | 82 (47) |
| 2 | 25 (14) |
| Missing | 0 (0) |
| Number of bolts used in oblique plane | |
| 0 | 144 (83) |
| 1 | 27 (16) |
| 2 | 2 (1) |
| Missing | 1 (1) |
| Number of blocking screws used | |
| 0 | 138 (79) |
| 1 | 31 (18) |
| 2 | 3 (2) |
| 3 | 2 (1) |
| 4 | 0 (0) |
| Missing | 0 (0) |
| Reduction technique used | |
| Open | 12 (7) |
| Closed | 106 (61) |
| Skeletal traction | 20 (11) |
| No traction | 34 (20) |
| Missing | 2 (1) |
| Surgical approach used | |
| Medial parapatella | 69 (40) |
| Lateral parapatella | 0 (0) |
| Tendon splitting | 102 (58) |
| Suprapatella approach | 2 (1) |
| Missing | 1 (1) |
| Locking plate (n = 142) | |
| Number of locking screws used distal to fracture | |
| 1 | 0 (0) |
| 2 | 8 (6) |
| 3 | 24 (17) |
| 4 | 53 (37) |
| 5 | 36 (25) |
| 6 | 16 (11) |
| > 6 | 4 (3) |
| Missing | 1 (1) |
| Number of locking screws used proximal to fracture | |
| 0 | 36 (25) |
| 1 | 4 (3) |
| 2 | 16 (11) |
| 3 | 46 (32) |
| 4 | 33 (23) |
| 5 | 7 (5) |
| > 5 | 0 (0) |
| Missing | 0 (0) |
| Number of non-locking screws used distal to fracture | |
| 1 | 60 (42) |
| 2 | 50 (35) |
| 3 | 21 (15) |
| 4 | 6 (4) |
| 5 | 2 (1) |
| 6 | 2 (1) |
| > 6 | 1 (1) |
| Missing | 0 (0) |
| Number of non-locking screws used proximal to fracture | |
| 0 | 43 (30) |
| 1 | 38 (27) |
| 2 | 17 (12) |
| 3 | 19 (13) |
| 4 | 21 (15) |
| 5 | 4 (3) |
| > 5 | 0 (0) |
| Missing | 0 (0) |
| Reduction technique used | |
| Open | 73 (51) |
| Closed | 53 (37) |
| Skeletal traction | 11 (8) |
| No traction | 5 (4) |
| Missing | 0 (0) |
| Surgical approach used | |
| Longitudinal over medial malleolus | 93 (65) |
| Other | 49 (35) |
| Missing | 0 (0) |
It was of note that the mean duration of the operations was the same for both treatment groups.
Treatment allocation
A total of 91% (293/321) of participants received their allocated treatment (Table 9). Among those participants allocated to the IM nail fixation group, 97% of whom received their allocated treatment and in those allocated to the locking plate group, 86% of whom received their allocated treatment. There were two participant withdrawals before any intervention was undertaken, two were treated with external fixation only and one was treated with manipulation under anaesthetic only.
| Received | Allocated (n) | ||
|---|---|---|---|
| IM nail fixation | Locking plate | Total | |
| IM nail fixation | 156 | 19 | 175 |
| Locking plate | 4 | 137 | 141 |
| Other | 1 | 4 | 5 |
| Total | 161 | 160 | 321 |
In total, there were 28 participants who received a treatment that was not their allocated treatment; more participants deviated from their allocated treatment in the locking plate group (n = 23) than in the IM nail fixation group (n = 5). The most common reasons why participants did not receive their allocated treatment was because of either surgeon choice (n = 10, 36%) or a clinical decision intraoperatively (n = 13, 46%) (Table 10).
| Reason | Allocated (n) | ||
|---|---|---|---|
| IM nail fixation | Locking plate | Total | |
| Surgeon choice | 3 | 7 | 10 |
| Clinical decision intraoperatively | 1 | 12 | 13 |
| Lack of equipment | 0 | 2 | 2 |
| Patient choice | 0 | 1 | 1 |
| Withdrawal from trial before treatment | 1 | 1 | 2 |
| Total | 5 | 23 | 28 |
The baseline demographics of patients receiving their allocated treatment were broadly similar to those not receiving allocated treatment, with mean age 45 versus 47 years, although patients who did not receive their allocated treatment were more likely to be male (75%).
Outcomes
Primary outcome
Figure 5a shows the trend in group DRI score means over the trial. Figure 5b shows the distribution of the DRI score at each time point, in which the middle bar is the median, the box represents the interquartile range and the whiskers extend to 1.5 times the interquartile range, with observations outside this range presented individually. Figure 5b demonstrates there is a treatment group difference in favour of the IM nail fixation group at 3 months, but this is reduced and not statistically significant at the 6-month time point and decreases further at the 12-month time point. Model assumptions were checked and appeared to be appropriate.
FIGURE 5.
The DRI. (a) Box plots of baseline and follow-up scores; and (b) overall trend in means and 95% CIs.
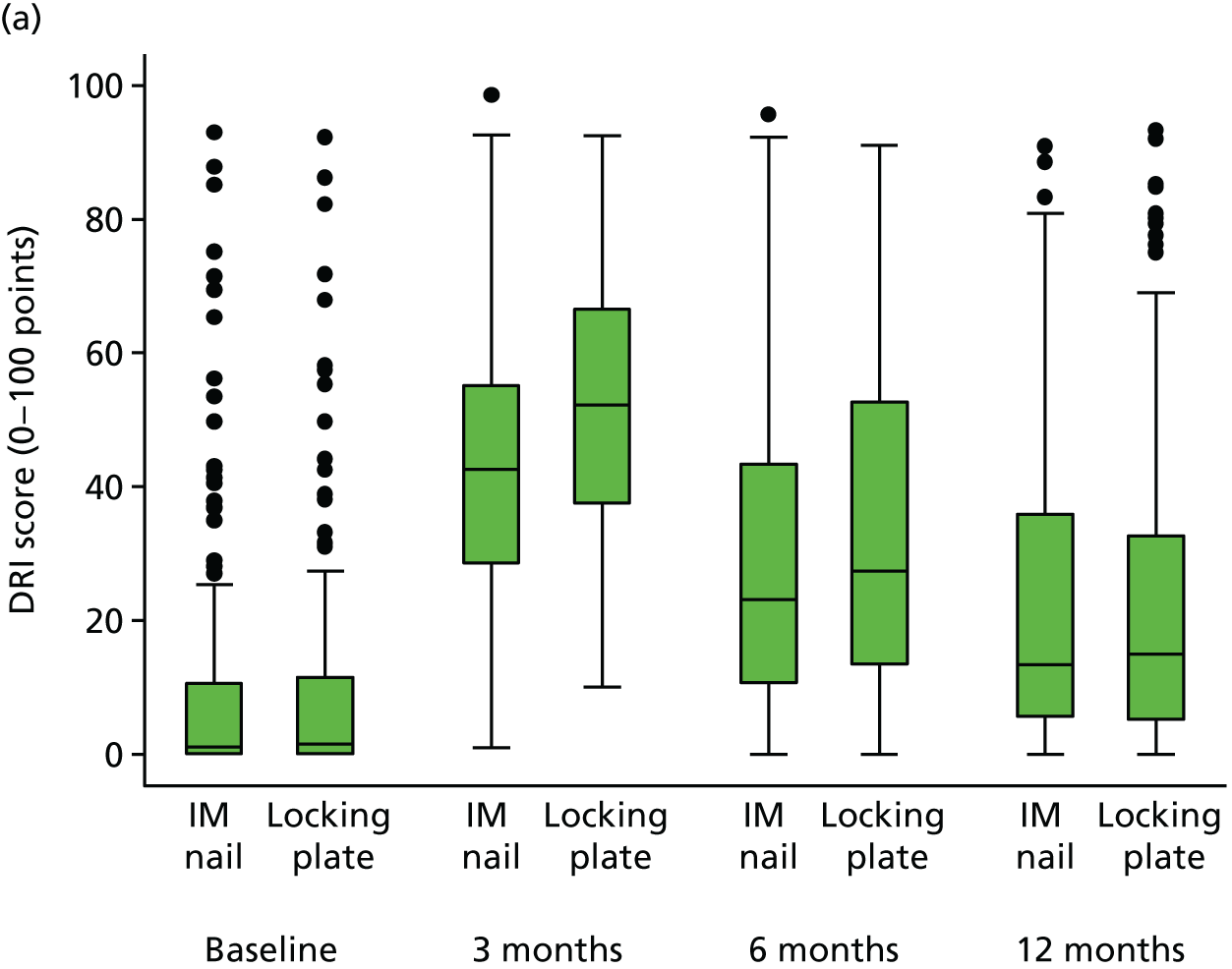
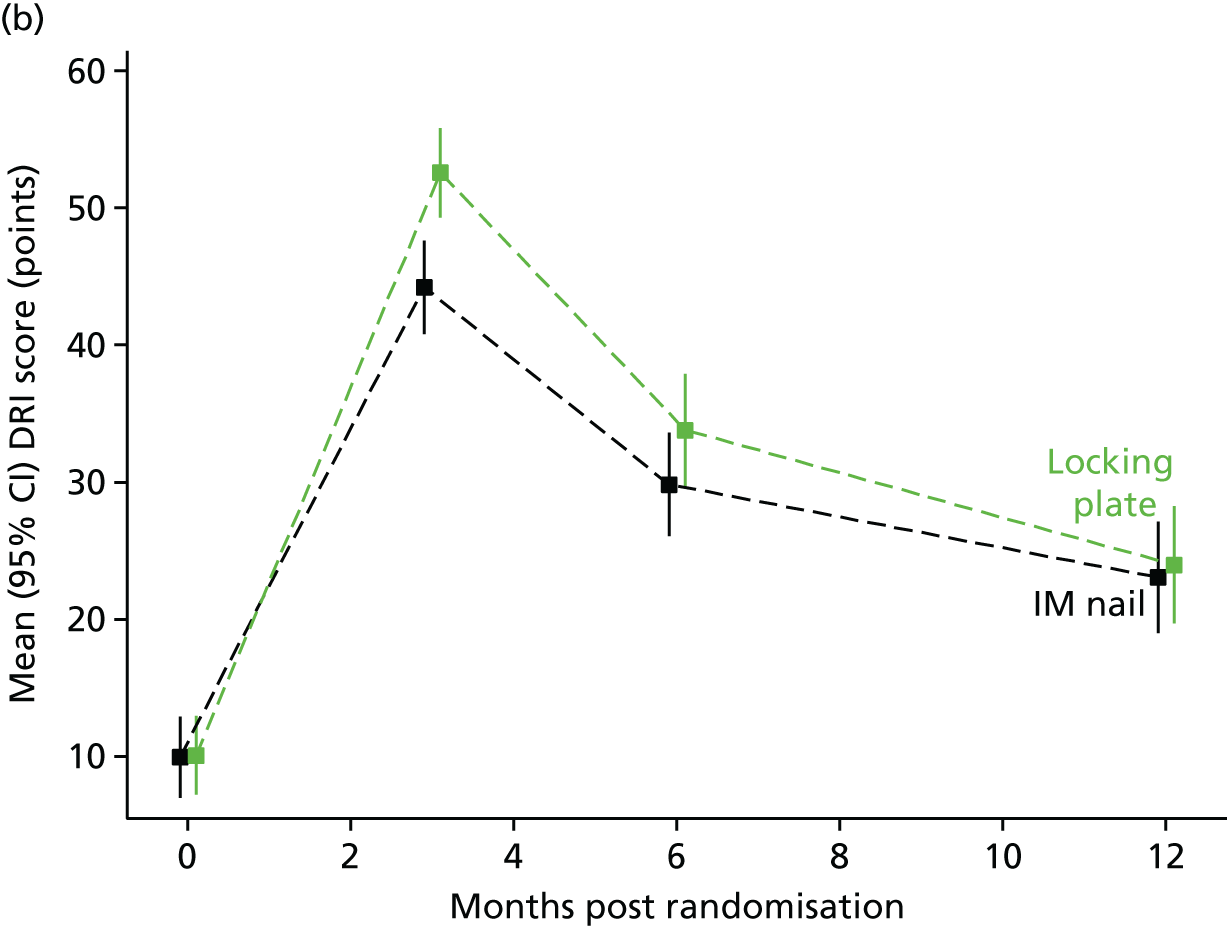
Table 11 shows the treatment estimates modelled using mixed-effects linear regression model, as previously described. The adjusted estimate of the treatment effect for the DRI score, at the 6-month post randomisation time point based on an intention-to-treat analysis, is 4.0 points (95% CI –1.0 to 9.0 points) in favour of the IM nail fixation group compared with the locking plate group. The p-value of 0.114 indicates that there is no evidence for a statistically significant difference in the DRI score between the two treatment groups at the 6-month post-randomisation time point. The prespecified MCID for the DRI is 8 points; therefore, at the 6-month time point we conclude that if there is a difference in the disability outcomes of the two groups, it is likely to be appropriately small as to be clinically unimportant. However, the 95% CI does include the prespecified MCID.
| Time point (months) | Treatment group | Difference (95% CI) | p-value | ||||
|---|---|---|---|---|---|---|---|
| IM nail fixation | Locking plate | ||||||
| Mean (SD) | n | Mean (SD) | n | Raw | Adjusteda | ||
| 3 | 44.2 (19.9) | 132 | 52.6 (19.9) | 141 | 8.4 | 8.8 (4.3 to 13.2) | < 0.001 |
| 6 | 29.8 (23.1) | 142 | 33.8 (24.7) | 140 | 4.0 | 4.0 (–1.0 to 9.0) | 0.114 |
| 12 | 23.1 (23.3) | 125 | 24.0 (24.6) | 129 | 0.9 | 1.9 (–3.2 to 6.9) | 0.468 |
The adjusted estimate of the treatment effect at 3 months is 8.8 (95% CI 4.3 to 13.2) in favour of the IM nail fixation group compared with the locking plate group. The p-value of < 0.001 indicates that there is strong evidence for a statistically significant difference in treatment group means at 3 months. The estimated treatment effect is larger than the prespecified MCID for the DRI of 8 points, so this difference is likely to be clinically important to patients. At the 12-month time point, the p-value of 0.468 indicates that there is no evidence for a statistically significant difference in the DRI score between the two treatment groups at the 12-month post-randomisation time point, and the adjusted treatment difference is 1.9 points (95% CI 3.2 to 6.9 points) in favour of the IM nail fixation group compared with the locking plate group.
Secondary outcomes
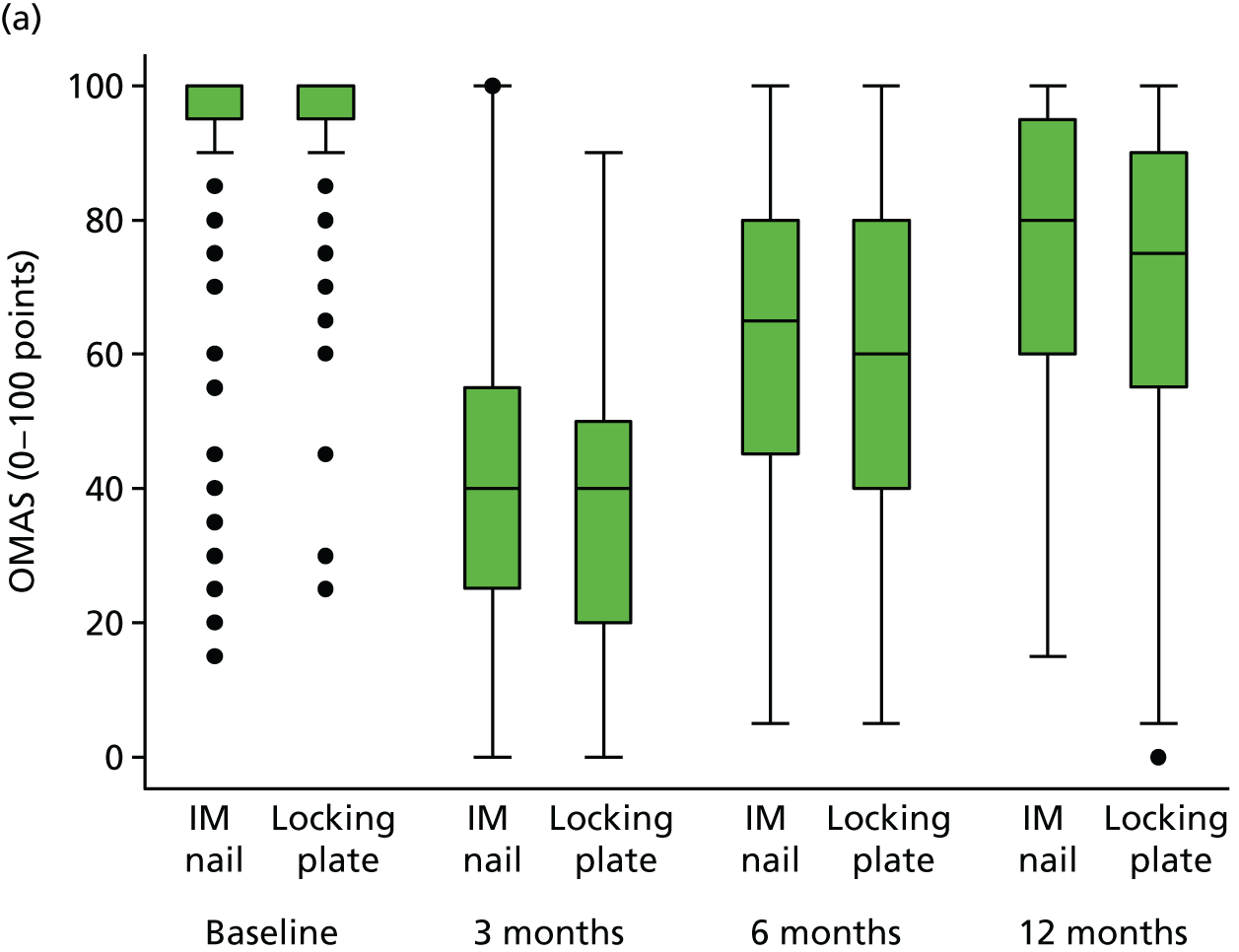
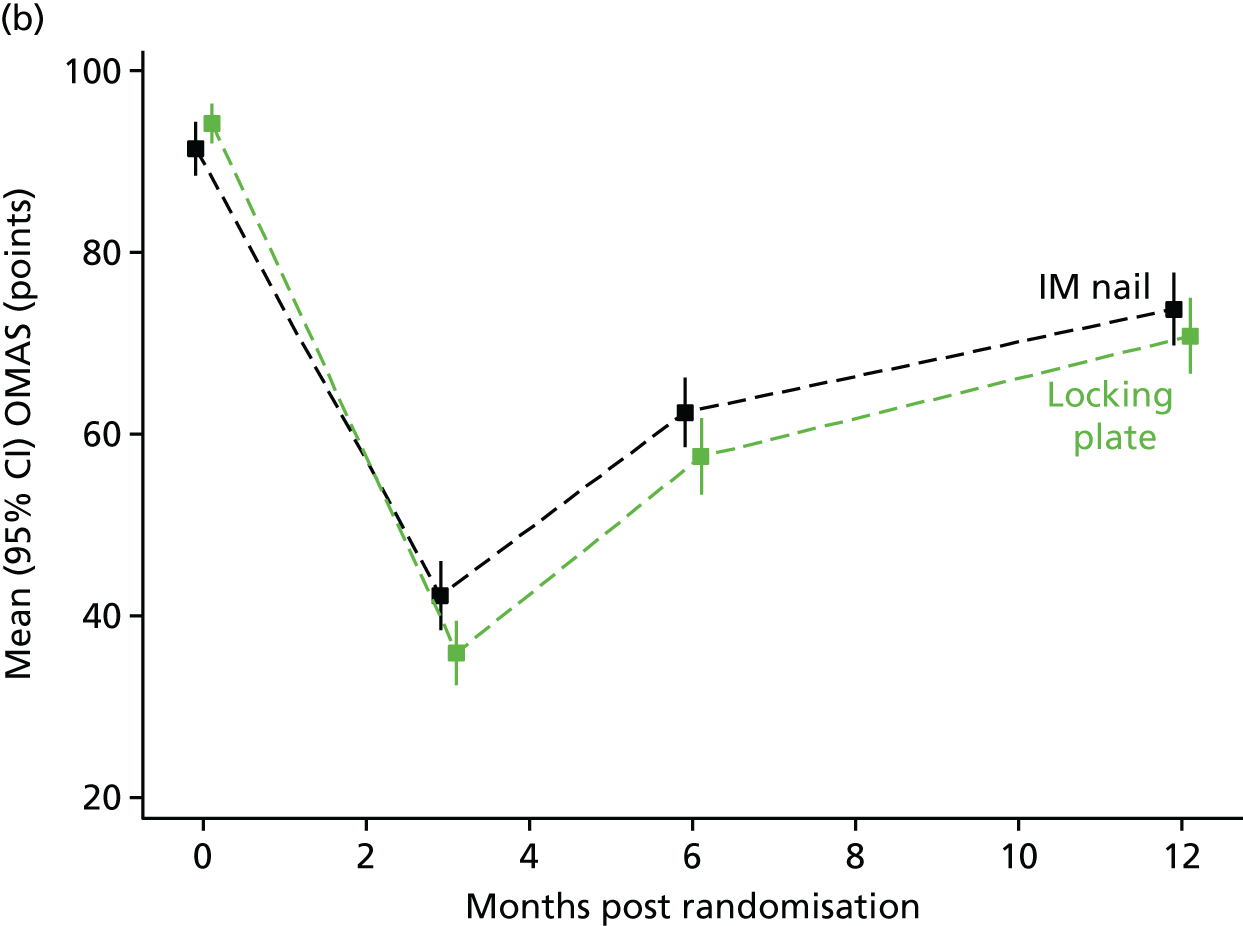
Olerud–Molander Ankle Score questionnaire
The adjusted estimate of the treatment effect for the OMAS, at the 6-month post-randomisation time point based on an intention-to-treat analysis, is –6.0 points (95% CI –11.2 to –0.7 points) in favour of the IM nail fixation group compared with the locking plate group (Figure 6 and Table 12). The p-value of 0.026 indicates that there is evidence for a statistically significant difference in the OMAS between the two treatment groups at the 6-month time point.
FIGURE 6.
The OMAS questionnaire. (a) Box plots of baseline and follow-up scores; and (b) overall trend in means and 95% CIs.
| Outcome measure, time point | Treatment group | Difference (95% CI) | p-value | ||||
|---|---|---|---|---|---|---|---|
| IM nail fixation | Locking plate | ||||||
| Mean (SD) | n | Mean (SD) | n | Raw | Adjusteda | ||
| OMAS (points) | |||||||
| 3 months | 42.3 (22.1) | 130 | 36.0 (21.3) | 139 | –6.3 | –7.0 (–12.0 to –2.0) | 0.006 |
| 6 months | 62.4 (23.1) | 139 | 57.6 (24.9) | 135 | –4.9 | –6.0 (–11.2 to –0.7) | 0.026 |
| 12 months | 73.8 (22.5) | 20 | 70.8 (24.2) | 29 | –3.0 | –3.6 (–9.1 to 1.9) | 0.195 |
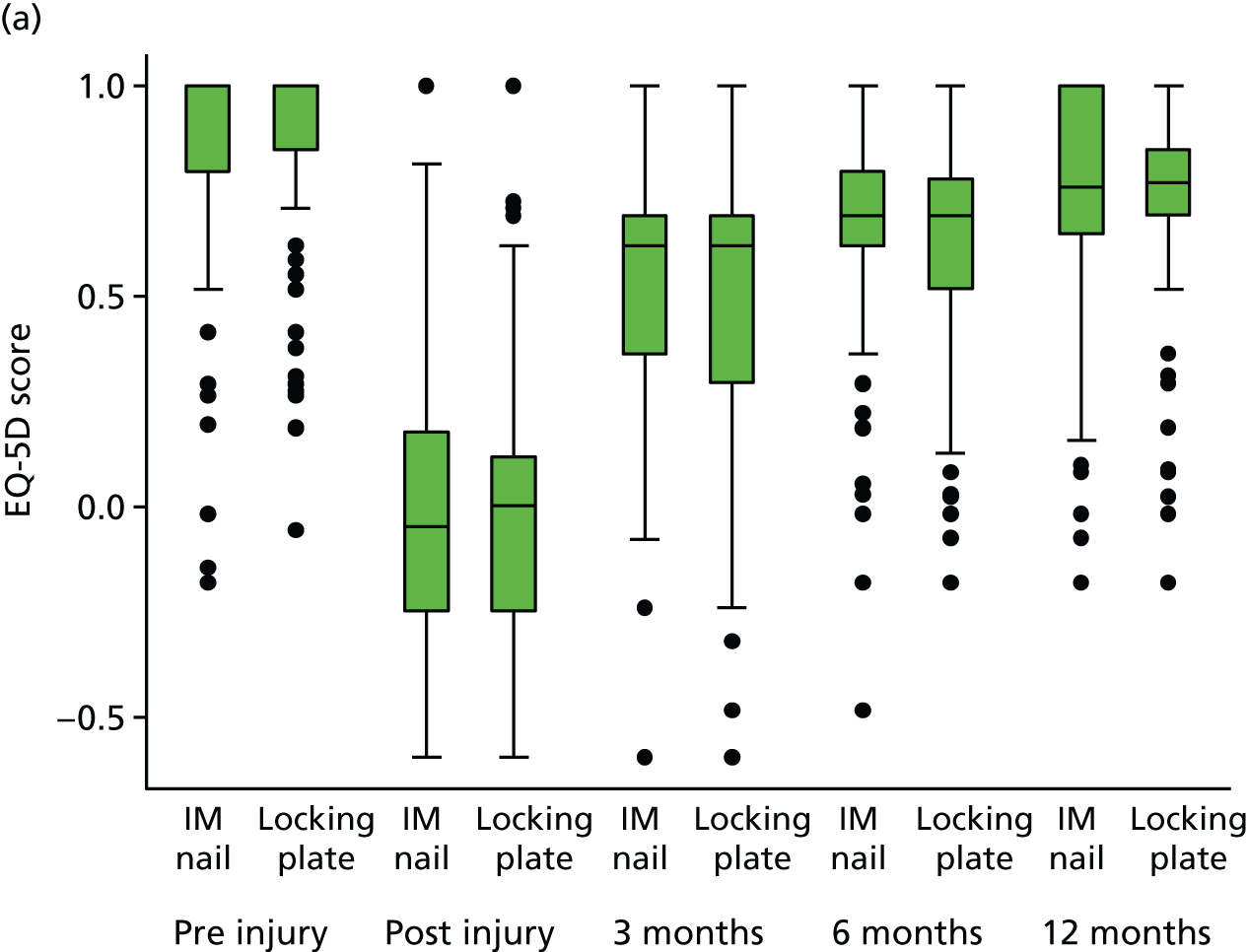
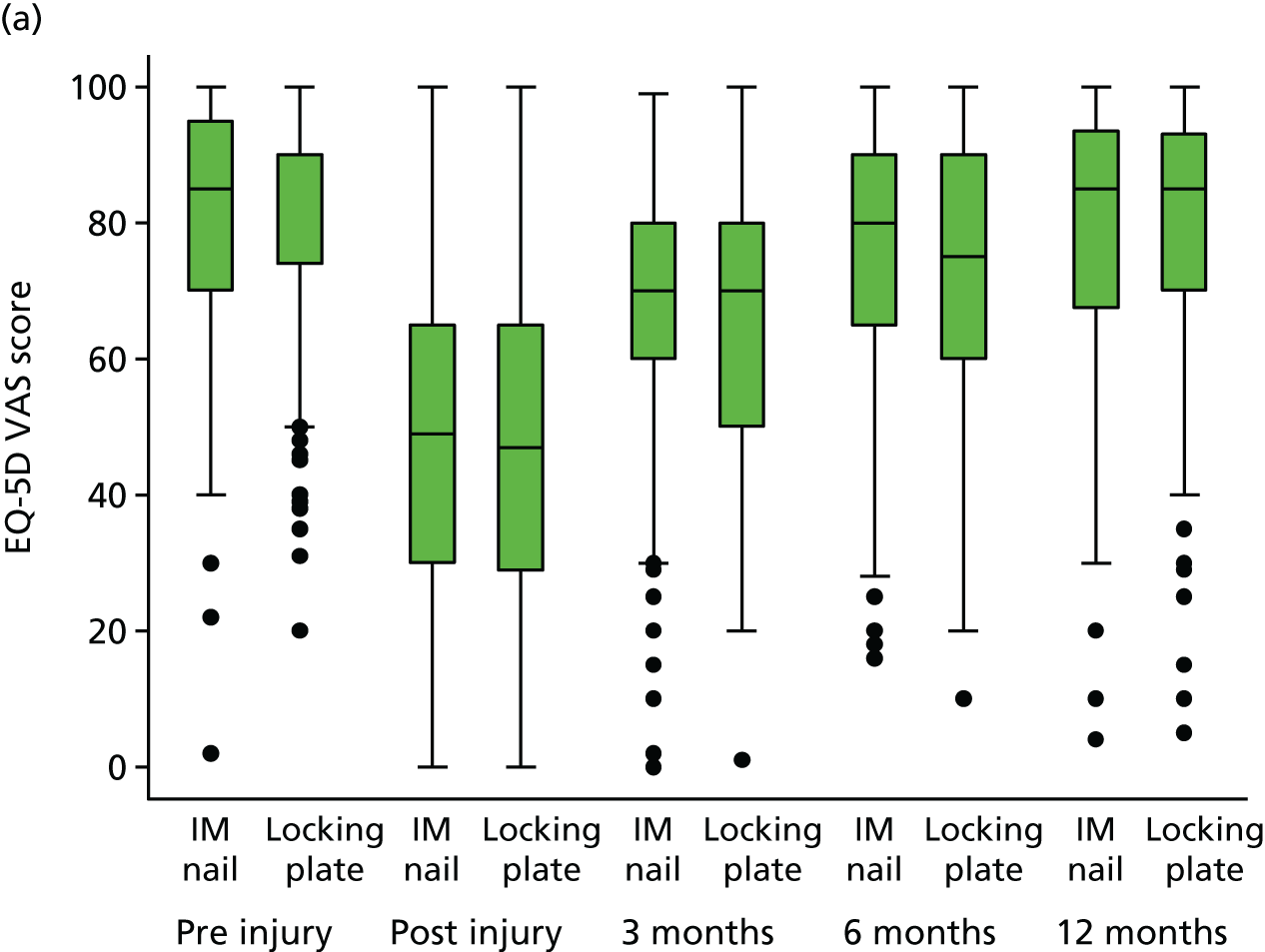
| EQ-5D index score | |||||||
| Post injury | –0.003 (0.334) | 158 | –0.024 (0.311) | 156 | –0.021 | –0.030 (–0.09 to 0.03) | 0.331 |
| 3 months | 0.546 (0.273) | 134 | 0.499 (0.302) | 142 | –0.047 | –0.058 (–0.12 to 0.00) | 0.067 |
| 6 months | 0.670 (0.265) | 143 | 0.622 (0.275) | 141 | –0.048 | –0.064 (–0.12 to –0.01) | 0.029 |
| 12 months | 0.722 (0.278) | 128 | 0.731 (0.246) | 130 | 0.009 | –0.018 (–0.07 to 0.05) | 0.525 |
| EQ-5D VAS score | |||||||
| Post injury | 46.6 (24.5) | 158 | 45.3 (24.8) | 157 | –1.3 | –0.8 (–5.7 to 4.0) | 0.735 |
| 3 months | 66.7 (20.5) | 134 | 64.4 (21.1) | 142 | –2.3 | –1.9 (–6.4 to 2.6) | 0.418 |
| 6 months | 75.0 (19.6) | 143 | 71.6 (21.2) | 141 | –3.4 | –2.5 (–6.8 to 1.8) | 0.247 |
| 12 months | 78.3 (20.5) | 128 | 78.4 (20.8) | 129 | 0.1 | –0.2 (–4.6 to 4.2) | 0.935 |
EuroQol-5 Dimensions index score
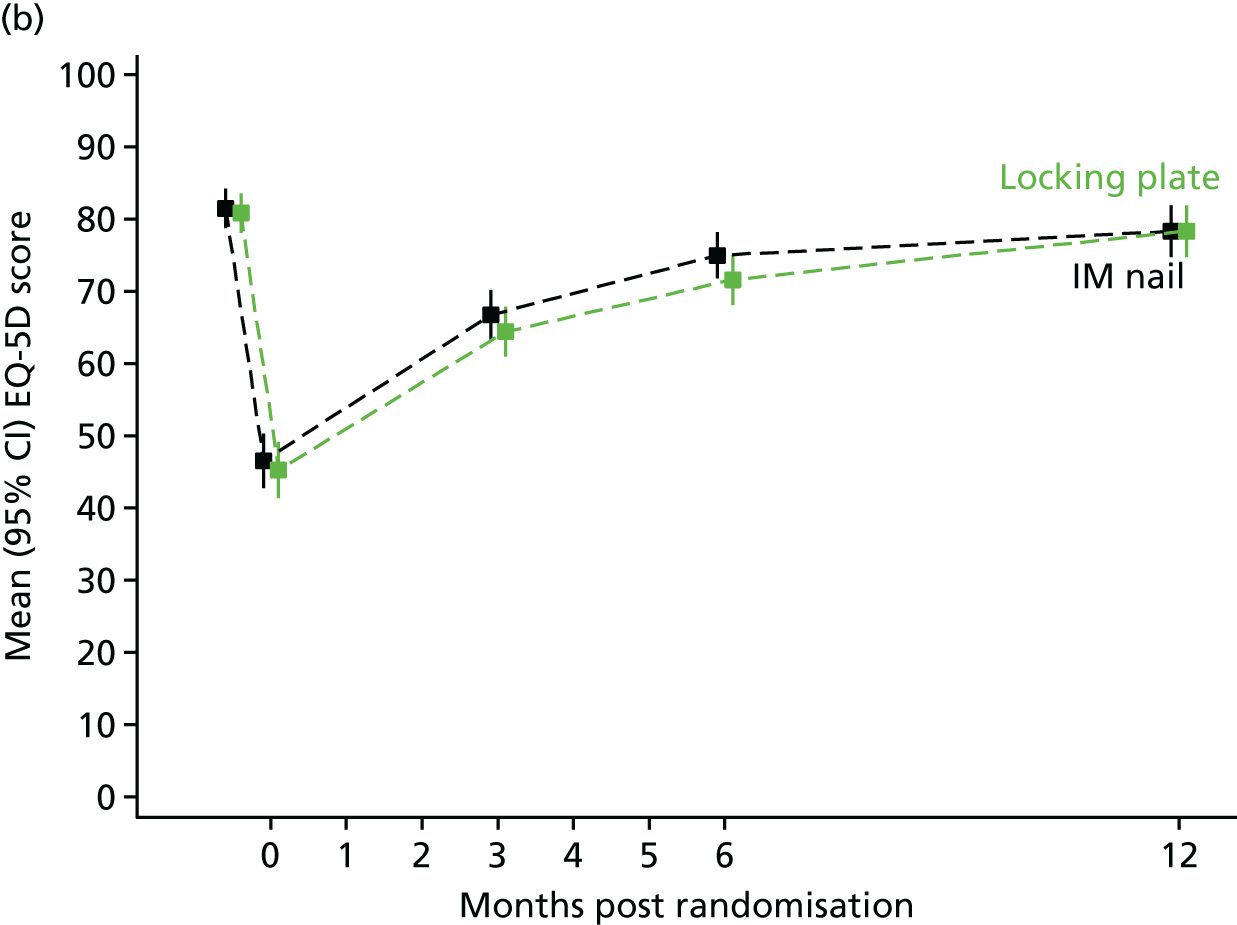
The adjusted estimate of the treatment effect for the EQ-5D index score, at the 6-month post-randomisation time point based on an intention-to-treat analysis, is –0.063 points (95% CI –0.12 to –0.01 points) in favour of the IM nail fixation group compared with the locking plate group (Figure 7 and see Table 12). The p-value of 0.033 indicates that there is evidence for a statistically significant difference in the EQ-5D score between the two treatment groups at the 6-month time point.
FIGURE 7.
The EQ-5D index. (a) Box plots of baseline and follow-up scores; and (b) overall trend in means and 95% CIs.
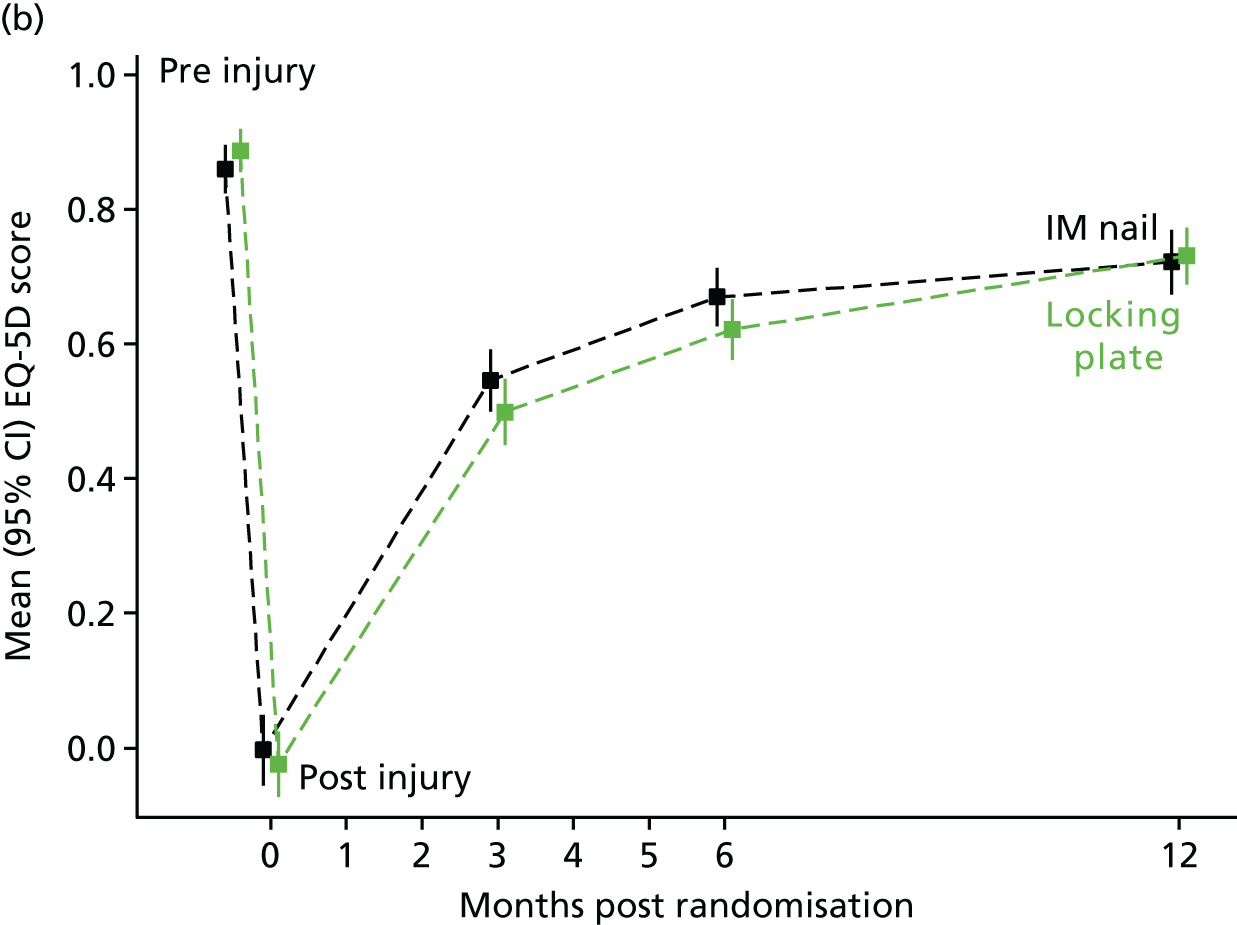
EuroQol-5 Dimensions visual analogue scale score
The adjusted estimate of the treatment effect for the EQ-5D VAS score, at the 6-month post-randomisation time point based on an intention-to-treat analysis, is –2.5 (95% CI –6.8 to 1.8) in favour of the IM nail fixation group compared with the locking plate group (Figure 8 and see Table 12). The p-value of 0.247 indicates that there is no evidence of a statistically significant difference in the EQ-5D VAS score between the two treatment groups at the 6-month time point.
FIGURE 8.
The EQ-5D VAS. (a) Box plots of EQ-5D VAS baseline and follow-up scores; and (b) overall trend in EQ-5D VAS means and 95% CIs.
Per-treatment analysis
Table 13 shows the results of per-treatment analyses, in which participants were analysed in per-treatment groups, that is, those who received IM nails compared with those who received locking plates. The five participants who did not receive either treatment were excluded from these analyses. An adjusted per-treatment analysis of the DRI scores at 6 months gave an adjusted treatment effect of 4.2 (95% CI –0.9 to 9.2) and a p-value equal to 0.103. Adjusted analysis at 3 and 12 months also gave similar results to the intention-to-treat analysis in Primary outcome.
| Outcome measure, time point | Treatment group | Difference (95% CI) | p-value | ||||
|---|---|---|---|---|---|---|---|
| IM nail fixation | Locking plate | ||||||
| Mean (SD) | n | Mean (SD) | n | Raw | Adjusteda | ||
| DRI score (points) | |||||||
| 3 months | 44.5 (20.8) | 148 | 53.2 (18.9) | 123 | 8.7 | 9.0 (4.5 to 13.5) | < 0.001 |
| 6 months | 29.9 (23.4) | 154 | 34.3 (24.6) | 126 | 4.5 | 4.2 (–0.9 to 9.2) | 0.103 |
| 12 months | 23.5 (23.5) | 136 | 24.0 (24.5) | 116 | 0.5 | 0.9 (–4.2 to 6.0) | 0.727 |
| OMAS (points) | |||||||
| 3 months | 42.1 (23.1) | 144 | 35.3 (19.9) | 123 | –6.8 | –7.2 (–12.3 to –2.2) | 0.005 |
| 6 months | 61.9 (23.8) | 150 | 57.5 (24.5) | 122 | –4.5 | –4.9 (–10.2 to 0.4) | 0.073 |
| 12 months | 73.2 (23.2) | 129 | 70.8 (23.7) | 118 | –2.3 | –2.4 (–7.9 to 3.1) | 0.395 |
| EQ-5D index score | |||||||
| 3 months | 0.533 (0.30) | 150 | 0.507 (0.28) | 124 | –0.025 | –0.046 (–0.11 to 0.02) | 0.158 |
| 6 months | 0.672 (0.27) | 155 | 0.614 (0.28) | 127 | –0.058 | –0.067 (–0.12 to –0.01) | 0.023 |
| 12 months | 0.718 (0.28) | 138 | 0.732 (0.24) | 118 | 0.014 | –0.004 (–0.06 to 0.05) | 0.900 |
| EQ-5D VAS score | |||||||
| 3 months | 66.5 (20.6) | 150 | 64.5 (21.2) | 124 | –2.0 | –2.0 (–6.5 to 2.6) | 0.399 |
| 6 months | 75.0 (19.9) | 155 | 71.2 (21.1) | 127 | –3.7 | –2.5 (–6.8 to 1.8) | 0.254 |
| 12 months | 78.1 (20.9) | 137 | 78.4 (20.5) | 118 | 0.3 | 0.6 (–3.9 to 5.0) | 0.803 |
Adjusted per-treatment analysis of the secondary outcome measures are also given in Table 13. All analyses yielded similar results to the equivalent intention-to-treat analysis.
Missing outcome data
The follow-up questionnaire completion rate was very good at all time points of the UK FixDT study. The expected loss to follow-up rate at the 6-month primary outcome time point was 20%; the actual rate was 12%. A summary of status at each follow-up time point is given in Table 5. In total, 284 out of 321 participants (88.4%) completed a DRI at the 6-month time point. The item-level missingness for the DRI score, and the secondary outcome measures, is given in Tables 32–34, Appendix 2. There were very few missing items in the DRI questionnaire at baseline (one item from 3816 items; < 0.1%), 3 months (1/3312; < 0.1%), 6 months (2/3408; < 0.1%) and 12 months (5/2640; 0.2%). Similar levels of missing data were seen across the OMAS questionnaire and the EQ-5D, with item-level missingness below 0.2% for all scales.
Table 14 shows the impact that including partial completion of the DRI using 11 or fewer items had on calculating the overall DRI score. There is very little difference in the adjusted treatment differences compared with the results given in Primary outcome based on fully completed questionnaires only. The largest differences are seen in the 12-month questionnaire data but this is because there are fewer observations and marginally more missing items than at 3- and 6-month data collection, resulting in a slightly larger treatment difference but being still in favour of IM nail fixation, as per the results in Primary outcome.
| Outcome measure, time point | Treatment group | Difference (95% CI) | p-value | ||||
|---|---|---|---|---|---|---|---|
| IM nail fixation | Locking plate | ||||||
| Mean (SD) | n | Mean (SD) | n | Raw | Adjusted | ||
| DRI score (points) | |||||||
| 3 months | 44.2 (20.1) | 134 | 52.7 (19.9) | 142 | 8.5 | 8.7 (4.2 to 13.2) | < 0.001 |
| 6 months | 30.0 (23.0) | 143 | 33.9 (24.6) | 141 | 3.9 | 4.0 (–1.0 to 8.9) | 0.119 |
| 12 months | 22.8 (23.1) | 127 | 24.1 (24.6) | 130 | 1.3 | 2.2 (–2.8 to 7.2) | 0.386 |
Subgroup analysis
At 6 months, the p-value of 0.516 indicates that there is no evidence for a significant interaction effect between age group and treatment group. The results of this analysis, and the subgroup analyses performed at 3 and 12 months, are given in Table 15.
| Time point, age (years) | Treatment group | Difference (95% CI) | p-valueb | ||||
|---|---|---|---|---|---|---|---|
| IM nail fixation | Locking plate | ||||||
| Mean (SD) | n | Mean (SD) | n | Raw | Adjusteda | ||
| 3 months | |||||||
| < 50 | 41.3 (19.4) | 76 | 51.5 (19.6) | 84 | 10.2 | 10.8 (4.9 to 16.6) | 0.290 |
| ≥ 50 | 48.2 (20.2) | 56 | 54.2 (20.5) | 57 | 6.0 | 5.9 (–1.1 to 12.8) | |
| 6 months | |||||||
| < 50 | 25.6 (21.8) | 84 | 31.1 (24.5) | 87 | 5.5 | 5.4 (–1.0 to 11.8) | 0.516 |
| ≥ 50 | 35.9 (23.7) | 58 | 38.2 (24.6) | 53 | 2.3 | 2.0 (–6.0 to 10.0) | |
| 12 months | |||||||
| < 50 | 18.6 (22.6) | 71 | 21.8 (22.8) | 79 | 3.2 | 3.4 (–3.1 to 10.0) | 0.465 |
| ≥ 50 | 28.8 (23.0) | 54 | 27.4 (27.3) | 50 | –1.5 | –0.4 (–8.3 to 7.5) | |
Neither was there any evidence for a significant interaction effect between sex and treatment group (p-value of the interaction term = 0.384).
Exploratory analyses
Area under the curve analysis for the Disability Rating Index score
To complement the preplanned analysis, a post hoc exploratory analysis using DRI score at all four time points was conducted. This analysis simplified longitudinal data collected at four time points to a single value, namely the AUC, and facilitated comparisons of the AUCs between treatment groups.
The group-specific time point means were used to calculate AUCs for treatment groups, as described in the Methods. Using the predicted model parameter, the calculated AUC for those participants who were allocated to the IM nail fixation group was 350 (SE 16.4) and for the locking plate group was 407 (SE 16.3), yielding a between-group difference of 57, 95% CI 12 to 103. Larger DRI scores represent higher levels of disability; therefore, larger AUCs are also associated with increased levels of disability. A t-test comparing the values between groups yielded a p-value of 0.013, indicating that there is a statistically significant difference in AUC between treatment groups. Clinically, this result may be interpreted as evidence that those allocated to locking plates experienced more disability over the 12-month trial follow-up period than those allocated to the IM nail fixation.
Complications
Local complications related to the fracture or its treatment
Complications were assessed by the research team at the 6-week time point for almost all randomised participants (n = 314; 99% of participants who had a surgical procedure) and, again, in the patient reported questionnaires at 3, 6 and 12 months. Table 16 shows these complications by allocated treatment group.
| Complication | Treatment group | p-valuea | |
|---|---|---|---|
| IM nail fixation (n = 157) | Locking plate (n = 157) | ||
| Any infection symptoms identified, n (%) | |||
| Yes | 20 (13) | 32 (20) | 0.094 |
| No | 137 (87) | 125 (80) | |
| Which symptoms?b | |||
| Erythema | 16 | 27 | |
| Persistent serous drainage | 4 | 12 | |
| Purulent drainage | 4 | 6 | |
| Dehiscence | 2 | 8 | |
| Treated with antibiotics, n (%) | |||
| Yes | 14 (9) | 21 (13) | 0.209 |
| No | 143 (91) | 136 (87) | |
| Neurological injury, n (%) | |||
| Yes | 8 (5) | 4 (3) | 0.378 |
| No | 149 (93) | 153 (96) | |
| Vascular injury, n (%) | |||
| Yes | 1 (1) | 0 (0) | 1.000 |
| No | 156 (97) | 157 (98) | |
| Tendon injury, n (%) | |||
| Yes | 0 (0) | 2 (1) | 0.498 |
| No | 157 (98) | 155 (97) | |
| Complex regional pain syndrome, n (%) | |||
| Yes | 0 (0) | 1 (1) | 1.000 |
| No | 157 (98) | 155 (98) | |
| Deep-vein thrombosis (within 6 weeks), n (%) | |||
| Yes | 1 (1) | 2 (1) | 1.000 |
| No | 156 (97) | 155 (97) | |
| Pulmonary embolism (within 6 weeks), n (%) | |||
| Yes | 1 (1) | 0 (0) | 1.000 |
| No | 156 (97) | 157 (98) | |
| Patient fully weight-bearing, n (%) | |||
| Yes | 53 (33) | 23 (14) | < 0.001 |
| No | 104 (65) | 134 (84) | |
| Missing | 4 (2) | 3 (2) | |
The number of patients with symptoms related to infection was higher in the locking plate group (n = 32; 20%) than in the nail fixation group (n = 20; 13%), although this was not statistically significant (Fisher’s exact test p = 0.094). Twenty-one (13%) patients in the locking plate group and 14 (9%) in the IM nail fixation group were treated with antibiotics.
Other local complications were rare in both groups.
Data on ability/inability to bear weight on the injured leg were also collected at the 6-week visit in Table 16. In total, 33% of those allocated to nail fixation reported being fully weight-bearing at the 6-week visit, compared with only 14% of those allocated to locking plates. The difference in proportions is 0.19, 95% CI 0.10 to 0.41. The p-value for the difference is these proportions is p < 0.001, indicating strong evidence of a difference in the proportion of participants weight-bearing at 6 weeks.
Further surgery related to the fracture or its treatment is shown in Table 17. Where patients reported any further surgery, full details of the operation were requested and provided from the treating centre. There was more further surgery in the locking plate group (n = 19; 12%) than in the nail fixation group (n = 14; 9%), although this was not statistically significant (Fisher’s exact test p-value = 0.363).
| Surgical procedure | Treatment group | p-valuea | |
|---|---|---|---|
| IM nail fixation (n = 161) | Locking plate (n = 160) | ||
| Any additional surgical procedure on trial distal tibia, n (%) | |||
| Yes | 14 (9) | 19 (12) | 0.363 |
| No | 148 (92) | 141 (88) | |
| If so, which procedure?,b n (%) | |||
| Metalwork removal | |||
| Yes | 11 (7) | 14 (9) | 0.540 |
| No | 150 (93) | 146 (146) | |
| Surgical debridement | |||
| Yes | 1 (1) | 5 (3) | 0.121 |
| No | 160 (99) | 155 (97) | |
| Revision of internal fixation | |||
| Yes | 2 (1) | 5 (3) | 0.283 |
| No | 159 (99) | 155 (97) | |
| Other operative procedure | |||
| Yes | 4 (2) | 3 (2) | 1.000 |
| No | 157 (98) | 157 (98) | |
Radiographic outcomes
An independent orthopaedic surgeon assessed the radiographic images, when available. The results of these independent assessments are given in Tables 18 and 19 for 6-week and 12-month images, respectively.
| Deformity | Trial group, n (%) | p-valuea | |
|---|---|---|---|
| IM nail fixation | Locking plate | ||
| Lateral deformity (> 5°) | |||
| Yes | 5 (3) | 5 (2) | 1.000 |
| No | 135 (84) | 140 (88) | |
| Missing | 21 (13) | 15 (10) | |
| Anteroposterior deformity (> 10°) | |||
| Yes | 12 (7) | 5 (3) | 0.081 |
| No | 128 (80) | 142 (89) | |
| Missing | 21 (13) | 13 (8) | |
| Shortening (> 10 mm) | |||
| Yes | 5 (3) | 0 (0) | 0.028 |
| No | 136 (84) | 146 (91) | |
| Missing | 20 (13) | 14 (9) | |
| Deformity | Treatment group, n (%) | p-valuea | |
|---|---|---|---|
| IM nail fixation | Locking plate | ||
| Lateral deformity (> 5°) | |||
| Yes | 1 (1) | 0 (0) | 0.469 |
| No | 82 (51) | 94 (59) | |
| Missing | 78 (48) | 66 (41) | |
| Anteroposterior deformity (> 10°) | |||
| Yes | 11 (7) | 8 (5) | 0.339 |
| No | 72 (45) | 86 (54) | |
| Missing | 78 (48) | 66 (41) | |
| Shortening (> 10 mm) | |||
| Yes | 0 (0) | 0 (0) | 1.000 |
| No | 83 (52) | 94 (59) | |
| Missing | 78 (48) | 66 (41) | |
| Ankle osteoarthritis | |||
| Yes | 10 (6) | 7 (4) | 0.320 |
| No | 73 (45) | 87 (54) | |
| Missing | 78 (48) | 66 (41) | |
In addition to the independently assessed radiographs, the principal investigator at each recruiting site assessed key radiographic outcomes and reported these on the 6-week postoperative form. Comparisons between these site assessments and independent assessments were investigated, and there were good levels of agreement between assessors.
Systemic complications potentially related to the fracture or its treatment
Information regarding complications was also given through the SAE reporting pathway over the full 12 months of the trial. Data from related SAEs have been included in these complication profiles, with cross-referencing to ensure that appropriate counts are taken using multiple data sources. Not all of the venous thromboses or infections of the chest, urinary system, etc., will be related to the treatment but we have included all ‘potentially’ related events here for completeness. These data are summarised by treatment group in Tables 17 and 20.
| Complication | Treatment group, n (%) | p-valuea | |
|---|---|---|---|
| IM nail fixation (n = 161) | Locking plate (n = 160) | ||
| Deep-vein thrombosis | |||
| Yes | 7 (4) | 6 (4) | 1.000 |
| No | 154 (96) | 15 (96) | |
| Infection treated with antibiotics (not wound related) | |||
| Yes | 24 (15) | 31 (19) | 0.303 |
| No | 137 (85) | 129 (81) | |
Serious adverse event unrelated to the fracture or its treatment
There was a total of 126 unrelated SAEs, which were reported by 83 participants. ‘Relatedness’ was assessed by the principal investigator at each centre. In total, 60 participants reported only one SAE, 14 reported two SAEs and nine reported more than two SAEs. The maximum number of unique SAE reports by a participant was nine. The reasons for SAE reporting are given in Table 21, by treatment group. More than one reason can be selected for each report of a SAE (e.g. both hospitalisation and persistent disability may be reasons); therefore, for reporting purposes, the most severe reason is presented.
| Reason | Treatment group (n) | Total | |
|---|---|---|---|
| IM nail fixation | Locking plate | ||
| Death | 2 | 4 | 6 |
| Life-threatening condition | 0 | 3 | 3 |
| Hospitalisation or prolongation of existing hospitalisation | 24 | 47 | 71 |
| Persistent disability/incapacity | 1 | 1 | 2 |
| Required medical intervention to prevent one of above | 11 | 15 | 26 |
| Otherwise medically significant | 8 | 10 | 18 |
| Total | 46 | 80 | 126 |
Chapter 4 Economic evaluation
Methods
Aim and perspective
The main objective of the health economic evaluation was to assess the cost-effectiveness of treating displaced extra-articular fractures of the distal tibia using IM nail fixation versus locking plate fixation. The primary analysis was undertaken from the perspective of the NHS and PSS, as recommended by the National Institute for Health and Care Excellence (NICE). 31 A societal perspective for costs was adopted for the sensitivity analysis and this included private costs incurred by trial participants and their families, as well as productivity losses and loss of earnings as a result of work absences.
The primary health economic outcome was the ICER attributable to IM nail fixation, which was calculated as the incremental cost per QALY gained 12 months after randomisation. No discounting of costs or health consequences was required as the trial-based economic evaluation was limited to a 12-month time horizon.
Measurement of resource use and costs
A comprehensive strategy was adopted to estimate the costs associated with distal tibia fixation using either locking plate or IM nail fixation. This included the (1) estimation of the initial fixation surgery costs and (2) estimation of broader health and personal social service resource inputs and broader societal resource inputs. All costs were expressed in pounds sterling and valued in 2014–15 prices. When appropriate, costs were inflated or deflated to 2014–15 prices using the Hospital and Community Health Services (HCHS) Pay and Price Inflation. 32
Costing of distal tibia fixation
The initial fixation surgery costs (intervention costs) were based on the initial hospital stay and associated operative costs, as reported in Table 22. The cost of distal tibia fracture fixation surgery was estimated using the NHS reference costs, specifically Healthcare Resource Group (HRG) code HT23D (major knee procedures for trauma). 33 According to this HRG code, operative costs for distal tibia fixation were £5315.47 for cases with a mean length of hospital stay of 5 days. Patient-specific costs for the initial operative period were identified using the average length of stay following primary surgery, as reported in the patient records. The mean length of hospital stay was 3.87 days for IM nail fixation versus 3.85 days for locking plate fixation and SEs were 0.34 and 0.33 days, respectively. The surgery cost of patients who stayed longer than 5 days was adjusted using the cost per excess bed-day figure of £327.00 for the same HRG code. For patients who stayed in hospitals < 5 days, we assumed that treatment costs were disproportionately weighted towards the first 3 days of each initial hospital admission. Thus, the cost to the NHS of a patient who stayed in hospital for 3 days was calculated as £5315.47 – (2 × £327), that is, the 5-day tariff minus the bed-day cost of £327 per each day not spent in hospital.
| Item | Unit cost (£) | Source |
|---|---|---|
| Surgery costsa | ||
| Average surgery cost of distal tibia fracture fixation (based on a mean length of stay of 5 daysb) | 5315.47 | Reference Costs 2014–15, ‘major knee procedures for trauma, 19 years and over, with a CC score of 0’, HT23D33 |
| Cost per excess bed-day | 327.00 | Reference Costs 2014–15, ‘major knee procedures for trauma, 19 years and over, with a CC score of 0’, HT23D33 |
| Implants: IM nail fixation | ||
| Guide wire 3.2 × 300 | 43.11 | UHCW finance department |
| Reaming rod 2.5 × 1000 | 63.47 | UHCW finance department |
| Distal bolts | 45.88 | UHCW finance department |
| End cap | 37.93 | UHCW finance department |
| Blocking screw | 29.80 | UHCW finance department |
| Nail | 265.53 | UHCW finance department |
| Implants: locking plate fixation | ||
| Medial distal tibia plate | 358.41 | UHCW finance department |
| Anterolateral distal tibia plate | 412.81 | UHCW finance department |
| Lock screw (3.5-mm diameter) | 37.79 | UHCW finance department |
| Lock screw (2.7-mm diameter) | 26.79 | UHCW finance department |
| Non-lock screw (3.5-mm diameter) | 6.98 | UHCW finance department |
| Non-lock screw (2.7-mm diameter) | 14.00 | UHCW finance department |
In addition, operative costs included the implants used during the surgery, namely nails, plates, locking screws/bolts, blocking screws and non-locking screws. Estimation of the number of each of these implants used involved prospectively recording the number of items used for each patient from the operation notes and radiographs. The total cost of implants for each patient was calculated by combining the resource inputs with their unit cost values; the unit cost values were derived from NHS trust finance departments.
Measuring broader resource use
Individual-level data on all significant health and personal social service and broader societal resource inputs were collected during the trial using follow-up questionnaires completed by trial participants. These data were collected at 3, 6 and 12 months post randomisation. The questionnaires captured the number and duration of admissions to inpatient hospital wards by ward type, number and type of diagnostic tests, use and type of outpatient hospital services, frequency of use and type of community-based health and social care services, medication use and aids and devices provided. In addition, the questionnaires captured the direct non-medical costs (including travel expenses) incurred by patients and their carers, as well as number of days off work and gross loss of earnings, attributable to the trial participant’s health state or contacts with care providers. Copies of the resource use questionnaires administered at each time point are provided in Appendix 3.
Valuation of resource use
The derivation of unit cost values was consistent with NICE’s Guide to the Methods of Technology Appraisal 201331 and included values extracted from the Department of Health and Social Care’s Reference Costs 2014–15,33 the Personal Social Services Research Unit (PSSRU)’s Unit Costs of Health and Social Care 2015,34 NHS Prescription Cost Analysis and the British National Formulary. 35 Table 35, Appendix 4, summarises the unit cost values and data sources for the broader resource use categories.
Further inpatient admissions following the initial operation were costed as minor knee procedures for non-trauma (HRG code HN25A) if the inpatient care involved procedures of the leg. However, if the inpatient admission was related to a surgical complication of the primary surgery, individual HRG codes that related to the subsequent operation procedures undertaken (e.g. debridement, metalwork removal, revision of internal fixation) were derived using the NHS HRG4 2014/15 Reference Cost Grouper software version RC1415 (NHS Digital, Leeds, UK). The Department of Health and Social Care’s Reference Costs 2014–1533 was used to assign the costs for each of the derived HRG codes. Subsequent inpatient care that was unrelated to procedures of the leg were also costed using Reference Costs 2014–1533 (Table 35, Appendix 4). The same approach was taken to cost subsequent hospital outpatient care, with resource use data on frequency of outpatient care being combined with the relevant unit costs.
Costs for community-based health services and PSS were calculated by applying unit costs extracted from national tariffs to resource volumes. Costs of medications for individual participants were estimated based on their reported doses and frequencies, when these were available, or based on an assumed daily dose using British National Formulary35 recommendations. When a dose range was reported as ‘as required’ or when the quantities were not recorded, we assumed a mean cost for that medication item based on the prescription cost analysis values (net ingredient cost per item). If the dose of the medication was missing, we assumed the patient received the same dosage as other trial participants who reported taking the same medication.
The costs of equipment that trial participants received to make their daily lives easier and manage their injury (aids and adaptations) were derived by combining the data on number and type of items received with their unit cost values. Unit costs were obtained from the NHS supply chain catalogue (https://my.supplychain.nhs.uk/catalogue; accessed 11 October 2017).
The costs of time taken off work were estimated by applying sex-specific median earnings data from the annual survey of hours and earnings for part-time and full-time work. 36 The employment status of trial participants was derived from self-reported work status information. Broader societal costs were calculated by combining the productivity losses and associated loss of earnings as a result of work absences and any privately incurred costs as a attributable to participants’ surgeries or impaired health states.
Calculation of utilities and quality-adjusted life-years
Participants’ health-related quality of life was assessed using the EQ-5D37 obtained at baseline and at 3, 6 and 12 months post randomisation. The EQ-5D defines health-related quality of life in terms of five dimensions: (1) mobility, (2) self-care, (3) usual activities, (4) pain/discomfort and (5) anxiety/depression. Responses in each dimension are divided into three ordinal levels coded: (1) no problems, (2) moderate problems and (3) extreme problems.
The EQ-5D health states are converted into a single summary index by applying a utility algorithm, which attaches values (weights) to each permutation of responses to the EQ-5D descriptive system. 37 EQ-5D preference weights have been elicited from general population samples in the UK using the time trade-off method. The resulting utility scores range from –0.594 to 1.0, with 0 representing death and 1.0 representing full health; values below 0 indicate health states worse than death. QALYs were calculated as the area under the baseline-adjusted utility curve and were calculated using linear interpolation between baseline and follow-up utility scores.
Missing data
Incomplete data are a particular issue in within-trial health economic evaluations and can result from item-level missingness; for example, when data for visit 2 are missing but data for visit 1 and all visits after visit 2 are available. 38 Consequently, a base-case analysis was constructed when missing data were imputed using fully conditional multiple imputation made chained equations, under the missing at random assumption. Multiple imputation under the missing at random assumption provides unbiased estimates of costs and health consequences. The missing at random assumption was tested through logistic regressions of missingness of costs and QALYs against baseline covariates.
Regression models were used to impute unobserved costs and QALYs at each time point and by treatment allocation using the baseline covariates (age, sex) as predictor variables. Costs and EQ-5D utility scores at each time point contributed as both predictors and imputed variables. The imputation was run 50 times, following the rule of thumb that the number of imputations should be similar to the percentage of incomplete cases. 39 The multiple imputation generated 50 data sets using predictive mean matching. Predictive mean matching provides plausible values when costs and QALYs are non-normally distributed. 40 In line with best practice, the MI model was validated by comparing the distributions of the imputed data with the observed data. 40
The multiply imputed data sets were analysed independently with bivariate regressions using a seemingly unrelated regression model (Sureg) to estimate the costs and QALYs in each treatment group over the 12-month trial horizon. Non-parametric bootstrapping was used to generate joint distributions of costs and outcomes from the original data set, and changes in costs and QALYs were calculated for each sample. A total of 1000 bootstrap samples were drawn and means for both incremental costs and incremental QALYs (with associated 95% CIs) were calculated.
The final step involved combining estimates from each imputed data set using Rubin’s rule to generate an overall mean estimate of costs and QALYs and the SEs. 40 The SE calculated through Rubin’s rules reflects the variability within and across imputations.
Analyses of resource use, costs and outcome data
Resource use items were summarised by trial allocation group and follow-up period and differences between groups were analysed using t-tests for continuous variables and Pearson chi-squared (χ2) test for categorical variables. Means and SEs for values of each cost category were estimated by treatment allocation and follow-up period. Statistical differences in mean costs by treatment allocation were assessed using Student t-tests. Mean total costs by treatment allocation and follow-up period were also estimated. Statistically significant differences in the mean total costs were assessed using non-parametric bootstrapping, based on 10,000 replications.
We calculated the proportion of patients reporting suboptimal health for each of the five dimensions of the EQ-5D. Patients were considered to be in suboptimal health if they reported moderate or extreme problems. We explored whether or not any statistical differences in suboptimal health-related quality of life existed between the two treatment arms at the different time points, using a Pearson chi-squared (χ2) test.
Cost-effectiveness analyses
Cost-effectiveness results are expressed in terms of the ICER and calculated as the difference between treatments in mean total costs divided by mean total QALYs. The bootstrap replicates from the non-parametric bootstrapping, described in Analyses of resource use, costs and outcome data, were used to populate cost-effectiveness scatterplots. Cost-effectiveness acceptability curves, which showed that the probability that IM nail fixation is cost-effective relative to locking plate fixation across a range of cost-effectiveness thresholds, were also generated based on the proportion of bootstrap replicates with positive incremental net benefits. The net monetary benefit (NMB) of using IM nail fixation versus locking plate fixation was also calculated across three cost-effectiveness thresholds, namely £15,000 per QALY, £20,000 per QALY and £30,000 per QALY. A positive incremental NMB indicates that the intervention is cost-effective compared with the alternative at the given cost-effectiveness threshold.
Sensitivity and subgroup analyses
Several sensitivity analyses were undertaken to assess the impact that uncertain parameters had on components of the economic evaluation. These involved re-estimating the main cost-effectiveness outcomes under the following scenarios: (1) restricting the analyses to complete cases (i.e. those with complete cost and outcome data over the 12-month follow-up period); (2) adopting a wider societal perspective that included private costs incurred by trial participants and their families, as well as productivity losses and loss of earnings owing to work absences; (3) estimating the cost-effectiveness under a per-treatment analysis; and (4) additionally adjusting the baseline analysis for pre-injury health-related quality of life, which was assessed using the EQ-5D at baseline.
Subgroup analyses were also conducted for the main cost-effectiveness results to explore heterogeneity in the trial population. These were conducted by (1) age group (< 50 and ≥ 50 years) and (2) sex (male and female).
Longer-term economic modelling
The study protocol allowed for decision-analytic modelling to extend the cost-effectiveness of IM nail fixation, drawing on best-available secondary data sources, supplemented when necessary by expert opinion.
Results of economic analysis
Table 36, Appendix 4, shows the degree of missing health economic data by treatment allocation and follow-up time point. The missing data pattern is non-monotonic, as individuals with missing data at one follow-up time point may return to the trial subsequently. For example, there are more missing EQ-5D data at 3 months than at 6 months. A similar pattern can be observed for costs.
Health-care resource use
Table 8 summarises the key resource inputs associated with the initial treatment of displaced extra-articular fractures of the distal tibia. Table 37, Appendix 4, presents details of broader health and social care resource use over the 12-month follow-up period for complete cases, disaggregated by resource category and period of follow-up. Generally, resource use at the aggregate level was higher for participants allocated to the locking plate than those allocated to IM nail fixation, but this was not always statistically significant. The exceptions were differences in mean total inpatient stay at 6 months (0 vs. 0.11 months), which was statistically significant at the 5% level (p-value of 0.03), and mean total outpatient care contacts at 6 months (3.64 vs. 4.78 mean outpatient contacts), which was also significant at the 5% level (p-value of 0.04). The reported number of days taken off work was generally higher for the locking plate arm. However, the mean difference (46.12 vs. 54.46) was significant at a 10% significance level at 3 months (p-value of 0.07). Regarding components of the resource categories, patients in the locking plate arm were more likely to use walking frames at 3 months (0.20 vs. 0.34), utilise more NHS physiotherapy (1.84 vs. 2.53) at 6 months and report higher use of ‘other’ medicines at 12 months (0.08 vs. 0.29).
Costs
Table 23 summarises the total costs associated with resource use during the trial period among complete cases by cost category and follow-up period. The mean intervention costs from admission until discharge were £5585 for IM nail fixation compared with £5615 for locking plate fixation; the mean difference of £30 was not statistically significant. The mean total NHS and PSS cost throughout the first 6 months post randomisation was £5876 for IM nail fixation and £6814 for locking plate fixation; the mean cost difference of £939 was statistically significant at the 5% level. The mean total NHS and PSS cost for the entire 12-month follow-up period was £6107 for IM nail fixation and £7102 for locking plate fixation; the mean cost difference of £995 was statistically significant at the 10% significance level. Total societal costs among cases with complete data are summarised in Table 24. The mean total societal costs throughout the first 6 months was £9793 for IM nail fixation compared with £12,178 for locking plate fixation; the mean cost difference of £2385 was statistically significant at the 10% significance level. The mean total societal costs are £9490 for IM nail fixation and £12,886 for locking plate fixation; the mean cost difference of £3396 was statistically significant at the 5% significance level.
| Cost category by period | Treatment arm, mean (SE) cost | Mean difference | p-valuea | Bootstrap 95% CIb | |
|---|---|---|---|---|---|
| IM nail fixation | Locking plate | ||||
| Baseline to discharge (total, n = 318: IM nail group; n = 158; locking plate group, n = 160) | |||||
| Intervention costs (includes initial surgery costs + initial hospital stay + implants) | 5584.86 (107.84) | 5615.52 (106.59) | –30.66 | 0.84 | –328.02 to 266.70 |
| Discharge to 3 months (total, n = 210: IM nail group, n = 104; locking plate group, n = 106) | |||||
| Subsequent inpatient care | 66.22 (49.31) | 229.53 (162.97) | –163.31 | 0.34 | –376.63 to 222.79 |
| Outpatient care | 137.64 (5.95) | 140.71 (7.86) | –3.07 | 0.78 | –15.49 to 19.21 |
| Community care | 49.01 (9.82) | 371.58 (318.06) | –322.57 | 0.31 | –764.66 to 242.61 |
| Medications | 25.30 (8.36) | 32.06 (13.12) | –6.76 | 0.51 | –26.01 to 52.51 |
| PSS | 0.23 (0.23) | 0.85 (0.51) | –0.62 | 0.27 | –1.49 to 0.54 |
| Aids and adaptations | 8.65 (1.93) | 9.02 (1.35) | –0.37 | 0.87 | –4.58 to 3.33 |
| Total cost | 287.05 (51.42) | 783.75 (358.54) | –496.70 | 0.17 | –1201.39 to 208.00 |
| Subsequent inpatient care | 11.27 (11.20) | 121 (63.34) | –109.73 | 0.09 | –235.82 to 16.37 |
| Outpatient care | 81.43 (7.39) | 106.74 (12.98) | –25.31 | 0.09 | –54.60 to 3.99 |
| Community care | 54.13 (20.35) | 154.97 (110.55) | –100.84 | 0.37 | –321.55 to 119.87 |
| Medications | 8.00 (2.99) | 4.28 (1.13) | 3.72 | 0.25 | –1.98 to 8.17 |
| PSS | 0.56 (0.32) | 0.37 (0.26) | 0.19 | 0.361 | –0.62 to 1.00 |
| Aids and adaptations | 1.40 (0.57) | 1.33 (0.49) | 0.07 | 0.92 | –1.40 to 1.55 |
| Total cost | 156.79 (25.84) | 388.70 (128.21) | –231.90 | 0.08 | –487.94 to 22.80 |
| 6–12 months (total, n = 219: IM nail, n = 108; locking plate group, n = 111) | |||||
| Subsequent inpatient care | 168.00 (66.46) | 293.51 (102.88) | –125.51 | 0.31 | –331.86 to 147.03 |
| Outpatient care | 52.61 (7.79) | 58.98 (9.72) | –6.37 | 0.61 | –33.08 to 12.48 |
| Community care | 15.45 (5.39) | 42.37 (28.60) | –26.92 | 0.36 | –89.66 to 31.29 |
| Medications | 12.53 (9.89) | 30.74 (24.58) | –18.21 | 0.49 | –48.54 to 23.01 |
| PSS | 0.61 (0.44) | 0. 64 (0.44) | –0.03 | 0.99 | –1.33 to 1.30 |
| Aids and adaptations | 0.38 (0.19) | 0.35 (0.21) | 0.03 | 0.93 | –0.65 to 0.60 |
| Total cost | 249.58 (72.38) | 426.59 (119.86) | –177.01 | 0.21 | –420.89 to 137.92 |
| 0–6 months (n = 189 total: IM nail group, n = 91; locking plate group, n = 98) | |||||
| Initial operation cost | 5460.04 (137.92) | 5600.11 (137.92) | –140.07 | 0.19 | –684.24 to 262.61 |
| Subsequent Inpatient care | 40.73 (29.35) | 313.14 (187.55) | –272.41 | 0.08 | –648.97 to 104.13 |
| Outpatient care | 218.66 (11.46) | 249.01 (19.49) | –30.35 | 0.09 | –75.00 to 14.31 |
| Community care | 106.91 (28.42) | 601.69 (371.42) | –494.78 | 0.10 | –1233.98 to 244.42 |
| Medications | 37.73 (10.18) | 38.83 (14.28) | –1.11 | 0.47 | –35.73 to 33.52 |
| PSS | 0.52 (0.52) | 0.98 (0.59) | –0.46 | 0.28 | –2.02 to 1.10 |
| Aids and adaptations | 10.97 (2.30) | 10.45 (1.61) | 0.52 | 0.58 | –5.02 to 6.06 |
| Total costs throughout first 6 months | 5875.56 (124.85) | 6814.22 (425.71) | –938.66 | 0.04* | –1795.46 to –83.62 |
| 0–12 months (total, n = 160: IM nail group, n = 70; locking plate group, n = 78) | |||||
| Initial operation costs | 5428.47 (112.00) | 5528.72 (114.25) | –100.26 | 0.53 | –671.23 to 298.66 |
| Subsequent inpatient care | 234.91 (92.68) | 596.25(237.18) | –361.34 | 0.16 | –848.35 to 211.12 |
| Outpatient care | 268.94 (16.90) | 299.14 (26.25) | –30.20 | 0.34 | –100.29 to 27.88 |
| Community care | 107.09 (23.30) | 588.22 (410.64) | –481.13 | 0.25 | –1401.81 to 361.51 |
| Medications | 58.14 (19.60) | 78.45 (35.95) | –20.31 | 0.62 | –111.91 to 62.76 |
| PSS | 0.32 (0.32) | 0.91 (0.64) | –0.59 | 0.40 | –2.16 to 0.88 |
| Aids and adaptations | 9.45 (2.08) | 10.77 (1.89) | –1.28 | 0.65 | –7.90 to 2.03 |
| Total costs throughout first 12 months | 6107.32 (158.56) | 7102.46 (485.18) | –995.14 | 0.05 | –2069.63 to –74.93 |
| Cost category by period | Treatment arm, mean (SE) cost | Mean difference | p-valuea | |
|---|---|---|---|---|
| IM nail fixation | Locking plate | |||
| Follow-up period: 0–6 months | ||||
| NHS and PSS costs | 5875.56 (124.85) | 6814.22 (425.71) | –938.66 | 0.04 |
| Private costs | 16.36 (8.02) | 12.46 (3.74) | 3.90 | 0.65 |
| Cost of lost productivity | 3901.13 (759.48) | 5351.80 (814.56) | –1450.67 | 0.20 |
| Societal costs | 9793.05 (761.66) | 12,178.48 (1003.33) | –2385.43 | 0.07 |
| Follow-up period: 0–12 months | ||||
| NHS resource use costs | 6107.32 (158.56) | 7102.46 (485.18) | –995.14 | 0.06 |
| Private costs | 49.52 (35.72) | 24.65 (7.80) | 24.87 | 0.48 |
| Cost of lost productivity | 3333.28 (649.45) | 5758.62 (1032) | –2425.34 | 0.05 |
| Societal costs | 9490.12 (658.07) | 12,885.73 (1174.33) | –3395.61 | 0.01 |
Health outcomes
Table 25 details the number and proportion of individuals reporting each of the EQ-5D dimension levels at each time point. The proportion of trial participants reporting suboptimal health (moderate to extreme health outcomes) is also indicated for each dimension and the difference between the two treatment arms shown by p-values. With the exception of mobility at 3 months [IM nail fixation (81%) vs. locking plate fixation (89%)], which was statistically significant at the 10% significance level, there were no significant differences in the proportions of individuals reporting suboptimal health within dimensions between the two arms at each time point.
| Time point | EQ-5D domain level, n (%)a | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mobility | Self-care | Anxiety/depression | Usual activities | Pain/discomfort | ||||||||||||||||
| Level 1 | Level 2 | Level 3 | Suboptimal | Level 1 | Level 2 | Level 3 | Suboptimal | Level 1 | Level 2 | Level 3 | Suboptimal | Level 1 | Level 2 | Level 3 | Suboptimal | Level 1 | Level 2 | Level 3 | Suboptimal | |
| Baseline: IM (n = 157); locking plate (n = 158) | ||||||||||||||||||||
| IM nail | 3 (2) | 44 (28) | 110 (70) | 154 (98) | 19 (12) | 109 (69) | 29 (18) | 138 (88) | 64 (41) | 74 (47) | 18 (11) | 92 (59) | 5 (3) | 28 (18) | 124 (79) | 152 (97) | 6 (4) | 92 (59) | 59 (38) | 151 (96) |
| Locking plate | 2 (1) | 41 (26) | 115 (73) | 156 (99) | 19 (12) | 109 (69) | 30 (19) | 139 (88) | 76 (48) | 70 (44) | 12 (8) | 82 (52) | 4 (3) | 29 (18) | 124 (78) | 153 (97) | 11 (7) | 103 (65) | 44 (28) | 147 (93) |
| p-value | 0.65 | 0.98 | 0.94 | 0.73 | 0.12 | |||||||||||||||
| 3 months: IM (n = 135); locking plate (n = 141) | ||||||||||||||||||||
| IM nail | 25 (19) | 107 (79) | 3 (2) | 110 (81) | 96 (71) | 38 (28) | 2 (1) | 40 (29) | 71 (53) | 58 (43) | 7 (5) | 65 (48) | 12 (9) | 99 (73) | 25 (19) | 124 (92) | 21 (16) | 104 (77) | 11 (8) | 115 (85) |
| Locking plate | 15 (11) | 125 (89) | 1 (1) | 126 (89) | 92 (65) | 49 (35) | 0 | 49 (35) | 76 (54) | 53 (38) | 12 (9) | 124 (88) | 6 (4) | 102 (72) | 33 (23) | 135 (96) | 16 (11) | 107 (76) | 18 (13) | 125 (89) |
| p-value | 0.07 | 0.34 | 0.42 | 0.12 | 0.31 | |||||||||||||||
| 6 months: IM (n = 142); locking plate (n = 142) | ||||||||||||||||||||
| IM nail | 64 (45) | 77 (54) | 1 (1) | 78 (55) | 116 (82) | 26 (18) | 0 | 26 (18) | 81 (57) | 52 (37) | 9 (6) | 142 (43) | 53 (37) | 77 (54) | 12 (8) | 89 (63) | 34 (24) | 98 (69) | 10 (7) | 108 (76) |
| Locking plate | 57 (40) | 85 (60) | 0 | 85 (60) | 114 (80) | 28 (20) | 0 | 28 (20) | 85 (60) | 50 (35) | 7 (5) | 142 (40) | 41 (29) | 85 (6) | 16 (11) | 101 (71) | 29 (20) | 108 (76) | 5 (4) | 113 (80) |
| p-value | 0.401 | 0.762 | 0.72 | 0.13 | 0.28 | |||||||||||||||
| 12 months: IM (n = 116); locking plate (n = 118) | ||||||||||||||||||||
| IM nail | 73 (63) | 43 (37) | 0 | 43 (37) | 98 (84) | 18 (16) | 0 | 18 (16) | 77 (66) | 35 (30) | 3 (3) | 38 (33) | 61 (53) | 51 (44) | 4 (3) | 55 (47) | 37 (32) | 73 (63) | 6 (5) | 79 (68) |
| Locking plate | 71 (60) | 46 (39) | 1 (1) | 47 (40) | 105 (89) | 13 (11) | 0 | 13 (11) | 82 (69) | 31 (26) | 5 (4) | 36 (31) | 68 (58) | 43 (36) | 7 (6) | 50 (42) | 41 (35) | 72 (61) | 5 (4) | 77 (65) |
| p-value | 0.66 | 0.31 | 0.55 | 0.44 | 0.87 | |||||||||||||||
Cost-effectiveness results
The cost-effectiveness results are presented in Table 26 with locking plate fixation selected as the comparator. The analytic time horizon covers the entire 12-month follow-up period of the trial. Table 26 shows the joint distribution of incremental costs and outcomes for the base-case analysis, sensitivity analyses and subgroup analyses. The joint distribution of costs and outcomes for the base-case analysis, sensitivity analyses and subgroup analyses are graphically represented in Figure 9 using the NMB metric and in Figure 10 using scatterplots and cost-effectiveness acceptability curves. Plots for the remaining of the sensitivity analyses that are not shown in Figure 10 mirror the base-case analysis plot. As such, we elected not to present them.
| Scenario | Incremental cost (95% CI) | Incremental QALYs (95% CI) | ICERa | Probability of cost-effectiveness (willingness-to-pay threshold) | NMB (willingness-to-pay threshold) | ||||
|---|---|---|---|---|---|---|---|---|---|
| £15,000 per QALY | £20,000 per QALY | £30,000 per QALY | £15,000 per QALY (95% CI) | £20,000 per QALY (95% CI) | £30,000 per QALY (95% CI) | ||||
| Base-case analysis | |||||||||
| Imputed attributable costs and QALYs, covariate adjusted | –970 (–1685 to –256) | 0.01 (–0.03 to 0.06) | Dominant | 0.98 | 0.97 | 0.94 | 1204 (43 to 2465) | 1273 (–82 to 2689) | 1410 (–385 to 3190) |
| Sensitivity analyses | |||||||||
| Complete-case attributable costs and QALYs, covariate adjusted | –1791 (–3986 to –225) | 0.04 (–0.02 to 0.09) | Dominant | 0.99 | 0.98 | 0.98 | 1429 (146 to 2818) | 1558 (118 to 3069) | 1818 (36 to 3626) |
| Societal perspective | –2230 (–4626 to 167) | 0.014 (–0.03 to 0.06) | Dominant | 0.97 | 0.97 | 0.96 | 2423 (–26 to 5173) | 2493 (–93 to 5337) | 2626 (–270 to 5706) |
| Per-treatment analysis – imputed attributable costs and QALYs, covariate adjusted | –875 (–1725 to –26) | –0.01 (–0.06 to 0.04) | 172,857 (south-west quadrant) | 0.92 | 0.88 | 0.81 | 923 (–347 to 2353) | 909 (–570 to 2508) | 872 (–1032 to 2861) |
| Imputed attributable costs and QALYs, additionally controlling for pre-injury utility | –1188 (–2266 to –110) | 0.02 (–0.02 to 0.06) | Dominant | 0.99 | 0.99 | 0.98 | 1518 (212 to 2940) | 1633 (180 to 3194) | 1862 (66 to 3738) |
| Subgroup analyses | |||||||||
| Base case: aged < 50 years | –1468 (–3547 to –291) | 0.08 (0 to 0.17) | Dominant | 0.99 | 0.98 | 0.98 | 1730 (207 to 3320) | 1953 (166 to 3804) | 2402 (55 to 4830) |
| Base case: aged ≥ 50 years | –821 (–2760 to 1110) | –0.022 (–0.09 to 0.05) | 60,000 (south-west quadrant) | 0.71 | 0.67 | 0.62 | 709 (–1960 to 3480) | 630 (–2320 to 3610) | 473 (–3065 to 3930) |
| Base case: males | –1651 (–5042 to –682) | 0.05 (–0.07 to 0.17) | Dominant | 0.71 | 0.68 | 0.62 | 745 (–1945 to 3612) | 670 (–2305 to 3741) | 520 (–3043 to 4075) |
| Base case: females | –1193 (–5243 to 102) | 0.02 (–0.05 to 0.10) | Dominant | 0.71 | 0.68 | 0.62 | 746 (–1950 to 3643) | 673 (–2307 to 3781) | 529 (–3049 to 4157) |
FIGURE 9.
Forest plots of base-case, sensitivity and subgroup analyses showing the impact on incremental NMB at cost-effectiveness thresholds of (a) £15,000 per QALY, (b) £20,000 per QALY and (c) £30,000 per QALY.
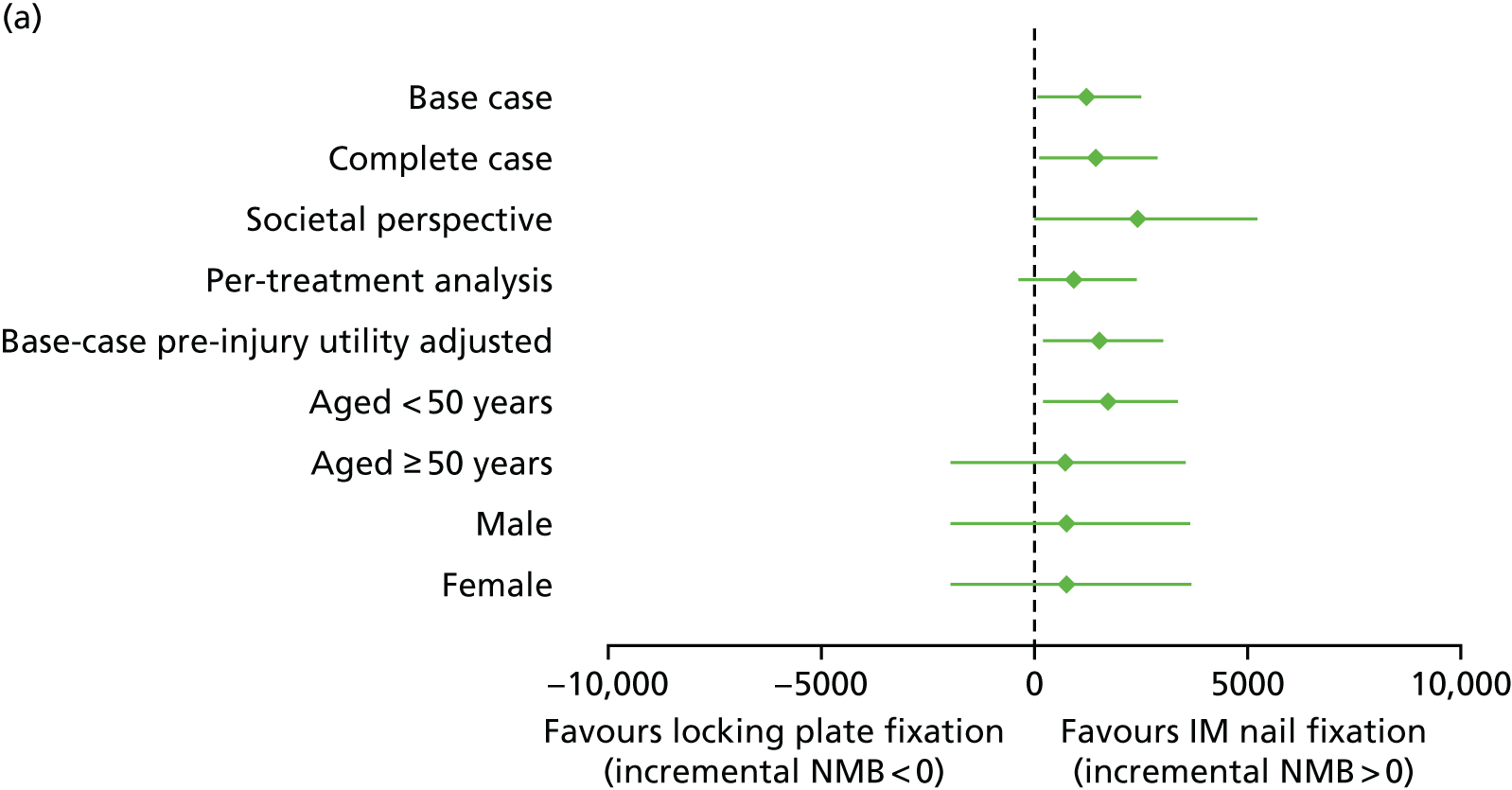
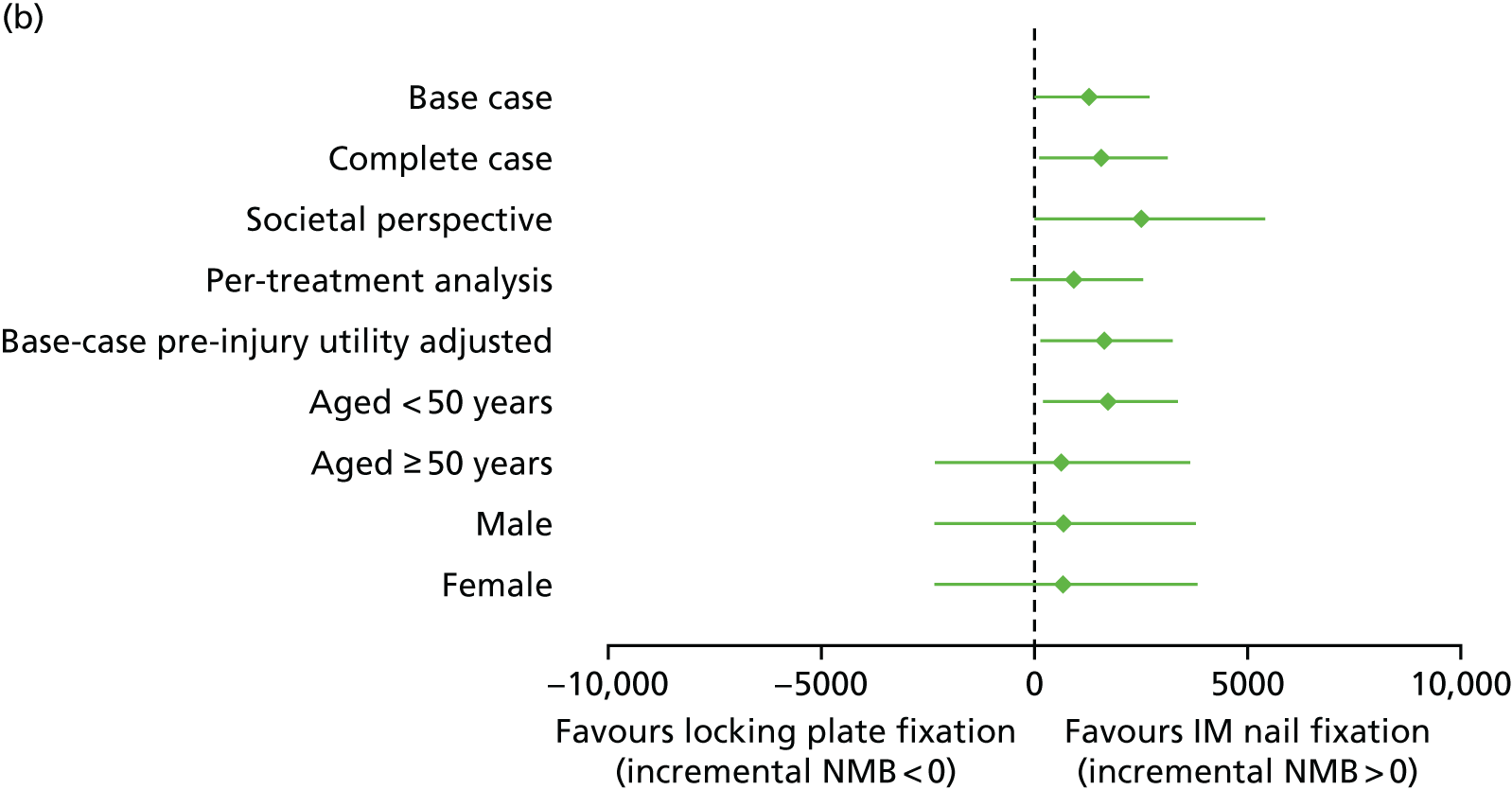
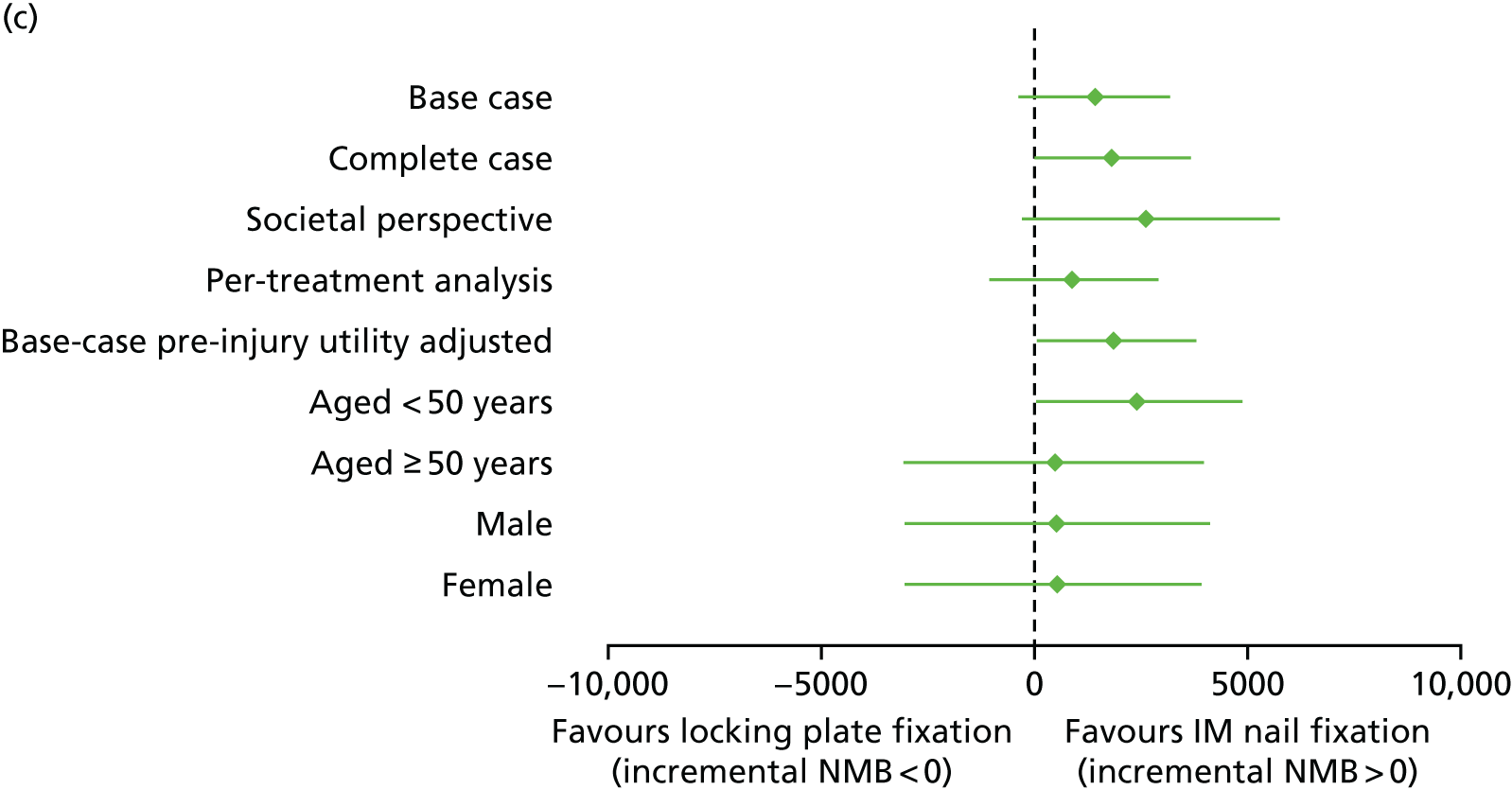
FIGURE 10.
Cost-effectiveness scatterplots and acceptability curves at 12 months. Base-case analysis (NHS and personal social service perspective, imputed, intention-to-treat analysis): (a) scatterplot and (b) cost-effectiveness acceptability curve; complete-case analysis – (c) scatterplot and (d) cost-effectiveness acceptability curve; and imputed per-treatment analysis – (e) scatterplot and (f) cost-effectiveness acceptability curve.
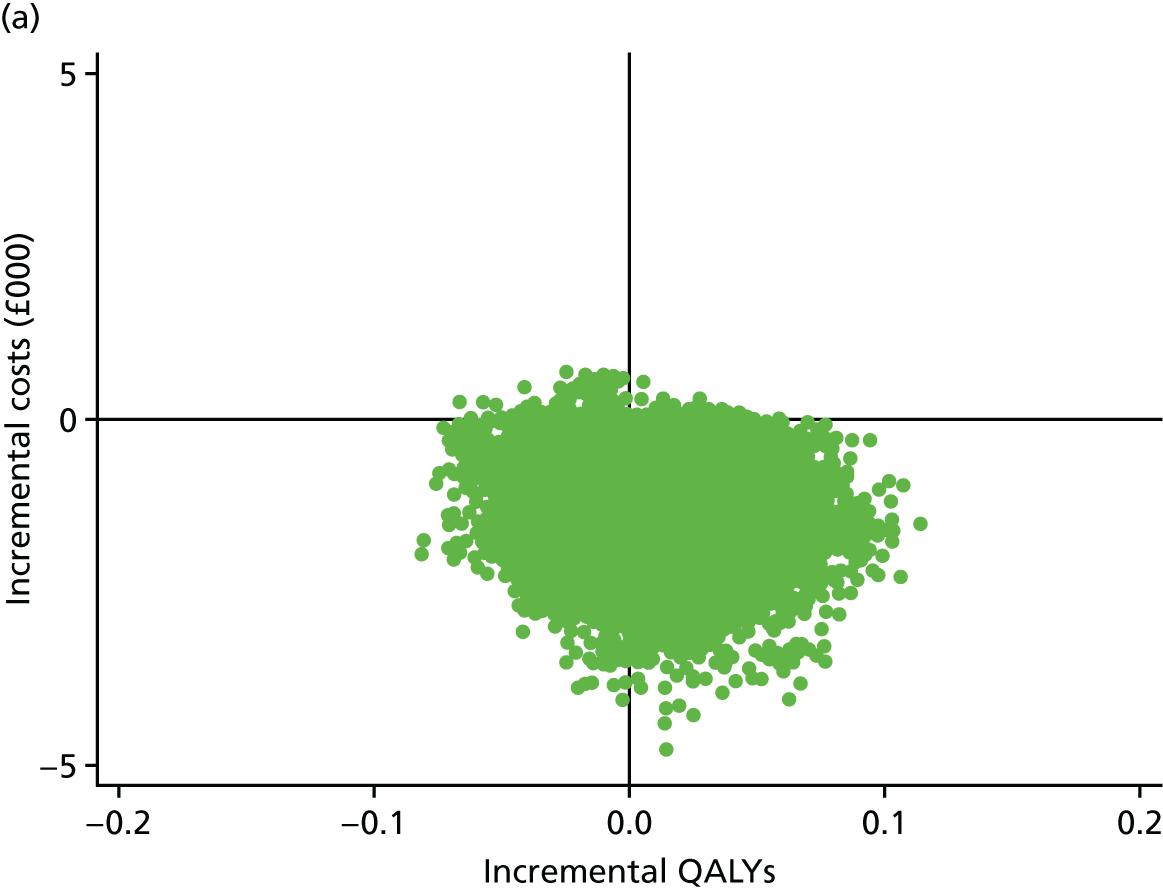
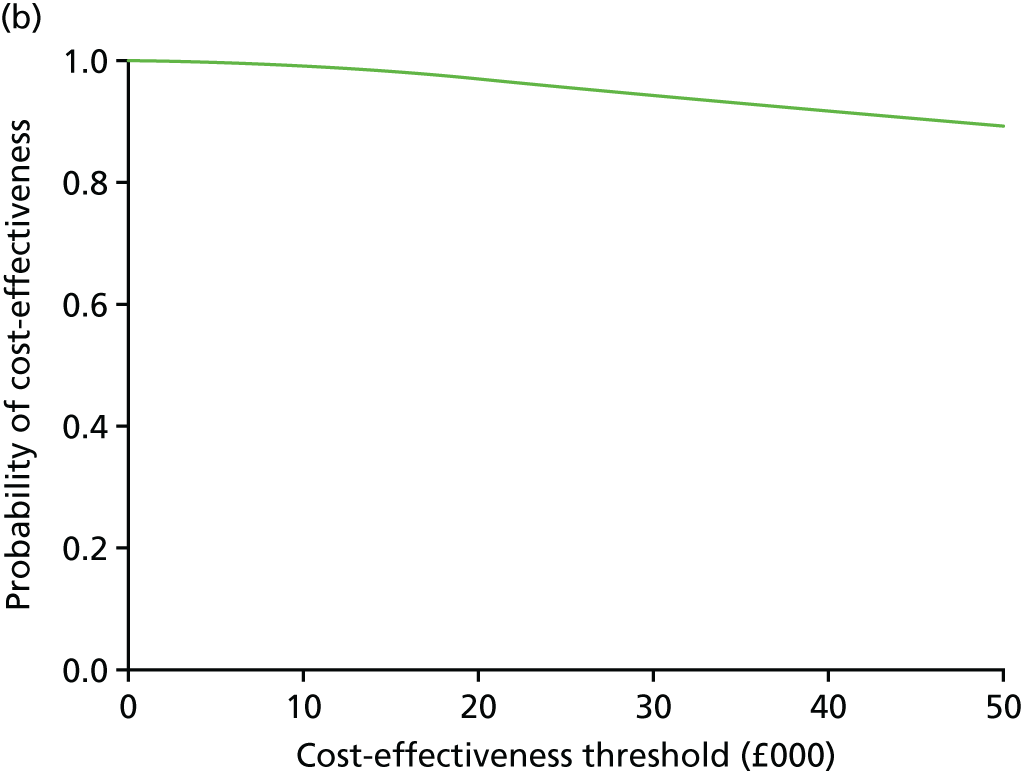
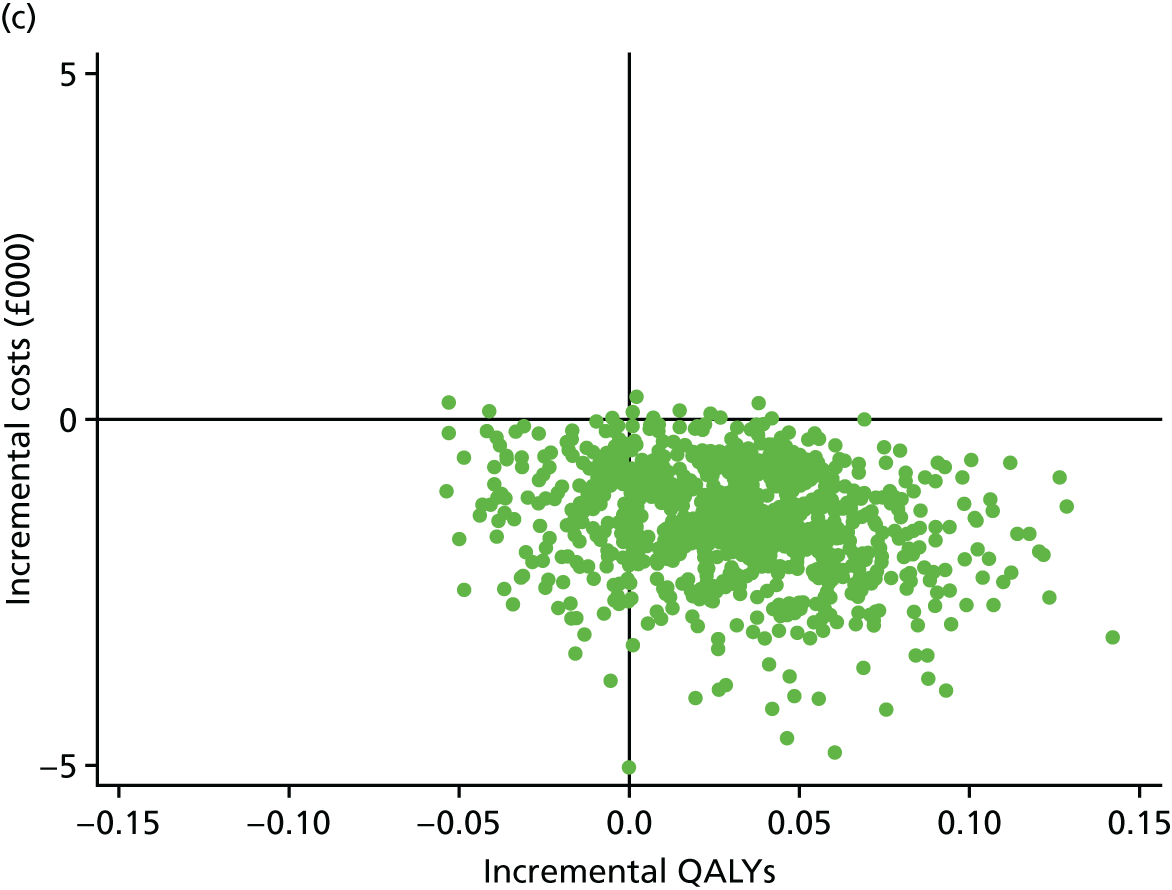
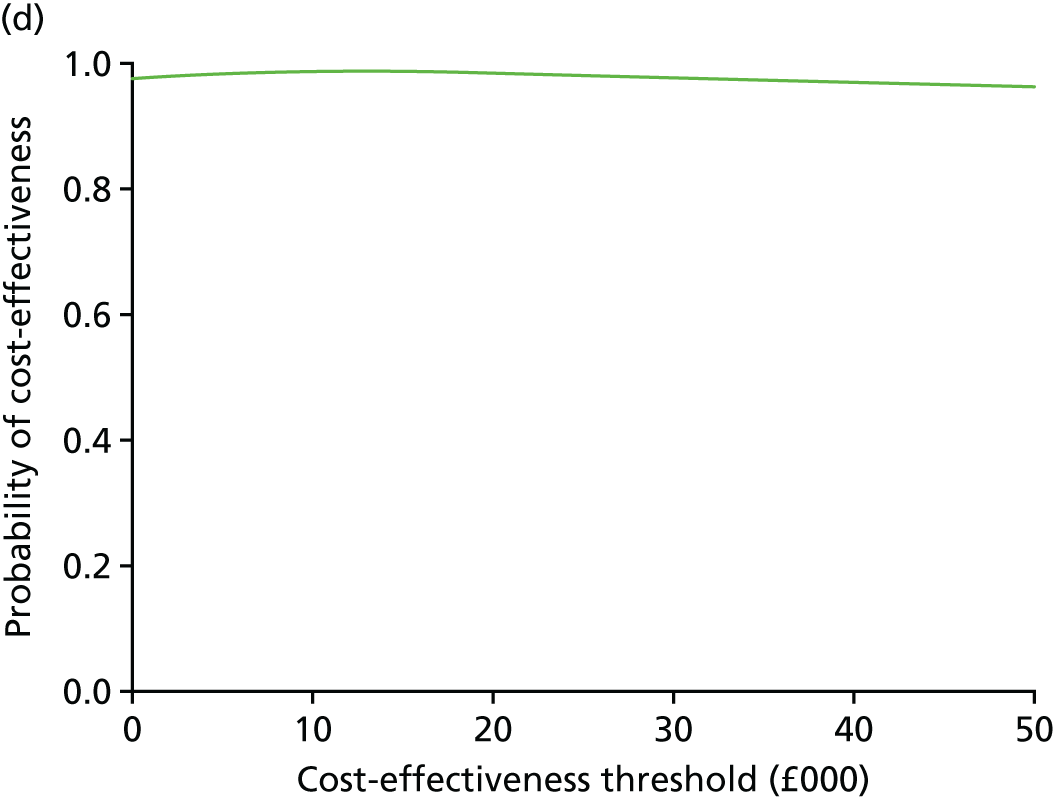
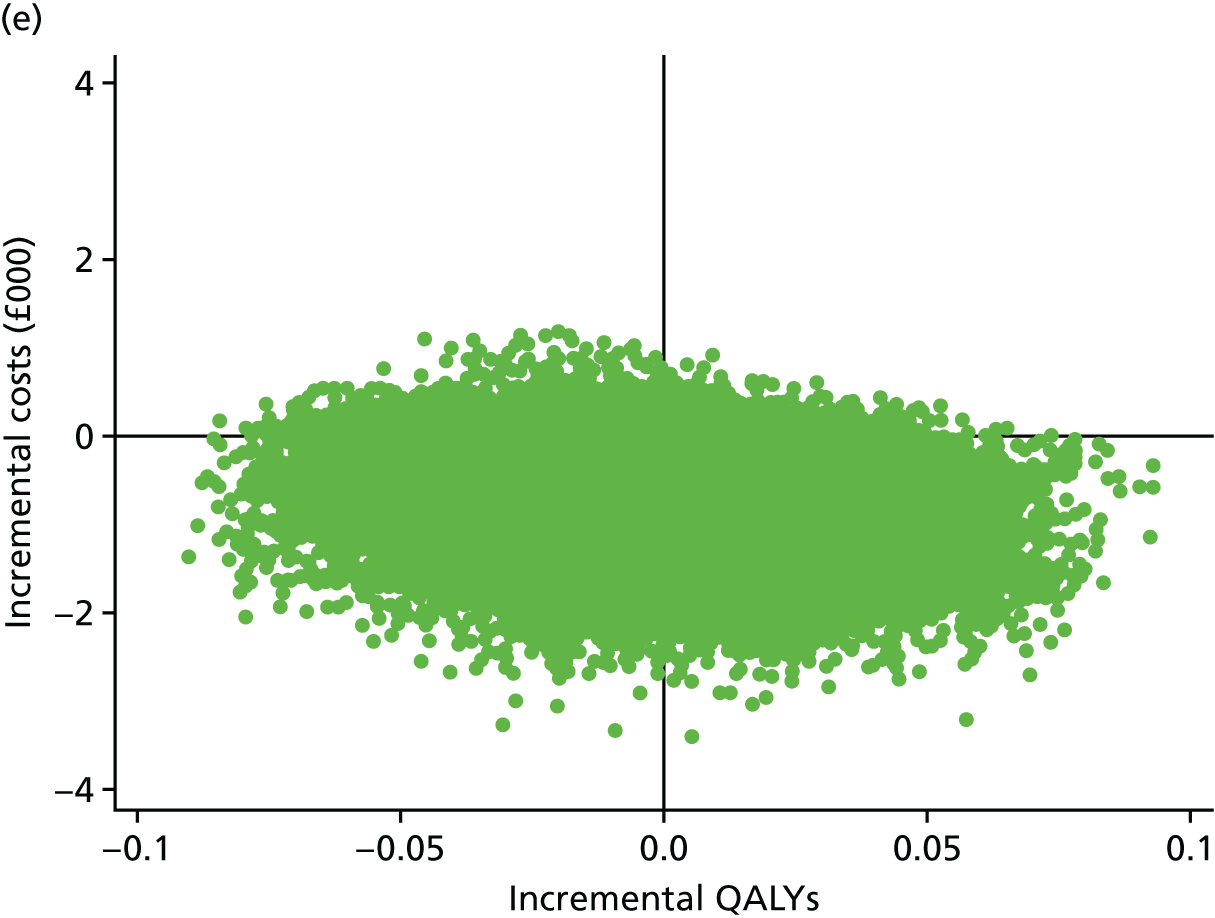
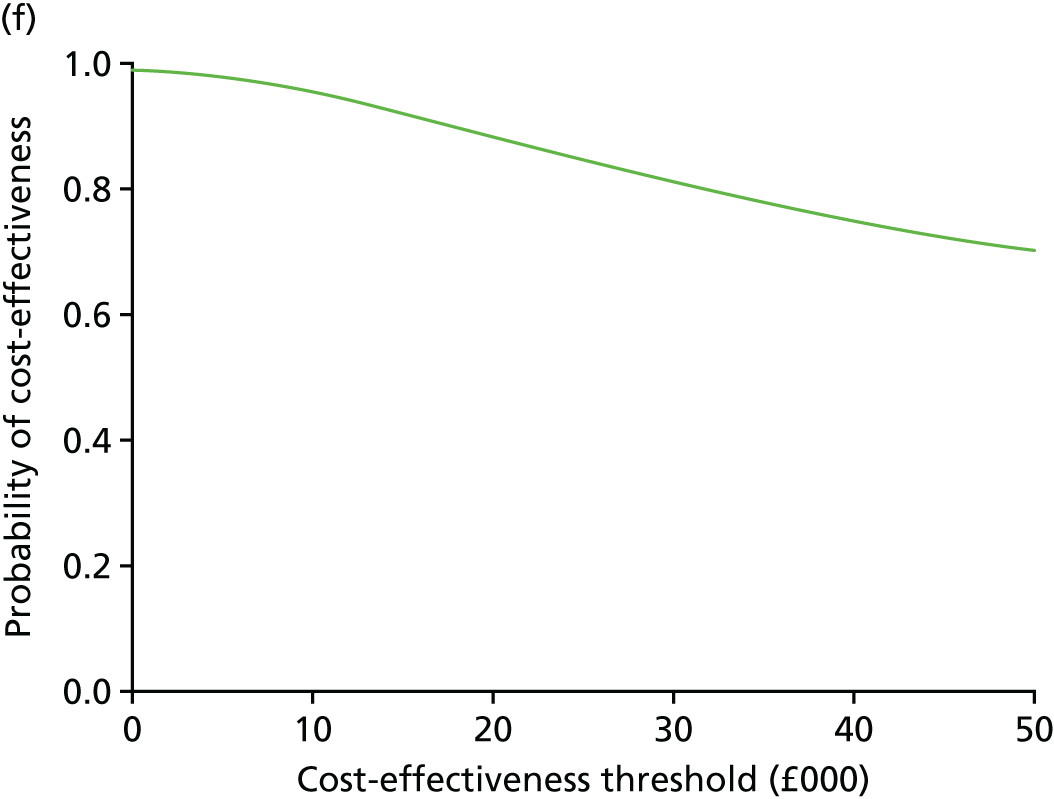
Base-case analysis
Patients allocated IM nail fixation experienced a non-statistically significant increase in QALYs in the base case (0.01 QALYs, 95% CI –0.03 to 0.06 QALYs) over a 12-month period. Mean NHS and PSS costs were significantly lower in the IM nail fixation group (–£970, 95% CI –£1685 to –£256). The ICER for the base-case analysis indicates that IM nail fixation is the dominant procedure, as average costs for this intervention were lower and average benefits were greater than those for locking plate fixation.
Assuming cost-effectiveness thresholds of £15,000 per QALY, £20,000 per QALY and £30,000 per QALY, the probability of cost-effectiveness for IM nail fixation ranged from 0.94 to 0.98 and the NMB associated with IM nail fixation was positive (see Figure 9). However, the 95% confidence levels for the NMB statistics overlapped the zero mark; the exception was the NMB at a cost-effectiveness threshold of £15,000 per QALY, for which the upper and lower limits for the 95% CI were both positive.
Sensitivity analyses
Comparing the mean costs and QALY estimates using different analytical scenarios [complete case, societal perspective and imputed attributable costs (additionally controlled for pre-injury utility)] supported the base-case finding (see Table 26, Figures 9 and 10]. However, the per-treatment analysis showed a slightly different pattern for QALY outcomes (see Table 26 and Figure 10). The results for this analysis indicated that participants in the IM fixation arm experienced slightly worse health-related quality-of-life outcomes. However, the result was not statistically significant. The cost difference remained in the same direction as that for the base-case analysis and indicated that IM fixation was significantly less costly than locking plate fixation.
Subgroup analyses
The subgroup analyses for age and sex revealed that there was significant interaction between treatment effect and age group, but this was significant at the 10% significance level (p-value of 0.09); the sex subgroup analysis did not reveal any statistically significant interactions. IM nail fixation lowered costs for patients aged < 50 years (–£1468, 95% CI –£3547 to –£291) and moderately increased QALY benefits (see Table 26). For patients aged ≥ 50 years, IM fixation reduced costs and moderately reduced QALY outcomes, with an ICER of £60,000 per QALY that fell within the south-west quadrant of the cost-effectiveness plane, that is, the average costs were less and average benefits were also lower for IM nail fixation than for locking plate fixation. The 95% CIs for both the costs and QALY estimates suggest considerable uncertainty surrounding the effects of IM nail fixation for this category of patients; this is graphically depicted in the NMB forest plot (see Figure 9). Cost-effectiveness acceptability curves for the subgroup analyses show the differences in probability of cost-effectiveness of IM nail fixation versus locking plate fixation (Figure 11). According to Figure 11, the probability that IM nail fixation is more cost-effective is higher for individuals aged < 50 years. There is no observable difference in probability of cost-effectiveness of IM nail fixation between male and female participants.
FIGURE 11.
Cost-effectiveness acceptability curves at 12 months (NHS and personal social service perspective, imputed). (a) Age; and (b) sex.
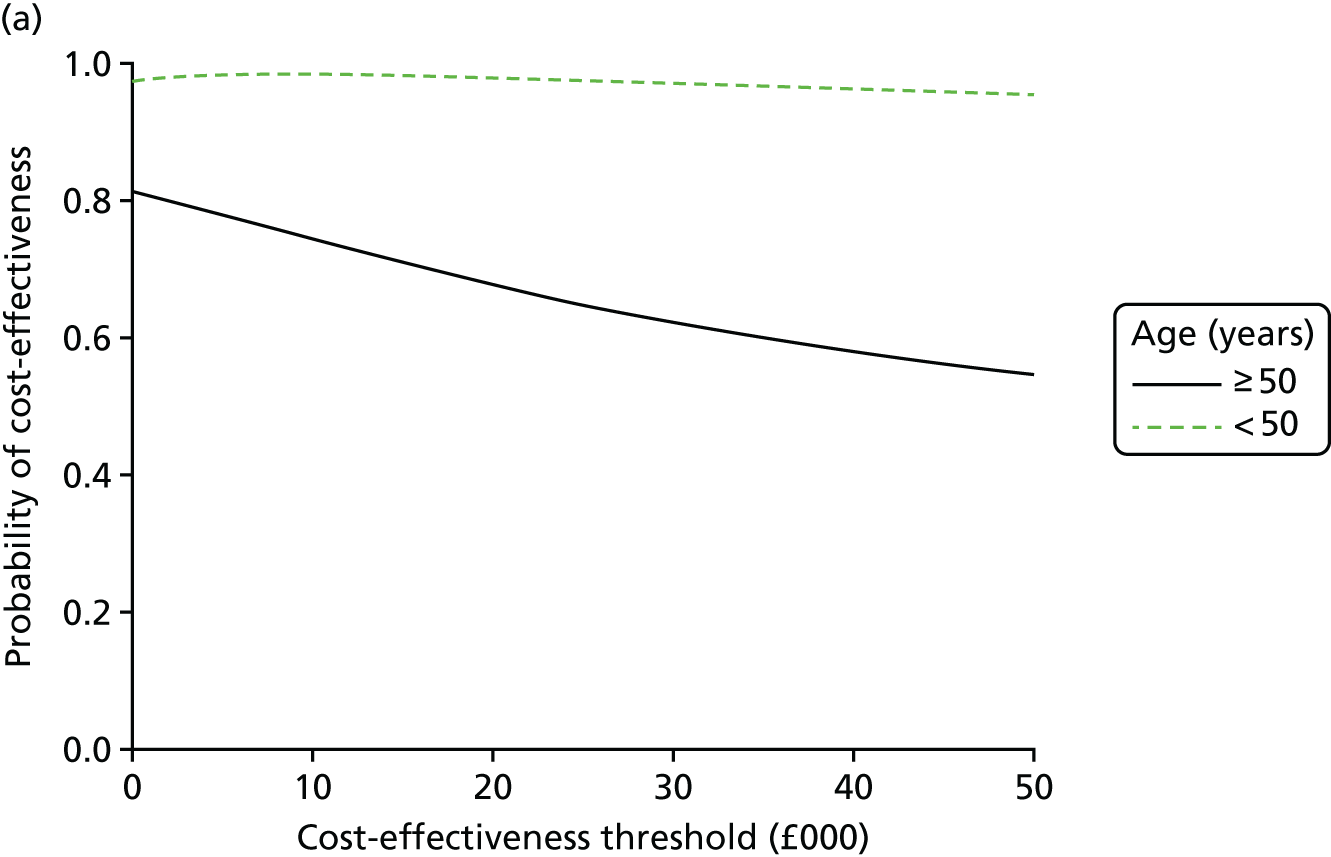
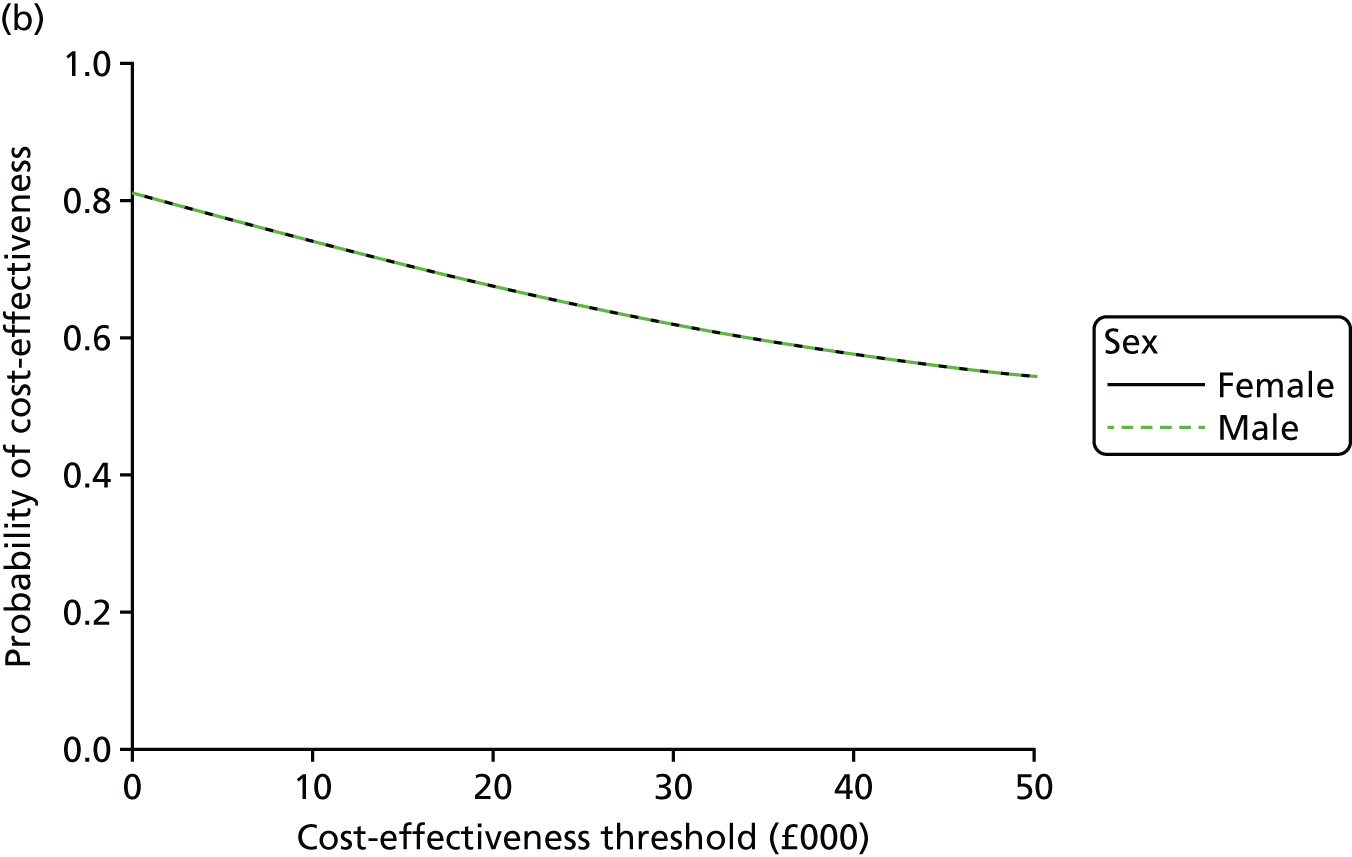
Long-term economic modelling
The protocol allowed for long-term decision-analytic modelling of the economic outcomes. We conducted a further analysis of the health-related quality-of-life outcomes of the trial participants using extended follow-up data for this trial. This analysis indicated that EQ-5D utility scores for the IM nail fixation and locking plate groups were similar at 24 months post randomisation. This analysis was based on sample of 74 (out of 113) participants who had reached the 24-month follow-up time point at the time of writing. The mean EQ-5D utility score in the IM nail fixation group was 0.76 (95% CI 0.69 to 0.82) versus 0.80 (95% CI 0.74 to 0.85) in the locking plate group at 24 months post randomisation. The p-value for the utility score difference of 0.36 was not statistically significant. This indicated that the benefits of IM nail fixation are very likely to be concentrated in the first year following the treatment of displaced, extra-articular fractures of the distal tibia. In addition, external studies were systematically searched for comparisons of locking plate and IM nail fixation, but no good-quality evidence on differences in functional outcomes and health-related quality of life beyond 12 months post surgery could be found. The available studies were based on a short follow-up period,41 had a small sample size,12,42,43 and was a non-randomised study that relied on retrospective reviews or case series, which tend to suffer from selection bias,11,12,43 or had a combination of these factors. It was, therefore, concluded that longer-term extrapolation of the cost-effectiveness of IM nail fixation would not be appropriate.
Chapter 5 Summary and discussion
Screening
A large number of patients were screened for eligibility to enter the trial, which is testament to the hard work of the research teams at each centre. As all patients with a fracture of the tibia are seen by specialist surgeons on the day that they attend the emergency department and because the great majority of patients with this fracture are admitted to the hospital, we can be confident that the research teams screened all potentially eligible patients.
Table 27, Appendix 1, shows the reasons why screened potential patients were not eligible (n = 1581). The most commonly used exclusion criteria were as expected: the fracture was too proximal (did not extend within 2 Müller squares of the ankle joint 375/1581, 24%), the fracture was open (369/1581, 23%) or the fracture extended into the ankle joint (329/1581, 21%). However, the wide variation in totals, by centre, indicates that some sites screened extensively and recorded any patient with a fracture involving the tibia; however, others only recorded fractures of the ‘distal’ tibia on the screening logs. Some centres also included children in their screening log; however, other adult-only trauma centres did not admit any children to their hospital.
Eligible but did not participate
The reasons why eligible potential participants were not randomised (n = 216) are given in Table 28, Appendix 1. This information is key to determining the external validity of the trial, that is, the degree to which the result of the UK FixDT trial can be generalised to the broader population of patients with a fracture of the distal tibia.
Some of the reasons were inevitable and are unlikely to have created a selection bias within the trial. The NIHR Clinical Research Network is, generally, unable to provide routine weekend research associate support for clinical trials, so 53 out of these 216 patients (25%) were not recruited for the reason of ‘no research staff being available’. Similarly, there were 18 potential participants for whom the reason for non-participation was on obvious clinical grounds; these reasons included skin around ankle precluded locking plate fixation (n = 4), primary amputation (n = 3) and hind foot nails used (n = 2). Thirteen patients (13/216, 6%) declined any surgery, despite this being offered by the clinical team. The number of patients who declined the trial as they ‘did not want to be part of a research study’ (25/216, 12%) or ‘did not want to fill in a questionnaire’ (9/216, 4%) was small, which, once again, goes to show that patients with even severe injuries are keen to take part in research projects.
Patients who were not included in the trial because of a preference for one treatment or the other were of more potential concern. However, preference for a treatment did not seem to be a important issue for the patients; only 38 patients (38/216, 18%) expressed a preference, of whom 23 preferred a IM nail fixation and 15 a locking plate fixation. By contrast, there was a stronger treatment preference among the surgeons and 57 potentially eligible patients were excluded because the surgeon had a treatment preference for the patient. Of these 57 participants, 54 were because the surgeon had a preference to use an IM nail and three were because the surgeon had a preference to use a locking plate. The breakdown of patients who were potentially eligible but who did not participate by centre is informative. Some centres had no such patients; however, two centres had 13 (Royal Sussex County Hospital) and eight (Frenchay Hospital), suggesting that there was a ‘centre’ preference for IM nail fixation in those centres. The Royal Infirmary of Edinburgh demonstrated this phenomenon very early in their recruitment period and decided to withdraw from the trial completely after only one patient was recruited.
Overall, 60% of patients who were potentially eligible to take part in the trial were approached and agreed to take part. Only 17% of patients who were potentially eligible did not take part in the trial because of a preference for one treatment or the other; the majority as a result of surgeon preference rather than a patient preference. Table 3 showed that the baseline characteristics of those patients who were eligible and recruited versus those who were potentially eligible but not recruited were well matched.
Therefore, in summary, we can be confident that the results of this trial can be extrapolated to the wider population with a fracture of the distal tibia.
Treatment according to allocation
The CONSORT flow diagram (see Figure 3) shows that 156 out of the 161 patients allocated to IM nail fixation received the allocated treatment. Of the 160 patients allocated to locking plate fixation, 137 received the allocated treatment. Therefore, in total, 91% (293/321) of the patients who were randomised received their allocated treatment.
The fact that fewer patients crossed over from IM nail to locking plate fixation than from locking plate to IM nail fixation may, again, reflect a surgeon preference for IM nail fixation. However, the number of crossovers is too small to comment in any meaningful way. Importantly, the small number of crossovers overall makes it very unlikely that surgeon preference will have affected the result of the trial.
Recruitment by centre
The rate of recruitment by centres varied between < 0.1 pcpm (Basingstoke & North Hampshire Hospital) and > 1.4 pcpm (University Hospitals of Leicester). To a large degree this was determined by the size of the catchment area (population served) by the hospital. University Hospitals of Leicester has a very large catchment compared with Basingstoke & North Hampshire Hospital. Given that some centres were only open for a few months (Basingstoke & North Hampshire Hospital), and the number of patients presenting to each centre per month was relatively low, the variation in recruitment rate may also have been affected by simple variation in presentations over a short period of time.
However, some large-catchment hospitals were open for a relatively long time and still had a low rate of recruitment, for example Frenchay Hospital and University Hospitals Coventry & Warwickshire. Therefore, it is more likely that the rate of recruitment in those centres was affected by local recruitment issues. Several centres reported being affected by staff shortages (King’s College Hospital, Aintree University Hospital). Only one centre (Royal Infirmary of Edinburgh) withdrew because of lack of equipoise in the local surgeons.
Baseline characteristics of the two groups
Patients
The baseline demographic and clinical characteristics of both treatment groups were well balanced by the randomisation process (see Table 6). The baseline patient-reported outcome measures also showed good balance, with similar mean scores being seen across all of the outcomes measures.
Of the 321 patients randomised into the trial, 70% had no preference for which treatment they received. This is further evidence that the patients did appear to have equipoise having read the participant information sheet and discussed the trial with the clinical team, as well as with their friends and relatives.
The most common mechanism of injury was a ‘low-energy fall’ and the great majority of patients did not have any other injuries at the time of their fracture, that is, the majority of distal tibial fractures are isolated injuries rather than one of multiple injuries in the context of high-energy polytrauma (see Table 6).
Surgeons
Surgery for fracture of the distal tibia is potentially complicated and may be technically challenging, depending on the fracture pattern and associated soft-tissue injury. It is, therefore, unsurprising that the majority of operations in both groups were performed by consultant surgeons: 90 (56%) of IM nail fixations and 99 (62%) of locking plate fixations. The great majority of the other operations being performed by a trainee surgeon under supervision by a consultant. As surgery to fix the distal tibia is technically demanding, surgical assistants are often required. There was, on average, 2.5 surgeons present in the operating theatre for both the IM nail fixations and locking plate fixations.
Surgery
Full details of the surgery performed are given in Table 8. Of note, the duration of surgery was exactly the same in both groups of patients, with a mean duration of 2 hours and 4 minutes of operating time. This contrasts with some previous reports, in which IM nail fixation was found to be a quicker procedure. 14
The use of locking plate fixation provides more options for screw fixation distal to the fracture than IM nail fixation. This is inherent in the design of the implants and, indeed, is one of the theoretical advantages of locking plate fixation. As expected, the number of screws used in the distal part of the plates was greater than the number used in the nails. Five or six distal locked screws were used most commonly in the locking plate fixation group.
The use of blocking (Poller) screws to augment the IM nail fixation of metaphyseal fractures, such as those in the distal tibia, is the subject of much debate in the orthopaedic trauma community. However, surgeons in this trial only used blocking screws in 21% of fractures fixed with a tibial nail. The number of cases in which blocking screws were used is too small to comment on differences between centres and certainly too small to identify preferences between surgeons.
Intraoperative complications, including extension of the distal tibial fracture into the ankle joint, were rare: 2% in both groups. This is reassuring as one of the often quoted ‘risks’ associated with IM nail fixation is that the nail may propagate the fracture into the weight-bearing portion of the distal tibial articular surface at the ankle.
Table 9 shows that the number of patients who crossed over to the other treatment group after randomisation; this is inevitable in trials of surgical interventions and may be because of intraoperative clinical reasons or surgeon preference. Of course, there may be some overlap between these reasons, as an individual surgeon may feel more confident using one technique over another. In technically demanding surgery, such as fixation of fractures of the distal tibia, this may be a large effect. However, in the UK FixDT trial, over 91% (293/321) of participants received their allocated treatment. Therefore, we can be confident that the results of the trial were not unduly affected by crossover of treatment. Even so, we used the conservative intention-to-treat approach as the primary analysis.
Among those allocated to the IM nail fixation group, 97% (156/161) of participants received their allocated treatment, and in the locking plate group, 86% (137/160) of participants received their allocated treatment (there were three participant withdrawals before any intervention was undertaken: two were treated with external fixation and one was treated with manipulation under anaesthetic only). The small number of patients who crossed over were spread across all of the centres; the highest being eight patients (University Hospitals of Leicester), although this centre also had the highest overall recruitment (45 participants). No other centre had more than three patients crossover treatment, so there did not appear to be a centre-specific effect. A centre-specific effect in surgical trials may be because of the particular philosophy and/or training issues in that centre/regional training programme. Again, a preference for one technique may be more common in technically demanding surgery. The one centre (Royal Infirmary of Edinburgh) that withdrew from the trial after only one patient was recruited, cited a preference for tibial nail over locking plate and, therefore, a lack of equipoise. Surgeons at this centre have written a large number of the published literature on tibial nail fixation, so there may have been an unconscious bias towards this technique.
Follow-up rate
The sample size for the UK FixDT trial allowed for 20% loss to follow-up. We achieved > 80% follow-up at each time point. Therefore, we can be very confident that we have achieved sufficient statistical power according to our prespecified sample size calculation.
Outcomes
Primary outcome
The adjusted estimate of the treatment effect for the DRI score at 3 months, on an intention-to-treat basis, is 8.8 points (95% CI 4.3 to 13.2 points) in favour of the nail group compared with the locking plate group. The p-value of < 0.001 indicates that there is strong evidence for a statistically significant difference in treatment group means at 3 months. The estimated treatment effect was larger than the prespecified MCID for the DRI score of 8 points. Therefore, at the 3-month time point, the difference between treatment groups is likely to be clinically important to patients.
However, the adjusted estimate of the treatment effect at 6 months was only 4.0 (95% CI –1.0 to 9.0) in favour of the IM nail group compared with the locking plate group. Six months was the primary end point for the trial and is the point upon which the sample size calculation was based. The p-value of 0.114 indicates that there is no evidence for a statistically significant difference in the DRI score between the two treatment groups at 6 months. The 95% CIs suggest that if there is a difference in the DRI score, it is unlikely to be clinically important to patients. However, the upper 95% CI does include the prespecified MCID of 8 points.
At the 12-month time point, the p-value of 0.468 indicates that there is no evidence for a statistically significant difference in the DRI score between the two treatment groups, the adjusted treatment difference being 1.9 (95% CI –3.2 to 6.9) in favour of the IM nail fixation group compared with the locking plate group. At 12 months, the upper 95% CI excludes the MCID.
To complement the preplanned analysis, a post hoc exploratory analysis using DRI score at all four time points was conducted. This analysis simplified longitudinal data collected at four time points to a single value, namely the AUC, and facilitated comparisons of the AUCs between treatment groups. Using the predicted model parameter, the calculated AUC for those allocated to IM nail fixation was 350 units (SE 16.4 units) and for the locking plate group was 407 units (SE 16.3 units), yielding a between-group difference of 57 units (95% CI 12 to 103 units). Larger DRI scores represent higher levels of disability, so larger AUCs are also associated with increased levels of disability. A t-test comparing the values between groups yielded a p-value of 0.013, indicating there is a statistically significant difference in AUC between treatment groups. Clinically, this result may be interpreted as evidence that those allocated to locking plates experienced more disability over the 12-month follow-up period than those allocated to the IM nail fixation.
In designing the trial, we expected that any difference between these two treatments would most likely occur around 6 months. However, in the light of uncertainty about the time course of recovery, we also made assessments at 3 and 12 months. The results show that the largest difference in DRI score actually occurred at the earlier time point of 3 months. The difference in disability reduced at 6 months, and there was very little difference at 12 months. In retrospect, we could perhaps have used 3 months as the primary end point, although traditionally later time points have been used in all trials involving fractures. The very similar results at 12 months are not too surprising, as the great majority of fractures of the tibia would be expected to have achieved bony union at this time point; only very large differences in other aspects of recovery – for instance, muscle strength – would be demonstrated using any outcome measurement tool at this later time point. However, a minimum of 12-month follow-up is important in such trials so that the disability associated with delayed or non-union of the fracture can be assessed. Although rare in the context of this trial, non-union may be more much common in other fractures.
Overall, the primary outcome result of this trial is good news for patients, in that IM nail fixation is associated with faster recovery, that is, there is less disability during the early stages of recovery following a fracture of the distal tibia. This is also an important observation for the design of future trials in fracture healing.
However, it is important for patients to note that, although the DRI scores improve in both groups of patients over the 12 months following the fracture, they did not return to their pre-injury levels. The average DRI score at 12 months was still 23 points out of a maximum disability of 100 points.
To set these results into context, we repeated the systematic review of the evidence regarding this question at the end of the UK FixDT trial. As noted in Chapter 1, Background, there was little evidence in the literature regarding the pattern of recovery before the trial began. Our updated review found that four trials have reported since the UK FixDT trial. 41,44–47
Vallier et al. 44 randomised 104 patients with an extra-articular fracture of the distal tibia to either IM nail fixation or plate fixation. However, the plates used in this study were ‘non-locking’ plates, that is, traditional ‘large fragment medial plates’. The authors did not include any patient-reported outcome measures in the initial report of the trial. They noted a high rate of complications in both arms, including non-union and infection, which may have affected functional outcome but their results are confounded by the inclusion of patients with open fractures. The same group subsequently reported later functional outcomes from the participants in their trial using the Foot Function Index and Musculoskeletal Function Assessment questionnaires. 45 They found that ‘scores were not related to plate or nail fixation’ but that both Musculoskeletal Function Assessment and Foot Function Index scores ‘were worse when knee pain or ankle pain was present’.
Fang et al. 46 compared the results of external fixation combined with limited internal fixation with a plate, minimally invasive percutaneous plate fixation and IM nailing for distal tibia fractures. They concluded that ‘all achieved similar good functional results’. The authors did not report a disability rating, although there was no evidence of a difference between groups in the American Orthopaedic Foot and Ankle Society score. However, there were only 28 patients in each group in this trial.
Li et al. 41 compared external fixation with both plate and nail fixation. This trial concluded that all three methods were ‘efficient methods for treating distal tibia fractures’. There was no evidence of difference in the Mazur ankle score; no disability rating was reported. Again, this study was too small to draw firm conclusions, with only 137 patients distributed across all three groups.
Polat et al. 47 compared IM nail fixation with minimally invasive plate fixation. This trial did not find any difference in the Foot Function Index, but only 25 patients were included.
Therefore, there is little, if any, evidence with which to compare the main result of the UK FixDT trial. No other trial reported a disability rating. Other patient-reported scores were used in three trials, each showing no evidence of a difference between the treatment groups. However, each of these trials was considerably smaller than the UK FixDT trial and so subject to an increased risk of type II error, that is, these four trials may not have been large enough to detect a clinically important difference between IM nail fixation and locking plate fixation, even though one existed.
Secondary outcomes
Patient reported
The secondary patient-reported outcome measures showed the same effect and the same pattern over time as the DRI score. Each measure showed a large difference in favour of IM nail fixation at 3 months, which gradually reduced at 6 months and then 12 months after the injury.
This is powerful corroborating evidence that the main result of the UK FixDT trial is real and important to patients.
The OMAS is used to assess pain and function of the ankle joint specifically. As the ankle is the closest joint to the distal tibia, it is likely to be the most affected by both the fracture and the surrounding soft-tissue injury. The adjusted estimate of the treatment effect for the OMAS, at the 6-month post-randomisation primary time point, based on an intention-to-treat analysis, was –6.0 points (95% CI –11.2 to –0.7 points) in favour of the IM nail group compared with the locking plate group. The p-value of 0.026 indicates that there is evidence for a statistically significant difference in the OMAS between the two treatment groups at 6 months. However, a difference of 6 points on the OMAS scale is unlikely to be particularly important to patients. Six points on the OMAS scale has been used as an equivalence margin in previous NIHR Health Technology Assessment trials. 25
Similarly, the adjusted estimate of the treatment effect for the EQ-5D index (utility) score, at the 6-month post-randomisation time point, on an intention-to-treat analysis, was –0.063 (95% CI –0.12 to –0.01) in favour of the nail group compared with the locking plate group. The p-value of 0.033 indicates that there is also evidence for a statistically significant difference in the EQ-5D utility score between the two treatment groups at the 6-month time point.
Weight-bearing status
Data on weight-bearing status were collected at the 6-week follow-up appointment. Only 33% of patients allocated to the IM nail group reported being fully weight-bearing. However, even fewer (15%) of the patients in the locking plate group reported being fully weight-bearing.
The p-value for the difference is p < 0.001, indicating strong evidence of a difference between groups. It is possible that the postoperative instructions given to the two groups of patients were different, although recent evidence strongly suggests that patients start to bear weight on their leg when they feel comfortable to do so rather than when the clinical team advise. 25
Weight-bearing mobilisation is thought to prevent stiffness in the ankle joint as well as reduced wasting (loss of strength) in the muscles of the lower leg. It is impossible to know how much of the difference in disability, ankle function and health-related quality of life noted in the UK FixDT trial at 3 months resulted from the difference in early weight-bearing status, and we did not record weight-bearing status at 3 months, but it seems likely that the ability to fully bear weight in the IM nail fixation group did at least contribute to the faster recovery in this group.
Complications
When interpreting the primary outcome of any surgical trial, it is important to take account of the complication profile of the two procedures. Therefore, we also preplanned a secondary analysis of the complications occurring in the two groups of patients. We have broken these down into ‘local complications related to the fracture or its treatment’ and ‘systemic complications potentially related to the fracture or its treatment’ during the 12 months after the injury.
Local complications related to the fracture or its treatment
In terms of superficial wound healing complications, we expected that there may be more of these in the locking plate group, as the plate sits on the surface of the distal tibia where there is only a thin soft-tissue envelope. There were 20 (13%) superficial wound healing complications in the IM nail group and 32 (20%) in the locking plate group (p = 0.094). Of these superficial wound healing complications,14 (9%) in the IM nail group and 21 (13%) in the locking plate group were treated with antibiotics in the first 6 weeks after surgery.
Superficial wound complications are uncomfortable and inconvenient for the patient, but usually resolve in a few days. Of greater concern are deep surgical site infections, in which the metalwork and, potentially, the underlying bone are infected. By 12 months, one (1%) of the patients in the IM nail group and five (3%) in the locking plate group required surgical debridement for deep infection (p = 0.121).
These findings suggest that, although there were more wound- and infection-related complications in the locking plate group than the IM nail group, both groups were at risk, including an overall 2% risk of deep infection.
Other local complications were rare in both groups. There was only one vascular injury, two tendon injuries and one case of complex regional pain syndrome reported in all 321 patients who took part in the trial. Deficits in the function of local nerves were reported in the period up to 6 weeks by eight (5%) patients in the IM nail group and four (3%) in the locking plate group (p = 0.378), but none of these cases required surgical intervention. We did not specifically ask patients to record symptoms related to nerve injury that persisted after 6 weeks. However, we expected that any functional deficit or pain related to such a persistent nerve deficit would affect the patient-reported outcome scores at 3 months and later.
As noted earlier, there have been four trials reported since the UK FixDT trial began. 41,45–48 In the most recent, Fang et al. 46 compared the results of external fixation combined with limited internal fixation, minimally invasive percutaneous plate fixation and IM nailing for distal tibia fractures. 46 They concluded that ‘all achieved similar good functional results’ but that the different surgical techniques may have different complication profiles. The other trials came to essentially the same conclusion, comparing plate and nail fixation, although these results may be confounded by the use of non-locking plates in some cases. Non-locking plates generally require larger incisions and greater soft-tissue ‘stripping’ than ‘locking’ plates, which can be inserted using ‘minimally invasive’ techniques.
External fixation leads to the least soft-tissue stripping of any surgical intervention; the external fixation pins/wires being inserted through tiny wounds in the skin. This should, in theory at least, lead to lower rates of infection. However, Fang et al. 46 noted that 14% of patients receiving external fixation in their trial, had ‘pin tract’ infections, that is, infections in the skin around the entry point of the external fixation pin/wire. This is similar to the number of patients requiring antibiotics for wound complications in the locking plate group of the UK FixDT trial. Other recent studies have specifically compared external fixation using ‘fine-wire’ Ilizarov external fixation with plate fixation. 48 This trial, although not directly relevant to the results of the UK FixDT trial, did indicate a lower complication rate with external fixation than with plate fixation. However, again, the plate fixation group of participants in this trial had an open reduction and internal fixation with the sort of non-locking plate associated with high wound complication rates.
Therefore, in summary, the most current literature is in keeping with the results of the UK FixDT trial in terms of complications, that is, the type of complication may differ between interventions but the overall rate of complications remains high, including in studies using the alternative intervention of external fixation.
In terms of radiographic malunion, we looked at three parameters to assess ‘deformity’: shortening (> 10 mm), anteroposterior angulation (> 10°) and lateral angulation (> 5°). We also looked for the presence or absence of arthritis in the ankle at 12 months.
As one of the theoretical advantages of locking plates is that they provide more options for fixation and, therefore, more control over the distal segment of the tibia, we expected that there would be more cases of angular deformity in the IM nail group than the locking plate group. At 6 weeks, there were 12 cases (7%) of lateral (coronal plane) deformity in the nail group and five (3%) in the locking plate group. There were five cases of anteroposterior (sagittal plane) deformity in each of the groups. The overall number of angular deformities was low and there was no statistical evidence of a difference between the groups in terms of angular deformity. However, at 6 weeks, there were five cases (3%) of shortening of the tibia in the IM nail group and none in the locking plate group. This difference was statistically significant (p = 0.028) but it is not clear if this was clinically important to the patients. Overall, as there were very few deformities in either group, it is difficult to draw any conclusions about the relationship between radiographic deformity and patient-reported outcome.
In terms of arthritis in the ankle joint, this was assessed using the radiographs taken at 12 months after the injury. Ten radiographs (6%) in the IM nail group showed radiological signs of arthritis and 7 (4%) in the locking plate group, which was not statistically different (p = 0.320). Again, it is not possible to tell if these cases led to deteriorating function or pain. Longer-term follow-up may answer this question, but given the low number of cases in either group it is unlikely that long-term review will be able to detect clinically important differences between treatment groups.
Further surgery related to the distal tibia fracture
Reassuringly, revision of the internal fixation was uncommon in both group: two patients (1%) in the IM nail group and five patients (3%) in the locking plate group (p = 0.283). Similarly, other (unspecified) unplanned surgery occurred in only four (2%) and three patients (2%) of the nail and ‘locking’ plate groups, respectively (p = 1.000).
We anticipated that routine removal of metalwork would be reasonably common in this trial. As any metalwork inserted in the region of the distal tibia is easily palpable under the patient’s skin, it is more likely to cause symptoms than in other areas of the body. However, removal of metalwork was required in only 11 (7%) of the patients in the nail group and 14 (9%) in the ‘locking’ plate group. Of course, these figures may rise as some patients wait until after 12 months before returning with symptoms related to their metalwork.
Systematic complications potentially related to the fracture or its treatment
Deep-vein thrombosis occurred in six patients (4%) in the nail group and five patients (3%) in the ‘locking’ plate group (p = 1.000) in the 12 months after the fracture. However, only three deep-vein thromboses (one in the nail group and two in the locking plate group) occurred in the first 6 weeks following surgery, when the patients were considered most at risk. It is not possible to know if the later thromboses were related to the fracture of the distal tibia, but we have included them here for completeness. Of note, there was only one pulmonary embolus reported in the 321 participants during the 12 months of follow-up. In terms of systemic but potentially related infections, for example chest, urinary infections, etc., these were more common; infection treated with antibiotics occurred in 24 patients (15%) of the IM nail group and 31 patients (19%) of the locking plate group (p = 0.303).
Unrelated adverse events
The principal investigator at each centre assessed the ‘relatedness’ of each adverse event. SAEs were reported by 83 participants, with 23 participants reporting more than one SAE.
Preplanned subgroup and secondary analyses
We preplanned a per-treatment analysis, expecting that some patients allocated to IM nail fixation would crossover to plate fixation, and vice versa. However, as the number of crossovers was actually small, we did not expect a difference between the intention-to-treat analysis and the per-treatment analysis. In keeping with this suggestion, the adjusted per-treatment analysis of the DRI scores at 6 months gave an adjusted treatment effect of 4.2 points (95% CI –0.9 to 9.2 points; p = 0.103). Adjusted analysis at 3 and 12 months also gave similar results to the intention-to-treat analysis.
We also preplanned a secondary analysis of the primary outcome measure, taking into account missing data. As there was very few missing data in the DRI forms at any time point, this analysis did not show any difference from the complete data analysis.
We also done preplanned subgroup analyses based upon sex and age, using < and ≥ 50 years as a surrogate for high-energy injuries in younger patients with normal bone density and lower-energy injuries in older patients with reduced bone density. At the primary outcome time point of 6 months, the p-value of 0.516 indicated there is no evidence for a significant interaction effect between age group and treatment group. Similarly, the p-value of 0.384 indicates there was no evidence for a significant interaction effect between sex and treatment group.
Health economic evaluation
The health economic evaluation is vital to the interpretation of the trial and not only for analysis of the initial cost of the implants and surgery. As the clinical data presented indicate that patients with a fracture of the distal tibia have persistent, measurable disability, even 1 year after their fracture, this injury is likely to have longer-term cost implications for both the health and social care systems.
Cost
The pre-pilot trial that informed the design of the UK FixDT trial suggested that there was considerable cost related to the choice of implant; at the time the cost of an IM nail and locking bolts was in the region of £350 and a distal tibia locking plate with screws was around £1200. Interestingly, in addition, operative costs included the implants used during the surgery, namely nails, plates, locking screws/bolts, blocking screws and non-locking screws. The estimation of the number of each of these implants used involved prospectively recording the number of items used for each patient from the operation notes and radiographs. The total cost of implants for each patient was calculated by combining the resource inputs with their unit cost values; the latter were derived from NHS trust finance departments.
Table 22 shows that the cost of the nail and four locking bolts had risen a little to approximately £450, whereas the cost of the medial distal tibial locking plate and eight locking screws had actually fallen to approximately £650. When the cost of disposable items (guidewire, reaming rod, etc.) is added to the cost of the IM nail, the difference between the costs of the two types of implant has greatly reduced in the last few years.
As a consequence, the trial found little difference in the cost of the initial surgical interventions. Neither was there much difference in the length of the index hospital stay. The total cost of the first admission to hospital was £5585 in the IM nail group and £5616 in the locking plate group.
However, between discharge from the index hospital stay and 6 months, both the inpatient and the outpatient health service costs were significantly greater in the locking plate group. The total NHS and PSS cost to 6 months was £5876 in the nail group and £6814 in the locking plate group, with a mean difference of £938, which was statistically significant (95% CI £84 to £1795; p = 0.04).
The difference in costs reflects the increased number of investigations, therapy visits and secondary interventions required in the locking plate group in the early phases of recovery. This fits with the clinical outcome data presented earlier, in that the number of patients having ‘problems’ was higher in the locking plate group than the IM nail fixation group. For example, patients with symptoms of wound infection would have more outpatient appointments, more blood and radiological tests and more in the way of antibiotic treatment than those without. Another factor contributing to the higher costs in the locking plate group may have been the higher proportion of patients who were not able to bear weight on their leg at 6 weeks. It is likely that this explains, at least in part, the increased number of therapy appointments in the locking plate fixation group.
Between 6 months and 12 months, there are, again, slightly higher costs in the locking plate group, but the difference between the groups was less than in the earlier phases of recovery. The mean cost difference to 12 months was £995.14, 95%CI £74.93 to £2069.63; p = 0.05. Further surgery, most commonly the removal of symptomatic metalwork, is likely to have happened later in the recovery phase when the surgeon and the patient were confident that the underlying fracture had healed. This may account for the increased costs in the locking plate group in the later phases of the trial.
A fracture of the distal tibia also has costs for the patient beyond the NHS and PSS perspective. The number of days off work in the first 3 months after injury was borderline statistically significant in favour of the IM nail fixation: 46 days in the IM nail group compared with 54 days in the locking plate group (p = 0.07). Depending upon the patient’s occupation, this may simply be a manifestation of the number of patients who were weight-bearing at this stage in their recovery, which was higher in the group having IM nail fixation. It may also reflect the greater number of days off work required to attend therapy, outpatient and inpatients visits in the locking plate group, or, most likely, a combination of the two.
Cost-effectiveness
As there is a small QALY gain in the nail group over the 12-month time frame of the trial, and the IM nail group incurred less cost, the cost-effectiveness evaluation is relatively straightforward to interpret; IM nail fixation dominates locking plate fixation. Assuming a cost-effectiveness threshold of £20,000 per QALY, there is a 97% probability that IM nail fixation is cost-effective.
The preplanned sensitivity analyses support this interpretation. The same result was noted with a complete-case analysis, an analysis including a societal perspective (i.e. including indirect costs, such as those associated with time off work) and an imputed attributable cost analysis. In the per-treatment analysis, there was a marginal QALY gain in the locking plate group, so IM nail fixation does not dominate in this scenario. However, the cost difference remained in the same direction and indicated that IM fixation was generally less costly than locking plate fixation.
In terms of the preplanned subgroup analyses, sex did not alter the interpretation; IM nail fixation dominates locking plate fixation in both men and women, that is, on average, it generates QALY gains and lower costs. The situation was not quite so clear in terms of age. For patients aged < 50 years, IM nail fixation again dominates, but there is much more uncertainty in patients aged ≥ 50 years. In this subgroup, although the costs of IM nail fixation were still lower, there were marginally fewer QALY gains, so the ICER was £60,000 per QALY gained in older patients.
Overall, the health economic evaluation provides strong evidence that IM nail fixation incurs less cost than locking plate fixation and marginally greater QALY gains. So, at any level of the cost-effectiveness threshold, IM nail fixation can be considered cost-effective.
Limitations
There are, of course, some limitations to the trial. Two hundred and sixteen potentially eligible participants were not randomised, which could pose a risk to the external validity (generalisability) of the trial. However, most of these patients were excluded for logistical reasons (e.g. no research staff available at the weekend), for good clinical reasons (e.g. declined any surgery) or because the patient ‘did not want to be’ part of a research study or fill out questionnaires’. There is no reason to suspect that these patients created a selection bias within the trial.
Patients who had a preference for one treatment or the other were of more concern. However, preference of treatment did not seem to be common among the patients; only 38 patients expressed a preference, of whom 23 preferred a IM nail and 15 a locking plate fixation. However, there was a stronger treatment preference among the surgeons, by whom 57 potentially eligible patients were excluded; 54 of these patients were excluded because the surgeon had a preference to use an IM nail. This does suggest that there was a preconceived preference for IM nail fixation, at least among surgeons in some centres. However, if patients deemed ‘suitable only for a nail’ were excluded, despite being eligible according to the trial criteria, this is only likely to have reduced the relative benefit of IM nail fixation compared with locking plate fixation. Despite this possible effect, the trial still showed an overall benefit of IM nail fixation.
Other possible limitations included post-randomisation crossover of patients from one group to the other. However, there were fewer than expected. Ninety-one per cent of patients received the treatment to which they had been allocated.
Similarly, some loss to follow-up was expected. However, the sample size was inflated to account for loss to follow-up of ≥ 20%, and < 20% of participants were lost from the primary outcome analysis at every time point.
Finally, as wound dressings after surgery are clearly visible, it was not possible to blind the patients to their treatment allocation.
Chapter 6 Conclusion
Among adults with an acute fracture of the distal tibia who were randomised to IM nail fixation or locking plate fixation, there were similar disability ratings at 6 months. However, recovery across all outcomes was faster in the IM nail fixation group and costs were lower.
Future work should address the potential clinical effectiveness and cost-effectiveness benefit of IM nail fixation in other metaphyseal fractures, such as the distal and proximal femur. Research is also required into the role of adjuvant treatment and different mobilisation strategies to accelerate recovery in tibial fractures treated with IM nail fixation. The patients in this trial will remain in longer-term follow-up.
Acknowledgements
The Fixation of Distal Tibia Fractures trial team
Chief investigator and applicant
Professor Matthew Costa.
Trial co-applicants
Dr Juul Achten, Dr Nick Parsons, Professor Stavros Petrou, Professor Ian Pallister and Professor Sarah E Lamb.
Senior project manager
Susie Hennings.
Trial co-ordinators and data entry clerk
Nafisa Boota, Katie McGuiness, Ann-Marie Brennan and Jo Walter.
Trial statisticians
James Griffin and Dr Nick Parsons.
Health economists
Mandy Maredza, Professor Stavros Petrou and Melina Dritsaki.
Rehabilitation lead
Professor Sarah E Lamb.
Collaborators
Mr Alan Johnstone (Aberdeen Royal Infirmary); Mr Andrew Carrothers (Addenbrookes Hospital); Mr Mike McNicholas (Aintree University Hospital); Mr Nigel Rossiter (Basingstoke & North Hampshire Hospital); Mr Nikhil Kharwadkar and Miss Anna Chapman (Heartlands Hospital); Mr Tim White (Royal Infirmary of Edinburgh); Mr James Murray (Frenchay Hospital); Mr Mark Blyth (Glasgow Royal Infirmary); Mr Shivkumar Gopal (Hull Royal Infirmary); Mr Ian McMurtry (James Cook Hospital); Mr David Noyes (John Radcliffe Hospital); Mr Adel Tavakkolizadeh (King’s College Hospital); Professor Peter Giannoudis (Leeds Teaching Hospital); Mr Aradhyula Murty (North Tyneside General Hospital & Wansbeck General); Mr Ben Ollivere (Nottingham University Hospitals); Mr Mark Westwood (Derriford Hospital); Mr Mark Farrar (Poole Hospital); Miss Charlotte Lewis (Queen Alexandra Hospital); Mr Andrew McAndrew (Royal Berkshire Hospital); Mr Benedict Rogers (Royal Sussex County Hospital); Mr Andrew Gray and Mr Stephen Aldridge (Royal Victoria Infirmary); Mr Paul Dixon (Sunderland Royal Hospital); Miss Caroline Hing (St George’s Hospital); Mr John Kendrew (University Hospitals of Birmingham); Mr Jonathan Young (University Hospitals Coventry & Warwickshire); Mr Ashwin Kulkarni (University Hospitals of Leicester); Mr Gorav Datta (Southampton General Hospital); and Mr Kevin Smith (Royal Stoke University Hospital).
Research associates/fellows/nurses/assistants
Carol Carnegie, Simone Hargreaves, Melanie Harrison, Cara Kennelly, Safia Begum, Ewan Goudie, Steven Barnfield, Emma Sharp, Lisa Wilson, Alanna Milne, Louise Spoors, Sarah Brannigan, Bernadette Cook, Chris Herriot, Jessica Nightingale, Rosalyn Squire, Carrie Colvin, Sheeba Babu, Emily Bannister, Carrie Ridley, Karen Smith, Tracey Robson, Agne Sekmokaite, Lauren Day-Cooper, Louise Clarkson, Manjit Attwal, Maria Letts and Racquel Carpio.
Trial Steering Committee
Professor Matthew Costa, chief investigator.
Professor James Mason, chairperson.
Professor Simon Donell, independent member.
Mr Tim Chesser, independent member (subsequently chairperson).
Mrs Suzanne Jones-Griffith, independent lay member.
Mrs Ceri Jones, sponsor representative (observing).
Data Monitoring Committee
Dr Dawn Teare (chairperson).
Mr Richard Gibson.
Mrs Smitaa Patel.
Contributions of authors
Matthew L Costa (Professor of Orthopaedic Trauma Surgery, Chief Investigator) participated in the study conception and design, clinical responsibility, writing and reviewing the report.
Juul Achten (Research Manager, Co-Applicant) developed the protocol, is a member of the TMG, and participated in writing and reviewing the report.
Susie Hennings (Senior Project Manager) is a member of the TMG, and participated in writing and reviewing the report.
Nafisa Boota (Trial Co-Ordinator) is a member of the TMG, and participated in writing and reviewing the report.
James Griffin (Research Associate, Trial Statistician) is a member of the TMG, was responsible for the statistical analysis of the trial, and participated in writing and reviewing the report.
Stavros Petrou (Professor of Health Economics, Co-Applicant) participated in the protocol development and writing and reviewing the report, was a member of the TMG and is responsible for the economic analysis of the trial.
Mandy Maredza (Research Fellow, Health Economist) is a member of the TMG, was responsible for the economic analysis of the trial, and participated in writing and reviewing the report.
Melina Dritsaki (Senior Research Fellow, Health Economist) was a former member of the TMG, conducted the early stages of the economic analysis of the trial, and participated in writing and reviewing the report.
Thomas Wood (Clinical Research Fellow) conducted the main radiographic analysis and participated in writing and reviewing the report.
James Masters (Clinical Research Fellow) participated in the review of the operation details and late infection data and writing and reviewing the report.
Ian Pallister (Professor of Trauma Surgery, Co-Applicant) participated in protocol development and writing and reviewing the report.
Sarah E Lamb (Professor of Rehabilitation, Co-Applicant) was a member of the TMG and participated in protocol development and in writing and reviewing the report.
Nick R Parsons (Associate Professor Medical Statistics, Co-Applicant) developed the protocol, is a member of the TMG and is responsible for the statistical analysis of the trial and writing and reviewing the report.
Publications
Mauffrey C, McGuinness K, Parsons N, Achten J, Costa ML. A randomised pilot trial of ‘locking plate’ fixation versus intramedullary nailing for extra-articular fractures of the distal tibia. J Bone Joint Surg 2012;94-B:704.
Achten J, Parsons NR, McGuinness KR, Petrou S, Lamb SE, Costa ML. UK Fixation of Distal Tibia Fractures (UK FixDT): protocol for a randomised controlled trial of ‘locking’ plate fixation versus intramedullary nail fixation in the treatment of adult patients with a displaced fracture of the distal tibia. BMJ Open 2015;5:e009162.
Costa ML, Achten J, Griffin J, Petrou S, Pallister I, Lamb SE, et al. Effect of locking plate fixation vs intramedullary nail fixation on 6-month disability among adults with displaced fracture of the distal tibia: the UK FixDT randomized clinical trial. JAMA 2017;318:1767–76.
Data sharing statement
Requests for data sharing for secondary research purposes can be addressed to the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Achten J, Parsons NR, McGuinness KR, Petrou S, Lamb SE, Costa ML. UK Fixation of Distal Tibia Fractures (UK FixDT): protocol for a randomised controlled trial of ‘locking’ plate fixation versus intramedullary nail fixation in the treatment of adult patients with a displaced fracture of the distal tibia. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009162.
- Sarmiento A, Burkhalter WE, Latta LL. Functional bracing in the treatment of delayed union and nonunion of the tibia. Int Orthop 2003;27:26-9.
- Böstman O, Vainionpää S, Saikku K. Infra-isthmal longitudinal fractures of the tibial diaphysis: results of treatment using closed intramedullary compression nailing. J Trauma 1984;24:964-9. https://doi.org/10.1097/00005373-198411000-00007.
- Digby JM, Holloway GM, Webb JK. A study of function after tibial cast bracing. Injury 1983;14:432-9. https://doi.org/10.1016/0020-1383(83)90094-3.
- Drosos G, Karnezis IA, Bishay M, Miles AW. Initial rotational stability of distal tibial fractures nailed without proximal locking: the importance of fracture type and degree of cortical contact. Injury 2001;32:137-43. https://doi.org/10.1016/S0020-1383(00)00157-1.
- Kneifel T, Buckley R. A comparison of one versus two distal locking screws in tibial fractures treated with unreamed tibial nails: a prospective randomized clinical trial. Injury 1996;27:271-3. https://doi.org/10.1016/0020-1383(95)00116-6.
- Obremskey WT, Medina M. Comparison of intramedullary nailing of distal third tibial shaft fractures: before and after traumatologists. Orthopedics 2004;27:1180-4.
- Boenisch UW, de Boer PG, Journeaux SF. Unreamed intramedullary tibial nailing – fatigue of locking bolts. Injury 1996;27:265-70. https://doi.org/10.1016/0020-1383(95)00150-6.
- Mosheiff R, Safran O, Segal D, Liebergall M. The unreamed tibial nail in the treatment of distal metaphyseal fractures. Injury 1999;30:83-90. https://doi.org/10.1016/S0020-1383(98)00213-7.
- Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res 1993;292:108-17.
- Vallier HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): plating versus intramedullary nailing. J Orthop Trauma 2008;22:307-11. https://doi.org/10.1097/BOT.0b013e31816ed974.
- Janssen KW, Biert J, van Kampen A. Treatment of distal tibial fractures: plate versus nail: a retrospective outcome analysis of matched pairs of patients. Int Orthop 2007;31:709-14. https://doi.org/10.1007/s00264-006-0237-1.
- Im GI, Tae SK. Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma 2005;59:1219-23. https://doi.org/10.1097/01.ta.0000188936.79798.4e.
- Guo JJ, Tang N, Yang HL, Tang TS. A prospective, randomised trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia. J Bone Joint Surg Br 2010;92:984-8. https://doi.org/10.1302/0301-620X.92B7.22959.
- Zelle BA, Bhandari M, Espiritu M, Koval KJ, Zlowodzki M. Evidence-Based Orthopaedic Trauma Working Group . Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures. J Orthop Trauma 2006;20:76-9. https://doi.org/10.1097/01.bot.0000202997.45274.a1.
- Mauffrey C, McGuinness K, Parsons N, Achten J, Costa ML. A randomised pilot trial of ‘locking plate’ fixation versus intramedullary nailing for extra-articular fractures of the distal tibia. J Bone Joint Surg Br 2012;94:704-8. https://doi.org/10.1302/0301-620X.94B5.28498.
- Salén BA, Spangfort EV, Nygren AL, Nordemar R. The Disability Rating Index: an instrument for the assessment of disability in clinical settings. J Clin Epidemiol 1994;47:1423-35. https://doi.org/10.1016/0895-4356(94)90086-8.
- Müller AO Classification of Fractures – Long Bones. Davos: AO Foundation; n.d.
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Rosenberger WF, Sverdlov O, Hu F. Adaptive randomization for clinical trials. J Biopharm Stat 2012;22:719-36. https://doi.org/10.1080/10543406.2012.676535.
- Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT. Statistical assessment of the learning curves of health technologies. Health Technol Assess 2001;5. https://doi.org/10.3310/hta5120.
- Berntsen GK, Fønnebø V, Tollan A, Søgaard AJ, Magnus JH. Forearm bone mineral density by age in 7620 men and women: the Tromsø study, a population-based study. Am J Epidemiol 2001;153:465-73. https://doi.org/10.1093/aje/153.5.465.
- Court-Brown CM, Rimmer S, Prakash U, McQueen MM. The epidemiology of open long bone fractures. Injury 1998;29:529-34. https://doi.org/10.1016/S0020-1383(98)00125-9.
- Parsons H, Bruce J, Achten J, Costa ML, Parsons NR. Measurement properties of the Disability Rating Index in patients undergoing hip replacement. Rheumatology 2015;54:64-71. https://doi.org/10.1093/rheumatology/keu293.
- Keene DJ, Mistry D, Nam J, Tutton E, Handley R, Morgan L, et al. The Ankle Injury Management (AIM) trial: a pragmatic, multicentre, equivalence randomised controlled trial and economic evaluation comparing close contact casting with open surgical reduction and internal fixation in the treatment of unstable ankle fractures in patients aged over 60 years. Health Technol Assess 2016;20. https://doi.org/10.3310/hta20750.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. https://doi.org/10.1016/0168-8510(96)00822-6.
- Stata 14 Base Reference Manual. College Station, TX: Stata Press; 2015.
- Bell ML, King MT, Fairclough DL. Bias in area under the curve for longitudinal clinical trials with missing patient reported outcome data: summary measures versus summary statistics. SAGE Open 2014;4:1-12. https://doi.org/10.1177/2158244014534858.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Value Health 2013;16:e1-5. https://doi.org/10.1016/j.jval.2013.02.010.
- Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Department of Health and Social Care . Hospital and Community Health Services (HCHS) Pay and Price Inflation n.d. www.info.doh.gov.uk/doh/finman.nsf/af3d43e36a4c8f8500256722005b77f8/360a47827991d10a80258036002d8d9f/$FILE/2015.16%20Pay%20&%20Price%20series.xlsx (accessed 11 October 2017).
- Reference Costs 2014–15. London: DHSC; 2015.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: PSSRU, University of Kent; 2015.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2015.
- Annual Survey of Hours and Earnings: 2015. Newport: ONS; 2015.
- van Reenen M, Oppe M. EQ-5D-3L User Guide EUROQOL. Rotterdam: EuroQol Research Foundation; 2015.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2014.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011;30:377-99. https://doi.org/10.1002/sim.4067.
- Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. PharmacoEconomics 2014;32:1157-70. https://doi.org/10.1007/s40273-014-0193-3.
- Li Y, Jiang X, Guo Q, Zhu L, Ye T, Chen A. Treatment of distal tibial shaft fractures by three different surgical methods: a randomized, prospective study. Int Orthop 2014;38:1261-7. https://doi.org/10.1007/s00264-014-2294-1.
- Yang SW, Tzeng HM, Chou YJ, Teng HP, Liu HH, Wong CY. Treatment of distal tibial metaphyseal fractures: Plating versus shortened intramedullary nailing. Injury 2006;37:531-5. https://doi.org/10.1016/j.injury.2005.09.013.
- Yavuz U, Sökücü S, Demir B, Yıldırım T, Ozcan C, Kabukçuoğlu YS. Comparison of intramedullary nail and plate fixation in distal tibia diaphyseal fractures close to the mortise. Ulus Travma Acil Cerrahi Derg 2014;20:189-93. https://doi.org/10.5505/tjtes.2014.92972.
- Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma 2011;25:736-41. https://doi.org/10.1097/BOT.0b013e318213f709.
- Vallier HA, Cureton BA, Patterson BM. Factors influencing functional outcomes after distal tibia shaft fractures. J Orthop Trauma 2012;26:178-83. https://doi.org/10.1097/BOT.0b013e31823924df.
- Fang JH, Wu YS, Guo XS, Sun LJ. Comparison of 3 minimally invasive methods for distal tibia fractures. Orthopedics 2016;39:e627-33. https://doi.org/10.3928/01477447-20160606-01.
- Polat A, Kose O, Canbora K, Yanık S, Guler F. Intramedullary nailing versus minimally invasive plate osteosynthesis for distal extra-articular tibial fractures: a prospective randomized clinical trial. J Orthop Sci 2015;20:695-701. https://doi.org/10.1007/s00776-015-0713-9.
- Fadel M, Ahmed MA, Al-Dars AM, Maabed MA, Shawki H. Ilizarov external fixation versus plate osteosynthesis in the management of extra-articular fractures of the distal tibia. Int Orthop 2015;39:513-19. https://doi.org/10.1007/s00264-014-2607-4.
- Reference Costs 2013–14. London: DHSC; 2014.
- Curtis LA. Unit Costs of Health and Social Care 2010. Canterbury: PSSRU, University of Kent; 2010.
- Curtis LA. Unit Costs of Health and Social Care 2014. Canterbury: PSSRU, University of Kent; 2014.
- The Income of the Self-Employed. London: Department for Business Innovation & Skills; 2016.
Appendix 1 Site-specific details
| Reason | Site (n) | Total, n (%) | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| University Hospitals Coventry & Warwickshire | Addenbrookes Hospital | Frenchay Hospital | University Hospitals of Leicester | Nottingham University Hospitals | James Cook Hospital | John Radcliffe Hospital | Aberdeen Royal Infirmary | Derriford Hospital | Royal Stoke University Hospital | Royal Sussex County Hospital | Royal Victoria Infirmary | Glasgow Royal Infirmary | Royal Berkshire Hospital | Poole Hospital | Queen Alexandra Hospital | King’s College Hospital | Aintree University Hospital | Southampton General Hospital | University Hospitals of Birmingham | Leeds Teaching Hospital | St George’s Hospital | Hull Royal Infirmary | North Tyneside General Hospital & Wansbeck General | Heartlands Hospital | Sunderland Royal Hospital | ||
| Aged < 16 years | 13 | 0 | 36 | 5 | 0 | 19 | 23 | 0 | 0 | 0 | 0 | 0 | 2 | 4 | 9 | 10 | 0 | 0 | 0 | 0 | 7 | 1 | 0 | 3 | 2 | 0 | 134 (8) |
| Fracture does not extend within 2 Müller squares | 28 | 23 | 76 | 27 | 7 | 35 | 26 | 2 | 4 | 21 | 19 | 5 | 3 | 7 | 15 | 11 | 1 | 13 | 14 | 25 | 8 | 0 | 2 | 3 | 0 | 0 | 375 (24) |
| Surgeon thinks patient would not benefit | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 (< 1) |
| Surgeon believes no operation preferable | 6 | 0 | 22 | 6 | 4 | 0 | 12 | 7 | 2 | 1 | 2 | 7 | 1 | 3 | 12 | 0 | 0 | 1 | 0 | 7 | 6 | 0 | 3 | 3 | 3 | 0 | 108 (7) |
| Surgeon believes external fixation preferable | 5 | 1 | 0 | 1 | 2 | 4 | 4 | 0 | 0 | 4 | 1 | 0 | 0 | 2 | 3 | 0 | 0 | 0 | 2 | 2 | 23 | 0 | 5 | 1 | 1 | 2 | 63 (4) |
| Surgeon believes contraindication to nail | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 4 (< 1) |
| Fracture too low for distal locking screws | 8 | 1 | 11 | 4 | 0 | 5 | 1 | 3 | 1 | 1 | 1 | 2 | 3 | 0 | 6 | 3 | 0 | 3 | 0 | 5 | 4 | 0 | 0 | 3 | 0 | 0 | 65 (4) |
| Obstruction to IM nail | 4 | 0 | 3 | 1 | 0 | 2 | 1 | 2 | 2 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 5 | 2 | 2 | 0 | 1 | 0 | 0 | 27 (2) |
| Fracture is open | 21 | 16 | 84 | 8 | 4 | 22 | 61 | 18 | 0 | 4 | 22 | 22 | 19 | 0 | 7 | 2 | 0 | 0 | 6 | 4 | 6 | 41 | 0 | 2 | 0 | 0 | 369 (23) |
| Patient contraindication to anaesthesia | 1 | 0 | 6 | 2 | 1 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 16 (1) |
| Patient has permanent cognitive impairment | 4 | 9 | 11 | 0 | 3 | 5 | 7 | 9 | 1 | 5 | 1 | 3 | 12 | 1 | 1 | 2 | 1 | 1 | 2 | 2 | 5 | 0 | 0 | 3 | 0 | 1 | 89 (6) |
| Fracture extends in to the ankle joint | 5 | 7 | 39 | 4 | 6 | 25 | 19 | 23 | 5 | 9 | 37 | 14 | 18 | 2 | 17 | 7 | 3 | 4 | 1 | 22 | 33 | 4 | 12 | 12 | 1 | 0 | 329 (21) |
| Total | 95 | 57 | 289 | 59 | 27 | 117 | 157 | 66 | 15 | 45 | 83 | 54 | 58 | 21 | 72 | 36 | 5 | 22 | 25 | 73 | 94 | 48 | 22 | 31 | 7 | 3 | 1581 |
| Reason | Site (n) | Total, n (%) | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| University Hospitals Coventry & Warwickshire | Addenbrookes Hospital | Frenchay Hospital | University Hospitals of Leicester | Nottingham University Hospitals | James Cook Hospital | John Radcliffe Hospital | Aberdeen Royal Infirmary | Derriford Hospital | Royal Stoke University Hospital | Royal Sussex County Hospital | Royal Victoria Infirmary | Glasgow Royal Infirmary | Royal Berkshire Hospital | Poole Hospital | Queen Alexandra Hospital | King’s College Hospital | Aintree University Hospital | Southampton General Hospital | University Hospitals of Birmingham | Leeds Teaching Hospital | St George’s Hospital | Hull Royal Infirmary | North Tyneside General Hospital & Wansbeck General | Heartlands Hospital | Sunderland Royal Hospital | ||
| Patient wants nail | 3 | 1 | 1 | 1 | 3 | 0 | 1 | 4 | 0 | 0 | 0 | 0 | 3 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 23 (11) |
| Patient wants plate | 0 | 0 | 1 | 2 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 6 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 15 (7) |
| Patient does not want surgery | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 5 | 0 | 2 | 0 | 0 | 0 | 13 (6) |
| Patient does not want to be part of research study | 3 | 2 | 1 | 1 | 0 | 0 | 0 | 5 | 0 | 2 | 0 | 0 | 3 | 3 | 0 | 0 | 0 | 0 | 0 | 1 | 3 | 0 | 1 | 0 | 0 | 0 | 25 (12) |
| Patient does not want to complete questionnaires | 1 | 0 | 1 | 0 | 0 | 3 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9 (4) |
| Research staff unavailable | 1 | 2 | 13 | 2 | 0 | 2 | 3 | 0 | 0 | 1 | 4 | 3 | 4 | 1 | 5 | 2 | 0 | 1 | 4 | 3 | 1 | 0 | 0 | 1 | 0 | 0 | 53 (25) |
| Surgeon preferred nail | 0 | 5 | 8 | 0 | 3 | 1 | 2 | 5 | 3 | 1 | 13 | 0 | 3 | 3 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 3 | 0 | 0 | 0 | 54 (25) |
| Surgeon preferred plate | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 (1) |
| Other | 1 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 2 | 0 | 0 | 4 | 1 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 18 (8) |
| No reason given | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 (1) |
| Total | 10 | 10 | 29 | 8 | 6 | 8 | 8 | 17 | 3 | 12 | 17 | 7 | 14 | 8 | 17 | 10 | 0 | 1 | 9 | 6 | 16 | 0 | 6 | 1 | 0 | 0 | 216 |
| Site | Date open | Year (n) | Total (n) | Months (n) | Rate (n) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | |||||||||||||||||||
| January | February | March | April | May | June | July | August | September | October | November | December | January | February | March | April | |||||||
| University Hospitals Coventry & Warwickshire | 8 April 2013 | 9 | 14 | 0 | 0 | 0 | 1 | 2 | 4 | 2 | 0 | 1 | 2 | 0 | 1 | 0 | 1 | 1 | 0 | 38 | 36 | 1.06 |
| Addenbrookes Hospital | 2 May 2013 | 2 | 7 | 3 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 15 | 35 | 0.43 |
| Frenchay Hospital | 12 June 2013 | 3 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 34 | 0.24 |
| University Hospitals of Leicester | 16 July 2013 | 6 | 19 | 2 | 1 | 1 | 0 | 2 | 2 | 1 | 3 | 1 | 0 | 2 | 1 | 1 | 1 | 1 | 1 | 45 | 32 | 1.41 |
| Nottingham University Hospitals | 25 July 2013 | 4 | 5 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 15 | 32 | 0.47 |
| James Cook Hospital | 5 September 2013 | 1 | 6 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 31 | 0.29 |
| John Radcliffe Hospital | 20 December 2013 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 0 | 1 | 0 | 1 | 0 | 3 | 3 | 0 | 1 | 15 | 28 | 0.54 |
| Aberdeen Royal Infirmary | 14 January 2014 | 8 | 2 | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 17 | 27 | 0.63 | |
| Derriford Hospital | 15 January 2014 | 8 | 0 | 1 | 0 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 13 | 27 | 0.48 | |
| Royal Stoke University Hospital | 31 January 2014 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 27 | 0.22 | |
| Royal Sussex County Hospital | 3 February 2014 | 5 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 26 | 0.27 | |
| Royal Infirmary of Edinburgh | 10 February 2014 | 1 | 1 | 10 | 0.10 | |||||||||||||||||
| Royal Victoria Infirmary | 10 February 2014 | 8 | 1 | 0 | 0 | 1 | 2 | 1 | 1 | 0 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 18 | 26 | 0.69 | |
| Glasgow Royal Infirmary | 11 March 2014 | 7 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 5 | 1 | 0 | 2 | 0 | 1 | 0 | 1 | 0 | 20 | 26 | 0.77 | |
| Royal Berkshire Hospital | 8 May 2014 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 6 | 24 | 0.25 | |
| Poole Hospital | 13 May 2014 | 2 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 9 | 24 | 0.38 | |
| Queen Alexandra Hospital | 29 May 2014 | 2 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 1 | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 13 | 24 | 0.54 | |
| King’s College Hospital | 10 June 2014 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 23 | 0.09 | |
| Aintree University Hospital | 15 July 2014 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 22 | 0.09 | |
| Southampton General Hospital | 4 August 2014 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 21 | 0.10 | |
| University Hospitals of Birmingham | 6 August 2014 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 21 | 0.24 | |
| Leeds Teaching Hospital | 12 August 2014 | 2 | 3 | 1 | 2 | 0 | 3 | 2 | 1 | 0 | 1 | 1 | 1 | 2 | 2 | 0 | 0 | 0 | 21 | 21 | 1.00 | |
| St George’s Hospital | 10 September 2014 | 2 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 20 | 0.30 | |
| Hull Royal Infirmary | 13 October 2014 | 0 | 0 | 0 | 3 | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 8 | 19 | 0.42 | |
| North Tyneside General Hospital & Wansbeck General | 20 November 2014 | 2 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 11 | 18 | 0.61 | |
| Heartlands Hospital | 3 February 2015 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 15 | 0.13 | |||
| Sunderland Royal Hospital | 4 March 2015 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 6 | 14 | 0.43 | ||||
| Basingstoke & North Hampshire Hospital | 1 April 2015 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 13 | 0.08 | |||||
| Total | 25 | 114 | 16 | 12 | 15 | 11 | 17 | 17 | 8 | 17 | 16 | 8 | 11 | 10 | 8 | 6 | 5 | 5 | 321 | 676 | 0.47 | |
| Site | Treatment group (n) | Total | |
|---|---|---|---|
| IM nail fixation | Locking plate | ||
| Aberdeen Royal Infirmary | 9 | 8 | 17 |
| Addenbrookes Hospital | 7 | 8 | 15 |
| Aintree University Hospital | 1 | 1 | 2 |
| Heartlands Hospital | 1 | 1 | 2 |
| Basingstoke & North Hampshire Hospital | 1 | 0 | 1 |
| Royal Infirmary of Edinburgh | 1 | 0 | 1 |
| Frenchay Hospital | 4 | 4 | 8 |
| Glasgow Royal Infirmary | 10 | 10 | 20 |
| Hull Royal Infirmary | 5 | 5 | 10 |
| James Cook Hospital | 5 | 4 | 9 |
| John Radcliffe Hospital | 7 | 8 | 15 |
| King’s College Hospital | 1 | 1 | 2 |
| Leeds Teaching Hospital | 10 | 11 | 21 |
| North Tyneside General Hospital & Wansbeck General | 5 | 4 | 9 |
| Nottingham University Hospitals | 8 | 7 | 15 |
| Derriford Hospital | 6 | 7 | 13 |
| Poole Hospital | 4 | 5 | 9 |
| Queen Alexandra Hospital | 7 | 6 | 13 |
| Royal Berkshire Hospital | 3 | 3 | 6 |
| Royal Sussex County Hospital | 3 | 4 | 7 |
| Royal Victoria Infirmary | 8 | 10 | 18 |
| St George’s Hospital | 3 | 3 | 6 |
| Sunderland Royal Hospital | 3 | 3 | 6 |
| University Hospitals of Birmingham | 3 | 2 | 5 |
| University Hospitals Coventry & Warwickshire | 19 | 19 | 38 |
| University Hospitals of Leicester | 23 | 22 | 45 |
| Southampton General Hospital | 1 | 1 | 2 |
| Royal Stoke University Hospital | 3 | 3 | 6 |
| Total | 161 | 160 | 321 |
| Site | Age (years) group (n) | |||
|---|---|---|---|---|
| < 50 | ≥ 50 | |||
| IM nail fixation | Locking plate | IM nail fixation | Locking plate | |
| Aberdeen Royal Infirmary | 7 | 6 | 2 | 2 |
| Addenbrookes Hospital | 4 | 4 | 3 | 4 |
| Aintree University Hospital | 1 | 0 | 0 | 1 |
| Heartlands Hospital | 0 | 1 | 1 | 0 |
| Basingstoke & North Hampshire Hospital | 0 | 0 | 1 | 0 |
| Royal Infirmary of Edinburgh | 0 | 0 | 1 | 0 |
| Frenchay Hospital | 2 | 2 | 2 | 2 |
| Glasgow Royal Infirmary | 5 | 4 | 5 | 6 |
| Hull Royal Infirmary | 2 | 4 | 3 | 1 |
| James Cook Hospital | 3 | 3 | 2 | 1 |
| John Radcliffe Hospital | 5 | 6 | 2 | 2 |
| King’s College Hospital | 1 | 1 | 0 | 0 |
| Leeds Teaching Hospital | 3 | 6 | 7 | 5 |
| North Tyneside General Hospital & Wansbeck General | 3 | 4 | 2 | 0 |
| Nottingham University Hospitals | 6 | 5 | 2 | 2 |
| Derriford Hospital | 3 | 5 | 3 | 2 |
| Poole Hospital | 4 | 2 | 0 | 3 |
| Queen Alexandra Hospital | 5 | 2 | 2 | 4 |
| Royal Berkshire Hospital | 3 | 1 | 0 | 2 |
| Royal Sussex County Hospital | 3 | 3 | 0 | 1 |
| Royal Victoria Infirmary | 8 | 7 | 0 | 3 |
| St George’s Hospital | 2 | 2 | 1 | 1 |
| Sunderland Royal Hospital | 3 | 2 | 0 | 1 |
| University Hospitals of Birmingham | 1 | 1 | 2 | 1 |
| University Hospitals Coventry & Warwickshire | 11 | 12 | 8 | 7 |
| University Hospitals of Leicester | 11 | 11 | 12 | 11 |
| Southampton General Hospital | 1 | 0 | 0 | 1 |
| Royal Stoke University Hospital | 0 | 3 | 3 | 0 |
| Total | 97 | 97 | 64 | 63 |
Appendix 2 Details of missing data
| DRI item | Time point (n) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | |||||
| IM nail fixation (n = 160) | Locking plate fixation (n = 158) | IM nail fixation (n = 134) | Locking plate fixation (n = 142) | IM nail fixation (n = 143) | Locking plate fixation (n = 141) | IM nail fixation (n = 128) | Locking plate fixation (n = 130) | |
| Dressing | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Outdoor walks | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Climbing stairs | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Sitting longer time | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Standing bent over a sink | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Carrying a bag | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Making a bed | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Running | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Light work | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Heavy work | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 |
| Lifting heavy objects | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Participating in exercise or sports | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| OMAS item | Time point (n) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | |||||
| IM nail fixation (n = 159) | Locking plate fixation (n = 158) | IM nail fixation (n = 134) | Locking plate fixation (n = 142) | IM nail fixation (n = 140) | Locking plate fixation (n = 140) | IM nail fixation (n = 123) | Locking plate fixation (n = 130) | |
| Pain | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| Stiffness | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| Swelling | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| Stairs | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Running | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Jumping | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 |
| Squatting | 2 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| Supports | 0 | 1 | 1 | 2 | 0 | 1 | 2 | 0 |
| Daily life | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| EQ-5D domain | Time point (n) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline pre injury | Baseline post injury | 3 months | 6 months | 12 months | ||||||
| IM nail fixation (n = 160) | Locking plate fixation (n = 158) | IM nail fixation (n = 158) | Locking plate fixation (n = 158) | IM nail fixation (n = 134) | Locking plate fixation (n = 143) | IM nail fixation (n = 143) | Locking plate fixation (n = 140) | IM nail fixation (n = 129) | Locking plate fixation (n = 130) | |
| Mobility | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Self care | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Usual activities | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Pain and discomfort | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Anxiety and depression | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| VAS | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 |
Appendix 3 Example follow-up questionnaire
The EQ-5D-3L has been reproduced with permission.
Appendix 4 Economic supplementary data
| Resource item | Unit cost (£) | Unit of analysis | Source of unit cost |
|---|---|---|---|
| Subsequent inpatient care | |||
| Orthopaedics (your leg) | |||
| Cost per average LoS of 1 day | 1780.34 | Per procedure | Reference Costs 2014–15; ‘minor knee procedures for non-trauma, 19 years and over’ – HN25A33 |
| Day case | 1349.10 | Per procedure | Reference Costs 2014–15; ‘minor knee procedures for non-trauma, 19 years and over’ – HN25A33 |
| Orthopaedics (any other bones) | |||
| Cost per average LoS of 4 days | 2648.56 | Per procedure | Reference Costs 2014–15; ‘other muscle, tendon, fascia or ligament procedures’ – HN93Z33 |
| Day case | 965.19 | Per procedure | Reference Costs 2014–15; ‘other muscle, tendon, fascia or ligament procedures’ – HN93Z33 |
| Adjustment per day ± average LoS (excess bed-days) | 278.52 | Per day | Reference Costs 2014–15; ‘other muscle, tendon, fascia or ligament procedures’ – HN93Z33 |
| Other inpatient | |||
| Rehabilitation unit | 335.00 | Per session | Reference Costs 2013–14; ‘rehabilitation for other trauma’ – V636Z49 |
| Outpatient care | |||
| Orthopaedics | 112.50 | Per session | Reference Costs 2014–15 33 |
| Blood tests/phlebotomy | 3.00 | Per test | Reference Costs 2014–15 33 |
| Radiology | |||
| Radiography | 30.23 | Per test | Reference Costs 2014–15 33 |
| Magnetic resonance imaging | 146.00 | Per test | Reference Costs 2014–15 33 |
| Computerised tomography | 111.00 | Per test | Reference Costs 2014–15 33 |
| Hospital physiotherapist (NHS) | 38.00 | Per session | Unit Costs of Health and Social Care 2015, p. 217 34 |
| Physiotherapist (private) | 70.00 | Per hour | The Physio Centre (URL: www.thephysiocentre.co.uk/how_much/; accessed 3 October 2017) |
| Emergency department | |||
| Orthopaedics and trauma | 112.50 | Per session | Reference Costs 2014–15 33 |
| Other | 140.59 | Per session | Reference Costs 2014–15 33 |
| Primary and community care | |||
| GP | |||
| Surgery consultation | 225.00 | Per hour | Unit Costs of Health and Social Care 2015, p. 17834 |
| Home visit | 5.20 | Per home visit minute | Unit Costs of Health and Social Care 2010, p. 16750 |
| Telephone call | 27.00 | Per telephone consultation lasting 7.1 minutes | Unit Costs of Health and Social Care 2015, p. 17834 |
| Practice nurse | 56.00 | Per hour of face-to-face contact | Unit Costs of Health and Social Care 2015, p. 17434 |
| District nurse | 67.00 | Per hour of patient related work | Unit Costs of Health and Social Care 2015, p. 16934 |
| Community physiotherapist | 36.00 | Per hour of consultation | Unit Costs of Health and Social Care 2015, p. 17934 |
| Occupational therapist | 44.00 | Per hour | Unit Costs of Health and Social Care 2015, p. 19134 |
| PSS | |||
| Meals on Wheels | |||
| Frozen, daily | 46.00 | Per weekly meal | Unit Costs of Health and Social Care 2014, p. 12751 |
| Hot, daily | 44.00 | Per weekly meal | Unit Costs of Health and Social Care 2014, p. 12751 |
| Laundry services | 4.55 | Per load | North Yorkshire Country Council (URL: www.northyorks.gov.uk/article/23988/Paying-for-social-care-services-in-the-community; accessed 3 October 2017) |
| Social worker contacts | 42.00 | Per hour | Unit Costs of Health and Social Care 2015, p. 9534 |
| Care worker contacts including help at home | 24.00 | Per hour | Unit Costs of Health and Social Care 2015, p. 19234 |
| Aids and adaptations | |||
| Crutches | 5.06 | Per unit | NHS Supply Chain 2016 (URL: https://my.supplychain.nhs.uk/catalogue; accessed 3 October 2017) |
| Stick | 3.94 | Per unit | NHS Supply Chain 2016 (URL: https://my.supplychain.nhs.uk/catalogue; accessed 18 July 2016) |
| Walking frame | 35.99 | Per unit | NHS Supply Chain 2016 (URL: https://my.supplychain.nhs.uk/catalogue; accessed 18 July 2016) |
| Grab rail | 1.61 | Per unit | NHS Supply Chain 2016 (URL: https://my.supplychain.nhs.uk/catalogue; accessed 18 July 2016) |
| Dressing aids | 1.66 | Per unit | NHS Supply Chain 2016 (URL: https://my.supplychain.nhs.uk/catalogue; accessed 18 July 2016) |
| Long-handle shoe horn | 1.66 | Per unit | NHS Supply Chain 2016 (URL: https://my.supplychain.nhs.uk/catalogue; accessed 18 July 2016) |
| Productivity losses | |||
| Median wage rate | |||
| Full time, male | 567.00 | Per week | Annual Survey of Hours and Earnings: 2015 36 |
| Full time, female | 471.00 | Per week | Annual Survey of Hours and Earnings: 2015 36 |
| Part time, male | 156.00 | Per week | Annual Survey of Hours and Earnings: 2015 36 |
| Part time, female | 171.00 | Per week | Annual Survey of Hours and Earnings: 2015 36 |
| Median earnings (self-employed) | 10,800.00 | Per year | The Income of the Self-Employed 52 |
| Variable | Description | Treatment group, missing values, n (%) | ||
|---|---|---|---|---|
| IM nail fixation (n = 158) | Locking plate (n = 160) | Total | ||
| eq5db | EQ-5D index score pre injury | 1 (1) | 1 (1) | 2 (1) |
| eq5d0 | EQ-5D index score post injury | 2 (1) | 3 (2) | 5 (2) |
| eq5d1 | EQ-5D at 3 months | 23 (15) | 19 (12) | 42 (13) |
| eq5d2 | EQ-5D at 6 months | 16 (10) | 18 (11) | 34 (11) |
| eq5d3 | EQ-5D at 12 months | 43 (27) | 42 (26) | 85 (27) |
| c0 | Operative costs (surgery cost including initial hospital stay and implants) | 0 (0) | 0 (0) | 0 (0) |
| c1 | Total resource use between baseline and 3 months | 54 (34) | 54 (34) | 108 (34) |
| c2 | Total resource use between 3 and 6 months | 30 (19) | 31 (19) | 61 (19) |
| c3 | Total resource use between 6 and 12 months | 60 (38) | 58 (36) | 118 (37) |
| c4 | Total resource use between 0 and 6 months | 67 (42) | 62 (39) | 129 (41) |
| c5 | Total resource use between 0 and 12 months | 88 (56) | 82 (51) | 170 (54) |
| Health-care resource | Treatment group | Difference: p-value of t-test | |
|---|---|---|---|
| IM nail fixation | Locking plate | ||
| Six-week follow-up | |||
| Inpatient care, mean length of stay in days (SE) | |||
| Intensive care | 0.11 (0.06) | 0.41 (0.39) | 0.45 |
| Acute trauma | 5.78 (0.36) | 5.83 (0.35) | 0.92 |
| Rehabilitation | 0.55 (0.30) | 0.19 (0.09) | 0.26 |
| Other | 0.17 (0.07) | 0.21 (0.12) | 0.78 |
| Total inpatient care use | 6.61 (0.47) | 6.64 (0.39) | 0.62 |
| Proportion of participants prescribed antibiotics at 6 weeks (SD) | 0.14 (0.35) | 0.13 (0.03) | 0.69 |
| Three-month follow-up | |||
| Subsequent inpatient care, mean length of stay in days (SE) | |||
| Orthopaedics | |||
| Leg | 0.09 (0.05) | 0.18 (0.12) | 0.25 |
| Other bones | 0 | 0 | |
| Rehabilitation unit | 0 | 0.09 (0.09) | 0.16 |
| Other | |||
| Surgery | 0.03 (0.03) | 0.11 (0.11) | 0.24 |
| Non-surgery | 0 | 0.01 (0.01) | 0.16 |
| Total inpatient care use | 0.12 (0.06) | 0.38 (0.24) | 0.16 |
| Outpatient care, mean number of contacts (SE) | |||
| Orthopaedics | 1.66 (0.12) | 1.93 (0.15) | 0.09 |
| Pathology | 0.07 (0.03) | 0.08 (0.03) | 0.85 |
| Radiology | |||
| Radiography | 1.26 (0.21) | 1.38 (0.11) | 0.21 |
| Magnetic resonance imaging | 0.01 (0.01) | 0.03 (0.01) | 0.09 |
| Computerised tomography | 0 | 0.03 (0.01) | 0.02 |
| Physiotherapy | |||
| NHS | 1.82 (0.21) | 1.69 (0.19) | 0.67 |
| Private | 3.59 (3.26) | 0.16 (0.10) | 0.86 |
| Emergency department | |||
| Fracture related | 0.10 (0.03) | 0.08 (0.03) | 0.66 |
| Other reasons | 0.02 (0.01) | 0.03 (0.02) | 0.25 |
| Other | 0.06 (0.02) | 0.08 (0.03) | 0.30 |
| Total outpatient care use | 8.59 (3.25) | 5.50 (0.33) | 0.83 |
| Community health care, mean number of contacts (SE) | |||
| GP contacts | |||
| Surgery consultation | 0.92 (0.13) | 0.97 (0.16) | 0.39 |
| Home visit | 0.14 (0.06) | 0.11 (0.05) | 0.62 |
| Telephone call | 0.36 (0.10) | 0.46 (0.10) | 0.24 |
| Practice nurse contacts | 0.64 (0.19) | 0.39 (0.10) | 0.88 |
| District nurse contacts | 2.61 (0.92) | 1.13 (0.49) | 0.92 |
| Community physiotherapy contacts | 0.59 (0.15) | 0.71 (0.18) | 0.31 |
| Occupational therapy contacts | 0.29 (0.13) | 0.26 (0.11) | 0.56 |
| Other | 0.10 (0.10) | 0.22 (0.17) | 0.27 |
| Total community health-care use | 5.64 (0.97) | 4.25 (0.56) | 0.89 |
| Aids and adaptations, mean count (SE) | |||
| Crutches | 1.05 (0.09) | 1.21 (0.10) | 0.11 |
| Stick | 0.12 (0.03) | 0.06 (0.03) | 0.91 |
| Walking frame | 0.20 (0.04) | 0.34 (0.06) | 0.03* |
| Grab rail | 0.12 (0.04) | 0.09 (0.04) | 0.70 |
| Dressing aids | 0.33 (0.24) | 0.11 (0.08) | 0.80 |
| Long-handle shoe horn | 0.03 (0.02) | 0.01 (0.01) | 0.81 |
| Other | 0.70 (0.10) | 0.68 (0.10) | 0.57 |
| Total use – aids and adaptations | 2.55 (0.30) | 2.51 (0.18) | 0.65 |
| Medicines, proportion of participants prescribed each class of drug (SD) | |||
| Analgesics | 0.58 (0.35) | 0.56 (0.37) | 0.60 |
| Antibiotics | 0.08 (0.19) | 0.13 (0.0.28) | 0.34 |
| Anti-inflammatories | 0.14 (0.0.21) | 0.16 (0.0.27) | 0.24 |
| Anticoagulant | 0.05 (0.16) | 0.03 (0.14) | 0.84 |
| Anti-inflammatory gels | 0.01 (0.06) | 0 (0.04) | 0.74 |
| Other | 0.15 (0.29) | 0.11 (0.25) | 0.82 |
| All medicines | 1.00 | 1.00 | 0.98 |
| PSS, number of contacts (SE) | |||
| Laundry services | 0 | 0 | |
| Social worker contacts | 0 | 0.01 (0.01) | 0.16 |
| Care worker/home help | 0.43 (0.43) | 0.74 (0.56) | 0.33 |
| Other | 0.60 (0.42) | 0 | 0.92 |
| Total PSS use | 1.02 (0.60) | 0.75 (0.56) | 0.63 |
| Productivity losses (SD) | |||
| Number of days off work | 46.12 (4.21) | 54.46 (3.72) | 0.07* |
| Six-month follow-up | |||
| Subsequent inpatient care, mean length of stay in days (SE) | |||
| Orthopaedics | |||
| Leg | 0 | 0.08 (0.08) | 0.04 |
| Other bones | 0 | 0 | |
| Rehabilitation unit | 0 | 0 | |
| Other | |||
| Surgery | 0 | 0.03 (0.03) | 0.16 |
| Non-surgery | 0 | 0.01 (0.01) | |
| Total inpatient care use | 0 | 0.11 (0.06) | 0.03** |
| Outpatient care, mean number of contacts (SE) | |||
| Orthopaedics | 0.71 (0.10) | 1.17 (0.25) | 0.04 |
| Pathology | 0.05 (0.02) | 0.02 (0.02) | 0.89 |
| Radiology | |||
| Radiography | 0.53 (0.09) | 0.71 (0.10) | 0.1 |
| Magnetic resonance imaging | 0.01 (0.01) | 0.01 (0.01) | 0.5 |
| Computerised tomography | 0.02 (0.01) | 0.02 (0.01) | 0.5 |
| Physiotherapy | |||
| NHS | 1.84 (0.28) | 2.53 (0.36) | 0.07* |
| Private | 0.27 (0.12) | 0.12 (0.06) | 0.88 |
| Emergency department | |||
| Fracture related | 0.02 (0.01) | 0.01 (0.01) | 0.72 |
| Other reasons | 0.02 (0.01) | 0.07 (0.05) | 0.18 |
| Other | 0.16 (0.09) | 0.13 (0.06) | 0.59 |
| Total outpatient care use | 3.64 (0.35) | 4.78 (0.53) | 0.04** |
| Community health care | |||
| GP contacts | |||
| Surgery consultation | 1.09 (0.18) | 0.89 (0.25) | 0.74 |
| Home visit | 0.06 (0.04) | 0.11 (0.08) | 0.30 |
| Telephone calls | 0.18 (0.09) | 0.14 (0.08) | 0.62 |
| Practice nurse contacts | 0.06 (0.04) | 0.07 (0.05) | 0.43 |
| District nurse contacts | 0.18 (0.13) | 0.43 (0.43) | 0.29 |
| Community physiotherapy contacts | 1.70 (0.59) | 1.04 (0.38) | 0.82 |
| Occupational therapy contacts | 0.15 (0.09) | 0.46 (0.43) | 0.24 |
| Other | 0.15 (0.10) | 0.54 (0.37) | 0.16 |
| Total community health-care use | 3.58 (0.61) | 3.68 (0.67) | 0.46 |
| Aids and adaptations | |||
| Crutches | 0.16 (0.04) | 0.19 (0.05) | 0.32 |
| Stick | 0.09 (0.03) | 0.05 (0.02) | 0.91 |
| Walking frame | 0.02 (0.01) | 0.04 (0.02) | 0.26 |
| Grab rail | 0.06 (0.04) | 0.01 (0.01) | 0.90 |
| Dressing aids | 0.03 (0.03) | 0 | 0.84 |
| Long-handle shoe horn | 0.01 (0.01) | 0 | 0.84 |
| Other | 0.09 (0.04) | 0.13 (0.04) | 0.24 |
| Total use – aids and adaptations | 0.47 (0.12) | 0.41 (0.09) | 0.65 |
| Medicines, proportion prescribed each class of drug (SD) | |||
| Analgesics | 0.51 (0.45) | 0.56 (0.46) | 0.32 |
| Antibiotics | 0.08 (0.24) | 0.13 (0.34) | 0.50 |
| Anti-inflammatories | 0.07 (0.23) | 0.02 (0.10) | 0.79 |
| Anticoagulant | 0.01 (0.08) | 0.01 (0.05) | 0.50 |
| Anti-inflammatory gels | 0.06 (0.23) | 0.04 (0.18) | 0.68 |
| Other | 0.27 (0.42) | 0.25 (0.39) | 0.58 |
| All medicines | 1.00 | 1.00 | |
| PSS, number of contacts (SE) | |||
| Laundry services | 0 | 0 | |
| Social worker contacts | 0 | 0 | |
| Care worker/home help | 2.43 (1.75) | 0.71 (0.71) | 0.82 |
| Other | 0 | 0 | |
| Total PSS use | 2.43 (1.75) | 0.71 (0.71) | 0.82 |
| Productivity losses (SD) | |||
| Number of days off work | 24.59 (5.22) | 32.80 (5.89) | 0.15 |
| Twelve-month follow-up | |||
| Subsequent inpatient care, mean length of stay in days (SE) | |||
| Orthopaedics | |||
| Leg | 0.16 (0.10) | 0.15 (0.09) | 0.95 |
| Other bones | 0 | 0 | |
| Rehabilitation unit | 0 | 0 | |
| Other | |||
| Surgery | 0.01 (0.01) | 0.10 (0.08) | 0.28 |
| Non-surgery | 0 | 0 | |
| Total inpatient care | 0.17 (0.11) | 0.25 (0.15) | 0.71 |
| Outpatient care, mean number of contacts (SE) | |||
| Orthopaedics | 0.46 (0.13) | 0.71 (0.18) | 0.28 |
| Pathology | 0.13 (0.07) | 0.27 (0.17) | 0.46 |
| Radiology | |||
| Radiography | 0.38 (0.09) | 0.30 (0.08) | 0.50 |
| Magnetic resonance imaging | 0 | 0.03 (0.01) | 0.08 |
| Computerised tomography | 0. 75 (0.46) | 0.11 (0.06) | 0.17 |
| Physiotherapy | |||
| NHS | 0.55 (0.22) | 0.70 (0.28) | 0.67 |
| Private | 0.07 (0.05) | 0.07 (0.05) | 0.97 |
| Emergency department | |||
| Fracture related | 0.03 (0.02) | 0.17 (0.16) | 0.36 |
| Other reasons | 0.01 (0.01) | 0. 03 (0.03) | 0.38 |
| Other | 0.10 (0.03) | 0.31 (0.21) | 0.33 |
| Total outpatient care use | 2.47 (0.71) | 2.70 (0.58) | 0.80 |
| Community health care, mean number of contacts (SE) | |||
| GP contacts | |||
| Surgery consultation | 0.91 (0.26) | 1.64 (0.37) | 0.11 |
| Home visit | 0.06 (0.04) | 0 | 0.16 |
| Telephone call | 0.91 (0.75) | 0.03 (0.03) | 0.25 |
| Practice nurse contacts | 0.09 (0.07) | 0.42 (0.20) | 0.14 |
| District nurse contacts | 0 | 0 | |
| Community physiotherapy contacts | 0.69 (0.33) | 1.11 (0.59) | 0.54 |
| Occupational therapy contacts | 0 | 0.89 (0.68) | 0.20 |
| Other | 0.09 (0.09) | 0.28 (0.22) | 0.45 |
| Total community health-care use | 2.75 (0.95) | 4.36 (1.02) | 0.25 |
| Aids and adaptations, mean number of items (SE) | |||
| Crutches | 0.13 (0.05) | 0.06 (0.03) | 0.30 |
| Stick | 0.03 (0.02) | 0.07 (0.02) | 0.13 |
| Walking frame | 0 | 0.02 (0.01) | 0.58 |
| Grab rail | 0.01 (0.01) | 0.02 (0.01) | 0.10 |
| Dressing aids | 0.02 (0.02) | 0 | 0.32 |
| Long-handle shoe horn | 0 | 0.02 (0.01) | 0.16 |
| Other | 0.14 (0.05) | 0.10 (0.04) | 0.53 |
| Total use – aids and adaptations | 0.35 (0.09) | 0.27 (0.07) | 0.45 |
| Medicines, proportion prescribed each class of drug (SD) | |||
| Analgesics | 0.55 (0.43) | 0.47 (0.42) | 0.73 |
| Antibiotics | 0.08 (0.24) | 0.05 (0.14) | 0.66 |
| Anti-inflammatories | 0.20 (0.34) | 0.19 (0.35) | 0.42 |
| Anticoagulant | 0.03 (0.11) | 0 | 0.84 |
| Anti-inflammatory gels | 0.08 (0.24) | 0 | 0.91 |
| Other | 0.08 (0.24) | 0.29 (0.43) | 0.03** |
| All medicines | 1.00 | 1.00 | |
| PSS, mean number of contacts (SE) | |||
| Laundry services | 0 | 0.02 (0.02) | 0.16 |
| Social worker contacts | 0.01 (0.01) | 0.04 (0.04) | 0.24 |
| Care worker/home help | 0 | 0.01 (0.01) | 0.16 |
| Other | 0 | 0.01 (0.01) | 0.16 |
| Total PSS use | 0.01 (0.01) | 0.08 (0.05) | 0.09* |
| Productivity losses (SD) | |||
| Mean number of days off work | 12.99 (5.84) | 15.59 (4.91) | 0.73 |
Appendix 5 Follow-up data
| Time point | Number of participants (%) | |||
|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | |
| C | C | C | C | 240 (75) |
| C | C | C | M | 18 (6) |
| C | C | M | M | 11 (3) |
| C | M | C | C | 11 (3) |
| C | M | M | M | 10 (3) |
| C | M | C | M | 10 (3) |
| C | M | W | W | 3 (1) |
| C | M | M | C | 4 (1) |
| C | C | C | D | 2 (1) |
| M | W | W | W | 2 (1) |
| C | C | M | C | 2 (1) |
| C | C | D | D | 1 (< 1) |
| C | D | D | D | 1 (< 1) |
| C | M | M | W | 1 (< 1) |
| M | M | C | C | 1 (< 1) |
| C | C | C | W | 1 (< 1) |
| C | W | W | W | 1 (< 1) |
| C | M | C | W | 1 (< 1) |
| C | C | M | D | 1 (< 1) |
Appendix 6 Protocol amendments
| Version | Date of approval | Reason for change | |
|---|---|---|---|
| Amendment number | Date | ||
| 1 | 19 December 2012 | 2 January 2013 | Alteration of filter question 7 |
| 2 | 17 March 2013 | 5 April 2013 | Changes in participant ‘consent’ |
| 3 | N/A | N/A | N/A |
| 4 | 14 August 2013 | 14 October 2013 | Data collection in clinic |
| 5 | 30 October 2013 | 22 November 2013 | Change in eligibility criteria |
| 6 | 1 March 2014 | 12 March 2014 | Clarification of eligibility criteria |
| 7 | N/A | N/A | N/A |
| 8 | 21 May 2014 | 20 June 2014 | Updated the contact details of the sponsor and trial staff details and added main phase sites |
| 9 | 24 June 2014 | 22 July 2014 | Clarification on how the randomisation is implemented |
| 10 | 26 February 2015 | 20 April 2015 | Opt-in option for long-term follow-up at the outset of the study and addendum foot pressure walking study |
Appendix 7 Patient information sheet
Appendix 8 Consent form
Appendix 9 Background information
Appendix 10 Baseline questionnaire
The EQ-5D-3L has been reproduced with permission.
Appendix 11 Randomisation process
Appendix 12 Operation note
Appendix 13 Six-week follow-up form
Appendix 14 Serious adverse event form
Appendix 15 Diagnostic plots for primary outcome model
FIGURE 12.
Quantile–quantile plot evaluating residuals against the inverse normal distribution, using residuals from the primary outcome analyses (DRI score at 12 months).
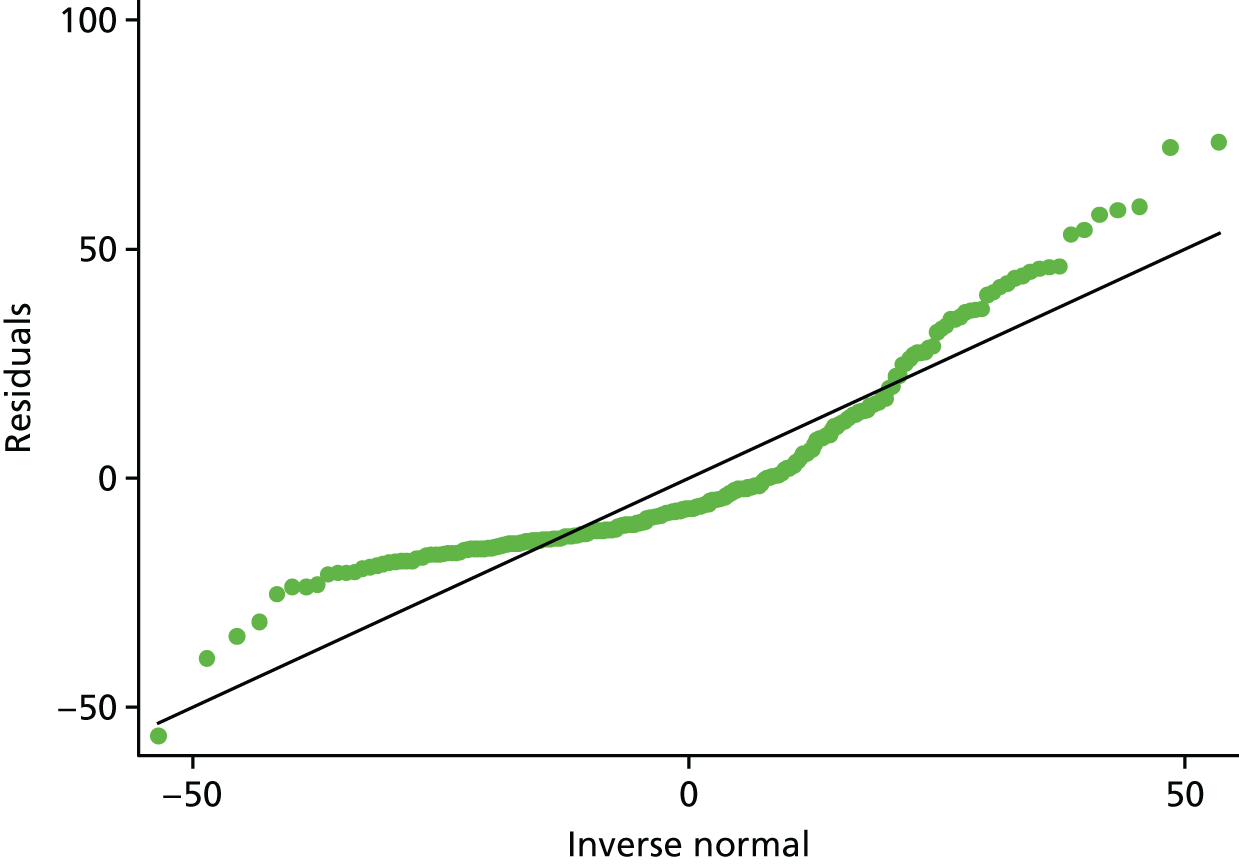
List of abbreviations
- AUC
- area under the curve
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DMC
- Data Monitoring Committee
- DRI
- Disability Rating Index
- EQ-5D
- EuroQol-5 Dimensions
- FixDT
- Fixation of Distal Tibia Fractures
- HRG
- Healthcare Resource Group
- ICER
- incremental cost-effectiveness ratio
- IM
- intramedullary
- MCID
- minimum clinically important difference
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NMB
- net monetary benefit
- OMAS
- Olerud–Molander Ankle Score
- pcpm
- per centre per month
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- SAE
- serious adverse event
- SD
- standard deviation
- SE
- standard error
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
- VAS
- visual analogue scale
- WCTU
- Warwick Clinical Trials Unit
