Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 10/104/34. The contractual start date was in January 2013. The draft report began editorial review in March 2017 and was accepted for publication in March 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Christopher Williams reports personal fees from Taylor and Francis (Abingdon, UK) and from Five Areas Ltd (Clydebank, UK) outside the submitted work and is president of the British Association for Behavioural and Cognitive Psychotherapies (BABCP). Sally-Ann Cooper reports grants from the National Institute for Health Research Health Technology Assessment programme during the conduct of the study.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Jahoda et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Depression and learning disabilities
Depression is common and places a significant burden on health services. For example, in 2011/12 the cost of prescribed antidepressant medication alone was £31.4M in Scotland1 and in 2015 it was £284.7M in England. 2 From 2008–12, of all psychiatric hospital discharges, mood disorders were the most common discharge diagnosis in women. 3 Depression is clearly a major public health challenge: it is the third leading contributor to the global burden of disease, and is expected to rise; the World Health Organization predicts that it will be the second leading contributor to the global burden of disease by 2020. 4
The term ‘learning disability’ refers to people who have significant impairments of both intellectual and functional ability, with age at onset occurring before adulthood. A significant proportion of the UK population has learning disabilities. Approximately 2% of adults and 3.5% of children have an intelligence quotient (IQ) of < 70. 5,6 Individuals with learning disabilities have higher levels of mental ill health than the general population, with a point prevalence of 40% for adults. 7
Depression is at least as common in adults with learning disabilities as in the general population, with a point prevalence of ≈5%. 8,9 Indeed, depression is the most common type of mental ill health experienced by adults with learning disabilities;7 anxiety disorders are also common, with a point prevalence of ≈4%. 10 Depression is more enduring than for the general population,11 suggesting that it is either a more severe condition, or more poorly managed. For example, a study with a British cohort found that adults with learning disabilities were four times more likely than the population without a learning disability to meet criteria for chronic depression over a 28-year period. 12 The US 2000 incident cohort with learning disabilities has been calculated to have lifetime costs (in excess of costs for people without learning disabilities) of US$44.1B. 13 Poorly addressed depression makes a clear contribution to these costs. Hence, as well as the human suffering that depression brings to people with learning disabilities, their families, local communities and society more widely, inadequately managed depression is a financial burden.
Psychological therapies for depression
In recent years there have been important innovations in the treatment of depression. A number of high-intensity psychosocial interventions are as effective as, and longer lasting than, medications in the treatment of non-psychotic depression. 14 This was confirmed in a recent individual patient-level meta-analysis with over 1700 patients treated in randomised controlled trials (RCTs). 15 The National Institute for Health and Care Excellence (NICE) recommends cognitive–behavioural therapy (CBT) to treat mild to moderate depression,16 and high-intensity forms of CBT delivered by mental health experts are recommended to treat moderate and severe levels of depression. 17 There is now an increasing emphasis on low-intensity delivery, as used in the Improving Access to Psychological Therapies (IAPT) programme in England. These include written self-help books, computerised CBT and self-help groups. 18–22 The evidence base for these approaches continues to grow, given the attraction of therapies that are less resource intensive.
In behavioural activation, the focus is on behaviour more than on cognition, emphasising engagement with potential environmental reinforcers. Behavioural activation also takes account of valued activities,23 emphasising the importance of purposeful routine activities such as household chores and self-care, as well as achievement, pleasure and closeness to others. Avoidance is a key target for change, with the aim of breaking the vicious cycle linked to mood and activity, whereby reduced activity lowers mood. In turn, the worse people feel, the more withdrawn they become. Behavioural activation has been shown to be at least as effective as antidepressant medications, and superior or non-inferior to CBT, placebo pills and treatment as usual (TAU) among patients with more severe depression,24–27 with effects as lasting as CBT following treatment termination. 28 Behavioural activation appears to be less complicated to learn than CBT, it is possible to train non-specialist nurses to deliver it26 and it can be delivered as a high-intensity or low-intensity therapy. 29,30
Psychological therapies for depression in adults with learning disabilities
Although psychological therapies have become established first-line interventions for depression in the general population, this has not been the case for adults with learning disabilities, owing to the additional complexities involved in making these interventions accessible to adults with cognitive and verbal communication impairments. Arguably, psychological therapies are more advisable than pharmacotherapy for adults with learning disabilities than for the general population, as limitations in verbal communication skills reduce their ability to report and describe adverse effects of drugs, which can be further disabling or potentially have serious health effects. Perhaps more importantly, people with learning disabilities should have the opportunity to access effective psychological therapies just like anyone else. Awareness of the inequity in provision of psychological therapies has grown, but there remain considerable limitations in the existing evidence base, and in its implementation. This was recently synthesised by the NICE guideline31 on mental health problems in people with learning disabilities. A key point is the need for modifications to the treatment interventions, depending on the type and extent of need of each adult with learning disabilities. 32
In 2016, NICE identified that the only available evidence on psychological interventions for depression in people with learning disabilities was for CBT, adapted for people with learning disabilities. Only three RCTs (total participants, n = 130)33–35 and three controlled before-and-after studies (total participants, n = 130)36–38 were identified that explored the use of CBT for the treatment, or prevention, of depression in adults with learning disabilities. These included only participants with mild, or mild and moderate, learning disabilities. Only two studies reported outcomes beyond the immediate end of treatment. 35,36 Although the trials had variations in the adaptations made to the intervention – and suffered from inadequate power as a result of the small size (being feasibility or pilot studies), leading to imprecise estimates – NICE concluded that CBT may result in a clinically meaningful reduction in depressive symptoms over TAU at 38 weeks’ follow-up. However, the combined evidence was assessed, using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach, as being of very low quality. One feasibility RCT with 32 participants also evaluated the cost-effectiveness (from the perspective of the NHS and social care services) of individual CBT constituting 16 weekly 1-hour sessions. 35 The cost difference between the two arms was £5650 but given the small size of the study, it is unclear whether or not CBT is a cost-effective option for people with mild to moderate learning disabilities. NICE recommended adapted CBT for depression be considered for adults with mild/moderate learning disabilities, but were not confident enough in the evidence to make a strong recommendation.
There are possible advantages to considering the use of behavioural activation for people with learning disabilities, given that it is less complicated to learn than CBT and can be delivered by non-specialists. However, the only study on behavioural activation with people with learning disabilities and depression was the feasibility study we undertook to inform the design of the study reported here. It was a pre–post trial with 22 participants recruited over a 12-month period, at one site. 39 Outcomes showed evidence of positive change on depressive symptoms for those able to self-report on the Glasgow Depression Scale40 pre- and post-intervention, and at 3 months’ follow-up after end of treatment. We therefore used this study to inform the design of the trial reported here.
Trial objectives
Primary objective
To measure the clinical effectiveness of BeatIt, a behavioural activation intervention adapted for adults with learning disabilities and depression, compared with a guided self-help intervention (StepUp), in reducing self-reported depressive symptoms.
Secondary objectives
-
Does BeatIt lead to a greater reduction in carer-reported depressive symptoms than StepUp?
-
Does BeatIt lead to a greater reduction in self-reported anxiety symptoms than StepUp?
-
Does BeatIt lead to a greater reduction in carer-reported aggressiveness than StepUp?
-
Does BeatIt lead to more significant and sustainable changes in participants’ activity levels than StepUp?
-
Does BeatIt lead to a significantly greater improvement in participants’ quality of life (QoL) than StepUp?
-
Does BeatIt improve carers’ sense of self-efficacy in supporting adults with learning disabilities who are depressed, compared with StepUp?
-
Is BeatIt a cost-effective intervention for the management of depression experienced by adults with learning disabilities, compared with StepUp?
-
Does BeatIt improve carers’ reported relationships with the adults with learning disabilities and depression that they support, compared with StepUp?
In addition, qualitative methods were used to address process issues, which could help to inform the future uptake of BeatIt or StepUp in practice. We explored the perspectives of:
-
participants receiving BeatIt and StepUp
-
carers supporting participants receiving BeatIt and StepUp
-
therapists delivering BeatIt and StepUp.
Chapter 2 Trial design and methods
Study design
This was the first large-scale RCT of an adapted individual psychological therapy for people with learning disabilities and a mental health problem. The design was a multicentre, single-blind RCT of adapted behavioural activation compared with an adapted, guided self-help intervention. The behavioural activation intervention was referred to as ‘BeatIt’, and the guided self-help intervention was called ‘StepUp’.
To ensure that it would be possible to recruit to the study, there was an internal pilot phase. Consequently, there were two phases of data collection:
-
Phase 1 – there was an initial 7-month internal pilot phase in Scotland, in which the criterion for success was to recruit a minimum of 20 participants (approximately three per month).
-
Phase 2 – following the successful completion of the internal pilot phase, the study sites in England and Wales were opened and recruitment continued at all three sites for an additional 11 months.
The trial was supplemented with an economic evaluation to consider the cost-effectiveness of providing the intervention compared with the attention control (see Chapter 6). There was also a qualitative study to explore the views and experiences of participants, their supporters and therapists who took part in the trial (see Chapter 7). The trial protocol has been published. 41 A description of all approved changes to the original protocol that were submitted are shown in Table 1.
| Version | Changes made to the protocol |
|---|---|
| From version 1 to 2 | The SSQ3 was added to the self-report measures |
| The Guernsey Community and Leisure Participation Assessment was removed | |
| Proxy-reported measures of aggression (BPI-S) and of selected aspects of adaptive behaviour (ABS-RC2) were added | |
| An 8-month follow-up call to the carer was added, to collect data on service and medication use | |
| A procedure and questionnaire for screening suicidal participants was added and suicidal intent was added to the exclusion criteria | |
| The separate consent forms for participation in the main study and participation in the qualitative interviews were combined into one form | |
| The Depression Carer Self-Efficacy Scale was removed and replaced with the EDSE scale | |
| Activity data were to be collected from the participant and carer jointly, rather than from the carer alone | |
| From version 2 to 3 | The timing of the qualitative interviews was changed from 12 months post randomisation to between 4 and 8 months post randomisation, to allow better recall |
| Decision to accept self-referrals | |
| Originally, it was specified that the supporter had to have known/worked with the participant for a minimum of 6 months. This was changed to 6 months OR is able to obtain information for the 4 months before randomisation | |
| Exclusion criteria: factors that prevent the participant from interacting with the carer and therapist or retaining information from the therapy – changed ‘dementia’ to ‘late-stage dementia’ | |
| To carry out inter-rater reliability checks on the fidelity ratings | |
| The need to communicate any potential risks to researchers and therapists was added to the protocol: Risk information regarding visiting participants at home will be communicated to researchers and therapists by the referring individual/organisation. The participant should be informed of this. If the allocated participant is not previously known to services, the therapist should follow their service’s standard procedure for seeing new clients safely | |
| The period of time for follow-up interviews was amended to ‘between 2 weeks before and 4 weeks after the due date’ |
Ethics approval and research governance
Multicentre approval was granted by the West of Scotland Research Ethics Committee 3. Research and development approval was granted in all study sites: Cumbria Partnership NHS Foundation Trust, Lancashire Care NHS Foundation Trust, Betsi Cadwaladr University Health Board, South Staffordshire and Shropshire Healthcare NHS Foundation Trust, NHS Lanarkshire, NHS Ayrshire and Arran, and NHS Greater Glasgow and Clyde. The International Standard Randomised Controlled Trial Number (ISRCTN) reference for the study is ISRCTN09753005.
Participants
A multipoint recruitment strategy was adopted with the aim of recruiting participants with mild to moderate learning disabilities and clinical depression across three study sites: (1) Scotland (Greater Glasgow and Clyde, Lanarkshire and Ayrshire), (2) England (Cumbria and Lancashire) and (3) North Wales (Betsi Cadwaladr University Health Board). Participants were also recruited from Shropshire and Staffordshire specialist learning disability services. For pragmatic reasons, Shropshire and Staffordshire were administered by the North Wales site. The recruitment sites comprised both rural and urban areas.
Potential participants were screened by research assistants and considered eligible for recruitment if they met all of the following inclusion criteria and did not meet any of the exclusion criteria.
Inclusion criteria
-
Had mild/moderate learning disabilities as assessed using the Wechsler Abbreviated Scale of Intelligence™ (WASI™)42 and a modified version of the Adaptive Behavior Scale – Residential and Community: Second Edition (ABS-RC2)43 to assess adaptive behaviour skills.
-
Aged ≥ 18 years.
-
Had clinically significant unipolar depression as determined using the Diagnostic Criteria for Psychiatric Disorders for use with Adults with Learning Disabilities (DC-LD),44 which was assessed by research assistants at screening who were trained in the use of the diagnostic assessment.
-
Gave informed consent to participate.
-
Had a level of expressive and receptive communication skills in English to allow for participation in treatment (reading skills were not required).
-
Had a family member, paid carer or other support person who could complete screening and baseline visits and had supported them ideally for a minimum of 6 months OR who was able to obtain information for the 4 months before randomisation.
-
Had a carer or other named individual who could accompany the participant to weekly or fortnightly treatment sessions with the therapist and who was providing them with a minimum of 2 hours support per week.
Exclusion criteria
-
Was suicidal as assessed during the screening process.
-
Had a measured IQ of > 75.
-
Experienced difficulties that prevented them from interacting with the carer and therapist or retaining information from the therapy (e.g. late-stage dementia, significant agitation, withdrawal arising from psychosis).
-
Did not consent to have their general practitioner (GP) contacted about their participation in the study.
Additional participants
As stated in the inclusion criteria above, a support person who had known the participant for at least 4 months was also recruited to take part in the trial as an informant for each individual participant.
Recruitment procedure
Although a multipoint recruitment strategy was adopted, most participants were recruited through specialist community health teams for people with learning disabilities. A smaller number of participants were recruited through social work colleagues, third sector organisations working alongside the community teams and IAPT services in Lancashire, which are open to anyone with mental health problems.
The approach to recruitment was for members of the research team to meet with members of the community teams or other organisations and provide an explanation about the study and suitable participants. This was a critical task, as few people with learning disabilities self-refer or are given psychological help for depression. Most receive help because their difficulties have become a problem for someone else. Referrals to health services are often for behavioural difficulties such as anger management problems or anxiety disorders that are proving disruptive or difficult for others to manage or support. Therefore, when describing who might be suitable participants, members of the research team highlighted that it would be important to bear in mind individuals whose depressive symptoms might be overshadowed by other presenting problems. Members of the community teams or other organisations were then able to identify potential participants, provide them with a brief explanation of the study and give them an information pack. These packs contained a letter, information sheets and a Freepost envelope that they could return if they were interested in finding out more about the study. It was suggested to participants that they might find it useful to discuss the study information with a friend or supporter.
Adults with learning disabilities are often supported by several people. For example, they may have multiple paid carers working in shifts or different supporters in their home and day-centre environments. This means that the potential participant may not have known who they could discuss the study with. This could have created a situation in which information sheets went missing before potential participants were able to discuss the study with supporters and make an informed decision about whether or not they wanted to participate. To take account of this, as in previous studies, the member of staff who gave out the information sheet was asked to notify a NHS secretary in the learning disabilities team (who was independent of the research study) that an information sheet had been handed out. After 2 weeks, if no tear off reply slip had been received, the NHS secretary contacted the individual once, by telephone, to check that they still had the information pack. If the information pack had gone missing, a second information pack was sent out.
On receiving a reply slip, a member of the research team arranged to meet the potential participant at their home or another convenient location for them. The participant was also asked if they would like someone to support them when they met to discuss the research project. When the member of the research team met with the participant, they talked through the information sheet and invited questions. If the participant was satisfied with the responses obtained, they would then be invited to participate in the study.
Advice about the information sheets and the approach taken to recruitment was provided by the Trial Steering Committee. The views of the Committee members with intellectual disabilities and a family member proved particularly helpful.
Informed consent
Individuals who chose to take part in the study were asked to complete a written consent form by members of the research team. The consent form was read to the individual with learning disabilities, they were asked to sign it, and this was witnessed by a carer or another individual who was independent of the study. Those who did not have the capacity to consent to participate were excluded from the study. The researchers all received training on assessing capacity to consent in adults with learning disabilities based on the relevant UK legislation45,46 and established best practice.
Randomisation, concealment and blinding
Participants who provided informed consent were screened and provided baseline data before being randomised. The flow diagram for the study is shown in Figure 1. Individuals were allocated to the BeatIt arm or the StepUp arm in a 1 : 1 ratio, using a blocked randomisation within each study centre. Mixed block sizes of length four and six were used at random. The randomisation was stratified by study centre and the use of antidepressants. At the design stage, several potential stratification variables were considered but ultimately not used, including the use by participants of other drugs that may have some mood-stabilising properties and are commonly prescribed in this population. For example, an estimated 25% of the population have comorbid epilepsy and may be taking carbamazepine, sodium valproate, lamotrigine or pindolol. Changes in the prescription of antidepressants and other mood-stabilising drugs were monitored over the duration of the study.
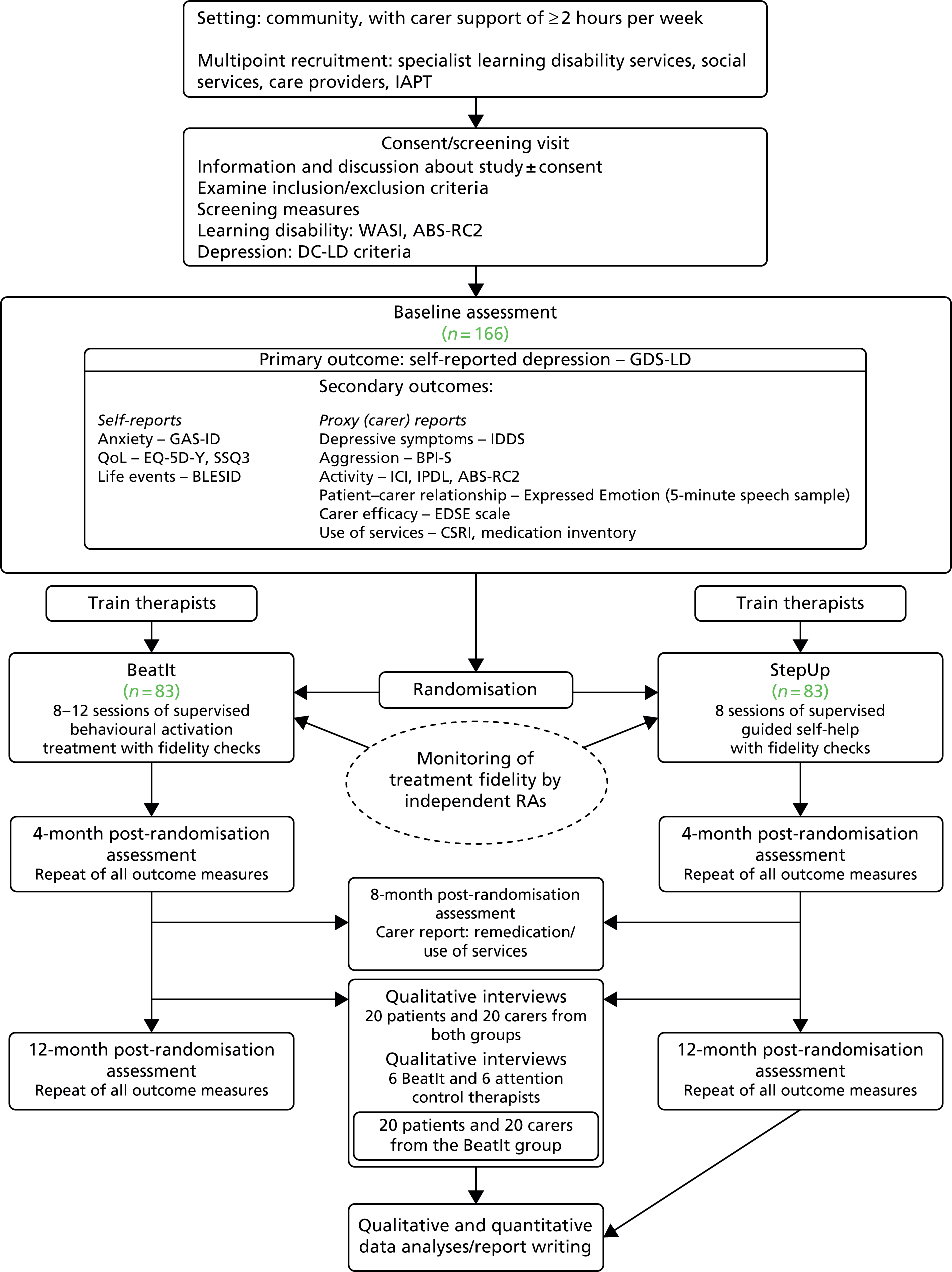
FIGURE 1.
Flow chart showing BeatIt study design and participant follow-up. BLESID, Bangor Life Events Schedule for Intellectual Disabilities; BPI-S, Behavior Problems Inventory for Individuals with Intellectual Disabilities – Short Form; CSRI, Client Service Receipt Inventory; EDSE, Emotional Difficulties Self-Efficacy; EQ-5D-Y, EuroQol-5 Dimensions – youth version; GAS-ID, Glasgow Anxiety Scale for people with an Intellectual Disability; GDS-LD, Glasgow Depression Scale for People with Learning Disabilities; ICI, Index of Community Involvement; IDDS, Intellectual Disabilities Depression Scale; IPDL, Index of Participation in Domestic Life; RA, research assistant; SSQ3, Social Support Questionnaire – three questions.
To conceal the allocation of participants from the research team, researchers randomised each participant to a treatment arm using an automated system run by the Robertson Centre for Biostatistics (RCB). The system did not reveal the random allocation to the researcher but notified the study coordinator, who then contacted the clinicians to arrange subsequent treatment visits. Thus, the researchers collecting outcome data remained unaware of the study arm to which participants had been assigned.
Interventions
Therapists
To avoid contamination, there were separate therapists for the behavioural activation (BeatIt) and the guided self-help intervention (StepUp). BeatIt and StepUp therapists were recruited from specialist community teams for people with a learning disability and, in Lancashire, they were also recruited from mainstream mental health IAPT services. Hence, the therapists were assistant and trainee psychologists, community nurses and occupational therapists who all had prior training and experience of working with people who have learning disabilities and mental health problems. The IAPT therapists who worked on the trial were low-intensity workers, who were trained to deliver brief, manualised psychological interventions for depression and anxiety disorders but did not necessarily have experience of working with adults with learning disabilities.
The therapists received 1–2 days of training about the delivery of the intervention and were given a manual and packs of materials for use in each treatment session. The training was delivered separately for BeatIt and StepUp therapists. All trainers completed an initial training course in collaboration with the curriculum developer (AJ) before training independently. The training provided (1) a background to the interventions and the underpinning theory, (2) an overview of the content and structure of the interventions, (3) an introduction to each of the exercises and self-report materials, and training and practice in their delivery and use, (4) how to deal with potential barriers to progress and (5) how to work alongside both clients with learning disabilities and their carers.
Supervisors
The supervisors were clinical psychologists with experience of delivering psychological therapies to people with learning disabilities. They all received 2 days of training in the intervention they supervised. The training followed the same format as the therapists’ training but included further guidance about supervision of participants. Time was spent highlighting issues that could cause confusion or may need particular support from the supervisor (e.g. producing the BeatIt formulation; delivery of the problem-solving StepUp booklet). Finally, care was taken to emphasise the limits of each intervention to avoid contamination and ensure that the core ingredients of BeatIt and StepUp remained distinct. For example, the StepUp therapy did not include homework tasks, with the exception of the problem-solving booklet. Hence, the therapists needed to be reminded to avoid following up on plans discussed in previous sessions.
Supporters
Table 2 shows the relationship of the supporters to the participants. Of the 161 participants at the outset, both residential (n = 49) and non-residential (n = 33) support workers featured most commonly, while parents were the next largest group (n = 34). The friends were other individuals with learning disabilities. When possible, participants chose who they wanted to support them in therapy sessions but some individuals had very limited formal or informal support, and in certain instances a visiting professional offered to help.
| Relationship | Site (n) | All (n) | ||
|---|---|---|---|---|
| Scotland | England | Wales and SSSFT | ||
| Parent | 15 | 13 | 6 | 34 |
| Sibling | 6 | 1 | 1 | 8 |
| Other family member | 2 | 1 | 1 | 4 |
| Support worker (residential) | 22 | 8 | 19 | 49 |
| Visiting social care assistant | 3 | 0 | 1 | 4 |
| Visiting professional (community nurse) | 7 | 5 | 2 | 14 |
| Spouse or partner | 3 | 2 | 2 | 7 |
| Support worker (non-residential) | 13 | 13 | 7 | 33 |
| Grandparent | 1 | 0 | 0 | 1 |
| Advocate | 1 | 0 | 0 | 1 |
| Social worker | 1 | 0 | 0 | 1 |
| Housing officer | 0 | 1 | 0 | 1 |
| Friend | 0 | 1 | 2 | 3 |
| Supervisor | 0 | 1 | 0 | 1 |
| Total | 74 | 46 | 41 | 161 |
Behavioural activation (BeatIt)
BeatIt was adapted from Lejeuz et al. ’s47 behavioural activation intervention. The underpinning theory of behavioural activation is that a negative cycle of withdrawal and avoidance of activity plays a key role in the development and maintenance of depression and low mood. Consequently, the main goal of the intervention was to break this negative cycle and bring the individual into contact with positive environmental contingencies that produce a corresponding improvement in mood. The focus was not on pleasurable activity but rather on regular activities that were purposeful, sustainable and consistent with life goals. For example, volunteering for a charity might provide someone with a reason to get up in the morning and take care of their personal appearance, as well as bringing them into contact with others and providing them with a valued social role.
BeatIt was delivered on an outreach basis, face to face at the participant’s home, except when participants chose to meet elsewhere or their living circumstances made it impossible to deliver the intervention at home. Sessions were scheduled to last for between 1 and 2 hours and were delivered on a weekly to fortnightly basis, to help build rapport and ensure continuity across sessions. When it was anticipated that sessions would last > 1 hour, a break was scheduled. The sessions were delivered to the participant alongside someone who provided regular support in their life. The participants were asked to choose who they would like to join them during sessions. A meeting was held with the supporter before starting therapy proper, to help them understand what the therapy involved and what their role in the sessions would be.
The overarching aim in the BeatIt intervention was to foster a collaborative approach, with an agenda agreed by the client and the supporter at the beginning of each session. The repetition and structure was designed to aid memory and understanding, helping the client to anticipate what was going to happen both within and across sessions and to play a more active role in therapy.
Adaptations to BeatIt
A number of adaptations was made to ensure that the behavioural activation intervention was both accessible to clients with a learning disability and sensitive to their life circumstances. There was careful piloting of the intervention and the views of people with learning disabilities and their families played a crucial role in determining the adaptations.
Supporter involvement
One of the main changes to the existing intervention was to involve a significant other in the client’s life in therapy sessions. People with learning disabilities are likely to rely on others for support in their everyday lives, including engagement in activity. They may lack the agency or the ability to recall and follow through with plans for activity without support. Involving a significant other in the therapy sessions helps to ensure ecological validity (i.e. that the intervention makes sense in the context of their wider lives).
Adapting materials and exercises
Adapting materials and therapeutic activities was designed to ensure that they were accessible and engaging. All exercises and forms were carefully developed and piloted before use. Using visual materials, such as photographs of activities, allowed participants to make active choices and helped to scaffold the therapeutic dialogue.
Assessing level and salience of activity
Care was required when examining a participant’s pattern of activity to avoid making assumptions about what level of activity was satisfactory. For example, a participant attending a college course several afternoons a week and going to a drama group on a weekly basis might have only 6 hours of regular purposeful daytime activity per week. However, this may be regarded as a relatively substantial package of support compared with that of other people with intellectual disabilities. Therefore, therapists were encouraged to carefully chart a participant’s ratio of activity and inactivity. Another issue the therapists were asked to consider was a participant’s level of control and engagement with the activities in which they took part. Being present at an activity does not necessarily mean that someone takes part or interacts with others who are there.
Formulation
A formulation was presented to the participant and their supporter using a behavioural activation framework to explain the participant’s difficulties and provide a shared ‘story’ or common frame of reference for joint work with the participant and supporter.
Barriers
Few participants presented with depression alone and most had other emotional, interpersonal and practical difficulties that needed to be addressed to allow people to increase their purposeful activity. Thus, another adaptation of the intervention was to tackle other barriers to change; the manual included guidance about how to deal with the most common barriers that were identified when the intervention was piloted.
These common barriers included (1) anxiety, (2) self-confidence and negative self-perceptions related to having a learning disability, (3) anger management/interpersonal difficulties, (4) chronic pain, (5) needing to learn or re-learn skills and (6) organisational barriers, such as a lack of support or inflexible support, which prevented participants from carrying out planned activities.
The manual made clear that this was not an exhaustive list of barriers and that this aspect of the intervention needed to be tailored to the individual concerned.
Ending therapy and final booklet
Twelve weeks of therapy were not considered to be sufficient to solve all clients’ difficulties, which it was thought would fluctuate in relation to the ongoing challenges they faced in their lives. Therefore, steps were taken to help maintain or build on therapeutic change. First, care was taken to avoid an abrupt end to therapy. Second, the participant and supporter were given a final booklet at the end of therapy, detailing the progress made, how this had been achieved and how progress could be maintained. Third, the presence of the supporter meant that there would be continuing support when the therapist input ended.
BeatIt materials
A comprehensive set of materials was provided to facilitate therapy session activities, including pictures and post boxes for an initial activity to gain insight into the participant’s pattern of activity, worksheets for a life-goals task and forms to chart a hierarchy of activities to work on. There were also mood and activity diaries for participants to complete between sessions with the help of supporters and activity sheets to be used to plan and schedule activities to be carried out between sessions. Templates were also provided for the formulation and final booklets to be produced for participants and supporters.
BeatIt: the therapy sessions
The manual describes 12 sessions, which can be divided into three main phases: (1) assessment and formulation, (2) working towards change and (3) finishing therapy. There was sufficient flexibility within the manual to allow the intervention to be tailored to the individual’s particular difficulties and life circumstances. The therapist could also make telephone contact between sessions to prompt participants about planned activities between sessions.
The first phase consisted of five sessions and involved socialising the client into the approach, identifying key areas to work on in relation to increasing activity/overcoming avoidance, and developing an individual formulation. The first three sessions involved key exercises: (1) to develop an understanding of the person’s activities, in the past and present, and what they would like to do in the future, (2) to help identify their main life goals and (3) to develop a hierarchy of potential activities in the areas of purposeful daytime, domestic and social activities, along with a plan of how these could be accessed.
In this first phase, the therapist also introduced mood and activity diaries, which the clients were asked to complete with the assistance of their supporter between sessions. Activity scheduling was also gradually introduced. Self-monitoring and scheduled activities were core features of the intervention.
Information gleaned from the first three therapy sessions furnished the therapist with material to develop an outline formulation. Session 4 was used to review what had been covered in the first three sessions and to check whether or not ideas for the formulation resonated with the participant and supporter. This feedback helped to finalise the illustrated formulation booklet, which was delivered in session 5. The formulation included the agreed plan to increase the participant’s activity or engagement through scheduled activity in three life domains: (1) domestic tasks, (2) purposeful daytime activity and (3) social/recreational activity. The plans may have included (1) recovering lost skills and interests, (2) graded exposure to reduce avoidant behaviours and (3) targeting inherently reinforcing activity and activity likely to increase access to other positive reinforcers through a programme of scheduled activity.
In the second phase of therapy (sessions 6–10), the participant, therapist and supporter worked to follow through with their plans, although these could be altered in light of new information or changing circumstances. For cases in which progress was limited, care was taken to highlight whatever achievements had been made, and activities and goals could be renegotiated to make them more achievable. The advantage of having the supporters present in sessions was that the scheduled activities were negotiated with both the supporters and participants, thereby helping to avoid making plans that the participant was not motivated to carry through or the supporter was unwilling or unable to support.
As stated above, the challenge of the approach was to overcome the barriers to change; the main issues faced by participants were tackled in the second phase of the therapy. These barriers included gaps in skills or lost skills, tackling emotional or interpersonal problems such as anxiety or anger difficulties, low self-esteem and chronic pain. Of course, the barriers were not all to do with the participants themselves and work also had to be carried out with supporters and organisations to ensure that people received the sensitive and flexible support that they required. For example, in some settings participants were not even allowed to engage in domestic tasks such as cooking or making themselves a snack.
If rapid progress was made, the number of sessions in this middle phase could be reduced.
The third and final phase (sessions 11 and 12) concerned the end of therapy. The first of these sessions involved recapping on the work that had been completed and highlighting progress made. At the final session, a booklet was given to the participant and supporter, describing their achievements and including a plan for maintenance and continued improvement.
Guided self-help (StepUp)
Guided self-help (StepUp) was chosen as an active control intervention because it is comparable to BeatIt in terms of receipt of some therapist attention, the use of a structured approach and the presence of a supporter in all therapy sessions. StepUp also offered an ethical alternative in the absence of any other evidence-based psychological therapies for people with learning disabilities and depression and a lack of information about the outcomes of usual care. Guided self-help is a psychoeducational approach, providing new knowledge and skills to help participants deal with common difficulties associated with depression to help lift their mood.
Once again, this intervention was delivered on an outreach basis, face to face at the participant’s home, unless they asked to meet elsewhere or their living circumstances made it impossible to deliver the intervention at home. Sessions were scheduled to last for 1 to 1.5 hours, with a break scheduled for sessions that continued beyond 1 hour. The sessions were delivered on a weekly to fortnightly basis to help build rapport and ensure continuity across sessions.
StepUp adaptations
Accessibility
The self-help booklets were developed in Glasgow with the assistance of people with learning disabilities from Enable, a third-sector organisation in Scotland. The resources were designed to be used by people with learning disabilities alongside a supporter. Most study participants had few, if any, literacy skills. Care was taken to ensure that the topics covered, the language used and the format, including the use of case examples, helped to make the booklets comprehensible for individuals with learning disabilities.
Relevance
The involvement of people with learning disabilities from Enable also helped to ensure that the content of the booklets and the examples used would be familiar and relevant to individuals with a learning disability.
As this was a manualised approach, the therapist went through all of the booklets in the same order with each participant and supporter. The drawback was that the different booklets were perceived to be more or less salient to different participants. Hence, when someone stated that they slept well, the booklet on sleep was delivered in light of this and reframed as reviewing the participant’s strengths and as a way of keeping well.
StepUp materials
This was a manualised approach, and the main accompanying materials were the four booklets concerning (1) feeling down, (2) sleep, (3) exercise and (4) problem-solving. There were also worksheets for the therapists to record the main points that the client and supporter had taken from the sessions, and worksheets to plan and review a problem-solving exercise to be used with the final self-help booklet. Paperwork was provided for the final two sessions, to draw together key points from across the different booklets and to produce a plan for the continued use of the booklets.
StepUp: the therapy sessions
Therapists attempted to promote a spirit of collaboration with the participant and supporter, and an agenda was agreed at the beginning of each session.
Setting the scene
The therapy started (session 1) with an initial meeting with the participant and carer to build rapport, explain the materials and provide coaching in the use of the materials.
Going through the booklets
In the subsequent five meetings (sessions 2–6), the therapist went through the booklets with the clients and supporters. The first three booklets were read within one session each, starting with ‘feeling down’, which provided an explanation of depression and depressive symptoms. The next two booklets concerned ‘sleep’ and ‘exercise’, describing how they are linked to depression and how improving sleep and increasing exercise can help to lift someone’s mood. The final booklet dealt with the more complicated topic of problem-solving and how such skills can help in overcoming depression. Owing to the complexity of this final topic, the problem-solving booklet was delivered over two sessions.
The booklets were designed to be made personally relevant to individuals. Characters were introduced to illustrate particular points and participants were asked how their experiences compared with those of the characters. The booklets also prompted discussion about whether or not the suggested changes or plans could be helpful for the participants and supporters. However, with the exception of the problem-solving booklet, in which the participant was asked to complete an exercise between sessions, a clear instruction was given to therapists to avoid returning to any particular plans or ideas that were discussed in previous sessions. It was important for therapists to avoid creating any expectation that clients and supporters were being set specific tasks to carry out between sessions.
Ending therapy
The two final sessions (7 and 8) helped to avoid an abrupt ending to therapy and gave time to consider the continued use of the booklets moving forward. The aim of the penultimate session was to review key messages from each booklet for participants, before going on to consider how the booklets could complement each other. For example, doing more exercise could help with sleep. In the same vein, better problem-solving abilities could help someone to manage their finances better, leaving sufficient funds to get out on a more regular basis.
At the final session, plans were made with the patient and supporter for the continued use of the booklets.
To clarify areas of overlap and difference between the behavioural activation and guided self-help interventions used in the study, an overview of the two interventions is shown in Table 3.
| Characteristic | Trial arm | |
|---|---|---|
| BeatIt | StepUp | |
| Type of intervention | Behavioural activation | Guided self-help |
| Number of sessions | 12 | 8 |
| Supporter present during sessions | Yes | Yes |
| Manualised | Yes | Yes |
| Review progress made between sessions | Yes | No |
| Address barriers to change | Yes | No |
| Intervention-specific materials | Mood and activity diaries to be completed between sessions; worksheets and identifying meaningful activities (post boxes and pictures); worksheets for identifying life goals and values; worksheets for planning and reviewing activities between sessions; individualised formulation booklet; list of common barriers to change with suggested materials for addressing them; final end-of-therapy booklet |
Four self-help booklets about In addition, summary sheets to identify key messages from each booklet and worksheets for problem-solving booklet homework task; and worksheets for making plans for continued use of booklets |
| Homework between sessions | Homework activities planned each session from session 3 to 11 and reviewed at following session | One homework task set during session 5 after reading through problem-solving booklet |
Fidelity to the intervention
Development of the fidelity measure
The first part of the fidelity measure concerned the presence of techniques and elements that were essential components of the described interventions. Each session for the two interventions had a different structure and content, with a greater variation in content for BeatIt than for StepUp. A simple descriptive rating of three core key activities specific to each session was developed for both interventions. For example, the core items for session 3 of BeatIt were: ‘Review of first homework activities and consider strategies for increasing motivation’, ‘Collaboratively draw up hierarchy of activities that include each target life domain’ and ‘Use a pictorial or other prompt that successfully engages the client’, with each item scored as simply present or absent. For StepUp, items for sessions 2, 3 and 4 were ‘The therapist asks the client and supporter what they can remember from the last session and reviews and discusses the topic’, ’The booklet for the current session is read through together with the client and supporter’ and ‘The client and supporter are asked what they think are the most important messages from the booklet that has been read’. For BeatIt there were additional items regarding homework and the use of diaries, which were unique aspects of this intervention.
The second part of the fidelity assessment concerned the ‘quality’ of therapy delivery. This was designed as a quality and non-specific therapy process measure for structured and manualised therapies. The structure of the measure was based on fidelity scales such as those described by Hepner et al. 48 and reported in Hunter et al. ,49 themselves based on the Cognitive Therapy Scale50 which is a precursor of the Cognitive Therapy Scale – Revised (CTS-R). 51 The 10 items in the current measure assessed whether or not the therapist:
-
creates an agenda and agrees what will be covered in the session
-
maintains a focus and clear structure to the session
-
avoids offering therapy outside the remit of the intervention
-
asks for feedback from the previous session
-
asks for feedback and reaction to the current session
-
conveys understanding by checking and rephrasing
-
adjusts content and style of own communication
-
communicates clearly without hesitations and with good pace
-
shows empathy
-
shows warmth and respect.
The rating of these was accompanied by an extended description of the factor addressed by the item, with the addition of clear operationalisation as part of the manual for the measure. For example, the descriptor for item 7, ‘adjusts content and style of own communication’ was as follows:
A core skill in working with people with learning disabilities is the ability to adjust how the therapist communicates to ensure that the client understands the communication. This is a complex skill and requires the therapist to be very aware of the client’s responses as clients may not communicate a lack of understanding in an obvious manner; this item may involve therapists using shorter sentences, breaking information into smaller chunks, using pictures and drawings.
The operationalisation aid was as follows:
There is a difficulty in judging adjustment, as many clients seem to follow the interaction well, and on that basis it could be argued that the therapist is adjusting the interaction to meet the client’s needs. To rate this, we should be listening for clear signs of the therapist using a different language, shorter statements and more pauses and that this might vary at key points in the interaction when new information or a more complex part of the process is introduced. Some therapists have difficulty doing this and use very complex language. In cases of very high complexity, speed or very long passages of speech by the therapist, it should be safe to assume that adjustment is not happening (all people with learning disability will struggle with multiple complex concepts without the opportunity to adjust and repeat). An additional complexity is that the therapist may be speaking to the carer in a different manner than they do to the client. This will demonstrate adaptation of delivery; however, it may be seen as excluding the client from parts of the therapy. This item will be judged on the complexity of delivery (some delivery may be so complex that it will not be possible for any person with a learning disability to understand even if they appear to do so) and evidence of rephrasing and adjusting language to explain and repeat a point.
The scale was rated on a four-point anchored scale, specific to each item. Thus, for item 7 the anchors were as follows:
-
The therapist does not adjust their communication style and communicates in a way that seems to be too complex for the client (and carer) or overcompensates and communicates in a way that seems condescending.
-
The therapist makes some adjustment to their communication style at some points in the session, but this is not based on how the client and carer respond and is not consistent throughout the session.
-
The therapist adjusts their communication style throughout most of the session and this appears to be well matched to the level of understanding of the client (and carer).
-
The therapist adjusts their communication style throughout the session and clearly reflects the client’s understanding in their adjustments in a way that shows accommodation to the client’s needs in each part and activity of the session.
The fidelity measures were then piloted by Dave Dagnan and Andrew Jahoda to assess six recorded sessions (three BeatIt and three StepUp). Each recording was separately rated by Dave Dagnan or Andrew Jahoda and then discussed to identify challenges in the wording of the items, their descriptors and operationalisation information. These processes enabled the further development of operationalisation information. A consensus rating of these recordings was agreed and used to develop criteria for training raters.
When each participant was allocated to a therapist, the therapist was instructed to record two particular sessions for fidelity purposes. These were selected to ensure that an early and a later session were recorded and that exemplars from every session would be equally available across both arms of the study. The recordings were returned to the research centre and uploaded. To avoid unblinding, researchers from one centre were allocated recordings from a different centre to rate for fidelity. Training for fidelity raters was delivered as follows:
-
Each researcher rated each of the six criterion recordings. After each recording was rated, a discussion was held with Dave Dagnan in which the reasoning behind each rating was discussed. Criteria for satisfactory agreement was set as full agreement on the technical presence or absence of treatment components and disagreement by no more than one point on four or fewer items in the 10-item therapy quality scale. A minimum of four recordings were rated in the training. If a researcher achieved criterion in less than four recordings, further recordings were rated and discussed until four recordings had been rated. Six raters were trained, although only four contributed to the final data set, with one rater carrying out ratings for inter-rater reliability; all achieved criterion between three and six recordings.
-
To ensure consistency and prevent drift throughout the fidelity rating process, a further recording was jointly rated by Dave Dagnan and the researcher every 20 fidelity ratings; the same criteria for agreement was applied as in the original training.
-
Inter-rater reliability data were generated by a further rater who rated 48 recordings with a balanced number of ratings from each site in each arm of the study. This rater was trained using the same procedure as the primary fidelity raters with the same consistency rating every 20 ratings.
Supervision
To help ensure that the therapy was delivered with fidelity to the manual, therapists received supervision from a clinical psychologist experienced in delivering psychological therapies to people with a learning disability on a weekly or fortnightly basis, with face-to-face supervision meetings at least once a month. In some locations, supervision was given to small groups of therapists (two to four). A supervision agreement was made with each of the therapists at the outset. The therapists brought therapy logs to supervision that they had completed after meeting with clients. The therapist used the logs to record (1) what tasks had been carried out in the session, (2) what had been carried out successfully, (3) barriers faced and (4) their plan for the next session. There was also a space for any other notes or thoughts to be recorded and an additional section for the BeatIt participants about any homework set for the participant to complete between sessions. The logs provided a structure for the supervision and notes were kept to provide a record of each supervision meeting and signed by both supervisor and therapist.
Data management
The trial was conducted in accordance with the principles of Good Clinical Practice (GCP) to ensure quality of data and protection of participants. These matters were carefully discussed with members of the Trial Steering Committee; members of the Committee with learning disabilities requested to run through the measures with the researchers in Scotland. When doing so, the Committee members offered helpful advice about ensuring that the process of data collection was engaging and accessible for participants. Data were collected by trained researchers and health professionals, using detailed standard operating procedures. Any inconsistencies were investigated and resolved in a timely manner. Careful quality checks were made before data were submitted to RCB. Once data had been submitted, further independent quality checks were performed by RCB before database lock. After database lock, the final statistical analyses were carried out.
Data collection and blinding
As shown in Figure 1, data were collected at three time points:
-
baseline
-
time 1 – 4 months post randomisation (post intervention)
-
time 2 – 12 months post randomisation (follow-up/maintenance).
The data were collected on an outreach basis, face to face, and this ordinarily occurred at a participant’s home, unless another location that offered privacy was preferable. As data were also collected from carers, arrangements were made to have separate meetings with both carers and participants when the researcher visited. There was one additional data collection point at 8 months via telephone with the carer alone, to chart any changes in the participant’s medication use and receipt of services.
Both treatments were of similar duration and included a support person. Moreover, both groups of participants were told that they were joining the BeatIt trial, rather than being told that they were being allocated to the BeatIt or StepUp intervention. These key similarities helped prevent research assistants from becoming unblinded if participants made reference to their therapy sessions during follow-up meetings. In addition, none of the researchers conducted qualitative interviews or was involved in the fidelity checks for participants from whom they collected outcome data. Qualitative interviews and therapy fidelity ratings were carried out by a researcher other than the researcher who gathered the outcome data from the participant concerned.
Measures
Primary outcome measure
The primary outcome was the Glasgow Depression Scale for people with a Learning Disability (GDS-LD),40 a self-reported measure of depressive symptoms. The GDS-LD is a 20-item scale that asks participants to indicate how often they have experienced particular depressive symptoms over the previous week using a three-point scale (never/sometimes/always).
Secondary outcome measures
Measures of depression and anxiety
Depressive symptoms (carer rating)
Carers completed the Intellectual Disabilities Depression Scale (IDDS)52 to provide an informant view of participants’ depressive symptoms. This is a 38-item behavioural checklist designed to measure the frequency of observable depressive behaviours within a 4-week period.
Anxiety symptoms (self-rating)
Self-reported anxiety symptoms were measured using the Glasgow Anxiety Scale for people with an Intellectual Disability (GAS-ID). 53 This scale has three sections dealing with worries, specific fears and physiological symptoms that the respondent may have experienced over the previous week and grades them using a three-point scale (never/sometimes/always).
Level of aggressive behaviour
The aggressive/destructive behaviour subscale of the Behavior Problems Inventory for Individuals with Intellectual Disabilities – Short Form (BPI-S)54 was completed by carers and used to examine the frequency with which the participants displayed different aggressive behaviours.
Quality of life
Quality of life (self-report)
The EuroQol-5 Dimensions – Youth version (EQ-5D-Y)55 was used to measure QoL outcomes. This version was developed for young people aged ≥ 8 years. Although the language is not childish, it is more straightforward and comprehensible. 56 The five questions are accompanied by a 100-point visual analogue scale [EuroQol Visual Analogue Scale (EQ-VAS)], on which participants are asked to rate how good or bad their health is on that day.
Community involvement
The Index of Community Involvement (ICI)57 recorded the frequency of participation in social, community-based and domestic and leisure activities over a 4-week period.
Domestic activity
The Index of Participation in Domestic Life (IPDL)58 was designed to record changes to participation in 13 household tasks during the previous 4 weeks.
Perceived social support
The Social Support Questionnaire – three questions (SSQ3)59 is a three-item questionnaire that examines perceived social support (PSS). It recorded both the size of participants’ social networks and their satisfaction with the levels of support that they received.
Adaptive behaviour
Four subscales of part 1 of the ABS-RC2,43 concerning the motivation to engage in tasks and to take responsibility, were used as a proxy measure of activity avoidance. These subscales were (1) domestic activity (six items), (2) self-direction (five items), (3) responsibility (three items) and (4) socialisation (seven items).
Carer self-efficacy and carer–patient relationship
Carer self-efficacy
The carers’ perceptions of their ability to provide support to adults with a learning disability was examined using the Emotional Difficulties Self-Efficacy (EDSE) scale. 60,61 This is a four-item questionnaire that asks carers to rate their confidence in supporting the emotional difficulties of the person with a learning disability.
Carer–patient relationship
The Expressed Emotion: Five-Minute Speech sample (FMSS)62 was used to assess the relationships between carers and participants by asking carers to speak about their thoughts and feelings towards the people whom they support, uninterrupted for 5 minutes, and rating their responses.
Life events
Finally, the Bangor Life Events Schedule for Intellectual Disabilities (BLESID)63 self-report version was used to record participants’ recent life events. This questionnaire was used to record the important life events that had taken place in participants’ lives over the previous 12 months and the impact that these events had on their lives. This allowed for the analysis of potential changes in the reactions to life events over time, such as a reduction in the negative impact experienced in response to new events that occurred during the course of the study. Because BLESID records events experienced over a period of 12 months, it was used only at baseline and the 12-month follow-up.
Health economics
Resource use
The Client Service Receipt Inventory (CSRI)64 is a validated tool to measure total package resource use and has been used in evaluations involving service users with psychiatric problems and service users with learning disabilities. It records items such as contacts with community-based primary care, other health or social services, educational services, and outpatient and inpatient attendances. Unit costs for most of these are available.
Medication inventory
Both prescription and over-the-counter (OTC) medication use was recorded. Any changes in the use of medication over the course of the intervention and during follow-up were noted to determine if there were treatment differences between the two arms of the study. In combination with the CSRI, medication use was costed.
Expectations of therapy
Participants’ expectations of the potential of therapy to be successful were assessed before starting the intervention using two questions rated on a four-point scale. The questions were taken from the Therapy Expectation Measure,65 developed for use with people who have learning disabilities.
Sample items from the primary outcome measure and selected secondary outcome measures can be found in Appendix 1.
Sample size
In the first 18 months of an earlier pre–post trial of BeatIt, the mean reduction in GDS-LD39 scores at 3 months’ follow-up was 8.50 points [standard deviation (SD) 5.24 points].
The present study was powered to detect a mean between-group difference of 0.6 SD units, or 3.14 points on the GDS-LD.
If the BeatIt group in this study could achieve an 8.5-point improvement in GDS-LD scores at 12 months, then this allows for the StepUp group showing 5.36-point improvement over the same time period (i.e. 63% of the improvement in the BeatIt group).
Alternatively, this allows for a small improvement in the StepUp group, in conjunction with a large short-term improvement in the BeatIt group, followed by some regression. For example, if the BeatIt group show an improvement from baseline to 12 months of 6 points, then the study would be powered to detect a difference if the mean improvement in the StepUp group was 2.86 points.
To have 90% power to detect this difference, the study required 60 participants in each arm to provide outcome data at 12 months post randomisation. The primary analysis was to be an analysis of covariance, adjusting for baseline GDS-LD score, which would have the power to detect smaller intervention effects, depending on the level of correlation in scores over time.
There were no data to inform the effect of clustering of outcomes for participants with learning disabilities seen by each therapist. The assumption was made that each therapist would work with an average of nine participants (i.e. several part-time therapists at each site) and an intraclass correlation of 0.025 was assumed, resulting in the sample size being increased by 20% to 72 per group, or 144 in total. A recruitment target of 166 participants allowed for a loss to follow-up of ≤ 13.3%. A meta-analysis of research with the general population66 found a post-intervention effect size on self-reported depression symptoms of behavioural activation therapy versus supportive therapy of 0.75. These designs were similar to our own attention control design. However, they did not report data regarding long-term follow-up in comparison with supportive therapy. The effects relative to brief psychotherapy were 0.56 post intervention and 0.50 after an average follow-up of 4 months, suggesting that the effects of behavioural activation therapy might persist for some time. Our follow-up at 12 months post randomisation was approximately 9 months post intervention, so we would be able to detect differences between groups only if they persisted over a longer time frame than usually studied. Therefore, we believed that an effect size for sample size estimation purposes of 0.60 was realistic given the results of this meta-analysis for behavioural activation versus supportive therapy, and this would also be considered to be of ‘moderate’ size and thus meaningful from a clinical perspective for an individual therapeutic intervention.
Statistical analyses
The statistical analyses were specified in a statistical analysis plan (SAP) (see Appendix 2), which was approved before database lock.
The primary analysis compared GDS-LD scores at 12 months post randomisation between intervention groups, adjusting for baseline GDS-LD scores, study centre and use of antidepressants at baseline within a mixed-effects linear regression model, including therapist as a random effect. Similar methods were applied to the primary outcome measure at the immediate post-intervention assessment (4 months post randomisation) and to secondary outcome measures at each assessment point. These models were used to estimate between-group differences at each follow-up time point, and to estimate mean changes from baseline within each intervention group. Repeated measures analyses, adjusting for stratification factors, were also applied to each outcome measure. These models were used to confirm the results of analyses looking at each follow-up time point separately, as well as estimating mean changes in outcomes between 4 and 12 months. In general, analyses were carried out using the available data. However, analyses of the primary outcome were repeated using multiple imputation, to assess whether or not the results were sensitive to missing data. To impute missing values at each time point, prediction models were based on age, antidepressant use and any previous or subsequent measurements of the primary outcome; prediction models did not include randomised group. Models for the primary outcome were extended to explore the effects of baseline characteristics, including the stratification factors, chronicity of depressive symptoms, life events and history of previous psychological intervention. The moderating effects of these factors were explored by using appropriately constructed interaction terms within linear regression models. These moderation analyses were exploratory only and designed to inform future translation of the intervention into routine clinical practice. Selected analyses were repeated using a per-protocol population of participants who attended at least eight BeatIt therapy sessions or at least six StepUp sessions.
Additional exploratory analyses were outlined in the SAP as potential avenues for future investigation. These analyses have not yet been carried out and are not included in this report.
Chapter 3 Participants
This chapter describes the characteristics and circumstances of participants recruited to the trial. This includes:
-
the flow of participants into the trial, including referral sources
-
demographic characteristics and circumstances of participants across the two therapy arms
-
characteristics of carers across the two therapy arms
-
the services people were receiving in the 4 months before baseline across the two therapy arms.
Flow of participants into the trial
Figure 2 reports the flow of participants into the trial. In total, 934 information packs were sent out, from which 233 reply slips were received (four of these slips indicated that the potential participant was not interested in taking part). In total, 186 people gave their consent to take part in the study, and at that point their eligibility was assessed. Of these 186 people, 19 people were excluded, most as a result of not meeting depression criteria (eight people) or the IQ being above the threshold for inclusion in the trial (six people). An additional three people withdrew before randomisation, and three people were randomised but no therapist was available.
FIGURE 2.
Participant flow diagram. Data were removed from analysis. (a) Intention-to-treat population; and (b) per-protocol population. SSSFT, South Staffordshire and Shropshire Healthcare NHS Foundation Trust. a, Includes one participant initially allocated to StepUp in error.
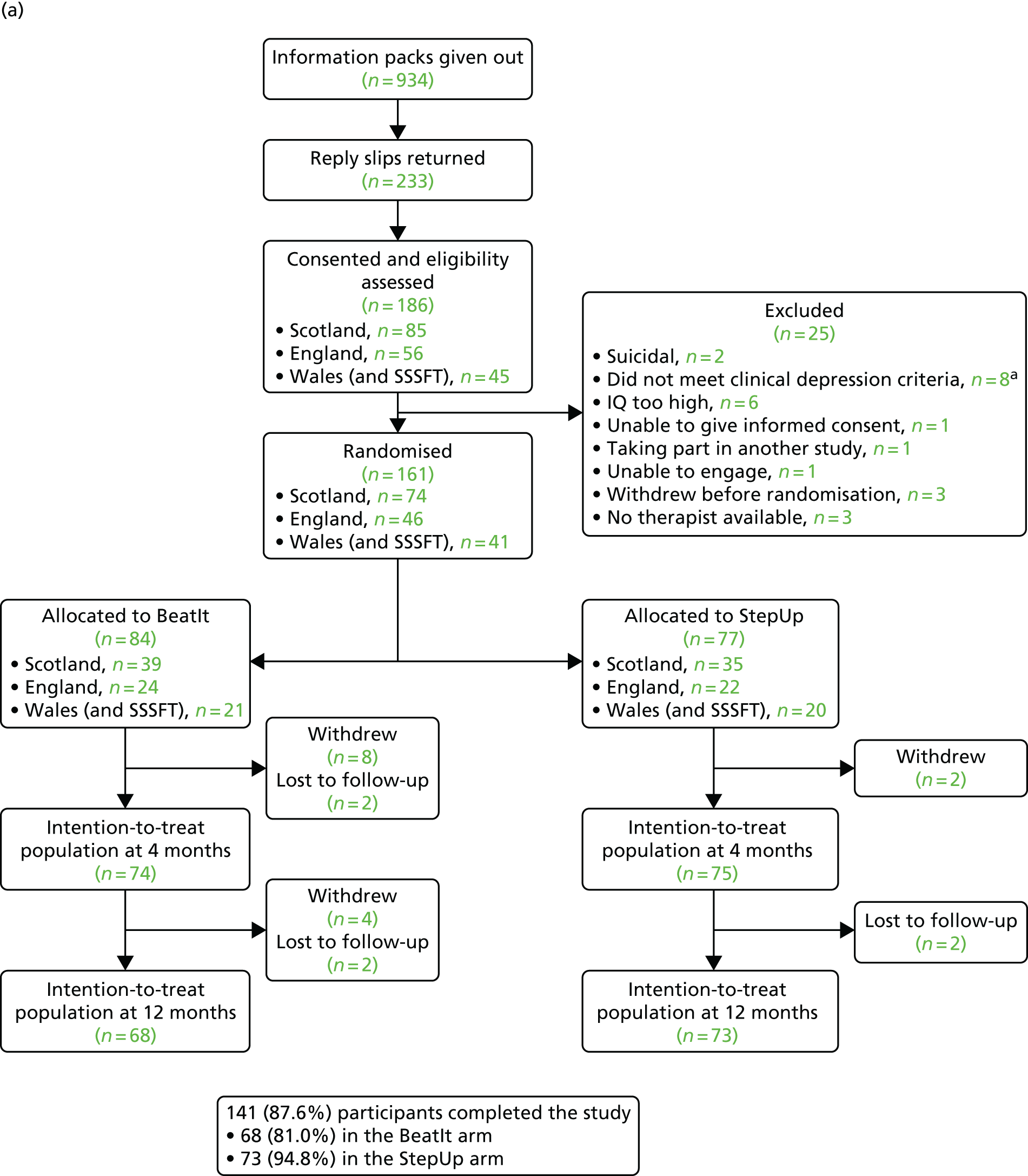
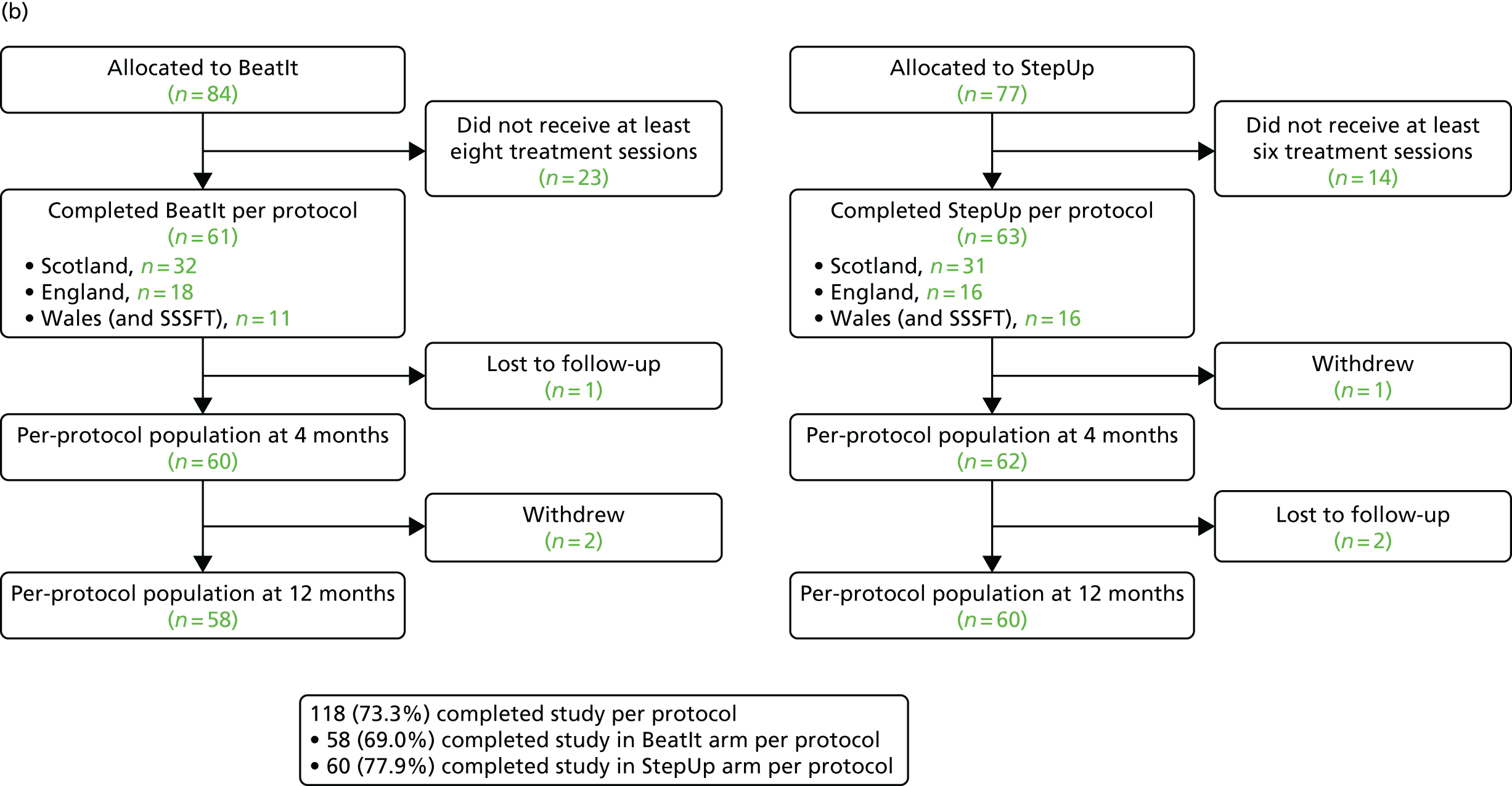
This resulted in 161 people being randomised into the trial. Six people were lost to follow-up and 14 people withdrew during the trial, resulting in a total of 141 participants who completed the trial. Sixty-nine of these 141 participants were recruited in Scotland, 38 in England and 34 in Wales.
Table 4 shows that two-thirds of the participants were referred by community nurses, psychologists and psychiatrists who worked in community teams for people with learning disabilities.
| Profession | Site (n) | Total (n) | ||
|---|---|---|---|---|
| Scotland | England | Wales | ||
| Nurse | 30 | 23 | 30 | 83 |
| Psychologist | 27 | 0 | 1 | 28 |
| Psychiatrist | 11 | 0 | 4 | 15 |
| Social worker | 4 | 0 | 4 | 8 |
| Dietitian | 2 | 0 | 0 | 2 |
| Self-referral | 0 | 6 | 0 | 6 |
| IAPT therapist | 0 | 9 | 0 | 9 |
| Clinical studies officer | 0 | 5 | 0 | 5 |
| Support worker | 0 | 3 | 0 | 3 |
| Reviewing officer | 0 | 0 | 2 | 2 |
| Unknown | 0 | 0 | 0 | 0 |
| Total | 74 | 46 | 41 | 161 |
Participants at baseline
Seventy-seven participants were randomised to receive StepUp and 84 participants were randomised to receive BeatIt. The imbalance of seven participants was a result of using a stratified randomisation scheme. Participants were randomised in six strata defined by recruitment site (Scotland, England, Wales) and whether or not participants were taking antidepressants at baseline (yes/no). Within these strata, participants were randomised in blocks of length four (two to each arm) and six (three to each arm), with block lengths occurring at random. Therefore, within each stratum, the imbalance between treatment groups could be at most three in either direction (if the study stopped midway through a block of six allocations, and that block had consisted of three allocations to one group by three allocations to the other group). Across the six strata, at the end of the trial, the balance of randomisations were as follows:
-
Scotland, taking antidepressants: 29 to BeatIt and 27 to StepUp; difference = +2
-
Scotland, not taking antidepressants: 10 to BeatIt and eight to StepUp; difference = +2
-
England, taking antidepressants: 12 to BeatIt and 13 to StepUp; difference = –1
-
England, not taking antidepressants: 12 to BeatIt and nine to StepUp; difference = +3
-
Wales, taking antidepressants: 12 to BeatIt and 11 to StepUp; difference = +1
-
Wales, not taking antidepressants: nine to BeatIt, and nine to StepUp; difference = 0.
Table 5 describes demographic and health characteristics of the 161 participants who began the trial at baseline, broken down across the two therapy arms. Overall, a slight majority of participants were female, with a mean age of 40 years. Most participants were white and single. The mean Full Scale IQ was 58.34 for StepUp participants and 55.44 for BeatIt participants.
| Variable | Trial arm | |
|---|---|---|
| StepUp (N = 77) | BeatIt (N = 84) | |
| Gender, n (%) | ||
| Male | 38 (49.4) | 38 (45.2) |
| Female | 39 (50.6) | 46 (54.8) |
| Age (years) | ||
| Mean (SD) | 40.1 (12.0) | 40.3 (11.7) |
| IQ, mean (SD) | ||
| Verbal | 63.14 (10.15) | 58.87 (8.67) |
| Performance | 58.45 (8.11) | 57.84 (9.18) |
| Full Scale | 58.34 (8.38) | 55.44 (8.02) |
| Ethnicity, n (%) | ||
| White | 75 (97.4) | 81 (96.4) |
| Other | 1 (1.3) | 2 (2.4) |
| Unknown | 1 (1.3) | 1 (1.2) |
| Marital status, n (%) | ||
| Married/live-in partner | 7 (9.1) | 5 (6.0) |
| Separated/divorced/widowed | 1 (1.3) | 6 (7.1) |
| Single | 67 (87.0) | 73 (86.9) |
| Unknown | 2 (2.6) | 0 (0.0) |
| Vision, n (%) | ||
| Visual impairment | 45 (58.4) | 55 (65.5) |
| No visual impairment | 32 (41.6) | 29 (34.5) |
| Hearing, n (%) | ||
| Hearing impairment | 8 (10.4) | 20 (23.8) |
| No hearing impairment | 69 (89.6) | 64 (76.2) |
| Mobility problems, n (%) | ||
| Mobility problems | 20 (26.0) | 19 (22.6) |
| No mobility problems | 57 (74.0) | 65 (77.4) |
| Antiepileptic medication, n (%) | 9 (11.7) | 4 (4.8) |
A majority of participants (58.4% of StepUp participants and 65.5% of BeatIt participants) had some degree of visual impairment, with smaller proportions (10.4% of StepUp participants; 23.8% of BeatIt participants) having some degree of hearing impairment. Approximately one-quarter of participants (26.0% of StepUp participants; 22.6% of BeatIt participants) had mobility problems.
Table 6 describes selected circumstances of the 161 participants who began the trial at baseline, broken down by therapy arm. In terms of deciles of neighbourhood deprivation (where 1 is the most deprived and 10 is the least deprived) based on participants’ postcodes, participants on average were living in slightly more deprived postcodes than the median. In terms of negative life events, participants in both therapy arms had experienced on average more than one negatively experienced life event in the 12 months before baseline (mean 1.36 events for StepUp participants; mean 1.48 events for BeatIt participants).
| Variable | Trial arm | |
|---|---|---|
| StepUp (N = 77) | BeatIt (N = 84) | |
| Deprivation decile, mean (SD) | 3.8 (2.1) | 4.5 (2.6) |
| BLESID (life events): number of life events experienced negatively, mean (SD) | 1.36 (1.60) | 1.48 (1.59) |
| Degree of service support, n (%) | ||
| Less than daily support | 24 (31.2) | 25 (29.8) |
| Daily support | 53 (68.8) | 59 (70.2) |
| PSS: number of family members, mean (SD) | 1.32 (1.5) | 1.98 (2.3) |
| PSS: number of non-family members, mean (SD) | 3.30 (2.6) | 2.92 (2.3) |
| Previous therapy for depression, n (%) | ||
| Yes | 14 (18.2) | 17 (20.2) |
| No | 63 (81.8) | 67 (79.8) |
| Use of antidepressants, n (%) | ||
| Yes | 51 (66.2) | 53 (63.1) |
| No | 26 (33.8) | 31 (36.9) |
| Use of mood stabilisers, n (%) | ||
| Yes | 15 (19.5) | 11 (13.1) |
| No | 62 (80.5) | 73 (86.9) |
| Antiepileptic medication, n (%) | ||
| Yes | 9 (11.7) | 4 (4.8) |
| No | 68 (88.3) | 80 (95.2) |
Service receipt in the 4 months prior to baseline
Over two-thirds of participants (68.8% of StepUp participants; 70.2% of BeatIt participants) were receiving support from services at least daily. According to the PSS scale, participants were receiving social support from an average of fewer than two family members (1.32 for StepUp participants; 1.98 for BeatIt participants) and social support from an average of approximately three non-family members (3.30 for StepUp participants; 2.92 for BeatIt participants).
Approximately one-fifth of participants had previously received therapy for depression (18.2% of StepUp participants; 20.2% of BeatIt participants). Approximately two-thirds of participants were being prescribed antidepressant medication (66.2% of StepUp participants; 63.1% of BeatIt participants). In terms of mood-stabilising medication, 19.5% of StepUp participants and 13.1% of BeatIt participants were prescribed this medication. It was also established that 11.7% of StepUp participants and 4.8% of BeatIt participants were taking antiepileptic medication.
Table 7 describes the services used by participants in the 4 months prior to baseline, broken down by therapy type. This was collected using the Client Service Receipt Inventory (CSRI) and gives some indication of the context of participants’ lives as they entered the trial.
| Resource | Trial arm | Difference | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | |||||
| Mean (SD) | Used by, n (%) | Mean (SD) | Used by, n (%) | Mean (SE) | 95% CI | |
| Daytime activities | ||||||
| Day centre | ||||||
| Weeks attended | 14.9 (3.93) | 10 (13.7) | 15.3 (2.69) | 13 (19.1) | –0.41 (1.45) | –3.49 to 2.68 |
| Hours per week | 18.4 (8.14) | 10 (13.7) | 20.8 (11.61) | 13 (19.1) | –2.46 (4.12) | –11.0 to 6.12 |
| Voluntary work | ||||||
| Weeks attended | 12.7 (6.25) | 18 (24.7) | 13.6 (4.87) | 13 (19.1) | –0.89 (2.0) | –4.98 to 3.20 |
| Hours per week | 4.69 (5.99) | 18 (24.7) | 5.31 (4.12) | 13 (19.1) | –0.61 (1.82) | –4.33 to 3.10 |
| Adult education | ||||||
| Weeks attended | 15.4 (1.81) | 7 (9.6) | 8.71 (5.62) | 7 (10.3) | 6.71 (2.23) | 1.47 to 12.0 |
| Hours per week | 4.93 (2.32) | 7 (9.6) | 8.57 (10.9) | 7 (10.3) | –3.64 (4.22) | –13.8 to 6.48 |
| Social club | ||||||
| Weeks attended | 13.1 (5.67) | 23 (31.5) | 13.4 (5.56) | 22 (32.4) | –0.32 (1.67) | –3.70 to 3.06 |
| Hours per week | 3.28 (2.01) | 23 (31.5) | 3.32 (1.96) | 22 (32.4) | –0.04 | –1.23 to 1.16 |
| Hospital services: number of contacts | ||||||
| Other hospital outpatient visit | 5.31 (11.2) | 13 (17.8) | 2.94 (3.55) | 16 (23.5) | 2.37 (3.23) | –4.55 to 9.30 |
| A&E visit | 1.56 (1.01) | 9 (12.3) | 1 (0) | 7 (10.3) | 0.56 (0.34) | –0.22 to 1.33 |
| Community-based services: number of contacts | ||||||
| Community psychiatrist | 1.77 (1.07) | 26 (35.6) | 2.43 (2.17) | 28 (41.2) | –0.66 (0.46) | –1.59 to 0.271 |
| Psychologist | 5.41 (8.14) | 17 (23.3) | 5.14 (6.68) | 14 (20.6) | 0.27 (2.66) | –5.17 to 5.71 |
| GP | 3.17 (3.40) | 48 (65.8) | 3.07 (2.33) | 46 (67.6) | 0.10 (0.60) | –1.09 to 1.29 |
| Community psychiatric nurse | 5.25 (3.20) | 4 (5.5) | 8.20 (5.85) | 5 (7.4) | –2.95 (3.07) | –10.3 to 4.45 |
| Community learning disability nurse | 5.91 (4.84) | 32 (43.8) | 6.21 (5.76) | 24 (35.3) | –0.30 (1.45) | –3.23 to 2.63 |
| Other community nurse | 28.8 (66.5) | 12 (16.4) | 3.27 (4.71) | 11 (16.2) | 25.6 (19.3) | –16.8 to 67.9 |
| Physiotherapist | 6.29 (6.02) | 7 (9.6) | 4.6 (6.95) | 5 (7.4) | 1.69 (3.85) | –7.21 to 10.6 |
| Occupational therapist | 6.10 (6.40) | 10 (13.7) | 5.40 (6.58) | 5 (7.4) | 0.70 (3.57) | –7.56 to 8.96 |
| Social worker/care manager | 3.16 (4.08) | 32 (43.8) | 3.72 (4.12) | 25 (36.8) | –0.56 (1.09) | –2.76 to 1.63 |
| Home help/home care worker | 80.3 (53.1) | 23 (31.5) | 84.3 (57.1) | 24 (35.3) | –4.07 (16.01) | –36.5 to 28.3 |
| Advocate/counsellor | 5.30 (6.36) | 10 (13.7) | 4.67 (5.89) | 9 (13.2) | 0.63 (2.81) | –5.30 to 6.57 |
| Dentist | 1.95 (1.81) | 37 (50.7) | 1.48 (0.77) | 25 (36.8) | 0.466 (0.335) | –0.21 to 1.14 |
| Optician | 1.45 (0.69) | 11 (15.1) | 1.08 (0.29) | 12 (17.6) | 0.37 (0.22) | –0.11 to 0.85 |
| Chiropodist | 1.80 (1.01) | 15 (20.5) | 2.31 (1.03) | 13 (19.1) | –0.51 (0.39) | –1.31 to 0.291 |
| Employment services/job centre | 5.60 (6.50) | 5 (6.8) | 6.57 (7.35) | 7 (10.3) | –0.97 (4.02) | –10.0 to 8.07 |
In cases in which < 5% of participants at baseline had received a particular service in the 4 months before baseline (eight participants or fewer), full data are excluded from Table 7. Specific services used by eight or fewer participants in total in the 4 months before baseline were sheltered work (used by three people in total); drop-in centre (four people); learning disabilities centre (zero people); psychiatric intensive care ward (zero people); acute psychiatric ward (one person); psychiatric rehabilitation ward (one person); general medical ward (seven people); other hospital specialties (two people); day hospital (two people); psychiatric outpatient visits (five people); community mental health team member (one person); healthcare assistant (three people); speech therapist (one person); art/drama/music therapist (one person); alternative therapist (two people); social work assistant (two people); and audiologist (five people).
Table 7 shows 25 indicators of service use, used by nine or more participants in the trial in the 4 months prior to baseline. For specific types of daytime activity, the number of weeks a service was used in the 4 months prior to baseline, the mean number of hours per week the service was used, and the number of people who used the service are presented. For hospital services and community-based services, the mean number of contacts with the service in the 4 months prior to baseline and the number of people having contact with the service are presented.
There was a statistically significant difference between BeatIt and StepUp participants in one of these indicators – StepUp participants had been attending adult education for more weeks than BeatIt participants.
In terms of daytime activities, across both therapy arms, 23 participants had attended a day centre in the 4 months prior to baseline, 31 participants had engaged in voluntary work, 14 participants had attended adult education and 45 participants had attended a social club. For those participants that had engaged in each daytime activity, participants spent 18–21 hours per week attending a day centre (mean 18.4 hours for StepUp participants; mean 20.8 hours for BeatIt participants), 5 hours per week engaged in voluntary work (mean 4.7 hours for StepUp participants; mean 5.3 hours for BeatIt participants), 5–9 hours per week attending adult education (mean 4.9 hours for StepUp participants; mean 8.6 hours for BeatIt participants), and 3 hours per week attending a social club (mean 3.3 hours for both StepUp and BeatIt participants).
In terms of contact with hospital services, across both therapy arms, 29 participants had attended other hospital outpatient visits in the 4 months prior to baseline, with StepUp participants having a mean of 5.3 contacts and BeatIt participants having a mean of 2.9 contacts. Sixteen participants had visited accident and emergency (A&E) in the 4 months prior to baseline, with StepUp participants having a mean of 1.6 contacts with A&E and BeatIt participants having 1 contact with A&E.
In terms of contacts with community-based services in the 4 months prior to baseline, most participants (94 across both therapy arms) had had contact with a GP, with a mean of 3.2 contacts for StepUp participants and 3.1 contacts for BeatIt participants).
Across both therapy arms 54 participants had had contact with a community psychiatrist (mean 1.8 contacts for StepUp participants; mean 2.4 contacts for BeatIt participants), 31 participants had had contact with a psychologist (mean 5.4 contacts for StepUp participants; mean 5.1 contacts for BeatIt participants), and nine participants had had contact with a community psychiatric nurse (mean 5.3 contacts for StepUp participants; mean 8.2 contacts for BeatIt participants).
In total, 56 participants had had contact with a learning disability nurse (mean 5.9 contacts for StepUp participants; mean 6.2 contacts for BeatIt participants), 23 participants had had contact with another community nurse (mean 28.8 contacts for StepUp participants; mean 3.3 contacts for BeatIt participants), 12 participants had had contact with a physiotherapist (mean 6.3 contacts for StepUp participants; mean 4.6 contacts for BeatIt participants) and 15 participants had had contact with an occupational therapist (mean 6.1 contacts for StepUp participants; mean 5.4 contacts for BeatIt participants).
Across both therapy arms, 57 participants had had contact with a social worker or care manager in the 4 months prior to baseline (mean 3.2 contacts for StepUp participants; mean 3.7 contacts for BeatIt participants), 47 participants had had contact with a home help or home care worker (mean 80.3 contacts for StepUp participants; mean 84.3 contacts for BeatIt participants), and 19 participants had had contact with an advocate or counsellor (mean 5.3 contacts for StepUp participants; mean 4.7 contacts for BeatIt participants).
Overall, 62 participants had had contact with a dentist (mean 2.0 contacts for StepUp participants; mean 1.5 contacts for BeatIt participants), 23 had had contact with an optician (mean 1.5 contacts for StepUp participants; mean 1.1 contacts for BeatIt participants), and 28 participants had had contact with a chiropodist (mean 1.8 contacts for StepUp participants; mean 2.3 contacts for BeatIt participants). In total, 12 participants had had contact with employment services or a job centre in the 4 months prior to baseline (mean 5.6 contacts for StepUp participants; mean 6.6 contacts for BeatIt participants).
Carers at baseline
Table 8 describes characteristics of the carers of the 161 participants who began the trial, broken down by therapy arm. Carers were those who had a significant caring responsibility for the participant and knew the participant sufficiently well to complete the informant measures in the study. A carer could also be the supporter for the participant in the therapy, but this was not a requirement, and a participant could have several people in their lives with significant caring roles.
| Variable | Trial arm | |
|---|---|---|
| StepUp (N = 77) | BeatIt (N = 84) | |
| Gender, n (%) | ||
| Male | 20 (26.0) | 21 (25.0) |
| Female | 57 (74.0) | 63 (75.0) |
| Age (years), mean (SD) | 47.0 (13.0) | 46.7 (12.6) |
| Ethnicity, n (%) | ||
| White | 77 (100.0) | 82 (97.6) |
| Other | 0 (0.0) | 2 (2.4) |
| Relationship to participant, n (%) | ||
| Family | 22 (28.6) | 24 (28.6) |
| Worker | 32 (41.6) | 35 (41.7) |
| Other | 23 (29.9) | 25 (29.8) |
| Average weekly contact with participant, n (%) | ||
| Less than daily | 50 (64.9) | 57 (67.9) |
| Daily | 9 (11.7) | 8 (9.5) |
| Lives with participant | 18 (23.4) | 19 (22.6) |
Table 8 shows that approximately three-quarters of carers were female (74.0% of carers of StepUp participants; 75.0% of carers of BeatIt participants), with an average age of 47 years. Almost all carers were white. In terms of their relationship to the participant, over one-quarter were family members (28.6% of carers of participants in each therapy arm), over two-fifths were workers (41.6% of carers of StepUp participants; 41.7% of carers of BeatIt participants), and over one-quarter were ‘other’ carers (29.9% of carers of StepUp participants; 29.8% of carers of BeatIt participants). In terms of average weekly contact between the carer and the participant, approximately two-thirds of carers had less than daily contact with participants (64.9% of carers of StepUp participants; 67.9% of carers of BeatIt participants); a small proportion had daily contact with participants (11.7% of StepUp participants; 9.5% of BeatIt participants); and almost one-quarter of carers were living with the participant (23.4% of carers of StepUp participants; 22.6% of carers of BeatIt participants).
Chapter 4 Fidelity
Training and supervision
The therapy was provided by 76 therapists. Sixteen (21.1%) therapists were men (BeatIt, n = 8 men; StepUp, n = 8 men) and 60 (78.9%) were women (BeatIt, n = 35 women; StepUp, n = 25 women), with a mean age of 40.5 years (SD 10.5 years) [BeatIt therapist mean age = 40.4 years (SD 11.4 years); StepUp therapist mean age = 41.8 years (SD 9.7 years)]. There were no significant differences in sex [χ2 = 0.36, degrees of freedom (df) = 1, not significant] or age (t = 0.55, df = 73, not significant) of therapist. Fifty (65.8%) therapists were nurses (BeatIt, n = 28 nurses; StepUp, n = 22 nurses), 13 (17.1%) were psychology assistants or trainees (BeatIt, n = 9 assistants or trainees; StepUp, n = 4 assistants or trainees), 4 (5.3%) were occupational therapists (BeatIt, n = 1 occupational therapist; StepUp, n = 3 occupational therapists) and 6 (7.9%) were CBT therapists (BeatIt, n = 3 CBT therapists; StepUp, n = 3 CBT therapists). There were three therapists whose profession was not recorded. There was no significant difference in distribution of professions between the arms of the study (χ2 = 2.6, df = 3, not significant). Forty-six (60.5%) therapists had worked with people with learning disabilities for > 5 years (BeatIt, n = 26 therapists; StepUp, n = 20 therapists), 10 (13.2%) for 1 to 5 years (BeatIt, n = 7 therapists; StepUp, n = 3 therapists) and 18 (23.7%) for < 1 year (BeatIt, n = 10 therapists; StepUp, n = 8 therapists). These data were not available for two therapists. There was no significant difference between the arms of the study in the distribution of the duration that therapists had been working with people who have learning disabilities (χ2 = 0.68, df = 2, not significant). Twenty-nine (38.2%) of the therapists had no previous therapy training (BeatIt, n = 14 therapists; StepUp, n = 15 therapists); 13 (17.1%) had attended an accredited training course (BeatIt, n = 6 therapists; StepUp, n = 7 therapists); 10 (13.2%) had received ‘in-house’ training (BeatIt, n = 4 therapists; StepUp, n = 6 therapists), 10 (13.2%) had received training as part of their professional training (BeatIt, n = 5 therapists; StepUp, n = 5 therapists) and 4 (4.8%) had received training from other sources (BeatIt, n = 4 therapists; StepUp, n = 0 therapists). These data were not available for 10 therapists. There was no significant difference between the arms of the study in the distribution of previous therapy training (χ2 = 4.38, df = 4, not significant).
The manual stipulated that there should be one supervision meeting for every two therapy sessions. All supervisors in the study were clinical psychologists. Therapists in the BeatIt arm received a mean of 6.4 supervision sessions (SD 0.37 sessions, range 1–13 sessions), and those in the StepUp arm had a mean of 4.7 supervision sessions (SD 0.29 sessions, range 1–10 sessions). However, these data can be misleading, as not all participants received the full number of sessions (as a result of drop-out etc.), and preferred levels of supervision were actually defined in terms of the ratio of supervision meetings to therapy sessions. Excluding participants who received no sessions, the mean ratio of supervision meetings to therapy sessions delivered was 1.9 (SD 1.36). The expected ratio was 2.0, and a mean of < 2.0 indicates a slightly higher than expected level of supervision. Ninety-eight (73.1%) cases met the criterion of at least one supervision meeting for every two therapy sessions, whereas 36 (25.5%) did not. The lowest ratio of supervision to therapy was 4.0, which occurred in one BeatIt case in which only three supervision meetings were recorded for 12 therapy sessions.
The measurement of fidelity during the course of the intervention
There were 144 fidelity recordings available for analysis. These constituted recordings for 93 participants, 49 from StepUp and 44 from BeatIt, with 51 participants having two recordings available. There are multiple reasons why recordings were not always completed: 21 participants refused consent for recording, 39 participants did not provide recordings because they withdrew from the study before being recorded, 12 recordings were not made because the participant or carer refused to have the recording made on the day and two recordings were lost in transfer or as a result of other technical difficulties with recording equipment. The baseline scores for GDS-LD, IDDS and BPI-S Aggressive Behaviour subscale and age for the 93 participants for whom fidelity recordings were available were compared with the 68 participants for whom they were not, and there were no statistically significant differences. There was also no association between the availability of fidelity recording and the sex of the participants. A second researcher rated 48 recordings to determine inter-rater reliability; the intraclass correlation for agreement was 0.76 (df = 43; p < 0.001).
Therapy quality and non-specific factors
When looking at the first available recording from each of the 93 participants who provided recordings, the 10-item fidelity scale had a mean total score of 33.1 points (SD 4.1 points, range 18–39 points). Table 9 shows that there was a very similar pattern of findings for both the BeatIt and StepUp arms. The highest scoring items were those relating to empathy, warmth and not including therapy activity that was not part of the manual; the lowest scoring items were for including the client and supporter in the process of setting the session agenda and asking for feedback at the end of the session. The scale had an alpha of 0.76 and a mean-adjusted item-total correlation of 0.42 (SD 0.1, range 0.31–0.58). The stability of fidelity was 0.64, estimated through a Pearson’s correlation of first and second fidelity ratings for the 51 participants with two recordings. There was no significant difference in the fidelity scores between the two arms (BeatIt: mean = 32.3, SD 4.1; StepUp: mean = 33.9, SD 3.9; t = 1.5, not significant).
| Scale items | Total group (n = 93) | Trial arm | |||||
|---|---|---|---|---|---|---|---|
| BeatIt | StepUp | ||||||
| Minimum, maximum | Mean | Corrected item-total correlation | Mean | SD | Mean | SD | |
| 1. Creates agenda, agrees what will be covered in session | 1, 4 | 2.74 | 0.35 | 2.75 | 1.04 | 2.73 | 0.79 |
| 2. The presence of a focus and clear structure to the session | 1, 4 | 3.44 | 0.58 | 3.32 | 0.77 | 3.55 | 0.65 |
| 3. Avoids offering therapy outside the remit of the intervention | 2, 4 | 3.73 | 0.31 | 3.64 | 0.69 | 3.82 | 0.49 |
| 4. Asks for feedback from previous session | 1, 4 | 3.19 | 0.43 | 3.14 | 0.73 | 3.24 | 0.72 |
| 5. Asks for feedback and reaction to the current session | 1, 4 | 2.89 | 0.43 | 2.84 | 0.75 | 2.94 | 0.88 |
| 6. Conveys understanding by checking and rephrasing | 1, 4 | 3.13 | 0.52 | 3.09 | 0.80 | 3.16 | 0.85 |
| 7. Adjusts content and style of own communication | 2, 4 | 3.28 | 0.31 | 3.14 | 0.73 | 3.41 | 0.61 |
| 8. Communicates clearly without hesitations and with good pace | 1, 4 | 3.48 | 0.51 | 3.45 | 0.70 | 3.51 | 0.77 |
| 9. Shows empathy | 2, 4 | 3.58 | 0.45 | 3.55 | 0.50 | 3.61 | 0.57 |
| 10. Shows warmth and respect | 1, 4 | 3.65 | 0.56 | 3.68 | 0.47 | 3.61 | 0.64 |
Covering key elements/activities in individual therapy sessions
For the session-specific technical ratings, each session could gain a score that ranged from 3, if all elements were conformed to, to 0 if none of the elements was conformed to. For BeatIt, 33 sessions obtained a score of 3, 10 sessions obtained a score of 2, one session obtained a score of 1 and no sessions received a score of 0. In the StepUp arm, 42 sessions obtained a score of 3, seven sessions obtained a score of 2 and no sessions received a score of 1 or 0. The differences in distribution of scores between the groups is not significant (Fisher’s exact test p = 0.23). For the purpose of further analysis, the data were collapsed across both arms and treated as dichotomous, with 75 sessions gaining a full score of 3 and 18 obtaining a score of < 3. The 75 sessions with a score of 3 had a mean therapy quality scale score of 33.7 (SD 3.6); the 18 sessions with a score of < 3 had a mean score of 33.1 (SD 4.7). This is a statistically significant difference (t = 2.5, df = 91; p = 0.014), showing a significant relationship between two measures of fidelity.
Delivery and consistency of support
Patients randomised to the BeatIt arm of the trial began their therapy sessions a median of 36 days (interquartile range 28–49 days) after randomisation, compared with 27 days (interquartile range 21–42 days) for those randomised to StepUp; this was a statistically significant difference (p = 0.003, Mann–Whitney U-test). This difference was because the BeatIt intervention began with a session for the supporters alone, to provide them with information about therapy and their role in sessions.
There was excellent attendance of the sessions, with participants in the BeatIt arm attending an average of 9.9 sessions (SD 3.2 sessions) and StepUp participants attending an average of 7.1 sessions (SD 2.1 sessions). Sixty-six per cent of the BeatIt therapy sessions were delivered as scheduled and 77% of the StepUp sessions were delivered as planned.
For BeatIt, 38 (51%) participants had the same supporter throughout their therapy, 16 (23%) had two supporters, 10 (14%) had three supporters, 1 (1%) had four supporters and 2 (3%) had five supporters. For StepUp, 42 (61%) participants had one supporter throughout their therapy, 16 (23%) had two supporters, 6 (9%) had three supporters, 1 (1%) had four supporters and 2 (3%) had five supporters.
Chapter 5 Trial results
Primary outcome
A reduction in the GDS-LD total score represents an improvement in symptoms of depression. In the analyses reported here, a positive intervention effect indicates a greater reduction in depression symptoms in the BeatIt group compared with the StepUp group. The GDS-LD scores post intervention (4 months after randomisation) and at follow-up (12 months after randomisation – the primary end point) were analysed in adjusted mixed-effects linear regression models (Table 10) that adjusted for baseline GDS-LD scores, therapist effects (as a random effect), study centre and baseline antidepressant use.
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 16.90 (6.73) | 84 (0) | 16.60 (7.91) | ||
| Post intervention (4 months) | 72 (5) | 12.94 (7.77) | 68 (16) | 11.91 (7.43) | 1.03 (–1.51 to 3.58) | 0.424a |
| Follow-up (12 months) | 70 (7) | 12.43 (7.64) | 65 (19) | 12.03 (7.99) | 0.40 (–2.26 to 3.06) | 0.768a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | –4.40 (–5.89 to –2.91); < 0.001b | –5.15 (–6.70 to –3.60); < 0.001b | –0.75 (–2.80 to 1.31) | 0.471c | ||
| Follow-up (12 months) | –4.46 (–6.21 to –2.70); < 0.001b | –4.20 (–6.0 to –2.40); < 0.001b | 0.26 (–2.18 to 2.70) | 0.833c | ||
There were no statistically significant unadjusted or adjusted group differences in the effects of the StepUp or BeatIt interventions on GDS-LD scores at 12 months (primary end point) or 4 months (p-value column of Table 10).
The same analysis models were also applied to the changes in GDS-LD scores between 4 and 12 months to examine whether or not the treatments may have had different effects on GDS-LD scores from post intervention to follow-up. There was no overall change in GDS-LD scores from 4 to 12 months [estimate –0.42, 95% confidence interval (CI) –2.30 to 1.47; p = 0.663] and no interaction between treatment group and data collection point (4 vs. 12 months) (estimate 0.56, 95% CI –2.15 to 3.27; p = 0.685).
All of the above reported analyses were repeated using multiple imputation for missing data. Although the estimates for effects changed slightly, the overall pattern of findings was identical.
Secondary, within-group analyses (see Table 10) showed that participants in both treatment groups reported significant reductions in GDS-LD scores at both 4 and 12 months. The analysis of 4- to 12-month change summarised above suggests that these changes from baseline are accounted for mainly by reductions in GDS-LD scores from baseline to post intervention (4 months), with no change from post intervention (4 months) to follow-up (12 months).
Secondary outcomes
Measures of depression and anxiety
Carers of participants were asked to complete the IDDS as a secondary measure of the effects of StepUp and BeatIt on behavioural symptoms of depression (Table 11). As with the primary outcome, reductions in IDDS scores represent improvement and, in the analyses reported here, a positive intervention effect indicates a greater reduction in depression symptoms in the BeatIt group compared with the StepUp group.
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 73.57 (31.37) | 84 (0) | 83.87 (32.70) | ||
| Post intervention (4 months) | 70 (7) | 59.66 (34.13) | 65 (19) | 60.37 (29.01) | –0.71 (–11.54 to 10.11) | 0.897a |
| Follow-up (12 months) | 66 (11) | 55.02 (30.06) | 63 (21) | 61.02 (31.82) | –6.00 (–16.78 to 4.78) | 0.273a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | –17.01 (–23.71 to –10.31); < 0.001b | –21.50 (–28.51 to –14.49); < 0.001b | –4.49 (–13.72 to 4.75) | 0.336c | ||
| Follow-up (12 months) | –22.01 (–29.62 to –14.40); < 0.001b | –20.65 (–28.3 to –12.98); < 0.001b | 1.36 (–9.19 to 11.92) | 0.797c | ||
There were no statistically significant unadjusted or adjusted group differences in the effects of StepUp and BeatIt on IDDS scores at 12 months (primary end point) or 4 months (p-value column of Table 11).
The same analysis models were also applied to the changes in IDDS scores between 4 and 12 months to examine whether or not the treatments may have had different effects on IDDS scores from post intervention to follow-up. There was no overall change in IDDS scores from 4 to 12 months, and no interaction between treatment group and data collection point (4 vs. 12 months).
Within-group analyses (see Table 11) showed that participants in both treatment groups reported significant reductions in IDDS scores at both 4 and 12 months. The analysis of 4- to 12-month change summarised above suggests that these changes from baseline are accounted for mainly by reductions in IDDS scores from baseline to post intervention (4 months), with no change from post intervention (4 months) to follow-up (12 months).
To examine potential effects on participants’ anxiety symptoms, they were asked to complete the self-report GAS-ID as a secondary measure (Table 12). Reductions in GAS-ID scores represent improvement and, in the analyses reported here, a positive intervention effect indicates a greater reduction in anxiety symptoms in the BeatIt group compared with the StepUp group.
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 24.71 (11.00) | 83 (1) | 25.05 (11.15) | ||
| Post intervention (4 months) | 70 (7) | 21.39 (11.70) | 65 (19) | 20.96 (11.18) | 0.43 (–3.39 to 4.26) | 0.823a |
| Follow-up (12 months) | 70 (7) | 20.07 (11.15) | 65 (19) | 20.77 (11.36) | –0.70 (–4.53 to 3.14) | 0.719a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | –3.96 (–5.86 to –2.06); < 0.001b | –4.73 (–6.71 to –2.75); < 0.001b | –0.77 (–3.38 to 1.84) | 0.559c | ||
| Follow-up (12 months) | –4.83 (–7.00 to –2.66); < 0.001b | –4.40 (–6.61 to –2.20); < 0.001b | 0.43 (–2.59 to 3.45) | 0.776c | ||
There were no statistically significant unadjusted or adjusted group differences in the effects of StepUp and BeatIt on GAS-ID scores at 12 months (primary end point) or 4 months (p-value column of Table 12).
The same analysis models were also applied to the changes in GAS-ID scores between 4 and 12 months. Again, there was no overall change in GAS-ID scores from 4 to 12 months, and no interaction between treatment group and data collection point (4 vs. 12 months).
Within-group analyses (see Table 12) showed that participants in both treatment groups reported significant reductions in GAS-ID scores at both 4 and 12 months. The analysis of 4- to 12-month change summarised above suggests that these changes from baseline are accounted for mainly by reductions in GAS-ID scores from baseline to post intervention (4 months), with no change from post intervention (4 months) to follow-up (12 months).
Level of aggressive behaviour
Carers of participants were asked to complete the Aggressive and Destructive Behaviour subscale from the BPI-S as a secondary measure of the effects of StepUp and BeatIt on aggressive behaviour (Table 13). Reductions in BPI-S scores represent improvement and, in the analyses reported here, a positive intervention effect indicates a greater reduction in depression symptoms in the BeatIt group compared with the StepUp group.
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 2.10 (3.61) | 84 (0) | 1.96 (2.74) | ||
| Post intervention (4 months) | 69 (8) | 2.09 (3.84) | 66 (18) | 1.24 (2.19) | 0.84 (–0.22 to 1.91) | 0.118a |
| Follow-up (12 months) | 67 (10) | 1.82 (3.42) | 64 (20) | 1.09 (1.85) | 0.73 (–0.22 to 1.67) | 0.131a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | –0.17 (–0.82 to 0.48); 0.861b | –0.82 (–1.49 to –0.15); 0.017b | –0.65 (–1.55 to 0.25) | 0.154c | ||
| Follow-up (12 months) | –0.22 (–0.80 to 0.36); 0.447b | –0.89 (–1.49 to –0.30); 0.004b | –0.67 (–1.46 to 0.12) | 0.093c | ||
There were no statistically significant unadjusted or adjusted group differences in the effects of StepUp and BeatIt on BPI-S scores at 12 months (primary end point) or 4 months (p-value column of Table 13). The same analysis models were also applied to the changes in BPI-S scores between 4 and 12 months. There was no overall change in BPI-S scores from 4 to 12 months, and no interaction between treatment group and data collection point (4 vs. 12 months).
Within-group analyses (see Table 13) showed that participants in the BeatIt group, but not in the StepUp group, reported significant reductions in BPI-S scores at both 4 and 12 months. The analysis of 4- to 12-month change summarised above suggests that these changes from baseline are accounted for mainly by reductions in BPI-S scores from baseline to post intervention (4 months), with no change from post intervention (4 months) to follow-up (12 months).
Quality-of-life measures
A range of self-reported and assisted-completion QoL measures were included as secondary outcomes. Higher EQ-5D-Y and EQ-VAS scores equated to better QoL, as did higher scores on the total and subdomains of the ICI and IPDL. Higher scores on the PSS scale indicated a larger social network and increased satisfaction with the social support received. All of these QoL indicators were analysed using the same approaches as for the primary outcome and other secondary outcomes reported in preceding sections.
For outcomes at 12 months (primary end point) and 4 months (post intervention), there were no treatment group differences for any QoL measure except the ICI domestic and leisure subscale (Tables 14–22). Participants in the BeatIt group had a statistically significant higher mean score on this outcome domain at the 12-month follow-up.
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 76 (1) | 0.62 (0.38) | 84 (0) | 0.46 (0.44) | ||
| Post intervention (4 months) | 72 (5) | 0.69 (0.36) | 68 (16) | 0.64 (0.41) | 0.05 (–0.08 to 0.18) | 0.411a |
| Follow-up (12 months) | 70 (7) | 0.70 (0.35) | 65 (19) | 0.68 (0.41) | 0.02 (–0.11 to 0.15) | 0.742a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 0.15 (0.06 to 0.24); 0.002b | 0.16 (0.06 to 0.25); 0.001b | 0.01 (–0.12 to 0.14) | 0.878c | ||
| Follow-up (12 months) | 0.12 (0.04 to 0.21); 0.005b | 0.16 (0.07 to 0.25); < 0.001b | 0.04 (–0.08 to 0.15) | 0.546c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 56.96 (29.53) | 84 (0) | 46.56 (28.63) | ||
| Post intervention (4 months) | 72 (5) | 56.64 (29.61) | 68 (16) | 48.72 (28.21) | –4.54 (–14.76 to 5.67) | 0.381a |
| Follow-up (12 months) | 70 (7) | 57.36 (28.92) | 65 (19) | 49.23 (28.76) | –3.32 (–13.48 to 6.85) | 0.520a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 4.96 (–1.81 to 11.72); 0.149b | 13.10 (6.11 to 20.09); < 0.001b | 8.15 (–1.16 to 17.45) | 0.085c | ||
| Follow-up (12 months) | 0.48 (–6.60 to 7.55); 0.893b | 7.22 (–0.11 to 14.56); 0.053b | 6.75 (–3.07 to 16.56) | 0.174c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 51.26 (17.35) | 84 (0) | 49.81 (15.94) | ||
| Post intervention (4 months) | 72 (5) | 51.47 (17.44) | 68 (16) | 53.71 (16.80) | –2.23 (–7.96 to 3.49) | 0.442a |
| Follow-up (12 months) | 69 (8) | 48.52 (16.95) | 66 (18) | 51.45 (15.34) | –2.93 (–8.44 to 2.58) | 0.294a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 1.53 (–1.06 to 4.12); 0.243b | 4.76 (2.07 to 7.45); < 0.001b | 3.23 (–0.33 to 6.78) | 0.074c | ||
| Follow-up (12 months) | –2.11 (–4.89 to 0.67); 0.135b | 1.00 (–1.84 to 3.85); 0.483b | 3.11 (–0.68 to 6.90) | 0.106c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 22.51 (10.51) | 84 (0) | 21.63 (9.02) | ||
| Post intervention (4 months) | 72 (5) | 23.53 (10.42) | 68 (16) | 23.99 (10.90) | –0.46 (–4.02 to 3.11) | 0.800a |
| Follow-up (12 months) | 69 (8) | 22.04 (9.61) | 66 (18) | 22.20 (9.77) | –0.15 (–3.45 to 3.15) | 0.927a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 1.23 (–0.40 to 2.85); 0.137b | 2.86 (1.18 to 4.55); 0.001b | 1.64 (–0.59 to 3.87) | 0.148c | ||
| Follow-up (12 months) | –0.69 (–2.42 to 1.04); 0.427b | 0.12 (–1.65 to 1.89); 0.892b | 0.81 (–1.55 to 3.18) | 0.495c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 16.21 (5.66) | 84 (0) | 15.55 (5.32) | ||
| Post intervention (4 months) | 72 (5) | 16.17 (5.28) | 68 (16) | 16.34 (5.62) | –0.17 (–1.99 to 1.65) | 0.853a |
| Follow-up (12 months) | 69 (8) | 14.81 (5.72) | 66 (18) | 16.21 (5.55) | –1.40 (–3.32 to 0.52) | 0.151a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 0.62 (–0.38 to 1.61); 0.220b | 0.86 (–0.17 to 1.89); 0.101b | 0.24 (–1.12 to 1.60) | 0.722c | ||
| Follow-up (12 months) | –1.16 (–2.31 to –0.01); 0.049b | 0.46 (–0.72 to 1.63); 0.441b | 1.62 (0.04 to 3.19) | 0.045c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 12.55 (8.05) | 84 (0) | 12.63 (7.78) | ||
| Post intervention (4 months) | 72 (5) | 11.78 (8.21) | 68 (16) | 13.38 (6.64) | –1.60 (–4.11 to 0.90) | 0.207a |
| Follow-up (12 months) | 69 (8) | 11.52 (7.46) | 66 (18) | 12.42 (7.72) | –1.38 (–4.02 to 1.26) | 0.303a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | –0.28 (–1.56 to 0.99); 0.660b | 1.16 (–0.16 to 2.48); 0.085b | 1.44 (–0.32 to 3.19) | 0.107c | ||
| Follow-up (12 months) | –0.22 (–1.53 to 1.08); 0.732b | 0.37 (–0.97 to 1.70); 0.586b | 0.59 (–1.19 to 2.37) | 0.511c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 18.19 (9.03) | 84 (0) | 19.07 (8.46) | ||
| Post intervention (4 months) | 72 (5) | 18.46 (8.45) | 68 (16) | 18.34 (9.24) | 0.12 (–2.84 to 3.08) | 0.936a |
| Follow-up (12 months) | 69 (8) | 15.86 (7.97) | 66(18) | 16.47 (8.01) | –0.61 (–3.34 to 2.11) | 0.656a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 0.82 (–0.38 to 2.03); 0.176b | 0.31 (–0.94 to 1.57); 0.620b | –0.51 (–2.16 to 1.14) | 0.539c | ||
| Follow-up (12 months) | –1.58 (–2.94 to –0.22); 0.024b | –0.83 (–2.22 to 0.56); 0.238b | 0.75 (–1.11 to 2.61) | 0.424c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 4.62 (2.6) | 83 (1) | 4.89 (3.2) | ||
| Post intervention (4 months) | 72 (5) | 4.92 (2.99) | 68 (16) | 5.31 (2.95) | –0.39 (–1.39 to 0.60) | 0.436a |
| Follow-up (12 months) | 69 (8) | 4.71 (2.74) | 65 (19) | 4.92 (2.91) | –0.21 (–1.18 to 0.75) | 0.663a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 0.353 (–0.203 to 0.910); 0.210b | 0.440 (–0.136 to 1.016); 0.132b | 0.087 (–0.682 to 0.856) | 0.823c | ||
| Follow-up (12 months) | 0.150 (–0.447 to 0.747); 0.616b | 0.186 (–0.431 to 0.803); 0.550b | 0.035 (–0.786 to 0.857); 0.98 | 0.932c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 2.62 (0.55) | 83 (1) | 2.48 (0.53) | ||
| Post intervention (4 months) | 72 (5) | 2.65 (0.53) | 68 (16) | 2.59 (0.49) | 0.07 (–0.11 to 0.24) | 0.448a |
| Follow-up (12 months) | 69 (8) | 2.66 (0.44) | 65 (19) | 2.62 (0.50) | 0.04 (–0.12 to 0.20) | 0.627a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 0.08 (–0.03 to 0.18); 0.168b | 0.05 (–0.06 to 0.16); 0.369b | –0.02 (–0.17 to 0.12) | 0.741c | ||
| Follow-up (12 months) | 0.11 (–0.002 to 0.22); 0.054b | 0.11 (–0.004 to 0.22); 0.059b | 0.001 (–0.15 to 0.15) 0.98 | 0.987c | ||
The change in QoL scores across all measures between the 4- and 12-month follow-ups was associated with no significant effects and no interaction with treatment group, with two exceptions. First, there was a reduction overall in ICI domestic and leisure scores between 4 and 12 months (estimate –1.44, 95% CI –2.78 to –0.09; p = 0.037), but no interaction between treatment group and data collection point (4 vs. 12 months) (estimate 1.35, 95% CI –0.58 to 3.28; p = 0.170). Second, there was a reduction overall in IPDL scores between 4 and 12 months (estimate –2.43, 95% CI –4.04 to –0.83; p = 0.003), but no interaction between treatment group and data collection point (4 vs. 12 months) (estimate 1.29, 95% CI –1.01 to 3.59; p = 0.271).
In terms of changes from baseline scores in each treatment group separately, the EQ-5D-Y scores were more positive than at baseline at both 4 and 12 months in both treatment groups. The lack of evidence for change between 4 and 12 months suggests that this change occurred during the therapies and not afterwards. The EQ-VAS scores improved in the BeatIt group at 4 months but not in the StepUp group. At 12 months, neither treatment group had EQ-VAS scores that were different from those at baseline.
For two measures (ICI total score and ICI community subscale), the BeatIt group but not the StepUp group had higher scores at 4 months than at baseline, but neither group differed from baseline by 12-month follow-up. For two other measures (ICI domestic and leisure, and the IPDL), neither treatment group’s scores differed from baseline at 4 months but for both measures the StepUp group had scores lower at 12 months than at baseline, whereas the BeatIt group scores at 12-month follow-up were not different from baseline. For the final three measures (ICI social, PSS network size, PSS satisfaction), neither the BeatIt nor the StepUp group had scores different from baseline at either 4 or 12 months.
Adaptive behaviour
The ABS-RC2 subscales on socialisation, self-direction and responsibility were used to measure change in participants’ adaptive skills/functioning. Higher scores on each of these scores indicate higher levels of skills/functioning.
For the socialisation score (Table 23), there was a treatment group difference at 4 months, but not by the time of the 12-month follow-up. For the self-direction (Table 24) and responsibility scores (Table 25), there were no treatment group differences at either 12 months’ follow-up (primary end point) or at 4 months. Participants in the BeatIt group had higher socialisation scores at 4 months than participants in the StepUp group.
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 20.75 (3.12) | 84 (0) | 20.92 (3.55) | ||
| Post intervention (4 months) | 71 (6) | 20.20 (3.57) | 67 (17) | 21.37 (3.19) | –1.18 (–2.32 to –0.03) | 0.044a |
| Follow-up (12 months) | 68 (9) | 21.47 (2.52) | 66 (18) | 21.59 (3.17) | –0.12 (–1.10 to 0.86) | 0.808a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | –0.29 (–0.96 to 0.37); 0.379b | 0.82 (0.13 to 1.51); 0.021b | 1.11 (0.20 to 2.02) | 0.017c | ||
| Follow-up (12 months) | 0.76 (0.12 to 1.39); 0.020b | 0.89 (0.25 to 1.54); 0.007b | 0.14 (–0.72 to 1.00) | 0.750c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 14.60 (5.49) | 84 (0) | 15.38 (5.41) | ||
| Post intervention (4 months) | 71 (6) | 15.54 (4.83) | 67 (17) | 16.87 (4.68) | –1.33 (–2.93 to 0.27) | 0.103a |
| Follow-up (12 months) | 68 (9) | 16.59 (4.28) | 66 (18) | 16.94 (4.50) | –0.35 (–1.85 to 1.15) | 0.644a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 0.80 (–0.03 to 1.62); 0.059b | 1.78 (0.92 to 2.64); < 0.001b | 0.98 (–0.15 to 2.12); 0.089 | 0.089c | ||
| Follow-up (12 months) | 1.92 (0.99 to 2.84); < 0.001b | 2.04 (1.10 to 2.99); < 0.001b | 0.13 (–1.13 to 1.39) | 0.838c | ||
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 7.62 (2.10) | 84 (0) | 8.27 (1.77) | ||
| Post intervention (4 months) | 71 (6) | 7.72 (2.02) | 67 (17) | 8.28 (1.84) | –0.23 (–0.85 to 0.39) | 0.466a |
| Follow-up (12 months) | 68 (9) | 8.40 (1.51) | 67 (17) | 8.20 (1.76) | 0.20 (–0.36 to 0.76) | 0.481a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 0.32 (0.008 to 0.63); 0.045b | 0.16 (–0.17 to 0.48); 0.336b | –0.16 (–0.59 to 0.27); 0.4 | 0.452c | ||
| Follow-up (12 months) | 0.68 (0.33 to 1.03); < 0.001b | 0.24 (–0.11 to 0.60); 0.176b | –0.44 (–0.92 to 0.05) | 0.076c | ||
Focusing on changes between 4 and 12 months, there were no significant interactions between treatment group and outcome point. For both socialisation (estimate 1.29, 95% CI 0.41 to 2.17; p = 0.004) and self-direction scores (estimate 1.15, 95% CI 0.01 to 2.30; p = 0.049), but not for responsibility scores, there was a main effect of time, with higher scores at 12-month follow-up than at 4 months post intervention.
Within the BeatIt group, socialisation and self-direction scores showed a statistically significant increase from baseline to 4- and 12-month data collection points, but responsibility scores did not differ from baseline at either point (see Tables 23–25). Within the StepUp group, socialisation and self-direction scores were significantly higher than baseline at the 12-month follow-up only, whereas responsibility scores were higher at both 4- and 12-month follow-ups (see Tables 23–25). Considering these findings, in contrast to several of the other secondary outcomes, there is some evidence that participants’ adaptive skills increased during the course of study participation.
Self-efficacy and carer–patient relationship
Carers of participants completed the EDSE scale to report on their confidence in supporting participants with their emotional difficulties, including depression. Higher scores indicate higher levels of self-efficacy in this domain.
There were no statistically significant unadjusted or adjusted group differences in the effects of the StepUp or BeatIt interventions on EDSE scores at 12 months (primary end point) or 4 months (see p-value column of Table 26).
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 76 (1) | 21.04 (4.68) | 84 (0) | 20.73 (4.98) | ||
| Post intervention (4 months) | 70 (7) | 22.01 (4.80) | 66 (18) | 22.45 (4.06) | –0.44 (–1.95 to 1.07) | 0.566a |
| Follow-up (12 months) | 67 (10) | 22.67 (3.83) | 64 (20) | 21.98 (4.34) | 0.69 (–0.73 to 2.10) | 0.338a |
| Change in mean scores from baseline (95% CI); p-value | ||||||
| Post intervention (4 months) | 1.16 (0.21 to 2.10); 0.017b | 2.01 (1.03 to 2.99); < 0.001b | 0.86 (–0.44 to 2.16) | 0.192c | ||
| Follow-up (12 months) | 1.76 (0.87 to 2.64); < 0.001b | 1.37 (0.46 to 2.28); 0.004b | –0.39 (–1.60 to 0.83) | 0.527c | ||
The same analysis models were also applied to the changes in EDSE scores between 4 and 12 months to examine whether or not the treatments may have had different effects on EDSE scores from post intervention to follow-up. There was no overall change in EDSE scores from 4 to 12 months, and no interaction between treatment group and data collection point (4 vs. 12 months).
Within-group analyses (Table 26) showed that supporters in both treatment groups reported significant increases in EDSE scores at both 4 and 12 months. The analysis of 4- to 12-month change summarised above suggests that these changes from baseline are accounted for mainly by increases in EDSE scores from baseline to post intervention (4 months), with no change from post intervention (4 months) to follow-up (12 months).
Carers also provided a FMSS focusing on their relationship with the participant. The presence of evidence for a high or low level of criticism (a dichotomous code) in the relationship from the speech sample was coded following standard criteria. 62 These data could not be analysed using mixed-effect logistic regression models. The models failed to fit owing to very small numbers with the high criticism code. Overall, speech sample data were available for 139 supporters at baseline (missing, n = 22) and 97% of supporters were coded low for criticism in the relationship with the participant at baseline. Missing data were more problematic at 4 months (missing, n = 63) and at 12-month follow-up (missing, n = 80). Overall, 94% of supporters whose data were available were given the same criticism code at 4- and 12-month follow-ups (i.e. the vast majority evidenced no change).
Life events
At the 12-month follow-up, BLESID was used as an outcome, because it asks participants to report life events experienced over the previous 12 months. The score used for analysis was the product of the frequency scores for each life event experienced that had a negative impact on the participant. Each life event is rated as not experienced over the 12-month period (score 0), experienced once only (score 1), or experienced more than once (score 2). Each life event experienced is also rated on whether it had a positive impact, no impact, or a negative impact on the person. Thus, a reduced score over time represents, overall, a less negative impact of life events on the participant.
The same approach to statistical data analysis was used as for all continuous outcomes, except that data were available at baseline and at 12-month follow-up only (Table 27). There was no treatment group difference for life event scores at 12-month follow-up after controlling for baseline life event scores and other factors. Within-group analysis showed reductions in life event scores from baseline to 12-month follow-up in both the StepUp and BeatIt groups.
| Time point | Trial arm | Statistics | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | Intervention effects (95% CI) | p-value | |||
| n (n missing) | Mean (SD) | n (n missing) | Mean (SD) | |||
| Baseline | 77 (0) | 1.79 (2.03) | 84 (0) | 2.04 (2.35) | ||
| Follow-up (12 months) | 69 (8) | 1.29 (1.72) | 66 (18) | 1.56 (1.86) | –0.27 (–0.88 to 0.34) | 0.380a |
| Change in mean scores from baseline (95% CI) p-value | ||||||
| Follow-up (12 months) | –0.670 (–1.130 to –0.270); 0.002b | –0.45 (–0.89 to –0.01); 0.044b | 0.25 (–0.34 to 0.83) | 0.406c | ||
Exploratory moderator analyses
For the primary outcome measure, measured using the GDS-LD, exploratory moderator analyses were conducted on a number of variables at baseline for outcomes at 4 months and 12 months. These analyses investigated whether or not there were main effects at 4 months and 12 months related to the baseline variable, and whether there were interaction effects at 4 months and 12 months between the baseline variable and the therapy arm.
Table 28 presents the exploratory moderator analyses for the following baseline variables: participant age, gender, Full Scale IQ, expectations of change and ABS-RC2 domains (personal self-sufficiency, community self-sufficiency, personal social responsibility, self-direction, responsibility and socialisation), study site, neighbourhood deprivation, relationship of carer to participant, level of service support for participant, BLESID impact of negative life events in the 12 months before baseline, whether or not the participant had received any previous psychological therapy for depression, prescribed usage of antidepressants and prescribed usage of mood-stabilising medication.
| Predictor variable | Change in GDS-LD score at | |||
|---|---|---|---|---|
| 4 months | 12 months | |||
| Predictor effect, estimate (95% CI); p-value | Interaction, p-value | Predictor effect, estimate (95% CI); p-value | Interaction, p-value | |
| Age | –0.05 (–0.14 to 0.04); 0.243 | 0.445 | –0.05 (–0.15 to 0.05); 0.299 | 0.119 |
| Gender (male vs. female) | –0.84 (–2.87 to 1.19); 0.412 | 0.933 | 1.54 (–0.71 to 3.80); 0.176 | 0.343 |
| Full Scale IQ | 0.07 (–0.06 to 0.20); 0.260 | 0.204 | 0.12 (–0.03 to 0.26); 0.115 | 0.795 |
| Expectations of change | –0.2 (–0.87 to 0.47); 0.555 | 0.443 | –0.97 (–1.71 to –0.24); 0.010 | 0.088 |
| ABS-RC2 subscales | ||||
| Personal self-sufficiency | 0.06 (–0.12 to 0.23); 0.516 | 0.535 | 0.21 (0.02 to 0.40); 0.032 | 0.346 |
| Community self-sufficiency | –0.04 (–0.17 to 0.08); 0.497 | 0.646 | 0.01 (–0.13 to 0.15); 0.869 | 0.782 |
| Personal social responsibility | –0.15 (–0.31 to 0.02); 0.080 | 0.492 | –0.06 (–0.25 to 0.12) 0.491 | 0.882 |
| Self-direction | –0.15 (–0.34 to 0.04); 0.109 | 0.188 | –0.06 (–0.27 to 0.15); 0.586 | 0.738 |
| Responsibility | –0.48 (–0.99 to 0.03); 0.065 | 0.838 | –0.31 (–0.88 to 0.25); 0.276 | 0.863 |
| Socialisation | –0.33 (–0.63 to –0.03); 0.034 | 0.417 | –0.09 (–0.42 to 0.25); 0.608 | 0.982 |
| Neighbourhood deprivation | –0.27 (–0.69 to 0.15); 0.202 | 0.970 | –0.09 (–0.56 to 0.39); 0.715 | 0.816 |
| Study site | Overall 0.048 | 0.312 | Overall 0.837 | 0.008 |
| England vs. Scotland | 2.61 (–0.25 to 5.48); 0.073 | –0.354 (–3.682 to 2.974); 0.832 | ||
| England vs. Wales | 3.33 (0.67 to 5.99); 0.015 | –0.894 (–4.022 to 2.234); 0.570 | ||
| Site-specific intervention effect estimates (BeatIt vs. StepUp) | ||||
| England | 1.16 (–2.96 to 5.29); 0.575 | |||
| Scotland | –3.14 (–6.21 to –0.08); 0.045 | |||
| Wales | 5.79 (1.02 to 10.57); 0.018 | |||
| Relationship of carer to participant | Overall 0.763 | 0.984 | Overall 0.257 | 0.351 |
| Family vs. other | 0.36 (–2.32 to 3.04); 0.791 | 1.11 (–1.88 to 4.11); 0.461 | ||
| Worker vs. other | –0.55 (–2.99 to 1.89); 0.655 | –1.24 (–3.92 to 1.45); 0.361 | ||
| Level of support (less than daily vs. daily) | 1.69 (–0.46 to 3.84); 0.122 | 0.181 | –1.33 (–3.77 to 1.11); 0.281 | 0.450 |
| BLESID life events negative impact | –0.34 (–1.05 to 0.37); 0.344 | 0.385 | –0.13 (–0.92 to 0.66); 0.748 | 0.773 |
| Previous therapies for depression | –1.50 (–4.01 to 1.02); 0.240 | 0.691 | 0.72 (–2.08 to 3.52); 0.610 | 0.610 |
| Use of antidepressants | –0.76 (–2.93 to 1.40); 0.485 | 0.051 | –0.91 (–3.32 to 1.51); 0.457 | 0.817 |
| Use of mood stabilisers | –1.03 (–3.76 to 1.70); 0.453 | 0.222 | 1.85 (–1.14 to 4.84); 0.220 | 0.825 |
Out of 18 potential predictor variables of change in GDS-LD score from baseline to 4 months, there were two statistically significant main effects. For participants with higher ABS-RC2 socialisation scores at baseline, there were bigger reductions in GDS-LD scores at 4 months. There was also a main effect of study site: for participants in Wales there were bigger reductions in GDS-LD scores at 4 months compared with participants in Scotland. There were no interaction effects of baseline variables by therapy type for change in GDS-LD scores at 4 months.
Out of 18 potential predictor variables of change in GDS-LD scores from baseline to 12 months, there were two statistically significant main effects. For participants with lower ABS-RC2 personal self-sufficiency scores at baseline, there were bigger reductions in GDS-LD scores at 12 months. For participants with higher expectations of change at baseline, there were bigger reductions in GDS-LD scores at 12 months. There was also one interaction effect of study site: in Scotland there were bigger decreases in GDS-LD scores from baseline to 12 months for participants in the BeatIt group, whereas in Wales there were bigger decreases in GDS-LD scores from baseline to 12 months for participants in the StepUp group.
Per-protocol analyses
Per-protocol analyses were also conducted; however, there were no differences in the pattern of results from those reported in this chapter. Given that there were virtually no treatment group differences found that could be examined in terms of the effects of a per-protocol approach, these analyses are not described further here.
Adverse events
Following randomisation, there were 19 adverse events reported by 15 participants allocated to StepUp and 21 adverse events reported by 18 participants allocated to BeatIt (Table 29).
| Adverse event categories | Trial arm | |
|---|---|---|
| StepUp (N = 77) | BeatIt (N = 84) | |
| Participants with any adverse event, n (%) | 15 (19.5) | 18 (21.4) |
| Total number of adverse events, n | 19 | 21 |
| Mild, n | 4 | 2 |
| Moderate, n | 8 | 9 |
| Severe, n | 7 | 10 |
| Number of serious adverse events, n | 12 | 12 |
| Hospitalisation, n | 12 | 12 |
| Death, n | 0 | 0 |
| Other, n | 0 | 0 |
All 24 serious adverse events reported during the trial were hospitalisations.
Five participants in the StepUp group were admitted to a mental health ward, of whom three presented with suicidal ideation. Four participants in the BeatIt group were admitted to a mental health ward, of whom two presented with suicidal ideation.
There was one reported episode of attempted suicide by overdose during the trial. The participant had been randomised into the study but had not yet started therapy sessions. The participant was subsequently withdrawn based on previously undisclosed suicide attempts.
Chapter 6 Economic evaluation
Introduction
This chapter outlines the health economics analysis of BeatIt. The objective of the analysis was to evaluate whether or not BeatIt is cost-effective compared with a guided self-help intervention (StepUp), as determined by an incremental cost per quality-adjusted life-year (QALY).
Methods
Overview
The cost-effectiveness analysis was carried out from a NHS and social services perspective, in line with the NICE guidelines;67 it was also anticipated that social care might be an important resource use in this population. The target population was adults with mild to moderate learning disabilities and clinical depression who had a supporter or family member available to attend treatment sessions with them and provide a minimum of 2 hours of support per week. The outcome used in the cost-effectiveness analyses was the QALY.
The intention-to-treat population was used for the economic analysis. Comparative results are presented as an incremental cost-effectiveness ratio (ICER), which is calculated by dividing the difference in mean costs by the difference in mean QALYs. The NICE threshold of £20,000–£30,000 was used when judging whether or not the intervention was cost-effective. 67
Health-care resource use
Resource use for hospital and community costs were collected using a CSRI. 64 The CSRI was adapted, based on a similar previous study for a population with learning disabilities,68 in conjunction with the research team. The CSRI was completed at baseline and 4 and 12 months post randomisation with the participant and supporter to record resource use over the previous 4 months. An additional CSRI was completed at 8 months by the supporter alone (for the previous 4 months). Resource use included daytime activities (measured in hours), hospital-based services (measured in units received) and community-based services (measured in hours). The timing of the data collection is illustrated in Table 30.
| Type of data | Source | Time point within trial | |||
|---|---|---|---|---|---|
| Baseline | 4 months | 8 months | 12 months | ||
| QoL | EQ-5D-Y | ✓ | ✓ | ✓ | |
| Resource use | CSRI | ✓ | ✓ | ✓ | ✓ |
| Therapist time sheets | ✓ | ||||
| Medication inventory | ✓ | ✓ | ✓ | ✓ | |
The therapist and supervisor time was collected using therapist and supervisor time sheets. These were completed by the supervisors and therapists during the trial and included time spent on supervision and on preparation and delivery of treatment sessions, in addition to time spent travelling and mileage travelled.
Medication, both prescribed and OTC, use was collected using a medication inventory, which was completed at baseline and at 4-, 8- and 12-month follow-up visits.
All resource use is reported for the 12-month follow-up (primary end point).
Costs: valuing resources
Costs for prescribed medication were taken from the British National Formulary. 69 Other resource costs were obtained from the Personal Social Services Research Unit (PSSRU),70 NHS Reference Costs 2014 to 201571 and the literature. 68 Intervention material costs were obtained from expert opinion (Dr Kim Appleton, University of Glasgow, 2016, personal communication). Resources were valued at 2015 costs in Great British Pounds (GBP), and any costs that needed to be raised were adjusted using the Hospital and Community Health Services index. 70 Unit costs and their sources are presented in Table 31.
| Resource (sector) | Unit cost (£) | Source |
|---|---|---|
| Daytime activities | ||
| Day centre (NHS) | 38.41/hour | PSSRU70 |
| Day centre (LA) | 24.44/hour | PSSRU70 |
| Day centre (voluntary) | 24.44/hour | PSSRU70 |
| Day centre (private) | 19.42/hour | PSSRU70 |
| Sheltered work | 8.51/hour | PSSRU70 |
| Voluntary work (LA) | 24.44/hour | PSSRU70 |
| Voluntary work (voluntary) | 24.44/hour | PSSRU70 |
| Voluntary work (private) | 19.42/hour | PSSRU70 |
| Adult education | 21.70/hour | PSSRU70 |
| Drop in centre | 11.53/hour | PSSRU70 |
| Social club | 11.53/hour | PSSRU70 |
| Learning disabilities centre | 24.44/hour | PSSRU70 |
| Hospital based | ||
| Psychiatric intensive care ward | 638/inpatient day | PSSRU70 |
| Acute psychiatric ward | 322/inpatient day | PSSRU70 |
| Psychiatric rehabilitation ward | 296/inpatient day | PSSRU70 |
| General medical ward | 260/inpatient day | PSSRU70 |
| Other specialties | 276/inpatient day | PSSRU70 |
| Day hospital | 157/attendance | PSSRU70 |
| Psychiatric outpatient visit | 172/appointment | PSSRU70 |
| Other hospital outpatient visit | 166/appointment | PSSRU70 |
| A&E visit | 124/attendance | PSSRU70 |
| Community based | ||
| Community psychiatrist | 357.92/hour | PSSRU70 |
| Psychologist | 88.39/hour | PSSRU70 |
| GP (clinic/surgery) | 39.28/hour | PSSRU70 |
| GP (day centre) | 57.83/hour | PSSRU70 |
| GP (home) | 130.95/hour | PSSRU70 |
| Community psychiatric nurse | 99.30/hour | PSSRU70 |
| Learning disability nurse | 99.30/hour | PSSRU70 |
| Other community nurse | 79.66/hour | PSSRU70 |
| Community mental health team member | 99.30/hour | PSSRU70 |
| Health care assistant | 25.10/hour | PSSRU70 |
| Therapist: speech, physiotherapist, occupational, art/drama/music, alternative | ||
| Clinic/surgery | 45.83/hour | PSSRU70 |
| Day centre | 37.10/hour | PSSRU70 |
| Home visit | 48.01/hour | PSSRU70 |
| Social worker/care manager | 94.94/hour | PSSRU70 |
| Social work assistant | 36.01/hour | PSSRU70 |
| Home help/home care worker | 19.00/hour | PSSRU70 |
| Advocate/counsellor | 48.01/hour | PSSRU70 |
| Dentist | 337.19/hour | PSSRU70 |
| Optician | 45.18/hour | PSSRU70 |
| Audiologist | 45.18/hour | PSSRU70 |
| Chiropodist | 24.01/hour | PSSRU70 |
| Employment services/job centre | 68.18/hour | PSSRU70 |
| Medication | ||
| Prescribed/OTC medication | Various | BNF69 |
| Materials for delivery of intervention | ||
| BeatIt | 59.13/participant | Expert opinion |
| StepUp | 41.25/participant | Expert opinion |
| Therapist/supervisor | ||
| Supervisor time | 50/hour | PSSRU70 |
| Therapist time | 24/hour | PSSRU70 |
| Mileage | 0.56/mile | PSSRU70 |
| Cost of therapist training per participant StepUp | 279 | Expert opinion |
| Cost of therapist training per participant BeatIt | 462 | Expert opinion |
| Carers | ||
| Carers time, average hourly wage rate | 13.49/hour | ONS72 |
Costs are grouped into daytime activities, hospital-based services, community-based services, medication and intervention costs. Medication costs include prescribed and OTC medication. Intervention costs include the cost of therapists and supervisors along with therapist training and the costs of materials for therapists and participants. Therapist and supervisor costs consist of direct contact, travelling and administrative/preparation costs, and include on-costs. The cost per participant for therapist training was calculated using within-trial information; during the trial a total of 45 therapists were trained in the StepUp arm and 51 in the BeatIt arm. An average of 3.5 therapists in the StepUp arm and 3.4 in the BeatIt arm were trained in each training session. Of the 76 therapists who were assigned participants, each therapist in the StepUp arm saw an average of 2.3 participants, and each therapist in the BeatIt arm saw an average of 2.0 participants.
Outcome measures
Health-related QoL data were generated using the EQ-5D-Y,55 a simplified version of the EuroQol-5 Dimensions, three-level version (EQ-5D-3L). EQ-5D-Y questionnaires are aimed at young people aged ≥ 8 years and are adapted directly from the EQ-5D-3L using simplified wording. The language is accessible and straightforward but not childlike, a good match for patients with learning disabilities. 56 The EQ-5D-Y is a generic, preference-based QoL measure designed for children and adolescents, comprising five questions and a visual analogue scale. The questions cover five dimensions: (1) mobility, (2) ‘looking after myself’, (3) usual activities, (4) pain/discomfort and (5) ‘feeling worried, sad or unhappy’. There are three possible responses for each dimension (i.e. ‘no pain’, ‘some pain’ and ‘a lot of pain’) giving a total of 243 possible health states. Participants were asked to complete the questionnaire at baseline and 4 and 12 months post randomisation.
At present there is no child-friendly preference-based scoring algorithm value set available for the EQ-5D-Y, and EuroQol are not advising a value set to use. As a result, an adult value set was used to value the responses. 73 Participant-reported health-related QoL obtained from EQ-5D-Y questionnaires was valued in terms of utilities on a scale of –0.59 to 1 (in which 1 represents full health). Utilities were converted into QALYs using standard area-under-the-curve methods. QALYs are a measure combining both quality and length of life; patient-specific QALYs were estimated using utility measurements at each follow-up point and weighting each time interval by the patient’s utility during that period. Discrete changes in utility values between follow-up points were assumed to be linear.
Analysis
Resource use for each resource item in each group is presented using descriptive statistics.
The cost per participant was estimated by applying the unit cost of a resource to the number of uses. These costs were summed and divided by the number of participants in each arm to give the mean cost per participant in each arm. Differences in these mean costs were calculated and are presented along with a 95% CI to illustrate uncertainty in the mean costs.
The mean QALY per participant for each intervention was estimated by summing all participants’ QALYs and dividing by the number of participants in that intervention arm. The difference in means was calculated along with 95% CIs.
The analysis was carried out using Stata® 14.0 (StataCorp, College Station, TX, USA).
Missing data
Two analyses were carried out: (1) a complete-case analysis of participants who had complete data and (2) a separate analysis in which missing data were replaced using multiple imputation techniques to explore the effect of missing data on results. The multiple imputation technique used was multiple imputation using chained equations. Multiple imputation assumes that data are missing at random; missing data may depend on observed data.
Costs were replaced at a disaggregated level (intervention and non-intervention in order to explore whether or not there were cost savings associated with the non-intervention costs), and EQ-5D-Y QoL data were replaced at utility score level at baseline and 4- and 12-month follow-ups. The regression analysis used to impute costs comprised age, treatment arm, baseline costs and therapist. For QALYs the analysis included age, treatment arm, baseline GDS-LD score and therapist. These variables were associated with missing data and were strong predictors of costs and QALYs.
During the trial, 20 participants did not complete treatment (2 as a result of adverse events, 6 lost to follow-up, 1 supporter unwilling to continue in the study and 11 participants unwilling to continue in the study). These participants were excluded from the analyses on the grounds that it would not be meaningful to include them in a multiple imputation model.
Assumptions
The following assumption was made: the duration of medication was truncated at 365 days, as the follow-up period was 365 days.
Uncertainty
To explore the robustness of the results and address the uncertainty of the point estimates, sensitivity analyses were carried out:
-
Resource use was collected at each visit for the previous 17-week period (4 months); however, 41 participants had their resource-use data collected over a 16-week period at each visit, and a further 15 had a mix of 16 and 17 weeks between visits. The effect this had on results was explored in a sensitivity analysis in which all the resource-use data collection periods were converted to 17 weeks for a 4-month period.
-
The sensitivity to within-trial training costs was explored in two ways. First, by including a more ideal scenario of nine therapists trained per training session with each therapist seeing nine participants, and second, by using a scenario in which no training costs were included.
To assess the impact of uncertainty and to strengthen the validity of the results, a non-parametric bootstrapping technique was employed with 1000 samples, with results presented on a cost-effectiveness plane and cost-effectiveness acceptability curve.
To account for any difference at baseline in costs and QALYs, results were adjusted using a generalised linear model (GLM).
Results
Missing data
Table 32 presents the proportion of missing data in the QoL and resource-use questionnaires. The percentage of missing data was < 5% in all areas. In addition to this, one participant in the BeatIt arm had missing therapist data.
| Time point | % (n) of participants | ||
|---|---|---|---|
| EQ-5D-Y | Daytime activities and hospital-based services | Community-based services | |
| Baseline | 0.71 (1) | 0 (0) | 0 (0) |
| 4 months | 4.26 (6) | 4.26 (6) | 4.26 (6) |
| 8 months | 3.55 (5) | 3.55 (5) | |
| 12 months | 4.26 (6) | 4.26 (6) | 4.26 (6) |
Resources
Total resource use by participants for complete cases, at 12-month follow-up, is presented in Table 33 (for more detail see Appendix 3, Table 51).
| Resource type | Trial arm | Mean difference (95% CI) | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | |||||
| Mean (SD) | Used by n (%) | Mean (SD) | Used by n (%) | |||
| Number of medications | 5.52 (3.69) | 66 (90.4) | 5.52 (4.29) | 65 (95.6) | 0.008 (0.700) | –1.39 to 1.38 |
| Daytime activities | ||||||
| Weeks attended | 54.8 (32.8) | 51 (69.9) | 65.6 (34.4) | 39 (57.4) | –10.7 (7.18) | –25.0 to 3.54 |
| Mean hours per week | 8.07 (7.71) | 51 (69.9) | 8.46 (7.59) | 39 (57.4) | –0.388 (1.63) | –3.62 to 2.85 |
| Hospital-based services (number of contacts) | 6.90 (12.6) | 40 (54.8) | 7.03 (9.88) | 32 (47.1) | –0.131 (2.65) | –5.41 to 5.15 |
| Community-based services | ||||||
| Contacts | 134.8 (236.9) | 68 (93.2) | 135.8 (181.2) | 59 (86.8) | –1.03 (37.17) | –74.6 to 72.5 |
| Mean duration of contact (minutes) | 67.4 (55.8) | 68 (93.2) | 61.5 (46.1) | 59 (86.8) | 5.87 | –12.0 to 23.8 |
The results from Table 33 indicate that there is no significant difference between the two arms for any of the resource groupings. It can be seen that 90.4% of participants in the StepUp arm and 95.6% in the BeatIt arm used medication, and the mean number of medications reported was 5.52 in both arms. In total, 69.9% of participants in the StepUp arm and 57.4% in the BeatIt arm reported participating in daytime activities, with a mean number of 54.8 and 65.6 weeks of daytime activities in StepUp and BeatIt, respectively. The mean hours per week spent participating in daytime activities was 8.07 in the StepUp arm and 8.46 in the BeatIt arm. The mean number of contacts with hospital services was 6.90 and 7.03 in the StepUp and BeatIt arms, respectively, with 54.8% in the StepUp arm and 47.1% in the BeatIt arm using hospital services. Community-based services were used by 93.2% of StepUp participants and 86.8% of BeatIt participants; the mean number of community-based contacts during the 12-month trial period was 134.8 in the StepUp arm and 135.8 in the BeatIt arm. The mean duration (minutes) of these contacts were 67.4 minutes in the StepUp arm and 61.5 in the BeatIt arm.
Costs
Total mean costs are presented in Table 34 below.
| Resource type | Trial arm | Mean difference (95% CI) | ||
|---|---|---|---|---|
| StepUp [used by n = 68 (93.2%)] | BeatIt [used by n = 58 (85.3%)] | |||
| Mean (SD) | Mean (SD) | Mean (SE) | 95% CI | |
| Medication | 807 (1409) | 862 (1718) | –55 (283) | –616 to 506 |
| Daytime activities | 8096 (11,301) | 8496 (11,766) | –400 (2065) | –4490 to 3689 |
| Hospital-based services | 1011 (3419) | 859 (2182) | 152 (504) | –846 to 1151 |
| Community-based services | 15,822 (36,193) | 15,512 (32,685) | 670 (6139) | –11,480 to 12,821 |
| Intervention | 1050 (310) | 1788 (506) | –738 (76) | –890 to –586 |
| Total costs | 26,786 (38,232) | 27,158 (35,751) | –371 (6598) | –13,432 to 12,689 |
Total costs favour StepUp by a difference of £371 [standard error (SE) £6598], but this difference is not significant. However, the difference in the mean costs of the interventions was highly significantly less expensive, in favour of StepUp, with mean StepUp intervention costs of £738 (SD £76) less than mean BeatIt costs. Conversely, there was no significant difference between the arms in any of the resource groups, suggesting that the extra cost of BeatIt does not translate into cost savings in any of the resource groups. This hypothesis can be further explored by aggregating non-intervention costs to see if there is any evidence of cost savings associated with either treatment. The results from this exploratory analysis are presented in Table 35.
| Costs | Trial arm | Mean difference (95% CI) | ||
|---|---|---|---|---|
| StepUp [used by n = 68 (93.2%)] | BeatIt [used by n = 58 (85.3%)] | |||
| Mean (SD) | Mean (SD) | Mean (SE) | 95% CI | |
| Intervention | 1050 (310) | 1788 (506) | –738 (76) | –890 to –586 |
| Non-intervention | 25,736 (38,228) | 25,370 (35,703) | 367 (6593) | –12,684 to 13,418 |
It can be seen from Table 35 that although there is no significant difference between arms for non-intervention costs, the results favour the StepUp arm.
A simple societal perspective was also assessed: the time burden associated with carers for accompanying participants to therapy sessions. Carers’ time was valued using the Office for National Statistics 2015 average hourly wage rate. 72 The results reflect that the BeatIt intervention requires more carers’ time than the StepUp intervention. Carers’ costs added £104 to the costs of the StepUp arm and £184 to the costs of the BeatIt arm.
Outcomes
Results of the EQ-5D-Y at each level, dimension and visit are presented in Table 36. For the mobility dimension, the proportion of participants who experienced ‘no problems walking about’ increased from 70.0% to 80.7%, and the proportion reporting ‘a lot of problems walking about’ decreased from 16.4% at baseline to 8.9% at the 12-month visit. For the self-care (‘looking after myself’) dimension, the proportion of participants reporting ‘no problems washing or dressing myself’ increased from 69.3% at baseline to 76.3% at the 12-month follow-up period, and the proportion reporting ‘a lot’ of problems decreased from 13.6% at baseline to 8.9% at follow-up. Although for the usual activities (hobbies, sports, etc.) dimension, the proportion of participants reporting ‘no problems’ decreased from 80.0% to 76.3% over the 12-month follow-up period, the proportion reporting ‘a lot’ of problems doing usual activities increased from 7.86% to 10.4%. The pain or discomfort domain returned to the previous trends seen in the mobility and ‘looking after myself’ dimensions: the proportion of participants reporting no pain or discomfort increased from 62.8% to 77.8% over the trial period, and those experiencing ‘a lot of pain or discomfort’ decreased from 11.4% to 7.4%. The final dimension of ‘feeling worried, sad or unhappy’ is arguably the most important one in this trial, with the proportion of participants reporting that they were ‘not worried, sad or unhappy’ increasing from 42.1% to 55.6%, and the proportion reporting that they felt ‘very worried, sad or unhappy’ decreasing from 20.7% to 13.3%.
| EQ-5D-Y dimension | n (%) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Mobility | |||
| Level 1 (no problems) | 98 (70.0) | 103 (76.3) | 109 (80.7) |
| Level 2 (some problems) | 19 (13.6) | 17 (13.6) | 14 (10.4) |
| Level 3 (a lot of problems) | 23 (16.4) | 15 (11.1) | 12 (8.9) |
| Looking after myself | |||
| Level 1 (no problems) | 97 (69.3) | 99 (73.3) | 103 (76.3) |
| Level 2 (some problems) | 24 (17.1) | 25 (18.5) | 20 (14.8) |
| Level 3 (a lot of problems) | 19 (13.6) | 11 (8.2) | 12 (8.9) |
| Usual activities | |||
| Level 1 (no problems) | 112 (80.0) | 101 (74.8) | 103 (76.3) |
| Level 2 (some problems) | 17 (12.1) | 24 (17.8) | 18 (13.3) |
| Level 3 (a lot of problems) | 11 (7.86) | 10 (7.4) | 14 (10.4) |
| Pain or discomfort | |||
| Level 1 (no pain) | 88 (62.8) | 92 (68.2) | 105 (77.8) |
| Level 2 (some pain) | 36 (25.7) | 29 (21.5) | 20 (14.8) |
| Level 3 (a lot of pain) | 16 (11.4) | 14 (10.4) | 10 (7.4) |
| Feeling worried, sad or unhappy | |||
| Level 1 (not worried, sad or unhappy) | 59 (42.1) | 79 (58.5) | 75 (55.6) |
| Level 2 (a bit worried, sad or unhappy) | 52 (37.1) | 44 (32.6) | 42 (31.1) |
| Level 3 (very worried, sad or unhappy) | 29 (20.7) | 12 (8.9) | 18 (13.3) |
The EQ-5D-Y results for utilities at baseline and 4 and 12 months post randomisation and QALYs for the 12-month trial period are presented in Table 37.
| Time point | Trial arm | Difference | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | |||||
| Mean (SD) | n (%) | Mean (SD) | n (%) | Mean (SE) | 95% CI | |
| Baseline | 0.638 (0.374) | 72 (98.6) | 0.474 (0.438) | 68 (100.0) | 0.163 (0.069) | 0.0270 to 0.300 |
| 4 months | 0.701 (0.358) | 71 (97.3) | 0.637 (0.412) | 64 (94.1) | 0.064 (0.067) | –0.069 to 0.196 |
| 12 months | 0.697 (0.349) | 70 (95.9) | 0.675 (0.410) | 65 (95.6) | 0.022 (0.066) | –0.109 to 0.152 |
| QALYs | 0.691 (0.287) | 68 (93.2) | 0.628 (0.361) | 61 (89.7) | 0.063 (0.058) | –0.052 to 0.178 |
It can be seen that there is no significant difference between arms in utilities at 4 months or 12 months; however, at baseline there is a significant difference of 0.163 (SE 0.069), with BeatIt participants reporting significantly lower QoL than StepUp participants. The results of the EQ-5D-Y scores are illustrated as a profile over time in Figure 3. This clearly illustrates the difference between the groups at baseline and 4 and 12 months. The area between the two lines represents the QALYs gained over the 12-month follow-up period between treatments. Figure 3 also presents the 95% CI (as bars) around StepUp and BeatIt EQ-5D-Y scores at baseline and 4 and 12 months. The scores and 95% CIs for both trial arms converge towards the 12-month follow-up point.
FIGURE 3.
The EQ-5D-Y scores over time, by group (all available data).
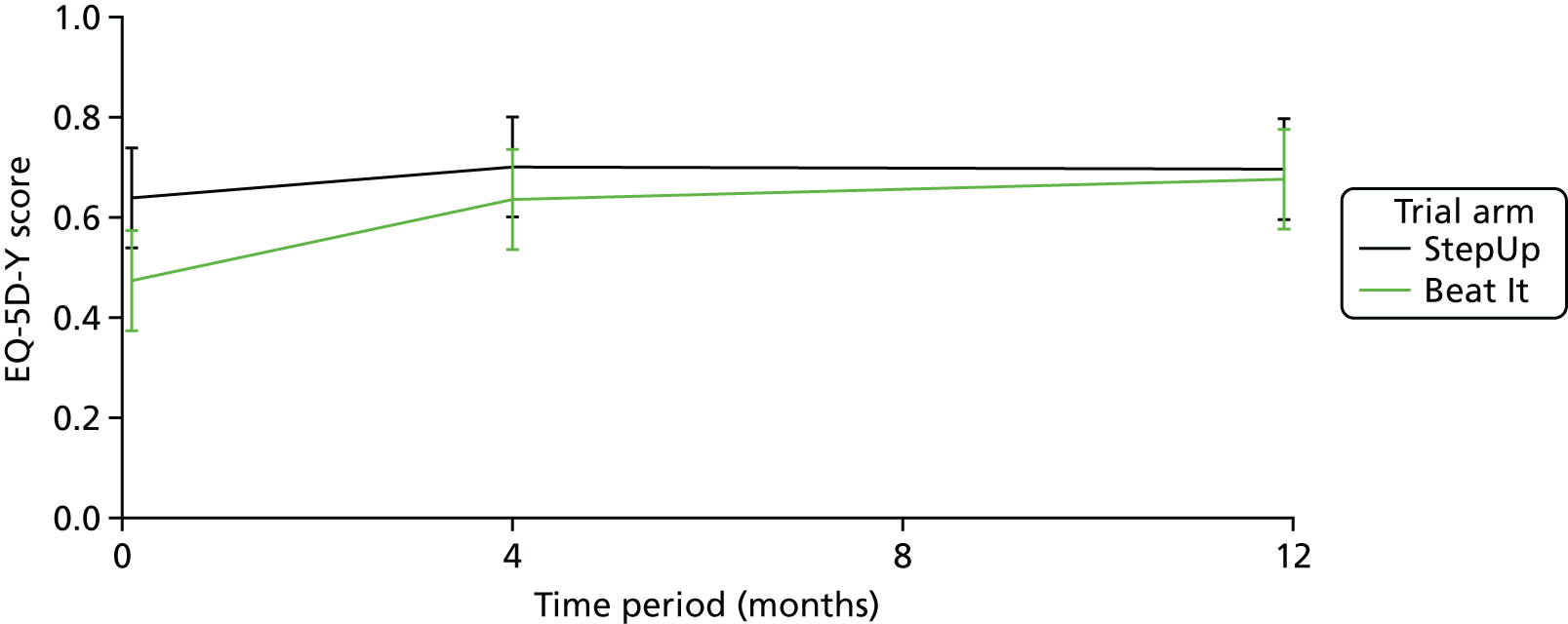
Multiple imputation results
The unadjusted multiple imputation results are presented in Table 38.
| Results | Trial arm | Difference (SE) | 95% CI | |
|---|---|---|---|---|
| StepUp (SE) | BeatIt (SE) | |||
| Intervention costs (£) | 1027 (36.70) | 1779 (68.20) | –751a (76.00) | –601 to –902 |
| Non-intervention costs (£) | 24,994 (4358) | 25,444 (4549) | –450 (6310) | –12,932 to 12,031 |
| Total costs (£) | 26,021 (4359) | 27,223 (4562) | –1201 (6319) | –13,702 to 11,299 |
| Total QALYs | 0.693 (0.034) | 0.617 (0.044) | 0.076 (0.055) | –0.033 to 0.185 |
It can be seen from the multiple imputation results in Table 38 that after imputing missing costs and QALYs, the differences in the intervention costs, total costs and QALYs remain consistent with the complete-case results. The difference between arms for intervention costs is £751, a significant difference; however, although the difference in total mean costs has increased to £1201 (SE £6319), this remains a statistically insignificant result. The mean difference in QALYs has increased slightly from the complete-case difference of 0.063 to 0.076, but again this mean difference is statistically insignificant. Non-intervention costs now favour StepUp; however, this difference is not significant.
Sensitivity analysis
The results of the sensitivity analysis are presented in Table 39.
| Sensitivity analysis | Trial arm, mean costs (£) (SE) | Difference (SE) | 95% CI | |
|---|---|---|---|---|
| StepUp | BeatIt | |||
| 17-week/4-month period for resource-use data collection | 25,489 (4362) | 26,478 (4354) | –989 (6181) | –13,216 to 11,238 |
| Nine therapists trained in each training session and nine participants per therapist | 25,451 (4362) | 26,428 (4354) | –977 (6181) | –13,204 to 11,250 |
| No therapist training costs included | 25,989 (4382) | 27,172 (4396) | –1183 (6225) | –13,499 to 11,133 |
It can be observed from the sensitivity analysis results that altering unit costs do not alter the results in any scenario from complete case or multiple imputation results; total mean cost differences in all three scenarios favour StepUp, but this difference is not significant. This indicates that the point estimates used as unit costs are robust.
The incremental cost-effectiveness results are presented in Table 40, and include multiple imputation results, both unadjusted and adjusted. Costs are split between intervention and non-intervention to explore whether or not the increased intervention costs have any effect on non-intervention costs. As a result of the imbalance in EQ-5D-Y scores at baseline, multiple imputation results for QALYs were adjusted as planned, using baseline EQ-5D-Y score and baseline GDS-LD score (both significant predictors of QALYs). Costs were adjusted for baseline costs and therapist (both significant predictors of costs). The model used to adjust for costs and QALYs was a GLM.
| Outcomes | Analysis, mean (SE) | Difference (SE) | 95% CI | |||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | |||||
| Trial arm | Trial arm | |||||
| StepUp | BeatIt | StepUp | BeatIt | |||
| Intervention costs (£) | 1027 (36.70) | 1779 (68.20) | 1019 (36.40) | 1789 (65.90) | –769a (75.10) | –622 to –917 |
| Non-intervention costs (£) | 24,994 (4358) | 25,444 (4549) | 27,181 (2491) | 24,630 (2503) | 2552 (1807) | –1021 to 6215 |
| Total costs (£) | 26,021 (4359) | 27,223 (4562) | 27,962 (2347) | 26,369 (2382) | 1593 (1827) | –2008 to 5194 |
| Total QALYs | 0.693 (0.034) | 0.617 (0.044) | 0.655 (0.029) | 0.657 (0.031) | –0.002 (0.043) | –0.085 to 0.082 |
| Incremental costs (£) | –1201 (6319) | 1593 (1827) | ||||
| Incremental adjusted QALYs | 0.076 (0.055) | –0.002 (0.043) | ||||
| ICER | StepUp dominates | BeatIt dominates | ||||
Unadjusted results show that BeatIt is more costly than StepUp and results in lower QALYs, which indicate that BeatIt is dominated by StepUp; however, it should be noted that the difference in both mean costs and QALYs is not significant. As expected, the intervention costs are greater for BeatIt, and this is a significant difference. The non-intervention costs are also higher for BeatIt, but this difference is not significant. The adjusted results indicate that the intervention costs are significantly higher for BeatIt, as in the unadjusted results; however, the non-intervention and total costs for BeatIt are lower than those for StepUp. Adjusted QALYs are higher in the BeatIt arm than in the StepUp arm; however, neither cost nor QALY differences are significant. This would suggest that BeatIt is a dominant intervention compared with StepUp for adjusted results: it is less costly with higher QALYs; however, this is the case only if non-significant non-intervention cost differences are allowed to over-ride the significant intervention differences in cost. The uncertainty in these results is explored further in Uncertainty.
Uncertainty
The complete-case and multiple imputation analyses both show no statistical differences between mean costs or QALYs. To explore the robustness of these results, 1000 non-parametric bootstrapping samples (unadjusted) were taken from the observed data and the resultant cost-effectiveness pairs are used in this exploratory analysis.
The cost-effectiveness plane presented in Figure 4 illustrates the 1000 bootstrap samples, showing the mean difference in costs and QALYs between the StepUp and BeatIt interventions. It can be seen that the samples fall into all four quadrants of the cost-effectiveness plane, showing that the difference in mean costs and QALYs can favour either intervention and that there is no evidence to show that one intervention is more cost-effective than the other.
FIGURE 4.
Cost-effectiveness plane showing mean difference in costs and QALYs between StepUp and BeatIt.
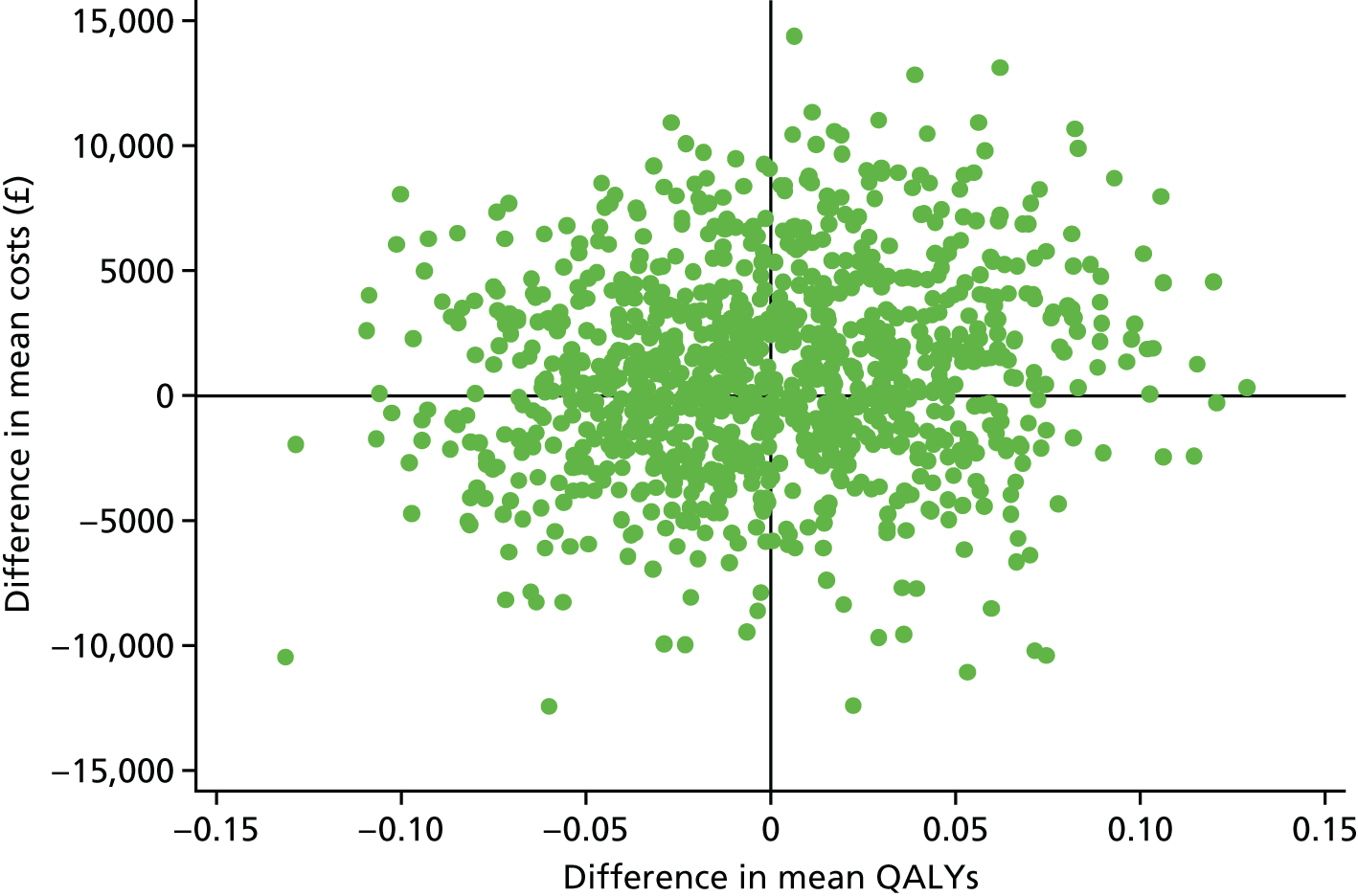
The likelihood of cost-effectiveness at various thresholds is illustrated in the cost-effectiveness acceptability curve presented in Figure 5.
FIGURE 5.
Cost-effectiveness acceptability curve for the BeatIt intervention.
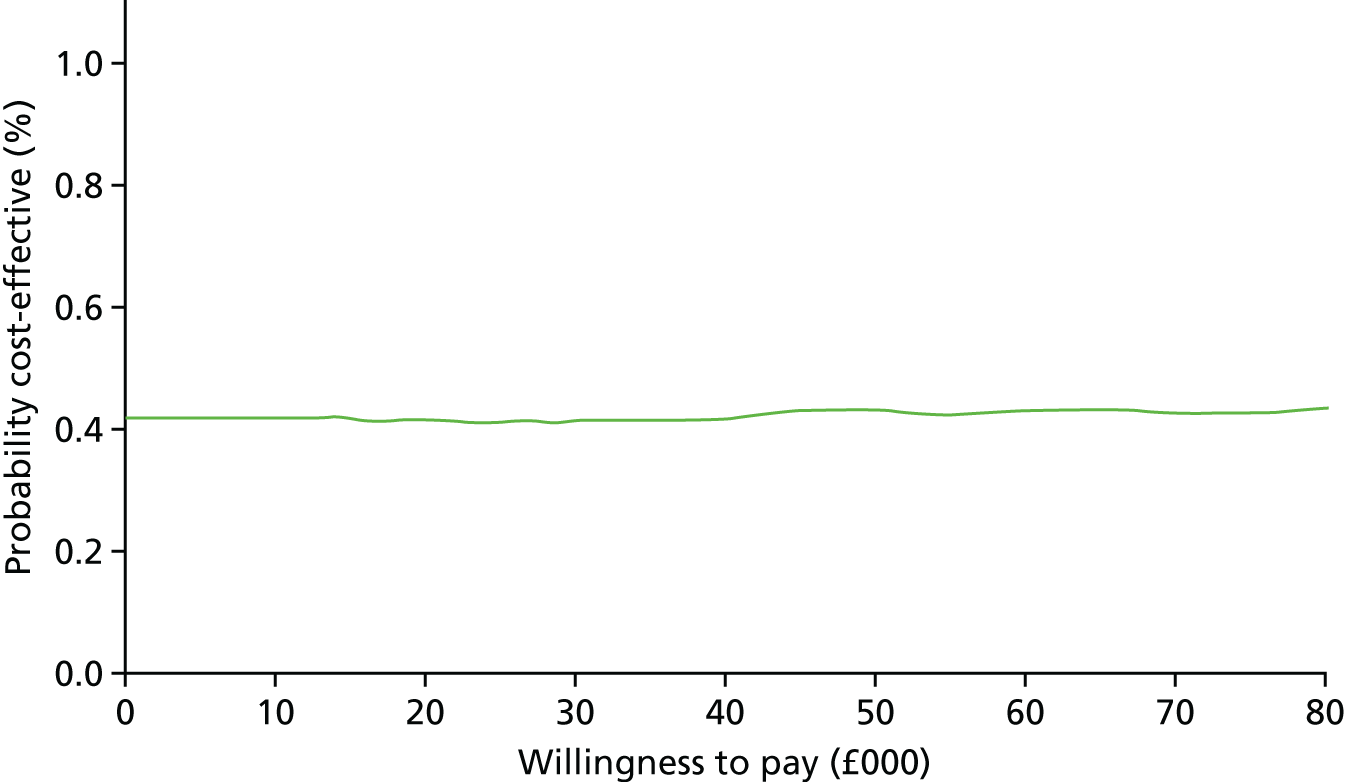
Figure 5 illustrates that at a willingness-to-pay (WTP) threshold of £0, there is a 41.7% likelihood of BeatIt being cost-effective compared with StepUp, and at the current NICE WTP threshold of £30,000, there is a 41.1% chance of BeatIt being cost-effective compared with StepUp. Conversely, StepUp has a 58.9% likelihood of being cost-effective at the £30,000 WTP threshold. The results in Figure 5 show that BeatIt is not likely to be cost-effective compared with StepUp at any WTP threshold: at £120,000 the likelihood of BeatIt being cost-effective compared with StepUp is 44.1%. This reflects the huge uncertainty in the results.
A further exploratory bootstrapping exercise has been carried out using only the intervention costs; we are certain that BeatIt is more costly than StepUp to deliver, but there is no significant difference in the other cost data collected. The results of the exploratory bootstrapping are presented on a cost-effectiveness plane in Figure 6.
FIGURE 6.
Cost-effectiveness plane, for intervention costs only.
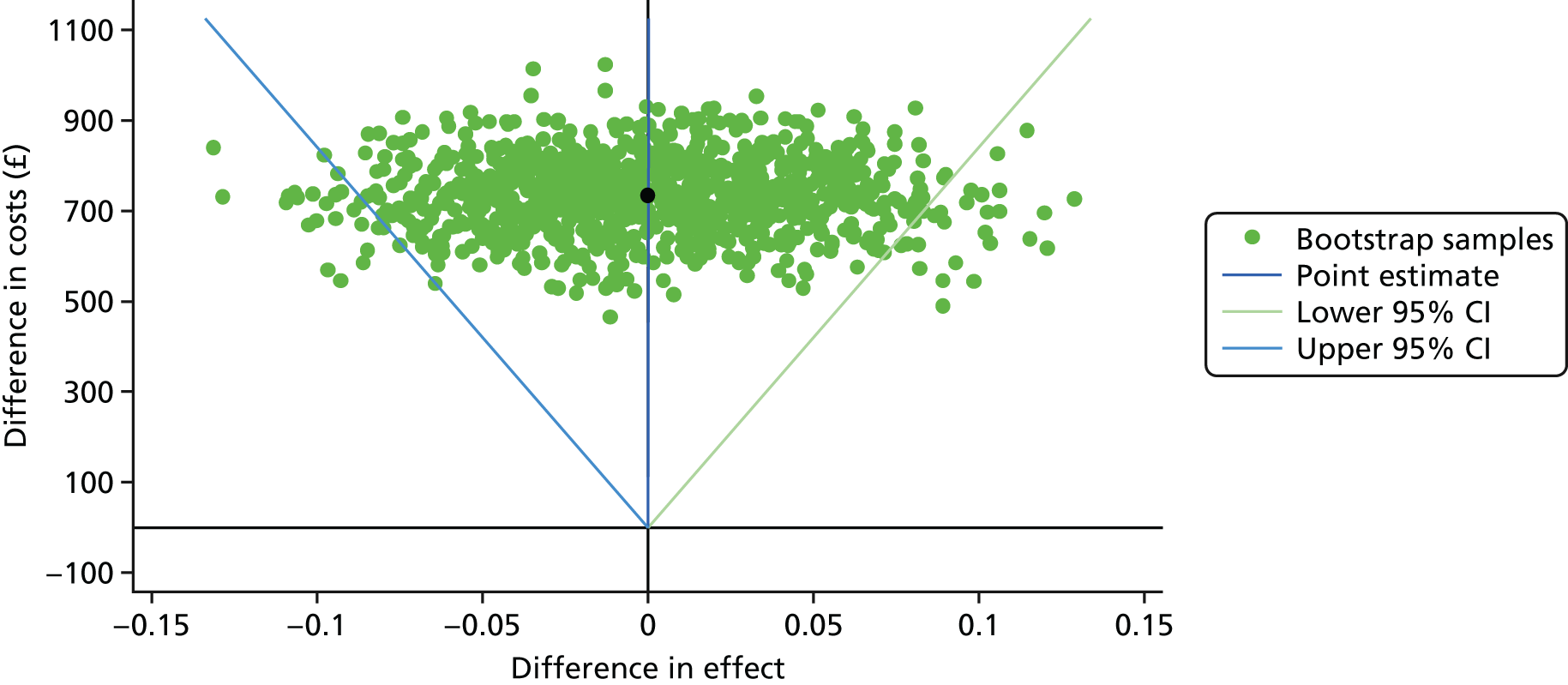
It can be seen from Figure 6 that, although we can be certain that BeatIt is costlier than StepUp to deliver, we cannot be certain that the QALYs differ between arms, as is the same for the primary outcome of GDS-LD score. The 95% CI for the ICER ranges from –£307,000 to £211,000, indicating that at no point does the ICER fall below £211,000 for BeatIt compared with StepUp, which is not considered cost-effective.
These exploratory bootstrapping results have also been presented on a cost-effectiveness acceptability curve in Figure 7.
FIGURE 7.
Cost-effectiveness acceptability curve, for intervention costs only.
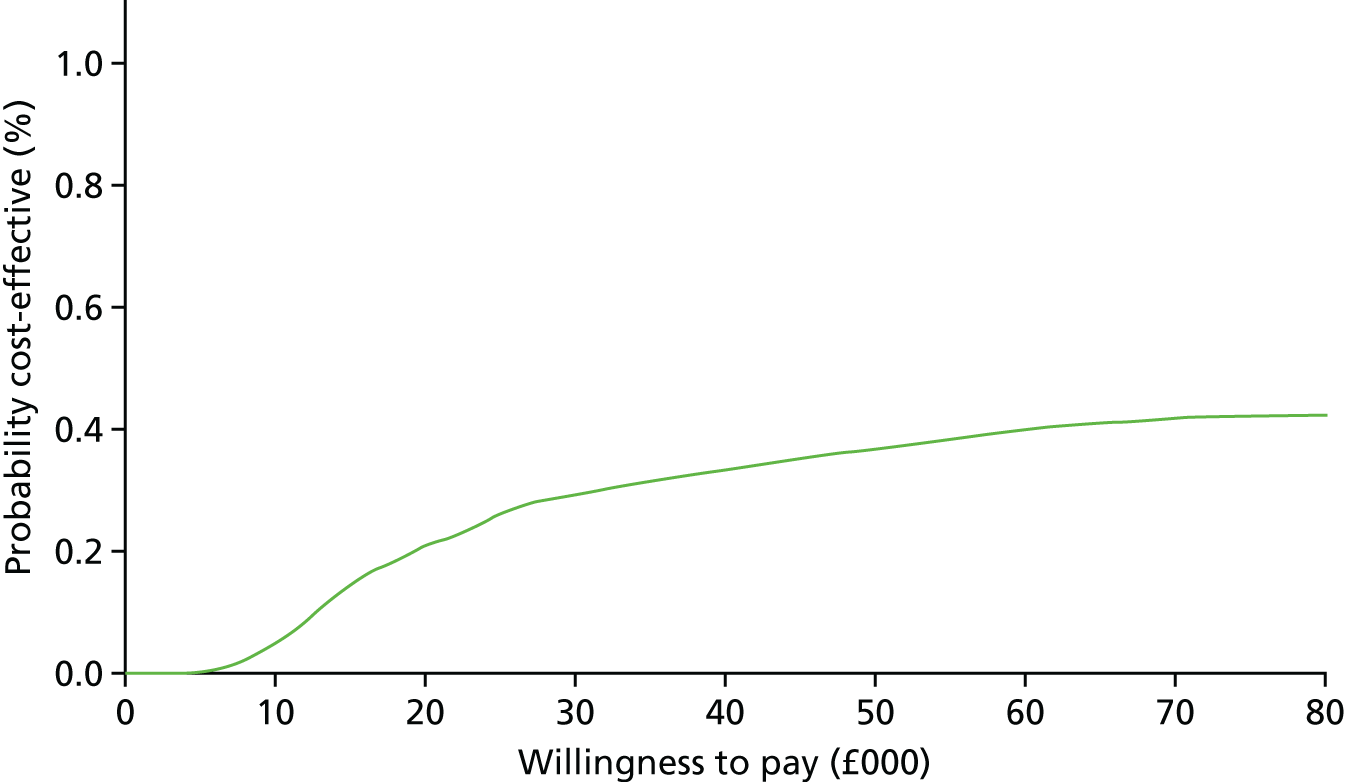
It can be seen from Figure 7 that at a WTP threshold of £0, there is an 0% likelihood of BeatIt being cost-effective compared with StepUp; however, as the WTP threshold increases, the probability of BeatIt being cost-effective compared with StepUp increases. At the current NICE WTP threshold of £30,000 there is a 29.5% chance of BeatIt being cost-effective compared with StepUp.
Chapter 7 Qualitative study
Introduction
When examining the cost-effectiveness of psychological interventions for mental health problems in people with learning disabilities, it is important to seek to understand the experiences of people centrally involved in the intervention alongside the quantitative data. This may illuminate facilitators of and barriers to change and offer insights about how to implement interventions effectively. This component of the study garnered qualitative data separately from people with learning disabilities who had received therapy, supporters in therapy sessions and therapists (all across both types of intervention) to understand the experiences of the therapy process from each perspective.
Previous research asking people with learning disabilities about their experiences of undergoing psychological therapy has found that people valued specific techniques used as part of the particular intervention they were receiving, but placed more emphasis on the non-specific aspects of their therapy such as the therapeutic relationship, being listened to and respected by the therapist, and being able to talk about their lives. 74,75 People with learning disabilities participating in a group intervention found it challenging to talk about their individual feelings in a group context. 75
Having a supporter (whether a family member or a paid carer) with the person with learning disabilities during at least part of a psychological intervention has been suggested as an important adjustment to the routine therapy process, to assist people undergoing the therapy with motivation and activities between therapy sessions. 76–78 Research on the impact of the presence of a member of staff as a supporter during psychological interventions with people with learning disabilities is mixed;74,79 however, research asking supporters directly about their experiences is lacking.
There has also been very little research concerning the experience of therapists trained to deliver manualised psychological interventions to people with learning disabilities. Stimpson et al. 80 explored the views of lay therapists who ran anger management groups as part of a trial of a group anger management intervention for people with learning disabilities. Although the therapists had some trepidation about taking on the role, they were largely positive about running the groups. Obtaining the views of more experienced professionals, trained to deliver individual psychological interventions, has the potential to provide important insights that would help with the wider roll-out of the interventions by services.
Method
Participants
People with learning disabilities
A purposive sample of 26 people with learning disabilities was interviewed, all of whom had received either the BeatIt or StepUp intervention. Participants were purposively sampled to reflect diversity in intervention type (BeatIt, n = 16; StepUp, n = 10), living situation (living independently, n = 13; living in family home, n = 5; living in group home, n = 3; living in supported accommodation, n = 5), location (England, n = 9; Scotland, n = 7; Wales, n = 10), gender (women, n = 18; men, n = 8) and participant–supporter relationship (family member, n = 7; non-family member, n = 19).
Participants’ ages ranged from 21 to 66 years. Participants’ WASI42 IQ scores ranged from 44 to 75.
Supporters
A purposive sample of 21 carers was interviewed, all of whom had supported an adult with learning disabilities through either the BeatIt or StepUp intervention. One supporter had supported two people through therapy. Of the 21 supporters, 11 had supported someone through the BeatIt intervention and 10 had supported someone through the StepUp intervention. Nineteen supporters were women and two were men. Fourteen supporters were paid support workers and seven were parents of the person with learning disabilities in therapy. Four supporters were from Scotland, nine from England and eight from Wales.
Therapists
Within each location (Scotland, Wales, England) separate focus groups were conducted with BeatIt therapists and therapists for the StepUp intervention. In total, 15 therapists (England, n = 7; Scotland, n = 5; Wales, n = 3) trained to deliver BeatIt took part across three focus groups, and 11 therapists (England, n = 2; Scotland, n = 6; Wales, n = 3) trained to deliver the StepUp intervention took part across three focus groups.
Materials
People with learning disabilities
A semistructured interview schedule was developed to explore people’s experiences of receiving either the BeatIt or StepUp intervention, as outlined in the protocol. 41 An initial interview schedule, based on the aims outlined in the protocol, was piloted in three interviews and then revised by the project team to focus more on exploring participants’ experiences of various aspects of the therapy process. The final interview schedule was divided into four topics, with opening questions that could be followed up with open-ended questions or prompts: (1) participants’ expectations of therapy, (2) participants’ views of the therapy sessions, (3) working relationships with the therapist and supporter and (4) perceived changes and maintenance of change. The aim was to establish a dialogue with participants, using the schedule to ensure that key topics were covered while having the flexibility to follow up other salient issues they raised.
Supporters
The same process as described above was used to develop a semistructured interview schedule for supporters. This interview schedule also comprised four general topics that could be followed up with questions or prompts: (1) supporters’ expectations of therapy, (2) supporters’ views of the therapy sessions, (3) working relationships with the therapist and person with learning disabilities and (4) perceived changes and maintenance of change post therapy.
Therapists
Semistructured focus group topic guides (with similar topics but some tailoring to the specific intervention being discussed) were developed. Topics covered included the following: (1) therapists’ initial expectations and understanding of the therapy, including views of the therapist training, (2) therapists’ views of the therapy process, (3) therapists’ views of helpful and unhelpful aspects of the therapy and how they might be improved and (4) therapists’ views of whether or not the therapy had any impact on the person’s life.
Procedure
People with learning disabilities and supporters
All participants (people with learning disabilities and supporters) had agreed to be interviewed as part of their consent when first agreeing to take part in the wider study. Those selected to be interviewed, using a purposive sampling grid, were contacted again by researchers to check that they were still willing to take part in the qualitative component of the study. For participants with learning disabilities who did not want their supporter to be interviewed, the supporters were not approached.
All interviews with people with learning disabilities and supporters took place within 8 weeks of participants completing therapy, to increase the probability that participants and supporters would clearly recall their experiences of therapy. Interviews were conducted by a team of four researchers, each in a different location to where they were collecting quantitative data for the wider study, to ensure that they were not unblinded to the therapy type assigned to participants within their location. Participants with learning disabilities and supporters were interviewed at a location of their choosing, either the home of the person with learning disabilities or a day centre they attended. All interviews with participants who had learning disabilities and supporters were carried out in person by one of the researchers.
Interviews were audio-recorded using digital recording equipment and transcribed verbatim. Interviews were 20- to 80-minutes long. Two people with learning disabilities and two supporters opted for the interviewer to take written notes of the interview rather than have the interview audio-recorded and transcribed. At the start of the interviews, the researchers made it clear to the participants with learning disabilities and supporters that their views were of great interest and would be kept confidential, and they could therefore speak openly about their experiences.
Therapists
A focus group with therapists took place after all therapeutic activity in that location (Scotland, England or Wales) had been completed. All therapists who were still currently working in that location were invited to a focus group in their area (Scotland, Wales or England) concerning the specific type of therapy that they had been delivering. At the point of the initial invitation, therapists were sent information about the focus groups. Before the focus group started, the information was repeated to those who attended and their signed consent was obtained.
All focus groups were face to face, and were facilitated by one or two senior members of the research team. Focus groups were audio-recorded using digital recording and transcribed verbatim. Focus groups were between 35 and 113 minutes long, with a mean length of 81 minutes.
Data analysis
Framework analysis81 was selected as the analytic approach to allow for comparisons to be made across the sample and also within individual interviews, meaning that although comprehensive analyses of key themes arising across the entire data set were possible, individual participants’ views remained. 82 In addition, a key aim of this qualitative component of the wider trial was to increase our understanding of how participants and supporters experienced therapy processes, to add to our interpretation of the quantitative data. Framework analysis allowed some specification of the dimensions of interest while retaining the potential for emergent themes to revise or add to the framework. Using framework analysis also made it possible for each of the researchers to code their own interviews and subsequently merge them together when applying the thematic framework. This process was made easier by the highly structured way in which the data were synthesised using a framework analysis. Summarising the data was particularly helpful owing to the large number of interviews in this study: 26 interviews with people with learning disabilities and 21 interviews with supporters.
People with learning disabilities
Once the interviews were transcribed, an initial thematic framework, closely related to the interview schedule, was developed. The framework was agreed by the team carrying out the analyses, which consisted of three researchers who conducted the bulk of the interviews, the researcher responsible for merging coded interviews, and two researchers with experience in conducting qualitative research. The three researchers who conducted the interviews then coded two interview transcripts each, with a fourth researcher responsible for merging these coded interviews into the agreed framework. At this point, the merged document was reviewed and discussed by the whole team, including the two experienced qualitative researchers, and the framework was modified to encompass themes and subthemes missing from the original framework. The researchers then coded the transcripts of all their interviews and all coded responses were subsequently merged into the revised framework by the fourth researcher using NVivo 11 (QSR International, Warrington, UK). 83 The same overall framework of themes and subthemes was used for participants receiving either the BeatIt or StepUp intervention, although specific aspects of subthemes could vary in accordance with the type of intervention experienced.
Supporters
The same data analysis process as described previously was used with transcripts from the supporters’ interviews. A similar overall framework, in terms of themes, was developed, with similarities and differences in subthemes and specific aspects of subthemes.
Therapists
Framework analysis was also used to analyse transcripts from the focus groups with therapists. An initial framework of themes and subthemes was developed by a researcher within the team who is experienced in conducting qualitative research, and then revised by an independent researcher, who is also experienced in analysing qualitative data. The same overall framework of themes and subthemes was used for therapists delivering the BeatIt intervention and for those delivering the StepUp intervention, although specific aspects of subthemes could vary in accordance with the type of intervention delivered.
Findings
Findings from the qualitative analyses are outlined in terms of themes, subthemes and specific issues within subthemes. As the overall thematic structure derived from framework analysis was the same for people with learning disabilities and supporters, these findings will be presented together. The thematic structure for therapists was different from that for people with learning disabilities and supporters; therefore, findings from therapists will be presented separately.
Findings from people with learning disabilities and supporters
The overall framework relating to the experiences of people with learning disabilities and supporters consisted of six themes: (1) before therapy, (2) the therapy process, (3) relationships in therapy, (4) ending and after therapy, (5) the impact of therapy and (6) views on the therapy. Table 41 presents the themes, subthemes and specific issues mentioned within each subtheme. Most of the specific issues were mentioned in relation to both the BeatIt and StepUp interventions. When specific issues relate to one or the other type of intervention, they are clearly indicated.
| Theme/subtheme | Specific issues | |
|---|---|---|
| People with learning disabilities | Supporters | |
| Theme 1: before therapy | ||
| Subtheme | Participants’ problems
|
Participants’ problems
|
| Subtheme | Participants’ expectations
|
Supporters’ expectations
|
| Theme 2: the therapy process | ||
| Subtheme | Important aspects of therapy process
|
Supporters’ role in therapy process
|
| Subtheme | Therapy materials
|
Therapy materials
|
| Subtheme | Between sessions
|
Between sessions
|
| Subtheme | Learning about the person receiving therapy
|
|
| Subtheme | Suitability of therapy
|
|
| Subtheme | What worked well in the therapy
|
|
| Theme 3: relationships in therapy | ||
| Subtheme | Relationship with therapist
|
Supporter relationship with therapist
|
| Subtheme | Relationship with supporter in therapy
|
Supporter relationship with person in therapy
|
| Subtheme | Working with therapist and supporter
|
|
| Theme 4: ending and after therapy | ||
| Subtheme | Feelings about ending therapy
|
|
| Subtheme | Maintaining change
|
Maintaining change
|
| Subtheme | Barriers
|
|
| Subtheme | Helpful factors
|
|
| Theme 5: the impact of therapy | ||
| Subtheme | Impact on the person
|
Impact on the person
|
| Subtheme | Broader impacts
|
|
| Theme 6: views on the therapy | ||
| Subtheme | Ideas for improving the therapy
|
Ideas for improving the therapy
|
| Subtheme | Would recommend the therapy to others | |
Theme 1: before therapy
People with learning disabilities and supporters across both therapy arms mentioned the participant feeling depressed or down before the therapy started. Supporters also mentioned the person experiencing negative life events and/or bereavements, but focused more on observable issues such as the person’s weight, a lack of energy/mobility, and/or withdrawal from other people. In addition, people with learning disabilities mentioned experiencing bereavements and bullying or victimisation, as well as feelings of loneliness, a lack of confidence and anger and/or anxiety:
That’s what made me so depressed at one time, because I kept being bullied at work and that’s why I didn’t go in [to work] for a couple of days . . . Mum thought it was great joining the programme because I was feeling down at the time.
StepUp; participant 295
People with learning disabilities across both therapy arms mentioned a range of feelings and expectations before the therapy started, from not being worried, and feeling the therapy might help with their mood and the achievement of life goals, through to nervousness and uncertainty. Similarly, supporters across both therapy arms hoped that the therapy would have a positive impact on the person and thought it was worth giving the therapy a try. This was in a context in which there was nothing else available for the person, or other approaches had been tried without success. However, they remained unclear about what to expect:
I’d not really heard about anything else for people with learning disabilities who had got depression, so yeah, I thought it was a good idea and I’d give it a try.
BeatIt; Supporter of participants 218 and 219
Theme 2: the therapy process
People with learning disabilities who received the BeatIt intervention described important aspects of the therapy as having the time and space to talk and be listened to, getting ideas about activities and making plans, building their confidence and understanding the materials and paperwork used within the therapy. For people with learning disabilities who received the StepUp intervention, important aspects of therapy were the process of reading and understanding the self-help booklets and making them relevant to their own situations:
I liked that I could explain more in the sessions to the therapist and supporter, you knew what you were talking about . . . I felt listened to.
BeatIt; participant 200
One week we did one book about sleeping and then we went through all the books we were given. We were given lots of books to read through . . . The other ones were to do with things like getting up and moving, things like dancing, go to groups, socialising, getting out and about, doing different things, getting in the community, doing things you don’t normally do.
StepUp; participant 211
Supporters across both therapy arms described their role in the therapy process as being an advocate for the person receiving therapy and also providing moral support and encouragement to the person. Supporters in the BeatIt intervention described acting as a liaison between the therapy and the person’s home, and supporters in the StepUp intervention mentioned learning more about the person and about depression:
I’m just here to support [name] because I know [name] wants to please and just wants to tell you things that he knows will make you smile and so my job I think really is just to say ‘is that really what you think [name]?’ I did try to let [name] be himself and say what he wanted but it’s just on the odd occasion to be a bit supportive and remind him about different things.
BeatIt; supporter of participant 186
In terms of the materials used in the therapies, both people with learning disabilities and supporters involved in the BeatIt intervention reported that the diaries were useful if the person was supported to use them, although they could be hard to complete within the person’s daily routine. Some supporters reported the mood ratings to be helpful, whereas others felt them to be too simplistic. Other activity materials and formulation booklets were also mentioned as useful, and the plan that was developed with the person at the end of therapy was seen as person centred. However, there were sometimes problems with remembering to use the materials:
I remember the cards, the things that you say what you do day to day. I had the two boxes and the cards rather than the pictures and things like that. So that was quite fun. And drawings and diaries as well.
BeatIt; participant 290
Both people with learning disabilities and supporters involved in the StepUp intervention reported that the booklets were useful when they were accessible and relevant to the person’s situation but that the use of the booklets within the context of a research trial could be inflexible:
I do think she could have done with a little bit longer because, personally, the first couple of booklets weren’t really too relevant, it just wasn’t amazingly relevant, but the last couple, you know where you tackle the problems head on, they were better I think and we could have done with a bit longer on them because with them coming at the end, there was only a couple of weeks to really tackle the problems.
StepUp; supporter of participant 209
People with learning disabilities receiving the BeatIt intervention reported using the diaries between sessions, getting out more, doing more and taking control of their lives, although they needed support to do this. People with learning disabilities receiving the StepUp intervention reported reading through the booklets with their supporter between sessions and using coping strategies discussed in the therapy sessions. Supporters across both types of intervention mentioned that the therapy stimulated activities between sessions, although supporting these activities could be difficult within people’s daily routines and because of the amount of support available to the person:
And then I started taking meself off instead of going to the pub because Susan helped me get a pass from my doctor so I get free travel and all that . . . Days out, going to different places and just having a wander round and some dinner and coming back . . . That’s when I used to see them [diaries] and write it down . . . I used to love those little booklet [diaries] things.
BeatIt; participant 182
There were additional subthemes from supporters’ interviews about the therapy process. Supporters involved in both types of intervention reported that being involved in the therapy helped them learn more about the person they were supporting and brought them closer. Supporters also mentioned that both therapies were generally pitched at the right level for the person they were supporting and that the person enjoyed participating in the therapy. In terms of what worked well in therapy, supporters involved in both types of intervention mentioned being able to have honest, open conversations with the person; the therapist being on the right wavelength; and the availability of materials that were accessible to the person. Some supporters appreciated the therapy taking place in the person’s home. Supporters of people receiving the BeatIt intervention thought that activities worked well when they were both tailored to the person and helped to instil a more active routine. Supporters of people receiving StepUp talked about the booklets and thought the focus on task-oriented problem-solving was particularly helpful:
The problem-solving book is really good, I’ve actually found it beneficial for myself. Definitely the sleeping one was good, it’s good to recognise depression as well in the initial booklet because I think people don’t realise, so I think all of the booklets were informative in different ways, but particularly I think it is important to recognise that you have a problem and that other people recognise that you have a problem as well.
StepUp; supporter of participant 289
Theme 3: relationships in therapy
Across both types of intervention, people with learning disabilities generally reported positive relationships with the therapist. They felt that they could talk openly and trust the therapist, and reported that they had developed a close relationship with the therapist. People with learning disabilities also generally reported that having a supporter in the therapy sessions helped to put them at ease and was very important in terms of achieving change. People with learning disabilities also mentioned that their therapy sessions generally involved joint working between them, the therapist and the supporter, with the supporter providing the scaffolding for the therapy session to go well:
Everything she [therapist] did, she explained, so it wasn’t so bad. I got into it, like you know. Because the therapist let me talk about what I wanted to talk about, you know, I felt more comfortable being that way.
StepUp; participant 252
However, supporters were not universally seen as helpful:
When my support worker was there I didn’t really like that bit of it to tell the truth, I have to be honest with that. ‘Cause I had to sort of watch what I was saying as maybe stuff that I want to talk about but my support worker was there all the time, it was like she took control in a way, about how she thinks I am. But when you know how you’re feeling, you know that’s how you’re feeling . . . I am an adult, do you know what I mean?
BeatIt; participant 075
Supporters involved in both types of intervention also reported positive relationships with the therapist, feeling that the therapist put them at ease, and that it was helpful to work together with the therapist and person with learning disabilities. Supporters also mentioned having to find the right balance within therapy sessions between intervening and staying quiet, a balance that sometimes resulted in less need for them to intervene as the therapy progressed:
I really liked the fact that as the weeks went by I could withdraw a little bit because [in] the first session, everything was coming through me and [name] was quite shy and would address things to me for me to pass back to the therapist but as the weeks went by she was quite confident to talk to the therapist.
StepUp; supporter of participant 204
Theme 4: ending and after therapy
People with learning disabilities across both types of therapy described how they felt at the end of the therapy sessions. They said that they were sad to end the relationship with the therapist and felt that the therapy was too short or that they wanted to do it again, with some people expressing a reluctant acceptance that therapy was at an end:
I was quite sad that it finished because I could have done with some more sessions of therapy to be honest, but sadly these things have to come to an end. So you have to make the most of what you’ve got, don’t you?
StepUp; participant 211
People with learning disabilities talked about maintaining changes they had made after therapy had finished. Those who had received the BeatIt intervention mentioned keeping their activities going and continuing to complete diaries and use the formulation booklets. They also talked about maintaining work towards the goals identified in the therapy. Some people who had received the StepUp intervention mentioned continuing to use the booklets and the coping strategies developed during therapy. Although others said that they had not used the booklets since the therapy had finished, they knew where they were in case they were needed:
No I don’t use the diaries any more. I’ve got my own diary in my bag. I usually write what I do and then if mum and dad, what they do . . . but I think it’s fun to.
BeatIt; participant 097
My favourite one is the activity. If I do feel down I can drag myself out and then just go somewhere and that . . . Yeah, go for a long walk or maybe have a bath or just go to [nearby town] or something for a day.
StepUp; participant 209
Supporters talked in similar terms to the people with learning disabilities across both types of intervention, talking about how they still supported people to use the materials (sometimes adapting them specifically for the person). They also described how the person (with encouragement) maintained activities and other progress that had been made. Some supporters reported that the person had not used the materials since the end of therapy.
Supporters identified barriers and helpful factors they had experienced when it came to maintaining change beyond the end of therapy. Barriers included the person facing negative life events or physical illness, a lack of encouragement or prompts required to sustain change or a lack of support/services needed for planned activities to happen. Helpful factors identified by supporters included feeling that they were more receptive to the person asking them for help, encouraging the person to do more activities and adapting the therapy materials to suit the individual person they supported:
We adapted the problem-solving worksheet, we talked about it together, it was very soon after it [therapy] finished so we adapted it and made it a little bit simpler with less ideas and I think we had some more prompting-type questions in there to explain, so that it wasn’t just like ‘What’s the problem? How do you solve it? What’s the idea to solve it?’ It’s really given me the confidence to try something different and move it on so we are still taking bits from it.
StepUp; supporter of participant 203
Theme 5: the impact of therapy
Both people with learning disabilities and supporters involved in both types of intervention reported similar positive effects of therapy on people’s lives. Supporters mentioned participants being happier, more confident and showing improved social skills. The supporters thought people talked more, engaged in more activities, were more empowered and used new problem-solving skills. The supporters also observed that the individuals they supported had better relationships with their friends, families and with the supporter themselves.
A small number of supporters also reported broader impacts of the therapy beyond the individual who had received it, in terms of them using some of the approach (whichever therapy it was) with other people and the importance of taking a more proactive approach to addressing people’s mental health:
A really big difference with her, more brighter, happier, she sings away (she never used to sing away before) she loves her singing, wanting to help everybody now. She got more social skills, going out more, which she’ll never say no. She’ll always go out. She’s more happier anyway, she’s more brighter. She’s just a pleasure to have now. Everyone says she’s a ray of sunshine when she comes in here. She gained a lot of confidence, she can express herself more now, she’s more happier.
BeatIt; supporter of participant 196
People with learning disabilities mentioned experiencing improvements in their mood, having a more positive sense of self and being more independent. They also said that they had more active lives and better relationships, and that bullying or victimisation had stopped:
But since I’ve been to therapy it’s totally different because I’ve started cleaning up my flat, cleaning myself up and going shopping. I have come on [in] leaps and bounds and it’s all because of this. I don’t think I’d have got through it otherwise. If I wouldn’t have had the therapist I wouldn’t have got through it . . . If it wasn’t for this and a couple of other friends, I think I’d be dead by now.
BeatIt; participant 182
I wanted it so that I didn’t have to be spoken to like a child and that people understood me and not, like, treated me differently. The therapy definitely did that.
StepUp; participant 272
Theme 6: views on the therapy
Relatively few people with learning disabilities or supporters mentioned specific ideas for improving the therapy that they had received. People with learning disabilities mentioned wanting aspects of the therapy to be simpler, and people who had received the StepUp intervention specifically mentioned wanting more booklets covering a wider range of topics, the booklets to be better presented, more sessions and more time within sessions. Supporters across both types of therapy wanted to tailor the therapy more to the specific needs of the person, and have shorter and simpler sessions. Some supporters suggested having an extra review session after the end of therapy, and to involve the person’s family more. Supporters involved in StepUp mentioned the need for more in-depth therapy and wanted more booklets covering a wider range of topics. Supporters across both therapy types also generally said that they would recommend the therapy to others:
I do think it was helpful. Yeah I think they would recommend it yeah, they were helpful. I don’t think it was too intense which was good, it was on a level that [name] could understand which was good, it sometimes can be different.
BeatIt; supporter of participant 302
It should be supported, I think it should be supported and offered to people, a lot more people. Because it does really, really help. I just can’t believe that there is nothing out there for people with depression bar from going to the doctors and they say ‘have some tablets’. It proves that it can work without tablets. So there should be funding for it. So let’s hope they do something about it.
StepUp; supporter of participant 295
Findings from therapists
For reasons of space, selected themes from the overall framework for therapist transcripts are reported here: (1) positive aspects of delivering the therapy (those common to both interventions, those related to the BeatIt intervention and those related to the StepUp intervention), (2) challenges of delivering the therapy (those common to both interventions, those related to the BeatIt intervention and those related to the StepUp intervention), (3) working with supporters and (4) therapist experience and supervision.
Theme 1: positive aspects of delivering the therapy
Therapists delivering either type of intervention reported positive perceptions of aspects of the therapies that were common across interventions, particularly the structured format and manualised nature of the interventions and the use of accessible materials throughout both interventions. Therapists generally reported that the structured nature of sessions facilitated rather than constrained the therapy and enabled them to quickly establish a therapeutic relationship. Having a fixed number of sessions helped therapists to keep on track and know when to end treatment:
My experience, obviously I’ve not done a set programme therapy before, so it was quite nice to have a bit of structure, made me feel quite comfortable, I was like ‘yes a bit of structure finally’, I’m all over the place with lots of my clients so this was quite nice, I knew what I’m doing.
BeatIt; therapist 2
Therapists also reported positive aspects specifically tied to the intervention that they were delivering. For example, some therapists delivering BeatIt reported that the intervention allowed them to tailor the sessions to the particular issues faced by the person with learning disabilities, thereby facilitating the person’s involvement in the therapeutic process:
My first participant, he had specific ideas of what he wanted to engage with himself, and that was his goal at the very end. We got really quite far with that. At the end he was able to meet that. He made little steps, he found it very, very useful. He asked for more copies of Make a Plan and How Did It Go? after all the sessions completed, he wanted in order that he could plan his time, he found that useful.
BeatIt; therapist 3
Therapists delivering the StepUp intervention reported that the consistent structure of the sessions was helpful to the person with learning disabilities. The intervention helped people to solve problems and see their situation differently, and the intervention provided valuable tools for the person to use after therapy had ended:
And it’s tools for not just that period or eight sessions, it’s tools for the future; that’s what it’s there for, not just those 8 weeks, so hopefully what I was trying to get across to mine was we might have addressed the problem that you want to discuss, that you identified, and we worked through that in sessions 5, 6 and . . . can’t remember. But also if anything does happen in the future when you start feeling a bit . . . which is highly likely to happen – there’s no point in saying otherwise, that StepUp is going to cure you now, that you’re never going to suffer from depression again, you’ve got the tools there.
StepUp; therapist 52
Theme 2: challenges of delivering the therapy
Therapists delivering either type of intervention reported some challenges in delivering the therapy that were common to both interventions. These challenges were often the flip side of those aspects of the interventions they viewed positively. For example, some therapists reported that the manualised, structured approach used in both interventions made it difficult for the therapy to be flexible enough to deal with the particular issues that a person might bring to a therapy session. The highly structured nature of the interventions, particularly within the context of a research trial, was reported by some therapists to constrain them in adapting and individualising the intervention and materials to suit the person’s needs or circumstances:
I had trouble with one family though, the sisters were saying, ‘but she doesn’t have sleep problems, why do you keep going on about this?’, and I’m rigid in that way, that I’m saying, ‘well I have to go through it ‘cause it’s research based and it’s part of it, let’s just do it’. And they just didn’t want it, they were just not interested and I still went through it, it ended up being pulled out ‘cause they were just saying it wasn’t relevant ‘cause they were saying ‘none of this is relevant, my sister doesn’t have depression and anxiety’.
StepUp; therapist 54
Community-based learning disability nurses who had taken on a therapist role delivering either intervention found the focus of delivering a specific, structured intervention both frustrating (in their therapist role they could not address other needs that the person had) and valuable (it enabled them to work with the person with learning disabilities towards a specific goal):
So the structure was good, to have it to not only guide but restrict as well, ‘cause half the time I would be sitting there going, ‘oh this is a problem, I’ll make a referral to this’, I’m not doing it, I’m not a nurse, I’m a therapist and so it was nice to have a very defined role to be within and a goal that was also quite clear.
BeatIt; therapist 1
Therapists also reported challenges more specifically tied to the intervention that they were delivering. For example, some therapists delivering the BeatIt intervention reported that the later sessions could be too repetitive and that the intervention might be less appropriate for people with learning disabilities who already led active lives:
. . . but it’s that gap of where you’re repeating the session, 6–10 is repetitive for that client. So we’re doing what we did last week and what are the problems with that? So I just felt that really that’s dependent on your individual.
BeatIt; therapist 4
Some therapists delivering the StepUp intervention reported that it was difficult to hold back from making suggestions or following up with the person on what had happened since the previous session:
Especially when you get to the problem-solving part I think, you know you could feel it was on the tip of your tongue all the time to prompt them, to help them, to come up with ideas that you know is going to make a massive difference to their lives, but you can’t and that was just very frustrating. I don’t know if it’s just part of being a nurse and that’s what we’re made to do so that was very difficult in the sense of not doing that.
StepUp; therapist 53
Theme 3: working with supporters
Therapists delivering either intervention reported that the level and nature of supporter engagement within the therapy process was a crucial factor in the progress of therapy. Within therapy sessions, supporters had an important role in encouraging and supporting the person to fully engage in the session. Supporters also had a vital role between sessions in reminding and supporting people to carry out tasks between sessions:
The support worker was absolutely brilliant with the lady that I was working with, she was very encouraging and in the sessions she’d support the lady, if she’d forgotten what she’d done she’d say, ‘do you remember what we did?’ and she’d sort of jog her memory, so that was really, really useful.
BeatIt; therapist 5
Therapists reported supporters to be most effective when they knew the person well, spent time with the person on a daily basis, reliably accompanied the person to therapy sessions and took responsibility for supporting the person between therapy sessions. Supporter negativity and lack of commitment could be active barriers to progress. However, therapists recognised that paid supporters in particular were sometimes under severe time constraints:
. . . and the supporter takes ownership and sees it as their responsibility to support the person to carry through this therapy. They end up reading up on it between the weeks and stuff as well so that’s quite good, prompting them to do that.
StepUp; therapist 54
. . . you could tell from the offset that the support worker thought that it was not any use at all. ‘Why are we here? Why have we got to do that?’ And I think my client picked up on that, didn’t engage, didn’t do any of the homework that he was supposed to do and I would spend most of the hour session trying to get him to engage rather than actually doing the work.
BeatIt; therapist 4
Some therapists reported that the therapy would have benefited from having a portion of the session without the supporter present, so that the person with learning disabilities could talk more freely:
There was one boy who was 17 or 18 and we were doing things on relationships and his mum was sitting there and it just wasn’t appropriate. I felt like he was embarrassed and didn’t want to speak in front of his mum, whereas if his mum had left for kind of 20 minutes and came back and recapped on what we had done, I might have got a bit more out of him.
BeatIt; therapist 6
Theme 4: therapist experience and supervision
Therapists mentioned the importance of gaining experience in delivering therapy, helping to make it feel like a more natural process:
From the therapy’s point of view though, the more you did it the more, I mean if it was rolling on and we were on our sixth client, it got easier and easier and easier, it got far more flexible, it got more client focused, it just became quite natural as a process and enthusiasm and looking at everything else just pops into your head as you mature in it, that’s how I felt out, I’d love to have had a third and a fourth, ‘cause you just felt like you were getting into your stride.
BeatIt; therapist 7
Although there could be challenges in arranging regular supervision sessions, therapists delivering both interventions valued supervision as an opportunity to focus, reflect and move on when ‘stuck’:
It was really good at helping you to look at things, if you’re faced with a specific difficulty, and it being from a psychologist as opposed to a nurse you just get slightly different perspectives in what we were doing. I really liked the resource, the way it was set up with your steps, what to do in the booklets, just the amount of conversation that that generates.
StepUp; therapist 55
Content analysis of therapists’ logs
The therapy logs that were completed after each session by the therapists contained a section in which they were asked to identify barriers that they faced when delivering the therapy. Barriers recorded on all of the therapy logs completed by therapists were extracted and the content analysed.
For the BeatIt intervention, the most frequently reported barriers were participants’ lack of interest in activities (reported at least once for 61 participants), a lack of resources between sessions (reported at least once for 35 participants), the non-completion of diaries (reported at least once for 28 participants), issues with supporters in sessions (reported at least once for 26 participants) and a lack of continuity with carers (reported at least once for 25 participants). For the StepUp intervention, the most frequently reported barriers were distractibility (reported at least once for 38 participants), understanding of materials (reported at least once for 16 participants), booklets not seeming relevant (reported at least once for 13 participants) and lack of continuity with carers (reported at least once for 11 participants).
The BeatIt therapists also recorded the participants’ planned homework activities on the therapy logs. All these planned homework activities were also extracted from the logs and the content was analysed. Of these, 51% were day-time activities, 26% were domestic or daily living activities, 7% were social activities and 16% were preparatory activities.
Summary
The accounts of people with learning disabilities undergoing therapy, their supporters and the therapists delivering the therapies increase our understanding of how people experienced the interventions in this study.
People with learning disabilities and their supporters clearly described the circumstances they were in before therapy and their perceived need for an intervention, focused on the person’s depression. Both people with learning disabilities and their supporters reported a range of feelings and perspectives about starting therapy, from nervousness and uncertainty to an attitude that it was worth trying the intervention, particularly in the absence of other mental health interventions.
For both interventions, people with learning disabilities, supporters and therapists generally (but not universally) described good working relationships being quickly established, and all agreed on the importance of these therapeutic relationships. When supporters were committed, positive, reliable and had time, their advocacy/scaffolding role within sessions and encouragement/reminders between therapy sessions were highly valued by people with learning disabilities and therapists.
Most people with learning disabilities, supporters and therapists generally viewed the materials in either intervention as accessible and useful, although more adaptability and flexibility in their use were also recommended.
In addition to these non-specific factors, people with learning disabilities, supporters and therapists clearly described specific aspects of each intervention. People with learning disabilities receiving the BeatIt intervention described important aspects of the therapy as having the time and space to talk and be listened to, generating ideas about activities and making plans, building their confidence, and understanding the materials and paperwork used within the therapy. Supporters described having a liaison function and encouraging/reminding the person to engage in activities between sessions. Therapists discussed being able to tailor aspects of the intervention towards the circumstances and interests of the person.
For people with learning disabilities receiving the StepUp intervention, important aspects of the therapy were the process of using the self-help booklets and making them relevant to themselves. Supporters thought that the intervention gave them new insights into the person they were supporting and gave them a greater understanding of depression more generally. Therapists also discussed how the intervention could be made personally relevant, and how they helped the person to solve problems that he/she faced and to think differently about his/her situation. They felt that the intervention provided useful tools for the person beyond the end of therapy.
The highly structured, manualised and time-limited nature of both interventions was valued by supporters and therapists. Although both these groups mentioned wanting to adapt and individualise interventions more to suit individuals’ needs, therapists mentioned the importance of a clear structure in keeping them focused. People with learning disabilities reported feeling sadness and disappointment when the therapy came to an end, although some reluctantly accepted that this had to happen.
Some people with learning disabilities and supporters reported continuing changes beyond the end of therapy, with materials (often individually adapted) continuing to be used and activities and coping strategies being maintained in accordance with the specific intervention. Others reported that these had not been maintained at the time of the interviews but mentioned that the materials would be used when they needed them.
Both people with learning disabilities and supporters involved in both types of intervention reported similar positive effects of the therapy on people’s lives. People with learning disabilities mentioned improvements in their mood, a more positive sense of self and more independence, more active lives and better relationships, and bullying or victimisation to have stopped. Supporters described people being happier and more confident, talking more and showing improved social skills, engaging in more activities, being more empowered and having better problem-solving skills. They also reported that people had better relationships with friends, family and with themselves (the supporters).
Chapter 8 Discussion
Primary objective
There were no statistically significant differences between the StepUp and BeatIt groups in GDS-LD scores at the 12-month primary outcome point. Therefore, there is no evidence that BeatIt is effective when compared with StepUp as an active control condition.
Although this was not designed as a non-inferiority study, an important consideration is that the study resulted in the outcomes of two active interventions being compared (see Chapter 7). Similarly designed trials conducted with the general population provide supportive evidence to add to the available armoury of effective interventions for use in depression. For example, the Cost and Outcome of Behavioural Activation versus Cognitive Behavioural Therapy for Depression (COBRA)27 non-inferiority trial promotes behavioural activation as being as equally effective as CBT. People with learning disabilities and their therapists are in a different position: there are no existing trials showing any psychological interventions to be effective in the treatment of depression in people with learning disabilities, including no high-quality evidence base for CBT. Ours is the first large-scale RCT conducted on psychological interventions for depression, and, other than our own feasibility study,39 is the only RCT of any size concerning behavioural activation with adults with learning disabilities. This is also the only trial involving an adapted, guided self-help treatment for depression for adults with learning disabilities. On the main outcome measure, participants in our trial had marked improvements in depressive symptoms in both conditions.
So how do we interpret these findings? We cannot conclude that either intervention is effective. However, both BeatIt and StepUp recipients reported considerable improvements in their symptoms of depression at 4 months post randomisation (following end of treatment), and this was sustained for both groups 12 months post randomisation. These findings could be explained by a regression of scores to the mean over time and a range of non-specific effects of receiving therapy and being involved in a clinical trial, but improvement in depression could suggest a successful response to both interventions, given the following factors:
-
The ‘unsuccessful’ previous treatment histories of the participants. At baseline, 66% of the participants with learning disabilities who were allocated to the StepUp intervention, and 63% who were allocated to the BeatIt intervention, were taking antidepressants. A total of 19% of the participants allocated to the StepUp intervention were taking mood-stabilising drugs (primarily for the management of epilepsy, but still with a theoretically mood-stabilising effect), and 13% allocated to the BeatIt intervention were taking mood-stabilising drugs [with 69% taking drugs of one or both of these classes (i.e. antidepressants and mood-stabilising drugs)]. In addition, 18% of the participants allocated to the StepUp intervention and 20% of the participants allocated to the BeatIt intervention had received prior psychological therapy (not specifically defined). Despite these ‘interventions’, all participants were depressed at baseline. This is suggestive of a view that these adults might have been at the severe and/or more enduring end of the depression spectrum.
-
The natural history of depression in the population with learning disabilities. It is apparent from previously published literature that people with learning disabilities are more likely to have enduring depression than those without learning difficulties. For example, reports from the longitudinal UK 1958 birth cohort found that at 33 years of age, adults with learning disabilities had significantly higher depressive scores than the adults without learning disabilities,84 and 15% of the cohort with learning disabilities, compared with only 3% of those without, had chronic depression (high depressive scores at ages 23, 33 and 43 years). 11 Similar evidence comes from the longitudinal study of the UK 1946 birth cohort. When aged 15, 36, and 43 years, individuals with learning disabilities were found to have significantly more depression and anxiety symptoms than those without learning disabilities,12 suggesting a more severe and enduring pattern of depressive illness.
-
Six previous small pilot trials of psychological interventions for depression in people with mild/moderate learning disabilities,33–38 reviewed by NICE,31 have reported depression data from TAU conditions. For participants in TAU in all six studies, there was virtually no change in depression scores from baseline to follow-up, including up to 11 months after baseline.
Although it cannot be discounted, it seems unlikely that the pattern of improvements in self-reported depressive symptoms in both BeatIt and StepUp groups – improvements by 4 months that were sustained at 12 months – could be just as a result of a natural history of spontaneous recovery of symptoms; however, participation in the trial may have had an effect.
Alongside these findings from the study, there were no related serious adverse events reported, suggesting that neither intervention carries any notable risk to participants.
Secondary objectives
Other psychological outcomes followed a similar pattern of results to the primary outcome. Again, there was no evidence that the BeatIt intervention is effective when compared with the StepUp intervention.
For carer-reported depression in the participants, self-reported anxiety and carer-reported aggressive behaviour, there were no treatment group differences at the 12-month follow-up (primary end point) or at 4 months post baseline. Within-treatment group analyses showed significant reductions from baseline in carer-reported depression and self-reported anxiety at both 4 and 12 months, associated primarily with reductions from baseline to 4 months that were maintained to follow-up. Similar analyses for carer-reported aggression showed a reduction from baseline to 4 months, but only for the BeatIt group.
Considering QoL outcomes together (self-reported health-related QoL, community and domestic activity measures, PSS), there were again no treatment group differences at the 12-month follow-up (primary outcome) or at 4 months after baseline. The one exception was increased participation in domestic and leisure activities among the BeatIt group participants at 12-month follow-up compared with the StepUp group participants. Although self-reported health-related QoL (measured using the EQ-5D) followed a similar pattern of within-group changes (improvements compared with baseline in both treatment groups), other QoL indicators demonstrated a more mixed pattern of results, with some showing no change from baseline, some a positive change in the BeatIt group, and some a positive change in the StepUp group.
Two of the three indicators of participants’ adaptive behaviour skills showed no treatment group differences at either the 4- or 12-month follow-ups, but BeatIt participants had higher socialisation scores at 4 months only (i.e. not at the 12-month follow-up primary end point). Within-group analyses suggested generally increased adaptive skills in the two treatment groups in comparison with baseline, including added increases following therapy up to the 12-month follow-up point.
Carers’ sense of self-efficacy in supporting adults with learning disabilities and depression increased within both treatment groups from baseline, but again there were no treatment group differences at either 4 or 12 months. Carers’ relationships with participants were almost universally lacking evidence of negativity on the basis of analysis of FMSSs, showing very little change, and analysis models could not be appropriately fitted.
Exploratory analyses of predictors and potential moderators of outcome suggested that the two treatments worked equally well across a variety of participant characteristics. Notably, IQ scores were unrelated to outcome. One interesting finding was that the participants’ positive expectation of change at the outset predicted a better outcome.
Health economics
The results of the economic evaluation indicate that there was no difference in outcomes between arms as measured by changes in mean QALYs between baseline and the 12-month follow-up, which is reflected by the lack of difference between arms in the primary outcome of change to GDS-LD score.
Although there was no significant difference in mean total costs between arms, this masks a highly significant difference in intervention costs. An alternative interpretation, therefore, is that the increased intervention cost in the BeatIt arm did not result in any significant cost savings in non-intervention-related costs.
The uncertainty around the complete-case and multiple imputation analyses results was explored using bootstrapping techniques. The results of the bootstrapping exercise confirmed the results: there was no evidence to suggest either intervention was cost-effective compared with the other if the focus was on the total costs. However, if non-significant, non-intervention costs were excluded, the bootstrap analysis confirmed that the BeatIt intervention never entered the cost-effectiveness range.
A review by Romeo and Molosankwe85 in 2010 found a paucity of economic evaluations carried out on people with learning disabilities. They found 10 papers reporting economic studies in learning disability, 4 of which reported costs and outcomes, and the areas covered included service use, community living and challenging behaviour. None of these studies had a cost–utility analysis, in which the outcome is preference-based, such as a QALY. In 2011, Ekers et al. 86 reported on a small pragmatic RCT (n = 47 participants) comparing behavioural activation with TAU for depression in adults with learning difficulties. Ekers et al. 86 found that behavioural activation resulted in a gain of 0.20 QALYs, producing an ICER of £5756 per QALY, which is considered cost-effective using NICE’s current threshold of £20,000 to £30,000 per QALY. 87 More recently, a report was published by Willner et al. 68 in 2013 exploring how costs are affected by challenging behaviour in people with learning disabilities. The participants were randomised to either a CBT manualised intervention or TAU ‘waiting list’ control arm. Willner et al. 68 concluded that there were no statistically significant differences in costs between groups, and because of lack of power, the study was not able to detect economic differences between groups. We have not found any previous studies looking at the cost-effectiveness of depression treatments for people with learning disabilities.
The strengths of this study are that < 5% of data were missing in all questionnaires for resource use and QoL, and cost-effectiveness results are consistent across all analyses carried out.
Limitations of the study include the imbalance in EQ-5D-Y utilities at baseline, with the BeatIt group participants reporting significantly lower QoL than those in the StepUp group. The generic EQ-5D-Y may not be sufficiently sensitive for this population. We found a small association between GDS-LD and EQ-5D-Y scores, but note that the analysis suggests a high amount of unexplained variability.
It was possible to administer the EQ-5D-Y to a population with learning difficulties. However, there is no tariff available to value the EQ-5D-Y for children and adolescents, or for those with a learning disability. Future research could include investigating whether or not there is a need for a learning-disability tariff.
In summary, given the lack of differences between the BeatIt and StepUp groups at the primary end point (12-month follow-up), it is not surprising that there was also no economic evidence to suggest that BeatIt may be more cost-effective than StepUp. No differences in resource use were found at 12 months, although the BeatIt intervention did cost more to deliver than the StepUp intervention. Overall, the vast majority of the support costs for participants in both treatment groups were not related to the treatments themselves: intervention costs were approximately 4%–6.5% of the total support costs.
Qualitative study
Results of the qualitative research with participants, supporters and therapists were in concert with the quantitative findings. In particular, both treatments were perceived as active interventions, and both treatments were valued in terms of their structure, content and perceived impact/outcomes. The qualitative data from supporters did offer additional insight into the impact of taking part in therapy on carer–participant relationships. Supporters reported understanding more about the person and/or his/her depression following either treatment, and reported more positive relationships with participants following either treatment.
Delivery of the interventions
Data from multiple sources across the study are consistent in showing that both therapies were conducted to the criteria set out in the protocol, and that participants, supporters and therapists viewed both interventions positively.
From fidelity ratings of therapy sessions, therapists across the BeatIt and StepUp interventions demonstrated similar high levels of fidelity to non-specific aspects of both interventions, and also demonstrated high fidelity to specific aspects of the intervention that they were delivering. This high level of therapist fidelity was achieved with a large cohort of 84 therapists who generally saw very few participants as part of the trial. From the qualitative interviews and focus groups, participants, supporters and therapists in both interventions agreed that good therapeutic working relationships were established quickly and maintained throughout therapy, and were an important component of the clinical effectiveness of either intervention.
In the qualitative study, both participants and supporters sometimes talked about feeling nervous and uncertain about starting either intervention, yet they were also generally positive because there was a perceived absence of other therapeutic options available for people with learning disabilities and mental health problems or depression. From therapist logs, participant adherence to both interventions, in terms of attending therapy sessions, was high and for most participants the presence of a supporter in therapy sessions was relatively reliable and stable. Supervision was also delivered to therapists in both interventions approximately once every two therapy sessions, as specified in the protocol.
The majority of therapists in the study (67.1%) were community learning disability nurses. Most therapists (63.1%) were experienced in working with people with learning disabilities (having experience of ≥ 5 years) and most therapists (60.7%) had received some previous therapy training.
In the qualitative interviews, community learning disability nurses valued the structure, clear focus and goals, and clinical supervision – which were seen as contrasts to their usual working practices – of both interventions. The highly structured, manualised and time-limited nature of both interventions was also valued by the supporters in the qualitative interviews. People with learning disabilities in qualitative interviews reported feeling sadness and disappointment when the therapy came to an end, although some reluctantly accepted that this had to happen. For some supporters and therapists there was a tension between the utility of a highly structured, manualised intervention and a desire to individualise the structure of the intervention to focus more on the issues facing specific participants with whom they were working.
In terms of adaptations to the interventions to make them more accessible to people with learning disabilities, both interventions used extensively adapted materials. Supporters and therapists generally reported that these adapted materials were accessible and useful. Nevertheless, participants, supporters and therapists all suggested specific changes to the materials in each intervention – some of the main changes being put forward were about making the materials more accessible and flexible to suit individual participants’ circumstances and preferences. Some supporters from both interventions reported that they had continued to use therapy materials, which they had personalised for the individual they were supporting.
A further adaptation to both interventions was to involve a supporter in therapy sessions. In the qualitative study, participants, supporters and therapists generally (although not universally) agreed that when supporters were committed, positive, reliable and had time, their advocacy/scaffolding role within sessions and encouragement/reminders between therapy sessions were highly valued and an important component of the clinical effectiveness of either intervention. Obtaining reliable, consistent and effective supporter involvement was problematic for a minority, as reported in therapist logs.
In terms of specific therapy factors, the participants in the BeatIt group valued having the time and space to talk and be listened to, generating ideas about activities and making plans, and building their confidence. Supporters described having a liaison function, and encouraging/reminding the person to engage in activities between sessions. Therapists discussed being able to tailor aspects of the intervention towards the circumstances and interests of the person. In therapist logs, barriers specific to the BeatIt intervention included a lack of resources to support participants to engage in activities and the non-completion of diaries between therapy sessions.
For the StepUp intervention, participants described using the self-help booklets and making them relevant. Supporters thought that the intervention gave them new insights into the person they were supporting and a greater understanding of depression. Therapists discussed how the intervention helped the person solve problems and think differently about their situation, and felt that the intervention provided useful tools for the person beyond the end of therapy. In therapist logs, barriers specific to the StepUp intervention included participants getting distracted, participants’ understanding of the materials and some of the booklets not being relevant for the individual participant.
Although participants and supporters described some aspects specific to each intervention, across both interventions participants and supporters reported similar positive impacts of either therapy on people’s lives, including improvements in their mood, a more positive sense of self, more independence, more active lives and better relationships with others.
Summary of findings
Primary and secondary outcomes, economic data and qualitative results all clearly demonstrate that there was no evidence for the BeatIt intervention being more effective than the StepUp intervention.
Based on these results, we cannot conclude that either intervention is effective. However, patients in both arms of the trial showed improvements in outcomes during the intervention phase that were maintained at 12 months; this may indicate that both the BeatIt and StepUp interventions are beneficial. There is a need for the clinical effectiveness of these (or similar) interventions to be compared with TAU in future RCT evaluations.
Conduct of the trial
Important insights and data were also obtained concerning the delivery of the trial. The ratio of trial information packs sent out to initial responses received was 4–5 : 1. Working through intermediaries to recruit participants was one of the challenges of conducting the trial. The main source of participants was from community learning disability teams, with smaller numbers of participants recruited from mainstream IAPT services and care providers. One drawback was that some professionals in IAPT services appeared to lack knowledge of people with learning disabilities and mistakenly referred people with specific learning difficulties such as dyslexia to the trial. Differences in the main referral sources between England, Wales and Scotland is likely to have reflected the different service patterns and practices. This highlights that a multipoint recruitment strategy, responsive to different service contexts, is vital in a multicentre trial.
We successfully recruited and randomised 161 participants into the trial and informed consent was obtained with the use of carefully developed accessible materials. There was good adherence and retention: 86% of participants in the BeatIt arm completed therapy (a minimum of 8 sessions), 82% of participants in the StepUp arm completed therapy (a minimum of 6 sessions) and 141 (87.6%) participants were followed up for 12 months. Community nurses and other professionals working in specialist community learning disability teams and IAPT services were trained as therapists to deliver the interventions. However, competing work demands meant that therapists had limited time available to deliver therapy as part of the trial and they were generally able to work with only one or two participants at any one point in time. This could pose a problem if therapists lacked capacity to take on new participants, as a therapist for each arm of the trial needed to be available at a location before a participant could be randomised to that location. Consequently, to ensure that there were sufficient numbers of therapists to allow new participants to be randomised in a timely fashion, a far higher number of therapists needed to be trained than originally anticipated: 95 in total. In the end, 76 of the trained therapists were assigned participants to work with. Importantly, it proved feasible to deliver the training to this large number of therapists. Supervisors were also recruited from local services and trained to supervise the delivery of the interventions.
The two manuals developed for the interventions provided comprehensive guidance and support materials for the therapists and it proved possible to deliver the therapies, at scale, with good fidelity to the manuals. Audio-recordings of therapy sessions were rated for fidelity. Although the inter-rater agreement for the fidelity ratings was good, it proved challenging to obtain audio-recordings, because of a reluctance on the part of some participants and therapists to consent to the audio-recording of sessions.
Overall, the successful delivery of the BeatIt trial contradicts a widely held contention that it is not possible to recruit to a large-scale RCT of an individual psychological therapy for people who have a learning disability. 88–90 The lessons learned may have important implications for the conduct of future trials of psychological therapies involving people with learning disabilities.
Limitations
The major limitation of the trial was the absence of a TAU condition, which would have been required to establish the clinical effectiveness of the BeatIt intervention. This was the original design suggested by the research team but was rejected by the funder, who asked for an attention control group to be recruited instead. The decision was made to use guided self-help (StepUp) as the attention control arm because it was seen as a less person-centred and more rigid approach with a different set of active ingredients, that is, psychoeducation rather than activity based. It was also chosen because it was an ethical option, as guided self-help is a NICE-recommended91 intervention for general adult mental health and we had a package available, with carefully adapted materials for people with learning disabilities. The StepUp intervention was also designed to involve a supporter in therapy sessions, thereby incorporating a key element of attention for which we wanted to control. The research team and funder-approved protocol failed to anticipate the ability of the therapists to personalise the materials or the agency shown by the participants and their supporters to follow through on ideas and plans made in therapy sessions.
Although, in retrospect, comparing TAU with the BeatIt intervention would have been a preferable design in terms of examining the clinical effectiveness of the BeatIt intervention, there remains the question of whether or not this would have made recruitment to the trial more challenging. Participants randomised to the trial knew that they would be receiving one of two interventions, making participation in the trial a more attractive proposition. Moreover, working through intermediaries meant that the researchers were not only having to recruit the participants themselves but were also having to make the case to carers or professionals working with the individual with learning disabilities that the study was worthwhile. Carers and professionals might have been less likely to engage with the recruitment process knowing that the person they supported or worked with may not have received an intervention.
There were a greater number of withdrawals from the BeatIt arm (n = 12) of the study than the StepUp arm (n = 2). This may have reflected the greater number of BeatIt sessions and the more active nature of the intervention, in which the aim was to support the participants and supporters to engage in scheduled activities between sessions. However, it is also worth noting that three of the BeatIt withdrawals happened before the participants entered therapy and another BeatIt participant withdrew when they were contacted for the 12-month follow-up visit, after the intervention had finished.
Lessons for trials with people who have learning disabilities
Our feasibility study helped to inform careful advanced planning of recruitment to our study, with a further opportunity to refine the strategy during the internal pilot. Consequently, when implementing our RCT, we achieved our target recruitment within the planned time frame. This was despite the fact that recruitment of people with learning disabilities to participate in trials is notoriously difficult. For example, a Health Technology Assessment (HTA) programme-funded study92 on antipsychotic medication for adults with learning disabilities had substantial recruitment problems: only 72% of the total number of intended participants were recruited, despite an increase in the recruitment time from 2 to 4 years and extending recruitment outside the UK. In addition, a HTA programme-funded study93 on antipsychotic drug withdrawal in adults with learning disabilities closed at the internal pilot stage because of recruitment problems. Even in general population trials, recruitment is often a challenge. A study94 of 114 UK trials funded by the Medical Research Council and the HTA programme found that only 31% of trials recruited successfully, whereas 45% recruited < 80% of the intended number of participants, and more than half required an extension. A Cochrane review synthesised the evidence around strategies to improve recruitment to RCTs,95 and concluded that triallists should include evaluations of their recruitment strategies in their trials, and funders should support this because the number of interventions that have been rigorously evaluated in the context of a real trial is low.
The challenges of recruitment in learning disability studies include a smaller population base and need for multiple sites, the randomisation process itself, the need to recruit through third-party intermediaries and via multiple sources to engage with enough people for the message to be passed on to potential participants, concerns by paid carers of the legalities of supporting consent to participate and the need for information to be accessible for the potential participants. 92,96–98 We have demonstrated that these potential obstacles can be successfully navigated and overcome across three countries of the UK, now significantly divergent in terms of the provision of health and social care services. This requires careful planning and ensuring that adequate human resources are available to devote to the time-consuming recruitment process, which is expensive but essential when conducting trials within this population. Finding and training sufficient numbers of therapists to allow participants to be randomised in a timely fashion to either arm of the trial also emerged as a significant consideration. Established links with existing services proved vital in obtaining the numbers of therapists required. An advantage of this strategy was that the trial demonstrated the delivery of the interventions by relevant professionals in routine clinical practice.
Clinical implications and future directions
There have been no previous large trials of psychological interventions for adults with learning disabilities. Hence, the lack of difference between the BeatIt and StepUp interventions means it is too early to say if both interventions are equally effective, or not effective.
Recruitment to our study was mostly from practitioners in community learning disability teams; the participants were already receiving considerable input from team members, including community nurses, psychologists and psychiatrists, and a higher proportion of participants in this study were receiving antidepressants than in previous population-based studies of adults with learning disabilities. 99 Despite this, the qualitative interviews on supporters’ expectations before the study identified that supporters perceived that there was nothing else available specifically to help with the depression being experienced by the person whom they supported. Participants were depressed at entry to the study, and there was an overall group-level clinical improvement associated with both the BeatIt and StepUp interventions. The interventions were also relatively low cost, in the context of the wider ongoing support that the participants were receiving.
It proved difficult to recruit via IAPT services in England (there is no direct equivalent in Scotland or Wales), and of the potential 14 participants who were referred, only 9 were suitable to be randomised. There appeared to be a poor understanding of learning disability by IAPT services and this is consistent with other research findings. 100 Perhaps this is in part explained by the lack of any psychological interventions for treatment of depression specifically recommended for use with adults with learning disabilities. However, it does indicate a training need within IAPT, and the need to support research and development initiatives to make IAPT services more accessible to people with learning disabilities. 101
Difficulties with assessment also arose in the study. For example, it was challenging to measure meaningful change in activity for people with learning disabilities, given that small and statistically insignificant increases may have considerable personal salience. Furthermore, it is also worth noting that the mean baseline GDS-LD40 score (16.7 points) for the study participants, although in the published clinically significant range, was lower than the mean scores reported by the 19 participants involved in the original development of the measure (23.4 points). This suggests that it might be important for further work to be carried out on concerning the clinical cut-off scores for the GDS-LD.
The next step in the research agenda will be to better understand whether or not the BeatIt and StepUp interventions could be effective with adults who have learning disabilities, exploring ethical trial designs to do so. Given the very similar outcomes found for both the BeatIt and StepUp interventions in the present study, it may be possible to examine the clinical effectiveness of both interventions in one trial, compared with TAU. The participants randomised to the intervention arm could be offered a choice of either the BeatIt or StepUp intervention, allowing a comparison of both interventions with TAU. This would be an ethical and cost-effective design.
It is also important to note that this study was conducted with people with mild/moderate learning disabilities. Adults with severe/profound learning disabilities also experience depression. The communicative and cognitive demands of CBT-based interventions place such interventions out of the reach of adults with severe/profound learning disabilities. These adults are also more at risk of adverse effects of pharmacotherapy, which can be both disabling and potentially serious, because of limited or no verbal communication skills to describe their symptoms of adverse effects, hence late and more severe presentations of such effects. NICE31 made a specific recommendation that research should be undertaken with people with severe learning disabilities to determine the clinical and cost-effectiveness of psychosocial interventions to treat mental health problems such as depression. We strongly endorse this, and consider further modification of the BeatIt intervention to be ideally suited for, and a high priority to trial with, adults with severe/profound learning disabilities.
Acknowledgements
We would like to thank all the participants and their supporters, who gave so generously of their time to take part in the trial. The therapists and supervisors are also owed a debt of gratitude by the research team, along with the unstinting efforts of the local principal investigators at each of the local sites: Dr Helen Lynn, Dr Ian Smith, Dr Ken MacMahon and Dr Gail Thomas. Thanks are also owed to past members of the research team who made an invaluable contribution: Marcela Gavigan, Emilly Scott, Felicity Larson and Kevanne Sanger.
The guidance and encouragement of members of the Trial Steering Committee and Data Monitoring Committee have been greatly appreciated and essential to the completion of this trial.
Contributions of authors
Professor Andrew Jahoda was the chief investigator, contributed to the design of the study and was part of the writing team.
Professor Richard Hastings was a co-applicant, contributed to the design of the study and was part of the writing team.
Professor Chris Hatton was a co-applicant, contributed to the design of the study and was part of the writing team.
Professor Sally-Ann Cooper was a co-applicant, contributed to the design of the study and was part of the writing team.
Ms Nicola McMeekin was the health economist working on the study and part of the writing team.
Professor Dave Dagnan was a co-applicant, contributed to the design of the study and was part of the writing team.
Dr Kim Appleton was the trial manager and part of the writing team.
Ms Katie Scott was a researcher on the project and contributed to the report.
Ms Lauren Fulton was a researcher on the project and part of the writing team.
Professor Robert Jones was a co-applicant, contributed to the design of the project and reviewed the report.
Dr Alex McConnachie was a co-applicant and the senior trial statistician and reviewed and contributed to the report.
Ms Rachel Zhang is a statistician who worked on the trial and contributed to this report.
Ms Rosie Knight was a researcher on the trial and contributed to the report.
Ms Dawn Knowles was a researcher on the trial and contributed to the report.
Professor Christopher Williams was a co-applicant who contributed to the design of the study and to this report.
Professor Andy Briggs was a co-applicant who designed the health economic component of the study and reviewed the report.
Professor Craig Melville was a co-applicant, contributed to the design of the study and was part of the writing team.
Publications
Jahoda A, Melville C, Cooper SA, Hastings R, Briggs A, Dagnan D, et al. BEAT-IT: comparing a behavioural activation treatment for depression in adults with intellectual disabilities with an attention control: study protocol for a randomised controlled trial. Trials 2015;16:595.
Jahoda A, Hastings R, Hatton C, Cooper SA, Dagnan D, Zhang R, et al. Comparison of behavioural activation with guided self-help for treatment of depression in adults with intellectual disabilities: a randomised controlled trial. Lancet Psychiatry 2017;4:909–19
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Prescribing Statistics – Medicines Used in Mental Health. Edinburgh: NHS Scotland; 2013.
- Prescription Cost Analysis England 2015: Prescription Items Dispensed in the Community in England and Listed Alphabetically Within Chemical Entity by Therapeutic Class. Leeds: NHS Digital; 2016.
- Mental Health (Psychiatric) Hospital Activity Statistics. Edinburgh: NHS Scotland; 2012.
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, et al. Grand challenges in global mental health. Nature 2011;475:27-30. https://doi.org/10.1038/475027a.
- Bittles AH, Petterson BA, Sullivan SG, Hussain R, Glasson EJ, Montgomery PD. The influence of intellectual disability on life expectancy. J Gerontol A Biol Sci Med Sci 2002;57:M470-2. https://doi.org/10.1093/gerona/57.7.M470.
- Morris J. The National Down Syndrome Cytogenetic Register 2007/8 Annual Report. London: Barts and The London School of Medicine and Dentistry; 2009.
- Cooper SA, Smiley E, Morrison J, Williamson A, Allan L. Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry 2007;190:27-35. https://doi.org/10.1192/bjp.bp.106.022483.
- Cooper SA, Smiley E, Morrison J, Williamson A, Allan L. An epidemiological investigation of affective disorders with a population-based cohort of 1023 adults with intellectual disabilities. Psychol Med 2007;37:873-82. https://doi.org/10.1017/S0033291707009968.
- Buckles J, Luckasson R, Keefe E. A systematic review of the prevalence of psychiatric disorders in adults with intellectual disability, 2003–2010. J Mental Health Res Intellect Disabil 2013;6:181-207. https://doi.org/10.1080/19315864.2011.651682.
- Reid KA, Smiley E, Cooper SA. Prevalence and associations of anxiety disorders in adults with intellectual disabilities. J Intellect Disabil Res 2011;55:172-81. https://doi.org/10.1111/j.1365-2788.2010.01360.x.
- Collishaw S, Maughan B, Pickles A. Affective problems in adults with mild learning disability: the roles of social disadvantage and ill health. Br J Psychiatry 2004;185:350-1. https://doi.org/10.1192/bjp.185.4.350.
- Richards M, Maughan B, Hardy R, Hall I, Strydom A, Wadsworth M. Long-term affective disorder in people with mild learning disability. Br J Psychiatry 2001;179:523-7. https://doi.org/10.1192/bjp.179.6.523.
- Honeycutt AA, Grisse SD, Dunlap LJ, Chen H, al Homis G, Schendel D, et al. Using Survey Data to Study Disability: Results from the National Health Interview Survey on Disability. London: Elsevier Science; 2003.
- DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry 2005;62:409-16. https://doi.org/10.1001/archpsyc.62.4.409.
- Weitz ES, Hollon SD, Twisk J, van Straten A, Huibers MJ, David D, et al. Baseline depression severity as moderator of depression outcomes between cognitive behavioral therapy vs pharmacotherapy: an individual patient data meta-analysis. JAMA Psychiatry 2015;72:1102-9. https://doi.org/10.1001/jamapsychiatry.2015.1516.
- Depression: Management of Depression in Primary And Secondary Care. London: NICE; 2009.
- Wiles N, Thomas L, Abel A, Ridgway N, Turner N, Campbell J, et al. Cognitive behavioural therapy as an adjunct to pharmacotherapy for primary care based patients with treatment resistant depression: results of the CoBalT randomised controlled trial. Lancet 2013;381:375-84. https://doi.org/10.1016/S0140-6736(12)61552-9.
- Lewinsohn PM AD, Steinmetz J, Teri L. The Coping with Depression Course: A Psychoeducational Intervention for Unipolar Depression. Eugene, OR: Castalia Publishing Company; 1984.
- Ridgway N, Williams C. Cognitive behavioural therapy self-help for depression: an overview. J Ment Health 2011;20:593-60. https://doi.org/10.3109/09638237.2011.613956.
- Cavanagh K, Seccombe N, Lidbetter N. The implementation of computerized cognitive behavioural therapies in a service user-led, third sector self help clinic. Behav Cogn Psychother 2011;39:427-42. https://doi.org/10.1017/S1352465810000858.
- Cuijpers P, Donker T, van Straten A, Li J, Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med 2010;40:1943-57. https://doi.org/10.1017/S0033291710000772.
- Gellatly J, Bower P, Hennessy S, Richards D, Gilbody S, Lovell K. What makes self-help interventions effective in the management of depressive symptoms? Meta-analysis and meta-regression. Psychol Med 2007;37:1217-28. https://doi.org/10.1017/S0033291707000062.
- Skinner BF. Beyond Freedom and Dignity. New York, NY: Alfred A. Knopf, Inc.; 1971.
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol 2006;74:658-70. https://doi.org/10.1037/0022-006X.74.4.658.
- Moradveisi L, Huibers MJ, Renner F, Arasteh M, Arntz A. Behavioural activation v. antidepressant medication for treating depression in Iran: randomised trial. Br J Psychiatry 2013;202:204-11. https://doi.org/10.1192/bjp.bp.112.113696.
- Ekers D, Richards D, McMillan D, Bland JM, Gilbody S. Behavioural activation delivered by the non-specialist: phase II randomised controlled trial. Br J Psychiatry 2011;198:66-72. https://doi.org/10.1192/bjp.bp.110.079111.
- Richards DA, Ekers D, McMillan D, Taylor RS, Byford S, Warren FC, et al. Cost and Outcome of Behavioural Activation versus Cognitive Behavioural Therapy for Depression (COBRA): a randomised, controlled, non-inferiority trial. Lancet 2016;388:871-80. https://doi.org/10.1016/S0140-6736(16)31140-0.
- Dobson KS, Hollon SD, Dimidjian S, Schmaling KB, Kohlenberg RJ, Gallop RJ, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the prevention of relapse and recurrence in major depression. J Consult Clin Psychol 2008;76:468-77. https://doi.org/10.1037/0022-006X.76.3.468.
- Lejuez CW, Hopko DR, Hopko SD. The Brief Behavioural Activation Treatment For Depression: A Comprehensive Patient Guide. Boston, MA: Pearson Custom Publishing; 2003.
- Martell CR, Addis ME, Jacobson NS. Depression in Context: Strategies for Guided Action. New York, NY: W. W. Norton and Company; 2001.
- Mental Health Problems in People with Learning Disabilities: Prevention, Assessment and Management. London: NICE; 2016.
- Lindsay WR, Jahoda A, Willner P, Taylor J, Lindsay W, Hastings R, et al. Psychological Therapies for Adults with Intellectual Disabilities. Chichester: Wiley-Blackwell; 2013.
- McCabe MP, McGillivray JA, Newton DC. Effectiveness of treatment programmes for depression among adults with mild/moderate intellectual disability. J Intellect Disabil Res 2006;50:239-47. https://doi.org/10.1111/j.1365-2788.2005.00772.x.
- McGillivray JA, McCabe MP, Kershaw MM. Depression in people with intellectual disability: an evaluation of a staff-administered treatment program. Res Dev Disabil 2008;29:524-36. https://doi.org/10.1016/j.ridd.2007.09.005.
- Hassiotis A, Serfaty M, Azam K, Strydom A, Blizard R, Romeo R, et al. Manualised individual cognitive behavioural therapy for mood disorders in people with mild to moderate intellectual disability: a feasibility randomised controlled trial. J Affect Disord 2013;151:186-95. https://doi.org/10.1016/j.jad.2013.05.076.
- Hartley SL, Esbensen AJ, Shalev R, Vincent LB, Mihaila I, Bussanich P. Cognitive behavioral therapy for depressed adults with mild intellectual disability: a pilot study. J Ment Health Res Intellect Disabil 2015;8:72-97. https://doi.org/10.1080/19315864.2015.1033573.
- Lindsay WR, Tinsley S, Beail N, Hastings RP, Jahoda A, Taylor JL, et al. A preliminary controlled trial of a trans-diagnostic programme for cognitive behaviour therapy with adults with intellectual disability. J Intellect Disabil Res 2015;59:360-9. https://doi.org/10.1111/jir.12145.
- McGillivray JA, Kershaw MM. The impact of staff initiated referral and intervention protocols on symptoms of depression in people with mild intellectual disability. Res Dev Disabil 2013;34:730-8. https://doi.org/10.1016/j.ridd.2012.11.005.
- Jahoda A, Melville CA, Pert C, Cooper SA, Lynn H, Williams C, et al. A feasibility study of behavioural activation for depressive symptoms in adults with intellectual disabilities. J Intellect Disabil Res 2015;59:1010-21. https://doi.org/10.1111/jir.12175.
- Cuthill FM, Espie CA, Cooper SA. Development and psychometric properties of the Glasgow Depression Scale for people with a Learning Disability. Individual and carer supplement versions. Br J Psychiatry 2003;182:347-53. https://doi.org/10.1192/bjp.182.4.347.
- Jahoda A, Melville C, Cooper SA, Hastings R, Briggs A, Dagnan D, et al. BEAT-IT: comparing a behavioural activation treatment for depression in adults with intellectual disabilities with an attention control: study protocol for a randomised controlled trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-1103-5.
- Wechsler D, Hsiao-pin C. WASI®-II: Wechsler Abbreviated Scale Of Intelligence. New York, NY: Pearson; 2011.
- Nihira K, Lambert NM, Leland H. Adaptive Behavior Scale: Residential and Community. Examiner’s Manual. Austin, TX: Pro-ed; 1993.
- Cooper SA, Melville CA, Einfeld SL. Psychiatric diagnosis, intellectual disabilities and Diagnostic Criteria for Psychiatric Disorders for Use with Adults with Learning Disabilities/Mental Retardation (DC-LD). J Intellect Disabil Res 2003;47:3-15. https://doi.org/10.1046/j.1365-2788.47.s1.2.x.
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Adults with Incapacity (Scotland) Act 2000. Edinburgh: Scottish Government; 2000.
- Lejuez CW, Hopko DR, Acierno R, Daughters SB, Pagoto SL. Ten year revision of the brief behavioral activation treatment for depression: revised treatment manual. Behav Modif 2011;35:111-61. https://doi.org/10.1177/0145445510390929.
- Hepner KA SS, Paddock SM, Hunter SB, Osilla KC, Watkins KE. A Fidelity Coding Guide for a Group Cognitive Behavioral Therapy for Depression. Santa Monica, CA: RAND Corporation; 2011.
- Hunter SB, Watkins KE, Hepner KA, Paddock SM, Ewing BA, Osilla KC, et al. Treating depression and substance use: a randomized controlled trial. J Subst Abuse Treat 2012;43:137-51. https://doi.org/10.1016/j.jsat.2011.12.004.
- Vallis TM, Shaw BF, Dobson KS. The Cognitive Therapy Scale: psychometric properties. J Consult Clin Psychol 1986;54:381-5. https://doi.org/10.1037/0022-006X.54.3.381.
- Blackburn IM, James IA, Milne DL, Baker C, Standart S, Garland A, et al. The Revised Cognitive Therapy Scale (CTS-R): psychometric properties. Behav Cogn Psychother 2001;29:431-46. https://doi.org/10.1017/S1352465801004040.
- Evans KM, Cotton MM, Einfeld SL, Florio T. Assessment of depression in adults with severe or profound intellectual disability. J Intellect Dev Disabil 1999;24:147-60. https://doi.org/10.1080/13668259900033941.
- Mindham J, Espie CA. Glasgow Anxiety Scale for people with an Intellectual Disability (GAS-ID): development and psychometric properties of a new measure for use with people with mild intellectual disability. J Intellect Disabil Res 2003;47:22-30. https://doi.org/10.1046/j.1365-2788.2003.00457.x.
- Rojahn J, Rowe EW, Sharber AC, Hastings R, Matson JL, Didden R, et al. The Behavior Problems Inventory – Short Form for individuals with intellectual disabilities: part II: reliability and validity. J Intellect Disabil Res 2012;56:546-65. https://doi.org/10.1111/j.1365-2788.2011.01506.x.
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. https://doi.org/10.1007/s11136-010-9648-y.
- Am I Making Myself Clear? Mencap’s Guidelines for Accessible Writing. London: Mencap; 2002.
- Raynes N, Sumpton R, Pettipher C. The Index of Community Involvement. Manchester: Manchester University Department of Social Policy and Social Work; 1989.
- Raynes N, Sumpton R, Pettipher C. Index of Participation in Domestic Life. Manchester: University Department of Social Policy and Social Work; 1989.
- Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: practical and theoretical implications. J Soc Pers Relat 1987;4:497-510. https://doi.org/10.1177/0265407587044007.
- Hastings RP, Brown T. Behavior problems of children with autism, parental self-efficacy, and mental health. Am J Ment Retard 2002;107:222-32. https://doi.org/10.1352/0895-8017(2002)107<0222:BPOCWA>2.0.CO;2.
- Hastings RP, Brown T. Behavioural knowledge, causal beliefs and self-efficacy as predictors of special educators’ emotional reactions to challenging behaviours. J Intellect Disabil Res 2002;46:144-50. https://doi.org/10.1046/j.1365-2788.2002.00378.x.
- Magaña AB, Goldstein JM, Karno M, Miklowitz DJ, Jenkins J, Falloon IR. A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Res 1986;17:203-12. https://doi.org/10.1016/0165-1781(86)90049-1.
- Hulbert-Williams L, Hastings RP, Crowe R, Pemberton J. Self-reported life events, social support and psychological problems in adults with intellectual disabilities. J Applied Res Intellect Disabil 2011;24:427-36. https://doi.org/10.1111/j.1468-3148.2011.00624.x.
- Chisholm D, Knapp MR, Knudsen HC, Amaddeo F, Gaite L, van Wijngaarden B. Client Socio-Demographic and Service Receipt Inventory – European Version: development of an instrument for international research. EPSILON Study 5. European Psychiatric Services: inputs linked to outcome domains and needs. Br J Psychiatry Suppl 2000;39:s28-33. https://doi.org/10.1192/bjp.177.39.s28.
- Kilbane AL, Jahoda A. Therapy expectations: preliminary exploration and measurement in adults with intellectual disabilities. J Applied Res Intellect Disabil 2011;24:528-42. https://doi.org/10.1111/j.1468-3148.2011.00630.x.
- Ekers D, Richards D, Gilbody S. A meta-analysis of randomized trials of behavioural treatment of depression. Psychol Med 2008;38:611-23. https://doi.org/10.1017/S0033291707001614.
- Guide to the Methods of Technology Appraisal: 2013. London: NICE; 2013.
- Willner P, Rose J, Jahoda A, Stenfert Kroese B, Felce D, MacMahon P, et al. A cluster randomised controlled trial of a manualised cognitive behavioural anger management intervention delivered by supervised lay therapists to people with intellectual disabilities. Health Technol Assess 2013;17. https://doi.org/10.3310/hta17210.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2016.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: PSSRU, University of Kent; 2015.
- NHS Reference Costs 2014 to 2015. London: Department of Health and Social Care; 2016.
- Average Usual and Paid Hours be Gender and Average Hourly Pay by Ethnicity and Disability. Newport: ONS; 2017.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Pert C, Jahoda A, Stenfert Kroese B, Trower P, Dagnan D, Selkirk M. Cognitive behavioural therapy from the perspective of clients with mild intellectual disabilities: a qualitative investigation of process issues. J Intellect Disabil Res 2013;57:359-69. https://doi.org/10.1111/j.1365-2788.2012.01546.x.
- Westerhof GJ, Beernink J, Sools A. Who am I? A life story intervention for persons with intellectual disability and psychiatric problems. Intellect Dev Disabil 2016;54:173-86. https://doi.org/10.1352/1934-9556-54.3.173.
- Jahoda A, Beail N. Psychological Therapies and People who have Intellectual Disabilities. Leicester: The British Psychological Society; 2016.
- Lindsay WR, Jahoda AJ, Willner P, Taylor J, Lindsay W, Hastings R, et al. Psychological Therapies for Adults with Intellectual Disabilities. Chichester: Wiley-Blackwell; n.d.
- Willner P. Readiness for cognitive therapy in people with intellectual disabilities. J Applied Res Intellect Disabil 2006;19:5-16. https://doi.org/10.1111/j.1468-3148.2005.00280.x.
- Rose J, Loftus M, Flint B, Carey L. Factors associated with the efficacy of a group intervention for anger in people with intellectual disabilities. Br J Clin Psychol 2005;44:305-17. https://doi.org/10.1348/014466505X29972.
- Stimpson A, Kroese BS, MacMahon P, Rose N, Townson J, Felce D, et al. The experiences of staff taking on the role of lay therapist in a group-based cognitive behavioural therapy anger management intervention for people with intellectual disabilities. J Appl Res Intellect Disabil 2013;26:63-70. https://doi.org/10.1111/jar.12006.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1994.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Jupp V. The SAGE Dictionary of Social Research Methods. London: SAGE Publications; 2006.
- Maughan B, Collishaw S, Pickles A. Mild mental retardation: psychosocial functioning in adulthood. Psychol Med 1999;29:351-66. https://doi.org/10.1017/S0033291798008058.
- Romeo R, Molosankwe I. Economic evidence in intellectual disabilities: a review. Curr Opin Psychiatry 2010;23:427-31. https://doi.org/10.1097/YCO.0b013e32833ad946.
- Ekers D, Godfrey C, Gilbody S, Parrott S, Richards DA, Hammond D, et al. Cost utility of behavioural activation delivered by the non-specialist. Br J Psychiatry 2011;199:510-11. https://doi.org/10.1192/bjp.bp.110.090266.
- Guide to the Methods of Technology Appraisal: 2008. London: NICE; 2008.
- Becker H, Roberts G, Morrison J, Silver J. Recruiting people with disabilities as research participants: challenges and strategies to address them. Ment Retard 2004;42:471-5. https://doi.org/10.1352/0047-6765(2004)42<471:RPWDAR>2.0.CO;2.
- Iacono T. Ethical challenges and complexities of including people with intellectual disability as participants in research. J Intellect Dev Disabil 2006;31:173-9. https://doi.org/10.1080/13668250600876392.
- Evenhuis H, van Splunder J, Vink M, Weerdenburg C, van Zanten B, Stilma J. Obstacles in large-scale epidemiological assessment of sensory impairments in a Dutch population with intellectual disabilities. J Intellect Disabil Res 2004;48:708-18. https://doi.org/10.1111/j.1365-2788.2003.00562.x.
- Depression: The Treatment and Management of Depression in Adults (Update). London: NICE; 2009.
- Oliver-Africano P, Dickens S, Ahmed Z, Bouras N, Cooray S, Deb S, et al. Overcoming the barriers experienced in conducting a medication trial in adults with aggressive challenging behaviour and intellectual disabilities. J Intellect Disabil Res 2010;54:17-25. https://doi.org/10.1111/j.1365-2788.2009.01195.x.
- Kerr M. Anti-Psychotic Drug Reduction in Primary Care for Adults With Learning Disabilities n.d. http://dx.doi.org/10.1186/ISRCTN38126962 (accessed 28 October 2016).
- McDonald AM, Knight RC, Campbell MK, Entwistle VA, Grant AM, Cook JA, et al. What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies. Trials 2006;7. https://doi.org/10.1186/1745-6215-7-9.
- Treweek S, Pitkethly M, Cook J, Kjeldstrøm M, Taskila T, Johansen M, et al. Strategies to improve recruitment to randomised controlled trials. Cochrane Database Syst Rev 2010;4. https://doi.org/10.1002/14651858.MR000013.pub5.
- Lennox N, Taylor M, Rey-Conde T, Bain C, Purdie DM, Boyle F. Beating the barriers: recruitment of people with intellectual disability to participate in research. J Intellect Disabil Res 2005;49:296-305. https://doi.org/10.1111/j.1365-2788.2005.00618.x.
- Nicholson L, Colyer M, Cooper SA. Recruitment to intellectual disability research: a qualitative study. J Intellect Disabil Res 2013;57:647-56. https://doi.org/10.1111/j.1365-2788.2012.01573.x.
- Cooper SA, Caslake M, Evans J, Hassiotis A, Jahoda A, McConnachie A, et al. Toward onset prevention of cognitive decline in adults with Down syndrome (the TOP-COG study): study protocol for a randomized controlled trial. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-202.
- Bowring DL, Totsika V, Hastings RP, Toogood S, McMahon M. Prevalence of psychotropic medication use and association with challenging behaviour in adults with an intellectual disability. A total population study. J Intellect Disabil Res 2017;61:604-17. https://doi.org/10.1111/jir.12359.
- Chinn D, Abraham E. Using ‘candidacy’ as a framework for understanding access to mainstream psychological treatment for people with intellectual disabilities and common mental health problems within the English Improving Access to Psychological Therapies service. J Intellect Disabil Res 2016;60:571-82. https://doi.org/10.1111/jir.12274.
- Dagnan D, Burke CK, Davies J, Chinn D. Improving Access to Psychological Therapies: Learning Disabilities Positive Practice Guide. London: Foundation for People with Learning Disabilities; 2015.
- Jahoda A, Melville C, Hastings R, Cooper SA, Briggs A, Dagnan D, et al. BEAT-IT: A Randomised Controlled Trial Comparing a Behavioural Activation Treatment for Depression in Adults With Learning Diabilities With an Attention Control n.d. www.journalslibrary.nihr.ac.uk/programmes/hta/1010434/#/ (accessed 25 September 2018).
Appendix 1 Questionnaires
Glasgow Depression Scale for people with a Learning Disability
The GDS-LD is a series of 20 self-rating questions asking a participant about their experiences in the previous week.
For each question, there are three possible answers: (1) never/no, (2) sometimes and (3) always/a lot, each being scored 0, 1 or 2, resulting in a range of possible scores from 0 to 40.
| In the last week . . . | Never/no | Sometimes | Always/a lot | |
|---|---|---|---|---|
| 1 | Have you felt sad? | 0 | 1 | 2 |
| Have you felt upset? | ||||
| Have you wished you could die? | ||||
| Have you felt you do not want to go on living? | ||||
Glasgow Anxiety Scale for people with an Intellectual Disability
The GAS-ID is a series of 27 questions asking a participant about their experiences in the previous week.
It is divided into three categories: (1) worries (10 questions), (2) specific fears (9 questions) and (3) physiological symptoms (8 questions). For each question there are three possible answers: (1) never/no, (2) sometimes and (3) always/a lot, each being scored 0, 1 or 2, resulting in a range of possible scores from 0 to 54.
| Worries | Never/no | Sometimes | Always/a lot | |
|---|---|---|---|---|
| 1 | Do you worry a lot? | 0 | 1 | 2 |
| (. . . feel worked up/wound up/uptight/up to high doh) | ||||
The Index of Community Involvement
The ICI is a list of 48 activities divided into three categories: (1) domestic and leisure (8 activities), (2) social (11 activities) and (3) community (19 activities). Participants are asked which activities they took part in over the previous month and how often they took part in those activities.
Each item is scored from 0 (never did activity) to 5 (daily) based on frequency of participation. There is a range of possible scores from 0 to 240.
| Activity in the past month | No | Yes | ||||
|---|---|---|---|---|---|---|
| Never | Once in the month | 2–3 times in the month | Once a week | 2–6 times a week | Daily | |
| Domestic/leisure | ||||||
| 1. Doing crafts (knitting) | ||||||
Emotional Difficulties Self-Efficacy scale
Supporters are asked four questions about their responses to emotional difficulties, experienced by the participants whom they support, over the previous month. Each item is scored from 1 (not at all confident) to 7 (very confident). There is a range of possible scores from 4 to 28.
| How confident are you in dealing with the emotional difficulties of the person you support? | ||||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Not at all confident | Very confident | |||||
Behavior Problems Inventory for Individuals with Intellectual Disabilities – Short Form
The BPI-S has a list of 10 aggressive behaviours. Supporters were asked how often in the previous month they observed the participants whom they support display each behaviour. Each item is scored from 0 (never) to 5 (more than once per hour). There is a range of possible scores from 0 to 50.
| Aggressive behaviours are offensive actions or deliberate overt attacks directed towards other individuals or objects | Never | About once per month | About once per week | About once per day | About once per hour | More than once per hour | |
|---|---|---|---|---|---|---|---|
| 1 | Hitting others | ||||||
Intellectual Disabilities Depression Scale
The IDDS consists of questions on 38 behaviours. The supporters were asked how often the participants whom they support experienced each of the behaviours, over the previous 4 weeks. Each item is scored from 0 (never) to 6 (always). There is a range of possible scores from 0 to 228.
| Symptoms of depression | Never | Almost never | Seldom | Half the time | Usually | Almost always | Always | |
|---|---|---|---|---|---|---|---|---|
| 15 | Difficulty falling asleep |
Adaptive Behavior Scale at screening visit
The Adaptive Behavior Scale (ABS) questionnaire is adapted from the ABS-RC2. It is directed to the supporter at the screening visit as a series of 39 questions from six categories: (1) personal self-sufficiency, (2) community self-sufficiency, (3) social responsibility, (4) self-direction, (5) responsibility and (6) socialisation.
Supporters were asked to rate the participants whom they support on each of the items.
| Item 67 | Co-operation (circle highest level) | Total | ||
|---|---|---|---|---|
| Offers assistance to others | 2 | |||
| Is willing to help if asked | 1 | |||
| Never helps others | 0 | |||
| Item 68 | Consideration for others (circle all answers) | Yes | No | Total |
| Shows interest in the affairs of others | 1 | 2 | ||
| Takes care of others’ belongings | 1 | 2 | ||
| Directs or manages the affairs of others when needed | 1 | 2 | ||
| Shows consideration for others’ feelings | 1 | 2 | ||
Adaptive Behavior Scale at the 4- and 12-month visits
At the 4- and 12-month visits, the supporters were asked to rate those whom they support in three of the six categories measured at screening:
-
Self-direction (five items), with a range of possible total scores from 0 to 23.
-
Responsibility (three items), with a range of possible scores from 0 to 10.
-
Socialisation (seven items), with a range of possible total scores from 0 to 26.
Bangor Life Events Schedule for Intellectual Disabilities
The BLESID consists of 24 significant life events from five categories. It is used to determine the life events that participants have experienced over the previous 12 months, the frequency of these events and the impact the events have had on the participants’ lives.
Each event receives a score of 0 (did not happen), 1 (happened once), or 2 (more than once) for frequency. If an event occurred, it then receives a score of –1 (bad), 0 (in the middle) or 1 (good) for impact.
| Life events | Do not know | Frequency | Impact | When? | ||||
|---|---|---|---|---|---|---|---|---|
| Did not happen | Happened once | More than once | ‘Bad’ | ‘In the middle’ | ‘Good’ | |||
| Health | ||||||||
| Illness or injury requiring hospitalisation | Do not know | 0 | 1 | 2 | – | 0 | + | |
Social Support Questionnaire – three questions
This was previously referred to as PSS.
The participant was asked to name people who they can count on to help them in each of the three ways described. They were then asked how happy they are with the support they receive.
Their satisfaction with the help they receive is given a score of 3 (very happy), 2 (quite happy) or 1 (not happy).
| Who can you really count on to be there for you when you need help? | |||
| No one | 1) | 4) | 7) |
| 2) | 5) | 8) | |
| 3) | 6) | 9) | |
| How happy are you with their help? | |||
| Very happy 3 | Quite happy 2 | Not happy 1 | |
Appendix 2 Statistical analysis plan
A randomised controlled trial comparing a behavioural activation treatment for depression in adults with learning disabilities with an attention control (BeatIt) statistical analysis plan
| Study title: | A randomised controlled trial comparing a behavioural activation treatment for depression in adults with learning disabilities with an attention control | ||||
| Short title: | BeatIt | ||||
| IDs: | REC number: 12/WS/0297; ISRCTN09753005 | ||||
| Funded by: | HTA Clinical Evaluation and Trials: 10 104 34 | ||||
| Protocol version: | V3.0 | Date | 5 March 2015 | ||
| SAP version: | V1.0 | Date | 23 November 2016 | ||
| Signature | Date | ||||
| Prepared by | Rachel Zhang | ||||
| Trainee Biostatistician, Robertson Centre for Biostatistics, University of Glasgow | |||||
| Approved by | Dr Alex McConnachie | ||||
| Assistant Director of Biostatistics, Robertson Centre for Biostatistics, University of Glasgow | |||||
| Professor Andrew Jahoda | |||||
| Professor of Learning Disabilities Psychology, Institute of Health and Wellbeing, University of Glasgow | |||||
Introduction
Study background
Adults with learning disabilities are as likely to have depression as adults who do not have learning disabilities. However, not much is known about what treatments help adults with learning disabilities and depression.
Psychological therapies, such as CBT, are recommended as the best treatment for most people with depression. However, psychological therapies require good verbal communication. Studies have shown that adults with learning disabilities do not have the communication skills to participate in most available psychological therapies. Therefore, adults with learning disabilities and depression experience inequitable access to treatments for depression.
Behavioural activation is a psychological therapy that has been shown to be as effective as CBT. Behavioural activation is less dependent on verbal communication. The BeatIt study is designed to test whether or not a behavioural activation treatment developed for adults with learning disabilities and depression is effective.
Study objectives
Primary objective:
-
To measure the clinical effectiveness of BeatIt in reducing self-reported depressive symptoms for adults with learning disabilities and depression, compared with an attention control intervention.
Secondary objectives:
-
Comparison between groups of carer-reported depressive symptoms and aggressiveness, self-reported anxiety symptoms, activity levels and QoL.
-
Comparison between groups of carers’ sense of efficacy and relationship with participants.
-
Comparison between groups of cost-effectiveness.
-
Comparison between groups of process issues.
Study design
Multicentre, single-blind randomised controlled trial.
Sample size and power
Section 12.2 of the study protocol102 states:
In the open trial of BEAT-IT, the mean (standard deviation, SD) reduction in GDS-LD scores at 3 month post-intervention follow-up was 8.50 (5.24). We have powered the study to detect a mean change of 3.14, or 0.6 SD units between study groups. This makes the conservative assumption that the 4 month post-randomisation change over that in the control group in the proposed design will be 60% of that observed from pre-test to follow-up in the intervention group during the open trial. To detect this effect size difference, the study requires 60 patients in each arm to provide outcome data at 12 months post randomisation (see below for a more detailed justification). The primary analysis will be an analysis of covariance adjusting for the baseline GDS score, which will have power to detect smaller intervention effects, depending on the level of correlation in scores over time.
There are no data to inform the effect of clustering of outcomes for patients seen by each therapist. Assuming each therapist works with an average of 9 participants (i.e. several part-time therapists at each site), and assuming an intraclass correlation of 0.025, the sample size must be increased by 20% to 72 per group, or 144 in total. Recruitment of 166 participants will allow for up to 13.3% loss to follow-up. The study would then be the largest behavioural activation evaluation to date (based on the studies included in recent reviews of the non-disability literature), despite targeting a difficult to reach population often excluded from research.
Study population
Inclusion criteria
-
Mild/moderate learning disabilities.
-
Aged ≥ 18 years.
-
Clinically significant unipolar depression.
-
Able to give informed consent to participate.
-
Has a level of expressive and receptive communication skills in English (reading skills not required) to allow participation in treatment.
-
Has a family member or paid carer, who has supported them for ideally a minimum of 6 months, with whom to complete the screening and baseline visits OR is able to obtain information for the 4 months previous to randomisation. The carer, or another named individual, should be available for weekly/fortnightly treatment sessions with the practitioner, and should currently provide ≥ 2 hours of support per week to the participant.
Exclusion criteria
-
Suicidal.
-
A measured IQ of > 75.
-
Factors that prevent the participant from interacting with the carer and therapist or retaining information from the therapy (e.g. late-stage dementia, significant agitation, withdrawal arising from psychosis).
-
Does not consent to her/his GP being contacted about her/his participation in the study.
Statistical analysis plan
Statistical analysis plan objectives
The objective of this SAP is to describe the statistical analyses to be carried out for the final analysis of the BeatIt trial.
General principles
All data will first be summarised and analysed by intention to treat, that is, on the basis of randomised treatment group, regardless of treatment actually received. Per-protocol analysis will be repeated in those who have attended at least eight BeatIt treatment sessions or six attention control sessions.
Study data will be summarised as a whole and by treatment group at each study assessment point. Changes over baseline will be reported for outcome measures. Continuous variables will be summarised by the number of observations, number of missing values, mean, SD, median, quartiles and range. Categorical variables will be summarised by the number of observations, number of missing values, and the number and percentage of individuals in each category.
Current protocol
The current study protocol at the time of writing is version 3.0, dated 5 March 2015. Future amendments to the protocol will be reviewed for their impact on this SAP, which will be updated only if necessary.
Deviations to those specified in the protocol
There are no planned deviations from the protocol. In case of non-convergence for the mixed-effect models as a result of higher-than-anticipated therapist numbers, the therapist random effect will be removed from the models and general linear models will be used instead.
Software
Analyses will be conducted using SAS® software (SAS Institute Inc., Cary, NC, USA. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc. in the USA and other countries. ® indicates USA registration.) for Microsoft Windows® v9.2 (Microsoft Corporation, Redmond, WA, USA) and/or R (The R Foundation for Statistical Computing, Vienna, Austria) for Windows v3.0.0 or higher.
Analyses
Study populations
The total number of participants screened will be summarised by region. The number of participants randomised to each treatment group will be presented. Attendance of those randomised to treatment sessions will be summarised by treatment group.
The number and percentage of those randomised who completed the trial or were prematurely withdrawn will be reported by treatment group, with reasons for withdrawal summarised. Other planned analyses will be provided for all randomised subjects.
Baseline characteristics
Summaries will be provided for the following baseline characteristics, by treatment group:
-
Patient –
-
demographic characteristics (age in years at randomisation, sex, ethnicity, marital status, Scottish Index of Multiple Deprivation (SIMD) decile, support with living)
-
expectations of therapy
-
health (epilepsy, vision, hearing, mobility problems, type and length of previous depression therapies)
-
GDS-LD
-
BLESID
-
EQ-5D-Y
-
GAS-ID
-
PSS scores
-
use of antidepressants, St John’s wort, lithium, carbamazepine, sodium valproate, lamotrigine and pindolol.
-
-
Carer –
-
demographic characteristics (age in years at randomisation, sex, ethnicity, education, employment status)
-
relationship to, and average weekly contact with, subject
-
experience and formal training (paid carers only)
-
IDDS
-
The BPI-S Aggressive Behaviour subscale
-
EDSE scale
-
Expressed emotion: FMSS
-
activity measures [ICI, IPDL, Adaptive Behavior subscale (self-direction, responsibility, socialisation)].
-
Primary outcome
The primary outcome is the change in self-rated depressive symptoms, measured by the GDS-LD score at 12 months.
Primary analysis
The GDS-LD will be summarised at baseline and 12 months, overall and by study group. The change in GDS-LD score at 12 months from baseline will also be summarised by group.
The primary analysis will be a mixed-effects regression model, including randomised group, study centre, antidepressant use and baseline GDS-LD score as fixed effects, and therapist as a random effect. This will be carried out for the change in GDS-LD scores from baseline to 12 months. The mean value (change from baseline) at 12 months for each treatment group and difference in mean change between the groups, 95% CI and p-value will be estimated from this model.
Secondary analysis
The GDS-LD scores at 4 months will be analysed in a similar manner as the 12-month GDS-LD scores.
In addition, a repeated-measures analysis will be carried out, using a mixed-effects regression model, including randomised group, time point, study centre and antidepressant use as fixed effects, and participant and therapist as random effects. The mean change from baseline and between-group difference in mean change, with a 95% CI and p-value, will be estimated from this model. The model will be extended to include a treatment-by-time interaction, to estimate the mean changes from baseline and between-group differences at each time point.
Sensitivity analyses
Any missing data for the primary outcome at 4 and 12 months will be imputed using multiple imputations when possible to further test the sensitivity of the results. Data are assumed to be missing at random. To impute missing values at each time point, prediction models will be derived based on age, antidepressant use and any previous or subsequent measurements of GDS-LD.
Secondary outcomes
Secondary outcomes will be analysed by the same method as the primary outcome; non-normally distributed outcomes will be transformed prior to analysis, or analysed by appropriate mixed-effects regression models. The type of model used for each outcome will be reported in the final statistical outputs.
The secondary outcomes are the change from baseline for:
-
Patient –
-
BLESID score
-
EQ-5D-Y
-
total GAS-ID score
-
PSS scores.
-
-
Carer –
-
IDDS
-
The BPI-S Aggressive Behaviour subscale
-
total EDSE scale score
-
Expressed emotion: FMSS
-
activity measures:
-
subscales and total ICI frequency
-
IPDL
-
subscale of the Adaptive Behavior Scale.
-
-
Safety outcomes
The numbers of serious adverse events will be reported as a whole and by treatment group. For those events that have resolved, the event duration will also be summarised.
The numbers and percentages of participants experiencing at least one serious adverse event will be reported as a whole and by treatment group for all events, and for events classified by the Medical Dictionary for Regulatory Activities (MedDRA) System Organ Class and Preferred Term.
Exploratory analyses
Mixed-effect models for the primary outcome will be extended to explore the effects of the following baseline characteristics on 4- and 12-month outcomes:
-
age
-
sex
-
study centre
-
use of antidepressants, St John’s wort, lithium, carbamazepine, sodium valproate, lamotrigine and pindolol
-
negative product total BLESID measured life events
-
history of previous failed psychological intervention (yes vs. no for different therapies)
-
SIMD
-
relationship to carer (family vs. others)
-
level of support (daily vs. other)
-
locus of control.
The moderating effects of these factors will be explored using interaction terms.
Per-protocol analyses
The analyses described in Baseline characteristics, Primary outcome and Secondary outcomes will be repeated in a per-protocol analysis. The analysis population included will be those who have attended at least eight BeatIt treatment sessions or six attention control sessions.
Additional analyses
The analyses in the previous sections constitute the main SAP analyses, and will be programmed and validated prior to database lock and release of the randomisation codes to the study statisticians. The following analyses will be carried out after database lock.
Potential mediation effects will be explored through extensions to the primary analysis regression model. Changes in outcome measures to 4 months post randomisation will be explored as mediators of effects to follow-up at 12 months post randomisation. Attendance at therapy sessions and therapist-rated session data will be explored as potential mediators of short- and long-term intervention effect differences.
In addition, sensitivity analyses for the secondary outcomes will be analysed by the same method as the primary outcome outlined in Sensitivity analyses.
Depending on the results of the main analyses, complier-average causal effect (CACE) analysis may be explored to account for missed therapy sessions.
The scope of these analyses will be agreed with the study team after review of the main SAP analysis results and documented prior to carrying out any additional analyses.
Document history
This is v1.0 of the SAP for the final analysis of the BeatIt study, dated 23 November 2016, and is the initial creation of this document.
Tables
Dummy tables will be produced during the development of the statistical analysis programs for review and feedback. Approval of the content of the final statistical outputs will be a requirement for database lock.
Figures
Dummy figures will be produced during the development of the statistical analysis programs for review and feedback. Approval of the content of the final statistical outputs will be a requirement for database lock.
Listings
No formal data listings will be produced as part of the final statistical outputs. Raw and derived datasets will be made available to the study team after the final statistical outputs have been produced.
Appendix 3 Health economics tables
| Resource | Trial arm | Difference | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | |||||
| Mean (SD) | Used by, n (%) | Mean (SD) | Used by, n (%) | Mean (SE) | 95% CI | |
| Daytime activities | ||||||
| Day centre | ||||||
| Weeks attended | 46.5 (4.74) | 13 (17.8) | 40.4 (13.5) | 17 (25) | 6.19 (3.53) | –1.17 to 13.5 |
| Mean hours per week | 19.3 (8.22) | 13 (17.8) | 17.3 (9.95) | 17 (25) | 1.95 (3.32) | –4.85 to 8.75 |
| Sheltered work | ||||||
| Weeks attended | 21.7 (7.23) | 3 (4.1) | 37.5 (4.95) | 2 (2.9) | –15.8 (5.45) | –33.5 to 1.79 |
| Mean hours per week | 11.75 (10.6) | 3 (4.1) | 17.25 (5.30) | 2 (2.9) | –5.5 (7.19) | –28.6 to 17.6 |
| Voluntary work | ||||||
| Weeks attended | 26.6 (17.0) | 27 (37.0) | 32.0 (16.8) | 14 (20.6) | –5.37 (5.55) | –16.8 to 6.03 |
| Mean hours per week | 7.44 (8.01) | 27 (37.0) | 7.01 (8.79) | 14 (20.6) | 0.433 (2.81) | –5.36 to 6.23 |
| Adult education | ||||||
| Weeks attended | 25.7 (16.0) | 13 (17.8) | 21.8 (18.3) | 8 (11.8) | 3.94 (7.83) | –12.9 to 20.8 |
| Mean hours per week | 6.91 (7.23) | 13 (17.8) | 7.31 (7.05) | 8 (11.8) | –0.402 (3.20) | –7.21 to 6.40 |
| Drop-in centre | ||||||
| Weeks attended | 11.8 (11.2) | 6 (8.2) | 19.6 (16.9) | 5 (7.4) | –7.77 (8.81) | –28.8 to 13.2 |
| Mean hours per week | 1.92 (1.11) | 6 (8.2) | 3.4 (2.51) | 5 (7.4) | –1.48 (1.21) | –4.54 to 1.58 |
| Social club | ||||||
| Weeks attended | 34.8 (15.5) | 26 (35.6) | 35.7 (14.1) | 27 (39.7) | –0.895 (4.08) | –9.09 to 7.30 |
| Mean hours per week | 3.30 (2.11) | 26 (35.6) | 3.60 (1.94) | 27 (39.7) | –0.304 (0.558) | –1.42 to 0.817 |
| Learning disabilities centre | ||||||
| Weeks attended | 48 (0) | 2 (2.7) | 24 (9.90) | 2 (2.9) | 24 (7) | –64.9 to 112.9 |
| Mean hours per week | 15.75 (19.4) | 2 (2.7) | 7 (7.07) | 2 (2.9) | 8.75 (14.6) | –107.1 to 124.6 |
| Hospital services – number of contacts | ||||||
| Psychiatric intensive care ward | 9.5 (10.6) | 2 (2.7) | 0 (N/A) | 0 (N/A) | 9.5 (N/A) | N/A |
| Acute psychiatric ward | 57 (N/A) | 1 (1.4) | 20.5 (20.5) | 2 (2.9) | 36.5 (N/A) | N/A |
| Psychiatric rehabilitation ward | 20 (N/A) | 1 (1.4) | 28 (N/A) | 1 (1.5) | –8 (N/A) | N/A |
| General medical ward | 5.17 (3.19) | 6 (8.2) | 10.3 (11.8) | 3 (4.4) | –5.17 (6.96) | –33.2 to 22.9 |
| Other specialties | 2 (1.41) | 2 (2.7) | 0 (0) | 0 (0) | 2 (N/A) | N/A |
| Day hospital | 1 (0) | 2 (2.7) | 1.2 (0.447) | 5 (7.4) | –0.2 (0.2) | –0.755 to 0.355 |
| Psychiatric outpatient visit | 1.6 (0.894) | 5 (6.8) | 1.6 (0.894) | 5 (7.4) | 0 (0) | –1.30 to 1.30 |
| Other hospital outpatient visit | 4.22 (4.15) | 27 (37.0) | 4.0 (4.08) | 25 (36.8) | 0.222 (1.14) | –2.07 to 2.52 |
| A&E visit | 1.75 (1.71) | 12 (16.4) | 1.38 (0.518) | 8 (11.8) | 0.375 (0.527) | –0.757 to 1.51 |
| Community based | ||||||
| Community psychiatrist | ||||||
| Contacts | 3.29 (2.42) | 31 (42.5) | 3.9 (3.18) | 30 (44.1) | –0.610 (0.725) | –2.06 to 0.844 |
| Mean duration of contact (minutes) | 36.16 (16.73) | 31 (42.5) | 36.78 (17.82) | 30 (44.1) | –0.622 (4.43) | –9.48 to 8.24 |
| Psychologist | ||||||
| Contacts | 8.31 (12.1) | 13 (17.8) | 12.2 (14.7) | 9 (13.2) | –3.91 (5.94) | –16.6 to 8.75 |
| Mean duration of contact (minutes) | 54.6 (13.1) | 13 (17.8) | 45.0 (18.4) | 9 (13.2) | 9.62 (7.13) | –5.72 to 24.9 |
| GP | ||||||
| Contacts | 6.83 (7.95) | 64 (87.7) | 6.89 (6.47) | 55 (80.9) | –0.063 (1.32) | –2.68 to 2.56 |
| Mean duration of contact (minutes) | 11.7 (0) | 64 (87.7) | 11.7 (0) | 55 (80.9) | 0 (N/A) | N/A |
| Community psychiatric nurse | ||||||
| Contacts | 4 (3.83) | 4 (5.5) | 16.3 (14.0) | 3 (4.4) | –12.3 (8.31) | –44.8 to 20.2 |
| Mean duration of contact (minutes) | 58.75 (43.7) | 4 (5.5) | 45 (15) | 3 (4.4) | 13.75 (23.5) | –52.3 to 79.8 |
| Learning disability nurse | ||||||
| Contacts | 15.9 (15.2) | 36 (49.3) | 14.1 (16.4) | 28 (41.2) | 1.75 (4.0) | –6.25 to 9.76 |
| Mean duration of contact (minutes) | 54.4 (19.5) | 36 (49.3) | 54.1 (19.0) | 28 (41.2) | 0.349 (4.84) | –9.34 to 10.0 |
| Other community nurse | ||||||
| Contacts | 46.6 (158.0) | 21 (28.8) | 8.05 (12.1) | 22 (32.4) | 38.6 (34.6) | –33.5 to 110.6 |
| Mean duration of contact (minutes) | 24.6 (15.2) | 21 (28.8) | 24.9 (19.8) | 22 (32.4) | –0.361 (5.36) | –11.2 to 10.5 |
| Community mental health team member | ||||||
| Contacts | 6.5 (4.95) | 2 (2.7) | 0 (N/A) | 0 (N/A) | 6.5 (N/A) | N/A |
| Mean duration of contact (minutes) | 60 (0) | 2 (2.7) | 0 (N/A) | 0 (N/A) | 60 (N/A) | N/A |
| Health-care assistant | ||||||
| Contacts | 64 (82.0) | 2 (2.7) | 8 (7.87) | 5 (7.4) | 56 (58.1) | –670 to 781 |
| Mean duration of contact (minutes) | 750 (976) | 2 (2.) | 72 (26.8) | 5 (7.4) | 678 (690) | –8078 to 9434 |
| Speech therapist | ||||||
| Contacts | 0 (0) | 0 (0) | 2.5 (0.707) | 2 (2.9) | –2.5 (N/A) | N/A |
| Mean duration of contact (minutes) | 0 (0) | 0 (0) | 45 (21.2) | 2 (2.9) | –45 (N/A) | N/A |
| Physiotherapist | ||||||
| Contacts | 7.20 (9.04) | 10 (13.7) | 6.63 (7.21) | 8 (11.8) | 0.575 (3.83) | –7.54 to 8.69 |
| Mean duration of contact (minutes) | 47.8 (11.9) | 10 (13.7) | 39.7 (11.7) | 8 (11.8) | 8.15 (5.59) | –3.74 to 20.0 |
| Occupational therapist | ||||||
| Contacts | 12.9 (15.6) | 9 (12.3) | 3 (2.83) | 4 (5.9) | 9.90 (5.37) | –2.25 to 22.0 |
| Mean duration of contact (minutes) | 51.7 (15.2) | 9 (12.3) | 55.0 (33.2) | 4 (5.9) | –3.33 (17.3) | –53.8 to 47.2 |
| Art/drama/music therapist | ||||||
| Contacts | 26.0 (12.7) | 2 (2.7) | 4.50 (2.12) | 2 (2.9) | 21.5 (9.12) | –81.0 to 124 |
| Mean duration of contact (minutes) | 30.0 (0) | 2 (2.7) | 85.0 (0) | 2 (2.9) | –55.0 (35.0) | –500 to 390 |
| Alternative therapist | ||||||
| Contacts | 3 (N/A) | 1 (1.4) | 5 (4.24) | 2 (2.9) | –2.0 (N/A) | N/A |
| Mean duration of contact (minutes) | 30.0 (N/A) | 1 (1.4) | 45.0 (21.2) | 2 (2.9) | –15.0 (N/A) | N/A |
| Social worker/care manager | ||||||
| Contacts | 5.21 (6.63) | 39 (53.4) | 4.63 (5.66) | 35 (51.5) | 0.577 (1.43) | –2.27 to 3.43 |
| Mean duration of contact (minutes) | 54.0 (24.0) | 39 (53.4) | 59.3 (22.3) | 35 (51.5) | –5.31 (5.38) | –16.0 to 5.40 |
| Social work assistant | ||||||
| Contacts | 0 (0) | 0 (0) | 1.76 (10.1) | 3 (4.4) | –1.76 (N/A) | N/A |
| Mean duration of contact (minutes) | 0 (0) | 0 (0) | 133 (15.3) | 3 (4.4) | –133 (N/A) | N/A |
| Home help/home care worker | ||||||
| Contacts | 205 (192) | 29 (39.7) | 285 (185) | 21 (30.9) | –79.5 (53.8) | –188 to 28.9 |
| Mean duration of contact (minutes) | 357 (439) | 29 (39.7) | 338 (393) | 21 (30.9) | 19.3 (118) | –219 to 258 |
| Advocate/counsellor | ||||||
| Contacts | 6.92 (10.6) | 13 (17.8) | 6.44 (5.66) | 9 (13.2) | 0.479 (3.49) | –6.82 to 7.78 |
| Mean duration of contact (minutes) | 58.5 (19.2) | 13 (17.8) | 55.4 (13.2) | 9 (13.2) | 3.09 (6.90) | –11.3 to 17.5 |
| Dentist | ||||||
| Contacts | 2.73 (1.98) | 49 (67.1) | 2.55 (1.95) | 40 (58.8) | 0.184 (0.418) | –0.646 to 1.02 |
| Mean duration of contact (minutes) | 21.8 (11.7) | 49 (67.1) | 20.2 (8.36) | 40 (58.8) | 1.61 (2.13) | –2.63 to 5.85 |
| Optician | ||||||
| Contacts | 1.92 (1.22) | 25 (34.2) | 1.83 (1.15) | 23 (33.8) | 0.094 (0.343) | –0.597 to 0.784 |
| Mean duration of contact (minutes) | 26.5 (12.8) | 25 (34.2) | 24.5 (14.1) | 23 (33.8) | 2.00 (3.89) | –5.84 to 9.85 |
| Audiologist | ||||||
| Contacts | 2.5 (0.707) | 2 (2.7) | 1.5 (0.577) | 4 (5.9) | 1.0 (0.577) | –1.93 to 3.93 |
| Mean duration of contact (minutes) | 40.0 (0) | 2 (2.7) | 28.1 (9.44) | 4 (5.9) | 11.9 (4.72) | –3.14 to 26.9 |
| Chiropodist | ||||||
| Contacts | 3.88 (2.26) | 25 (34.2) | 3.96 (2.53) | 24 (35.3) | –0.078 (0.686) | –1.46 to 1.30 |
| Mean duration of contact (minutes) | 24.0 (10.1) | 25 (34.2) | 19.9 (6.02) | 24 (35.3) | 4.11 (2.36) | –0.663 to 8.87 |
| Employment services/job centre | ||||||
| Contacts | 6.60 (9.86) | 5 (6.8) | 14.9 (19.2) | 7 (10.3) | –8.26 (8.48) | –27.3 to 10.8 |
| Mean duration of contact (minutes) | 53.3 (14.0) | 5 (6.8) | 54.3 (37.2) | 7 (10.3) | –0.952 (15.4) | –36.4 to 34.5 |
| Medication (mean of participants using medication) | ||||||
| Prescribed medication | ||||||
| Number of medications | 4.95 (3.41) | 66 (90.4) | 5.06 (4.01) | 64 (94.1) | –0.108 (0.653) | –1.40 to 1.19 |
| Duration (days) | 316.3 (69.6) | 66 (90.4) | 285.7 (93.6) | 64 (94.1) | 30.7 (14.5) | 1.95 to 59.4 |
| ‘Use when necessary’ – number of medications | 1.53 (0.697) | 19 (26.0) | 1.42 (0.692) | 19 (27.9) | 0.105 (0.225) | –0.352 to 0.562 |
| OTC – number of medications | 2.67 (2.08) | 3 (4.1) | 1.33 (0.516) | 6 (8.8) | 1.33 (1.22) | –3.63 to 6.30 |
| Therapist and supervisor timesheets (hours) | ||||||
| Therapist session time | 7.67 (3.08) | 73 (100) | 13.6 (5.87) | 68 (100) | –5.93 (0.797) | –7.51 to –4.35 |
| Therapist time travelling (to session) | 126.2 (102.7) | 71 (97.3) | 214.0 (161.0) | 67 (98.5) | –87.8 (23.1) | –133.7 to –42.0 |
| Therapist time travelling (to supervisor) | 24.02 (34.3) | 65 (89.0) | 35.4 (52.7) | 63 (92.6) | –11.33 (7.89) | –26.98 to 4.31 |
| Therapist administration time | 5.88 (3.46) | 73 (100) | 13.56 (8.39) | 68 (100) | –7.68 (1.10) | –9.86 to –5.51 |
| Supervisor (preparation, supervision and travel) | 2.54 (2.32) | 73 (100) | 3.94 (2.83) | 68 (100) | –1.40 (0.438) | –2.27 to –0.53 |
| Resource | Trial arm | Difference (£) | ||||||
|---|---|---|---|---|---|---|---|---|
| StepUp | BeatIt | |||||||
| Mean cost (£) (SD) | Used by, n (%) | Total cost (£) | Mean cost (£) (SD) | Used by, n (%) | Total cost (£) | Mean (SE) | 95% CI | |
| Daytime activities | ||||||||
| Day centre | 21,223 (9052) | 13 (17.8) | 275,899 | 18,667 (13,607) | 17 (25) | 317,339 | 2556 (4147) | –5944 to 11,056 |
| Sheltered work | 1986 (1319) | 3 (4.1) | 5958 | 5393 (966) | 2 (2.9) | 10,786 | –3408 (1023) | –6770 to –44.7 |
| Voluntary work | 5367 (7533) | 27 (39) | 144,909 | 5113 (5597) | 14 (20.6) | 71,582 | 253 (2083) | –3981 to 4487 |
| Adult education | 3616 (3758) | 13 (17.8) | 47,008 | 4482 (6152) | 8 (11.8) | 35,856 | –866 (2412) | –6221 to 4489 |
| Drop-in centre | 292 (308) | 6 (8.2) | 1752 | 936 (1295) | 5 (7.4) | 4680 | –644 (593) | –2235 to 947 |
| Social club | 1463 (1301) | 26 (35.6) | 38,038 | 1578 (1141) | 27 (39.7) | 42,606 | –116 (337) | –792 to 560 |
| Learning disabilities centre | 18,477 (22,812) | 2 (2.7) | 36,954 | 4961 (5841) | 2 (2.9) | 9922 | 13,515 (16,650) | –148,214 to 175,244 |
| Total daytime cost (mean for complete cases) (£) | 500,518 (8096) | 492,771 (8496) | ||||||
| Hospital based | ||||||||
| Psychiatric intensive care ward | 6061 (6767) | 2 (2.7) | 12,122 | 0 (0) | 0 (0) | 0 | 6061 (N/A) | N/A |
| Acute psychiatric ward | 18,354 (N/A) | 1 (1.4) | 18,354 | 6601 (6603) | 2 (2.9) | 13,202 | 11,753 (N/A) | N/A |
| Psychiatric rehabilitation ward | 5920 (N/A) | 1 (1.4) | 5920 | 8288 (N/A) | 1 (1.5) | 8288 | –2368 (N/A) | N/A |
| General medical ward | 1343 (829) | 6 (8.2) | 8058 | 2687 (3080) | 3 (4.4) | 8061 | 1343 (1810) | –8644 to 5958 |
| Other specialties | 552 (390) | 2 (2.7) | 1104 | 0 (0) | 0 (0) | 0 | 552 (N/A) | N/A |
| Day hospital | 157 (0) | 2 (2.7) | 314 | 188 (70) | 5 (7.4) | 940 | –31 (31) | –119 to 56 |
| Psychiatric outpatient visit | 275 (154) | 5 (6.8) | 1375 | 275 (154) | 5 (7.4) | 1375 | 0 (97) | –224 to 224 |
| Other hospital outpatient visit | 701 (690) | 27 (37.0) | 18,927 | 664 (678) | 25 (0) | 16,600 | 37 (190) | –344 to 418 |
| A&E visit | 217 (212) | 12 (16.4) | 2604 | 171 (64) | 8 (11.8) | 1368 | 47 (65) | –94 to 187 |
| Total hospital cost (mean for complete cases) (£) | 68,778 (1011) | 49,834 (859) | ||||||
| Community based | ||||||||
| Community psychiatrist | 775 (839) | 31 (42.5) | 24,025 | 931 (980) | 30 (44.1) | 27,930 | –155 (234) | –623 to 313 |
| Psychologist | 757 (1217) | 13 (17.8) | 9841 | 804 (817) | 9 (13.2) | 7236 | –48 (434) | –952 to 857 |
| GP | 274 (313) | 64 (87.7) | 17,536 | 297 (293) | 55 (80.9) | 16,335 | –24 (56) | –134 to 87 |
| Community psychiatric nurse | 232 (150) | 4 (5.5) | 928 | 1324 (1475) | 3 (4.4) | 3972 | –1092 (855) | –4717 to 2532 |
| Learning disability nurse | 1561 (2019) | 36 (49.3) | 56,196 | 1468 (1853) | 28 (41.2) | 41,104 | 93 (486) | –878 to 1065 |
| Other community nurse | 1129 (3329) | 21 (28.8) | 23,709 | 300 (403) | 22 (32.4) | 6600 | 829 (731) | –695 to 2352 |
| Community mental health team member | 645 (492) | 2 (2.7) | 1290 | 0 (0) | 0 (0) | 0 | 645 (N/A) | N/A |
| Health-care assistant | 36,822 (51,861) | 2 (2.7) | 73,644 | 261 (269) | 5 (7.4) | 1305 | 36,561 (36,671) | –429,369 to 502,490 |
| Speech therapist | 0 (0) | 0 (0) | 0 | 75.8 (28.5) | 2 (2.9) | 152 | –75.8 (N/A) | N/A |
| Physiotherapist | 305 (438) | 10 (13.7) | 3050 | 251 (330) | 8 (11.8) | 2008 | 54.0 (181) | –330 to 438 |
| Occupational therapist | 549 (742) | 9 (12.3) | 4941 | 166 (236) | 4 (5.9) | 664 | 382 (274) | –224 to 989 |
| Art/drama/music therapist | 596 (292) | 2 (2.7) | 1192 | 252 (32) | 2 (2.9) | 504 | 344 (207) | –2147 to 2835 |
| Alternative therapist | 72.0 (N/A) | 1 (1.4) | 72 | 144 (68) | 2 (2.9) | 288 | –72 (N/A) | N/A |
| Social worker/care manager | 408 (600) | 39 (53.4) | 15,912 | 413 (474) | 35 (51.5) | 14,455 | –4.85 (125) | –254 to 244 |
| Social work assistant | 0 (0) | 0 (0) | 0 | 3055 (2936) | 3 (4.4) | 9165 | –3055 (N/A) | N/A |
| Home help/home care worker | 28,184 (47,039) | 29 (39.7) | 817,336 | 34,601 (46,795) | 21 (30.9) | 726,621 | –6417 (13,437) | –33,510 to 20,675 |
| Advocate/counsellor | 302 (459) | 13 (17.8) | 3926 | 238 (201) | 9 (13.2) | 2142 | 64.1 (144) | –239 to 367 |
| Dentist | 374 (358) | 49 (67.1) | 18,326 | 309 (318) | 40 (58.8) | 12,360 | 65.3 (71.8) | –77.5 to 208 |
| Optician | 37.2 (25.6) | 25 (34.2) | 930 | 43.1 (56.0) | 23 (33.8) | 991 | –5.85 (12.7) | –31.9 to 20.2 |
| Audiologist | 100 (28.3) | 2 (2.7) | 200 | 45.0 (27.4) | 4 (5.9) | 180 | 55.0 (24.2) | –48.8 to 159 |
| Chiropodist | 35.9 (22.1) | 25 (34.2) | 898 | 30.3 (19.4) | 24 (35.3) | 727 | 5.67 (5.93) | –6.26 to 17.6 |
| Employment services/job centre | 398 (668) | 5 (6.8) | 1990 | 1459 (2186) | 7 (10.3) | 10,213 | –1061 (879) | –3112 (990) |
| Total community cost (mean for complete cases) (£) | 10,759,452 (15,822) | 884,952 (15,512) | ||||||
| Medication | ||||||||
| Prescribed medication | 866 (1489) | 66 (90.4) | 57,156 | 1002 (2029) | 64 (94.1) | 64,128 | –136 (308) | –748 to 475 |
| ‘Use when necessary’ | 21.6 (26.6) | 19 (26.0) | 410 | 6.76 (11.8) | 19 (27.9) | 128 | 14.9 (6.67) | 1.14 to 28.6 |
| OTC | 193 (182) | 3 (4.1) | 579 | 14.4 (13.9) | 6 (8.8) | 86 | 179 (105.0) | –270 to 629 |
| Total medication cost (mean for complete cases) (£) | 58,145 (807) | 64,343 (862) | ||||||
| Intervention costs | ||||||||
| Supervisor costs | 143 (136) | 72 (98.6) | 10,296 | 225 (183) | 65 (95.6) | 14,625 | –82.0 (27.8) | –137 to –27.0 |
| Therapist costs | 566 (256) | 73 (10) | 41,318 | 1058 (484) | 67 (98.5) | 70,886 | –491 (66) | –623 to –360 |
| Therapist training | 279 (0) | 73 (100) | 20,367 | 462 (0) | 68 (100) | 31,416 | –183 (0) | N/A |
| Materials | 41.25 (0) | 73 (100) | 3011 | 59.1 (0) | 68 (100) | 4019 | –183 (0) | N/A |
| Total intervention cost (mean for complete cases) (£) | 74,992 (1050) | 120,946 (1788) | ||||||
| Resource | Trial arm | Difference | ||||
|---|---|---|---|---|---|---|
| StepUp | BeatIt | |||||
| Mean (SD) | Used by, n (%) | Mean (SD) | Used by, n (%) | Mean (SE) | 95% CI | |
| Daytime activities | ||||||
| Day centre | ||||||
| Weeks attended | 14.9 (3.93) | 10 (13.7) | 15.3 (2.69) | 13 (19.1) | –0.408 (1.45) | –3.49 to 2.68 |
| Mean hours per week | 18.4 (8.14) | 10 (13.7) | 20.8 (11.61) | 13 (19.1) | –2.46 (4.12) | –11.0 to 6.12 |
| Sheltered work | ||||||
| Weeks attended | 16 (N/A) | 1 (1.4) | 16 (0) | 2 (2.9) | 0 (N/A) | N/A |
| Mean hours per week | 35 (N/A) | 1 (1.4) | 21.5 (9.19) | 2 (2.9) | 13.5 (0) | N/A |
| Voluntary work | ||||||
| Weeks attended | 12.7 (6.25) | 18 (24.7) | 13.6 (4.87) | 13 (19.1) | –0.893 (2.0) | –4.98 to 3.20 |
| Mean hours per week | 4.69 (5.99) | 18 (24.7) | 5.31 (4.12) | 13 (19.1) | –0.613 (1.82) | –4.33 to 3.10 |
| Adult education | ||||||
| Weeks attended | 15.4 (1.81) | 7 (9.6) | 8.71 (5.62) | 7 (10.3) | 6.71 (2.23) | 1.47 to 12.0 |
| Mean hours per week | 4.93 (2.32) | 7 (9.6) | 8.57 (10.9) | 7 (10.3) | –3.64 (4.22) | –13.8 to 6.48 |
| Drop-in centre | ||||||
| Weeks attended | 16 (0.577) | 3 (4.1) | 17 (N/A) | 1 (1.5) | –1.0 (N/A) | N/A |
| Mean hours per week | 4.17 (2.75) | 3 (4.1) | 9 (N/A) | 1 (1.5) | –4.83 (N/A) | N/A |
| Social club | ||||||
| Weeks attended | 13.1 (5.67) | 23 (31.5) | 13.4 (5.56) | 22 (32.4) | –0.322 (1.67) | –3.70 to 3.06 |
| Mean hours per week | 3.28 (2.01) | 23 (31.5) | 3.32 (1.96) | 22 (32.4) | –0.036 (0.591) | –1.23 to 1.16 |
| Learning disabilities centre | ||||||
| Weeks attended | 13.6 (5.37) | 5 (6.8) | 0 (0) | 0 (0) | N/A | N/A |
| Mean hours per week | 17.2 (13.9) | 5 (6.8) | 0 (0) | 0 (0) | N/A | N/A |
| Hospital services – number of contacts | ||||||
| Psychiatric intensive care ward | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A | N/A |
| Acute psychiatric ward | 122 (N/A) | 1 (1.4) | 0 (0) | 0 (0) | 122 (N/A) | N/A |
| Psychiatric rehabilitation ward | 0 (0) | 0 (0) | 10 (N/A) | 1 (1.5) | –10 (N/A) | N/A |
| General medical ward | 6.67 (8.14) | 3 (4.1) | 2.25 (0.5) | 4 (5.9) | 4.42 (4.71) | –15.7 to 24.6 |
| Other specialties | 3.5 (2.12) | 2 (2.7) | 0 (0) | 0 (0) | 3.5 (N/A) | N/A |
| Day hospital | 1 (N/A) | 1 (1.4) | 1 (N/A) | 1 (1.5) | 0 (N/A) | N/A |
| Psychiatric outpatient visit | 2 (N/A) | 2 (2.7) | 1 (N/A) | 3 (4.4) | 1 (0) | N/A |
| Other hospital outpatient visit | 5.31 (11.2) | 13 (17.8) | 2.94 (3.55) | 16 (23.5) | 2.37 (3.23) | –4.55 to 9.30 |
| A&E visit | 1.56 (1.01) | 9 (12.3) | 1 (0) | 7 (10.3) | 0.556 (0.338) | –0.224 to 1.33 |
| Community based | ||||||
| Community psychiatrist | ||||||
| Contacts | 1.77 (1.07) | 26 (35.6) | 2.43 (2.17) | 28 (41.2) | –0.660 (0.460) | –1.59 to 0.271 |
| Mean duration of contact (minutes) | 38.7 (19.5) | 26 (35.6) | 47.5 (23.9) | 28 (41.2) | –8.85 (5.91) | –20.7 to 3.02 |
| Psychologist | ||||||
| Contacts | 5.41 (8.14) | 17 (23.3) | 5.14 (6.68) | 14 (20.6) | 0.269 (2.66) | –5.17 to 5.71 |
| Mean duration of contact (minutes) | 58.2 (25.4) | 17 (23.3) | 47.9 (15.4) | 14 (20.6) | 10.4 (7.40) | –4.82 to 25.6 |
| GP | ||||||
| Contacts | 3.17 (3.40) | 48 (65.8) | 3.07 (2.33) | 46 (67.6) | 0.101 (0.600) | –1.09 to 1.29 |
| Mean duration of contact (minutes) | 11.07 (0) | 48 (65.8) | 11.07 (0) | 46 (67.6) | 0 (N/A) | N/A |
| Community psychiatric nurse | ||||||
| Contacts | 5.25 (3.20) | 4 (5.5) | 8.20 (5.85) | 5 (7.4) | –2.95 (3.07) | –10.3 to 4.45 |
| Mean duration of contact (minutes) | 45.0 (17.3) | 4 (5.5) | 50.0 (14.1) | 5 (7.4) | –5.0 (10.7) | –31.4 to 21.4 |
| Learning disability nurse | ||||||
| Contacts | 5.91 (4.84) | 32 (43.8) | 6.21 (5.76) | 24 (35.3) | –0.302 (1.45) | –3.23 to 2.63 |
| Mean duration of contact (minutes) | 55.6 (29.7) | 32 (43.8) | 54.6 (26.8) | 24 (35.3) | 1.04 (7.58) | –14.2 to 16.2 |
| Other community nurse | ||||||
| Contacts | 28.8 (66.5) | 12 (16.4) | 3.27 (4.71) | 11 (16.2) | 25.6 (19.3) | –16.8 to 67.9 |
| Mean duration of contact (minutes) | 23.8 (19.2) | 12 (16.4) | 27.3 (18.4) | 11 (16.2) | –3.52 (7.83) | –19.8 to 12.8 |
| Community mental health team member | ||||||
| Contacts | 0 (0) | 0 (0) | 16.0 (N/A) | 1 (1.5) | –16.0 (N/A) | N/A |
| Mean duration of contact (minutes) | 0 (0) | 0 (0) | 60.0 (N/A) | 1 (1.5) | –60.0 (N/A) | N/A |
| Health-care assistant | ||||||
| Contacts | 122.0 (N/A) | 1 (1.4) | 14.5 (7.78) | 2 (2.9) | 107.5 (N/A) | N/A |
| Mean duration of contact (minutes) | 1440 (N/A) | 1 (1.4) | 150 (127) | 2 (2.9) | 1290 (N/A) | N/A |
| Speech therapist | ||||||
| Contacts | 0 (0) | 0 (0) | 1.0 (N/A) | 1 (1.5) | –1.0 (N/A) | N/A |
| Mean duration of contact (minutes) | 0 (0) | 0 (0) | 90.0 (N/A) | 1 (1.5) | –90.0 (N/A) | N/A |
| Physiotherapist | ||||||
| Contacts | 6.29 (6.02) | 7 (9.6) | 4.6 (6.95) | 5 (7.4) | 1.69 (3.85) | –7.21 to 10.6 |
| Mean duration of contact (minutes) | 42.9 (16.0) | 7 (9.6) | 34.0 (15.2) | 5 (7.4) | 8.86 (9.10) | –11.7 to 29.4 |
| Occupational therapist | ||||||
| Contacts | 6.10 (6.40) | 10 (13.7) | 5.40 (6.58) | 5 (7.4) | 0.70 (3.57) | –7.56 to 8.96 |
| Mean duration of contact (minutes) | 64.5 (44.7) | 10 (13.7) | 51.0 (13.4) | 5 (7.4) | 13.5 (15.4) | –20.1 to 47.1 |
| Art/drama/music therapist | ||||||
| Contacts | 0 (0) | 0 (0) | 8.0 (N/A) | 1 (1.5) | –8.0 (N/A) | N/A |
| Mean duration of contact (minutes) | 0 (0) | 0 (0) | 60.0 (N/A) | 1 (1.5) | –60.0 (N/A) | N/A |
| Alternative therapist | ||||||
| Contacts | 0 (0) | 0 (0) | 1 (N/A) | 2 (2.9) | –1 (N/A) | N/A |
| Mean duration of contact (minutes) | 0 (0) | 0 (0) | 60.0 (42.4) | 2 (2.9) | –60.0 (N/A) | N/A |
| Social worker/care manager | ||||||
| Contacts | 3.16 (4.08) | 32 (43.8) | 3.72 (4.12) | 25 (36.8) | –0.564 (1.09) | –2.76 to 1.63 |
| Mean duration of contact (minutes) | 49.8 (20.8) | 32 (43.8) | 51.5 (14.8) | 25 (36.8) | –1.68 (4.725) | –11.1 to 7.79 |
| Social work assistant | ||||||
| Contacts | 1.0 (N/A) | 1 (1.4) | 42.0 (N/A) | 1 (1.5) | –41.0 (N/A) | N/A |
| Mean duration of contact (minutes) | 60.0 (N/A) | 1 (1.4) | 90.0 (N/A) | 1 (1.5) | –30.0 (N/A) | N/A |
| Home help/home care worker | ||||||
| Contacts | 80.3 (53.1) | 23 (31.5) | 84.3 (57.1) | 24 (35.3) | –4.07 (16.01) | –36.5 to 28.3 |
| Mean duration of contact (minutes) | 408 (449) | 23 (31.5) | 366 (439) | 24 (35.3) | 41.8 (130) | –219 to 303 |
| Advocate/counsellor | ||||||
| Contacts | 5.30 (6.36) | 10 (13.7) | 4.67 (5.89) | 9 (13.2) | 0.633 (2.81) | –5.30 to 6.57 |
| Mean duration of contact (minutes) | 62.0 (23.9) | 10 (13.7) | 66.7 (46.9) | 9 (13.2) | –4.67 (17.4) | –42.7 to 33.3 |
| Dentist | ||||||
| Contacts | 1.95 (1.81) | 37 (50.7) | 1.48 (0.770) | 25 (36.8) | 0.466 (0.335) | –0.206 to 1.14 |
| Mean duration of contact (minutes) | 25.3 (19.9) | 37 (50.7) | 24.2 (22.4) | 25 (36.8) | 1.07 (5.55) | –10.1 to 12.2 |
| Optician | ||||||
| Contacts | 1.45 (0.688) | 11 (15.1) | 1.08 (0.289) | 12 (17.6) | 0.371 (0.223) | –0.111 to 0.853 |
| Mean duration of contact (minutes) | 26.4 (15.2) | 11 (15.1) | 39.2 (47.5) | 12 (17.6) | –12.8 (14.4) | –43.9 to 18.3 |
| Audiologist | ||||||
| Contacts | 4 (N/A) | 1 (1.4) | 1.75 (1.5) | 4 (5.9) | 2.25 (N/A) | N/A |
| Mean duration of contact (minutes) | 30.0 (N/A) | 1 (1.4) | 16.3 (9.46) | 4 (5.9) | 13.75 (N/A) | N/A |
| Chiropodist | ||||||
| Contacts | 1.80 (1.01) | 15 (20.5) | 2.31 (1.03) | 13 (19.1) | –0.508 (0.388) | –1.31 to 0.291 |
| Mean duration of contact (minutes) | 24.3 (12.8) | 15 (20.5) | 19.2 (6.07) | 13 (19.1) | 5.10 (3.71) | –2.62 to 12.8 |
| Employment services/job centre | ||||||
| Contacts | 5.60 (6.50) | 5 (6.8) | 6.57 (7.35) | 7 (10.3) | –0.971 (4.02) | –10.0 to 8.07 |
| Mean duration of contact (minutes) | 37.2 (23.0) | 5 (6.8) | 72.9 (54.4) | 7 (10.3) | –35.7 (23.0) | –88.0 to 16.7 |
| Resource | Trial arm | Difference (£) | ||||||
|---|---|---|---|---|---|---|---|---|
| StepUp | BeatIt | |||||||
| Mean cost (£)(SD) | Used by, n (%) | Total cost (£) | Mean cost (£) (SD) | Used by, n (%) | Total cost (£) | Mean (SE) | 95% CI | |
| Daytime activities | ||||||||
| Day centre | 6694 (3727) | 10 (13.7) | 66,940 | 7723 (4912) | 13 (19.1) | 100,399 | –1028 (1801) | –4775 to 2718 |
| Sheltered work | 4766 (N/A) | 1 (1.4) | 4766 | 2927 (1252) | 2 (2.9) | 5854 | 1838 (N/A) | N/A |
| Voluntary work | 1515 (2443) | 18 (24.7) | 27,270 | 1686 (1524) | 13 (19.1) | 21,918 | –171 (714) | –1633 to 1291 |
| Adult education | 1623 (775) | 7 (9.6) | 11,361 | 1482 (1423) | 7 (10.3) | 10,374 | 141 (613) | –1239 to 1521 |
| Drop-in centre | 757 (468) | 3 (4.1) | 2271 | 1764 (N/A) | 1 (1.5) | 1764 | –1007 (N/A) | N/A |
| Social club | 548 (460) | 23 (31.5) | 12,604 | 551 (432) | 22 (32.4) | 12,122 | –2.65 (133) | –271 to 266 |
| Learning disabilities centre | 6550 (5676) | 5 (6.8) | 32,750 | 0 (0) | 0 (0) | 0 | N/A | N/A |
| Total daytime cost (mean for complete cases) (£) | 157,962 (2323) | 152,431 (2628) | ||||||
| Hospital based | ||||||||
| Psychiatric intensive care ward | 0 (0) | 0 (0) | 0 | 0 (0) | 0 (0) | 0 | N/A | N/A |
| Acute psychiatric ward | 39,284 (N/A) | 1 (1.4) | 39,284 | 0 (0) | 0 (0) | 0 | 39,284 (N/A) | N/A |
| Psychiatric rehabilitation ward | 0 (0) | 0 (0) | 0 | 2960 (N/A) | 1 (1.5) | 2960 | –2960 (N/A) | N/A |
| General medical ward | 1733 (2118) | 3 (4.1) | 5199 | 585 (130) | 4 (5.9) | 2340 | 1148 (1224) | –4091 to 6388 |
| Other specialities | 966 (585) | 2 (2.7) | 1932 | 0 (0) | 0 (0) | 0 | 966 (N/A) | N/A |
| Day hospital | 157 (N/A) | 1 (1.4) | 157 | 157 (N/A) | 1 (1.5) | 157 | 0 (N/A) | N/A |
| Psychiatric outpatient visit | 344 (0) | 2 (2.7) | 688 | 172 (0) | 3 (4.4) | 516 | 172 (0) | N/A |
| Other hospital outpatient visit | 881 (1858) | 13 (17.8) | 11,453 | 488 (589) | 16 (23.5) | 7808 | 393 (536) | –756 to 1543 |
| A&E visit | 193 (125) | 9 (12.3) | 1737 | 124 (0) | 7 (10.3) | 868 | 69 (42) | –28 to 166 |
| Total hospital cost (mean for complete cases) (£) | 60,450 (889) | 14,649 (252) | ||||||
| Community based | ||||||||
| Community psychiatrist | 431 (364) | 26 (35.6) | 11,206 | 672 (746) | 28 (41.2) | 18,816 | –241 (158) | –560 to 78.7 |
| Psychologist | 477 (725) | 17 (23.3) | 8109 | 392 (542) | 14 (20.6) | 5488 | 84.6 (228) | –382 to 551 |
| GP | 142 (186) | 48 (65.8) | 6816 | 120 (91.6) | 46 (67.6) | 5520 | 21.2 (30.1) | –38.9 to 81.2 |
| Community psychiatric nurse | 385 (293) | 4 (5.5) | 1540 | 741 (620) | 5 (7.4) | 3705 | –357 (313) | –1126 to 412 |
| Learning disability nurse | 610 (909) | 32 (43.8) | 19,520 | 549 (605) | 24 (35.3) | 13,176 | 61 (203) | –345 to 468 |
| Other community nurse | 433 (530) | 12 (16.4) | 5196 | 194 (396) | 11 (16.2) | 2134 | 239 (194) | –166 to 643 |
| Community mental health team member | 0 (0) | 0 (0) | 0 | 1589 (N/A) | 1 (1.5) | 1589 | –1589 (N/A) | N/A |
| Health-care assistant | 73,493 (N/A) | 1 (1.4) | 73,493 | 1117 (1260) | 2 (2.9) | 2234 | 72,376 (N/A) | N/A |
| Speech therapist | 0 (0) | 0 (0) | 0 | 72.0 (N/A) | 1 (1.5) | 72 | –72.0 (N/A) | N/A |
| Physiotherapist | 185 (157) | 7 (9.6) | 1295 | 84.7 (98.3) | 5 (7.4) | 424 | 100 (74.0) | –64.9 to 265 |
| Occupational therapist | 458 (752) | 10 (13.7) | 4580 | 209 (234) | 5 (7.4) | 1045 | 249 (260) | –318 to 815 |
| Art/drama/music therapist | 0 (0) | 0 (0) | 0 | 367 (N/A) | 1 (1.5) | 367 | –367 (N/A) | N/A |
| Alternative therapist | 0 (0) | 0 (0) | 0 | 46.4 (31.6) | 2 (2.9) | 93 | –46.4 (N/A) | N/A |
| Social worker/care manager | 253 (382) | 32 (43.8) | 8096 | 292 (348) | 25 (36.8) | 7300 | –38.5 (97.0) | –233 to 156 |
| Social work assistant | 36.0 (N/A) | 1 (1.4) | 36 | 2269 (N/A) | 1 (1.5) | 2269 | –2233 (N/A) | N/A |
| Home help/home care worker | 12,540 (18,071) | 23 (31.5) | 288,420 | 12,530 (17,642) | 24 (35.3) | 300,720 | 9.85 (5212) | –10,489 to 10,509 |
| Advocate/counsellor | 262 (320) | 10 (13.7) | 2620 | 243 (316) | 9 (13.2) | 2187 | 19.7 (145) | –288 to 328 |
| Dentist | 289 (306) | 37 (50.7) | 10,693 | 254 (417) | 25 (36.8) | 6350 | 35.3 (97.3) | –161 to 232 |
| Optician | 31.1 (23.6) | 11 (15.1) | 342 | 30.4 (35.4) | 12 (17.6) | 364 | 0.71 (12.4) | –25.3 to 26.7 |
| Audiologist | 90.4 (N/A) | 1 (1.4) | 90 | 17.9 (10.4) | 4 (5.9) | 72 | 72.5 (N/A) | N/A |
| Chiropodist | 16.4 (12.1) | 15 (20.5) | 246 | 17.7 (9.56) | 13 (19.1) | 230 | –1.29 (4.09) | –9.71 to 7.12 |
| Employment services/job centre | 124 (91.8) | 5 (6.8) | 620 | 862 (1302) | 7 (10.3) | 6034 | –738 (494) | –1943 to 467 |
| Total community cost (mean for complete cases) (£) | 442,919 (6513) | 380,189 (6450) | ||||||
Appendix 4 Qualitative interview schedules
Interview schedule for supporter interviews
-
What were their initial expectations, beliefs and emotions about the intervention?
-
What can they remember about the intervention and what they did in the sessions (and between the sessions)?
-
Materials (activity diaries, etc.).
-
Activities in sessions.
-
Homework tasks.
-
Formulation and final booklets.
-
-
Aspects of intervention found most helpful.
-
Aspects of intervention found least helpful.
-
What they learned about depression and how to support people with depressive symptoms?
-
Did their involvement in sessions change their confidence about supporting their relative/client?
-
Did their involvement in sessions change how they support their relative/client?
-
Process issues:
-
relationship with therapist
-
joint working with client and therapist
-
continuity across sessions
-
a sense of whether or not the intervention was sufficiently tailored to the individual.
-
-
Perceived changes for client, if any, as a consequence of the therapy:
-
their feelings
-
their ability to cope/sense of self-efficacy
-
engagement with the world – in terms of activities and social relationships.
-
-
Perceived changes for the supporter in terms of:
-
their relationship with their relative/client
-
their confidence in supporting their relative/client
-
how they support their relative/client
-
the support person’s QoL.
-
-
How could the intervention be improved?
-
Do they think the intervention is suitable for other clients?
-
What has happened since the therapy finished?
-
building on any progress made/or going backwards
-
continuing any aspect of the therapeutic work
-
other life changes linked to the initial therapy.
-
Interview schedule for participants with learning disabilities
I am going to ask you some questions about the psychological therapy you are receiving through the meetings with <insert the name of therapist>. There are no right answers to these questions and different people might say different things. I would like you to think about these sessions and how it feels for you.
Warm-up questions/establishing presence of alliance
-
You are seeing <insert the name of therapist> to help you with some problems. How do you feel these sessions are going?
-
Tell me about what happens during these sessions.
-
What have you done together/talked about that has really helped you feel better?
-
Is there anything about these sessions that has not helped you or made you feel worse?
Goals
-
What do you hope to get out of your sessions with <insert the name of therapist>? What would you like to get better? What would you like to be able to do after these sessions finish?
Example prompts
-
What does <insert the name of therapist> want you to be able to do after these sessions?
-
How did you decide what you wanted to get out of sessions? Was this the best thing?
-
Have there been any differences between what <insert the name of therapist> wants you to get out of sessions and what you want? What was it like to agree/disagree? What did you think about this? How did this feel?
-
Was what you wanted listened to by <insert the name of therapist>? Did you listen to what they thought? How did this feel?
Tasks
-
Tell me about the kinds of things you do/tasks you do when you meet with <insert the name of therapist>? How do you decide what kinds of tasks you will do?
Example prompts
-
What tasks have been good? How have they helped you?
-
Was there any task that was not helpful or did not feel good? Why did it not help?
-
Do you understand why you talk about certain issues/do certain tasks?
-
Did you get control over the tasks you do? If yes, what was this like?
-
If no, what was it like to be told by <insert the name of therapist> what tasks you would do?
Bond
-
Can you tell me about what <insert the name of therapist> is like? How do you feel when you meet with them?
Example prompts
-
How do you get on with <insert the name of therapist>?
-
What qualities do you think makes a therapist be able to help someone in therapy?
-
What is it like speaking to <insert the name of therapist> about your problems? Can you trust them?
-
What things help you to feel relaxed talking to them?
-
What would make it hard to talk to them about your problems? Have there been times you did not want to go to sessions?
-
Do you think they can help you with your problems? Why/why not?
-
How do you think they feel about meeting with you? Do you think they care about how you are getting on?
(When appropriate, photographs and drawings can be used by the interviewer to help illustrate the questions and stimulate discussion.)
Interview schedule for therapist focus groups
-
What were their initial expectations, beliefs and emotions about the intervention?
-
Views of the therapy training.
-
Understanding and views of the behavioural activation model.
-
Views about the manual and different materials and exercises:
-
materials (activity diaries etc.)
-
activities in sessions
-
homework tasks
-
formulation and final booklets.
-
-
View about working with clients to overcome barriers to change and the challenges they faced with this.
-
Aspects of intervention that they thought the clients and support persons found most helpful and engaging.
-
Aspects of intervention that they thought the clients and support persons found least helpful or engaging.
-
Process issues:
-
relationship with therapist
-
joint working with client and therapist
-
continuity across sessions
-
a sense of whether or not it was possible to tailor the intervention to the individual’s particular difficulties and life circumstances.
-
-
Perceived changes for client, if any, as a consequence of the therapy:
-
their feelings
-
their ability to cope/sense of self-efficacy
-
engagement with the world in terms of activities and social relationships.
-
-
Perceived changes for the support person in terms of:
-
their relationship with their relative/client
-
their confidence in supporting their relative/client
-
how they support their relative/client
-
the support person’s QoL.
-
-
Therapist views of supervision:
-
What have been the most helpful aspects of supervision?
-
What has been least helpful about supervision?
-
How could the supervision be improved?
-
-
If they delivered the therapy to more than one client, how did their approach and confidence change over time?
-
Overall, what, if anything, do they think they have gained from being a therapist in the study?
-
In their view, what could be done to improve the intervention?
-
What clients, if any, do they think the intervention is suitable for?
Glossary
- BeatIt
- A behavioural activation intervention adapted for adults with learning disabilities and depression, delivered to participants over 12 sessions by a therapist alongside a supporter, ordinarily within a 4-month period.
- StepUp
- A guided self-help intervention.
List of abbreviations
- A&E
- accident and emergency
- ABS-RC2
- Adaptive Behavior Scale – Residential and Community: Second Edition
- BLESID
- Bangor Life Events Schedule for Intellectual Disabilities
- BPI-S
- Behavior Problems Inventory for Individuals with Intellectual Disabilities – Short Form
- CBT
- cognitive–behavioural therapy
- CI
- confidence interval
- CSRI
- Client Service Receipt Inventory
- df
- degrees of freedom
- EDSE
- Emotional Difficulties Self-Efficacy
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-Y
- EuroQol-5 Dimensions – youth version
- EQ-VAS
- EuroQol Visual Analogue Scale
- FMSS
- Five-Minute Speech Sample
- GAS-ID
- Glasgow Anxiety Scale for people with an Intellectual Disability
- GCP
- Good Clinical Practice
- GDS-LD
- Glasgow Depression Scale for people with a Learning Disability
- GLM
- generalised linear model
- GP
- general practitioner
- IAPT
- Improving Access to Psychological Therapies
- ICER
- incremental cost-effectiveness ratio
- ICI
- Index of Community Involvement
- IDDS
- Intellectual Disabilities Depression Scale
- IPDL
- Index of Participation in Domestic Life
- IQ
- intelligence quotient
- NICE
- National Institute for Health and Care Excellence
- OTC
- over the counter
- PSS
- perceived social support
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCB
- Robertson Centre for Biostatistics
- RCT
- randomised controlled trial
- SAP
- statistical analysis plan
- SD
- standard deviation
- SE
- standard error
- SIMD
- Scottish Index of Multiple Deprivation
- TAU
- treatment as usual
- WASI™
- Wechsler Abbreviated Scale of Intelligence™
- WTP
- willingness to pay
