Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 14/157/06. The contractual start date was in January 2016. The draft report began editorial review in May 2017 and was accepted for publication in September 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Roz Shafran is on the Health Technology Assessment Mental, Psychological and Occupational Health Panel and Stuart Logan is on the Open Call Assessment Board – Medicines for Children.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Moore et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Preface
Watching a child suffer from a long-term health condition is awful. They may be in pain, feel ill or be unable to do the things that other young people do. They may need surgery and lengthy stays in hospital. They need medication, the side effects of which can be a challenge all by themselves. Watching a child have to cope with all this, and then put their fist through their bedroom door in anger, refuse to leave the house for weeks through social isolation or be unable to sleep/eat properly because of anxiety, is heartbreaking.
Children and young people with long-term health conditions – be it cancer, brain injury, muscular dystrophy or any of a myriad of physical conditions that cannot be cured, only managed – face enormous challenges. As well as their physical illness, many of these young people suffer from mental health problems as a consequence of their condition. These include anxiety, depression, anger, social isolation and poor self-esteem. Children and young people with long-term health conditions may be four times more likely to suffer mental health problems than their physically healthy peers.
It is vital that the mental ill health of these young people is treated alongside their physical condition. A range of strategies are currently in use, and this study aims to evaluate how effective different types of intervention are in improving mental health.
The quality, and accessibility, of these strategies vary greatly. Those young people lucky enough to have accessed top-quality mental health provision may overcome their anxieties and worries completely. They may recover to become confident and happy once again. Others may still not be able to attend school, engage socially or live without dark thoughts years after their physical condition began. There is no justification for this disparity. Every single child or young person suffering from a long-term health condition must receive top-quality interventions to improve their mental health – it should not be down to chance as to which technique or provider they are given. Some parents have been able to see their child’s anguished mental state healed. Others, on a daily basis, do not know what they will find when they return home each day.
In looking at the effectiveness of the various strategies, it is hoped that excellent practice can be identified and used to improve all mental health provision for our young people with long-term physical conditions. They deserve nothing less.
Fiona Lockhart
Chapter 1 Background
Description of the health problem
Defining long-term physical conditions
A 2007 systematic review1 of definitions of chronic health conditions in childhood found 25 different definitions of long-term physical conditions (LTCs), with relatively few appearing across multiple publications. For the current project, the team drew from some of the most frequently cited definitions2–4 to define LTCs as any diagnosed physical health condition with an expected duration of at least 3 months for which a cure is considered unlikely and which results in limitations in ordinary activities and necessitates the use of medical care or related services beyond what is usual for someone of the age of the affected individual.
This definition was used to select conditions that were included in searches for the systematic reviews. To fit the definition, physical conditions could not be psychiatric disorders found in Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition. 5 Aside from this, the definition was inclusive, with conditions including structural or functional central nervous system disorders [e.g. acquired brain injury (ABI), epilepsy], disability (e.g. cerebral palsy, spina bifida) or those with unclear aetiology [e.g. chronic pain, inflammatory bowel disease (IBD)]. It is acknowledged that LTCs may be referred to as chronic illness/disease/conditions or complex/special health needs and that most often these terms include mental health conditions. In the current review LTC refers to children and young people’s (CYP’s) physical health conditions only.
Defining mental health
The term ‘mental health’ captures far more than the absence of psychiatric disorders6 to include adjustment, well-being and coping. 7 Although we take this view of mental health, for the purposes of this project we needed to define mental health in different ways. When we refer to mental health conditions or psychiatric illness, we use the term ‘mental health disorder’, for instance depression or conduct disorder. As the reviews conducted do not focus only on mental health disorders, we use the term ‘mental ill health’ to refer to elevated symptoms that may or may not relate to a particular mental health disorder, but indicate difficulties experienced by an individual, for example anxiety or stress. Finally, we use the term ‘mental health and well-being’ to refer to mental health in its broad sense as indicated above, to include coping and adjustment. This is necessary when we have been inclusive in terms of how interventions may aim to improve mental health and the wide range of mental health outcomes that such interventions may affect.
Prevalence
Despite advances in medicine leading to improved prognosis and/or cures for many conditions, LTCs continue to be common in CYP. van der Lee et al. 1 considered a range of definitions of chronic conditions, but identified an overall prevalence of around 15% in CYP in the international literature. In the USA, prevalence of LTCs is high and has increased over time; the US National Health Interview Survey (NHIS) has annually collated information about the health of CYP across the nation, and, in 2014, 42% of CYP suffered from one or more LTCs (NHIS data, childhealthdata.org; accessed 9 February 2017), whereas in 1988 this figure stood at 31%. 8 Although the majority of reported data relate to the USA, a high prevalence of LTCs is experienced across the globe. In England, 23% of secondary school age pupils reported that they had a long-term medical illness or disability in 2014,9 with similar proportions of youths reporting a LTC in New Zealand in 200710 as well as in Canada and Finland in 2002. 11 Inconsistency in the methods used to survey the health of CYP exists, for example in the definition of LTCs, the sample inclusion criteria or the reporting method; in spite of uncertainty regarding the prevalence of LTCs according to our definition, there is strong evidence that there is an international burden related to LTCs in CYP. 12
Having a LTC places strain on the individual and their family, as well as placing demands on societal systems such as health care and education. A mental health disorder in addition to the LTC therefore poses a significant problem for some CYP and those around them. The challenges associated with childhood mental disorders alone can be significant and have the potential to exert a more negative impact than certain LTCs. 13
There is extensive evidence that links the presence of a LTC with increased risk of the development of a mental health diagnosis in CYP. Although the overall risk of a mental health disorder is reportedly around four times greater in CYP with LTCs than in their physically healthy counterparts,14,15 this risk varies because of a number of factors. For example, the duration,10,16,17 severity and progression11,18,19 of a LTC are associated with the risk of mental ill health or of mental health disorder.
For a variety of LTCs, there is evidence to support increased risk of mental health disorder, for example asthma,20,21 gastrointestinal disorders,22 functional abdominal pain,23 kidney disease,17,24,25 chronic headache,26 type 1 diabetes mellitus (T1DM)27 and epilepsy. 28 However, for a range of LTCs there is limited evidence of any association with mental health disorders and many studies suffer from poor quality. For example, the literature regarding CYP with cancer is particularly equivocal. There is research showing little difference in depressive symptoms between CYP with cancer and healthy comparators (e.g. Weschler and Sánchez-Iglesias,29 Arabiat et al. ,30 Myers et al. 31), although some aspects, such as the stage of treatment32 or undertaking certain distressing procedures, such as stem cell transplants,33,34 can influence the mental health of cancer patients.
How long-term physical conditions may increase risk of mental ill health
Although the prevalence of mental health disorder in populations with LTCs may be greater than in populations without such physical health concerns, the mechanisms for this are not fully understood. Physical and mental health conditions can share the same pathology,35 or the stress and/or treatment associated with having a LTC can adversely affect mental health. For instance, LTCs and their treatment may involve pain; invasive, complicated or time-consuming treatment regimens; time away from school and peers for hospital visits; restrictions on activity or diet; and a sense of isolation from friends and family. 36
There are several empirical models that attempt to explain why children with a LTC are at risk of mental ill health, including the risk resistance model developed by Wallander and Varni. 37,38 This model was intended to guide interventions to support children to adapt to living with a LTC. It suggests that aspects of disease severity, the impact a LTC has on the child’s functional independence and other psychosocial stressors within the child’s life are a set of risk factors that can increase the risk of a child developing some form of mental, social or physical maladjustment associated with their LTC. The model also proposes a set of personal and family factors that may act as factors protecting against mental ill health. Both risk and protective factors identified by this model are proposed to be applicable across different types of LTC, but their relevance to specific illness groups has not been widely tested.
An alternative theory is Thompson and Gustafson’s39 transactional stress and coping model, which views chronic illness using a systems theory approach and sees a LTC as a stressor requiring adaptation. This model identifies processes that contribute to the adjustment of both children with chronic disorders and their mothers. Adaptation to a LTC is seen to involve psychological, biomedical and developmental processes and, therefore, there are similarities to Wallander and Varni’s model. 38 Thompson’s model has been tested primarily with sickle cell disease and cystic fibrosis. 40
Moos and Holahan’s41 conceptual model for the determinants of health-related outcomes of chronic illness and disability builds on the previous models by integrating the influence of personal and social factors on the course of illness. It demonstrates how different adaptive tasks can influence the development of coping skills and mediate potential health outcomes. The model emphasises the inter-relationship between risk and protective factors and health-related outcomes, resulting in the concept of adjustment to a LTC as a process rather than an end point. Although aimed at adults and thus omitting the important influences of developmental stage and family and social dynamics for CYP, the model notes the importance of building relationships with health-care providers as one of seven ‘adaptive tasks’ for the chronically ill person to complete.
Haase et al. 42 put forward a resilience in illness model, which focuses on adolescents and young adults, identifying risk and protective factors that influence the resilience shown by those experiencing illness-related distress. In common with the above models, the model considers family factors and coping capabilities, which have been the subject of exploratory and confirmatory evaluations among young people with cancer.
Aside from theoretical models of the interaction between physical and mental ill health, aspects of the experience of living with a LTC highlight the stress that CYP face. The initial diagnosis of a LTC is often very distressing for both the child and their family, and is associated with feelings of shock, sadness and confusion. 43 At the time of diagnosis, children and families must take in information regarding the child’s immediate treatment needs, which can feel confusing and frustrating, but also consider the possible impact of the diagnosis on the child’s future. 44
The daily experience of living with a LTC can be physically unpleasant for CYP, and this may have a detrimental effect on their mental health via several mechanisms. Venning et al. 45 conducted a qualitative metasynthesis focusing on the experiences of children diagnosed with a LTC and noted how LTCs made children ‘feel uncomfortable in their body and the world’.
Impact of mental health on physical health and economic consequences
Cottrell46 describes the vicious cycle of comorbid LTCs and mental health diagnosis, in which one condition exacerbates the other. Mental ill health may also be associated with poor treatment adherence, which may exacerbate the physical condition, impair self-management and worsen long-term outcomes. 47,48 For example, depression in children with diabetes mellitus is associated with poorer control of blood sugar, increasing the risk of later serious complications such as loss of vision. 49 It is estimated that between 12% and 18% of all NHS spending on LTCs is linked to poor mental health and well-being50 and that psychological interventions can reduce care costs by up to 20%. 51
Interventions
Numerous highly effective psychological interventions for mental ill health in CYP are available but pay no explicit regard to physical illnesses, with > 750 treatment protocols cited in one systematic review. 52 For instance, the National Institute for Health and Care Excellence (NICE) recommends the use of group or individual parenting interventions for children with conduct disorder53 and cognitive–behavioural therapy (CBT) for children with depression. 54 It is important to know whether or not such interventions are also effective in children with physical illnesses. However, children with some LTCs are often excluded from trials of such interventions; for example, in a large trial of CBT for children with anxiety disorders, children with a disabling medical condition were excluded. 55
Various characteristics of a LTC may make traditional interventions for mental ill health more challenging and/or less effective, necessitating a modified approach to treatment. Cottrell46 suggests that, although existing evidence-based treatments for mental health diagnoses in CYP should be effective in the presence of LTCs, there are circumstances in which this may not be the case. For example, in CYP with T1DM, the strong link between blood glucose control and mood disorders56 may mean that management of diabetes mellitus should be targeted first. 57 In CYP with epilepsy in whom seizure control is challenging, it is recommended that any treatment for depression is carefully managed by an interdisciplinary team and adapted to the individual’s needs, particularly when pharmacological management is warranted for either condition. 58 Patients with comorbid gastrointestinal disorders and depression may be unsuitable candidates for pharmacological treatments, as these treatments may exacerbate physical symptoms, whereas approaches such as CBT may need to be adapted to focus on maladaptive thinking related to the LTC. 59 The additional costs of treatment for mental ill health can be significant. For example, one study60 suggested that, in the USA, the presence of comorbid depression increases the treatment cost in adolescents with asthma by 51%. This was largely attributable to non-asthma and non-mental health costs related to primary care and laboratory/radiology expenditure.
Treatment guidance
The closer integration of mental and physical health care is a priority for the NHS,61 and the NHS Confederation has highlighted the social, health and economic benefits that arise from the integration of physical and mental health treatments. 62 NICE calls for access to mental health professionals with an understanding of diabetes mellitus to address psychological and social issues in CYP with diabetes mellitus63 and states that the psychological needs of children with epilepsy should be considered as part of routine care. 64 A 2014 Department of Health and Social Care (DHSC) policy paper65 builds on the government’s mental health strategy for mental and physical health to have ‘parity of esteem’. 61 It explicitly states the DHSC’s ambition for mental health care and physical health care to be better integrated at every level and mandates best practice approaches to caring for patients to include potential psychological care needs. 65 However, at present we do not know what ‘best practice’ consists of in relation to the treatment of mental ill health in CYP with LTCs.
In 2015, the DHSC and NHS England released a policy document, Future in Mind,66 which aimed to comprehensively evaluate the current picture of children’s mental health in the UK and outline plans to improve the care provided. Within this document, the prevalence of comorbid mental health diagnosis in CYP with LTCs is highlighted, but the associated treatment difficulties are not discussed and the only recommendations related to this topic are aimed at holistic school-based promotion of mental and physical self-care. NICE has not produced any general guidance for the treatment of CYP with LTCs and comorbid mental health diagnosis, although it exists for the treatment of adults with LTCs and depression. 67 One document specifically considers mental health services referral in diabetes mellitus patients,63 but this is focused more on management of the physical condition. Specifically, NICE guideline NG1863 acknowledges the increased risk of emotional and behavioural difficulties in CYP with T1DM, and promotes awareness of these risks in health-care professionals. The availability of mental ill health screening and referral to mental health professionals with expertise in diabetes mellitus is recommended in the NICE guidelines. 63
This represents a gap in policy development and research activity. In adults with cancer, the collaborative care model implemented by Sharpe et al. 68 led to large improvements in depressive symptoms compared with usual care. The model involved the integration of cancer nurses and psychiatrists into the hospital environment alongside primary care physicians, and, given the improvements shown in treatment of depression in the adult population, primary evidence is needed to assess such an approach with CYP with LTCs.
Evidence for adults cannot simply be applied to CYP. A wide range of factors may influence the clinical effectiveness of interventions for CYP,69 for example the developmental stage of the child; aspects relating to parents; accessibility requirements, such as relying on others to access treatment; attentional requirements, such as keeping children engaged and interested; the need to work around education; and different social aspects of being a child compared with being an adult. It is clear that separate research is required for CYP with LTCs.
Measurement of mental health and other outcomes
A range of different outcome measures can be used to measure the clinical effectiveness of mental health interventions for CYP with LTC. There are several reasons for this. First, the range of mental health disorders that might coexist with LTCs is wide and, likewise, the varied symptoms of mental ill health can be measured using a large number of validated scales. Second, there are no gold standard outcome measures. For example, a Cochrane review70 of CBT for anxiety in CYP that was restricted to studies using validated and reliable diagnostic interviews and symptom rating scales identified four diagnosis tools and more than eight different outcome measures in 41 studies. Third, some more generic measures of mental health and well-being are used to measure clinical effectiveness. Finally, interventions that aim to improve the mental health of CYP might also be predicted to improve markers of physical health, whether as a result of improved mental health or components of the intervention.
Previous systematic reviews
Systematic reviews of mental health interventions rarely separately consider the clinical effectiveness of these interventions in populations with LTCs. A Cochrane systematic review by James et al. 70 included 41 studies to assess the effectiveness of CBT for anxiety in CYP. Despite this relatively large number of studies, none considered a sample or subgroup in which a comorbid LTC was present. Similarly, systematic reviews of non-pharmacological treatments for depression in CYP with traumatic brain injury71 and congenital heart disease72 found no relevant randomised controlled trials (RCTs) in CYP.
There are a number of existing, well-executed systematic reviews in the broader area of psychological interventions for people with LTCs, including several Cochrane reviews. 73–76 However, these reviews are highly targeted, focusing on, for example, one particular physical and/or one particular psychiatric comorbidity, rather than exclusively on CYP or parenting interventions.
The majority of other reviews in this area have concerned either adult populations or specific disorders, and have often focused on the distress arising from having a LTC rather than the treatment of a comorbid mental health disorder. 57,77 Reviews of psychological interventions in CYP with LTC have been undertaken, but many of these have focused on coping, treatment adherence and/or use of health-care resources in populations without elevated mental ill health (e.g. Yorke et al. ,78 Sansom-Daly et al.,79 Thompson et al. 80). There have been some reviews81 of pharmacological interventions for children with mental health diagnoses and physical illness that have considered particular physical illnesses and mental health symptoms (e.g. depression in epilepsy).
The most relevant attempt to systematically review psychological interventions to treat symptoms of mental health disorder in CYP with LTCs was by Bennett et al. 82 This review targeted only psychotherapeutic interventions in which child-related mental health measures were the primary outcome. A total of 10 relevant studies were identified, of which two were RCTs. These RCTs trialled CBT for subthreshold depression in CYP with epilepsy83 or IBD. 84 Although the review provides preliminary evidence that CBT can be a clinically effective treatment for depression and anxiety in CYP with LTCs, the reviewers concluded that the existing evidence base was weak.
The current review fills a gap in the literature by synthesising studies investigating interventions aiming to improve mental health in CYP with LTCs who exhibit elevated symptoms of mental ill health and studies reporting cost and cost-effectiveness evidence. In addition, this review synthesises evidence from qualitative research studies in order to understand how children with LTCs experience interventions aimed at improving their mental health and well-being and their attitudes towards them.
Aim and research questions
We aimed to evaluate the effectiveness of interventions aimed at improving the mental health of children and young people with LTCs and to explore the factors that may enhance or limit the delivery of such interventions. This necessitated reviewing both quantitative and qualitative research. The systematic reviews addressed the following research questions:
-
What are the clinical effectiveness and cost-effectiveness of interventions targeting mental health for CYP with LTCs and symptoms of mental ill health?
-
What are the effects of such interventions on other key aspects of individual and family functioning?
-
What are the factors that may enhance, or hinder, the clinical effectiveness of interventions and/or the successful implementation of interventions intended to improve mental health for CYP with LTCs?
Chapter 2 Review 1: clinical effectiveness of interventions aiming to improve mental health in children and young people with long-term physical conditions
Research questions
This chapter describes the first systematic review and addresses the following research questions:
-
What are the clinical effectiveness and cost-effectiveness of interventions aiming to improve mental health for CYP with LTCs and symptoms of mental ill health?
-
What are the effects of such interventions on other key aspects of individual and family functioning?
Methods
The methods used to identify and select evidence followed recommended best practice. 85,86 A protocol for the systematic reviews across the project was registered on the PROSPERO database (PROSPERO CRD42011001716).
Identification of evidence
Inclusion/exclusion criteria
The following inclusion and exclusion criteria were used to determine eligibility of articles. The inclusion criteria specified RCTs or economic evaluations involving CYP aged 0–25 years with LTCs and symptoms of mental ill health. Participants needed to have received any type of intervention that targeted their mental health. Clinical effectiveness had to be measured in terms of impact on at least one measure of the young person’s mental health. Additional details of inclusion and exclusion criteria are shown in Report Supplementary Material 1, Table 1.
Search strategy
A search strategy was developed and tested in the databases to be searched. The strategy used both controlled headings [e.g. medical subject heading (MeSH)] and free-text searching. Terms were grouped according to four concepts:
-
children and young people terms
-
mental health terms
-
long-term physical conditions terms
-
study design terms (using a Cochrane filter for locating RCT87).
The LTC terms were informed by previous reviews that included studies with populations with LTCs or chronic conditions,79,82,88–105 as well as discussion with experts among the wider project team. Thirteen electronic databases were searched: MEDLINE including MEDLINE in-process (via OvidSP), EMBASE (via OvidSP), PsycINFO (via OvidSP), Cochrane Database of Systematic Reviews (CDSR) (via The Cochrane Library), Cochrane Central Register of Controlled Trials (CENTRAL) (via The Cochrane Library), Database of Abstracts of Reviews of Effects (DARE) (via The Cochrane Library), Health Technology Assessment (HTA) database (via The Cochrane Library), NHS Economic Evaluation Database (NHS EED) (via The Cochrane Library), Cumulative Index of Nursing and Allied Health Literature (CINAHL) (via EBSCOhost), British Nursing Index (via ProQuest), Health Management Information Consortium (HMIC) (via OvidSP), Conference Proceedings Citation Index (via Web of Science) and Science Citation Index (via Web of Science). No language or date restrictions were applied. Searches were conducted between 28 January and 4 February 2016. An example search strategy used for the MEDLINE database is shown in Appendix 1. All references identified by the searches were exported into EndNote X7 (Thomson Reuters, New York, NY, USA) prior to deduplication and screening.
A second search strategy was designed to locate studies relating to cost-effectiveness using the University of York’s Centre for Reviews and Dissemination (CRD) search strategy for economic evaluations in place of the RCTs filter. 106 The economic evaluation filter for this search was applied to MEDLINE and EMBASE from April 2015 only as the NHS EED was updated using these databases up until 31 March 2015. Searches for economic evaluations were carried out on 3 May 2016. The search strategy used for EMBASE to locate economic evaluations is shown in Appendix 2.
Supplementary searches were also conducted. Backward citation-chasing (searching the references of included articles) was conducted by three researchers (DM, MN and LS) to locate further potentially relevant articles. Alongside backward citation-chasing, these researchers checked lists of included studies from related reviews. Forward citation-chasing (searching articles citing included articles) was conducted by an information specialist (JTB) using Web of Science and Google Scholar (Google Inc., Mountain View, CA, USA). In addition, three researchers (DM, LS and MN) searched websites that had been identified by the project team and the children and young people advisory group (CYPAG) for relevant research (see Appendix 3 for a list of websites searched). Targeted searches to identify ‘sibling’ papers (further outcomes, process evaluations, economic studies and qualitative research) associated with included trials and based on trial names and first and last authors were conducted by Juan Talens-Bou. Michael Nunns e-mailed all contact authors of included studies to request any articles associated with included articles. The databases CINAHL, HMIC and Conference Proceedings Citation Index were searched, all of which index grey literature. The website OpenGrey was also searched via www.opengrey.eu/ on 23 June 2016.
Study selection
Relevant studies were identified in two stages based on the inclusion/exclusion criteria given above. First, independent double screening of titles and abstracts for each record was conducted (seven researchers shared this screening: MN, LS, DM, JTC, MR, VB and IR). Endnote X7 was used to perform this screening. Disagreements were resolved through discussion between two reviewers, with referral to a third reviewer as necessary (DM, MN and LS). Full texts of records that appeared to meet the inclusion criteria on the basis of titles and abstracts were then obtained whenever possible via the University of Exeter online library, web searching and the British Library. Each full-text article was screened independently by two reviewers (six researchers shared this screening: MN, LS, DM, JTC, VB and IR). Reasons for exclusion at this stage were recorded. Disagreements were again resolved as for title and abstract screening. To assess population eligibility at full-text screening, reviewers often needed to locate information regarding cut-off scores for validated measures of mental health outcomes. These were rarely reported in screened records and, therefore, reviewers searched for publications including cut-off scores for these measures or manuals for the scale in question. Whenever possible a threshold indicating symptoms of clinical distress in a previous CYP sample was used. These thresholds were collated so that reviewers applied them consistently. Screening for the additional economic search proceeded in the same manner.
Methods of analysis/synthesis
Data extraction
A data extraction form was developed and piloted. Three researchers (MN, LS and DM) each extracted one article and checked one colleague’s extraction before discussing and amending the form. Data on article details and aims, participants, mental health measures at baseline, intervention, outcome measures, findings and study quality were extracted into Microsoft Office Excel® 2010 (Microsoft Corporation, Redmond, WA, USA) by three researchers (MN, DM and LS) and checked (by either DM or MN). When data were missing that would have allowed for meta-analysis, authors were contacted for information alongside our request for sibling papers.
Quality appraisal
Quality appraisal was conducted simultaneously with data extraction using criteria adapted from the Cochrane risk-of-bias tool. 86 In addition to criteria on randomisation, allocation concealment, blinding of assessors and selective outcome reporting from the existing tool, we included items on intention-to-treat analysis, between-group similarities at baseline, dropouts, response rates, intervention details and manuals, adherence, follow-up measures and psychometric properties of outcome measures (see Richardson et al. 107). This gave 15 items on which risk of bias and quality of included articles were assessed, providing additional insight into study quality and reporting. Assessment of quality and risk of bias was performed at the article level to evaluate any differences on account of the different outcomes reported in articles from the same study. Quality appraisal decisions were made by two reviewers (from DM, MN and LS) and disagreements resolved through discussion. The appraisals were used to evaluate risk of bias and study quality and were not used to exclude papers.
Categorisation of interventions and outcomes
During data extraction, interventions were categorised according to similarities in terms of broad intervention type and intervention content. The label and definition of these intervention categories were developed using the descriptions of interventions in the included studies and with reference to previous general classifications of interventions. The categories were developed by Darren Moore and Michael Nunns and discussed with the wider team. The categorisation was primarily used to organise the presentation of the synthesis by intervention type, with sections synthesising the findings from studies relating to each intervention category.
Owing to the diversity of outcomes used to measure the clinical effectiveness of interventions in the included studies, outcome categories were determined in response to the constructs measured by the instruments used. These categories and, therefore, each measure were also categorised at a broad level as either a ‘CYP mental health outcome’ or ‘other outcome’, given that the focus of the review is on interventions that aim to improve CYP mental health. Outcomes were categorised as CYP mental health when they appeared to meet our broad definitions of mental health and well-being given in Chapter 1. Other outcomes were extracted and analysed in order to include all clinical effectiveness outcomes and, therefore, address our second research question (what are the effects of such interventions on other key aspects of individual and family functioning?). These categories and the measures used within included studies are shown in the tables in Analysis of included study findings. These outcome categories were refined after data extraction by Michael Nunns and then reduced by Darren Moore before they were shared with experts among the wider team. These outcome categories were primarily used to determine when results for outcomes measuring similar constructs could be meta-analysed and as a way to compare similar outcomes for each intervention category, without necessitating knowledge of individual measures.
Data analysis and synthesis
The principal summary measure used to compare clinical effectiveness findings in included studies was differences in mean between intervention and control group post test and, when available, at the longest follow-up time point. For each outcome, mean, standard deviation (SD) and sample size (or figures that could be used to derive these when available) for the relevant intervention and control groups were used to assess differences between groups. When we did not receive necessary data for outcomes from either articles or correspondence with authors, we did not synthesise these outcomes. When such figures were not available for any CYP mental health outcomes in a study, we synthesised findings narratively. Effect sizes for each study were calculated post intervention using Cohen’s d, that is, the difference between the means in the two groups divided by their pooled SD. 108 Ninety-five per cent confidence intervals (CIs) for the effect sizes were also calculated, along with p-values. Effect sizes and CIs were calculated using the ‘metan’ command in Stata® v13 (StataCorp LP, College Station, TX, USA). The p-values for each effect size were calculated using the ‘ttesti’ command in Stata. Cohen’s guidelines were used to aid interpretation of effect sizes. 108 Thresholds above which effect sizes are considered to be ‘small’, ‘medium’ and ‘large’ are d = 0.20, d = 0.50 and d = 0.80, respectively. Although these classifications are widely used, it is acknowledged that these guidelines do not take account of how the clinical or practical importance of effects might vary between outcome measures. 109
Meta-analysis was considered feasible if multiple studies examined the same intervention type and used the same outcome category and a similar comparator and participant LTC. Random-effects meta-analysis models were fitted to pool effect sizes across the studies, based on the assumption that no two studies were addressing the same research questions in exactly the same way. We calculated 95% CIs for each pooled effect size estimate. The I2 statistic (possible range 0–100%) was used to quantify statistical heterogeneity, with higher values indicating greater heterogeneity. 110 When two or more measures assessing the same outcome category were reported in a study, the effects were combined into a single summary effect for that study, calculating the standard error for this effect using the correlation between the measures obtained from the paper itself or other research. 111 When different studies used identical measures, we conducted additional meta-analysis using raw mean differences. All meta-analyses and associated forest plots were produced using the ‘metan’ command in Stata.
We intended to assess publication bias by examining funnel plots for asymmetry using the ‘metafunnel’ command in Stata. However, we were unable to assess funnel plots properly or use more advanced regression-based assessments to assess publication bias owing to the substantial heterogeneity identified across studies and the small number of studies with similar characteristics that could be entered into a given meta-analysis. 112 Therefore, we cannot comment on publication bias in this review.
Results
Tables and figures described below are available in Report Supplementary Material 1.
Study selection
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram113 in Figure 1 summarises the process of study selection. Approximately 5% of the 18,360 records were identified by methods other than searches of academic databases, including citation-chasing searches, searching relevant reviews and websites, searches for sibling papers and author contact. After the removal of duplicates, a total of 11,706 records were screened at title and abstract stage. We attempted to retrieve the full text of 343 records for further consideration, and were successful in 336 cases (98%). After full-text screening, 312 articles were excluded for reasons provided in Figure 1. The majority of articles were excluded because CYP mental health measures did not indicate that the sample was above an established cut-off at baseline, no recognised cut-off was available for the measures used or there was not enough information to determine inclusion because only an abstract had been published. A number of articles were excluded because they did not meet inclusion criteria for one of intervention target, population or study design. Only one paper was excluded on account of the sample having moderate intellectual disabilities. A list of reasons for the exclusion of each article screened at full-text screening is given in Report Supplementary Material 1, Table 2.
FIGURE 1.
The PRISMA flow chart recording review 1’s study selection.
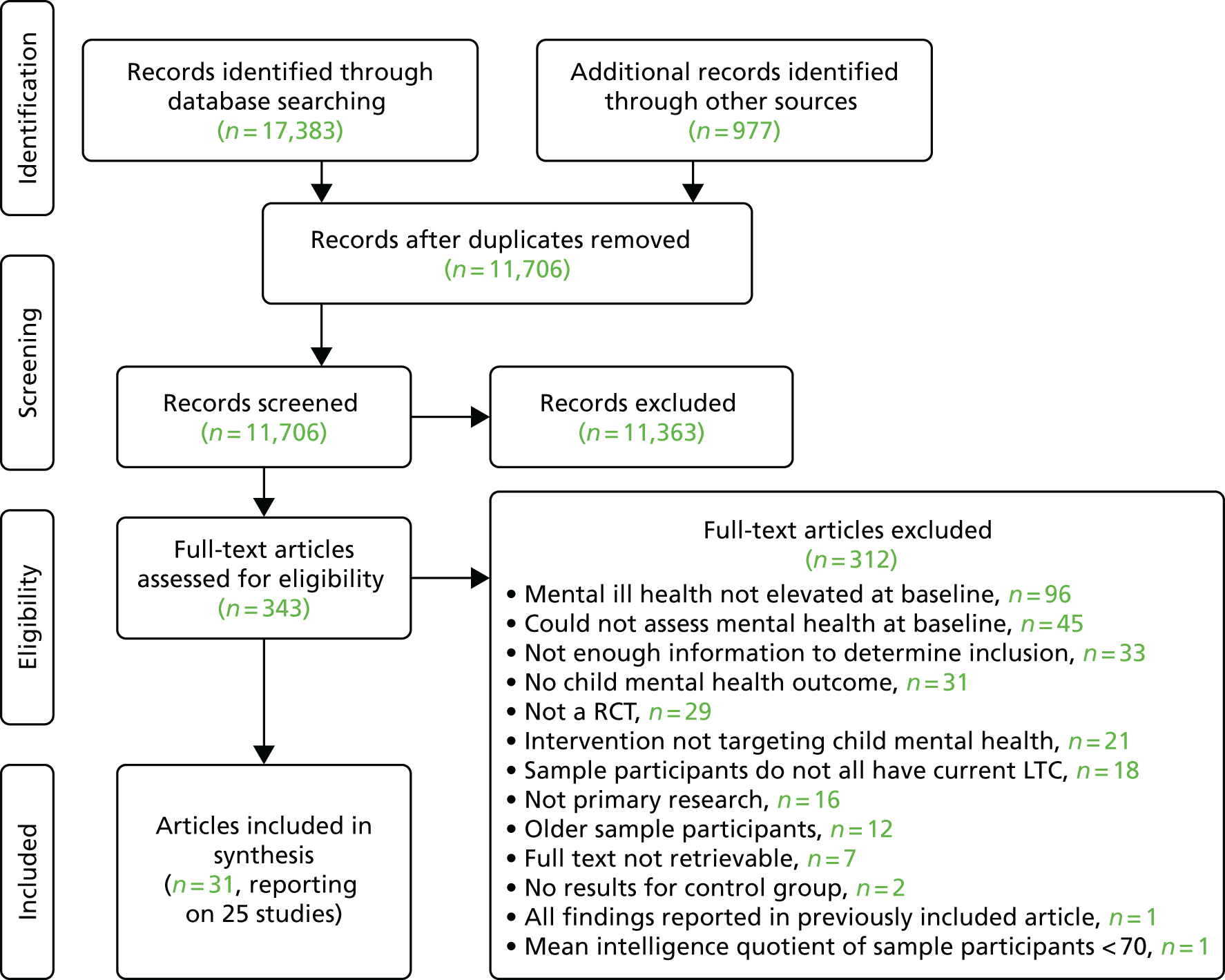
Thirty-one articles met our inclusion criteria and were included in the synthesis. Six of the articles were additional papers relating to studies already reported in included papers. These papers were included if they provided any additional relevant data not seen in other study articles. Eight of the 31 included articles were located through additional searching (forward citation-chasing, backward citation-chasing, author contact, included in previous reviews). We e-mailed 22 authors from the 25 included studies to ask for details of any other articles associated with the studies. Ten authors responded. Ten e-mails to authors included specific data queries. Six authors replied to the data queries, allowing additional effect sizes to be calculated. None of the 31 articles that met the full-text screening criteria reported economic outcomes such as costs or cost-effectiveness.
Economic evaluation
The PRISMA flow diagram in Figure 2 summarises the study selection after the second database search for economic evaluations and targeted search for sibling studies of the 31 articles included in the review. The majority (78%) of the 207 records were identified from the search of databases. Thirteen records were considered relevant after title and abstract screening. Both reviewers agreed that none of the 13 articles met the inclusion criteria for this part of the review. Two studies identified among the screened articles are worthy of note. Whittemore et al. 114 provided a single-cost estimate of providing a 5-week Teencope intervention that met the intervention inclusion criteria (see Report Supplementary Material 2, Table 5), but provided no breakdown of this cost or description of how it was calculated. In another study,115 figures on the use of ‘integrated psychological therapies’ to increase treatment adherence (the Shine intervention; see Report Supplementary Material 2, Table 5) allowed us to estimate the cost of providing the intervention/therapy to 12 patients as £4260. However, some costs (such as hospital staff training and costs of staff from the social enterprise) appear to have been excluded, and there were insufficient data presented for the stated net cost savings to be seen as reliable.
FIGURE 2.
The PRISMA flow chart recording review 1’s economic evaluation study selection.
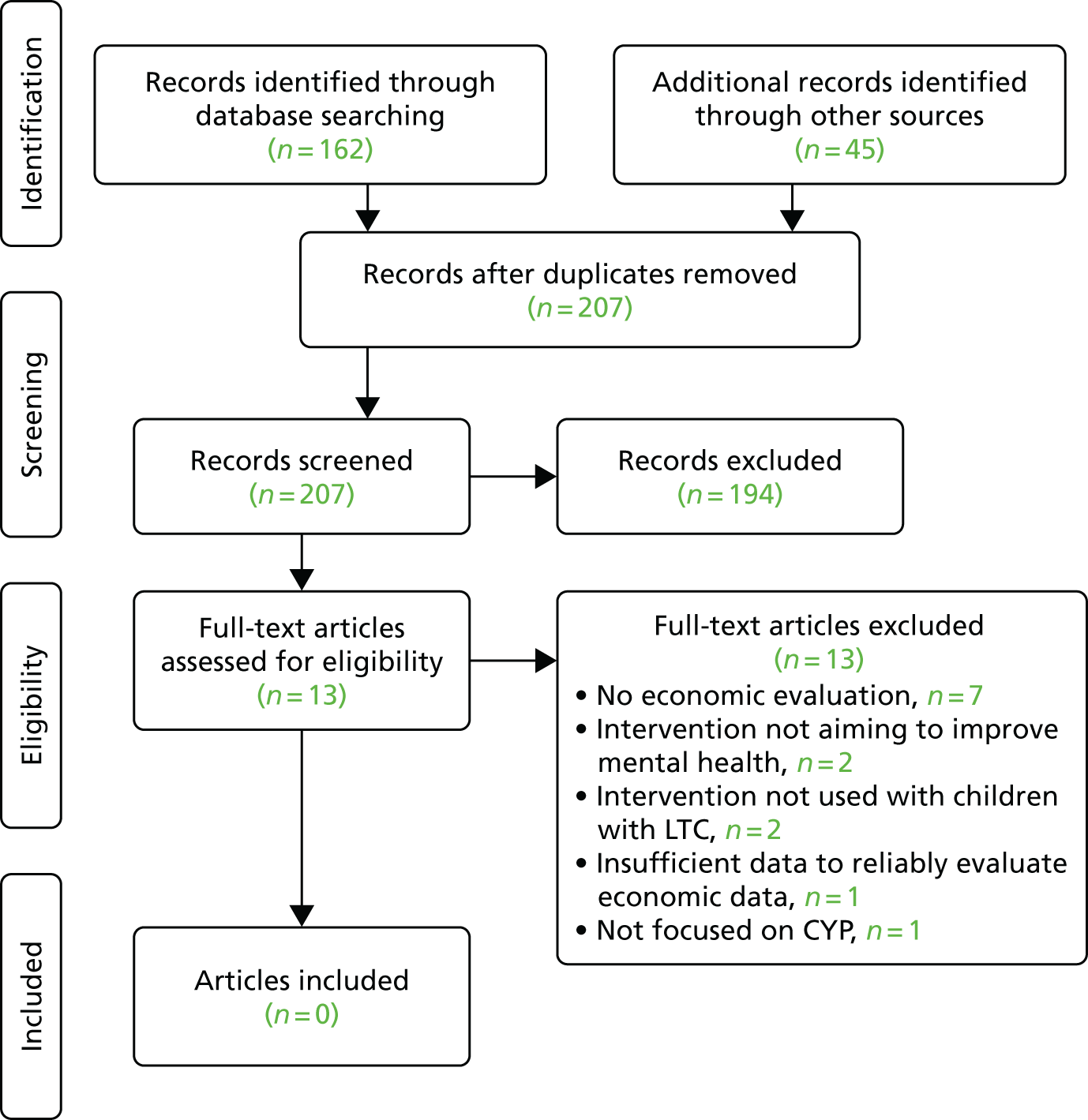
It was noted that two of the screened economic studies assessed the cost of the Positive Parenting Programme (Triple P) parenting intervention (i.e. Foster et al. 116 in the USA and Mihalopoulos et al. 117 in Australia), which was also evaluated in one of the effectiveness studies included in review 1 (i.e. Westrupp et al. 118). However, some features of the intervention used in these two studies differed from that used in the study by Westrupp et al. 118 (which would have made the costs different). In addition, both the study by Foster et al. 116 and that by Mihalopoulos et al. 117 targeted all families with at least one child below a particular age, rather than specifically families with children with LTCs. For these reasons, their findings would not be comparable to the findings of Westrupp et al. 118 or the results of similar parenting interventions targeting only families with children with LTCs. Therefore, this study was also excluded.
Descriptive statistics
Report Supplementary Material 1, Table 3, provides details about the study location, participants’ LTC, intervention type, comparator, qualifying baseline mental health status and other reported CYP mental health outcomes for the 25 studies included in this review. Studies were conducted in eight different countries, with the USA (n = 10)84,119–127 most common, followed by Australia (n = 5)118,128–131 and Iran (n = 4). 132–135 Studies included children and/or young people with 12 different LTCs, with cancers (n = 5)123,133,135–137 receiving the most attention. T1DM (n = 4),118,120,122,130 asthma (n = 3),119,138,139 IBD (n = 3)84,125,126 and hearing loss (n = 2)132,134 were also the subject of multiple studies, with all other LTCs featuring in one study each. Only one article was published before 2000,120 with 13 articles (52%) being published since 2010. 118,119,123–128,130–134,137,138
Five included studies were reported in more than one included journal article reporting on different study details or findings. Brown et al. 140 reported additional parent and family function outcomes from their 2014 trial. 128 We excluded one article associated with this study as it did not provide any effectiveness outcomes that were not seen in the previous articles. 128 Lyon et al. 123 included detailed information about the content of their intervention in 2013, with outcome data reported in the 2014 article. 123 The earliest Szigethy et al. 84 trial was linked with two additional papers. These reported on correlates of treatment with individual items on the Child Depression Inventory (CDI)141 and long-term follow-up data for the original trial. 142 For Szigethy et al. ’s143 later trial, the article reported secondary outcomes from a subset (those with Crohn’s disease) of the 2014 sample, which included both Crohn’s disease and ulcerative colitis patients. 126 Finally, the two papers from Whittingham et al. 131,144 reported different outcomes from their trial of a parenting and acceptance and commitment therapy (ACT) for children with cerebral palsy. The 2014 paper131 focused directly on child behaviour outcomes and parenting skills, whereas the 2015 paper144 reported child quality of life (QoL) related to physical functioning, and further parenting and parent mental health outcomes.
A range of interventions was evaluated, with those categorised as CBT the most frequent (n = 7). 83,84,124–126,130,145 After CBT, interventions categorised as parenting programmes133,142,145–147 and group play therapy148–150 were most commonly evaluated. Emotional intelligence training,132,134 stress management programmes120,122 and palliative care123,137 also featured in two studies each. Most often, the comparator involved ‘usual care’ (e.g. regular schooling, usual sedation, usual hospital care) within a given setting (n = 20),83,84,118,120,122–124,127,128,130–139,145 with five of these studies employing a waiting list control group. 122,124,127,131,137 Active comparators in the remaining five studies included asthma education,119 progressive muscle relaxation,121 aerobic exercise129 and non-directive supportive therapy. 125,126
Two studies contained in their inclusion criteria a mental health diagnosis (principal anxiety disorder in Masia-Warner et al. ,124 mild or major depression in Szigethy et al. 126). All other studies included samples from which reviewers found that symptoms of mental ill health were above an established threshold or included a sample at risk of a mental health disorder. 83 At baseline, elevated symptoms of anxiety119,121–125,127,136,137,139 and depression83,84,121,126,129,133,135,137,139,145 were most common, each present in 10 studies. The participants in seven studies showed elevated symptoms in more than one mental health domain. 84,121,124,132,134,137,139 Additional CYP mental health outcomes were reported in 15 studies,84,120,122,123,126–128,130–133,137,138,140,144,145 crossing a wide range of categories including anxiety and depression, coping measures, emotional difficulties, adjustment and general mental health.
Sample characteristics
The studies included a total of 1198 participants, of whom 48.1% were female, with a mean age of 12.2 years (when data were available: gender not reported by Gordon et al. 129 and mean age not reported by Hains et al. 122 and Zareapour et al. 135). The ethnicity of the sample was predominantly (> 66%) white in seven studies84,120,122,124–126,128 and predominantly black or African American in two studies. 119,121 Lyon et al. 123 and Yetwin127 recruited samples from a more diverse mix of ethnicities, but ethnicity was not reported in 12 studies. Report Supplementary Material 1, Table 4, provides details about the sample size, gender, age, ethnicity and inclusion criteria for each study.
Eleven studies provided some information about the socioeconomic status of participants. 84,118,120,121,123–126,128,131,137 The method of classifying socioeconomic status was inconsistent, with family income,84,124–126,128,131 federal poverty level,123 parental education,84,123,128,131 parental employment status,128 social class,137 a socioeconomic index118 and the Hollingshead Index120,121 all reported, preventing comparison across the included studies.
Thirteen studies recruited subjects from hospitals. 84,118,120–123,126,130,133,135–137,145 Referrals by specialists or general practitioners, with or without additional advertising in clinics or waiting rooms (flyers, online posts, etc.), was the second most common method of recruitment, used in six studies. 83,124,125,127–129 Three further studies recruited from schools119,132,134 and two by consulting patient databases. 131,139 In total, 111 (9.2%) participants dropped out from studies after the intervention delivery had commenced, which appears low. 151
Typically, inclusion criteria in included studies required diagnosis of the relevant LTC, lack of intellectual disability that would prevent understanding of interventions or assessments and willingness/availability to participate. Five studies had specific requirements of elevated mental health symptoms for inclusion. 83,84,124,126,128 Martinović et al. 83 required ‘subthreshold’ depression scores (just below a validated cut-off point on three scales) whereas Szigethy et al. 84 required a minimum score of 9 on the CDI. In the 2014 study by Szigethy et al. ,126 diagnosis of minor or major depression was required and confirmed using the Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (K-SADS-PL) diagnostic interview. Brown et al. 128 included parents who subjectively considered their child to have behavioural problems. Masia-Warner et al. 124 recruited participants with a previously diagnosed principal anxiety disorder. However, 13 studies excluded participants with certain mental health diagnoses or issues. 83,84,118,123–127,130,132,135,138,139 Therefore, some studies excluded particular mental health diagnoses, even when other diagnoses or elevated symptoms were required.
Intervention characteristics
Report Supplementary Material 1, Table 5, provides details about the interventions reported in the included studies. The intervention aims and structure, as well as details of the delivery site and personnel, the intended recipients and the comparator group, are shown. Eleven intervention categories were used to group together similar interventions. The label and definition of these intervention categories are shown, along with the studies evaluating them, in Appendix 4. Interventions based on CBT were the most frequently studied (n = 7),83,84,124–126,130,145 with 267 participants randomised to this type of intervention. The two studies reported by Szigethy et al. 84,126 explored the effects of the CBT programme PASCET-PI (Primary and Secondary Control Enhancement Therapy-Physical Illness) on various outcomes in children with IBD84 or Crohn’s disease. 143 Masia-Warner et al. 124 and Reigada et al. 125 used versions of TAPS (treatment of anxiety and physical symptoms), the latter authors modifying the intervention to include management of specific symptoms of IBD. Adapted intervention content was seen in eight studies. 84,119,120,124–126,130,145 All but two of these were trials of CBT, with Bignall et al. ’s119 relaxation intervention and Boardway et al. ’s120 stress management training also including adapted content. For each study, Appendix 5 describes the content of each intervention, and whether it was adapted or delivered flexibly. Only Szigethy et al. 126 specifically allowed flexibility in delivery, allowing for individual changes to content based on the developmental stage of the recipient.
The parenting programmes Triple P118 and its modified subsidiary for families in which a child has a disability and behavioural problems, Stepping Stones Triple P (SSTP),128,131 were assessed in three studies, with 93 parents randomised to these intervention conditions. The study by Whittingham et al. 131 was the only one to include more than one intervention condition, as both SSTP with and without additional ACT featured. Group play therapy featured in three studies,133,135,138 with 44 participants randomised to these treatment arms. Palliative care (n = 49),123,137 emotional intelligence training (n = 40)132,134 and stress management programmes (n = 16)120,122 featured in two studies each.
Progressive muscle relaxation (PMR) techniques featured in three studies. 119,133,139 However, they formed part of only two intervention arms, with 47 participants receiving such interventions. Specifically, Bignall et al. 119 trialled an intervention containing breathing retraining with PMR, asthma education and guided imagery, whereas Yang et al. 139 used 30 minutes of audio-recorded guided muscle relaxation nightly before going to sleep. PMR was also an active comparator in the intervention trialled by Diego et al. ,121 in which the intervention was massage therapy. Sometimes the intervention label used in the study indicated that more than one intervention category might be relevant, for instance Hains et al. ’s122 cognitive restructuring and problem solving and Nekah et al. ’s133 structured cognitive–behavioural group play therapy both suggest CBT. The descriptions of interventions provided in articles were used to assess which category was most suitable.
The most common comparator involved treatment as usual (TAU) or usual care (e.g. regular schooling, usual sedation, usual hospital care) within a given setting (n = 20),83,84,118,120,122–124,127,128,130–139,145 with five of these studies employing a waiting list design. 122,124,127,131,137 In total, 393 participants were randomised to standard or usual care control groups. Active comparators in the remaining six studies (n = 157 participants) included asthma education,119 PMR,121 aerobic exercise129 and non-directive supportive therapy. 125,126 Standard care/TAU was often described only roughly and varied considerably between studies, to the extent that determining common components was not possible. During the waiting period of studies with waiting list designs, all participants received usual care.
Interventions were received by parents alone in three studies,118,128,131 by parents and children together in five studies84,123,125,126,145 and by CYP alone in the remainder. When both parents and CYP received the intervention, the goal was usually to give parents skills to help them encourage positive behaviours at home and develop skills to maintain positive effects beyond the intervention end. This occurred as a component of CBT interventions, with the exception of Lyon et al. ’s123 palliative care intervention, in which the aim was to include the family in decision-making. The delivery of interventions occurred across a variety of settings and through a range of personnel. Twelve studies delivered at least part of their intervention in a hospital setting. 84,118,120,122,123,126,128–130,133,136,145 Five interventions took place in other medical centres or university outpatient departments,83,124,125,127,135 three were delivered in school settings119,132,134 and one at home. 139 In Shoshani et al. ’s137 study, which assessed the Make-A-Wish (Make-A-Wish Foundation® UK, Reading, UK) intervention, children’s wishes were ascertained in their own home, but the nature of their delivery was not reported. Seven studies included some component that required delivery, receipt or practice of the intervention at home. 84,119,123,126–128,131
Interventions were delivered by researchers, clinicians, therapists, psychologists, postgraduate students and teachers. Specific training in the delivery of the intervention was reported in 12 studies. 84,123,125–128,131,132,136,137,139,145 Intervention manuals were referred to in only nine studies. 84,118,123,125–128,130,131
Quality appraisal and risk of bias
Table 1 provides a summary of the quality and risk-of-bias appraisal of included articles. Risk of bias was performed at the article, rather than study, level, as data collection and/or outcomes differed across articles and, therefore, risk of bias may vary where there were several publications reporting on a single study. Eight of the 15 criteria allowed a rating of ‘Yes’, ‘No’ or ‘unclear’. An additional ‘not applicable’ option was available for four criteria (whether or not intention-to-treat analysis was performed, the longest follow-up was at ≥ 6 months, dropouts were described and missing data were explained). For comparative purposes, a response rate at the longest follow-up of ≥ 85% was considered high, 70–84% as moderate and < 70% was considered a poor response rate. For the assessment of outcome measures, only when all outcomes had good psychometric properties was the score deemed positive.
| Study author and year of publication | Adequate method of randomisation? | Allocation concealed? | Intention-to-treat analysis performed? | Blinding of outcome assessor in at least one measure? | Group outcomes similar at baseline, or imbalances accounted for? | Response rate at longest follow-up (%) | Intervention well described? | Adherence, compliance or fidelity measured? | Included follow-up beyond post treatment? | Longest follow-up ≥ 6 months? | Were any dropouts and attrition described? | Proportion of outcome measures with good psychometric properties? | Was missing data explained? | Is the study free of suggestion of selective outcome reporting? | Was there a treatment manual for the intervention? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ashori et al.,132 2013 | ? | ? | n/a | N | Y | ≥ 85 | N | N | N | n/a | n/a | 1/1 | n/a | Y | N |
| Bignall et al.,119 2015 | Y | ? | N | N | N | ≥ 85 | Y | N | N | n/a | Y | 4/4 | n/a | Y | N |
| Boardway et al.,120 1993 | ? | ? | N | ? | Y | ≥ 85 | Y | N | Y | N | N | 11/12 | N | Y | N |
| Brown et al.,128 2014 | Y | Y | Y | N | N | < 70 | Y | Y | Y | Y | Y | 3/3 | Y | Y | Y |
| Brown et al.,140 2015 | Y | Y | Y | N | N | < 70 | Y | Y | Y | Y | Y | 7/7 | Y | Y | Y |
| Bufalini136 2009 | ? | ? | n/a | N | N | ≥ 85 | N | N | N | n/a | n/a | 3/4 | n/a | Y | N |
| Diego et al.,121 2001 | ? | ? | n/a | ? | ? | ≥ 85 | Y | N | N | n/a | n/a | 4/4 | n/a | Y | N |
| Gordon et al.,129 2010 | Y | Y | Y | Y | N | ≥ 85 | N | N | N | n/a | Y | 5/7 | Y | Y | N |
| Hains et al.,122 2000 | N | ? | N | ? | Y | ≥ 85 | Y | N | Y | N | n/a | 5/5 | N | Y | N |
| Lyon et al.,123 2014 | Y | ? | Y | N | Y | ≥ 85 | Y | N | N | n/a | n/a | 4/4 | Y | Y | Y |
| Lyon et al.,123 2014 | Y | ? | Y | N | Y | ≥ 85 | Y | Y | N | n/a | n/a | 2/3 | Y | Y | Y |
| Martinović et al.,83 2006 | Y | ? | n/a | N | Y | ≥ 85 | N | N | Y | N | N | 4/5 | n/a | Y | N |
| Masia-Warner et al.,124 2011 | Y | ? | N | Y | Y | ≥ 85 | N | N | Y | N | Y | 4/5 | Y | Y | N |
| Nekah et al.,133 2015 | ? | ? | N | N | Y | 70–84 | Y | N | N | N | Y | 1/1 | n/a | Y | N |
| Pourmohamadreza-Tajrishi et al.,134 2013 | ? | ? | n/a | N | Y | ≥ 85 | N | N | N | n/a | n/a | 1/1 | n/a | Y | N |
| Reigada et al.,125 2015 | Y | ? | Y | Y | Y | ≥ 85 | Y | Y | Y | N | Y | 4/4 | N | Y | Y |
| Serlachius et al.,130 2016 | Y | Y | Y | ? | Y | < 70 | Y | N | Y | Y | N | 4/4 | N | Y | Y |
| Shoshani et al.,137 2016 | Y | ? | N | N | Y | ≥ 85 | N | N | Y | N | Y | 5/5 | N | Y | N |
| Szigethy et al.,84 2007 | ? | ? | N | Y | Y | < 70 | Y | Y | N | n/a | Y | 6/6 | N | Y | Y |
| Szigethy et al.,141 2009 | ? | ? | N | Y | Y | < 70 | Y | Y | N | n/a | N | 3/3 | N | Y | Y |
| Szigethy et al.,126 2014 | ? | ? | Y | Y | Y | 70–84 | Y | Y | N | n/a | N | 7/7 | N | Y | Y |
| Szigethy et al.,143 2015 | ? | ? | Y | Y | Y | 70–84 | Y | Y | N | n/a | N | 5/5 | N | N | Y |
| Thompson et al.,142 2012 | ? | ? | N | Y | Y | 70–84 | Y | Y | Y | Y | N | 3/3 | N | Y | Y |
| Wang et al.,138 2012 | Y | ? | N | N | Y | ≥ 85 | Y | N | N | n/a | Y | 2/2 | n/a | Y | N |
| Westrupp et al.,118 2015 | Y | Y | Y | N | Y | 70–84 | N | N | Y | Y | N | 9/9 | N | Y | Y |
| Whittingham et al.,131 2014 | Y | Y | Y | N | Y | < 70 | Y | Y | Y | Y | Y | 3/3 | Y | Y | Y |
| Whittingham et al.,144 2016 | Y | Y | Y | N | Y | < 70 | Y | Y | Y | Y | Y | 4/4 | Y | Y | Y |
| Wicksell et al.,145 2009 | Y | ? | Y | N | Y | 70–84 | Y | N | Y | Y | N | 7/9 | N | Y | N |
| Yang et al.,139 2004 | ? | ? | n/a | Y | Y | ≥ 85 | N | N | N | n/a | n/a | 2/8 | n/a | Y | N |
| Yetwin,127 2011 | N | ? | N | ? | Y | 70–84 | N | N | N | n/a | Y | 8/8 | N | N | Y |
| Zareapour,135 2009 | ? | ? | N | N | Y | ≥ 85 | N | N | N | N | Y | 1/1 | n/a | Y | N |
The included articles were often free from risk of bias on freedom from selective outcome reporting, with 33 out of 35 papers rated ‘yes’. Lack of differences or adjustment for differences between groups at baseline was present in 28 out of 35 articles. Twenty-seven articles included only outcomes with good psychometric properties, and five of the eight articles not meeting this criterion were marked down on only one outcome measure. 83,120,123,124,136 Seventeen articles reported a response rate at the longest follow-up of ≥ 85%; however, none of these articles collected follow-up data at a period ≥ 6 months following the intervention. For those eight articles that did include longer follow-ups, response rates were 70–84% in three articles118,142,145 and < 70% in the rest. 128,130,131,140,144
The criteria that indicated risk of bias most often across articles were the assessment of adherence, compliance or fidelity (20/31 ‘no’); explaining missing data (13/31 ‘no’); blinding of assessors and inclusion of a follow-up after treatment (both 17/31 ‘no’). In addition, only half of those articles including a follow-up assessment did this at ≥ 6 months. The selection bias domains scored poorly, largely because of a lack of clarity in reporting.
Four articles were rated as being at a particularly high risk of bias (were judged to be of poor quality in relation to ≥ 50% criteria). 83,127,135,136 There were five other articles in which < 50% of criteria scored positively and > 15% of criteria were unclear, indicating potential risk of bias. 120,121,132,133,139 In all five articles, it was not possible to determine whether or not randomisation was adequate or allocation was concealed. However, these articles were rated as being free from bias in relation to the suggestion of selective reporting, and had a ≥ 85% response rate at follow-up (except Nekah et al. 133), although none included a follow-up assessment at ≥ 6 months.
The articles by Yetwin127 and Hains et al. 122 were rated as being at risk of bias on adequacy of randomisation because both allowed two participants to swap groups after allocation.
The articles demonstrating as being at the lowest risk of bias were by Whittingham et al. ,131,144 both of which were rated positively on 13 criteria. The only risk of bias in the Whittingham articles arose because outcomes were self-reported, therefore assessors were not blinded, and the response rate at the longest follow-up was < 70%. This poor response rate was symptomatic of the few studies to collect data at the 6-month follow-up interval. The two articles reporting on the study by Brown et al. 128,140 performed similarly to the Whittingham articles. The article by Reigada et al. 125 was also rated as being at low risk of bias overall, with only two negative scores.
Analysis of included study findings
Effectiveness of cognitive–behavioural therapy interventions
Interventions categorised as CBT were the most common type of intervention, featuring in 10 articles reporting on seven studies across a range of LTCs: epilepsy, persistent functional somatic complaints, IBD, T1DM and chronic pain. 83,84,124–126,130,145 Across the seven studies, 531 participants were randomised. Comparators were TAU, waiting list or non-directive supportive therapy (NDST). 84,125,126 Despite being the most common intervention type, there was no opportunity to meta-analyse data because of differing LTCs, control groups and outcomes. The included studies were also characterised by small samples and varying risk of bias. Six different CBT interventions were assessed across the seven studies. All interventions in this category shared components of typical CBT interventions and/or were identified as a CBT intervention. All of these interventions aimed to improve both mental and physical health. Mental health variables included depression,83,84,126,145 anxiety124,125 and stress. 130 Parent sessions were included in all but two of the interventions. 83,130 Exposure and ACT in Wicksell et al. ’s study145 were categorised as CBT because exposure exercises were seen in other CBT interventions,124,125 and the authors145 characterised ACT as a development of CBT.
Five of the interventions [Best of Coping (BOC),130 TAPS,124 TAPS+IBD,125 PASCET-PI84,126 and Exposure and ACT145] contained content adapted for the LTC of the sample in the study (T1DM,130 persistent functional somatic complaints,124 IBD84,125,126 or chronic pain145) by the inclusion of intervention content such as tasks identifying IBD-specific stressors and developing ways to cope with symptoms,125 addressing fears specifically related to physical pain124 and integrating illness narratives and working on the development of healthy IBD-related cognitions and behaviours. The intervention trialled by Martinović et al. 83 targeted depressive thoughts and did not contain any LTC-specific (epilepsy) content.
Children and young people mental health outcomes
Depression was assessed in the four studies whose intervention aimed to improve this outcome. 83,84,126,145 Three of the studies measured depression using multiple measures,83,84,126 meaning that this was the most frequently occurring outcome category for CBT interventions. General mental health was assessed in four studies,84,124,126,145 and two studies whose interventions aimed to improve anxiety also measured it as an outcome. 124,125
Report Supplementary Material 1, Table 6, displays means and SD for control and intervention groups for each CYP mental health outcome assessed post intervention, in which sample size, mean and SD were reported or calculable. Effect sizes (Cohen’s d), 95% CIs and p-values are included, with a positive effect size representing improvement on the measure.
Evidence of the beneficial effect of CBT for measures of CYP mental health can be found in six out of the seven studies featuring this type of intervention. Evidence of the beneficial effect of CBT on depression across all outcomes is provided by one study83 in which large positive effect sizes are seen for all depression measures, although wide 95% CIs for two of the measures include negligible effect sizes, reflecting the imprecision of the estimate of effect [Beck Depression Inventory (BDI): d = 0.85, 95% CI 0.10 to 1.60; p = 0.03; Centre for Epidemiological Studies Depression scale (CES-D): d = 0.86, 95% CI 0.11 to 1.61; p = 0.03]. Evidence for the beneficial effect of CBT on depression from other studies is less clear; although small to large positive effect sizes were seen for the other studies reporting depression outcomes, these effects tended to be imprecise, with 95% CIs typically including negligible or even slightly harmful effects. Reigada et al. 125 provide evidence of a large beneficial effect of CBT on IBD-specific anxiety (d = 1.31, 95% CI 0.36 to 2.27; p = 0.007). However, there was little evidence for a beneficial effect of CBT on anxiety in the study by Masia-Warner et al. 124 (d = 0.27, 95% CI –0.38 to 0.92; p = 0.41). There was some evidence for a large beneficial effect of CBT on general mental health according to Masia-Warner et al. 124 (d = 1.11, 95% CI 0.42 to 1.81; p = 0.002) and Szigethy et al. 84 (d = 0.91, 95% CI 0.25 to 1.56; p = 0.007), although the wide CIs in the latter study include small effect sizes reflecting the imprecision of the estimate of effect. However, Wicksell et al. 145 report a lack of evidence for the beneficial effect of CBT on general mental health (d = 0.40, 95% CI –0.40 to 1.13; p = 0.41) in their trial. There was no opportunity to meta-analyse CYP mental health outcomes for these interventions evaluating CBT because of differing LTCs or comparators across studies in which outcome categories were shared.
Other outcomes
Report Supplementary Material 1, Table 7, displays findings for other outcomes assessed post intervention. Conflicting evidence regarding the beneficial effect of CBT on LTC-specific QoL and LTC symptoms can be seen across the studies featuring CBT interventions. For instance, although the study by Martinović et al. 83 provides evidence of a large beneficial effect of CBT for epilepsy-specific QoL (d = 1.55, 95% CI 0.72 to 2.37; p < 0.001), a lack of evidence for such a beneficial effect on diabetes mellitus control was reported by Serlachius et al. 130 (d = 0.32, 95% CI –0.08 to 0.73; p = 0.12). The study by Masia-Warner et al. 124 provides evidence of some medium to large beneficial effect sizes for CBT on measures of LTC symptoms. Large beneficial effect sizes for self-reported (d = 1.33, 95% CI 0.61 to 2.05; p < 0.001) and parent-reported (d = 0.98, 95% CI 0.30 to 1.67; p = 0.005) pain were found, as well as a medium beneficial effect on somatisation (d = 0.75, 95% CI 0.08 to 1.42; p = 0.03), although the wide CI for somatisation includes negligible effect sizes, reflecting the imprecision of this estimate of effect. The study by Wicksell et al. 145 provides evidence of large beneficial effects of CBT for pain (d = 1.25, 95% CI 0.45 to 2.05; p = 0.002) and pain-related emotional discomfort (d = 1.46, 95% CI 0.63 to 2.28; p < 0.001). However, there was little evidence for a beneficial effect of CBT on other pain and LTC symptoms outcomes measured by Wicksell et al. 145 There was little evidence for a beneficial effect of CBT on LTC symptoms in other studies. 125,126,130
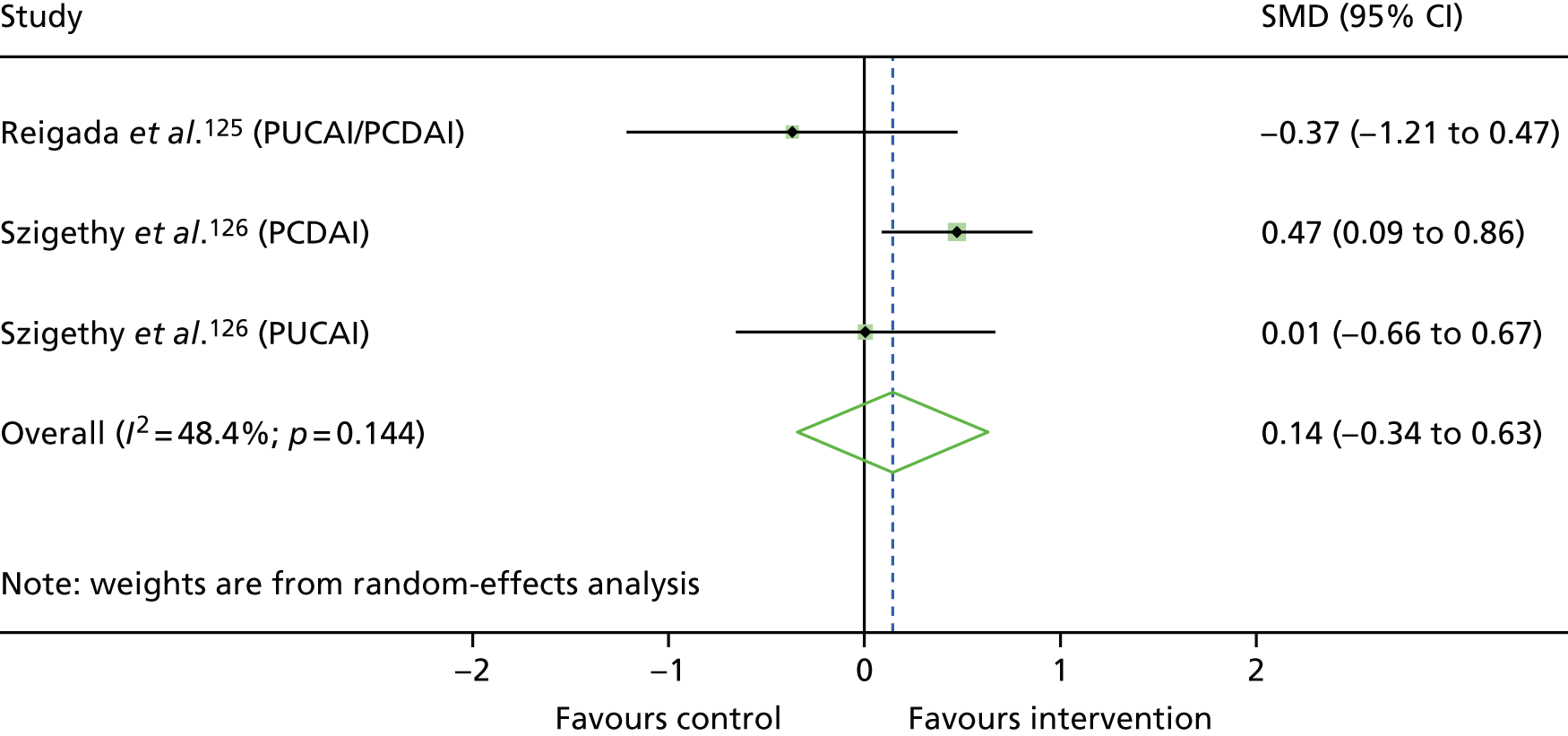
Evidence for the effect of CBT on LTC symptom severity could be investigated further by meta-analysing outcomes from Szigethy et al. 126 and Reigada et al. ,125 both of which studied patients with IBD and used NDST as the comparator. Reigada et al. 125 reported pooled data for the Paediatric Ulcerative Colitis Activity Index (PUCAI) and Paediatric Crohn’s Disease Activity Index (PCDAI) outcomes,125 whereas Szigethy et al. 126 reported separately for participants with ulcerative colitis and Crohn’s disease. Figure 3 is a forest plot of the effects of CBT on these disease activity measures reported in these studies. This meta-analysis demonstrated little evidence of an effect of CBT on LTC symptoms (d = 0.14, 95% CI –0.34 to 0.63; p = 0.56).
FIGURE 3.
Forest plot showing the results of meta-analysis of the effects of CBT on IBD symptoms post intervention for included studies. SMD, standardised mean difference (Cohen’s d).
Overall, the seven included studies that evaluated the clinical effectiveness of interventions categorised as CBT aiming to improve the mental health of CYP with LTCs show some promising effects. A number of large beneficial effects for CYP mental health and other outcomes were seen, although effects for particular outcomes were rarely consistent across all studies. The heterogeneity in study characteristics prevented meta-analysis of CYP mental health outcomes. The available sample of studies is small, targeting different aspects of mental health for children with different LTCs. There was also diversity in quality and risk of bias across these studies.
Effectiveness of parenting interventions
Parenting interventions without acceptance and commitment therapy
Of the four parenting interventions assessed in included studies, two were parenting without ACT (Westrupp et al. 118 and Whittingham et al. 131,144). Westrupp et al. 118 assessed the Triple P in families with a child with diabetes mellitus, whereas one of the intervention arms in Whittingham et al. 131,144 was SSTP alone. SSTP is tailored towards families with pre-adolescent children with a disability, which may be physical or intellectual, and behavioural problems. 148 The sample in the study by Whittingham et al. 131,144 had cerebral palsy. Both studies had similar aims, including improving aspects of CYP mental health, with a focus on behavioural and emotional problems in Whittingham et al. 131,144 as well as improving parenting. A total of 50 participants were randomised to intervention or control arms, with all control participants (n = 32) receiving TAU (Whittingham et al. 131,144 used a waiting list control). In both studies, the primary aim was to reduce child behavioural problems through improved parenting skills. Westrupp et al. 118 examined the effects of Triple P in a group of families with children who had elevated behavioural problems at baseline, as well as a group without elevated behavioural symptoms. We were unable to obtain raw data for the subgroup analysis of families with children with behaviour problems and, therefore, could not calculate effect sizes for the study.
Report Supplementary Material 1, Table 8, shows the findings for each CYP mental health outcome assessed post intervention by Whittingham and colleagues. 131,144 Despite a medium-sized beneficial effect for the Eyberg Child Behavior Inventory (ECBI): Problems subscale (d = 0.72, 95% CI 0.04 to 1.40; p = 0.04), there was a lack of evidence for the beneficial effect of a parenting programme on child behaviour, with 95% CIs on the other measures of child behaviour all including harmful effects. There was conflicting evidence of the effect of parenting on social dysfunction, with a large beneficial effect seen for the Strengths and Difficulties Questionnaire (SDQ) peer problems subscale, although a wide 95% CI includes negligible effect sizes, reflecting the imprecision of the estimate of effect (d = 0.88, 95% CI 0.19 to 1.57; p = 0.01), but there was little evidence of a beneficial effect on the prosocial subscale (d = –0.19, 95% CI –0.84 to 0.47). A medium effect size was also found in this study for the SDQ emotional behaviour subscale (d = 0.64, 95% CI –0.03 to 1.31; p = 0.06), but the imprecise 95% CI includes negligibly harmful effects. Although it was not possible to calculate effect sizes for the outcomes reported by Westrupp et al. ,118 the article reports medium to large and statistically significant beneficial effects for externalising problems, internalising problems and disruptive behaviours for the participants with behaviour problems receiving the intervention. Because of the different LTCs in the two studies and the lack of necessary statistics reported in the study by Westrupp et al. ,118 a meta-analysis was not performed for these CYP mental health outcomes or others reported below.
Numerous secondary outcomes were also reported. Given the parent-focused nature of the interventions, the studies by both Westrupp et al. 118 and Whittingham et al. 131,144 assessed parenting styles and parent mental health. A number of outcomes related to LTC symptoms and LTC-specific QoL were also reported. Report Supplementary Material 1, Table 9, displays findings for these other outcomes. Overall, the study by Whittingham et al. 131,144 demonstrates a lack of evidence of a beneficial effect of this parenting intervention on other outcomes, except parenting confidence, which recorded a medium-sized beneficial effect, but the wide 95% CI included negligible effect sizes (d = 0.69, 95% CI 0.02 to 1.37; p < 0.05). 131,144 Westrupp et al. 118 found statistically significant medium effect sizes for parent mental health, but only evidence of the benefit of a parenting intervention for some measures of parenting and family functioning for participants with behaviour problems.
Westrupp et al. 118 included follow-up assessments of all outcomes 12 months post intervention. They reported large statistically significant favourable effects for parent anxiety and stress at 12 months, but not for the CYP mental health and other outcomes assessed.
These two studies investigated the effect of parenting programmes on a wide range of outcomes, yet clear evidence for benefits was rarely seen. The study by Whittingham et al. 131,144 provides conflicting evidence relating to child behaviour and social dysfunction across different measures used. For other outcomes, reported effect sizes were typically small with wide CIs, reflecting imprecision in effect estimates. Overall, with only two RCTs assessing parenting interventions without an ACT component and only one providing data that allowed the calculation of effect sizes, there is weak evidence relating to the effectiveness of parenting programmes for improvement of child or parent outcomes.
Parenting interventions with acceptance and commitment therapy
The study by Whittingham et al. 131,144 included two intervention groups; as well as SSTP, summarised in Parenting interventions without acceptance and commitment therapy, the authors assessed the clinical effectiveness of SSTP plus ACT. Brown et al. 128,140 also evaluated the clinical effectiveness of SSTP plus ACT. Whittingham et al. 131,144 investigated SSTP plus ACT in children with cerebral palsy, whereas the sample of children in the trial by Brown et al. 128,140 had an ABI, of whom a proportion (7%) had cerebral palsy. Both studies compared the parenting intervention with TAU, with Whittingham et al. 131,144 employing a waiting list control group. Both studies aimed to reduce child behaviour and emotional problems and dysfunctional parenting. Because of the consistent comparator and LTC between studies, similar outcomes were considered eligible for meta-analysis. In total, the parents of 92 children were randomised equally between SSTP plus ACT and control groups. Whittingham was a co-author on both Brown et al. 128,140 papers whereas Boyd and McKinlay were co-authors on all four included papers across both studies. 128,131,140,144
Report Supplementary Material 1, Table 10, summarises findings for each CYP mental health outcome assessed post intervention. As for the SSTP intervention discussed in the previous section, evidence of improvement on the ECBI: Problems subscale is provided in the study by Whittingham et al.,131,144 in which a large beneficial effect size was observed (d = 1.34, 95% CI 0.65 to 2.03; p < 0.001). There was a lack of evidence for the beneficial effect of SSTP plus ACT on other behaviour outcomes. Only for the ECBI: Intensity subscale was a medium beneficial effect reported, but the wide 95% CI included negligible beneficial effect sizes (d = 0.78, 95% CI 0.14 to 1.43; p = 0.02). Brown et al. 128,140 observed a slightly larger effect for the same measure (d = 0.82, 95% CI 0.25 to 1.38; p = 0.005), although they did not mirror the evidence from Whittingham et al. 131,144 of a large beneficial effect for the ECBI: Problems subscale. Brown et al. 128,140 also found a medium beneficial effect for a measure of emotion problems (d = 0.76, 95% CI 0.19 to 1.32; p = 0.009), although the wide CI reflects the imprecision of the estimate. There was little evidence for a similar beneficial effect for emotional problems in the study by Whittingham and colleagues. 131,144
As these studies had the same intervention, LTC and comparator, a meta-analysis was performed on behaviour (Figure 4) and emotional problems outcomes (Figure 5). For the meta-analysis of child behaviour the effects from ECBI: Problems and ECBI: Intensity were combined into a single summary effect for each study, calculating the standard error for this effect using an estimate of the correlation between the subscales, obtained from other research. 152 There was evidence of the beneficial effect of SSTP plus ACT for both outcomes with a large beneficial effect for child behaviour problems (d = 0.81, 95% CI 0.38 to 1.23; p < 0.001) and a medium beneficial effect for emotional problems, although the latter in particular was characterised by wide CIs that included small effect sizes (d = 0.58, 95% CI 0.17 to 1.00; p < 0.006). As both Brown et al. 128,140 and Whittingham et al. 131,144 used the SDQ: Emotional problems subscale, meta-analysis using mean differences was feasible and the results can be seen in Appendix 6.
FIGURE 4.
Forest plot showing the results of meta-analysis of the effects of parenting programmes with ACT on child behaviour post intervention for CYP with ABI and/or cerebral palsy. SMD, standardised mean difference (Cohen’s d).
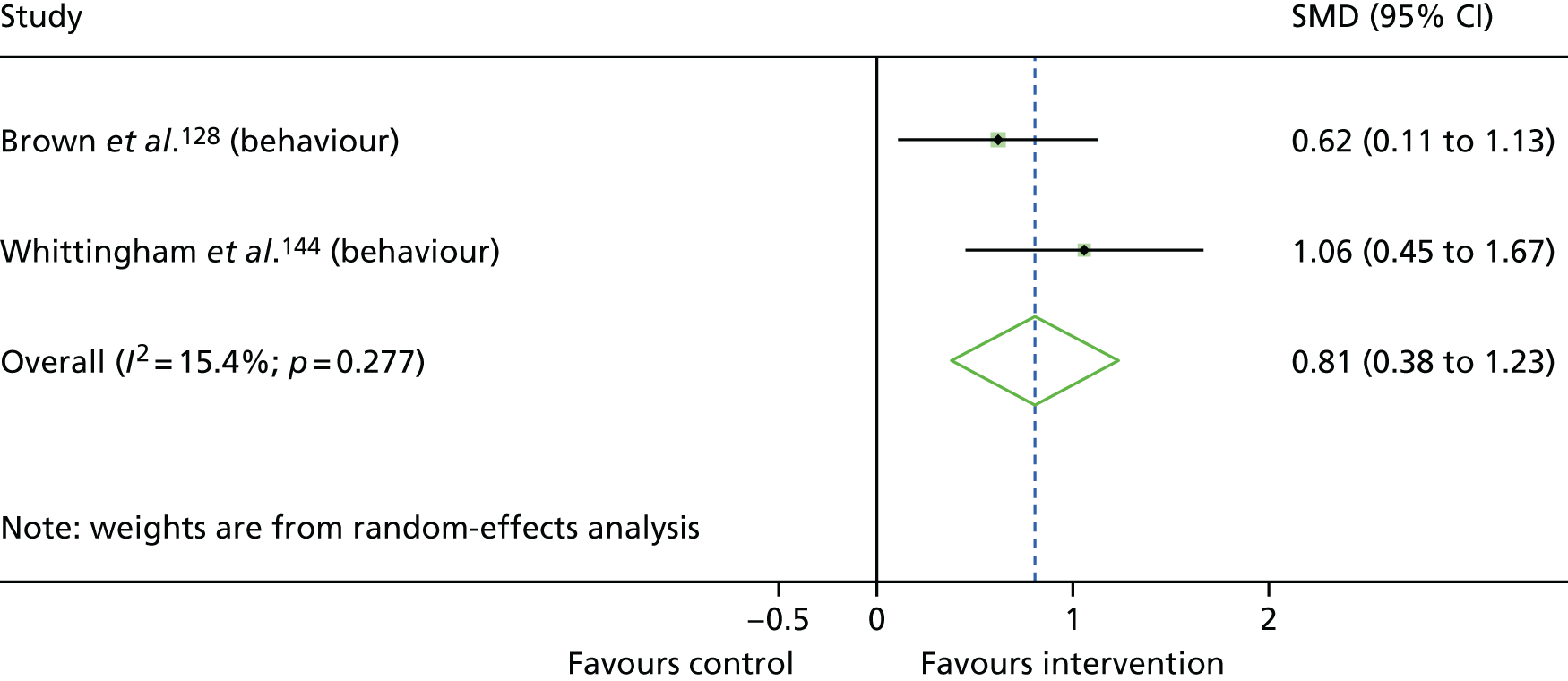
FIGURE 5.
Forest plot showing the results of meta-analysis of the effects of parenting programmes with ACT on child emotional problems post intervention for CYP with ABI and/or cerebral palsy. SMD, standardised mean difference (Cohen’s d).
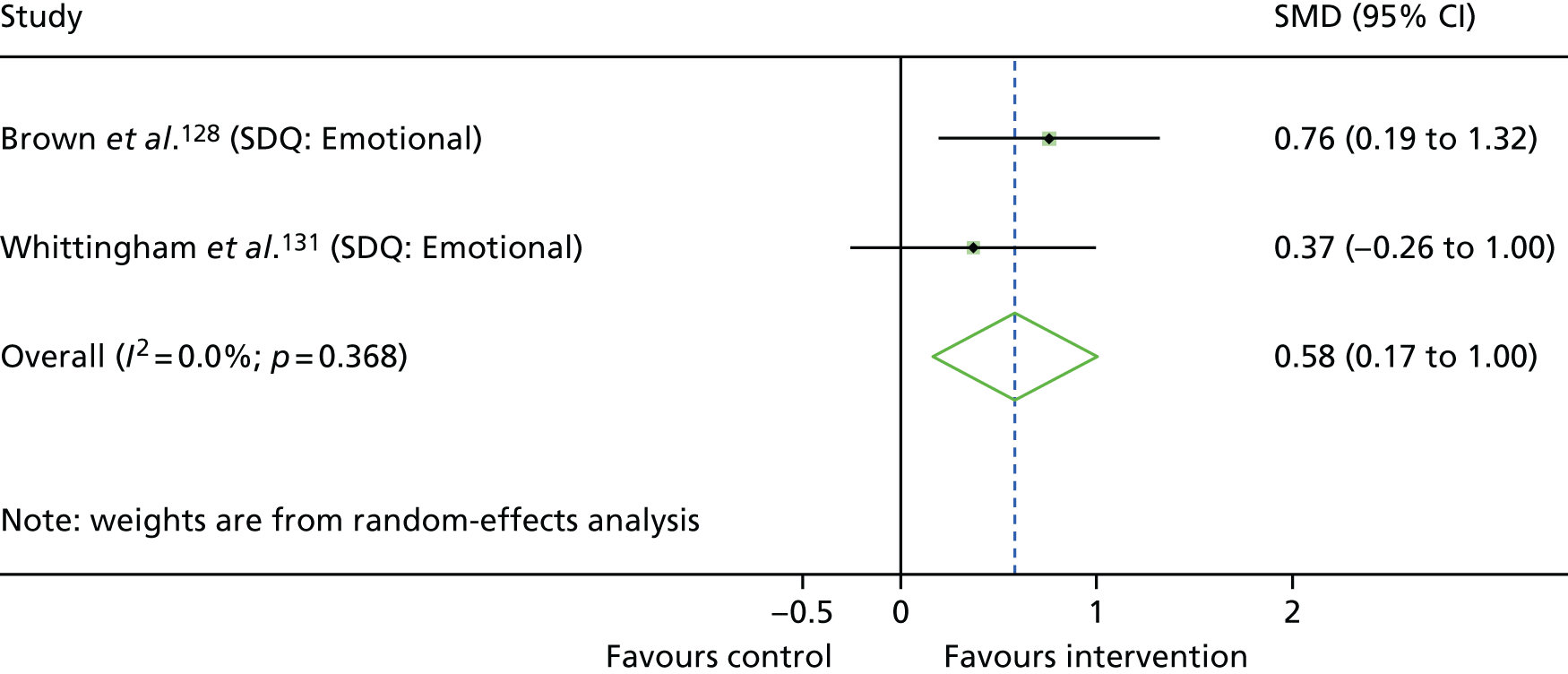
Report Supplementary Material 1, Table 11, shows findings for other outcomes assessed post intervention in these studies. There is some evidence for the beneficial effect of SSTP plus ACT for some outcomes relating to parenting styles, parenting health and LTC-specific QoL. The largest effect size was for parenting laxness (a measure of parents’ inconsistent or permissive parenting style) (d = 1.20, 95% CI 0.61 to 1.79; p < 0.001) in the study by Brown et al. ,128,140 although this was not mirrored in Whittingham et al. ’s131,144 study. A large beneficial effect on parenting over-reactivity was seen in the studies of both Brown et al. 128,140 (d = 0.83, 95% CI 0.26 to 1.40; p = 0.004) and Whittingham et al. 131,144 (d = 1.11, 95% CI 0.44 to 1.78; p = 0.001). Further evidence of a beneficial effect of SSTP plus ACT on parenting was provided by Brown et al. 128,140 (Parent Thoughts and Feelings Questionnaire: d = 0.88, 95% CI 0.31 to 1.45; Parenting Tasks Checklist Behaviour subscale: d = 0.91, 95% CI 0.33 to 1.48). A range of other measures of parenting were used in both studies, and many others produced medium to large effects, although these effects tended to be imprecise, with 95% CIs typically including negligible effect sizes. There was less evidence from Whittingham et al. 131,144 for the beneficial effect of SSTP plus ACT on LTC-specific QoL and LTC symptoms.
Meta-analysis was performed for parent mental health (Figure 6) and parenting outcomes (Figure 7). The range of individual measures reported above for each outcome category were combined into a single summary effect for each study. There was evidence of a beneficial effect of SSTP plus ACT on parent mental health with a medium-sized effect (d = 0.57, 95% CI 0.30 to 0.83; p < 0.001), and a large beneficial effect size was reported for parenting (d = 0.90, 95% CI 0.57 to 1.24; p < 0.001). Meta-analysis using mean differences for parent mental health and parenting outcomes can be seen in Appendix 6.
FIGURE 6.
Forest plot showing the results of meta-analysis of the effects of parenting programmes with ACT on parent mental health post intervention for parents of CYP with ABI and/or cerebral palsy. SMD, standardised mean difference (Cohen’s d).
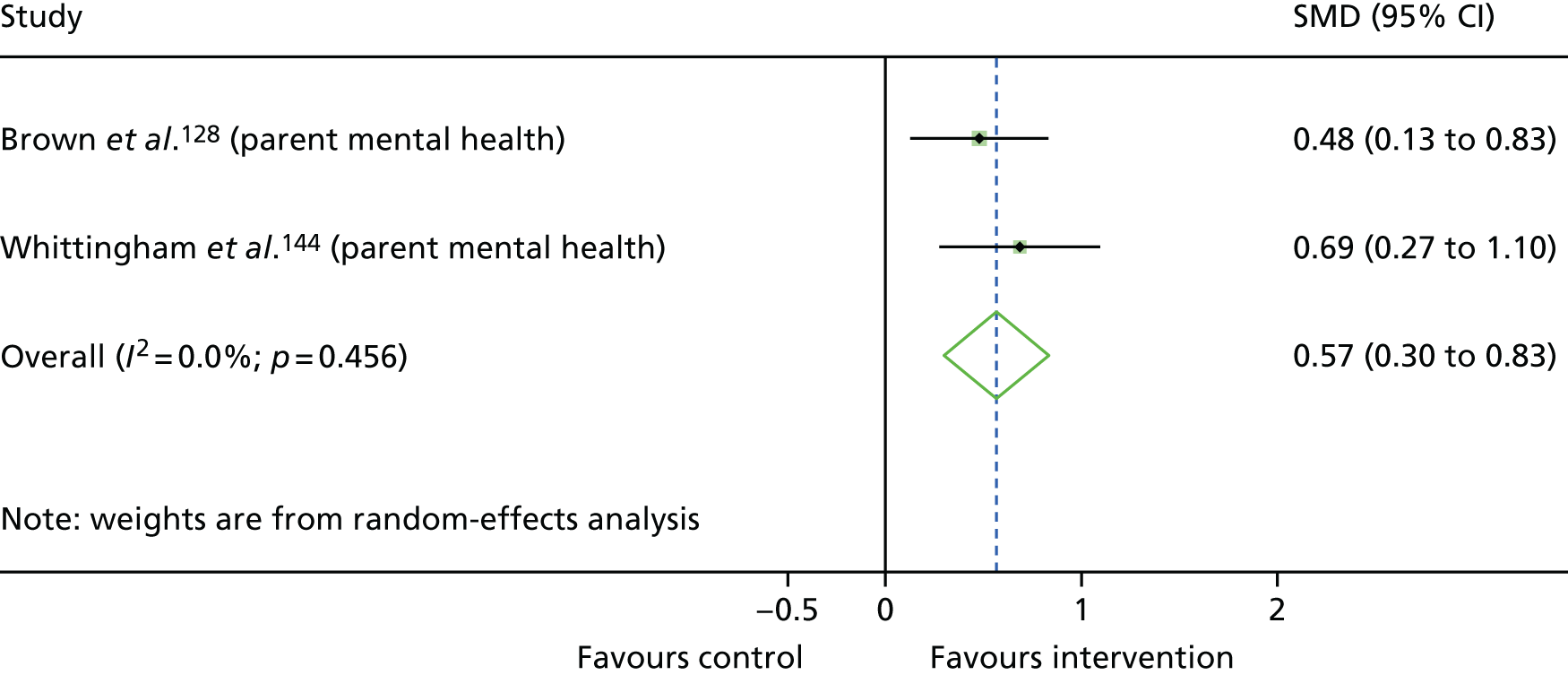
FIGURE 7.
Forest plot showing the results of meta-analysis of the effects of parenting programmes with ACT on parenting post intervention for parents of CYP with ABI and/or cerebral palsy. SMD, standardised mean difference (Cohen’s d).
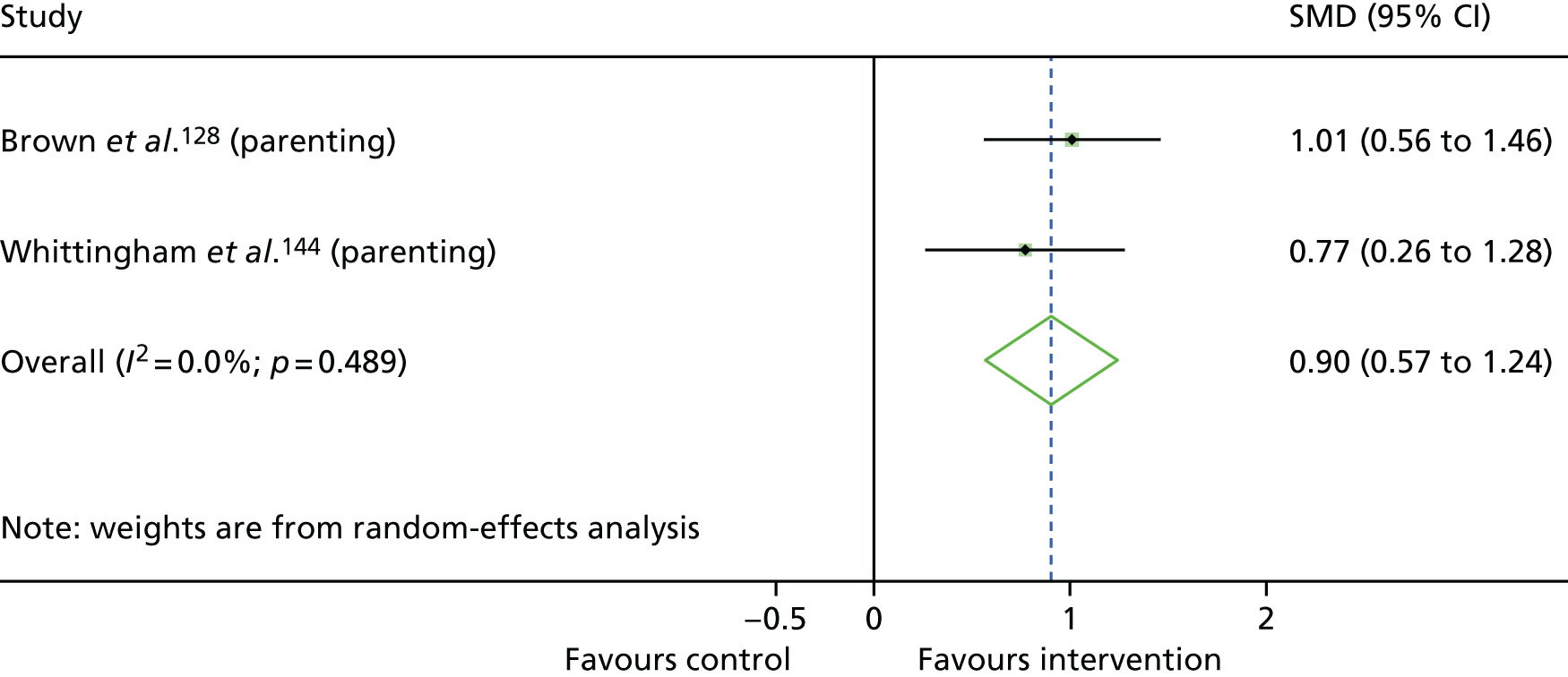
The two studies that assessed the clinical effectiveness of SSTP plus ACT128,131 provide tentative evidence that it may have beneficial effects on some outcomes, including child behaviour, emotional problems, parenting and parent mental health. Although the meta-analyses summarise these overall effects, there were contrasting effects from the range of different measures used to quantify the effectiveness of SSTP plus ACT, so conclusions relating to more fine-grained outcomes are unclear. Notwithstanding the small number and size of trials of parenting interventions, the findings may indicate the benefit of the addition of ACT to the SSTP programme. Although the included articles scored well on quality appraisal, it is noted that there was some risk of bias because blinding of participants was not possible, and outcomes were rated by parents. 128,131,140,144
Overall, there is a lack of research investigating the clinical effectiveness of parenting programmes that measured CYP mental health outcomes aside from Triple P. We know from other systematic reviews that trials have delivered other parenting programmes, but not measured the effects on child mental health. 73
Effectiveness of group play therapy interventions
Three studies evaluated the effectiveness of group play therapy interventions, with Nekah et al. 133 and Zareapour et al. 135 studying children with cancer and elevated symptoms of depression, and Wang et al. 138 sampling children with asthma and behavioural problems. All three group play therapy studies took place in countries that are not members of the Organisation for Economic Co-operation and Development (OECD) (Iran and China) and were translated from Persian or Chinese. The study by Zareapour et al. 135 utilised daily art-based play over the course of 1 week. Art and crafts featured in Nekah et al. ’s133 trial of a play programme, which contained aspects of storytelling and performance supplemented with a behavioural therapy focus. Wang et al. 138 placed greater emphasis on team building, development of confidence and learning through games and activities in their trial. A total of 88 participants were included, of whom 48 were randomised to the intervention arms. All control participants received TAU. The study by Zareapour et al. 135 primarily aimed to improve depression, whereas Nekah et al. 133 targeted depression and anxiety. Wang et al. 138 aimed to improve mental coping ability in their trial. It is notable that the studies reporting group play therapy interventions scored relatively poorly on quality.
Children and young people mental health outcomes
Report Supplementary Material 1, Table 12, shows the findings for each CYP mental health outcome assessed post intervention. Nekah et al. 133 observed a large beneficial effect for anxiety; however, the wide CI includes negligible effect sizes and raises uncertainty about the effect (d = 1.29, 95% CI 0.11 to 2.46; p = 0.04). Similarly, this study reported a large beneficial effect for depression, although the wide CI includes slightly harmful effects (d = 1.04, 95% CI –0.10 to 2.17; p = 0.08). On the other hand, the study by Zareapour et al. 135 reported a particularly large beneficial effect on depression of art-based group play therapy (d = 3.40, 95% CI 2.12 to 4.69; p < 0.001). In the study by Wang et al. ,138 coping improved with a large effect size (d = 0.93, 95% CI 0.27 to 1.59; p = 0.006), but there was little evidence for the beneficial effect of the intervention on behaviour problems (d = 0.31, 95% CI –0.32 to 0.94; p = 0.32).
Given that Nekah et al. 133 and Zareapour et al. 135 both studied patients with cancer and TAU control groups, meta-analysis was possible for their depression outcomes. Figure 8 shows a forest plot for the effects of group play therapy on child depression post intervention. Meta-analysis revealed that the large beneficial effect size was characterised by very wide CIs that include slightly harmful effect sizes (d = 2.20, 95% CI –0.12 to 4.52; p = 0.06) and large heterogeneity between the two studies’ findings (I2 = 86.3%), limiting the evidence for positive effects.
FIGURE 8.
Forest plot showing the results of meta-analysis of the effects of group play therapy on child depression post intervention for CYP with cancer. CDS-A, Child Depression Scale Abbreviated; HADS, Hospital Anxiety and Depression Scale; SMD, standardised mean difference (Cohen’s d).
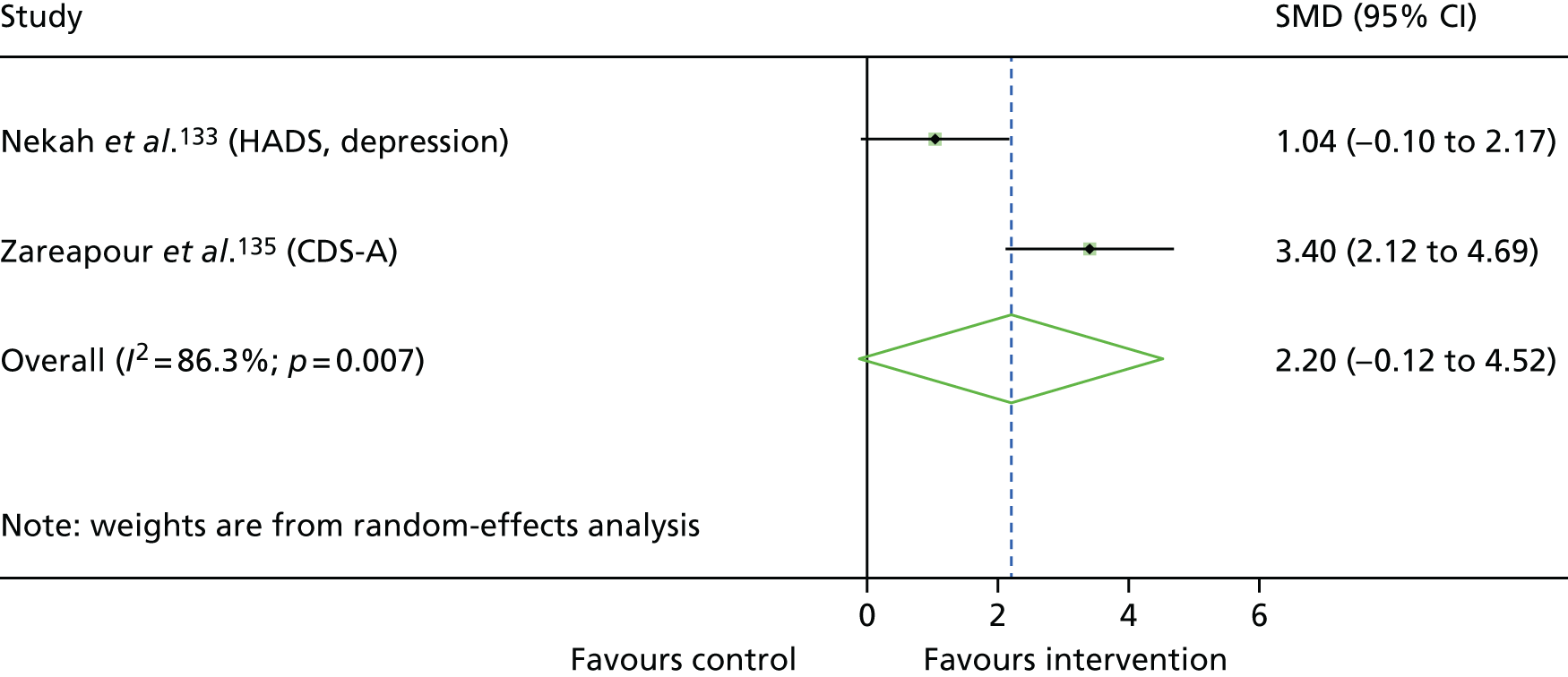
Overall, the included studies cannot tell us with precision whether or not group play therapy interventions are beneficial for depression or anxiety. Despite the individual findings of a large beneficial effect in the study by Zareapour et al. ,135 when meta-analysed, this effect is uncertain. Behaviour outcomes did not improve in the study by Wang et al. ;138 however, there may be a beneficial effect for coping. The low quality and high risk of bias across the three studies further weakens the strength of conclusions drawn from the evidence.
Effectiveness of palliative care interventions
Two studies evaluated the clinical effectiveness of interventions that we have categorised broadly as palliative care, both studying a sample of children with cancer. 123,137 Lyon et al. 123 evaluated Family-Centred Advance Care Planning for Teens with Cancer (FACE-TC) and elevated symptoms of anxiety, whereas Shoshani et al. 137 evaluated the Make-a-Wish programme in CYP with mixed mental health symptoms (anxiety, depression, general mental health). FACE-TC emphasises a family-centred approach to discussions about the future, whereas the Make-a-Wish programme aims to identify and deliver an activity that the child wants, without influence from their parents. Although these interventions clearly differ in content, they both fit broad definitions of palliative care149 and share some intervention targets, including hope. Control participants in both studies received TAU, with Shoshani et al. 137 employing a waiting list design in their study. A total of 96 participants were included, of whom 47 were randomised to the intervention arms. The majority of outcomes were assessed 3 months post intervention in the study by Lyon et al. 123 and 5 weeks post Wish in Shoshani et al. ’s137 study. There were no further follow-up assessments.
Children and young people mental health outcomes
Both palliative care studies assessed child anxiety and depression. Shoshani et al. 137 also measured emotional problems, hope and optimism. Report Supplementary Material 1, Table 13, displays findings for CYP mental health outcomes assessed post intervention. Taking the results of Lyon et al. ’s123 trial in isolation gives little evidence of the beneficial effect of FACE-TC for anxiety and depression outcomes. The trial by Shoshani et al. 137 found that the Make-a-Wish intervention had a large, beneficial effect on positive emotions (d = 1.03, 95% CI 0.52 to 1.55; p < 0.001), but evidence for reduction in negative emotions was lacking. Shoshani et al. 137 also reported medium-sized beneficial effects on range of measures, including anxiety, depression, general mental health and hope, but all of these effects were characterised by imprecision, with wide CIs including small effect sizes.
As the study characteristics were similar, meta-analyses were conducted when outcome categories were shared. Figure 9 is a forest plot of the effects of palliative care on child anxiety post intervention reported by Lyon et al. 123 and Shoshani et al. 137 Figure 10 is a forest plot of the effects of palliative care on child depression post intervention reported in these studies. 123,137 Meta-analysis revealed that palliative care interventions show a medium-sized beneficial effect on both child anxiety (d = 0.61, 95% CI 0.19 to 1.02; p = 0.004) and depression (d = 0.61, 95% CI 0.19 to 1.03; p = 0.05). However, there is uncertainty in concluding a positive effect of palliative care interventions on these aspects of child mental health, as wide CIs included small effect sizes.
FIGURE 9.
Forest plot showing the results of meta-analysis of the effects of palliative care on child anxiety post intervention for CYP with cancer. BAI, Beck Anxiety Inventory; BSI-18, Brief Symptom Inventory-18 item version; SMD, standardised mean difference (Cohen’s d).
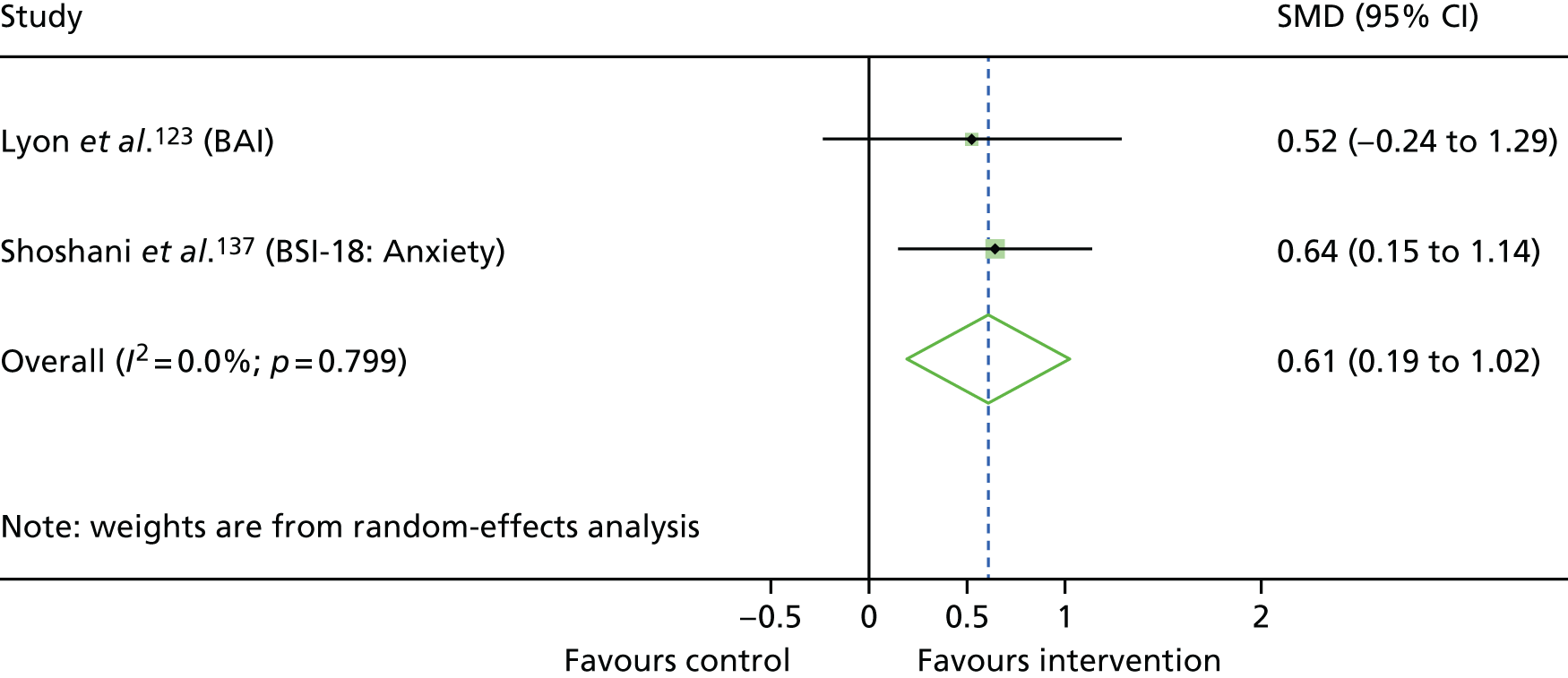
FIGURE 10.
Forest plot showing the results of meta-analysis of the effects of palliative care on child depression post intervention for CYP with cancer. BAI, Beck Anxiety Inventory; BSI-18, Brief Symptom Inventory-18 item version; SMD, standardised mean difference (Cohen’s d).
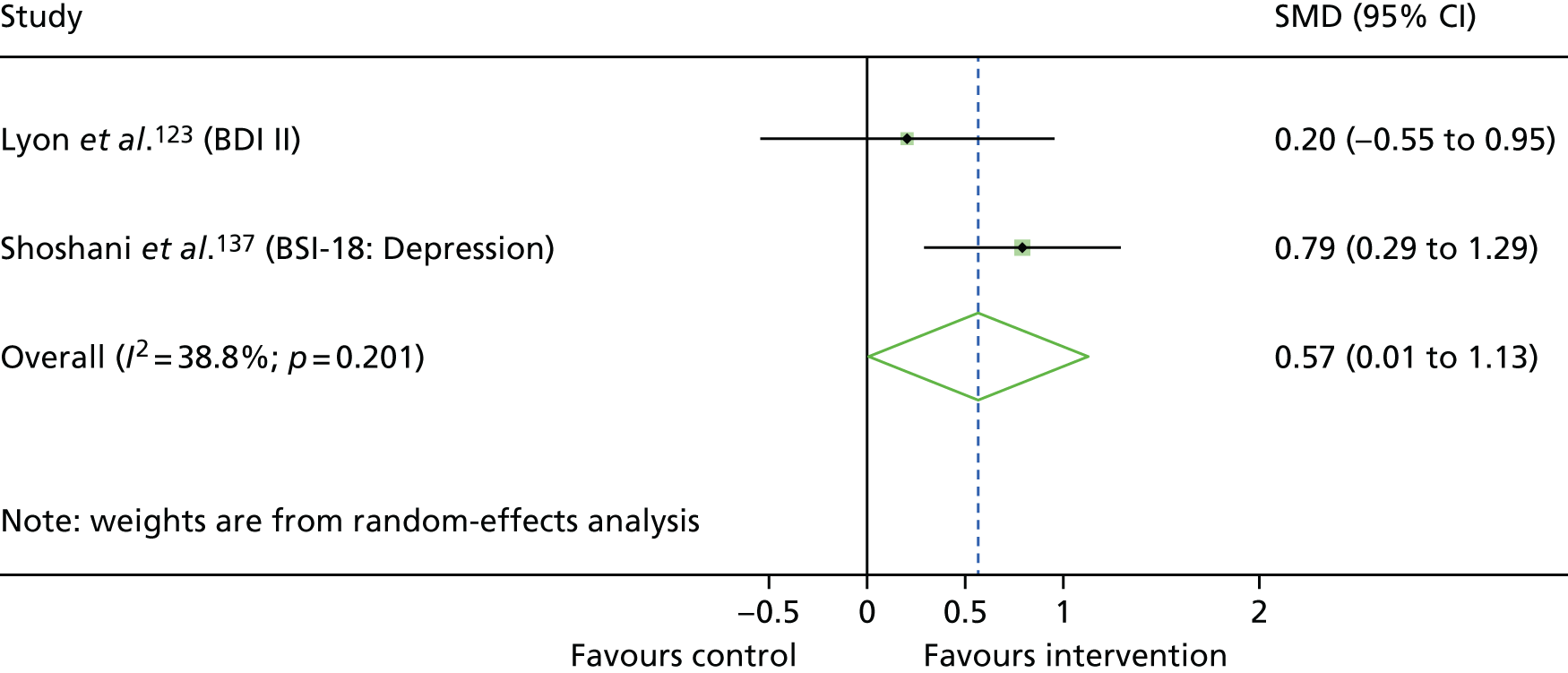
Other outcomes
Report Supplementary Material 1, Table 14, provides the findings for all other outcomes assessed post intervention. There was little evidence of a beneficial effect of FACE-TC on the majority of outcomes reported. However, Lyon et al. 123 did find a large beneficial effect for spirituality (d = 0.99, 95% CI 0.19 to 1.78; p = 0.02), albeit with imprecision in the estimate of effect, with the CI including small effect sizes. Shoshani et al. 137 provided evidence of a large beneficial effect for the Make-a-Wish intervention for physical QoL (d = 0.87, 95% CI 0.37 to 1.38; p < 0.001). Both studies measured intervention effects using the Paediatric Quality of Life Inventory (PedsQL) 4.0: Physical functioning subscale, and, therefore, physical QoL specifically could be meta-analysed across the two studies (Figure 11). The result of this meta-analysis provides evidence for a medium-sized beneficial effect of these palliative care interventions on physical aspects of QoL in CYP with cancer (d = 0.73, 95% CI 0.31 to 1.15; p = 0.001). As both studies used the PedsQL 4.0: Physical functioning subscale, meta-analysis using mean differences can be seen in Appendix 6.
FIGURE 11.
Forest plot showing the results of meta-analysis of the effects of palliative care on child physical quality of life post intervention for CYP with cancer. SMD, standardised mean difference (Cohen’s d).
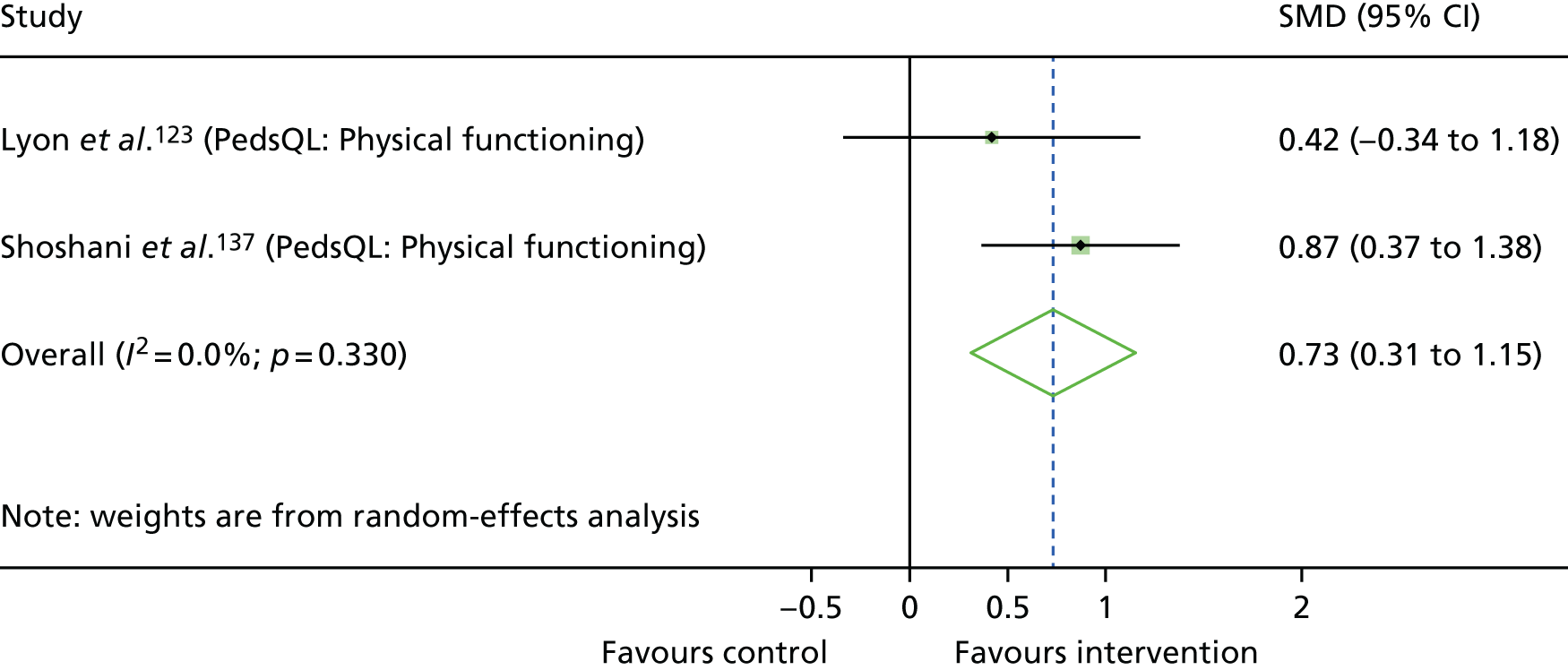
Overall, analysis of the clinical effectiveness of palliative care interventions for CYP with cancer provides tentative evidence that there may be some benefits for child depression and anxiety, child physical QoL and child spirituality. Only two studies investigated the clinical effectiveness of this type of intervention, with differences in findings perhaps reflecting the different intervention content. 123,137 The relatively low quality of the two articles further limits the confidence of evidence regarding whether or not palliative care interventions show beneficial effects in children with mental ill health and cancer.
Effectiveness of relaxation interventions
Two studies evaluated the clinical effectiveness of relaxation interventions, and both included children with asthma. 119,139 The sample studied by Bignall et al. 119 had elevated symptoms of anxiety, whereas the CYP in Yang et al. ’s139 study had elevated depression and anxiety symptoms. Both interventions assessed included PMR. 119,139 The study by Yang et al. 139 was conducted in China, and assessed 30 minutes per night of audio-taped PMR for 4 weeks versus a TAU control. The study by Bignall et al. 119 was based in the USA and compared a programme of asthma education, breathing exercises, guided imagery and CD-guided PMR to a control group receiving the asthma education alone. A total of 94 participants were included, of whom 47 were randomised to the intervention arms. Both studies aimed to reduce anxiety, with the relaxation intervention trialled by Yang et al. 139 also targeting depression. It is notable that the two studies reporting relaxation interventions scored poorly on quality appraisal.
Children and young people mental health outcomes
Report Supplementary Material 1, Table 15, displays findings for CYP mental health outcomes assessed post intervention. Evidence for the positive effect of PMR is provided by the study by Yang et al. ,139 in which a large, beneficial effect on depression (d = 1.01, 95% CI 0.48 to 1.43; p < 0.001) was observed. Yang et al. 139 also reported a medium beneficial effect on anxiety (d = 0.70, 95% CI 0.19 to 1.20; p = 0.007), although the CI for this effect includes some small beneficial effect sizes. In contrast, there was little evidence reported by Bignall et al. 119 for the effect of their relaxation intervention on anxiety, with small harmful effect sizes reported, although CIs were wide and included positive effects (state anxiety: d = –0.39, 95% CI –1.11 to 0.34; p = 0.30; trait anxiety: d = –0.21, 95% CI –0.93 to 0.51; p = 0.58).
Given that the same asthma education appeared in both Bignall et al. ’s119 intervention and control groups, we meta-analysed the anxiety outcomes alongside the data from Yang et al. ’s139 study, whose control group received TAU (Figure 12). The trait anxiety subscale of the Spielberger State–Trait Anxiety Inventory (STAI) was more aligned with the Screen for Child Anxiety Related Emotion Disorder (SCARED) assessment tool than the state subscale data from Bignall et al. ,119 and thus was entered into meta-analysis instead. Meta-analysis of these outcomes provides a lack of evidence for the effect of relaxation interventions on anxiety (d = 0.28, 95% CI –0.60 to 1.16; p = 0.53). Heterogeneity across the two papers was wide (I2 = 75.3%), further impacting the confidence in the pooled effect.
FIGURE 12.
Forest plot showing the results of meta-analysis of the effects of relaxation on child anxiety post intervention for CYP with asthma. SMD, standardised mean difference (Cohen’s d); STAI-T, Spielberger State–Trait Anxiety Index-Trait subscale.
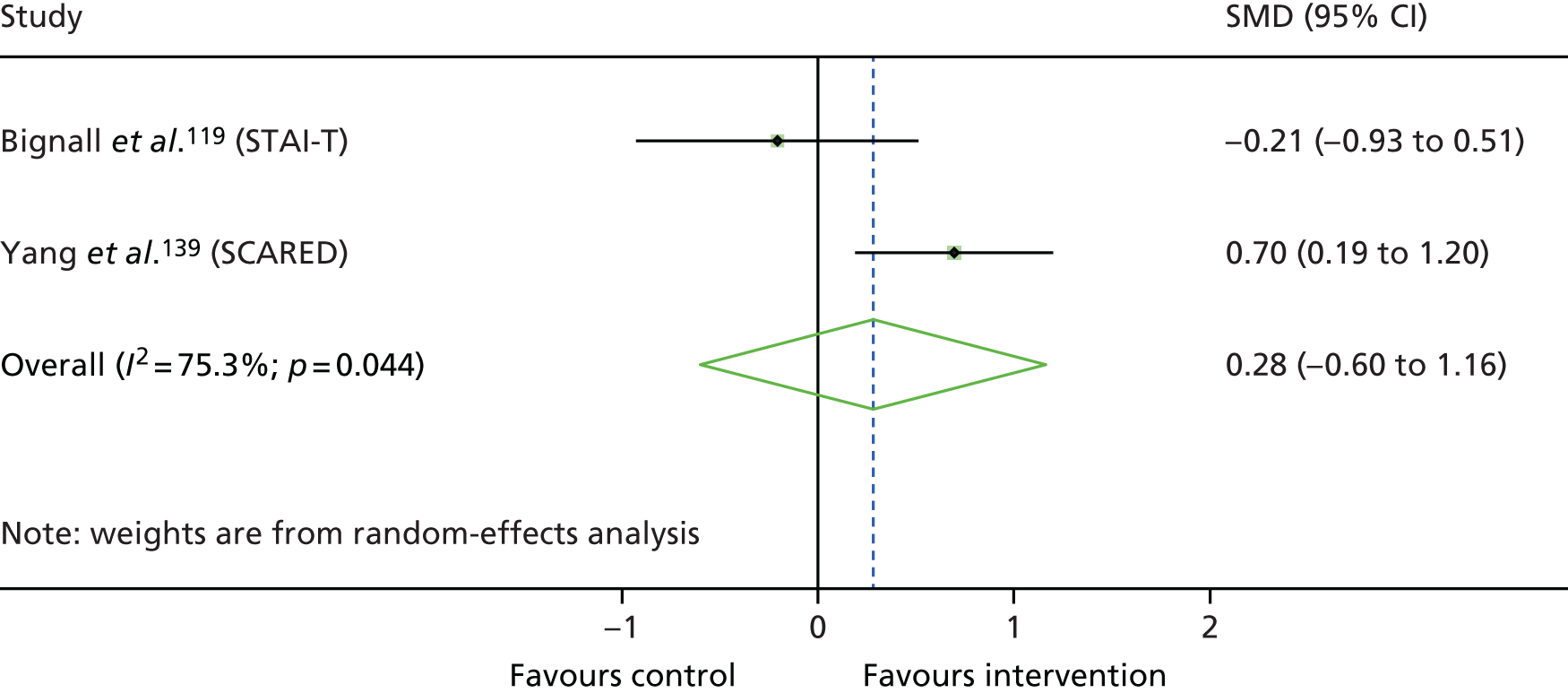
Other outcomes
Both studies included assessments of asthma symptoms. Yang et al. 139 recorded the incidence of daytime and night-time symptoms, as well as the percentages of days without asthma symptoms and of participants experiencing one or more asthma attacks. However, these outcomes were not reported in terms of means and SDs, and so were not included in data synthesis. In addition, Bignall et al. 119 included a measure of LTC-specific QoL, the PedsQL: Asthma module.
Report Supplementary Material 1, Table 16 displays findings for other outcomes assessed post intervention. Evidence for the effect of PMR on asthma symptoms is provided by Yang et al. ,139 with large beneficial effects on the number of daytime (d = 2.32, 95% CI 1.68 to 2.96; p < 0.001) and night-time (d = 1.91, 95% CI 1.31 to 2.50; p < 0.001) symptoms reported. However, this was only corroborated by one measure of asthma symptoms in Bignall et al. ’s119 study, in which a large effect size was found for asthma control, although the wide CIs included some negligible effect sizes (d = 0.80, 95% CI 0.05 to 1.54; p = 0.04). There was a lack of evidence from the study by Bignall et al. 119 for other measures of asthma symptoms. For asthma-specific QoL there was a medium effect size, although this estimate of effect is uncertain, with a wide CI including negligible effect sizes.
Combined LTC symptom outcomes were produced for each study and entered into a meta-analysis (Figure 13), which showed a lack of evidence for the effect of relaxation interventions on LTC symptoms. Despite a large pooled effect, it was characterised by very wide CIs, including harmful effects as well as very large heterogeneity (I2 = 97.4%) on account of the differences between each study’s findings (d = 1.10, 95% CI –0.88 to 3.08; p = 0.28).
FIGURE 13.
Forest plot showing the results of meta-analysis of the effects of relaxation on asthma symptoms post intervention for included studies. SMD, standardised mean difference (Cohen’s d).
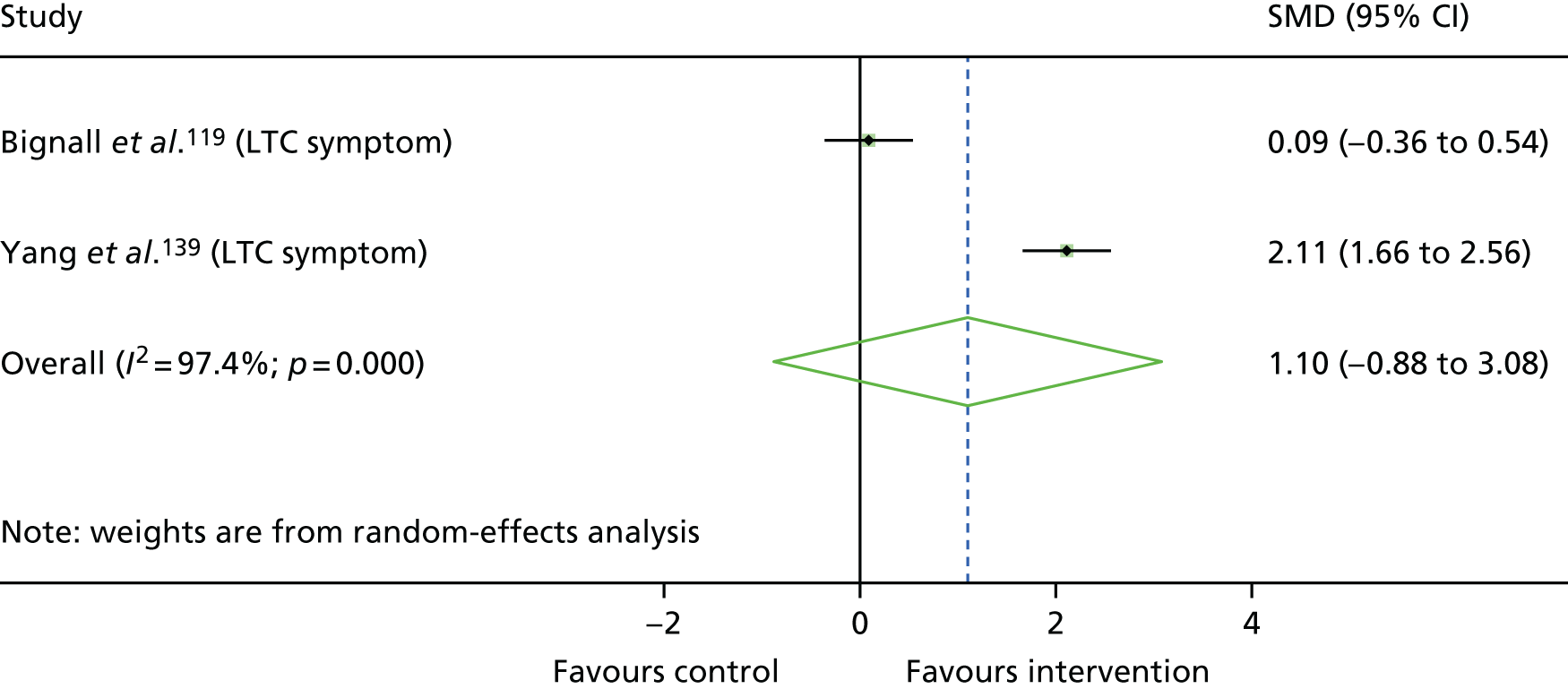
Overall, the included studies provide mixed evidence regarding the benefits of relaxation interventions for depression, anxiety and LTC symptoms. Yang et al. 139 reported medium to large beneficial effects across these domains. Bignall et al. 119 reported little evidence for the beneficial effects of a combined relaxation intervention. A reason for this may be the asthma education active comparator group in the trial by Bignall et al. ,119 which did improve asthma symptoms compared with baseline. Both studies were rated as being of low quality and high risk of bias. We recommend that the positive effects from Yang et al. 139 are treated with caution.
Effectiveness of stress management training interventions
Two studies conducted in the USA evaluated the effectiveness of stress management training (SMT) interventions in children with T1DM and elevated stress120 and anxiety. 122 Hains et al. 122 structured a SMT programme over 6 weekly 1-hour sessions, whereas Boardway et al. 120 began with 10 sessions of SMT delivered over 12 weeks, followed by 3 monthly sessions focused on dietary compliance and insulin administration. The SMT trialled by Hains et al. 122 was described as a cognitive–behaviour stress inoculation training programme, in that there was an emphasis on identifying potential illness-related stressors and thinking about them in a more positive way. Boardway et al. 120 used a somewhat similar approach, but developed problem-solving or coping activities in response to identified stressors. Across the two studies, 15 participants received SMT and 16 control participants received TAU, with Hains et al. 122 employing a waiting list design. Both studies targeted diabetes mellitus-specific stress as their primary outcome. The included studies are the oldest in this review, and both scored relatively poorly on quality appraisal.
Children and young people mental health outcomes
Report Supplementary Material 1, Table 17 displays findings for each CYP mental health outcome assessed post intervention. There was little evidence across both studies regarding the clinical effectiveness of stress management programmes on CYP mental health outcomes. On the occasions when medium-sized effects were recorded, these were characterised by wide 95% CIs that included harmful effect sizes. This was the case for state anxiety (d = 0.69, 95% CI –0.41 to 1.78; p = 0.23) and behavioural coping (d = 0.65, 95% CI –0.44 to 1.74; p = 0.25) in the study by Hains et al. 122
Meta-analysis was possible for their LTC-specific stress and coping outcomes. Figure 14 shows a forest plot for the effects of SMT on diabetes mellitus-specific stress post intervention. Meta-analysis revealed little evidence of a beneficial clinical effect for LTC-specific stress (d = 0.10, 95% CI –0.62 to 0.82; p = 0.80). As both studies used the Diabetes Stress Questionnaire (DSQ), meta-analysis using mean differences can be seen in Appendix 6. Figure 15 is a forest plot of the effects of SMT on coping post intervention reported by Boardway et al. 120 and Hains et al. 122 Negative coping from the KidCOPE measure was selected from Hains et al. ,122 as this subscale has most similarities with Boardway et al. ’s120 Ways of Coping checklist. Meta-analysis again revealed little evidence of a clinical effect of the intervention on coping (d = –0.09, 95% CI –0.83 to 0.64; p = 0.81).
FIGURE 14.
Forest plot showing the results of meta-analysis of the effects of SMT on T1DM-specific stress post intervention for CYP with diabetes mellitus. SMD, standardised mean difference (Cohen’s d).
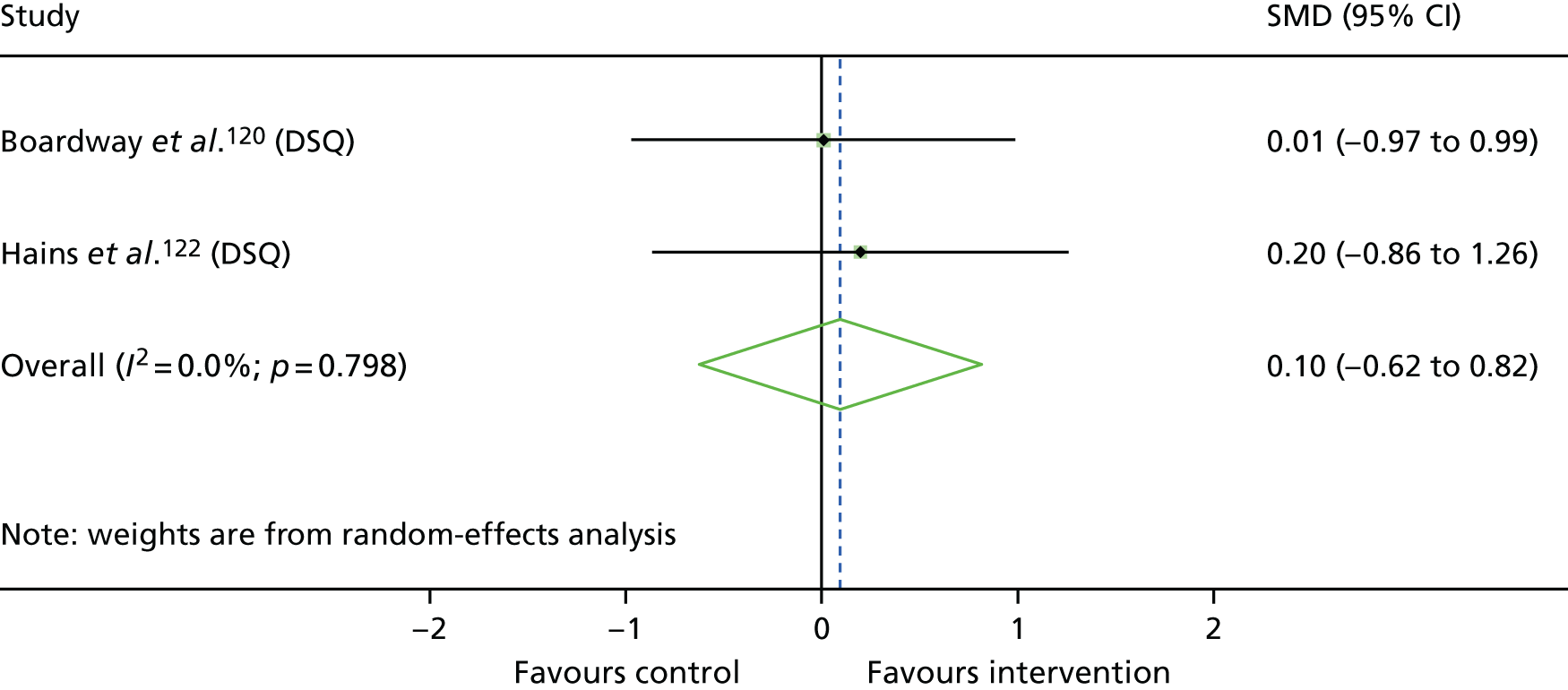
FIGURE 15.
Forest plot showing the results of meta-analysis of the effects of SMT on coping post intervention for CYP with diabetes mellitus. SMD, standardised mean difference (Cohen’s d).
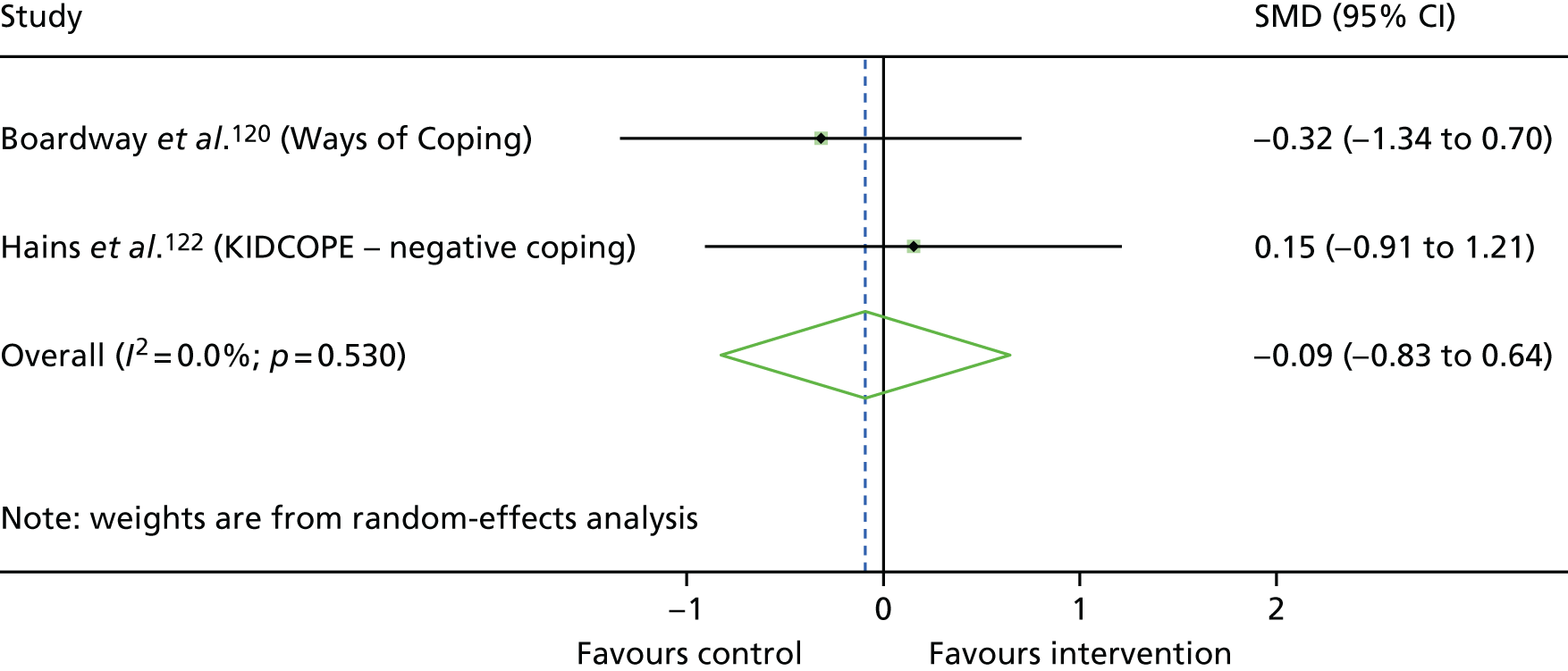
Other outcomes
Report Supplementary Material 1, Table 18, displays findings for each other outcome assessed post intervention. There was again a lack of evidence for the effect of stress management interventions on any outcome. LTC symptoms were meta-analysed for the two studies using the most similar glycaemic control outcomes [i.e. level of total glycosylated haemoglobin (GHb) in Boardway et al. ,120 level of glycated haemoglobin (HbA1C) in Hains et al. 122]. This meta-analysis (Figure 16) provides little evidence of an effect of SMT on LTC symptoms (d = –0.10, 95% CI –1.77 to 1.57; p = 0.91), showing imprecise effects owing to a wide CI and large heterogeneity across the two studies (I2 = 79.9%).
FIGURE 16.
Forest plot showing the results of meta-analysis of the effects of SMT on CYP diabetes mellitus symptoms at post intervention. SMD, standardised mean difference (Cohen’s d).
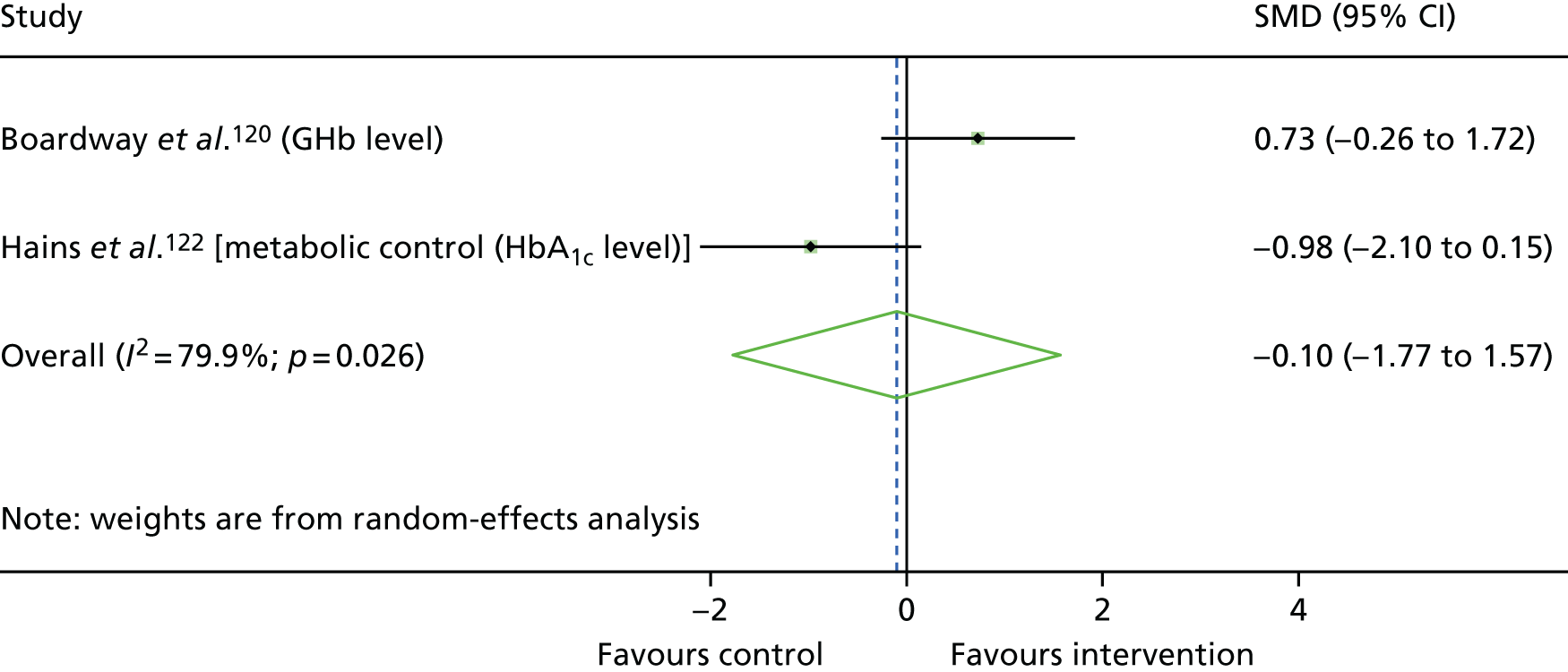
Overall, the two included studies provide very little evidence regarding the effect of SMT on a wide range of outcomes. Effect sizes ranged from medium-sized and beneficial to large harmful effects, but all were characterised by imprecision in the estimate with large effect sizes, at least in part due to the small sample sizes in these studies. 120,122
Clinical effectiveness of emotional intelligence training interventions
Two studies based in Iran evaluated the clinical effectiveness of emotional intelligence training (EIT) in children with hearing loss, elevated distress and general mental health symptoms. 132,134 The article by Ashori et al. 132 was translated from Persian; it tested a programme based on nine modules related to understanding and controlling emotions, whereas the study by Pourmohamadreza-Tajrishi et al. 134 featured 11 similar modules. Each study contained 40 participants recruited from specialist schools for the deaf, equally split between EIT and TAU. The two included studies were of very poor quality.
Children and young people mental health outcomes
Both EIT studies used the 28-item version of the General Health Questionnaire (GHQ) and reported subscales for anxiety, depression, social dysfunction, somatic symptoms and overall mental health. No other outcomes were reported.
Report Supplementary Material 1, Table 19, displays findings for these study outcomes. Both studies reported very large, positive beneficial effects for each outcome domain. Effect sizes ranged from 2.41 (95% CI 1.58 to 3.23; p < 0.001) for depression to 6.79 (95% CI 5.14 to 8.44; p < 0.001) for overall mental health in the study by Pourmohamadreza-Tajrishi et al. ,134 whereas Ashori et al. 132 reported effect sizes in the range 11.0–17.4 for the same outcomes.
Initial assessment of the two papers suggested that they were reporting on different studies, because of differences in the EIT programme outline and age of the sample. On inspection of the raw data presented for each study, the review team decided that the mean scores were too similar to be confident that these were in fact different samples and, therefore, meta-analysis was not performed. It is also noted that extremely large effect sizes are evident, in part because of the very small standard deviations presented. We attempted to contact the authors for clarification but received no reply.
Despite the reports of very large beneficial effects in the individual studies of Ashori et al. 132 and Pourmohamadreza-Tajrishi et al. ,134 both studies scored poorly on quality appraisal, notwithstanding the conspicuous similarities between the studies. Overall, there is a lack of evidence to confidently determine the effect of EIT on the mental health of CYP with hearing loss.
Clinical effectiveness of massage therapy interventions
The study by Diego et al. 121 was the only study to assess a massage therapy intervention, studying its effects in adolescents infected with human immunodeficiency virus (HIV) and symptoms of depression and anxiety. The study hypothesised that HIV infection symptoms, anxiety and depression would be improved in the massage therapy group compared with the PMR control group after 12 weeks of the intervention. Twenty-four adolescents were randomised equally to massage therapy or relaxation involving PMR.
Children and young people mental health outcomes
Diego et al. 121 assessed anxiety using the Spielberger State–Trait Anxiety Inventory-State subscale (STAI-S) and depression using the CES-D. Report Supplementary Material 1, Table 20, displays these findings. There is evidence that massage therapy had a beneficial effect on child anxiety, with a large positive effect size calculated (d = 1.23, 95% CI 0.35 to 2.10; p = 0.007). Despite a medium positive effect size for depression, there is a lack of evidence for this beneficial effect, given the wide CI that includes negligible effect sizes (d = 0.75, 95% CI –0.08 to 1.58; p = 0.08).
Other outcomes
Diego et al. 121 reported the effects of massage therapy on markers of immune function. Medical charts were reviewed to assess HIV infection progression (CD4 cells per mm3, CD8 cells per mm3, CD4-to-CD8 ratio) and protection against viruses associated with HIV (CD56 cells per mm3, CD56-to-CD3 ratio). Overall, there is a lack of evidence for the effects of massage therapy on symptoms of HIV infection.
The evidence provided in the study by Diego et al. 121 suggests that massage therapy may reduce anxiety and, to a lesser extent, depression in adolescents infected with HIV. However, there was a lack of evidence for effects on markers of immune function. This was the only study reporting massage therapy, and it was of low quality; therefore, there is a lack of unequivocal evidence regarding the effects of this intervention on the mental health of CYP with LTCs. It is notable that the comparator in this study was similar to components of interventions tested in the studies by Bignall et al. 119 and Yang et al. ,139 which were earlier categorised as relaxation interventions.
Clinical effectiveness of heart rate variability biofeedback interventions
Yetwin’s was the only included study to assess a heart rate variability biofeedback intervention, studying its effects in a sample of 19 adolescents with chronic pain and elevated anxiety symptoms. 127 The nine participants in the intervention group practised the use of breathing and relaxation to control their heart rate while linked to a heart rate monitor. The control group was enrolled in a waiting list design.
Children and young people mental health outcomes
Child anxiety and depression were self-reported using the Children’s Anxiety Sensitivity Index and Child Depression Inventory-Short Form, respectively. Report Supplementary Material 1, Table 21, shows findings for these outcomes as measured post intervention. There was little evidence of an effect of heart rate variability biofeedback on either anxiety or depression.
Other outcomes
Yetwin127 assessed QoL, quality of sleep and LTC symptoms (pain). Report Supplementary Material 1, Table 22, shows findings for these other outcomes measured post intervention. There were a couple of medium to large effect sizes reported for both LTC symptom and sleep outcomes; however, these were characterised by imprecision in the estimates, with CIs including negligible effect sizes (e.g. Faces Pain Scale: d = 0.86, 95% CI –0.09 to 1.81; p = 0.08; and Child/Adolescent Sleep–Wake Scale: Falling Asleep: d = 0.78, 95% CI –0.16 to 1.72; p = 0.11). This tentative evidence of beneficial effect also conflicted with other measures of these outcomes that showed a lack of evidence of beneficial effects (e.g. Varni/Thompson Paediatric Pain Questionnaire Worst Pain: d = –0.05, 95% CI –0.95 to 0.85; p = 0.92; Child/Adolescent Sleep–Wake Scale total score: d = 0.27, 95%CI –0.63 to 1.18; p = 0.56).
Overall, the one paper assessing heart rate variability biofeedback provides a lack of evidence for its effect on child anxiety, depression, sleep, QoL or pain in adolescents with chronic pain. In addition to being the sole study to use this type of intervention, Yetwin127 scored very poorly on quality appraisal; therefore, there is insufficient evidence to assess the clinical effectiveness of heart rate variability biofeedback for improving either mental health or other outcomes in CYP with LTCs.
Clinical effectiveness of resistance training interventions
One study investigated the influence of a resistance training programme on depression and physical symptoms in a sample of 22 adolescents with chronic fatigue syndrome (CFS). 129 The programme was progressive (gradually increasing in difficulty), utilising exercises such as weightlifting and sit-ups, and was compared with a programme consisting of aerobic exercises alone.
Children and young people mental health outcomes
Depression was self-reported using the BDI. Report Supplementary Material 1, Table 23, shows the findings for this measure and other measures (described in the following section) post intervention. There was a lack of evidence for the effect of resistance training on depression (d = –0.23, 95% CI –1.07 to 0.60; p = 0.59) compared with an aerobic exercise programme.
Other outcomes
Gordon et al. 129 assessed QoL using the physical subscale of the Short Form questionnaire-36 items (SF-36). LTC symptoms were measured using the Fatigue Severity Scale, and several exercise tests were chosen to assess exercise tolerance and muscular endurance, including the number of push-ups completed until fatigue, the sit-to-stand test, the time to fatigue on a submaximal walking test and the metabolic equivalent during the walking test (ratio of energy expenditure during the test to energy expenditure at rest). There was a lack of evidence for the effects of resistance training on these outcomes.
Overall, the one paper assessing the effects of a resistance training programme on depression, physical indices and QoL provides little evidence of a benefit compared with aerobic training. It should be noted that Gordon et al. 129 scored moderately well on quality appraisal, describing randomisation, allocation concealment, blinding of outcome assessors and using an intention-to-treat analysis. However, groups were imbalanced at baseline, when the resistance training group had performed statistically significantly better on the sit-to-stand test, and this was not adjusted for; the intervention was not well described and adherence, compliance and fidelity were not assessed. For this reason, there is insufficient evidence to state with confidence whether or not resistance training has any benefit on the mental health of CYP with LTCs.
Clinical effectiveness of music therapy interventions
The study by Bufalini136 was the only one included to assess a music therapy intervention. It also differed from other included studies as it was written in Italian and aimed to alleviate procedural anxiety rather than general anxiety. It included 39 adolescents with cancer undergoing painful procedures in Italy. The intervention consisted of actively listening to music and playing instruments, and then having background music playing prior to sedation. The 19 participants randomised to the control group received usual sedation.
Children and young people mental health outcomes
Bufalini136 assessed anxiety at four time points using the modified Yale Preoperative Anxiety Scale. Report Supplementary Material 1, Table 24, shows the findings post intervention, just prior to sedation. There is evidence that music therapy had a large beneficial effect on child anxiety (d = 1.47, 95% CI 0.76 to 2.18; p < 0.001). No other outcomes were measured in this study.
The evidence provided by Bufalini136 suggests that there may be a benefit of music therapy in reducing procedural anxiety. However, in addition to being the sole paper reporting on this intervention, it scored the lowest of all included studies on quality appraisal. Therefore, more evidence is required to increase confidence in the clinical effectiveness of music therapy for improving the mental health of CYP with LTCs.
Discussion
Summary of findings
This review synthesised RCTs studying the clinical effectiveness of interventions that aim to reduce the mental ill health of CYP with LTCs. The primary focus of the review is the mental health of CYP, yet all secondary outcomes were synthesised in order to evaluate any wider benefits of interventions, including key aspects of individual and family functioning.
Of the 11 reported intervention types, CBT was the subject of the greatest volume of research, with seven studies evaluating CBT-based interventions. These studies provide tentative evidence that CBT-based interventions could be beneficial for the mental health of CYP with LTCs, with six out of seven studies of CBT interventions reporting improvements in CYP mental health outcomes. However, the heterogeneity of the included study characteristics (comparators, LTCs and outcomes) meant that no meta-analyses could be conducted for CYP mental health outcomes in our main analysis, leading to a reliance on individual study outcomes.
Parenting programmes featured in four interventions, tested in three studies. 118,128,131 Two interventions included ACT with the SSTP parenting programme, and there appeared to be evidence of beneficial effects of this combined programme on child behaviour, emotional problems, parenting and parent mental health compared with SSTP alone. Group play therapy interventions were assessed in three studies. 133,135,138 Quality appraisal indicated each study being rated at a high risk of bias, and large positive effect sizes, when seen, were all characterised by uncertainty about the true effect of these interventions. It should be noted that reliance on parent-reported outcomes introduced further potential for bias when assessing parenting programmes.
The effects of SMT,120,122 EIT,132,134 palliative care123,137 and relaxation interventions119,139 were each reported in two studies, with four further interventions reported in single studies (biofeedback,127 music therapy,136 resistance training129 and massage therapy121). Although there were some beneficial effects reported for EIT, palliative care and massage therapy, risk of bias in these studies limits the conclusions that can be drawn regarding these interventions.
The 25 included studies reported on 269 individual outcomes; however, there were relatively few opportunities to meta-analyse studies with similar interventions, comparators, LTCs and outcomes. No more than two studies shared particular combinations of these study characteristics and could be meta-analysed in the main analysis. Even when we considered pooling studies across LTCs for supplementary analyses, this allowed for further pooling only of CBT interventions (see Appendix 7). Trials were typically small, with only two including more than 100 CYP participants. 126,130 Effect sizes across the board were therefore characterised by wide CIs, meaning that in many cases estimates of standardised mean differences that indicated medium or large effects were imprecise. The evidence for particular interventions used with similar samples of CYP is very limited.
Results in context
Despite the high prevalence of CYP with LTCs and comorbid mental illness, this review highlights the lack of RCTs aiming to address the problem. It is notable that 21 of the 31 included papers were published after 2010 and 13 after 2014, perhaps suggesting that this lack of research is beginning to be addressed. However, the quality of the relatively small amount of research to date is poor, with 19 of the 25 studies having at least four separate indicators of risk of bias.
The suggestion that CBT shows promise for improving the mental health of CYP with LTCs is supported by existing evidence. The most relevant previous review, by Bennett et al. ,82 was a systematic review of psychological interventions for symptoms of mental health disorders in CYP with LTCs, finding preliminary evidence that CBT interventions may be beneficial. The authors located only two RCTs,83,84 both of which appear in the current review, and both of which reported beneficial effects for depression outcomes. Bennett et al. 82 required the presence of symptoms of a Diagnostic and Statistical Manual of Mental Disorders, Fourth or Fifth Edition, mental health disorder for inclusion in their review, and had narrower inclusion criteria regarding LTCs and mental health outcome measures than the present review. In addition to those studies identified by Bennett et al. ,82 we found two later RCTs that included participants with a diagnosed mental health disorder: Reigada et al. 125 included participants with principal anxiety disorder and Szigethy et al. 126 included those with a major or minor depression diagnosis. As highlighted previously, ours is the first systematic review to consider all treatments for elevated symptoms of mental ill health in CYP with LTCs. By examining this literature, our findings add to the evidence from the small number of trials of participants with diagnosed mental health disorders. Extending the criteria to include CYP with clinically significant levels of mental health difficulties, as well as those with a mental health diagnosis, enabled a wider range of studies to be included and acknowledges the significant psychological impact of LTCs on some children.
Wider evidence of the clinical effectiveness of CBT for improving mental health has informed NICE guidelines54 recommending CBT for CYP with depression. James et al. 70 published a Cochrane systematic review of CBT for childhood anxiety disorders in CYP without comorbid LTCs, reporting that, despite a limited evidence base, there was a suggestion that CBT is a more effective treatment than TAU or active comparators. Given our own findings, there is tentative evidence that this recommendation may hold for CYP with LTCs.
It was observed that five of the six CBT interventions included in this review had been adapted prior to delivery to contain LTC-specific content relevant to the CYP in the study. 84,124–126,130,145 Content was adapted to the extent that the intervention would be suitable only for a sample with that LTC. In these studies, beneficial effects on CYP mental health outcomes were observed following four of the interventions, with only BOC failing to produce any benefits. 130 Of the other intervention types evaluated in studies included in this review, only two were adapted to the LTC, with neither showing evidence of benefit to CYP mental health outcomes. 119,120 The mixed evidence for interventions that are adapted to the LTC means that it is unclear how this should be done to best effect. Studies in populations with a LTC assessing the effects of CBT that has not been modified or adapted to the LTC were lacking. Although Martinović et al. 83 demonstrated some positive effects of CBT for depression in a sample with epilepsy, there were issues with study quality, indicating a lack of RCTs assessing how well CBT interventions that have been shown to be clinically effective in physically well CYP populations work for CYP with LTCs.
The strengths and limitations of the review, and the implications and recommendations for future work, are discussed in Chapter 6.
Chapter 3 Review 2: experience of interventions targeting mental health for children and young people with long-term physical conditions
Research questions
This chapter describes the second systematic review and addresses the following research questions:
-
What are the perceived effects of interventions aiming to improve mental health and well-being for CYP with LTCs on mental health and other key aspects of individual and family functioning?
-
What are the factors that may enhance, or hinder, the clinical effectiveness of interventions and/or the successful implementation of interventions intended to improve mental health and well-being for CYP with LTCs?
For definitions of the key terms used in this chapter, see Chapter 1.
Methods
Identification of evidence
The inclusion criteria shown in Report Supplementary Material 2, Table 1, were agreed among the wider project team and used to determine eligibility of articles. The inclusion criteria specified primary qualitative studies that explore attitudes and experiences regarding interventions aiming to improve the mental health and well-being of CYP with LTCs from the perspectives of CYP with LTCs, their families and/or practitioners. Articles did not have to report elevated symptoms of mental ill health among participants at baseline to be eligible for inclusion, as was the case for review 1. Owing to the nature of qualitative research, it was anticipated that it would have been unlikely that mental health symptoms would have been measured. This would have severely limited the number of studies eligible for inclusion in our review, as highlighted in Quality Appraisal.
Search strategy
A search strategy using both controlled (e.g. medical subject headings) and free-text searching was developed and tested in the databases to be searched. Terms were grouped according to four concepts:
-
children and young people terms
-
mental health terms
-
long-term physical conditions terms
-
study design terms (qualitative research).
Children and young people terms and LTC terms were the same as those used for review 1. Mental health terms included those used for review 1 as well as additional terms capturing intervention targets informed by discussion with experts among the wider project team (see Appendix 8 for list of project team and advisory group members). Additional mental health terms such as ‘well-being’ and ‘coping’ were added to the search strategy to reflect the terminology it was anticipated would be used by authors and participants of studies to be included in the review. These search terms were consistent with the broad definition of mental health used within this linked evidence synthesis (see Chapter 1).
MEDLINE including MEDLINE in-process (via OvidSP), PsycINFO (via OvidSP) and CINAHL (via EBSCOhost) were searched. These databases were selected because of their known coverage of qualitative literature. 153,154 The other databases from review 1 were not searched because of their focus on quantitative literature, but any qualitative studies identified during study selection in review 1 were marked for possible inclusion in this review. No date restrictions were applied to the search. Searches were conducted on 19 April 2016. An example search strategy used for the MEDLINE database is shown in Appendix 9. All references identified by the searches were exported into EndNote X7 prior to screening and eliminating duplication.
Supplementary searches were also conducted. Backward citation-chasing (searching the references of included articles) searches were conducted by four reviewers (DM, MN, LS, ZK) to locate additional primary articles of potential relevance. Included studies from relevant reviews located during title and abstract screening for both reviews 1 and 2 were also checked. Forward citation-chasing (searching articles citing included articles using Web of Knowledge) searches were conducted by an information specialist (JTB) using Web of Science and Google Scholar. In addition, three researchers (DM, LS and MN) searched websites that had been identified by the project team and advisory group for relevant research (see Appendix 3 for a list of websites searched). The databases CINAHL, HMIC and Conference Proceedings Citation Index (CPCI) were searched, all of which index grey literature.
Relevant studies were identified in two stages based on the inclusion and exclusion criteria given above. First, two reviewers conducted title/abstract screening independently for each record (eight researchers shared this screening: LS, DM, MN, IR, JTB, JTC, MR and VB). EndNote X7 software was used to perform screening. Disagreements were resolved through discussion between two reviewers, with referral to a third reviewer as necessary (DM, MN or LS). Full texts of records that appeared to meet the inclusion criteria on the basis of titles and abstracts were then obtained whenever possible. Full texts were screened independently by two reviewers (nine researchers shared this screening: DM, LS, MN, JTB, JTC, MR, LL, VB and IR) for inclusion and exclusion. Disagreements were again resolved through discussion between two reviewers, with referral to a third reviewer as necessary (DM, MN or LS).
Methods of analysis/synthesis
Data extraction
A data extraction form was developed and piloted. Three researchers (LS, MN and DM) each extracted one article and checked one colleague’s extraction before discussing and amending the form. Data on article details and aims, participants, methods, intervention, summary of findings and study quality were extracted into Microsoft Excel 2010 by four researchers (LS, MN, IR and DM) and checked (by either DM or LS). Full articles were uploaded to NVivo 11 (QSR International, Warrington, UK) software, which was used to aid coding of the findings and interpretation.
Quality appraisal
Quality appraisal was conducted simultaneously with data extraction using criteria from the Wallace checklist. 147 The checklist includes 13 questions covering research questions, underpinning theory, study design, context, the sample, data collection, analysis, relationships between data and findings, limitations, generalisability and ethics. We used questions regardless of whether they were considered essential or desirable in the checklist and separated questions falling under the same category. The question, ‘are the interventions of interest clearly described?’ was added in line with a previous review of intervention experience. 155 Questions were assigned a response of ‘yes’, ‘no’, ‘cannot tell’ or ‘not applicable’ for each article. Quality appraisal decisions were made by two reviewers (LS, MN, IR or DM) and disagreements resolved through discussion. The appraisals were used to evaluate study quality and were not used to exclude articles, our inclusion criteria requiring recognised methods of qualitative data collection and analysis provided a basic quality threshold.
Data analysis and synthesis
Data analysis and synthesis followed the principles of metaethnography. This approach was developed by Noblit and Hare156 and has proved to be a useful method to interpret findings across multiple qualitative studies in health research. 157–159 Metaethnography aims to create new interpretations through a process of reciprocal translation and refutation across studies. Translation involves establishing a common language of interpretation between or among the included studies and refutation involves the explanation of contradictory findings. If applicable, a ‘line of argument’ synthesis is created that produces a model that synthesises various reciprocal and refutational relationships into a coherent whole.
A challenge faced was the large number of articles and breadth/diversity of interventions, LTCs and participant groups. Noblit and Hare156 speak of the danger that the inclusion of too many studies may lead to ‘trite conclusions’. This was dealt with by grouping articles on the basis of similarities in participant perspective and level of interpretation in article findings to create a staged process of synthesis. Articles were grouped according to the quantity of relevant findings available and the level of interpretation used by individual study authors when generating themes from their primary patient data, as judged and agreed by reviewers (LS and DM). Synthesis began using articles that had a greater degree of interpretive findings. Report Supplementary Material 2, Table 2, provides examples of interpretative and descriptive themes from primary studies included in this review.
This meant that a smaller number of articles were initially synthesised separately before being combined into an overall synthesis, assuming that there were similarities that allowed for some translation of ideas between articles. Different participant perspectives were initially analysed separately as follows: CYP, parents, practitioners, mixed perspectives. Interventions targeting procedural anxiety were initially synthesised separately. This allowed for any potential differences in the experiences of procedural interventions aiming to alleviate anxiety in the short term and interventions that aim to address CYP’s mental health and/or well-being over a longer period of time to be identified.
We then used purposive sampling to select additional included articles with LTCs, interventions and participant perspectives that had not been represented in the synthesis of articles thus far. Purposive sampling has been used in previous qualitative evidence syntheses to manage the analytical process when many studies are included. 160 We used a form of maximum variation sampling to decide whether or not studies that included interventions and LTCs not seen in the synthesis thus far ought to be synthesised next161 and to ensure that LTCs and interventions included in review 1 were prioritised for inclusion in the current synthesis. Studies were ranked according to the degree to which they met these three criteria. Studies that met these criteria (n = 30) were synthesised, which left 12 articles with descriptive findings related to interventions and LTCs previously included in the synthesis whose findings were compared with the existing synthesis. A summary of the stages of the synthesis and articles included at each stage is provided in Table 2.
| Stage of synthesis | Articles included | Rationale for stage of inclusion in synthesis |
|---|---|---|
| 1. Synthesis of articles with a large volume of interpretative findings | Barnetz and Feigin;162 Bluebond-Langer et al.;163 Brodeur;164 Bultas et al.;165 Desai;166 Gillard and Allsop;167 Hosek et al.;168 Moola et al.;169 Stewart et al.;170 Barlow et al.;171 Fair et al.;172 Gillard and Watts;173 Gillard et al.;174 Lewis et al.;175 Muskat et al.;176 Nicholas et al.;177 Stewart et al.;178 Tiemens et al.;179 White et al.;180 and Wright et al.181 | Articles with more than two pages of interpretative data relating to experience of or attitude towards an intervention. Provision of a rich source of data to begin process of reciprocal translation |
| 2. Purposive sampling | Bignall et al.;119 Dennison et al.;182 Kirk and Milnes et al.;183 Serlachius et al.;184 White;185 Kashikar-Zuck et al.;186 Campbell et al.;187 Curle et al.;188 Gan et al.;189 Jaser et al.;190 Marsac et al.;191 Masuda et al.;192 Nieto et al.;193 Nilsson et al.;194 Reme et al.;195 Sibinga et al.;196 Whittemore et al.;114 Wolf Bordonaro;197 Ayers et al.;198 Barry et al.;199 Baruch;200 Burns et al.;201 Docherty et al.;202 O’Callaghan et al.;203 O’Callaghan et al.;204 O’Callaghan et al.;205 Shrimpton et al.;206 and Weekes et al.207 |
Interventions or LTC seen in review 1 Types of intervention or LTC not yet seen within the review 2 synthesis Interventions focused on procedural distress |
| 3. Read through of descriptive articles | Barnfather et al.;208 Brothers et al.;209 Gaysynsky et al.;210 Griffiths et al.;211 Macdonald and Greggans et al.;212 Nicholas et al.;213 Nicholas et al.;214 Romero;215 Stewart et al.;216 Stewart et al.;217 Stinson et al.;218 and Stinson et al.219 | These articles did not meet previous criteria. Checked for data to support or refute existing analysis |
The process used for the metaethnography, as a whole, included the following:
Reading and re-reading the included studies
This initial stage involved the careful reading of all of the included articles in order for reviewers to familiarise themselves with the studies and their findings. This process began in the screening phase and continued through data extraction and analysis.
Determining how the studies are related
Following data extraction, structured summaries were created to juxtapose the same type of information across articles for consideration of similarities and differences. 159 Information tabulated included study aims, samples, methods, interventions and themes. These summaries included information on participant perspective and whether or not the intervention targeted procedural anxiety to allow categorising of articles for synthesis. Themes from all included studies presented in their findings sections were also tabulated and colour coded separately to allow for early comparison of themes across different studies.
Reciprocal translation of studies
Each article was rated by two reviewers (DM and LS) according to whether the analysis was interpretive or descriptive and whether or not there were more than two pages of findings focused on the experience of the intervention. This facilitated a more in-depth consideration of the quantity and quality of interpretive findings available within each article for analysis. This process identified a smaller number of studies with a large volume of interpretive information on which to focus the initial synthesis.
The reciprocal translation stage involved the extraction of first- and second-order constructs from the studies identified as having a large volume of interpretive findings available for synthesis. First-order construct data were identified as efforts to make sense of daily experiences, often illustrative participant quotes within studies. Second-order construct data consisted of author analysis and interpretation in included articles. Third-order constructs were our interpretations as reviewers, which go further than first- and second-order constructs in individual articles. 220 Table 3 displays examples of first-, second- and third-order constructs contributing towards the analysis. Concept maps showing the relationships between analytical ideas and themes across articles were then developed.
| Construct | ||
|---|---|---|
| First order | Second order | Third order |
| ‘It was fun like it’s never been before, I saw someone who is in control of the situation and isn’t afraid of diabetes. If he can do it, I’ve got to succeed . . . I’m less afraid because of the project; I met people there with amazing abilities.’ (CYP quote)162 | The mentees admired their mentors. Numerous mentees reported adopting and emulating parts of their mentors’ behaviour regarding diabetes mellitus162 | Hope and inspiration: meeting peers who were managing to live successfully with a LTC provided CYP with a source of hope and inspired CYP that they too could live a fulfilling life |
Initially, articles that focused on young people, parents or practitioners were synthesised separately. However, as we observed considerable overlap between perspectives, all of the articles with large amounts of interpretive findings were synthesised. We compared the findings and interpretations of each article to the concept map developed to that point, adding new constructs and themes when relevant. NVivo software was used to code findings and interpretations, line by line, in articles against the ideas seen in the concept maps, as well as new ideas. Refutational translation was conducted when any quotations, metaphors, themes and concepts that offered oppositional or counterarguments to current findings were specifically searched for and incorporated into the findings. This process was completed with the articles in the initial synthesis, and repeated with findings and interpretations from studies selected through the purposive sampling process. When new constructs and themes emerged, studies previously examined were checked to see if they could contribute to these new ideas. Studies evaluating procedural mental health interventions were initially considered separately, but, because of the similarity in the concepts across these articles and other articles focusing on broader interventions, they were then included in the reciprocal translation process during this purposive sampling phase. The remaining articles that neither had large amounts of interpretive findings nor were included in the purposive sampling were then read to see which constructs and themes were supported by the data and if there was any material that refuted the content of these themes. NVivo was used to code any relevant information from these remaining articles. Feedback and ideas relevant to the synthesis from the CYPAG and parent meetings were considered before the reciprocal translation process began and incorporated throughout the different stages of the synthesis, as outlined in Table 2.
Synthesising translations/creating a line of argument
By considering relationships and overlap among the constructs and themes within the synthesis, a line of argument was developed. A line of argument synthesis attempts to make sense of the synthesis as a whole through the development of a new theory or model of understanding. The line of argument consisted of a model that captured how the overarching themes, and the categories that contributed towards them, related to one another and captured the experience of participants with a LTC receiving mental health and well-being interventions, their families and the professionals involved in their care.
Results
Study selection
The PRISMA flow diagram in Figure 17 summarises study selection. Database searches identified 12,285 records, with a further 1118 of the total records identified by other means, including citation-chasing, included articles from relevant reviews, websites, searches for sibling articles of those included in review 1 and author contact. After the removal of duplicates, the titles and abstracts of a total of 10,364 records were screened against inclusion and exclusion criteria. We attempted to retrieve the full text of 355 records for further consideration and were successful in 342 (96%) cases. After full-text screening, 295 articles were excluded for reasons provided in Figure 17. A list of reasons for the exclusion of each article screened at full text is given in Supplementary Material 2, Table 3.
FIGURE 17.
The PRISMA flow chart recording review 2’s study selection.
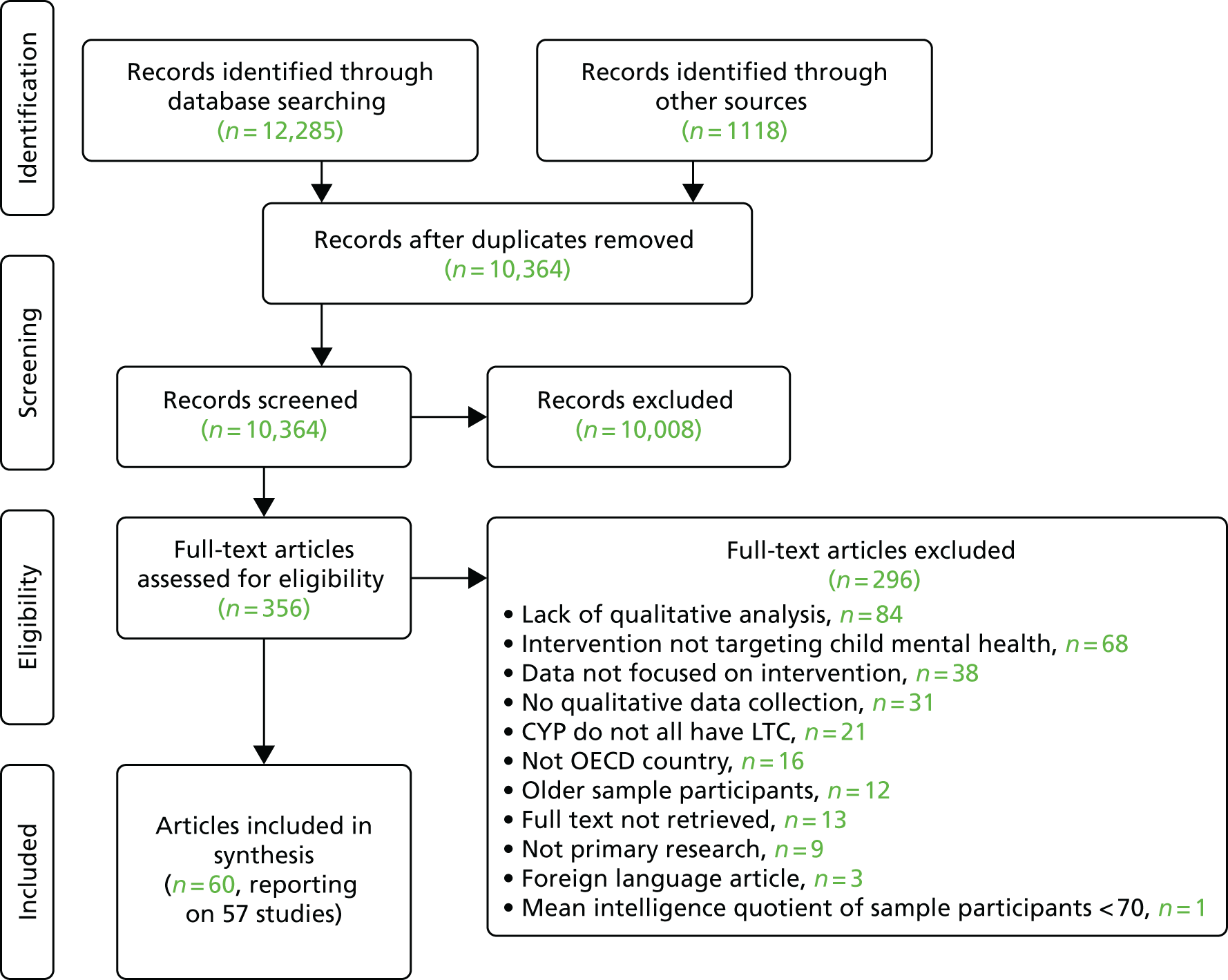
Three studies were each represented by two articles published about the qualitative findings. 170,178,180,185,208,216 Twenty-two of the 60 included articles were located through additional searching.
Included articles were categorised in terms of the quantity and quality of interpretive findings, participant perspective, intervention and LTC focus. This allowed a stepped approach to synthesis, given the large number of included articles. Twenty articles entered the synthesis at the first stage, all of which include a large number of interpretive findings. Of these, eight reported the views of CYP participants only,162,163,165–169,178 11 included a mix of participant perspectives164,171–179,181 and two included parent participants only. 165,180 The different participant perspectives were initially synthesised separately, but considered together on account of the overlap between findings across the articles. In the second stage, 19 articles were selected using a purposive sampling method. Twelve of these articles focused on interventions aiming to alleviate procedural distress. 191,194,198–207 These were initially synthesised separately, but were added to the main synthesis on account of the overlap in the ideas that were included. In the final stage of the synthesis, the remaining 12 (see Table 2) articles that held descriptive findings were compared with the constructs and themes resulting from the synthesis after the first two stages.
Study characteristics
Report Supplementary Material 2, Table 4, provides details about the study location, publication type, focus of the study, method of data collection, method of analysis and intervention type for the 57 included studies. Studies were conducted in seven different countries, with the USA being the most common (n = 25114,119,163–168,172–174,181,186,189–191,196,197,200–202,207,209,210,215), followed by Canada (n = 13169,176–179,185,192,208,213,214,217–219), the UK (n = 9171,182,183,187,188,195,198,211,212) and Australia (n = 7175,184,199,203–206). All included articles were published in peer-reviewed journals, except for five dissertations, four at PhD level164,197,200,215 and one at masters level. 185 Three studies were published before 2000,163,171,207 with over three-quarters of included studies (76.7%) published since 2010. The majority of studies evaluated an intervention received by CYP with a LTC; 10 studies either asked participants about an intervention in development or did this as well as evaluating the intervention once received. 114,168,171,184,191–193,211,218,219 Two studies relied on participants’ recollections of interventions previously received,171,198 the remainder collected data about current intervention experience.
Twenty-four out of the 57 included studies used only qualitative research methods; the remainder also used quantitative methods, although only 20 of these collected quantitative measures of clinical effectiveness alongside qualitative data collection. 114,119,164,170,175,181,186,189,190,193–199,207,213,214,216 Forty-eight of the included studies involved interviews. The remainder used focus groups,114,168,184,205,211 online posts in discussion forums made as part of the intervention183,210,211,215 and/or observations. 197 The median sample size was 23 participants (range 3–100); only 18 studies included > 30 participants. 164,170,172,178,183,187,189,193,200,203,206,208,211,215–219
Twenty-two out of the 57 studies included only CYP participants. 114,119,162,163,166–169,184,186,187,194–197,204,207,210,211,213,215,219 One study collected data only from practitioners who delivered the intervention. 205 Four studies collected data from parents only;185,201,202,206 the remaining 30 studies included a mix of participant types. 164,165,170–179,181–183,188–193,198–200,203,209,212,214,217,218 The most commonly studied intervention types were:
Qualitative data analysis methods typically involved thematic analysis (22/57 studies). In 15 studies, the authors described the analysis as based on grounded theory or used constant comparative methods. 162,172–174,179,181,183,188,196,199,203–205,207,217 In nine studies, the authors reported that they used some form of qualitative content analysis only. 114,189,190,193,194,200,210,213,218
Few details about populations studied were consistently provided. Over half of the 57 included studies did not report the ethnicity of participants providing qualitative data (n = 31),162,163,165,166,171,173,177–179,183,184,186,189,192–195,199,201,203–205,208,211–215,217–219 and only 10 studies provided socioeconomic information about participants or their families. 169,178,180,190,191,197,198,209,214,218 None of the included studies reported that CYP with LTCs had received a mental health diagnosis. One study, which was also included in review 1, indicated that participants had clinically significant levels of anxiety. 119 The study by Curle et al. 188 included CYP showing signs of emotional distress related to their LTC. Aside from these two examples, the mental health of CYP participants was not assessed on entry into the study. CYP with an LTC who provided qualitative data were between 8 and 17 years of age in 25 studies. 114,119,162,165–167,169,171,175,179,184,186,187,189,190,192,193,200,207,208,212,213,215,218,219 Only three studies focused solely on the views of young adults (≥ 18 years old), two of which were conducted in young adults living with a HIV infection in the USA. 168,204,210
The most frequently seen LTC in CYP in the 57 included studies was cancer (n = 14). 163,173,191,194,199–207,211 HIV-positive intervention recipients were the focus of eight studies,168,172,174,176,187,196,209,210 and a further 10 studies included CYP with a mix of LTCs. 164,167,170,175,177,188,192,207,208,217 Five studies focused on CYP with T1DM. 114,162,184,190,213 Included studies commonly explored the perceptions and experiences of interventions aimed at improving coping (n = 26),163,166,174,177,184,186–193,199–203,207,208,210,211,213,214,216,217 self-esteem (n = 13)163,165,166,173,175,179,181,200,204,209–212 and emotional support (n = 11)171–173,182,183,187,189,208–211 rather than targeting mental health symptoms, for example depression (n = 1)176 or anxiety (n = 8). 119,165,176,177,196–198,206 Some interventions also aimed to improve symptoms related to the LTC (n = 35)114,119,162,166–168,171,172,174,176,177,181–184,186,187,190,193–196,198,203,205,208–211,213–215,217–219 and social skills (n = 16). 114,163,164,168,174,181,182,187,200–202,206,208,209,216,217 Mental ill health, often referred to as psychiatric problems, was an exclusion criterion in nine studies. 186,189,193,196,203,204,209,218,219
Interventions were delivered in a variety of settings and by a range of personnel (see Report Supplementary Material 2, Table 5). Twenty of the 57 studies reported on interventions delivered in a hospital or clinical setting. 119,175,176,181,182,186,188,189,191,194,196,197,199,200,202,203,205–207,209 Other frequent settings were online (13 studies)114,170,177,183,192,193,210,211,213,215,217–219 and campsites (10 studies);163,165–167,169,173,174,179,185,214 this included one psychoeducation intervention214 delivered during a residential camp. Interventions were delivered by mentors, various clinicians, music therapists, researchers, counsellors, volunteers, students, social workers, the recipient themselves, parents and a martial arts instructor. Twenty-six studies involved interventions delivered at least in part by clinicians with specialised training. 164,170,172,174,176,178,179,181,186–189,195–197,199,201–205,208,209,211,213,214 In 10 studies interventions were multidisciplinary, delivered by more than one specialist. 164,173–175,181,186–189,214 Although not widely reported, 17 studies reported that practitioners delivering the intervention received supervision or training. 162,164,166,174,175,177,178,185,186,188–190,195,200,202,208,212
Among studies that reported the structure of interventions (n = 42114,119,162–167,172–181,184–197,199–202,208–214,216–218), the length of interventions was often at least 2 months, commonly with weekly or twice-weekly sessions. One-off interventions were typically camps that lasted for around 1 week or procedural interventions that after introductory session(s) lasted for the length of the procedure. A number of interventions were ongoing and continued after completion of the study in question. 164,172,175–177,183,188,189,191,195–197,200–204,206,209–212,215,219
Quality appraisal
The results of the quality appraisal of included articles are summarised in Table 4. Quality ratings were based on individual articles rather than studies to allow for the different research questions across articles. Only one of the 60 articles, a PhD dissertation,164 scored a ‘Yes’ against every quality appraisal question. Thirteen articles scored a ‘yes’ for at least 12 quality appraisal questions. 164,166,169,178,184,188,195,199–201,203,208,216 Whittemore et al. 114 scored poorest, with nine ‘no’ ratings indicating that study quality was rather lower than in other articles. The Stewart et al. 170 article reported on the same study as Barnfather et al. ;208 the latter article scored well on quality appraisal, with a ‘no’ only for consideration of limitations of methods and a ‘cannot tell’ rating for rigorous data collection. This discrepancy in quality appraisals illustrates the difficulty in rating quality when different journals, authors and disciplines may have different criteria for reporting. The Bignall article119 is a RCT included in review 1.
| Study first author and publication year | Is the research question clear? | Is the theoretical or ideological perspective of the author (or funder) explicit? | Has this influenced the study design, methods or research findings? | Is the study design appropriate to answer the question? | Is the context or setting adequately described? | Is the sample adequate to explore the range of subjects and settings, and has it been drawn from an appropriate population? | Was the data collection adequately described? | Was data collection rigorously conducted to ensure confidence in the findings? | Was there evidence that the data analysis was rigorously conducted to ensure confidence in the findings? | Are the findings substantiated by the data? | Has consideration been given to any limitations of the methods or data that may have affected the results? | Do any claims to generalisability follow logically and theoretically from the data? | Have ethical issues been addressed and confidentiality respected? | Are the interventions of interest clearly described? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ayers et al., 2011198 | Y | N | ?a | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Barlow et al., 1999171 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N |
| Barnetz et al., 2012162 | Y | N | ? | Y | N | Y | Y | N | Y | Y | Y | Y | ? | Y |
| Barnfather et al., 2011208 | Y | Y | Y | Y | Y | Y | Y | ? | Y | Y | N | Y | Y | Y |
| Barry et al., 2010199 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Baruch, 2010200 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | N |
| Bignall et al., 2015119 | Y | N | ? | ? | N | Y | N | ? | N | Y | Y | N | N | Y |
| Bluebond-Langer et al., 1991163 | N | N | ? | Y | Y | Y | Y | ? | N | Y | N | Y | Y | Y |
| Brodeur, 2005164 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Brothers et al., 2014209 | Y | N | ? | Y | N | Y | N | Y | N | Y | Y | N | N | Y |
| Bultas et al., 2015165 | Y | N | ? | Y | N | Y | Y | ? | Y | Y | Y | N | Y | N |
| Burns et al., 2010201 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Campbell et al., 2010187 | Y | N | ? | Y | Y | N | Y | Y | Y | Y | Y | Y | N | N |
| Curle et al., 2005188 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Dennison et al., 2010182 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Desai et al., 2014166 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Docherty et al., 2013202 | Y | N | ? | Y | N | Y | Y | Y | Y | Y | Y | N | Y | N |
| Fair et al., 2012172 | N | N | ? | Y | Y | Y | Y | ? | Y | Y | Y | Y | N | Y |
| Gan et al., 2010189 | Y | N | ? | Y | Y | Y | Y | ? | N | Y | Y | Y | Y | Y |
| Gaysynsky et al., 2015210 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Gillard et al., 2011174 | Y | N | ? | Y | N | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Gillard et al., 2013173 | Y | N | ? | Y | N | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Gillard et al., 2016167 | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | N | Y | N |
| Griffiths et al., 2015211 | Y | Y | Y | Y | N | Y | Y | ? | Y | Y | Y | Y | Y | N |
| Hosek et al., 2012168 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | N | N |
| Jaser et al., 2014190 | Y | N | ? | Y | N | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Kashikar-Zuck et al., 2016186 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Kirk et al., 2016183 | Y | N | ? | Y | N | Y | Y | Y | N | Y | N | Y | Y | N |
| Lewis et al., 2016175 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y |
| MacDonald et al., 2010212 | Y | N | ? | Y | N | Y | N | Y | Y | Y | Y | N | Y | N |
| Marsac et al., 2012191 | Y | N | ? | Y | N | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Masuda et al., 2013192 | Y | N | ? | Y | N | Y | Y | ? | N | Y | N | N | Y | Y |
| Moola et al., 2015169 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Muskat et al., 2016176 | Y | N | ? | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Nicholas et al., 2007177 | Y | N | ? | N | N | Y | N | Y | Y | Y | N | N | ? | Y |
| Nicholas et al., 2009214 | N | N | ? | Y | N | Y | N | ? | Y | N | Y | ? | Y | Y |
| Nicholas et al., 2012213 | N | N | ? | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Nieto et al., 2015193 | Y | N | ? | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Nilsson et al., 2009194 | Y | N | ? | Y | Y | Y | Y | ? | Y | Y | N | Y | Y | Y |
| O’Callaghan et al., 2011203 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| O’Callaghan et al., 2012204 | N | N | ? | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N |
| O’Callaghan et al., 2013205 | Y | N | ? | Y | Y | N | Y | Y | Y | Y | Y | N | Y | N |
| Reme et al., 2013195 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Romero, 2014215 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Serlachius et al., 2012184 | N | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Shrimpton et al., 2013206 | Y | N | ? | Y | N | N | Y | Y | Y | Y | Y | Y | Y | N |
| Sibinga et al., 2011196 | Y | N | ? | Y | N | N | Y | Y | N | N | Y | Y | Y | Y |
| Stewart et al., 2013b178 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Stewart et al., 2013a216 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Stewart et al., 2011a217 | Y | N | ? | Y | N | Y | Y | Y | Y | Y | N | N | Y | N |
| Stewart et al., 2011b170 | Y | N | ? | Y | N | Y | N | ? | N | Y | N | Y | ? | N |
| Stinson et al., 2010218 | Y | N | ? | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
| Stinson et al., 2008219 | Y | N | ? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Tiemens et al., 2007179 | Y | N | ? | Y | N | Y | N | Y | Y | Y | Y | Y | N | Y |
| Weekes et al., 1993207 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | N | N |
| White et al., 2016180 | Y | N | ? | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| White, 2014185 | N | Y | Y | N | Y | N | Y | Y | Y | Y | Y | Y | Y | Y |
| Whittemore et al., 2010114 | Y | N | ? | Y | N | N | N | N | N | Y | N | N | N | Y |
| Wolf Bordonaro, 2005197 | Y | Y | Y | N | N | N | Y | ? | N | N | Y | N | Y | Y |
| Wright et al., 2004181 | Y | N | ? | Y | N | N | Y | Y | Y | Y | Y | N | Y | Y |
With regard to the criteria against which articles were appraised, articles were most likely to score positively in relation to findings being substantiated by data, clarity of research question, study design appropriateness, adequacy of sample and description of data collection. We were not able to determine whether or not the authors’ theoretical perspective had influenced the study design, methods or research findings in 45 articles, suggesting a lack of reflexivity in the reporting of the included studies. Twenty-nine articles were rated as being at risk of bias in relation to the context or setting of qualitative research being inadequately described. 114,119,162,165,167,168,170,173,174,176,177,179,181,183,184,190–193,196,197,202,206,209,211–214,217 Twenty-two articles were rated as being of poor quality regarding the clarity of description of interventions. 165,167,168,170,171,176,182,183,187,198,200,202–207,211,212,215,217,219 After excluding theoretical or ideological perspective, which was rarely reported by included articles, five articles were of excellent quality, scoring a ‘yes’ or ‘cannot tell’ for all other quality appraisal items. 164,166,195,199,216
Qualitative synthesis
The translation of first- and second-order construct data across all 60 articles yielded five third-order constructs: ‘a therapeutic foundation’, ‘social support’, ‘a hopeful alternative’, ‘resilience’ and ‘getting in and staying in’. A number of third-order themes contribute to each construct. The line of argument that suggests how the constructs and themes are related to one another is represented pictorially in Figure 18. This line of argument is described in detail at the end of the qualitative synthesis. Important areas of overlap between themes are illustrated by intersecting circles. Arrows between constructs and themes suggest how they may relate to one another.
FIGURE 18.
Line of argument synthesis.
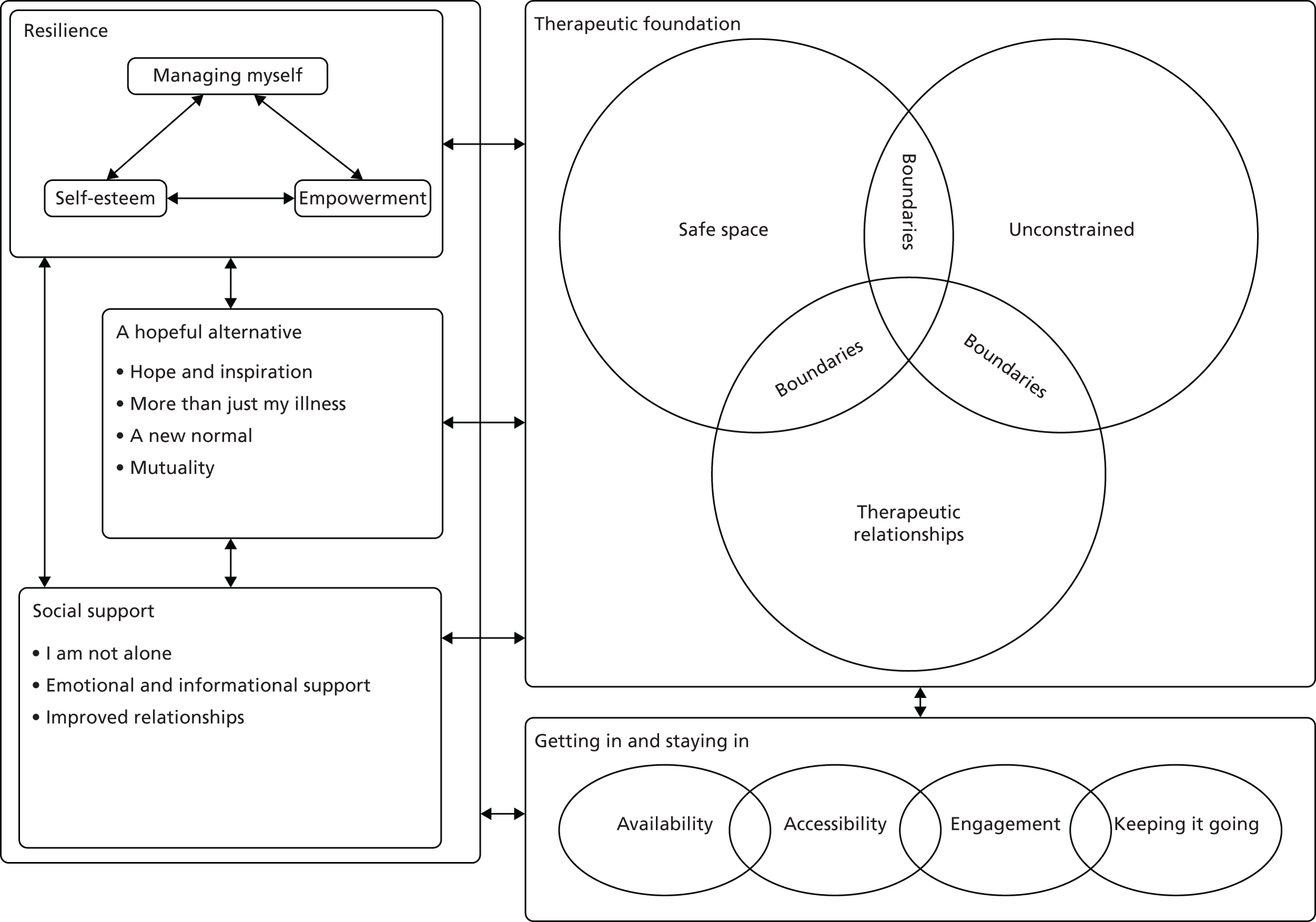
Report Supplementary Material 2, Table 6, provides an overview of the themes within each construct and the articles that contribute to each theme. The author interpretations or second-order ideas that contributed towards each third-order theme are discussed within each section, with first-order quotations in italics presented for illustration purposes and to maintain the link with participants’ voices. Each quotation is accompanied by a label within square brackets, acknowledging the type of participant providing the quote and the LTC under consideration within the study the quotation was taken from (e.g. ‘[parent, juvenile idiopathic arthritis]’). Additional interpretation is provided when necessary after first-order construct data, to explore its contribution to the theme.
Further detail regarding the third-order ideas that contribute towards each theme and the first- and second-order data that these ideas are based on can be found in Report Supplementary Material 2, Table 7.
Construct: a therapeutic foundation
‘A therapeutic foundation’ describes how mental health interventions can confer a sense of safety for CYP, through the provision of an environment that is perceived as physically and emotionally secure. The content of the four themes within this construct explores a range of factors that may contribute towards the development of a therapeutic space. The first theme, ‘a safe space’, discusses the importance for CYP of knowing what to expect and/or prior experience of an environment as safe. To perceive a space as safe, CYP need to know what is expected of them and have their privacy respected; these needs are explored within the second theme, ‘boundaries’. The third theme, ‘unconstrained’, explores how CYP value the opportunity to escape from the worries and everyday routine associated with their LTC. ‘Therapeutic relationships’ is the fourth theme and explores different aspects of the relationship between CYP and their peers or practitioners that may be considered therapeutic. Overall, the ‘therapeutic foundation’ construct aims to emphasise the importance of CYP having access to somewhere they feel able to express themselves fully and be listened to and understood by empathetic people.
Figure 19 indicates how some second-order construct data contribute towards more than one theme. This overlap between ‘a safe space’, ‘unconstrained’, ‘boundaries’ and ‘therapeutic relationships’ aims to illustrate how the experience of one of these aspects may facilitate the occurrence, or experience, of another.
FIGURE 19.
Inter-relationship between ‘a safe space’, ‘unconstrained’, ‘therapeutic relationships’ and ‘boundaries’ in creating a ‘therapeutic foundation’ and links with other constructs.
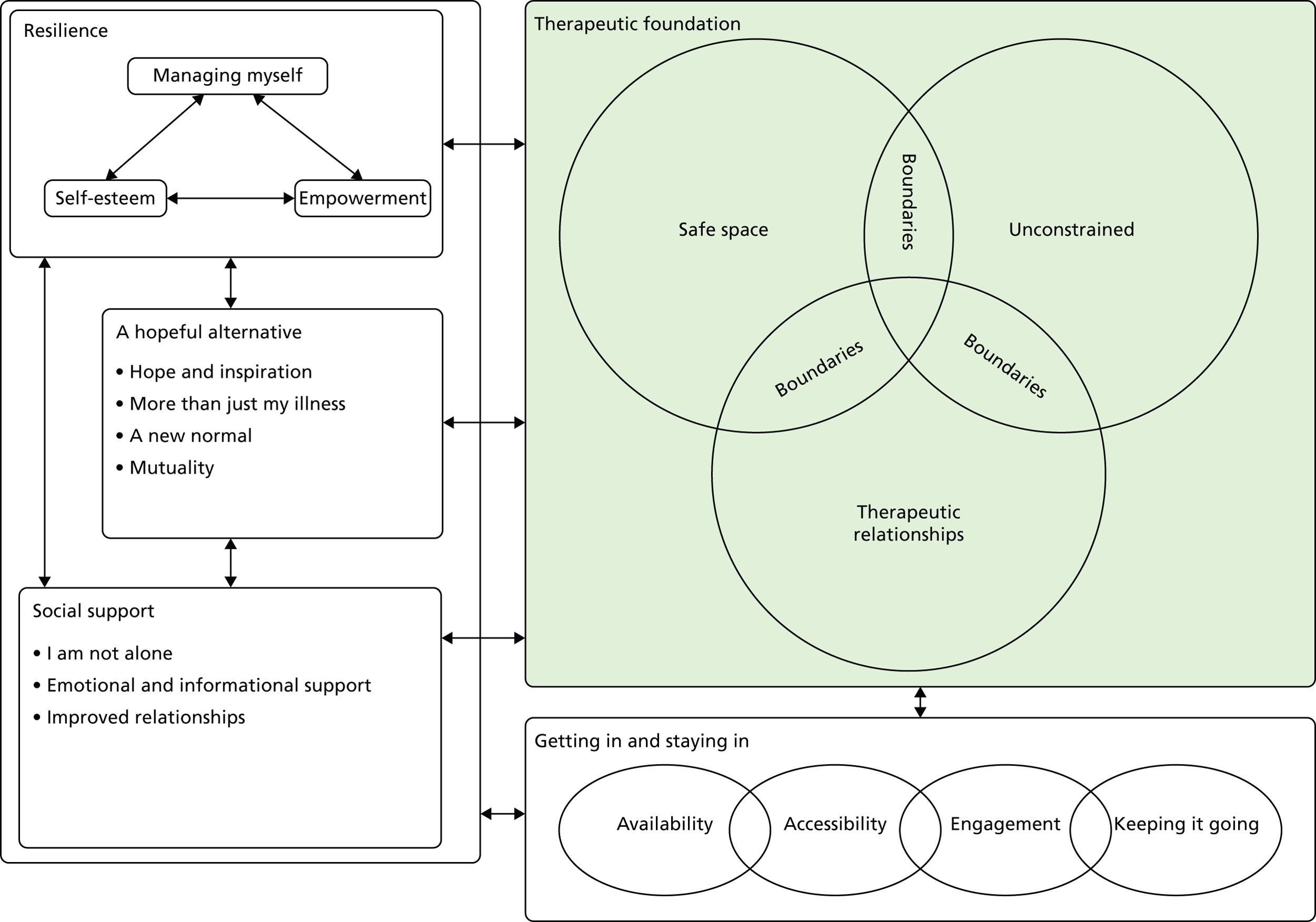
Theme: a safe space
‘A safe space’ illustrates how the presence of familiar family or staff within a setting that is already known to them can result in CYP feeling reassured and comforted. These feelings are necessary if CYP are to feel receptive to, and thus benefit from, an intervention. The people who deliver an intervention, or ‘intervention deliverers’, have an important role in helping CYP familiarise themselves with the intervention setting and with other people taking part. These factors, together with an understanding of what the intervention entails, may help reduce anxiety about entering an unfamiliar environment and enable CYP to experience the setting as somewhere that is both emotionally and physically ‘safe’. Nineteen articles contributed to this theme (see Report Supplementary Material 2, Table 6).
The authors of three studies found that CYP may experience anxiety at the prospect of meeting unknown people prior to an intervention172,177,182 and that the presence of a parent or support of a known staff member, such as a social worker, can reduce this anxiety and enable CYP to engage with a previously unknown intervention (see Report Supplementary Material 2, Table 7). A young person with T1DM illustrates this when discussing their anxiety about meeting the person delivering their psychoeducation intervention for the first time:
. . . I hadn’t met anybody and didn’t know where I was going and all those kinds of things, ummm, being quite young, being very ill, very worried. And I personally wouldn’t have coped very well if they had just invited me to go to somewhere. I needed my mum there.
Young person, T1DM182
The above quotation suggests that the involvement of someone who is known to the young person is comforting. The reduction in anxiety as a result of the presence of someone familiar may potentially ‘mask’ a mental health need of CYP taking part. However, within the initial stages of an intervention, a familiar person could transform a previously feared space into one that is ‘safer’, allowing CYP to better engage with the intervention being delivered. The following quotation from a young person taking part in a study examining different management techniques for needle-related distress illustrates this:
If I actually knew the nurse it would be OK, but if I didn’t I would be like ‘what’s going on? I don’t even know you!’
Young person, cystic fibrosis198
Making an environment feel safer may be an important intervention itself, especially for CYP with anxiety around medical procedures. This may depend on the frequency and duration of medical treatments and related levels of distress for the young person.
Fears about not knowing anyone else who was taking part were also acknowledged at the start of a creative writing group172 and online peer-support interventions. 177 Authors of three studies suggest that CYP valued the opportunity to get to know peers more. 162,174,179 As CYP became more acquainted with one another, a feeling of acceptance was created, giving the intervention space a sense of being familiar and safe, helping CYP feel able to share their feelings and experiences with one another. This is illustrated by a participant from a camp:
The camp did help with that [to talk about our different experiences] by bringing us all together and letting us get to know each other for a couple of days so that we felt that we were comfortable enough to go up to each other and just talk about it.
Young person, craniofacial differences179
First- and second-order data from 11 studies suggests that the individuals who delivered the interventions played a key role in supporting the initial recognition of similarity between peers and encouraging interaction and engagement during the early stages of group interventions. 114,166,172–177,179,184,192 Second-order data from five studies suggests that deliverers of interventions should plan to allow sufficient time for CYP to get to know each other. 166,169,174,175,179
Report Supplementary Material 2, Table 7, indicates that prior experience of a setting as somewhere safe was viewed positively by CYP. 175,176 Below, a young person indicates how they perceived coming back to a hospital environment with which they were already familiar for an introduction to a peer-support programme:
. . . for me, the hospital became like a second home. It was my safe haven. I always felt safe in the hospital. I always felt comforted in the hospital. So having the 8-week group in the hospital, I saw it as somewhere safe that I could come back to.
Young person, mixed175
Authors identified that CYP valued knowing what to expect from an intervention, either through explanation regarding the content of the intervention and its aims by the intervention deliverer182,185,195 or through provision of the opportunity to observe others participating before taking part themselves. 205 Wolf Bordonaro197 discusses how the process of asking for information from the intervention deliverer about the time and place of follow-up sessions by CYP may be a method used by CYP to feel in control within the intervention situation. Many CYP with LTCs experience unpredictable symptom fluctuations and are expected to attend appointments to manage their physical health – aspects of their life over which they may have little control. Feeling in control of a situation related to their LTC could be a novel experience for CYP, providing an opportunity to distance themselves from anxiety associated with their LTC and its management. CYP may feel reassured by the presence of a predictable intervention structure, as illustrated by Gillard et al. ,174 who discuss the use of ground rules and set format within their ‘TeenTalk’ intervention. This use of predictability to help CYP feel safe within the intervention setting is explored further within Theme: boundaries.
This theme indicates that CYP may find it helpful to invite their family members and familiar staff to attend distressing procedures and accompany them in unfamiliar intervention situations. It is also important that CYP are given enough time to get to know one another in group settings and are supported to familiarise themselves with the setting and staff beforehand. Knowing what to expect from an intervention through the use of a predictable routine and requesting information may also help reduce CYP’s worries about attendance and help them feel safe and in control of the intervention situation.
Theme: boundaries
This section considers the theme ‘boundaries.’ Authors of the 34 articles included in this theme (see Report Supplementary Material 2, Table 6) describe the efforts made by the deliverers and/or recipients of an intervention to set certain rules for one another. These boundaries may include maintaining the privacy and anonymity of intervention recipients; setting rules for behaviour or acceptable discussion topics; and having an established meeting time, structure and setting. As indicated within Figure 19, the setting of boundaries appears to facilitate the experience of a setting as ‘safe’, which may in turn enable CYP and their families to discuss their emotions and sensitive issues connected to living with their LTC. This is an example of CYP feeling ‘unconstrained’ by their LTC, an idea that is explored in Theme: unconstrained.
Seven studies suggest that among CYP with LTCs there appears to be a fear of their diagnosis, or other issues they regard as private, being disclosed to others. 167,172,174,177,178,187,196 Authors describe health and social care professionals playing an important role in advertising interventions to an appropriate audience,172 monitoring those who are able to access the intervention210 and locating a secure, safe environment in which to discuss sensitive topics. 176
Three study authors suggest that there is a demand for intervention deliverers to respect the privacy of CYP by creating opportunities for CYP to talk without parents or the deliverer present,179,182,202 as recognised by a parent supporting their child to attend a CBT intervention:
I did wonder whether they should have spoken to her by herself . . . I just felt like there could be things going on that are of worry and whether friends like you etc. that may not want to be said in front of parents.
Parent, T1DM182
This appears to contradict the observation made under the theme of ‘a safe space’ that the presence of a familiar person may enable CYP to access an intervention and talk about their experiences. As CYP become familiar with an intervention and its setting, they become more open to meeting with an intervention deliverer, or other young people, without the support of family or known staff members.
Two studies suggested that online interventions provide the opportunity for greater anonymity than face-to-face interventions, which some CYP and their parents felt facilitated participation and engagement among less confident attendees. 177,178 This is evidenced by a quotation from a young person who took part in an online support and education intervention, supported by older peer mentors:
The internet was better because you’re not looking at them straight in the eye. I guess it is a bit easier. I think I shared my feelings better. Face to face would be hard.
Young person, asthma/allergies178
Three studies suggest that the use of certain rules, such as the use of a deliberate turn-taking structure within sessions, can help CYP feel safe enough to express their emotions,174,189 as well as ensure that these emotions are appropriately managed. 187 This is illustrated by a family member discussing taking part in a family system intervention:
I liked how each of us had a turn to speak and share our experiences. I also liked how everybody else listens on what you have to say.
Sibling, ABI189
Although Gan et al. 189 do not indicate how the precedence for this turn-taking was established, the topic manual developed to guide the implementation of their family intervention indicates that time to introduce the intervention and develop an agreed contract between participants and intervention deliverers was included during the early stages of the intervention. One mother taking part in a family art therapy intervention agreed that boundaries around acceptable behaviour should be established early on in the intervention:
The kids, you know, I think it’s extremely important when you are dealing with children, regardless of illness or age, that they know from the get go, what is expected, and what their limitations are . . . then when they are imposed after the fact, it feels restrictive.
Parent, mixed164
Here, the late introduction of boundaries to curb potentially disruptive behaviour appears to have been experienced as critical and restraining. Perhaps the introduction of boundaries at an earlier stage of an intervention may ensure that the CYP’s behaviour remains respectful of others and also enables them to relax, have fun and feel ‘uncontrolled’. This possibility is supported by Gillard and Watts,173 who highlight how camp staff supported CYP to take part in ‘transgressive activity’ while attending camp, such as the challenge to overcome ‘security’ measures to win a box of sweets for their cabin group. This was seen as an opportunity to engage in risk-taking behaviour within set appropriate limits. Four studies highlighted how behavioural rules ensured that CYP respected the personal space and boundaries of others,173,181,185 which contributed towards the creation of a supportive community within peer group interventions:
That it’s got a sense of community . . . that everybody respects everybody . . . and you can talk about everything and anything . . . Some people disagree with you, but they don’t bark at you.
Young person, cerebral palsy/spina bifida170
One topic in which discussion appeared to be restricted was in relation to life-threatening LTCs. Within some interventions, the avoidance of the discussion of death and dying was noticeable. For one study, this was a result of the intervention’s explicit aim to provide the child with respite from worries regarding their LTC,173 whereas within an online support site for CYP with cystic fibrosis and their parents, the avoidance of discussing the life-limiting nature of the LTC was not explicitly discussed. 183 Perhaps this reflects the desires of participants within this group and may highlight the need to discuss ground rules at the beginning of an intervention, to ensure that participants know what to expect.
The conscious or unconscious avoidance of discussions of death may reflect the need for CYP with certain diagnoses, and those involved with their care, to change the focus of mental health and well-being interventions to consider ‘how to make the best’ of the time left and live as normal a life as possible. In contrast, two studies aimed at alleviating distress for CYP with cancer undergoing stem cell transplantation suggest that the interventions provided the opportunity for CYP to confront their own mortality and the possibility of dying. 201,202 These two apparently contradictory concepts illustrate the important role mental health interventions may play in facilitating both the acceptance of the possibility of death and ensuring that life is as fulfilling as possible for CYP with potentially terminal diagnoses. The balance between these two alternative outcomes may be affected by LTC type and prognosis, as well as by the choice of coping strategy preferred by the CYP and their family. The evocative nature of the work, particularly in supporting CYP at the end stage of their illness, necessitates the presence of an intervention deliverer who is adequately trained and the resources to ensure that they are provided with adequate supervision. The need for an intervention to be adequately resourced and consider the type of LTC and personal preferences of CYP is discussed within the ‘availability’ and ‘engagement’ themes under Construct: getting in and staying in.
Setting aside time to spend together can be difficult because of the challenges of meeting the needs of different family members and balancing family life alongside the demands of managing a LTC. 164,188 First- and second-order construct data from two studies evaluating family-orientated interventions indicated that CYP and their parents appreciated having a scheduled opportunity to spend time together as a family. 164,189 This appeared to facilitate communication between family members, as described by two parents taking part in a family system intervention, facilitated by a social worker/rehabilitation counsellor:
Opened my eyes as to what [the adolescent with the ABI] was thinking.
Parent 1, ABI189
Helped us to discuss concerns and feelings that otherwise might not surface.
Parent 2, ABI189
This opportunity to communicate more openly facilitated insight into what the young person with the LTC was thinking and meant that the family could use the space to better understand each other’s feelings. Authors of two studies also indicated that CYP valued the opportunity to meet with peers. 163,174 This may prove beneficial for CYP in building respectful, understanding and empathetic relationships with family and peers with a LTC, as discussed in Construct: social support.
In this section we discuss the value of establishing boundaries, and their role in ensuring that CYP experience an intervention setting as safe and feel able to express their emotions. Intervention deliverers and participants can be involved in the creation of boundaries, which through the sharing of experiences can facilitate the development of understanding and caring relationships.
Theme: unconstrained
This theme explores how the opportunity to meet similar peers seemed to be important to CYP. This experience appeared to provide CYP with the freedom to fully express their emotions without being constrained by the expectations or views of others. The theme also discusses how mental health and well-being interventions can provide an experience of freedom or respite from the constraints and daily routine of having a LTC and the anxiety and distress that can result. Twenty-eight articles contributed to this theme (see Report Supplementary Material 2, Table 6).
Although the idea of an intervention setting being both ‘safe’ and ‘unconstrained’ appears to be contradictory, there is a large degree of overlap in the 12 studies that contribute towards both of these categories,162,164,166,173–177,179,181,182,205 across a diverse range of interventions and LTCs. The ‘boundaries’ category suggests that a therapeutic space must have limits if it is to be experienced as safe by CYP. This may account for these two different sets of ideas from the same studies. The use of ‘boundaries’ within an intervention may need to be flexible to consider the changing needs of participants and facilitate their ability to access ‘a safe space’ or feel ‘unconstrained’ as required. A possible example of this is that CYP may wish to think about the risk of dying on some occasions, but not others.
Interventions that provided the opportunity for CYP to be themselves, speak openly and experience freedom from stigma or judgement were particularly valued163,166,167,169,173,174,176,187 and facilitate a safe space in which CYP felt able to talk and share their experiences:
I feel open that I could talk to whoever, however I want like I can talk open about what I feel and what I need.
Young person, HIV176
One way in which this appears to have been achieved is by CYP interacting face to face with peers with similar LTCs (see Report Supplementary Material 2, Table 7). Six of these interventions were residential camps;163,166,167,169,173,174 however, this opportunity was also provided during two weekly peer support group interventions. 176,187
The opportunity to feel free from the perceived judgement of others appeared to be particularly relevant for CYP whose LTCs result in a visible difference in their appearance or which are associated with high levels of perceived stigma. 163,166,167,172–174,176,187 Although the majority of the interventions included in this review were delivered to CYP with the same LTC, there was some evidence to suggest that CYP, including those with stigmatised diagnoses,167 also enjoyed and benefited from interacting with peers with different LTCs. 164,177,178,217 This evidence suggests that the ability of CYP to empathise with others who are experiencing similar difficulties to them may transcend diagnosis.
In addition to the positive benefits of spending time with peers in similar situations, the authors of five studies explicitly discussed the value of CYP having the opportunity to access an ‘adult-free space’ to meet by themselves169,179 or separately with the intervention deliverers. 164,182,202 Four of these studies interviewed participants between 9 and 24 years of age; thus, the developmental stage of participants may have influenced their expressed need and comfort with a space separate from their parents. 169,179,182,202 A flexible approach, depending on timing and needs of CYP, might be appropriate, as suggested by CYP with craniofacial conditions receiving a camp-based intervention:
It is good to have a leader [adult deliverer] but maybe not [one] who does everything . . . like especially when we didn’t know each other at first it was really tough to get us to talk . . . So it might be good to have a leader at first but once we got to know each other it was a little easier.
Young person, craniofacial conditions179
These peer relationships also appeared to provide CYP with a release from perceived pressure from health professionals and parents, as illustrated by a young person with T1DM talking about their relationship with their mentor, a slightly older peer with lived experienced of their LTC:
The mentor manages to come into both worlds, the world of the adults and the world of my worries, he knows them, you can choose what to share with him and what not to share, he’s tolerant. He doesn’t pressure me.
Young person, T1DM162
In contrast with the need for structure highlighted within ‘boundaries’, Barnetz and Feigin162 highlight how young adolescents can learn to accept their condition through relationships based on enjoyment and interest, unconstrained by an adult-orientated approach to relationships that emphasises structure, contribution and development. This apparent freedom from adult rules offers a contrast to life as usual for CYP, when opportunities for experiencing autonomy may be complicated or limited by the LTC. The ability to learn and express feelings through unstructured, informal contact with peers was also identified by studies evaluating camp-163,166,169,174,179,185 and technology-based interventions. 177,183 The role of CYP being able to express themselves emotionally to receive emotional support and learn new skills is discussed in more detail in Theme: emotional and informational support and Theme: managing myself.
Another way CYP were able to feel ‘unconstrained’ by their LTC was through interventions that provided respite from the ‘daily suffering and uncertainty’ associated with treatment for a LTC,202 as well as a temporary reprieve from worries about daily life and the limitations enforced on them by the LTC. This is illustrated by a quotation from a parent of a child receiving music therapy:
He looked forward to the [therapeutic music session]. He knew it was going to be a day where he didn’t have to worry about if they were coming in to give him a pill or if they’re coming in to start the chemotherapy.
Parent, cancer201
Interventions associated with feelings of respite seem to be those that are not part of routine treatment, such as camps, or interventions that aim to provide an alternative environment or distraction from the hospital setting. 177,201,205 This release from the daily burden of living with a LTC could potentially improve the mental health of CYP. CYP taking part in camp interventions spoke of the bodily freedom they experienced in being able to take part in activities that they had never tried before because of the physical limitations placed on them by their LTC and risk management strategies used by adults they came into contact with. 165,166,169,173,174 Authors of five camp studies discussed how, owing to adaptations such as the provision of trained staff and specialist equipment to support physical health needs,165,166,173,174,185 CYP were able to take part in an activity commonly available to American CYP without LTCs. This brief opportunity to experience being like any other child may be a novel experience for CYP with LTCs and is discussed further under Theme: a new normal.
The emphasis on how much CYP enjoy fun and engaging activities was acknowledged by 18 studies114,162–168,172–174,177,178,185,187,189,205,206 and could be considered as another important factor that allows CYP to relax and ‘just be a kid’. 173 This is an important component to consider when designing interventions that CYP find engaging, discussed later in Theme: engagement. However, it may not always be appropriate to incorporate an element of ‘fun’ into a mental health intervention. For example, in the case of CYP receiving procedural interventions, the focus of a mental health intervention may be on reducing the distress of CYP enough to support them to engage with the procedure. In addition, three study authors acknowledged that there was the risk of CYP learning information about their illness or those of others that may upset them while interacting with peers with similar LTCs. 163,177,185 For example, one CYP with cancer talks about the uncertainty created through meeting peers at camp who had experienced a relapse in their illness:
It worries me sometimes, because they [campers who relapsed] thought that some day they’d be sure, and they could go on with their lives. And it didn’t turn out that way. So once in a while, I think, ‘Well, maybe I will relapse, and I won’t be around very long.’
Young person, cancer163
Nicholas et al. 177 highlight the importance of having a member of staff to address any anxiety or distress that may be created through peer interaction.
The studies contributing to this theme indicated that CYP appreciated the chance to speak openly, particularly when they did not often have this opportunity within their everyday lives. 167,174 CYP also valued opportunities to escape the routine and pain associated with their LTC through new environments, having fun and trying new activities.
Theme: therapeutic relationships
This theme, receiving contributions from 42 articles (see Report Supplementary Material 2, Table 6), characterises therapeutic relationships as the availability of trustworthy individuals who make CYP feel cared for, respected and valued. These relationships offer CYP the opportunity to share their stories and be listened to in a respectful environment. Studies included in this review indicate that relationships of this quality are not just limited to interactions between CYP and a trained intervention deliverer. This theme also considers the importance of relationships with peers and families in similar situations in helping them to feel secure within the intervention setting.
The authors of seven studies162,166,174,175,183,186,197 note that CYP receiving interventions valued the knowledge that helpful people were consistently available (see Report Supplementary Material 2). This is illustrated by the following quotation from a young person, describing their perception of counsellors at their camp:
That is what camp means to me, I love the counsellors. They are awesome and if you need help just ask them a question and they will help you.
Young person, congenital heart disease (CHD)166
Within the camps included in this review, camp counsellors referred to volunteers, often previous camp attendees,167,173 who provided support and supervised CYP while they completed activities. This suggests that therapeutic relationships can exist between CYP and individuals without specialised mental health training.
Along with interest and understanding,186,190,196,210,219 Report Supplementary Material 2, Table 7, indicates that mental health and well-being interventions provided the opportunity to build empathetic connections with both peers and intervention delivers. 114,183,205 This opportunity is evidenced by a young person discussing an internet-based coping skills programme with a discussion board component:
The scene presented was true . . . but, most of all I liked knowing that other teenagers know how I feel. That made me feel good.
Young person, T1DM114
These empathetic interactions appeared to provide the opportunity for CYP to receive recognition and validation of their experiences. 163,164,172,175,177–179,186 First- and second-order construct data from 10 studies suggest that these connections may elicit feelings of being cared for and valued. 164,167,169,172–174,176,178,185,197 This is evidenced by a young person describing the emotional effect of their relationship with fellow campers:
I would probably take that feeling of like being wanted because I know, like, for some kids . . . they don’t feel as, like, wanted or like people want to be around them. . . . it’s not, like, very often that you’re included in a lot of stuff.
Young person, mixed167
This suggests that it is important that CYP feel that they matter to other people, who can see and value them for the person they are, beyond their LTC. This may help CYP build trusting relationships with their peers and intervention deliverers and to express themselves and thus create the opportunity for them to receive social support from peers, as discussed in Construct: social support.
This opportunity for self-expression and being heard by an empathetic audience may in turn have reinforced the experience of the intervention space as safe and trustworthy. For example, a parent observed the following of the relationship between their child and the deliverer of a movie-making programme designed to reduce CYP’s anxiety while receiving radiotherapy:
She placed a lot of trust in them and she really loved them. . . . And I think because of that she felt safe. She felt she was not going to be let down and that she could go through the process with the people around her.
Parent, cancer206
These therapeutic relationships, including the positive regard of both peers and those delivering the intervention,197 influence both how the child feels about themselves and their coping outside the intervention setting. This is illustrated by a young person discussing how their camp experience could affect them during their everyday life:
The love that I received here made me a better person because I was able to have more independence yet still have a lot of fun whenever I want and always find the bright side of things instead of things that are negative and pessimistic . . . [I] have more confidence in myself.
Young person, mixed167
The evidence within this theme suggests that relationships with empathetic peers, intervention deliverers and family members can play an important role in helping CYP feel validated, cared for and valued. This appears to facilitate the expression of emotions and increase the likelihood that CYP’s psychological needs will be met. As a result, high-quality therapeutic relationships could be considered as a critical component of mental health interventions in their own right.
Summary: therapeutic foundation
The importance of a sense of familiarity, feeling unconstrained, establishing boundaries and developing therapeutic relationships has been discussed in the context of creating a ‘therapeutic foundation’. The creation of such a foundation is something that is needed to form the basis of an intervention. It provides a healing space in which CYP can be themselves, reinforces the engagement of CYP with an intervention and enables them to access social support from their peers and intervention deliverers. In turn, this social support, as discussed within Construct: social support, may reinforce that it is safe for CYP to talk about their feelings and experiences. Having a safe space and supportive peer network can also enable CYP to learn new skills and fresh perspectives to help them manage their LTC that can contribute towards the building of resilience and hope, concepts that are explored within the overarching themes below.
Construct: social support
Three themes contribute to the construct of ‘social support’: ‘I am not alone’; ‘emotional and informational support’ and ‘improved relationships’. Theme: I am not alone details how CYP can experience feelings of connectedness and belonging through contact with peers with a LTC. Theme: emotional and informational support discusses how CYP can gain access to emotional reassurance and receive information to help them to manage their relationships with peers and family through contact with empathetic, understanding peers and intervention deliverers. The final them, ‘improved relationships’ discusses how an intervention may improve CYP’s relationships with peers who do not share their illness experience and family members.
The concepts identified within the themes that contribute towards the ‘social support’ construct can influence CYP’s experience of a ‘therapeutic foundation’ but can also potentially affect CYP’s lives outside the intervention setting. The emotional and informational support received as part of the intervention may enable CYP to communicate more freely with family and peers and have a positive impact on these relationships. These improved relationships may both reinforce the experience of an intervention setting as therapeutic and potentially extend this experience of a therapeutic safe space beyond the intervention setting into their daily lives in the form of social support. This may have important implications for maintaining engagement with the intervention and any effect beyond its end point, as suggested within the overarching construct ‘getting in and staying in’, which are described in detail in later sections. Figure 20 depicts the relationship between the construct ‘social support’ and the other constructs.
FIGURE 20.
Therapeutic foundation and social support.
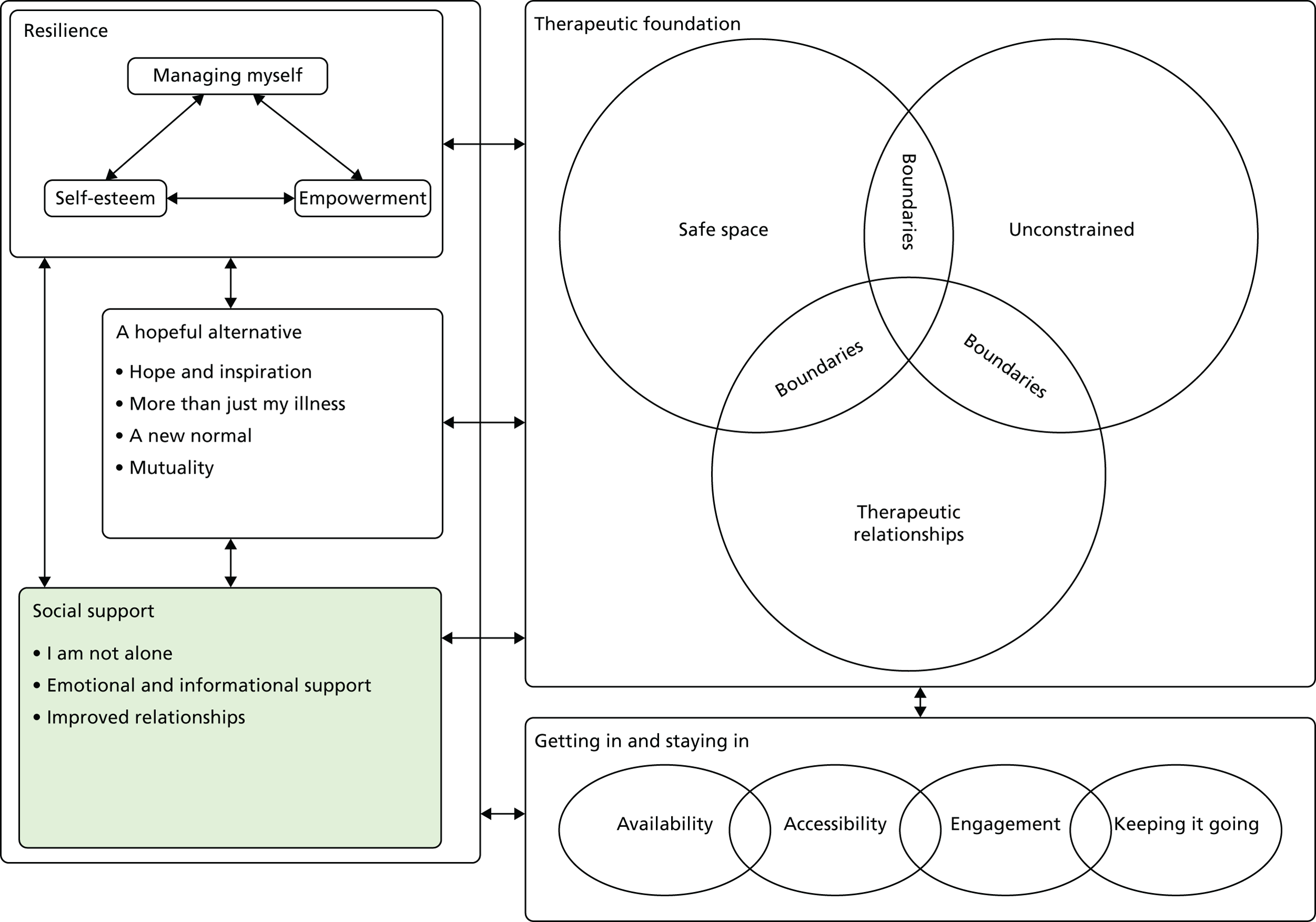
Theme: I am not alone
This theme discusses how CYP value the opportunity to connect with others who are similar to them, and the feelings of safety and belonging that this can provide. Meeting and interacting with peers helped CYP to realise that they were not the only ones living with such difficulties and normalised their experiences. This experience can help reassure CYP and reduce feelings of loneliness and isolation. Forty-six articles contributed towards this theme (see Supplementary Material 2, Table 6).
Six study authors discuss how, for some CYP, meeting people with similar experiences was a novel experience. 162,166,169,172,176,185 Conditions such as cystic fibrosis actively prevent CYP from meeting face to face in groups because of the potential risk to their physical health. 183 Other LTCs such as HIV infection and sickle cell disease can be associated with high levels of stigma, poor understanding and grief within the wider community, which can prevent CYP with these LTCs from connecting with peers with the same conditions. 167,176
Ten studies indicated that CYP valued the sense of being understood and accepted through interactions with peers with similar conditions. 162,163,166,171,174–176,179,216,217 This is illustrated by a quotation from a young person accessing a week-long camp intervention:
At home I’m like Clark Kent . . . but like here, I’m Superman. I’m just like, I’m more open, more talkative, more inspired . . . ’Cause when I’m at my home it’s like I’m hiding from everybody else . . . I just don’t communicate. Camp is more open, it’s just friends all over.
Young person, HIV174
The quotation suggests that feelings of being understood and accepted by similar peers may be related to CYP’s perception that they were free from stigma or judgement from others, facilitating feelings of safety and self-expression as discussed in Theme: unconstrained.
Nineteen studies suggested that the opportunity to connect with others who share their experiences appears to facilitate feelings of belonging in CYP. 114,162,164–166,169,171,172,174,177,179,183,186,187,189,200,202,216,217 This is evidenced by experiences of a variety of interventions, which ranged from structured family art therapy-style or support groups for CYP164,172,176,189 to more unstructured interventions, such as camps:166,169,174,179
Here it’s like a happy home so it’s like, . . . we are all like a family and our grandma lived here, and grandma invited us all over for dinner every 3 months, that’s how it is, like whenever we come it’s like ‘Hey, good to see you’.
Young person, HIV176
The authors of five studies indicate that the communication of experiences with peers or understanding that intervention deliverers can help reduce feelings of isolation within CYP,162,166,171,186,202 as supported by a quotation from a young person experiencing an online peer-mentoring intervention:
When I was doing the chats, I was involved with the conversation, and I wasn’t thinking about [loneliness] . . . [The chats] made me realise that I’m not alone; like with my disability . . . there’s lots of people out there that go through the exact same thing as I do.
Young person, CP/SB170
These reduced feelings of isolation also occurred through use of online interventions,114,177,178,183,216,217 although some parents suggested that the inclusion of an opportunity to meet either before or after commencement of online sessions would enhance bonding between CYP. 178,216
The reduced isolation through recognition that there were other people who were similar to them and the validation achieved by connecting through shared experiences could also be thought of as a form of ‘affirmational support’ as conceptualised by Stewart et al. 178 Stewart et al. 178 describe affirmational support as CYP sharing challenges and solutions and thus receiving validation of their concerns and reassurance that they are not alone and are able to cope well with their LTC.
Theme: emotional and informational support
Forty articles contributed to this theme (see Report Supplementary Material 2, Table 6), which explores how both emotional and informational support are important components of social support experienced by CYP. We used Stewart et al. ’s178 model of social support and their conceptualisation of ‘emotional’ and ‘informational’ support to inform the set of ideas within this theme. In this section, ‘emotional support’ aims to encompass the relief and reassurance experienced by CYP as a result of expressing their feelings to peers who can empathise with them. Access to people with similar stories to tell and experienced intervention deliverers also enabled CYP to receive information and advice on how to manage and cope with their LTC. This informational and emotional support may reinforce CYP’s experience of the intervention setting as a safe space where they can express their emotions freely and enable them to acquire skills and knowledge, as discussed later in Construct: resilience.
Report Supplementary Material 2, Table 7, indicates that the opportunity to be in the same environment and share experiences with similar others enabled CYP to access emotional support and reassurance,162,172–174,176–178,183,207,216,217 as illustrated by this quotation from a participant attending a camping intervention for CYP infected with HIV:
You’re just always getting reassured that it’s OK that you have this [HIV], and it’s just a good feeling.
Young person, HIV174
Children and young people appeared to experience the sharing of their emotions with peers as a form of stress relief174,217 and valued the opportunity to talk about anxieties they worried that parents would not understand. This is illustrated by a young person with T1DM discussing their older peer mentor:
You can share deep experiences and fears that other people won’t understand or don’t know how to calm.
Young person, T1DM168
This suggests that the presence of peers may facilitate emotional self-expression for CYP, owing to their perception that their peers can understand what they have been going through, as discussed under Theme: unconstrained. CYP may perceive that it is safe to discuss difficult feelings if they know others will be able to understand and empathise with them.
The authors of three studies suggest that those delivering interventions have an important role in maintaining the ‘emotional safety’ of CYP during discussion of sensitive topics and reassuring CYP that other people will understand and listen to them. 178,187,189 Peers and intervention deliverers also provided CYP with the opportunity to express their emotions and think about how to manage them:
When I used to get angry, I just handle matters myself. I’d get in trouble. Here I don’t get in trouble. They just talk to me for a while, about like, how it’s not worth it.
Young person, HIV174
In addition to emotional support, CYP also expressed a desire for information on what to expect in the future, including information on medications; activity limitations; variations in disease severity; and possible impact on family, friend and romantic relationships. 168,171,189 This is indicated by a young person discussing what they would like as part of a psychoeducation programme:
I’d like to know what could happen, so you’ve got no surprises later on.
Young person, juvenile idiopathic arthritis (JIA)171
This suggests that informational support gained from individuals delivering an intervention may help to reduce anxiety associated with not knowing what could happen next or how their LTC may impact on their lives in the future. The quotation below from a young person infected with HIV illustrates how they intended to use the knowledge from a peer support group intervention to prepare them to answer questions from others in the future:
. . . I always had to ask how do I get it again, how do I transmit it . . . and yeah cause I always had to ask the second questions because I always have to make sure that I’m at a point where if someone asked me, I’m ready to answer their questions.
Young person, HIV176
Second-order construct data suggest that CYP valued information from same-age peers, older peer mentors and intervention deliverers on how to manage relationship challenges, such as teasing because of appearance, or LTC management issues166,178,216,217 and how to manage issues of disclosure and sexual relationships. 168,172 Listening to how peers managed these difficult situations may help to inspire CYP through the recognition that they may be able to do this too, an idea explored in Theme: hope and inspiration.
The data within this theme suggest that mental health interventions should aim to incorporate emotional and informational support components, as there is evidence that this may benefit CYP’s mental health and well-being. These components may be delivered through contact with peers with similar conditions and/or intervention deliverers.
Theme: improved relationships with family and healthy friends
This theme discusses how an intervention targeting CYP mental health may also improve connections with family members and healthy peers. This may occur through enabling CYP to help their family members and peers better understand their feelings and the impact of the LTC on their lives. Alternatively, interventions can directly target communication styles between CYP and family members or peers. Both of these approaches can improve relationships between CYP and key people in their lives. This may in turn result in increased social support for CYP outside the intervention setting. Thirty-four articles contributed towards this theme (see Report Supplementary Material 2, Table 6).
The authors of four studies suggest that one method of changing dynamics within the family is by altering parenting styles through both family-directed interventions164,184,189 and those focused on CYP. 185 Changes reported by parents as a result of these interventions included improved recognition of protective parenting styles185,189 and increased attempts to focus on aspects of family life other than their child’s LTC. 164
Seven studies suggest that an intervention can provide a distraction from the LTC. 164,177,181,190,201,205,206 One young person discussed how they enjoyed the alternative focus provided by a family art therapy intervention:
It’s a lot of fun. And I get to do things with my mum. And there are things, finally, that we can have fun at doing. When I was going through so much of my sickness, I wasn’t able to do fun things. It’s just a healthy experience.
Young person, mixed164
The idea that CYP appreciate interventions that consider other areas of their life in addition to their LTC is discussed further under Theme: more than just my illness.
Interventions that aim to improve CYP mental health and well-being may also indirectly improve relationships between the CYP and other members of their family. The authors of 12 studies indicated that improved communication between family members and increased empathy for the child with a LTC resulted from interventions aimed at individual CYP184,190,196,200–202,205,206 or peer groups. 172,175,177,181 CYP receiving peer support interventions valued advice from peers with similar conditions, which helped them to resolve communication and relationship issues with family members. 178,216,217 Communication skills training may be an important component of a mental health intervention and be particularly relevant to young people transitioning into adulthood, with the resulting change in family dynamics.
The impact of interventions that directly and indirectly target family communication is illustrated by two quotations below. The first is from a parent describing the impact that attending a creative writing group for CYP infected with HIV had on her child; the second is from a young person discussing the impact that a family intervention to support them with their ABI had on their family:
She opens up more to her mother and her family. She used to be pretty shy, but now she’s like so talkative!
Parent, HIV172
We as a family were able to come together to better understand my brain injury and how I live my life . . .
Young person, ABI189
The above quotations suggest that increased empathy and understanding of the impact of LTCs on CYP and their communication can improve family relationships.
Seven studies reported that CYP and parents noted that relationships with healthy peers could also improve following an intervention:163,172,178,201,202,206,217
Lisa was facing some bullying so she showed the DVD [digital versatile disc] to her class to help them comprehend what was going . . . So as far as coping and being accepted at school I think it helped a lot.
Parent, cancer220
These improved relationships could stem from the creation of an age-appropriate means to tell their story and increase peer empathy (e.g. Baruch200) or through the acquisition of social skills learnt through communication with peers with LTCs (e.g. Stewart et al. 178,217).
The authors of nine studies discuss how the interventions evaluated helped CYP ask for the support they needed from family, peers and practitioners, or improved relationships with health professionals. 164,177,178,191,197,200–202,217 This is illustrated by a quotation from a parent of a young person taking part in an online intervention, discussing how the intervention influenced their child’s relationship with his health-care provider outside the online setting:
[through the online network the ill child] has gotten to know [a health-care provider] a lot better so he feels much freer . . . to go ask her for help.
Parent, mixed177
Thus, interventions that can support CYP to tell their story and engage in supportive interactions with peers and intervention deliverers may enable them to seek support from parents, healthy peers and health professionals when required.
There was some evidence (see Report Supplementary Material 2, Table 6) to suggest that the impact of these interventions on family and peer relationships endured beyond the end of the intervention period,164,174 as illustrated by a parent discussing the impact of a family art intervention:
I’ve changed because it does not have to be the first thing I tell my husband about when he calls me at night – about what’s going on with [ill child] . . . I’ve really tried to make a conscience [sic] effort not to do that . . .
Parent, T1DM164
The integration of changes to family lifestyle and relationships into daily life may be an important component for maintaining the effects of the intervention on CYP’s mental health over time. This will be explored further in Theme: keeping it going. The potential improvements to family and peer relationships in terms of increased empathy and understanding, which are achieved through enhanced communication, may have a significant impact on CYP’s mental health and well-being in the long term.
Summary: social support
The affirmational, informational and emotional support described above are all components of social support as described by Stewart et al. 178 The social support received by peers may facilitate their experience of an intervention setting as a safe space, which in turn may increase the likelihood of receiving emotional and informational support. Support to share their experiences can result in feelings of reduced isolation and improved relationships with healthy peers and family. This may have important implications for extending the impact of an intervention on CYP mental health and well-being beyond the intervention setting. Social support seems to be an important mechanism that may facilitate the development of new skills and knowledge and help CYP create a more hopeful view for the future, as discussed below.
Construct: a hopeful alternative
This construct explores how the creation of a sense of hope is important to CYP with LTC and their families when considering how to reduce symptoms of mental ill health. The first theme discusses how a sense of ‘hope and inspiration’ can be created through exposure to people who are managing to live successfully with similar conditions. Theme: more than just my illness explains how interventions aimed at improving CYP mental health can also address other factors in addition to management of their LTC symptoms and that this is valued by CYP. Theme: a new normal considers the importance of continuing taking part in ‘normal’ day-to-day activities while encouraging an acceptance of the limitations caused by the LTC. Theme: mutuality details how it is important that mental health and well-being interventions help CYP recognise that they too have something to offer other people in their relationships with peers and intervention deliverers. Figure 21 shows how this construct interacts with the findings of the previous two sections.
FIGURE 21.
‘A hopeful alternative’ and its relationship to other constructs.
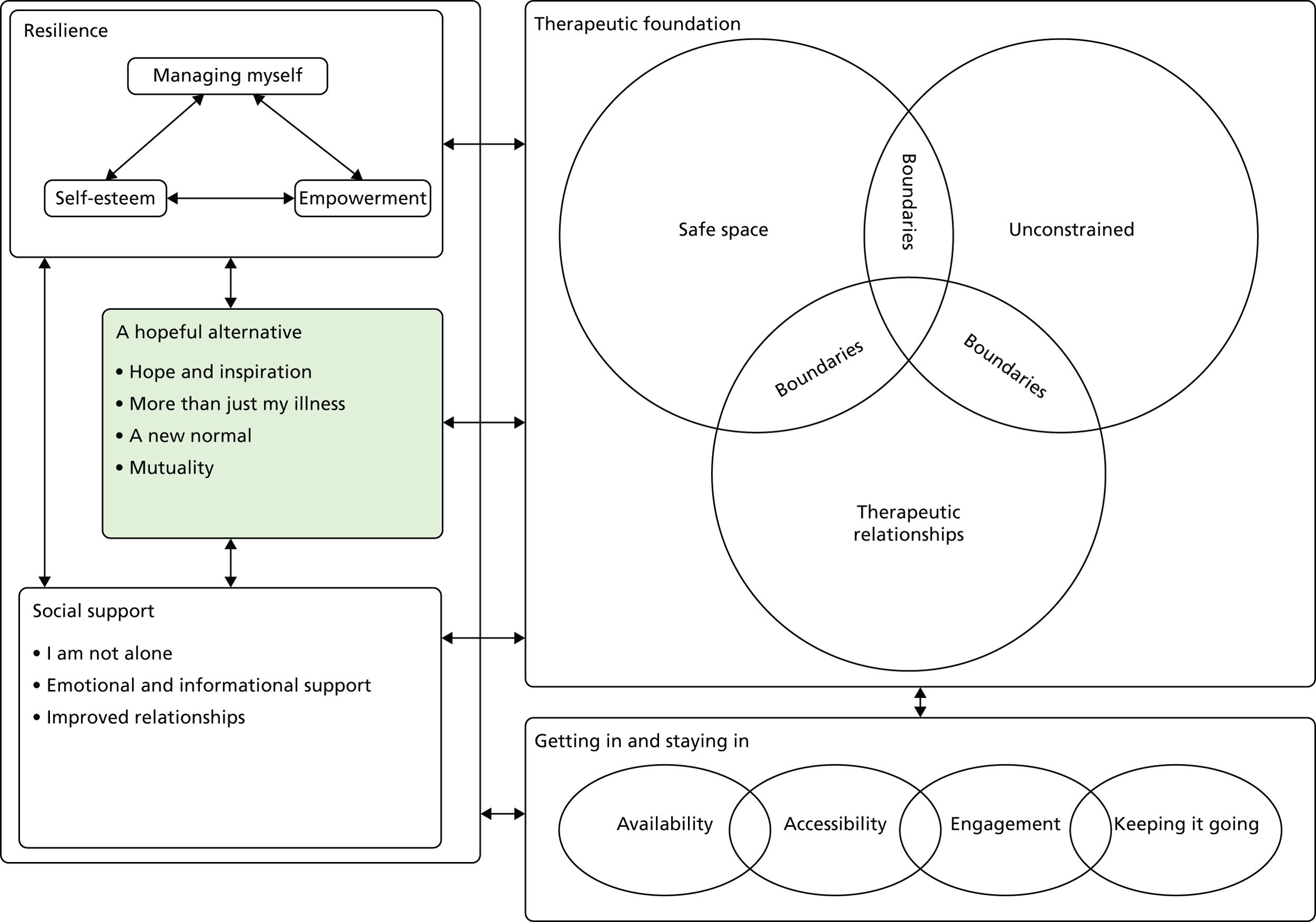
Theme: hope and inspiration
This theme discusses how CYP value having a sense of hope while living with a LTC. Hope and inspiration can be provided through access to role models who are living successfully with a LTC. Alternatively, mental health and well-being interventions may provide opportunities to experience success and mastery by encouraging CYP to persevere with challenging situations. A sense of inspiration may also be elicited by interventions that encourage CYP to focus on positive activities. Thirty articles contributed towards this theme (see Report Supplementary Material 2, Table 6).
Twenty studies focused on CYP’s interactions with peers who have an LTC as a source of encouragement, motivation and inspiration. 162–165,167,168,171–175,181,183,185–187,201,214,216,219 CYP appeared to find it particularly powerful seeing an example of someone older who was leading a fulfilling life despite their illness,162,178,216 as illustrated by the recipient of a peer-mentoring intervention below:
It was fun like it’s never been before, I saw someone who is in control of the situation and isn’t afraid of diabetes. If he can do it, I’ve got to succeed.
Young person, T1DM162
The advice received through contact with peers of the same age in both formal and informal settings also showed that it was possible for others in the same position to overcome difficulties associated with the LTC or challenges within the intervention itself:
. . . makes you want to do something and get up and go for it. Because you see all these kids, the kids in wheelchairs and they’re doing all this stuff, and they’re not letting anything get in their way.
Young person, cancer173
I saw that the other girls were fine with exercises I was like, ‘OK you are worrying over nothing’.
Young person, fibromyalgia186
Role models did not have to be someone CYP had met personally. Barlow et al. 171 suggest that CYP could watch vignettes of peers online to observe people who are managing to live successfully with the disease. Role models may also help encourage CYP to think about goals for other areas of their life, outside managing their LTC, as suggested by a young woman discussing important components for a group intervention for young women infected with HIV:
Ask them who their role models are. They could be somebody famous or something like that. Be like, you see how they work hard to get that, you want to do that for yourself. You want that life for yourself.
Young person, HIV168
This quotation suggests that feelings of hope and inspiration may encourage CYP that they too can affect positive changes within their own lives outside the interventions setting. This interpretation is supported by three studies whose authors suggest that the inspiration provided by peers can also provide CYP with the motivation to persevere with intervention activities or physical health procedures they perceive to be difficult. 184–186 This is illustrated by a parent discussing their views on the impact that attending camp will have on their child:
I think that [friendships among children with CHD] will inspire him . . . when he sees other kids do things that he might be afraid of, I think it will help him to take that leap of faith and inspire him. And he might think ‘oh well let me try that’.
Parent, CHD185
The inspiration provided by peers may encourage CYP to achieve success within challenging situations. The potential feelings of empowerment and improved self-esteem that may result could be considered as important protective factors against mental ill health, as discussed further in Construct: resilience. However, there was some evidence that CYP found talking about their emotions with peers uncomfortable1,92 and advice from peers was perceived as irrelevant if CYP felt that they were in a worse position than their peers. 171
The authors of four studies suggest that activity-based interventions that provide CYP with an opportunity to receive positive feedback, such as receiving beads following a painful procedure,200 or provide an alternative focus through taking part in a creative activity can provide CYP with a sense of comfort and positivity. 197,201,204 This positive feedback may inspire CYP to continue with challenging procedural treatments and/or have a beneficial effect on their mental well-being.
The evidence above illustrates how hope and inspiration can be created through contact with peers with a similar illness whether face to face, online or by video. Interventions that provide CYP with a source of hope may also inspire increased feelings of self-confidence that they too can live a fulfilling life with a LTC.
Theme: more than just my illness
This theme draws on data from 33 articles (see Report Supplementary Material 2, Table 6) and discusses how CYP value interventions that consider more than just their LTC and explores to what extent certain interventions included in the review tried to meet this need.
Eleven studies indicated that CYP valued interventions that focus on other aspects of their lives in addition to their LTC. 114,167,168,174,176,178,184,187,195,205,206 In addition to addressing psychosocial or educational needs162,171,177,183,189 and acknowledging how CYP’s physical and mental health could affect one another,114,186,195 interventions also created opportunities for CYP to exercise control and self-expression. 189,197 However, there was also some evidence that some interventions failed to adequately address CYP’s psychosocial needs. 171,178,182,183,216 Below, a young person describes what she would like to see as part of a group intervention for young women infected with HIV:
My perfect programme wouldn’t just not only [sic] be focused on the infection. It would just really be building self-worth, building self-esteem like all the way around.
Young person, HIV168
Second-order construct data indicate that CYP appeared to particularly value interventions that lead to them feeling recognised as a ‘normal’ person,206 and let them explore other aspects of their identities. 167,169,174,205,217 One intervention deliverer discussed how CYP used a peer support group to explore how they wanted to incorporate HIV into their identity:
So really a means for them to figure things out on their own and figure out how they wanted to represent themselves and HIV or if they wanted that to be a part of who they were.
Group leader, HIV172
This suggests that CYP value the opportunity to explore who they are in addition to their LTC, and services that reflect their additional needs.
The authors of five studies indicated that interventions that affect or involve other family members may also have a positive impact on the mental health of the CYP by addressing family interaction styles:171,177,185,189,206
My mum and dad get stressed out too and I learned some things to try to calm down when I am frustrated.
Young person, ABI189
Consideration of the impact of family on CYP’s mental health ensures that CYP are not burdened with the expectation to manage their LTC and psychosocial needs by themselves. It may also encourage family members to access appropriate support for their own needs and enable them to support their child. This could be a relief for CYP and may lead to increased empathy and understanding between family members, creating the opportunity for improved family relationships, as discussed in Construct: social support.
Theme: a new normal
This theme explores the importance of an intervention enabling CYP to continue taking part in day-to-day activities, while accepting any limitations resulting from their LTC. The impact of CYP being able to observe how other CYP cope and adjust to life with a LTC is also discussed. Thirty-nine articles contributed towards this theme (see Report Supplementary Material 2, Table 6).
Thirteen studies found that CYP value interventions that enable them to take part in everyday activities, whether that is household tasks or doing things that friends or family members without a LTC also do. 165,167,169,171,173,177,181,182,185,186,196,197,201 Below, a parent talks about the importance of a karate class that her child with cerebral palsy could attend with his healthy brothers:
There are things that go on that normal kids with no disabilities do that he can enjoy also. This helps him out the most. His brother and other kids can take karate, and so can he.
Parent, cerebral palsy181
Online interventions also help CYP to have a link with their normal life, as illustrated by one parent who talked about how an online environment allowed their hospitalised child to engage in fun activities as he would at home:
Because he can’t always go out and play, I think to be able to do it vicariously through the computer has been really good for him.
Parent, mixed177
The data above suggest that interventions that reduce CYP’s sense of being different may help them feel more ‘normal’ and reduce their sense that they are excluded by their LTC. However, O’Callaghan et al. 204 suggest that some CYP may feel stigmatised by being asked to take part in a mental health and well-being intervention, which may act as a barrier to participation.
Eleven interventions supported CYP to accept the limitations that their LTC imposes on their lifestyle and to acknowledge that, although their LTC is a part of their lives, it does not necessarily need to take over. 162,165,169,172,176,180–182,186,187,202 Below a parent discusses how camp could help their child to realise that having a LTC does not need to stop him from doing the things that he wants to do:
[interacting with children with CHD] is good for Adam to see that just because you have [CHD] doesn’t mean that you can’t live a full life . . . the activities that they will do together will just help them to see that you can just be as normal as others kids . . .
Parent, CHD185
In contrast to the above, parents from two studies evaluating interventions to relieve procedural distress in CYP with cancer reported that the interventions could provide CYP with the opportunity to come to terms with their own mortality. 201,202 For CYP with a terminal illness, an intervention should focus less on creating hope and more on achieving a sense of peace and acceptance.
Having the opportunity to meet or observe peers with similar difficulties to their own meant that CYP were able to compare the impact the LTC had on the lives of their peers and the coping strategies used by others to their own. Sometimes this encouraged CYP to develop a new, more positive, perspective on their personal circumstances. 162,164,167,169,171,173–175,177,178,185,187,200,201,216,217 This is illustrated by a young person with JIA comparing themselves with peers they saw in a psychoeducational video:
Well, I haven’t got it in many places so I thought that I was lucky because other people have got it worse.
Young person, JIA171
Despite the apparent desire to feel normal, second-order construct data from six studies suggest that, at times, CYP may enjoy the opportunity to feel ‘special’ as a result of an intervention. This may be through the recognition that an intervention is specifically for them181,191 or through recognition by others that they are ‘brave’ or ‘special’. 166,173,200,206 This is a possible extension on the typical developmental need to feel valued by others.
Theme: mutuality – I have something to offer to others
This theme focuses on the realisation that some CYP experienced while receiving an intervention that they too had something to bring to their relationships with peers or those delivering the intervention. This included input on setting up new interventions or providing information, advice or empathy. This helped CYP view themselves differently, as an equal part of the relationship, instead of passive recipients of care. This has implications for CYP’s feelings of empowerment and self-esteem. Thirty-three articles contributed to this theme (see Report Supplementary Material 2, Table 6).
As later acknowledged under Theme: engagement, CYP and their families have a wealth of experience that can be called on when designing an intervention. 114,168,170,171,175,184,191–193,211,218,219 CYP draw on their knowledge and experience to provide social support to their peers,178,216,217 as illustrated by an adolescent discussing how they were asked to provide a peer with some informational support at camp:
His parents wanted me to . . . give him some advice and help him relate to how it is going to be. That really makes me feel important . . . I get to share my life experience and relate to him with his life experience.
Young person, CHD166
Children and young people were able to recognise that they were able to provide support to both peers with a LTC and the intervention deliverers who had been asked to support them,162–164,166,186,217 as highlighted by a young person talking about their relationship with their peer mentor:
I know him no less than he knows me, I help him, he doesn’t only help me.
Young person, T1DM162
This represents an alternative, more positive, way of viewing their LTC and the impact it has on their identity, and indicates that CYP can have an impact on the lives of others. This is a possible alternative identity that may offer a source of hope for the future for CYP and act as a protective factor against mental ill health. The recognition that they too can offer beneficial advice to others can have a positive impact on how CYP see themselves within the context of their relationships. The LTC is no longer the reason for needing help from others; rather, it is also a rich source of experience to draw on so that the CPY can be ‘the helpers’ instead. This may improve CYP’s self-esteem and sense of empowerment and have a beneficial impact on their mental well-being.
Data shown in Report Supplementary Material 2, Table 7, indicate that by recognising that they too had something to bring to their personal relationships, CYP were empowered in their interactions with people outside the intervention setting, exemplified by teaching others new skills119 or challenging the stigma narratives around their illness:
It has influenced me to become more active in AIDS [acquired immune deficiency syndrome] and HIV [sic] in teaching others about AIDS and HIV, becoming more open about my disease because I do live in a community where I have certain people around me who will not judge me for my disease.
Young person, HIV172
The realisation that they too have something to offer others may facilitate behaviour change and give CYP a voice within the wider community. The impact of having their voice heard within an intervention is discussed in Theme: empowerment.
Summary: a hopeful alternative
This construct encapsulates how valuable CYP find the hope that it is possible for them to live fulfilling lives with a LTC. In addition to the importance of social support and the positive influence on peer mentors in providing a source of inspiration, it is also important for interventions to focus on more than just CYP’s physical illness. Interventions should consider how CYP can be encouraged to take part in activities that make them feel ‘normal’ despite their physical limitations. CYP also appear to value the opportunity to recognise that they too have something to offer other people and are not just the passive recipients of help. These factors can help CYP to feel empowered and to develop positive self-esteem, factors that may contribute towards improved mental well-being, discussed in Construct: resilience, and may help CYP develop and maintain links with peers and family, as discussed in Construct: social support.
Construct: resilience
This construct conceptualises resilience as a process that occurs through CYP’s involvement with an intervention and interaction with the environment/systems around them, which influences how CYP perceive themselves and their abilities. The themes described below focus on issues that may influence CYP well-being, in addition to potentially impacting on clinical symptoms of mental ill health. The first of the inter-related categories, ‘managing myself’, discusses how CYP benefit from interventions that equip them with skills and knowledge to help them manage their emotions and relationships and take responsibility for managing their LTC. This can help them feel empowered and develop positive self-esteem. The second theme discusses how being given opportunities for choice and encouragement to be more involved in their care is key to develop feelings of ‘empowerment’. The third and final theme discusses how positive ‘self-esteem’ may be promoted through positive interactions with others and experiences of mastery, which in turn further promotes the use of positive coping strategies. Figure 22 shows the relationship between ‘resilience’ and the other constructs in the synthesis.
FIGURE 22.
Resilience and its relationship to other constructs.
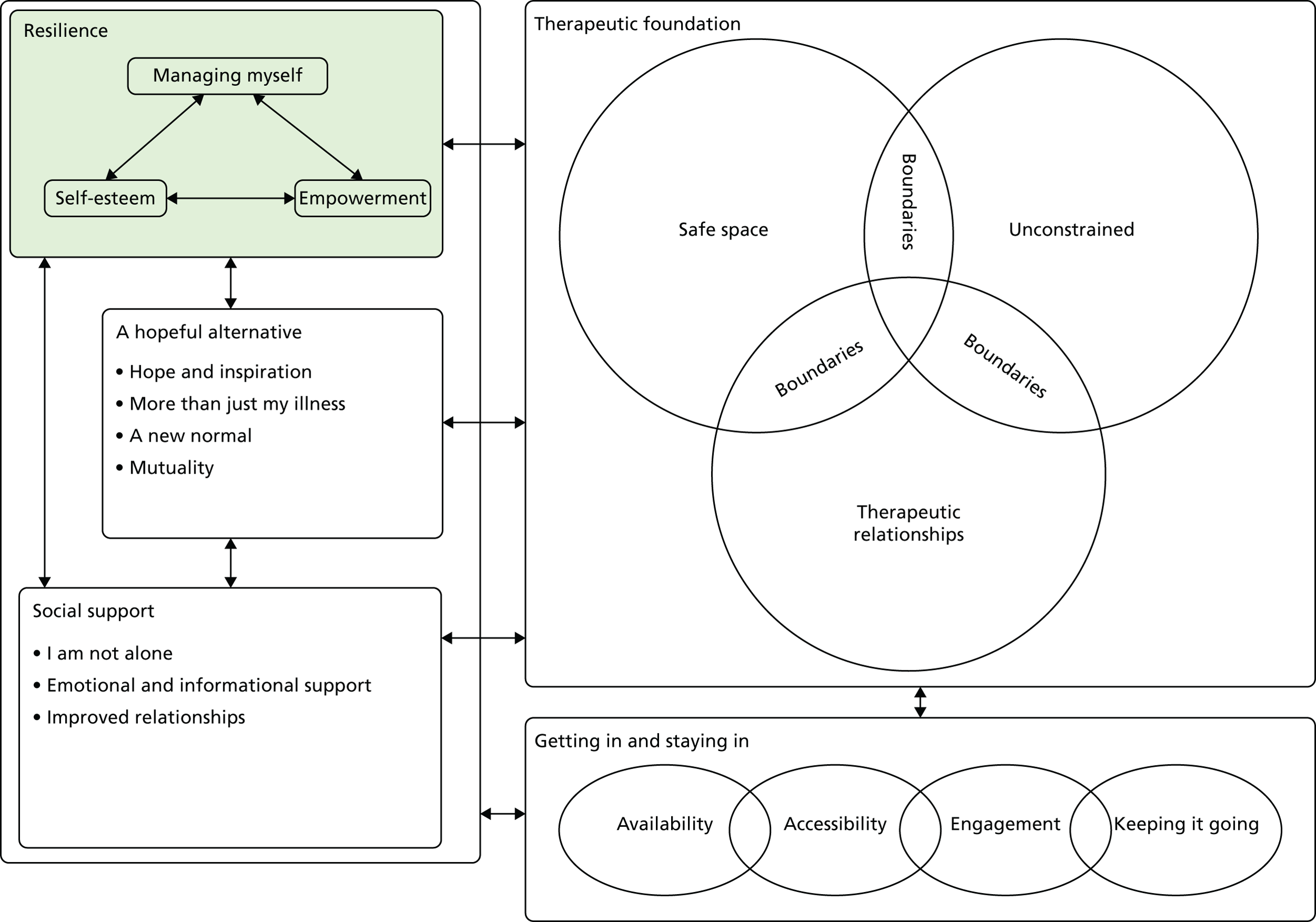
Theme: managing myself
This theme explores how being taught skills and knowledge to manage both their physical and mental well-being can enhance CYP’s ability to cope with difficult life circumstances and lead to a sense of empowerment and improved self-esteem. Forty-nine articles contributed to this theme (see Report Supplementary Material 2, Table 6).
Twenty-three studies indicate that CYP seemed to find it helpful to have the opportunity to learn skills that would allow them to take responsibility for managing their LTC as part of an intervention aiming to improve their mental health. 114,119,162,163,166,168,171,172,174,176–178,182–184,186,190,191,193,195–197,214 Such learning appeared to take place through interventions in one-to-one, group and online settings and increased CYP’s confidence to manage their LTC in the future:192,199,211
Learning the techniques helped my asthma and me as a person, because if I know how to control my asthma now, I can help in the future and stop things from occurring.
Young person, asthma119
One CYP receiving CBT described how the skills they learned provided them with a sense of control over their fibromyalgia:
It gave me something to work with, which is something I haven’t had since I was in school.
Young person, fibromyalgia182
Three studies highlighted how learning how to manage their LTC and what to expect in the future could help CYP feel prepared and increase feelings of self-efficacy, mastery and being in control. 168,171,177 This may have important implications for helping reduce CYP’s anxiety around not knowing if they will be able to cope with physical, emotional and social challenges arising from their LTC.
Children and young people and their parents also appreciated skills learnt during mental health and well-being interventions that directly enabled CYP to manage stress114,119,162,171,177,183,184,189–191,196,200,205 and in some cases showed that they were able to use these new skills when required during their day-to-day life,178,182,186,190,196,216 as illustrated by two participants of a neuromuscular and CBT training programme:
Mini-relaxation I would do all the time when I felt a little tense . . . muscle relaxation I would usually do in the morning or at night before I went to bed.
Young person 1, CFS186
Pleasant imagery I usually did before bed or if I was having a lot of pain . . . calming statements . . . I did mostly when I felt . . . anxious or when I couldn’t sleep.
Young person 2, CFS186
Interventions that acknowledged the interaction between physical symptoms and mental well-being seemed to be appreciated,114 particularly for LTCs such as fibromyalgia and CFS. 186,195
Acquiring skills to manage challenging social situations seemed to be particularly important for CYP living with LTCs associated with a high degree of stigma, such as HIV infection for which there were issues around managing intimate relationships and disclosure. 168,176,187 Hosek et al. 168 highlighted a demand for group interventions that support young women who have a HIV infection to manage the emotional distress resulting from negative consequences following disclosure:
It doesn’t mean that because I told my friend that I’m HIV positive she’s gonna accept me. It doesn’t mean that because I told her I have to accept that she has to accept me . . . She’s out of my picture. So how do we deal with it?
Young person, HIV168
Eleven studies included in this review indicated that distraction can be a valuable skill that CYP can use to cope with distress and pain and escape the boredom or uncertainty associated with long hospital stays. 164,169,173,174,177,191,201,202,205–207 The evidence presented within this theme suggests that gaining skills to managing their LTC, social situations and distressing procedures through a mental health intervention can help CYP to take responsibility for managing their physical and mental well-being.
Theme: empowerment
Forty-seven articles contributed to this theme (see Report Supplementary Material 2, Table 6), which discusses how mental health and well-being interventions can empower CYP to take responsibility for their own health-care needs on day-to-day and health-care settings, enable them to have a voice within their local community and increase their confidence in managing tasks of everyday living. CYP can feel empowered as a result of an intervention that includes the incorporation of activities that allow them to experience mastery and achievement, and by having their voices heard within an environment that encourages reflection on progress. The experience of feeling empowered within the intervention setting can have an impact on how able CYP feel to effect change in their day-to-day lives and is thus an important component of resilience. Feeling empowered can also affect how CYP view themselves in relation to others and thus relates to the ‘mutuality’ theme above. Other third-order constructs that contributed towards this theme can be seen in Report Supplementary Material 2, Table 8.
Evidence from 11 studies suggest that interventions can offer opportunities for CYP to make choices and exercise autonomy by deciding how they would like others to interact with and support them. 162,170,173,177,178,183,185,195,197,198,207 An example of this is provided by a parent describing how their child instructed staff on how best to support her while she was undergoing needle insertions:
[The child] wrote out a needle plan, and she talked it through at home and worked it out with the psychotherapist here at the hospital . . . every time there was a new nurse or doctor she’d hand the card to them and they had to read it . . .
Parent, cystic fibrosis198
It appeared to be important for interventions to provide opportunities for CYP to experience having their voices heard. This could be achieved through allowing CYP to vote on important decisions as part of the wider group and giving them the chance to tell their story. 171,173,176,181,197,198,200,202 These experiences enabled children to make their voices heard within the wider community. 164,172,176 One parent observed how a camp for CYP with CHD allowed their child to develop confidence in her ability to speak up for what she needed later while attending school:
Since going back to school . . . she knows that from camp as well, that she has to be an advocate for herself. That she’s the one that has to kind of put the foot down and say ‘this is why I need to stop and I’m going to stop’.
Parent, CHD185
Data from Report Supplementary Material 2, Table 7, also indicate that activities incorporated into interventions that promote recognition of achievement and mastery of challenges may help CYP gain a sense of confidence in their abilities. 119,165–167,169,171,173–175,177,179,185,186,198,200,201,205,206 This is supported by a quotation from an intervention deliverer from a camp intervention:
For some of these people, they’re very sheltered and their parents don’t let them do anything, and they’re climbing rock walls and going down zip lines, and the fact is that they’re overcoming their fears and obstacles.
Intervention deliverer, cancer173
Having this sense of confidence in their own abilities may enable CYP to feel empowered outside the intervention setting. Some of the outcomes that were less directly related to mental health included the willingness of CYP to become more involved in their care,198 to take responsibility for completing homework exercises119 and to complete other tasks in order to manage their health needs. 119,162,171,176,178,184,185,187,195,197,216 For example, in a study that examined the clinical effectiveness of breathing retraining for asthma, one adolescent reported that it was they who took responsibility for remembering to do the exercises:
Nothing has gotten in the way, I just remember, no one reminds me.
Young person, asthma119
Overall, this theme illustrates how mental health interventions that offer opportunities for CYP to exert control, gain experiences of mastery and feel that their voices are heard can enable them to feel empowered within their everyday lives beyond the intervention setting. This may contribute towards CYP’s development of ‘resilience’ and a positive view of themselves.
Theme: empowerment
This theme details how improved self-esteem may contribute towards the development of resilience. A young person’s self-esteem may be improved by an intervention that encourages them to recognise their capabilities and areas of achievement, as well as providing opportunities to interact with others who can reflect the positive parts of their identity. Twenty-seven studies contributed to this theme (Report Supplementary Material 2, Table 6).
Data from four studies indicate that taking part in those interventions reinforced CYP’s belief in their own ability to manage their condition, emotions and negative responses from other people. 178,185,197,206
The authors of six studies suggested that CYP value the opportunity to recognise positive things about themselves. 164,168,179,186,189,190 One study encouraged CYP to practise making positive affirmations about themselves during the day, and there was some evidence to suggest that CYP could then use this to ameliorate emotional distress in other settings:
Thought about what I was proud of or what made me happy, which helped me to calm down and be happy again.
Young person, T1DM190
The above quotation demonstrates the impact of CYP having the opportunity to learn skills to manage their emotions on their sense of well-being and suggests that opportunities to build CYP’s self-esteem can provide a valuable resource for CYP to draw on in times of emotional need.
The authors of 17 studies suggested that positive recognition and affirmation from peers, family, intervention deliverers and themselves were found to be important for improving CYP’s self-esteem and/or mood. 114,162,164,166,173,178,179,181–183,185–187,189,200,201,206 One parent felt that their child found it valuable to recognise that he was capable of offering support to peers through a computer-based intervention and that other people also recognised this:
I think it encouraged [the ill adolescent] . . . to know that he had the ability to ‘do’. I think it really boosted his confidence, knowing that he had something to offer other kids, and that someone saw that while he was on the computer.
Parent, mixed177
The authors of three studies indicate that opportunities for CYP to tell their story to others help CYP communicate their experiences and receive positive recognition from others. 200,201,206 Kashikar-Zuck et al. 186 indicate that CYP appreciated the tailoring of intervention tasks to their individual abilities, alongside the opportunity for progression through stages of increasing difficulty. One quotation suggests that this structure provided CYP with the chance to reflect on their achievements with pride:
I am glad that I went through it . . . now I can look back . . . at how far I have come . . . today that stuff, wasn’t hard. It just gives you this sense of pride, like if I can overcome that, what else can I overcome?
Young person, fibromyalgia186
The importance of the individual delivering an intervention being able to relinquish control in an intervention setting to help CYP recognise that they too have something to offer is highlighted in Report Supplementary Material 2, Table 7, under Theme: empowerment. The below quotation highlights the emotional impact on CYP if they perceive an intervention deliverer as being unable to acknowledge their views as equal to their own:
I spoke to [therapist’s name] about it . . . and I said to him that it wasn’t working and I didn’t know why, he basically told me it was my fault and that if it wasn’t working it must be because I wasn’t doing it properly.
Young person, CFS195
This quotation suggests that this young person was left feeling blamed and criticised when they felt that the intervention deliverer had not respected their views. This highlights the need for empathetic, supportive, therapeutic relationships with intervention deliverers, as discussed in Construct: a therapeutic foundation, and the potential impact of these relationships on CYP’s self-esteem.
Second-order construct data from four studies indicate that having the opportunity to reflect on what they have been through may be meaningful for CYP. 167,173,174,200 Such reflection appeared to be facilitated through the receipt or creation of ‘mementos’ documenting their LTC and treatment story and the chance to observe change over the course of an intervention. Combined with the positive responses these mementos elicit from others, they may reinforce CYP’s self-concept as someone who is brave, special and resilient. This may bolster their sense of self-esteem, which could be a protective factor against the development of mental ill health.
Having the opportunity to achieve a sense of mastery by successfully completing activities not only empowered CYP, as described above, but also improved their mood181,186 and/or increased their sense of self-esteem:167,177,179
I have to say my favorite [sic] memory from camp would probably be climbing the tower. It was an incredible experience. When I got to the top I felt like I accomplished, you know, what I wanted to do. The zip line was probably the best part also.
Young person, mixed167
Quotations from five studies suggest that interventions that encouraged focus on areas of ability within the individual child, rather than what they were not able to do, were also valued. 166,168,181,185,201 This is illustrated by a parent describing the importance of a karate class to provide an example of what they could do for their CYP with cerebral palsy:
I don’t want his sister or brother to be in a private karate class. This has really helped him a lot. Even during the week when they do things that he can’t do, we mention the karate thing. I tell him that he does karate and they don’t.
Parent, cerebral palsy181
Opportunities that allow CYP to feel capable and included may boost CYP self-esteem by supporting them to develop a more hopeful view of their capabilities and of the future, as described in Construct: a hopeful alternative.
This section discusses the role of mental health and well-being interventions that encourage positive recognition and experiences of mastery in boosting the self-esteem of CYP. This may result in CYP having a more positive image of themselves, which may act as a preventative factor against experiencing symptoms of mental ill health.
Summary: resilience
This theme explored three inter-related components that may promote resilience within CYP with LTCs. Theme: managing myself detailed how it is necessary that CYP are supported to gain the relevant skills and knowledge they need to be able to take age-appropriate responsibility and have a voice within the intervention process and the wider community. This knowledge transfer can occur both through formally ‘taught’ interventions and by more informal social learning through contact with peers in group interventions. Having the appropriate skills may facilitate the development of ‘empowerment’. In Theme: empowerment the importance of allowing CYP opportunities to make choices about the care they receive and take responsibility for managing the different areas of their lives affected by their illness was explored. The recognition of both their success in managing their LTC and achievement in other areas of their life facilitates a sense of positive self-esteem, the third theme conceptualised here as being necessary to promote resilience.
Construct: getting in and staying in
This construct details the different continuous/overlapping stages as a young person accesses an intervention, from the development of interventions aiming to improve the mental health and well-being of CYP with LTCs to CYP being able to access and stay engaged with the intervention. Theme: availability explores how issues such as the initial recognition of mental health need and provision of required resources are necessary for an intervention to be considered. The different factors required to ensure that CYP and their families can access these interventions are discussed under Theme: accessibility. Issues that may affect ongoing engagement with mental health and well-being interventions are detailed in Theme: engagement. The final theme, ‘keeping it going’, discusses the need for interventions to have components that can be adopted into everyday life, ensuring that beneficial effects are not confined to intervention sessions. The inter-relationship between ‘getting in and staying in’ and the other four constructs is shown in Figure 23.
FIGURE 23.
Getting in and staying in and its relationship to other constructs.
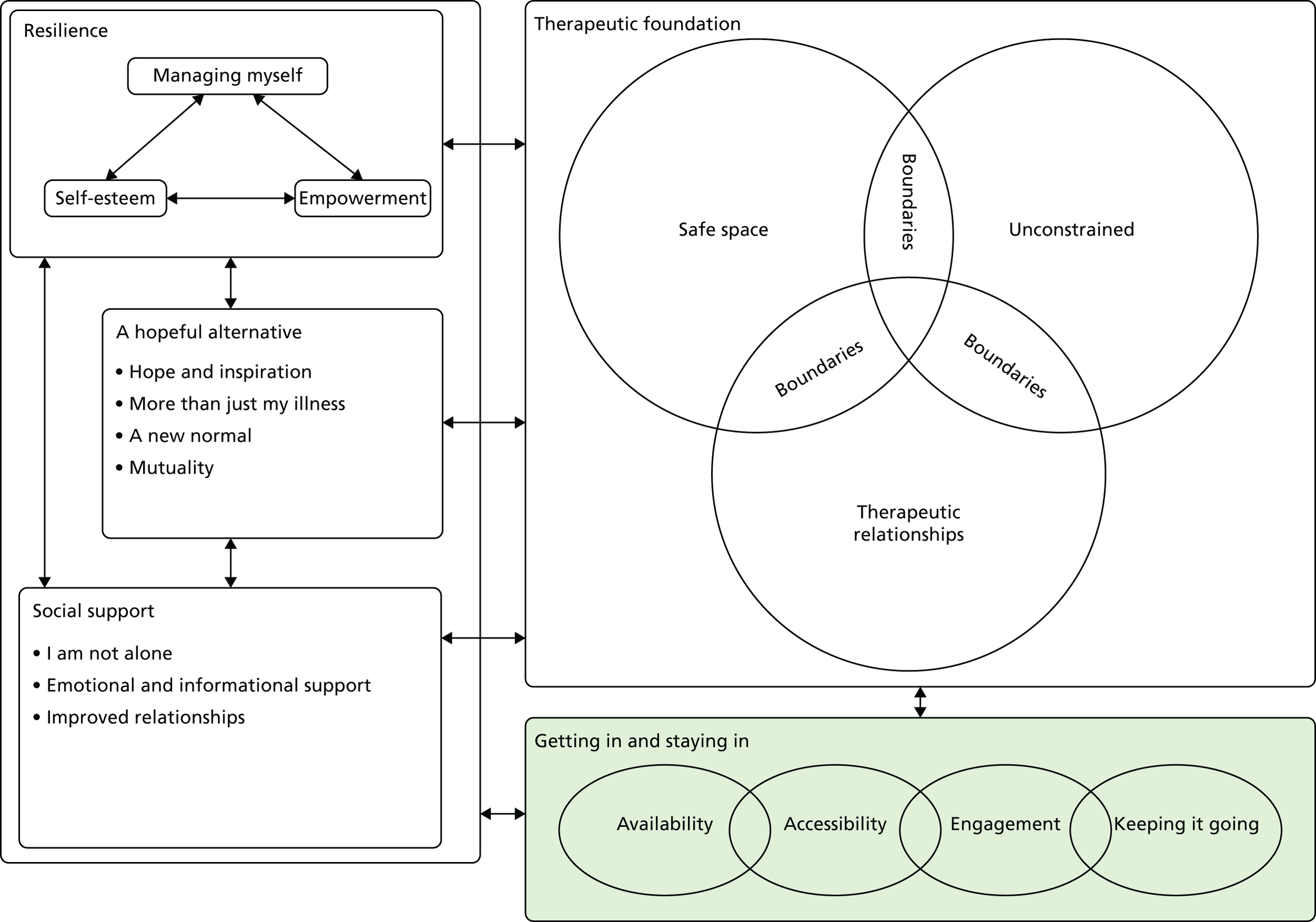
Theme: availability
This theme draws on 30 articles (see Report Supplementary Material 2, Table 6) and centres on the need to recognise the mental health needs of children with a LTC and ensure the availability of relevant resources to address them.
The authors of three articles acknowledge the difficulty that health services face in identifying CYP and/or their families in need of support to maintain their well-being. 162,171,187 One parent expressed frustration at the difficulty of getting the mental health needs of their child recognised by health professionals focusing on physical symptom management:
They really don’t understand the problems you have at home . . . The doctors see them for half an hour . . . and examine the joints . . . but, it doesn’t just affect their joints. It affects them mentally and that’s what we have to put up with.
Parent, JIA177
In seven studies it was reported that participants commented that, when mental health interventions are provided, the availability or range of options offered is sometimes limited:168,171,175,176,186,189,197
[The intervention] wasn’t easy to find. I was looking for some support for [my son] because he was struggling last year . . . They said they only had one social worker for the outpatient department and it was all very difficult for them to see him.
Parent, mixed175
The authors of two studies highlight the need for staff expertise to design and set up an intervention114,171 and to ensure that a suitable space for the intervention to take place in is available. 114,176 The authors of a further nine studies highlighted the need to ensure that staff delivering the intervention have the appropriate skills, experience and training so that the intervention is delivered as planned and that the emotional or behavioural needs of the CYP are met. 162,166,171–174,178,189,197
Second-order construct data from three studies suggest that, when mental health and well-being interventions are available, some CYP may not feel able to seek support for their well-being. 162,182,207 This may be for a variety of reasons: a desire not to discuss their anxieties or their LTC in front of parents,162 fear of physically hurting someone by holding their hand while undergoing painful procedures207 or the view that the setting in which they are being seen is not appropriate to their perceived needs. 182 Overall, this theme highlights the need for CYP’s mental health needs to be recognised by staff that they may come into contact with and relevant interventions to be provided to CYP in a timely manner.
Theme: accessibility
This theme focuses on factors that may affect whether or not CYP and their families are able to access an available intervention. Factors that may facilitate access include pre-existing relationships with health and social care staff, ensuring that interventions consider the individual needs of the CYP and addressing practical issues such as ensuring that the intervention setting, duration and timing are convenient. Fifty-two articles contributed to this theme (see Report Supplementary Material 2, Table 6).
Seven studies suggest that both health and social care professionals play an important role in identifying CYP who may benefit from existing interventions, ensuring that families are aware of the support available and inviting them to participate in the intervention. 166,169,172,175,177,187,197
Approaching CYP directly via text message or letter was an effective means of supporting them to access an intervention,175,187 and CYP may observe others taking part and wish to participate. 172,177,182,205 There was the suggestion that more formal processes could ensure that interventions are accessible by those who need them, including introduction of referral systems197,211 and ensuring that CYP from certain ethnic minorities or with more severe illness are able to attend. 169 Parents felt that the means of introducing mental health interventions relevant to their child should be incorporated into inpatient discharge processes:
You’ve got the teachers, you’ve got the wards, you’ve got the social workers. It should be just part and parcel of coming around on discharge, you know that you are aware that there is support for young people, maybe not now, but when it may be appropriate.
Parent, mixed175
The idea that the unpredictable nature of a LTC can prevent CYP from accessing, or participating fully in, treatment for their mental health was recognised by 14 studies. 164,165,173–175,177,182,183,185,186,191,201,202,205 Therefore, the recognition of physical health needs by those planning mental health and well-being interventions and consideration of how the intervention can be altered accordingly is required to ensure that the intervention is accessible to those who need it. 173
By ensuring that CYP’s physical health needs are met, intervention deliverers and services can reduce some of the anxiety around attending an intervention, which may help it to be perceived as a safe space for CYP and their families.
Facilitators in online interventions may also play an important role in stimulating discussion and ensuring the relevance of the material to those taking part. 114,178,216 This may help CYP who are less confident access intervention material and maintain their engagement. Six studies suggested that the communication skills and understanding of those delivering the intervention are also key in making the material accessible. 162,166,185,186,195,200 One young person highlights how they felt that the person delivering the intervention did not understand the material and this meant that the information delivered was not fully understood:
The physiology stuff at the beginning I didn’t find helpful because I don’t think it was fully explained, ’cause to be honest I don’t think they fully understand it themselves.
Young person, CFS195
This has important implications for CYP acquiring the skills and knowledge required to manage their physical and mental well-being as described under Theme: managing myself. First- and second-order data in Report Supplementary Material 2, Table 7, suggest that interventions within this synthesis used different ways to ensure that their material was accessible through considering the age, educational and developmental level of the CYP. 114,119,164,168,171,174,182,184,187,191,197,200,201
Second-order construct data from 13 studies also suggest that the timing of the intervention and choice of venue need to be considered to ensure that the intervention does not interfere with CYP’s education or parents’ employment and that the duration and financial burden of travel does not prevent attendance. 119,164,172,175,176,182,183,186,187,191,195,201,216 The usefulness of co-ordinating delivery of physical and mental health interventions was highlighted,176,191 and is illustrated by a quotation from a young person who had attended a hospital-based support group:
It’s convenient and just you can do everything all in one day and see everybody in one day, and just get everything done.
Young person, HIV176
Considering CYP’s physical, psychosocial and family needs together may not only reduce the burden of attending multiple appointments, but also reinforce that CYP and their families have other needs in addition to their LTC and are part of a wider family system, as discussed in Theme: more than just my illness. This may help CYP feel validated as a whole person and make them feel supported and understood by services, necessary components to build a therapeutic foundation.
Interventions delivered online can overcome some of the practical issues around access. One of the perceived benefits of such interventions was that they enabled children to access the intervention independently and overcome the physical limitations of their illness, although sometimes technological issues hindered this:177,178,183,216
[a window with a picture of] a dog comes up and says that they’re unable to locate their site or for safety purposes it’s been blocked. And a lot of the time they go to put on a game and they can’t get it to work. So that gets frustrating.
Health-care provider, mixed177
However, the authors of six studies suggest that CYP and their families would like flexibility in terms of how an intervention is delivered. 114,168,178,179,189,190 Parents acknowledged the convenience of interventions supported by technology, but stated that they would also like CYP to have the opportunity to meet peers and/or intervention deliverers face to face. 178,189,190,216
Care is required that the intervention itself is not too burdensome for CYP or their families. The authors of four studies suggest that the pace and duration of interventions should be considered to ensure that interventions are not too long, yet allow enough time for the material to be covered without overwhelming participants. 164,178,186,195 The quotation below describes how a particularly long intervention session became too burdensome:
It was . . . really taxing the first day because it started at 10 and didn’t finish until about 7 in the evening, and there were also about seven other people there which is like . . . considering I had been like housebound for years I hadn’t really . . . saw anyone . . . I was absolutely shattered.
Young person, CFS195
This quotation suggests that a balance is needed between the convenience of holding multiple appointments at the same time and ensuring that CYP and their families do not feel overwhelmed.
The perceived burden of sessions may be affected by the type of LTC experienced by CYP as well as the stage of their illness. Studies in this review support this idea by discussing the perceived importance of ensuring that a mental health and well-being intervention acknowledges that the LTC may affect the mental health of CYP and address this by considering LTC-specific challenges or worries166,167,171,173–175,182,184,186,187,189,197,205 and stage of illness. 171,178,180,184,187,189,195,197,201,205,217 An example of the role of the intervention deliverer in ensuring that exercises and activities are within the physical capabilities of CYP is given below, within a cognitive–behavioural neuromuscular training programme for CYP with fibromyalgia:
[The exercise physiologist] would work with you personally to make sure you were comfortable with where you were . . . make sure the exercise wasn’t too easy or too hard.
Young person, fibromyalgia186
The role of the intervention deliverer in establishing boundaries to ensure that participants feel safe enough to discuss emotive subjects is discussed in Construct: a therapeutic foundation. Having opportunities to chat before the interventions and including activities that CYP and their families find enjoyable also appears to make the more formal therapeutic aspects of intervention accessible. 164,204 As an example, the art activities provided as part of a family intervention seemed to provide an alternative focus and aid disclosure:
Was Living Well what you expected it to be?
Actually, it wasn’t. And that’s good. I thought about everybody talking about their kids would be kind of depressing, but it turned out, the artwork and everything kind of opened everybody up.
Parent, mixed164
The authors of five studies acknowledged that the interventions being evaluated were not able to address CYP’s every need or replace other interventions that may be useful. 114,178,182,183,189 This highlights how CYP with LTCs have other needs in addition to their physical health, as discussed under Theme: more than just my illness.
This theme summarises different factors that may influence how accessible CYP and their families find an intervention and the role of the intervention deliverer in adapting the intervention to ensure that it meets CYP’s psychosocial needs.
Theme: engagement
Although the availability of an accessible intervention is necessary for its provision, CYP may not necessarily want to engage. Different factors that may influence engagement with an intervention are explored next. Fifty-four articles contributed to this theme (see Report Supplementary Material 2, Table 6).
The role of the intervention deliverer in adapting the intervention to ensure its relevance to CYP is discussed in Theme: accessibility. Report Supplementary Material 2, Table 7, indicates that there are multiple ways in which mental health and well-being interventions can be flexibly delivered according to the needs and individual characteristics of CYP. The authors of six studies suggest that interventions that consider the individual behavioural, social and emotional needs are valued by CYP and their families. 168,173,179,181,182,202 Interventions included in the review also considered stage of illness,171,187,189,195 gender162,168,169,184,197,205,217 and the individual interests of CYP taking part in the intervention162,172,177,182,191,201,206 as factors that could ensure a mental health intervention’s relevance to CYP and help sustain their engagement with the intervention.
In contrast, the authors of seven studies suggest that CYP can engage with an intervention at a level that meets their needs, sometimes with no formal adaptation of the intervention process. 162,163,167,174,177,183,206 For example, Gillard and Allsop167 discuss how a camp intervention appears to meet differing needs among CYP, as influenced by their type of LTC. This fluid interaction of CYP with the interventions may be because the design of the interventions allows for it. CYP can choose which aspects of the intervention are relevant to their needs and access the intervention at this ‘level’. Not only can this be empowering for CYP, as discussed above, but it may also mean that some interventions could meet the mental health needs of CYP as they change over time. This idea is explored further in Theme: keeping it going.
Explaining the rationale or theory behind an intervention can also facilitate the engagement of CYP with an intervention. 167,195,205 One young person discusses how helpful they found understanding the rationale behind an intervention to treat their CFS:
The explaining of the process, the background information definitely helped because it helps you realise how the process works, and there is no point doing something unless you understand how it works . . . otherwise you won’t believe in it enough.
Young person, CFS195
Both CYP and their families appeared to engage with interventions that were evidence based or developed through consultation with other families, as this appeared to give the interventions validity and made them worth ‘buying into’:
This would be a very good tool. [This has] techniques developed through research with other families and [would be] very beneficial.
Parent, cancer191
The above suggests that CYP and their families feel able to trust and perhaps put their faith in interventions that are tailored to meet their needs and ‘make sense’. This could be considered an important part of knowing what to expect from an intervention, as discussed earlier in Theme: a safe space.
Second-order construct data from Report Supplementary Material 2, Table 7, indicate that CYP and their families can have a variety of different expectations prior to the beginning of an intervention182,195,196 and the extent to which these expectations match their experience of the interventions may affect how effective the intervention is perceived to be. 195 CYP expressed anxieties about encountering new health professionals, not knowing anyone else or what to expect and a fear of not knowing what to say to someone who was going through difficult experiences or dying. 163,164,182
Most CYP’s concerns appeared to dissipate over the course of the various interventions. 175,179,181,186 Some CYP and authors of studies believed that an initial tolerance of anxiety, discomfort or frustration was necessary to both begin and maintain engagement with an intervention:171,172,177,186,197
Don’t be shy because if you’re shy you miss out on a lot.
Young person, HIV172
The below quote from a young person attending a camp intervention aimed at CYP with CHD emphasises that it is important that CYP are given enough time to develop relationships with peers:
It’s not long enough, you know we don’t get enough time to bond, but it’s like, ‘how much can you do in 1 week right’?
Young person, CHD169
First- and second-order construct data from Report Supplementary Material 2, Table 7, suggest that fun or pleasant activities appeared to be important in motivating CYP, particularly those who are younger, to engage with an intervention. 114,162–168,172–174,177,178,181,185,187,189,197,201,205,206,216 Other components that enhanced engagement with, or adherence to, an intervention included the provision of a meal during the session, the receipt of rewards or ‘gifts’, and the opportunity to keep a product of the intervention as a memento or display it for others to see. 164,173,174,187,190,200,201,211
Some evaluations of online support interventions acknowledged the importance of clear website layout and attractive graphics to maximise user engagement. 177,190,218,219 A quotation from a young person evaluating an online self-management programme for CYP with JIA emphasises how large amounts of text can be off-putting for young people:
Like this, it looks like a lot of stuff to read, and I probably, as a teenager . . . wouldn’t take the time to read it.
Young person, JIA218
Information from six studies indicates that many families appreciated telephone calls or text messages from intervention deliverers or researchers to remind them to attend appointments, carry out the intervention at home or use the intervention when required. 114,177,186,190,191,201 Three additional studies suggested that CYP and their families may benefit from information that they can refer back to at the end of an appointment or intervention. 119,171,189 In addition to facilitating engagement with an intervention, these memory aids can also help CYP and their families to incorporate advice and skills practice into their daily lives. This may extend any potential benefits of a mental health and well-being intervention beyond the scheduled end of the intervention, a concept which is discussed below in Theme: keeping it going.
Theme: keeping it going
The content of this theme draws on 42 articles (see Report Supplementary Material 2, Table 6) and discusses the importance of ensuring that interventions are adequately resourced and have components that can be adopted into everyday life by CYP and their families. Some interventions may encourage the development of skills such as emotional management by CYP, which may increase the likelihood that any benefits on CYP’s mental health and well-being can be sustained beyond the end point of an intervention.
The importance of ongoing training or supervision with peers or colleagues with specialised mental health training, particularly for intervention deliverers with non-mental health backgrounds, was recognised by the authors of three studies. 162,178,197 It was observed that individuals delivering more specialised mental health interventions, such as art therapy, receive a higher degree of training. 172,189,197 Without such ongoing support, it would be difficult to sustain delivery of an intervention long term and maintain engagement with CYP by ensuring that the intervention meets their mental health and well-being needs.
The need for training prior to the onset of an intervention to ensure that intervention deliverers are able to meet the psychosocial needs of CYP taking part was implied in a further three studies. 166,172,200 This is illustrated by a quotation describing how intervention deliverers needed to be able to respond quickly to manage the disclosures of CYP during a group creative writing intervention:
And then there’s the risk that a kid starts to write something that maybe puts them in a precarious situation that we have to address in the class. We didn’t know what was going to come out, what kids were going to write, what they were going to say.
Intervention deliverer, HIV172
This interpretation is closely linked to the need to provide appropriately trained staff to deliver an intervention, as discussed in Theme: availability. The skills of individual intervention deliverers and the support provided to them may determine how well an intervention of longer duration can meet the needs of CYP as these needs change over time. Manualised protocols may also help facilitate the training of health/social care staff and consistent delivery of mental health interventions. 186,189,200
Financial support to buy appropriate equipment that CYP can use if required173,177,205 and to fund staff time189,191,198,206 was also recognised as essential to ensuring that an intervention is sustainable. One young person from a family art therapy intervention indicated their concern regarding issues relating to the funding of an intervention:
I worry that they’re not going to get funded because there might not be a huge change in someone, but when you’re chronically ill, you don’t need a huge change to make a difference . . . I think whoever grants you all the money needs to know that . . .
Young person, mixed164
The above quotation hints at the need for services to prove their efficacy in order to receive funding, and the potential impact on the mental health of CYP who are aware that funding for an intervention they find helpful may not be secure. 189 Resource and funding issues may have implications for the ability of intervention deliverers and services to provide an intervention that can be experienced as a ‘therapeutic foundation’ by those who access it.
Data from 16 studies suggest that, over time, the psychosocial impact of a mental health intervention may be seen outside the original intervention setting, as discussed in Theme: improved relationships with family and healthy friends and Theme: managing myself. 162,166,167,172–175,177,178,185,186,196,197,205,206,217 One factor that appears to facilitate this is the opportunity for CYP to practise the skills they have learnt, both in an intervention setting186,195 and in their everyday lives. 119,164,186,191,195 One young person describes how having materials to support practice of relaxation skills was helpful for encouraging practice outside a formal intervention setting:119,189,190
I found the CD [compact disc] to be most helpful. I practiced twice a week. Will still use it even after the study.
Young person, asthma119
The authors of 10 studies suggested that technology, including social networking sites, can provide the opportunity for CYP to continue supportive relationships developed during peer-based interventions. 163,165,166,169,174,175,179,183,185,217 A quotation from a young person indicates how these relationships can endure across time, despite relatively little face-to-face contact:
She was the one I called when I got cancer. I don’t know. Even though like we never see each other, I feel like she is one of my closest friends. Like, closer than the ones I have at school.
Young person, CHD165
The authors of six studies suggest that intervention deliverers can play a role in extending the impact of the intervention beyond its time-limited delivery period, by creating opportunities to meet again after the intervention has ended166,174 or by providing ‘top up’ intervention sessions based on the changing needs of the child. 171,189,195,205
Positive feelings regarding interventions can permeate CYP’s lives. Six studies suggest that merely the memory, facilitated by mementos or anticipation, of the intervention could have a positive impact on their feelings of well-being for both the CYP and their family:166,167,173,174,200,203
The meaning of camp in my life is everything. It’s what I want to do every single summer. I look forward to it every single summer . . . So it’s really, really fun.
Young person, mixed167
I’ll tell you that it’s something we won’t forget. It will be a memory that we will share. Together, the four of us. And you know, we talk about things that we did at Living Well.
Parent, mixed164
Four studies suggest that having a memory from the intervention to think about, or an object, such as a toy, to use, can be a source of comfort for CYP, particularly those undergoing distressing procedures. 174,191,200,205 These physical objects or memories can act as a reminder to CYP of their resilience by reminding them of how they have successfully overcome challenges in their physical health treatment and in an intervention setting. 174,200 These ‘transitional objects’ may act as a source of emotional comfort191,205 and be utilised in times of stress to improve emotional well-being.
Summary: getting in and staying in
‘Getting in and staying in’ acknowledges that getting CYP involved with an intervention that may benefit their mental health is a process, requiring the availability of an accessible intervention that is both tailored to the needs and characteristics of the CYP it intends to support and capable of adapting over time if their needs change. To ensure that an intervention is sustainable, adequate resources must be available to both implement the intervention and continue delivery over time. Interventions demonstrate sustainability when CYP are using aspects of the intervention or developing relationships outside sessions. It appears that both parents and service professionals have an important role in supporting CYP to access and engage with an intervention and encourage long-term behaviour/emotional change.
Line of argument synthesis
The line of argument presented in Figure 18 aims to illustrate the relationships between the different themes discussed in this chapter. Overall, it describes the process of CYP with LTCs accessing and maintaining engagement with a relevant mental health and well-being intervention, acquiring a sense of hope for the future and increasing resilience, all against the backdrop of a safe space with adequate social support. However, this relationship is tentative and does not necessarily mean that increased experience of a safe space and social support leads to increased hope and resilience, as other factors may modify this relationship.
The process illustrated within Construct: getting in and staying in shows CYP’s journey from the recognition of their mental health needs to being offered an available intervention, and the potential barriers to accessing an intervention and continued engagement if appropriate. Maintaining engagement with an intervention and the experience of an intervention setting as a ‘therapeutic foundation’ seem to be closely interlinked. In particular, the aspects of the ‘engagement’ and ‘a safe space’ that encourage addressing worries prior to the intervention and the use of a familiar routine and structure within intervention settings so that CYP know what to expect are inter-related. The more CYP engage with a setting, the more familiar that setting becomes, thus reinforcing both the potential for continued future engagement and the experience of that setting as safe. Not only does this have a positive impact on CYP’s anxiety about meeting new people, but it also allows them to develop relationships with empathetic intervention deliverers and peers, which can aid the CYP in telling their stories and expressing their feelings to an empathetic audience. This process of speaking and being heard can allow CYP to access the affirmational, emotional and informational support detailed under the social support theme, which can further reinforce the experience of a setting as being a safe space. This opportunity to discuss feelings and experiences can be a positive release. The evidence indicates that CYP highly value the sense of reduced isolation that accompanies the chance to meet peers with similar experiences to themselves.
Alongside the relationships being developed within the intervention setting among CYP, their peers and those delivering the intervention, the informational support acquired as a result of these relationships also enables CYP to acquire skills to address challenges in their relationships with healthy peers and their family. The resulting improved relationships between CYP, their families and both peers with a LTC and peers without, may contribute to the continued engagement of CYP and their family with an intervention and maintenance of the effects beyond its scheduled end.
Having access to a ‘therapeutic foundation’ also allows CYP to utilise the informational support offered by peers and intervention deliverers to develop new skills and knowledge to manage their LTC and emotions. This can help facilitate feelings of empowerment, as can the experience of mastery of tasks both related and unrelated to managing their LTC. These experiences of mastery, alongside encouragement to recognise positive aspects about themselves, can also contribute to feelings of improved self-esteem and empowerment. As indicated in Figure 18, this inter-related set of themes can contribute to the overall resilience of the CYP and their ability to cope with both their LTC and their mental health difficulties. In addition to increased resilience, having the opportunity to observe other people who are able to successfully manage their LTC and live a fulfilling life alongside it can provide a sense of hope to CYP. Their interaction with supportive others in an intervention that considers their LTC within the context of their daily lives appears to reinforce to CYP that they are more than just their illness and that they too have something to contribute in their relationships with peers and intervention deliverers. This sense of mutuality can also contribute towards developing feelings of empowerment. Having a sense of hope may provide the motivation for CYP to engage with an intervention and implement the knowledge that they have learnt, and increased resilience may further contribute to their sense of hope for the future.
Figure 18 indicates a cyclical relationship between the themes and suggests that the impact of an intervention may affect future engagement. One of the key factors that may be associated with maintaining engagement over time is the ability of the intervention to flexibly adapt to the physical and mental health needs of the CYP for whom it is intended. This reflects an important point raised by our study-specific CYP public and patient involvement group members, who were consulted on emerging preliminary overarching themes identified by this review. They emphasised that they prefer individuals delivering the intervention to listen to what the young people themselves feel was the main issue, rather than trying to impose an intervention that CYP feel is irrelevant. There is a tension between the need for an intervention to be flexible and provide a sense of being unconstrained and the need for boundaries. The evidence we collected suggests that, although CYP welcome the opportunity to escape the worries and constraints associated with living with a LTC in everyday life, they require certain limits on behaviour, discussion topics and physical activity to experience a space as safe, with the limits reinforced by both intervention deliverers and peers. The apparent balance required to ensure that these two concepts are incorporated into an intervention may represent a challenge to those who design and deliver it.
Discussion
Summary of findings
Among the 60 articles included in this review, 21 types of intervention were evaluated. These included online interventions, camps, music therapy, psychoeducation and development of coping skills. The LTCs seen most frequently within the studies were cancer (14 studies163,164,173,191,199–205,207,211,214), a mix (10 studies164,167,170,175,177,178,188,192,196,207,208,217), HIV infection (eight studies168,172,174,176,187,196,209,210) and T1DM (five studies114,162,184,190,213). Although no formal mental health diagnosis was required for inclusion in the review, reported mental health and well-being aims of interventions included goals to promote adjustment, reduce anxiety and depression and improve coping skills. Articles typically reported on studies of good quality; the general weaknesses in this literature included a failure to make the theoretical perspective of the author explicit, inadequate description of the context or setting of qualitative research and lack of clarity in the description of the intervention.
Results in context
Relation to previous reviews
This review is the first to examine the experiences of participants regarding interventions aiming to improve the mental health of CYP with LTCs. The majority of studies (52/57) evaluated interventions that aimed to improve others aspects of CYP functioning. This synthesis has brought together previously suggested theoretical understandings of the mechanisms underlying how the development and prevention of mental health in CYP with LTCs and expanded on them.
Wallander and Varni’s disability-stress coping model of adjustment to chronic illness (see Chapter 1) acknowledges the importance of involving the family and social support under social-ecological factors that may have an impact on the coping strategies used to moderate the stress of having an LTC. 38 They also discuss the importance of ‘perceived competence’, ‘effectance motivation’ (‘a desire for understanding, predictability and control over one’s environment’221) and ‘problem-solving ability’ in how an individual appraises a stressor and the type of coping strategy they use to manage it. 38 These concepts appear to be similar to the themes of ‘empowerment’ and ‘skills and knowledge’ discussed above. The line of argument presented in Figure 18 shares specific resistance factors in Wallander et al. ’s37 model that may affect adjustment to life with a LTC.
The concept of social support was common within the studies included in this review and, as could be expected, was mentioned most often with regard to interventions that encouraged interactions with peers and family members. Stewart et al. 178,216 propose that social support can be thought of as consisting of several components, including affirmational, emotional and informational support. Gaysynsky et al. 210 go further and draw on the typology of social support proposed by Cutrona and Suhr222 by suggesting that there are multiple types of social support, including encouragement, esteem, network support and tangible assistance. The content of esteem support encompasses ideas such as relief of blame, validation and compliment, which could be considered as being related to the ‘empowerment’ theme under Construct: resilience from the synthesis of this review.
Venning et al. 45 conducted a systematic review that focused on young people’s experiences of chronic illness. Their objective was to make recommendations regarding ways in which mental health difficulties could be prevented in this population. Their results link closely with the results of the synthesis in this review in several areas. First, in Venning et al. ’s review,45 CYP discussed how a LTC made them feel different and reported that other people did not understand them. This relates to the themes ‘I am not alone’ and ‘therapeutic relationships’ in the current review, which explore how much CYP valued feelings of connectedness and belonging with similar peers and empathy/validation from intervention deliverers. The themes ‘unconstrained’ and ‘a new normal’ in this review appear to be supported by Venning et al. ’s45 findings that CYP view the LTC as something that restricts their participation in ‘normal’ life and everyday activities and is a source of uncertainty both in the present and with regard to worries about their future. The importance of social support, development of coping strategies and a sense of hope and acceptance are also discussed in both reviews. The synthesis in this review evaluates whether or not existing interventions are perceived to meet the needs identified by Venning et al. 45 across a broader range of LTCs and identifies additional themes, such as the role of ‘hope and inspiration’ for health and social care professionals to consider when designing an intervention.
Relation to the UK health setting
Mental and physical health services for CYP in England are often commissioned and delivered separately. 223 Although some integration of psychological services into physical health wards for CYP with LTCs does exist, the extent to which this takes place is influenced by available funding and perceived clinical need/importance/priority and thus is subject to regional variation. In 2012/13, only 6% of NHS mental health funding was allocated to services for CYP,224 and between 2013/14 and 2014/15 services providing mental health and social care services to CYP saw cuts to funding of £35M. 225 Thus, recommendations made by this review regarding the need for easily accessible, evidence-based interventions that are sustainable with limited resources over time, with an effect that can be sustained beyond the end of an intervention, appear particularly relevant.
The difficulty in funding and accessing holistic services may make it more challenging for mental health service providers to meet some of the conditions recommended by the ‘availability’, ‘a safe space’ and ‘more than just my illness’ themes. Opportunities to meet peers with LTCs outside physical health wards can vary according to different service providers. This may limit opportunities for CYP with a LTC to access the social support offered by similar peers and, in turn, develop a sense of hope and resilience. The finding that mental health interventions can be delivered effectively by individuals without specialist mental health training, across a variety of settings, could overcome this limitation. Proposals to increase the mental health support for CYP in schools and other health-care settings offer the potential for the delivery of mental health interventions to be more flexible, with more opportunities for CYP with a LTC to meet each other. 223 However, the issue of ensuring that adequate resources are available to provide the training and ongoing supervision to ensure that the appropriate, sustainable delivery of these services remains.
Interventions in online and/or group settings may be another way of meeting the mental health needs of CYP with LTCs; however, these approaches will not be suitable or acceptable to all CYP. Care is needed to ensure that alternative options are available when appropriate and that the design of an intervention can be adapted to meet the needs of individual members. A potential challenge for health and social care services will be how to ensure that an intervention space is experienced as safe and allows the development of empathetic, supportive relationships with peers and intervention deliverers over time in a system in which waiting times for routine appointments within Child and Adolescent Mental Health Services (CAMHS) have reached 32 weeks (2015/16). 226
The inclusion of nine American camp interventions also raises the issue of how transferable some of the themes are to UK health and social care settings. This is particularly relevant for the themes ‘a safe space’ and ‘unconstrained’. Camps could be considered as a respite intervention,185 which is a familiar concept in UK services supporting individuals with learning disabilities and can include the provision of holidays for carers and/or those they care for. 227 This suggests that there may be a potential need to evaluate the psychosocial benefits of respite opportunities for CYP with LTCs in the UK.
The strengths and limitations of the review and the implications and recommendations for future work are discussed in Chapter 6.
Chapter 4 Overarching synthesis
An integration of insights generated via studies addressing different types of questions contributes to a more synergistic, holistic utilisation of research evidence. 228
Aims
The aim of this overarching synthesis was to draw together the findings from the previously reported systematic reviews.
A mixed-methods synthesis approach was used to analyse the evidence from review 1 and review 2 together. Although all studies included in review 1 involved CYP with elevated symptoms of mental ill health, the majority of studies in review 2 did not assess the mental health of participants. Thus, the degree to which CYP with elevated mental ill health were represented in the studies included in review 2 cannot be determined. Based on the author-reported mental health aims of the studies, the mental health aims of interventions tested in review 1 more often sought to improve symptoms of mental health disorders, whereas in review 2 interventions more often aimed at benefiting broader aspects of mental health and well-being, such as coping, self-esteem and reducing stress.
Although different intervention types appear in the two systematic reviews, the factors that may enhance, or hinder, the clinical effectiveness of interventions and/or the successful implementation of interventions suggested by review 2 can be used to help interpret some of the review 1 findings. Likewise, review 1 evidence can help verify or refute ideas about beneficial intervention components proposed by review 2.
Background
There are few established methods for the integration of findings from quantitative and qualitative systematic reviews of interventions. One mixed-methods approach to conducting systematic reviews involves the completion of comprehensive syntheses of two or more types of data (e.g. quantitative and qualitative) before these reviews are aggregated into a final, combined synthesis. Sandelowski et al. 229 refer to this framework for conducting mixed-methods systematic reviews as ‘segregated’. Published examples of syntheses that combine separate quantitative and qualitative systematic reviews tend to take the findings of one of the reviews as their start point. 230–232 For instance, Thomas et al. 233 identified participant views in their qualitative synthesis of barriers to and facilitators of fruit and vegetable eating in children. These qualitative recommendations formed a framework for analysing the extent to which findings from controlled trials were in agreement.
Owing to the differences in research questions and interventions that were included in each of the systematic reviews in this project, it was felt that it would be limiting to use a model where one review was used to explain the findings from the other review only. Therefore, a similar method to the initial step used by Richardson et al. 107 in their overarching synthesis of attention-deficit/hyperactivity disorder (ADHD) interventions in school settings to consider the findings of each review in the light of the other was used.
Method
We conducted the overarching synthesis by undertaking a collaborative question-and-answer exercise with preliminary findings from each review. This allowed for the issues raised during the question-and-answer exercise to also contribute to the synthesis of the individual reviews (Figure 24). This was a deductive approach as questions based on the findings of each review were generated and used to interrogate the other review for information that could potentially inform the findings or explain gaps in the literature. Questions were framed using the format ‘Review 1 found X; can Review 2 inform these findings?’ Questions were related to either the synthesised review findings or descriptive details regarding included studies.
FIGURE 24.
The overarching synthesis process. R1, review 1; R2, review 2.
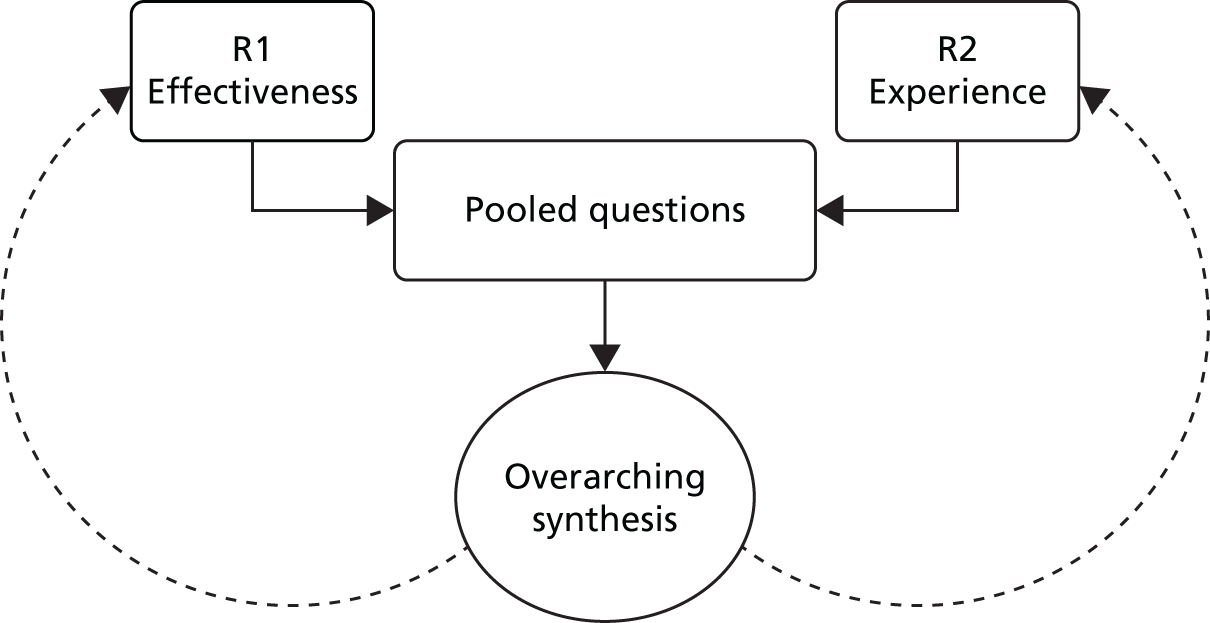
Michael Nunns and Liz Shaw wrote questions arising from review 1 and review 2, respectively. Michael Nunns answered questions posed to review 1 in written form and Darren Moore answered questions from the perspective of review 2. The initial drafts of these questions and answers were shared with the other reviewers (MN, LS, DM) for comments and edits. In answering the questions, reviewers consulted both the systematic review findings and the data extraction forms from included studies. The resultant sets of questions and answers were grouped into categories according to shared ideas within the questions and/or answers. Each category was written up in narrative form.
Findings
Nine categories emerged from the analysis. Descriptions of the categories, the contribution of each systematic review and the implications are tabulated later in this chapter.
Degree of overlap between the two reviews
Because of a difference in inclusion criteria and search terms in review 1 and review 2, one would have predicted differences in terms of populations and interventions included. The requirement for the studies in review 1, but not review 2, to include samples with elevated symptoms of mental ill health indicates that samples for review 1 are likely to have more severe symptoms of mental ill health than samples for review 2, in which this information was unknown in all but one study that did assess mental health at baseline. 119 The database search for review 2 included broader mental health and well-being terms to locate literature that may have focused on participant views rather than intervention aims in abstracts. Therefore, a broader range of mental health intervention aims may have been seen in review 2, although review 1 included interventions with broader mental health aims that included improvement in stress, adjustment, coping and well-being. 120,122,123,130
Specific combinations of intervention types and LTCs were rarely seen in either review 1 or review 2 (see Report Supplementary Material 3 – intervention and LTC map). The only time this occurred was when the same researchers conducted both quantitative and qualitative evaluations of interventions. 119,130,184 Otherwise, cancer and music therapy was the only LTC intervention dyad seen in both reviews, with Bufalini136 conducting a RCT and six qualitative studies exploring experiences of music therapy for CYP with cancer. 199,201–205 This meant that the available evidence often prevented direct comparison of quantitative and qualitative research findings across similar interventions and populations.
There were also noticeable differences in the type of interventions studied in review 1 and review 2. CBT was the most frequently studied intervention in review 1, with seven included studies,83,84,124,126,130,145 whereas only four studies in review 2 featured interventions that included an element of CBT182,184,186,193 and these were commonly combined with other intervention approaches including psychoeducation and physical activity. Parenting interventions118,128,131 and group play therapy133,135,138 were each the subject of three included studies in review 1 and no studies in review 2. Conversely, the most common intervention categories in review 2 were online support interventions targeting various mental health and well-being constructs (n = 13),114,177,178,183,192,208,210,211,213,215–219 camp (n = 9),163,165–167,169,173,174,179,185 music therapy (n = 6),199,201–205 face-to-face peer support (n = 4),162,175,176,212 psychoeducation (n = 3)171,193,214 and coping skills (n = 3). 114,184,191
There were more similarities between the two reviews in terms of the populations studied. In both reviews CYP with cancer was the most commonly studied population (five studies in review 1,123,133,135–137 13 studies in review 2 that included CYP with only cancer163,167,173,191,194,199,201–206,211 and five studies in review 2 that included CYP with cancer alongside CYP with other LTCs164,167,175,177,207). CYP with T1DM were included in four review 1 studies118,120,122,130 and also frequently appeared in review 2 (n = 5),114,162,184,190,213 and asthma appeared in three review 1 studies119,138,139 and five review 2 studies. 119,178,192,214,217 There were, however, a larger number of studies in review 2 that included CYP who are HIV positive (n = 8)168,172,174,176,187,196,209,210 and different CYP with different LTCs (n = 10). 164,167,175,177,178,188,192,207,208,217 Only one study in review 1 included CYP who are HIV positive121 and no review 1 studies included different CYP with different LTCs.
What is noticeable from the map of interventions and LTCs studied across reviews (see Report Supplementary Material 3) are the pockets of research that have been conducted for certain intervention–LTC dyads. For instance, qualitative studies of camp interventions are most often focused on cancer163,173,174 and heart disease. 165,166,169,185 In review 1, three studies focused on CBT for IBD, although this may be partially explained by shared authorship across the three studies. 84,125,126 In review 1, both trials evaluating stress management did so in samples with T1DM. 120,122 It is unclear why there is a focus on particular combinations of intervention and LTC in these instances. On the other hand, online support group interventions, appearing frequently in review 2, were evaluated across populations with 10 different LTCs. This may indicate that online support groups target aspects of mental health that are common across populations. Clearer reporting of the rationale for interventions, as well as proposed mechanisms of effect, may help explain why certain interventions are used with particular LTCs.
Availability of up-to-date, good-quality research
Seventy-six per cent of studies included in review 1 and 82% in review 2 were initially published after 2008, and 36% in review 1 and 26% in review 2 were published after 2014. Despite the relatively recent body of research, in approximately one-third of the studies (n = 983,119,122,127,132,135,136,139,152) included in review 1 there were multiple areas for concern in terms of study quality. In particular, assessment of adherence, compliance or fidelity, explaining missing data, blinding of assessors and inclusion of a follow-up after treatment were identified as areas of weakness. In review 2, there were also a number of areas of concern with the quality of the qualitative articles, including adequacy of description of the theoretical or ideological perspective, the context or setting of qualitative research and the clarity of intervention description. Our findings in terms of the quantity and quality of evidence available echo those of Bennett et al. 82
What works for whom?
As mentioned above, there was a lack of overlap between the two reviews, meaning that it was rarely the case that qualitative research could suggest why certain interventions may or may not have been effective for specific LTC populations. However, it may be that commonalities in intervention experience revealed across studies in review 2 can tentatively suggest reasons for some effectiveness results in review 1, or suggest areas of focus for future effectiveness studies.
Relaxation
Two studies found beneficial effects of relaxation for asthma, one of which119 included both a RCT and qualitative data about their intervention, which aimed to improve asthma outcomes and reduce anxiety symptoms. Although the relaxation techniques used in the study, including breathing retraining exercises, progressive muscle relaxation and guided imagery, were considered acceptable and feasible in young people with asthma and reduced anxiety compared with baseline, there was no benefit when compared with standard asthma education materials received by the comparator group. The authors suggest that this was indicative of a general lack of confidence in symptom management, and that interaction with the research team, regardless of intervention, immediately reduced anxiety symptoms. This is somewhat contradicted by interview quotations from participants in the study, which suggested that they used the techniques while feeling angry, upset and breathless. Looking beyond this study, the ‘social support’ and ‘resilience’ constructs from review 2 suggest that CYP appreciate being able to learn techniques and strategies to manage both their LTC and their emotions, which might provide a theoretical underpinning for the effectiveness of relaxation interventions more broadly.
Music therapy for procedural anxiety
The use of music therapy in CYP with cancer to assist with their procedural anxiety featured in one study in review 1136 and six in study in review 2. 199,201–205 Studies included in review 2 identified that CYP had positive experiences of music therapy utilised during medical treatment/procedures, indicating that music therapy may provide a distraction from the burden of having a LTC;201,202,205 provide an emotional outlet and regulation tool for CYP undergoing treatment;204 and facilitate the development of relationships between CYP and their family, health professionals and peers. 201,202,205 The one study in review 1 to assess music therapy found that interacting with music (making music, playing with instruments) prior to a painful treatment procedure (such as a lumbar puncture) and listening to background music during the procedure were effective in reducing procedural anxiety in comparison with the control group, who were sedated, although this study was methodologically weak. 136
Cognitive–behavioural therapy
Synthesis of the four studies featuring components of CBT in review 2182,184,186,193 suggests that CYP may have appreciated an approach that addressed both mental and physical health needs as well as the behavioural components of CBT interventions, as they can provide an easily understood process for CYP to follow. The specific CBT intervention that was evaluated across both reviews was BOC, aiming to both improve glycaemic control and psychosocial well-being. The RCT demonstrated that it was the least effective CBT intervention in terms of CYP mental health outcomes, with no evidence to show that it reduced LTC-specific stress or improved self-efficacy compared with treatment as usual. 130 The authors commented on the poor study recruitment and retention, implying that the requirement for weekly travel was a deterrent, but also that the explicit focus of the intervention on mental health was a problem for potential participants concerned about associated stigma. Access to interventions and the potential for stigma related to intervention attendance and health needs are evidenced clearly in the review 2 themes ‘accessibility’ and ‘a new normal’.
Other physical and biofeedback interventions
Review 1 included two single studies evaluating the clinical effectiveness of interventions in CYP with CFS and chronic pain, conditions for which there is no determined physical cause. There was no evidence that resistance training was more effective than aerobic exercise training in reducing anxiety in adolescents with CFS. 129 Heart rate variability biofeedback therapy supplemented by at-home breathing practice had no beneficial effect on anxiety and potentially detrimental effects on depression outcomes in CYP with chronic pain. 127
An evaluation of a combined CBT and neuromuscular training programme in CYP with fibromyalgia, a diagnosis associated with physical symptoms of uncertain origin, was included in review 2. 186 The intervention was well received by participants, who valued the opportunity to address both the physical and cognitive factors that have an impact on their LTC, in addition to gradually increasing their physical exercise alongside a group of similar peers. The interventions studied by Gordon et al. 129 and Yetwin127 appear not to have included both the cognitive and social components addressed by the intervention evaluated by Kashikar-Zuck et al. 186
Moderators of effectiveness
Review 2 suggests that the way CYP engage with an intervention is affected by age; for instance, Nicholas et al. 177 noted that younger and older children had different preferences regarding an intervention that included online games, education and a peer support network. However, no review 1 studies investigated differences in effectiveness outcomes by variables such as age. There were also too few studies investigating similar populations and interventions in review 1 to allow moderator analyses at the review level. In review 2, eight studies assessed the clinical effectiveness of the intervention, although seven of these were not RCTs and, therefore, were excluded from review 1. 119,190,193,194,196,199,209,213 But, aside from Bignall et al. 119 discussed above, there was no clear indication from any of these studies as to why interventions may or may not have been effective and how individuals’ experiences differed.
Category summary
Overall, owing to the lack of crossover between the types of intervention and LTC populations included in review 1 and review 2, the ability to explain what works and for whom is limited. Future research needs to include qualitative process evaluations alongside RCTs and vice versa to investigate reasons for effectiveness and any individual differences.
Adaptations to interventions and flexibility
This category considers evidence from both reviews pertaining to whether or not and how interventions are adapted to respond to participants’ LTC or other needs. In review 1, the majority of the interventions assessed were not described as including content adapted for the LTC of samples (see Appendix 5). However, six out of seven CBT studies included intervention content that was adapted to respond to the LTC of recipients. The clearest example of flexible delivery in review 1 was the study by Szigethy et al. ,126 in which the PASCET-PI intervention was simplified for younger participants.
Review 2 suggests the need for flexibility in intervention content, delivery or structure so that CYP with LTCs can access and engage with interventions. There was evidence for a wider range of adaptations to make sure interventions were accessible to individuals, including changes according to age, development and education levels, as well as LTC. There is the issue of how to tailor programmes without loss of fidelity to the intervention. In review 1 the fidelity of, or adherence to, adapted CBT interventions was measured in several studies, including the one study that delivered the intervention flexibly according to participant age. 84,125,126 There is a balance between ensuring that the effective components of an intervention are delivered as intended and ensuring that the individual needs of those receiving the intervention and the context in which the intervention is being delivered are acknowledged. 234
Examples of the adaptation of CBT in review 1 include the identification of LTC-specific stressors and developing coping strategies that adapt to IBD symptoms,125 addressing fears specifically related to physical pain124 and integrating illness narrative techniques and emphasising healthy IBD-related cognitions and behaviours. 84,126 CBT interventions for IBD and functional somatic complaints (TAPS,124 TAPS and IBD,125 PASCET-PI84,126) showed evidence of some beneficial effect on CYP mental health outcomes. However, one ‘cognitive behaviour intervention’83 showed large improvements in depression outcomes for CYP with epilepsy who were at risk of depression, and this intervention was not adapted to the LTC.
The BOC CBT intervention assessed in the study by Serlachius et al. 130 began as a generic CBT intervention aimed at improving coping and reducing stress. 235 Following patient feedback analysed in a qualitative study included in review 2,184 a number of diabetes mellitus-specific components were integrated into the intervention, including diabetes mellitus-specific goal setting and self-efficacy. Despite these components, Serlachius et al. 130 reported no improvement across any outcome for their intent-to-treat analysis as reported in review 1. But a ‘per-protocol’ analysis suggests a significant reduction in stress at the 3-month assessment for those who attended sessions compared with the control group.
A tenet of the review 2 ‘getting in and staying in’ construct is that interventions need to be relevant to young people and, if applicable, their families. A key component of interventions being considered applicable and engaging was perceived to be the ability to use the interventions flexibly according to the LTC. Within a camp167 and online intervention177 that were open to CYP with different diagnoses and ages, CYP were able to choose what activities they took part in to meet their own psychosocial needs at a developmentally appropriate level. Review 2 highlights the need to be flexible according to more than just the LTC of CYP. Factors to consider also include participant age and developmental level,114,164,168,171,174,177,182,184,187,191,197,200,201 and personal interests. 162,172,177,182,191,201,206
When considering whether or not an intervention meets certain recipient needs, it should be acknowledged that these needs may change over time, as alluded to in several studies from review 2. 171,179,189,200,202,205 Developmental, educational and LTC changes could affect participation in, or effectiveness of, an intervention. A number of review 1 studies cite a wide variety of reasons for dropping out of programmes, such as parental break-ups,128 being too busy,137 moving from the local area,84 worsening symptoms133 or simply lack of interest. 84 Although there may not be a solution to all of these potential challenges, interventions that are more adaptable to the situation of the recipients and can be adapted accordingly may benefit from greater retention over time.
Further evidence is needed to understand whether or not and how interventions should be adapted for the LTCs of CYP and the extent to which interventions can be used flexibly without compromising fidelity. When aiming to meet the needs of the intervention’s recipient, it is important to consider how these may change over time.
Accessibility and delivery of interventions
Setting
Review 2 findings suggest that participation can be facilitated by utilising families’ existing links with health and social care professionals. There was some evidence that future accessibility had sometimes been considered during interventions developed for research included in the reviews. In the case of the intervention targeting anxiety in CYP with IBD, as tested by Reigada et al.,125 part of the rationale was to increase accessibility to mental health treatment in clinical health settings. Review 2 provides evidence that CYP and their families appreciate the delivery of mental health interventions in familiar settings, inclusive in terms of travel and any other costs,119,172,175,176,178,182,183,186,187,201 when they could access multiple services relevant to their needs. 175,176
Evidence from both reviews suggest that, in addition to the physical location of the intervention, the familiarity of the environment136,175 and staff to CYP198 and the extent to which the intervention creates a therapeutic atmosphere may influence the extent to which it is perceived as accessible and may thus affect the degree to which CYP and their families engage with the intervention. There is little evidence from review 1 that familiarity was taken into consideration when delivering interventions, other than in Bufalini’s study136 in which the child was shown around the room where their painful procedure would take place. A number of review 1 interventions may have encouraged practice in convenient settings, for instance home119,139 or school,119,132 or delivered over the telephone. 84,126,128
Role of technology
Although it was not possible to determine whether or not interventions delivered online or by telephone are as effective as those delivered in face-to-face settings in review 1, the review does provide some evidence that interventions delivered, at least in part, over the telephone can be effective in relieving mental health difficulties. 84,126,190
Results from review 2 suggest that some CYP and parents appreciate online interventions that CYP can access with minimal support from parents and the freedom of expression that can be facilitated by perceived anonymity. 177,178 However, other studies suggest that, despite the convenience of online interventions, CYP and their families may still prefer face-to-face meetings. 189 Some staff noted that, in the case of interventions delivered online, it was harder to monitor how the intervention was received as a result of being unable to read the body language of the participants. 178 It was also noted that, although some participants actively engaged with online interventions, it could be difficult for shy children to join in initially,178 whereas others participated only when they had a specific problem. 183 Studies in review 2 also noted the importance of a facilitator in encouraging initial engagement and discussion, particularly in the early stages of an online intervention. 114,177,178,211 Review 1 does not include any studies that take advantage of technologies CYP use in everyday life.
Delivery
The ‘unconstrained’ theme in review 2 suggests that CYP value opportunities to feel that they can ‘escape’ from worries and everyday routines associated with their LTC, including hospital visits. 166,167,187,201 Interventions that allowed CYP to try fun activities or enabled them to ‘be themselves’167 with similar peers were also highly valued. In review 1, group play therapy interventions promoted interaction with peers in similar situations and potentially elements of ‘fun’. 133,135,138
It is not possible to determine whether or not there were any differences in effectiveness according to individuals’ specialist training as there were too many confounding variables. Review 2 suggests that some interventions delivered by individuals without specialist training, such as peer mentors, were acceptable to CYP and in some cases were perceived as being more approachable or trustworthy when based on the deliverer’s own experience. 174 Evidence from the ‘keeping it going’ theme suggests that adequate training is required to ensure that both specialist and non-specialist individuals deliver the intervention in the way that it is intended and that the benefit of the intervention is sustained over time.
Stress and coping
The following section considers concepts that emerge from the two reviews that relate to managing the stress of living with a LTC, and evidence for strategies to help CYP cope.
Managing physical symptoms alongside daily life
The ‘hope and inspiration’ and ‘a new normal’ themes in review 2 indicate that having one or several role models who are living successfully with a LTC and being able to incorporate the realities of living with a LTC into everyday life, as well as taking part in ‘normal’ activities, can provide CYP with a sense of hope.
Eleven interventions from review 2 included components that focused on supporting CYP to improve control of LTC symptoms, whereas the effect of interventions on LTC symptoms was measured in 13 out of 25 review 1 studies. The ‘resilience’ construct from review 2 showed that CYP perceive learning skills that allow them to take responsibility for managing their LTC as improving their confidence and empower them to move forward with their lives. 182,186 There is evidence from review 1 that interventions that successfully supported CYP to manage physical health symptoms also had a beneficial impact on CYP’s mental health,124,126,139 although this was not always the case. 119
Choice, mastery and having a voice
Review 2 suggests that interventions that support CYP to make choices can facilitate feelings of empowerment. Despite the inclusion of two palliative care interventions that encouraged CYP to make decisions about their care,123,137 it was not possible to assess the extent to which the availability of choice as a component of the intervention was beneficial or not.
Review 2 indicated that CYP reported benefits in terms of empowerment and self-esteem from opportunities to experience mastery and personal autonomy. These experiences were not restricted to management of LTCs, but were also achieved through taking part in fun or challenging activities and having the opportunity to reflect on their illness journey. 179,200,201 None of the studies in review 1 explicitly evaluated the impact of interventions on self-esteem outcomes, although developing a sense of ‘positive self’ and LTC-specific self-esteem were components of some CBT interventions. 84,130
Review 2 also suggests that interventions that encourage children to have a voice in the intervention are important components of empowerment. Studies in review 1 that encouraged CYP to voice their opinions included two palliative care interventions that asked children about their wishes137 and included CYP in advanced decision-making for end-of-life care. 123 Although several review 1 interventions incorporated aspects of problem-solving or goal-setting, it was often unclear to what extent this was led by CYP themselves, which is something that might offer a greater sense of empowerment. 184,189,195 It was also unclear whether or not these intervention components had an influence on outcomes.
Distraction
Both reviews offer some support for the use of distraction as an effective intervention when CYP are undergoing distressing procedures. From review 1, Bufalini136 reported large beneficial effects of music therapy as a distraction during a painful procedure, although the study was rated as being at high risk of bias. Likewise, review 2 indicated that interventions such as music therapy and making videos are perceived to reduce anxiety. 201,205,206 Distraction alleviates the boredom associated with long hospital stays. 177 Distraction was also seen outside the context of procedural distress. In review 1, Szigethy et al. 84 included distraction in an attempt to avoid negative cognitions. However, review 2 suggests that being able to tolerate some distress is important for CYP to access and maintain engagement with an intervention. 171
Coping over time
To sustain the impact of interventions on CYP well-being over time, the ‘keeping it going’ theme in review 2 proposed that interventions should incorporate the use of new skills into the daily routine. There is evidence of interventions across both reviews that encourage this through homework tasks for parents to practise new skills and manage CYP behavioural problems128,131 and CYP to practise exercises, relaxation, CBT techniques and stress management skills between sessions. 114,119,127,129,139,186,190,195
There are a number of proposed methods for reducing stress and improving coping in the short and long term that arise from the two reviews. Although having a role model who represents an achievable, ‘normal’ life appears to be valued by CYP, none of the review 1 studies incorporated this into their interventions. Encouraging active decision-making, autonomy and participation in discussions about the child’s own illness is one strategy that may lead to increased self-esteem; review 1 was unable to effectively evaluate these suggestions.
Working with family and peers
This category explores the importance of involving others in mental health interventions for CYP with LTCs, including interventions that involve members of the CYP’s family or members of their community, such as teachers. Studies included in review 2 indicated that interventions that aim to treat the mental health of CYP are perceived to improve the quality of family relationships164 and provide families with the opportunity of meeting others in similar situations, which may provide a sense of community and support. 164,171,185 Parents stated that it was sometimes challenging to answer their children’s questions when they did not know the answer171 and that they appreciated interventions that enabled them to support their child. 191 Some interventions appeared to enable parents to cope with daily stressors and adopt a more positive perspective with regard to the family’s situation/health of the ill child. 164,166,177,184,187
Review 1 suggests that parenting interventions may help improve parents’ feeling of parenting competence and confidence, as well as improving their own mental health. 118,128,131 Review 2 also provides some evidence to suggest that skills learnt by families may in turn have a positive impact on the mental health of their child by promoting positive coping strategies within the family. 185,189,191
The potential for tension between providing the opportunity for CYP to become empowered via learning to manage their LTC versus involvement of parents in the intervention process is acknowledged. Parents have an important role in supporting CYP to manage their LTC, attend interventions and practise techniques that may benefit their mental and physical health, as acknowledged within the ‘getting in and staying in’ construct in review 2. However, some studies in review 2 also acknowledge how parents value the opportunity to step back and how CYP may benefit from accessing ‘adult-free’ spaces. 169,180,185 In review 1, five interventions had components that were delivered to parents as well as CYP,84,123,125,126,145 although only Lyon et al. 123 intervened in a way that simultaneously involved both CYP and their parents.
Reigada et al. 125 educated parents about the LTC and actively encouraged parents to foster a sense of independence in their children. The findings of review 2 suggest that Reigada et al. ’s125 approach could be perceived as effective and, indeed, it reported large beneficial effects on LTC-specific anxiety, although this was of course a small element of the overall intervention.
There was also evidence that involving affected peers in interventions might be beneficial. Review 1 included three studies that encouraged group play or activities with affected peers. 133,135,138 Synthesis suggests that the group play interventions were effective, producing large beneficial effects on mental health; however, the quality of these studies was poor and no firm conclusion regarding the efficacy of studies emphasising group interaction compared with individual-based delivery could be made owing to study heterogeneity. However, review 2 indicated that group interventions allowing interaction with affected peers, particularly older mentors, was highly valued by CYP because it reduced the feeling of isolation and provided access to support. 162,166,170,183
Therapeutic relationships
Review 2 identified the theme of ‘therapeutic relationships’ as an important component for making the participants in an intervention feel as though it is taking place in a safe and secure environment, where they can express themselves freely without fear of judgement. The ‘therapeutic relationships’ theme discussed how CYP can feel valued, respected and cared for if the relationships with fellow recipients or whoever is delivering the intervention are understanding, validating and respectful of their needs. Review 2 suggested that it may take time to develop these relationships and establish trust through the exchange of personal information. This process may facilitate the expression of emotions and could be a key component of a successful mental health intervention, as a result of its role in enabling CYP to access social support.
Some interventions in review 1 incorporated opportunities for discussion about experiences and emotions, such as group discussions, one-to-one sessions and tasks that required participants to identify typical stressors. Although this could facilitate the development of key therapeutic relationships, there is little available evidence to examine the extent to which the sharing of experiences occurred, or whether or not the CYP felt that other people understood and empathised with them. The only insight available emerges from the intervention rating/satisfaction data reported in four studies. 120,123–125 Each of these papers included findings regarding ratings of the clinician involved in delivery of the intervention. Lyon et al. 123 administered a satisfaction questionnaire to families receiving FACE-TC, who rated all three sessions as ‘worthwhile’, with the vast majority of adolescents finding the sessions helpful.
Children and young people and parents in the study conducted by Masia-Warner et al. 124 were highly satisfied with the therapist delivering the intervention, reporting high levels of satisfaction and treatment benefit. Boardway et al. 120 reported high levels of satisfaction with several components including staff, content, equipment, patient improvement and overall satisfaction; however, their stress management training programme was ineffective across all outcome domains. The limited information from review 1 studies cannot tell us whether or not clinical effectiveness is affected by relationship with the therapist.
Holistic approach
Although both reviews only included interventions that aimed to improve CYP’s mental health, it was clear that the majority of interventions aimed to improve other aspects of CYP’s health, most often outcomes related to their LTC. In review 1, 2083,84,118–131,136,137,139,145 out of the 25 included studies also aimed to improve other outcomes aside from those categorised as child mental health. Sixteen out of these 20 interventions aimed to improve LTC symptoms as well as mental health. Despite this evidence that interventions aiming to improve mental health assessed in RCTs tend to have a more holistic focus, there was a lack of evidence of clinical effectiveness for intervention targets beyond mental health.
In review 2, all but five of the 57 included studies focused on interventions that also targeted outcomes other than those categorised as mental health. Frequently seen targets for interventions included social support or relationships (22 interventions), LTC symptoms (13 interventions), LTC self-management (11 interventions) or education or knowledge about the LTC (nine interventions). Review 2 intervention targets were therefore broader than those in review 1.
In terms of improvement in child mental health outcomes, the interventions targeting only this domain almost exclusively reported large beneficial effects. The three group play therapy interventions,133,135,138 two emotional intelligence training interventions132,134 and a single music therapy intervention136 reported large, beneficial effects on most mental health outcomes, although these findings may be limited by the lower quality of these studies. However, this raises the suggestion that focusing solely on child mental health outcomes might be an effective approach.
Conclusion
This chapter drew together the evidence presented by the quantitative and qualitative systematic reviews and presented nine overarching synthesis categories, which enabled a structured discussion of findings. Table 5 summarises the findings from the overarching synthesis and their implications. Despite the lack of good-quality evidence, we are able to use the evidence presented to make a number of suggestions regarding what may have an impact on the clinical effectiveness of interventions aiming to improve the mental health of CYP with LTCs, as well as make recommendations for further research in the field.
| Category | Summary | Contribution | Implications | |
|---|---|---|---|---|
| Review 1 | Review 2 | |||
| Degree of overlap between the two reviews | Limited amount of overlap between reviews. Small pockets of LTC population–intervention dyads seen | Range of LTCs and interventions studied, many gaps for specific LTC population–intervention dyads | Shared study on asthma/relaxation. Qualitative studies on cancer and music therapy. Differences in interventions and LTCs studied |
Research needed that includes clinical effectiveness and qualitative research for same LTC and intervention Investigate whether or not certain interventions are suited to particular LTCs |
| Availability of up-to-date, good-quality research | Much recent research in both reviews, but lack of UK-based studies for review 1 in particular and issues regarding limited quality of research | Many recent RCTs. No UK research. Risk of bias evident for a number of RCTs | Majority of qualitative studies published since 2008. Some UK studies. A few issues with study quality | Need for good-quality research relevant to the UK context |
| What works for whom? | Although review 1 indicates some evidence of benefit for interventions in particular LTC populations, neither review can go further to explain why this may be and how intervention effectiveness may vary between individuals | Provide examples of LTC population–intervention dyads where evidence for effectiveness, as well as highlighting where there is a lack of evidence | Can suggest reasons why interventions may be effective or not, but often using evidence across interventions | Both RCTs and qualitative studies ought to explore variables that may affect whether or not a particular intervention is effective for individuals |
| Adaptations to interventions and flexibility | There is some evidence from both reviews that adapting interventions to the needs of individuals, particularly their LTC, may be beneficial | Some evidence that CBT and parenting programmes that are adapted to the needs of individuals are beneficial | Perceived effectiveness for interventions that are relevant to CYP’s needs and can adapt to CYP’s goals | Comparison of adapted interventions vs. generic interventions yet to be performed |
| Accessibility and delivery of interventions | Considers the role of the setting, use of technology and flexibility of an intervention in ensuring that it can be accessed by CYP with LTCs | Some evidence that accessibility and familiarity of interventions may be beneficial, but hard to tease out from other components of interventions | Familiar setting, use of technology and interventionists who can relate to the needs of young people all perceived to be effective | Research that can investigate the relative importance of accessibility and how interventions are delivered vs. other intervention components |
| Stress and coping | Details evidence from both reviews about elements of interventions that may support CYP to manage their LTC within their daily life, in the short and long term | Some effectiveness of interventions for which CYP having a voice was an intervention component. A small number of interventions improve physical as well as mental health. Lack of evidence of effect for SMT | Adjusting to LTC key for CYP. CYP want choice and a voice. Distraction may be a useful intervention component. Different stressors experienced over time, so coping may change | Relative importance of stress and coping with LTC highlighted by review 2 suggests that more high-quality research into interventions addressing adjustment should address this. Effective stress management is needed |
| Working with family and peers | Evidence from reviews that interventions ought to include family, particularly parents, and that there are benefits of group settings where CYP meet peers with LTCs | Parenting interventions may be beneficial for parents. Unclear if parent components of CYP interventions beneficial | Tension between involving parents and empowering CYP. Interaction with peers with LTCs was highly valued by CYP | Further research on how to include family in interventions and whether or not including mentors or peers with LTC experience is a beneficial intervention component |
| Therapeutic relationships | Explores the evidence available from both reviews about the impact of CYPs relationships with their therapists, ill and healthy peers on intervention effectiveness | Range of different interventions often incorporate opportunities for sharing experiences and emotions, although effectiveness of this component cannot be isolated | Therapeutic relationships are an important component of interventions. Many review 2 interventions aimed to improve social support | Research that investigates how therapeutic relationships are established before or as part of interventions is needed |
| Holistic approach | Reviews included interventions that targeted mental health; however, the majority of interventions also targeted other outcomes | Majority of RCTs investigated interventions that also aimed to improve LTC outcomes | Interventions often targeted social support and aspects of the LTC, such as knowledge and self-management | High-quality future research is needed on the broad range of interventions that might be relevant to CYP with LTCs, which should include a wider range of outcomes including both physical and psychological outcomes, rather than just diagnosed mental health conditions or aspects of mental health, but not always mental disorders |
The main challenge for comparison in this overarching synthesis relates to the different inclusion criteria across the reviews, which may have led to a focus on different interventions. Review 1 included studies in which participants had elevated mental ill health scores at baseline measured using a validated and standardised scale and, therefore, interventions were likely to be more focused on improving clinical symptoms. In review 2, the nature of qualitative studies meant that participants’ symptoms of mental ill health were very rarely measured. Including any samples in review 1 regardless of mental health measures at baseline would have significantly increased the size of the review. Future reviews might consider this and make the review manageable by focusing on particular interventions or LTCs.
It is clear from both the quantitative and the qualitative evidence that interventions aiming to improve the mental health of CYP with LTCs often take a holistic approach, rarely focusing on only one aspect of mental health. Many interventions in the included studies also targeted aspects of CYP’s physical health, and the qualitative review interventions frequently aimed to improve social support. Although there is no strong evidence that these interventions are effective for the range of targets, it does appear that there is a preference that interventions focus more broadly on the range of issues faced by CYP experiencing both mental and physical health difficulties. This is expressed by those involved in delivering and receiving the interventions and indicated by the aims of the interventions developed. Additional research is required to investigate whether or not a holistic approach to interventions is beneficial. Tentative evidence suggests that interventions ought to be used flexibly to meet the various needs of CYP when possible, including accounting for the specific nature of their LTC. A balance is required between the need to manualise an intervention to ensure that delivery is standardised and delivered with fidelity and the need for flexibility of delivery to ensure that the needs of individual CYP are met. Although some interventions are associated with populations with certain LTCs, for example CBT for CYP with IBD, there currently is not enough evidence to ascertain whether or not the effectiveness of certain interventions aiming to improve mental health is moderated by the LTC. Review 2 suggests that, to improve the accessibility and long-term effectiveness of interventions for the mental health of CYP with LTCs, future research should consider ways in which technology could improve intervention delivery.
In summary, this overarching synthesis of qualitative and quantitative evidence highlights a number of implications regarding interventions for the mental health of CYP with LTCs, although this is to some extent limited by the lack of high-quality evidence. Therefore, further research is warranted generally, particularly research that makes use of both high-quality quantitative and qualitative evaluation in the same study and investigates further some of the messages from this synthesis.
Chapter 5 End-user involvement
Introduction
The inclusion of end-users within health-care research is encouraged because of the valuable insight they can provide during the research process. 236,237 Incorporating the knowledge and experiences of these groups into each stage of a project’s conceptualisation, development, implementation and dissemination of findings ensures that the research remains relevant and accessible to the people whom it is intended to benefit. 238 Thompson Coon et al. 239 conceptualise end-user involvement to include not only service users, carers and service user representatives, typically considered in the literature to exemplify patient and public involvement, but also health and social care professionals who may utilise the research findings in their daily practice. 240
A full account of the involvement of topic experts, including psychiatrists, psychologists, paediatricians, young people and parents at each stage of this project can be found in Report Supplementary Material 4. In Table 6 we provide a summary of the involvement at each stage and the impact their experience and insight had on the project.
| Activity | Date; method | Who? | End-user perspectives represented | Impact |
|---|---|---|---|---|
| Planning stage | ||||
| Finalising search terms | January 2016; e-mail | Co-applicants and expert advisory group (n = 16) | Paediatric psychiatry, paediatric psychology, paediatrics, patient and public involvement, parent, researchers – child mental health | Terms including ‘Crohn’s’, ‘fibromyalgia’, additional cerebral palsy terms and broad mental health terms such as ‘psychiatric/psychological/emotional disorder’ added to the search |
| Defining key terms and refining inclusion criteria | 11 February 2016; meeting in London | Co-applicants (n = 12) | Paediatric psychiatry, paediatric psychology, patient and public involvement, parent, researchers – child mental health and evidence synthesis |
Definition of ‘long-term condition’ finalised Eligibility criteria for long-term conditions finalised Eligibility criteria for mental health interventions finalised |
| Checking relevance of the project and definitions of key concepts | 20 February 2016; meeting in London | Review team and CYPAG (n = 12) | Patient and public involvement, CYP, researchers – evidence synthesis |
Reinforced the importance of acknowledging the link between physical and mental health and how interventions aimed at treating one aspect of mental health may have an impact on another Strengthened our justification for including all outcomes in the synthesis of review 1 |
| Review methods stage | ||||
| Study selection | 14 April 2016; teleconference | Co-applicants (n = 11) |
Refined our interpretation of the eligibility criteria for the reviews By sharing some of the challenges of identifying relevant information at this early stage of the process, we were able to use the experience of the entire team in planning alternative approaches |
|
| Categorising interventions and outcomes for review 1; planning dissemination | 10 September 2016; meeting in London | Review team and CYPAG (n = 11) | Patient and public involvement, CYP, researchers – evidence synthesis |
Reinforced the importance of a wide range of outcomes and the effects of interventions on relationships with friends and family members Children and young people emphasised the importance of school attendance and coping with school, outcomes that were not frequently reported in the included studies. This discussion highlighted the importance of this type of outcome to CYP and informed our implications for future research Decided to consider a podcast as a dissemination activity involving the CYP and to include time for editing plain-language summaries for different end-users in the final CYP meeting |
| Discussing preliminary findings and approach to synthesis; identifying consultation opportunities | 3 October 2016; meeting in Exeter and subsequent e-mail dialogue | Co-applicants and expert advisory group (n = 16) | Paediatric psychiatry, paediatric psychology, paediatrics, patient and public involvement, parent, researchers – child mental health and evidence synthesis |
Provided a practice-based verification of our interpretation of the emerging findings. The need for caution owing to small numbers of studies was emphasised Several opportunities for consultation were identified and facilitated as a result of this meeting |
| Consultation stage | ||||
| Discussing preliminary review findings; planning dissemination | 28 January 2017: meeting in London | Review team, CYPAG and their parents (n = 15) | Patient and public involvement, CYP, parents, researchers – evidence synthesis |
Reinforced ideas that were emerging from the analysis in review 2, such as the importance of having a voice within the wider community. Some points that challenged the initial synthesis were also raised by members of the CYPAG. An example of this was the suggestion that mental health interventions should acknowledge that the needs of CYP were serious and, therefore, did not always need to contain an element of ‘fun’. This encouraged the researchers to check the studies included within review 2 for any refutational data Ideas from the parent group regarding the impact of school environment, long-term effectiveness of interventions and the need for an age-appropriate approach reinforced ideas presented by the CYPAG, which were drawn on to inform the analysis for review 2 and the overarching synthesis The parent group highlighted the need for interventions to involve systems around the child and the challenges in having the mental health needs of CYP recognised and met by schools and primary care clinicians. This feedback validated the decision to keep ‘availability’ as a separate theme within review 2 and the category ‘holistic approach’ within the overarching synthesis The views of parents and CYP helped researchers bring together the results from the two reviews within the overarching synthesis by providing an alternative viewpoint through which to conduct a secondary interpretation of their results |
| Discussing preliminary findings; establishing links for dissemination | Various dates between 10 January and 15 March 2017; meetings, Skype™ (Microsoft Corporation, Redmond, WA, USA) calls, conference presentations; teleconference (n = 11) | Variousa | Researchers – child mental health and evidence synthesis, patient and public involvement, CYP, paediatric psychiatry, third-sector organisations, paediatric psychology, paediatrics, parents, conference attendees at the MQ Mental Health Science meeting |
Highlighted methodological decisions that required additional detail within the write-up of the report. Examples include: The Paediatric Liaison Group suggested some additional studies to check for eligibility for review 1. All suggested studies had been excluded during screening as they did not meet the inclusion criteria Consideration of the availability of evidence from samples of CYP with learning disabilities was requested by the CYPMHC At least one young person from the YPMHAG had a precise definition of a mental health intervention as something that is used as a preventative-type tool distinguished from treatment, indicating the need to define ‘intervention’ in the final report and particularly in the plain-language summaries Feedback through consultation events also had some influence on the synthesis for results in review 2. Interest shown by members of the CYPMHC regarding how much the synthesis of review 2 focused on CYP’s experience of transition between child and adult mental health services led to us re-examining the data set for relevant information Presentation of the results of review 1 and 2 at the MQ Science Meeting provided the opportunity to disseminate our results to an interested audience of clinicians, researchers and CYP who use mental health services. During this conference, The Mental Elf (National Elf Service, Minervation Ltd) expressed interest in writing a blog post about the project, creating an additional opportunity to disseminate the results in a format accessible to the wider public The consultation process also created opportunities for collaboration with other organisations. We shared our methods for review 2 with the Mental Health Foundation (London, UK) who were undertaking a qualitative systematic review in a similar topic area. CLIC Sargent (London, UK) offered to share the results of several reports they had recently been working on and we reciprocated by sharing information located through our literature searches Through discussing preliminary results with organisations working in the area of CYP mental health we were able to explore opportunities for using their communication channels as a platform for disseminating our findings. CLIC Sargent, the Mental Health Foundation, the ERG, MQ and the Paediatric Psychology Network all indicated that they would be willing to provide a platform for the dissemination of our podcasts and plain-language summaries |
| Dissemination stage | ||||
| Creating dissemination products | 18 March 2017; meeting in London | Review team, CYPAG and their parents, podcast recording specialist (n = 15) | Researchers – evidence synthesis, patient and public involvement, CYP, parents |
Children and young people and their parents recorded material for two podcasts – the first discusses the findings of the project, the second their experiences of being involved Children and young people and their parents also co-wrote plain-language summaries of the findings – one for the final report and adapted versions for their respective audiences |
Impact of end-user involvement
On the children and young people and their parents
One of our main concerns was to ensure that, just as the research benefited from the involvement of CYP, the CYP and their parents should also benefit. CYPAG members and parents were provided with £20 vouchers following each event to acknowledge their contribution and time commitment. It was reiterated at every meeting that participants should contribute towards the project in whatever way was comfortable and meaningful for them.
Throughout the course of the project we discussed and reflected on the balance between burden and benefit. There is evidence that the young people benefited from their involvement simply by meeting one another through this process. At the first meeting, two of the young people discovered that they shared the same rare physical health condition and each appeared to value the opportunity to meet someone else in the same situation. This impression was reinforced by e-mail feedback received following the first CYPAG meeting from two group members:
It was good to hear other people’s points of view.
CYPAG member
I think it was really helpful having other people who have gone through the same things as you that understand you.
CYPAG member
It was not the intention to have a dedicated parent group providing input into the project, but we observed that, when parents came to collect their children from the meeting, they spontaneously discussed their experiences of accessing care for their child, issues with school attendance and their children’s health conditions. Although it was not part of the original patient and public involvement plans for the project, this presented an opportunity to access the experiences and knowledge of the parents and we henceforth held separate parent group meetings in tandem with the young people’s meeting. In the parent group, parents commented how ‘meetings like this’ (parent, third meeting) were good for CYP to share experiences and meet people who could ‘get on with their lives’ (parent, third meeting). One example provided was how one young person met an older peer who was in a romantic relationship, which the younger child had thought was a slim possibility for themselves given their physical condition.
The parents agreed that sometimes it was difficult to get their children out of the house, but that they were always keen to attend these research meetings. Overall, the experience of witnessing how enthusiastic CYP were in having the opportunity to meet each other outside a treatment setting was extremely powerful for the researchers. This observation later contributed towards the decision to have ‘social support’ as an overarching construct within review 2, rather than a theme within ‘a therapeutic foundation’.
On the report findings
Involvement of end-users in each stage of the systematic review process has made a valuable contribution towards the creation of a robust evidence synthesis by incorporating the experiences of those whose lives the project intends to influence. As a result of this contribution, this report is grounded in the experiences of CYP with LTCs and mental health problems and the health-care professionals who provide their care, and appears to be relevant to their needs. This is reflected by the degree to which the preliminary findings from review 2 and overarching synthesis appeared to be transferable across different end-user groups and in keeping with practitioners’ approaches to providing mental health interventions.
There was agreement across different stakeholders that the separation of mental and physical health when developing interventions was artificial and unhelpful. The views of the people consulted have also highlighted implications for areas of future research, which are explored in the final chapter of the report.
Chapter 6 Discussion and conclusions
The aim of this research project was to evaluate the clinical effectiveness and cost-effectiveness of interventions aiming to improve the mental health of CYP with LTCs and to explore the factors that may enhance, or limit, the beneficial delivery of such interventions. To address these aims we conducted two systematic reviews, one focused on quantitative studies and one on the qualitative evidence related to relevant interventions. We then brought together findings from each review in an overarching synthesis. As part of the project we consulted with a range of end-users about preliminary findings, strengthening the main arguments and developing key implications on the basis of these activities. A CYPAG was formed and met four times during the project to provide input into methodological decisions, to consult on preliminary findings and to help prepare dissemination materials. This final chapter summarises the findings of each review and the overarching synthesis and describes the strengths and limitations of the work conducted, outlining the implications for practice and recommendations for further research.
Summary of findings
Summary of review 1
In review 1 (see Chapter 2), we synthesised 25 RCTs (31 articles) that assessed the clinical effectiveness of interventions aiming to improve the mental health of CYP with LTCs and elevated symptoms of mental ill health. These studies evaluated 11 types of intervention provided to CYP with 12 different types of LTC. We extracted 269 outcome measures from the 31 articles. Although the primary focus of the review was the impact of interventions on the mental health of CYP, all secondary outcomes were synthesised to evaluate any benefits of interventions on other aspects of young people’s lives, including key aspects of individual and family functioning. As many different measures of similar underlying constructs were reported, we categorised them into 28 categories. Seventeen categories related to CYP mental health; the rest related to ‘other outcomes’.
The greatest volume of research focused on the clinical effectiveness of CBT, which was evaluated in seven studies (10 articles). These studies provide tentative evidence that CBT-based interventions could be beneficial for the mental health of CYP with IBD, chronic pain, epilepsy and persistent functional somatic complaints, but not T1DM. The majority of the CBT interventions had content that was adapted to the needs of the LTC of CYP in the sample. In addition, four parenting programme interventions were tested in three studies. Group play therapy interventions were also assessed in three studies. Other intervention types (palliative care, relaxation, SMT, emotional intelligence training, massage therapy, biofeedback, resistance training and music therapy) were reported in only one or two studies.
We calculated effect sizes for each study outcome whenever data allowed. Trials were typically small, so effect sizes across the included studies were characterised by wide CIs. Therefore, the evidence for particular interventions used with similar samples of CYP is very limited. There were relatively few opportunities to meta-analyse studies with similar intervention, comparator, LTC and outcomes. No more than two studies shared particular combinations of these study characteristics and could be meta-analysed.
Study quality of the relatively small amount of research to date is poor, with 19 out of the 25 studies having at least four separate indicators of potential bias. Blinding of assessors and evaluation of adherence, fidelity and compliance were often neglected, and reporting of randomisation methods and allocation concealment was largely unclear. Fewer than half of the studies included a follow-up assessment, with only one-half of those occurring beyond 6 months post intervention. The quality of future research in the field should therefore be improved. Although findings from review 1 are tentative, they support previous research. A systematic review by Bennett et al. 82 of psychological interventions for mental health disorders in CYP with chronic conditions also reported preliminary evidence that CBT interventions may be beneficial. Review 1 is the first systematic review to consider all interventions for elevated symptoms of mental ill health in CYP with LTCs.
National Institute for Health and Care Excellence guidelines recommend CBT for CYP with depression. 54 James et al. 70 published a Cochrane systematic review of CBT for childhood anxiety disorders in CYP without comorbid LTCs, reporting a suggestion that CBT is a more effective treatment than treatment as usual or active controls. Given our own findings, there is tentative evidence that these recommendations may hold for CYP with LTCs. Review 1 does not explain why CBT has promising effects, or whether or not and how to adapt it to CYP with LTCs for the best effect. Future research should seek to explore these questions.
The findings of review 1 point to the need for large, high-quality RCTs with consistency in intervention, design and outcome reporting. Rigorous testing of interventions across a range of conditions and locations, including fidelity and process evaluation measures, would aid comparison of the components of different interventions. It would be particularly useful to examine whether or not intervention types that show some promise (e.g. CBT) are clinically effective across a range of LTCs, including whether or not (and how) they should be adapted to specific LTCs. Although we included studies of interventions that aimed to improve mental health, the majority also targeted other outcomes, particularly LTC symptoms. Therefore, future research might consider treatment integrating both physical and mental health care and its effects across a wider range of outcomes, rather than focus primarily on mental health in terms of population, intervention and outcome.
Summary of review 2
In review 2 (see Chapter 3), 57 studies were reviewed, which included qualitative data collection and analysis on the experience of, and attitude towards, interventions aiming to improve the mental health and well-being of CYP with LTCs. These studies evaluated a more diverse range of interventions (n = 21) than that seen in review 1. The most frequently seen LTC in the 57 included studies was cancer (n = 14). HIV-positive intervention recipients were the focus of eight studies, whereas a further 10 studies included CYP with a mix of LTCs, something that was not seen in review 1. Included studies commonly explored the perceptions and experiences of interventions that aimed to improve aspects of mental health and well-being such as coping (n = 26), self-esteem (n = 13) and emotional support (n = 11) rather than targeting a mental health disorder, for example depression (n = 1) or anxiety (n = 8). Interventions also often aimed to improve symptoms related to the LTC (n = 35) and social skills (n = 16). Included studies represented views from a range of different participants involved in the delivery and receipt of relevant interventions.
We used metaethnography to synthesise the 57 included studies (60 articles). The synthesis revealed five main constructs: ‘a therapeutic foundation’, ‘social support’, ‘a hopeful alternative’, ‘resilience’ and ‘getting in and staying in’. A number of themes contributed to each construct. We developed a line of argument (a model explaining how themes and constructs related to each other) that offers an explanatory model of the experience of receiving and delivering interventions to improve the mental health of CYP with LTCs (see Figure 18). The model describes the process by which CYP with LTCs access and maintain engagement with a relevant intervention aiming to improve mental health and well-being. Some interventions can help CYP to acquire a sense of hope for the future and increase their resilience. Interventions are often perceived to be effective when they offer participants a safe space and social support. The relationship between these constructs is not fully defined, as other factors may have an impact on the experience of interventions and participants’ attitudes.
A young person’s sense of resilience, hope and social support as created through taking part in an intervention may help them and encourage them to maintain their engagement with the intervention. Their experience may also encourage CYP and their carers to build positive relationships and use these relationships and the skills learnt during interventions to develop techniques to manage emotions, physical symptoms and other relationships. Interventions that can respond flexibly to the physical and mental health needs of the CYP for whom it is intended may also help keep the CYP engaged with the intervention over time. Such flexibility, along with the acquisition of new skills, may help build and maintain the effects of interventions beyond the intervention setting. There is a tension between (1) the perceived need for an intervention to be flexible in content and delivery to respond to individual needs and also provide a sense of being unconstrained and (2) the need for boundaries. Evidence suggests that, although CYP welcome the opportunity to escape from the worries and constraints associated with living with a LTC in everyday life, they require certain limits on behaviour, discussion topics and physical activity to experience an intervention as safe. The balance required to ensure that these two concepts are incorporated into an intervention may represent a challenge to those who design and deliver it.
The quality of included articles was generally good. At least 10 high-quality articles contributed to each theme in the synthesis. However, general weaknesses included a failure to make the theoretical perspective of the author explicit, a failure to adequately describe the context or setting of qualitative research and a lack of clarity in the description of the intervention.
This is the first attempt to examine the experiences of participants in interventions that aim to improve the mental health and well-being of CYP with LTCs. However, our synthesis shares features with some previous literature. Concepts from Wallander et al. ’s37 disability-stress coping model of adjustment to chronic illness (e.g. problem solving and perceived competence) appear to be similar to our themes of ‘empowerment’ and ‘skills and knowledge’. Some of the specific resistance factors seen within Wallander et al. ’s37 model, including the role of improved family relationships, sense of competence and use of coping strategies, are also seen in our line of argument.
Our themes ‘I am not alone’ and ‘therapeutic relationships’, which explore how CYP valued feelings of connectedness and belonging with peers and empathy/validation from intervention deliverers, fit with the findings of a systematic review of young people’s experience of mental health in chronic illness. 45 Our themes ‘unconstrained’ and ‘a new normal’ are also reflected in findings from this previous review that CYP view their LTC as something that restricts participating in ‘normal’ life and everyday activities and is a source of uncertainty both in the present and with regard to worries about their future. 45 The importance of social support, development of coping strategies and a sense of hope and acceptance are also acknowledged in both our review 2 and the previous review. 45
There was only one study in which qualitative data collection and analysis occurred alongside a RCT, which was also included in review 1;119 there is a need for this type of mixed-methods process evaluation conducted according to best practice guidance to improve our understanding of how interventions are experienced and how this may link to effectiveness. 241
Summary of the overarching synthesis
The overarching synthesis (see Chapter 4) integrated the findings from review 1 and review 2. A deductive approach was used, whereby questions based on the emerging findings of each review were generated and used to interrogate the other review for information that could potentially inform the findings or explain gaps in the literature. Despite the different review questions, methods of synthesis and types of interventions seen across the two systematic reviews, the overarching synthesis allowed us to raise a number of tentative implications.
Nine categories emerged from the analysis:
-
degree of overlap between the two reviews
-
availability of up-to-date, good-quality research
-
what works for whom
-
adaptations to interventions and flexibility
-
accessibility and delivery of interventions
-
stress and coping
-
working with family or peers
-
therapeutic relationships
-
holistic approach.
There is a limited amount of overlap between the reviews, particularly when focusing on interventions used for particular populations. Much of the research included in both reviews was published in the 10 years prior to the review, but there is a noticeable lack of studies conducted in the UK. Although there is some evidence of benefit for interventions in CYP with particular LTC populations, for example CBT in populations with IBD and music therapy for procedural distress in CYP with cancer, neither the quantitative nor qualitative evidence can explain why this may be or suggest how intervention effectiveness may vary between individuals.
The review work suggests that further evidence is needed to understand whether or not and how interventions should be adapted for the LTCs of CYP. The accessibility and familiarity of an intervention’s setting, use of technology and flexibility of delivery can have an impact on perceived effectiveness and may warrant consideration as to how such issues affect effectiveness in terms of mental health outcomes and wider functioning. There was evidence from both reviews that interventions that include family, particularly parents, may be beneficial. Relationships between CYP with LTCs and their therapists, and with their ill and healthy peers, seem important. Although both reviews include interventions that aim to improve mental health in some way, the majority of interventions also targeted other outcomes including LTC symptoms, social support, knowledge and self-management.
Strengths and limitations
There are a number of strengths of the project’s reviews, overarching synthesis and end-user involvement:
-
Review 1 represents the first (to our knowledge) systematic review of RCTs evaluating interventions targeting mental health of CYP with LTCs. It was conducted and is reported in accordance with best practice guidelines. 85,113
-
We have used comprehensive search strategies and made extensive efforts to locate research outside academic databases.
-
We have also broadened the scope of review 1 compared with previous attempts to synthesise this evidence base by including populations with elevated symptoms of mental ill health in samples as opposed to only symptoms of mental health disorders or diagnoses.
-
For review 1, searches were not limited to English-language papers, date or study location, and authors were contacted for supplementary materials and missing data when necessary. Although we targeted papers reporting on interventions that primarily sought to improve CYP mental health, we included and synthesised all wider outcomes, therefore providing a fuller picture of the effects of interventions.
-
Review 2 is the first attempt (to our knowledge) to synthesise research on the experience of those involved in the delivery and receipt of interventions that aim to improve the mental health of CYP with LTCs. A strength of the review is that studies included the views of a range people with an interest in such interventions, namely CYP, caregivers and intervention deliverers on interventions at different stages in development.
-
The synthesis within review 2 considered a large number of papers in a time-effective manner and prioritised richer, interpretive findings, before using the descriptive studies to support or refute aspects of the synthesis.
-
Our overarching synthesis brought together findings from both reviews. In doing so, we were able to highlight clearer implications for practice and gaps for further research.
-
We consulted with a wide range of end-users about our preliminary findings and used feedback to refine our analysis and write-up of the final report.
-
We convened a CYPAG that met at four points during the project. This group gave feedback on the use of terminology for the project, commented on preliminary findings, co-produced the Plain English summary and recorded audio for a podcast disseminating the work.
We also acknowledge the following limitations, which predominantly stemmed from the primary research reviewed:
-
The breadth of outcomes reported in review 1 presented a challenge for analysis and interpretation. For example, depression was assessed using 14 different instruments across 14 different studies. The breadth of measures used made comparability across samples challenging when different scales assessing the same construct were used, as the meaning of established cut-off points may differ across scales. When it was not possible to find an established cut-off score in the literature for measures used, the article was considered not to have met inclusion criteria, even though it is possible the sample may have had unreported elevated symptoms.
-
There were insufficient studies to allow meaningful moderator analysis of intervention type and LTC population or assess publication bias.
-
No economic evaluations related to the included trials or that otherwise fitted our inclusion criteria were located, which indicates a need for measures of cost-effectiveness to be incorporated in trials.
-
No UK studies were included in review 1, therefore limiting the applicability of review findings to the UK context.
-
There may be subjectivity in the categorisation of interventions. For instance, we may have grouped progressive muscle relaxation, heart rate variability biofeedback and massage together if there was an argument for these intervention targets or active ingredients being similar. Categorisation was on the basis of similar content and targets, meaning that several interventions could not be categorised with any others.
-
Each study included in this review sampled CYP participants with particular LTCs, with the result that we do not have a clear sense regarding the applicability of particular interventions for improving mental health across a range of LTCs.
-
Relevant interventions may have been excluded from the synthesis because of our inclusion criterion that the intervention had to be described as aiming to improve the mental health or well-being of CYP with a LTC.
-
Owing to the potential impact of misinterpretation of abstract concepts following translation from other languages, only English-language articles were included in review 2. There was a wide range in the type of qualitative analysis used within the studies, which meant that the analyses conducted in individual studies were not always directly comparable. The categorisation of study findings and purposive sampling strategy as described in Chapter 3, Methods, Methods of analysis/synthesis, Data analysis and synthesis, meant that all studies meeting inclusion criteria were able to contribute towards the synthesis.
-
It is not known how the final synthesis would have been affected if included studies had been synthesised in a different sequence. The translation component of metaethnography, whereby components of themes are compared with one another across articles, and the line-by-line coding in NVivo meant that the synthesis captured concepts that appear across included studies, as well as ideas that refuted the existing synthesis. Owing to the wide range of interventions, utilising metaethnography may have meant that the constructs and themes generated from the synthesis reflect core therapeutic components common across a range of interventions. It cannot be assumed that these are applicable across all LTCs, mental health conditions or ages.
-
Establishing the mental health and well-being focus of an intervention was not always straightforward. Only seven included studies evaluated interventions that focused on only the mental health and well-being of the child. In 24 studies, additional focus was on some aspect of controlling the LTC, and in 22 studies on provision of social support. The small number of interventions that had a sole mental health focus may have influenced the (sub)themes that emerged from the synthesis.
-
None of the studies included in review 2 sampled participants with a diagnosed mental health disorder, and only two considered the current mental ill health of participants on study entry. The number of CYP who received interventions who were experiencing mental ill health is therefore uncertain.
-
Information from the quality appraisal was considered during the synthesis, rather than used to exclude studies based on quality as only three articles received more negative than positive study quality ratings. At least 10 of the highest quality articles (10/14 ‘yes’ ratings on quality criteria or better) contributed to each theme. This implies that lower-quality articles alone did not determine any of the themes, but did provide support for them. This is common in qualitative evidence syntheses, in which higher-quality articles are found to contribute more to the synthesis (e.g. Moore et al. 155).
-
The overarching synthesis was challenged by the different inclusion criteria across review 1 and review 2. Review 2 interventions more often focused on improving coping, stress and self-esteem than review 1 interventions, which more often aimed to improve symptoms of mental health disorders, such as anxiety and depression.
Implications for policy and practice
Given the nature of the review findings and challenges in synthesising across reviews considered in the previous chapters, recommendations for research and, in particular, implications for policy and practice, can only be tentative. There is evidence that CBT may be beneficial in some of the LTC populations in which it has been evaluated (epilepsy, persistent somatic functional complaints, IBD, chronic pain). Implications for practice regarding adapting CBT for the LTC and for the effectiveness of other interventions are far less clear, although the overarching synthesis category ‘adapting interventions’ highlights a need for further research into any potential benefits of adapted content.
There was some evidence from review 1 for parenting programme interventions to reduce behavioural problems in children with ABI and/or cerebral palsy, particularly when combined with acceptance and commitment therapy. However, only four parenting interventions were included, and effects were inconsistent across studies. Three studies examining the clinical effectiveness of group play therapy in children with cancer and asthma showed beneficial effects for anxiety, depression or coping; however, these were studies of low methodological quality. Overall, the evidence from review 1 highlights the need for further, rigorous research to be conducted, rather than recommendations for practice.
From review 2, the ‘availability’ theme indicates that it may not always be straightforward for CYP to access interventions that explicitly target their mental health. Recognition of mental health needs by physical health clinicians appears to be a particular barrier to the access of relevant interventions. Once engaged with an intervention, the importance of access was further highlighted in the ‘accessibility and delivery’ category of the overarching synthesis. This described the need for consideration of CYP’s needs in delivery of intervention content and the possible benefit of flexible and/or technology-based content delivery. Additional research on methods that might assist paediatric health-care services to detect the mental health needs of CYP with LTCs and provide services in which physical and mental health needs are managed in a genuinely integrated way would help to plan future services to support the mental health needs of CYP with LTCs. Twenty-five of the interventions from review 2 were delivered by someone with some degree of specialist training. Sixteen of the interventions included in this study were delivered by intervention deliverers with no specialist training. Eight of these required supervision by personnel qualified in mental health and/or additional training to deliver the intervention. This indicates that it may be possible to deliver mental health and well-being interventions outside mental health settings and potentially ease demand on waiting lists for mental health services. However, the training and support needs of those who will be delivering an intervention would need to be considered alongside the resources required for setting up and sustaining the intervention.
Both review 2 and the overarching synthesis category ‘holistic approach’ shows that CYP value interventions that consider a range of needs (e.g. coping with school, as our CYPAG members informed us), as opposed to, for example, purely their mental health. Therefore, consideration of collaborative approaches between different treatment providers and educators may be of benefit. Research examining the extent to which collaboration already occurs in different paediatric physical and mental health-care settings could be valuable alongside an exploration of factors that may support or hinder co-ordinated approaches.
Evidence from review 2 and the overarching synthesis also suggests that the creation of opportunities for CYP to access social support and to share feelings and experiences may result in reduced feelings of isolation and improved relationships with both peers and family members. This suggests that integration of opportunities to build supportive relationships with peers and meet people who are successfully managing their LTC may be useful for some CYP. The constructs and themes identified in review 2 may be considered as a framework to aid intervention development.
The varying methods and varying locations for delivery of interventions in both reviews indicate that interventions aiming to improve mental health can be delivered outside mental health service settings. Review 2 also highlights the importance of the involvement of family members in the engagement of CYP with an intervention and encouraging the incorporation of intervention components into daily life so that the beneficial effects are maintained over time. CYP discussed how they wanted interventions to address expectations placed on them by wider society. This included educating teachers and friends regarding what they were physically capable of171 to address the stigma surrounding certain diagnoses. 172 These findings support an important issue raised during consultation with our CYPAG, which felt that interventions should attempt to relieve the burden of feeling solely responsible for ‘coping’ with their LTC from the child. Given the importance of social support highlighted by review 2 and the overarching synthesis, relationships CYP establish with those who deliver interventions, family and peers are an important component of interventions. The relationship between CYP and provider should be considered for future evaluation in trials.
Suggested research priorities
The findings of review 1 suggest the need for further large, high-quality, well-reported RCTs. In particular, improved reporting of the methods used to randomise participants and conceal their group allocation and blinding of outcome assessors is required. The production of manualised interventions would allow for more rigorous testing of interventions across a range of conditions and locations and would aid comparison of intervention components across different interventions. Likewise, to evaluate the beneficial components of interventions across trials, better description of the content of interventions is necessary. Adherence to the many available design and reporting guidelines would facilitate this (e.g. Schulz et al. 242). UK-based research is also crucial to ensure that the findings are relevant to the UK health-care system and UK CYP.
Combining the collection of effectiveness research with that of the views and experiences of those giving and receiving the intervention within the same study is necessary to explore why certain interventions may (or may not) be effective and to identify the moderators of effectiveness. Mixed-methods process evaluations conducted in accordance with best practice guidance are required in this field as none was located as part of RCTs. Future intervention trials should clearly specify the aims of interventions and primary outcomes and should preferably include logic models to demonstrate the theoretical framework of the intervention. 243 This work should also include analysis regarding the impact of different moderators such as age, ethnicity, mental health difficulty and LTC on intervention effectiveness.
Review 1 raises implications for a research programme when an intervention with promise, such as CBT, is delivered across a range of LTCs, including variation of how the intervention is adapted to specific LTCs versus the recommended treatment for mental ill health. Such research would still need to take account of the recommendations above.
Stress and coping skills are recognised as important in both reviews, which indicates that the focus of interventions should not be just on mental health disorders and their symptoms. Future research might focus on integrated treatment targeting mental and physical health and its effects across a wide range of outcomes for those with a LTC, rather than primarily on mental health in terms of population, intervention and outcome.
To improve the accessibility and long-term effectiveness of interventions for the mental health of CYP with LTCs, review 2 and the overarching synthesis suggest that future research should consider ways in which technology could improve intervention delivery. For example, the use of the telephone or internet to deliver therapeutic content or keep appointments with clinicians could be beneficial, whereas top-up or booster sessions, including those giving skills to parents, might help in sustaining intervention effects. Meanwhile, built-in flexibility to adapt to the changing developmental or LTC needs of the patient is important. Additional research that evaluates the long-term effects of interventions that meet these needs is required.
Review 2 in particular notes the part that family, peers (both ill and healthy) and practitioners can play in the experience of interventions, in terms of relationships with CYP or as fellow intervention recipients. Additional research should consider this either as part of interventions being tested or by investigating the impact of actively involving peers in interventions.
Consensus on the use of outcome measures should also be considered a priority. 244 Having agreed gold standard outcome measures for particular mental health constructs in specific situations would further aid the production of comparable data across research outputs, strengthening future evidence synthesis. The lack of identification of primary and secondary outcomes in many RCTs, along with the large numbers of measures typically used per study, raises the question of the extent to which interventions were targeting different aspects of mental health compared with wider individual and family functioning. Future trials should clearly indicate primary and secondary outcomes.
Some outcomes (e.g. LTC knowledge, self-management, school attendance, goal-setting, self-harm, hope) were identified as important in review 2 and in our consultation with end-users, but were not commonly assessed in the effectiveness studies. Consideration should be given to the best way to measure and incorporate these into future trials. Patient and other end-user involvement in trials may assist the selection of outcomes that are pertinent for those involved.
No relevant cost-effectiveness studies were located by review 1. Although this is an obvious gap in the literature, the tentative nature of the evidence of effectiveness suggests that further work is needed to establish evidence of clinical effectiveness before cost-effective studies will provide meaningful results. However, costs should be included in intervention trials and there may be scope for modelling of potential cost-savings in terms of cost-effectiveness as well as economic modelling to include broader societal costs such as education, parent employment and incremental savings as CYP grow up.
Owing to the apparent importance of social support to the emotional well-being of CYP with a LTC highlighted in review 2, a systematic review that examined the effectiveness and experiences of social support interventions for CYP with LTCs could be valuable. The review could expand on the conceptualisation of social support discussed in this review by considering the model used by Gaysynsky et al. 210 It could potentially consider which methods of social support are experienced as most useful and effective in improving mental health in this population and effective ways of incorporating it into care for CYP with LTCs, and could inform the design of future interventions and studies of their effectiveness.
Involving CYP in an advisory group that met throughout the course of the project to advise on methods and preliminary findings and assist with dissemination material was considered a clear strength of the project and it is recommended that future systematic reviews form an advisory group of true end-users whenever possible.
Closing messages from children and young people advisory group
Before my diagnosis of SLE [systemic lupus erythematosus] at the age of 9 (I am now 17), my life was relatively normal. For the past 9 years I have battled with having to take daily medications, continual check-ups, and various mental health problems mainly around anxiety and depression. Over the years my biggest struggles have been the lack of control I have felt over my physical and mental health. Both these things affected my ability to socialise, go to school and college consistently and take part in activities that other teenagers of my age might do. At times this has made life difficult and isolating, with professionals around me not really listening to me. Being part of this research project has been important, because over the years I have used mental health services with varying affect and they have felt forced rather than a choice. I hope the findings in the research will enable future interventions to be more creative for all young people but particularly for those like me who have long-term illnesses. It felt good to think that my experiences and contributions can make a difference.
Living with a long-term medical condition is often much harder than many people think it is. Not only do you have to cope with the health condition itself, but you also have to tackle all the other issues it brings along with it, such as psychological disorders or simply chronic pain, and in a young teenager’s normal life of long, tiring days and constantly fluctuating moods, these are enough to really push you over the edge.
I think one of the main issues concerning this are those of awareness and flexibility within conventional activities in a young person’s life, such as school. Many teachers in my time at the school have struggled to adjust their policies to my condition. This is the same with many young people coping with long-term health conditions.
I think researchers need to develop effective methods of improving mental health, and these need to be implemented in schools, as well as outside. This would have a big impact on the young person’s welfare. Perhaps teachers should be better informed about young people’s conditions and taught how to support them. Tackling mental health problems before they become too overwhelming would be beneficial to the young person’s physical health and life in general. Better, more effective methods of intervention need to be found, and be readily accessible. With more research and better awareness in general, the problem of mental health difficulties in children with a long-term health condition can be easily solved.
I was diagnosed with juvenile dermatomyositis in April 2015, which is inflammation of the skin and weakness of the muscles. This results in daily life being very difficult for me because I’m stiff getting out of bed every morning, I struggle climbing stairs, getting out of a bath and walking and standing is very tough as well. I haven’t had a complete pain-free day in over 2 years.
One of the drugs that I have to take is . . . a type of chemotherapy which is meant to reduce the inflammation. I have to inject this into me every Friday night, but every week it makes me feel very nauseas [sic] and sick. Every Saturday I feel sick and I can’t enjoy my weekend like everybody else and I can miss out on meeting up with family or friends. At first, I was very apprehensive about injecting it into myself because every Friday night I would get myself so worked up and feel very sick, but now I’ve just learnt to accept it and it has become a part of my routine. However, . . . it doesn’t help with the pain. So, they say that I have chronic pain syndrome, where I’m always in constant pain.
At the moment, I’m in year 13 and will soon be completing my A Levels, so the stress of the exams, revision and feeling sick from [chemotherapy] hasn’t helped with my pain or my mood. I was diagnosed with depression in January 2017 because for about 6 months prior to this I have been feeling very low and have just felt like I’d had enough because of the stress with school, the pressure of not knowing what I want to do once I’d finished my A Levels and the hospital kept telling me the way to deal with chronic pain syndrome was to have good sleep, to eat, drink, take part in mindfulness and do exercise. I was doing all this but I’m still in so much pain and no one seemed to understand and doctors just say I would feel better in time, but time has no end.
I believe that researchers should work to develop more treatment to help with depression because when you’re diagnosed with a long-term physical condition, no one tells you that you could be at risk of developing a mental health problem because you deal with so much; the condition, the medication, the side effects of the medication, the hospital appointments and missing school due to the hospital appointments.
Acknowledgements
We would like to thank the young people and their parents who attended and contributed to advisory group meetings during the project and a range of end-users from organisations who took part in consultation activities. The young people and their parents helped to edit the Plain English summary and several of the young people contributed to the closing messages from the CYPAG. We are also grateful to:
-
Juan Talens-Bou for assistance in screening, forward citation-chasing, full-text retrieval and proofreading
-
Ingrid Romero de Jager for assistance in screening, data extraction, backward citation-chasing and proofreading
-
Pam Bowman for commenting on an early draft of Chapter 1 and attending a project meeting and consultation event
-
Vashti Berry for assistance screening and discussing review 2 preliminary synthesis
-
Linda Long for assistance screening
-
Oana Mitrofan for commenting on an early draft of Chapter 1
-
Zohrah Khan for backward citation-chasing
-
Katie Finning and Jean Burrows for proofreading final report chapters
-
William Wong, Nancy Liu, Elaine Meng, Mitra Tavakoli and Ross Watkins for translating foreign-language papers and/or data extracting them for review 1
-
Cath Hopkins for administrative support throughout the project
-
Heather Boult for consulting with us on the project individually.
We also thank Paula Lavis for her work in setting up and participating in consultation activities.
Contributions of authors
Darren A Moore (Research Fellow) was involved in the design and conception of the project, co-ordinated review work, led reviews and the overarching synthesis, wrote and edited the final report and planned and conducted end-user involvement and consultation events.
Michael Nunns (Research Fellow) led review 1 and the overarching synthesis, wrote and edited the final report and planned and conducted the end-user involvement and consultation events.
Liz Shaw (Associate Research Fellow) led review 2 and the overarching synthesis, wrote and edited the final report and planned and conducted the end-user involvement and consultation events.
Morwenna Rogers (Information Specialist) was involved in the design and conception of the project, designed and conducted searches for review 1, review 2 and economic studies, retrieving records for screening and title and abstract screening, and edited draft chapters.
Erin Walker (Patient and Public Involvement Lead) co-ordinated the CYPAG, organised young people and parent meetings, conducted end-user involvement and consultation events and edited draft chapters.
Tamsin Ford (Professor) was involved in the design and conception of the project, provided mental health topic advice and edited draft chapters.
Ruth Garside (Senior Lecturer) was involved in the design and conception of the project, provided qualitative synthesis topic advice, assisted in qualitative synthesis and edited the review 2 draft chapter.
Obi Ukoumunne (Associate Professor) provided quantitative synthesis topic advice, assisted in quantitative synthesis and edited draft chapters.
Penny Titman (Consultant Clinical Psychologist) was involved in the design and conception of the project, provided mental and physical health topic advice and edited draft chapters.
Roz Shafran (Professor) was involved in the design and conception of the project, provided mental health topic advice and edited draft chapters.
Isobel Heyman (Professor) was involved in the design and conception of the project, provided mental health topic advice, conducted a consultation event and edited draft chapters.
Rob Anderson (Associate Professor) provided health economic topic advice, wrote the economic evaluation section and edited draft chapters.
Chris Dickens (Professor) provided mental health topic advice and edited draft chapters.
Russell Viner (Professor) provided paediatric topic advice and edited draft chapters.
Sophie Bennett (Research Associate) was involved in the design and conception of the project, provided mental health topic advice, conducted a consultation event and edited the overarching synthesis draft chapter.
Stuart Logan (Professor) provided paediatric topic advice and edited the overarching synthesis draft chapter.
Fiona Lockhart (Parent advisory group member) was involved in the design and conception of the project, attended team meetings and consultation events, wrote the Preface and edited the Plain English summary.
Jo Thompson Coon (Associate Professor) provided overall supervision of the project, was involved in the design and conception of the project, provided evidence synthesis topic advice, edited draft chapters and planned and conducted end-user involvement and consultation events.
Data-sharing statement
This is a systematic review and, therefore, the data used for each analysis are present within the report or supplementary materials. Further information and requests for access to the data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- van der Lee JH, Mokkink LB, Grootenhuis MA, Heymans HS, Offringa M. Definitions and measurement of chronic health conditions in childhood: a systematic review. JAMA 2007;297:2741-51. https://doi.org/10.1001/jama.297.24.2741.
- Perrin EC, Newacheck P, Pless IB, Drotar D, Gortmaker SL, Leventhal J, et al. Issues involved in the definition and classification of chronic health conditions. Pediatrics 1993;91:787-93.
- Stein RE, Bauman LJ, Westbrook LE, Coupey SM, Ireys HT. Framework for identifying children who have chronic conditions: the case for a new definition. J Pediatr 1993;122:342-7. https://doi.org/10.1016/S0022-3476(05)83414-6.
- Pless IB, Douglas JW. Chronic illness in childhood: part I. Epidemiological and clinical characteristics. Pediatrics 1971;47:405-14.
- Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Association; 2013.
- Keyes CL. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol 2005;73:539-48. https://doi.org/10.1037/0022-006X.73.3.539.
- Nastasi BK, Borja AP. International Handbook of Psychological Well-Being in Children and Adolescents. New York, NY: Springer-Verlag New York; 2016.
- Newacheck PW, Taylor WR. Childhood chronic illness: prevalence, severity, and impact. Am J Public Health 1992;82:364-71. https://doi.org/10.2105/AJPH.82.3.364.
- Brooks FMJ, Klemera E, Chester K, Spencer N, Smeeton N. HBSC England National Report: Health Behaviour in School-aged Children (HBSC): World Health Organization Collaborative Cross National Study. Hatfield: University of Hertfordshire; 2015.
- Denny S, de Silva M, Fleming T, Clark T, Merry S, Ameratunga S, et al. The prevalence of chronic health conditions impacting on daily functioning and the association with emotional well-being among a national sample of high school students. J Adolesc Health 2014;54:410-15. https://doi.org/10.1016/j.jadohealth.2013.09.010.
- Boyce WF, Davies D, Raman SR, Tynjälä J, Välimaa R, King M, et al. Emotional health of Canadian and Finnish students with disabilities or chronic conditions. Int J Rehabil Res 2009;32:154-61. https://doi.org/10.1097/MRR.0b013e32831e452e.
- Newacheck PW, Halfon N. Prevalence and impact of disabling chronic conditions in childhood. Am J Public Health 1998;88:610-17. https://doi.org/10.2105/AJPH.88.4.610.
- Dey M, Wang J, Jorm AF, Mohler-Kuo M. Children with mental versus physical health problems: differences in perceived disease severity, health care service utilization and parental health literacy. Soc Psychiatry Psychiatr Epidemiol 2015;50:407-18. https://doi.org/10.1007/s00127-014-0944-7.
- Hysing M, Elgen I, Gillberg C, Lie SA, Lundervold AJ. Chronic physical illness and mental health in children. Results from a large-scale population study. J Child Psychol Psychiatry 2007;48:785-92. https://doi.org/10.1111/j.1469-7610.2007.01755.x.
- Pinquart M, Shen Y. Depressive symptoms in children and adolescents with chronic physical illness: an updated meta-analysis. J Pediatr Psychol 2011;36:375-84. https://doi.org/10.1093/jpepsy/jsq104.
- Gupta V, Singh A, Singh TB, Upadhyay S. Psychological morbidity in children undergoing chemotherapy for acute lymphoblastic leukemia. Indian J Pediatr 2014;81:699-701. https://doi.org/10.1007/s12098-013-1211-8.
- Esmaeeli MR, Erfani Sayar R, Saghebi A, Elmi S, Rahmani S, Elmi S, et al. Screening for depression in hospitalized pediatric patients. Iran J Child Neurol 2014;8:47-51.
- Kogon AJ, Vander Stoep A, Weiss NS, Smith J, Flynn JT, McCauley E. Depression and its associated factors in pediatric chronic kidney disease. Pediatr Nephrol 2013;28:1855-61. https://doi.org/10.1007/s00467-013-2497-5.
- Merikangas KR, Calkins ME, Burstein M, He JP, Chiavacci R, Lateef T, et al. Comorbidity of physical and mental disorders in the neurodevelopmental genomics cohort study. Pediatrics 2015;135:e927-38. https://doi.org/10.1542/peds.2014-1444.
- Katon W, Lozano P, Russo J, McCauley E, Richardson L, Bush T. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. J Adolesc Health 2007;41:455-63. https://doi.org/10.1016/j.jadohealth.2007.05.023.
- Acosta-Pérez E, Canino G, Ramírez R, Prelip M, Martin M, Ortega AN. Do Puerto Rican youth with asthma and obesity have higher odds for mental health disorders?. Psychosomatics 2012;53:162-71. https://doi.org/10.1016/j.psym.2011.07.011.
- Greenley RN, Hommel KA, Nebel J, Raboin T, Li SH, Simpson P, et al. A meta-analytic review of the psychosocial adjustment of youth with inflammatory bowel disease. J Pediatr Psychol 2010;35:857-69. https://doi.org/10.1093/jpepsy/jsp120.
- Shelby GD, Shirkey KC, Sherman AL, Beck JE, Haman K, Shears AR, et al. Functional abdominal pain in childhood and long-term vulnerability to anxiety disorders. Pediatrics 2013;132:475-82. https://doi.org/10.1542/peds.2012-2191.
- Moreira JM, Bouissou Morais Soares CM, Teixeira AL, Simões E, Silva AC, Kummer AM. Anxiety, depression, resilience and quality of life in children and adolescents with pre-dialysis chronic kidney disease. Pediatr Nephrol 2015;30:2153-62. https://doi.org/10.1007/s00467-015-3159-6.
- Kogon AJ, Matheson MB, Flynn JT, Gerson AC, Warady BA, Furth SL, et al. Chronic Kidney Disease in Children (CKiD) Study Group . Depressive symptoms in children with chronic kidney disease. J Pediatr 2016;168:164-70.e1. https://doi.org/10.1016/j.jpeds.2015.09.040.
- Rousseau-Salvador C, Amouroux R, Annequin D, Salvador A, Tourniaire B, Rusinek S. Anxiety, depression and school absenteeism in youth with chronic or episodic headache. Pain Res Manag 2014;19:235-40. https://doi.org/10.1155/2014/541618.
- Wändell P, Ljunggren G, Wahlström L, Carlsson AC. Diabetes and psychiatric illness in the total population of Stockholm. J Psychosom Res 2014;77:169-73. https://doi.org/10.1016/j.jpsychores.2014.06.012.
- Plioplys S, Dunn DW, Caplan R. 10-year research update review: psychiatric problems in children with epilepsy. J Am Acad Child Adolesc Psychiatry 2007;46:1389-402. https://doi.org/10.1097/chi.0b013e31815597fc.
- Wechsler AM, Sánchez-Iglesias I. Psychological adjustment of children with cancer as compared with healthy children: a meta-analysis. Eur J Cancer Care 2013;22:314-25. https://doi.org/10.1111/ecc.12031.
- Arabiat DH, Elliott B, Draper P. The prevalence of depression in pediatric oncology patients undergoing chemotherapy treatment in Jordan. J Pediatr Oncol Nurs 2012;29:283-8. https://doi.org/10.1177/1043454212451524.
- Myers RM, Balsamo L, Lu X, Devidas M, Hunger SP, Carroll WL, et al. A prospective study of anxiety, depression, and behavioral changes in the first year after a diagnosis of childhood acute lymphoblastic leukemia: a report from the Children’s Oncology Group. Cancer 2014;120:1417-25. https://doi.org/10.1002/cncr.28578.
- von Essen L, Enskär K, Kreuger A, Larsson B, Sjödén PO. Self-esteem, depression and anxiety among Swedish children and adolescents on and off cancer treatment. Acta Paediatr 2000;89:229-36. https://doi.org/10.1111/j.1651-2227.2000.tb01221.x.
- Chang G, Ratichek SJ, Recklitis C, Syrjala K, Patel SK, Harris L, et al. Children’s psychological distress during pediatric HSCT: parent and child perspectives. Pediatr Blood Cancer 2012;58:289-96. https://doi.org/10.1002/pbc.23185.
- Phipps S, Dunavant M, Lensing S, Rai SN. Acute health-related quality of life in children undergoing stem cell transplant: II. Medical and demographic determinants. Bone Marrow Transplant 2002;29:435-42. https://doi.org/10.1038/sj.bmt.1703376.
- Beyenburg S, Mitchell AJ, Schmidt D, Elger CE, Reuber M. Anxiety in patients with epilepsy: systematic review and suggestions for clinical management. Epilepsy Behav 2005;7:161-71. https://doi.org/10.1016/j.yebeh.2005.05.014.
- Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Diez Roux AV, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA 2008;299:2751-9. https://doi.org/10.1001/jama.299.23.2751.
- Wallander JL, Varni JW, Babani L, Banis HT, Wilcox KT. Family resources as resistance factors for psychological maladjustment in chronically ill and handicapped children. J Pediatr Psychol 1989;14:157-73. https://doi.org/10.1093/jpepsy/14.2.157.
- Wallander JL, Varni JW, La Greca AM, Siegel LJ, Wallander JL, Walker CE. Stress and Coping in Child Health. New York, NY: Guilford Press; 1992.
- Thompson R, Gustafson K. Adaptation to Chronic Childhood Illness. Washington, DC: American Psychological Association; 1996.
- Thompson RJ, Gustafson KE, Gil KM, Kinney TR, Spock A. Change in the psychological adjustment of children with cystic fibrosis or sickle cell disease and their mothers. J Clin Psychol Med Settings 1999;6:373-92. https://doi.org/10.1023/A:1026219831205.
- Moos RH, Holahan CJ, Martz E, Livneh H. Coping with Chronic Illness and Disability: Theoretical, Empirical, and Clinical Aspects. New York, NY: Springer US; 2007.
- Haase JE, Kintner EK, Monahan PO, Robb SL. The resilience in illness model, part 1: exploratory evaluation in adolescents and young adults with cancer. Cancer Nurs 2014;37:E1-12. https://doi.org/10.1097/NCC.0b013e31828941bb.
- Gannoni AF, Shute RH. Parental and child perspectives on adaptation to childhood chronic illness: a qualitative study. Clin Child Psychol Psychiatry 2010;15:39-53. https://doi.org/10.1177/1359104509338432.
- Christie D, Romano G, Barnes J, Madge N, Nicholas DB, Koot HM, et al. Exploring views on satisfaction with life in young children with chronic illness: an innovative approach to the collection of self-report data from children under 11. Clin Child Psychol Psychiatry 2012;17:5-15. https://doi.org/10.1177/1359104510392309.
- Venning A, Eliott J, Wilson A, Kettler L. Understanding young peoples’ experience of chronic illness: a systematic review. Int J Evid Based Healthc 2008;6:321-36. https://doi.org/10.1111/j.1744-1609.2008.00107.x.
- Cottrell D. Prevention and treatment of psychiatric disorders in children with chronic physical illness. Arch Dis Child 2015;100:303-4. https://doi.org/10.1136/archdischild-2014-307866.
- Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complicat 2005;19:113-22.
- Chavira DA, Garland AF, Daley S, Hough R. The impact of medical comorbidity on mental health and functional health outcomes among children with anxiety disorders. J Dev Behav Pediatr 2008;29:394-402. https://doi.org/10.1097/DBP.0b013e3181836a5b.
- Kovacs M, Mukerji P, Drash A, Iyengar S. Biomedical and psychiatric risk factors for retinopathy among children with IDDM. Diabetes Care 1995;18:1592-9. https://doi.org/10.2337/diacare.18.12.1592.
- Naylor C, Parsonage M, McDaid D, Knapp M, Fossey M, Galea A. Long-Term Conditions and Mental Health: The Cost of Co-morbidities. London: The King’s Fund; 2012.
- Chiles JA, Lambert MJ, Hatch AL. The impact of psychological interventions on medical cost offset: a meta-analytic review. Clin Psychol Sci Pract 1999;6:204-20. https://doi.org/10.1093/clipsy.6.2.204.
- Chorpita BF, Daleiden EL, Ebesutani C, Young J, Becker KD, Nakamura BJ, et al. Evidence-based treatments for children and adolescents: an updated review of indicators of efficacy and effectiveness. Clin Psychol Sci Pract 2011;18:154-72. https://doi.org/10.1111/j.1468-2850.2011.01247.x.
- Antisocial Behaviour and Conduct Disorders in Children and Young People: Recognition and Management. London: NICE; 2013.
- Depression in Children and Young People: Identification and Management. London: NICE; 2005.
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: a randomized clinical trial evaluating child and family modalities. J Consult Clin Psychol 2008;76:282-97. https://doi.org/10.1037/0022-006X.76.2.282.
- Johnson B, Eiser C, Young V, Brierley S, Heller S. Prevalence of depression among young people with type 1 diabetes: a systematic review. Diabet Med 2013;30:199-208. https://doi.org/10.1111/j.1464-5491.2012.03721.x.
- Markowitz SM, Gonzalez JS, Wilkinson JL, Safren SA. A review of treating depression in diabetes: emerging findings. Psychosomatics 2011;52:1-18. https://doi.org/10.1016/j.psym.2010.11.007.
- Ekinci O, Titus JB, Rodopman AA, Berkem M, Trevathan E. Depression and anxiety in children and adolescents with epilepsy: prevalence, risk factors, and treatment. Epilepsy Behav 2009;14:8-18. https://doi.org/10.1016/j.yebeh.2008.08.015.
- Szigethy E, Whitton SW, Levy-Warren A, DeMaso DR, Weisz J, Beardslee WR. Cognitive-behavioral therapy for depression in adolescents with inflammatory bowel disease: a pilot study. J Am Acad Child Adolesc Psychiatry 2004;43:1469-77. https://doi.org/10.1097/01.chi.0000142284.10574.1f.
- Richardson LP, Russo JE, Lozano P, McCauley E, Katon W. The effect of comorbid anxiety and depressive disorders on health care utilization and costs among adolescents with asthma. Gen Hosp Psychiatry 2008;30:398-406. https://doi.org/10.1016/j.genhosppsych.2008.06.004.
- No Health Without Mental Health: A Cross-Government Outcomes Strategy. London: DHSC; 2011.
- Investing in Emotional and Psychological Wellbeing for Patients With Long-Term Conditions. London: NHS Confederation; 2012.
- Diabetes (Type 1 and Type 2) in Children and Young People: Diagnosis and Management. London: NICE; 2015.
- Epilepsies: Diagnosis and Management. London: NICE; 2012.
- Closing the Gap: Priorities for Essential Change in Mental Health. London: Department of Health and Social Care; 2014.
- Future In Mind: Promoting, Protecting and Improving Our Children and Young People’s Mental Health and Wellbeing. London: Department of Health and Social Care; 2015.
- Depression in Adults with a Chronic Physical Health Problem: Recognition and Management. London: NICE; 2009.
- Sharpe M, Walker J, Holm Hansen C, Martin P, Symeonides S, Gourley C, et al. Integrated collaborative care for comorbid major depression in patients with cancer (SMaRT Oncology-2): a multicentre randomised controlled effectiveness trial. Lancet 2014;384:1099-108. https://doi.org/10.1016/S0140-6736(14)61231-9.
- Owens PL, Hoagwood K, Horwitz SM, Leaf PJ, Poduska JM, Kellam SG, et al. Barriers to children’s mental health services. J Am Acad Child Adolesc Psychiatry 2002;41:731-8. https://doi.org/10.1097/00004583-200206000-00013.
- James AC, James G, Cowdrey FA, Soler A, Choke A. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst Rev 2015;2. https://doi.org/10.1002/14651858.CD004690.pub4.
- Gertler P, Tate RL, Cameron ID. Non-pharmacological interventions for depression in adults and children with traumatic brain injury. Cochrane Database Syst Rev 2015;12. https://doi.org/10.1002/14651858.CD009871.pub2.
- Lane DA, Millane TA, Lip GY. Psychological interventions for depression in adolescent and adult congenital heart disease. Cochrane Database Syst Rev 2013;10. https://doi.org/10.1002/14651858.CD004372.pub2.
- Eccleston C, Palermo TM, Fisher E, Law E. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev 2012;8. https://doi.org/10.1002/14651858.CD009660.pub2.
- Glasscoe CA, Quittner AL. Psychological interventions for people with cystic fibrosis and their families. Cochrane Database Syst Rev 2008;3. https://doi.org/10.1002/14651858.CD003148.pub2.
- Ramaratnam S, Baker GA, Goldstein LH. Psychological treatments for epilepsy. Cochrane Database Syst Rev 2008;3. https://doi.org/10.1002/14651858.CD002029.pub3.
- Timmer A, Preiss JC, Motschall E, Rücker G, Jantschek G, Moser G. Psychological interventions for treatment of inflammatory bowel disease. Cochrane Database Syst Rev 2011;2. https://doi.org/10.1002/14651858.CD006913.pub2.
- Gandy M, Sharpe L, Perry KN. Cognitive behavior therapy for depression in people with epilepsy: a systematic review. Epilepsia 2013;54:1725-34. https://doi.org/10.1111/epi.12345.
- Yorke J, Fleming SL, Shuldham C. A systematic review of psychological interventions for children with asthma. Pediatr Pulmonol 2007;42:114-24. https://doi.org/10.1002/ppul.20464.
- Sansom-Daly UM, Peate M, Wakefield CE, Bryant RA, Cohn RJ. A systematic review of psychological interventions for adolescents and young adults living with chronic illness. Health Psychol 2012;31:380-93. https://doi.org/10.1037/a0025977.
- Thompson RD, Delaney P, Flores I, Szigethy E. Cognitive-behavioral therapy for children with comorbid physical illness. Child Adolesc Psychiatr Clin N Am 2011;20:329-48. https://doi.org/10.1016/j.chc.2011.01.013.
- Thomé-Souza MS, Kuczynski E, Valente KD. Sertraline and fluoxetine: safe treatments for children and adolescents with epilepsy and depression. Epilepsy Behav 2007;10:417-25. https://doi.org/10.1016/j.yebeh.2007.01.004.
- Bennett S, Shafran R, Coughtrey A, Walker S, Heyman I. Psychological interventions for mental health disorders in children with chronic physical illness: a systematic review. Arch Dis Child 2015;100:308-16. https://doi.org/10.1136/archdischild-2014-307474.
- Martinović Z, Simonović P, Djokić R. Preventing depression in adolescents with epilepsy. Epilepsy Behav 2006;9:619-24. https://doi.org/10.1016/j.yebeh.2006.08.017.
- Szigethy E, Kenney E, Carpenter J, Hardy DM, Fairclough D, Bousvaros A, et al. Cognitive-behavioral therapy for adolescents with inflammatory bowel disease and subsyndromal depression. J Am Acad Child Adolesc Psychiatry 2007;46:1290-8. https://doi.org/10.1097/chi.0b013e3180f6341f.
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York: CRD, University of York; 2009.
- Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. London: John Wiley & Sons; 2011.
- Glanville JM, Lefebvre C, Miles JN, Camosso-Stefinovic J. How to identify randomized controlled trials in MEDLINE: ten years on. J Med Libr Assoc 2006;94:130-6.
- Eccleston C, Palermo TM, Williams AC, Lewandowski Holley A, Morley S, Fisher E, et al. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2014;5. https://doi.org/10.1002/14651858.CD003968.pub4.
- Canter KS, Roberts MC. A systematic and quantitative review of interventions to facilitate school re-entry for children with chronic health conditions. J Pediatr Psychol 2012;37:1065-75. https://doi.org/10.1093/jpepsy/jss071.
- Taylor SJ, Pinnock H, Epiphaniou E, Pearce G, Parke HL, Schwappach A, et al. A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions: PRISMS–Practical systematic Review of Self-Management Support for long-term conditions. Health Serv Deliv Res 2014;2.
- Sattoe JN, Bal MI, Roelofs PD, Bal R, Miedema HS, van Staa A. Self-management interventions for young people with chronic conditions: a systematic overview. Patient Educ Couns 2015;98:704-15. https://doi.org/10.1016/j.pec.2015.03.004.
- Fisher E, Law E, Palermo TM, Eccleston C. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2015;3. https://doi.org/10.1002/14651858.CD011118.pub2.
- Galdas P, Fell J, Bower P, Kidd L, Blickem C, McPherson K, et al. The effectiveness of self-management support interventions for men with long-term conditions: a systematic review and meta-analysis. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006620.
- Lambert V, Keogh D. Striving to live a normal life: a review of children and young people’s experience of feeling different when living with a long term condition. J Pediatr Nurs 2015;30:63-77. https://doi.org/10.1016/j.pedn.2014.09.016.
- Schwartz L, Drotar D. Defining the nature and impact of goals in children and adolescents with a chronic health condition: a review of research and a theoretical framework. J Clin Psychol Med Settings 2006;13:390-402. https://doi.org/10.1007/s10880-006-9041-8.
- Spencer NJ, Blackburn CM, Read JM. Disabling chronic conditions in childhood and socioeconomic disadvantage: a systematic review and meta-analyses of observational studies. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-007062.
- Braam KI, van der Torre P, Takken T, Veening MA, van Dulmen-den Broeder E, Kaspers GJ. Physical exercise training interventions for children and young adults during and after treatment for childhood cancer. Cochrane Database Syst Rev 2013;4. https://doi.org/10.1002/14651858.CD008796.pub2.
- Nightingale R, Friedl S, Swallow V. Parents’ learning needs and preferences when sharing management of their child’s long-term/chronic condition: a systematic review. Patient Educ Couns 2015;98:1329-38. https://doi.org/10.1016/j.pec.2015.05.002.
- Smith J, Cheater F, Bekker H. Parents’ experiences of living with a child with a long-term condition: a rapid structured review of the literature. Health Expect 2015;18:452-74. https://doi.org/10.1111/hex.12040.
- Orrskog S, Medin E, Tsolova S, Semenza JC. Causal inference regarding infectious aetiology of chronic conditions: a systematic review. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0068861.
- Ludvigsen MS, Fegran L, Aagaard H, Meyer G, Uhrenfeldt L. Parents’ experiences of the transfer from pediatric to adult care for their adolescent or young adult children with chronic conditions: a systematic review protocol. JBI Database Syst Rev Implement Rep 2014;12:102-11. https://doi.org/10.11124/jbisrir-2014-1565.
- Quiñones A, Richardson J, Freeman M, O’Neil ME, Kansagara D. Group Visits Focusing on Education for the Management of Chronic Conditions in Adults: A Systematic Review. USA: US Department of Veteran Affairs; 2012.
- Brown CA, Kuo M, Phillips L, Berry R, Tan M. Non-pharmacological sleep interventions for youth with chronic health conditions: a critical review of the methodological quality of the evidence. Disabil Rehabil 2013;35:1221-55. https://doi.org/10.3109/09638288.2012.723788.
- Hardelid P, Dattani N, Gilbert R. Programme Board of the Royal College of Paediatrics and Child Health. Estimating the prevalence of chronic conditions in children who die in England, Scotland and Wales: a data linkage cohort study. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005331.
- Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr 2014;14. https://doi.org/10.1186/1471-2431-14-199.
- Glanville J, Kaunelis D, Mensinkai S. How well do search filters perform in identifying economic evaluations in MEDLINE and EMBASE. Int J Technol Assess Health Care 2009;25:522-9. https://doi.org/10.1017/S0266462309990523.
- Richardson M, Moore DA, Gwernan-Jones R, Thompson Coon J, Ukoumunne O, Rogers M, et al. Non-pharmacological interventions for attention-deficit/hyperactivity disorder (ADHD) delivered in school settings: systematic reviews of quantitative and qualitative research. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19450.
- Cohen J. A power primer. Psychol Bull 1992;112:155-9. https://doi.org/10.1037/0033-2909.112.1.155.
- Glass GV, McGaw B, Smith M. Meta-analysis in Social Research. Beverly Hills, CA: Sage Publications, Inc.; 1981.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. https://doi.org/10.1136/bmj.327.7414.557.
- Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to Meta-Analysis. Chichester: John Wiley & Sons, Ltd; 2009.
- Ahmed I, Sutton AJ, Riley RD. Assessment of publication bias, selection bias, and unavailable data in meta-analyses using individual participant data: a database survey. BMJ 2012;344. https://doi.org/10.1136/bmj.d7762.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Whittemore R, Grey M, Lindemann E, Ambrosino J, Jaser S. Development of an internet coping skills training program for teenagers with type 1 diabetes. Comput Inform Nurs 2010;28:103-11. https://doi.org/10.1097/NCN.0b013e3181cd8199.
- Foundation H. Doing Diabetes Differently: A Novel Way of Contracting Integrated Psychological Therapies to Increase Treatment Adherence. Milton Keynes: Health Foundation; 2014.
- Foster EM, Prinz RJ, Sanders MR, Shapiro CJ. The costs of a public health infrastructure for delivering parenting and family support. Child Youth Serv Rev 2008;30:493-501. https://doi.org/10.1016/j.childyouth.2007.11.002.
- Mihalopoulos C, Sanders MR, Turner KM, Murphy-Brennan M, Carter R. Does the triple P-Positive Parenting Program provide value for money?. Aust N Z J Psychiatry 2007;41:239-46. https://doi.org/10.1080/00048670601172723.
- Westrupp EM, Northam E, Lee KJ, Scratch SE, Cameron F. Reducing and preventing internalizing and externalizing behavior problems in children with type 1 diabetes: a randomized controlled trial of the Triple P-Positive Parenting Program. Pediatr Diabetes 2015;16:554-63. https://doi.org/10.1111/pedi.12205.
- Bignall WJ, Luberto CM, Cornette AF, Haj-Hamed M, Cotton S. Breathing retraining for African-American adolescents with asthma: a pilot study of a school-based randomized controlled trial. J Asthma 2015;52:889-96. https://doi.org/10.3109/02770903.2015.1033724.
- Boardway RH, Delamater AM, Tomakowsky J, Gutai JP. Stress management training for adolescents with diabetes. J Pediatr Psychol 1993;18:29-45. https://doi.org/10.1093/jpepsy/18.1.29.
- Diego MA, Field T, Hernandez-Reif M, Shaw K, Friedman L, Ironson G. HIV adolescents show improved immune function following massage therapy. Int J Neurosci 2001;106:35-4. https://doi.org/10.3109/00207450109149736.
- Hains AA, Davies WH, Parton E, Totka J, Amoroso-Camarata J. A stress management intervention for adolescents with type 1 diabetes. Diabetes Educ 2000;26:417-24. https://doi.org/10.1177/014572170002600309.
- Lyon ME, Jacobs S, Briggs L, Cheng YI, Wang J. A longitudinal, randomized, controlled trial of advance care planning for teens with cancer: anxiety, depression, quality of life, advance directives, spirituality. J Adolesc Health 2014;54:710-17. https://doi.org/10.1016/j.jadohealth.2013.10.206.
- Masia-Warner C, Colognori D, Kim RE, Reigada LC, Klein RG, Browner-Elhanan KJ, et al. Cognitive-behavioral treatment of persistent functional somatic complaints and pediatric anxiety: an initial controlled trial. Depress Anxiety 2011;28:551-9. https://doi.org/10.1002/da.20821.
- Reigada LC, Polokowski AR, Walder DJ, Szigethy EM, Benkov KJ, Bruzzese J-M, et al. Treatment for comorbid pediatric gastrointestinal and anxiety disorders: a pilot study of a flexible health sensitive cognitive-behavioral therapy program. Clin Pract Ped Psych 2015;3:314-26. https://doi.org/10.1037/cpp0000116.
- Szigethy E, Bujoreanu SI, Youk AO, Weisz J, Benhayon D, Fairclough D, et al. Randomized efficacy trial of two psychotherapies for depression in youth with inflammatory bowel disease. J Am Acad Child Adolesc Psychiatry 2014;53:726-35. https://doi.org/10.1016/j.jaac.2014.04.014.
- Yetwin AK. Heart Rate Variability Biofeedback Therapy for Children and Adolescents with Chronic Pain. San Diego, CA: Alliant International University; 2011.
- Brown FL, Whittingham K, Boyd RN, McKinlay L, Sofronoff K. Improving child and parenting outcomes following paediatric acquired brain injury: a randomised controlled trial of Stepping Stones Triple P plus Acceptance and Commitment Therapy. J Child Psychol Psychiatry 2014;55:1172-83. https://doi.org/10.1111/jcpp.12227.
- Gordon BA, Knapman LM, Lubitz L. Graduated exercise training and progressive resistance training in adolescents with chronic fatigue syndrome: a randomized controlled pilot study. Clin Rehabil 2010;24:1072-9. https://doi.org/10.1177/0269215510371429.
- Serlachius AS, Scratch SE, Northam EA, Frydenberg E, Lee KJ, Cameron FJ. A randomized controlled trial of cognitive behaviour therapy to improve glycaemic control and psychosocial wellbeing in adolescents with type 1 diabetes. J Health Psychol 2016;21:1157-69. https://doi.org/10.1177/1359105314547940.
- Whittingham K, Sanders M, McKinlay L, Boyd RN. Interventions to reduce behavioral problems in children with cerebral palsy: an RCT. Pediatrics 2014;133:e1249-57. https://doi.org/10.1542/peds.2013-3620.
- Ashori M, Hasanzadeh S, Pourmohamadreza-Tajrishi M. Effectiveness of life skill instruction on the mental health of hearing loss students. J Rehabil 2013;13:48-57.
- Nekah A, Mohsen S, Kamali F, Jansouz F. The effects of structured cognitive-behavioral group play therapy on anxiety and depression in children with cancer: a pilot study. Evid-Based Care J 2015;5:39-50.
- Pourmohamadreza-Tajrishi M, Ashori M, Jalilabkenar SS. The effectiveness of emotional intelligence training on the mental health of male deaf students. Iran J Public Health 2013;42:1174-80.
- Zareapour A, Khoshknab MF, Kashaninia A, Biglarian A, Babashahabi R. Effect of group play therapy on depression in children with cancer. Sci J Kurdistan University Med Sci 2009;14:64-72.
- Bufalini A. Role of interactive music in oncological pediatric patients undergoing painful procedures. Minerva Pediatr 2009;61:379-89.
- Shoshani A, Mifano K, Czamanski-Cohen J. The effects of the Make a Wish intervention on psychiatric symptoms and health-related quality of life of children with cancer: a randomised controlled trial. Qual Life Res 2016;25:1209-18. https://doi.org/10.1007/s11136-015-1148-7.
- Wang Q, Zhang J, Mei Q, Huang Y, Liu Y, Yuan X, et al. [Group play therapy for improving mental coping ability in children with asthma.]. PLAMJ 2012;37:623-9.
- Yang HB, Tang YQ, Yi ZW. Effect of relaxation training on psychosomatic symptoms of children with asthma. Chin J Clin Rehabil 2004;8:8392-3.
- Brown FL, Whittingham K, Boyd RN, McKinlay L, Sofronoff K. Does Stepping Stones Triple P plus Acceptance and Commitment Therapy improve parent, couple, and family adjustment following paediatric acquired brain injury? A randomised controlled trial. Behav Res Ther 2015;73:58-66. https://doi.org/10.1016/j.brat.2015.07.001.
- Szigethy E, Craig AE, Iobst EA, Grand RJ, Keljo D, DeMaso D, et al. Profile of depression in adolescents with inflammatory bowel disease: implications for treatment. Inflamm Bowel Dis 2009;15:69-74. https://doi.org/10.1002/ibd.20693.
- Thompson RD, Craig A, Crawford EA, Fairclough D, Gonzalez-Heydrich J, Bousvaros A, et al. Longitudinal results of cognitive behavioral treatment for youths with inflammatory bowel disease and depressive symptoms. J Clin Psychol Med Settings 2012;19:329-37. https://doi.org/10.1007/s10880-012-9301-8.
- Szigethy E, Youk AO, Gonzalez-Heydrich J, Bujoreanu SI, Weisz J, Fairclough D, et al. Effect of 2 psychotherapies on depression and disease activity in pediatric Crohn’s disease. Inflamm Bowel Dis 2015;21:1321-8. https://doi.org/10.1097/MIB.0000000000000358.
- Whittingham K, Sanders MR, McKinlay L, Boyd RN. Parenting intervention combined with acceptance and commitment therapy: a trial with families of children with cerebral palsy. J Pediatr Psychol 2016;41:531-42. https://doi.org/10.1093/jpepsy/jsv118.
- Wicksell RK, Melin L, Lekander M, Olsson GL. Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quality of life in longstanding pediatric pain – a randomized controlled trial. Pain 2009;141:248-57. https://doi.org/10.1016/j.pain.2008.11.006.
- Robb SL, Clair AA, Watanabe M, Monahan PO, Azzouz F, Stouffer JW, et al. A non-randomized [corrected] controlled trial of the active music engagement (AME) intervention on children with cancer. Psycho-Oncology 2008;17:699-708. https://doi.org/10.1002/pon.1301.
- Wallace A, Croucher K, Quilgars D, Baldwin S. Meeting the challenge: developing systematic reviewing in social policy. Policy Polit 2004;32:455-70. https://doi.org/10.1332/0305573042009444.
- Sanders MR, Mazzucchelli TG, Studman LJ. Stepping Stones Triple P: the theoretical basis and development of an evidence-based positive parenting program for families with a child who has a disability. J Intellect Dev Disabil 2004;29:265-83. https://doi.org/10.1080/13668250412331285127.
- Ewing B. Wish fulfillment: palliative care and end-of-life intervention. Pediatr Nurs 2009;35:81-5.
- Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res 2011;63:467-72. https://doi.org/10.1002/acr.20561.
- Karlson CW, Rapoff MA. Attrition in randomized controlled trials for pediatric chronic conditions. J Pediatr Psychol 2009;34:782-93. https://doi.org/10.1093/jpepsy/jsn122.
- Abrahamse ME, Junger M, Leijten PH, Lindeboom R, Boer F, Lindauer RJ. Psychometric properties of the Dutch Eyberg Child Behavior Inventory (ECBI) in a community sample and a multi-ethnic clinical sample. J Psychopathol Behav Assess 2015;37:679-91. https://doi.org/10.1007/s10862-015-9482-1.
- Subirana M, Solá I, Garcia JM, Gich I, Urrútia G. A nursing qualitative systematic review required MEDLINE and CINAHL for study identification. J Clin Epidemiol 2005;58:20-5. https://doi.org/10.1016/j.jclinepi.2004.06.001.
- Wright K, Golder S, Lewis-Light K. What value is the CINAHL database when searching for systematic reviews of qualitative studies?. Syst Rev 2015;4. https://doi.org/10.1186/s13643-015-0069-4.
- Moore DA, Gwernan-Jones R, Richardson M, Racey D, Rogers M, Stein K, et al. The experiences of and attitudes toward non-pharmacological interventions for attention-deficit/hyperactivity disorder used in school settings: a systematic review and synthesis of qualitative research. Emotional Behav Difficulties 2016;21:61-82. https://doi.org/10.1080/13632752.2016.1139296.
- Noblit GW, Hare RD. Meta-ethnography: Synthesizing Qualitative Studies. Sage Publications, Inc.: Newbury Park, CA; 1988.
- Morton K, Dennison L, May C, Murray E, Little P, McManus RJ, et al. Using digital interventions for self-management of chronic physical health conditions: a meta-ethnography review of published studies. Patient Educ Couns 2017;100:616-35. https://doi.org/10.1016/j.pec.2016.10.019.
- Evans R, Hurrell C. The role of schools in children and young people’s self-harm and suicide: systematic review and meta-ethnography of qualitative research. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3065-2.
- Frost J, Garside R, Cooper C, Britten N. A qualitative synthesis of diabetes self-management strategies for long term medical outcomes and quality of life in the UK. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-348.
- Ames HM, Glenton C, Lewin S. Parents’ and informal caregivers’ views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database Syst Rev 2017;2. https://doi.org/10.1002/14651858.CD011787.pub2.
- Suri H. Purposeful sampling in qualitative research synthesis. Qual Res J 2011;11:63-75. https://doi.org/10.3316/QRJ1102063.
- Barnetz Z, Feigin R. ‘We didn’t have to talk’: adolescent perception of mentor-mentee relationships in an evaluation study of a mentoring program for adolescents with juvenile diabetes. Child Adolesc Soc Work J 2012;29:463-83. https://doi.org/10.1007/s10560-012-0273-1.
- Bluebond-Langer M, Perkel D, Goertzel T. Pediatric cancer patients’ peer relationships: the impact of an oncology camp experience. J Psychosoc Oncol 1991;9:67-80. https://doi.org/10.1300/J077v09n02_05.
- Brodeur SS. Treating families coping with chronic illness: an evaluation of the ‘Living Well’ program. Dissert Abst Int Sect B Sci Engin 2005;66.
- Bultas MW, Steurer LM, Balakas K, Brooks C, Fields H. Psychosocial outcomes of a summer overnight recreational experience for children with heart disease. J Child Health Care 2015;19:542-9. https://doi.org/10.1177/1367493514540350.
- Desai PP, Sutton LJ, Staley MD, Hannon DW. A qualitative study exploring the psychosocial value of weekend camping experiences for children and adolescents with complex heart defects. Child Care Health Dev 2014;40:553-61. https://doi.org/10.1111/cch.12056.
- Gillard A, Allsop J. Camp experiences in the lives of adolescents with serious illnesses. Child Youth Serv Rev 2016;65:112-19. https://doi.org/10.1016/j.childyouth.2016.04.001.
- Hosek S, Brothers J, Lemos D. Adolescent Medicine Trials Network for HIV/AIDS Interventions. What HIV-positive young women want from behavioral interventions: a qualitative approach. AIDS Patient Care STDS 2012;26:291-7. https://doi.org/10.1089/apc.2011.0035.
- Moola FJ, Faulkner G, White L, Kirsh J. Kids with special hearts: the experience of children with congenital heart disease at Camp Willowood. Qual Res Sport Exercise Health 2015;7:271-93. https://doi.org/10.1080/2159676X.2014.926968.
- Stewart M, Barnfather A, Magill-Evans J, Ray L, Letourneau N. Brief report: an online support intervention: perceptions of adolescents with physical disabilities. J Adolesc 2011;34:795-800. https://doi.org/10.1016/j.adolescence.2010.04.007.
- Barlow JH, Shaw KL, Harrison K. Consulting the ‘experts’: children’s and parents’ perceptions of psycho-educational interventions in the context of juvenile chronic arthritis. Health Educ Res 1999;14:597-610. https://doi.org/10.1093/her/14.5.597.
- Fair CD, Connor L, Albright J, Wise E, Jones K. ‘I’m positive, I have something to say’: assessing the impact of a creative writing group for adolescents living with HIV. The Arts in Psychotherapy 2012;39:383-9. https://doi.org/10.1016/j.aip.2012.06.010.
- Gillard A, Watts CE. Program features and developmental experiences at a camp for youth with cancer. Child Youth Serv Rev 2013;35:890-8. https://doi.org/10.1016/j.childyouth.2013.02.017.
- Gillard A, Witt PA, Watts CE. Outcomes and processes at a camp for youth with HIV/AIDS. Qual Health Res 2011;21:1508-26. https://doi.org/10.1177/1049732311413907.
- Lewis P, Klineberg E, Towns S, Moore K, Steinbeck K. The effects of introducing peer support to young people with a chronic illness. J Child Fam Stud 2016;25:2541-53. https://doi.org/10.1007/s10826-016-0427-4.
- Muskat B, Salter R, Shindler S, Porter M, Bitnun A. ‘Here you feel like it’s not taboo’: an evaluation of a pediatric hospital-based HIV support group. J HIV AIDS Soc Serv 2016;15:353-70. https://doi.org/10.1080/15381501.2015.1124310.
- Nicholas DB, Darch J, McNeill T, Brister L, O’Leary K, Berlin D, et al. Perceptions of online support for hospitalized children and adolescents. Soc Work Health Care 2007;44:205-23. https://doi.org/10.1300/J010v44n03_06.
- Stewart M, Letourneau N, Masuda JR, Anderson S, McGhan S. Online support for children with asthma and allergies. J Fam Nurs 2013;19:171-97. https://doi.org/10.1177/1074840713483573.
- Tiemens K, Beveridge HL, Nicholas DB. Evaluation of a therapeutic camp program for adolescents with a facial difference. Soc Work Groups 2007;30:57-71. https://doi.org/10.1300/J009v30n02_06.
- White LC, Moola FJ, Kirsh JA, Faulkner GE. A therapeutic recreation camp for children with congenital heart disease: examining impact on the psychosocial well-being of parents. J Child Fam Stud 2016;25:3034-43. https://doi.org/10.1007/s10826-016-0474-x.
- Wright PM, White K, Gaebler-Spira D. Exploring the relevance of the personal and social responsibility model in adapted physical activity: a collective case study. J Teach Phys Educ 2004;23:71-87. https://doi.org/10.1123/jtpe.23.1.71.
- Dennison L, Stanbrook R, Moss-Morris R, Yardley L, Chalder T. Cognitive behavioural therapy and psycho-education for chronic fatigue syndrome in young people: reflections from the families’ perspective. Br J Health Psychol 2010;15:167-83. https://doi.org/10.1348/135910709X440034.
- Kirk S, Milnes L. An exploration of how young people and parents use online support in the context of living with cystic fibrosis. Health Expect 2016;19:309-21. https://doi.org/10.1111/hex.12352.
- Serlachius A, Northam E, Frydenberg E, Cameron F. Adapting a generic coping skills programme for adolescents with type 1 diabetes: a qualitative study. J Health Psychol 2012;17:313-23. https://doi.org/10.1177/1359105311415559.
- White L. A Therapeutic Recreation Camp for Children with Congenital Heart Disease: Examining Impact on the Psycho-social Well-being of Caregivers and their Children. Toronto, ON: University of Toronto; 2014.
- Kashikar-Zuck S, Tran ST, Barnett K, Bromberg MH, Strotman D, Sil S, et al. A qualitative examination of a new combined cognitive-behavioral and neuromuscular training intervention for juvenile fibromyalgia. Clin J Pain 2016;32:70-81. https://doi.org/10.1097/AJP.0000000000000221.
- Campbell T, Beer H, Wilkins R, Sherlock E, Merrett A, Griffiths J. ‘I look forward. I feel insecure but I am ok with it’. The experience of young HIV+ people attending transition preparation events: a qualitative investigation. AIDS Care 2010;22:263-9. https://doi.org/10.1080/09540120903111460.
- Curle C, Bradford J, Thompson J, Cawthron P. Users’ views of a group therapy intervention for chronically ill or disabled children and their parents: towards a meaningful assessment of therapeutic effectiveness. Clin Child Psychol Psychiatry 2005;10:509-27. https://doi.org/10.1177/1359104505056315.
- Gan C, Gargaro J, Kreutzer JS, Boschen KA, Wright FV. Development and preliminary evaluation of a structured family system intervention for adolescents with brain injury and their families. Brain Inj 2010;24:651-63. https://doi.org/10.3109/02699051003692142.
- Jaser SS, Patel N, Linsky R, Whittemore R. Development of a positive psychology intervention to improve adherence in adolescents with type 1 diabetes. J Pediatr Health Care 2014;28:478-85. https://doi.org/10.1016/j.pedhc.2014.02.008.
- Marsac ML, Hildenbrand AK, Clawson K, Jackson L, Kohser K, Barakat L, et al. Acceptability and feasibility of family use of The Cellie Cancer Coping Kit. Support Care Cancer 2012;20:3315-24. https://doi.org/10.1007/s00520-012-1475-y.
- Masuda JR, Anderson S, Letourneau N, Sloan Morgan V, Stewart M. Reconciling preferences and constraints in online peer support for youth with asthma and allergies. Health Promot Pract 2013;14:741-50. https://doi.org/10.1177/1524839912465083.
- Nieto R, Hernández E, Boixadós M, Huguet A, Beneitez I, McGrath P. Testing the feasibility of DARWeb: an online intervention for children with functional abdominal pain and their parents. Clin J Pain 2015;31:493-50. https://doi.org/10.1097/AJP.0000000000000199.
- Nilsson S, Finnström B, Kokinsky E, Enskär K. The use of Virtual Reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. Eur J Oncol Nurs 2009;13:102-9. https://doi.org/10.1016/j.ejon.2009.01.003.
- Reme SE, Archer N, Chalder T. Experiences of young people who have undergone the Lightning Process to treat chronic fatigue syndrome/myalgic encephalomyelitis – a qualitative study. Br J Health Psychol 2013;18:508-25. https://doi.org/10.1111/j.2044-8287.2012.02093.x.
- Sibinga EM, Kerrigan D, Stewart M, Johnson K, Magyari T, Ellen JM. Mindfulness-based stress reduction for urban youth. J Altern Complement Med 2011;17:213-18. https://doi.org/10.1089/acm.2009.0605.
- Wolf Bordonaro GP. Art therapy with hospitalized pediatric patients. Dissert Abst Int Sect A Human Soc Sci 2005;66.
- Ayers S, Muller I, Mahoney L, Seddon P. Understanding needle-related distress in children with cystic fibrosis. Br J Health Psychol 2011;16:329-43. https://doi.org/10.1348/135910710X506895.
- Barry P, O’Callaghan C, Wheeler G, Grocke D. Music therapy CD creation for initial pediatric radiation therapy: a mixed methods analysis. J Music Ther 2010;47:233-63. https://doi.org/10.1093/jmt/47.3.233.
- Baruch JM. The Beads of Courage Program for Children Coping with Cancer. Tucson, AZ: University of Arizona; 2010.
- Burns DS, Robb SL, Phillips-Salimi C, Haase JE. Parental perspectives of an adolescent/young adult stem cell transplant and a music video intervention. Cancer Nurs 2010;33:E20-7. https://doi.org/10.1097/NCC.0b013e3181d4b671.
- Docherty SL, Robb SL, Phillips-Salimi C, Cherven B, Stegenga K, Hendricks-Ferguson V, et al. Parental perspectives on a behavioral health music intervention for adolescent/young adult resilience during cancer treatment: report from the Children’s Oncology Group. J Adolesc Health 2013;52:170-8. https://doi.org/10.1016/j.jadohealth.2012.05.010.
- O’Callaghan C, Baron A, Barry P, Dun B. Music’s relevance for pediatric cancer patients: a constructivist and mosaic research approach. Support Care Cancer 2011;19:779-88. https://doi.org/10.1007/s00520-010-0879-9.
- O’Callaghan C, Barry P, Thompson K. Music’s relevance for adolescents and young adults with cancer: a constructivist research approach. Support Care Cancer 2012;20:687-97. https://doi.org/10.1007/s00520-011-1104-1.
- O’Callaghan C, Dun B, Baron A, Barry P. Music’s relevance for children with cancer: music therapists’ qualitative clinical data-mining research. Soc Work Health Care 2013;52:125-43. https://doi.org/10.1080/00981389.2012.737904.
- Shrimpton BJ, Willis DJ, Tongs CD, Rolfo AG. Movie making as a cognitive distraction for paediatric patients receiving radiotherapy treatment: qualitative interview study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-001666.
- Weekes DP, Kagan SH, James K, Seboni N. The phenomenon of hand holding as a coping strategy in adolescents experiencing treatment-related pain. J Pediatr Oncol Nurs 1993;10:19-25. https://doi.org/10.1177/104345429301000105.
- Barnfather A, Stewart M, Magill-Evans J, Ray L, Letourneau N. Computer-mediated support for adolescents with cerebral palsy or spina bifida. Comput Inform Nurs 2011;29:24-33. https://doi.org/10.1097/NCN.0b013e3181f9db63.
- Brothers J, Harper GW, Fernandez MI, Hosek SG. Adolescent Trials Network for HIV/AIDS Interventions. EVOLUTION – taking charge and growing stronger: the design, acceptability, and feasibility of a secondary prevention empowerment intervention for young women living with HIV. AIDS Patient Care STDS 2014;28:33-42. https://doi.org/10.1089/apc.2013.0085.
- Gaysynsky A, Romansky-Poulin K, Arpadi S. ‘My YAP Family’: analysis of a Facebook group for young adults living with HIV. AIDS Behav 2015;19:947-62. https://doi.org/10.1007/s10461-014-0887-8.
- Griffiths C, Panteli N, Brunton D, Marder B, Williamson H. Designing and evaluating the acceptability of Realshare: an online support community for teenagers and young adults with cancer. J Health Psychol 2015;20:1589-601. https://doi.org/10.1177/1359105313519154.
- MacDonald K, Greggans A. ‘Cool friends’: an evaluation of a community befriending programme for young people with cystic fibrosis. J Clin Nurs 2010;19:2406-14. https://doi.org/10.1111/j.1365-2702.2010.03294.x.
- Nicholas DB, Fellner KD, Frank M, Small M, Hetherington R, Slater R, et al. Evaluation of an online education and support intervention for adolescents with diabetes. Soc Work Health Care 2012;51:815-27. https://doi.org/10.1080/00981389.2012.699507.
- Nicholas DB, Williams M, MacLusky IB. Evaluating group work within a summer camp intervention for children and adolescents with asthma. Soc Work Group 2009;32:209-21. https://doi.org/10.1080/01609510802527425.
- Romero SL. The development and impact of an online social networking community for adolescents with cystic fibrosis. Dissert Abst Int Sect B Sci Engin 2014;74.
- Stewart M, Letourneau N, Masuda JR, Anderson S, McGhan S. Impacts of online peer support for children with asthma and allergies: it just helps you every time you can’t breathe well’. J Pediatr Nurs 2013;28:439-52. https://doi.org/10.1016/j.pedn.2013.01.003.
- Stewart M, Masuda JR, Letourneau N, Anderson S, McGhan S. ‘I want to meet other kids like me’: support needs of children with asthma and allergies. Issues Compr Pediatr Nurs 2011;34:62-78. https://doi.org/10.3109/01460862.2011.572638.
- Stinson J, McGrath P, Hodnett E, Feldman B, Duffy C, Huber A, et al. Usability testing of an online self-management program for adolescents with juvenile idiopathic arthritis. J Med Internet Res 2010;12. https://doi.org/10.2196/jmir.1349.
- Stinson JN, Toomey PC, Stevens BJ, Kagan S, Duffy CM, Huber A, et al. Asking the experts: exploring the self-management needs of adolescents with arthritis. Arthritis Rheum 2008;59:65-72. https://doi.org/10.1002/art.23244.
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-21.
- Waytz A, Gray K, Epley N, Wegner DM. Causes and consequences of mind perception. Trends Cogn Sci 2010;14:383-8. https://doi.org/10.1016/j.tics.2010.05.006.
- Cutrona CE, Suhr JA. Controllability of stressful events and satisfaction with spouse support behaviors. Commun Res 1992;19:154-74. https://doi.org/10.1177/009365092019002002.
- Guidance for Commissioners of Child and Adolescent Mental Health Services. London: Joint Commissioning Panel for Mental Health; 2013.
- Thorley C. Education, Education, Mental Health: Supporting Secondary Schools to Play a Central Role in Early Intervention Mental Health Services. London: Institute for Public Policy Research; 2016.
- YoungMinds . Mental Health Statistics 2017. www.youngminds.org.uk/training_services/policy/mental_health_statistics (accessed 10 April 2017).
- The Five Year Forward View for Mental Health. London: NHS England; 2016.
- NHS Choices . Carers’ Breaks and Respite Care n.d. www.nhs.uk/Conditions/social-care-and-support-guide/Pages/breaks-for-carers-respite-care.aspx (accessed 21 March 2017).
- Richards DA, Hallberg IR. Complex Interventions in Health: An Overview of Research Methods. London: Routledge; 2015.
- Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Res Sch 2006;13.
- Whitaker R, Hendry M, Aslam R, Booth A, Carter B, Charles JM, et al. Intervention Now to Eliminate Repeat Unintended Pregnancy in Teenagers (INTERUPT): a systematic review of intervention effectiveness and cost-effectiveness, and qualitative and realist synthesis of implementation factors and user engagement. Health Technol Assess 2016;20. https://doi.org/10.3310/hta20160.
- Noyes J, Popay J. Directly observed therapy and tuberculosis: how can a systematic review of qualitative research contribute to improving services? A qualitative meta-synthesis. J Adv Nurs 2007;57:227-43. https://doi.org/10.1111/j.1365-2648.2006.04092.x.
- Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev 2013;10. https://doi.org/10.1002/14651858.CD010414.pub2.
- Thomas J, Harden A, Oakley A, Oliver S, Sutcliffe K, Rees R, et al. Integrating qualitative research with trials in systematic reviews. BMJ 2004;328:1010-12. https://doi.org/10.1136/bmj.328.7446.1010.
- Harn B, Parisi D, Stoolmiller M. Balancing fidelity with flexibility and fit: what do we really know about fidelity of implementation in schools?. Except Child 2013;79:181-93. https://doi.org/10.1177/001440291307900204.
- Frydenberg E, Lewis R, Bugalski K, Cotta A, McCarthy C, Luscombe-smith N, et al. Prevention is better than cure: coping skills training for adolescents at school. Educ Psych Pract 2004;20:117-34. https://doi.org/10.1080/02667360410001691053.
- Beresford P. User involvement, research and health inequalities: developing new directions. Health Soc Care Community 2007;15:306-12. https://doi.org/10.1111/j.1365-2524.2007.00688.x.
- Boote J, Baird W, Beecroft C. Public involvement at the design stage of primary health research: a narrative review of case examples. Health Policy 2010;95:10-23. https://doi.org/10.1016/j.healthpol.2009.11.007.
- Thompson J, Barber R, Ward PR, Boote JD, Cooper CL, Armitage CJ, et al. Health researchers’ attitudes towards public involvement in health research. Health Expect 2009;12:209-20. https://doi.org/10.1111/j.1369-7625.2009.00532.x.
- Thompson Coon J, Gwernan-Jones R, Moore D, Richardson M, Shotton C, Pritchard W, et al. End-user involvement in a systematic review of quantitative and qualitative research of non-pharmacological interventions for attention deficit hyperactivity disorder delivered in school settings: reflections on the impacts and challenges. Health Expect 2016;19:1084-97. https://doi.org/10.1111/hex.12400.
- Mockford C, Staniszewska S, Griffiths F, Herron-Marx S. The impact of patient and public involvement on UK NHS health care: a systematic review. Int J Qual Health Care 2012;24:28-3. https://doi.org/10.1093/intqhc/mzr066.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Schulz KF, Altman DG, Moher D. CONSORT Group . CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-18.
- Logic Model Development Guide. Battle Creek, MI: W. K. Kellogg Foundation; 2001.
- Williamson PR, Altman DG, Blazeby JM, Clarke M, Gargon E. The COMET (core outcome measures in effectiveness trials) initiative. Trials 2011;12. https://doi.org/10.1186/1745-6215-12-S1-A70.
- Slaski M, Cartwright S. Emotional intelligence training and its implications for stress, health and performance. Stress and Health 2003;19:233-9. https://doi.org/10.1002/smi.979.
Appendix 1 Search strategy used for review 1 with the Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) database
Search strategy
-
Chronic Disease/px [Psychology] (4269)
-
Neoplasms/px [Psychology] (15,475)
-
Diabetes Mellitus/px [Psychology] (2700)
-
Asthma/px [Psychology] (3457)
-
exp Respiratory Tract Diseases/px [Psychology] (12,446)
-
Cystic Fibrosis/px [Psychology] (854)
-
Cerebral Palsy/px [Psychology] (1058)
-
exp Epilepsy/px [Psychology] (7330)
-
exp Muscular Diseases/px [Psychology] (4743)
-
exp Endocrine System Diseases/px [Psychology] (14,089)
-
exp Immune System Diseases/px [Psychology] (33,503)
-
exp HIV Infections/px [Psychology] (16,557)
-
exp Cardiovascular Diseases/px [Psychology] (27,191)
-
exp Nervous System Diseases/px [Psychology] (128,905)
-
exp Skin Diseases/px [Psychology] (14,730)
-
exp Digestive System Diseases/px [Psychology] (11,110)
-
exp Hematologic Diseases/px [Psychology] (2320)
-
exp Otorhinolaryngologic Diseases/px [Psychology] (6693)
-
exp Stomatognathic Diseases/px [Psychology] (5416)
-
exp Eye Diseases/px [Psychology] (4290)
-
exp Pain/px [Psychology] (23,130)
-
Disabled Children/px [Psychology] (941)
-
((chronic* or longterm or long-term or “long standing” or physical) adj2 (condition* or ill* or disease* or disorder* or syndrome*)).ti,ab. (204,183)
-
(cancer* or neoplas* or tumor* or tumour* or malignan* or carcinoma* or “bone marrow” or leukaemia or leukemia).ti,ab. (2,710,274)
-
“spina bifada”.ti,ab. (458,788)
-
asthma*.ti,ab. (127,105)
-
(respiratory adj2 (illness* or disease* or condition*)).ti,ab. (32,642)
-
cystic fibrosis.ti,ab. (35,054)
-
cerebral palsy.ti,ab. (16,321)
-
quadriplegi*.ti,ab. (3604)
-
tetraplegi*.ti,ab. (3450)
-
diplegi*.ti,ab. (1995)
-
spinal cord injur*.ti,ab. (27,628)
-
muscular dystrophy.ti,ab. (17,776)
-
epilep*.ti,ab. (105,645)
-
seizure*.ti,ab. (932,77)
-
spina bifida.ti,ab. (5893)
-
(heart adj2 (condition* or disease* or disorder* or defect*)).ti,ab. (147,955)
-
(cardiac adj2 (condition* or disease* or disorder* or defect*)).ti,ab. (27,109)
-
(cardiovascular adj2 (condition* or disease* or disorder* or defect*)).ti,ab. (121,138)
-
(skin adj2 (condition* or disease* or disorder*)).ti,ab. (27,379)
-
eczema.ti,ab. (13,093)
-
(allergies or allergy).ti,ab. (60,164)
-
dermatitis.ti,ab. (44,017)
-
(gastrointestinal adj (disorder* or disease*)).ti,ab. (11,476)
-
((stomach or abdominal or gastrointestinal) adj pain).ti,ab. (41,843)
-
(bowel* adj2 inflammatory adj2 (condition* or disease* or illness*)).ti,ab. (31,340)
-
(liver adj (disease* or transplant*)).ti,ab. (104,995)
-
hepatitis.ti,ab. (175,155)
-
(disabilit* adj5 child*).ti,ab. (7935)
-
(human immunodeficiency virus or HIV).ti,ab. (262,555)
-
AIDS.ti,ab. (127,472)
-
(hyperthyroidism or hypothyroidism).ti,ab. (38,333)
-
an?emia.ti,ab. (113,434)
-
h?emophilia.ti,ab. (15,632)
-
sickle.ti,ab. (20,240)
-
((renal or kidney) adj (disease* or disorder*)).ti,ab. (87,486)
-
nephrotic syndrome.ti,ab. (15,366)
-
encephalomyelitis.ti,ab. (15,778)
-
chronic fatigue syndrome.ti,ab. (4389)
-
((cleft or palate) adj lip).ti,ab. (10,349)
-
craniofacial.ti,ab. (17,695)
-
(deaf or deafness).ti,ab. (24,812)
-
(hearing adj (defect* or disorder*)).ti,ab. (1915)
-
blindness.ti,ab. (20,927)
-
((vision or visually or visual) adj (impaired or impairment*)).ti,ab. (9360)
-
((persistent or chronic or recurring or frequent) adj (headache* or migraine*)).ti,ab. (3532)
-
chronic pain.ti,ab. (23,794)
-
fibromyalgia.ti,ab. (7465)
-
medically unexplained symptoms.ti,ab. (505)
-
(spinal adj injur*).ti,ab. (4324)
-
or/1-71 (4,906,406)
-
(child or children*).ti,ab. (959,407)
-
(adolescent or adolescents).ti,ab. (174,139)
-
teen*.ti,ab. (23,472)
-
(young adj (adult* or people)).ti,ab. (81,908)
-
youth*.ti,ab. (46,618)
-
73 or 74 or 75 or 76 or 77 (1,146,540)
-
exp Mental Disorders/pc, rh, th [Prevention & Control, Rehabilitation, Therapy] (219,183)
-
exp Self-Injurious Behavior/pc, th [Prevention & Control, Therapy] (10,462)
-
(mental adj (health or illness* or disorder* or distress or problem*)).ti,ab. (123,672)
-
(psychiatric adj (illness* or disorder* or difficulties or problems or distress or adjustment)).ti,ab. (37,713)
-
(psychological adj (illness* or disorder* or difficulties or problems or distress)).ti,ab. (18,705)
-
psychopathology.ti,ab. (23,584)
-
(depression or depressed or depressive).ti,ab. (321,415)
-
adjustment disorders.ti,ab. (578)
-
(anxiety or anxious).ti,ab. (131,581)
-
(behavio*ral adj (condition* or disturb* or disorder*)).ti,ab. (7142)
-
mood disorder*.ti,ab. (12,037)
-
(emotional adj (disorder* or distress or adjustment or problem* or health)).ti,ab. (11,716)
-
psychosocial adjustment.ti,ab. (1720)
-
internali?ing.ti,ab. (5832)
-
(self adj (harm* or injur* or mutilation)).ti,ab. (7223)
-
bipolar.ti,ab. (47,112)
-
conduct disorder*.ti,ab. (3658)
-
externali?ing.ti,ab. (5649)
-
oppositional defiant.ti,ab. (1599)
-
((disruptive or challenging or antisocial) adj behavio?r).ti,ab. (5296)
-
eating disorder*.ti,ab. (13,689)
-
anorexia.ti,ab. (23,853)
-
bulimia.ti,ab. (6163)
-
mutism.ti,ab. (1712)
-
obsess*.ti,ab. (15,553)
-
panic disorder*.ti,ab. (8123)
-
phobia*.ti,ab. (7304)
-
post traumatic stress disorder.ti,ab. (6641)
-
PTSD.ti,ab. (14,726)
-
(psychosis or psychotic).ti,ab. (44,807)
-
personality disorder*.ti,ab. (15,416)
-
mania.ti,ab. (8238)
-
schizophrenia.ti,ab. (83,194)
-
(self harm or self injur*).ti,ab. (5930)
-
(suicide or suicidal).ti,ab. (54,111)
-
or/79-113 (896,398)
-
(substance adj (misuse or abuse)).ti,ab. (20,418)
-
((drug or alcohol) adj (addiction or abuse or misuse)).ti,ab. (33,943)
-
115 or 116 (51,906)
-
12 or 49 or 51 or 52 (486,920)
-
117 not 118 (46,257)
-
114 or 119 (917,885)
-
randomized controlled trial.pt. (404,549)
-
controlled clinical trial.pt. (90,003)
-
exp Randomized Controlled Trials as Topic/(101,462)
-
randomi?ed.ti,ab. (426,544)
-
randomly.ab. (240,673)
-
trial.ti,ab. (407,141)
-
groups.ab. (1,507,035)
-
or/121-127 (2,247,880)
-
72 and 78 and 120 and 128 (4473)
Appendix 2 Search strategy used for review 1 economic search with the Ovid EMBASE database
Search strategy
-
exp childhood disease/cn, dm, rh, th [Congenital Disorder, Disease Management, Rehabilitation, Therapy] (10,053)
-
diabetes mellitus/rh, th [Rehabilitation, Therapy] (13,071)
-
asthma/rh, th [Rehabilitation, Therapy] (10,837)
-
respiratory tract disease/rh, th [Rehabilitation, Therapy] (2064)
-
cystic fibrosis/dm, rh, th [Rehabilitation, Therapy] (3304)
-
cerebral palsy/dm, rh, th [Rehabilitation, Therapy] (4379)
-
epilepsy/rh, th [Rehabilitation, Therapy] (5014)
-
heart disease/dm, rh, th [Rehabilitation, Therapy] (4816)
-
skin disease/rh, th [Rehabilitation, Therapy] (3943)
-
muscle disease/rh, th [Rehabilitation, Therapy] (838)
-
endocrine disease/rh, th [Rehabilitation, Therapy] (428)
-
neurologic disease/rh, th [Rehabilitation, Therapy] (4281)
-
hematologic disease/rh, th [Rehabilitation, Therapy] (1991)
-
mouth disease/rh, th [Rehabilitation, Therapy] (1958)
-
ear disease/rh, th [Rehabilitation, Therapy] (341)
-
eye disease/rh, th [Rehabilitation, Therapy] (2159)
-
handicapped child/ (7141)
-
((chronic* or longterm or long-term or “long standing” or physical) adj2 (condition* or ill* or disease* or disorder* or syndrome*)).ti,ab. (295,589)
-
(cancer* or neoplas* or tumor* or tumour* or malignan* or carcinoma* or “bone marrow” or leukaemia or leukemia).ti,ab. (3,623,580)
-
diabet*.ti,ab. (684,993)
-
asthma*.ti,ab. (185,088)
-
(respiratory adj2 (illness* or disease* or condition*)).ti,ab. (44,620)
-
cystic fibrosis.ti,ab. (50,040)
-
cerebral palsy.ti,ab. (23,043)
-
quadriplegi*.ti,ab. (4721)
-
tetraplegi*.ti,ab. (4658)
-
diplegi*.ti,ab. (2764)
-
spinal cord injur*.ti,ab. (36,614)
-
muscular dystrophy.ti,ab. (22,965)
-
epilep*.ti,ab. (157,765)
-
seizure*.ti,ab. (140,681)
-
spina bifida.ti,ab. (7573)
-
(heart adj2 (condition* or disease* or disorder* or defect*)).ti,ab. (204,821)
-
(cardiac adj2 (condition* or disease* or disorder* or defect*)).ti,ab. (39,924)
-
(cardiovascular adj2 (condition* or disease* or disorder* or defect*)).ti,ab. (178,430)
-
(skin adj2 (condition* or disease* or disorder*)).ti,ab. (40,227)
-
eczema.ti,ab. (19,576)
-
(allergies or allergy).ti,ab. (94,945)
-
dermatitis.ti,ab. (62,293)
-
(gastrointestinal adj (disorder* or disease*)).ti,ab. (16,480)
-
((stomach or abdominal or gastrointestinal) adj pain).ti,ab. (67,844)
-
(bowel* adj2 inflammatory adj2 (condition* or disease* or illness*)).ti,ab. (50,014)
-
(liver adj (disease* or transplant*)).ti,ab. (162,025)
-
hepatitis.ti,ab. (238,818)
-
(disabilit* adj5 child*).ti,ab. (10,810)
-
(human immunodeficiency virus or HIV).ti,ab. (325,933)
-
AIDS.ti,ab. (146,763)
-
(hyperthyroidism or hypothyroidism).ti,ab. (51,321)
-
an?emia.ti,ab. (160,099)
-
h?emophilia.ti,ab. (24,268)
-
sickle.ti,ab. (27,249)
-
((renal or kidney) adj (disease* or disorder*)).ti,ab. (125,441)
-
nephrotic syndrome.ti,ab. (19,220)
-
encephalomyelitis.ti,ab. (19,754)
-
chronic fatigue syndrome.ti,ab. (5809)
-
((cleft or palate) adj lip).ti,ab. (11,586)
-
craniofacial.ti,ab. (21,025)
-
(deaf or deafness).ti,ab. (30,007)
-
(hearing adj (defect* or disorder*)).ti,ab. (2285)
-
blindness.ti,ab. (26,167)
-
((vision or visually or visual) adj (impaired or impairment*)).ti,ab. (13,041)
-
((persistent or chronic or recurring or frequent) adj (headache* or migraine*)).ti,ab. (6194)
-
chronic pain.ti,ab. (36,382)
-
fibromyalgia.ti,ab. (12,217)
-
medically unexplained symptoms.ti,ab. (666)
-
(spinal adj injur*).ti,ab. (5422)
-
or/1-66 (6,477,448)
-
(child or children*).ti,ab. (1,248,757)
-
(adolescent or adolescents).ti,ab. (232,830)
-
teen*.ti,ab. (31,160)
-
(young adj (adult* or people)).ti,ab. (109,824)
-
youth*.ti,ab. (58,783)
-
68 or 69 or 70 or 71 or 72 (1,487,904)
-
mental disease/dm, pc, rh, th [Disease Management, Prevention, Rehabilitation, Therapy] (30,502)
-
automutilation/dm, pc, rh, th [Disease Management, Prevention, Rehabilitation, Therapy] (1490)
-
depression/dm, pc, rh, th [Disease Management, Prevention, Rehabilitation, Therapy] (28,465)
-
exp anxiety disorder/dm, rh, th [Disease Management, Rehabilitation, Therapy] (22,583)
-
exp eating disorder/dm, pc, rh, th [Disease Management, Prevention, Rehabilitation, Therapy] (6782)
-
(mental* adj2 (ill* or disorder*)).ti,ab. (71,484)
-
(psychiatric adj (illness* or disorder* or difficulties or problems or distress or adjustment)).ti,ab. (55,442)
-
(psychological adj (illness* or disorder* or difficulties or problems or distress)).ti,ab. (25,749)
-
psychopathology.ti,ab. (32,344)
-
(depression or depressed or depressive).ti,ab. (440,151)
-
adjustment disorders.ti,ab. (904)
-
(anxiety or anxious).ti,ab. (193,926)
-
(behavio*ral adj (condition* or disturb* or disorder*)).ti,ab. (10,574)
-
mood disorder*.ti,ab. (18,825)
-
(emotional adj (disorder* or distress or adjustment or problem* or health)).ti,ab. (16,428)
-
psychosocial adjustment.ti,ab. (2176)
-
internali?ing.ti,ab. (7243)
-
(self adj (harm* or injur* or mutilation)).ti,ab. (9543)
-
bipolar.ti,ab. (68,758)
-
conduct disorder*.ti,ab. (4850)
-
externali?ing.ti,ab. (7009)
-
oppositional defiant.ti,ab. (2086)
-
((disruptive or challenging or antisocial) adj behavio?r).ti,ab. (6916)
-
eating disorder*.ti,ab. (19,058)
-
anorexia.ti,ab. (33,225)
-
bulimia.ti,ab. (8250)
-
mutism.ti,ab. (2429)
-
obsess*.ti,ab. (22,459)
-
panic disorder*.ti,ab. (10,807)
-
phobia*.ti,ab. (10,326)
-
post traumatic stress disorder.ti,ab. (9149)
-
PTSD.ti,ab. (20,214)
-
(psychosis or psychotic).ti,ab. (69,543)
-
personality disorder*.ti,ab. (21,402)
-
mania.ti,ab. (12,209)
-
schizophrenia.ti,ab. (118,359)
-
(self harm or self injur*).ti,ab. (7961)
-
(suicide or suicidal).ti,ab. (70,596)
-
(substance adj (misuse or abuse)).ti,ab. (27,665)
-
((drug or alcohol) adj (addiction or abuse or misuse)).ti,ab. (47,759)
-
or/74-111 (998,337)
-
112 or 113 (72,030)
-
44 or 46 or 47 (618,316)
-
115 not 116 (64,343)
-
114 or 117 (1,041,237)
-
67 and 73 and 118 (23,307)
-
health economics (35,400)
-
exp Economic Evaluation (241,708)
-
exp Health Care Cost (232,673)
-
pharmacoeconomics (6278)
-
(econom* or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic*).ti,ab. (733,411)
-
(expenditure$ not energy).ti,ab. (28,398)
-
(value adj2 money).ti,ab. (1693)
-
budget*.ti,ab. (28,298)
-
120 or 121 or 122 or 123 or 124 or 125 or 126 or 127 (959,359)
-
119 and 128 (1258)
-
limit 129 to yr = “2015 -Current” (129)
Appendix 3 List of websites searched
-
Mental Health Foundation: www.mentalhealth.org.uk/
-
YoungMinds: www.youngminds.org.uk/
-
Department of Child and Adolescent Mental Health Services at Great Ormond Street Hospital: www.gosh.nhs.uk/medical-information/clinical-specialties/child-and-adolescent-mental-health-services-camhs-information-parents-and-visitors/research-and-publications
-
Child & Adolescent Mental Health Services Research Unit: www.cpcs.org.uk/index.php?page = high-needs-project
-
National Institute for Health Research Clinical Research Network: www.crn.nihr.ac.uk/mentalhealth/about-mental-health-research/children-and-young-peoples-mental-health-research/
-
National Institute for Mental Health. Child and Adolescent Mental Health: www.nimh.nih.gov/health/topics/child-and-adolescent-mental-health/index.shtml#part_152583
-
Royal College of Physicians Child and Adolescent Mental Health Services Resource Library: www.rcpsych.ac.uk/quality/qualityandaccreditation/childandadolescent/communitycamhsqncc/camhsresourcelibrary.aspx
-
National Child and Maternal Health Intelligence Network: www.chimat.org.uk/camhs
-
National Children’s Bureau: www.ncb.org.uk/healthy-care/useful-links/mental-health-and-emotional-well-being
-
Association for Children’s Mental Health: www.acmh-mi.org/get-information/
-
Substance Abuse and Mental Health Services Administration: www.samhsa.gov/data/
-
American Academy of Pediatrics: www.aap.org/en-us/professional-resources/Research/Pages/Research.aspx
-
Child and Youth Health: www.cyh.com/HealthTopics/HealthTopicDetails.aspx
-
The King’s Fund. Mental Health: www.kingsfund.org.uk/topics/mental-health
-
Young Epilepsy: www.youngepilepsy.org.uk/
-
Epilepsy Society: www.epilepsysociety.org.uk/young-people-and-epilepsy#.Vz8FjuTAN_A
-
Epilepsy Action: www.epilepsy.org.uk/info/young-people
-
Cancer Research UK: www.cancerresearchuk.org/health-professional/cancer-statistics/teenagers-and-young-adults-cancers
-
Macmillan: www.macmillan.org.uk/cancerinformation/teensandyoungadults/infoforteensandyoungadults.aspx
-
Teenage Cancer Trust: www.teenagecancertrust.org/get-help/ive-got-cancer/stories-others
-
Teenagers and Young Adults with Cancer: www.tyac.org.uk/
-
Sickle Cell and Young Stroke Survivors: www.scyss.org/
-
Sickle Cell Society: http://sicklecellsociety.org/resources/did-you-know-age-11–16-an-information-booklet-for-young-people/
-
AVERT (HIV): www.avert.org/living-with-hiv/health-wellbeing/being-young-positive
-
Young People with AIDS: www.amfar.org/about-hiv-and-aids/young-people-and-hiv/young-people-and-hiv-aids/
-
Pozitude: www.pozitude.co.uk/
-
Children and Young People HIV network: www.ncb.org.uk/hiv
-
Child’s Brain Injury Trust: http://childbraininjurytrust.org.uk/how-we-help/young-people/
-
Stroke Association: www.stroke.org.uk/finding-support/information-about-stroke-childhood
-
National Institute of Neurological Disorders and Stroke: www.ninds.nih.gov/disorders/tbi/detail_tbi.htm
-
Cerbera: http://w3.cerebra.org.uk/
-
Association of Young People with ME: www.ayme.org.uk/
-
Away with Pain: www.awaywithpain.co.uk/young-people
-
Fibromyalgia: www.fmauk.org/information-packs-mainmenu-58/booklet-mainmenu-135/232-children-and-young-people; www.fmscommunity.org/paediatric.htm
-
Healing Well: www.healingwell.com/community/default.aspx?f = 24&m = 1813258
-
Arthritis Research UK: www.arthritisresearchuk.org/arthritis-information/young-people.aspx
-
Youth Health: www.healthtalk.org/young-peoples-experiences/arthritis/what-arthritis-and-what-are-early-symptoms
-
Arthritis Care: www.arthritiscare.org.uk/managing-arthritis/children-with-arthritis
-
CLIC Sargent: www.clicsargent.org.uk/content/help-and-support
-
Cerebral Palsy: www.cerebralpalsy.org/information/child-care
-
Asthma UK: www.asthma.org.uk/research/
-
British Lung Foundation: www.blf.org.uk/what-we-do/research
-
Diabetes UK: www.diabetes.org.uk/Research/
-
British Deaf Association: www.bda.org.uk/publications
-
Mental Elf: www.nationalelfservice.net/
URLs were last accessed in March 2017.
Appendix 4 Categories of intervention, their definition and included studies that use them
| Intervention | Definition | Studies |
|---|---|---|
| CBT | Structured programme that aims to identify negative thought processes, which may be triggered by certain situations or physical feelings, and learn to think and act on them in a positive way (www.nhs.uk/Conditions/Cognitive-behavioural-therapy/Pages/How-does-it-work.aspx) | 83,84,124–126,130,145 |
| Parenting programmes | Family interventions aiming to reduce child behavioural and emotional difficulties by targeting improvement in parenting skills, knowledge and confidence (from Brown et al.128) | 118,131 |
| Parenting programmes with ACT | As above, but with the addition of ACT. ACT is a variation of CBT incorporating mindfulness techniques that aim to increase psychological flexibility and decrease experiential avoidance (from Brown et al.128) | 128,131 |
| Palliative care | Interventions that focus on making the patient as comfortable as possible by helping to manage pain and symptoms, and provide psychological, social and spiritual support for the patient, their family or their carers. Commonly thought of as end of life care, but this is not always true (www.nhs.uk/Planners/end-of-life-care/Pages/what-it-involves-and-when-it-starts.aspx) | 123,137 |
| Group play therapy | Interventions in which children and therapists use games and play activities as the main medium of communication, with the aim of achieving a psychological interaction that conveys therapeutic benefit (from Wang et al.138) | 133,135,138 |
| EIT | Programmes designed to improve emotional intelligence, which is the skills with which to perceive and regulate emotions, particularly with regard to the development of stress (Slaski and Cartwright, 2003245) | 132,134 |
| Relaxation | Interventions using one or more generic techniques for relaxation, including breathing exercises, progressive muscle relaxation or guided imagery, to reduce psychological distress | 119,139 |
| SMT | A structured programme aiming to improve coping with stress. Although aspects of other interventions may be used (e.g. CBT/cognitive restructuring), they form one of an array of coping strategies. Other SMTs may involve goal setting, medical adherence, emotional control, etc. | 120,122 |
| Music therapy | Interventions in which music is delivered by therapists in a way that provides psychosocial support. Involves creating music with instruments or voice, and is distinct from passively listening to music (www.bamt.org/) | 136 |
| Massage therapy | Manual manipulation of soft body tissues (muscle, connective tissue, tendons and ligaments) to enhance a person’s health and well-being (www.nwhealth.edu/school-of-massage-therapy/massage-therapy-definition/) | 121 |
| Heart rate variability biofeedback | Combines the use of relaxation techniques with non-invasive technology providing real-time feedback on heart rate (from Yetwin127) | 127 |
| Resistance training | A graded exercise programme involving sets of lifting, pushing or pulling activities (including free weights/objects, resistance training machines or participant body weight) | 129 |
Appendix 5 Categories of intervention, and details of delivery and adapted components
| Intervention | Study author and year of publication | Content adapted to sample LTC? | Notes on delivery (e.g. was it manual based, flexible delivery, individually focused?) | Details of adapted components |
|---|---|---|---|---|
| CBT (CBI) | Martinović et al., 200683 | No | No manual. Delivered ‘as part of individual treatment plan’, but no details | Individual treatment plan aimed at distorted automatic thoughts related to negative depressive thinking |
| CBT (TAPS) | Masia-Warner et al., 2011124 | Yes | Modified from ‘Coping Cat’. Option to receive CBT at one of two locations | Jointly addresses anxiety and physical symptoms. Identifies contexts in which symptoms occur, targets fears related to physical pain and anxiety-inducing situations |
| CBT (TAPS + IBD) | Reigada et al., 2015125 | Yes | Adapted from TAPS. Delivered to all from a treatment manual | Specifically focuses on interaction of anxiety and IBD symptoms. Includes content designed to assist CYP with academic and social activities when physical symptoms present, as well as IBD management and reacting positively to pain. Parents encouraged to foster independence in the young person |
| CBT (BOC) | Serlachius et al., 2014130 | Yes | Based on manualised BOC, with added components. Not explicit, but diaries and goals probably individualised | Diabetes mellitus-specific components were added to the standard BOC intervention to specifically address the needs of CYP with T1DM. Added components: conflict resolution, health-behaviour diaries to support T1DM management and goals, positive reinforcement and modelling to increase T1DM-related self-efficacy, T1DM-specific information and resources. |
| CBT (PASCET-PI) | Szigethy et al., 200784 | Yes | Based on PASCET. Allowed telephone delivery | Adaptation of PASCET, with addition of physical illness narrative. Targets depression, but has specific content related to IBD to improve cognitions and behaviours related to IBD. Includes information about IBD and techniques for coping with abdominal pain, identifying negative cognitions about IBD and eliciting and later reassessing the young person’s physical illness narrative (belief about how IBD influences their life) |
| CBT (PASCET-PI) | Szigethy et al., 2014126 | Yes | Content was simplified or made more child friendly for younger participants (age 9–13 years). More telephone delivery than 2007 version – allowed greater flexibility for participants | As above, but specifically states that the programme was ‘tailored to a youth’s individual developmental stage’. This appears to be manifested in simplifying materials for 9–13 year olds – in the CBT group, ‘handouts and practice assignments were simplified; pictures were used to illustrate concepts; skills became part of games; and parents were involved after each individual session to review practice assignments’; the control group received non-directive supportive therapy in which ‘conversations with participants [. . .] were conducted during games, and parents were involved after each session to review their child’s progress’. They also considered the delivery of CBT over the telephone when possible, as a response to the wide catchment area of participating families |
| CBT (ACT) | Wicksell et al., 2009145 | Yes | Participants received intervention individually. Unclear whether or not all received exactly the same content – no manual | Entire intervention focused on changing CYP’s response to chronic pain. Included thinking about pain differently and trying to accept it but not let it limit activities, and thus reduce avoidant behaviours |
| Parenting programme (SSTP) | Whittingham et al., 2014131 | No | Based on SSTP manual | Parenting skills for CYP with behavioural problems and a disability. No mention of content specifically related to LTC (cerebral palsy) |
| Parenting programme (Triple P) | Westrupp et al., 2015118 | No | Based on Triple P manual | Standard Triple P. No diabetes mellitus-specific content |
| Parenting programme with ACT (SSTP + ACT) | Whittingham et al., 2014131 | No | Based on SSTP manual, but with added ACT | As with SSTP,131 but with additional ACT exercises designed to improve parent coping with stress and improvement in psychological skills. ACT contains no description of any content specifically related to having a young person with a LTC (cerebral palsy) |
| Parenting programme with ACT (SSTP + ACT) | Brown et al., 2014128 | No | Based on SSTP manual, but with added ACT | No content was adapted specifically to the LTC (ABI) |
| Palliative care (ACP) | Lyon et al., 2013123 | No | Structured delivery based on Lyon family-centred ACP. Five Wishes exercise was part of shared decision-making for under 18s | Only LTC-specific component was increasing understanding of the medical condition. In this study it was cancer, but could be any condition. Remaining content not LTC specific |
| Palliative care (Make a Wish) | Shoshani et al., 2015137 | No | All CYP interviewed at home. No variation in interview | No suggestion that the intervention would be different for other LTCs. In addition, the CYP determine their own intervention content |
| Group play therapy | Nekah et al., 2015133 | No | No manual. Includes four sessions of ‘flexible play’, which sounds like free play. Little detail provided | Nothing suggested by data extraction form (check translation). Focus appears to be on mental health, not LTC |
| Group play therapy | Wang et al., 2012138 | No | No manual. No suggestion of flexibility in delivery | Nothing to suggest that there is LTC-specific content |
| Group play therapy | Zareapour et al., 2009135 | No | Little detail, no manual | Not enough detail, but sounds like generic play |
| EIT | Ashori et al., 2013132 | No | No manual, structured intervention. No mention of how content was adapted for delivery to deaf children | No LTC-specific content |
| EIT | Pourmohamadreza-Tajrishi et al., 2013134 | No | No manual, structured intervention. No mention of how content was adapted for delivery to deaf children | As in Ashouri et al., 2013132 |
| Relaxation | Bignall et al., 2015119 | Yes | Script developed to train all CYP to practise exercises. Home-based practise | Included asthma-specific guided imagery. Breathing exercises and PMR were not LTC specific |
| Relaxation | Yang et al., 2004139 | No | All CYP listened to same audio tape to guide relaxation at home | PRM only, no mention of asthma-specific content |
| SMT | Boardway et al., 1993120 | Yes | Structured intervention, but no manual. Individual diet plans introduced towards end of intervention | Included content around the identification and management of diabetes mellitus-specific stressors. Included a 3-month programme focusing on treatment regimen adherence. Additional content focused on diet plans, insulin injection and timing related to meals, etc. |
| SMT | Hains et al., 2000122 | No | Structured intervention, but no manual. All participants receive the same intervention | Although activities such as identifying recent stressors would inevitably focus on LTC stressors, there is nothing to suggest that activities could not be carried out in samples with other LTCs |
| Music therapy | Bufalini 2009136 | No | All CYP go through the same process, but choose/make their own music | Music therapy was arranged around a painful procedure for cancer. Could be applied for painful procedures related to other LTCs |
| Massage therapy | Diego et al., 2001121 | No | Same intervention for all | Although massage therapy was proposed to have physiological benefits for people infected with HIV (boosting immune function), the same massage could be delivered to CYP with other LTCs |
| Heart rate variability biofeedback | Yetwin 2011127 | No | Manualised protocol. No flexibility | Nothing to suggest that intervention could not be applied to other LTCs |
| Resistance training | Gordon 2010129 | No | All performed same exercises, but progressed in difficulty according to individual ability | General exercise programme set to a level appropriate for the participants |
Appendix 6 Non-standardised meta-analyses
Non-standardised meta-analyses of outcomes following parenting programme with acceptance and commitment therapy intervention
Brown et al. 128 and Whittingham et al. 131 used the same outcome measures to assess child behavioural problems, parenting styles and parent mental health; therefore, non-standardised mean difference meta-analyses were performed on these outcomes (Figures 25–32). There was statistically significant improvements for the intensity (mean difference 27.5 points, 95% CI 13.4 to 41.6 points; p < 0.001) and number (mean difference 6.58 points, 95% CI 1.50 to 11.7 points; p = 0.01). Emotional difficulties improved by a mean of 1.21 points on the SDQ: Emotional Symptoms Subscale (95% CI 0.38 to 2.05 points; p = 0.004). There were also statistically significant improvements in parent mental health, as measured by the three Depression, Anxiety, Stress Scale subscales: anxiety (mean difference 3.26 points, 95% CI 0.71 to 5.81 points; p = 0.01); depression (mean difference 3.75 points, 95% CI 0.30 to 7.21 points; p = 0.03); and stress (mean difference 5.24 points, 95% CI 2.13 to 8.35 points; p = 0.001). There were similar statistically significant improvements in parenting laxness (mean difference 0.79 points, 95% CI 0.36 to 1.21 points; p ≤ 0.001) and over-reactivity (mean difference 0.77 points, 95% CI 0.43 to 1.11 points; p ≤ 0.001). There was < 25% heterogeneity for all outcomes, with the exception of the ECBI: Problems Scale, for which heterogeneity was moderate but not statistically significant (I2 = 59.7%; p = 0.12).
FIGURE 25.
Forest plot showing the results of non-standardised meta-analysis of the effects of parenting programmes with ACT on the intensity of child behavioural problems post intervention for included studies. MD, mean difference.
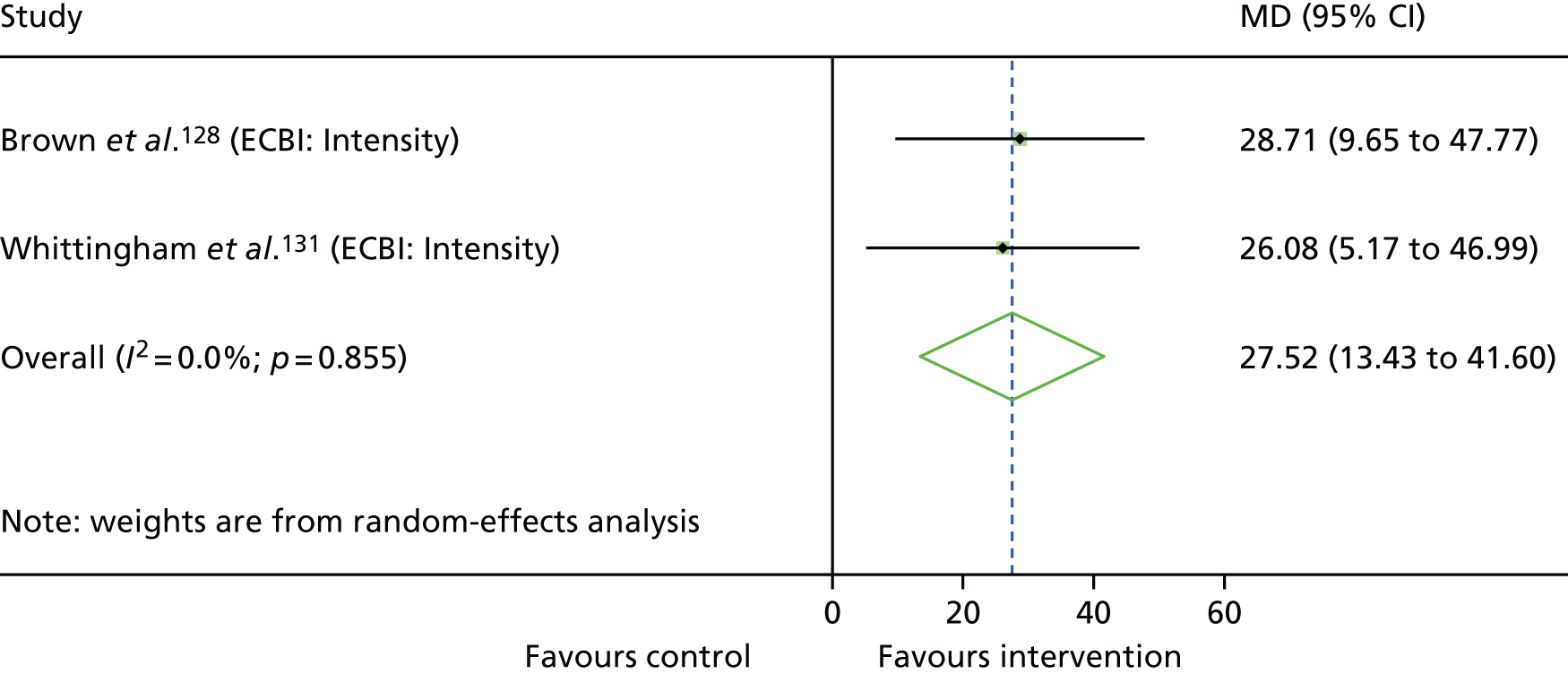
FIGURE 26.
Forest plot showing the results of non-standardised meta-analysis of the effects of parenting programmes with ACT on the number of child behavioural problems post intervention for included studies. MD, mean difference.
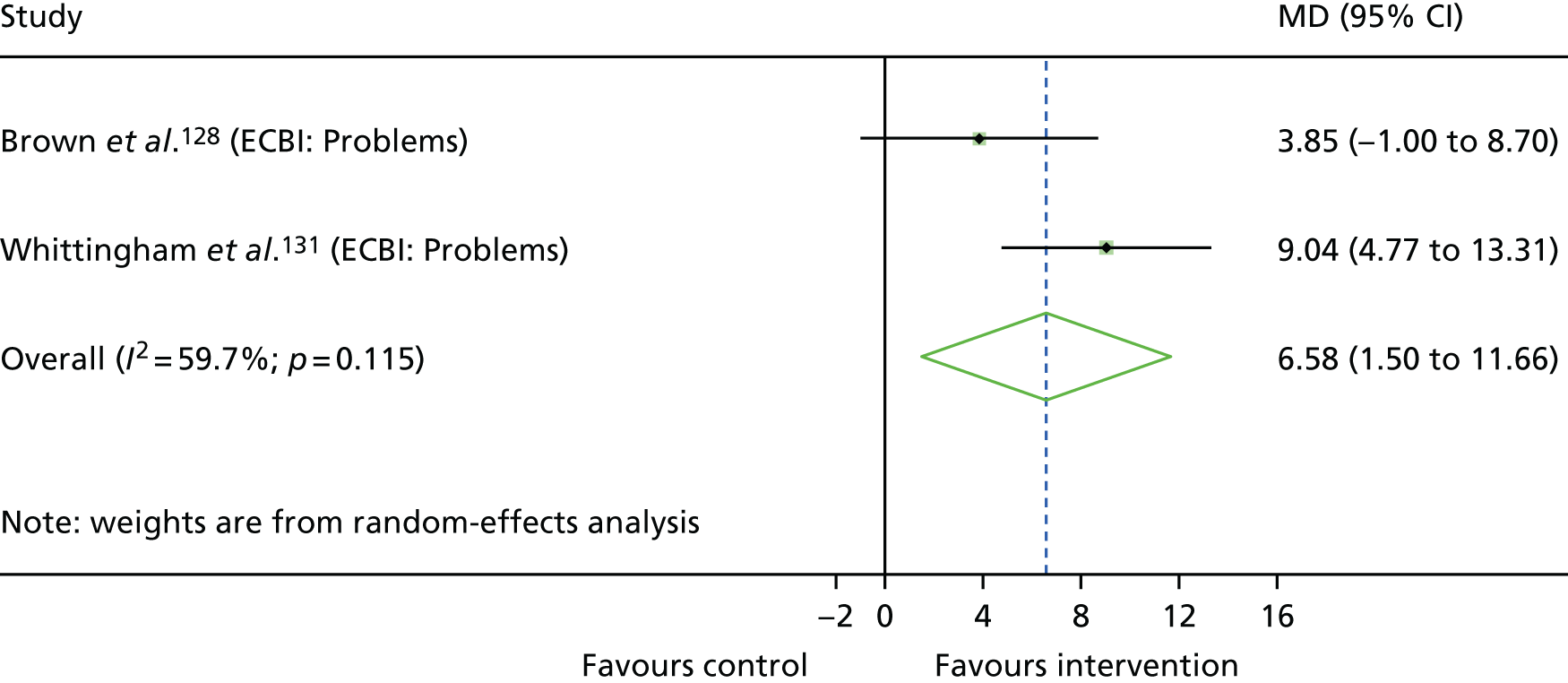
FIGURE 27.
Forest plot showing the results of non-standardised meta-analysis of the effects of parenting programmes with ACT on child emotional problems post intervention for included studies. MD, mean difference.
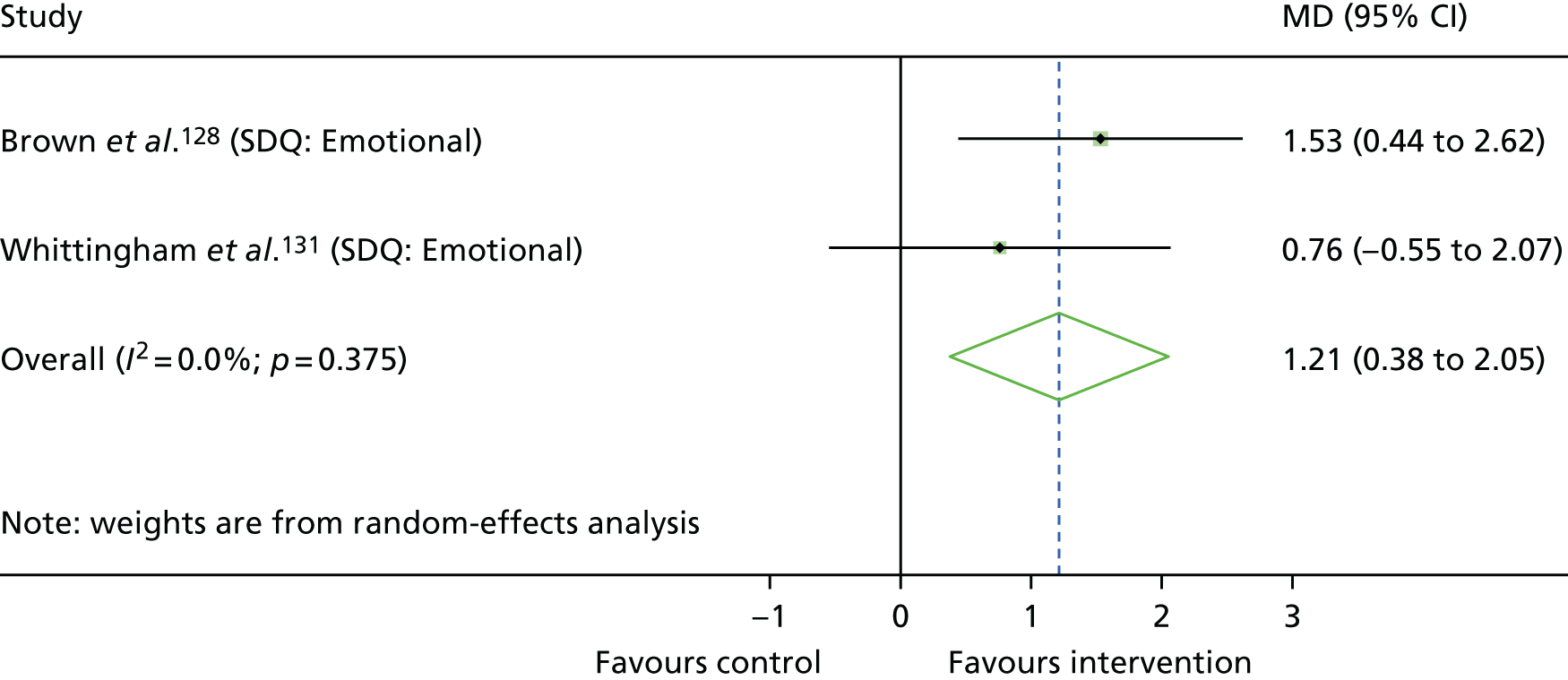
FIGURE 28.
Forest plot showing the results of non-standardised meta-analysis of the effects of parenting programmes with ACT on parent anxiety post intervention for included studies. DASS, Depression, Anxiety, Stress Scale; MD, mean difference.
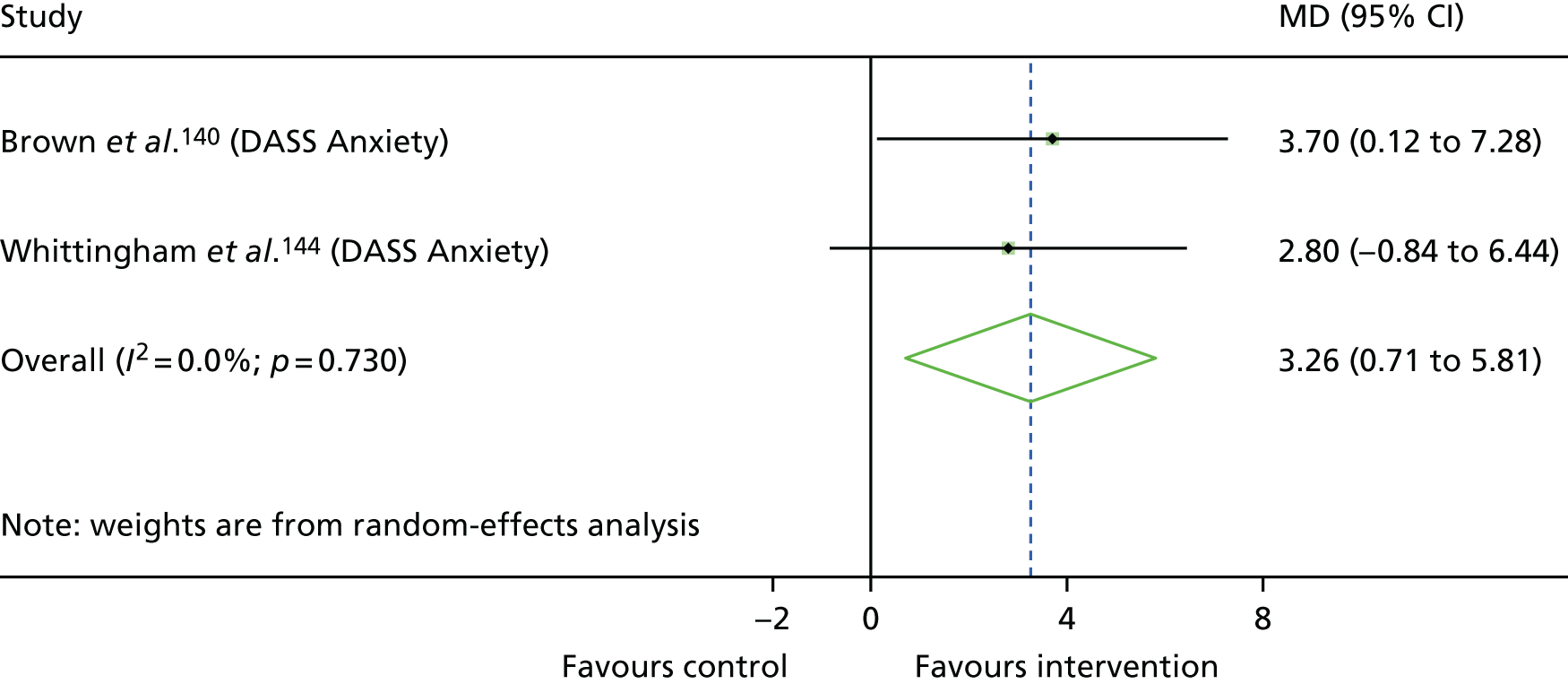
FIGURE 29.
Forest plot showing the results of non-standardised meta-analysis of the effects of parenting programmes with ACT on parent depression post intervention for included studies. DASS, Depression, Anxiety, Stress Scale; MD, mean difference.
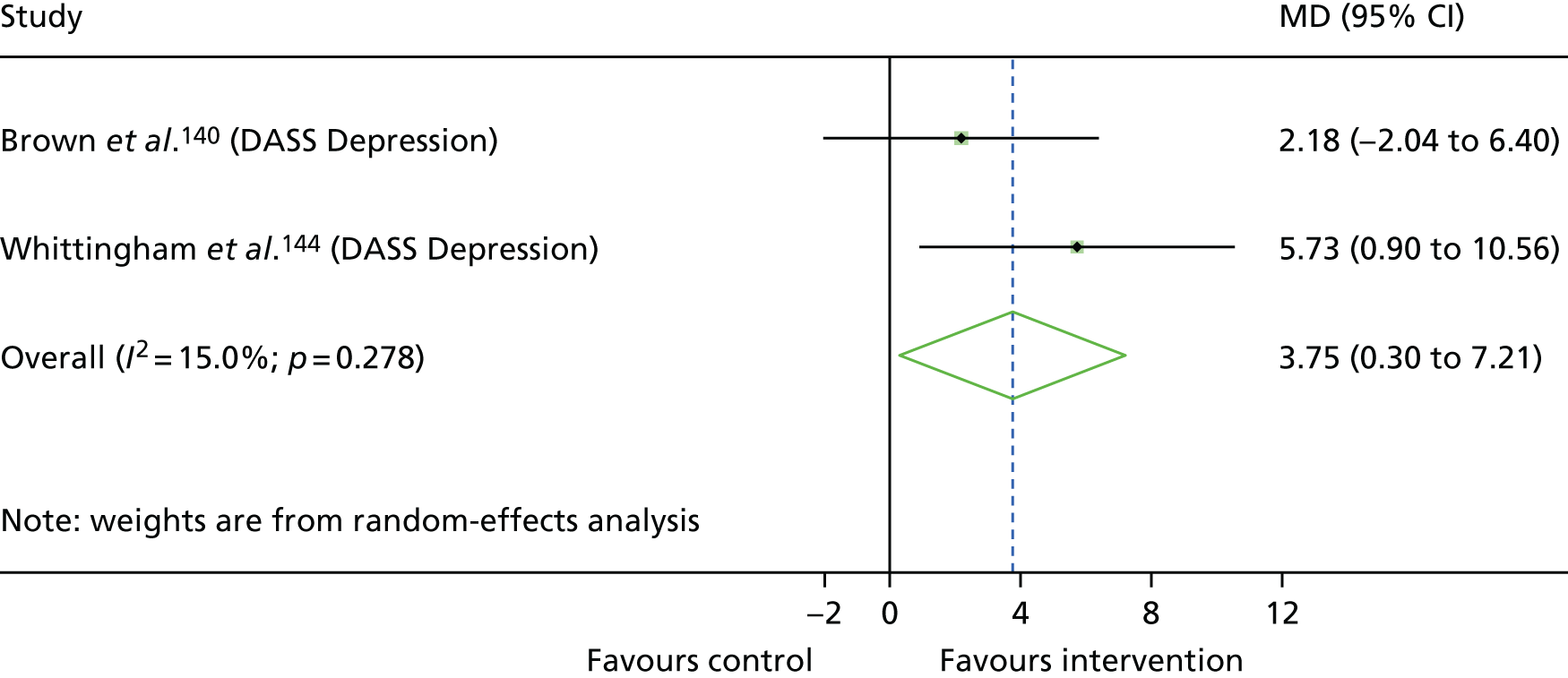
FIGURE 30.
Forest plot showing the results of non-standardised meta-analysis of the effects of parenting programmes with ACT on parent stress post intervention for included studies. DASS, Depression, Anxiety, Stress Scale; MD, mean difference.
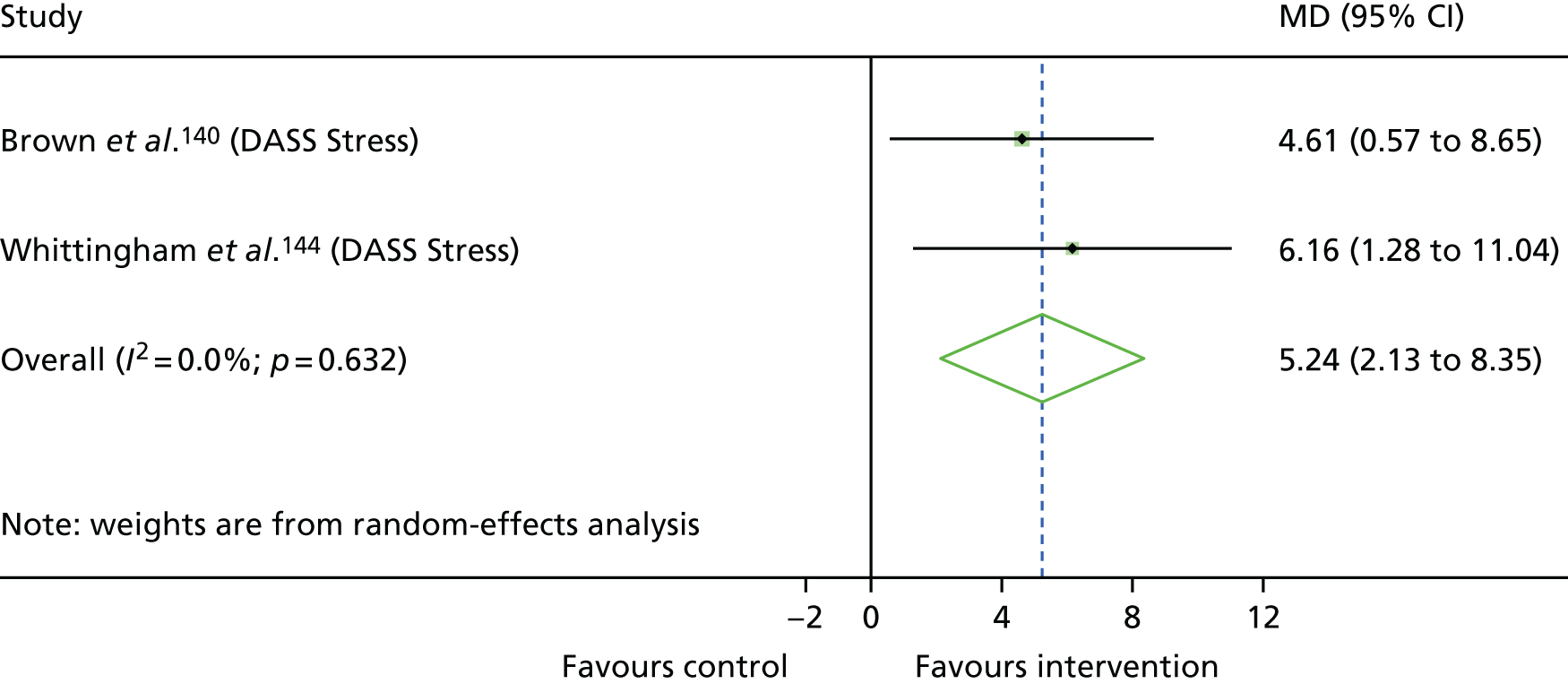
FIGURE 31.
Forest plot showing the results of non-standardised meta-analysis of the effects of parenting programmes with ACT on parenting laxness post intervention for included studies. MD, mean difference; PS, Parenting Scale.
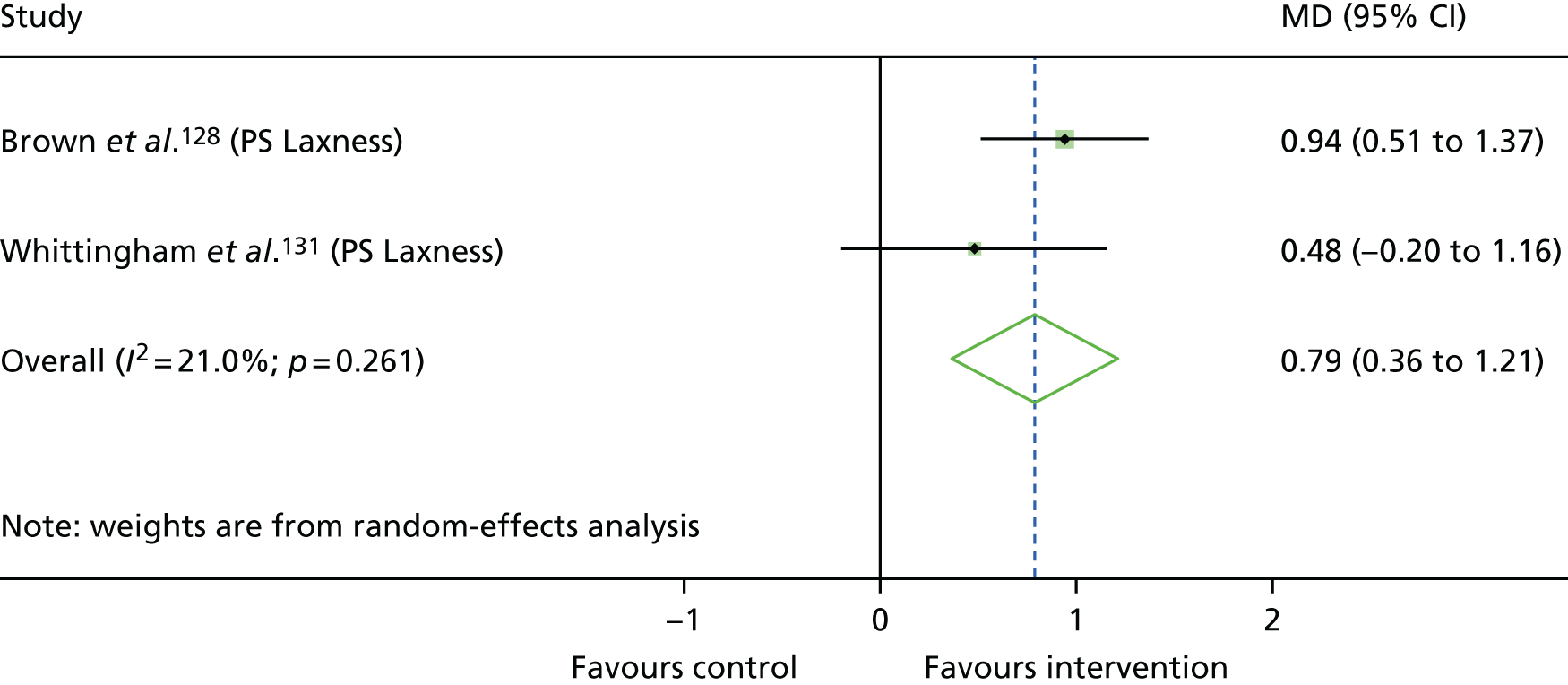
FIGURE 32.
Forest plot showing the results of non-standardised meta-analysis of the effects of parenting programmes with ACT on parenting over-reactivity post intervention for included studies. MD, mean difference; PS, Parenting Scale.
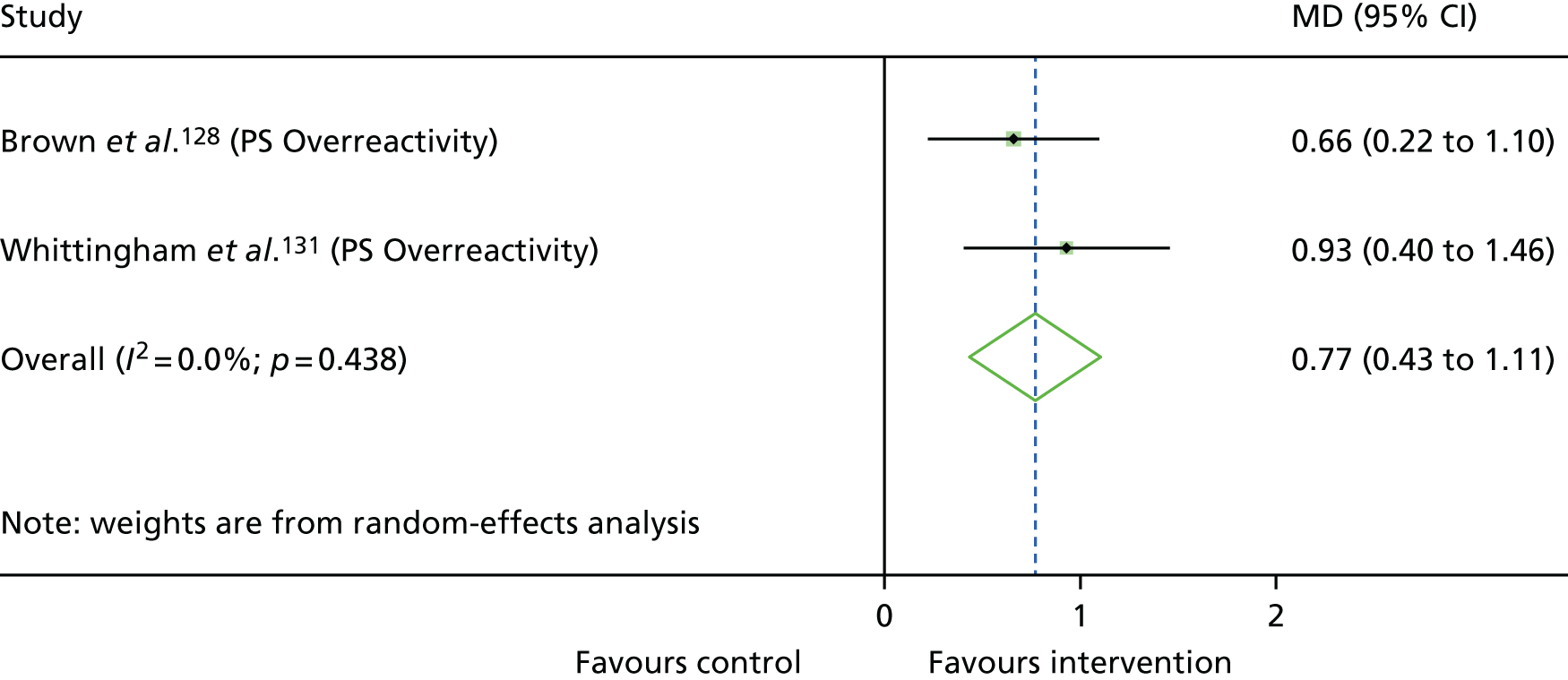
Non-standardised meta-analyses of outcomes following palliative care intervention
Child physical functioning was assessed using the PedsQL: Physical Functioning Scale by both Lyon et al. 123 and Shoshani et al. ;137 therefore, a non-standardised mean difference meta-analysis was performed (Figure 33). Overall, there was a statistically significant 15.8-point increase on the scale following palliative care intervention (95% CI 7.18 to 24.5 points; p < 0.001).
FIGURE 33.
Forest plot showing the results of non-standardised meta-analysis of the effects of palliative care on child physical quality of life post intervention for included studies. MD, mean difference.
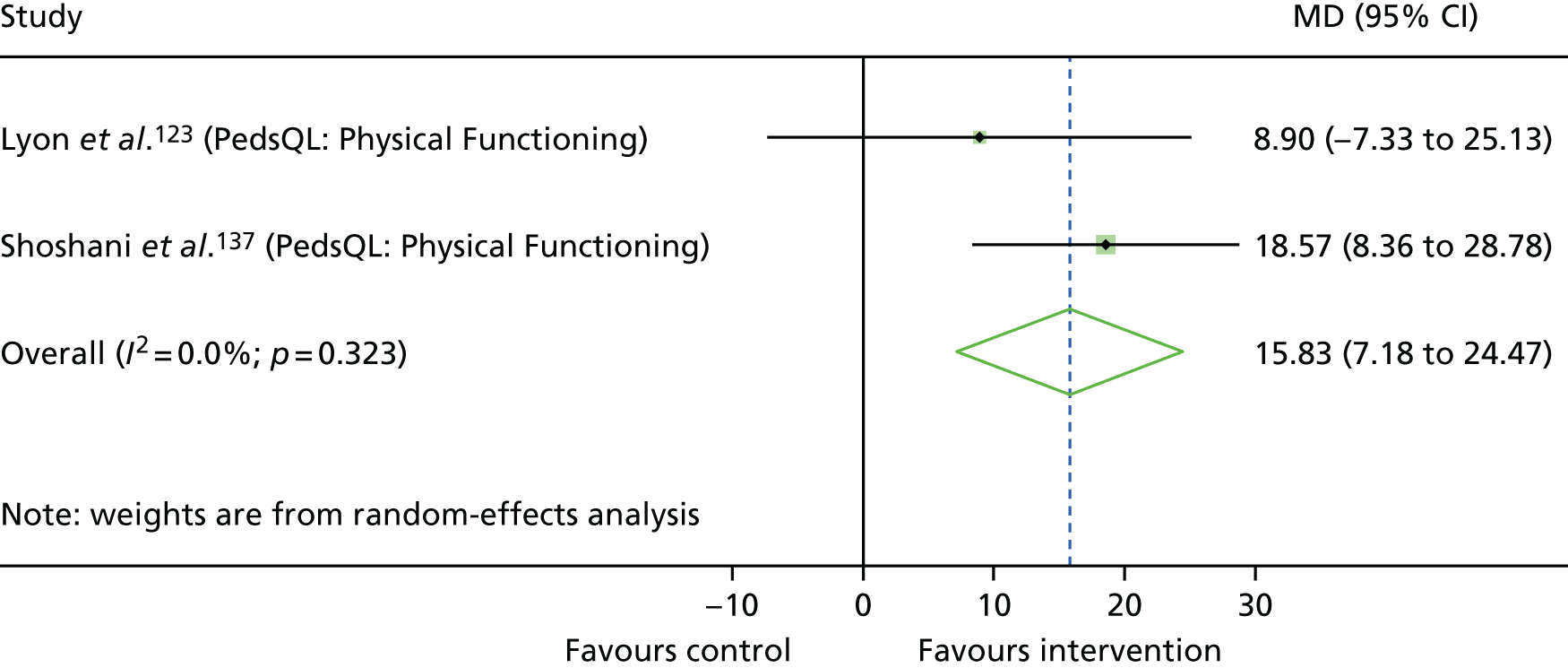
Non-standardised meta-analyses of outcomes following stress management training intervention
LTC-specific stress was measured using the DSQ in the included studies that trialled SMT (Boardway et al. ,120 Hains et al. 122), therefore a non-standardised mean difference meta-analysis was performed on this outcome (Figure 34). There was an increase of 3.51 points on the measure; however, this was not statistically significant, being associated with wide CI (mean difference 3.51, 95% CI –18.4 to 25.4 points; p = 0.75).
FIGURE 34.
Forest plot showing the results of non-standardised meta-analysis of the effects of SMT on child LTC-specific stress post intervention for included studies.
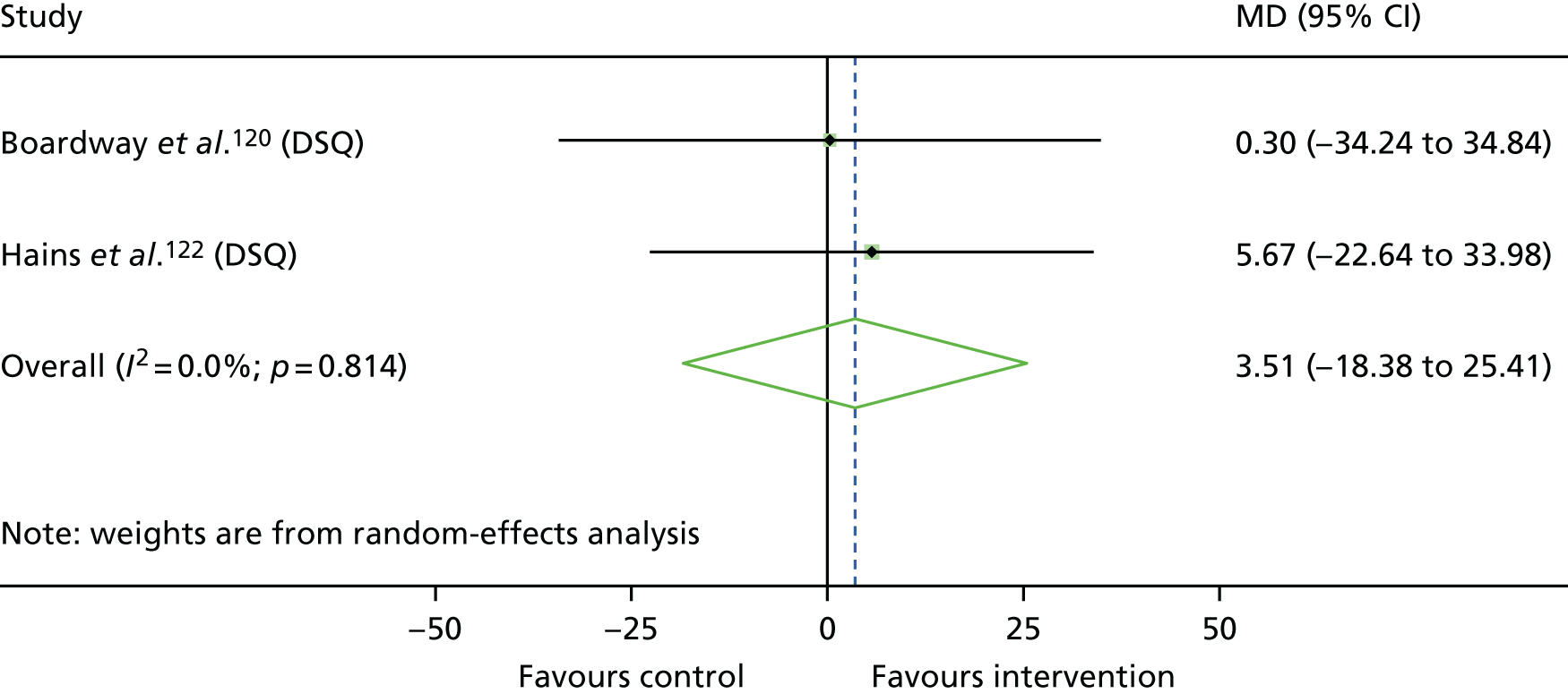
Appendix 7 Supplementary analysis: meta-analyses for cognitive–behavioural therapy across long-term conditions
When the same intervention, comparator and outcome category were used, a meta-analysis was performed across LTCs. This opportunity was only presented for CBT across five LTCs.
Figure 35 shows a forest plot for the effect of CBT on outcomes post intervention across patients with epilepsy (i.e. Martinović et al. 83), chronic pain (i.e. Wicksell et al. 145), persistent functional somatic complaints (i.e. Masia-Warner et al. 124), IBD (i.e. Szigethy et al. 84) and diabetes mellitus (i.e. Serlachius et al. 130). The plot is arranged by groups of outcomes, with depression, general mental health, LTC-specific QoL and LTC symptoms displayed. For depression, three measures (CES-D, BDI, Hamilton Depression Scale) were combined to produce a single outcome for Martinović et al. 83 For LTC symptoms, parent- and self-report of pain and the Children’s Somatization Inventory were combined to produce a single outcome for Masia-Warner et al. ,124 whereas five outcomes were combined to produce one single effect for Wicksell et al. 145 These were the Pain and Impairment Rating Scale, Pain Intensity Visual Analogue Scale, Pain Interference Scale and Functional Disability Index (child and parent reports).
FIGURE 35.
Forest plot showing the results of meta-analysis of the effects of CBT on depression, general mental health, LTC-specific QoL and LTC symptoms post intervention for included studies. CDI-CP, Child Depression Inventory-Child and Parent version; CGAS, Children’s Global Assessment Scale; DQOL, Diabetes Quality of Life scale; QOLIE-31, Quality of Life In Epilepsy Inventory-31 item version; SMD, standardised mean difference (Cohen’s d).
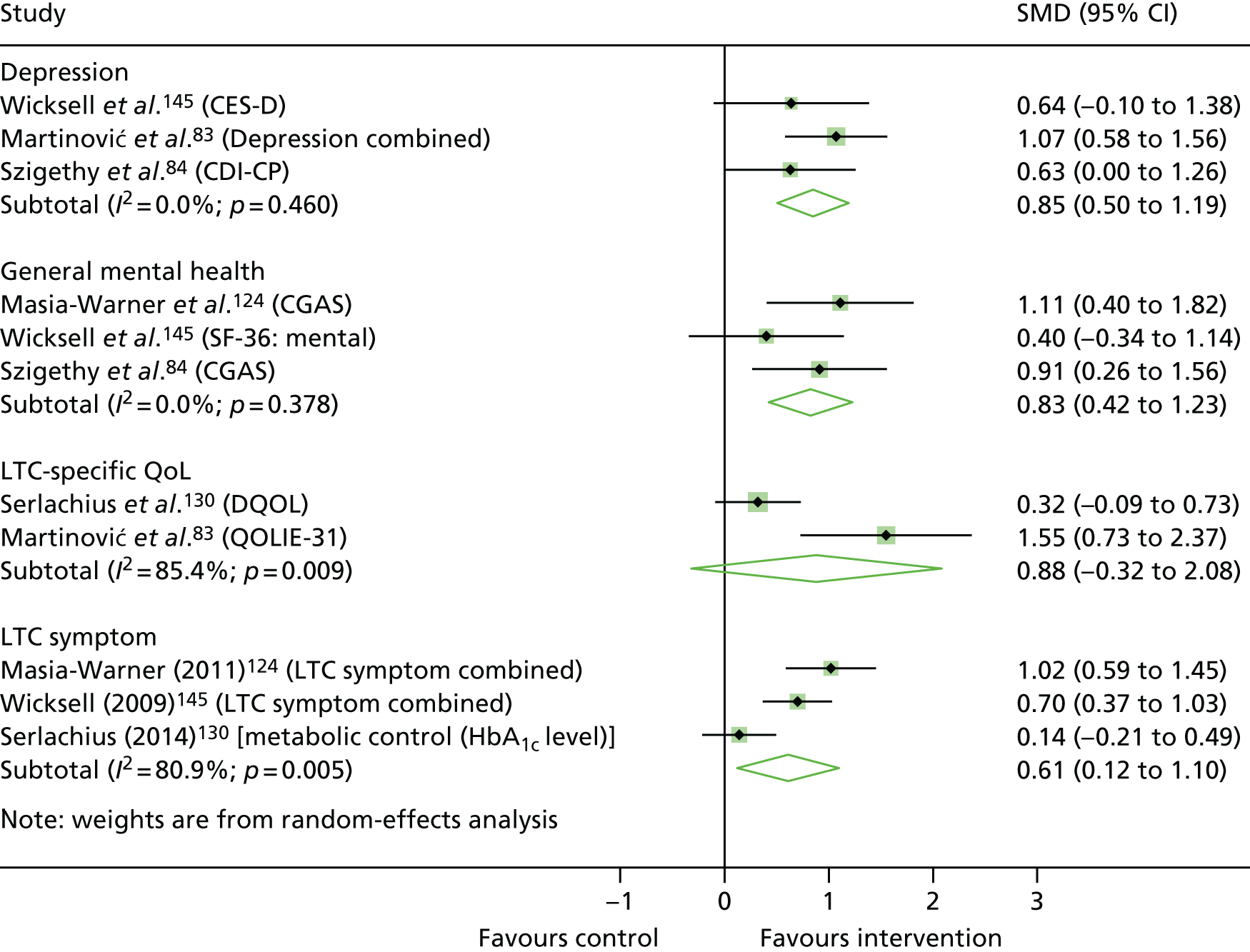
A statistically significant large beneficial effect was observed for depression (d = 0.85, 95% CI 0.50 to 1.19; p < 0.001) and general mental health (d = 0.83, 95% CI 0.42 to 1.23; p < 0.001) outcomes. In both cases, statistical heterogeneity was zero, providing further confidence in this effect. There was a large positive effect size for LTC-specific QoL; however, this was not supported at the 5% statistical significance level (d = 0.88, 95% CI –0.32 to 2.08; p = 0.15). The wide CIs and high heterogeneity (I2 = 85.4%; p = 0.009) reflect the imprecision and uncertainty for this outcome. LTC symptoms were improved with a medium-sized statistically significant effect (d = 0.61, 95% CI 0.12 to 1.10; p = 0.02); however, the CIs suggest uncertainty as to whether this effect is likely to be small or large. High heterogeneity further reflects the imprecision of this estimate (I2 = 80.9%; p = 0.005).
Appendix 8 Project team and expert advisory group who contributed to whole-team meetings
| Member | Area of expertise | Membership |
|---|---|---|
| Professor Rob Anderson | Health economics | Project team |
| Dr Sophie Bennett | Clinical psychology | Project team |
| Professor Chris Dickens | Psychological medicine | Project team |
| Professor Tamsin Ford | Child and adolescent mental health | Project team |
| Dr Ruth Garside | Evidence synthesis | Project team |
| Professor Isobel Heyman | Consultant child and adolescent psychiatrist | Project team |
| Ms Paula Lavis | Co-ordinator children and young people mental health coalition | Expert advisory group |
| Ms Fiona Lockhart | Parent of a young person with lived experience of a LTC and mental health difficulties | Expert advisory group |
| Professor Stuart Logan | Paediatric epidemiology | Expert advisory group |
| Dr Darren Moore | Evidence synthesis | Project team |
| Dr Michael Nunns | Evidence synthesis | Project team |
| Morwenna Rogers | Information specialist | Project team |
| Professor Roz Shafran | Clinical psychology | Project team |
| Dr Liz Shaw | Evidence synthesis | Project team |
| Professor Jo Thompson Coon | Evidence synthesis | Project team |
| Dr Penny Titman | Consultant clinical psychologist | Project team |
| Professor Obioha Ukoumunne | Statistics | Project team |
| Professor Russell Viner | Adolescent health | Project team |
| Dr Erin Walker | Patient and public involvement lead | Project team |
Appendix 9 Search strategy used for review 2 search with the PsycINFO (via OvidSP) database
| # | Searches | Results |
|---|---|---|
| 1 | Chronic Disease/ | 0 |
| 2 | Neoplasms/ | 28,712 |
| 3 | Diabetes Mellitus/ | 4470 |
| 4 | Asthma/ | 4034 |
| 5 | exp Respiratory Tract Diseases/ | 0 |
| 6 | Cystic Fibrosis/ | 732 |
| 7 | Cerebral Palsy/ | 4202 |
| 8 | exp Epilepsy/ | 22,725 |
| 9 | exp Muscular Diseases/ | 0 |
| 10 | exp Endocrine System Diseases/ | 0 |
| 11 | exp Immune System Diseases/ | 0 |
| 12 | exp HIV Infections/ | 0 |
| 13 | exp Cardiovascular Diseases/ | 0 |
| 14 | exp Nervous System Diseases/ | 0 |
| 15 | exp Skin Diseases/ | 0 |
| 16 | exp Digestive System Diseases/ | 0 |
| 17 | exp Hematologic Diseases/ | 0 |
| 18 | exp Otorhinolaryngologic Diseases/ | 0 |
| 19 | exp Stomatognathic Diseases/ | 0 |
| 20 | exp Eye Diseases/ | 0 |
| 21 | exp Pain/ | 47,653 |
| 22 | Disabled Children/ | 0 |
| 23 | ((chronic* or longterm or long-term or “long standing” or physical) adj2 (condition* or ill* or disease* or disorder* or syndrome*)).ti,ab. | 45,152 |
| 24 | (cancer* or neoplas* or tumor* or tumour* or malignan* or carcinoma* or “bone marrow” or leukaemia or leukemia).ti,ab. | 63,603 |
| 25 | diabet*.ti,ab. | 23,493 |
| 26 | asthma*.ti,ab. | 6465 |
| 27 | (respiratory adj2 (illness* or disease* or condition*)).ti,ab. | 1201 |
| 28 | cystic fibrosis.ti,ab. | 993 |
| 29 | cerebral palsy.ti,ab. | 5460 |
| 30 | quadriplegi*.ti,ab. | 491 |
| 31 | tetraplegi*.ti,ab. | 291 |
| 32 | diplegi*.ti,ab. | 378 |
| 33 | spinal cord injur*.ti,ab. | 4595 |
| 34 | muscular dystrophy.ti,ab. | 1123 |
| 35 | epilep*.ti,ab. | 33,297 |
| 36 | seizure*.ti,ab. | 25,791 |
| 37 | spina bifida.ti,ab. | 868 |
| 38 | (heart adj2 (condition* or disease* or disorder* or defect*)).ti,ab. | 9188 |
| 39 | (cardiac adj2 (condition* or disease* or disorder* or defect*)).ti,ab. | 1390 |
| 40 | (cardiovascular adj2 (condition* or disease* or disorder* or defect*)).ti,ab. | 8891 |
| 41 | (skin adj2 (condition* or disease* or disorder*)).ti,ab. | 966 |
| 42 | eczema.ti,ab. | 330 |
| 43 | (allergies or allergy).ti,ab. | 1529 |
| 44 | dermatitis.ti,ab. | 532 |
| 45 | (gastrointestinal adj (disorder* or disease*)).ti,ab. | 669 |
| 46 | ((stomach or abdominal or gastrointestinal) adj pain).ti,ab. | 1342 |
| 47 | (bowel* adj2 inflammatory adj2 (condition* or disease* or illness*)).ti,ab. | 602 |
| 48 | (liver adj (disease* or transplant*)).ti,ab. | 1621 |
| 49 | hepatitis.ti,ab. | 3515 |
| 50 | (disabilit* adj5 child*).ti,ab. | 13,184 |
| 51 | (human immunodeficiency virus or HIV).ti,ab. | 42,006 |
| 52 | AIDS.ti,ab. | 30,925 |
| 53 | (hyperthyroidism or hypothyroidism).ti,ab. | 1635 |
| 54 | an?emia.ti,ab. | 1617 |
| 55 | h?emophilia.ti,ab. | 368 |
| 56 | sickle.ti,ab. | 1162 |
| 57 | ((renal or kidney) adj (disease* or disorder*)).ti,ab. | 1900 |
| 58 | nephrotic syndrome.ti,ab. | 55 |
| 59 | encephalomyelitis.ti,ab. | 1604 |
| 60 | chronic fatigue syndrome.ti,ab. | 1946 |
| 61 | ((cleft or palate) adj lip).ti,ab. | 295 |
| 62 | craniofacial.ti,ab. | 527 |
| 63 | (deaf or deafness).ti,ab. | 13,257 |
| 64 | (hearing adj (defect* or disorder*)).ti,ab. | 347 |
| 65 | blindness.ti,ab. | 5420 |
| 66 | ((vision or visually or visual) adj (impaired or impairment*)).ti,ab. | 4261 |
| 67 | ((persistent or chronic or recurring or frequent) adj (headache* or migraine*)).ti,ab. | 1720 |
| 68 | chronic pain.ti,ab. | 11,547 |
| 69 | fibromyalgia.ti,ab. | 2541 |
| 70 | medically unexplained symptoms.ti,ab. | 452 |
| 71 | (spinal adj injur*).ti,ab. | 301 |
| 72 | or/1-71 | 335,060 |
| 73 | (child or children*).ti,ab. | 529,036 |
| 74 | (adolescent or adolescents).ti,ab. | 169,875 |
| 75 | teen*.ti,ab. | 18,103 |
| 76 | (young adj (adult* or people)).ti,ab. | 53,922 |
| 77 | youth*.ti,ab. | 73,029 |
| 78 | 73 or 74 or 75 or 76 or 77 | 701,901 |
| 79 | Mental Health/ | 47,847 |
| 80 | (psychological adj (illness* or disorder* or difficulties or problems or distress)).ti,ab. | 23,105 |
| 81 | (mental adj (health or illness* or disorder* or distress or problem*)).ti,ab. | 186,832 |
| 82 | (depression or depressed or depressive).ti,ab. | 235,411 |
| 83 | ((disruptive or challenging or antisocial) adj behavio?r).ti,ab. | 11,412 |
| 84 | (behavio?r adj problem*).ti,ab. | 12,771 |
| 85 | (anxiety or anxious).ti,ab. | 157,623 |
| 86 | feelings.ti,ab. | 57,562 |
| 87 | Internali*.ti,ab. | 3 |
| 88 | (wellbeing or well being).ti,ab. | 61,891 |
| 89 | happiness.ti,ab. | 11,767 |
| 90 | worry.ti,ab. | 7030 |
| 91 | distress.ti,ab. | 48,777 |
| 92 | satisfaction.ti,ab. | 82,607 |
| 93 | emotional.ti,ab. | 174,569 |
| 94 | coping.ti,ab. | 61,721 |
| 95 | or/79-94 | 828,319 |
| 96 | qualitative research/ | 6724 |
| 97 | Ethnology/ | 1943 |
| 98 | exp Questionnaires/ | 15,996 |
| 99 | phenomenology/ | 11,126 |
| 100 | Attitudes/ | 23,102 |
| 101 | interviewing/ | 3181 |
| 102 | interview*.ti,ab. | 250,183 |
| 103 | qualitative.ti,ab. | 110,757 |
| 104 | (talked or asked).ti,ab. | 81,112 |
| 105 | focus group*.ti,ab. | 24,246 |
| 106 | ethnograph*.ti,ab. | 20,873 |
| 107 | grounded theory.ti,ab. | 11,222 |
| 108 | thematic.ti,ab. | 14,905 |
| 109 | (barriers and (facilitators or enablers)).ti,ab. | 2521 |
| 110 | process evaluation.ti,ab. | 1094 |
| 111 | group discussion*.ti,ab. | 7342 |
| 112 | perception*.ti,ab. | 232,038 |
| 113 | attitude*.ti,ab. | 171,590 |
| 114 | views.ti,ab. | 56,281 |
| 115 | experience*.ti,ab. | 486,970 |
| 116 | or/96-115 | 1,107,429 |
| 117 | intervention.ti,ab. | 171,181 |
| 118 | psychotherapy.ti,ab. | 77,346 |
| 119 | (support adj3 (group* or network)).ti,ab. | 13,125 |
| 120 | therapy.ti,ab. | 194,016 |
| 121 | counselling.ti,ab. | 9299 |
| 122 | peer support.ti,ab. | 2673 |
| 123 | social support.ti,ab. | 35,639 |
| 124 | program*.ti,ab. | 318,905 |
| 125 | (mental adj3 service*).ti,ab. | 22,848 |
| 126 | training.ti,ab. | 210,131 |
| 127 | technique*.ti,ab. | 158,051 |
| 128 | treatment*.ti,ab. | 508,051 |
| 129 | or/117-128 | 1,226,579 |
| 130 | 72 and 78 and 95 and 116 and 129 | 4011 |
List of abbreviations
- ABI
- acquired brain injury
- ACT
- acceptance and commitment therapy
- AIDS
- acquired immune deficiency syndrome
- BDI
- Beck Depression Inventory
- BOC
- Best of Coping
- CAMHS
- Child and Adolescent Mental Health Services
- CBT
- cognitive–behavioural therapy
- CDI
- Child Depression Inventory
- CES-D
- Centre for Epidemiological Studies Depression scale
- CFS
- chronic fatigue syndrome
- CHD
- congenital heart disease
- CI
- confidence interval
- CINAHL
- Cumulative Index of Nursing and Allied Health Literature
- CRD
- Centre for Reviews and Dissemination
- CYP
- children and young people
- CYPAG
- children and young people advisory group
- DHSC
- Department of Health and Social Care
- DSQ
- Diabetes Stress Questionnaire
- ECBI
- Eyberg Child Behavior Inventory
- EIT
- emotional intelligence training
- FACE-TC
- Family-Centred Advance Care Planning for Teens with Cancer
- GHb
- total glycosylated haemoglobin
- GHQ
- General Health Questionnaire
- HbA1C
- glycated haemoglobin
- HIV
- human immunodeficiency virus
- HMIC
- Health Management Information Consortium
- HTA
- Health Technology Assessment
- IBD
- inflammatory bowel disease
- JIA
- juvenile idiopathic arthritis
- K-SADS-PL
- Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version
- LTC
- long-term physical condition
- NDST
- non-directive supportive therapy
- NHIS
- National Health Interview Survey
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OECD
- Organisation for Economic Co-operation and Development
- PASCET-PI
- Primary and Secondary Control Enhancement Therapy-Physical Illness
- PCDAI
- Paediatric Crohn’s Disease Activity Index
- PedsQL
- Paediatric Quality of Life Inventory
- PMR
- progressive muscle relaxation
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PUCAI
- Paediatric Ulcerative Colitis Activity Index
- QoL
- quality of life
- RCT
- randomised controlled trial
- SCARED
- Screen for Child Anxiety Related Emotion Disorder
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SF-36
- Short Form questionnaire-36 items
- SMT
- stress management training
- SSTP
- Stepping Stones Triple P
- STAI
- Spielberger State–Trait Anxiety Inventory
- STAI-S
- Spielberger State–Trait Anxiety Inventory-State subscale
- T1DM
- type 1 diabetes mellitus
- TAPS
- Treatment of Anxiety and Physical Symptoms
- TAU
- treatment as usual
