Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/59/22. The contractual start date was in June 2016. The draft report began editorial review in March 2018 and was accepted for publication in June 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Matthew L Costa is a member of the UK National Institute for Health Research Health Technology Assessment General Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Griffin et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
Fractures of the distal femur are increasingly common injuries. They account for 5% of all fractures of the femur with an estimated incidence of 10 per 100,000. 1 The optimal management of these fractures remains controversial. There is a bimodal distribution of the incidence of these fractures with age. 2 The majority, approximately 85%, are fragility fractures sustained by elderly patients after a fall from a standing height, and the remainder are typically sustained by multiply injured patients after massive trauma. 2 This study will investigate the most common fracture subtype: fragility fractures sustained in the elderly population, often as a consequence of osteoporosis.
Fragility fractures of the distal femur occur in the same population as hip fractures. 3 Similar to hip fractures, these are significant injuries in a vulnerable group of patients, causing considerable morbidity and mortality as well as placing a major financial burden on the NHS. 4 Hip fracture is approximately 10 times more common than fracture of the distal femur. 1 However, the overall incidence of fragility fractures associated with osteoporosis is rising steadily, promising an increasing challenge to future health-care provision. 5
It is current practice to manage displaced fractures with operative fixation if the patient is medically fit enough to undergo surgery. 3,6 Surgery reduces the substantial complications associated with non-operative treatment, such as prolonged immobilisation and bed rest, as well as the problems of non-union and malunion. 7
Since the operative treatment of these fractures was popularised, a wide variety of implants have been employed to achieve fixation. Despite the significant advancements in implant design and manufacture, operative fixation is still associated with substantial complications similar to those seen with hip fractures. 6,8 This reflects the common pathology underlying these injuries, that the bone is weakened by osteoporosis, undermining the stability of the bone–implant construct.
There has been very little research comparing operative technologies for treating distal femoral fractures in this population. A recent Cochrane review9 found few trials in this area, most of which compared outdated implants, such as non-anatomical, non-locking plating systems or earlier-generation nails. Furthermore, important limitations in the methodology of each of the trials were identified, leading to substantial risks of bias. 9 It was suggested that in order to optimise patient functional recovery following this debilitating injury ‘a well-designed, adequately powered, randomised controlled trial (RCT) comparing modern treatments is required’. 9
The two interventions most commonly used in UK practice are intramedullary fixation with a locked retrograde nail (nail) and extramedullary fixation with an anatomical locking plate (plate). 3 Nails offer twin theoretical advantages: the mechanical impact of a long, intramedullary device that is close to the axis of the femur10 and the biological advantages of minimum disruption of the fracture site and stimulation of blood supply through reaming. 11 However, nails provide only limited options for distal locking screws, as all screws must pass through the centre of the nail, so the stability of the bone–implant construct may be suboptimal. Locking plate fixation has been facilitated by recent advances in implant technology that allow the screws to be screwed into the bone as well as the plate itself (‘locked’). This produces a ‘fixed-angle’ bone–plate construct. These plates were designed specifically for use in osteoporotic bone and have been shown to exhibit excellent biomechanical properties. 12 However, they are more expensive than nails and require larger surgical wounds to apply. There are few clinical data available to guide clinicians9 and it is clear that there is no current consensus concerning the best management of these injuries. 3
Relevance of the research
We performed a multicentre retrospective study to review the current management of distal femoral fractures at four UK major trauma centres. 3 We found that only two devices are now used for fixation: retrograde nails and locking plates. In addition, > 80% of these injuries in a population were fragility fractures, which matched those sustaining hip fracture. Furthermore, mortality in this frail elderly group of patients was 20% at 1 year and the prevalence of cognitive impairment was 30% as reported at baseline. 3 The overall annual incidence in each centre was 20 fractures per year. This retrospective study shows the patient demographics, the variability in treatment of these fractures in the UK and the considerable morbidity associated with the injury.
Crucially, we have found that there may be an important difference in outcomes following the choice of surgical management of these patients. The mean benefit of a nail over locking plates may be as great as 0.12 in EuroQol-5 Dimensions (EQ-5D) (p = 0.019). 13 The minimum clinically important difference in EQ-5D score is estimated to be 0.08. 14 Similar effect sizes are demonstrated in other measures of function and quality of life, such as the Glasgow Outcome Scale (extended) and Short Form questionnaire-12 items. 13 These findings have also been reported by other groups. A small pilot study in the USA comparing these technologies found some evidence of a similar benefit in quality of life in favour of nails (mean difference in EQ-5D score was 0.1; p = 0.07). 15
Below we present the null hypothesis and trial objectives for both the proposed definitive trial and the current feasibility trial.
Definitive trial null hypothesis
There is no difference in the EuroQol-5 Dimensions, five-level version (EQ-5D-5L), at 4 months after injury between adults aged > 18 years with an acute, extra-articular fragility fracture of the distal femur treated with ‘locking’-plate fixation (plate) versus retrograde intramedullary nail fixation (nail).
Definitive trial objectives
The objectives of any subsequent definitive trial will be to:
-
quantify and draw inferences on observed differences in health-related quality of life (HRQoL) at 4 months between the study intervention groups (nail versus plate)
-
quantify and draw inferences on observed differences in functional status at 4 weeks, 4 months and 12 months
-
quantify and draw inferences on observed differences in the radiological outcomes of non-union, malalignment and shortening
-
determine the complication profile associated with nail fixation versus locking plate fixation in the first year after the injury
-
investigate, using appropriate statistical and economic analytical methods, the resource use, costs and comparative cost-effectiveness of nail fixation versus locking plate fixation.
Feasibility trial objectives
The objectives of this feasibility study were to:
-
estimate the number of eligible patients in the UK population and the proportion of those eligible who are willing to consent to take part in the study
-
optimise the protocol, procedures and CRFs in preparation for a future definitive trial
-
perform a process evaluation to better understand the implementation, mechanisms of impact and context of the interventions and the generalisability and likely success of any future definitive trial
-
explore the validity of self and proxy reporting of the primary outcome measure in this specific population.
Strict recruitment criteria, against which a decision to determine the feasibility of a definitive trial can be judged, are given below. If these criteria are not met a full trial will not be pursued. These criteria were:
-
an average recruitment rate of 1.0 participants per month per centre
-
appropriate recruitment performance across all feasibility sites.
Chapter 2 Methods
Trial design
Phase I (feasibility study) was designed to determine the expected rate of recruitment in a large-scale multicentre RCT in this complicated area of trauma research. Phase II (definitive trial) is a proposed multicentre RCT in the UK. This report concerns Phase I only.
This feasibility study was a multicentre controlled trial, stratified by centre and cognitive impairment, with balanced randomisation 1 : 1.
In parallel with the conduct of the feasibility study, we also performed a process evaluation in line with the recommendations of the Medical Research Council (MRC)’s guidance. 16 The evaluation focused on investigating the fidelity and quality of implementation, clarifying the causal mechanisms and identifying the contextual factors that might be important in variation of outcome.
Important changes after commencement
Eligibility criteria
The trial protocol17 aimed to include all patients with fragility fracture. Fragility was initially defined using age as a surrogate marker. After reviewing the screening data during recruitment, the Trial Steering Committee (TSC) recommended that an assessment of the feasibility of using a mechanistic definition of fragility should be made within the trial. The minimum age was therefore revised from 50 to 18 years to ensure that all possible fragility fractures were included. The mechanism of injury was recorded during screening and defined using the World Health Organization (WHO)’s definition as a fall from standing height or less.
Participants
Inclusion criteria
Patients were eligible for this study if they:
-
were ≥ 18 years
-
had a fracture of the femur involving the distal two ‘Müller’ squares18
-
would, in the opinion of the attending surgeon, benefit from internal fixation of the fracture.
Many of the patients who sustain this injury have some degree of cognitive impairment, similar to patients sustaining hip fracture. Some have chronic cognitive impairment3 and some develop acute delirium at the time of presentation to hospital. 19 Cognitive status is an important independent predictor of patients’ baseline functional, quality-of-life status and likely outcome in this population. 19,20 This is possibly related to patients’ pre-injury independence, post-injury expectations and ability to participate fully in their rehabilitation. Inclusion of these patients was essential to determine specific effect sizes in this subgroup and so that the sample properly reflected the population sustaining this injury.
Exclusion criteria
Patients were excluded from this trial if they had:
-
a loose knee or hip arthroplasty requiring revision
-
pre-existing femoral deformity
-
an arthroplasty that precluded nail fixation.
Patients who sustained injuries to areas of the body other than the lower limbs, which may affect the primary outcome measure, were still included in the analysis. For patients with bilateral fractures of the distal femur, a rare event, both fractures were recorded but only one fracture was included in the trial. The treating surgeon decided which injury to include in the study prior to randomisation.
All patients who were eligible for inclusion in Trial of Acute Femoral Fracture Fixation (TrAFFix) and their personal consultees, as well as all staff members involved in the research and intervention delivery, were eligible to be approached about participating in qualitative interviews as part of the process evaluation.
Screening and trial recruitment
The clinical care team notified the research team of any potentially eligible patients. Non-identifiable patient details were then used for screening in the emergency department and trauma wards at the trial centres. Reasons for patients’ exclusion or ineligibility were recorded.
Consent to trial participation
The nature of these injuries meant that the great majority of patients were operated on immediately or on the next available trauma operating list, depending on access to an appropriate operating theatre. Some patients were unconscious, all were distracted by the injury to their lower limb and its subsequent treatment and all had large doses of opiates for pain relief, potentially affecting their ability to process information. Similarly, patients’ next of kin, carers and friends were often anxious at this time and had difficulty in weighing the large amount of information that they were given about the injury and plan for treatment. In this emergency situation, the focus was on obtaining consent for surgery (when possible) and informing the patient and any next of kin about immediate clinical care. The consent procedure for this trial reflected that of the surgery, with the clinical team assessing capacity before taking consent for the surgical procedure and this capacity assessment then being used to decide on the proper approach to consenting to the research. The appropriate method, as described below, was used to gain either prospective or retrospective consent from the patient or appropriate consultee by a good clinical practice-trained, appropriately delegated, member of the research team.
Conducting research in this ‘emergency setting’ is regulated by the Mental Capacity Act 2005. 21 As patients may have lacked capacity as described above, and because the urgent nature of the treatment limited access to and appropriate discussion with personal consultees, we proposed to act in accordance with section 32, subsection 9b of the Mental Capacity Act 2005 following a process approved by the relevant Research Ethics Committee (REC): the clinical team would make an assessment of capacity as per usual procedures for obtaining consent for a surgical procedure. The clinical team then provided guidance to the research team as to whether the patient had capacity to consent prospectively or if consultee agreement should be sought.
When the clinical team advised that prospective patient consent was appropriate, this was sought by the research team. If the clinical team advised that prospective patient consent was not appropriate, the research team approached an appropriate consultee. When a personal consultee was available, they were provided with the study information. The personal consultee was given the opportunity to ask questions and discuss the study, after which their written agreement was recorded. When a personal consultee was not available then a nominated consultee was identified to advise the research team. The nominated consultee was the patient’s treating surgeon. If that surgeon was a member of the research team, another independent surgeon was identified. Consent or agreement for further participation into the study after surgery was then sought by the patient themselves or a personal/nominated consultee.
Those patients who were able to consent before their operation were always approached for consent before surgery. For those patients who did not consent prior to surgery, the research associate (RA) provided the patients with all of the study information at the first appropriate time when the patient regained capacity. The patients were given the opportunity to ask questions and discuss the study with their family and friends. They were then asked to provide written consent for continuation in the study. Patients were asked to consent to long-term follow-up and data linkage to routine NHS data sets.
For those patients who did not prospectively consent or who had a nominated consultee give prospective agreement and still lacked capacity after their surgery, a personal consultee was contacted to advise the research team about the patient’s continued participation in the study.
Patients or personal consultees who preferred not to be actively involved in the study follow-up were asked if they were willing to consent to the research team using their routinely collected NHS data for the study.
Responsibility for recording and dating both oral and written informed consent or agreement was with the investigator, or persons delegated by the investigator, who conducted the informed consent discussion. Permission was sought to inform the patient’s general practitioner (GP) of their participation in the study.
Recruitment and consent to process evaluation
As part of the initial consent process, patients and their personal consultees were asked whether or not they could be approached about participating in interviews regarding their views on participating in this trial. Written agreement from participants or their personal consultees to be approached for an interview was sent to the TrAFFix research office. Participants who did not consent to the main trial were also given the opportunity to participate in an interview with a member of the research team.
Participants who agreed to be approached underwent a separate informed consent discussion for the interviews with a member of the research team either in person, by telephone, or by post. Written informed consent was provided when the interviews were face to face and verbal informed consent was recorded if the interviews took place by telephone.
NHS staff were initially invited for an interview by telephone or e-mail, and if they agreed to be approached an informed consent discussion took place with a researcher from the TrAFFix office by telephone or in person.
As part of the process evaluation, conversations between researchers and participants or personal consultees were audio recorded. This included the initial discussion about TrAFFix, before informed consent for the main study has been given. When patients agreed, their verbal consent was recorded at the start of the recording. When patients did not agree, the informed consent conversation continued as usual without being recorded.
Settings
The trial was run in seven NHS hospitals across the UK (Box 1).
John Radcliffe Hospital, Oxford University Hospitals NHS Foundation Trust (PI: Mr David Noyes).
Leeds General Infirmary, The Leeds Teaching Hospitals NHS Trust (PI: Professor Peter Giannoudis).
Queen’s Medical Centre, Nottingham University Hospitals NHS Trust (PI: Professor Ben Ollivere).
Queen Alexandra Hospital, Portsmouth Hospitals NHS Trust (PI: Ms Charlotte Lewis).
Royal Berkshire Hospital, Royal Berkshire NHS Foundation Trust (PI: Mr Andrew McAndrew).
Royal Stoke Hospital, University Hospitals of North Midlands NHS Trust (PIs: Mr Haroon Majeed and Mr Damian McClelland).
Leicester Royal Infirmary, University Hospitals of Leicester NHS Trust (PI: Mr Ashwin Kulkarni).
PI, principal investigator.
Sample size
Data from this feasibility study can be used to calculate estimates of the standard deviation (SD) of the primary outcome measure (EQ-5D-5L) to drive a formal power analysis and sample size calculation for a definitive trial. Evidence from other relevant sources for EQ-5D-5L22,23 can also be used to inform this process.
We anticipated that each of the participating centres would treat approximately 1.5 eligible patients per month. 3 Taking a conservative approach, we expected, to ensure feasibility, to be able to recruit 1.0 patients per month per centre. Given our schedule for centre opening times and recruitment length, we had 52 centre.months available to recruit for this study. Assuming that the recruitment rate was 1.0 per month per centre, and that monthly centre counts of patient recruitment numbers were approximately Poisson distributed and independent of one another, would allow us to estimate the recruitment rate with a 95% confidence interval (CI) of 0.73 to 1.28. 24 Therefore, recruiting 52 patients in total would provide sufficiently precise estimates of the monthly recruitment rate to decide if a definitive trial was feasible.
For the qualitative interviews with participants, convenience sampling was used. We intended to sample participants until data saturation was achieved; however, as there were fewer than anticipated potential participants, we approached all participants who were willing to be interviewed. For the interviews with staff, we used a purposive sampling strategy that included an interview with at least one surgeon [i.e. the principal investigator (PI)] and a RA at each of the seven participating centres.
Randomisation
Sequence generation
Stratification by centre ensured that any clustering effects related to the centre itself were equally distributed across the trial arms. This would not eliminate centre- or surgeon-specific effects, but, because between 10 and 30 surgeons were likely to be involved in the management of the patient group, any one surgeon would treat only two or three patients enrolled in the trial. Patients were also stratified by chronic cognitive impairment, which was judged by the clinical team on randomisation, to ensure that participants with cognitive impairment were allocated evenly across the treatment groups.
Allocation implementation
Eligible participants were recruited by a trial RA or member of the clinical team using a secure online registration and randomisation system provided by the Oxford Clinical Trials Research Unit (OCTRU). Basic information, including the patient’s initials and age and eligibility checks, was entered. The patient then received a trial identifier (ID) that was used on all non-public-facing trial documentation. The treatment allocation was generated prior to surgery, allowing randomisation outside working hours.
Blinding
Participants were informed of their treatment allocation only at the end of the trial. For this trial, surgical scars were evident, which could have given informed participants knowledge of their allocation. The treating surgeons were not blind to the treatment but took no part in the post-operative assessment of the patients. The functional outcome data were collected and entered onto the trial central database by a research assistant/data clerk in the trial central office. The radiographs collected were reviewed by independent assessors.
Post-randomisation withdrawals
Participants could decline to continue to take part in the trial at any time without prejudice. A decision to decline consent or withdraw did not affect the standard of care the patient received. Once withdrawn, the patients were advised to discuss their further care plan with their surgeon. Data collected up to the point of withdrawal were included in the final analysis. Post-randomisation withdrawals were not replaced.
Interventions
Participants were usually assessed in the emergency department. Diagnosis of a fracture of the distal femur was confirmed from plain radiographs of the femur. When there was doubt over the radiological pattern of the fracture, for example whether or not it extends into the knee, participants were reviewed by the on-call orthopaedic surgeon and, if clinically indicated, computed tomography (CT) was performed; this constituted standard of care practice.
As a minimum, all participants underwent electrocardiography, had a full blood count, underwent group and save investigations, had a coagulation screen, and underwent urea, creatinine and electrolytes tests. Routine thromboprophylaxis was started in all participants who were not already receiving anticoagulant therapy. Pharmaceutical and mechanical prophylaxis measures were used in accordance with the current practice agreed at each centre. A regional or general anaesthesia technique was used and routine analgesia was provided in accordance with local practice.
All participants received perioperative prophylactic antibiotics in accordance with the current practice agreed at each centre. Appropriate preparation, positioning and fracture reduction were left to the discretion of the operating surgeon, as per their normal clinical practice. Participants were randomly allocated to fixation using either intramedullary nailing or locking plate fixation.
All of the hospitals involved in this trial used both methods of fixation3 and all of the consulting surgeons involved will be familiar with both techniques.
Retrograde intramedullary nailing
Fixation of the fracture was achieved with a proximally and distally locked nail that spanned the entire diaphysis of the femur. All nails were introduced retrograde through the knee joint. In this pragmatic trial, the details of surgical incision and approach, fracture reduction and supplementary fixation with wires or screws were at the surgeon’s discretion as per their normal clinical practice.
Locking plate fixation
Fixation of the fracture was achieved with anatomical distal femoral locking plate and screws. Locking plates were defined as those in which at least one fixed-angle locking screw was placed distal to the fracture. The operating surgeon determined the length, number and type of additional screws. Additional fixation with lag screws and cerclage wires was at the surgeon’s discretion. In this pragmatic trial, the details of surgical incision and approach, fracture reduction, number and type of other screws and supplementary fixation with wires or screws were at the surgeon’s discretion as per their normal clinical practice.
Patients received the same standardised written physiotherapy advice detailing the exercises they need to perform for rehabilitation following their injury regardless of which group they were randomised to. All of the patients were advised to move their toes, ankle and knee joints fully within the limits of their comfort. Weight-bearing status was decided by the treating surgeon, with a preference for early weight-bearing mobilisation immediately or as soon as the surgeon felt appropriate. In this pragmatic trial, any other rehabilitation input beyond the written physiotherapy advice (including a formal referral to physiotherapy) was left to the discretion of the treating clinicians. However, a record of any additional rehabilitation input (type of input and number of additional appointments) together with a record of any other investigations/interventions was requested as part of the 6-week and 4-month postal follow-ups and formed part of the trial data set.
Outcomes
Primary
The primary outcome measures for this study were the participant recruitment rate and the completion rate of the EQ-5D-5L at 4 months post surgery.
Other measurements
Other measurements that were made during the trial are summarised in Table 1.
| Pre-randomisation | Time point | |||
|---|---|---|---|---|
| Pre-surgery | Baseline | 6 weeks | 4 months | |
| Fracture classification18 | ✓ | |||
| Cognitive impairment | ✓ | ✓ | ||
| Age | ✓ | |||
| Personal details | ||||
| Contact details | ✓ | |||
| Baseline characteristics | ||||
| Date of birth | ✓ | |||
| Sex | ✓ | |||
| Current medications | ✓ | |||
| Comorbidities | ✓ | |||
| Current/previous occupation | ✓ | |||
| Educational attainment | ✓ | |||
| Grip strength | ✓ | ✓ | ✓ | |
| Self-efficacy report | ✓ | |||
| Rockwood Frailty Scale score | ✓ | |||
| MOS social support | ✓ | |||
| Government benefits | ✓ | |||
| Residential status | ✓ | |||
| Discharge destination | ✓ | |||
| Mobility | ✓ | |||
| Treatment | ||||
| Additional fixation | ✓ | |||
| Anaesthesia | ✓ | |||
| Grade of surgeon | ✓ | |||
| Prescribed medications | ✓ | |||
| Rehabilitation assessment | ✓ | |||
| Outcomes | ||||
| EQ-5D-5L | Pre and post injury | ✓ | ✓ | |
| DEMQoLa | Pre and post injury | ✓ | ✓ | |
| DRIb | Pre and post injury | ✓ | ✓ | |
| Radiographs | ✓ | ✓ | ||
| Complications | ✓ | ✓ | ✓ | |
| Resource use | ✓ | |||
| Qualitative interviewsc | ✓ | ✓ | ✓ | |
Baseline characteristics
Routine baseline characteristics were recorded for all participants to describe the nature of the participants. Additional measurements (described below) were made to more fully describe the groups.
Grip strength
Grip strength is a measure of muscle strength and gives an indication of sarcopenia, a predictor of frailty, and was measured as previously described by Roberts et al. 25
Frailty
The degree of frailty can provide useful predictive information26 and was measured using the Rockwood Frailty Scale. The Rockwood Frailty Scale is a quick nine-point index used to measure frailty. 26
Social support
The Medical Outcomes Survey social support survey is a brief multidimensional, self-administered social support survey. 27
Self-efficacy
Self-efficacy is a measure of an individual’s confidence in their ability to accomplish tasks and overcome problems. Low levels of self-efficacy are associated with less optimal health behaviours. 28
Health-related quality of life
The EQ-5D-5L29 is a validated generalised and standardised instrument comprising a visual analogue scale measuring self-rated health and a health status instrument, consisting of a five-level response (no problems, some problems, moderate problems, severe problems and unable) for five domains related to daily activities:29 (1) mobility, (2) self-care, (3) usual activities, (4) pain and discomfort and (5) anxiety and depression. Responses to the health status classification system are converted into an overall score using a published utility algorithm for the UK population. 30 The EuroQol visual analogue scale scores self-rated health on a scale on which the end points are labelled ‘best imaginable health state’ (100) and ‘worst imaginable health state’ (0). The EQ-5D-5L has some important advantages in this study. It has been validated for use in patients with cognitive impairment, for whom an appropriate proxy may respond to the questions. 31 It can be administered by mail or by telephone. Our recent work has demonstrated it to have excellent measurement properties in comparison with other commonly used disease- and region-specific outcome tools in the similar cohort of patients with fragility hip fracture. 22,23 The EQ-5D-5L scores were collected at baseline (for pre and post surgery), 6 weeks post surgery and 4 months post surgery.
The Dementia Quality of Life Measure (DEMQoL)32 score is a validated questionnaire specifically designed to assess quality of life in patients with dementia. A large minority of the participants in this study are expected to have coexisting dementia. The score can be self- or proxy-reported and comprises 28 or 31 items, respectively. These data were collected at baseline and at 6 weeks and 4 months post surgery in participants who had cognitive impairment. Recently, preference-based utility scores for a UK population have also been published. 33
Lower limb function
The Disability Rating Index (DRI)34 score is a validated self-reported questionnaire. It comprises 12 items specifically related to function of the lower limb. These data will be collected at baseline and at 6 weeks and 4 months post surgery in participants who do not have cognitive impairment. The DRI34 has been proven to be a robust, practical clinical and research instrument with good responsiveness and acceptability for assessment of disability caused by impairment in the lower limb. 35
Complications
All complications were recorded. Complications were classified as either:
-
unrelated to the trial protocol
-
related systemic complications (including venous thromboembolic phenomena, death, pneumonia, urinary tract infection, blood transfusion, acute cerebrovascular accident, acute cardiac event, other)
-
related local complications (superficial/deep infection, non-/mal-union, failure/removal/revision of metalwork, injury to adjacent structures, such as nerves/tendons/blood vessels, other).
Radiographic evaluation
Standard anteroposterior and lateral radiographs of the femur were assessed for malunion at 6 weeks post injury. Radiographs were those routinely used for the investigation of patients with a suspected fracture of the distal femur and for the follow-up of such patients following any intervention, so that there would be no need for any additional or special investigations. Radiographs were assessed by an independent researcher at each site for:
-
evidence of early loss of fixation
-
varus/valgus of > 5°
-
re/procurvatum of > 10°
-
shortening of > 1 cm.
Semistructured interviews
Patients, carers and staff were asked to participate in qualitative interviews to discuss their experience of participating in the trial and the intervention. Interviews were semistructured, based on a semistructured interview guide (see Appendix 1).
Adverse event management
An adverse event (AE) was defined as any untoward medical occurrence in a clinical trial subject that did not necessarily have a causal relationship with the treatment. All AEs were listed on the appropriate clinical reporting form (CRF) for routine return to the TrAFFix central office. A serious adverse event (SAE) was defined as any untoward and unexpected medical occurrence that:
-
resulted in death
-
was life-threatening
-
required hospitalisation or prolongation of existing inpatients’ hospitalisation
-
resulted in persistent or significant disability or incapacity
-
was a congenital anomaly or birth defect
-
was any other important medical condition that, although not included in the above, may have required medical or surgical intervention to prevent one of the outcomes listed.
Some SAEs were expected as part of the surgical interventions and did not need to be reported to the trial co-ordinating centre, provided that they were recorded on the ‘complications’ section of the CRFs. These included:
-
wound infection
-
venous thromboembolic phenomena
-
blood transfusion
-
death
-
pneumonia
-
urinary tract infection
-
cerebrovascular accident
-
myocardial infarction/acute coronary syndrome
-
damage to a nerve, tendon or blood vessel.
All other SAEs were entered onto the SAE reporting form and sent to the TrAFFix office by e-mail within 24 hours of the principal investigator (or delegated clinician) becoming aware of them. Once received, causality and expectedness were confirmed by the chief investigator. The SAEs that were deemed to be unexpected and related to the trial were notified to the REC within 15 days of being reported to the TrAFFix office. Any such events were be reported to the TSC and Data Monitoring Committee at its next meeting.
All participants experiencing SAEs were followed up as per protocol until the end of the trial.
Risks and benefits
The risks associated with this study were predominantly the risks associated with the surgery: infection, bleeding and damage to the adjacent structures, such as nerves, blood vessels and tendons. Participants in both groups underwent surgery and were potentially at risk from any/all of these complications. There were no data to suggest that the risk is greater in one group than another. We believe that the overall risk profile was similar for the two interventions.
Statistical analysis
Analysis plan
The statistical analysis plan was agreed with the Data Safety Monitoring Committee (DSMC) at the start of the study.
Software
The main analyses were conducted using specialist mixed-effects modelling functions available in the software package R (The R Foundation for Statistical Computing, Vienna, Austria), for which EQ-5D-5L29 data were assumed to be normally distributed, possibly after appropriate variance-stabilising transformation.
Data validation
Data returned to the trial office were entered into an OpenClinica database (version 3.7; OpenClinica LLC, Waltham, MA, USA) and data that were missing or failed to pass automatic validation checks were queried with researchers at participating sites. A random sample of 10% of CRFs were checked against the database to ensure accuracy of data entry.
Missing data
The reasons and patterns of any missing data, loss to follow-up and participant withdrawals were carefully considered and reported.
Final statistical analyses
The primary outcome measures for this feasibility study were the participant recruitment rate and the completion rate of the EQ-5D-5L during follow-up. The overall monthly recruitment rate was estimated using Poisson regression analysis, with 95% CIs to assess the likely range of rates in a future main study. Data completeness for the primary EQ-5D-5L outcome was calculated as the percentage of randomised participants completing the HRQoL at baseline and at 6 weeks and 4 months after operation.
Baseline demographics (e.g. age, sex, cognitive status) were compared between groups to ensure that an approximate balance was achieved. This was a small study so group treatment effects were unlikely to be estimated with much precision and, consequently, inferences were tentative and reported as such.
The main analysis of the effects of the intervention investigated differences in the primary outcome measure, EQ-5D-5L29 score at 4 months, between the two treatment groups (nail and plate) on an intention-to-treat basis. In addition, a per-protocol analysis was also reported and early EQ-5D-5L status assessed and reported at 6 weeks. Differences between groups were based on a normal approximation for EQ-5D-5L. 22,23 Tests were two-sided and considered to provide evidence for a significant difference if p-values were < 0.05 (5% significance level). The stratified randomisation procedure ensured a balance in cognitive impairment and recruiting centre between test treatments. Although generally we had no reason to expect that clustering effects would be important for this study, in reality the data would be hierarchical in nature, with patients naturally clustered into groups by recruiting centre. Therefore, we accounted for this by generalising the conventional linear (fixed-effects) regression approach to a mixed-effects modelling approach, in which participants are naturally grouped by recruiting centres (random effects). This model formally incorporated terms that allowed for possible heterogeneity in responses for patients from different recruiting centres, in addition to the fixed effects of the treatment groups, cognitive impairment and other participant characteristics that might prove to be important moderators of the treatment effect (e.g. age and sex).
Secondary analyses were undertaken using the above strategy for approximately normally distributed outcome measures, such as DRI. 34 For dichotomous outcome variables, such as complications related to the trial interventions, mixed-effects logistic regression analyses were undertaken with results presented as odds ratios (and 95% CIs) between the trial groups.
In order to assess the relative performance and merits of EQ-5D-5L and DEMQoL in the study population, we planned to compare the two measures in the subgroup of study participants who were unable to self-report EQ-5D. Given the relatively small size of this study, and minority of participants who were unable to self-report, we anticipated that there would be insufficient data to undertake formal statistical testing for differences between measures. However, graphical presentation of the distribution and relationship (correlation) between measures for individuals would provide some assessment of the merits and metric properties (e.g. variance) of the two measures. Agreement or moderate to strong correlation between measures would indicate that the instruments measure the same underlying trait, which we take to be the true HRQoL of the study participants.
Null hypothesis
For the purposes of analysis for the data collected in the feasibility study the following null hypothesis was proposed:
-
There is no difference in EQ-5D-5L score at 4 months after injury between adults aged > 18 years with an acute, extra-articular fragility fracture of the distal femur treated with ‘locking’-plate fixation (plate) and those treated with retrograde intramedullary nail fixation (nail).
Health economics analysis
The economic analysis investigated the feasibility of a definitive economic evaluation within a large RCT of treatment with modern intramedullary nails or anatomical locking plates for fragility fractures of the distal femur.
A NHS and Personal Social Services perspective was adopted for the costing component of the feasibility study. The main analysis reports the practicalities and difficulties associated with an assessment of the cost to providers, to individuals and, more broadly, to society consequent on the intervention, along with the identification of appropriate sources of unit cost data.
Process evaluation
We evaluated intervention implementation, mechanisms of impact and context in line with the MRC guidance on process evaluation of complex interventions using a mixed-methodology approach. 16 Process evaluation enables us to understand how the interventions work and under what circumstances effectiveness is achieved.
In this feasibility study, we developed and tested methods for process evaluation that might then be modified in the subsequent definitive trial. The findings of the process evaluation could also lead to modifications in the plan for outcomes evaluation and so we did not separate research team members conducting process and outcomes evaluation in the way that might be appropriate in a definitive trial.
Implementation
Evaluation of intervention implementation focused on four areas. These were (1) the reach of the interventions, (2) the fidelity of delivering the interventions, (3) the acceptability of the interventions and study procedures and (4) understanding how delivery was achieved.
The reach of the intervention, that is whether or not the intended audience came into contact with the intervention, was assessed through the rates of screening and recruitment at each centre over the 10-month period. The fidelity of delivering the intervention considered the procedures for screening patients and application of the study eligibility criteria, the content of consent discussions, deviations from the study protocol and delivery and compliance with post-operative rehabilitation instructions. In addition to our evaluation of intervention implementation, we examined the implementation of the study processes in order to inform the development of a definitive trial.
Mechanisms of impact
Process evaluations seek to identify how the delivered intervention produces change. From our process evaluation data and patient and public involvement (PPI) workshop, we identified relevant intermediate outcomes that might be associated with the effect of the interventions on the primary outcomes of interest. These were used to develop a logic model for the feasibility study that worked from the hypothesis that nail fixation is associated with better outcomes then locking plate fixation.
Context
Understanding of the context in which the intervention is delivered is important to understand how the outcome was achieved. Our evaluation of context focused on three areas. These were the national context, contextual similarities and differences between the participating centres and patient factors.
Screening logs and enhanced screening
Screening logs were kept at each site to determine the number of patients assessed for eligibility. As fewer than expected fractures of the distal femur were recorded on the screening logs, the TSC recommended further screening to ascertain whether or not any distal femoral fractures had been missed. Trainee PIs at each participating centre were asked to review hospital records and rescreen all patients who were admitted with fractures of the distal femur during the recruitment window for their institution. It was recommended that this was done by searching electronic records for fractures of both intra- and extra-articular distal femur [Arbeitsgemeinschaft für Osteosynthesefragen (AO)/Orthopaedic Trauma Association (OTA) 33]. 18
Trauma Audit and Research Network data
We requested admissions data from Trauma Audit and Research Network (TARN)36 in order to monitor the accuracy of the screening logs and enhanced screening. This allowed us to compare the screening information returned by the participating centres with the information returned to TARN. Clinical leads for TARN at each site gave us permission to receive anonymised aggregate patient demographic data that corresponded to our screening data. These screening data were compared with screening data supplied by research teams at each site to help confirm the completeness of the screening logs. The TARN database was queried using a search string that included the site ID, the recruitment window for which the site was open for TrAFFix and the AO/OTA classification 33A, B and C.
We also requested some additional data, such as operation(s) performed, injury severity score and comorbidity index, in order to determine whether or not recruitment may have been biased against certain patient groups. We collected some basic information about the provision of rehabilitation for patients after a distal femoral fracture, specifically the rehabilitation recommended and received.
Clinical reporting forms
The CRFs, comprising data collected from participants and their medical notes, were completed at the time of recruitment (which included pre- and post-injury information) and at 6 weeks and 4 months post injury.
NHS data
We used data from NHS Digital, NHS England Statistics and the annual reports of the participating NHS trusts to describe the context for each participating hospital. From NHS Digital, we used the NHS Hospital and Community Health Service (HCHS) Workforce Statistics in England, Summary of staff in the NHS 2003–201337 and Hospital Admitted Patient Care Activity. 38 This provides details on workforces within NHS organisations, including numbers of consultants, registrars and other doctors in training by specialty. It is provisionally published monthly and data are extracted from NHS human resources and payroll system. Hospital-admitted patient care activity reports the number of finished consultant episodes and admissions. It is published annually and uses data collected from the Hospital Episodes Statistics, which contains records of all admissions, appointments and attendances for patients at NHS hospitals in England. From NHS England Statistics, we used The NHS Quarterly Bed Availability39 and Supporting Facilities Dataset. 40 The former gives data on the number of available beds and occupied beds. The latter provides information on operating theatres and dedicated day case theatres. These data sets are published quarterly; we looked for information about the populations they serve from the annual reports of the participants NHS trusts.
Questionnaire
A brief questionnaire, comprising six questions, was used to assess surgical expertise and preference. The questionnaire was sent to consultant trauma and orthopaedic surgeons by e-mail using the distribution lists of the Orthopaedic Trauma Society and PIs at each of the participating centres. The questionnaire content can be found in Appendix 2.
Interviews
Qualitative interviews adopted a phenomenological approach that has been used successfully in other trauma studies. 41,42 This approach seeks to understand individuals’ lived experience of a phenomenon of interest, and in this study staff and participants’ experience of TrAFFix and participants’ experience of being injured was explored. To enable interviewees to tell us what was important to them, the interviews were semistructured and used a brief topic guide. Topics covered during participant interviews were their experience of (1) injury, (2) recovery and (3) taking part in TrAFFix. Interviews with RAs covered (1) their experience of recruiting to TrAFFix and other trauma trials, (2) their experience of explaining research studies to patients, (3) their experience of nominated consultee consent, (4) their experience of follow-up questionnaires and (5) their views on their colleagues’ engagement with research and TrAFFix. Surgeon interviews covered the following topics: (1) their experience of recruiting to TrAFFix and other trauma trials, (2) their experience of the two interventions, (3) their views on rehabilitation, (4) their views on blinding and (5) their colleagues’ engagement with research and TrAFFix. Owing to the small number of patients recruited to the study, staff interviews explored experiences of trauma trials in general, as well as staff experiences of TrAFFix. Interviews were conducted face to face or by telephone. The majority of staff were interviewed towards the end of the recruitment period or shortly after, with 22 of the 24 interviews conducted between May and October 2017.
Patient and public involvement workshop
We held a 1-day workshop with PPI representatives to learn about the factors other than surgery that influence patients’ recovery from this injury. The workshop aimed to identify what is important for patients and their families/carers during treatment and recovery. Factors identified form this workshop contributed to the development of a logic model for the feasibility study. The patient pathway, from before the fracture to returning home from hospital, was used as a guide to discuss what might be important for patients at each stage. The PPI representatives from the Oxford Trauma PPI group were invited to attend the workshop by e-mail. The workshop was also advertised on the Patients Active in Research (PAIR) website. Six PPI representatives and four members of the study team attended. The workshop was audio-recorded with consent from the attendees.
Audio-recordings of consent discussion
The intention was for RAs to record their discussions with patients about the study, with agreement from the patient. However, there were limited opportunities for RAs to do this and it proved difficult in a trauma setting. Consequently, only one discussion about the study was audio-recorded.
Data analyses
Quantitative data
Discrete data were summarised as absolute values and proportions; continuous data as means and SDs. No inferential statistical tests were performed but comparisons were facilitated through tabulation of the data.
Qualitative data
When participants agreed, interviews were audio-recorded and transcribed verbatim. Data analysis was conducted alongside data collection to enable refinement of the interview topic guide. NVivo 10 (QSR International, Warrington, UK) was used to manage the data. All data relating to trauma trials and the study processes were analysed inductively using thematic analysis. 43 This involved grouping sentences or paragraphs of similar meaning into codes. Similar codes were then grouped together into categories by comparing within and across the codes. For example, the category enabling participation comprised codes that described involving family or nominated consultee consent procedures. Three themes relating to trial recruitment were developed by comparing within and across the emerging categories. Within this approach, we acknowledge that the researcher’s interpretation of codes, categories and themes is shaped by their own experience and knowledge. To enable reflection on this process throughout analysis, Emma Phelps, Elizabeth Tutton, Janis Baird and Xavier L Griffin met regularly to discuss the emerging themes. Data saturation occurred when the team agreed that no new elements were arising from the interviews or within the themes. Data saturation was achieved within the staff interviews but the degree of frailty in the patient population limited the degree of saturation that was achieved. The thematic framework and the themes and categories within it are presented in Table 2. The audio-recorded consent discussion was transcribed verbatim. The transcript was used to see what information patients were given about the study and how patients responded.
| Item | Component | Data sources | Indicator |
|---|---|---|---|
| Reach |
|
|
|
| Fidelity |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Acceptability |
|
|
|
|
|
|
|
| How is delivery achieved? |
|
|
|
Integration
Qualitative and quantitative data relating to each aspect of the process evaluation are presented within the process evaluation framework. The themes and categories identified from the thematic analysis were also mapped onto the process evaluation framework to demonstrate how they relate to each aspect of the process evaluation. Tables 2–4, which summarise the process evaluation results, demonstrate how the qualitative themes relate to the process evaluation findings.
| Item | Component | Data sources | Indicator |
|---|---|---|---|
| Existing factors | Factors relating to the patients, such as health, social support, levels of self-efficacy, which may influence their recovery |
|
|
| Injury and treatment | Factors relating to the injury, treatment and time in hospital, which may influence patients’ recovery |
|
|
| Post-discharge factors | Factors relating to the patients, such as access to support and place of discharge, which may influence their recovery |
|
|
| Item | Component | Data sources | Indicator |
|---|---|---|---|
| National context |
|
|
|
| Contextual similarities and differences between the participating centres |
|
|
|
| Patient factors |
|
|
|
Ethics approval and monitoring
Ethics committee approval
TrAFFix was approved by the Wales REC (reference number 16/WA/0225), study-wide NHS approval was given by the Health Research Authority (Integrated Research Application System 206745) and participating NHS trusts provided local approvals. The study protocol has been published. 17
Trial Management Group
The day-to-day management of the trial was the responsibility of the trial co-ordinator, based at Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), and supported by the OCTRU administrative staff. This was overseen by the Trial Management Group, which met monthly to assess progress. It was also the responsibility of the trial co-ordinator to undertake training of the RAs at each of the trial centres. The trial statistician and health economist were closely involved in the setting up of data capture systems and the design of databases and CRFs.
Trial Steering Committee
A TSC, which included independent members, was responsible for monitoring and supervising the progress of TrAFFix. The terms of reference were agreed with the Health Technology Assessment (HTA) programme manager and was drawn up in a TSC charter that outlined its roles and responsibilities. Meetings of the TSC took place at the beginning and end of the feasibility study and once during recruitment.
An outline of the remit of the TSC was to:
-
monitor and supervise the progress of the trial towards its interim and overall objectives
-
review, at regular intervals, relevant information from other sources
-
consider the recommendations of the DSMC
-
inform the funding body on the progress of the trial.
The TSC consisted of five independent experts, a lay member and the chief investigator. Membership of the TSC is given in Acknowledgements.
Data Safety and Monitoring Committee
The study DSMC agreed and adopted an appropriate charter, structured in accordance with DAMOCLES principles,45 which defined its terms of reference and operation in relation to oversight of the trial. The DSMC was not asked to perform any formal interim analyses of effectiveness. The committee did, however, review accruing data and summaries of the data presented by treatment group and assessed the screening algorithm against the eligibility criteria. The DSMC reviewed all related SAEs that were reported and could advise the TSC if, in its view, the trial should be stopped for ethics reasons. The DSMC meetings were held once during the recruitment phase of the study and once at the end of the trial. The trial statistician provided data and analyses requested by the DSMC at each of the meetings. Membership of the DSMC is given in Acknowledgements.
Chapter 3 Results of the process evaluation
Introduction
This section is divided into three parts. We will first present the logic model developed for this feasibility study. Second, we will describe the characteristics of the patients and staff groups who were interviewed during the process evaluation. This will be followed by our evaluation of implementation, mechanisms of impact and context.
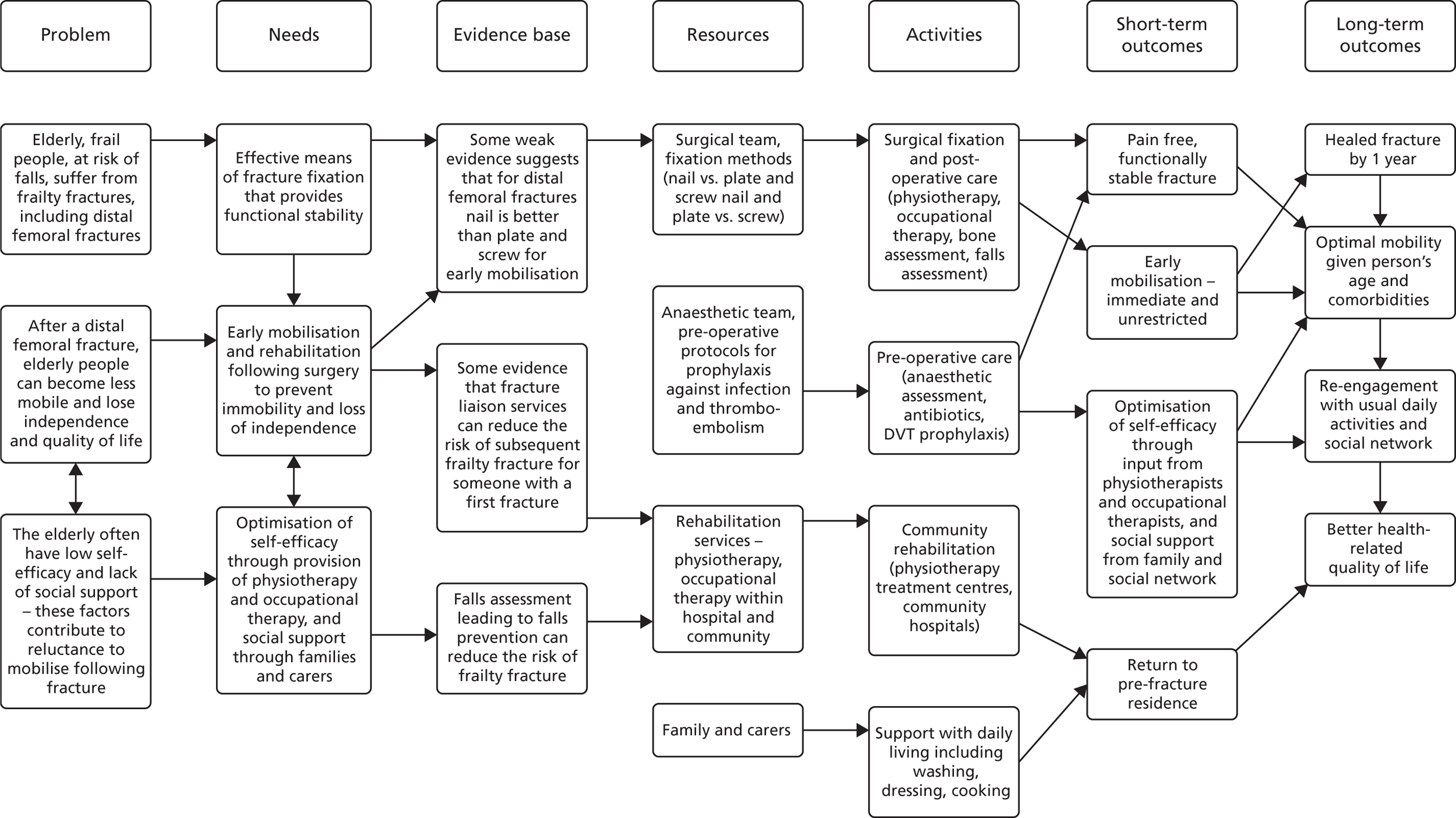
Logic model
We developed a draft logic model for TrAFFix through discussions with clinical members of the research team. The model summarised the problem posed by fractures of the distal femur, which tend to occur in frail older patients, and the resulting need for effective methods of fixation combined with support for rehabilitation and recovery in this group of patients. Logic models provide a diagrammatic representation of the relationships between an intervention’s resources, activities and intended outcomes. 46 The model outlined the evidence in support of the two approaches to fracture fixation and the resources and activities required to deliver the treatment. Short- and long-term outcomes were identified. We then used the content of the draft logic model to inform discussion at a 1-day workshop with PPI representatives. The workshop aimed to identify factors, other than surgery, that are important for patients and their families/carers during treatment and recovery from this injury (see Chapter 2). The themes that emerged from the workshop informed our findings relating mechanisms of impact summarised in Tables 5–7, but also fed into the logic model. Many of the factors that the clinical team had identified as potentially important pre- and post-operatively, such as patient frailty, lack of confidence (self-efficacy) and comorbidities, were also identified by the PPI representatives. The resulting version of the logic model (Figure 1) will form the basis for the full-scale trial of acute femoral fracture fixation.
| Item | Component | Data sources | Findings | |
|---|---|---|---|---|
| Quantitative | Qualitative | |||
| Reach |
|
|
|
|
| Fidelity |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Acceptability |
|
|
|
|
|
|
|
|
|
| How is delivery achieved? |
|
|
|
|
| Item | Component | Data source | Findings | |
|---|---|---|---|---|
| Quantitative | Qualitative | |||
| Existing factors | Factors relating to the patients, such as health, social support, levels of self-efficacy, which may influence their recovery |
|
|
|
| Injury and treatment | Factors relating to the injury, treatment and time in hospital, which may influence patients’ recovery, for example grade of operating surgeon |
|
|
|
| Post-discharge factors | Factors relating to the patients, such as access to support and place of discharge, which may influence patients’ recovery |
|
|
|
| Item | Component | Data source | Findings | |
|---|---|---|---|---|
| Quantitative | Qualitative | |||
| National context |
|
|
|
|
| Contextual similarities and differences between the participating centres |
|
|
|
|
| Patient factors |
|
|
|
|
FIGURE 1.
Logic model for TrAFFix.
Interview participant characteristics
A convenience sample of 11 study participants, or their personal consultees, from five out of the seven centres participating in the study were interviewed. Seventeen participants agreed to be approached about taking part in an interview. One participant died and another withdrew from the study prior to being contacted about the interview. Two participants declined to be interviewed when contacted by the researcher and two could not be reached. The sample of participants interviewed included two consultees who provided consent for their relative to participate in the study. Of the participants who were interviewed or whose consultee was interviewed on their behalf, two were male and nine were female. All participants, or their carers where interviewed, were of white ethnicity and aged between 54 and 93 years (mean age of participants 76.3 years). Participants were interviewed up to 5 months after surgery. Three participants were interviewed twice. The majority of participant interviews were conducted by telephone (n = 9). One participant went through the interview questions with her daughter, who gave the answers to the researcher in writing.
A purposive sample of 24 members of staff from each of the seven sites were also interviewed. Of the 24 members of staff interviewed, 10 were surgeons. The remaining 14 members of staff, hereafter referred to as RAs to protect anonymity, included research nurses, a RA, a physiotherapist, a research manager and a trial co-ordinator. The majority of staff were interviewed face to face (n = 21).
Process evaluation results
For each aspect of the process evaluation framework we present a brief synopsis of the relevant quantitative and qualitative findings at the beginning of the section (see Tables 5–7). Within these tables we also demonstrate how the themes developed from the qualitative analysis relate to the process evaluation framework.
Implementation
Our evaluation of implementation considered the implementation of the surgical and rehabilitative components of the intervention and the implementation of the study procedures.
In relation to intervention implementation, we evaluated whether or not potentially eligible patients received the interventions. This is described within the sections Reach, Applying the study eligibility criteria, Protocol deviations and Patient compliance with rehabilitation instructions. Our evaluation of intervention implementation also explored the acceptability of the interventions as presented in the sections Acceptability of the interventions to staff and patients (referring to fixation with nail or plate) and Patient compliance with rehabilitation instructions.
In order to inform the development of a definitive trial, we also examined the fidelity of applying the study procedures and the acceptability of the study procedures, as described within the sections Reach, Applying the study eligibility criteria, Consent discussions, How was delivery achieved? and Acceptability of study procedures.
Our evaluation of intervention implementation and implementation of the study procedures overlaps with some components, such as ‘reach’, aiding our understanding of both areas. For reason this, we have not separated these two areas within our results. For a summary of our findings regarding implementation, see Table 5.
Reach
Screening and recruitment
[The quotations throughout this chapter were produced in the course of research and also appear in Griffin et al. 44 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/.]
Ninety-one patients were screened and recorded on screening logs during the 10-month recruitment period. Of these, 54 were eligible to participate in the study. After review by the TSC, this number seemed too small given the assumptions made in the development of the protocol. The TSC recommended revisiting screening with the sites to confirm the incident fracture population size. Trainee PIs and PIs at each of the sites were asked to revisit their local clinical databases to confirm the number of potentially eligible patients and, when additional patients were identified, to conduct screening based on the clinical records. This enhanced screening found a further 82 unscreened patients with distal femur fractures who were not included on the screening logs. Of these, 31 met the eligibility criteria for inclusion in the study.
The number of patients added from enhanced screening varied by centre, with between 0 and 34 patients added. In four centres, ≥ 40% of distal femoral fractures were not included on the screening logs and were added after enhanced screening. At interview, staff were confident that few patients were eligible for the study, suggesting that they were unaware that potentially eligible patients were being missed. Some staff appeared confident that they were not missing patients, even in centres that were subsequently found to have missed many patients. Some research teams were unable to provide a fully integrated daily provision to the clinical teams:
With the TrAFFix study, well we just never had the numbers come through and I think the only two that we actually missed were during weekends and I think one was when I was on annual leave and obviously, research nurses don’t work 7 days a week and that was the issue for recruiting.
Staff (RA) 19
Differences in the number of patients missed from screening logs may relate to the experience of the research teams and the research culture within the centres, which are discussed further in the sections Procedures for screening patients and Contextual similarities and differences between the participating centres. For example, in some centres, not all surgeons within the team screened and identified eligible patients and this may have contributed to patients being missed:
Generally it is mainly the PI that screens for them and that would be identifying them. We do if we find them on the trauma list but it would be mainly the PI that would be identifying if the patient was eligible for us and obviously the PI wants to have people in the trial.
Staff (RA) 4
In addition, patients deemed ineligible might not have been recorded on the screening logs in some centres. One surgeon felt he had ‘a very big screening log to actual recruitment’ (staff, surgeon 18) despite having very few patients recorded on the log.
Figure 2 shows the number of patients screened, the number of patients deemed eligible for inclusion in the study and the reasons for exclusion. Of the 85 eligible patients, 23 were included in the study. Thirty-nine eligible patients were excluded because of surgeon preference, two declined to participate, five were missed as a result of staffing (e.g. the PI was not present to confirm eligibility, or the patient was admitted and operated on over the weekend) and one was missed owing to failure of the randomisation programme. The reasons for missing the remaining 15 patients are unknown. Further details of screening are reported by site in Appendix 3.
FIGURE 2.
Summary of screening. RRAMP, Registration/Randomisation and Management of Product. Adapted from Griffin et al. 44 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/.
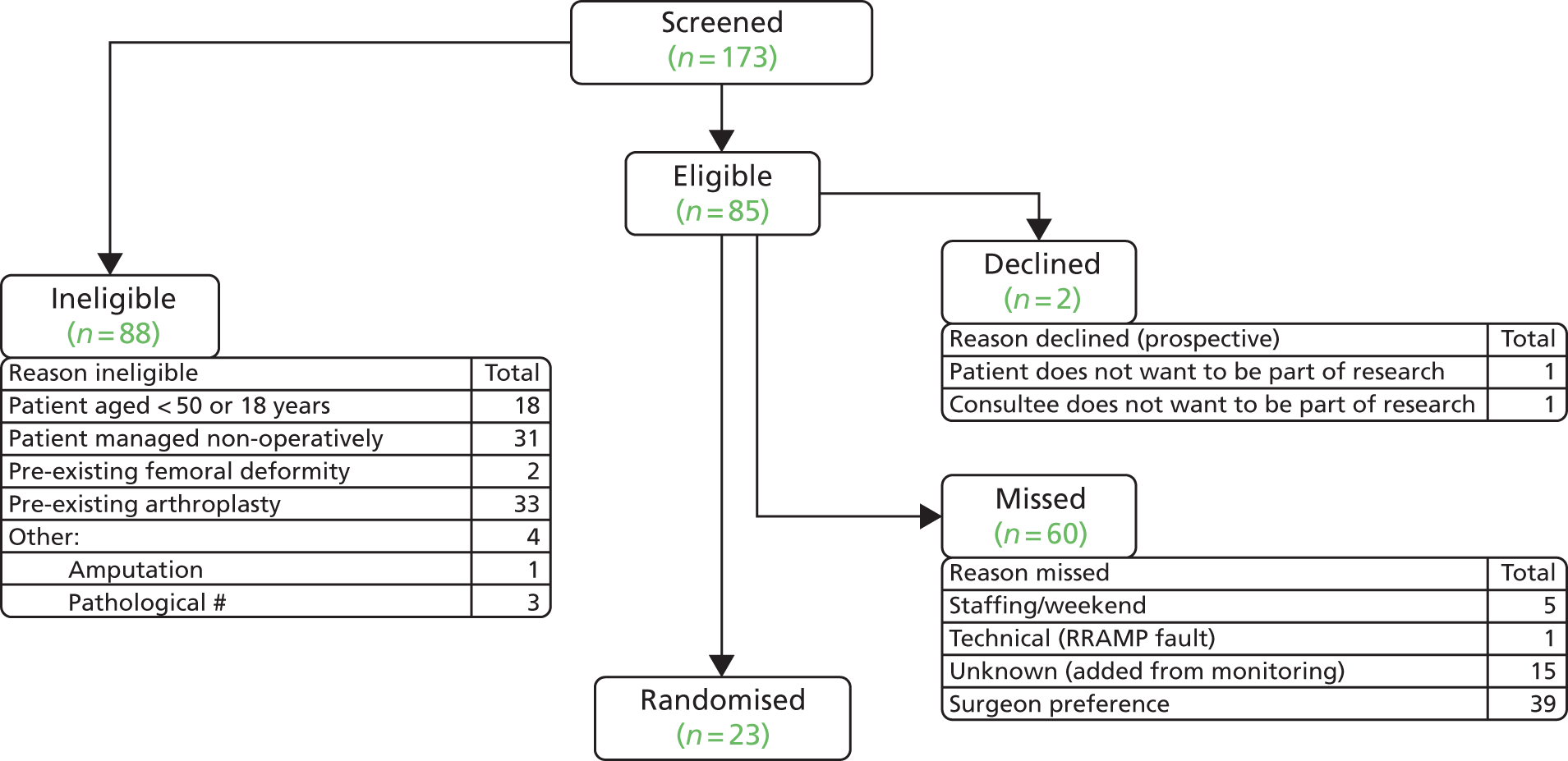
After the TSC recommended that the age limit be lowered, a further 69 patients were screened. In this group, eligibility increased from 44% to 60% but this did not translate into an increase in successful recruitment into the study. Only 18 out of the 88 ineligible patients were excluded because of age. After the change in eligibility criteria, only two participants were recruited who were < 50 years of age. Only 3 of the 69 patients screened after the change sustained their fracture from an injury involving more energy transfer than a fall from standing height.
The reasons for ineligibility and missed patients varied between sites. Of the 39 patients treated non-operatively, 18 were from a single site, whereas another site did not report any patients treated non-operatively. Similarly, the proportion of eligible patients excluded because of surgeon preference ranged from 0–10 to 15–19 between sites, although two sites did not completely report the reasons why patients were not included as some patients were screened retrospectively during monitoring activities after the study had closed.
Two centres did not record reasons for missing the majority of patients eligible for inclusion in the study. In the remaining five centres, surgeon preference was the most common reason for eligible patients not being included. The proportion of eligible patients excluded because of surgeon unwillingness to randomise in these five centres varied from 43% (three out of seven eligible patients) to 79% (15 out of 19 eligible patients). In three centres, < 50% of eligible patients were excluded because of surgeon preference, and in two centres > 70% of eligible patients were excluded because of surgeon preference. Several factors may have contributed to this variation. Differences in surgeons’ interpretation of the eligibility criteria were evident at interview and are discussed fully in Applying the study eligibility criteria. Some surgeons felt that patients could be ‘borderline’ or not appropriate for both of the treatments and this might have influenced the number of patients they excluded. Research culture and the experience of the research teams may have also influenced the number of patients excluded because of surgeon preference. In addition, of these five centres, the three that were major trauma centres excluded a smaller proportion of eligible patients because of surgeon preference, perhaps reflecting a greater willingness among specialist trauma surgeons to use both technologies.
Combining the baseline demographic data collected for all screened patients with the hospital data supplied from TARN demonstrated that the screened population was over two-thirds women, one-fifth of whom had cognitive impairment and were aged approximately 70 years. Although a little younger than the hip fracture population, which has a mean age in the UK of 83 years,47 this cohort was similar to a hip fracture population.
Fidelity
Procedures for screening patients
The ideal method of screening patients was for the clinical care teams to identify eligible patients in the emergency department and trauma wards and notify the research team during the daily trauma meeting. Interviews with surgeons and RAs revealed that in several centres the clinical teams tended not to notify the research teams of eligible patients. These centres relied on strong research teams to screen patients and promote studies. The presence of members of the research team (PIs and RAs) in the daily trauma meeting also facilitated screening, as they were able to prompt the clinical teams to consider whether or not patients were eligible. PIs were usually unable to attend every trauma meeting because of other commitments and RA attendance varied. In one centre, the RA attended two or three times per week but was supported by a specialist trainee, while in two centres RAs did not attend the trauma meeting. For one centre, this was as a result of staffing. Staff interviewed at this site felt that RA attendance at this meeting was important for identifying eligible patients, promoting studies and building a rapport with clinical teams:
We have a research nurse in the trauma meeting every morning to screen for patients and so yes they are infrequent and as such the treating surgeons don’t necessarily have it in mind but the research team always do. They have 8–10 studies on their list and they screen the trauma meeting for those patients so . . . I think from the surgeons perspective, because they are not very common, they wouldn’t necessarily phone up the research nurses as we would like them to do and just say someone has come in, I have already mentioned the study to them, so there is a little bit of a scuffle round in the morning because obviously the consultant concerned needs to say to the patient would you mind if the research team approach you about this study and so on, so on that side of logistics yes but not terrible. I think if we didn’t have enough studies running to have a fully funded research team then it would be tricky.
Staff (surgeon) 20
I’m keen to see what is going to happen when we do get the other research nurses going to the trauma meeting because I feel that that’s going to make a big difference and I think our recruitment will increase quite a lot but I might be completely wrong in thinking that. It’s just that I always think having somebody there and having a face to face and having a nurse that is going to see. We have orthopaedic nurse practitioners as well who run the department in the daytime clinically with beds and things and they always know what’s coming in, but they also do some of the clinical stuff for the patients that is more advanced as well. They know everybody that’s coming in and if we get them on boards as well to tell us when patients come in that’s even better. Through emails and just popping in every now and then it’s just difficult to get that rapport whereas actually if you really get to know somebody then they’ll let you know if anybody comes in . . . I’m hoping that they’ll just get to know them because they’ll see them every day and it should help with building that relationship with them as well and the consultants seeing a research nurse every day.
Staff (RA) 4
In addition to the trauma meeting, building relationships with staff who have up-to-date knowledge of admissions could aid RAs in finding eligible patients.
Given the rarity of eligible patients, some centres found it difficult for the clinical care team to keep the study in mind. Other, unspecified, research studies being conducted at the same time as TrAFFix, in which eligible patients were common, were more easily remembered and in one centre were prioritised over TrAFFix:
So I think because we’ve been trying to put more effort into an area that we know is going to guarantee a better outcome. We’ve put more effort into that and sacrificed a study that’s a bit more complicated and harder to recruit to. So yes, it has gone a little bit into the background I would say.
Staff (RA) 16
More often than not they’ve not discussed whether or not the patient is eligible for TrAFFix in their morning meeting and so I’m then ringing them and chasing it up and you’re racing against time and when you are given an answer that they are going to do this one that’s better I don’t know whether that’s because it is better or whether it wasn’t discussed early in the meeting, it’s now half eight and we just need to get on with it and we’ve decided it’s too much hassle to think about randomising them now. I don’t know the reasons behind that and it is sort of infrequent, it’s not in the front of their mind.
Staff (RA) 11
One team described using anonymised instant messaging to prompt and engage surgeons in recruitment to trauma trials. This meant that the PI could encourage recruitment even when unable to attend the trauma meeting in person.
Applying the study eligibility criteria
Obtaining confirmation from treating surgeons that patients were eligible for inclusion was a challenge. The majority of staff interviewed considered there to be few patients eligible for the study, but some also felt that there was lack of equipoise and unwillingness from treating surgeons to randomise patients. Staff emphasised that there were fewer patients with distal femur fractures than they had expected, and many who did were ineligible either because they did not meet the age criterion, which was at least 50 years old at the beginning of the study, or because they had had a total hip replacement, which meant that they were not suitable for a nail. In fact, there was no increase in recruitment rate when the age restriction was removed despite staff beliefs that this was a major contributing factor. Surgeons’ beliefs about the suitability of both interventions for certain fractures (namely periprosthetic, intra-articular and comminuted fractures) also influenced their interpretation of eligibility criteria. Patients with these fractures were considered eligible by some surgeons but borderline by others:
This study is focusing on a very narrow range of patients so they are very infrequent patients. Not all patients are suitable for either or categories so patient selection is very difficult sometimes they are borderline.
Staff (surgeon) 18
So there are certain patients that would be eligible based on the criteria but whom people are saying no but this obviously needs a plate or no but this obviously needs a nail you would never do the other thing for this fracture. Now I appreciate that this may not be across sites but certainty within this site my perception is that that patients are screened eligible but aren’t included because people are going that just shouldn’t have either nail or plate?
Staff (surgeon) 8
Consent discussions
Interviews with participants and staff, along with data from the CRFs, showed that patients eligible to participate in TrAFFix were typically frail, older patients. Their traumatic injury and the effects of drugs and anaesthesia often caused confusion and reduced their capacity to make sense of the study.
Drawing on their experience of TrAFFix along with other musculoskeletal trauma trials, staff described encountering difficulty assessing and handling patients’ limited capacity. They felt that some patients were ‘borderline’ in terms of their ability to consent to research participation. On the surface, ‘borderline’ patients appeared to have capacity to consent to the study as they were judged to have capacity to consent to surgery and could participate well in everyday conversations or seemed to understand the study information. However, staff sensed that they might have been unable to weigh up or retain the information. They acknowledged that having capacity to participate in an everyday conversation or to consent to surgery did not always translate into capacity to comprehend, weigh up and make an informed decision about research participation. During discussions about research studies with this group of patients, RAs sought cues to confirm whether or not they could make an informed decision about participation. These included checking that patients could recall the study, spending time chatting with them and paying attention to the questions they asked:
I remember initially when we started doing the WHiTE [World Hip Trauma Evaluation] study[48] and it was set as black and white and you just looked at the consent form and you based it on the same thing and you followed the guidance of the surgeons and if the surgeon had used the lack of capacity consent form you followed that consent trail and if the surgeon said they’d got capacity you followed that consent trail. But that didn’t really translate because I think most people can understand the concept of you need to have an operation, is that OK yes/no. It’s quite a binary established thing whereas with research they have much more of a choice and much less of an obligation and they don’t know automatically that it’s something of benefit to them whereas I think surgery people it’s an easier decision, it’s a much more clear cut decision. Whereas the research one is a much more complex decision and the people that can make a surgery decision can’t necessarily make the research decision. So I do think you have to make a bit of a judgement on case by case basis and that can be a bit tricky. Sometimes but I can’t think of many occasions where I feel that I’ve got it completely wrong and there have been issues where you come back to a patient say 3 or 4 days later and they can’t remember you or something like that and it’s not happened particularly frequently and so it can be tricky but I don’t think its unsurpassably tricky.
Staff (RA) 7
We have a technique now. The ones without capacity go to consultee, the ones with capacity are very clear. With the borderline patients, we’re doing this new technique now where, and this is retrospectively obviously, when it’s prospective you’re under a time pressure trying to get consent prior to surgery. If they’re already in a study or it’s an observational study what we do when we’re not time pressured we actually go to see them one day, give them the information sheet, have a chat about the study, we go back the next day and if they’ve retained any of that conversation from yesterday or they remember who we are or they say they’ve read that sheet we gave them yesterday then that’s our little method of assessing their capacity. We find that’s really useful for the borderline patients.
Staff (RA) 12
The majority of staff found involving relatives in the discussion about the study to be helpful as it enabled patients to be supported in their decision-making. Some patients, particularly older patients, were concerned about signing or agreeing to something without the involvement of their relative (typically their adult son or daughter) and were worried they may be ‘told off’ for agreeing to something without checking with them beforehand. On the other hand, some staff felt that it was easier to consent patients to studies without involving relatives. Relatives could be protective, concerned that their family member is being used as a guinea pig, and were aware that they are going through something traumatic and felt that a research study may be too much for them at this time:
It depends on the person and sometimes you find that people can be quite nervous because they think a lot of older people are trained aren’t they so they’re told by their children and whatever that if somebody rings you up over the phone don’t agree to do anything, don’t sign up for any contracts, don’t do anything. I think particularly with women when they’re used to having husbands who do a lot of the signing of paperwork and they don’t have to sign for anything and all of a sudden you’re saying sign this and you can tell that they’re a bit guarded because it’s not something that they would normally do. Sometimes you can find it easier if you approach them to try and time it around their visiting hours and so they’ve got a relative with them and so you can kind of talk to them as a family and a lot more patients feel more comfortable with that but it’s about making a decision and again you don’t want to pressurise them.
Staff (RA) 7
Through family, I have experienced more people declining generally for the fact that they’ve got a relative that’s undergoing something that’s really quite traumatic for the family and they don’t feel that they would want to put them through something else that is going to mean follow-up or something else like that. I think if you’re going family consent you’re probably more likely to get people declining depending on what it is and depending upon what the follow-up is.
Staff (RA) 4
I spoke to her [daughter] about it and she said well you know if you feel satisfied with it and it doesn’t include any more cuts and bumps and things and so I said well I did ask that and the answer is no they won’t be doing anything extra. So she said well ok if you feel you want to do it. I think if it helps people, I’ll just as well do it.
Participant 3
Staff avoided jargon and described the study in simple terms, using phrases such as ‘50/50’, ‘computer decides’ and ‘heads or tails’ to explain randomisation. They also emphasised that both treatments are routinely used and that their surgeon was happy for them to receive either intervention, as they believed that these aspects were important to patients:
I think we make sure that they have understanding but I think a lot of it is quite self-explanatory and the trials I find very easy to do and I don’t find them difficult because generally they’re quite simple and you’re offering one standard or another standard. When you explain to the patients that actually the consultant thinks you’re appropriate for both then they would just make that decision but instead it’s the computer making that decision and a lot of people are more than happy to take part really so I find the type of trials very simple to do which makes it a lot easier for the patients to understand.
Staff (RA) 4
They’re going to have surgery anyway and then like I said if you say we don’t know which the better one is and the surgeon is happy, I think is the key point is that the surgeon is happy for them to be part of the study.
Staff (RA) 1
At interview, participants’ recollection of the study tended to be vague. The majority of participants could recall that the study involved a ‘nail or a plate’ but they could rarely describe the study in their own words. Several participants described their struggle to engage with information about the study around the time of their surgery. When discussing the study with a RA, participants were not ‘in a fit state’ (participant 5) to ask questions or were ‘trying to so hard to be normal’ (participant 3):
Yes because one is on the outside and one is a rod through the middle isn’t it?
Participant 4
One discussion of the study between two RAs and a patient was audio-recorded. This patient declined to participate in the trial. During the discussion, the RAs explained that both treatments are routinely used and that the surgeon was happy that either treatment would provide a good outcome for her. The patient appeared uncomfortable with randomisation, explaining that she wanted the surgeon to decide the operation that would be most appropriate for her and would allow her to recover quickly so that she could return to work.
Protocol deviations
Two deviations from protocol were recorded. One patient allocated a plate received a nail and one patient allocated a nail was treated non-operatively.
Some staff described strategies that may help avoid crossovers in surgical trials. If the treating surgeon was uncomfortable or unwilling to perform one of the interventions then another surgeon who was comfortable would take that patient onto their operating list instead. This could prevent missing eligible patients and protocol deviations:
There’s been a couple of others where the operating surgeon has said no and [another surgeon] has taken them on to his list because [he] is happy to treat them equivocally so if he’d have gone we would have put less in if we hadn’t had that additional support where we’ve been able to redirect them.
Staff (RA) 7
Of course, if somebody is not comfortable doing something then we either find somebody who is comfortable or in rarer situations we overrule and let the surgeon do what they wish to do for that patient.
Staff (surgeon) 18
Weight-bearing status was decided by the treating surgeons. Fifteen participants were mobilised on the day of or day after surgery. Postoperative weight-bearing instructions varied, with eight participants instructed to weight-bear as tolerated, three participants instructed to weight-bear as required to survive, seven participants instructed to weight-bear only partially and five participants instructed not to bear weight.
The interviews with surgeons suggested that they held different views about the most appropriate rehabilitation instructions for patients with this fracture. Many favoured early weight-bearing while a minority explained that weight-bearing instructions depended on either the intervention or the fracture. Early weight-bearing was favoured as surgeons felt that elderly patients cannot non-weight-bear or do not have sufficient upper limb strength for partial weight-bearing:
I’m probably pretty much of the theory that they’re elderly and so therefore they can’t non weight-bear anyway and so therefore I’d let them walk if they can, or certainly let them transfer. That’s my theory and I know if I say to them go non-weight-bearing for 6 months or whatever they are not going to do it and so I’m pretty pragmatic that they can deal with one but others will say no non-weight-bearing for weeks on end because that’s the general teaching that was in the past.
Staff (surgeon) 10
Patient compliance with rehabilitation instructions
Of the 15 participants who completed 6 weeks’ follow-up, six were weight-bearing and nine were not. At 4 months’ follow-up, of the 14 participants who completed the questionnaire, nine were weight-bearing and five were not.
For participants, rehabilitation was typically slow and for some it was a frustrating process. At the time of their interview, the majority of participants were trying to walk or stand with frames, crutches or walking sticks. Many were not fully weight-bearing, either because they had been instructed not to do so or because they experienced a lack of confidence after their fracture or were in pain. A few participants had experienced several falls leading up to their injury or they were frightened of falling again, and on the baseline CRF many (n = 16) reported limited mobility prior to their fracture. For some of these participants, support from physiotherapists, particularly while in hospital, helped them to gain confidence. Others were still struggling or had lost confidence since returning home:
Yes, I have got a sheet of exercises to do while lying on my bed and standing up with a frame and rocking from side to side trying to be able to put more weight on that leg . . . the bed ones come natural now, I mean they don’t even hurt any more when I am lying on the bed and I am showing you with my feet now doing my legs and bringing my knees up and pushing my knees back down into the bed but it’s the standing, the standing and putting the weight on that side and I am just no confidence in myself at all.
Participant 9
When the physio came to me I was absolutely shaking from head to foot because I knew I had got to have the [walking frame] on my bad leg if you know what I mean my faulty leg and I was terrified to go on a [walking frame] or anything and they gave me confidence. They were absolutely brilliant with me and they usually come once a day and I said can you come twice a day because obviously I want to get confident so I could get back home and they came to me twice a day and I couldn’t fault them at all.
Participant 7
Acceptability of the interventions to staff and patients
Surgeons’ preferences
Thirty-nine patients were excluded based on surgeon preference. At interview, some staff (surgeons and RAs) felt that many surgeons had strong preferences for one of the two interventions and were unwilling to randomise patients:
TrAFFix wise I think it’s a been quite a controversial study because the surgeons do have quite a strong feeling about what, it’s not evidence based but through experience, is best for this fracture and so I think they’re being challenged because they might be doing an operation that they wouldn’t have first thought would have been the one they would choose and then you get a bit of resistance.
Staff (RA) 5
Several staff who were interviewed explained that preferences varied between individual surgeons and depending on the fracture and that there was no clear overall preference. However, although they tended to say there was no overall preference, they typically indicated that plates are overwhelmingly favoured:
It’s almost universally preferences for plates so the two occasions are periprosthetics around the knee where they are concerned about the nail going in through the box and for patients with unstable fractures people become concerned about them, the intra-articular splits coming displaced or complicating the fracture.
Staff (surgeon) 20
Four of the surgeons interviewed expressed a personal preference for one intervention over the other but were comfortable performing both methods and were willing to randomise patients. Meanwhile, some surgeons described their colleagues as reluctant to accept randomising patients to their less preferred treatment. These findings suggest that some surgeons were able to accept community equipoise and proceed with their less preferred intervention if required:
We haven’t had that many but there have been, so for example I randomised a patient that I was going to operate on and then the list changed such that I wasn’t and so I had to tell one of my colleagues you have to do a plate on this and he said he really wouldn’t want to but I will because they’ve already been put in the study.
Staff (surgeon) 3
Equipoise and surgical skills
Surgeons’ unwillingness to randomise patients stemmed from their beliefs about whether or not both methods of fixation were appropriate for a patient’s specific fracture and their own surgical skills. Interviews with surgeons suggested that, for simple distal femoral fractures (extra-articular fractures in patients with their native knee), surgeons were typically in equipoise, were confident that they could perform both procedures and were willing to randomise patients. For more complex fractures, such as periprosthetic, intra-articular and comminuted fractures, surgeons were less willing to randomise patients as they lacked equipoise or experience of both interventions. Some surgeons believed that these fractures were more appropriate for one method of fixation than the other or that only one method of fixation was appropriate and ‘you would never do the other thing for this fracture’ (staff surgeon 8). Furthermore, in one centre, treating surgeons were not only unwilling to use a nail to fix periprosthetic fractures themselves, but they were also unwilling for their colleagues to do so, reflecting their strong belief that plates were more appropriate for these patients:
I think that there is a lot of resistance to try and get a nail up a knee replacement . . . I think you would physically be able to get a nail up it if you wanted but people don’t just seem generally to be that happy for us doing that and similarly with the intra articular splits people just don’t seem to be that happy with us nailing them, they just don’t think it is the right thing to do.
Staff (surgeon) 8
Because I think with TrAFFix there doesn’t seem to be that equipoise and there seems to be a clear decision about what they would do in their own heads it doesn’t ever seem to be a huge question mark on what you would do and so when you approach them about whether you can put this patient into the study you can see a look go across their face and they go I really want to do this [the study] but this is going to be quicker and its easier and they look at you and go well and they know they should be supporting the research studies and so they probably think about it.
Staff (RA) 7
Some surgeons and RAs believed that the treating surgeons’ own surgical skill influenced their willingness to take part in the study. To include a patient in the study, surgeons needed to be certain that they could use both techniques. Some fractures were considered too difficult to nail and some surgeons had little, if any, experience of using nails to fix some of the types of fractures eligible for inclusion in the study:
To give you an example the other day a patient came in with a periprosthetic knee and people felt unhappy to put a nail in . . . because they had never done it before.
Staff (surgeon) 20
That’s why I said personality because some surgeons they only know how to do a plate and what you will see is plate plate plate plate so it comes down to also what you are good at sometimes and you don’t want something else.
Staff (surgeon) 16
Furthermore, distal femoral fractures were described as difficult to fix in comparison with other fractures, with two surgeons explaining that these operations, unlike many others, are not performed from implicit memory. Some surgeons felt that this might make it more difficult for surgeons to accept randomisation and use their less preferred method of fixation:
The case when they have to ponder and think about things is one when they get a bit stressed out. Distal femur fractures are in that group of it’s a bit more complicated than average and can really be quite difficult and as soon as the surgeon concentrates on that case they start thinking about reasons why they prefer one technique over another and so the uncertainty on the surgeon’s side is much more difficult to establish.
Staff (surgeon) 23
This is a fracture you might only do once a year or once every other year and you’re not very familiar with this kit or the approach and the operation is difficult and now I don’t even want you to choose what kit you’re going to use and it’s one more step along the pathway and so people are more resistant. Whereas when we ask people to do different interventions for hip fracture everyone is doing lots of hip fracture fixations and so they’re comfortable with the overall operation and the additional thing you’re asking them to release from their control and it’s not such a big deal.
Staff (surgeon) 13
Patients’ experience of the interventions
The majority of staff (surgeons and RAs) found patients to be accepting of the study interventions. They felt that this was typical for trials in which two routinely used surgical interventions were compared. Patients were thought to typically understand and accept that their surgeon is recommending that they have an operation and they trusted their surgeon to fix them. Staff reflected that patients were unlikely to recall and understand all elements of the study given their frail and confused state. They felt reassured that patients understood the aim of the study or remembered that it involved ‘nail versus plate’ but acknowledged that it would be difficult for patients to appreciate the differences between these two interventions. Staff understood that the type of metalwork used to fix their fracture was unlikely to be a priority for patients who were in pain and at times worried about their future after injury:
Remember we are talking about the specific cohort of patients before they changed it, I mean sometimes you don’t remember what you ate yesterday especially when you have got after surgery, the drugs, the painkillers, a bit of fear, uncertainty all of these might be more important than whether you had a plate or a nail.
Staff (surgeon) 16
Some people are very trusting of the surgeons and don’t really care and don’t really understand the difference between a plate and a nail and as long as their problem gets fixed and something is being done they’re happy with either one or the other. It would be different if it was like you’re either getting a cast or an operation, that’s the difference but if they have an operation anyway . . .
Staff (RA) 1
The interviews with participants revealed that they were rarely able to describe the study in their own words but typically recognised or recalled the ‘nail versus plate’. They asked few questions about the study and tended to be indifferent to the two interventions. One participant, however, commented that with hindsight she preferred the intervention she received, as she knew someone who had a complication after the other intervention:
Yes I think one is like two metal pieces either side whereas this one the rod goes right through.
I think I prefer the one they have done. I mean I didn’t have a say in it, they decided what they thought was best, you know but I preferred the one they have done definitely.
OK, is there a reason for that?
I don’t know, well there is one reason for that, when I broke my ankle in three places and I was in hospital there was a lady in the bed next to me who had done exactly what I had done to my leg. She was in there about 3 weeks and she had the plates and one day she just moved all of a sudden and she said ooo something moved in my leg and when they X-rayed it her plates had moved and she had to have it all redone and that made me want the rod.
Acceptability of study procedures
Twenty-five patients were invited to participate in the study. Two declined to participate when approached prior to surgery and two declined when approached for retrospective consent to continue in the study after surgery. One participant who consented to participate prior to surgery withdrew from the study after surgery.
Overall, participants were accepting of the study procedures. They expressed altruistic motivations for participation, wanting to help future patients or science. The acceptability of the following study procedures are discussed in turn: (1) nominated consultee agreement, (2) randomisation, (3) blinding and (4) completing clinical reporting forms.
Nominated consultee agreement
Patients who were entered into the study under nominated consultee agreement because of a lack of capacity prior to surgery were approached to continue in the study when they regained capacity. Seven patients were entered into the study under nominated consultee agreement, two of whom withdrew when they were approached after surgery to consent to continue in the study. Of the participants interviewed, only one was approached to consent to continue in the study after surgery, the others were all consented prospectively. They acknowledged that prior to surgery they did not have the capacity to make a decision and expressed no dissatisfaction with being included.
The RAs were familiar with this procedure for patients with reduced capacity from other trauma trials. They described feeling nervous, uncomfortable and guilty about approaching patients after surgery for consent to continue in research studies including TrAFFix. However, they found that in the majority of cases people were accepting of this procedure and did not mind having been included already. They described occasions in other studies when patients became defensive or upset at being included without being asked prior to their operation or withdrew straight away, but this was atypical. Although RAs expected patients to be upset to learn that they had been included in a study, on reflection they found that for some patients this took away a difficult decision in the context of stressful decision-making in an emergency setting. The RAs emphasised the importance of reassuring patients that the study involved no experimental techniques and that the doctor was happy for them to participate when approaching them after surgery. RAs also felt that it was important for the study to be discussed at the earliest opportunity after surgery:
At first we were quite sort of worried approaching people saying you’ve been randomised but actually I think what’s different with the prospective is that they don’t like the idea of making that decision, so making a decision to be randomised is still making a decision whereas if it’s after they still feel like it was ultimately the doctor who made that decision so they still feel like they’re in the best hands, the doctor made that decision to this, I’ve had surgery and I don’t think we’ve had anyone that’s been miffed or upset.
Staff (RA) 11
I find it a bit difficult and guilty as well that the patient has been included in the trial without their consent. There was one patient who straightaway withdrew and he didn’t want to be part of the trial and he was unhappy that he was being included in the trial.
Staff (RA) 2
Randomisation
The majority of staff found randomisation to be acceptable to most patients. Some staff believed that it was considered acceptable because of the explanation that the surgeon thought both treatments were appropriate for them. They understood that after injury many patients, including those eligible to participate in TrAFFix, just wanted to be fixed and trusted their surgeon to fix them. In contrast, two RAs found that patients disliked randomisation and wanted their surgeons to choose the treatment that they felt was most appropriate for them.
As described above, participants were rarely able to describe the study in their own words. When randomisation was described to them during their interview, participants typically seemed to be accepting of this procedure or indifferent towards it. Several participants demonstrated the therapeutic misconception: ‘when a research subject fails to appreciate the distinction between the imperatives of clinical research and of ordinary treatment and, therefore, inaccurately attributes therapeutic intent to research procedures’. 49 They believed that they or their relative would receive the intervention most appropriate for them, suggesting a misunderstanding of randomisation and appeared confused about the alternative to trial participation, which they understood to mean no surgery rather than the surgeon choosing a method of fixation:
Well I think it was the right decision because up until she had the accident she was . . . she’s not at home being miserable you know she had lots of family go round to see her and things and you know if, I didn’t want her to be in pain and obviously I wanted the best that she could get and that’s what has happened and I think it was her right decision to have her leg because obviously you couldn’t leave her and it seems to have worked quite well it just really getting the aftercare that is the problem.
Participant 4
I don’t mind, I don’t know what else they would have done with it. I know they didn’t put a plaster on my leg or anything like that when I came round you could see the bandage and everything my leg weren’t restrained or anything. I just sat in the bed and over a week later, I just had the clips out.
Participant 9
Confusion over randomisation was also evident in the audio-recording of a discussion about the study with a patient who declined to participate. For this patient, the confusion related to the role of the computer, as found in similar studies. They believed that randomisation involved the computer making a decision about the best treatment for them based on her clinical information. They were concerned that the computer may not be able to understand their individual circumstances to the extent that the surgeon could.
Blinding
Not all participants were blind to their treatment allocation at the time of their interview. Five participants described the intervention they received when asked about the study. Some had been told of their allocation following surgery or had seen radiographs when they returned for follow-up. Some staff felt that blinding participants to their treatment allocation would be difficult. This was because patients could see their allocation in the letter sent to their GP, they may be told of their allocation by another member of staff or they may work out their allocation based on their surgical scars. Some staff wanted to tell their patients which intervention they were allocated to if they asked and one felt uncomfortable blinding patients. In addition, some staff questioned how important blinding participants is in a trial, such as this one, in which both interventions are well established and participants are unlikely to hold any preferences or preconceptions about them:
I wouldn’t be particularly comfortable [blinding patients], on a personal level . . . I would want to tell them what they have had. Because they want to see their X-rays by and large and so they will know as soon as they come round before a follow-up what they have had. I don’t think you gain that much by blinding so I wouldn’t try and blind them. The patients aren’t going to have any preconception.
Staff (surgeon) 8
As far as I know they’re blinded but a lot of them ask and if they ask someone will tell them and so I’ve got a feeling that a lot of them know what they’ve got and with TrAFFix they would certainly have known what they got by the scars.
Staff (surgeon) 10
Completing clinical reporting forms
Of the 23 participants entered in to the study, three withdrew at or before their 6-week follow-up, one consented to the collection of routine data only and one died. Fifteen of the remaining 18 participants completed 6 weeks’ follow-up and 14 participants completed 4 months’ follow-up. However, not all follow-up questionnaires were complete.
The RAs found that completing CRFs with patients could be challenging and time-consuming. This group of patients and their consultees needed support to complete the questionnaires, which were lengthy and tiring for patients, and some RAs found that it was occasionally too much for patients to answer all in one go. The RAs felt that many of the questions (EQ-5D and DRI) required talking through because patients were often unable to express their experience using the responses in the scales or were unable to quantify their health. The RAs tended to ask the questions as part of a conversation to pull out the information for the questionnaire, and felt that some questions were not appropriate (e.g. ‘How often is each of the following kinds of support available to you: someone who hugs you?’, ‘Which of the following benefits are you receiving?’); some RAs found that they needed to explain the purpose of the questions, but this could add another layer of complexity to the study. Questionnaires were also considered burdensome for relatives, who also struggled with the questions (pre/post injury) or could not answer them all. At times, RAs needed to contact several relatives to complete one questionnaire or speak to carers to find out the information. Several RAs felt that when patients were wary of participating in studies, such as TrAFFix, this was usually because of the burden of follow-up rather than a dislike of randomisation or a preference for one of the two interventions:
They want to tell you everything so a simple EQ-5D where you literally asking how’s your mobility, can you wash and dress yourself and things like that and I’ve had people go well about 5 years ago I started using a stick and all I need to know is right now, can you walk? It’s nice for them because sometimes you’re the only person that they’ve spoken to for a really long time. If they live by themselves and don’t often have people come into them they want to tell you about the whole journey and you listen because of course you do but sometimes it can be difficult.
Staff (RA) 4
In terms of the follow-up I think maybe if the questionnaires that we’re asking the patients were not so extensive that might help just because of the age category of the patients and I think they struggle a little bit with a lot of questions particularly when, I know obviously they’re separate questionnaires that are used within research, but some of them ask really similar questions and I think they feel like you’ve just asked me that about my mobility so why are you asking me again. Obviously we rate them in a different way and they tell us different things but I think for them they see it as, ‘Why do you keep asking me the same question?’ and so I think that would possibly be something to look at because actually although the patient might go in the trial it could prevent them from follow-up because although the questionnaires aren’t quite so extensive for the other follow-ups I think it could put them off.
Staff (RA) 4
One patient withdrew from the study and another consented to the collection of their routine clinical data only, as they did not want to complete study questionnaires. A minority of participants interviewed found the study questionnaires repetitive, but others explained that completing questionnaires helped pass the time or gave them something to think about while they recovered.
How was delivery achieved?
The overarching concept of facilitating trial recruitment was identified from the interview data collected from participants and staff as part of this process evaluation. This was developed from a phenomenological approach and a thematic analysis (see Chapter 2). Facilitating trial recruitment was defined as the proactive process of navigating patient and family involvement, knowing that it is the right decision to include patients in the trial, and making it work by juggling an array of activities in order to fit in with normal everyday practice. This overarching concept and the three themes it encompasses highlight facilitators of, and barriers to, delivering a complex trauma trial, such as TrAFFix, and aid understanding of how delivery was achieved. Table 8 presents the definitions of the themes and the categories encompassed within the themes along with one example finding for each category.
| Theme | Category | Description | Illustrative example |
|---|---|---|---|
| Theme 1: navigating research with patients after orthopaedic trauma | |||
| Navigating involved actively engaging with patients and their family (carers/friends) to guide them through the process of making sense of the study and enabling their participation in the trial | Making sense of the study | Staff helped patients to make sense of the study by:
|
Staff emphasised that both treatments are routinely used and that their surgeon was happy for them to receive either intervention, as they believed that these aspects were important to patients |
| Enabling participation | Staff enabled participation by:
|
RAs sought cues to confirm whether or not they could make an informed decision about participation, which included checking that patients could recall the study, spending time chatting with them and paying attention to the questions they asked | |
| Theme 2: knowing it is the right decision | |||
| Knowing that it is the right decision involved a process of interpretation of the eligibility criteria, consideration of surgical preferences, skill and beliefs about equipoise with the intent of providing the best care for patients | Making sense of the eligibility criteria | Individual interpretation of the eligibility criteria influenced willingness to include patients in the study | Surgeons’ beliefs about the suitability of both interventions for certain fractures influenced their interpretation of eligibility criteria. Patients with periprosthetic or intra-articular fractures were considered eligible by some surgeons, but ‘borderline’ by others |
| Surgeon preferences | Surgeons’ own surgical preferences influenced their experience of the study and their willingness to take part in the study | Some surgeons and RAs believed that the treating surgeons’ own surgical skill influenced their willingness to take part in the study | |
| Equipoise | Challenges existed as clinical uncertainty varied between individual surgeons, groups of surgeons and the wider surgical community | Some surgeons were willing to include patients in the study despite a personal preference for one intervention as they accepted that as a community there is uncertainty as to which treatment is better | |
| Theme 3: making it work | |||
| Making it work involved juggling a range of activities, balancing recruitment with concerns regarding study burden, and fitting in with staff and normal team practice | Juggling activities | RAs juggle an array of different activities to ensure that recruitment is maximised and fits in with clinical staff and their activities | RAs endeavoured to minimise the impact of research on clinical staff, trying to help where they could, for example by taking patients to the toilet or asking for pain relief or medications for patients |
| Balancing their own beliefs with their recruiting role | Balancing being a practitioner and being a RA could cause conflict and concern regarding the burden of research for patients | RAs felt that for some patients (e.g. those with a terminal diagnosis) research participation was inappropriate and felt uncomfortable approaching them | |
| Research culture | Fitting in with normal ways of working in a busy acute surgical environment could cause tension if the study was not part of normal everyday practice | The presence of RAs in the daily trauma meeting could facilitate recruitment by prompting surgeons to consider whether or not a patient is eligible | |
Navigating research after orthopaedic trauma
Staff understood the complexity of engaging patients in research after injury and were considerate of their confusion, frailty and the trauma that they had endured. They sought cues to assess whether or not patients could recall and comprehend information about the study and adopted appropriate strategies to enable participation. These included using personal or nominated consultee consent when appropriate and by involving relatives to support patients with capacity in their decision-making. The theme navigating is evident in Consent discussions, Acceptability of the interventions to staff and patients and Acceptability of study procedures.
Knowing it is the right decision
Surgeons’ interpretation of the eligibility criteria, their individual treatment preferences and the presence of clinical uncertainty within individual departments and the wider surgical community influenced the delivery of the study. This theme, described below, is captured briefly within Procedures for screening patients and Acceptability of the interventions to staff and patients.
Expertise and confidence to perform both techniques within the team of surgeons could aid recruitment. By taking on tricky cases, surgeons who were confident using both techniques could demonstrate to their colleagues that a good result can be achieved with an intervention that they may not normally choose. Familiarity with the study may also make the decision easier over time. In addition, as described in Protocol deviations, if one surgeon felt uncomfortable performing one intervention, another surgeon could take that patient onto their operating list instead:
We did a couple of cases where people thought we were really completely off our rockers because they ended up being nailed and they were quite tricky. But they went on and were absolutely fine and actually that meant that the rest of the group were much happier to participate in the study because someone else had blazed the way and so that was good. We had a couple of difficult nailings right at the beginning and then they came back to clinic and they’d all done well and we showed the pictures [radiographs] and people knew that it was described in text books and you could do that. But it wouldn’t be what they would normally do and so the degree of acceptance has substantially moved a long way since we started.
Staff (surgeon) 13
There is probably always a little bit of an uptick . . . as people get more used to us repeatedly asking, are you happy to randomise this, perhaps a decision gets made slightly easier.
Staff (surgeon) 8
Some surgeons held strong views about their preferred method of fixation for some distal femur fractures, particularly the more complex fractures. Their lack of equipoise was considered to be one of the main barriers to delivering the study by the RAs and surgeons who participated in interviews. Two surgeons emphasised the importance of accepting community equipoise in the absence of individual equipoise. As described in the section above, they explained that individual equipoise can be difficult to achieve in surgical trials. However, the presence of uncertainty about which of the two interventions is best within the community could give surgeons a reason to randomise their patients:
I think people really generally don’t know which is best, nails or plates. I think they think the idea of the study is fine and they think that it’s a good idea and we should answer the question and I think if you were able to write a paper and give it to them and say X is better than Y then they would be pleased to know that but I do think that they worry about their individual participation in the study because of the complexity of the fracture fixation.
Staff (surgeon) 13
I don’t think when it comes to individual patients then surgeons can have that [equipoise], they always have an opinion about what they prefer to do because that’s what we’re trained to do. But I think the big real change for me over the last 10 years really working in trauma research is that people have embraced this idea that as a community it’s OK for me to randomise my patient because as a group we don’t know. So the fact that I might have a preference individually at that particular moment for that particular patient with that particular fracture it’s still OK to randomise because as a community we don’t know.
Staff (surgeon) 23
Some staff spoke of developing ‘group think’ among surgeons, when surgeons made decisions about treatment and trial participation as a group. They described a consensus between the consultants as to which patients they were prepared to include and in some centres formed collective preferences. Collective preference for one of the two interventions could hinder recruitment as it may be difficult to make the decision to randomise patients without the support of the group. In contrast, disagreement within the group as to which intervention a patient should receive could reinforce the need for the study. In addition, agreement within the team about participation in trials could take away the burden of decision-making from the individual surgeon. If teams agreed that, as a centre, they would include all eligible patients in a trial individual, then surgeons may feel more comfortable to accept randomisation to an intervention that they would not personally choose:
. . . and someone else would pipe up well they’re eligible for TrAFFix and there’s a collective sigh of let’s hope it’s a plate then and so they have their preferences.
Staff (RA) 5
If you say ‘OK well the unit’s going to participate in the trial at unit level then no-one has to make too many individual decisions . . .’ I think one of the advantages of a trial is that it takes away some of your decision-making ability and it takes away some of your personal responsibilities. You still obviously have responsibilities to the patient clinically but one of the key things about surgery is decision-making and so if you can just turn around and say the decision-making is random that’s the whole point and I could participate in that then, it unburdens you a little bit.
Staff (surgeon) 13
For me I think that the real issue is that a consensus opinion falls before [TrAFFix is considered], so everyone says this is what I think we should do so when you say so would you be happy to be randomised the consensus is no.
Staff (surgeon) 8
Making it work
To deliver the study, RAs juggled a variety of activities that allowed them to maximise recruitment and follow-up and balanced their own beliefs with the role of recruiting to research studies. Developing a research culture where clinical teams are engaged in research could also facilitate the delivery of the study. In some centres, this was a ‘work in progress’, with surgeons slowly becoming more involved. In other centres, staff described research to be routine. This theme, described below, is noted within our evaluation of context:
Definitely yes and I think those that have been quite resistant are gradually, very slowly coming round to it and so I think it is improving.
Staff (RA) 4
The consultant colleagues, because we run so many studies, are well rehearsed about patients entering the trials, they know how these people can be managed. There are no issues about anybody getting a bit upset about having a patient on the study that is randomised to one particular method of treating compared to the other. Although they personally might want to do that particular method but they would follow what is in the trial because they know that this is how trials work.
Staff (surgeon) 18
Staff across all sites experienced some degree of resistance from treating surgeons to engaging in trials. For some, this was resistance to specific studies, such as this one, where the treating surgeons did not feel that there was equipoise, but others (surgeons, particularly consultants) were unenthusiastic or unengaged in research more generally. Two reasons for this were suggested. First, research is difficult and not a priority for clinical staff when the department is busy:
I work in a department where (1) it’s really busy and (2) my colleagues will go through the path of least resistance. So if they are going to have to do anything that’s slightly more work than necessary or if you’ve got a busy trauma list they’re not going to start looking. On the days that I’m working and I’m on the trauma list, as in trauma meeting and seeing the trauma list, then it’s easy because I can get people to recruit but the days when I’m not here then nothing happens.
Staff (surgeon) 3
Yes we’re busy and it is a bit relentless for surgeons too, we went through a phase about two months ago and it was a really good meeting and it was this patient can go on this study and that patient to that study and it was really felt that it was being considered but now at the minute it’s a bit of a struggle . . . because the doctors are shattered because they’re working two or three [surgeons] short at the minute and so they’re all doing extra clinical hours and they haven’t got the capacity to really sit back and think about the luxuries of research.
Staff (RA) 5
Second, surgical training may unintentionally inhibit enthusiasm for research by focusing on surgical judgement, decision-making and confidence. Surgeons may feel that the uncertainty required to participate in RCTs is counterintuitive to their everyday role:
So they [the consultants] were used to doing what they thought was good and they just think that what they do is the best and so why do they have to do things, we have consultants who think like that but we cannot do anything.
Staff (RA) 22
I’d given up on individual surgeon equipoise, I don’t think it exists because we’re all trained and probably a little bit personality wise as well to make decisions because that’s what the job requires really.
Staff (surgeon) 23
Three features that may foster the development of a research culture with departments were raised. These were (1) participating in a variety of studies, (2) effective communication between the research team and clinical staff and (3) a strong research team to support clinical teams.
Interviews suggested that participating in several studies might lead to more surgeons becoming involved in research and identifying or recruiting patients eligible for their colleagues’ studies as well as their own. Getting involved in the ‘right’ trials, when the surgeons are interested in the research question, was highlighted by one RA as important, with surgeons who were previously uninvolved in research becoming more active when they considered the research question relevant to their practice:
However, that’s changing and we’ve got a lot more of the consultants on board now and a lot more involved in the trial . . . there’s consultants that are running trials in hand orthopaedics, the more elective side of things but also do the trauma lists and so are getting more involved with what’s going on in research and, therefore, they’re more happy to be involved in it and identifying the patients and things like that.
Staff (RA) 4
And it’s taken a couple of years, there’s been a bit of resistance but now the PIs are getting on board and it’s I’ll recruit to your trial if you recruit to my trial and it’s a snowball effect and so now they argue far less than they used to.
Staff (surgeon) 13
Communication from research teams was a way in which clinical staff could gain a better understanding of the research going on and so did not feel uninformed. In addition to informing staff of research during meetings, one centre described using anonymised instant messaging to communicate as described in Fidelity, Procedures for screening patients. Others put up posters or gave positive feedback to show appreciation and encourage input:
I think in the bigger department there’s a lot of scepticism, people can be quite – not obstructive exactly but maybe they feel the researchers don’t communicate very well to them and so there seems to be this issue that people feel the studies happen and they weren’t told about it. Likewise when they’re told about it they push back and say well how’s this going to work, I don’t have time for this and so you have to spend a lot of time reassuring them and that actually you don’t have to do anything, it’s just happening and so you know about it and so I think there can be those issues and I think sometimes they can be a bit of a struggle.
Staff (RA) 14
Because there’s more, and again I think the communication’s there . . . I think if you’re constantly getting these messages it’s actually oh I will need to get involved in this, what is it. Also, when you read through the messages its gives you a better understanding and idea of what is actually going on and how they can be involved I think and the discussion within the trauma meetings about them and things like that.
Staff (RA) 4
Staff emphasised the importance of strong, integrated clinical and research teams to facilitate the development of a research culture and maximise recruitment rates into studies. Research teams endeavoured to promote studies, prompt recruitment and do the groundwork for surgeons. They could also provide a point of contact for clinical staff:
I think we do quite well generally because there’s a sort of assumption that we do all the groundwork for the surgeons, we highlight all the patients, we go prepared to the morning meetings so that we know what to expect and again its having that knowledge behind you that gives you the confidence to do that.
Staff (RA) 5
We definitely want to be growing in orthopaedic research and we’ve struggled. We would like to have a separate orthopaedic research nurse but we’re employing generic nurses now into our team so that they can work across different areas . . . but I think having that link there as the one person that everybody can go to and who’s going to be there are the right time of day and that kind of thing is going to be really helpful moving forward.
Staff (RA) 4
Some staff felt that recruitment to research often falls away when the PI is not there to promote the studies. Some surgeons needed prompting to include patients in research studies and were willing to be involved when they were reminded by the research team:
For example, today there was a patient eligible for the study, not TrAFFix but one of the WHiTE4 study, I arrived 15 minutes late for the meeting and said OK what’s happening with this patient and they said DHS [dynamic hip screw] and I said why are not they going in the study, well they can if you want, OK they need to go into the study.
Staff (surgeon) 3
RAs endeavoured to minimise the impact of research on clinical staff, appreciating that they were extremely busy. They avoided taking too much of consultants’ time and tried to help where they could, for example by taking patients to the toilet or asking for pain relief or medications for patients:
You’ve got to try and make sure you’re not taking up their time because if the consultants have been delayed because of research and things their clinics are running over, the staff are having to stop later and it impacts everybody and so I’m trying to make as little impact in the clinics as much as possible and on the ward areas. If you try and help for example with taking people to the toilet, you might go and see a patient and they say they want the bed pan and so you end up helping.
Staff (RA) 16
The RAs endeavoured to balance their role of recruiting to research with their own beliefs about patient care. Some RAs described feeling caught between trial managers who wanted numbers and patients who needed care and time to reach a decision. For RAs, an important part of their role was building a relationship with patients; they wanted to show patients that they were cared for and listened to. Patients were often bored and lonely in hospital and at times felt uninformed. RAs spent time chatting with them and giving them information about their injury and what to expect while recovering. This was time-consuming for RAs, who spoke of blanking out the clock or spending days involving patient and families who then chose not to take part in studies. However, they felt that showing reciprocity and care to patients who had been approached about research during a time of vulnerability was important:
Yes if I am with patients I am with patients and that’s it because I want to have something with them and they deserve my time, I have to be there for them and to answer all their questions no matter how long it takes. When I’m done I can go back to my office and my colleagues and say oh my god it took me ages to deal with it but it’s OK.
Staff (RA) 1
And because we have time with the patient rather than being just a nurse . . . and you can see the time that we have with the patients and they appreciate it very much. They can tell us things and we are there for them and so that keeps them coming back for the follow-up.
Staff (RA) 21
They also considered the appropriateness of research participation for certain patients, such as those with terminal diagnoses or multiple injuries:
I’m a nurse and so obviously it’s a big consideration of mine if it’s not appropriate, if patients have had a terminal diagnosis then it’s very tricky when some of our studies follow the patients up for 4 months or 6 months. To then approach them to discuss a study where we want to follow them up and see the outcomes from their injury and they are what we know as a terminal patient that I don’t feel is appropriate to say we’ll call at 4 months to see how they’re doing and things, that’s very difficult.
Staff (RA) 12
For two RAs, being aware that their surgeons may not have equipoise was troubling. They explained they would feel uncomfortable approaching patients or their relatives about participation in a trial if they were aware that their surgeon might prefer one of the two treatments. They tried to avoid learning the surgeons’ opinions about of which of the two interventions was better. Although they trusted the surgeons’ judgement, they needed to know that they were not causing harm to patients by asking them to participate:
Yes for a surgical thing I would be very uncomfortable to approach someone saying the doctor’s happy to do either knowing that surgeon had said I wouldn’t want to do that, I would rather do that. I wouldn’t like that at all.
Staff (RA) 11
No, I think we need to know as well that the surgeons themselves could and will do either quite happily to a high quality because from our own emotional state that’s someone’s mother, someone’s daughter, someone’s loved one. You really want to know that what we’re doing is not causing any harm. As far as we’re aware of and preliminary research is pointing in the direction that we still need more research because it’s not clear that if it ever becomes a point when it starts to become clear then that would change our emotional feelings about doing what we do.
Staff (RA) 12
Our evaluation of implementation identified key considerations for intervention implementation and the delivery of the study; these are summarised in Box 2.
Intervention implementation was hindered by surgeon preferences, which resulted in some eligible patients not being included in the study.
Patients found the surgical interventions acceptable as they trusted their surgeon to fix their fracture and were not overly concerned about how this was achieved.
Surgeons implemented a variety of rehabilitation instructions, with some patients instructed to weight-bear following surgery but others instructed not to weight-bear.
Delivering the studyThe presence of RAs at the trauma meeting and communication between research and clinical staff aided delivery of the study.
Working closely with clinical staff, seeking cues from patients to assess capacity and involving family in the consent process or using personal or nominated consultees where appropriate aided recruitment to the study.
Obtaining confirmation of a patient’s eligibility from surgeons was a challenge in this study and some surgeons have strong treatment preferences and were unwilling to include patients.
There was increased degree of uncertainty with complex fractures, as some surgeons preferred not to include them in the study.
For some surgeons, a sense of community equipoise helped them to take part. However, for others, it remained an individual decision.
Mechanisms of impact
In this feasibility study, we aimed to identify relevant intermediate outcomes that might be associated with the effect of the interventions on the primary outcomes of interest; Table 6 shows a summary of our findings. The relationship between the factors identified in this feasibility study, the intervention and the outcome of interest would be explored in a definitive trial, which would have a larger sample and so potentially sufficient statistical power to assess such associations.
Thirty factors that might influence patients’ recovery after a fracture of the distal femur were identified at our workshop with PPI contributors and from data collected from interviews with participants and staff. These factors can be collected into three groups: (1) existing factors, for example patients’ age and health prior to their fracture, (2) factors relating to injury, treatment and experience while in hospital and (3) post-discharge factors (Table 9).
| Factors | ||
|---|---|---|
| Existing | Injury and treatment | Post-discharge |
|
|
|
Existing factors
Patients’ age and health prior to their fracture might contribute to their recovery. The mean age of the study participants was 74 years, and only six were able to move about freely without aids prior to their fracture. Nine participants were classified as frail [either mildly (n = 3), moderately (n = 2), severely (n = 3) or very severely (n = 1)] at baseline. During their interview, some participants described limited mobility prior to their fracture and other health concerns that they felt may have an impact on their recovery:
I could get out on my scooter and I could get to town. I have got a three-wheeler as well and I used to take that on the bus to town.
Participant 5
I have got no feeling in the right leg at all and I am not sure whether that actually let me down or whether I slipped. I just went out the back door across to put some recycling in the bin and next thing I am on the floor. As I say I have got no feeling in the ride side, right leg at all from the outside it is numb so I am assuming that I didn’t pick it up high enough and it just gave way.
OK, so you have had trouble with that leg for a while?
Yes, a long while. I have had a knee replacement that went wrong about 15 years ago something like that.
Very slowly, because I had bronchitis when I came out and they thought it was perhaps due to the heat but my legs, both my legs swelled up very much and so I couldn’t get around an awful lot, but um I took water tablets and they have more or less gone down now but I realised that my left leg, which I broke, the fracture was near where I had osteoarthritis in the knee and I had that before I broke the leg and that is what is holding me back now I think.
Participant 5
With him losing the ability to walk it has really hindered him every which way but I don’t think that’s because of the operation I don’t think that’s because of the treatment he got I just think it’s his age, dementia and just having that time not walking I think it affected his walking ability.
Participant 11
Two surgeons identified factors that may result in patients being treated non-operatively. These were existing comorbidities that cause a patient to be unfit for surgery and a strong preference from patients for a non-operative treatment:
There will be some people who are unfit for surgery for one reason or another, sometimes it may be cardiovascular problems or sometimes it may be that they have skin issues and sometimes they are simply too obese or have other comorbidities, including dementia. Whether to operate or not operate is a decision made on the balance based on the entire patient and not based on the fracture.
Staff (surgeon) 18
Very occasionally, very occasionally they’ll listen to you and say they just really don’t want an operation and I accept the risks that come with that and the potential benefits, I just don’t want an operation. They’re generally very elderly patients or patients who have had bad experiences of operations or things where their spouses have died during an operation and they just want to have a plaster and go home and I get that.
Staff (surgeon) 13
Injury and treatment
Several factors relating to the patients’ injury and the treatment they receive in hospital could have an impact on their recovery after a distal femur fracture. These relate to the injury event, surgery, rehabilitation and care in hospital.
Patients’ recovery might be influenced by the severity of their fracture, the mechanisms of injury and whether or not they sustained other injuries at the time of their fracture. For example, two participants from this study sustained other injuries at the time of their fracture:
But they are very pleased from the hospital anyway, the consultant is pleased with how it is healing, you know what I mean, because they said it was going to be a really tricky operation because I had smashed it in several places. When I came home and looked on the internet you normally only smash it, break your femur if you have a really bad car accident so the thing was as well, I have had a knee replacement in that knee . . . I have had a knee replacement on both my knees prior to this happening.
Participant 7
The time between a patient’s injury and surgery might be important. Two relatives who were interviewed described a delay between their relatives’ injury and surgery. One participant was not taken to hospital until 3 days after he fell, as paramedics did not suspect he had sustained a fracture, and the other participant waited several days for an operating theatre to become available as more emergencies were prioritised:
She had the accident on a Thursday and she was on standby for the theatre all the time until they could operate but obviously as more emergencies came in she kept going down the list so she was actually in hospital from the Thursday to the Monday waiting to operate on . . . well the first problem is because of her age, her skin is very thin and it has caused quite bad pressure sores because obviously they had to put her in traction. The other thing is it has caused a lot of problems with being constipated and things because she didn’t eat hardly anything in that period of time she was on standby to go to the theatre. We have had quite a lot of problems you know and also she lost weight because she was very small anyway and she sort of lost weight because you know she hadn’t eaten a lot before she had the operation.
Participant 6
In addition to the intervention that patients were randomised to, several other factors relating to surgery could be important. This includes the experience of the surgeon, for example the grade of the supervising surgeon, the number of trauma lists the surgeon routinely supervises and the number of distal femoral fractures the surgeon has fixed. In this study, 15 participants were operated on by a consultant, six by a specialist trainee (level 3) and two by a staff associate specialist (SAS).
Surgeons’ preferences for one intervention over the other could also influence patients’ outcomes. Interviews with surgeons revealed that some may not be confident with both techniques, with preferences often based on surgical skill and experience. These fractures are not common and were described by surgeons as difficult to fix. Two surgeons explained that this operation, unlike many others, is not performed from implicit memory. It may, therefore, be more difficult to use their less preferred technique:
Distal femoral fractures are not common and so there are only about 10% of fractures of the femur overall and so no-one is doing lots unless you put your hand up to do them.
Staff (surgeon) 13
Distal femur fractures are in that group of it’s a bit more complicated than average and can really be quite difficult.
Staff (surgeon) 23
It’s not like a routine thing like an ankle fracture that you don’t really think about, it’s not like a brain stem reflex.
Staff (surgeon) 10
Surgeons’ beliefs about rehabilitation and the rehabilitation instructions that they give to patients could influence how quickly patients mobilise following surgery. As described in Protocol deviations, surgeons held different views about the most appropriate rehabilitation instructions for these patients. Although early weight-bearing was favoured by many, some surgeons restricted weight-bearing for some patients:
Personally, I do bed to chair for the first 4 weeks and I don’t allow them to fully weight-bear if they’ve had a plate, which I know is different to a lot of people. It depends a little on what their bone quality is like at surgery and nails will be weight-bear as tolerated. A lot of them will stay in for quite a long time and they rehabilitate pretty slowly on the whole.
Staff (surgeon) 3
In the elderly group I think you’ve got to let them walk straightaway. I just don’t think it’s meaningful to ask a 90-year-old man or woman to walk around on crutches and so I just get the physios [physiotherapists] to get them walking.
Staff (surgeon) 13
Many participants described receiving support from physiotherapists while in hospital. Several participants spoke of the exercises and support they were given to walk enthusiastically:
They gave me the confidence to do it. I don’t know what I would have done if they didn’t . . . if I hadn’t had a good team of physios [physiotherapists], they were really great as I say I was shaking from head to foot because I knew I had got, that this bad leg was going to have to be the leg that I was going to have to use to support me . . . they have got some bigger [walking frames] you know where you put your arms on to and I used those first off and originally they said I could bring one home because I was terrified to go on a normal [walking frame] and they had said I could bring one home, not the one they were using in the hospital but an older model but eventually they got me on to a [walking frame], they gave me the confidence they were absolutely great.
Participant 7
I had to do exercises this morning and they were painful but you know once they got too painful you just stop and then I went downstairs to the gym and with the help . . . of one of those pushers I was able to walk using my wonky leg and my good leg. I couldn’t put too much weight on that one and I walked the length of the gym and back again and they were very pleased with me. I was pleased with myself.
Participant 3
For some participants, their time in hospital was difficult. One participant described being moved to another hospital the day after surgery as other patients were waiting for a bed:
Well I didn’t like it. I wanted out because I don’t like hospitals and so I wanted out.
Participant 8
It was a horrendous feeling for my daughter and for me, you know not knowing where we were going and they just came on the wards and started packing my stuff up and said we want this bed, you have got to go to the [hospital name] and there was no warning, no nothing, no it was awful and when I went to the [hospital name] they more or less said we weren’t expecting you, so they had got no pads or anything.
Participant 9
In contrast, others described being cared for and were pleased with their experience in hospital:
You know nothing is too much for them no matter what time of the night or day because I have got a [call nurse button] . . . So as I say I am quite pleased with them. You know they don’t treat you as an idiot you know they consider that you have got some intelligence left.
Participant 3
Post-discharge factors
Several factors were identified that might influence a patient’s recovery once they were discharged from hospital. These were post-discharge living arrangements, access to carers, loss of independence, family support, access to physiotherapy, psychological factors, such as resilience, self-efficacy and confidence, and pain.
For some participants, recovery was slow and frustrating. At interview, several participants described spending a long time in hospitals, rehabilitation units or care homes before returning to their pre-fracture residence. Ten participants were discharged to their own home or sheltered housing, nine were discharged to rehabilitation units, one to a residential care home and one to an acute hospital. At the 4-month follow-up, 8 out of the 11 participants who completed the health economics questionnaire were living in their own home or sheltered accommodation and three were living in residential care:
I was, I was in there what nearly 6 weeks and then I had the enablement team from the hospital for about 2 or 3 weeks for a couple of weeks or so and now, I have got carers full you know full time.
Participant 2
I am back at home with my bed downstairs. Obviously, I haven’t been upstairs since they actually did the operation.
Participant 7
At the interview, participants described trying to ‘muddle through’ at home but often needed support from family, carers and cleaners to manage. The majority needed help with household chores and a few also needed help washing, dressing and cooking. Their loss of independence could be frustrating and they did not like to be reliant on others or ask for help:
To be honest I don’t want to be where I can’t do things for myself. It’s very frustrating when you have to keep asking people and you know they are thinking what now but they don’t say so half the time and I want to be able to get back up and go shopping if I want to you know . . . well just do what I always did.
Participant 6
Yes, I am back at home, I have a carer in the morning because I can’t stand and wash myself yet and I am incontinent so that makes it difficult because I am not walking on me leg yet. I am walking with a frame just like toe touch toe touch sort of thing with a frame but most of the time I just sit in a wheelchair.
Participant 10
Several participants found ways to contribute to the housework and overcome the restrictions their injury imposed, suggesting resilience. For example, as they struggled to stand for long without support, they ironed sitting down, hoovered from their wheelchair or washed the dishes from a stool:
So I am very pleased with what has happened at home so hopefully I can start . . . I mean I can walk with a frame but you can’t carry a cup of tea or you can’t carry a meal to where you sit to have your meal. So I have to more or less have to stay in the wheelchair whereas the physiotherapist wants me walking everywhere if you know what I mean, to make my legs stronger but I just find it easier to skim around in my wheelchair. I even do the hoovering in the wheel chair, well it’s only a little granny annex so it’s not a big carpet space to do but . . . and I sit and do my own washing up and everything on my perching stool so yea I am quite happy at home.
Participant 9
I have got a cleaner that comes in three times a week for an hour Monday and Tuesday and Thursday and she does the house cleaning because I can’t bend down and get up again. I do my own washing but I am going to try and do my own ironing. It’s the fact that I can’t stand for a long time but my daughter has given me one of those table tops that you can sit down on a chair and iron on it so I am going to try that.
Participant 3
In contrast, some participants became isolated and depressed after their fracture:
Well she was actually getting quite depressed because obviously she can’t get to the front door and obviously I used to take her round in her wheelchair to see her sister and things like that and she wouldn’t do it because she is frightened of . . . You know she has had nobody since she got home she was doing quite well to start with but then as I say we were expecting a physiotherapist to come round but then gradually because nobody has come to assess her or . . . she was getting quite depressed about not being able to get up and things like that and not being able to move round like she could before.
Participant 4
Our interview data highlighted the role of family and carers in supporting patients’ recovery. We also assessed patients’ social support using the Medical Outcomes Study, Social Support Survey. 27 We calculated an overall support score by averaging the scores for the 19 items included in the survey. This provides a score between 1 and 5, with higher scores indicating more support available. Within our sample, the mean overall support score (the average of the 19 items in the Medical Outcomes Survey scale) was 4.18 (SD 0.76). In addition to providing an overall support score, the survey comprises four separate social support subscales: (1) tangible support, (2) emotional/informational support, (3) affectionate support and (4) positive social interaction. The mean scores for the subscales were (1) 4.28 (SD 0.66) for tangible support, (2) 4.22 (SD 0.86) for emotional/informational support, (3) 4.28 (SD 0.75) for affectionate support and (4) 3.87 (SD 1.10) for positive social interaction. These data show that, within the sample, levels of social support varied but tended to be high.
As described in Patient compliance with rehabilitation instructions, some participants experienced a loss of confidence after their fracture or struggled with pain and needed help to move forward with their rehabilitation:
She has also lost confidence after several falls and although she has been able to stand up on the patient turner and even holding onto the gutter frame, she has not been able to move either of her feet when standing.
Participant 10
Just if I walk too far, that’s when I feel it you know, I need to sit down sort of thing give it a rest, at night-time, that’s when I get the pain, at night-time.
Participant 8
Self-efficacy may be an important factor in patients’ recovery as low self-efficacy may result in patients being reluctant to mobilise following surgery. We assessed self-efficacy using an adapted five-item version of the General Self Efficacy scale, which gives respondents a score between 5 and 20, with higher scores indicating more self-efficacy. Within our sample, patients’ levels of self-efficacy varied. The mean self-efficacy score was 13.4 (SD 4.1).
Of the 12 participants who completed the health economics questionnaire, which asked about services they had received, four reported receiving physiotherapy after discharge from hospital. Some families advocated for support for their injured relatives, particularly during the transition from hospital to home. They sought access to physiotherapy, which was not easily available for all patients owing to long waiting lists or in one case because it was initially believed that the patient would not be able to weight-bear again:
No. They haven’t done nothing [sic.] to be honest. Because they were supposed to send me for therapy but I never had nothing.
Participant 8
After the fall which caused the present fracture to her right femur, the physios [physiotherapists] initially said that she wouldn’t be able to weight-bear again and would probably need to be hoisted everywhere for the rest of her life. I objected and said that I planned to have her come to live in my home but would need her to be able to stand up using a patient turner. From that point, efforts were made to help mum to learn to stand and she was allowed to spend a few weeks in an NHS-funded bed for rehabilitation.
Participant 10
Participants also described the difficulty in accessing transport for rehabilitation activities:
I missed the last [physiotherapy] appointment because the ambulance didn’t turn up to take me. Other than that, I have been going to hydrotherapy. I did a 4-week course at hydrotherapy and they offered me to go to the self-help hydrotherapy thing and then they told me that if I go to that they will probably ban me from the ambulance because you are not allowed to have an ambulance for that and if you can get to that without an ambulance then you can get to any other appointment without an ambulance.
Participant 1
There were many challenges for the TrAFFix study that might have affected the mechanism of impact of the intervention, highlighted in Box 3.
Participants were older and they could be frail. Some, according to the surgeons, might not be suitable to be treated operatively.
The complexity of the injury often required more thought and energy to treat and was perceived as a ‘difficult’ surgical procedure rather than one that was done routinely.
The severity of the fracture could make decisions about treatment difficult as being constrained by a particular approach to treatment could be a source of stress for surgeons.
The proximity of the fracture to the knee and pre-existing knee replacements increased the complexity of the surgery and was a cause of concern.
The experience and training of the surgeon may impact on their comfort with undertaking both treatments.
Care of the patient because of their age and frailty could be challenging, with delays to surgery increasing the risk of dehydration, constipation and bed sores, as noted by participants and relatives.
There was a range of professional views about the best approach to take in relation to the degree of weight-bearing and rehabilitation required.
Participants and their relatives were appreciative of physiotherapy interventions but in general felt they had to fight for help and it was not readily available. Some functioned well in wheelchairs or with aids but were concerned about moving forward and regaining mobility.
Post-hospital recovery was a long, slow, frustrating process with notable lack of mobility, pain and other problems, such as incontinence.
Participants felt they muddled through by finding ways of maintaining normal activities with support from family, carers and cleaners.
Context
Contextual factors can influence outcomes for this group of patients and will also affect the feasibility and conduct of this research. Relevant contextual factors can be grouped at three levels: (1) the national context identified through surgeon views of the frequency of occurrence of distal femoral fractures and preferred treatment, (2) the contextual similarities and differences between the participating centres and (3) the contextual factors specific to this group of patients, which are discussed in turn. Table 7 shows a summary of our findings regarding context.
National context
To provide a national view of the occurrence of this injury and differing treatments, a brief questionnaire to elicit surgeons’ views was administered. The findings suggest that surgeons perceive distal femoral fractures to be uncommon and hold different preferences for their treatment. Seventy-nine surgeons responded to the questionnaire (details of the questionnaire are reported in Appendix 2), of whom 57% (n = 45) worked in major trauma centres and 76% (n = 60) defined themselves as specialist trauma surgeons; 82% (n = 65) reported that they personally operate on < 10 distal femoral fractures per year (Table 10). Distal femoral fractures are less common than some other fractures and individual surgeons are unlikely to regularly operate on them. This may therefore influence their experience and confidence to perform both interventions noted in the interview data.
| Context | Participating centre | ||||||
|---|---|---|---|---|---|---|---|
| Leeds Teaching Hospitals | Oxford University Hospitals | Nottingham University Hospitals | Portsmouth Hospitals | Royal Berkshire Hospital | University Hospitals of Leicester | University Hospitals of the North Midlands | |
| Workforce (FTE) (trauma and orthopaedics March 2017) (multiples of FTEs) | |||||||
| Consultant | 36.3 | 26.4 | 38.1 | 21.6 | 17.5 | 38.4 | 23.0 |
| Associate specialist | – | – | – | – | 1 | 2 | 1.29136 |
| Specialty registrar | 31.5 | 32.6 | 39.6 | 12 | 11 | 35.9 | 22.4 |
| Specialty doctor | 1 | – | – | 2 | 3 | – | 3 |
| Foundation year 2 | 4 | 12 | 9 | 4 | 4 | 8 | 4 |
| Foundation year 1 | 6 | 2 | 2.6 | 4 | 4 | – | 4 |
| Core training | 4 | 3 | 15 | 4 | 4 | 18 | 5 |
| Hospital-facilities (October–December 2016) | |||||||
| Bed occupancy (trauma and orthopaedics) | 145 | 146 | 144 | 114 | 52 | 115 | 98 |
| Number of operating theatres (of which, number of dedicated day case theatres) | 60 (8) | 46 (1) | 53 (6) | 31 (10) | 24 (4) | 51 (7) | 40 (6) |
| Hospital-admitted patient care activity, 2015–16 | |||||||
| Finished consultant episodes | 235,129 | 222,948 | 253,110 | 166,404 | 138,089 | 308,946 | 263,438 |
| Admissions | 198,980 | 199,059 | 209,171 | 137,629 | 104,807 | 255,895 | 206,728 |
| Population served | |||||||
| Major trauma centre | Yes | Yes | Yes | No | No | No | Yes |
| Local population served | 770,000 | 805,000 | 2.5 million | 675,000 | 500,000+ | 1 million+ | 900,000 |
| Wider population served | 5.4 million | 2.5 million | 4 million+ | 2 million+ | 1 million | 2–3 million | 3 million |
Seventy-eight respondents answered the question ‘do you have a preference for operative fixation of most distal femoral fractures?’, with the option of answering anatomical locking plate, retrograde intramedullary nail or no preference. Just over half (54%, n = 42) of the respondents expressed a preference for one method of fixation. Of those who expressed a preference, 62% (95% CI 46% to 76%, n = 26) preferred anatomical locking plates.
Based on limited data from this questionnaire and our interviews with surgeons, there is a sense that anatomical locking plates may be preferred, although most surgeons say that they do not have a preference.
Contextual similarities and differences between the participating centres
Contextual similarities and differences between the participating centres can influence how the study is delivered and how patients recover. These will be discussed in turn.
Seven centres participated in this feasibility study. Four major trauma centres were included. As demonstrated in Table 10, they differed in the size of population served and number of consultants and mix of full-time equivalent staff. This demonstrates that this feasibility study was conducted in a range of settings.
Contextual differences between the participating centres that may have led to differences in how the study was implemented were evident within our evaluation of intervention implementation. These relate to the degree of development of a research culture identified through (1) surgeons’ willingness to randomise patients, (2) a range of ongoing research studies, occurring at the same time as TrAFFix, (3) the frequency of occurrence of injury and (4) the research teams.
Surgeons’ willingness to randomise patients, shaped by their surgical skill, equipoise and beliefs about the appropriateness of research participation for their patients as described in acceptability of study interventions, could influence recruitment. Strong surgeon preference, or in some centres a group preference, for one of the two interventions could lead to some centres including different patients to others. This is discussed in How was delivery achieved?. Centres where there was a range of surgical expertise may have been better equipped to avoid potential protocol deviations or missed patients.
Surgeons’ willingness to randomise patients was also influenced by the emergency nature of trauma work. The fast pace, nature of trauma work and complexity of major trauma meant that, although a patient may have met the eligibility criteria, not all surgeons were prepared to include them. For example, patients with open fractures require surgery urgently to minimise the risk of infection:
There’s been a couple [of eligible patients not included], I remember a lady she had an open tibial fracture and the distal femur as well and I’d spoken to the PI about it and he felt she was eligible but I think that the surgeon who was doing it . . . thought he had the two big injuries to deal with at the same time and it was all very time pressured because she’d got an open fracture and to go to theatre straight away.
Staff (RA) 7
The level of surgeon input required for a study such as TrAFFix is challenging. Some RAs contrasted recruitment to TrAFFix with that of less challenging studies, for example dressing studies, which they believed surgeons were more amenable to as they require less input:
I do feel that at different levels we’ve got quite an open environment to research and they’re very happy us doing it so long as it doesn’t really involve them. So all these new studies that are the more interventional studies that you have to get more of an input from the surgeon, it’s harder. Today we’ve got two who are eligible and it was a struggle to get them to say they were eligible and then a struggle for the surgeon to say yes I’ll do it. So the surgeon will do it as long as someone else will do all the decision-making, does all the paperwork behind him and just literally at the final hour tells him which bit to do because he hasn’t got capacity in his brain to take on the responsibility.
Staff (RA) 5
You find the consultant response is variable, they always seem much more amenable with something like WHIST [Wound Healing in Surgery for Trauma], which is just a dressing and not interfering with what they’re doing whatsoever and they really couldn’t care less and anything you find physio [therapy] orientated never received a huge amount of objection.
Staff (RA) 7
The research culture varied across sites in the degree to which research was embedded in daily trauma activity. A range of studies facilitated recruitment by increasing opportunities for engagement. As described in How was delivery achieved?, surgeons working in departments where several trials are running may be more engaged in research and inclined to participate:
So we’ve got surgeons who are doing a couple of other hand studies and so they would be involved and they’re keen to do them partly because they are doing their own bits of research and they want to get involved with it and partly because we’re doing the WHiTE studies and all of a sudden it is like we’re a team, an orthopaedic research team so I think that’s moving forward.
Staff (RA) 4
The infrequent occurrence of distal femoral fractures inhibited the study from fitting in with the existing research culture. Patients who were eligible to participate in TrAFFix did not present frequently enough for the clinical team to keep the study in mind and the study did not become routine, as described in Procedures for screening patients:
We’ve only been getting one every month or 6 weeks. For example, 6 weeks goes past and the patient comes in and they’ve forgotten about the study because it’s not in the front of their minds and then I have had to pretty much ring every time to speak to the consultant to say have you considered this study, if not why.
Staff (RA) 11
TrAFFix hasn’t been regular enough for it to be routine to some extent.
Staff (RA) 11
An effective research culture required all clinical staff to be aware of the study. If patients were told that they would receive one intervention before they were informed of the study, it could be difficult for them to accept being randomised to one of two different treatments:
I think the only challenge we have is when someone’s already spoken to them about a treatment option and then you suddenly come saying you might do something different . . . If they’ve been told something different to what you then tell them in terms of nail and plate and don’t notice any difference they say the last surgeon they saw said it was definitely going to be better with a plate it’s then very difficult to convince them otherwise.
Staff (surgeon) 3
The research culture was facilitated by experienced RAs, who could facilitate research activity and make things easier for clinical staff. Differences in the size of the research team, their workload and working hours could influence the implementation of the interventions. For example, as described under implementation, the presence of RAs in the trauma meeting could facilitate screening but required RAs to start work before 08.00, which was not possible in every centre. Such structural issues are substantial barriers to the integration of the clinical and research teams, development of a strong research culture and effective delivery of these studies. Meanwhile, some centres relied on one RA or part-time RAs. This might result in patients being missed (at consent or follow-up) either when the RA was away or because they were struggling with their workload:
Yes so for instance the Friday before there were two patients coming in but there was nobody available because either the surgeon was in theatre, the surgeon was on annual leave, the registrar was on annual leave who normally helps with clinic, who helps recruit and so yes that does happen but not all the time. There was nobody in this Friday just gone and it can happen because I’ve got to be everywhere.
Staff (RA) 15
I did once have nine patients in a morning clinic and they were seeing two different consultants so it was trying to be with one consultant and patient doing a follow-up and my other patient I might have missed because they were at the same time with simultaneous appointments.
Staff (RA) 15
For RAs, familiarity with the paperwork was an important factor. For centres that were unfamiliar with Oxford trauma studies,51–54 some staff thought that paperwork could be difficult to get to grips with. Not only was the paperwork considered lengthy, but there were also multiple versions of information sheets and questionnaires. Although complex, many RAs commented on the logical and familiar structure of the paperwork, which facilitated data collection:
I mean I think from a paperwork point of view we’re very well versed in Oxford paperwork so you’ve got the prospective PIS, prospective CIS, retrospective and then you’ve got all the consent forms that go with all the various options and then you’ve got the dementia self-reporting, dementia non-reporting. But we’re quite familiar with that so that’s not an issue and I don’t think it would have been an issue, maybe for some centres that don’t do as many Oxford studies, the level of paperwork and different categories of patients might be a little bit overwhelming, it hasn’t been for us.
Staff (RA) 11
The development of a research culture appears crucial to the success of a study such as TrAFFix. This varied across the centres, with some sites further on than others in their development of a research culture.
Contextual factors relating to the participating centres also had potential to influence patient outcomes after a distal femoral fracture. For example, surgeons’ views about rehabilitation instructions for these patients and the instructions they gave differed between the centres, as described in Protocol deviations. The National Institute for Health and Care Excellence (NICE) recommends that health-care professionals should consider advising patients who have had a distal femoral fracture to immediately weight-bear as tolerated following surgery. 55 Differences in the delivery of this post-operative component could have an impact on patients’ recovery and quality of life after their fracture, as discussed in Chapter 2, Mechanisms of impact:
My whole argument about why I do the operation is because you want to get them to walk, you could treat them with a plaster and you can walk on that so I think if your concept is to treat the patient in a way that allows them to walk immediately then you end up allowing them to walk immediately and I’m strongly of the view that that is what we’re trying to do and so I’m happy to take the risk that some will fail because I let them walk.
Staff (surgeon) 13
Further contextual factors relating to the participating centres that might influence patient outcomes are discussed in Chapter 2, Mechanisms of impact.
Patient factors
Contextual factors relating to the group of patients who were eligible to participate in this study could have the potential to inhibit recruitment and also influence patients’ outcomes after a distal femoral fracture. These factors include frailty, attitudes towards research and access to support.
Patient frailty was the main contextual factor for this population. Despite reducing the minimum age for patients eligible to participate to 18 years, participants were typically older (mean age of 74.1 years). Many were frail, compounded by the shock of injury and surgery, and often experienced some confusion or memory loss following their fracture, as described in Chapter 2, Mechanisms of impact:
No, I don’t [remember] because it was when I was coming through you know being up there and I was trying so hard to be normal.
Participant 3
I probably wasn’t in a fit state to ask anyway but I don’t remember wanting to know anything.
Participant 5
They understand the main idea however . . . they forget easily. They can remember the plate or the nail but it is difficult to remember everything.
Staff (surgeon) 17
Interviews with staff and participants revealed that patients were typically accepting of research. Many participants expressed altruistic motivations for participation and trusted their surgeon to fix them:
They don’t have any idea about what you’re talking about and nor do they particularly care. I think they just think that you’re recommending an operation, they buy into that idea and then you’ll just do a technically sound operation. So when you say well there’s these two different ways of fixing your fracture and one is a nail and one is a plate and we’re not a 100% sure which is better and so we’re doing a study comparing the two where you might end up with either one and I can do both and its reasonable we could do either then they just say yes fine.
Staff (surgeon) 13
Although accepting of research, some participants demonstrated confusion over randomisation and few could describe the study in their own words:
Yes, yes they had to decide because they know what they are doing and I don’t so, they have done hundreds haven’t they.
Participant 5
Well because it helps other people and obviously it would obviously help her the best way you know . . . obviously because of her age her bones weren’t going to mend properly and the doctors did explain and they said that they would give her the best which they thought would help her.
Participant 4
These factors highlight the need for consideration of the information given to this group of patients and how best to approach and engage them in research. In the participating centres, RAs were typically experienced at navigating consent with this group of patients. They understood the complexity of approaching these patients about research participation and sought strategies to mitigate these factors as described in How was delivery achieved?.
Several participants described a loss of confidence following their fracture. This, along with their frailty and limited mobility prior to their injury, as described in Chapter 2, Mechanisms of impact, may make recovery difficult for this group:
When she was in hospital she was actually getting on very well with walking while she was in hospital but as soon as she came home she was frightened of doing it on her own without . . . you know she needed somebody like the lady who came today [name] was very good because she started to get her doing things.
Participant 4
Yes but I did have a walking stick . . . and if I go down town say to [a shop] or anywhere I use three wheels to walk with because I can’t do it for long on my own natural sources if you know what I mean. I have arthritis in both knees and I have got arthritis in my lumber region, so walking isn’t my best thing but when you have to do it you have to find the easiest way don’t you. I think the three wheels have been all right for me up to now but I still haven’t tried them yet [since the surgery], I am still trying with the frame.
Participant 9
These participants required support to aid their recovery and allow them to live independently. As described in Chapter 2, Mechanisms of impact, participants received support from their families and from paid carers. Of those who completed the health economics questionnaire, eight reported receiving unpaid care from relatives or friends, most frequently their adult children (n = 5). Several participants also received resources from charities to enable them to manage at home. As described in Chapter 2, Mechanisms of impact, access to physiotherapy was difficult. Several participants explained that they did not receive physiotherapy after discharge from hospital while two personal consultees described advocating for their relative to ensure that they received physiotherapy. It would seem that access to support from physiotherapists, family and carers is important to these patients during recovery as their frailty may cause them to struggle to manage alone:
Obviously it would have been a lot better if we’d have had the physiotherapists out straight away, which is what I thought was going to happen. But we have actually had to have the doctor out to her because she was getting the bed sores as well due to the not moving round enough, which is why I kept chasing the physiotherapist to come out and sort of assess her and things which is as I say what has happened today so I feel a lot happier today.
Participant 4
The contextual challenges are summarised in Box 4.
Patient frailty was notable, with confusion evident, a loss mobility, lack of confidence and little evidence of return to pre-injury state; most managed at home or in other care facilities with support.
The general view was that distal femoral fractures are not a common fracture and are often complex in nature. There was a sense that plates might be the preferred method of fixation, but many surgeons did not state a preference.
Views on weight-bearing varied and the degree of rehabilitation differed but it was noted that more was required.
Contextual challenges for the studyWillingness to include patients at different centres could be influenced by individual and team views about how these injuries should be treated.
The emergency nature of trauma work, speed of treatment required and complexity of multiply injured patients could limit the willingness of surgeons to randomise to this study.
This study required higher surgical input from surgeons than some other trials, which could make it more difficult to implement.
A research culture was noted in some centres. Recruiting to multiple trauma trials with an increased number of staff involved contributed to research activity becoming routine to daily trauma work.
Experienced RAs make research fit in more easily with routine clinical care but some struggle with workload and covering all areas of practice.
Trial paperwork could be a challenge but familiarity helped to facilitate its completion.
Participants’ involvement in the study was based on their need to be fixed, trust in the surgeon and feelings of altruism. Navigating their consent was a lengthy process undertaken by RAs and understanding was limited generally to the two types of metal work, nail and plate.
Summary
This study adds to existing literature by identifying the overarching concept of facilitating trial recruitment identified through three themes. We have identified challenges of undertaking a study in which surgeons, at an individual or collective level, are concerned that the care they provide patients may be compromised by the trial despite a sense of community equipoise. We have also identified the importance of having embedded in the trauma service RAs who understand the specialty, the impact of injury on patients’ and families’ lives and who know how things work in trauma. This enables them to navigate patient and family involvement and make the study work by juggling an array of activities, making it easier for surgeons and fitting it into every day clinical practice.
Strengths and limitations
We followed the MRC’s framework for process evaluations of complex interventions. This framework provides a systematic approach for evaluation of implementation, mechanisms of impact and context. We used a concurrent mixed-method design, allowing us to address multiple aspects of the process evaluation. Data collected from qualitative interviews complemented the quantitative data to enable us to gain a more complete understanding of how the interventions were delivered and the feasibility of the TrAFFix study.
Our qualitative sample included a range of good informants with experience of the study, namely participants, personal consultees, surgeons and RAs. This was achieved by inviting all participants who expressed interest to participate in an interview and by including staff from all of the seven participating centres. Although our interview sample used a convenience sampling strategy, the characteristics of the interview participants were similar to those of the study sample.
We adopted several strategies to ensure the trustworthiness of our qualitative findings. 56 This was accomplished through our sampling strategy, methods of data analysis and presentation of results. As described above, we included a range of informants to capture the breadth of experience and allow corroboration of ideas. Emerging themes were discussed by four researchers, from differing backgrounds, throughout the analysis to ensure that our findings reflected the experience and ideas of our participants. Verbatim quotes were presented to allow mediation between the researchers’ interpretation and participants’ accounts. A detailed description of our methods and the TrAFFix study are provided to allow transferability of findings.
We evaluated the implementation and acceptability of both the interventions and the study procedures. This allowed us to understand both how the interventions were implemented and how the study was delivered. However, these areas do overlap and consequently are intertwined within our results.
Owing to the small number of participants in the study and the loss of participants to follow-up, our quantitative data related to a relatively small sample. The number of surgeon responses to our questionnaire was also low.
Our sample of interviewees included participants, personal consultees, surgeons and RAs. No patients who declined to participate in the TrAFFix study agreed to be approached about the interview study. The experience of these patients may have provided a useful contribution to our understanding of what it is like to be approached about research after sustaining a fracture. Furthermore, inclusion of a wider range of staff, such as physiotherapists and other multidisciplinary clinical staff, may have allowed us to collect additional data about factors that may influence patient outcomes after this type of fracture.
Interviews with participants were conducted up to 5 months post surgery. Although efforts were made to interview participants at earlier time points, this proved difficult. Interviewing participants earlier may have afforded a greater understanding of patients’ experience of being approached to participate in a study and the consent process.
We intended to interview participants at two time points, with the aim of the first interview being to gain an understanding of participants’ experience of the study and the second interview aiming to understand participants’ experience of recovery. Only 3 out of the 11 participants were interviewed twice because of the difficulty of interviewing participants in the first few weeks following surgery.
We intended to record discussions about the study between RAs and potential participants. There were limited opportunities to do this given the small number of potentially eligible patients. RAs’ ability to do this was also impaired by the nature of consent discussion with frail patients who have sustained a traumatic injury. Discussions of the study often involved multiple interactions as there was a limit to how much information patients could assimilate in one discussion. The complexity of explaining the purpose of recording the discussion before the study had been discussed was also challenging.
We created a brief questionnaire to ascertain surgical caseload and surgeon preferences. Including questions about surgeon willingness to randomise patients to a trial comparing plates and nails and surgeon preferences for different types of distal femoral fractures may have provided additional useful information to help us understand the national context.
Chapter 4 Results
Recruitment rate and data completeness
Recruitment commenced in October 2016 and by February 2017 was taking place at seven sites and ceased in July 2017, after sampling 54.8 centre.months of recruiting time in total. During this time period, 23 patients were recruited to the study. Figure 3 shows the distribution of monthly recruitment, which ranges from 0 to 3 patients.
FIGURE 3.
Observed distribution of monthly recruitment (bars), with predicted numbers from Poisson count model (•).
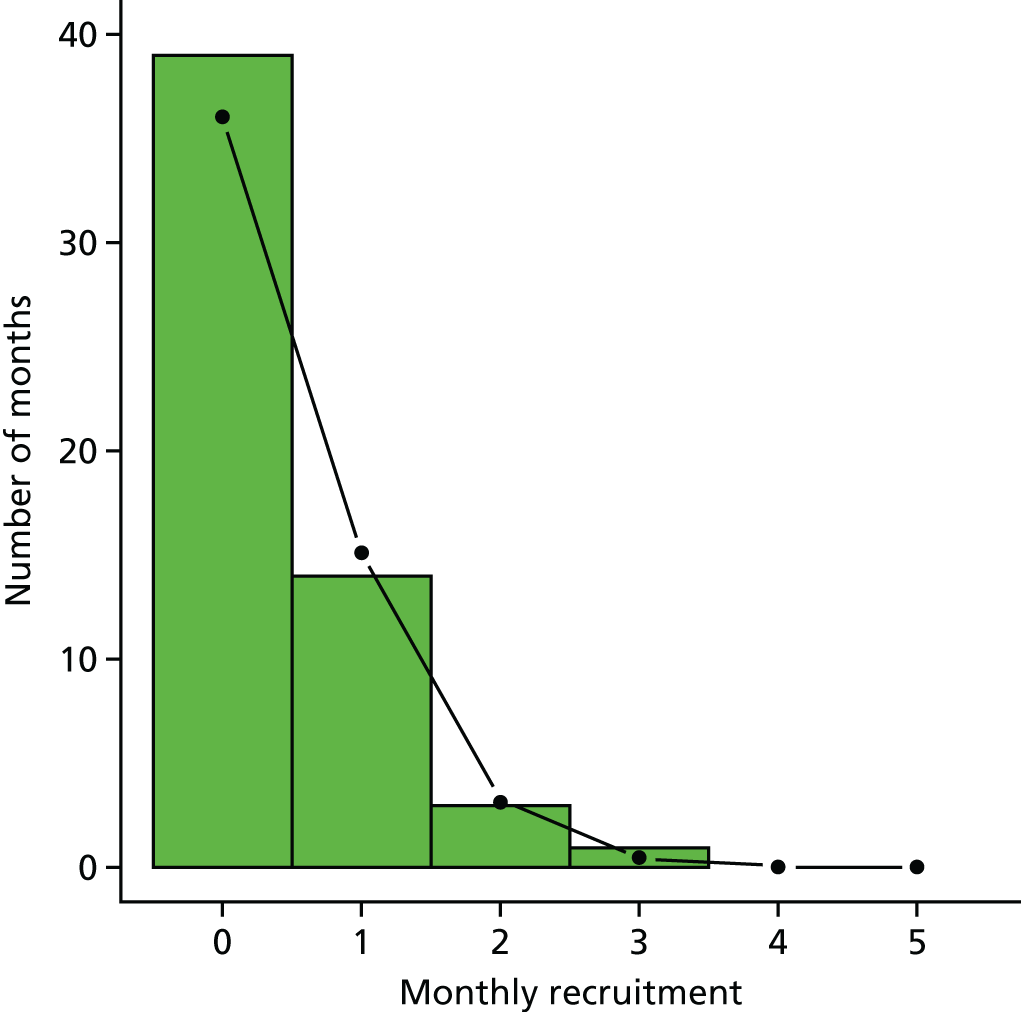
Fitting a Poisson model to the monthly count data provided a reasonable model for the observed numbers (see Figure 3) and gave an estimated recruitment rate of 0.42 (95% CI 0.27 to 0.62) participants per site per month.
Data completeness was calculated as the proportion of the randomised participants who completed the EQ-5D-5L study primary outcome at baseline and at 6 weeks and 4 months. Of the 23 study participants, 20, 15 and 14 participants completed the EQ-5D-5L assessment at baseline and at 6 weeks and 4 months [87% (95% CI 65% to 97%), 65% (95% CI 43% to 83%) and 61% (95% CI 39% to 80%)], respectively.
Participants
Twenty-three participants were randomised to either retrograde intramedullary nailing (the nail intervention group) or locking plate fixation (the plate intervention group) using a 1 : 1 allocation ratio. Randomisation was stratified by recruiting site and cognitive impairment and used fixed blocks of size four to achieve improved balance within each stratum. Table 11 shows the breakdown of study participants by the stratification factors. Figure 4 shows the flow of participants through the trial.
| Stratification factor | Intervention group, n (%) | |
|---|---|---|
| Nail (N = 11) | Plate (N = 12) | |
| Site | ||
| Leeds Teaching Hospitals | 2 (18.2) | 1 (8.3) |
| Leicester University Hospitals | 1 (9.1) | 2 (16.7) |
| Nottingham University Hospital | 2 (18.2) | 1 (8.3) |
| Oxford University Hospitals | 4 (36.4) | 6 (50) |
| Portsmouth University Hospitals | 1 (9.1) | 2 (16.7) |
| Stoke University Hospital | 1 (9.1) | 0 (0) |
| Cognitive impairment | ||
| No | 10 (90.9) | 11 (91.7) |
| Yes | 1 (9.1) | 1 (8.3) |
FIGURE 4.
Flow of participants through the trial. a, The minimum eligible age was changed from 50 to 18 years during the trial. Reproduced from Griffin et al. 44 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. This figure contains minor formatting changes to the original text.
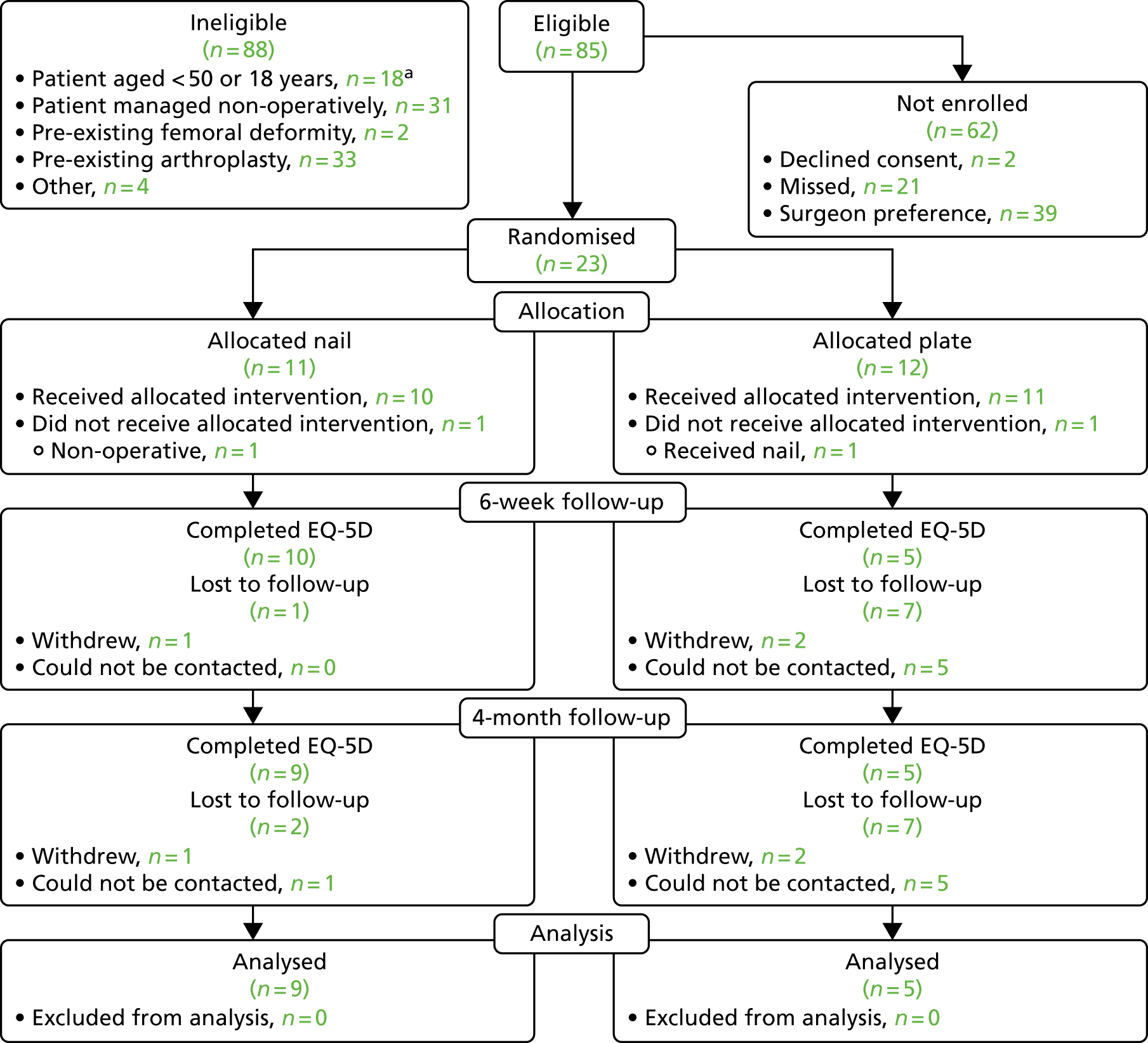
The baseline characteristics of the study participants were well matched between groups (Table 12). Participants were older adults with features that were consistent with frailty, for example relatively poor grip strength and low Rockwood Frailty Scale scores. There was a good representation of educational attainment groupings, suggesting a reasonable representation across socioeconomic groups.
| Variable | Intervention group | |
|---|---|---|
| Nail (N = 11) | Plate (N = 12) | |
| Continuous variables; mean (SD; n) | ||
| Age (years) | 70.1 (13.6; 10) | 78.7 (14.9; 11) |
| BMI (kg/m2) | 32.7 (6.3; 10) | 28.3 (7.4; 11) |
| Grip strength (kg) | 16.8 (4.6; 4) | 18.7 (1.2; 3) |
| Rockwood Frailty Scale score (1–9) | 3.7 (2.2; 10) | 4.5 (2.1; 12) |
| Categorical variables, n (%) | ||
| Pre-operation Abbreviated mental test score | ||
| < 7 | 3 (27.3) | 1 (8.3) |
| ≥ 7 | 4 (36.4) | 7 (58.3) |
| Post-operation Abbreviated mental test score | ||
| < 7 | 0 (0.0) | 1 (8.3) |
| ≥ 7 | 2 (18.2) | 3 (25.0) |
| Gender | ||
| Female | 7 (63.6) | 9 (75) |
| Male | 4 (36.4) | 3 (25) |
| Ethnicity | ||
| Indian | 1 (9.1) | 0 (0) |
| White | 9 (81.8) | 11 (91.7) |
| Analgesia | ||
| No | 6 (54.5) | 4 (33.3) |
| Yes | 4 (36.4) | 7 (58.3) |
| Regular medications | ||
| No | 2 (18.2) | 0 (0) |
| Yes | 8 (72.7) | 11 (91.7) |
| Diabetes | ||
| No | 5 (45.5) | 9 (75) |
| Yes | 5 (45.5) | 2 (16.7) |
| Regular smoker | ||
| No | 9 (81.8) | 10 (83.3) |
| Yes | 1 (9.1) | 1 (8.3) |
| Alcohol | ||
| 0–7 units | 7 (63.6) | 9 (75) |
| 8–14 units | 0 (0) | 2 (16.7) |
| 14–21 units | 0 (0) | 0 (0) |
| > 21 units | 3 (27.3) | 0 (0) |
| Renal failure | ||
| No | 10 (90.9) | 9 (75) |
| Yes | 0 (0) | 2 (16.7) |
| Living arrangement | ||
| Care home | 1 (9.1) | 1 (8.3) |
| Live alone | 3 (27.3) | 4 (33.3) |
| Live with relatives | 1 (9.1) | 1 (8.3) |
| Live with wife/husband/partner | 5 (45.5) | 5 (41.7) |
| Annual income (£) | ||
| 0–19,999 | 7 (63.6) | 7 (58.3) |
| 20,0000–39,999 | 0 (0) | 0 (0) |
| 40,0000–59,999 | 0 (0) | 1 (8.3) |
| 60,0000–79,000 | 0 (0) | 0 (0) |
| 80,0000–99,999 | 0 (0) | 0 (0) |
| ≥ 100,000 | 0 (0) | 1 (8.3) |
| Unknown | 3 (27.3) | 2 (16.7) |
| Qualifications | ||
| None | 3 (27.3) | 2 (16.7) |
| Primary school | 1 (9.1) | 1 (8.3) |
| Secondary school | 4 (36.4) | 6 (50) |
| GCSE/O levels | 1 (9.1) | 0 (0) |
| Advanced Subsidiary or A level | 1 (9.1) | 0 (0) |
| Bachelor degree | 0 (0) | 1 (8.3) |
After recruitment, all study participants proceeded to operation to repair the fracture (details of the fracture and the operation are shown in Table 13). One study participant in the nail group did not receive either of the study interventions and one participant in the plate group received a nail rather than a plate.
| Variable | Intervention group | |
|---|---|---|
| Nail (N = 11) | Plate (N = 12) | |
| Time (days) from admission to surgery median (IQR) | 2 (1–3) | 2 (1–3) |
| Side fracture, n (%) | ||
| Left | 3 (27.3) | 6 (50) |
| Right | 8 (72.7) | 6 (50) |
| Classification, n (%)18 | ||
| A1 | 7 (63.6) | 5 (41.7) |
| A2 | 3 (27.3) | 2 (16.7) |
| A3 | 0 (0) | 1 (8.3) |
| B1 | 0 (0) | 1 (8.3) |
| C2 | 1 (9.1) | 1 (8.3) |
| C3 | 0 (0) | 2 (16.7) |
| CT scan, n (%) | ||
| No | 5 (45.5) | 3 (25) |
| Yes | 6 (54.5) | 9 (75) |
| Periprosthetic fracture, n (%) | ||
| No | 8 (72.7) | 9 (75) |
| Yes | 3 (27.3) | 3 (25) |
| Ortho-geriatrician review, n (%) | ||
| No | 5 (45.5) | 7 (58.3) |
| Yes | 6 (54.5) | 5 (41.7) |
| Pre-fracture mobility, n (%) | ||
| Freely mobile without aids | 4 (36.4) | 3 (25) |
| Mobile outdoors with one aid | 4 (36.4) | 6 (50) |
| Mobile outdoors with two aids | 0 (0) | 2 (16.7) |
| Indoor mobility but not outside without help | 3 (27.3) | 1 (8.3) |
| Other surgery, n (%) | ||
| No | 10 (90.9) | 11 (91.7) |
| Yes | 1 (9.1) | 1 (8.3) |
| Anaesthesia, n (%) | ||
| General + nerve block | 4 (36.4) | 5 (41.7) |
| General + spinal anaesthesia | 0 (0) | 2 (16.7) |
| GA only | 6 (54.5) | 3 (25) |
| Other | 1 (9.1) | 0 (0) |
| Spinal anaesthesia only | 0 (0) | 2 (16.7) |
| American Society of Anaesthesiologist Physical Status Classification grade, n (%) | ||
| 1 or 2 | 3 (27.3) | 4 (33.3) |
| 3 or 4 | 8 (72.8) | 6 (50) |
| Method fixation, n (%) | ||
| Intramedullary nail | 10 (90.9) | 1 (8.3) |
| Locking plate | 0 (0) | 11 (91.7) |
| Other | 1 (9.1) | 0 (0) |
| Grade senior surgeon, n (%) | ||
| Consultant | 11 (100) | 12 (100) |
| Grade operating surgeon, n (%) | ||
| Consultant | 7 (63.6) | 8 (66.7) |
| SAS | 1 (9.1) | 1 (8.3) |
| Trainee | 3 (27.3) | 3 (25) |
| Physiotherapist assessment, n (%) | ||
| Yes | 11 (100) | 12 (100) |
| Post-operative mobilisation, n (%) | ||
| No | 2 (18.2) | 6 (50) |
| Yes (other staff) | 1 (9.1) | 0 (0) |
| Yes (physiotherapist) | 8 (72.7) | 6 (50) |
| Post-operation weight-bearing, n (%) | ||
| Non-weight-bearing | 1 (9.1) | 4 (33.3) |
| Partial weight-bearing | 5 (45.5) | 2 (16.7) |
| Weight-bearing as required to survive | 1 (9.1) | 2 (16.7) |
| Weight-bearing as tolerated | 4 (36.4) | 4 (33.3) |
| Rehabilitation assessment, n (%) | ||
| No | 4 (36.4) | 2 (16.7) |
| Yes | 7 (63.6) | 10 (83.3) |
| Pre-discharge weight-bearing, n (%) | ||
| No | 6 (54.5) | 8 (66.7) |
| Yes | 4 (36.4) | 4 (33.3) |
| Orthopaedic ward discharge, n (%) | ||
| No | 0 (0) | 1 (8.3) |
| Yes | 10 (90.9) | 11 (91.7) |
| Orthopaedic ward destination, n (%) | ||
| Acute hospital | 0 (0) | 1 (8.3) |
| Own home/sheltered housing | 5 (45.5) | 5 (41.7) |
| Rehabilitation unit – other trust | 2 (18.2) | 3 (25) |
| Rehabilitation unit – this trust | 2 (18.2) | 2 (16.7) |
| Residential care | 1 (9.1) | 0 (0) |
| NHS care discharge, n (%) | ||
| No | 1 (9.1) | 3 (25) |
| Yes | 9 (81.8) | 9 (75) |
| NHS care destination, n (%) | ||
| Care home | 2 (18.2) | 1 (8.3) |
| Live alone | 2 (18.2) | 3 (25) |
| Live with wife/husband/partner | 5 (45.5) | 3 (25) |
| Other | 0 (0) | 2 (16.7) |
At baseline, participants were assessed using the self-efficacy questionnaire, EQ-5D-5L, DRI and DEMQoL (the last three measures were used both pre and post operation). Here, for the purposes of statistical analysis of the self-efficacy questionnaire, the scores 1 to 4 were assigned to the categories (1) strongly disagree, (2) disagree, (3) agree and (4) strongly agree, for the first five items in the questionnaire, and summed to give a score between 5 and 20. These data, together with the numbers of friends and relatives, are summarised by means and SDs in Table 14, together with EQ-5D-5L, DRI and DEMQoL outcomes. A more complete report of the self-efficacy questionnaire is presented in Appendix 4.
| Measurement | Intervention group, mean (SD; n) | |
|---|---|---|
| Nail (N = 11) | Plate (N = 12) | |
| Friends and relatives | 6.2 (5.4; 9) | 10.9 (18.9; 9) |
| Self-efficacy score (5–20) | 13.3 (3.9; 9) | 13.6 (4.6; 9) |
| Pre-operation EQ-5D-5L | 0.59 (0.29; 10) | 0.56 (0.22; 10) |
| Pre-operation EQ VAS | 50.5 (25.5; 10) | 58 (13.4; 10) |
| Post-operation EQ-5D-5La | –0.05 (0.28; 10) | –0.04 (0.16; 10) |
| Post-operation EQ VASa | 41.1 (21.9; 9) | 40.5 (12.8; 10) |
| Pre-operation DRI | 45.4 (36.7; 9) | 67.5 (10.1; 10) |
| Post-operation DRIa | 86.5 (15.5; 9) | 92.5 (5.3; 10) |
| Pre-operation DEMQoL Proxy | 102 (0; 1) | – |
| Pre-operation DEMQoL Self | – | 78.2 (0; 1) |
| Post-operation DEMQoL Proxya | 97 (0; 1) | – |
| Post-operation DEMQoL Selfa | – | 84 (0; 1) |
The planned comparison between DEMQoL and EQ-5D-5L was not possible as there were insufficient DEMQoL data reported by participants to estimate even the simplest possible metrics, such as the variance.
Outcomes and analyses
Study participants were followed up at 6 weeks and 4 months; outcomes for these occasions are shown in Tables 15 and 16.
| Measurement | Intervention group | |
|---|---|---|
| Nail (N = 11) | Plate (N = 12) | |
| Weight-bearing, n (%) | ||
| No | 5 (45.5) | 4 (33.3) |
| Yes | 5 (45.5) | 1 (8.3) |
| Early loss of fixation, n (%) | ||
| No | 9 (81.8) | 5 (41.7) |
| Yes | 1 (9.1) | 1 (8.3) |
| Varus/valgus > 5°, n (%) | ||
| Neither | 10 (90.9) | 5 (41.7) |
| Recurvatum/procurvatum > 10°, n (%) | ||
| Neither | 8 (72.7) | 5 (41.7) |
| Procurvatum | 1 (9.1) | 0 (0) |
| Recurvatum | 1 (9.1) | 0 (0) |
| Shortening, n (%) | ||
| No | 8 (72.7) | 5 (41.7) |
| Yes | 2 (18.2) | 0 (0) |
| EQ-5D-5L; mean (SD; n) | 0.35 (0.30; 10) | 0.05 (0.16; 5) |
| EQ VAS; mean (SD; n) | 58.5 (24.6; 10) | 62.0 (21.7; 5) |
| DRI; mean (SD; n) | 78.0 (16.9; 9) | 87.3 (3.1; 5) |
| DEMQoL proxy; mean (SD; n) | 87 (0; 1) | – |
| DEMQoL self; mean (SD; n) | – | – |
| Measurement | Intervention group | |
|---|---|---|
| Nail (N = 11) | Plate (N = 12) | |
| Weight-bearing, n (%) | ||
| No | 2 (18.2) | 3 (25) |
| Yes | 7 (63.6) | 2 (16.7) |
| Discharged, n (%) | ||
| No | 0 (0) | 1 (8.3) |
| Yes | 9 (81.8) | 4 (33.3) |
| EQ-5D-5L; mean (SD; n) | 0.38 (0.36; 9) | 0.37 (0.41; 5) |
| EQ VAS; mean (SD; n) | 50.4 (29.0; 9) | 50.0 (21.5; 5) |
| DRI; mean (SD; n) | 60.9 (23.1; 8) | 82.8 (2.9; 4) |
| DEMQoL proxy; mean (SD; n) | 89 (0; 1) | – |
| DEMQoL self; mean (SD; n) | – | – |
| Grip strength (kg); mean (SD; n) | 25.3 (8.3; 3) | 16 (0; 1) |
The main study outcome variable is EQ-5D-5L score. Overall temporal trends in EQ-5D-5L score during the course of the study are shown in Figure 5 and for DRI are shown in Figure 6.
FIGURE 5.
Temporal trends in EQ-5D-5L, by intervention group. Boxes show IQR, bars medians, whiskers 1.5 times the IQR and potential outliers as individual symbols (◦). Means are shown as solid symbols (•), with 95% CIs. (a) Nail; and (b) plate. IQR, interquartile range.
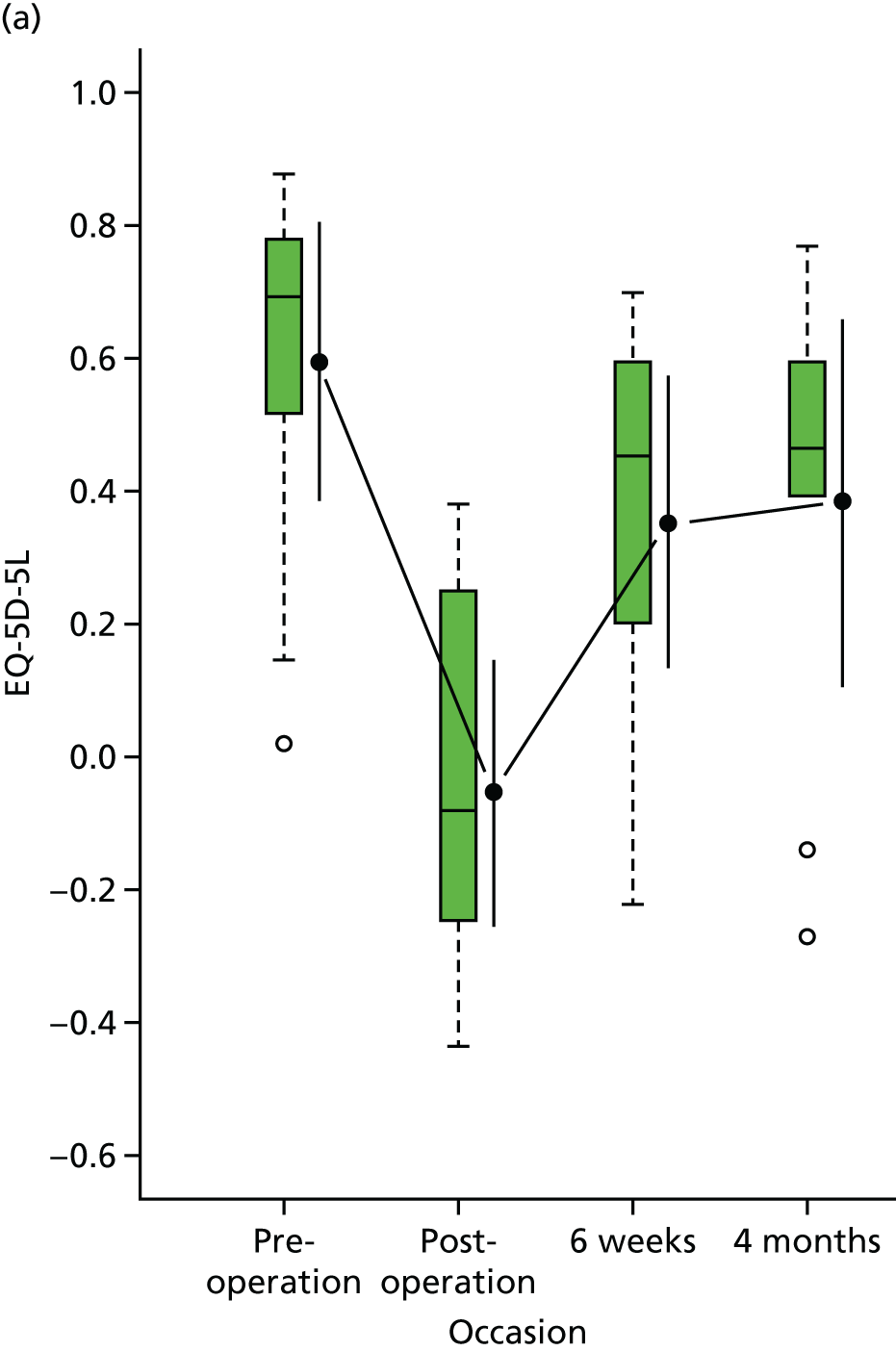
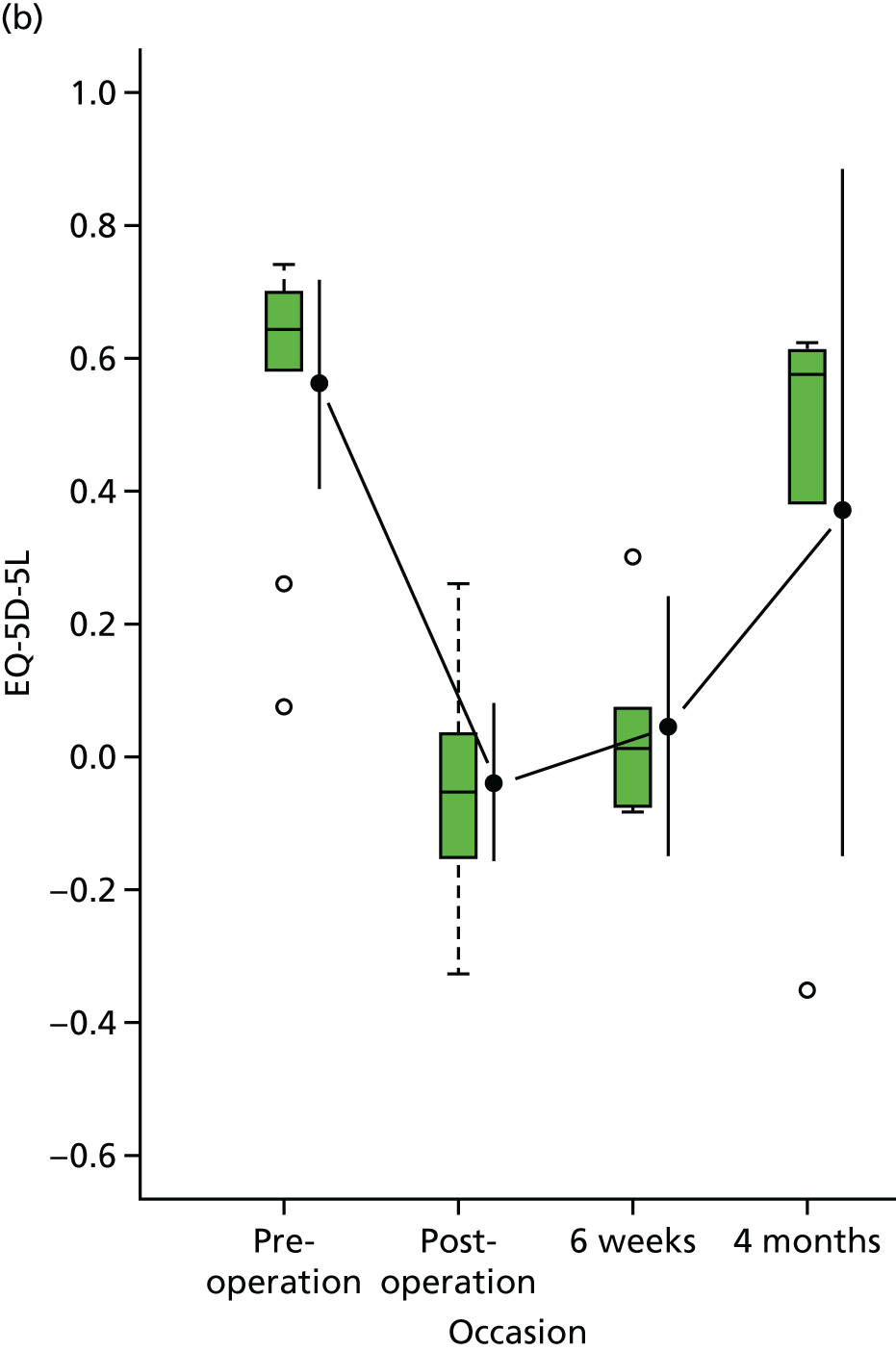
FIGURE 6.
Temporal trends in DRI, by intervention group. Boxes show IQR, bars medians, whiskers 1.5 times the IQR and potential outliers as individual symbols (◦). Means are shown as solid symbols (•), with 95% CIs. (a) Nail; and (b) plate. IQR, interquartile range.
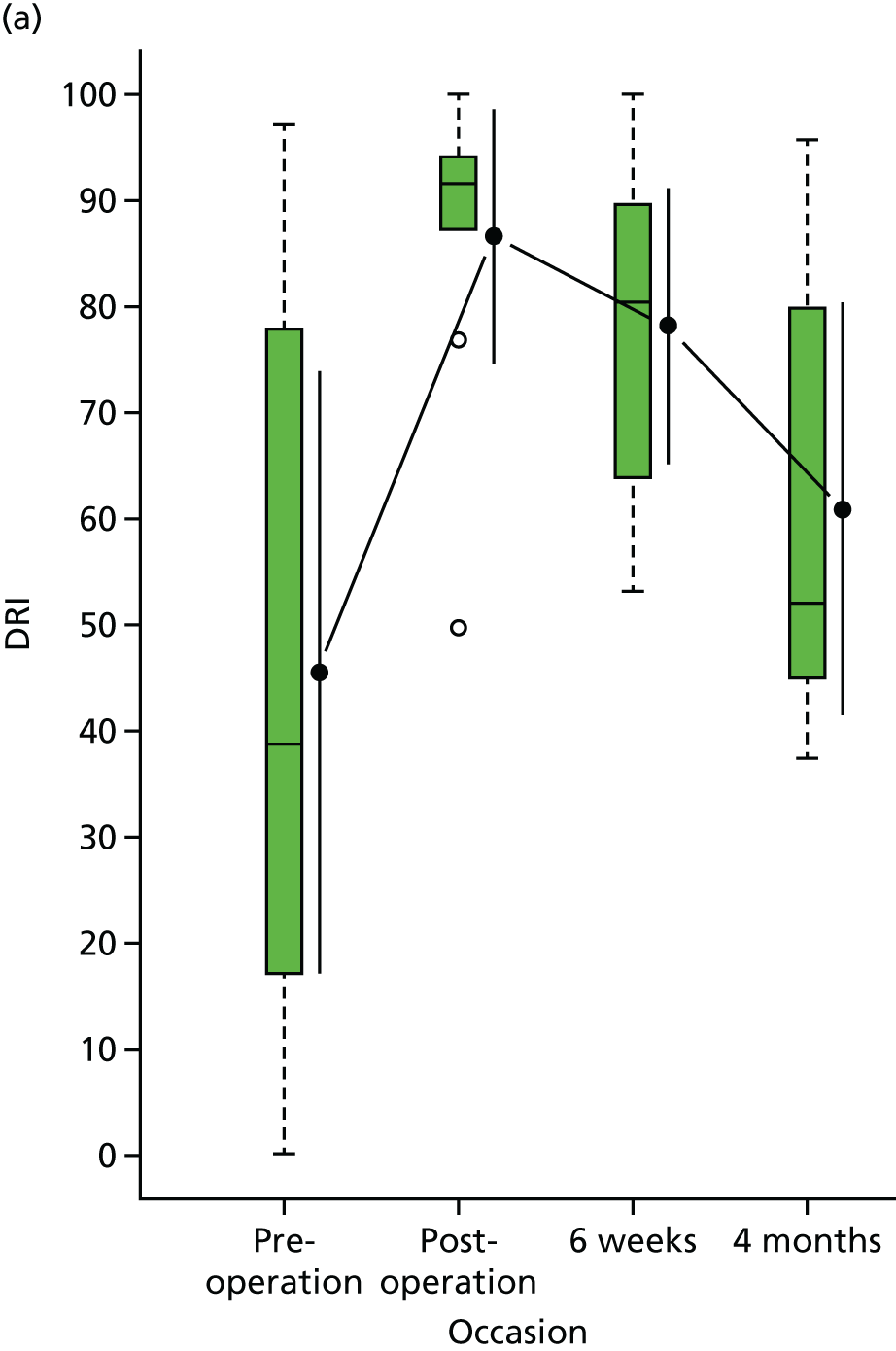
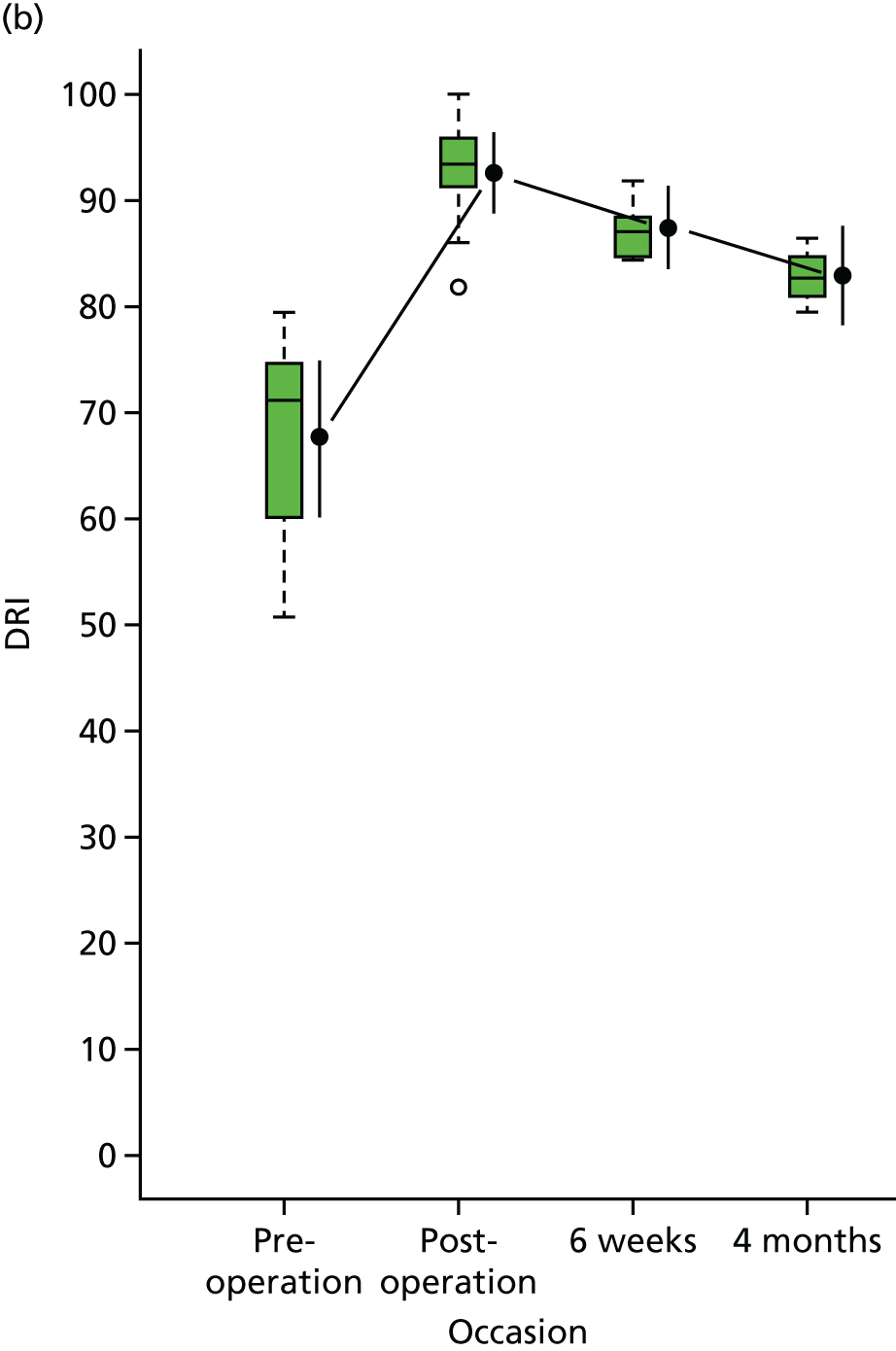
Table 17 shows raw and adjusted estimates of treatment effects, on an intention-to-treat (ITT) basis, for EQ-5D-5L at 4 months and earlier occasions; a negative value is in favour of the nail treatment, as a higher EQ-5D-5L score indicates less disability. The opposite was true for DRI, as a lower DRI score indicates less disability. It was not possible to adjust for cognitive impairment for DRI as all participants who reported a DRI were not cognitively impaired. The adjusted estimate of the treatment effect for the primary outcome of the 4-month EQ-5D-5L is –0.00 (95% CI –0.53 to 0.53). The p-value of 0.987 (see Table 17) indicates that there is no evidence of a statistically significant difference in EQ-5D-5L scores between the treatment groups at 4 months post injury. The minimum clinically important difference for the EQ-5D is 0.08 points.
| Outcome | Intervention group | Difference (95% CI) | p-value | ||||
|---|---|---|---|---|---|---|---|
| Nail | Plate | ||||||
| Mean (SD) | n | Mean (SD) | n | Rawa | Adjustedb | ||
| Primary outcome | |||||||
| EQ-5D-5L (4 months) | 0.38 (0.36) | 9 | 0.37 (0.41) | 5 | –0.01 | –0.00 (–0.53 to 0.53) | 0.987 |
| Secondary and early outcomes | |||||||
| DRI (4 months) | 60.9 (23.1) | 8 | 82.8 (2.9) | 4 | 21.9 | 21.9 (–7.1 to 50.9) | 0.114 |
| EQ-5D-5L (6 weeks) | 0.35 (0.30) | 10 | 0.05 (0.16) | 5 | –0.31 | –0.32 (–0.68 to 0.05) | 0.077 |
| DRI (6 weeks) | 78.0 (16.9) | 9 | 87.3 (3.1) | 5 | 9.3 | 9.3 (–9.1 to 27.6) | 0.271 |
There was also no evidence (p-value = 0.114; see Table 17) of a statistically significant difference in DRI scores between the treatment groups at 4 months post injury. There was some weak, statistically non-significant, evidence (p-value = 0.077; see Table 17) of EQ-5D-5L being lower in the plate group than in the nail group at 6 weeks. However, given the small sample size, there was insufficient power to make any strong inferential statements from these analyses.
There were few post-operative complications reported for this study (Table 18).
| Complications | Intervention group, n (%) | |
|---|---|---|
| Nail (N = 11) | Plate (N = 12) | |
| Wound infection | 0 (0) | 0 (0) |
| Venous thromboembolism | 0 (0) | 0 (0) |
| Pneumonia | 1 (9.1) | 0 (0) |
| Urinary tract infection | 1 (9.1) | 0 (0) |
| Cerebrovascular accident | 0 (0) | 0 (0) |
| Myocardial infarction | 1 (9.1) | 0 (0) |
| Blood transfusion | 2 (18.2) | 2 (16.7) |
| Malunion | 0 (0) | 0 (0) |
| Failure of fixation | 0 (0) | 1 (8.3) |
Chapter 5 Health economic analyses
Currently, there is no evidence to estimate the cost of fragility fractures of the distal femur in the UK. However, injuries of the distal femur occur in the same population as the hip fracture3 and are comparable in severity, allowing for some indicative costs to be presented. There is evidence to suggest that the incidence of hip fractures may rise substantially over the next 5–10 years in the UK. 57 A recent study by Leal et al. 58 used incident hip fracture cases to estimate the cost of hospital services for hip fractures in the UK to be £1.1B per year and expected to rise to £1.5B per year in 2025. Following patients to 1 year post surgery, the authors found that acute hospitalisation as a result of a hip fracture accounted for 61% of these total first-year costs. For comparison, the estimated incidence of distal fractures is 10 per 100,000, accounting for 5% of all fractures of the femur and in a ratio of 1 : 10 with hip fracture. 1
We undertook an exploratory health economic analysis at 4 months post surgery to more accurately estimate resource use and costs associated with the treatment of distal femoral fractures and the feasibility of collection of these data.
Methods
Collection of resource use
This study collected data on the use of services within the health-care system, as well as on broader costs to society, in an attempt to capture relevant components of the overall cost of treating fractures of the distal femur. Key outcomes included data completeness and the main cost drivers of the interventions under investigation.
Valuation of resource use
Estimation of unit costs followed recent NICE guidelines on costing health and social care services. 59 All costs presented are in 2017/18 Great British pounds. For unit costs obtained before 2017, prices were inflated to 2017/18 prices as necessary using the NHS Hospital and Community Health Services (HCHS) index for health service resources. 60
The cost of the distal femur fracture surgery was assessed using the latest NHS Reference Costs 2015 to 201661 and Healthcare Resource Group code for ‘Major Knee Procedures for Trauma’ (Table 19). If a patient experienced a length of stay greater than the average length of the stay (i.e. 5 days) reported from the NHS reference costs, then the inpatient excess day cost from the NHS reference cost was used to compute the direct medical cost associated with the trial. 61
| Item | Unit cost (£) | Source |
|---|---|---|
| Surgerya | ||
| Average surgery cost of distal femur fracture fixation (mean length of stay of 5 days)b | 5978.52c | National schedules of NHS Reference Costs 2015 to 201661 – Major Knee Procedures for Trauma with CC Score 1 (code HT23C) |
| Cost per excess bed-day | 172.31c | National schedules of NHS Reference Costs 2015 to 201661 – Major Knee Procedures for Trauma with CC Score 1 (code HT23C) |
| Major implant cost component | ||
| Nail | 1010.48 | NHS Supply Chain Catalogue 62 |
| Guide wire | 61.86 | NHS Supply Chain Catalogue 62 |
| Locking bolts | 83.14 | NHS Supply Chain Catalogue 62 |
| Helical blade plate | 360.56 | NHS Supply Chain Catalogue 62 |
| Distal femoral locking plate | 1364.04 | NHS Supply Chain Catalogue 62 |
| Locking screw | 136.82 | NHS Supply Chain Catalogue 62 |
| Cable (e.g. Dall–Miles cable) | 241.24 | NHS Supply Chain Catalogue 62 |
The NHS reference cost is the average unit secondary health-care cost to the NHS and would in fact include the implant cost but we have included unit costs of major implant cost components here for future trials that might utilise microcosting (or bottom-up costing). These unit costs were obtained from the 2018 NHS Supply Chain Catalogue62 (see Table 19). Similarly, use of additional implants for the operative treatment of distal femur fractures (e.g. number of screws, wires or cables) was reported in the trial CRFs.
Data on further resource use were collected within the trial at 4 months post surgery via self-reported patient questionnaires and appropriate proxies (when necessary). 29,63 Questionnaires captured the frequency of use of community-based health and social care services (classified as general practitioner, practice nurse, community nurse, physiotherapist, occupational therapist), number and duration of admissions to inpatient wards, number of diagnostic tests, use of outpatient services [classified as orthopaedics (injured bone), orthopaedics (any other bones), rehabilitation unit, physiotherapy, emergency department], medication use and equipment provided, indirect costs borne by partners and carers as a result of attending hospital visits, as well as direct non-medical costs (including travel expenses) attributable to the participants’ health state. Unit cost data were obtained from the latest available national databases, such as the NHS Reference Costs 2015 to 2016,61 NHS Supply Chain Catalogue62 and Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care,64,65 or other sources, such as North Yorkshire County Council’s Paying for Care at Home,66 Independent People Homecare Services’ The Cost of Live in Care67 and the Office for National Statistics’68 Annual Survey of Hours and Earnings: 2017 Provisional and 2016 Revised Results (Table 20), and used to compute the direct medical costs that are not directly related to the trial.
| Resource item | Unit | Unit cost (£) | Source of unit cost |
|---|---|---|---|
| Readmitted inpatient care | |||
| Orthopaedic: cost per average length of stay of 1 day | Procedure | 520.62a | NHS Reference Costs 2015 to 2016,61 ‘Minor Knee Procedures for Non-Trauma, 19 years and over’ (code HN25A) |
| Outpatient care | |||
| Orthopaedic | Session | 111.96a | NHS Reference Costs 2015 to 2016:61 code 110 |
| Pathology (blood) | Test | 3.05a | NHS Reference Costs 2015 to 2016:61 code DAPS05 |
| Radiology | Test | 30.77a | NHS Reference Costs 2015 to 2016:61 code DAPF |
| Imaging | Test | 39.70a | NHS Reference Costs 2015 to 2016:61 code YH30Z |
| Hospital physiotherapist | Session | 49.87a | NHS Reference Costs 2015 to 2016:61 code A08A1 |
| Emergency department | Session | 149.48a | NHS Reference Costs 2015 to 2016:61 code 180 |
| Community and social care | |||
| GP consultation (surgery) | Consultation (9.22 minutes) | 37.00 | PSSRU,65 p. 162 |
| GP consultation (home) | Consultation (9.22 minutes) | 37.00 | PSSRU,65 p. 162 |
| GP consultation (telephone) | Consultation (4 minutes) | 14.75 | PSSRU,65 p. 164 |
| Practice nurse | Hour | 43.00 | PSSRU,65 p. 117 |
| District/community nurse | Hour | 39.39a | PSSRU,69 p. 159 |
| Community physiotherapist | Hour | 34.00 | PSSRU,65 p. 203 (band 5) |
| Ambulance/paramedic | Consultation | 119.00 | PSSRU,65 p. 110 |
| Community occupational therapist | Hour | 45.00 | PSSRU,65 p. 177 |
| Community psychiatrist | Hour | 44.00 | PSSRU,65 p. 185 |
| Personal Social Services | |||
| Meals on Wheels (hot, daily) | Week | 47.87a | PSSRU,64 p. 127 |
| Laundry services | Load | 4.60 | North Yorkshire County Council66 |
| Home care worker (professional) | Hour | 26.00 | PSSRU,65 p. 125 |
| Medication | |||
| 50 mg of tramadol | Pack of 60 tablets | 4.60 | WHOCC ATC:70 code N02AX02, BNF 74 |
| 100 mg of morphine | Pack of 60 tablets | 28.54 | WHOCC ATC:70 code N02AA01, BNF 74 |
| 500 mg of paracetamol | Pack of 16 tablets | 0.16 | WHOCC ATC:70 code N02BE01, BNF 74 |
| 400 units of vitamin D (colecalciferol) | Pack of 60 tablets | 15.50 | WHOCC ATC:70 code A11CC05, BNF 74 |
| 10 mg of bisoprolol | Pack of 28 tablets | 5.89 | WHOCC ATC:70 code C07AB07, BNF 74 |
| 250 mg of flucloxacillin | Pack of 28 tablets | 1.25 | WHOCC ATC:70 code J01CF05, BNF 74 |
| 5 mg of prednisolone | Pack of 28 tablets | 9.86 | WHOCC ATC:70 code H02AB06, BNF 74 |
| Mobility aids | |||
| Crutches | Each | 18.30 | NHS Supply Chain Catalogue 62 |
| Stick | Each | 5.50 | NHS Supply Chain Catalogue 62 |
| Walking frame | Each | 18.25 | NHS Supply Chain Catalogue 62 |
| Long-handle shoehorn | Each | 2.72 | NHS Supply Chain Catalogue 62 |
| Other: four-wheeled walking frame | Each | 45.48 | NHS Supply Chain Catalogue 62 |
| Other: rotastand | Each | 364.95 | NHS Supply Chain Catalogue 62 |
| Other: wheelchair | Each | 195 | PSSRU,65 p. 111 |
| Other: commode | Each | 65.32 | NHS Supply Chain Catalogue 62 |
| Formal care | |||
| Live in carer | Week | 695.00 | Independent People Homecare Services67 |
| Home adaptations | |||
| Grab rail | Each | 7.86 | NHS Supply Chain Catalogue 62 |
| Fixed hoist | Each | 1113.40 | NHS Supply Chain Catalogue 62 |
| Other: profiling bed | Each | 728.05 | NHS Supply Chain Catalogue 62 |
| Other: bed rail | Each | 25.45 | NHS Supply Chain Catalogue 62 |
| Informal care | |||
| Median gross earnings: men | Hour | 14.48 | Office for National Statistics68 |
| Median gross earnings: women | Hour | 13.16 | Office for National Statistics68 |
For medications, the defined daily dose for each medication was obtained from the World Health Organization Collaborating Centre for Drug Statistics Methodology website70 using the relevant Anatomic Therapeutic Chemical code. Unit cost of each medication was then sourced using the British National Formulary71 and either tablet or capsule form (if tablet form was not available) of the medication was assumed.
The human capital approach was adopted to estimate the cost of informal caregiving. As the age group of the caregivers was not collected in the CRFs, we assumed the wage to differ by sex only.
Missing data
The reasons for and patterns of any missing data, loss to follow-up and participant withdrawals have been carefully considered and reported, with particular emphasis on how these may impinge on any future trial.
Analysis
A data analysis was conducted on an ITT basis and aimed to determine the main cost drivers of the trial from the NHS and Personal Social Services perspectives. The mean cost and SD were reported for each resource item by treatment allocation.
Health economics outcomes
Response rate and data completeness
Of the 23 participants who were randomised, 52% (n = 12) responded to the health resource use questionnaires. Participants’ perception of the resource use questionnaires in terms of their content and length is reported in Chapter 3, Results of the process evaluation. The quality of response to the resource use questionnaires was acceptable with no missing items in most of the resource categories (Tables 21–23).
| Cost | Intervention group | |||
|---|---|---|---|---|
| Nail (n = 12) | Plate (n = 11) | |||
| Mean (SD) | Number missing | Mean (SD) | Number missing | |
| Length of stay (days) | 28.3 (45.2) | 1 | 19.4 (9.3) | 1 |
| Cost per excess bed-day (£) | 4025.79 (7785.80) | 2481.26 (1610.69) | ||
| Total surgery cost (£) | 33,374.89 (8287.41) | 32,373.86 (1610.69) | ||
| Cost | Intervention group | |||
|---|---|---|---|---|
| Nail (n = 9) | Plate (n = 3) | |||
| Mean cost (SD) (£) | Number missing | Mean cost (SD) (£) | Number missing | |
| Readmitted inpatient care | ||||
| Orthopaedic | 2603.10 | 0 | 5466.51 (2576.94) | 0 |
| Outpatient care | ||||
| Orthopaedic | 251.91 (115.89) | 0 | 223.92 (111.96) | 0 |
| Pathology (blood) | 3.05 | 2 | – | 0 |
| Radiology | 48.35 (24.21) | 0 | 51.28 (17.77) | 0 |
| Imaging | 39.70 | 0 | – | 0 |
| Physiology | 249.35 (211.58) | 0 | 274.29 (105.79) | 0 |
| Emergency department | 149.48 | 0 | – | 0 |
| Rehabilitation | – | 2 | – | 0 |
| Emergency department: not related to injury | – | 1 | – | 0 |
| Other | – | 1 | – | 0 |
| Community and social care | ||||
| GP surgery | 74.00 (37.00) | 0 | – | 1 |
| GP home visit | 92.50 (78.49) | 1 | 37.00 | 0 |
| GP telephone | 24.58 (17.03) | 0 | – | 0 |
| Practice nurse | 43.00 | 0 | – | 0 |
| District/community nurse | 216.65 (139.26) | 2 | 393.90 | 0 |
| Community physiologist | 136.00 (96.17) | 0 | 187.00 (72.12) | 0 |
| Ambulance/paramedic | 119.00 | 0 | 119.00 | 0 |
| Community occupational therapist | 157.50 (159.10) | 1 | – | 0 |
| Community psychiatry | 44.00 | 0 | – | 0 |
| Other | – | 2 | – | 0 |
| Personal Social Services | ||||
| Hot Meals on Wheels | 335.09 | 0 | 670.18 | 0 |
| Laundry | 32.20 | 1 | – | 0 |
| Home care worker (professional) | 455.00 (386.08) | 0 | 182.00 | 0 |
| Social worker | – | 1 | – | 0 |
| Medication | 2 | 1 | ||
| Paracetamol | 2.40 | – | ||
| Tramadol | 46.92 | – | ||
| Morphine | 8.16 | – | ||
| Vitamin D | 31.20 | – | ||
| Bisoprolol | – | – | ||
| Flucloxacillin | 2.52 | – | ||
| Prednisolone | 3.50 | – | ||
| Mobility aids | ||||
| Crutch | 27.45 (10.57) | 0 | – | 0 |
| Stick | 5.50 | 0 | 8.25 (3.89) | 0 |
| Walking frame | 18.25 | 0 | 18.25 | 0 |
| Shoehorn | – | 0 | 2.72 | 0 |
| Other: four-wheeled walking frame | 45.48 | – | ||
| Other: rotastand (e.g. rotunda, turner) | 364.95 | 364.95 | ||
| Other: wheelchair | 195.00 | 195.00 | ||
| Other: commode | 65.32 | 65.32 | ||
| Formal care | ||||
| Live in carer | 5041.07 | 0 | 1572.24 (1111.47) | 0 |
| Cost | Intervention group | |||
|---|---|---|---|---|
| Nail (n = 9) | Plate (n = 3) | |||
| Mean cost (SD) (£) | Number missing | Mean cost (SD) (£) | Number missing | |
| Home adaptations | 3 | 1 | ||
| Grab rail | 7.86 | 7.86 | ||
| Fixed hoist | 1113.40 | – | ||
| Other: profiling bed | 728.05 | – | ||
| Other: bed support rail | – | 25.45 | ||
| Informal care | 0 | 0 | ||
| Men | 5495.16 (5334.47) | 8615.60 | ||
| Women | 13,709.43 (16,338.02) | 1645.00 (837.50) | ||
| Income loss | 3000.00 | 2 | – | 0 |
Estimation of resource use and costs
The mean usage and cost of the major implant cost components of each intervention per patient are provided in Table 24. The mean total implant cost per patient of the locking plate intervention was higher than that of the intramedullary nail intervention.
| Item | Intervention group | |||||
|---|---|---|---|---|---|---|
| Nail (n = 12) | Plate (n = 11) | |||||
| Number of patients | Mean quantity (SD) | Mean cost (SD) (£) | Number of patients | Mean quantity (SD) | Mean cost (SD) (£) | |
| Nail | 12 | 1 | 1010.48 | – | – | – |
| Guide wire | 12 | 1 | 61.86 | – | – | – |
| Three locking bolts | 12 | 3 | 249.41 | – | – | – |
| Additional locking bolt/blocking screw | 7 | 1.4 (0.5) | 116.39 (41.57) | – | – | – |
| Helical blade plate | 1 | 1 | 360.56 | – | – | – |
| Distal femoral locking plate | – | – | – | 11 | 1 | 1364.04 |
| 10 locking screws | – | – | – | 11 | 8 | 1094.56 |
| Additional locking screws | – | – | – | 6 | 2.5 (1.0) | 342.05 (136.82) |
| Cable | 1 | 1 | 241.24 | 3 | 1.7 (0.6) | 410.11 (144.74) |
| Total implant cost per patient (£) | 2039.93 | 3210.76 | ||||
The total inpatient cost of intramedullary nail fixation seemed to be higher than that of locking plate fixation as one participant had a much longer length of stay (of 233 days) than the rest of the participants in the same group (length of stay of ≤ 25 days) (see Table 21). Removing this participant would result in a mean length of stay of 14.8 days (SD 7.4 days) and a total surgery cost of £31,000.62 (SD £2722.85).
In terms of direct medical cost that was not directly related to the trial (i.e. broader NHS and Personal Social Services resource use utilisation) (see Table 22), inpatient care following readmission constituted the largest component of direct medical cost for both interventions. Two participants reported the use of outpatient care, such as rehabilitation and attendance at emergency departments, not related to their injury. The costs of formal social care was also a very substantial cost driver compared with the other relatively small costs incurred.
Table 23 depicts the direct non-medical (home adaptations not funded by NHS) and indirect costs (informal caregiving and income loss) borne by the study caregivers and participants. The largest single-cost item associated with the interventions other than the surgery cost was informal caregiving from the participants’ relatives. One participant in the nail group reported that a relative was providing informal care for 24 hours per week for 17 weeks. Removing this participant’s response in a sensitivity analysis would result in a mean cost of £5750.92 (SD £4513.19).
The resource item that had the most number of missing responses was home adaptations. This could be due to the order of the mobility aids and home adaptations questions in the questionnaire. As the mobility aids and home adaptations questions were not in sequence, two participants had reported their home adaptations under other response categories.
Summary
The current feasibility study suggests that it is possible to collect the resource use data necessary for a full economic evaluation of locking plates and retrograde intramedullary nail fixation. There were no difficulties in relation to accessing information to evaluate the interventions under investigation. Estimations of health and social care service resource utilisation were also feasible through patient self-reported resource use questionnaires. Other than the direct medical cost of the trial interventions, the main cost drivers were formal and informal caregiving and readmission for participants who underwent nail fixation and locking plate fixation. Future trials might consider removing the section on ‘living arrangements’ as it was not used at all in the computation of costs associated with the trial; similarly, the medication section contributed little compared with the other costs. The response rate to the health economics questionnaires at 4 months was slightly more than 50%; this indicates that the design of the health resources questionnaire should be revised to reduce the burden of follow-up.
Chapter 6 Discussion
Screening and recruitment
Screening
A total of 173 patients were screened during the course of the feasibility study, 85 of whom were potentially eligible for inclusion in the study. This very closely matched our estimate of approximately 1.5 eligible patients per centre per month,3 which predicted a total eligible population of approximately 80 patients. Initial screening estimates of the incident population fell short of this number. The process evaluation revealed that in some centres screening was being conducted by only a subgroup of the clinicians, and often eligibility assessment and screening were confused. Centres with a stronger research culture and a more embedded research team that was organic to the trauma and orthopaedic department provided more complete screening data.
The distribution of baseline demographic characteristics, including mechanism of injury, sex and degree of cognitive impairment, in the screened population was similar to that observed in the hip fracture population. The assumptions underpinning the development of the protocol were in part based on the more highly investigated hip fracture population.
As expected, there were a small number of patients in whom a pre-existing femoral deformity precluded fixation. Nineteen per cent of the screened population were ineligible owing to the presence of an ipsilateral femoral component of a hip arthroplasty. We are not aware of any existing data that describe the proportion of patients with a distal femoral fracture who have an ipsilateral femoral component. More surprising was the finding that a further 18% were excluded as they were managed non-operatively. Not only is this not the practice described in multicentre audits,3 but there is evidence in favour of operative treatment for fractures of the distal femur. 7
A total of 85 patients were eligible for inclusion in the study, which greatly exceeded our specified definition of feasibility of 1.0 participants per centre per month. The most important reason for missing eligible patients was a lack of willingness among surgeons to enter patients into the trial, accounting for 39 out of the 60 missed patients. The reasons for 15 missed patients could not be determined but it is likely that the majority of these were also lost because of surgeon-related factors. Therefore, between 54% and 65% of all eligible patients were lost because of surgeon-related factors: principally, a lack of confidence with both interventions.
The screening data demonstrated very marked variation in practice across the centres. This was most apparent in the variation in surgical decision-making. For example, in one centre 18 patients were managed non-operatively whereas in another there were no patients who were managed non-operatively. In two centres, > 70% of those missed were because of surgeon preference whereas in another two centres < 40% of those missed were because of surgeon preference.
The process evaluation identified that the interaction at surgeon level between a lack of individual equipoise and an imbalance in their confidence in the use of the two technologies posed a very significant barrier for surgeons to participate fully in a trial investigating what is perceived to be a technically demanding procedure. An integrated qualitative recruitment intervention based on the theme of community equipoise, to support surgeons in their decision-making to recruit participants, could substantially overcome this major barrier to the successful delivery of a definitive trial.
If all the participants who were missed because of lack of surgeon equipoise had in fact been recruited, which is a reasonable assumption as so few patients declined to participate, then the recruitment rate would have risen to 1.1 participants per centre per month, exceeding the prespecified definition of feasibility.
During the recruitment phase of the study, the TSC took the decision to widen the eligibility criteria to all adults in an effort to understand whether or not age as a proxy for fragility was leading to a substantial loss of eligible patients at screening. Thirty-one out of 88 ineligible patients were excluded because of their age. The eligibility change did lead to a change in eligibility rate from 44% to 60%, although this did not translate into an increase in the recruitment rate. Throughout the duration of the study, only two participants < 50 years of age were recruited.
The mechanistic criterion reported in the screening process of a fall from standing height (defined as < 2 m) successfully identified fragility fractures and was the commonest cause of injury. Only 3 out of the 69 eligible participants for whom these data were recorded sustained their fracture from higher-energy injuries. This definition is concordant with the WHO’s definition of fragility fracture and may be an eligibility criterion for a future definitive trial. We suggest eligibility criteria that include both surrogates for fragility.
Recruitment
As expected, recruitment in the lead centre outstripped that in other centres, exceeding twice the rate of recruitment in the best-performing other centres. Approximately half of all the participants were recruited in the lead centre.
One of the centres failed to recruit any participants and four centres recruited only three participants, despite screening larger numbers of eligible patients. Further exploration of the reasons for this in the process evaluation showed that the surgeons’ personal preferences were the principal barrier to recruitment. Recruitment was also hindered by the procedures for identifying and screening patients; our findings suggest that a strong research culture and integrated clinical and research teams within the centres may facilitate the identification of potential patients and recruitment.
We found that gaining confirmation from the treating surgeons that their patient was eligible for inclusion and that they were willing to randomise them was the greatest barrier to delivering this study. As demonstrated throughout the results of our process evaluation, although patients tended to be accepting of the study interventions and procedures and research teams were successful at recruiting eligible patients, surgeons held strong views about the two interventions and their appropriateness for individual patients. When integrating these data, it was apparent that recruitment is enhanced in specialist trauma centres. This is probably because of an interaction of greater confidence with both technologies among specialist trauma surgeons and more fully integrated research teams with a more complete understanding of community equipoise at these sites.
The development of a research culture appears crucial to the success of a study such as TrAFFix. TrAFFix was particularly difficult to implement because of the comparatively uncommon number of injuries seen in any one centre by each treating surgeon. RAs commonly reported that the infrequent presentation of eligible patients challenged their established structures for screening and recruitment. The data from the process evaluation suggest that a supportive and experienced research team may contribute to the success of delivering difficult studies. Experienced RAs may make things easier for surgeons by undertaking activities that limit the amount of research-related activity required and prompt recruitment through attendance in the daily trauma meeting and understanding of the eligibility criteria. Furthermore, in this study, by understanding how best to involve this group of patients in research, RAs enabled the majority of patients who were approached to participate.
Overall, the estimate of recruitment rate for the definitive trial was 0.42 [95% confidence interval (CI) 0.27 to 0.62] participants per centre per month. This estimate falls short of the prespecified definition of feasibility, which was 1.0 participants per centre per month. However, it very closely mirrors the recruitment rate observed in a successfully completed trial of similar technologies used in the tibia. 72,73 It is therefore likely that the recruitment rate observed here could be sufficient to deliver a successful definitive study given modifications in the design of that future trial.
For the future success of a definitive trial, it is important that surgeons are confident to recruit participants. This is facilitated by sharing the existing community equipoise found in this study with individual surgeons who may not have a sense of equipoise. Furthermore, the perceived operative complexity of these fracture patterns is real and recruitment could be substantially improved if an integrated qualitative recruitment intervention was adopted.
Declined to participate
Only five patients declined to participate or withdrew from the study. This suggests that the patient and consultee materials and the consent discussions conducted by the RAs were effective. However, patients often recalled the consent discussions and details of the study incompletely.
Treatment according to allocation
Twenty-one out of the 23 participants received their allocation treatment according to protocol. Although the randomised numbers were small, this is a reassuring proportion and suggests that once allocation had been assigned the majority of participants and surgeons were happy to proceed with the study intervention.
Baseline characteristics of the participants
We hypothesised, based on existing multicentre audits,3 that the population of patients sustaining distal femoral fractures might be very similar to that sustaining hip fracture. However, despite the similarity of the screened population to the population with hip fracture, important differences were observed between the recruited and screened samples in this study.
Recruited participants were younger and the proportion with chronic cognitive impairment was < 5%. 47 In addition, the great majority of participants were ambulant both inside and outside their homes, only two lived in a supported care environment and the measures of frailty were considerably better than expected. The reasons for these discrepancies between screened and recruited groups seem to largely be explained by the exclusion of a large proportion of patients from the screened sample because of non-operative management. During the process evaluation, it was reported that in the trial sites patients with substantial comorbidities, such as chronic cognitive impairment or low functional demand, were often treated non-operatively. This is in contrast with the low rate of non-operative treatment for hip fracture, which is < 1%. 47 It likely reflects that non-operative treatment of injuries to the leg is more feasible than that for hip fracture because splinting or casting of these more distal fractures is technically easier. In this feasibility trial, this was an unanticipated loss of participants as it is contrary to previous published audits of practice. 3 Future decisions on recruitment strategies will need to take this reduced availability of potential trial patients into consideration.
The initial flawed assumption that a substantial proportion of patients would have chronic cognitive impairment also had a substantial impact on the feasibility study design because the choice of primary and secondary outcome measures reflected the need for proxy reporting. It is now clear that such considerations are largely unnecessary because the generality of surgeons included in this study do not offer operative treatment to this frailer subgroup. This greatly simplifies a future definitive trial design, with a wider choice of outcome measures being available for consideration.
The distribution of fracture types within the recruited sample was similar to that seen in other small trials in this area. 15 Approximately two-thirds of participants were treated for extra-articular fractures and one-third for periprosthetic fractures around an existing total knee arthroplasty. Initial concerns that surgeons would be unwilling to randomise very proximal simple fractures (AO/OTA A1)18 and complex distal fractures (AO/OTA C1–3)18 were not borne out in this feasibility study. It is likely that the eligibility criterion relating to the fracture type is appropriate for a future trial design.
Interventions
Only two deviations from protocol were recorded. One patient who was allocated a plate received a nail and one patient who was allocated a nail was treated non-operatively.
All of the surgeries were supervised by consultant surgeons and in 15 out of 23 cases the lead surgeon was a consultant. All participants received a physiotherapy assessment and 15 participants were mobilised on the day of or day following surgery. Post-operative instructions by the treating surgeon for 11 out of the 23 participants allowed immediate unrestricted weight-bearing following surgery and eight participants self-reported that they were successfully weight-bearing before discharge.
During the design of the feasibility study, there were concerns that, despite an increasing recognition by some proponents of early weight-bearing in fragility fractures of the lower limb, this practice did not extend universally or even widely across the range of clinical practice in the UK. The results of this study would suggest that there is substantial variation among surgeons in post-operative weight-bearing instructions. Any definitive trial would need to be pragmatic in terms of weight-bearing status for rehabilitation.
A little over half of the surgeons who responded to our national survey expressed a preference for one method of fixation; of those who expressed a preference, there was a similar distribution of surgeons who preferred each technology. These data are concordant with our finding that a large proportion of eligible patients were lost because of surgeon preference. The distribution of preferences in our survey, coupled with the time window available prior to most participants receiving the interventions, is such that a surgeon-preference design is feasible for this research question.
Follow-up
Of the 23 participants entered in to the study, three withdrew at or before their 6-week follow-up, one consented to the collection of routine data only and one died. Fifteen of the remaining 18 participants completed 6 weeks’ follow-up and 14 participants completed 4 months’ follow-up.
Unanticipated loss to follow-up was therefore similar to that of other trauma trials (16%). Data from the putative primary outcome to determine clinical effectiveness in a future study were available from 70% of participants. Similar to our finding that the recruited sample differed from our comparison group of patients with hip fracture, this rate of attrition of primary outcome data is lower than has been observed in recent hip fracture trials (WHiTE 3: Hemi and WHiTE4). 51,74 This would suggest that any future definitive sample size calculation might reasonably be adjusted to account for 30% overall attrition rather than the 50% anticipated when designing this feasibility study.
Measurements
Completion rates
Seventy per cent of the participants were available at the primary outcome time point but not all follow-up questionnaires were complete. Some research staff reported that for this group of patients the length of the CRFs could be burdensome. Research staff stated that the burden of questions at baseline exceeded what could be easily completed during a single consultation and felt this may deter patients from completing the CRFs at follow-up. The majority of the participants were followed up in hospital with clinical and radiographic assessments. This is distinctly different from the hip fracture population, among whom patients are infrequently followed up in outpatient settings. Therefore, collection of face-to-face instruments and radiographs has been demonstrated in this study to be feasible, but the number of the data to be collected should be reduced to a minimum data set.
Baseline characteristics
Generally, baseline data were completed adequately, but research staff commented that measurement of some of the effect modifiers, such as social support, was time-consuming, complex and intrusive. It is likely that in a larger trial a perceived burden of entry into the trial by both researchers and participants could be a barrier to successful delivery. We would therefore recommend reducing the number of additional measurements included at baseline.
Measures of clinical effectiveness
Staff reported that they perceived a duplication between the EQ-5D-5L and DRI, instruments that are designed to measure quality of life and function, respectively; however, participants did not often recall the detail of their contacts with research staff.
Insufficient numbers of participants with chronic cognitive impairment were available in the recruited sample to draw any inferences about the relative merits of DEMQoL versus EQ-5D-5L in determining HRQoL in this group. It is likely that any future trial would not include participants with chronic cognitive impairment owing to the very low rate of operative treatment in this group and, therefore, such considerations would no longer be relevant.
The collection of radiographical outcomes and AEs was uncomplicated with good data completeness. It is not anticipated that the collection of these data need be removed from a definitive trial.
Measures of cost-effectiveness
Approximately half of all the participants provided complete responses to the resource use questionnaires. Researchers reported that they found the length of the questionnaires to be excessive for this group of patients. It is likely that the main drivers of cost within a definitive analysis would reduce the questionnaires to a much smaller subset of questions so that the burden of follow-up could be reduced.
Readmission to hospital for inpatient care and use of social care services in the community dwarfed all of the other costs collected in the study. The majority of the resource use categories, such as pathology services, yielded costs that were negligible in comparison. This information could be used to reduce the size of questionnaires and burden of follow-up and promote better data completeness without compromising the validity of a definitive health economic evaluation.
The estimation of health states using EQ-5D-5L was very successful, with an overall attrition rate of only 30%. The requirement to collect a separate instrument in the cognitively impaired subgroup is likely not to be relevant in any future definitive trial.
Process evaluation of the interventions
Implementation
Some surgeons had strong treatment preferences, which could be considered a barrier to future intervention implementation. Surgeons’ willingness to implement their less preferred intervention in their practice, should it be found more effective in a definitive trial, could be questioned. However, the results of a definitive trial may overcome surgeons’ concerns about the appropriateness of both interventions for these fractures. Furthermore, surgeons have been found to change their practice in response to the results of musculoskeletal trauma trials. 75
Mechanisms of impact
A variety of factors may interact with the interventions to influence patient outcomes after a distal femoral fracture. Most notably, we found that, among our sample of participants, recovery was difficult. In some cases, recovery was inhibited by limited mobility prior to the fracture, a loss of confidence after the fracture and limited access to physiotherapy. Support from relatives or carers enabled some participants to manage at home.
Context
Contextual factors may influence the implementation of the interventions and may affect intervention outcomes. Important factors include the frailty of patients who sustain distal femoral fractures. These patients need support to rehabilitate and to manage after surgery and post discharge.
Logic model
We developed a logic model that summarised the problem posed by fractures of the distal femur. The logic model highlights key factors, in addition to the surgical and rehabilitative interventions, that may have an impact on patients’ HRQoL after distal femoral fractures. These include mediators such as self-efficacy and social support, as well as intermediate outcomes such as being pain free or returning to a pre-fracture residence.
Chapter 7 Conclusions and implications for future research
Conclusion
This feasibility study has challenged many of the assumptions that underpinned the development of the proposed definitive trial protocol. We conclude that the trial design tested in this study could not be successfully delivered. We propose a modified protocol here that would be feasible given the recruitment rate observed, which is equal to that reported in the similar FixDT trial,73 which delivered to target and budget. Similar surgeon barriers to recruitment were encountered in the FixDT trial, and concerns regarding the technical delivery of the nail intervention and the eligibility criteria were commonly reported (personal communication with FixDT trial chief investigator).
Recommendations for further research
A modified protocol could successfully deliver a trial to answer this research question. We recommend a definitive trial, with embedded internal pilot to test the assumptions found in this feasibility study. The trial design would be as follows.
Design
A RCT reporting a two-sided test for superiority with an integrated qualitative recruitment intervention based on the theme of community equipoise. The trial should be made up of two phases: an internal pilot to test recruitment assumptions and a main recruitment study. Clear stop–go criteria should be defined for the pilot phase, with a mean recruitment cut-off point specified at 0.5 participants per centre per month.
Population
We have modified the inclusion criteria to accommodate a clinical definition of fragility fracture. Patients are potentially eligible if they:
-
are aged ≥ 60 years or
-
are aged ≥ 18 years or have sustained a fragility fracture defined as a fall from standing height and
-
have a fracture of the femur involving the distal two ‘Müller’ squares18 that would, in the opinion of the treating surgeon, benefit from internal fixation of the fracture.
We have modified the exclusion criteria to exclude patients with cognitive impairment. This reflects the findings that few such patients undergo operative treatments. Patients will be excluded if they:
-
have a loose knee or hip arthroplasty requiring revision
-
have a pre-existing femoral deformity
-
have an arthroplasty that precludes nail fixation
-
are unable to adhere to trial procedures, for example as a result of chronic cognitive impairment.
Interventions
Retrograde intramedullary nailing
Fixation of the fracture will be achieved with a proximally and distally locked nail that spans the entire diaphysis of the femur. All nails will be introduced retrograde through the knee joint.
Locking plate fixation
Fixation of the fracture will be achieved with an anatomical distal femoral locking plate and screws. Locking plates will be defined as those in which at least one fixed angle locking screw is placed distal to the fracture.
Patients allocated to either of the two groups will receive standardised written physiotherapy advice detailing the exercises they need to perform for rehabilitation following their injury. Weight-bearing status will be decided by the treating surgeon, with a preference for early weight-bearing mobilisation immediately or as soon as the surgeon feels appropriate.
Outcomes
The primary outcome should be a patient-reported functional outcome, such as DRI, assessed at 4 months. Our patient and public representatives at the workshop reported that this instrument had suitable face validity; it is a general measure of lower limb function capturing important global domains of function34 and has performed well in previous HTA studies in lower limb trauma. 72,73 We found that patients with chronic cognitive impairment were under-represented in the recruited sample as surgeons tend not to treat them operatively. Hence, there is no requirement for a proxy-reported instrument in the proposed definitive trial. Secondary outcomes would include HRQoL measured using the EQ-5D-5L, AEs and resource use questionnaires focused on key drivers of cost, such as readmission to hospital and use of social care services.
Sample size
The best available evidence for what constitutes a minimally important difference for DRI comes from a recent large trial. 72 The minimally important difference used in the FixDT trial was 8 points on a 100-point scale. On an individual patient level, a difference of 8 points represents the ability to climb stairs with ‘some difficulty’ versus with ‘great difficulty’. Using an estimate of the SD of 21 points from other studies,72 this suggests a standardised effect size of approximately 0.38, which is a ‘moderate effect’ based on Cohen’s criteria. 12
Assuming that the DRI at 4 months post surgery has an approximate normal distribution (which our data suggest is reasonable), a 1 : 1 allocation ratio and an attrition rate of 30%, then, if the true difference between the experimental and control group EQ-5D-5L means is 8 points, 211 participants would need to be recruited in each group (422 in total) to be able to reject the null hypothesis that the population means are equal with probability (power) 0.9 and type I error rate of 5% (significance).
Recruitment
Given a sample size of 422 and a plausible recruitment rate, based on the findings here, of approximately 0.5 participants per centre per month, a recruitment window of approximately 2.5 years would be required across 28 centres.
Acknowledgements
Trial co-ordinator
Dr Robin Lerner, Oxford Trauma, Kadoorie Centre, NDORMS, University of Oxford, John Radcliffe Hospital, Oxford, UK.
Trial Management Group
-
Mr Xavier Griffin.
-
Professor Matthew L Costa.
-
Dr Juul Achten.
-
Dr Nick Parsons.
-
Dr Robin Lerner.
-
Mr Damian Haywood.
-
Dr Melina Dritsaki.
-
Professor Janis Baird.
-
Mrs Alwin McGibbon.
-
Dr Liz Tutton.
-
Dr Emma Phelps.
Trial Steering Committee
-
Mr Mike Kelly (chairperson).
-
Mr Graham Smith (independent clinician).
-
Dr Ada Keding (independent statistician).
-
Dr Philip Bell (independent lay member).
-
Dr Sarah Morgan-Trimmer (independent implementation researcher).
-
Mr Xavier Griffin (chief investigator).
Data Monitoring Committee
-
Mr Dan Perry (chairperson).
-
Mr Tim White (independent clinician).
-
Dr Nikki Totton (independent statistician).
Principal collaborators
-
Mr David Noyes, John Radcliffe Hospital, Oxford University Hospitals NHS Foundation Trust.
-
Professor Peter Giannoudis, Leeds General Infirmary, The Leeds Teaching Hospitals NHS Trust.
-
Professor Ben Ollivere, Queen’s Medical Centre, Nottingham University Hospitals NHS Trust.
-
Ms Charlotte Lewis, Queen Alexandra Hospital, Portsmouth Hospitals NHS Trust.
-
Mr Andrew McAndrew, Royal Berkshire Hospital, Royal Berkshire NHS Foundation Trust.
-
Mr Haroon Majeed, Mr Damian McClelland, Royal Stoke Hospital, University Hospitals of North Midlands NHS Trust.
-
Mr Ashwin Kulkarni, Leicester Royal Infirmary, University Hospitals of Leicester NHS Trust.
Contributions of authors
Xavier L Griffin (Associate Professor Trauma Surgery) contributed to the conception, design, conduct and reporting of the study.
Matthew L Costa (Professor of Orthopaedic Trauma Surgery) contributed to the conception, design and reporting of the study.
Emma Phelps (Postdoctoral RA in Mixed Methods Research) contributed to the design, conduct and analysis of the process evaluation and the reporting of the study.
Nicholas Parsons (Principal Research Fellow, Statistics and Epidemiology) contributed to the design, conduct, analysis and reporting of the study.
Melina Dritsaki (Senior Health Economist) contributed to the design, conduct and reporting of the study.
May Ee Png (Health Economist) performed the health economics analysis and contributed to the reporting of the study.
Juul Achten (Research Fellow) contributed to the conception, design, conduct and reporting of the study.
Elizabeth Tutton (Senior Research Fellow) contributed to the design, conduct and analysis of the process evaluation and the reporting of the study.
Robin Lerner (Clinical Trial Manager) contributed to the conduct and reporting of the study.
Alwin McGibbon (Patient & Public Representative) contributed to the design, conduct and reporting of the study.
Janis Baird (Professor of Public Health and Epidemiology) contributed to the conception, design, conduct, reporting and analysis of the study.
Publication
Griffin XL, Costa ML, Achten J, Dritsaki M, Baird J, Parsons N. Trial of Acute Femoral Fracture Fixation (TrAFFix): study protocol for a randomised controlled feasibility trial. Trials 2017;18:538.
Griffin XL, Costa ML, Phelps E, Parsons N, Dritsaki M, Achten J, et al. Intramedullary nails versus distal locking plates for fracture of the distal femur: results from the Trial of Acute Femoral Fracture Fixation (TrAFFix) randomised feasibility study and process evaluation. BMJ Open 2019;9:e026810.
Phelps EE, Tutton E, Griffin X, Baird J, TrAFFix research collaborators. A qualitative study of patients’ experience of recovery after a distal femoral fracture [published online ahead of print July 22 2019]. Injury 2019.
Phelps EE, Tutton E, Griffin X, Baird J, TrAFFix study co-applicants. Facilitating trial recruitment: a qualitative study of patient and staff experiences of an orthopaedic trauma trial. Trials 2019;20:492.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Please note that exclusive use will be retained until the publication of major outputs. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006;37:691-7. https://doi.org/10.1016/j.injury.2006.04.130.
- Martinet O, Cordey J, Harder Y, Maier A, Bühler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury 2000;31:C62-3. https://doi.org/10.1016/S0020-1383(00)80034-0.
- Smith JR, Halliday R, Aquilina AL, Morrison RJ, Yip GC, McArthur J, et al. Distal femoral fractures: the need to review the standard of care. Injury 2015;46:1084-8. https://doi.org/10.1016/j.injury.2015.02.016.
- Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 2004;15:897-902. https://doi.org/10.1007/s00198-004-1627-0.
- Bleibler F, Konnopka A, Benzinger P, Rapp K, König HH. The health burden and costs of incident fractures attributable to osteoporosis from 2010 to 2050 in Germany – a demographic simulation model. Osteoporos Int 2013;24:835-47. https://doi.org/10.1007/s00198-012-2020-z.
- Zlowodzki M, Bhandari M, Marek DJ, Cole PA, Kregor PJ. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005). J Orthop Trauma 2006;20:366-71. https://doi.org/10.1097/00005131-200605000-00013.
- Butt MS, Krikler SJ, Ali MS. Displaced fractures of the distal femur in elderly patients. Operative versus non-operative treatment. J Bone Joint Surg Br 1996;78:110-14. https://doi.org/10.1302/0301-620X.78B1.0780110.
- Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am 1994;76:15-2. https://doi.org/10.2106/00004623-199401000-00003.
- Griffin XL, Parsons N, Zbaeda MM, McArthur J. Interventions for treating fractures of the distal femur in adults. Cochrane Database Syst Rev 2015;8. https://doi.org/10.1002/14651858.CD010606.pub2.
- Harma A, Germen B, Karakas HM, Elmali N, Inan M. The comparison of femoral curves and curves of contemporary intramedullary nails. Surg Radiol Anat 2005;27:502-6. https://doi.org/10.1007/s00276-005-0019-2.
- Browner BD, Edwards CC. The Science and Practice of Intramedullary Nailing. Philadelphia, PA: Lea & Febiger; 1987.
- Miller DL, Goswami T, Prayson MJ. Overview of the locking compression plate and its clinical applications in fracture healing. J Surg Orthop Adv 2008;17:271-81.
- Hoskins W, Sheehy R, Edwards ER, Hau RC, Bucknill A, Parsons N, et al. Nails or plates for fracture of the distal femur?. Bone Joint J 2016;98–B:846-50. https://doi.org/10.1302/0301-620X.98B6.36826.
- Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 2005;14:1523-32. https://doi.org/10.1007/s11136-004-7713-0.
- Tornetta P, Egol KA, Ertl JP, Mullis B, Collinge CA, Ostrum RF. Locked Plating Versus Retrograde Nailing for Distal Femur Fractures: A Multicentre Randomized Trial n.d.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Griffin XL, Costa ML, Achten J, Dritsaki M, Baird J, Parsons N. Trial of Acute Femoral Fracture Fixation (TrAFFix): study protocol for a randomised controlled feasibility trial. Trials 2017;18. https://doi.org/10.1186/s13063-017-2265-0.
- Kellam JF, Meinberg EG, Agel J, Karam MD, Roberts CS. Introduction: Fracture and Dislocation Classification Compendium-2018: International Comprehensive Classification of Fractures and Dislocations Committee. J Orthop Trauma 2018;32:1-10. https://doi.org/10.1097/BOT.0000000000001063.
- Dolan MM, Hawkes WG, Zimmerman SI, Morrison RS, Gruber-Baldini AL, Hebel JR, et al. Delirium on hospital admission in aged hip fracture patients: prediction of mortality and 2-year functional outcomes. J Gerontol A Biol Sci Med Sci 2000;55:M527-34. https://doi.org/10.1093/gerona/55.9.M527.
- Griffin XL, Achten J, Parsons N, Costa ML. Platelet-rich therapy in the treatment of patients with hip fractures: a single centre, parallel group, participant-blinded, randomised controlled trial. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-002583.
- Great Britain . Mental Capacity Act 2005 2005.
- Griffin XL, Parsons N, Achten J, Fernandez M, Costa ML. Recovery of health-related quality of life in a United Kingdom hip fracture population. The Warwick Hip Trauma Evaluation – a prospective cohort study. Bone Joint J 2015;97–B:372-82. https://doi.org/10.1302/0301-620X.97B3.35738.
- Parsons N, Griffin XL, Achten J, Costa ML. Outcome assessment after hip fracture: is EQ-5D the answer?. Bone Joint Res 2014;3:69-75. https://doi.org/10.1302/2046-3758.33.2000250.
- Cocks K, Torgerson DJ. Sample size calculations for pilot randomized trials: a confidence interval approach. J Clin Epidemiol 2013;66:197-201. https://doi.org/10.1016/j.jclinepi.2012.09.002.
- Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing 2011;40:423-9. https://doi.org/10.1093/ageing/afr051.
- Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173:489-95. https://doi.org/10.1503/cmaj.050051.
- Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32:705-14. https://doi.org/10.1016/0277-9536(91)90150-B.
- Schwarzer R, Bäßler J, Kwiatek P, Schröder K, Zhang JX. The assessment of optimistic self-beliefs: comparison of the German, Spanish, and Chinese versions of the general self-efficacy scale. Appl Psychol 1997;46:69-88. https://doi.org/10.1111/j.1464-0597.1997.tb01096.x.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. https://doi.org/10.1016/0168-8510(96)00822-6.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Hounsome N, Orrell M, Edwards RT. EQ-5D as a quality of life measure in people with dementia and their carers: evidence and key issues. Value Health 2011;14:390-9. https://doi.org/10.1016/j.jval.2010.08.002.
- Smith SC, Lamping DL, Banerjee S, Harwood RH, Foley B, Smith P, et al. Development of a new measure of health-related quality of life for people with dementia: DEMQOL. Psychol Med 2007;37:737-46. https://doi.org/10.1017/S0033291706009469.
- Mulhern B, Rowen D, Brazier J, Smith S, Romeo R, Tait R, et al. Development of DEMQOL-U and DEMQOL-PROXY-U: generation of preference-based indices from DEMQOL and DEMQOL-PROXY for use in economic evaluation. Health Technol Assess 2013;17. https://doi.org/10.3310/hta17050.
- Salén BA, Spangfort EV, Nygren AL, Nordemar R. The Disability Rating Index: an instrument for the assessment of disability in clinical settings. J Clin Epidemiol 1994;47:1423-35. https://doi.org/10.1016/0895-4356(94)90086-8.
- Parsons H, Bruce J, Achten J, Costa ML, Parsons NR. Measurement properties of the Disability Rating Index in patients undergoing hip replacement. Rheumatology 2015;54:64-71. https://doi.org/10.1093/rheumatology/keu293.
- Lecky F. Twenty-five years of the trauma audit and research network: a continuing evolution to drive improvement. Emerg Med J 2015;32:906-8. https://doi.org/10.1136/emermed-2015-205460.
- NHS Digital . NHS Hospital and Community Health Service (HCHS) Workforce Statistics in England, Summary of Staff in the NHS 2003–2013 2014.
- NHS Digital . Hospital Admitted Patient Care Activity 2017.
- NHS . The NHS Quarterly Bed Availability.
- NHS . Supporting Facilities Dataset.
- Keene DJ, Mistry D, Nam J, Tutton E, Handley R, Morgan L, et al. The Ankle Injury Management (AIM) trial: a pragmatic, multicentre, equivalence randomised controlled trial and economic evaluation comparing close contact casting with open surgical reduction and internal fixation in the treatment of unstable ankle fractures in patients aged over 60 years. Health Technol Assess 2016;20. https://doi.org/10.3310/hta20750.
- Achten J, Parsons NR, Bruce J, Petrou S, Tutton E, Willett K, et al. Protocol for a randomised controlled trial of standard wound management versus negative pressure wound therapy in the treatment of adult patients with an open fracture of the lower limb: UK Wound management of Lower Limb Fractures (UK WOLLF). BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009087.
- Taylor SJ, Bogdan R. Introduction to Qualitative Research Methods: The Search for Meanings. Hoboken, NJ: John Wiley & Sons Inc.; 1984.
- Griffin XL, Costa ML, Phelps E, Parsons N, Dritsaki M, Achten J, et al. Intramedullary nails versus distal locking plates for fracture of the distal femur: results from the Trial of Acute Femoral Fracture Fixation (TrAFFix) randomised feasibility study and process evaluation. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-026810.
- Damocles Study Group . A proposed charter for clinical trial data monitoring committees: helping them to do their job well. Lancet 2005;365:711-22. https://doi.org/10.1016/S0140-6736(05)70939-9.
- WK Kellogg Foundation . Logic Model Development Guide 2004.
- Royal College of Physicians (RCP) . National Hip Fracture Database Annual Report 2016 2016.
- Costa ML, Griffin XL, Achten J, Metcalfe D, Judge A, Pinedo-Villanueva R, et al. World Hip Trauma Evaluation (WHiTE): framework for embedded comprehensive cohort studies. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011679.
- Lidz CW, Appelbaum PS. The therapeutic misconception: problems and solutions. Med Care 2002;40:V55-63. https://doi.org/10.1097/01.MLR.0000023956.25813.18.
- Phelps EE, Tutton E, Griffin X, Baird J. TrAFFix study co-applicants . Facilitating trial recruitment: a qualitative study of patient and staff experiences of an orthopaedic trauma trial. Trials 2019;20. https://doi.org/10.1186/s13063-019-3597-8.
- Griffin XL, Achten J, Sones W, Cook J, Costa ML. Randomised controlled trial of the sliding hip screw versus X-Bolt Dynamic Hip Plating System for the fixation of trochanteric fractures of the hip in adults: a protocol study for WHiTE 4 (WHiTE4). BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019944.
- International Standard Randomised Controlled Trial Number Registry . World Hip Trauma Evaluation Five: A Randomised Controlled Trial Comparing Cemented and Uncemented Implants for the Treatment of Displaced Intracapsular Hip Fractures n.d. https://doi.org/10.1186/ISRCTN18393176 (accessed 25 October 2018).
- Masters JPM, Achten J, Cook J, Dritsaki M, Sansom L, Costa ML. Randomised controlled feasibility trial of standard wound management versus negative-pressure wound therapy in the treatment of adult patients having surgical incisions for hip fractures. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020632.
- Achten J, Vadher K, Bruce J, Nanchahal J, Spoors L, Masters JP, et al. Standard wound management versus negative-pressure wound therapy in the treatment of adult patients having surgical incisions for major trauma to the lower limb – a two-arm parallel group superiority randomised controlled trial: protocol for Wound Healing in Surgery for Trauma (WHIST). BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-022115.
- National Institute for Health and Care Excellence (NICE) . Fractures (Non-complex): Assessment and Management 2016.
- Lincoln YS, Guba E. Naturalistic Inquiry. Newbury Park, CA: Sage Publications Inc; 1985.
- Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 2013;8. https://doi.org/10.1007/s11657-013-0136-1.
- Leal J, Gray AM, Prieto-Alhambra D, Arden NK, Cooper C, Javaid MK, et al. REFReSH study group . Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int 2016;27:549-58. https://doi.org/10.1007/s00198-015-3277-9.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013.
- Curtis L, Burns A. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2016.
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2015 to 2016 2016.
- National Health Service . NHS Supply Chain Catalogue n.d. https://my.supplychain.nhs.uk/catalogue (accessed March 2018).
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Curtis L. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2014.
- Curtis L, Burns A. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2017.
- North Yorkshire County Council . Paying for Care at Home n.d. https://www.northyorks.gov.uk/paying-care-home (accessed March 2018).
- Independent People Homecare Services . The Cost of Live in Care n.d. https://www.ip-live-in-care.co.uk/care-costs/live-in-care-costs/ (accessed Mar 2018).
- Office for National Statistics (ONS) . Annual Survey of Hours and Earnings: 2017 Provisional and 2016 Revised Results 2017.
- Curtis L. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2014.
- World Health Organization Collaborating Centre for Drug Statistics Methodology . ATC/DDD/Index/2018 n.d. www.whocc.no/atc_ddd_index/ (accessed March 2018).
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2017.
- Costa ML, Achten J, Griffin J, Petrou S, Pallister I, Lamb SE, et al. FixDT Trial Investigators . Effect of Locking plate fixation vs intramedullary nail fixation on 6-month disability among adults with displaced fracture of the distal tibia: the UK FixDT Randomized Clinical Trial. JAMA 2017;318:1767-76. https://doi.org/10.1001/jama.2017.16429.
- Costa ML, Achten J, Hennings S, Boota N, Griffin J, Petrou S, et al. Intramedullary nail fixation versus locking plate fixation for adults with a fracture of the distal tibia: the UK FixDT RCT. Health Technol Assess 2018;22. https://doi.org/10.3310/hta22250.
- Sims AL, Parsons N, Achten J, Griffin XL, Costa ML, Reed MR. The world hip trauma evaluation study 3: hemiarthroplasty evaluation by multicentre investigation – WHITE 3: HEMI – an abridged protocol. Bone Joint Res 2016;5:18-25. https://doi.org/10.1302/2046-3758.51.2000473.
- Costa ML, Jameson SS, Reed MR. Do large pragmatic randomised trials change clinical practice?: assessing the impact of the Distal Radius Acute Fracture Fixation Trial (DRAFFT). Bone Joint J 2016;98–B:410-13. https://doi.org/10.1302/0301-620X.98B3.36730.
Appendix 1 Interview guide
Appendix 2 Surgeon questionnaire
Consultant trauma and orthopaedic surgeons were asked to answer the following six multiple-choice questions.
-
How long have you been a consultant trauma and orthopaedic surgeon?
-
Would you define yourself as a specialist trauma surgeon?
-
Do you work in a major trauma centre, trauma unit or other institution?
-
How many trauma lists do you routinely supervise per calendar month?
-
How many distal femoral fractures do you personally operate on per year?
-
Do you have a preference for operative fixation of most distal femoral fractures?
Appendix 3 Screening and recruitment by site
FIGURE 7.
Flow chart of screening and recruitment, by site. LDS, Leeds Teaching Hospitals; LEI, University Hospitals Leicester; NUH, Nottingham University Hospitals; POR, Portsmouth Hospitals; RAD, Oxford University Hospitals; RBK, Royal Berkshire Hospital; STO, Royal Stoke University Hospital.
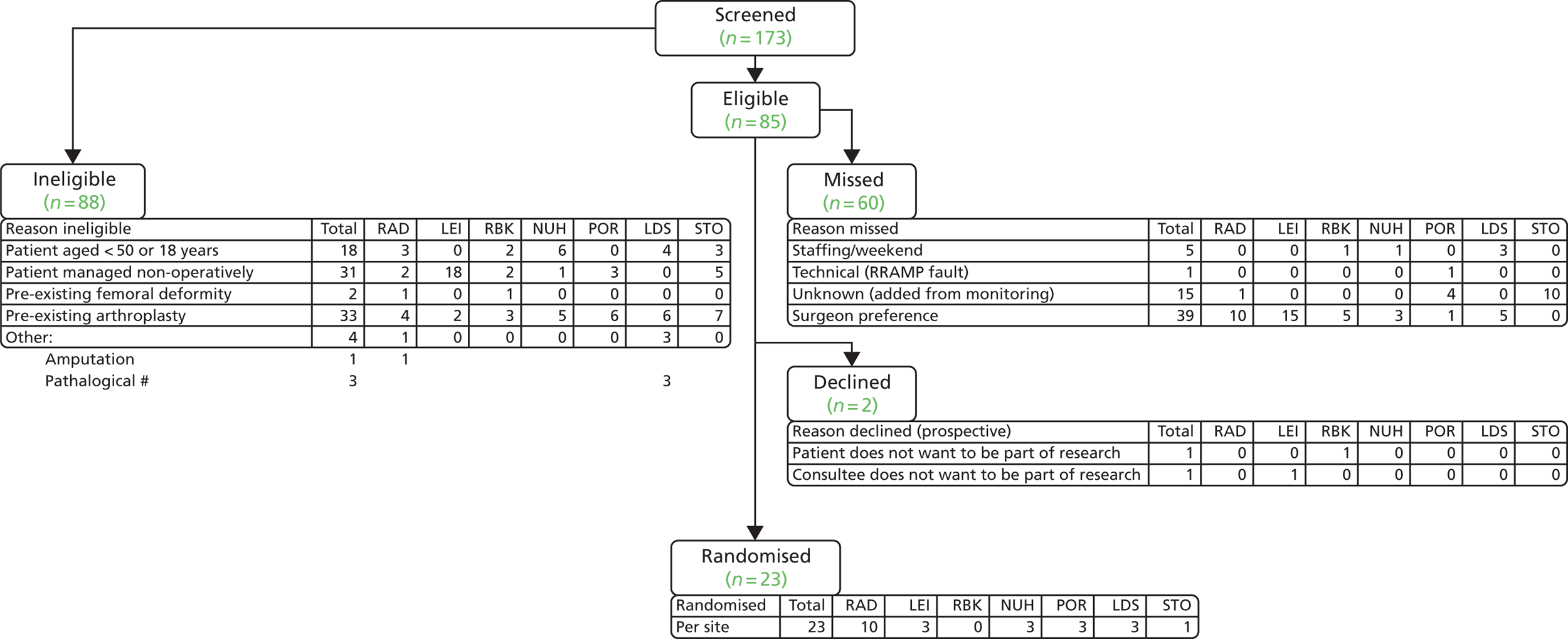
Appendix 4 Breakdown of self-efficacy questionnaire by group
| Self-efficacy (self-reporting) | Intervention group, n (%) | |
|---|---|---|
| Nail (N = 11) | Plate (N = 12) | |
| Solve problems | ||
| Strongly agree | 2 (18.2) | 2 (16.7) |
| Agree | 6 (54.5) | 3 (25) |
| Disagree | 1 (9.1) | 3 (25) |
| Strongly disagree | 0 (0) | 1 (8.3) |
| Own way | ||
| Strongly agree | 3 (27.3) | 4 (33.3) |
| Agree | 2 (18.2) | 1 (8.3) |
| Disagree | 3 (27.3) | 2 (16.7) |
| Strongly disagree | 1 (9.1) | 2 (16.7) |
| Stick aims | ||
| Strongly agree | 2 (18.2) | 1 (8.3) |
| Agree | 2 (18.2) | 4 (33.3) |
| Disagree | 5 (45.5) | 2 (16.7) |
| Strongly disagree | 0 (0) | 2 (16.7) |
| Calm difficulty | ||
| Strongly agree | 2 (18.2) | 0 (0) |
| Agree | 1 (9.1) | 6 (50) |
| Disagree | 3 (27.3) | 3 (25) |
| Strongly disagree | 3 (27.3) | 0 (0) |
| Trouble solving | ||
| Strongly agree | 2 (18.2) | 3 (25) |
| Agree | 2 (18.2) | 4 (33.3) |
| Disagree | 4 (36.4) | 1 (8.3) |
| Strongly disagree | 1 (9.1) | 1 (8.3) |
| Preinjury walking speed | ||
| Fast | 0 (0) | 0 (0) |
| Fairly brisk | 1 (9.1) | 0 (0) |
| Normal speed | 1 (9.1) | 0 (0) |
| Stroll at an easy pace | 3 (27.3) | 3 (25) |
| Very slow | 4 (36.4) | 6 (50) |
| Confined bed | ||
| None of the time | 0 (0) | 0 (0) |
| A little of the time | 0 (0) | 0 (0) |
| Some of the time | 2 (18.2) | 4 (33.3) |
| Most of the time | 4 (36.4) | 2 (16.7) |
| All of the time | 3 (27.3) | 3 (25) |
| Listen talk | ||
| None of the time | 0 (0) | 0 (0) |
| A little of the time | 1 (9.1) | 1 (8.3) |
| Some of the time | 1 (9.1) | 1 (8.3) |
| Most of the time | 3 (27.3) | 2 (16.7) |
| All of the time | 4 (36.4) | 5 (41.7) |
| Advice crisis | ||
| None of the time | 1 (9.1) | 0 (0) |
| A little of the time | 0 (0) | 0 (0) |
| Some of the time | 3 (27.3) | 1 (8.3) |
| Most of the time | 3 (27.3) | 2 (16.7) |
| All of the time | 2 (18.2) | 6 (50) |
| Take doctor | ||
| None of the time | 0 (0) | 0 (0) |
| A little of the time | 0 (0) | 0 (0) |
| Some of the time | 2 (18.2) | 0 (0) |
| Most of the time | 2 (18.2) | 3 (25) |
| All of the time | 5 (45.5) | 6 (50) |
| Love affection | ||
| None of the time | 0 (0) | 0 (0) |
| A little of the time | 0 (0) | 0 (0) |
| Some of the time | 2 (18.2) | 1 (8.3) |
| Most of the time | 2 (18.2) | 0 (0) |
| All of the time | 5 (45.5) | 8 (66.7) |
| Good time | ||
| None of the time | 1 (9.1) | 1 (8.3) |
| A little of the time | 1 (9.1) | 0 (0) |
| Some of the time | 1 (9.1) | 2 (16.7) |
| Most of the time | 3 (27.3) | 1 (8.3) |
| All of the time | 3 (27.3) | 5 (41.7) |
| Information | ||
| None of the time | 1 (9.1) | 0 (0) |
| A little of the time | 0 (0) | 0 (0) |
| Some of the time | 0 (0) | 0 (0) |
| Most of the time | 5 (45.5) | 2 (16.7) |
| All of the time | 3 (27.3) | 7 (58.3) |
| Confide in | ||
| None of the time | 0 (0) | 0 (0) |
| A little of the time | 0 (0) | 0 (0) |
| Some of the time | 2 (18.2) | 0 (0) |
| Most of the time | 3 (27.3) | 2 (16.7) |
| All of the time | 4 (36.4) | 7 (58.3) |
| Hugs you | ||
| None of the time | 0 (0) | 1 (8.3) |
| A little of the time | 1 (9.1) | 0 (0) |
| Some of the time | 1 (9.1) | 1 (8.3) |
| Most of the time | 4 (36.4) | 2 (16.7) |
| All of the time | 3 (27.3) | 5 (41.7) |
| Relaxation | ||
| None of the time | 1 (9.1) | 1 (8.3) |
| A little of the time | 0 (0) | 0 (0) |
| Some of the time | 2 (18.2) | 1 (8.3) |
| Most of the time | 4 (36.4) | 4 (33.3) |
| All of the time | 2 (18.2) | 3 (25) |
| Prepare meals | ||
| None of the time | 0 (0) | 0 (0) |
| A little of the time | 0 (0) | 1 (8.3) |
| Some of the time | 2 (18.2) | 1 (8.3) |
| Most of the time | 1 (9.1) | 1 (8.3) |
| All of the time | 6 (54.5) | 6 (50) |
| Valued advice | ||
| None of the time | 1 (9.1) | 0 (0) |
| A little of the time | 0 (0) | 0 (0) |
| Some of the time | 2 (18.2) | 2 (16.7) |
| Most of the time | 3 (27.3) | 2 (16.7) |
| All of the time | 3 (27.3) | 5 (41.7) |
| Help distract | ||
| None of the time | 0 (0) | 0 (0) |
| A little of the time | 1 (9.1) | 1 (8.3) |
| Some of the time | 1 (9.1) | 1 (8.3) |
| Most of the time | 4 (36.4) | 2 (16.7) |
| All of the time | 3 (27.3) | 5 (41.7) |
| Daily chores | ||
| None of the time | 0 (0) | 1 (8.3) |
| A little of the time | 0 (0) | 0 (0) |
| Some of the time | 3 (27.3) | 0 (0) |
| Most of the time | 2 (18.2) | 2 (16.7) |
| All of the time | 4 (36.4) | 6 (50) |
| Share private | ||
| None of the time | 0 (0) | 0 (0) |
| A little of the time | 1 (9.1) | 0 (0) |
| Some of the time | 0 (0) | 1 (8.3) |
| Most of the time | 4 (36.4) | 2 (16.7) |
| All of the time | 4 (36.4) | 6 (50) |
| Personal problems | ||
| None of the time | 1 (9.1) | 0 (0) |
| A little of the time | 1 (9.1) | 2 (16.7) |
| Some of the time | 1 (9.1) | 0 (0) |
| Most of the time | 2 (18.2) | 2 (16.7) |
| All of the time | 4 (36.4) | 5 (41.7) |
| Enjoyable | ||
| None of the time | 1 (9.1) | 0 (0) |
| A little of the time | 0 (0) | 2 (16.7) |
| Some of the time | 2 (18.2) | 1 (8.3) |
| Most of the time | 1 (9.1) | 1 (8.3) |
| All of the time | 5 (45.5) | 5 (41.7) |
| Understand problems | ||
| None of the time | 1 (9.1) | 0 (0) |
| A little of the time | 0 (0) | 1 (8.3) |
| Some of the time | 1 (9.1) | 0 (0) |
| Most of the time | 4 (36.4) | 1 (8.3) |
| All of the time | 3 (27.3) | 7 (58.3) |
| Love feel wanted | ||
| None of the time | 0 (0) | 1 (8.3) |
| A little of the time | 1 (9.1) | 0 (0) |
| Some of the time | 1 (9.1) | 0 (0) |
| Most of the time | 3 (27.3) | 1 (8.3) |
| All of the time | 4 (36.4) | 7 (58.3) |
Appendix 5 Statistical analysis plan
Appendix 6 Health economics analysis plan
List of abbreviations
- AE
- adverse event
- AO
- Arbeitsgemeinschaft für Osteosynthesefragen
- CI
- confidence interval
- CRF
- clinical reporting form
- CT
- computed tomography
- DEMQoL
- Dementia Quality of Life Measure
- DRI
- Disability Rating Index
- DSMC
- Data Safety Monitoring Committee
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GP
- general practitioner
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- ID
- identifier
- ITT
- intention to treat
- MRC
- Medical Research Council
- NDORMS
- Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OCTRU
- Oxford Clinical Trials Research Unit
- OTA
- Orthopaedic Trauma Association
- PI
- principal investigator
- PPI
- patient and public involvement
- PSSRU
- Personal Social Services Research Unit
- RA
- research associate
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- SAE
- serious adverse event
- SAS
- staff associate specialist
- SD
- standard deviation
- TARN
- Trauma Audit and Research Network
- TrAFFix
- Trial of Acute Femoral Fracture Fixation
- TSC
- Trial Steering Committee
- WHiTE
- World Hip Trauma Evaluation
- WHO
- World Health Organization
