Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/94/01. The contractual start date was in June 2013. The draft report began editorial review in December 2017 and was accepted for publication in April 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Ira Madan reports being the chairperson of the National Institute for Health Research (NIHR)’s Health Technology Assessment (HTA) Mental Health panel from 1 January 2018 to December 2020. Vaughan Parsons reports personal fees from the magazine Occupational Health at Work during the conduct of the trial. Alison Wright reports other grants from the NIHR HTA programme during the conduct of the study. Julia Smedley reports other grants from NIHR via Guy’s and St Thomas’ NHS Foundation Trust (lead centre) during the conduct of the study (HTA reference number 15/107/02). Hywel Williams is Director of the HTA programme and chairperson of the HTA Commissioning Board. From 1 January 2016, he became Programme Director for the HTA programme.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Madan et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Parts of this chapter have been adapted from Madan et al. 1 This is an open-access article distributed under the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Scientific background
Irritant hand dermatitis is an important occupational disease in health professionals. A study in Sweden found the 1-year prevalence of self-reported hand dermatitis among 9051 health-care workers to be 21%,2 slightly lower than the 24% found among health-care workers in an earlier study in the Netherlands. This compares to < 10% in the general population. 3 Past history of atopy (childhood or adult eczema, asthma or allergic rhinitis), female sex and occupational exposure are well recognised as predictive risk factors for future hand dermatitis,4,5 with studies showing that history of atopy can also negatively affect the prognosis of hand dermatitis in later life. 6,7
Among health professionals, nurses are the group at highest risk of hand dermatitis, with an estimated point prevalence of 12–30%;8–10 this is often attributed to frequent exposure to wet work, including hand-washing. 11 Moreover, in a study of German geriatric nurses, two-thirds of those who reported hand dermatitis stated that it had developed after they had joined the profession. 8 Consistent with this, among Korean nursing students, the prevalence of self-reported hand dermatitis increased from 7% in the first year to 23% in the fourth year of training. 12 The costs of hand dermatitis to the individual and employer are high. It not only affects quality of life, but also can lead to loss of employment. 13,14 Once an individual has developed irritant hand dermatitis, the prognosis is poor. In a 15-year follow-up study of a Swedish general population sample, about one-third of those people with hand dermatitis needed ongoing medical treatment and 5% experienced long periods of sickness absence, loss or change of job, or retirement due to ill health. 6 Affected individuals may also experience negative psychosocial consequences, such as sleep disturbance and interference with leisure activities,6 as well as economic implications. 15 Recent evidence from the UK suggests that, although the incidence of allergic contact dermatitis is decreasing, probably because of an improvement in working practices, the incidence of irritant contact dermatitis remains unchanged. 16
Health-care settings are known to expose health-care workers to a variety of irritants that can cause and exacerbate skin abnormalities. Current hand-cleansing improvement policies in the NHS are driven by efforts to reduce colonisation and transmission of infections, and the emphasis is on frequent use of hand rubs before and after patient contact, and washing with soap and water if the hands are visibly soiled or potentially contaminated with bodily fluids. 17 However, to date, little attention has been paid to the prevention of hand dermatitis.
For a nurse who develops irritant hand dermatitis, the condition is likely to be aggravated by exposure to recommended hand-hygiene measures. The presence of hand dermatitis may discourage nurses from undertaking adequate hand decontamination because of discomfort or concern about exacerbating skin lesions. It is known that 50% of people with hand dermatitis are colonised with Staphylococcus aureus18 and, accordingly, there is a risk that nurses with hand dermatitis infected with S. aureus or indeed antimicrobial-resistant strains, such as those resistant to meticillin [i.e. meticillin-resistant Staphylococcus aureus (MRSA)], could transmit these organisms and cause infections in patients. 19 Occupational health-care workers often have to advise nurses with active dermatitis to refrain from working in clinical areas until the lesions are healed, as it is difficult for them to avoid frequent hand-washing unless they are redeployed to a non-clinical area. This workplace adjustment may become temporary or permanent.
Existing literature and interventional studies
Several studies on the primary and secondary prevention of hand dermatitis have been conducted in the last decade, with variable success, as detailed in the following section.
Moisturisers
Two systematic reviews of the management of occupational dermatitis20,21 have concluded that moisturisers contributed importantly to both prevention and treatment of hand dermatitis at work. The review commissioned by NHS Plus focused on the evidence for managing established occupational dermatitis and found a small body of consistent evidence that hand moisturisers used before and during work improved skin condition in health-care workers with damaged skin,22,23 and concluded that there was sufficient evidence to recommend that skin-care programmes should include the use of hand moisturisers. 24,25
Guidelines produced by the British Occupational Health Research Foundation21 recommended the regular application of emollients to help prevent the development of occupational dermatitis, citing three high-quality studies: a systematic review26 and two randomised controlled trials (RCT). 27,28 One RCT found an improvement in all outcomes, including visible dermatitis. In the other RCT, transepidermal water loss improved among construction workers who used pre- and after-work creams compared with controls, but there was no difference in the workers’ clinically assessed skin condition. 28 Moisturisers also improved skin condition in health-care workers with damaged skin. 29 More recent reviews, including a Cochrane review,30 concluded that there is some evidence to support the use of educational interventions that include moisturisers to prevent occupational hand dermatitis, but, as the evidence came from only a small number of studies, the authors strongly recommended that larger high-quality RCTs in different occupational groups were needed. 30,31 Following these recommendations, Soltanipoor et al. 11 conducted a RCT in the Netherlands that examined the effectiveness of an educational programme together with the provision of moisturisers in dispensers. The dispensers were fitted with electronic usage monitors, allowing the researchers to give feedback to the participants on their moisturiser use. The effectiveness of the intervention was measured from the assessment of skin conditions in participants before and after the interventions. The study found higher levels of self-reported use of hand moisturising cream among nurses before and during shifts in the intervention group than in the control group. However, the self-reported prevalence of hand dermatitis was similar in both study groups at follow-up. Notwithstanding, evidence from the study suggests that electronic tracking of hand cream usage coupled with feedback has a positive impact on skin-care behaviour among health-care workers.
In the experience of the dermatologists and occupational health physicians in this research team, moisturisers are not widely used by health-care workers in the UK. This anecdotal observation is supported by a study of nurses working in intensive care units (ICUs) in Germany that found that only 15% of the 204 respondents reported that they applied moisturising creams after hand-washing and only 2% after skin disinfection with hand rubs. Furthermore, 9% of respondents never applied skin care to their hands and 72% reported that they did not perform final skin care after the last hand wash of the day. 32
Hand cleansing
The use of antibacterial (alcohol-based) hand rubs, with the addition of moisturisers for hand hygiene, reduces the drying and cracking of the skin that commonly results from repeated hand cleansing with soap and water. 33,34 This has the added benefit of also reducing rates of some health-care-associated infections, such as S. aureus bacteraemia and Clostridium difficile infections. 35 Moreover, antibacterial hand rubs have been associated with increased hand-hygiene compliance and reduced rates of nosocomial infection. 17,36 Although the benefits of using antibacterial hand rubs as a safe and effective dermatitis prevention strategy have now been established,2 a notable difficulty faced by occupational health-care workers and dermatologists is to challenge the misconceptions among nurses that antibacterial hand rubs are more damaging to the skin integrity than hand-washing and, therefore, more likely to cause hand dermatitis. 37 There is a misconception among some health-care workers that alcohol-based hand rubs are more irritating and drying than cleaning hands using soap and water; therefore, they are less likely to use them. 38 Accordingly, Stutz et al. 37 argue that hand-hygiene education and training should focus on promoting the use of antibacterial hand rubs as an effective protective behaviour for reducing the prevalence of hand dermatitis in nurses. The implementation of the World Health Organization (WHO)’s guidelines among physicians working in Ireland, which promoted the use of alcohol-based hand rubs by senior management and infection control teams, had a positive impact on changing attitudes and practices towards the use of hand rubs without damaging the epidermis. 39
Hand drying and glove use
The appropriate use of gloves during clinical work and proper drying of the hands after washing is pivotal to good hand hygiene and care, particularly as wet skin is more likely than dry skin to facilitate the transmission of bacteria. A recent review of hand-drying processes,40 which included 12 studies, concluded that paper towels are superior to electric air dryers in drying hands in clinical environments. The ensuing recommendation that paper towels should be used for hand drying in clinical environments, where hand hygiene is vital, was supported by The Royal College of Physicians20 and WHO. 17
Effectiveness of skin-care programmes
Various skin-care programmes that incorporated the provision of hand moisturisers, hand rubs and paper towels have shown a beneficial effect in the prevention of hand dermatitis in health-care workers. 22,23,41–44 However, as John and Kezic45 pointed out, although effective preventative strategies are available, these are often limited by poor understanding of the causes of occupational skin diseases among at-risk workers. Furthermore, others have argued the need to reconsider what is deemed acceptable levels of hand-hygiene compliance, as, for example, a 70% hand-hygiene compliance rate among health-care workers is as effective at reducing infections as 90% compliance. 46
Educational programmes (individual or part of hand health programmes)
Previous studies examining the effectiveness of educational programmes designed to influence and encourage optimal hand-care behaviours among health-care workers22 including ICU nurses47 have yielded only moderately promising results. However, Ibler et al. 43 found that an educational programme coupled with individual counselling focusing on good hand dermatitis prevention behaviours had a positive impact on the secondary prevention of hand dermatitis. The intervention reduced the frequency with which participants washed their hands and increased the frequency of their use of protective gloves during wet work, when compared with their usual treatment. However, this intervention was delivered on a one-to-one basis and so might be difficult to scale up across the health service.
A recent systematic review suggested that educational programmes could benefit from being more strongly informed by psychological theories of behaviour, as programme success relies on employees adopting appropriate preventative and protective behaviours. 31 Furthermore, other studies have also investigated interventions specifically designed to facilitate behaviour change, with an emphasis on improving hand care among health professionals. The Hands4U RCT trial in the Netherlands examined a multifaceted intervention that comprised (1) a leaflet containing evidence-based hand dermatitis prevention recommendations, (2) a participatory working group to explore facilitators of and barriers to adopting recommendations, (3) provision of trained role models (dermacoaches) to encourage and model good hand dermatitis prevention behaviours at a departmental level and (4) provision of education and training to promulgate preventative measures in the workplace. 44 The main outcome measures assessed were self-reported hand dermatitis and adoption of preventative behaviours over a 12-month period. The study found that health-care workers in the intervention group were significantly more likely to engage in positive preventative behaviours to protect themselves from hand dermatitis. That is, the health-care workers reported significantly less hand-washing and more frequent use of hand moisturisers and wearing of cotton under gloves than colleagues in the control arm. However, the intervention group reported a higher prevalence of hand dermatitis than the control group at 12 months. This may have been due to an increased awareness of hand dermatitis as a consequence of the intervention. A notable limitation of this study was the use of self-reported measures to assess hand dermatitis, as opposed to more objective measures. Moreover, no cost-effectiveness analysis of the intervention was undertaken. A prominent observation with many skin-protection programmes is that sustained compliance among at-risk workers is poor and so programmes that promote sustained behaviour change are required. 48
Although there are good reasons to expect that well-designed skin-care programmes would be beneficial for nurses, their clinical effectiveness and cost-effectiveness remain uncertain. Trials to date have been limited by size and the possibility that the control group was aware of the intervention,44 or by a failure to address cost-effectiveness. 49 Furthermore, trials have been hampered by lack of sustainability of behaviour change. Psychological theory suggests that knowledge transfer coupled with a behaviour change programme would be effective in changing the beliefs and behaviours of at-risk nurses in relation to hand care and, if accompanied by provision of hand moisturisers, would lead to a reduction in the prevalence of hand dermatitis.
The use of psychological theory to improve hand hygiene and hand care
Hand dermatitis prevention requires the adoption and maintenance of several protective behaviours. Changing behaviour requires an understanding of its determinants. Interventions to prevent hand dermatitis have not always drawn sufficiently on psychological theories of behaviours. 31 Psychological theory has, however, proved useful in understanding the behavioural determinants of hand hygiene among health-care workers. 17,50–52 Several trials have employed behavioural theoretical frameworks to modify and improve hand-hygiene behaviours among health-care workers,51,53 including one study of critical care nurses that used the theory of planned behaviour (TPB) as a theoretical framework. 54 Moreover, a meta-analysis of internet-based behaviour change interventions found that interventions that focused more on behaviour were more effective,55 suggesting that theories may help interventions better target key influences on the behaviour they wish to change. In contrast, hand dermatitis prevention interventions have often focused only on improving nurses’ knowledge of the condition. Larger effects on behaviour, and so on hand dermatitis prevention, might be achieved if a broader range of the psychological determinants of behaviour were targeted. One of the few studies applying psychological theory to occupational hand dermatitis examined the ability of the TPB to predict the behaviour of a sample of German patients with occupational hand dermatitis receiving an inpatient tertiary prevention programme. 56 The TPB57 suggests that behaviour is directly influenced by intentions (motivation, in the form of a conscious plan or decision to try to perform the behaviour) and perceived behavioural control (the individual’s belief concerning how easy or difficult performing the behaviour will be). Moreover, intentions are influenced by three constructs: attitudes (the degree to which the person has a favourable or unfavourable evaluation of the behaviour), subjective norms (beliefs about whether important others want one to perform the behaviour) and perceived behavioural control. In the study of German patients with occupational dermatitis, the TPB variables explained 30% of the variance in post-intervention dermatitis prevention behaviour and 38% of the variance in intentions for preventative behaviours. 56 Therefore, an intervention targeting attitudes, subjective norms and perceived behavioural control over hand dermatitis prevention behaviours may lead to risk-reducing behaviour change and reduced prevalence of hand dermatitis. Systematic review evidence suggests that the TPB may perform somewhat better at predicting intentions than behaviour. 58 One particular issue is ‘inclined abstainers’, individuals with positive intentions who subsequently fail to act in line with those intentions. 59 However, systematic review evidence shows that forming implementation intentions and specific plans about how, when and where health-promoting behaviours will be performed increases the likelihood of individuals acting on their positive intentions. Furthermore, evidence suggests that reminding individuals of their implementation intentions can facilitate longer-term behaviour change. 60,61 Therefore, adding an implementation intentions component to a dermatitis prevention behaviour change intervention may promote greater protective behaviour change.
Approaches to diagnosing hand dermatitis and use of photographic methods as a diagnostic tool
Various techniques have been used to diagnose hand dermatitis in dermatological research. Some studies have relied on visual inspections of hands by clinicians, whereas others have based diagnoses on information collected about symptoms from questionnaires or used self-diagnosis by participants. 37,62,63 The merits of these different techniques, in terms of sensitivity and specificity, were evaluated by Smit et al. 62 Smit et al. 62 found a prevalence of hand dermatitis of 18% based on visual examination, 19% based on self-diagnosis and 48% by symptom-based diagnosis. The study also found varying degrees of overestimation regarding disease prevalence, namely that, although there was 100% sensitivity in the symptom-based questionnaire, the specificity was found to be low, at 64%, whereas the sensitivity of the self-diagnosis questionnaire was found to be lower (65%), with a higher degree of specificity (93%).
Teledermatology (a method of assessing and diagnosing skin conditions from photographic images) is a validated procedure, which yields results similar to those from face-to-face consultations64–67 and can be used by patients to self-assess their own hand dermatitis severity. 65,68 Researchers have found that face-to-face (‘live’) diagnoses by specialist dermatologists were in agreement with retrospective diagnoses by resident dermatologists based on digital photographs in 22 of the 29 cases (76% of the time). 65 Furthermore, the ‘live’ diagnoses by the specialist dermatologists agreed with the definitive diagnoses (by biopsy) in 73% of occasions. Interpretation of digital photographs is sufficiently sensitive to detect early signs of dermatitis. 66 Teledermatology has been shown to have high intra- and inter-rater reliability when compared with face-to-face assessment in NHS ICU nurses and nursery nurses,64 with a slight tendency to overestimate the prevalence of hand dermatitis. 64,66 Teledermatology based on images from a mobile phone camera has been shown to have > 70% diagnostic agreement with face-to-face assessments by dermatologists. 69,70 Furthermore, Shin et al. 70 found that images taken on mobile phones for diagnosing dermatitis had a sensitivity of 78% [standard deviation (SD) 0%] and a specificity of 93.1% (SD 5.2%). 70
Rationale for research
Hand dermatitis in nurses is an important clinical and occupational issue in the NHS: treatment is costly, and hand dermatitis affects service delivery. It may increase in importance in the future given that hand-hygiene measures will continue to be rigorously enforced in health care. At the same time, retention of highly trained nurses in the workforce is likely to become increasingly important as fewer people are being trained to become nurses. Given the current economic climate, it is vital that new interventions implemented in the NHS are both clinically effective and cost-effective. As there was genuine equipoise about the suggested intervention, the study assembled a multidisciplinary team to deliver a high-quality study to test whether or not an intervention based on the TPB and implementation intentions could lead to enhanced hand-care behaviours and reduce the incidence of hand dermatitis in the NHS. We chose to employ a cluster RCT design to avoid contamination during the study as we recognised the potential problems that would occur if individual nurses at each site were randomised to either the intervention plus or the intervention light arm.
Objectives
-
The study tested the hypothesis that a bespoke, web-based behaviour change intervention to improve hand care, together with provision of hand moisturisers, could produce a clinically useful reduction in the prevalence of hand dermatitis after 1 year, when compared with standard care, among nurses working in the NHS who are particularly at risk.
-
Secondary aims were to assess impacts on participants’ beliefs and behaviour regarding hand care, days off sick over a 1-year follow-up period and use of hand moisturisers.
-
In addition, the study assessed the cost-effectiveness of the intervention compared with normal care.
Chapter 2 Trial design and methods
Parts of this chapter have been adapted from Madan et al. 1 This is an open-access article distributed under the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Design overview
The study used a cluster RCT design, with sites as the unit of randomisation. This was a pragmatic multicentre study in which participating sites were randomly allocated to the ‘intervention light’ or ‘intervention plus’ arm. See Madan et al. 1 for a full description of the trial protocol. Participants were newly recruited student nurses and ICU or special-care baby unit (SCBU) nurses.
Inclusion criteria
Included individuals were:
-
student nurses who –
-
were first-year student nurses, and
-
had a history of atopic tendency (i.e. had ever had, or received treatment for, asthma, hay fever, eczema anywhere on the body or dermatitis of the hands)
-
-
ICU nurses (including SCBU nurses) who –
-
worked on ICUs (or SCBUs)
-
worked full-time (i.e. ≥ 30 hours per week)
-
had no extended periods of leave of > 3 months in the following 12 months.
-
Exclusion criteria
The study excluded individuals who:
-
were first-year mental health student nurses
-
were ICU nurses (or SCBU nurses) working on a part-time basis (i.e. < 30 hours per week), or
-
had extended periods of leave of > 3 months planned in the following 12 months.
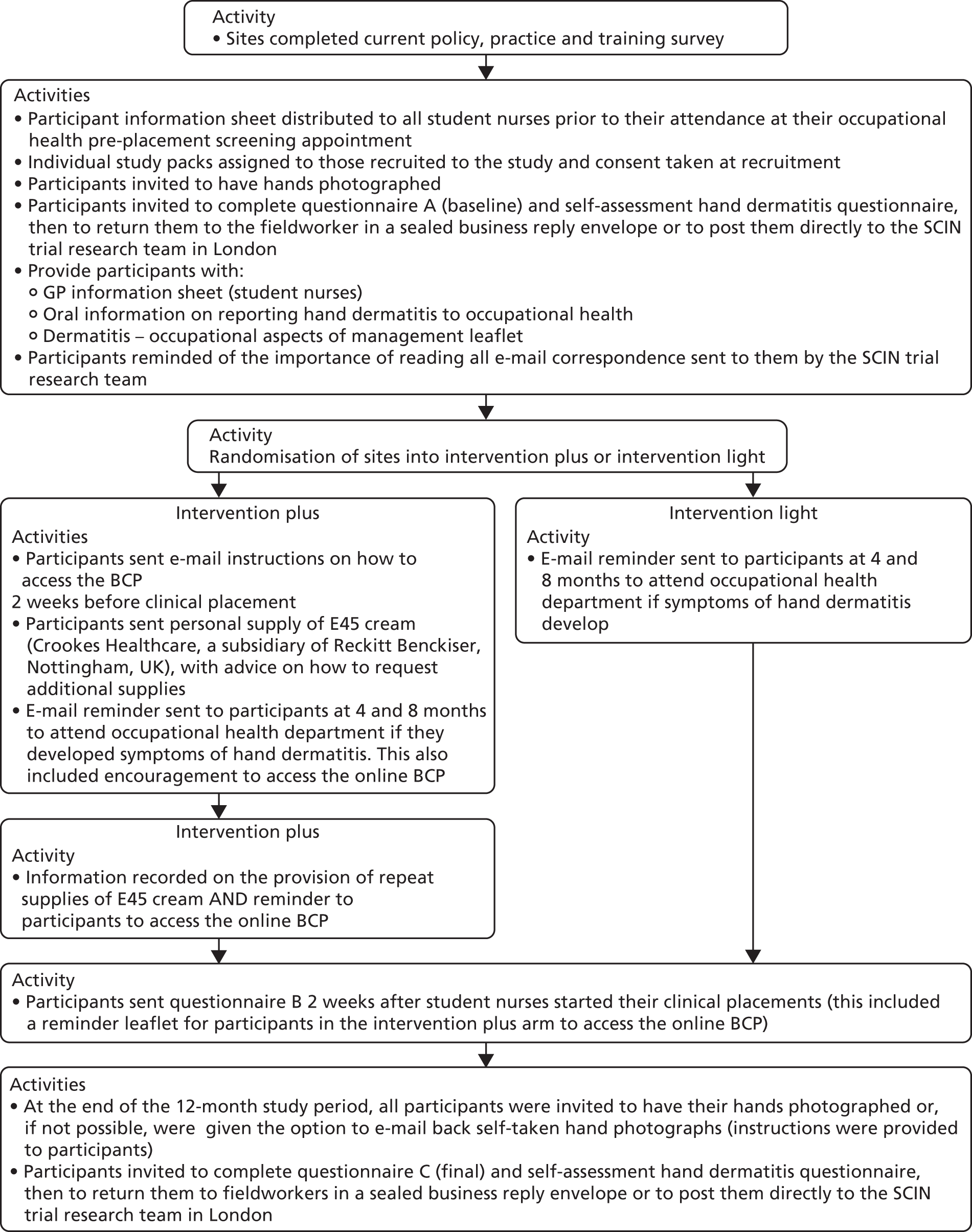
Student nurses were recruited during their occupational health pre-placement screening appointments in the occupational health departments located at either their local NHS trusts/health boards or their respective universities. ICU/SCBU nurses were recruited on-site at their respective NHS trust/health board. Figures 1 and 2 outline the trial procedures for ICU/SCBU nurses and student nurses, respectively.
FIGURE 1.
Flow chart of the trial procedures for ICU/SCBU nurses. BCP, behaviour change package; GP, general practitioner; SCIN, Skin Care Intervention in Nurses.
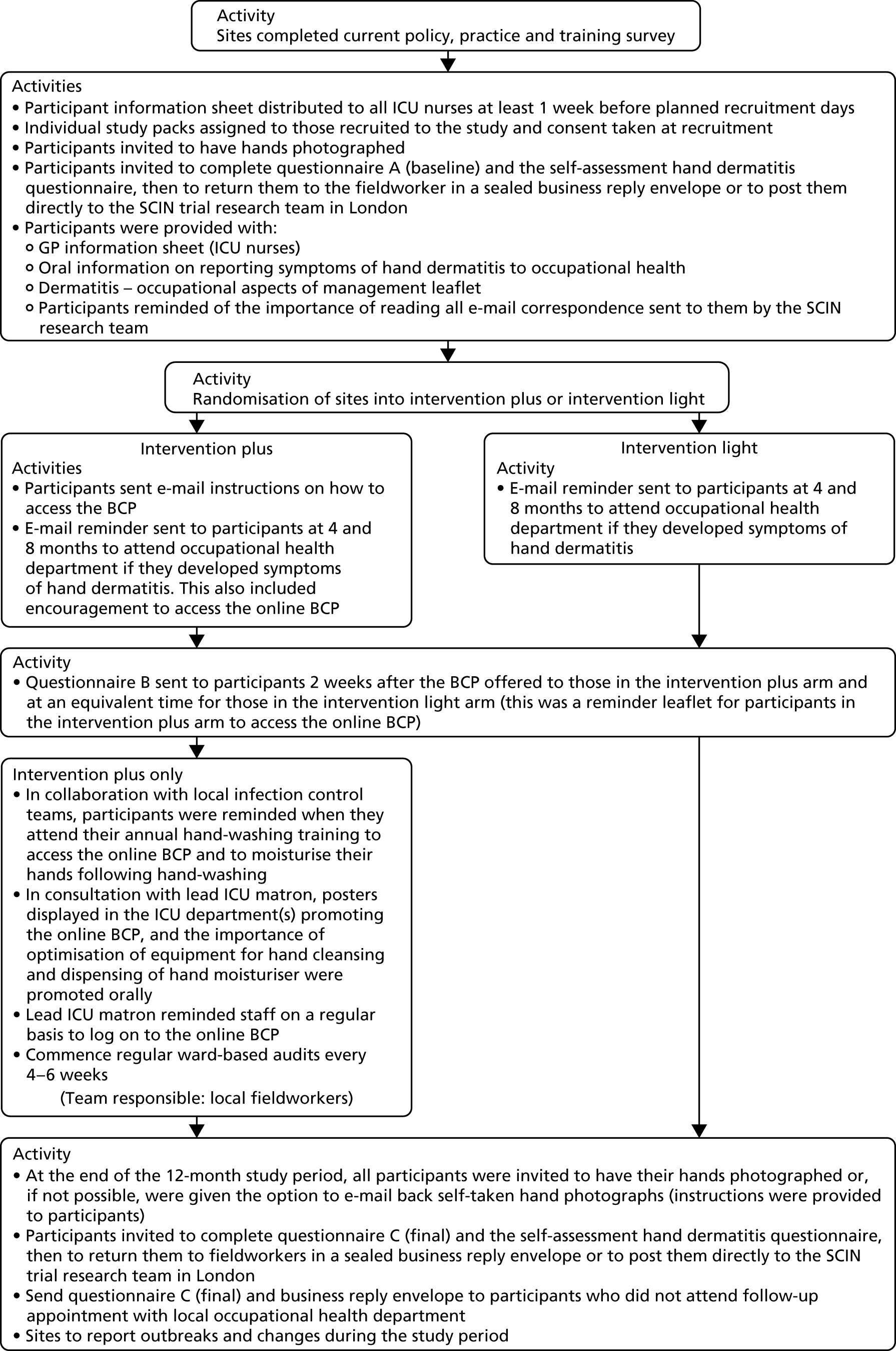
FIGURE 2.
Flow chart for the trial procedures for student nurses. BCP, behaviour change package; GP, general practitioner; SCIN, Skin Care Intervention in Nurses.
Preliminary work
Questionnaire development and management
Careful consideration was given when designing the study questionnaires to ensure that the study was able to collect reliable measures of TPB variables in relation to hand dermatitis prevention behaviours among the study participants, for example ‘When I start clinical work I intend to apply hand cream before and after work and during each of my breaks’ (intentions), ‘Contacting occupational health if I get symptoms which I think might be hand dermatitis would be worthwhile’ (behavioural belief) and ‘Other nurses at my placement would approve of me using hand rubs, when appropriate for infection control, instead of washing my hands with soap and water’ (subjective norms).
Three study questionnaires were developed and administered at 0, 3 and 12 months during the study. Participant questionnaires comprised a modified version of the Nordic Occupational Skin Questionnaire – 2002 (NOSQ-2002) to measure, before and after randomisation, participants’ self-reported behaviours relating to hand care and dermatitis prevention practices, and activities both inside and outside the workplace. The questionnaires also asked about participants’ rating of their overall health status using the validated EuroQol-5 Dimensions (EQ-5D) questionnaire and their views on the behaviour change package (BCP) (participants in the intervention plus arm of the study only). In addition, the study separately gathered site-level data on the use of moisturising cream (i.e. ad hoc requests for further personal supplies by student nurses and monthly estimates of moisturising creams available in each dispenser on the ICUs and SCBUs).
Local fieldworkers at each participating site made use of individual ‘study packs’ when recruiting participants to the study. Study packs contained each of the research documents (e.g. data collection worksheets, consent forms, questionnaire A booklet, a one-page self-assessment dermatitis questionnaire, business reply envelope) that required completion at the time of recruitment. The second questionnaire booklet (i.e. questionnaire B) was not included in these packs as these were posted directly to participants by the SCIN trial research team based in London. A matching preassigned participant identification number (PIN) was recorded on all research documents contained in each pack and these were numbered sequentially to reflect the order in which they were to be completed. A unique PIN was allocated to each participant as they were recruited to the study. The local fieldworkers then recorded the PIN, participant initials and date of birth on a separate participant registration log sheet as participants were recruited to the study.
Hand photography protocol development
Photographs of hands that were taken by trained personnel using high-resolution digital cameras were considered to be a cost-effective and practical method for collecting data on the presence or absence and severity of dermatitis. Developing a photographic guide to assist with diagnosing hand dermatitis and for use when assessing self-taken photographs of hands (i.e. ‘selfies’) was previously proposed by van der Meer et al. 44 In developing this photographic guide for diagnosing hand dermatitis and assessing its severity, the study team had the following requirements:
-
The method had to measure presence or absence of any form of hand dermatitis, as well as severity.
-
The method could not involve physical examination of the participants, as that would be logistically very difficult, expensive and likely to result in poor response rates.
-
The method had to be objective and not based on self-report as self-reporting tends to over-report hand dermatitis.
-
The severity scale needed to be able to distinguish dermatitis towards the milder end of the disease spectrum.
For the purpose of this study, three distinct stages were undertaken when developing the new hand photography method for use in the study. Accordingly, this new method for diagnosing hand dermatitis and assessing its severity offered a multidisciplinary method for diagnosing hand dermatitis and its severity. The method relied solely on dermatologist and research nurse inspection of hand photographs from research participants (in lieu of physical examinations), with comparisons from standardised images contained in Coenraads et al. ’s photographic guide. 71 The stages were:
-
developing a standardised procedure for hand photography
-
a stepwise validation process of rules for the study dermatologists to diagnose and determine the severity of the hand dermatitis
-
training, by a dermatologist, of the research nurse to screen out hand photographs of study participants without dermatitis (‘clear cases’).
The method for taking high-resolution digital photographs of the participants’ hands was developed in conjunction with a medical photographer and is consistent with the views required for the photographic assessment scale, for use in clinical trials, described by Coenraads et al. 71 When participants were unable to return to have their hands photographed by the trained fieldworkers, they were asked to provide, via e-mail, self-taken photographs of their hands, with a stipulation that self-taken photographs were taken against a grey or white background.
Hand dermatitis was assessed through photographs taken of each of the two sides of both hands (i.e. palm and dorsum). The presence of hand dermatitis was based on comparisons made with the standardised images of severity at various stages of diseases, which were contained in Coenraads et al. ’s photographic severity guide. 71 In accordance with this guide, for each combination of sides of the hand, the study dermatologists were required to indicate whether dermatitis was clear (absent), almost clear, moderate, severe or very severe. These four variables (i.e. dermatitis in the right hand at the dorsum, right hand in the palm, left hand at the dorsum and left hand in the palm) were then dichotomised as clear versus almost clear/moderate/severe/very severe. A single binary variable was generated for the presence of dermatitis (i.e. no/yes). Agreement or disagreement on the severity of hand dermatitis was not assessed during the validation process, as it was realised early on in the study that the likelihood of two dermatologists agreeing on the severity grading (five grades) at four different sites was likely to be poor and that perfect agreement on each site was not necessary for this study, which sought to establish a global estimate of hand dermatitis severity. Therefore, a pragmatic view was taken that severity would be defined as the combined score from the two dermatologists. Agreement between the two dermatologists on the binary rating (yes/no) was assessed using Cohen’s kappa statistic. Each participant’s overall severity of hand dermatitis was defined as the most severe combined score from both dermatologists on Coenraads et al. ’s scale from their four hand photographs. The levels of severity of dermatitis, as these were assessed by the two dermatologists, were 1 = clear, 2 = almost clear, 3 = moderate, 4 = severe and 5 = very severe. For each participant positive for dermatitis, a severity score by each of the two dermatologists was defined as the maximum score across the four photographs, then an overall severity of dermatitis score was derived as the average value of the two severity scores given by the two dermatologists. Overall severity was dichotomised using 3 as a cut-off point. Overall severity scores of < 3 (including those without dermatitis) indicated no severe dermatitis, whereas scores of ≥ 3 indicated severe dermatitis. Only two participants had severe dermatitis at baseline and only three participants had severe dermatitis at follow-up. As the prevalence of severe dermatitis was so low, this secondary outcome was not analysed further.
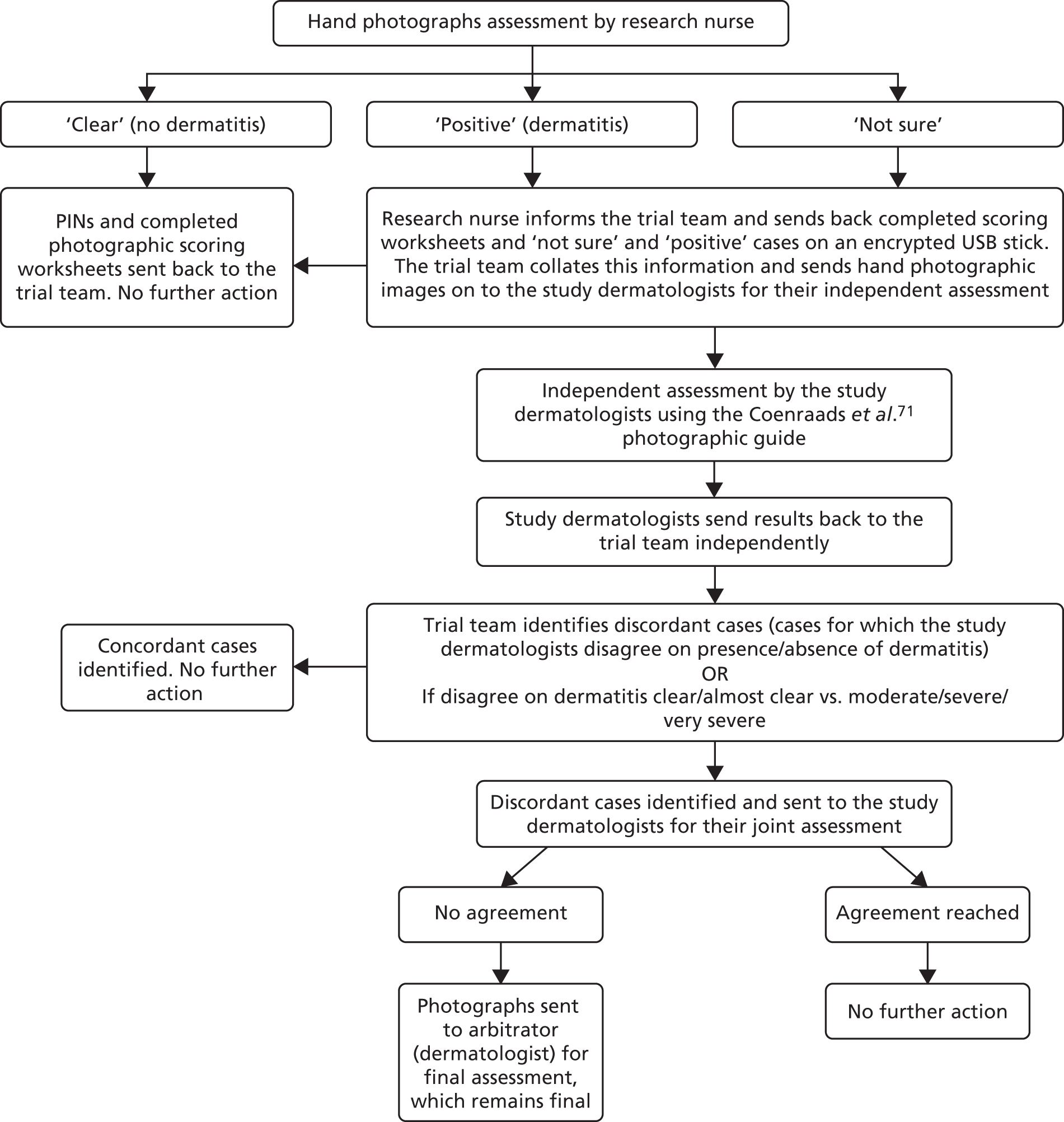
Figure 3 outlines the procedure that the dermatologists and dermatology research nurses used for assessing the hand photographs.
FIGURE 3.
Flow chart for assessing hand photographs. USB, universal serial bus.
Development of the behaviour change package
A key component of the study’s intervention was the BCP, which provided nurses with evidence-based information on good hand dermatitis prevention behaviours and encouraged them to form implementation intentions regarding specific hand-care behaviours, such as when and where they would use hand moisturising cream and when they would regularly check their hands for signs of hand dermatitis. The BCP employed the TBP, supplemented by implementation intentions, as its key theoretical framework. As described previously, the TPB postulates that a person’s behaviour is influenced by their intentions and perceived behavioural control (PBC). For example, whether or not a nurse uses hand moisturiser at the start and end of a shift is influenced by his/her intentions (e.g. ‘I strongly intend to use hand moisturiser at the start and end of a shift’) and his/her PBC (e.g. ‘I find it quite easy to use hand moisturiser at the start and end of a shift’). Intentions are influenced by attitudes towards the behaviour (e.g. ‘I believe using hand moisturiser at the start and end of a shift will be beneficial’) and subjective norms (e.g. ‘the matron wants me to use hand moisturiser at the start and end of a shift’) as well as PBC (as before).
Prior to the development of the BCP, the trial’s health psychologist conducted a focus group meeting with first-year student nurses, exploring their beliefs about the different hand dermatitis prevention behaviours likely to be targeted by the intervention. This work partly used open-ended belief elicitation questions recommended by Ajzen,57 but also explored student nurses’ perceptions of the practicality of performing behaviours frequently and their understanding of the consequences of hand dermatitis. For practising nurses, similar work was performed using an online questionnaire (with open-ended questions), so that the data could be collected at a time that was convenient for each nurse. Importantly, the early work revealed that nurses perceived that applying hand cream more frequently than at the start and end of shifts and before going on breaks was an impractical recommendation; therefore, making such a recommendation would damage the credibility of the BCP. It also allowed the health psychologist to identify misconceptions relating to hand dermatitis, such as alcohol-based hand rubs being more harmful to skin than hand-washing, and to ensure that specific information was included in the BCP to help to challenge these beliefs.
The BCP was designed to target four key hand dermatitis prevention behaviours:
-
using hand moisturising cream
-
using disinfectant hand rubs rather than hand-washing, while remaining in line with infection control guidance
-
using gloves for the shortest time possible while still conforming with infection control guidance
-
checking oneself regularly for hand dermatitis symptoms and seeking support from occupational health if required.
Different versions were developed for student nurses with an atopic tendency and ICU/SCBU nurses, given their differing levels of nursing experience and working environments.
The intervention was intended to be delivered primarily online, as this would allow good scalability if it proved to be effective. A web-based intervention standardises treatment delivery, thereby enhancing intervention fidelity. 72 Moreover, given that nurses work a variety of shift patterns, an online intervention allowed participants to access the BCP at a time that was convenient for them. Given the demands on nurses’ time, the intervention consisted of a single session with two brief follow-up reminder e-mails to access the intervention.
The intervention aimed to increase each of the behaviours by targeting relevant attitudes, subjective norms, PBC and implementation intentions. Specific change techniques73 were selected to target each construct, based on published expert consensus regarding which behaviour change techniques (BCTs) were most effective at changing particular psychological constructs. Where the expert consensus suggested a number of possible BCTs, the ultimate selection was based on feasibility of delivery in an online intervention and likely acceptability to participants. 73
Content of the BCP was intended to reflect current evidence-based guidelines and scientific literature on hand dermatitis prevention and infection control, at the time the intervention was developed, and to be appropriate for nurses working in NHS settings.
Patient and public involvement
The patient involvement in this study differs from that in other studies in that the ‘patients’ are NHS nurses. During the set-up and conduct of the trial, the research team actively consulted with representatives from the nursing (including student) profession. In particular, the trial involved a patient representative, Wendy Taylor, who:
-
ensured that the proposed interventions and data collection tools were acceptable
-
provided her expertise on the planning and management of the trial
-
provided her expertise on the optimum dissemination of the trial results to ensure that they reach the target audience.
Wendy Taylor is a midwife with a history of hand dermatitis acquired during her nurse training. She commented on the draft proposal, was a member of the Trial Steering Committee and attended one of the training workshops for fieldworkers.
During the intervention development stage, the study also conducted focus group sessions involving student nurses and registered nurses for the purpose of seeking their views on hand dermatitis, including prevention strategies, approaches to hand hygiene in the workplace and their preference for hand moisturisers to use during the trial.
Participating sites
The study identified all NHS sites in the UK that train nurses and have an in-house occupational health service and at least one ICU. The lead occupational physician in each eligible site was written to in December 2011, asking their willingness, in principle, to collaborate in a trial; again, the lead occupational physician was written to in May 2012 and January 2014 asking them to confirm their willingness to collaborate. In addition, additional sites were invited to sign up to the study via national occupational health newsletters. This included some sites that had an ICU but did not train nurses, and vice versa. To avoid the risk of student nurses moving placements from an intervention to a control site (or vice versa) during the study period, only one site, in general, was invited in each city or town to participate in the study. The exceptions were London and Manchester. In London, three sites were identified in which student nurses did not move to neighbouring sites during their training. In Manchester, sites were identified where students at three local universities undertake their clinical placements during their first year of nursing training, and it was ensured that these sites were clustered appropriately to prevent cross-contamination in the study:
-
12 sites recruiting both ICU nurses (including SCBU nurses) and student nurses
-
18 sites recruiting ICU nurses (including SCBU nurses) only
-
five sites recruiting student nurses only.
Participant recruitment procedure
Study group 1 student nurses
All student nurses are required to attend an occupational health assessment before starting their clinical work. At participating sites, with permission from the universities concerned, all student nurses in one or more year groups (excluding mental health nursing students) who were due to start their first clinical placement were provided with a participant information sheet by their university or their occupational health department, before or at the time of their mandatory assessment. Those student nurses who had a history of atopic tendency or hand dermatitis were identified by the occupational health department at the assessment from information that they provided in a generic pre-placement health screening questionnaire or during screening conversations the fieldworkers had with potential participants. An occupational health clinician explained to the student nurses that, because of their constitution, they are at increased risk of hand dermatitis. Student nurses who met the inclusion criteria were then invited to participate in the study. The local fieldworker obtained written consent from those nurses who agreed to take part in the study (the lead occupational health practitioner at the study site and the trial manager were available to answer questions when necessary). The consent form asked participants to provide a preferred e-mail address and telephone number to facilitate follow-up, and so that those at intervention plus sites could be sent a link to the online BCP. Paper copies of the BCP were provided at sites where participants were unable to access the online version. One copy of the signed consent form was filed in the nurse’s occupational health notes, one copy was sent to the trial manager and a third copy was given to the participant. Participants were also provided with an information sheet to give to their general practitioner (GP).
Study group 2 intensive care unit nurses (including special-care baby unit nurses)
The investigators, trial manager and lead occupational health clinicians from each site identified all critical care nurses who were suitable for the study. A local occupational health clinician or senior ICU nurse explained to all nurses working on the selected ICUs that they are at increased risk of hand dermatitis because of frequent hand-washing with cleansers and water. Full-time ICU nurses (i.e. those working ≥ 30 hours per week) were provided with a participant information sheet and, when possible, given a week to decide whether or not they wished to participate in the study. Consent to take part was obtained by the fieldworker, who, along with the trial manager, was available to answer any queries about the study. The consent form asked participants to provide a preferred e-mail address to facilitate follow-up, and so that those participants at the intervention plus sites could be sent a link to the online BCP. Paper copies of the BCP were provided at sites where participants were unable to access the online version. Participants were provided with an information sheet to give to their GP.
The study was presented to both study groups as research to assess the causes, consequences and ways of managing hand dermatitis in nurses who are at increased risk, either because of a personal history of atopy disease or because of the type of work that they do. However, to minimise the chance of bias, the nurses were not told that they were in an intervention plus or intervention light group. During the recruitment phase, fieldworkers reinforced the importance of participants being able to commit fully to the study, particularly with respect to the completion of the study questionnaires.
To check that rates of participation did not differ importantly between sites randomised to the two arms of the study, the recruitment process was carefully documented. The total number of eligible student and critical care nurses was recorded, as was the number who were consented to take part. In addition, the numbers and dates of those who dropped out of the study were recorded.
The recruitment period was between September 2014 and December 2015 and the follow-up period was between September 2015 and March 2017.
Informed consent
Participants were provided with an opportunity to read through the participant information sheet and to ask any clarifying questions before consent for entry into the study was taken. Informed written consent was obtained from participants at the time they were recruited into the study. In addition, all participants were required to provide written consent for the collection of hand photographs at the time of recruitment in the study (i.e. t = 0) and when photographs were collected during the follow-up period (i.e. t = 12 months). The participants who provided self-taken hand photographs via e-mail were taken to have provided consent by way of their self-initiated e-mail correspondence to the research team. Participants were provided with a copy of the consent forms and copies were also retained in the site file, the trial management file and occupational health records. All participants were provided with a GP information sheet, so that their GPs were aware of their participation in the trial.
Interventions
Intervention plus
The intervention plus in both staff groups centred on a bespoke BCP that targeted the behaviours of appropriate glove use, use of antibacterial hand rubs versus hand-washing, regular use of moisturising cream and contacting occupational health early if hand dermatitis occurred.
The BCP was developed by members of the study team with expertise in dermatology, occupational medicine, nursing and health psychology. As described earlier in this report, the intervention aimed to change relevant attitudes, subjective norms, PBC and implementation intentions. Copies of the BCP interventions screenshots (from the online platform: see Report Supplementary Materials 1 and 2) for the student nurses and ICU nurses are provided as supplementary documents. When participants were asked to form implementation intentions for performing the behaviours in their workplace, a record of each participant’s implementation intentions was generated by the online BCP package and e-mailed to her/him.
If a participant reported being unable to access the online BCP, she/he was posted a paper-based magazine version of the BCP, which reflected the information provided in the online BCP. Participants were asked to read through the material provided and write down their action plans in the spaces provided. The participants were then asked to keep the paper-based BCP in a convenient place so that, as required, they could refer back to it. The BCP was supported by provision of facilities to encourage adherence. These included personal supplies of moisturising cream for at-risk student nurses and provision of (1) optimal equipment for cleaning hands and (2) moisturising cream dispensers on ICUs and SCBUs.
The BCP was made available to ICU/SCBU nurse participants within 12 weeks of their recruitment to the study and for student nurse participants 2 weeks before they started their first clinical attachment. However, for many participants, access to the BCP occurred within a shorter timeframe (i.e. 2–4 weeks from their recruitment). It was actively reinforced over the course of the study by consistent messages on skin care from the local occupational health and control of infection teams, and from local line management. Research has shown that senior role models have important effects on more junior health professionals’ hand-hygiene behaviours,74,75 and it seemed reasonable to assume that this influence would extend to behaviours preventing dermatitis. To facilitate this, when implementing intervention plus, a dialogue was engaged in with local occupational health staff and line managers about the nature and purpose of the study and information was provided to them on the content provided in the BCP to ensure that they promoted consistent messages on skin care.
The online BCP was offered to allow nurses to access it at a time convenient to their schedules, to permit standardisation of the delivery of key information across all intervention plus sites and to reduce the potential burden on occupational health staff. Moreover, it was considered that, if the BCP was found to be effective in this trial, it would be simple to scale up access to the website to deliver the BCP across the country.
In the early stages of the trial, responses from the intermediate questionnaires and electronic user activity data showed that the initial uptake of the BCP was poor for both study groups. The most commonly cited reasons for this were that most participants forgot to, or did not have time to, access the BCP. In response to this, the research team implemented a targeted strategy to further promote and encourage uptake of the BCP. This comprised attaching a leaflet to the intermediate questionnaire that contained the website link and encouragement for participants to access the material; additional specific information in the follow-up reminder e-mails that were sent to participants; and displaying BCP information on posters in prominent locations in clinical areas.
Intervention light
Nurses at the intervention light sites were managed in accordance with what was currently regarded as best practice, with the provision of an advice leaflet about optimal hand care entitled Dermatitis: Occupational Aspects of Management. Evidence-based Guidance for Employees (which was also provided to the intervention plus group) and encouragement to contact their occupational health department early if hand dermatitis occurred. However, the nurses did not receive the BCP or active reinforcement of its messages. Nor were the nurses routinely offered supplies of moisturising cream over and above what was already standard practice at their site.
During the recruitment phase, fieldworkers reinforced to participants the importance of being able to fully commit to the study, particularly with respect to the completion of each of the study questionnaires.
Study groups
Study group 1 student nurses
At both the intervention plus and the intervention light sites, all first-year student nurses were given the participant information sheet about the study. Student nurses who agreed to take part were invited to complete a consent form, a self-administered baseline questionnaire booklet and a one-page hand dermatitis self-assessment form (t = 0 months). The completed questionnaires were then placed into a sealed business reply envelope and returned to the fieldworker, who forwarded them on to the SCIN trial research team in London. If the student nurses preferred, they could send the completed questionnaires directly back to the SCIN trial team in London. After the two questionnaires had been completed, all student nurses were invited to have their hands photographed as per a standard operating procedure developed for use in the study. Separate consent was obtained from the participating nurses each time their hands were photographed. In addition, the fieldworkers provided participants with oral information about hand dermatitis and with the Dermatitis: Occupational Aspects of Management. Evidence-based Guidance for Employees written leaflet. Participants were also told that they may be sent a link to access a BCP that they should undertake in the week before starting their first clinical attachment. Participants were required to log on to the online BCP package and register as a first-time user. At that time, the nurses would also be sent (by post) three personal tubes of moisturising cream, with guidance on how to request further supplies if needed.
All participants in both the intervention plus and the intervention light sites were encouraged (orally, through the written advice leaflet and by e-mail reminders at 4 and 8 months) to attend their local occupational health department at an early stage if they developed hand dermatitis during the study period. One week after starting their first clinical attachment, all nurses were asked to complete a further short self-administered questionnaire booklet (t = 3 months), covering beliefs and plans regarding dermatitis prevention behaviours. At intervention plus sites, it also asked about participation in, and views on, the BCP. The intermediate questionnaire was sent by post to participants by the SCIN trial research team along with a business reply envelope so that completed questionnaires could be returned. E-mail reminders were also sent to participants containing a positive reinforcement message to encourage ongoing participation in the study. At the intervention sites, the e-mail reminders also reinforced the BCP.
To account for seasonal variations in the prevalence of dermatitis, the final study data collection tools were administered 12 months after questionnaire A. All participants were asked to complete the final self-administered questionnaire booklet and a one-page dermatitis self-assessment form and to have their hands photographed. The questionnaires were sent out in the post to fieldworkers 2 months before the end of the study by the SCIN trial research team. The fieldworkers gave the student nurses the questionnaires at the time that they recalled them to have their hands photographed. The questionnaire C booklet covered clinical attachments undertaken in the previous year; hours worked per week over the previous year; beliefs and plans regarding dermatitis prevention behaviours; participation in, and views about, the BCP (only at intervention plus sites); activities outside work that predispose to hand dermatitis; recent practices regarding use of gloves; recent practices regarding hand cleansing; recent use of moisturising creams; history of hand dermatitis in the previous 12 months (including its investigation and treatment, and any consequent loss of time from work or restriction of duties); and the EQ-5D questionnaire.
At the follow-up time point (i.e. t = 12 months), participants who were unable to attend to have hand photographs taken by a fieldworker were provided with an opportunity to send the SCIN trial research team self-taken photographs, taken with their mobile phones, of their hands. If it was not possible for a student nurse to complete the questionnaire at the time, then they were asked to return the completed questionnaire to the SCIN trial team directly using a business reply envelope.
Information on the number of attendances at occupational health with symptoms of hand dermatitis and requests for extra provisions of emollients was also recorded.
Study group 2 intensive care unit nurses (including special-care baby unit nurses)
At both the intervention plus and the intervention light sites, all nurses who worked on selected ICU/SCBU wards were given the participant information sheet. Those who agreed to participate were asked to complete a consent form and self-administered questionnaire booklet (t = 0 months). This was similar to the baseline questionnaire booklet administered to student nurses, but also included items on current occupation; recent practices regarding the use of gloves; recent practices regarding hand cleansing; recent use of moisturising creams; and any sickness absence or modification of duties during the previous 12 months because of hand dermatitis. At the time of the photograph, ICU/SCBU nurses were asked to complete a one-page dermatitis self-assessment form evaluating whether or not they considered themselves to have dermatitis and the extent to which it interfered with work and hobbies. ICU/SCBU nurses were asked to return the completed questionnaires either to the fieldworkers or (by post) directly back to the SCIN trial research team in London. All ICU/SCBU nurses had their hands photographed as per protocol. All ICU/SCBU nurses, including those at intervention light sites, were provided with the Dermatitis: Occupational Aspects of Management. Evidence-based Guidance for Employees written leaflet. Participants were also told that they may be sent a link to access a BCP in due course that they should use. Participants were required to log on to the online BCP package and register as a first-time user.
At the intervention plus sites, once participants had been recruited, fieldworkers (occupational health clinicians) promoted the importance of optimisation of equipment for hand cleansing and use of moisturising cream. An e-mail was also sent via the lead ICU/SCBU nurses to all staff on the wards, with a link to the BCP. Two weeks after the BCP was offered (or at a similar interval after recruitment in the intervention light sites), participants were asked to complete an intermediate questionnaire about beliefs regarding prevention of dermatitis and (at intervention plus sites) participation in and views on the BCP. Questionnaire B was sent by post to participants by the SCIN trial research team along with a business reply envelope. All participants, at both the intervention plus and intervention light sites, were encouraged (orally, through the written advice leaflet and by e-mail reminders sent out by the SCIN trial research team at 4 and 8 months) to attend their local occupational health department at an early stage should they develop hand dermatitis. E-mail reminders were also sent to participants containing a positive reinforcement message to encourage ongoing participation in the study. At the intervention sites, the e-mail reminders also reinforced the BCP.
To account for seasonal variations in the prevalence of dermatitis, the final study data collection tools were administered 12 months after questionnaire A. All participants were asked to have their hands photographed and invited to complete questionnaire C. At the time of the photograph, ICU/SCBU nurses were asked to complete a one-page dermatitis self-assessment form evaluating whether or not they considered themselves to have dermatitis and the extent to which it interfered with work and hobbies. The questionnaires were sent to fieldworkers 2 months before the end of the study by the SCIN trial research team. The fieldworkers gave the ICU/SCBU nurses the questionnaires at recall for hand photographs. Completed questionnaires were returned to the fieldworker or directly (by post) to the SCIN trial research team in London. If it was not possible for an ICU/SCBU nurse to complete the questionnaires at the time, then they were asked to return the completed questionnaire to the SCIN trial team directly using a business reply envelope. At the follow-up time point (i.e. t = 12 months), participants who were unable to attend to have hand photographs taken by the fieldworker could send the SCIN trial research team self-taken photographs of their hands.
All participants who decided to withdraw from the study were asked to complete a shortened version of questionnaire C and were invited to have follow-up hand photographs taken after giving further consent. The collection of these data enabled the researchers to report further on the study’s primary objective measure (i.e. changes in the point prevalence of visible hand dermatitis from baseline).
Optimising response date to questionnaires and follow-up hand photographs
Study questionnaires were identified by the unique PIN assigned at the time of recruitment. For security reasons, contact details were kept separately. The content of the questionnaire was described above. Throughout the study, non-responders to any of the three study questionnaires were sent an e-mail reminder from the SCIN trial research team. If questionnaires remained outstanding, another copy of the paper questionnaire and a reply envelope were posted to participants’ preferred postal address. Non-responding participants were sent up to two reminder text messages (or landline telephone messages). 76
At the end of the study period, participants who had completed and returned all three study questionnaire booklets (i.e. questionnaires A, B and C) were entered into a prize draw for one study camera (a total of 26 cameras were offered). Information about the draw and prizes had been provided on the participant information sheets.
If local fieldworkers were unable to follow up participants at the end of the trial, the central research team then sent participants an information sheet with easy step-by-step instructions to follow on how to take and send in self-taken photographs of their hands.
Extension to the follow-up period
To optimise the response rate at follow-up, the research team felt that it was important to adopt a pragmatic approach that encouraged fieldworkers to try and follow up as many participants as practicable beyond the 12- to 15-month time point. As described in Chapters 3 and 4, an ancillary analysis (sensitivity analysis II) was conducted for the purpose of excluding the sample of participants who were followed up between 12 and 15 months.
Measure outcomes
Primary outcome
-
Difference between intervention plus and intervention light sites in the change in point prevalence of visible hand dermatitis from baseline to the end of follow-up, as assessed by two dermatologists.
Secondary outcomes
-
The difference between intervention and control sites in the change in point prevalence of severity of visible hand dermatitis from baseline to the end of follow-up (as ascertained by the dermatologists).
-
Days lost from sickness absence and days of modified duties because of hand dermatitis per 100 days of nurse time during the 12 months of follow-up.
-
The change from baseline to after completion of the BCP, and to the end of the 12-month follow-up period, in beliefs about dermatitis prevention behaviours.
-
The change from baseline to the end of follow-up in the reported frequency of:
-
use of hand rubs for hand cleansing
-
hand-washing with water
-
use of moisturising creams (for student nurses, who had not started clinical attachments at the beginning of the study, this was reduced to differences between the intervention and control sites at the end of the follow-up).
-
-
The change from baseline to the end of follow-up in quality-of-life score.
-
The use of moisturiser provided for the intervention (in terms of requests for further supplies by student nurses and orders for supplies of moisturisers by ICUs).
Sample size
Original sample size calculations
The aim was to recruit at least 40 student nurses and 40 nurses from the ICUs at each trust. To give an indication of power, it was assumed that:
-
the expected baseline prevalence of hand dermatitis, overall, was 5% in student nurses and 25% in ICU nurses
-
the expected rates, overall, at the control trusts at the end of follow-up were 25% for student nurses and 23% for ICU nurses; these estimated rates allow for limited impact in control trusts
-
the expected prevalence rates for individual trusts varied by a multiplying factor, which was normally distributed with a mean of 1.0 and a SD of 0.2
-
after allowance for other variables, hand dermatitis at baseline in an individual carried a relative risk of 2.5 for the presence of hand dermatitis at follow-up.
With these assumptions and a 5% level of statistical significance (two-sided), the study would have approximately 89% power to detect a prevalence at follow-up in the intervention trusts of 10% in student nurses and 95% power to detect a prevalence of 10% at follow-up in ICU nurses. For final prevalence rates of 12%, the corresponding power values would be 73% for student nurses and 82% for ICU nurses.
Revised sample size calculations
Fieldworkers were encouraged to recruit as many eligible student nurses and ICU/SCBU nurses as possible, with the expectation that they would recruit at least 40 student nurses and 40 critical care nurses at each site. From the outset it was acknowledged that, as a result of the low workforce populations, a number of smaller sites would not reach this target. To give an indication of power, it was assumed that, at the end of follow-up, the expected prevalence rates overall at the intervention light sites would be 24% in both student and ICU/SCBU nurses, the intraclass correlation coefficient (ICC) would be 0.05 and 20% of participants would be lost to follow-up. With a 5% level of statistical significance (two-sided), the study would have approximately 83% power to detect a reduction in prevalence of dermatitis at follow-up in the intervention plus sites to 10% in student nurses and a 91% power to detect a reduction in prevalence to 10% at follow-up in ICU nurses. For final prevalence rates of 12%, the power values would be 68% for student nurses and 78% for ICU/SCBU nurses, whereas for final prevalence rates of 14%, the corresponding power values would be 51% and 61%, respectively. The power would be higher if the ICC was < 0.05. [These calculations were carried out using the ‘clustersampsi’ command in Stata® (version 12.1; StataCorp LP, College Station, TX, USA) for difference in proportions.]
Randomisation
A total of 54 sites were assessed as eligible for entry into the study. However, 10 sites subsequently declined to participate, citing capacity reasons. No site-level data were collected from these 10 sites. Following this, the trial methodologist and statistician developed a formal strategy for randomisation based on the remaining list of 44 participating sites, and King’s Clinical Trials Unit (CTU) was responsible for conducting the randomisation procedure. Randomisation was carried out in four blocks as a single step at the beginning of the study. The blocks were defined according to the types of nurses who the centres planned to recruit (i.e. student nurses, ICU nurses or both) and by the size of the centres to ensure an approximate balance of numbers of nurses in the two arms of the trial. Five clusters contained more than one site, as the sites were geographically close to each other and student nurses may go on placement to another. This was done to avoid contamination between sites. The three clusters that comprised more than one site were all randomised to the control arm. If the sites in these clusters recruited ICU nurses only or student nurses only, the clusters were recorded twice on the Consolidated Standards of Reporting Trials (CONSORT) flow diagram, which needs to be taken into account in its interpretation (see Figure 5).
The output of the randomisation resulted in 19 clusters being randomised to be intervention plus sites and 19 clusters being randomised to be intervention light sites. The 19 clusters comprised the 44 participating sites. Following randomisation, nine sites either lost interest in taking part or withdrew from participating in the trial for capacity reasons. This included two clusters that contained more than one site, that is, the number of clusters taking part reduced by seven. No participant data were collected from the nine sites that withdrew after randomisation, as no participants were recruited at these sites. Of these nine sites, five completed a site survey of current policy, practice and training. Regarding the dropout of sites, it is important to note that the original list of proposed sites was devised as part of the initial funding application period in 2012. However, there was a period of > 12 months between their commitment and the commencement of the trial, and the sites that dropped out did so because they no longer felt that they had the capacity to participate in trial. Furthermore, the nature of occupational health departments is such that business contracts are usually awarded on a short-term basis and it is not uncommon for frequent changes of management to occur. With these factors in mind, there is no reason to believe that the dropout of these sites was influenced by concerns related to the potential uptake of the intervention.
The final number of clusters in the trial was 31, comprising 35 individual sites. Of the 31 clusters, 14 were randomised to intervention plus and 17 were randomised to intervention light. As the three clusters that contained more than one site were randomised to intervention light, the final ratio of intervention plus to intervention light sites was 21 : 14.
(When possible, before randomisation, the fieldworkers at each participating site provided information about current arrangements to minimise the occurrence of hand dermatitis in nurses and the procedure to manage it when it occurs. Among other things, this covered general training regarding dermatitis; guidance on when and when not to use gloves; guidance on washing and drying hands and on use of hand rubs; information on the use of moisturising creams; and provision of moisturising creams for staff. Sites were stratified to ensure that sample sizes were similar in the intervention light and intervention plus arms. This helped to address issues such as low recruitment numbers at specific sites, which were anticipated.)
As described above, to ensure that the nurses were not influenced by prior knowledge of treatment allocation, the study ensured that only the CTU knew if sites had been randomised to the intervention light or intervention plus arm of the study at the time when study participants were recruited and completed baseline questionnaire A. At all sites, we recorded the number of nurses who did not participate in the study for whatever reason (e.g. those who declined or who were not eligible). Numbers of all potential participants in each site were obtained so that assessment could be undertaken to see if there had been differential uptake in intervention plus and intervention light sites.
For the purpose of the intention-to-treat (ITT) analysis, the date of entry into the study for all participants was the date when they signed the consent form for the research study. Although the research team acknowledged that student nurses could contribute useful information only once they started clinical work, in practice, very few failed to start their clinical work once they commenced their nursing studies.
Fieldworkers at sites were informed of the outcome of the randomisation via e-mail, when practicable, after all of the participants had been recruited into the trial. Study team members were informed of the randomisation in a blinded or unblinded manner, depending on their role in the trial. The trial statistician (GN), methodologist (DC), infection control expert (BC), dermatologists (HW and JE) and health economist (PM) remained blinded to treatment allocation until after the primary analysis.
Ethics approval and research governance
Ethics approval to conduct the trial was granted by the National Research Ethics Service (NRES) Committee London – City Road and Hampstead (Research Ethics Committee reference number 13/LO/0981). Subsequent substantial and minor amendments are outlined in Appendix 1. Ethics approval applied to all research sites taking part in the study. In addition, local site-specific assessments were conducted at participating research sites and approval obtained by their respective research and development departments. A full list of participating sites is given in Table 4. The trial was registered with the International Standard Randomised Controlled Trial Number (ISRCTN) registry, on 21 June 2013, as ISRCTN53303171.
Statistical methods
The primary analysis was an ITT comparison of the two study arms (i.e. intervention plus and intervention light) in change of objectively assessed dermatitis, health beliefs and health prevention measures, and was run separately for student and ICU nurses. All outcomes, primary and secondary, were initially described using means, SDs and percentages, separately for each of the trial arms.
The difference between the two trial arms in change in the primary outcome of the trial (i.e. prevalence of objectively assessed dermatitis) from baseline to follow-up was assessed using logistic regression modelling, with hand dermatitis assessed at follow-up used as an outcome variable after adjusting for hand dermatitis assessed at baseline. The effect of intervention on change in prevalence of hand dermatitis was summarised by odds ratios (ORs) and 95% confidence intervals (CIs).
Health belief variables were used as continuous measures with their scores ranging from 1 to 5, with higher scores indicating more positive beliefs. The difference between the two trial arms in change in health beliefs was assessed using linear regression models, with all of the 25 measures assessed at follow-up used as outcome variables in separate regression models after adjusting for the corresponding measures assessed at baseline. The effect of the intervention on change in health beliefs from baseline to follow-up was summarised by regression coefficients and 95% CIs.
The variables for use of dermatitis prevention measures were used in their ordinal form; scores for hand-washing with soap and water and for the use of hand rubs ranged from 1 to 4 and scores for use of moisturising creams (before, during and after shifts) ranged from 1 to 6. Higher scores for dermatitis prevention measures indicated more frequent use. The difference between the two trial arms in change in frequency of use of dermatitis prevention measures from baseline to follow-up in ICU nurses was assessed using ordinal logistic regression models, with each measure assessed at follow-up used as an outcome variable and adjusting for the measure assessed at baseline. As student nurses started their clinical placement at the beginning of the trial, the difference in frequency of use of dermatitis prevention measures from baseline to follow-up could not be assessed. Thus, for student nurses, the differences in the two trial arms were explored in relation to the frequency of use of dermatitis prevention measures at the end of the study. The effect of intervention was summarised by ORs and 95% CIs.
All analyses were further adjusted for participants’ age, sex and follow-up time, and were repeated after excluding those nurses who reported that they did not access the BCP intervention. Clustering of the outcome among student nurses was very low, so that the ICC approximated zero. Therefore, the final model fitted was a single-level model, adjusted for sex, age and follow-up time. For ICU nurses, a random-intercept model was used to account for clustering by site. The estimated ICCs were 0.01 (95% CI 0.00 to 0.95) and 0.03 (95% CI 0.00 to 0.36) for the ‘adjusted for baseline dermatitis’ and the ‘adjusted for baseline dermatitis, sex, age and follow-up time’ models, respectively. All analyses were run using Stata (version 12.1).
With respect to the approach used for missing data, all analyses were restricted to participants with data on the relevant outcomes. The main adjusted analysis of the primary outcome (i.e. presence of dermatitis at follow-up) was further restricted to participants with complete data on all relevant independent variables.
To explore potential attrition biases in the results, the numbers of participants who completed the baseline, intermediate and the 12-month follow-up questionnaires were compared by categories of their characteristics and the primary outcome variable assessed at baseline and separately for the two intervention arms. In addition, health behaviour and belief variables assessed at baseline were compared between those nurses who completed the baseline, intermediate and follow-up questionnaires using medians, interquartile ranges (IQRs) and ranges, and separately for the two intervention arms.
Per-protocol analysis
As the primary research question was whether or not the change in the prevalence of hand dermatitis was different between those nurses who were in the intervention plus arm and those nurses in the intervention light arm, in the analysis it was important to consider the possibility that participants in the intervention plus group did not access the intervention at all (intervention access rates described above). If the number of participants who did not access intervention was large, it is likely that the intervention effect was underestimated. For this reason, the main analysis for the primary outcome, and that for health beliefs, was repeated, after restricting the intervention plus group to those nurses who accessed the intervention.
Sensitivity analysis I
If photos of hands could not be taken using the trial’s standard camera, participants were asked to take their own photographs of their hands. The information taken from the self-taken photographs was used in the main analysis. However, a separate analysis was repeated for the main outcome after exclusion of participants for whom information about dermatitis was based on self-taken photographs.
Sensitivity analysis II
As inclusion of participants with shorter or longer follow-up times was likely to increase bias in the effect estimate of the intervention on the primary outcome, the analysis for hand dermatitis at follow-up was repeated after restricting the sample to participants with a follow-up time of between 12 and 15 months.
Sensitivity analysis III
It was expected that the number of recruited nurses in some trusts would be considerably higher than that in other trusts. In addition, there was the possibility that clusters with high numbers of recruited nurses were different from those with low numbers of recruited nurses, especially in terms of participants’ beliefs. To explore that possibility, the size of trust was plotted against average values of health beliefs for the trust, and correlation coefficients were to be calculated. If any association between the size of trust and health beliefs scores was apparent from the descriptive statistics (i.e. scatterplots and correlation coefficients), the participating trusts were categorised according to the distribution of their size and the main models, including that of the primary outcome and those of health beliefs, and were repeated separately for small, average and large clusters.
Process evaluation
The intervention process was evaluated by describing the:
-
uptake of the intervention, as measured by the proportion of eligible nurses who accessed the BCP (online or paper based), determined by responses in the study questionnaires
-
acceptability of the intervention, as measured by the perceived interest, relevance to role and likelihood of recommending it to colleagues.
These data were collected from study questionnaires B and C at intervention plus sites only.
Health economics
Methods
A cost-effectiveness analysis was conducted combining intervention and other costs with quality-adjusted life-years (QALYs). Costs were measured from the perspective of the NHS, with secondary analyses also considering societal costs by including lost work days.
Service use and costs
The intervention costs were based on an estimate of the resources required to set up the BCP, the provision of creams and the time spent by nurses accessing the material in the BCP. The development costs were estimated at £5020, the software hosting fee was £1200 and the E45 cream costs were £4 per student nurse. Creams were assumed to be already available for ICU nurses. These costs were apportioned over all intervention group nurses in the trial. This potentially overestimates the costs as a larger number of nurses would presumably use the intervention if it proved to be effective. Time spent accessing the BCP by nurses was recorded, but it was not possible to allocate this to specific nurses. For those nurses for whom data were available, it was estimated that 13 minutes was spent, on average, accessing the BCP. The 13 minutes was applied to all intervention nurses and so, again, this may lead to an overestimation of costs. This time was valued using average salaries of nurses. Overall, the intervention cost per ICU nurse was estimated at £13 and the cost per student nurse was estimated at £14. The higher cost was as a result of the creams provided to student nurses.
Other health service use was measured using an adapted version of the Client Service Receipt Inventory (CSRI) at baseline and at the 12-month follow-up. 77 The CSRI recorded the number of contacts during the previous 12 months with GPs, dermatologists, practice nurses, pharmacists, other doctors, physiotherapists and complementary health-care practitioners. These contacts were categorised as skin related and skin unrelated. The duration of contacts was not recorded and so unit costs of contacts were used (see Appendix 2). These were derived from the annual compendium published by the University of Kent’s Unit Costs of Health and Social Care 201178 and the Department of Health and Social Care’s NHS Reference Costs 2015 to 2016. 79 When these documents did not provide a cost per contact but rather a cost per hour, a typical duration was assumed based on previous work. It was assumed that a practice nurse contact would last 10 minutes, a pharmacist contact 10 minutes and a complementary health-care practitioner contact 60 minutes. Medication for skin-related conditions was recorded and costed using the British National Formulary80 and tests were costed using NHS Reference Costs 2015 to 2016. 79 The number of days lost from work during the previous 12 months was recorded. This was costed at £173 per day for student nurses and £263 per day for ICU nurses. These costs are based on salaries for typical grades plus on-costs and overheads. Unit costs are listed in Appendix 2. Costs are reported in 2015–16 Great British pounds.
Quality-adjusted life-years
Quality-adjusted life-years were calculated using the EuroQol-5 Dimensions, five-level version (EQ-5D-5L). This questionnaire includes five domains (mobility, self-care, usual activities, pain/discomfort and anxiety/depression), which score 1 (no problems) to 5 (major problems). The resulting five-figure score (e.g. 11111 to 55555) relating to a specific health-state then had a re-calculated population-rated weight attached to it. A weight of 1 represents full health and 0 represents death. Negative values indicate health states considered by the population sample as worse than death. Baseline and follow-up EQ-5D-5L scores were combined using the area under the curve approach to generate QALYs over the follow-up period.
Analyses
The number and percentage of participants using specific services and having lost work days are reported, as are the mean and SD of the number of contacts by those using them (i.e. excluding those with zero use), and the mean and SD of costs (including those with zero costs). Tests of significance were not conducted for the group differences in use and cost of individual services. The significance of the difference in total service costs and societal costs was tested between groups using regression models, controlling for baseline costs. QALY differences were compared, controlling for baseline EQ-5D-5L scores. Differences were assessed for nurses with QALY data and also for those with both QALY and cost data.
For nurses with both cost and QALY data, the cost and QALY differences were used in the cost-effectiveness analyses. If either treatment arm resulted in lower costs and more QALYs, then it would be seen as ‘dominant’. If one arm resulted in higher costs and more QALYs, then an incremental cost-effectiveness ratio (ICER) was to be calculated by dividing the extra cost by the extra outcome. This shows the extra cost incurred to achieve one more QALY. Uncertainty around the cost-effectiveness results was explored by generating cost-effectiveness planes in which 1000 cost–QALY differences, obtained using the aforementioned bootstrapped regression models, were combined in scatterplots. There was no imputation for missing data; instead, a complete-case analysis was conducted. Health economic analyses were conducted using Stata (version 14).
Feasibility study
Prior to the commencement of the full trial, a feasibility study was conducted in Swansea from February 2014 to May 2014. The aims of the feasibility study were to assess the process, response rates and data collection tools to be used in the main study.
Method
Study procedures were followed as for the first stages of the main study at an intervention plus site. In addition, the hands of participants were swabbed to look for the carriage of pathogenic bacteria. As the web version of the BCP was not developed at the time of the feasibility study, a paper version of the BCP was tested. As in the main study, all student nurses who were due to start their first clinical placement, and who had a history of atopic disease or hand dermatitis (as indicated on the responses provided on a standard health questionnaire), were identified by the occupational health department in the course of its routine occupational health assessment and invited to take part. In addition, all full-time ICU nurses (i.e. those working ≥ 30 hours per week) on the ICU unit at the local health board were invited to participate. Those nurses who agreed to participate were asked to complete questionnaire A (with modifications for ICU nurses, as in the main study), and their hands were photographed and swabbed for organisms using the proposed methodology for the main study.
Once the student nurses started clinical work, they were offered the written leaflet Dermatitis: Occupational Aspects of Management. Evidence-based Guidance for Employees and a paper version of the BCP. The nurses were asked to develop implementation plans and were provided with personal supplies of emollients for use during the study period. Once ICU nurses were recruited to the study, optimal equipment for hand cleansing and drying was placed on their ward, along with dispensers of moisturising cream. The written leaflet and paper version of the BCP were then offered to all ICU staff of the ward concerned (i.e. not only those individuals who had consented to take part in the study), and the uptake was documented.
Two weeks after the paper version of the BCP was offered, the nurses were asked to complete questionnaire B about beliefs regarding prevention of dermatitis and participation in, and views on, the BCP.
At the end of the study period, a number of participants recruited to the study were invited to take part in an in-depth telephone semistructured interview designed to seek qualitative feedback on the acceptability and user-friendliness of the methods of data collection and the BCP. The lead occupational health clinician from the trust was also asked for feedback on the ease of implementation of the study procedures, data collection tools and study protocols.
Results of the feasibility study
Thirty-two student nurses were identified as being eligible for the study, 22 (69%) of whom were recruited into the study. Twenty-two (100%) of those nurses recruited returned a completed questionnaire A and 10 out of 22 (45%) nurses returned a completed questionnaire B. Two (20%) of those nurses who returned questionnaire B did not participate in the BCP. One hundred and forty-eight ICU nurses were identified as being eligible for the study (including those not on shift). Twenty-six eligible ICU nurses were on shift on the day of recruitment and all 26 (100%) were recruited into the study. Twenty-two (77%) of those nurses recruited returned a completed questionnaire A and 13 out of 22 (60%) returned a completed questionnaire B. One (8%) of those nurses who returned questionnaire B did not participate in the BCP. The baseline prevalence of hand dermatitis, as diagnosed by the dermatologists, was 5 out of 21 (23.8%) student nurses (one had missing data) and 10 out of 26 (38.5%) ICU nurses. The photographic method for assessing the presence and severity of hand dermatitis was found to be easy to implement by the fieldworker and the dermatologists. However, as one of the dermatologists was found to have a lower threshold for diagnosing hand dermatitis, the dermatologists considered it necessary to develop a set of mini consensus rules that they would follow during the main trial. (One dermatologist tended to diagnose erythema in isolation as evidence of dermatitis and the other diagnosed dermatitis only when erythema was present in association with dryness of the skin.) The development of these mini rules ensured that a consistent and uniform approach was followed by the dermatologists when assessing the hand photographs. Without prior agreement of the rules of diagnosing dermatitis between the dermatologists, the interobserver agreement in the assessment of photographs was 0.5%. Importantly, there was poor correlation between the participants’ self-assessment of the presence of hand dermatitis and between the fieldworkers and the dermatologists. All participants agreed to have their hands swabbed, but only one swab (from a student nurse) was positive for a mild growth of Streptococcus pyogenes (Lancefield group A); the other swabs were negative for the organisms looked for. The paper version of the BCP that was piloted was acceptable in format and appeared to be clearly understood by the study participants.
None of the study participants agreed to be interviewed after the feasibility study, but the fieldworker was interviewed by the trial manager and gave valuable feedback on the practicalities of running the study at a grass-roots level. The fieldworker’s feedback allowed the research team to address ambiguities with respect to several of the data collection tools, the procedure for setting up study material prior to commencement of participant recruitment, the practicalities associated with the taking of hand photographs and for conducting physical inspections of hands.
Changes to the main study protocol as a result of the feasibility study
The feasibility study provided a valuable opportunity to test the study protocol/procedures and to identify and address issues that were likely to arise in the main trial. As a consequence, minor but important amendments, as outlined below, were made to the study protocol to enhance trial processes and procedures, and the study team is confident that these amendments contributed to the overall success of the main trial.
As there was poor agreement in the diagnosis of dermatitis between the fieldworkers, the study participants and the dermatologists, the requirement for fieldworkers to assess whether or not hand dermatitis was present was removed. As a result, the dermatologists’ assessment to report on the primary outcome measure was relied on solely. As a consequence, all participants’ hands were photographed at baseline (when questionnaire A was administered) and 12–15 months after the BCP was delivered in intervention plus sites (and at an equivalent time at the intervention light sites). The trial dermatologists agreed a set of rules by which they would diagnose hand dermatitis from the photographs and assessed a further 100 hand photographs to ensure that they achieved a good agreement between themselves (kappa > 0.6). In addition, an experienced dermatology research nurse was employed to conduct an initial screening assessment of all hand photographs collected during the trial. The swabbing of the participants’ hands yielded little useful information. As a consequence, it was a recommendation from the Trial Steering Committee that the collection of swab samples be removed from the main study. This recommendation was upheld by the National Institute for Health Research Health Technology Assessment programme.
Chapter 3 Results
The reporting of the results of this study was guided by the CONSORT statement, including the statement’s extensions on the reporting of cluster randomised trials. 81 Owing to the pragmatic nature of this trial, this report describes the results from the ITT analysis.
Recruitment of participating sites
A total of 54 sites were assessed for eligibility for the study. Of these, 35 sites agreed to participate and 19 were not able to participate. Of the 35 participating sites, five recruited student nurses only, 18 recruited ICU/SCBU nurses only and 12 recruited both student and ICU/SCBU nurses.
Approximately half (47%) of the participating sites recruiting student nurses (n = 17) and most (70%) of the participating sites recruiting ICU/SCBU nurses (n = 30) had a written policy on the management of hand dermatitis in staff. Most sites provided nurses with ward-based moisturisers (13/17 and 28/30 sites recruiting student and ICU/SCBU nurses, respectively) and guidance on washing and drying hands, and fewer sites provided nurses with hand-care leaflets or individual moisturisers. In addition, most of the participating sites provided information on whom nurses should inform if they developed hand dermatitis or if they experienced deterioration in their current dermatitis (15/17 and 28/30 participating sites recruiting student and ICU/SCBU nurses, respectively). Most of the sites encouraged nurses to contact occupational health services in the event of such an occurrence.
The outbreak and policy change for the participating sites recruiting ICU/SCBU nurses was recorded at the end of the study. Most of the sites reported no outbreak or changes to hygiene policies.
Study sample: numbers analysed
All analyses were carried out in accordance with ITT principles. As this was a cluster randomised trial, ITT applied to the clusters. The sites/clusters that withdrew after randomisation did so before participant data had been collected (see Chapter 2, Randomisation), before any intervention was implemented, and without any knowledge of the intervention to which they would be allocated. The sites/clusters can therefore be considered effectively as never having entered the trial. The numbers analysed are described in the following sections.
Questionnaires
A total of 1825 participants returned at least one of the three questionnaires (at t = 0 months, t = 3 months and t = 6 months). The sample breakdown of participants by questionnaires returned, for all nurses and separately for student and ICU/SCBU nurses, is shown in Table 1. Participants who did not return the baseline questionnaire and returned only the intermediate and/or follow-up questionnaires (n = 97) were excluded from any further analysis. The overall sample suitable for analysis of data collected from questionnaires was 1728.
| Time point of questionnaire return | Nurses (n) | ||
|---|---|---|---|
| Student | ICU/SCBU | All | |
| Baseline only | 248 | 165 | 413 |
| Follow-up only | 6 | 71 | 77 |
| Intermediate only | 1 | 9 | 10 |
| Baseline and intermediate (no follow-up) | 147 | 123 | 270 |
| Follow-up and intermediate (no baseline) | 3 | 7 | 10 |
| Baseline and follow-up | 57 | 168 | 225 |
| All three | 337 | 483 | 820 |
| Total | 799 | 1026 | 1825 |
Photographs
Overall, photographs were available for 1903 participants (794 student nurses and 1109 ICU nurses). Just over half of the participants (n = 1105) had photographs taken at both baseline and follow-up, whereas 40% had photographs taken only at baseline. Less than 2% (28 student nurses and nine ICU/SCBU nurses) of the participants had hand photographs taken only at follow-up. These were dropped from any further analysis of hand photograph data. The overall sample suitable for analysis of objectively assessed dermatitis by hand photographs was 1866.
Questionnaires and photographs
Overall, 1638 participants had valid data from both sources of information in the trial: the questionnaires and the hand photographs. A further 90 participants returned at least the baseline questionnaire, but hand photographs were not available for them, and 228 participants had at least baseline hand photographs but did not return any questionnaire. In total, 1956 participants had either data from at least the baseline questionnaire or the objective dermatitis assessment from at least baseline hand photographs. The above figures are broken down by type of nurses and intervention arm in Table 2. (Note that two sites in the intervention plus arm achieved a very high rate of recruitment among the student nurse population. Both of these sites were in the intervention plus arm of the trial and this resulted in an unequal number of student nurse participants in the intervention plus and intervention light sites.) The proportion of participants in each of the three categories of source of information (questionnaire returned but no hand photographs, hand photographs but no questionnaire or both questionnaires returned and hand photographs taken) is shown by type of nurse and intervention arm in Figure 4.
| Source of information | Nurses, n (%) | |||
|---|---|---|---|---|
| Student | ICU/SCBU | |||
| Light | Plus | Light | Plus | |
| At least the baseline questionnaire returned, but no objective dermatitis assessment from the hand photographs | 12 (4.1) | 67 (12.2) | 7 (1.2) | 4 (0.8) |
| Objective dermatitis assessment from at least the baseline hand photographs, but no questionnaires returned | 44 (15.0) | 12 (2.2) | 105 (17.8) | 67 (12.9) |
| Both the baseline questionnaire returned and the objective dermatitis assessment from baseline hand photographs | 238 (81.0) | 472 (85.7) | 478 (81.0) | 450 (86.4) |
| Total | 294 | 551 | 590 | 521 |
FIGURE 4.
Proportion of participants in each of the three categories of source of information by type of nurse and intervention arm.
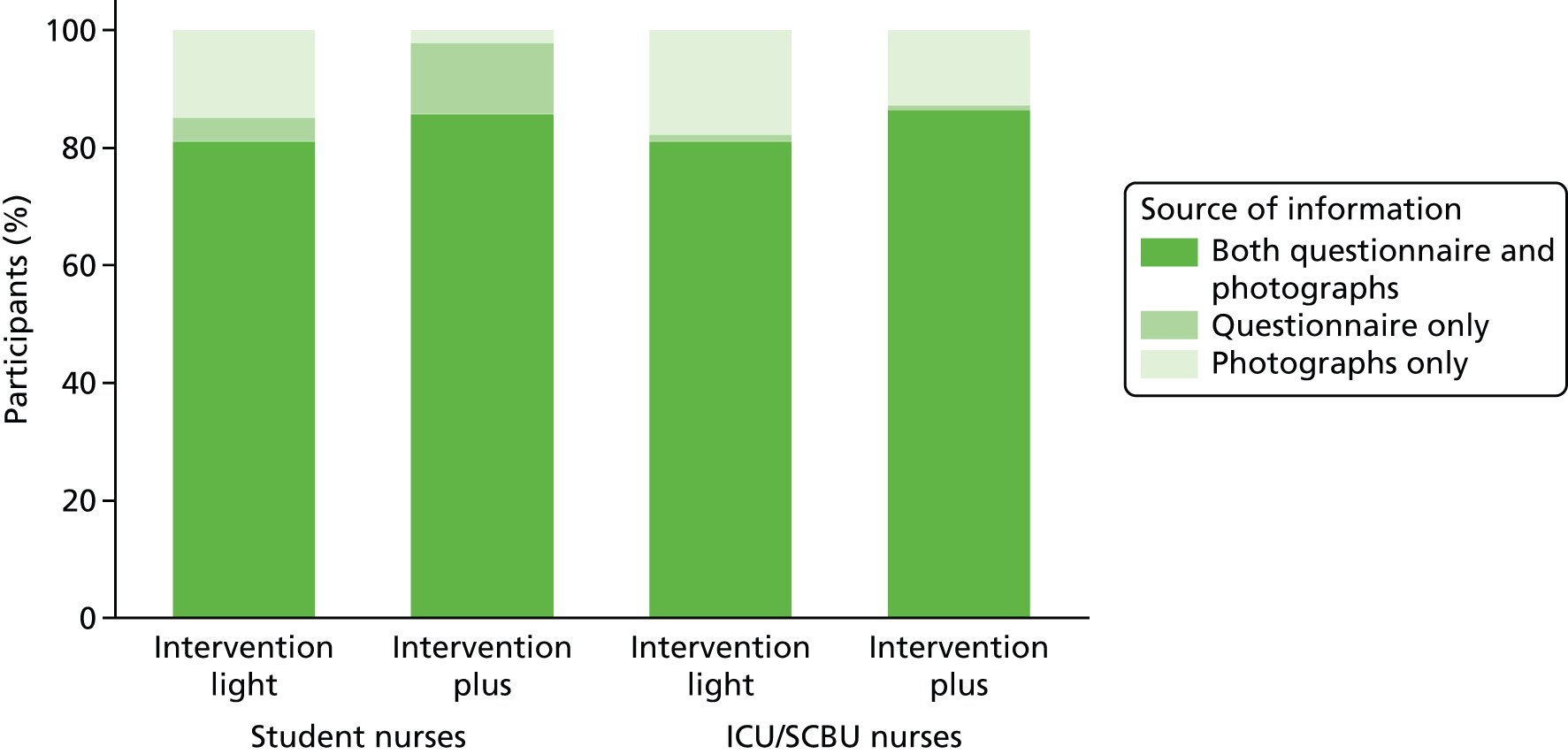
The 789 student nurses with data from at least the baseline questionnaire were distributed across the 17 sites that recruited student nurses. Site sizes for student nurses ranged from 7 to 362. The 939 ICU nurses with data from at least the baseline questionnaire were distributed across the 30 sites that recruited ICU nurses. Site sizes for ICU nurses ranged from 6 to 99.
Consolidated Standards of Reporting Trials flow diagram
The numbers of study participants as presented above, including information about the numbers of participants who returned the baseline, intermediate and final questionnaires, the number of hand photographs collected at baseline and at follow-up and the number of participants who accessed the BCP, are shown in the CONSORT flow diagram presented in Figure 5. Figures in the CONSORT flow diagram relating to ‘total screened’ are broad estimates based on the data captured on the screening log forms. It is acknowledged that these screening logs may not have accurately captured all those who were initially approached to take part in the trial.
FIGURE 5.
Flow diagram of participants at the different stages of the study.
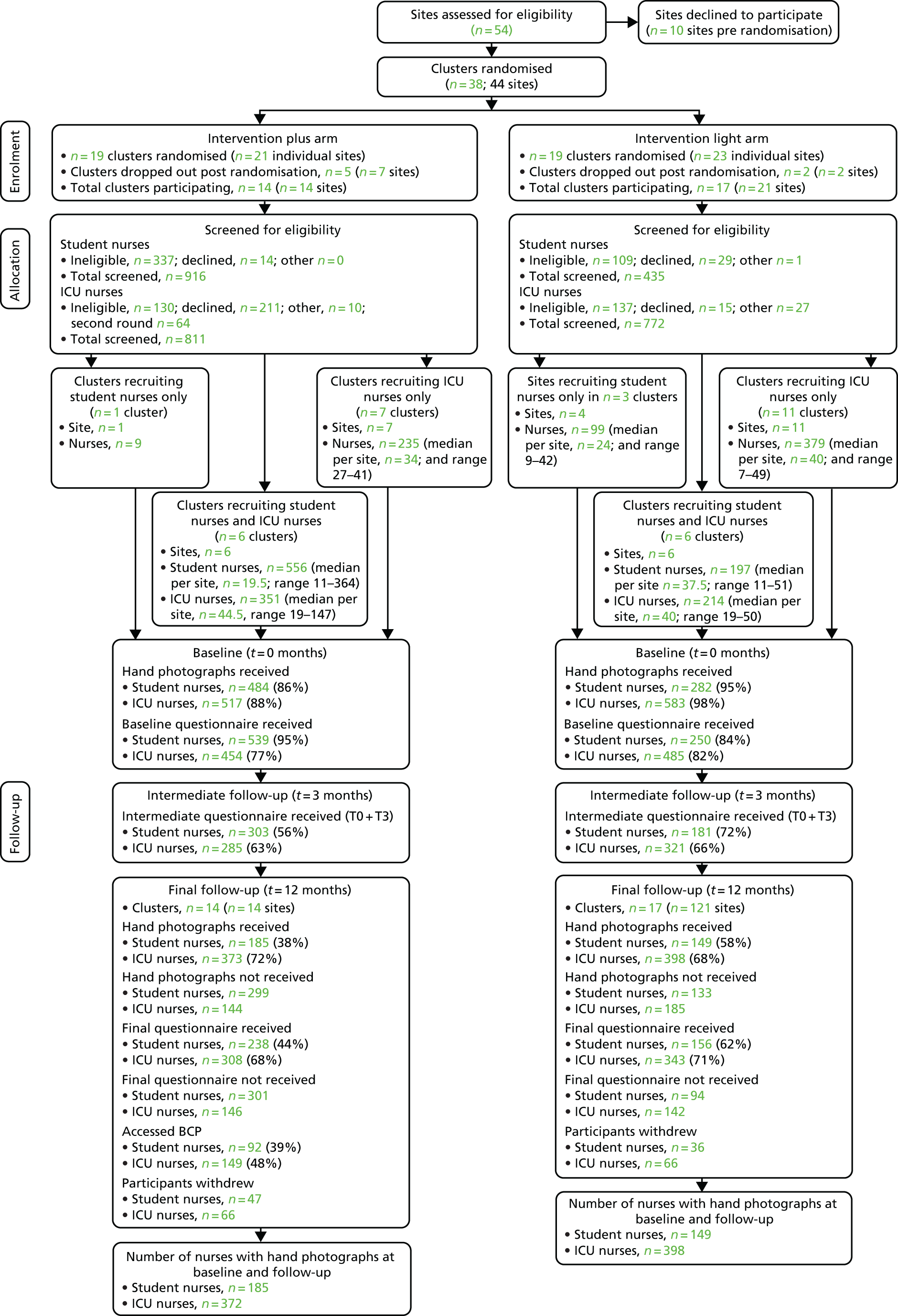
It is important to note that, in the analysis of the results, each site was analysed separately, that is, 35 sites rather than 31 clusters. The rationale for this decision was that two clusters each comprised two sites, one site that recruited ICU nurses only and the other site that recruited student nurses only. As a result, sites would have been analysed separately. Using site-level analysis rather than cluster-level analysis may have influenced only one cluster, which contained three sites. Within this cluster, one site recruited ICU nurses only and two sites recruited student nurses. As the analysis of the primary outcome for student nurses was ordinary logistic regression (rather than multilevel logistic regression because of the failure for the latter to converge), results for the primary outcome would not be changed if cluster-level analysis was used. Secondary outcomes, health beliefs and behaviours for these two sites were analysed as if they were one cluster and there was no difference in the results.
Baseline data
Table 3 describes baseline information about participants’ characteristics and (primary and secondary) outcomes separately for student and ICU/SCBU nurses and by intervention group. The outcomes included dermatitis assessed at baseline, subjective norms and attitudes towards use of hand cream, hand rubs and gloves and towards hand-washing and contacting occupational health. For both types of nurses, demographic characteristics and outcomes were very similar between the two intervention groups, showing that the randomisation achieved adequate balance. The only exception was the difference in baseline prevalence of the primary outcome among student nurses (15.1% vs. 8.1% in the intervention plus and light arms, respectively). This difference could be attributed only to chance.
| Characteristics | Nurses | |||||
|---|---|---|---|---|---|---|
| Student | ICU/SCBU | |||||
| Intervention | All (N = 789 in 17 clusters) | Intervention | All (N = 939 in 30 clusters) | |||
| Plus (N = 539 in seven clusters) | Light (N = 250 in 10 clusters) | Plus (N = 454 in 13 clusters) | Light (N = 485 in 17 clusters) | |||
| Sex, n (%) female | 510 (94.6) | 233 (93.2) | 743 (94.2) | 389 (85.7) | 410 (84.5) | 799 (85.1) |
| Age (years), median (IQR) | 21 (19–26) | 22 (19–29) | 22 (19–27) | 36 (27–45) | 36 (27–45) | 36 (27–45) |
| Hours worked per week, mean (SD) | – | – | – | 36.7 (2.6) | 36.7 (2.6) | 36.7 (2.6) |
| Atopic tendency, n (%) | 531 (98.5) | 238 (95.2) | 769 (97.5) | 283 (62.3) | 289 (59.6) | 572 (60.9) |
| Self-reported atopic dermatitis, n (%) | 145 (26.9) | 65 (26.0) | 210 (26.6) | 58 (12.8) | 63 (13.0) | 121 (12.9) |
Procedure to check for bias
A full list of participating sites is given in Table 4.
| Intervention and participating sites | Nurses | |||||||
|---|---|---|---|---|---|---|---|---|
| Student | ICU/SCBU | |||||||
| n | Sex, % female | Age in years, median (IQR) | Dermatitis (%) | n | Sex, % female | Age in years, median (IQR) | Dermatitis (%) | |
| Intervention plus | ||||||||
| East Kent Hospitals University NHS Foundation Trust | – | – | – | – | 25 | 80.0 | 36 (30–47) | 10.3 |
| Guy’s and St Thomas’ NHS Foundation Trust | 124 | 92.7 | 23 (19–26) | 13.6 | 99 | 86.9 | 30 (26–40) | 9.7 |
| Kettering General Hospital NHS Foundation Trust | 15 | 86.7 | 23 (19–28) | 20.0 | 47 | 91.7 | 38 (29–49) | 20.8 |
| Lancashire Teaching Hospitals NHS Foundation Trust | 8 | 87.5 | 26 (20–36) | 12.5 | – | – | – | – |
| Luton and Dunstable University Hospital NHS Foundation Trust | – | – | – | – | 22 | 81.8 | 42 (37–48) | 11.1 |
| Norfolk and Norwich University Hospitals NHS Foundation Trust | – | – | – | – | 27 | 96.3 | 38 (26–47) | 28.6 |
| Plymouth Hospitals NHS Trust | – | – | – | – | 36 | 69.4 | 38 (34–45) | 17.1 |
| Ipswich Hospital NHS Trust | 11 | 90.9 | 25 (21–34) | 9.1 | 36 | 83.3 | 39 (28–45) | 8.9 |
| Newcastle Upon Tyne Hospitals NHS Foundation Trust | 7 | 71.4 | 28 (23–32) | 36.4 | 9 | 77.8 | 32 (24–40) | 16.7 |
| University Hospital Southampton NHS Foundation Trust | 362 | 96.1 | 21 (19–26) | 14.4 | 22 | 90.9 | 28 (24–37) | 25.6 |
| York Teaching Hospital NHS Foundation Trust | – | – | – | – | 30 | 90.0 | 30 (25–43) | 33.3 |
| Peterborough and Stamford Hospitals NHS Foundation Trust | 12 | 100.0 | 33 (25–37) | 13.3 | 40 | 90.0 | 44 (36–49) | 5.0 |
| NHS Lanarkshire | – | – | – | – | 26 | 80.8 | 45 (35–49) | 14.3 |
| Frimley Health NHS Foundation Trust | – | – | – | – | 34 | 85.3 | 36 (27–43) | 14.7 |
| Intervention light | ||||||||
| Hywel Dda University Health Board | – | – | – | – | 30 | 93.3 | 40 (30–49) | 26.8 |
| Cambridge University Hospitals NHS Foundation Trust | 17 | 88.2 | 20 (19–25) | 35.5 | 49 | 73.5 | 31 (27–40) | 16.0 |
| Hull and East Yorkshire Hospitals NHS Trusta | – | – | – | – | 36 | 91.7 | 36 (26–47) | 17.5 |
| Industrial Diagnosticsa (University of Nottingham) | 22 | 95.5 | 24 (20–29) | 0.0 | – | – | – | – |
| Milton Keynes University Hospital NHS Foundation Trust | 11 | 100.0 | 19 (18–29) | 18.2 | 19 | 94.7 | 43 (29–51) | 21.1 |
| Northampton General Hospital NHS Trust | 41 | 90.2 | 21 (19–31) | 3.9 | 16 | 81.0 | 30 (26–41) | 4.2 |
| North Tees and Hartlepool NHS Foundation Trust | – | – | – | – | 49 | 89.8 | 38 (27–45) | 28.6 |
| Nottingham University Hospitals NHS Trusta | – | – | – | – | 23 | 69.6 | 33 (25–44) | 33.3 |
| Royal Papworth Hospital NHS Foundation Trust | – | – | – | – | 38 | 86.8 | 37 (28–42) | 17.5 |
| Pennine Acute Hospitals NHS Trusta | – | – | – | – | 16 | 81.3 | 38 (36–43) | 17.6 |
| Royal Berkshire NHS Foundation Trust | – | – | – | – | 40 | 82.5 | 39 (29–47) | 8.9 |
| St George’s University Hospitals NHS Foundation Trust | 20 | 90.0 | 22 (20–27) | 5.4 | 23 | 91.3 | 29 (24–42) | 5.1 |
| University Hospitals Birmingham NHS Foundation Trust | 24 | 100.0 | 21 (19–28) | 16.3 | 25 | 80.0 | 29 (26–41) | 10.0 |
| University Hospitals of Leicester NHS Trust | 37 | 91.9 | 24 (20–30) | 8.1 | 32 | 75.0 | 29 (25–41) | 7.3 |
| University of Manchestera | 9 | 100.0 | 20 (19–22) | 11.1 | – | – | – | – |
| University of Hulla | 42 | 95.2 | 23 (19–29) | 2.4 | – | – | – | – |
| University of Salforda | 17 | 88.2 | 29 (26–34) | 4.2 | – | – | – | – |
| Wye Valley NHS Trust | – | – | – | – | 24 | 95.8 | 37 (29–50) | 7.1 |
| West Suffolk NHS Foundation Trust | – | – | – | – | 24 | 79.2 | 46 (30–51) | 47.1 |
| Salisbury NHS Foundation Trust | – | – | – | – | 29 | 90.0 | 39 (31–45) | 6.5 |
| Homerton University Hospital NHS Foundation Trust | – | – | – | – | 6 | 83.3 | 25 (23–30) | 0.0 |
To explore any potential sources of bias, follow-up completion rates were calculated separately for student and ICU/SCBU nurses and for the two arms of the trial (Table 5). The table shows counts of participants for each category of baseline characteristics and objectively assessed dermatitis among nurses who returned baseline questionnaires (n = 1728), nurses who returned baseline and intermediate questionnaires (n = 1090), and nurses who returned baseline and follow-up questionnaires (n = 1045). For the last two groups (i.e. nurses who returned baseline and intermediate questionnaires and nurses who returned baseline and follow-up questionnaires), the proportion of participants in each category of baseline characteristics is also presented as a proportion of the total number of participants (those who returned baseline questionnaires) in the same category (completion rate) and shown in brackets. Completion rates of the intermediate and follow-up questionnaires were 61% and 50%, respectively, among student nurses, and 65% and 69%, respectively, among ICU nurses. The completion rates were slightly higher in females than in males, and higher for higher age categories. The rates were also somewhat higher among those nurses with dermatitis assessed at baseline. Overall, the difference in completion rates were small between the different baseline categories, indicating that a bias as a result of a loss to follow-up was unlikely.
| Characteristics | Sample, n (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline questionnaire (N = 1728) | Baseline and intermediate questionnaire (N = 1090) | Baseline and follow-up questionnaire (N = 1045) | ||||||||||
| Nurses | Nurses | Nurses | ||||||||||
| Student | ICU | Student | ICU | Student | ICU | |||||||
| Intervention plus (n = 539) | Intervention light (n = 250) | Intervention plus (n = 454) | Intervention light (n = 485) | Intervention plus (n = 303; 56.2) | Intervention light (n = 181; 72.4) | Intervention plus (n = 285; 62.8) | Intervention light (n = 321; 66.2) | Intervention plus (n = 238; 44.2) | Intervention light (n = 156; 62.4) | Intervention plus (n = 308; 67.8) | Intervention light (n = 343; 70.7) | |
| Sex | ||||||||||||
| Female | 510 | 233 | 389 | 410 | 290 (56.9) | 168 (72.1) | 249 (64.0) | 279 (68.0) | 227 (44.5) | 147 (63.1) | 266 (68.4) | 286 (69.8) |
| Male | 29 | 17 | 65 | 75 | 13 (44.8) | 13 (76.5) | 36 (55.4) | 42 (56.0) | 11 (37.9) | 9 (52.9) | 42 (64.6) | 57 (76.0) |
| Age (years) | ||||||||||||
| 18–24 | 361 | 143 | 59 | 61 | 185 (51.2) | 105 (73.4) | 34 (57.6) | 38 (62.3) | 149 (41.3) | 89 (62.2) | 35 (59.3) | 43 (70.5) |
| 25–35 | 140 | 72 | 154 | 170 | 91 (65.0) | 51 (70.8) | 96 (62.3) | 102 (60.0) | 68 (48.6) | 45 (62.5) | 97 (63.0) | 107 (62.9) |
| 35–66 | 38 | 25 | 240 | 248 | 27 (71.1) | 23 (92.0) | 155 (64.6) | 179 (72.2) | 21 (55.3) | 21 (84.0) | 176 (73.3) | 193 (77.8) |
| Hours worked per week | ||||||||||||
| < 38 | – | – | 434 | 465 | – | – | 273 (62.9) | 307 (66.0) | – | – | 291 (67.1) | 330 (71.0) |
| ≥ 38 | – | – | 16 | 15 | – | – | 9 (56.3) | 10 (66.7) | – | – | 13 (81.3) | 11 (73.3) |
| Atopic tendency | ||||||||||||
| No | 8 | 12 | 171 | 195 | 5 (62.5) | 7 (58.3) | 110 (64.3) | 130 (66.7) | 5 (62.5) | 8 (66.7) | 123 (71.9) | 136 (69.7) |
| Yes | 531 | 238 | 283 | 289 | 298 (56.1) | 174 (73.1) | 175 (61.8) | 190 (65.7) | 233 (43.9) | 148 (62.2) | 185 (65.4) | 206 (71.3) |
| Self-reported atopic dermatitis | ||||||||||||
| No | 251 | 125 | 272 | 289 | 136 (54.2) | 91 (72.8) | 167 (61.4) | 202 (69.9) | 107 (42.6) | 77 (61.6) | 179 (65.8) | 213 (73.7) |
| Yes | 145 | 65 | 58 | 63 | 83 (57.2) | 48 (73.8) | 37 (63.8) | 41 (65.1) | 61 (42.1) | 45 (69.2) | 42 (72.4) | 36 (57.1) |
| Self-rated health score | ||||||||||||
| 9–85 | 241 | 100 | 173 | 191 | 129 (53.5) | 75 (75.0) | 99 (57.2) | 129 (67.5) | 104 (43.2) | 59 (59.0) | 113 (65.3) | 130 (68.1) |
| 86–95 | 229 | 110 | 184 | 188 | 126 (55.0) | 76 (69.1) | 124 (67.4) | 125 (66.5) | 102 (44.5) | 73 (66.4) | 128 (69.6) | 137 (72.9) |
| 96–100 | 63 | 36 | 96 | 99 | 46 (73.0) | 26 (72.2) | 61 (63.5) | 63 (63.6) | 31 (49.2) | 22 (61.1) | 67 (69.8) | 71 (71.7) |
| Objectively assessed dermatitis | ||||||||||||
| No | 404 | 215 | 376 | 400 | 225 (55.7) | 150 (69.8) | 235 (62.5) | 263 (65.8) | 176 (43.6) | 133 (61.9) | 255 (67.8) | 281 (70.3) |
| Yes | 68 | 23 | 74 | 78 | 45 (66.2) | 19 (82.6) | 48 (64.9) | 51 (65.4) | 38 (55.9) | 13 (56.5) | 51 (68.9) | 56 (71.8) |
To assess sources of bias further, summary statistics [means (SDs)] were produced for the 25 health belief outcomes in the three samples of participants [i.e. those nurses who returned baseline questionnaires (n = 1728), those nurses who returned baseline and intermediate questionnaires (n = 1090) and those nurses who returned baseline and follow-up questionnaires (n = 1045)] and separately for the two types of nurses and the two arms of the trial. For those nurses with baseline and intermediate questionnaires (n = 1090), and for those nurses with baseline and follow-up questionnaires (n = 1045), differences in baseline health beliefs from those nurses who were lost to follow-up (i.e. did not complete intermediate or follow-up questionnaires) were calculated. Overall, baseline health belief scores were very similar among those nurses who completed the baseline and intermediate questionnaires and those who did not. In addition, baseline health belief scores were very similar among those nurses who completed the baseline and follow-up questionnaires and those who did not.
Primary outcome
The primary outcome, that is objective dermatitis, was assessed at two time points (i.e. baseline and follow-up). The numbers of student and ICU/SCBU nurses with dermatitis at baseline and/or follow-up are shown in Table 6. The prevalence rates of dermatitis at each of the two time points of assessment, by intervention arm and separately for student and ICU/SCBU nurses, are also illustrated in Figure 6. Among student nurses in the intervention light arm, the prevalence of dermatitis was 8.1% at baseline and it increased to 11.4% at follow-up, whereas the prevalence of dermatitis in the intervention plus arm decreased slightly from 15.1% at baseline to 10.3% at follow-up (see Figure 6). Among ICU/SCBU nurses in the intervention light arm, the prevalence of dermatitis was very similar at both time points (16%), whereas among those nurses in the intervention plus arm the prevalence of dermatitis decreased from 16.4% to 10.5% (see Figure 6).
| Dermatitis cases as diagnosed by the dermatologist | Nurses (n) | |||
|---|---|---|---|---|
| Student | ICU/SCBU | |||
| Plus (N = 185) | Light (N = 149) | Plus (N = 372) | Light (N = 398) | |
| Nurses without hand dermatitis at either baseline or follow-up | 146 | 124 | 292 | 304 |
| Nurses with hand dermatitis at baseline only | 20 | 8 | 41 | 40 |
| Nurses with hand dermatitis at follow-up only | 11 | 13 | 19 | 30 |
| Nurses with hand dermatitis at both baseline and follow-up | 8 | 4 | 20 | 24 |
FIGURE 6.
Prevalence of objectively assessed dermatitis by intervention arm and time point when dermatitis was assessed (baseline and follow-up), for (a) student and (b) ICU/SCBU nurses.
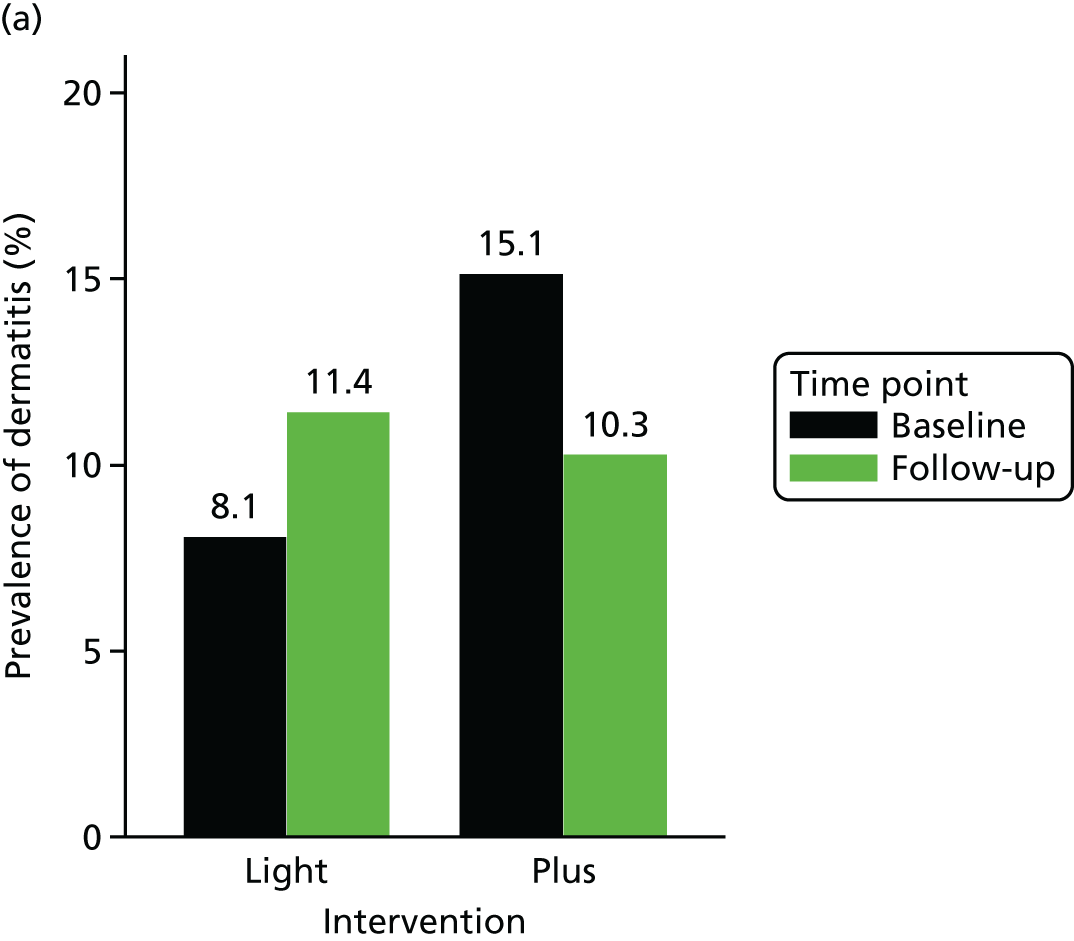
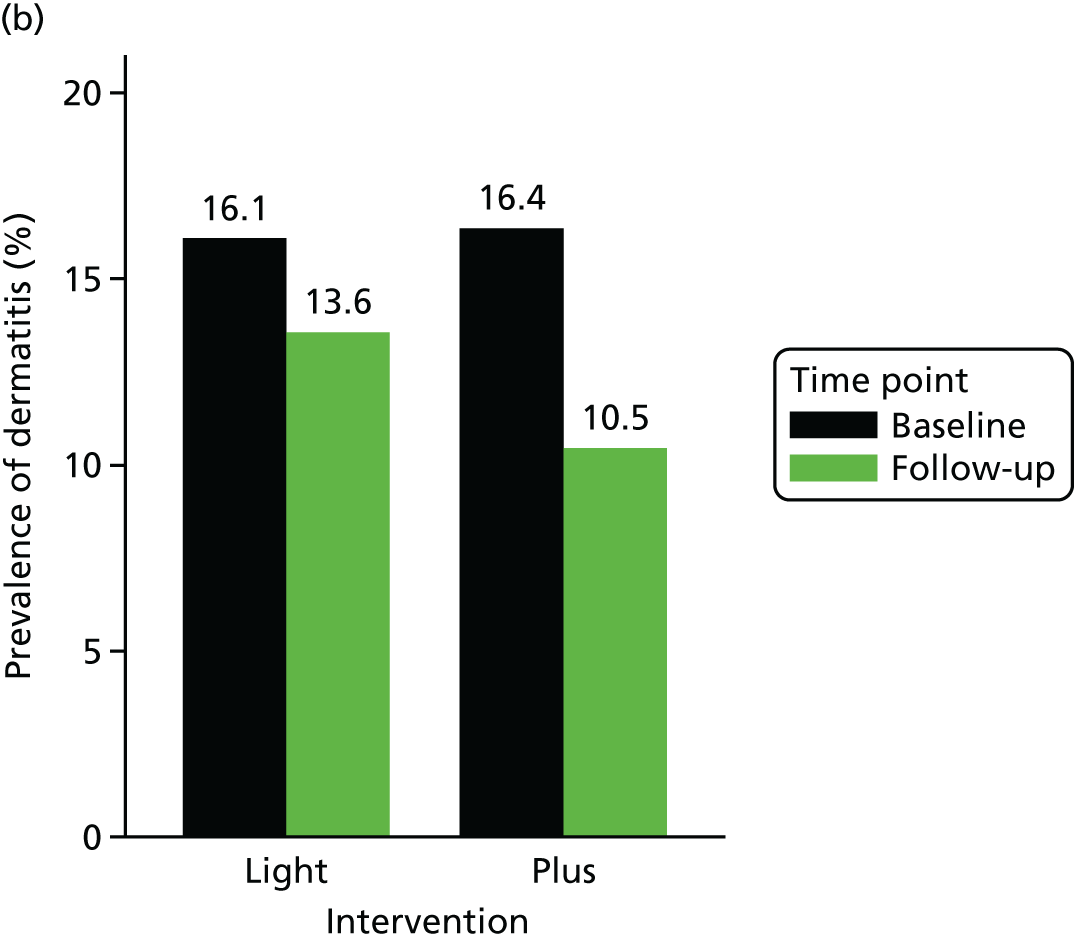
Effect estimates indicated that the intervention was more beneficial (less dermatitis) for those nurses in the intervention plus arm than for those nurses in the intervention light arm, even though the effect was not statistically significant for either student or ICU/SCBU nurses (Table 7). The effect of the intervention was slightly attenuated after adjusting for age, sex and follow-up time among student nurses, whereas it did not change after adjustment among ICU nurses.
| Nurses | Dermatitis | n | OR (95% CI) |
|---|---|---|---|
| Student nursesa | For baseline dermatitis | 334 | 1.35 (0.66 to 2.80) |
| For baseline dermatitis, age and follow-up time | 327 | 1.26 (0.59 to 2.69) | |
| ICU nurses | For baseline dermatitis | 770 | 1.39 (0.86 to 2.25) |
| For baseline dermatitis, sex, age and follow-up time | 744 | 1.41 (0.81 to 2.44) |
Secondary outcomes
Severity of hand dermatitis
At follow-up, 2 out of 36 (5.6%) student nurses and 1 out of 93 (1.1%) ICU nurses with dermatitis at follow-up had severe dermatitis. Owing to the very low number of cases of dermatitis, it was not possible to conduct further analysis of this secondary outcome.
Days lost
The basic descriptive statistical analysis found that of the 324 out of 337 (96.1%) student nurses who answered the days lost question, only four in the intervention plus arm and four in the intervention light arm reported having taken sick leave because of dermatitis. Likewise, of the 459 out of 483 (95.0%) of ICU nurses who answered the days lost question, only three in the intervention plus arm and four in the intervention light arm reported having taken sick leave because of dermatitis. The sparsity of the data meant that this aspect of the data would not be analysed in regression modelling.
Health beliefs
Table 8 shows descriptive statistics for each of the 25 health belief scores separately for the two arms of the trial and the two types of nurses among those nurses who returned the baseline and intermediate questionnaires (n = 1090). Similar to Table 8, descriptive statistics of health beliefs scores among those nurses who returned the baseline and 12-month follow-up questionnaires are presented in Table 9. Figure 7 shows a graphical illustration of the change in health beliefs from baseline (x-axis) to the 12-month follow-up (y-axis) separately for those in the intervention light arm (green dots) and intervention plus arm (blue dots), and for student (Figure 7a) and ICU/SCBU nurses (Figure 7b). Among student nurses, those in the intervention light arm had health beliefs scores that were very similar at both baseline and follow-up (green dots lying on the line of equality). In contrast, student nurses in the intervention plus arm had higher health belief scores at follow-up than at baseline (blue dots lying on the left side of the line of equality), indicating a shift towards more positive health beliefs. For ICU/SCBU nurses, the change in health beliefs from baseline to follow-up was smaller and parallel for both nurses in the intervention light and those in the intervention plus arm (both green and blue dots lying to the left side of, but very close to, the line of equality).
| Nurses | Intervention | Time point | |||
|---|---|---|---|---|---|
| Baseline | Intermediate | ||||
| Mean (SD) | Median (range) | Mean (SD) | Median (range) | ||
| Student nurses | |||||
| Use of hand cream | |||||
| Attitude | Plus | 4.2 (0.7) | 4 (4–5) | 4.5 (0.6) | 5 (4–5) |
| Light | 4.2 (0.7) | 4 (4–5) | 4.4 (0.7) | 5 (4–5) | |
| Subjective norm | Plus | 3.7 (0.8) | 4 (3–4) | 4.3 (0.7) | 4 (4–5) |
| Light | 3.8 (0.8) | 4 (3–4) | 4.1 (0.8) | 4 (4–5) | |
| PBC | Plus | 3.8 (0.8) | 4 (3–4) | 4.2 (0.9) | 4 (4–5) |
| Light | 3.9 (0.8) | 4 (3–4) | 4.0 (0.9) | 4 (4–5) | |
| Intentions | Plus | 3.8 (0.9) | 4 (3–4) | 4.2 (0.9) | 4 (4–5) |
| Light | 3.9 (0.9) | 4 (3–4) | 3.9 (1.0) | 4 (4–5) | |
| Action plans | Plus | 2.3 (1.0) | 2 (2–3) | 2.8 (1.2) | 3 (2–4) |
| Light | 2.4 (1.0) | 2 (2–3) | 2.6 (1.1) | 2 (2–3) | |
| Consulting occupational health if symptoms occur | |||||
| Attitude | Plus | 4.2 (0.6) | 4 (4–5) | 4.3 (0.8) | 4 (4–5) |
| Light | 4.2 (0.7) | 4 (4–5) | 4.3 (0.8) | 4 (4–5) | |
| Subjective norm | Plus | 4.1 (0.7) | 4 (4–5) | 4.2 (0.7) | 4 (4–5) |
| Light | 4.0 (0.8) | 4 (4–5) | 4.1 (0.8) | 4 (4–5) | |
| PBC | Plus | 4.2 (0.7) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) |
| Light | 4.2 (0.7) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) | |
| Intentions | Plus | 4.1 (0.7) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) |
| Light | 4.0 (0.9) | 4 (4–5) | 4.1 (1.0) | 4 (4–5) | |
| Action plans | Plus | 2.7 (1.0) | 3 (2–3) | 2.9 (1.2) | 3 (2–4) |
| Light | 2.8 (1.0) | 3 (2–3) | 2.8 (1.1) | 3 (2–3) | |
| Use of hand rubs | |||||
| Attitude | Plus | 3.4 (1.0) | 4 (3–4) | 3.8 (1.0) | 4 (3–5) |
| Light | 3.5 (1.0) | 4 (3–4) | 3.8 (0.9) | 4 (3–4) | |
| Subjective norm | Plus | 3.6 (0.9) | 4 (3–4) | 4.0 (0.9) | 4 (4–5) |
| Light | 3.7 (0.9) | 4 (3–4) | 4.0 (0.9) | 4 (4–5) | |
| PBC | Plus | 3.6 (1.0) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.8 (1.0) | 4 (3–4) | 4.0 (1.0) | 4 (4–5) | |
| Intentions | Plus | 3.6 (1.1) | 4 (3–4) | 3.9 (1.1) | 4 (3–5) |
| Light | 3.6 (1.1) | 4 (3–4) | 4.0 (1.0) | 4 (4–5) | |
| Action plans | Plus | 2.6 (1.0) | 3 (2–3) | 3.0 (1.2) | 3 (2–4) |
| Light | 2.7 (0.9) | 3 (2–3) | 2.9 (1.1) | 3 (2–4) | |
| Use of gloves | |||||
| Attitude | Plus | 3.9 (0.9) | 4 (4–4) | 4.3 (0.8) | 4 (4–5) |
| Light | 4.0 (0.8) | 4 (4–5) | 4.2 (0.7) | 4 (4–5) | |
| Subjective norm | Plus | 3.8 (0.9) | 4 (3–4) | 4.2 (0.8) | 4 (4–5) |
| Light | 3.9 (0.8) | 4 (3–5) | 4.1 (0.8) | 4 (4–5) | |
| PBC | Plus | 3.9 (0.8) | 4 (4–4) | 4.3 (0.8) | 4 (4–5) |
| Light | 4.0 (0.8) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) | |
| Intentions | Plus | 3.9 (0.9) | 4 (3–4) | 4.2 (0.8) | 4 (4–5) |
| Light | 4.0 (0.9) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) | |
| Action plans | Plus | 2.8 (1.0) | 3 (2–3) | 3.2 (1.2) | 3 (2–4) |
| Light | 3.0 (1.1) | 3 (2–4) | 3.0 (1.1) | 3 (2–4) | |
| Hand-washing | |||||
| Attitude | Plus | 3.5 (1.1) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.8 (1.0) | 4 (3–5) | 4.0 (1.0) | 4 (4–5) | |
| Subjective norm | Plus | 3.4 (1.1) | 3 (3–4) | 4.0 (1.0) | 4 (4–5) |
| Light | 3.7 (1.0) | 4 (3–4) | 4.0 (1.0) | 4 (3–5) | |
| PBC | Plus | 3.5 (1.2) | 4 (3–4) | 4.0 (1.0) | 4 (4–5) |
| Light | 3.8 (1.1) | 4 (3–5) | 3.9 (1.0) | 4 (4–5) | |
| Intentions | Plus | 3.1 (1.3) | 3 (2–4) | 3.7 (1.1) | 4 (3–5) |
| Light | 3.3 (1.2) | 4 (2–4) | 3.7 (1.2) | 4 (3–5) | |
| Action plans | Plus | 2.9 (1.1) | 3 (2–4) | 3.2 (1.2) | 3 (2–4) |
| Light | 3.0 (1.1) | 3 (2–4) | 3.0 (1.2) | 3 (2–4) | |
| ICU/SCBU nurses | |||||
| Use of hand cream | |||||
| Attitude | Plus | 4.2 (0.7) | 4 (4–5) | 4.4 (0.6) | 4 (4–5) |
| Light | 4.1 (0.8) | 4 (4–5) | 4.3 (0.7) | 4 (4–5) | |
| Subjective norm | Plus | 3.9 (0.8) | 4 (3–4) | 4.1 (0.8) | 4 (4–5) |
| Light | 4.0 (0.8) | 4 (4–4) | 4.1 (0.8) | 4 (4–5) | |
| PBC | Plus | 3.6 (1.0) | 4 (3–4) | 3.8 (1.0) | 4 (3–4) |
| Light | 3.5 (1.1) | 4 (3–4) | 3.6 (1.0) | 4 (3–4) | |
| Intentions | Plus | 3.4 (1.2) | 4 (3–4) | 3.9 (1.0) | 4 (4–5) |
| Light | 3.4 (1.2) | 4 (3–4) | 3.6 (1.1) | 4 (3–4) | |
| Action plans | Plus | 2.3 (1.0) | 2 (2–3) | 2.9 (1.1) | 3 (2–4) |
| Light | 2.3 (1.1) | 2 (1–3) | 2.6 (1.1) | 2 (2–3) | |
| Consulting occupational health if symptoms occur | |||||
| Attitude | Plus | 4.0 (0.8) | 4 (4–4) | 4.2 (0.8) | 4 (4–5) |
| Light | 4.0 (0.8) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) | |
| Subjective norm | Plus | 4.1 (0.7) | 4 (4–4) | 4.3 (0.7) | 4 (4–5) |
| Light | 4.1 (0.7) | 4 (4–5) | 4.3 (0.7) | 4 (4–5) | |
| PBC | Plus | 4.1 (0.7) | 4 (4–4) | 4.3 (0.6) | 4 (4–5) |
| Light | 4.2 (0.7) | 4 (4–5) | 4.4 (0.7) | 4 (4–5) | |
| Intentions | Plus | 3.8 (0.9) | 4 (3–4) | 4.2 (0.8) | 4 (4–5) |
| Light | 3.9 (0.9) | 4 (4–4) | 4.2 (0.8) | 4 (4–5) | |
| Action plans | Plus | 2.8 (1.1) | 3 (2–4) | 3.2 (1.1) | 3 (3–4) |
| Light | 2.9 (1.1) | 3 (2–4) | 3.0 (1.1) | 3 (2–4) | |
| Use of hand rubs | |||||
| Attitude | Plus | 3.6 (1.0) | 4 (3–4) | 3.9 (0.9) | 4 (3–5) |
| Light | 3.4 (1.1) | 4 (3–4) | 3.5 (1.1) | 4 (3–4) | |
| Subjective norm | Plus | 3.9 (0.8) | 4 (4–4) | 4.0 (0.8) | 4 (4–5) |
| Light | 3.8 (0.9) | 4 (3–4) | 3.9 (1.0) | 4 (3–5) | |
| PBC | Plus | 3.8 (0.9) | 4 (4–4) | 4.1 (0.8) | 4 (4–5) |
| Light | 3.7 (1.1) | 4 (3–4) | 3.9 (1.1) | 4 (4–5) | |
| Intentions | Plus | 3.6 (1.1) | 4 (3–4) | 3.9 (1.0) | 4 (4–5) |
| Light | 3.4 (1.2) | 4 (2–4) | 3.6 (1.1) | 4 (3–4) | |
| Action plans | Plus | 2.9 (1.1) | 3 (2–4) | 3.3 (1.1) | 3 (3–4) |
| Light | 2.9 (1.1) | 3 (2–4) | 2.9 (1.1) | 3 (2–4) | |
| Use of gloves | |||||
| Attitude | Plus | 4.1 (0.7) | 4 (4–5) | 4.2 (0.7) | 4 (4–5) |
| Light | 4.1 (0.8) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) | |
| Subjective norm | Plus | 4.0 (0.8) | 4 (4–4) | 4.1 (0.8) | 4 (4–5) |
| Light | 3.9 (0.9) | 4 (4–4) | 4.0 (1.0) | 4 (4–5) | |
| PBC | Plus | 4.0 (0.8) | 4 (4–4) | 4.1 (0.8) | 4 (4–5) |
| Light | 3.9 (0.9) | 4 (4–5) | 4.0 (0.9) | 4 (4–5) | |
| Intentions | Plus | 4.1 (0.8) | 4 (4–5) | 4.1 (0.8) | 4 (4–5) |
| Light | 4.0 (0.9) | 4 (4–5) | 4.1 (0.9) | 4 (4–5) | |
| Action plans | Plus | 3.1 (1.1) | 3 (2–4) | 3.4 (1.1) | 3 (3–4) |
| Light | 3.1 (1.1) | 3 (2–4) | 3.2 (1.1) | 3 (2–4) | |
| Hand-washing | |||||
| Attitude | Plus | 3.8 (1.0) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.8 (1.1) | 4 (3–5) | 4.0 (1.0) | 4 (4–5) | |
| Subjective norm | Plus | 3.8 (0.9) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.8 (1.0) | 4 (3–5) | 4.0 (1.0) | 4 (4–5) | |
| PBC | Plus | 3.8 (1.1) | 4 (3–5) | 4.1 (1.0) | 4 (4–5) |
| Light | 3.7 (1.1) | 4 (3–5) | 3.9 (1.0) | 4 (4–5) | |
| Intentions | Plus | 3.5 (1.2) | 4 (2–4) | 3.9 (1.0) | 4 (4–5) |
| Light | 3.5 (1.2) | 4 (2–4) | 3.7 (1.1) | 4 (3–5) | |
| Action plans | Plus | 3.0 (1.1) | 3 (2–4) | 3.3 (1.1) | 3 (3–4) |
| Light | 3.1 (1.2) | 3 (2–4) | 3.1 (1.2) | 3 (2–4) | |
| Nurses | Intervention | Time point | |||
|---|---|---|---|---|---|
| Baseline | 12-month follow-up | ||||
| Mean (SD) | Median (range) | Mean (SD) | Median (range) | ||
| Student nurses | |||||
| Use of hand cream | |||||
| Attitude | Plus | 4.2 (0.7) | 4 (4–5) | 4.6 (0.6) | 5 (4–5) |
| Light | 4.2 (0.7) | 4 (4–5) | 4.5 (0.7) | 5 (4–5) | |
| Subjective norm | Plus | 3.8 (0.8) | 4 (3–4) | 4.2 (0.7) | 4 (4–5) |
| Light | 3.8 (0.8) | 4 (3–4) | 4.1 (0.7) | 4 (4–5) | |
| PBC | Plus | 3.8 (0.9) | 4 (3–4) | 4.2 (0.9) | 4 (4–5) |
| Light | 3.9 (0.8) | 4 (3–4) | 4.0 (0.9) | 4 (4–5) | |
| Intentions | Plus | 3.8 (0.9) | 4 (3–4) | 4.2 (0.9) | 4 (4–5) |
| Light | 3.9 (0.9) | 4 (3–4) | 3.9 (1.0) | 4 (4–5) | |
| Action plans | Plus | 2.3 (1.0) | 2 (2–3) | 2.9 (1.3) | 3 (2–4) |
| Light | 2.4 (1.0) | 2 (2–3) | 2.5 (1.0) | 2 (2–3) | |
| Consulting occupational health if symptoms occur | |||||
| Attitude | Plus | 4.2 (0.7) | 4 (4–5) | 4.3 (0.8) | 4 (4–5) |
| Light | 4.2 (0.7) | 4 (4–5) | 4.3 (0.8) | 4 (4–5) | |
| Subjective norm | Plus | 4.1 (0.7) | 4 (4–5) | 4.2 (0.7) | 4 (4–5) |
| Light | 4.1 (0.8) | 4 (4–5) | 4.1 (0.8) | 4 (4–5) | |
| PBC | Plus | 4.2 (0.7) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) |
| Light | 4.3 (0.7) | 4 (4–5) | 4.2 (0.9) | 4 (4–5) | |
| Intentions | Plus | 4.1 (0.8) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) |
| Light | 4.1 (0.9) | 4 (4–5) | 4.1 (0.9) | 4 (4–5) | |
| Action plans | Plus | 2.8 (1.1) | 3 (2–3) | 2.9 (1.2) | 3 (2–4) |
| Light | 2.8 (1.0) | 3 (2–3) | 2.7 (1.0) | 3 (2–3) | |
| Use of hand rubs | |||||
| Attitude | Plus | 3.4 (1.0) | 4 (3–4) | 3.8 (1.0) | 4 (3–5) |
| Light | 3.5 (1.0) | 4 (3–4) | 3.8 (0.9) | 4 (3–4) | |
| Subjective norm | Plus | 3.5 (1.0) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.7 (0.9) | 4 (3–4) | 4.0 (0.9) | 4 (4–5) | |
| PBC | Plus | 3.6 (1.0) | 4 (3–4) | 4.2 (0.8) | 4 (4–5) |
| Light | 3.8 (1.0) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) | |
| Intentions | Plus | 3.5 (1.1) | 4 (3–4) | 4.0 (1.0) | 4 (4–5) |
| Light | 3.6 (1.1) | 4 (3–4) | 4.0 (0.9) | 4 (4–5) | |
| Action plans | Plus | 2.5 (1.0) | 3 (2–3) | 3.0 (1.2) | 3 (2–4) |
| Light | 2.7 (0.9) | 3 (2–3) | 2.9 (1.1) | 3 (2–4) | |
| Use of gloves | |||||
| Attitude | Plus | 3.9 (0.9) | 4 (4–5) | 4.3 (0.8) | 4 (4–5) |
| Light | 4.0 (0.9) | 4 (4–5) | 4.2 (0.7) | 4 (4–5) | |
| Subjective norm | Plus | 3.8 (0.9) | 4 (3–4) | 4.2 (0.8) | 4 (4–5) |
| Light | 3.9 (0.9) | 4 (3–5) | 4.1 (0.7) | 4 (4–5) | |
| PBC | Plus | 3.9 (0.9) | 4 (3–4) | 4.3 (0.8) | 4 (4–5) |
| Light | 4.0 (0.8) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) | |
| Intentions | Plus | 3.9 (0.9) | 4 (3–4) | 4.2 (0.8) | 4 (4–5) |
| Light | 4.0 (0.9) | 4 (4–5) | 4.2 (0.7) | 4 (4–5) | |
| Action plans | Plus | 2.9 (1.0) | 3 (2–3) | 3.2 (1.3) | 3 (2–4) |
| Light | 3.0 (1.1) | 3 (2–4) | 2.9 (1.1) | 3 (2–4) | |
| Hand-washing | |||||
| Attitude | Plus | 3.5 (1.1) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.8 (1.0) | 4 (3–5) | 3.9 (1.0) | 4 (3–5) | |
| Subjective norm | Plus | 3.4 (1.1) | 3 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.8 (1.0) | 4 (3–5) | 3.9 (1.0) | 4 (3–5) | |
| PBC | Plus | 3.5 (1.1) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.8 (1.1) | 4 (3–5) | 3.9 (1.0) | 4 (4–5) | |
| Intentions | Plus | 3.1 (1.2) | 3 (2–4) | 3.7 (1.1) | 4 (3–5) |
| Light | 3.3 (1.3) | 4 (2–4) | 3.7 (1.1) | 4 (3–5) | |
| Action plans | Plus | 2.8 (1.1) | 3 (2–4) | 3.2 (1.3) | 3 (2–4) |
| Light | 3.1 (1.1) | 3 (2–4) | 2.9 (1.2) | 3 (2–4) | |
| ICU/SCBU nurses | |||||
| Use of hand cream | |||||
| Attitude | Plus | 4.2 (0.8) | 4 (4–5) | 4.5 (0.6) | 5 (4–5) |
| Light | 4.1 (0.8) | 4 (4–5) | 4.3 (0.7) | 4 (4–5) | |
| Subjective norm | Plus | 3.9 (0.8) | 4 (3–4) | 4.1 (0.8) | 4 (4–5) |
| Light | 3.9 (0.8) | 4 (3–4) | 4.1 (0.8) | 4 (4–5) | |
| PBC | Plus | 3.6 (1.0) | 4 (3–4) | 3.9 (0.9) | 4 (4–5) |
| Light | 3.5 (1.1) | 4 (3–4) | 3.6 (1.0) | 4 (3–4) | |
| Intentions | Plus | 3.5 (1.1) | 4 (3–4) | 3.9 (1.0) | 4 (4–5) |
| Light | 3.4 (1.2) | 4 (3–4) | 3.6 (1.1) | 4 (3–4) | |
| Action plans | Plus | 2.4 (1.0) | 2 (2–3) | 3.0 (1.1) | 3 (2–4) |
| Light | 2.3 (1.1) | 2 (1–3) | 2.6 (1.1) | 2 (2–3) | |
| Consulting occupational health if symptoms occur | |||||
| Attitude | Plus | 4.0 (0.8) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) |
| Light | 4.0 (0.8) | 4 (4–4) | 4.2 (0.8) | 4 (4–5) | |
| Subjective norm | Plus | 4.1 (0.7) | 4 (4–5) | 4.3 (0.7) | 4 (4–5) |
| Light | 4.1 (0.7) | 4 (4–5) | 4.3 (0.7) | 4 (4–5) | |
| PBC | Plus | 4.1 (0.7) | 4 (4–5) | 4.3 (0.7) | 4 (4–5) |
| Light | 4.1 (0.8) | 4 (4–5) | 4.3 (0.7) | 4 (4–5) | |
| Intentions | Plus | 3.8 (0.9) | 4 (3–4) | 4.2 (0.8) | 4 (4–5) |
| Light | 3.8 (0.9) | 4 (4–4) | 4.2 (0.8) | 4 (4–5) | |
| Action plans | Plus | 2.9 (1.1) | 3 (2–4) | 3.2 (1.1) | 3 (3–4) |
| Light | 2.9 (1.1) | 3 (2–4) | 3.0 (1.1) | 3 (2–4) | |
| Use of hand rubs | |||||
| Attitude | Plus | 3.5 (1.1) | 4 (3–4) | 3.9 (0.9) | 4 (3–5) |
| Light | 3.4 (1.1) | 4 (3–4) | 3.5 (1.1) | 4 (3–4) | |
| Subjective norm | Plus | 3.8 (0.9) | 4 (3–4) | 4.0 (0.8) | 4 (4–5) |
| Light | 3.7 (0.9) | 4 (3–4) | 3.9 (1.0) | 4 (4–5) | |
| PBC | Plus | 3.7 (1.0) | 4 (4–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.7 (1.1) | 4 (3–4) | 3.9 (1.0) | 4 (4–5) | |
| Intentions | Plus | 3.5 (1.1) | 4 (3–4) | 3.9 (1.0) | 4 (4–5) |
| Light | 3.4 (1.2) | 4 (2–4) | 3.6 (1.2) | 4 (3–4) | |
| Action plans | Plus | 3.0 (1.1) | 3 (2–4) | 3.2 (1.0) | 3 (3–4) |
| Light | 2.9 (1.1) | 3 (2–4) | 2.9 (1.1) | 3 (2–4) | |
| Use of gloves | |||||
| Attitude | Plus | 4.1 (0.8) | 4 (4–5) | 4.3 (0.7) | 4 (4–5) |
| Light | 4.1 (0.8) | 4 (4–5) | 4.2 (0.8) | 4 (4–5) | |
| Subjective norm | Plus | 4.0 (0.8) | 4 (4–4) | 4.1 (0.8) | 4 (4–5) |
| Light | 3.9 (0.9) | 4 (4–5) | 4.0 (1.0) | 4 (4–5) | |
| PBC | Plus | 4.0 (0.8) | 4 (4–5) | 4.1 (0.8) | 4 (4–5) |
| Light | 4.0 (0.9) | 4 (4–5) | 4.1 (0.9) | 4 (4–5) | |
| Intentions | Plus | 4.0 (0.8) | 4 (4–5) | 4.1 (0.9) | 4 (4–5) |
| Light | 4.0 (0.9) | 4 (4–5) | 4.1 (0.9) | 4 (4–5) | |
| Action plans | Plus | 3.2 (1.1) | 3 (2–4) | 3.4 (1.1) | 4 (3–4) |
| Light | 3.1 (1.1) | 3 (2–4) | 3.2 (1.1) | 3 (2–4) | |
| Hand-washing | |||||
| Attitude | Plus | 3.8 (1.0) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.7 (1.2) | 4 (3–5) | 3.9 (1.0) | 4 (4–5) | |
| Subjective norm | Plus | 3.8 (1.0) | 4 (3–4) | 4.1 (0.9) | 4 (4–5) |
| Light | 3.8 (1.1) | 4 (3–5) | 3.9 (1.0) | 4 (3–5) | |
| PBC | Plus | 3.8 (1.1) | 4 (3–5) | 4.1 (1.0) | 4 (4–5) |
| Light | 3.7 (1.2) | 4 (3–5) | 3.9 (1.0) | 4 (3–5) | |
| Intentions | Plus | 3.4 (1.2) | 4 (2–4) | 3.9 (1.0) | 4 (4–5) |
| Light | 3.5 (1.3) | 4 (2–4) | 3.7 (1.2) | 4 (3–5) | |
| Action plans | Plus | 3.1 (1.1) | 3 (2–4) | 3.3 (1.1) | 3 (3–4) |
| Light | 3.0 (1.1) | 3 (2–4) | 3.1 (1.2) | 3 (2–4) | |
FIGURE 7.
Scatterplot of health belief scores assessed at follow-up against health belief scores assessed at baseline separately for (a) student and (b) ICU/SCBU nurses and for the two arms of the trial. The dashed line represents the line of equality.
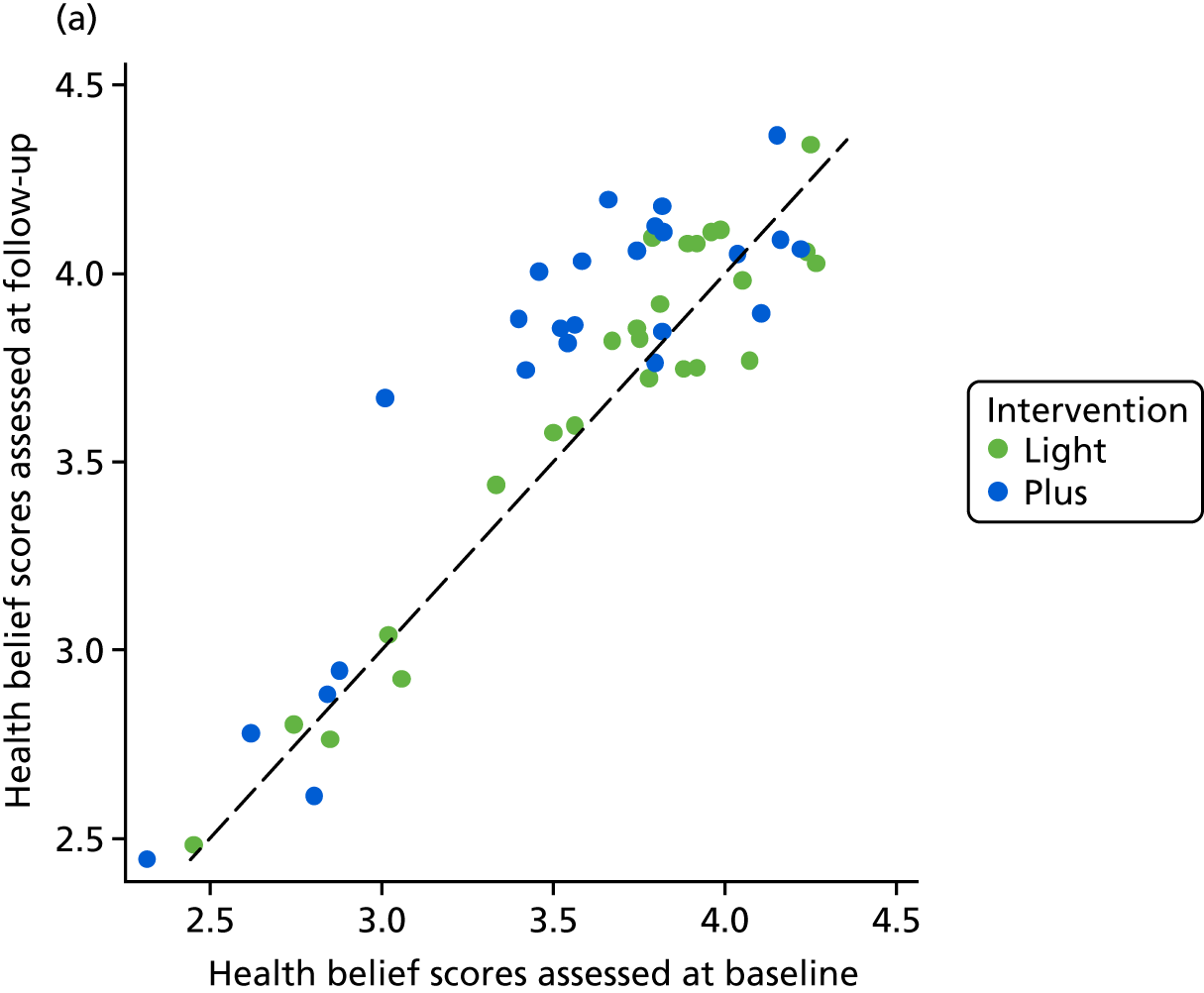
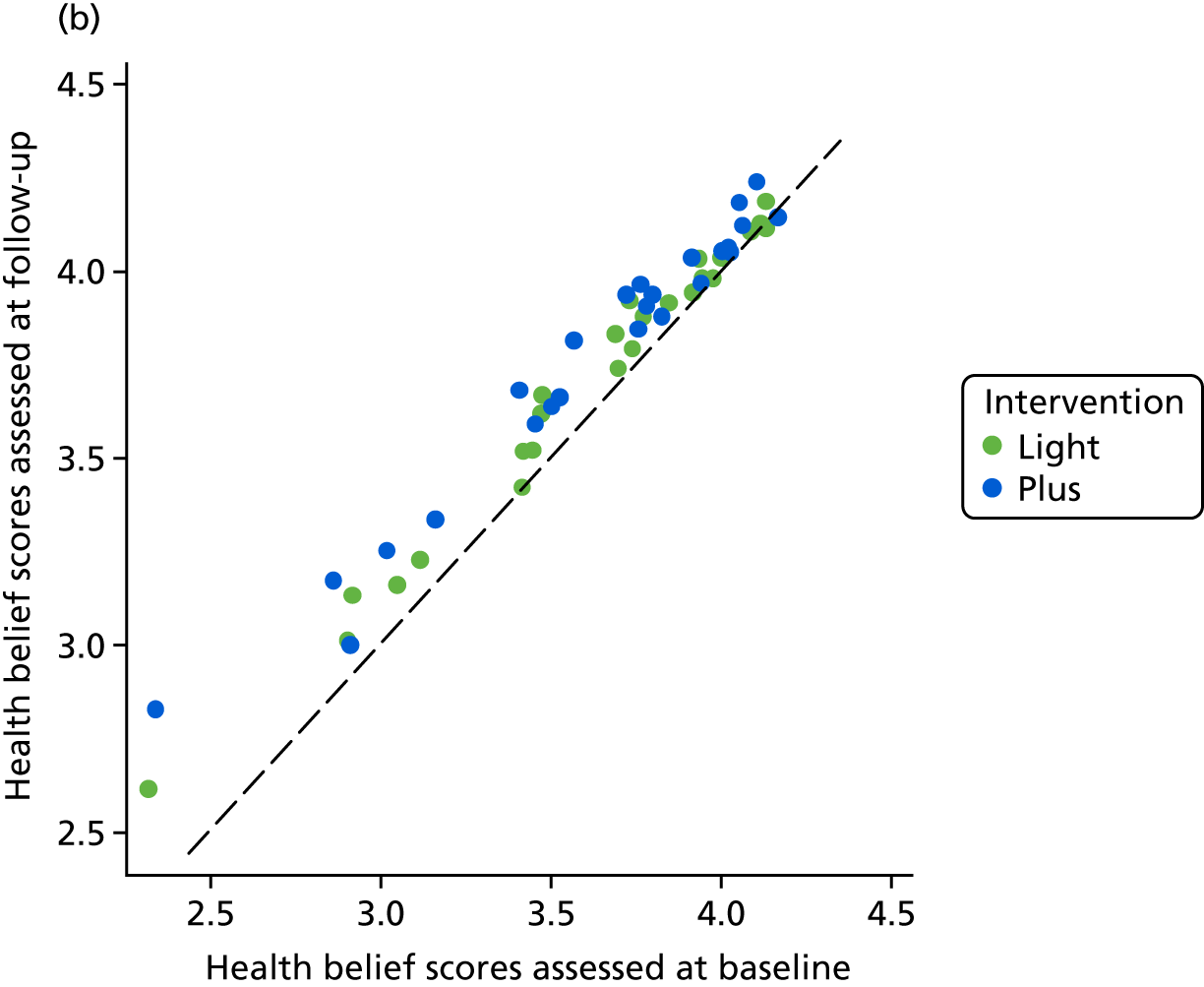
The change in health beliefs was assessed further through regression modelling before and after adjusting for age, sex and follow-up time. In regression modelling, both changes from baseline to after accessing the online BCP and from baseline to the 12-month follow-up were explored. As for the primary outcome (i.e. objectively assessed dermatitis), the change in each health belief score was modelled by using the score at follow-up as the outcome variable, adjusting for the corresponding score at baseline. Effect estimates summarised by regression coefficients and their corresponding 95% CIs are presented in Table 10. A regression coefficient of value β indicates that those nurses in the intervention plus arm changed their average score in the given health belief variable by β units from baseline to follow-up compared with those nurses in the intervention light arm. A graphical display of the effect of intervention on change in health belief scores from baseline to the 12-month follow-up for each type of nurse is shown in Figure 8. In Figure 8, for each of the two graphs (for student nurses and ICU/SCBU nurses), regression coefficients to the left side of the vertical line (regression coefficient 0 = 0) indicate higher scores in the intervention light arm than in the intervention plus arm by a value of β. Regression coefficients to the right side of the vertical line indicate higher scores in the intervention plus arm than in the intervention light arm by a value of β. For student nurses, change was more positive for those in the intervention plus arm than for those in the intervention light arm for almost all health beliefs, except for action plans about consulting occupational health services if symptoms occur. However, almost none of those changes in health belief scores was significantly different between the two intervention arms. An exception to this was change in PBC for use of hand rubs and in intentions to wash hands only when appropriate; both changes were significantly more positive for those nurses in the intervention plus arm than for those in the intervention light arm. Similar to student nurses, ICU/SCBU nurses in the intervention plus arm had a more positive change than ICU/SCBU nurses in the intervention light arm in most of the health beliefs assessed. However, almost none of the changes was statistically different between the two trial arms. The only exception was the change in action plans for use of hand cream, for which the change from baseline to the 12-month follow-up was more positive for nurses in the intervention plus arm than for those in the intervention light arm.
| Nurses | Change period | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| From baseline to after accessing the BCP packagea | From baseline to the 12-month follow-upb | |||||||||||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||||
| ICC | n | β (95% CI) | ICC | n | β (95% CI) | ICC | n | β (95% CI) | ICC | n | β (95% CI) | |
| Student nurses | ||||||||||||
| Use of hand cream | ||||||||||||
| Attitude | 0.03 | 481 | 0.11 (–0.06 to 0.27) | 0.02 | 463 | 0.08 (–0.08 to 0.25) | 0 | 392 | 0.03 (–0.09 to 0.16) | 0 | 383 | 0.04 (–0.09 to 0.17) |
| Subjective norm | 0.03 | 480 | 0.11 (–0.09 to 0.31) | 0.05 | 462 | 0.11 (–0.13 to 0.34) | 0 | 392 | 0.1 (–0.04 to 0.23) | 0 | 383 | 0.08 (–0.06 to 0.22) |
| PBC | 0 | 482 | 0.14 (–0.01 to 0.30) | 0 | 464 | 0.15 (–0.02 to 0.31) | 0 | 393 | 0.1 (–0.09 to 0.30) | 0 | 384 | 0.13 (–0.07 to 0.34) |
| Intentions | 0.01 | 482 | 0.23 (0.02 to 0.44) | 0.004 | 464 | 0.22 (0.03 to 0.41) | 0.02 | 391 | 0.11 (–0.18 to 0.39) | 0 | 382 | 0.08 (–0.13 to 0.29) |
| Action plans | 0.17 | 480 | 0.63 (0.10 to 1.16) | 0.11 | 462 | 0.54 (0.10 to 0.99) | 0.03 | 391 | 0.12 (–0.18 to 0.42) | 0 | 382 | 0.02 (–0.19 to 0.23) |
| Consulting occupational health if symptoms occur | ||||||||||||
| Attitude | 0.003 | 483 | 0 (–0.15 to 0.14) | 0 | 464 | –0.01 (–0.15 to 0.14) | 0.01 | 393 | 0.02 (–0.17 to 0.20) | 0.03 | 384 | 0.04 (–0.20 to 0.27) |
| Subjective norm | 0.07 | 483 | 0.08 (–0.19 to 0.34) | 0.09 | 464 | 0.06 (–0.24 to 0.35) | 0 | 393 | 0.07 (–0.08 to 0.21) | 0 | 384 | 0.06 (–0.09 to 0.21) |
| PBC | 0.01 | 482 | 0.1 (–0.09 to 0.28) | 0.003 | 463 | 0.1 (–0.06 to 0.27) | 0.05 | 392 | 0.19 (–0.06 to 0.44) | 0.04 | 383 | 0.22 (–0.02 to 0.46) |
| Intentions | 0.08 | 482 | 0.2 (–0.10 to 0.50) | 0.07 | 463 | 0.19 (–0.11 to 0.50) | 0.03 | 391 | 0.18 (–0.08 to 0.44) | 0.03 | 382 | 0.21 (–0.06 to 0.48) |
| Action plans | 0.10 | 483 | 0.18 (–0.22 to 0.58) | 0.08 | 464 | 0.14 (–0.24 to 0.52) | 0.08 | 392 | –0.01 (–0.42 to 0.40) | 0.07 | 383 | –0.04 (–0.44 to 0.37) |
| Use of hand rub | ||||||||||||
| Attitude | 0.004 | 484 | –0.01 (–0.21 to 0.18) | 0.03 | 465 | 0 (–0.28 to 0.27) | 0.03 | 393 | 0.18 (–0.09 to 0.44) | 0.01 | 384 | 0.19 (–0.05 to 0.42) |
| Subjective norm | 0.04 | 483 | 0.09 (–0.19 to 0.36) | 0.03 | 464 | 0.09 (–0.16 to 0.34) | 0 | 391 | 0.06 (–0.10 to 0.22) | 0 | 382 | 0.04 (–0.13 to 0.22) |
| PBC | 0.01 | 482 | 0.08 (–0.11 to 0.27) | 0.01 | 463 | 0.08 (–0.13 to 0.29) | 0 | 391 | 0.21 (0.04 to 0.37) | 0.01 | 382 | 0.21 (0.01 to 0.41) |
| Intentions | 0 | 483 | –0.11 (–0.29 to 0.07) | 0.01 | 464 | –0.1 (–0.33 to 0.14) | 0.14 | 392 | 0.12 (–0.32 to 0.56) | 0.16 | 383 | 0.11 (–0.37 to 0.59) |
| Action plans | 0.06 | 484 | 0.26 (–0.11 to 0.62) | 0.05 | 465 | 0.25 (–0.11 to 0.61) | 0 | 393 | 0.03 (–0.17 to 0.24) | 0 | 384 | 0.08 (–0.13 to 0.29) |
| Use of gloves | ||||||||||||
| Attitude | 0 | 484 | 0.1 (–0.04 to 0.24) | 0 | 465 | 0.07 (–0.07 to 0.22) | 0 | 393 | 0.09 (–0.06 to 0.23) | 0 | 384 | 0.06 (–0.09 to 0.20) |
| Subjective norm | 0 | 484 | 0.11 (–0.03 to 0.26) | 0 | 465 | 0.08 (–0.07 to 0.23) | 0 | 392 | 0.01 (–0.15 to 0.18) | 0 | 383 | 0 (–0.17 to 0.16) |
| PBC | 0 | 484 | 0.09 (–0.05 to 0.23) | 0 | 465 | 0.07 (–0.08 to 0.22) | 0 | 393 | 0.03 (–0.12 to 0.18) | 0 | 384 | –0.01 (–0.16 to 0.15) |
| Intentions | 0 | 484 | 0.01 (–0.13 to 0.15) | 0 | 465 | 0.01 (–0.14 to 0.16) | 0 | 392 | 0.07 (–0.08 to 0.22) | 0 | 383 | 0.01 (–0.14 to 0.16) |
| Action plans | 0.07 | 484 | 0.44 (0.05 to 0.83) | 0.06 | 465 | 0.43 (0.06 to 0.79) | 0.02 | 393 | 0.02 (–0.26 to 0.30) | 0.01 | 384 | 0.02 (–0.22 to 0.27) |
| Hand-washing | ||||||||||||
| Attitude | 0 | 483 | 0.16 (–0.00 to 0.33) | 0 | 464 | 0.09 (–0.08 to 0.27) | 0 | 391 | 0.15 (–0.02 to 0.33) | 0 | 382 | 0.17 (–0.01 to 0.34) |
| Subjective norm | 0 | 484 | 0.13 (–0.05 to 0.30) | 0 | 465 | 0.07 (–0.11 to 0.26) | 0 | 392 | 0.12 (–0.06 to 0.30) | 0 | 383 | 0.13 (–0.06 to 0.32) |
| PBC | 0 | 482 | 0.13 (–0.05 to 0.30) | 0 | 463 | 0.04 (–0.15 to 0.22) | 0 | 390 | 0.17 (–0.02 to 0.37) | 0 | 381 | 0.19 (–0.02 to 0.39) |
| Intentions | 0 | 481 | 0.05 (–0.16 to 0.26) | 0.004 | 462 | 0.01 (–0.23 to 0.25) | 0 | 388 | 0.25 (0.04 to 0.45) | 0 | 379 | 0.25 (0.03 to 0.47) |
| Action plans | 0.09 | 483 | 0.42 (–0.02 to 0.86) | 0.09 | 464 | 0.43 (–0.02 to 0.89) | 0 | 392 | 0.02 (–0.19 to 0.24) | 0 | 383 | 0.07 (–0.15 to 0.30) |
| ICU/SCBU nurses | ||||||||||||
| Use of hand cream | ||||||||||||
| Attitude | 0 | 605 | 0.11 (0.02 to 0.21) | 0 | 543 | 0.12 (0.02 to 0.22) | 0 | 648 | 0 (–0.10 to 0.10) | 0.01 | 608 | 0 (–0.12 to 0.12) |
| Subjective norm | 0.04 | 605 | 0.06 (–0.06 to 0.18) | 0.02 | 543 | 0.04 (–0.11 to 0.18) | 0.004 | 648 | –0.01 (–0.12 to 0.11) | 0 | 608 | –0.01 (–0.13 to 0.10) |
| PBC | 0.01 | 604 | 0.12 (–0.03 to 0.27) | 0.02 | 542 | 0.11 (–0.06 to 0.27) | 0 | 648 | 0.13 (–0.00 to 0.26) | 0 | 608 | 0.12 (–0.02 to 0.25) |
| Intentions | 0 | 605 | 0.28 (0.14 to 0.41) | 0 | 543 | 0.28 (0.14 to 0.43) | 0 | 650 | 0.09 (–0.04 to 0.23) | 0 | 610 | 0.06 (–0.08 to 0.20) |
| Action plans | 0.05 | 603 | 0.34 (0.12 to 0.55) | 0.05 | 541 | 0.34 (0.11 to 0.58) | 0.01 | 644 | 0.2 (0.03 to 0.37) | 0 | 604 | 0.17 (0.01 to 0.33) |
| Consulting occupational health if symptoms occur | ||||||||||||
| Attitude | 0 | 605 | –0.03 (–0.14 to 0.07) | 0 | 542 | –0.02 (–0.14 to 0.09) | 0 | 650 | –0.01 (–0.12 to 0.11) | 0 | 610 | –0.02 (–0.14 to 0.11) |
| Subjective norm | 0 | 605 | –0.04 (–0.14 to 0.06) | 0 | 542 | –0.03 (–0.14 to 0.08) | 0 | 650 | 0.06 (–0.05 to 0.16) | 0 | 610 | 0.04 (–0.07 to 0.15) |
| PBC | 0 | 606 | –0.05 (–0.15 to 0.05) | 0 | 543 | –0.07 (–0.17 to 0.04) | 0 | 649 | 0.05 (–0.06 to 0.15) | 0 | 609 | 0.04 (–0.07 to 0.15) |
| Intentions | 0.03 | 606 | 0.03 (–0.12 to 0.17) | 0.04 | 543 | 0.01 (–0.16 to 0.18) | 0 | 646 | 0 (–0.14 to 0.14) | 0 | 606 | –0.01 (–0.15 to 0.13) |
| Action plans | 0.01 | 604 | 0.27 (0.10 to 0.45) | 0 | 541 | 0.26 (0.10 to 0.42) | 0 | 648 | 0.05 (–0.11 to 0.20) | 0 | 608 | 0.05 (–0.11 to 0.21) |
| Use of hand rub | ||||||||||||
| Attitude | 0.02 | 605 | 0.31 (0.13 to 0.48) | 0.004 | 542 | 0.32 (0.16 to 0.48) | 0 | 649 | 0.11 (–0.03 to 0.26) | 0 | 609 | 0.12 (–0.03 to 0.28) |
| Subjective norm | 0.02 | 605 | 0.07 (–0.09 to 0.23) | 0 | 543 | 0.07 (–0.07 to 0.21) | 0 | 649 | 0.06 (–0.06 to 0.19) | 0.06 | 609 | 0 (–0.20 to 0.21) |
| PBC | 0.01 | 603 | 0.16 (0.01 to 0.30) | 0 | 541 | 0.12 (–0.03 to 0.27) | 0 | 648 | 0.09 (–0.05 to 0.22) | 0 | 608 | 0.08 (–0.06 to 0.22) |
| Intentions | 0.02 | 604 | 0.16 (–0.00 to 0.33) | 0 | 541 | 0.15 (–0.00 to 0.30) | 0 | 650 | 0.08 (–0.07 to 0.22) | 0.001 | 610 | 0.07 (–0.08 to 0.22) |
| Action plans | 0.02 | 602 | 0.29 (0.11 to 0.47) | 0.01 | 539 | 0.34 (0.15 to 0.53) | 0.001 | 645 | –0.04 (–0.20 to 0.12) | 0 | 605 | –0.03 (–0.19 to 0.14) |
| Use of gloves | ||||||||||||
| Attitude | 0 | 604 | 0.04 (–0.07 to 0.15) | 0 | 541 | 0.04 (–0.08 to 0.15) | 0 | 649 | 0.02 (–0.09 to 0.14) | 0 | 609 | 0.01 (–0.11 to 0.13) |
| Subjective norm | 0 | 604 | 0.08 (–0.05 to 0.20) | 0 | 541 | 0.04 (–0.09 to 0.18) | 0 | 649 | 0.01 (–0.11 to 0.13) | 0 | 609 | –0.04 (–0.17 to 0.09) |
| PBC | 0 | 604 | 0.04 (–0.09 to 0.17) | 0 | 541 | 0.02 (–0.12 to 0.16) | 0.01 | 651 | 0.06 (–0.08 to 0.20) | 0 | 611 | 0.04 (–0.09 to 0.17) |
| Intentions | 0 | 603 | 0.02 (–0.10 to 0.15) | 0 | 540 | 0 (–0.13 to 0.14) | 0.01 | 650 | 0.07 (–0.08 to 0.21) | 0 | 610 | 0.05 (–0.09 to 0.18) |
| Action plans | 0 | 603 | 0.25 (0.09 to 0.40) | 0 | 540 | 0.27 (0.11 to 0.44) | 0 | 644 | 0.08 (–0.08 to 0.24) | 0 | 604 | 0.08 (–0.08 to 0.24) |
| Hand-washing | ||||||||||||
| Attitude | 0 | 605 | 0.09 (–0.05 to 0.23) | 0 | 542 | 0.06 (–0.09 to 0.21) | 0.01 | 650 | 0.02 (–0.13 to 0.18) | 0 | 610 | 0.02 (–0.13 to 0.16) |
| Subjective norm | 0 | 604 | 0.08 (–0.06 to 0.22) | 0 | 541 | 0.07 (–0.08 to 0.22) | 0 | 650 | 0.06 (–0.08 to 0.19) | 0 | 610 | 0.04 (–0.10 to 0.19) |
| PBC | 0 | 605 | 0.12 (–0.03 to 0.26) | 0 | 542 | 0.1 (–0.06 to 0.26) | 0 | 650 | 0.09 (–0.05 to 0.23) | 0 | 610 | 0.1 (–0.05 to 0.24) |
| Intentions | 0 | 603 | 0.15 (–0.01 to 0.32) | 0 | 540 | 0.13 (–0.05 to 0.30) | 0 | 649 | 0.03 (–0.12 to 0.19) | 0 | 609 | 0.01 (–0.16 to 0.17) |
| Action plans | 0 | 605 | 0.24 (0.08 to 0.39) | 0 | 542 | 0.27 (0.10 to 0.43) | 0.005 | 650 | 0.08 (–0.09 to 0.26) | 0.01 | 610 | 0.09 (–0.09 to 0.27) |
FIGURE 8.
Associations between change in health beliefs scores from baseline to the 12-month follow-up and intervention group after adjusting for age, sex and follow-up time. For each of the two graphs (for student nurses and ICU/SCBU nurses), regression coefficients to the left side of the vertical line (regression coefficient = 0) indicate higher scores in the intervention light arm, and regression coefficients to the right side of the vertical line indicate higher scores in the intervention plus arm.
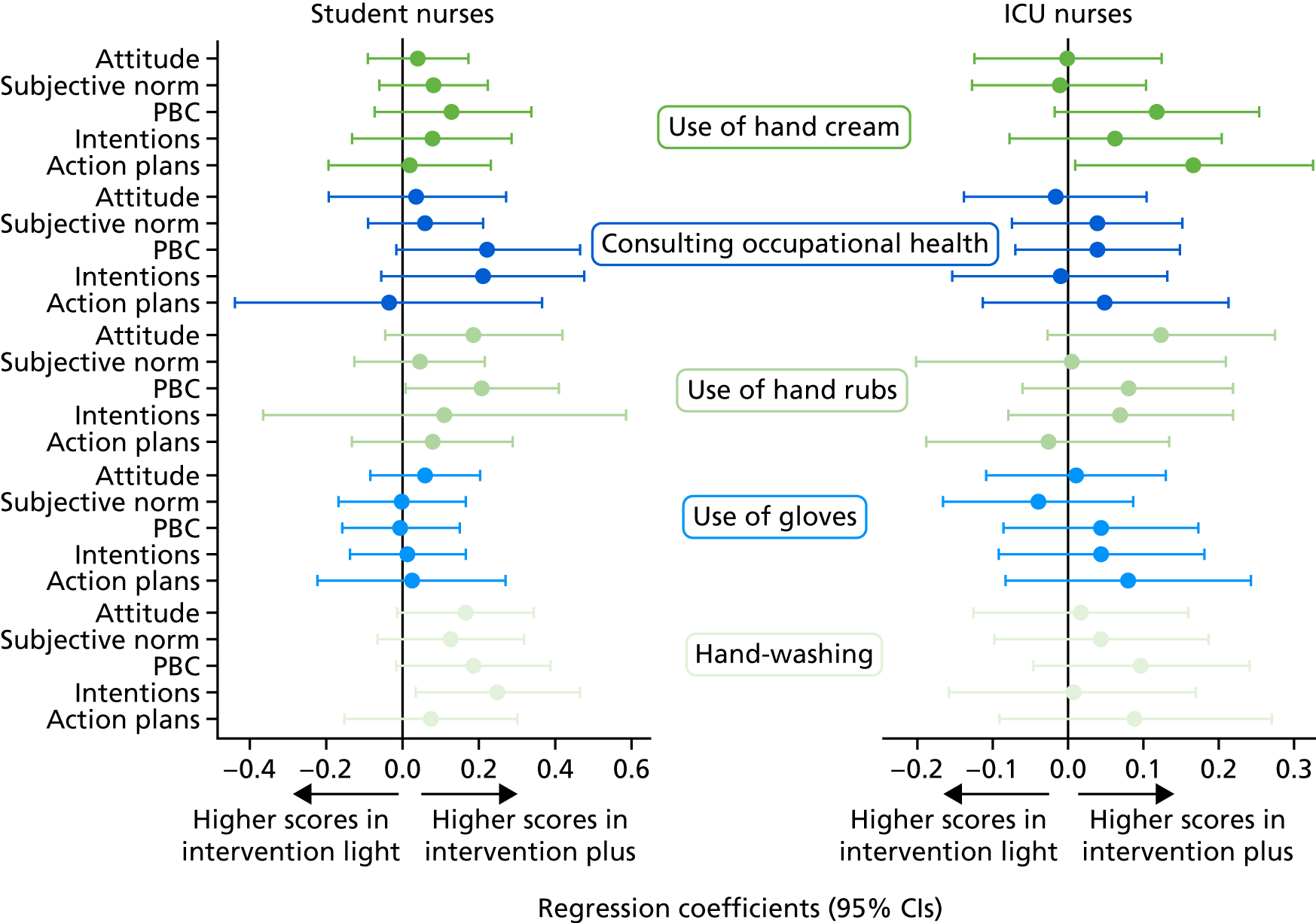
Health behaviours
Five health behaviours were assessed in the trial (frequency of hand-washing with soap and water, use of hand rubs, use of moisturising creams before shifts, use of moisturising creams during shifts and use of moisturising creams after shifts). These were assessed at both baseline and the 12-month follow-up for ICU/SCBU nurses and only at the 12-month follow-up for student nurses, as they had not started their placement yet.
Considering the ordinal responses to these questions as a continuous measure, the average scores for each of the five measures assessed at follow-up (and their corresponding 95% CIs) are illustrated in Figure 9. For most of the protective measures, frequency of use of hand rubs and hand creams at the 12-month follow-up was higher for nurses in the intervention plus trial arm than for those in the intervention light arm. Differences were more marked for frequency of use of moisturising creams before, during and after shifts among ICU/SCBU nurses. Estimates from the regression analysis (Table 11) confirmed this observation (the proportionality of odds assumption of the model was tested). However, the differences in frequency of use of hand-protective measures between those nurses in the intervention plus and light arms were mostly non-significant in the adjusted models. The only exception was the difference between the two trial arms in the frequency of use of moisturising creams during shifts among ICU/SCBU nurses, which was statistically higher in the intervention plus arm. The composite score of frequency of use of hand cream (before, during and after shifts) was statistically higher in the intervention plus arm.
FIGURE 9.
Mean scores and 95% CIs for use of dermatitis preventative measures at the 12-month follow-up for (a) student nurses and (b) ICU nurses.
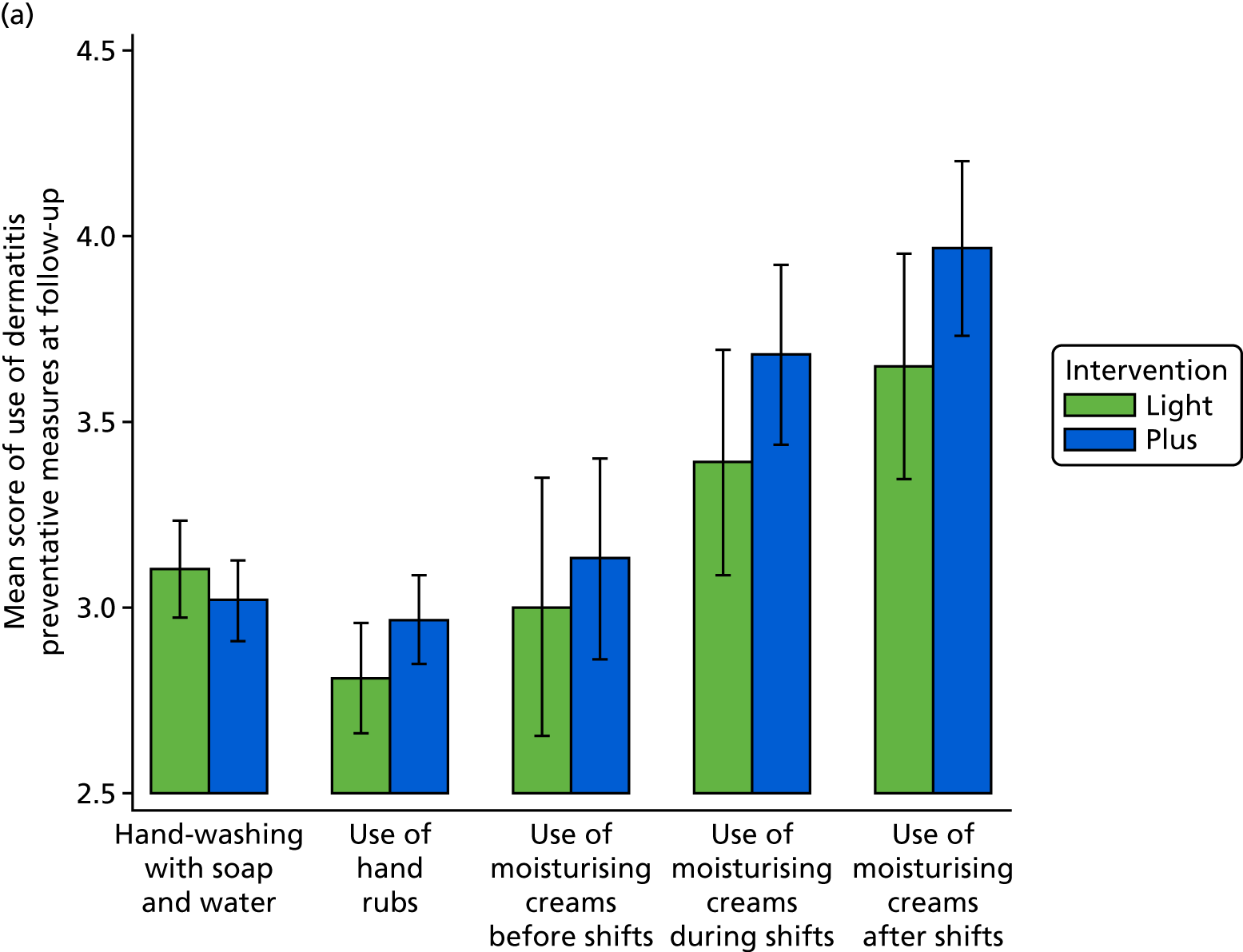
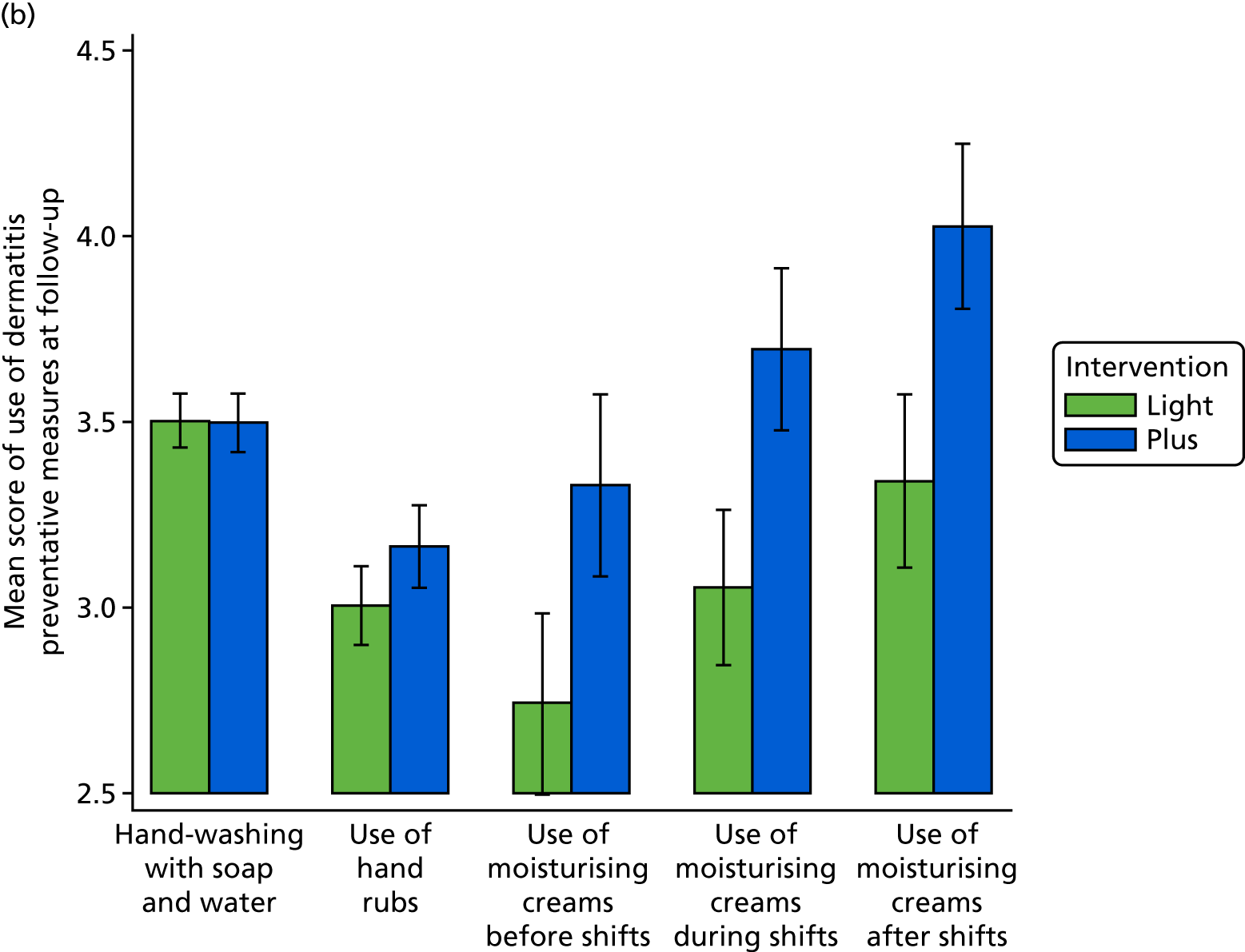
| Nurses | Frequency of . . . | Model | |||
|---|---|---|---|---|---|
| Unadjusteda | Adjustedb | ||||
| n | OR (95% CI) | n | OR (95% CI) | ||
| Student | . . . hand-washing with soap and water | 392 | 1.23 (0.72 to 2.12) | 383 | 1.2 (0.71 to 2.04) |
| . . . use of hand rubs | 393 | 0.73 (0.50 to 1.05) | 384 | 0.71 (0.49 to 1.05) | |
| . . . use of moisturising cream before shifts | 394 | 0.88 (0.61 to 1.26) | 385 | 0.82 (0.56 to 1.19) | |
| . . . use of moisturising cream during shifts | 394 | 0.76 (0.45 to 1.26) | 385 | 0.73 (0.50 to 1.07) | |
| . . . use of moisturising cream after shifts | 394 | 0.74 (0.52 to 1.05) | 385 | 0.72 (0.50 to 1.05) | |
| . . . use of moisturising creamsc | 394 | –0.74 (–1.77 to 0.30) | 385 | –0.91 (–1.98 to 0.16) | |
| ICU/SCBU | . . . hand-washing with soap and water | 645 | 1.24 (0.76 to 2.02) | 605 | 1.18 (0.70 to 1.99) |
| . . . use of hand rubs | 643 | 0.77 (0.55 to 1.06) | 603 | 0.76 (0.55 to 1.05) | |
| . . . use of moisturising cream before shifts | 644 | 0.8 (0.60 to 1.06) | 604 | 0.8 (0.60 to 1.08) | |
| . . . use of moisturising cream during shifts | 644 | 0.59 (0.43 to 0.80) | 604 | 0.62 (0.46 to 0.84) | |
| . . . use of moisturising cream after shifts | 645 | 0.76 (0.52 to 1.11) | 605 | 0.77 (0.54 to 1.11) | |
| . . . use of moisturising creamsc | 643 | –1.87 (–2.96 to –0.78) | 603 | –1.61 (–2.92 to –0.31) | |
Quality of life
See Health economics.
Use of moisturising (in terms of requests for further supplies by student nurses and orders for supplies of moisturisers by intensive care units)
Because of logistical difficulties, it was not possible to reliably collect data on orders for supplies of moisturisers by ICUs, that is supplies of moisturisers were replenished from the main hospital stock rather than being ordered separately by ICUs. As an alternative, monthly inspections were conducted of all wall dispensers available on the ICUs and crude measures were recorded of the quantity of moisturising cream, as seen through the clear display field on each dispenser. However, at the end of the study it was agreed that this was not a robust method for taking reliable measures because it was not possible to ascertain how many times each dispenser may have been refilled between inspections and the dispensers were used by all ward staff and not just by those nurses taking part in the study.
Among student nurses in the intervention plus arm, only 10 nurses from four sites returned completed forms with information regarding requests for an extra supply of moisturising creams. The overall quantity requested was 33 tubes in total. As the reason for the additional supply request, the nurses reported that the existing supply had been used.
Ancillary analysis
Per-protocol analysis
The main analysis presented above is the ITT analysis. However, a large proportion of the nurses in the intervention plus arm reported that they did not access the BCP intervention, although they may have accessed other components of the intervention (e.g. provision of moisturising creams). The per-protocol analysis is based on those nurses who reported that they did not access the BCP. The number of participants who did not access the BCP intervention are shown by categories of baseline characteristics in Table 12. Among student nurses, fewer of the females accessed the BCP intervention than those who did not (38% vs. 61%). Nurses who did not access the BCP were slightly younger and were more likely to have atopic tendency and self-reported atopic dermatitis at baseline. Among ICU/SCBU nurses, all baseline characteristics were well balanced between those who accessed the BCP intervention and those who did not. For both student and ICU/SCBU nurses, the outcome variables, including the primary outcome and health beliefs about action plans, were very similar between those nurses who accessed the BCP intervention and those who did not.
| Characteristics | Nurses | |||||
|---|---|---|---|---|---|---|
| Student | ICU/SCBU | |||||
| Completed the follow-up questionnaire | Accessed the BCP intervention? | Completed the follow-up questionnaire | Accessed the BCP intervention? | |||
| Yes | No | Yes | No | |||
| Participants, n (%)a | 238 | 92 | 143 | 308 | 149 | 158 |
| Sex, n (%)a | ||||||
| Males | 11 | 6 (55) | 5 (45) | 42 | 19 (45) | 23 (55) |
| Females | 227 | 86 (38) | 138 (61) | 266 | 130 (49) | 135 (51) |
| Age (years), median (IQR) | 22 (19–27) | 24 (19–31.5) | 22 (19–26) | 38 (28.5–47) | 37 (28–46) | 38 (29–47) |
| Atopic tendency, n (%)a | 233 | 91 (39) | 139 (60) | 185 | 90 (49) | 95 (51) |
| Self-reported atopic dermatitis, n (%)a | 61 | 24 (39) | 35 (57) | 42 | 21 (50) | 21 (50) |
| Self-rated health score, median (IQR) | 90 (80–95) | 90 (80–95) | 90 (80–94) | 90 (80–95) | 90 (80–95) | 90 (80–95) |
| Outcomes assessed at baseline | ||||||
| Objectively assessed dermatitis at baseline, n (%)a | 38/214b | 17 (45) | 21 (55) | 51/306 | 26 (51) | 25 (49) |
| Action plans for . . . , mean (SD) | ||||||
| . . . hand cream use | 2.32 (1.00) | 2.28 (0.95) | 2.34 (1.03) | 2.38 (1.04) | 2.39 (1.05) | 2.37 (1.04) |
| . . . consulting occupational health if symptoms occur | 2.75 (1.07) | 2.70 (1.16) | 2.78 (1.02) | 2.90 (1.07) | 2.97 (1.09) | 2.83 (1.05) |
| . . . hand rub use | 2.54 (1.00) | 2.50 (1.04) | 2.58 (0.97) | 2.96 (1.11) | 2.95 (1.13) | 2.96 (1.09) |
| . . . appropriate glove use | 2.86 (1.04) | 2.87 (1.14) | 2.85 (0.98) | 3.18 (1.10) | 3.28 (1.08) | 3.08 (1.11) |
| . . . appropriate hand-washing | 2.83 (1.14) | 2.84 (1.29) | 2.83 (1.04) | 3.08 (1.13) | 3.08 (1.12) | 3.07 (1.14) |
The trial participants reported the main reasons for not accessing the BCP intervention. The predominant reason for student nurses was that they forgot (55%), whereas for ICU/SCBU nurses it was a lack of time (40%). Many (student and ICU/SCBU) nurses also reported that they wanted to access the BCP intervention but did not get around to it (23% for both student and ICU nurses), whereas a few nurses also reported that they were not interested (10% among student and 13% among ICU nurses).
Primary outcome
When the analysis was repeated after excluding those nurses who reported that they did not access the BCP intervention, the change observed in objectively assessed dermatitis from baseline to the 12-month follow-up was more pronounced. As shown in Figure 10, dermatitis among student nurses increased from 8.1% at baseline to 11.4% at follow-up in the intervention light arm, but it decreased from 17.1% at baseline to 3.9% at follow-up in the intervention plus arm. Among ICU/SCBU nurses, dermatitis prevalence decreased from 16.1% at baseline to 13.6% at follow-up in the intervention light arm, whereas in the intervention plus arm it decreased from 16.4% at baseline to 10.2% at follow-up. The greater difference between the two intervention arms, especially for student nurses, after excluding participants who reported not having accessed the BCP intervention, is also depicted in the effect estimates from regression analysis shown in Table 13.
FIGURE 10.
Prevalence of objectively assessed dermatitis by intervention arm and time point when dermatitis was assessed (baseline and follow-up), for (a) student and (b) ICU/SCBU nurses after excluding participants who reported not having accessed the BCP intervention.
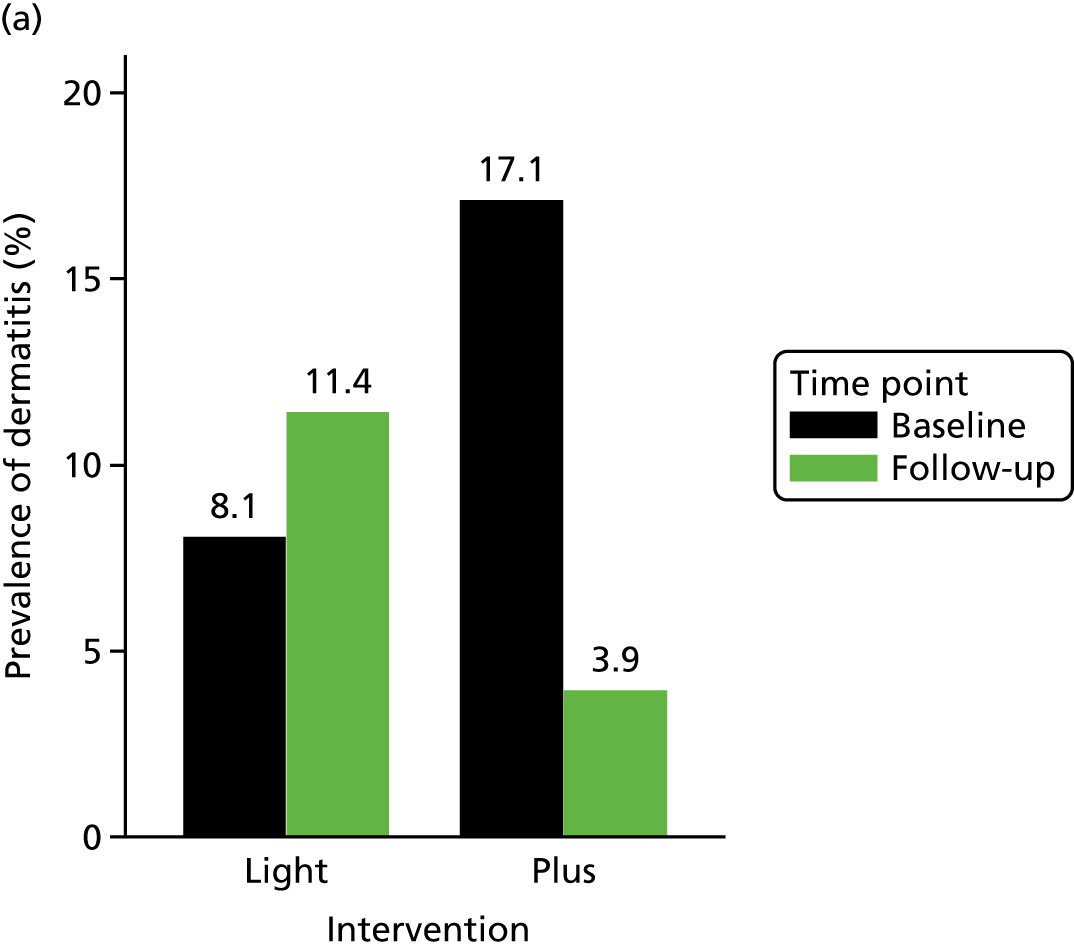
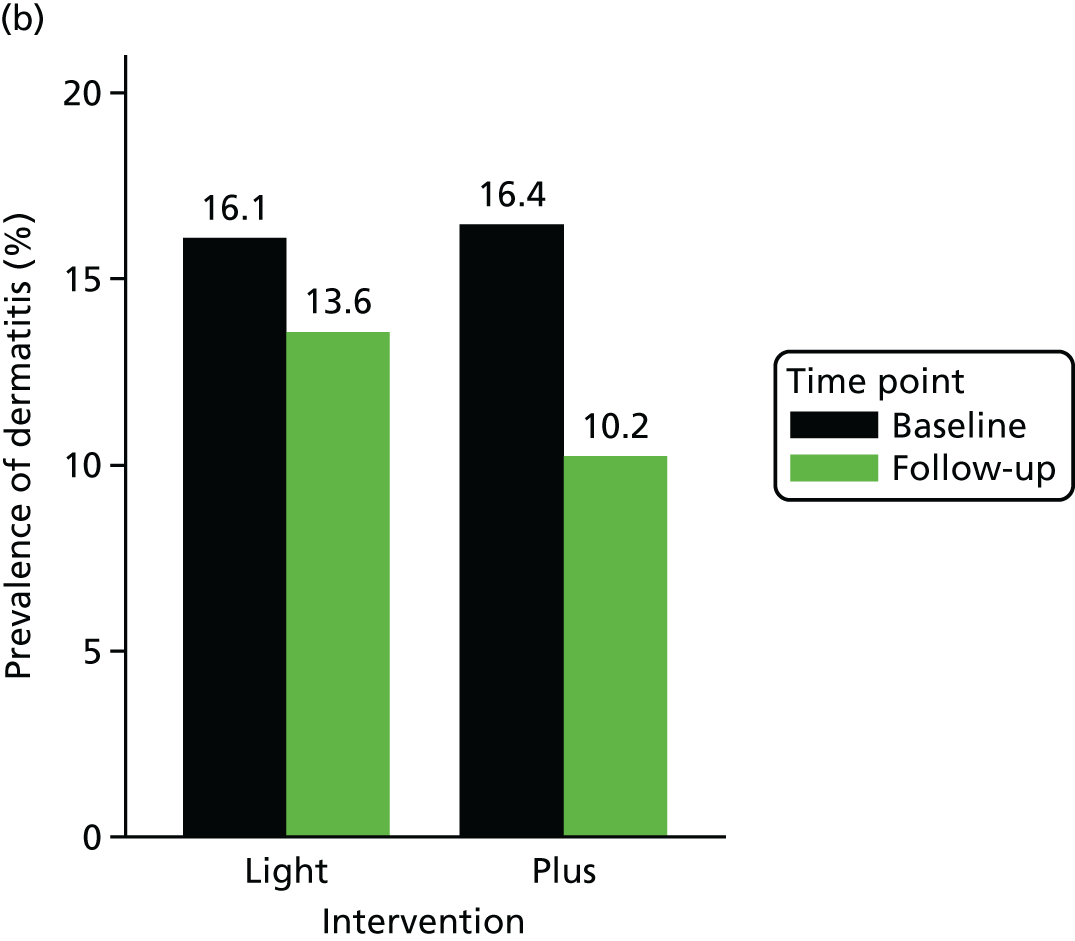
| Nurses | Dermatitis | n | OR (95% CI) |
|---|---|---|---|
| Studenta | For baseline dermatitis | 225 | 4.31 (1.14 to 16.29) |
| For baseline dermatitis, age and follow-up time | 218 | 3.85 (1.00 to 14.76) | |
| ICU/SCBU | For baseline dermatitis | 623 | 1.44 (0.81 to 2.54) |
| For baseline dermatitis, sex, age and follow-up time | 599 | 1.43 (0.75 to 2.74) |
Sensitivity analyses
The main analysis for the primary outcome was repeated after (1) excluding self-taken photographs, (2) restricting the sample to those nurses who were followed up between 12 and 15 months and (3) excluding two big trusts, namely University Hospital Southampton NHS Foundation Trust and Guy’s and St Thomas’ NHS Foundation Trust, on the basis that these were considered to have achieved very high rates of participant recruitment. For each of the three sets of sensitivity analyses, a bar chart of prevalence of objectively assessed dermatitis by intervention arm is shown and the (unadjusted and adjusted) effect estimates of intervention on change in dermatitis from baseline to follow-up are presented.
Sensitivity analysis I (after excluding self-taken photographs)
Among student nurses, the prevalence of dermatitis increased from baseline to follow-up among those in the intervention light arm, but it decreased among those nurses in the intervention plus arm (Figure 11). Among ICU/SCBU nurses, prevalence of dermatitis decreased from baseline to follow-up for both arms. However, the decrease was somewhat larger among those nurses in the intervention plus arm. Regression analysis (Table 14) confirmed this observation, with effect estimates being stronger for student nurses and closer to the null value of 1 (OR = 1) for ICU/SCBU nurses. None of the calculations reached the threshold of statistical significance.
FIGURE 11.
Prevalence of objectively assessed dermatitis by intervention arm and time point when dermatitis was assessed (baseline and follow-up), for (a) student and (b) ICU/SCBU nurses, after excluding self-taken photographs.
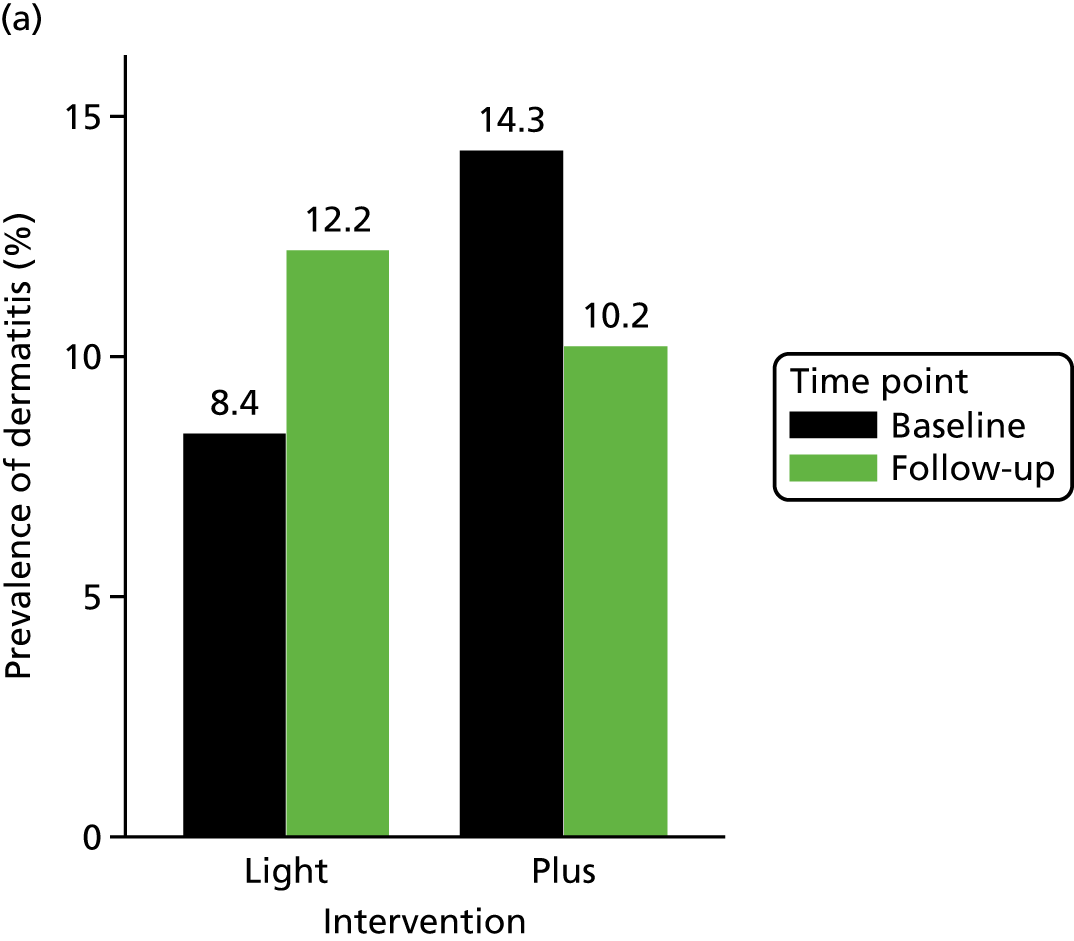
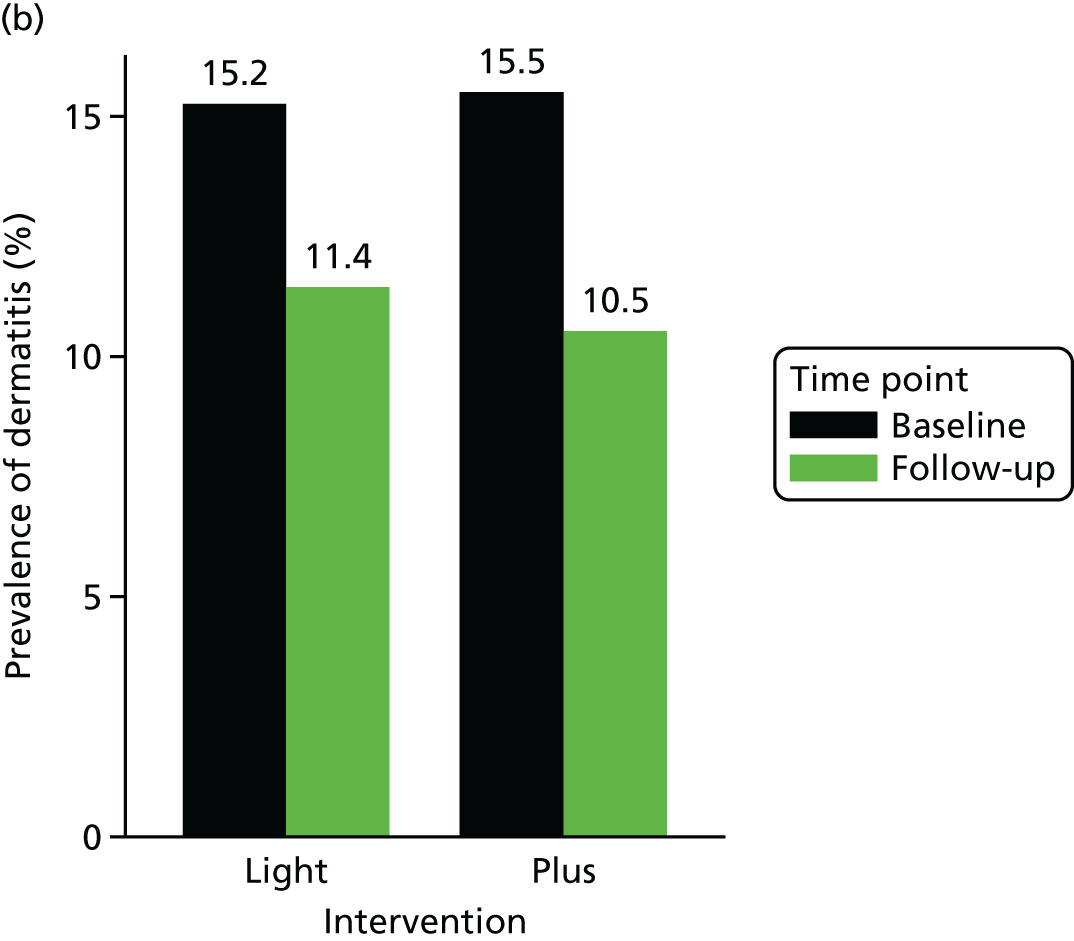
| Nurses | Dermatitis | n | OR (95% CI) |
|---|---|---|---|
| Studenta | For baseline dermatitis | 278 | 1.44 (0.66 to 3.14) |
| For baseline dermatitis, age and follow-up time | 271 | 1.42 (0.62 to 3.26) | |
| ICU/SCBU | For baseline dermatitis | 683 | 1.10 (0.63 to 1.93) |
| For baseline dermatitis, sex, age and follow-up time | 658 | 1.13 (0.60 to 2.11) |
Sensitivity analysis II (after restricting the sample to those who were followed up between 12 and 15 months)
Among student nurses, the prevalence of dermatitis increased from baseline to follow-up for both the intervention light and intervention plus arms (Figure 12). However, the increase in prevalence of dermatitis was smaller in the intervention plus group. Among ICU/SCBU nurses, prevalence of dermatitis decreased from baseline to follow-up for both trial arms, but the decrease was larger in the intervention plus arm. In the fully adjusted model, effect estimates (Table 15) were stronger for ICU/SCBU nurses than for student nurses. None of the calculations reached the threshold of statistical significance.
FIGURE 12.
Prevalence of objectively assessed dermatitis by intervention arm and time point when dermatitis was assessed (baseline and follow-up), for (a) student and (b) ICU/SCBU nurses, after restricting the sample to those who were followed up between 12 and 15 months.
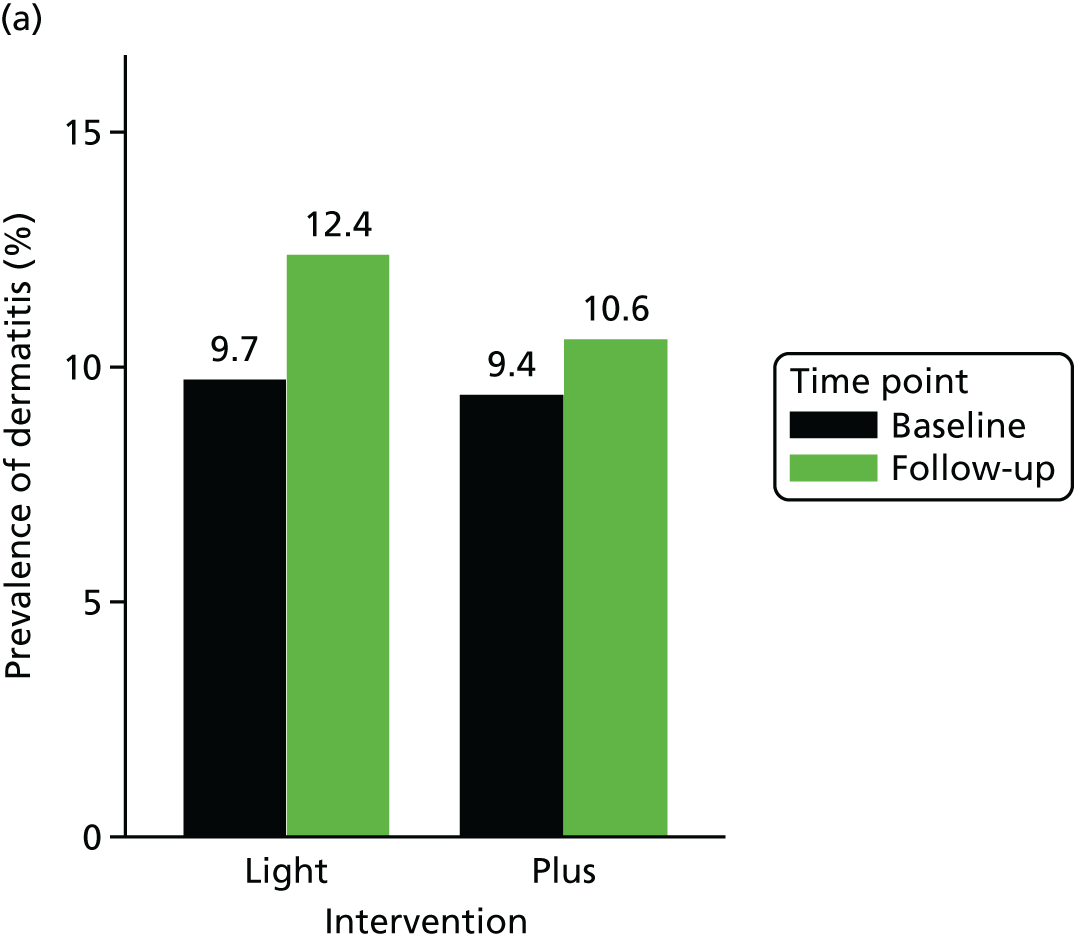
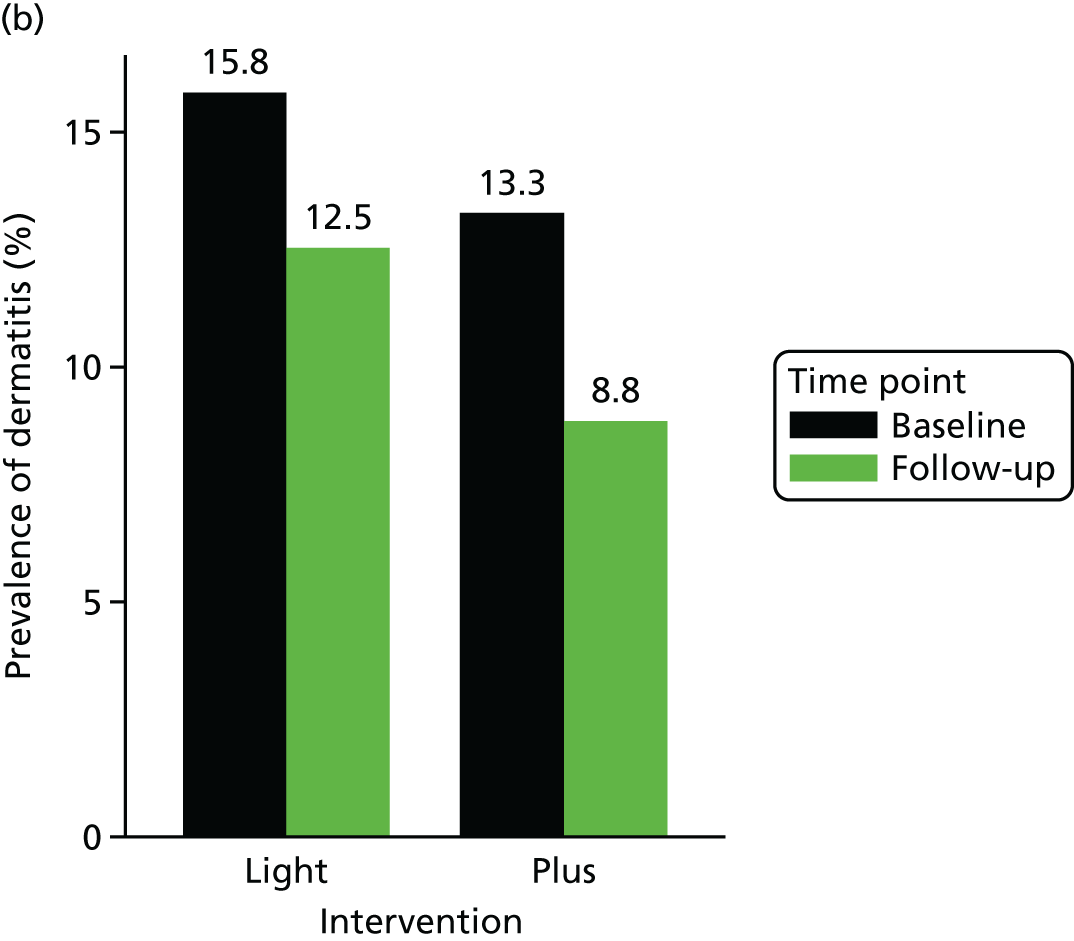
| Nurses | Dermatitis | n | OR (95% CI) |
|---|---|---|---|
| Studenta | For baseline dermatitis | 198 | 1.2 (0.47 to 3.06) |
| For baseline dermatitis, age and follow-up time | 198 | 1.21 (0.47 to 3.12) | |
| ICU/SCBU | For baseline dermatitis | 529 | 1.42 (0.73 to 2.77) |
| For baseline dermatitis, sex, age and follow-up time | 529 | 1.29 (0.64 to 2.60) |
Sensitivity analysis III (after excluding University Hospital Southampton NHS Foundation Trust and Guy’s and St Thomas’ NHS Foundation Trust)
The University Hospital Southampton NHS Foundation Trust and Guy’s and St Thomas’ NHS Foundation Trust achieved a very high rate of recruitment among the student nurse population. Both these sites were in the intervention plus arm of the trial and this resulted in unequal numbers of student nurse participants in the intervention plus and intervention light sites.
In student nurses, the prevalence of dermatitis increased from baseline to follow-up in those in the intervention light arm, and it decreased considerably in those in the intervention plus arm (Figure 13). In ICU/SCBU nurses, prevalence of dermatitis decreased from baseline to follow-up, but decrease was larger in those in the intervention plus arm. Fully adjusted effect estimates for both student and ICU/SCBU nurses were 1.2 (Table 16). None of the associations reached statistical significance.
FIGURE 13.
Prevalence of objectively assessed dermatitis by intervention arm and time point when dermatitis was assessed (baseline and follow-up), for (a) student and (b) ICU/SCBU nurses, after excluding University Hospital Southampton NHS Foundation Trust and Guy’s and St Thomas’ NHS Foundation Trust.
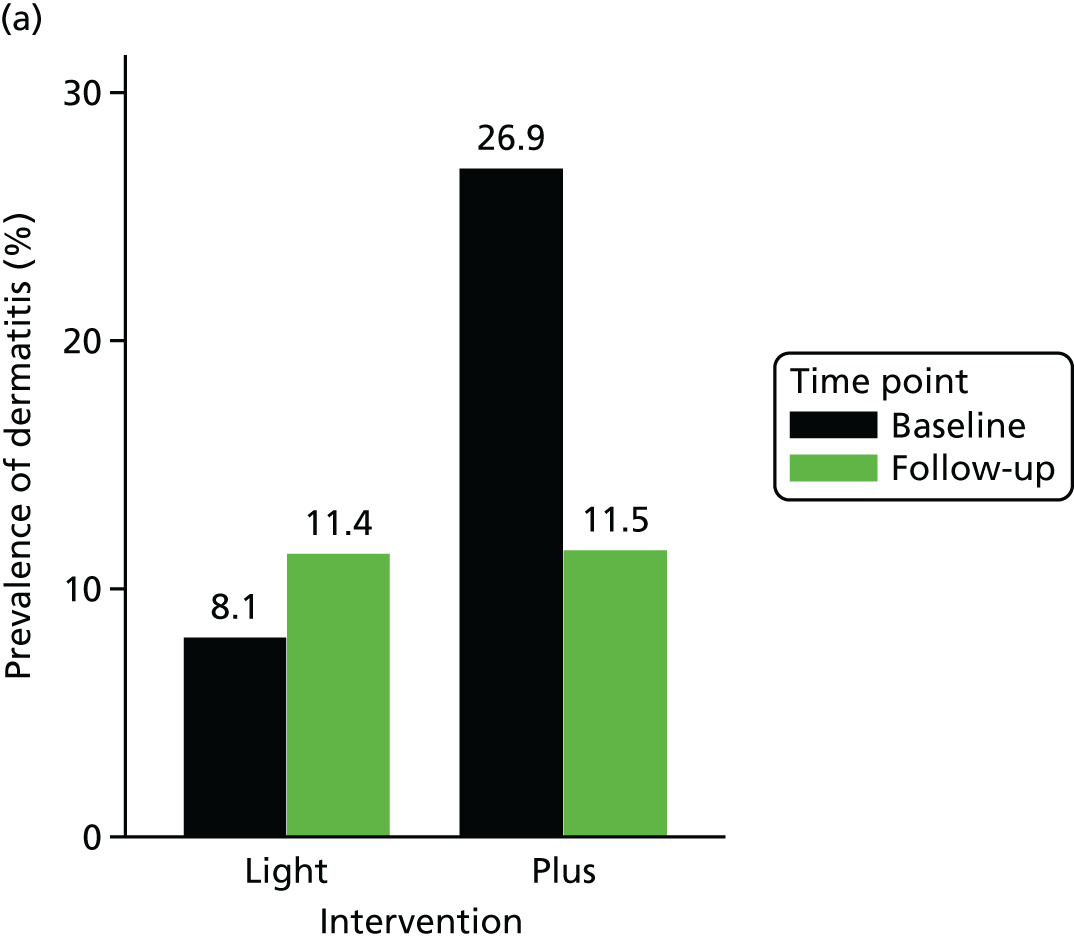
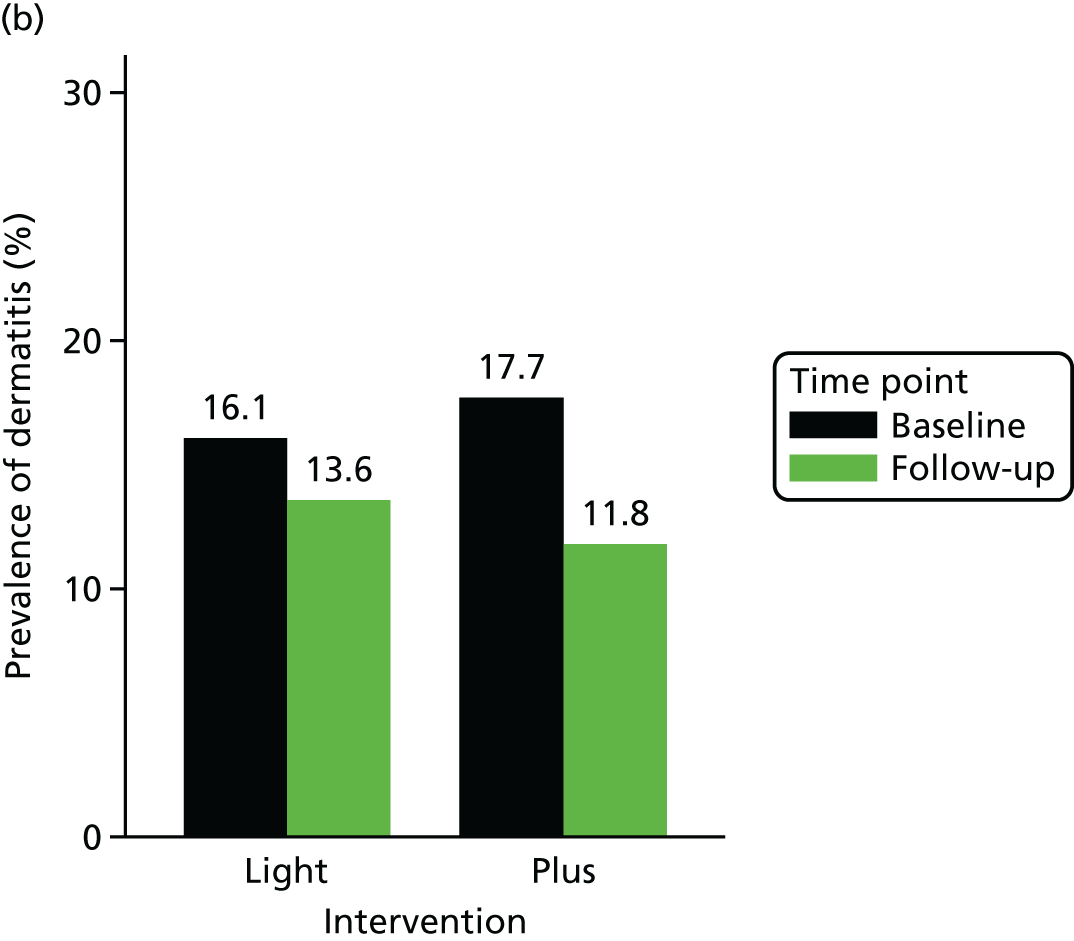
| Nurses | Dermatitis | n | OR (95% CI) |
|---|---|---|---|
| Studenta | For baseline dermatitis | 175 | 1.54 (0.37 to 6.35) |
| For baseline dermatitis, age and follow-up time | 170 | 1.27 (0.30 to 5.43) | |
| ICU | For baseline dermatitis | 669 | 1.26 (0.75 to 2.13) |
| For baseline dermatitis, sex, age and follow-up time | 646 | 1.23 (0.69 to 2.21) |
As anticipated, the number of recruited nurses was considerably higher in some trusts than in other trusts. To explore the possibility that clusters of sites with higher numbers of recruited nurses were different from those with lower numbers of recruited nurses in terms of health beliefs and behaviours, correlation coefficients between size of the cluster and mean scores of health beliefs and behaviours were calculated (Table 17). Correlation coefficients between size of the cluster and health beliefs and behaviours were predominantly negative, suggesting that the larger the size of the cluster, the more negative the health beliefs and the lower the frequency of use of dermatitis prevention measures. In most cases, the correlation coefficients were weak and not statistically significant. The exception was the association between size of the cluster and attitude towards appropriate hand-washing in student nurses, cluster size and subjective norm for use of hand rub and subjective norm for appropriate glove use in ICU/SCBU nurses.
| Nurses | ||||
|---|---|---|---|---|
| Student | ICU/SCBU | |||
| Correlation coefficient | p-value | Correlation coefficient | p-value | |
| Health behaviours | ||||
| Average frequency of use of moisturising creams | –0.31 | 0.23 | –0.11 | 0.55 |
| Average frequency of cleansing hands with hand rub | 0.06 | 0.82 | 0.18 | 0.34 |
| Average frequency of washing hands with soap and water | 0.29 | 0.26 | 0.35 | 0.06 |
| Use of hand cream | ||||
| Attitude towards hand cream use | –0.38 | 0.13 | –0.16 | 0.39 |
| Subjective norm for hand cream use | –0.39 | 0.12 | –0.02 | 0.93 |
| PBC for hand cream use | –0.26 | 0.31 | –0.06 | 0.76 |
| Intentions to use hand cream | –0.12 | 0.66 | –0.08 | 0.67 |
| Action plans for hand cream use | –0.10 | 0.69 | –0.21 | 0.26 |
| Consulting occupational health if symptoms occur | ||||
| Attitude towards consulting occupational health if symptoms occur | –0.29 | 0.26 | –0.10 | 0.60 |
| Subjective norm for consulting occupational health if symptoms occur | –0.07 | 0.79 | –0.05 | 0.80 |
| PBC for consulting occupational health if symptoms occur | –0.23 | 0.38 | –0.03 | 0.88 |
| Intentions to consult occupational health if symptoms occur | –0.39 | 0.12 | –0.33 | 0.07 |
| Action plans for consulting occupational health if symptoms occur | 0.09 | 0.73 | 0.29 | 0.13 |
| Use of hand rub | ||||
| Attitude towards hand rub use | 0.13 | 0.61 | –0.29 | 0.13 |
| Subjective norm for hand rub use | 0.22 | 0.40 | –0.44 | 0.01 |
| PBC for hand rub use | 0.04 | 0.87 | –0.29 | 0.12 |
| Intentions to use hand rub | 0.09 | 0.73 | 0.03 | 0.87 |
| Action plans for hand rub use | –0.25 | 0.32 | –0.32 | 0.09 |
| Use of gloves | ||||
| Attitude towards appropriate glove use | –0.08 | 0.77 | –0.25 | 0.19 |
| Subjective norm for appropriate glove use | –0.33 | 0.19 | –0.41 | 0.03 |
| PBC for appropriate glove use | –0.12 | 0.64 | –0.22 | 0.24 |
| Intentions to use gloves appropriately | –0.32 | 0.21 | –0.27 | 0.16 |
| Action plans for appropriate glove use | –0.16 | 0.54 | –0.33 | 0.08 |
| Hand-washing | ||||
| Attitude towards appropriate hand-washing | –0.57 | 0.02 | –0.26 | 0.17 |
| Subjective norm for appropriate hand-washing | –0.17 | 0.52 | –0.29 | 0.12 |
| PBC for appropriate hand-washing | –0.29 | 0.25 | –0.02 | 0.90 |
| Intentions to wash hands only when appropriate | –0.18 | 0.49 | –0.17 | 0.38 |
| Action plans for appropriate hand-washing | –0.11 | 0.68 | –0.17 | 0.37 |
Process evaluation
In terms of uptake of the BCP intervention, the study found that 39% of the student nurses and 48% of the ICU/SCBU nurses in the intervention plus arm reported that they had accessed the BCP intervention during the study. (Note that these figures are based on the number of nurses who returned the final questionnaire and not the total number of nurses in the intervention plus arm who were given access to the BCP.) More than 90% of the nurses who accessed BCP agreed or strongly agreed that the information was easy to understand, it was sufficiently detailed, was relevant and was presented clearly, and that the intervention itself was easy to use.
Missing data
There were various reasons for the missing data. In relation to the study questionnaires, the research team implemented a three-tiered reminder strategy to optimise the response rate among nurses. This included sending reminder e-mail and text messages, and also replacement copies to nurses who had not returned completed questionnaires within specific time frames, that is, at 2-week intervals. When practicable, all nurses were encouraged to complete and return the study questionnaires to fieldworkers when recruitment and follow-up activities were being conducted, rather than taking the questionnaires away to complete at a later date. This was not always possible because of time constraints in the critical care settings (for critical care nurses) and between lectures (for student nurses).
In relation to the photographic images, all nurses were invited to have their hands photographed immediately after consent was taken at the time of recruitment. Photographic images at baseline were collected for all nurses who were recruited into the study. Photographic images at follow-up (t = 12–15 months) were either collected by local fieldworkers who were able to make personal contact with nurses or sent by nurses who agreed to e-mail self-taken hand photographs directly to the research team.
Health economics
The number and percentage of nurses using specific services and the number of work days lost at baseline and follow-up are given in Table 18. Within the student nurse group, over 80% had seen a GP in the previous year and about half had also seen a practice nurse. There was a relatively high rate of pharmacist contact. Days off work occurred for just under 40% of student nurses. In the ICU/SCBU nurse group, GP, nurse and pharmacist contacts were the most commonly used services, but the rates were lower than for student nurses. However, lost work days were more common (54–59%). There were no major differences between the intervention and control groups in either nurse group at baseline. (Differences in the use of specific services and lost employment were not tested for statistical significance and are seen as descriptive.) During the 1-year follow-up period, the above service patterns were generally repeated and, again, there were no clear differences between trial arms. Lost work days were, again, more probable for the ICU/SCBU nurses.
| Time point | Nurses, n (%) | |||
|---|---|---|---|---|
| Student | ICU/SCBU | |||
| Intervention light (N = 249) | Intervention plus (N = 539) | Intervention light (N = 246) | Intervention plus (N = 245) | |
| Baseline | ||||
| GP | 209 (84) | 451 (84) | 335 (69) | 312 (69) |
| Dermatologist | 15 (6) | 25 (5) | 22 (5) | 13 (3) |
| Practice nurse | 118 (47) | 241 (45) | 145 (30) | 137 (30) |
| Pharmacist | 98 (39) | 205 (38) | 104 (22) | 99 (22) |
| Other doctors | 34 (14) | 98 (18) | 78 (16) | 79 (17) |
| Complementary health care | 5 (2) | 25 (5) | 36 (7) | 29 (6) |
| Physiotherapist | 13 (5) | 53 (10) | 73 (15) | 61 (13) |
| Medication | 82 (33) | 184 (34) | 120 (25) | 103 (23) |
| Tests | 8 (3) | 25 (5) | 15 (3) | 13 (3) |
| Lost work days | 97 (39) | 206 (39) | 262 (54) | 266 (59) |
| 12-month follow-up | (N = 163) | (N = 238) | (N = 340) | (N = 307) |
| GP | 122 (75) | 164 (69) | 215 (63) | 189 (62) |
| Dermatologist | 5 (3) | 9 (4) | 13 (4) | 11 (4) |
| Practice nurse | 68 (42) | 91 (38) | 82 (24) | 67 (22) |
| Pharmacist | 62 (38) | 74 (31) | 74 (22) | 61 (20) |
| Other doctors | 25 (15) | 30 (13) | 39 (11) | 43 (14) |
| Complementary health care | 5 (3) | 16 (7) | 21 (6) | 28 (9) |
| Physiotherapist | 11 (7) | 15 (6) | 50 (15) | 36 (12) |
| Medication | 60 (37) | 98 (41) | 70 (21) | 66 (22) |
| Tests | 7 (4) | 14 (6) | 9 (3) | 10 (3) |
| Lost work days | 54 (33) | 78 (33) | 168 (49) | 164 (53) |
For those nurses with specific service contacts, the mean and SD of those contacts are shown in Table 19. Most services were used, on average, between one and three times, with no large differences between trial arms. At baseline, the number of days lost from work for those nurses for whom this occurred was greater in the intervention light arm for students than in the intervention plus arm. At follow-up, it is interesting that the ICU/SCBU nurses had more time off work than the student nurses.
| Time point | Nurses, mean (SD) | |||
|---|---|---|---|---|
| Student | ICU/SCBU | |||
| Intervention light | Intervention plus | Intervention light | Intervention plus | |
| Baseline | ||||
| GP | 2.4 (1.7) | 2.3 (1.9) | 2.2 (1.5) | 2.3 (1.6) |
| Dermatologist | 1.4 (1.1) | 1.2 (0.4) | 1.8 (1.8) | 1.1 (0.3) |
| Practice nurse | 1.3 (0.7) | 1.4 (1.2) | 1.1 (0.5) | 1.4 (3.4) |
| Pharmacist | 1.5 (1.2) | 1.6 (1.9) | 1.5 (1.5) | 1.3 (1.4) |
| Other doctors | 1.4 (1.1) | 1.6 (1.3) | 1.6 (2.2) | 2.3 (4.0) |
| Complementary health care | 1.8 (0.4) | 2.4 (2.2) | 2.6 (2.1) | 2.2 (1.0) |
| Physiotherapist | 2.5 (1.2) | 2.5 (2.7) | 2.3 (1.3) | 2.8 (3.2) |
| Lost work days | 11.3 (26.2) | 7.8 (13.9) | 12.9 (31.4) | 13.8 (34.1) |
| 12-month follow-up | ||||
| GP | 2.0 (2.2) | 1.9 (1.9) | 1.5 (1.2) | 1.4 (1.2) |
| Dermatologist | 1.4 (0.5) | 1.3 (0.7) | 1.3 (0.9) | 1.6 (1.2) |
| Practice nurse | 1.3 (0.9) | 1.2 (0.7) | 1.1 (0.3) | 1.1 (0.2) |
| Pharmacist | 1.4 (1.5) | 1.4 (1.3) | 1.4 (1.0) | 1.3 (1.0) |
| Other doctors | 1.5 (0.9) | 1.7 (1.7) | 1.6 (1.0) | 1.3 (0.6) |
| Complementary health care | 2.0 (2.2) | 1.5 (1.2) | 1.7 (1.6) | 1.3 (0.7) |
| Physiotherapist | 1.5 (0.8) | 1.6 (1.6) | 1.6 (1.6) | 1.7 (3.2) |
| Lost work days | 5.9 (8.2) | 5.6 (9.8) | 10.5 (21.5) | 11.3 (22.5) |
Costs are shown in Table 20. The services that seemed to contribute most to total health-care costs at both baseline and follow-up were GPs, other doctors and physiotherapists. The intervention costs were, on average, £14 for the student nurses and £13 for the ICU/SCBU nurses. Societal costs in both trial arms, in both groups of nurses and at both time points were dominated by the cost of lost work days.
| Time point | Nurses, mean cost (SD) (£) | |||
|---|---|---|---|---|
| Student | ICU/SCBU | |||
| Intervention light | Intervention plus | Intervention light | Intervention plus | |
| Baseline | ||||
| GP | 68 (59) | 65 (64) | 50 (53) | 51 (56) |
| Dermatologist | 11 (56) | 7 (35) | 11 (71) | 4 (25) |
| Practice nurse | 6 (8) | 6 (10) | 3 (6) | 4 (18) |
| Pharmacist | 10 (18) | 11 (24) | 5 (16) | 5 (14) |
| Other doctors | 27 (86) | 39 (109) | 35 (143) | 53 (253) |
| Complementary health care | 2 (13) | 6 (36) | 10 (46) | 7 (31) |
| Physiotherapist | 18 (84) | 34 (152) | 46 (129) | 51 (204) |
| Medication | 14 (33) | 11 (27) | 9 (25) | 8 (23) |
| Tests | 2 (9) | 7 (40) | 9 (113) | 4 (36) |
| Total health-care cost | 157 (177) | 184 (269) | 179 (330) | 187 (374) |
| Lost work days | 760 (2973) | 516 (1622) | 1835 (6300) | 2124 (7076) |
| Total societal cost | 918 (3014) | 700 (1707) | 2013 (6461) | 2312 (7253) |
| 12-month follow-up | ||||
| Intervention | 0 (0) | 14 (0) | 0 (0) | 13 (0) |
| GP | 50 (69) | 43 (61) | 31 (40) | 29 (38) |
| Dermatologist | 6 (35) | 7 (39) | 7 (40) | 8 (51) |
| Practice nurse | 5 (8) | 4 (7) | 3 (5) | 2 (4) |
| Pharmacist | 9 (20) | 7 (16) | 5 (13) | 5 (12) |
| Other doctors | 31 (87) | 29 (111) | 24 (81) | 26 (69) |
| Complementary health care | 3 (26) | 5 (25) | 6 (30) | 6 (22) |
| Physiotherapist | 14 (59) | 14 (74) | 32 (114) | 27 (164) |
| Medication | 30 (77) | 27 (61) | 15 (40) | 19 (61) |
| Tests | 11 (71) | 11 (59) | 6 (56) | 8 (51) |
| Total health-care cost | 159 (225) | 162 (234) | 128 (215) | 142 (265) |
| Lost work days | 334 (943) | 315 (1069) | 1360 (4192) | 1580 (4551) |
| Total societal cost | 494 (1030) | 477 (1171) | 1489 (4303) | 1723 (4642) |
Analysis of total health-care costs
At baseline, the total mean health-care costs for student nurses were £184 in the intervention plus arm and £157 in the intervention light arm. The difference was not statistically significant (bootstrapped 95% CI –£4 to £58). For ICU/SCBU nurses, the costs were £187 and £179 for the intervention plus and intervention light arms, respectively. This difference was not statistically significant (bootstrapped 95% CI –£35 to £55).
At follow-up, the mean total health-care costs for the student nurses were £162 for the intervention plus arm and £159 for the intervention light arm. After adjusting for baseline, it was found that the intervention plus arm had mean costs that were £2 less than for the intervention light arm, a difference that was not statistically significant (bootstrapped 95% CI –£44 to £45). The mean costs for the ICU/SCBU nurses were £142 for the intervention plus arm and £128 for the intervention light arm. The intervention plus arm had costs that were, on average, £3 higher after adjusting for baseline, which again was not statistically significant (bootstrapped 95% CI –£31 to £34).
When only cases for which there were QALY data were included, it was found that the student nurses in the intervention plus arm still had costs that were £2 less than for the intervention light arm (bootstrapped 95% CI –£44 to £49) and the ICU/SCBU nurses in the intervention plus arm had costs that were £4 higher than for the intervention light arm (bootstrapped 95% CI –£23 to £38).
Analysis of total societal costs
At baseline, the student nurses in the intervention plus arm had mean societal costs of £700, whereas the intervention light arm had costs of £918. The difference of £218 was not statistically significant (bootstrapped 95% CI –£160 to £649). The ICU/SCBU nurses in the intervention plus arm had mean societal costs of £2312 compared with £2013 in the intervention light arm, a difference of £298 (bootstrapped 95% CI –£637 to £1173).
During the follow-up period, the societal costs in the student nurse group were, on average, £477 for the intervention plus arm and £494 for the intervention light arm. After adjustment for baseline, the intervention plus arm was shown to have costs £32 higher than for the intervention light arm (bootstrapped 95% CI –£159 to £234). The ICU/SCBU nurses in the intervention plus arm had mean societal costs at follow-up of £1723, compared with £1489 for the intervention light arm. The intervention plus arm costs were £250 higher after adjustment (bootstrapped 95% CI –£484 to £943).
When only cases for which QALY data were included, it was found that the student nurses in the intervention plus arm still had costs that were £33 more than for the intervention light group (bootstrapped 95% CI –£156 to £231) and the ICU/SCBU nurses in the intervention plus arm had costs that were £233 higher than for the intervention light arm (bootstrapped 95% CI –£417 to £922).
Quality-adjusted life-years
The baseline and follow-up EQ-5D-5L scores are shown in Table 21. There was virtually no difference in the EQ-5D-5L scores between trial arms at baseline or at follow-up or for QALYs over the follow-up period. Adjusting for baseline EQ-5D-5L scores among student nurses in the intervention plus arm resulted in just 0.0002 more QALYs (bootstrapped 95% CI –0.0054 to 0.0062 QALYs). Among ICU/SCBU nurses, the intervention plus arm had 0.0015 fewer QALYs (bootstrapped 95% CI –0.0018 to 0.0049 QALYs).
| Time point | Nurses, mean score (SD) | |||
|---|---|---|---|---|
| Student | ICU/SCBU | |||
| Intervention light | Intervention plus | Intervention light | Intervention plus | |
| Baseline EQ-5D-5L score | 0.969 (0.053) | 0.972 (0.052) | 0.967 (0.065) | 0.971 (0.054) |
| Follow-up EQ-5D-5L score | 0.963 (0.064) | 0.967 (0.058) | 0.974 (0.049) | 0.972 (0.051) |
| QALYs | 0.966 (0.050) | 0.971 (0.044) | 0.973 (0.043) | 0.973 (0.043) |
For student nurses for whom baseline and follow-up costs were available, the intervention plus arm had 0.00002 more QALYs (bootstrapped 95% CI –0.0051 to 0.0055 QALYs). For ICU/SCBU nurses, the intervention plus arm had 0.0016 fewer QALYs (bootstrapped 95% CI –0.0018 to 0.0046 QALYs).
Cost-effectiveness analysis
Using complete cases (baseline and follow-up costs and QALYs available), the above results show that, from a health-care perspective, the intervention plus arm for student nurses dominated the intervention light arm in that it resulted in lower mean costs (by £2) and more QALYs (0.00002). For ICU/SCBU nurses, the intervention plus arm was dominated – it had higher costs (by £4) and fewer QALYs (0.0016) than the intervention light arm. The ICERs are, consequently, both negative. However, the CIs around the cost and QALY differences are very wide. Figures 14 and 17 show the uncertainty around these estimates. Each point on the scatterplots represents a cost and QALY difference obtained from 1 of 1000 bootstrapped resamples. The spread of replications in Figure 15 means that there is a 31% likelihood that intervention plus is cost-saving and outcome-improving for student nurses, 23% likelihood of lower costs and worse outcomes, 23% likelihood of worse outcomes and higher costs and 20% likelihood of higher costs and better outcomes. The corresponding cost-effectiveness acceptability curve shows that at a threshold of £20,000 per QALY there is a 53% likelihood that intervention plus was cost-effective (Figure 15).
FIGURE 14.
Cost-effectiveness plane for student nurses (health-care perspective).
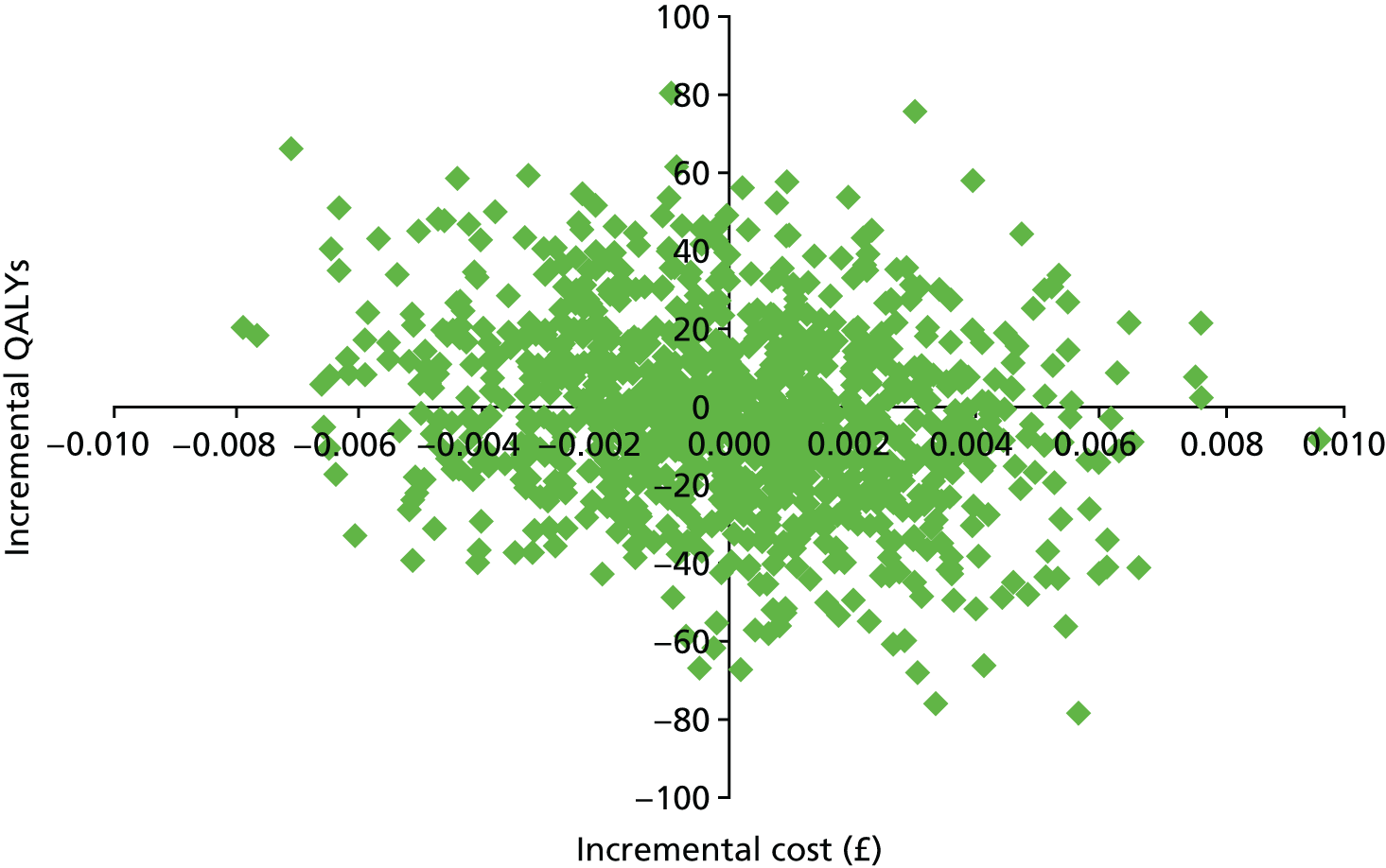
FIGURE 15.
Cost-effectiveness acceptability curve for student nurses.
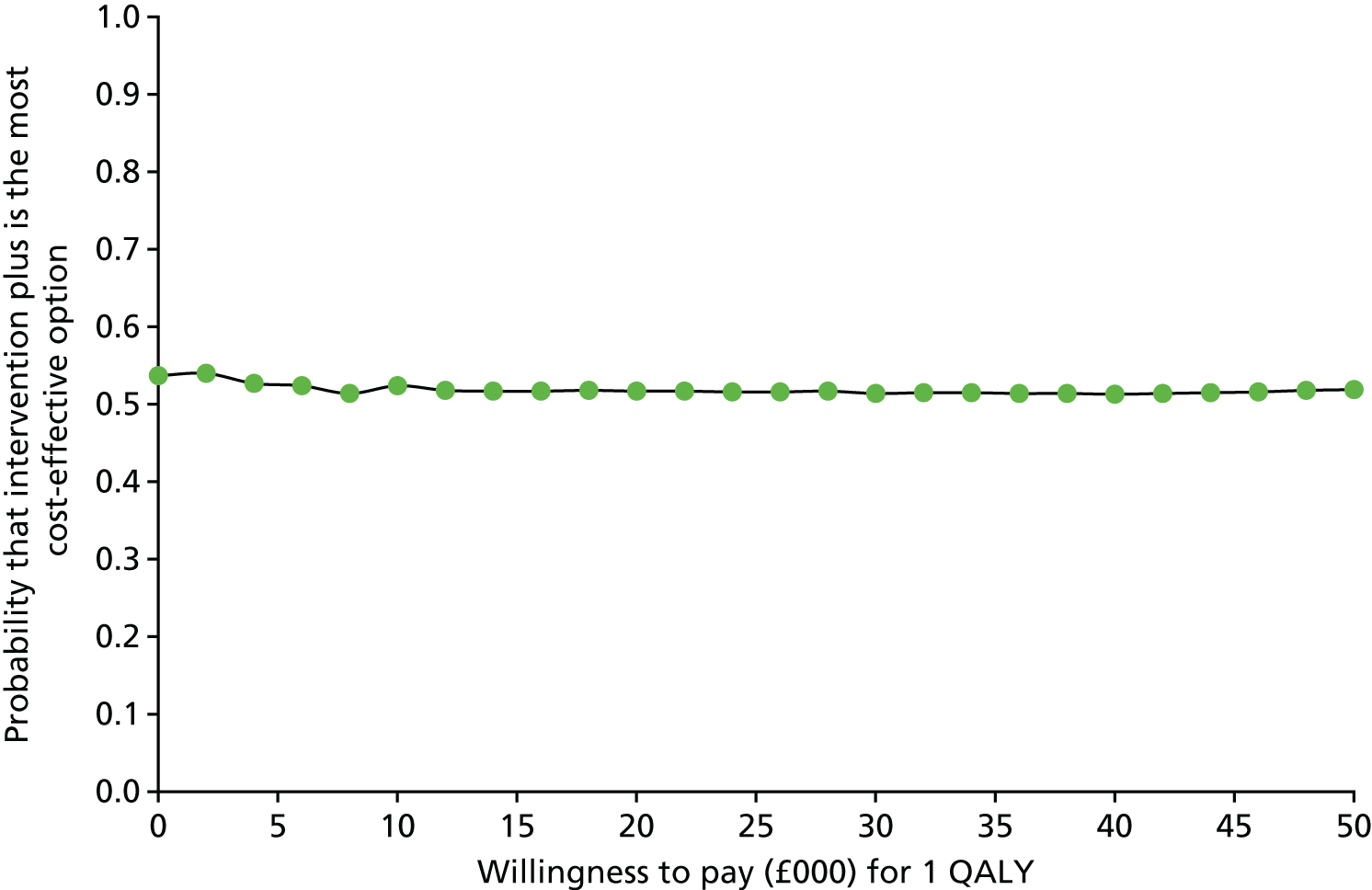
Figure 16 shows that, for ICU/SCBU nurses, intervention plus has a probability of 10% of resulting in lower costs and better outcomes, a 29% probability of resulting in lower costs and worse outcomes, a 53% probability of resulting in worse outcomes and higher costs and an 8% probability of resulting in higher costs and better outcomes. At a threshold of £20,000 per QALY, there is a 19% likelihood that intervention plus was cost-effective (Figure 17).
FIGURE 16.
Cost-effectiveness plane for ICU/SCBU nurses.
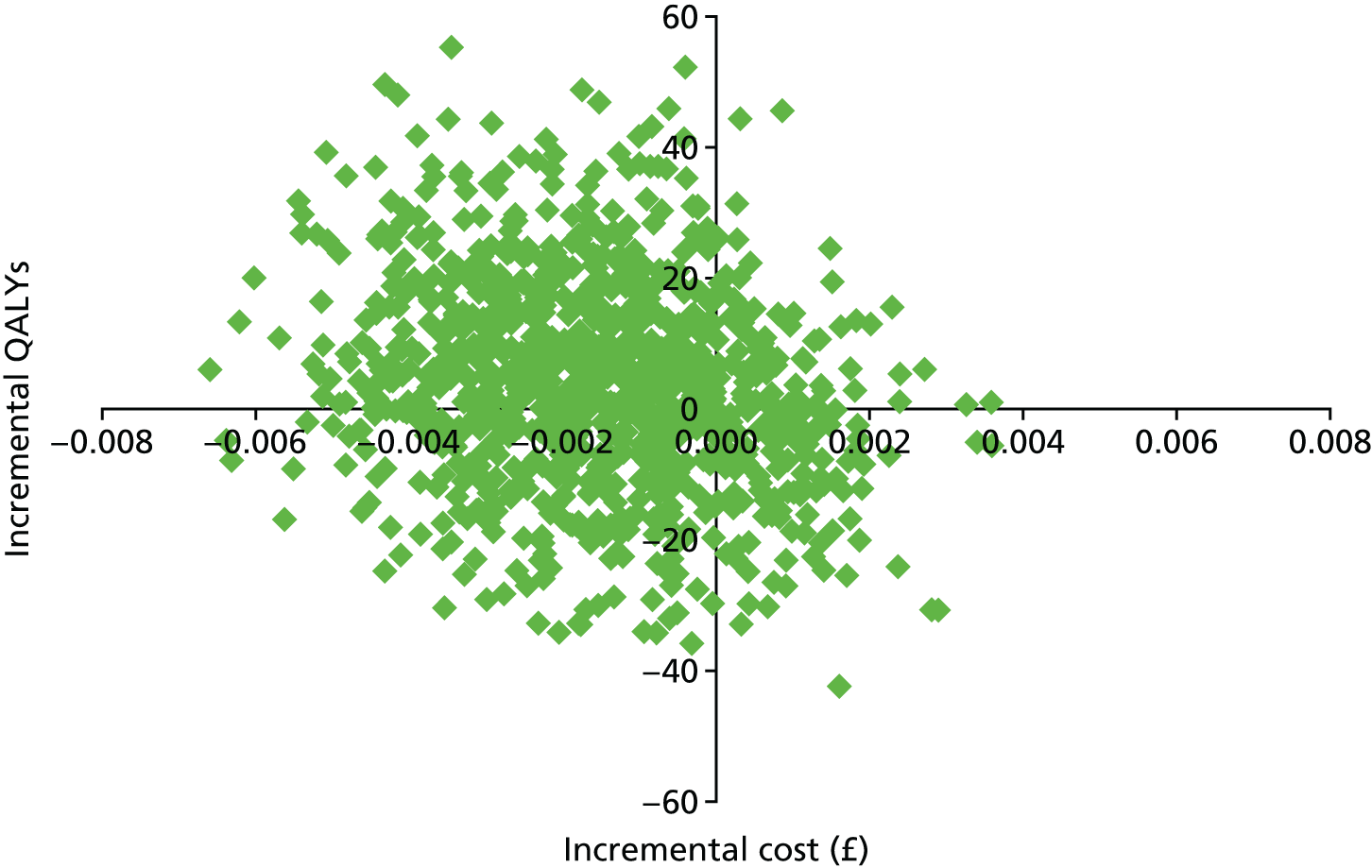
FIGURE 17.
Cost-effectiveness acceptability curve for ICU/SCBU nurses.
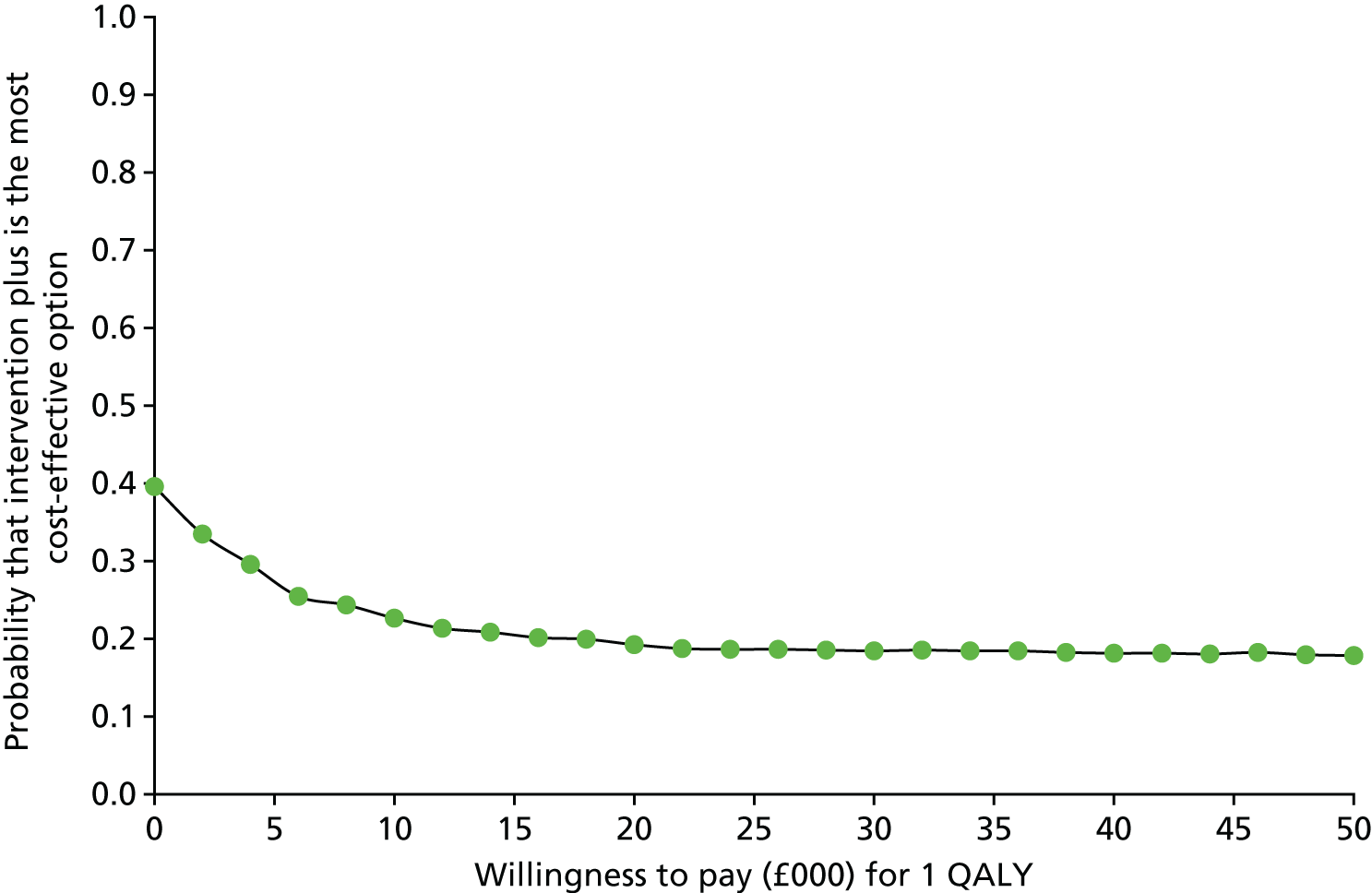
As stated earlier, societal cost differences were higher for intervention plus by £33 for student nurses and £233 for ICU/SCBU nurses. For student nurses, intervention plus has an ICER of £1.65M (£33 divided by 0.00002), whereas for ICU/SCBU nurses, intervention plus is dominated by intervention light.
Elsewhere it has been observed that intervention plus, relative to intervention light, resulted in a smaller proportion of nurses having dermatitis. The incremental percentage point difference between baseline and follow-up was 8.1 for student nurses and 3.4 for ICU/SCBU nurses. The intervention plus arm was therefore ‘dominant’ for student nurses (i.e. lower costs and a higher proportion of nurses free of dermatitis than with intervention light). For the ICU/SCBU nurses, the average extra cost for one more nurse to avoid dermatitis was £3 (the incremental cost) divided by 0.034 (the incremental outcome), resulting in a cost of £88 per case averted.
Sensitivity analyses
When intervention plus arm participants from the student nurse group who declared that they had not accessed the intervention were assigned a zero time cost, the mean health-care cost savings increased from £2 to £5. This makes intervention plus more likely to be cost-effective. For ICU/SCBU nurses, intervention plus resulted in costs that were £2 higher than for intervention light (compared with £3 for the base-case analysis).
Chapter 4 Discussion and conclusions
Changes in health beliefs
Of the 25 health beliefs measured, the change between baseline and the end of the study was only statistically significantly improved in the intervention plus group in two health beliefs for student nurses and one health belief for ICU nurses. Caution should be applied in interpretation of the results of the three health beliefs in which the change was statistically significant as they were only just significant and may have arisen by chance because of multiple testing. However, the increase in action-planning for use of hand cream in ICU nurses may be an explanatory factor in their change in behaviour in use of hand creams (see Changes in health behaviours).
Student and ICU/SCBU nurse participants in both trial arms tended to have positive attitudes towards all five hand dermatitis prevention behaviours, even at baseline, demonstrating that they were aware of the behaviours’ potential benefits. This is an important finding in itself and there may have been little scope for the intervention plus arm to further enhance attitudes. In contrast, action-planning scores tended to be below that scale mid-point at baseline and the scores were significantly improved only in the intervention plus arm in the case of ICU/SCBU nurses’ hand cream use.
Changes in health behaviours
An important finding from the trial was that the intervention had a statistically significant positive effect on increasing the repeated use of hand moisturising creams before, during and after shifts from baseline to follow-up among the ICU/SCBU nurses. There is a possibility that their reported increase was due to the nurses reporting what they perceived they should have done; this is unlikely as the nurses did not report an increase in use of hand rubs or a decrease in hand-washing with soap and water, behaviours that had also been emphasised in the intervention. Furthermore, the ICU/SCBU nurses in the intervention plus arm reported significantly higher actions for hand cream use, which may have resulted in the reported change in behaviour. Moreover, the intervention included enhanced provision of hand cream, which may have made it easier for ICU/SCBU nurses to enact their plans.
The hand-care behaviours of student nurses were enquired about only at follow-up once the student nurses had been on the wards. None of the changes in behaviour of the student nurses was statistically significant.
Changes in assessed hand dermatitis
Results from the ITT analysis showed no significant reduction in hand dermatitis after adjusting for dermatitis at baseline in the student and ICU/SCBU nurses in the intervention plus arm of the study from baseline to follow-up.
Other than occurring by chance, there was no plausible explanation to account for the lower prevalence of hand dermatitis observed at baseline in student nurses in the intervention light arm than in the student nurses in the intervention plus arm.
Therefore, although the intervention resulted in an increased action-planning and use of hand creams in ICU/SCBU nurses, this did not translate to a decrease of hand dermatitis at follow-up. It could be argued that the follow-up was not long enough to show a change, but equally it is not known if the use of hand creams by ICU/SCBU nurses would have been sustained after the end of the trial.
Uptake of the behaviour change package
Although the study made use of champions (i.e. lead ICU matrons and School of Nursing teams) to promote key messages contained in the BCP and to encourage participants to access the BCP intervention, no data were captured to measure the extent to which the champions’ involvement influenced either participants’ health behaviours relating to hand care or participants’ decisions on whether or not to access the BCP intervention. In the earlier Hands4U study,44 role models were not found to have an effect on social influence with respect to hand care among health-care workers. Like the Hands4U study, it is possible that our champions did not actively promote the key messages contained in the BCP or failed to promote or encourage participants to access the BCP itself. It is likely that this could have been one of contributory reasons to explain the low rate of uptake to the BCP observed during the study.
Important lessons were learned regarding engagement with the BCP intervention among the study groups. In keeping with the pragmatic nature of this trial, access to the BCP by participants was voluntary. However, the study found that the reminder strategy to improve uptake of the BCP had a positive effect for both student and ICU/SCBU nurses as the trial progressed. Notwithstanding, the barriers found to affect uptake of the BCP (i.e. ‘forgetting’ or ‘not having sufficient time’ to engage with the BCP) will need to be carefully considered in future trials using web-based technology as part of an intervention. Of those who did access the BCP component of the intervention, 90% reported that they found the BCP relevant and informative as well as enjoyable and easy to navigate. This suggests that the BCP intervention was of benefit to those who chose to access it.
Ancillary analyses
The low compliance with the intervention is a limitation of the study. In retrospect, a more appropriate method for the per-protocol analysis would have been the complier average causal effect (CACE) method. It is difficult to interpret the results of the per-protocol analysis as the subgroup non-compliant with the randomised intervention received other interventions that cannot be measured in retrospect (e.g. encouragement from the line manager to use moisturising creams and availability of moisturising cream on the wards). Therefore, compliance is not a binary yes or no. As the ITT analyses were not significant and the study’s participant compliance was low, it was decided not to carry out a CACE analysis retrospectively as the results would be difficult to interpret and would be unlikely to change the interpretation of the results of the trial.
The results from sensitivity analysis I (excluding self-taken hand photographs) were similar to those observed in the ITT analyses with respect to the changes in hand dermatitis from baseline to follow-up in both trial arms. In the light of this, we are confident that the inclusion of self-taken hand photographs did not inadvertently affect the size of the intervention’s effect. This provides further important evidence to support existing research that has shown that smartphone technology can be used to aid reliable diagnostic skin assessment in dermatological research. 70
The results from sensitivity analysis II (restricting the sample to those who were followed up between 12 and 15 months) for the ICU/SCBU nurses were broadly similar to those observed in the ITT; among the student nurse participants, the effects of the intervention were attenuated. This suggests that there may have been a delay beyond 15 months in the intervention leading to a decrease in hand dermatitis. Moreover, it is likely that student nurses may not have been working in clinical placements on a similar full-time equivalent basis as their ICU/SCBU nurse counterparts and so did not have the same opportunities to perform hand dermatitis prevention behaviours.
The results of sensitivity analysis III (after excluding two high-recruiting sites) were broadly similar to those observed in the ITT.
Process evaluation
In addition to the comments provided in Uptake of the behaviour change package, feedback from participants suggests that once individuals accessed the BCP they reported a high degree of positive user satisfaction.
Health economics
The cost-effectiveness analysis found that intervention plus was low cost and that rolling it out would be unlikely to have major cost implications. It was also found that intervention plus had little impact on the use of health-care services. Given the low cost of the intervention and the reduction in hand dermatitis achieved, it is likely to be a cost-effective intervention. However, the National Institute for Health and Care Excellence (NICE) makes recommendations on how to use NHS resources by considering alternative demands for them and, for this purpose, the QALY is the preferred outcome measure. For student nurses, intervention plus saved money and increased QALYs, although these effects were very small. For ICU nurses, intervention plus resulted in higher costs and decreased QALYs, again with these effects being small. Uncertainty around estimates was substantial. The intervention plus was not cost-effective if lost employment costs were included. However, days off work were rarely due to dermatitis and NICE does not generally consider these costs when making recommendations.
There were limitations with the analyses. The study relied on self-report of service use and that may have led to recall inaccuracy. However, this was the best option as a comprehensive approach to service use measurement was wanted. Inpatient costs were excluded. If these costs were included, then they would have had a large impact on costs even if only a small number were admitted. However, it was felt that admission would be unlikely to be related to dermatological problems. Finally, QALYs were used as the main outcome measure in the analyses. EQ-5D-5L scores were high at each time point and did not differ between groups. This means that either the EQ-5D-5L was not sensitive to clinical change or clinical change was limited. Our view is that the EQ-5D is not sensitive to detect clinical change, such as reduced cases of hand dermatitis. The impact of the intervention on outcomes for patients seen by nurses was not examined. This would be problematic to measure and beyond the scope of the study.
In conclusion, there is evidence to suggest that the BCP is a cost-effective intervention if the outcome of reduced hand dermatitis is the main concern. If broader outcomes are to be considered, such as QALYs, then there is little evidence that it is cost-effective.
Consistency with other studies
The baseline prevalence of hand dermatitis in our study was lower than has been reported in other studies. 2,3,8,9 This may be because other studies determined the prevalence of hand dermatitis by self-report rather than by hand photography. The increased prevalence of hand dermatitis among the student nurses after they commenced clinical work is consistent with other studies that found that hand dermatitis becomes more prevalent and problematic after nurses enter the nursing profession. 8,12
A particular benefit of exposure to the BCP was that ICU/SCBU nurses were more likely to report a subsequent increase in their usage of hand moisturiser cream. This change in behaviour was considered encouraging as it is well recognised in the literature that regular application of hand moisturising cream forms an important dermatitis prevention strategy in health-care workers. 21,26–28
The study found that the BCP provided a user-friendly platform from which to provide nurses with evidence-based dermatitis prevention information. Earlier work has shown that workplace behaviour change interventions are effective tools to promote using hand cream as a protective barrier to hand dermatitis, which then, as a consequence, results in an increase in hand cream usage among health-care workers. 30,31,44 Importantly, the study findings are consistent with results from the Hands4U study, which examined changes in hand dermatitis over time following delivery of a multifaceted implementation strategy, including education about hand care delivered by dermacoaches to prevent hand dermatitis. In the Hands4U study, van der Meer et al. 44 found changes in health behaviours relating to hand dermatitis among health-care workers randomised to the intervention arm of the study. These changes included an increase in the reporting of hand dermatitis as well as an increase in the wearing of cotton under-gloves and the use of hand moisturising cream and a decrease in hand-washing activity. Results from the Hands4U study showed that, although the multifaceted implementation strategy had a positive effect in changing health behaviours relating to hand dermatitis in the intervention group, that there was also a corresponding increase in the self-reported prevalence of hand dermatitis at 12 months’ follow-up in the same group. van der Meer et al. 44 argued that the increase in self-reported symptoms in the intervention group at follow-up was probably due to an increase in participants’ knowledge, understanding and, importantly, recognition of hand eczema. A limitation with this earlier study was that it relied solely on participants’ self-assessments of hand dermatitis. In the light of the limitations of using self-reported measures of hand dermatitis identified during the feasibility study, it was decided in this study to use hand dermatitis diagnosed by dermatologists using high-quality hand photographs.
The results from this study build on previous research that used psychological theory to explore the behavioural determinants that are associated with dermatitis prevention. 43,51,54 In particular, the results were similar to those found in the Feedback Intervention Trial (FIT) in the UK, which examined a feedback intervention grounded in a behavioural theoretical framework (i.e. operant learning theory) coupled with personalised action-planning to improve hand hygiene in health-care workers. 51 Although FIT examined a different primary outcome (i.e. hand-hygiene compliance, e.g. use of antibacterial hand rubs by covert direct observation), the results showed that the intervention had a positive effect on facilitating behaviour change with respect to sustained improvements in hand-hygiene practices among the participants. However, unlike the BCP used in the SCIN trial, which was grounded in the TPB and implementation intentions and did not require staff to deliver the intervention, FIT relied on specially trained observers (ward sisters or infection control nurses) to intervene and help participants to formulate their own hand-hygiene goals and to assist nurses to make their own action plans to improve hand-hygiene measures. Furthermore, FIT made use of ward meetings and annual professional development appraisals to assist health-care workers to set their own hand-hygiene goals and to make action plans. In our study, participants were encouraged to access the BCP material (mostly via an e-mail link) at a time convenient to themselves. It was suspected that, for many participants, this was likely to have occurred outside the workplace setting and during non-clinical times. Of particular relevance to the present study were the results from FIT that also showed that the intervention had a much stronger effect in intensive therapy units (as opposed to acute care of the elderly wards) where intervention effectiveness was shown to increase with fidelity to the intervention.
Internet-based interventions have the advantage of being easily and consistently delivered to participants at many different sites, they are scalable and are available to participants at times convenient to them, an important consideration when targeting nurses. The present study provides some evidence that this medium of delivery can be an effective platform from which to promote behaviour change in health professionals, given the positive effects on hand cream use in ICU/SCBU nurses. One of the challenges that affected this present study was the uptake of the online BCP by participants, with fewer than half of the participants reporting that they had accessed the BCP. It is possible that the rate of uptake of the BCP intervention may have been hampered because access to the online version of the BCP was optimised for a desktop browser. Given the increase in people accessing the web via their smartphones, having a version of the website optimised for mobile browsing might have made the BCP intervention more readily accessible, which, in turn, would have increased its overall uptake during the study period. It is also possible that uptake of the intervention would have been greater if the intervention been incorporated as part of existing mandatory hand-hygiene initiatives.
Previous research has also shown that internet-based interventions can be further enhanced by making use of short message service (SMS) or text messages as additional methods of communicating with participants and reminding them to access the intervention. 55 In this present study, a variety of methods were used, including a text message at specific time points to remind and encourage participants to access the online intervention;76 however, it was not possible to ascertain the extent to which these additional methods were responsible for prompting participants to access the intervention.
Generalisability
Although this trial did not result in a statistically significant reduction in hand dermatitis among the participants, the results have contributed to the literature on complex behavioural interventions as a method of changing individual behaviour in occupational settings. Although this present study focused on the nursing profession in the public health-care setting, it is reasonable to argue that the results and their interpretations may provide a degree of generalisability to other health professionals at risk of hand dermatitis and, particularly, to those employed in other health-care settings as well as other non-health professionals who are also at risk of hand dermatitis. It is acknowledged that the occupational health departments that participated in the study may be larger and more proactive than those that did not. However, participating sites were geographically diverse, and there is no reason to believe that the results would be reproducible in other NHS sites across the UK.
As shown in the demographic profile of the participants who took part in this study (in terms of age and gender), we are confident that we successfully recruited a representative sample for each participant group. Moreover, although a significantly large number of female nurses (both student nurses and ICU/SCBU nurses) were recruited into the study, this broadly reflected current nursing workforce characteristics.
Harms
This study assessed the effectiveness of a BCP to improve hand care in nurses and to reduce the prevalence of hand dermatitis in this at-risk population. In the light of the defined scope of this study, it was deemed a very low-risk study to conduct in terms of any potential harms to participants. No adverse events were reported during the study.
Strengths and limitations
A strength of this study was the large number of participating sites that took part in the study and the large number of participants who volunteered. The study initially planned to recruit 26 participating sites, but for various reasons (i.e. staff changes and lack of resources) many of the sites that initially expressed a willingness to take part were subsequently unable to proceed. The dropout of sites was mainly due to changes in management or contracts of the occupational health departments and the trusts. It is not uncommon for occupational health services to trusts to be put out to tender every 3–5 years. The uncertainty surrounding regaining tenders or change in management structure was the main reason for sites dropping out. Site dropout was not thought to be related to the acceptability of the intervention. As a result, a large number of additional sites across the UK were approached to scope out their interest and capacity to take part. In response to this, it was possible to recruit a total of 35 participating sites. Moreover, a number of sites that took part in the study had approached the trial team directly to request involvement in the study after hearing about the study from a third party. Overall, this enthusiasm contributed to the success of the implementation of the trial. In addition, the trial benefited from the recruitment of participants that exceeded our initial target. Common feedback from fieldworkers was that participants considered this a very important study for their profession that they were keen to support.
The trial had a reasonable response rate to the study questionnaires and to the collection of hand photographs at baseline and follow-up, particularly among the ICU/SCBU nurse population. However, in relation to the student nurse population, one of the major challenges local fieldworkers faced during the follow-up period was the difficulty co-ordinating suitable times to collect the follow-up data from participants. This difficulty was mainly because the student nurses were on clinical placements out of the area or because the study team was not in receipt of updated residential address details. The study implemented a regular reminder system comprising an e-mail, SMS and telephone contact to encourage completion and return of the study questionnaires. In addition, participants who completed all three questionnaires were entered into a prize draw to win one of the study cameras. Information relating to the prize draw was included in all correspondence sent to the participants. The benefits of using questionnaires and surveys to measure key beliefs among health-care workers relating to hand-hygiene practice and to seek their feedback on issues relating to the availability and accessibility of hand-care products has been previously acknowledged. 38,82 However, it is acknowledged that self-report questionnaires have the potential to yield inaccurate information, most notably because responders have a tendency to overestimate their adherence to hand-hygiene requirements17 or because their memories of past events and behaviours are prone to recall bias.
With respect to the collection of hand photographs, participants who could not be followed up by the local fieldworkers (because of logistical difficulties or other reasons) were provided with an opportunity to send in self-taken hand photographs via e-mail. This strategy helped to increase the overall response rate at follow-up. However, one of the main challenges that was faced during the study was the means by which local fieldworkers were able to successfully collect follow-up data from student nurses, who were geographically dispersed by the end of the trial; for example, they had returned to their parental residence or had gone travelling.
Another important strength of the study was the development of a novel hand photography protocol to support the delivery of the study. This proved to be an efficient and convenient method for collecting standardised hand photographs from each of the participating sites. The hand photography protocol comprised the development of a detailed procedure for setting up and taking hand photographs and a practical training session provided to local fieldworkers. Moreover, an experienced dermatology research nurse was trained in the procedure for screening all hand photographs collected during the study into three distinct categories (‘clear’, ‘positive dermatitis’ or ‘unsure’). The training of a dermatology research nurse was shown to be a cost-effective and reliable method for processing a large number of hand photographs. As described previously, the study dermatologists also developed a set of guiding mini assessment rules that they followed when diagnosing hand dermatitis from the hand photographs. Collectively, the hand photography protocol has been shown to be a suitable and reliable method for use in clinical practice (e.g. hand dermatitis health surveillance activities), as well as for other future research studies.
The major limitation of the study was the low compliance with the BCP and an inability to estimate the compliance with other aspects of the intervention, for example the use of hand moisturising cream. It was found to be difficult to conduct accurate indirect assessments of the usage of hand moisturising cream from ward-based dispensers in ICU and SCBUs because the supplies available from individual dispensers were typically replenished from hospital general stock and were not ordered locally. This made it impossible to collect reliable procurement data specific to the ICUs/SCBUs. As a consequence, visual proxy measures were relied on for usage measurements at 4- to 6-week time intervals. The reliance on crude estimates of usage of hand moisturising cream is also prone to inaccurate or misleading results. For instance, it does not account for spillage or wastage of the product, or intentional or deliberate inflation of usage, particularly if participants were motivated by a desire to be seen to be increasing their uptake of hand-hygiene behaviours. Furthermore, there is the likelihood of poor inter-rater and intra-rater reliability when taking indirect measures and such measures do not provide any information on when and why usage of hand moisturising cream occurred. In addition, participants may have had a preference for using alternative personal supplies of hand moisturising cream to the products made available to them during the study. It is possible that participants may have over-reported their adoption of hand-care behaviours, for example increasing their use of hand moisturising cream, to appear more compliant with hand-care requirements. The limitations associated with indirect measurements of hand-hygiene adherence have been highlighted by others. 38,83 In response to this limitation in reporting, Boyce84 suggested that the use of multiple measurement methods, such as electronic reporting, in conjunction with direct observations may provide a more robust approach to improve and sustain hand-hygiene compliance rate, although the practicalities of this have yet to be fully realised.
As described elsewhere in this report, the validity of self-reported measures of hand-hygiene behaviours has attracted considerable attention in the literature in recent years,85 with some suggesting that their limitations outweigh their benefits in producing reliable information. 54,86 For example, some studies have shown overall inconsistency between self-reported and observed hand-hygiene behaviours among nurses and physicians. 87,88 In one study, physicians self-reported greater compliance with hand-hygiene practices than observers noted, whereas in contrast nurses self-reported lower compliance with hand-hygiene requirements than observers noted. 89 In a later study comparing nurses’ self-reported adherence to hand hygiene with observations of their behaviours, the results showed that nurses had a tendency to self-report greater adherence to hand-hygiene requirements than observers recorded. 54 As Larson et al. 87 further point out, when two methods are used to measure hand hygiene and produce different results, it is impossible to confidently ascertain which measurement method is more accurate, particularly because direct observations to measure hand hygiene can be greatly influenced by a range of variables. In this study, it is acknowledged that participants may have had a preference or motivation to report more positive or socially desirable responses when completing the study questionnaires. It is also important to recognise that, in this study, salient workload, staffing or environmental factors were not measured, which may influence participants’ health beliefs and health behaviours associated with hand care. In retrospect, the research team acknowledges that the collection and analyses of these types of data would have assisted us in better understanding the effects these salient organisational influences may have had on the participants taking part in the study. Accordingly, the need for future research to be undertaken in order to better understanding the impact these factors may have on individuals and cultural drivers associated with hand dermatitis prevention among health-care workers is recognised. In particular, future studies may benefit from supplementing questionnaires about hand-care beliefs with qualitative interviews with nurses and other key informants to explore the origins of, and influences on, nurses’ beliefs and hand-care behaviours in more depth. This would provide a more nuanced understanding of how the intervention achieved its effects.
The possible impact of non-responder bias at follow-up is acknowledged and it is recognised that there may have been circumstances in which some participants may have been reluctant to provide follow-up data, for example if they had concerns that any potential signs of active hand dermatitis present at follow-up may have been reported by the research team to local management. To mitigate this, participants were posted a letter of reassurance that information obtained at follow-up would not be shared with local management along with a brief questionnaire seeking the reason why they did not wish to provide follow-up hand photographs (‘I forgot’, ‘I currently have hand eczema/dermatitis’, ‘I don’t want to’). In addition, participants who were leaving their positions were asked if they were doing so as a result of hand dermatitis. Furthermore, we do not think that there would be any reason why such non-responder bias would have a larger adverse impact on participation at follow-up in the intervention plus sites than in the intervention light sites. An important limitation with the hand photography protocol was that the study dermatologists experienced difficulties assessing borderline or ambiguous cases of hand dermatitis from hand photographs, even when using a validated assessment guide. However, the establishment of mini assessment rules helped to address this issue. Another limitation with the hand photographs related to the poor digital quality of some of the images. This occurred because, in some cases, hand photographs taken by the fieldworkers or by participants (i.e. self-taken photographs) did not follow the instructions outlined in their respective standard operating procedures; some photographs were under- or over-exposed, in others there was glare/reflection from the surrounding environment or images were taken from a side angle. This made it difficult for the study dermatologists to conduct accurate assessments. The health economic analysis had limitations. The cost-effectiveness was based on QALYs gained, as derived from the EQ-5D-5L. This measure may not have been sufficiently sensitive to change in this clinical area. A complete-case analysis was conducted and, to some extent, this may have introduced bias to the results. However, there was little difference between the groups, and it is unlikely that imputation would have altered this.
Conclusions
There was no evidence that the risk of developing dermatitis in the intervention light group was greater than in the intervention plus group. However, the intervention led to a statistically significant increase in the use of hand moisturising creams before, during and after shifts in the ICU nurse participants. An important finding from the secondary outcomes was the high level of knowledge, at baseline, in both groups of study participants, about the use of hand moisturisers to prevent hand dermatitis. The intervention is cheap to deliver. These results have added to the understanding of how best to change nurses’ beliefs and behaviour towards hand care and, ultimately, how to reduce the prevalence of hand dermatitis in this at-risk occupational group. Future research should focus on how workplace culture can be changed to enable nurses’ knowledge of the importance of good hand care, particularly the use of hand moisturisers before, during and after shifts, to be put into action in the face of busy shifts.
Implications for health care
-
As our results did not show a statistically significant reduction in hand dermatitis in the intervention plus group, we are unable to recommend that the intervention is rolled out across the NHS. However, the Royal College of Nursing has decided to host the BCP component of the intervention on the education section of its website.
-
The success of any future initiative that aims to change health-care workers’ beliefs, attitudes and behaviours should involve strong leadership and support from management and infection control teams. In the present study, the role and influence of managers in the promotion of hand care among health-care workers are recognised and so their involvement in should be further recognised and promoted.
Acknowledgements
We would like to take this opportunity to thank all of the participants who agreed to give up their valuable time to take part in this study. In addition, we acknowledge the hard work of all of the local fieldworkers at participating sites who assisted with the study. Their tireless effort throughout the study was a reflection of their dedication to their profession and their commitment to advancing the knowledge and understanding of dermatitis prevention among health professionals.
We are grateful to members of the SCIN Trial Steering Committee for their oversight and expertise:
-
Dr Ira Madan
-
Dr Christopher Harling (chairperson)
-
Dr Graham Johnston
-
Dr Guduru Gopal Rao
-
Dr Isabel Reading
-
Dr Lesley Rushton
-
Ms Wendy Taylor
-
Dr Peter White
-
Dr Vaughan Parsons
-
Mrs Barbara Smiley
-
Mrs Mopelola Jegede (minute taker).
We also extend our thanks and appreciation of the Trial Management Committee for its support and guidance throughout the trial:
-
Dr Ira Madan
-
Professor Hywel Williams
-
Professor David Coggon
-
Dr Barry Cookson
-
Dr Paul McCrone
-
Ms Caroline Murphy
-
Dr Georgia Ntani
-
Dr Vaughan Parsons
-
Dr Alison Wright
-
Mrs Barbara Smiley
-
Mrs Mopelola Jegede (minute taker).
In addition, we appreciate the oversight and guidance with respect to trial governance and data collection and monitoring requirements that was provided by the King’s CTU (Ms Caroline Murphy, Ms Joanna Kelly and Mrs Beverley Aloa-White) and for participation in regular SCIN trial Operational Management group meetings along with the addition of Dr Alison Wright.
We would like to also extend our appreciation to the management team at Guy’s and St Thomas’ NHS Foundation Trust for their willingness to sponsor the trial, in particular, to the Research and Development Unit for its research governance and financial management support (Miss Ceri Potts, Miss Elizabeth Bruna, Miss Samantha Roper, Mr Ernie Finch and Mr Mariusz Marcinkowski) and to the management team and staff in the Guy’s and St Thomas’ NHS Foundation Trust Occupational Health Service for hosting the SCIN trial research team.
We also thank NRES Committee London – Hampstead and City Road for providing ethics oversight, review and approval: Ms Maeve Groot Bluemink and Ms Jess Vlieland-Boddy.
Contributions of authors
Ira Madan (Chief Investigator, Consultant Occupational Physician and Reader from the specialty of occupational medicine) brought expertise in NHS occupational health, pragmatic research and translating research findings into policy.
Vaughan Parsons (Trial Manager from the specialty of psychology and health management) was responsible for the operational management of the trial.
Georgia Ntani (Medical Statistician from the specialty of medical statistics) was responsible for formulating the trial analysis plan and undertaking the analysis.
Alison Wright (Lecturer from the specialty of health psychology) brought expertise in psychological aspects of intervention design and evaluation and developed the BCP.
John English (Consultant Dermatologist from the specialty of dermatology) brought expertise in the field of occupational dermatology. He was responsible for assessing the presence or absence of dermatitis from the photographic images collected from participants during the trial.
David Coggon (Professor of Occupational and Environmental Medicine from the specialty of occupational medicine) brought expertise in the epidemiological aspects of design, analysis and interpretation.
Paul McCrone (Director from the specialty of health economics) assisted with the trial design and economic evaluation.
Julia Smedley (Consultant Occupational Physician from the specialty of occupational medicine) advised on occupational health operational aspects of methodology and aided with the identification and recruitment of participating sites.
Lesley Rushton (Reader in Occupational Epidemiology from the Medical Research Council Centre for Environment and Health) advised on occupational epidemiology and statistics.
Caroline Murphy (Operational Manager) manages the UK Clinical Research Collaboration-registered King’s CTU at King’s College London and assisted with drafting the study protocol, randomisation and governance of the trial.
Barry Cookson (Director from the specialty of microbiology) brought expertise in hand hygiene, medical microbiology, infection prevention and control of infection.
Tina Lavender (Director, Midwifery Research Group and from the specialty of nursing/midwifery) brought expertise in clinical trials in relation to skin-care practices.
Hywel Williams (Professor of Dermato-epidemiology from the specialty of dermatology) brought expertise in the design and delivery of dermatology clinical trials plus content expertise as a clinical dermatologist. He was responsible for assessing the presence or absence of dermatitis from the photographic images collected from participants during the trial.
All co-investigators provided input into the development of the protocol and during the design and conduct of the study and provided ongoing advice as required. In addition, all co-investigators contributed to the production of the final report.
Publications and conference proceedings
Publications (up to the time of publication of the final report)
Parsons V, Madan I. From vision to action part 1: building an evidence-base in occupational health. Occup Health Work 2015;12(4).
Parsons V, Madan I. Developing a successful national occupational health research proposal. Part 2. Occup Health Work 2015;12(5).
Madan I, Parsons V, Cookson B, English J, Lavender T, McCrone P, et al. A behavioural change package to prevent hand dermatitis in nurses working in the National Health Service. The SCIN trial: study protocol for a cluster randomised controlled trial. Trials 2016;17:145.
Parsons V, Madan I. Implementing a national OH clinical trial. Part 3: the national SCIN trial – roll out and lessons learned. Occup Health Work 2016;13(5).
Weston D, Parsons V, Ntani G, Rushton L, Madan I. Mixed contact methods to improve response to a postal questionnaire. Occup Med 2017;67:305–7.
Parsons V, Williams H, English J, Llewellyn J, Ntani G, Madan I. The development of a protocol for diagnosing hand dermatitis from photographic images. Contact Derm 2018;79:270–5.
Conference proceedings (up to the time of publication of the final report)
Parsons V, Coggon D, Cookson B, English J, Lavender T, McCrone P, et al. The SCIN (Skin Care Intervention in Nurses) Trial. A Cross-sectional Feasibility Study in Wales (Stage 1). Poster presentation at the 8th Georg Rajka International Symposium on Atopic Dermatitis, Nottingham, UK, 22 May 2014.
Parsons V, Din S, Wright A, Coggon D, Ntani G, Williams H, et al. The SCIN (Skin Care Intervention in Nurses) Trial. A Cross-sectional Feasibility Study in Wales. Poster presentation at the Society of Occupational Medicine Scientific Meeting, London, UK, 28 May 2014.
Madan I, Parsons V, Cookson B, English J, Lavender T, McCrone P, et al. The SCIN (Skin Care Intervention in Nurses) Trial. A Cluster Randomised Trial. Oral presentation at the Epidemiology in Occupational Health (EPICOH) Conference, Barcelona, Spain, 5 September 2016.
Weston D, Parsons V, Madan I. The Use of Mixed Methods of Contact to Improve Response rate to a Postal Questionnaire. Poster presentation at the Epidemiology in Occupational Health (EPICOH) Conference, Barcelona, Spain, 5 September 2016.
Madan I, Parsons V, Cookson B, English J, Lavender T, McCrone P, et al. The SCIN (Skin Care Intervention in Nurses) Trial. A Cluster Randomised Trial. Poster presentation at the 13th Congress European Society of Contact Dermatitis (ESCD) Conference, Manchester, UK, 15 September 2016.
Madan I, Parsons V. Update on the Conduct of the SCIN Trial. Oral presentation at the Eczema and Contact Dermatitis: An Evidence-based Update Meeting, Nottingham, UK, 17 May 2017.
Madan I, Parsons V. Development of the Hand Photography Protocol. Oral and poster presentation at the StanDerm workshop, Berlin, Germany, 18 May 2017.
Madan V, Parsons V, Ntani G, Harling C, McCrone P, Brough C, et al. Presentation of the SCIN Trial Results. Paper presented at the SCIN trial dissemination conference, London, UK, 12 July 2017.
Madan I, Parsons V, Cookson B, English J, Lavender T, McCrone P, et al. SCIN Trial (Skin Care Intervention in Nurses). Dissemination of results. Oral presentation at the 32nd Triennial Congress of the International Commission on Occupational Health (ICOH), Dublin, Ireland, 29 April–4 May 2018.
Data-sharing statement
Access to the study data is available from the corresponding author. The study data will be made available to other researchers on request and if deemed appropriate.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Madan I, Parsons V, Cookson B, English J, Lavender T, McCrone P, et al. A behavioural change package to prevent hand dermatitis in nurses working in the national health service (the SCIN trial): study protocol for a cluster randomised controlled trial. Trials 2016;17. https://doi.org/10.1186/s13063-016-1255-y.
- Hamnerius N, Svedman C, Bergendorff O, Björk J, Bruze M, Pontén A. Wet work exposure and hand eczema among healthcare workers: a cross-sectional study. Br J Dermatol 2018;178:452-61. https://doi.org/10.1111/bjd.15813.
- Thyssen JP, Johansen JD, Linneberg A, Menné T. The epidemiology of hand eczema in the general population – prevalence and main findings. Contact Derm 2010;62:75-87. https://doi.org/10.1111/j.1600-0536.2009.01669.x.
- Meding B, Swanbeck G. Predictive factors for hand eczema. Contact Derm 1990;23:154-61. https://doi.org/10.1111/j.1600-0536.1990.tb04776.x.
- Coenraads PJ, Diepgen TL. Risk for hand eczema in employees with past or present a topic dermatitis. Int Arch Occup Environ Health 1998;71:7-13. https://doi.org/10.1007/s004200050243.
- Meding B, Wrangsjö K, Järvholm B. Fifteen-year follow-up of hand eczema: persistence and consequences. Br J Dermatol 2005;152:975-80. https://doi.org/10.1111/j.1365-2133.2005.06494.x.
- Lerbaek A, Kyvik KO, Ravn H, Menné T, Agner T. Clinical characteristics and consequences of hand eczema – an 8-year follow-up study of a population-based twin cohort. Contact Derm 2008;58:210-16. https://doi.org/10.1111/j.1600-0536.2007.01305.x.
- Skudlik C, Dulon M, Wendeler D, John SM, Nienhaus A. Hand eczema in geriatric nurses in Germany – prevalence and risk factors. Contact Derm 2009;60:136-43. https://doi.org/10.1111/j.1600-0536.2008.01496.x.
- Smit HA, Burdorf A, Coenraads PJ. Prevalence of hand dermatitis in different occupations. Int J Epidemiol 1993;22:288-93. https://doi.org/10.1093/ije/22.2.288.
- Visser MJ, Verberk MM, van Dijk FJ, Bakker JG, Bos JD, Kezic S. Wet work and hand eczema in apprentice nurses; part I of a prospective cohort study. Contact Derm 2014;70:44-55. https://doi.org/10.1111/cod.12131.
- Soltanipoor M, Kezic S, Sluiter JK, Rustemeyer T. The effectiveness of a skin care program for the prevention of contact dermatitis in health care workers (the Healthy Hands Project): study protocol for a cluster randomized controlled trial. Trials 2017;18. https://doi.org/10.1186/s13063-017-1803-0.
- Smith DR, Choe MA, Jeong JS, An GJ, Chae YR, Jeon MY. Hand dermatitis among Korean nursing students. Int J Nurs Pract 2006;12:160-5. https://doi.org/10.1111/j.1440-172X.2006.00564.x.
- Hutchings CV, Shum KW, Gawkrodger DJ. Occupational contact dermatitis has an appreciable impact on quality of life. Contact Derm 2001;45:17-20. https://doi.org/10.1034/j.1600-0536.2001.045001017.x.
- Fowler JF, Ghosh A, Sung J, Emani S, Chang J, Den E, et al. Impact of chronic hand dermatitis on quality of life, work productivity, activity impairment, and medical costs. J Am Acad Dermatol 2006;54:448-57. https://doi.org/10.1016/j.jaad.2005.11.1053.
- Diepgen TL, Scheidt R, Weisshaar E, John SM, Hieke K. Cost of illness from occupational hand eczema in Germany. Contact Derm 2013;69:99-106. https://doi.org/10.1111/cod.12038.
- Stocks SJ, McNamee R, van der Molen HF, Paris C, Urban P, Campo G, et al. Trends in incidence of occupational asthma, contact dermatitis, noise-induced hearing loss, carpal tunnel syndrome and upper limb musculoskeletal disorders in European countries from 2000 to 2012. Occup Environ Med 2015;72:294-303. https://doi.org/10.1136/oemed-2014-102534.
- World Health Organization . WHO Guidelines on Hand Hygiene in Health Care 2009.
- Haslund P, Bangsgaard N, Jarløv JO, Skov L, Skov R, Agner T. Staphylococcus aureus and hand eczema severity. Br J Dermatol 2009;161:772-7. https://doi.org/10.1111/j.1365-2133.2009.09353.x.
- Brans R, Kolomanski K, Mentzel F, Vollmer U, Kaup O, John SM. Colonisation with methicillin-resistant Staphylococcus aureus and associated factors among nurses with occupational skin diseases. Occup Environ Med 2016;73:670-5. https://doi.org/10.1136/oemed-2016-103632.
- NHS Plus . Dermatitis: Occupational Aspects of Management: A National Guideline 2009 2009.
- Nicholson PJ. Evidence-based guidelines: occupational contact dermatitis and urticaria. Occup Med 2010;60:502-4. https://doi.org/10.1093/occmed/kqq075.
- Held E, Wolff C, Gyntelberg F, Agner T. Prevention of work-related skin problems in student auxiliary nurses: an intervention study. Contact Derm 2001;44:297-303. https://doi.org/10.1034/j.1600-0536.2001.440509.x.
- Held E, Mygind K, Wolff C, Gyntelberg F, Agner T. Prevention of work related skin problems: an intervention study in wet work employees. Occup Environ Med 2002;59:556-61. https://doi.org/10.1136/oem.59.8.556.
- Berndt U, Wigger-Alberti W, Gabard B, Elsner P. Efficacy of a barrier cream and its vehicle as protective measures against occupational irritant contact dermatitis. Contact Derm 2000;42:77-80. https://doi.org/10.1034/j.1600-0536.2000.042002077.x.
- McCormick RD, Buchman TL, Maki DG. Double-blind, randomized trial of scheduled use of a novel barrier cream and an oil-containing lotion for protecting the hands of health care workers. Am J Infect Control 2000;28:302-10. https://doi.org/10.1067/mic.2000.107425.
- Saary J, Qureshi R, Palda V, DeKoven J, Pratt M, Skotnicki-Grant S, et al. A systematic review of contact dermatitis treatment and prevention. J Am Acad Dermatol 2005;53. https://doi.org/10.1016/j.jaad.2005.04.075.
- Arbogast JWFEJ, Hammond BS, Cartner TJ, Dolan MD, Ali Y, Maibach HI. Effectiveness of a hand care regimen with moisturizer in manufacturing facilities where workers are prone to occupational irritant dermatitis. Dermatitis 2004;15. https://doi.org/10.2310/6620.2004.20420.
- Winker R, Salameh B, Stolkovich S, Nikl M, Barth A, Ponocny E, et al. Effectiveness of skin protection creams in the prevention of occupational dermatitis: results of a randomized, controlled trial. Int Arch Occup Environ Health 2009;82:653-62. https://doi.org/10.1007/s00420-008-0377-2.
- Graham M, Nixon R, Burrell LJ, Bolger C, Johnson PD, Grayson ML. Low rates of cutaneous adverse reactions to alcohol-based hand hygiene solution during prolonged use in a large teaching hospital. Antimicrob Agents Chemother 2005;49:4404-5. https://doi.org/10.1128/AAC.49.10.4404-4405.2005.
- Bauer A, Schmitt J, Bennett C, Coenraads PJ, Elsner P, English J, et al. Interventions for preventing occupational irritant hand dermatitis. Cochrane Database Syst Rev 2010;6. https://doi.org/10.1002/14651858.CD004414.pub2.
- van Gils RF, Boot CR, van Gils PF, Bruynzeel D, Coenraads PJ, van Mechelen W, et al. Effectiveness of prevention programmes for hand dermatitis: a systematic review of the literature. Contact Derm 2011;64:63-72. https://doi.org/10.1111/j.1600-0536.2010.01825.x.
- Große-Schütte K, Assadian O, Hübner NO, Löffler H, Kramer A. Practices of skin care among nurses in medical and surgical intensive care units: results of a self-administered questionnaire. GMS Krankenhhyg Interdiszip 2011;6. https://doi.org/10.3205/dgkh000165.
- Larson E, Friedman C, Cohran J, Treston-Aurand J, Green S. Prevalence and correlates of skin damage on the hands of nurses. Heart Lung 1997;26:404-12. https://doi.org/10.1016/S0147-9563(97)90027-3.
- Pedersen LK, Held E, Johansen JD, Agner T. Less skin irritation from alcohol-based disinfectant than from detergent used for hand disinfection. Br J Dermatol 2005;153:1142-6. https://doi.org/10.1111/j.1365-2133.2005.06875.x.
- Stone SP, Fuller C, Savage J, Cookson B, Hayward A, Cooper B, et al. Evaluation of the national Cleanyourhands campaign to reduce Staphylococcus aureus bacteraemia and Clostridium difficile infection in hospitals in England and Wales by improved hand hygiene: four year, prospective, ecological, interrupted time series study. BMJ 2012;344. https://doi.org/10.1136/bmj.e3005.
- Boyce JM, Pittet D. Hand Hygiene Task Force . Guideline for Hand Hygiene in Health-Care Settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Infect Control Hosp Epidemiol 2002;23:3-40. https://doi.org/10.1086/503164.
- Stutz N, Becker D, Jappe U, John SM, Ladwig A, Spornraft-Ragaller P, et al. Nurses’ perceptions of the benefits and adverse effects of hand disinfection: alcohol-based hand rubs vs. hygienic handwashing: a multicentre questionnaire study with additional patch testing by the German Contact Dermatitis Research Group. Br J Dermatol 2009;160:565-72. https://doi.org/10.1111/j.1365-2133.2008.08951.x.
- Consensus Measurement in Hand Hygiene Project Expert Advisory Panel . Measuring Hand Hygiene Adherence: Overcoming the Challenges 2009.
- Kingston LM, Slevin BL, O’Connell NH, Dunne CP. Attitudes and practices of Irish hospital-based physicians towards hand hygiene and hand rubbing using alcohol-based hand rub: a comparison between 2007 and 2015. J Hosp Infect 2017;97:17-25. https://doi.org/10.1016/j.jhin.2017.05.010.
- Huang C, Ma W, Stack S. The hygienic efficacy of different hand-drying methods: a review of the evidence. Mayo Clin Proc 2012;87:791-8. https://doi.org/10.1016/j.mayocp.2012.02.019.
- Löffler H, Bruckner T, Diepgen T, Effendy I. Primary prevention in health care employees: a prospective intervention study with a 3-year training period. Contact Derm 2006;54:202-9. https://doi.org/10.1111/j.0105-1873.2006.00825.x.
- Dulon M, Pohrt U, Skudlik C, Nienhaus A. Prevention of occupational skin disease: a workplace intervention study in geriatric nurses. Br J Dermatol 2009;161:337-44. https://doi.org/10.1111/j.1365-2133.2009.09226.x.
- Ibler KS, Jemec GB, Diepgen TL, Gluud C, Lindschou Hansen J, Winkel P, et al. Skin care education and individual counselling versus treatment as usual in healthcare workers with hand eczema: randomised clinical trial. BMJ 2012;345. https://doi.org/10.1136/bmj.e7822.
- van der Meer EW, Boot CR, van der Gulden JW, Knol DL, Jungbauer FH, Coenraads PJ, et al. Hands4U: the effects of a multifaceted implementation strategy on hand eczema prevalence in a healthcare setting. Results of a randomized controlled trial. Contact Derm 2015;72:312-24. https://doi.org/10.1111/cod.12313.
- John SM, Kezic S. Occupational skin diseases – development and implementation of European standards on prevention of occupational skin diseases. J Eur Acad Dermatol Venereol 2017;31:3-4. https://doi.org/10.1111/jdv.14276.
- Oliver C, Thompson A, Cooke RPD. In defence of high hand-hygiene compliance rates. J Hosp Infect 2017;97:31-2. https://doi.org/10.1016/j.jhin.2017.06.009.
- Dubbert PM, Dolce J, Richter W, Miller M, Chapman SW. Increasing ICU staff handwashing: effects of education and group feedback. Infect Control Hosp Epidemiol 1990;11:191-3. https://doi.org/10.1086/646148.
- Norman P, Conner M, Conner M, Norman P. Predicting and Changing Health Behaviour: Research and Practice with Social Cognition Models. Maidenhead: Open University Press; 2015.
- Ibler KS, Agner T, Hansen JL, Gluud C. The Hand Eczema Trial (HET): design of a randomised clinical trial of the effect of classification and individual counselling versus no intervention among health-care workers with hand eczema. BMC Dermatol 2010;10. https://doi.org/10.1186/1471-5945-10-8.
- Dyson J, Lawton R, Jackson C, Cheater F. Does the use of a theoretical approach tell us more about hand hygiene behaviour? The barriers and levers to hand hygiene. J Infect Prev 2011;12:17-24. https://doi.org/10.1177/1757177410384300.
- Fuller C, Michie S, Savage J, McAteer J, Besser S, Charlett A, et al. The Feedback Intervention Trial (FIT) – improving hand-hygiene compliance in UK healthcare workers: a stepped wedge cluster randomised controlled trial. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0041617.
- Srigley JA, Corace K, Hargadon DP, Yu D, MacDonald T, Fabrigar L, et al. Applying psychological frameworks of behaviour change to improve healthcare worker hand hygiene: a systematic review. J Hosp Infect 2015;91:202-10. https://doi.org/10.1016/j.jhin.2015.06.019.
- McAteer J, Stone S, Fuller C, Charlett A, Cookson B, Slade R, et al. NOSEC/FIT group . Development of an observational measure of healthcare worker hand-hygiene behaviour: the hand-hygiene observation tool (HHOT). J Hosp Infect 2008;68:222-9. https://doi.org/10.1016/j.jhin.2007.12.009.
- O’Boyle CA, Henly SJ, Larson E. Understanding adherence to hand hygiene recommendations: the theory of planned behavior. Am J Infect Control 2001;29:352-60. https://doi.org/10.1067/mic.2001.18405.
- Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res 2010;12. https://doi.org/10.2196/jmir.1376.
- Matterne U, Diepgen TL, Weisshaar E. A longitudinal application of three health behaviour models in the context of skin protection behaviour in individuals with occupational skin disease. Psychol Health 2011;26:1188-207. https://doi.org/10.1080/08870446.2010.546859.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179-211. https://doi.org/10.1016/0749-5978(91)90020-T.
- McEachan RRC, Conner M, Taylor NJ, Lawton RJ. Prospective prediction of health-related behaviours with the theory of planned behaviour: a meta-analysis. Health Psychol Rev 2011;5:97-144. https://doi.org/10.1080/17437199.2010.521684.
- Orbell S, Sheeran P. ‘Inclined abstainers’: a problem for predicting health-related behaviour. Br J Soc Psychol 1998;37:151-65. https://doi.org/10.1111/j.2044-8309.1998.tb01162.x.
- Soureti A, Murray P, Cobain M, Chinapaw M, van Mechelen W, Hurling R. Exploratory study of web-based planning and mobile text reminders in an overweight population. J Med Internet Res 2011;13. https://doi.org/10.2196/jmir.1773.
- Prestwich A, Perugini M, Hurling R. Can the effects of implementation intentions on exercise be enhanced using text messages?. Psychol Health 2009;24:677-87. https://doi.org/10.1080/08870440802040715.
- Smit HA, Coenraads PJ, Lavrijsen AP, Nater JP. Evaluation of a self-administered questionnaire on hand dermatitis. Contact Derm 1992;26:11-6. https://doi.org/10.1111/j.1600-0536.1992.tb00861.x.
- Kavli G, Angell E, Moseng D. Hospital employees and skin problems. Contact Derm 1987;17:156-8. https://doi.org/10.1111/j.1600-0536.1987.tb02697.x.
- Steiner M. Workplace Health Surveillance for Occupational Skin Diseases: Diagnostic Accuracy and Reliability of a Teledermatology Tool 2011.
- Scheinfeld N, Kurz J, Teplitz E. A comparison of the concordance of digital images, live examinations, and skin biopsies for the diagnosis of hospitalized dermatology consultation patients. Skinmed 2003;2:14-9. https://doi.org/10.1111/j.1540-9740.2003.01866.x.
- Baumeister T, Weistenhöfer W, Drexler H, Kütting B. Prevention of work-related skin diseases: teledermatology as an alternative approach in occupational screenings. Contact Derm 2009;61:224-30. https://doi.org/10.1111/j.1600-0536.2009.01606.x.
- Scheinfeld NS, Flanigan K, Moshiyakhov M, Weinberg JM. Trends in the use of cameras and computer technology among dermatologists in New York City 2001–2002. Dermatol Surg 2003;29:822-5. https://doi.org/10.1097/00042728-200308000-00009.
- Hald M, Veien NK, Laurberg G, Johansen JD. Severity of hand eczema assessed by patients and dermatologist using a photographic guide. Br J Dermatol 2007;156:77-80. https://doi.org/10.1111/j.1365-2133.2006.07565.x.
- Ebner C, Wurm EM, Binder B, Kittler H, Lozzi GP, Massone C, et al. Mobile teledermatology: a feasibility study of 58 subjects using mobile phones. J Telemed Telecare 2008;14:2-7. https://doi.org/10.1258/jtt.2007.070302.
- Shin H, Kim DH, Ryu HH, Yoon SY, Jo SJ. Teledermatology consultation using a smartphone multimedia messaging service for common skin diseases in the Korean army: a clinical evaluation of its diagnostic accuracy. J Telemed Telecare 2014;20:70-4. https://doi.org/10.1177/1357633X14524151.
- Coenraads PJ, Van Der Walle H, Thestrup-Pedersen K, Ruzicka T, Dreno B, De La Loge CT, et al. Construction and validation of a photographic guide for assessing severity of chronic hand dermatitis. Br J Dermatol 2005;152:296-301. https://doi.org/10.1111/j.1365-2133.2004.06270.x.
- Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 2004;23:443-51. https://doi.org/10.1037/0278-6133.23.5.443.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Sax H, Uçkay I, Richet H, Allegranzi B, Pittet D. Determinants of good adherence to hand hygiene among healthcare workers who have extensive exposure to hand hygiene campaigns. Infect Control Hosp Epidemiol 2007;28:1267-74. https://doi.org/10.1086/521663.
- Whitby M, McLaws ML, Ross MW. Why healthcare workers don’t wash their hands: a behavioral explanation. Infect Control Hosp Epidemiol 2006;27:484-92. https://doi.org/10.1086/503335.
- Weston D, Parsons V, Ntani G, Rushton L, Madan I. Mixed contact methods to improve response to a postal questionnaire. Occup Med 2017;67:305-7. https://doi.org/10.1093/occmed/kqx032.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
- Curtis L, Beecham J. Unit Costs of Health and Social Care 2011. Canterbury: Personal Social Services Research Unit, University of Kent; 2016.
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2015 to 2016 2016. www.gov.uk/government/publications/nhs-reference-costs-2015-to-2016 (accessed 16 July 2019).
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2017.
- Campbell MK, Piaggio G, Elbourne DR, Altman DG. CONSORT Group . Consort 2010 statement: extension to cluster randomised trials. BMJ 2012;345. https://doi.org/10.1136/bmj.e5661.
- Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med 2004;141:1-8. https://doi.org/10.7326/0003-4819-141-1-200407060-00008.
- Bradley CW, Holden E, Garvey MI. Hand hygiene compliance targets: what are we actually targeting?. J Hosp Infect 2017;95:359-60. https://doi.org/10.1016/j.jhin.2017.02.004.
- Boyce JM. Electronic monitoring in combination with direct observation as a means to significantly improve hand hygiene compliance. Am J Infect Control 2017;45:528-35. https://doi.org/10.1016/j.ajic.2016.11.029.
- Parsons V, Williams HC, English J, Llewellyn J, Ntani G, Madan I. The development of a protocol for diagnosing hand dermatitis from photographic images. Contact Derm 2018;79:27-5. https://doi.org/10.1111/cod.13053.
- Haas JP, Larson EL. Measurement of compliance with hand hygiene. J Hosp Infect 2007;66:6-14. https://doi.org/10.1016/j.jhin.2006.11.013.
- Larson EL, Aiello AE, Cimiotti JP. Assessing nurses’ hand hygiene practices by direct observation or self-report. J Nurs Meas 2004;12:77-85. https://doi.org/10.1891/jnum.12.1.77.66322.
- Moret L, Tequi B, Lombrail P. Should self-assessment methods be used to measure compliance with handwashing recommendations? A study carried out in a French university hospital. Am J Infect Control 2004;32:384-90. https://doi.org/10.1016/j.ajic.2004.02.004.
- Tibballs J. Teaching hospital medical staff to handwash. Med J Aust 1996;164:395-8. https://doi.org/10.5694/j.1326-5377.1996.tb124899.x.
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2016 17 2008. https://improvement.nhs.uk/resources/reference-costs/ (accessed 9 September 2019).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- Office for National Statistics . Annual Survey of Hours and Earnings: 2016 Provisional Results 2016. www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/bulletins/annualsurveyofhoursandearnings/2016provisionalresults (accessed 9 September 2019).
Appendix 1 Summary of substantial and non-substantial amendments
| Amendment date | Amendment type: substantial/minor | Documents covered |
|---|---|---|
| 3 September 2014 | Substantial 1 |
|
| 8 September 2014 | Minor 1 |
|
| 18 September 2015 | Minor 2 |
|
| 19 September 2015 | Minor 3 |
|
| 9 October 2014 | Minor 4 |
|
| 20 October 2014 | Minor 5 |
|
| 30 October 2014 | Minor 6 |
|
| 3 November 2014 | Minor 7 |
|
| 7 November 2014 | Minor 8 |
|
| 17 December 2015 | Minor 9 |
|
| 9 February 2015 | Minor 10 |
|
| 16 February 2015 | Substantial 2 |
|
| 20 March 2015 | Minor 11 |
|
| 23 March 2015 | Minor 12 |
|
| 10 April 2015 | Minor 13 |
|
| 10 April 2015 | Minor 14 |
|
| 23 April 2015 | Minor 15 |
|
| 28 April 2015 | Minor 16 |
|
| 30 April 2015 | Minor 17 |
|
| 8 May 2015 | Minor 18 |
|
| 15 May 2015 | Minor 19 |
|
| 29 June 2015 | Minor 20 |
|
| 30 June 2015 | Minor 21 |
|
| 17 July 2015 | Minor 22 |
|
| 16 July 2015 | Substantial 3 |
|
| 10 September 2015 | Minor 23 |
|
| 12 October 2015 | Substantial 4 |
|
| 4 May 2016 | Substantial 5 |
|
| 27 May 2016 | Substantial 6 |
|
Appendix 2 Unit costs used in the economic analyses
| Service | Unit cost (2015/16; £) |
|---|---|
| GP | 33 |
| Dermatologist | 135 |
| Other doctors | 135 |
| Practice nurse (assuming a 10-minute visit) | 9 |
| Pharmacist (assuming a 10-minute visit) | 17 |
| Physiotherapist | 135 |
| Complementary health care | 52 |
| Student nurse – lost work (per day) | 173 |
| ICU nurse – lost work (per day) | 263 |
| Medication | Depends on drug |
| Blood test (depending on reason) | Either 9 or 47 depending on the type of blood test |
| Skin prick test | 51 |
| Patch test | 303 |
| Biopsy | 145 |
Glossary
- Intervention light
- Participants in the intervention light arm received only the written leaflet with advice on dermatitis prevention.
- Intervention plus
- Participants received access to a behaviour change package intervention to improve hand care, and a written leaflet with advice on dermatitis prevention and optimisation of hand moisturising cream.
List of abbreviations
- BCP
- behaviour change package
- BCT
- behaviour change technique
- CACE
- complier average causal effect
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CSRI
- Client Service Receipt Inventory
- CTU
- clinical trials unit
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FIT
- Feedback Intervention Trial
- GP
- general practitioner
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- ICU
- intensive care unit
- IQR
- interquartile range
- ITT
- intention to treat
- NICE
- National Institute for Health and Care Excellence
- NRES
- National Research Ethics Committee
- OR
- odds ratio
- PBC
- perceived behavioural control
- PIN
- participant identification number
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SCBU
- special-care baby unit
- SCIN
- Skin Care Intervention in Nurses
- SD
- standard deviation
- SMS
- short message service
- TPB
- theory of planned behaviour
- WHO
- World Health Organization
Notes
-
A BCP (intensive care unit nurse) screenshot
-
A BCP (student nurse) screenshot
Supplementary material can be found on the NIHR Journals Library report project page (www.journalslibrary.nihr.ac.uk/programmes/hta/119401/#/documentation).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
