Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/187/06. The contractual start date was in April 2017. The draft report began editorial review in April 2018 and was accepted for publication in August 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Steve Goodacre is chairperson of the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme Clinical Evaluation and Trials Board and a member of the HTA Funding Boards Policy Group. Tim Nokes received personal fees from Bayer Pharmaceuticals (Bayer AG, Leverkusen, Germany), personal fees from the Bristol-Myers Squibb Company (New York City, NY, USA)–Pfizer Inc. (New York City, NY, USA) Alliance and personal fees from Daiichi Sankyo Company Ltd (Tokyo, Japan) outside the submitted work. Kerstin de Wit reports grants from Bayer Pharmaceuticals outside the submitted work.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Pandor et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Description of the health problem
Venous thromboembolism (VTE) is a condition in which a blood clot (a thrombus) forms in a vein. It predominantly occurs in the large veins of the legs and causes a deep-vein thrombosis (DVT). When part or all of the thrombus dislodges from its site of origin, it can travel to the lungs and disrupt or block the blood flow in a pulmonary artery, causing a pulmonary embolism (PE). 1 VTE encompasses a range of clinical presentations. Thrombosis in the venous circulation may be asymptomatic (no clinical symptoms), whether a DVT or a PE, or symptomatic (clinically apparent e.g. DVT may cause leg pain or swelling, whereas PE may lead to sudden death or cause symptoms such as breathlessness or chest pain). 2
If patients survive the acute episode of VTE, they may go on to develop long-term problems. Post-thrombotic syndrome (PTS) can occur if DVT causes damage to the valves in the leg veins that prevent backflow of blood, resulting in pain, swelling, itching, discolouration of the skin and, in some cases, an ulcer on the leg. Chronic thromboembolic pulmonary hypertension (CTEPH) can occur if a PE blocks blood flow to the lungs and increases the blood pressure in the arteries supplying the lungs, resulting in chronic shortness of breath and fatigue.
Despite modern advances in care, both asymptomatic and symptomatic VTE are still associated with significant morbidity and mortality. 3,4 In the past decade, VTE has resulted in more deaths than prostate cancer, breast cancer, road traffic accidents and acquired immune deficiency syndrome combined. 5 It is the second most common cause of vascular death after heart attack. 6 In 2005, the total cost (comprising direct and indirect costs) to the UK for the management of VTE was estimated at approximately £640M. 6
Temporary immobilisation of lower-limb injury is an important cause of potentially preventable VTE. In this context, injury is defined as physical trauma caused by an external force (e.g. a fall or a direct blow), abnormal movement (e.g. twisting or overstretching) or normal movement applied to a weakened limb structure (e.g. rupture of an inflamed tendon). Immobilisation is defined as involving a temporary splint, cast or boot that prevents movement in the knee and/or ankle joint. It is temporary insofar as it is applied after the injury and then removed when the injury has healed. For the purposes of this report, removable splints that are used only at times of activity during healing and hinged splints or bandages that allow joint movement while they are in place are not included.
Case reports, observational cohort studies and randomised controlled trials (RCTs) suggest that patients with lower-limb immobilisation due to injury have a significant risk of VTE, morbidity and death. 7–16 A typical type one emergency department (ED) is likely to see, immobilise and discharge around 360 patients per year with lower-limb injury, with an overall subsequent VTE rate approaching 2%. 16–18 There are currently 194 type one EDs in the English NHS that generate a relevant annual patient population of just under 70,000 patients. The exclusion of type two EDs, minor injury units and walk-in centres, probably renders this an underestimate of the population. The incidence of VTE in ambulatory trauma patients with lower-limb immobilisation is ≈11%. However, this rate can vary from 2% to 30%, depending on the type of injury and the immobilisation used. 19 Although the majority of these events will be asymptomatic distal DVT, there is a small risk of clot propagation, potentially leading to fatal PE19 in 20–30% of patients receiving no prophylaxis,14 reducing to 0.3–2.0% in those with prophylaxis. 20
Description of the technology under assessment
Thromboprophylaxis, both mechanical [e.g. antiembolism stockings or VTE compression devices (not the subject of this report, as plaster cast immobilisation precludes the application of devices to support the calf muscle pump and/or stimulate blood flow in the leg)] and pharmacological, has been the routine standard of care after lower-limb immobilisation. The main goal of administering thromboprophylaxis is to prevent PE and DVT and their sequelae. Pharmacological thromboprophylaxis in patients with lower-limb immobilisation due to injury has been principally studied using subcutaneous low-molecular-weight heparin (LMWH). Several different agents are available [e.g. dalteparin (Fragmin®, Pfizer Inc., New York City, NY, USA), enoxaparin (Clexane®, Sanofi Genzyme, Cambridge, MA, USA) and tinzaparin (Innohep®, Leo Pharma A/S, Copenhagen, Denmark)]21 and equivalent doses are used for hospital inpatients, extended spectrum groups (e.g. post-operative orthopaedic cases) and pregnant patients. LMWH is well tolerated in these groups and has clear acceptability to staff and patients, given its widespread utilisation across the NHS. LMWH has some limitations. As an injection-only agent, it causes a degree of pain and discomfort, which are poorly tolerated by some. It also requires administration; therefore, patients unhappy to self-inject, or elderly patients, often require expensive and time-consuming additional district nursing support to facilitate home medication. Finally, there are associated complications with LMWH, principally bleeding and, rarely, heparin-induced thrombocytopenia.
Aspirin use has also been studied in this patient group, albeit with limited evidence of efficacy. 22,23 The attractions and benefits of aspirin include familiarity and availability, cost and a clearly understood side-effect profile. Despite this, the National Institute for Health and Care Excellence (NICE) guidelines on VTE (clinical guideline number 9224 and NICE guideline number 891) do not consider aspirin or other antiplatelet agents to be appropriate for VTE prophylaxis. In addition, aspirin is not indicated as a treatment for VTE prophylaxis in lower-limb immobilisation. 21,25,26
Fondaparinux (Arixtra®, Aspen Pharma Trading Ltd, Dublin, Ireland) is a synthetic pentasaccharide antithrombotic that inactivates factor X (Xa) and results in a strong inhibition of thrombin generation and clot formation without affecting thrombin or platelets. It is administered subcutaneously and has similar limitations to LMWH. However, it is not widely used in the UK for VTE prophylaxis.
Finally, direct oral anticoagulant (DOAC) medications [e.g. apixaban (Eliquis®, Bristol-Myers Squibb Company, New York City, NY, USA), dabigatran etexilate (Pradaxa®, Boehringer Ingelheim GmbH, Ingelheim am Rhein, Germany) and rivaroxaban (Xarelto®, Bayer AG, Leverkusen, Germany)] are of increasing interest to clinicians and offer an option for thromboprophylaxis. DOACs present an attractive option based on applicable evidence from extrapolated orthopaedic surgical thromboprophylaxis trials, in addition to their inherent acceptability and practicality. 27–29 Oral anticoagulant prophylaxis regimens can be taken orally once or twice daily, have no additional specific contraindications to LMWH, are convenient and reliable, and appear acceptable to staff and patients. However, they are currently more expensive and are associated with more limited clinical experience than heparin products; furthermore, the management of bleeding complications may be challenging, given the lack of an agent to reverse DOACs’ anticoagulant effect. 30
Preventative treatment with anticoagulant drugs (thromboprophylaxis) could reduce the risk of VTE, but these drugs carry risks of adverse events, in particular an increased risk of intracranial or gastrointestinal (GI) bleeding. Thromboprophylaxis can be justified only if the benefits of reducing VTE outweigh the risks of bleeding and other side effects. Furthermore, the considerable expense of providing thromboprophylaxis to all patients with lower-limb immobilisation can be justified only if this treatment delivers meaningful improvements in health at an acceptable cost. The risk to benefit and cost to benefit ratios of thromboprophylaxis could be improved if patients were selected for treatment on the basis of risk factors for VTE, but this requires accurate and usable risk assessment methods.
A number of risk assessment models (RAMs) have been developed to select patients with lower-limb cast immobilisation due to injury for thromboprophylaxis. 17,31–33 These models aim to target high-risk patients who stand to gain maximal health benefit on treatment and avoid treatment in low-risk groups. However, the methodology for deriving and validating these RAMs is often poorly described, limited in validity or based on expert consensus only. 17,31–33
In general, risk prediction tools use clinical information from a patient’s history and examination to identify those with an increased risk of VTE who could be selected for thromboprophylaxis. Existing risk prediction rules use either a flow chart or a checklist to guide the user through risk assessment and lead him or her to a decision regarding thromboprophylaxis. Tools may take the form of rules that simply categorise patients by whether or not they need thromboprophylaxis, or scores that estimate the risk of VTE but leave the decision to provide thromboprophylaxis in the hands of the user. The tools may be paper based or electronic. The latter can potentially facilitate more complex risk assessment based on weighting of risk factors, if appropriate data are available to support such weighting.
Current service provision
Extended spectrum thromboprophylaxis for outpatients immobilised in plaster following lower-limb injury continues to generate international debate. There is substantial variation in both the use of thromboprophylaxis and the use of RAMs. Although VTE events are potentially preventable with prophylaxis, international guidance offers conflicting advice, from no intervention, to pragmatic shared decision-making, all the way to routine chemical thromboprophylaxis. 17,34,35
In many European countries, thromboprophylaxis is routine,35 whereas, in North America, recent guidelines interpret the literature as too weak to justify intervention, and actively discourage thromboprophylaxis. 34 Current UK guidance from NICE recommends that clinicians consider pharmacological VTE prophylaxis with LMWH or fondaparinux for people with lower-limb immobilisation whose risk of VTE outweighs their risk of bleeding, but does not provide guidance on how these risks can be determined. 24 This may foster clinical uncertainty and has led to a UK position of variable practice, using variable drug regimens throughout the NHS, with limited understanding of the safety, efficacy or cost-effectiveness of local protocols. Since 2015, there has been a move towards using the DOACs for this indication, despite the lack of applicable research or licence, based on convenience and cost implications. Personal correspondence from the Royal College of Emergency Medicine (RCEM) Clinical Studies Group suggests that DOAC drugs are currently being used for this indication in at least four NHS trusts (Catherine Roberts, Lancashire Teaching Hospitals, 2018, personal communication).
In the UK, risk assessment strategies in current use include the Plymouth VTE risk assessment tool (derived by expert consensus),31 the Guidelines in Emergency Medicine Network (GEMNet) guidance (produced in 2012 for RCEM, following a rapid review of the applicable literature and expert consensus)17 and several expert-derived pathways supported by the British Orthopaedic Association Standards for Trauma. 33 However, uptake of these RAMs seems to be poor as a result of equipoise/uncertainty, and many centres utilising these tools have pragmatically amended them without published supporting evidence.
Chapter 2 Research questions
Rationale for the study
Venous thromboembolism is a documented global health burden. 4,5 Preventative treatment with anticoagulant drugs (thromboprophylaxis) has the potential to reduce the risk of symptomatic or asymptomatic VTE in patients with lower-limb immobilisation due to injury; however, it is not clear whether or not this translates into meaningful health benefit for patients, justifies the risk of treatment-related adverse events (in particular, an increased risk of intracranial or GI bleeding) or is cost-effective. Risk assessment strategies could improve the ratios of benefit to risk and benefit to cost, but the evidence to support VTE RAMs for lower-limb immobilisation has not been robustly evaluated.
International guidelines have made clear recommendations for research in this area. Previous NICE clinical guidelines (CG92)24 made a specific recommendation of research into the clinical effectiveness and cost-effectiveness of pharmacological prophylaxis for reducing the risk of VTE in patients with lower-limb plaster casts, which this research proposal was designed to address. The 2012 American College of Chest Physicians guidance contains a grade 2C recommendation (i.e. weak recommendation, low- or very-low-quality evidence) on the topic and highlights the extensive list of exclusion criteria from previous research. 34 In addition, the RCEM guidelines17 and several additional review papers published in specialist journals have called for further research to address the equipoise. 13,36
Primary research could reduce uncertainty around decision-making, but carries substantial risks of failure. A large pragmatic trial could estimate the benefits and harms of thromboprophylaxis and determine whether or not it is effective, but the low rates of symptomatic VTE events and bleeding events mean that a very large sample would be required. Furthermore, it may not be ethical to randomise patients to no treatment if convincing evidence of the effectiveness of thromboprophylaxis already exists. It is also not clear whether or not a risk-based approach might be better than thromboprophylaxis for all, and, if it is, what RAM should be used. A cohort study could be used to derive or validate a RAM but it is not clear whether or not participants in such a study should receive thromboprophylaxis or how a RAM should weigh the relative benefits of optimising sensitivity and specificity when there is inevitably a trade-off between these parameters.
In these circumstances, an evidence synthesis project, involving systematic review, meta-analysis, elicitation of expert consensus, decision-analytic modelling and value-of-information analysis, provides a relatively quick and inexpensive way of drawing together all of the existing evidence in a rational and explicit manner, exploring the trade-off between treatment harms and benefits, and between sensitivity and specificity in risk assessment, estimating the cost-effectiveness of different strategies and the cost-effectiveness of different options for future primary research.
Overall aims and objectives of assessment
The overall aim was to determine the clinical effectiveness and cost-effectiveness of different strategies for providing thromboprophylaxis to people with lower-limb immobilisation due to injury and identify priorities for future research. More specifically, the objectives were as follows:
-
To undertake systematic reviews and meta-analysis (when appropriate) to (1) assess the effectiveness of pharmacological thromboprophylaxis for preventing any VTE, clinically detected (symptomatic) DVT, clinically relevant (symptomatic, proximal or extensive) DVT, PE and asymptomatic DVT in people with lower-limb immobilisation due to injury; (2) identify individual risk factors associated with VTE risk in patients with temporary lower-limb immobilisation due to injury; and (3) identify RAMs that predict the risk of VTE in people with lower-limb immobilisation due to injury and estimate the accuracy of these models.
-
To undertake a modified Delphi survey of expert opinion to augment reviews 2 and 3 above, on the assumption that the available evidence will be very limited and expert opinion will be required to identify risk factors and RAMs for VTE in lower-limb immobilisation due to injury.
-
To develop an economic model to estimate the (i) clinical effectiveness of thromboprophylaxis, in terms of overall adverse outcomes avoided or incurred by treatment and quality-adjusted life-years (QALYs); (ii) cost-effectiveness of different strategies for providing thromboprophylaxis (including thromboprophylaxis for all, thromboprophylaxis for none and risk-based strategies), in terms of the incremental cost per QALY gained by each strategy compared with the next most effective strategy on the efficiency frontier; and (iii) expected value of information provided by further primary research and to determine the optimal direction of future research.
Chapter 3 Assessment of clinical effectiveness
A series of systematic reviews of the literature and (network) meta-analysis (when appropriate) were undertaken to (1) assess the effectiveness of pharmacological thromboprophylaxis for preventing VTE, (2) identify individual risk factors associated with VTE risk and (3) identify RAMs for the prediction of VTE risk in people with temporary lower-limb immobilisation due to injury.
All reviews of the evidence were undertaken in accordance with the general principles recommended in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement37 and were registered on the PROSPERO international prospective register of systematic reviews (CRD42017058688). 38 The full protocol is available on the project web page [URL: www.journalslibrary.nihr.ac.uk/programmes/hta/1518706/#/ (accessed 3 December 2018)].
Review of pharmacological thromboprophylaxis for preventing venous thromboembolism
Objective
The objective was to assess the effectiveness of pharmacological thromboprophylaxis for preventing any VTE, clinically detected (symptomatic) DVT, clinically relevant (symptomatic, proximal or extensive) DVT, PE and asymptomatic DVT in patients with temporary lower-limb immobilisation due to injury. In this study, proximal DVT is defined as disease at or above the level of the popliteal trifurcation. Distal DVT is defined as disease below the popliteal trifurcation, confined to the calf veins (e.g. peroneal, posterior, anterior tibial and muscular veins).
Methods of reviewing effectiveness
Identification of studies
Studies were identified by searching the following electronic databases and research registers:
-
Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily, MEDLINE and Versions(R) (OvidSP), 1946 to April 2017.
-
EMBASE (OvidSP), 1974 to April 2017.
-
Cochrane Database of Systematic Reviews (Wiley Online Library), 1996 to April 2017.
-
Database of Abstracts of Review of Effects (Wiley Online Library), 1995 to March 2015.
-
Cochrane Central Register of Controlled Trials (Wiley Online Library), 1898 to April 2017.
-
Health Technology Assessment (HTA) database (Wiley Online Library), 1995 to April 2017.
-
NHS Economic Evaluation Database NHS EED (Wiley Online Library), 1995 to March 2015.
-
Science Citation Index Expanded (Web of Science), 1900 to April 2017.
-
ClinicalTrials.gov (US National Institutes of Health), 2000 to April 2017.
-
International Clinical Trials Registry Platform (World Health Organization), 1990 to April 2017.
The search strategy used free text and thesaurus terms and combined synonyms relating to the condition (i.e. VTE in people with lower-limb immobilisation) with synonyms relating to the interventions (e.g. LMWH, aspirin and oral anticoagulants). No language restrictions were used. However, as the search strategy of the current review updated the search strategy of an existing review on LMWH,15 searches were limited by date from 2013 (the last search date from the earlier review) to April 2017 for this intervention. For the other interventions, the search strategy was amended to include terms for aspirin and oral anticoagulants and searched from inception to April 2017. Further details of the search strategy can be found in Appendix 1. Searches were supplemented by hand-searching the reference lists of all relevant studies (including existing systematic reviews), performing a citation search of relevant articles, contacting key experts in the field and undertaking systematic keyword searches of the internet using the Google search engine (Google Inc., Mountain View, CA, USA).
All identified citations from the electronic searches and other resources were imported into and managed using EndNote bibliographic software version X8 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA].
Inclusion and exclusion criteria
The inclusion of potentially relevant articles was undertaken using a two-step process. First, all titles were examined for inclusion by one reviewer (AP) and any citations that clearly did not meet the inclusion criteria (e.g. non-human, unrelated to VTE) were excluded. Second, all abstracts and full-text articles were examined independently by two reviewers (AP and DH). When necessary, non-English-language studies were translated using Google Translate (Google Inc., Mountain View, CA, USA) to facilitate study selection and subsequent data extraction. Any disagreements in the selection process were resolved through discussion or, if necessary, arbitration by a third reviewer (SG), and articles were included by consensus.
Studies were considered eligible for inclusion if they met the following criteria: (1) study design – RCTs and controlled clinical trials; (2) population – adults (aged > 16 years) requiring temporary immobilisation (e.g. leg cast or brace in an ambulatory setting) for an isolated lower-limb injury; (3) interventions – chemical thromboprophylaxis with LMWH (e.g. dalteparin, enoxaparin, tinzaparin), fondaparinux or oral anticoagulants (e.g. apixaban, dabigatran etexilate, rivaroxaban); (4) comparators – these included placebo, no treatment, aspirin or alternative treatment (although the original protocol considered aspirin to be an option for VTE prophylaxis, NICE guidelines on venous thromboembolism (CG92)24 do not consider aspirin or other antiplatelet agents to be appropriate for VTE prophylaxis; in addition, aspirin is not indicated as a treatment for VTE prophylaxis in lower-limb immobilisation);21,25,26 and (5) outcomes – these included symptomatic or asymptomatic DVT, PE, major bleeding or mortality. Exclusion criteria for selection included studies that had not been designed as experimental studies (e.g. cohort studies and case–control studies), studies that had involved hospital inpatient care or any patient requiring hospital admission of > 5 days and studies in which patients received mechanical thromboprophylaxis or underwent ambulant orthopaedic surgery (e.g. arthroscopy, arthroscopic surgery).
Data abstraction and quality assessment strategy
Data relating to study design, methodological quality and outcomes were extracted by one reviewer (AP) into a standardised data extraction form and independently checked for accuracy by a second reviewer (DH). Any discrepancies were resolved through discussion or, if necessary, arbitration by a third reviewer (SG), and articles were included by consensus. If required, authors of primary studies were contacted to obtain additional data, clarify uncertainties and/or confirm data that had been extracted. When multiple publications of the same study were identified, data were extracted and reported as a single study.
The methodological quality of each included study was evaluated using a revised Cochrane Risk of Bias tool for randomised trials (RoB 2.0). 39 The original tool40 was updated because of questionable inter-rater agreement, subjectivity in assigning risk-of-bias judgements and bias judgements assigned at the trial level. 41–44 In general, RoB 2.0 redefined the potential for bias to five domains: (1) bias arising from the randomisation process, (2) bias as a result of deviations from intended interventions, (3) bias as a result of missing outcome data, (4) bias in the measurement of the outcome and (5) bias in the selection of the reported result. To limit subjectivity in assigning bias judgements, the RoB 2.0 tool provides detailed guidance and contains decision algorithms. An overall judgement of bias was assigned as ‘low risk’ if all domains were judged as being at a low risk of bias, a judgement of bias was assigned as ‘high risk’ if at least one domain was judged to be at a high risk of bias (or if the study had some concerns for multiple domains in a way that substantially lowers confidence in the result) and as ‘some concerns’ if some concerns of bias were noted in at least one domain. 39 The methodological quality of each included study was independently evaluated by two reviewers (AP and DH). Any discrepancies were resolved through discussion or, if necessary, the involvement of a third reviewer (SG). Blinding of the quality assessor to author, institution or journal was not considered necessary.
Methods of data synthesis and analysis
The extracted data and quality assessment variables were presented for each included study, both in structured tables and as a narrative description. For each outcome of interest, a network meta-analysis (NMA) was performed to allow a simultaneous comparison between interventions using all available studies. The data were the number of events out of the number of patients randomised to each intervention, which were assumed to arise from an underlying binomial distribution. The probabilities of an event for each intervention were modelled using a logistic model to estimate odds ratios (ORs). The control intervention was defined as placebo, no treatment or aspirin, and the reference intervention defined in the NMA was the control intervention. Aspirin was grouped with placebo and no treatment on the basis that aspirin is not indicated as a treatment for VTE prophylaxis in lower-limb immobilisation21,25 and NICE guidelines on VTE (CG9224 and NG891) do not consider aspirin or other antiplatelet agents to be appropriate for VTE prophylaxis. It was planned to analyse different types of thromboprophylaxis drugs as separate interventions (i.e. LMWH, DOACs and fondaparinux) in the NMA on the basis of having different mechanisms of action and, therefore, potentially different effects.
The analysis was implemented using a Markov chain Monte Carlo simulation using WinBUGS software version 1.4.3 (MRC Biostatistics Unit, Cambridge, UK). 45 A fixed-effect model was used to estimate the effects of LMWH and fondaparinux relative to control in the available studies, namely a conditional inference. In addition, a random-effects model was used to allow for heterogeneity in the effects of interventions between studies and to estimate whether or not the interventions can have an effect in future studies. The random-effects model was the primary analysis. The baseline log odds in each study were given normally distributed prior distributions with mean 0 and variance 1000, namely N(0, 1000). The log-odds ratios for LMWH and fondaparinux versus control were given normally distributed prior distributions with a mean of 0 and variance of 1000, namely N(0, 1000). The between-study standard deviation (SD) was given a half-normal prior distribution with a mean of 0 and precision of 1.82, namely HN(0, 0.5495); this prior distribution was chosen to have, a priori, 95% of the study-specific odds ratios lie within a factor of 5 from the median odds ratio for each comparison. Convergence of the Markov chains to their stationary distributions was assessed using the Gelman–Rubin convergence statistic. 46 For all outcomes other than major bleeding, convergence occurred within 30,000 iterations of the Markov chain and within 100,000 samples for major bleeding; a burn-in of 100,000 iterations was used in all analyses. There was some evidence of high autocorrelation between successive iterations of the Markov chain; parameters were estimated after retaining every 10th sample of the Markov chain to limit the number of unnecessary runs of the decision model that are informed by the results of the NMA. Results were presented using ORs, 95% credible intervals (CrIs) and the 95% predictive intervals47 for the OR in a randomly chosen study relative to the control, and the probability of each intervention being the best. 48
It was planned to assess the following potential treatment effect modifiers in a series of meta-regressions: (1) population characteristics (e.g. proportion who were male, baseline risk of VTE), (2) type of injury (i.e. fractures, Achilles tendon rupture, other soft-tissue injury), (3) treatment of injury (surgical vs. conservative, above- vs. below-knee immobilisation), (4) thromboprophylactic agent used and (5) duration of thromboprophylaxis.
Results
Quantity and quality of research available
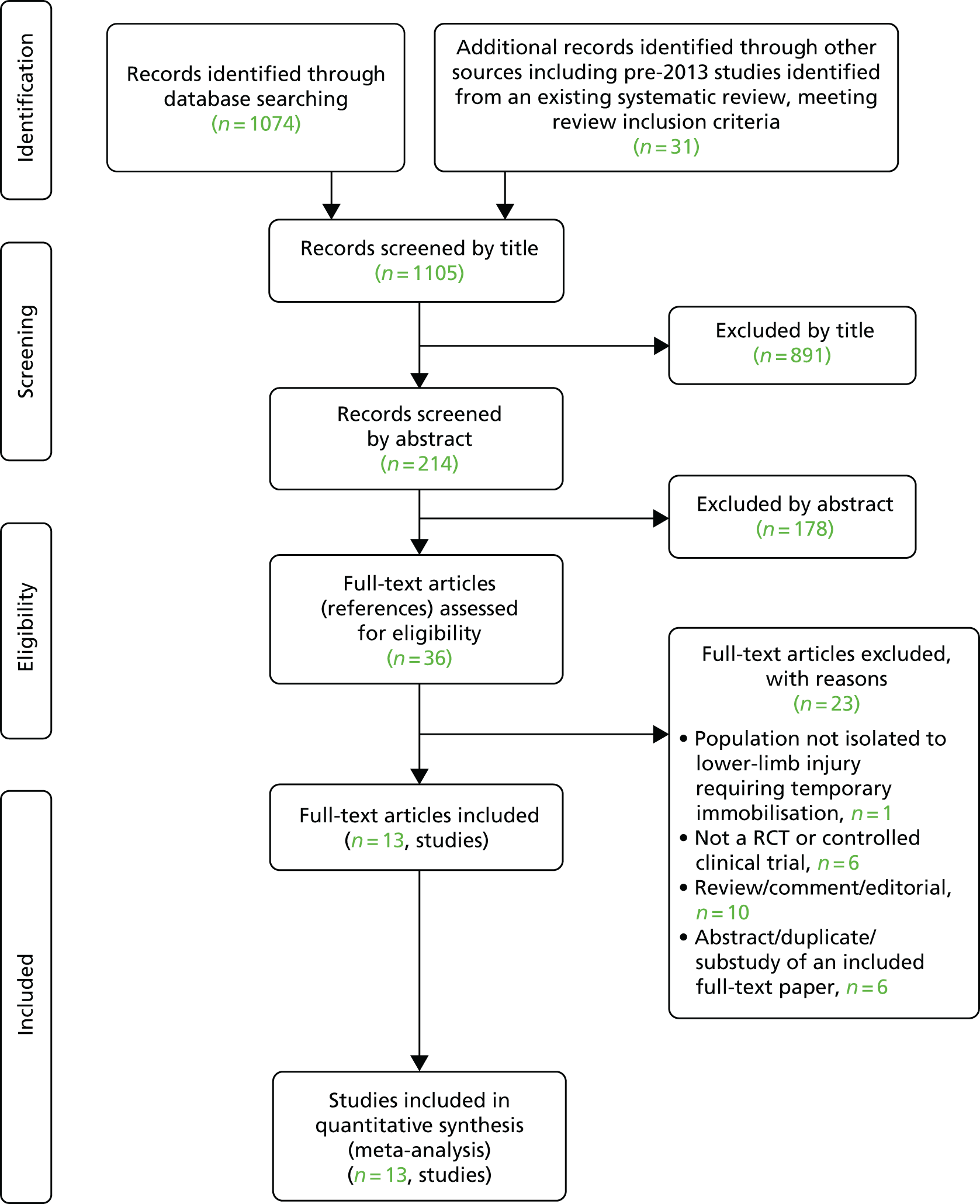
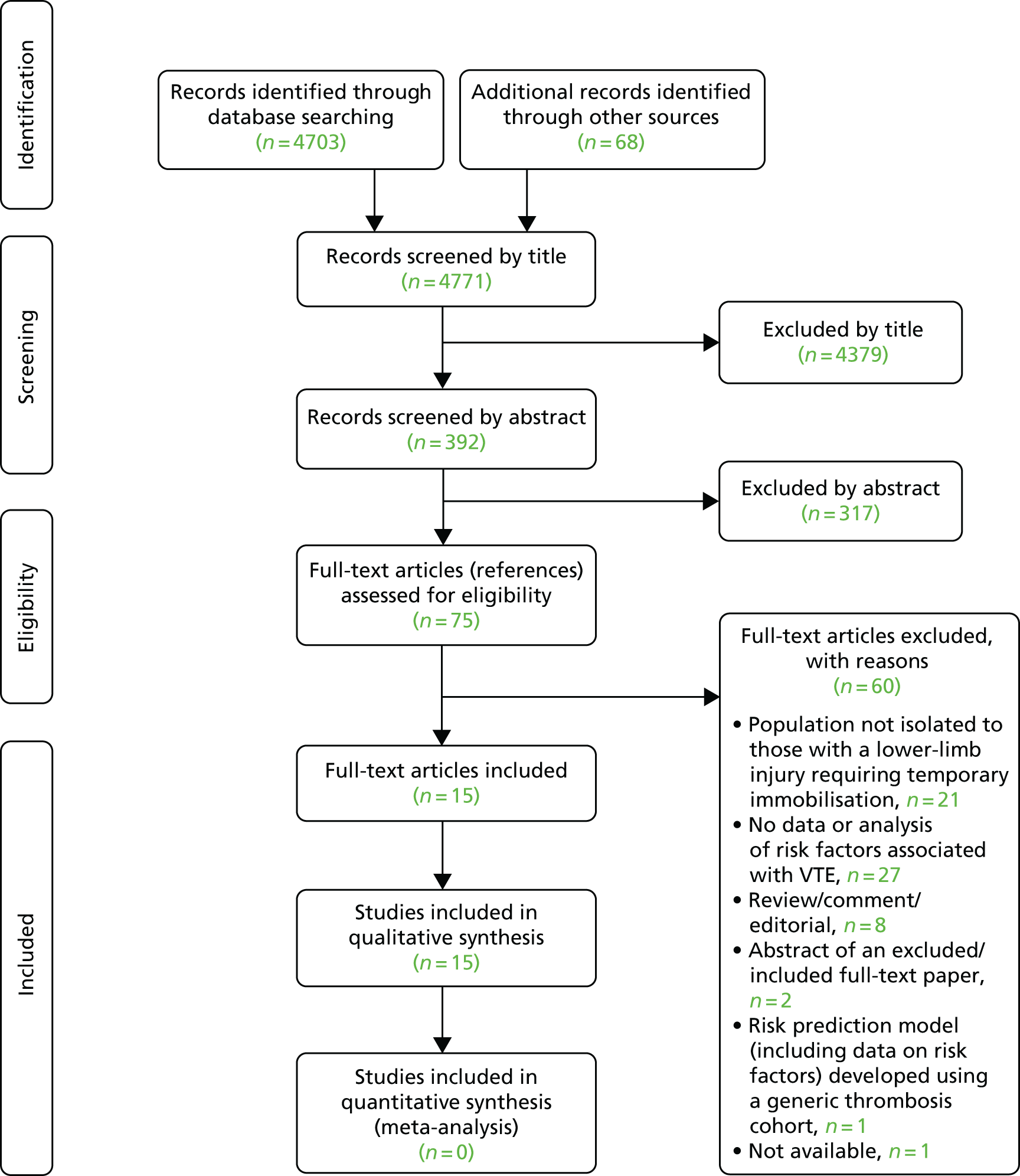
The literature searches identified 1105 citations. Of these, 13 studies (all RCTs) met the inclusion criteria. 23,49–60 A flow chart describing the process of identifying relevant literature can be found in Figure 1. A total of 23 full-text articles were excluded as they did not meet all of the prespecified inclusion criteria. The majority of the articles were excluded primarily on the basis of inappropriate study design (i.e. non-randomised controlled trial or controlled clinical trial), wrong target population (i.e. not isolated lower-limb injury requiring temporary immobilisation) or unsuitable publication type (i.e. reviews, commentaries, editorials or multiple publications of the same study). A full list of excluded studies with reasons for exclusion is presented in Appendix 2.
FIGURE 1.
Study flow chart (adapted):37 review of pharmacological thromboprophylaxis for preventing VTE. © 2009 Moher et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Description of included studies (design and participant characteristics)
The design and participant characteristics of the 13 included studies23,49–60 that evaluated the effectiveness of pharmacological thromboprophylaxis for preventing VTE in ambulatory trauma patients with temporary lower-limb immobilisation are summarised in Table 1.
| Authors, year | Country (sites) | Design | Population | Exclusion criteria (main) | Time between injury and recruitment/immobilisation duration (mean) | Prophylaxis before randomisation | Intervention | Comparator | Outcome measure (primary) |
|---|---|---|---|---|---|---|---|---|---|
| Goel et al., 200950 | Canada (NR) | RCT, DBa |
|
History of VTE, foot fractures, contraindications to surgery, anticoagulant medication, platelet counts of < 100, elevated serum creatinine of > 200 µmol/l |
|
No | LMWH (dalteparin: 5000 IU/day for 14 days, administered by s.c. injection; compliance: > 95%) | Matching placebo for 14 days (compliance with injections: > 95%) | Incidence of DVT determined by bilateral venography at end of treatment |
| Jørgensen et al., 200251 | Denmark (three centres) | RCT, OLa |
|
Pregnancy, allergy to heparin or contrast media, renal or liver impairment, uncontrolled hypertension, bleeding disorders, recent GI bleeding, inability to perform self-injection |
|
No | LMWH (tinzaparin: 3500 IU/day for duration of cast immobilisation, administered by s.c. injection; compliance: NR) | No treatment | Incidence of DVT determined by unilateral venography after plaster cast removal |
| Kock et al., 199552 | Germany (NR) | RCT, OL |
|
Previous DVT, pregnancy, clotting disorders or anticoagulant medication, bleeding, chronic venous insufficiency, contraindication to heparin, surgical treatment |
|
No | LMWH [certoparin (Mono-Embolex®, Novartis International AG, Basel, Switzerland): 3000 IU/day for duration of cast immobilisation, administered by s.c. injection; compliance: NR] | No treatment | Incidence of DVT determined by duplex sonography and confirmed by phlebography after plaster cast removal |
| Kujath et al., 199353 | Germany (one hospital) | RCT, OL |
|
Known thrombopathy, oral anticoagulation, recent brain or GI bleeding, acute pancreatitis, inflammatory heart disease |
|
No | LMWH [nadroparin (Fraxiparine®, Sanofi SA, Paris, France): 2850 IU/day for duration of cast immobilisation, administered by s.c. injection; compliance: NR] | No treatment | Incidence of DVT determined by compression ultrasonography and phlebography (positive findings only) after plaster cast removal |
| Lapidus et al., 200755 | Sweden (one centre) | RCT, DBa |
|
Anticoagulant medication, contrast media allergy, kidney disorder, VTE in preceding 3 months, surgery in preceding month, malignancy, bleeding disorder, pregnancy, high-dose aspirin or platelet inhibitors |
|
No | LMWH (dalteparin: 5000 IU/day for 6 weeks, administered by s.c. injection; compliance: NR) | Matching placebo for 6 weeks (compliance with injections: NR) | Incidence of DVT determined by unilateral duplex sonography and confirmed by phlebography |
| Lapidus et al., 200754 | Sweden (one centre) | RCT, DBa |
|
Anticoagulant medication, allergy to contrast media, renal disorders (including transplant), VTE in preceding 3 months, surgery in preceding month, malignancy, bleeding disorder, pregnancy, high-dose aspirin or platelet inhibitors, multitrauma |
|
Yes, all patients received 1 week of initial treatment with dalteparin (5000 IU/day) before randomisation | LMWH (dalteparin: 5000 IU/day for 5 weeks, administered by s.c. injection; compliance: 94.6%) | Matching placebo for 5 weeks (compliance with injections: 94.6%) | Incidence of DVT confirmed by unilateral phlebography after cast removal or compression ultrasonography if the phlebography failed |
| Lassen et al., 200256 | Denmark (six hospitals) | RCT, DBa |
|
Current VTE, hypertension, cerebral aneurysm, CVA in preceding 3 weeks, active GI ulcer, bleeding disorder, previous heparin use, contraindication to heparin or contrast allergy, venography, kidney disorder, MI in the preceding 3 months, multiple myeloma, pregnancy, body weight of < 35 kg, history of drug or alcohol abuse |
|
Yes, approximately one-third of participants in each group received other LMWH for up to 4 days before randomisation | LMWH [reviparin (Clivarin®, Abbott Laboratories, Lake Bluff, IL, USA): 1750 IU/day for the duration of cast immobilisation, administered by s.c. injection; compliance: approximately 100%] | Matching placebo for the duration of cast immobilisation (compliance with injections: approximately 100%) | Incidence of DVT determined by unilateral venography after plaster cast removal (or earlier if clinical symptoms of thrombosis suspected) |
| Selby et al., 201558 | Canada (13 hospitals) | RCT, DBa |
|
Major trauma, other anticoagulant use, allergy to LMWH, pregnancy, active cancer, previous VTE, hypercoagulable state, active bleeding or bleeding disorder, intracranial bleeding in preceding 4 weeks, vascular injury needing repair |
|
No | LMWH (dalteparin: 5000 IU/day for 14 days, administered by s.c. injection; compliance: 90%) | Matching placebo for 14 days (compliance with injections: 92%) | Symptomatic VTE within 3 months after surgery or asymptomatic proximal DVT determined by bilateral Doppler ultrasonography at end of treatment |
| van Adrichem et al., 201759 | The Netherlands (eight hospitals) | RCT, OLa |
|
History of VTE, contraindications to LMWH therapy, pregnancy, current use of anticoagulant therapy for other indications (use of antiplatelet drugs was allowed) |
|
No | LMWH [nadroparin: 2850 IU/day or dalteparin (2500 IU/day for < 100 kg or 5000 IU/day for > 100 kg) for the duration of cast immobilisation, administered by s.c. injection; compliance: 87%] | No treatment | Incidence of symptomatic VTE within 3 months after the procedure. DVT determined by abnormal compression ultrasonography |
| Zheng et al., 201660 | China (three hospitals) | RCT, DBa |
|
Multiple fractures; history of VTE; a tibial, fibular, femoral or hip fracture that required operative treatment or had casts or splints; history of thromboembolic event; anticoagulation; active cancer; or known hypercoagulability and pilon fractures |
|
No | LMWH (NR but given once daily for 14 days, administered by s.c. injection; compliance: NR) | Matching placebo for 14 days (compliance with injections: NR) | Incidence of VTE. DVT determined by bilateral Doppler ultrasonography |
| Gehling et al., 199823 | Germany (one hospital) | RCT |
|
Patients aged < 40 years without lower-limb injury and risk factors, contraindication to LMWH or aspirin anticoagulation, thrombocytopenia, pregnancy, kidney damage, apoplectic insult, haemorrhagic diathesis, gastric ulcer, hypertension, acute thrombosis |
|
NR | LMWH (reviparin: 1750 IU/day, administered by s.c. injection; compliance: NR) | Aspirin (1000 mg/day, administered orally; compliance: NR) | Incidence of DVT determined by duplex sonography (all) or phlebography (if thrombosis suspected) |
| Bruntink et al., 201749 (three-arm study) | The Netherlands (seven hospitals) | RCT, SBa |
|
History of VTE, hypersensitivity to nadroparin or fondaparinux, anticoagulation, hypercoagulability, bleeding tendency/disorder (including previous or active bleeding from the digestive tract), pregnancy or lactation, ‘active’ malignancy, severe hepatic or renal impairment, retinopathy, haemorrhagic stroke, major surgery in the preceding 2 months, severe hypertension |
|
No | LMWH (nadroparin: 2850 IU/day for the duration of cast immobilisation, administered by s.c. injection; compliance: approximately 100%) |
|
Incidence of DVT determined by duplex sonography after the removal of the cast (or earlier if thrombosis was suspected) |
| Samama et al., 201357 | France, Russia, the Netherlands, Spain, Germany and Italy (93 centres) | RCT, OLa |
|
Antithrombotic therapy; bleeding tendency/disorder; peptic ulcer disease; haemorrhagic stroke, brain, spinal or ophthalmological surgery (in the preceding 12 months); severe head injury in the preceding 3 months; uncontrolled arterial hypertension; severe hepatic impairment; body weight of < 50 kg; contraindication to anticoagulant therapy; pregnancy/lactation or not using a reliable contraceptive method |
|
No | LMWH (nadroparin: 2850 IU/day for the duration of cast immobilisation, administered by s.c. injection; compliance: NR) | Fondaparinux (2.5 mg/day for the duration of cast immobilisation, administered by s.c. injection; compliance: NR) | Incidence of VTE. Compression ultrasonography and/or venography performed for suspected DVT after cast removal |
All studies were published between 1993 and 2017. In total, 6857 patients were included and randomised across 10 countries (i.e. Canada,50,58 China,60 Denmark,51,56 France,57 Germany,23,52,53,57 Italy,57 the Netherlands,49,57,59 Russia,57 Spain57 and Sweden54,55) to receive either intervention or control treatment. LMWH injections were the primary intervention, using variable agents (i.e. certoparin,52 dalteparin,50,54,55,58 nadroparin,49,53,57,59 reviparin23,56 and tinzaparin51) and dosing regimes (e.g. administered once daily without dose adjustment for bodyweight), but two studies used fondaparinux. 49,57 One study used aspirin as a control group treatment,23 with others using placebo injections or nothing dependent on design. 50–56,58–60 In general, most studies excluded patients at highest risk of VTE, namely those with active cancer,49,54,55,58,60 previous VTE49,50,52–56,58–60 or first-degree family history of VTE. 59,60
Five identified studies used open-label methodology with subjective screening outcomes (duplex sonography or phlebography on cast removal). 51–53,57,59 Six studies used double blinding within the design. 50,54–56,58,60 The single largest study had symptomatic VTE only as an identified primary outcome, confirmed with imaging. 59 Although all studies included adult patients with an isolated lower-limb injury requiring temporary immobilisation, there was wide variation in terms of injury type. Five studies focused on patients with fractures,49,50,54,58,60 one focused on Achilles tendon ruptures55 and the remaining seven studies included patients with mixed pathology. 23,51–53,56,57,59 Depending on the type of injury, the management of lower-limb injury included conservative treatment,49,52,53,57 surgical management50,54,55,58,60 or both. 51,56,59 In eight studies,49,50,54–58,60 patients were recruited within 4 days of injury, whereas, in the remaining studies,23,51–53,59 the time to recruitment was not stated. The duration of immobilisation ranged from 14 days50 to 44 days. 54,56 In two studies, all54 or some (approximately one-third)56 patients first received prophylaxis prior to randomisation; these studies were included, as any final impact on outcome would be likely to take the form of a reduction in VTE outcome events. In addition, the results of these trials remain relevant to the study question in the light of current regimes, suggesting that prophylaxis continue for the duration of immobilisation (usually 4–6 weeks). The sample sizes of the included studies ranged from 10555 to 151959 patients, with the mean age of participants ranging from 34 years52,53 to 49 years. 58 The number of male participants ranged from 42%58 to 79%. 55
Quality characteristics
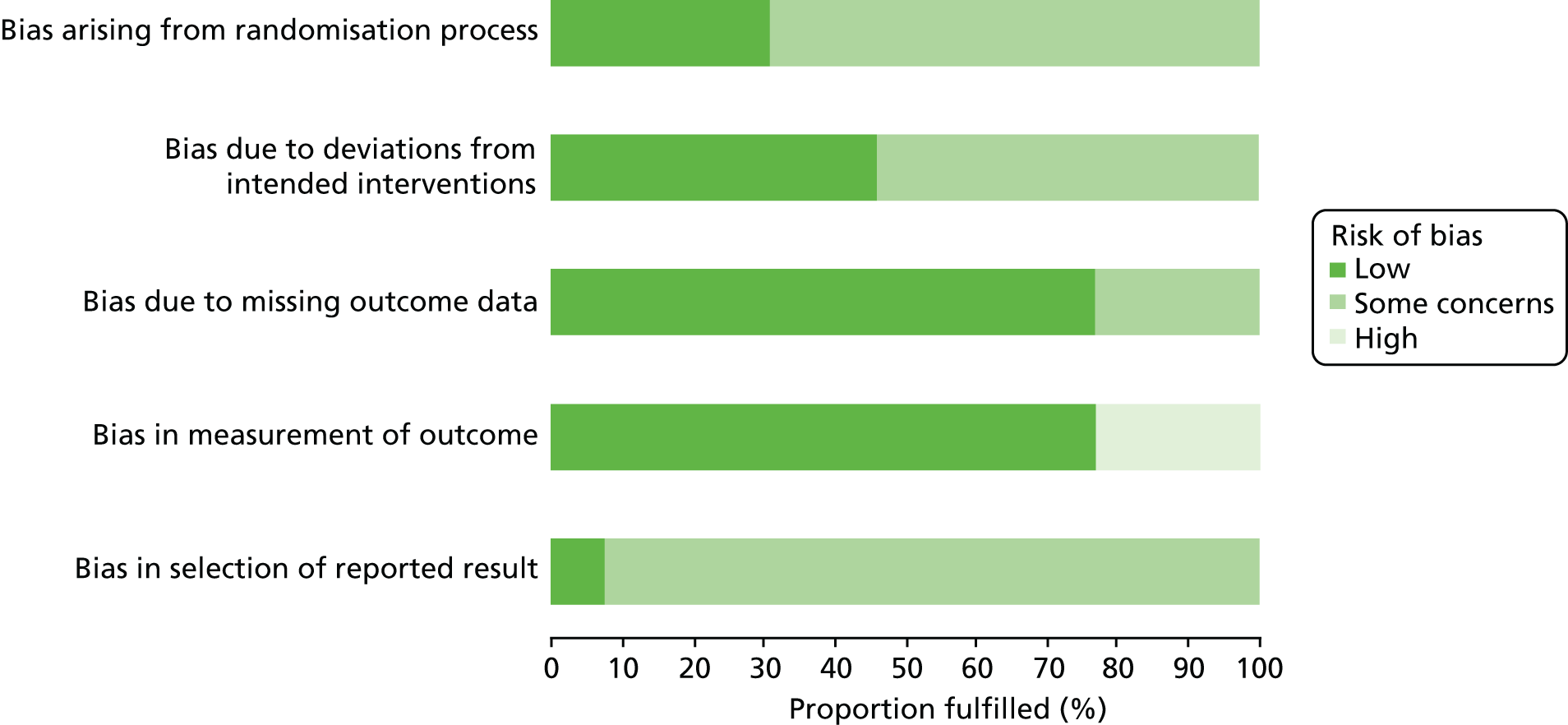
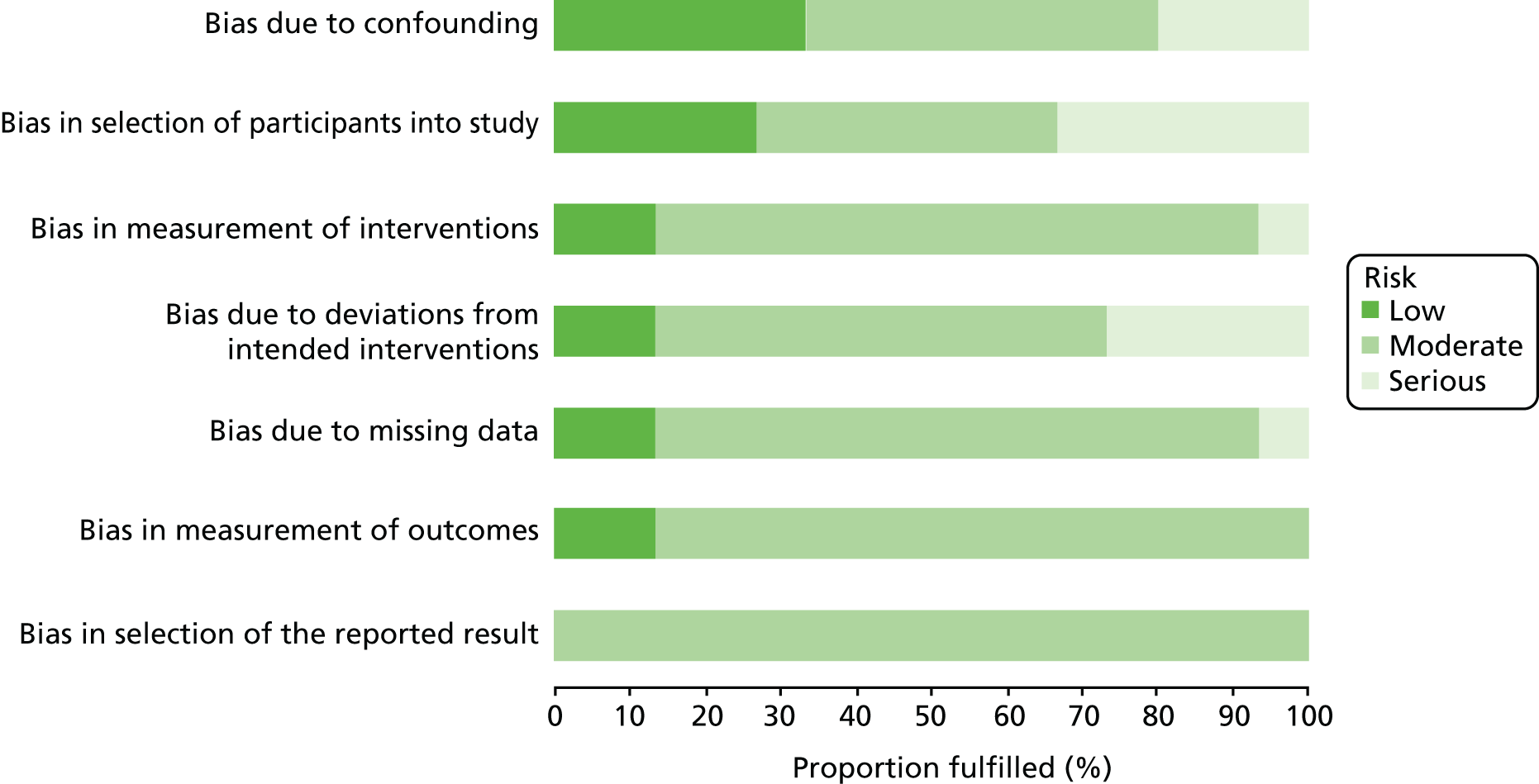
The overall methodological quality of the 13 included studies is summarised in Figure 2 and Table 2. Overall, risk of bias was present in all studies. Ten studies raised some concerns of bias. 49–51,54–60 The potential sources of bias most frequently identified included concerns about the randomisation process (allocation concealment was not reported in nine studies),23,50–56,60 blinding (open-label design)23,49,51–53,57,59 and analyses intentions (only one study provided sufficient information on the selection of the reported result). 59 A high risk of bias was noted in three studies. 23,52,53 High risk of bias was principally attributable to outcome assessment; in three open-label studies,23,52,53 outcome assessment was performed on all patients with routine screening compression ultrasonography and phlebography for confirmation of positive findings. Finally, all of the included studies were conducted outside the UK, making generalisability of the findings to the UK setting uncertain.
FIGURE 2.
Risk-of-bias assessment graph:39 review authors’ judgements about each methodological quality item across all included studies – review of pharmacological thromboprophylaxis for preventing VTE.
| Study authors, year | Area of potential bias | Overalla | ||||
|---|---|---|---|---|---|---|
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported result | ||
| Goel et al., 200950 | Some concerns | Low | Low | Low | Some concerns | Some concerns |
| Jørgensen et al., 200251 | Some concerns | Some concerns | Low | Low | Some concerns | Some concerns |
| Kock et al., 199552 | Some concerns | Some concerns | Low | High | Some concerns | High |
| Kujath et al., 199353 | Some concerns | Some concerns | Some concerns | High | Some concerns | High |
| Lapidus et al., 200755 | Some concerns | Low | Low | Low | Some concerns | Some concerns |
| Lapidus et al., 200754 | Some concerns | Low | Low | Low | Some concerns | Some concerns |
| Lassen et al., 200256 | Some concerns | Low | Low | Low | Some concerns | Some concerns |
| Selby et al., 201558 | Low | Low | Low | Low | Some concerns | Some concerns |
| van Adrichem et al., 201759 | Low | Some concerns | Low | Low | Low | Some concerns |
| Zheng et al., 201660 | Some concerns | Low | Some concerns | Low | Some concerns | Some concerns |
| Gehling et al., 199823 | Some concerns | Some concerns | Some concerns | High | Some concerns | High |
| Bruntink et al., 201749 | Low | Some concerns | Low | Low | Some concerns | Some concerns |
| Samama et al., 201357 | Low | Some concerns | Low | Low | Some concerns | Some concerns |
Quantitative data synthesis
Details of the results of the primary studies are provided in Appendix 3. All 13 studies reported outcomes for any VTE, PE and major bleeding. The rate of any VTE in the control group ranged from 1.8% to 40.4% with a median of 12.2%. The rate of PE in the control group was zero in eight studies and ranged from 0.7% to 2.1% in the other four. There was only one bleeding event across all the control groups. Clinically relevant (proximal or symptomatic) DVTs were reported in 10 out of 13 studies, with control event rates ranging from 0.0% to 6.4% (median 1.5%). Clinically detected (symptomatic) DVTs were reported in all 13 studies, with control event rates ranging from 0.0% to 5.5% (median 0.7%). Any proximal or distal asymptomatic DVTs were reported in 10 out of 13 studies, with control event rates ranging from 1.6% to 25.7% (median 6.9%). Asymptomatic proximal DVTs were reported in 8 out of 13 studies, with control event rates ranging from 0.0% to 6.4% (median 0.7%). Asymptomatic distal DVTs were reported in 8 out of 13 studies, with control event rates ranging from 0.8% to 16.0% (median 3.0%).
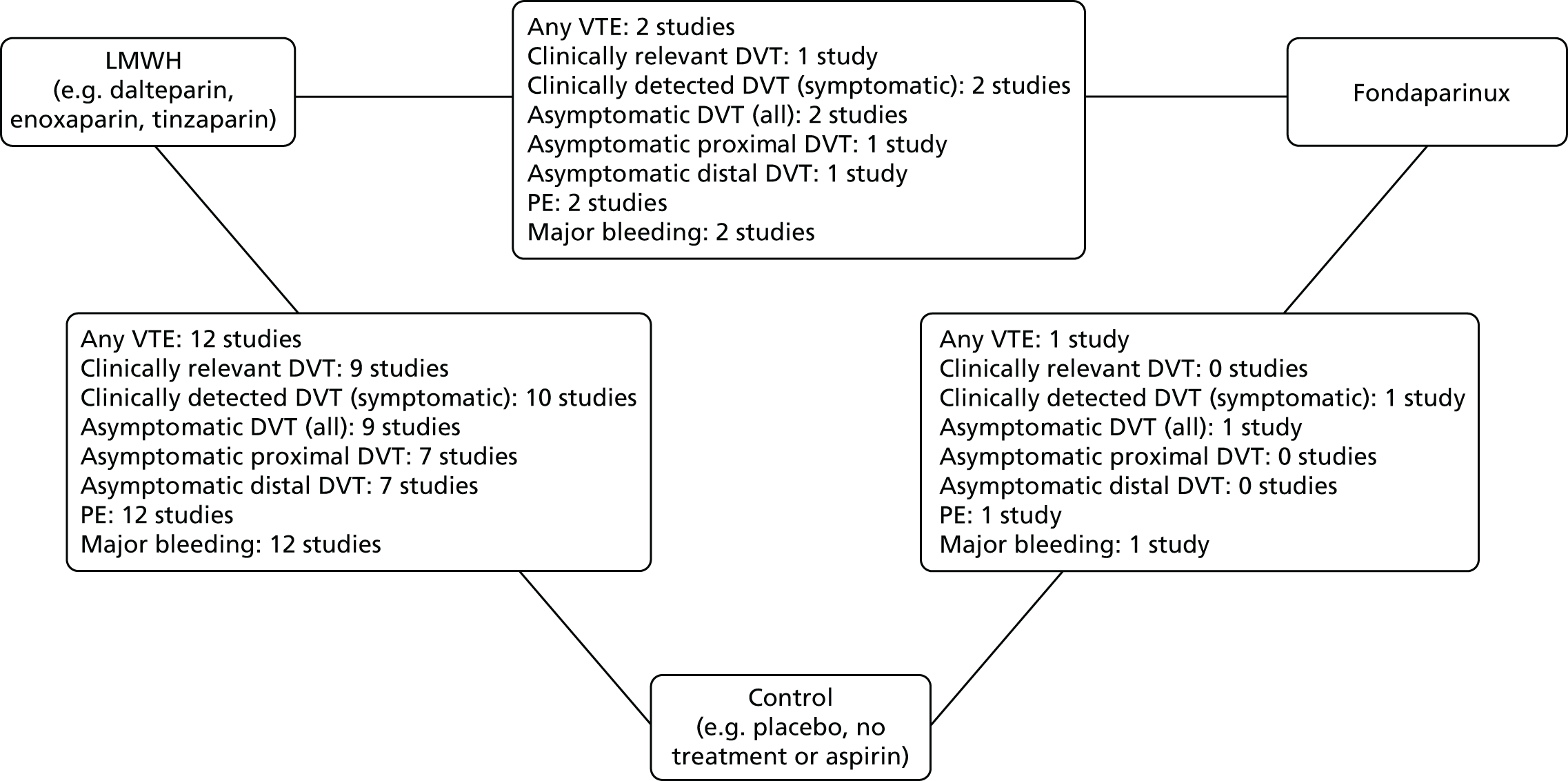
A NMA was undertaken to compare the effectiveness of two alternative forms of thromboprophylaxis (i.e. LMWH or fondaparinux) with no thromboprophylaxis (i.e. aspirin, placebo or no treatment). Figure 3 presents the network of evidence. All 13 studies were included in the analysis and provided information on at least one of the outcomes being analysed. Eleven of the studies compared LMWH thromboprophylaxis with no thromboprophylaxis, one three-arm study compared LMWH with fondaparinux with no thromboprophylaxis, and one study compared LMWH with fondaparinux. A summary of the key results of fixed-effect and random-effects NMA are provided in Table 3.
FIGURE 3.
Network diagram of different pharmacological thromboprophylaxis interventions vs. no thromboprophylaxis for preventing VTE. The nodes are the interventions. The numbers against each outcome represent the number of times that each pair of interventions has been compared. There was one multiarm study comparing LMWH vs. fondaparinux vs. control. Diagrams for specific outcomes depend on the number of studies that provide data and the number of non-zero event studies; not all outcomes involve feedback loops.
| Treatment | NMA, OR (95% CrI) | Probability of being best | ||
|---|---|---|---|---|
| Fixed effect | Random effects | OR (95% PrI) | ||
| Clinically detected DVT (symptomatic) | ||||
| LMWH | 0.45 (0.22 to 0.89) | 0.40 (0.12 to 0.99) | 0.41 (0.05 to 2.31) | 0.09 |
| Fondaparinux | 0.11 (0.01 to 0.60) | 0.10 (0.01 to 0.94) | 0.10 (0.00 to 1.46) | 0.91 |
| None | – | – | – | 0.00 |
| Asymptomatic DVT (proximal segment) | ||||
| LMWH | 0.22 (0.05 to 0.71) | 0.21 (0.04 to 0.82) | 0.21 (0.02 to 1.34) | 0.63 |
| Fondaparinux | 0.29 (0.03 to 2.35) | 0.28 (0.02 to 3.42) | 0.28 (0.01 to 4.49) | 0.36 |
| None | – | – | – | 0.01 |
| Asymptomatic DVT (distal) | ||||
| LMWH | 0.69 (0.47 to 1.01) | 0.69 (0.43 to 1.12) | 0.69 (0.29 to 1.62) | 0.00 |
| Fondaparinux | 0.11 (0.04 to 0.27) | 0.11 (0.03 to 0.35) | 0.11 (0.03 to 0.42) | 1.00 |
| None | – | – | – | 0.00 |
| Asymptomatic DVT (all) | ||||
| LMWH | 0.57 (0.42 to 0.77) | 0.57 (0.39 to 0.82) | 0.57 (0.28 to 1.12) | 0.00 |
| Fondaparinux | 0.14 (0.07 to 0.27) | 0.14 (0.05 to 0.31) | 0.14 (0.05 to 0.38) | 1.00 |
| None | – | – | – | 0.00 |
| PE | ||||
| LMWH | 0.30 (0.07 to 0.96) | 0.17 (0.01 to 0.88) | 0.18 (0.00 to 1.79) | 0.74 |
| Fondaparinux | 0.64 (0.05 to 7.26) | 0.47 (0.01 to 9.54) | 0.48 (0.01 to 17.53) | 0.25 |
| None | – | – | – | 0.01 |
| Major bleeding | ||||
| LMWH | 1.60 (0.14 to 25.67) | 1.45 (0.08 to 32.17) | 1.46 (0.06 to 42.87) | 0.37 |
| Fondaparinux | 14,380 (0.48 to 9.9 × 1014) | 8422 (0.32 to 1.3 × 1014) | 8421 (0.29 to 1.3 × 1014) | 0.03 |
| None | – | – | – | 0.59 |
| Clinically relevant DVTa | ||||
| LMWH | 0.43 (0.22 to 0.79) | 0.40 (0.16 to 0.85) | 0.40 (0.07 to 1.76) | 0.22 |
| Fondaparinux | 0.25 (0.07 to 0.82) | 0.23 (0.03 to 1.36) | 0.23 (0.02 to 2.11) | 0.77 |
| None | – | – | – | 0.01 |
| Any VTE | ||||
| LMWH | 0.53 (0.41 to 0.67) | 0.52 (0.37 to 0.71) | 0.52 (0.23 to 1.12) | 0.00 |
| Fondaparinux | 0.14 (0.07 to 0.25) | 0.13 (0.05 to 0.30) | 0.13 (0.04 to 0.39) | 1.00 |
| None | – | – | – | 0.00 |
Clinically detected deep-vein thrombosis (symptomatic)
Data were available from all 13 studies. 23,49–60 The risk of clinically detected DVT (symptomatic) was lower in adult outpatients with lower-limb immobilisation who received LMWH (OR 0.40, 95% CrI 0.12 to 0.99) and fondaparinux (OR 0.10, 95% CrI 0.01 to 0.94) than those in the control group. Fondaparinux is likely to be the most effective treatment (probability of being the most effective = 0.91). However, the heterogeneity in treatment effects between studies suggests that the true effects may vary depending on study characteristics (between-study SD 0.55, 95% CrI 0.03 to 1.59).
Asymptomatic deep-vein thrombosis (proximal segment)
Data were available from eight studies. 23,50–52,55,57,58,60 The risk of asymptomatic DVT (proximal segment) was lower in adult outpatients with lower-limb immobilisation who received LMWH (OR 0.21, 95% CrI 0.04 to 0.82) than those in adults in the control group. A similar effect was found for fondaparinux, although the results were inconclusive (OR 0.28, 95% CrI 0.02 to 3.42). The heterogeneity in treatment effects between studies suggests that the true effects may vary depending on study characteristics (between-study SD 0.42, 95% CrI 0.02 to 1.44).
Asymptomatic deep-vein thrombosis (distal)
Data were available from eight studies. 23,50–52,56–58,60 The risk of asymptomatic DVT (distal) was lower in adult outpatients with lower-limb immobilisation who received fondaparinux (OR 0.11, 95% CrI 0.03 to 0.35) than in those in the control group; fondaparinux is likely to be the most effective treatment (probability of being the most effective = 1.00). There was insufficient evidence of an effect of LMWH (OR 0.69, 95% CrI 0.43 to 1.12) compared with control, although the effect favoured treatment with LMWH. There was evidence of mild to moderate heterogeneity between studies, suggesting that the true effects may vary depending on study characteristics (between-study SD 0.20, 95% CrI 0.01 to 0.83).
Asymptomatic deep-vein thrombosis (all)
Data were available from 10 studies. 23,49–52,54,56–58,60 The risk of asymptomatic DVT (all) was lower in adult outpatients with lower-limb immobilisation who received LMWH (OR 0.57, 95% CrI 0.39 to 0.82) and fondaparinux (OR 0.14, 95% CrI 0.05 to 0.31) than in those in the control group. Fondaparinux is likely to be the most effective treatment (probability of being the most effective = 1.00). There was evidence of mild to moderate heterogeneity in treatment effects between studies, suggesting that the true effects may vary depending on study characteristics (between-study SD 0.17, 95% CrI 0.01 to 0.70).
Pulmonary embolism
Data were available from all 13 studies. 23,49–60 The risk of PE was lower in adult outpatients with lower-limb immobilisation who received LMWH (OR 0.17, 95% CrI 0.01 to 0.88) than in those in the control group. A reduction in risk was also found for fondaparinux, although the results were inconclusive (OR 0.47, 95% CrI 0.01 to 9.54). The heterogeneity in treatment effects between studies suggests that the true effects may vary depending on study characteristics (between-study SD 0.81, 95% CrI 0.05 to 2.04).
Major bleeding
Data were available from all 13 studies,23,49–60 but, with only four events across all the studies, estimates of the effects of LMWH (OR 1.45, 95% CrI 0.08 to 32.17) and fondaparinux on the risk of major bleeding were inconclusive. Control had the highest probability of being the best treatment (probability of being the best = 0.59). The between-study SD was 0.50 (95% CrI 0.02 to 1.64).
Clinically relevant deep-vein thrombosis
Data were available from 10 studies. 23,50–52,55,57,58,60 The risk of clinically relevant DVT was lower in adult outpatients with lower-limb immobilisation who received LMWH (OR 0.40, 95% CrI 0.16 to 0.85) than in those in the control group. The risk was also lower in patients treated with fondaparinux, although the results were inconclusive (OR 0.23, 95% CrI 0.03 to 1.36). The heterogeneity in treatment effects between studies suggests that the true effects may vary depending on study characteristics (between-study SD 0.45, 95% CrI 0.02 to 1.39).
Any venous thromboembolism
Data were available from all 13 studies. 23,49–60 The risk of any VTE was lower in adult outpatients with lower-limb immobilisation who received LMWH (OR 0.52, 95% CrI 0.37 to 0.71) and fondaparinux (OR 0.13, 95% CrI 0.05 to 0.30) than in those not receiving thromboprophylaxis. Fondaparinux is likely to be the most effective treatment (probability of being the most effective = 1.00). There was mild to moderate heterogeneity in treatment effects between studies. Although the results suggest that the true effects may vary depending on study characteristics, the predictive distribution still favoured fondaparinux relative to control (between-study SD 0.23, 95% CrI 0.01 to 0.75).
There were few reported adverse effects in the treated patients. Minor bleeding event rates varied from 0.0% to 10.5% in the LMWH intervention groups, 0.0% to 1.5% in the fondaparinux intervention groups and 0.0% to 6.8% in the control groups. In the largest RCT to date,59 the most common adverse event (of infection) occurred at a similar rate in the intervention and control groups (1.6% vs. 2.0%, respectively). When assessed in the trials, compliance appeared good, with only a single open-label study49 recording pain on injection, which was seen in 1.4% of participants in the intervention group. In studies monitoring for the incidence of heparin-induced thrombocytopaenia, no cases were found. 58 No deaths in any study were deemed attributable to either VTE or the use of an intervention.
The results of the network meta-regressions are detailed in Appendix 4. A network meta-regression of population characteristics (e.g. proportion of males, baseline risk of VTE), type of injury (i.e. fractures, Achilles tendon rupture, other soft-tissue injury), treatment of injury (surgical vs. conservative, above- vs. below-knee immobilisation) and the duration of thromboprophylaxis was undertaken for each available outcome. This showed that no covariate improved model fitted and, therefore, explained the variation in treatment effects.
The effect of the type of thromboprophylactic agent used (i.e. dalteparin, tinzaparin, certoparin, nadroparin, reviparin) was assessed using a separate NMA. This suggested that there were differences in the effects of the type of thromboprophylactic agent used, including between the different types of LMWH, with certoparin having the highest probability of having the greatest effect on any VTE. However, this finding was based on the effect of certoparin being used in one study,52 so it is not possible to draw any reliable conclusions.
Summary of key findings
-
Thromboprophylaxis with LMWH approximately halves the risk of any VTE. The effects on different types of VTE are variable and uncertain (in accordance with random error), but all are consistent with a halving of risk.
-
Thromboprophylaxis with fondaparinux appears to have a greater effect on the risk of VTE and a greater probability than LMWH of being the more clinically effective, but estimates for fondaparinux are based on only two trials.
-
Major bleeding is very uncommon; therefore, the effect of thromboprophylaxis on major bleeding in this group is uncertain.
-
Meta-regression did not identify any reliable evidence of effect modification by key covariates.
Review of individual risk factors associated with venous thromboembolic risk
Objectives
To identify individual, patient identifiable risk factors associated with VTE risk in patients with temporary lower-limb immobilisation due to injury.
Methods of reviewing effectiveness
Identification of studies
Studies were identified by searching the following electronic databases and research registers:
-
Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily, MEDLINE and Versions(R) (via OvidSP), 1946 to May 2017.
-
EMBASE (via OvidSP), 1974 to May 2017.
-
Cochrane Database of Systematic Reviews (via Wiley Online Library), 1996 to May 2017.
-
Database of Abstracts of Review of Effects (via Wiley Online Library), 1995 to March 2015.
-
Cochrane Central Register of Controlled Trials (via Wiley Online Library), 1898 to May 2017.
-
HTA database (via Wiley Online Library), 1995 to May 2017.
-
NHS EED (via Wiley Online Library), 1995 to March 2015.
-
Science Citation Index Expanded (via Web of Science), 1900 to May 2017.
-
ClinicalTrials.gov (via US National Institutes of Health), 2000 to May 2017.
-
International Clinical Trials Registry Platform (via World Health Organization), 1990 to May 2017.
The search strategy used free-text and thesaurus terms and combined synonyms relating to the condition (i.e. VTE in people with lower-limb immobilisation) with risk factor assessment or risk prediction modelling terms (used in the searches of MEDLINE, The Cochrane Library and EMBASE only). No language or date restrictions were used on any database. Further details on the search strategy can be found in Appendix 5. Searches were supplemented by hand-searching the reference lists of all relevant studies (including existing systematic reviews), performing a citation search of relevant articles, contacting key experts in the field and undertaking systematic keyword searches of the internet using the Google search engine.
All identified citations from the electronic searches and other resources were imported into and managed using EndNote bibliographic software.
Inclusion and exclusion criteria
The inclusion of potentially relevant articles was undertaken using a two-step process. First, all titles were examined for inclusion by one reviewer (AP) and any citations that clearly did not meet the inclusion criteria (e.g. non-human, unrelated to VTE) were excluded. Second, all abstracts and full-text articles were then examined independently by two reviewers (AP and DH). When necessary, non-English-language studies were translated using Google Translate to facilitate study selection and subsequent data extraction. Any disagreements in the selection process were resolved through discussion or, if necessary, arbitration by a third reviewer (SG), and articles were included by consensus.
Studies were considered eligible for inclusion if they met the following criteria: (1) any study design that included a measurement of VTE patient outcome, (2) a study population of adults (aged > 16 years) requiring temporary immobilisation (e.g. leg cast or brace in an ambulatory setting) for an isolated lower-limb injury, (3) any studies that reported and analysed data on individual risk factors associated with DVT or PE. Exclusion criteria for the selection included studies that involved hospital inpatient care or any patient requiring hospital admission for > 5 days, or studies that involved patients undergoing ambulant orthopaedic surgery (e.g. arthroscopy, arthroscopic surgery).
Data abstraction and quality assessment strategy
Data relating to study design, methodological quality and outcomes were extracted by one reviewer (AP) into a standardised data extraction form and independently checked for accuracy by a second reviewer (DH). Any discrepancies were resolved through discussion to achieve agreement. When differences were unresolved, the opinion of a third reviewer (SG) was sought. When multiple publications of the same study were identified, data were extracted and reported as a single study.
The methodological quality of each included study was assessed using the Risk Of Bias In Non-randomized Studies – of Interventions tool (ROBINS-I) [formerly called A Cochrane Risk of Bias Assessment Tool for Non-Randomized Studies of Interventions (ACROBAT-NRSI)]. 61 The tool is based on the original Cochrane Risk of Bias tool for randomised studies40 and also builds on related tools, such as the quality assessment of diagnostic accuracy studies (QUADAS-2). 62
The ROBINS-I61 tool provides a detailed framework for assessment and judgement of risk-of-bias domains that may arise in three phases: (1) at pre-intervention, bias arising from confounding and selection of participants into the study; (2) at intervention, bias in measurement of interventions; and (3) at post-intervention, bias due to deviations from intended interventions, missing data, measurement of outcomes and selection of reported results. Each domain is rated as being at low, moderate, serious or critical risk of bias. A low risk of bias indicates that the study is comparable to a well-performed randomised trial in the domain being evaluated. A moderate risk of bias indicates that the study is sound for a non-randomised study but is not comparable to a well-performed randomised trial. A serious risk of bias indicates the presence of important problems in the domain and a critical risk of bias indicates that the study is too problematic to provide any useful evidence on the intervention effects. If insufficient information is provided to determine the risk of bias of a certain domain, the domain is marked as having no information. In general, the overall risk of bias of each study was determined to be equal to that of the most severe level of bias found in any domain.
All studies were analysed using ROBINS-I,61 regardless of whether or not the original study design included randomisation to other exposures, thus ensuring that risk of bias was assessed specifically for the comparisons of interest to this review. It is important to note that the quality assessment reflects how well a specific result evaluated the association of interest to this review, regardless of the objectives of the original study.
Methods of data synthesis and analysis
Venous thromboembolism was considered to comprise any subsequent recorded diagnosis of DVT or PE, or death attributable to either pathology. No attempt was made to distinguish between anatomical location, thrombus burden or clinical sequelae of VTE for this project, in accordance with the definitions of hospital-acquired thrombosis produced by NHS England. 63 Individual risk factors highlighted through regression, OR analysis or parametric testing as significantly associated with an increased or decreased likelihood of subsequent VTE were extracted. In particular, each paper was scrutinised for evidence of individual risk factors, especially those highlighted within current risk stratification tools,17,31–33 and their predictive performance was recorded, when available. Other risk factors demonstrating an association with VTE in the context of individual studies were also reported. A meta-analysis was not possible owing to significant levels of heterogeneity between studies, variable reporting items and the high risk of attributable bias. Descriptive statistics and thematic analysis were used to synthesise risk factors acting in a reproducible fashion across studies. Thematic analysis took an inductive/semantic form, using familiarisation and coding directed by data content. Consistent risk factor themes were then highlighted in ordinal fashion. All analyses were conducted using Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA).
Results
Quantity and quality of research available
The literature searches identified 4771 citations. Of these, 15 studies9,11,23,50,52,53,60,64–71 met the inclusion criteria. Figure 4 presents a flow chart describing the process of identifying relevant literature. Sixty full-text articles were excluded as they did not meet all the prespecified inclusion criteria. The majority of the articles were excluded primarily on the basis of an inappropriate target population (not isolated lower-limb injury requiring temporary immobilisation), no data or analysis of risk factors associated with VTE, or an unsuitable publication type (i.e. reviews, commentaries, editorials or abstracts of excluded/included full-text papers). More specifically, two potentially relevant papers72,73 were excluded as they included a specific elective surgical population who were not considered to meet the inclusion criterion of lower-limb injury. A potentially relevant prospective observational cohort study74 was excluded, based on the authors’ conclusion of a low event rate precluding any subsequent analysis for predictors of VTE. Finally, a case–control study32 specifically seeking to derive a decision rule for the cohort of interest was excluded, based on the creation of this rule from a generic thrombosis cohort rather than a subgroup of patients with temporary lower-limb immobilisation. A full list of excluded studies with reasons for exclusion is presented in Appendix 6.
FIGURE 4.
Study flow chart (adapted):37 review of individual risk factors associated with VTE risk. © 2009 Moher et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Description of included studies (design and patient characteristics)
The design and patient characteristics of the 15 included studies9,11,23,50,52,53,60,64–71 that provided data on individual patient identifiable risk factors associated with VTE risk in ambulatory trauma patients with temporary immobilisation following lower-limb injury is summarised in Table 4.
| Study authors, year; country | Design, setting | Inclusion criteria (main) | Patients, sex, age (years) | Incidence of VTE | Prophylaxis | Duration of follow-up | Risk factor ascertainment | Outcome ascertainment | Statistical analysis |
|---|---|---|---|---|---|---|---|---|---|
| Gehling et al., 1998; Germany23 |
|
Age > 16 years with lower-limb injury requiring immobilisation with plaster or bandages (and at least one risk factor for VTE) |
|
|
NR | NR | Physician assessment (prospective) | Clinical assessment, screening sonography and confirmation phlebography | NR (appears descriptive) |
| Goel et al., 2009; Canada50 |
|
Adults aged 18–75 years with unilateral displaced fractures below the knee requiring operative intervention |
|
LMWH group: 8.7% Control group: 12.6% |
No prophylaxis prior to randomisation | Minimum of 3 months following surgery or until the fracture had united | Physician assessment (prospective) | Clinical assessment and bilateral lower-leg venography for all patients | Univariate and multivariate logistic regression |
| Kock et al., 1995; Germany52 |
|
Adults aged 18–65 years undergoing conservative treatment for below-knee injury with cylinder or below-knee cast |
|
LMWH group: 0.0% Control group: 4.3% |
No prophylaxis prior to randomisation | NR (however, duration of casting: LMWH group, 15.2 days; control group, 18.8 days) | Physician assessment (prospective) | Clinical assessment, screening sonography and confirmation phlebography | NR (appears descriptive) |
| Kujath et al., 1993; Germany53 |
|
Aged > 16 years undergoing conservative treatment for lower-limb injury with below-knee plaster applied for > 7 days |
|
LMWH group: 4.8% Control group: 16.5% |
No prophylaxis prior to randomisation | NR (however, duration of casting: LMWH group, 15.6 days; control group, 15.8 days) | Physician assessment (prospective) | Compression ultrasonography by two examiners and confirmation phlebography | NR (appears descriptive) |
| Zheng et al., 2016; China60 |
|
Adults aged > 18 years with any fracture of the lower limb requiring operative treatment |
|
LMWH group: 1.5% Control group: 3.2% |
No prophylaxis prior to randomisation | 3 months | Physician assessment (prospective) | Blinded bilateral Doppler compression ultrasonography | Logistic regression |
| Riou et al., 2007; France69 |
|
Aged > 18 years with isolated lower-limb injury (below the knee) managed conservatively (immobilisation duration of > 7 days) |
|
6.4% | Antithrombotic prophylaxis was given to 61% of patients | 3 months | Physician assessment (prospective) | Adjudication committee | Logistic regression with propensity score analysis |
| Hanslow et al., 2006; Australia64 |
|
Patients who had an operative intervention to the foot or ankle |
|
5.3% | Antithrombotic prophylaxis was given to 31% of patients | 4.4 months | Collected from clinical records (retrospectively) | Case note search, including hospital reattendance and diagnostic imaging | Logistic regression |
| Jameson et al., 2014; UK66 |
|
Patients with isolated unilateral closed ankle fracture, managed conservatively |
|
0.22% (PE only) | No data recorded | 3 months | NR, assumed to be collected from clinical records (retrospective) | Inpatient mortality or coded diagnosis of PE within 90 days of injury | Logistic regression |
| Makhdom et al., 2013; Canada9 |
|
All patients undergoing Achilles tendon repair |
|
23.5% | No peri- or post-operative prophylaxis | 3 months | Collected from electronic medical record system (retrospectively) | Case note search, including hospital reattendance and diagnostic imaging | Non-parametric testing using Fisher’s exact test |
| Meek and Tong, 2012; Australia11 |
|
Aged > 18 years with acute lower-limb injury requiring temporary immobilisation (ED discharge within 24 hours of presentation) |
|
2.9% | No prophylaxis (excluded if received at any dose) | NR | Electronic notes screened for eligibility by one investigator (retrospective) | Case note search, including hospital reattendance and diagnostic imaging | Logistic regression |
| Patel et al., 2012; USA68 |
|
All patients who had Achilles tendon rupture |
|
0.77% | Nil routine, assumed to be none provided | 3 months | Collected from electronic medical record system (retrospective) | Case note search, including hospital reattendance and diagnostic imaging | Logistic regression |
| Wahlsten et al., 2015; Denmark71 |
|
Aged > 18 years undergoing an operative procedure for a fracture of the foot, ankle, tibia or patella |
|
1.0% | Routine perioperative prophylaxis with nil post operative prophylaxis | 180 days | Collected from five different cross-linked registries (retrospective) | Case note search, including hospital reattendance and diagnostic imaging | Multivariate Cox regression |
| van Adrichem et al., 2014; the Netherlands70 |
|
|
|
NR | No data recorded | 3 months | Participant completed questionnaire (prospective collection) | Case note search, including hospital reattendance and diagnostic imaging | Logistic regression |
| Ho and Omari, 2017; Australia65 |
|
Aged > 18 years with fracture to foot/ankle with conservative management |
|
11.0% | Nil routine, assumed to be none provided | 6 months | Questionnaire (unclear if physician or patient completed) | Prospective compression ultrasonography | Parametric and non-parametric testing with bootstrapping |
| Manafi Rasi et al., 2013; Iran67 |
|
Aged > 15 years with stable foot/ankle fracture or grade 3 sprain (non-surgical treatment) |
|
3.0% | NR | 7–14 days | NR | Compression ultrasonography by two independent examiners | NR (appears descriptive) |
All studies were published between 1993 and 2017 (five were RCTs with conservative arms,23,50,52,53,60 three were prospective observational cohort or cross-sectional studies,65,67,69 one was a case–control study70 and six were retrospective cohort studies)9,11,64,66,68,71 and conducted in 10 countries (Australia,11,64,65 Canada,9,50 China,60 Denmark,71 France,69 Germany,23,52,53 Iran,67 the Netherlands,70 the UK66 and the USA). 68 Most of the studies (n = 11) were entirely outpatient based,11,23,50,52,53,60,64–67,69 whereas the remaining studies9,68,70,71 included patients with a short-duration inpatient stay to facilitate day-case surgery. In total, data were collated on 80,678 patients with a subsequent reported outcome of VTE positive or negative following temporary lower-limb immobilisation. The incidence of VTE across the studies with interpretable outcome data (79,202 patients) ranged from 0.22%66 to 23.5%9 (median 4.8%), mean age ranged from 33.8 years52 to 52.6 years71 and the proportion of male patients ranged from 45.8%65 to 86.1%,9 with a median across those studies with reported data of 56.3%.
The duration of follow-up varied between studies. Ten studies reported follow-up over a period of at least 3 months9,50,60,64–66,68–71 and one study followed up patients for up to 14 days. 67 Although four studies failed to record the duration of follow-up,11,23,52,53 two of these appeared to report follow-up only for the duration of the plaster cast, which averaged at 15.7 days53 and 17 days. 52 Eight studies collected data on risk factors prospectively via physician assessment or questionnaire,23,50,52,53,60,65,69,70 whereas six studies collected these data through clinical records, electronic patient notes or registries. 9,11,64,66,68,71 One study did not report the methodology for this aspect of data collection. 67 Analysis and methodology of VTE diagnosis subsequent to immobilisation varied markedly across studies and included prospective screening in all patients following plaster cast removal (seven studies),23,50,52,53,60,65,67 adjudicated diagnostic evaluation in those with symptoms (two studies)69,70 and retrospective identification of VTE through the interrogation of clinical records/health databases (six studies). 9,11,64,66,68,71 A single study66 looked only at the subsequent diagnosis of PE as an outcome, with reduced prevalence as expected. The association of individual risk factors with subsequent VTE was highlighted through regression analyses (nine studies),11,50,60,64,66,68–71 non-parametric tests (two studies)9,65 and descriptive statistics (four studies). 23,52,53,67
Quality characteristics
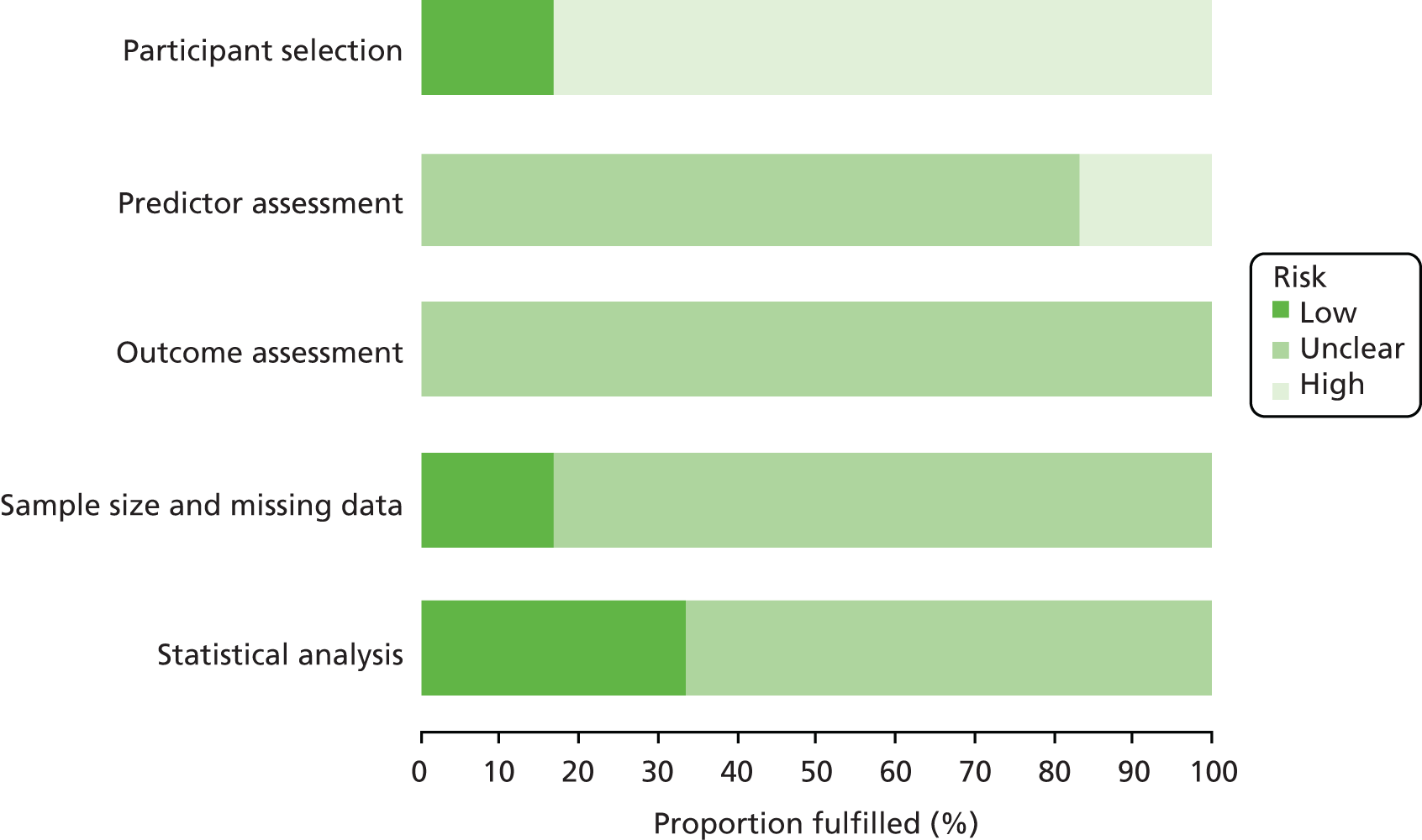
The overall methodological quality of the 15 included studies is summarised in Figure 5 and Table 5.
FIGURE 5.
ROBINS-I61 risk-of-bias assessment graph: review authors’ judgements about each methodological quality item across all included studies – review of individual risk factors associated with VTE risk.
| Study authors, year | Cause/area of bias | Overalla | ||||||
|---|---|---|---|---|---|---|---|---|
| Confounding | Selection of participants into the study | Classification/measurement of interventions | Deviations from intended interventions | Missing data | Measurement of outcomes | Selection of the reported result | ||
| Gehling et al., 199823 | Low | Low | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Goel et al., 200950 | Low | Low | Low | Low | Low | Low | Moderate | Moderate |
| Kock et al., 199552 | Low | Low | Moderate | Moderate | Low | Moderate | Moderate | Moderate |
| Kujath et al., 199353 | Low | Low | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Zheng et al., 201660 | Low | Moderate | Low | Low | Moderate | Low | Moderate | Moderate |
| Riou et al., 200769 | Moderate | Moderate | Moderate | Serious | Moderate | Moderate | Moderate | Serious |
| Hanslow et al., 200664 | Moderate | Moderate | Moderate | Serious | Moderate | Moderate | Moderate | Serious |
| Jameson et al., 201466 | Moderate | Serious | Moderate | Serious | Moderate | Moderate | Moderate | Serious |
| Makhdom et al., 20139 | Serious | Serious | Moderate | Moderate | Moderate | Moderate | Moderate | Serious |
| Meek and Tong, 201211 | Moderate | Serious | Moderate | Moderate | Moderate | Moderate | Moderate | Serious |
| Patel et al., 201268 | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Wahlsten et al., 201571 | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| van Adrichem et al., 201470 | Moderate | Serious | Serious | Serious | Moderate | Moderate | Moderate | Serious |
| Ho and Omari, 201765 | Serious | Serious | Moderate | Moderate | Serious | Moderate | Moderate | Serious |
| Manafi Rasi et al., 201367 | Serious | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Serious |
All studies were deemed to be at overall moderate (seven studies)23,50,52,53,60,68,71 or serious (eight studies)9,11,64–67,69,70 risk of bias, using the ROBINS-I61 framework for assessment and judgement. Studies scoring a serious risk of bias did so predominantly on the selection of participants into the study, perhaps highlighting the issue with retrospective observational work into VTE outcomes; patients deemed to be at high risk in these cohorts are often treated with thromboprophylaxis (as highlighted in Table 4), or managed in a different manner from other patients. If this is not highlighted within a prospective analysis plan, a false low event rate is seen and risk is marginalised.
Narrative data synthesis
Age was the most consistent individual risk prediction factor, highlighted across 11 studies. 9,11,50,52,53,60,65,68–71 ORs reported for age varied from 1.0560 to 3.48,11 with limited estimates of precision. Meta-analysis was not undertaken owing to limitations in the data reported and concerns about the heterogeneous nature of the study populations. Injury type was the second most highlighted risk factor across six studies,11,50,52,53,69,70 all using multivariate logistic regression to suggest that severe traumatic injuries and fractures (when compared with soft-tissue injuries) were independently associated with VTE. Body mass index (BMI) was the third most consistent individual risk highlighted, noted as independently predictive of VTE across four studies,53,60,70,71 with ORs ranging from 1.20160 to 17.2. 70 Other risk factors were highlighted in fewer than four studies. Despite being present within several currently used risk stratification tools, pregnancy, recent hospital admission and preceding immobility prior to injury failed to demonstrate an independent association with VTE in any of the selected studies. Individual risk factors currently used within risk stratification tools and their association with VTE across all studies are shown in Table 6.
| Study authors, year | Risk factors associated with developing VTE | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Permanent (present before episode of lower-limb immobilisation) | Transient (during injured period) | ||||||||||||||
| Age | BMI | Active cancer | Pregnancy | Smoking | Varicosities | Prior or family history of VTE | Significant comorbidity | Known thrombophilia | Exogenous oestrogen therapy | Recent hospital admission or surgery | Preceding immobility | Injury type | Immobilisation type | Weight-bearing status | |
| Using an end point of asymptomatic VTE, detected by routine screening | |||||||||||||||
| Gehling et al., 199823 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Goel et al., 200950 | PSARa | NSARa | NSARa | N/A | NSARa | N/A | N/A | NSARa | NSARa | NSARa | N/A | N/A | PSARa | N/A | N/A |
| Kock et al., 199552 | PSARb | NSARb | N/A | N/A | NSARb | NSARb | N/A | N/A | N/A | NSARb | N/A | N/A | PSARb | PSARb | N/A |
| Kujath et al., 199353 | PSARc | PSARc | N/A | N/A | N/A | PSARc | N/A | N/A | N/A | N/A | N/A | N/A | PSARc | N/A | N/A |
| Zheng et al., 201660 | PSARd | PSARd | N/A | N/A | N/A | N/A | N/A | NSARd | N/A | N/A | N/A | N/A | N/A | NSARd | N/A |
| Ho and Omari, 201765 | PSARe | NSARe | N/A | N/A | NSARe | N/A | NSARe | N/A | N/A | NSARe | N/A | N/A | N/A | NSARe | NSARe |
| Manafi Rasi et al., 201367 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Using an end point of symptomatic VTE, detected by clinical follow-up and targeted investigation | |||||||||||||||
| Riou et al., 200769 | PSARf | NSARf | N/A | N/A | NSARf | NSARf | NSARf | NSARf | N/A | NSARf | N/A | N/A | PSARf | PSARf | PSARf |
| Hanslow et al., 200664 | N/A | N/A | N/A | N/A | N/A | N/A | PSARg | PSARg | N/A | N/A | N/A | N/A | N/A | PSARg | PSARg |
| Jameson et al., 201466 | NSARh | N/A | N/A | N/A | N/A | N/A | N/A | PSARh | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Makhdom et al., 20139 | PSARi | NSARi | N/A | N/A | NSARi | N/A | N/A | NSARi | N/A | NSARi | N/A | N/A | N/A | N/A | N/A |
| Meek and Tong, 201211 | PSARj | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | PSARj | NSARj | N/A |
| Patel et al., 201268 | PSARk | NSARk | N/A | N/A | N/A | N/A | NSARk | NSARk | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Wahlsten et al., 201571 | PSARl | PSARl | PSARl | N/A | NSARl | N/A | PSARl | N/A | N/A | PSARl | N/A | N/A | N/A | N/A | N/A |
| van Adrichem et al., 201470 | PSARm | PSARm | N/A | N/A | N/A | N/A | N/A | N/A | PSARm | PSARm | N/A | N/A | PSARm | N/A | N/A |
Other potential risk factors associated with subsequent development of VTE after lower-limb immobilisation included recent air travel (one study),64 coagulopathy and peripheral arterial disease (one study). 71 A single paper67 looked at the cumulative incidence of risk factors per patient and reported the presence of three or more factors to be significantly associated with the development of VTE. Methodology of reporting individual variables to have no association with subsequent VTE was inconsistent and heterogeneous. Six studies reported no association between sex and VTE in this cohort,11,50,52,65,66,70 five studies reported no association between exogenous oestrogen use and VTE9,50,52,53,65 and six studies reported no association between smoking and subsequent VTE. 9,50,52,65,69,71 Several papers produced conflicting results; six studies reported no association between raised BMI and subsequent risk of VTE9,50,52,65,68,69 and one study reported no association of VTE with increasing age. 66 These other identified risk factors and all negative associations are reported in Table 7.
| Study authors, year | Other risk factors shown to be associated with VTE | Risk factors shown to have no association with VTE | Other key findings/author conclusions |
|---|---|---|---|
| Gehling et al., 199823 | NR | Unable to demonstrate association between cumulative risk factors and thrombosis | Non-relevant |
| Goel et al., 200950 | NR |
|
Given the overall number of fractures, it is difficult to define a specific type as increasing the risk for DVT, but those fractures of the tibial plateau did display a tendency towards higher rates of DVT in the study |
| Kock et al., 199552 | NR |
|
Treatment procedures involving less immobilisation should be used whenever possible |
| Kujath et al., 199353 | NR |
|
The patients who did not develop a thrombosis had an average of 1.24 risk factors, whereas the patients with thrombosis had an average of 1.96 risk factors. The patients who suffered a thrombosis despite prophylaxis had 2.7 risk factors |
| Zheng et al., 201660 | NR | NR | The study was not statistically powered to properly cull out any additional potential risk factors that might affect VTE incidence in this population |
| Riou et al., 200769 | Non-weight-bearing status (OR 4.11, 95% CI 1.72 to 9.86) | No association seen on multivariate regression with:
|
Owing to a very low incidence of certain variables (e.g. cancer, severe diseases and hormonal treatment), the power of the study was not sufficient to identify their roles as potential risk factors. Because the incidence of obesity was not high in the study population, the results may not apply to morbidly obese patients |
| Hanslow et al., 200664 |
|
Tourniquet use and mode of anaesthesia for those undergoing operative intervention | The incidence of thromboembolic disease after foot and ankle surgery could be higher than that previously reported, particularly if a patient has certain risk factors |
| Jameson et al., 201466 | Charlson score of ≥ 1 gives OR 11.97 (95% CI 5.14 to 27.87; p < 0.001) |
|
Comorbidities elevate the risk of PE and these data can be utilised by clinicians when considering whether or not to prescribe LMWH for VTE prophylaxis with the attendant risks of the therapy itself borne in mind |
| Makhdom et al., 20139 | NR |
|
Patient education is necessary regarding anticipated complications, and early mobilisation should be advocated, especially for patients aged > 40 years |
| Meek and Tong, 201211 | Achilles tendon rupture (descriptive) |
|
Increasing age and a diagnosis of Achilles tendon rupture appeared to increase the risk of VTE |
| Patel et al., 201268 | NR |
|
Congestive heart failure, history of DVT or PE, and obesity might be risk factors, but perhaps the study did not have an adequate number of patients to show this difference |
| Wahlsten et al., 201571 |
|
|
Patients with risk factors, especially previous DVT or PE, use of oral contraceptives and mobid obesity, have an increased risk of DVT/PE that exceeds the risk of DVT/PE in healthy patients undergoing total hip or knee replacement |
| van Adrichem et al., 201470 | The presence of two or more acquired or genetic risk factors in patients with below-knee cast immobilisation produced an OR of 43.4 (95% CI 13.4 to 141.0) | Sex | Patients with below-knee cast immobilisation have a substantially increased risk of venous thrombosis, namely a 56-fold increased risk, compared with patients with no cast, corresponding to an estimated incidence of 1% in the first 3 months after cast application |
| Ho and Omari, 201765 | Subsequent presentation with symptoms suggestive of DVT (p = 0.006) |
|
This pilot study unveiled limitations and logistical issues to be addressed in the future. Notably, the limitations include the small number of patients and the low adherence to attending ultrasonography assessment |
| Manafi Rasi et al., 201367 | Cumulative number of risk factors: presence of ≥ 3 risk factors reported as being significantly associated with VTE development (p = 0.01) | NR | The incidence of DVT significantly increased in the presence of ≥ 3 risk factors (p = 0.01) |
Summary of key findings
-
Increasing age and injury severity were the most consistent risk factors associated with the development of VTE in patients with lower-limb injury and temporary immobilisation.
-
Many clinical features considered to be risk factors for VTE were not examined or associated with VTE in the studies.
-
All studies included in the review were deemed to be at moderate or serious risk of bias.
-
The evidence base for tailored risk prediction in people with lower-limb immobilisation due to injury is very weak.
Review of risk assessment models for predicting venous thromboembolic risk
Objective
The objective was to identify RAMs that predict the risk of VTE in ambulatory trauma patients with temporary immobilisation following lower-limb injury.
Methods of reviewing effectiveness
Identification of studies
Studies were identified by searching the following electronic databases and research registers:
-
Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily, MEDLINE and Versions(R) (via OvidSP), 1946 to May 2017.
-
EMBASE (via OvidSP), 1974 to May 2017.
-
Cochrane Database of Systematic Reviews (via Wiley Online Library), 1996 to May 2017.
-
Database of Abstracts of Review of Effects (via Wiley Online Library), 1995 to March 2015.
-
Cochrane Central Register of Controlled Trials (via Wiley Online Library), 1898 to May 2017.
-
HTA database (via Wiley Online Library), 1995 to May 2017.
-
NHS EED (via Wiley Online Library), 1995 to March 2015.
-
Science Citation Index Expanded (via Web of Science), 1900 to May 2017.
-
ClinicalTrials.gov (via US National Institutes of Health), 2000 to May 2017.
-
International Clinical Trials Registry Platform (via Word Health Organization), 1990 to May 2017.
The search strategy used free text and thesaurus terms and combined synonyms relating to the condition (i.e. VTE in people with lower-limb immobilisation) with risk factor assessment or risk prediction modelling terms (used in the searches of MEDLINE, The Cochrane Library and EMBASE only). No language or date restrictions were used on any database. Further details on the search strategy can be found in Appendix 5. Searches were supplemented by hand-searching the reference lists of all relevant studies (including existing systematic reviews), performing a citation search of relevant articles, contacting key experts in the field and undertaking systematic keyword searches of the World Wide Web using the Google search engine.
All identified citations from the electronic searches and other resources were imported into and managed using EndNote bibliographic software.
Inclusion and exclusion criteria
The inclusion of potentially relevant articles was undertaken using a two-step process. First, all titles were examined for inclusion by one reviewer (AP) and any citations that clearly did not meet the inclusion criteria (e.g. non-human, unrelated to VTE) were excluded. Second, all abstracts and full-text articles were then examined independently by two reviewers (AP and DH). When necessary, non-English-language studies were translated using Google Translate to facilitate study selection and subsequent data extraction. Any disagreements in the selection process were resolved through discussion or, if necessary, arbitration by a third reviewer (SG), and articles were included by consensus.
Studies were considered eligible for inclusion if they met the following criteria: (1) any study design that included a measurement of VTE patient outcome, (2) studies that recruited adults (aged > 16 years) who required temporary immobilisation (e.g. leg cast or brace in an ambulatory setting) for an isolated lower-limb injury and (3) any studies that reported any validation, or estimates of utility and performance of VTE risk assessment models for people with lower-limb cast immobilisation.
Data abstraction and quality assessment strategy
Data relating to study design, methodological quality and outcomes were extracted by one reviewer (AP) into a standardised data extraction form and independently checked for accuracy by a second reviewer (DH). Any discrepancies were resolved through discussion or, if necessary, arbitration by a third reviewer (SG) and included by consensus. When multiple publications of the same study were identified, data were extracted and reported as a single study.
There are no validated (or widely agreed on) tools for the assessment of prognosis research studies and there is little empirical evidence to support the importance of particular study features affecting the reliability of findings, including the avoidance of bias. 75 For this review, a generic list of important methodological features recommended by Altman76 and Moons et al. 77 for prediction modelling studies was deemed to be the most appropriate (i.e. useful) to assess the internal validity of the included studies. In general, five domains were considered important for assessing biases sufficiently large to distort the findings of prognosis research. These included (1) participant selection, (2) predictor assessment, (3) outcome assessment, (4) sample size and missing data and (5) statistical analysis. An overall judgement of bias was assigned as ‘low risk’ if all domains were judged as low risk, as ‘high risk’ if at least one domain was judged to be at high risk and as ‘unclear risk’ if an unclear risk of bias was noted in at least one domain and it was ‘low risk’ for all other domains. The methodological quality of each included study was independently evaluated by two reviewers (AP and DH). Any discrepancies were resolved through discussion or, if necessary, through the involvement of a third reviewer (SG). Blinding of the quality assessor to author, institution or journal was not considered necessary.
Methods of data synthesis and analysis
Venous thromboembolism was considered to comprise any subsequent recorded diagnosis of DVT, PE or death attributable to either pathology. No attempt was made to distinguish between anatomical location, thrombus burden or clinical sequelae of VTE for this project, in accordance with the definitions of hospital-acquired thrombosis produced by NHS England. 63 A narrative review of all identified scoring systems was performed, to compare design characteristics with thresholds for prophylaxis. Estimates of sensitivity, specificity, predictive values or likelihood ratios were directly extracted from validation studies or retrospectively calculated using available baseline data when applicable. All analyses were conducted using Microsoft Excel 2010.
Results
Quantity and quality of research available
The literature searches identified 4771 citations. In total, only six studies32,78–82 met the inclusion criteria. Of these, one paper32 focused on prediction model development with external validation in independent data. The remaining papers focused on external model validation without model updating. 78–82 A flow chart describing the process of identifying relevant literature is given in Figure 6. A total of 69 full-text articles were excluded as they did not meet all of the prespecified inclusion criteria. The majority of the articles were excluded on the basis of inappropriate target population (i.e. not isolated lower-limb injury requiring temporary immobilisation), having no relevant RAMs or outcome evaluations and being an unsuitable publication type (i.e. reviews, commentaries, editorial or abstracts of included full-text papers). A full list of excluded studies with reasons for exclusion is presented in Appendix 7.
FIGURE 6.
Study flow chart (adapted):37 review of RAMs that predict the risk of VTE. © 2009 Moher et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
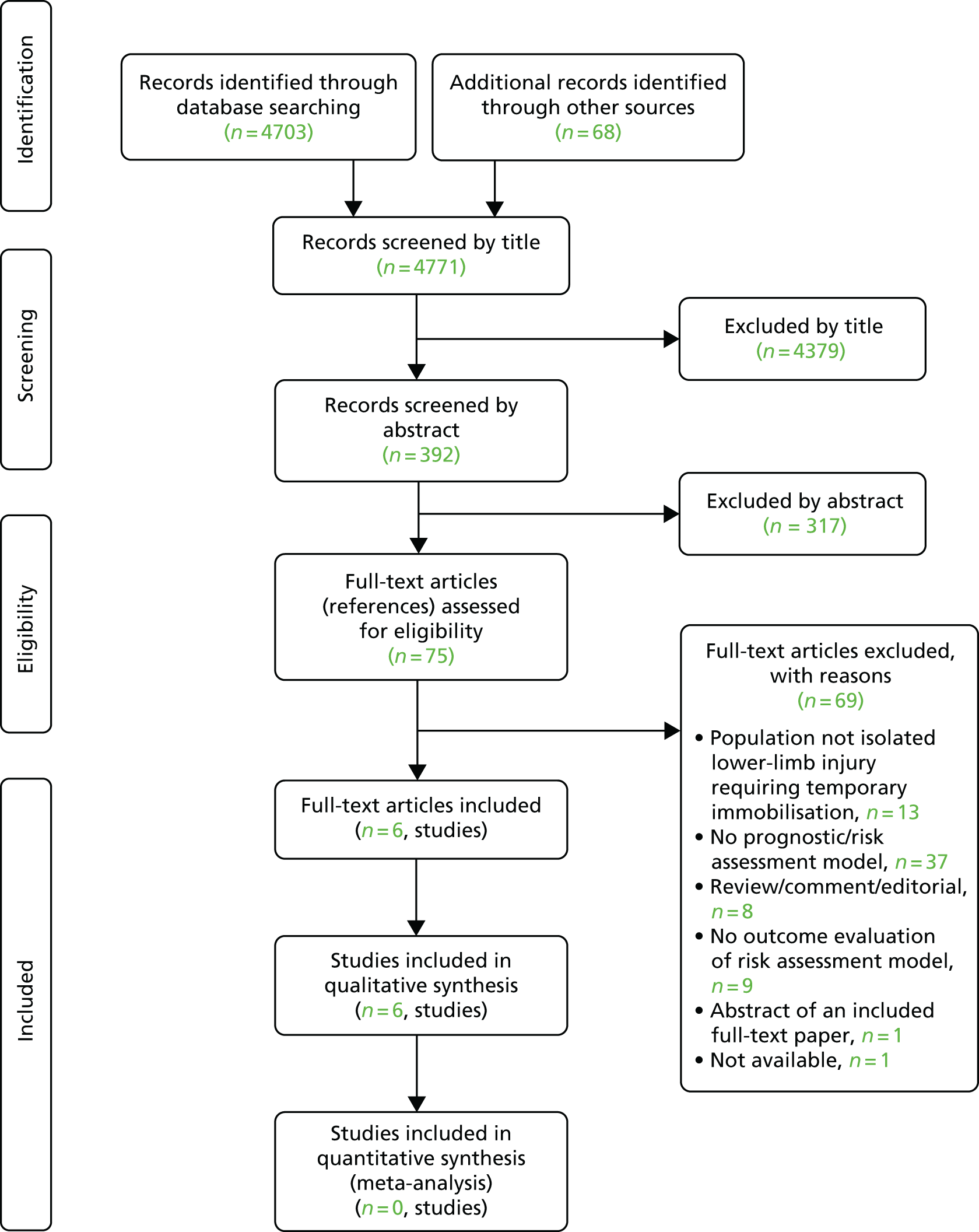
Description of included studies (design and patient characteristics)
Study characteristics are described in Table 8. Two case–control studies32,82 and four observational studies78–81 that described the evaluation of seven RAMs were found. A single study32 presented data on derivation and validation; this study used a generic thrombosis database (including all acute thrombosis patients seen in an outpatient clinic matched with partner controls) to derive a new rule, rather than a relevant cohort of patients with temporary lower-limb immobilisation. All other papers looked to provide measures of external validation or implementation metrics regarding previously derived scores, with no description of the initial derivation methodology.
| Authors, year | Study objective/type | Source of data | Recruitment method | Study dates | Setting, country | Eligibility criteria | Study population | Outcome to be predicted | Candidate predictors | Sample size (events) | Missing data | Model development | Model performance | Model evaluation | Results (key comparisons) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nemeth et al., 201532 |
|
Case–control study | Consecutive recruitment | 1 March 1999 to 31 August 2004 | Six clinics, the Netherlands | Patients aged 18–70 years with a first DVT, PE or both. Control group consisted of partners of participating patients or individuals identified via random digit dialling (controls were frequency matched to cases with respect to sex and age). Information on thromboprophylaxis use during plaster cast immobilisation was missing |
|
|
|
Multiple imputation was used to complete missing predictor values |
Modelling method: logistic regression Predictor selection: full model (32 predictors), forward selection procedure, and if p ≤ 0.25 in the univariate analysis of all participants or a well-established association with VTE Restricted model (11 predictors) and clinical model (14 environmental predictors) also developed. Based on the regression coefficients in the clinical logistic regression model, L-TRiP(cast) score developed for plaster cast patients Shrinkage of predictor weight or regression coefficient: NR |
|
Internal validation: test set for derivation and two separate validation data sets | Comparison of sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios | |
| Watson et al., 201682 |
|
Case–control study | Consecutive recruitment | 1 November 2010 to 31 May 2011 | Single centre (fracture clinic), Wales | Patients aged 19–75 years with lower-limb casts who developed symptomatic VTE (confirmed by Doppler ultrasonography, CT pulmonary angiography or a pulmonary V/Q scan within 5 months of application of cast). Control group consisted of patients (case matched to age, sex and injury) who were treated with casts during the same date range, but did not develop symptomatic VTE. Routine thromboprophylaxis was not used | Validation: n = 42 |
|
21 symptomatic VTE cases | NR |
Modelling method: NA Predictor selection: Roberts et al. 17 11 predictor variables (environmental factors with a well-established association with the occurrence of VTE in the literature); Keenan et al. 31 14 predictor variables (no details provided) Shrinkage of predictor weight or regression coefficient: NA |
Discrimination, calibration, classification measures: NR | No recalibration; no adjustment or update | Comparison of sensitivity, specificity and positive and negative predictive values | |
| Saragas et al., 201781 |
|
Prospective cohort study without control | Consecutive recruitment | March 2014 to April 2015 | NR, South Africa | All patients aged > 18 years who underwent foot and ankle surgery requiring the combination of below-knee immobilisation in a cast and non-weight bearing for ≥ 4 weeks. Patients who were already on anticoagulants or had previously had a DVT were excluded | Validation: n = 142 |
|
|
Three DVT cases (2.1%) | NR |
Modelling method: NA Predictor selection: 36 risk factors (no details provided on how these were selected/derived) Shrinkage of predictor weight or regression coefficient: NA |
Discrimination, calibration, classification measures: NR | No recalibration; no adjustment or update | Incidence of VTE following prophylactic anticoagulation for 4–6 weeks, namely until non-weight bearing or cast removal, whichever came first (non-comparative study) |
| Haque et al., 201680 |
|
Prospective cohort study without control | Consecutive recruitment | NR | Single centre, UK | Patients aged ≥ 18 years with isolated foot and ankle fractures who were treated non-operatively and immobilised in a plaster cast (weight bearing as well as non-weight bearing) and managed as outpatients. Patients were excluded if they had a known bleeding disorder, renal disorder, multiple injury/polytrauma, complex pilon fracture or if they had a known allergy to LMWH (minimum of 6 months following injury) | Validation: n = 150 |
|
|
Three symptomatic VTE (two distal DVT’s and one PE) cases (2.0%) | NR |
Modelling method: NA Predictor selection: 14 predictor variables (consensus selection of predictors from NICE guidelines24 and GEMNet,17 which focuses on patients managed as outpatients, with an arbitrary cut-off point) Shrinkage of predictor weight or regression coefficient: NA |
Discrimination, calibration, classification measures: NR | No recalibration; no adjustment or update | Incidence of VTE in those considered to be at high risk, namely with a score of ≥ 3 (non-comparative study) |
| Giannadakis et al., 200079 |
|
Prospective cohort study without control | NR | March 1994 to March 1996 | Single centre, Germany | Selected patients (aged > 16 years) with minor lower-limb injuries and at low risk of DVT, who required cast immobilising and did not receive medical thromboprophylaxis, were included. Patients who required medical thromboprophylaxis were excluded | Validation: n = 178 |
|
|
Two DVT cases (1.1%) | NR |
Modelling method: NA Predictor selection: 12 predictor variables (no details provided on how these were selected/derived) Shrinkage of predictor weight or regression coefficient: NA |
Discrimination, calibration, classification measures: NR | No recalibration; no adjustment or update | Incidence of thrombosis in low-risk patients who received no thromboprophylaxis, namely no risk factors (non-comparative study) |
| Eingartner et al., 199578 |
|
NR | NR | July 1993 to February 1994 | Single centre, Germany | Outpatients with an immobilising cast of a lower-limb after an injury | Validation: n = 305 |
|
|
No VTE events | NR |
Modelling method: NA Predictor selection: nine predictor variables (no details provided on how these were selected/derived) Shrinkage of predictor weight or regression coefficient: NA |
Discrimination, calibration, classification measures: NR | No recalibration; no adjustment or update | Incidence of thrombosis (non-comparative study) |
The seven identified RAMs varied in design, structure, output and threshold for prophylaxis. Several scores were dichotomous, with others providing ordinal measure of risk. Design characteristics and threshold levels for each RAM are presented for comparison in Table 9. The majority of RAMs focused solely on the estimate of thromboembolic risk; a single method featured characteristics designed to balance the risk of bleeding with thromboprophylaxis. 17 The individual predictors and their weighting varied markedly between RAMs. Variables (and their definitions) for each RAM are presented for comparison in Table 10.
| Risk assessment model | Acronym/descriptor | Derivation | Design | Incorporation of bleeding risk? | Number of variables | Threshold (suggested cut-off point) | Attempted validation? |
|---|---|---|---|---|---|---|---|
| Roberts et al.17 | The GEMNet guideline | EC | Dichotomous | Yes | 11 | N/A | Yes |
| Keenan et al.31 | The Plymouth Rule | EC | Ordinal | No | 14 | > 2 | Yes |
| Nemeth et al.32 | The L-TRiP(cast) score | Regression | Ordinal | No | 14 | > 8 | Yes |
| Saragas et al.81 | The modified Caprini score | EC | Ordinal | No | 36 | > 1 | No |
| Eingartner et al.78 | N/A | EC | Ordinal | No | 9 | > 1 | No |
| Haque et al.80 | N/A | EC | Ordinal | No | 14 | > 2 | No |
| Giannadakis et al.79 | N/A | EC | Dichotomous | No | 12 | N/A | No |
| Variable | Study authors, year | ||||||
|---|---|---|---|---|---|---|---|
| Nemeth et al., 201532 L-TRiP(cast) | Watson et al., 201682 | Saragas et al., 201781 | Haque et al., 201680 | Giannadakis et al., 200079 | Eingartner et al., 199578 | ||
| Keenan et al., 200931 | Roberts et al., 201317 | ||||||
| Brief details of RAMs | VTE risk scoring model for thromboprophylaxis in patients after cast immobilisation of the lower extremity (14 clinical predictor variables) | VTE risk scoring model for thromboprophylaxis in patients after lower-limb cast/boot immobilisation [14 clinical predictor variables (patient completed)] | VTE risk assessment for thromboprophylaxis in ambulatory trauma patients requiring temporary lower-limb plaster cast immobilisation after acute severe injury (11 clinical predictor variables) | Thrombosis risk factor assessment in foot and ankle surgery patients requiring below-knee cast immobilisation and non-weight bearing for ≥ 4 weeks (36 predictor variables) | VTE risk scoring model for thromboprophylaxis in patients requiring lower-limb immobilisation [14 clinical predictor variables (patient completed)] | Checklist for pharmacological thromboprophylaxis for outpatients who required cast immobilisation after lower-limb injury (12 clinical predictor variables) | VTE risk scoring system for thromboprophylaxis in patient with lower-limb immobilisation [9 clinical predictor variables (patient completed)] |
| Predictor variables included in RAMs | |||||||
| Age | Yes (≥ 35 and < 55 years; ≥ 55 years) | Yes (≥ 60 years) | Yes (> 60 years) | Yes (≥ 41 years) | Yes (≥ 60 years) | Yes (> 40 years) | Yes (> 60 years) |
| Sex | Yes (male sex) | – | – | – | – | – | – |
| Overweight/obese | Yes (BMI of ≥ 25 kg/m2 and < 35 kg/m2; ≥ 35 kg/m2) | Yes (very overweight, BMI of ≥ 30 kg/m2) | Yes (BMI of ≥ 30 kg/m2) | Yes (BMI of > 25 kg/m2) | Yes (BMI of ≥ 30 kg/m2) | Yes (Broca Index of > 20%) | Yes (overweight, > 100 kg) |
| Cancer | Yes (within previous 5 years) | Yes (active) | Yes (active) | Yes (malignancy present or previous) | Yes (active or cancer treatment including tamoxifen and raloxifen) | Yes (malignancies) | Yes (ongoing malignancy) |
| Pregnancy or puerperium | Yes | Yes | Yes | Yes (including history of unexplained stillborn infant, recurrent spontaneous abortion, premature birth with toxaemia or growth-restricted infant) | Yes | – | – |
| Smoking | – | – | Yes (active) | – | – | Yes (> 20 cigarettes per day) | Yes (active) |
| Varicosities | Yes (superficial vein thrombosis) | Yes (varicose veins) | Yes (extensive varicosities) | Yes (varicose veins, large) | Yes (varicose veins) | Yes (varicose veins) | Yes (varicose veins even after varicose vein surgery) |
| Prior or family history of VTE | Yes [family history (first-degree relative)] | Yes [family history (brother, sister, father, mother) or personal history of DVT/PE] | Yes (personal history or first-degree relative) | Yes (personal history of DVT/PE, family history of thrombosis) | Yes [personal or family history (brother, sister, father, mother, child) of blood clot in leg or lung] | Yes (personal history of previous thrombosis/PE, family history of thrombosis/PE) | Yes (personal history of previous DVT/PE) |
| Significant comorbidity | Yes (rheumatoid arthritis, chronic kidney disease, COPD, multiple sclerosis) | Yes (heart disease, lung disease, bowel disease, hormone disease or other long-term medical condition requiring treatment) | Yes (any serious medical comorbidity including cardiac failure, COPD, chronic renal failure or inflammatory bowel disease) | Yes (history of inflammatory bowel disease, acute MI, CHF for < 1 month, COPD, stroke with lower-extremity weakness for < 1 month) | Yes (active heart, lung, bowel or joint disease) | Yes (diabetes mellitus, CHD) | Yes (history of cardiovascular disease, including arterial hypertension) |
| Known thrombophilia | – | – | Yes | Yes (positive factor V Leiden, positive prothrombin G20210 A, other congenital or acquired thrombophilia) | Yes (thrombophilia associated with increased risk of blood clots) | ||
| Exogenous oestrogen therapy | Yes (oral contraceptives) | Yes (oral contraceptive pill or HRT) | Yes [hormone therapy (combined oral contraceptive pill/HRT/tamoxifen)] | Yes (oral contraceptives or HRT) | Yes (on HRT or taking oestrogen-containing contraceptive) | Yes (contraception use) | Yes (oral contraceptives) |
| Hospital admission or surgery | Yes (hospital admission or surgery within the previous 3 months) | Yes (abdominal surgery in previous 6 weeks) | Yes (any recent hospital admission/major surgery) | Yes (minor surgery planned, major surgery < 1 month previously, major surgery > 45 minutes previously, arthroscopic surgery, elective major lower-extremity arthroplasty) | Yes (hospital admission within the previous 6 weeks, including lower-limb surgery) | – | Yes (lower-limb, pelvic or lower-abdominal surgery over the previous 6 months) |
| Preceding immobility | Yes (bedridden within previous 3 months) | Yes (unable to walk before accident/injury) | – | Yes [medical patient currently at bed rest, patient confined to bed (> 72 hours)] | – | – | – |
| Injury type | – | Yes (Achilles tendon rupture) | – | Yes [hip, pelvis or leg fracture of < 1 month, acute spinal-cord injury (paralysis) of < 1 month] | Yes (Achilles tendon rupture) | Yes (soft-tissue injury of higher than grade 1) | – |
| Immobilisation type | Yes (plaster cast: complete leg, circular knee cast – ankle free, foot, lower leg) | – | – | Yes (immobilising plaster cast for < 1 month) | Yes (plaster cast extending above the knee) | Yes (thigh bandage) | – |
| Pneumonia | Yes | – | – | Yes (serious lung disease including pneumonia < 1 month) | – | – | – |
| Travel | – | – | – | – | Yes [continuous travel of ≥ 3 hours (road, rail or air travel) in the previous 4 weeks or needing to travel while wearing plaster cast] | – | – |
| Swollen legs | – | – | – | Yes (current) | – | – | – |
| Sepsis | – | – | – | Yes (occurred < 1 month previously) | – | – | – |
| Central venous access | – | – | – | Yes | – | – | – |
| Antiphospholipid antibodies | – | – | – | Yes (positive lupus anticoagulant, elevated anticardiolipin antibodies) | – | – | – |
| Multiple trauma | – | – | – | Yes (multiple trauma occurring < 1 month previously) | – | – | – |
Quality characteristics
The overall methodological quality of the six included studies is summarised in Figure 7 and Table 11. The majority of studies were deemed to be at high risk of bias,32,78,79,81,82 based primarily on participant selection; all reviewed studies attempted validation of proposed decision rules in heterogeneous cohorts, with pragmatic observational follow-up only. Outcomes were also non-standardised and varied by site in terms of description and inclusion.
| Study author, year | Participant selection | Predictor assessment | Outcome assessment | Sample size and missing data | Statistical analysis | Overalla |
|---|---|---|---|---|---|---|
| Nemeth et al., 201532 | High | Unclear | Unclear | Low | Low | High |
| Watson et al., 201682 | High | High | Unclear | Unclear | Low | High |
| Saragas et al., 201781 | High | Unclear | Unclear | Unclear | Unclear | High |
| Haque et al., 201680 | Low | Unclear | Unclear | Unclear | Unclear | Unclear |
| Giannadakis et al., 200079 | High | Unclear | Unclear | Unclear | Unclear | High |
| Eingartner et al., 199578 | High | Unclear | Unclear | Unclear | Unclear | High |
Both case–control studies32,82 had specific and notable limitations in methodology. The larger study, by Nemeth et al. ,32 used three distinct generic thrombosis data sets to derive and validate the proposed RAM. As such, the tool is derived from a group of patients with unprovoked or hospital-acquired VTE and has limited potential generalisability to the cohort of interest in this study. The authors looked at a subgroup of patients with temporary lower-limb immobilisation within the study data, finding only a small proportion in whom to attempt validation (230 patients, 2% of the original derivation data set). The smaller study, by Watson et al. ,82 derived case–control data using an equal measure of appropriate patients with thrombosis following cast immobilisation, alongside a separate cohort of those without. As such, the prevalence of thrombosis within this study cohort was 50%. This is 20 times the estimated prevalence within the literature and, therefore, renders their estimates of predictive value at high risk of error.
Narrative data synthesis
The study by Nemeth et al. 32 derived and validated a clinical risk score for plaster cast patients: the Leiden thrombosis risk in plaster (cast) [L-TRiP(cast)] score. In this study,32 data from a large population-based case–control study of approximately 10,000 patients (4446 consecutive patients with a first episode of venous thrombosis and 6118 controls) were used in developing the model (included in patients with disease and many other confounding factors). After minimising the variables in an attempt to produce a clinical (14 environmental predictor variables) and pragmatic rule (11 predictor variables), the authors validated this rule in two subsequent VTE case–control data sets.
Watson et al. 82 assessed the diagnostic accuracy of five RAMs (only two of these, the GEMNet model17 and the Plymouth model,31 were specific to patients with lower-limb trauma and cast immobilisation) in a case–control study of 42 patients with lower-limb immobilisation following injury (21 cases and 21 controls). The reported sensitivity and specificity of the GEMNet model (85.7% and 47.6%, respectively) did not seem to be compatible with the numbers of cases and controls, so contact was made with the authors for clarification. They identified an error in the sensitivity, which should have been reported as 4.76%, and provided the raw numbers for both RAMs, which were used to calculate all diagnostic parameters and confidence intervals (CIs).
Prognostic accuracy measures for the three scores evaluated in these two studies are presented in Table 12. Sensitivity ranged from 57.1% to 92.6% across the RAMs and specificity ranged from 4.76% to 60.8%. The L-TRiP(cast) data are displayed in this table using thresholds denoting optimal performance and to allow direct comparison with other validated scores. The estimates of positive and negative predictive value for the L-TRiP(cast) score were modelled using an appropriately low prevalence of VTE, whereas the estimates for the GEMNet and Plymouth models used the artificial 50% prevalence from the case–control study. This explains the relatively high positive predictive values and the relatively low negative predictive values for these scores.
| Author | RAM | Sensitivity, % (95% CI) | Specificity, % (95% CI) | Positive predictive value, % (95% CI) | Negative predictive value, % (95% CI) | Likelihood ratio positive (95% CI) | Likelihood ratio negative (95% CI) | Percentage receiving thromboprophylaxis (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Roberts et al.17 | GEMNet | 85.7 (62.6 to 96.2) | 4.76 (0.2 to 25.9) | 47.4 (31.3 to 64.0) | 25.0 (1.3 to 78.1) | 0.90 (0.73 to 1.10) | 3.00 (0.16 to 55.31) | 90.5 (76.5 to 96.9) |
| Keenan et al.31 | Plymouth | 57.1 (33.4 to 77.4) | 52.4 (30.3 to 73.6) | 54.5 (32.7 to 74.9) | 55.0 (32.0 to 76.2) | 1.20 (0.67 to 2.15) | 0.81 (0.46 to 1.46) | 52.4 (36.6 to 67.7) |
| Nemeth et al.32 | L-TRiP(cast) with a cut-off point of ≥ 8 | 92.6 | 39.7 | 3.8 | 99.5 | 1.5 | 0.2 | 87.8 |
| L-TRiP(cast) with a cut-off point of ≥ 9 | 80.8 | 60.8 | 5.0 | 99.2 | 2.1 | 0.3 | 74.7 |
The area under the curve (AUC) for the L-TRiP(cast) score ranged from 0.77 (95% CI 0.66 to 0.87) in the derivation cohort to 0.77 (95% CI 0.58 to 0.96) and 0.95 (95% CI 0.91 to 0.99) in the two subsequent validation cohorts.
In addition to these rules, four additional models were identified (Saragas et al. ,81 Haque et al. ,80 Giannadakis et al. 79 and Eingartner et al. 78). No measures of external validation of these RAMs were found. All were found as single-centre small-scale implementation studies, revealing no further additional information on performance, utility or reliability.
Summary of key findings
-
A number of RAMs have been developed using a variety of methods and based on a variety of predictor variables.
-
External validation studies have weak designs and limited generalisability, so estimates of prognostic accuracy are very uncertain.
-
The limited data available suggest that the L-TRiP(cast) score with a cut-off point of 8 can achieve reasonable sensitivity for predicting VTE without an excessive loss of specificity.
Identifying key variables to assess thromboembolic risk: a Delphi consensus exercise
Objectives
The systematic reviews revealed a lack of evidence relating to individual risk predictors and RAMs for VTE in lower-limb immobilisation due to trauma. Therefore, expert consensus methods were used to identify potential risk factors for VTE and expert consensus was sought on which were considered to be the most useful predictors. The aim was to bring together topic experts from haematology, orthopaedics and emergency medicine and achieve consensus through serial rounds and facilitated discussion. The results of this Delphi exercise would then be compared with current risk prediction models and consensus opinion on clinical engagement, utility and acceptability to patients would be gauged. Delphi methodology has been previously described85–87 and used throughout health services research for similar indications. 88,89
Methods
Delphi methodology
A three-round Delphi study was conducted between August 2017 and April 2018 using a panel of international topic experts, identified from the published literature and national clinical research network (injuries and emergency theme).
Expertise was ascribed using two criteria: (1) evidence of experience in relevant guideline or risk assessment tool design and (2) routine clinical experience with the relevant patient cohort and topic of interest. These criteria were selected to allow disclosure of unpublished methodology deriving existing rules, confer practicality of any rule and to ensure broad dissemination and uptake of consensus findings. Experts were identified through national bodies, relevant literature and local thrombosis committee groups. National bodies included The British Orthopaedic Association, The Royal College of Emergency Medicine and The Clinical Research Network Injuries and Emergencies Specialty group. Additional national or international societies were not approached for independent representation owing to time constraints and workload. All individuals approached agreed to participate and provided written informed consent. Experts were entirely independent of the core review team (n = 11), local colleagues independent of the review work (n = 3) and members of the core review team (n = 6).
The open first round of the classical Delphi approach was replaced with a systematic literature review to identify possible VTE predictors, as previously described. Round 1 of the Delphi study was then delivered via a web-based platform using SmartSurvey Ltd (Tewkesbury, UK)90 through a subscribed account. All potential individual predictor variables identified through the previous systematic review of existing decision rules and the wider literature on risk prediction in the relevant cohort were presented to participants as potential candidate predictors. Participants were then asked to rate the strength of the VTE prediction risk for each variable using a four-point Likert scale, with the option to record uncertainty. Their replies were collated into quantitative and qualitative output for each individual question. An opportunity to identify new relevant predictor variables was provided and participants were encouraged to identify missing themes.
New candidate variables were proposed, and those failing to achieve consensus in round 1 of the Delphi exercise were carried forward to a second round. Participants were presented with these variables together with a summary of the panel results from round 1, when applicable. Participants were asked to complete the same Likert scale as before, with the advantage of having additional insight into comments and quantitative results revealed by the rest of the group.
At the end of round 2 of the Delphi exercise, all variables were carried forward to a facilitated round-table discussion where consensus results and comments were provided to all participants. Data were collated and analysed to calculate frequencies, mean and range of scores.
Data synthesis and analysis
Criteria for inclusion in the decision rule were defined by a variable identified as a moderate or strong predictor by consensus between two, three or more respondents. Variables identified as uncertain or not or weakly predicting VTE risk by consensus between two, three or more respondents were likewise excluded from the exercise. Quantitative data from rounds 1 and 2 were presented to participants as bar charts with percentages. All analyses were conducted using Microsoft Excel 2010.
Results
Expert engagement
Twenty participants were identified to participate in the study. All (100%) completed round 1; 19 participants (95.0%) completed round 2. Ten participants (50.0%) contributed to the final facilitated round-table discussion. A list of participants and the clinical scope of the Delphi panel is provided in Appendix 8.
Systematic review and identification of candidate predictors
Trial flow results from the relevant systematic reviews prior to the Delphi exercise have been previously described (see Review of individual risk factors associated with venous thromboembolic risk and Review of risk assessment models for predicting venous thromboembolic risk). Thirty-five individual candidate predictors were identified and included for dissemination in round 1. Predictors were subdivided into risks related to injury/immobilisation and generic thrombosis risks. Initial proposed candidate predictors are shown in Table 13, which also shows the results of subsequent Delphi rounds.
| Consensus as predictor | Consensus as non-predictor | No consensus | Additional suggested variables |
|---|---|---|---|
| Delphi consensus exercise: round 1 results | |||
| Thrombophilia | Smoker | Age | Non-weight-bearing status |
| Prior VTE | Hepatitis | Intravenous drug use | Partial weight-bearing status |
| Surgery in the preceding 3 months | Dehydration | Hospital admission in the preceding 3 months | Significant soft-tissue injury |
| BMI of > 30 kg/m2 | Sex | Pneumonia | Baseline D-dimer level |
| Above-knee plaster cast | Antipsychotic drug use | Exogenous oestrogen/hormone therapy | |
| Pregnant/puerperium | Extensive varicosities | Preceding immobility | |
| Active cancer | Non-type O blood | Superficial thrombophlebitis | |
| Aircast® boot (DJO, LLC, Dallas, TX, USA) | Ankle fracture/dislocationa | ||
| Complete ligament rupture (non-Achilles tendon) | Family history of VTE (first-degree relative) | ||
| Red cell distribution width | Significant injury in the preceding 3 months | ||
| Factor 8 activity | Significant medical comorbidity | ||
| Factor 11 activity | Lower-limb paralysis | ||
| von Willebrand factor antigen levels | Achilles tendon rupture | ||
| Comminuted injury | |||
| Rigid immobilisation in plaster | |||
| Delphi consensus exercise: round 2 results | |||
| Age | Hospital admission within the preceding 3 months | Intravenous drug use | |
| Exogenous oestrogen/hormone therapy | Baseline D-dimer level | Significant injury in the preceding 3 months | |
| Lower-limb paralysis | Pneumonia | Significant medical comorbidity | |
| Superficial thrombophlebitis | Partial weight-bearing status | Preceding immobility | |
| Achilles tendon rupture | Significant soft-tissue injury | Comminuted injury | |
| Rigid immobilisation in plaster | Non-weight-bearing status | ||
| Family history of VTE (first-degree relative) | |||
Round 1 results
Seven variables were identified as predictive of VTE risk by consensus criteria during round 1. Thirteen variables were identified as not predictive of VTE by consensus criteria and excluded from the exercise. No consensus was achieved on 15 variables; 14 predictors were carried forward to the second round, with moderated peer feedback and tabular display. A single variable was excluded from the exercise after collated comments, group discussion and feedback regarding the lack of primary suitability for inclusion. Four new variables were suggested during the round 1 exercise and these were also carried forward. All candidate predictors and their round 1 results are presented in Table 13.
Round 2 results
In the second round, consensus was achieved on six further variables as predictive of VTE risk. Five variables were identified on reflection as not predictive of VTE risk by consensus criteria and these were excluded from the exercise. No consensus remained for 7 of the 17 variables carried forward from round 1. No further risk predictors were suggested by participants during round 2. Candidate variables taken forward and their round 2 results are presented in Table 13.
Variables failing to achieve consensus
Of the seven variables failing to achieve consensus, two failed because of a dichotomous split with clear unresolvable disagreement by experts (intravenous drug use and comminuted fracture). The other five variables appeared to be categorised as weakly to moderately predictive by all, but fell short of agreed criteria for inclusion. Further rounds were deemed unlikely to generate further consensus at this stage and the trial team proposed a move to the facilitated round-table discussion to achieve consensus.
Facilitated round-table discussion
There was general round-table agreement about all variables for which consensus had been achieved by the Delphi exercise. A specific point was made by the group regarding the inclusion of several variables depicting the degree of immobilisation of the calf pump, and whether or not this should become a single ordinal variable. A single variable (active intravenous drug use) on which the group did not reach consensus was discussed in further detail, with the majority of the round table proposing that the variable be refined or this entire cohort of patients be excluded based on safety concerns. Several discussion points followed regarding the need for strict inclusion criteria when applying any decision rule, with particular regard to the type of immobilisation in this group. The final agreed variables considered to be predictors of VTE risk via the Delphi expert consensus were eight generic VTE risk predictors (i.e. thrombophilia, pregnancy/puerperium, active cancer, surgery in the preceding 3 months, prior VTE, exogenous oestrogen/hormone therapy, lower-limb paralysis and superficial thrombophlebitis), two patient demographics (i.e. age and BMI) and three variables specific to lower-limb immobilisation or injury (i.e. Achilles tendon rupture, rigid immobilisation and above-knee cast).
Table 14 compares the expert consensus variables to those included in the RAMs. Most of the expert consensus variables were included in one or more of the RAMs but the RAMs also included many variables that were not supported by expert consensus.
| Variable | RAM | |||||||
|---|---|---|---|---|---|---|---|---|
| L-TRiP(cast)32 | Plymouth31 | GEMNet17 | Saragas et al.81 | Haque et al.80 | Giannadakis et al.79 | Eingartner et al.78 | Delphi | |
| Predictor variables included in risk assessment models | ||||||||
| Age | Yes (≥ 35 and ≥ 55 years) | Yes (≥ 60 years) | Yes (> 60 years) | Yes (≥ 41 years) | Yes (≥ 60 years) | Yes (> 40 years) | Yes (> 60 years) | Yes (> 60 years) |
| Sex | Yes (male sex) | – | – | – | – | – | – | No |
| Overweight/obese | Yes (BMI of ≥ 25 kg/m2 and ≥ 35 kg/m2) | Yes (BMI of ≥ 30 kg/m2) | Yes (BMI of ≥ 30 kg/m2) | Yes (BMI of > 25 kg/m2) | Yes (BMI of ≥ 30 kg/m2) | Yes (Broca Index of > 20%) | Yes (overweight, > 100 kg) | Yes (BMI of > 30 kg/m2) |
| Cancer | Yes (within previous 5 years) | Yes (active) | Yes (active) | Yes (malignancy present or previous) | Yes (active or cancer treatment) | Yes (malignancies) | Yes (ongoing malignancy) | Yes (active) |
| Pregnancy or puerperium | Yes | Yes | Yes | Yes | Yes | – | – | Yes |
| Smoking | – | – | Yes (active) | – | – | Yes (> 20 cigarettes per day) | Yes (active) | No |
| Varicosities | – | Yes (varicose veins) | Yes (extensive varicosities) | Yes (varicose veins, large) | Yes (varicose veins) | Yes (varicose veins) | Yes (varicose veins even after surgery) | No |
| Superficial thrombophlebitis | Yes (superficial vein thrombosis) | – | – | – | – | – | – | Yes |
| Prior or family history of VTE | Yes [family history (first-degree relative)] | Yes [family history (brother, sister, father, mother) or personal history of DVT/PE] | Yes (personal history or first-degree relative) | Yes (personal history of DVT/PE, family history of thrombosis) | Yes [personal or family history (brother, sister, father, mother, child) of blood clot in leg or lung] | Yes (personal history of previous thrombosis/PE, family history of thrombosis/PE) | Yes (personal history of previous DVT/PE) | Yes (prior VTE only) |
| Significant comorbidity | Yes (rheumatoid arthritis, chronic kidney disease, COPD, multiple sclerosis) | Yes (heart disease, lung disease, bowel disease, hormone disease or other long-term medical condition requiring treatment) | Yes (any serious medical comorbidity, including cardiac failure, COPD, chronic renal failure or inflammatory bowel disease) | Yes [history of inflammatory bowel disease, acute MI, CHF (diagnosed < 1 month previously), COPD, stroke with lower-extremity weakness < 1 month] | Yes (active heart, lung, bowel or joint disease) | Yes (diabetes mellitus, CHD) | Yes (history of cardiovascular disease, including arterial hypertension) | No |
| Known thrombophilia | – | – | Yes | Yes (positive factor V Leiden, positive prothrombin G20210 A, other congenital or acquired thrombophilia) | Yes (thrombophilia associated with increased risk of blood clots) | – | – | Yes |
| Exogenous oestrogen therapy | Yes (oral contraceptives) | Yes (oral contraceptive pill or HRT) | Yes [hormone therapy (combined oral contraceptive pill/HRT/tamoxifen)] | Yes (oral contraceptives or HRT) | Yes (on HRT or taking oestrogen-containing contraceptive) | Yes (contraception use) | Yes (oral contraceptives) | Yes (exogenous oestrogen or hormone therapy) |
| Hospital admission or surgery | Yes (hospital admission or surgery within the previous 3 months) | Yes (abdominal surgery in last 6 weeks) | Yes (any recent hospital admission/major surgery) | Yes [minor surgery planned, major surgery (occurring < 1 month previously), major surgery (occurring > 45 minutes previously) arthroscopic surgery, elective major lower-extremity arthroplasty] | Yes (hospital admission within the previous 6 weeks, including lower-limb surgery) | – | Yes (lower limb, pelvic or lower-abdominal surgery over the previous 6 months) | Yes (surgery in the preceding 3 months only) |
| Preceding immobility | Yes (bedridden within previous 3 months) | Yes (unable to walk before accident/injury) | – | Yes [medical patient currently at bed rest, patient confined to bed (> 72 hours)] | – | – | – | No |
| Injury type | – | Yes (Achilles tendon rupture) | – | Yes [hip, pelvis or leg fracture (occurring < 1 month previously), acute spinal-cord injury (paralysis) < 1 month] | Yes (Achilles tendon rupture) | Yes (soft-tissue injury of higher than grade 1) | – | Yes (Achilles tendon rupture) |
| Immobilisation type | Yes (plaster cast: complete leg, circular knee cast – ankle free, foot, lower leg) | – | – | Yes (immobilising plaster cast acquired < 1 month previously) | Yes (plaster cast extending above the knee) | Yes (thigh bandage) | – | Yes (rigid immobilisation and/or above-knee plaster cast) |
| Pneumonia | Yes | – | – | Yes (serious lung disease including pneumonia, diagnosed < 1 month previously) | – | – | – | No |
| Travel | – | – | – | – | Yes [continuous travel of ≥ 3 hours (road, rail or air travel) in the previous 4 weeks or needing to travel while wearing plaster cast] | – | – | No |
| Swollen legs | – | – | – | Yes (current) | – | – | – | No |
| Sepsis | – | – | – | Yes (occurring < 1 month previously) | – | – | – | No |
| Central venous access | – | – | – | Yes | – | – | – | No |
| Antiphospholipid antibodies | – | – | – | Yes (positive lupus anticoagulant, elevated anticardiolipin antibodies) | – | – | – | No |
| Multiple trauma | – | – | – | Yes (multiple trauma occurring < 1 month previously) | – | – | – | No |
Originally, it was planned to use the expert consensus methods to refine existing RAMs or construct up to five new RAMs from the selected risk factors, and then produce a consensus estimate of sensitivity and specificity for each RAM that would allow the exploration of the trade-off between sensitivity and specificity in decision-analytic modelling. It was decided not to proceed with this for the following reasons:
-
The difficulty of achieving consensus on individual risk factors (which was felt to be unsurprising given the limited available evidence) suggested that it would not be possible to achieve the necessary consensus on the content and structure required to refine an existing RAM or construct a new RAM.
-
The receiver operating characteristic (ROC) analysis of the L-TRiP(cast) score published by Nemeth et al. 32 (identified in the systematic review of RAMs) provided an estimate of the trade-off between sensitivity and specificity that could be used in decision-analytic modelling, and would be more credible and usable than expert-derived estimates of sensitivity and specificity for expert-derived RAMs.
Summary of key findings
-
Expert consensus on 13 variables most likely to predict VTE risk for outpatients with lower-limb injury and temporary immobilisation has been established: eight generic VTE risk predictors (i.e. thrombophilia, pregnancy/puerperium, active cancer, surgery in the preceding 3 months, prior VTE, exogenous oestrogen/hormone therapy, lower-limb paralysis and superficial thrombophlebitis), two patient demographics (i.e. age and BMI) and three variables specific to lower-limb immobilisation or injury (i.e. Achilles tendon rupture, rigid immobilisation and above-knee cast).
-
It was not possible to achieve expert consensus on the following seven variables: intravenous drug use, significant injury in the preceding 3 months, significant medical comorbidity, preceding immobility, comminuted injury, non-weight-bearing status and family history of VTE.
-
Injury- and plaster-associated risk was proposed as a single ordinal variable based primarily on the degree of calf pump immobilisation.
Chapter 4 Assessment of cost-effectiveness
Systematic review of existing cost-effectiveness evidence
A systematic review was undertaken to identify any existing studies on the cost-effectiveness of thromboprophylaxis for lower-limb immobilisation due to injury.
Methods of reviewing cost-effectiveness
Identification of studies
Studies were identified by searching the following electronic databases and research registers:
-
Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily, MEDLINE and Versions(R) (via OvidSP), 1946 to October 2017.
-
EMBASE (via OvidSP), 1974 to October 2017.
-
Cochrane Database of Systematic Reviews (via Wiley Online Library), 1996 to October 2017.
-
Database of Abstracts of Review of Effects (via Wiley Online Library), 1995 to March 2015.
-
HTA database (via Wiley Online), 1995 to October 2017.
-
NHS EED (via Wiley Online Library), 1995 to March 2015.
For the MEDLINE and EMBASE searches, the aim was to maximise the specificity of the search in these databases that do not target economic evaluations. In these searches, the keyword strategies developed in the review of clinical effectiveness (see Chapter 3, Objective), which combined terms related to VTE with terms related to lower-limb immobilisation, were used with sensitive economic evaluation, quality of life and cost search filters91–93 aimed at restricting search results to economic and cost-related studies. For the searches of HTA and NHS EED, terms for lower-limb immobilisation were not included, in order to maximise sensitivity and find all economic evaluations relating to VTE. All resources were searched initially from inception to October 2017 (or, in the case of discontinued sources such as NHS EED, the date at which coverage ceased). Further details on the search strategy can be found in Appendix 9.
All identified citations from the electronic searches and other resources were imported into and managed using EndNote bibliographic software.
Inclusion and exclusion criteria
The inclusion of potentially relevant articles was undertaken using a two-step process by a single reviewer. During the screening stage, all titles were examined for inclusion by the health economist and any citations that clearly did not meet the inclusion criteria (e.g. non-human, unrelated to VTE) were excluded. During the screening stage, abstracts were also examined if the paper could not be excluded based on the title alone. During the eligibility stage, all full-text articles that could not be excluded based on title and abstract were examined.
Studies were selected for inclusion on the basis of pre-determined inclusion and exclusion criteria. The population, interventions and comparators were defined as per the clinical effectiveness review of pharmacological thromboprophylaxis for preventing VTE (see Chapter 3, Inclusion and exclusion criteria). In addition, the study population was restricted to patients treated in the UK NHS because estimates of resource use and costs may not be transferable between different health-care settings. Criteria for the study design and outcomes were specified to identify studies meeting the NICE reference case. 94 In terms of study design, the review was restricted to cost-effectiveness studies, thereby excluding cost-minimisation studies. In terms of outcomes, the review was restricted to studies that measured benefits using QALYs because the QALY has been defined by NICE as the reference case measure for benefit for UK cost-effectiveness studies94 and the NICE methods guide94 provides guidance on the range of cost-per-QALY values that can be considered to represent good value for money within the UK NHS. Studies reporting alternative outcomes, such as cost per VTE avoided, were therefore excluded. Cost-consequence studies and other studies that reported data on costs, resource use or utility values in relevant populations were excluded from the cost-effectiveness review but were examined for relevant data that might inform the modelled estimates of cost-effectiveness (described in Independent economic assessment methods).
Results of cost-effectiveness review
The literature searches identified 1299 citations. Of these, no relevant published cost-effectiveness studies were identified. A flow chart describing the process of identifying relevant literature can be found in Figure 8. A total of three full-text articles were excluded as they did not meet all the prespecified inclusion criteria. 95–97 The articles were excluded for the following reasons: inappropriate study design (not a cost-effectiveness analysis)96 and wrong target population (not isolated lower-limb injury requiring temporary immobilisation). 95,97 A full list of excluded studies with reasons for exclusion is presented in Appendix 10. One study was identified that examined the costs of providing thromboprophylaxis following lower-limb injuries but benefits were not assessed. This study was retained as a potential source of cost inputs for the analysis described in Independent economic assessment methods.
FIGURE 8.
Study flow chart (adapted):37 cost-effectiveness review of pharmacological thromboprophylaxis for preventing VTE in patients having lower-limb immobilisation due to injury. © 2009 Moher et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
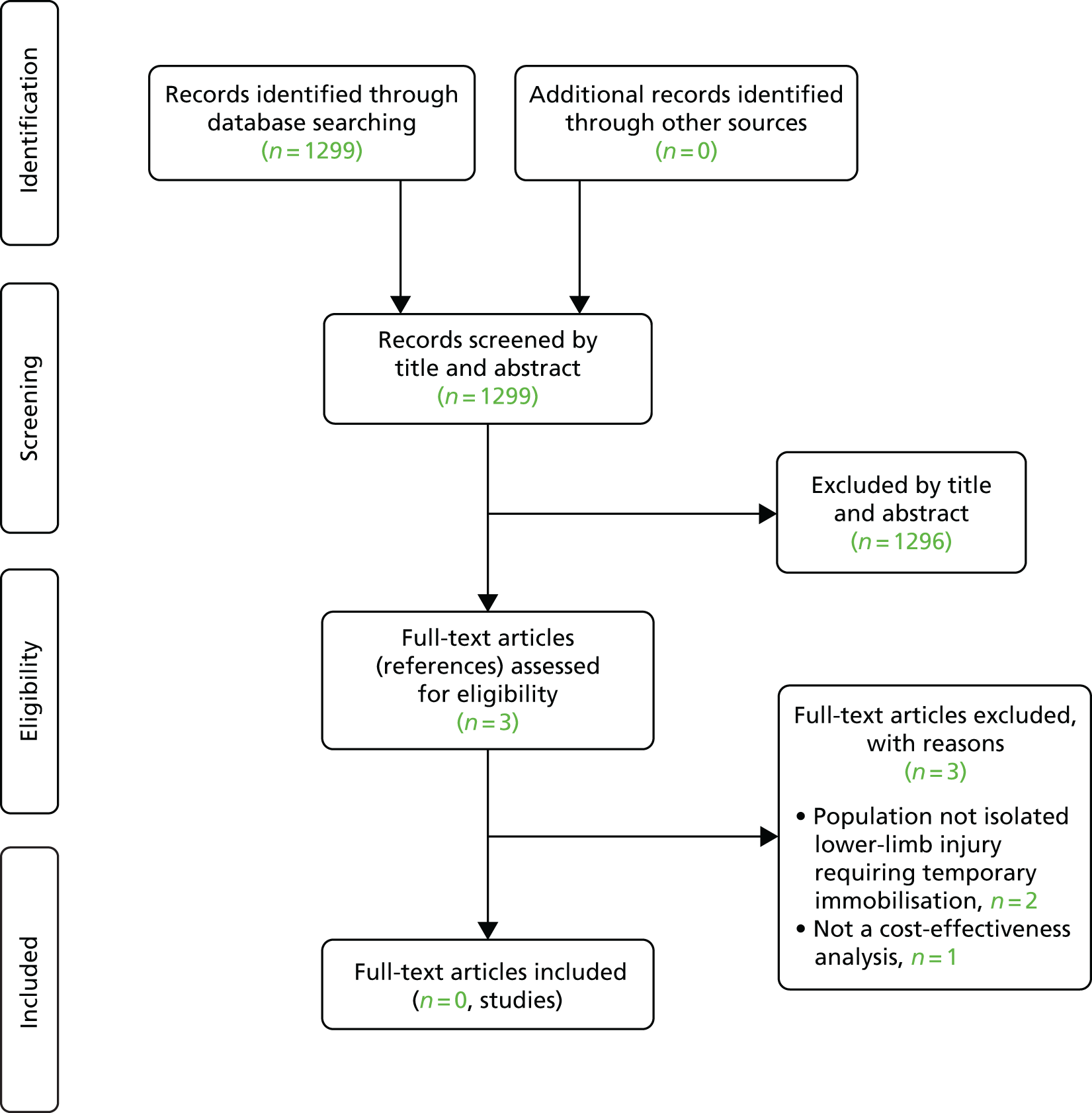
Given the lack of published analyses in directly relevant populations, it was decided to retain papers describing cost-effectiveness analyses in related populations for the purpose of identifying suitable model inputs. Based on clinical advice, only those studies examining the cost-effectiveness of thromboprophylaxis in patients having elective knee surgery were retained, as these patients are more likely to be generally fit and well prior to surgery, do not have long periods of hospitalisation, will have some degree of reduced mobility in the lower limb during their recovery from surgery and the impact of surgery may mimic, to some extent, the trauma of lower-limb injury. Although two papers98,99 were identified that reported the cost-effectiveness for thromboprophylaxis in patients having elective knee surgery, both corresponded to the same study, namely main analysis99 and subgroup analysis98 of patients aged > 75 years or with moderate renal impairment. Given that the parameter sources of interest did not vary between these two citations, only the paper reporting the main analysis was retained. 99 The parameters identified from this paper are described in the next section.
Independent economic assessment methods
Given the lack of published analyses examining the cost-effectiveness of thromboprophylaxis in patients having lower-limb immobilisation due to injury (see Systematic review of existing cost-effectiveness evidence), a de novo economic evaluation was conducted using decision-analytic modelling.
Decision problem
The aim of the decision-analytic model was to estimate the incremental cost-effectiveness of different strategies for thromboprophylaxis in patients with lower-limb injury requiring immobilisation. The thromboprophylaxis strategies examined were based on treating all patients or treating patients in accordance with the application of the RAMs identified in the review of RAMs described in Chapter 3, Review of risk assessment models for predicting venous thromboembolic risk. Based on the estimates of sensitivity and specificity identified in the review, it was decided to examine the L-TRiP(cast) tool, published by Nemeth et al. ,32 using cut-off scores ranging from 6 to 10. The Plymouth tool, published by Keenan et al. ,31 and the GEMNet tool, published by Roberts et al. ,17 were not included in the economic analysis. The only available estimates of the sensitivity and specificity for these RAMs, from an evaluation by Watson et al. ,82 suggested that both of these tools would be outperformed by the L-TRiP(cast) tool. The comparator considered in the economic analysis was no thromboprophylaxis. The base-case economic analysis assumes that prophylaxis consists of LMWH being given for the duration of lower-limb immobilisation (e.g. duration of casting or splinting).
Context
The model estimates lifetime costs and QALYs for the different thromboprophylaxis strategies and the comparator of no thromboprophylaxis under a NHS and Personal Social Services perspective. Future costs and benefits are discounted from their net present value at a rate of 3.5% per annum in accordance with the NICE Guide to the Methods of Technology Appraisal. 94 Costs are reported in Great British pounds, based on 2017 prices. To achieve this, historical prices used as model inputs were inflated using the hospital and community health services pay and prices index. 100
Conceptual model
The clinical events that are expected to be affected by whether or not thromboprophylaxis is given to patients with lower-limb immobilisation due to injury are as follows:
-
bleeding events during the period of prophylaxis, including fatal bleeds, non-fatal intracranial bleeds, other major bleeds and clinically relevant non-major bleeds
-
VTE events, which includes distal and proximal DVT, both of which may be either symptomatic or asymptomatic, and PE, which may be either fatal or non-fatal
-
bleeding events during the treatment of symptomatic VTE with anticoagulants
-
long-term complications of VTE, such as PTS and CTEPH
-
long-term complications of bleeds, such as disability following non-fatal intracranial bleeds.
It should be noted that, within the modelling framework, symptomatic DVTs include any DVTs causing symptoms that result in the patient seeking medical care and any DVTs categorised as asymptomatic would include those with minor symptoms that are not sufficient for the patient to seek medical care. In the context of lower-limb injury and immobilisation, some DVTs may be categorised as asymptomatic in this analysis despite symptoms being present if these symptoms are attributed to the injury and do not prompt the patient to seek medical care.
Model structure
The model structure consists of a decision tree followed by a Markov model. The decision tree captures outcomes related to prophylaxis and VTE events in the first 6 months. The Markov model is used to extrapolate the QALY losses from fatal events and the costs and QALY losses from long-term complications that develop or persist beyond 6 months. The model estimates outcomes for a cohort of identical patients with average characteristics.
The decision tree captures the impact of alternative strategies on thromboprophylaxis rates, the impact of thromboprophylaxis on VTE events (e.g. symptomatic/asymptomatic DVT and PE) and bleeding complications related to either the initial thromboprophylaxis or anticoagulants used in the management of VTE in symptomatic patients. Bleeding complications are split into fatal bleeds, non-fatal intracranial haemorrhage (ICH) and other (i.e. non-fatal non-intracranial) major bleeds. The decision tree captures the first 6 months after lower-limb injury as this is considered a sufficient time frame to capture both 6–8 weeks of thromboprophylaxis during lower-limb immobilisation and 3 months of anticoagulant treatment for any VTEs arising during lower-limb immobilisation. All costs and health effects related to major bleeds that are non-fatal and non-intracranial are assumed to resolve within the 6-month timeframe of the decision tree model. Any chronic complications of VTE are assumed not to be diagnosed until after the completion of VTE treatment as it is difficult to distinguish PTS and CTEPH from acute symptoms during the first 3 months after VTE. Therefore, PTS and CTEPH are assumed not to occur during the decision tree phase of the model. The decision tree structure is shown in Figure 9. The key model assumptions were as follows:
-
Bleeding events during immobilisation are possible in both those having thromboprophylaxis and those having no thromboprophylaxis.
-
Bleeds associated with thromboprophylaxis are assumed to occur before VTE associated with immobilisation and both are assumed to occur within 12 weeks of the start of lower-limb immobilisation.
-
Patients who have major bleeding will stop thromboprophylaxis immediately, but the treatment effect of thromboprophylaxis is assumed to be the same as for those who completed treatment, as patients who bleed are assumed to be adequately anticoagulated.
-
The risk of VTE is the same whether or not prophylaxis caused bleeding.
-
All patients with symptomatic DVT receive accurate diagnosis and initiate treatment with anticoagulants (3 months of either DOACs or phased anticoagulation).
-
Asymptomatic DVTs are not detected and are not treated.
-
All PEs are symptomatic and lead to detection and treatment with anticoagulants in all cases.
-
Patients treated for symptomatic DVT and PE have a bleed risk associated with treatment, which is assumed to occur during the 3-month treatment period (i.e. within 6 months of the start of lower-limb immobilisation).
-
Chronic complications of VTE (e.g. CTEPH following PE and PTS following DVT) are assumed to be diagnosed at least 3 months after VTE and, therefore, occur after any bleeds associated with VTE treatment.
-
Deaths caused by PE occur before any bleeding associated with the treatment of PE.
-
Risk of bleeding during treatment of VTE is independent of whether or not the patient bled during prophylaxis.
-
Risk of VTE, risk of bleeding and risk of PTS/CTEPH are not dependent on patient characteristics.
FIGURE 9.
Decision tree structure.
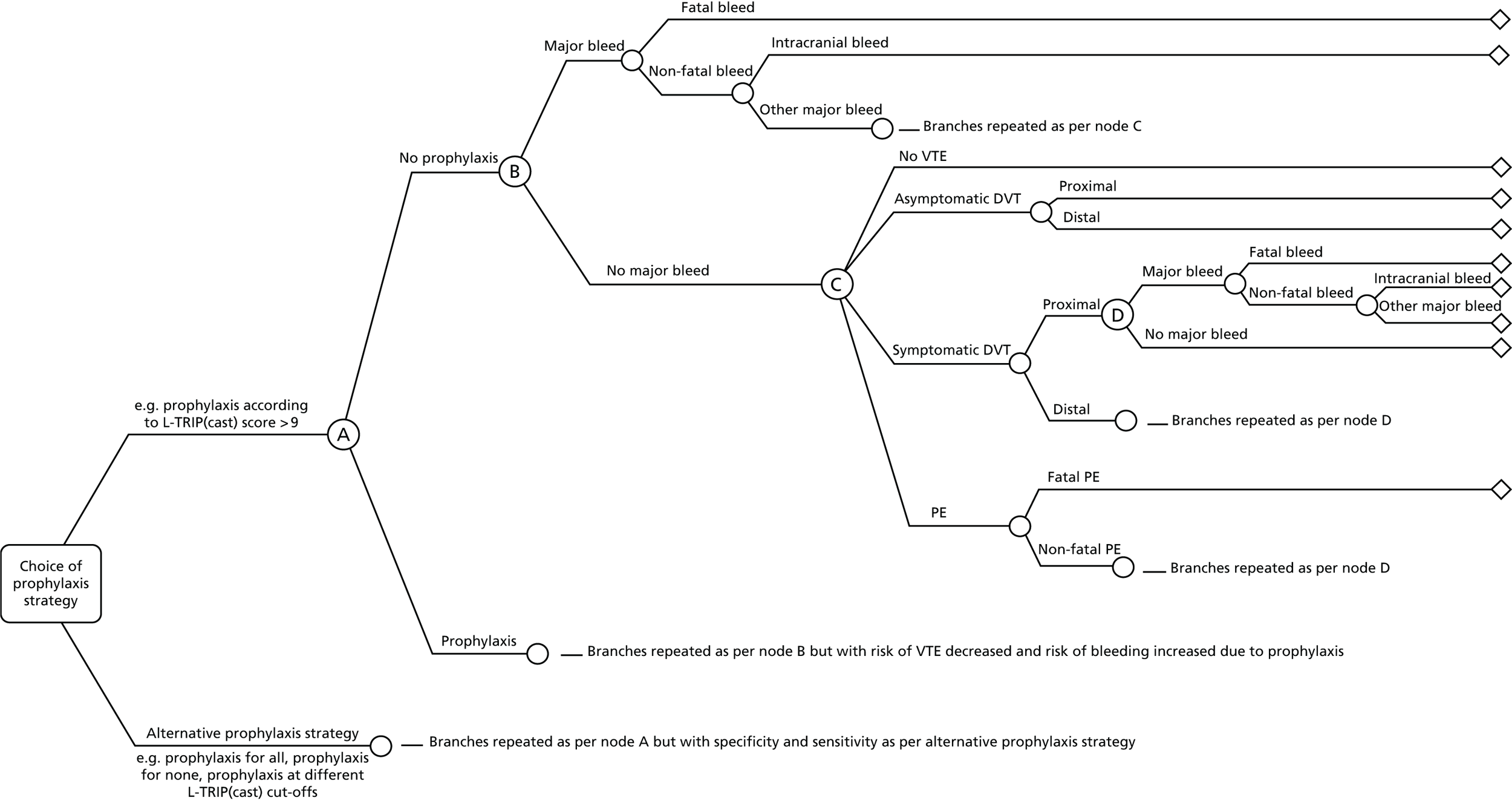
A key structural assumption within the model is the use of a cohort modelling approach that assumes that all patients have identical characteristics based on the average characteristics of those having lower-limb immobilisation due to injury. Depending on the RAMs used, the likelihood of receiving prophylaxis may be dependent on patient characteristics, leading to the treated and untreated populations having different characteristics, which is not captured in a cohort model. Based on clinical advice, it was expected that age would be the only relevant patient characteristic that would predict different outcomes. A scenario analysis was conducted to explore whether or not patient heterogeneity would affect the conclusions by varying the age of the cohort. Based on this, it was concluded that the cohort-level modelling approach was adequate and would not introduce significant bias.
Clinically relevant non-major bleeding (CRNMB), which is any non-major bleeding that results in contact with a health-care professional, was not expected to be a significant driver of cost-effectiveness. It was therefore excluded from the base-case analysis, but the impact of this assumption was explored in a scenario analysis. As CRNMB has no long-term implications, it was not modelled using a separate branch in the decision tree. Instead, it was included in a scenario analysis by applying a simple one-off cost for consultation to a proportion of the population having thromboprophylaxis.
Outcomes related specifically to surgical site wounds, such as wound infection and wound breakdown, were excluded from the model as there is substantial uncertainty as to whether or not thromboprophylaxis influences wound healing. Furthermore, only a small proportion of the lower-limb immobilisation population would have surgical intervention or open fractures. This is supported by data from the largest RCT to date,59 in which only 12% of participants across both arms had surgery and the rate of infections was similar across arms (12/719 for treatment vs. 14/716 for control).
The aim of the Markov model is to capture QALY losses due to fatal PEs or fatal bleeds and the costs and QALY losses associated with chronic complications following VTE events (e.g. PTS or CTEPH) or bleeds (e.g. disability following ICH). At 6 months, patients enter one of eight Markov states: (1) well, (2) dead, (3) post-ICH, (4) asymptomatic proximal DVT, (5) asymptomatic distal DVT, (6) symptomatic proximal DVT, (7) symptomatic distal DVT or (8) PE. The Markov model is then used to estimate the number of patients from the DVT and PE states who develop either PTS or CTEPH, respectively, and the long-term survival in each health state. Separate DVT states were required to capture differences in PTS risk depending on whether the DVT was proximal or distal and whether it was symptomatic and treated or was asymptomatic and, therefore, remained undiagnosed and untreated. The prevalence of PTS and CTEPH is captured by having separate health states for patients with these long-term complications. All patients with PTS are combined in a single health state, as costs, utilities and survival are not expected to be affected by whether or not PTS occurred following proximal or distal DVT. The PTS state is not split into different severity levels as the utility estimates are based on the average across severity levels and the costs are not expected to differ by severity. Separate Markov states were required for medically and surgically managed CTEPH as the type of management affects life expectancy, costs and utilities in patients with CTEPH. The health states are shown in Figure 10.
FIGURE 10.
Markov model structure.
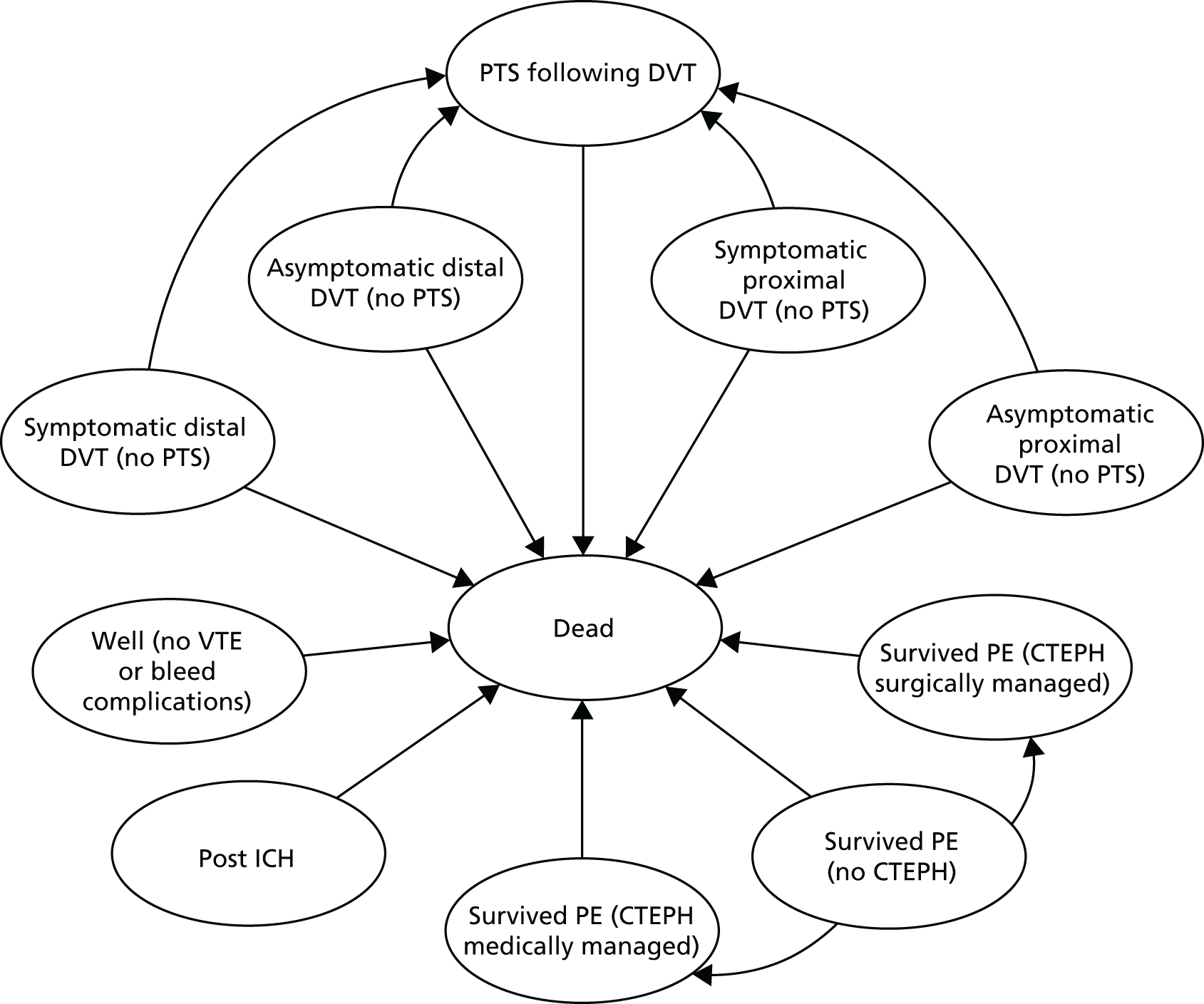
The Markov model has one 6-month cycle, to extrapolate the decision tree outcomes to the end of the first year, followed by annual cycles thereafter. All-cause mortality during the first year is assumed to occur at 6 months (i.e. between the end of the decision tree and the start of the Markov model) and then mid-way through each annual cycle thereafter. The CTEPH and post-ICH health states have state-specific mortality risks, whereas the other states experience general population mortality rates. Average costs and QALYs across each model cycle were calculated by applying a half-cycle correction.
Assumptions related to the Markov phase of the model are as follows:
-
All symptomatic DVTs are associated with a risk of PTS but the rate is allowed to differ depending on whether the DVT is distal or proximal and whether it is symptomatic and treated or asymptomatic and untreated.
-
There is no risk of PTS for PE.
-
CTEPH is possible only after PE.
-
Further outcomes (i.e. VTE, CTEPH and PTS) are not modelled for those who experience ICH, as lifetime cost and QALYs will be determined predominantly by disability related to the ICH.
-
All-cause mortality is applied to all Markov states with state-specific mortality rates possible for patients who have experienced ICH or who have CTEPH that is either medically or surgically managed.
-
Recurrent VTE is not modelled as it is not likely to be related to the initial provoked VTE and, therefore, would occur equally regardless of whether or not thromboprophylaxis was given during immobilisation.
Data sources
Identification of data sources
A summary of the model parameters and data sources used to populate the model are provided in Table 15, with the exception of utility values, which are provided in Treatment-related utility decrement. The number of patients receiving thromboprophylaxis under the various treatment strategies is estimated by combining data on sensitivity and specificity, from the systematic review of RAMs (see Chapter 3, Review of risk assessment models for predicting venous thromboembolic risk), with data on the risk in untreated patients, from the review of RCTs comparing thromboprophylaxis with no thromboprophylaxis (see Chapter 3, Review of pharmacological thromboprophylaxis for preventing venous thromboembolism). Parameters relating to the relative risk (RR) of VTE events in patients receiving thromboprophylaxis compared with those not receiving thromboprophylaxis have been taken from the review of clinical effectiveness of thromboprophylaxis to prevent VTE in lower-limb immobilisation. For all other parameters, data were obtained by reviewing the data sources used in published cost-effectiveness analyses and other published sources. As no relevant models were identified that were specific to the population having lower-limb immobilisation, the search for parameter sources was broadened to models in related populations or indications. This search focused, first, on models used to inform NICE guidance on anticoagulants to prevent and treat VTE as the models used to inform any existing NICE guidance were considered highly likely to contain data relevant to the UK context and the NICE reference case, and have been critically scrutinised by independent academic groups. Second, the additional studies identified in the literature review for the related population of patients having elective knee surgery were used (as discussed in Results of cost-effectiveness review). Finally, ad hoc searches were conducted using the reference lists of recently published reviews to identify any relevant sources not identified during the review of published models and clinical experts were consulted to see if any key data sources known to them had been missed. This included any sources used in relevant models known to the authors. The published cost-effectiveness analyses identified as potential sources of model inputs are summarised in Appendix 11.
| Parameter description | Mean value | 95% CIa | Source | Notes |
|---|---|---|---|---|
| Clinical parameters | ||||
| Sensitivity of decision tools | See Chapter 3, Narrative data synthesis | |||
| L-TRiP(cast) score of | ||||
| ≥ 6 | 98.4% | Assumed fixed | ||
| ≥ 7 | 95.3% | Assumed fixed | ||
| ≥ 8 | 92.6% | Assumed fixed | ||
| ≥ 9 | 80.8% | Assumed fixed | ||
| ≥ 10 | 65.1% | Assumed fixed | ||
| Specificity of decision tools | See Chapter 3, Narrative data synthesis | |||
| L-TRiP(cast) score of | ||||
| ≥ 6 | 14.2% | Assumed fixed | ||
| ≥ 7 | 26.2% | Assumed fixed | ||
| ≥ 8 | 39.7% | Assumed fixed | ||
| ≥ 9 | 60.8% | Assumed fixed | ||
| ≥ 10 | 72.2% | Assumed fixed | ||
| Probabilities of VTE in patients having lower-limb immobilisation without thromboprophylaxis | Systematic review of thromboprophylaxis effectiveness | Average proportion across 12 RCTs (see Table 16) | ||
| PE | 0.4% | 0.2% to 0.7% | ||
| Symptomatic DVT | 0.9% | 0.5% to 1.3% | ||
| Asymptomatic DVT | 7.1% | 6.0% to 8.1% | ||
| Proportion of asymptomatic DVTs that are distal | 83.9% | 73.3% to 92.2% | Systematic review of thromboprophylaxis effectiveness | Average proportion across six RCTs (see Table 16) |
| Proportion of symptomatic DVTs that are distal | 50% | 26.5% to 73.4% | Systematic review of thromboprophylaxis effectiveness | Based on a single RCT that focused exclusively on symptomatic DVTs (see Table 16) |
| Effectiveness of prophylaxis: OR for VTE | 0.52 | 0.37 to 0.71 | Systematic review of decision tools for identifying patients at risk of VTE | OR for LMWH vs. placebo for all VTE based on random-effects Bayesian NMA |
| Risk of major bleed with no prophylaxis | 1.89 per 1000 person-years | 1.86 to 1.92 per 1000 patient years | Hippisley-Cox and Coupland101 | Age-standardised incidence across whole cohort used to derive the QBleed101 risk score:
|
| Bleed risk for prophylaxis vs. no prophylaxis: HR | 1.64 | 0.98 to 2.75 | Pooled analysis of bleed risks across all VTE prophylaxis studies in NICE CG9224 | Data presented in CG92 reanalysed on log-odds scale using random-effects Bayesian meta-analysis |
| Proportion of major bleeds during lower-limb immobilisation that are fatal (with and without prophylaxis) | 21.0% | 17.0% to 25.0% | Average fatality across GI and ICH bleeds with case fatality rates of 10% (95% CI 9.7% to 10.4%) and 49% (95%CI 37% to 60%), respectively | |
| Proportion of non-fatal major bleeds during lower-limb immobilisation that are ICH (with and without prophylaxis) | 19.0% | 15.4% to 22.2% | Fang et al.,102 Button et al.103 and Hippisley-Cox and Coupland101 | Estimated based on incidence and case fatality rates for GI and ICH bleeds |
| Risk of bleeding during 3-month anticoagulant treatment for VTE | 0.9% | 0.2% to 2.0% | Kooiman et al.104 | 6-month incidence pooled across patients with HAS-BLED score of 0 or 1 |
| Proportion of major bleeds during VTE treatment that are fatal | 25.0% | 21.0% to 28.0% | Nieto et al.105 | Based on case fatality rates for major bleeds within RIETE (Nieto et al.)105 |
| Proportion of non-fatal major bleeds during VTE treatment that are ICH | 9.0% | 6.5% to 11.9% | Nieto et al.105 | Based on proportion of major non-fatal bleeds within RIETE that were ICH (Nieto et al.)105 |
| All-cause (non-VTE-related) mortality | Varies by age | N/A | ONS lifetables106 | Risk applied each year is based on current age and is not adjusted to account for contribution of VTE to population mortality |
| SMR for patients surviving ICH, compared with general population | Ranges for SMRs not stated so ± 20% on the logged scale is assumed | Fogelholm et al.107 | Assumed no increased mortality risk after 6 years | |
| Year 1 after ICH | 4.5 | |||
| Years 2 to 6 after ICH | 2.2 | |||
| Probability of PE being fatal | 2.9% | 2.5% to 3.3% | Maestre et al.108 |
|
| Cumulative risk of PTS for treated symptomatic DVT at 3 years | Hach-Wunderle et al.109 (TULIPA PLUS registry) | Cumulative incidence at 3 years based on the TULIPA PLUS registry. Distribution of risk across years 1 to 3 based on van Dongen et al.110 Zero risk assumed from year 4 onwards | ||
| Proximal | 32.4% | 22.1% to 43.6% | ||
| Distal | 15.6% | 7.9% to 25.3% | ||
| Cumulative risk of PTS for untreated asymptomatic DVT at 3 years | Hach-Wunderle et al.109 and van Dongen et al.110 |
|
||
| Proximal | 56.5% | 29.0% to 79.8% | ||
| Distal | 15.6% | Fixed relative to symptomatic | ||
| Risk of CTEPH per annum applied in the first 2 years after PE | 1.6% | 1.0% to 2.2% | Ende-Verhaar et al.111 |
|
| Proportion of CTEPH treated surgically | 59.5% | 55.8% to 63.2% | Delcroix et al.113 | |
| Mortality for CTEPH | ||||
| Medically treated | Exponential survival curve with mean hazard of 0.1168 | SE of mean hazard 0.0123 | Original data from Delcroix et al.113 but curves taken from Goodacre et al.114 |
|
| Surgically treated | Log-normal survival curve with mean 5.081 and SD of 3.343 |
|
Original data from Delcroix et al.113 but curves taken from Goodacre et al.114 |
|
| Cost parameters | ||||
| Application of RAM to patient | £8.83 | Fixed | Curtis and Burns100 | Cost for 5 minutes of hospital consultant time |
| Prophylaxis: 6 weeks of LMWH (dalteparin), including costs of initiating treatment and district nurse administration for 4% of patients | £224.64 | £197 to £267 | ||
| Treatment of symptomatic proximal DVT | £687.69 | £660 to £715 |
NHS reference costs116 Drug Tariff21 |
Clinical expert discussion regarding the likelihood of resource use, combined with NHS reference cost data116 for health-care contacts and Drug Tariff21 costs for treatments (see Table 19 for a more detailed costing breakdown) |
| Treatment of symptomatic distal DVT | £559.62 | £536 to £584 |
NHS reference costs116 Drug Tariff21 |
Clinical expert discussion regarding the likelihood of resource use, combined with NHS reference cost data116 for health-care contacts and Drug Tariff21 costs for treatments (see Table 19 for more detailed costing breakdown) |
| Treatment of non-fatal PE | £1788.44 | £1995 to £2168 |
NHS reference costs116 Drug Tariff21 |
Clinical expert discussion regarding the likelihood of resource use, combined with NHS reference cost data116 for health-care contacts and Drug Tariff21 costs for treatments (see Table 19 for more detailed costing breakdown) |
| Fatal PE | £1498.14 | £1430 to £1571 | NHS reference costs116 | As per non-fatal bleed, minus drug therapy for PE |
| Fatal bleed | £1802.48 | £322 to £3283 | Luengo-Fernandez et al.117 |
|
| Non-fatal, non-ICH bleed | £1197.88 | £1118 to £1288 | NHS reference costs 2015/16116 | Weighted average of reference costs for GI bleed (HRG codes FZ38G – FZ38P) |
| Post non-fatal ICH: first 90 days | £21,255.00 | £16,814 to £26,217 | Luengo-Fernandez et al.117 |
Weighted average of costs for non-fatal haemorrhagic strokes Uplifted to current prices using inflation indices100 |
| Post non-fatal ICH: post acute (beyond 90 days) costs per annum | £8013.00 | £5300 to £11,271 | Luengo-Fernandez et al.117 |
|
| PTS cost per annum: year 1 (mild/moderate/severe) | £308 in year 1 | £294 to £323 | NHS reference costs 2015/16116 |
One first and one follow-up vascular surgery outpatient appointment Weighted average of consultant-led and non-consultant-led outpatient appointments for non-admitted face-to-face first attendance (WF01B) and follow-up (WF01A) for vascular surgery (service code 107) |
| PTS cost per annum: year 2 (mild/moderate/severe) | £74 in each subsequent year | Fixed | Curtis and Burns100 | Two GP surgery consultations with qualification costs including direct-care staff costs at £37 per appointment |
| CTEPH cost per annum | ||||
| Medically managed | £17,942 each year | Fixed | NICE CG9224 | |
| Surgically managed | £9890 in year 1 and zero in year 2 onwards | £9471 to £10,370 | NHS reference costs 2015/16116 |
|
Characteristics of population having lower-limb immobilisation
The Prevention of Thrombosis after Lower Leg Plaster Cast (POT-CAST) trial by van Adrichem et al. 59 was selected as being representative of the population having lower-limb immobilisation due to injury who are at risk of thrombosis. This was selected as it is a recent, large RCT conducted exclusively in Europe (the Netherlands) and the inclusion and exclusion criteria were not too restrictive; patients with a prior history of VTE were excluded but those with cancer or family history of DVT were not excluded. The starting age in the model was set to be 46 years of age and 51.5% of the starting population were male.
Risk of venous thromboembolism and types of venous thromboembolism
The risk of VTE was based on data taken from the systematic review of clinical effectiveness for LMWH versus control (see Chapter 3, Review of pharmacological thromboprophylaxis for preventing venous thromboembolism). The rate of any form of VTE (i.e. PE, symptomatic DVT or asymptomatic DVT) was 8.39% across the 12 studies23,49–56,58–60 reporting data for control (i.e. placebo, aspirin, no thromboprophylaxis). The risk of PE, including those that experienced PE with DVT, was 0.43%. Therefore, the risk of DVT without PE was 7.96%. Only nine studies23,49–52,54,56,58,60 reported outcomes for both symptomatic and asymptomatic DVT. From these studies, it was estimated that 11.4% of DVT are symptomatic (16/140), giving an absolute incidence of 0.91% for symptomatic DVT and 7.05% for asymptomatic DVT in patients having lower-limb immobilisation without thromboprophylaxis. These are slightly higher than the raw figures (Table 16) as three studies53,55,59 did not report outcome data for both symptomatic and asymptomatic DVT but did report data for all VTE and PE. These estimates effectively assume the same split of symptomatic and asymptomatic DVT for the three studies with missing data to achieve the total VTE rate observed across all 12 studies. For asymptomatic DVT, only six studies23,50–52,58,60 reported outcomes for both distal and proximal asymptomatic DVT. From these six studies, it was estimated that 16% (9/56) of asymptomatic DVTs are proximal (and, therefore, 84% are distal). The data on the location of symptomatic DVTs (distal or proximal) were very sparse, with only 46 events reported across all trial arms and many studies not reporting the location. It was possible to extract data on the location of symptomatic DVTs for four studies54,57–59 included in the review, covering a total of 34 events across all trials arms. The proportion of symptomatic DVTs that were proximal varied from 14% to 100% across these four studies, with a median estimate of 36%. The POT-CAST trial59 was the only one of these four studies that focused exclusively on symptomatic VTE. The other three studies54,57,58 screened patients for asymptomatic DVTs as well as recording the number of DVTs that were symptomatic. There is a risk that the process of screening patients for asymptomatic DVTs may lead to patients attributing symptoms to screening-detected DVTs that may otherwise not have been sufficiently symptomatic to result in the patient presenting with symptoms in routine care. For this reason, it was decided to use the POT-CAST trial59 as the single source of estimates for the proportion of symptomatic DVTs that are proximal, as no routine screening was used in this trial to detect asymptomatic DVTs. As this single study provided a low number of events, it was decided to pool the data across trial arms. This resulted in 50% of the 16 symptomatic DVTs being proximal. Given that these data were based on a single study and a small number of events, two extreme scenarios were examined, assuming that either 0% or 100% of symptomatic DVTs are proximal, to see if the overall conclusions were sensitive to uncertainty around this parameter.
| Event type | n with event | N at risk | Rate based on studies (%) | Number of studies | Data applied in model (%) |
|---|---|---|---|---|---|
| Any VTE | 196 | 2336 | 8.39 | 1223,49–56,58–60 | 8.39 |
| PE risk | 10 | 2336 | 0.43 | 1223,49–56,58–60 | 0.43 |
| DVT without PEa | 186 | 2336 | 7.96 | 1223,49–56,58–60 | |
| Asymptomatic DVT | 124 | 1466 | 8.58 | 923,49–52,54,56,58,60 | 7.05b |
| Symptomatic DVT | 16 | 1466 | 1.11 | 923,49–52,54,56,58,60 | 0.91b |
| Asymptomatic proximal DVT | 9 | 1055 | 0.85 | 623,50–52,58,60 | 1.13c |
| Asymptomatic distal DVT | 47 | 1055 | 4.45 | 623,50–52,58,60 | 5.59c |
| Symptomatic proximal DVT | 8 | 1435 | 0.56 | 159 | 0.45d |
| Symptomatic distal DVT | 8 | 1435 | 0.56 | 159 | 0.45d |
All-cause mortality
It was not considered necessary to model males and females separately as the risks of VTE during lower-limb immobilisation were not expected to vary according to sex. However, life-expectancy is dependent on sex and, consequently, any QALY gains from deaths prevented would be dependent on sex. For this reason, a weighted mortality risk was applied, based on the proportion of males (51.5%) in the POT-CAST trial,59 using data on the risk of death for males and females by age obtained from lifetables. The weighting across males and females was allowed to vary over the course of the model to allow for the fact that lower mortality risks in females leads to a slight increase in the proportion of people alive who are female over time.
Case fatality rate for pulmonary embolism
None of the studies included in the review of clinical effectiveness reported any fatal PEs. Given that 14 PEs were reported within the 13 studies23,49–60 included in the review, this suggests that the rate of fatality due to PE is < 7% in the population having lower-limb immobilisation due to injury. The research team looked for alternative data sources on the case fatality rate of PE. Data were identified from the Computerized Registry of Patients with Venous Thromboembolism (RIETE) (an extensive data registry of consecutive patients with VTE), which found that the rate of all-cause mortality at 30 days had fallen over time from 6.6% in 2001–05 to 4.9% in 2010–13 (reported by Jiménez et al. 118). However, some of this mortality may not be related to PE. When looking at only PE-related mortality, the rate at 30 days was 1.8%. Another analysis of RIETE, by Maestre et al. ,108 found that rates of fatal PE at 90 days were lower for outpatients than inpatients. They found that of 7591 outpatients with clinically overt PE, 219 (2.9%) had fatal PE at 90 days; this was lower than the 4.1% (119/2870) rate with clinically overt PE having a fatal PE in the inpatient population. Given that patients having lower-limb immobilisation due to injury would generally be managed as outpatients, this suggests that a lower risk may be seen in this population.
The Emergency Medicine Pulmonary Embolism in the Real World Registry (EMPEROR) cohort study (reported by Pollack et al. 119), which recruited patients with PE from EDs in the USA, reported a 30-day all-cause mortality rate of 5.4% for patients with confirmed PE, but the rate of mortality was only 1.1% when restricted to PE-related in-hospital mortality. These data seem reasonably consistent with the 30-day data from RIETE.
It was decided to apply the case fatality rate for outpatients from the RIETE study (2.9%) in the model, as patients having lower-limb immobilisation would be managed as outpatients and there was a slight increase from 30 days to 90 days, which is captured in the analysis by Maestre et al. 108 but not in the other two analyses, which were limited to 30 days.
Combining the incidence and case fatality rate for PE, it is estimated that one fatal PE per 8097 patients having lower-limb immobilisation without thromboprophylaxis would be expected, which is consistent with there being no fatal PEs observed in the studies included in the systematic review for treatment effectiveness.
Effectiveness of thromboprophylaxis on prevention of venous thromboembolism during lower-limb immobilisation
We applied the OR for LMWH versus control for the outcome of any VTE estimated from the NMA to all forms of VTE within the model. Although the NMA provides estimates of clinical effect that are specific to different types of VTE (i.e. symptomatic DVT, asymptomatic DVT and PE) the estimates for these specific VTE types are more uncertain as they are based on fewer events. The pooled effect for the OR (0.52, 95% CrI 0.37 to 0.71) was converted to a RR and applied to the baseline risk within the model.
For the sensitivity analyses examining thromboprophylaxis using alternative drug classes, it was assumed that DOACs would have the same effectiveness as LMWH, as no studies examining the effectiveness of DOACs in this population were included in the systematic review. For the analysis assuming that fondaparinux is used, the OR for fondaparinux versus control from the NMA was applied (0.13, 95% CrI 0.05 to 0.30). In both cases, the same adverse effects profile for LMWH, DOACs and fondaparinux were implicitly assumed, as the only adverse event included in the model was bleeding and it was assumed that all prophylaxis had the same impact on bleeding rates.
Risk of bleeding during lower-limb immobilisation
There is a risk of major bleeding within the general population regardless of whether or not they receive treatment with anticoagulants. A cohort study (reported by Hippisley-Cox and Coupland101), conducted in a large primary care population using data from 4.4 million patients with 16.4 million person-years of follow-up, estimated an age-standardised incidence rate of 1.34 (95% CI 1.32 to 1.36) per 1000 person-years for upper GI bleeding and 0.55 (95% CI 0.54 to 0.56) per 1000 person-years for intracranial bleeds for patients not taking anticoagulants. Given that the study cohort was patients aged 21–99 years registered with a general practice and that the only relevant exclusion criteria appears to be existing anticoagulated patients, this study was considered to be reflective of the risk of GI bleeds and ICH in the general population at risk of lower-limb injury who are not currently taking anticoagulants. The baseline characteristics of patients not taking anticoagulants in the study by Hippisley-Cox and Coupland101 were compared with the characteristics of those in the comparator arm of the POT-CAST trial59 (Table 17). Although Hippisley-Cox and Coupland101 did not present a mean age, a weighted mean age was calculated using the distribution across age bands and the mid-point ages for each band: this was found to be 40 years (with a range of 36–45 years when using the lower and upper limits of the age bands), which is lower than the mean age of 46 years from the POT-CAST trial. 59 The proportion of non-smokers was slightly lower in the POT-CAST trial and the proportion of patients with previous cancer was slightly higher.
| Characteristic | QBleed (no anticoagulation)101 | POT-CAST59 |
|---|---|---|
| Male (%) | 48.9 | 51.5 |
| Age (years), mean (SD) | NRa | 46 (16) |
| Age group (years) (%) | ||
| 21–24 | 54.6 | NR |
| 45–64 | 29.0 | NR |
| 65–74 | 8.5 | NR |
| 75–84 | 5.4 | NR |
| ≥ 85 | 2.5 | NR |
| BMI (kg/m2), mean (SD) | 26 (4.8) | 26 (4.4) |
| Smoking status (%) | ||
| Non-smoker | 55.9 | 46.5 |
| Former smoker | 18.7 | 26.8 |
| Current smoker | 21.7 | 26.8 |
| Previous cancer (%) | 2.7 | 4.3 |
To see if the rates of major bleeding in the RCTs included in the clinical effectiveness review were similar, data on the rates of major bleeding (see Appendix 3) were combined with data on the number of person-years people were at risk of bleeding within each study. It was assumed that the period at risk was the period of cast immobilisation, unless the study explicitly reported a longer duration of follow-up. The number of person-years at risk could be estimated for only 11 of the 13 studies. 23,49–56,59,60 One study used an active control group,57 whereas another did not explicitly report the duration of follow-up. 23 There was only one episode of major bleeding across 447 person-years, giving an incidence of major bleeding of two per 1000 person-years. This appears to be relatively consistent with the estimates for ICH and GI bleeds combined from the cohort reported by Hippisley-Cox and Coupland. 101 Therefore, it was decided to use the age-standardised estimates from the cohort reported by Hippisley-Cox and Coupland101 within the model.
Thromboprophylaxis would be expected to increase the risk of a major bleed but the very small number of major bleeding events in the systematic review meant that the estimate of the risk of major bleeding due to thromboprophylaxis in people with lower-limb immobilisation was very uncertain (OR 1.45, 95% CrI 0.08 to 32.17). Although the baseline risk of bleeding will vary between patient groups, there is no strong reason to believe that the relative effect of thromboprophylaxis will vary. Therefore, data from the NICE clinical guideline (CG) on reducing the risk of VTE (NICE CG92)24 was used, which pooled all indications into a single meta-analysis. 24 These data were reanalysed to use a random-effects approach. In this meta-analysis, the median OR was found to be 1.643 (95% CrI 0.90 to 2.53). The OR was converted to a RR and applied to the baseline risk within the model.
The significance of major bleeding depends primarily on whether or not it is fatal; for non-fatal bleeds, the significance depends on whether or not it is intracranial, as ICH has the potential to result in long-term disability. Fang et al. 102 examined death and disability following bleeds associated with warfarin (Coumadin®, Bristol-Myers Squibb Company, New York City, NY, USA). These data were used to estimate the proportion of major bleeding episodes that were fatal. Fang et al. 102 found that 48.6% of patients having ICH died within 30 days, whereas only 5.1% of patients having non-intracranial bleeds died within 30 days. 102 Although it is acknowledged that bleeds associated with warfarin use may be more likely to result in fatalities than bleeds in patients not having anticoagulation,120 it seemed reasonable to apply the case fatality rates from bleeds associated with warfarin use in the model as these would be directly applicable to the additional cases of bleeding associated with thromboprophylaxis. Any overestimation of mortality in those having bleeds not related to anticoagulant use would be similar across arms and, therefore, would affect estimates of absolute QALYs for each thromboprophylaxis strategy but not the incremental QALY gains when comparing thromboprophylaxis strategies.
The case fatality rate for non-intracranial bleeds reported by Fang et al. 102 was lower than the case fatality rates observed for GI bleeds by Rockall et al. 121 and Button et al. ,103 but this may be because GI bleeds have a greater mortality risk than other non-ICHs. Although Button et al. 103 found that the case fatality rate had fallen over time, the case fatality rate of 10% estimated by Button et al. 103 appears to be consistent with a 2015 report122 from the National Confidential Enquiry into Patient Outcome and Death, based on data collected in 2013. As the data from QBleed101 related only to the incidence of ICH and GI bleeds, the 10% risk of mortality from Button et al. 103 was used instead of the 5% for extracranial bleeds from Fang et al. 102
In addition to the risk of ICH being fatal at the time of the bleed itself, there is an increased risk of death in patients having ICH compared with population norms. Fogelholm et al. 107 found that patients with primary ICH who survived to 28 days had a standardised mortality rate that was 4.5-fold higher in the first year and 2.2-fold higher in years 2–6 than that of age- and sex-matched controls. These figures were applied as RRs to the all-cause mortality rates to increase the risk of mortality in those patients who survived ICH. Although Fogelholm et al. 107 reported a 10% reduction in mortality compared with general population norms in years 7–16, no increased or decreased risk beyond 6 years was assumed as there was doubt over the clinical plausibility of a reduced risk of death following ICH.
Risk of bleeding during anticoagulation treatment of venous thromboembolism
Several sources of data on bleeding risks during treatment of VTE were identified. These included the RIETE105 and Prevention of thromboembolic events – European registry in venous thromboembolism (PREFER-VTE)123 studies and a systematic review of RCTs and cohort studies by Carrier et al. 124 In the review by Carrier et al. ,124 56 of the 69 studies included were RCTs, which the authors say are not generalisable to all patients with VTE because those with additional comorbid conditions are often excluded from clinical trials. Carrier et al. 124 reported a rate of major bleeding for any VTE of 1.6% (95% CI 1.3% to 2.0%) at 3 months and a rate of fatal bleeding of 0.2% (95% CI 0.1% to 0.3%). The case fatality rate for bleeding following any VTE was 11.3%. RIETE reports a rate of major bleeding of 2.24% (95% CI 2.05% to 2.42%) at 3 months and a rate of fatal major bleeding of 0.55% (95% CI 0.46% to 0.65%) giving a case fatality rate equivalent to 24.7%. 105 This higher case fatality rate may be because of a higher rate of comorbidities in an unselected cohort. In the PREFER-VTE cohort, the rate of major bleeds was 1.5% at 12 months but the rate of fatal bleeds was not reported. 123 In addition, the timing of the bleeds was not reported so it is unclear what the rate of bleeding would have been during the treatment period. The data from PREFER-VTE were considered to be more applicable to current UK practice than the data from RIETE as PREFER-VTE included only European sites, included UK patients and recruited patients after the introduction of DOACs. However, it was noted that only 56.7% of patients in the PREFER-VTE cohort had a low risk of bleeding at baseline [a HAS-BLED (Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile international normalised ratio, Elderly, Drugs/alcohol concomitantly) score of 0 or 1]. 123 As thromboprophylaxis for lower-limb injury is likely to be limited to those with a low risk of bleeding, the research team looked for alternative data sources. A study by Kooiman et al. 104 estimated the incidence of major bleeding at 6 months for patients having treatment for VTE stratified by HAS-BLED score. The combined incidence for patients with a HAS-BLED score of 0 or 1 was 0.9% (3/335). Kooiman et al. 104 did not report risks separately for PE and DVT but Cohen et al. 123 reported that, in PREFER-VTE, the rates of major bleeds were not significantly different after PE and DVT, so the same rate of 0.9% has been applied to both DVT and PE. This seems reasonable given that the same treatment is assumed in both groups.
Owing to the greater detail reported by RIETE, the breakdown of major bleeding events into fatal events, non-fatal ICH and other non-fatal major bleeds was based on the event rates from RIETE. 105 The analysis of RIETE also found that symptomatic PE was not a significant predictor of whether a fatal bleed occurred and the site of DVT was not a significant predictor unless the DVT was distal when the OR was 0.39 (95% CI 0.16 to 0.95). This lower rate may be as a result of less aggressive anticoagulation therapy or another confounding factor not accounted for in the analysis. It was decided to apply the same rates of fatal bleeding in all patients treated for VTE regardless of the VTE event type.
Clinically relevant non-major bleeding during prophylaxis
Clinically relevant non-major bleeding was not included in the base-case analysis as it has a low impact on quality of life and would be likely to incur a relatively small cost compared with major bleeding. However, to test whether or not the model was sensitive to this structural assumption, the cost of one ED attendance was applied to those experiencing CRNMB. To estimate the rate of CRNMB, the ratio of CRNMB to major bleeding (2.05) from Cohen et al. 123 (PREFER-VTE) was applied to the rate of major bleeding for those having prophylaxis to estimate the proportion of patients having CRNMB during prophylaxis. Owing to the low rate of bleeding during prophylaxis, the cost of CRNMB was only £0.19 for each patient receiving prophylaxis. Therefore, the exclusion of this cost from the base-case analysis is not expected to have significantly biased the base-case results.
Risk of chronic thromboembolic pulmonary hypertension
The incidence of CTEPH following PE was based on a systematic review by Ende-Verhaar et al. ,111 which reported an overall incidence of CTEPH of 2.3% (95% CI 1.5% to 3.1%). The review111 also reported the incidence separately for all patients with PE (0.56%, 95% CI 0.13% to 0.98%) and for those who survived the initial 3- to 6-month treatment period for PE (3.2%, 95% CI 2.0% to 4.4%). The follow-up period in the studies included in the review varied from 3 months to 8 years, with most reporting follow-up of ≈2 years. One study, by Pengo et al. ,112 which followed patients prospectively for 10 years, found that no cases occurred beyond 2 years, despite a median follow-up of 94 months. It is therefore assumed in the model that all cases are diagnosed between 6 months and 2 years after PE. The rate of CTEPH for those surviving the initial 3- to 6-month treatment period (3.2%) was considered to be the most relevant estimate for the model as no diagnoses of CTEPH are assumed until patients complete their anticoagulant treatment, and deaths during VTE and during anticoagulation are already accounted for in the decision tree part of the model.
Mortality risks in patients with CTEPH were based on data from an international prospective registry reported by Delcroix et al. 113 A recent HTA report by Goodacre et al. 114 used data from this registry to estimate survival curves for patients having medical or surgical management of CTEPH. The same survival curves were used in this model to estimate the hazard of death over time for patients diagnosed with CTEPH. The proportion having surgical management in the registry was 60% and this was applied in the model. Given that deaths related to PE occurring within 6 months of PE are already accounted for in the model, all-cause mortality has been applied to those with PE in the first year regardless of whether or not CTEPH occurs and the rate of mortality for those with CTEPH is applied from year 2 onwards. To ensure that the risk of death in the CTEPH group was not artificially low compared with the risk of death in the general population, general population mortality risks were applied whenever these were higher than the risk in the CTEPH population, based on the survival curves.
Risk of post-thrombotic syndromes
A review of epidemiological studies by Galanaud et al. 125 describes how the incidence of PTS is dependent on the scoring system used to diagnose PTS, the location and extent of the DVT (e.g. proximal vs. distal), and the duration of time since DVT. Galanaud et al. 125 also discuss how pre-existing chronic venous insufficiency and the symptomatic versus asymptomatic nature of the DVT may also affect the risk of PTS.
The risk of PTS in patients with symptomatic DVT in the model was estimated from a prospective registry [Thrombosis and Pulmonary Embolism in Out-Patients – plus (TULIPA-PLUS)], reported by Hach-Wunderle et al. 109 This source was chosen as the study design excluded patients with previous DVT or signs of PTS prior to the index DVT. The incidence is reported separately for proximal and distal DVT and is stratified into mild, moderate and severe PTS using a validated scoring system (Villalta scale), which is the scale preferred by the International Society on Thrombosis and Haemostasis. 126 The prevalence of symptomatic PTS at 3 years was 24.4% for all DVTs, 32.4% for proximal DVT and 15.6% for distal DVT, with 70% being mild, 24% being moderate and 6% being severe (average across both proximal and distal). 109
One applicability issue related to this study was that patients received anticoagulation for a whole year, which is longer than the period of anticoagulation assumed in the model. Therefore, the rates of PTS may be underestimated if longer anticoagulation is protective of PTS. However, as it was not known if longer anticoagulation was protective, and the risk of PTS in this study may reasonably be lower than other estimates as a result of careful exclusion of PTS symptoms at the time of the index DVT, it was decided that it was reasonable to apply the incidence from Hach-Wunderle et al. 109 in the model given that the incidence was in the range generally reported (20–50%). 125
There are only limited data on the incidence of PTS in patients with asymptomatic DVT because these patients are less likely to be followed up for a PTS diagnosis as their DVT is less likely to be diagnosed outside a research setting. However, a study by Persson et al. 127 examining PTS incidence in 83 patients operated on for Achilles tendon rupture, which prospectively identified DVT using colour duplex scanning 3 and 6 weeks after surgery and assessed PTS (assessors were blinded to DVT diagnosis) 5 years post operatively, reported a low rate of a PTS diagnosis (Villalta score of ≥ 5) of 8% (3/38) in the DVT group and 4% (2/45) in the no-DVT group. All of the diagnosed cases had a Villalta score of < 15 and were therefore of mild to moderate severity. However, it should be noted that most of those patients with asymptomatic DVT diagnosed post operatively received warfarin for 3 months and were advised to wear compression stockings for 1 year. As a result, the rate of PTS in asymptomatic, undiagnosed and, therefore, untreated DVT is unknown but is likely to be at least 8%. Furthermore, only three of the 38 DVTs were proximal, making it difficult to estimate the rate of PTS in patients with asymptomatic proximal DVTs from this study. 127
A study by Schindler and Dalziel128 in a related population (those having total hip or knee arthroplasty) found that four of 34 (11%) with asymptomatic distal DVT and three of eight (32.5%) with asymptomatic proximal DVT developed PTS 15 to 24 months after surgery. In the knee arthroplasty subgroup (which is considered to be more clinically relevant to those having lower-limb immobilisation), 28 patients had distal DVT with one of these having clot propagation leading to proximal DVT. Four of these 28 patients (14.3%) with DVT developed PTS, with one of these being the patient who had clot propagation. However, PTS was also diagnosed in 5.3% of those patients without DVT. In this study,128 all those with proximal DVT were treated with anticoagulants (i.e. 3 months of warfarin), whereas those with distal DVT received 3 months of aspirin. Therefore, the rate of PTS in untreated asymptomatic DVT following hip and knee surgery remains unknown.
van Dongen et al. 110 studied the relationship between inadequate anticoagulation with vitamin K antagonist (VKA) and the risk of PTS with symptomatic proximal DVT and found that patients who spend > 50% of their time beneath the international normalised ratio (INR) level of 2.0 are at a higher risk for PTS (OR 2.71, 95% CI 1.44 to 5.10). Based on this, one would expect a higher risk of PTS in patients with asymptomatic proximal DVT that is untreated than in those with treated asymptomatic proximal DVT. Although van Dongen et al. 110 did not include untreated patients in their study, they reported a fourfold increase (OR 3.69, 95% CI 1.29 to 10.53) for those patients spending > 90% of their time outside the target INR range, which suggests that the risks may be higher still in those patients not offered any anticoagulation.
The rate of PTS in patients with asymptomatic proximal DVTs reported by Schindler et al. 128 (32.5%) was similar to that reported in symptomatic proximal DVT by Hach-Wunderle et al. 109 (32.4%). This suggests that the risk of PTS is similar regardless of whether or not the proximal DVT is symptomatic, provided that it is treated with anticoagulants. However, given that patients who are asymptomatic in the model will not receive any anticoagulant treatment as they are not being proactively screened for asymptomatic DVT, a higher rate for asymptomatic proximal DVT was applied using the OR reported by van Dongen et al. 110 for good versus poor anticoagulation (OR 2.71 for those patients spending > 50% of their time outside the target INR). This gave a rate of PTS of 56.5% for untreated asymptomatic proximal DVT. It is recognised that the rate of PTS may be higher still for those receiving no anticoagulation at all, as discussed in the previous paragraph, but this may be partially offset by asymptomatic DVTs being less extensive and, therefore, less likely to cause PTS.
The rate of PTS in asymptomatic untreated distal DVT was set as equal to that for treated symptomatic distal DVT, namely 15.6% as reported by Hach-Wunderle et al. 109 Inflating this risk further by applying the OR from van Dongen et al. 110 did not seem appropriate, given that this would give a risk of 33.4% and the clinical experts believed that the rate for untreated distal DVT should be lower than for treated proximal DVT. Furthermore, it is noted that the rate from Hach-Wunderle et al. 109 of 15.6% is nearly twice the rate reported for treated asymptomatic distal DVT by Persson et al. ,127 which would support not inflating the rate further.
The timing of PTS within the model has been based on data reported by van Dongen et al. ,110 who reported the incidence of PTS at 0.5, 1, 2 and 4 years (Figure 11). The shape of the curve for incidence over time was compared with that reported by Prandoni et al. 129 and was found to be similar, although the magnitude better matched the upper 95% CI of the estimates of incidence reported by Prandoni et al. 129 The hazards based on the incidence reported by van Dongen et al. 110 were scaled to match the rate reported at 3 years by Hach-Wunderle et al. 109 for symptomatic proximal and distal DVT. As van Dongen et al. 110 reported no further incidence beyond 4 years, no new incidence of PTS from 4 years was assumed. The prevalence of PTS over time incorporated within the model is shown in Figure 12.
FIGURE 11.
Prevalence of PTS in years following proximal DVT from studies.
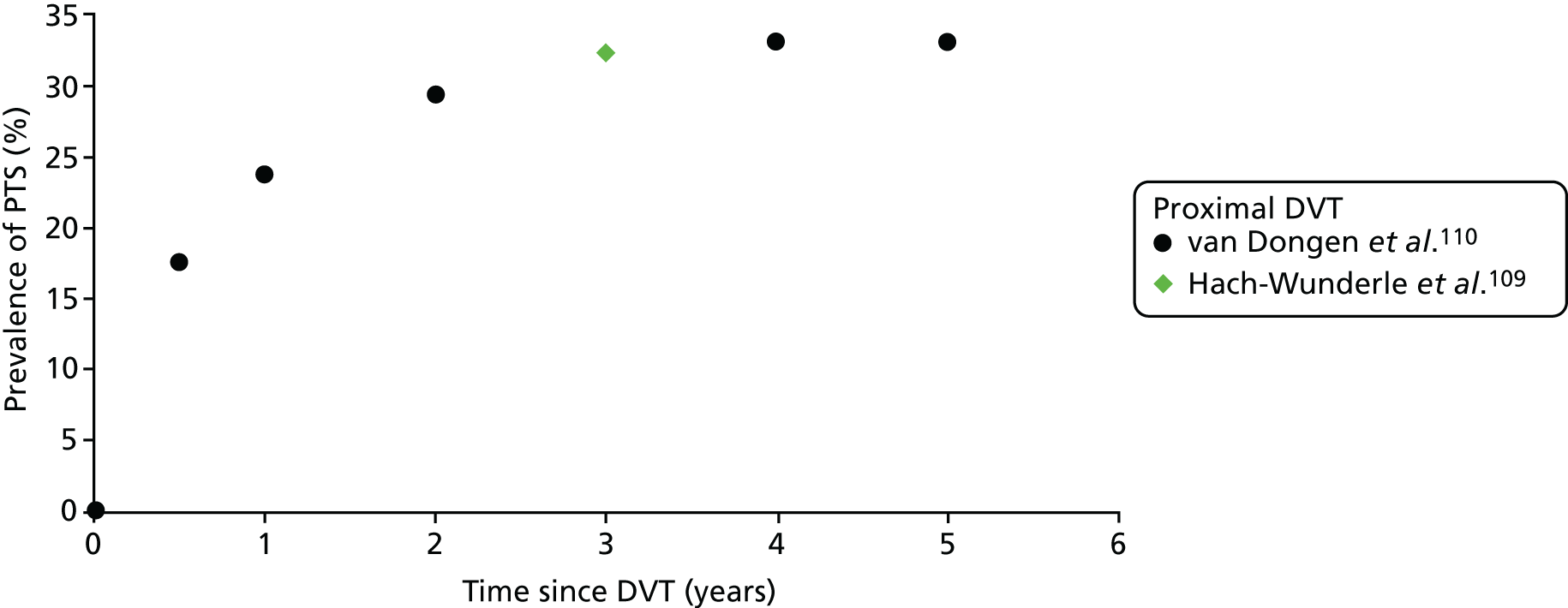
FIGURE 12.
Prevalence of PTS in the model for treated symptomatic and untreated asymptomatic DVTs.
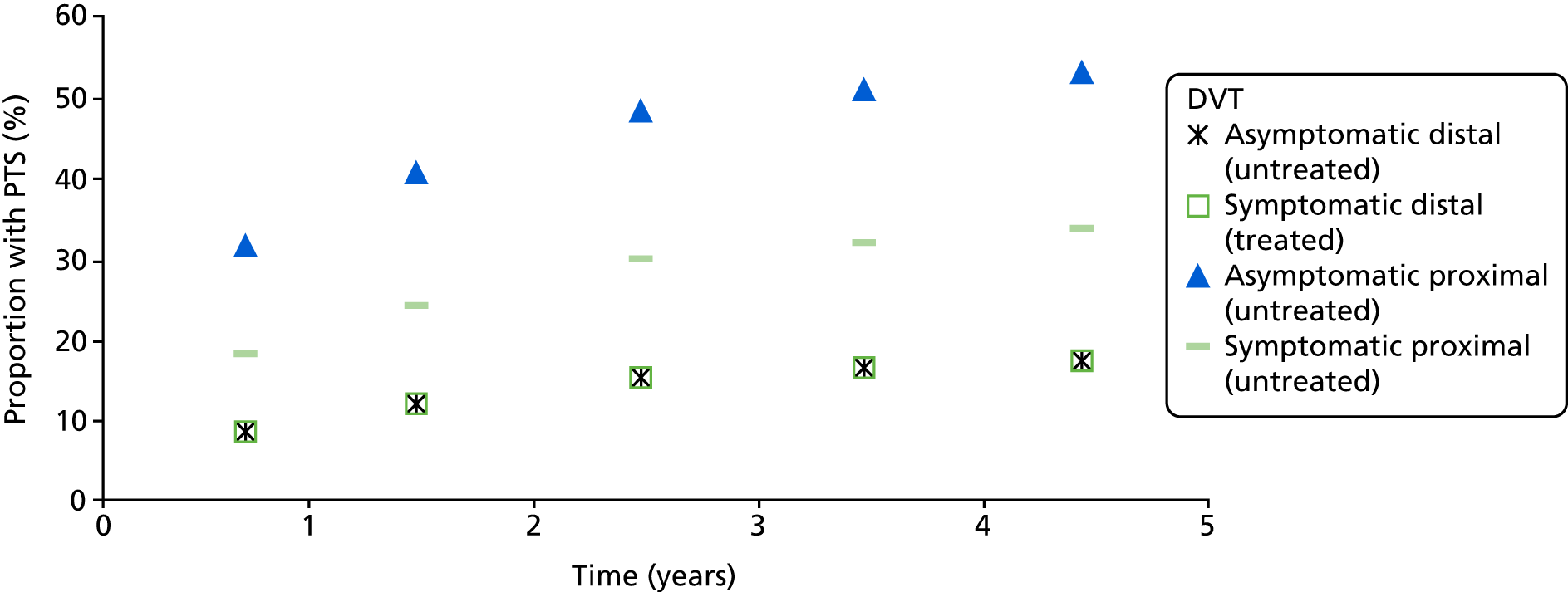
Costs of prophylaxis
For thromboprophylaxis during lower-limb immobilisation, it was assumed that patients receive 6 weeks of treatment using LMWH at the dose recommended for long-term treatment after hip or knee replacement. In the base-case analysis, it was assumed that the lowest-cost formulation of LMWH would be used (dalteparin), but the impact of treatment with either fondaparinux or dabigatran was explored in sensitivity analyses as these represented the highest- and lowest-cost alternatives to LMWH. The dosages and drug costs are summarised in Table 18.
| Drug | Dosing and delivery21 | Product and cost21 | Cost per day (£) | Cost per course (assuming 42 days treatment) (£) | Administration cost per course (£) | Total cost per course (£) |
|---|---|---|---|---|---|---|
| Dalteparin | 5000 units every 24 hours by subcutaneous injection for 4–6 weeks | Dalteparin sodium 5000 units/0.2 ml solution for injection: £28.23 for 10 pre-filled syringes | 2.82 | 118.57 | 105.13 | 223.70 |
| Exonaparin | 40 mg every 24 hours by subcutaneous injection for 4–6 weeks | Enoxaparin sodium 40 mg/0.4 ml: £30.27 for 10 pre-filled syringes | 3.03 | 127.13 | 105.13 | 232.26 |
| Tinzaparin | 4500 units every 24 hours by subcutaneous injection for 4–6 weeks | Tinzaparin sodium 4500 units/0.45 ml solution for injection: £35.63 for 10 pre-filled syringes | 3.56 | 149.65 | 105.13 | 254.78 |
| Fondaparinux | 2.5 mg every 24 hours by subcutaneous injection for 4–6 weeks |
|
5.97 (assuming that the lowest-cost formulation was prescribed) | 250.53 | 105.13 | 355.66 |
| Apixaban | 2.5 mg orally twice daily | Eliquis 2.5 mg tablets | 1.90 | 79.80 | 12.83 | 92.63 |
| Dabigatran | 220 mg orally daily | Pradaxa 110 mg capsules: £51.00 for 60 capsules (same cost per capsule for 10) | 1.70 | 71.40 | 12.83 | 84.23 |
| Rivaroxaban | 10 mg orally daily | Xarelto 10 mg tablets: £54.00 for 30 tablets (same cost per tablet for 10) | 1.80 | 75.60 | 12.83 | 88.43 |
Menakaya et al. 115 estimated the costs of outpatient VTE prophylaxis for patients having lower-limb injuries based on 388 patients receiving prophylaxis who were recruited from 7048 patients attending a fracture clinic in England. The total cost for an average of 46 days of anticoagulant treatment was £107.54 for the self-administration of LMWH, with £46 of this being the drug cost (the authors assumed £1 per day). Therefore, the total cost of administration was £61.54. This covered clinical time for counselling and taking blood samples (including a 5-day platelet count), pharmacy dispensing and initial administration. For patients requiring district nurse administration (£23 per home visit), the average cost of administration across the treatment course was £1096.54 but this was required in only 4% of cases, giving an average cost of £102.94 across the cohort. Adjusting the number of doses from 46 to 42, which affects only the district nurse administration costs, and updating this from 2011/12 to 2016/17 prices (Curtis and Burns100), gives a total administration cost of £105.13. The total cost for the 6-week course of dalteparin, including administration costs, was £223.70.
For the sensitivity analysis on fondaparinux, the same administration costs as those required for LMWH were assumed. Patients initiating treatment with a DOAC were assumed to require one nurse-led telephone consultation at 10 days. The range tested in sensitivity analysis for the whole course of treatment was £84.23 for dabigatran to £355.66 for fondaparinux.
When assessing the cost-effectiveness of using RAMs to determine thromboprophylaxis, it is necessary to include the cost of the time spent by the clinician to determine the individual’s risk score. It was assumed that this would require 5 minutes of time by a hospital consultant, which was estimated to be £8.83 based on an hourly cost of £106. 100 This was applied to all patients in the RAM-based thromboprophylaxis strategies but to none of the patients in the treat-all and treat-none strategies.
Cost of treatment
Patients who have lower-limb immobilisation may later present with symptomatic DVT or PE, requiring diagnosis and treatment. The costs of VTE have been estimated for three broad categories of costs: health-care contacts, diagnostic costs and drug treatment costs. It was assumed that all patients presenting with symptomatic VTE would require an ED assessment, but that a proportion would present first to a general practitioner (GP) before attending an ED, and that only a proportion of those attending an ED would require admission. It was assumed that those patients requiring admission would also be likely to require ambulance transfer to the ED. The proportion of patients attending GPs prior to ED attendance and the proportion requiring admission (Table 19) were based on clinical expert opinion. Discussions with clinical experts were informed by the assumptions used in the model described in the 2017 draft update to the NICE guideline on managing VTE130 and the assumptions used in relevant NICE single technology appraisals (STAs). 131–139
| Resource item | Proportion using resource (%) | Unit cost per patient using this resource (£) | Description | ||
|---|---|---|---|---|---|
| Non-fatal PE | Symptomatic proximal DVT | Symptomatic distal DVT | |||
| Health-care contacts/admission | |||||
| GP visit | 20 | 50 | 50 | 37 | Curtis and Burns,100 GP cost per surgery consultation with qualification costs, including direct care staff costs |
| Ambulance transfer to ED | 60 | 10 | 0 | 236 | NHS Schedule of Reference Costs 2015–16.116 ‘See and treat and convey’, code ASS02 |
| ED visit leading to admission | 60 | 10 | 0 | 228 | NHS Schedule of Reference Costs 2015–16.116 VB05Z type 01 admitted (category 2 investigation with category 3 treatment) |
| ED visit without admission | 40 | 90 | 100 | 196 | NHS Schedule of Reference Costs 2015–16.116 VB05Z type 01 non-admitted (category 2 investigation with category 3 treatment) |
| Short stay admission for PE | 60 | 0 | 0 | 1498 | NHS Schedule of Reference Costs 2015–16.116 Weighted average cost of non-elective inpatient (short and long stay with excess bed-days) for ‘pulmonary embolus with interventions’, codes DZ09 J to DZ09 N and DZ09P and DZ09Q |
| Short stay admission for DVT | 0 | 10 | 0 | 1012 | NHS Schedule of Reference Costs 2015–16.116 Weighted average cost of non-elective inpatient (short and long stay with excess bed-days) for ‘deep-vein thrombosis’, CC score 0 to ≥ 12, codes YQ51 A to YQ51E |
| Critical care unit stay | 10 | 0 | 0 | 1012 | NHS Schedule of Reference Costs 2015–16.116 Weighted average cost of adult critical care, 0 to 6 or more organs supported, codes XC01Z to XC01Z |
| Subtotal for health-care contacts (£) | 1365 | 342 | 214 | ||
| Diagnostic costs | |||||
| Risk assessment tool (Wells score) | Included in an ED episode of care so not costed separately | ||||
| D-dimer | Included in an ED episode of care so not costed separately | ||||
| ECG | Included in an ED episode of care so not costed separately | ||||
| Chest radiography | |||||
| Proximal leg vein ultrasonography | 0 | 100 | 100 | 55 | RD40Z, outpatient ultrasound scan (duration of < 20 minutes), without contrast, cost £55 [RD47Z may be more relevant for the diagnosis of distal DVTs, but cost is similar (£58)]116 |
| CTPA | 90 | 0 | 0 | 102 | RD21A, outpatient computerised tomography scan of one area, with post contrast only, patients aged ≥ 19 years116 |
| V/Q SPECT | 5 | 0 | 0 | 261 | RN08A, outpatient SPECT, patients aged ≥ 19 years116 |
| V/Q planar | 5 | 0 | 0 | 274 | RN18A, outpatient lung ventilation or perfusion scan, patients aged ≥ 19 years116 |
| Echocardiography | 20 | 0 | 0 | 72 | RD51A, outpatient simple echocardiography116 |
| Subtotal for unbundled diagnostics (£) | 133 | 55 | 55 | ||
| Subtotal for drug treatment (£) | 290 | 290 | 290 | See Table 20 | |
| Total (£) | 1788a | 688 | 560 | ||
Diagnostic tests that occur during the ED episode of care, such as electrocardiography monitoring and chest radiography, are not costed separately. However, scans occurring later as outpatient activity were costed separately as these diagnostic tests are ‘unbundled’ within the NHS reference cost data. 116 Assumptions regarding the use of diagnostic tests to assess patients with suspected DVT and PE were based on clinical expert opinion. The main costs not covered within the ED episode of care are assumed to be leg vein ultrasonography for patients with a suspected DVT and computerised tomography pulmonary angiography (CTPA) or ventilation/perfusion scans for patients with a suspected PE. A minority of patients (20%) with suspected PE are also assumed to require echocardiography. The diagnostic tests are summarised in Table 19. It was assumed that all patients presenting with PE or symptomatic DVT (proximal or distal) would be treated with anticoagulants.
Treatment for VTE was assumed to consist of 3 months of either a VKA (warfarin) or a DOAC. Patients being treated with a VKA would also require initial anticoagulation with LMWH until adequate oral anticoagulation is established. The proportion receiving DOACs versus VKA was informed by data from the PREFER-VTE study,123 which found that 40% of patients in countries where DOACs had been launched were receiving a DOAC as their initial treatment following DVT. The split between drugs in the LMWH class was informed by assumptions used in a previous appraisal. 140 The costs of administering treatment with LMWH are based on the costs estimated by Menakaya et al. 115 for initiating prophylaxis using LMWH but with a reduction in district nurse administration based on the shorter duration of treatment (7 vs. 42 days). Patients receiving VKA are assumed to require nine visits to an anticoagulation service in 3 months to monitor their INR. Patients initiating treatment with a DOAC are assumed to require one nurse-led telephone consultation at 10 days. All patients are assumed to require a consultant-led face-to-face visit at 3 months to assess the need for ongoing treatment. The overall cost, including monitoring, when averaged across the treatment strategies was £290.24 (Table 20).
| Drug | Dosing and delivery | Product and cost | Cost (£) | Percentage using treatment | |
|---|---|---|---|---|---|
| Drug, per course | Monitoring/administration | ||||
| Apixaban | Initially, 10 mg twice daily for 7 days, orally, followed by 5 mg twice daily, orally, for the remainder of the 3-month (91-day) treatment period | Apixaban, 5 mg: £53.20 for 56 tablets (cost per tablet is the same for the 28-tablet pack size) | 186.20 | 50.00a | 20% (half of the 40% using DOACs) |
| Rivaroxaban | Initially, 15 mg twice daily for 21 days, to be taken orally with food. This is followed by 20 mg once daily, to be taken orally with food for the remainder of the 3-month (91-day) treatment period | Rivaroxaban, 20 mg: £50.40 for 28 tablets (cost per tablet is the same for 15 mg tablets and larger and smaller pack sizes) | 201.60 | 50.00a | 20% (half of the 40% using DOACs) |
| Enoxaparin | 1.5 mg/kg every 24 hours by subcutaneous injection until adequate oral anticoagulation established (7 days) (i.e. 120 mg of enoxaparin if assuming weight of 80 kg) |
|
61.55 | 70.26b | 30% (45% of heparin use) |
| Dalteparin | 15,000 units (assuming body weight of 80 kg) once daily until adequate oral anticoagulation established (7 days) | Dalteparin sodium, 15,000 units/0.6 ml solution: £42.34 for five pre-filled syringes | 59.28 | 70.26b | 18% (35% of heparin use) |
| Tinzaparin | 175 units/kg once daily until adequate oral anticoagulation established (7 days) (i.e. 14,000 units if assuming body weight of 80 kg) | Innohep, 14,000 units/0.7 ml solution: £83.30 for 10 pre-filled syringes | 58.31 | 70.26b | 6% (20% of heparin use) |
| Warfarin | 5 mg twice daily orally for 3 months (91 days) | Warfarin sodium, 5 mg (various suppliers): £0.70 for 28 tablets | 4.55 | 186.27c | 60% |
| Average across those using DOACs and those using LMWH/VKA | 116.35 | 173.89 | Total: £290.24 | ||
The total cost for non-fatal PE was estimated to be £1788, which includes health-care contacts, diagnostic costs and 3 months of drug treatment for VTE. Fatal PE was assumed to incur the same costs for health-care contacts and diagnostics, but without the cost of VTE treatment, giving a cost of £1498. Symptomatic proximal and distal DVTs had a total cost of £688 and £560, respectively, with the higher cost of proximal DVTs driven by a greater likelihood of admission.
Cost of bleeding complications
A paper by Luengo-Fernandez et al. 117 on the acute and long-term costs of care after stroke in patients with atrial fibrillation (AF) was identified as a source of costs in those having ICH from the NICE appraisal of edoxaban tosylate (Lixiana®; Daiichi Sankyo UK Ltd, Gerrards Cross, UK) for the treatment and secondary prevention of DVT and/or PE. 140 The paper117 provides estimates of acute (up to 90-day) and long-term costs (average annual costs up to 5 years post stroke) using data from the Oxford Vascular Study (OXVASC), which was a prospective study of 91,000 UK patients registered with general practices in Oxfordshire. The paper by Luengo-Fernandez et al. 117 reports costs for the subset of patients who experienced a stroke during the study and who had a history of AF prior to that index stroke (n = 153). The mean age of patients in this subset was 80 years, with 26% of patients having previous stroke and 20% of patients having pre-morbid warfarin use.
The costs were reported separately on the basis of disability level and whether the type of stroke was ischaemic, haemorrhagic or not known. Only 17 of the 191 strokes experienced by the 153 patients were haemorrhagic. The mean acute cost of fatal haemorrhagic strokes was £1592 (SD £1886; n = 8). This mean cost was substantially lower than the average for all haemorrhagic strokes, which was £10,683 (SD £12,885; n = 17). Given that these estimates were based on a small number of patients, the estimates for all stroke types were also considered. The cost of fatal strokes across all types was also lower, at £2680 (SD £2661; n = 40), than the average for all strokes (mean £10,413, SD £15,105; n = 191), suggesting that fatal strokes do incur a lower acute cost than non-fatal strokes. The cost of fatal haemorrhagic strokes was used in the base-case analysis for fatal intracranial bleeds. The cost was updated from 2008/9 prices to 2016/17 prices (using Curtis and Burns100), giving an acute cost of £1802 over 3 months.
The paper by Luengo-Fernandez et al. 117 also provided relevant data on the cost of non-fatal ICHs. The cost of a non-fatal haemorrhagic stroke was estimated to range from £3401 to £24,234, depending on the level of disability following the stroke. A weighted average cost for non-fatal haemorrhagic strokes of £18,764 was calculated across the non-disabling, moderately disabling and totally disabling haemorrhagic strokes. However, it was noted that these estimates were based on only nine non-fatal haemorrhagic strokes. The equivalent average across all non-fatal strokes was £12,461. The higher cost for haemorrhagic non-fatal strokes appeared reasonable given that haemorrhagic strokes appeared to result in higher than average costs across all categories except fatal strokes. This is supported by data presented by Fernando et al. ,141 which show that patients with haemorrhagic stroke who are admitted to an intensive care unit (ICU) incur higher costs than matched patients (matched for age, sex and comorbidity) admitted to an ICU for other (non-ICH) reasons. Furthermore, ICHs associated with oral anticoagulant use were also found to be significantly more costly than those not associated with oral anticoagulant use. 141 The weighted average cost for non-fatal haemorrhagic stroke from Luengo-Fernandez et al. 117 was used in the base-case analysis for the acute cost of non-fatal ICH. This cost was updated from 2008/9 prices to 2016/17 prices (using Curtis and Burns100), giving non-fatal ICH a cost of £21,245 over 3 months.
It was noted that this cost for non-fatal ICH is significantly higher than the weighted average cost of stroke based on NHS reference costs for non-elective long- and short-stay inpatients (including excess bed-days), which was £3290 [average of reference costs116 for Healthcare Resource Group (HRG) codes AA35A to AA35F]. However, the average NHS reference cost is similar to the cost reported by Luengo-Fernandez et al. 117 for non-disabling stroke costs. This may reflect the fact that rehabilitation costs are reported separately in NHS reference costs and these costs are between £332 and £402 per day for admitted rehabilitation. These rehabilitation costs would have been included in the hospitalisation costs reported by Luengo-Fernandez et al. 117 and would be much higher for moderately and totally disabling strokes, which may explain the higher costs in these groups than the NHS reference cost for admitted care in stroke patients, which excludes rehabilitation.
The model also required post-acute costs (post 90 days) for patients having non-fatal ICH. Luengo-Fernandez et al. 117 estimated the post-acute costs per annum relative to the year before stroke (baseline). The total post-acute costs were found to be non-significantly higher versus baseline costs at £804 (95% CI –£832 to £2440). However, the GP and emergency care components were significantly higher at £98 (95% CI £27 to £169) and £99 (95% CI £56 to £141), respectively. In addition, the paper separately reported long-term residential care costs for patients not previously admitted to residential care. They reported that 18% of strokes resulted in a new admission to long-term care (i.e. warden housing, residential care or nursing home care), with an average annual cost of £6880 across all patients surviving the acute period (90 days). Post-acute and long-term costs were not reported separately by stroke type (haemorrhagic vs. other) by Luengo-Fernandez et al. 117 The total costs of GP, emergency care and long-term care were averaged across all stroke types and uplifted to current prices (using inflation indices from Curtis and Burns100) to give a total cost per year for non-fatal ICH patients of £8013 in the post-acute (beyond 90 days) period. This was applied in the Markov phase of the model to patients in the non-fatal ICH health state. It was also applied pro rata to patients having non-fatal ICH more than 90 days before the end of the decision tree model.
The cost of non-fatal extracranial bleeds was estimated using average inpatient costs for GI bleeds, based on the approach taken in the NICE Technology Appraisal (TA) 354. 140 A weighted average was taken across bleeds requiring single, multiple or no intervention and across short- and long-stay non-elective inpatients (including excess bed-days). This gave an average cost of £1198 based on 2015/16 reference costs (HRG codes FZ38G to FZ38P). 116
Cost of post-thrombotic syndrome and chronic thromboembolic pulmonary hypertension
Several reviews of studies relating to PTS were examined to identify any cost papers cited. 125,142–145 None of the cost papers identified were specific to the UK NHS. Three examined costs from a US perspective (Caprini et al. ,146 MacDougall et al. 147 and Olin et al. 148), one examined costs from a Brazilian perspective (Ramacciotti et al. 149), one examined costs from a Swedish perspective (Bergqvist et al. 150) and one examined costs from a Canadian perspective (Guanella et al. 151). Although the paper by Bergqvist et al. 150 was from a European country, the data related to patients diagnosed between 1970 and 1985.
Several of the NICE STAs identified in Appendix 11 cited cost assumptions from Goodacre et al. 152 One cited the US study by Caprini et al. 146 and another cited costs from a 2001 abstract by Cohen et al. 153
It was assumed in the model that management of PTS would involve one first and one follow-up vascular surgery outpatient appointment in the first year after diagnosis and two follow-up GP appointments every year thereafter. This was based on clinical expert advice regarding current management of PTS in the UK and is consistent with the assumptions made by Goodacre et al. ,152 which have been applied in several previous NICE STAs. 131,132,140,154
A review by Grosse et al. 143 on the costs attributable to VTE in the USA identified one paper155 on the cost burden of CTEPH. Kirson et al. 155 compared costs for patients with CTEPH with those for controls (matched for age, sex, employee status and geographical region) in a cohort of privately insured US patients. They found that costs per month were US$2368 (p < 0.0001) higher in patients with CTEPH than in matched controls, but they also found higher rates of comorbidities, suggesting that some of the differences may not be directly attributable to CTEPH. Grosse et al. 143 commented that CTEPH patients are far more likely to have chronic heart failure or chronic pulmonary disease, and no risk-adjusted treatment cost estimates were identified in their review.
The cost of CTEPH was based on the approach taken in technology appraisal (TA) number 354 (i.e. TA354)140 in which pulmonary endarterectomy costs were applied based on reference costs for complex thoracic procedures. Updating this estimate by using current reference costs116 gave a cost of £7898. The Evidence Review Group’s preferred assumption for TA354140 was to use the cost of drugs from CG92,24 which estimated a cost of £1219 per 4 weeks, giving a cost of £17,942 per annum when uplifted to 2016/17 prices (using inflation indices from Curtis and Burns100). Data from Delcroix et al. 113 were used to estimate the proportion having surgical management and the proportion receiving medical management. The fact that some surgical patients receive bridging therapy, as reported by Delcroix et al. ,113 was taken into account by allowing them 4.6 months of medical therapy based on the average time to surgery for these patients. This increased the costs in the first year for patients having surgical management to £9890. It was assumed that no further costs are incurred in year 2 and beyond for those having surgical management.
Summary of methods used to identify studies reporting utility values relevant to the model
The searches for the systematic review of published cost-effectiveness studies included a filter to identify health-related quality of life (HRQoL) data. While sifting these studies, one study156 reporting HRQoL data in patients with lower-limb immobilisation was identified; this study by Arverud et al. ,156 reported EuroQol-5 Dimensions (EQ-5D)157 scores in patients who had an Achilles tendon rupture. The study reported mean EQ-5D scores at 1 year for patients who did and patients who did not experience DVT following surgical repair and immobilisation. The average EQ-5D score was lower in patients with DVT but the difference was not statistically significant (p = 0.6). A second study158 identified in the search reported the validation of a disease-specific HRQoL measure, Deep Venous Thrombosis Quality of Life (DVTQoL), in patients with DVT but this study reported only the correlation between the EQ-5D and the domains of the DVTQoL; utility values based on EQ-5D scores could not be extracted. No other studies reporting preference-based measures of utility in patients with lower-limb immobilisation were identified from the searches conducted for the economic review.
One published study by Wolowacz et al. 99 was identified from the literature review that examined the cost-effectiveness of thromboprophylaxis for a similar, but not directly relevant, population (elective knee replacement) as described in Results of cost-effectiveness review. This was supplemented by searches of the NICE website to identify models developed to inform NICE TAs and CGs, as these models would be expected to have a relevant setting and methodological approach and would not always be identified through database searches. The cost-effectiveness analyses identified are summarised in Appendix 11.
In addition, ad hoc searches for systematic reviews of utilities for relevant model states (e.g. PTS) were conducted using the Google Scholar search engine (Google Inc., Mountain View, CA, USA). This identified a published systematic review of HRQoL studies for VTE and related complications by Lubberts et al. 159 This review focused on studies with a minimum follow-up of 1 year in order to capture the long-term impact of complications such as PTS and CTEPH. Only two of the studies included by Lubberts et al. 159 reported a generic preference-based utility measure (EQ-5D). One of the two studies reporting EQ-5D was conducted in patients with subclavian DVT and is therefore less applicable to this population. The other study, by Haig et al. ,160 reported EQ-5D scores for patients with and without PTS following DVT.
In addition, the systematic review by Lubberts et al. 159 reports outcomes for 15 studies that used either the Short Form questionnaire-36 items (SF-36)161 or the Short Form questionnaire-12 items (SF-12). Data from these studies were meta-analysed to assess the difference in HRQoL between patients and members of the general population matched by country, age and sex. Lubberts et al. 159 report the meta-analysed decrement in SF-36/SF-12 mental component summary (MCS) and physical component summary (PCS) scores compared with general population norms (matched by country, age and sex) using the standardised mean difference (SMD) as a common currency across studies. These meta-analyses by Lubberts et al. 159 do not provide a preference-based utility measure that can be used directly in the model, but their outcomes are summarised below as they provide evidence as to whether or not each VTE-related outcome has an important impact on long-term HRQoL based on more than a single study. They are therefore useful in interpreting the utility estimates from individual studies identified from existing cost-effectiveness models.
Although Lubberts et al. 159 included only studies reporting outcomes more than 1 year after VTE, they also listed nine studies158,162–169 that were excluded for reporting outcomes at shorter follow-up points. Of these, one study by Hogg et al. 163 reported useful data (see Appendix 12); the remaining eight studies did not report utility values for relevant health states. 158,162,164–169
One additional HRQoL study170 was identified from ad hoc searches; Roberts et al. 170 examined the predictors of HRQoL for patients following DVT using the SF-36. This is also discussed below as it provides useful additional information on PTS as a determinant of HRQoL.
The sources of utility data identified from both the published models listed in Appendix 11 and the systematic review by Lubberts et al. 159 are summarised in Appendix 12.
Utility values in pulmonary embolism
Lubberts et al. 159 report that PE is associated with a significant reduction in SF-36 PCS score (SMD –0.30, 95% CI –0.45 to –0.14) but not SF-36 MCS score (SMD 0.14, 95% CI –0.01 to 0.30), relative to general population norms at time periods of > 1 year based on an analysis of two studies. 171,172 This suggests that PE has an important long-term impact on patients. Three studies173–175 reported EQ-5D outcomes for patients with PE, although two of these studies173,174 were published only in abstract form and the other study175 used Danish rather than UK population norms. One study used an alternative generic preference-based measure, the Short Form questionnaire-6 Dimensions (SF-6D). 163 In addition, two studies176,177 reported utility values for PE measured directly using either standard gamble or time trade-off (TTO). Data from the study abstract by Cohen et al. 173 were reported in additional detail in the company submission for TA354140,178 (Figure 13).
The data from Cohen et al. 153 were selected for use in the model because these were measured using the EQ-5D, were sourced from a large registry database (PREFER-VTE) including patients recruited in the UK and the paper included estimates of the change in utility over time (see Figure 13). The data reported by Cohen et al. 173 demonstrated that utility values varied depending on the time since PE, with utility values appearing to stabilise at between 3 and 6 months. The average utility in patients with PE during the 6 months following PE was calculated using the data from Cohen et al. 173 This was compared with the utility value at 6 months in patients with DVT (who do not have a long-term utility decrement according to the review Lubberts et al. 159) to calculate the utility multiplier for PE, which was then applied to the age appropriate utility for patients without PE. A linear change in utility between the points measured was assumed, giving an average utility of 0.775 over the 6 months after PE, which is a 9% decrement relative to utility at 6 months post DVT. Given that there was some evidence of a reduction in HRQoL for patients with PE found by Lubberts et al. 159 at 1 year, it was decided to use the 6-month utility decrement for PE relative to DVT, when no long-term reduction was found, to estimate the long-term utility reduction for patients following PE. This gave a 5% reduction in utility beyond 6 months for a patient surviving PE beyond 6 months. Tavoly et al. 175 reported mean EQ-5D values of 0.8 in patients post PE versus 0.86 in age- and sex-matched general population controls, suggesting a 7% reduction in utility despite a median time since diagnosis of 3.8 years. This supports the assumption that there are some ongoing post-PE symptoms beyond 6 months.
Utility values in deep-vein thrombosis
The data sources for utility values in DVT were similar to those identified for PE, except that the study by Tavoly et al. 175 was not relevant because it examined only patients with PE. However, a similar study by Utne et al. 179 examining DVT outcomes from the same hospital registry was identified instead. One additional study by Arverud et al. 156 examining DVT versus no DVT after lower-limb immobilisation due to injury was also identified. This study found that DVT identified by screening (colour duplex sonography) 2 weeks post operatively was a non-statistically significant predictor of worse EQ-5D scores (0.918 vs. 0.906; p = 0.604). This may be expected given that the DVTs were detected by screening and, therefore, may have been asymptomatic. Utne et al. 179 found that EQ-5D score was statistically significantly lower for patients with DVT compared with age- and sex-matched buddy controls. However, these patients were recruited any time after DVT, and a significant proportion had PTS, so the reduction compared with controls may have been partly due to PTS symptoms, which are likely to be persistent beyond 6 months. In the first 6 months of the model, the data from Cohen et al. 173 were used to estimate the average utility, which was compared with the utility at 6 months. This gave a utility decrement of 4%, on average, during the first 6 months after DVT. Beyond 6 months, no utility decrement for patients without PTS was assumed, as the systematic review by Lubberts et al. 159 reported that there was no statistically significant difference in SF-36 PCS and MCS scores for DVT at time periods of > 1 year based on an analysis of nine studies. 172,180–187 Utne et al. 179 did not find a statistically significant difference in the odds of having impaired HRQoL, measured by EQ-5D, depending on whether the DVT was proximal or distal. In the absence of any other data on the difference in HRQoL impact of proximal versus distal DVT, the same utility loss was assumed during the first 6 months for symptomatic proximal DVT and symptomatic distal DVT.
Utility values in post-thrombotic syndrome
Lubberts et al. 159 reported that patients with PTS had significantly lower MCS and PCS scores than matched population norms (SMD for MCS score –0.27, 95% CI –0.43 to –0.11; SMD for PCS score –0.89, 95% CI –1.21 to –0.57), based on an analysis of seven studies. 180–182,184–186,188 Five studies reported utility values for patients with PTS,160,177,189–191 with two studies160,189 reporting EQ-5D scores and three studies177,190,191 using direct measures of utility such as standard gamble or TTO. The data reported by Haig et al. 160 and Enden et al. 189 were the 2-year and 5-year follow-up points from the catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (CaVenT) study that compared catheter-directed thrombolysis (with 24 months of compression stockings) against standard treatment (6 months of anticoagulant and 24 months of compression stockings) for patients with high proximal DVT. The CaVenT study189 found no difference in EQ-5D scores between treatment arms at 6 months, 2 years or 5 years, but did find a statistically significant difference in HRQoL between those with PTS (n = 92) and those without PTS (n = 97) at 24 months and 5 years. At 6 months, the mean EQ-5D scores were lower for those with PTS but the difference was not statistically significant (p = 0.062).
The decrement measured at 2 years in the CaVenT study189 was applied to all patients with PTS in the Markov phase of the model. It was decided not to model a change in HRQoL for patients with PTS over time as some HRQoL decrement is likely to be present from the time of diagnosis of PTS (i.e. 6 months after DVT) and the HRQoL impact of PTS appears to remain apparent at 5 years. Therefore, a 10% decrement was applied based on the 24-month data from Enden et al. 189
Supportive evidence is provided in the study by Roberts et al. ,170 which reported that patients without PTS recovered their SF-36 PCS scores from below population norms by 6 months, whereas those with mild or moderate/severe PTS did not experience a similar recovery. This study170 also reported that the location of DVT (i.e. proximal or distal) was not an independent predictor of HRQoL, with only sex, comorbidities and PTS being significant predictors in the multivariate analysis.
As the CaVenT study189 reported the average utility decrement across all PTS, without stratifying by PTS severity, this value was applied in the model for all patients with PTS. This may overestimate the utility decrement if patients in the CaVenT study had more severe PTS than would be seen in the modelled population and severity was a predictor of utility decrement. However, in the study by Roberts et al. ,170 the coefficients for mild versus no PTS and for moderate/severe versus no PTS were similar in the regressions for SF-36 PCS and MCS scores, suggesting that both mild and moderate/severe PTS had similar implications for HRQoL. Furthermore, the review by Lubberts et al. 159 shows that the 5-year estimates from the CaVenT study reported by Haig et al. 160 are fairly consistent with the average across the 10 studies160,180–182,184–186,188,192,193 that reported outcomes for the disease-specific measure of HRQoL Venous Insufficiency Epidemiological and Economic Study – Quality of life (VEINES-QoL). A sensitivity analysis was conducted to see if halving the utility decrement for PTS had a significant impact on the model results. A sensitivity analysis was also conducted using the data from Lenert and Soetikno190 and estimating a weighted average utility across severe and mild/moderate PTS using the data from Hach-Wunderle et al. 109 to estimate the proportion of PTS that is severe (6%). This gave an average utility decrement of 2% rather than the 10% assumed in the base-case analysis.
Utility values in chronic thromboembolic pulmonary hypertension
Only one study included in the review by Lubberts et al. 159 reported outcomes for CTEPH, and this reported statistically significantly lower MCS (SMD –0.31, 95% CI –0.54 to –0.08) and PCS scores (SMD –1.72, 95% CI –1.95 to –1.48) than matched population norms. Six studies were identified as providing information on preference-based measures of HRQoL in patients with CTEPH. Three of these studies reported data based on the EQ-5D,194–196 a fourth reported data from an alternative generic preference-based measure, the SF-6D197 and a fifth reported data from a condition-specific preference-based measure, the Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR). 198 Finally, one study reported values based on a standard gamble. 199 Only one of the papers reported values specifically for patients with CTEPH195 but this paper was restricted to those with resistant/recurrent or inoperable CTEPH (i.e. those in whom pulmonary endarterectomy had failed or was not possible). The paper by Ara and Brazier194 reported data for ‘other heart problems’ (i.e. not heart attack/angina). The study by Keogh et al. 197 only included patients with idiopathic pulmonary arterial hypertension (PAH) or PAH related to connective tissue disease. Two studies, by Olschewski et al. 196 and Meads et al. ,198 included patients with CTEPH and other forms of PAH but Meads et al. 198 reported utility outcomes separately for those with CTEPH. Meads et al. 198 also reported a statistically significant difference in utility between CTEPH and those with PAH associated with connective tissue disorder. There was some inconsistency in the estimates provided by Ghofrani et al. 195 and Meads et al. ,198 with higher baseline scores in the population with inoperable/recurrent resistant CTEPH (0.66 for placebo arm) in Ghofrani et al. 195 than in the CTEPH subgroup reported by Meads et al. 198 (0.56). This may be because patients accepted into trials have slightly better general health than those receiving treatment in general practice. It was decided to use the data from Meads et al. 198 in the model; this was calculated based on the difference between the average utility for patients with CTEPH (0.56) and the average utility for those with New York Heart Association (NYHA) class 1 (0.89), who would be expected to have minimal HRQoL impact. This gave a multiplier of 0.63 or, equivalently, a 37% decrement relative to patients who are well. The decrement was applied for a patient’s lifetime for those who were medically managed but only applied for the first year for those being surgically managed, who had the decrement for PE applied thereafter.
Utility values following intracranial haemorrhage
Of the 10 studies177,190,194,200–206 reporting utility values for stroke patients, six studies 194,200–204 measured utility using the EQ-5D. Another four studies177,190,205,206 reported utility values using a direct standard gamble or TTO measure, but these were disregarded as generic measures of HRQoL are preferred by NICE. 94 The values based on the EQ-5D ranged from 0.31 (as reported by Pickard et al. )203 to 0.70 (as reported by Lunde et al. ). 202 Luengo-Fernandez et al. 201 reported that the decrement ranged from 0.22 at 1 month to 0.09 at 5 years. Studies that reported multiple time points found that the absolute utility value increased and the decrement versus controls decreased over time. The study with the longest follow-up201 found that utility values were relatively stable from 6 months to 5 years post stroke. The data from the 5-year follow-up of the OXVASC study201 were chosen for application in the model as this was the largest sample of stroke patients, the population was selected from the UK, the duration of follow-up allowed time since stroke to be accounted for, and a comparison was made against general population norms. A decrement of 0.22 was assumed in the decision tree part of the model where time since stroke was < 6 months and a decrement of 0.09 was assumed in the long-term part of the model.
Utility values for major non-intracranial haemorrhage bleeds
For major non-ICH bleeds, no studies were identified that measured utility using the EQ-5D or another generic preference-based measure. Two studies176,206 reported values using the standard gamble and a third used TTO. 177 Two of the studies that recruited at least some patients with VTE reported a utility value of 0.65,176,177 whereas the study in patients with AF reported a much higher value of 0.841. 206 The study by Locadia et al. 177 (median 0.65, interquartile range 0.49 to 0.86) was considered to be the most relevant as it used TTO, which is the same method used to generate utility vales for the EQ-5D, and it explicitly included patients with experience of major bleeding episodes during VKA treatment in addition to some patients with VTE. However, using the data from Locadia et al. 177 directly would have resulted in a lower utility value for non-ICH bleeds than for ICH, which would not have had face validity. As the study by Locadia et al. 177 showed similar valuations for the PE and GI bleed health states, and these states were ranked as equivalent, it was decided to use the data for PE from Cohen et al. 173 in the model as the longer-term data provided by Cohen et al. 173 allows the utility multiplier to be calculated relative to a patient who has recovered from VTE (i.e. relative to a patient 6 months after a DVT). The utility multiplier was, therefore, estimated to be 0.80 (0.68/0.84). As major non-ICH bleeds are not expected to lead to long-term disability, the utility multiplier for major bleeding was applied for 28 days.
Treatment-related utility decrement
Given that thromboprophylaxis involves giving patients treatment even though they may not go on to experience a VTE event without treatment, it is important to include in the model the possibility that treatment itself is associated with harm.
Several sources of data were identified for the decrement associated with prophylaxis and treatment of VTE. Six studies reported the utility decrement for warfarin or other VKAs. Four of these studies177,205–207 used a direct measure of utility (e.g. TTO or standard gamble) and two of these studies173,208 measured utility using the EQ-5D. The study by Monz et al. 208 examined HRQoL in a subset of the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial, which was a randomised comparison of dabigatran and warfarin in patients with AF. Therefore, it was unable to measure the utility impact of warfarin alone. However, it did report that there was no statistically significant difference in HRQoL based on treatment type (DOAC vs. warfarin) and the utility scores observed were similar to age-comparable population norms. Cohen et al. 173 reported EQ-5D data by treatment type (heparin only, heparin/VKA, DOAC) from the PREFER-VTE registry. However, it was not clear whether or not patients receiving heparin alone in the PREFER-VTE registry would have different characteristics from those receiving other forms of treatment for VTE, in which case the difference in utility between heparin and other VTE treatments may have been confounded by patient characteristics and their influence on clinicians’ choice of anticoagulant.
Only two studies173,207 provided data on the disutility associated with heparin. Given the potential bias described above for Cohen et al. ,173 it was decided to use the data provided by Marchetti et al. ;207 in this study, a TTO exercise was used in 48 patients attending an anticoagulation clinic who had experience of LMWH. The trade-off was based on clinical vignettes for hypothetical patients receiving LMWH. The average number of days they were willing to trade was 2.7 days over a 1-year time frame. Therefore, a mean decrement of 0.007 was applied during thromboprophylaxis.
Four studies provided directly elicited measures of utility for warfarin therapy. Two were in patients with AF. 205,206 Marchetti et al. 207 was the only study conducted exclusively in patients with a history of VTE. Half of the patients recruited by Marchetti et al. 207 had previous experience of receiving warfarin. All of the patients in the study reported by Locadia et al. 177 had been treated previously with a VKA, but not all had previous VTE. The utility decrement for VKA versus no VKA was 4% for Locadia et al. 177 (0.92 vs. 0.96) based on median estimates of utility for both states, whereas it was 1% for Marchetti et al. 207 based on a willingness to trade 4 of 365 days of full health to avoid warfarin. The estimate from Marchetti et al. 207 is similar to the estimates from Gage et al. 205 in patients with AF, whereas the estimate from Locadia et al. 177 is close to the estimate from Robinson et al. 206 It was decided to use the data from Marchetti et al. 207 to provide an estimate consistent with the methodology used to estimate the utility decrement for LMWH.
In the sensitivity values exploring the use of DOACs as prophylaxis, no utility decrement has been assumed, as DOACs are taken orally and do not require frequent blood tests to monitor INR levels. In the sensitivity analysis exploring the use of fondaparinux as prophylaxis, the same utility decrement as for LMWH was assumed as both treatments are given by subcutaneous injection.
The utility values applied in the model are summarised in Tables 21 and 22.
| Health state value | Absolute utility value | Range | Source | Notes |
|---|---|---|---|---|
| Well/asymptomatic DVT without prophylaxis | 0.879 | 0.878 to 0.882 | Ara and Brazier194 | Population mean utility values based on person (average for male and females) with starting age of 46 years |
| Symptomatic proximal or distal DVT | 0.848 | 0.846 to 0.850 | Cohen et al.173 (using additional detail reported in TA354,140 Daiichi Sankyo company submission, table B78178) | 5% reduction relative to well patients based on comparison of average utility over 6 months for DVT (0.819) vs. utility at 6 months (0.850) for patients with DVT |
| Non-fatal PE | 0.80 | 0.780 to 0.825 | Cohen et al.173 (using additional detail reported in TA354,140 Daiichi Sankyo company submission, table B78178) | 9% reduction relative to well patients based on comparison of average utility over 6 months (0.775) for PE vs. utility at 6 months (0.850) for patients with DVT |
| Non-fatal ICH | 0.66 | 0.616 to 0.701 | Luengo-Fernandez 2013201 | Absolute decrement of 0.22 measured at 1 month |
| Non-fatal non-ICH bleed | 0.69 | 0.652 to 0.688 | Cohen et al.173 |
|
| Prophylaxis: absolute decrement applied to utility values of well/asymptomatic DVT | 0.007 | 0.000 to 0.050 | Marchetti et al.207 | Patients willing to trade average of 2.7 days per year to avoid treatment with LMWH |
| Treatment: absolute decrement applied to utility values for non-fatal PE or symptomatic DVT | 0.011 | 0.000 to 0.081 | Marchetti et al.207 | Patients willing to trade average of 4 days per year to avoid treatment with warfarin |
| Fatal PE | 0 | NA | Assumption |
| Health state(s) | Utility multiplier relative to well | Range | Source | Notes |
|---|---|---|---|---|
| PE survivor without CTEPH and PE survivor > 1 year after surgery for CTEPH | 0.95 | 0.927 to 0.978 | Cohen et al.173 | 5% reduction relative to well patients based on comparison of average utility at 6 months for patients with PE (0.81) vs. utility at 6 months (0.85) for patients with DVT |
| Any DVT without PTS | 1 | N/A | Assumption | Supported by Lubberts et al.’s159 systematic review finding no significant HRQoL decrement in nine long-term studies based on SF-36 outcomes |
| Non-fatal ICH | 0.89 | 0.810 to 0.955 | Luengo-Fernandez et al.201 | Multiplier calculated based on absolute decrement of 0.09 at 5 years (utility values stable from 6 months to 5 years) relative to absolute utility for well state of 0.88 from general population values |
| PTS | 0.90 | 0.855 to 0.944 | Enden et al.189 | Multiplier calculated based on absolute decrement of 0.09 relative to absolute utility for well state of 0.86 |
| CTEPH: first year for surgically managed and every year for medically managed | 0.63 | 0.579 to 0.690 | Meads et al.198 | Multiplier calculated based on comparison of utility for CTEPH (0.56) vs. utility for NYHA class I (0.89) |
| Dead | 0 | Assumption |
Timing and duration of utility decrements applied in the decision tree
To calculate the QALYs gained by patients having different paths through the decision tree, it is necessary to make some assumptions regarding the timing of events, as these are not explicitly modelled in a decision tree. The following assumptions were made when estimating QALYs in the decision tree:
-
Baseline utilities using general population utility values for the starting age are applied to those not having treatment and not having any clinical events (e.g. VTE, bleeds).
-
Bleeds during lower-limb immobilisation are assumed to occur halfway through the immobilisation period, which is assumed to last 8 weeks (56 days), namely bleeds occur at 28 days.
-
VTEs occurring during lower-limb immobilisation are assumed to be diagnosed at the end of immobilisation (i.e. at 56 days) and utility decrements for PE and DVT are applied from diagnosis until the end of the decision tree period.
-
Bleeds occurring during treatment for VTE are assumed to occur at 13, 32 and 12 days post diagnosis of VTE for fatal, ICH and other major bleeds, respectively (based on data from RIETE, reported by Nieto et al. 105).
-
Disutilities for ICH are applied lifelong, but separate disutilties are applied in decision tree and Markov phases of the model (i.e. before and after 6 months post lower-limb immobilisation).
-
Disutility of GI bleeding is assumed to last a maximum of 28 days.
-
Disutility of prophylaxis applies for the duration of prophylaxis (6 weeks) and is therefore less in those stopping early because of major bleeding.
-
Disutility of treatment for VTE applies for the duration of treatment (3 months) and is therefore less in those stopping early because of major bleeding.
The following assumptions were made when estimating QALYs in the Markov model:
-
Utility values for patents without any long-term sequelae (e.g. ICH, CTEPH, PTS) are taken from general population values and decrease as patients age in the model.
-
All other utility values are applied as multipliers, such that the absolute utility value decreases for all patients as a result of ageing.
-
Utility decrements continue in the Markov model for the remainder of a patient’s lifetime for PE but not for DVT, for which patients are assumed to return to general population utility values at 6 months.
-
Patients with CTEPH who are treated medically have a lifelong utility decrement, whereas those treated surgically return after 1 year to the same utility as those surviving PE without CTEPH.
-
Patients with PTS have the same utility decrement from diagnosis to death.
-
Patients with ICH have the same utility decrement from 6 months (i.e. the start of Markov model) to death.
Methods used to quantify decision uncertainty
A probabilistic sensitivity analysis (PSA) was used to estimate the impact of parameter uncertainty on the estimates of costs and QALYs. For each input parameter, a probability distribution was assigned that reflected the degree of uncertainty surrounding the mid-point parameter estimate and we sampled from the distribution 10,000 times. This number of runs was deemed sufficient because it ensured that the coefficient of variation was < 2% for both incremental costs and incremental QALYs. In general, utility values, which must be < 1, and probabilities, which are bounded by 0 and 1, were sampled from beta distributions, and costs, which must be > £0, were sampled from gamma distributions. Uncertainty surrounding the ORs for efficacy (all VTE events) and adverse events (major bleeds) were captured using the convergence diagnostics and output analysis (CODA) samples from the NMA. When parameters were calculated from regression equations, multivariate normal sampling was used to incorporate the covariance between the regression parameters. The estimates of sensitivity and specificity were fixed within the PSA as the uncertainty around these parameters was not reported by Nemeth et al. 32 Table 39 in Appendix 13 presents the distributions for each parameter included in the PSA. For each of the 10,000 sets of parameter inputs, the costs and QALYs of each thromboprophylaxis strategy were re-estimated.
The 10,000 PSA estimates of costs and QALYs were used to estimate the mean costs and QALYs for each thromboprophylaxis strategy. From this, the incremental net monetary benefit (INMB) was estimated when using a willingness-to-pay threshold of £20,000 or £30,000 per QALY, which is the range of thresholds used by NICE when assessing value for money in the context of the UK NHS. 94 The strategy with the maximum INMB at a given threshold is considered to have the optimal cost-effectiveness. The INMB was used to calculate the optimal thromboprophylaxis strategy at both of these thresholds and the proportion of times, within the 10,000 PSA samples, that each strategy is optimal across a range of thresholds was estimated in order to generate the cost-effectiveness acceptability curve (CEAC).
The global expected value of perfect information (EVPI) was estimated, which tells a decision-maker the value of reducing all current decision uncertainty associated with the parameters included in the PSA. This was estimated across all the complete set of possible thromboprophylaxis strategies. The parameter EVPI analysis was also used to assess the importance of each individual parameter in generating uncertainty around the optimal strategy. The Sheffield Accelerated Value of Information (SAVI) tool was used to calculate parameter EVPI. 209
It should be noted that a PSA and an EVPI analysis can capture only uncertainty related to parameters included in the PSA and will not capture any uncertainty associated with structural assumptions or the choice of data inputs used to estimate parameter uncertainty. These uncertainties are quantified instead using deterministic sensitivity analyses, in which a range of alternative parameter inputs and assumptions are explored within the model to see whether or not the conclusions are robust under these changes.
Results of the de novo economic evaluation
Clinical outcomes predicted by the model
The symptomatic adverse clinical outcomes predicted by the model at 6 months (based on mid-point parameter values) are summarised in Figures 14 and 15. As patients may have more than one adverse outcome during the 6-month time period of the decision tree model, patients are summarised on the basis of the worst outcome experienced, such that those recorded as having non-fatal PE or symptomatic DVT are those who did not also have fatal bleed, fatal PE or ICH. In Figure 14 it can be seen that prophylaxis for all is the strategy that minimises the total number of symptomatic adverse outcomes at 6 months. The numbers of the most serious adverse clinical outcomes (e.g. fatal bleeds, fatal PEs or ICHs) are similar across the prophylaxis strategies and the differences are too small to see based on Figure 14. Figure 15 focuses solely on these serious adverse clinical outcomes and shows that giving prophylaxis based on a L-TRiP(cast) score of ≥ 9 minimises the total number of these outcomes, although the rate is very low (≈1 in 4000) and shows little variation between strategies.
FIGURE 14.
Symptomatic clinical outcomes predicted at 6 months for 10,000 patients having lower-limb immobilisation due to injury.
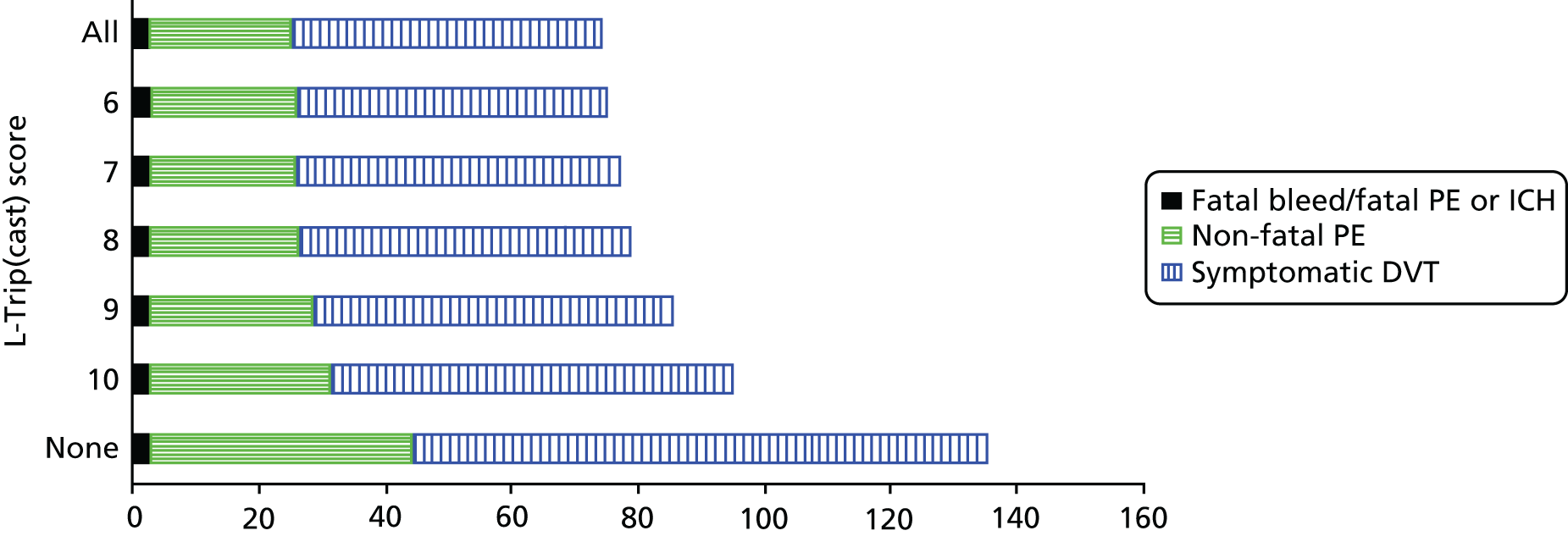
FIGURE 15.
Serious adverse clinical outcomes predicted at 6 months for 10,000 patients having lower-limb immobilisation due to injury.
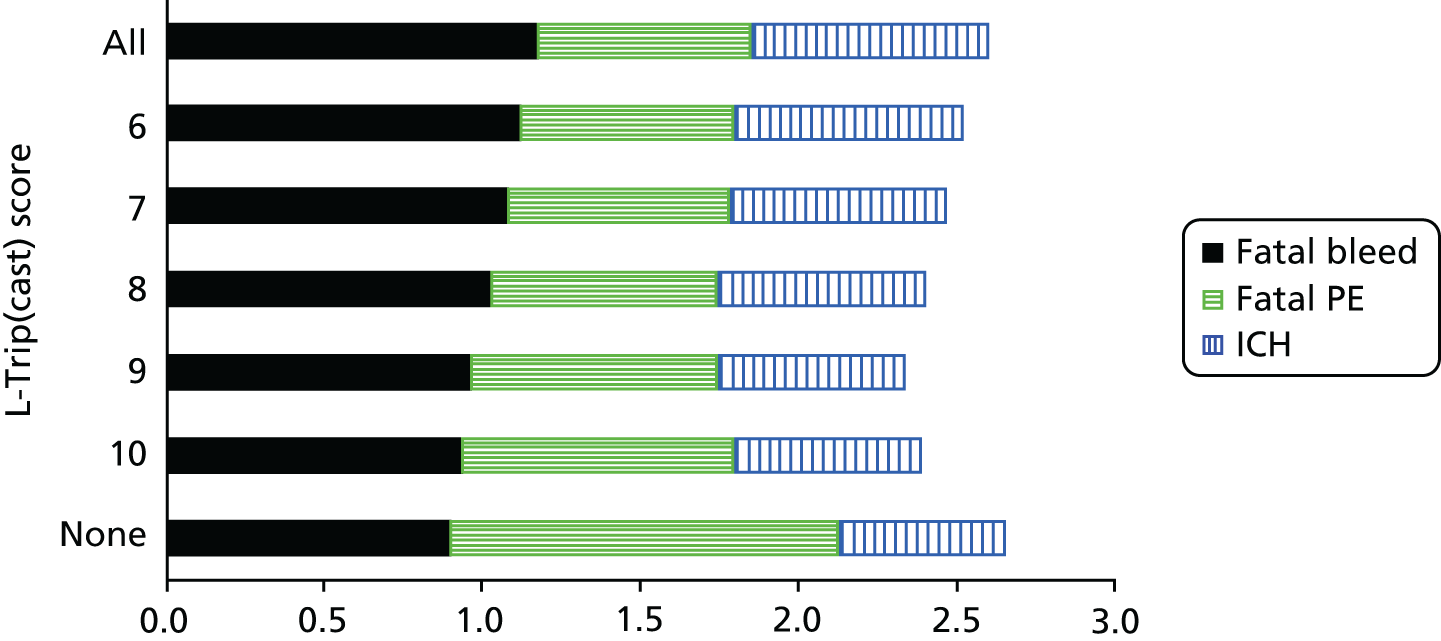
It should be noted that major bleeds that are non-fatal and not ICHs are assumed to resolve within 6 months and are, therefore, not included in Figure 14. The number of major bleeding outcomes is summarised in Figure 16, which shows that the total number of major bleeds, including fatal and non-fatal ICHs, increased from 4.03 per 10,000 having lower-limb immobilisation when no prophylaxis is given to 5.38 per 10,000 when prophylaxis is given to all. Giving prophylaxis to all patients with lower-limb immobilisation, therefore, results in fewer than two additional cases of major bleeding per 10,000 patients receiving prophylaxis. The increase in major bleeding is smaller than would be expected based solely on the RR of 1.64 for bleeding with prophylaxis versus bleeding without prophylaxis, because prophylaxis prevents VTE, thereby lowering the rate of bleeding experienced during VTE treatment.
FIGURE 16.
Major bleeding predicted at 6 months for 10,000 patients having lower-limb immobilisation due to injury.
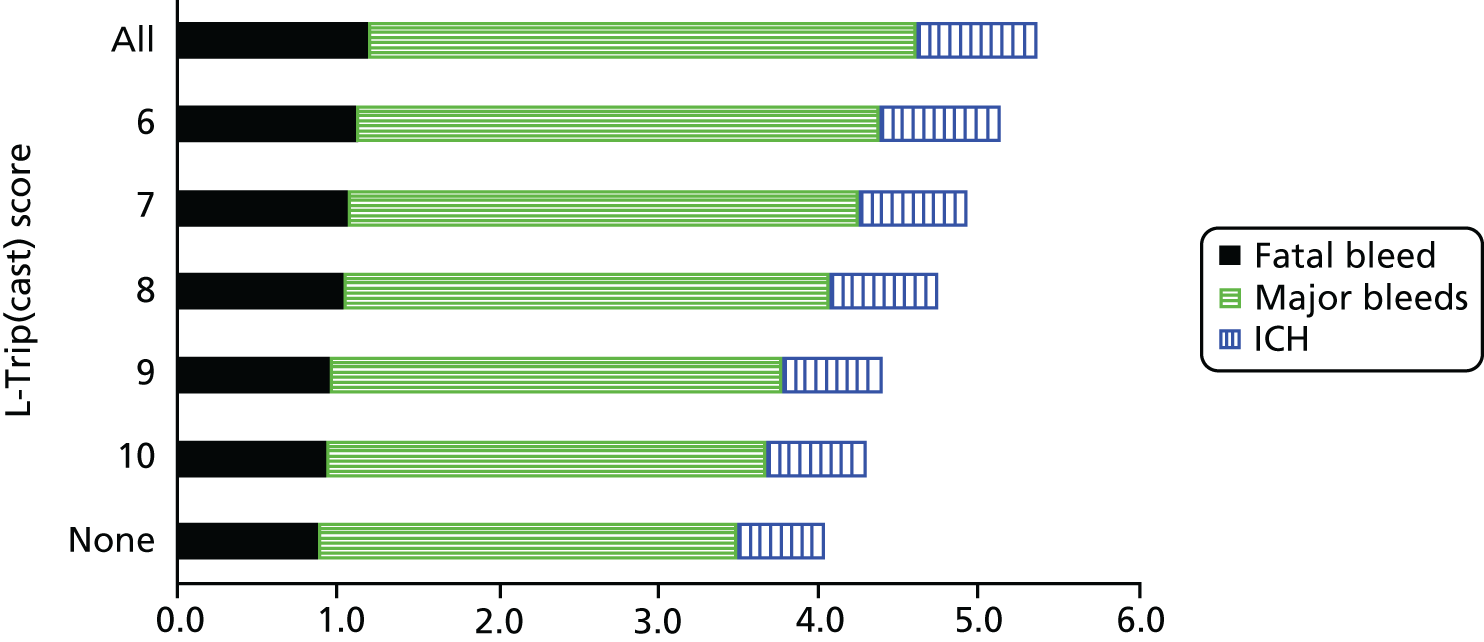
The adverse clinical outcomes predicted by the model at 5 years (based on mid-point parameter values) are summarised in Figure 17. Only those outcomes resulting in long-term morbidity are included; therefore, patients who experience DVTs without any subsequent PTS are not included in the adverse clinical outcomes shown. It can be seen that the number of people surviving to 5 years is fairly similar across all the thromboprophylaxis strategies. The strategy of thromboprophylaxis for all results in the smallest number of people surviving with CTEPH, PTS or ongoing morbidity due to previous ICH or PE. The numbers surviving with either ongoing morbidity due to ICH or CTEPH following PE are relatively small, at ≈1 per 10,000 patients for each outcome.
FIGURE 17.
Adverse clinical outcomes predicted at 5 years for 10,000 patients having lower-limb immobilisation due to injury.
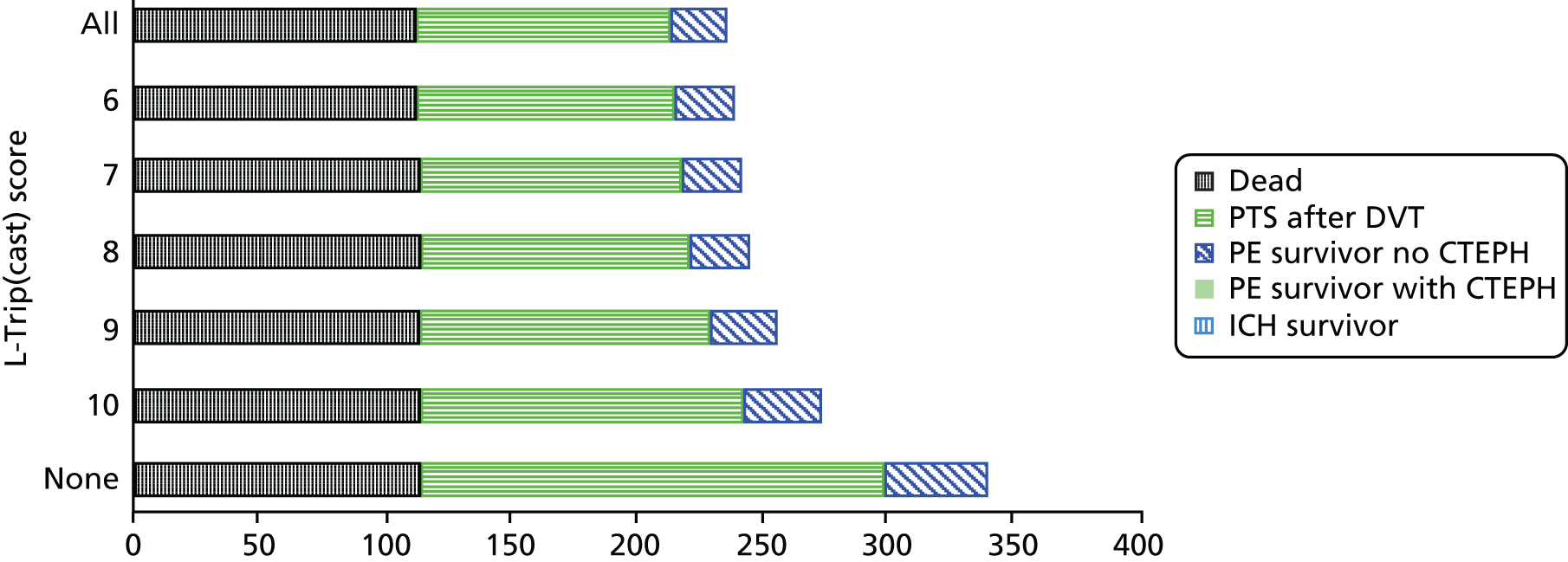
Cost-effectiveness of thromboprophylaxis for all compared with thromboprophylaxis for none
Figure 18 shows the estimates of incremental costs and QALYs for the comparison of thromboprophylaxis for all with thromboprophylaxis for none for 10,000 PSA samples. The mean incremental costs and QALYs from the 10,000 PSA samples are shown as an × on the cost-effectiveness plane. The mean QALY gain is 0.015, but it can be seen that there is a wide spread of incremental QALY estimates, with 95% of the incremental QALYs falling in the range of 0.004 to 0.029 but with some PSA samples (0.53%) having a negative QALY gain. The mean incremental cost is £203 with 95% of the PSA estimates falling in the range £172–245. The incremental cost-effectiveness ratio (ICER) for thromboprophylaxis for all compared with thromboprophylaxis for none based on the mean costs and QALYs is £13,524. Therefore, if a decision-maker is willing to pay £20,000 per QALY, it would be cost-effective to give thromboprophylaxis to all patients with lower-limb immobilisation due to injury if this was the only alternative to giving thromboprophylaxis to none. However, it can be seen that a significant proportion of the PSA estimates fall above the £20,000 per QALY threshold; therefore, there is a 24% probability that thromboprophylaxis for all is not cost-effective.
FIGURE 18.
Cost-effectiveness plane for the comparison of thromboprophylaxis for all vs. thromboprophylaxis for none.
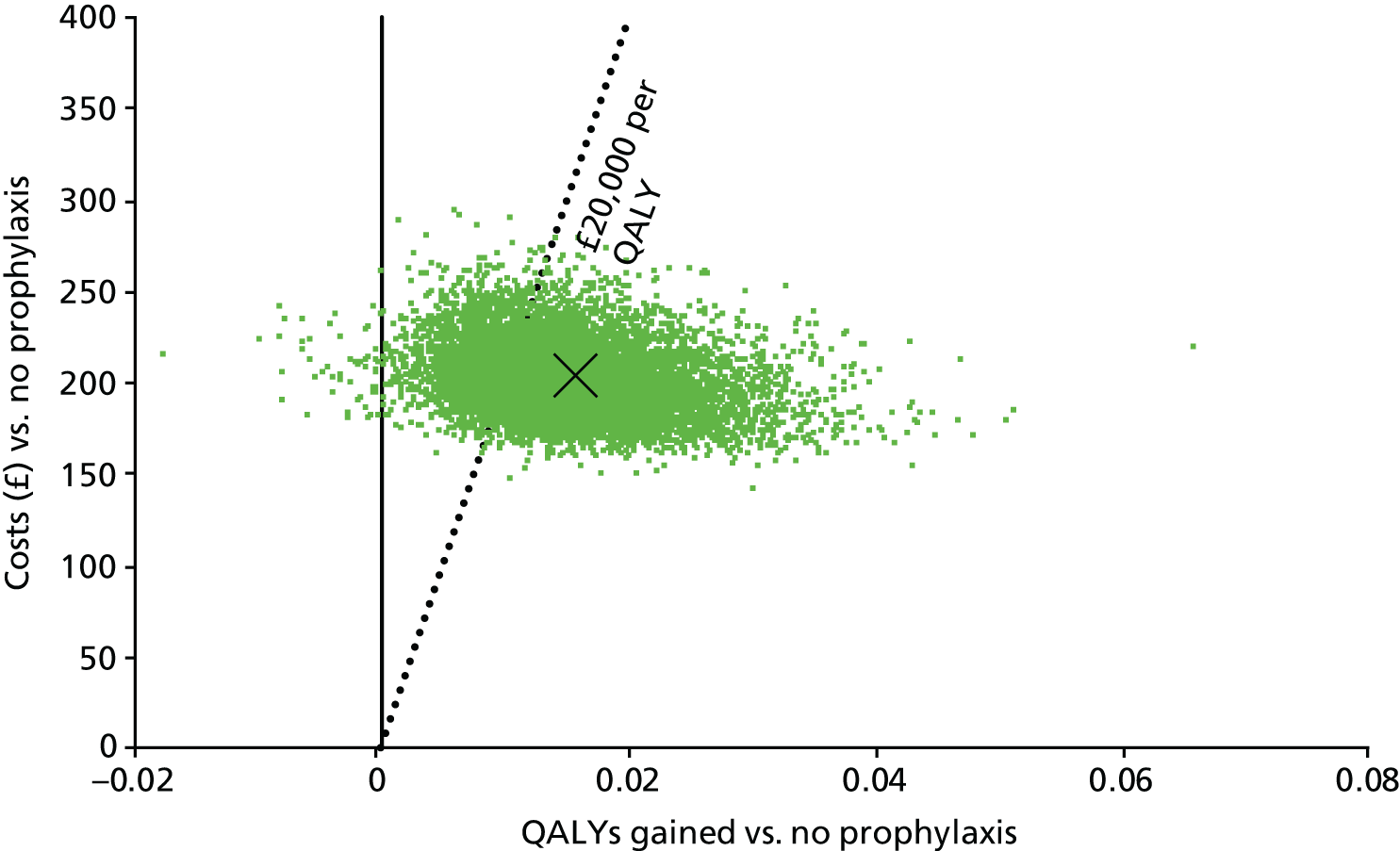
Cost-effectiveness of using a risk assessment model to determine thromboprophylaxis
The results of all of the thromboprophylaxis strategies considered in the model (based on the mean outputs of the PSA for 10,000 samples) are summarised in Table 23 and Figure 19. It can be seen in Figure 19 that, generally, the QALYs increase as the proportion receiving prophylaxis increases across the decision tools, with the QALY gains becoming more marginal as the proportion receiving prophylaxis increases. Furthermore, it can be seen in Figure 19 that L-TRiP(cast)-7 is extendedly dominated, as the ICER to move from L-TRiP(cast)-8 to L-TRiP(cast)-6 would be lower than the ICER to move from L-TRiP(cast)-8 to L-TRiP(cast)-7, but more QALYs are gained by L-TRiP(cast)-6. However, it should be noted that the point for L-TRiP(cast)-7 is close to falling on the cost-effectiveness frontier [i.e. on the line between L-TRiP(cast)-8 and L-TRiP(cast)-6]. The incremental analysis for the remaining non-dominated strategies is shown in Table 24. The optimal strategy would be L-TRiP(cast)-9 if the decision-maker values QALYs at £20,000 and L-TRiP(cast)-8 if the decision-maker values QALYs at £30,000.
| Prophylaxis strategy | % receiving prophylaxis | Sensitivity | Specificity | Absolute costs (£) | Absolute QALYs | Cost vs. no prophylaxis (£) | QALYs vs. no prophylaxis | ICER vs. prophylaxis for none (£) | INMB vs. prophylaxis for none, at £20,000 per QALY (£)a | INMB vs. prophylaxis for none, at £30,000 per QALY (£)a |
|---|---|---|---|---|---|---|---|---|---|---|
| Prophylaxis for none | 0 | 0 | 1 | 65.37 | 16.6198 | N/A | N/A | N/A | N/A | N/A |
| L-TRiP(cast)-10 | 31 | 0.651 | 0.722 | 128.11 | 16.6301 | 62.73 | 0.0103 | 6085 | 143.44 | 246.53 |
| L-TRiP(cast)-9 | 43 | 0.808 | 0.608 | 150.96 | 16.6326 | 85.58 | 0.0127 | 6724 | 168.96 | 296.23 |
| L-TRiP(cast)-8 | 63 | 0.926 | 0.397 | 194.41 | 16.6342 | 129.04 | 0.0144 | 8984 | 158.24 | 301.88 |
| L-TRiP(cast)-7 | 76 | 0.953 | 0.262 | 222.55 | 16.6345 | 157.17 | 0.0146 | 10,755 | 135.10 | 281.23 |
| L-TRiP(cast)-6 | 87 | 0.984 | 0.142 | 247.51 | 16.6348 | 182.14 | 0.0150 | 12,183 | 116.87 | 266.38 |
| Prophylaxis for all | 100 | 1 | 0 | 268.35 | 16.6348 | 202.98 | 0.0150 | 13,524 | 97.20 | 247.29 |
FIGURE 19.
Base-case results on CE plane (mean from 10,000 PSA samples).
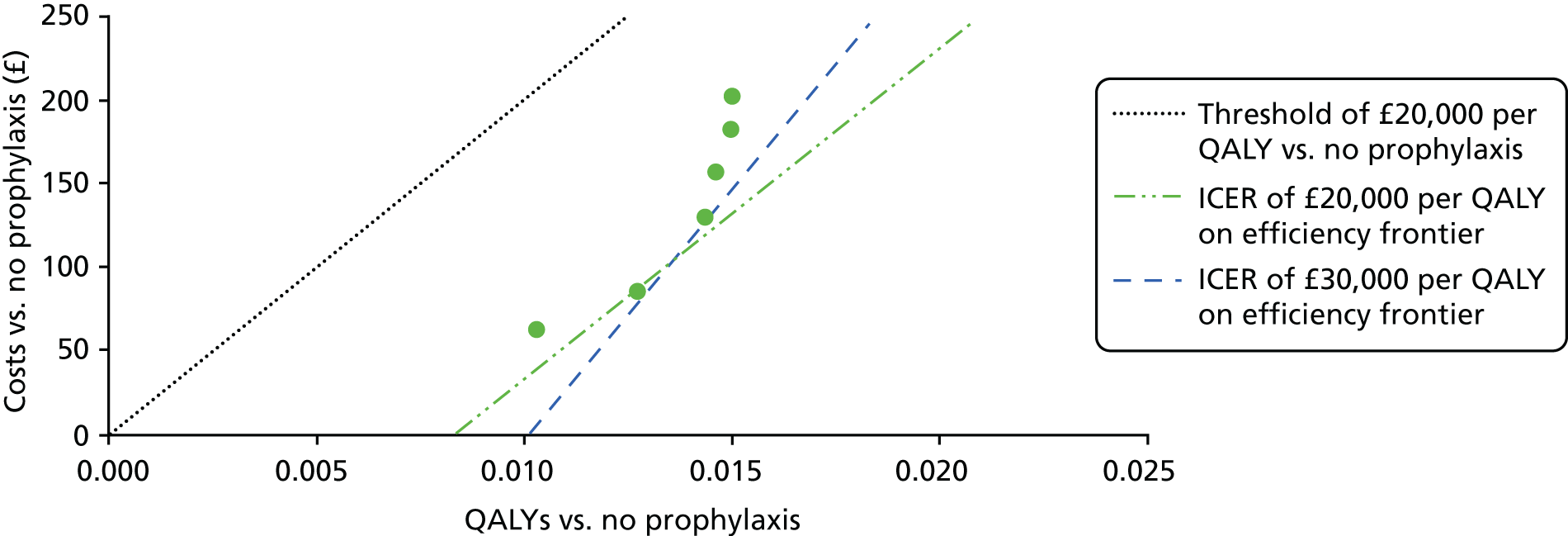
| Absolute costs (£) | Absolute QALYs | Cost vs. previous row (£) | QALY vs. previous row | ICER vs. previous row (£) | |
|---|---|---|---|---|---|
| No prophylaxis | 65.37 | 16.6198 | N/A | N/A | N/A |
| L-TRiP(cast)-10 | 128.11 | 16.6301 | 62.73 | 0.01031 | 6085 |
| L-TRiP(cast)-9 | 150.96 | 16.6326 | 22.85 | 0.00242 | 9448 |
| L-TRiP(cast)-8 | 194.41 | 16.6342 | 43.46 | 0.00164 | 26,550 |
| L-TRiP(cast)-6 | 247.51 | 16.6348 | 53.09 | 0.00059 | 90,554 |
| Prophylaxis for all | 268.35 | 16.6348 | 20.84 | 0.00006 | 357,026 |
Optimal balance of sensitivity and specificity for a risk assessment model
From the base-case results, it can be seen that as we move from higher to lower thresholds of the L-TRiP(cast) score, the QALYs gained increase as the sensitivity of the risk assessment tool increases but the cost increases as the specificity decreases. The ROC curve for the L-TRiP(cast) score provided by Nemeth et al. 32 allows us to explore where the optimal balance of sensitivity and specificity lies when assuming that it lies somewhere on the ROC curve provided by L-TRiP(cast). To do this, a linear regression on the logit scale was fitted to the points on the ROC plane from L-TRiP(cast)-6 to L-TRiP(cast)-10 (intercept = –1.5256, gradient = 0.8098, R2 = 0.9926). The sensitivity and specificity values were then varied between the L-TRiP(cast)-9 and L-TRiP(cast)-8 points of the curve to maximise the INMB using the deterministic model that uses mid-point parameter estimates. It was identified that, when valuing a QALY at £20,000, the INMB is maximised for a sensitivity of 84% and a specificity of 55%, resulting in 48% of patients being treated. When valuing a QALY at £30,000, the INMB is maximised for a sensitivity of 89% and a specificity of 46%, resulting in 57% of patients being treated. Therefore, even when using an optimised balance between sensitivity and specificity on the ROC curve predicted by the data from Nemeth et al. ,32 between 43% and 52% of patients would not receive thromboprophylaxis. The incremental costs and QALYs for these optimal points are shown in Figure 20. It can be seen from this that the optimal points on the ROC curve are actually extendedly dominated by the points for LTRiP(cast)-9 and LTRiP(cast)-8. This is because the ROC curve predicted by the linear regression on the logit scale passes below the data points for LTRiP(cast) scores of 9 and 8.
FIGURE 20.
Cost-effectiveness plane showing optimal points on the ROC curve when valuing a QALY at either £20,000 or £30,000 (generated using mid-point parameter values).
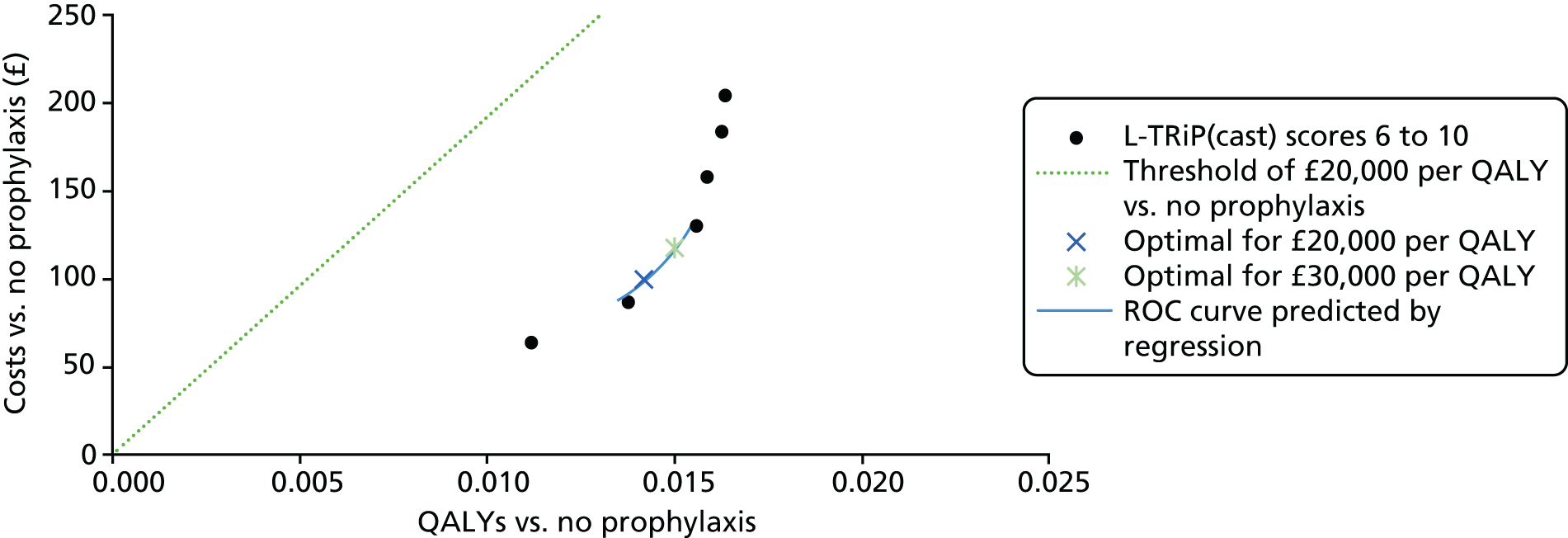
Uncertainty surrounding base-case results
Figure 21 shows the cost-effectiveness plane for L-TRiP(cast)-9 (the optimal strategy when valuing QALYs at £20,000) versus no prophylaxis. It can be seen that there is considerable uncertainty in the size of the QALY gain but there is a low chance of the optimal strategy resulting in QALY losses, compared with no prophylaxis, with 95% of the incremental QALYs falling in the range of 0.005 to 0.024. In terms of costs savings, 95% of the incremental costs fell in the range of £69 to £107, suggesting that the optimal strategy is unlikely to result in cost savings compared with no prophylaxis. This is expected, as prophylaxis results in definite costs to those receiving it but the benefits of preventing VTE are small and uncertain when averaged over the whole population receiving prophylaxis. Similar distributions of incremental costs and QALYs were seen for the other L-TRiP(cast) cut-off scores, with all predicting additional costs and additional QALYs and a mean ICER of < £20,000 relative to a strategy of no prophylaxis.
FIGURE 21.
Cost-effectiveness plane for L-TRiP(cast)-9 showing incremental costs and QALYs relative to no prophylaxis.
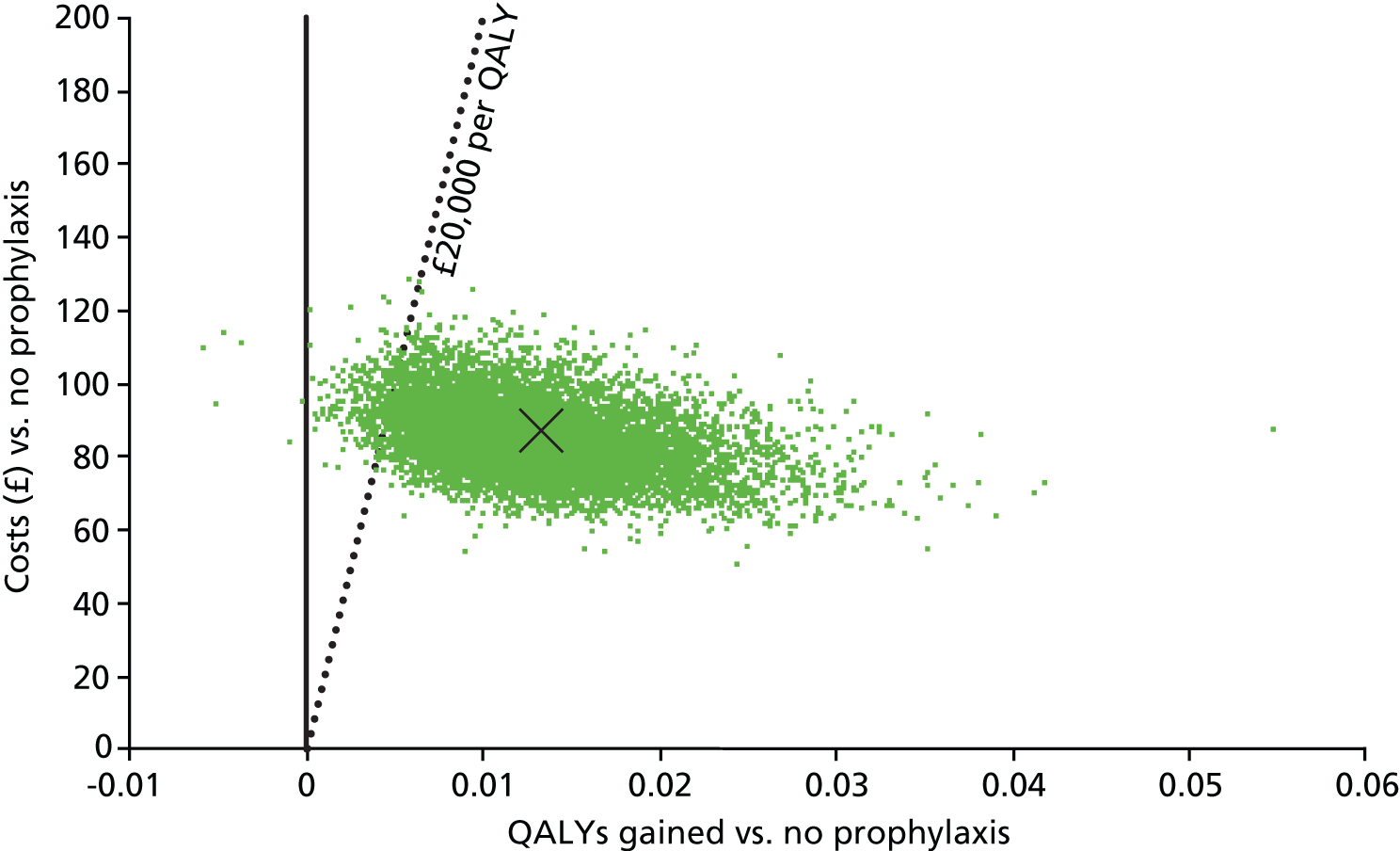
Figure 22 is the CEAC, which shows the probability that each strategy is optimal when varying the amount that the decision-maker is willing to pay for a QALY. It can be seen that L-TRiP(cast)-9 has the highest probability (66.8%) of being optimal when valuing a QALY at £20,000, which is consistent with the results in Table 24. L-TRiP(cast)-8 has a slightly higher probability of being optimal when valuing a QALY at £30,000, but there is also a high probability of L-TRiP(cast)-9 remaining optimal. This makes sense given that the ICER for L-TRiP(cast)-8 versus L-TRiP(cast)-9 is only just under £30,000 per QALY. It can also be seen that L-TRiP(cast)-7 always has a low probability of being optimal regardless of what the decision-maker is willing to pay and that the decision-maker would need to be willing to pay more than £100,000 per QALY before prophylaxis for all is the optimal strategy. This is interesting because if the risk-stratifying decision tools had not been included in the analysis, then prophylaxis for all would have been cost-effective compared with prophylaxis for none. This demonstrates the potential value of using decision tools to target prophylaxis in a cost-effective manner instead of focusing on evaluating all or nothing prophylaxis options.
FIGURE 22.
Cost-effectiveness acceptability curve.
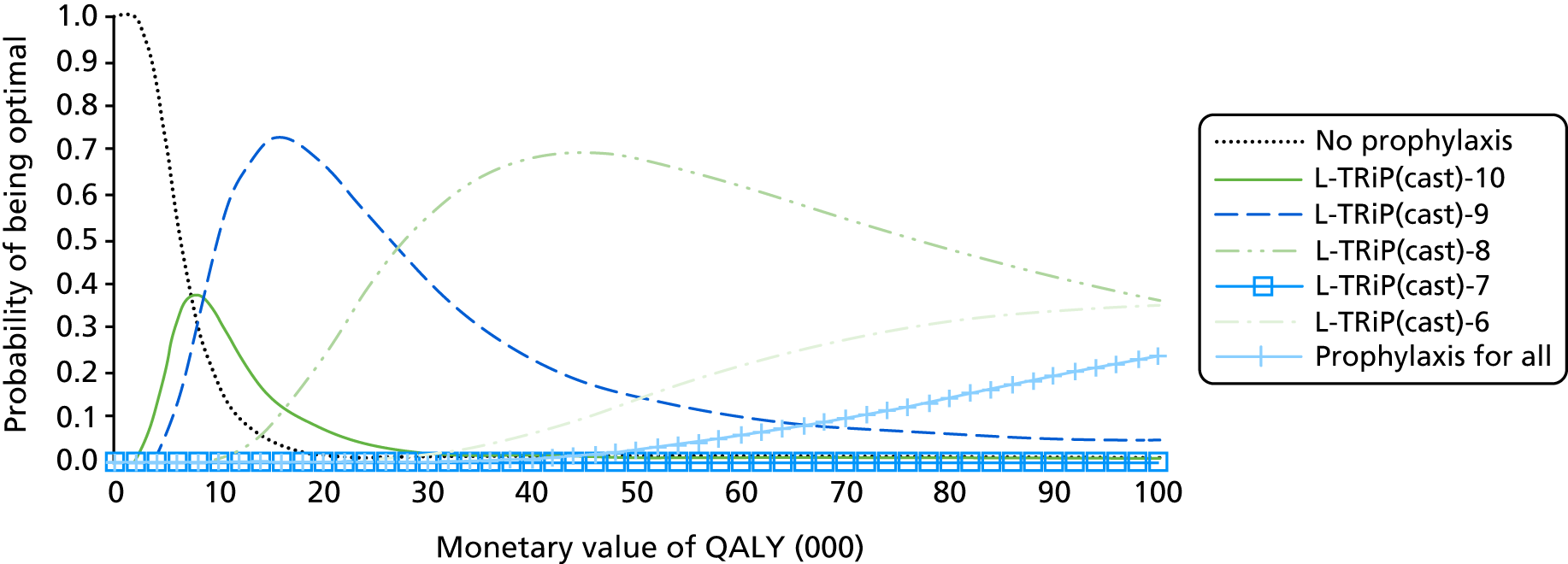
To demonstrate the impact of different strategies on a health service, L-TRiP(cast)-9 can be compared with a strategy of using prophylaxis for all across the English NHS. In Chapter 1, Description of the health problem, it was estimated that 70,000 people per year across the English NHS experience temporary lower-limb immobilisation due to injury as an outpatient. Using the mean outputs from the PSA, it is found that prophylaxis for all would result in an additional 0.0023 QALYs per person, but for an additional cost of £117.40 per person when compared with L-TRiP(cast)-9. Applied to the 70,000 annual population for the English NHS, the cost saving that could be achieved by giving prophylaxis to only those with a L-TRiP(cast) score of ≥ 9 would be £8.2M pounds and the QALYs lost would be 160. Conversely, if the impact of giving prophylaxis to patients at a L-TRiP(cast) score of 9 compared with treatment for none is considered, it is found that the additional cost to the NHS is £6.0M, with QALY gains of 891 for a population of 70,000 patients having lower-limb immobilisation. One-tenth of this additional cost to the NHS is the upfront cost of performing risk assessment in all patients with lower-limb immobilisation following injury to identify those requiring prophylaxis.
Value to the decision maker of reducing uncertainty in the estimates of cost-effectiveness
The global EVPI was estimated, which tells a decision-maker the value of reducing all current decision uncertainty associated with the PSA parameters. It was found that the overall EVPI was £4.12 per patient treated, suggesting that although treating patients at the L-TRiP(cast)-9 cut-off score would be expected to achieve an INMB of £168.96 per patient compared with no prophylaxis, based on current information, only 2.4% more INMB could be achieved with perfect information. This suggests that the value of reducing the decision uncertainty further is low on a per-patient basis. However, if the EVPI is estimated over 5 years, assuming that 70,000 patients have lower-limb immobilisation due to injury every year, then the overall discounted population EVPI is £1.3M.
Parameter EVPI analysis was also used to assess the importance of each individual parameter in generating uncertainty around the optimal strategy. Based on this, the most important parameters for decision uncertainty were the utility value for PTS, the efficacy of thromboprophylaxis in reducing VTE, the probability of PTS for patients with distal DVT and the utility decrement associated with taking prophylaxis. This suggests that the main factors driving uncertainty in the model are the efficacy and disutility of receiving prophylaxis, and the long-term complications of PTS. The incidence of PTS in patients with distal DVT is particularly important probably because asymptomatic DVT is more common than symptomatic DVT and the majority of asymptomatic DVTs are expected to be distal in this population. However, the magnitude of the overall EVPI suggests that a large-scale RCT comparing thromboprophylaxis with no thromboprophylaxis would be unlikely to be cost-effective.
It should be noted that EVPI analysis can capture only uncertainty related to parameters included in the PSA and will not capture any uncertainty associated with structural assumptions or the choice of data inputs used to estimate parameter uncertainty. These uncertainties are quantified instead using deterministic sensitivity analyses.
Important factors driving the cost-effectiveness estimates identified during model validation were:
-
incidence, long-term costs and utility decrement for PTS
-
baseline risks of VTE and the proportion of DVTs that are distal
-
costs and efficacy of prophylaxis and prophylaxis-related disutility.
These have been explored in deterministic sensitivity analyses by examining changes in the outputs of the deterministic model (the values produced when assuming mid-point parameter inputs) when changing one or more selected parameter inputs.
Scenario analyses and threshold analyses
The results of the individual scenario analyses are summarised in Table 25 by reporting the optimal thromboprophylaxis strategy when valuing a QALY at £20,000 and £30,000 for each scenario.
| Scenario description | Base-case parameter value | Alternative parameter value | Optimal strategy when valuing a QALY at £20,000 | Optimal strategy when valuing a QALY at £30,000 |
|---|---|---|---|---|
| Base case | N/A | N/A | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| High starting age | 46 years | 70 years | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| Low starting age | 46 years | 20 years | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| DOACS used for prophylaxis | LMWH with cost of £223.70 and utility decrement of 0.007 and an OR for preventing VTE of 0.52 | DOACs with cost of £84.23 and no utility decrement and an OR for preventing VTE of 0.52 | L-TRiP(cast)-8 | Prophylaxis for all |
| Fondaparinux used for prophylaxis | LMWH with cost of £223.70 and utility decrement of 0.007, and an OR for preventing VTE of 0.52 | Fondaparinux with cost of £355.66 and utility decrement of 0.007 and an OR for preventing VTE of 0.13 | L-TRiP(cast)-8 | L-TRiP(cast)-8 |
| Double utility decrement for LMWH | Utility decrement of 0.007 | Utility decrement of 0.015 | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| Cost of patients with CRNMB attending ED | £0 (costs of CRNMB excluded in base-case analysis) | £196 per patient having CRNMB | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| Discounting | 3.5% costs and 3.5% QALYs | 1.5% costs and 1.5% QALYs | L-TRiP(cast)-8 | L-TRiP(cast)-8 |
| Discounting | 3.5% costs and 3.5% QALYs | 3.5% cost and 1.5% QALYs | L-TRiP(cast)-8 | L-TRiP(cast)-8 |
| Utility decrement of PTS based on data from Lenert and Soetikno190 | 10% utility decrement for PTS vs. no PTS | 2% utility decrement for PTS vs. no PTS | L-TRiP(cast)-10 | L-TRiP(cast)-9 |
| Costs of PTS based on US estimates by Caprini et al.146 |
|
|
L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| Time to complete risk assessment scoring tool | 5 minutes of consultant time | 20 minutes of consultant time | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| Risk of PTS in patients with asymptomatic distal DVT | 15.6% at 3 years | None | L-TRiP(cast)-9 | L-TRiP(cast)-9 |
| Risk of PTS in patients with asymptomatic proximal DVT | 56.4% at 3 years (inflated vs. symptomatic as untreated) | Same as symptomatic proximal DVT: 32.4% at 3 years | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| Higher risk of bleeding without prophylaxis | 0.03% in 8 weeks | Five times base-case value, namely 0.15% in 8 weeks | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| Higher risk of bleeding without prophylaxis | 0.03% in 8 weeks | 10 times base-case value, namely 0.29% in 8 weeks | L-TRiP(cast)-9 | L-TRiP(cast)-9 |
| Proportion of symptomatic DVTs that are distal | 50% distal | 0% distal (all proximal) | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| Proportion of symptomatic DVTs that are distal | 50% distal | 100% distal (none proximal) | L-TRiP(cast)-9 | L-TRiP(cast)-8 |
| Proportion of asymptomatic DVTs that are distal | 84% distal | 0% distal (all proximal) | L-TRiP(cast)-8 | L-TRiP(cast)-8 |
| Proportion of asymptomatic DVTs that are distal | 84% distal | 100% distal (none proximal) | L-TRiP(cast)-9 | L-TRiP(cast)-9 |
| Increased VTE baseline risk | 8.39% total VTE with 1.34% symptomatic DVT or PE | Three times baseline, namely 25% total VTE with 4.01% symptomatic DVT or PE | L-TRiP(cast)-6 | Prophylaxis for all |
| Decreased VTE baseline risk | 8.39% total VTE with 1.34% symptomatic DVT or PE | One-third of baseline, namely 2.8% total VTE risk with 0.45% symptomatic DVT or PE | Prophylaxis for none | L-TRiP(cast)-10 |
Whether or not the age of the cohort being offered prophylaxis would alter the conclusions was examined, as it is likely that those receiving prophylaxis under the various decision tools would be older than the mean age of the whole group who have lower-limb immobilisation due to injury. It was found that increasing the mean starting age of the whole cohort to 70 years increased the ICERs but L-TRiP(cast)-9 remained optimal at £20,000 and L-TRiP(cast)-8 remained optimal at £30,000 with an ICER of £29,555 versus L-TRiP(cast)-9. This suggests that the decision to use a cohort approach based on average age is unlikely to have over- or underestimated prophylaxis benefits sufficiently to alter the key conclusions regarding the optimal strategy.
A threshold analysis was conducted to see how much the mid-point estimates of efficacy for LMWH in preventing VTE would need to change to alter the optimal prophylaxis strategies. It was found that a decrease in the hazard ratio (HR) (improvement in efficacy) from 0.54 to 0.44 would make L-TRiP(cast)-8 the optimal strategy at both £20,000 and £30,000 per QALY, whereas an increase in the HR (decrease in efficacy) to 0.60 would make L-TRiP(cast)-9 optimal at both £20,000 and £30,000 per QALY. An increase in the HR to 0.76 would be required for L-TRiP(cast)-9 to no longer be optimal at £20,000 per QALY. An increase in the HR to 0.84 would be required for treatment for none to be the optimal strategy at £20,000 per QALY.
It was examined whether or not the conclusions would differ if all patients were assumed to receive either fondaparinux or DOACs instead of LMWH for prophylaxis. For this, no difference in adverse event rates was assumed across the different prophylaxis options. Costs were assumed to vary in each case as per the costing analysis in Table 18. For DOACs, equivalent efficacy to LMWH was assumed and no utility decrement for DOACs was assumed because they are taken orally. For fondaparinux, the efficacy estimates from the NMA for fondaparinux versus control (OR 0.1, 95% predictive interval 0.05 to 0.3, from the random effects analysis) were used and the same utility decrement as applied for LMWH was assumed because both drugs are given by subcutaneous injection. Using DOACs shifted the optimal strategy when valuing a QALY at £20,000 from L-TRiP(cast)-9 to L-TRiP(cast)-8 and shifted the optimal strategy when valuing a QALY at £30,000 to treat all. Using fondaparinux resulted in the ICER for L-TRiP(cast)-8 versus L-TRiP(cast)-9 falling under £20,000 per QALY but L-TRiP(cast)-8 remained optimal when valuing a QALY at £30,000. It should be noted that these two scenarios are fairly crude and do not fully explore differences between the different drug classes in terms of adverse events. Furthermore, in the case of DOACs the analysis is based on an assumption of equivalent efficacy. The intention here was to explore whether or not the optimal cut-off point for providing thromboprophylaxis would differ when using a different drug class, rather than determining the optimal drug class to use for thromboprophylaxis.
In addition to a lack of precision in the estimates of utility decrement associated with PTS, there were differences in the estimates provided by different papers. The data from Lenert and Soetikno190 were used, which had lower decrements for PTS and showed that the optimal strategy when willing to pay £20,000 per QALY became L-TRiP(cast)-10, with L-TRiP(cast)-9 having an ICER of just under £30,000 in this scenario. This suggests that there is considerable decision uncertainty associated with the choice of utility data for PTS.
An assumption was made regarding the resource use associated with management of PTS based on clinical expert advice. A costing study from the USA146 reported higher costs, possibly related to more aggressive management of PTS. Whether or not using these higher cost estimates changed the conclusions was tested; it was found that the optimal strategies did not change, suggesting that the costs of managing PTS are not an important source of decision uncertainty.
It should also be noted that the PSA does not incorporate any uncertainty related to the estimates of sensitivity and specificity. Therefore, a scenario analysis was conducted in which, for each strategy, the specificity was fixed and the sensitivity was reduced so that it fell half-way between the observed value and the line on the ROC curve, which represents a tool that is no better than random selection. The alternative points are shown in Figure 23. The approximate AUC for the alternative points is 0.62, which is in the lower range of the CI for the AUC for the L-TRiP(cast) score is the plaster cast subgroup of the derivation cohort (AUC mean 0.76, 95% CI 0.66 to 0.86). 32 A similar AUC was achieved when L-TRiP(cast) score was validated in a subgroup of patients having plaster cast in the THE-VTE study (0.77, 95% CI 0.58 to 0.96) but a much better AUC was achieved when it was validated in the Milan study (0.95, 95% CI 0.91 to 0.99). 32 It can be seen in Figure 24 that, in this scenario assuming a lower AUC, the ICER for moving from each L-TRiP(cast) cut-off score to the next is fairly constant, such that the gains in QALYs when increasing the numbers treated are fairly proportional to the gains in cost across all L-TRiP(cast) cut-off scores. In this scenario, treatment for all is the optimal strategy when valuing a QALY at either £20,000 or £30,000. This tells us that the shape of the ROC curve is important in determining whether or not risk assessment tools can be used to target treatments more cost-effectively. If the tool used is less efficient at identifying the patients at risk, as indicated by a lower AUC, then a strategy of treating all patients would be most cost-effective. It was examined how much the sensitivity and specificity values could change before the RAM based thromboprophylaxis became extendedly dominated by treatment for all (i.e. when the ICER vs. no treatment was the same for both). It was found that for a specificity of 55%, the sensitivity would need to fall to 49% before thromboprophylaxis using a RAM became extendedly dominated by thromboprophylaxis for all. However, the absolute QALY gains would be 42% lower than the optimal point on the ROC curve and the costs would be only 16% lower.
FIGURE 23.
The ROC curve for the observed sensitivity and specificity values for L-TRiP(cast)-6 to L-TRiP(cast)-10 and the alternative values used in the sensitivity analysis.
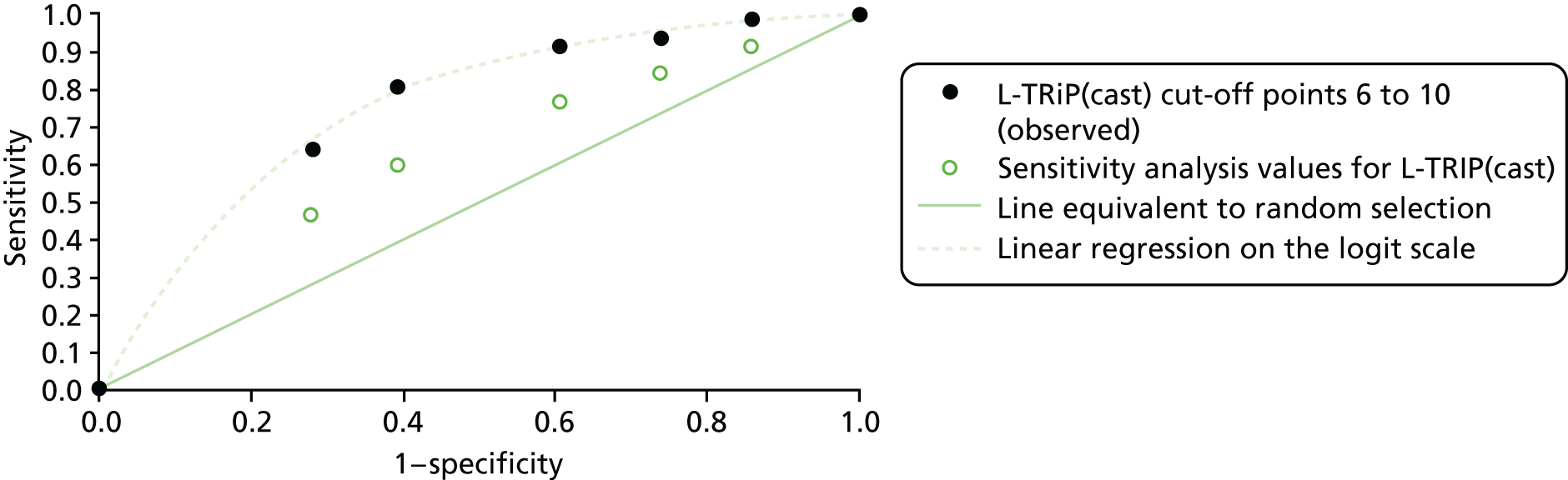
FIGURE 24.
Cost-effectiveness plane when assuming that L-TRiP(cast) performs less well than observed by Nemeth et al. 32 (AUC of 0.62 instead).
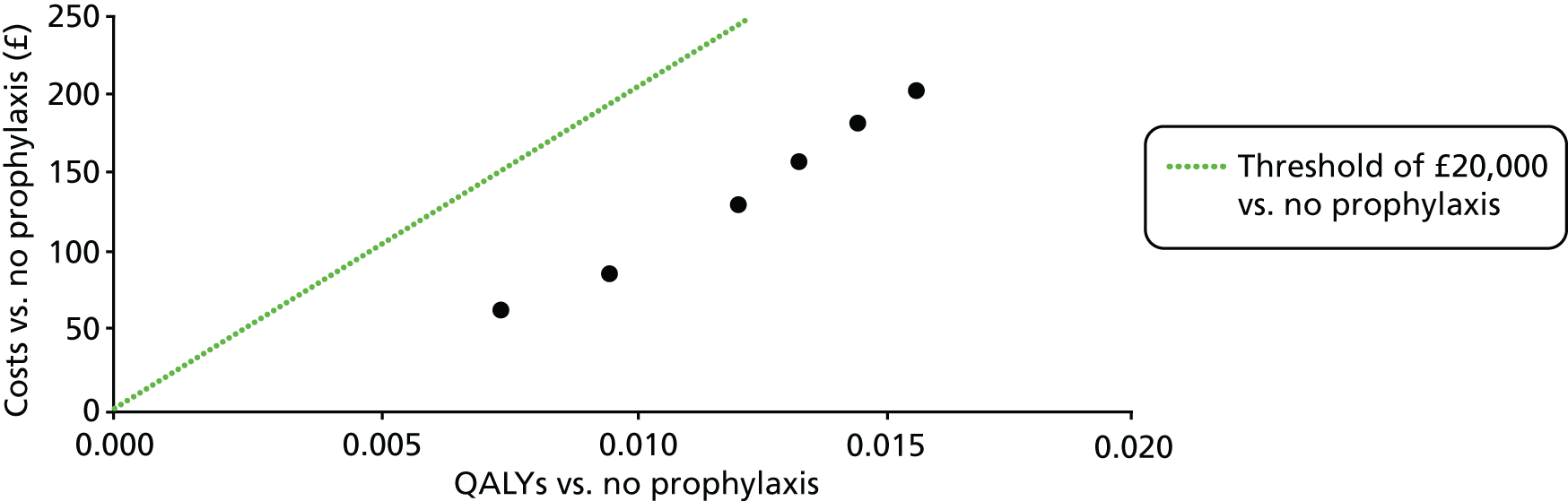
Given that the use of a decision tool would result in clinical time being spent for every patient who has lower-limb immobilisation, it was important to evaluate whether or not the assumption regarding the time taken for risk assessment was associated with significant decision uncertainty. The time taken was changed from 5 minutes to 20 minutes and it was found that this had an impact on the ICER only for L-TRiP(cast)-10 versus no prophylaxis; as this remained < £20,000, L-TRiP(cast)-9 remained optimal.
Whether or not the exclusion of costs related to CRNMB had an important impact on the model conclusions was examined and it was found that the optimal strategies did not change when assuming that all patients with CRNMB attended ED for assessment.
It was initially planned to have a zero rate of PTS in patients with asymptomatic distal DVT based on clinical expectations that the rate of PTS would be low in this group. Given that we had identified that PTS following distal DVT was an important driver of uncertainty in the model, a scenario analysis was conducted with a zero rate of PTS for asymptomatic distal DVT. Under this assumption, L-TRiP(cast)-9 was still the optimal strategy when willing to pay £20,000 per QALY but L-TRiP(cast)-8 had an ICER of > £50,000 compared with L-TRiP(cast)-9. In addition, under this scenario, prophylaxis for all had an ICER of £26,962 versus prophylaxis for none. This is because the marginal gains of preventing VTE are smaller when PTS risk is limited to the minority with proximal DVTs or symptomatic distal DVTs.
There was some uncertainty regarding the rate of PTS in asymptomatic proximal DVT that remains undetected and untreated, as most of the studies that identified asymptomatic proximal DVT treated patients. It was examined whether or not the conclusions varied if assuming the same rate of PTS as observed in symptomatic proximal DVT but it was found that the optimal strategies were unchanged.
The estimates of the proportion of symptomatic DVTs that are proximal were based on 16 DVTs reported in a single study. 59 To determine if this factor was an important driver of cost-effectiveness, the proportion was varied from 0% to 100%; it was found that this had no impact on the optimal strategy when valuing a QALY at either £20,000 or £30,000.
Similarly, as the estimates of the proportion of asymptomatic DVTs that are distal was based on a small number of events, an extreme analysis was conducted to see if varying the proportion from 0% to 100% had a large impact on the conclusions. It was found that, when assuming that all asymptomatic DVTs are distal, the optimal strategy was L-TRiP(cast)-9 when valuing a QALY at either £20,000 or £30,000. Conversely, when assuming that all asymptomatic DVTs are proximal, the optimal strategy was L-TRiP(cast)-8 when using a willing-to-pay threshold of either £20,000 or £30,000 per QALY.
Given that the major risk of adverse effects to patients is the risk of a bleed following prophylaxis, a threshold analysis was conducted to see how much higher the bleed risk in the general population would need to be to change the optimal strategy. It was found that L-TRiP(cast)-9 was optimal at £20,000 per QALY until the bleed risk reached 30 times that assumed in the base-case analysis. However, a sixfold increase in bleed risk in the population was required to make L-TRiP(cast)-8 have an ICER of > £30,000 per QALY. Furthermore, when the bleed risk is 15-fold higher than assumed in the base-case analysis, the treat-all strategy is no longer cost-effective relative to the treat-none strategy at a threshold of £20,000 per QALY.
The risk of VTE without prophylaxis was increased and decreased threefold; it was found that this had a significant impact on the optimal strategy, with a threefold increase resulting in treating all being the optimal strategy when valuing a QALY at £30,000, and a threefold decrease resulting in treat none being optimal when valuing a QALY at £20,000. For a strategy of treat all to result in fewer QALYs gained than lost, namely for there to be a net harm to patients, the VTE risk would need to be < 9% of its base-case value, suggesting that baseline risks would need to be substantially lower than thought before prophylaxis would be at risk of doing more harm than good to a patient’s health. However, at this level of risk, none of the prophylaxis strategies would be cost-effective.
Summary of key findings
-
The benefits of thromboprophylaxis in terms of reducing VTE outweigh the harms in terms of increased bleeding risk in the modelled population.
-
Thromboprophylaxis for all has an ICER of £13,524 compared with thromboprophylaxis for none.
-
When considering whether or not the cost-effectiveness of thromboprophylaxis can be improved by using a RAM to target thromboprophylaxis, the optimal strategy would be to use the L-TRiP(cast) score with a threshold score of 9 if the £20,000-per-QALY threshold is used and with a threshold score of 8 if the £30,000-per-QALY threshold is used.
-
An optimal RAM would be expected to operate with a sensitivity of 84–89% and specificity of 46–55%, assuming the ROC curve for the L-TRiP(cast) score reflects the typical trade-off between sensitivity and specificity in risk assessment.
Chapter 5 Discussion
Statement of principal findings
Clinical effectiveness reviews
Pharmacological thromboprophylaxis for preventing venous thromboembolism
In the meta-analysis, it was found that thromboprophylaxis with LMWH reduced any VTE (OR 0.52, 95% CrI 0.37 to 0.71), clinically detected DVT (OR 0.40, 95% CrI 0.12 to 0.99) and PE (OR 0.17, 95% CrI 0.01 to 0.88) compared with no thromboprophylaxis. The effect of LMWH thromboprophylaxis varied between different VTE outcomes but all estimates were consistent with an approximate halving of risk. The number of deaths and bleeding events were too small to draw reliable conclusions. Thromboprophylaxis with fondaparinux also reduced any VTE (OR 0.13, 95% CrI 0.05 to 0.30) and clinically detected DVT (OR 0.10, 95% CrI 0.01 to 0.94) compared with no thromboprophylaxis, but the effect on PE was inconclusive (OR 0.47, 95% CrI 0.01 to 9.54). Event rates for symptomatic DVT and PE were generally low across the studies, so an approximate halving of risk may result in a small absolute risk reduction. Network meta-regression did not identify evidence of effect modification associated with population characteristics, type of injury, type of immobilisation or duration of treatment. There was evidence of difference in the effect of different types of LMWH used, with certoparin having the highest probability of the greatest effect on any VTE, but this was based on findings from one study. 52
Individual risk factors associated with venous thromboembolism risk
In the systematic review, it was found that only older age was consistently associated with increased risk of VTE across the included studies. Four studies53,60,70,71 showed that higher BMI was associated with increased risk and six studies11,50,52,53,69,70 show associations between injury type and risk of VTE. All studies were deemed to be at moderate23,50,52,53,60,68,71 or serious9,11,64–67,69,70 risk of bias overall following structured quality assessment. The use of individual risk factors to predict VTE risk in people with lower-limb immobilisation due to injury is, therefore, based on limited and weak evidence.
Risk assessment models for prediction of venous thromboembolism risk
The systematic review identified a number of RAMs but only two studies32,82 (both case–control design) provided estimates of sensitivity and specificity for three of the RAMs. The L-TRiP(cast) score32 using a threshold score of 8 (sensitivity 92.6%, specificity 39.7%) or 9 (sensitivity 80.8%, specificity 60.8%) may have appropriate accuracy for use in practice but these estimates are subject to considerable uncertainty.
Expert consensus study
The Delphi study resulted in agreement that the following were potentially useful predictors of VTE in lower-limb immobilisation due to injury: age, BMI of > 30 kg/m2, active cancer, pregnancy/puerperium, thrombophilia, prior VTE, surgery in the previous 3 months, exogenous oestrogen, lower-limb paralysis, superficial thrombophlebitis, Achilles tendon rupture, above-knee plaster cast and rigid immobilisation in a cast (as opposed to removable immobilisation). Most of the predictors agreed by the experts were not supported by evidence in the systematic review. Therefore, it appears that experts are willing to draw on evidence from other patient groups, pathophysiological knowledge and their clinical experience to identify predictors of VTE.
Most of the agreed predictors were included in one or more of the RAMs, presumably reflecting the role of clinical expertise in developing most of the RAMs. However, the expert group were unable to reach consensus on many potential predictors, including many variables that were included in one or more RAMs. The differences between RAMs are likely to reflect differences in expert opinion, which may, in turn, reflect the lack of available evidence for VTE predictors in lower-limb immobilisation due to injury.
Economic evaluation
Decision-analytic modelling compared thromboprophylaxis for all people with lower-limb immobilisation due to injury with thromboprophylaxis for none and risk-based approaches [i.e. the L-TRIP(cast) score was used to select higher-risk patients for thromboprophylaxis]. Effectiveness analysis suggested that the rate of serious adverse outcomes (ICH or death from VTE or bleeding) would be very low regardless of the approach used (around 1 in 4000). Rates of symptomatic DVT and non-fatal PE would be higher (around 22 to 41 per 10,000 and 49 to 91 per 10,000, respectively) and varied across the strategies. The total number of major bleeds, including fatal and non-fatal ICHs, ranged from 4.03 per 10,000 with no thromboprophylaxis (reflecting baseline population rates and bleeding as a result of treatment of subsequent VTE) to 5.38 per 10,000 when thromboprophylaxis is given to all. The higher rates of VTE events compared with bleeding events meant that overall quality-adjusted life expectancy increased in accordance with the proportion of the population receiving thromboprophylaxis with each strategy. It therefore appears that the benefits of thromboprophylaxis in terms of reducing VTE outweigh the harms in terms of increased bleeding risk in the modelled population.
Cost-effectiveness analysis comparing thromboprophylaxis for all with thromboprophylaxis for none showed that thromboprophylaxis for all gained a mean of 0.0147 QALYs at a mean cost of £204 per patient, with an ICER of £13,524. This suggests that, if no acceptable RAM is available, then thromboprophylaxis for all would be cost-effective according to NICE thresholds, but there was some uncertainty in this estimate, with a 24% probability that thromboprophylaxis for all is not cost-effective at the £20,000-per-QALY threshold.
Cost-effectiveness analysis comparing thromboprophylaxis for all, thromboprophylaxis according to varying thresholds of the L-TRiP(cast) score and thromboprophylaxis for none showed that the optimal strategy would use the L-TRiP(cast) score with a threshold of 9 if the £20,000-per-QALY threshold is used and with a threshold of 8 if the £30,000-per-QALY threshold is used. Analyses to determine the optimal trade-off between sensitivity and specificity suggested that INMB is maximised when sensitivity is 84% and specificity is 55% when the £20,000-per-QALY threshold is used, or when sensitivity is 89% and specificity is 46% when the £30,000-per-QALY threshold is used. An optimal RAM would therefore be expected to operate with a sensitivity of 84–89% and a specificity of 46–55%, assuming that the ROC curve of the L-TRiP(cast) score is typical of RAMs.
The EVPI analysis suggested that the most important parameters for decision uncertainty were the utility value for PTS, the effectiveness of thromboprophylaxis in reducing VTE, the probability of PTS for patients with distal DVT and the utility decrement associated with taking thromboprophylaxis. The value of reducing the decision uncertainty further was low on a per-patient basis. However, the uncertainty surrounding estimates of RAM accuracy in the PSA could not be appropriately reflected. As noted in the review of RAMs, these estimates are based on very weak and limited data, and are therefore likely to be subject to substantial uncertainty.
Strengths and limitations of the assessment
Clinical effectiveness review
Pharmacological thromboprophylaxis for preventing venous thromboembolism
The meta-analysis synthesised data from 6857 participants in 13 randomised trials that were judged to have a low risk of bias or some concerns only for most quality criteria. This represents a large, methodological robust data set across a variety of settings that allows us to draw generalisable conclusions. Reasonably precise estimates of the effect of thromboprophylaxis compared with control could be produced for most outcomes. Statistical power was more limited for uncommon outcomes, such as PE, but even here it was possible to generate an estimate that suggested a statistically significant effect. It was also possible to undertake a NMA to compare across three alternatives: (1) LMWH, (2) fondaparinux and (3) no thromboprophylaxis.
A recent Cochrane meta-analysis by Zee et al. 18 reported data from eight trials,49,51–56,59 including 3680 participants, that compared thromboprophylaxis with no treatment or placebo. They found that LMWH was associated with a significantly reduced risk of any DVT (OR 0.45, 95% CI 0.33 to 0.61) and symptomatic VTE (OR 0.40, 95% CI 0.21 to 0.76) but not PE (OR 0.50, 95% CI 0.17 to 1.47). Zee et al. 18 excluded four trials that were included in this analysis (Goel et al. ,50 Selby et al. ,58 Gehling et al. 23 and Samama et al. 57), and one additional trial was published after their updated meta-analysis (Zheng et al. 60). Two of the trials were excluded because they focused on operatively treated fractures rather than immobilisation (Goel et al. 50 and Selby et al. 58), one because the comparator was aspirin (Gehling et al. 23) and one because the intervention was fondaparinux rather than LMWH (Samama et al. 57). The inclusion of these trials has ensured that this analysis is more comprehensive and provides more precise estimates of effectiveness, but at the expense of greater heterogeneity.
This analysis was inevitably limited by the primary data. The variety of settings and patient groups may be a strength in terms of increasing generalisability; there was evidence of heterogeneity of effect for many of the outcomes, suggesting that effects may differ between populations. Three trials23,52,53 were judged as having a high risk of bias on the basis of outcome ascertainment being potentially subject to bias in an open-label trial. One trial that administered aspirin to the control group was included on the basis that NICE guidelines on VTE1,24 do not consider aspirin or other antiplatelet agents to be appropriate for VTE prophylaxis and aspirin is not indicated as a treatment for VTE prophylaxis in lower-limb immobilisation. 21,25,26 If aspirin has a significant prophylactic effect, then this trial may underestimate the effect of thromboprophylaxis.
The primary studies had a number of selection criteria that limit the ability to apply the findings to certain populations. Patients at a high risk of VTE (such as those with active cancer, thrombophilia, previous VTE or pregnancy/puerperium) and those with an increased risk of bleeding were often excluded. The studies generally included patients with rigid immobilisation rather than those with a degree of movement or a removable cast or splint, so the findings may be applicable only to those with full immobilisation.
The analysis included a substantial number of participants but the event rates for some outcomes were very low. As a consequence, it was not possible to produce reliable estimates of the effect of thromboprophylaxis on major bleeding or death. The low rate of bleeding provides some reassurance that thromboprophylaxis is not causing a clinically important rate of serious adverse outcome in this population but this may not be applicable to patients at a higher risk of bleeding.
Individual risk factors associated with venous thromboembolism risk
This is the first systematic review conducted to look directly at individual risk factors increasing the risk of VTE in patients with lower-limb injury immobilised in plaster, discharged to an outpatient setting. This is an important distinction, as the population of interest differs markedly from generic thrombosis data sets; patients with lower-limb injury tend to be younger, more active and devoid of comorbidity than those presenting with unprovoked or cancer-associated thrombosis. Previous work has attempted to address a similar issue in patients undergoing elective foot and ankle surgery. 72,73,81 We consider this to be a different population because of the absence of acute blunt trauma causing local vessel/endothelial injury, expert postoperative immobilisation and often bespoke immobilisation regimes.
The review was undertaken in accordance with guidelines published by the Centre for Reviews and Dissemination75 and the protocol was registered with the PROSPERO register. 38 Clinical experts were involved throughout as checkers and to assess the validity and applicability of research during the project. Descriptive statistics were reported to provide plain insight into the limited evidence base applicable to the subject matter and the scientific concerns regarding validity of the data.
The review was limited by a lack of studies specifically examining risk prediction in lower-limb immobilisation due to injury. Therefore, studies, such as RCTs, that were designed for another purpose but reported risk predictors in their analyses were included. The studies of risk prediction were a combination of prospective cohorts and retrospective health database registries. Both have significant limitations. Retrospective studies of health database registries may have large numbers but may be limited by poor data quality and failure to accurately ascertain outcomes. Prospective cohorts may have better-quality data but lack statistical power because of smaller numbers. The included studies demonstrated high levels of heterogeneity, so a meta-analysis could not be undertaken.
Several studies included patients receiving operative intervention and short inpatient stays. Following the introduction of NICE guidance on thromboprophylaxis to reduce the risk of hospital-acquired thrombosis, it is reasonable to assume that, in a modern health-care environment, all these patients would receive some form of routine thromboprophylaxis. 24 For this reason, inclusion of these patients could lead to false reassurance regarding low incidence of VTE. However, patients with a short inpatient stay (< 5 days) were considered to fit within the scope of interest; these patients often remain temporarily immobilised for a period of 4–8 weeks in total, and debate persists about the role of thromboprophylaxis that is similar to debate around patients discharged directly from the ED.
All the studies within the review were classed as being at moderate or severe risk of bias. Therefore, any conclusions regarding the influence of risk factors on the subsequent development of VTE drawn are based on weak evidence and have the potential to be inaccurate.
Risk assessment models for prediction of venous thromboembolism risk
This review had strengths of following recognised guidance, prospective registration, a clear protocol and drawing on appropriate clinical and reviewing expertise. It was anticipated that the data would not allow meta-analysis; therefore, descriptive analyses only were planned.
A previous review by Watson et al. 82 identified two of the RAMS included in this review (Keenan et al. 31 and Roberts et al. 17), along with three generic RAMs that could be applied to people with lower-limb immobilisation due to injury. 210–212 Watson et al. ’s82 review then undertook primary analysis of these two RAMs to estimate sensitivity and specificity for predicting VTE. This review included these data and a number of other studies32,78–81 but only the study of Nemeth et al. 32 provided estimates of sensitivity and specificity.
The review is, therefore, limited by the paucity of data. Furthermore, case–control designs are known to be associated with a risk of bias,213 so sensitivity and specificity may have been overestimated. The study by Watson et al. 82 was relatively small (21 cases and 21 controls), so estimates of sensitivity and specificity are imprecise. The study by Nemeth et al. 32 involved validation using two data sets but each only contained a small number of patients with lower-limb immobilisation (32 cases, 7 controls, and 143 cases, 8 controls, respectively).
Expert consensus study
The Delphi study involved a wide range of experts from emergency medicine, orthopaedics and haematology, and used recognised techniques to attempt to achieve consensus without supressing divergent views. There were acceptable levels of participation and the experts seemed to understand and engage with the process.
Expert consensus is considered to represent weak evidence and is usually sought only when (as in the case of VTE risk prediction in lower-limb immobilisation) other forms of evidence are weak or absent. It is hoped that experts will draw on weak evidence appropriately and combine it with clinical experience and pathophysiological understanding. However, experts may be subject to a number of cognitive biases that may influence their judgement. For example, the availability heuristic may lead experts to place undue emphasis on a risk predictor if they have seen a case in which a patient with that characteristic developed VTE after lower-limb immobilisation.
The Delphi process achieved consensus on 13 predictors but failed to achieve consensus on many more. This is perhaps unsurprising in the light of the limited evidence base relevant to the population of interest. It could be argued that achieving consensus on 13 predictors reflects undue certainty in the light of the limited evidence to support these judgements.
Economic evaluation
A key strength of the de novo economic analysis is that it is able to synthesise the evidence on both benefits and harms to assess the overall impact of different thromboprophylaxis strategies in people having lower-limb immobilisation. Therefore, it was possible to explore the trade-off between preventing VTE and the adverse effects associated with prophylaxis, including the direct impact of subcutaneous injections of anticoagulants on patient quality of life. The estimates of clinical effectiveness were based on the systematic review and meta-analysis and the decision uncertainty associated with the uncertainty in the estimates of clinical effectiveness was captured in the model. The availability of the ROC curve for the L-TRiP(cast) score allowed us to explore what the optimal sensitivity and specificity might be for a tool to identify patients needing thromboprophylaxis when assuming that any future tool would have similar characteristics to L-TRiP(cast).
The main limitation of the economic analysis was that it was not possible to incorporate the uncertainty in the sensitivity and specificity estimates for the RAMs within the PSA as these were not reported. A scenario analysis was conducted, which suggested that the cost-effectiveness of using a RAM to guide thromboprophylaxis is dependent on the performance characteristics of the RAM, but it was not possible to quantify the decision uncertainty associated with the RAMs currently available.
Another potential limitation of the economic analysis is that a cohort modelling approach was used, which estimates outcomes based on average patient characteristics and, therefore, does not allow for heterogeneity in patient outcomes on the basis of patient characteristics. However, whether or not variation in outcomes on the basis of age would significantly alter the conclusions of the model was explored; it was found that the optimal thromboprophylaxis strategy was not sensitive to variations in age.
The estimate of the incidence of major bleeds during thromboprophylaxis was based solely on the incidence of GI bleeds and ICHs; therefore, this may have underestimated the impact on costs and QALYs of major bleeds at other sites. In addition, CRNMBs were excluded from the model. However, the sensitivity analyses suggest that neither of these factors is likely to have significantly biased the results, as incorporating costs for CRNMBs and increasing the risk of bleeding during thromboprophylaxis fivefold did not alter the main conclusions.
Another potential limitation is that many of the data sources quantifying the impact of VTE on patients, such as the incidence and quality-of-life impact of post-thrombotic syndrome following DVT, were not specific to patients having lower-limb immobilisation. Therefore, the benefits of thromboprophylaxis in this population may have been overestimated if the risks of complications following DVT are lower in patients having lower-limb immobilisation than in other groups at risk of VTE.
Uncertainties
The main uncertainty identified in the analysis related to the prognostic accuracy of RAMs. The estimates were based on very weak data but suggested that L-TRiP(cast) score, using a threshold score of 8 or 9, would be an optimal strategy. However, this conclusion holds only if the prognostic accuracy of L-TRiP(cast) is confirmed. More precise and accurate estimates of the prognostic accuracy of RAMs are required but this may be difficult to achieve if higher-risk patients receive thromboprophylaxis as standard care.
Most of the effectiveness data for thromboprophylaxis relate to LMWH, with a smaller number relating to fondaparinux. LMWH is administered by injection, thereby incurring additional costs and inconvenience for patients. DOACs are taken orally and, therefore, do not incur these additional costs and inconvenience. However, no studies evaluating the effectiveness of DOACs as thromboprophylaxis for lower-limb immobilisation were found. DOACs have been used for thromboprophylaxis in other conditions and have been shown to be generally as safe and effective as LMWH. 214–216 On this basis, a secondary economic analysis was undertaken, assuming that DOACs were as effective as LMWH and could be delivered at lower cost and with less inconvenience. This suggested that at the £30,000-per-QALY threshold, DOACs would be cost-effective in a thromboprophylaxis-for-all strategy, even compared with an optimal RAM. The obvious uncertainty affecting this conclusion is whether or not it can be assumed that DOACs are at least as effective and safe as LMWH.
The value-of-information analysis showed that the most important parameters for decision uncertainty were the utility value for PTS, the effectiveness of thromboprophylaxis in reducing VTE, the probability of PTS for patients with distal DVT and the utility decrement associated with taking prophylaxis. The importance of uncertainty around PTS is consistent with the observation from the modelling that the benefit of thromboprophylaxis lies in avoiding long-term complications rather than avoiding short-term adverse outcomes. The utility decrement associated with taking prophylaxis is relevant to the potential role of DOACs discussed in the paragraph above, because most of the decreased utility is assumed to be as a result of the need to administer LMWH by injection.
The primary studies for the review of effectiveness, and, by implication, the economic model, excluded a number of important patient groups. Patients at a high risk of VTE, because of active cancer, previous VTE, pregnancy/puerperium or thrombophilia, were excluded but, as they have a higher risk of VTE, these patients are even more likely to benefit from thromboprophylaxis. Patients with an increased risk of bleeding were also excluded; these represent a more difficult group with regard to guiding recommendations. The model assumed a low risk of bleeding so, clearly, the findings of modelling analysis cannot be applied to this group. It may be possible to develop the model to provide estimates of overall effectiveness if bleeding risk is higher, but increased bleeding risk is often associated with conditions that also increase the risk of VTE. It is, therefore, unlikely that general recommendations can be made for those with an increased risk of bleeding and decisions will have to be made on an individual case-by-case basis.
The primary studies for the review of effectiveness were also generally limited to patients with full, rigid immobilisation and did not include those with more limited immobilisation, such as splints that allow a degree of movement and removable splints or casts. There are pathophysiological reasons for expecting the VTE risk to be lower for these patients and the benefit of thromboprophylaxis to be consequently lower or even negligible. However, current evidence is insufficient to determine whether or not this is the case and what, if any, role there may be for thromboprophylaxis.
Patient and public involvement
The patient and public involvement (PPI) representatives were involved in a number of elements of the study and met regularly with the project team to discuss the interpretation and implications of the emerging findings. The PPI representatives identified the following issues at these meetings:
-
The risks and benefits of thromboprophylaxis need to be explained to patients in clear and comprehensible terms so that they can participate in decision-making. It would be helpful to provide this information in written form, along with information about the symptoms of VTE and what to do if they have concerns.
-
It was considered acceptable to provide thromboprophylaxis in accordance with the patient’s risk of VTE. It may be acceptable for patients to be involved in assessing their risk of VTE but this should be done in consultation with a health professional.
-
If a risk-based approach was used and a patient was assessed as not requiring thromboprophylaxis on the basis of lack of cost-effectiveness when the risk is low, then they should be informed of the possible benefit of thromboprophylaxis in case they wish to arrange their own treatment.
-
Use of LMWH for thromboprophylaxis has clear disadvantages related to the inconvenience and discomfort of injections. Oral treatment would be much more acceptable but the risks of DOACs need to be explained to patients, specifically the lack of a means of reversing DOACs in the event of bleeding. The lack of research into the use of DOACs as thromboprophylaxis for lower-limb immobilisation was also a concern.
-
If the risk of adverse outcome is low (i.e. < 1 in 100), then patients may not think the benefit of thromboprophylaxis is worth the inconvenience and discomfort of LMWH.
-
An implementation study of risk-based thromboprophylaxis, potentially involving comparison of different approaches, would be acceptable provided it was justified on the basis of current practice being variable and the need to identify best practice.
Assessment of factors relevant to the NHS and other parties
Current NICE guidance1 recommends that clinicians consider pharmacological VTE prophylaxis with LMWH or fondaparinux for people with lower-limb immobilisation whose risk of VTE outweighs their risk of bleeding. This analysis suggests that the risk of VTE outweighs the risk of bleeding for any patient who does not have risk factors for bleeding. The review for the NICE guidance1 did not identify any relevant economic evidence and only considered the unit costs for different agents (LMWH and fondaparinux). This economic analysis showed that thromboprophylaxis with LMWH is cost-effective compared with no thromboprophylaxis and a risk-based strategy is potentially optimal, when valuing a QALY at £20,000 to £30,000. The NICE guidance1 also recommends that clinicians assess all patients to identify the risk of VTE and bleeding, but does not identify or recommend any specific RAM for lower-limb immobilisation. This analysis suggests that the L-TRiP(cast) score with a threshold score of 8 or 9 could have appropriate prognostic accuracy for cost-effective risk stratification in lower-limb immobilisation but the available estimates of prognostic accuracy are very uncertain.
Chapter 6 Conclusions
Implications for service provision
The meta-analysis of effectiveness suggested that thromboprophylaxis in lower-limb immobilisation due to injury approximately halves the risk of any VTE and is associated with reductions in the risks of symptomatic DVT and PE. However, the evidence is limited to LMWH and fondaparinux, so it is unclear whether or not the findings can be extrapolated to DOACs. This in an important consideration as the absolute risks of clinically relevant VTE are low and patients may not be willing to submit to the inconvenience of parenteral treatment to reduce a relatively small risk.
The economic analysis suggested that thromboprophylaxis is effective and cost-effective compared with no thromboprophylaxis, so it would be reasonable to offer thromboprophylaxis to patients undergoing lower-limb immobilisation due to injury. This is based on the potential for thromboprophylaxis to reduce the risk of DVT and PE, with their long-term sequelae, rather than any meaningful reduction in the risk of mortality. The economic analysis also suggested that risk-based thromboprophylaxis using a RAM with a sensitivity of 84–89% and specificity of 46–55% is, potentially, the most cost-effective approach. This is similar to the prognostic accuracy of the L-TRiP(cast) score using a threshold score of 8 or 9, although estimates of sensitivity and specificity are very uncertain.
The cost-effectiveness of using an appropriate RAM is based on (1) reducing the number of people requiring thromboprophylaxis (and thus costs) compared with thromboprophylaxis for all, with only a small reduction in effectiveness and (2) increasing the number of VTE events prevented (and this effectiveness) compared with no thromboprophylaxis, with only a small increase in costs. Assuming universal acceptance by patients, a risk-based strategy, as outlined in the previous paragraph, would cost the English NHS £6M per year and gain 891 QALYs compared with no thromboprophylaxis. Compared with this, providing thromboprophylaxis for all would cost an additional £8.2M per year and gain an additional 160 QALYs. These estimates are not intended to be precise figures, as strategies are unlikely to be implemented perfectly and patients may decline treatment, but they provide an indication of the potential implications of different strategies for service provision.
The PPI representatives highlighted the importance of patient involvement in decision-making and the need for clear and comprehensible information to be provided. This has important implications for service provision. To participate in shared decision-making, patients need to understand that the risk of clinically important VTE is relatively low but that it can be reduced by thromboprophylaxis. The effectiveness of thromboprophylaxis relies on the benefits of reducing DVT and PE (and their sequelae), outweighing a small increase in the risk of bleeding, but VTE events may still occur despite thromboprophylaxis. The risks of death from VTE or bleeding after immobilisation due to injury are very small regardless of the treatment strategy, and thromboprophylaxis is unlikely to have any significant impact on the risk of death.
Suggested research priorities
This analysis suggested that risk-based thromboprophylaxis using a RAM with sensitivity of 84–89% and specificity of 46–55% would be the most cost-effective strategy. However, the current evidence base for RAMs is very limited and estimates of sensitivity and specificity are subject to substantial uncertainty. Improving the evidence base for RAMs is therefore a key priority.
Ideally, a large prognostic cohort study of people experiencing lower-limb immobilisation due to injury would be undertaken to estimate the prognostic accuracy of existing RAMs for VTE and possibly derive a new RAM. However, the evidence of effectiveness and cost-effectiveness provided by this analysis suggests that thromboprophylaxis should be offered to patients in this cohort, or at least those considered as being at a higher risk. Administration of thromboprophylaxis would be expected to reduce the risk of VTE and thus lead to underestimation of the prognostic accuracy of RAMs. Furthermore, the VTE events that were prevented by thromboprophylaxis would be precisely those that we would want a RAM to predict.
A large cohort study could still provide useful information if it is used to evaluate implementation rather than accuracy. It could determine the proportion of the cohort receiving thromboprophylaxis with different RAMs or different thresholds for treatment. It could be used to determine whether or not the low rate of bleeding events is confirmed in practice and, if risk-based thromboprophylaxis were provided, it could be used to determine whether or not the low rate of VTE events is confirmed in low-risk patients who do not receive treatment.
Direct oral anticoagulants could provide the benefits of thromboprophylaxis without the costs, inconvenience and discomfort of injections, which the PPI representatives identified as a potential barrier to patient acceptance. However, all the evidence of effectiveness in this review related to LMWH or fondaparinux. Ideally, an appropriately powered RCT comparing thromboprophylaxis of DOACs with LMWH would provide evidence of equivalent effectiveness, but such a trial may be prohibitively expensive, especially if it were felt that evidence of effectiveness of DOAC for other indications could be reasonably extrapolated to lower-limb immobilisation.
The most important parameters for decision uncertainty in the value-of-information analysis were related to the efficacy and disutility of receiving prophylaxis, and the long-term complications of PTS, so estimating these parameters should be a priority for future research. The disutility of receiving LMWH injections or oral DOACs could be investigated as part of a cohort study or trial of different types of thromboprophylaxis. The uncertainty around the long-terms effects of PTS mainly relate to subclinical DVT rather than clinically detected and treated DVT, so research to reduce uncertainty around the incidence and disutility of PTS would need to involve long-term follow-up or a retrospective observational study of people following lower-limb immobilisation due to injury.
It is currently unclear whether or not people with limited lower-limb immobilisation (such as splints that allow some movement or removable splints or casts) carry similar risks of VTE to those with full immobilisation. A cohort study of this population, perhaps undertaken alongside a cohort study evaluating risk-based thromboprophylaxis, could determine the risk of VTE and identify risk predictors.
All of these research suggestions would require large numbers of participants to generate meaningful results. There are plenty of eligible participants presenting to the NHS but an efficient research design would be required, using standardised collection of predictor variables and routine data sources for outcomes, to ensure that any study was not prohibitively expensive.
Finally, the PPI representatives identified the need for patients to receive clear and comprehensible communication of the risks and benefits of thromboprophylaxis, including written materials. Research is required to develop information for patients and ways of communicating benefits and risks.
Acknowledgements
The authors are grateful to Joanne Hinde for her clerical support. The authors would like to thank members of the expert clinical advisory group for their participation in the expert consensus work and the PPI representatives for their advice.
Patient and public involvement representatives
-
Shan Bennet (Sheffield Emergency Care Forum).
-
Robin Pierce-Williams (Thrombosis UK).
Expert advisory group
-
Professor Matt Costa (Orthopaedic Surgery, Oxford).
-
Associate Professor Xavier Griffin (Orthopaedic Surgery, Oxford).
-
Mr David Johnson (Orthopaedic Surgery, Stockport).
-
Mr Dilraj Sandher (Orthopaedic Surgery, Stockport).
-
Ms Vicky Lyle (Orthopaedic Surgery, Salford).
-
Dr Gordon Fuller (Emergency Medicine, Sheffield).
-
Professor Jason Smith (Emergency Medicine, Derriford).
-
Professor Rick Body (Emergency Medicine, Manchester).
-
Dr Graham Johnson (Emergency Medicine, Derby).
-
Dr Jamie Cooper (Emergency Medicine, Aberdeen).
-
Dr Catherine Roberts (Emergency Medicine, Preston).
-
Dr Rowena Thomas-Dewing (Haematology, Salford).
-
Dr Rhona Maclean (Haematology, Sheffield).
-
Dr Jecko Thachil (Haematology, Manchester).
-
Dr Henry Watson (Haematology, Aberdeen).
We would also like to extend our thanks to Professor Matt Stevenson (University of Sheffield), who was a co-applicant on the bid and provided advice, as necessary, relating to health economics.
Contributions of authors
Abdullah Pandor (Senior Research Fellow) co-ordinated the review and was responsible for the design of the study, acquisition of data, analysis and interpretation of data (for the systematic review), and drafting and revision of the final report.
Daniel Horner (Professor at the Royal College of Emergency Medicine and Substantive NHS Consultant Emergency Physician) was responsible for the conception and design of the study, acquisition of data, analysis and interpretation of data (for the systematic reviews and health economic evaluations), and drafting and revision of the final report.
Sarah Davis (Senior Lecturer) was responsible for the design of the study, acquisition of data, analysis and interpretation of data and model construction (for the health economic evaluations), and drafting and revision of the final report.
Steve Goodacre (Professor of Emergency Medicine) was responsible for the conception and design of the study, acquisition of data, analysis and interpretation of data (for the systematic reviews and health economic evaluations), and drafting and revision of the final report.
John W Stevens (Reader in Decision Science) was responsible for the design of the study, statistical analyses, interpretation of data, and drafting and revision of the final report.
Mark Clowes (Information Specialist) was responsible for developing and undertaking the electronic literature searches.
Beverley J Hunt (Professor of Thrombosis and Haemostasis) was responsible for the design of the study, interpretation of data (for the systematic reviews and health economic evaluations), and drafting and revision of the final report.
Tim Nokes (Consultant Haematologist) was responsible for the design of the study, interpretation of data (for the systematic reviews and health economic evaluations), and drafting and revision of the final report.
Jonathan Keenan (Consultant Orthopaedic Surgeon) was responsible for the design of the study, interpretation of data (for the systematic reviews and health economic evaluations), and drafting and revision of the final report.
Kerstin de Wit (Assistant Professor and Thrombosis Physician) was responsible for the design of the study, interpretation of data (for the systematic reviews and health economic evaluations), and drafting and revision of the final report.
Publications
Horner D, Pandor A, Goodacre S, Clowes M, Hunt BJ. Individual risk factors predictive of venous thromboembolism in patients with temporary lower limb immobilisation due to injury: a systematic review. J Thromb Haemost 2019;17:329–44.
Davis S, Goodacre S, Pandor A, Horner D, Stevens JW, de Wit K, Hunt BJ. Decision-analysis modelling of the effects of thromboprophylaxis for people with lower limb immobilisation for injury. Br J Haematol 2019;186:130–95.
Horner D, Stevens J, Pandor A, Nokes T, Keenan J, de Wit K, Goodacre S. Pharmacological thromboprophylaxis to prevent venous thromboembolism in patients with temporary lower limb immobilisation after injury: a systematic review and network meta-analysis [published online ahead of print October 26 2019]. J Thromb Haemost 2019.
Horner D, Goodacre S, Pandor A, Nokes T, Keenan J, Hunt BJ, et al. Thromboprophylaxis in Lower Limb Immobilisation after Injury (TiLLI) [published online ahead of print November 6 2019]. Emergency Medicine Journal 2019.
Data-sharing statement
Most of the data used in this study are already publicly available. Requests for access to other data should be addressed to the corresponding author for consideration.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- National Institute for Health and Care Excellence . Venous Thromboembolism in Over 16s – Reducing the Risk of Hospital-Acquired Deep Vein Thrombosis or Pulmonary Embolism 2018. www.nice.org.uk/guidance/ng89 (accessed 9 April 2018).
- Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 1999;353:1386-9. https://doi.org/10.1016/S0140-6736(98)07534-5.
- Prandoni P, Lensing AW, Cogo A, Cuppini S, Villalta S, Carta M, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med 1996;125:1-7. https://doi.org/10.7326/0003-4819-125-1-199607010-00001.
- Cohen AT, Agnelli G, Anderson FA, Arcelus JI, Bergqvist D, Brecht JG, et al. Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb Haemost 2007;98:756-64. https://doi.org/10.1160/TH07-03-0212.
- Raskob GE, Angchaisuksiri P, Blanco AN, Buller H, Gallus A, Hunt BJ, et al. Thrombosis: a major contributor to global disease burden. Arterioscler Thromb Vasc Biol 2014;34:2363-71. https://doi.org/10.1161/ATVBAHA.114.304488.
- House of Commons Health Committee . The Prevention of Venous Thromboembolism in Hospitalised Patients – Second Report of Session 2004–05 2005. www.publications.parliament.uk/pa/cm200405/cmselect/cmhealth/99/99.pdf (accessed 15 March 2018).
- Chen L, Soares D. Fatal pulmonary embolism following ankle fracture in a 17-year-old girl. J Bone Joint Surg Br 2006;88:400-1. https://doi.org/10.1302/0301-620X.88B3.17152.
- Healy B, Levin E, Perrin K, Weatherall M, Beasley R. Prolonged work- and computer-related seated immobility and risk of venous thromboembolism. J R Soc Med 2010;103:447-54. https://doi.org/10.1258/jrsm.2010.100155.
- Makhdom AM, Cota A, Saran N, Chaytor R. Incidence of symptomatic deep venous thrombosis after Achilles tendon rupture. J Foot Ankle Surg 2013;52:584-7. https://doi.org/10.1053/j.jfas.2013.03.001.
- Makhdom AM, Garceau S, Dimentberg R. Fatal pulmonary embolism following Achilles tendon repair: a case report and a review of the literature. Case Rep Orthop 2013;2013. https://doi.org/10.1155/2013/401968.
- Meek R, Tong RL. Venous thromboembolism in emergency department patients with rigid immobilization for lower leg injury: incidence and risk factors. Emerg Med Australas 2012;24:277-84. https://doi.org/10.1111/j.1742-6723.2012.01539.x.
- Nilsson-Helander K, Thurin A, Karlsson J, Eriksson BI. High incidence of deep venous thrombosis after Achilles tendon rupture: a prospective study. Knee Surg Sports Traumatol Arthrosc 2009;17:1234-8. https://doi.org/10.1007/s00167-009-0727-y.
- Nokes TJ, Keenan J. Thromboprophylaxis in patients with lower limb immobilisation – review of current status. Br J Haematol 2009;146:361-8. https://doi.org/10.1111/j.1365-2141.2009.07737.x.
- Patil S, Gandhi J, Curzon I, Hui AC. Incidence of deep-vein thrombosis in patients with fractures of the ankle treated in a plaster cast. J Bone Joint Surg Br 2007;89:1340-3. https://doi.org/10.1302/0301-620X.89B10.19241.
- Testroote M, Stigter WA, Janssen L, Janzing HM. Low molecular weight heparin for prevention of venous thromboembolism in patients with lower-leg immobilization. Cochrane Database Syst Rev 2014;4. https://doi.org/10.1002/14651858.CD006681.pub3.
- Horner D, Bennett P, Ryan A, Gillet A. Thromboprophylaxis for ambulatory patients with immobilised lower limb trauma: a closed audit loop. Emerg Med J 2015;32. https://doi.org/10.1136/emermed-2015-205372.46.
- Roberts C, Horner D, Coleman G, Maitland L, Curl-Roper T, Smith R, et al. Guidelines in Emergency Medicine Network (GEMNet): guideline for the use of thromboprophylaxis in ambulatory trauma patients requiring temporary limb immobilisation. Emerg Med J 2013;30:968-82. https://doi.org/10.1136/emermed-2013-203134.
- Zee AA, van Lieshout K, van der Heide M, Janssen L, Janzing HM. Low molecular weight heparin for prevention of venous thromboembolism in patients with lower-limb immobilization. Cochrane Database Syst Rev 2017;8. https://doi.org/10.1002/14651858.CD006681.pub4.
- Smith R, Wood E. BET 4: quantifying the risk of venous thromboembolism for temporary lower limb immobilisation in ambulatory patients. Emerg Med J 2012;29:779-80. https://doi.org/10.1136/emermed-2012-201686.5.
- Hill AB, Garber B, Dervin G, Howard A. Heparin prophylaxis for deep vein thrombosis in a patient with multiple injuries: an evidence-based approach to a clinical problem. Can J Surg 2002;45:282-57.
- Joint Formulary Committee . British National Formulary n.d. www.medicinescomplete.com (accessed 24 January 2018).
- Braithwaite I, Dunbar L, Eathorne A, Weatherall M, Beasley R. Venous thromboembolism rates in patients with lower limb immobilization after Achilles tendon injury are unchanged after the introduction of prophylactic aspirin: audit. J Thromb Haemost 2016;14:331-5. https://doi.org/10.1111/jth.13224.
- Gehling H, Giannadakis K, Lefering R, Hessmann M, Achenbach S, Gotzen L. Prospective randomized pilot study of ambulatory prevention of thromboembolism. 2 times 500 mg aspirin (ASS) vs. clivarin 1750 (NMH). Unfallchirurg 1998;101:42-9. https://doi.org/10.1007/s001130050231.
- National Clinical Guideline Centre – Acute and Chronic Conditions (UK) . Venous Thromboembolism: Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Hospital 2010. www.ncbi.nlm.nih.gov/books/NBK116518/ (accessed 4 March 2018).
- Electronic Medicines Compendium (eMC) . Aspirin 75 mg Tablets – Summary of Product Characteristics (SmPC) n.d. www.medicines.org.uk/emc/product/2408 (accessed 12 March 2018).
- Electronic Medicines Compendium (eMC) . Aspirin Tablets BP 300 mg – Patient Leaflet n.d. www.medicines.org.uk/emc/product/8006 (accessed 12 March 2018).
- Lassen MR, Gallus A, Raskob GE, Pineo G, Chen D, Ramirez LM. ADVANCE-3 Investigators. Apixaban versus enoxaparin for thromboprophylaxis after hip replacement. N Engl J Med 2010;363:2487-98. https://doi.org/10.1056/NEJMoa1006885.
- Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Hornick P. ADVANCE-2 investigators. Apixaban versus enoxaparin for thromboprophylaxis after knee replacement (ADVANCE-2): a randomised double-blind trial. Lancet 2010;375:807-15. https://doi.org/10.1016/S0140-6736(09)62125-5.
- Raskob GE, Gallus AS, Pineo GF, Chen D, Ramirez LM, Wright RT, et al. Apixaban versus enoxaparin for thromboprophylaxis after hip or knee replacement: pooled analysis of major venous thromboembolism and bleeding in 8464 patients from the ADVANCE-2 and ADVANCE-3 trials. J Bone Joint Surg Br 2012;94:257-64. https://doi.org/10.1302/0301-620X.94B2.27850.
- Klarenbach S, Lee K, Boucher M, So H, Manns B, Tonelli M. Direct Oral Anticoagulants for the Treatment of Venous Thromboembolic Events: Economic Evaluation. Ottawa, ON: Canadian Agency for Drugs and Technologies in Health; 2016.
- Keenan J, Hall M, Nokes T. A practical VTE risk assessment score tool for patients treated with lower limb cast immobilization. Injury Extra 2009;40:199-200. https://doi.org/10.1016/j.injury.2009.06.211.
- Nemeth B, van Adrichem RA, van Hylckama Vlieg A, Bucciarelli P, Martinelli I, Baglin T, et al. Venous thrombosis risk after cast immobilization of the lower extremity: derivation and validation of a clinical prediction score, L-TRiP(cast), in three population-based case-control studies. PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001899.
- Stockport NHS Foundation Trust . Lower Limb Immobilisation VTE Risk Assessment Tool and Treatment Protocol 2013. www.boa.ac.uk/wp-content/uploads/2014/01/Stockport-VTE-Lower-limb-immobilisation.pdf (accessed 9 January 2018).
- Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e278-325.
- Struijk-Mulder MC, Ettema HB, Verheyen CC, Büller HR. Comparing consensus guidelines on thromboprophylaxis in orthopedic surgery. J Thromb Haemost 2010;8:678-83. https://doi.org/10.1111/j.1538-7836.2009.03728.x.
- Ettema HB, Kollen BJ, Verheyen CC, Büller HR. Prevention of venous thromboembolism in patients with immobilization of the lower extremities: a meta-analysis of randomized controlled trials. J Thromb Haemost 2008;6:1093-8. https://doi.org/10.1111/j.1538-7836.2008.02984.x.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Pandor A, Goodacre S, Horner D, Stevens JW, Clowes M, Davis S, et al. Systematic Review and Cost-Effectiveness Analysis of Thromboprophylaxis for Lower Limb Immobilisation n.d. www.crd.york.ac.uk/prospero/display_record.php?RecordID=58688 (accessed 3 April 2018).
- Higgins JPT, Sterne JAC, Savović J, Page MJ, Hróbjartsson A, Boutron I, et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev 2016:29-31.
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d5928.
- Hartling L, Hamm MP, Milne A, Vandermeer B, Santaguida PL, Ansari M, et al. Testing the risk of bias tool showed low reliability between individual reviewers and across consensus assessments of reviewer pairs. J Clin Epidemiol 2013;66:973-81. https://doi.org/10.1016/j.jclinepi.2012.07.005.
- Hartling L, Ospina M, Liang Y, Dryden DM, Hooton N, Krebs Seida J, et al. Risk of bias versus quality assessment of randomised controlled trials: cross sectional study. BMJ 2009;339. https://doi.org/10.1136/bmj.b4012.
- Jørgensen L, Paludan-Müller AS, Laursen DR, Savović J, Boutron I, Sterne JA, et al. Evaluation of the Cochrane tool for assessing risk of bias in randomized clinical trials: overview of published comments and analysis of user practice in Cochrane and non-Cochrane reviews. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0259-8.
- Savović J, Weeks L, Sterne JA, Turner L, Altman DG, Moher D, et al. Evaluation of the Cochrane Collaboration’s tool for assessing the risk of bias in randomized trials: focus groups, online survey, proposed recommendations and their implementation. Syst Rev 2014;3. https://doi.org/10.1186/2046-4053-3-37.
- Lunn D, Thomas A, Best N, Spiegelhalter D. WinBUGS – a Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput 2000;10:325-37. https://doi.org/10.1023/A:1008929526011.
- Brooks SP, Gelman A. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat 1998;7:434-55.
- Dias S, Sutton AJ, Welton NJ, Ades AE. NICE DSU Technical Support Document 3: Heterogeneity – Subgroups, Meta-Regression, Bias and Bias-Adjustment. Sheffield: Decision Support Unit; 2012.
- Dias S, Sutton AJ, Welton NJ, Ades AE. NICE DSU Technical Support Document 2: A Generalised Linear Modelling Framework for Pairwise and Network Meta-Analysis of Randomised Controlled Trials. Sheffield: Decision Support Unit; 2016.
- Bruntink MM, Groutars YME, Schipper IB, Breederveld RS, Tuinebreijer WE, Derksen RJ. PROTECT study group . Nadroparin or fondaparinux versus no thromboprophylaxis in patients immobilised in a below-knee plaster cast (PROTECT): a randomised controlled trial. Injury 2017;48:936-40. https://doi.org/10.1016/j.injury.2017.02.018.
- Goel DP, Buckley R, deVries G, Abelseth G, Ni A, Gray R. Prophylaxis of deep-vein thrombosis in fractures below the knee: a prospective randomised controlled trial. J Bone Joint Surg Br 2009;91:388-94. https://doi.org/10.1302/0301-620X.91B3.20820.
- Jørgensen PS, Warming T, Hansen K, Paltved C, Vibeke Berg H, Jensen R, et al. Low molecular weight heparin (Innohep) as thromboprophylaxis in outpatients with a plaster cast: a venografic controlled study. Thromb Res 2002;105:477-80. https://doi.org/10.1016/S0049-3848(02)00059-2.
- Kock HJ, Schmit-Neuerburg KP, Hanke J, Rudofsky G, Hirche H. Thromboprophylaxis with low-molecular-weight heparin in outpatients with plaster-cast immobilisation of the leg. Lancet 1995;346:459-61. https://doi.org/10.1016/S0140-6736(95)91320-3.
- Kujath P, Spannagel U, Habscheid W. Incidence and prophylaxis of deep venous thrombosis in outpatients with injury of the lower limb. Haemostasis 1993;23:20-6. https://doi.org/10.1159/000216905.
- Lapidus LJ, Ponzer S, Elvin A, Levander C, Lärfars G, Rosfors S, et al. Prolonged thromboprophylaxis with dalteparin during immobilization after ankle fracture surgery: a randomized placebo-controlled, double-blind study. Acta Orthop 2007;78:528-35. https://doi.org/10.1080/17453670710014185.
- Lapidus LJ, Rosfors S, Ponzer S, Levander C, Elvin A, Lärfars G, et al. Prolonged thromboprophylaxis with dalteparin after surgical treatment of Achilles tendon rupture: a randomized, placebo-controlled study. J Orthop Trauma 2007;21:52-7. https://doi.org/10.1097/01.bot.0000250741.65003.14.
- Lassen MR, Borris LC, Nakov RL. Use of the low-molecular-weight heparin reviparin to prevent deep-vein thrombosis after leg injury requiring immobilization. N Engl J Med 2002;347:726-30. https://doi.org/10.1056/NEJMoa011327.
- Samama CM, Lecoules N, Kierzek G, Claessens YE, Riou B, Rosencher N, et al. Comparison of fondaparinux with low molecular weight heparin for venous thromboembolism prevention in patients requiring rigid or semi-rigid immobilization for isolated non-surgical below-knee injury. J Thromb Haemost 2013;11:1833-43. https://doi.org/10.1111/jth.12395.
- Selby R, Geerts WH, Kreder HJ, Crowther MA, Kaus L, Sealey F. D-KAF (Dalteparin in Knee-to-Ankle Fracture) Investigators . A double-blind, randomized controlled trial of the prevention of clinically important venous thromboembolism after isolated lower leg fractures. J Orthop Trauma 2015;29:224-30. https://doi.org/10.1097/BOT.0000000000000250.
- van Adrichem RA, Nemeth B, Algra A, le Cessie S, Rosendaal FR, Schipper IB, et al. Thromboprophylaxis after knee arthroscopy and lower-leg casting. N Engl J Med 2017;376:515-25. https://doi.org/10.1056/NEJMoa1613303.
- Zheng X, Li DY, Wangyang Y, Zhang XC, Guo KJ, Zhao FC, et al. Effect of chemical thromboprophylaxis on the rate of venous thromboembolism after treatment of foot and ankle fractures. Foot Ankle Int 2016;37:1218-24. https://doi.org/10.1177/1071100716658953.
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355. https://doi.org/10.1136/bmj.i4919.
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529-36. https://doi.org/10.7326/0003-4819-155-8-201110180-00009.
- Rowswell HR, Nokes TJC. Significant reduction in hospital-acquired thrombosis: impact of national risk assessment and real-time feedback. Open Heart 2017;4. https://doi.org/10.1136/openhrt-2017-000653.
- Hanslow SS, Grujic L, Slater HK, Chen D. Thromboembolic disease after foot and ankle surgery. Foot Ankle Int 2006;27:693-5. https://doi.org/10.1177/107110070602700907.
- Ho E, Omari A. Prevalence of acute deep vein thrombosis in patients with ankle and foot fractures treated with nonoperative management – a pilot study. Int J Angiol 2017;26:53-9. https://doi.org/10.1055/s-0035-1556054.
- Jameson SS, Rankin KS, Desira NL, James P, Muller SD, Reed MR, et al. Pulmonary embolism following ankle fractures treated without an operation – an analysis using National Health Service data. Injury 2014;45:1256-61. https://doi.org/10.1016/j.injury.2014.05.009.
- Manafi Rasi A, Kazemian G, Emami Moghadam M, Tavakoli Larestani R, Fallahi A, Nemati A, et al. Deep vein thrombosis following below knee immobilization: the need for chemoprophylaxis. Trauma Mon 2013;17:367-9. https://doi.org/10.5812/traumamon.9158.
- Patel A, Ogawa B, Charlton T, Thordarson D. Incidence of deep vein thrombosis and pulmonary embolism after Achilles tendon rupture. Clin Orthop Relat Res 2012;470:270-4. https://doi.org/10.1007/s11999-011-2166-6.
- Riou B, Rothmann C, Lecoules N, Bouvat E, Bosson JL, Ravaud P, et al. Incidence and risk factors for venous thromboembolism in patients with nonsurgical isolated lower limb injuries. Am J Emerg Med 2007;25:502-8. https://doi.org/10.1016/j.ajem.2006.09.012.
- van Adrichem RA, Debeij J, Nelissen RG, Schipper IB, Rosendaal FR, Cannegieter SC. Below-knee cast immobilization and the risk of venous thrombosis: results from a large population-based case-control study. J Thromb Haemost 2014;12:1461-9. https://doi.org/10.1111/jth.12655.
- Wahlsten LR, Eckardt H, Lyngbæk S, Jensen PF, Fosbøl EL, Torp-Pedersen C, et al. Symptomatic venous thromboembolism following fractures distal to the knee: a nationwide Danish cohort study. J Bone Joint Surg Am 2015;97:470-7. https://doi.org/10.2106/JBJS.N.00307.
- Saragas NP, Ferrao PN, Saragas E, Jacobson BF. The impact of risk assessment on the implementation of venous thromboembolism prophylaxis in foot and ankle surgery. Foot Ankle Surg 2014;20:85-9. https://doi.org/10.1016/j.fas.2013.11.002.
- Mizel MS, Temple HT, Michelson JD, Alvarez RG, Clanton TO, Frey CC, et al. Thromboembolism after foot and ankle surgery. A multicenter study. Clin Orthop Relat Res 1998;348:180-5.
- Selby R, Geerts WH, Kreder HJ, Crowther MA, Kaus L, Sealey F. Symptomatic venous thromboembolism uncommon without thromboprophylaxis after isolated lower-limb fracture: the Knee-to-Ankle Fracture (KAF) cohort study. J Bone Joint Surg Am 2014;96. https://doi.org/10.2106/JBJS.M.00236.
- Centre for Reviews and Dissemination . Systematic Reviews. CRD’s Guidance for Undertaking Reviews in Health Care 2009. www.york.ac.uk/crd/SysRev/!SSL!/WebHelp/SysRev3.htm (accessed 14 August 2017).
- Altman DG. Systematic reviews of evaluations of prognostic variables. BMJ 2001;323:224-8. https://doi.org/10.1136/bmj.323.7306.224.
- Moons KG, de Groot JA, Bouwmeester W, Vergouwe Y, Mallett S, Altman DG, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLOS Med 2014;11. https://doi.org/10.1371/journal.pmed.1001744.
- Eingartner C, Hontzsch D, Lang E, Weller S. [Individualized prophylaxis for thromboembolism in outpatients – a practical way out between ‘ever’ and ‘never’?]. Aktuelle Traumatologie 1995;25:1-5.
- Giannadakis K, Gehling H, Sitter H, Achenbach S, Hahne H, Gotzen L. [Is medicamentous thrombosis prophylaxis necessary in conservative outpatient therapy with lower limb injuries?]. Unfallchirurg 2000;103:475-8. https://doi.org/10.1007/s001130050568.
- Haque S, Bishnoi A, Khairandish H, Menon D. Thromboprophylaxis in ambulatory trauma patients with foot and ankle fractures: prospective study using a risk scoring system. Foot Ankle Spec 2016;9:388-93. https://doi.org/10.1177/1938640016640892.
- Saragas NP, Ferrao PN, Jacobson BF, Saragas E, Strydom A. The benefit of pharmacological venous thromboprophylaxis in foot and ankle surgery. S Afr Med J 2017;107:327-30. https://doi.org/10.7196/SAMJ.2017.v107i4.10843.
- Watson U, Hickey BA, Jones HM, Perera A. A critical evaluation of venous thromboembolism risk assessment models used in patients with lower limb cast immobilisation. Foot Ankle Surg 2016;22:191-5. https://doi.org/10.1016/j.fas.2015.08.003.
- van Hylckama Vlieg A, Baglin CA, Luddington R, MacDonald S, Rosendaal FR, Baglin TP. The risk of a first and a recurrent venous thrombosis associated with an elevated D-dimer level and an elevated thrombin potential: results of the THE-VTE study. J Thromb Haemost 2015;13:1642-52. https://doi.org/10.1111/jth.13043.
- Ribeiro DD, Bucciarelli P, Braekkan SK, Lijfering WM, Passamonti SM, Brodin EE, et al. Seasonal variation of venous thrombosis: a consecutive case series within studies from Leiden, Milan and Tromsø. J Thromb Haemost 2012;10:1704-7. https://doi.org/10.1111/j.1538-7836.2012.04811.x.
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs 2000;32:1008-15.
- Jones J, Hunter D. Consensus methods for medical and health services research. BMJ 1995;311:376-80. https://doi.org/10.1136/bmj.311.7001.376.
- McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm 2016;38:655-62. https://doi.org/10.1007/s11096-016-0257-x.
- Crawford IW, Mackway-Jones K, Russell DR, Carley SD. Delphi based consensus study into planning for chemical incidents. Emerg Med J 2004;21:24-8. https://doi.org/10.1136/emj.2003.003087.
- Fuller GW, Nelson-Piercy C, Hunt BJ, Lecky FE, Thomas S, Horspool K, et al. Consensus-derived clinical decision rules to guide advanced imaging decisions for pulmonary embolism in pregnancy and the postpartum period. Eur J Emerg Med 2018;25:221-2. https://doi.org/10.1097/MEJ.0000000000000477.
- SmartSurvey Ltd . Make Smarter Decisions n.d. www.smartsurvey.co.uk/ (accessed 2 October 2017).
- Canadian Agency for Drugs and Technologies in Health (CADTH) . Strings Attached: CADTH Database Search Filters 2016. www.cadth.ca/resources/finding-evidence (accessed 1 August 2017).
- Centre for Reviews and Dissemination . NHS Economic Evaluation Database Search Strategy 2014. www.crd.york.ac.uk/crdweb/searchstrategies.asp (accessed 1 August 2017).
- McKinlay RJ, Wilczynski NL, Haynes RB. Hedges Team . Optimal search strategies for detecting cost and economic studies in EMBASE. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-67.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013.
- Brasel KJ, Borgstrom DC, Weigelt JA. Cost-effective prevention of pulmonary embolus in high-risk trauma patients. J Trauma 1997;42:456-60. https://doi.org/10.1097/00005373-199703000-00013.
- Lu JP, Knudson MM, Bir N, Kallet R, Atkinson K. Fondaparinux for prevention of venous thromboembolism in high-risk trauma patients: a pilot study. J Am Coll Surg 2009;209:589-94. https://doi.org/10.1016/j.jamcollsurg.2009.08.001.
- Velmahos GC, Oh Y, McCombs J, Oder D. An evidence-based cost-effectiveness model on methods of prevention of posttraumatic venous thromboembolism. J Trauma 2000;49:1059-64. https://doi.org/10.1097/00005373-200012000-00014.
- Wolowacz SE, Roskell NS, Plumb JM, Clemens A, Noack H, Robinson PA, et al. Economic evaluation of dabigatran etexilate for the prevention of venous thromboembolism in patients aged over 75 years or with moderate renal impairment undergoing total knee or hip replacement. Thromb Haemost 2010;103:360-71. https://doi.org/10.1160/TH09-08-0579.
- Wolowacz SE, Roskell NS, Maciver F, Beard SM, Robinson PA, Plumb JM, et al. Economic evaluation of dabigatran etexilate for the prevention of venous thromboembolism after total knee and hip replacement surgery. Clin Ther 2009;31:194-212. https://doi.org/10.1016/j.clinthera.2009.01.001.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: PSSRU, University of Kent; 2017.
- Hippisley-Cox J, Coupland C. Predicting risk of upper gastrointestinal bleed and intracranial bleed with anticoagulants: cohort study to derive and validate the QBleed scores. BMJ 2014;349. https://doi.org/10.1136/bmj.g4606.
- Fang MC, Go AS, Chang Y, Hylek EM, Henault LE, Jensvold NG, et al. Death and disability from warfarin-associated intracranial and extracranial hemorrhages. Am J Med 2007;120:700-5. https://doi.org/10.1016/j.amjmed.2006.07.034.
- Button LA, Roberts SE, Evans PA, Goldacre MJ, Akbari A, Dsilva R, et al. Hospitalized incidence and case fatality for upper gastrointestinal bleeding from 1999 to 2007: a record linkage study. Aliment Pharmacol Ther 2011;33:64-76. https://doi.org/10.1111/j.1365-2036.2010.04495.x.
- Kooiman J, van Hagen N, Iglesias Del Sol A, Planken EV, Lip GY, van der Meer FJ, et al. The HAS-BLED score identifies patients with acute venous thromboembolism at high risk of major bleeding complications during the first six months of anticoagulant treatment. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0122520.
- Nieto JA, Solano R, Ruiz-Ribó MD, Ruiz-Gimenez N, Prandoni P, Kearon C, et al. RIETE Investigators . Fatal bleeding in patients receiving anticoagulant therapy for venous thromboembolism: findings from the RIETE registry. J Thromb Haemost 2010;8:1216-22. https://doi.org/10.1111/j.1538-7836.2010.03852.x.
- Office for National Statistics . National Life Tables, England 1980–82 to 2014–16 2017.
- Fogelholm R, Murros K, Rissanen A, Avikainen S. Long term survival after primary intracerebral haemorrhage: a retrospective population based study. J Neurol Neurosurg Psychiatry 2005;76:1534-8. http://doi.org/10.1136/jnnp.2004.055145.
- Maestre A, Sánchez R, Rosa V, Aujesky D, Lorenzo A, Barillari G, et al. RIETE Investigators . Clinical characteristics and outcome of inpatients versus outpatients with venous thromboembolism: findings from the RIETE Registry. Eur J Intern Med 2010;21:377-82. https://doi.org/10.1016/j.ejim.2010.07.004.
- Hach-Wunderle V, Bauersachs R, Gerlach HE, Eberle S, Schellong S, Riess H, et al. Post-thrombotic syndrome 3 years after deep venous thrombosis in the Thrombosis and Pulmonary Embolism in Out-Patients (TULIPA) PLUS Registry. J Vasc Surg Venous Lymphat Disord 2013;1:5-12. https://doi.org/10.1016/j.jvsv.2012.07.003.
- van Dongen CJ, Prandoni P, Frulla M, Marchiori A, Prins MH, Hutten BA. Relation between quality of anticoagulant treatment and the development of the postthrombotic syndrome. J Thromb Haemost 2005;3:939-42. https://doi.org/10.1111/j.1538-7836.2005.01333.x.
- Ende-Verhaar YM, Cannegieter SC, Vonk Noordegraaf A, Delcroix M, Pruszczyk P, Mairuhu AT, et al. Incidence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism: a contemporary view of the published literature. Eur Respir J 2017;49. https://doi.org/10.1183/13993003.01792-2016.
- Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med 2004;350:2257-64. https://doi.org/10.1056/NEJMoa032274.
- Delcroix M, Lang I, Pepke-Zaba J, Jansa P, D’Armini AM, Snijder R, et al. Long-term outcome of patients with chronic thromboembolic pulmonary hypertension: results from an international prospective registry. Circulation 2016;133:859-71. https://doi.org/10.1161/CIRCULATIONAHA.115.016522.
- Goodacre S, Horspool K, Shephard N, Pollard D, Hunt B, Fuller G, et al. Selecting pregnant or postpartum women with suspected pulmonary embolism for diagnostic imaging: the DiPEP diagnostic study with decision-analysis modelling. Health Technol Assess 2018;22. https://doi.org/10.3310/hta22470.
- Menakaya CU, Pennington N, Muthukumar N, Joel J, Ramirez Jimenez AJ, Shaw CJ, et al. The cost of outpatient venous thromboembolism prophylaxis following lower limb injuries. Bone Joint J 2013;95–B:673-7. https://doi.org/10.1302/0301-620X.95B5.30555.
- Department of Health and Social Care . NHS Reference Costs 2015 to 2016 2016.
- Luengo-Fernandez R, Yiin GS, Gray AM, Rothwell PM. Population-based study of acute- and long-term care costs after stroke in patients with AF. Int J Stroke 2013;8:308-14. https://doi.org/10.1111/j.1747-4949.2012.00812.x.
- Jiménez D, de Miguel-Díez J, Guijarro R, Trujillo-Santos J, Otero R, Barba R, et al. Trends in the management and outcomes of acute pulmonary embolism: analysis from the RIETE registry. J Am Coll Cardiol 2016;67:162-70. https://doi.org/10.1016/j.jacc.2015.10.060.
- Pollack CV, Schreiber D, Goldhaber SZ, Slattery D, Fanikos J, O’Neil BJ, et al. Clinical characteristics, management, and outcomes of patients diagnosed with acute pulmonary embolism in the emergency department: initial report of EMPEROR (Multicenter Emergency Medicine Pulmonary Embolism in the Real World Registry). J Am Coll Cardiol 2011;57:700-6. https://doi.org/10.1016/j.jacc.2010.05.071.
- Rosand J, Eckman MH, Knudsen KA, Singer DE, Greenberg SM. The effect of warfarin and intensity of anticoagulation on outcome of intracerebral hemorrhage. Arch Intern Med 2004;164:880-4. https://doi.org/10.1001/archinte.164.8.880.
- Rockall TA, Logan RFA, Devlin HB, Northfield TC. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. BMJ 1995;311:222-6. https://doi.org/10.1136/bmj.311.6999.222.
- McPherson SJ, Mason MT, Smith NCE, Kelly K, Ellis D, Mason M. Time to Get Control? A Review of the Care Received by Patients Who Had a Severe Gastrointestinal Haemorrhage. London: National Confidential Enquiry into Patient Outcome and Death; 2015.
- Cohen AT, Gitt AK, Bauersachs R, Fronk EM, Laeis P, Mismetti P, et al. The management of acute venous thromboembolism in clinical practice. Results from the European PREFER in VTE Registry. Thromb Haemost 2017;117:1326-37. https://doi.org/10.1160/TH16-10-0793.
- Carrier M, Le Gal G, Wells PS, Rodger MA. Systematic review: case-fatality rates of recurrent venous thromboembolism and major bleeding events among patients treated for venous thromboembolism. Ann Intern Med 2010;152:578-89. https://doi.org/10.7326/0003-4819-152-9-201005040-00008.
- Galanaud JP, Monreal M, Kahn SR. Epidemiology of the post-thrombotic syndrome. Thromb Res 2018;164:100-9. https://doi.org/10.1016/j.thromres.2017.07.026.
- Kahn SR, Partsch H, Vedantham S, Prandoni P, Kearon C. Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis . Definition of post-thrombotic syndrome of the leg for use in clinical investigations: a recommendation for standardization. J Thromb Haemost 2009;7:879-83. https://doi.org/10.1111/j.1538-7836.2009.03294.x.
- Persson LM, Lapidus LJ, Lärfars G, Rosfors S. Asymptomatic deep venous thrombosis is associated with a low risk of post-thrombotic syndrome. Eur J Vasc Endovasc Surg 2009;38:229-33. https://doi.org/10.1016/j.ejvs.2008.03.021.
- Schindler OS, Dalziel R. Post-thrombotic syndrome after total hip or knee arthroplasty: incidence in patients with asymptomatic deep venous thrombosis. J Orthop Surg 2005;13:113-19. https://doi.org/10.1177/230949900501300202.
- Prandoni P, Villalta S, Bagatella P, Rossi L, Marchiori A, Piccioli A, et al. The clinical course of deep-vein thrombosis. Prospective long-term follow-up of 528 symptomatic patients. Haematologica 1997;82:423-8.
- National Institute for Health and Care Excellence (NICE) . Venous Thromboembolism in Over 16s – Reducing the Risk of Hospital-Acquired Deep Vein Thrombosis or Pulmonary Embolism: Draft NICE Guideline for Consultation 2017.
- Copley V, Pickett K, Cooper K, Shepherd J. Rivaroxaban for the Treatment of Pulmonary Embolism and the Prevention of Recurrent Venous Thromboembolism: Evidence Review Group Report 2012.
- Edwards S, Wakefield V, Thurgar E, Karner C, Marceniuk G. Dabigatran Etexilate for the Treatment and Secondary Prevention of Deep Vein Thrombosis and Or Pulmonary Embolism: A Single Technology Appraisal – Evidence Review Group Report 2014.
- Greenhalgh J, Bagust A, Beale S, Boland A, Richardson M, Dwan K, et al. Apixaban for the Treatment and Secondary Prevention of Deep Vein Thrombosis and Or Pulmonary Embolism: Evidence Review Group Report 2014.
- Holmes M, Carroll C, Papaioannou D. Dabigatran Etexilate for the Prevention of Venous Thromboembolism in Patients Undergoing Elective Hip and Knee Surgery: A Single Technology Appraisal – Evidence Review Group Report 2008.
- Riemsma R, Joore M, Grutters J, Armstrong N, Misso K, Noake C, et al. Apixaban for the Prevention of Venous Thromboembolism in People Undergoing Elective Knee and Hip Replacement Surgery: Evidence Review Group Report 2011.
- Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E. Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal. Health Technol Assess 2009;13. https://doi.org/10.3310/hta13suppl3/07.
- Bristol-Myers Squibb Company, Pfizer Inc . Apixaban (Eliquis®) for the Prevention of Venous Thromboembolic Events in Adult Patients Who Have Undergone Elective Hip or Knee Replacement Surgery: Company Submission 2011.
- Bristol-Myers Squibb Company, Pfizer Inc . Apixaban (Eliquis®) for the Treatment of Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE) and Prevention of Recurrent DVT and PE in Adults: Company Submission 2014.
- Bayer Schering Pharma AG . Single Technology Appraisal (STA) of Rivaroxaban (Xarelto®) for the Prevention of Venous Thromboemobolism (VTE) in Adult Patients Undergoing Elective Hip or Knee Replacement Surgery: Company Submission 2008.
- National Institute for Health and Care Excellence . Edoxaban Tosylate for the Treatment and Secondary Prevention of Deep Vein Thrombosis and Or Pulmonary Embolism 2015.
- Fernando SM, Reardon PM, Dowlatshahi D, English SW, Thavorn K, Tanuseputro P, et al. Outcomes and costs of patients admitted to the ICU due to spontaneous intracranial hemorrhage. Crit Care Med 2018;46:e395-e403. https://doi.org/10.1097/CCM.0000000000003013.
- Ashrani AA, Heit JA. Incidence and cost burden of post-thrombotic syndrome. J Thromb Thrombolysis 2009;28:465-76. https://doi.org/10.1007/s11239-009-0309-3.
- Grosse SD, Nelson RE, Nyarko KA, Richardson LC, Raskob GE. The economic burden of incident venous thromboembolism in the United States: a review of estimated attributable healthcare costs. Thromb Res 2016;137:3-10. https://doi.org/10.1016/j.thromres.2015.11.033.
- Prandoni P. Healthcare burden associated with the post-thrombotic syndrome and potential impact of the new oral anticoagulants. Eur J Haematol 2012;88:185-94. https://doi.org/10.1111/j.1600-0609.2011.01733.x.
- Ruppert A, Steinle T, Lees M. Economic burden of venous thromboembolism: a systematic review. J Med Econ 2011;14:65-74. https://doi.org/10.3111/13696998.2010.546465.
- Caprini JA, Botteman MF, Stephens JM, Nadipelli V, Ewing MM, Brandt S, et al. Economic burden of long-term complications of deep vein thrombosis after total hip replacement surgery in the United States. Value Health 2003;6:59-74. https://doi.org/10.1046/j.1524-4733.2003.00204.x.
- MacDougall DA, Feliu AL, Boccuzzi SJ, Lin J. Economic burden of deep-vein thrombosis, pulmonary embolism, and post-thrombotic syndrome. Am J Health Syst Pharm 2006;63:5-15. https://doi.org/10.2146/ajhp060388.
- Olin JW, Beusterien KM, Childs MB, Seavey C, McHugh L, Griffiths RI. Medical costs of treating venous stasis ulcers: evidence from a retrospective cohort study. Vasc Med 1999;4:1-7. https://doi.org/10.1177/1358836X9900400101.
- Ramacciotti E, Gomes M, de Aguiar ET, Caiafa JS, de Moura LK, Araújo GR, et al. A cost analysis of the treatment of patients with post-thrombotic syndrome in Brazil. Thromb Res 2006;118:699-704. https://doi.org/10.1016/j.thromres.2005.12.005.
- Bergqvist D, Jendteg S, Johansen L, Persson U, Odegaard K. Cost of long-term complications of deep venous thrombosis of the lower extremities: an analysis of a defined patient population in Sweden. Ann Intern Med 1997;126:454-7. https://doi.org/10.7326/0003-4819-126-6-199703150-00006.
- Guanella R, Ducruet T, Johri M, Miron MJ, Roussin A, Desmarais S, et al. Economic burden and cost determinants of deep vein thrombosis during 2 years following diagnosis: a prospective evaluation. J Thromb Haemost 2011;9:2397-405. https://doi.org/10.1111/j.1538-7836.2011.04516.x.
- Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al. Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis. Health Technol Assess 2006;10. https://doi.org/10.3310/hta10150.
- Cohen ABM, Nadipelli V, Stephens J, Ewing M, Collier P, . Estimating the Economic Burden of PTS and Recurrent VTE Following DVT in the UK n.d.
- Harnan S, Rafia R, Poku E, Stevens JW, Stevenson M, Wong R. Rivaroxaban for the Treatment of Deep Vein Thrombosis and Secondary Prevention of Venous Thromboembolism. London: NICE; 2012.
- Kirson NY, Birnbaum HG, Ivanova JI, Waldman T, Joish V, Williamson T. Excess costs associated with patients with chronic thromboembolic pulmonary hypertension in a US privately insured population. Appl Health Econ Health Policy 2011;9:377-87. https://doi.org/10.2165/11592440-000000000-00000.
- Arverud ED, Anundsson P, Hardell E, Barreng G, Edman G, Latifi A, et al. Ageing, deep vein thrombosis and male gender predict poor outcome after acute Achilles tendon rupture. Bone Joint J 2016;98–B:1635-41. https://doi.org/10.1302/0301-620X.98B12.BJJ-2016-0008.R1.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Hedner E, Carlsson J, Kulich KR, Stigendal L, Ingelgård A, Wiklund I. An instrument for measuring health-related quality of life in patients with deep venous thrombosis (DVT): development and validation of Deep Venous Thrombosis Quality of Life (DVTQOL) questionnaire. Health Qual Life Outcomes 2004;2. https://doi.org/10.1186/1477-7525-2-30.
- Lubberts B, Paulino Pereira NR, Kabrhel C, Kuter DJ, DiGiovanni CW. What is the effect of venous thromboembolism and related complications on patient reported health-related quality of life? A meta-analysis. Thromb Haemost 2016;116:417-31. https://doi.org/10.1160/TH16-02-0152.
- Haig Y, Enden T, Grøtta O, Kløw NE, Slagsvold CE, Ghanima W, et al. Post-thrombotic syndrome after catheter-directed thrombolysis for deep vein thrombosis (CaVenT): 5-year follow-up results of an open-label, randomised controlled trial. Lancet Haematol 2016;3:e64-71. https://doi.org/10.1016/S2352-3026(15)00248-3.
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 1992;30:473-83. https://doi.org/10.1097/00005650-199206000-00002.
- Harzheim D, Klose H, Pinado FP, Ehlken N, Nagel C, Fischer C, et al. Anxiety and depression disorders in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Respir Res 2013;14. https://doi.org/10.1186/1465-9921-14-104.
- Hogg K, Shaw J, Coyle D, Fallah P, Carrier M, Wells P. Validity of standard gamble estimated quality of life in acute venous thrombosis. Thromb Res 2014;134:819-25. https://doi.org/10.1016/j.thromres.2014.07.029.
- Kline JA, Nordenholz KE, Courtney DM, Kabrhel C, Jones AE, Rondina MT, et al. Treatment of submassive pulmonary embolism with tenecteplase or placebo: cardiopulmonary outcomes at 3 months – multicenter double-blind, placebo-controlled randomized trial. J Thromb Haemost 2014;12:459-68. https://doi.org/10.1111/jth.12521.
- Mathias SD, Prebil LA, Putterman CG, Chmiel JJ, Throm RC, Comerota AJ. A health-related quality of life measure in patients with deep vein thrombosis: a validation study. Drug Inf J 1999;33:1173-87. https://doi.org/10.1177/009286159903300421.
- O’Brien B, Levine M, Willan A, Goeree R, Haley S, Blackhouse G, et al. Economic evaluation of outpatient treatment with low-molecular-weight heparin for proximal vein thrombosis. Arch Intern Med 1999;159:2298-304. https://doi.org/10.1001/archinte.159.19.2298.
- Roman A, Barbera JA, Castillo MJ, Muñoz R, Escribano P. Health-related quality of life in a national cohort of patients with pulmonary arterial hypertension or chronic thromboembolic pulmonary hypertension. Arch Bronconeumol 2013;49:181-8. https://doi.org/10.1016/j.arbres.2012.12.007.
- Shrier I, Kahn SR, Steele RJ. Effect of early physical activity on long-term outcome after venous thrombosis. Clin J Sport Med 2009;19:487-93. https://doi.org/10.1097/JSM.0b013e3181bd11a3.
- Stewart LK, Peitz GW, Nordenholz KE, Courtney DM, Kabrhel C, Jones AE, et al. Contribution of fibrinolysis to the physical component summary of the SF-36 after acute submassive pulmonary embolism. J Thromb Thrombolysis 2015;40:161-6. https://doi.org/10.1007/s11239-014-1155-5.
- Roberts LN, Patel RK, Donaldson N, Bonner L, Arya R. Post-thrombotic syndrome is an independent determinant of health-related quality of life following both first proximal and distal deep vein thrombosis. Haematologica 2014;99:e41-3. https://doi.org/10.3324/haematol.2013.089870.
- van Es J, den Exter PL, Kaptein AA, Andela CD, Erkens PM, Klok FA, et al. Quality of life after pulmonary embolism as assessed with SF-36 and PEmb-QoL. Thromb Res 2013;132:500-5. https://doi.org/10.1016/j.thromres.2013.06.016.
- Lukas PS, Krummenacher R, Biasiutti FD, Begré S, Znoj H, von Känel R. Association of fatigue and psychological distress with quality of life in patients with a previous venous thromboembolic event. Thromb Haemost 2009;102:1219-26. https://doi.org/10.1160/TH09-05-0316.
- Cohen AT, Bauersachs R, Gitt AK, Mismetti P, Monreal M, Willich SN, et al. Health state in patients with venous thromboembolism on conventional and non-VKA oral anticoagulants as assessed with the EQ-5D-5L questionnaire: PREFER in VTE registry. Value Health 2014;17:A493-4. https://doi.org/10.1016/j.jval.2014.08.1465.
- Sullivan P, Fraessdorf M, Feuring M, Schulman S, Hass B. Health-related quality of life after venous thromboembolism. Value Health 2011;14. https://doi.org/10.1016/j.jval.2011.08.830.
- Tavoly M, Utne KK, Jelsness-Jørgensen LP, Wik HS, Klok FA, Sandset PM, et al. Health-related quality of life after pulmonary embolism: a cross-sectional study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-013086.
- Hogg K, Kimpton M, Carrier M, Coyle D, Forgie M, Wells P. Estimating quality of life in acute venous thrombosis. JAMA Intern Med 2013;173:1067-72. https://doi.org/10.1001/jamainternmed.2013.563.
- Locadia M, Bossuyt PM, Stalmeier PF, Sprangers MA, van Dongen CJ, Middeldorp S, et al. Treatment of venous thromboembolism with vitamin K antagonists: patients’ health state valuations and treatment preferences. Thromb Haemost 2004;92:1336-41. https://doi.org/10.1160/TH04-02-0075.
- Daiichi Sankyo. Edoxaban for the Treatment and Secondary Prevention of Deep Vein Thrombosis and/or Pulmonary Embolism. Company Submission. London: NICE; 2015.
- Utne KK, Tavoly M, Wik HS, Jelsness-Jørgensen LP, Holst R, Sandset PM, et al. Health-related quality of life after deep vein thrombosis. SpringerPlus 2016;5. https://doi.org/10.1186/s40064-016-2949-z.
- Kahn SR, Shbaklo H, Lamping DL, Holcroft CA, Shrier I, Miron MJ, et al. Determinants of health-related quality of life during the 2 years following deep vein thrombosis. J Thromb Haemost 2008;6:1105-12. https://doi.org/10.1111/j.1538-7836.2008.03002.x.
- Kahn SR, Elman EA, Bornais C, Blostein M, Wells PS. Post-thrombotic syndrome, functional disability and quality of life after upper extremity deep venous thrombosis in adults. Thromb Haemost 2005;93:499-502. https://doi.org/10.1160/TH04-10-0640.
- Czihal M, Paul S, Rademacher A, Bernau C, Hoffmann U. Impact of the postthrombotic syndrome on quality of life after primary upper extremity deep venous thrombosis. Vasa 2012;41:200-4. https://doi.org/10.1024/0301-1526/a000186.
- Berzaczy D, Popovic M, Reiter M, Puchner S, Weber M, Minar E, et al. Quality of life in patients with idiopathic subclavian vein thrombosis. Thromb Res 2010;125:25-8. https://doi.org/10.1016/j.thromres.2009.04.015.
- Broholm R, Sillesen H, Damsgaard MT, Jørgensen M, Just S, Jensen LP, et al. Postthrombotic syndrome and quality of life in patients with iliofemoral venous thrombosis treated with catheter-directed thrombolysis. J Vasc Surg 2011;5:18-25. https://doi.org/10.1016/j.jvs.2011.06.021.
- Kahn SR, Hirsch A, Shrier I. Effect of postthrombotic syndrome on health-related quality of life after deep venous thrombosis. Arch Intern Med 2002;162:1144-8. https://doi.org/10.1001/archinte.162.10.1144.
- Kahn SR, Hirsch A, Shrier I. Predictors of the post-thrombotic syndrome during long-term treatment of proximal deep vein thrombosis. J Thromb Haemost 2005;3:718-23. https://doi.org/10.1111/j.1538-7836.2005.01216.x.
- Zhang X, Ren Q, Jiang X, Sun J, Gong J, Tang B, et al. A prospective randomized trial of catheter-directed thrombolysis with additional balloon dilatation for iliofemoral deep venous thrombosis: A single-center experience. Cardiovasc Interv Radiol 2014;37:958-68. https://doi.org/10.1007/s00270-013-0747-3.
- Kahn SR, Shrier I, Shapiro S, Houweling AH, Hirsch AM, Reid RD, et al. Six-month exercise training program to treat post-thrombotic syndrome: A randomized controlled two-centre trial. Canad Med Assoc J 2011;183:37-44. https://doi.org/10.1503/cmaj.100248.
- Enden T, Wik HS, Kvam AK, Haig Y, Kløw NE, Sandset PM. Health-related quality of life after catheter-directed thrombolysis for deep vein thrombosis: secondary outcomes of the randomised, non-blinded, parallel-group CaVenT study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-002984.
- Lenert LA, Soetikno RM. Automated computer interviews to elicit utilities: potential applications in the treatment of deep venous thrombosis. J Am Med Inform Assoc 1997;4:49-56. https://doi.org/10.1136/jamia.1997.0040049.
- O’Meara JJ, McNutt RA, Evans AT, Moore SW, Downs SM. A decision analysis of streptokinase plus heparin as compared with heparin alone for deep-vein thrombosis. N Engl J Med 1994;330:1864-9. https://doi.org/10.1056/NEJM199406303302605.
- O’Donnell MJ, McRae S, Kahn SR, Julian JA, Kearon C, Mackinnon B, et al. Evaluation of a venous-return assist device to treat severe post-thrombotic syndrome (VENOPTS): a randomized controlled trial. Thromb Haemost 2008;99:623-9. https://doi.org/10.1160/TH07-09-0546.
- Holmes CE, Bambace NM, Lewis P, Callas PW, Cushman M. Efficacy of a short course of complex lymphedema therapy or graduated compression stocking therapy in the treatment of post-thrombotic syndrome. Vasc Med 2014;19:42-8. https://doi.org/10.1177/1358863X14521883.
- Ara R, Brazier JE. Using health state utility values from the general population to approximate baselines in decision analytic models when condition-specific data are not available. Value Health 2011;14:539-45. https://doi.org/10.1016/j.jval.2010.10.029.
- Ghofrani HA, D’Armini AM, Grimminger F, Hoeper MM, Jansa P, Kim NH, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension. N Engl J Med 2013;369:319-29. https://doi.org/10.1056/NEJMoa1209657.
- Olschewski H, Simonneau G, Galiè N, Higenbottam T, Naeije R, Rubin LJ, et al. Inhaled iloprost for severe pulmonary hypertension. N Engl J Med 2002;347:322-9. https://doi.org/10.1056/NEJMoa020204.
- Keogh AM, McNeil KD, Wlodarczyk J, Gabbay E, Williams TJ. Quality of life in pulmonary arterial hypertension: improvement and maintenance with bosentan. J Heart Lung Transplant 2007;26:181-7. https://doi.org/10.1016/j.healun.2006.11.009.
- Meads DM, McKenna SP, Doughty N, Das C, Gin-Sing W, Langley J, et al. The responsiveness and validity of the CAMPHOR Utility Index. Eur Respir J 2008;32:1513-19. https://doi.org/10.1183/09031936.00069708.
- Shafazand S, Goldstein MK, Doyle RL, Hlatky MA, Gould MK. Health-related quality of life in patients with pulmonary arterial hypertension. Chest 2004;126:1452-9. https://doi.org/10.1378/chest.126.5.1452.
- Lindgren P, Kahan T, Poulter N, Buxton M, Svarvar P, Dahlöf B, et al. ASCOT investigators . Utility loss and indirect costs following cardiovascular events in hypertensive patients: the ASCOT health economic substudy. Eur J Health Econ 2007;8:25-30. https://doi.org/10.1007/s10198-006-0002-9.
- Luengo-Fernandez R, Gray AM, Bull L, Welch S, Cuthbertson F, Rothwell PM. Oxford Vascular Study . Quality of life after TIA and stroke: ten-year results of the Oxford Vascular Study. Neurology 2013;81:1588-95. https://doi.org/10.1212/WNL.0b013e3182a9f45f.
- Lunde L. Can EQ-5D and 15D be used interchangeably in economic evaluations? Assessing quality of life in post-stroke patients. Eur J Health Econ 2013;14:539-50. https://doi.org/10.1007/s10198-012-0402-y.
- Pickard AS, Johnson JA, Feeny DH, Shuaib A, Carriere KC, Nasser AM. Agreement between patient and proxy assessments of health-related quality of life after stroke using the EQ-5D and Health Utilities Index. Stroke 2004;35:607-12. https://doi.org/10.1161/01.STR.0000110984.91157.BD.
- Rivero-Arias O, Ouellet M, Gray A, Wolstenholme J, Rothwell PM, Luengo-Fernandez R. Mapping the modified Rankin scale (mRS) measurement into the generic EuroQol (EQ-5D) health outcome. Med Decis Making 2010;30:341-54. https://doi.org/10.1177/0272989X09349961.
- Gage BF, Cardinalli AB, Owens DK. The effect of stroke and stroke prophylaxis with aspirin or warfarin on quality of life. Arch Intern Med 1996;156:1829-36. https://doi.org/10.1001/archinte.1996.00440150083009.
- Robinson A, Thomson R, Parkin D, Sudlow M, Eccles M. How patients with atrial fibrillation value different health outcomes: a standard gamble study. J Health Serv Res Policy 2001;6:92-8. https://doi.org/10.1258/1355819011927288.
- Marchetti M, Pistorio A, Barone M, Serafini S, Barosi G. Low-molecular-weight heparin versus warfarin for secondary prophylaxis of venous thromboembolism: a cost-effectiveness analysis. Am J Med 2001;111:130-9. https://doi.org/10.1016/S0002-9343(01)00793-8.
- Monz BU, Connolly SJ, Korhonen M, Noack H, Pooley J. Assessing the impact of dabigatran and warfarin on health-related quality of life: results from an RE-LY sub-study. Int J Cardiol 2013;168:2540-7. https://doi.org/10.1016/j.ijcard.2013.03.059.
- Strong M, Brennan A, Oakley J. How to calculate value of information in seconds using ‘SAVI’, the Sheffield Accelerated Value of Information web app. Value Health 2015;18:A725-6. https://doi.org/10.1016/j.jval.2015.09.2759.
- Caprini JA, Arcelus JI, Reyna JJ. Effective risk stratification of surgical and nonsurgical patients for venous thromboembolic disease. Semin Hematol 2001;38:12-9. https://doi.org/10.1016/S0037-1963(01)90094-0.
- Department of Health and Social Care . Venous Thromboembolism (VTE) Risk Assessment 2010.
- Nygaard A, Nelson AS, Pick A, Danekas PL, Massoomi F, Thielen J, et al. Inter-rater reliability in the evaluation of a thrombosis risk assessment tool. Hospital Pharmacy 2009;44:1089-94. https://doi.org/10.1310/hpj4412-1089.
- Lijmer JG, Mol BW, Heisterkamp S, Bonsel GJ, Prins MH, van der Meulen JH, et al. Empirical evidence of design-related bias in studies of diagnostic tests. JAMA 1999;282:1061-6. https://doi.org/10.1001/jama.282.11.1061.
- Gómez-Outes A, Terleira-Fernández AI, Suárez-Gea ML, Vargas-Castrillón E. Dabigatran, rivaroxaban, or apixaban versus enoxaparin for thromboprophylaxis after total hip or knee replacement: systematic review, meta-analysis, and indirect treatment comparisons. BMJ 2012;344. https://doi.org/10.1136/bmj.e3675.
- Lassen MR, Ageno W, Borris LC, Lieberman JR, Rosencher N, Bandel TJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med 2008;358:2776-86. https://doi.org/10.1056/NEJMoa076016.
- Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Portman RJ. Apixaban or enoxaparin for thromboprophylaxis after knee replacement. N Engl J Med 2009;361:594-60. https://doi.org/10.1056/NEJMoa0810773.
- López-Reyes R, Nauffal D, Ballester M, Martín-Antorán JM, de Sousa MS, Riera-Mestre A, et al. Venous thromboembolism in patients immobilised at home. Eur Respir J 2015;45:1728-31. https://doi.org/10.1183/09031936.00220114.
- Blackwell JR, Raval P, Quigley JP, Patel A, McBride D. Patient compliance with venous thromboembolism prophylaxis (VTE). J Clin Orthop Trauma 2017;8:201-5. https://doi.org/10.1016/j.jcot.2017.03.009.
- Calder JD, Freeman R, Domeij-Arverud E, van Dijk CN, Ackermann PW. Meta-analysis and suggested guidelines for prevention of venous thromboembolism (VTE) in foot and ankle surgery. Knee Surg Sports Traumatol Arthrosc 2016;24:1409-20. https://doi.org/10.1007/s00167-015-3976-y.
- Chapelle C, Rosencher N, Jacques Zufferey P, Mismetti P, Cucherat M, Laporte S. Meta-Embol Group . Prevention of venous thromboembolic events with low-molecular-weight heparin in the non-major orthopaedic setting: meta-analysis of randomized controlled trials. Arthroscopy 2014;30:987-96. https://doi.org/10.1016/j.arthro.2014.03.009.
- Doggrell SA. Reviparin as prophylaxis for thromboembolism after leg injury and hip replacement. Expert Opin Pharmacother 2003;4:285-8. https://doi.org/10.1517/14656566.4.2.285.
- Griffiths JT, Matthews L, Pearce CJ, Calder JD. Incidence of venous thromboembolism in elective foot and ankle surgery with and without aspirin prophylaxis. J Bone Joint Surg Br 2012;94:210-14. https://doi.org/10.1302/0301-620X.94B2.27579.
- Haque S, Davies MB. Oral thromboprophylaxis in patients with ankle fractures immobilized in a below the knee cast. Foot Ankle Surg 2015;21:266-8. https://doi.org/10.1016/j.fas.2015.02.002.
- Hickey BA, Watson U, Cleves A, Alikhan R, Pugh N, Nokes L, et al. Does thromboprophylaxis reduce symptomatic venous thromboembolism in patients with below knee cast treatment for foot and ankle trauma? A systematic review and meta-analysis. Foot and Ankle Surgery 2018;24:19-27. https://doi.org/10.1016/j.fas.2016.06.005.
- Kaye ID, Patel DN, Strauss EJ, Alaia MJ, Garofolo G, Martinez A, et al. Prevention of venous thromboembolism after arthroscopic knee surgery in a low-risk population with the use of aspirin. A randomized trial. Bull Hosp Jt Dis 2015;73:243-8.
- Kock HJ, Schmit-Neuerburg KP, Hanke J, Hakmann A, Althoff M, Rudofsky G, et al. Ambulatory prevention of thrombosis with low molecular weight heparin in plaster immobilization of the lower extremity. Chirurg 1993;64:483-91.
- Little MTM. Low-molecular-weight heparin did not differ from placebo in preventing clinically important deep venous thrombosis after surgical repair of leg fracture. J Bone Joint Surg Am 2016;98. https://doi.org/10.2106/JBJS.15.01442.
- Mangwani J, Sheikh N, Cichero M, Williamson D. What is the evidence for chemical thromboprophylaxis in foot and ankle surgery? Systematic review of the English literature. Foot 2015;25:173-8. https://doi.org/10.1016/j.foot.2014.07.007.
- Menakaya CU, Boddice T, Malhotra R, Ingoe H, Shah M, Muthukumar N, et al. Outpatients thromboprophylaxis following lower limb immobilisation: an institution’s experience. Eur Orthopaed Traumatol 2013;5:335-9. https://doi.org/10.1007/s12570-013-0240-0.
- Metz R, Verleisdonk EJ, van der Heijden GJ. Insufficient evidence for routine use of thromboprophylaxis in ambulatory patients with an isolated lower leg injury requiring immobilization: results of a meta-analysis. Eur J Trauma Emerg Surg 2009;35:169-75. https://doi.org/10.1007/s00068-008-8015-y.
- Ramos J, Perrotta C, Badariotti G, Berenstein G. Interventions for preventing venous thromboembolism in adults undergoing knee arthroscopy. Cochrane Database Syst Rev 2008;4. https://doi.org/10.1002/14651858.CD005259.pub3.
- Samama CM, Lecoules N, Kierzek G, Claessens YE, Riou B, Rosencher N, et al. Comparison of fondaparinux with low-molecular-weight heparin for venous thromboembolism prevention in patients requiring rigid or semi-rigid immobilization for isolated non-surgical below-knee injury. Ann Fr Med ’Urg 2014;4:153-66.
- Samama CM, Riou B, Roy PM, Sautet A, Mismetti P. Prevention of venous thromboembolism after an isolated, non-surgical below-knee injury. Benefit/risk of fondaparinux vs. low molecular weight heparin: the FONDACAST study. J Thromb Haemost 2013;11.
- Samama CM, Riou B, Roy PM, Sautet A, Mismetti P, Van Der Veen A. Subgroup analysis of the FONDACAST study comparing fondaparinux to low-molecular-weight heparin for the prevention of venous thromboembolism after an isolated, non-surgical below-knee injury. J Thromb Haemost 2013;11:88-9.
- Spannagel U, Kujath P. Low molecular weight heparin for the prevention of thromboembolism in outpatients immobilized by plaster cast. Semin Thromb Hemost 1993;19:131-41.
- Walenga JM, Kaiser PC, Prechel MM, Hoppensteadt D, Jeske WP, Misselwitz F, et al. Sustained release of tissue factor following thrombosis of lower limb trauma. Clin Appl Thromb Hemost 2014;20:678-86. https://doi.org/10.1177/1076029614545212.
- Ajwani SH, Shaw A, Naiz O, Bhaskar D, Charalambous CP. Venous thromboembolism prophylaxis in outpatient lower limb fractures and injuries. Ortop Traumatol Rehabil 2016;18:263-8. https://doi.org/10.5604/15093492.1212870.
- Batra S, Kurup H, Gul A, Andrew JG. Thromboprophylaxis following cast immobilisation for lower limb injuries – survey of current practice in United Kingdom. Injury 2006;37:813-17. https://doi.org/10.1016/j.injury.2006.03.016.
- Bertoletti L, Righini M, Bounameaux H, López-Jiménez L, Tiraferri E, Visonà A, et al. Acute venous thromboembolism after non-major orthopaedic surgery or post-traumatic limb immobilisation. Findings from the RIETE registry. Thromb Haemost 2011;105:739-41. https://doi.org/10.1160/TH10-11-0751.
- Caprini JA. Identification of patient venous thromboembolism risk across the continuum of care. Clin Appl Thromb Hemost 2011;17:590-9. https://doi.org/10.1177/1076029611404217.
- Cirlincione AS, Mendicino R, Catanzariti AR, Grossman J. Low-molecular-weight heparin for deep vein thrombosis prophylaxis in foot and ankle surgery: a review. J Foot Ankle Surg 2001;40:96-100. https://doi.org/10.1016/S1067-2516(01)80050-8.
- Decramer A, Lowyck H, Demuynck M. Parameters influencing thromboprophylaxis management of a lower leg trauma treated with a cast/splint. Acta Orthop Belg 2008;74:672-7.
- Douna F. Minor injuries as a risk factor for venous thrombosis. Medecine Therapeutique – Cardio 2008;4:129-32.
- Dyall L, Munireddy S, Tams L, Strong J, Best A, Pavord S. Venous-thromboembolism in patients with plaster casts for lower leg fracture: experience in a large teaching hospital trust. Br J Haematol 2012;157.
- Engbers MJ, Blom JW, Cushman M, Rosendaal FR, Van Hylckama Vlieg A. The contribution of immobility risk factors to the risk of venous thrombosis in the older population. J Thromb Haemost 2013;11:440-1.
- Fall AO, Proulle V, Sall A, Mbaye A, Ba PS, Diao M, et al. Risk factors for thrombosis in an African population. Clin Med Insights Blood Disord 2014;7:1-6. https://doi.org/10.4137/CMBD.S13401.
- Felcher AH, Mularski RA, Mosen DM, Kimes TM, DeLoughery TG, Laxson SE. Incidence and risk factors for venous thromboembolic disease in podiatric surgery. Chest 2009;135:917-22. https://doi.org/10.1378/chest.08-1631.
- Fleischer AE, Abicht BP, Baker JR, Boffeli TJ, Jupiter DC, Schade VL. American College of Foot and Ankle Surgeons’ clinical consensus statement: risk, prevention, and diagnosis of venous thromboembolism disease in foot and ankle surgery and injuries requiring immobilization. J Foot Ankle Surg 2015;54:497-50. https://doi.org/10.1053/j.jfas.2015.02.022.
- Gearhart MM, Luchette FA, Proctor MC, Lutomski DM, Witsken C, James L, et al. The risk assessment profile score identifies trauma patients at risk for deep vein thrombosis. Surgery 2000;128:631-40. https://doi.org/10.1067/msy.2000.108224.
- Healy B, Beasley R, Weatherall M. Venous thromboembolism following prolonged cast immobilisation for injury to the tendo Achillis. J Bone Joint Surg Br 2010;92:646-50. https://doi.org/10.1302/0301-620X.92B5.23241.
- Jiang Y, Li J, Liu Y, Li YC, Zhang WG. Risk factors for deep vein thrombosis after orthopedic surgery and the diagnostic value of D-dimer. Ann Vasc Surg 2015;29:675-81. https://doi.org/10.1016/j.avsg.2014.12.022.
- Kocialkowski C, Bhosale A, Pillai A. Venous thromboembolism prophylaxis in patients immobilised in plaster casts. Clin Res Foot Ankle 2016;4. https://doi.org/10.4172/2329-910X.1000203.
- Lawall H, Matthiessen A, Hohmann V, Bramlage P, Haas S, Schellong S. Venous thromboembolism in medical outpatients – a cross-sectional survey of risk assessment and prophylaxis. Thromb Haemost 2011;105:190-6. https://doi.org/10.1160/TH10-03-0191.
- Lim TK, Goh XL, Tay HC, Goh HFJ, Kang YK. Evaluation of risk assessment models (padua and caprini) in the prediction of venous thromboembolism events: a retrospective review. Ann Acad Med Singapore 2016;45.
- Micheli LJ. Thromboembolic complications of cast immobilization for injuries of the lower extremities. Clin Orthop Relat Res 1975;108:191-5. https://doi.org/10.1097/00003086-197505000-00031.
- Nemeth B, Van Adrichem RA, Le Cessie S, Van Hylckama Vlieg A, Bucciarelli P, . Prediction of risk of venous thrombosis after cast immobilization of the lower extremity. J Thromb Haemost 2013;11:438-9.
- Nesheiwat F, Sergi AR. Deep venous thrombosis and pulmonary embolism following cast immobilization of the lower extremity. J Foot Ankle Surg 1996;35:590-4. https://doi.org/10.1016/S1067-2516(96)80135-9.
- Park MS, Perkins SE, Spears GM, Ashrani AA, Leibson CL, Boos CM, et al. Risk factors for venous thromboembolism after acute trauma: a population-based case-cohort study. Thromb Res 2016;144:40-5. https://doi.org/10.1016/j.thromres.2016.03.026.
- Park SJ, Kim CK, Park YS, Moon YW, Lim SJ, Kim SM. Incidence and factors predicting venous thromboembolism after surgical treatment of fractures below the hip. J Orthop Trauma 2015;29:e349-54. https://doi.org/10.1097/BOT.0000000000000336.
- Parsonage I. Venous thromboembolism in patients with below-knee plaster casts. Emerg Nurse 2009;16:32-5. https://doi.org/10.7748/en2009.03.16.10.32.c6852.
- Persson A, Wredmark T. The treatment of total ruptures of the Achilles tendon by plaster immobilisation. Int Orthop 1979;3:149-52.
- Randelli F, Romanini E, Biggi F, Danelli G, Della Rocca G, Laurora NR, et al. II Italian intersociety consensus statement on antithrombotic prophylaxis in orthopaedics and traumatology: arthroscopy, traumatology, leg immobilization, minor orthopaedic procedures and spine surgery. J Orthop Traumatol 2013;14:1-13. https://doi.org/10.1007/s10195-012-0214-y.
- Rogers FB, Shackford SR, Horst MA, Miller JA, Wu D, Bradburn E, et al. Determining venous thromboembolic risk assessment for patients with trauma: the Trauma Embolic Scoring System. J Trauma Acute Care Surg 2012;73:511-15. https://doi.org/10.1097/TA.0b013e3182588b54.
- Samama MM. An epidemiologic study of risk factors for deep vein thrombosis in medical outpatients: the Sirius study. Arch Intern Med 2000;160:3415-20. https://doi.org/10.1001/archinte.160.22.3415.
- Simon MA, Mass DP, Zarins CK, Bidani N, Gudas CJ, Metz CE. The effect of a thigh tourniquet on the incidence of deep venous thrombosis after operations on the fore part of the foot. J Bone Joint Surg Am 1982;64:188-91. https://doi.org/10.2106/00004623-198264020-00006.
- Slaybaugh RS, Beasley BD, Massa EG. Deep venous thrombosis risk assessment, incidence, and prophylaxis in foot and ankle surgery. Clin Podiatr Med Surg 2003;20:269-89. https://doi.org/10.1016/S0891-8422(03)00007-7.
- Solis G, Saxby T. Incidence of DVT following surgery of the foot and ankle. Foot Ankle Int 2002;23:411-14. https://doi.org/10.1177/107110070202300507.
- Spencer FA, Emery C, Joffe SW, Pacifico L, Lessard D, Reed G, et al. Incidence rates, clinical profile, and outcomes of patients with venous thromboembolism. The Worcester VTE study. J Thromb Thrombolysis 2009;28:401-9. https://doi.org/10.1007/s11239-009-0378-3.
- Spyropoulos AC. Venous thromboembolism risk factors in acutely ill hospitalized medical patients. Haematologica Meeting Reports 2009;3:21-2.
- Spyropoulos AC, Anderson FA, FitzGerald G, Decousus H, Tapson V. Venous Thromboembolism Risk Factors in Acutely Ill Hospitalized Medical Patients: Findings From the Improve Registry (OC-MO-052) n.d.
- Tan L, Qi B, Yu T, Wang C. Incidence and risk factors for venous thromboembolism following surgical treatment of fractures below the hip: a meta-analysis. Int Wound J 2016;13:1359-71. https://doi.org/10.1111/iwj.12533.
- Toure AO. Risk factors of thrombosis in an African population. J Thromb Haemost 2014;12.
- True VL, Williamson DM. Do patients receive the appropriate assessment and implementation of venous thromboembolism prophylaxis for lower leg trauma and surgery?. Br J Haematol 2014;165.
- van Adrichem RA, Nelissen RG, Schipper IB, Rosendaal FR, Cannegieter SC. Risk of venous thrombosis after arthroscopy of the knee: results from a large population-based case-control study. J Thromb Haemost 2015;13:1441-8. https://doi.org/10.1111/jth.12996.
- van Adrichem RA, Debeij J, Nelissen GHH, Schipper IB, Rosendaal FR, Cannegieter SC. Lower leg cast immobilisation and risk of venous thrombosis: results from the MEGA study. J Thromb Haemost 2013;11.
- Vollans S, Chaturvedi A, Sivasankaran K, Madhu T, Hadland Y, Allgar V, et al. Symptomatic venous thromboembolism following circular frame treatment for tibial fractures. Injury 2015;46:1108-11. https://doi.org/10.1016/j.injury.2015.04.003.
- Wang J, Zhao CP, Wei J, Wang CM. An analysis of risk factors for lower limb deep venous thrombosis in patients with tibial plateau fractures. Chin J Bone Joint 2015;2:86-90.
- Simpson EL, Stevenson MD, Rawdin A, Papaioannou D. Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis. Health Technol Assess 2009;13. https://doi.org/10.3310/hta13020.
- Ingelgard A, Hedner E, Stigendal J, Carlsson J. Patient-Reported Outcomes in Patients With Deep Vein Thrombosis Treated With Warfarin 2002.
- Ghanima W, Wik HS, Tavoly M, Enden T, Jelsness-Jorgensen LP. Late consequences of venous thromboembolism: measuring quality of life after deep vein thrombosis and pulmonary embolism. Thromb Res 2018;164:170-6. https://doi.org/10.1016/j.thromres.2017.07.025.
Appendix 1 Literature search strategies for the review of pharmacological thromboprophylaxis for preventing venous thromboembolism
Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily, Ovid MEDLINE and Versions(R)
Platform or provider used: Ovid SP.
Date range searched: 1946 to April 2017.
Date searched: April 2017.
Search strategy
-
thrombosis/ or exp venous thrombosis/
-
Venous Thromboembolism/ or Thromboembolism/
-
exp Pulmonary Embolism/
-
(thromboprophyla* or thrombus* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol*).ti,ab,kw.
-
((vein* or ven*) adj7 thromb*).ti,ab,kw.
-
(PE or DVT or VTE).ti,ab,kw.
-
1 or 2 or 3 or 4 or 5 or 6
-
exp Immobilization/
-
exp Mobility Limitation/
-
Splints/
-
Braces/
-
exp Casts, Surgical/
-
immobili*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
brace*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
splint*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
plaster*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
cast.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(leg* or tibia* or fibula* or ankle*).mp. and (fracture*.hw. or su.fs.) and co.fs.
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
-
exp Heparin, Low-Molecular-Weight/
-
(heparin* or LMWH or nadroparin* or fraxiparin* or enoxaparin or Clexane or klexane or lovenox or dalteparin or Fragmin or ardeparin or normiflo or tinzaparin or logiparin or Innohep or certoparin or sandoparin or reviparin or clivarin* or danaproid or danaparoid or bemiparin or bioparin or Alphaparin or Troparin).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(antixarin or ardeparin* or bemiparin* or Zibor or cy 222 or embolex or monoembolex or Mono-embolex or parnaparin* or “rd 11885” or tedelparin or Kabi-2165 or Kabi 2165).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(emt-966 or emt-967 or pk-10169 or pk10169).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(cy-216 or cy216 or seleparin* or tedegliparin or seleparin* or tedegliparin* or tedelparin or Boxol or Liquemine).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
fr-860.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(wy90493 or wy-90493).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(kb-101 or kb101 or lomoparan or orgaran).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(parnaparin or fluxum or lohepa or lowhepa or “op 2123” or parvoparin).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(AVE5026 or M118 or RO-14).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29
-
(Rivaroxaban or xarelto or Apixaban or eliquis or Edoxaban or lixiana or Dabigatran or pradaxa or prazaxa or Praxibind or idaricuzimab).mp.
-
(novel oral anticoagulant* or novel oral anti-coagulant* or (new adj3 (anticoagulant* or anti-coagulant*))).mp.
-
(direct oral anticoagulant* or direct oral anti-coagulant*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(NOAC* or DOAC*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
exp Aspirin/
-
(acetylsalicylic acid* or aspirin).mp.
-
31 or 32 or 33 or 34 or 35 or 36
-
7 and 19 and 30
-
limit 38 to yr=“2013 -Current”
-
7 and 19 and 37
-
39 or 40
Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Database of Abstracts of Review of Effects, Health Technology Assessment Database and NHS Economic Evaluation Database
Platform or provider used: Wiley Online Library.
Date range searched: 1898 to April 2017.
Date searched: April 2017.
Search strategy
-
#1 MeSH descriptor: [Thrombosis] explode all trees
-
#2 MeSH descriptor: [Venous Thrombosis] explode all trees
-
#3 MeSH descriptor: [Thromboembolism] explode all trees
-
#4 MeSH descriptor: [Venous Thromboembolism] explode all trees
-
#5 MeSH descriptor: [Pulmonary Embolism] explode all trees
-
#6 (thromboprophyla* or thrombus* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol*):ti,ab,kw (Word variations have been searched)
-
#7 ((vein* or ven*) near/7 thromb*):ti,ab,kw
-
#8 (PE or DVT or VTE):ti,ab,kw
-
#9 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8
-
#10 MeSH descriptor: [Immobilization] explode all trees
-
#11 MeSH descriptor: [Mobility Limitation] explode all trees
-
#12 MeSH descriptor: [Splints] explode all trees
-
#13 MeSH descriptor: [Braces] explode all trees
-
#14 MeSH descriptor: [Casts, Surgical] explode all trees
-
#15 (immobili* or brace* or splint* or plaster* or cast):ti,ab,kw
-
#16 ((leg* or tibia* or fibula* or ankle*) and (fracture* or surg*) and complication*):ti,ab,kw
-
#17 #10 or #11 or #12 or #13 or #14 or #15 or #16
-
#18 MeSH descriptor: [Heparin, Low-Molecular-Weight] explode all trees
-
#19 (heparin* or LMWH or nadroparin* or fraxiparin* or enoxaparin or Clexane or klexane or lovenox or dalteparin or Fragmin or ardeparin or normiflo or tinzaparin or logiparin or Innohep or certoparin or sandoparin or reviparin or clivarin* or danaproid or danaparoid or bemiparin or bioparin or Alphaparin or Troparin):ti,ab,kw
-
#20 (antixarin or ardeparin* or bemiparin* or Zibor or cy 222 or embolex or monoembolex or Mono-embolex or parnaparin* or “rd 11885” or tedelparin or Kabi-2165 or Kabi 2165):ti,ab,kw
-
#21 (emt-966 or emt-967 or pk-10169 or pk10169):ti,ab,kw
-
#22 fr-860:ti,ab,kw
-
#23 (wy90493 or wy-90493 or kb-101 or kb101 or lomoparan or orgaran or parnaparin or fluxum or lohepa or lowhepa or “op 2123” or parvoparin or AVE5026 or M118 or RO-14):ti,ab,kw
-
#24 #18 or #19 or #20 or #21 or #22 or #23
-
#25 #9 and #17 and #24 Publication Year from 2013 to 2017
-
#26 MeSH descriptor: [Anticoagulants] explode all trees
-
#27 (Rivaroxaban or xarelto or Apixaban or eliquis or Edoxaban or lixiana or Dabigatran or pradaxa or prazaxa or praxibind or idaricuzimab):ti,ab,kw
-
#28 (novel oral anticoagulant* or novel oral anti-coagulant* or (new near/3 (anticoagulant* or anti-coagulant*))):ti,ab,kw
-
#29 (direct oral anticoagulant* or direct oral anti-coagulant*):ti,ab,kw
-
#30 (NOAC* or DOAC*):ti,ab,kw
-
#31 MeSH descriptor: [Aspirin] explode all trees
-
#32 (acetylsalicylic acid* or aspirin):ti,ab,kw
-
#33 #26 or #27 or #28 or #29 or #30 or #31 or #32
-
#34 #9 and #17 and #33
-
#35 #25 or #34
EMBASE
Platform or provider used: Ovid SP.
Date range searched: 1974 to April 2017.
Date searched: April 2017.
Search strategy
-
thrombosis/ or exp vein thrombosis/ or deep vein thrombosis/
-
Venous Thromboembolism/ or Thromboembolism/
-
exp lung embolism/
-
(thromboprophyla* or thrombus* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol*).ti,ab,kw.
-
((vein* or ven*) adj7 thromb*).ti,ab,kw.
-
(PE or DVT or VTE).ti,ab,kw.
-
1 or 2 or 3 or 4 or 5 or 6
-
exp Immobilization/
-
exp Mobility Limitation/
-
Splints/
-
Braces/
-
exp Casts, Surgical/
-
immobili*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
brace*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
splint*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
plaster*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
cast.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(leg* or tibia* or fibula* or ankle*).mp. and (fracture*.hw. or su.fs.) and co.fs.
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17
-
exp Heparin, Low-Molecular-Weight/
-
(heparin* or LMWH or nadroparin* or fraxiparin* or enoxaparin or Clexane or klexane or lovenox or dalteparin or Fragmin or ardeparin or normiflo or tinzaparin or logiparin or Innohep or certoparin or sandoparin or reviparin or clivarin* or danaproid or danaparoid or bemiparin or bioparin or Alphaparin or Troparin).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(antixarin or ardeparin* or bemiparin* or Zibor or cy 222 or embolex or monoembolex or Mono-embolex or parnaparin* or “rd 11885” or tedelparin or Kabi-2165 or Kabi 2165).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(emt-966 or emt-967 or pk-10169 or pk10169).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(cy-216 or cy216 or seleparin* or tedegliparin or seleparin* or tedegliparin* or tedelparin or Boxol or Liquemine).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
fr-860.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(wy90493 or wy-90493).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(kb-101 or kb101 or lomoparan or orgaran).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(parnaparin or fluxum or lohepa or lowhepa or “op 2123” or parvoparin).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(AVE5026 or M118 or RO-14).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29
-
(Rivaroxaban or xarelto or Apixaban or eliquis or Edoxaban or lixiana or Dabigatran or pradaxa or prazaxa or Praxibind or idaricuzimab).mp.
-
(novel oral anticoagulant* or novel oral anti-coagulant* or (new adj3 (anticoagulant* or anti-coagulant*))).mp.
-
(direct oral anticoagulant* or direct oral anti-coagulant*).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(NOAC* or DOAC*).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
acetylsalicylic acid/
-
(acetylsalicylic acid* or aspirin).mp.
-
31 or 32 or 33 or 34 or 35 or 36
-
7 and 19 and 30
-
limit 38 to yr=“2013 -Current”
-
7 and 19 and 37
-
39 or 40
Appendix 2 Excluded studies: review of pharmacological thromboprophylaxis for preventing venous thromboembolism
| Number | Authors, year | Reason for exclusion |
|---|---|---|
| 1 | Blackwell et al.,218 2017 | Not a randomised or controlled clinical trial |
| 2 | Braithwaite et al.,22 2016 | Not a randomised or controlled clinical trial |
| 3 | Calder et al.,219 2016 | Systematic review |
| 4 | Chapelle et al.,220 2014 | Systematic review |
| 5 | Doggrell et al.,221 2003 | Review (non-systematic) |
| 6 | Ettema et al.,36 2008 | Systematic review |
| 7 | Griffiths et al.,222 2012 | Not a randomised or controlled clinical trial |
| 8 | Haque and Davies,223 2015 | Not a randomised or controlled clinical trial |
| 9 | Hickey et al.,224 2016 | Systematic review |
| 10 | Kaye et al.,225 2015 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| 11 | Kock et al.,226 1993 | Duplicate of included full-text study: Kock et al.52 |
| 12 | Little,227 2016 | Commentary |
| 13 | López-Reyes et al.,217 2015 | Not a randomised or controlled clinical trial (letter to the editor) |
| 14 | Mangwani et al.,228 2015 | Systematic review |
| 15 | Menakaya et al.,229 2013 | Not a randomised or controlled clinical trial |
| 16 | Metz et al.,230 2009 | Systematic review |
| 17 | Ramos et al.,231 2008 | Systematic review |
| 18 | Samama et al.,232 2014 | Duplicate of an included full-text study: Samama et al.,57 2013 |
| 19 | Samama et al.,233 2013 (abstract) | Abstract of an included full-text study: Samama et al.,57 2013 |
| 20 | Samama et al.,234 2013 | Subgroup results of an included full-text study: Samama et al.,57 2013 |
| 21 | Spannagel and Kujath,235 1993 | Duplicate of included full text study: Kujath et al.,53 1993 |
| 22 | Testroote et al.,15 2014 | Systematic review |
| 23 | Walenga et al.,236 2014 | Substudy of an included full-text study (Lassen et al.,56 2002) – focus on biomarker evaluation |
Appendix 3 Summary of trials included in the base-case network meta-analysis of pharmacological thromboprophylaxis for preventing venous thromboembolism
| Authors, year | Comparison | Any VTE | Clinically relevant DVT (i.e. symptomatic or proximal/extensive) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LMWH | Fondaparinux | Control | LMWH | Fondaparinux | Control | ||||||||
| Events, n | Total, n (%) | Events, n | Total, n (%) | Events, n | Total,a n (%) | Events, n | Total, n (%) | Events, n | Total, n (%) | Events, n | Total,b n (%) | ||
| Goel et al.,50 2009 | LMWH vs. placebo | 11 | 127 (8.7) | – | – | 14 | 111 (12.6) | 0 | 127 (0.0) | – | – | 0 | 111 (0.0) |
| Jørgensen et al.,51 2002 | LMWH vs. no treatment | 10 | 99 (10.1) | – | – | 18 | 106 (17.0) | 0 | 99 (0.0) | – | – | 1 | 106 (0.9) |
| Kock et al.,52 1995 | LMWH vs. no treatment | 0 | 176 (0) | – | – | 7 | 163 (4.3) | 0 | 176 (0.0) | – | – | 5 | 163 (3.1) |
| Kujath et al.,53 1993 | LMWH vs. no treatment | 6 | 126 (4.8) | – | – | 21 | 127 (16.5) | – | – | – | – | – | – |
| Lapidus et al.,55 2007 | LMWH vs. placebo | 18 | 49 (36.7) | – | – | 19 | 47 (40.4) | 1 | 49 (2.0) | – | – | 3 | 47 (6.4) |
| Lapidus et al.,54 2007 | LMWH vs. placebo | 24 | 117 (20.5) | – | – | 34 | 109 (31.2) | 2 | 117 (1.7) | – | – | 6 | 109 (5.5) |
| Lassen et al.,56 2002 | LMWH vs. placebo | 17 | 183 (9.3) | – | – | 35 | 188 (18.6) | – | – | – | – | – | – |
| Selby et al.,58 2015 | LMWH vs. placebo | 4 | 130 (3.1) | – | – | 4 | 128 (3.1) | 2 | 130 (1.5) | – | – | 2 | 128 (1.6) |
| van Adrichem et al.,59 2017 | LMWH vs. no treatment | 10 | 719 (1.4) | – | – | 13 | 716 (1.8) | 7 | 719 (1.0) | – | – | 9 | 716 (1.3) |
| Zheng et al.,60 2016 | LMWH vs. placebo | 6 | 411 (1.5) | – | – | 13 | 403 (3.2) | 1 | 411 (0.2) | – | – | 6 | 403 (1.5) |
| Gehling et al.,23 1998 | LMWH vs. aspirin | 9 | 143 (6.3) | – | – | 7 | 144 (4.9) | 2 | 143 (1.4) | – | – | 1 | 144 (0.7) |
| Bruntink et al.,49 2017 | LMWH vs. fondaparinux vs. no treatment | 2 | 92 (2.2) | 1 | 92 (1.1) | 11 | 94 (11.7) | – | – | – | – | – | – |
| Samama et al.,57 2013 | LMWH vs. fondaparinux | 49 | 622 (7.9) | 14 | 621 (2.3) | – | – | 10 | 622 (1.6) | 6 | 621 (1.0) | – | – |
| Authors, year | Comparison | Clinically detected DVT (i.e. symptomatic) | Asymptomatic DVT (all) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LMWH | Fondaparinux | Control | LMWH | Fondaparinux | Control | ||||||||
| Events, n | Total, n (%) | Events, n | Total, n (%) | Events, n | Total,a n (%) | Events, n | Total,b n (%) | Events, n | Total, n (%) | Events, n | Total,b n (%) | ||
| Goel et al.,50 2009 | LMWH vs. placebo | 0 | 127 (0.0) | – | – | 0 | 111 (0.0) | 11 | 127 (8.7) | – | – | 14 | 111 (12.6) |
| Jørgensen et al.,51 2002 | LMWH vs. no treatment | 0 | 99 (0.0) | – | – | 0 | 106 (0.0) | 10 | 99 (10.1) | – | – | 18 | 106 (17.0) |
| Kock et al.,52 1995 | LMWH vs. no treatment | 0 | 176 (0.0) | – | – | 4 | 163 (2.5) | 0 | 176 (0.0) | – | – | 3 | 163 (1.8) |
| Kujath et al.,53 1993 | LMWH vs. no treatment | – | – | – | – | – | – | – | – | – | – | – | – |
| Lapidus et al.,55 2007 | LMWH vs. placebo | – | – | – | – | – | – | – | – | – | – | – | – |
| Lapidus et al.,54 2007 | LMWH vs. placebo | 2 | 117 (1.7) | – | – | 6 | 109 (5.5) | 22 | 117 (18.8) | – | – | 28 | 109 (25.7) |
| Lassen et al.,56 2002 | LMWH vs. placebo | 0 | 183 (0.0) | – | – | 4 | 188 (2.1) | 17 | 183 (9.3) | – | – | 31 | 188 (16.5) |
| Selby et al.,58 2015 | LMWH vs. placebo | 1 | 130 (0.8) | – | – | 1 | 128 (0.8) | 3 | 130 (2.3) | – | 2 | 128 (1.6) | |
| van Adrichem et al.,59 2017 | LMWH vs. no treatment | 7 | 719 (1.0) | – | – | 9 | 716 (1.3) | – | – | – | – | – | – |
| Zheng et al.,60 2016 | LMWH vs. placebo | 0 | 411 (0.0) | – | – | 0 | 403 (0.0) | 6 | 411 (1.5) | – | – | 13 | 403 (3.2) |
| Gehling et al.,23 1998 | LMWH vs. aspirin | 2 | 143 (1.4) | – | – | 1 | 144 (0.7) | 7 | 143 (4.9) | – | – | 6 | 144 (4.2) |
| Bruntink et al.,49 2017 | LMWH vs. fondaparinux vs. no treatment | 0 | 92 (0.0) | 0 | 92 (0.0) | 0 | 94 (0.0) | 2 | 92 (2.2) | 1 | 92 (1.1) | 9 | 94 (9.6) |
| Samama et al.,57 2013 | LMWH vs. fondaparinux | 7 | 622 (1.1) | 2 | 621 (0.3) | – | – | 42 | 622 (6.8) | 11 | 621 (1.8) | – | – |
| Authors, year | Comparison | Asymptomatic DVT (proximal) | Asymptomatic DVT (distal) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LMWH | Fondaparinux | Control | LMWH | Fondaparinux | Control | ||||||||
| Events, n | Total, n (%) | Events, n | Total, n (%) | Events, n | Total,a n (%) | Events, n | Total, n (%) | Events, n | Total, n (%) | Events, n | Total,b n (%) | ||
| Goel et al.,50 2009 | LMWH vs. placebo | 0 | 127 (0.0) | – | – | 0 | 111 (0.0) | 11 | 127 (8.7) | – | – | 14 | 111 (12.6) |
| Jørgensen et al.,51 2002 | LMWH vs. no treatment | 0 | 99 (0.0) | – | – | 1 | 106 (0.9) | 10 | 99 (10.1) | – | – | 17 | 106 (16.0) |
| Kock et al.,52 1995 | LMWH vs. no treatment | 0 | 176 (0.0) | – | – | 1 | 163 (0.6) | 0 | 176 (0.0) | – | – | 2 | 163 (1.2) |
| Kujath et al.,53 1993 | LMWH vs. no treatment | – | – | – | – | – | – | – | – | – | – | – | – |
| Lapidus et al.,55 2007 | LMWH vs. placebo | 1 | 49 (2.0) | – | – | 3 | 47 (6.4) | – | – | – | – | – | – |
| Lapidus et al.,54 2007 | LMWH vs. placebo | – | – | – | – | – | – | – | – | – | – | – | – |
| Lassen et al.,56 2002 | LMWH vs. placebo | – | – | – | – | – | 14 | 183 (7.7) | – | – | 21 | 188 (11.2) | |
| Selby et al.,58 2015 | LMWH vs. placebo | 1 | 130 (0.8) | – | – | 1 | 128 (0.8) | 2 | 130 (1.5) | – | – | 1 | 128 (0.8) |
| van Adrichem et al.,59 2017 | LMWH vs. no treatment | – | – | – | – | – | – | – | – | – | – | – | – |
| Zheng et al.,60 2016 | LMWH vs. placebo | 1 | 411 (0.2) | – | – | 6 | 403 (1.5) | 5 | 411 (1.2) | – | – | 7 | 403 (1.7) |
| Gehling et al.,23 1998 | LMWH vs. aspirin | 0 | 143 (0.0) | – | – | 0 | 144 (0.0) | 7 | 143 (4.9) | – | – | 6 | 144 (4.2) |
| Bruntink et al.,49 2017 | LMWH vs. fondaparinux vs. no treatment | – | – | – | – | – | – | – | – | – | – | – | – |
| Samama et al.,57 2013 | LMWH vs. fondaparinux | 3 | 585 (0.5) | 4 | 582 (0.7) | – | – | 39 | 585 (6.7) | 7 | 582 (1.2) | – | – |
| Authors, year | Comparison | PE | Major bleeding | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LMWH | Fondaparinux | Control | LMWH | Fondaparinux | Control | ||||||||
| Events, n | Total, n (%) | Events, n | Total, n (%) | Events, n | Total,a n (%) | Events, n | Total, n (%) | Events, n | Total, n (%) | Events, n | Total,b n (%) | ||
| Goel et al.,50 2009 | LMWH vs. placebo | 0 | 127 (0.0) | – | – | 0 | 111 (0.0) | 0 | 127 (0.0) | – | – | 0 | 111 (0.0) |
| Jørgensen et al.,51 2002 | LMWH vs. no treatment | 0 | 99 (0.0) | – | – | 0 | 106 (0.0) | 0 | 99 (0.0) | – | – | 0 | 106 (0.0) |
| Kock et al.,52 1995 | LMWH vs. no treatment | 0 | 176 (0.0) | – | – | 0 | 163 (0.0) | 0 | 176 (0.0) | – | – | 0 | 163 (0.0) |
| Kujath et al.,53 1993 | LMWH vs. no treatment | 0 | 126 (0.0) | – | – | 0 | 127 (0.0) | 0 | 126 (0.0) | – | – | 0 | 127 (0.0) |
| Lapidus et al.,55 2007 | LMWH vs. placebo | 0 | 49 (0.0) | – | – | 0 | 47 (0.0) | 0 | 49 (0.0) | – | – | 0 | 47 (0.0) |
| Lapidus et al.,54 2007 | LMWH vs. placebo | 0 | 117 (0.0) | – | – | 0 | 109 (0.0) | 0 | 117 (0.0) | – | – | 0 | 109 (0.0) |
| Lassen et al.,56 2002 | LMWH vs. placebo | 0 | 183 (0.0) | – | – | 2 | 188 (1.1) | 2 | 217 (0.9) | – | – | 1 | 221 (0.5) |
| Selby et al.,58 2015 | LMWH vs. placebo | 0 | 130 (0.0) | – | – | 1 | 128 (0.8) | 0 | 134 (0.0) | – | – | 0 | 131 (0.0) |
| van Adrichem et al.,59 2017 | LMWH vs. no treatment | 4 | 719 (0.6) | – | – | 5 | 716 (0.7) | 0 | 719 (0.0) | – | – | 0 | 716 (0.0) |
| Zheng et al.,60 2016 | LMWH vs. placebo | 0 | 411 (0.0) | – | – | 0 | 403 (0.0) | 0 | 411 (0.0) | – | – | 0 | 403 (0.0) |
| Gehling et al.,23 1998 | LMWH vs. aspirin | 0 | 143 (0.0) | – | – | 0 | 144 (0.0) | 0 | 143 (0.0) | – | – | 0 | 144 (0.0) |
| Bruntink et al.,49 2017 | LMWH vs. fondaparinux vs. no treatment | 0 | 92 (0.0) | 0 | 92 (0.0) | 2 | 94 (2.1) | 0 | 92 (0.0) | 0 | 92 (0.0) | 0 | 94 (0.0) |
| Samama et al.,57 2013 | LMWH vs. fondaparinux | 0 | 622 (0.0) | 2 | 621 (0.3) | – | – | 0 | 670 (0.0) | 1 | 674 (0.1) | – | – |
Appendix 4 Details of the network meta-regressions
The following potential treatment effect modifiers were assessed: (1) population characteristics (i.e. proportion that were male, baseline risk of VTE), (2) type of injury (i.e. fractures, Achilles tendon rupture, other soft-tissue injury), (3) treatment of injury (surgical vs. conservative, above- vs. below-knee immobilisation), (4) thromboprophylactic agent used and (5) duration of thromboprophylaxis.
For each outcome of interest, except for major bleeding, a network meta-regression of the potential treatment effect modifiers 1–3 and 5 was performed separately for each covariate using an approach similar to that described in Chapter 3, Methods of data synthesis and analysis. The analyses were performed by centring the covariates at their mean values of the reference treatment (i.e. placebo, no treatment and aspirin) to improve mixing of the Markov chain Monte Carlo chains. In each model, the regression parameter was given a normally distributed prior distribution with mean 0 and variance 1000, that is N(0, 1000). Only Lassen et al. 56 and Samama et al. 57 provided information about major bleeding. Consequently, a meta-regression of major bleeding was not performed.
The analysis of the effect of the baseline risk of VTE was performed with respect to the true baseline rather than the sample estimate of the baseline in order to avoid regression to the mean. Simultaneously assessing the effect of three types of injury would have involved a model with two covariates to estimate in relatively sparse data sets; in practice, only the effect of fractures versus other types of injury was assessed. The effect of the management of the injury using a surgical or conservative approach, and the method of immobilisation (i.e. whether above or below the knee), were assessed separately. Several studies (i.e. Kujath et al. ,53 Samama et al. ,57 Selby et al. ,58 van Adrichem et al. 59 and Zheng et al. 60) provided insufficient information to allow a classification of whether the immobilisation was above or below the knee; these studies were excluded from the meta-regression.
In a network meta-regression, three assumptions can be made about the interaction between a covariate and each treatment effect: (1) independent – treatment-specific interaction terms for each pair of treatments, (2) exchangeable – treatment-specific but related interaction terms and (3) identical interaction effects for all treatments. Given the relative sparseness of the data, the analysis was performed by only assuming identical interaction terms for all treatments.
The effect of the type of thromboprophylactic agent used (i.e. dalteparin, tinzaparin, certoparin nadroparin, reviparin) was assessed using a separate NMA. Van Adrichem et al. 59 allowed nadroparin or dalteparin to be used in accordance with the preference of each hospital and no further information was provided as to what was actually used. No information was available on the LMWH used in Zheng et al. 60 Therefore, Van Adrichem et al. 59 and Zheng et al. 60 were excluded from the analysis.
The unadjusted and covariate-adjusted models were compared using the deviance information criterion. Models fitted to a particular data set that have lower deviance information criterion values provide the best predictions. However, differences in deviance information criterion values of < 5 are generally not important and the simpler model is generally preferred, irrespective of the estimated effect of individual parameters. In addition, deviation information criterion values can only be compared for models applied to the same data sets. Consequently, it is not possible to compare unadjusted and adjusted models with respect to the effect of immobilisation above or below the knee, or the type of thromboprophylactic agent used, because the analyses make use of data from different studies.
It was not possible to use data from all the studies in all the analyses. Gehling et al. 23 and Goel et al. 50 had no asymptomatic DVT proximal events and, consequently, provided no information with which to estimate treatment effects or the effects of potential treatment effect modifiers. Jørgensen et al. ,51 Goel et al. ,50 Bruntink et al. 49 and Zheng et al. 60 had no clinically detected DVT events and, consequently, provided no information with which to estimate treatment effects or the effects of potential treatment effect modifiers. Goel et al. 50 had no clinically relevant DVT events and, consequently, provided no information with which to estimate treatment effects or the effects of potential treatment effect modifiers. Only Lassen et al. ,56 Samama et al. ,57 Selby et al. ,58 Bruntink et al. 49 and van Adrichem et al. 59 had PEs; all other studies provided no information with which to estimate treatment effects or the effects of potential treatment effect modifiers.
Table 31 shows the results of the network meta-regression for all potential effect modifiers except thromboprophylactic agent used. Results according to the proportion of patients with immobilisation below the knee should be treated with caution as the model is fitted to a subset of the data and it is not possible to compare the fit of this model with that of the unadjusted model. The adjusted deviance information criterion suggested that no covariate improved the model fits.
| Covariate | No treatmenta | Adjusted DIC | Regression parameter coefficient (95% CI) |
|---|---|---|---|
| Any VTE (unadjusted DIC = 157.6) | |||
| Proportion male | 56 | 159.1 | 0.007 (–0.029 to 0.043) |
| Baseline VTE (%; logit) | 0.10 (–2.214) | 159.5 | –0.024 (–0.358 to 0.299) |
| Type of injury: proportion fractures | 68 | 158.9 | 0.003 (–0.007 to 0.015) |
| Treatment of injury: proportion surgery | 63 | 153.6 | 0.009 (0.002 to 0.018) |
| Treatment of injury: proportion below knee | 91 | N/A | –0.001 (–0.043 to 0.041) |
| Duration of thromboprophylaxis (days) | 28 | 159.2 | 0.005 (–0.021 to 0.033) |
| Asymptomatic DVT (all) (unadjusted DIC = 113.9) | |||
| Proportion male | 54 | 115.8 | –0.005 (–0.064 to 0.053) |
| Baseline VTE (%; logit) | 0.12 (–2.039) | 172.1 | –0.003 (–0.452 to 0.445) |
| Type of injury: proportion fractures | 85 | 114.6 | 0.015 (–0.011 to 0.050) |
| Treatment of injury: proportion surgery | 71 | 112.1 | 0.012 (–0.000 to 0.026) |
| Treatment of injury: proportion below knee | 90 | N/A | –0.005 (–0.045 to 0.034) |
| Duration of thromboprophylaxis (days) | 27 | 115.6 | –0.005 (–0.035 to 0.025) |
| Asymptomatic DVT (distal) (unadjusted DIC = 84.4) | |||
| Proportion male | 56 | 85.6 | –0.040 (–0.153 to 0.059) |
| Baseline VTE (%; logit) | 0.10 (–2.249) | 128.8 | –0.172 (–0.879 to 0.510) |
| Type of injury: proportion fractures | 81 | 84.7 | 0.022 (–0.011 to 0.070) |
| Treatment of injury: proportion surgery | 77 | 85.1 | 0.013 (–0.009 to 0.044) |
| Treatment of injury: proportion below knee | 85 | N/A | –0.003 (–0.057 to 0.050) |
| Duration of thromboprophylaxis (days) | 23 | 86.2 | –0.005 (–0.045 to 0.038) |
| Asymptomatic DVT (proximal) (unadjusted DIC = 44.8) | |||
| Proportion male | 60 | 46.6 | –0.018 (–0.205 to 0.148) |
| Baseline VTE (%; logit) | 0.11 (–2.141) | 89.3 | –0.060 (–1.467 to 1.123) |
| Type of injury: proportion fractures | 69 | 46.5 | 0.003 (–0.032 to 0.045) |
| Treatment of injury: proportion surgery | 84 | 43.9 | 0.900 (0.045 to 2.650) |
| Treatment of injury: proportion below knee | 87 | N/A | 1.289 (–0.128 to 4.068) |
| Duration of thromboprophylaxis (days) | 23 | 46.5 | –0.007 (–0.146 to 0.111) |
| Clinically detected (DVT) (unadjusted DIC = 64.4) | |||
| Proportion male | 53 | 63.8 | –0.209 (–0.685 to 0.056) |
| Baseline VTE (%; logit) | 0.10 (–2.229) | 127.0 | –0.514 (–1.505 to 0.303) |
| Type of injury: proportion fractures | 85 | 62.6 | 0.080 (0.003 to 0.267) |
| Treatment of injury: proportion surgery | 65 | 64.9 | 0.007 (–0.017 to 0.041) |
| Treatment of injury: proportion below knee | 90 | N/A | 1.247 (0.101 to 4.133) |
| Duration of thromboprophylaxis (days) | 28 | 65.5 | –0.018 (–0.119 to 0.076) |
| Clinically relevant (DVT) (unadjusted DIC = 80.9) | |||
| Proportion male | 58 | 81.0 | –0.062 (–0.176 to 0.029) |
| Baseline VTE (%; logit) | 0.10 (–2.229) | 137.3 | –0.267 (–0.983 to 0.377) |
| Type of injury: proportion fractures | 75 | 81.1 | 0.017 (–0.008 to 0.052) |
| Treatment of injury: proportion surgery | 77 | 82.1 | 0.002 (–0.017 to 0.027) |
| Treatment of injury: proportion below knee | 88 | N/A | 2.056 (0.128 to 7.393) |
| Duration of thromboprophylaxis (days) | 27 | 82.2 | 0.010 (–0.063 to 0.082) |
| PE (unadjusted DIC = 38.2) | |||
| Proportion male | 56 | 37.7 | 0.308 (–0.269 to 1.062) |
| Baseline VTE (%; logit) | 0.09 (–2.277) | 104.2 | –15.190 (–36.670 to –3.094) |
| Type of injury: proportion fractures | 74 | 38.3 | –0.058 (–0.309 to 0.191) |
| Treatment of injury: proportion surgery | 63 | 38.8 | –0.057 (–0.263 to 0.028) |
| Treatment of injury: proportion below knee | 91 | N/A | 0.060 (–0.212 to 0.488) |
| Duration of thromboprophylaxis (days) | 28 | 38.9 | 0.060 (–0.212 to 0.488) |
Table 32 shows the results according to the type of thromboprophylactic agent used. These findings should be treated with caution as the model is fitted to a subset of the data and it is not possible to compare the fit of this model with the original model. In the case of an asymptomatic DVT (distal) outcome, the study by Samama et al. 57 is not connected; consequently, it is not possible to estimate the effects of nadroparin or fondaparinux on an asymptomatic DVT (distal) outcome. In the case of an asymptomatic DVT (proximal segment) outcome, the study by Samama et al. 57 is not connected and the Gehling et al. 23 study had no events; consequently, it is not possible to estimate the effects of nadroparin, reviparin or fondaparinux on an asymptomatic DVT (proximal segment) outcome. In the case of a clinically detected (symptomatic) outcome, Jørgensen et al. 51 and Bruntink et al. 49 had no events and provide no information about relative treatment effect; in addition, the study by Samama et al. 57 is connected in the network only via the nadroparin and fondaparinux arms of the study by Bruntink et al. 49 Consequently, it is not possible to estimate the effect of nadroparin, tinzaparin or fondaparinux on a clinically detected (symptomatic) outcome. In the case of a clinically relevant DVT outcome, the study by Samama et al. 57 is not connected; consequently, it is not possible to estimate the effects of nadroparin or fondaparinux on a clinically relevant DVT outcome.
| OR (95% CrI) | OR (95% PrI) | Probability of being the best | |
|---|---|---|---|
| Clinically detected DVT (symptomatic) | |||
| Dalteparin | 0.38 (0.05 to 2.60) | 0.38 (0.03 to 5.28) | 0.01 |
| Tinzaparin | NE | NE | NE |
| Certoparin | 7.2 × 10–10 (3.6 × 10–31 to 0.09) | 7.0 × 10–10 (3.5 × 10–31 to 0.11) | 0.98 |
| Nadroparin | NE | NE | NE |
| Reviparin | 0.35 (0.03 to 2.71) | 0.35 (0.02 to 4.99) | 0.01 |
| Fondaparinux | NE | NE | NE |
| None | – | – | 0.00 |
| Asymptomatic DVT (proximal segment) | |||
| Dalteparin | 0.43 (0.04 to 3.26) | 0.42 (0.03 to 5.23) | 0.00 |
| Tinzaparin | 6.4 × 10–10 (1.0 × 10–29 to 0.66) | 6.1 × 10–10 (1.0 × 10–29 to 0.69) | 0.51 |
| Certoparin | 5.8 × 10–10 (1.5 × 10–32 to 0.59) | 5.8 × 10–10 (1.5 × 10–32 to 0.65) | 0.49 |
| Nadroparin | NE | NE | NE |
| Reviparin | NE | NE | NE |
| Fondaparinux | NE | NE | NE |
| None | – | – | 0.01 |
| Asymptomatic DVT (distal) | |||
| Dalteparin | 0.79 (0.25 to 3.13) | 0.79 (0.15 to 5.36) | 0.00 |
| Tinzaparin | 0.58 (0.13 to 2.48) | 0.58 (0.08 to 3.96) | 0.01 |
| Certoparin | 1.4 × 10–10 (2.5 × 10–30 to 0.20) | 1.5 × 10–10 (2.6 × 10–30 to 0.22) | 0.99 |
| Nadroparin | NE | NE | NE |
| Reviparin | 0.81 (0.29 to 2.41) | 0.80 (0.16 to 4.40) | 0.00 |
| Fondaparinux | NE | NE | NE |
| None | – | – | 0.00 |
| Asymptomatic DVT (all) | |||
| Dalteparin | 0.72 (0.35 to 1.59) | 0.72 (0.23 to 2.54) | 0.00 |
| Tinzaparin | 0.54 (0.16 to 1.84) | 0.54 (0.11 to 2.54) | 0.00 |
| Certoparin | 3.5 × 10–10 (4.7 × 10–31 to 0.13) | 3.5 × 10–10 (4.6 × 10–31 to 0.13) | 0.96 |
| Nadroparin | 0.23 (0.04 to 1.06) | 0.23 (0.03 to 1.31) | 0.00 |
| Reviparin | 0.66 (0.29 to 1.70) | 0.66 (0.20 to 2.63) | 0.00 |
| Fondaparinux | 0.06 (0.01 to 0.33) | 0.06 (0.01 to 0.40) | 0.04 |
| None | – | – | 0.00 |
| PE | |||
| Deltaparin | 4.2 × 10–10 (9.0 × 10–31 to 0.43) | 4.2 × 10–10 (9.3 × 10–31 to 0.47) | 0.27 |
| Tinzaparin | NE | NE | NE |
| Certoparin | NE | NE | NE |
| Nadroparin | 2.8 × 10–13 (8.8 × 10–28 to 1.6 × 10–3) | 2.7 × 10–13 (8.7 × 10–28 to 1.9 × 10–3) | 0.48 |
| Reviparin | 6.5 × 10–10 (1.6 × 10–27 to 0.26) | 6.4 × 10–10 (1.4 × 10–27 to 0.28) | 0.25 |
| Fondaparinux | 1.6 × 10–6 (5.9 × 10–15 to 62) | 1.6 × 10–6 (5.3 × 10–15 to 0.70) | 0.00 |
| None | – | – | 0.01 |
| Major bleeding | |||
| Deltaparin | NE | NE | NE |
| Tinzaparin | NE | NE | NE |
| Certoparin | NE | NE | NE |
| Nadroparin | NE | NE | NE |
| Reviparin | NE | NE | NE |
| Fondaparinux | NE | NE | NE |
| None | – | – | NE |
| Clinically relevant DVT | |||
| Deltaparin | 0.40 (0.10 to 1.46) | 0.40 (0.06 to 2.52) | 0.00 |
| Tinzaparin | 3.4 × 10–10 (7.5 × 10–32 to 0.67) | 3.3 × 10–10 (7.0 × 10–32 to 0.70) | 0.46 |
| Certoparin | 1.3 × 10–11 (1.9 × 10–31 to 0.05) | 1.3 × 10–11 (1.8 × 10–31 to 0.06) | 0.54 |
| Nadroparin | NE | NE | NE |
| Reviparin | 2.35 (0.14 to 92.18) | 2.35 (0.11 to 112.10) | 0.00 |
| Fondaparinux | 0.23 (0.03 to 1.36) | 0.23 (0.02 to 2.11) | 0.00 |
| None | – | – | 0.01 |
| Any VTE | |||
| Dalteparin | 0.69 (0.40 to 1.23) | 0.68 (0.27 to 1.83) | 0.00 |
| Tinzaparin | 0.54 (0.17 to 1.61) | 0.54 (0.13 to 2.95) | 0.00 |
| Certoparin | 8.5 × 10–12 (9.9 × 10–29 to 0.02) | 8.6 × 10–12 (9.8 × 10–29 to 0.02) | 0.99 |
| Nadroparin | 0.22 (0.08 to 0.54) | 0.22 (0.06 to 0.69) | 0.00 |
| Reviparin | 0.63 (0.31 to 1.42) | 0.62 (0.23 to 1.97) | 0.00 |
| Fondaparinux | 0.06 (0.02 to 0.19) | 0.06 (0.01 to 0.24) | 0.01 |
| None | – | – | 0.00 |
There was evidence to suggest that there were differences in the effects based on the type of thromboprophylactic agent used, including between the different types of LMWH, with certoparin having the highest probability of the greatest effect on any VTE. However, this is based on the effect of certoparin being used in one study (Kock et al. ),52 so it is not possible to draw any reliable conclusions.
The meta-regression used in this assessment was a between-study comparison and lacked information with which to estimate parameters compared with a within-study comparison using patient data. In addition, comparisons between treatments involving zero events within a study provide no information about the relative treatment effect or the relationship between a potential treatment effect modifier and treatment effect. The between-study meta-regression has the potential to suffer from an ecological fallacy, such that the estimate of the relationship between a potential treatment effect modifier and treatment effect in a between-study comparison may be qualitatively different from the relationship between the treatment effect modifier and treatment effect within studies. Potential treatment effect modifiers were assessed separately, whereas they could be affecting treatment effect simultaneously; there is insufficient information with which to estimate potential treatment effect modifiers simultaneously. An adjusted model that is indistinguishable from an unadjusted model may reflect a lack of evidence rather than a lack of a relationship between potential treatment effect modifier and treatment. Estimates of the regression parameter should be interpreted with caution when they indicate evidence of a relationship between a potential treatment effect modifier and treatment but the adjusted model is indistinguishable from the unadjusted model.
There was insufficient evidence to suggest that any of the potential treatment effect modifiers defined in the protocol affected the treatment effect.
There was evidence to suggest that there were differences in the effects based on the type of thromboprophylactic agent used, including between the different types of LMWH.
Appendix 5 Literature search strategies for the review of individual risk factors associated with venous thromboembolism risk and risk assessment models for prediction of venous thromboembolism
Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily, Ovid MEDLINE and Versions(R)
Platform or provider used: Ovid SP.
Date range searched: 1946 to May 2017.
Date searched: May 2017.
Search strategy
-
thrombosis/ or exp venous thrombosis/
-
Venous Thromboembolism/ or Thromboembolism/
-
exp Pulmonary Embolism/
-
(thromboprophyla* or thrombus* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol*).ti,ab,kw.
-
((vein* or ven*) adj7 thromb*).ti,ab,kw.
-
(PE or DVT or VTE).ti,ab,kw.
-
1 or 2 or 3 or 4 or 5 or 6
-
exp Immobilization/
-
exp Mobility Limitation/
-
Splints/
-
Braces/
-
exp Casts, Surgical/
-
immobili*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
brace*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
splint*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
plaster*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
cast.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(leg* or tibia* or fibula* or ankle*).mp. and (fracture*.hw. or su.fs.) and co.fs.
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
-
7 and 19
-
predict:.mp. or scor:.tw. or observ:.mp.
-
(validation or validate).tw.
-
predict:.tw. or validat:.mp. or develop.tw.
-
21 or 22 or 23
-
(risk assess* or risk predict* or risk stratif*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
exp *Risk/ or exp Models, Statistical/ or exp Risk Assessment/ or *Postoperative Complications/ or risk model*.mp. or *Risk Factors/
-
24 or 25 or 26
-
(Risk model* or prognostic model* or prediction model* or predictive model* or risk assessment model* or prediction score* or algorithm* or matrix or matrices or assessment tool* or prediction rule* or decision rule* or risk score*).mp.
-
27 or 28
-
20 and 29
Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Database of Abstracts of Review of Effects, Health Technology Assessment Database and NHS Economic Evaluation Database
Platform or provider used: Wiley Online Library.
Date range searched: 1898 to May 2017.
Date searched: May 2017.
Search strategy
-
#1 MeSH descriptor: [Thrombosis] explode all trees
-
#2 MeSH descriptor: [Venous Thrombosis] explode all trees
-
#3 MeSH descriptor: [Venous Thromboembolism] explode all trees
-
#4 MeSH descriptor: [Pulmonary Embolism] explode all trees
-
#5 (thromboprophyla* or thrombus* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol*):ti,ab,kw
-
#6 ((vein* or ven*) and thromb*):ti,ab,kw
-
#7 (PE or DVT or VTE):ti,ab,kw
-
#8 MeSH descriptor: [Immobilization] explode all trees
-
#9 MeSH descriptor: [Mobility Limitation] explode all trees
-
#10 MeSH descriptor: [Splints] explode all trees
-
#11 MeSH descriptor: [Braces] explode all trees
-
#12 MeSH descriptor: [Casts, Surgical] explode all trees
-
#13 immobili* or brace* or splint* or plaster* or cast*:ti,ab,kw (Word variations have been searched)
-
#14 ((leg* or tibia* or ankle* or fibula*) and (fracture* or surg*) and complicat*):ti,ab,kw
-
#15 #1 or #2 or #3 or #4 or #5 or #6 or #7
-
#16 #8 or #9 or #10 or #11 or #12 or #13 or #14
-
#17 #15 and #16
-
#18 MeSH descriptor: [Risk] explode all trees
-
#19 MeSH descriptor: [Models, Statistical] explode all trees
-
#20 MeSH descriptor: [Risk Assessment] explode all trees
-
#21 MeSH descriptor: [Postoperative Complications] explode all trees
-
#22 MeSH descriptor: [Risk Factors] explode all trees
-
#23 (risk and (assess* or predict* or model* or stratif*)):ti,ab,kw
-
#24 (predict* or scor* or observ* or validat* or develop* or Risk model* or prognostic model* or prediction model* or predictive model* or risk assessment model* or prediction score* or algorithm* or matrix or matrices or assessment tool* or prediction rule* or decision rule* or risk score*):ti,ab,kw
-
#25 #18 or #19 or #20 or #21 or #22 or #23 or #24
-
#26 #17 and #25
EMBASE
Platform or provider used: Ovid SP.
Date range searched: 1974 to May 2017.
Date searched: May 2017.
Search strategy
-
thrombosis prevention/ or exp thrombosis/ or exp deep vein thrombosis/ or exp vein thrombosis/ or leg thrombosis/ or lower extremity deep vein thrombosis/
-
exp thromboembolism/ or exp venous thromboembolism/
-
exp lung embolism/
-
(thromboprophyla* or thrombus* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol*).ti,ab,kw.
-
((vein* or ven*) adj7 thromb*).ti,ab,kw.
-
(PE or DVT or VTE).ti,ab,kw.
-
1 or 2 or 3 or 4 or 5 or 6
-
exp Immobilization/
-
exp Mobility Limitation/
-
exp splint/
-
exp brace/
-
exp plaster cast/
-
immobili*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
brace*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
splint*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
plaster*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
cast.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(leg* or tibia* or fibula* or ankle*).mp. and (fracture*.hw. or su.fs.) and co.fs.
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
-
7 and 19
-
predict:.mp. or scor:.tw. or observ:.mp.
-
(validation or validate).tw.
-
predict:.tw. or validat:.mp. or develop.tw.
-
21 or 22 or 23
-
(risk assess* or risk predict* or risk stratif*).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(Risk model* or prognostic model* or prediction model* or predictive model* or risk assessment model* or prediction score* or algorithm* or matrix or matrices or assessment tool* or prediction rule* or decision rule* or risk score*).mp.
-
statistical model/
-
exp *risk factor/
-
exp *postoperative complication/
-
exp *risk/
-
exp risk assessment/
-
25 or 26 or 27 or 28 or 29 or 30 or 31
-
24 or 32
-
20 and 33
Appendix 6 Excluded studies: review of individual risk factors associated with venous thromboembolism risk
| Authors, year | Reason for exclusion |
|---|---|
| Ajwani et al.,237 2016 | No data or analysis of risk factors associated with VTE |
| Batra et al.,238 2006 | No data or analysis of risk factors associated with VTE |
| Bertoletti et al.,239 2011 | No data or analysis of risk factors associated with VTE |
| Caprini,240 2011 | Narrative review |
| Caprini et al.,210 2001 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Cirlincione et al.,241 2001 | Narrative review |
| Decramer et al.,242 2008 | No data or analysis of risk factors associated with VTE |
| Department of Health and Social Care,211 2010 | No data or analysis of risk factors associated with VTE |
| Douna,243 2008 | Commentary |
| Dyall et al.,244 2012 (abstract) | No data or analysis of risk factors associated with VTE |
| Eingartner et al.,78 1995 | No data or analysis of risk factors associated with VTE |
| Engbers et al.,245 2013 | No data or analysis of risk factors associated with VTE |
| Fall et al.,246 2014 | No data or analysis of risk factors associated with VTE |
| Felcher et al.,247 2009 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Fleischer et al.,248 2015 | No data or analysis of risk factors associated with VTE |
| Gearhart et al.,249 2000 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Giannadakis et al.,79 2000 | No data or analysis of risk factors associated with VTE |
| Haque et al.,80 2016 | No data or analysis of risk factors associated with VTE |
| Healy et al.,250 2010 | No data or analysis of risk factors associated with VTE |
| Jiang et al.,251 2015 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Kocialkowski et al.,252 2016 | No data or analysis of risk factors associated with VTE |
| Lawall et al.,253 2011 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Lim et al.,254 2016 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Mangwani et al.,228 2015 | Systematic review |
| Micheli,255 1975 | No data or analysis of risk factors associated with VTE |
| Mizel et al.,73 1998 | Population: not isolated lower-limb injury requiring temporary immobilisation (elective surgical population) |
| Nemeth et al.,32 2015 | RAM (including data on risk factors) developed using a generic thrombosis cohort rather than a subgroup of patients with temporary lower-limb immobilisation. However, based on regression coefficients in a clinical logistic regression model, a RAM was developed for individuals with a plaster cast of the lower extremity |
| Nemeth et al.,256 2013 (abstract) | Abstract of an excluded full-text study: Nemeth et al.32 |
| Nesheiwat and Sergi,257 1996 | No data or analysis of risk factors associated with VTE |
| Nilsson-Helander et al.,12 2009 | No data or analysis of risk factors associated with VTE |
| Nokes,31 2010 | No data or analysis of risk factors associated with VTE |
| Nygaard et al.,212 2009 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Park et al.,258 2016 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Park et al.,259 2015 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Parsonage,260 2009 | Narrative review |
| Persson and Wredmark,261 1979 | No data or analysis of risk factors associated with VTE |
| Randelli et al.,262 2013 | No data or analysis of risk factors associated with VTE |
| Roberts et al.,17 2013 | No data or analysis of risk factors associated with VTE |
| Rogers et al.,263 2012 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Samama,264 2000 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Saragas et al.,81 2017 | No data or analysis of risk factors associated with VTE |
| Saragas et al.,72 2014 | Population: not isolated lower-limb injury requiring temporary immobilisation (elective surgical population) |
| Selby et al.,58 2015 | No data or analysis of risk factors associated with VTE (authors reported that a low event rate precluded any subsequent analysis of predictors for VTE) |
| Simon et al.,265 1982 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Slaybaugh et al.,266 2003 | Review |
| Solis and Saxby,267 2002 | Population: not isolated lower-limb injury requiring temporary immobilisation (elective surgical population) |
| Spannagel and Kujath,235 1993 | No data or analysis of risk factors associated with VTE |
| Spencer et al.,268 2009 | Population: not isolated lower-limb injury requiring temporary immobilisation (elective surgical population) |
| Spyropoulos,269 2009 | Population: not isolated lower-limb injury requiring temporary immobilisation (elective surgical population) |
| Spyropoulos et al.,270 2009 | Population: not isolated lower-limb injury requiring temporary immobilisation (elective surgical population) |
| Stockport NHS Trust Foundation,33 2013 | No data or analysis of risk factors associated with VTE |
| Tan et al.,271 2016 | Systematic review |
| Testroote et al.,15 2014 | Systematic review |
| Toure,272 2014 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| True and Williamson,273 2014 | No data or analysis of risk factors associated with VTE |
| van Adrichem et al.,274 2015 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| van Adrichem et al.,275 2013 (abstract) | Abstract of included full-text study: van Adrichem et al.70 |
| Vollans et al.,276 2015 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Wang et al.,277 2015 | Not available |
| Watson et al.,82 2016 | No data or analysis of risk factors associated with VTE |
Appendix 7 Excluded studies: review of risk assessment models for prediction of venous thromboembolism risk
| Authors, year | Reason for exclusion |
|---|---|
| Ajwani et al.,237 2016 | No outcome evaluation of RAM |
| Batra et al.,238 2006 | No prognostic model/RAM |
| Bertoletti et al.,239 2011 | No prognostic model/RAM (letter to the editor) |
| Caprini,240 2011 | Narrative review |
| Caprini et al.,210 2001 | Generic RAM (no outcome evaluation) |
| Cirlincione et al.,241 2001 | Narrative review |
| Decramer et al.,242 2008 | No prognostic model/RAM |
| Department of Health and Social Care,211 2010 | Generic RAM (no outcome evaluation) |
| Douna,243 2008 | Commentary |
| Dyall et al.,244 2012 (abstract) | No prognostic model/RAM |
| Engbers et al.,245 2013 | No prognostic model/RAM |
| Fall et al.,246 2014 | No prognostic model/RAM |
| Felcher et al.,247 2009 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Fleischer et al.,248 2015 | No outcome evaluation of RAM |
| Gearhart et al.,249 2000 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Gehling et al.,23 1998 | No prognostic model/RAM |
| Goel et al.,50 2009 | No prognostic model/RAM |
| Hanslow et al.,64 2006 | No prognostic model/RAM |
| Healy et al.,250 2010 | No prognostic model/RAM (letter to the editor) |
| Ho and Omari,65 2017 | No prognostic model/RAM |
| Jameson et al.,66 2014 | No prognostic model/RAM |
| Jiang et al.,251 2015 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Kocialkowski et al.,252 2016 | No outcome evaluation of RAM |
| Kock et al.,52 1995 | No prognostic model/RAM |
| Kujath et al.,53 1993 | No prognostic model/RAM |
| Lawall et al.,253 2011 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Lim et al.,254 2016 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Makhdom et al.,9 2013 | No prognostic model/RAM |
| Manafi Rasi et al.,67 2013 | No prognostic model/RAM |
| Mangwani et al.,228 2015 | Systematic review |
| Meek and Tong,11 2012 | No prognostic model/RAM |
| Micheli,255 1975 | No prognostic model/RAM |
| Mizel et al.,73 1998 | No prognostic model/RAM |
| Nemeth et al.,256 2013 (abstract) | Abstract of an included full-text study: Nemeth et al.32 |
| Nesheiwat and Sergi,257 1996 | No prognostic model/RAM |
| Nilsson-Helander et al.,12 2009 | No prognostic model/RAM |
| Nokes,31 2010 | No outcome evaluation of RAM |
| Nygaard et al.,212 2009 | Generic RAM (no outcome evaluation) |
| Park et al.,258 2016 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Park et al.,259 2015 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Parsonage,260 2009 | Narrative review |
| Patel et al.,68 2012 | No prognostic model/RAM |
| Persson and Wredmark,261 1979 | No prognostic model/RAM |
| Randelli et al.,262 2013 | No prognostic model/RAM |
| Riou et al.,69 2007 | No prognostic model/RAM |
| Roberts et al.,17 2013 | No outcome evaluation of RAM |
| Rogers et al.,263 2012 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Samama,264 2000 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Saragas et al.,72 2014 | No prognostic model/RAM |
| Selby et al.,58 2015 | No prognostic model/RAM |
| Simon et al.,265 1982 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Slaybaugh et al.,266 2003 | Review |
| Solis and Saxby,267 2002 | No prognostic model/RAM |
| Spannagel and Kujath,235 1993 | No prognostic model/RAM |
| Spencer et al.,268 2009 | No prognostic model/RAM |
| Spyropoulos,269 2009 | No prognostic model/RAM |
| Spyropoulos et al.,270 2009 | No prognostic model/RAM |
| Stockport NHS Trust Foundation,33 2013 | No outcome evaluation of RAM |
| Tan et al.,271 2016 | Systematic review |
| Testroote et al.,15 2014 | Systematic review |
| Toure,272 2014 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| True and Williamson,273 2014 | No prognostic model/RAM |
| van Adrichem et al.,70 2014 | No prognostic model/RAM |
| van Adrichem et al.,274 2015 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| van Adrichem et al.,275 2013 (abstract) | No prognostic model/RAM |
| Vollans et al.,276 2015 | Population: not isolated lower-limb injury requiring temporary immobilisation |
| Wahlsten et al.,71 2015 | No prognostic model/RAM |
| Wang et al.,277 2015 | Not available |
| Zheng et al.,60 2016 | No prognostic model/RAM |
Appendix 8 Delphi panel
| Participant number | Initials | Specialty | Title/scope of practice |
|---|---|---|---|
| 1 | MC | Orthopaedic surgery | Professor |
| 2 | VL | Orthopaedic surgery | Advanced nurse practitioner |
| 3 | XG | Orthopaedic surgery | Consultant |
| 4 | JK | Orthopaedic surgery | Consultant |
| 5 | DJ | Orthopaedic surgery | Consultant |
| 6 | RS | Orthopaedic surgery | Consultant |
| 7 | SG | Emergency medicine | Professor |
| 8 | DH | Emergency medicine | Professor |
| 9 | RB | Emergency medicine | Professor |
| 10 | GJ | Emergency medicine | Consultant |
| 11 | JC | Emergency medicine | Consultant |
| 12 | CR | Emergency medicine | Consultant |
| 13 | JS | Emergency medicine | Professor |
| 14 | JT | Thrombosis and haemostasis | Consultant |
| 15 | BH | Thrombosis and haemostasis | Professor |
| 16 | KdW | Thrombosis and haemostasis | Assistant professor |
| 17 | TN | Thrombosis and haemostasis | Consultant |
| 18 | HW | Thrombosis and haemostasis | Consultant |
| 19 | RT-D | Thrombosis and haemostasis | Consultant |
| 20 | RM | Thrombosis and haemostasis | Consultant |
Appendix 9 Literature search strategies for review of economic studies
Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily, Ovid MEDLINE and Versions(R)
Platform or provider used: Ovid SP.
Date range searched: 1946 to October 2017.
Date searched: October 2017.
Search strategy
-
thrombosis/ or exp venous thrombosis/
-
Venous Thromboembolism/ or Thromboembolism/
-
exp Pulmonary Embolism/
-
(thromboprophyla* or thrombus* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol*).ti,ab,kw.
-
((vein* or ven*) adj7 thromb*).ti,ab,kw.
-
(PE or DVT or VTE).ti,ab,kw.
-
1 or 2 or 3 or 4 or 5 or 6
-
exp Immobilization/
-
exp Mobility Limitation/
-
Splints/
-
Braces/
-
exp Casts, Surgical/
-
immobili*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
brace*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
splint*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
plaster*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
cast.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(leg* or tibia* or fibula* or ankle*).mp. and (fracture*.hw. or su.fs.) and co.fs.
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
-
exp “costs and cost analysis”/ or costs.tw. or cost effective:.tw.
-
(cost: or cost benefit analys: or health care costs).mp.
-
Economics/
-
exp “costs and cost analysis”/
-
Economics, Dental/
-
exp economics, hospital/
-
Economics, Medical/
-
Economics, Nursing/
-
Economics, Pharmaceutical/
-
(economic$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab.
-
(expenditure$ not energy).ti,ab.
-
value for money.ti,ab.
-
budget$.ti,ab.
-
22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32
-
((energy or oxygen) adj cost).ti,ab.
-
(metabolic adj cost).ti,ab.
-
((energy or oxygen) adj expenditure).ti,ab.
-
34 or 35 or 36
-
33 not 37
-
letter.pt.
-
editorial.pt.
-
historical article.pt.
-
or/39-41
-
38 not 42
-
exp animals/ not humans/
-
43 not 44
-
bmj.jn.
-
“cochrane database of systematic reviews”.jn.
-
health technology assessment winchester england.jn.
-
or/46-48
-
45 not 49
-
“Value of Life”/
-
Quality of Life/
-
quality of life.ti,kf.
-
((instrument or instruments) adj3 quality of life).ab.
-
Quality-Adjusted Life Years/
-
quality adjusted life.ti,ab,kf.
-
(qaly* or qald* or qale* or qtime* or life year or life years).ti,ab,kf.
-
disability adjusted life.ti,ab,kf.
-
daly*.ti,ab,kf.
-
(sf36 or sf 36 or short form 36 or shortform 36 or short form36 or shortform36 or sf thirtysix or sfthirtysix or sfthirty six or sf thirty six or shortform thirtysix or shortform thirty six or short form thirtysix or short form thirty six).ti,ab,kf.
-
(sf6 or sf 6 or short form 6 or shortform 6 or sf six or sfsix or shortform six or short form six or shortform6 or short form6).ti,ab,kf.
-
(sf8 or sf 8 or sf eight or sfeight or shortform 8 or shortform 8 or shortform8 or short form8 or shortform eight or short form eight).ti,ab,kf.
-
(sf12 or sf 12 or short form 12 or shortform 12 or short form12 or shortform12 or sf twelve or sftwelve or shortform twelve or short form twelve).ti,ab,kf.
-
(sf16 or sf 16 or short form 16 or shortform 16 or short form16 or shortform16 or sf sixteen or sfsixteen or shortform sixteen or short form sixteen).ti,ab,kf.
-
(sf20 or sf 20 or short form 20 or shortform 20 or short form20 or shortform20 or sf twenty or sftwenty or shortform twenty or short form twenty).ti,ab,kf.
-
(hql or hqol or h qol or hrqol or hr qol).ti,ab,kf.
-
(hye or hyes).ti,ab,kf.
-
(health* adj2 year* adj2 equivalent*).ti,ab,kf.
-
(pqol or qls).ti,ab,kf.
-
(quality of wellbeing or quality of well being or index of wellbeing or index of well being or qwb).ti,ab,kf.
-
nottingham health profile*.ti,ab,kf.
-
sickness impact profile.ti,ab,kf.
-
exp health status indicators/
-
(health adj3 (utilit* or status)).ti,ab,kf.
-
(utilit* adj3 (valu* or measur* or health or life or estimat* or elicit* or disease or score* or weight)).ti,ab,kf.
-
(preference* adj3 (valu* or measur* or health or life or estimat* or elicit* or disease or score* or instrument or instruments)).ti,ab,kf.
-
disutilit*.ti,ab,kf.
-
rosser.ti,ab,kf.
-
willingness to pay.ti,ab,kf.
-
standard gamble*.ti,ab,kf.
-
(time trade off or time tradeoff).ti,ab,kf.
-
tto.ti,ab,kf.
-
(eq or euroqol or euro qol or eq5d or eq 5d or euroqual or euro qual).ti,ab,kf.
-
duke health profile.ti,ab,kf.
-
functional status questionnaire.ti,ab,kf.
-
dartmouth coop functional health assessment*.ti,ab,kf.
-
(hui or hui1 or hui2 or hui3).ti,ab,kf.
-
or/51-87
-
20 or 21 or 50 or 88
-
7 and 19 and 89
EMBASE
Platform or provider used: Ovid SP.
Date range searched: 1974 to October 2017.
Date searched: October 2017.
Search strategy
-
thrombosis prevention/ or exp thrombosis/ or exp deep vein thrombosis/ or exp vein thrombosis/ or leg thrombosis/ or lower extremity deep vein thrombosis/
-
exp thromboembolism/ or exp venous thromboembolism/
-
exp lung embolism/
-
(thromboprophyla* or thrombus* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol*).ti,ab,kw.
-
((vein* or ven*) adj7 thromb*).ti,ab,kw.
-
(PE or DVT or VTE).ti,ab,kw.
-
1 or 2 or 3 or 4 or 5 or 6
-
exp Immobilization/
-
exp Mobility Limitation/
-
exp splint/
-
exp brace/
-
exp plaster cast/
-
immobili*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
brace*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
splint*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
plaster*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
cast.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word]
-
(leg* or tibia* or fibula* or ankle*).mp. and (fracture*.hw. or su.fs.) and co.fs.
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
-
7 and 19
-
cost effectiveness analysis.sh. or randomized.tw. or economic.tw.
-
(cost or costs).tw.
-
Economics/
-
Cost/
-
exp Health Economics/
-
Budget/
-
budget*.ti,ab,kw.
-
(economic* or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic* or pharmaco-economic* or expenditure or expenditures or expense or expenses or financial or finance or finances or financed).ti,kw.
-
(economic* or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic* or pharmaco-economic* or expenditure or expenditures or expense or expenses or financial or finance or finances or financed).ab. /freq=2
-
(cost* adj2 (effective* or utilit* or benefit* or minimi* or analy* or outcome or outcomes)).ab,kw.
-
(value adj2 (money or monetary)).ti,ab,kw.
-
Statistical Model/
-
economic model*.ab,kw.
-
Probability/
-
markov.ti,ab,kw.
-
monte carlo method/
-
monte carlo.ti,ab,kw.
-
Decision Theory/
-
Decision Tree/
-
(decision* adj2 (tree* or analy* or model*)).ti,ab,kw.
-
23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40
-
21 or 22 or 41
-
20 and 42
-
socioeconomics/
-
exp Quality of Life/
-
quality of life.ti,kw.
-
((instrument or instruments) adj3 quality of life).ab.
-
Quality-Adjusted Life Year/
-
quality adjusted life.ti,ab,kw.
-
(qaly* or qald* or qale* or qtime* or life year or life years).ti,ab,kw.
-
disability adjusted life.ti,ab,kw.
-
daly*.ti,ab,kw.
-
(sf36 or sf 36 or short form 36 or shortform 36 or short form36 or shortform36 or sf thirtysix or sfthirtysix or sfthirty six or sf thirty six or shortform thirtysix or shortform thirty six or short form thirtysix or short form thirty six).ti,ab,kw.
-
(sf6 or sf 6 or short form 6 or shortform 6 or sf six or sfsix or shortform six or short form six or shortform6 or short form6).ti,ab,kw.
-
(sf8 or sf 8 or sf eight or sfeight or shortform 8 or shortform 8 or shortform8 or short form8 or shortform eight or short form eight).ti,ab,kw.
-
(sf12 or sf 12 or short form 12 or shortform 12 or short form12 or shortform12 or sf twelve or sftwelve or shortform twelve or short form twelve).ti,ab,kw.
-
(sf16 or sf 16 or short form 16 or shortform 16 or short form16 or shortform16 or sf sixteen or sfsixteen or shortform sixteen or short form sixteen).ti,ab,kw.
-
(sf20 or sf 20 or short form 20 or shortform 20 or short form20 or shortform20 or sf twenty or sftwenty or shortform twenty or short form twenty).ti,ab,kw.
-
(hql or hqol or h qol or hrqol or hr qol).ti,ab,kw.
-
(hye or hyes).ti,ab,kw.
-
(health* adj2 year* adj2 equivalent*).ti,ab,kw.
-
(pqol or qls).ti,ab,kw.
-
(quality of wellbeing or quality of well being or index of wellbeing or index of well being or qwb).ti,ab,kw.
-
nottingham health profile*.ti,ab,kw.
-
nottingham health profile/
-
sickness impact profile.ti,ab,kw.
-
sickness impact profile/
-
health status indicator/
-
(health adj3 (utilit* or status)).ti,ab,kw.
-
(utilit* adj3 (valu* or measur* or health or life or estimat* or elicit* or disease or score* or weight)).ti,ab,kw.
-
(preference* adj3 (valu* or measur* or health or life or estimat* or elicit* or disease or score* or instrument or instruments)).ti,ab,kw.
-
disutilit*.ti,ab,kw.
-
rosser.ti,ab,kw.
-
willingness to pay.ti,ab,kw.
-
standard gamble*.ti,ab,kw.
-
(time trade off or time tradeoff).ti,ab,kw.
-
tto.ti,ab,kw.
-
(hui or hui1 or hui2 or hui3).ti,ab,kw.
-
(eq or euroqol or euro qol or eq5d or eq 5d or euroqual or euro qual).ti,ab,kw.
-
duke health profile.ti,ab,kw.
-
functional status questionnaire.ti,ab,kw.
-
dartmouth coop functional health assessment*.ti,ab,kw.
-
44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82
-
21 or 22 or 41 or 83
-
20 and 84
NHS Economic Evaluation Database, Health Technology Assessment Database
Platform or provider used: The Cochrane Library.
Date range searched: inception to 2015.
Date searched: October 2017.
Search strategy
-
ID Search
-
#1 MeSH descriptor: [Thrombosis] explode all trees
-
#2 MeSH descriptor: [Venous Thrombosis] explode all trees
-
#3 MeSH descriptor: [Venous Thromboembolism] explode all trees
-
#4 MeSH descriptor: [Pulmonary Embolism] explode all trees
-
#5 (thromboprophyla* or thrombus* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol*):ti,ab,kw
-
#6 ((vein* or ven*) and thromb*):ti,ab,kw
-
#7 (PE or DVT or VTE):ti,ab,kw
-
#8 #1 or #2 or #3 or #4 or #5 or #6 or #7
Appendix 10 Excluded studies: review of cost-effectiveness evidence
Appendix 11 Supplementary table
| Model identifier | Population | Interventions and comparators | How found |
|---|---|---|---|
| TA354140 | People with DVT and/or PE (treatment and secondary prevention) |
|
Search of NICE website for models that informed NICE guidance on VTE prevention or treatment |
| TA341133 | People with DVT and/or PE (treatment and secondary prevention) |
|
Search of NICE website for models that informed NICE guidance on VTE prevention or treatment |
| TA327132 | People with DVT and/or PE (treatment and secondary prevention) (Subpopulation with cancer also considered but not considered relevant here) |
|
Search of NICE website for models that informed NICE guidance on VTE prevention or treatment |
| TA261154 | People with a confirmed symptomatic DVT |
|
Search of NICE website for models that informed NICE guidance on VTE prevention or treatment |
| TA245135 | People having elective hip or knee replacement surgery |
|
Search of NICE website for models that informed NICE guidance on VTE prevention or treatment |
| TA287131 | People with an acute symptomatic PE |
|
Search of NICE website for models that informed NICE guidance on VTE prevention or treatment |
| TA157134 | People having elective hip or knee replacement surgery |
|
Search of NICE website for models that informed NICE guidance on VTE prevention or treatment |
| TA170136 | People having elective hip or knee replacement surgery |
|
Search of NICE website for models that informed NICE guidance on VTE prevention or treatment |
| NICE CG9224 | This guideline examined many populations but the group having elective knee surgery is the most relevant (note: the NG89 is more likely to include up-to-date sources) | Search of NICE website for models that informed NICE guidance on VTE prevention or treatment | |
| NG89130 | People having elective hip or knee replacement surgery | Search of NICE website for models that informed NICE guidance on VTE prevention or treatment | |
| Goodacre et al.,114 2017 (draft, not final) | Women with suspected PE during pregnancy | Alternative diagnostic pathways | Known to authors |
| Simpson et al.,278 2009 | People with VTE | Thrombophilia testing strategies | Known to authors |
| Goodacre et al.,152 2006 | People with suspected DVT | Alternative diagnostic pathways | Known to authors |
| Wolowacz et al.,99 2009 | People having total knee and hip replacement surgery | Dabigatran etexilate | Published study for related population identified during economic review |
Appendix 12 Sources of utility data
| Authors, year | Participants | HRQoL tool and valuation method | Health state(s) valued | Utility estimate, mean (SD)a | Cited by |
|---|---|---|---|---|---|
| Ara and Brazier,194 2011 | General population sample with utilities reported according to whether or not responders were affected by particular conditions (stroke and other heart conditions reported here) | EQ-5D UK tariff |
|
|
Goodacre et al.114 |
|
|
||||
|
|
||||
|
|
||||
|
|
||||
| Cohen et al.,173 2014 (abstract) | 2790 patients with VTE taking anticoagulants (1640 with DVT and 1150 with PE at baseline; 443 with DVT and 280 with PE at 6 months) | EQ-5D-5L |
|
|
|
|
|
||||
|
|
||||
|
|
||||
|
|
||||
| Arverud et al.,156 2016 | 111 patients 1 year after surgery and immobilisation for Achilles tendon injury | EQ-5D (valuation set not stated) |
|
|
Searches conducted for the systematic review of published cost-effectiveness studies (see Chapter 4, Systematic review of existing cost-effectiveness evidence) |
| Enden et al.,189 2013 (same study as Haig et al.160) | 189 with proximal DVT | EQ-5D |
|
|
TA354140 |
|
|
||||
| Gage et al.,205 1996 | 70 patients aged ≥ 50 years with AF (community dwelling), half of whom were taking warfarin | TTO and standard gamble |
|
|
|
| Ghofrani et al.,195 2013 | 259 people with CTEPH (inoperable or persistent post surgically) | EQ-5D (valuation set not stated) |
|
|
TA341133 |
| Haig et al.,160 2016 | 176 patients with DVT (mid-thigh level or higher) | EQ-5D |
|
|
Data as reported by Lubberts et al.159 |
| Hogg et al.,176 2013 | 215 thrombosis clinic patients with a history of VTE (at any time, i.e. 56% of patients were diagnosed > 12 months previously) | Standard gamble for vignettes, not patient’s own health state |
|
Mean (IQR)
|
|
|
|
||||
|
|
||||
|
|
||||
|
|
||||
| Hogg et al.,163 2014 | 44 patients with previous experience of VTE (PE or proximal DVT) within 12 months of diagnosis | SF-6D (standard gamble also reported) |
|
Median (IQR)
|
Lubberts et al.’s159 systematic review |
|
|
||||
| Ingelgard et al.,279 2002 | 121 outpatients with DVT | EQ-5D (tariff not reported) | Patients with PE or DVT treated with warfarin | 0.08 decrement for both |
TA245135 Wolowacz et al. 99 |
| Keogh et al.,197 2006 | 177 patients with PAH (idiopathic or related to connective tissue disease, i.e. not CTEPH) | SF-6D UK valuation set |
|
|
TA327132 (company compared class 1 mean with HSE data to calculate decrement of 0.1) |
| Lenert and Soetikno,190 1997 | 30 healthy volunteers (all female) and 30 physicians (not selected by specialty) | Standard gamble |
|
|
|
| Lindgren et al.,200 2007 | 60 patients with mild to moderate hypertension, of whom 18 experienced a stroke event during the study | EQ-5D UK tariff | Stroke over 1 year | Decrement of 0.145 (0.145) (95% CI 0.059 to 0.249) | TA327132 |
| Locadia et al.,177 2004 | Patients with VTE on VKA (n = 53), a bleeding episode during VKA therapy (n = 23) or PTS treated with VKA (n = 48) | TTO for clinical vignettes |
|
Median (IQR)
|
|
|
|
||||
|
|
||||
|
|
||||
|
|
||||
|
|
||||
|
|
||||
|
|
||||
|
|
||||
| Luengo-Fernandez et al.,201 2013 | 1188 stroke and TIA patients (748 stroke patients) | EQ-5D UK TTO tariff |
|
|
Follow-up of OXVASC cohort reported by Rivero-Arias et al.204 |
|
|
||||
|
|
||||
|
|
||||
| Lunde,202 2013 | 345 stroke patients (6 months post stroke) | EQ-5D UK TTO valuation set | Post stroke | 0.70 (0.30) (also reports values for independent yes/no) | |
| Marchetti et al.,207 2001 | 48 patients attending an anticoagulation clinic with experience of heparin and half with experience of VKA | Direct TTO using clinical vignettes |
|
|
|
|
|
||||
| Meads et al.,198 2008 | 308 patients with CTEPH | CAMPHOR QoL, which was valued by 249 members of the UK general population using TTO | CTEPH | 0.56 (0.29) (ERG in TA327132 calculated disutility relative to age-matched general population as 0.22 = 0.78–0.56) | |
| Monz et al.,208 2013 | 1435 patients having dabigatran or warfarin during RE-LY study (AF patients) | EQ-5D UK TTO tariff |
VKA treated DOAC treated |
No statistically significant difference in HRQoL substudy as a whole | TA327132 |
| Olschewski et al.,196 2002 | 203 patients with primary PAH and CTEPH (n = 57) (NYHA class III or IV) | EQ-5D index |
|
Improved from 0.49 ± 0.28 to 0.58 ± 0.27 in drug treatment group | Reference list of Keogh et al.197 |
| O’Meara et al.,191 1994 | 36 patients > 50 years, of which 20 had no history of DVT | Standard gamble |
|
|
|
| Pickard et al.,203 2004 | 124 patients hospitalised following ischaemic stroke | EQ-5D with UK TTO tariff (HUI3 also reported) | Ischaemic stroke at
|
|
|
|
|
||||
|
|
||||
|
|
||||
| Rivero-Arias et al.,204 2010 | 1293 stroke and TIA patients (subset of the OXVASC data set) | EQ-5D UK TTO tariff |
Stroke and TIA (average over 2 years) Stroke data points (n = 1359) |
|
|
| Robinson et al.,206 2001 (data from abstract) | 57 patients with AF | Standard gamble |
|
|
|
| Shafazand et al.,199 2004 | 53 patients with pulmonary hypertension (not specifically CTEPH) | Standard gamble | All participants’ current health | 0.71 (95% CI 0.64 to 0.78) | TA327132 |
| Sullivan et al.,174 2011 | 2299 patients with VTE taking secondary prophylaxis | EQ-5D UK valuation set |
|
|
|
| Tavoly et al.,175 2016 | 213 patients with PE (median 3.8 years since diagnosis) | EQ-5D with Danish tariff |
|
|
TA327132 (cites 2013 abstract but data here from full paper) |
|
|
||||
| Utne et al.,179 2016 | 254 patients with DVT during previous 1 to 10 years | EQ-5D with Danish tariff |
|
|
Review by Ghanima et al.280 |
Appendix 13 Parameter sampling
| Parameter description | Mid-point value | Uncertainty measure | Distribution | Source | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Probability of PE in those having lower-limb immobilisation | 0.4% | 95% CI 0.2% to 0.7% | Beta(10, 2326) | Rates across placebo arms of 12 studies included in the systematic review of clinical effectiveness (see Table 16) | ||||||||||||||||
| Probability of DVT in those having lower-limb immobilisation not having PE | 8.0% | 95% CI 6.9% to 9.1% | Beta(186, 2140) | Rates across placebo arms of 12 studies included in the systematic review of clinical effectiveness (see Table 16) | ||||||||||||||||
| Proportion of DVT that is symptomatic | 11.4% | 95% CI 6.7% to 17.2% | Beta(16, 124) | Rates across placebo arms of 9 studies included in the systematic review of clinical effectiveness (see Table 16) | ||||||||||||||||
| Proportion of asymptomatic DVTs that are distal | 83.9% | 95% CI 73.3% to 92.2% | Beta(47, 9) | Rates across placebo arms of 6 studies included in the systematic review of clinical effectiveness (see Table 16) | ||||||||||||||||
| Proportion of symptomatic DVTs that are distal | 50% | 95% CI 26.5% to 73.4% | Beta(8, 8) | Rates across placebo arms of a single study (see Table 16) | ||||||||||||||||
| Effectiveness of prophylaxis: OR for VTE | 0.52 | 95% CI 0.37 to 0.71 | Not applicable | Systematic review of decision tools for identifying patients at risk of VTE. CODA samples from NMA used directly to characterise uncertainty around OR (see Methods used to quantify decision uncertainty) | ||||||||||||||||
| Risk of major GI bleed with no prophylaxis (per 1000 person-years) | 1.34 | 95% CI 1.32 to 1.36 | Norm(1.34, 0.010) | Hippisley-Cox et al.101 | ||||||||||||||||
| Risk of ICH with no prophylaxis (per 1000 person-years) | 0.55 | 95% CI 0.54 to 0.56 | Norm(0.56, 0.005) | Hippisley-Cox et al.101 | ||||||||||||||||
| Bleed risk for prophylaxis vs. none: OR (OR is converted to RR using baseline risks for no prophylaxis) | 1.64 | 95% CI 0.90 to 2.53 | Not applicable | Pooled analysis of bleed risks across all VTE prophylaxis studies in NICE CG92 re-analysed on log-odds scale using random-effects Bayesian meta-analysis. CODA samples used directly to characterise uncertainty around OR | ||||||||||||||||
| Case fatality rate for GI bleeds | 10.0% | 95% CI 9.7% to 10.4% | Beta(2452, 21,969) | Case fatality rate of GI bleeds taken from Button et al.103 | ||||||||||||||||
| Case fatality rate for ICH | 49.0% | 95% CI 37% to 60% | Beta(35, 37) | Case fatality rate of ICH bleeds taken from Fang et al.102 | ||||||||||||||||
| Risk of bleeding during 3-month anticoagulant treatment for VTE | 0.9% | 95% CI 0.2% to 2.0% | Beta(3, 352) | Kooiman et al.104 | ||||||||||||||||
| Proportion of major bleeds during VTE treatment that are fatal | 25.0% | 95% CI 21% to 28% | Beta(135, 411) | Nieto et al.105 | ||||||||||||||||
| Proportion of non-fatal major bleeds during VTE treatment that are ICH | 9.0% | 95% CI 6.5% to 11.9% | Beta(37, 374) | Nieto et al.105 | ||||||||||||||||
| SMR for patients surviving ICH compared with general population | ||||||||||||||||||||
| Year 1 after ICH | 4.5 | 95% CI 3.7 to 5.5 | Log(SMR) = norm(1.5, 0.1) |
Fogelholm et al. 107 CIs around SMR not reported, so have assumed ± 20% on the log scale |
||||||||||||||||
| Years 2–6 after ICH | 2.2 | 95% CI 1.8 to 2.7 | Log(SMR) = norm(0.8, 0.1) | |||||||||||||||||
| Probability of PE being fatal | 2.9% | 95% CI 2.5% to 3.3% | Beta(219, 7372) | Maestre et al.108 | ||||||||||||||||
| Cumulative risk of PTS for treated symptomatic DVT at 3 years | ||||||||||||||||||||
| Proximal | 32.4% | 95% CI 22.1% to 43.6% | Beta(23, 48) | Hach-Wunderle et al.109 | ||||||||||||||||
| Distal | 15.6% | 95% CI 7.9% to 25.3% | Beta(10, 54) | |||||||||||||||||
| OR for PTS in asymptomatic untreated proximal DVT vs. treated proximal DVT | 2.71 | 95% CI 1.44 to 5.1 | Log(OR) = norm(0.99, 0.32) | van Dongen et al.110 | ||||||||||||||||
| Incidence of CTEPH at 2 years (converted to annual risk of 1.6%) | 3.2% | 95% CI 2.0% to 4.4% | Beta(32, 967) | Ende-Verhaar et al.,111 based on incidence in those surviving the initial treatment period of 3–6 months | ||||||||||||||||
| Proportion of CTEPH patients treated surgically | 59.5% | 95% CI 55.8% to 63.2% | Beta(404, 275) | Delcroix et al.113 | ||||||||||||||||
| Proportion of those patients with CTEPH who are surgically treated who also received bridging medical care | 30.0% | 95% CI 24.6% to 33.5% | Beta(117, 287) | Delcroix et al.113 | ||||||||||||||||
| Mean hazard for exponential survival curve in medically treated patients with CTEPH | 0.1168 | SE 0.0123 | Norm(0.1168, 0.0123) | Original data from Delcroix et al.113 but curves taken from Goodacre et al.114 | ||||||||||||||||
| Mean and SD for log-normal survival curve in surgically treated patients with CTEPH | Mean 5.08 (SD 3.34) |
|
Multivariate normal |
Original data from Delcroix et al. 113 but curves taken from Goodacre et al. 114 Variance–covariance matrix Mean logSD logMean0.017708–0.05572SD–0.055720.230935 |
Mean log | SD log | Mean | 0.017708 | –0.05572 | SD | –0.05572 | 0.230935 | ||||||||
| Mean log | SD log | |||||||||||||||||||
| Mean | 0.017708 | –0.05572 | ||||||||||||||||||
| SD | –0.05572 | 0.230935 | ||||||||||||||||||
| Ambulance transfer to ED | £236 | IQR £211–256, n = 11 | Gamma(551, 0.43) |
|
||||||||||||||||
| ED visit leading to admission | £228 | IQR £184–261, n = 139 | Gamma(2210, 0.10) |
|
||||||||||||||||
| ED visit not leading to admission | £196 | IQR £165–220, n = 138 | Gamma(3203, 0.06) |
|
||||||||||||||||
| DVT admission: weighted average of following HRG costs | ||||||||||||||||||||
| YQ51A | £4632 | IQR £2394–5794, n = 122 | Gamma(42.4, 109) |
|
||||||||||||||||
| YQ51B | £2943 | IQR £1595–3629, n = 130 | Gamma(30.0, 98.3) | |||||||||||||||||
| YQ51C | £2406 | IQR £1559–2773, n = 136 | Gamma(41.5, 57.9) | |||||||||||||||||
| YQ51D | £1731 | IQR £1267–1903, n = 141 | Gamma(48.5, 35.7) | |||||||||||||||||
| YQ51E | £1453 | IQR £1041–1574, n = 134 | Gamma(35.7, 40.6) | |||||||||||||||||
| PE admission: weighted average of following HRG costs | ||||||||||||||||||||
| DZ09J | £5903 | IQR £3012–7602, n = 129 | Gamma(45, 129) |
|
||||||||||||||||
| DZ09K | £3440 | IQR £2116–4204, n = 137 | Gamma(41, 84) | |||||||||||||||||
| DZ09L | £3795 | IQR £2369–4741, n = 136 | Gamma(48, 79) | |||||||||||||||||
| DZ09M | £2851 | IQR £1997–3291, n = 142 | Gamma(65, 44) | |||||||||||||||||
| DZ09N | £2276 | IQR £1751–2507, n = 143 | Gamma(92, 25) | |||||||||||||||||
| DZ09P | £1837 | IQR £1473–2077, n = 144 | Gamma(73, 25) | |||||||||||||||||
| DZ09Q | £1550 | IQR £1270–1724, n = 141 | Gamma(76, 20) | |||||||||||||||||
| Critical care: weighted average of HRG costs for codes | ||||||||||||||||||||
| XC01Z | £2588 | n = 1 | Fixed |
|
||||||||||||||||
| XC02Z | £1682 | IQR £1478–2014, n = 6 | Gamma(107, 15.7) | |||||||||||||||||
| XC03Z | £1705 | IQR £1419–1944, n = 11 | Gamma(211, 8.1) | |||||||||||||||||
| XC04Z | £1581 | IQR £1423–1781, n = 17 | Gamma(605, 2.6) | |||||||||||||||||
| XC05Z | £1195 | IQR £1133–1381, n = 21 | Gamma(884, 1.4) | |||||||||||||||||
| XC06Z | £820 | IQR £481–1001, n = 23 | Gamma(104, 7.9) | |||||||||||||||||
| XC07Z | £521 | IQR £188–868, n = 15 | Gamma(16.0, 32.5) | |||||||||||||||||
| Proximal leg vein ultrasonography | £55 | IQR £41–61, n = 149 | Gamma(2135, 0.03) |
|
||||||||||||||||
| CTPA | £102 | IQR £71–135, n = 137 | Gamma(635, 0.16) |
|
||||||||||||||||
| V/Q SPECT | £261 | IQR £118–337, n = 78 | Gamma(202, 1.29) |
|
||||||||||||||||
| V/Q planar | £274 | IQR £153–270, n = 106 | Gamma(1045, 0.26) |
|
||||||||||||||||
| Echocardiography | £72 | IQR £38–94, n = 47 | Gamma(146, 0.50) |
|
||||||||||||||||
| Proportion receiving LMWH who need district nurse administration | 4% | 95% CI 1.3% to 7.8% | Beta(5, 123) | Menakaya et al.229 | ||||||||||||||||
| Fatal bleed | £1592 | SD 1886, n = 8 | Gamma(5.70, 279) | Luengo-Fernandez et al.117 (cost before inflation) | ||||||||||||||||
| Acute costs for non-fatal ICH (first 90 days) – weighted average of | ||||||||||||||||||||
| Non-disabling non-fatal stroke | £9903 | SD 4510, n = 5 | Gamma(24, 411) | Luengo-Fernandez et al.117 (cost before inflation) | ||||||||||||||||
| Moderately disabling non-fatal stroke | £25,442 | SD 9635, n = 3 | Gamma(21, 1216) | |||||||||||||||||
| Totally disabling non-fatal stroke | £43,036 | SD N/A, n = 1 | Fixed | |||||||||||||||||
| Residential costs for non-fatal ICH (first 90 days) | £6880 | SD £15,600, n = 136 | Gamma(26, 260) | Luengo-Fernandez et al.117 (cost before inflation) | ||||||||||||||||
| GP costs for non-fatal ICH (first 90 days) | £98 | 95% CI £27 to £169 | Norm(98, 36) | Luengo-Fernandez et al.117 (cost before inflation) | ||||||||||||||||
| Emergency care costs for non-fatal ICH (first 90 days) | £99 | 95% CI £56 to £141 | Norm (99, 22) | Luengo-Fernandez et al.117 (cost before inflation) | ||||||||||||||||
| Non-fatal non-ICH bleed (weighted average of HRG costs) | ||||||||||||||||||||
| FZ38G | £5369 | IQR £3097–6235, n = 134 | Gamma(63, 85) |
|
||||||||||||||||
| FZ38H | £3172 | IQR £2054–3876, n = 131 | Gamma(35, 90) | |||||||||||||||||
| FZ38J | £3667 | IQR £2100–4636, n = 135 | Gamma(32, 115) | |||||||||||||||||
| FZ38K | £2630 | IQR £1793–3153, n = 134 | Gamma(39, 67) | |||||||||||||||||
| FZ38L | £2084 | IQR £1655–£2332, n = 135 | Gamma(72, 29) | |||||||||||||||||
| FZ38M | £2531 | IQR £1646–3061, n = 136 | Gamma(38, 66) | |||||||||||||||||
| FZ38N | £1882 | IQR £1496–2051, n = 140 | Gamma(94, 20) | |||||||||||||||||
| FZ38P | £1406 | IQR £1161–1542, n = 142 | Gamma(78, 18) | |||||||||||||||||
| Anticoagulant service | ||||||||||||||||||||
| Face-to-face follow-up, consultant led | £37 | IQR £21–41, n = 58 | Norm(37, 3.7) with minimum of zero |
|
||||||||||||||||
| Face-to-face follow-up, non-consultant led | £16 | IQR £9–16, n = 46 | Norm(16, 1.6) with minimum of zero |
|
||||||||||||||||
| First face-to-face attendance, non-consultant led | £22 | IQR £8–17, n = 40 | Norm(22, 2.2) with minimum of zero |
|
||||||||||||||||
| Non-face-to-face follow-up, non-consultant led | £13 | IQR £5–7, n = 10 | Norm(13, 1.3) with minimum of zero |
|
||||||||||||||||
| Vascular surgery | ||||||||||||||||||||
| First appointment face to face, consultant led | £167 | IQR £124–211, n = 112 | Gamma(759, 0.22) |
|
||||||||||||||||
| Follow-up appointment face to face, consultant led | £140 | IQR £100–165, n = 111 | Gamma(942, 0.15) |
|
||||||||||||||||
| First appointment face to face, non-consultant led | £173 | IQR £100–240, n = 48 | Gamma(312, 1.39) |
|
||||||||||||||||
| Follow-up appointment face to face, non-consultant led | £139 | IQR £173–230, n = 55 | Gamma(79, 1.76) |
|
||||||||||||||||
| Surgical management of CTEPH: average of following HRG costs | ||||||||||||||||||||
| DZ02H | £9871 | IQR £7694–10,623, n = 35 | Gamma(723, 13.7) |
|
||||||||||||||||
| DZ02J | £7772 | IQR £6437–9086, n = 40 | Gamma(627, 12.4) | |||||||||||||||||
| DZ02K | £6702 | IQR £5048–7597, n = 46 | Gamma(579, 11.6) | |||||||||||||||||
| Utility decrement for stroke up to 6 months | –0.22 | 95% CI –0.26 to –0.18 | Norm(–0.22, 0.02) | Luengo-Fernandez et al.201 | ||||||||||||||||
| Utility decrement for stroke from 6 months | –0.09 | 95% CI –0.13 to –0.05 | Norm(–0.09, 0.02) | Luengo-Fernandez et al.201 | ||||||||||||||||
| Utility immediately after DVT | 0.71 | SD 0.26, n = 1640 | Beta(3545, 1448) | Cohen et al.173 | ||||||||||||||||
| Utility immediately after PE | 0.67 | SD 0.24, n = 1150 | Beta(1663, 819) | Cohen et al.173 | ||||||||||||||||
| Utility for DVT without PTS | 0.86 | 95% CI 0.823 to 0.903 | Beta(248, 40.3) | Enden et al.189 | ||||||||||||||||
| Utility decrement for PTS vs. no PTS after DVT | 0.09 | 95% CI 0.03 to 0.15 | Beta(7.78, 78.6) | Enden et al.189 | ||||||||||||||||
| Utility for CTEPH | 0.56 | SD 0.29, n = 308 | Beta(505, 397) | Meads et al.198 | ||||||||||||||||
| Utility for NYHA class I | 0.86 | SD 0.17, n = 35 | Beta(105, 12.9) | Meads et al.198 | ||||||||||||||||
| Utility for LMWH | 0.993 | SD 0.016 | Beta(27.5, 0.205) | Marchetti et al.207 | ||||||||||||||||
| Utility for warfarin | 0.989 | SD 0.024 | Beta(17.6, 0.195) | Marchetti et al.207 | ||||||||||||||||
| Utility regression for age-related decrement: coefficients for | ||||||||||||||||||||
| Age | –0.0001728 | SE 0.0003737 | Multivariate normal |
Ara and Brazier194 Variance–covariance matrix AgeAge × ageConstantAge1.4 × 10–7Age × age–1.5 × 10–91.6 × 10–11Constant–2.80 × 10–62.8 × 10–86 × 10–5 |
Age | Age × age | Constant | Age | 1.4 × 10–7 | Age × age | –1.5 × 10–9 | 1.6 × 10–11 | Constant | –2.80 × 10–6 | 2.8 × 10–8 | 6 × 10–5 | ||||
| Age | Age × age | Constant | ||||||||||||||||||
| Age | 1.4 × 10–7 | |||||||||||||||||||
| Age × age | –1.5 × 10–9 | 1.6 × 10–11 | ||||||||||||||||||
| Constant | –2.80 × 10–6 | 2.8 × 10–8 | 6 × 10–5 | |||||||||||||||||
| Age × age | –0.000034 | SE 3.96 × 10–6 | ||||||||||||||||||
| Constant | 0.9584588 | SE 0.0077431 | ||||||||||||||||||
Glossary
- Chronic thromboembolic pulmonary hypertension
- Persistent increased blood pressure in the arteries supplying the lungs, which is caused by pulmonary embolism and results in long-term shortness of breath and fatigue.
- Cost-effectiveness acceptability curve
- A way of illustrating cost-effectiveness results by plotting the probability that the intervention is cost-effective (y-axis) against the maximum that society is willing to pay for an improvement in health (x-axis).
- Cost-effectiveness plane
- A way of illustrating cost-effectiveness results by plotting the mean incremental cost and effectiveness on a four-quadrant graph. Interventions that are more costly and more effective fall in the north-east quadrant.
- Deep-vein thrombosis
- A blood clot that develops within a deep vein in the body, usually in the leg.
- Incremental cost-effectiveness ratio
- The difference in the mean costs in the population of interest divided by the differences in the mean outcomes in the population of interest.
- L-TRiP(cast)–N
- A strategy of giving thromboprophyalxis to patients with a L-TRiP(cast) score of N or above.
- Post-thrombotic syndrome
- Pain, swelling, itching, skin discolouration and leg ulcers occurring after a deep-vein thrombosis, caused by damage to the valves in the leg veins that prevent backflow of blood.
- Predictor
- Throughout this report, ‘predictor’ is used to refer to any clinical, laboratory or demographic characteristic. The term ‘predictor’ encompasses other similar terms, such as prognostic factor, covariate and variable.
- Prophylaxis
- A measure taken to prevent a disease.
- Pulmonary embolism
- A blood clot that breaks off from the deep veins and travels around the circulation to block the pulmonary arteries (arteries in the lung). Most deaths arising from deep-vein thrombosis are caused by pulmonary embolism.
- Quality-adjusted life-year
- A measure of the benefit of health care that combines the impact of both the expected length of life and quality of life.
- Risk assessment models
- In this report, defined as a combination of at least two predictors within a statistical model that is used to predict an individual’s risk of outcome, for example venous thromboembolism. Other terms also related to risk assessment models may include prognostic model, prediction models, clinical decision rules and clinical prediction guides. The term ‘risk assessment model’ is used in this report to encompass all of these terms; therefore, all are considered to refer to the same thing.
- Thromboprophylaxis
- A measure taken to reduce the risk of thrombosis.
- Vein thrombosis
- A condition in which a blood clot (thrombus) forms in a vein.
- Venous thromboembolism
- The blocking of a blood vessel by a blood clot dislodged from its site of origin. It includes both deep-vein thrombosis and pulmonary embolism.
List of abbreviations
- AF
- atrial fibrillation
- AUC
- area under the curve
- BMI
- body mass index
- CaVenT
- catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep-vein thrombosis
- CEAC
- cost-effectiveness acceptability curve
- CG
- clinical guideline
- CI
- confidence interval
- CrI
- credible interval
- CRNMB
- clinically relevant non-major bleeding
- CTEPH
- chronic thromboembolic pulmonary hypertension
- DOAC
- direct oral anticoagulant
- DVT
- deep-vein thrombosis
- DVTQoL
- Deep Venous Thrombosis Quality of Life
- ED
- emergency department
- NHS EED
- NHS Economic Evaluation Database
- EQ-5D
- EuroQoL-5 Dimensions
- EVPI
- expected value of perfect information
- GEMNet
- Guidelines in Emergency Medicine Network
- GI
- gastrointestinal
- GP
- general practitioner
- HAS-BLED
- Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile international normalised ratio, Elderly, Drugs/alcohol concomitantly
- HR
- hazard ratio
- HRG
- Healthcare Resource Group
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- HUI-3
- Health Utilities Index – 3
- ICER
- incremental cost-effectiveness ratio
- ICH
- intracranial haemorrhage
- INMB
- incremental net monetary benefit
- INR
- international normalised ratio
- LMWH
- low-molecular-weight heparin
- L-TRiP(cast)
- Leiden thrombosis risk in plaster (cast)
- MCS
- mental component summary
- NICE
- National Institute for Health and Care Excellence
- NMA
- network meta-analysis
- OR
- odds ratio
- OXVASC
- Oxford Vascular Study
- PAH
- pulmonary arterial hypertension
- PCS
- physical component summary
- PE
- pulmonary embolism
- POT-CAST
- Prevention of Thrombosis after Lower Leg Plaster Cast
- PPI
- patient and public involvement
- PREFER-VTE
- Prevention of thromboembolic events – European registry in venous thromboembolism
- PSA
- probabilistic sensitivity analysis
- PTS
- post-thrombotic syndrome
- QALY
- quality-adjusted life-year
- RAM
- risk assessment model
- RCEM
- Royal College of Emergency Medicine
- RCT
- randomised controlled trial
- RIETE
- Computerized Registry of Patients with Venous Thromboembolism
- RoB
- Cochrane Risk of Bias tool
- ROBINS-I
- Risk Of Bias In Non-randomized Studies – of Interventions
- ROC
- receiver operating characteristic
- RR
- relative risk
- SD
- standard deviation
- SF-6D
- Short-Form questionnaire-6 Dimensions
- SF-12
- Short-Form questionnaire-12 items
- SF-36
- Short-Form questionnaire-36 items
- SMD
- standardised mean difference
- STA
- single technology appraisal
- TA
- technology appraisal
- TTO
- time trade-off
- VKA
- vitamin K antagonist
- VTE
- venous thromboembolism