Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 14/49/34. The contractual start date was in October 2015. The draft report began editorial review in February 2019 and was accepted for publication in November 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Fiona Lobban reports grants from the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme during the conduct of the study. Fiona Lobban and Lesley Chapman were involved in the design and development of the Relatives’ Education And Coping Toolkit (REACT); hence, this is not an independent evaluation. Bruce Hollingsworth reports that he was a NIHR Health Services and Delivery Research Commissioned Board member (2013–15). Paula Williamson reports grants from NIHR during the conduct of the study, and that the Clinical Trials Research Centre at the University of Liverpool was in receipt of NIHR Support Funding during the conduct of the study.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Lobban et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
This chapter provides the background and rationale for the present study. We present an overview of the challenges faced by relatives of people with psychosis or bipolar disorder (BD), describe what support is currently available for this group and outline why we developed the Relatives’ Education And Coping Toolkit (REACT). We briefly describe previous work in developing REACT and explain the context for the current study.
This chapter draws on some material previously published by the report’s authors during the course of the study,1–3 and reproduced here under a Creative Commons licence (https://creativecommons.org/licenses/by/4.0/). Honary et al. 1 © Mahsa Honary, Naomi Ruth Fisher, Roisin McNaney, Fiona Lobban. Originally published in JMIR Mental Health (http://mental.jmir.org), 07.12.2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Mental Health, is properly cited. The complete bibliographic information, a link to the original publication on http://mental.jmir.org/, as well as this copyright and license information must be included.
Challenges faced by relatives of people with psychosis or bipolar disorder
Psychosis is an umbrella term that covers many different conditions, the common feature of which is that people perceive or interpret the world around them very differently. The most frequent ways this manifests are having beliefs that are not shared by others and do not have a basis that is understandable to others (often called delusions); not being able to think clearly, and so sounding muddled and hard to follow (often called thought disorder); or experiencing, for example hearing or seeing, things that other people cannot (often called hallucinations).
As well as the presence of these unusual experiences, many people with psychosis also report a loss of valued experiences, most notably pleasure in everyday activities (anhedonia) and loss of motivation (apathy). These losses are sometimes referred to as ‘negative symptoms’, and are particularly challenging for relatives, not least because they are hard to differentiate from normal ‘teenage angst’, side effects of medication or depression. It is difficult to report exact figures on the number of people who will experience psychosis as many may never have contact with mental health services, but most recent estimates have calculated worldwide prevalence to be approximately 1 in 13 people (7.7%),4 and up to 10% of people in the UK report some kind of psychotic experiences. 5 Only a fraction of these people (approximately 1% of the general population) will ever come into contact with mental health services and receive a diagnosis of a mental health condition. In general, these are likely to be people for whom these experiences are particularly distressing or cause significant changes in behaviour.
Bipolar disorder is the third most common mental health cause of disability globally,6 affecting 1–4.5% of adults7 and costing the English economy £5.2B annually, largely owing to inadequate treatment. 8 BD is characterised by episodes of extreme low mood (depression) and extreme high or irritable mood (mania, or hypomania in its milder form). Challenging behaviours, such as increased self-harm and suicidal behaviour, excessive spending, sexual disinhibition and heightened irritability, can all occur during mood episodes, which are often accompanied by psychotic symptoms. Between episodes, functioning may return to normal levels, although many people report problematic subsyndromal levels of depression that affect their functioning and relationships. 9
Psychosis and BD present significant challenges to relatives, particularly in recognising and understanding what is happening, living with the elevated risk of suicide, the impact on relationships within the family, and having to balance caring, work and other family commitments. These challenges are exacerbated by difficulties in accessing mental health services, which delay access to effective treatment, leading to worse long-term outcomes. 10,11 It has been estimated that more than one-third of relatives of people with psychosis experience clinically significant levels of distress and burden,12 and estimates from more recent studies with relatives from early intervention in psychosis (EIP) services are even higher, at > 60%. 2,13
Almost half of relatives of people with psychosis experience post-traumatic stress symptoms associated with their caring roles,14 particularly linked to episodes of violence, disruptive behaviour and forced admission. 15
Key factors that increase the negative impact of psychosis on carers include being a female carer;16 living with the person with psychosis; young patient age and awareness of suicidal ideation;17 reduced social support and family resources;17,18 use of emotion-focused coping strategies;19 and beliefs that relatives hold about the psychosis, particularly those concerning cause and control. 20–22
In BD, symptoms associated with depressive episodes result in increased burden of caring, poorer general health, and depressive symptoms in carers. 23–25 The frequency of suicide attempts among the BD population is higher than in many other populations affected by mental health issues, creating a distressing situation for carers. 26 During periods of mania, extravagant spending, irritability and inappropriate and disproportionate behaviour become more frequent and extreme. 27–29 The challenge of learning to cope with symptoms associated with manic and depressive episodes can not only negatively affect the service user, but also diminish carers’ and their families’ quality of life, with carers expressing feelings of helplessness, anger and anxiety. 30,31
Importantly, many relatives also report positive aspects of caring for someone with a severe mental health problem, including identifying personal strengths; feeling a sense of love, caring and compassion; developing new insights about their lives and living; and greater intimacy with others as a result of their journey coping with mental illness. 32,33
We have chosen to focus on the needs of relatives of people with psychosis or BD together in the REACT project, as they face many common challenges. These include how best to support someone in their recovery journey, how to deal with a mental health crisis, how to manage difficult situations, how to manage stress and how to understand and navigate mental health services and the treatments they offer. Mental health services are often structured such that people with a diagnosis of psychosis or BD are managed in the same teams (e.g. community mental health teams, EIP teams). Therefore, having interventions to support relatives that work across these conditions also makes practical sense.
Support for relatives
Relatives of people with psychosis or BD provide a large amount of unpaid care,34,35 but at high personal cost in terms of distress and burden. 12,36,37 Without this unpaid care, the NHS would not be able to cope. Historically, the impact of severe mental health problems on relatives has been ignored, or included as a secondary outcome to service user outcomes. 38 However, more recently, there has been increasing recognition of the importance of understanding the impact on the carer of supporting someone with a mental health problem, and of the need for effective interventions to address this impact. 39
There is now good evidence that interventions that support relatives can improve outcomes both for service users38,40,41 and for carers. 39,42–44 The exact nature of these interventions for carers varies. Some are psychoeducational, aiming to empower relatives with information and coping strategies. 45 Others are more systemic and, in addition to psychoeducation, work with the family on approaches to problem-solving and communication (e.g. Miklowitz46). Interventions also vary in how many sessions are offered, over what period sessions are offered, whether or not the service user also takes part in the intervention and whether the programme is offered to individual families or in groups. To date, there are no good-quality data sets that determine which content or format is most effective.
The exact mechanism underlying the improvements in carer outcomes as a result of family-focused support is not well understood. However, studies have identified several factors associated with improved outcomes for relatives, including the following:
Implementing support for relatives
The UK government recognises the need to support relatives in a caring role,52 and the National Institute for Health and Care Excellence (NICE) recommends that all relatives be given carer-focused education and support and offered a structured family intervention to enhance family coping and communication. 53,54
However, a recent national audit of EIP services in the UK showed poor implementation, with only 50% of relatives receiving a carer-focused education and support programme and only 31% being offered a structured intervention (of whom only 12% took up the offer). 55 A survey of > 1100 families across 22 European countries showed that half were dissatisfied with how they were involved by mental health services,56 suggesting that it is unlikely that services are better elsewhere.
The challenges services face in providing structured family interventions are likely to include cost and the practicalities of delivery. Many require two trained therapists, available at the same time weekly for up to 9 months with regular access to supervision, as well as a family whose members can all commit to attending face-to-face sessions, often during office hours, and have a sufficiently open and robust relationship with the service user.
However, these factors do not account for the lack of more straightforward psychoeducational approaches and emotional support for relatives. It is likely that additional organisational factors also play a role in poor implementation.
For example, staff workload is often measured in terms of the number of service user contacts, which may not adequately recognise time spent with family members. Under pressure, this may be the first thing to go. As well as highlighting the need for organisation-wide change, a study by Eassom et al. 57 identified staff reservations about the level of involvement family members should be given in the recovery process, fear of negative outcomes as a result of involving family members and the need for an exclusive patient–professional relationship.
Attempts have been made to improve access to support for relatives. Achieving Better Access to Mental Health Services by 2020,58 published in October 2014 by NHS England and the Department of Health and Social Care, sets a key standard that ‘more than 50% of people experiencing a first episode of psychosis will be treated with a NICE approved care package within two weeks of referral’ (contains public sector information licensed under the Open Government Licence v3.0). This includes carer-focused education and access to structured family interventions. Clinical Commissioning Groups (CCGs) have been directed to allocate funding to EIP teams to support efforts to meet this standard, the success of which is being audited by the College Centre for Quality Improvement in the Royal College of Psychiatrists. 55
In addition to government policy, the Triangle of Care59 has been developed by the Carers Trust and the Mental Health Development Unit as a ‘guide to best practice’ to help mental health services improve collaboration and partnership with carers. The Triangle of Care sets out six key standards, which have already been adopted by a significant number of NHS trusts. However, the extent to which these are being met is currently monitored through self-audit only, which may limit their impact on practice.
In this context, our aim was to develop a user-friendly, easily accessible self-management intervention, based on the principles of psychoeducation and family intervention, that could overcome some of the identified barriers to implementation, and be made available to all relatives of people with psychosis or BD across the UK. Specifically, we were keen that the intervention would target key appraisals and coping strategies, be empowering for relatives, not require extensive staff time or training, be low-cost and require little input from mental health services. Self-management interventions that have the flexibility to be used alongside other work and family commitments and augment other forms of support are ideally suited to meet the needs of relatives, and have the potential to be widely available in an increasingly resource-restricted health service.
Initial development of REACT
REACT was first developed as a paper-based self-management intervention for relatives of people with psychosis in EIP services as part of a National Institute for Health Research (NIHR) Research for Patient Benefit-funded study. 60 The content was informed3 by:
-
our systematic review of interventions for relatives of people with psychosis,39 highlighting the distinguishing features of effective interventions
-
focus groups of relatives3
-
cognitive–behavioural therapy models highlighting the importance of helping relatives to understand psychosis and build on existing strategies
-
the research team’s own expertise.
REACT consisted of 13 sections, designed to be used flexibly depending on the individual needs of relatives. The 13 sections were as follows:
-
Introduction to REACT
-
What is psychosis?
-
Managing positive symptoms
-
Managing negative symptoms
-
Dealing with crises
-
Dealing with difficult behaviour
-
Managing stress: thinking differently
-
Managing stress: doing things differently
-
Understanding mental health services
-
Treatment options
-
The future
-
Resource directory (RD)
-
Jargon terms.
Through this combination of modules and the directory, the toolkit aimed both to support users directly, by providing advice, information and case studies, and to connect them to other sources of advice and support. The toolkit was printed in A5 format and given to each participant. It could also be read online or downloaded from a website made available to participants, although this was very little used and relatives made clear in feedback that they preferred a resource that they could hold in their hands. Most sections were < 24 pages: the shortest was 11 pages, the longest was the RD, at 43 pages. The large number of links to other services and resources meant that the toolkit required constant editing and updating to maintain its accuracy.
Support in using the toolkit came from EIP support workers, who conducted one-to-one introductory sessions with each participant, with ongoing support available for 6 months by telephone or e-mail, as preferred, limited to 60 minutes per week. Participants who did not contact their support worker or who missed appointments were called at least monthly to maintain engagement. The intention of this personalised support was to help relatives to identify their greatest challenges and to then navigate the toolkit to find information or useful strategies that could be used. The focus was on practical engagement rather than transmission of information, with relatives encouraged to adopt and adapt new strategies, acquire and use new skills and reflect on the results: an active rather than passive approach.
The feasibility and acceptability of the toolkit were tested in a randomised controlled trial (RCT), in which the toolkit was offered in addition to treatment as usual (TAU). Relatives’ distress and well-being outcomes were compared at 6 months’ follow-up against those receiving TAU. This trial showed that relatives were very keen to engage with the intervention, that staff could integrate delivery of REACT into existing EIP services, and that relatives who received REACT were significantly less distressed than those receiving TAU at 6 months, as measured by the General Health Questionnaire-28 items (GHQ-28)61 [regression coefficient –6.59, 95% confidence interval (CI) –12.55 to –0.64]. They also had higher levels of perceived support [measured using the Carer Well-being and Support (CWS) Questionnaire:62 regression coefficient 4.86, 95% CI 0.77 to 8.96] and perceived ability to cope (measured using the Family Questionnaire:63 regression coefficient –4.89, 95% CI –9.34 to –0.44) than those receiving TAU.
As well as strongly preferring the printed toolkit over the online version, relatives showed a slight preference for accessing support by telephone rather than e-mail. There were practical challenges in retaining trained NHS staff for the trial and in maintaining their allocated time to support the intervention.
Qualitative feedback from relatives who used REACT was extremely positive. 64 Relatives reported feeling less isolated and more supported as a result of REACT:
Say it were a Saturday night and they aren’t available, I still know, come Monday morning, I could ring that number, and that could help me through that weekend.
When asked what they felt REACT had changed for them, relatives reported changes in their ways of thinking about the service user’s behaviour:
[It] made me see things differently from a different point of view.
They also reported changes in their coping strategies:
I now know how to say things to David – rather than, I would have said, ‘Oh David, do you have to smoke? Your teeth are going to be yellow,’ I will say something now like, ‘Oh David, you know, you are so nice looking, you would be even nicer if you didn’t smoke because smoking can actually make your teeth go yellow.’ So I know how to word things more to make him feel not guilty about the smoking.
They also reported feeling more supported as a result of the intervention:
Oh, very reassuring. It [support] saved my life. I know that sounds melodramatic, but it saved my life; I feel as if it saved my sanity in a way.
Subsequent development of REACT
Based on qualitative feedback from relatives using REACT in the feasibility trial, as well as input from the patient and public involvement (PPI) group and from clinical academic experts in our research team, we proposed the following goals for the next version of the intervention:
-
to adapt REACT for a broader range of relatives, including those outside EIP and those supporting people with BD
-
to make a more interactive version of REACT, available online to relatives
-
to have expert relatives offer REACT support rather than NHS staff.
The reasons for these goals are explained in the following sections.
Adapt REACT for a broader range of relatives
Although targeted early interventions have been successful in improving outcomes, these improvements are not sustained when service users move from specialist EIP services into routine mental health services. 65,66 There are also many relatives supporting people with psychosis who are not accessing mental health services at all. There is an urgent need to develop interventions that can be extended beyond EIP services, to include relatives outside mental health services and to support people with a broader range of diagnoses.
A more interactive, online REACT
In the feasibility trial, relatives preferred the paper version of REACT. However, the online version was restricted to static Portable Document Formats (PDFs), with none of the advantages that interactive online interventions can offer. The paper version was also very difficult to update regularly, and had high production costs, which might limit dissemination.
Because of the general increase in the use of the internet to access health-care interventions, the advantages of being able to update information quickly as required and the opportunity to add more interactive components and multimedia formats, such as video clips, we proposed delivering REACT as an online intervention, despite the preferences stated in the feasibility study.
Online interventions are well established for many mental health conditions, including depression and anxiety,67 and some have now been developed for psychosis68 and BD. 69 Such interventions are particularly suited to delivering standardised information together with a platform for sharing ideas through online forums. Online support is also being developed for relatives of people with other chronic health conditions,70 and may be particularly useful for these groups because of the flexibility of use and the empathy and support available from other carers. 71 There is some evidence that online interventions would be well received by carers,72 although acceptability, along with clinical effectiveness and cost-effectiveness, needs further testing.
Have expert relatives offer the REACT support rather than NHS staff
Offering REACT to all relatives, including those not in contact with mental health services, and putting it online allowed us to develop a single dedicated team to support the intervention. This gave us greater control over the nature and design of the support. We chose to employ peer workers – relatives with lived experience of supporting someone with a mental health problem – for several reasons.
Our PPI group strongly favoured this approach. Our co-applicant (LCh) had worked with the charity Rethink for many years, sharing her knowledge and experience to support other relatives. There was a shared perception that peer workers would be highly knowledgeable, empathetic and motivated to support other relatives. This was reiterated in the design workshops that we conducted to develop the online version of REACT (see Chapter 2).
Qualitative and observational studies have identified a number of benefits of using peer workers, both for those receiving support and for the peers themselves. 73 For service users, these benefits include reduced admission rates; greater empowerment, empathy, acceptance and hope; better social functioning; and less stigma. Benefits reported by peer workers include support for their own recovery and personal growth, acquisition of new skills and the therapeutic effect of helping others. For paid peer workers, there are also financial benefits. 74,75 Employing relatives as REACT supporters to support the REACT website was an opportunity to develop the strategic role of service users and carers in delivery of services and explore the benefits and challenges of this role. It also circumvented the difficulty of identifying existing staff who had the expertise, time and support to take on this role. Developing the peer worker role as part of the NHS workforce was also consistent with recommendations from NICE in 2016. 76
Securing funding to evaluate REACT
In January 2013, we applied to NIHR for Health Technology Assessment (HTA) programme funding to deliver these adaptations and test the clinical effectiveness and cost-effectiveness of the new version of REACT in a large definitive trial. The application was rejected (13 December 2013), as the trial was seen as too expensive to deliver, at £2,032,667. Given the positive outcomes we had already demonstrated and the correspondence of the intervention to NICE guidance requirements to offer all carers psychoeducational and emotional support, the HTA programme funding committee suggested that we consider how best to deliver REACT in the NHS.
We then responded to the HTA programme efficient design call for RCTs that tested efficient trial designs to address the problem of the escalating costs of large-scale definitive trials. This offered the opportunity to test the online REACT intervention in an entirely online trial. Advantages of online trial design include the potential to reach a greater number and range of participants; to reach a population more representative of those likely to use an online intervention; to recruit more people over a shorter time frame; to simplify protocols for secure randomisation and data entry; and to deliver a trial much more cheaply because fewer staff are needed. 77 However, retention rates for such trials can be low,77,78 compromising internal validity of the trial.
This efficient design reduced the costs of the trial to £633,404. We were awarded funding for 36 months, to begin in October 2015.
In parallel, we applied to the NIHR Health Services and Delivery Research (HSDR) programme for funding for an implementation study to identify the factors affecting successful delivery of an online intervention within EIP services. This study was also funded for 30 months, starting in March 2016. The two studies were complementary. The HSDR study explored factors affecting implementation of a clinician-supported intervention in EIP services in the NHS, in contrast to this study’s peer worker-supported intervention. It also included an evaluation of outcomes for the relatives, using the same measures and follow-up period as this study. We thus had the potential to compare both the reach and the outcomes achieved by providing REACT through two very different study designs. This allowed us to answer questions about which was likely to be the most effective service provision model, as well as to compare the effectiveness of peer worker- and clinician-supported approaches. The HSDR report was submitted for publication in December 2018.
Trial design
The REACT trial is a single-blind, parallel online RCT to determine the clinical effectiveness and cost-effectiveness of REACT, including an online RD, compared with the RD only, for relatives of people with psychosis or BD. No changes were made to any other support that relatives received outside the trial. See Chapter 3 for the specific objectives of the trial.
Research team
The team included relatives, clinicians, academics and methodologists from a range of disciplines, with a common interest in developing and evaluating new ways to support people with mental health problems and their relatives. Team members were all UK based, and, although some had worked together previously, the team in its entirety came together specifically for this project. Although the team all differed in background, training, epistemological and ontological stance, some important factors underpinned the team in working together successfully:
-
a commitment to improving the lives of people with mental health problems and their relatives in non-stigmatising, empowering, and recovery-focused ways
-
a recognition of the huge role that relatives play in supporting people with health problems, and of the current lack of adequate support available to them
-
a belief in the importance of evidence-based health care and the need to carry out high-quality research to inform how NHS funding is spent
-
an interest in testing the potential of digital technology to increase accessibility and reduce costs of clinical interventions, while also exploring the challenges of and barriers to this approach
-
a commitment to identify efficient ways to carry out publicly funded research to provide value for money to the UK taxpayer.
Trial monitoring
Trial Management Group
The Trial Management Group (TMG) was involved in developing the trial ideas and was responsible for delivering the project. This group included the trial co-applicants: a relative with many years supporting a family member with a diagnosis of schizophrenia (LCh); two clinical academic psychologists (FL and SHJ) based in Lancaster; a clinical academic psychiatrist with a lead role nationally in EIP services (SJo) and a clinical academic general practitioner (GP) who is an expert in development and evaluation of digital health interventions (EM); a trial statistician who is director of the Clinical Trials Research Centre (CTRC) in Liverpool, which oversaw the data management and statistical analysis (PW); and a health economist based in Lancaster (CM).
The TMG met monthly and also included the trial managers (HR and BM), information technology (IT) experts who built and maintained REACT and the data collection systems (DA and AW) and lead and support statisticians who managed the data collection and recruitment and retention reporting, as well as conducting the final analysis (SD and NR). To accommodate the geographical spread, and consistent with our efficient design, all meetings took place by teleconference.
REACT was supported by a team of trained relatives [SF, Alison Hankinson (see Acknowledgements), LC, NA] and supervised by two clinical psychologists (SHJ, WS).
Trial Steering Committee and Data Monitoring and Ethics Committee
The trial was overseen by an independent Trial Steering Committee (TSC) and a separate Data Monitoring and Ethics Committee (DMEC). The TSC was chaired by an expert in clinical trials testing psychological interventions (Shirley Reynolds) and included two academic clinical psychologists (Gillian Hardy and Pete Langdon), a statistician (Alex McConnachie), a service user and a relative. It also included a representative of the sponsoring organisation Lancaster University (SD) and the NIHR Clinical Research Network (MW). The TSC met before the start of the trial, at 10 months to review progress with recruitment, at 15 months to determine whether or not the findings from the internal pilot supported the continuation of the trial, and then annually to the end of the trial.
The DMEC was chaired by a statistician who directs a clinical trials unit (Kerry Hood), and included another academic clinical psychologist with expertise in developing and evaluating digital health interventions (Cathy Creswell). The role of the DMEC was to monitor the data and, specifically, to assess whether or not we had met the stop/go criteria set for our internal pilot (see Chapter 3), and to monitor any ethics or safety concerns. The DMEC met before the start of the study, at 10, 12 and 15 months and then annually, timed to feed reports into meetings of the TSC. All meetings were by teleconference.
Patient and public involvement
Consistent with A Framework for Mental Health Research,79 this project was developed and conducted in partnership with service users and carers.
Co-investigator
One of the trial investigators and co-author is a parent of someone living with psychosis and was extensively involved in the development of REACT, the RD and the data collection processes. She was part of the supervisory team for the REACT supporters. She was also invited to attend the TMG meetings.
Development of REACT
Relatives were involved in the development of the initial content for the toolkit,80 and in subsequent iterations to develop an online toolkit;1 see Chapter 2.
Relatives’ advisory group
At the start of the project, we set up the relatives’ advisory group (RAG) of 13 relatives or close friends of someone with BD and/or psychosis and one individual with lived experiences of BD. Their role was to provide consultative input to each stage of the research.
Consistent with the online nature of the trial, members of the group worked mainly remotely, providing detailed feedback on REACT (reviewing its content and format) and the online data collection process (including selection of questionnaires and items used for eligibility screening), and advising on strategies for maximising recruitment and retention.
In addition to independent review work, the group met three times during the trial: before the start of the trial, to familiarise themselves with the REACT and trial and data collection tools; at 12 months, to review the recruitment strategy; and at 22 months, to advise on the follow-up strategy. The first meeting was held face to face at Lancaster University; the other meetings were held online, which facilitated the involvement of people from a wider geographic area and a greater diversity of relatives’ experiences. RAG members were also invited to write blogs for the website to stimulate discussions on the REACT forum. The results of the trial have been presented to the RAG members, and work continues with this group on interpretation and broader dissemination of the data.
The RAG members received a high-street shopping voucher for £10–50 (depending on the length of the task undertaken) as a thank-you for their time.
The REACT supporter role
The REACT supporters were relatives with lived experience of supporting someone with psychosis or BD. They were employed by the host NHS trust as NHS band 5 staff. See Chapter 2 and the project web page [www.journalslibrary.nihr.ac.uk/programmes/hta/144934/#/ (accessed 28 October 2019)] for more details on their role.
Trial Steering Committee
One relative and one service user were appointed to the TSC at the start of the trial. They both had experience of using services, but also had research expertise. The service user was employed as a research associate on another NIHR-funded study, and the relative was a retired academic.
Chapter 2 Intervention development
Introduction
In this chapter, we describe how the paper-based REACT intervention (see Chapter 1) was adapted to an online version, and describe the resulting content. The three key adaptations, based on learning from the feasibility trial, were to:
-
broaden REACT to make it suitable for relatives outside EIP services and for relatives supporting people with BD
-
make REACT more interactive and directly available online to relatives
-
offer REACT with support from trained relatives.
In the feasibility trial of the paper-based REACT, modules were posted online as PDFs to aid availability. Clearly, this is not the same as an online intervention, which would typically be more structured, self-guided, interactive, visually rich and personally tailored. Therefore, considerable work was needed.
Following guidance from the Consolidated Standards of Reporting Trials of Electronic and Mobile HEalth Applications and onLine TeleHealth (CONSORT-EHEALTH) checklist, version 1.6.1,81 we describe the history, development and initial formative evaluations of REACT, details of how the dynamic components worked and how the site was updated. We provide relevant screenshots and have archived the site (access available on request). We also present the development and content of the RD that was offered as our active control intervention. As required by the Consolidated Standards of Reporting Trials (CONSORT), we identify the sponsorship and ownership of the site.
The aim was to involve relatives, clinicians and the clinical academic team in co-developing content and design to ensure that both would be of high quality, user friendly, meet the needs of relatives and engender confidence in potential referrers. The importance of understanding the needs of users and involving them in design has been well reported. 82 We carried out a series of workshops with users (relatives) and drew on the expertise within our clinical academic team to develop a list of design features, which guided our development of REACT.
Understanding user perspectives: method
We held two workshops (workshops 1 and 2, with 13 and 11 participants, respectively) to explore the needs of relatives outside EIP services, and their views about how REACT should be developed. We aimed to recruit participants from diverse backgrounds in terms of age, gender, relationship with the service user, length of experience as a caregiver and computer literacy. Workshop participants were invited if they identified as supporting a relative or close friend with psychosis or BD. Our recruitment strategy was to advertise locally to obtain a convenience sample that could attend face-to-face workshops. Advertisements were circulated via Lancaster University’s Spectrum Centre for Mental Health Research,83 using e-mail, social media and post. The Spectrum Centre is a multidisciplinary research centre focusing on the development and evaluation of psychosocial interventions for people with long-term mental health problems.
In accordance with our approval from the Lancaster University Ethics Committee, those who indicated interest were sent an information sheet by e-mail or post before the workshop, allowing them to raise any questions in advance. This information included the purpose of the workshop, its location and duration, that participation was voluntary, and what would happen to their audio-recorded data.
Participants were offered a £20 Amazon (Amazon.com, Inc., Bellevue, WA, USA) voucher in recognition of their time and input. Two researchers facilitated each workshop, using a semistructured topic guide to lead discussion and ask open questions to elicit a range of views.
First, the participants were encouraged to reflect and share their lived experiences as caregivers of people with psychosis or BD. This included how their relative was first diagnosed, how they became involved as caregivers, the impact of mental health problems on their family and daily life, and their current sources of support, as well as the types of support or strategies they found most useful.
Second, they were asked their views on gaps in the support system for caregivers, how to fill these and whether or not online support could play a role in this. Finally, they reviewed the REACT booklets together and discussed whether or not and how these could be redesigned as a web-based intervention, and what additional support might be needed to facilitate REACT’s use online. Each workshop was audio-recorded with participants’ permissions, and transcribed verbatim for later analysis (see the data analysis section).
We conducted an additional workshop (workshop 3) with two participants to scope the types of features that could be included in the web-based REACT intervention. Both participants were comfortable using computers, used social media frequently and were interested in helping with the design of REACT. Before the workshop, participants were given access to the website of the PDFs. They were also asked to identify other websites that they liked or disliked, both related and unrelated to mental health. We explored their aesthetics and functionalities together. This was followed by a visual demonstration of a series of design prototypes for the web-based REACT intervention, based on our findings from workshops 1 and 2. The prototypes were developed in conjunction with a web design company and mainly focused on aesthetic aspects of the web interface, such as logo, font style and size, navigation menu, colour scheme and multimedia choices.
We wanted to know how to translate the values and needs that participants had highlighted in workshops 1 and 2 into functionalities. In particular, we wanted to understand how best to give users a positive experience. We therefore asked participants in workshop 3 to discuss how to design the web-based REACT to be more engaging, what features might motivate users to keep returning and what types of support could be offered only online.
A full description of the findings of all three workshops is reported elsewhere,1 and is summarised in the next section.
Understanding user perspectives: results
The majority of participants in workshops 1 and 2 were female, aged > 45 years, parents and infrequent computer users. Most had had many years’ experience of caring for relatives with severe mental illness (on average, about 10 years). In workshop 3, one participant had taken part in workshop 1 and was typical of that group, whereas the second participant was aged 21 years and new to the study. In total, 25 participants took part in this qualitative study across all three workshops (18 females, age range 21–75 years, n = 20 parents). Participants comfortably shared their experiences, and no prompting was required for conversation to flow. Key findings covered their caregiving experiences, the support that they believed was needed, the potential role of online interventions and the design of such interventions.
Caregiving experiences
Identity as a carer
Relatives talked about feeling a loss of sense of self in their journey to becoming a carer. They felt that they had been pushed into a ‘carer’ role and found it hard to maintain their identity as a father, wife, etc:
I don’t want to be a carer, I don’t like the word. I’m a mother. I know somebody has me down as a carer even if they don’t give me a decision. But in my head, I’m not.
Workshop 1, participant 9
The role of carer was particularly unappealing as it came with no formal training or guidance, so, as well as being imposed, it was also very challenging. Many relatives described it taking years for them to learn strategies to cope with the impact of psychosis or BD on the rest of the family.
Impact on the whole family
Participants described the very broad impact mental health problems had on the wider family, and the need for support for all family members:
Our youngest son didn’t understand what his brother was going through . . . It must have been terrible for him and, in fact, not long ago, he actually left the family.
Workshop 1, participant 1
In addition, caregivers discussed needing support, not just as caregivers, but as individuals in their own right, with other responsibilities in their lives:
I might have had a right morning with my son, threatening suicide or wrestling for my own life. And I’d have to go in work . . . change into my uniform and drive to work and I’ve got a lump in my throat. And I’d phone my partner [saying] ‘I’m going to cry’.
Workshop 2, participant 3
Social isolation
Caregivers of people with physical illness may have little opportunity for social interaction because of the need for constant caring. In mental health, social isolation can be further exacerbated by stigma and lack of public awareness about mental health. Participants talked about finding it difficult to open up to their friends and families:
My children used to say to me ‘what do we say to our friends about [relative]?’ And I told them to [deny relative has a mental health problem], which I don’t know is right, because I thought they’ll get bullied. Or otherwise they will say your relative’s crazy or . . .
Workshop 2, participant 10
Many had found it challenging initially to find others with similar lived experiences. Once they were in contact with other caregivers, they found this invaluable not only for emotional support, but also for signposting to important information and guidance. Many were part of charity-run face-to-face peer support groups facilitated by an ‘expert caregiver’:
The person who runs our small group is a godsend. What’s worrying is, if she couldn’t do that job, what would we do with it? That’s what I always think about, because there’s got to be a system there that does what she does.
Workshop 1, participant 1
Although valuable, these groups were considered scarce, and almost invisible to newly diagnosed caregivers.
Support needed
Information
Participants reflected on the knowledge and information that they wished they had had as they first adapted to the caregiver role:
We’ve been caring for so many years, I thought there’s nothing I can learn now. I know it all. But actually a lot of what was in [the REACT booklet] was kind of new to me and if somebody had told me that at the beginning, you know, how to – how to break through the system, then I think things wouldn’t have got so bad.
Workshop 1, participant 1
They acknowledged that it could take years for relatives to learn about the mental health condition, and, on reflection, identified three types of educational sources that newly diagnosed caregivers would greatly benefit from:
-
A comprehensive list of available sources of support, such as local support groups and national charities –Workshop 1, participant 6
This exists. That exists. You can read this. You can read that. You can go here. You can go there. You’ve got a right to this – this is practical help, not the general pat you on the back and say everything’s alright and happy clappy, and let’s be friends, but actual hard practical, meaningful.
-
Information about medication, including types, side effects and how to manage doses –Workshop 2, participant 5
We’re never given, sort of, like, a comparative – information about the various antipsychotics. They had awful side effects.
-
Legal rights –Workshop 1, participant 1
I think actually what carers are entitled to under the law is very different from what they get in real life. And you’ve got to know.
Overall, participants agreed that knowledge is power and that less experienced relatives would benefit from guidance on how to get help, and from being directed to trusted and up-to-date resources.
Emotional support
Participants talked about the emotional impact of supporting someone with psychosis, and the importance of emotional, as well as practical, support:
I had some professional experience [in mental health], but it’s completely different when you are emotionally involved . . . It’s literally like somebody’s just parachuted you into a foreign country. You’ve no idea of what should be happening, what is available. And you need to know that sometimes, to be able to get it.
But the peer support is about emotional support. And I think what health professionals sometimes don’t understand is, by the time you get to them, you’ve been doing this for months, 24 hours a day, 7 days a week. And the emotional toll on you . . .
Workshop 2, participant 2
They talked about the importance of hearing that their experiences were not unique, as well as the need for explicit reassurance that the development of mental health problems within the family was not their fault and that they were doing all they could to manage the situation:
My mum never forgets this nurse who said to her ‘it could happen to anybody. This is not your fault. You’re doing everything you can’. And that just lifted that guilt off my parents. But sadly that was the only time.
Workshop 2, participant 7
Opportunities to have social contact with similar caregivers, to share experiences and feel connected and supported, were particularly valued:
There’s nothing better than seeing that somebody else has had the same fears and guilt to start with. Worries about the future and practical travel problems.
Workshop 3, participant 1
A recovery-focused approach
Although most of the discussion revolved around the challenges relatives faced, the need to focus on positive outcomes was also evident. One participant explained how she desperately struggled to find positive role models for her son:
Then I realised that the positive role models don’t want to go back and look again. And there’s got to be thousands of recovered or people who are managing their condition but they don’t really want to join the club. And that would be priceless, to have more positive role models. People who have managed and are managing their conditions or have completely recovered.
Workshop 3, participant 1
There was a general feeling that caregivers and service users would benefit from hearing positive stories to give them hope that recovery was possible.
The role of online interventions
For the majority of relatives, online support was seen as part of a ‘big scary virtual world’. They described several practical challenges regarding using the internet, including limited access and skills:
I live in the country and my internet doesn’t work half the time and my computer is probably my biggest source of stress.
Workshop 1, participant 10
However, it was not only practical issues that concerned them. There was a lot of fear associated with online activity, and many relatives felt reluctant to post personal information on any website. They feared that, once shared, it could never be removed and would always be ‘Googleable’. There was also an ethical dilemma that, in sharing their experiences online, they could also be sharing their relatives’ experiences, without their explicit consent. Participants felt that it was often unclear ‘whose story’ it was:
I don’t mind saying anything about my own medical symptoms or if I had a mental health problem, but . . . if my anxiety and stress and my needs are because my relative’s issues aren’t being addressed, then it is about me, but it’s still about her . . . But everybody’s different, so I think there needs to be a number of ways to access this information.
Workshop 1, participant 10
This dilemma was exacerbated by fear of the impact their posts might have on their relative if they saw them:
If my relative happened to get access to it, it could trigger a major episode.
Workshop 1, participant 8
This led to limits in how open relatives felt they could be online:
My relative has now got access to all my Facebook [Facebook, Inc., Menlo Park, CA, USA] discussions. But I’ve always feared letting [my relative] know how I’m feeling about things . . . I’m not sure how far we can open up.
Workshop 1, participant 5
Overall, participants had mixed views about the value of online support, but felt that people in the generation after them might be more positive, and might even be put off by paper-based support:
We’re all of a certain age. And what I’m finding is that, the people in the group who are a lot younger are actually perfectly happy to go all over Facebook.
Workshop 1, participant 1
It’s often a generational thing, and a lot of younger carers are siblings and would never dream of getting something off paper; they would automatically go online.
Workshop 2, participant 6
Online design of REACT
Most of the specific ideas for design features came from workshop 3, whose two participants were more frequent and confident users of computers. The key design issues that they identified are summarised in this section.
The paper-based REACT PDFs are too text-heavy for online
Initially, participants were presented with the website containing the PDF versions of the REACT booklets. Unsurprisingly, they found these too text-heavy, and felt that relatives would not have time to read them and would quickly lose interest. Their suggestion was for much more use of video to convey factual information and sharing of experiences.
Importance of vicarious learning in addition to didactic instruction
One challenge of a self-management toolkit for long-term health conditions is that it is difficult to make concrete recommendations when there is often no right or wrong answer. One participant felt that a limitation of many sites they had reviewed was that they tried to provide checklists:
A lot of websites will say, ‘oh why don’t you try meditation [or] going for a walk’.
Workshop 3, participant 2
Instead it was suggested that online support needed to be thought-provoking, to facilitate ‘thinking and reflecting’ exercises that enabled users to learn problem-solving strategies that could then be applied to their own particular context:
Stuff that helps you ask questions and helps you think about what you’re feeling rather than, like, ‘try this, try [that]’, because there’s only, like, so much a hot bath can cure.
Workshop 3, participant 2
Sometimes relatives had questions for which Google (Google Inc., Mountain View, CA, USA), and online interventions, could provide no useful answer:
How much am I supposed to do? What’s too much? What’s not enough? How strict am I supposed to be? When’s the point when I back off? And that’s not really a question that I felt I could ask Google, ‘cause I’m not going to get anything useful from that.
Workshop 3, participant 2
Need for a personalised record of support
Supporting someone with a mental health problem is often a long, episodic journey. Participants suggested offering a personal space where relatives could save useful and interesting information to revisit easily:
Like some kind of like scrapbook section . . . where, like, people just put different stuff in.
Workshop 3, participant 2
The value of this would be not only having a useful place to store things, but also facilitating a process of reflection on progress over time:
It’s very affirming to go back to some of the earlier learning content to realise that you have learnt, you know, I’ve acted correctly. You have been a good carer.
Workshop 3, participant 1
Attractive, appealing and easy-to-navigate design
Participants were keen that we retain the colour-coded modular design of the toolkit, and suggested more emphasis be given to the invitation to dip in and out in an order and frequency of the user’s choosing, without the need to complete modules in sequence:
Instead of having to go through it in, like, a sequence, you can just, like, go onto the ones you choose . . . Like you can do it quite easily with the hard copy.
Workshop 3, participant 1
They recommended including a ‘how to use the intervention’ section to explain that REACT covered a wide range of topics and to encourage shorter sessions, selecting the modules that were most relevant to the challenges they faced at that time.
When asked about frequency and mode of delivery of prompts, participants felt that this would vary and that users should be able to customise this. They both disliked receiving too many prompts and would feel ‘suffocated’ or ‘pressured’, especially if they were having a good day. They therefore recommended ‘reject’ and ‘unsubscribe’ buttons. They also preferred to receive person-centred prompts:
What’s your question this week? What are you worrying about this week? You never get any e-mails that just say, ‘How are you doing? How are you?’
Workshop 3, participant 2
Participants recommended using colourful, positive images and artworks throughout the toolkit:
I’m just thinking right the way back to 2000; I think probably what my family were given were ‘Here’s these leaflets’, which weren’t even colour leaflets at that point, you know. You can imagine what it was like [to] read that info[rmation].
Workshop 3, participant 1
Trustworthiness
The design of the toolkit was felt to be very important in engendering a sense of trust in participants. Simplicity, ease of navigation and a professional look were all seen as qualities that would attract users by assuring them that the intervention was legitimate:
’Cause you look at it and you go ‘Oh wow, this looks legitimate’, like, ‘I can trust this’. And then you start building up that trust and start using it.
Workshop 3, participant 2
Participants compared the look of a website to a building and suggested aiming, not for a slick look, like a building with shiny floors that felt corporate, but instead for something simple and professional that provided information.
Creating the design brief
Based on these findings, we drew on the expertise of the TMG to create a design brief for building REACT. The TMG included a relative with extensive experience of supporting other relatives through a leading charity, and a consultant psychiatrist, two consultant clinical psychologists and a GP, all with expertise in supporting people with mental health problems and their families, and some with expertise in designing and delivering digital health interventions (SJo, EM). The brief was as follows.
The modules
The content of the paper versions of the modules was updated and rewritten for a broader range of relatives. Large sections of text were replaced by video material whenever possible. Videos included experts sharing their clinical expertise on each topic, and actors sharing the personal experiences of relatives and service users.
We were very keen to ensure that the personal experience videos felt authentic to people using the site. We considered filming real relatives and service users, but were concerned that subjects might change their mind over time about sharing their story, and that removing a story already uploaded to the internet might not be possible. Relatives’ questions in workshops about the ownership of stories also made us wary. We therefore invited relatives and service users to talk on video, and then, supplemented by face-to-face discussions with relatives and service users at the Spectrum Centre in Lancaster University, worked with the actors to create hybrid characters who shared their ‘experiences’ on camera.
Additional modules were added, including ‘What is bipolar disorder?’ and ‘Managing mood swings’, and new introductory sections were created: a welcome page, ‘meet the team’ and a ‘how-to’ module that outlined the aims and structure of REACT and how it could be used. All new and revised modules were shared with the RAG, which gave detailed feedback on the language and structure.
Signposting
We specified the need for a comprehensive signposting page, which could be updated regularly, containing direct links to other useful organisations and websites providing information or support.
Peer-to-peer support
The strong desire to meet and learn from the lived experiences of other relatives led to us specifying the need for an online function to allow this. We chose to allow people to be anonymous in this space, because of their fears around confidentiality. We were also keen that this be moderated to ensure that any negative responses could be managed, and any risk issues quickly identified and responded to (see Protocols and policies).
Confidential support
In addition to peer-to-peer support, we also specified the need for direct, confidential support for those relatives who did not want to share their experiences with peers, but had specific questions they wanted answered.
A place to store the history
We really liked the idea of an online place where relatives could securely store any documents they found relevant to their supporting role and might want to revisit. We hoped this would also allow them to reflect on their caring journey by providing reminders of events over time and the challenges they had overcome.
Look and feel
The site should be simple and easy to use, create a positive tone and include images relevant to the content. We reused many of the images from the paper-based toolkit. Furthermore, one of the relatives who took on a REACT supporter role was a professional artist and created additional images for the site.
Building and hosting the REACT intervention
REACT was initially built in WordPress (Automattic Inc., San Francisco, CA, USA) by a web design and hosting company local to Lancaster; initially, the plan was for the company to host and maintain the REACT site during the trial. However, owing to difficulties in establishing a sustainable plan to do this, the site was brought in-house and is now located on a dedicated virtual server at Lancaster University. It is maintained and updated bimonthly by a digital technology developer from the REACT team (AW).
To meet the design brief, the WordPress site required a number of plug-ins. These included standard ones, such as bbPress (Automattic Inc.) to run the REACT group forum, and some built bespoke for the REACT site.
REACT
The content of the toolkit was informed by family intervention models that underpin effective face-to-face treatments for people with psychosis. 84–88 The key components of the toolkit were as follows: 12 information modules, a comprehensive RD, and peer support through a group forum and a confidential direct messaging service. A ‘meet the team’ page ensured that relatives were fully informed about who was delivering the content of the site. Logos for Lancaster University, Lancashire Care NHS Trust, University College London, Liverpool CTRC, and the McPin Foundation (London, UK) were prominently displayed on the log-in page. ‘Mytoolbox’ offered users a confidential space to save links to any information they might want to access easily later, including specific toolkit content, their self-reflection tasks and external web links. A blog page offered a flexible space for additional communication with site users, which could be edited by the REACT supporters.
The REACT information modules
Each of the 12 modules contained evidence-based written information, videos of clinical experts and/or content from experts by experience to illustrate key points, and self-reflection tasks to ensure that content was personalised to the user. The 12 modules were as follows:
-
What is psychosis? – information about psychosis, what it feels like, possible causes and common misconceptions.
-
What is BD? – an overview of BD, its main features, different presentations and how it feels to experience it.
-
Managing ‘positive’ symptoms – an explanation of the term ‘positive symptoms’, how these might be experienced, how they might appear to relatives and friends and how they can be managed.
-
Managing ‘negative’ symptoms – a detailed description of signs that make up ‘negative symptoms’, how these can manifest and how relatives can spot them, how they might make relatives feel and suggestions for helping the person experiencing these symptoms.
-
Managing mood swings – how to help people avoid extreme lows and highs, maintain a stable mood and support a relapse prevention or a staying-well plan, with suggestions for creating a low-stress environment in a friendly, non-judgemental way.
-
Dealing with difficult situations – describes the difficult situations that relatives and friends can encounter, including risky, illegal or embarrassing behaviours, and suggests ways to manage these.
-
Managing stress – doing things differently – helps relatives consider what stresses they have in their own lives and how to adapt their behaviour to manage.
-
Managing stress – thinking differently – helps relatives to consider how they think about the stresses in their lives, and whether or not different perspectives might help reduce their distress; explores the many common thinking traps, such as jumping to conclusions or mind-reading; and helps relatives to test their own thoughts.
-
Understanding mental health services – supports relatives in navigating services, helping to ensure that they talk to the right people to get the right information and the support they need.
-
Treatment options – information on the medication, psychological interventions and other therapies that people with psychosis or BD and their relatives should be offered, according to the NICE guidelines53,54; aims to empower relatives by outlining choices.
-
Dealing with crisis – clear suggestions about what to do in a crisis, where to turn to for help and what to expect from services; creates a useful personalised ‘what to do in a crisis’ plan.
-
The future and recovery – focuses on supporting recovery, with useful tips on how to help people with BD or psychosis to develop confidence and gain independence, including finding a balance between support and enabling independence, looking for positive changes to celebrate, accepting new goals and challenges and focusing on the bigger picture.
The resource directory
The RD provided to participants in the REACT and control arms of the REACT trial contained a comprehensive list, with website addresses and telephone numbers, of national organisations that support people with psychosis or BD and their relatives [e.g. Rethink (London, UK), Mind (Stratford, UK), Carers UK (London, UK) and Bipolar UK (London, UK)] and organisations that provide support for related conditions [e.g. Anxiety UK (Manchester, UK) and Samaritans (Ewell, UK)]. The RD also listed government websites that offer information and guidance about mental health and related topics, such as NHS Choices, Care Quality Commission, NICE guidelines and the Department of Work and Pensions, and gave contact details for emergency services and Samaritans, and a link for finding contact details for each user’s local NHS mental health services out-of-hours crisis team.
The RD given to those in the REACT arm of the trial also contained additional elements, including extensive information on topics such as advance directives, advocacy, benefits, direct payments, carer’s allowance, carer’s breaks, confidentiality, mental health law and an interactive map of support groups in different geographical areas. This content was developed in consultation with the REACT supporters and the RAG, and was added to over the period of the trial in response to information from users.
Support
Support was offered through confidential direct messaging with trained relatives (REACT supporters), and peer support was provided through a moderated online forum. The REACT supporters were available on the site Monday–Friday, from 09.00 to 16.30, excluding bank holidays and university holiday closures. Their key role was to provide emotional support and to guide relatives to relevant parts of the toolkit or other resources, as appropriate. They were also trained to moderate the forum and could hide posts or withdraw access in response to inappropriate use. They were trained to identify and report risk, and were supervised by two clinical psychologists and an expert relative. A REACT supervision manual and a REACT supporter manual [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/144934/#/ (accessed 28 October 2019)] were provided.
Reminders
Participants allocated to REACT were e-mailed reminders to visit the website after a week of inactivity. Participants could change the frequency of these reminders or turn them off.
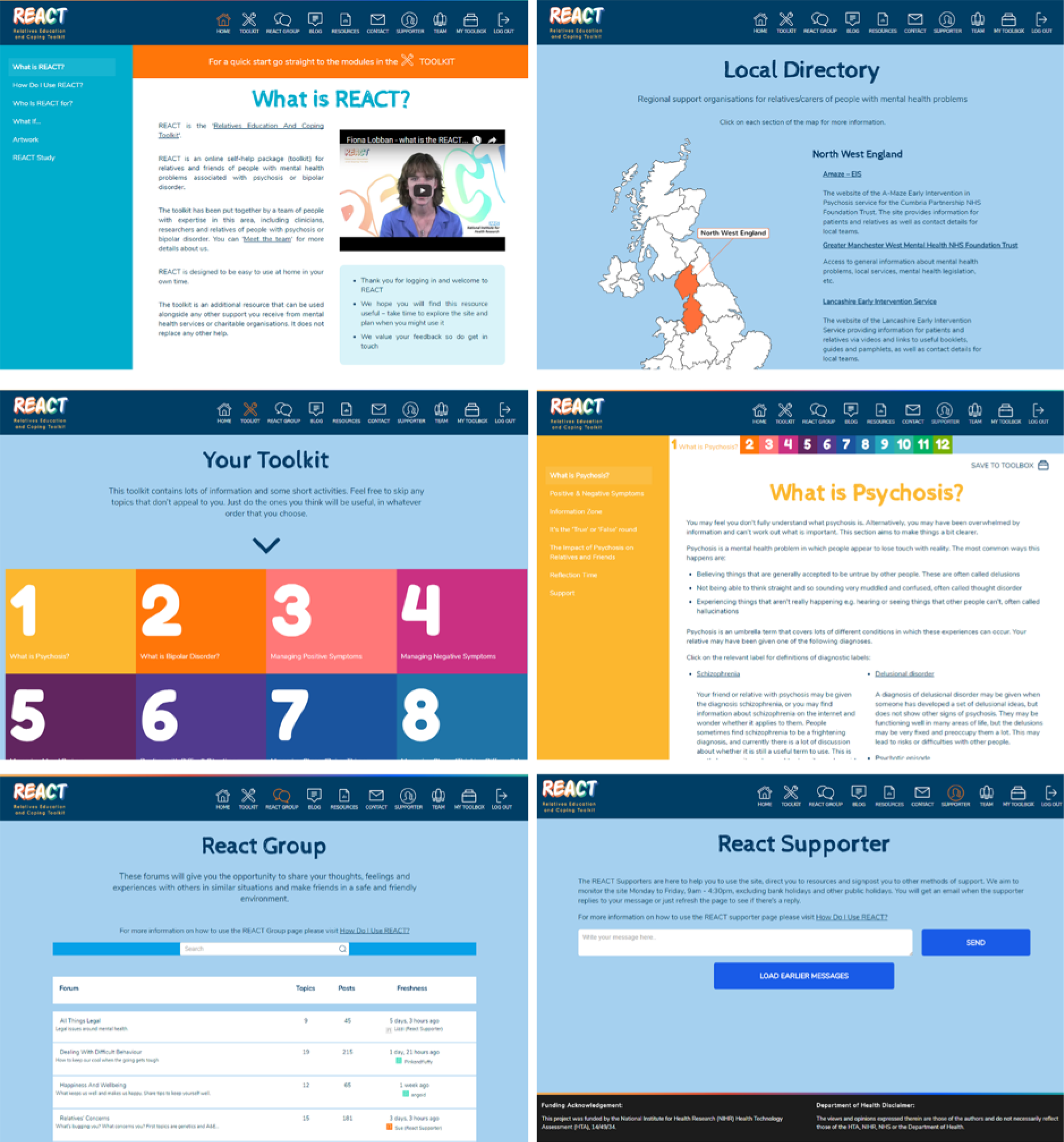
Appearance
Screenshots in Figure 1 show the look and feel of the REACT intervention.
FIGURE 1.
Screenshots of the REACT intervention website.
The REACT supporters
The role, training and supervision of the REACT supporters are briefly summarised in the following paragraphs. The detailed manuals for the REACT supervisors and the REACT supporters, as well as the REACT risk protocol, can be found on the project web page [www.journalslibrary.nihr.ac.uk/programmes/hta/144934/#/ (accessed 28 October 2019)].
Role
The REACT supporters were carers with lived experience of supporting a relative with psychosis or BD. Their role was to offer support to REACT participants through forum posts, direct messages and blogs. The REACT supporters did not give direct advice, but provided empathetic support while helping participants access relevant information and resources. They also moderated forum activity to ensure that there were no inappropriate posts and checked forums and direct messages for risk (see Protocols and policies). Carers, rather than clinicians, were selected to support the intervention so that supporters had personal experience of the issues raised by people using the site, and so could readily empathise with these issues in a sensitive and appropriate manner.
Training
The primary focus of the REACT supporter training was on familiarising supporters with REACT’s content and functions and giving them confidence to make timely forum posts and respond to personal messages from relatives while logging any risk issues. There were three intended domains for training: clinical, technical and co-worker sharing.
Clinical training was provided by the clinical supervisor (SHJ) and chief investigator (FL) before REACT was launched, and supplemented with ongoing clinical supervision (see Supervision). As the REACT supporters were able to draw on their personal experience of caring, clinical supervision helped train them in providing empathetic support and guiding relatives to the best use of the toolkit and associated resources to deal with their concerns.
Technical training was provided by the IT/digital support lead (AW) and clinical supervisor (SHJ). This was intended to ensure that the REACT supporters were very familiar with the REACT site and module content, the RD and how to access the automated e-mails informing them about posts.
Co-worker sharing was intended to offer a supportive environment in which supporters could share information and learning and develop ideas to increase site activity.
The REACT supporter role was relatively novel and there were, therefore, few training and supervision models to draw on at the beginning of the programme. The REACT supporters indicated that they would have appreciated more in-depth structured training in how to moderate peer-to-peer interactions on the forum and offer support, more detail on site functionality and longer access to training around clinical issues in mental health. Although the REACT supporters did successfully execute their roles with the training provided, the REACT supporter and supervision manuals provide additional information on how such training could be improved in future.
Supervision
Supervision was led by an experienced clinician fortnightly for up to 1.5 hours to provide a space for the REACT supporters to discuss relevant issues in a supportive environment. Issues typically covered in supervision included clinical issues, site cover and supporter well-being, with other issues discussed as required. Supervisors and the REACT supporters would review topics raised in direct messaging and the forum, including any risk issues. Urgent risk issues between sessions were dealt with in accordance with the risk protocol (see Protocols and policies).
Site cover issues included planned site closures such as Christmas, as well as staff leave, training and sickness absence. It was important to ensure that adequate time was allocated to supporter well-being. This included consideration of how personal and work factors might affect different supporters at different times and reviewing approaches to address this. Other issues covered as required included reviews of planned blog posts, ideas for updates, refinement of site materials, technical issues and site promotion.
Protocols and policies
All forum posts and private messages were reviewed by REACT supporters for potential risk, in accordance with the risk protocol [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/144934/#/ (accessed 28 October 2019)]. Risk was categorised as being low or high. Low-risk posts and messages were defined as showing no indication of immediate or serious threat of severe harm or risk to life, but showing either:
-
clear evidence of high levels of distress
-
concerns about risk of harm or abuse towards participants or others (safeguarding risks).
The REACT supporters who detected low-risk posts in which distress was the primary issue responded with a standardised e-mail to the carer. For potential safeguarding issues, the supporter consulted their clinical supervisor and used their NHS trust safeguarding team to discuss potential risks, if appropriate.
High-risk posts and messages were defined as those with clear evidence of immediate and serious risk to life or child welfare. If immediate risk of severe harm or death was detected, the protocol stipulated that an emergency call should be made to police (risk to life) or social services (other risk to child). Any concerns that might constitute a risk issue but that fell outside these definitions were discussed as urgent with the clinical supervisor to decide on a course of action. All risks were logged by the relevant REACT supporter on the REACT system to provide a record of the level of risk identified, where the risk was identified (forum post, direct message or other source), which supporter identified the risk, what action was undertaken and what follow-up actions were performed, including the name of the clinical supervisor consulted. Steve Jones was the lead clinical supervisor. To allow for leave and other commitments, a rota of alternative clinically qualified contacts was employed, including William Sellwood, Sonia Johnson and Fiona Lobban. Fiona Lobban was the contact of last choice, to avoid unblinding, and was never required. Steve Jones and William Sellwood dealt with the vast majority of risk queries, none of which met the high-risk criterion.
As part of their role, REACT supporters also monitored the site for inappropriate posts in line with an agreed posting policy [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/144934/#/ (accessed 28 October 2019)]. If the supporter believed a post might cause significant distress to participants, they had authority to remove it temporarily. It was then discussed with the clinical supervisor at supervision, or at an earlier ad hoc meeting if required. This discussion was used to reach a final decision as to whether the post would be removed permanently or reinstated.
Resource directory-only intervention
Participants allocated to the RD arm logged in to the same website, but were able to see only the ‘meet the team’ and RD pages. At the end of the trial, those in the RD-only arm were given access to the modules, without the forum or direct messaging.
Logic model for REACT
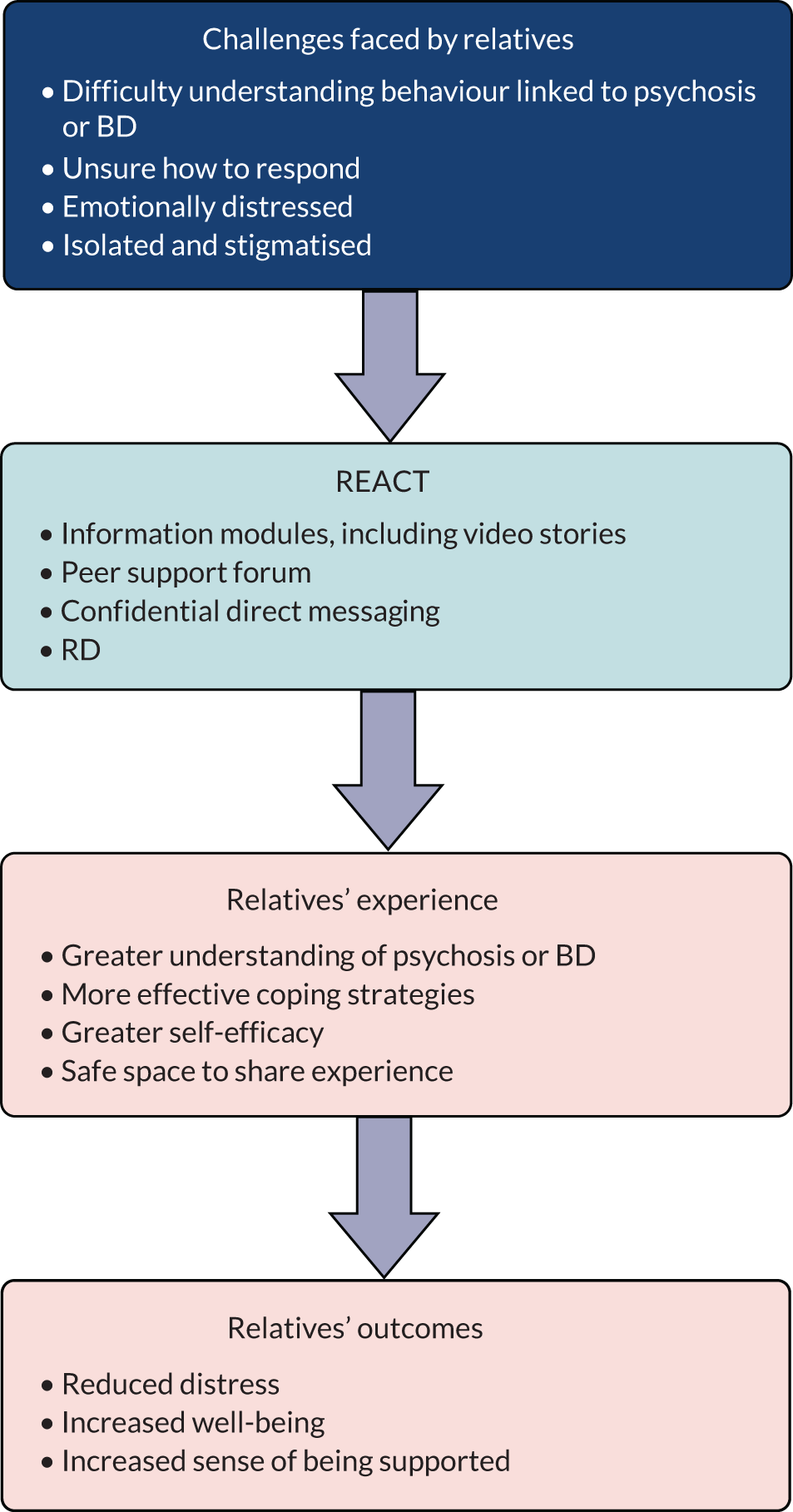
For any intervention, it is important to make explicit the underlying theoretical basis. Figure 2 outlines the process by which we hypothesised that REACT would benefit relatives.
FIGURE 2.
Hypothesised mechanism for REACT.
Reflections on developing REACT
REACT drew on evidence-based cognitive and behavioural psychological theories and clinical practice. The content had been developed and refined over many years, with extensive input from relatives, clinicians and service users in an early-intervention context. Therefore, in building the online version, we already had a good idea of the problems faced by relatives and an understanding of the processes underlying these difficulties and the strategies that could be successfully used to address them.
Even so, in broadening the reach of REACT to relatives of people outside EIP services and those with bipolar experiences, we felt that it was important to explore further what challenges these groups experienced and what support they valued. We also wanted to investigate relatives’ views about online interventions. This information was invaluable in helping us to build a design brief, and, ultimately, to develop the online version of REACT in time to start the trial. However, there were many challenges along the way, and we learnt a lot in overcoming them.
The drive to translate REACT from a paper-based to digital intervention came primarily from the practical need to have something that was easy to update, cheap to deliver and consistent with the NHS’ direction of travel towards digital NHS. 89 However, the extent to which service users and relatives wanted to receive support online was not clear. Many studies showed support for digital health interventions (DHIs) in mental health, but none of the studies was from representative samples of the service-using population, and most studies had recruited small convenience samples of people interested in digital health. 90,91 The relatives in our workshops were also a convenience sample, but were invited to the study to talk more broadly about their experiences of supporting someone with a mental health problem, and so may have been less biased in their views about online support. They had many reservations about the use of online interventions, but also suggested that this might be a cohort effect, and that a younger population would perhaps be less concerned and more comfortable with this mode of delivery.
Although all the relatives in our sample could access online support, some were limited in their access to private spaces to use computers, and in their connectivity, skills and confidence. There is some concern that, rather than broadening access, online interventions might, in fact, narrow access, dividing those with and those without easy access to online computers, and also those with and those without the skills, confidence and motivation to go online. 92 In many ways, it was helpful to hear the concerns of these relatives, as it made us think about how to address these in our design. However, involving more regular users of online technology might have generated ideas for additional functionality. For example, live social media feeds are now a standard feature of many online interventions and, with hindsight, might have been of benefit by ensuring constant new material that brought people back to the site.
Drawing on the extensive work done to develop the paper-based REACT also gave us a text-heavy starting point, which required a lot of reverse engineering to produce content more relevant to an online intervention. Starting from scratch might, in some ways, have been easier and led to a more digitally friendly product.
We wanted REACT to be built by experts who could work face to face with the relatives in our RAG. We did not have an existing relationship with any digital health companies, and Lancaster University did not, at the time, have a list of preferred providers. We therefore put the build of REACT out to tender among local companies. We had a limited budget, which proved to be well below the costs quoted by many companies offering bespoke builds. We knew that REACT would need to evolve, with edits made over time, and that staff would need training in how to use the site, all of which would make us reliant on those who could write the code, further increasing ongoing costs. We also recognised that many web-development businesses do not survive, and so we were wary of stranding ourselves with a bespoke site built in a code we could not then edit.
Therefore, we employed a local digital technology company that quoted within our budget, with some experience of building attractive websites using the open-source WordPress programme. However, during the build process, we became concerned about the company’s ability to deliver secure storage and regular updates for the website; therefore, we decided to bring the project in-house. The site was moved to the university server, we ensured that all identifiable user data were stored separately at the Liverpool CTRC, and all edits and updates were done by IT experts in the REACT team. This proved to be a wise decision as the company ceased to trade fewer than 12 months later.
Although a genuine partnership with a digital technology company would have offered many advantages, including greater investment in the product design and support for wider dissemination, there were also many challenges with this model. Digital technology companies are rarely run as not-for-profit social enterprises; therefore, they will look to maximise profit from the NHS. Given the NHS’s increasing reliance on digital technology, costs to the NHS are likely to rise exponentially. This may cause serious financial problems in the future.
Finally, we know that having people to support digital interventions is crucial to the success of such interventions,93,94 but how and by whom this is best done remains to be answered. The relatives in our workshops talked extensively about the power of peer-to-peer support. This is consistent with feedback from our feasibility trial, and with growing support for the development of peer worker roles in mental health services around the world. 95–100 In developing the design brief for this role, we identified a range of new skills that need to be learnt (e.g. managing online forums and communicating effectively in text format) and existing protocols that need to be adapted, such as risk management. These were new to and challenging for not only the REACT supporters, but also supervisors. Considerable time and effort were therefore needed to provide training, support and development for all members of the team.
Chapter 3 Clinical effectiveness: methods
Introduction
This chapter outlines the methods used to assess the clinical effectiveness of REACT. This chapter follows the structure of the CONSORT statement,101 including the extensions for pragmatic trials102 and for eHealth interventions. 81 As our data were collected online, we have also reported data collection in line with the Checklist for Reporting Results of Internet E-Survey. 103
Trial design
This was a primarily online two-arm, pragmatic, single-blind, individually randomised controlled superiority trial. The trial is described as primarily online because all of the intervention and most of the data collection occurred online. However, some text, telephone and postal reminders were used to support the registration process and to maximise retention.
Setting
This trial took place online in the UK. It was hosted by one NHS foundation trust, and other trusts and CCGs were eligible to take part as participant identification centres (PICs). Recruitment also took place through local and national mental health charities, media, social media and Google Ads (Google Inc.). REACT was built using WordPress open-source software, and hosted and maintained at Lancaster University. Data were collected using a bespoke web-based system at the Liverpool CTRC.
Participants
Eligibility criteria were designed to be as broad as possible. Inclusion criteria were (according to self-report):
-
Aged ≥ 16 years.
-
Living in the UK.
-
Relative or close friend of someone with psychosis or BD.
-
Currently experiencing distress due to their relative or close friend (determined as selecting ‘rather more than usual’ or ‘much more than usual’ on the GHQ-28 item ‘Have you recently been feeling nervous and strung up all the time?’). This was included to avoid a floor effect on levels of distress at baseline, and was the item that correlated most highly with the GHQ-28 total score in the REACT feasibility trial.
-
Currently seeking help (self-identified), and, therefore, likely to engage with support offered.
-
Access to an internet-enabled computer.
-
Sufficient English fluency to comprehend the intervention content.
Exclusion criteria included living in any of the six geographical areas by postcode taking part in the parallel IMPART study104 of the same intervention. In addition, only one relative per service user was allowed to participate, to avoid a clustering effect.
Recruitment strategy
Recruitment took place from 22 April 2016 to 30 September 2017. Before this, relatives who visited the website were invited to leave a contact e-mail address. A range of online and offline recruitment strategies was used, all directing potential participants to the trial home page (www.reacttoolkit.co.uk; accessed 1 June 2019), which provided information about the trial and how to take part.
At registration, participants were asked how they had found out about the REACT trial. The number of participants coming into the trial through each avenue was monitored by the TMG at its monthly meetings, and the recruitment strategy was adapted accordingly.
Social media
Twitter (Twitter, Inc., San Francisco, CA, USA)
Studies of Twitter (www.twitter.com) as a recruitment tool for online studies have been mixed: some found it unsuccessful,105 others successful. 106 Given its large reach and free nature, we set up a REACT Twitter account. The research team posted several times a week about the trial and relevant mental health news, and encouraged colleagues with Twitter accounts to tweet or retweet. We posted or retweeted 325 times and gained 711 followers.
Facebook (www.facebook.com) has been used successfully for recruitment in previous studies. 107 We set up a REACT Facebook page to post relevant mental health and trial-related news. After an expensive and fruitless attempt at creating Facebook advertisements ourselves, we enlisted an agent for this purpose, funded by one regional clinical research network for 13 months and by another five networks across the UK for the last 7 months.
In all, 70 carousel and standard-type advertisements were used, targeting seven geographical areas. We split test each variant, reallocating the spend to the best-performing advertisements. The standard advertisement type outperformed the carousel advertisements, and the more obvious images, containing text that reiterated the messaging, outperformed other advertisements. The best-performing advertisements are shown in Figure 3.
FIGURE 3.
Screenshots of Facebook advertisements.


Advertisements were viewed on mobile devices over desktops by 40 : 1. Over 13 months, we reached 873,096 individuals; 53,216 people engaged with an advertisement (liking, commenting or sharing) and there were 71,026 clicks through to the REACT website.
Websites and forums
Recommendations from previous studies77 led us to increase our online presence through promotion on websites, within online forums and through Google Ads. We encouraged PICs to display information on their NHS websites (the outcome of this is unknown as this was not specifically monitored). Promotion via forums proved difficult owing to restrictions on joining as a researcher.
Google Ads were suggested by previous research into online recruitment to online intervention. 108 Google displayed a short advertisement whenever browsers searched for our keywords (e.g. bipolar disorder, relative, carer and information), depending on our budget and on competition with other advertisers for our keywords. We set our budget at £10 per day for 12 months, reviewing our strategy and keywords regularly. Google Ads data showed that our advertisement was seen 1,323,900 times and received 11,448 clicks.
Charitable organisations
Promotion through trusted charity sites can ensure high numbers of visitors,77 and endorsement by the charities can reassure participants, increasing the likelihood of sign-up. 77 The REACT trial was promoted by Bipolar UK, Rethink Mental Illness, Mind, Sane, the McPin Foundation, National Survivor User Network, National Centre for Mental Health, and Carers Link through a combination of websites, social media, blogs, e-newsletters, mail-outs, offline magazine adverts and dissemination of material at events and meetings. Charitable organisations were invited to be included in the RD listing of support services.
Universities
Promotion through universities was focused locally. An e-mail was sent to all members of the Faculty of Health and Medicine at Lancaster University. Posters were displayed on plasma screens and stickers were placed in the university building. The REACT trial was also promoted in the monthly university e-newsletter and at Lancaster University community day. REACT supporters also presented the trial at the University of Central Lancashire PPI group.
Newspaper and radio
Local and national newspapers and radio stations were contacted, but the trial was covered by only one local radio station and one local newspaper, so the strategy was not pursued.
NHS
As with charities, previous studies suggested that promotion through health-care providers would reassure and encourage participants to sign up. 91 We therefore targeted the NHS strongly. However, NHS trusts and GP surgeries rarely have an accurate, up-to-date way of identifying relatives. Contact with relatives is often documented only in patient notes, not recorded against a separate code in the electronic record. Listed next-of-kin may not be the person offering day-to-day support (our target population). Therefore, recruitment is often through the patient, who may forget or not wish to pass information on.
We invited 54 NHS mental health trusts in England (out of 60, six trusts being participants in the parallel IMPART study), two trusts in Wales and two in Scotland to become PICs for the REACT trial. We also invited 124 primary care trusts (which later became CCGs). Across the UK, 54 mental health trusts (50 in England, two in Wales and two in Scotland) and > 74 primary care trusts or CCGs gave approval. Lancashire Care NHS Foundation Trust was the host trust.
Given the challenge of persuading busy clinical services to engage in research, we offered PICs an incentive to recruit to the REACT trial by allocating accruals to the PIC (based on participant postcode), rather than to the host trust (which is sometimes the case when sites are operating as PICs).
The research team gave presentations, put up posters and disseminated flyers and business cards at NHS trust sites, general practices and support groups locally (in the north-west of England). The trial manager hosted two webinars for NHS staff involved in recruitment (numbers were not recorded but participants described them as helpful). The trial manager periodically sent e-newsletter updates to PIC staff and responded to any contact from clinical studies officers, including requests for recruitment material. The REACT supporters presented the trial at clinical team meetings and NHS support groups.
Across England, the clinical research networks supported recruitment through clinical studies officers and research nurses in secondary care mental health trusts, and promotion and database searches in general practices. Practices were asked by clinical studies officers in their area to display posters, flyers and business cards in waiting areas; however, we did not keep a record of how many did this.
Across the UK, 35 general practices searched their databases for patients with a diagnosis of ‘psychosis/schizophrenia/schizophreniform disorder/psychotic disorder/schizoaffective disorder/bipolar disorder/manic depression/cyclothymia’, and sent invitations and participant information sheets to these patients to pass on to a relative. The 35 practices sent 2377 letters in total (range 5–451; median 34). At least two practices included the REACT trial on their websites; we did not keep a record of this activity, so the number may be greater.
The PICs also did their own online promotion via social media, intranets and websites. We did not monitor this activity in detail.
To maximise efficiency of resources within NHS services, our recruitment focused initially on England and then moved into Wales and Scotland. We reached our target before moving on to Northern Ireland.
Service user and carer support groups
The REACT supporters presented the trial at two local non-NHS service user and carer support groups. These groups were attended by both service users and carers, but not in large numbers.
Consent
We adhered to the British Psychological Society’s guidelines for taking informed consent online. 109 These included taking a record of valid consent; including checkboxes relating to specific consent statements; limiting the number of consent items; and ensuring participants were fully informed of trial procedures, risks, confidentiality and right to withdraw. Capacity to consent was assumed, as there is little scope to assess it in an online trial. All participants were e-mailed a Microsoft Word (Microsoft Corporation, Redmond, WA, USA) copy of the completed consent form, with a version kept on a secure server and in the trial database.
Participants were informed that they were free to withdraw at any time, but that online questionnaire data could be removed only within 2 weeks of data collection, and web usage data, online forum posts and direct messages could not be removed and would be used for research purposes. Participants were informed that data would be stored on secure servers at the Liverpool CTRC and Lancaster University. Note that the trial predated the European Union General Data Protection Regulation. 110
Interventions
The design and delivery of the REACT trial were described in detail in Chapter 2. Participants were randomly allocated either to the REACT arm (TAU plus toolkit including the RD) or to TAU plus the RD. Those in the REACT arm could access the toolkit with a username and password, without charge, whenever they wished throughout the trial (for a minimum of 24 weeks after the final participant was recruited). REACT supporters were available on weekdays from 9.00 to 16.30, excluding public holidays and university closures (1.5 weeks at Christmas and 1 week at Easter). Participants were advised to use the intervention as they needed. No changes were made to existing support and treatment.
Participants allocated to the RD-only arm logged on to the same website, but could see only the ‘meet the team’ and RD pages. At the end of the trial, they were given access to the modules, without the forum or direct messaging.
Objectives and hypotheses
The aim of this RCT was to determine the clinical effectiveness and cost-effectiveness of REACT (including online RD) and TAU, compared with TAU and the RD only. This comparator was chosen to test the effect of offering REACT as an additional intervention to the support that relatives could already access. Relatives were likely to access support from a wide range of services. In this context, TAU was used to indicate that no attempts were made to make any changes to any of these other sources of support.
The objectives were to determine the following:
-
the impact of the REACT intervention on relatives’ distress
-
the impact of the REACT intervention on relatives’ well-being and support
-
the impact of the REACT intervention on hypothesised mediators of change, including relatives’ beliefs, perceived coping and amount of use of REACT
-
the delivery and maintenance costs of the REACT intervention
-
the incremental cost-effectiveness ratio (ICER) of the REACT intervention
-
the key issues for which relatives seek support.
The primary hypothesis was that there would be a significant difference (p < 0.05) between the two arms of the trial in the GHQ-28 scores at the 24-week follow-up.
Outcomes
All outcomes were collected online using a closed system available only to participants with an account on the REACT site. Questionnaires were all validated self-reporting measures, although not originally designed for use online. These were presented in order of priority to the study (primary outcome first) and used drop-down options and checkboxes. Participants were required to respond to all items before moving on to the next measure. At baseline, participants were required to complete all measures before being randomised. Following completion of each questionnaire, the data were submitted and participants were unable to edit them.
Primary outcome
The primary outcome was relatives’ distress at 24 weeks, assessed using an online version of the GHQ-28 with Likert scoring (0–3). 61 The GHQ-28 showed sensitivity to change2,111 and had shown significant associations with important functional outcomes in the general population, including GP visits,112 absence from work,113 incapacity benefits114 and severe adverse health outcomes, including death. 115 We chose 24 weeks to allow the content of the website to be processed and to have an effect on cognition and behaviour, and for these effects to have an impact on distress.
The Likert scoring method assigns a value of 0 to 3 to each possible multiple choice answer (higher scores indicate more severe distress), and results in a total score of between 0 and 84.
The total 28-item score can be divided into four subscales of seven items each. These were explored for secondary analyses:
-
somatic symptoms (items 1–7)
-
anxiety/insomnia (items 8–14)
-
social dysfunction (items 15–21)
-
severe depression (items 22–28).
The alternative ‘caseness’ scoring method (assigning either 0 to the first two categories of response and 1 to the last two categories) was presented as a secondary analysis.
Secondary outcomes
Secondary outcomes included relatives’ experience of caring, assessed online at the 24-week follow-up using the CWS Questionnaire,116 and distress (measured using the GHQ-28) and carer experience (measured using the CWS Questionnaire), assessed online at the 12-week follow-up. The CWS Questionnaire covers all aspects of the carer’s experience of caring for someone with a serious mental health problem, including relationships, roles, financial concerns, physical and emotional health, stigma, worries about safety, satisfaction with support offered and ease of obtaining information.
The CWS Questionnaire consists of two separate scales. The well-being scale consists of 32 questions about the user’s caring or support role, relationship with the person they care for or support, relationship with family and friends, financial situation, physical health, emotional well-being, experiences of stigma and discrimination, personal safety and the safety of the person they care for or support. Carers rate their level of concern in each area using a five-point Likert scale (from ‘a lot’ to ‘not at all’). The overall well-being score is derived by assigning a score of 0 to the most negative answer (‘a lot of concern’) and a score of 4 to the most positive answer (‘not at all’), then summing the scores from all 32 questions, creating an overall score of between 0 and 128; a higher score indicates greater well-being.
Similarly, the support scale consists of 17 questions relating to the carer’s level of satisfaction with the information and advice they receive, their involvement in treatment and care planning, and support from medical and care staff, each measured on a four-point Likert scale (from ‘very dissatisfied’ to ‘very satisfied’). The overall support score is derived by summing scores from these 17 questions, with a score of 0 assigned to the most negative answer (‘very dissatisfied’) and 3 to the most positive answer (‘very satisfied’), creating an overall score of between 0 and 51; a higher score indicates better support.
Mediators
To test the proposed mediators of change in relatives’ outcomes, participants also completed online versions of the Brief Illness Perception Questionnaire (Brief IPQ),117 a 15-item Likert scale assessment of beliefs about psychosis and BD, with an additional single item to assess perceived coping; and the Brief Coping Orientation to Problems Experienced (Brief COPE),118 a 28-item measure widely used to assess coping styles.
The REACT was designed using a cognitive–behavioural framework, which proposes that the way in which relatives think about the challenges they face, and the things they do in response, will determine their levels of distress. 119 The Brief IPQ allowed us to assess the way in which relatives made sense of the psychosis or BD, namely their cognitive models. The Brief COPE inventory allowed us to assess the specific strategies they were using to manage their distress.
Brief Illness Perception Questionnaire
The Brief IPQ consists of 16 questions (rated by the carer between 0 and 10) regarding perceptions of illness, some focusing on the service user experience (e.g. ‘how much control do you feel your relative/close friend has over their mental health problems?’), others on the carer (e.g. ‘how much control do you feel you have over your relative/close friend’s mental health problems?’). It can, therefore, be summarised as two total scores: one relating to the service user and the other to the carer. Answers to seven of the questions (items 4–7, 10, 11 and 15) must be inverted according to the formula where x becomes 10–x). Therefore, a higher total score indicates that, overall, the illness was perceived as more severe (e.g. more negative consequences, longer timeline, less control).
The service user score was derived by summing the ratings (between 0 and 10) for questions 1, 3, 8, 12 and 13, resulting in a total score of between 0 and 80 (with a higher score indicating that the illness was perceived as being more severe). The carer score was derived by summing the ratings (between 0 and 10) for questions 2, 9, 14 and 16, resulting in a total score of between 0 and 70 (with a higher score indicating that the illness was perceived as being more severe).
An additional item was added to the Brief IPQ (question 6: ‘how able do you feel to cope with your relative/close friend’s mental health problem?’).
Brief Coping Orientation to Problems Experienced inventory
The Brief COPE inventory consists of 28 questions (rated by the carer from 1 to 4) about the methods used by the relative to cope with the stress of their caring role. Values are assigned to the answers to each question as follows:
-
‘I haven’t been doing this at all’ = 1
-
‘I’ve been doing this a little bit’ = 2
-
‘I’ve been doing this a medium amount’ = 3
-
‘I’ve been doing this a lot’ = 4.
There is no overall score for the Brief COPE; instead the following subscales are computed:
-
self-distraction – questions 1 and 19
-
active coping – questions 2 and 7
-
denial – questions 3 and 8
-
substance use – questions 4 and 11
-
use of emotional support – questions 5 and 15
-
use of instrumental support – questions 10 and 23
-
behavioural disengagement – questions 6 and 16
-
venting – questions 9 and 21
-
positive reframing – questions 12 and 17
-
planning – questions 14 and 25
-
humour – questions 18 and 28
-
acceptance – questions 20 and 24
-
religion – questions 22 and 27
-
self-blame – questions 13 and 26.
Web usage
Website usage data for each participant were downloaded from the intervention site and summarised for participants in each intervention arm. Data were available for the website as a whole, and for each of the 12 information modules, forum, direct messaging and the RD, to investigate which components were used most.
These data were then condensed into a small number of summary covariates over the 24 weeks to determine causal effects of the intervention for each participant:
-
total number of web page downloads
-
total number of log-ins to the REACT website
-
total time spent logged on to the REACT website.
Inactivity (when the user was logged in but with no evidence of activity) on any given page was capped at 20 minutes. Given that these capped values were not likely to reflect the true time spent on a given page and were likely to skew the data, imputation of the mean total time spent per page was performed for REACT participants with capped values. The imputed mean values were considered to be more realistic than using capped values of 20 minutes; however, it is acknowledged that the use of imputed values inflates the precision of summary estimates (as unknown values are assumed to be known), as would the assumption of 20 minutes for these capped values.
The time spent on the final web page of any given session was not available; therefore, it had to be imputed. For pages with a video, video feedback data allowed calculation of this time to within 5 seconds. If there was no video, it was assumed that the time spent on this page was equal to the mean time the participant had spent on all previous pages to date.
The number (%) of participants who did not log in to their assigned intervention was presented for each randomised arm, as well as the number (%) of participants in each randomised arm who did not log in again after their initial log-in.
To assess the hypothesis that DHIs provide a distinct advantage in allowing ‘out-of-hours’ access, the timing of web access was summarised relative to the working week (defined as 9.00–17.00, Monday–Friday, excluding public holidays, UK time).
We explored whether or not reminders would increase intervention use by comparing participants’ patterns of use (using measures of frequency and time spent on intervention) within 1 day, 3 days and 7 days of reminders being sent with their intervention use during the period prior to their first reminder.
Sample size
We aimed to recruit 666 relatives of people with psychosis or BD to accurately test the primary hypothesis that there would be a significant difference (p < 0.05) between the trial arms in distress, measured by GHQ-28 scores at the 24-week follow-up.
Our feasibility trial2 had shown a mean difference between arms at 6 months (controlling for baseline) of 6.59 units [standard deviation (SD) 16.6 units] in favour of the REACT arm.
To build a degree of protection against pilot results proving optimistic, and to accommodate adaptations to the design of the study and the intervention, we reduced our estimate of the mean difference in this trial from 6.59 to 5.0 units. A detailed qualitative and quantitative analysis of our feasibility data suggests that a (within-relative) reduction of 3 units on the GHQ-28 can indicate clinically meaningful change; however, the minimum difference required for the between-arm comparison (of change in GHQ-28 score from baseline) was set at 5 units, to justify the staff and resource costs associated with delivery of the intervention.
We retained our estimate of the SD of 16.60 from the feasibility study, consistent with other studies using this measure with relatives in EIP services13 and somewhat higher than those from other mental health or dementia services. 120,121 A total of 666 (333 per arm) participants provided 90% power to reject the null hypothesis (p < 0.05) with an effect size of 5.0 units, assuming a 30% dropout rate by 24 weeks. Although dropout was only 17% in our feasibility trial, it tends to be higher in online trials. 78
Recruitment rate
Recruitment to face-to-face trials often starts slowly; recruitment online is often very fast. Given that we planned to recruit both via clinical providers and through online marketing, we hypothesised a steady rate of recruitment and set our criteria using an average monthly rate of > 37 relatives per month over an 18-month recruitment period.
Internal pilot
Monthly recruitment rates were monitored under a 9-month internal pilot with the following criteria:
-
go – ≥ 100% of anticipated recruitment at 9 months (≥ 333 participants per arm)
-
amend – 80–100% of anticipated recruitment (267–333 participants per arm): review and amend recruitment strategies
-
stop – < 80% of target for 9 months (< 267 relatives per arm): inform funders, who would determine whether or not to stop trial.
An assessment of the SD of GHQ-28 scores was also planned for the 24-week follow-up at the end of the internal pilot. We planned that a higher SD than the estimated 16.6 units would result in the sample size being increased; a lower SD would result in an unchanged recruitment target. If GHQ-28 retention at 24 weeks had been < 70%, the recruitment target would have been increased.
Randomisation
Sequence generation
Eligible participants were randomised using a 1 : 1 ratio to either ‘REACT (including the RD) plus TAU’ or ‘RD plus TAU’ by the Liverpool CTRC. We used a web-based variable block randomisation, in which the unit of randomisation was the relative. Given the lack of convincing evidence that the effectiveness of REACT would be associated with any baseline variables, we did not stratify randomisation.
Allocation concealment
Following randomisation, participants received an e-mail telling them which arm of the trial they had been allocated to. The e-mail included a link to REACT, and their username and password. All participants were aware that the RD was one component of the intervention, and therefore were likely to perceive REACT as the ‘intervention of interest’ and the RD as the ‘comparator’.
Once participants had completed their baseline questionnaires, they were asked to click a button that enabled them to be randomly allocated to an arm and their account on the intervention site was created. Access to the intervention site was dependent on randomisation having taken place.
Data collection
Registration
The REACT landing page included text about what the trial involved and the eligibility criteria. Based on PPI feedback, text was kept short, and a video of the chief investigator was included. To reduce attrition, the landing page also highlighted the need to commit to follow-ups at 12 and 24 weeks.
Participants who clicked ‘register’ moved to a second page outlining the next stages and a video of REACT supporters explaining what taking part would involve. The random allocation design of the trial was also described here, to reduce attrition from the control arm.
The online registration process comprised an eligibility check (by checkboxes relating to essential criteria); consent form (by checkboxes confirming that they had read and agreed to a series of statements); recording of participants’ e-mail, telephone and postal contact details; and an identity check via text message.
Applicants found to be not eligible for the trial were given an explanation and pointed to other potentially relevant studies. As in traditional trials, flow through the study was recorded and monitored.
Participants were informed that we needed their contact details to allow follow-up contact to increase retention, and in case a safety issue was identified; their encrypted details would be stored on the trial database. E-mail addresses were verified by sending an e-mail with a confirmation link, and at the activation stage a code was sent to each participant by mobile phone [by short message service (SMS)] or landline (in a call by the trial manager, who would then enter the code into the system). This also allowed the research team to ensure that the registrant was not a robot.
To ensure that each randomisation was a unique participant and to prevent multiple registrations by individuals, we checked each new registration against existing data.
Baseline measures
Demographic information and baseline measures were completed before randomisation. To make the process less daunting, questionnaires were paginated rather than appearing as one long web page. Validating algorithms ensured that all questions were completed and inappropriate answers minimised. These methods were reviewed by the RAG to ensure that they were fit for purpose. Demographic data included age, gender, ethnicity, marital status, education, employment, living arrangements (including dependents), the primary diagnosis of the service user, length of time in caring role, number of people they were caring for, relationship to person(s) with mental health problem, whether or not they lived with the person(s), level and type of contact, whether or not they received support from NHS services and internet access.
On completion of the baseline questionnaires, participants were randomised to either the REACT arm or the RD-only arm, using a list generated by the statistical team.
At the 12- and 24-week follow-ups, up to three reminder emails were sent at 5-day intervals. If data entry had still not started, the trial manager was prompted to send a personalised e-mail, and, finally, to try to make contact by telephone to ask if the participant would complete the GHQ-28 (primary outcome) over the telephone (with the trial manager entering the data) or in writing, in which case the researcher would download and post a personalised letter and questionnaire. Returned data would be entered manually by the researcher. Towards the end of the trial, the researcher was also able manually to trigger a SMS with a unique URL for the GHQ-28. To identify participants who had completed some of the measures but stopped mid-way through the process, the trial manager’s dashboard displayed how many questionnaires had been completed at each stage.
The REACT participant information sheet, available on the website, explained the withdrawal process. A link to withdraw from the trial featured in all reminder emails, and in the toolkit. Withdrawing participants were required to select from a drop-down menu of options:
-
‘I don’t want to complete the 12-week follow-up questionnaires but I am happy to be contacted for the 24-week follow-up’.
-
‘I don’t want to complete ANY more follow-up questionnaires but I would like to continue to use the website. Note that any data inputted to the website will continue to be used for research purposes’.
-
‘I don’t want to complete ANY more follow-up questionnaires and DO NOT want to use the website anymore. Note that your access to the website will cease’.
Participants were also invited to provide an optional reason for withdrawing:
-
‘I don’t have time due to other commitments’.
-
‘I didn’t like the website I was given’.
-
‘I don’t like filling in the questionnaires’.
-
‘I don’t feel well enough to take part’.
-
‘Other (please specify)’.
Researchers would ask the same sets of questions of participants who withdrew over the telephone or by e-mail, and enter this information into the system. Withdrawal also blocked further automated reminders.
The data collection process is shown in Figure 4.
FIGURE 4.
Data collection process. a, Accessed 1 September 2018.
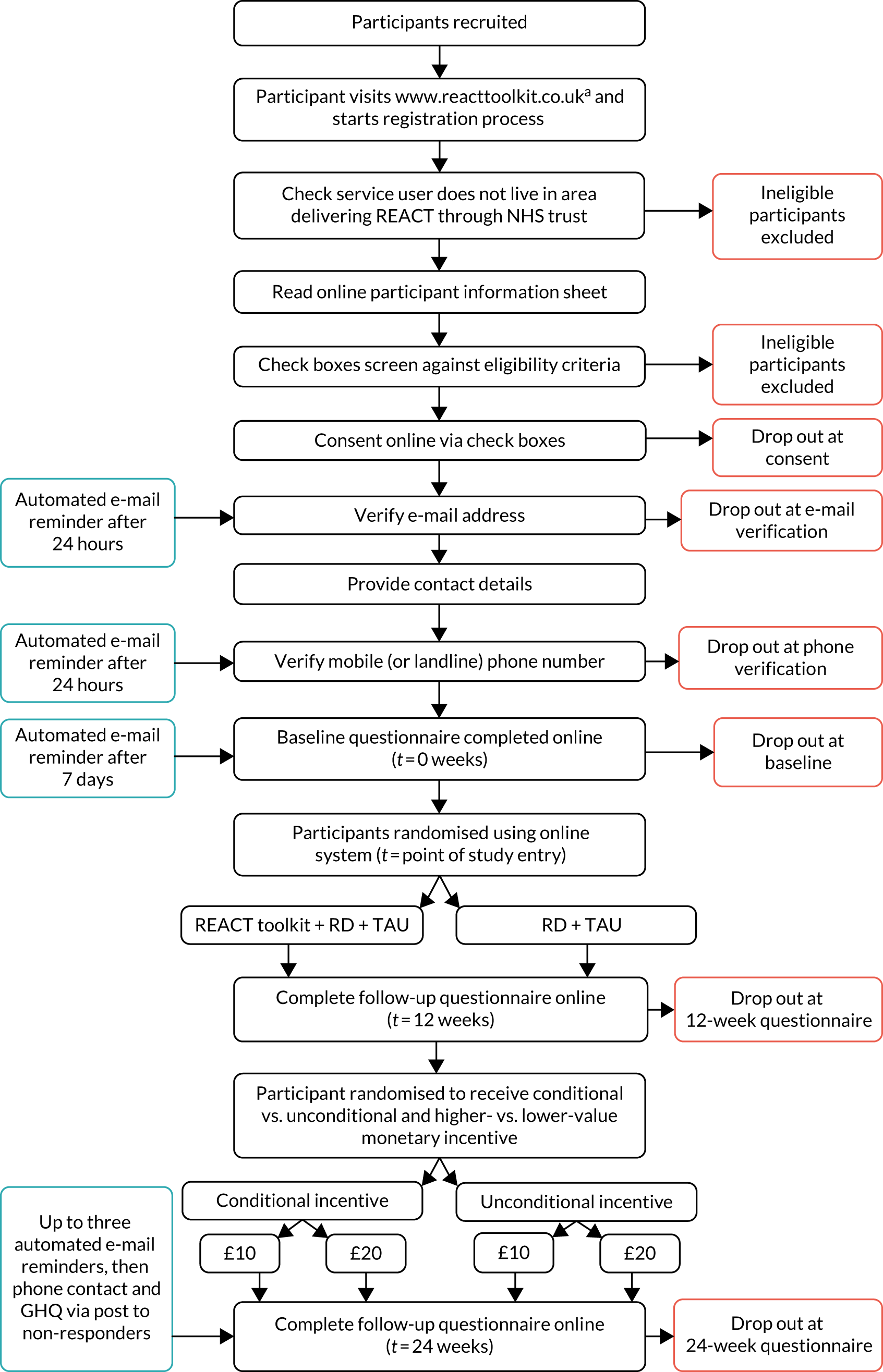
The REACT trial registration process incorporated a number of strategies to enhance engagement:
-
lay-language speech bubbles
-
a progress bar appeared at the top of each registration page, and there was an indication of how long each stage should take
-
an automated e-mail reminder with detailed instructions was sent if participants had not progressed within 24 hours of giving consent
-
an automated e-mail reminder was sent 24 hours after participants completed activation and 7 days after starting the baseline questionnaire
-
e-mail reminders were copied to the trial manager to check that the registration process was working correctly
-
the option to e-mail the trial manager during registration to get e-mail or telephone support through the process
-
a dashboard that allowed the trial manager to monitor progress and identify those who needed chasing.
Retention strategy
Dropout from follow-up is a particular problem in online trials. 78 Drawing on lessons from previous studies,77,107,122–124 we used the following strategies to maximise follow-up:
-
We randomised participants only once baseline assessment measures were completed.
-
We included detailed explanations in our recruitment materials about why data completion at follow-up was so important.
-
We obtained multiple contact details at registration.
-
We sent multiple reminders by different methods and with different options for completing online measures, based on PPI feedback, striking a balance between cost, data and burden on participants.
-
We gave £10 or £20 vouchers as incentives to complete follow-up questionnaires (see Appendix 2).
-
We informed RD-only participants that they would be able to access toolkit modules after the final follow-up.
Blinding
All data were self-reported and predominantly entered online by participants. Outcome questionnaires submitted by post were recorded as such and inputted by the trial manager, who was blinded to allocation. Data were uploaded directly to the CTRC database. The system allowed only valid values to be entered. To prevent any bias in the conduct of the trial, the chief investigator, trial manager and statisticians were blinded to treatment assignment. The REACT supporters, clinical supervisors, qualitative interviewer, one CTRC analyst of web usage data and technical staff (AW) were unblinded. Participants were also unblinded.
To minimise unblinding, all contact with participants was prefaced by a reminder not to disclose their trial arm. If the trial manager was unblinded regarding a particular participant, another blinded team member delivered any non-automated reminders and carried out any data entry for that participant. All instances of unblinding were recorded.
Statistical analysis
A full statistical analysis plan was published on 22 March 2017, before the start of data collection, and updated on 20 December 2017, before the end of data collection. Both versions are available online. 125
Updates to the plan are listed in Appendix 1. All analyses were done using SAS® statistical analysis software version 9.4 (SAS Institute Inc., Cary, NC, USA; SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc. in the USA and other countries. ® indicates USA registration) or Stata® version 14 (StataCorp LP, College Station, TX, USA).
Primary outcome
The mean scores and SDs of the GHQ-28 at 24 weeks were calculated separately for each arm and compared between arms using analysis of covariance (ANCOVA), adjusting for baseline score and including all participations according to the randomisation scheme.
The baseline characteristics of those who provided 12-week and 24-week follow-up data were compared, to investigate whether missingness could be assumed to be random for the 12- and 24-week follow-up data (at least with respect to baseline characteristics). A joint modelling approach was used to check for any difference in GHQ-28 scores (see Report Supplementary Material 1, section 6.6.4).
Of the four subscales, somatic symptoms and anxiety/insomnia were summarised for each randomised arm by mean and SD, and were compared between randomised arms using ANCOVA, adjusting for the corresponding baseline subscale score. Severity of depression and social dysfunction were summarised for each randomised arm using medians and interquartile ranges (IQRs) and were compared between randomised arms using Mann–Whitney U-tests, as the distributions of these subscales were non-normal. Multivariate analysis of variance (‘MANOVA’ in Stata) was used to assess the impact of intervention arm on each of these subscales, while taking into account correlation between the subscales.
Secondary outcomes
Relatives’ distress at 12 weeks was assessed using the GHQ-28, and analysed using the same methods as described for analysing the GHQ-28 at 24 weeks. Relatives’ well-being at 12 and 24 weeks was assessed using the CWS Questionnaire measure on both the well-being and support scales and summarised for each arm using means and SDs. They were also analysed using the same methods as described for the primary outcome GHQ-28 scores, using ANCOVA and joint modelling.
Causal analysis
To investigate the relationship between website use and outcome, we recorded data on baseline covariates (correlated with website use and outcome) and relevant website use (from participants in both randomised arms). Instrumental variable (IV) regression was used to estimate the impact of intervention use on the outcome using the IV regression (ivreg) command in Stata.
Intervention use (i.e. web page downloads from the REACT intervention site excluding the RD) was summarised as a single continuous covariate derived from web usage data. Given the extensive password protection of the REACT site, it was assumed that participants in the control arm had null intervention use.
Exploratory analyses of the total number of log-ins and the total time spent logged in over 24 weeks as other measures of use were also conducted, and the suitability of randomisation as the instrument in this regression was assessed (see Report Supplementary Material 1).
Testing mediators
The hypothesised mechanism of change for the REACT intervention was that participants’ distress levels (the primary outcome) would be mediated by their understanding of the service user’s disorder, their insight into the service user’s experiences and their own perceived ability to cope.
These potential mediators were measured using the Brief IPQ and Brief COPE at 12 weeks and 24 weeks. Baseline characteristics of those who did not provide data were compared with those who did (as for the primary outcome), to determine whether or not absent data could be assumed to be missing at random. Collected data sets were then summarised for each treatment arm by mean and SD or by median and IQR, depending on whether or not they were normally distributed. We then compared the arms and analysed the impact of the intervention on subscales using ANCOVA and MANOVA.
To test whether these potential mediators actually predicted change in outcome, mediation analysis was carried out using ivreg in Stata, as for causal analysis, adjusting for each baseline variable that was included in the final regression model (along with baseline GHQ-28 score) for the primary outcome. This analysis was not successful, as the ‘instrument’ was not useful (very weak) in each case, so, instead, we performed post hoc mediation analysis along with sensitivity analyses to check the robustness of the model results in terms of the assumption of no unmeasured confounders.
Each potential mediator was assessed individually in this exploratory analysis:
-
overall Brief IPQ score
-
additional IPQ coping question
-
Brief COPE summary scores (each individual score assessed individually).
Owing to the number of variables being considered, this mediation analysis was entirely exploratory, in order to generate hypotheses for confirmation in future studies.
Additional analyses
Exploratory analyses were conducted to determine the impact of the following baseline factors on the intervention effect on total GHQ-28 score at 24 weeks, by including the following baseline factors in the linear regression model along with baseline GHQ-28 score and randomised intervention:
-
age (older relatives are likely to have been caring for longer and have their own physical health needs)
-
gender (in society, women tend to spend more time on the caring role and take greater responsibility for caregiving)
-
ethnicity (minority ethnic groups may experience barriers to receiving support)
-
marital status (a relationship may provide support for the carer or relative)
-
living arrangements (a relationship may provide support for the carer or relative)
-
dependents (may add to the carer’s or relative’s stress)
-
highest education (the intervention may be overly complex for those without sufficient reading or cognitive ability)
-
employment (work commitments may impede use of the intervention)
-
home internet access (aids ease of use of the intervention)
-
caring role (the intervention’s impact is likely to relate to the burden of care).
Results from each individual model (i.e. the regression coefficient, 95% CI and p-value associated with each baseline factor when added to the model containing baseline GHQ-28 score and randomised intervention) were presented for each of these baseline factors separately. A stepwise selection procedure (with entry/exit criterion based on p-values of 0.05/0.1, respectively) was used to determine which baseline variables to include in the final multivariable regression model (along with baseline GHQ-28 score and randomised intervention).
This exploratory analysis included a formal test of treatment–covariate interaction to assess the effect of relationship with service user (i.e. according to whether or not the relationship was parental) by including the ‘intervention service user (non-parental/parental) relationship’ interaction term in the linear regression model [along with baseline GHQ-28 score, randomised intervention and main effect of service user (non-parental/parental) relationship].
The impact of ‘lurking’ on social forums
We tested the hypothesis that reading but not posting (‘lurking’)126 on social forums would lead to worse outcomes than posting (or not logging on at all) to social forums. In the absence of a second instrument to facilitate this three-way comparison (lurking vs. non-use vs. use), ordinary least squares regression was used at 24 weeks to assess the impact on the GHQ-28 score of lurking.
The validity of this analysis was assessed by repeating this model for the binary comparison between users and non-users (with lurkers included as users), adjusting for the same baseline covariates, and comparing the group effect from this model with that obtained using ivreg for the users versus non-users comparison (with randomisation as the instrument).
Lurkers were defined as those who logged on to the forum at least once over the 24 weeks but posted no comments, users were defined as those who logged on and posted at least once on the forum over 24 weeks and non-users were defined as those who never logged on to the forum over 24 weeks.
Participants’ experiences of the intervention
Participants in the REACT intervention arm were asked to respond to the following statements at 12 and 24 weeks post randomisation (based on previously published studies):127
-
‘I always feel supported by the REACT supporters’.
-
‘I always feel supported by the REACT group’.
-
‘I always feel the REACT site is a safe and confidential environment’.
Options for each answer were ‘strongly disagree’, ‘disagree’, ‘agree’, and ‘strongly agree’.
Appropriate use of the site
The following data were collected automatically via the site and summarised for the REACT intervention arm only:
-
number of times a relative flagged content as requiring attention
-
number of times a REACT supporter hid a comment from the site
-
number of participants’ accounts suspended.
Missing data
Participants were asked to complete the primary outcome measure (GHQ-28) before being presented with any other measures, to maximise primary outcome data collection. In addition, participants were unable to submit any questionnaire with a missing field; therefore, by design, no data were missing from questionnaires completed online. (This was not true for some items assessing the relatives’ caring role owing to an error in design and testing; hence, there are some missing values for these variables.)
The only instances of missing outcome data occurred when the GHQ-28 was returned by post. These questionnaires were included in the analysis if more than half of the questions in each of the four subscales had been completed; missing answers were given the mean value of given answers within that subscale for that participant. This approach was chosen following discussions with the TSC, with guidance provided by the Patient Health Questionnaire-9 items. 128
This simple approach was chosen as there were very few missing data entries (four missing questions from three patients at 12 weeks, and one missing question at 24 weeks) on which to base multiple imputation.
Data entered up to 18 weeks post randomisation were considered to be 12-week data; data entered beyond 18 weeks and up to 30 weeks post randomisation were considered to be 24-week data. Any duplication of 24-week data entered by a given participant (i.e. if the participant provided ‘12-week’ data beyond 18 weeks and later entered 24-week data) was addressed by choosing the data entered closest in time to 24 weeks post randomisation.
Missing completion dates for postal GHQ-28s were estimated using the mid-point between the date sent and the date received. If not recorded, the date of receipt was imputed using the mean number of days between sending and receiving questionnaires for all accurately recorded postal GHQ-28s.
Joint modelling of the longitudinal outcome data and the time to dropout was carried out using the stjm command in Stata, to demonstrate any association between these two processes. A longitudinal trajectory plot was produced using the subsidiary command ‘stjmgraph’; the graph showed dependence between the longitudinal profiles and dropout.
Monitoring of adverse events
Adverse events were assessed in terms of the number of participants for whom it was necessary to trigger the risk protocol, for both low-risk and high-risk events [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/144934/#/ (accessed 28 October 2019)]. Risks were identified in one of three ways:
-
‘red flags’ raised by the system in response to answers to GHQ-28 items D3, D4, D6 or D7 that indicated possible risk to self, or to CWS Questionnaire questions 29 or 30 indicating possible risk from the person cared for, with the trial manager notified via the dashboard
-
by a REACT supporter through the forum or direct messaging
-
by the trial manager when contacting non-responders for follow-up (in both arms, with strategies to ensure that blinding was not broken).
Low-risk alerts triggered a standardised e-mail to the participant, expressing concern, checking they were OK, and pointing them to appropriate support. High-risk alerts, defined as clear evidence of immediate and serious risk to life or to child welfare, and referred to as ‘serious adverse events’, led to immediate contact with police or social services, as appropriate, including sharing participant details. Safeguarding concerns were also covered by the protocol.
Add-on studies
We conducted a study within a trial (SWAT) to investigate factors influencing the impact of incentives to participants (see Appendix 2) and a qualitative study to understand participants’ experiences of using REACT (see Chapter 6). We also plan to conduct a qualitative analysis of the posts on the REACT forum to identify the key issues that relatives raised in the online forum (see Chapter 6 for initial themes).
Ethics approval and research governance
Ethics approval was given by Lancaster National Research Ethics Service committee (reference number 15/NW/0732) on 21 September 2015. The eight ethics amendments (current version 1.8, dated 6 December 2017) can be found on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/144934/#/ (accessed 28 October 2019).
Patient and public involvement strategy
One of the study investigators is a parent of someone living with psychosis and was extensively involved in the development of REACT, the RD and data collection processes. She was part of the supervisory team for REACT supporters.
We established a RAG, working primarily online, to give detailed feedback on REACT, the online data collection processes and the recruitment strategy.
Our REACT supporters were people with lived experience of supporting someone with psychosis or BD; as well as supporting the REACT intervention, they were involved in promotion, recruitment, interpretation and writing up the findings. A REACT supporter presented a paper as part of a symposium about REACT at the World Congress for Behavioural and Cognitive Therapies in Berlin in July 2019. The TSC included a relative and service user.
Data management, storage and security
All participant trial data were collected through an online system at Liverpool CTRC and stored on secure servers physically located in access-controlled server rooms and backed up nightly to a separate physical location. All identifiable data were encrypted using a 256-bit encryption algorithm. CTRC servers were subject to penetration-testing audits undertaken by University of Liverpool central IT staff. Website usage data, qualitative data from the REACT group forum and direct messages to REACT supporters were taken from the REACT website and hosted on a dedicated virtual private server at Lancaster University. All communication with website users was limited to Secure Sockets Layer- (SSL-)protected Hypertext Transfer Protocol Secure (HTTPS) protocol, to protect passwords and data in transit over the internet.
The REACT data are stored on a secure server at Lancaster University, which complies with relevant statutory provisions including the Data Protection Act 2018129 and the EU General Data Protection Regulation. 110 Data held on Lancaster servers are stored in a resilient storage infrastructure that is dual-housed in the university’s data centres (on site). There are multiple levels of redundancy built in to these storage arrays: snapshots and backups are automated and taken regularly.
University single sign-on (SSO) credentials are required to access the shared network drive; the principal investigator controls access to specific folders and ensures that this is monitored regularly.
Chapter 4 Clinical effectiveness: results
Introduction
This chapter reports the findings from analyses to test the clinical effectiveness of REACT. The structure follows the CONSORT guidelines and the methods outlined in Chapter 3. A full statistical analysis is available in Report Supplementary Material 1.
First, we describe the flow of participants through the trial. We then list any deviations from our published protocol. 130 We describe the levels of intervention use in both arms of the trial. Next, we present our rate of recruitment, report the findings of the internal pilot, test the effectiveness of the online and offline strategies to maximise recruitment and explore the impact of the reminders protocol on retention.
We then present the baseline data for each of the key outcomes: distress (measured using the GHQ-28), carer well-being (measured using the CWS Questionnaire) and carer support (also measured with the CWS Questionnaire). We test the impact of the REACT intervention on each of the main outcomes (primary outcome: GHQ-28 score at 24 weeks; secondary outcomes: GHQ-28 score at 12 weeks and CWS Questionnaire scores at 12 and 24 weeks), and explore evidence for any causal impact. We test whether or not illness perceptions and coping strategies mediate any relationship between the intervention and GHQ-28 score, as hypothesised.
We present two additional analyses: testing the impact of participants’ baseline characteristics on the primary outcome and the impact of ‘lurking’ on the REACT group forum. Finally, we report the adverse events that occurred during the trial.
Technical issues that arose during the trial are set out in Report Supplementary Material 1, Table 6–6. The resulting deviations from protocol are set out in Appendix 1, Table 54.
Participant flow
The total number of visits to the REACT trial page from 22 April 2016 to 30 September 2017 was 451,832. The total number of visits to the trial registration page was 4348.
Figure 5 shows the flow of participants through each stage of the trial.
FIGURE 5.
The CONSORT flow diagram. Reproduced from Lobban et al. 131 © The Author(s). 2020 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.
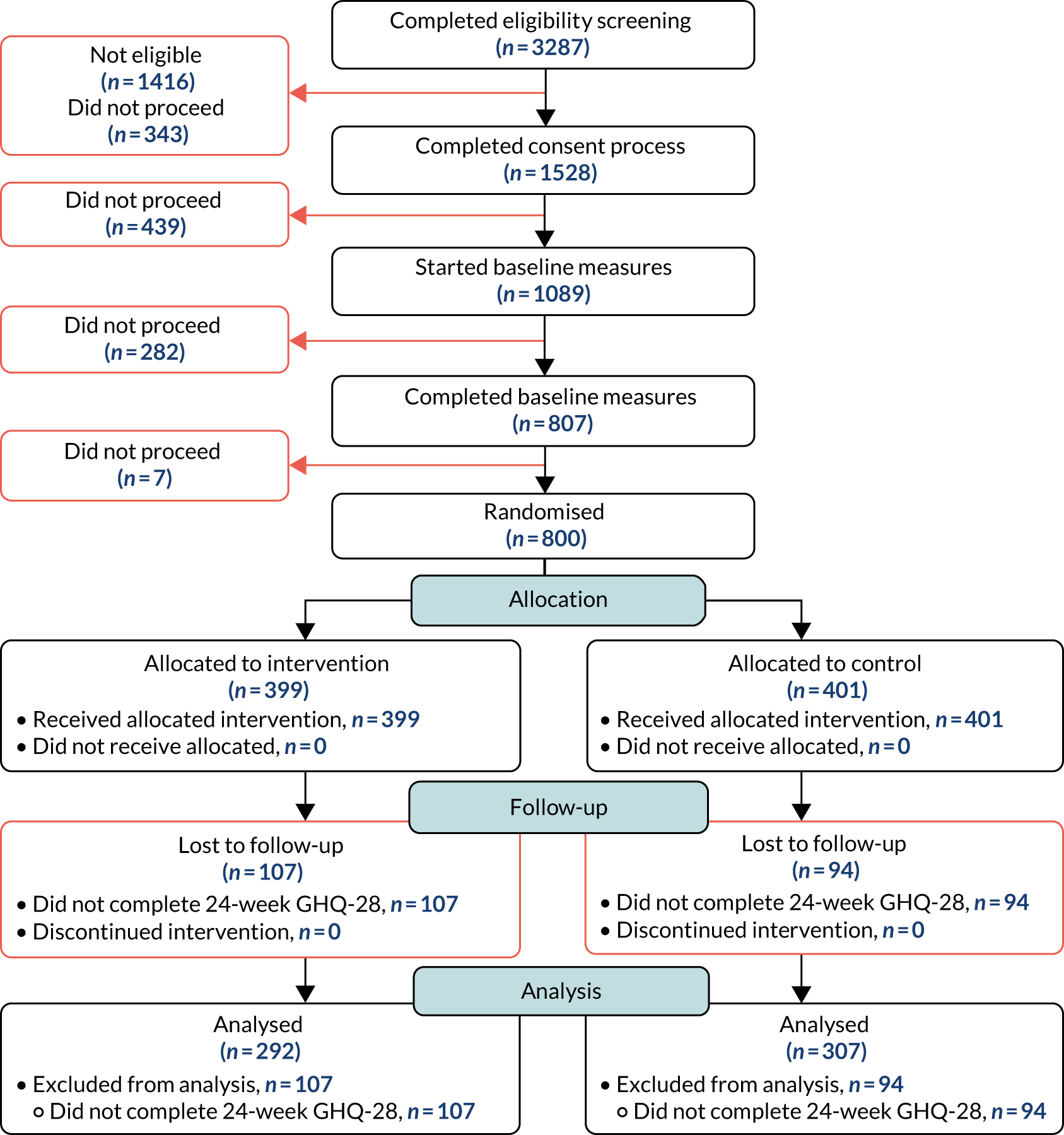
Of the 3287 people who completed the eligibility screening, 1528 (46%) consented to the trial. Of these, 343 failed to proceed through the registration process and 1416 people failed on at least one of the eligibility items. The number failing on each eligibility item is shown in Table 1 (note that 55 people failed on more than one criterion).
| Question | Number failing (% of total ineligible) |
|---|---|
| I am aged ≥ 16 years | 10 (0.7) |
| I am a relative (or close friend providing regular support) of someone with psychosis or BD | 88 (6.2) |
| Have you recently been feeling nervous and strung-up all the time? | 1146 (80.9) |
| I would like to receive help for my distress through an online toolkit | 118 (8.3) |
| I have regular access to a computer that is connected to the Internet | 28 (2.0) |
| I have a good working knowledge of written and spoken English language | 13 (0.9) |
| I live in the UK | 13 (0.9) |
| To the best of my knowledge, I am the only relative/close friend of the person I support taking part in the REACT trial | 67 (4.7) |
The most frequently failed item was the requirement for participants to score 2 (‘rather more than usual’) or 3 (‘much more than usual’) on the GHQ-28 item ‘Have you recently been feeling nervous and strung-up all the time?’.
Of the 1528 who consented, 1089 started the baseline measures but 282 did not proceed; 807 completed the measures. Seven did not proceed at this point; the remaining 800 (52% of those consenting) were randomised.
Use of the intervention (compliance with treatment)
Table 2 shows the level of intervention use in each arm of the trial. These data were available for only 700 of the 800 people, as page view numbers began to be recorded only part-way through the trial. The number of participants who logged in to the site at least once was similar in both arms of the trial, but the total number of log-ins after the first visit was much higher in the REACT arm than in the RD-only arm. The median time spent on the REACT site in the REACT arm was 50.8 minutes (IQR 12.4–172.1 minutes), with a large amount of variation between individuals (range 0.1–4505.5 minutes). The median time spent on the RD in the RD-only arm was 0.5 minutes, again with large variation, ranging from 0 to 42.9 minutes.
| Descriptive statistics | Trial arm | Overall (n = 700) | |
|---|---|---|---|
| REACT (n = 348) | RD only (n = 352) | ||
| REACT site | |||
| Total number of web page downloads from intervention sitea | |||
| n | 51,416 | 4276 | 55692 |
| Mean (SD) | 149.9 (266) | 12.7 (39.1) | 82 (202.9) |
| Median (IQR) | 69 (18–179) | 6 (3–13) | 14 (5–76) |
| Minimum, maximum | 1, 3501 | 1, 651 | 1, 3501 |
| Total number of times participants logged on to intervention sitea | |||
| Number of participants who logged in | 343 | 336 | 679 |
| Total number of log-ins | 2724 | 681 | 3405 |
| Mean (SD) | 7.9 (13.3) | 2 (1.7) | 5 (10) |
| Median (IQR) | 4 (2–9) | 1 (1–2) | 2 (1–5) |
| Minimum, maximum | 1, 159 | 1, 12 | 1, 159 |
| Total time spent on REACT intervention page per person (minutes)b | |||
| Number of people who accessed the website | 343 | N/A | N/A |
| Total time (minutes) (across all participants) | 46,531.5 | N/A | N/A |
| Mean (SD) time on page per person (minutes) | 135.7 (296.8) | N/A | N/A |
| Median (IQR) time on page per person (minutes) | 50.8 (12.4–172.1) | N/A | N/A |
| Minimum, maximum time spent on page (minutes) | 0.1, 4505.5 | N/A | N/A |
| Number of participants who did not log in to the intervention site | 5 | 16 | 21 |
| Number of participants who did not log in to the intervention site after the initial log-in | 75 | 184 | 259 |
| RD | |||
| Page hits | |||
| Total number of page hits | 971 | 645 | 1616 |
| Mean (SD) page hits per person | 5.1 (5.6) | 2.5 (3.9) | 3.7 (4.9) |
| Median (IQR) page hits per person | 3 (2–7) | 2 (1–3) | 2 (1–4) |
| Minimum, maximum page hits per person | 1, 37 | 1, 58 | 1, 58 |
| Total time spent on page | |||
| Number of people who accessed page | 189 | 253 | 442 |
| Total time (minutes) (across all participants) | 159.7 | 189.0 | 348.7 |
| Mean (SD) time on page per person (minutes) | 4.7 (7.9) | 2.2 (5.2) | 3.3 (6.6) |
| Median (IQR) time on page per person (minutes) | 1.4 (0.5–5.5) | 0.5 (0–1.6) | 0.9 (0–3) |
| Minimum, maximum time spent on page (minutes) | 0, 55.8 | 0, 42.9 | 0, 55.8 |
Detailed statistics on the use of the intervention, split by module, are provided in Report Supplementary Material 1, Tables 6–9.
The most popular module (i.e. most people visited at least once) was the REACT arm: the online forum. More than half of the people allocated to the REACT visited this module (n = 207, 52%). The least popular modules were ‘Recovery: looking to the future’ (n = 108, 27%) and ‘Managing stress; thinking differently’ (n = 108, 27%).
Timing of intervention access
Table 3 shows how site use varied by the time of week. Both online interventions (REACT and the RD) were accessed considerably more outside the working week (09.00 to 17.00, Monday–Friday, excluding public holidays, UK time) than during it. This provides evidence for the need for online interventions to be available 24 hours per day.
| Descriptive statistics | Working-week accessa | Out-of-hours accessa | ||||
|---|---|---|---|---|---|---|
| REACT arm (n = 343) | RD-only arm (n = 336) | Overall (n = 679b) | REACT arm (n = 343) | RD-only arm (n = 336) | Overall (n = 679b) | |
| Total number of web page downloads from the intervention site | ||||||
| Mean (SD) | 49.3 (99.0) | 4.9 (12.2) | 27.3 (74.2) | 100.6 (193.3) | 7.9 (30.3) | 54.7 (146.4) |
| Median (IQR) | 14 (0–57) | 0 (0–5) | 3 (0–19) | 44 (9–124) | 3 (1–8) | 8 (2–48) |
| Minimum, maximum | 0, 890 | 0, 128 | 0, 890 | 0, 2611 | 0, 523 | 0, 2611 |
| Total number of times participants logged in to the allocated intervention | ||||||
| Mean (SD) | 2.8 (5.7) | 0.8 (1.1) | 1.8 (4.2) | 5.1 (8.8) | 1.3 (1.3) | 3.2 (6.6) |
| Median (IQR) | 1 (0–3) | 0 (0–1) | 1 (0–2) | 3 (1–6) | 1 (1–2) | 1 (1–3) |
| Minimum, maximum | 0, 54 | 0, 6 | 0, 54 | 0, 105 | 0, 9 | 0, 105 |
| Total time spent on allocated intervention per person (minutes) | ||||||
| Mean (SD) | 58.9 (109.6) | 6.6 (11.7) | 37.4 (88.2) | 97.3 (231.6) | 6.2 (8.9) | 56.3 (177.5) |
| Median (IQR) | 24.5 (4.8–64.9) | 3 (0.9–6.7) | 7.1 (2.2–35.6) | 33.6 (7.2–110.2) | 2.7 (1.1–7.0) | 8 (1.8–45.4) |
| Minimum, maximum | 0.1, 1054.3 | 0, 97.3 | 0, 1054.3 | 0, 3445.8 | 0, 61 | 0, 3445.8 |
Impact of e-mail reminders to visit the REACT site
This analysis explores whether or not reminders led to an increase in intervention use by comparing participants’ patterns of intervention use within 1, 3 and 7 days of the first reminder being sent (standardised to a daily rate) with their intervention use during the period before the first reminder. Data prior to the first reminder are standardised by the number of days from randomisation to the first reminder, when appropriate. Data summarised in Table 4 are based on 246 participants in the REACT arm who had available web usage data and received a reminder.
| Intervention use | Daily rate of intervention use | |||
|---|---|---|---|---|
| Within 1 day of first reminder | Within 3 days of first remindera | Within 7 days of first reminderb | Prior to first reminderc | |
| Page hits (average number per person per day) | ||||
| Mean (SD) | 2.9 (10.2) | 2.0 (5.3) | 1.3 (2.8) | 3.0 (4.4) |
| Median (IQR) | 0 (0–0) | 0 (0–0.7) | 0 (0–1.6) | 1.6 (0.5–4.0) |
| Minimum, maximum | 0, 94 | 0, 38.7 | 0, 24.6 | 0, 49.4 |
| Total time spent on the intervention (average per person per day in minutes) | ||||
| Mean (SD) | 0.1 (0.4) | 0.1 (0.3) | 0.04 (0.1) | 2.6 (3.6) |
| Median (IQR) | 0 (0–0) | 0 (0–0.02) | 0 (0–0. 1) | 1.0 (0.2–4.1) |
| Minimum, maximum | 0, 4.8 | 0, 4.5 | 0, 0.7 | 0, 30.3 |
Participants’ experiences of the intervention
Participants’ experiences of the REACT intervention were assessed at 12 and 24 weeks. Results are shown in Table 5. At the end of the intervention period, 88% of participants reported having always felt supported by the REACT supporters, 89% always felt supported by the REACT group (forum), and an even greater proportion (96%) always felt that the REACT site was a safe and confidential environment.
| Experience | Response, n (%) | |||
|---|---|---|---|---|
| Strongly agree | Agree | Disagree | Strongly disagree | |
| Always feel supported by the REACT supporters | ||||
| 12 weeks (N = 226) | 65 (28.76) | 132 (58.41) | 24 (10.62) | 5 (2.21) |
| 24 weeks (N = 239) | 69 (28.87) | 141 (59.00) | 24 (10.04) | 5 (2.09) |
| Always feel supported by the REACT group | ||||
| 12 weeks (N = 226) | 58 (25.66) | 138 (61.06) | 27 (11.95) | 3 (1.33) |
| 24 weeks (N = 239) | 67 (28.03) | 145 (60.67) | 24 (10.04) | 3 (1.26) |
| Always feel that the REACT site is a safe and confidential environment | ||||
| 12 weeks (N = 226) | 118 (52.21) | 95 (42.04) | 10 (4.42) | 3 (1.33) |
| 24 weeks (N = 239) | 125 (52.30) | 105 (43.93) | 6 (2.51) | 3 (1.26) |
Appropriate use of the site
Users had the option to flag content on the forum as ‘requiring attention’ if they felt that it was inappropriate or hostile. REACT supporters were able to hide posts. Only two posts were hidden during the trial. These were posted by the same participant, and were felt to have the potential to put unreasonable burden on other participants in the forum. No user accounts were suspended during the trial.
Recruitment
Rate
Recruitment took place from 22 April 2016 to 30 September 2017. The rate of recruitment is shown in Figure 6. Recruitment was steady and close to target for the first 8 months, and then rose above target. Ethics approval was granted to continue recruitment throughout the recruitment phase, despite the target having been reached, to ensure we had an adequate sample size to test the primary and secondary hypotheses. The increase in recruitment in July 2016 may have been due to circulation of a Bipolar UK e-newsletter at this time, and the accelerating rate from December 2016 may have been as a result of increasing Facebook activity.
FIGURE 6.
Recruitment rate.
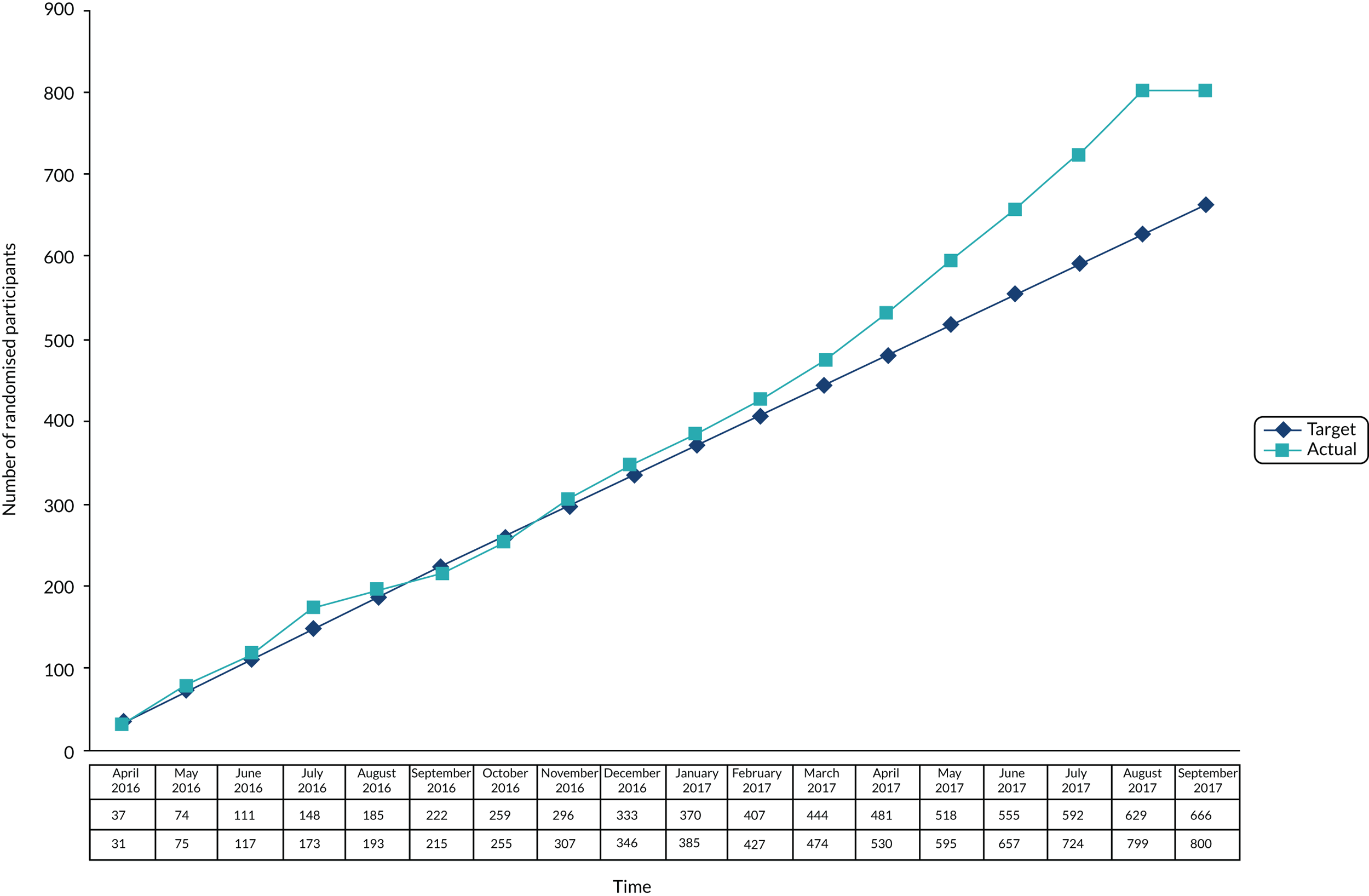
Effectiveness of recruitment strategies
The success of each recruitment strategy used is indicated by the number of randomised participants who were recruited via each strategy (Table 6). Each strategy has been categorised as being primarily online or offline. Of the randomised participants, 421 (53%) were recruited through five, primarily online, strategies and 379 (47%) were recruited through 10, primarily offline, strategies. Thus, combining online and offline recruitment was important in meeting the recruitment target.
| Number | Recruitment strategies for randomised participants | Online/offline | n (%) |
|---|---|---|---|
| 1 | Online | 206 (25.8) | |
| 2 | Mental health teams/professionals | Offline | 151 (18.9) |
| 3 | Internet search | Online | 121 (15.1) |
| 4 | Mental health charities | Online | 77 (9.6) |
| 5 | Recommended by a friend/family | Offline | 74 (9.3) |
| 6 | GP | Offline | 59 (7.4) |
| 7 | Carer or service user support group | Offline | 42 (5.3) |
| 8 | NHS contacts | Offline | 25 (3.1) |
| 9 | Online | 15 (1.9) | |
| 10 | Employer | Offline | 8 (1.0) |
| 11 | Other third-sector organisation | Offline | 8 (1.0) |
| 12 | Not classifiable | Offline | 6 (0.8) |
| 13 | Other public adverts (excluding NHS adverts) | Offline | 4 (0.5) |
| 14 | Local newspaper | Online | 2 (0.3) |
| 15 | Research team | Offline | 2 (0.3) |
Internal pilot
At 9 months into recruitment, we had recruited 368 participants. The pooled SD of the GHQ-28 score at the 24-week follow-up (based on 134 participants who had completed it by this point) was 11.91. This result was reviewed by the independent data and safety monitoring committee; it was agreed that we had met our ‘go’ criteria and that no changes to the sample size were needed. The trial continued.
Effect of reminders on retention
With ethics committee approval, participants received the following series of reminders to complete follow-ups (until follow-up was completed):
-
Up to three automated e-mail reminders at 5-day intervals.
-
A manual text message from the trial manager 3 days after the final automated e-mail, with the participant’s log-in details and instructions on how to complete the follow-up.
-
A telephone call from the trial manager 3 days after the text message, asking the participant to complete the questionnaires online, but offering to complete the primary questionnaire over the telephone. If the participant did not answer, a second attempt was made; an answer-machine message left if this too was unsuccessful.
-
A postal pack containing a letter, the primary questionnaire and a reply-paid envelope, and an automated text message triggered by the trial manager through the trial dashboard. The message contained prespecified text and a link to complete the primary questionnaire on their mobile phone.
Participants who indicated any reluctance to remain in the sample were withdrawn from the trial immediately. Table 7 shows the number of participants who completed the primary outcome measure after each reminder for each time point. Most participants who completed follow-ups did so after the first automated e-mail reminder (n = 399). However, all reminders (online and offline) increased completion, suggesting that multiple reminders and different options for completion (online and offline) have a positive, cumulative effect on follow-up rate. There was no obvious difference in the impact of reminders at the 12- and 24-week follow-ups.
| Reminder | Online or offline retention strategy | Number (%) completed (%) | |
|---|---|---|---|
| At 12 weeks (n = 594) | At 24 weeks (n = 599) | ||
| Completed online after first reminder e-mail | Online | 177a (30) | 162 (27) |
| Completed online after second reminder e-mail | Online | 114 (19) | 71 (12) |
| Completed online after third reminder e-mail | Online | 61 (10) | 93 (16) |
| Completed online after manual text message | Offline | 80 (13) | 94 (16) |
| Completed GHQ-28 over the telephone or online after telephone call | Offline | 68 (11) | 81 (14) |
| Completed GHQ-28 via post or online after receiving a postal pack | Offline | 84 (14) | 76 (13) |
| Completed GHQ-28 via auto-text | Online | 10 (2) | 22 (4) |
Baseline data
The demographic and situational characteristics of the participants are presented in Table 8 (a fuller version can be found in Report Supplementary Material 1).
| Characteristic | Trial arm | Overall (n = 800) | |
|---|---|---|---|
| REACT (n = 399) | RD only (n = 401) | ||
| Age (years) | |||
| < 30, n (%) | 39 (9.77) | 36 (8.98) | 75 (9.38) |
| 30–39, n (%) | 50 (12.53) | 73 (18.20) | 123 (15.38) |
| 40–49, n (%) | 95 (23.81) | 104 (25.94) | 199 (24.88) |
| 50–59, n (%) | 111 (27.82) | 112 (27.93) | 223 (27.88) |
| 60–69, n (%) | 88 (22.06) | 61 (15.21) | 149 (18.63) |
| ≥ 70, n (%) | 16 (4.01) | 15 (3.74) | 31 (3.88) |
| Mean (SD) | 49.4 (13.3) | 47.9 (12.7) | 48.6 (13.00) |
| Minimum, maximum | 16, 84 | 18, 86 | 16, 86 |
| Gender, n (%) | |||
| Male | 82 (20.55) | 69 (17.21) | 151 (18.88) |
| Female | 317 (79.45) | 331 (82.54) | 648 (81.00) |
| Missing | 0 (0.00) | 1 (0.25) | 1 (0.13) |
| How many people do you support?, n (%) | |||
| 1 | 296 (74.19) | 295 (73.57) | 591 (73.88) |
| 2 | 68 (17.04) | 72 (17.96) | 140 (17.50) |
| 3 | 20 (5.01) | 21 (5.24) | 41 (5.13) |
| ≥ 4 | 15 (3.76) | 13 (3.24) | 28 (3.50) |
| Relationship to service user (n) | |||
| Mother | 187 | 200 | 387 |
| Father | 17 | 10 | 27 |
| Partner | 149 | 143 | 292 |
| Daughter | 56 | 62 | 118 |
| Son | 6 | 1 | 7 |
| Sibling | 41 | 38 | 79 |
| Friend | 31 | 26 | 57 |
| Grandparent | 8 | 2 | 10 |
| Wider family member | 17 | 17 | 34 |
| Other | 10 | 12 | 22 |
| Undefined | 38 | 52 | 90 |
| Ethnicity, n (%) | |||
| White British | 361 (90.48) | 366 (91.27) | 727 (90.88) |
| White Irish | 5 (1.25) | 6 (1.50) | 11 (1.38) |
| Any other white background | 15 (3.76) | 13 (3.24) | 28 (3.50) |
| Mixed | 6 (1.50) | 6 (1.50) | 12 (1.50) |
| Asian or Asian British | 11 (2.76) | 3 (0.75) | 14 (1.75) |
| Other ethnic group | 1 (0.25) | 5 (1.25) | 6 (0.75) |
| Rather not say | 0 (0.00) | 2 (0.50) | 2 (0.25) |
| Marital status, n (%) | |||
| Single | 88 (22.06) | 77 (19.20) | 165 (20.63) |
| Married | 219 (54.89) | 239 (59.60) | 458 (57.25) |
| Civil partnership | 14 (3.51) | 13 (3.24) | 27 (3.38) |
| Separated | 8 (2.01) | 15 (3.74) | 23 (2.88) |
| Divorced | 47 (11.78) | 40 (9.98) | 87 (10.88) |
| Widowed | 10 (2.51) | 8 (2.00) | 18 (2.25) |
| Rather not say | 13 (3.26) | 9 (2.24) | 22 (2.75) |
| Living arrangements, n (%) | |||
| Spouse or partner | 275 (68.92) | 289 (72.07) | 564 (70.50) |
| Living alone | 82 (20.55) | 80 (19.95) | 162 (20.25) |
| Parent(s) | 17 (4.26) | 11 (2.74) | 28 (3.50) |
| Other | 20 (5.01) | 17 (4.24) | 37 (4.63) |
| Rather not say | 5 (1.25) | 4 (1.00) | 9 (1.13) |
| Dependents, n (%) | |||
| None | 168 (41.90) | 175 (43.86) | 343 (42.88) |
| 1 | 99 (24.69) | 117 (29.32) | 216 (27.00) |
| 2 | 91 (22.69) | 57 (14.29) | 148 (18.50) |
| 3 | 30 (7.48) | 28 (7.02) | 58 (7.25) |
| ≥ 4 | 13 (3.26) | 22 (5.49) | 35 (3.48) |
| Highest education level, n (%) | |||
| School level | 65 (16.29) | 73 (18.20) | 138 (17.25) |
| Further education (college) | 108 (27.07) | 117 (29.18) | 225 (28.13) |
| Higher education (university) | 226 (56.64) | 211 (52.62) | 437 (54.63) |
| Employment status, n (%) | |||
| Employed full-time (≥ 35 hours per week) | 150 (37.59) | 151 (37.66) | 301 (37.63) |
| Employed part-time | 92 (23.06) | 96 (23.94) | 188 (23.50) |
| Unable to work because of caring responsibilities | 33 (8.27) | 33 (8.23) | 66 (8.25) |
| Unable to work because of ill health/disability | 30 (7.52) | 20 (4.99) | 50 (6.25) |
| Unemployed | 10 (2.51) | 8 (2.00) | 18 (2.25) |
| Student | 7 (1.75) | 8 (2.00) | 15 (1.88) |
| Retired | 53 (13.28) | 58 (14.46) | 111 (13.88) |
| Voluntary work | 12 (3.01) | 11 (2.74) | 23 (2.88) |
| Housewife/house husband | 12 (3.01) | 16 (3.99) | 28 (3.50) |
| Home internet access, n (%) | |||
| Yes | 395 (99.00) | 400 (99.75) | 795 (99.38) |
| No | 1 (0.25) | 0 (0.00) | 1 (0.13) |
| Intermittent or of poor quality | 3 (0.75) | 1 (0.25) | 4 (0.50) |
| Paid work affected by caring role | |||
| No, I did not have paid work before, n (%) | 120 (30.08) | 125 (31.17) | 245 (30.63) |
| No, I still perform the same amount of paid work, n (%) | 198 (49.62) | 195 (48.63) | 393 (49.13) |
| Yes, I stopped work completely, n (%) | 40 (10.03) | 33 (8.23) | 73 (9.13) |
| Yes, I reduced my working hours, n (%) | 41 (10.28) | 48 (11.97) | 89 (11.13) |
| Mean (SD) | 13.5 (9.3) | 11.4 (6.6) | 12.4 (8.0) |
| Minimum, maximum | 2, 48 | 1, 30 | 1, 48 |
Participants were typically middle-aged (53% were aged between 40 and 60 years), white British (91%), female (81%), mothers (48%), highly educated (55% were educated to university level) and supporting a young adult aged ≤ 35 years (61%). More than half (58%) were supporting someone with BD. Most were supporting only one person with a mental health problem, but 26% reported supporting two or more people, and 57% had other dependents. A total of 61% were married or in a civil partnership. Most were in full-time, part-time or voluntary work (64%), but 8.5% reported being unable to work specifically because of their caring responsibilities. All but four participants had home internet access.
Baseline scores on the main outcomes are presented in Table 9. These scores showed very high levels of distress. Using Likert scoring, a mean total score of 40 points on the GHQ-28 (SD 14) suggested that the majority of the sample scored above the 23/24 cut-off point for psychiatric caseness. 132,133 The highest scores were on the anxiety/insomnia subscale.
| Assessment | Trial arm | Overall (n = 800) | |
|---|---|---|---|
| REACT (n = 399) | RD only (n = 401) | ||
| GHQ-28 | |||
| Mean (SD) | 40.3 (14.6) | 40.0 (14.0) | 40.2 (14.3) |
| Minimum, maximum | 5, 83 | 11, 81 | 5, 83 |
| Somatic symptoms subscale | |||
| Mean (SD) | 10.3 (4.4) | 10.4 (4.0) | 10.3 (4.2) |
| Minimum, maximum | 1, 21 | 1, 21 | 1, 21 |
| Anxiety/insomnia subscale | |||
| Mean (SD) | 13.0 (4.1) | 12.9 (4.0) | 13.0 (4.1) |
| Minimum, maximum | 0, 21 | 1, 21 | 0, 21 |
| Social dysfunction subscale | |||
| Median (IQR) | 11 (8–13) | 11 (8–14) | 11 (8–13.5) |
| Minimum, maximum | 1, 21 | 3, 21 | 1, 21 |
| Severe depression subscale | |||
| Median (IQR) | 4 (1–9) | 4 (1–9) | 4 (1–9) |
| Minimum, maximum | 0, 21 | 0, 21 | 0, 21 |
| CWS Questionnaire | |||
| Well-being | |||
| Mean (SD) | 55.9 (25.9) | 55.8 (26.4) | 55.9 (26.1) |
| Minimum, maximum | 0, 125 | 0, 114 | 0, 125 |
| Support | |||
| Mean (SD) | 19.5 (11.6) | 18.8 (11.7) | 19.1 (11.7) |
| Minimum, maximum | 0, 51 | 0, 51 | 0, 51 |
| Brief IPQ | |||
| Carer | |||
| Mean (SD) | 41.0 (7.4) | 41.4 (6.9) | 41.2 (7.2) |
| Minimum, maximum | 21, 65 | 19, 63 | 19, 65 |
| Service user | |||
| Mean (SD) | 44.4 (8.5) | 44.2 (8.6) | 44.3 (8.6) |
| Minimum, maximum | 19, 70 | 18, 75 | 18, 75 |
| Additional item on coping | |||
| Mean (SD) | 5.6 (2.2) | 5.6 (2.3) | 5.6 (2.2) |
| Minimum, maximum | 0, 10 | 0, 10 | 0, 10 |
| Brief COPE | |||
| Self-distraction | |||
| Median (IQR) | 5 (4–6) | 5 (4–7) | 5 (4–6) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Active coping | |||
| Median (IQR) | 5 (4–7) | 6 (4–7) | 5 (4–7) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Denial | |||
| Median (IQR) | 2 (2–3) | 2 (2–3) | 2 (2–3) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Substance use | |||
| Median (IQR) | 2 (2–4) | 2 (2–4) | 2 (2–4) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Use of emotional support | |||
| Median (IQR) | 4 (3–5) | 4 (3–5) | 4 (3–5) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Use of instrumental support | |||
| Median (IQR) | 4 (3–6) | 4 (3–6) | 4 (3–6) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Behavioural disengagement | |||
| Median (IQR) | 3 (2–4) | 3 (2–4) | 3 (2–4) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Venting | |||
| Median (IQR) | 4 (3–5) | 4 (3–5) | 4 (3–5) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Positive reframing | |||
| Median (IQR) | 4 (3–5) | 4 (3–5) | 4 (3–5) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Planning | |||
| Median (IQR) | 6 (4–8) | 6 (4–7) | 6 (4–7) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Humour | |||
| Median (IQR) | 3 (2–4) | 3 (2–4) | 3 (2–4) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Acceptance | |||
| Median (IQR) | 6 (5–7) | 6 (5–7) | 6 (5–7) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Religion | |||
| Median (IQR) | 2 (2–4) | 2 (2–4) | 2 (2–4) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
| Self-blame | |||
| Median (IQR) | 4 (3–6) | 4 (3–6) | 4 (3–6) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 |
Well-being and support scores measured using the CWS Questionnaire were also very low compared with other studies using this measure with groups of relatives of people with psychosis, although there are no clinical thresholds or established norms for this scale. The mean well-being scores were in the 50s at baseline (possible range is 0–128; higher scores indicate greater well-being). The mean support scores at baseline were < 20 in each arm (possible range 0–51; higher scores indicate greater support). Other studies of relatives of people with mental health problems report CWS Questionnaire mean scores in the 70s for well-being and 30s for support. 2,62,134 This pattern is likely to be a result of the stringent eligibility criteria used to prevent a floor effect on distress scores.
There are no clinical thresholds or published norms for scores on the Brief IPQ or the Brief COPE. These measures are used to assess change over time, and to assess the relationship between illness perceptions and coping styles and relevant outcomes.
Outcomes and estimated effect sizes
Table 10 sets out summary scores for the overall GHQ-28 and for each of its four subscales at baseline and at the 12- and 24-week follow-ups (primary end point).
| GHQ-28 | REACT arm | RD-only arm | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (n = 399) | 12 weeks (n = 287) | 24 weeks (n = 292) | Baseline (n = 401) | 12 weeks (n = 307) | 24 weeks (n = 307) | Baseline (n = 800) | 12 weeks (n = 594) | 24 weeks (n = 599) | |
| Mean (SD) | 40.3 (14.6) | 30.6 (15.2) | 29.6 (15.9) | 40.0 (14.0) | 32.9 (15.4) | 31.3 (15.2) | 40.2 (14.3) | 31.8 (15.3) | 30.5 (15.6) |
| Minimum, maximum | 5, 83 | 3, 80 | 2, 79 | 11, 81 | 1, 77 | 3, 81 | 5, 83 | 1, 80 | 2, 81 |
| Somatic symptoms subscale | |||||||||
| Mean (SD) | 10.3 (4.4) | 8.1 (4.3) | 7.9 (4.7) | 10.4 (4.0) | 8.7 (4.4) | 8.3 (4.5) | 10.3 (4.2) | 8.4 (4.4) | 8.1 (4.6) |
| Minimum, maximum | 1, 21 | 0, 21 | 0, 21 | 1, 21 | 0, 21 | 0, 21 | 1, 21 | 0, 21 | 0, 21 |
| Anxiety/insomnia subscale | |||||||||
| Mean (SD) | 13.0 (4.1) | 9.5 (4.7) | 9.2 (4.9) | 12.9 (4.0) | 10.1 (4.8) | 9.9 (4.9) | 13.0 (4.1) | 9.8 (4.7) | 9.6 (4.9) |
| Minimum, maximum | 0, 21 | 0, 21 | 0, 21 | 1, 21 | 0, 21 | 0, 21 | 0, 21 | 0, 21 | 0, 21 |
| Social dysfunction subscale | |||||||||
| Median (IQR) | 11 (8–13) | 8 (7–11) | 8 (7–11) | 11 (8–14) | 9 (7–13) | 8 (7–11) | 11 (8–13.5) | 9 (7–12) | 8 (7–11) |
| Minimum, maximum | 1, 21 | 0, 21 | 0, 21 | 3, 21 | 0, 21 | 0, 20 | 1, 21 | 0, 21 | 0, 21 |
| Severe depression subscale | |||||||||
| Median (IQR) | 4 (1–9) | 2 (0–7) | 2 (0–6) | 4 (1–9) | 3 (0–7) | 2 (0–7) | 4 (1–9) | 2 (0–7) | 2 (0–7) |
| Minimum, maximum | 0, 21 | 0, 21 | 0, 21 | 0, 21 | 0, 21 | 0, 21 | 0, 21 | 0, 21 | 0, 21 |
Primary efficacy assessment: General Health Questionnaire-28 items score at 24 weeks
Table 11 shows the analysis of covariance that was used to compare GHQ-28 scores between the two arms at the 24-week follow-up, adjusting for baseline scores. The estimated mean difference between the two arms favoured REACT, but was small (–1.39, 95% CI –3.60 to 0.83), not statistically significant (p = 0.2189) and unlikely to be of clinical significance. The same pattern was observed in the individual subscales (see Report Supplementary Material 1, section 6.6.1).
| Covariate | Coefficient (95% CI) | F-statistic | p-value |
|---|---|---|---|
| Baseline GHQ-28 score | 0.53 (0.45 to 0.61) | 165.27 | < 0.0001 |
| Treatment (REACT vs. control) | –1.39 (–3.60 to 0.83) | 1.51 | 0.2189 |
Secondary efficacy end point: General Health Questionnaire-28 items score at 12 weeks
Table 12 shows that the estimated mean difference between the two arms at the 12-week follow-up favoured REACT, but was small and, although statistically significant, was likely to be of limited clinical significance. The same pattern was observed in all of the individual subscales, but without significant differences between the two arms (see Report Supplementary Material 1, section 6.6.3).
| Covariate | Coefficient (95% CI) | F-statistic | p-value |
|---|---|---|---|
| Baseline GHQ-28 score | 0.61 (0.53 to 0.68) | 265.18 | < 0.0001 |
| Treatment (REACT vs. control) | –2.08 (–4.14 to –0.03) | 4.91 | 0.0271 |
Joint modelling analysis: General Health Questionnaire-28 items score
Details of the joint modelling analysis for the GHQ-28 scores can be found in Report Supplementary Material 1, section 6.6.4.
In summary, baseline GHQ-28 scores were very high, with a mean of 40.2 (SD 14.3). The highest subscale was anxiety. The GHQ-28 score fell over time in both arms of the trial. Most of this occurred during the first 12 weeks. At the 12-week follow-up, the GHQ-28 scores were statistically significantly lower in the REACT arm than in the RD-only arm, but this difference was small and likely to be of limited clinical significance. There was no statistically significant difference between the arms by 24 weeks.
Retention at 12 weeks was 74%; at 24 weeks, it was 75%. Although similar numbers of participants dropped out in each arm, those who dropped out of the REACT arm were more distressed than those who remained. The joint model estimates that the REACT arm participants who dropped out were, on average, 0.33 (95% CI –0.27 to 0.93; p = 0.279) GHQ-28 units more distressed than those who did not drop out; note, however, that this is the average over the entire 24-week period, that is this model assumes that the difference in distress between those REACT participants who did and those did not drop out was constant over the entire period. In the RD-only arm, the equivalent result for those who did/those who did not drop out was 0.12 (95% CI –0.52 to 0.77; p = 0.707).
This meant that data could not be assumed to be missing at random in both arms. When missing data were taken into account, using joint modelling methods (jointly accounting for time to drop-out and longitudinal GHQ-28 measurements), there was no statistically significant difference between the REACT and RD-only arms over the 24-week follow-up period.
Despite the significant (statistical and clinical) reduction in GHQ-28 scores over time in both arms, mean scores at the 12- and 24-week follow-ups remained higher than the 23/24 threshold score suggestive of clinical caseness.
Secondary efficacy end point: carer well-being and support
The number of respondents and summary scores for the CWS Questionnaire well-being and support scales at baseline and at the 12- and 24-week follow-ups are presented in Table 13.
| CWS Questionnaire | REACT arm | RD-only arm | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (n = 399) | 12 weeks (n = 233) | 24 weeks (n = 249) | Baseline (n = 401) | 12 weeks (n = 271) | 24 weeks (n = 275) | Baseline (n = 800) | 12 weeks (n = 504) | 24 weeks (n = 524) | |
| Well-being | |||||||||
| Mean (SD) | 55.9 (25.9) | 72.0 (27.0) | 77.0 (26.6) | 55.8 (26.4) | 68.9 (27.7) | 72.6 (30.5) | 55.9 (26.1) | 70.3 (27.4) | 74.7 (28.8) |
| Minimum, maximum | 0, 125 | 15, 127 | 8, 124 | 0, 114 | 0, 128 | 0, 127 | 0, 125 | 0, 128 | 0, 127 |
| Support | |||||||||
| Mean (SD) | 19.5 (11.6) | 26.0 (12.0) | 25.7 (11.7) | 18.8 (11.7) | 22.6 (12.0) | 23.2 (12.2) | 19.1 (11.7) | 24.2 (12.1) | 24.4 (12.0) |
| Minimum, maximum | 0, 51 | 0, 51 | 0, 51 | 0, 51 | 0, 50 | 0, 51 | 0, 51 | 0, 51 | 0, 51 |
Well-being and support at 12 weeks
The ANCOVA at the 12-week follow-up is presented in Table 14. The estimated mean difference in well-being between the two arms of the trial favoured REACT, but was small, was not statistically significant (p = 0.4225) and was unlikely to be clinically significant.
| Covariate | Coefficient (95% CI) | F-statistic | p-value |
|---|---|---|---|
| Well-being | |||
| Baseline | 0.66 (0.59 to 0.74) | 326.79 | < 0.0001 |
| Treatment (REACT vs. control) | 1.53 (–2.21 to 5.27) | 0.64 | 0.4225 |
| Support | |||
| Baseline | 0.68 (0.61 to 0.76) | 351.15 | < 0.0001 |
| Treatment (REACT vs. control) | 2.50 (0.87 to 4.12) | 16.83 | < 0.0001 |
The estimated mean difference in support at 12 weeks also favoured REACT and was statistically significant (p < 0.0001).
Well-being and support at 24 weeks
The ANCOVA at the 24-week follow-up is presented in Table 15. The estimated mean difference in wellness between the two arms favoured REACT at the 24-week follow-up, but was not statistically significant (p = 0.2582) and was unlikely to be of clinical significance.
| Covariate | Coefficient (95% CI) | F-statistic | p-value |
|---|---|---|---|
| Well-being | |||
| Baseline | 0.61 (0.53 to 0.69) | 219.13 | < 0.0001 |
| Treatment (REACT vs. control) | 2.39 (–1.76 to 6.54) | 1.28 | 0.2582 |
| Support | |||
| Baseline | 0.64 (0.57 to 0.71) | 321.52 | < 0.0001 |
| Treatment (REACT vs. control) | 1.65 (0.04 to 3.27) | 4.03 | 0.0451 |
The estimated mean difference in support between the arms at the 24-week follow-up also favoured REACT, and this was statically significant (p = 0.0451).
Joint modelling analysis: Carer Well-being and Support Questionnaire, well-being and support scores
Details of the joint modelling analysis for the CWS Questionnaire well-being and support scores can be found in Report Supplementary Material 1, section 6.6.7.
In summary, the CWS Questionnaire well-being and support scores were very low at baseline, with a well-being mean score of 55.9 and a support mean score of 19.1, but both improved significantly over time in both arms; most of this improvement occurred during the first 12 weeks.
There was no statistically significant difference in well-being scores between the two arms at the 12- or 24-week follow-up. However, support scores were significantly higher in the REACT arm than in the RD-only arm at both 12 and 24 weeks.
Retention at 12 weeks was 63%; at 24 weeks, it was 66%. More people dropped out of the REACT arm than out of the RD-only arm, and those who dropped out were more likely to have lower well-being scores. This meant that data could not be assumed to be missing at random in both arms.
When missing data were taken into account, there was no statistically significant difference between the REACT and RD-only arms for well-being or support over the 24-week follow-up period. However, the mean difference between the two arms on the support scale was 1.51 points; the clinical significance of this remains unknown.
Causal analysis
Instrumental variable regression
Instrumental variable regression was used to estimate the association between intervention use and GHQ-28 score at 24 weeks, using a number of measures of website use, principally the number of web page downloads during the 24 weeks of follow-up, but also participants’ total number of log-ins over the same period and their total time logged in to the REACT site. Scores for those in the control arm were taken to be 0 because they were not granted access to the intervention.
For web page downloads, randomised arm was chosen as the IV, as it was assumed to satisfy the following criteria:
-
association with web page downloads
-
an indirect effect on GHQ-28 score (via web page downloads)
-
no common causes of randomisation and GHQ-28 score.
A two-stage least squares estimator was used: the first stage was to fit a model regressing web page downloads on randomisation and the second stage was to regress GHQ-28 score at 24 weeks on the fitted values of web page downloads predicted in the previous step. The model was adjusted for baseline GHQ-28 score.
Table 16 shows the outcome of IV regression of GHQ-28 scores at 24 weeks, based on web page downloads in the 24 weeks of follow-up, adjusted for baseline GHQ-28 score.
| Covariate | Coefficient (95% CI) | Z-statistic | p-value |
|---|---|---|---|
| Baseline GHQ-28 score | 0.53 (0.44 to 0.62) | 12.0 | < 0.001 |
| Web page downloads | –0.01 (–0.02 to 0.01) | –1.1 | 0.295 |
The mean number of web page downloads in the REACT arm was 149.9. For each additional download, there was a mean reduction in GHQ-28 score at 24 weeks of 0.01; however, this effect was not statistically significant (p = 0.295).
Similarly, the mean number of log-ins to the REACT site was 7.9, with each additional log-in seeing a mean reduction in GHQ-28 score at 24 weeks of 0.17; again, this was not a statistically significant effect (p = 0.296).
Finally, the median number of minutes spent on REACT was 50.8; there was a mean reduction in GHQ-28 score at 24 weeks of 0.01 for each additional minute on the site there, which, again, was not statistically significant (p = 0.296).
Details of the analysis of all three measures of website use, including the suitability of using randomisation as the instrument in this regression, can also be found in Report Supplementary Material 1, section 6.6.8.1.
Mediation analysis
Brief Illness Perception Questionnaire
Table 17 shows scores on the Brief IPQ subscales at baseline and at 12 and 24 weeks. Scores on the carer and service user subscales show a pattern of decrease over time in both arms. Lower scores on this measure indicate a more benign perception of illness and its impact on both service user and carer. The additional item on coping also shows a pattern of decrease over time, suggesting that carers feel more able to cope over time.
| Brief IPQ | REACT arm | RD-only arm | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (n = 399) | 12 weeks (n = 228) | 24 weeks (n = 244) | Baseline (n = 401) | 12 weeks (n = 263) | 24 weeks (n = 268) | Baseline (n = 800) | 12 weeks (n = 491) | 24 weeks (n = 512) | |
| Carer | |||||||||
| Mean (SD) | 41.0 (7.4) | 38.7 (7.5) | 37.5 (7.7) | 41.4 (6.9) | 39.2 (7.0) | 68.0 (7.7) | 41.2 (7.2) | 39.0 (7.2) | 37.8 (7.7) |
| Minimum, maximum | 21, 65 | 16, 59 | 10, 61 | 19, 63 | 16, 55 | 10, 62 | 19, 65 | 16, 59 | 10, 62 |
| Service user | |||||||||
| Mean (SD) | 44.4 (8.5) | 42.6 (8.5) | 41.5 (8.7) | 44.2 (8.6) | 42.6 (8.1) | 41.8 (8.4) | 44.3 (8.6) | 42.6 (8.3) | 41.6 (8.5) |
| Minimum, maximum | 19, 70 | 18, 66 | 15, 65 | 18, 75 | 20, 69 | 13, 66 | 18, 75 | 18, 69 | 13, 66 |
| Additional item on coping | |||||||||
| Mean (SD) | 5.6 (2.2) | 5.0 (2.3) | 4.5 (2.1) | 5.6 (2.3) | 5.0 (2.2) | 4.9 (2.2) | 5.6 (2.2) | 5.0 (2.2) | 4.7 (2.2) |
| Minimum, maximum | 0, 10 | 0, 10 | 0, 10 | 0, 10 | 0, 10 | 0, 10 | 0, 10 | 0, 10 | 0, 10 |
Multivariate ANCOVA was used to assess the impact of the intervention arm on each of the subscales, at 12 weeks and at 24 weeks, while taking into account correlation between the subscales. The results of the MANOVA and ANCOVA tables for individual subscales at each time point are shown in Report Supplementary Material 1. The p-values for all tests are non-significant, indicating no evidence of a difference between randomised arms for one or more of the outcomes at either time point.
Instrumental variable regression, with the interaction between randomised arm and baseline score of the mediator as the instrument, was performed to assess whether or not the 24-week mediator score was a predictor of the 24-week GHQ-28 score. These were found to be weak instruments; therefore, causal mediation analysis was instead performed to estimate the average causal mediated effect (ACME) of GHQ-28 score at 24 weeks. None of the putative mediators had a significant mediation effect on outcome. Details of the analysis are in Report Supplementary Material 1, section 6.6.9.
Brief Coping Orientation to Problems Experienced
Table 18 shows scores on the subscales of the Brief COPE at 12 and 24 weeks. There was very little change in COPE scores in either arm at any time point throughout the study. Active coping, planning, and acceptance remained the most commonly used strategies. Denial, substance use, and religion, were the least common strategies in both arms.
| Brief COPE | REACT arm | RD-only arm | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (n = 399) | 12 weeks (n = 228) | 24 weeks (n = 244) | Baseline (n = 401) | 12 weeks (n = 263) | 24 weeks (n = 265) | Baseline (n = 800) | 12 weeks (n = 491) | 24 weeks (n = 508) | |
| Self-distraction | |||||||||
| Median (IQR) | 5 (4–6) | 5 (4–6) | 5 (4–6) | 5 (4–7) | 5 (4–6) | 5 (4–6) | 5 (4–6) | 5 (4–6) | 5 (4–6) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.3654 | 0.9350 | |||||||
| Active coping | |||||||||
| Median (IQR) | 5 (4–7) | 6 (4–7) | 5 (4–6) | 6 (4–7) | 5 (4–7) | 5 (4–6) | 5 (4–7) | 5 (4–7) | 5 (4–6) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.6969 | 0.8700 | |||||||
| Denial | |||||||||
| Median (IQR) | 2 (2–3) | 2 (2–3) | 2 (2–2) | 2 (2–3) | 2 (2 -2) | 2 (2–2) | 2 (2–3) | 2 (2–3) | 2 (2–2) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 7 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.2837 | 0.7378 | |||||||
| Substance use | |||||||||
| Median (IQR) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.8157 | 0.4303 | |||||||
| Use of emotional support | |||||||||
| Median (IQR) | 4 (3–5) | 4 (3–6) | 4 (3–6) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.0028 | 0.3877 | |||||||
| Use of instrumental support | |||||||||
| Median (IQR) | 4 (3–6) | 4 (3.5–6) | 4 (3–5) | 4 (3–6) | 4 (3–5) | 4 (3–5) | 4 (3–6) | 4 (3–6) | 4 (3–5) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.0559 | 0.9637 | |||||||
| Behavioural disengagement | |||||||||
| Median (IQR) | 3 (2–4) | 2 (2–4) | 2 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 2 (2–4) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.3561 | 0.2335 | |||||||
| Venting | |||||||||
| Median (IQR) | 4 (3–5) | 3.5 (3–4) | 4 (3–5) | 4 (3–5) | 3 (3–5) | 3 (3–4) | 4 (3–5) | 3 (3–4) | 3 (3–4) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.5816 | 0.3243 | |||||||
| Positive reframing | |||||||||
| Median (IQR) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.5805 | 0.3890 | |||||||
| Planning | |||||||||
| Median (IQR) | 6 (4–8) | 6 (4–7) | 5 (4–7) | 6 (4–7) | 6 (4–7) | 5 (4–7) | 6 (4–7) | 6 (4–7) | 5 (4–7) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.6936 | 0.9400 | |||||||
| Humour | |||||||||
| Median (IQR) | 3 (2–4) | 2 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 2 (2–4) | 3 (2–4) | 3 (2–4) | 2 (2–4) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.1743 | 0.9358 | |||||||
| Acceptance | |||||||||
| Median (IQR) | 6 (5–7) | 6 (5–7) | 6 (5–7) | 6 (5–7) | 6 (5–8) | 6 (5–7) | 6 (5–7) | 6 (5–7) | 6 (5–7) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.4409 | 0.4331 | |||||||
| Religion | |||||||||
| Median (IQR) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) | 2 (2–4) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.4568 | 0.2450 | |||||||
| Self-blame | |||||||||
| Median (IQR) | 4 (3–6) | 4 (3–5) | 4 (3–5) | 4 (3–6) | 4 (3–5) | 4 (2–5) | 4 (3–6) | 4 (3–5) | 4 (3–5) |
| Minimum, maximum | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 | 2, 8 |
| Mann–Whitney U-test p-value | 0.3386 | 0.6988 | |||||||
Multivariate ANCOVA was used to assess the impact of intervention arm on each of these subscales, at 12 weeks and 24 weeks, while taking into account correlation between the subscales. The results of the MANOVA and ANCOVA tables for each subscale at each timepoint are shown in Report Supplementary Material 1. The p-values for all the tests are non-significant, indicating no evidence of a difference that is significant at the p = 0.05 level between randomised arms for one or more of the outcomes at either time point.
Instrumental variable regression, with the interaction between randomised arm and baseline score of the mediator as the instrument, was performed to assess whether or not the 24-week mediator score was a predictor of the 24-week GHQ-28 score. These were found to be weak instruments; therefore, causal mediation analysis was instead performed to estimate the ACME of GHQ-28 score at 24 weeks. None of the putative mediators had a significant mediation effect on outcome. Details of the analysis are in Report Supplementary Material 1, section 6.6.9.
Additional analyses
The following analyses were conducted in addition to the testing of our main trial hypotheses, which were prespecified in the published statistical analysis plan.
Impact of baseline factors on intervention effect
When each baseline variable was added to the model separately (see Report Supplementary Material 1), the variables of gender, marital status, education level and employment status each had a statistically significant effect on the 24-week GHQ-28 score (adjusting for baseline GHQ-28 score and treatment). For the multivariable analysis, a stepwise selection process was performed to determine the significant predictors of outcome that should be included in the final model (using p-value criteria of 0.05 for entry and 0.1 for removal). When controlling for baseline GHQ-28 scores, gender, marital status and employment were all significant predictors of GHQ-28 scores, but treatment arm was not. Being male, single and unemployed (or in unpaid work) were all associated with greater levels of distress. There was no significant impact of a treatment–mother interaction. Full details of the analysis are set out in Report Supplementary Material 1, section 6.6.10.
Impact of ‘lurking’ on the REACT forum
Users were defined as participants who left at least one comment on the forum in the 24 weeks of follow-up. ‘Lurkers’ accessed the forum but left no comments. Non-users did not access the forum. Those in the RD-only arm were all classed as non-users. Table 19 gives the proportion of participants in each category.
| Status | Trial arm, n (%) | Overall (n = 700), n (%) | |
|---|---|---|---|
| REACT (n = 348) | RD (n = 352) | ||
| Non-users | 141 (41) | 352 (100) | 493 (70.4) |
| ‘Lurkers’ | 140 (40) | 0 (0) | 140 (20.0) |
| Users | 67 (19) | 0 (0) | 67 (9.6) |
| Total | 348 (100) | 352 (100) | 700 (100) |
In the absence of an additional instrument (other than randomisation), it was not possible to employ IV regression to assess the impact of ‘lurking’ versus non-use versus use of the forum. Therefore, a three-way (non-users vs. ‘lurkers’ vs. users) ordinary least squares regression model was employed, adjusting for baseline covariates. Users were estimated to have lower GHQ-28 scores at 24 weeks than non-users (–2.0, 95% CI –5.9 to 1.9) and lurkers to have a similar effect size to non-users (–0.1, 95% CI –3.2 to 2.9), but with no evidence of a significant difference for this covariate (p = 0.5949). However, an assessment of this model using binary comparisons suggested that the effect size estimated in the three-way ordinary least squares model might be conservative and that the true effect might be larger than estimated (see Report Supplementary Material 1, section 6.6.8.1.3).
Adverse events
During the trial, 363 participants received a low-risk response (an automated e-mail sent in response to a report of distress, but with no threat to self or others) and 185 participants had more than one. No high-risk events (serious adverse events) were reported. The trial manager identified three low-risk events, all of which were in the RD-only arm. The REACT supporters reported 16 low-risk events (eight forum posts, five direct messages and three in e-mail correspondence from people outside the intervention). Table 20 shows the number of participants scoring a low-risk item in each arm, and across each time point.
| Baseline, n (%) | 12 weeks, n (%) | 24 weeks, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| REACT arm (n = 399) | RD-only arm (n = 401) | Overall (n = 800) | REACT arm (n = 399) | RD-only arm (n = 401) | Overall (n = 800) | REACT arm (n = 399) | RD-only arm (n = 401) | Overall (n = 800) | |
| Participants with at least one red flag | 156 (39.1) | 139 (34.7) | 295 (36.9) | 51 (12.8) | 52 (13.0) | 103 (12.9) | 49 (12.3) | 57 (14.2) | 106 (13.3) |
| GHQ-28 (D3) | 22 (5.5) | 24 (6.0) | 46 (5.8) | 10 (2.5) | 12 (3.0) | 22 (2.8) | 11 (2.8) | 11 (2.7) | 22 (2.8) |
| GHQ-28 (D4) | 14 (3.5) | 19 (4.7) | 33 (4.1) | 4 (1.0) | 9 (2.2) | 13 (1.6) | 6 (1.5) | 7 (1.7) | 13 (1.6) |
| GHQ-28 (D6) | 27 (6.8) | 25 (6.2) | 52 (6.5) | 11 (2.8) | 11 (2.7) | 22 (2.8) | 12 (3.0) | 9 (2.2) | 21 (2.6) |
| GHQ-28 (D7) | 19 (4.8) | 18 (4.5) | 37 (4.6) | 5 (1.3) | 7 (1.7) | 12 (1.5) | 11 (2.8) | 8 (2.0) | 19 (2.4) |
| CWS Questionnaire Q29 | 58 (14.5) | 54 (13.5) | 112 (14.0) | 14 (3.5) | 12 (3.0) | 26 (3.3) | 6 (1.5) | 19 (4.7) | 25 (3.1) |
| CWS Questionnaire Q30 | 111 (27.8) | 100 (24.9) | 211 (26.4) | 26 (6.5) | 35 (8.7) | 61 (7.6) | 30 (7.5) | 41 (10.2) | 71 (8.9) |
Chapter 5 Health economic analysis
Introduction
This chapter presents the health economic analysis of REACT: a within-trial incremental cost-effectiveness analysis of using REACT and the RD compared with access to the RD only. Both interventions were offered in addition to TAU.
In accordance with NICE guidance,135 our analysis adopted an NHS and Personal Social Services perspective. Costs for REACT and the RD were considered, as well as costs related to health care provided in a hospital setting, primary care, community health, emergency services, Personal Social Services and community mental health services. For health outcomes, relatives’ distress was assessed using the GHQ-28, and quality of life was assessed using a generic measure of health-related quality of life: the EuroQol-5 Dimensions, five-level version (EQ-5D-5L). Intervention costs were measured with a microcosting approach. Results were also presented for the societal perspective, including relatives’ time off work due to their caring role.
In addition, we also reported the burden to carers as time spent in caring role, using data about participants’ unpaid hours spent looking after their relatives and time off work due to their caring role.
Information about the use of medicines was also collected, but, owing to errors in the data collection process that resulted in data about the length of time each medicine was used for, these data could not be included in the analyses.
All costs are presented in Great British pounds using 2018 available costs.
Aims and objectives
The aim of the health economic analysis was to determine the cost-effectiveness of TAU plus REACT and the RD in reducing distress for relatives, compared with TAU and access to only the RD. The specific objectives were to determine:
-
the cost of delivering TAU plus REACT plus the RD, compared with NHS and productivity cost savings in the use of health services, and paid work adapted from the Client Service Receipt Inventory (CSRI)
-
cost-effectiveness – the cost of significant unit changes (defined as 3-point reduction) in the primary outcome (GHQ-28 score)
-
cost–utility – the marginal cost of any marginal change in quality-adjusted life-years (QALYs), measured by the EQ-5D-5L.
Method: costs
Information about the trial design, setting, participants, recruitment, randomisation, data collection and effectiveness outcomes are reported in Chapter 3. Following NICE guidance,135 the economic analysis was undertaken from an NHS and Personal Social Services perspective. Costs of real-world delivery in the trial were used. A microcosting approach136 was undertaken to value REACT and the RD.
Costs of REACT and the RD were calculated separately. Health-care and Personal Social Services use, and health outcomes, including a generic measure of health and well-being (GHQ-28) and a generic health-related quality-of-life outcome (EQ-5D-5L), were assessed online.
REACT intervention cost
The REACT intervention cost included the following components:
-
cost of developing the intervention
-
cost of delivering the intervention
-
cost of recruiting participants
Development costs
REACT was developed over many years, first in a paper version and subsequently adapted for the online version used in this trial. We assessed all costs relevant to content development, including the initial paper version. Development costs included:
-
conception and design of the toolkit
-
consultation with service users, relatives and professionals to identify user requirements
-
staff time to develop content
-
production of videos and images
-
design and development of the website
-
website infrastructure during development.
The most significant cost was the research and academic staff time incurred throughout the conception and design of the toolkit. The time spent by each person in each development activity was estimated. Detailed records and a retrospective analysis of invoices allowed us to assess the various activities and costs incurred.
The second substantive cost lay in employing an external web design company to build the REACT website. Other substantive costs included costs related to domain name registration, SSL certification fees, web hosting and exclusive Internet Protocol (IP) address during development. All these were obtained from invoices and receipts.
Costs associated with the development of the intervention could be considered as ‘sunk costs’, as they had already been incurred but were impossible to recover; previous researchers have taken this approach. 137 However, we decided to follow a more conservative approach by including them in the analysis.
The REACT delivery costs
Delivery of REACT was described in Chapter 2. Related costs included general infrastructure for hosting the REACT website and the costs of training, supervision and employment of REACT supporters for 6 months.
The most significant costs related to the REACT supporters’ time spent on each clinical task (forum posts, direct messages, supervision and other activities), which we derived from staff time sheets. The second most significant cost was associated with supporter training.
Hourly rates for staff were obtained from national pay scales, with additional costs calculated for superannuation and national insurance, or from invoices when the staff involved were not directly employed by Lancaster University. Costs of relatives’ contributions to toolkit delivery were obtained from invoices. Reimbursement was based on organisational policy at the time of activity.
Other costs in this phase related to web hosting, IP address, software used to send automated e-mails to participants and technical maintenance to keep the website working properly; all these costs were obtained from invoices and receipts. These activities are required for regular maintenance and delivery of REACT.
Costs related to training, supervision, and employment of REACT supporters are for 6 months and 400 participants, based on the maximum number of people who were supported at any one time; this was considered to be at or near capacity for the number of REACT supporters employed. Costs of the infrastructure are also for 6 months, divided equally between the two arms of the trial (intervention and comparator), as both arms used equal amounts of infrastructure.
Recruitment costs
Recruitment of participants was necessary to deliver the intervention. As participants were relatives or carers of people with psychosis or BD – not the service users themselves – social media and the internet were used to disseminate information. Online adverts on Facebook, Google and Bipolar UK were the most successful in recruiting participants, but there were also costs related to offline recruitment, such as printing flyers and leaflets. These recruitment methods would be unnecessary were the intervention to be delivered through the NHS in routine practice, but some method of referring relatives to the intervention would still be needed. We decided to use available data on costs incurred, in line with our in-trial analytical approach, rather than hypothetical data on costs of an NHS model of referral to the intervention. Total recruitment costs were divided by the number of people who completed eligibility screening for the trial (n = 3287).
Resource directory (comparator arm) costs
Participants in the control arm were given access only to the online RD. Costs associated with the development and delivery of the directory included time spent in developing materials and infrastructure costs of domain registration and web hosting. There were also costs to supporters editing and updating RD content during the trial. As for REACT, staff and relative costs were calculated from the product of time spent on development and delivery by cost per unit of time.
Considerably less time was spent on developing the RD than on developing REACT. Some of the REACT supporter time was allocated to updating the RD in both arms of the trial.
Costs of health care and Personal Social Services
Participants were asked about their use of a wide range of health-care and social services; this information was collected at baseline and at the 12- and 24-week follow-ups. Data collected at baseline referred to the 12 weeks before entering the trial; data collected at each of the follow-up points covered the previous 12 weeks of the trial.
Participants self-reported their use of health-care services, Personal Social Services and medicines, using a CSRI developed for this trial. Data collected covered the use of hospital services such as accident and emergency (A&E), general hospital, community hospital, day hospital, outpatient visits and clinics based at hospital sites. For primary and community services, participants were asked about their use of ambulance services, community matrons, community or district nurses, GPs, practice nurses and specialist nurses. Questions focused on the type of contact (home, clinic/office or telephone), number of contacts and duration.
Personal Social Services use was identified through questions about the number and duration of home, clinic/office or telephone contacts with social workers or care managers, home care or home help workers, private home helps or cleaners, or respite care.
Another set of questions covered community mental health services: psychiatrist/psychogeriatrician, community psychiatric nurse or community mental health nurse and other mental health professionals. Once again, people were asked the number and duration of home, clinic/office or telephone contacts.
Participants were also asked about the number and duration of face-to-face and telephone contacts with other community-based services they might have used in the previous 12 weeks.
Use of activities such as day care, lunch clubs and social clubs was collected. Participants were asked about use, number of contacts per week, total number of contacts over the previous 12 weeks and how the service was paid for (i.e. by the participant, NHS trust, charity, social services or other).
Participants were asked about their use of any voluntary or third-sector support services and given the opportunity to select from a list > 40 organisations, including Anxiety UK, Bipolar UK, Big White Wall and Samaritans. Questions were asked about the number and duration of contacts in the previous 12 weeks and if those had been face to face, by telephone or online.
The last group of questions was about use of medications. Participants were asked whether or not they had taken any medication in the previous 12 weeks and, if so, the name, dose, frequency and duration of use.
Service use was costed by applying national average unit costs, obtained from Unit Costs of Health and Social Care 2017,138 NHS reference costs139 or other sources, as appropriate (Table 21). The unit costs used included overheads, capital and infrastructure costs, allocated according to staff time. The average distance or time for home visits was not available; it was decided to use 10 minutes per visit based on the estimates made in the Unit Costs of Health and Social Care 2017. 138 Travel expenses were not accounted for.
| Resource | Cost (£) | Unit | Source |
|---|---|---|---|
| A&E | 160.00 | Attendance | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, table 2 (p. 5) |
| General hospital inpatient | 3894.00 | Admission | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, table 2 (p. 5) |
| Community hospital inpatient | 3894.00 | Admission | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, table 2 (p. 5) |
| Day hospital | 742.00 | Admission | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, table 2 (p. 5) |
| Outpatient services | 125.00 | Appointment | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, table 2 (p. 5) |
| Paramedic (ambulance service) | 98.00 | Service | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, AMB |
| Ambulance calls | 7.00 | Calls | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, table 6 (p. 9) |
| Specialist nursing, active case management (community matrons), adult, face to face | 99.00 | Contact | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, N06AN |
| Specialist nursing, active case management (community matrons), adult, non-face to face | 45.00 | Contact | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, AMB |
| District nurse, adult, face to face | 38.00 | Contact | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, N02AF |
| District nurse, adult, non-face to face | 19.00 | Contact | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, N02AN |
| Practice nurse | 36.00 | Hour | Unit Costs of Health and Social Care 2017,138 table 2, (p. 117) |
| Specialist nurse (respiratory, diabetes, cardiac or other) | 62.00 | Hour | Unit Costs of Health and Social Care 2017138 (cost per working hour) |
| Occupational therapist, adult, one to one | 81.31 | Contact | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, A06A1 |
| Physiotherapist, adult, one to one | 57.26 | Contact | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, A08AG |
| GP | 183.00 | Hour | Unit Costs of Health and Social Care 2017,138 10.3b GP (p. 162) |
| Social worker or care manager | 43.00 | Hour | Unit Costs of Health and Social Care 2017,138 11.2 social worker (adult services) (p. 174) |
| Home care/home help worker | 21.00 | Hour | Unit Costs of Health and Social Care 2017,138 11.6 home care worker, (p. 178) |
| Private home help/cleaner | 12.50 | Hour | Market price |
| Psychiatrist/psychogeriatrician | 108.00 | Hour | Unit Costs of Health and Social Care 2017,138 consultant psychiatric |
| Community psychiatric nurse/community mental health nurse | 62.00 | Hour | Unit Costs of Health and Social Care 2017,138 10.1 nurses (p. 159) |
| Other mental health professional, please specify | 39.00 | Hour | Unit Costs of Health and Social Care 2017,138 12.2 community mental health team for adults with mental health problems (p. 186) |
| Day care – voluntary organisation | 34.00 | Per client attendance | Unit Costs of Health and Social Care 2017,138 2.4 private and voluntary sector day care (p. 46) |
| Day care – NHS (community based) | 104.00 | Contact | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, DCF30 |
| Dentist | 127.00 | Hour | Unit Costs of Health and Social Care 2017,138 10.5 NHS dentist – performer only (p. 165) |
| Optician | 25.00 | Appointment | Boots UK Ltd (Nottingham, UK) |
| Mental health care clusters initial assessments | 307.00 | Assessment | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, table 3 (p. 6) |
| IAPT | 353.00 | Episode | National Schedule of Reference Costs 2017/18,139 NHS trusts and NHS foundation trusts, IAPTMHCC |
The unit cost of inpatient episodes covered only elective inpatient admissions. Unit costs of A&E visits included admitted and non-admitted patients. Information about clinical tests was not collected; therefore, it is not considered in the analysis.
Health outcomes
Two health outcomes were used in the analysis: GHQ-28 score and QALYs derived from the EQ-5D-5L. Both measures were collected at baseline and at 12 and 24 weeks.
The EQ-5D-5L sets out five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression), each with five levels: no problems, slight problems, moderate problems, severe problems and extreme problems. The tariff for the UK population140 was used to compute the index score, with a range of –0.285 (worst health) to 1 (perfect health).
From EQ-5D-5L data collected at baseline and at 12 and 24 weeks, the respective index scores were computed based on the results of Devlin et al. 140 To calculate the QALYs gained by the intervention index, scores for baseline and week 24 were divided by number of weeks in 1 year (365.25 ÷ 7) and multiplied by 12 to match the time horizon of 24 weeks (the interpolation method).
The GHQ-28 is described in Chapter 3.
Carers’ productivity losses
Carers were asked at baseline and at weeks 12 and 24 to report any additional time off work due to their caring role, with a recall period of 12 weeks.
Burden of disease on carers: time spent in caring role
Carers were asked at baseline and at weeks 12 and 24 about the number of unpaid hours spent looking after their relative each week, with a recall period of 12 weeks. For the same recall period, they were asked to report any additional time off work due to their caring role.
Methods: analysis
A health economics analysis plan was developed and approved by the TMG before the analysis began (see Report Supplementary Material 2).
Analysis of the intervention costs
The costs of developing and delivering REACT and the RD were calculated separately. Half of the costs of developing and delivering the RD were allocated to the intervention arm and half were allocated to the comparator arm, reflecting the trial design of TAU plus REACT plus the RD versus TAU plus the RD only. This meant that the total cost for development and delivery of REACT without the RD was divided by 400 (number of participants in the intervention arm), whereas total cost of the RD was divided by 800, to obtain an average per participant cost for each. Infrastructure costs were divided by 800 to reflect the total number of trial participants, and divided between the intervention and comparator arms.
Recruitment costs were calculated over the total trial period and divided by 3287 (the number of people who completed eligibility screening for the trial). Cost included an average per participant in both arms of the trial, as both required recruitment.
All costs were computed for a 6-month period, which was the length of time that each participant took part in the trial.
Missing data
The EQ-5D-5L data sets obtained at baseline and at weeks 12 and 24 were used in the primary analysis. The imputation of missing values was based on age, gender and baseline EQ-5D-5L scores. We implemented a multiple imputation by chained equations system. 141 This involves first imputing each variable and then deleting the imputed values for the first variable and replacing them with values imputed from a regression, using as independent variables all remaining imputed ones. Subsequently, we deleted the imputed values for the second variable and replaced them with the values imputed from a regression controlling for the remaining variables. This process was repeated iteratively. The estimation process used predictive mean matching with five ‘nearest neighbours’ over 50 imputations by treatment arm. As the percentage of missing data was, at worst, 50%, we calculated 50 imputed values for each observation. Multiple imputation for missing data was undertaken for the total cost of the use of hospital services at baseline and at weeks 12 and 24, and for the EQ-5D-5L at weeks 12 and at 24. Further to this, we undertook an analysis using the chained equation imputation combined with a seemingly unrelated regression model method. 141 This method takes into account the possible correlation between the error terms in the two equations (the QALYs and the costs) and can bring efficiency gains compared with ordinary least squares when estimating QALYs and costs adjusting for a different set of variables.
Cost–utility analysis
Each EQ-5D-5L index score was converted to QALYs to perform a cost–utility analysis. QALYs were calculated over the duration of the trial.
The ICER was calculated by determining the difference in the mean cost per participant in the two arms of the trial, and dividing this difference by the mean difference in QALYs (Equation 1). The total cost per participant in the REACT arm comprised the costs of developing and delivering REACT with the RD plus recruitment costs plus the cost of health-care and Personal Social Services use. The total cost per participant in the RD arm comprised the cost of developing and delivering the RD plus the cost of health-care and Personal Social Services use:
We performed both unadjusted and adjusted estimations. A linear model was fitted with the 24-week outcome as the dependent variable, adjusting for the baseline outcome. The differences in the mean 24-week costs and outcomes were estimated based on the model. In the adjusted model, we controlled for age, gender and utility at baseline in the QALY equation, and only for age and gender in the costs model. This is because the utility is likely to be influenced by age, gender and its baseline value. Health-care use is influenced by age and gender.
To address the uncertainty present in the results obtained for the differences in mean costs and outcomes at 24 weeks, the non-parametric bootstrapping technique was employed. A total of 1000 bootstrapped samples were created and the total costs and outcomes estimated from each. The results from bootstrap resampling were used to construct 95% CIs for incremental costs and incremental QALYs. Those results were also used to plot the cost-effectiveness plane and cost-effectiveness acceptability curve (CEAC) to show the uncertainty surrounding conclusions (see Figures 7–10).
Sensitivity analyses
The use of modelling can introduce uncertainty around the assumptions used, such as the health states described and data sources selected. We tested the robustness of the ICER by also undertaking a complete-case analysis as a secondary analysis, as this uses alternative assumptions from those informing the multiple imputation.
Valuing carers’ productivity losses
A value was ascribed to the mean time taken off work by carers using the average (median) hourly pay in 2017. 142
Valuing burden of disease on carers: time spent in caring role
The mean numbers of hours lost by carers at baseline and at weeks 12 and 24 in the REACT and the RD arms were valued according to the latest average hourly pay published data. 142 The t-test for independent samples was used to assess differences reported at each time by participants in the REACT and RD arms. The t-test for paired samples was used to assess differences between baseline and week 24 in each arm.
Results
Costs
Development costs of REACT
The largest development cost for REACT was £22,599 for staffing (Table 22), covering time spent by three professors of clinical psychology, one professor of psychiatry, two experienced clinical psychologists, two research assistants and one research fellow.
| Type of cost | Total number of hours or units | Cost (£) per hour or unit | Total cost (£) |
|---|---|---|---|
| Content generation | 5574.40 | ||
| Staff | 3699.40 | ||
| Professor of clinical psychology | 54 hours | 55.81 | 3013.74 |
| Clinical psychologist | 17 hours | 29.66 | 504.22 |
| Research assistant | 18 hours | 10.08 | 181.44 |
| Relatives | 1875.00 | ||
| Relative co-applicant | 29 hours | 20.00 | 580.00 |
| Relatives in focus groups and advisory role | 118 hours | 10.00 | 1180 |
| Relatives travelling | 23 persons | 5.00 | 115.00 |
| Producing videos and images | 18,422.78 | ||
| Staff | 14,326.13 | ||
| Research fellow | 450 hours | 23.76 | 10,692 |
| Research assistant | 157.5 hours | 15.83 | 2493.23 |
| Information officer | 37.5 hours | 30.43 | 1141.13 |
| Communications and information manager | 56.25 hours | 31.36 | 1764.00 |
| Actors | 2112.65 | ||
| Relatives | 11 persons | 20.00 per person | 220.00 |
| Developing and designing the website | 12,499.59 | ||
| Staff | 10,901.11 | ||
| Professor of clinical psychology | 36 hours | 55.81 | 2009.16 |
| Professor of clinical psychology | 26 hours | 69.80 | 1814.80 |
| Professor of psychiatry | 26 hours | 68.00 | 1768.00 |
| Research assistant | 10 hours | 12.29 | 122.90 |
| Digital technologist/web developer | 225 hours | 23.05 | 5186.25 |
| Relatives | 1598.48 | ||
| Relatives’ focus groups | 56 hours | 20.00 | 1120.00 |
| Other relatives | 8 hours | 59.81 | 478.48 |
| Website infrastructure during development (until going live) | 28,039.00 | ||
| Domain name | 9.00 | ||
| SSL certificate fees | 30.00 | ||
| Web hosting and exclusive IP address | 100.00 | ||
| Website development | 27,900.00 | ||
| Total | 64,535.99 | ||
The total costs for the information officer, communications and information manager and web developer were £8091, including time spent designing the website, filming, editing and post-processing videos and managing the content. The actors hired for the website videos cost £2112. These actors worked closely with relatives whose own involvement in the design cost £3693.
The costs associated with website infrastructure during development, including domain name, SSL certificate fees, web hosting and exclusive IP address, and costs related to the private website developer were slightly higher than £28,000. The total development costs were £64,535.99.
Delivery costs of REACT
We calculated the delivery costs for the 6 months the intervention lasted per individual (Table 23). Costs associated with website infrastructure totalled £5119. The cost of employing REACT supporters (based on the 400 participants recruited to the trial) was £14,178; training was close to £4500 and supervision cost £2135. The recruitment costs totalled £12,635; the costliest component related to the advertisements.
| Type of costs | Total number of hours or units | Cost (£) per hour or unit | Total cost (£) |
|---|---|---|---|
| General infrastructure for hosting REACT | 5119.00 | ||
| Digital technology/web developer | 180 hours | 23.05 | 4149.00 |
| Secure web hosting and exclusive IP address | 6 months | 100.00 | 600.00 |
| Software for bulk e-mails | 2 blocks | 185.00 | 370.00 |
| Training, supervision and employment (6 months) of REACT supporters | 20,813.05 | ||
| REACT supporters | 756 hours | 15.83 | 11,967.48 |
| Back-up REACT supporter | 94 hours | 13.52 | 1270.88 |
| Expert relative REACT supporter | 47 hours | 20.00 | 940.00 |
| Supervision | 33 hours | 64.71 | 2135.52 |
| In-house training | 224.75 hours | 18.33 | 4119.17 |
| External training | 380.00 | ||
| Recruitment | 12,635.56 | ||
| Advertisements (Facebook, Google and Bipolar UK) | 11,059.56 | ||
| Printing | 1526.00 | ||
| Flyers and postage | 50.00 | ||
| Total | 38,567.61 | ||
Total development and operating costs of REACT to the end of the trial period came to £103,103.60.
Average costs were calculated as follows:
-
total development costs – 800 users (total number of trial participants)
-
general website infrastructure costs – 800 users (total number of trial participants)
-
REACT supporter costs – 400 users (number of participants in the REACT arm)
-
recruitment costs – 3287 users (number that initiated a registration in the REACT website).
This gives an average cost of £142.95 per participant in the REACT arm. (Note that, if we cost delivery only, the cost is £62.27 per relative.)
Resource directory costs
Participants in the comparator arm were given access to the RD. Development and delivery costs were therefore divided by the 800 participants in both arms of the trial, calculated for the 6 months of each participant’s involvement (Table 24). The most significant component related to staff (£530). The average participant cost was £0.84. (Note that delivery only would require the infrastructure and REACT supporter time, and would cost £0.43 per participant.)
| Type of costs | Total number of hours or units | Cost (£) per hour or unit | Total cost (£) |
|---|---|---|---|
| Development costs | 463.50 | ||
| Staff | 324.50 | ||
| Research assistant | 20 hours | 10.08 | 201.60 |
| Research assistant | 10 hours | 12.29 | 122.90 |
| Infrastructure | 139.00 | ||
| Domain name | 1 | 9.00 | 9.00 |
| SSL certificate fees | 1 | 30.00 | 30.00 |
| Web hosting and exclusive IP address | 1 | 100.00 | 100.00 |
| Delivery costs | 205.79 | ||
| REACT supporter | 13 hours | 15.83 | 205.79 |
| Total | 669.29 | ||
Use of hospital and Personal Social Services
Our starting point was a crude analysis of the number of visits to and users of hospital services; primary care, community health and emergency services; community mental health services; and other community-based services at baseline and at 12 and 24 weeks (Tables 25–28). This showed, as expected, that hospital admissions were the type of service least used by carers, with a significant decrease from week 12 onwards, and outpatient visits at hospital sites were the most used in both arms. As for primary care, community health and emergency services, there was a decrease in the quantity of services used over time; however, at 24 weeks, the participants in the REACT arm were using more services than the participants in the control arm. As perhaps could be expected, the most used service by participants in the REACT arm at baseline was GP services. This was followed by ambulance services (both face-to-face and telephone contacts). The control arm had a different usage pattern at baseline. GP visits were still the most used service, followed by specialist nurse services, face-to-face ambulance services and occupational therapists. At 24 weeks, GP services was clearly the most used service by both arms.
| Hospital service | Baseline | 12 weeks | 24 weeks | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |||||||
| Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | |
| A&E visits | 63 | 44 | 87 | 51 | 18 | 14 | 22 | 16 | 23 | 16 | 25 | 20 |
| General hospital inpatient days | 55 | 20 | 162 | 26 | 4 | 3 | 9 | 5 | 80 | 12 | 9 | 7 |
| Community hospital inpatient days | 42 | 2 | 40 | 4 | 30 | 3 | 0 | 0 | 33 | 3 | 1 | 1 |
| Day hospital | 25 | 18 | 44 | 24 | 19 | 9 | 15 | 11 | 17 | 10 | 34 | 17 |
| Outpatient visits at hospital site | 266 | 115 | 298 | 110 | 128 | 57 | 159 | 68 | 170 | 67 | 159 | 58 |
| Other | 118 | 37 | 180 | 57 | 78 | 28 | 80 | 29 | 65 | 19 | 51 | 22 |
| Service | Baseline | 12 weeks | 24 weeks | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |||||||
| Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | |
| Paramedic (ambulance service – face to face) | 47 | 10 | 92 | 11 | 10 | 4 | 2 | 1 | 0 | 12 | 4 | |
| Paramedic (ambulance service – telephone) | 39 | 4 | 4 | 2 | 0 | 0 | 0 | 0 | ||||
| Community matron (telephone) | 1 | 1 | 0 | 0 | 0 | 0 | 0 | |||||
| Community/district/practice nurse (face to face) | 15 | 4 | 59 | 6 | 0 | 66 | 3 | 7 | 1 | 3 | 1 | |
| Community/district/practice nurse (telephone) | 0 | 10 | 3 | 0 | 3 | 2 | 5 | 2 | 0 | |||
| Specialist nurse (face to face) | 27 | 4 | 96 | 9 | 10 | 3 | 8 | 2 | 24 | 2 | 7 | 1 |
| Specialist nurse (telephone) | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | ||||
| Occupational therapist | 0 | 83 | 3 | 0 | 6 | 2 | 0 | 1 | 2 | 1 | ||
| Physiotherapist | 10 | 5 | 22 | 5 | 13 | 3 | 29 | 4 | 29 | 4 | 19 | 3 |
| GP | 309 | 67 | 267 | 47 | 213 | 52 | 154 | 42 | 151 | 38 | 89 | 26 |
| Community mental health service | Baseline | 12 weeks | 24 weeks | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |||||||
| Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | |
| Psychiatrist/psychogeriatrician | 21 | 21 | 16 | 16 | 11 | 11 | 5 | 5 | 7 | 7 | 6 | 6 |
| Community psychiatric nurse or community mental health nurse | 32 | 31 | 19 | 18 | 12 | 12 | 23 | 23 | 14 | 14 | 16 | 16 |
| Other mental health professional | 28 | 24 | 29 | 29 | 15 | 14 | 10 | 10 | 12 | 12 | 18 | 18 |
| Other community-based service | Baseline | 12 weeks | 24 weeks | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |||||||
| Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | Quantity (n) | Users (n) | |
| Dentist | 19 | 19 | 9 | 9 | 10 | 10 | 14 | 14 | 6 | 6 | 14 | 14 |
| Optician | 2 | 2 | 5 | 5 | 1 | 1 | 1 | 1 | 3 | 3 | 2 | 2 |
Community mental health services were used at baseline by more participants in the REACT arm than in the control arm. However, there was a reduction throughout the duration of the trial: by week 24, participants in the control arm were using more services provided by community psychiatric or mental health nurses or other mental health-care professionals. Dental services were used more than opticians, and there was a shift in the pattern of use. More participants in the REACT arm were using these services at baseline; however, at week 24, more participants in the control arm were using these services.
We then calculated the mean frequency of use of hospital services; primary care, community health and emergency services; community mental health services; and other community-based services at each time point (Tables 29–32). At baseline, all but one participant had complete data. Around 40% of data were missing at 12 and 24 weeks.
| Hospital service | Baseline | 12 weeks | 24 weeks | |||
|---|---|---|---|---|---|---|
| REACT arm (n = 398) | RD-only arm (n = 401) | REACT arm (n = 233) | RD-only arm (n = 267) | REACT arm (n = 245) | RD-only arm (n = 268) | |
| A&E | 0.16 (0.534) | 0.22 (0.735) | 0.08 (0.326) | 0.08 (0.348) | 0.09 (0.389) | 0.09 (0.390) |
| General hospital inpatient days | 0.14 (1.237) | 0.40 (4.886) | 0.02 (0.160) | 0.03 (0.292) | 0.33 (3.197) | 0.03 (0.218) |
| Community hospital inpatient days | 0.11 (1.788) | 0.10 (1.707) | 0.13 (1.836) | 0.00 (–) | 0.13 (1.438) | 0.00 (0.061) |
| Day hospital | 0.06 (0.307) | 0.11 (0.581) | 0.08 (0.593) | 0.06 (0.301) | 0.07 (0.394) | 0.13 (0.749) |
| Outpatient visits at hospital site | 0.67 (1.487) | 0.74 (1.994) | 0.55 (1.447) | 0.60 (1.304) | 0.69 (0.112) | 0.59 (1.650) |
| Other | 0.30 (1.433) | 0.45 (1.64) | 0.33 (1.306) | 0.30 (1.095) | 0.27 (1.581) | 0.19 (0.782) |
| Service | Baseline | 12 weeks | 24 weeks | |||
|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |
| Paramedic (ambulance service – face to face) | 0.12 (0.89) | 0.24 (2.10) | 0.04 (0.34) | 0.01 (0.12) | 0.05 (0.43) | |
| Paramedic (ambulance service – telephone) | 0.13 (1.9) | 0.01 (0.18) | ||||
| Community matron (telephone) | ||||||
| Community/district/practice nurse (face to face) | 0.04 (0.49) | 0.15 (1.43) | 0.26 (3.76) | 0.03 (0.46) | 0.01 (0.18) | |
| Community/district/practice nurse (telephone) | 0.03 (0.33) | 0.01 (0.15) | 0.02 (0.25) | |||
| Specialist nurse (face to face) | 0.07 (0.76) | 0.25 (2.37) | 0.04 (0.44) | 0.03 (0.36) | 0.10 (1.44) | 0.03 (0.43) |
| Specialist nurse (telephone) | 0.005 (0.07) | 0.005 (0.07) | ||||
| Occupational therapist | 0.21 (3.64) | 0.02 (0.27) | 0.004 (0.06) | 0.01 (0.12) | ||
| Physiotherapist | 0.03 (0.22) | 0.06 (0.52) | 0.06 (0.65) | 0.11 (0.98) | 0.12 (1.21) | 0.07 (0.75) |
| GP | 0.78 (2.81) | 0.67 (3.53) | 0.93 (2.98) | 0.58 (2.05) | 0.62 (2.75) | 0.33 (1.17) |
| Community mental health service | Baseline | 12 weeks | 24 weeks | |||
|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |
| Psychiatrist or psychogeriatrician | 0.06 (0.23) | 0.04 (0.20) | 0.05 (0.21) | 0.02 (0.14) | 0.03 (0.17) | 0.02 (0.15) |
| Community psychiatric nurse or community mental health nurse | 0.09 (0.29) | 0.05 (0.23) | 0.05 (0.22) | 0.09 (0.28) | 0.06 (0.23) | 0.06 (0.24) |
| Other mental health professional | 0.07 (0.31) | 0.08 (0.27) | 0.07 (0.27) | 0.04 (0.19) | 0.05 (0.22) | 0.07 (0.25) |
| Other community-based service | Baseline | 12 weeks | 24 weeks | |||
|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |
| Dentist | 0.06 (0.23) | 0.03 (0.16) | 0.05 (0.22) | 0.06 (0.23) | 0.03 (0.17) | 0.06 (0.24) |
| Optician | 0.01 (0.08) | 0.01 (0.12) | 0.01 (0.07) | 0.004 (0.06) | 0.01 (0.12) | 0.01 (0.09) |
Overall use of health services was very low and highly skewed, with a very small number of participants reporting very high levels of service use. At least one participant in each arm reported at least one visit per week to an outpatient clinic. At baseline, the mean use of outpatient clinics was slightly higher in the control arm.
For the intervention arm, the mean use increased slightly for all hospital services except A&E from baseline to week 24. However, in the control arm, we observed a decrease in the use of all types of hospital service, except day hospital services, over the same period. For all other services, the mean values were very small at all time points, the exception being the mean value of GP visits. Participants in the intervention arm used more GP services than participants in the control arm.
There was no information to report about the use of Personal Social Services or the use of other community-based services, with the exception of dentist and optician services. For all other services, too few participants reported any use, and, when use was reported, the information about the number of times the service was accessed was often missing. Furthermore, it proved almost impossible to identify which services provided by the voluntary or third sector were paid for by the NHS and which were paid for by Personal Social Services. Many of these services were registered charities, and so were likely to be funded by a whole range of government grants, donations and other sources of income, with funding changing over time. Furthermore, the levels of use were not accurately recorded. Therefore, these data were not included in the analysis.
Costs of health services and Personal Social Services used
We applied the unit costs in Table 21 to the service use reported in Table 25 to calculate the cost of hospital and social services (presented in Tables 33–36). Given the diversity of services reported in the ‘other’ category, these were not included. For some items, we observed very large SDs, consistent with the reported use patterns (many participants reported no use of health-care services and some participants reported very high use of such services).
| Hospital service | Baseline | 12 weeks | 24 weeks | |||
|---|---|---|---|---|---|---|
| REACT arm (n = 398) | RD-only arm (n = 401) | REACT arm (n = 233) | RD-only arm (n = 267) | REACT arm (n = 245) | RD-only arm (n = 268) | |
| A&E | 25.33 (85.37) | 34.71 (117.61) | 12.36 (52.11) | 13.18 (55.66) | 15.02 (62.17) | 14.93 (62.44) |
| General hospital inpatient days | 207.15 (1854.16) | 605.58 (7324.68) | 25.73 (239.68) | 50.52 (437.87) | 489.47 (4792.33) | 50.34 (326.90) |
| Community hospital inpatient days | 158.19 (2680.63) | 149.53 (2559.33) | 193.01 (2752.34) | N/A | 201.91 (2155.58) | 5.59 (91.57) |
| Day hospital | 46.61 (227.83) | 81.42 (431.34) | 60.51 (439.65) | 41.69 (223.61) | 51.49 (292.13) | 94.13 (555.57) |
| Outpatient visits at hospital site | 83.54 (185.92) | 92.89 (249.26) | 68.67 (180.86) | 74.44 (163.00) | 86.84 (220.06) | 74.16 (206.22) |
| Service | Baseline | 12 weeks | 24 weeks | |||
|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |
| Paramedic (ambulance service – face to face) | 12.03 (87.31) | 23.12 (205.73) | 4.32 (32.96) | 0.77 (12.25) | 4.47 (41.71) | |
| Paramedic (ambulance service – telephone) | 0.90 (13.33) | 0.09 (1.25) | ||||
| Community matron (telephone) | 0.13 (2.41) | |||||
| Community/district/practice nurse (face to face) | 1.49 (18.69) | 5.73 (54.50) | 9.80 (142.84) | 1.13 (17.32) | 0.43 (7.03) | |
| Community/district/practice nurse (telephone) | 0.61 (6.25) | 0.26 (2.85) | 0.45 (4.73) | |||
| Specialist nurse (face to face) | 6.98 (75.66) | 24.37 (234.17) | 4.38 (43.56) | 3.09 (36.02) | 142.31 (10.07) | 2.63 (42.73) |
| Specialist nurse (telephone) | 0.20 (3.02) | 0.22 (3.11) | ||||
| Occupational therapist | 17.00 (296.10) | 1.83 (22.26) | 0.33 (5.22) | 0.61 (9.97) | ||
| Physiotherapist | 1.45 (12.84) | 3.17 (29.73) | 3.24 (37.13) | 6.24 (56.04) | 6.83 (69.01) | 4.09 (42.74) |
| GP | 29.98 (119.26) | 34.02 (284.29) | 47.77 (276.44) | 32.82 (283.00) | 21.78 (129.00) | 10.69 (41.00) |
| Community mental health service | Baseline | 12 weeks | 24 weeks | |||
|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |
| Psychiatrist or psychogeriatrician | 3.04 (12.46) | 2.34 (11.00) | 2.59 (11.57) | 1.02 (7.35) | 1.57 (9.09) | 1.23 (8.06) |
| Community psychiatric nurse or community mental health nurse | 2.66 (8.99) | 1.59 (7.22) | 1.62 (6.92) | 2.68 (8.73) | 1.80 (7.26) | 1.88 (7.41) |
| Other mental health professional | 1.46 (6.05) | 1.52 (5.24) | 1.28 (5.17) | 0.73 (3.72) | 0.97 (4.25) | 1.32 (4.92) |
| Other community-based service | Baseline | 12 weeks | 24 weeks | |||
|---|---|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | REACT arm | RD-only arm | |
| Dentist | 2.46 (9.92) | 1.13 (6.85) | 2.23 (9.48) | 2.48 (9.96) | 1.23 (7.14) | 2.52 (10.04) |
| Optician | 0.15 (1.95) | 0.37 (3.03) | 0.13 (1.81) | 0.10 (1.62) | 0.36 (3.00) | 0.21 (2.30) |
Costs related to general hospital admissions were the largest component, as is usual in this type of analysis, followed by the cost of admissions to community hospitals. The total average costs decreased for the participants in the control arm and increased for participants in the intervention arm between baseline and week 24.
The other category with meaningful costs is primary care, community health and emergency services. At baseline, the most relevant costs for the participants in the REACT arm were the ones associated with GP services and face-to-face ambulance services. For the participants in the control arm, the costs incurred with GP services were closely followed by those with specialist nurses, face-to-face paramedic services and occupational therapists. At 12 weeks, for both arms, the most significant costs were associated with GP services. However, at 24 weeks, only specialist nurse costs were relevant for the participants in the REACT arm.
The mean costs of observed cases for community mental health services and other community-based services can be considered negligible for both arms. All data are provided in Report Supplementary Material 3.
Health-related quality of life
EuroQol-5 Dimensions, five-level version
At baseline, the mean EQ-5D-5L index score was lower for the REACT intervention arm than for the control arm (Table 37). However, by 24 weeks, participants in the REACT arm reported higher EQ-5D-5L index scores (indicating better health). However, none of the differences was statistically significant.
| Time point | REACT arm | RD-only arm | ||
|---|---|---|---|---|
| Mean (SD) score | Participants (n) | Mean (SD) score | Participants (n) | |
| Baseline | 0.757 (0.211) | 399 | 0.764 (0.191) | 401 |
| 12 weeks | 0.795 (0.185) | 235 | 0.788 (0.180) | 273 |
| 24 weeks | 0.799 (0.187) | 247 | 0.792 (0.184) | 270 |
Primary outcome
Results for outcomes and incremental costs and effectiveness based on imputed data sets are presented in Tables 38–40 as means with standard errors (SEs). Except at baseline, the mean costs were always higher for the intervention arm (Table 38). Overall, participants in the intervention arm had higher costs than participants in the control arm, but the difference was not statistically significant. Incremental costs, adjusted for participants’ baseline age and gender, came to £286.77 (95% CI –£858.81 to £1432.36; p = 0.624).
| Cost | Trial arm (£) | |
|---|---|---|
| REACT | RD only | |
| Mean intervention cost | 142.95 | 0.84 |
| Baseline, mean (SE) | 651.29 (116.37) | 1263.70 (402.50) |
| 12 weeks, mean (SE) | 681.61 (110.48) | 505.41 (27.55) |
| 24 weeks, mean (SE) | 998.72 (209.77) | 450.14 (41.13) |
| Total mean cost | 2474.57 | 2220.09 |
| Mean unadjusted incremental cost | 254.47 | |
| Incremental cost adjusted for age and gender, mean (95% CI) | 286.77 (–858.81 to 1432.36) | |
At baseline, estimated GHQ-28 scores were similar in the control arm and in the intervention arm. At 12 and 24 weeks, GHQ-28 scores were lower in the intervention arm.
The incremental GHQ-28 score over the 24 weeks of the trial, unadjusted, was –1.067. Adjusted for baseline GHQ-28 score, it was –1.160 (95% CI –3.371 to 1.051), indicating that participants in the intervention arm were more likely to have a lower GHQ-28 score than participants in the control arm; however, the difference was very small and not statistically significant (p = 0.304). Further adjusting GHQ-28 scores for age and gender, the difference between arms decreased slightly, to –1.152 (95% CI –3.370 to 1.065), but was still small and not significant (p = 0.308).
In terms of GHQ-28 scores, the REACT intervention was costlier and more effective than the RD only (Table 39), suggesting that REACT users had a marginally better outcome than RD users. However, the 95% CI for costs and GHQ-28 scores include zero, making this conclusion uncertain. For a reduction of 3 points in the GHQ-28 score, an additional £746.80 per relative had to be spent (calculated as if the cost per –1.152 is £286.77; thus, a reduction of 3 points corresponds to £746.80).
| GHQ-28 | Trial arm | |
|---|---|---|
| REACT | RD only | |
| Baseline score, mean (SE) | 40.25 (0.5145) | 40.05 (0.4942) |
| 12-week score, mean (SE) | 31.27 (0.4882) | 32.80 (0.4882) |
| 24-week score, mean (SE) | 30.36 (0.5123) | 31.43 (0.4844) |
| Mean unadjusted incremental score | –1.067 | |
| Incremental score adjusted for baseline score, mean (SE) | –1.160 (1.127) | |
| Incremental score adjusted for baseline score, age and gender, mean (95% CI) | –1.152 (–3.370 to 1.065) | |
Estimated EQ-5D-5L scores (Table 40) were always higher in the control arm than in the intervention arm.
| EQ-5D-5L and QALY | REACT arm | RD-only arm |
|---|---|---|
| EQ-5D-5L index score, mean (SE) | ||
| Baseline | 0.7570 (0.2113) | 0.7637 (0.1908) |
| 12 weeks | 0.7743 (0.1886) | 0.7849 (0.1676) |
| 24 weeks | 0.7812 (0.1890) | 0.7925 (0.1666) |
| Mean QALYs | ||
| QALYs 12 weeks | 0.176 | 0.178 |
| QALYs 24 weeks | 0.179 | 0.181 |
| Total QALYs | 0.355 | 0.359 |
| Mean incremental QALYs | ||
| Unadjusted | –0.0045 | |
| Adjusted for baseline EQ-5D-5L index score | –0.0021 | |
| Adjusted for baseline EQ-5D-5L index score, age and gender, mean (95% CI) | –0.0024 (–0.0088 to 0.0039) | |
The incremental QALY over the 24 weeks of the trial, unadjusted, was –0.0045. Adjusted for baseline EQ-5D-5L score, it was –0.0021 (95% CI –0.0084 to 0.0042), indicating that participants in the intervention arm were more likely to have lower QALY gains than participants in the control arm; however, the difference was very small and not statistically significant (p = 0.517). Further adjusting QALYs for age and gender, the difference between arms increased slightly, to –0.0024 (95% CI –0.0088 to 0.0039), but was still small and not significant (p = 0.448).
In terms of EQ-5D-5L scores, the REACT intervention was costlier and less effective than the RD only (Table 41), suggesting that REACT users had health-related quality-of-life losses at extra cost compared with RD users. However, the 95% CI for costs and QALYs include zero, making this conclusion uncertain.
| Cost and QALY | Mean (95% CI) |
|---|---|
| Incremental cost (£) adjusted for baseline age and gender | 286.77 (–858.81 to 1432.36) |
| Incremental QALYs adjusted for baseline EQ-5D-5L score, age and gender | –0.0024 (–0.0088 to 0.0039) |
| ΔCost/ΔQALY | Intervention dominated by control as being costlier and less effective |
The cost-effectiveness plane (Figure 7) illustrated this point: the uncertainty surrounding the point estimates of the incremental costs and incremental QALYs from the primary analysis was important, with the majority of the distribution scattered in the northern quadrants of the plane, supporting the conclusion that the intervention was costlier. The magnitude of the incremental QALYs was rather small.
FIGURE 7.
Cost-effectiveness plane, intervention arm vs. control arm.
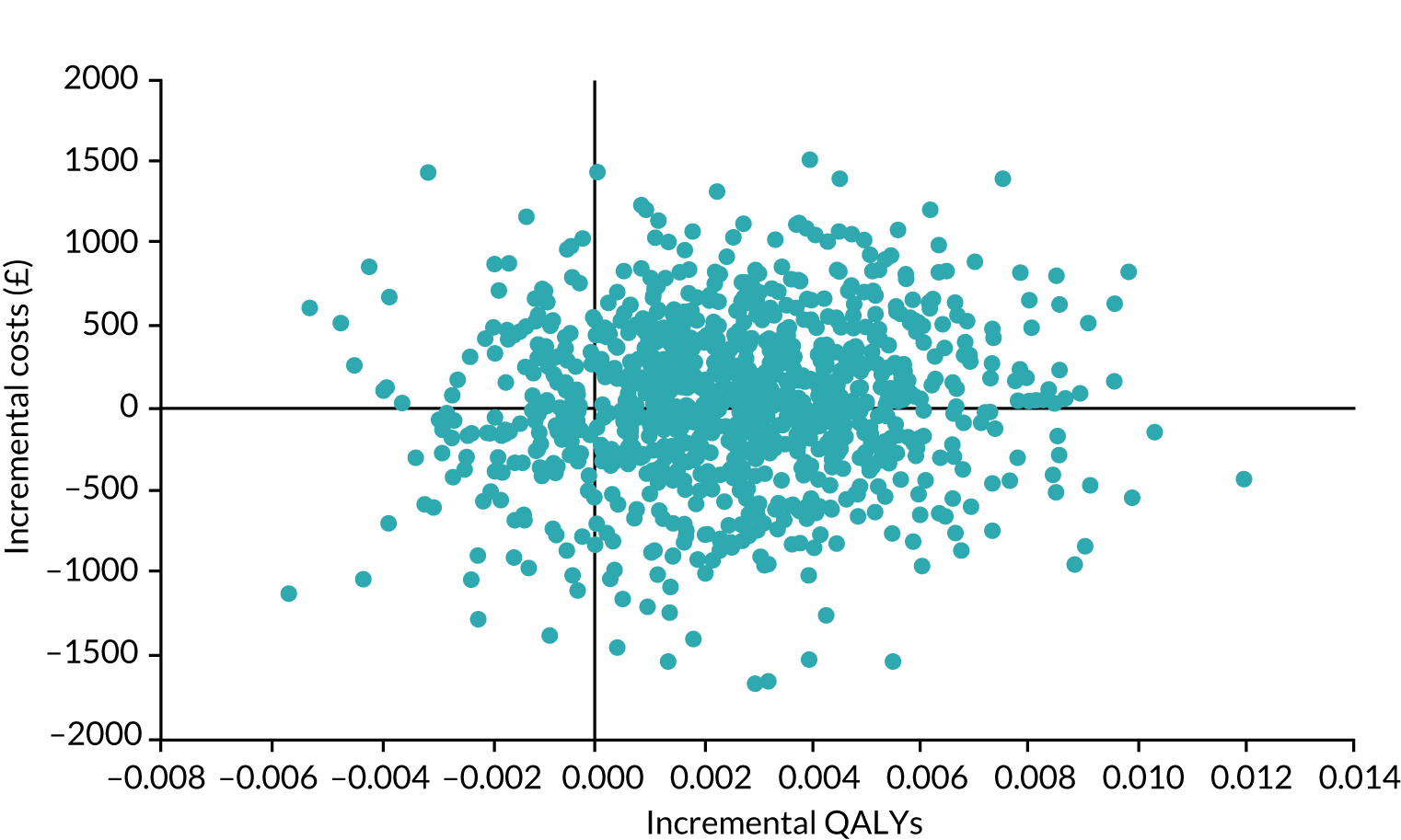
The CEAC (Figure 8) was constructed using the bootstrapped data and showed that the probability that REACT was cost-effective within the existing willingness-to-pay threshold of £20,000–30,000 was ≈50% when compared with the RD.
FIGURE 8.
The CEAC for the intervention.
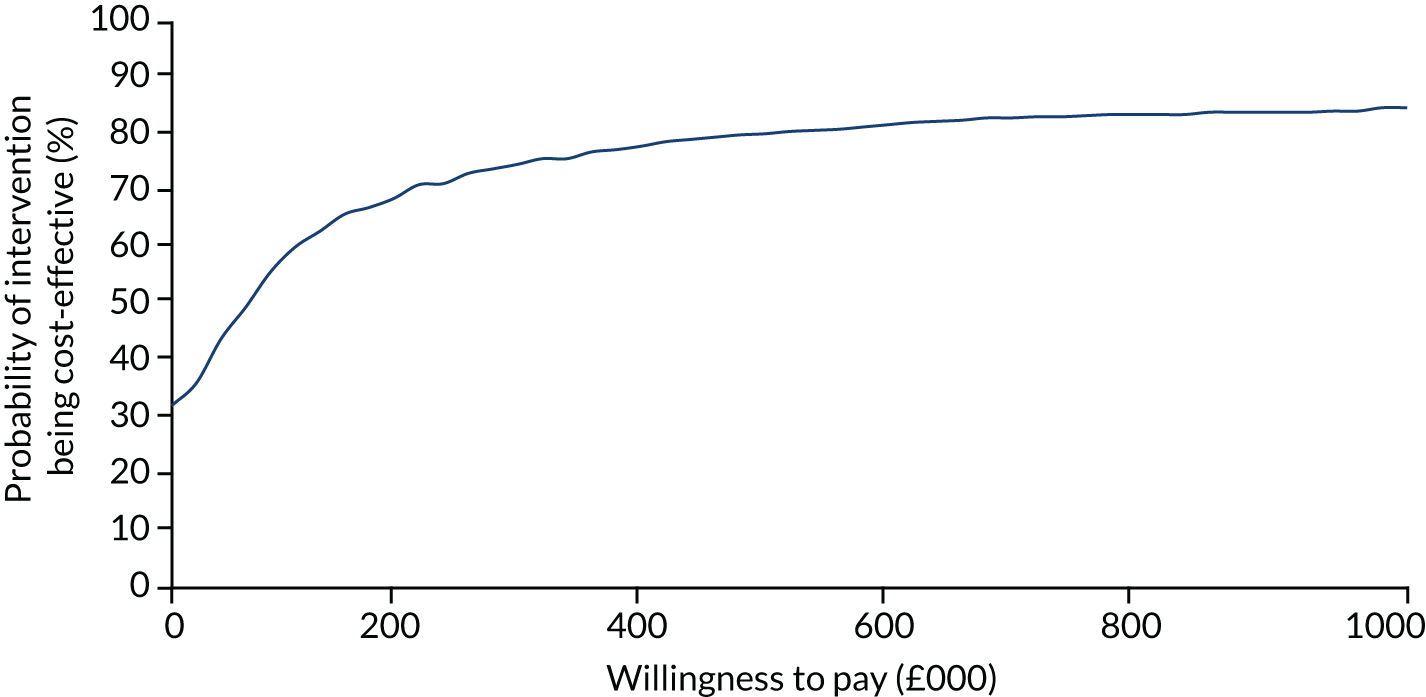
Societal perspective
The societal perspective was added to the health and social services analysis to assess productivity losses associated with the caring role of the relatives. To account for those losses, we considered the number of hours people currently working had to take off work because of their caring roles.
The EQ-5D-5L scores were the same as those estimated for the NHS and Personal Social Services perspective. In this section, we added to the costs estimated for the health and Personal Social Services perspective the costs associated with productivity losses of those in work.
The pattern observed for costs in the societal perspective (Tables 42 and 43) was similar to that observed for complete cases in the REACT arm: increasing costs from baseline to week 24. In the control arm, the opposite behaviour was observed: costs decreased from baseline to week 24. Costs reported by participants in the REACT arm were higher than the costs reported by participants in the RD-only arm, as expected; however, the adjusted incremental costs were similar to the ones observed in the NHS and Personal Social Services perspective, at £309.93 (95% CI –£861.04 to £1480.90), but were not statistically significant.
| Cost | Trial arm (£) | |
|---|---|---|
| REACT | RD only | |
| Costs (£) | ||
| Mean intervention cost | 142.95 | 0.84 |
| Baseline, mean (SE) | 891.52 (167.60) | 1507.46 (403.24) |
| 12 weeks, mean (SE) | 909.81 (110.76) | 734.61 (28.01) |
| 24 weeks, mean (SE) | 1243.32 (211.15) | 662.96 (40.94) |
| Total cost | 3187.60 | 2905.86 |
| Incremental costs | ||
| Unadjusted incremental costs | 281.73 | |
| Adjusted incremental costs for age and gender, mean (95% CI) | 309.93 (–861.04 to 1480.90) | |
| Cost and QALY | Mean (95% CI) |
|---|---|
| Incremental cost (£) adjusted for age and gender | 309.93 (–861.04 to 1480.90) |
| Incremental QALYs adjusted for baseline EQ-5D-5L index score, age and gender | –0.0026 (–0.0089 to 0.0037) |
| ΔCost/ΔQALY | Intervention dominated by control as being costlier and less effective |
Figures 9 and 10 present the cost-effectiveness plane and CEAC for the societal perspective using imputed cases. It is clear from the distribution of the dots in the cost-effectiveness plane that the intervention can be costlier and less effective than the control.
FIGURE 9.
Cost-effectiveness plane, intervention arm vs. control arm (imputed cases, societal perspective).
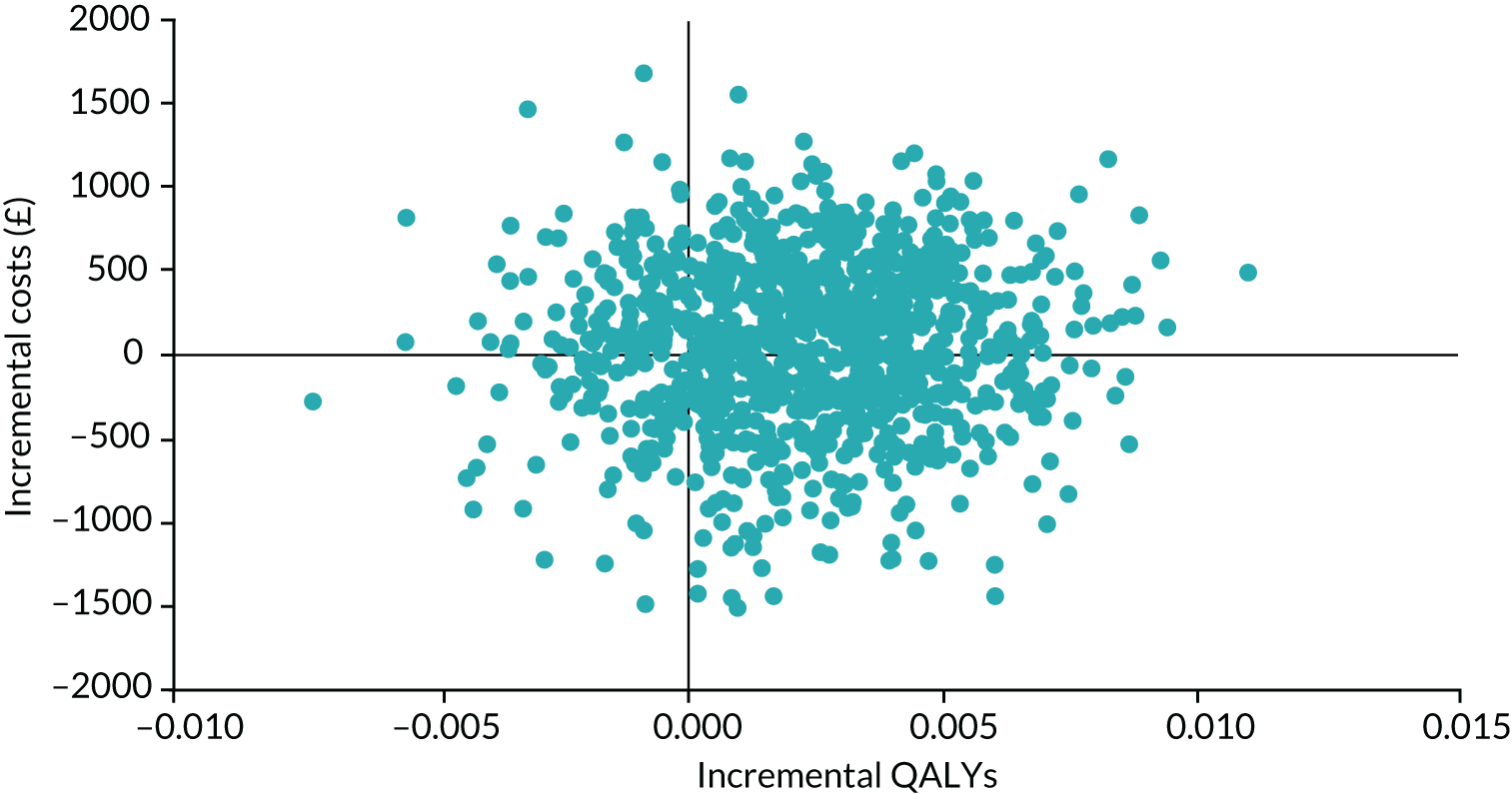
FIGURE 10.
The CEAC for the intervention (imputed cases, societal perspective).
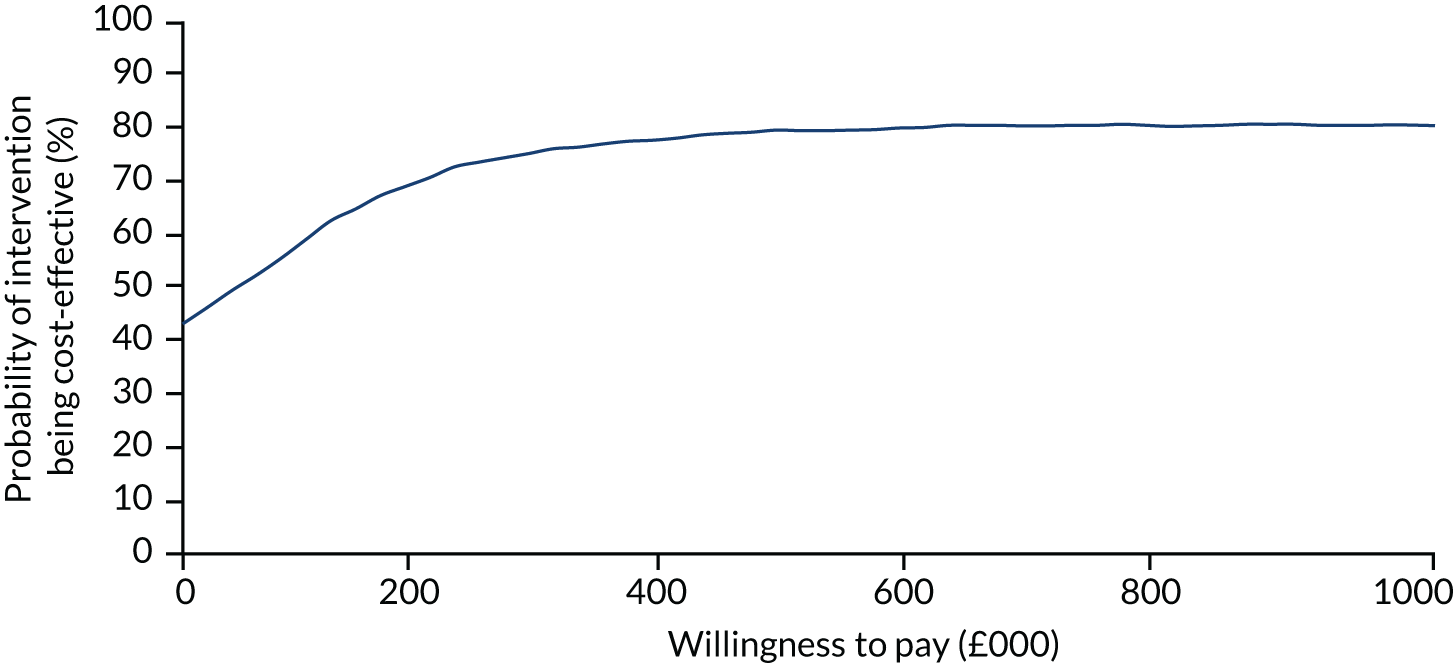
The probability of the intervention being cost-effective (see Figure 10) was similar to what had been estimated from imputed data in the NHS and Personal Social Services perspective. The probability of the intervention being cost-effective at £20,000 was 46%.
Sensitivity analysis
Complete-case analysis
The extent of completeness varied for the outcomes used in the primary analysis (Table 44). We considered complete cases to be participants who had information for all three data points.
| Trial arm | ||
|---|---|---|
| REACT | RD only | |
| Total costs (n participants) | 196 | 236 |
| EQ-5D-5L (n participants) | 197 | 238 |
The EQ-5D-5L was completed at all three time points by 193 participants in the REACT arm and 233 participants in the control arm (Table 45). The REACT participants who completed the EQ-5D-5L at all three time points had higher mean scores at all three time points than the REACT participants who did not complete the EQ-5D-5L at all three time points. This difference was not seen in the RD-only arm, where index score values were similar.
| EQ-5D-5L index scores and QALYs | REACT (n = 193) | RD only (n = 233) |
|---|---|---|
| EQ-5D-5L index score, mean (SD) | ||
| Baseline | 0.781 (0.186) | 0.764 (0.196) |
| 12 weeks | 0.797 (0.181) | 0.788 (0.185) |
| 24 weeks | 0.806 (0.182) | 0.793 (0.183) |
| QALYs, mean (SD) | ||
| QALYs 12 weeks | 0.182 (0.040) | 0.178 (0.040) |
| QALYs 24 weeks | 0.184 (0.040) | 0.182 (0.040) |
| Total QALYs | 0.366 (0.078) | 0.361 (0.079) |
| Incremental QALYs | ||
| Unadjusted (mean) | 0.0057 | |
| Adjusted for baseline EQ-5D-5L index score (mean) | –0.0011 | |
| Adjusted for baseline EQ-5D-5L index score, age and gender, mean (95% CI) | –0.0013 (–0.0079 to 0.0053) | |
The pattern observed for costs for complete cases (Tables 46 and 47) was different from that obtained with imputed cases. Costs reported by participants in the REACT arm were higher than the costs reported by participants in the RD-only arm, as expected, and the adjusted incremental costs were only somewhat higher than the costs observed for imputed cases, at £715.83 (95% CI –£328.48 to £1760.14).
| Trial arm (£) | ||
|---|---|---|
| REACT | RD only | |
| Costs, mean (SD) | ||
| Intervention cost | 142.95 | 0.84 |
| Baseline | 252.00 (587.92) | 613.52 (3675.92) |
| 12 weeks | 507.15 (3026.46) | 263.44 (681.02) |
| 24 weeks | 935.07 (5851.86) | 225.10 (553.60) |
| Total | 1837.17 | 1102.90 |
| Incremental costs | ||
| Unadjusted incremental costs | 734.27 | |
| Adjusted incremental costs for age and gender | 715.83 | |
| Cost and QALY | Mean (95% CI) |
|---|---|
| Incremental cost (£) adjusted for age and gender | 715.83 (–328.48 to 1760.14) |
| Incremental QALYs adjusted for baseline EQ-5D-5L index score, age and gender | –0.0013 (–0.0079 to 0.0053) |
| ΔCost/ΔQALY | Intervention dominated by control as being costlier and less effective |
The unadjusted incremental QALY gain was 0.0057 (95% CI –0.0091 to 0.02067; p = 0.447) when we compare the REACT participants with the RD-only participants. When we adjust for baseline EQ-5D-5L index score, age and gender, there is no difference between the arms.
Figures 11 and 12 present the cost-effectiveness plane and CEAC as for the primary analysis, but using only data from the 426 complete cases. It is clear from the distribution of the dots in the cost-effectiveness plane that the intervention can be costlier and less effective than the control.
FIGURE 11.
Cost-effectiveness plane, intervention arm vs. control arm (complete cases).
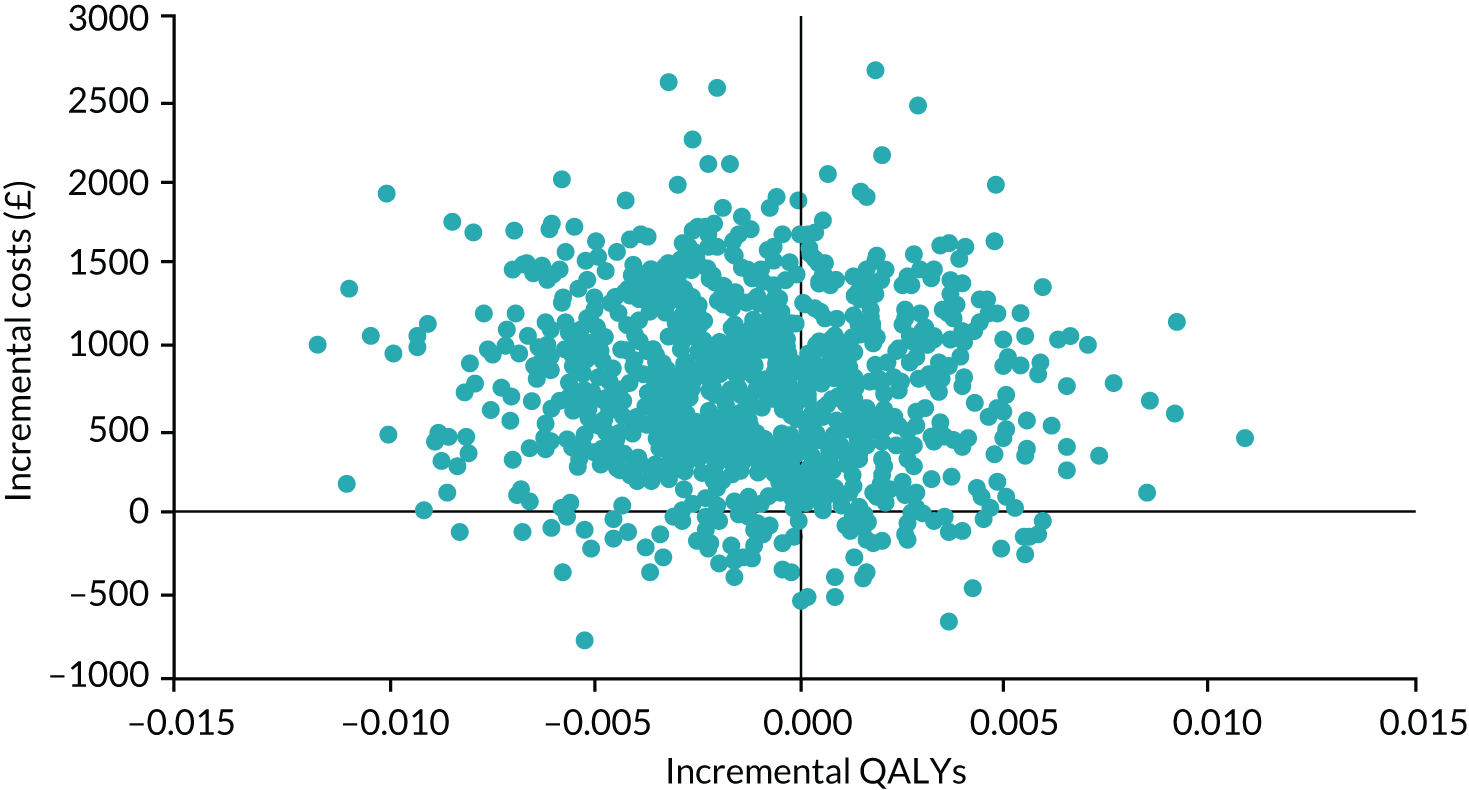
FIGURE 12.
The CEAC for the intervention (complete cases).
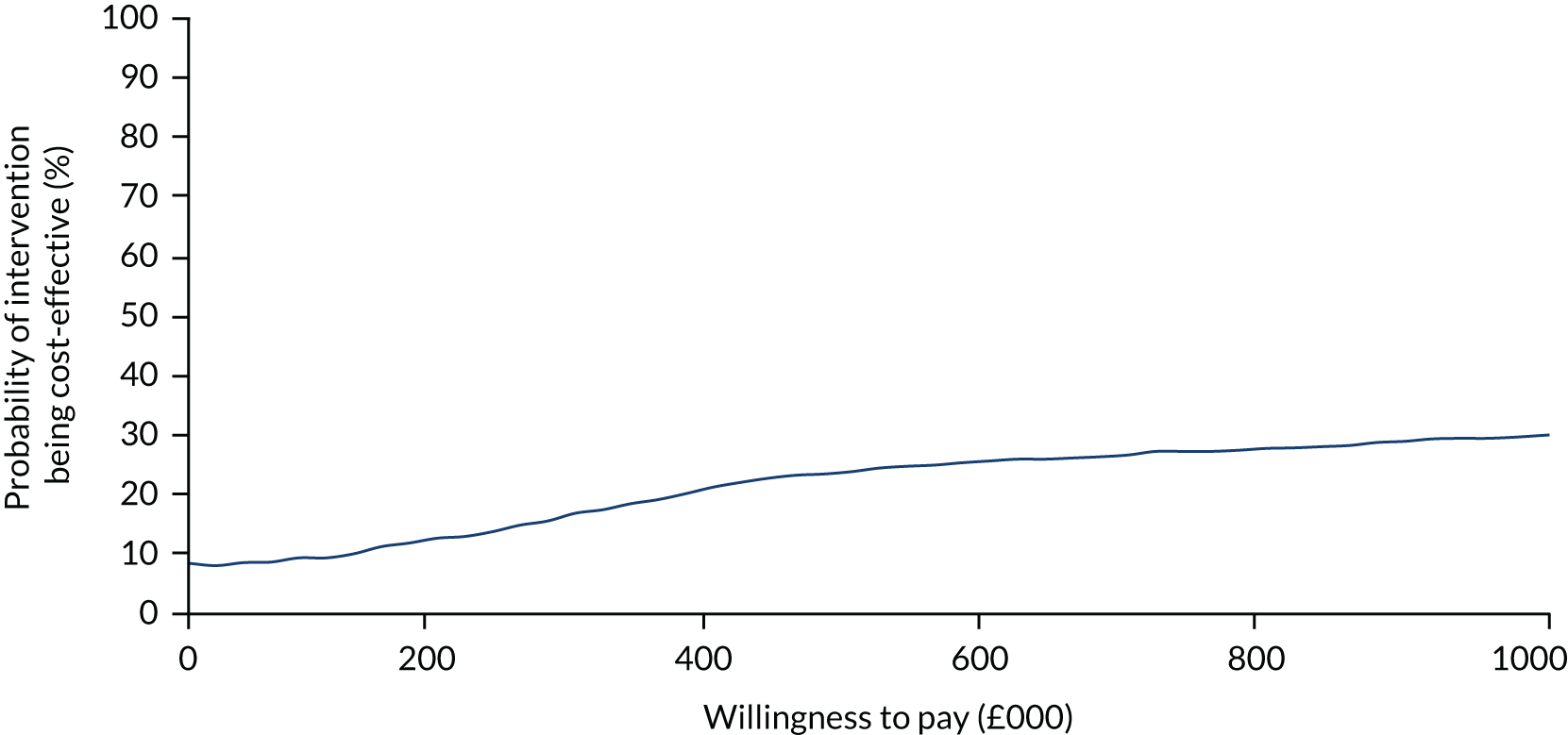
Taking this into account, it is not surprising that the probability of the intervention being cost-effective (see Figure 12) was much lower than estimated from imputed data. The probability of the intervention being cost-effective at £20,000 was only 8%.
Burden of disease on carers: time spent in caring role
In addition to the societal perspective, we considered it relevant to report on the burden of the disease to carers, based on the time spent in their caring role. It is widely accepted that carers’ income and work life are affected by their caring role. Participants in the trial were asked about the number of unpaid hours spent each week looking after their relative(s). The number of hours spent caring was higher than the typical 40-hour week of a full-time job. The number decreased in both arms during the trial (Table 48).
| Time point | REACT arm | RD-only arm | ||
|---|---|---|---|---|
| Participants (n) | Hours, mean (SD) | Participants (n) | Hours, mean (SD) | |
| Baseline | 399 | 43.92 (46.40) | 401 | 44.58 (45.77) |
| 12 weeks | 231 | 42.87 (47.63) | 266 | 45.17 (44.18) |
| 24 weeks | 243 | 41.00 (45.29) | 265 | 39.03 (41.59) |
Using a paired samples t-test, we observed that, for carers in the REACT arm (n = 243), the differences between the number of hours reported at baseline and at week 24 had no statistical significance (3.40 hours, 95% CI –1.272 to 8.063 hours; p = 0.153). However, for participants in the RD-only arm (n = 265), the decrease was greater and had statistical significance (5.14 hours, 95% CI 0.703 to 9.576 hours; p = 0.023).
Participants were also asked about time taken off work due to their caring role in the previous 12 weeks. The number of hours off work decreased in both arms from baseline to week 24 (Table 49).
| Time point | REACT arm | RD-only arm | ||
|---|---|---|---|---|
| Participants (n) | Hours, mean (SD) | Participants (n) | Hours, mean (SD) | |
| Baseline | 118 | 21.28 (15.81) | 117 | 21.49 (15.80) |
| 12 weeks | 63 | 19.71 (15.10) | 61 | 21.15 (17.93) |
| 24 weeks | 51 | 20.06 (14.72) | 46 | 19.17 (18.27) |
Differences between the arms were not statistically significant. The mean difference at baseline was 0.208 hours (95% CI –3.855 to 4.270 hours; p = 0.920) in favour of the REACT arm. At week 24, it was –0.88 hours (95% CI –7.543 to 5.773; p = 0.792) in favour of the RD-only arm.
Using a paired-samples t-test for the 29 participants reporting in the REACT arm, the mean change in the number of hours off work from baseline to week 24 was 0.448 (SD 13.45 hours, 95% CI –4.668 to 5.564 hours; p = 0.859), showing no statistical significance. For the 34 participants reporting in the RD-only arm, the mean change over the same period was 0.706 hours (SD 20.84 hours, 95% CI –6.567 to 7.979 hours; p = 0.845), which, again, was not statistically significant.
The number of hours was fairly constant over time, showing the impact on family life. By multiplying the average number of hours at each time point by the number of participants completing data for each arm, we reached a total of 9462.13 hours off work due to caring duties among the participants reporting in the trial. If we consider the average (median) hourly pay in 2017 was £11.31,142 we can estimate productivity losses of, potentially, > £100,000 in the 36-week period under analysis, for those providing data.
Across the whole trial sample from baseline to week 24, there was a reduction in the mean number of unpaid hours spent per week looking after a relative; this difference was statistically significant (Table 50). A reduction was also observed in the number of hours off work for caring in the previous 12 weeks, but without statistical significance.
| Time spent in caring role | Paired samples t-test for the difference | |||||
|---|---|---|---|---|---|---|
| n | Baseline, mean (SE) | Week 24, mean (SE) | Mean (SE) | 95% CI | p-value | |
| Number of unpaid hours spent per week looking after relative | 508 | 44.28 (2.02) | 39.97 (1.92) | 4.30 (1.63) | 1.10 to 7.51 | 0.009 |
| Number of hours off work due to caring role in the previous 12 weeks | 63 | 21.02 (1.63) | 20.43 (2.14) | 0.59 (2.23) | –3.87 to 5.04 | 0.793 |
Discussion
Main results
As set out in Aims and objectives, the health economic analysis sought to determine the costs and cost-effectiveness of the intervention using three measures:
-
cost of delivery versus NHS and productivity cost savings in use of health services and paid work
-
cost of significant unit changes (defined as a 3-point reduction) in the primary outcome (GHQ-28 score)
-
marginal cost of any marginal change in QALYs, measured using the EQ-5D-5L.
Cost of delivery versus NHS and productivity cost savings
REACT and the RD were inexpensive interventions, compared with face-to-face family support or pharmacological interventions attempting to address the same type of problems. REACT cost £142.95 per participant to design and deliver (£62.27 per participant for delivery only). The RD cost only £0.84 per participant to develop and deliver (£0.43 per participant for delivery only).
The overall use of health services and Personal Social Services was very low and highly skewed, with a very small number of participants reporting very high levels of service use. Participants in the intervention arm had higher costs than participants in the control arm.
This within-trial health economic analysis of NHS, health services and Personal Social Services outcomes found that REACT had higher costs of £286.77 (95% CI –£858.81 to £1432.36; p = 0.624), slightly better GHQ-28 scores (incremental GHQ-28 score adjusted for baseline GHQ-28 score, age and gender = –1.152, 95% CI –3.370 to 1.065) and slightly fewer QALYs (incremental QALYs adjusted for baseline EQ-5D-5L index score, age and gender = –0.0024, 95% CI –0.0088 to 0.0039), but none of these differences was statistically significant.
Cost of significant change in primary outcome (GHQ-28 score)
REACT (including the RD) added to TAU resulted in a decrease of –1.152 in GHQ-28 score, compared with the RD only added to TAU. This was at an additional cost of £286.77. Therefore, the cost of a reduction of 3 points in the GHQ-28 score would be £746.80 per relative.
Marginal cost of any marginal change in quality-adjusted life-years
REACT cost more money for poorer outcomes on the EQ-5D-5L. The probability that REACT was cost-effective at the existing willingness-to-pay threshold of £20,000–30,000 was ≈50%, when compared with the RD.
The results of the additional analysis of societal perspective (including time off paid work) were based on imputed data. The incremental total cost was in line with that observed for the NHS and social care perspective (£309.93, 95% CI –£861.04 to £1480.90), and the difference in health outcomes was slightly lower (–0.0026 QALYs, 95% CI –0.0089 to 0.0073). The probability of REACT being cost-effective for a willingness-to-pay threshold of £20,000 fell from 50% in the primary analysis to 46% in the societal perspective analysis. Once again, these analyses suggest that participants in the intervention arm incurred higher costs and experienced no better health outcomes, making it very unlikely that the intervention was cost-effective at a standard willingness-to-pay threshold of £20,000.
The results of the analysis of complete cases were more uncertain than those obtained in primary analysis, which were based on imputed data. The incremental total cost was much higher, but still not statistically significant (£715.83, 95% CI –£328.48 to £1760.14), and the difference in health outcomes was slightly lower but not statistically significant (–0.0013 QALYs, 95% CI –0.0079 to 0.0053). The probability of REACT being cost-effective for a threshold of £20,000 fell from 50% in the primary analysis to 8% in the complete-case analysis. Taken together, these analyses suggest that participants in the intervention arm incurred higher costs and experienced no better health outcomes, making it very unlikely that the intervention was cost-effective at a standard willingness-to-pay threshold of £20,000.
The burden of disease to carers, based on time spent in the caring role, is significant. This burden is not taken into account in NICE guidance135 but should perhaps be considered in a broader assessment of the burden of psychosis and BD on families. The data showed that, on average, among those participants reporting the information, carers spent 6 hours per day looking after their relative(s) and had taken 1.75 hours off work per week because of their caring role in the previous 12 weeks.
Strengths and limitations
The analysis was undertaken following NICE guidance,135 and used actual data on costs incurred in the development and delivery of the intervention and comparator and in the recruitment of participants. We adopted a very conservative approach to the costs of developing the intervention, and included these real data in the analysis, even though they might be considered ‘sunk costs’. We opted to do this as, otherwise, we would have needed to include maintenance and updating costs, which would have been hypothetical. However, this does mean that the estimates of costs associated with the intervention are at the upper end of plausibility. We collected and presented the costs of the individual, as recommended. 143 Using the NHS and Personal Social Services perspective, complete cases or the societal perspective, the results obtained were always in the same direction: that the intervention was more expensive than the alternative, and with negligible effects in terms of health-related quality of life.
The analysis has some weaknesses. As is common practice, we relied on self-reported data on health service use. 144,145 This may have been subject to recall bias. Because of problems in the data collection process, information about the use of medicines could not be used. However, given the consistent pattern across all the previous analyses, it is unlikely that adding the costs of medicines would materially alter the overall conclusion.
Fit with existing literature
This makes a significant addition to the literature on health economic analyses of DHIs, which, overall, remains scarce. A 2017 systematic review143 identified 39 health economic analyses of mHealth applications, but found that many did not report all the factors recommended by the Consolidated Health Economic Evaluation Reporting Standards checklist,146 and none of the reported interventions was in the field of mental health. We found one other study, reporting results of a DHI for carers of people with dementia,147 whose impact in terms of QALYs was similar to that obtained here. Our study is particularly important as it shows that a more complex DHI was no more effective in reducing distress (as measured using the GHQ-28) or improving quality of life, and probably less cost-effective, than a simple online RD that signposted users to existing sources of help.
Chapter 6 Relatives’ experiences of using REACT
Introduction
The main aim of the trial was to assess the clinical effectiveness and cost-effectiveness of REACT. However, we also wanted to understand participants’ experiences of REACT, how they interacted with the website and how both could be improved. Therefore, we conducted a qualitative study to understand relatives’ experiences of using REACT. The qualitative interviews explored how people experienced REACT, the factors that influenced their levels of use, which areas of the toolkit were most used and how people experienced the support offered via the forum and personal messaging.
Method
We conducted a qualitative study using thematic framework analysis to understand participants’ experiences of REACT, how they interacted with the website and how it could be improved. In addition to the formal qualitative interviews with participants described in this chapter, we also explored how people used the REACT forum and the types of topic covered; this was a preliminary analysis conducted during the trial. As per protocol, we are seeking additional funding to conduct further analysis on these data.
Sampling participants
Participants were drawn from a pool of 76 people who had:
-
been randomised to the intervention arm
-
already completed the 24-week follow-up
-
consented to be contacted about further research.
The aim was to recruit 20–25 participants and to ensure variation across the levels of REACT website use (high, low and mid). For the 76 potential participants, median web use was 207.98 minutes (range 1.43–12,476.3 minutes, IQR 55.54–564.78 minutes). Using the IQR, usage was classed as follows:
-
low use: ≤ 55.54 minutes
-
mid use: just over 55.54 minutes to just under 564.78 minutes
-
high use: ≥ 564.78 minutes.
Development of the topic guide
A topic guide for the interviews was developed by the REACT team, with input from relatives on the relevance and appropriateness of the questions [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/144934/#/ (accessed 28 October 2019)]. Open questions explored relatives’ general experiences of REACT, factors influencing levels of use, which parts of REACT were used, experience of support from the REACT supporters and any suggestions for improvements. Draft questions and prompts were shared with a REACT supporter, who offered feedback from a carer’s perspective. The interview schedule provided a flexible structure for each interview around the key domains of interest.
Procedure
Participants who had consented to being contacted for further research as part of the REACT trial were e-mailed an invitation along with the participant information sheet and consent form [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/144934/#/ (accessed 28 October 2019)]. Participants were also given the option of receiving material as hard copies by post. If there was no response to the e-mail, the interviewer attempted to contact participants by telephone to invite them to the interview. Effort was targeted at recruiting participants based on their levels of use, in an attempt to recruit similar numbers in each of the low, mid and high categories.
Following receipt of the completed consent forms, a telephone or Skype™ (Microsoft Corporation, Redmond, WA, USA) interview was arranged at a time suitable for each participant. Interviews typically lasted 30–60 minutes, followed by a short debrief. All participants were offered an optional follow-up call the next day to discuss any concerns arising from the interview.
All interviews (including verbal consent) were recorded with an encrypted digital recorder. Recordings were downloaded to the Lancaster University secure server and deleted from the audio device after each interview. Interviews were transcribed verbatim by a professional transcriber. Interviews were conducted between 8 September 2017 and 23 February 2018 by Katerina Panagaki, a psychologist with a specialist research interest in mental health who had not been directly involved in the development of REACT.
Data management
Hard copies of the consent form were kept in a lockable filing cabinet in a secure office at Lancaster University and were scanned as soon as possible on receipt. All electronic consents and scanned copies were saved under the participant’s randomisation number (given by Liverpool CTRC). Recordings of interviews were kept in folders and under the participant’s randomisation number on the same password-protected shared drive in their original format and in Waveform Audio File Format.
Recordings were sent to the transcriber via ZendTo, a secure file transfer service, after being encrypted and password protected using 7-Zip. Transcripts were returned to the interviewer by e-mail in the same encrypted and password-protected format (7-Zip). Transcripts were also saved on the shared drive using participants’ randomisation numbers.
All digital data from the study was stored on the Lancaster University shared network drive, in a resilient storage infrastructure that is dual-housed in the university data centres (on site). Multiple levels of redundancy are built into these storage arrays; snapshots and backups are automated and taken regularly. Files with identifying information (e.g. electronic copies of consent forms) were protected with an additional password. Data were accessed by the interviewer using an encrypted computer and were clearly labelled to avoid contamination of blinded researchers. Qualitative analysis was conducted using NVivo qualitative data analysis software, version 11 (QSR International, Warrington, UK) for Windows® (Microsoft Corporation).
Analysis
Analysis of interviews followed the framework approach as described by Ritchie and Spencer. 148 The initial framework was created a priori, based on the research team’s interest in answering the main research questions of how participants experienced REACT, including patterns of use and experience of the website, and how the toolkit could be improved. This framework evolved during familiarisation and indexing to create the final themes used to understand the data.
We anticipated that high-level users would be more positively inclined towards REACT than low-level users, and would be more motivated to share their insights. We were particularly keen to understand the reasons for forum use and what functions it served, although we were aware that this would not be relevant to all participants. Finally, we expected that the experiences of the relatives would be applicable to online interventions for carers more widely, rather than applicable to just REACT.
The initial analysis of topics discussed on the forum consisted of grouping thread titles thematically into main topic areas. In addition, we used online software Wmatrix149 to analyse the vocabulary used on the forum. This software allocates words to semantic fields and makes it possible to obtain the most frequently used semantic fields in a data set, and to compare one’s data with a larger ‘reference’ corpus and, thus, obtain a ranked list of semantic fields that are relatively more frequent in the former than the latter, to a statistically significant extent.
Results
Participant characteristics
Fifty-five eligible participants were approached: 10 declined, 10 did not respond and 11 were unavailable at the time or agreed but were then unreachable. Of the remaining 24 who took part, six were low-level users, three were mid-level users and 15 were high-level users.
All participants were invited to provide basic descriptive details, shown in Table 51 (some participants were supporting more than one family member or close friend). Of the 24 participants, 20 were female; 21 were white British, two were Indian, one was Irish and one was of ‘any other white’ background. The lack of ethnic diversity in the sample was consistent with the pattern in the overall trial sample, in which > 95% of participants were white British, Irish or of ‘any other white’ background. The average participant age was 51 years. Although we attempted to sample across the range of web usage, it was easier to recruit high-level users, and much more difficult to engage low-level users.
| Identifier | Relationship to person with mental health problem | Diagnosis of relative/friend | Age (years) | Gender | Ethnicity | Web use level |
|---|---|---|---|---|---|---|
| T0001 | Mother | Schizophrenia | 60 | Female | Other white | High |
| T0002 | Mother | Schizophrenia | 57 | Female | White British | High |
| T0003 | Not completed | Undefined | 54 | Female | White British | Medium |
| T0004 | Mother | Schizophrenia | 65 | Female | White British | Medium |
| T0005 | Mother | BD | 60 | Female | White British | High |
| T0006 | Mother, daughter | Schizophrenia, other | 54 | Female | White British | Low |
| T0007 | Not completed | Undefined | 42 | Female | White British | Medium |
| T0008 | Partner | BD | 35 | Male | White British | Low |
| T0009 | Father | Schizoaffective disorder | 57 | Male | White British | High |
| T0010 | Mother | Psychosis | 48 | Female | White British | High |
| T0011 | Mother | Schizophrenia | 58 | Female | White British | Low |
| T0012 | Sibling | Psychosis | 30 | Male | Indian | Low |
| T0013 | Mother | Schizophrenia | 57 | Female | White British | High |
| T0014 | Mother, partner | BD, schizophrenia | 65 | Female | White British | High |
| T0015 | Sibling, wider family member | Psychosis, other | 57 | Female | White British | High |
| T0016 | Partner | BD | 43 | Female | White British | High |
| T0017 | Partner | BD | 44 | Female | White British | High |
| T0018 | Partner | BD | 43 | Female | Irish | High |
| T0019 | Mother, partner, wider family member | BD, other, schizophrenia | 54 | Female | White British | High |
| T0020 | Mother | Schizophrenia | 64 | Female | White British | High |
| T0021 | Mother, partner, friend | BD, other, other | 69 | Female | White British | High |
| T0022 | Partner | Schizoaffective disorder | 37 | Female | White British | High |
| T0023 | Partner | BD | 48 | Male | White British | Low |
| T0024 | Sibling | Psychosis | 26 | Female | Indian | Low |
Overview
Participants seemed to feel able to talk openly about both positive and negative aspects of their experience. Some interviewees chose to have the website open in front of them during the interview to help trigger their memories. All participants responded positively to the opportunity to share their experiences and thoughts about REACT and found the questions appropriate. During the debrief, no concerns were reported, other than queries about the future of REACT. Interviews typically lasted 30–40 minutes. Key themes were derived from interpretation of the mapped data obtained from participants. This was informed by an initial framework of wanting to understand how relatives experienced REACT, and what improvements they would suggest. Table 52 provides a summary of the a priori framework themes and the final framework themes and subthemes.
| A priori framework themes | Final framework themes and sub-themes |
|---|---|
| How did people use REACT? | Is REACT really needed?
|
| Experience of REACT | What facilitates use of REACT?
|
| How could REACT be improved? | What hinders use of REACT?
|
Who did REACT help?
|
|
How did REACT work?
|
|
Peer support: the active ingredient
|
|
Ways to improve
|
Key themes
Is REACT really needed?
REACT was welcomed. For some relatives, this was because of a general lack of support experienced from services and a lack of carer-specific information online. For others, it was because the kind of help they had received was felt to be too demanding to be useful alongside the challenges of caring; thus, the simplicity of access to REACT support was important:
I did have a carer’s assessment but it’s proved to be more stressful than helpful . . . this lovely social worker came and spoke to me and then I said what I needed, which was practical help more than anything, and then he e-mailed me to say ‘can you give me a timetable of your day?’ and again me head started to explode and I’m thinking ‘oh God this is too stressful, I can’t cope with it’. So I’ve decided not to bother with it because I don’t think it’s going to be that much help; I think it’s just a paper exercise more than anything.
T0011 – mother, aged 58 years
Negative experiences with services and health professionals led to feelings of exclusion for many participants. Moreover, when support was offered, it commonly failed to acknowledge the systemic context for the service user and carer. This could create an additional burden and trigger for the person experiencing mental health difficulties, leading, at times, to a vicious cycle of increasing distress for the carer and service user:
Doctors, they . . . look at the medical side of things. I worked for a consultant psychiatrist when I was within the NHS so I know that their interests were the patient and getting the patient to feel better, but it wasn’t so much around the family life and what was happening at home . . . In a way, that’s where people fail, because if they don’t look at the whole picture of what’s going on, then they can’t assess what’s going on with that patient.
T0003 – female, aged 54 years
REACT was a useful support option even for individuals who had access to appropriate local support. A key attraction was that it was accessed anonymously, in contrast to local support groups, which by their nature cannot provide anonymity. The need for anonymity was often driven by the service user more than the relative:
He . . . made the request that I don’t tell my family that he has bipolar one, so it curtails where I can get support. So I have a number of friends who know about it and they’re very supportive and very understanding of it, but . . . to be able to go online whenever I needed to and know I . . . would probably get a reply within 24 hours was really helpful.
T0004 – mother, aged 65 years
REACT was compared with other mental health websites and was seen as a useful addition. For some it was helpful to have information concentrated in one trusted site, whereas others found it helpful to have multiple websites that signposted to each other, of which REACT could be one. Furthermore, REACT was thought to address a gap in the written literature, which predominantly referred to systems in other countries, particularly the USA, which were of limited relevance to these UK-based participants:
I know that sounds really really bad, but the majority of the books seemed to be American and they definitely deal with things in a different way and the medication they have over there is different, the health service and the psychiatric system over there [are] very different to what we have here.
T0023 – male partner, aged 48 years
What facilitates use of REACT?
Most participants were regular users of the internet and familiar with accessing online material. This made incorporating REACT into their routine relatively straightforward in principle:
I do use online a lot and it’s convenient for me ‘cause you can go jump on and off whenever you [have] a spare moment.
T0019 – mother, partner and wider family member, aged 54 years
Participants liked the flexibility of being able to access REACT when and where they wanted, and being able to progress through the site at their own pace, which could be altered as other demands required. They also appreciated it being a free service. Relatives were encouraged to use REACT as often, and access as many of its features, as they found personally useful without feeling penalised or excluded. For example, access to the forum could vary from reading posts to responding to comments and creating new threads:
The great thing is that you can just go when you need to, as opposed to having to make appointments and get to a place.
T0003 – female, aged 54 years
Flexibility was also appreciated in the range of media that REACT used – relatives could focus on text, forum or video formats as they chose:
I also have learning difficulties and dyslexia, so I actually found having both [text and videos] was more useful because sometimes I wouldn’t always take the text in, but watching the video as well kind of would reinforce and make it easier to understand.
T0004 – mother, aged 65 years
The videos were really helpful because it wasn’t constant reading, so I like that. I loved the depth of information that was available. The layout itself was absolutely great as well, it was easy to read, it was eye-catching enough and quite interactive as well . . . The opportunity for me to be able to write notes and things like that, I thought that was really, really good.
T0024 – sister, aged 26 years
The privacy and anonymity built into REACT were highly valued. Participants appreciated being able to have non-identifying usernames and to privately message REACT supporters, as well as having the option of posting in the community forum. The desire for anonymity was often a result of fear and stigma, and could be more prominent in certain communities and cultures. The ability to access REACT’s information and personalised advice on a range of devices, especially mobile phone, enhanced privacy and anonymity:
You are anonymous. And you can leave when you want, whereas if you go to a group you tend to be there for at least a polite amount of time.
T0002 – mother, aged 57 years
Certainly in the BME [black and minority ethnic] community it’s very taboo, you’re not allowed to talk about it, you pretend it doesn’t exist, you ignore it, and, therefore, the more they deal with people like me the better, I think.
T0012 – brother, aged 30 years
What hinders use of REACT?
Participants appeared to start off keen to explore the site, initially going through the modules one by one, for example. However, after an initial burst of curiosity, other considerations began to affect use, especially lack of time, workload and levels of distress. One challenge people reported was that they would sometimes forget to use the site when under pressure or distressed. In those situations, e-mail reminders or notifications of responses to a forum post could point them back to REACT as a resource that could help them address their current difficulties:
I suppose I did need a little bit of reminding every now and again to keep going into the site to look . . . but that’s probably because I had a lot on and couldn’t find the time to do it.
T0020 – mother, aged 64 years
Participants varied in how they used the site. Some used it in a preventative way; others were more ad hoc, using it as they felt the need. Most appeared to return as needed, triggered by circumstances.
There were two key reasons for using REACT less than intended. Either the person(s) for whom they cared became better, or the person(s) became unwell, and so the carer lacked time and energy to use REACT and, under stress, felt less able to process new information or even to remember their password:
When things are a little bit more, kind of, stable and things are ticking along OK, you kind of forget about it [REACT] in the sense because you kind of don’t need as much support.
T0005 – mother, aged 60 years
I was engaging with it [REACT] and then he then went into crisis and then went into hospital and, in fact, he was in hospital until the following January, and I was then caught up in that. And then, you know, after that I needed reminders. So I think that’s your difficulty really, is that the very people that you’re trying to help have so much on their plates really.
T0002 – mother, 57 years
Although most participants found it useful to read that others were in a similar situation, this was not always straightforward. Some seemed to experience ‘impostor syndrome’, feeling that their situation was less complex than those of other contributors and that they therefore had less right to share their concerns online. Others identified so strongly with being a carer (professionally or personally) that asking for support for themselves felt very difficult:
I am a support worker . . . [but] that wasn’t something that I found that I wanted to use because, when it comes to my carer’s role, it is very stressful, it is something that you do kind of just do, so when it comes to asking for the help, often you kind of do feel a little bit ashamed because you’re sitting there and . . . you’re meant to be helping.
T0024 – sister, aged 26 years
Who did REACT help?
To meet criteria for participation in the REACT trial, relatives had to self-identify as a carer of a person with BD or psychosis, and to report experiencing significant levels of distress. In addition to being a carer, some of the participants worked in mental health-related jobs, and it was particularly interesting to hear how REACT helped them. Some felt familiar with much of the information shared, but found it helpful to be reminded of it and to read about other people’s experiences. In particular, it reminded relatives to take care of themselves and encouraged them to reflect on their own mental health and well-being.
Clearly, having a professional mental health background is no guarantee of looking after oneself well; in fact, there was some evidence that this group faced additional hurdles (personal and practical) to opening up and getting the support they needed from local services. REACT’s anonymity helped participants to address those needs:
When I first got it, I read all the text of everything, and looked at my plan . . . My daughter’s been ill for 17 years so I’m pretty clued up about all these things and I do research in mental health myself, so it reminded me of what to do and helped me stay positive and things like that, you know. And reinforced things I should be doing and trying not to forget the important stuff, taking respite and keeping things in proportion.
T0014 – mother and partner, aged 65 years
I can’t really get support in this area because I am a health professional for other people with mental health difficulties, so I would be on very dodgy ground confidentiality-wise if I went to a support group in this area . . . So, in that sense, being able to tap into that [online] group was good. I’m a bit of a complex client, I think.
T0002 – mother, aged 57 years
For some participants, using REACT had a knock-on effect on those whom they cared for, or on other relatives. Some used information they had accessed on REACT to initiate discussions with their relative, or showed service users or other family members elements of the site that they had found useful:
It had plenty of information in it . . . It obviously, overall, benefits the person that the relative’s looking after if they’re more informed.
T0020 – mother, aged 64 years
Yeah, he didn’t feel as isolated . . . ’cause there’s still that kind of [stigma] and he’s obviously felt isolated, he’s not wanted to talk about it, and it did actually make him open up a bit more . . . so that had a really positive effect for him.
T0016 – female partner, aged 43 years
How did REACT work?
Many participants expressed an interest in knowing more about their relative’s condition and its consequences, as well keeping up to date with information on mental health in general. Consistent with the logic model for REACT (see Chapter 2), participants linked learning more about their relative’s conditions to changes in how they perceived and responded to it:
The layout was quite easy to use and stuff like that, it broke down everything that you need from, you know, different kinds of mental illness – my wife was diagnosed with bipolar so . . . while I knew about depression or I had a little understanding of depression, bipolar I didn’t know at all. And it was quite good to . . . get an eye-opener on different treatments and it was the first place I went to when my wife went through ECT [electroconvulsive therapy] treatment as well, because it kind of helped me cope with it.
T0008 – male partner, aged 35 years
In general, I felt that I got a lot of information from it and I felt that it kind of changed my perspective.
T0010 – mother, aged 48 years
Most participants had very high levels of distress at inception and had been caring for someone for long periods of time. They said that they valued gaining more knowledge and a more practical understanding of how to manage challenging situations.
Even with improved understanding, there was acknowledgement that it was a continuing challenge to respond constructively, and that REACT’s round-the-clock availability helped. Much of the most valued content involved practical advice about services and processes, and about how to communicate effectively with a person experiencing a mental health problem. This was done most effectively by learning from other people’s stories, which had the added benefit of reducing feelings of isolation:
It’s almost at the point at which their behaviour is most challenging, [that] you’re sort of required to be most understanding, and that’s when you sort of have the least capacity to be, you know, insightful and understanding about it. So that’s where I went to the toolkit to almost try and force myself to have that.
T0004 – mother, aged 65 years
But you know it’s incredibly difficult because their behaviour can be . . . intensely challenging and confronting, and so it’s trying to get that balance of being passionate while also looking after yourself.
So I got the responses from the REACT supporters about . . . how to navigate the system differently and language to use and so on and so forth, and then [from] people who had had . . . much worse experiences than my experience. So it was that ability to connect with people who kind of have some empathy with what’s going on in your life and how difficult it can be in those moments.
T0004 – mother, aged 65 years
Even for participants who chose not to use REACT, knowing that it was available and accessible offered comfort and reassurance. Participants also appreciated the existence of a forum and the more private direct messaging service that allowed them to seek tailored information. The personalised nature of the intervention was highly valued and set REACT apart from other websites and professional advice.
A key purpose in accessing the forum or direct messaging was to offload frustrations with current services and to feel heard and supported in a non-judgemental environment. This may have been facilitated by the fact that REACT supporters were trained relatives, not health professionals:
I think there’s that sense of almost, with the direct messaging, of someone looking out for you, at I guess a more personal level, and, in the forum, that sense of shared community experience of being in the same boat and . . . that other people are unfortunately experiencing some pretty shitty things too.
T0004 – mother, aged 65 years
Sometimes it’s, it’s like releasing the frustrations to say all this . . . and, you know, sometimes just having somebody say, ‘that must be hard, that’s . . . a difficult situation to be in’, it’s enough to at least relieve some of my distress that the system seems to be causing.
T0001 – mother, aged 60 years
Overall, participants reported that REACT helped them to cope better with difficult situations by offering emotional support in a safe space and practical advice, and by teaching them improved coping mechanisms, consistent with our logic model. However, a consistent message was that REACT was most useful when offered early in the recovery journey. Introduced later in the journey, it was still helpful but mostly by confirming knowledge gained and by providing an outlet to offload pent-up feelings of loneliness and frustration:
We only had a diagnosis last year, so actually I was really desperate for any resources and any further information that I could find, so I was literally soaking everything up as much as I could, and I found REACT through Bipolar UK and . . . it has been really helpful because I think what I really struggled to find was anybody else in a similar situation who had a recent diagnosis, you know early forties and [with] a young family.
T0018 – female partner, aged 43 years
I was 8 years or 7 years into my daughter’s journey by the time I’d come into the REACT study and I think I had a lot of stored-up questions, topics, things that I had no one to talk to about, so I got to get that all off my chest and I think it still took another while after my period of the study ended, but I do feel that that’s parked now, I don’t have to think about those things all the time anymore.
T0001 – mother, aged 60 years
There was some evidence to suggest that the needs of long-term carers are different, and more emotion-focused. For some, REACT had not been able to meet this need:
If I’d had the REACT toolkit when my daughter first went to hospital, I would have gotten a huge amount more out of it. I think the videos then would have been absolutely essential. [Now] . . . I didn’t need that section as much because it was stuff I was familiar with because it’s just a long trip. My problem is it’s a long trip, that’s forever as far as I can see, and that’s the bit I was having trouble with. So it wasn’t where to find some information, it was how to get that emotional support.
T0001 – mother, aged 60 years
Support: the active ingredient
The REACT supporters were identified as different from health professionals, yet treated as a specialist, trained and knowledgeable group that stood apart from other relatives using the website. Access to them and peer support appeared to be the most highly valued aspect of the website. In particular, REACT supporters were given high praise for the advice they offered and their empathy in the forum and in direct messages. Furthermore, participants felt cared for, valued and safe when REACT supporters individually followed up with them if they were concerned, and maintained a continuous yet not intrusive level of contact. The prompt responses of REACT supporters were particularly valued during periods of crisis:
They got back to me really quick, and it was like, sort of, experts getting back to you and people that had been through things, people that knew more, different websites where I could go, they could offer more support that way.
T0003 – female, aged 54 years
I think one of them even followed up with me ‘cause I then wasn’t on the forum for a couple of days, and she just . . . said something to the effect of ‘I just want to check that you’re OK’. So it was a really sweet thing and it was just like, ‘I am OK, I’ve just had my hands full’.
T0004 – Mother, aged 65 years
Participants also appreciated the support from other relatives. Even when they disagreed with responses, they valued receiving a plethora of opinions and thoughts. They also perceived benefits in sometimes being able to offer support themselves. This seemed to link to the logic model’s proposal that REACT would increase relatives’ sense of self-efficacy, which, in part, would be realised through helping others:
It was quite encouraging to hear other people’s points of views, even though, on some occasions, I didn’t actually agree with them.
T0010 – mother, aged 48 years
If I got a reply to a forum post, then I would go and look at that because there’s partly a sense of wanting to help other people who are in the same boat as you . . . Even if [their reply] was like 3 or 4 months afterwards, then I would reply to their post.
T0004 – mother, aged 65 years
Ways to improve
Participants were invited to suggest specific ways that they would like to see REACT improved. These can be grouped under three headings: overall feel of the website, technical improvements and content improvement.
Overall feel of the website
Suggestions for improving the feel of the website included:
-
make the site more interactive
-
add less academic ways of learning, for example cartoons
-
update the interface – change fonts and colours (e.g. blue is too clinical)
-
make tabs more visible
-
turn blog into newsfeed
-
offer opportunity to contribute to blogs and directory
-
use pop-up windows to attract attention to specific elements.
Technical improvements
These included:
-
easier navigation in the forum
-
direct links to comments in the notification e-mails
-
a function to download or print personal or private discussions for future reference
-
extend search function to all pages including forum subsections
-
snooze function for reminder e-mails
-
make the site an application, obviating the need for multiple log-ins and problems with forgotten passwords
-
support note-making during videos
-
offer Skype call option for support for those with dyslexia
-
allow recording of messages as alternative to typing.
Content improvement
Most responses concerned the toolkit’s content, with suggestions for:
-
additional teaching on coping strategies
-
help with deciding where a topic fits in a forum
-
positive topics
-
spaces for planned interaction that do not relate to problems
-
more frequent blog updates, with e-mail notifications
-
more detail on how services work and the functions of different team roles
-
a module on improving communication with services (e.g. what to ask whom)
-
more information on additional local sources of support, with e-mail prompts for these events
-
more medication information, especially on supporting someone to manage side effects
-
updates on relevant news events such as legislation changes or topical television programmes
-
more information for children and adolescents
-
allow support workers and carers to interact on the forums to share good practice
-
allow creative input from participants.
Analysis of the REACT forum topics
We also explored how participants in the REACT arm used the REACT forum and what sorts of topics were covered.
Thread titles
As of November 2018, the forum contained 171 different threads. These could be grouped into the following main topics:
-
problems with the cared-for relative (e.g. ‘How to deal with verbal abuse and aggression’, ‘Think partner is getting worse again’)
-
medication (e.g. ‘Coming off medication’, ‘Medication changes and drug abuse’)
-
emotions and stress (e.g. ‘Blues after helping my wife through an episode’, ‘Stress and stressors’)
-
hobbies and leisure activities (e.g. ‘Swimming’, ‘The power of gardening’)
-
relationships (e.g. ‘Retaining a relationship while being your partner’s carer’)
-
work (e.g. ‘Disclosing mental illness at work’)
-
legal issues (e.g. ‘Mental health law’)
-
dealing with the health and social care system (e.g. ‘Can anyone support me with complaint?’, ‘Use and abuse of “confidentiality” by NHS staff’)
-
communication (e.g. ‘The power of words’)
-
the forum itself (e.g. ‘So I’m new to REACT . . . how am I feeling?’).
Preliminary corpus linguistic analysis
Corpus linguistic analysis revealed the following additional themes:
-
help and advice – needing, asking and receiving help; supporters not being allowed to give advice
-
obligation – talking about one’s responsibility, duty, etc.
-
hypothesising – possibilities and wishes, for example ‘If only I could live by the sea’.
This approach also provided more detail for themes suggested by thread titles, for example:
-
illnesses and symptoms – for example bipolar, illness, psychosis, symptoms, psychotic, depression, drugs, mental, physical, ill, disorder, paranoia, adjective+ episode (e.g. psychotic episode)
-
medicine, medical actions – carers, psychiatrist, diagnosis, treatment, NHS, assessment, lithium, therapy, medications, valproate, confidentiality, meds [medications], dose, anti-psychotic
-
problems/negative emotions – stress, delusion, anxiety, crisis, issues, anxious, difficult, challenging
-
strategies/positive emotions – coping, managing, recover, wishes, exercise, hope, glad, love, well-being
-
kinship – son, relatives, husband, daughter, parent, wife, family, relationship.
Discussion
Chapter 2 reported on the development of REACT as an online toolkit, drawing on the insights of experts by experience at a series of workshops and the design brief created from this by the TMG. The logic model for REACT, based on well-established cognitive–behavioural principles, mapped out the challenges faced by relatives, the key features of REACT, the anticipated experiences of users and outcomes in response to such experiences. The in-depth interviews that were analysed were broadly consistent with the logic model.
Relatives reported multiple challenges in understanding the behaviours of the relative they cared for and how best to respond to these, resulting in distress, isolation, stigma and shame. REACT offered them psychoeducational information and interactive support through the forum and direct messaging, as well as additional information on where to seek further help on specific topics. Participants reported that they used REACT to learn more about BD and psychosis, to develop more effective ways of dealing with challenging situations, to share problems and solutions and to feel more able to manage their experiences.
A consistent message was that participants felt that REACT would be most useful early on in their relative’s recovery journey, when they were likely to be seeking information and strategies. Relatives later in this journey might need more emotion-focused interventions.
Relatives found prioritising time to use REACT difficult. The advantage of an online intervention is that it is always accessible. However, the corollary is that there is no dedicated time to engage. Overall, relatives reported feeling less isolated, more supported and, through better self-care, more able to attend to their own well-being without feeling ashamed to do so.
There were helpful suggestions about potential improvements and updates for REACT, consistent with digital formats rapidly evolving to become more interactive and integrated. Peer support and REACT supporter contributions were seen as crucial features of REACT, but not all participants accessed these. It is therefore crucial that future iterations of REACT optimise access to these elements. Linguistic analysis of the REACT forum indicated this platform was used to share information about living with mental health issues in a broad context, including, but not limited to, the clinical and behavioural features of psychosis and BD. Consistent with REACT’s recovery perspective, there were also discussions about how both a relative and the individual with the mental health diagnosis could best live well alongside BD and psychosis.
A key limitation of our qualitative findings was the difficulty in recruiting low-level users for interview, resulting in a high proportion of high-level users in the final sample. This was despite the invitation’s emphasis that we were very interested in talking to all participants in the trial, even those who had not used REACT at all. Although the views of medium- and low-level users have contributed to each of the key themes, the predominance of high-level users is likely to be linked to the primarily positive views we received. There remains a real need to understand better the views of those who do not engage with DHIs, to ensure that DHIs do not increase inequalities in access to mental health services.
Chapter 7 Discussion
Introduction
In this chapter, we summarise the main findings from the study and interpret these in the light of other relevant research and the clinical context. We highlight the key strengths and limitations of the research that need to be taken into account when considering these findings. We draw out implications for policy, practice and future research. As this study was funded by a specific call by the HTA for efficient trial designs, we comment on how the lessons from this study can be used to inform future online trials. Finally, we draw out the main conclusions from this work.
Summary and interpretation of key findings
To our knowledge, this was the first definitive RCT testing an online DHI for relatives of people with severe mental health problems. The aim was to develop and test the clinical effectiveness and cost-effectiveness of an online, supported self-management toolkit for relatives of people with psychosis and BD (which included a comprehensive RD), compared with a comprehensive RD alone. At baseline, participants reported very high levels of distress and low levels of well-being, both of which improved significantly, but there was no evidence of a difference between the arms. There was some evidence that those with access to REACT felt better supported than those with access to the RD only, but the difference was small and, after accounting for missing data, failed to reach statistical significance (p = 0.051).
REACT appeared to be highly acceptable, with users reporting feeling safe and supported. No serious adverse events were reported. REACT cost an estimated £142.95 per participant, including full development and delivery costs. These costs would reduce as the number of users grew. There was no evidence that REACT increased QALYs (incremental QALYS adjusted for baseline EQ-5D-5L score, age and gender: –0.0024, 95% CI –0.0088 to 0.0039) or would save money (incremental cost adjusted for baseline age and gender: £286.77, 95% CI –£858.81 to £1432.36; p = 0.624).
REACT was originally designed as a paper-based intervention for relatives of people with psychosis in EIP services;2 we were able to adapt it to create an online DHI that also supported relatives of people with BD. Modules relevant to understanding and managing BD experiences were added, and a forum to facilitate a peer support community was established, along with a confidential direct messaging system, both of which were successfully moderated by trained relatives with lived experience of supporting someone with psychosis or BD. The textual content was updated, and made more interactive through the use of videos of service users, relatives and professionals sharing their experiences and knowledge, and the use of reflective exercises to help relatives to think about how to apply the information they were gaining to their specific situations. Making the toolkit available online made it easier to disseminate widely, and to update content as required.
REACT was made available to relatives across the UK who agreed to take part in an online trial. Recruitment, eligibility, consent, randomisation, data collection and follow-up all occurred primarily online (with some face-to-face recruitment and some telephone or postal reminders for follow-up). A bespoke data collection system was built. Despite the huge increase in development and testing of DHIs for mental health problems across the world, to our knowledge, this was the first definitive RCT test in Europe of an online DHI for relatives of people with severe mental health problems. In the USA, Glynn et al. 150 and Rotondi et al. 151 both report proof-of-concept trials for online psychoeducation programmes for relatives of people diagnosed with schizophrenia, but neither arm reported a fully powered definitive evaluation.
There was a lot of interest from relatives in using REACT. Our aim was to recruit 666 relatives over 18 months. We recruited 800 relatives fairly easily during the recruitment phase of the study. This might indicate substantial unmet need in this area, and the potential for widespread use of an online support tool. Many more relatives were keen to take part, but 43% of those who completed the eligibility criteria questionnaire failed on at least one item, most commonly (81% of those failing) on the requirement to report ‘being strung up and nervous all the time’, ‘rather more than usual ‘ or ‘much more than usual’. This item was chosen as having the highest item-total correlation with total GHQ-28 scores in our feasibility study and was included to avoid a floor effect at baseline. However, as a consequence, most relatives in the trial were in crisis at the beginning of the study, but relatives who had been distressed for longer periods and so responded ‘no more than usual’ were ineligible.
Baseline GHQ-28 scores [mean 40.2 (SD 14.3)] were much higher than those reported for previous samples in studies of relatives of people with psychosis or BD who were seeking help,13,120 including our feasibility trial [mean 34.14 (SD 24.63)]. 2 The same pattern was evident for well-being and support scores, which were significantly lower than in our feasibility trial.
Over the study’s 24-week follow-up, there was a big reduction in distress and an increase in well-being and support in all relatives across both arms. This is likely to be because circumstances change over time and, for people recruited in crisis, the crisis is likely to have abated by follow-up, at least for some participants. This statistical regression to the mean makes it harder to see any impact from an intervention, as any difference needs to be significant, over and above the effect of time.
Furthermore, reducing distress using an online psychoeducation approach might have been an overly ambitious goal. Although psychoeducation has been reliably shown to improve knowledge outcomes, and is recommended by NICE,53,54 there is no evidence that it reduces distress, even when delivered face to face. 43 There is evidence that face-to-face interventions designed to improve outcomes for relatives are generally less effective for those with higher levels of distress. 39 Although many people flourish alongside psychosis or BD, these are potentially chronic mental health problems that, for some people, can have a devastating effect on their lives and the lives of their family and friends. REACT provides information and strategies to support relatives, but did not offer a cure for either condition, which might be what relatives were initially seeking to reduce their distress.
Although REACT showed no benefit over only the RD in reducing distress (as measured using the GHQ-28), relatives who had access to REACT did report feeling more supported than those who had access to the RD only at 12 weeks (2.50, 95% CI 0.87 to 4.12) and 24 weeks (1.65, 95% CI 0.04 to 3.27). However, this was a small effect and, after accounting for missing data in a longitudinal model, the difference between arms was no longer statistically significant at the cut-off point of p < 0.05 (1.51, 95% CI –0.005 to 3.01; p = 0.051), and unlikely to be of clinical significance. This is because, although similar numbers of relatives dropped out of follow-up in each arm of the trial, dropout in the RD-only arm was not linked to outcome, whereas those in the REACT arm who felt less supported were more likely to drop out. This pattern of informative dropout was consistent across all the outcome measures, and highlighted the importance of adequately accounting for missing data in RCTs.
We were able to test the hypothesised logic model that REACT would reduce distress by providing relatives with a working cognitive model of psychosis or BD (assessed using the Brief IPQ) and more adaptive coping (using the Brief COPE). Relatives in both arms of the trial developed more benign perceptions of illness and reported feeling more able to cope over the 24-week period. However, these changes did not differ between those receiving REACT and those receiving the RD only, and there was no evidence that these changes played a causal role in reduced levels of distress. Coping strategies assessed using the Brief COPE showed little change over time, but already favoured active coping, planning and acceptance at the outset.
REACT was valued by relatives for being comprehensive, relevant, easy to access, private and anonymous. The proactive support from REACT supporters was appreciated, as was the opportunity to learn about how best to support someone with a mental health problem through a variety of different mediums (text, video, forum). Relatives provided useful feedback about the content and design of REACT, all of which should be used to further develop the toolkit. A consistent message was that REACT would be most useful to relatives early on in the recovery journey, when they were likely to be seeking information and strategies. This suggested that more recruitment through GP surgeries and EIP teams would be beneficial. Some relatives found seeking help for their own needs difficult, and most found it hard to prioritise time to use REACT.
The problem of low levels of use is common across many DHIs. The flexibility of DHIs, in that they can be used any time, anywhere (with an internet connection), may paradoxically limit their effectiveness. The median time spent on REACT (excluding the RD) in the REACT arm was 50.8 minutes (IQR 12.4–172.1 minutes), with a large variation between individuals (range 0.1–4505.5 minutes). The median time spent on the RD in the RD-only arm was 0.5 minutes (IQR 0–1.6 minutes), again with wide variation from 0 to 42.9 minutes. However, as the purpose of the RD was to signpost relatives to other sources of support, and we do not have data on how much they used these alternative supports, these figures cannot be directly compared.
Causal analysis suggested a small but non-significant association between website use and outcome, suggesting the need to better understand factors that affect engagement with REACT, and DHIs more broadly.
All relatives were free to use REACT at their own convenience. The modules were openly accessible and we did not specify any ideal levels or order of use (although there was a logic to the presentation order). Although relatives were sent periodic reminders in response to low levels of activity, they did not report their levels of use to anyone directly. The REACT supporters moderated activity on the forum and responded to direct messages from relatives, but did not support use of the psychoeducation modules. The content was easy to follow, and each module had self-reflection exercises built in, to help relatives to think about how the information might apply to their specific situation. However, as Mohr et al. 152 reflect, it may be that users will more effectively engage with DHIs if there are clear expectations of use, and the presence of a respected individual to whom the individual is accountable. This may be similar to the effect of personal trainers for exercise: it’s not that we do not know how to exercise, or that we need to exercise, but that, for some people, being accountable to a respected person at a dedicated time and specific place makes us more likely to do it. This might, in part, account for evidence to suggest greater efficacy of supported interventions,153 and suggests that broadening the role of the REACT supporters to support all relatives to engage with all parts of REACT, including the modules, and as occurred in the feasibility study, might increase levels of use.
There were several ways in which this study differed from the REACT feasibility trial, which might account for the differences in findings. These differences might provide valuable insights into factors that affect the effectiveness of DHIs, but all require further testing:
-
Relatives in this study were more distressed at the outset and more likely to be in crisis.
-
Relatives had been caring for longer, and the information in REACT might have come too late.
-
REACT was online, rather than in paper form, and so might have been less accessible or visible, reducing triggers for use.
-
Relatives did not receive as much support to use REACT, in general. Only the forum and direct messaging were supported, and relatives not engaging with these components did not receive any support in using REACT.
-
REACT was offered in addition to TAU, but not as an integral part of a clinical service, in which clinicians working with relatives were also aware of the nature of the problems experienced by the people they were caring for.
-
REACT was supported by trained relatives rather than members of the clinical team.
-
REACT was compared with an active control (the RD).
Strengths of the trial
Despite the recent interest in use of DHIs in mental health, and the government’s backing of this agenda,154,155 there is still a lack of a robust evidence base to support the effectiveness of DHIs in mental health. This trial was rigorously conducted, with a large, broadly recruited sample, a clearly defined and theoretically based supported intervention, an active control arm, a good follow-up rate for an online trial, web-based randomisation, a robust blinding protocol to manage any direct contact with participants and a pre-published analysis plan that appropriately addresses missing data.
As a result of these strengths, our findings highlight three key dangers of current research in this area. The first is assuming that interventions adapted from those delivered face to face will be equally as effective as those delivered face to face: REACT was shown to be effective when offered in paper form and supported by telephone by staff linked to the relevant clinical team.
The second is the use of uncontrolled pre–post comparison to argue for effectiveness: REACT would have appeared very effective without comparison with an active control arm.
The third is the need to appropriately manage missing data. Dropout in online trials is often higher than in offline trials, and cannot be assumed to occur at random: relatives in the REACT arm who were more distressed were also more likely to drop out of follow-up. This may be true for other online interventions, as it may be harder to adapt the intervention to better meet individual user needs than would be the case in face-to-face support.
Limitations of the trial
The trial also had several limitations that need to be taken into account in interpreting the findings.
Accepting the need for rigour, there were limitations in selecting a traditional RCT design to evaluate REACT. RCTs were developed to test the effectiveness of static stand-alone interventions that can be easily defined (e.g. dose of a drug). DHIs, including REACT, are often designed to be one component of a comprehensive package of care, and their effectiveness should be evaluated as such. Their impact is likely to be very different when offered as part of a service, rather than in isolation. For example, REACT is one part of the support that NICE recommends to relatives, and may only be effective for relatives able to access other elements of this support (e.g. appropriate clinical and social support for the person with psychosis or BD, and/or family intervention). REACT educates relatives about the services they should be receiving. If they are unable to access these, it could increase rather than decrease distress. Alternatively, awareness that a relative is accessing REACT could lead to changes in behaviour among clinical staff, who may reduce other forms of input that they perceive as no longer necessary. Testing an intervention that is designed to be part of a package of care, using a RCT design, maximises internal validity, but is inherently problematic in ignoring the impact of the changes throughout the wider system. As recommended by the new guidance being developed by the Medical Research Council and NIHR for developing and evaluating complex interventions, study designs that take a more systems-based approach to the evaluation of interventions like REACT, which are just one component of a more complex health-care package, may be more appropriate than traditional RCTs. 156
Digital health interventions also need to be able to evolve and adapt at pace. The REACT trial took 3 years to deliver; by the end of the trial, the toolkit looked dated, but had not been adapted during the trial in an attempt to standardise the intervention across all participants. The way in which people used technology had evolved, such as increased use of mobile applications, and the content needed to be updated to reflect advances in the way in which mental health problems were understood and managed over time. REACT participants provided excellent ideas for updates as part of the qualitative data collection, described in Chapter 6. However, health research currently adopts a model of ‘definitive’ testing, using a large expensive trial lasting several years, and testing between-arm differences. If a trial shows no overall group benefit for the intervention after a defined period, it is likely to become very challenging to attract additional investment to develop it further.
This is in contrast to the iterative dynamic model of design, evaluate, adapt157 seen in other areas of digital development, in which real-time data collection informs continuous adaptations over time. Because DHIs can similarly facilitate the collection of large numbers of real-time data, within-person variation in the impact of the intervention can be explored, to identify what works for particular individuals in particular contexts.
A further limitation of this trial included the failure to recruit a broader range of relatives. Despite designing a broad recruitment strategy, incorporating a wide range of online and offline recruitment strategies, our sample predominantly comprised white British females. There was some evidence of a greater proportion of partners than in previous studies. 2,13,120 It is possible that the predominance of female participants partially reflects the continuing burden of care falling to women, but the lack of relatives from ethnic minority groups is likely to result from lack of cultural adaptation in content and language, both of which were beyond the scope of this trial. Cultural adaptation should be a key focus of future work in this area, to ensure that DHIs do not exacerbate existing inequalities in access to health care.
Treatment as usual was not well measured and, therefore, cannot be reliably defined. There were also some technical issues in data collection online using the CSRI, which meant that information about medication use and some service use was not reliable and could not be used. This made it difficult to understand exactly what services relatives were receiving, and if and how these changed as a result of their being offered REACT or accessing the RD. Given that both interventions were designed to be one component of a care package, and a key function of both is to inform and signpost relatives to other sources of support available, more rigorous and detailed data on how these additional data sources were accessed and used would have allowed us to better understand the impact of both REACT and the RD.
Retention to follow-up played a very important role in this trial. Online trials have historically reported higher dropout rates than those conducted face to face. 77 In anticipation of this, we over-recruited to the trial to ensure that the final analysis was adequately powered. This strategy was successful and there was no evidence of differential rates of dropout between the two arms. However, those who dropped out of the REACT arm were more distressed than those who remained. This was not the case in the RD-only arm. This meant that data could not be assumed to be missing at random in both arms. When missing data were taken into account, any statistically significant benefits of REACT over the RD were lost. We do not know why relatives who were more distressed were more likely to drop out of the REACT arm, but it may have been low satisfaction with the intervention. Those in the RD-only arm may have been less dissatisfied, or had lower expectations of the RD and remained involved for the promise of access to the REACT modules at the end of the trial (even though these were also made available to those who dropped out).
Recruitment to the nested qualitative study in this trial was also limited by a failure to interview those in the RD-only arm and those who dropped out of the trial prior to the 24-week follow-up. The focus was on understanding relatives’ experiences of using REACT; as the RD was one component of REACT, we did not recruit additionally from the RD-only arm. However, we acknowledge that their experiences of the RD may have been very different. We recruited only those who had completed the 24-week follow-up as we were keen to prioritise collection of the primary outcome data and so did not want to overburden those from whom we were still seeking data. However, given that retention was not random (see Chapter 4), this biased us to interview relatives who were less distressed at baseline.
Our intention was to recruit a sample across the range of levels of use of REACT so we could understand what factors might affect engagement. Inevitably, it proved easier to recruit those with higher levels of use; hence, our findings are likely to be positively biased in their impressions of REACT.
Practical limitations of this trial included underestimating the amount of IT resources needed to build and host REACT and the online trial methodology. Part-time support meant that we could not always address issues immediately, and led to protocol deviations (outlined in Chapter 4). Finally, PPI in the REACT trial was challenging. Despite extensive involvement of relatives in the clinical delivery of REACT (from REACT supporters and supervisors), it was much more difficult to engage relatives in the RAG or the oversight committees. Consistent with the online design of the trial, this work was conducted remotely via digital or telephone communication, and it was harder to create a sense of engagement.
Finally, this trial is not an independent evaluation as members of the research team were also involved in the design and delivery of REACT. This may have led to bias in interpretation of the findings. Extensive peer review has been used to mitigate this, but it is important that this remains acknowledged.
Implications for online trials
This trial was funded as part of a specific call by the HTA programme for efficient trial designs.
The key challenges and our suggested solutions are provided in Table 53. These recommendations build directly on previous research in this area. 77
| Task | Challenge | Solution |
|---|---|---|
| Recruitment | Reaching people who may not use the internet regularly | A combination of offline and online recruitment strategies was needed to reach our recruitment target, and there was no evidence that recruitment avenue affected dropout |
| Cost-effective advertising through social media, specifically Facebook | We outsourced Facebook advertising to an expert, which proved to be a very successful recruitment strategy. This is an example of new skills and expertise that are needed within a research team to deliver online trials | |
| Registration engagement | Ensuring that online registration effectively encourages trial participation | Based on PPI feedback, on our landing page, we limited text, included videos and highlighted the requirement of commitment to follow-ups |
| Strategies to enhance engagement beyond the landing page included lay language to explain processes and encourage continuation; a progress bar; automated reminder e-mails 24 hours after consent and telephone number activation, and 7 days after baseline questionnaires were started; and the option to contact the trial manager personally by telephone | ||
| Eligibility checks | Randomised participants must meet strict eligibility criteria to adhere to the protocol | Participant eligibility was validated using online checkboxes |
| Pop-ups were set up to explain to participants who failed to meet criteria why they could not take part, and to direct them to alternative opportunities | ||
| Participant identification and contact | Participants should be contactable throughout the trial to encourage follow-up and in case of risk | We ensured the collection of complete and valid contact details to be sure that participants were identifiable, contactable and real. Participants could not progress without providing e-mail, postal address and contact number. These details were also validated |
| Consent | Valid informed consent must be obtained online for all participants in line with ethics standards | We adhered to the British Psychological Society guidelines109 and received NHS ethics approval |
| Monitoring intervention use | Assessing the amount of intervention use accurately | Web use was measured by Google Analytics (Google Inc.) data showing activity on web pages (i.e. page downloads, number of log-ins and time spent on a page). Such data were limited as they did not tell us anything about how this information was being processed or used. We tried to account for pages that could have been left open and inactive, by restricting maximum time, but it was always possible that the page was open but not being actively engaged with, or was being used by another person |
| Retention | The remote nature of contact may reduce retention to follow-up – ‘out of sight, out of mind’ | A combination of e-mail reminders at follow-up points, along with additional postal, text and telephone contact, increased retention rates |
| Another possible solution to low retention rates in online trials is to offer financial incentives for follow-up. We tested the effectiveness of higher/lower and conditional/unconditional financial incentives in our SWAT (see Appendix 2). We found no effect for this population from varying the amount or conditionality of incentives to complete follow-up (see Appendix 2, Table 55). This finding was in contrast to previous studies,107,123 so may vary depending on population | ||
| Participant withdrawal | Studies must inform participants about the times at which, and ways in which, they can withdraw from a study | Information regarding withdrawal was included in the participant information sheet |
| A link to withdraw was contained in all follow-up reminder e-mails | ||
| Different levels of withdrawal were provided (data collection, intervention use, reminders, etc.) | ||
| We tried to collect data on reasons for withdrawal | ||
| PPI | PPI in online trials may require some new strategies to enhance engagement and ensure meaningful involvement | Relatives involved in the clinical delivery of REACT (REACT supporters and supervisors) were physically located with the research team; consequently, they had high levels of face-to-face contact with other members of the team |
| Online strategies to communicate with the RAG and oversight committees (the TSC and DMEC) were less effective at engaging members. Some face-to-face involvement of PPI participants is advisable | ||
| Risk management | Identifying and responding to risk during an online trial needs careful consideration because of the remote nature of contact | A clear risk strategy and protocol are needed. In the REACT trial, this included:
|
Implications for health-care delivery
Services aim to offer support and education to relatives of people with psychosis or bipolar disorder, as recommended by NICE guidelines. We assessed the effect of including REACT as one component of a comprehensive care package that addresses these guidelines. Relatives felt safe and well supported using REACT, which might facilitate better engagement with other aspects of the service. However, adding REACT to treatment as usual was no more effective than adding an online Resource Directory in reducing the level of relatives’ distress, as measured with the GHQ-28 items.
Key developments should include redesigning the content and presentation using feedback from participants; making the technology more interactive and user friendly; increasing the role of REACT supporters to include support to use the modules; specifying recommended levels of use; and offering REACT to relatives earlier in the recovery journey, alongside other components of care, particularly for those with high levels of distress. REACT can also help services to meet the NICE recommendation54 to increase the involvement of service users (including relatives) in peer worker roles to support the delivery of health-care services. However, in its current form, REACT is unlikely to reduce relatives’ distress or save money in terms of the use of other health-care services.
The need for DHIs to enhance, but not replace, face-to-face support is consistent with findings across other groups,158 including young people,159 who are often assumed to be more likely to embrace digital technology.
Recommendations for further research
-
Given the apparent unmet need and high acceptability of REACT, further work is needed to make the content of REACT more effective, by iteratively co-designing and testing each of the key developments, including redesigning the content and presentation using feedback from participants; making the technology more interactive and user friendly; increasing the role of REACT supporters to include support to use the modules; specifying recommended levels of use; and offering REACT to relatives earlier in the recovery journey, alongside other components of care, particularly for those with high levels of distress.
-
Psychoeducation and support are important and valued by relatives, but distress (as measured by the GHQ-28) may not be the most appropriate outcome to evaluate their effectiveness. Understanding more about a chronic health problem for which there is no immediate cure is important, but is unlikely to reduce distress without additional therapeutic input. Therefore, the effectiveness of psychoeducation interventions may be better tested against alternative outcomes, such as whether they support relatives to feel more knowledgeable, more empowered, better able to cope and more engaged with services, rather than on reducing distress. Further research could focus on working with relatives to understand their views about what should be the primary outcomes for future psychoeducation programmes.
-
Research is needed to understand how to increase the amount of engagement and use of REACT and other DHIs, to maximise their potential to improve outcomes.
-
Research is needed to understand how to improve uptake and reach of REACT (and other DHIs) by groups that currently show low levels of use of mental health services and support, including ethnic minority groups and men.
-
The impact of effective psychoeducation interventions for relatives on service user outcomes needs to be tested.
-
Randomised controlled trials can be delivered online at a lower cost. However, this methodology presents new challenges in keeping participants engaged throughout long-term follow-ups, and managing high-quality PPI; both need to be addressed by further research.
Conclusions
Despite being informed by evidence-based theory and extensive user-informed design, and having previously shown positive outcomes on relatives’ distress in a pilot study, REACT did not reduce relatives’ distress significantly more than a comprehensive RD listing nationally available support services for relatives, nor did it reduce resource use in other areas of health and social care. Distress reduced significantly in both arms, but, as there was no TAU-only arm, it is possible that both interventions were effective, but equally possible that neither was, and that this change was a function of time.
There are several reasons why REACT may have failed to show the benefits suggested in the feasibility study: the relatives taking part included those caring for people with BD, those who had been caring for longer and those who were more highly distressed at baseline; REACT was online rather than in paper form; REACT was supported by trained relatives rather than staff in the participant’s clinical team; REACT was tested against an active control (the RD) of unknown effectiveness; and there was less support targeted at using the modules rather than the forum. It is impossible to know which of these factors was crucial in determining these findings.
Notwithstanding these findings, relatives using REACT also reported feeling safe and supported, and no serious adverse events were reported. Qualitative feedback was very positive. Relatives need access to information and emotional support,53,54 even if it does not reduce their distress, as assessed using the GHQ-28.
Acknowledgements
Our thanks go to all the relatives who gave their time to take part in this research study. Without their generosity, none of this work would have been possible.
We are grateful to Emma Bedson for her very helpful consultancy on the set-up of the trial and Alison Hankinson for her role as a REACT supporter. We thank the Clinical Research Network for supporting recruitment, along with Bipolar UK, Rethink, staff in participating NHS trusts and Clinical Commissioning Groups, and Tim Slack at Nativve (Sheffield, UK) for supporting our social media recruitment. Thanks to Lancashire and South Cumbria NHS Foundation Trust for hosting the research. Additional thanks go to Professor Elena Semino for thematic analysis of the forum topics, and to Anthony Greenwood and Paul Dolby for filming and editing videos and website development. We thank the TSC, chaired by Professor Shirley Reynolds, and including Gillian Hardy, Pete Langdon and Alex McConnachie; and the DMEC, chaired by Professor Kerry Hood and including Cathy Creswell.
The background intellectual property (IP) for the content of the paper-based version of REACT was originally held by Lancashire and South Cumbria NHS Foundation Trust, which sponsored the feasibility trial. This IP was given freely to Lancaster University to develop the foreground IP for the online REACT site, with the understanding that, should the intervention be shown to be effective, further collaboration for delivery of REACT would first be explored with them as clinical host.
Contributions of authors
Fiona Lobban (https://orcid.org/0000-0001-6594-4350) was the chief investigator.
Nadia Akers (https://orcid.org/0000-0002-1276-6092) was a REACT supporter and provided administrative support.
Duncan Appelbe (https://orcid.org/0000-0003-1493-0391) provided IT design, and managed and supported the online data collection of trial participant data.
Rossella Iraci Capuccinello (https://orcid.org/0000-0002-6875-4867) conducted the health economics analysis.
Lesley Chapman was a co-investigator and an expert relative, responsible for training, supervision and support of the REACT supporters.
Lizzi Collinge (https://orcid.org/0000-0001-5297-4112) was a REACT supporter.
Susanna Dodd (https://orcid.org/0000-0003-2851-3337) (Institute of Child Health, Alder Hey Children’s NHS Foundation Trust) was the supervising statistician.
Sue Flowers (https://orcid.org/0000-0002-9302-3492) was a REACT supporter.
Bruce Hollingsworth (https://orcid.org/0000-0002-4314-6523) was a co-investigator and the lead for the health economics analysis.
Mahsa Honary (https://orcid.org/0000-0001-5966-2197) contributed to the development and design of the content for the online REACT.
Sonia Johnson (https://orcid.org/0000-0002-2219-1384) was a co-investigator, advising on intervention content and the design and implementation of the trial.
Steven H Jones (https://orcid.org/0000-0002-8801-5113) was a co-investigator, responsible for training and supervising the REACT supporters.
Ceu Mateus (https://orcid.org/0000-0001-6219-219X) conducted the health economics analysis.
Barbara Mezes (https://orcid.org/0000-0002-0799-2423) provided trial management and administrative support.
Elizabeth Murray (https://orcid.org/0000-0002-8932-3695) was a co-investigator, contributing to setting the research questions, designing the research methods and protocol, analysing and interpreting the data, and writing the final report.
Katerina Panagaki (https://orcid.org/0000-0002-0383-4890) conducted and analysed qualitative interviews with relatives in the REACT arm of the trial.
Naomi Rainford (https://orcid.org/0000-0002-5876-3946) (Institute of Child Health, Alder Hey Children’s NHS Foundation Trust) is a statistician who supported the management of the trial data.
Heather Robinson (https://orcid.org/0000-0002-3566-2253) was the trial manager.
Anna Rosala-Hallas (https://orcid.org/0000-0001-8012-9995) (Institute of Child Health, Alder Hey Children’s NHS Foundation Trust) is a statistician who supported the analysis of the trial data.
William Sellwood (https://orcid.org/0000-0001-8260-9503) supported the supervision of the REACT supporters.
Andrew Walker (https://orcid.org/0000-0001-6486-6135) is a digital technologist who was involved in the design and delivery of REACT and in data extraction, management and analysis.
Paula Williamson (https://orcid.org/0000-0001-9802-6636) (Institute of Child Health, Alder Hey Children’s NHS Foundation Trust) was a co-applicant and advisor on trial design and statistical analysis.
Publications
Robinson H, Lobban F, Honary M. Relatives’ Education and Coping Toolkit (REACT) Lessons learnt from developing a national online trial for relatives/friends of people with psychosis or bipolar disorder. Early Interv Psychia 2016;10:70.
Lobban F, Robinson H, Appelbe D, Barraclough J, Bedson E, Collinge L, et al. Protocol for an online randomised controlled trial to evaluate the clinical and cost-effectiveness of a peer-supported self-management intervention for relatives of people with psychosis or bipolar disorder: Relatives’ Education And Coping Toolkit (REACT). BMJ Open 2017;7:e016965.
Appelbe D, Robinson H, Dodd S, Walker A, Williamson P, Lobban F. Implementing and running an online trial – a case study using the REACT trial. Trials 2017;18(Suppl. 1):230.
Honary M, Fisher NR, McNaney R, Lobban F. A web-based intervention for relatives of people experiencing psychosis or bipolar disorder: design study using a user-centred approach. JMIR Mental Health 2018;5:e11473.
Lobban F, Collinge L, Robinson H, Flowers S, Minns V, Jones S. Approaches to service user engagement in the Relatives’ Education and Coping Toolkit (REACT) RCT. Bipolar Disord 2018;20:31.
Honary M, McNaney R, Lobban F. Designing Video Stories Around the Lived Experience of Severe Mental Illness. In NordiCHI ’18 Proceedings of the 10th Nordic Conference on Human–Computer Interaction. New York, NY: ACM; 2018. pp. 25–38.
Lobban F, Akers N, Appelbe D, Chapman L, Collinge L, Dodd S, et al. Clinical effectiveness of a web-based peer-supported self-management intervention for relatives of people with psychosis or bipolar (REACT): online, observer-blind, randomised controlled superiority trial. BMC Psychiatry 2020;20:160.
Data-sharing statement
Ownership of copyright and intellectual property rights for all research conducted for the REACT trial will ultimately be held by Lancaster University. We intend to make available the individual participant data that underlie the results reported in this article, after de-identification. Data will be made available on request 12 months following article publication, and only to researchers who provide a methodologically sound proposal and where the proposed use of the data has been approved by an independent ethics review committee (‘learned intermediary’) identified for this purpose. Proposals should be directed to the corresponding author at rdm@lancaster.ac.uk. Data will be available for 10 years at Lancaster University’s Research Directory (10.17635/lancaster/researchdata/306). The study protocol130 and statistical analysis plan125 are already published and freely available.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Honary M, Fisher NR, McNaney R, Lobban F. A web-based intervention for relatives of people experiencing psychosis or bipolar disorder: design study using a user-centered approach. JMIR Ment Health 2018;5. https://doi.org/10.2196/11473.
- Lobban F, Glentworth D, Chapman L, Wainwright L, Postlethwaite A, Dunn G, et al. Feasibility of a supported self-management intervention for relatives of people with recent-onset psychosis: REACT study. Br J Psychiatry 2013;203:366-72. https://doi.org/10.1192/bjp.bp.112.113613.
- Lobban F, Glentworth D, Haddock G, Wainwright L, Clancy A, Bentley R. React Team . The views of relatives of young people with psychosis on how to design a Relatives’ Education And Coping Toolkit (REACT). J Ment Health 2011;20:567-79. https://doi.org/10.3109/09638237.2011.593592.
- McGrath JJ, Saha S, Al-Hamzawi AO, Alonso J, Andrade L, Borges G, et al. Age of onset and lifetime projected risk of psychotic experiences: cross-national data from the World Mental Health Survey. Schizophr Bull 2016;42:933-41. https://doi.org/10.1093/schbul/sbw011.
- Johns LC, Kompus K, Connell M, Humpston C, Lincoln TM, Longden E, et al. Auditory verbal hallucinations in persons with and without a need for care. Schizophr Bull 2014;40:255-64. https://doi.org/10.1093/schbul/sbu005.
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013;382:1575-86. https://doi.org/10.1016/S0140-6736(13)61611-6.
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry 2007;64:543-52. https://doi.org/10.1001/archpsyc.64.5.543.
- McCrone PR, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying the Price: The Cost of Mental Health Care in England to 2026. London: The King’s Fund; 2008.
- Paykel ES, Abbott R, Morriss R, Hayhurst H, Scott J. Sub-syndromal and syndromal symptoms in the longitudinal course of bipolar disorder. Br J Psychiatry 2006;189:118-23. https://doi.org/10.1192/bjp.bp.105.013870.
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry 2005;62:975-83. https://doi.org/10.1001/archpsyc.62.9.975.
- Drancourt N, Etain B, Lajnef M, Henry C, Raust A, Cochet B, et al. Duration of untreated bipolar disorder: missed opportunities on the long road to optimal treatment. Acta Psychiatr Scand 2013;127:136-44. https://doi.org/10.1111/j.1600-0447.2012.01917.x.
- Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: a review. PharmacoEconomics 2008;26:149-62. https://doi.org/10.2165/00019053-200826020-00005.
- Barrowclough C, Gooding P, Hartley S, Lee G, Lobban F. Factors associated with distress in relatives of a family member experiencing recent-onset psychosis. J Nerv Ment Dis 2014;202:40-6. https://doi.org/10.1097/NMD.0000000000000072.
- Kingston C, Onwumere J, Keen N, Ruffell T, Kuipers E. Posttraumatic stress symptoms (PTSS) in caregivers of people with psychosis and associations with caregiving experiences. J Trauma Dissociation 2016;17:307-21. https://doi.org/10.1080/15299732.2015.1089969.
- Onwumere J, Bebbington P, Kuipers E. Family interventions in early psychosis: specificity and effectiveness. Epidemiol Psychiatr Sci 2011;20:113-19. https://doi.org/10.1017/s2045796011000187.
- Tennakoon L, Fannon D, Doku V, O’Ceallaigh S, Soni W, Santamaria M, et al. Experience of caregiving: relatives of people experiencing a first episode of psychosis. Br J Psychiatry 2000;177:529-33. https://doi.org/10.1192/bjp.177.6.529.
- McDonell MG, Short RA, Berry CM, Dyck DG. Burden in schizophrenia caregivers: impact of family psychoeducation and awareness of patient suicidality. Fam Process 2003;42:91-103. https://doi.org/10.1111/j.1545-5300.2003.00091.x.
- Magliano L, Fadden G, Madianos M, de Almeida JM, Held T, Guarneri M, et al. Burden on the families of patients with schizophrenia: results of the BIOMED I study. Soc Psychiatry Psychiatr Epidemiol 1998;33:405-12. https://doi.org/10.1007/s001270050073.
- Möller-Leimkühler AM. Burden of relatives and predictors of burden. Baseline results from the Munich 5-year-follow-up study on relatives of first hospitalized patients with schizophrenia or depression. Eur Arch Psychiatry Clin Neurosci 2005;255:223-31. https://doi.org/10.1007/s00406-004-0550-x.
- Lobban F, Barrowclough C, Jones S. Does expressed emotion need to be understood within a more systemic framework?. Soc Psychiatry Psychiatr Epidemiol 2006;41:50-5. https://doi.org/10.1007/s00127-005-0993-z.
- Onwumere J, Lotey G, Schulz J, James G, Afsharzadegan R, Harvey R, et al. Burnout in early course psychosis caregivers: the role of illness beliefs and coping styles. Early Interv Psychiatry 2017;11:237-43. https://doi.org/10.1111/eip.12227.
- Kuipers E, Watson P, Onwumere J, Bebbington P, Dunn G, Weinman J, et al. Discrepant illness perceptions, affect and expressed emotion in people with psychosis and their carers. Soc Psychiatry Psychiatr Epidemiol 2007;42:277-83. https://doi.org/10.1007/s00127-007-0165-4.
- Chessick CA, Perlick DA, Miklowitz DJ, Dickinson LM, Allen MH, Morris CD, et al. Suicidal ideation and depressive symptoms among bipolar patients as predictors of the health and well-being of caregivers. Bipolar Disord 2009;11:876-84. https://doi.org/10.1111/j.1399-5618.2009.00765.x.
- Ostacher MJ, Nierenberg AA, Iosifescu DV, Eidelman P, Lund HG, Ametrano RM, et al. Correlates of subjective and objective burden among caregivers of patients with bipolar disorder. Acta Psychiatr Scand 2008;118:49-56. https://doi.org/10.1111/j.1600-0447.2008.01201.x.
- Steele A, Maruyama N, Galynker I. Psychiatric symptoms in caregivers of patients with bipolar disorder: a review. J Affect Disord 2010;121:10-21. https://doi.org/10.1016/j.jad.2009.04.020.
- Chessick CA, Perlick DA, Miklowitz DJ, Kaczynski R, Allen MH, Morris CD, et al. Current suicide ideation and prior suicide attempts of bipolar patients as influences on caregiver burden. Suicide Life Threat Behav 2007;37:482-91. https://doi.org/10.1521/suli.2007.37.4.482.
- Fletcher K, Parker GB, Manicavasagar V. Coping profiles in bipolar disorder. Compr Psychiatry 2013;54:1177-84. https://doi.org/10.1016/j.comppsych.2013.05.011.
- Hosang GM, Uher R, Maughan B, McGuffin P, Farmer AE. The role of loss and danger events in symptom exacerbation in bipolar disorder. J Psychiatr Res 2012;46:1584-9. https://doi.org/10.1016/j.jpsychires.2012.07.009.
- Morriss R, Yang M, Chopra A, Bentall R, Paykel E, Scott J. Differential effects of depression and mania symptoms on social adjustment: prospective study in bipolar disorder. Bipolar Disord 2013;15:80-91. https://doi.org/10.1111/bdi.12036.
- Lowenstein JA, Butler DW, Ashcroft K. The efficacy of a cognitively orientated carers group in an early intervention in psychosis service – a pilot study. J Psychiatr Ment Health Nurs 2010;17:628-35. https://doi.org/10.1111/j.1365-2850.2010.01564.x.
- Zendjidjian X, Richieri R, Adida M, Limousin S, Gaubert N, Parola N, et al. Quality of life among caregivers of individuals with affective disorders. J Affect Disord 2012;136:660-5. https://doi.org/10.1016/j.jad.2011.10.011.
- Chen FP, Greenberg JS. A positive aspect of caregiving: the influence of social support on caregiving gains for family members of relatives with schizophrenia. Community Ment Health J 2004;40:423-35. https://doi.org/10.1023/b:comh.0000040656.89143.82.
- Veltman A, Cameron J, Stewart DE. The experience of providing care to relatives with chronic mental illness. J Nerv Ment Dis 2002;190:108-14. https://doi.org/10.1097/00005053-200202000-00008.
- Andrew A, Knapp M, McCrone P, Parsonage M, Trachtenberg M. Effective Interventions in Schizophrenia – The Economic Case. A Report Prepared for the Schizophrenia Commission 2012.
- Buckner L, Yeandle S. Valuing Carers 2015. London: Carers UK; 2015.
- Lowyck B, De Hert M, Peeters E, Wampers M, Gilis P, Peuskens J. A study of the family burden of 150 family members of schizophrenic patients. Eur Psychiatry 2004;19:395-401. https://doi.org/10.1016/j.eurpsy.2004.04.006.
- Perlick D, Clarkin JF, Sirey J, Raue P, Greenfield S, Struening E, et al. Burden experienced by care-givers of persons with bipolar affective disorder. Br J Psychiatry 1999;175:56-62. https://doi.org/10.1192/bjp.175.1.56.
- Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database Syst Rev 2010;12. https://doi.org/10.1002/14651858.CD000088.pub2.
- Lobban F, Postlethwaite A, Glentworth D, Pinfold V, Wainwright L, Dunn G, et al. A systematic review of randomised controlled trials of interventions reporting outcomes for relatives of people with psychosis. Clin Psychol Rev 2013;33:372-82. https://doi.org/10.1016/j.cpr.2012.12.004.
- Miklowitz DJ, George EL, Richards JA, Simoneau TL, Suddath RL. A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. Arch Gen Psychiatry 2003;60:904-12. https://doi.org/10.1001/archpsyc.60.9.904.
- Perlick DA, Miklowitz DJ, Lopez N, Chou J, Kalvin C, Adzhiashvili V, et al. Family-focused treatment for caregivers of patients with bipolar disorder. Bipolar Disord 2010;12:627-37. https://doi.org/10.1111/j.1399-5618.2010.00852.x.
- Yesufu-Udechuku A, Harrison B, Mayo-Wilson E, Young N, Woodhams P, Shiers D, et al. Interventions to improve the experience of caring for people with severe mental illness: systematic review and meta-analysis. Br J Psychiatry 2015;206:268-74. https://doi.org/10.1192/bjp.bp.114.147561.
- Sin J, Gillard S, Spain D, Cornelius V, Chen T, Henderson C. Effectiveness of psychoeducational interventions for family carers of people with psychosis: a systematic review and meta-analysis. Clin Psychol Rev 2017;56:13-24. https://doi.org/10.1016/j.cpr.2017.05.002.
- Geddes JR, Miklowitz DJ. Treatment of bipolar disorder. Lancet 2013;381:1672-82. https://doi.org/10.1016/S0140-6736(13)60857-0.
- Reinares M, Colom F, Sánchez-Moreno J, Torrent C, Martínez-Arán A, Comes M, et al. Impact of caregiver group psychoeducation on the course and outcome of bipolar patients in remission: a randomized controlled trial. Bipolar Disord 2008;10:511-19. https://doi.org/10.1111/j.1399-5618.2008.00588.x.
- Miklowitz DJ. Bipolar Disorder: A Family-focused Treatment Approach. New York, NY: Guilford Press; 2010.
- Addington J, McCleery A, Addington D. Three-year outcome of family work in an early psychosis program. Schizophr Res 2005;79:107-16. https://doi.org/10.1016/j.schres.2005.03.019.
- Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26:1-7. https://doi.org/10.1207/S15324796ABM2601_01.
- Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry 1998;55:547-52. https://doi.org/10.1001/archpsyc.55.6.547.
- Miklowitz DJ, Goldstein MJ, Nuechterlein KH, Snyder KS, Mintz J. Family factors and the course of bipolar affective disorder. Arch Gen Psychiatry 1988;45:225-31. https://doi.org/10.1001/archpsyc.1988.01800270033004.
- Kim EY, Miklowitz DJ. Expressed emotion as a predictor of outcome among bipolar patients undergoing family therapy. J Affect Disord 2004;82:343-52. https://doi.org/10.1016/j.jad.2004.02.004.
- Great Britain . Care Act 2014 2014.
- National Institute for Health and Care Excellence . Bipolar Disorder: Assessment and Management of Bipolar Disorder 2014.
- National Institute for Health and Care Excellence . Psychosis and Schizophrenia in Adults: Prevention and Management 2014.
- Healthcare Quality Improvement Partnership, Royal College of Psychiatrists . Report of the Early Intervention in Psychosis Audit 2016.
- Vermeulen B, Lauwers H, Spruytte N, Van Audenhove C, Magro C, Saunders J, et al. Experiences of Family Caregivers for Persons with Severe Mental Illness: An International Exploration. Leuven: LUCAS KU Leuven/EUFAMI; 2015.
- Eassom E, Giacco D, Dirik A, Priebe S. Implementing family involvement in the treatment of patients with psychosis: a systematic review of facilitating and hindering factors. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-006108.
- Department of Health and Social Care . Achieving Better Access to Mental Health Services by 2020 2014.
- Worthington A, Rooney P, Hannan R. The Triangle of Care. Carers Included: A Guide to Best Practice in Mental Health Care in England. London: Carers Trust; 2013.
- Lobban F, Glentworth D, Wainwright L, Pinfold V, Chapman L, Larkin W, et al. Relatives’ Education And Coping Toolkit – REACT. Study protocol of a randomised controlled trial to assess the feasibility and effectiveness of a supported self management package for relatives of people with recent onset psychosis. BMC Psychiatry 2011;11. https://doi.org/10.1186/1471-244X-11-100.
- Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med 1979;9:139-45. https://doi.org/10.1017/s0033291700021644.
- Quirk A, Smith SC, Hamilton S, Lamping DL, Lelliott P, Stahl D, et al. Development and Validation of the Carer Well-Being and Support (CWS) Questionnaire: Report for the National Institute for Health Research Service Delivery and Organisation Programme 2009.
- Quinn J, Barrowclough C, Tarrier N. The Family Questionnaire (FQ): a scale for measuring symptom appraisal in relatives of schizophrenic patients. Acta Psychiatr Scand 2003;108:290-6. https://doi.org/10.1034/j.1600-0447.2003.00156.x.
- Wainwright L. Relatives’ Experiences of Supporting and Caring for a Family Member with First Episode Psychosis, with or without a Self-management Intervention. Lancaster: Lancaster University; 2015.
- Gafoor R, Nitsch D, McCrone P, Craig TK, Garety PA, Power P, et al. Effect of early intervention on 5-year outcome in non-affective psychosis. Br J Psychiatry 2010;196:372-6. https://doi.org/10.1192/bjp.bp.109.066050.
- Bertelsen M, Jeppesen P, Petersen L, Thorup A, Øhlenschlaeger J, le Quach P, et al. Five-year follow-up of a randomized multicenter trial of intensive early intervention vs. standard treatment for patients with a first episode of psychotic illness: the OPUS trial. Arch Gen Psychiatry 2008;65:762-71. https://doi.org/10.1001/archpsyc.65.7.762.
- Arnberg FK, Linton SJ, Hultcrantz M, Heintz E, Jonsson U. Internet-delivered psychological treatments for mood and anxiety disorders: a systematic review of their efficacy, safety, and cost-effectiveness. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0098118.
- Alvarez-Jimenez M, Alcazar-Corcoles MA, González-Blanch C, Bendall S, McGorry PD, Gleeson JF. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophr Res 2014;156:96-106. https://doi.org/10.1016/j.schres.2014.03.021.
- Hidalgo-Mazzei D, Mateu A, Reinares M, Matic A, Vieta E, Colom F. Internet-based psychological interventions for bipolar disorder: review of the present and insights into the future. J Affect Disord 2015;188:1-13. https://doi.org/10.1016/j.jad.2015.08.005.
- Scott JL, Dawkins S, Quinn MG, Sanderson K, Elliott KE, Stirling C, et al. Caring for the carer: a systematic review of pure technology-based cognitive behavioral therapy (TB-CBT) interventions for dementia carers. Aging Ment Health 2016;20:793-80. https://doi.org/10.1080/13607863.2015.1040724.
- Ziebland S, Wyke S. Health and illness in a connected world: how might sharing experiences on the internet affect people’s health?. Milbank Q 2012;90:219-49. https://doi.org/10.1111/j.1468-0009.2012.00662.x.
- Sin J, Henderson C, Spain D, Cornelius V, Chen T, Gillard S. eHealth interventions for family carers of people with long term illness: a promising approach?. Clin Psychol Rev 2018;60:109-25. https://doi.org/10.1016/j.cpr.2018.01.008.
- Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health 2011;20:392-411. https://doi.org/10.3109/09638237.2011.583947.
- Faulkner A, Basset T. A helping hand: taking peer support into the 21st century. Ment Health Soc Incl 2012;16:41-7. https://doi.org/10.1108/20428301211205892.
- Walker G, Bryant W. Peer support in adult mental health services: a metasynthesis of qualitative findings. Psychiatr Rehabil J 2013;36:28-34. https://doi.org/10.1037/h0094744.
- National Institute for Health and Care Excellence . Implementing the Early Intervention in Psychosis Access and Waiting Time Standard: Guidance 2016.
- Murray E, Khadjesari Z, White IR, Kalaitzaki E, Godfrey C, McCambridge J, et al. Methodological challenges in online trials. J Med Internet Res 2009;11. https://doi.org/10.2196/jmir.1052.
- Mathieu E, McGeechan K, Barratt A, Herbert R. Internet-based randomized controlled trials: a systematic review. J Am Med Inform Assoc 2013;20:568-76. https://doi.org/10.1136/amiajnl-2012-001175.
- Department of Health and Social Care . A Framework for Mental Health Research 2017.
- Wainwright LD, Glentworth D, Haddock G, Bentley R, Lobban F. What do relatives experience when supporting someone in early psychosis?. Psychol Psychother 2015;88:105-19. https://doi.org/10.1111/papt.12024.
- Eysenbach G. CONSORT-EHEALTH Group . CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res 2011;13. https://doi.org/10.2196/jmir.1923.
- Norman DA, Norman DA, Draper SW. User Centered System Design: New Perspectives on Human–Computer Interaction. Hillsdale, NJ: Lawrence Erlbaum Associates Inc.; 1986.
- Lancaster University . The Spectrum Centre for Mental Health Research n.d. www.lancaster.ac.uk/shm/research/spectrum/ (accessed 28 October 2019).
- Anderson CM, Reiss DJ, Hogarty GE. Schizophrenia and the Family: A Practitioner’s Guide to Psychoeducation and Management. New York, NY: Guilford Press; 1986.
- Barrowclough C, Tarrier N. Families of Schizophrenic Patients: Cognitive Behavioural Intervention. Cheltenham: Stanley Thornes Publishers Ltd; 1992.
- Falloon IR. Handbook of Behavioural Family Therapy. London: Routledge; 1988.
- Kuipers L, Birchwood M, McCreadie RG. Psychosocial family intervention in schizophrenia: a review of empirical studies. Br J Psychiatry 1992;160:272-5. https://doi.org/10.1192/bjp.160.2.272.
- McFarlane WR. Family Therapy in Schizophrenia. New York, NY: Guilford Press; 1983.
- NHS England . Five Year Forward View 2014.
- Berry N, Lobban F, Emsley R, Bucci S. Acceptability of interventions delivered online and through mobile phones for people who experience severe mental health problems: a systematic review. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5250.
- O’Connor S, Hanlon P, O’Donnell CA, Garcia S, Glanville J, Mair FS. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: a systematic review of qualitative studies. BMC Med Inform Decis Mak 2016;16. https://doi.org/10.1186/s12911-016-0359-3.
- Van Dijk J. The International Encyclopedia of Media Effects. Hoboken, NJ: John Wiley & Sons; 2017.
- Christensen H, Griffiths KM, Farrer L. Adherence in internet interventions for anxiety and depression. J Med Internet Res 2009;11. https://doi.org/10.2196/jmir.1194.
- Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn Behav Ther 2009;38:196-205. https://doi.org/10.1080/16506070903318960.
- Kaufman L, Brooks W, Steinley-Bumgarner M, Stevens-Manser S. Peer Specialist Training and Certification Programs: A National Overview. Austin, TX: Center for Social Work Research, University of Texas at Austin; 2012.
- Mental Health Commission . Blueprint II: Improving Mental Health and Wellbeing for All New Zealanders: How Things Need To Be 2012.
- National Institute for Health and Care Excellence . Transition Between Inpatient Mental Health Settings and Community or Care Home Settings 2016.
- Joint Commissioning Panel for Mental Health . Guidance for Commissioners of Acute Care – Inpatient and Crisis Home Treatment 2012.
- Joint Commissioning Panel for Mental Health . Guidance for Commissioners of Community Specialist Mental Health Services 2012.
- Mental Health Commission of Canada . Changing Directions, Changing Lives: The Mental Health Strategy for Canada 2012.
- Schulz KF, Altman DG, Moher D. CONSORT Group . CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-18.
- Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B, et al. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ 2008;337. https://doi.org/10.1136/bmj.a2390.
- Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 2004;6. https://doi.org/10.2196/jmir.6.3.e34.
- Lobban F, Appleton V, Appelbe D, Barraclough J, Bowland J, Fisher NR, et al. IMPlementation of A Relatives’ Toolkit (IMPART study): an iterative case study to identify key factors impacting on the implementation of a web-based supported self-management intervention for relatives of people with psychosis or bipolar experiences in a National Health Service: a study protocol. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0687-4.
- Gu LL, Skierkowski D, Florin P, Friend K, Ye Y. Facebook, Twitter, & QR codes: an exploratory trial examining the feasibility of social media mechanisms for sample recruitment. Comput Hum Behav 2016;60:86-9. https://doi.org/10.1016/j.chb.2016.02.006.
- O’Connor A, Jackson L, Goldsmith L, Skirton H. Can I get a retweet please? Health research recruitment and the Twittersphere. J Adv Nurs 2014;70:599-60. https://doi.org/10.1111/jan.12222.
- Bailey JV, Pavlou M, Copas A, McCarthy O, Carswell K, Rait G, et al. The Sexunzipped trial: optimizing the design of online randomized controlled trials. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2668.
- Morgan AJ, Jorm AF, Mackinnon AJ. Internet-based recruitment to a depression prevention intervention: lessons from the Mood Memos study. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2262.
- British Psychological Society . Ethics Guidelines for Internet-Mediated Research 2013.
- European Parliament, Council of the European Union . Regulation (EU) 2016 679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons With Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95 46 EC (General Data Protection Regulation) n.d. https://eur-lex.europa.eu/eli/reg/2016/679/oj (accessed 28 January 2020).
- Harvey K, Catty J, Langman A, Winfield H, Clement S, Burns E, et al. A review of instruments developed to measure outcomes for carers of people with mental health problems. Acta Psychiatr Scand 2008;117:164-76. https://doi.org/10.1111/j.1600-0447.2007.01148.x.
- Whittaker W, Sutton M. Mental Health, Work Incapacity and State Transfers: An Analysis of the British Household Panel Survey. York: Department of Economics, University of York; 2010.
- Whittaker W, Sutton M, Macdonald S, Maxwell M, Smith M, Wilson P, et al. The effect of mental ill health on absence from work in different occupational classifications: analysis of routine data in the British Household Panel Survey. J Occup Environ Med 2012;54:1539-44. https://doi.org/10.1097/JOM.0b013e3182677d12.
- Whittaker W, Sutton M, Maxwell M, Munoz-Arroyo R, Macdonald S, Power A, et al. Predicting which people with psychosocial distress are at risk of becoming dependent on state benefits: analysis of routinely available data. BMJ 2010;341. https://doi.org/10.1136/bmj.c3838.
- Russ TC, Stamatakis E, Hamer M, Starr JM, Kivimäki M, Batty GD. Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. BMJ 2012;345. https://doi.org/10.1136/bmj.e4933.
- Quirk A, Smith S, Hamilton S, Lamping D, Lelliott P, Stahl D, et al. Development of the Carer Well-being and Support (CWS) Questionnaire. Ment Health Rev 2012;17:128-38. https://doi.org/10.1108/13619321211287184.
- Broadbent E, Petrie KJ, Main J, Weinman J. The Brief Illness Perception Questionnaire. J Psychosom Res 2006;60:631-7. https://doi.org/10.1016/j.jpsychores.2005.10.020.
- Carver CS. You want to measure coping but your protocol’s too long: consider the Brief COPE. Int J Behav Med 1997;4:92-100. https://doi.org/10.1207/s15327558ijbm0401_6.
- Beck JS. Cognitive Behavior Therapy: Basics and Beyond. New York, NY: Guilford Press; 2011.
- Szmukler GI, Herrman H, Colusa S, Benson A, Bloch S. A controlled trial of a counselling intervention for caregivers of relatives with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 1996;31:149-55. https://doi.org/10.1007/bf00785761.
- Woods RT, Bruce E, Edwards RT, Elvish R, Hoare Z, Hounsome B, et al. REMCARE: reminiscence groups for people with dementia and their family caregivers – effectiveness and cost-effectiveness pragmatic multicentre randomised trial. Health Technol Assess 2012;16. https://doi.org/10.3310/hta16480.
- Brueton VC, Tierney JF, Stenning S, Meredith S, Harding S, Nazareth I, et al. Strategies to improve retention in randomised trials: a Cochrane systematic review and meta-analysis. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-003821.
- Khadjesari Z, Murray E, Kalaitzaki E, White IR, McCambridge J, Thompson SG, et al. Impact and costs of incentives to reduce attrition in online trials: two randomized controlled trials. J Med Internet Res 2011;13. https://doi.org/10.2196/jmir.1523.
- David MC, Ware RS. Meta-analysis of randomized controlled trials supports the use of incentives for inducing response to electronic health surveys. J Clin Epidemiol 2014;67:1210-21. https://doi.org/10.1016/j.jclinepi.2014.08.001.
- Lobban F. REACT Statistical Analysis Plan v1.0; An Online Randomised Controlled Trial to Evaluate the Clinical and Cost Effectiveness of a Peer Supported Self-Management Intervention for Relatives of People With Psychosis or Bipolar Disorder: Relatives Education And Coping Toolkit (REACT) 2017. https://figshare.com/articles/REACT_Statistical_Analysis_Plan_v1_0_An_online_randomised_controlled_trial_to_evaluate_the_clinical_and_cost_effectiveness_of_a_peer_supported_self-management_intervention_for_relatives_of_people_with_psychosis_or_bipolar_disorder_Relatives_Education_And_/4775539 (accessed 28 October 2019).
- Nonnecke B, Andrews D, Preece J. Non-public and public online community participation: needs, attitudes and behavior. Electron Commerce Res 2006;6:7-20. https://doi.org/10.1007/s10660-006-5985-x.
- Gleeson JF, Lederman R, Wadley G, Bendall S, McGorry PD, Alvarez-Jimenez M. Safety and privacy outcomes from a moderated online social therapy for young people with first-episode psychosis. Psychiatr Serv 2014;65:546-50. https://doi.org/10.1176/appi.ps.201300078.
- NHS Digital . Patient Health Questionnaire-9 (PHQ-9) n.d. www.datadictionary.nhs.uk/data_dictionary/nhs_business_definitions/p/patient_health_questionnaire-9_de.asp (accessed 28 October 2019).
- Great Britain . Data Protection Act 2018 2018.
- Lobban F, Robinson H, Appelbe D, Barraclough J, Bedson E, Collinge L, et al. Protocol for an online randomised controlled trial to evaluate the clinical and cost-effectiveness of a peer-supported self-management intervention for relatives of people with psychosis or bipolar disorder: Relatives’ Education And Coping Toolkit (REACT). BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016965.
- Lobban F, Akers N, Appelbe D, Chapman L, Collinge L, Dodd S, et al. Clinical effectiveness of a web-based peer-supported self-management intervention for relatives of people with psychosis or bipolar (REACT): online, observer-blind, randomised controlled superiority trial. BMC Psychiatry 2020;20. https://doi.org/10.1186/s12888-020-02545-9.
- GL Assessment . General Health Questionnaire n.d. www.gl-assessment.co.uk/products/general-health-questionnaire-ghq/ (accessed 23 August 2019).
- Goldberg D. Manual of the General Health Questionnaire. Windsor: NFER Nelson; 1978.
- Jones CJ, Hayward M, Brown A, Clark E, Bird D, Harwood G, et al. Feasibility and participant experiences of a written emotional disclosure intervention for parental caregivers of people with psychosis. Stress Health 2016;32:485-93. https://doi.org/10.1002/smi.2644.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013 2013.
- Frick KD. Microcosting quantity data collection methods. Med Care 2009;47:76-81. https://doi.org/10.1097/MLR.0b013e31819bc064.
- Li J, Parrott S, Sweeting M, Farmer A, Ross J, Dack C, et al. Cost-effectiveness of facilitated access to a self-management website, compared to usual care, for patients with type 2 diabetes (HeLP-Diabetes): randomized controlled trial. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.9256.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- NHS Improvement . National Schedule of Reference Costs 2017 18 2017.
- Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ 2018;27:7-22. https://doi.org/10.1002/hec.3564.
- Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. PharmacoEconomics 2014;32:1157-70. https://doi.org/10.1007/s40273-014-0193-3.
- Department for Business, Energy and Industrial Strategy . Ethnicity Facts and Figures: Average Hourly Pay 2018.
- Iribarren SJ, Cato K, Falzon L, Stone PW. What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0170581.
- Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev 2006;63:217-35. https://doi.org/10.1177/1077558705285298.
- Petrou S, Murray L, Cooper P, Davidson LL. The accuracy of self-reported healthcare resource utilization in health economic studies. Int J Technol Assess Health Care 2002;18:705-10. https://doi.org/10.1017/s026646230200051x.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) – explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health 2013;16:231-50. https://doi.org/10.1016/j.jval.2013.02.002.
- Livingston G, Barber J, Rapaport P, Knapp M, Griffin M, King D, et al. Long-term clinical and cost-effectiveness of psychological intervention for family carers of people with dementia: a single-blind, randomised, controlled trial. Lancet Psychiatry 2014;1:539-48. https://doi.org/10.1016/S2215-0366(14)00073-X.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. Abingdon: Routledge; 2002.
- Rayson P. Wmatrix: A Web-based Corpus Processing Environment. Lancaster: Computing Department, Lancaster University; 2009.
- Glynn SM, Randolph ET, Garrick T, Lui A. A proof of concept trial of an online psychoeducational program for relatives of both veterans and civilians living with schizophrenia. Psychiatr Rehabil J 2010;33:278-87. https://doi.org/10.2975/33.4.2010.278.287.
- Rotondi AJ, Haas GL, Anderson CM, Newhill CE, Spring MB, Ganguli R, et al. A clinical trial to test the feasibility of a telehealth psychoeducational intervention for persons with schizophrenia and their families: intervention and 3-month findings. Rehabil Psychol 2005;50:325-36. https://doi.org/10.1037/0090-5550.50.4.325.
- Mohr DC, Cuijpers P, Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J Med Internet Res 2011;13. https://doi.org/10.2196/jmir.1602.
- Baumeister H, Reichler L, Munzinger M, Lin J. The impact of guidance on internet-based mental health interventions – a systematic review. Internet Interventions 2014;1:205-15. https://doi.org/10.1016/j.invent.2014.08.003.
- Mental Health Taskforce . The Five Year Forward View for Mental Health 2016.
- NHS Digital . Health Secretary: My Tech Vision Will Help Build Most Advanced Health and Care System in the World 2018. https://digital.nhs.uk/news-and-events/latest-news/nhs-technology-vision (accessed 18 February 2020).
- Craig P, Matthews L, Moore L, Simpson S, Skivington K, Baird J, et al. Developing and Evaluating Complex Interventions: Draft of Updated Guidance n.d. www.sphsu.gla.ac.uk/stakeholder-survey-2019/Full%20complex%20guidance%20draft%20for%20consultation%20v1.1%2026.03.19.pdf (accessed 28 February 2020).
- Mohr DC, Schueller SM, Riley WT, Brown CH, Cuijpers P, Duan N, et al. Trials of intervention principles: evaluation methods for evolving behavioral intervention technologies. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4391.
- Perle JG, Langsam LC, Randel A, Lutchman S, Levine AB, Odland AP, et al. Attitudes toward psychological telehealth: current and future clinical psychologists’ opinions of internet-based interventions. J Clin Psychol 2013;69:100-13. https://doi.org/10.1002/jclp.21912.
- Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, et al. Annual research review: digital health interventions for children and young people with mental health problems – a systematic and meta-review. J Child Psychol Psychiatry 2017;58:474-503. https://doi.org/10.1111/jcpp.12663.
- Queen’s University Belfast . SWAT 65: Strategies to Optimise Retention to an Online Randomised Controlled Trial for Relatives of People With Severe Mental Illness n.d. www.qub.ac.uk/sites/TheNorthernIrelandNetworkforTrialsMethodologyResearch/FileStore/Filetoupload,786657,en.pdf (accessed 28 October 2019).
- Deci E, Ryan RM. Intrinsic Motivation and Self-determination in Human Behavior. Berlin: Springer Science+Business Media; 1985.
Appendix 1 Changes to the protocol and statistical analysis plan
Protocol
The REACT trial protocol130 was published before the end of data collection.
The following amendments and clarifications were made to the published protocol paper:
-
We aimed to recruit 666 relatives. Ethics approval was granted to continue recruiting throughout the recruitment phase to ensure that we had an adequate sample size to test our primary and secondary hypotheses.
-
The RAG was involved in the development of REACT and the recruitment strategy for the trial. However, it was not involved in the data analysis or interpretation, and has not yet been involved in dissemination. The challenges of PPI in an entirely online trial are described in Chapter 7.
-
The protocol130 stated that one of the inclusion criteria was ‘a score’ of ≥ 3 on the GHQ-28 item ‘I feel nervous and strung-up all the time’. This should read ‘eligibility requires a response on the third (rather more than usual) or fourth (much more than usual) option’. The items were not scored. If they had been, this would have been a score of ≥ 2, as the GHQ-28 items are scored 0–3.
Protocol deviations
Full details of all the technical issues that arose during the trial are listed in Report Supplementary Material 1, Table 6–6. Table 54 summarises the cases in which this led to a protocol deviation and the number of participants affected in each arm. In addition, the University of Liverpool server, which hosted the data collection, was inaccessible from 21.00 on 15 November 2017 until 08.45 on 16 November 2017, which would have interrupted use of REACT for all participants.
| Protocol specification | Potential deviation(s) | Trial arm, n (%) | Total, n (%) (n = 800) | |
|---|---|---|---|---|
| REACT (n = 399) | RD only (n = 401) | |||
| Baseline demographic information | Missing baseline demographic information | 31 (7.8) | 31 (7.7) | 62 (7.8) |
| 12-week outcome measures | Missing 12-week outcome measures | 112 (28.1) | 94 (23.4) | 206 (25.8) |
| 24-week outcome measures | Missing 24-week outcome measures | 107 (26.8) | 94 (23.4) | 201 (25.1) |
| E-mail participants follow-up reminders or secondary randomisation allocation | Any inaccuracies associated with e-mail contact with participants | 26 (6.5) | 20 (5.0) | 46 (5.8) |
| Access to intervention | Times when participants unable to access assigned intervention (e.g. during maintenance or bug-fixing) | 3 (0.8) | 2 (0.5) | 5 (0.6) |
| Web use data will be recorded | Protocol to measure web use was activated only on 15 June 2017 | 51 (12.8) | 49 (12) | 100 (12.5) |
Statistical analysis plan
A full statistical analysis plan125 was published on 22 March 2017, before the start of data collection, and updated on 20 December 2017, before the end of data collection. Both versions are available. 125
Updates were as follows:
-
Clarification that the time spent on the final web page of a given log-in session for a participant would not be available; therefore, this would be imputed. If there was a video on this web page, video feedback data would allow calculation of the time, accurate to within 5 seconds, spent on this page. If there was no video on this page, it would be assumed that the time spent on this page was equal to the mean time that they had spent on all previous web pages to date.
-
Clarified that p-values would be reported to four decimal places [changed from ‘three decimal places (unless < 0.00001, in which the exact p-value will be reported up to a maximum of five decimal places, i.e. minimum reporting threshold of p < 0.00001)’].
-
To maximise retention, participants who did not complete the GHQ-28 online were sent postal versions. When completion dates were missing for postal GHQ-28s, we estimated them by calculating the mid-point between dates of sending and receiving the questionnaires. If not recorded, the date of receipt was imputed using the mean number of days between sending and receiving questionnaires for all postal GHQ-28s with accurately recorded sending and receiving dates.
-
An additional exploratory analysis was added to test the impact of ‘lurking’ in the forums, as this became a topic of growing interest during the trial.
All analyses were carried out using SAS version 9.4 and Stata version 14.
Appendix 2 Study within a trial
We embedded a methodological study within the REACT trial on the impact of higher incentives and conditional rewards on recruitment, and registered it as a SWAT protocol, which is available online. 160
The strongest evidence exists for payment incentives as supporting effectiveness in increasing follow-up completion rates. 122,124 However, the amount paid, and whether it is offered conditionally or unconditionally, remain areas of uncertainty. We compared the relative effectiveness and costs associated with a lower value (£10) with those associated with a higher value (£20) of reward, and whether the reward was conditional or unconditional. We embedded this SWAT in the REACT randomised trial, for the 24-week follow-up.
At 24 weeks’ follow-up, participants underwent a second randomisation to one of the following four intervention groups:
-
intervention 1 – £10 conditional (dependent on completion of the follow-up questionnaire)
-
intervention 2 – £10 unconditional (offered with the request, and so available even without completion)
-
intervention 3 – £20 conditional
-
intervention 4 – £20 unconditional.
To assess the impact of this second randomisation, the number (proportion) of participants providing 24-week follow-up data was calculated, presented and compared between arms using the χ2 test. The independent impact of intervention arm on retention rates over and above that of reward was explored by including the intervention arm along with the value of the reward (or un/conditional nature of the reward) as an explanatory variable in logistic regression.
Outcome
Table 55 shows the number of people completing the GHQ-28 at the 24-week follow-up in each arm of the trial, and in each category of £10 versus £20 reward, and unconditional versus conditional reward. A chi-squared test showed no significant benefit in offering people a higher level of reward, or a conditional reward.
| Randomised group | Completed GHQ-28 (n) | Did not complete GHQ-28 (n) | ||
|---|---|---|---|---|
| REACT arm | RD-only arm | REACT arm | RD-only arm | |
| Overall | 292 | 307 | 96 | 83 |
| Value of the reward | ||||
| £10 | 148 | 146 | 51 | 44 |
| £20 | 144 | 161 | 45 | 39 |
| Nature of the reward | ||||
| Unconditional | 145 | 158 | 41 | 45 |
| Conditional | 147 | 149 | 55 | 38 |
The independent impact of intervention arm on retention rates was explored by including intervention arm along with value of the reward (or un/conditional nature of the reward) as an explanatory variable in logistic regression. There was no significant impact of intervention arm on retention when allowing for either the value of reward (odds ratio 0.825, 95% CI 0.590 to 1.154) or the nature of reward (odds ratio 0.825, 95% CI 0.590 to 1.154) (see Report Supplementary Material 1, section 6.6.11).
Discussion
Retention in online trials is always a challenge. We used several strategies to maximise retention, including multiple strategies for follow-up, which showed some success. However, our SWAT showed that, for this population, there was no effect when varying the amount of financial incentive to complete follow-up or when making the incentive conditional on completion. This finding was in contrast to previous studies, such as the ‘Sexunzipped’ online trial,107 in which higher financial rewards (£20 vs. £10) increased response rates for both online self-report data and urine samples by post, and might reflect differences in the populations, highlighting the importance of understanding the motivations of the population being recruited. 123 It is possible that older relatives in a caring role are more motivated to take part in the trial by having access to the intervention and the opportunity to improve care for other relatives, whereas younger people recruited to a sexual health study may have less disposable income and be more motivated by the financial reward. However, this remains speculative and is an important area for future research, especially as misunderstanding motivation could result in retention strategies that, in fact, have a negative impact on retention. 161
Glossary
- Adverse event
- Any untoward medical occurrence in a patient or clinical investigation subject who has been administered a health intervention, but that does not necessarily have a causal relationship with this treatment.
- Analysis of covariance
- A model that evaluates whether or not the means of a dependent variable are equal across levels of a categorical independent variable (often called the treatment), while statistically controlling for the effects of covariates (other continuous variables that are not of primary interest).
- Bipolar disorder
- A mood disorder characterised by periods of low mood (depression) and periods of elevated mood (hypomania or mania).
- Brief Coping Orientation to Problems Experienced (COPE)
- A shorter version of the Coping Orientation to Problems Experienced (COPE) inventory, which is a questionnaire designed to assess a broad range of a subject’s coping responses.
- Consolidated Standards of Reporting Trials of Electronic and Mobile HEalth Applications and onLine TeleHealth (CONSORT-EHEALTH)
- A checklist designed to standardise the running of randomised controlled trials for digital health interventions.
- Covariance
- A measure of the joint variability of two random variables.
- Digital health intervention
- An intervention delivered via digital technologies such as smartphones, website, text messaging.
- eHealth
- Electronic health. An alternative term for digital health intervention.
- EuroQol-5 Dimensions, five-level version
- A measure of health-related quality of life, developed by the EuroQol Group. The latest version assesses five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Ratings can be given for each dimension across five levels of severity.
- Family intervention
- Structured help and support for carers and family members of a person with a mental health problem, either individually or together, delivered by health professionals.
- Instrumental variable
- A variable measure used to estimate a causal relationship when a treatment is not delivered to every participant in a randomised controlled trial.
- Likert scale
- A psychometric scale used in research questionnaires, measuring levels of agreement or disagreement with a given statement.
- Lurking
- Spending time on an online forum or social media, reading posts without posting.
- Mediator
- A variable measure posited to explain the relationship between an independent variable and a dependent variable, by investigating whether or not the influence of the independent variable on the mediator in turn influences the variable outcome.
- Mental health trust
- A health-care delivery organisation that provides specialist health and social care services for people with mental health problems in a defined geographical area in the UK.
- mHealth
- Mobile health: a form of digital health intervention accessed or delivered mainly by mobile phone or another mobile device.
- Multiple imputation
- A statistical process for replacing missing data in incomplete data sets, conducted multiple times and averaged to reduce noise in the data.
- NHS trust
- A health-care delivery organisation that covers a defined geographical area in England.
- Participant identification centre
- A centre that identifies potential participants for off-site research studies through patient records, speaking to patients or other means.
- Patient and public involvement
- Input from patients and members of the public into decisions about the design and delivery of health services or (in this instance) health research.
- Peer worker
- Someone with lived experience of (usually) mental health problems providing support or services to others with mental health problems.
- Psychoeducation
- Evidence-based provision of information and support to help patients and their relatives better understand and cope with illness, particularly serious mental illness.
- Psychosis
- A state in which people perceive or interpret the world around them very differently. Psychosis most frequently manifests as having beliefs that are not shared by others and do not have a basis that is understandable to others (often called delusions); not being able to think clearly and so sounding muddled and hard to follow (often called thought disorder); and experiencing, for example hearing or seeing, things that other people cannot (often called hallucinations).
- Quality-adjusted life-year
- A generic measure of disease burden, including both the quality and the quantity of life lived, used to assess the value for money of medical interventions. One quality-adjusted life-year equates to 1 year in perfect health.
- Randomised controlled trial
- A scientific investigation method whereby participants are allocated randomly to either a group receiving the treatment under investigation or a control group receiving standard treatment.
- Relative/carer
- A family member or other close person providing unpaid care and support to a person with psychosis or bipolar disorder.
- Relatives’ Education And Coping Toolkit (REACT)
- An online supported self-management toolkit for relatives or friends of people with psychosis or bipolar disorder.
- Technology-enabled service
- A health service in which technology plays a role alongside many other face-to-face components.
- Triangle of care
- The three-way collaboration of health professional, mental health service user and the user’s carer to provide therapeutic care.
List of abbreviations
- ACME
- average causal mediated effect
- A&E
- accident and emergency
- ANCOVA
- analysis of covariance
- BD
- bipolar disorder
- CCG
- Clinical Commissioning Group
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CONSORT-EHEALTH
- Consolidated Standards of Reporting Trials of Electronic and Mobile HEalth Applications and onLine TeleHealth
- COPE
- Coping Orientation to Problems Experienced
- CSRI
- Client Service Receipt Inventory
- CTRC
- Clinical Trials Research Centre
- CWS
- Carer Well-being and Support
- DHI
- digital health intervention
- DMEC
- Data Monitoring and Ethics Committee
- EIP
- early intervention in psychosis
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GHQ-28
- General Health Questionnaire-28 items
- GP
- general practitioner
- HSDR
- Health Services and Delivery Research
- HTA
- Health Technology Assessment
- ICER
- incremental cost-effectiveness ratio
- IMPART
- IMPlementation of A Relatives’ Toolkit
- IP
- Internet Protocol
- IPQ
- Illness Perception Questionnaire
- IQR
- interquartile range
- IT
- information technology
- IV
- instrumental variable
- ivreg
- instrumental variable regression
- MANOVA
- multivariate analysis of variance
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- Portable Document Format
- PIC
- participant identification centre
- PPI
- patient and public involvement
- QALY
- quality-adjusted life-year
- RAG
- relatives’ advisory group
- RCT
- randomised controlled trial
- RD
- resource directory
- REACT
- Relatives’ Education And Coping Toolkit
- SD
- standard deviation
- SMS
- short message service
- SSL
- Secure Sockets Layer
- SWAT
- study within a trial
- TAU
- treatment as usual
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hta24320).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
