Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/28/02. The contractual start date was in July 2016. The draft report began editorial review in April 2019 and was accepted for publication in January 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Paul Baker was a member of the National Institute for Health and Care Excellence (NICE) guideline committee (CG157: hip, knee and shoulder replacement clinical guideline) (2018–2020). He is also a member of the NICE Quality Assurance Committee (2019 to present), is a HTA Commissioning panel member (Panel B) (2019 to present) and a Royal College of Surgeons Specialty Lead for Orthopaedics (2019 to present). Avril Drummond is a member of the Health Education England/National Institute for Health Research (NIHR) Integrated Clinical Academic Programme Clinical Lectureship and Senior Clinical Lectureship Review Panel (2018 to present). Catriona McDaid is a member of the NIHR Health Technology Assessment (HTA) and Efficacy and Mechanism Evaluation (EME) Editorial Board (2017 to present). Catherine Hewitt is a member of the HTA Commissioning Board (2015 to present). Louise Thomson was a member of the NICE Public Health Advisory Committee on Workplace Health: long-term sickness absence and capability to work (NICE Guideline number 146) (2018–19). Amar Rangan is an NIHR grant holder [Partial Rotator Cuff Tear Repair (PRO CURE) trial, NIHR HTA project 128043 (co-investigator), subject to Department of Health and Social Care contracting; UKFROST, NIHR HTA project 13/26/01 (chief investigator); ProFHER) trial, NIHR HTA project 06/404/53 (chief investigator); HUSH trial, NIHR HTA project 127817 (co-investigator); Patch Augmented Rotator Cuff Surgery (PARCS) feasibility study, NIHR HTA project 15/103 (co-investigator); treatment of first time anterior shoulder dislocation, Clinical Practice Research Datalink analysis, NIHR HTA project 14/160/01 (co-investigator); SWIFFT, NIHR HTA project 11/36/37 (co-investigator); DRAFFT Trial, NIHR HTA project 08/116/97 (co-investigator); PRESTO feasibility study, NIHR HTA project 15/154/07 (mentor to chief investigator); and evidence synthesis on the frozen shoulder NIHR HTA project 09/13/02 (co-investigator)] and an Orthopaedic Research UK (London, UK) research grant holder, and research and educational grants were provided to his institution from DePuy Synthes [Raynham, MA, USA; a Johnson & Johnson (New Brunswick, NJ, USA) company].
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Baker et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background and study introduction
Is there a need for an occupational advice intervention for hip and knee replacement patients?
The impact of hip and knee osteoarthritis on employment
Decreased physical function associated with hip and knee osteoarthritis reduces the likelihood of employment, reduces household income and increases the number of missed workdays for those who are employed. 1 The magnitude of the impact varies according to the degree of activity limitation and disease severity. 2 A diagnosis of hip or knee osteoarthritis is associated with a reduction in work participation and productivity and an increased risk of work loss. 3,4 In a national study of patients in Finland, Kontio et al. 5 found that the age-adjusted incidence of disability retirement owing to knee osteoarthritis was 60 and 72 per 100,000 person-years for men and women, respectively. The highest rates of disability retirement in men were found in construction workers, electricians and plumbers, and in women they were found in building caretakers, cleaners, nurses and kitchen workers. 5
The cost of work-related musculoskeletal disorders that have an impact on a person’s ability to work is difficult to quantify. Direct (the cost of treatment) and indirect (costs related to the impact of the period of ill health) costs are borne by the individual (impact of ill health on quality of life), employers and society (loss of productivity, need for health care, rehabilitation and compensation). 6,7 The Health and Safety Executive calculates the annual cost of workplace injury and ill health on this basis by estimating both the financial cost and the ‘human’ cost. 7,8 The Health and Safety Executive estimates that the total annual cost of workplace ill health due to musculoskeletal disorders is £9.7B, equivalent to £18,400 per case. 7,8 However, these figures do not take account of non-work-related injuries and ill health and, therefore, are likely to be an underestimate of the total cost. In addition to its financial benefits, working has significant physical, mental and emotional health benefits. 9–11 Loss of employment is associated with a reduction in physical function, increased anxiety and depression and increased risk of mortality. 12,13 Therefore, earlier return to work (RTW) has potential health benefits as well as socioeconomic benefits.
The role of lower limb joint replacement in patients of working age
Lower limb joint replacements are successful and cost-effective treatments that relieve pain, restore physical function and improve health-related quality of life for patients with hip and knee arthritis. 14–17 Currently, > 1 million hip and knee replacements are carried out annually in the USA and > 190,000 are carried out annually in England, Wales and Northern Ireland. 18 Projections from 2005 suggest that, by 2030, the number of primary total hip replacements (THRs) and total knee replacements (TKRs) carried out will increase by 174% and 673%, respectively. 19
Recent changes to the state pension age, combined with an ageing UK workforce, resulted in a steady increase in the numbers of hip and knee replacements being carried out in patients of working age between 2007 and 2017. 18 These changes are also reflected in data from North America, which suggest that over half of all hip or knee replacement procedures will be carried out in patients aged < 65 years by 2030. 19 International estimates suggest that between 15% and 45% of patients undergoing either hip or knee replacements are of working age. 20,21
According to data published by the National Joint Registry (NJR) for England, Wales and Northern Ireland, 106,334 primary knee replacements22 and 96,717 primary hip replacements23 were carried out in 2017. Of the 91,923 hip replacement patients with available patient data, 18,812 (20.5%) were aged < 60 years (9778 females and 9034 males) and a further 26,295 were aged 60–69 years (28.6%; 15,375 females and 10,920 males). Of the 102,347 knee replacement patients with available patient data, 17,765 (17.4%) were aged < 60 years (10,259 females and 7506 males) and a further 33,523 were aged 60–69 years (32.8%; 18,161 females and 15,362 males).
Occupational advice for patients undergoing hip or knee replacement
There is currently a paucity of information and guidance to support patients returning to work after hip or knee replacement. Over the last 2 years [during the course of the Occupation advice for Patients undergoing Arthroplasty of the Lower limb (OPAL) study], the Royal College of Surgeons of England has produced written information resources to guide recovery including RTW after both hip replacement and knee replacement (example information is available at www.rcseng.ac.uk/patients/recovering-from-surgery/total-hip-replacement/returning-to-work; accessed 16 April 2019). We are not aware of any other currently available occupational advice or information resources specifically tailored to this patient group.
The UK Government currently funds the ‘Fit for Work’ service (in Scotland, the service is called ‘Fit for Work Scotland’). 24 This initiative is free for the public to use and is designed to support people in work with health conditions and help with sickness absence. It works alongside existing occupational health services and employer sickness absence policies. Patients can access this service via telephone line support, by visiting the ‘Fit for Work’ websites or by e-mailing the team. However, the patient-facing materials are generic and there is no specific information for hip or knee replacement patients. 24
Current evidence relating to return to work after hip or knee replacement
Two systematic reviews examined work status, time to return to work and determinants of RTW in patients undergoing hip or knee replacement. 20,21
The most recent and comprehensive review, by Tilbury et al. ,20 identified 19 articles:25–43 14 relating to hip replacements, four on knee replacements and one on both. All were cohort studies of either prospective (eight studies) or retrospective (11 studies) design and included the three studies from the earlier Kuijer et al. 21 review. Four of the included studies were from the UK. 38–41 Among these 19 studies, there was significant variation in the definition of work status both before surgery and after surgery. 20 The proportion of patients returning to work ranged from 25% to 95% at between 1 and 12 months after hip replacement and from 71% to 83% at 3–6 months after knee replacement. 20 Time to RTW ranged from 1.1 to 10.5 weeks after hip replacement and from 8 to 12 weeks after knee replacement. 20 Determinants of a worse ‘work outcome’ after hip replacement included female sex, older age, pain in other joints, failure of the procedure, employment involving physical work, unskilled work and being a farmer. 29,32,35 Better work outcomes after hip replacement were associated with younger age, a higher level of education, working within 1 month of surgery, primary osteoarthritis and earlier return of walking ability. 29,32,35 Determinants of a faster RTW after knee replacement included female sex, self-employment, better postoperative physical and mental health scores, a higher functional comorbidity index and a disability-accessible workplace. 42 Slower RTW after knee replacement was associated with the level of preoperative pain, a physically demanding job and being on workers’ compensation. 42
Of the work published in the UK, Mobasheri et al. 38 studied 86 hip replacement patients aged < 60 years at a mean of 3 years after surgery, of whom 51 were in work prior to surgery. After surgery, 49 patients (96%) returned to work and an additional 13 gained employment. 38 In a similar study, Lyall et al. 40 examined 56 knee replacement patients aged < 60 years at a mean of 5 years after surgery. Overall, 40 out of 41 (98%) patients who were employed before their operation returned to their previous work but none of the patients not working prior to surgery found work after their operation. Both studies suggest that high rates of RTW can be achieved in patients at mid-term follow-up (3–5 years). Of the 285 hip replacement patients aged < 65 years studied by Cowie et al. ,39 170 (71.1%) were working after their surgery and the mean time to RTW was 13.9 weeks. Of those who returned to work, 132 (78.1%) did so without any workplace restrictions. They also found a negative correlation between time to RTW and increasing age and body mass index (BMI). 39 Finally, Foote et al. 41 studied 109 patients aged < 60 years at a mean of 3 years post surgery who had previously had a total, unicondylar or patellofemoral knee replacement. The rate of and time to RTW varied by the type of operation, with the TKR (82% had returned to work at a median of 12 weeks) and unicondylar (82% had returned to work at a median of 11 weeks) patients returning significantly sooner than the patellofemoral knee replacement patients (54% had returned to work at a median of 20 weeks). 41
A number of additional studies examining RTW after hip or knee replacement have been published since these reviews.
Sankar et al. 44 studied RTW in a cohort of Canadian patients and found that the rate of RTW varied according to the joint replaced and the time since surgery. The proportion of patients returning to work was lower for knee replacement than for hip replacement at 1, 3 and 6 months, but by 12 months it was equivalent (1 month: TKR 24%, THR 34%; 3 months: TKR 57%, THR 66%; 6 months: TKR 78%, THR 85%; 12 months: TKR 85%, THR 87%). 44 They also reported that the time taken to return to work was improved in males and in patients with a higher level of education and in less physically demanding jobs. 44 Dutch researchers have also examined the rate of RTW, duration until RTW and determinants of RTW in patients undergoing total hip or knee replacement. 45,46 At 1 year post surgery, 90% of hip and 83% of knee replacement patients had returned to work, but 14% of the hip and 19% of the knee patients had returned to work on reduced hours. 45 The mean time to RTW was 12.5 [standard deviation (SD) 7.6] and 12.9 (SD 8.0) weeks for hip and knee replacement patients, respectively. 45 Factors associated with a RTW included self-employment and better preoperative activities of daily living subscale scores. 46 Preoperative absence from work reduced the chance of returning to work after surgery. 46
There have also been three recent publications from the UK. 47–49 Scott et al. 47 retrospectively reviewed 289 TKR patients aged < 65 years at a mean of 3.4 years after surgery. Overall, 261 patients (90%) were working prior to surgery, of whom 105 (40%) returned to work after surgery, with 89 (34%) returning to the same job at a mean of 13.5 weeks postoperatively. Factors predictive of a successful RTW included younger age and type of work undertaken. 47
Malviya et al. 48 summarised the qualitative and quantitative literature for RTW after hip or knee replacement. They found that patients have high expectations of the impact of joint replacement surgery on their ability to work and that unrealistic expectations lead to heightened frustration and a slower rate of recovery, preventing them from returning to work. In this setting, supportive care from health-care providers and family support after surgery were helpful in facilitating successful rehabilitation and satisfaction. 48 The same research team, Kleim et al. ,49 studied 83 patients undergoing hip or knee replacement who were employed prior to surgery. At review, 80 patients had returned to work at median of 12 (range 2–64) weeks. They found that those patients in more manual occupations, those without preoperative sick leave due to their hip or knee arthritis and those with a higher level of qualification returned to employment significantly quicker than the rest of the cohort. 49 In addition, hip replacement patients reported a greater improvement than patients after knee replacement did in terms of performance at work (63% vs. 44%) and job prospects (50% vs. 36%). 49
Summary of the current literature: key points
Current evidence suggests that:
-
A substantial proportion of patients undergoing hip or knee replacement are of working age and the majority are in work at the time of surgery. This number is set to increase in an increasingly aged workforce who will have to work for longer because of changes in the state pension age.
-
Lengthy sickness absence can have a negative impact on individual physical and mental health status.
-
The cost associated with sickness absence to the patient, employer and the state is significant.
-
Occupational advice interventions to support RTW after hip or knee replacement are limited.
-
The extent to which RTW is ‘full’ and ‘sustained’ is not known.
-
Given the lack of occupational advice interventions and associated resources, there is likely to be significant variation in the advice and information delivered to patients seeking to return to work after hip or knee replacement.
-
Return to work is influenced by a range of patient, health process and employment factors.
-
The underlying probability of employment varies by age, sex, education level and other factors, meaning that the economic implications of musculoskeletal limitations vary between patients and regions.
The OPAL study
In 2016, the National Institute for Health Research Health Technology Assessment programme commissioned a research call that asked ‘How feasible is a trial to evaluate whether occupational advice, initiated prior to planned surgery for major joint replacement within the lower limb, improves health outcomes in terms of faster recovery to usual activities, including work?’.
The Health Technology Assessment guidance described the need to develop a tailored occupational advice intervention that ensured targeted support and rehabilitation to facilitate RTW as part of this study. This intervention should be proactive and suitable for routine delivery in the NHS alongside the usual-care pathway. There was also a requirement to define the population group, describe usual care and explore important outcomes, such as time to RTW, health-related quality of life, health-care utilisation and proportion of patients requiring workplace occupational health interventions.
Preliminary work undertaken by the OPAL investigators demonstrated a number of evidence gaps related to RTW after major lower limb joint replacement that directed the format and direction of the study. These are described in the following sections.
Population
There is limited evidence about the population of patients undergoing hip or knee replacement who are in work and returning to work after surgery. Further information is required to understand the individualised workplace needs of this group, including an understanding of how job classifications (e.g. manual vs. non-manual), employment status (e.g. employed vs. self-employed), the type of employer (e.g. small and medium-sized enterprises vs. large companies; public- vs. private- or third-sector employer) and how the presence of an occupational health service within the organisational structure influences the potential for early RTW.
The target population for a clinical trial is, therefore, not clearly defined.
Intervention
-
Current recommendations guiding RTW are limited and inconsistent. Information is rarely individualised and generic information often fails to provide the patient, employers or health-care teams with the advice required.
-
The majority of patients undergoing hip or knee replacement undertake an integrated multidisciplinary team programme of education and rehabilitation spanning the surgical episode. The provision and utility of occupational advice within these ‘usual-care’ pathways is not established and the ability of this service to facilitate RTW has not been explored.
-
Studies suggested that the vast majority of ‘fit notes’ are not being used correctly. ‘Fit notes’ offer the patient and employer opportunities for early phased RTW. However, most are advising that patients are ‘not fit’ for work, with few doctors making use of the opportunity to advise on patient function and/or work modifications that might facilitate RTW after surgery. 50,51
-
There is limited information about the impact of addressing modifiable barriers that prevent RTW or how modifiable psychosocial factors influence RTW behaviours and the specific needs of the patients regarding perioperative care and advice. 48,52
There is, therefore, no appropriate occupational advice intervention available that could be used as the intervention in a clinical trial.
Comparison
There is no information about how and when occupational advice is delivered and who is delivering it to hip and knee replacement patients. The rapid and inconsistent adoption of enhanced recovery and early-discharge pathways has led to variations in provision of perioperative care and advice.
‘Standard care’ is therefore not currently defined for use as a study comparator.
Outcome
-
There is currently no standardised method of recording RTW. Dichotomous recording of work status (yes/no) is blunt and does not address important aspects of workplace behaviour including absenteeism, presenteeism, return to usual activities and interference with activities. In the UK, > 20% of patients do not return to usual activities and have restrictions in their ability to work after hip replacement. 39 Measuring RTW should ideally consider specific elements of the job, the duties and the hours worked.
-
Assessment of workplace disability and productivity is poorly reported after hip or knee replacement. Validated tools exist (e.g. the Workplace Activity Limitations Scale and Work Limitations Questionnaire) but little is known about their applicability to the UK workforce and their utility as outcome measures for clinical trials. 53
The appropriateness of individual RTW measures for use as primary outcome measures in a clinical trial is currently unclear.
Summary
There is a need for preliminary research to generate relevant evidence and develop an occupational advice intervention to support a future clinical trial. The OPAL study was commissioned to facilitate this.
Objectives
This section is reproduced from Baker et al. 54 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited (see https://creativecommons.org/licenses/by/4.0/). The OPAL study had nine objectives:
-
to evaluate the specific needs of the population of patients who are in work and intend to return to work following hip or knee replacement
-
to establish how individual patients return to work; the role of fit notes, clinical and workplace-based interventions; and how specific job demands influence workplace disability and productivity
-
to establish what evidence is currently available relating to RTW/occupational advice interventions following elective surgical procedures
-
to understand the barriers preventing RTW that need to be addressed by an occupational advice intervention
-
to determine current models of delivering occupational advice, the nature and extent of the advice offered and how tools to facilitate RTW are being currently used
-
to define a suitable measure of RTW through systematic review and evaluation of specific measures of activity, social participation and including specific validated workplace questionnaires
-
to construct a multistakeholder intervention development group to inform the design and establish the necessary components of an evidence-based occupational advice intervention initiated prior to elective lower limb joint replacement
-
to develop and manualise a multidisciplinary occupational advice intervention tailored to the needs of this patient group
-
to test the acceptability, practicality and feasibility and potential cost of delivering the manualised intervention within current care frameworks and as a potential trial intervention.
Chapter 2 Methodological overview: the OPAL intervention mapping framework
The OPAL study employed an intervention mapping (IM) framework to deliver the objectives listed in Chapter 1, Objectives.
Intervention mapping
Intervention mapping is a framework for developing effective theory- and evidence-based behaviour change interventions. 55–59 IM was developed for, and is widely used in, health promotion, but the process has also been applied to many other fields, including traffic safety and energy conservation. 60 It has also been used in rehabilitation, for example in the management of osteoarthritis and back pain61 and stroke,62 as well as in work disability prevention. 63
The IM framework was first used in work disability prevention in 2007. Interventions developed using this methodology have included self-management at work of chronic diseases64 and upper limb conditions,65 but the majority (six separate interventions) have been designed to promote RTW. 66–71 However, only one study has focused on RTW following surgery. 68 Furthermore, in three of these studies69–71 an intervention has been designed but has yet to be implemented/evaluated.
Only three of the interventions to assist RTW developed using an IM framework have been formally evaluated in a randomised controlled trial (RCT); these are van Oostrom et al. ,72 Vermeulen et al. 73 and Vonk Noordegraaf et al. 68 The details of these studies are described in Chapter 3 and they suggest that the IM framework being employed in the OPAL study can facilitate the development of an effective occupational advice intervention.
Intervention mapping is a useful approach as it acknowledges that health is a function of individuals and their environments. Many health-related behaviours are dependent on individual knowledge, motivation and skills, but are also determined by the actions of decision-making groups, such as organisations and health authorities. RTW interventions are complex and thus at higher risk of theory and/or implementation failure than simpler interventions, such as medication delivery or hospital-based rehabilitation. The main characteristics of the IM protocol are to consider the individual within all of the different levels of their environment, and to make explicit use of theories when defining the problem, the intended changes and how these changes will be achieved. In this way, IM has the potential to prevent both theory failures and execution failures when developing and implementing RTW interventions, with better chances of demonstrating effectiveness.
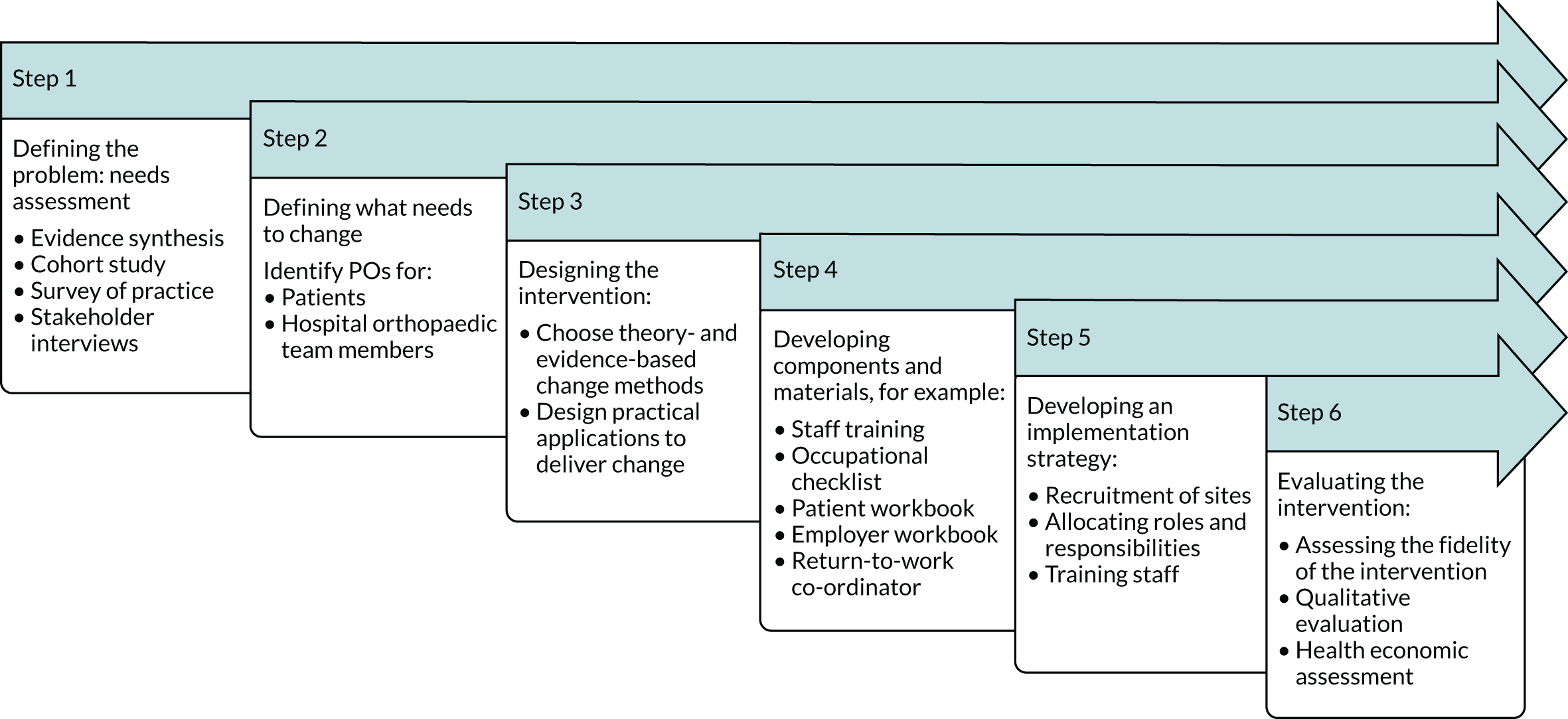
Intervention mapping is a stepwise approach to theory, evidence-based development and implementation of interventions. It consists of six stages: (1) needs assessment, (2) identification of intended outcomes and performance objectives (POs), (3) selection of theory-based methods and practical strategies, (4) development of intervention components, (5) development of an adoption and implementation plan, and (6) evaluation and feasibility testing.
The OPAL intervention mapping process
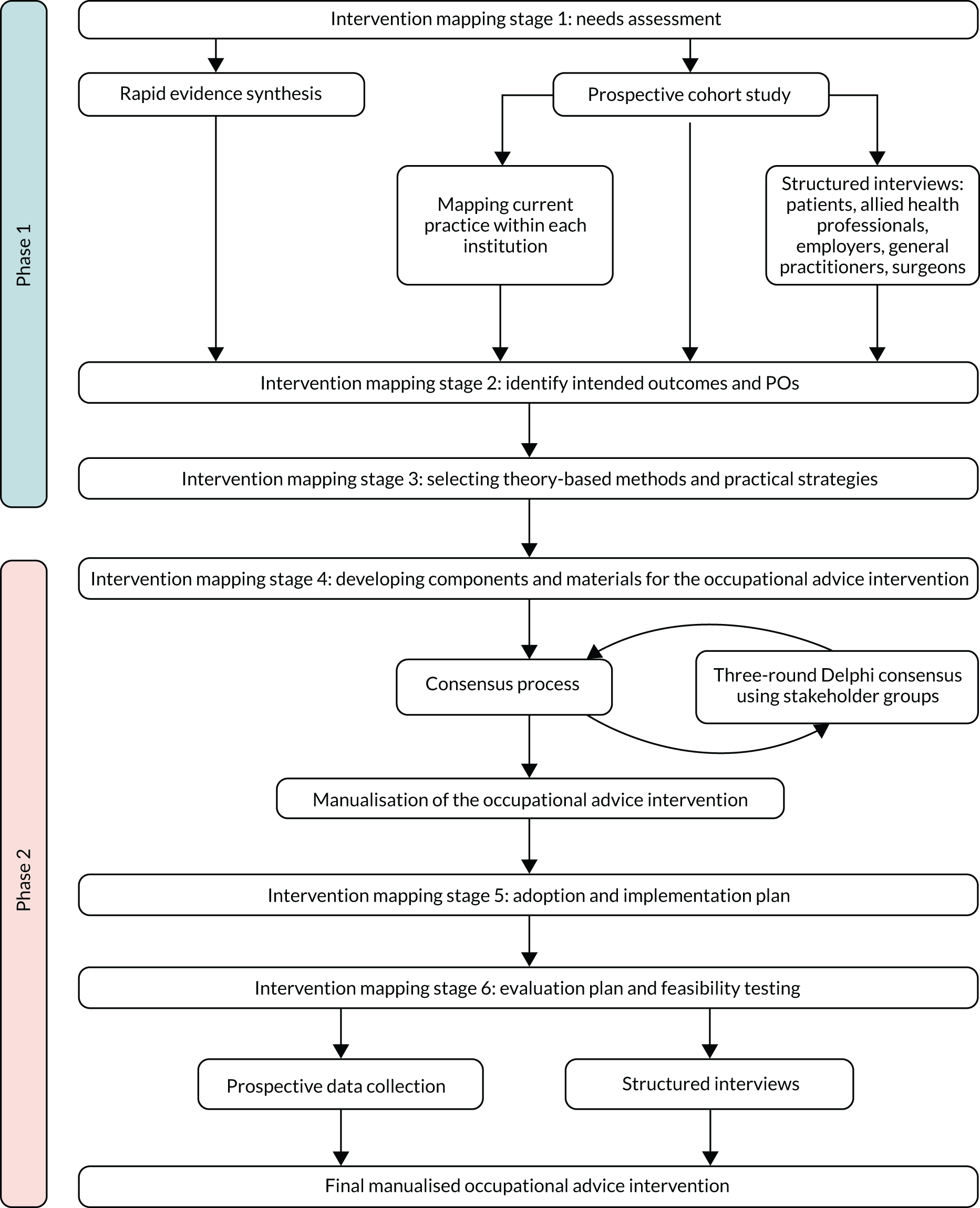
The OPAL study followed the six-stage IM approach (Figure 1). Stages 1–3 (phase 1) addressed objectives 1–6 (see Chapter 1, Objectives) by gathering information on current practice and barriers to change; stages 1–3 also provided a theoretical framework for intervention development. Stages 4–6 (phase 2) addressed objectives 7–9 (see Chapter 1, Objectives). An overview of the activity within each stage of the IM process is provided below, and further details can be found in each of the corresponding chapters.
FIGURE 1.
Overview of the OPAL IM methodology.
Intervention mapping stage 1: needs assessment (see Chapters 3–6)
Intervention mapping stage 1 established the rationale for an occupational advice intervention within the target population by evaluating the discrepancy between current and desired practice. It utilised a variety of approaches including a rapid evidence synthesis (see Chapter 3), a cohort study (see Chapter 4), a national survey of practice (see Chapter 4) and patient (see Chapter 5) and stakeholder (see Chapter 6) interviews. This information was then used to create a logic model of the problem considering how the behaviours of the target population increase the risk, prevalence, incidence and burden of the problem and how interpersonal, organisational, community and societal factors influence RTW directly or through influence on the behaviour of the target population. These behavioural and environmental factors were then mapped to specific theory- and evidence-based factors and determinants to help provide an overview of the problem and a framework to address it.
Intervention mapping stage 2: identify intended outcomes and performance objectives (see Chapter 7)
Stage 2 used the findings from stage 1 to specify who and/or what needs to change for patients to make a successful RTW following hip/knee replacement. A provisional matrix of POs for key stakeholder groups was constructed outlining the personal determinants, external determinants and expected outcomes for each objective.
Intervention mapping stage 3: selecting theory-based methods and practical strategies (see Chapter 7)
In stage 3, a list of possible components matched to each performance objective/determinant was generated. Using theory, evidence, experience and consensus, the most practical ways to implement these interventions were identified. These intervention ‘components’ formed the basis of the statements presented to stakeholders as part of the Delphi consensus process (see the next section on IM stage 4) and helped to develop the first iteration of the developed occupational advice intervention.
Intervention mapping stage 4: development of intervention components (see Chapters 8 and 9)
Stage 4 used the information and associated occupational advice strategies identified in the first three IM stages to develop specific tailored tools and materials. To help refine these components, a multistakeholder intervention development group was created to reach agreement about the design, content, delivery, format and timing of the proposed occupational advice intervention. To facilitate this process, a modified three-round Delphi consensus process was employed. Information from the Delphi consensus process was then used to refine and finalise the occupational intervention.
Intervention mapping stage 5: adoption and implementation plan (see Chapter 10)
In stage 5, strategies for the implementation and adoption of the intervention were developed. This stage ran concurrently with the final stages of intervention development as the content, format and method of delivery became finalised. The implementation plan focused on the delivery of the intervention within the realities of the NHS. Therefore, the intervention and the associated implementation plan had to be adaptable to current practice, infrastructure and staffing at each of the three feasibility sites. This flexibility permitted delivery alongside current ‘standard’ care while stipulating the achievement of specified POs, against which the fidelity of the intervention was assessed.
To facilitate the implementation and adoption of the intervention, education and training materials were developed for each of the staff groups involved in its delivery. Appropriate support and training systems were developed and an implementation plan was constructed to assist adoption at each site, which included a site visit and ongoing support from the OPAL investigators.
Intervention mapping stage 6: evaluation plan and feasibility testing (see Chapter 10)
The final stage of the IM process evaluated the intervention by assessing four complementary aspects of its delivery and performance:
-
assessment of intervention fidelity – quantitative evidence that the intervention was delivered against specific POs for both the hospital orthopaedic team (HOT) (staff objectives) and the patient (patient objectives)
-
assessment of intervention quality – qualitative assessment of the intervention delivery obtained by interviewing patients and staff groups about what worked and what did not, why it did not work or why it went well
-
assessment of feasibility data – preliminary comparison of outcomes using data obtained from IM stages 1 (pre intervention) and 6 (post intervention)
-
assessment of economic data – approximate cost estimates for the intervention using derived health economic data.
In addition, the feasibility stage collected information that would help to shape the design and development of a future clinical trial by assessing screening, recruitment, consent and follow-up procedures and rates at each of the study sites. A formal pilot study was not undertaken at this stage as per the commissioning brief.
The OPAL IM approach described above is outlined in Figure 1 and a diagram describing development of the OPAL occupational advice intervention is shown in Figure 2.
FIGURE 2.
Diagram of the stages of development of the OPAL occupational advice intervention.
Stakeholder engagement strategy
Five key stakeholder groups central to the development of an occupational advice intervention were identified: (1) patients, (2) employers and their associated occupational health departments, (3) allied health professionals (AHPs) (occupational therapists and physiotherapists) and nurses, (4) orthopaedic surgeons and (5) general practitioners (GPs).
To maximise engagement with these stakeholder groups, nominated OPAL investigators were responsible for the identification and engagement of stakeholders within their area of expertise. This included stakeholder recruitment from a number of professional bodies and employment institutions, providing the breadth of opinion and insight required to ensure generalisability and acceptability of findings and assist with dissemination of findings at various stages of the study (Table 1).
| Stakeholder group | Nominated OPAL investigator | Participants recruited via |
|---|---|---|
| Patients | Mrs J Fitch |
|
| Employers and occupation health services | Professor S Khan |
|
| Orthopaedic surgeons | Mr I McNamara |
|
| AHPs and nurses | Dr D McDonald and Dr C Coole |
|
| GPs | Mr P Baker and Professor A Rangan |
|
Data collection and handling
Personal data collected during the trial were handled and stored in accordance with the 199875 and 2018 Data Protection Acts. 76 All electronic patient-identifiable information was held on a secure, password-protected database accessible to only essential study personnel. Only OPAL investigators (University of York and University of Nottingham), the sponsor (South Tees Hospitals NHS Foundation Trust) and the recruiting NHS trust had access to the personal data. Written consent was taken for collected data to be linked to routinely collected health data stored in national databases (via NHS Number), although this activity did not form part of this research project.
Project management
The South Tees Hospitals NHS Foundation Trust was the sponsor for this project. This study was compliant with the research governance framework77 and Medical Research Council good clinical practice guidance. 78 The Trial Steering Committee, which met approximately 6-monthly during the OPAL study, oversaw the study.
Ethics approval
The OPAL study was approved by the East Midlands – Derby Research Ethics Committee (Integrated Research Application System ID 200852) on 18 August 2016. The employer/workplace representative interviews were approved by the University of Nottingham Ethics Committee on 25 July 2016. Health Research Authority approval was received on 4 October 2016. For ethics approvals and Health Research Authority correspondence documents, see www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/ (accessed 2 May 2020).
Project registration
-
Current Controlled Trials ISRCTN27426982 (date registered: 20 December 2016); URL: www.isrctn.com/ISRCTN27426982 (accessed 16 April 2019).
-
International prospective register of systematic reviews (PROSPERO) registration number CRD42016045235 (date registered: 4 August 2016).
Protocol management and version history
See study protocol version 4.0, which has been published. 54 Protocol version history is provided in Appendix 1.
Patient and public involvement
Active patient and public involvement (PPI) was ensured throughout the study. During the development of the grant application, PPI was sought from the NJR patient network and the British Orthopaedic Association (BOA) Patient Liaison Group. Six patients who had a joint replacement contributed to the initial proposal.
A recurring concern during initial discussions with patients was that a ‘one size fits all’ approach could be too generic. Other issues raised were variations across hospitals in the support provided; the needs of specific occupational groups, such as self-employed; different expectations among people about RTW; and the impact of the employer perspective, coupled with concerns about how early RTW interventions may result in pressure for people to return too early.
To address these concerns, the OPAL study specifically assessed individual patients’ experiences to enable an individualised intervention to be developed. Patient interviews explored individual patients’ needs, concerns and expectations related to the RTW process. This information, along with information from other stakeholders, shaped the development of the intervention during the rest of the study. In phase 2, patients were included in the Delphi consensus process, ensuring that we understood and addressed issues pertinent to them within the intervention. In addition to patients, engagement from other stakeholders was ensured during both phases of the OPAL study as part of the study design, maximising their engagement in the design and development of the intervention.
The study investigators included a patient representative as co-applicant (Mrs Judith Fitch). Mrs Fitch was involved in the ongoing management of the study through her involvement with the Trial Management Group, and intervention development meetings. In addition, a lay member sat on the Trial Steering Committee. Throughout the project, we continued to work with the NJR PPI group and the BOA patient network as well as PPI groups local to the sponsor site (South Tees). These groups helped us to develop study materials for the cohort study, patient interviews, Delphi consensus process and feasibility elements of the OPAL study. This included refining the study screening and consent processes, and developing the content of all patient-facing materials, ensuring that they were ethically sound, participant friendly and acceptable to the patient population. PPI members had the opportunity to contribute to the OPAL study via face-to-face meetings with the investigators and via telephone, e-mail or post. The costing for all PPI activity was calculated using the guidelines on the INVOLVE website. 79 PPI members were informed of the various resources and opportunities available for patient and public engagement with the NHS and research.
Once the study was complete, the chief investigator held a patient and public focus group meeting at which an outline of the study and the study outcomes were presented; this meeting included hip and knee arthroplasty patients, a carer and a patient ambassador. The intervention that was developed and its associated resources (patient and employer workbooks, and POs) were discussed and queries about specific aspects of the study findings and intervention were answered. The group agreed that the designed intervention was highly valuable to the patient population. They agreed that it should be tested in a larger setting and commented on its potential to be adapted to other areas. The group also discussed dissemination plans for the research findings and future research. The Plain English summary in this report was reviewed and edited by the group.
Chapter 3 Intervention mapping stage 1: needs assessment – rapid evidence synthesis
Introduction
A rapid evidence review of existing quantitative and qualitative evidence on occupational advice interventions for people undergoing any type of elective surgery was undertaken. This was to ensure that the best available evidence informed the OPAL occupational advice intervention. All elective surgery populations were included as it was considered likely that there would be some generalisability across different surgery populations. However, due to the paucity of information available on this population, established following initial screening of the database searches, the review was widened, following the advice of the Trial Steering Committee. It also therefore included systematic reviews evaluating occupational advice interventions supporting RTW for individuals with chronic musculoskeletal problems.
Objectives
The rapid evidence review supported study objectives 3–6 (see Chapter 1, Objectives).
Methods
Overview
A rapid review methodology was used. Given that the commissioner had already identified an evidence gap relating to occupational advice interventions for patients undergoing hip or knee replacement, and the need for primary research and a future trial (if feasible), a full systematic review was not warranted. The purpose of the rapid review was to identify interventions that showed evidence of benefit (or a signal of benefit where the study is underpowered) to explore the content of the interventions and identify aspects that could inform the development of the intervention for people undergoing lower limb joint replacement.
The term ‘rapid review’ covers a range of methods and there is no generally accepted definition, although generally the approach addresses a trade-off between time and methodological rigour and comprehensiveness of the end product. 80 We focused on the systematic review evidence in the first instance, included only English-language articles published in the last 20 years, restricted the range of databases searched and double-checked a proportion of the literature searches, rather than 100% (which is accepted practice for a full systematic review). The protocol for the rapid review is available on PROSPERO (protocol registration number CRD42016045235). 81
Literature searches
There were two sets of searches: one for systematic reviews and one for primary studies reported outside the search dates or remit of the reviews identified.
The Cochrane Database of Systematic Reviews and Database of Reviews of Effectiveness were searched in August 2016 for systematic reviews up to 2015. Additional supplementary searches were undertaken for the period 2015 to July 2016 in MEDLINE and EMBASE. The search combined various terms for ‘occupational advice’ and ‘return to work’ with terms for ‘systematic reviews’. There was no restriction for type of population (e.g. elective surgery) so that the searches were as comprehensive as possible. The following five databases were searched for primary studies in August 2016: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Central Register of Controlled Trials, MEDLINE, EMBASE and OTseeker. The strategy combined terms for ‘surgery’ and terms for ‘return to work’ and ‘occupational advice’. The full search strategies are reported in Appendix 2.
An information specialist undertook the searches. Both sets of searches were restricted to English-language studies published in the previous 20 years (since 1996). Records were downloaded, added to EndNote (Clarivate Analytics, Philadelphia, PA, USA) bibliographic software and deduplicated.
In addition, reference and citation checking of included studies was undertaken to identify further potentially relevant records.
Eligibility criteria
The eligibility criteria that were applied are displayed in Table 2. We anticipated the literature outside elective surgery to be vast and dominated by RTW following mental ill health and musculoskeletal problems, such as back and neck pain, where generalisability to hip and knee surgery is less certain; hence, we initially excluded studies in which the participants were not undergoing an elective surgical procedure.
| Criteria | Review of systematic reviews | Review of primary studies |
|---|---|---|
| Study type | Systematic reviews with no restriction on the types of primary studies they included | RCTs, non-randomised designs (e.g. non-randomised controlled trials, controlled before-and-after and interrupted time series studies) and qualitative studies that explore process issues, such as barriers to and facilitators of implementation, and stakeholder perspectives |
| Population |
|
People who have been on a period of sickness absence or where a prolonged absence is anticipated following an elective surgical procedure |
| Interventions | Any occupational advice intervention, where occupational advice includes occupational therapy advice and/or occupational health advice. No restriction on when the intervention was provided | |
| Comparator | No restriction on the types of comparators included in reviews | No intervention, usual care or another occupational advice intervention. Qualitative studies were not required to have a comparator |
| Context | Studies delivered in any setting were included (i.e. primary, secondary, community and workplace). This was to capture the widest evidence to inform the development of the intervention | |
| Outcomes | The outcomes of interest were those related to RTW, return to normal activities and social participation. Condition-specific measures were excluded, except where they were specifically related to people with hip or knee functional limitations. Also included were any process measures related to the delivery of interventions, such as barriers and facilitators, and any data on stakeholder perspectives. There was not a single primary outcome for the review, given its broad aims | |
However, following an initial screening of the search results, where only a small number of studies were identified for elective surgical populations, we widened our inclusion criteria for the population. Hence, the review also included systematic reviews that evaluated occupational advice interventions, aiming to support RTW, targeted at participants with chronic musculoskeletal problems as this population was considered most similar to our target population of interest. Owing to resource constraints, it was not feasible to widen the inclusion criteria in a similar way for the supplementary primary study searches.
Study selection
The titles and abstracts of all studies identified by the literature search were screened for inclusion by one reviewer, with 30% screened by a second researcher. The full texts of potentially eligible studies were retrieved and assessed for eligibility by a single reviewer, with 100% also being assessed by a second reviewer, following the development and piloting of a screening tool. Any disagreement between the reviewers regarding this sample was resolved via discussion with a third reviewer.
Data extraction
A standardised data extraction form was developed and piloted to record key information, such as population, study design, intervention details, outcomes, surgical procedure type and results. Items related to the intervention followed the Criteria for Reporting the Development and Evaluation of Complex Interventions in healthcare,82 with outcome data extracted from the primary studies, and summary information provided for the systematic reviews. The data extraction forms can be found in Appendix 2. Data extraction was undertaken by a single reviewer, and checked by a second reviewer.
-
For primary quantitative studies, the data extraction form recorded information including population; intervention (e.g. content of the intervention, material and tools used for delivery, who delivered, setting and any theoretical basis, such as behaviour change theory); process measures related to the delivery of interventions, such as barriers and facilitators; stakeholder perspectives (i.e. patients, health-care professionals and employers); study methods (e.g. study design, how outcomes were measured and length of follow-up); outcomes (e.g. what outcome measures are used in studies to assess RTW, return to normal activities and social participation?); and surgical procedure type.
-
For primary qualitative studies, data were extracted for the following items: population; study objective; surgical procedure type; method of evaluation and underpinning methodology, views and experiences (related to return to work, normal activities and social participation); and process measures related to delivery of interventions.
-
For reviews, the data extraction form also collected information such as objectives of the review; search strategies (e.g. searched databases, date of literature search, languages and inclusion/exclusion criteria); number of studies included in the review, sample sizes and details of data synthesis; types of studies included/setting, population, interventions assessed and outcomes assessed; quality assessment tools used; analysis (e.g. meta-analysis); results of the review; key conclusions; and limitations.
Assessment of risk of bias
Careful consideration was given to the risk-of-bias tools that were selected for use in our evidence synthesis, with a recent systematic review noting there being several limitations of existing tools regarding their scope, guidance for judgements on the risk of bias, and measurement properties. 83 Each of the tools listed below was considered to be appropriate for the different study type to adequately capture biases, with further information provided in the corresponding references for each tool. The quality of the included studies was assessed at the study level by one researcher and checked by a second. Specifically:
-
for systematic reviews – the Assessing the Methodological Quality of Systematic Reviews (AMSTAR) tool,84,85 a measurement tool to assess the methodological quality of systematic reviews
-
for RCTs – the Cochrane risk-of-bias tool86
-
for non-randomised studies (including non-randomised controlled trials, controlled before-and-after and interrupted time series studies) – the ROBINS-I (Risk Of Bias In Non-randomised Studies – of Interventions) tool87
-
for qualitative studies – the Critical Appraisal Skills Programme (CASP) qualitative checklist. 88
Data synthesis
Details of studies were tabulated and presented in a narrative synthesis to address the review questions. A meta-analysis was not possible owing to heterogeneity of studies and limited availability of RCTs. Key study characteristics have been tabulated, and the outcome domains investigated in the studies and specific outcome measures used have been mapped.
Many of the included systematic reviews had broad inclusion criteria and included primary studies outside the remit of interest (i.e. occupational advice interventions). Therefore, for the systematic reviews, the relevant primary studies were pulled out for closer examination, with the studies reported according to whether they featured a (1) surgical population or (2) wider musculoskeletal population. Mapping of the content of the interventions was also undertaken to allow exploration of all intervention components, materials and tools, any underlying theoretical basis, and any issues related to delivery and implementation. Data were explored and described by individual review question. No subgroup analysis was planned as part of this review.
Results
The results of the review are presented in two sections: the first relates to the included systematic reviews, for both surgical and musculoskeletal evidence, and the second refers to the review of primary studies of elective surgery populations.
Systematic reviews
Study selection
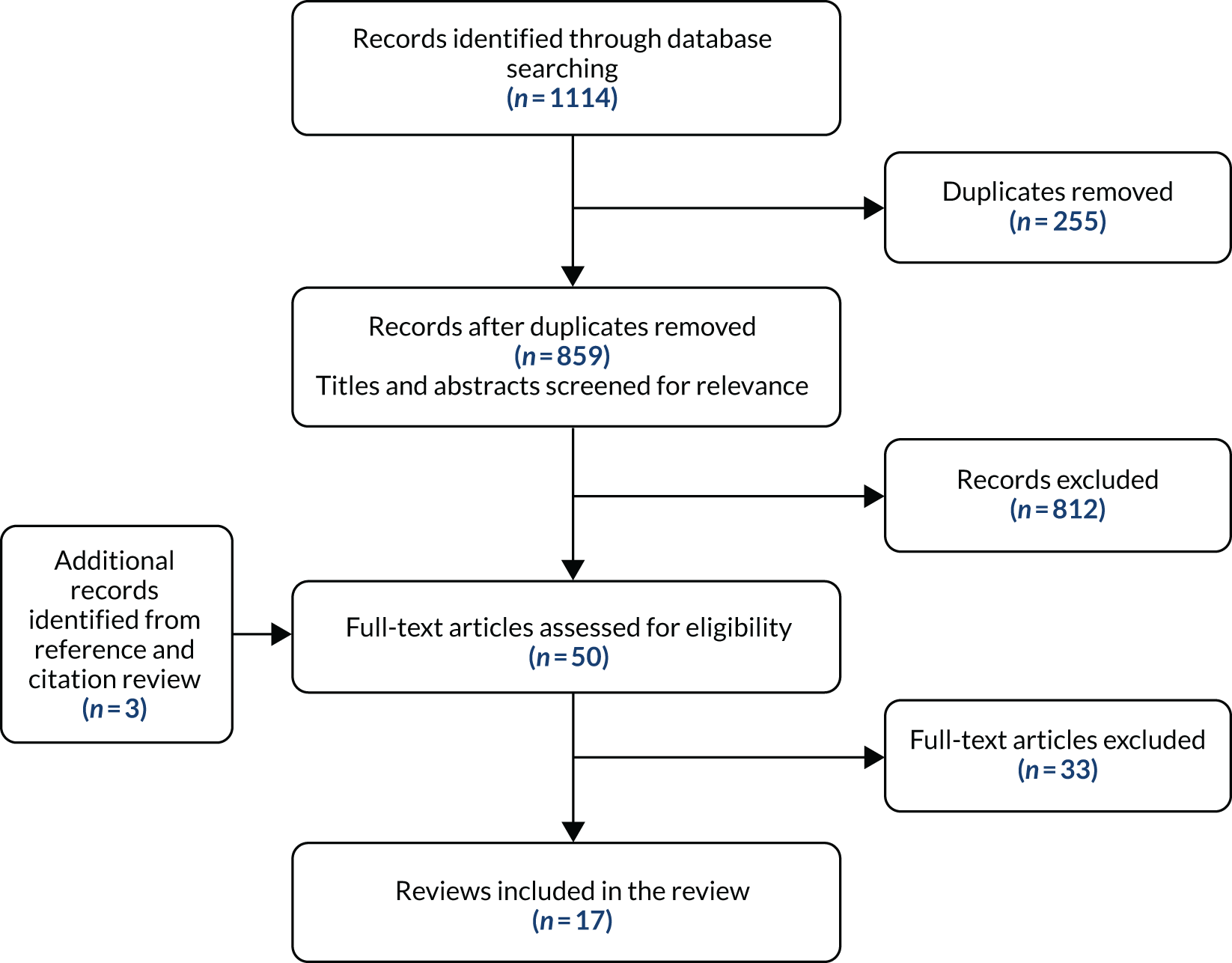
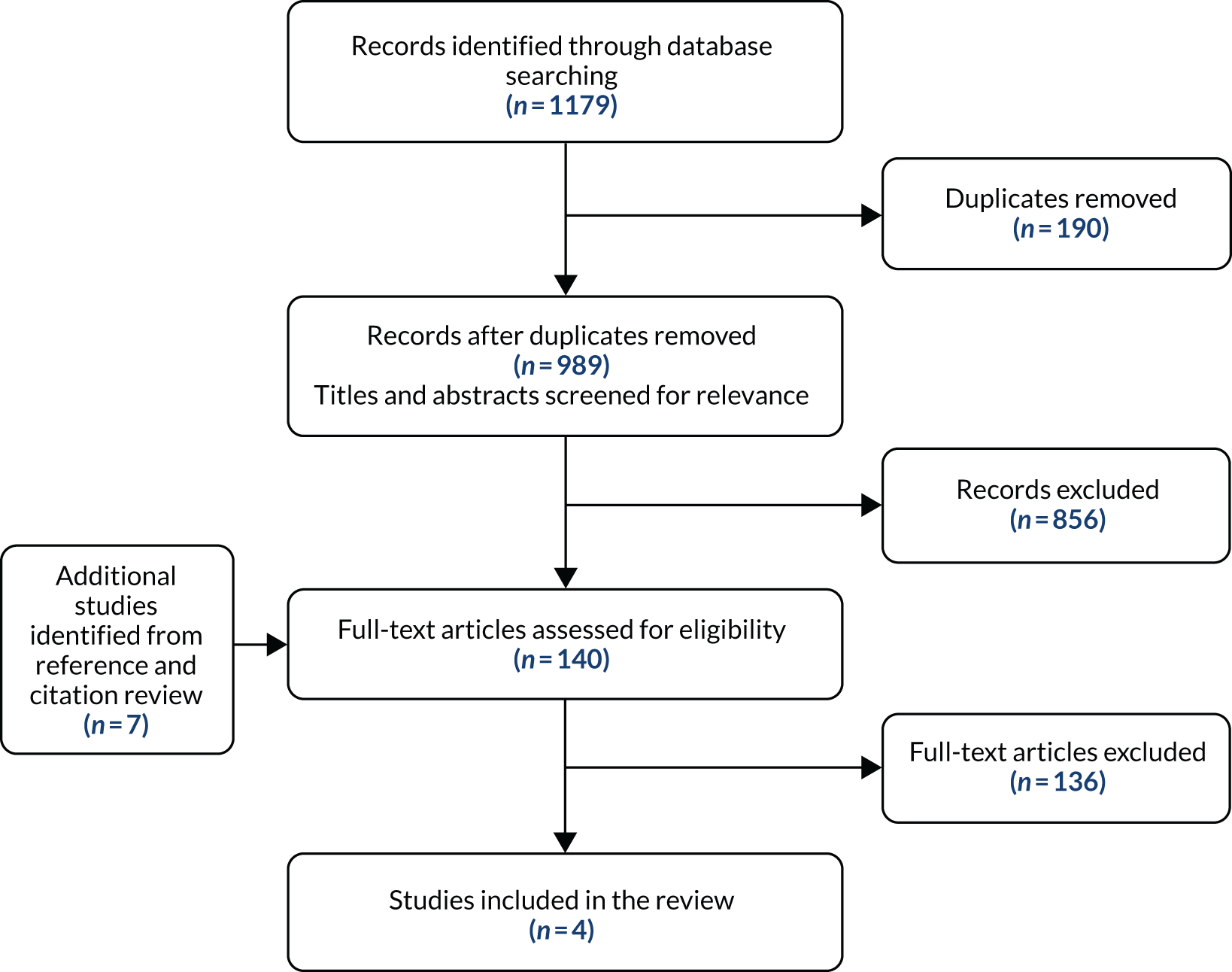
There were 859 records that were screened for relevance following deduplication of the results of the searches for systematic reviews (Figure 3). On reviewing titles and abstracts, 812 records were excluded, with 50 obtained in full-text form to assess eligibility for inclusion. A total of 17 systematic reviews were included, as listed in Appendix 2. The 33 excluded reviews and their associated reasons for exclusion are available in Appendix 2.
FIGURE 3.
Study selection for the review of systematic reviews.
Overview of included studies and reviews
The 17 systematic reviews included a total of 188 unique studies (242 before removing duplicated studies). Appendix 2 summarises the key review characteristics, the eligibility criteria, the work-related outcomes assessed and a summary of the review authors’ conclusions. The AMSTAR scores for the included systematic reviews are also provided in Appendix 2 alongside scores for individual items. These ranged from 3 to 9 out of a total of 11 possible points. The majority of reviews used robust methods to reduce risk of error and bias in study selection, data extraction and assessment of risk of bias. For some of the reviews, it was not possible to locate a protocol to verify that the review was conducted following a protocol. From the 188 included studies in the reviews, 30 were considered to be relevant to our review questions.
Only a single review was identified that focused on elective surgery (lumbar disc surgery patients);89 the remaining 16 included a range of musculoskeletal conditions:90–105 back pain (n = 6), neck and shoulder pain (n = 1), musculoskeletal issues/conditions more generally (i.e. musculoskeletal-related sickness absence and non-specific musculoskeletal complaints) (n = 2), neck pain (n = 1), repetitive strain injuries (n = 1) and fibromyalgia and musculoskeletal pain (n = 1). The remaining four reviews took a broader approach regarding the population, for example by specifying that individuals were of working age and participated in a rehabilitation programme, or by including patients with a range of permanent disabilities, or focusing on workers who were off work for reasons as specified in the review.
Type of return-to-work interventions
Almost half of the RTW interventions featured in the included reviews were of a multidisciplinary nature in a health-care setting, with seven involving multidisciplinary rehabilitation programmes,89,92,95–97,101,106 four of which featured a biopsychosocial element. 95–97,106 A further seven reviews focused on specifically workplace-based interventions,90,91,94,100,102,104,105 with the remaining three involving other types of interventions: one related to physical conditioning as part of a RTW strategy,103 one investigated secondary prevention for back disorders93 and the other featured interventions that fell into five different categories (detailed in Other interventions). 99
Workplace-based interventions
One review included interventions conducted at the workplace only (clinical and health-care interventions outside the workplace were excluded), which were either group based or individual and which were aimed at modifying body function, activity performance, participation, environmental factors or personal factors. 90 The interventions could comprise either a single strategy or a combination of strategies. The review by Franche et al. 94 included studies whose interventions were provided by the workplace, by an insurance company or by a health-care provider in very close collaboration with the workplace. Nevala et al. 100 focused on interventions comprising workplace accommodation, occupational rehabilitation, vocational rehabilitation and assistive technology interventions. Studies featuring workplace interventions implemented directly by the employer, including involvement from occupational health services, were included in the review by Vargas-Prada et al. 104
The review by Carroll et al. 91 considered interventions that featured either full or partial involvement of the workplace, or involved the intervention being delivered via direct employer/representative contact. Williams et al. 105 reviewed studies that featured interventions undertaken at the workplace, in addition to studies involving secondary prevention interventions for the condition under consideration. The review by Palmer et al. 102 focused on interventions delivered in a workplace or primary care setting, or in collaboration with employers or primary care providers.
Multidisciplinary rehabilitation programme interventions
Désiron et al. 92 focused on occupational therapy interventions as part of a multidisciplinary rehabilitation programme, with the review by Norlund et al. 101 specifying that the multidisciplinary interventions should involve two or more health-care disciplines. The surgical review89 included studies that focused on active rehabilitation programmes, where these included exercise therapy, strength and mobility training, physiotherapy and multidisciplinary programmes.
Multidisciplinary biopsychosocial rehabilitation programme interventions
The review by Kamper et al. 95 included studies that featured multidisciplinary biopsychosocial rehabilitation interventions, defined as involving a physical component and at least one of the following elements: biopsychosocial, social or occupational. The reviews by Karjalainen et al. 96,97,106,107 focused on studies whose interventions featured a biopsychosocial multidisciplinary inpatient or outpatient rehabilitation programme, specifically stating as part of their eligibility criteria that the programme should consist of a physician’s consultation, in addition to a psychological, social or vocational intervention, or a combination of these. Studies featuring rehabilitation interventions that were solely or predominantly medical were excluded. Note that the 1999 Karjalainen et al. 96 review did not state the word ‘biopsychosocial’ in the intervention description; however, the intervention was set out to incorporate the same elements, and because it was derived from the review on common musculoskeletal disorders by the same authors,97 it has been placed in the biopsychosocial category.
Other interventions
In their review, Elders et al. 93 included interventions relating to a secondary prevention intervention in a non-health-care setting for back pain or disorders. These comprised either organisational or administrative interventions (including modified work and early RTW); technical, engineering or ergonomic interventions; or personal interventions. The review by Meijer et al. 99 featured interventions that fell into the following five categories: knowledge conditioning, physical conditioning, psychological conditioning, social conditioning and work conditioning (e.g. vocational training and workplace-based interventions). Physical conditioning interventions, as part of RTW strategies, were reviewed by Schaafsma et al. ,103 which were specified as comprising advice about exercises for restoration of functionality (neurological, musculoskeletal, systemic or cardiopulmonary), with an intended improvement in work status, and a relationship between the intervention and functional job demands. In addition, the intervention could include further components, such as advice on RTW and workplace involvement.
Individual relevant studies from the included reviews
The systematic reviews were included based on the scope of the reviews and their inclusion criteria meeting the eligibility criteria for our rapid review. However, the primary studies that were identified and included in the reviews did not necessarily all provide relevant data or fit with our review question (i.e. have an occupational advice intervention). Hence, if conclusions were to be drawn solely from the overall messages of each of the reviews, this would not be of use for our review, as several irrelevant studies would be feeding into this. As a result, we screened the list of included studies in each review and the key details from the studies identified as being relevant have been extracted and summarised in Appendix 2, regarding work-related outcomes.
Effectiveness of interventions
The interventions that showed evidence of benefit are summarised in Appendix 2, comprising 14 musculoskeletal studies and one surgical study. The intervention content within the musculoskeletal studies varied, but generally featured rehabilitation, with multidisciplinary team involvement. The studies tended to relate to back pain or musculoskeletal pain in general. Specifically, six studies related to low back pain,108–115 one was for work-related thoracic/lumbar pain,116 one for upper extremity musculoskeletal disorders117 and one for rheumatic disease. 118 More generally, four studies related to musculoskeletal disorders/pain119–122 and one study investigated soft-tissue injuries,123 which involved back, shoulder, lower extremity, neck and thoracic pain.
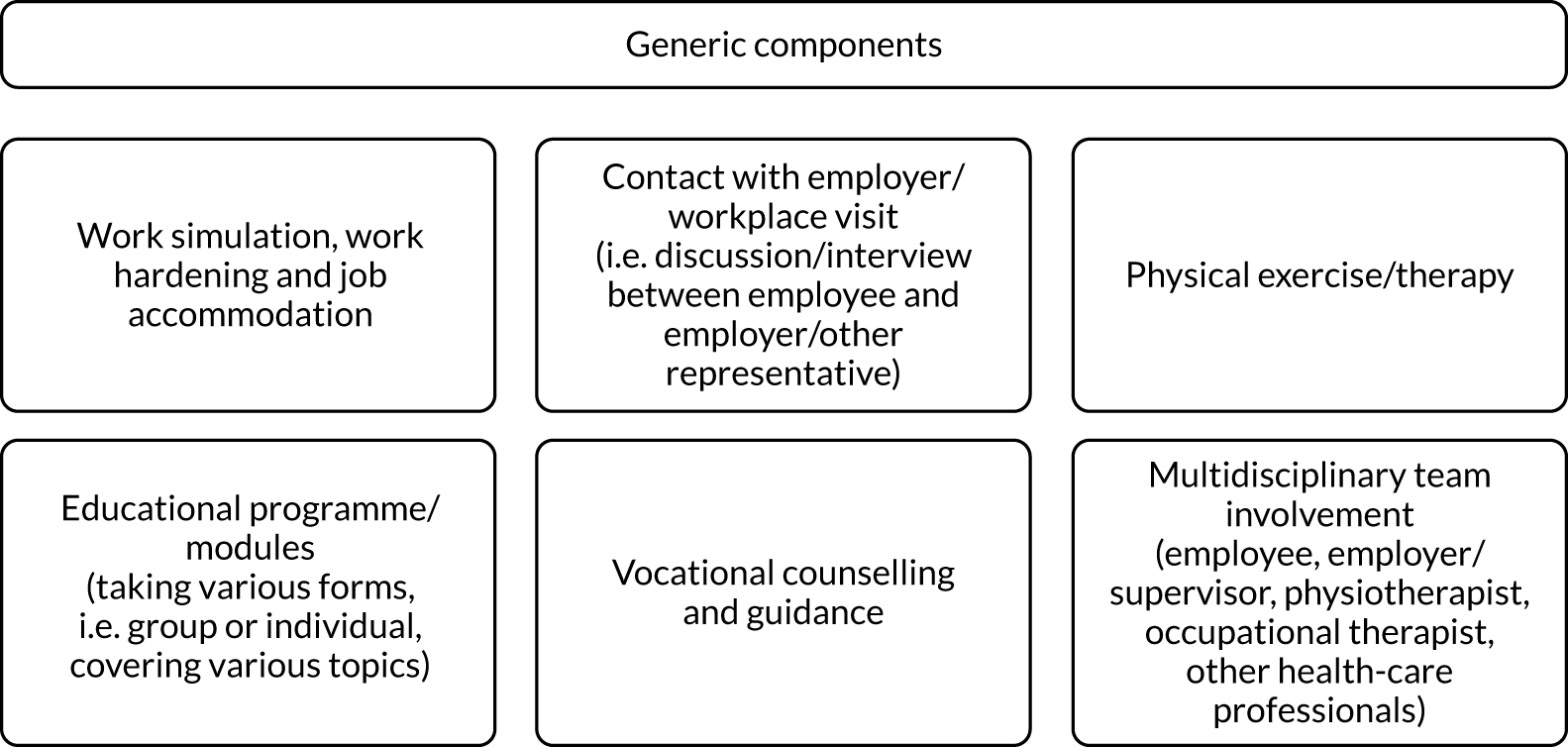
Duration and timing of the interventions varied, with participants often being on sick leave at entry to the programme. Some interventions were more intensive,108–111,114,115,117,121–123 for example being 6 hours per day, 5 days per week, for 5 weeks,110 whereas others involved only a few visits or sessions at longer time intervals. All of the interventions were delivered face to face. The multidisciplinary team involved in the effective interventions tended to comprise an occupational therapist, physiotherapist, other health-care professionals and the employer/workplace supervisor, in collaboration with the employee. The majority of the rehabilitation interventions included components such as job accommodation, work hardening/simulation, physical therapy/exercises, vocational advice, workplace visits and educational classes, with some covering pain management.
The intervention that featured in the one surgical study of herniated lumbar disc surgery124 followed a rehabilitation-orientated approach used by medical advisors to motivate patients and treating physicians towards social and professional reintegration. It was delivered face to face by medical advisors, with patients first visiting at 6 weeks post operation and then attending monthly follow-up consultations. The intervention also involved contacts with treating physicians and case discussion with medical advisors’ colleagues (see Appendix 2).
What components of the interventions are likely to be generic across conditions and surgical procedures and, therefore, generalisable to an occupational advice intervention prior to planned surgery for hip or knee replacement?
The effective interventions tended to involve rehabilitation programmes, which took a multidisciplinary approach in general. In the majority of cases, it was not possible to disentangle the separate elements to determine whether certain components were playing more of a role in the effectiveness than others. The key components of the interventions that kept appearing irrespective of the condition and/or surgical procedure under consideration are summarised in Figure 4.
FIGURE 4.
Summary of key components across effective interventions.
Outcome measures for return to work, return to normal activities and return to social activities
The outcome measures used in the relevant primary studies from the systematic reviews are mapped in Appendix 2 by study and type of outcome measure. Outcome measures were grouped in the following categories to aid mapping, although in reality there is overlap between these categories: (1) non-standardised return to work/activities measures, standardised scales for return to work/usual activities, measures focusing on musculoskeletal symptoms, quality-of-life measures, psychological measures and other measures.
Studies most commonly used some type of measure of RTW, although how this was assessed varied between studies. In some studies, the measure distinguished between whether participants returned to work at full capacity or whether this was in an altered capacity, whereas other studies had a more blunt measure, such as the proportion of participants who returned to work. Number of days of sick leave was also commonly used as an outcome measure. Patient-reported outcome measures tended to focus more broadly on activities of daily living, such as the disability component of the low back pain rating scale developed by Manniche et al. 125 This component of the scale assesses ability to perform daily activities, such as working, sleeping, housework, walking, sitting, lifting, dressing, driving and running. Other outcome measures focusing on ability to perform activities of daily living were the Oswestry Disability Index (ODI)126 and the Roland–Morris Disability Questionnaire. 127 There are multiple versions of the ODI and not all contain questions related to employment, and none of the multiple versions of the Roland–Morris Disability Questionnaire contains questions related specifically to employment. Two studies128,129 used measures that focused specifically on work using the Graded Reduced Work Ability Scale developed by Haldorsen et al. 130
Primary studies (surgical)
Study selection
The literature search of electronic databases identified 1179 potentially relevant records for the primary studies (Figure 5). After removal of duplicates, 989 primary studies were screened for relevance. A total of 856 primary studies were excluded on the basis of title and abstract and 140 full papers were retrieved for more detailed evaluation, which included seven obtained via reference and citation checking. A total of 136 papers were excluded and four studies met the inclusion criteria, with the included primary studies listed in Appendix 2. One of these studies had already been identified in the review of reviews and was also included here for the sake of completion so that it was quality assessed and discussed in conjunction with the only other identified study of a surgical population. 124 Details of excluded studies are also provided in Appendix 2.
FIGURE 5.
Study selection for review of primary studies.
Overview of included studies
The four included primary studies comprised two RCTs (n = 925 participants) conducted in the Netherlands131 and Belgium124 and two qualitative studies undertaken in England132 and Texas, USA. 133 The main study characteristics are presented in Appendix 2.
One RCT involved individuals who had undergone lumbar disc herniation surgery124 and the other featured participants following gynaecological surgery. 131 One of the qualitative studies explored perspectives of patients who had undergone knee replacement surgery,132 and the other focused on cancer care. 133
Risk of bias
The risk-of-bias assessments are reported in Appendix 2. The qualitative studies were of variable methodological quality; one study132 met all of the CASP criteria with the exception of one area being unclear regarding whether or not the relationship between researcher and participants had been adequately considered. The other study133 lacked detail in relation to data collection considerations, ethics issues and the researcher–participant relationship. One of the two RCTs was at an unclear risk of bias due to limited reporting on several elements of study design124 and the other was at unclear risk of bias due to lack of information about allocation concealment. 131
Type of return-to-work interventions
One RCT evaluated a personalised eHealth intervention in terms of the effect on recovery and RTW,131 and the second assessed a rehabilitation-oriented approach that focused on early mobilisation and early resumption of professional activities in terms of the effect on RTW. 124 The Criteria for Reporting the Development and Evaluation of Complex Interventions in healthcare82 were used for the interventions in the included studies (see Appendix 2).
The qualitative studies explored factors affecting RTW from the perspective of the patient following knee replacement,132 and factors influencing work disability following mastectomy through involvement of patients, therapists and employers. 133 Rather than discuss a defined intervention as such, both studies instead discuss individuals’ experiences of advice or education and rehabilitation received from health-care professionals132 and employers133 regarding RTW, among other issues relating to RTW.
Effectiveness of interventions
The RCT by Donceel et al. ,124 of early mobilisation and early resumption of professional activities versus usual practice (control) for lumbar disc surgery, reported that, at 52 weeks after surgery, a smaller proportion of patients in the intervention group (10.1%) than in the control group (18.1%) had not resumed work. The difference between the groups was found to be statistically significant (log-rank test: p < 0.001), with the intervention group being more successful (i.e. a higher rate of RTW was found for the intervention group).
When evaluating a personalised eHealth programme compared with a control website for recovery and RTW following gynaecological surgery, Vonk Noordegraaf et al. 131 estimated a hazard ratio of 1.43 (95% confidence interval 1.003 to 2.040; p = 0.048) in their adjusted intention-to-treat (ITT) analyses of RTW in favour of the eHealth intervention. Findings were comparable for the adjusted per-protocol analyses, but for the univariate crude ITT analyses, findings were not statistically significant.
Further details of the interventions are provided in Appendix 2. The two interventions (a rehabilitation-oriented approach and a personalised eHealth intervention) were very different in terms of the surgical population under consideration (lumbar disc surgery and hysterectomy) and the content of the interventions. The modes of delivery varied between studies, from the intervention being delivered face to face to being delivered purely online. In terms of the timing of the interventions, one was delivered 6 weeks after surgery whereas the other was delivered both before and after surgery.
Taken collectively, the two studies124,131 suggest that a multicomponent intervention with a focus on assisting RTW for individuals undergoing elective surgery is beneficial. However, owing to there being only two interventions from the included studies and because these were heterogeneous in nature, it was not possible to examine the components of the interventions that are likely to be generic across conditions and surgical procedures.
Outcome measures for return to work, return to normal activities and return to social activities
Donceel et al. 124 assessed the proportion of patients who had returned to work at 12 months’ follow-up. In Vonk Noordegraaf et al. ,131 the primary outcome was duration of sick leave until a full sustainable RTW, defined as the duration of sick leave in calendar days from the day of surgery until a full RTW to the same job, or to other work with equal pay, for at least 4 weeks without recurrence (partial or full). Other outcomes assessed in this study were quality of life (assessed by the RAND Short Form questionnaire-36 items), general recovery [measured by the Recovery Index 10 (RS-10), a validated recovery-specific quality-of-life questionnaire134] and pain intensity (measured by a visual analogue scale questionnaire).
Barriers to and facilitators of intervention delivery and stakeholder perspectives
Truncated data extraction tables from the two qualitative studies on stakeholder perspectives are provided in Appendix 2.
One UK study of 10 employed patients who had undergone TKR identified several facilitators and barriers from the patient perspective. 132 Three key themes were identified that have relevance for delivery of an occupational advice intervention:
-
Delays in surgical intervention and impact on work participation preoperatively. Patients felt that their employment status and need to remain in employment were not fully taken into consideration in the decision-making process about whether surgery should take place or be delayed until they were older. Perceived delays in surgery due to their age had a negative impact on their work before surgery and had the potential to have a negative impact on future employability.
-
Limited and inconsistent advice from health-care providers to optimise RTW. Patients reported that the advice they received focused mainly on the needs of an older retired population and covered the inpatient stay and immediate postoperative period but not RTW. Some patients thought that they should not return to work until they were advised to do so. Some reported that they could have returned to work earlier. Advice appeared to be generic rather than tailored.
-
Rehabilitation to optimise recovery and RTW. Patients reported that the postoperative rehabilitation they received was variable, that their need to return to work was not routinely considered and that they would have benefited from a more tailored approach. However, rehabilitation staff played an important role in giving them confidence to progress in their recovery.
One US study obtained the views of 31 mastectomy patients, 18 physical or occupational therapists and five employers. 133 Information provided about patients’ views on RTW was very limited. It is noteworthy that, although ‘many women’ described physical impairments that interfered with their ability to work, only one woman reported being asked by a health-care professional about the physical requirements of her job. However, 81% of therapists reported that job requirements were addressed in their treatment goals. Employers reported that they had written guidelines in place appropriate for people returning to work following surgery but that they would find it useful to have more tailored information about their employee’s physical restrictions, better patient education about expectations for recovery, more counselling services and better timing of clinic appointments to reduce disruption to work schedules. The authors commented that a common theme from all three stakeholder groups was the perceived dependence on doctors to guide the recovery process. It was suggested that some of this responsibility could be delegated to other health-care professionals.
Chapter 4 Intervention mapping stage 1: needs assessment – cohort study, health economic analysis and national survey of practice
Introduction
A cohort study was undertaken to collect information about the population of working patients undergoing elective primary hip or knee replacement and the care they currently receive. A national survey of current national practice was conducted concurrently to provide additional information about current practice.
Objectives
The cohort study and survey of practice supported study objectives 1, 2 and 5 (see Chapter 1, Objectives).
Methods
Cohort study
Overview
Participants undergoing hip or knee replacement (or who were on the waiting list) who had been working in the 6 months prior to surgery were prospectively recruited over a 5-month period at four centres (Middlesbrough, Nottingham, Norwich and Northumbria). Potential patients were identified by the clinical teams and screened by the local research teams at each site. Eligible patients were approached and given a patient information sheet (see Appendix 3), had an opportunity to ask the research team questions and then, if appropriate, were consented into the study.
Questionnaires were completed at baseline (either postoperatively on the inpatient ward or preoperatively in a pre-assessment clinic) and at 8 and 16 weeks post surgery (postal), and, for a subsample, at 24 weeks post surgery. Baseline questionnaires included:
-
patient demographic data
-
functional status in the workplace (Work Limitations Questionnaire135,136 and Workplace Design Questionnaire137)
-
health-related quality of life [EuroQol-5 Dimensions, five-level version (EQ-5D-5L)]
-
depression and anxiety [Patient Health Questionnaire-9 items (PHQ-9) and Generalised Anxiety Disorder-2 item (GAD-2)]
-
Brief Resilience Scale (BRS)
-
joint specific functional outcomes [Oxford Hip Score (OHS) or Oxford Knee Score (OKS)]
-
employment details
-
expectations of recovery and RTW after surgery.
Follow-up questionnaires included the same measures plus information about RTW, adaptions to hours and the workplace environment, use of fit notes, health-care utilisation, interaction with occupational health services and return to normal activities. The baseline hip questionnaire and postoperative knee questionnaire documents are available at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/ (accessed 2 May 2020).
Study inclusion/exclusion criteria
The inclusion criteria for patients recruited into the cohort study were:
-
aged ≥ 16 years
-
on the orthopaedic ward undergoing a primary hip or knee replacement or on the waiting list for a primary hip or knee replacement
-
in work in the 6 months prior to their joint replacement.
The exclusion criteria were:
-
lack of mental capacity
-
did not understand written and/or spoken English
-
emergency surgical procedure (e.g. surgery for an indication of trauma)
-
currently undergoing surgery for cancer
-
currently undergoing surgery for infection.
Sample size
A sample size of 150 patients was used as this number is sufficient for representative estimates within an 8% margin of error. 138 In addition, based on the rule of thumb of 10 events per variable in logistic and Cox regression, a sample size of 150 would allow a maximum of seven predictor variables to be included in the regression analyses, assuming that 50% of participants experienced the outcome of interest.
Data checking and transfer
The cohort questionnaires collected anonymised patient data linked to patient contact information forms (including patient identifiers) using a unique study number. The patient contact forms were used to administer follow-up and contact patients who had consented to be approached for interview. Once a participant completed the questionnaire, a researcher entered the anonymised data into an equivalent form in Qualtrics® [SAP (Systems, Applications & Products in Data Processing), Provo, UT, USA]. This process allowed the research team at the University of York to download a copy of the anonymised responses and conducted a blinded analysis.
To check for data entry errors, a selection of forms were second checked. For the first 10 participants at each site, a complete check of the questionnaires was carried out. After this initial check, a further 10% were then sampled randomly from each site to ensure that data quality was maintained. Any discrepancies were recorded and overall data error rates were calculated.
Data analysis
Analyses were undertaken in Stata® 15 (StataCorp LP, College Station, TX, USA). The baseline and follow-up questionnaires (8, 16 and 24 weeks) were summarised using descriptive statistics (continuous: n, mean, SD, median, first and third quartiles, minimum and maximum; categorical: counts and percentages). Logistic regression models were used to predict early RTW (within 6 weeks) using preoperative, operative and postoperative characteristics. In addition, a Cox proportional hazards model was used to predict time to RTW in days from the date of the operation using the same covariates as the logistic model.
Health economic analysis
We had originally intended to utilise information from the survey of practice to inform the mapping of the ‘standard care’ pathway. However, the findings from the survey highlighted considerable variation in what constitutes standard care at different institutions and according to different individuals (e.g. surgeons and physiotherapists), making it difficult to define and quantify standard care. Therefore, it was not possible to incorporate the survey data in the mapping of standard care for the economic analysis and this analysis was therefore based solely on the data collected from the cohort study.
Estimates of health-care resource use
The resource use items comprised visits to the GP, nurse, occupational therapist, physiotherapist and ‘other health service professional’, hospital inpatient attendances, day cases, outpatient attendances, accident and emergency (A&E) visits and physiotherapy hospital attendances. Participants were asked to answer the resource use questions and total resource use over 24 weeks estimated for each participant in relation to whether or not the visit was ‘about your joint replacement’ and also in relation to ‘another reason’. Unit costs (see Appendix 3) were obtained from established national costing sources [NHS Reference Costs139 and Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care140] and were applied to the resource use data up to the 16-week follow-up, given that only a subsample of participants were followed to 24 weeks. Total costs for the 41 participants who completed 24-week questionnaires are presented in Appendix 3. Costs are presented in Great British pounds at 2018 prices.
Return-to-work advice
The cohort questionnaires asked participants if they received any advice about returning to work following their operation, at all time points, from the following: surgeon, GP, occupational health, physiotherapist, occupational therapist, employer and ‘other’, where they were asked to state what this was. For the purpose of costing, there was some overlap with the health-care resource use items listed in the previous section; hence, the only items that were costed separately from this question are occupational health and employer. The corresponding unit costs and sources are presented in Appendix 3.
Estimates of health-related quality of life
The EQ-5D-5L141 was administered to the participants at baseline and 8 and 16 (and 24, for a subset of participants) weeks. The EQ-5D-5L, launched in 2009 by the EuroQol Group, consists of the EuroQol-5 Dimensions (EQ-5D) descriptive system and the EuroQol visual analogue scale (EQ VAS). 142 There are five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression), with each dimension having five levels (no problems, slight problems, moderate problems, severe problems and extreme problems). Following recommendations by the National Institute for Health and Care Excellence (NICE),143 the crosswalk between the EuroQol-5 Dimensions, three-level version, and the newer EQ-5D-5L was used to estimate utilities. 144
At baseline, the EQ-5D-5L was administered twice. One was the normal version of the questionnaire, which asked ‘Under each heading, please tick the one box that best describes your health today’. The additional version asked participants to ‘please think back to your health before your joint replacement operation. Under each heading, please tick the one box that best describes your health 4 weeks before your operation’. This was because at baseline we were aiming to capture participants’ health status prior to surgery, but owing to the timing of completion (i.e. before or after surgery) varying for different participants, we included an additional version that asked about 4 weeks prior to surgery.
Productivity loss
Cost estimates were attached to productivity losses using data from the cohort questionnaires regarding the number of days that participants missed from work because of the joint that required joint replacement surgery over the 6-month period prior to surgery. The number of days missed from work was multiplied by a daily wage of £114, which was based on median full-time gross weekly earnings of £569, sourced from the Office for National Statistics. 145 The same daily wage was attached to the number of days missed from work following the participant’s surgery, to generate a mean per-participant cost due to productivity loss over the period following surgery.
Data analysis and presentation of results
For each resource use item, data are presented for all available cases, and also according to complete cases, whereby participants with missing data at any of the questionnaire time points were excluded. The missing data were due to participants either not returning the questionnaire or not completing the relevant questions on the questionnaire. Similarly, the EQ-5D findings are displayed for all available cases. Analyses were undertaken in Stata 15. Data were summarised separately by type of replacement.
The cost of the intervention is presented in Chapter 10, as part of the feasibility assessment.
Survey of practice
A web-based electronic software (SurveyMonkey®, Palo Alto, CA, USA) was used to create the survey. To achieve national dissemination, a three-armed sampling strategy was used. First, the survey was e-mailed to the 149 individual trust leads for the NJR for England, Wales and Northern Ireland. Each lead was asked to disseminate the survey to relevant members of their clinical teams. Second, a link to the survey was embedded in an article about the OPAL study in the July edition of the NJR eBulletin (https://webactivate.hqip.org.uk/index.php?action=social%26c=284%26m=367; accessed 27 September 2017), which has an e-mail readership of > 3800 stakeholders. Third, to capture clinical teams in Scotland, the survey was distributed via the chairperson of the Scottish Committee for Orthopaedics and Trauma to members for dissemination within local organisations. The survey was available for completion for 6 weeks and collected information from all of the HOT involved in the treatment of hip and knee replacement patients.
The survey collected information specific to each member of the HOT. The survey explored (1) when each group interacted with patients as part of their preoperative pathway, (2) whether or not RTW advice was routinely given during this interaction, (3) the methods used to deliver RTW advice, (4) confidence in delivering advice and (5) the need for an occupational RTW advice intervention. The survey also offered the participants the opportunity to provide free-text comment. The survey was released on 1 July 2017 and responses were collated 6 weeks later, with the last response received on 11 August 2017. The OPAL survey of practice document is available at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/ (accessed 2 May 2020).
Each question was summarised using simple descriptive statistics and, where appropriate, by job role. Direct comments from the ‘free-text’ question were grouped based on positive or negative experiences of delivering RTW advice.
Results
Cohort
Screening data
Overall, 765 people were screened, of whom 202 (26.4%) were in work in the 6 months prior to surgery and were eligible for inclusion. All 202 patients in work met the other eligibility criteria. Figure 6 details the flow of participants through the study and details reasons for exclusion and non-participation. In total, 162 patients (80.2% of eligible patients) consented, of whom 154 (95.1%) provided baseline data (77 hip replacement patients and 77 knee replacement patients) and were followed up. Participants were recruited from all four sites over a 5-month period (1 November 2016 to 30 March 2017): Nottingham (n = 42), Norfolk and Norwich (n = 12), Middlesbrough (n = 62) and Northumbria (n = 38).
FIGURE 6.
Screening log data describing work status prior to surgery and intention to return to work after surgery.
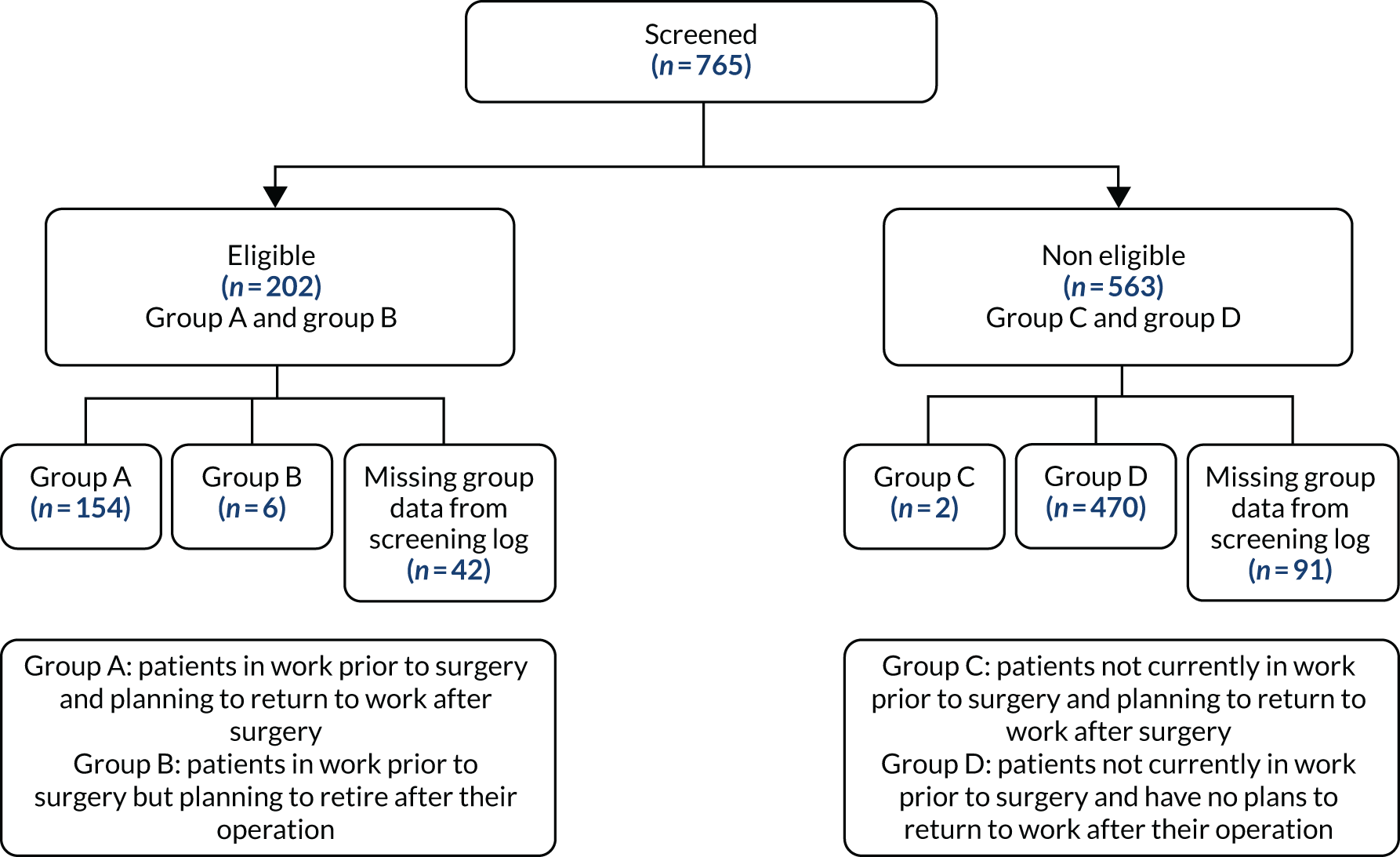
The OPAL study intended to capture data from two defined groups of patients (see Figure 6). Group A comprised patients in work prior to surgery and planning to return to work after surgery, and group B comprised patients in work prior to surgery but planning to retire after their operation. However, only six screened patients (three consenting) were in group B, limiting the ability to analyse data from this group.
Baseline data
Population characteristics
The participants in the cohort were aged, on average, 60.1 years (SD 9.4 years), this ranged from 31 to 86 years. The average ages were similar for the hip (58.9 years) and knee (61.3 years) replacement groups. There were slightly more males (n = 85, 55.2%) than females (n = 64, 41.6%) in this cohort, with balance across the two types of operation; some participants did not state their sex (n = 5). The median BMI was 28.2 kg/m2 (range 15.9–44.9 kg/m2). Almost all of the participants were of white ethnicity (94.2%), with one Asian participant and three in the ‘other’ ethnicity category.
When asked about their health, 81.2% of participants said that they did not suffer from chronic health problems, with a slight difference between those undergoing hip (85.7%) and those undergoing knee (76.6%) replacements. Of the participants undergoing hip replacements, 48.1% stated that they also had problems with their other hip joint, and, similarly, 54.6% of those undergoing knee replacement stated they also had problems with their other knee. Those undergoing hip arthroplasty seemed, in general, not to suffer from knee problems, with only 28.6% stating that they suffered from knee problems, and vice versa for the knee arthroplasty patients (18.2%). Only 24 participants (15.6%) stated that they suffered from chronic back or neck problems.
Type of employment and work environment prior to operation
Details of the type of employment, the number of hours participants worked per week and length of time in their current job are detailed in Table 3. The distribution of the type of employment was similar for hip and knee replacement patients. The majority stated that they worked for a ‘large’ employer (43.5%), with similar numbers saying that they worked for medium, small and micro employers, or worked alone (10.4%, 9.1%, 16.2% and 14.3%, respectively). As part of their job, 20.8% of participants were required to work rotating shifts and 40.3% were required to drive while at work. Overall, 72.7% reported that they had to drive to get to work (83.1% of the knee and 62.3% of the hip replacement groups). A list of all job types is provided in Appendix 3.
| Employment details | Group | Total (N = 154) | |
|---|---|---|---|
| Hip replacement (N = 77) | Knee replacement (N = 77) | ||
| Which of these best describes your usual work?, n (%) | |||
| Employed full time | 29 (37.7) | 30 (39.0) | 59 (38.3) |
| Employed part time | 21 (27.3) | 17 (22.1) | 38 (24.7) |
| Self-employed | 17 (22.1) | 20 (26.0) | 37 (24.0) |
| Unpaid work | 7 (9.1) | 8 (10.4) | 15 (9.7) |
| Other | 2 (2.6) | 1 (1.3) | 3 (2.0) |
| Missing | 1 (1.3) | 1 (1.3) | 2 (1.3) |
| Number of hours worked each week | |||
| Employed full time | n = 28 | n = 30 | n = 58 |
| Mean (SD) | 43.6 (11.5) | 43.4 (11.3) | 43.5 (11.3) |
| Median (Q1, Q3) | 40 (37, 48) | 38 (37, 45) | 39 (37, 48) |
| Minimum, maximum | 26, 80 | 33, 84 | 26, 84 |
| Employed part time | n = 21 | n = 17 | n = 38 |
| Mean (SD) | 21.1 (6.4) | 20.9 (15.8) | 21.0 (11.4) |
| Median (Q1, Q3) | 20 (16, 25) | 20 (14, 21.5) | 20 (15, 25) |
| Minimum, maximum | 10, 32 | 2, 75 | 2, 75 |
| Self-employed | n = 13 | n = 17 | n = 30 |
| Mean (SD) | 40.6 (24.3) | 41.9 (19.0) | 41.3 (21.1) |
| Median (Q1, Q3) | 45 (22, 55) | 50 (30, 50) | 45 (22, 55) |
| Minimum, maximum | 2, 84 | 6, 78 | 2, 84 |
| Unpaid work | n = 7 | n = 5 | n = 12 |
| Mean (SD) | 11.3 (6.0) | 31.8 (21.7) | 19.8 (17.4) |
| Median (Q1, Q3) | 12 (5, 18) | 20 (18, 50) | 16.5 (9, 19) |
| Minimum, maximum | 4, 18 | 11, 60 | 4, 60 |
| How long have you worked at your current job? (Years) | n = 38 | n = 37 | n = 75 |
| Mean (SD) | 13.4 (11.2) | 12.3 (12.6) | 12.8 (11.9) |
| Median (Q1, Q3) | 10.2 (4.3, 20.3) | 8 (4, 15.9) | 9.5 (4.1, 16.8) |
| Minimum, maximum | 1.1, 50.8 | 0.8, 61.1 | 0.8, 61.1 |
Eighty-six per cent of participants were working in their usual role right up to the day before their surgery. Those who did not work in their usual role were either working reduced hours or had amended work duties. The majority (72.1%) made no changes to their workplace in the 6 months before their operation. Further detail about the work habits of participants prior to surgery is given in Appendix 3.
Workplace sickness policy
The majority of participants (57.8%) did not have any periods of sick leave in the 6 months before their operation. Those who did reported having an average of 4.3 periods of sick leave due to their hip/knee and an average of 1.7 periods of sick leave for other reasons. On average, the participants took 13.1 days of leave because of their hip/knee (range 0–90 days) and 4.6 days for other reasons (range 0–60 days). Around half of the participants were aware of the sickness policy for their workplace. Approximately one-quarter said that they would receive statutory sick pay and one-quarter said that they would receive employer-based sick pay; however, around one-fifth of participants stated that they did not know about their sickness pay. The most common length of sickness payment was for > 6 months; however, the majority of respondents (36 of 92, 39%) were unaware of how long they would receive sickness payments for. Further details can be found in Appendix 3.
Workplace design questionnaire and workplace questionnaire
A summary of these responses can be found in Appendix 3. Responses suggested that patients had autonomy to structure how they worked. In response to questions relating to work ergonomics and work demands, 60% of participants agreed or strongly agreed that their seating arrangements in their job were adequate and 61% of participants agreed or strongly agreed that their workplace accommodated size differences between people in terms of clearance, reach, eye height, leg room, etc. Only 30% of participants agreed or strongly agreed that their job involved excessive reaching. Approximately half of the participants felt that their job was physically demanding. Overall, 44% agreed or strongly agreed that their job required a great deal of muscular endurance, 37% agreed or strongly agreed that their job required a great deal of muscular strength and 51% agreed or strongly agreed that their job required a lot of physical effort.
The majority of participants reported that they felt that their workplace gave them the opportunity for social interaction and that the people they worked with were friendly and supportive. Overall, 72% agreed or strongly agreed that they had the opportunity to develop close friendships in their job, and 88% agreed or strongly agreed that their job gave them the chance to get to know other people. Although 75% of participants agreed or strongly agreed that the people they worked with took a personal interest in them and 88% agreed or strongly agreed that the people they worked with were friendly, only 60% stated that their supervisor was concerned about the welfare of the people who worked for them.
Expectations of recovery after surgery
At baseline, participants thought that they would be back in work at an average of 9.5 weeks post surgery (range 1–68 weeks). Similarly, the average time they thought their employer would be happy for them to return was 9.6 weeks post surgery (range 0–78 weeks). In terms of their usual activities, participants stated that they expected to be performing these by, on average, 9.3 weeks post surgery, slightly earlier than returning to work, and, on average, expected to be driving after 6.3 weeks.
Baseline health measures
A total of 147 (95.5%) participants completed the PHQ-9 and the average score was 5.4 (range 0–24). The hip replacement participants had a slightly higher mean score (5.9) than knee replacement participants (4.9), but both were within the ‘mild’ depression category.
The GAD-2 was completed by 148 (96.1%) participants. Over 50% reported that they never felt nervous, anxious or on edge and over 60% stated that they had never felt uncontrollably worried. However, approximately 10% of participants did experience these symptoms more than every other day. A follow-up question was asked relating to how these problems affected their work, home and personal lives; 42.9% stated that these things were not made difficult at all, with only 3.3% saying that things were made extremely difficult by their anxiousness and worrying.
Scores were calculated for 148 (96.1%) participants at baseline, with an average score of 19.2 for hip patients and 20.9 for knee patients (range 6–44), which correspond to ‘moderate to severe’ hip/knee problems.
A total of 148 participants had valid responses for this questionnaire. The average score was 3.03, which falls just into the range for normal resilience (3.0–4.3). One participant had high resilience (0.7%), 106 participants had normal resilience (68.8%) and 40 participants had low resilience (26.0%) [data were missing for seven patients (4.6%)]. The results for this measure were similar for hip and knee participants.
Further information about the baseline health measures for the cohort participants is presented in Appendix 3.
Follow-up data
Follow-up rates
All participants who had not withdrawn from the study were followed up at weeks 8 and 16; however, a subsample of participants was followed up 24 weeks post surgery. In total, 148 participants were provided with week eight questionnaires (73 hip and 75 knee participants), 139 were provided with week 16 questionnaires (70 hip and 69 knee participants) and 87 were provided with week 24 questionnaires (51 from Middlesbrough and 36 from Nottingham; 41 knee and 46 hip participants) (Figure 7 and Table 4). The Middlesbrough and Nottingham sites were the first to open for the OPAL study, so the participants reached week 24 first and became the subsample at this time point. This differs from the plan of including only 45 participants, as stated in the protocol. It can be seen that 83.8% of the participants replied to at least one of the follow-up questionnaires; the average response rate to the follow-up questionnaires was 61.6%.
FIGURE 7.
Flow of patients through the cohort study.
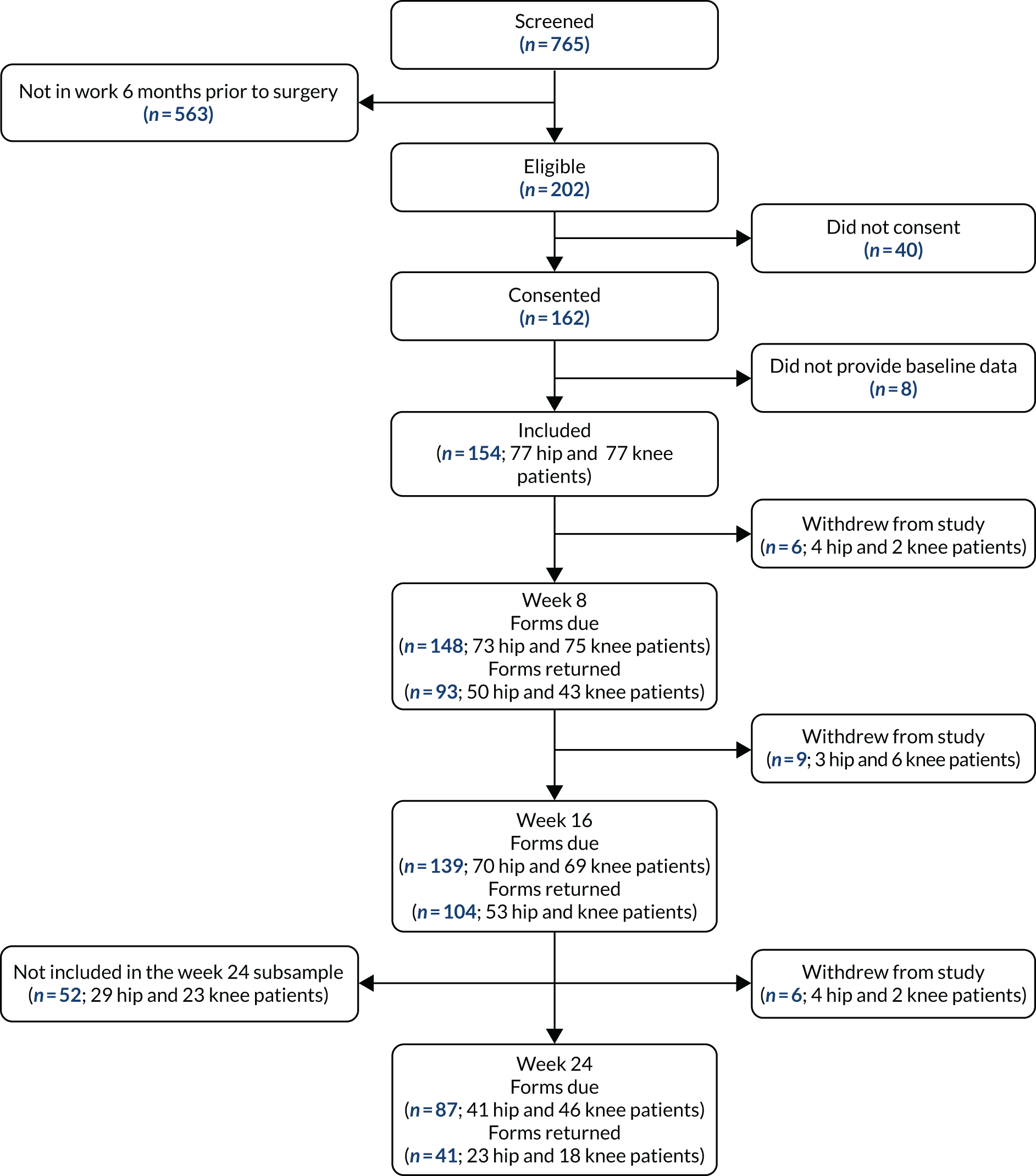
| Time point | Group | Total | ||||
|---|---|---|---|---|---|---|
| Hip replacement | Knee replacement | |||||
| Number sent | Number returned (%) | Number sent | Number returned (%) | Number sent | Number returned (%) | |
| Baseline | 80 | 77 (96.3) | 82 | 77 (93.9) | 162 | 154 (95.1) |
| Week 8 | 73 | 50 (68.5) | 75 | 43 (57.3) | 148 | 93 (62.8) |
| Week 16 | 70 | 53 (75.7) | 69 | 51 (73.9) | 139 | 104 (74.8) |
| Week 24 | 41 | 23 (56.1) | 46 | 18 (39.1) | 87 | 41 (47.1) |
| Completed at least one follow-up questionnaire, n (%)a | 65/77 (84.4) | 64/77 (83.1) | 129/154 (83.8) | |||
Oxford Hip and Knee Scores
The OHS/OKS raw scores and a categorised representation are provided in Appendix 3.
At week 8, 93 participants completed the questionnaire (62.8% of those who were sent the questionnaire) and the average score was 33.6 for hip and 28.3 for knee participants. This increased to 38.6 and 54.1 at week 16, and remained similar at 24 weeks (see Table 4). The proportions of participants who were classified as ‘satisfactory’ increased from 1.3% at baseline to 19.4% at week 8 and to 45.2% at week 16 (see Appendix 3). Similarly, the proportion of those who classified their joint symptoms as ‘severe’ decreased from 49.4% at baseline to around 6% at week 16.
Return to work
Only 78 participants (50.6%, 37 hip and 41 knee participants) indicated that they returned to work within their period of follow-up. Of these, 74 participants (94.9% of returnees, 48.1% of entire cohort) provided a return date, allowing time between surgery and RTW to be calculated. On average, those who did return did so 10 weeks after surgery, with a range of 1 to 27 weeks. Return times are presented in Figure 8, and detailed in Table 5, for those who returned to work and those classified as early returners.
FIGURE 8.
Time to RTW after surgery. Note that two participants returned their 24-week questionnaires late.
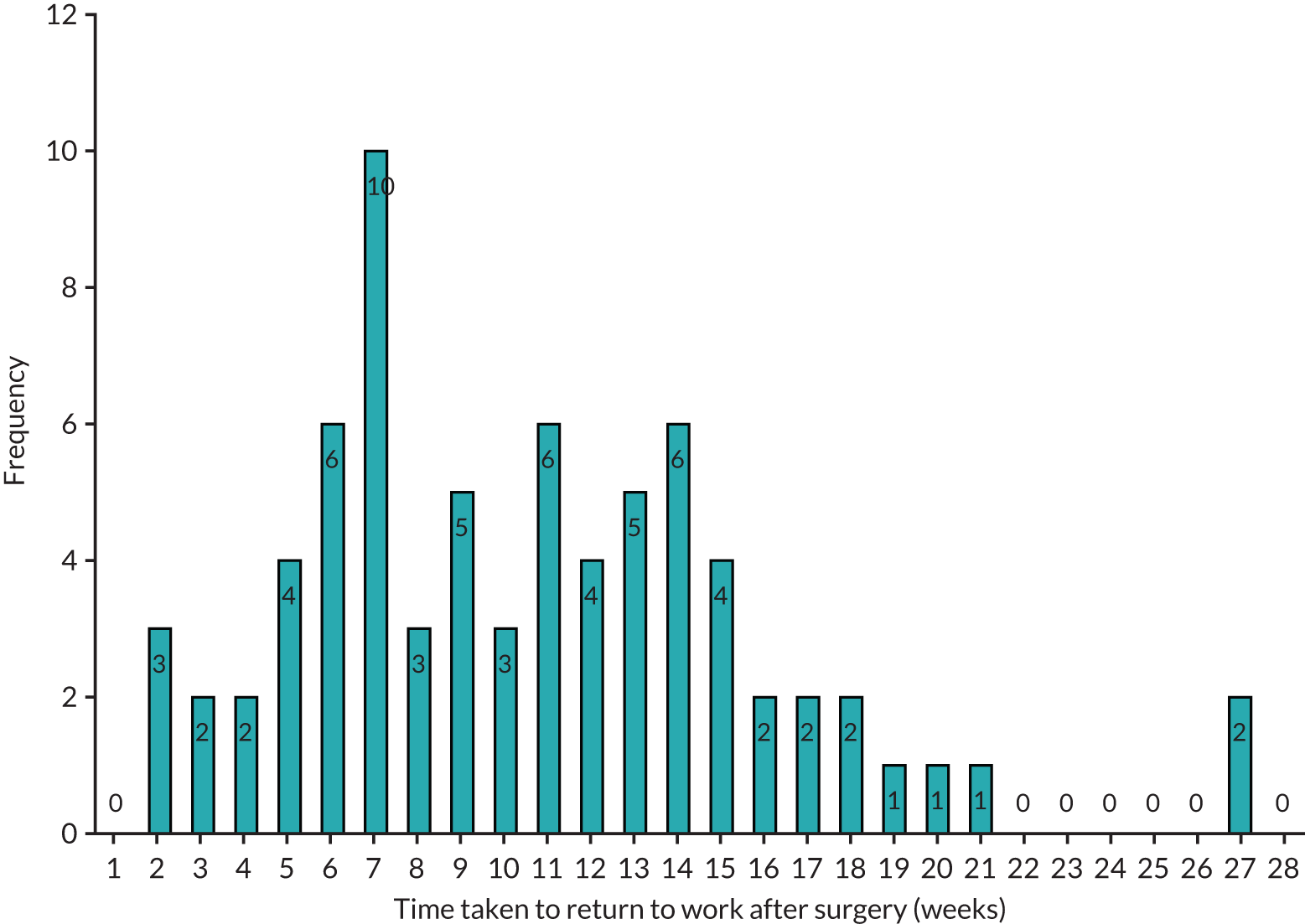
| Length of time (weeks) | Group | Total (N = 154) | |
|---|---|---|---|
| Hip replacement (N = 77) | Knee replacement (N = 77) | ||
| Participants who returned to work | n = 36 | n = 38 | n = 74 |
| Mean (SD) | 9.7 (5.5) | 10.3 (5.4) | 10.0 (5.4) |
| Median (Q1, Q3) | 8.5 (6.2, 13.1) | 10 (6.3, 13.1) | 9.4 (6.3, 13.1) |
| Minimum, maximum | 1, 26.9 | 1.9, 27 | 1, 27 |
| Participants who returned earlya to work | n = 8 | n = 9 | n = 17 |
| Mean (SD) | 3.6 (1.8) | 3.9 (1.3) | 3.8 (1.5) |
| Median (Q1, Q3) | 4.5 (1.9, 5) | 4.4 (3, 4.7) | 4.4 (2.7, 5) |
| Minimum, maximum | 1, 5.4 | 1.9, 5.7 | 1, 5.7 |
At 8 weeks’ follow-up, 27 of the 93 (29%) respondents had returned to work (12 hip and 15 knee replacement participants). Fifty-six (60.2%) respondents had not yet returned to work but intended to and nine (9.7%) stated that they no longer intended to return to work. At 16 weeks’ follow-up, 47 of the 103 (45.6%) participants stated that they had returned to work in the previous 8 weeks (23 hip and 24 knee participants), 17 (16.5%) had not yet returned to work but intended to and nine (8.7%) stated that they no longer intended to return to work.
Returning to work, workplace productivity and use of fit notes
When returning to work, 48.7% of the 78 participants who returned stated that they were working their usual hours and carrying out their usual duties in their first week, and a similar percentage (47.4%) returned with amended duties or hours. For those who had returned with reduced hours, the average amount of time worked in their first week back was 16.3 hours (range 3–40 hours). This is around half of the average amount of time worked before their operation (34 hours, range 6–65 hours). When asked about adaptations that had been made to their workplace and alterations to their pattern of work, only 16.7% (13/78) and 28.2% (22/78), respectively, said that any changes had been made.
Based on the Work Limitations Questionnaire, the average productivity loss in the 2 weeks prior to surgery was 30.4% for THR (SD 34.1%, range 0–100%) and 24.2% for TKR (SD 31.7%, range 0–100%) participants. For the patients who had returned to work after surgery, this had reduced to 19.7% and 5.1% for THR and 11.1% and 5.6% for TKR participants at 8 weeks and 16 weeks post surgery, respectively (Table 6).
| Percentage of time lost | Group | Total (N = 154) | |
|---|---|---|---|
| Hip replacement (N = 77) | Knee replacement (N = 77) | ||
| Baseline | n = 65 | n = 62 | n = 127 |
| Mean (SD) | 30.4 (34.1) | 24.2 (31.7) | 27.4 (32.9) |
| Median (Q1, Q3) | 25 (0, 50) | 0 (0, 50) | 0 (0, 50) |
| Minimum, maximum | 0, 100 | 0, 100 | 0, 100 |
| Week 8 | n = 19 | n = 18 | n = 37 |
| Mean (SD) | 19.7 (30.7) | 11.1 (26.0) | 15.5 (28.5) |
| Median (Q1, Q3) | 0 (0, 25) | (0, 0) | 0 (0, 25) |
| Minimum, maximum | 0, 100 | 0, 100 | 0, 100 |
| Week 16 | n = 39 | n = 36 | n = 75 |
| Mean (SD) | 5.1 (13.1) | 5.6 (12.1) | 5.3 (12.1) |
| Median (Q1, Q3) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Minimum, maximum | 0, 50 | 0, 50 | 0, 50 |
| Week 24a | n = 16 | n = 15 | n = 31 |
| Mean (SD) | 10.9 (22.3) | 11.7 (26.5) | 11.3 (24.0) |
| Median (Q1, Q3) | 0 (0, 12.5) | 0 (0, 25) | 0 (0, 25) |
| Minimum, maximum | 0, 75 | 0, 100 | 0, 100 |
Around half (50.5%) of those responding at week 8 stated that they had been given a fit note after their operation. The majority of these fit notes stated that the participant was not fit for work (87.2%) or may be fit to work taking into account a phased return (8.5%). Very few of these fit notes (n = 1 at 16 weeks) stated that amended duties may be needed. The mean length of time that the first fit note supplied to patients post surgery applied to was 5.6 weeks (range 2–10 weeks), and this was similar for hip (5.7 weeks) and knee (5.4 weeks) patients.
Further details about the mode of RTW and fit notes provided are in Appendix 3.
Returning to driving and normal activities
At week 16, 58 of the 79 (73.4%) participants had returned to driving when expected; at baseline, this was estimated to be 6 weeks. Similarly, 48 out of 85 (56.6%) participants said that they had returned to normal activities when they expected to (around 9.3 weeks as stated at baseline).
Access to occupational advice
Overall, 44 (28.6%) participants reported having access to an occupational health service through their employer at baseline. However, when asked at week 8, only 36 (23.4%) participants stated that they had received advice about returning to work post surgery. For those participants who received advice, the advice came from a variety of sources including surgeons, GPs, occupational health teams, physiotherapists, occupational therapists and employers (see Appendix 3).
Predictors of return to work
Because only 78 participants returned to work within our follow-up time frame, 74 of whom provided a return date, the number of variables to be included in the model was limited. Factors including age, sex, BMI, ethnicity, type of employer, number of hours worked and standardised outcome measures showed little or no evidence of predicting RTW. Size of employer, especially working for a micro employer, showed a sign of prediction when used solely in a model; however, when other factors were also included, this became non-statistically significant (see Appendix 3).
Although other studies found factors that were predictive of RTW within this population,42,44,48,146 our lack of predictive factors may be due to the relatively small sample size. Given the small numbers, no further statistical analyses were undertaken.
Health economics
Resource use and total costs
The health-care resource use in Table 7 refers to use relating to participants’ joint replacements. Resource use relating to ‘another reason’ is reported in Appendix 3. Participants predominantly visited health services in relation to their joint replacement, with low average resource use overall for ‘another reason’. The most commonly used resources for joint replacements were GP visits, physiotherapist attendances (both hospital and non-hospital), inpatient nights in hospital and outpatient attendances. The most notable resources for those who visited for ‘another reason’ were GP visits and nurse visits (both at the GP’s practice), physiotherapist visits (hospital and non-hospital), inpatient nights in hospital and outpatient attendances.
| Type of resource use | Group | |||||
|---|---|---|---|---|---|---|
| Hip replacement (N = 77) | Knee replacement (N = 77) | |||||
| Mean (SD) | Missing (%) | Mean (SD) | Missing (%) | |||
| GP visits at GP’s practice | ||||||
| Baselinea | 1.30 (3.85) | 8 (10.4) | 0.58 (0.96) | 11 (14.3) | ||
| 8 weeks | 0.32 (0.66) | 30 (39.0) | 0.28 (0.64) | 37 (48.1) | ||
| 16 weeks | 0.20 (0.63) | 32 (41.6) | 0.43 (0.90) | 33 (42.9) | ||
| 24 weeksb | 0.19 (0.40) | 20 (48.8) | 0.06 (0.24) | 29 (63.0) | ||
| GP visits at home | ||||||
| Baseline | 0.02 (0.12) | 11 (14.3) | 0.02 (0.13) | 14 (18.2) | ||
| 8 weeks | 0.00 (0.00) | 32 (41.6) | 0.00 (0.00) | 37 (48.1) | ||
| 16 weeks | 0.00 (0.00) | 32 (41.6) | 0.02 (0.15) | 34 (44.2) | ||
| 24 weeks | 0.00 (0.00) | 20 (48.8) | 0.00 (0.00) | 29 (63.0) | ||
| Nurse visits at GP’s practice | ||||||
| Baseline | 0.21 (0.60) | 11 (14.3) | 0.16 (0.51) | 13 (16.9) | ||
| 8 weeks | 0.41 (0.58) | 31 (40.3) | 0.36 (0.67) | 38 (49.4) | ||
| 16 weeks | 0.13 (0.40) | 31 (40.3) | 0.29 (0.99) | 35 (45.5) | ||
| 24 weeks | 0.05 (0.22) | 20 (48.8) | 0.06 (0.25) | 30 (65.2) | ||
| Community nurse visits at home | ||||||
| Baseline | 0.06 (0.38) | 10 (13.0) | 0.05 (0.38) | 14 (18.2) | ||
| 8 weeks | 0.80 (4.20) | 32 (41.6) | 0.20 (0.60) | 36 (46.8) | ||
| 16 weeks | 0.20 (0.73) | 22 (28.6) | 0.30 (1.55) | 34 (44.2) | ||
| 24 weeks | 0.00 (0.00) | 20 (48.8) | 0.12 (0.49) | 29 (63.0) | ||
| Occupational therapist visits | ||||||
| Baseline | 0.55 (0.79) | 11 (14.3) | 0.25 (0.53) | 12 (15.6) | ||
| 8 weeks | 0.13 (0.34) | 32 (41.6) | 0.18 (0.51) | 38 (49.4) | ||
| 16 weeks | 0.13 (0.34) | 11 (14.3) | 0.00 (0.00) | 34 (44.2) | ||
| 24 weeks | 0.05 (0.22) | 20 (48.8) | 0.18 (0.33) | 29 (63.0) | ||
| Physiotherapist visits | ||||||
| Baseline | 1.06 (2.34) | 8 (10.4) | 0.82 (2.20) | 11 (14.3) | ||
| 8 weeks | 0.87 (1.43) | 33 (42.9) | 3.68 (2.44) | 37 (48.1) | ||
| 16 weeks | 0.89 (1.69) | 33 (42.9) | 2.32 (2.61) | 33 (42.9) | ||
| 24 weeks | 1.43 (3.23) | 20 (48.8) | 0.76 (1.71) | 29 (63.0) | ||
| Other health service visits | ||||||
| Baseline | 0.45 (0.97) | 13 (16.9) | 0.25 (0.53) | 13 (16.9) | ||
| 8 weeks | 0.27 (0.65) | 32 (41.6) | 0.18 (0.39) | 38 (49.4) | ||
| 16 weeks | 0.16 (0.57) | 34 (44.2) | 0.17 (0.66) | 35 (45.5) | ||
| 24 weeks | 0.14 (0.36) | 20 (48.8) | 0.12 (0.33) | 29 (63.0) | ||
| Inpatient nights in hospital | ||||||
| Baseline | 2.34 (4.21) | 7 (9.1) | 1.66 (1.46) | 13 (16.9) | ||
| 8 weeks | 2.61 (3.19) | 28 (36.4) | 2.12 (1.82) | 35 (45.5) | ||
| 16 weeks | 1.19 (2.11) | 30 (39.0) | 1.13 (1.44) | 31 (40.3) | ||
| 24 weeks | 0.86 (1.56) | 20 (48.8) | 0.78 (1.22) | 28 (60.9) | ||
| Day-case visits to hospital | ||||||
| Baseline | 0.22 (1.05) | 12 (15.6) | 0.08 (0.42) | 17 (22.1) | ||
| 8 weeks | 0.00 (0.00) | 30 (39.0) | 0.03 (0.16) | 39 (50.6) | ||
| 16 weeks | 0.12 (0.55) | 33 (42.9) | 0.12 (0.55) | 35 (45.5) | ||
| 24 weeks | 0.00 (0.00) | 21 (51.2) | 0.00 (0.00) | 30 (65.2) | ||
| Outpatient attendances | ||||||
| Baseline | 1.34 (2.22) | 10 (13.0) | 0.87 (1.10) | 17 (22.1) | ||
| 8 weeks | 1.06 (0.94) | 30 (39.0) | 0.74 (1.08) | 39 (50.6) | ||
| 16 weeks | 0.64 (0.85) | 30 (39.0) | 0.60 (0.66) | 34 (44.2) | ||
| 24 weeks | 0.57 (0.68) | 20 (48.8) | 0.24 (0.44) | 29 (63.0) | ||
| A&E visits | ||||||
| Baseline | 0.07 (0.36) | 10 (13.0) | 0.07 (0.31) | 17 (22.1) | ||
| 8 weeks | 0.04 (0.21) | 22 (28.6) | 0.05 (0.23) | 40 (51.9) | ||
| 16 weeks | 0.02 (0.15) | 22 (28.6) | 0.05 (0.21) | 34 (44.2) | ||
| 24 weeks | 0.05 (0.22) | 21 (51.2) | 0.00 (0.00) | 29 (63.0) | ||
| Physiotherapy hospital attendances | ||||||
| Baseline | 0.74 (2.73) | 27 (35.1) | 0.44 (1.17) | 15 (19.5) | ||
| 8 weeks | 0.93 (1.08) | 31 (40.3) | 3.21 (2.58) | 38 (49.4) | ||
| 16 weeks | 0.82 (1.67) | 32 (41.6) | 1.60 (2.13) | 35 (45.5) | ||
| 24 weeks | 1.00 (3.16) | 21 (51.2) | 0.41 (0.80) | 29 (63.0) | ||
| Number of patients who received RTW advice from:c | Occupational health (n) | Employer (n) | Occupational health (n) | Employer (n) | ||
| Baseline | 4 | 3 | 5 (6.49) | 7 | 5 | 6 (7.79) |
| 8 weeks | 2 | 2 | 2 (2.60) | 0 | 4 | 7 (9.09) |
| 16 weeks | 4 | 5 | 9 (11.7) | 1 | 2 | 8 (10.39) |
| 24 weeks | 2 | 2 | 6 (14.63) | 0 | 1 | 2 (4.35) |
The total average costs for each item of resource use based on all available cases (for participants’ joint replacements) are summarised in Table 8. Average costs based on all available cases (for ‘another reason’) and based on cases with complete data at 16 weeks can be found in Appendix 3. The key cost driver was inpatient hospital stay, in addition to, to a lesser extent, outpatient attendances, physiotherapy hospital attendances and (non-hospital) physiotherapist visits, although physiotherapist costs were lower for hip replacement patients than for knee replacement patients.
| Cost item | Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Hip replacement (N = 77) | Knee replacement (N = 77) | |||||||
| Baseline–8 weeks | 8–16 weeks | Baseline–8 weeks | 8–16 weeks | |||||
| Mean cost (SD) (£) | n | Mean cost (SD) (£) | n | Mean cost (SD) (£) | n | Mean cost (SD) (£) | n | |
| GP visits at GP’s practice | 11.94 (24.79) | 47 | 7.48 (23.4) | 45 | 10.29 (23.94) | 40 | 16.15 (33.64) | 44 |
| GP visits at home | 0.00 (0.00) | 45 | 0.00 (0.00) | 43 | 0.00 (0.00) | 40 | 2.18 (14.27) | 43 |
| Nurse visits at GP’s practice | 4.48 (6.30) | 46 | 1.42 (4.35) | 46 | 3.89 (7.25) | 39 | 3.10 (10.79) | 42 |
| Community nurse visits – home | 30.76 (161.41) | 45 | 7.69 (27.92) | 45 | 7.50 (23.10) | 41 | 11.63 (59.65) | 43 |
| Occupational therapist visits | 6.27 (16.16) | 45 | 6.13 (16.00) | 46 | 8.44 (23.80) | 39 | 0.00 (0.00) | 43 |
| Physiotherapist visits | 49.79 (82.41) | 46 | 50.75 (96.61) | 44 | 210.42 (139.88) | 40 | 132.73 (149.60) | 44 |
| Other health service visits | 19.76 (48.44) | 45 | 12.06 (42.57) | 43 | 13.30 (28.81) | 39 | 12.35 (48.88) | 42 |
| Inpatient nights in hospital | 1058.84 (1291.93) | 49 | 482.95 (856.26) | 47 | 858.92 (739.33) | 42 | 458.21 (583.39) | 46 |
| Day-case visits to hospital | 0.00 (0.00) | 47 | 0.00 (0.00) | 44 | 35.97 (221.74) | 38 | 162.73 (751.87) | 42 |
| Outpatient attendances | 154.80 (137.06) | 47 | 92.88 (122.97) | 47 | 107.22 (157.54) | 38 | 87.98 (96.00) | 43 |
| A&E visits | 7.13 (33.41) | 45 | 3.56 (23.90) | 45 | 8.67 (36.75) | 37 | 7.46 (34.16) | 43 |
| Physiotherapy hospital attendances | 51.33 (59.48) | 46 | 45.15 (91.65) | 45 | 175.99 (141.50) | 39 | 87.59 (116.99) | 42 |
| Occupational health RTW advice | 0.18 (0.87) | 48 | 0.39 (1.25) | 44 | 0.00 (0.00) | 36 | 0.10 (0.66) | 43 |
| Employer RTW advice | 0.16 (0.79) | 48 | 0.44 (1.25) | 44 | 0.43 (1.24) | 36 | 0.18 (0.83) | 43 |
| Total costs | 1425.45 (1494.00) | 41 | 806.08 (1122.92) | 32 | 1324.09 (874.30) | 26 | 1029.15 (1216.09) | 34 |
Health-related quality-of-life outcomes
Over 90% of participants completed the EQ-5D-5L questionnaires at baseline; this was similar for hip and knee replacement participants (see Appendix 3 for tabular summaries of the health-related quality-of-life outcome data). At the 8-week follow-up, 65% of hip and 55% of knee participants had completed the EQ-5D-5L, and there were similar proportions at 16 weeks (61% for hip and 58% for knee participants). The 24-week follow-up questionnaire was completed by 51% of hip and 39% of knee participants. Among those who had incomplete EQ-5D-5L questionnaires, the majority missed out all five responses, three participants had one missing response and one participant had three missing responses (see Appendix 3).
The proportion of both hip and knee participants who reported any level of problem (i.e. levels 2–5) reduced over time on all five dimensions, with the exception of anxiety/depression, which initially reduced at 8 weeks but then increased slightly by 16 weeks among knee participants (see Appendix 3). The most marked change occurred on the self-care dimension: the proportion of hip participants who reported any problems reduced from 85% at baseline to 23% at 16 weeks.
Utility scores were higher for knee participants than for hip participants for all time points, with the exception of the baseline (today) time point. There was an upwards trend over time for the utility scores, apart from a slight dip at 24 weeks for hip participants, with utility scores beginning at around 0.3 at baseline and increasing to > 0.7 by 24 weeks’ follow-up.
The mean baseline EQ VAS scores were 60.0 for hip and 61.6 for knee replacement participants. At 8 and 16 weeks, there was an increase in mean score (across both groups); however, there was a slight drop in the 24-week EQ VAS score for hip participants, which is consistent with the utility score findings.
Productivity loss
It was estimated that the mean cost per participant attributable to productivity loss over the 6-month period prior to surgery was £1602 (£1977 for hip and £936 for knee participants). Converting this to a weekly cost indicates a mean cost attributable to absenteeism of £62 (SD £102) per week [£76 (SD £125) for hip and £36 (SD £31) for knee replacement participants]. 145 For the period following surgery, a cost was attached to the number of days missed from work after the participant’s operation; the mean cost of missed workdays was estimated to be £7761 (SD £4367) per hip replacement participant and £8194 (SD £4286) per knee replacement participant. Overall, the mean cost was found to be £7983 (SD £4301) per participant, ranging between £797 and £21,508.
Survey of practice
Responses were received from a total of 152 participants from 59 different public and private health providers across England (n = 47), Wales (n = 1), Scotland (n = 10) and Northern Ireland (n = 1). These included 78 surgeons, 20 physiotherapists, 25 occupational therapists and 25 nurses/specialist nurses/extended-scope practitioners. A further four participants who labelled their role as ‘other’ were excluded from the analysis as their role within the HOT and input into the orthopaedic surgical pathway was unclear.
General responses
There was variation across the 59 different health-care organisations in the professionals who were responsible for delivering pre-assessment and preoperative education prior to surgery. Most of the interactions between health-care teams and patients took place either during the patient’s outpatient clinic appointment when they were listed for surgery or at pre-assessment/education appointments, which typically took place 2–5 weeks prior to surgery. Only 28 of the 78 (36%) surgeons surveyed reported that they saw their patients again before the day of surgery after they had been listed.
For patients who were in work and intended to return to work, only 20% (n = 30) of health-care professionals reported that these patients were identified as a specific subset in need of additional support and information during their care episode (see Appendix 3). In total, 62% (n = 92) reported that this patient group did not receive any additional RTW advice and support during their inpatient stay or after discharge. Overall, 131 participants (89%) stated that they were confident delivering RTW advice either all or some of the time. However, the majority of these respondents did not routinely offer RTW advice. Overall, 116 (78%) felt that an occupational advice intervention was needed.
Specific stakeholder responses
Orthopaedic surgeons (n = 78)
Surgeons reported that 96% (n = 75) of their patients received written information (leaflets/booklets) relating to their upcoming joint replacement. However, only 40% (n = 31) reported that these documents included information about returning to work. Eleven surgeons (14%) routinely identified patients in need of RTW advice when they listed them for surgery. However, only nine (12%) routinely offered advice either verbally or as written information. Surgeons were asked how they would respond if their patient asked them for advice about returning to work after surgery. The majority (n = 75, 96%) said that they would offer verbal advice based on their experience and the patient’s circumstances. Only six surgeons (8%) said that they would offer additional advice in the form of written materials based on local pathways (n = 2), referral to occupational therapy or occupational health teams (n = 3), or directing the patient to external resources, such as those available via the Royal College of Surgeons of England website (n = 1).
Physiotherapists (n = 20)
Of the 20 physiotherapist respondents, 14 assessed hip patients and 10 saw knee patients preoperatively. Four physiotherapists (20%) reported giving advice to patients returning to work after surgery as part of their routine practice, with a further nine (45%) willing to offer advice if requested. If asked to provide information, 19 (95%) said that they would offer verbal advice, supplemented by written information in two cases (10%) or referral to occupational therapy or occupation health teams in five cases (25%).
Occupational therapists (n = 25)
Of the occupational therapy respondents, 22 were involved in the preoperative assessment of hip replacement patients and 15 were involved in the preoperative assessment of knee replacement patients. Only six (24%) respondents offered routine advice about returning to work and 12 (48%) stated that they would give advice if asked. All respondents said that they would offer verbal advice. In two cases (8%), the therapists stated that they would also supplement the verbal advice with a referral to occupational health services. No one in the occupational therapy group offered written advice and information.
Nurses/specialist nurses/extended-scope practitioners (n = 25)
Nineteen of the 25 (76%) respondents were involved in the preoperative assessment and education of patients, and the remainder (24%) delivered inpatient care. Only 6 of the 19 (32%) respondents who saw patients preoperatively offered routine advice about returning to work. A further six (32%) stated that they would give advice if asked. If asked to provide advice, respondents reported that they provided verbal advice in all cases. Again, a small number of respondents stated that they would supplement their verbal advice with either written advice (n = 2, 8%) or referral to occupational therapy or occupational health services (n = 4, 16%).
Chapter 5 Intervention mapping stage 1: needs assessment – patient interviews
Introduction
The cohort analysis was supplemented by qualitative data from semistructured patient interviews to obtain information about shortcomings in current care, barriers preventing RTW, how these might be overcome and how to translate this into an occupational advice intervention.
Objectives
The patient interviews supported study objectives 1, 2, 4 and 5 (see Chapter 1, Objectives).
Methods
Sampling
From the cohort, a purposive sample of 45 patients who intended to return to work following surgery were interviewed at approximately 16 weeks post surgery. Patients were sampled to provide an equal proportion of participants having had hip or knee surgery, representing a range of work roles and employing organisations. Interviews were conducted by telephone. We had originally planned to interview a subgroup of patients not intending to return to work; however, these did not take place as only three participants met the criteria (the cohort study screening information is available at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/; accessed 2 May 2020).
A framework approach was used to design the semistructured interviews and analyse data. 147,148 This method is widely used in health research and is particularly recommended for use in multidisciplinary health research teams. As a range of stakeholder groups and patients were to be interviewed, this was an appropriate design. The theoretical framework reflected an essentialist/realist perspective, reporting on the experiences, meanings and reality of the participants, rather than examining the ways in which the broader social context impinges on those meanings. Interview schedules informed by initial piloting with service users were used (see Appendix 4).
Data analysis
The analysis procedure followed the seven stages proposed by Gale et al. :148 transcription, familiarisation with the interview, coding, developing a working analytical framework, applying the analytical framework, charting the data in the framework matrix and interpreting the data.
The patient interviews were conducted by Carol Coole and Fiona Nouri (both occupational therapists by background). Both interviewers were experienced in conducting qualitative research, and in relation to the topic of work and health. Interviews were conducted individually and by telephone. This was a pragmatic decision made in order to recruit the intended sample and conduct the interviews using the resources available.
All interviews were digitally recorded and transcribed verbatim, and NVivo 10 (QSR International, Warrington, UK) was used to manage the data, which were analysed thematically. Following familiarisation, the first few transcripts were independently coded by the researchers who conducted the interviews, who then compared, revised and agreed a set of codes and/or categories to form a working analytical framework. This framework was used to code the remaining transcripts. Summarised data were charted into a matrix to facilitate comparison of data across cases as well as codes and categories. Potential themes were identified independently by the interviewers, who discussed, revised and agreed the final themes.
Characteristics of patient participants
In total, 45 telephone interviews were conducted between 28 February 2017 and 21 July 2017 (mean duration 36 minutes). The mean age was 59.8 years (range 43–76 years), with 25 females and 20 males. Twenty interviewees were employed in the private sector, 16 were employed in the public sector, six were self-employed and three were in unpaid work/carers. Twenty-six patients had undergone hip replacement and 19 had undergone knee replacement. The occupations of the participants are provided in Appendix 4. Interviews were conducted across all four study sites (mean 12 per site, range 8–14 per site).
Results
Themes identified from the interview analysis
The following themes were identified relating to RTW after hip or knee replacement:
-
preoperative context
-
postoperative context
-
advice received
-
GP role and fit note
-
barriers to and facilitators of RTW
-
perceptions of an occupational advice intervention.
Patient interview analysis
Summaries of the analysis for each identified theme (see previous section) are described in the following sections. Direct quotations supporting these themes are provided in Appendix 4.
The preoperative context
Prior to surgery, patients reported that reduced mobility and pain affected commuting to work and general travel. Although many struggled with driving, none reported being advised not to drive.
Symptoms affected patients’ ability to carry out their usual job demands effectively and resulted in considerable discomfort by the end of the day. Pain also affected sleep quantity and quality, which had an impact on work.
Some workplaces had made adjustments prior to surgery and others had assisted with travel/parking or enabled working from home. In other cases, colleagues were the main source of support. Although medication alleviated some symptoms, it could result in sleepiness or concerns about addiction, leading to patients not taking the full dose.
For many, the decision to proceed to surgery was based on health professional recommendation following unsuccessful non-surgical treatment. Other patients were motivated by pain, work concerns, the impact on interests/hobbies, and quality of life, and were keen to schedule surgery to accommodate work demands, family commitments and hobbies. Many had not considered the recovery period prior to surgery, whereas others had carried out their own research or gained insights from family/friends.
The postoperative context
There were mixed experiences of the inpatient stay. Problems such as fit notes and medication not being available at discharge, or feeling under pressure to vacate the hospital bed, were reported. Some patients received physiotherapy postoperatively and others wanted more rehabilitation than they received. Some organised their own physiotherapy, or had it arranged via their occupational health providers. Others were content to continue with the exercise routine recommended by the hospital.
Many patients were positive about the prospect, or experience, of RTW. Some believed that they should not work for at least 6 weeks. Others intended to return more quickly. Others wanted to wait until fully fit, or expressed uncertainty about RTW owing to anxieties about their ability to cope with physical work demands, functional impairments (e.g. ability to kneel), fear of harming their new joint or lack of workplace adjustments. When interviewed, some had returned to work sooner than expected, including those who felt bored at home. For others, RTW took longer than expected. For some patients, their ability to return to work was dependent on their ability to drive to, and at, work. Public transport was not always practical or accessible. Patients who needed to drive for work worked from home while recovering, arranged lifts from colleagues or initially hired automatic vehicles.
Advice received
Pre-surgical advice focused mainly on surgery, the hospital stay and aftercare: it was provided in a variety of formats. Opportunities to share experiences and concerns in preoperative group education sessions were valued.
The majority of patients received advice on driving. Some described having to gain ‘permission’ from health professionals to resume driving. The duration before the patient was able to resume driving varied between 2 and 10 weeks. Whether or not the patient was considered safe to drive was based on various measures, including range of movement, general recovery, balance and insurance policy terms. In many cases, the decision was left with the patient as to when they felt sufficiently capable to brake or conduct an emergency stop. Some patients cited prescribed analgesia as having a major influence on return to driving, with some reducing the dose in order to feel ‘safe’.
Some patients reported being advised to avoid activities such as kneeling. Others were given no restrictions. Not everyone was offered physiotherapy and some were uncertain as to the amount and duration of exercise they should be doing postoperatively. Patients were advised on the duration that they were likely to be off work (e.g. 6, 8 or 12 weeks), depending on the type of work and whether or not their work included driving. Some had been advised that they might not return to their normal work rate until much later, and to consider graded returns. Several patients recalled having helpful discussions about work with clinicians, whereas others had received little advice or information.
Perceptions of the current services were generally positive. Patients found information booklets and education sessions helpful. A number had accessed online resources for additional information.
The general practitioner role and fit notes
From respondent accounts, the GP role was primarily restricted to identifying the need for surgery and referral to secondary care and some did not feel that the GP had a role postoperatively. Making appointments was difficult, and many felt that they did not have a personal relationship with their GP.
The GP had a role in pain management and analgesia, and, in some cases, referral for interventions such as rehabilitation. GPs were also active in referring patients for scans and other investigative procedures. This process was sometimes prompt, with GPs identifying the problem and referring almost immediately. However, in other cases, GPs referred to patients being ‘too young’ for joint replacement or that the cost of surgery was too prohibitive to refer. Some patients reported having to be proactive and forceful to be referred. There was little discussion reported between GPs and patients about patients’ work demands.
General practitioners became involved postoperatively mainly if there were complications. The majority of participants did not consult their GP post surgery other than to request fit notes. Most were discharged from hospital with a fit note covering the first few weeks of absence, with the expectation that the GP would provide subsequent notes. Those not issued a fit note on discharge, due to either an oversight or the patient ‘forgetting’ to request one, had to contact their GP promptly after discharge to obtain one. Most patients requested fit notes by telephone, to be collected at reception. Few saw their GP face to face to discuss their RTW. GPs appeared to be led by the patient as to the duration of absence required, and completed the fit note accordingly.
Most fit notes completed by the GP were ‘not-fit’ notes. The work modifications section was rarely utilised, and the note was usually completed for a phased return, the detail of which was rarely described. The self-employed and contract workers did not require a fit note so rarely had contact with the GP post surgery.
Barriers to and facilitators of return to work
Prior to surgery
Some patients made their employers aware of their joint problems prior to surgery. Others felt that there was little point until they were actually on the waiting list, particularly if their symptoms were not affecting work. Once listed, it was thought important to give notice to allow the employer to arrange cover. Employers were generally supportive, with some actively encouraging patients to undergo surgery. Many participants reported being given time off work by their employer for presurgical appointments but others used annual leave.
Following surgery
Once the patient was on sick leave, several employers regularly kept in touch with a view to assessing the patient’s readiness to return to work. In other instances, the employee took the initiative, giving regular reports on progress and arranging meetings to discuss their return. Company policy often required patients to meet with their line manager/occupational health prior to RTW, but on some occasions the meeting actually took place after the patient had returned. Several patients did not have any workplace contact until they had returned.
Job demands
The most difficult jobs to return to were those with a significant physical component, for example those involving kneeling, bending, climbing and/or health and safety risks. Some jobs were physically demanding but person-centred, involving lifting and handling, for example in a care setting or child care. Occupations that might appear to be less physically demanding still involved physical components; working in a post office, petrol station or bank could involve considerable moving and handling. Other patients reported issues around prolonged sitting or standing.
Many patients had jobs involving significant travel, either on foot or by car, which meant that they had to be fit to drive before returning to work. Those employed in family businesses found it easier to adapt job demands as other family members covered for them. The demands of shift working, including length of shifts or shift patterns, also affected work ability.
Patients on zero-hours contracts had less control over tasks but were more able to adjust work patterns. Those in small businesses might feel pressured to return to work quickly, including while using crutches. Even those with managerial roles had environmental hazards to negotiate, for example when accessing construction sites.
Line management
Many patients were positive about the RTW role played by their line manager. Most reported that managers were happy to allow them to decide what they could or could not do, and work accordingly. Some patients were managed by members of their family or had managers whom they considered friends, leading them to feel more supported than they might otherwise.
Some participants reported being reassured by their line manager that they did not need to rush their RTW and that they were willing to be flexible. Those with greater experience of managing employees with joint replacement were considered to be more understanding and supportive. Some assisted employees by offering them lifts to and from work. Only one patient reported problems with their line manager.
Policies and procedures
Some participants thought that company policies and procedures delayed RTW, for example having to be seen by an occupational health practitioner prior to return or being signed ‘fit for work’ by their GP, or having limited work modification opportunities.
Sick pay and sick leave
Sick pay could be a major factor in the timing of RTW, particularly when there were limited days of sick pay available before going on to statutory sick pay. In addition, there were concerns that lengthy periods of sick leave might have an impact on the individual’s sickness absence record. Many people balanced the decision to undergo surgery against the duration for which they could afford to be off work. Those working in the public sector were eligible for full pay for up to 6 months of absence. Other patients negotiated their sick leave with their employer, incorporating annual leave and public holidays in order to cope financially.
Colleagues
Many patients reported that their immediate work colleagues were supportive before and after surgery, facilitating their RTW. However, one patient whose job was initially modified but was able to cycle to work felt that his colleagues perceived him as ‘swinging the lead’. Others reported that colleagues were vigilant, not allowing them to do too much too quickly. Those whose colleagues were also members of their family or friends felt particularly supported financially and practically.
Work modifications
Some participants stated that their manager was flexible and supportive about RTW plans, allowing them to decide on modifications. Others reported that their employer suggested modifications, such as prescriptive phased returns, but these did not necessarily address the employee’s needs, resulting in them implementing their own work modifications.
Although many employers being amenable to employees adopting a phased return to ‘ease’ them back into the workplace, others did not offer this facility. Some patients had not yet returned to their previous level of work when interviews took place.
Occupational health
Several patients had access to workplace occupational health, particularly in the public sector, either in-house or contracted in. Opinion was sought on fitness to return to work, safety to drive, work modifications and, in some cases, a change of role. Occupational health referrals might also include referral to physiotherapy. Other organisations operated a self-referral policy, particularly for patients who had not triggered the sickness absence duration point for automatic referral.
Some patients reported receiving multiple occupational health assessments both while they were off work and on their return. Occupational health was often involved in identifying appropriate changes to the work environment and in conducting risk assessments. Some patients felt that the wait to see someone from occupational health delayed their RTW. Protracted communication between the various parties involved was also reported to cause delays.
Occupational health could be time-consuming and inappropriate, or patients felt that they would have benefited from an on-site assessment. Other patients were seen by occupational health only after they had returned to work, resulting in no initial RTW plan, or one devised by the employee themselves in conjunction with their line manager. Some felt that they would have benefited from greater occupational health involvement whereas several others felt that their RTW was managed by their line manager, making occupational health involvement unnecessary. Most felt reassured that they could request occupational health input at any time. However, some preferred not to involve occupational health.
Perceptions of an occupational advice intervention
Perceived need
Many patients thought that more occupational advice was needed. Others did not consider it personally necessary, either because they had received sufficient support from their employer or because they felt able to manage their own RTW.
Format
Although many patients were positive about using online resources, others did not use computers. Even those in computer-based occupations sometimes preferred printed formats to refer to easily and share. Some were unable or unwilling to read or process much written information, and thought that a more personal, verbal approach (i.e. group/individual, face to face/telephone) could provide opportunities to ask questions and seek clarification. There was support for enabling employers to access information about the operation and advice given, rather than relying on patient report. Participants thought that employers might have little experience of arthroplasty, postoperative limitations or how to modify work. However, there were concerns over privacy and patient choice regarding information shared with employers.
Content
Patients valued the inclusion of realistic recovery time scales and functional milestones post surgery to better manage expectations. There was support for work-related advice, such as graded returns, modified duties and fit notes. Some felt that there should be more opportunities to seek reassurance following surgery, and more advice on home exercises.
Delivery
Some respondents believed that the GP or surgeon should be the main informant regarding RTW. Others felt that physiotherapists were better suited, and that occupational health teams should be involved if available. They thought that the information should be delivered by someone knowledgeable in arthroplasty. Many patients would prefer to receive information prior to surgery to aid with decision-making and planning. Others believed that they would be best placed to use this information post surgery.
Chapter 6 Intervention mapping stage 1: needs assessment – stakeholder interviews
Introduction
The patient interviews were supplemented by qualitative data from semistructured stakeholder interviews. Employer, surgeon, GP, AHP and nurse interviews were conducted.
Objectives
The stakeholder interviews supported study objectives 2, 4 and 5 (see Chapter 1, Objectives).
Methods
Sampling
A sample of eight employers (the term ‘employers’ is used in the broadest sense, encompassing a range of individuals within the workplace, including managers, human resources staff, occupational health staff and colleagues) around each study site were recruited from organisations of differing sizes and sectors via local employer organisations and contacts. Eligible participants had experience of employees undergoing THR or TKR in the previous 12 months. Data were also collected from HOTs and local GPs. A sample of 12 orthopaedic surgeons, 12 AHPs and nurses and 12 GPs were interviewed across the sites to provide sufficient diversity of views and experiences. Interviews with these stakeholders were conducted by telephone, face to face or in small focus groups. Interview schedules informed by initial piloting with stakeholders were used (see Appendix 5).
A methodology and framework approach similar to that described in Chapter 5 was used.
Data analysis
The stakeholder interviews were conducted by Carol Coole, Fiona Nouri (occupational therapists by background) and Melanie Narayanasamy (social scientist by background). All interviewers were experienced in conducting qualitative research, and in relation to the topic of work and health. Interviewees were offered face-to-face or telephone interviews, either as a group or individually, according to preference. This was a pragmatic decision made in order to recruit the intended sample and conduct the interviews using the resources available.
Interview conduct
Twenty-five workplace representatives were interviewed, 15 by telephone and 10 face to face, between September 2016 and June 2017 (mean duration 36 minutes). Recruitment was extended outside the geographical catchment of the study sites. The characteristics of the participants are listed in Appendix 5.
Twelve interviews were conducted with AHPs and nurses: six by telephone and six face to face. The mean interview duration was 52 minutes. Characteristics of the AHP/nurse participants are listed in Appendix 5.
Twelve interviews were conducted with consultant orthopaedic surgeons (mean duration 51 minutes). One was interviewed by telephone and 11 were interviewed face to face, either in a group or individually. Characteristics of the surgeon participants are listed in Appendix 5.
Sixteen interviews, 10 by telephone and 6 face to face, were conducted with GPs (mean duration 36 minutes). Characteristics of the GP participants are listed in Appendix 5.
Results
Themes identified from the interview analysis
The following themes were identified relating to RTW after hip or knee replacement.
Workplace representatives (n = 25):
-
experiences of accommodating patients undergoing THR and TKR in the workplace
-
barriers to and facilitators of RTW
-
perceptions regarding an occupational advice intervention.
Clinicians [AHPs/nurses (n = 12), surgeons (n = 12) and GPs (n = 16)]:
-
decision to have surgery and expectations of recovery
-
advising patients about work and other activities
-
barriers to and facilitators of RTW
-
perceptions regarding an occupational advice intervention.
Workplace representative interview analysis
Summaries of the qualitative analysis are provided below. Direct quotations supporting the themes are provided in Appendix 5.
Experiences of accommodating patients undergoing total hip replacement and total knee replacement in the workplace
Some employers reported arranging work modifications for employees prior to surgery. Others would have considered this if advised by the GP rather than signing employees off sick. Employers reported that some employees managed their usual work up until surgery without accommodations, although they were not necessarily working at full capacity. Employers described how they accommodated employees’ RTW. Alternative tasks and/or work areas/locations were provided, in some cases on a permanent basis, which might require additional training. Phased returns, amended duties and adaptive equipment for manual tasks were organised when needed. Adjustments to office furniture might be made for those in mainly sedentary occupations, or reductions in workload might be used for those with more mentally demanding roles and responsibilities.
Some employers were able to extend cover for the employee if their RTW was delayed, or allowed the employee to return as supernumerary. Employees whose work was mainly computer based were often able to work from home, and accommodations also included travel and parking, and facilitating general mobility in the workplace. Some employees used accrued annual leave to facilitate phased returns. Not all employees had returned to work as anticipated, even with adjustments. This happened for a variety of reasons, including recovery taking longer than expected, postoperative complications (e.g. deep-vein thrombosis), and being listed for a second joint replacement and deciding not to RTW in the interim.
Barriers to and facilitators of return to work
Occupational health
Employers felt that organisations with on-site occupational health could be at an advantage in supporting RTW owing to a better understanding of the job demands. Occupational health might help reassure employers that they were acting according to best practice. However, there were concerns that occupational health practitioners might have insufficient knowledge of the employees’ work tasks and employees might perceive occupational health negatively and not know what support was available. In some workplaces, all employees undergoing THR/TKR would be referred to occupational health; in others, referral was at the manager’s discretion, and not necessarily before the employee had returned to work. Occupational health was reported as helpful by many, although not all valued every occupational health intervention, but felt it necessary if insufficient medical advice was received.
Some occupational health department staff felt under-resourced and there was a perception that surgeons and GPs were not sufficiently trained in this area.
General practitioners
Employers reported that support provided by GPs was extremely varied. They thought that the GP role was limited by time and expertise, and that there was a reliance on the patient for work information. Although fit notes were perceived by some to be of benefit, others felt that the information provided was of little help, particularly regarding work modifications. There were concerns that GPs might be overcautious, could raise an employee’s expectations inappropriately or might consider only the employee’s current job rather than potential alternatives.
Concerns were expressed by employers that patients might see the fit note as ‘gospel’, rather than advisory, although this was also true for employers, who might also be reluctant to act against fit note advice. Some wanted GP approval for modifications, whereas others reported paying less attention to fit note advice.
The employee
Employees’ personal characteristics were perceived to help or hinder RTW. Some were keen to return to work as soon as possible – in some cases too early – owing to loss of their usual routine, boredom and difficulty adapting to not being at work. Others were keen to return owing to the demands and responsibilities of work, or for reasons of finance or job security. Employees might delay surgery because of anxiety about the operation. Employers recognised that it was important to re-establish a work routine as early as possible, and that some employees might be anxious about returning to work.
Employers reported that employees in manual jobs might struggle to consider ‘lighter duties’, or be reluctant to return to tasks that they felt had caused their osteoarthritis. Employee motivation, compliance with rehabilitation and self-management were considered key factors in enabling RTW. Employers stated that some employees needed more active support in recovery. Proximity to retirement was also felt to be a factor, and linked to concerns that RTW might have an impact on the new joint.
The workplace
Participants believed that the size of an organisation could have an impact on employees’ RTW. For example, managers in smaller organisations might be less skilled in the process, have little access to support systems and less experience of surgery. However, even in larger organisations, line managers might not be aware of the support available from the organisation. Some larger organisations had on-site rehabilitation services, which they perceived could enable line managers to better understand RTWs, with rehabilitation continuing at work.
Employers perceived that smaller organisations might have fewer options for work adjustments and reorganisation of workload. Very large organisations might have set RTW procedures following arthroplasty, or might provide access to physiotherapy or rehabilitation. Office-based and non-manual work roles were seen as easier to return to, although some interviewees perceived that adjustments might also be required for office-based work.
Employers considered that larger organisations could cope more easily with lengthy sickness absence, and that employees in smaller organisations/teams might feel less comfortable about taking sick leave because of the demands on colleagues or the business. Employers perceived that some organisations might be less supportive than others, and some posts more difficult to provide cover for. Even within the same organisation, employers reported that sick pay arrangements, phased returns or access to health schemes might differ, and have an impact on RTW.
Surgery
Employers identified a range of factors related to surgery that could help or hinder RTW. These included postsurgical complications, ongoing symptoms and after-effects of surgery, such as stiffness, pain, swelling, low mood and fatigue. The impact that successive joint replacements had on sick leave was also a consideration, and perceptions of insufficient or delayed postoperative care and physiotherapy. NHS delays and cancellations could be a hindrance for some; however, others had not experienced any problems. For large organisations with highly structured RTW policies, the variation in expected duration of sickness absence between different surgeons and trusts was seen as a potential hindrance.
Perceptions regarding an occupational advice intervention
There was widespread support for an intervention for both employees and employers. Currently, employers were reliant on employee feedback; employers might not be aware of the information patients received.
Timing
Many considered that the intervention should be initiated prior to the decision to have surgery, to inform and reassure the patient and facilitate RTW planning with their employer. However, others would prefer to wait until after surgery as plans might have to change, for example due to complications.
Format
Some favoured paper-based, rather than verbal, advice. The information needed to be of appropriate size and easy to navigate, as some employees might struggle with large amounts to read. Digital-based information could make information more widely available to staff considering or undergoing joint replacement. Digital methods, such as apps, would not suit all employees, who might not have a mobile phone or computer. A format that could be shared with the employer and with the employee’s family was supported, and one that other stakeholders could access and contribute to was suggested. There was a view that some employers’ anxieties might be raised by too much information.
Having a standardised intervention was seen as beneficial, as current practice might vary between hospitals. A more individualised or personalised approach might be required because of different employee characteristics and circumstances.
Delivery
Some considered surgeons best placed to deliver the intervention; others considered the GP or rehabilitation professionals and/or someone who could review progress regularly best placed. Others perceived that the workplace should have a role in delivering the intervention, and facilitating workplace and health-care communication.
Content
Participants thought that advice should include the psychosocial impacts of RTW, such as feelings of isolation, fatigue, loss of identity and confidence, and anxiety. They said that it should guide employees on how best to access support from others in the workplace, including information on attendance reviews and organisational services available to employees.
Employers said that they would benefit from access to both generic and individually targeted advice on supporting RTW, including expected time frames for recovery, milestones and restrictions. This could include advice on home working, managing unexpected complications and employees with other health conditions, including instances of consecutive joint replacement.
The intervention could include guidance on how organisations recorded sickness absence following surgery and the impact this might have on an employee’s absence record and potential job prospects. Existing occupational advice information for other health conditions could be used to inform the intervention.
Measuring impact
Key outcome measures could include RTW itself and days of sickness absence, including prior to surgery. Whether or not the employee had returned to their usual work and whether or not work ability improved following their operation were also important. Reasons why the intervention had been successful or failed were felt to be important, including recording why RTW had not proceeded as planned. The different nature of the individuals’ work tasks should be accounted for, in addition to the effect of other individual characteristics, including general health, and their approach to recovery. Evaluation should reflect the perspectives of employees and employers regarding the intervention and RTW process, and the resource implications for the employer.
Clinician interview analysis
The decision to have surgery, and expectations of recovery
Clinicians generally considered that advising patients when to have surgery was complex and that outcomes were difficult to predict. Patients might delay surgery until they had retired or until their function had deteriorated. With increased knowledge, patients might make a more informed decision about surgery in relation to their work situation. Patients’ expectations varied, but were often high, especially among younger patients. Surgeons perceived their role as being to manage and, at times, intentionally lower these expectations. Employers might also overestimate the speed of recovery. Patients might simply expect relief from pain; others might expect to increase functional activity. It was important to clarify whether patients expected to be able to function as well as or better than they were prior to surgery.
Work issues could influence patients’ decisions, including pressure of work demands, concerns about sickness absence records or potential inability to return to their existing role. These factors also affected the advice surgeons gave; however, they were unable to guarantee patients’ postoperative work ability. Patients’ expectations and decisions to have surgery could also be influenced by their GP and the referral system, which might impede patients having surgery at an optimum time. Patients might be concerned about joint longevity, although some surgeons perceived these concerns to be unfounded. The timing of surgery in relation to patients’ work schedules was important, for example preferences for surgery during holidays or quieter periods. It was not always possible to offer this because of issues around breaching waiting lists.
General practitioners perceived that patients’ decisions regarding surgery were often influenced by their friends and family, either positively or negatively. For example, some patients might anticipate a longer recovery time than needed. The impact of surgery on work was believed to be a consideration for patients. Anticipated recovery time scales and time away from paid work might dissuade patients from surgery, particularly the self-employed. Others felt that patients were willing to wait until retirement rather than inconvenience their employer, and might tolerate a painful joint if only experienced at work. Staged referrals and effective triage could help mitigate expectations. More accurate information on recovery might encourage patients to have surgery earlier. However, there was a perception among GPs that surgery would be offered only to patients in considerable discomfort or over a certain age.
Most GPs considered their main role to be managing pain and referring patients to physiotherapy and secondary care, and did not consider the provision of occupational advice to be a main responsibility, other than issuing ‘sickness certificates’. Many were reluctant to ‘interfere with’ or ‘jeopardise’ the patient’s recovery. GPs rarely communicated with patients’ employers other than through fit notes. GPs were uncertain as to the advice that patients actually received from the hospital, and communication from the hospital regarding occupational factors was limited.
Advising patients about work and other activities
Perceptions of roles
Most interviewees had only a superficial understanding of the occupational advice provided by the HOT, even within their own centre. There was little awareness of fit note provision or of written occupational advice.
Return-to-work interventions were not generally considered the role of the orthopaedic team. The onus was on the patient regarding requesting occupational advice. Interviewees reasoned that patients were focused on the operation, or assumed that RTW was not a topic they wished to discuss. They also felt that it was difficult to individualise this advice.
The fit note was considered the realm of doctors rather than AHPs or nurses.
Some surgeons reported actively enquiring about patients’ occupations as part of the decision to operate; however, it was not a priority, and the time available in clinic limited opportunities to discuss work. Other members of the team were perceived to have a greater role. Patients were often discharged by the surgeon before they had returned to work. In this situation, the surgeon would not know when or how they returned to work. Routine follow-up past 6 weeks was often not thought necessary.
Differing management of total hip replacement/total knee replacement patients
Opportunities for patients to receive advice from AHPs and nurses varied. In some hospitals, separate preoperative group education classes were held for THR/TKR patients; in others, these were combined and involved different professions. Occupational therapy mainly entailed screening hip replacement patients preoperatively, and was not provided routinely for knee replacement patients, because they rarely needed adaptive equipment. Postoperative physiotherapy for knee patients was supported, particularly in groups. However, patients might be unable to access physiotherapy at the main hospital where they had surgery. Hip patients were unlikely to receive routine physiotherapy postoperatively.
Advice provided
The AHPs and nurses frequently referred to occupational management in terms of set time scales of when a patient might return to work, rather than how they might do this. In some cases, these time scales were trust policies and were seen to offer medicolegal protection to staff. Usually, staff would defer to the consultant concerning these time scales. Individual advice about work activity was provided on an ad hoc, informal basis. In some cases, advice on modified work was given.
Surgeons also referred to ‘blanket’ RTW time scales – often 6 or 12 weeks of sickness absence – usually coinciding with follow-up appointments and advice on returning to driving. These time scales appeared to be based on a combination of convenience, clinical reasoning and experience. Advice regarding work could be given verbally to patients, or communicated to other stakeholders by letter or fit note. Surgeons might advise patients whether or not they would be able to do their job following surgery, including considering changing their occupation owing to its physical demands, but rarely told patients that they should not do a particular job. Surgeons recognised the value of modifications and adjustments; however, their advice tended to focus on whether or not someone would eventually return to their job.
Most GPs would consider advising patients on work modifications; however, their confidence to do this was variable.
Communication with other stakeholders
Communication with other stakeholders about RTW was limited. Contact with employers was rare and usually initiated by an organisation’s occupational health provider. Patients were the main conduit of information for employers. Clinic/discharge letters to the GP rarely documented work issues.
Fit notes
Fit notes were issued to patients on request, often by a junior doctor on discharge. These were routinely ‘not fit’ notes for a duration of 6 weeks, although patients might be advised that they could return earlier if they wished to, and a longer period might be written on request. Occasionally, fit notes might be issued post discharge, but usually this was perceived to be the role of the GP. There was frustration among some GPs when hospital fit notes were not issued at all, or for a very short period. GPs were inclined to rely on the patients to guide fit note completion.
Advice about driving
Hospital staff frequently advised patients on return to driving and reported that this had an impact on their RTW. Advice on refraining from driving varied in time scale, but generally coincided with the follow-up appointment, and ‘permission’ to return to work was conflated by some patients and AHPs/nursing staff with advice on driving and follow-up. Some surgeons routinely advised all patients not to drive for 6 weeks, and others were more flexible. Surgeons felt unable to assess fitness to drive, or used proxy assessments. However, no one else was perceived by surgeons to have the ability to assess this either. There were concerns about litigation and it was considered easier to adhere to a set time scale.
Most GPs perceived that patients should not drive for approximately 4 weeks postoperatively. They assumed, or expected, that patients would have received advice on driving from the hospital. Patients were referred by GPs to the Driver and Vehicle Licensing Agency (DVLA) website for advice. GPs felt unable to make a decision on patients’ ability to drive, and instead relied on the patient, or another health-care professional, to make this judgement. GPs tended to assume that patients who drove for their job would cover this aspect of their RTW in discussions with their employer.
Barriers to and facilitators of return to work
Workplace
The AHPs and nurses believed employers to be generally supportive, but might not see the cost benefits of supporting an earlier RTW or understand the magnitude of the surgery. Some perceived that limited sick pay facilitated RTW. Patients with ‘flexible’ employers were more likely to return to work sooner than those who expected employees to return fully fit. They felt that sickness absence policies might be a barrier to earlier return.
Surgeons perceived that employers could be a barrier to RTW (e.g. using surgery as a reason to terminate employment, and through restrictive sick leave allowances and phased returns), particularly in the private sector. Employers’ concerns about health and safety law might have an impact on RTW forming part of the rehabilitation process. Therefore, they felt that employers might respond better to a ‘worst-case scenario’ rather than have their expectations raised by promises of an earlier RTW.
The GPs believed that some employers could be very accommodating, particularly if the individual was perceived to make a key contribution to the business. However, modifications were not necessarily easy for the employer, and some employers needed encouragement or additional information. Others were unable or unwilling to make adjustments. Where employers had already made interim staffing arrangements to cover the employee’s work, they might prefer to wait for the individual to return to full hours and duties. The quality of patients’ jobs and work environments was perceived to have an impact on their motivation to return to work. There was a view that larger organisations were not necessarily more accommodating. Generally, GPs felt that most employers facilitated RTW, although they were cautious about RTW for any patients undergoing surgery. RTW planning prior to surgery by the employer was seen as a potential facilitator.
Job demands
Clinicians considered that physically demanding jobs necessitated a longer recovery period. Analgesia might preclude some work tasks, but there was a risk that, by reducing their analgesia to facilitate RTW, patients might hinder their full recovery.
Occupational health
Clinicians believed that not all patients had access to occupational health services. Smaller organisations might be in greater need of an occupational advice intervention. However, occupational health providers might be outdated in their management of THR/TKR, and would not necessarily have an in-depth knowledge of the patient’s job. Occupational health providers might be risk-averse and extend sick leave unnecessarily.
General practitioners encouraged patients to involve occupational health to facilitate their RTW, although patients might be reluctant if they thought that their sickness absence might be scrutinised. Contact between patients and occupational health might be made only at the point of RTW. GPs believed that large organisations would have their own systems in place for managing RTW. In some cases, occupational health might request GP reports on patients’ ability to work, which GPs found difficult to comment on and they doubted the usefulness of their responses.
General practitioners
There was a view among orthopaedic clinicians that GPs might delay referral if they believed that patients were unlikely to be offered surgery because they were too young, or might refer too early owing to patient pressure. Some queried the extent to which GPs would actively use occupational advice with this patient group, and there was a perceived need to educate GPs about THR/TKR.
Patients
Patient characteristics could help or hinder recovery, including age, adherence to recovery advice, comorbidities, social circumstances, recovery beliefs and expectations, interpretation of pain and motivation to return to work. Those who were self-employed or receiving limited sick pay, or believed that they were needed at work, might be motivated to return earlier, and perhaps too early.
Surgery
Postoperative symptoms of pain, swelling and fatigue, and restrictions such as hip precautions or resulting from particular surgical approaches, could be a barrier to RTW. The timing of surgery could be a barrier for patients, for example during busy work periods. Some GPs reported that their local hospital had listed patients to fit around work demands.
Resources
All clinicians felt restricted by a lack of resources, particularly time and skill set. There was a perceived lack of rehabilitation and support postoperatively in the hospital and the community. The demarcation between primary and secondary care was not necessarily helpful for the patient. Triaged referral systems for surgery were perceived to be resource led, and the reasoning generally understood and supported, although they did not always work well owing to waiting lists for physiotherapy.
Perceptions regarding an occupational advice intervention
Perceived need
Hospital staff reported that only a small number of patients might need an intervention because they believed that most patients had retired. Some questioned what constituted ‘work’ (e.g. if work was unpaid or for only a few hours per week). Some AHPs/nurses believed that employed patients were unlikely to be working to their full capacity before the operation and, therefore, did not consider providing an occupational advice intervention necessary. Being over a certain age might automatically be conflated by GPs and hospital clinicians with not working. There was uncertainty about whether or not there would be a future increase in the proportion of patients in work. Some considered that current practice was meeting patients’ needs, or that only those in more physically demanding occupations would need an intervention. Providing occupational advice was not seen as a priority, and participants thought that sufficient RTW plans were usually in place. Providing an occupational advice intervention might require increased resources, and existing service-level agreements could limit the extent of support available from the hospital team.
Advising on work was considered difficult because of variation in patients and their jobs, and a belief that the NHS was unable to offer work rehabilitation. Increasingly, clinicians felt that they had less time to spend with individual patients. Some believed that patients were able to access RTW support through occupational health or already received sufficient occupational advice and support from the HOT. Others implied that providing occupational advice and support was ‘common sense’ or believed that most patients were able to return to work.
Several GPs thought that patients would benefit from further occupational advice, and others thought that current care was adequate.
Timing
Some participants believed that the intervention should start in primary care; however, the GP would not necessarily know whether or not the patient would be listed for surgery, or have a good understanding of THR/TKR. Some thought that it should start at listing for surgery or at the first clinic appointment. Others felt that this was too early as patients did not always focus at the consultation, and considered the pre-assessment period best. However, this would depend on the timing of the appointment. Others thought that the intervention could start much later in the process, or should vary according to the patient’s circumstances. GPs perceived that some patients might have difficulty in focusing past the operation itself. There was uncertainty as to how long the intervention should last, and whether or not every patient might need it.
Some suggested a postoperative element to the intervention, with the facility for one-to-one communication between patients and hospital staff.
Format
Patient age, literacy and access to online resources needed consideration. There might be a limit to what patients would retain in a group educational setting, although it provided an opportunity for interaction. Patients could be given a booklet to bring to appointments that other stakeholders could contribute to (e.g. similar to the personal child health record ‘red book’), but they might forget to bring it and stakeholders might not have time to complete it. The use of currently available ‘joint replacement’ helplines could be extended to include work issues. Some believed that an individualised approach was essential.
Online information was considered a useful option, preferably tailored to the local service. A format that patients could refer to easily, in which information was reinforced as necessary and accessible to all stakeholders, was important. Delivering an individually tailored intervention was considered difficult in practice, but potentially of value to the NHS and employers. Where possible, it would be helpful to communicate advice about individual patients, for example in clinic/discharge letters, and information about the patient’s occupation could be included in the referral from the GP to secondary care.
Content
Hospital clinicians suggested that the intervention includes advice for manual and non-manual work demands, phased returns and general examples of recovery. Individual cases could be used to illustrate examples. GPs suggested information about occupational health, complications, restrictions, signposting, advice lines, negotiating modifications with employers, medication and work, and symptom management. As patient recovery rates were variable, GPs felt that providing an individualised intervention would be difficult. However, information on expected general milestones would be useful to both the patient and the GP.
Delivery
Some believed that the intervention was best delivered by physiotherapists, occupational therapists or nurses. Others perceived that the intervention should be delivered by a member of staff with sufficient time, knowledge and skills, and who saw the patient regularly. Information booklets, provided by surgeons in the clinic, could also help deliver information and advice to patients. Most GPs thought that the intervention should be delivered through secondary care, but professional background was less important than the required time and skills. The reinforcement of messages was important.
Measuring the impact of the intervention
Measurement could include comparing preoperative and postoperative work status, the time frame for RTW, relapse, use of analgesia, whether or not expectations were being met, patients’ perception of their RTW and the extent to which the intervention was used. Some surgeons believed that a successful operation and discharge remained the most important outcome. The timing and circumstances surrounding data collection might have an impact on results. GPs considered qualitative assessment of the intervention and the numbers of patients returning to full, sustained work to be important.
Chapter 7 Intervention mapping stages 2 and 3: identification of intended outcomes and performance objectives, and selection of theory-based methods and practical strategies
Introduction
Intervention mapping stages 2 and 3 used the information from the needs assessment (IM stage 1) to develop provisional POs for the occupational advice intervention and to select theory-based methods and practical strategies to support their development.
Objectives
Intervention mapping stages 2 and 3 supported study objective 8 (see Chapter 1, Objectives).
Summary of what was learned from intervention mapping stage 1
Parts of this text have been reproduced with permission from Coole et al. 149 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Prior to commencing IM stages 2 and 3, the investigators summarised the key information developed from IM stage 1. This information was summarised based on the participants, interventions, comparisons, outcomes, study design (PICO) format to mirror the knowledge gaps discussed in Chapter 1. Illustrative examples covering the ‘key’ information are given below, and are referenced against the source of evidence from IM stage 1 (please note that this is not an exhaustive list). This information formed the basis for developing the first draft of the POs for the proposed intervention in IM stages 2 and 3.
Population: the return-to-work population
The need for a return-to-work intervention
-
A substantial proportion (up to 25%) of patients are in work prior to surgery, including some past state pension age (cohort).
-
A minority of patients have access to occupational health services and knowledge about employer sickness policies and sick pay is poor (cohort and interviews).
-
A considerable proportion of patients return to work by 16 weeks, to their usual job and/or with amended hours and/or duties (cohort).
-
Although a significant proportion of patients might benefit from an occupational advice intervention, ‘standard care’ is currently sufficient to enable the majority of patients to go back to work after surgery (cohort and interviews).
Characteristics of the return-to-work population
-
Many patients are in full-time employment, in physically demanding roles and often at work until the day before surgery (cohort).
-
Most patients need to drive, either to or at work (cohort).
-
Patients report and stakeholders perceive that patients/employees often have a strong motivation to undergo joint replacement to improve their quality of life, reduce pain and continue work (interviews).
-
Some patients are keen to return to work as soon as possible, sometimes too early (particularly the self-employed), and struggle to consider ‘lighter duties’ (interviews).
-
Only around half of patients are provided with a fit note and most are given by the patient’s GP. The majority of fit notes prescribe the patients as ‘not fit for work’ for 6 weeks (cohort).
Expectations of patients and health-care teams
-
Although some patients want to be fully fit before returning to work, others are happy to return on a phased or amended return while they continued to recover (interviews).
-
Patients expect to be off work for between 2 and 3 months after surgery (cohort).
-
Many do not want to inconvenience their employer (interviews).
-
There is an overall perception among clinicians that RTW is a realistic goal for the majority of patients undergoing joint replacement. However, expectations need to be managed carefully (interviews).
Perceived barriers to and facilitators of return to work
-
The motivation of the employee is a key factor in returning to work and compliance with rehabilitation and self-management of health (interviews).
-
Patients feel that their employment status and need to remain in employment are not fully taken into consideration in the surgical decision-making process (interviews).
-
Patients often do not consider the impact that surgery will have on their ability to work until they are listed for surgery (interviews).
-
Workplaces are generally able to accommodate patients’ needs for workplace adaptions and changes in working patterns. The majority of patients have some autonomy over how their work is planned (cohort and interviews).
-
Office-based and non-manual work roles are considered easier to return to. The use of analgesia might preclude some work tasks (interviews).
-
Employers’ concerns about health and safety and potential litigation might have an impact on RTW (interviews).
-
Return-to-work planning prior to surgery by the employer is seen as a potential facilitator of RTW (interviews).
-
Organisations with on-site occupational health services are seen as having an advantage in supporting employees’ RTW following surgery. However there are concerns that occupational health might take an outdated approach to recovery, might not have an in-depth knowledge of the patient’s job, or be risk-averse and extend sick leave unnecessarily (interviews).
-
Surgery itself can be a barrier to returning to work, including postoperative symptoms of pain, oedema, low mood and fatigue, and restrictions such as hip precautions (interviews).
-
Patients mainly identify the physical demands of the job, the availability of modifications and the support of managers and colleagues as influencing factors, whereas employers and clinicians also perceive that the characteristics of the individual patient can help or hinder their RTW (interviews).
Invervention: an occupational advice intervention
Perceived need
-
Widespread workplace support for an occupational advice intervention is available for use by employees and employers; however, patients and clinicians perceive that not all patients might need an intervention (interviews).
-
Currently, employers are reliant on employee feedback, and are not necessarily aware of the content of the information patients receive until the employee has returned to work. Having a standardised, approved intervention is seen as potentially beneficial (interviews).
-
Accurate information about expected recovery might encourage patients to have surgery earlier, and prompt patients to discuss the timing of surgery with their employer, which could benefit their future health and work prospects (interviews).
-
Health-care providers do not see providing occupational advice as a priority compared with addressing other patient needs. The intervention might require increased resources, and existing service-level agreements might limit the extent of support available from the HOT (interviews and survey).
-
An occupational advice intervention that (1) helps those who would have returned to work using standard care go back to work earlier, (2) improves rates of full, sustained RTW, or (3) helps those patients who would not have returned to work using standard care get back to work is desirable as this would produce overall benefits to the patient, employer and society (evidence synthesis and interviews).
-
Any intervention should complement rather than replace existing preoperative information. Most trusts have invested significant time and resources in creating patient resources, and the occupational advice intervention should sit alongside these (interviews and survey).
-
Delivering a tailored intervention for individual patients is considered difficult in practice, but potentially of value to the NHS and to employers (interviews).
Content and format
-
An individualised or personalised approach to the intervention might be required because of the differences in employee characteristics and circumstances (interviews).
-
Suggestions for the content of the intervention include information about occupational health, complications, restrictions, signposting, advice lines, symptom management and information on expected recovery milestones, as well as advice regarding sick notes, negotiating modifications, and medication and work. Advice should include the psychosocial impacts of returning to work, such as feelings of isolation, fatigue, loss of identity and confidence, and anxiety (interviews).
-
Generic components of previously developed RTW interventions include work simulation, work hardening and job simulation; contact with the employers; physical therapy and exercise; educational content; vocational counselling and guidance; and multidisciplinary team involvement (evidence synthesis).
-
A printed format for information materials is favoured by patients, health practitioners and employers. Many are positive about using digital resources; however, computer literacy does not mean that patients would prefer to receive their advice exclusively by this method (interviews).
-
Employers favour information in a paper format that other stakeholders can access and contribute to at different stages in the process of RTW, which would aid clarity and transparency of information (interviews).
Delivery and timing
-
Some patients might not be able or willing to process a great deal of written one-way information, and a more personal, verbal approach (i.e. group and individual, face to face and by telephone) has advantages in terms of opportunities for asking questions and for seeking clarification and explanation (interviews).
-
Some GPs suggest using a format similar to that used for new parents (i.e. the ‘red book’), which other stakeholders could use and contribute to (interviews).
-
Employers are keen to be recipients of the intervention. There is support for designing the intervention in such a way that the employers can see or be provided with information about the operation, and a copy of any generic and individual work-related advice, rather than relying only on the patient to report that information. Employers also suggest that the intervention includes information for employees as to how they can help themselves at different stages of the surgical pathway (interviews).
-
There are differing views regarding who should be delivering the intervention and the timing of the intervention (interviews).
-
Evidence indicates that health-care-based RTW rehabilitation is best delivered by multidisciplinary teams using a biopsychosocial approach and a tailored ‘stepped care’ model (evidence synthesis).
-
Current NHS resources, including access to postoperative physiotherapy, are seen as a barrier to the advice and support available to those returning to work, because clinicians and therapists have less time to spend with individual patients (interviews).
Comparator: advice currently provided to return-to-work patients
Current delivery of return-to-work advice
-
Patients currently receive a range of written advice and information in a variety of formats from secondary care prior to surgery. However, the advice received does not usually include information about RTW, and tends to focus on the needs of an older, retired population (interviews and survey).
-
The delivery of occupational advice is not generally seen as the role of, or a priority for, the orthopaedic team. There is a perceived dependence on doctors to guide the recovery process, and some of this responsibility could be delegated to other health-care professionals (interviews and survey).
-
Occupational advice is generally given ad hoc, verbally and at patient request (survey).
-
Most clinicians have only a superficial understanding of any occupational advice provided to patients through the HOT (interviews and survey).
-
Many hospital orthopaedic staff feel unable to provide advice about returning to work, and most AHPs take their lead from, or defer to, the surgeon (interviews and survey).
-
Surgeons feel that they lack the necessary knowledge of patients’ occupations, and the skills to give more than general advice (interviews).
-
Surgeons frequently refer to RTW advice in terms of ‘blanket’ time scales – often 6 or 12 weeks of sickness absence – which usually coincides with follow-up appointments and advice on returning to drive. These time scales appear mainly to be used for the sake of convenience, with some basis in clinical reasoning and experience (interviews and survey).
-
Surgeons’ advice tends to focus on whether or not someone would eventually return to their job, and how long they might be on sick leave, rather than rehabilitation ‘on the job’ through adjustments (interviews).
Structure of current NHS services
-
The structure of existing pre-admission and preoperative education programmes is extremely varied in terms of content, timing and the health-care team members delivering this information. Resources are at a premium; therefore, any occupational advice intervention should be embeddable within existing pathways without the need for significant service restructure. An occupational advice intervention therefore needs to be pragmatic and deliverable within current health-care settings (interviews and survey).
-
Most surgeons do not see their patients again after listing for surgery until the day of surgery and then only once after surgery, limiting the opportunities to discuss RTW issues (interviews and survey).
-
Communication with other stakeholders about patients’ RTW or other occupational matters is limited. Patients are the main conduit of information and advice for employers, which depends on how the patient interprets and communicates the advice given by the surgeon. Clinic/discharge letters to the GP rarely focus on work issues (interviews).
-
General practitioners see their main role as supporting (and not ‘interfering’ with) the medical treatment of the patient after surgery. They assume that the main responsibility for advising on work rests with the hospital team and/or physiotherapists, or with occupational health departments. GPs report that their role with patients is restricted by a lack of resources, particularly time, and their skill set. Employers perceived that GPs are variable in the support they provided in RTW, and are inclined to be overcautious (interviews).
-
The opportunity for patients to receive advice/information from AHPs and nurses varies between trusts. In some cases, separate preoperative group education classes are held for hip and knee patients; in others, these are combined (interviews and survey).
-
Occupational therapy is generally not routinely provided for knee replacement patients, particularly those aged < 60 years, because they rarely need adaptive equipment on discharge (interviews).
-
Postoperative physiotherapy for knee patients is favoured. Hip patients are unlikely to receive physiotherapy postoperatively as routine, although individual patients might be referred depending on need (interviews).
Outcome: measurement of return to work
How is return to work measured?
-
There is no standardised method of measuring RTW (evidence synthesis).
-
A variety of tools have previously been used to assess RTW after surgery or for musculoskeletal conditions. Generally, measures used in the literature fall in to one of the following categories: non-standardised return-to-work/-activities measures, standardised scales for return to work/usual activities, measures focusing on musculoskeletal symptoms, and quality-of-life, psychological and other measures. Number of days of sick leave is also commonly used. Patient-reported outcome measures tend to focus more broadly on activities of daily living (evidence synthesis).
-
Other potential measures might include retention/relapse following RTW, sickness absence prior to surgery, work ability/performance, use of analgesia and whether or not expectations of surgery/RTW are met (interviews and survey).
-
Regarding measuring the impact of the intervention, potential measures included qualitative assessment of the process and the extent to which any intervention was accessed and perceived to be useful (interviews).
Logic model of the problem
Having explored the issues relating to RTW for people undergoing hip or knee replacement based on the information from IM stage 1, the next step was defining the problem to be addressed by an intervention by creating logic models to better understand the problem.
Failing to return to work when fit to do some work, or returning to work too soon, which may impede full recovery, potentially increases the risk of patients not achieving sustained return to their usual/expected work following THR/TKR. The theory- and evidence-based factors causally related to these patient behaviours include patients’ knowledge and beliefs about the recovery process in relation to RTW, their attitudes to and expectations of RTW, matters related to financial/job security and their confidence in managing their recovery and RTW.
Following the ecological model (Figure 9), several environmental factors were identified that could either directly or indirectly influence these patient behaviours. For example, these included interpersonal factors, such as the influence of friends and family; interpersonal health-care factors, such as the influence and practice of primary care clinicians; organisational health-care factors, such as hospital resources and commissioning decisions; workplace factors, such as the availability of modified work; and societal factors, such as NHS policies regarding work and health outcome measurement. As the study had neither the remit nor the resources to address all of the factors identified, its main focus was on the interpersonal (health-care) factor of work-focused advice and support provided by HOTs. The theory- and evidence-based factors causally related to the behaviour of HOTs included their knowledge and skills in offering work-focused advice, attitudes and beliefs about roles and resources, and patient need.
FIGURE 9.
Ecological model illustrating the outcomes to be addressed by IM in this study (in pink). Adapted from Kok et al. 150 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/, which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. This figure includes minor additions and changes to the original.
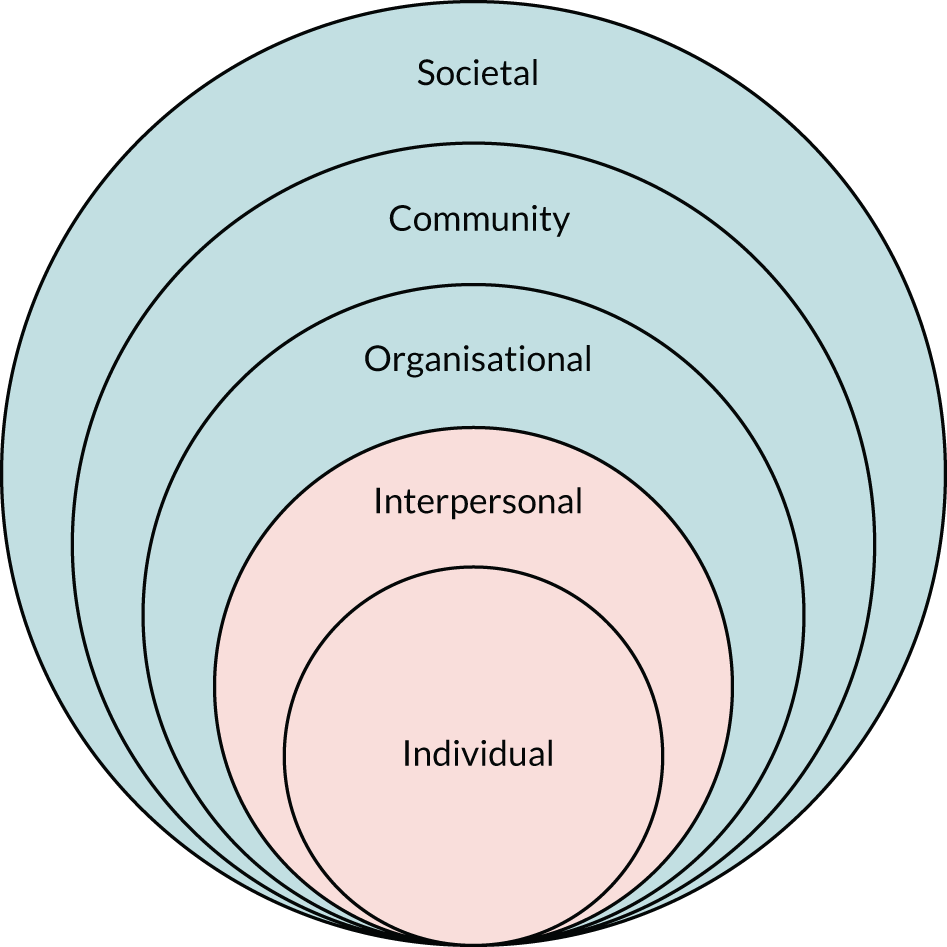
A logic model of the problem illustrates in detail the problem under investigation and the relationships and factors associated with it (Figure 10).
FIGURE 10.
Logic model of the problem. HCP, health-care professional. Reproduced with permission from Coole et al. 149 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
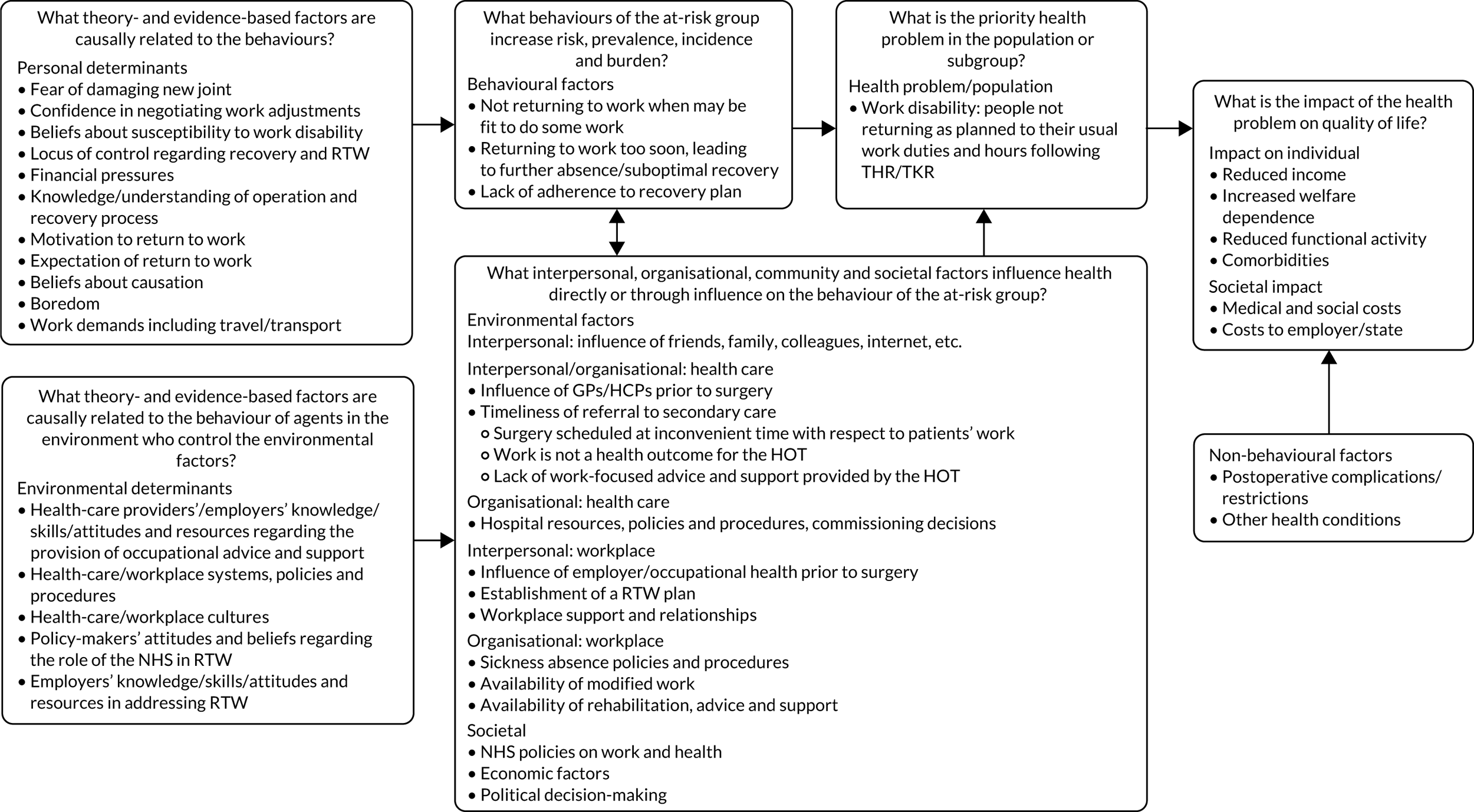
Intervention mapping stage 2
Stage 2 of the IM process involved the five elements described below.
The first element of stage 2 of the IM process involved stating the expected behavioural and environmental outcomes of the intervention. There were two:
-
The patient makes a safe and sustained return to usual work following surgery.
-
The HOT provides work-focused advice and support.
The second element of stage 2 was to specify the POs for patients and the members of the HOT. The needs assessment indicated that patients would benefit from occupational advice as early as possible in the hospital pathway, starting from the clinic appointment with the surgeon. It should also involve employers and continue post discharge. As well as containing generic information and advice, the intervention should also be individually targeted. A preliminary list of patient POs, and at what stage these might take place, was initially drawn up by Carol Coole, Fiona Nouri and Melanie Narayanasamy, then presented to/discussed/revised with Paul Baker, before it was circulated to the rest of the OPAL team for comment and further review (Table 9).
| Patient PO | Stage in pathway | Examples of unresolved questions |
|---|---|---|
| 1. Patient makes informed decision about surgery with respect to work | At/following first clinic appointment | How will this be done? Whose responsibility is it to enable this? What is the role of the GP/surgeon? |
| 2. Patient is provided with advice and information about recovery and RTW | Following first clinic appointment/listing | What information is important? How and when will the information be delivered? |
| 3. Patient provides employer with accurate information about their planned surgery and recovery | Prior to surgery | What information will the employers receive? How will this be delivered to employers? |
| 4. Patient completes RTW checklist detailing their work demands (with employer as required) | Prior to surgery | What information will be included in the checklist? When will it be completed? |
| 5. Patient identifies and prioritises potential barriers and solutions to a safe and appropriate RTW | Prior to surgery | How will patients do this? Will they do this with their employer? What skills to we need to equip them with to allow this to happen? |
| 6. Patient engages with hospital team, allowing preoperative development of a RTW plan | Prior to surgery | Which member of the hospital orthopaedic team and when will this happen? What training will be involved? |
| 7. Patient meets with their employer to discuss their recovery and provisional RTW plan | Prior to surgery | How long before surgery will this happen? Will it happen after the employer has received the information in PO3? |
| 8. ‘At-risk’ patient engages in a minimum of three preoperative follow-ups (telephone calls/meet-ups) with member of hospital staff to help develop a RTW plan and enable safe RTW | Prior to surgery | How do we identify ‘at-risk’ patients? Is it feasible to offer three preoperative appointments? What are the resource implications? Will patients be able to attend if they are continuing to work? |
| 9. Patient communicates with employer regarding surgical outcome and progress/recovery | Following surgery | How soon after surgery should they do this? How will the patient/employer get information about the postoperative recovery? |
| 10. Patient revises RTW plan following surgery as necessary with their employer and hospital staff | Following surgery | How will this happen (especially if patient is not routinely followed up/offered postoperative therapy)? |
| 11. ‘At-risk’ patient engages in a minimum of three postoperative follow-ups (telephone calls/meet-ups) with member of hospital staff to review progress with RTW plan | Following surgery | How do we identify ‘at-risk’ patients? Is it feasible to offer three preoperative appointments? What are the resource implications? |
| 12. Patient adheres to postoperative rehabilitation plan and advice | Following surgery | Can we monitor this? How do we ensure that it happens? |
| 13. Patient seeks help and support regarding RTW as required postoperatively | Following surgery | How do we facilitate this? What is the mechanism for support? |
For patients to change their behaviour, and thus achieve their POs, staff would also be required to change their behaviour. A preliminary list of staff POs and at what stage these might take place was therefore also drawn up by the OPAL investigators (Table 10). Drafting the POs for patients and staff led to a number of unresolved questions (see right-hand column of Tables 9 and 10). Uncertainty around these questions formed the basis of the initial draft questions put to the Delphi consensus group (see Chapter 8), with their responses allowing subsequent revision and refinement of each of the POs as the position around each was clarified.
| Staff PO | Stage in pathway | Examples of unresolved questions |
|---|---|---|
| 1. Staff screen patients who intend to return to work prior to meeting with surgeon | At first clinic appointment/listing | How will this be done? Which team member will be responsible? |
| 2. Surgeon asks patients about their usual work and expectations of RTW following surgery | At first clinic appointment/listing | How do we ensure that this is done? What tools can we develop to enable this process? |
| 3. Surgeon discusses pros and cons of surgery with patient, including time scales of surgery – in relation to patients’ usual work | At first clinic appointment/listing | Need to train and empower surgeons – how do we get them to engage? |
| 4. Surgeon considers patients’ work schedules when listing them for surgery | At listing | How do they get this information and is this possible? |
| 5. Staff screen patients to identify those who are perceived to be at risk of not making a safe and appropriate/expected RTW | At listing | How do we identify ‘at-risk’ patients and what tools could assist with this? |
| 6. Staff provide all patients with RTW advice manual and contact telephone number/e-mail address | At listing | What will the patient manual include? |
| 7. Staff provide patients with generic written information relating to surgery/RTW to give to their employer/colleagues | At listing | What will the employer manual include? |
| 8. Staff provide ‘at-risk’ patients with a RTW checklist to complete with their employer if necessary (i.e. if patient is unable to answer questions about availability of modified work) | At listing | How do we identify ‘at-risk’ patients and what tools could assist with this? What would the checklist include? |
9. Staff make a minimum of three preoperative follow-ups (telephone calls/meet-ups) with patients in the ‘at-risk’ group to:
|
Preoperative | Is this possible? What are the resource implications of three preoperative interactions? Will patients have time for this and be willing to engage with it? |
| 10. Staff routinely include the topic of RTW in group preoperative education and identify any ‘at-risk’ patients to . . . (as per PO9) | Preoperative | How do we signpost RTW patients to the preoperative education team? What information do they need to cover? |
| 11. Staff routinely ask patients at pre-assessment about RTW and identify any ‘at-risk’ patients to . . . (as per PO9) | Preoperative | How do we signpost RTW patients to the pre-assessment teams? What information do they need to cover? |
| 12. Surgeon liaises with treatment team regarding the patient’s postoperative recovery and how this may have an impact on the patient’s RTW | Postoperative prior to discharge | Will surgeons take an active interest? |
| 13. Staff complete a postoperative screening tool to identify ‘at-risk’ patients | Postoperative prior to discharge | When will this be done and who will do it? How do we identify ‘at-risk’ patients and what tools could assist with this? |
| 14. Staff advise on revision of the patient’s RTW plan as necessary following surgery | Postoperative | Which staff and when will this happen? |
| 15. Staff summarise patient’s expected RTW outcome and RTW plan in ward discharge letter | Postoperative | How will junior doctors on the ward find this information? What specific information will be sent to the GP? |
| 16. Staff give a copy of the ward discharge letter to the patient addressed to their employer to pass on if they wish to | Postoperative | Who will do this? Will patients be happy to share this information with their employers? |
| 17. Staff ask each patient whether or not they require a fit note on discharge | Postoperative prior to discharge | How can we make staff remember to do this? What prompts and tools might be needed? |
| 18. Staff complete fit notes in accordance with best-practice guidelines and hospital standard contract | Postoperative prior to discharge | How do we determine the duration of the fit note and what recommendations for work are included? |
| 19. Staff offer all RTW patients a minimum of three postoperative physiotherapy/rehabilitation appointments | Postoperative | Is this feasible? (Not routine care for all) |
| 20. Staff offer all ‘at-risk’ patients a minimum of six postoperative physiotherapy/rehabilitation appointments | Postoperative | Is this feasible? (Not routine care for all.) How do we identify ‘at-risk’ patients for this more intensive approach? |
| 21. Staff conduct a minimum of three follow-up telephone calls/meet-ups with ‘at-risk’ patients to review progress with RTW plan, support/signpost, liaise with employer as required | Postoperative | Is this feasible? (Not routine care for all.) How much staff time will be required? Are the resources available for this? |
| 22. Staff summarise and record patient’s RTW status/outcome in all outpatient clinic notes and following each appointment with therapists | Follow-up | When will they do this and where will they record the information so that it is visible? |
| 23. Staff discharge patient from the orthopaedic service when the patient has returned to work | Discharge | Some people may not return to work so this implies that they will remain under orthopaedics – for how long should orthopaedic teams offer follow-up for RTW issues? |
The third element of stage 2 was to select the determinants for the behavioural outcomes of both patients and hospital staff. Based on the literature, views and experiences of the investigators, and the findings of the needs assessment, the key determinants selected for both patients and hospital staff included:
-
knowledge and awareness
-
skills and self-efficacy
-
attitudes, beliefs and emotions
-
outcome expectations
-
perceived norms.
The fourth element of stage 2 was to specify the desired change objectives and to build matrices of change for every behaviour, target group and environmental agent that was required to be influenced. The change objectives were initially generated by Carol Coole, Fiona Nouri and Melanie Narayanasamy, then presented to/discussed/revised with Paul Baker, before they were circulated to the rest of the OPAL team for comment and further review. The choice of change methods was informed by IM texts,56,57 and the methods were reviewed and commented on by Christine Markham (in the USA), an international lead and trainer in IM. An example of the patient change objectives required to achieve a PO is shown in Table 11. A completed matrix for all patient change objectives linked to the final intervention patient POs can be found in Appendix 6. An example of the staff change objectives required to achieve a PO is shown in Table 12. A completed matrix for all staff change objectives in the final occupational advice intervention can be found in Appendix 6.
| PO | Determinants | ||||
|---|---|---|---|---|---|
| Knowledge and awareness | Skills and self-efficacy | Attitudes, beliefs and emotions | Outcome expectations | Perceived norms | |
| Patient makes informed decision about surgery with respect to their work |
Appraises the general risks/benefits of surgery and RTW rates Appraises the likely impact of surgery on their ability to do their job States that they have received sufficient information about surgery |
Expresses confidence in ability to make informed decision about surgery Demonstrates ability to process information about surgical procedure and make an informed choice |
Expresses willingness to take responsibility for the surgical decision Demonstrates appropriate response with regard to their decision |
Describes a realistic expectation of outcome following surgery |
Perceives that it is usual for patients to make an informed decision about surgery with respect to work Recognises that nowadays patients are encouraged to take an active part in their care Recognises that RTW is now considered a health outcome |
| PO | Determinants | ||||
|---|---|---|---|---|---|
| Knowledge and awareness | Skills and self-efficacy | Attitudes, beliefs and emotions | Outcome expectations | Perceived norms | |
| Staff screen patients who intend to return to work prior to meeting with surgeon using occupational checklist | Team members describe process of asking RTW patients to complete checklist and giving it to surgeon | Team members express confidence in ability to ask RTW patients to complete checklist and giving it to surgeon | Team members state that asking RTW patients to complete occupational checklist will help patient and surgeon make a more informed decision about surgery with regard to RTW | Team members recognise that preparing the patient and surgeon to discuss the patient’s RTW will aid their RTW | Team members perceived that preparing the patient and surgeon to discuss the patient’s RTW is usual practice |
The fifth and final element of stage 2 was to create a logic model of change to illustrate the proposed causal relations between theory- and evidence-based change methods, the determinants they are expected to influence, and behavioural and environmental outcomes that will address the health problem (Figure 11).
FIGURE 11.
Logic model of change (i.e. what needs to change in order to address the problem). Reproduced with permission from Coole et al. 149 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
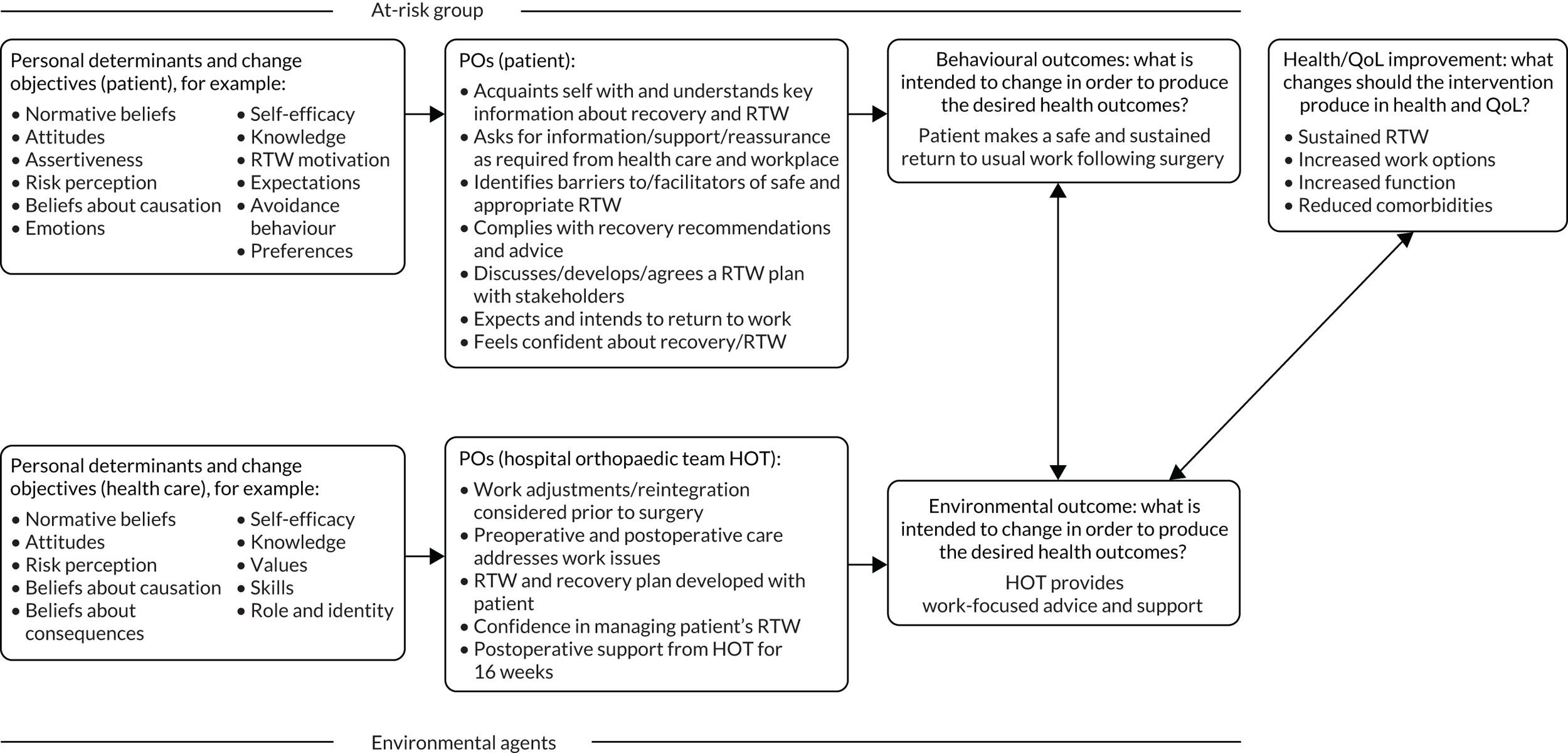
Intervention mapping stage 3
Stage 3 involved consolidation of ideas about the components, scope and sequence of the intervention. Change objectives organised by determinants in the matrices were reviewed (see Appendix 6). Theory- and evidence-based methods to influence the determinants in the desired direction were then identified. The parameters for each method were considered and the methods were translated into practical applications that matched the target group (patients). An example is shown in Table 13. A table showing the complete methods and applications for the patient group is provided in Appendix 6.
| Determinant: knowledge and awareness | ||||
|---|---|---|---|---|
| Change objective | Methods | Definition | Parameters | Application |
| 5. Patient identifies and prioritises potential barriers and solutions to a safe and appropriate RTW |
Modelling (social cognitive theory) Variety of media/elaboration (theory of information processing) |
Providing an appropriate model Stimulating the learner to add meaning to the information that is processed |
Identification with the model – receives positive reinforcement, coping vs. mastery model Messages that are personally relevant |
Examples of other patient barriers and solutions and RTW plans included in workbook/on website and at preoperative presentations given by staff Discussions with return-to-work co-ordinator and preoperative education and assessment team |
The parameters for each method were considered and the methods translated into practical applications that matched the target group (staff). An example is shown in Table 14. A table showing the complete methods and applications for the staff group is provided in Appendix 6.
| Determinant: knowledge and awareness | ||||
|---|---|---|---|---|
| Change objective | Methods | Definition | Parameters | Application |
2. Members of the outpatient clinic team know the process of identifying RTW patients before their appointment with a surgeon:
|
Discussion (elaboration likelihood model) Providing cues (theories of information processing) Individualisation/tailoring (transtheoretical model) |
Encouraging consideration of topic in open formal debate Ensuring that the same cues are present at the time of learning and time of retrieval Matching to participant characteristics |
Listening to the learner to ensure that the correct schemas are activated Work best when people select and provide own cues Tailoring to participant, relevant to learner’s needs |
Each member of the team has their own study pack containing this information Study pack uses chunking, advance organisers and imagery methods to aid learning Staff to suggest cues to action (e.g. posters/photos on ward/in clinic) Tailored staff training |
The methods, parameters and applications for both staff and patients were initially generated by Carol Coole, Fiona Nouri and Melanie Narayanasamy, then presented to/discussed/revised with Paul Baker, before they were circulated to the rest of the OPAL team for comment and review. The choice of methods and parameters was informed by IM texts,56,57 and they were also reviewed and commented on by Christine Markham.
Chapter 8 Intervention mapping stage 4: development of components and materials for the occupational advice intervention using a modified Delphi consensus process
Introduction
Intervention mapping stage 4 used a multistakeholder intervention development group to help address the areas of uncertainty around the preliminary patient and staff POs and potential intervention components identified in Chapter 7. The group’s remit was to help reach agreement about the content, delivery, format and timing of the proposed occupational advice intervention. A modified Delphi consensus process was used to facilitate this process.
Objectives
The Delphi consensus process supported study objectives 7 and 8 (see Chapter 1, Objectives).
Methods
During IM stages 1–3, potential POs and intervention components emerged within the IM development framework. However, there was considerable uncertainty related to these objectives, as described in Tables 9 and 10. These areas of uncertainty were used to create statements relating to the intervention that were explored using a modified Delphi consensus process. The Delphi process generated information about the level of agreement relating to these statements, which was subsequently used to refine the intervention.
Stakeholder recruitment
Five stakeholder groups were identified for inclusion in the modified Delphi process, mirroring the groups involved in IM stage 1. The sampling strategy for each stakeholder group is outlined in Table 1, with participants chosen to maximise patient, public and professional engagement. Participants were nationally sampled from across England and Scotland (see Appendix 7, Table 67). To ensure the validity of the consensus process, a minimum of five individuals from each stakeholder group were recruited. A maximum limit of 15 individuals from any given stakeholder group was chosen to ensure that one group’s opinions did not overwhelm the opinions of others in the consensus process. In total, 66 participants were invited to participate in round 1 of the Delphi process (see Appendix 7).
Statement development
Statements relating to the proposed content, format, delivery, timing and measurement of the occupational advice intervention were developed within the OPAL investigator group. Owing to the breadth of statements and their inter-related nature, a step-wise approach to the presentation of individual statements to the Delphi group was adopted.
Round 1 focused on defining the content of the intervention in two sections. Section 1 focused on the content (‘written’ advice and information) and section 2 focused on activities to deliver content (actions or processes for patients, employers and health-care members to undertake). These statements were piloted by two surgeons, two GPs and three patients prior to distribution to the Delphi panel.
The information from round 1 was then used to refine the statements for round 2, which focused on defining the format, delivery, timing and measurement of the content examined in round 1. The statements for round 2 were grouped under headings in order to enable the Delphi panel to explore different approaches to these specific areas. Round 3 was then used to clarify any areas of residual uncertainty from rounds 1 and 2 and to present the draft occupational advice intervention back to the Delphi participants for comment.
Definition of agreement
Participants were asked to rate individual statements in the Delphi questionnaire, with possible options being strongly agree, agree, disagree, strongly disagree and don’t know. Participants were asked to rate the importance of the content or action given in the statement. For a subset of statements in round 1, participants were also asked to rate the deliverability of the content or action alongside current health-care provision. This was done to assess whether or not the stakeholders felt that certain actions, despite being important, were achievable owing to their experience of current service delivery, funding and logistics. Therefore, for this subset of statements, the participants were asked to provide two ratings: one for ‘importance’ and one for ‘deliverability’.
At the end of each section, participants were also able to insert comments in a free-text box or provide additional suggestions relating to the intervention that could be evaluated in subsequent rounds. In rounds in which statements from a previous Delphi round were being re-presented, these were presented alongside controlled feedback, with modal round 1 rating for these statements; the proportion of each response option selected by the other participants; and a reminder of the participant’s own previous ratings.
Delivery of the Delphi survey
The Delphi survey was delivered via e-mail using an online web-based survey platform (SurveyMonkey). Round 1 was delivered between 25 September 2017 and 13 October 2017, round 2 between 22 November 2017 and 13 December 2017 and round 3 between 1 June 2018 and 22 June 2018. The OPAL Delphi questionnaires are available at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/ (accessed 2 May 2020). The survey included a covering e-mail to the participants and an electronic link to the questionnaires. This e-mail informed the participants of the details of each round and provided instructions on completing the survey. Round 1 and 2 questionnaires required respondents to provide their initials and occupation to assist the investigators in identifying respondents. Round 3 e-mails included four documents from the developed occupational advice intervention (a summary of the intervention, an occupational checklist, a patient ‘return-to-work’ workbook and an employer booklet) for participants to review and comment on. A minimum of two reminders were sent to non-responders during the final week of the surveys.
Analysis of data
An a priori consensus level of 70% (strongly agree/agree or strongly disagree/disagree) across all stakeholder groups combined was set. 151 For statements that failed to reach consensus across the overall group, further analysis was undertaken based on responses for each of the five stakeholder subgroups. The following rules were then employed to determine which statements were discarded and which were re-presented in the next round:
-
if no or only one stakeholder group reached concordant consensus (≥ 70% agreement or disagreement), then the statement was withdrawn
-
if two or more stakeholder groups reached concordant consensus (≥ 70% agreement or disagreement), then the statement was re-presented in the next round
-
in the situation in which one or more stakeholder group reached ‘agreement’ and another group reached ‘disagreement’, the statement was discussed among the investigators and a decision on inclusion/exclusion of the statement was made.
As stated previously, a subgroup of round 1 statements were rated for their deliverability in addition to their perceived importance. For these statements, consensus was reached if the 70% threshold was achieved for both the importance rating and the deliverability rating. Statements that reached consensus for one of the domains were analysed by stakeholder grouping as described above.
Round 1 statements relating to the content of the intervention were ranked according to the level of agreement to enable the investigators to determine which items of content were the most important to include in the intervention.
In round 3, the intervention documents created based on the results of the first two rounds were presented and descriptive open feedback from participants was recorded.
Results
The OPAL Delphi consensus process is summarised in Figure 12.
FIGURE 12.
Summary of the Delphi consensus process. Reproduced with permission from Baker et al. 74 This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/.4.0/. This figure includes minor additions and formatting changes to the original.
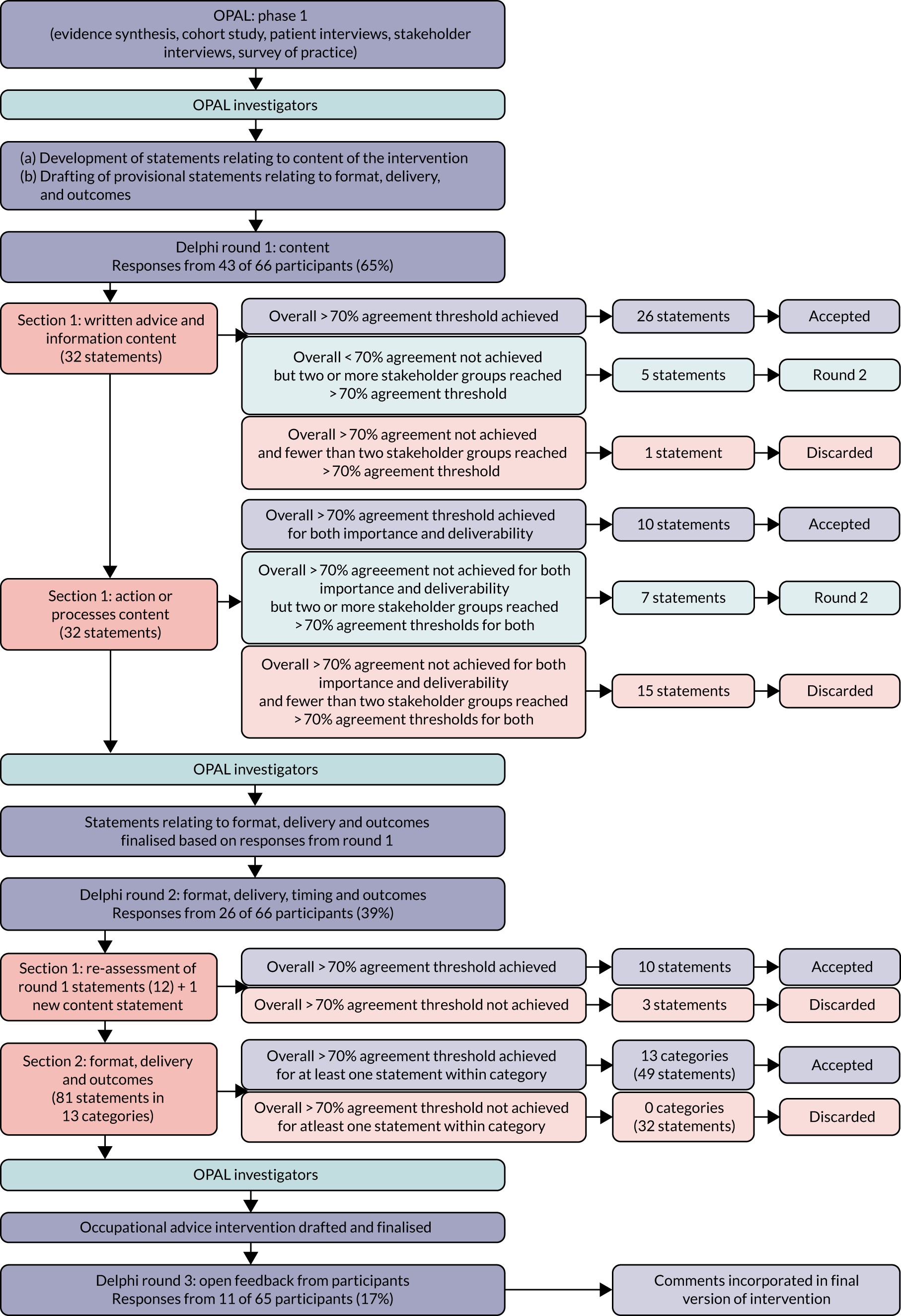
Round 1
Responses were received from 43 of the 66 invited participants (65%), comprising 14 patients, 8 surgeons, 6 GPs, 11 AHPs and nurses, and 4 employers. In section 1 (‘written’ advice and information), consensus was reached for 26 of 32 statements (81%). Of the remaining six statements, five reached consensus for two or more stakeholder groups and were therefore taken forward to round 2, and one statement was discarded. A full summary of all round 1, section 1, responses and analysis is reported in Appendix 7. The top 10 ‘section 1’ statements reaching consensus, ranked based on the level of agreement (percentage who responded strongly agree or agree), are listed below.
Question: is it important that an occupational advice intervention commenced prior to hip or knee replacement includes the following (percentage strongly agree or agree)?
-
information about exercises and rehabilitation following surgery (100%)
-
information about returning to driving (100%)
-
a broad overview written for all stakeholders, of what to expect following surgery (rates and timing of expected recovery) (98%)
-
information about managing pain, types of analgesia and side effects (98%)
-
information about postoperative precautions, restrictions and activities to avoid following surgery (95%)
-
information about symptom management in relation to RTW and specific occupations (e.g. expected levels of fatigue, pain and swelling) (95%)
-
tips and tricks to help the patient manage around their home with day-to-day activities immediately following surgery (95%)
-
information regarding postoperative complications and their management (95%)
-
signposting to DVLA guidance (95%)
-
information for the patient about who to ask if they are having a problem with returning to work (93%).
In section 2 (actions or processes for patients, employers and health-care staff to undertake), participants were asked to rate both the importance and the deliverability of each statement. Of the 32 components presented, 10 (31%) reached consensus for both importance and deliverability. Of the remaining 22 statements, 14 reached consensus for importance but not deliverability, two reached consensus for deliverability but not importance and six did not reach consensus for either. Of these statements, seven reached consensus for both importance and deliverability for two or more stakeholder groups and were therefore taken forward to round 2, and 15 statements were discarded. A full summary of all round 1, section 2, responses and analysis is reported in Appendix 7. The top 10 ‘section 2’ statements reaching consensus, ranked based on the level of agreement (percentage who responded very important or important), are listed below.
Question: how important/deliverable do you believe the following components are if an occupational advice intervention commencing prior to hip or knee replacement was to be developed (percentage who strongly agree or agree with the importance and deliverability of the statement)?
-
a postoperative mechanism for the identification of patients who are not progressing towards RTW as planned (important 95%, deliverable 71%)
-
guidance for health services defining ‘best practice’ for patients returning to work after hip or knee replacement surgery (important 93%, deliverable 82%)
-
training for members of the hospital orthopaedic care team to increase awareness about RTW issues (important 88%, deliverable 82%)
-
interaction between the health-care team and the patient by telephone, e-mail or ‘online’ so that members of the care team can monitor progress and help the patient use the advice and information provided (important 88%, deliverable 70%)
-
guidance on when in the RTW process patients can safely be discharged back to primary care for continued management of their RTW (important 86%, deliverable 80%)
-
a mechanism for preoperative identification of patients at ‘high risk’ of prolonged sickness absence following surgery (important 86%, deliverable 74%)
-
routine preoperative therapy assessment during which a RTW plan is developed between the patients and the hospital orthopaedic care team (important 84%, deliverable 80%)
-
a separate intervention for hip and knee replacement patients who are not progressing towards RTW as planned (important 84%, deliverable 79%)
-
a process by which work status can be included in referral information for all patients referred from primary care into secondary care for consideration of hip or knee replacement (important 79%, deliverable 79%)
-
information from patients who have experienced the process of returning to work after hip or knee replacement within the preoperative education process (important 76%, deliverable 73%).
Round 2
Responses were received from 26 of the 66 participants (39%), comprising eight patients, seven surgeons, three GPs, six AHPs and nurses, and two employers.
The 12 questions (five from section 1 and seven from section 2) carried forward from round 1 plus one additional question generated from the free-text comments (see Appendix 7) were presented to participants. In round 2, participants were asked to rate only the importance of these statements, having been made aware of the responses from round 1 and the overall group’s position regarding the deliverability of the component if applicable. Of the 13 statements, 10 reached the threshold for consensus (see Appendix 7).
Based on the responses to round 1, a further 81 statements grouped into 13 categories were generated. These statements related to the format, delivery, timing and measurement of the agreed content components from round 1. Each category included three to nine statements relating to a common category theme (see OPAL Survey questionnaires at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/; accessed 2 May 2020). This allowed the participants to compare different options presented within the category in the context of the other available options and reach a position on each statement accordingly. This allowed the investigators to explore different approaches to a given problem. For example, the first category asked participants to rate a set of five statements relating to which health-care team member should have responsibility for delivery and co-ordination of the occupational advice intervention. If at least one statement in a given category reached consensus, this was taken as representative of the Delphi group’s position relating to the given category and the remaining statements were discarded.
Overall, 49 statements (60%) reached consensus (44 agreement and 5 disagreement). At least one statement in every category reached consensus (see Appendix 7).
The 13 categories presented to participants and a summary of the responses are listed below:
-
Responsibility for delivery and co-ordination of the RTW intervention. Participants agreed that the orthopaedic surgeons should not be responsible for delivering and co-ordinating the RTW intervention (88% agreement). Surgeons and patients agreed (both > 70% agreement) that the intervention should be co-ordinated by primary care teams. However, GPs felt that the intervention should be co-ordinated in secondary care by a nominated member of the orthopaedic team (100% agreement).
-
Preoperative identification of patients at ‘higher risk’ of prolonged sickness absence following surgery who may require additional individualised help and support. There was agreement (80%) for a face-to-face assessment with a staff member trained in the RTW intervention to help identify patients at ‘higher risk’ of prolonged sickness absence following surgery. No agreement was reached on other forms of assessment, including written, telephone, patient’s self-referral and surgeon assessment.
-
Preoperative assessment. Participants felt that a greater level of involvement from the therapy team would be beneficial irrespective of whether or not the patient was deemed to be at ‘high risk’ of an extended period of sickness absence after surgery (80–88% agreement). They also felt that development of a RTW plan prior to surgery (80% agreement), discussion with employer (100% agreement) and routine inclusion of RTW information in pre-assessment/education classes (88% agreement) were important.
-
Postoperative identification of patients at risk of an extended period off work after surgery. There was overall agreement for additional monitoring for RTW patients after surgery, including routine physiotherapy (84% agreement), closer contact with the therapy team (92% agreement) and access to telephone support (92% agreement). Participants also felt that patients should meet with their employer after surgery to discuss their recovery and plan for RTW (72% agreement).
-
Additional care for patients identified as being at ‘higher risk’ of an extended period off work after surgery. Participants agreed that ‘high-risk’ patients should receive additional physiotherapy (92% agreement) and occupational therapy (76% agreement) input and that this should continue until RTW had been achieved (76% agreement). This could be supplemented by additional information (92% agreement) and referral to the Fit4Work (Leeds, UK) service (84% agreement).
-
Scope of training for staff. The group felt that all members of the HOT involved in the treatment of hip and knee replacement patients should receive training regarding the intervention (76% agreement) and that training should also be offered to local GP groups (72% agreement).
-
Communicating occupational status and progress between stakeholders. There was widespread agreement for statements relating to improved communication between stakeholders through greater information in referral, clinic, discharge and therapy service letters (84–96% agreement). Participants agreed that greater information sharing between primary and secondary care and employers would be beneficial (84–96% agreement). However, there was also a feeling that it was the patient’s and not the health-care team’s responsibility to communicate with their employer about their RTW (76% agreement).
-
Fit notes. Every patient should be offered a fit note (96% agreement) and it should be completed in accordance with Department for Work and Pensions Fit Note Guidance152 (96% agreement). Participants felt that providing short-duration fit notes (2 weeks) to discourage extended periods off work was wrong (72% agreement) but that GPs should be responsible for administering subsequent fit notes after the initial fit note given on discharge (76% agreement).
-
Format and delivery of patient information. Written materials were favoured (76% agreement), although participants felt that only the most ‘important’ information (based on round 1 ranking) needed to be included, with additional information made available through other sources (e.g. website) (80% agreement). It was felt that an interactive booklet in which information and progress could be recorded and shared (80% agreement) and interactions with their employer documented (92% agreement) would be beneficial. Online materials should be accessible by GPs prior to referral (88% agreement).
-
When should the intervention commence? There was uncertainty about the timing of the intervention. AHPs and GPs felt that it should start during the pre-assessment process. Overall, there was agreement that it should not start after surgery (88% agreement).
-
Defining RTW. Participants struggled to agree on a definition of RTW. However, they agreed (72%) that RTW should not be defined as the patient returning to the same job (usual hours and duties) and activities outside of work they were doing prior to surgery.
-
The aim of the intervention. There was agreement that the RTW intervention’s primary aim should be to return the patient to their preoperative work role and level of occupational performance (76% agreement).
-
Measuring RTW. There were a number of ideas about how RTW could be measured. The group felt that RTW was not a binary outcome (72% agreement). There was agreement on more detailed assessment, including the use of graded assessment based on specific work milestones, for example return to place of work, return to normal hours and return to normal workplace activities (92% agreement) or the resumption of specific work-related activities (e.g. climbing, lifting and manual tasks) based on a list of preoperative workplace activities (72% agreement). Rate of further sick leave (80% agreement), requirement and duration of occupational adjustments (84% agreement) and patients’ reports of their experiences and expectations were also felt to be important.
Following round 2, the investigator group convened to further refine the intervention and develop supporting materials and resources (discussed further in Chapter 9). During this process, a number of materials were drafted, which were subsequently shared with the Delphi participants in round 3.
Round 3
In round 3, the finalised occupational advice intervention along with selected patient and staff materials were circulated to 65 of the 66 Delphi participants for comment (one participant had withdrawn). Responses were received from 11 participants (four surgeons, one physiotherapist, one GP, three employers and two patients), comprising a constructive appraisal of the intervention from nine respondents (two employers responded but did not comment on the intervention) as well as highlighting typographical and formatting issues. The feedback was positive in all cases and all of the comments received are reported in Appendix 7.
Chapter 9 Intervention mapping stage 4: development of a draft occupational advice intervention
Introduction
The Delphi consensus process clarified the stakeholder position with respect to a number of the areas of uncertainty within the initial draft intervention. This information was used to finalise the intervention and create materials to support its delivery. The process of final intervention development ran alongside Delphi rounds 1 and 2 and prior to Delphi round 3.
Objectives
Intervention mapping stage 4 supported study objective 8 (see Chapter 1, Objectives).
Using information from the Delphi consensus process to refine the intervention
The Delphi process provided the OPAL investigators with additional information about what the occupational advice intervention should include (content) and how and when it should happen (format, delivery and timing).
Content, format and delivery
The majority of the written information presented to the Delphi group reached consensus either in round 1 (26 of 32 statements) or when re-presented in round 2 (three of five statements). During the interviews (see Chapters 5 and 6), both patients and employers had stated a preference for written materials, although there was a concern about patients becoming disengaged if the amount of information was overwhelmingly large. The Delphi process suggested that only the most ‘important’ information (based on Delphi ranking) needed to be included in any written materials and that information could be made available in other formats (e.g. a website).
There was support both from the interviews and through the Delphi process for an interactive booklet in which information and progress could be recorded and shared with other stakeholders invested in the RTW process. The OPAL investigators thought that this approach had the potential to allow patients to record individualised information about their workplace, the impact of their health condition, plans for returning to work and progress after surgery, providing an individualised intervention. This individualised approach also had the potential to avoid having a separate intervention for hip and knee replacement patients as long as patients who did not make the anticipated progress received individualised ‘joint-specific’ support after surgery. On this basis, the OPAL investigators created an interactive patient workbook that enabled the patient to develop a RTW plan, tailored to their own circumstances, that could be shared and agreed with their employer. The decision was made to provide key information in the booklet, with additional information available via a website that was signposted within the booklet.
There was greater uncertainty about the ‘active’ elements of the intervention. Two key areas that stakeholders felt were important were (1) the provision of additional preoperative and postoperative therapy (over and above standard care) in which RTW issues could be addressed and (2) the identification of ‘high-risk’ patients, with additional support made available for this group. The initial draft intervention (see Chapter 7) mirrored this position and aimed to provide three preoperative and three postoperative interactions between the patient and hospital team to discuss RTW, with additional input for ‘high-risk’ patients. However, the investigators identified difficulties with this approach.
First, our cohort data (see Chapter 4) failed to identify a ‘high-risk’ population and the current literature describing predictors of RTW after hip or knee replacement (see Chapter 1) was limited. 42,44,48,146 This meant that we were not able to confidently identify a ‘high-risk’ group in need of a more intensive intervention. The OPAL investigators therefore decided not to pursue a tiered high-/low-risk intervention and instead focused on developing an intervention that could be tailored to the patients’ needs with the ability to offer more or less support as required.
Second, there was concern about the cost, time and logistics associated with the implementation of a resource-intensive intervention requiring an additional six patient interactions. The survey of practice (see Chapter 4) and interviews (see Chapters 5 and 6) demonstrated that services varied significantly in their structure and the resources available, and concerns were expressed about the implementation and sustainability of an intervention requiring significant additional resources. Therefore, a flexible model that allows the intervention to be delivered at different times by different people in different trusts dependent on the timing and delivery of current standard care in individual trusts was considered desirable. Despite the need to limit resource use, the investigators felt that it was important to have a hospital team member actively engaging with RTW patients. This reflected a key aspect of RTW interventions reported in the rapid evidence review (see Chapter 3) in which there was an element of counselling and guidance and the ability to co-ordinate the wider multidisciplinary team. We therefore developed a return-to-work co-ordinator (RTWC) role that had a range of responsibilities including co-ordination of the RTW process, encouragement and supporting completion of the interactive patient workbook, being a point of access for problems and signposting and assisting with referrals to other existing services should this be required (see Staff roles).
The process to identify and support patients having problems and not making progress as expected was then considered. The Delphi group agreed that a postoperative mechanism for the identification of patients who were not progressing towards RTW as planned was required. They felt that the intervention should include the ability for the health-care team to interact with the patient by telephone, by e-mail or ‘online’ to help monitor progress. These actions were linked to the RTWC role through the requirement for the co-ordinator to contact patients prior to surgery to support and monitor their RTW process and be available after surgery via a dedicated RTW contact line (telephone or e-mail). This provided patients with access to a designated point of contact who could offer additional help and support if needed. This, in effect, was an extended version of ‘usual care’, in which problems after surgery are assessed by the patient’s clinical team and treated accordingly (e.g. group physiotherapy, one-to-one physiotherapy, referral to occupational therapy and referral to occupational health services). However, for the purpose of the intervention, this task was centralised and administered by the RTWC.
Issues relating to fit notes and communication between stakeholders were more easily accommodated within the intervention through the development of specific guidance and examples of correct completion (see Materials and resources). Although there was agreement that recording work status in referral information from primary care would be beneficial, the OPAL investigators felt that this was not logistically possible within the study time frame owing to the large number of general practices referring into secondary care teams.
Finally, throughout the needs assessment and Delphi process, there was a lack of clarity about who should be responsible for administering the intervention. The prevailing opinion was ‘anyone but me’. Therefore, as work-focused health-care is a relatively new concept and delivery of occupational advice is not perceived to be the role of any particular health professional, the OPAL investigators agreed that all members of staff should be encouraged to take an active part in the intervention and be aware of each other’s role in delivery. This would help to embed the concept within the pathway and supported ‘organisational’ change. Training for all members of the HOT was therefore provided to increase awareness about RTW issues.
Timing: when should the intervention be initiated?
Given the residual uncertainty following the Delphi process about when the intervention should start, the OPAL investigators reflected on the information from the IM stage 1 needs assessment. It was subsequently decided that the optimal time to initiate an occupational advice intervention was the outpatient consultation during which patients were listed for surgery. This was based on the following factors:
-
Patients and HOT members (AHPs and nurses) take the lead from their surgeon. Surgeons are integral to the delivery of information to their patients, who, in many cases, will not contemplate or consider returning to work without their permission. AHPs and GPs involved in the care of these patients often defer decisions relating to RTW to the surgeon (from interviews).
-
In over two-thirds of cases, the only time the patient sees their surgeon prior to surgery is in the initial outpatient consultation. Surgeons then do not see patients again until the morning of their operation, limiting the opportunity for interaction between the surgeon and their patients (from survey).
-
Over 90% of surgeons do not offer routine advice to patients returning to work after surgery and, when it is delivered, it is ad hoc verbal advice based on anecdote and personal experience. Patients, GPs and the HOT look to surgeons to lead the RTW process; however, they do not routinely provide advice and when they do it is not based on specific guidance or best practice (from survey/interviews).
-
The preoperative assessment process is extremely varied between trusts. The composition, timing (sometimes only 1 week before surgery) and staffing of these services would make it difficult to embed an intervention that fulfils the individualised needs of this patient group (from survey).
-
The outpatient consultation is a consistent step within the preoperative pathway in all institutions. Early discussion of RTW issues allows adequate time for patients and employers to develop, communicate and instigate a suitable plan to enable early and sustained RTW (from survey/interviews).
A pragmatic decision was made to allow access to the RTWC up to and including 16 weeks after surgery. Cohort data (see Chapter 4) suggested that the majority of patients had returned to work by 16 weeks and this, therefore, seemed an appropriate time point for the end of the intervention. This should allow some additional time to access the support following the standard postoperative review by the surgical team at 8–12 weeks after surgery when the patient was routinely either discharged back to primary care or offered further appointments (usually at 12 months post operation).
Summary of the occupational advice intervention
The OPAL investigators agreed on a final version of 13 patient objectives: nine prior to and four post surgery. A total of 20 objectives were agreed on for members of the HOT: 12 prior to and 8 post surgery. The final list of POs for patients and staff, alongside the matrices of change and determinants, can be found in Appendix 6. These POs form the ‘manual’ describing what, when, how and why the specific elements of the intervention are delivered. They are supported by the specific staff roles outlined in Staff roles and intervention resources and materials described in Materials and resources.
The key elements of the intervention are summarised in the following sections.
Timing
-
The intervention supported patients throughout their surgical pathway. It started in their outpatient appointment during which they are listed for surgery and continued until 16 weeks after their surgery.
Patient identification
-
All patients in work and intending to return to work after surgery were identified as RTW patients at their initial outpatient clinic appointment. The definition of ‘work’ included being in full-time or part-time employment or self-employment. It also included patients who are full- or part-time carers or who work as volunteers. The identification process was facilitated by the use of an occupational checklist completed by patients prior to their clinic appointment. The checklist was administered by a member of the outpatient clinic team when the patient arrived for their appointment.
-
The surgical team used the information on the occupational checklist to aid surgical decision-making with respect to surgery and allow an individualised preliminary discussion of RTW with the patient.
-
Patients who were subsequently listed for hip or knee replacement surgery (and consented to participate in the OPAL study) were signposted to the OPAL intervention resources (OPAL patient RTW workbook, employer information resource, website and local RTWC) by their surgical team.
Delivery of information
-
All patients in work and intending to return to work after surgery were provided with the following resources at the point at which they were recruited into the OPAL programme (in clinic after they are listed for surgery):
-
The patient RTW workbook. This was designed as an eight-step interactive workbook. Completion of the workbook helped patients to list and understand their current job demands, set a provisional RTW date, identify potential barriers and solutions to safe and appropriate RTW and develop a provisional RTW plan that could be shared with their employer/work colleagues. The completion of the workbook was the responsibility of the patient but was overseen by a designated RTWC who was a member of the orthopaedic team.
-
The employer RTW information resource. This mirrored the information in the patient workbook. It explained the OPAL project and the steps the patient will follow when completing their patient RTW workbook and provided useful information for employers and work colleagues with respect to returning to work after hip or knee replacement. The patient was provided with a copy to give to their employer, manager, occupational health link or other relevant work colleagues.
-
Signposting to the OPAL website: www.opalreturntowork.org.uk (accessed 1 April 2019). This contained additional information and advice for patients, employers, HOTs and GPs to access.
-
Assessment by a designated member of the orthopaedic team
-
All patients were contacted by a RTWC prior to surgery. The RTWC was a designated member of the orthopaedic team identified at each site who was involved in the assessment, management or education of hip and knee replacement patients. The RTWC offered support to patients, encouraged them to complete the patient RTW workbook and discussed the plans they have developed. This contact took place a minimum of 4 weeks prior to surgery.
-
The RTWC also encouraged patients to share their plans with their employer if they had not done so already.
Support, review and escalation
-
During the course of their assessment, the RTWC offered additional support to patients based on need. This decision was made on an individual patient basis having discussed and reviewed the information in the patient RTW workbook. Additional support could involve review and input from local therapy teams (in hospital or the community) and could be arranged either preoperatively or post discharge.
-
The RTWC facilitated a mechanism that allowed patients to contact them following their surgery (e.g. answerphone or e-mail). If indicated, this could prompt further review and referral back into local therapy services.
Communication
-
The intervention included mechanisms and guidance to support communication within the hospital team, between the hospital team and primary care and between the patient and their employer:
-
signposting ‘in-hospital’ teams (e.g. pre-assessment, ward nurses and doctors, inpatient and outpatient therapy services) to patients in the OPAL programme by the RTWC
-
guidelines for clinic letters, fit notes and discharge communication to support communication between secondary and primary care
-
the employer RTW information resource and specific instruction and advice in the patient RTW workbook to assist communication between the patient and their employer
-
communication between the patient and the RTWC via the telephone/e-mail service
-
a comprehensive training platform for staff to embed the OPAL programme within the participating unit’s/surgical team’s practices.
-
Training
-
The OPAL intervention provided training for members of the hospital orthopaedic care team who interact with RTW patients to increase awareness of RTW issues across the orthopaedic department.
Staff roles
The OPAL intervention was embedded within ‘usual’ care at each of the study sites. The OPAL intervention required a multidisciplinary team approach as evidence from IM stage 1 suggested that this was the most effective model for delivery. We therefore identified roles and responsibilities for key staff groups already involved in the care pathway (outpatient clinic staff, surgeons, ward nurses, ward doctors and therapy teams).
As well as adapting the work of existing staff, additional roles were created. These included the roles of the RTWC and deputy. A description of the proposed staff groups involved in delivery of the OPAL intervention and their roles and responsibilities is provided in Appendix 8.
Materials and resources
To support the delivery of the OPAL occupational advice intervention, a variety of resources for both patients and staff were developed. These are summarised in Table 15. An example of how these materials promoted the desired change objectives, applications and overall message is given in Table 16. See OPAL examples of developed materials, available at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/ (accessed 2 May 2020).
| Programme components | Description/content | Highlights |
|---|---|---|
| Patient programme components | ||
| Occupational checklist | Paper checklist to screen patient eligibility for feasibility study and guide consultation with surgeon at initial outpatient clinic appointment | Patient completes details of work situation and tasks |
| Patient RTW workbook | Workbook given to patients at outpatient clinic appointment | Stepped guidance on RTW; templates for patients to complete on job demands, impact (of joint problem) on work, RTW plan |
| Employer workbook | Workbook given to patients at outpatient clinic appointment to give to their employer/colleagues |
Information on joint replacement Guidance on how to support the employee’s RTW |
| Website | www.opalreturntowork.org.uk | Information about the OPAL study, hip and knee replacement surgery, advice on RTW |
| Helpline | Telephone/answerphone number for patients to contact RTWC for further guidance/support following surgery |
RTWC checks and responds to messages every 2 or 3 days Helpline accessible for 16 weeks following discharge |
| Staff programme components | ||
| Staff training |
PowerPoint® (Microsoft Corporation, Redmond, WA, USA) presentations. Generic training for all staff and targeted presentations for specific staff Training/study packs |
Overview of study and flow chart; POs for each job role; methods of behaviour change; work modifications; fit notes; occupational health advice |
| Occupational checklist | Paper checklist to screen patient eligibility for feasibility study and guide consultation with surgeon | Given to patients to complete by outpatient staff and then forwarded to RTWC |
| RTWC’s workbook | Booklet to guide RTWC in delivering the intervention | Stepped guidance on RTW; checklist of objectives; example templates for RTWC to complete to document job demands, impact (of joint problem) on work, RTW plan |
| Examples of fit notes | Completed examples of less/more appropriate fit notes to guide fit note completion by ward staff at discharge | Examples of ‘not fit’ fit notes and ‘maybe fit’ fit notes |
| Examples of job demands, impact on work, RTW plans | Completed examples of templates to be completed by patients in their RTW workbook, informed by experiences reported by actual patients interviewed in phase 1 | Six examples of each pertaining to different job roles and demands |
| Communication guidance | Written guidance on referring to RTW in clinic notes and discharge letters | A4 sheet giving examples of how to refer to patient’s RTW in medical documentation |
| GP letter | Letter to inform GP of patient’s enrolment in OPAL programme | Provides GP with information about OPAL programme |
| OPAL study posters, pens, newsletters | Branded study merchandise to increase visibility and awareness of the OPAL study | |
| Proposed vehicle | Change objectives grouped by determinant | Methods and practical applications | Message content |
|---|---|---|---|
| Patient materials | |||
| Occupational checklist |
Knowledge and awareness: completing a checklist informs the surgeon about work activities and demands Self-efficacy and skills: having the confidence and ability to complete the checklist Attitudes, beliefs and expectations: believing that completing an occupational checklist will facilitate RTW following surgery |
Consciousness raising by outpatient clinic staff Facilitation by outpatient clinic staff Information about others’ approval by outpatient clinic staff |
The surgeon is interested in my job and how surgery might have an impact on it The checklist is not too complex. We have pens and clipboards and we can help you if necessary The surgeon will be pleased that I have completed the checklist and it will help me return to work |
| RTW workbook |
Knowledge and awareness: knows key advice and information concerning recovery and RTW Self-efficacy and skills: able to acquaint self with key information about RTW Attitudes, beliefs and expectations: believes that revising RTW plan following surgery will aid RTW Perceived norms: recognises that RTW is now considered a positive health outcome |
Coherence and imagery sections of text have logical order and clearly related to graphics Verbal persuasion by outpatient clinic staff and RTWC Modelling provides examples of how patients have revised the RTW plan Consciousness raising: information about causes/consequences |
The HOT thinks that my RTW is important and that having this information will help The RTW book has been designed for and approved by patients as something they can use Other patients have revised their RTW plans and this has been helpful Getting back to work is good for health; this is why the health service is focusing on it |
| HOT materials | |||
| Staff training |
Knowledge and awareness: clinic staff know process of asking patients to complete checklist Self-efficacy and skills: RTWC expresses confidence in ability to support RTW Attitudes, beliefs and expectations: surgeon believes that they should encourage patients to take an active role in their decision about surgery in relation to RTW Perceived norms: asking patients about their RTW plans is good practice |
Individualisation through tailored staff training Facilitation: staff training at optimal times/places/methods Consciousness raising: information about causes/consequences of behaviour Shifting perspective: encourage the perspective of another |
The checklist is completed by the patient and taken into the consultation to aid their decision about surgery in relation to RTW The training has been delivered according to my needs and work context Surgery has an impact on RTW and patients need to be actively involved in the decision It is everyone’s role in the HOT to be actively interested in patients’ RTW |
| Examples of job demands, impact on work and RTW plans |
Knowledge and awareness: knowing what is expected from a completed template Self-efficacy and skills: enabling the RTWC to support the patient |
Modelling: appropriate examples provided for the RTWC to demonstrate completion Facilitation: creating an environment that makes the action easier |
These are some typical examples based on real patient experiences These will help you support the patient to plan their RTW |
Central to the intervention was the development of the patient RTW workbook. The workbook outlined an eight-step process that allowed the patient to record individualised information about their own RTW process, which they could then share with other members of the HOT, their employer and their GP.
The RTW process that they followed comprises the eight steps described below, which were presented in the workbook as a checklist and flow diagram (Figures 13 and 14):
-
assessment of the impact of their hip or knee on their ability to work, the specific demands of their workplace and how surgery might have an impact on these
-
setting an approximate date for their RTW
-
developing a RTW plan
-
discussing and reviewing their RTW plan with the RTWC
-
discussing and reviewing the RTW plan with their employer and/or their occupational health team
-
contacting their employer and/or occupational health team after surgery and updating them on their progress
-
amending their RTW plan based on the recovery after surgery and discussions with their employer, occupational health team and hospital staff
-
seeking help after surgery.
FIGURE 13.
Diagrammatic representation of the OPAL intervention and description of the eight-step process as described on pages 8 and 9 of the patient workbook.
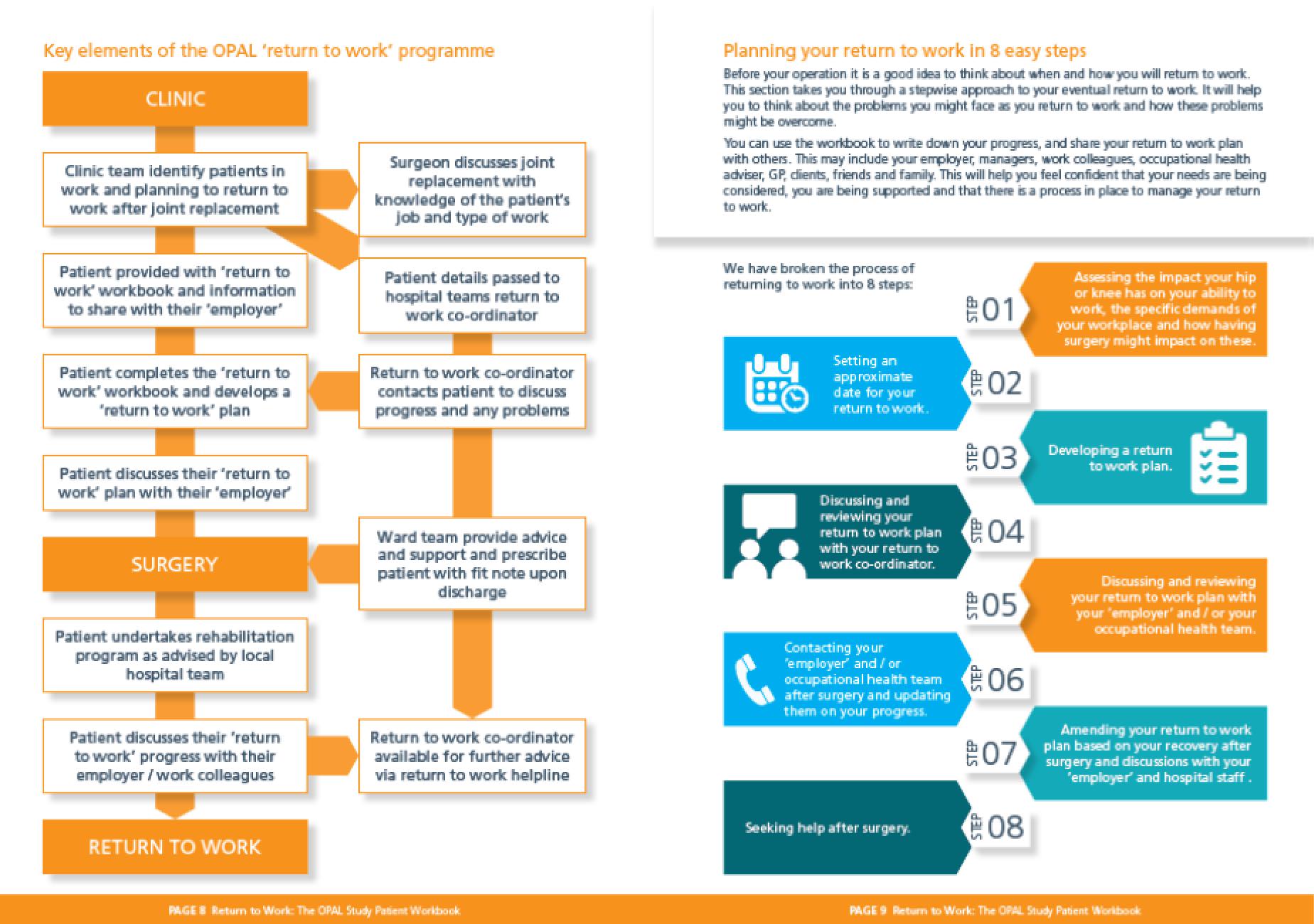
FIGURE 14.
Patient checklist for the eight-step RTW process as described on page 10 of the patient workbook.
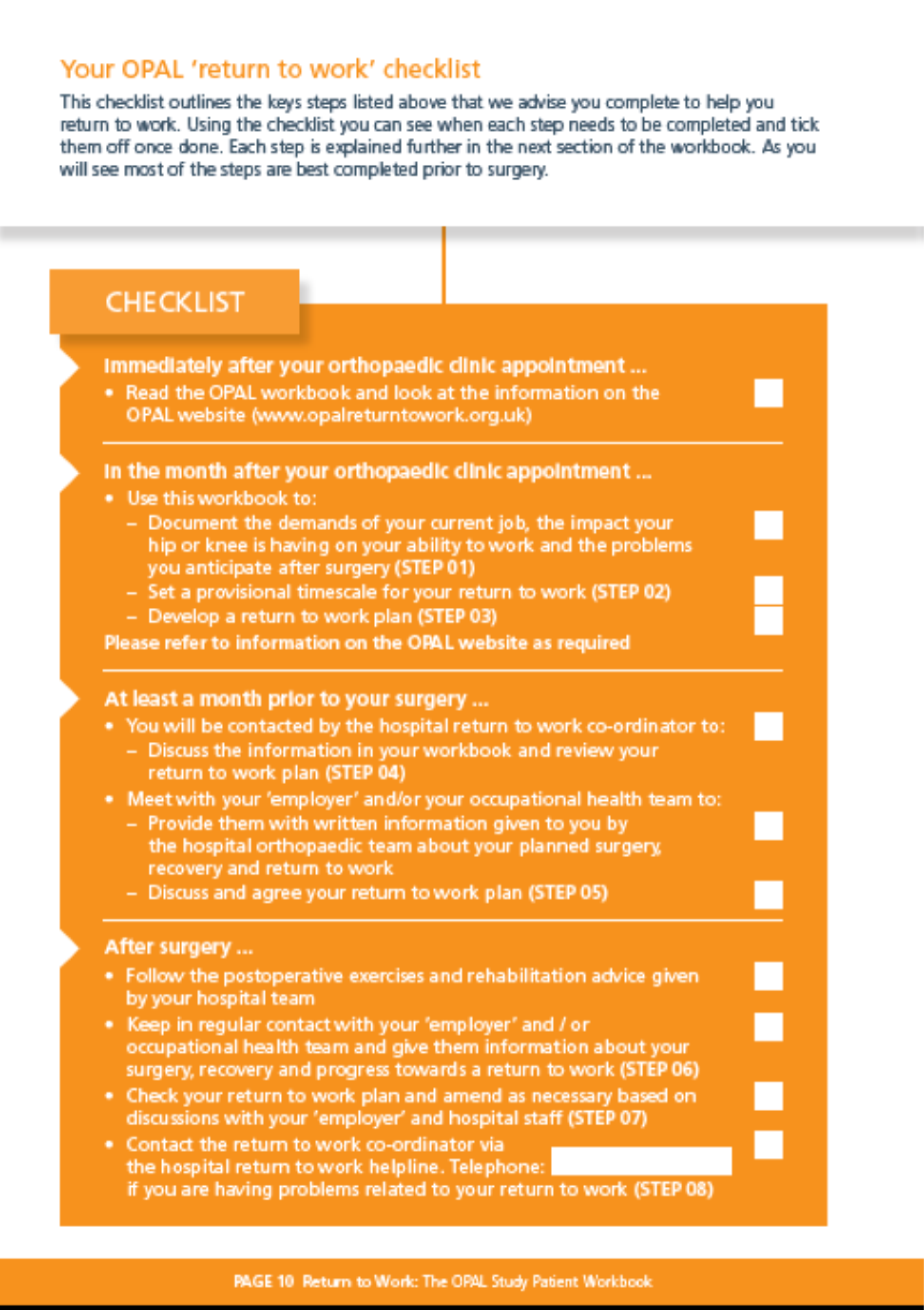
For examples of the specific tools developed for patients during steps 1–3, along with examples of completion, please see OPAL examples of developed materials at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/ (accessed 2 May 2020). The RTW plan (step 3) central to the patient workbook is illustrated in Figure 15.
FIGURE 15.
Step 3: development of a RTW plan as described on pages 16 and 17 of the patient workbook.
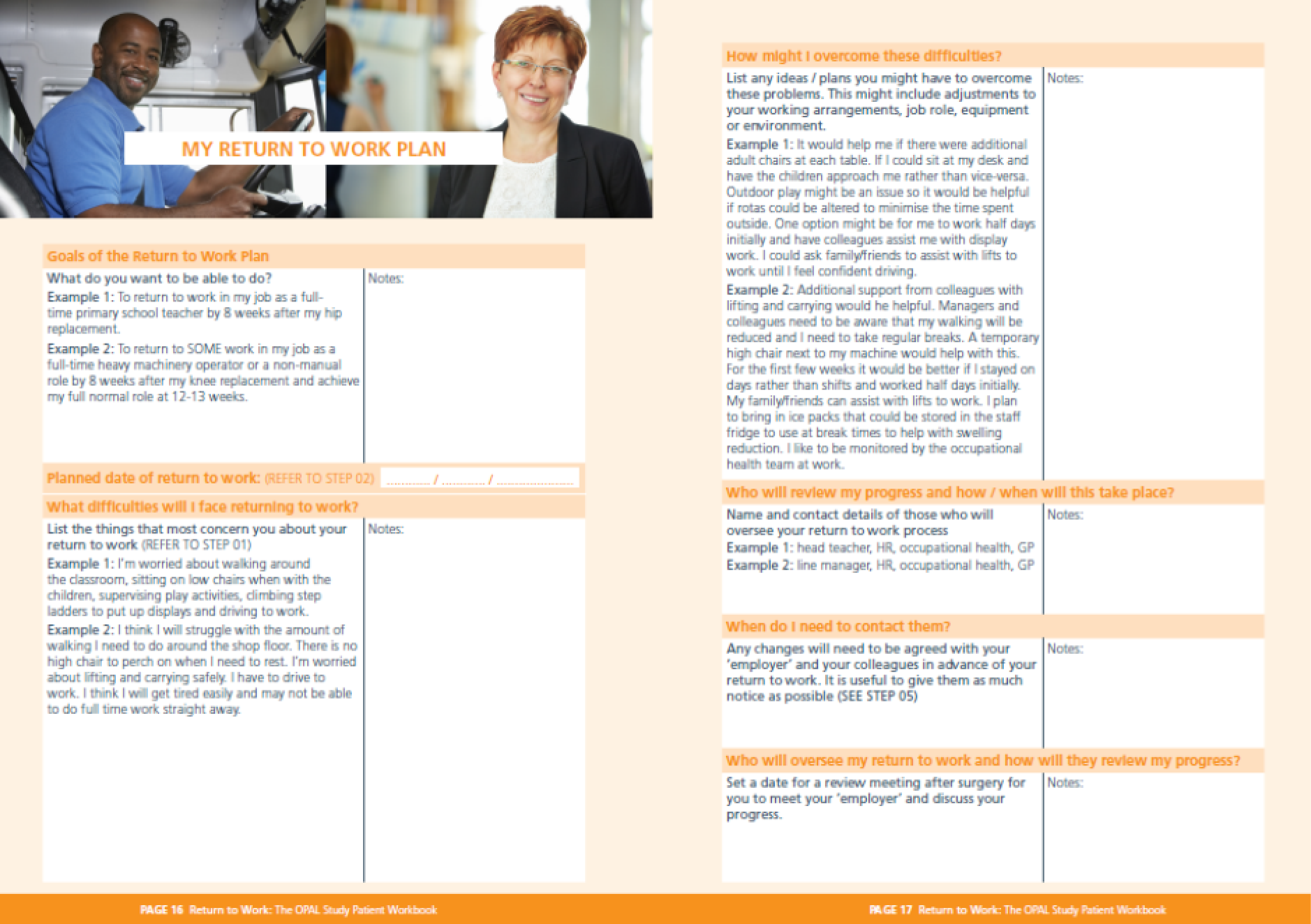
Chapter 10 Intervention mapping stages 5 and 6: implementation and feasibility assessment
Introduction
During IM stage 5, an implementation and adoption plan for the intervention was developed. This stage ran concurrently with the Delphi consensus process. The implementation plan focused on delivery within a small cohort of 5–10 patients at three sites and examined whether the intervention could be delivered alongside ‘standard’ care.
Intervention mapping stage 6 evaluated the fidelity of the intervention (was the intervention delivered as planned?) by assessing the intervention against the defined patient and staff POs. It also evaluated the quality of the intervention (how did patients, staff and employers feel about the intervention?) as well as establishing preliminary effectiveness and cost. Finally, the feasibility of undertaking a trial using the intervention was assessed using screening, recruitment, consent and follow-up procedures and rates at each of the study sites.
Objectives
Intervention mapping stages 5 and 6 supported study objectives 8 and 9 (see Chapter 1, Objectives).
Intervention mapping stage 5: implementation
Overview
An implementation strategy was developed to support the adoption and implementation of the OPAL intervention at three NHS hospital trusts in England. At each hospital, a principal investigator (PI) (a consultant orthopaedic surgeon) was identified to assist the OPAL investigators as they had knowledge of local service structure and personnel. The PIs identified staff members for the OPAL intervention roles (e.g. RTWC) based on local service structure and personnel. The person used in the RTWC role was chosen by the PI after discussion with the OPAL research team based on seniority, experience and time available for the role. The PI then planned how the intervention would work alongside ‘standard’ care at their institution.
Support and clarification were provided by the OPAL investigators when needed; however, the local delivery of the intervention was largely determined by the local teams through negotiation with the PI and nominated RTWC. In this way, the intervention could be delivered pragmatically alongside current care while also stipulating the achievement of specified POs against which the fidelity of the intervention could be assessed. The investigators were then able to support local implementation through training sessions and specific training resources tailored to the roles and clinical areas.
At each site, potential users of the intervention were identified using eligibility criteria similar to those used in phase 1: (1) placed on the waiting list for hip or knee replacement during their outpatient appointment with the surgical team, (2) in work in the 3 months prior to being added to the waiting list for joint replacement and (3) intending to return to work following surgery.
Training
The OPAL training for hospital staff was undertaken between May and July 2018. Different approaches were required at each site; training logs are provided in Appendix 9. At the Nottingham and Middlesbrough sites, visits were conducted on a number of occasions with staff groups from a variety of clinical areas, to ensure coverage within the department. In Middlesbrough, two or three large-group training sessions were held. In Nottingham, a more labour-intensive one-to-one approach was needed after an initial group session failed to include all of the required personnel. In contrast, the Northumbria site invited ‘key’ staff to the training (including the PI, nominated RTWC and members of the local research team). The RTWC then facilitated the implementation of the OPAL intervention at this site through a systematic series of training with the local team, collating the information and materials needed by each team member and cascading this internally as required.
To support training, the patient and staff materials produced to support the OPAL intervention were made available to each site as ‘site files’ that could be stored and used for reference in clinical areas delivering the intervention (outpatient departments, wards and the RTWC office). To supplement these materials, specific training resources were created, including worked examples of completed study paperwork and fit notes, and training PowerPoint slides. A full list of training resources can be found in Appendix 9. For examples, see OPAL examples of developed materials at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/ (accessed 2 May 2020).
Performance objectives to support implementation
As part of the implementation strategy, the OPAL investigators identified a number of POs required to facilitate adoption at each site.
The POs were to:
-
recruit the participating sites and PIs
-
recruit the RTWC
-
train staff in delivering the OPAL intervention
-
support the staff in delivering the OPAL intervention.
The POs for the local site PI and RTWCs were to:
-
familiarise themselves with the OPAL intervention and associated materials
-
inform and enthuse their HOT about the study, and promote engagement
-
identify potential RTWCs and deputies (PI role)
-
identify surgeons willing to support their patients’ involvement in the study
-
arrange training events/meetings between the HOT and the OPAL investigators
-
set up a helpline for patients to access a RTWC
-
support the team in identifying existing staff members to act as OPAL champions for their subteam (e.g. outpatient clinic, ward and therapy team).
As this was a feasibility study, the implementation strategy focused around adoption for a 6- to 8-week period during which the HOT was to deliver the intervention. Therefore, it was not necessary to identify future adopters and maintainers of the programme.
Determinant matrices for dissemination/adoption/implementation actions
Having identified POs, determinant matrices were created to support behaviour change and provide actions and outcomes to facilitate adoption. Change matrices for the OPAL investigators and for the PIs and RTWCs are shown in Tables 17 and 18. These matrices were then used as the framework for training at each site.
| POs for programme implementation | Personal determinants | |||
|---|---|---|---|---|
| Outcome expectation | Knowledge | Attitudes | Perceived norms | |
| Recruit the participating sites and PIs at each site | Expect that recruiting sites and PIs is possible and will facilitate the feasibility study | Can describe how and when site and PIs will be recruited | Believe that recruitment of sites and PIs is important and necessary for a study such as OPAL | Recognise that recruiting sites and PIs is a usual step when conducting a feasibility study |
| Recruit the RTWC at each site | Expect that recruiting a RTWC at each site is possible and will facilitate the feasibility study | Can describe how and when a RTWC can be recruited at each site | Believe that the recruitment of a RTWC at each site is important and necessary | Recognise that recruiting a RTWC at each site is a usual step when conducting a feasibility study |
| Train staff at the sites in delivering the OPAL intervention | Expect that training staff at each site in delivering OPAL is possible and will facilitate the feasibility study | Can describe how and when staff at each site will be trained in the delivery of the OPAL study | Believe that the training of staff to deliver the OPAL study at each site is important and necessary | Recognise that training staff in the delivery of the OPAL study at each site is a usual step when conducting a feasibility study |
| Support staff at the sites in delivering the OPAL intervention | Expect that supporting the staff at each site is possible and will facilitate the feasibility study | Can describe how and when staff at each site will be supported in the delivery of the OPAL study | Believe that supporting staff at each site to deliver the OPAL study is important and necessary | Recognise that supporting staff in the delivery of the OPAL study at each site is a usual step when conducting a feasibility study |
| POs for programme implementation | Personal determinants | |||
|---|---|---|---|---|
| Outcome expectation | Knowledge | Attitudes | Perceived norms | |
| Familiarise themselves with the OPAL intervention and associated materials | Expects that reading and learning about the OPAL intervention will facilitate adoption through the feasibility study | Can describe the structure, content, delivery and format of the OPAL intervention. Can describe how they will impart this information to their HOT | Believes that the OPAL intervention is useful and that the materials created support its adoption and implementation | Recognises that understanding the OPAL intervention enables them to lead the adoption and implementation at their site and that is a usual step when conducting a feasibility study |
| Inform and enthuse their HOT about the study and promote engagement | Expects that enthusing their HOT about the study is possible and will facilitate the feasibility study | Can describe how and when they will enthuse their HOT staff in the delivery of the OPAL study | Believes that enthusing their HOT staff to deliver the OPAL study at each site is important and necessary | Recognises that enthusing staff in the delivery of the OPAL study at each site is a usual step when conducting a feasibility study |
| Identify potential RTWCs at each site and deputies | Expects that identifying the RTWC and deputy at their site is possible and will facilitate the feasibility study | Can describe how and when they will identify a potential RTWC and their deputy at their site | Believes that enthusing their HOT staff to deliver the OPAL study at their site is important and necessary | Recognises that identifying a RTWC and deputy at their site is a usual step when conducting a feasibility study |
| Identify surgeons willing to support their patients’ involvement in the study | Expects that identifying surgeons who are willing to support their patients’ involvement in the study is possible and will facilitate the feasibility study | Can describe how and when they will identify surgeons at their site who are willing to support their patients’ involvement in the study | Believes that identifying surgeons at their site who are willing to support their patients’ involvement in the study is important and necessary | Recognising that identifying surgeons at their site who are willing to support their patients’ involvement in the study is a usual step when conducting a feasibility study |
| Arrange a training event/meeting at the site between the HOT and the OPAL investigators | Expects that arranging a training event/meeting at their site between the HOT and the OPAL investigators is possible and will facilitate the feasibility study | Can describe how and when they will arrange a training event/meeting at their site between the HOT and the OPAL investigators | Believes that arranging a training event/meeting at their site between the HOT and the OPAL investigators is important and necessary | Recognises that arranging a training event/meeting at their site between the HOT and the OPAL investigators is a usual step when conducting a feasibility study |
| Support the team in setting up a helpline for patients to access a RTWC | Expects that supporting their HOT in setting up a helpline for patients to access the RTWC is possible and will facilitate the feasibility study | Can describe how and when they will support their HOT in setting up a helpline for patients to access the RTWC | Believes that supporting their HOT in setting up a helpline for patients to access the RTWC is important and necessary | Recognises that supporting their HOT in setting up a helpline for patients to access the RTWC is a usual step when conducting a feasibility study |
Intervention mapping stage 6: feasibility
Methods
The methods used for the ‘feasibility’ stage were similar to the methods used in IM stage 1. 54 Questionnaire and interview data were collected from patients returning to work after hip or knee replacement. Assessment of the intervention considered four inter-related themes:
-
Assessment of intervention fidelity (were the stated POs delivered?). Data collected from participants were mapped against the final staff and patient POs. Evidence was collected from a variety of sources including the baseline and follow-up questionnaires, the patient RTW workbooks (evidence of patient activity) and the RTWC checklists (evidence of RTWC activity) for each patient. All POs were assessed except for PO10 (patient communicates with employer regarding surgical outcome and progress/recovery, by telephone, e-mail or face to face) and PO13 (patient adheres to postoperative rehabilitation plan and advice) owing to an omission on the postoperative questionnaires. Examples of the evidence sources used to determine intervention fidelity for the patient and staff POs are provided in Table 19. A complete description of the evidence sources for all POs is provided in Appendix 9.
-
Assessment of intervention quality (what did patients, staff and employers feel about the intervention and how it was delivered?). Structured interviews explored patient and stakeholder (HOT members and employers) perceptions of the intervention. Interviews explored the understanding, opinions and experiences of the intervention and the study processes associated with its delivery in the context of a research study.
-
Assessment of feasibility data (did the intervention facilitate early supported RTW?). Data collected from the feasibility study (rates and timing of RTW, functional outcomes scores, health utility measures and work-related scores) were compared with similar data collected in IM stage 1 to generate a preliminary comparison of patients who did (IM stage 6) and did not (IM stage 1) receive the OPAL intervention.
-
Assessment of economic data (how much does the intervention cost to deliver and what is the associated health utilisation?). Health-care utilisation data were collected using questionnaires, allowing costs to be assigned to activities. In addition, costs were attached to data collected in the RTWC checklist that documented the time spent by the RTWC supporting the delivery of the intervention. The timing of RTW after surgery in patients receiving the intervention was also explored.
| PO | Evidence of completion | Evidence source |
|---|---|---|
| Patient POs | ||
| PO1. Patient completes occupational checklist prior to appointment with surgeon |
|
|
| PO2. Patient makes informed decision about surgery with respect to work |
|
|
| PO3. Patient acquaints self with key information about recovery and RTW provided in the patient RTW workbook and associated online information resources |
|
|
| Staff POs | ||
| PO10. RTWC highlights RTW patients to ward teams managing preoperative education and assessment and records this action in the RTWC workbook | Evidence that the RTWC contacted pre-assessment teams (RTWC workbook) | RTWC workbook ‘task 4’ |
| PO11. RTWC highlights RTW patients to the ward teams when admitted for surgery and records this action in the RTWC workbook | Evidence that the RTWC contacted ward teams (RTWC workbook) | RTWC workbook ‘task 5’ |
Intervention mapping stage 6 also supported collection of other key information, such as (1) patients’ and surgeons’ views on their willingness to participate in a future trial, (2) potential rates of recruitment and the proportion of eligible patients consenting and (3) information about the behaviour and distributional characteristics of RTW outcomes that would inform the power calculation for any subsequent trial. It therefore captured data that allowed recommendations about the conduct of a future trial to be made.
Feasibility study
Participants were recruited from three sites (Middlesbrough, Nottingham and Northumbria). Participants were asked to complete questionnaires at baseline (preoperatively, when listed for surgery) and at 8 and 16 weeks after surgery as in IM stage 1, to allow comparison with data collected during this stage. The aim was to recruit 30 patients.
All patients attending hip and knee replacement clinics at the study sites were screened, prior to their surgical appointment, using the developed occupational checklist (see OPAL examples of developed materials at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/; accessed 2 May 2020). This checklist was taken into the appointment, providing the surgeon with information about their work and work-related activities that could be considered as part of the decision to offer surgery. Where patients were offered surgery, the surgeon confirmed eligibility and facilitated referral to the local research team for further information about the OPAL study, for consent and enrolment. Patients who consented were then provided with the OPAL resources (patient and employer workbooks, and website access) and their contact information was passed on to the RTWC. The design of the feasibility study is shown in Figure 16.
FIGURE 16.
Feasibility study design.
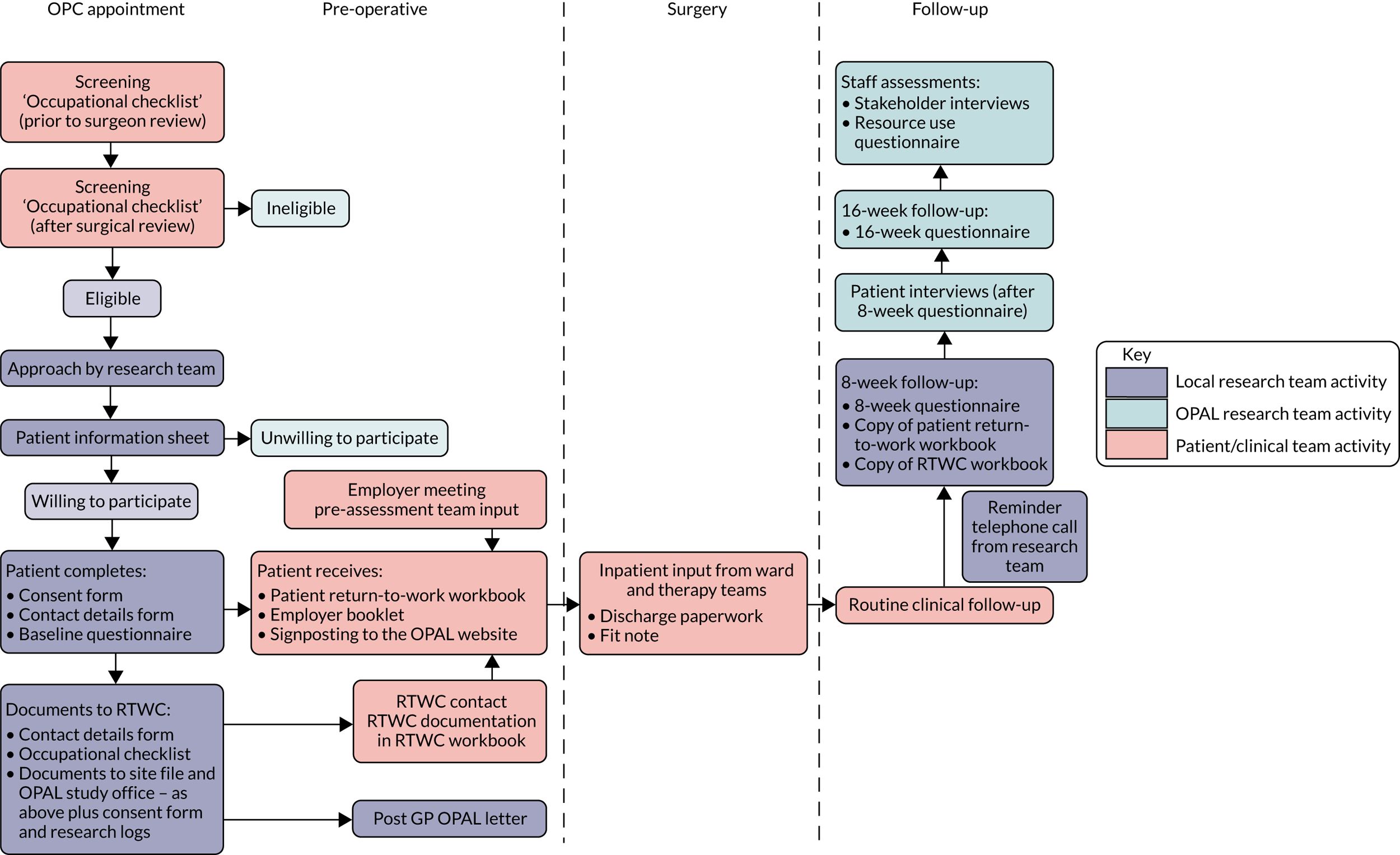
Inclusion/exclusion criteria for the cohort study
The inclusion criteria for patients recruited into the cohort/interview elements of the feasibility assessment during IM stage 6 were:
-
aged ≥ 16 years
-
listed for primary hip or knee replacement
-
in work in the 3 months prior to listing for surgery (including full-time, part-time, paid and unpaid job roles); equates to approximately 6 months prior to surgery
-
intending to return to work following surgery.
The exclusion criteria were:
-
lack of mental capacity to understand and participate in the cohort study
-
not understanding written and spoken English
-
emergency surgical procedure (e.g. surgery for an indication of trauma)
-
surgery for cancer or infection.
Patient and stakeholder interviews
The information from the feasibility study was supplemented by a further 15 patient and 12 stakeholder interviews (sampling from employers, AHPs, nurses, GPs and orthopaedic surgeons) across the study sites. Patient interviews were undertaken at 8 weeks post surgery. Stakeholder interviews were undertaken once all patients at the site had received surgery (i.e. once all patients were recruited and had been through the preoperative phase of the intervention). The sampling strategy for the stakeholder interviews is given in Table 20.
| Interviewees | Suggested time scale |
|---|---|
| RTWCs (× 3) | Once all patients had been recruited and had, as a minimum, been through the preoperative phase of the intervention |
| Employers (× 3) | To be interviewed post employee/patient interview (i.e. ≥ 8 weeks post surgery) |
| GPs (× 2) | Interview post patient interview (i.e. ≥ 8 weeks post surgery) |
| Surgeons (× 2) | Interview post 8-week follow-up |
| Rehabilitation/ward staff (× 2) | Once all patients had been recruited and had, as a minimum, been through the preoperative phase of the intervention |
Results
Feasibility recruitment commenced on 1 June 2018 and ended on 14 August 2018. A total of 147 patients were screened, of whom 35 (24%) were eligible for recruitment. In total, 26 of a planned 30 patients were recruited (11 in Northumbria, 8 in Middlesbrough and 7 in Nottingham) (Figure 17). Consent forms, contact details forms and baseline questionnaires were received from all 26 participants. Four participants were withdrawn from the study for the following reasons: participant’s care transferred to a neighbouring trust (n = 1), surgery deferred until later in the year at the participant’s request (n = 1) and participant requested withdrawal from the study (n = 2). A further participant had their surgery delayed for medical reasons and was still awaiting surgery when follow-up for the feasibility was closed (surgery date 22 March 2019). A total of 21 participants were included in the analysis. Follow-up data were received from 18 participants at 8 weeks and from 14 participants at 16 weeks. Copies of the patient workbooks and RTWC checklists were received for 10 and 19 of the 21 remaining participants, respectively. The results are presented under the headings of the four inter-related themes described in Methods.
FIGURE 17.
Flow of patients through the feasibility study.
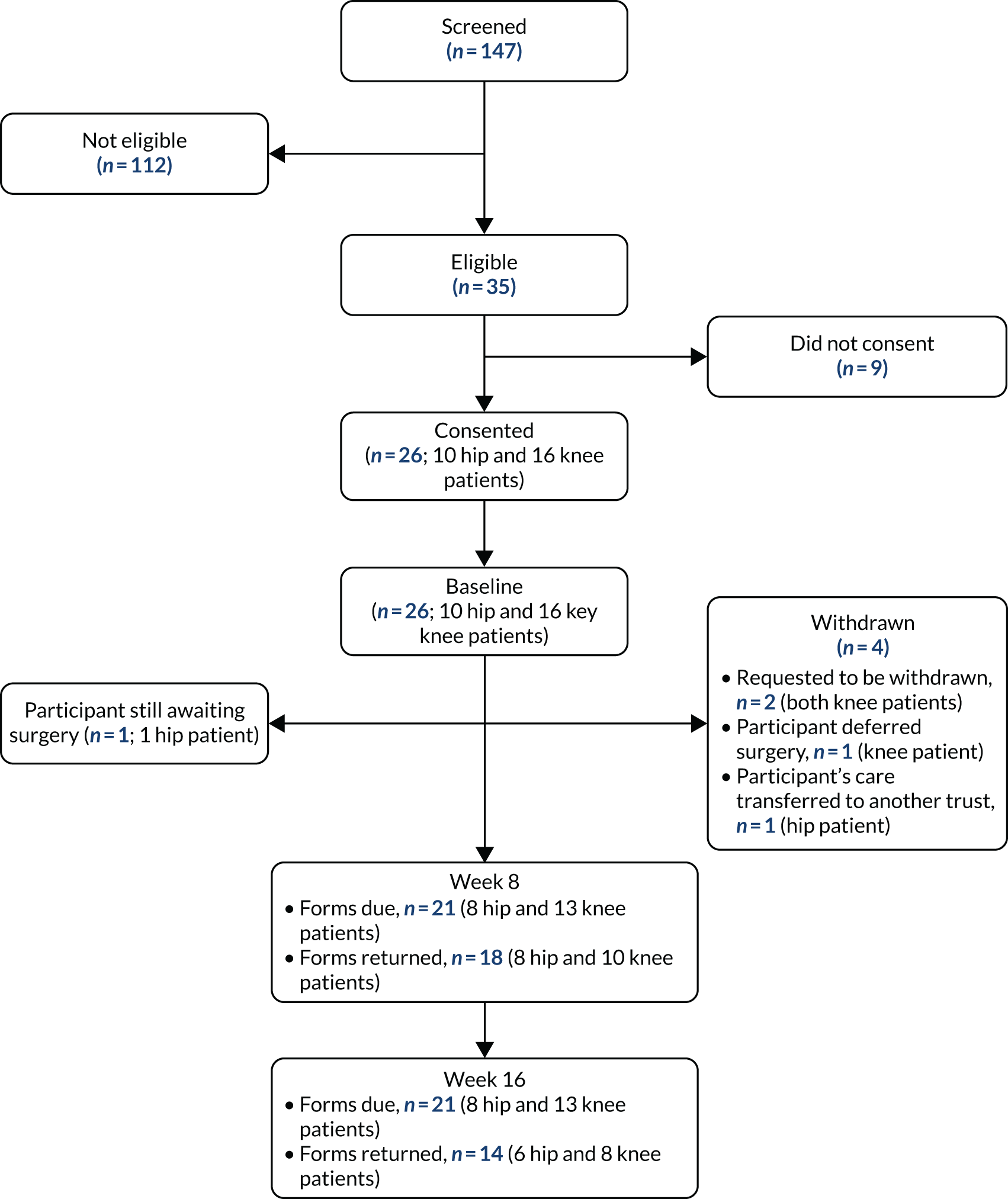
Assessment of intervention fidelity
Data from the questionnaires were mapped against each of the participant and staff POs for all 6 participants (Tables 21 and 22).
| Participant ID | Patient objectives fidelity assessment checklist | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PO1 | PO2 | PO3 | PO4 | PO5 | PO6 | PO7 | PO8 | PO9 | PO10 | PO11 | PO12 | PO13 | |
| 1060 | |||||||||||||
| 1061 | |||||||||||||
| 2060 | |||||||||||||
| 2061 | |||||||||||||
| 2062 | |||||||||||||
| 2063 | |||||||||||||
| 2064 | |||||||||||||
| 1262 | |||||||||||||
| 2260 | |||||||||||||
| 2262 | |||||||||||||
| 2265 | |||||||||||||
| 2266 | |||||||||||||
| 2267 | |||||||||||||
| 2268 | |||||||||||||
| 2269 | |||||||||||||
| 1360 | |||||||||||||
| 1361 | |||||||||||||
| 1362 | |||||||||||||
| 1363 | |||||||||||||
| 1364 | |||||||||||||
| 1366 | |||||||||||||
| 1367 | |||||||||||||
| 2363 | |||||||||||||
| 2364 | |||||||||||||
| 2366 | |||||||||||||
| 2367 | |||||||||||||
| Participant ID | Staff objectives fidelity assessment checklist | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PO1 | PO2 | PO3 | PO4 | PO5 | PO6 | PO7 | PO8 | PO9 | PO10 | PO11 | PO12 | PO13 | PO14 | PO15 | PO16 | PO17 | PO18 | PO19 | PO20 | |
| 1060 | ||||||||||||||||||||
| 1061 | ||||||||||||||||||||
| 2060 | ||||||||||||||||||||
| 2061 | ||||||||||||||||||||
| 2062 | ||||||||||||||||||||
| 2063 | ||||||||||||||||||||
| 2064 | ||||||||||||||||||||
| 1262 | ||||||||||||||||||||
| 2260 | ||||||||||||||||||||
| 2262 | ||||||||||||||||||||
| 2265 | ||||||||||||||||||||
| 2266 | ||||||||||||||||||||
| 2267 | ||||||||||||||||||||
| 2268 | ||||||||||||||||||||
| 2269 | ||||||||||||||||||||
| 1360 | ||||||||||||||||||||
| 1361 | ||||||||||||||||||||
| 1362 | ||||||||||||||||||||
| 1363 | ||||||||||||||||||||
| 1364 | ||||||||||||||||||||
| 1366 | ||||||||||||||||||||
| 1367 | ||||||||||||||||||||
| 2363 | ||||||||||||||||||||
| 2364 | ||||||||||||||||||||
| 2366 | ||||||||||||||||||||
| 2367 | ||||||||||||||||||||
Patient performance objectives
For the 21 participants with follow-up data, the rate of delivery of the 13 patient POs was 205 out of 273 (75%). This improved to 205 out of 231 (89%) if POs 10 and 13 were removed.
The rate of delivery for all the assessed POs was > 85% except for PO11 (patient revises RTW plan following surgery as necessary with their employer and hospital staff), in which the rate of delivery was only 9 out of 21 (43%). However, many participants might not have had to revise their RTW plan and so a negative response for this PO might simply reflect the fact that the RTW plan they made prior to surgery was adequate.
Staff performance objectives
For the 21 participants with follow-up data, the rate of delivery of the 20 staff POs was 312 out of 420 (74%). The rate of delivery for the POs was at least 85%, with the exception of PO10 (71%), PO11 (81%), PO16 (52%), PO17 (38%), PO18 (0%), PO19 (0%) and PO20 (33%). PO 10 and PO 11 related to the RTWC highlighting OPAL participants to the preoperative education and assessment teams and ward staff. This activity was evidenced from the RTWC checklist and was generally well recorded. PO16 covered fit note prescription on the ward after discharge and was assessed by the participant’s report of receiving a fit note. PO17 involved the RTWC checking the telephone line for participant contacts; however, in many cases the RTWC did not document in the individual participant RTWC checklists that they had checked the telephone line, although the RTWC interview data suggested that they undertook this task regularly. The observed rate of delivery may therefore be falsely low and not reflect actual practice. PO 18 and PO 19 related to communication between the HOT and the GP through the ward discharge and outpatient clinic letters. As it was not possible to obtain copies of all clinical correspondence from the study sites, this could not be investigated further.
Assessment of intervention quality
Patient interviews
Fifteen patients were interviewed across the three study sites. The patient interviews conducted in IM stage 6 explored the following three themes:
-
understanding of the OPAL intervention
-
views about the OPAL intervention
-
experience of participating in the OPAL study.
Summaries of the analysis for each identified theme are described below. Direct quotations supporting these themes are provided in Appendix 9.
Two patients felt that the OPAL study was an exercise in information collection; others felt that it was an attempt to help patients return to work and ‘normality’ after surgery. Some perceived the OPAL study as aiming to involve stakeholders and patients in the RTW process. One patient believed that earlier RTW was the goal and questioned whether the OPAL study was for the benefit of the employer rather than the patient. Some believed that it examined occupational health services and others believed that it would aid RTW through more intensive physiotherapy.
Several patients believed that the OPAL study provided advice and information about RTW after surgery. Some valued recording what their work entailed as it helped focus their RTW. As the intervention started preoperatively, it gave more time for the patient to engage. However, not all of the participants felt that work should be the primary focus and some prioritised ‘getting their life back’. Some questioned whether or not RTW was in the role of hospital clinicians. Others believed that the OPAL study did not apply to them because their ‘work’ was voluntary or their employers already had procedures in place. Some felt that they did not need help from the RTWC because they were able to manage their RTW, or perceived that the RTWC could not help them.
Twenty (76.9% of all participants, 95.2% of those followed up) participants reported being issued with OPAL patient and employer workbooks by the research nurse. Other than a telephone call, there was little reported engagement with the RTWC.
Participants who were in paid employment and completed the workbook were positive about it, although their employer did not always take up their RTW plan. This put the emphasis on the employee to implement the plan. Other participants found the RTW workbook informative and two reported that it had helped inform their fit note. Another saw the workbook as the opportunity to formalise plans, but did not consider it applicable to their employment situation, in which sickness absence procedures were in place.
One self-employed participant used the workbook to write down all their tasks, aiding their RTW by identifying components of the job they could do. Another self-employed participant found the workbook of limited value as they considered that they needed to go to back to work immediately for financial reasons. One participant stopped completing the workbook as they were concerned that it might be shared with their employer and used against their best interests. Another participant, who was office based, felt that not all the steps in the workbook applied to them, compared with someone in a more physically demanding role.
Participants reported passing the workbook to their employer. Some reported that their employer read the workbook and used it to direct their RTW interview. One participant saw that their employer had consulted the workbook but believed that organisational policies superseded it. Others reported that their employer looked at it but did not discuss the implications of the information with them. One participant felt that, owing to the size of the business and lack of opportunity for modifications, the employer considered the information inappropriate. Another thought that it might have intimidated their occupational health adviser.
Few patients reported using the helpline because either they did not need to or they were not aware of it. One used it to ask about fit notes and benefits.
The majority of patients did not visit the website.
Patients reported limited face-to-face contact with the RTWC. Most received telephone calls or e-mails from the RTWC prior to surgery as well as a follow-up call/e-mail that they had found helpful. A number of patients reported that OPAL interaction was mainly with the research nurse.
Participants expressed some disappointment that their expectations around the OPAL study were not realised. Some reported lack of knowledge and communication within the HOT regarding the OPAL study. Others felt that the orthopaedic team was doing an excellent job but that there was limited focus on RTW.
Stakeholder interviews
Summaries of the analysis for each stakeholder group are described below. Direct quotations supporting these analyses are provided in Appendix 9.
Two employers were interviewed from one study site. Both worked for public-sector organisations reporting comprehensive RTW procedures. One employer was responsible for 30 staff and the other was responsible for 125 staff.
Both were aware of their employee’s involvement in the OPAL study and felt that they understood its purpose. Both had seen the employer workbook. Both had used the workbooks to prompt discussion of the RTW plan and to inform their understanding of recovery. They believed that the workbook helped employees clarify and record the RTW process, and provided an opportunity for the two parties to agree the RTW plan. The information prompted consideration of work modifications/issues that might delay a full RTW. The workbooks were perceived as easy to use, although some language was considered over-technical. One respondent felt that there should be one combined employer/patient workbook, accessible to everyone involved. One felt that there should be more included about the individual, such as information about follow-up and seeking advice if the employee was not progressing as expected.
Both employers received fit notes from their employees, although neither reported that they were informative. One believed that interventions like that in the OPAL study could become standard practice in their organisation. The intervention gave more detail than their occupational health teams were able to provide, and they felt that it could be adapted for other health conditions.
Two surgeons, from two study sites, were interviewed. Both were aware of the OPAL study, and had patients receiving the intervention. Neither had attended face-to-face training. One reported viewing the online training, although they had difficulty recalling it. One surgeon felt that attending training would not be justified unless OPAL became embedded in the service, in which case face-to-face group training would be preferable.
Neither had had contact with the RTWC in relation to OPAL or seemed clear about the RTWC role. Both were aware of the patient workbook; one had looked at it and seemed to understand how it might be used. Neither had seen the employer workbook or was aware of the helpline.
One surgeon relied on the research nurses to implement OPAL, and the other reported a more active role and discussed the patient workbook with their patients. It seemed that OPAL did not change their documentation of patients’ work issues. Both considered OPAL a good idea. One felt that it made them more aware of RTW and changed their consultation practice. One thought that it should be of value to most patients, although one of their patients had not engaged even though they appeared to be in need of RTW support. One respondent felt the intervention should be restricted to those in paid employment who needed to negotiate their RTW with an employer. One saw the intervention as a tool for patients rather than surgeons. The other considered that, within their role and time available, it was not possible to provide occupational counselling, despite believing that this should happen.
Three RTWCs were interviewed, one from each site. All had received training. One RTWC, who received face-to-face training, felt that too much information was imparted, and another felt that the ward team should have been more involved. Another received individual training, which was viewed positively; however, they would have preferred group training to allow them to appreciate others’ roles.
In some cases, difficulties in obtaining surgical information led to delays in contacting patients. One RTWC attempted to meet every recruited patient preoperatively, preferring face-to-face contact. The RTWCs commented that it was difficult to contact all patients, particularly during office hours, so one RTWC mainly communicated by e-mail. Two RTWCs reported contacting patients again on the ward after surgery, and one also tried to contact each patient following discharge.
Completion of workbooks was seen as the responsibility of the patient, supported by the research nurses. RTWCs did not necessarily see the completed workbooks. Some RTWCs reported encouraging patients to bring workbooks to hospital appointments, although they were unsure of the purpose of doing this.
Two RTWCs informed patients about the OPAL website but none believed that patients had accessed this, and nor had the co-ordinators. All RTWCs reported making patients aware of a helpline but only one received a RTW-related call. Another had been contacted by e-mail, but had subsequently failed to reach the patient by telephone.
One RTWC found their role unclear. They were unsure if the purpose of OPAL was for patients to return to work earlier or in a ‘safe and structured’ way. The same RTWC understood that their role included answering patients’ work-related questions, but were not confident that they had all the necessary skills to do this. Another RTWC perceived their role to be administrative.
The RTWCs’ opinions of OPAL were positive. There was general support for OPAL, although there was a view that it might not be appropriate or necessary for all patients. More appropriate completion of the fit note was considered a benefit, and they thought that OPAL provided additional information and opportunities to discuss work in more detail, and that patients benefited from receiving more support preoperatively. Organisational issues were viewed as a problem, such as keeping track of the dates of surgery, preadmission and education groups, as these often changed. One interviewee reported having an insufficient number of information packs for all staff, and another reported that there was too much paperwork and the structure and format could be improved. One RTWC suggested a pro forma script to use when initially contacting patients.
Patient feedback to the RTWCs was generally good, although some patients were not keen on completing the paperwork, and felt that there was too much. Patients required varying levels of support. Not all patients wished to share information with their employer and some were influenced by their family. As regards the most appropriate person to carry out the RTWC role, one perceived that good communication skills and knowledge of orthopaedics were key. Another perceived it as an administrative role with back-up from the HOT. The other believed that therapists were more suited as they had the skill set to advise on work modifications.
Two senior members of nursing staff, from two study sites, were interviewed. One interviewee received face-to-face training from their PI, which they perceived positively. The other interviewee had not received any training and felt that they knew little about OPAL.
One interviewee was unaware of the RTWC at their site. The other knew the individual, but seemed uncertain about their role. Both were aware of the patient workbook but only one had seen it. This nurse reported advising patients about its completion and taking it to appointments. One nurse had seen patients completing the workbook in hospital rather than prior to admission.
One nurse believed that OPAL promoted discussions about RTW and reassured patients that their RTW was important. The other interviewee reported less involvement with the delivery of the study and felt that it had not changed their practice. The interviewee who had seen the workbook viewed it positively.
One interviewee believed that OPAL resulted in more patients being offered a fit note. This interviewee believed that the hospital should be supporting patients to return to work and that the process had been successful. The other interviewee felt that the OPAL information could be delivered by a nurse, but that patients preferred to get direction from the hospital consultant.
The intention was to interview two GPs of patients recruited to the feasibility study; however, there was no response from those contacted, despite reminders being sent.
Assessment of feasibility data
The participants in the feasibility phase were similar to those in the cohort phase; participant characteristics, job titles and details of the activities relating to their jobs can be found in Appendix 9. The flow of participants through the feasibility study is shown in Figure 17. The average questionnaire return rate was 69.6% (see Appendix 9).
Interaction with the intervention
At baseline, most participants completed the occupational checklist prior to their appointment with the surgical team and stated that it was referred to during their consolation (76.9% for both); on average, it took 10.7 minutes to complete. Twenty-two (84.6%) participants talked about their job when discussing the options for treatment, 23 (88.5%) stated that a surgical team member mentioned the OPAL programme, but only 18 (69.2%) discussed how and when they might return to work. All but one of the participants had the OPAL programme explained to them. These results suggest that the initial introduction to the OPAL programme was implemented.
By contrast, only two participants stated that they had contacted the RTWC by telephone following their operation (4.8% of those followed up), and two had used the website. Seventeen of the eighteen (94%) responders at 8 weeks had completed the workbook. Patients took an average of 38.6 minutes to complete the workbook (range 5–90 minutes). Twelve of the 18 (66.7%) participants found the workbook helpful, and nine (50.0%) said that it helped them to develop a RTW plan. Full details can be found in Appendix 9.
Returning to work
At 8 weeks, 7 of the 17 responders had returned to work. At 16 weeks, a further three participants had returned to work. Overall, 38.5% (10/26) of the participants in the feasibility phase stated that they had returned to work; however, 26.9% of the participants (including those who were not followed up) provided no data for this question. Of the returnees, there were five hip and five knee replacement patients.
The average return time was 7.4 weeks (ranging from 0.6 to 17.7 weeks) (Figure 18). This was approximately 2.6 weeks on average earlier than in the cohort phase; however, it should be noted that the sample size here was significantly smaller than in the phase 1 cohort study. There was a difference in return times for the two types of operation, with hip patients returning on average 5.2 weeks after surgery, compared with 9.7 weeks for knee patients. Of those who returned to work, seven (70.0%) did so with reduced hours, on average reducing to 13.7 hours in their first week back at work (ranging from 6 to 20 hours). Full details can be found in Appendix 9.
FIGURE 18.
Bar chart of time to RTW after surgery for the participants in the feasibility study.
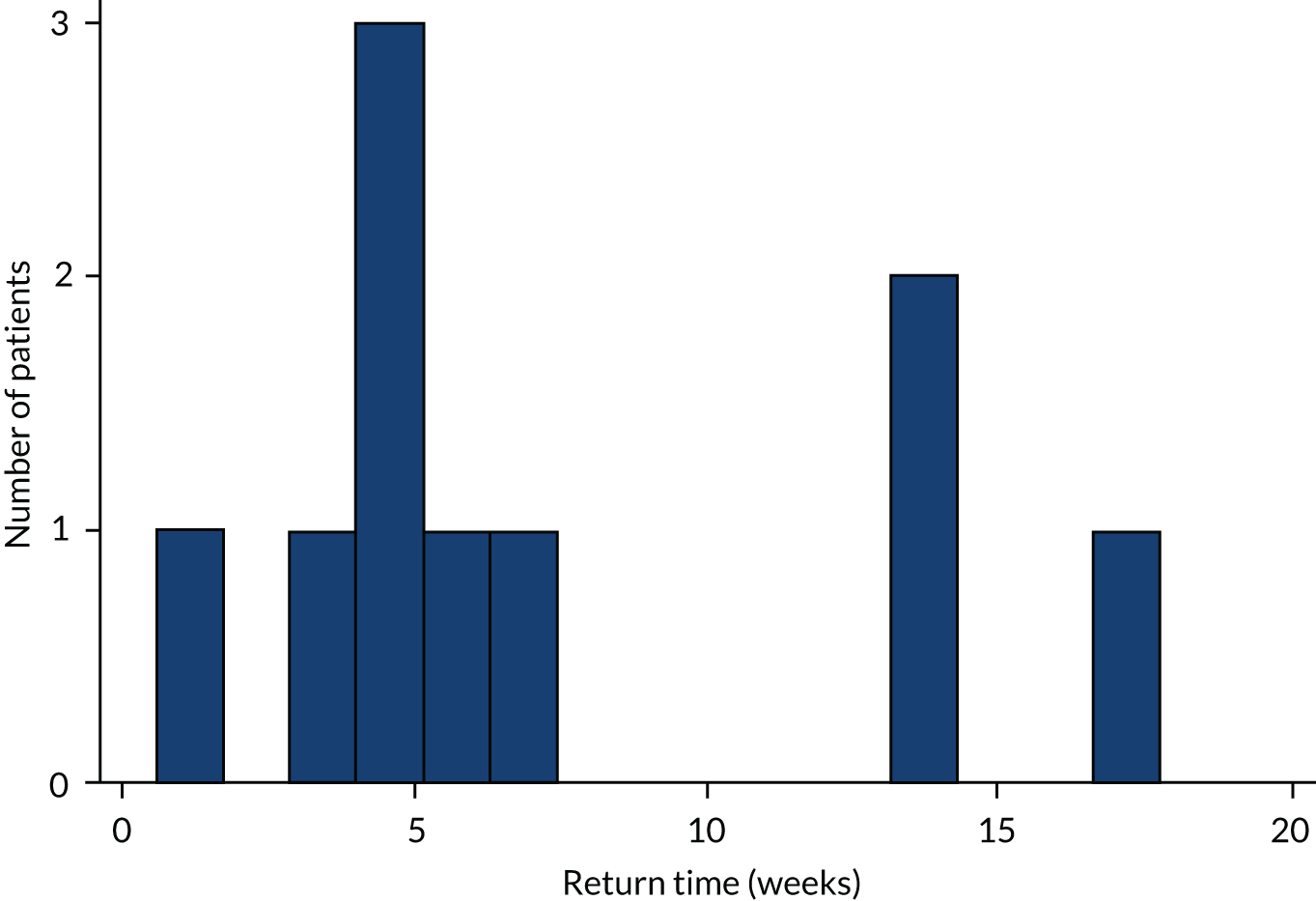
Fit notes
On average, participants requested 1.6 (range 1–3) additional fit notes after discharge. The average length of fit notes reported at 8 weeks was 6.1 weeks (ranging from 0 to 12 weeks) (see Appendix 9).
Oxford Hip and Knee Scores
At baseline, the average OHS and OKS were 17.4 and 17.3, respectively; this was comparable to the phase 1 cohort study. This increased to 35.6 for hip participants and 29.2 for knee participants 8 weeks post surgery, and to 43.0 for hip and 29.4 for knee participants at week 16. These follow-up results were similar to those in the phase 1 cohort (see Appendix 9).
Work Limitations Questionnaire
As in the initial cohort study, participants completed the Work Limitations Questionnaire135,153–155 at each time point, to indicate time lost at work. At baseline, there was an average of 41.4% time loss due to their joint problems; this decreased to 23.1% at week 8 and 17.6% at week 16. These results are similar to those seen in the phase 1 cohort (39.4%, 16.8% and 16.8% across the corresponding time points).
Self-efficacy
The General Self-Efficacy Scale156 was included in the feasibility phase baseline questionnaire. This was included on the advice of Trial Steering Committee members as it was a variable felt to be important that we failed to collect in the phase 1 cohort study. This scale ranges between 10 and 40, with higher scores indicating higher self-efficacy. The participants had an average score of 32.6 (range 22–40), implying good self-efficacy; the full results can be found in Appendix 9.
Readiness to return to work
The Readiness to Return to Work Scale157 was included in the follow-up questionnaires. This scale has two sections: one for those already back at work (13 questions) and one for those who are not yet there (nine questions). The scale asks participants to indicate how well they agree with a selection of statements, from ‘strongly disagree’ to ‘strongly agree’, and they are scored on a five-point Likert scale. Full results can be found in Appendix 9. In the case of those not back at work, the results indicated that participants wanted to get back to work, thought that it was possible and were working towards achieving it. At week 8, 50% of the respondents stated that they did not think that they were ready to go back to work, and 40% had not yet set a date for their return. Of those who had returned to work, the responses indicated that they were working towards staying at work, had found strategies to make it possible to be at work and were not concerned about having to take more time off.
Assessment of economic data
Health-care resource use and EQ-5D data were collected, with the items used being the same as those collected during phase 1. The findings are summarised in Appendix 9, separated according to whether the resource utilisation was in relation to participants’ joint replacement or for ‘another reason’. The intervention was costed using information from the RTWCs involved in the intervention and also using the cost of training and printing of the materials.
Return-to-work co-ordinator time and intervention costs
Information recorded by the three RTWCs detailed the individual tasks undertaken as part of their role. Costs were attached to the average total time spent on these tasks, to generate an average cost per participant of £52.87. This was based on the RTWC spending 1.01 hours per participant, on average, costed at £53.24 per hour of RTWC time (using details of the RTWC’s bands, with their associated salaries, sourced from PSSRU Unit Costs of Health and Social Care 2018;140 see Appendix 9).
In addition, the RTWC training cost associated with the intervention (£10.91) was incorporated, based on the cost of the RTWC for 1 day of their time (using the costs outlined in Appendix 9) and a trainer for 1.5 days (1 day at a training event plus 0.5 days of preparation time) (i.e. a total cost of £2181, divided by the number of individuals they would be likely to work with over 12 months, which was assumed to be 50 for each RTWC). The cost of printing the intervention materials (£6.37 per participant; see Appendix 9) was also estimated. The resulting estimated total cost of the intervention was £70.52 per participant.
Resource use and total costs
Summaries of participants’ resource use and the average costs for each item of resource use can be found in Appendix 9. Regarding health-care utilisation in relation to participants’ joint replacement, the key cost drivers were inpatient hospital stay and outpatient attendances. Knee participants encountered greater use of physiotherapist services and day-case visits. There were low levels of utilisation for ‘another reason’, with costs predominantly arising for occupational therapy visits and, to a lesser extent, for visiting a general practice nurse.
Productivity loss
Absenteeism was estimated using the number of days missed from work. This was based on the reported RTW date. Costs were attached to the missed workdays, for the 10 participants who returned to work, to generate a mean cost per participant attributable to productivity loss over the period following surgery. This average cost of days missed from work was found to be £5929 (SD £4388) per participant, with a large degree of variability between participants in their productivity losses (range £455–14,111). The mean cost was higher for knee replacement participants (£7738, SD £4521) than for hip replacement participants (£4120, SD £3833).
Health-related quality of life
All participants completed the EQ-5D questions at baseline, with completion rates falling to 70% and 63% at 8 weeks, and to 60% and 50% at 16 weeks, for hip and knee replacement participants, respectively (see Appendix 9). Mean utility scores and EQ VAS scores increased over time for hip and knee replacement participants. The proportion of hip replacement participants who reported any problems decreased with time, from baseline to 16 weeks, for all five dimensions. For knee replacement participants, however, the proportion reporting problems increased at 16 weeks for mobility and self-care, and remained the same as at 8 weeks for pain/discomfort.
Chapter 11 Discussion and conclusion
Overview
To our knowledge, the OPAL study was the first such research study to develop a tailored, occupational advice intervention to be delivered in the UK NHS to patients returning to work after hip or knee replacement surgery. The feasibility of delivering the developed intervention alongside usual-care pathways was subsequently tested. The study methodology allowed the OPAL investigators to collect a wide variety of data and perspectives across a number of NHS sites. It provided pertinent information about the target population and delivery of usual care, and explored outcomes of importance for this patient group, in keeping with the objectives defined at the beginning of the study (see Chapter 1, Objectives). In this section, the main findings of the study are summarised and discussed in the context of relevant published literature, and, based on the findings of the study, recommendations are made for further research.
Intervention mapping methodology
The IM approach proved complex and time-intensive, but did support the development of a clearly justified and structured intervention.
Several studies have reflected that IM is time- and resource-consuming. 66,69,158,159 Wolfers et al. 160 recommend a more flexible application of the method to make it more applicable in practice. Meng et al. 161 employed a ‘modified’ approach to IM, using ‘action plans’ as ‘a more practically feasible alternative to the matrices of change objectives’, which have been highlighted as particularly time-consuming by McEachen et al. 159 However, the main challenge reported when applying IM is the implementation of the action plans developed with this methodology.
OPAL experienced similar challenges with implementation (IM stage 5), particularly in the context of a feasibility study (IM stage 6). In stages 2–4, the investigators developed the performance and change objectives, methods, applications and materials for delivering the occupational advice intervention in a hospital setting. However, in the context of a research setting, these were not always appropriate as there was overlap in the tasks related to ‘intervention activity’ (as laid out in the POs) and ‘research activity’ (as required to fulfil ethics requirements). For example, in delivering the occupational advice intervention, the identification of RTW patients would have been the role of the outpatient clinic team, whereas in the feasibility study this was undertaken by a research nurse. Other implementation issues included the complexity of training a range of staff in several different processes, in a short space of time, to deliver the intervention to a very small number of patients. These issues are discussed further in Strengths and limitations.
In OPAL, it became clear that the occupational advice intervention could address outcomes based at only the individual and interpersonal levels of the ecological model; it could not address outcomes based at organisational, community or societal levels. For example, it could not address NHS commissioning or primary care practice. It could not directly influence employer or workplace practice; however, it had the potential to indirectly make changes at these levels driven by changes in the individuals’ (employees’) behaviour. In their systematic review, Fassier et al. 63 concluded that IM is not a ‘magic panacea to prevent theory and/or implementation failures of work disability prevention interventions’. They have suggested that the limited number of effective interventions in work disability prevention indicates that IM needs to be adapted to reflect the complex interaction between health care and the workplace. They also recommend exploring the value of the use of alternative paradigms to RCTs in the evaluation of interventions in this field, such as the theory-driven realist evaluation approach. 162 Given the complexity of the health-care setting, as well as the complexity of the intervention, evaluation methods that are sensitive to the adaptation of interventions in different health-care settings may be most appropriate,163,164 such as the use of dynamic logic models. 165
Given the complexity of the IM approach, the study might have benefited from a greater number of ‘participatory planning group’ meetings. At times, the amount of information generated, particularly in IM stage 1, was overwhelming. Having three different teams based at different locations leading on complementary aspects of this stage (cohort study and survey: South Tees; evidence synthesis: University of York; patient and stakeholder interviews and IM approach: University of Nottingham) added to the complexities of project management, and facilitating greater communication between the research teams may have made the overall process easier.
Future research
Is a future clinical trial feasible?
The feasibility study demonstrated that it was possible to collect relevant data to answer the research question and that an economic analysis could be conducted alongside a future definitive trial. The OPAL study has defined and clarified the following key components for a future trial.
Population
Information collected about patients returning to work after hip or knee replacement defined the target population for a future randomised control trial. The cohort study, structured interviews, evidence synthesis, Delphi consensus process and feasibility study provided information that allowed this population to be characterised and their needs assessed, and barriers to and facilitators of RTW after surgery to be defined. The findings confirmed that this population had varied and complex needs, which supported the use of an individualised approach to managing their RTW. Information collected from key stakeholders (employers, surgeons, AHPs, nurses and GPs) generated a more complete picture of this patient group. These interviews demonstrated that health-care teams and workplaces may not be prepared to, or understand how to, facilitate their patients’/employees’ RTW after surgery. The information generated has supplemented the previous literature20–49 to further define the target population that would benefit from an occupational advice intervention.
Intervention
An intervention was developed that addressed the key aspects of the commissioning brief; that is, it was based in hospital, started prior to surgery, was individualised, provided target support, was proactive and was designed in a pragmatic fashion to support delivery alongside routine care in an NHS setting. The intervention was designed using an iterative process using the IM approach,55–59 which allowed the OPAL investigators to revisit, revise and adapt the intervention as new information became available.
The intervention had a strong theoretical background and was underpinned by biopsychosocial models that supported behaviour change in the target groups (patients and stakeholders in the RTW process). It was manualised as a set of patient and staff POs that defined its content, format, delivery and timing while maintaining pragmatism in the ability for participating sites to administer the intervention alongside standard care. Central to the intervention was the development of an interactive patient workbook that supported the self-directed development of a RTW plan, similar to other recently developed RTW interventions. 166 Implementation during the feasibility stage highlighted specific issues relating to the introduction of a complex intervention. The OPAL intervention was generally well received by patients and stakeholders: positive feedback was received throughout and the developed study materials were reported to be informative and helpful. There was good evidence from the completed patient workbooks that the intervention supported individualised care and, through the development of a RTW plan, acted as a decision aid167–170 enabling shared decision-making in line with best practice. 171,172 The intervention also shared many of the characteristics of the occupational advice interventions identified in the rapid evidence synthesis, including advice about job accommodation; mechanisms to support workplace visits and contact with the employer; education and advice; counselling and guidance through the RTWC; and involvement of the multidisciplinary team.
Furthermore, the OPAL intervention has similarities to another recently tested occupational advice intervention. 166 Grunfeld et al. 166 recently reported on the feasibility and acceptability of a theoretically led workbook intervention designed to support patients with cancer returning to work and confirmed the feasibility of undertaking a definitive trial in this setting.
There is some overlap between the content of the written materials developed in OPAL and those available through the Royal College of Surgeons of England website (example at www.rcseng.ac.uk/patients/recovering-from-surgery/total-hip-replacement/returning-to-work; accessed 26 May 2020). The Royal College of Surgeons of England provides generic written resources covering recovery after both hip and knee replacement. Within these are sections providing information about RTW and timelined guides for recovery after surgery. Because they are designed for all patients, they do not provide the level of detail available in OPAL and cannot provide the individualised support that our phase 1 interviews suggest is needed. The structure, format and delivery of the OPAL intervention has been specifically designed to empower patients to take responsibility for their RTW and provides tools for them to develop an individualised RTW plan. It also encourages active engagement with employers and health-care teams via the OPAL booklets and RTWC role.
Comparison
Usual care that would be the comparator in a future definitive trial was evaluated in the cohort study, patient and stakeholder interviews and survey of practice. This demonstrated a haphazard approach to the delivery of RTW information and significant variation in the way preoperative services were configured. Most patients received little or no information about RTW from their HOT or GP, and only one-third of patients had access to occupational health support at work. These findings were counter to best practice as defined by NICE guideline 138171 and NICE quality standard 15172 (patient experience), which describe the need to ensure that ‘patients experience care that is tailored to their needs and personal preferences, taking into account their circumstances, their ability to access services and their coexisting conditions’ (© NICE 2012. Patient Experience in Adult NHS Services. 172 Available from www.nice.org.uk/guidance/qs15. All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication). Many patients did not have workplace contact until they returned to work. Despite this, a significant proportion of patients felt that current care was sufficient. This may reflect the fact that they returned to work (if they returned to work, this was seen as success) rather than any indication of the quality or timing of their RTW.
Outcome
The measurement of RTW is complex and the evidence synthesis demonstrated that there is currently no standardised method of recording it. Different approaches to measuring RTW were explored during the Delphi process and suggested that a number of complementary measures are needed. Dichotomous recording of work status is blunt and does not address important aspects of behaviour, such as how patients return, use of phased and adapted returns, timing of RTW and secondary sickness absence. Measures such as the Work Limitations Questionnaire135,153–155 and Readiness to Return to Work Scale157 were assessed during the feasibility stage. They provided useful information about time lost at work and information about where patients felt they were in their RTW process.
Study delivery and design
Approximately one-quarter of patients approached for the cohort and feasibility studies were eligible for inclusion, and consent rates for eligible patients were > 80%. This suggests that there are substantial numbers of patients willing to participate in research examining RTW after hip or knee replacement. The response rates for the questionnaires, which reduced with extended follow-up as participants returned to work, highlight a need to put additional efforts into improving the proportion of participants who return questionnaires.
The utility and resource use measures that were included in the questionnaires appear to have been appropriate for the purpose of collecting the health-related quality-of-life and cost data that fed into the economic analysis. The responses to such resource use and EQ-5D questions can be used to inform and improve the design of questionnaires in future research. For instance, participants reported that they had minimal or zero resource use for some items, which could be considered for removal from future questionnaires in order to reduce questionnaire completion burden for participants. Mean utility scores and EQ VAS scores increased over time, in line with what would be expected, which supports the face validity of using the EQ-5D measure.
Health-care resource use was broadly similar for the cohort and feasibility participants, with common key cost drivers; the most notable cost difference was for knee replacement participants over the period of baseline to 8 weeks, when the costs associated with inpatient stay and day-case visits were higher for cohort participants than for those in the feasibility study (who received the intervention). The cost associated with productivity loss following surgery was lower for the feasibility participants (£5929 per feasibility participant vs. £7983 per cohort participant). This cost saving has the potential to offset the cost associated with the intervention and the difference in health-care resource utilisation. It should be noted that, because there were only a small number of participants in the feasibility element, and the feasibility and cohort groups were not randomised to facilitate meaningful comparisons, firm conclusions could not be drawn here. However, a definitive trial would enable robust conclusions to be made regarding the cost-effectiveness of the RTW intervention.
The cost of training, which fed into the intervention cost (as part of the feasibility study), was based on the time spent by the RTWCs at the participating sites. It is acknowledged that this is a simplification of the costs involved, but owing to the variation in training across the sites and additional data not being available, the RTWC time was the focus for the training cost. As part of a definitive trial, more detailed information could be collected in order to estimate the training cost more accurately.
Other research recommendations
There are a number of opportunities for further research. Further research to define the optimal method of implementing the OPAL intervention would be essential before the intervention is formally tested in a RCT (see further discussion in Strengths and limitations).
Additional research could focus on how the intervention might integrate with primary care. This could allow RTW planning to start earlier and may provide support to additional patients seeking to remain in work who have symptomatic osteoarthritis below the threshold requiring joint replacement. If proven to be effective in a definitive trial, there is also the potential to investigate how the OPAL intervention could be implemented in other elective orthopaedic surgery and other surgical specialties undertaking planned surgical procedures. A significant proportion of the developed intervention has transferable content and the needs assessment conducted in OPAL is likely to be generalisable more widely to other specialties and settings, making this an important area for future research.
Strengths and limitations
Intervention mapping stages 1–4
Because our evidence synthesis followed rapid review methodology, there was a restriction on the range of databases that were searched. However, our searches were undertaken by an experienced information specialist in order to capture the most relevant databases, given this restriction. Preliminary results from the rapid evidence synthesis found only four papers for the elective surgery population. This finding was discussed with the Trial Steering Committee, which advised including the musculoskeletal literature even though this included patients with a range of chronic musculoskeletal conditions, not representative of our target population. This approach yielded useful results that were applicable to our hip and knee replacement patients.
We were initially unable to set up the cohort study within the planned time scales in the three originally proposed sites. To mitigate issues posed by the delays, we opened an additional site, which helped achieve our target recruitment and provided additional support during the feasibility study. Despite approaching all hip and knee replacement patients awaiting surgery at the study sites, we were able to identify only six patients intending to retire after surgery; this was a group we intended to examine. As a consequence, this part of the analysis was not carried out. Interestingly, 10% (n = 9) of patients at the 8-week follow-up stated that they no longer intended to return to work. It may be that these patients intended to retire after surgery but, for reasons that are unclear, did not state this during the baseline assessment.
The cohort study followed all patients until 16 weeks post surgery and a subset of patients for 24 weeks. Only 50% (n = 78) returned to work within the follow-up period. Extended follow-up studies have shown improvements in the observed rates of RTW;44,45 however, we were restricted by the study duration. Extended follow-up would be useful as part of a larger trial as it could evaluate other complementary aspects of RTW. These include evaluating RTW over time to understand whether or not it was sustained, periods of secondary sickness absence and whether or not patients returning to work on phased or adapted returns get back to full duties and the time frame for this. The study participant group included only a small number of black and minority ethnic patients. Their views and experiences were therefore not adequately represented in the cohort, patient interviews and feasibility testing, and the findings of these elements may not be generalisable to these patient groups. Consideration needs to be given to how black and minority ethnic patients are represented in a future trial.
Follow-up rates for the cohort study were 75% (n = 104) at 16 weeks and were lower at other time points. Similar issues with follow-up and dropout were observed during the feasibility study. Once patients had returned to work, they disengaged with follow-up procedures, instead seeming to focus on their work role. This may be a specific issue when conducting research on working patients who are possibly least likely to have time to participate in research and needs to be considered when designing a future study. We had initially hoped to use data to stratify patients into high and low risk of failed RTW as part of a tiered intervention. However, the failure to identify predictors, alongside the results from the Delphi consensus group and advice from the Trial Steering Committee, led us to design an intervention for everyone. The advantage of this approach was that the intervention was available for all patients, allowing engagement based on their individual need (described in Chapter 9).
The interviews demonstrated that current ‘usual care’ was frequently not following best practice in relation to the use of workplace adjustments and partial RTW, and the use of the fit note to advise on this. This suggests that there is room for improvement in how patients are supported in returning to work. Unfortunately, we were able to interview only a small number of self-employed patients. This meant that we were unable to provide a comprehensive commentary on the needs and behaviour of this group and to investigate whether or not they behave differently to those in other types of employment (e.g. because of lack of sick pay, pressure to get back to work sooner than employed patients, more options for workplace adaption and phased returns for employed people). Recruiting employers and GPs to interview was difficult. However, using a variety of strategies,173 we were able to achieve the recruitment required in IM stage 1, although we were unable to replicate this in the feasibility study. Whether or not interviews are conducted on a group or one-to-one basis is likely to change the dynamics of the interaction between researchers and participants. This may have influenced the nature of clinicians’ contributions and the data collected, and may thus be a limitation of the study.
Overall participation in the Delphi consensus process decreased from round 1 to round 3. Attrition through the Delphi process is well recognised;151,174 hence, various strategies were employed that were known to enhance response rates. 175,176 By round 3, fewer than 20% of our invited participants remained, and employers and GPs were poorly represented in the final two rounds. Round 3 responses comprised feedback from only one employer and one GP. To mitigate the potential response bias introduced by a stakeholder group being not represented,177 an employer representative (Unison, London, UK) was approached, who provided structured feedback on the intervention outside the Delphi process. This information was used alongside the comments from other participants to finalise the intervention prior to feasibility testing.
Intervention mapping stages 5 and 6
OPAL is a complex intervention that required considerable planning for its implementation and sufficient time to put in place the facilitators to embed it into practice and to remove potential barriers to its effectiveness. 178 Having developed the intervention using the IM framework, it was extremely challenging to effectively implement it within the time scale of the feasibility study. For it to be successfully embedded at each site, there was a need to involve all members of the HOT. However, in reality, owing to the limited time available for implementation and feasibility, it was difficult to train all staff and implement the intervention as intended. Consequently, some staff had no training or did not receive the training as intended.
The feasibility study suggested that patient experience of the intervention was positive and there was high adherence to the patient POs. However, some of the staff POs showed lower adherence. This may reflect that data sources were unable to ascertain if these POs had been adhered to but also may reflect the challenges of incorporating new behaviours and procedures into current health-care professional roles. It suggested that some of the implementation processes presented challenges and barriers to effective adoption. For future implementation and research studies, these barriers to implementation could be viewed within the Consolidated Framework for Implementation Research,179 which could help with understanding and overcoming them.
Throughout OPAL, and particularly in the Delphi study, we found evidence of reluctance among health-care professionals to take on the role of the provider of occupational advice: an ‘anyone but me’ attitude. This reluctance suggests that sufficient time needs to be provided to change the attitudes, norms and behaviours necessary to embed the roles and responsibilities for occupational advice in the OPAL intervention. Disappointingly, we were unable to interview GPs and therapy team members during the feasibility stage, which might have provided greater detail about their attitudes towards the OPAL intervention and might help to identify potential improvements. Time is also needed to prepare patients’ expectations with respect to the provision of RTW advice as part of routine health care.
The RTWC role was not fulfilled in all settings in the way we had expected. It is a key role in the OPAL intervention, delivering or facilitating a number of the POs. It would take a considerable time for someone to adapt and learn the competencies required for this role unless they had been recruited to specifically fulfil the required criteria for the role. There were contrasting experiences of the recruitment of the RTWCs. In one centre, there was uncertainty about whether or not funding was available to backfill posts, meaning that the local team found it difficult to predict how much time and resource would be required. By contrast, at another centre an experienced and enthusiastic senior nurse with a background in patient experience could be identified. Interviews suggested that some RTWCs accepted the role with reluctance. RTWCs were also required to be good clinical practice trained because the role was in the context of a research study, causing delays in their appointment. The feasibility study demonstrated that some members of staff were not fully committed to the intervention. However, evidence from the feasibility interviews suggested that if the occupational advice intervention were to be an agreed and funded component of routine treatment, a greater level of acceptance and adherence to delivery would be expected.
During the feasibility study, some of the trained staff rotated to other departments (junior doctors and AHPs), and others went on leave. This highlighted the need for ongoing training if the intervention was to become embedded and sustained in a department. In addition, some departments (e.g. outpatient departments) were reluctant to take on additional duties as they were already ‘overstretched’.
The barriers described above relate to the ‘readiness for implementations’ in the inner settings constructs of the Consolidated Framework for Implementation Research,179 suggesting that increased commitment and engagement among staff need to be ensured prior to implementation of the OPAL intervention. Given the time scales for implementation in the feasibility study, it is not surprising that the intervention was not fully embedded and that there were signs of a lack of commitment, resource issues and lack of awareness in some teams. However, these are all factors relating to the inner setting for implementation that could be improved on for a larger trial or full adoption of the intervention in a service. There was also variation among patients in understanding and perception of the aims of the OPAL intervention, which suggests that the intervention may need to be presented more clearly. This links into the Consolidated Framework for Implementation Research179 concept of intervention design quality and packaging, and is an area for further consideration beyond the OPAL study.
In hindsight, it may have been beneficial to pause the project after IM stage 4 once the final intervention had been drafted. This would have allowed time to develop a more robust implementation strategy that provided the necessary training and support to deliver individual, organisational and cultural change in the local orthopaedic teams. However, this was not an option given the protocol and the need to make recommendations about the feasibility of a future clinical trial as per the original commissioning brief. Other studies have similarly reported difficulties with applying IM stage 5. In a systematic review of interventions to prevent work disability developed using an IM approach,63 reviewers were unable to report the IM stage 5 outcomes because they were insufficiently reported in the studies they reviewed.
It is important to consider how a future study would evaluate the cost-effectiveness of a RTW intervention in terms of the study design and data collection considerations. The OPAL study found challenges around obtaining accurate cost information (e.g. cost of training) and achieving sufficient participant numbers to allow meaningful conclusions around the cost-effectiveness findings. Rather than the feasibility and cohort groups that were summarised here, a future definitive study should aim to randomise participants using a robust RCT design to enable a full comparison to be made.
The final intervention
The feasibility study and Delphi round 3 provided an opportunity for patients and stakeholders to comment on the intervention. Based on this feedback, the intervention will be further refined and updated. However, this has not yet happened as the follow-up for the feasibility study closed on 22 March 2019.
In the developed intervention, all patient and staff POs were equally important. Further review of the intervention may reveal key core POs that are essential to delivery and could define the essence of OPAL with supplementary peripheral POs that could be more flexibly delivered. This approach may further support adoption and ‘scaling up’ as teams have the ability to adapt the intervention so that it is fit for purpose in their own clinical settings. This fits with the approach already taken not to be overly prescriptive about the intervention and to allow pragmatism in delivery.
Content and format issues have also been identified, including the need to adapt the workbooks to include information for patients undergoing partial knee replacement procedures, requiring further detail on returning to driving and insurance after surgery, and further information for self-employed patients to make the workbooks more relevant for this group. The feasibility interview participants expressed some disappointment that their expectations around OPAL were not met/achieved or that they did not fully understand its purpose. This finding will also need to be addressed to provide clarity across the intervention and associated patient-facing materials.
Currently, a number of NHS patients are treated in the private sector. These patients are more likely to be younger and fitter and less likely to be obese;22,23 therefore, a greater proportion of patients than observed in this study could be expected to be working at the time of surgery. Furthermore, they often do not have to wait as long for surgery. Although it would have been beneficial to assess this patient group, it was not possible because of the challenges of conducting research in the private sector due to a lack of research infrastructure and research delivery support. We could not establish whether or not the needs or behaviours of this patient group differ from those of the observed NHS cohort. However, the OPAL intervention was designed to support delivery across a range of NHS settings and it is sympathetic to the variations in practice inherent in the NHS. Therefore, we feel confident that it should be possible to translate the intervention to patients having surgery in the private sector once its effectiveness has been established with further research.
Conclusions
OPAL had two key objectives: (1) to develop a multidisciplinary occupational advice intervention for working adults undergoing primary, elective, hip and knee replacement, and (2) to assess the delivery of the intervention and make recommendations about its further evaluation in a clinical trial. Both of these objectives were met. An IM approach was used to develop the RTW intervention and a series of methodologies were employed to underpin the development of the intervention and to test its feasibility clinically.
The OPAL intervention developed is an individualised RTW plan that is tailored to patients’ needs and involves them in decisions about their care, which supports best practice. 171,172 It was feasible to deliver the OPAL intervention with high levels of fidelity in current NHS care settings, although further preparatory research on implementation is still required. The effectiveness and cost-effectiveness of the OPAL intervention then needs to be formally tested in a definitive multicentre pragmatic RCT. Further research is warranted given that there are currently between 40,000 and 50,000 patients who might be eligible for a RTW intervention every year in the UK18,180 who could potentially benefit from the OPAL intervention.
Acknowledgements
We are very grateful for the assistance of Kath Wright (Centre for Reviews and Dissemination, University of York), who had an important role in defining the search strategies and conducted the searches for the rapid evidence synthesis; Dr Arabella Scantlebury, for undertaking the checking of the qualitative studies; and Dr Louise Gascoine, for study selection, checking the quality assessment of the RCTs and checking data extraction.
We acknowledge the contribution of Reece Walker (Research Data Assistant at South Tees Hospitals NHS Foundation Trust), who administered the survey of practice and Delphi consensus process and facilitated follow-up data collection and checking for the cohort study; and Amanda Goodman (South Tees), who provided administrative support for the project and arranged investigator and Trial Steering Committee meetings.
We acknowledge the help and support of Christine Markham, who provided guidance and assistance throughout the IM process.
We would like to thank the NJR PPI group, the BOA Patient Liaison Group and the South Tees Hospitals NHS Foundation Trust patient involvement group for their support and assistance.
The Trial Steering Committee comprised Professor Paul Gregg (Orthopaedic Surgeon and Chairperson), Professor Nadine Foster (Trial Methodologist and Physiotherapist), Dr Henry Waters [Commissioner and GP (Retired)], Dr Brian Blacklidge (GP) and Jo Fox (patient).
Contributions of authors
Paul Baker (https://orcid.org/0000-0001-8529-2417) contributed to the conception, design and delivery of the overall project, supervised the project as chief investigator and had specific responsibility for the cohort study, survey of practice, intervention development and feasibility study. He drafted the report.
Carol Coole (https://orcid.org/0000-0003-4147-5398) contributed to the conception, design and delivery of the overall project, led the IM process and led on the collection and analysis of qualitative data throughout the study. She drafted the report.
Avril Drummond (https://orcid.org/0000-0003-1220-8354) contributed to the conception, design and delivery of the overall project, and had specific responsibility for the patient and stakeholder interviews and Delphi consensus process. She commented on drafts of the report.
Sayeed Khan (https://orcid.org/0000-0002-9388-7063) contributed to the conception, design and delivery of the overall project, and had specific responsibility for employer engagement. He commented on drafts of the report.
Catriona McDaid (https://orcid.org/0000-0002-3751-7260) contributed to the conception, design and delivery of the overall project, and supervised the rapid evidence synthesis. She commented on drafts of the report.
Catherine Hewitt (https://orcid.org/0000-0002-0415-3536) contributed to the conception, design and delivery of the overall project, and supervised the statistical analysis of the cohort study and feasibility study. She commented on drafts of the report.
Lucksy Kottam (https://orcid.org/0000-0002-7976-2416) contributed to the design and delivery of the overall project, supervised all ethics requests and PPI engagement, and contributed to the cohort study, Delphi consensus process, survey of practice, intervention development and feasibility study. She drafted the report.
Sarah Ronaldson (https://orcid.org/0000-0001-8321-786X) contributed to the design and delivery of the overall project, performed the health economic evaluation and rapid evidence synthesis and contributed to the statistical analyses for the cohort study. She drafted the report.
Elizabeth Coleman (https://orcid.org/0000-0003-4210-1865) contributed to the delivery of the overall project, and performed the statistical analyses for the cohort study and feasibility study. She drafted the report.
David A McDonald (https://orcid.org/0000-0002-9805-7720) contributed to the design and delivery of the overall project, and contributed to the cohort study, survey of practice and feasibility study. He commented on drafts of the report.
Fiona Nouri (https://orcid.org/0000-0003-4151-1512) contributed to the delivery of the overall project, and to the IM process and the collection and analysis of qualitative data throughout the study. She commented on drafts of the report.
Melanie Narayanasamy (https://orcid.org/0000-0003-3483-0777) contributed to the delivery of the overall project, and to the IM process and the collection and analysis of qualitative data in phase 1 of the study.
Iain McNamara (https://orcid.org/0000-0002-2051-8451) contributed to the design and delivery of the overall project, and to the cohort study and survey of practice. He commented on drafts of the report.
Judith Fitch (https://orcid.org/0000-0002-6687-5200) contributed to the design of the overall project and facilitated PPI engagement. She commented on drafts of the report.
Louise Thomson (https://orcid.org/0000-0003-1736-7506) contributed to the design and delivery of the overall project, and to the intervention development and feasibility study. She drafted the report.
Gerry Richardson (https://orcid.org/0000-0002-2360-4566) contributed to the design and delivery of the overall project, and supervised the health economic evaluation. He commented on drafts of the report.
Amar Rangan (https://orcid.org/0000-0002-5452-8578) contributed to the conception, design and delivery of the overall project, supervised the Delphi consensus process and contributed to the intervention development. He drafted the report.
Publications
Baker P, Coole C, Drummond A, McDaid C, Khan S, Thomson L, et al. Development of an occupational advice intervention for patients undergoing lower limb arthroplasty (the OPAL study). BMC Health Serv Res 2018;18:504.
Drummond A, Nouri F, Narayanasamy M, Coole C, Baker P, Khan S. Engaging workplace representatives in research: what recruitment strategies work best? Occup Med 2018;68:282–5.
Coole C, Nouri F, Narayanasamy M, Baker P, Drummond A. Total hip and knee replacement and return to work: clinicians' perspectives [published online ahead of print August 23 2019]. Disabil Rehabil 2019.
Nouri F, Coole C, Narayanasamy M, Baker P, Khan S, Drummond A. Managing employees undergoing total hip and knee replacement: experiences of workplace representatives. J Occup Rehabil 2019;29:451–61.
Baker P, Kottam L, Coole C, Drummond A, McDaid C, Rangan A, et al. Development of an occupational advice intervention for patients undergoing elective hip and knee replacement: a Delphi study. BMJ Open 2020;10:e036191.
Coole C, Baker P, McDaid C, Drummond A. Using intervention mapping to develop an occupational advice intervention to aid return to work following hip and knee replacement in the United Kingdom. BMC Health Serv Res 2020;20:523.
Nouri F, Coole C, Baker P, Drummond A. Return to work advice after total hip and knee replacement. Occup Med 2020;70:113–18.
Tsang B, McDonald D, McNamara I, Kottam L, Rangan A, Baker P. National survey of occupational advice for lower limb arthroplasty patients. Occup Med 2020;70:123–6.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Li X, Gignac MA, Anis AH. The indirect costs of arthritis resulting from unemployment, reduced performance, and occupational changes while at work. Med Care 2006;44:304-10. https://doi.org/10.1097/01.mlr.0000204257.25875.04.
- Fautrel B, Hilliquin P, Rozenberg S, Allaert FA, Coste P, Leclerc A, et al. Impact of osteoarthritis: results of a nationwide survey of 10,000 patients consulting for OA. Joint Bone Spine 2005;72:235-40. https://doi.org/10.1016/j.jbspin.2004.08.009.
- Bieleman HJ, Bierma-Zeinstra SM, Oosterveld FG, Reneman MF, Verhagen AP, Groothoff JW. The effect of osteoarthritis of the hip or knee on work participation. J Rheumatol 2011;38:1835-43. https://doi.org/10.3899/jrheum.101210.
- Sharif B, Garner R, Sanmartin C, Flanagan WM, Hennessy D, Marshall DA. Risk of work loss due to illness or disability in patients with osteoarthritis: a population-based cohort study. Rheumatology 2016;55:861-8. https://doi.org/10.1093/rheumatology/kev428.
- Kontio T, Viikari-Juntura E, Solovieva S. To what extent do education and physical work load factors explain occupational differences in disability retirement due to knee OA? A nationwide register-based study in Finland. BMJ Open 2019;8. https://doi.org/10.1136/bmjopen-2018-023057.
- Bhattacharya A. Costs of occupational musculoskeletal disorders (MSDs) in the United States. Int J Ind Ergon 2014;44:448-54. https://doi.org/10.1016/j.ergon.2014.01.008.
- Health and Safety Executive . Lower Limbs: Information for Employees 2018. www.hse.gov.uk/msd/lld/employees.htm (accessed 18 September 2019).
- Health and Safety Executive . Costs to Great Britain of Workplace Injuries and New Cases of Work-Related Ill Health – 2016 17 2018. www.hse.gov.uk/statistics/cost.htm (accessed 18 September 2019).
- Waddell G, Burton KA. Is Work Good for your Health and Well-being?. London: The Stationery Office; 2006.
- Gignac MA, Badley EM, Lacaille D, Cott CC, Adam P, Anis AH. Managing arthritis and employment: making arthritis-related work changes as a means of adaptation. Arthritis Rheum 2004;51:909-16. https://doi.org/10.1002/art.20822.
- O’Brien GE, Feather NT. The relative effects of unemployment and quality of employment on the affect, work values and personal control of adolescents. J Occup Psychol 1990;63:151-65. https://doi.org/10.1111/j.2044-8325.1990.tb00517.x.
- Cook DG, Cummins RO, Bartley MJ, Shaper AG. Health of unemployed middle-aged men in Great Britain. Lancet 1982;1:1290-4. https://doi.org/10.1016/S0140-6736(82)92852-5.
- Linn MW, Sandifer R, Stein S. Effects of unemployment on mental and physical health. Am J Public Health 1985;75:502-6. https://doi.org/10.2105/AJPH.75.5.502.
- Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 2004;86:963-74. https://doi.org/10.2106/00004623-200405000-00012.
- Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. Health related quality of life outcomes after total hip and knee arthroplasties in a community based population. J Rheumatol 2000;27:1745-52.
- Fitzgerald JD, Orav EJ, Lee TH, Marcantonio ER, Poss R, Goldman L, et al. Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum 2004;51:100-9. https://doi.org/10.1002/art.20090.
- Bachmeier CJ, March LM, Cross MJ, Lapsley HM, Tribe KL, Courtenay BG, et al. A comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgery. Osteoarthr Cartil 2001;9:137-46. https://doi.org/10.1053/joca.2000.0369.
- National Joint Registry (NJR) . NJR 15th Annual Report; National Joint Registry for England, Wales, Northern Ireland and the Isle of Man, Surgical Data to 31 December 2017 2018.
- Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 2009;467:2606-12. https://doi.org/10.1007/s11999-009-0834-6.
- Tilbury C, Schaasberg W, Plevier JW, Fiocco M, Nelissen RG, Vliet Vlieland TP. Return to work after total hip and knee arthroplasty: a systematic review. Rheumatology 2014;53:512-25. https://doi.org/10.1093/rheumatology/ket389.
- Kuijer PP, de Beer MJ, Houdijk JH, Frings-Dresen MH. Beneficial and limiting factors affecting return to work after total knee and hip arthroplasty: a systematic review. J Occup Rehabil 2009;19:375-81. https://doi.org/10.1007/s10926-009-9192-1.
- National Joint Registry (NJR) . Knees – Primary Procedures – Patient Characteristics – Age and Gender of Primary Knee Replacement Patients 2018.
- National Joint Registry (NJR) . Hips – Primary Procedures – Patient Characteristics – Age and Gender of Primary Hip Replacement Patients 2018.
- Fit for Work . Fit for Work 2018. https://fitforwork.org/about/ (accessed 18 September 2019).
- Weingarten S, Riedinger MS, Sandhu M, Bowers C, Ellrodt AG, Nunn C, et al. Can practice guidelines safely reduce hospital length of stay? Results from a multicenter interventional study. Am J Med 1998;105:33-40. https://doi.org/10.1016/S0002-9343(98)00129-6.
- Tanavalee A, Jaruwannapong S, Yuktanandana P, Itiravivong P. Early outcomes following minimally invasive total hip arthroplasty using a two-incision approach versus a mini-posterior approach. Hip Int 2006;16:17-22. https://doi.org/10.5301/hip.2008.2460.
- Peak EL, Parvizi J, Ciminiello M, Purtill JJ, Sharkey PF, Hozack WJ, et al. The role of patient restrictions in reducing the prevalence of early dislocation following total hip arthroplasty. A randomized, prospective study. J Bone Joint Surg Am 2005;87:247-53. https://doi.org/10.2106/00004623-200502000-00002.
- Suarez J, Arguelles J, Costales M, Arechaga C, Cabeza F, Vijande M. Factors influencing the return to work of patients after hip replacement and rehabilitation. Arch Phys Med Rehabil 1996;77:269-72. https://doi.org/10.1016/S0003-9993(96)90110-0.
- Nunley RM, Ruh EL, Zhang Q, Della Valle CJ, Engh CA, Berend ME, et al. Do patients return to work after hip arthroplasty surgery. J Arthroplasty 2011;26:92-8.e1. https://doi.org/10.1016/j.arth.2011.03.038.
- Jensen JS, Mathiesen B, Tvede N. Occupational capacity after hip replacement. Acta Orthop Scand 1985;56:135-7. https://doi.org/10.3109/17453678508994338.
- Sarkar M, Billharz E, Wachter N, Kinzi L, Bischoff M. Long-term outcome of secondary joint replacement after acetabular fracture. Eur J Trauma 2001;27:301-8. https://doi.org/10.1007/s00068-001-1157-9.
- Nevitt MC, Epstein WV, Masem M, Murray WR. Work disability before and after total hip arthroplasty. Assessment of effectiveness in reducing disability. Arthritis Rheum 1984;27:410-21. https://doi.org/10.1002/art.1780270408.
- Bohm ER. The effect of total hip arthroplasty on employment. J Arthroplasty 2010;25:15-8. https://doi.org/10.1016/j.arth.2008.11.011.
- Johnsson R, Persson BM. Occupation after hip replacement for arthrosis. Acta Orthop Scand 1986;57:197-200. https://doi.org/10.3109/17453678608994374.
- Visuri T, Koskenvuo M, Lindholm TS. Return to work and working capacity after total hip replacement. Int J Rehabil Res 1987;10:434-8. https://doi.org/10.1097/00004356-198712000-00014.
- Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res 2004;429:239-47. https://doi.org/10.1097/01.blo.0000150127.80647.80.
- Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Patients preferred a mini-posterior THA to a contralateral two-incision THA. Clin Orthop Relat Res 2006;453:156-9. https://doi.org/10.1097/01.blo.0000238858.38992.2d.
- Mobasheri R, Gidwani S, Rosson JW. The effect of total hip replacement on the employment status of patients under the age of 60 years. Ann R Coll Surg Engl 2006;88:131-3. https://doi.org/10.1308/003588406X95129.
- Cowie JG, Turnbull GS, Turnball GS, Ker AM, Breusch SJ. Return to work and sports after total hip replacement. Arch Orthop Trauma Surg 2013;133:695-700. https://doi.org/10.1007/s00402-013-1700-2.
- Lyall H, Ireland J, El-Zebdeh MY. The effect of total knee replacement on employment in patients under 60 years of age. Ann R Coll Surg Engl 2009;91:410-13. https://doi.org/10.1308/003588409X391785.
- Foote JA, Smith HK, Jonas SC, Greenwood R, Weale AE. Return to work following knee arthroplasty. Knee 2010;17:19-22. https://doi.org/10.1016/j.knee.2009.06.001.
- Styron JF, Barsoum WK, Smyth KA, Singer ME. Preoperative predictors of returning to work following primary total knee arthroplasty. J Bone Joint Surg Am 2011;93:2-10. https://doi.org/10.2106/JBJS.I.01317.
- Lombardi AV, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA. Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty?. Clin Orthop Relat Res 2009;467:1450-7. https://doi.org/10.1007/s11999-009-0731-z.
- Sankar A, Davis AM, Palaganas MP, Beaton DE, Badley EM, Gignac MA. Return to work and workplace activity limitations following total hip or knee replacement. Osteoarthr Cartil 2013;21:1485-93. https://doi.org/10.1016/j.joca.2013.06.005.
- Tilbury C, Leichtenberg CS, Tordoir RL, Holtslag MJ, Verdegaal SH, Kroon HM, et al. Return to work after total hip and knee arthroplasty: results from a clinical study. Rheumatol Int 2015;35:2059-67. https://doi.org/10.1007/s00296-015-3311-4.
- Leichtenberg CS, Tilbury C, Kuijer P, Verdegaal S, Wolterbeek R, Nelissen R, et al. Determinants of return to work 12 months after total hip and knee arthroplasty. Ann R Coll Surg Engl 2016;98:387-95. https://doi.org/10.1308/rcsann.2016.0158.
- Scott CEH, Turnbull GS, MacDonald D, Breusch SJ. Activity levels and return to work following total knee arthroplasty in patients under 65 years of age. Bone Joint J 2017;99–B:1037-46. https://doi.org/10.1302/0301-620X.99B8.BJJ-2016-1364.R1.
- Malviya A, Wilson G, Kleim B, Kurtz SM, Deehan D. Factors influencing return to work after hip and knee replacement. Occup Med 2014;64:402-9. https://doi.org/10.1093/occmed/kqu082.
- Kleim BD, Malviya A, Rushton S, Bardgett M, Deehan DJ. Understanding the patient-reported factors determining time taken to return to work after hip and knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015;23:3646-52. https://doi.org/10.1007/s00167-014-3265-1.
- Shiels CHJ, Pollard E, Gabbay M. An Evaluation of the Statement of Fitness for Work (Fit Note): Quantitative Survey of Fit Notes. Research Report No 841 2013. www.employment-studies.co.uk/resource/evaluation-statement-fitness-work-fit-note-quantitative-survey-fit-notes (accessed 28 June 2020).
- Coole CDA, Watson PJ, Nouri F, Potgieter I. Getting the Best from the Fit Note – Investigating the Use of the Statement of Fitness for Work. Wigston: Institution of Occupational Safety and Health; 2015.
- Clayton M, Verow P. Advice given to patients about return to work and driving following surgery. Occup Med 2007;57:488-91. https://doi.org/10.1093/occmed/kqm063.
- Tang K, Beaton DE, Boonen A, Gignac MA, Bombardier C. Measures of work disability and productivity: Rheumatoid Arthritis Specific Work Productivity Survey (WPS-RA), Workplace Activity Limitations Scale (WALS), Work Instability Scale for Rheumatoid Arthritis (RA-WIS), Work Limitations Questionnaire (WLQ), and Work Productivity and Activity Impairment Questionnaire (WPAI). Arthritis Care Res 2011;63:337-49. https://doi.org/10.1002/acr.20633.
- Baker P, Coole C, Drummond A, McDaid C, Khan S, Thomson L, et al. Development of an occupational advice intervention for patients undergoing lower limb arthroplasty (the OPAL study). BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3238-z.
- Bartholomew LK, Parcel GS, Kok G. Intervention mapping: a process for developing theory- and evidence-based health education programs. Health Educ Behav 1998;25:545-63. https://doi.org/10.1177/109019819802500502.
- Bartholomew, Eldredge LK, Markham CM, Ruiter RAC, Fernández ME, Kok G, et al. Planning Health Promotion Programs: An Intervention Mapping Approach. San Francisco, CA: Jossey-Bass Inc.; 2016.
- Kok G, Schaalma H, Ruiter RA, van Empelen P, Brug J. Intervention mapping: protocol for applying health psychology theory to prevention programmes. J Health Psychol 2004;9:85-98. https://doi.org/10.1177/1359105304038379.
- Kok G. A practical guide to effective behavior change: how to apply theory- and evidence-based behavior change methods in an intervention. Eur Health Psychol 2014;16:156-70.
- Peters G-JY. A practical guide to effective behavior change: how to identify what to change in the first place. Eur Health Psychol 2014;16:142-55.
- Kok G, Lo SH, Peters G-JY, Ruiter RAC. Changing energy-related behavior: an intervention mapping approach. Energy Policy 2011;39:5280-6. https://doi.org/10.1016/j.enpol.2011.05.036.
- Hurley DA, Murphy LC, Hayes D, Hall AM, Toomey E, McDonough SM, et al. Using intervention mapping to develop a theory-driven, group-based complex intervention to support self-management of osteoarthritis and low back pain (SOLAS). Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0418-2.
- Sakakibara BM, Lear SA, Barr SI, Benavente O, Goldsmith CH, Silverberg ND, et al. Development of a chronic disease management program for stroke survivors using intervention mapping: the stroke coach. Arch Phys Med Rehabil 2017;98:1195-202. https://doi.org/10.1016/j.apmr.2017.01.019.
- Fassier JB, Sarnin P, Rouat S, Péron J, Kok G, Letrilliart L, et al. Interventions developed with the intervention mapping protocol in work disability prevention: a systematic review of the literature. J Occup Rehabil 2019;29:11-24. https://doi.org/10.1007/s10926-018-9776-8.
- Detaille SI, van der Gulden JW, Engels JA, Heerkens YF, van Dijk FJ. Using intervention mapping (IM) to develop a self-management programme for employees with a chronic disease in the Netherlands. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-353.
- Hutting N, Detaille SI, Engels JA, Heerkens YF, Staal JB, Nijhuis-van der Sanden MW. Development of a self-management program for employees with complaints of the arm, neck, and/or shoulder: an intervention mapping approach. J Multidiscip Healthc 2015;8:307-20. https://doi.org/10.2147/JMDH.S82809.
- van Oostrom SH, Anema JR, Terluin B, Venema A, de Vet HC, van Mechelen W. Development of a workplace intervention for sick-listed employees with stress-related mental disorders: Intervention Mapping as a useful tool. BMC Health Serv Res 2007;7. https://doi.org/10.1186/1472-6963-7-127.
- Vermeulen SJ, Anema JR, Schellart AJ, van Mechelen W, van der Beek AJ. Intervention mapping for development of a participatory return-to-work intervention for temporary agency workers and unemployed workers sick-listed due to musculoskeletal disorders. BMC Public Health 2009;9. https://doi.org/10.1186/1471-2458-9-216.
- Vonk Noordegraaf A, Huirne JA, Pittens CA, van Mechelen W, Broerse JE, Brölmann HA, et al. eHealth program to empower patients in returning to normal activities and work after gynecological surgery: intervention mapping as a useful method for development. J Med Internet Res 2012;14. https://doi.org/10.2196/jmir.1915.
- Ammendolia C, Cassidy D, Steensta I, Soklaridis S, Boyle E, Eng S, et al. Designing a workplace return-to-work program for occupational low back pain: an intervention mapping approach. BMC Musculoskelet Disord 2009;10. https://doi.org/10.1186/1471-2474-10-65.
- Munir F, Kalawsky K, Wallis DJ, Donaldson-Feilder E. Using intervention mapping to develop a work-related guidance tool for those affected by cancer. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-6.
- Désiron HA, Crutzen R, Godderis L, Van Hoof E, de Rijk A. Bridging health care and the workplace: formulation of a return-to-work intervention for breast cancer patients using an intervention mapping approach. J Occup Rehabil 2016;26:350-65. https://doi.org/10.1007/s10926-015-9620-3.
- van Oostrom SH, van Mechelen W, Terluin B, de Vet HC, Knol DL, Anema JR. A workplace intervention for sick-listed employees with distress: results of a randomised controlled trial. Occup Environ Med 2010;67:596-602. https://doi.org/10.1136/oem.2009.050849.
- Vermeulen SJ, Anema JR, Schellart AJ, Knol DL, van Mechelen W, van der Beek AJ. A participatory return-to-work intervention for temporary agency workers and unemployed workers sick-listed due to musculoskeletal disorders: results of a randomized controlled trial. J Occup Rehabil 2011;21:313-24. https://doi.org/10.1007/s10926-011-9291-7.
- Baker P, Kottam L, Coole C, Drummond A, McDaid C, Rangan A, et al. Development of an occupational advice intervention for patients undergoing elective hip and knee replacement: a Delphi study. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-036191.
- Great Britain . Data Protection Act 1998 1998.
- Great Britain . Data Protection Act 2018 2018.
- NHS Health Research Authority . UK Policy Framework for Health and Social Care Research 2020. www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/uk-policy-framework-health-social-care-research/ (accessed 7 April 2020).
- Medical Research Council . MRC Policy on the UK Health Departments’ Research Governance Framework n.d. https://mrc.ukri.org/research/policies-and-guidance-for-researchers/clinical-research-governance/health-departments-research-governance/ (accessed 7 April 2020).
- NIHR INVOLVE . How Do I Cost PPI in Research Projects? n.d. www.invo.org.uk/posttypefaq/how-do-i-cost-ppi-in-research-projects/ (accessed 7 April 2020).
- Featherstone RM, Dryden DM, Foisy M, Guise JM, Mitchell MD, Paynter RA, et al. Advancing knowledge of rapid reviews: an analysis of results, conclusions and recommendations from published review articles examining rapid reviews. Syst Rev 2015;4. https://doi.org/10.1186/s13643-015-0040-4.
- McDaid C, Ronaldson S, Wright K, Baker P. Occupational Advice Interventions for Elective Surgical Procedures: A Rapid Evidence Synthesis 2017. www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016045235 (accessed 18 September 2019).
- Möhler R, Köpke S, Meyer G. Criteria for Reporting the Development and Evaluation of Complex Interventions in healthcare: revised guideline (CReDECI 2). Trials 2015;16. https://doi.org/10.1186/s13063-015-0709-y.
- Page MJ, McKenzie JE, Higgins JPT. Tools for assessing risk of reporting biases in studies and syntheses of studies: a systematic review. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019703.
- Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 2007;7. https://doi.org/10.1186/1471-2288-7-10.
- Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol 2009;62:1013-20. https://doi.org/10.1016/j.jclinepi.2008.10.009.
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d5928.
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355. https://doi.org/10.1136/bmj.i4919.
- Critical Appraisal Skills Programme (CASP) . CASP Checklists 2014. https://casp-uk.net/casp-tools-checklists/ (accessed 18 September 2019).
- Oosterhuis T, Costa LO, Maher CG, de VHC, van TMW, Ostelo RW. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev 2014;3. https://doi.org/10.1002/14651858.CD003007.pub3.
- Aas RW, Tuntland H, Holte KA, Røe C, Lund T, Marklund S, et al. Workplace interventions for neck pain in workers. Cochrane Database Syst Rev 2011;4. https://doi.org/10.1002/14651858.CD008160.pub2.
- Carroll C, Rick J, Pilgrim H, Cameron J, Hillage J. Workplace involvement improves return to work rates among employees with back pain on long-term sick leave: a systematic review of the effectiveness and cost-effectiveness of interventions. Disabil Rehabil 2010;32:607-21. https://doi.org/10.3109/09638280903186301.
- Désiron HA, de Rijk A, Van Hoof E, Donceel P. Occupational therapy and return to work: a systematic literature review. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-615.
- Elders LA, Beek AJ, Burdorf A. Return to work after sickness absence due to back disorders: a systematic review on intervention strategies. Int Arch Occup Environ Health 2000;73:339-48. https://doi.org/10.1007/s004200000127.
- Franche RL, Cullen K, Clarke J, Irvin E, Sinclair S, Frank J. Workplace-based return-to-work interventions: a systematic review of the quantitative literature. J Occup Rehabil 2005;15:607-31. https://doi.org/10.1007/s10926-005-8038-8.
- Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst Rev 2014;9. https://doi.org/10.1002/14651858.CD000963.pub3.
- Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary rehabilitation for fibromyalgia and musculoskeletal pain in working age adults. Cochrane Database Syst Rev 1999;3. https://doi.org/10.1002/14651858.CD001984.
- Karjalainen KA, Malmivaara AO, Tulder MW, Roine RP, Jauhiainen MS, Hurri HO, et al. Biopsychosocial rehabilitation for repetitive-strain injuries among working-age adults. Scand J Work Environ Health 2000;26:373-81. https://doi.org/10.5271/sjweh.557.
- Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain among working age adults. Cochrane Database Syst Rev 2003;2. https://doi.org/10.1002/14651858.CD002193.
- Meijer EM, Sluiter JK, Frings-Dresen MH. Evaluation of effective return-to-work treatment programs for sick-listed patients with non-specific musculoskeletal complaints: a systematic review. Int Arch Occup Environ Health 2005;78:523-32. https://doi.org/10.1007/s00420-005-0622-x.
- Nevala N, Pehkonen I, Koskela I, Ruusuvuori J, Anttila H. Workplace accommodation among persons with disabilities: a systematic review of its effectiveness and barriers or facilitators. J Occup Rehabil 2014;25:432-48. https://doi.org/10.1007/s10926-014-9548-z.
- Norlund A, Ropponen A, Alexanderson K. Multidisciplinary interventions: review of studies of return to work after rehabilitation for low back pain. J Rehabil Med 2009;41:115-21. https://doi.org/10.2340/16501977-0297.
- Palmer KT, Harris EC, Linaker C, Barker M, Lawrence W, Cooper C, et al. Effectiveness of community- and workplace-based interventions to manage musculoskeletal-related sickness absence and job loss: a systematic review. Rheumatology 2012;51:230-42. https://doi.org/10.1093/rheumatology/ker086.
- Schaafsma FG, Whelan K, van der Beek AJ, van der Es-Lambeek LC, Ojajärvi A, Verbeek JH. Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database Syst Rev 2013;8. https://doi.org/10.1002/14651858.CD001822.pub3.
- Vargas-Prada S, Demou E, Lalloo D, Avila-Palencia I, Sanati KA, Sampere M, et al. Effectiveness of very early workplace interventions to reduce sickness absence: a systematic review of the literature and meta-analysis. Scand J Work Environ Health 2016;42:261-72. https://doi.org/10.5271/sjweh.3576.
- Williams RM, Westmorland MG, Lin CA, Schmuck G, Creen M. Effectiveness of workplace rehabilitation interventions in the treatment of work-related low back pain: a systematic review. Disabil Rehabil 2007;29:607-24. https://doi.org/10.1080/09638280600841513.
- Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults. Cochrane Database Syst Rev 2003;2. https://doi.org/10.1002/14651858.CD002194.
- Karjalainen K, Malmivaara A, Tulder M, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2001;26:174-81. https://doi.org/10.1097/00007632-200101150-00012.
- Bendix AE, Bendix T, Haestrup C, Busch E. A prospective, randomized 5-year follow-up study of functional restoration in chronic low back pain patients. Eur Spine J 1998;7:111-19. https://doi.org/10.1007/s005860050040.
- Bendix AF, Bendix T, Vaegter K, Lund C, Frølund L, Holm L. Multidisciplinary intensive treatment for chronic low back pain: a randomized, prospective study. Cleve Clin J Med 1996;63:62-9. https://doi.org/10.3949/ccjm.63.1.62.
- Jousset N, Fanello S, Bontoux L, Dubus V, Billabert C, Vielle B, et al. Effects of functional restoration versus 3 hours per week physical therapy: a randomized controlled study. Spine 2004;29:487-93. https://doi.org/10.1097/01.BRS.0000102320.35490.43.
- Kool J, Bachmann S, Oesch P, Knuesel O, Ambergen T, de Bie R, et al. Function-centered rehabilitation increases work days in patients with nonacute nonspecific low back pain: 1-year results from a randomized controlled trial. Arch Phys Med Rehabil 2007;88:1089-94. https://doi.org/10.1016/j.apmr.2007.05.022.
- Lambeek LC, Bosmans JE, Van Royen BJ, Van Tulder MW, Van Mechelen W, Anema JR. Effect of integrated care for sick listed patients with chronic low back pain: economic evaluation alongside a randomised controlled trial. BMJ 2010;341. https://doi.org/10.1136/bmj.c6414.
- Lambeek LC, van Mechelen W, Knol DL, Loisel P, Anema JR. Randomised controlled trial of integrated care to reduce disability from chronic low back pain in working and private life. BMJ 2010;340. https://doi.org/10.1136/bmj.c1035.
- Roche G, Ponthieux A, Parot-Shinkel E, Jousset N, Bontoux L, Dubus V, et al. Comparison of a functional restoration program with active individual physical therapy for patients with chronic low back pain: a randomized controlled trial. Arch Phys Med Rehabil 2007;88:1229-35. https://doi.org/10.1016/j.apmr.2007.07.014.
- Roche-Leboucher G, Petit-Lemanac’h A, Bontoux L, Dubus-Bausière V, Parot-Shinkel E, Fanello S, et al. Multidisciplinary intensive functional restoration versus outpatient active physiotherapy in chronic low back pain: a randomized controlled trial. Spine 2011;36:2235-42. https://doi.org/10.1097/BRS.0b013e3182191e13.
- Durand MJ, Loisel P. Therapeutic return to work: rehabilitation in the workplace. Work 2001;17:57-63.
- Feuerstein M, Callan-Harris S, Hickey P, Dyer D, Armbruster W, Carosella AM. Multidisciplinary rehabilitation of chronic work-related upper extremity disorders. Long-term effects. J Occup Med 1993;35:396-403.
- Allaire SH, Li W, LaValley MP. Reduction of job loss in persons with rheumatic diseases receiving vocational rehabilitation: a randomized controlled trial. Arthritis Rheum 2003;48:3212-18. https://doi.org/10.1002/art.11256.
- Arnetz BB, Sjögren B, Rydéhn B, Meisel R. Early workplace intervention for employees with musculoskeletal-related absenteeism: a prospective controlled intervention study. J Occup Environ Med 2003;45:499-506. https://doi.org/10.1097/01.jom.0000063628.37065.45.
- Bültmann U, Sherson D, Olsen J, Hansen CL, Lund T, Kilsgaard J. Coordinated and tailored work rehabilitation: a randomized controlled trial with economic evaluation undertaken with workers on sick leave due to musculoskeletal disorders. J Occup Rehabil 2009;19:81-93. https://doi.org/10.1007/s10926-009-9162-7.
- Haldorsen EM, Grasdal AL, Skouen JS, Risa AE, Kronholm K, Ursin H. Is there a right treatment for a particular patient group? Comparison of ordinary treatment, light multidisciplinary treatment, and extensive multidisciplinary treatment for long-term sick-listed employees with musculoskeletal pain. Pain 2002;95:49-63. https://doi.org/10.1016/S0304-3959(01)00374-8.
- Nordström-Björverud G, Moritz U. Interdisciplinary rehabilitation of hospital employees with musculoskeletal disorders. Scand J Rehabil Med 1998;30:31-7. https://doi.org/10.1080/003655098444291.
- Corey DT, Koepfler LE, Etlin D, Day HI. A limited functional restoration program for injured workers: a randomized trial. J Occup Rehabil 1996;6:239-49. https://doi.org/10.1007/BF02110886.
- Donceel P, Du Bois M, Lahaye D. Return to work after surgery for lumbar disc herniation. A rehabilitation-oriented approach in insurance medicine. Spine 1999;24:872-6. https://doi.org/10.1097/00007632-199905010-00007.
- Manniche C, Asmussen K, Lauritsen B, Vinterberg H, Kreiner S, Jordan A. Low Back Pain Rating scale: validation of a tool for assessment of low back pain. Pain 1994;57:317-26. https://doi.org/10.1016/0304-3959(94)90007-8.
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine 2000;25:2940-52. https://doi.org/10.1097/00007632-200011150-00017.
- Roland M, Morris R. A study of the natural history of back pain, part 1 & part 2: Roland-Morris Disability Questionnaire. Spine 1983;8:141-50. https://doi.org/10.1097/00007632-198303000-00004.
- Coole C, Drummond A, Watson PJ. Individual work support for employed patients with low back pain: a randomized controlled pilot trial. Clin Rehabil 2013;27:40-5. https://doi.org/10.1177/0269215512446839.
- Haldorsen EM, Kronholm K, Skouen JS, Ursin H. Multimodal cognitive behavioral treatment of patients sicklisted for musculoskeletal pain: a randomized controlled study. Scand J Rheumatol 1998;27:16-25. https://doi.org/10.1080/030097498441128.
- Haldorsen EM, Indahl A, Ursin H. Patients with low back pain not returning to work. A 12-month follow-up study. Spine 1998;23:1202-7. https://doi.org/10.1097/00007632-199806010-00004.
- Vonk Noordegraaf A, Anema JR, van Mechelen W, Knol DL, van Baal WM, van Kesteren PJ, et al. A personalised eHealth programme reduces the duration until return to work after gynaecological surgery: results of a multicentre randomised trial. BJOG 2014;121:1127-35. https://doi.org/10.1111/1471-0528.12661.
- Bardgett M, Lally J, Malviya A, Deehan D. Return to work after knee replacement: a qualitative study of patient experiences. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-007912.
- Hinman MR. Factors influencing work disability for women who have undergone mastectomy. Women Health 2001;34:45-60. https://doi.org/10.1300/J013v34n02_04.
- Kluivers KB, Riphagen I, Vierhout ME, Brölmann HA, de Vet HC. Systematic review on recovery specific quality-of-life instruments. Surgery 2008;143:206-15. https://doi.org/10.1016/j.surg.2007.08.017.
- Lerner D, Amick BC, Rogers WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Med Care 2001;39:72-85. https://doi.org/10.1097/00005650-200101000-00009.
- Munir F. The Work Limitation Questionnaire. Occup Med 2008;58:310-1. https://doi.org/10.1093/occmed/kqn039.
- Morgeson FP, Humphrey SE. The Work Design Questionnaire (WDQ): developing and validating a comprehensive measure for assessing job design and the nature of work. J Appl Psychol 2006;91:1321-39. https://doi.org/10.1037/0021-9010.91.6.1321.
- Bartlett JEI, Kotrlik JW, Higgins CC. Organizational research: determining appropriate sample size in survey research. Inf Technol Learn Perform J 2001;19:43-50.
- Department of Health and Social Care . NHS Reference Costs 2017 18 2018. https://improvement.nhs.uk/resources/reference-costs/ (accessed 18 September 2019).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2018. Canterbury: PSSRU, University of Kent; 2018.
- Dolan P, Gudex C, Kind P, Williams A. A Social Tariff for Euroqol: Results from a UK General Population Survey. York: Centre for Health Economics; 1995.
- Oemar MJB. EQ-5D-5L User Guide: Basic Information on How to Use the EQ-5D-5L Instrument 2013. www.unmc.edu/centric/_documents/EQ-5D-5L.pdf (accessed 28 June 2020).
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013.
- National Institute for Health and Care Excellence (NICE) . Position Statement on Use of the EQ-5D-5L Valuation Set for England (updated November 2018) 2018. www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l (accessed 18 September 2019).
- Office for National Statistics . Employee Earnings in the UK: 2018 2018. www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/bulletins/annualsurveyofhoursandearnings/2018 (accessed 18 September 2019).
- Barrack RL, Ruh EL, Chen J, Lombardi AV, Berend KR, Parvizi J, et al. Impact of socioeconomic factors on outcome of total knee arthroplasty. Clin Orthop Relat Res 2014;472:86-97. https://doi.org/10.1007/s11999-013-3002-y.
- Ritchie JLJ. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2003.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Coole C, Baker P, McDaid C, Drummond A. Using intervention mapping to develop an occupational advice intervention to aid return to work following hip and knee replacement in the United Kingdom. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05375-3.
- Kok G, Peters LWH, Ruiter RAC. Planning theory- and evidence-based behavior change interventions: a conceptual review of the intervention mapping protocol. Psicologia: Reflexão E Crítica 2017;30. https://doi.org/10.1186/s41155-017-0072-x.
- Sinha IP, Smyth RL, Williamson PR. Using the Delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLOS Med 2011;8. https://doi.org/10.1371/journal.pmed.1000393.
- Department for Work and Pensions . Fit Note: Guidance for Patients and Employees 2013. www.gov.uk/government/publications/the-fit-note-a-guide-for-patients-and-employees (accessed 26 May 2020).
- Lerner D, Amick BC, Lee JC, Rooney T, Rogers WH, Chang H, et al. Relationship of employee-reported work limitations to work productivity. Med Care 2003;41:649-59. https://doi.org/10.1097/01.MLR.0000062551.76504.A9.
- Lerner D, Reed JI, Massarotti E, Wester LM, Burke TA. The Work Limitations Questionnaire’s validity and reliability among patients with osteoarthritis. J Clin Epidemiol 2002;55:197-208. https://doi.org/10.1016/S0895-4356(01)00424-3.
- Lerner D, Rogers W, Chang H. The work limitations questionnaire. Qual Life 2002;28:9-10. https://doi.org/10.1037/t66378-000.
- Schwarzer R, Jerusalem M, Weinman J, Wright S, Johnston M. Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs. Slough: NFER-Nelson; 1995.
- Franche RL, Corbière M, Lee H, Breslin FC, Hepburn CG. The Readiness for Return-To-Work (RRTW) scale: development and validation of a self-report staging scale in lost-time claimants with musculoskeletal disorders. J Occup Rehabil 2007;17:450-72. https://doi.org/10.1007/s10926-007-9097-9.
- Ammendolia C, Côté P, Cancelliere C, Cassidy JD, Hartvigsen J, Boyle E, et al. Healthy and productive workers: using intervention mapping to design a workplace health promotion and wellness program to improve presenteeism. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3843-x.
- McEachan RR, Lawton RJ, Jackson C, Conner M, Lunt J. Evidence, theory and context: using intervention mapping to develop a worksite physical activity intervention. BMC Public Health 2008;8. https://doi.org/10.1186/1471-2458-8-326.
- Wolfers ME, van den Hoek C, Brug J, de Zwart O. Using intervention mapping to develop a programme to prevent sexually transmittable infections, including HIV, among heterosexual migrant men. BMC Public Health 2007;7. https://doi.org/10.1186/1471-2458-7-141.
- Meng A, Borg V, Clausen T. Enhancing the social capital in industrial workplaces: Developing workplace interventions using intervention mapping. Eval Program Plann 2019;72:227-36. https://doi.org/10.1016/j.evalprogplan.2018.11.007.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: SAGE Publications Ltd; 2013.
- Fletcher A, Jamal F, Moore G, Evans RE, Murphy S, Bonell C. Realist complex intervention science: applying realist principles across all phases of the Medical Research Council framework for developing and evaluating complex interventions. Evaluation 2016;22:286-303. https://doi.org/10.1177/1356389016652743.
- Ling T. Evaluating complex and unfolding interventions in real time. Evaluation 2012;18:79-91. https://doi.org/10.1177/1356389011429629.
- Mills T, Lawton R, Sheard L. Advancing complexity science in healthcare research: the logic of logic models. BMC Med Res Methodol 2019;19. https://doi.org/10.1186/s12874-019-0701-4.
- Grunfeld EA, Schumacher L, Armaou M, Woods PL, Rolf P, Sutton AJ, et al. Feasibility randomised controlled trial of a guided workbook intervention to support work-related goals among cancer survivors in the UK. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-022746.
- Boland L, Taljaard M, Dervin G, Trenaman L, Tugwell P, Pomey MP, et al. Effect of patient decision aid was influenced by presurgical evaluation among patients with osteoarthritis of the knee. Can J Surg 2018;61:28-33. https://doi.org/10.1503/cjs.003316.
- Bozic KJ, Belkora J, Chan V, Youm J, Zhou T, Dupaix J, et al. Shared decision making in patients with osteoarthritis of the hip and knee: results of a randomized controlled trial. J Bone Joint Surg Am 2013;95:1633-9. https://doi.org/10.2106/JBJS.M.00004.
- Ibrahim SA, Blum M, Lee GC, Mooar P, Medvedeva E, Collier A, et al. Effect of a decision aid on access to total knee replacement for black patients with osteoarthritis of the knee: a randomized clinical trial. JAMA Surg 2017;152. https://doi.org/10.1001/jamasurg.2016.4225.
- Stacey D, Taljaard M, Dervin G, Tugwell P, O’Connor AM, Pomey MP, et al. Impact of patient decision aids on appropriate and timely access to hip or knee arthroplasty for osteoarthritis: a randomized controlled trial. Osteoarthr Cartil 2016;24:99-107. https://doi.org/10.1016/j.joca.2015.07.024.
- National Institute for Health and Care Excellence (NICE) . Patient Experience in Adult NHS Services: Improving the Experience of Care for People Using Adult NHS Services. Clinical Guideline [CG138] 2012. www.nice.org.uk/guidance/cg138 (accessed 18 September 2019).
- National Institute for Health and Care Excellence (NICE) . Patient Experience in Adult NHS Services Quality Standard [QS15] 2012. www.nice.org.uk/guidance/qs15 (accessed 18 September 2019).
- Drummond A, Nouri F, Narayanasamy M, Coole C, Baker P, Khan S. Engaging workplace representatives in research: what recruitment strategies work best?. Occup Med 2018;68:282-5. https://doi.org/10.1093/occmed/kqy047.
- Cole ZD, Donohoe HM, Stellefson ML. Internet-based Delphi research: case based discussion. Environ Manage 2013;51:511-23. https://doi.org/10.1007/s00267-012-0005-5.
- Hall DA, Smith H, Heffernan E, Fackrell K. Core Outcome Measures in Tinnitus International Delphi (COMiT’ID) Research Steering Group . Recruiting and retaining participants in e-Delphi surveys for core outcome set development: evaluating the COMiT’ID study. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0201378.
- Hsu C-CS, Brian A. Minimizing non-response in the Delphi process: how to respond to non-response. Pract Assess Res Eval 2007;12.
- Williamson PR, Altman DG, Bagley H, Barnes KL, Blazeby JM, Brookes ST, et al. The COMET Handbook: version 1.0. Trials 2017;18. https://doi.org/10.1186/s13063-017-1978-4.
- Horton TJ, Illingworth JH, Warburton WHP. Overcoming challenges in codifying and replicating complex health care interventions. Health Aff 2018;37:191-7. https://doi.org/10.1377/hlthaff.2017.1161.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- ISD Scotland, NHS National Services Scotland . Scottish Arthroplasty Project Report 2018 2018. www.arthro.scot.nhs.uk/ (accessed 18 September 2019).
- Aas RW, Tuntland H, Holte KA, Røe C, Labriola M. Workplace interventions for low-back pain in workers. Cochrane Database Syst Rev 2009;4. https://doi.org/10.1002/14651858.CD008159.
- Åberg F. From prolonging life to prolonging working life: tackling unemployment among liver-transplant recipients. World J Gastroenterol 2016;22:3701-11. https://doi.org/10.3748/wjg.v22.i14.3701.
- Bigos SJ, Holland J, Holland C, Webster JS, Battie M, Malmgren JA. High-quality controlled trials on preventing episodes of back problems: systematic literature review in working-age adults. Spine J 2009;9:147-68. https://doi.org/10.1016/j.spinee.2008.11.001.
- Bond-Smith G, Belgaumkar AP, Davidson BR, Gurusamy KS. Enhanced recovery protocols for major upper gastrointestinal, liver and pancreatic surgery. Cochrane Database Syst Rev 2016;2. https://doi.org/10.1002/14651858.CD011382.pub2.
- Brown HE, Gilson ND, Burton NW, Brown WJ. Does physical activity impact on presenteeism and other indicators of workplace well-being?. Sports Med 2011;41:249-62. https://doi.org/10.2165/11539180-000000000-00000.
- Corbiere MSJ. A Systematic Review of Psychological Return-to-Work Interventions for People with Mental Health Problems and/or Physical Injuries. Database of Abstracts of Reviews of Effects: Quality-assessed Reviews. York: Centre for Reviews and Dissemination; 2006.
- Ebrahim S, Malachowski C, Kamal El Din M, Mulla SM, Montoya L, Bance S, et al. Measures of patients’ expectations about recovery: a systematic review. J Occup Rehabil 2015;25:240-55. https://doi.org/10.1007/s10926-014-9535-4.
- Ellis DJ, Mallozzi SS, Mathews JE, Moss IL, Ouellet JA, Jarzem P, et al. The relationship between preoperative expectations and the short-term postoperative satisfaction and functional outcome in lumbar spine surgery: a systematic review. Global Spine J 2015;5:436-52. https://doi.org/10.1055/s-0035-1551650.
- Engers A, Jellema P, Wensing M, van der Windt DA, Grol R, van Tulder MW. Individual patient education for low back pain. Cochrane Database Syst Rev 2008;1. https://doi.org/10.1002/14651858.CD004057.pub3.
- Euler U, Wegewitz UE, Schmitt J, Adams J, van Dijk JL, Seidler A. Interventions to support return-to-work for patients with coronary heart disease. Cochrane Database Syst Rev 2013;9. https://doi.org/10.1002/14651858.CD010748.
- Faber E, Kuiper JI, Burdorf A, Miedema HS, Verhaar JA. Treatment of impingement syndrome: a systematic review of the effects on functional limitations and return to work. J Occup Rehabil 2006;16:7-25. https://doi.org/10.1007/s10926-005-9003-2.
- Handoll HH, Elliott J. Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev 2015;9. https://doi.org/10.1002/14651858.CD003324.pub3.
- Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non-specific low-back pain. Cochrane Database Syst Rev 2004;4. https://doi.org/10.1002/14651858.CD000261.pub2.
- Hlobil H, Staal JB, Spoelstra M, Ariëns GA, Smid T, van Mechelen W. Effectiveness of a return-to-work intervention for subacute low-back pain. Scand J Work Environ Health 2005;31:249-57. https://doi.org/10.5271/sjweh.880.
- Hou WH, Chi CC, Lo HL, Kuo KN, Chuang HY. Vocational rehabilitation for enhancing return-to-work in workers with traumatic upper limb injuries. Cochrane Database Syst Rev 2013;10. https://doi.org/10.1002/14651858.CD010002.pub2.
- Huda A, Newcomer R, Harrington C, Keeffe EB, Esquivel CO. Employment after liver transplantation: a review. Transplant Proc 2015;47:233-9. https://doi.org/10.1016/j.transproceed.2014.10.022.
- Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain in working-age adults: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2001;26:262-9. https://doi.org/10.1097/00007632-200102010-00011.
- Krause NDL, Neuhauser F. Modified Work and Return To Work: A Review of the Literature. Database of Abstracts of Reviews of Effects: Quality-assessed Reviews. York: Centre for Reviews and Dissemination; 1998.
- Lin CW, Donkers NA, Refshauge KM, Beckenkamp PR, Khera K, Moseley AM. Rehabilitation for ankle fractures in adults. Cochrane Database Syst Rev 2012;11. https://doi.org/10.1002/14651858.CD005595.pub3.
- Lurati AR. Management of acute lumbar injuries in the workplace. Orthop Nurs 2016;35:152-8. https://doi.org/10.1097/NOR.0000000000000244.
- Ostelo RW, de Vet HC, Waddell G, Kerckhoffs MR, Leffers P, van Tulder M. Rehabilitation following first-time lumbar disc surgery: a systematic review within the framework of the cochrane collaboration. Spine 2003;28:209-18. https://doi.org/10.1097/01.BRS.0000042520.62951.28.
- Parreira P, Heymans MW, van Tulder MW, Esmail R, Koes BW, Poquet N, et al. Back schools for chronic non-specific low back pain. Cochrane Database Syst Rev 2017;8. https://doi.org/10.1002/14651858.CD011674.pub2.
- Petit A, Rozenberg S, Fassier JB, Rousseau S, Mairiaux P, Roquelaure Y. Pre-return-to-work medical consultation for low back pain workers. Good practice recommendations based on systematic review and expert consensus. Ann Phys Rehabil Med 2015;58:298-304. https://doi.org/10.1016/j.rehab.2015.08.001.
- Poquet N, Lin CW, Heymans MW, van Tulder MW, Esmail R, Koes BW, et al. Back schools for acute and subacute non-specific low-back pain. Cochrane Database Syst Rev 2016;4. https://doi.org/10.1002/14651858.CD008325.pub2.
- Schwarz B, Neuderth S, Gutenbrunner C, Bethge M. Multiprofessional teamwork in work-related medical rehabilitation for patients with chronic musculoskeletal disorders. J Rehabil Med 2015;47:58-65. https://doi.org/10.2340/16501977-1893.
- Smith TO, Jepson P, Beswick A, Sands G, Drummond A, Davis ET, et al. Assistive devices, hip precautions, environmental modifications and training to prevent dislocation and improve function after hip arthroplasty. Cochrane Database Syst Rev 2016;7. https://doi.org/10.1002/14651858.CD010815.pub2.
- Vogel N, Schandelmaier S, Zumbrunn T, Ebrahim S, de Boer WE, Busse JW, et al. Return-to-work coordination programmes for improving return to work in workers on sick leave. Cochrane Database Syst Rev 2017;3. https://doi.org/10.1002/14651858.CD011618.pub2.
- Vooijs M, Leensen MC, Hoving JL, Wind H, Frings-Dresen MH. Interventions to enhance work participation of workers with a chronic disease: a systematic review of reviews. Occup Environ Med 2015;72:820-6. https://doi.org/10.1136/oemed-2015-103062.
- Young AE, Besen E, Choi Y. The importance, measurement and practical implications of worker’s expectations for return to work. Disabil Rehabil 2015;37:1808-16. https://doi.org/10.3109/09638288.2014.979299.
- Altmaier EM, Lehmann TR, Russell DW, Weinstein JN, Kao CF. The effectiveness of psychological interventions for the rehabilitation of low back pain: a randomized controlled trial evaluation. Pain 1992;49:329-35. https://doi.org/10.1016/0304-3959(92)90240-c.
- Bendix AF, Bendix T, Ostenfeld S, Bush E, Andersen A. Active treatment programs for patients with chronic low back pain: a prospective, randomized, observer-blinded study. Eur Spine J 1995;4:148-52. https://doi.org/10.1007/BF00298239.
- Bendix T, Bendix A, Labriola M, Haestrup C, Ebbehøj N. Functional restoration versus outpatient physical training in chronic low back pain: a randomized comparative study. Spine 2000;25:2494-500. https://doi.org/10.1097/00007632-200010010-00012.
- Bethge M, Herbold D, Trowitzsch L, Jacobi C. Work status and health-related quality of life following multimodal work hardening: a cluster randomised trial. J Back Musculoskelet Rehabil 2011;24:161-72. https://doi.org/10.3233/BMR-2011-0290.
- Henchoz Y, de Goumoëns P, So AK, Paillex R. Functional multidisciplinary rehabilitation versus outpatient physiotherapy for non specific low back pain: randomized controlled trial. Swiss Med Wkly 2010;140. https://doi.org/10.4414/smw.2010.13133.
- Johansson C, Dahl J, Jannert M, Melin L, Andersson G. Effects of a cognitive-behavioral pain-management program. Behav Res Ther 1998;36:915-30. https://doi.org/10.1016/S0005-7967(98)00079-5.
- Lindh M, Lurie M, Sanne H. A randomized prospective study of vocational outcome in rehabilitation of patients with non-specific musculoskeletal pain: a multidisciplinary approach to patients identified after 90 days of sick-leave. Scand J Rehabil Med 1997;29:103-12.
- Marhold C, Linton SJ, Melin L. A cognitive-behavioral return-to-work program: effects on pain patients with a history of long-term versus short-term sick leave. Pain 2001;91:155-63. https://doi.org/10.1016/S0304-3959(00)00431-0.
- Meijer EM, Sluiter JK, Heyma A, Sadiraj K, Frings-Dresen MH. Cost-effectiveness of multidisciplinary treatment in sick-listed patients with upper extremity musculoskeletal disorders: a randomized, controlled trial with one-year follow-up. Int Arch Occup Environ Health 2006;79:654-64. https://doi.org/10.1007/s00420-006-0098-3.
- Meyer K, Fransen J, Huwiler H, Uebelhart D, Klipstein A. Feasibility and results of a randomised pilot-study of a work rehabilitation programme. J Back Musculoskelet Rehabil 2005;18:67-78. https://doi.org/10.3233/BMR-2005-183-403.
- Mitchell RI, Carmen GM. The functional restoration approach to the treatment of chronic pain in patients with soft tissue and back injuries. Spine 1994;19:633-42. https://doi.org/10.1097/00007632-199403001-00001.
- Skouen JS, Grasdal AL, Haldorsen EM, Ursin H. Relative cost-effectiveness of extensive and light multidisciplinary treatment programs versus treatment as usual for patients with chronic low back pain on long-term sick leave: randomized controlled study. Spine 2002;27:901-9. https://doi.org/10.1097/00007632-200205010-00002.
- Strand LI, Ljunggren AE, Haldorsen EM, Espehaug B. The impact of physical function and pain on work status at 1-year follow-up in patients with back pain. Spine 2001;26:800-8. https://doi.org/10.1097/00007632-200104010-00022.
- Lehmann TR, Brand RA, Gorman TW. A low-back rating scale. Spine 1983;8:308-15. https://doi.org/10.1097/00007632-198304000-00013.
- Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain 1975;1:277-99. https://doi.org/10.1016/0304-3959(75)90044-5.
- Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain 1985;23:345-56. https://doi.org/10.1016/0304-3959(85)90004-1.
- Cott CA, Gignac MA, Badley EM. Determinants of self rated health for Canadians with chronic disease and disability. J Epidemiol Community Health 1999;53:731-6. https://doi.org/10.1136/jech.53.11.731.
- Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 1987;18:233-7. https://doi.org/10.1016/0003-6870(87)90010-X.
- Geissner E. Fragebogen zur Erfassung der Schmerzspezifischen Selbstwirksamkeit (Pain Management Questionnaire). Göttingen: Hogrefe; 2001.
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473-83. https://doi.org/10.1097/00005650-199206000-00002.
- Snaith RP. The Hospital Anxiety And Depression Scale. Health Qual Life Outcomes 2003;1. https://doi.org/10.1186/1477-7525-1-29.
- Lauridsen HH, Hartvigsen J, Manniche C, Korsholm L, Grunnet-Nilsson N. Danish version of the Oswestry Disability Index for patients with low back pain. Part 1: Cross-cultural adaptation, reliability and validity in two different populations. Eur Spine J 2006;15:1705-16. https://doi.org/10.1007/s00586-006-0117-9.
- Lauridsen HH, Hartvigsen J, Manniche C, Korsholm L, Grunnet-Nilsson N. Danish version of the Oswestry Disability Index for patients with low back pain. Part 2: sensitivity, specificity and clinically significant improvement in two low back pain populations. Eur Spine J 2006;15:1717-28. https://doi.org/10.1007/s00586-006-0128-6.
- Linton SJ, Boersma K. Early identification of patients at risk of developing a persistent back problem: the predictive validity of the Orebro Musculoskeletal Pain Questionnaire. Clin J Pain 2003;19:80-6. https://doi.org/10.1097/00002508-200303000-00002.
- Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A, Oja G. Work Ability Index. Helsinki: Finnish Institute of Occupational Health; 1998.
- Ahlstrom L, Grimby-Ekman A, Hagberg M, Dellve L. The work ability index and single-item question: associations with sick leave, symptoms, and health – a prospective study of women on long-term sick leave. Scand J Work Environ Health 2010;36:404-12. https://doi.org/10.5271/sjweh.2917.
- Nicholas MK. Self-Efficacy and Chronic Pain n.d.
- Jensen MP, Karoly P, Turk DC, Melzack R. Handbook of Pain Assessment. New York, NY: Guildford Press; 2001.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993;52:157-68. https://doi.org/10.1016/0304-3959(93)90127-B.
- Murphy DF, McDonald A, Power C, Unwin A, MacSullivan R. Measurement of pain: a comparison of the visual analogue with a nonvisual analogue scale. Clin J Pain 1988;3:197-9. https://doi.org/10.1097/00002508-198712000-00003.
- Durand M, Loisel P, Durand P, Lussier A. Traduction en francais et étude de fidélité test-retest et de validité du Fear-Avoidance Beliefs Questionnaire. Méd Sci 1994;44.
- Kopec JA, Esdaile JM, Abrahamowicz M, Abenhaim L, Wood-Dauphinee S, Lamping DL, et al. The Québec Back Pain Disability Scale. Measurement properties. Spine 1995;20:341-52. https://doi.org/10.1097/00007632-199502000-00016.
- Durand MJ, Loisel P, Durand P. Le retour thérapeutique au travail comme une intervention de réadaptation centralisée dans le milieu de travail: description et fondements théoriques. Can J Occup Ther 1998;65:72-80. https://doi.org/10.1177/000841749806500107.
- Scott J, Huskisson EC. Vertical or horizontal visual analogue scales. Ann Rheum Dis 1979;38. https://doi.org/10.1136/ard.38.6.560.
- Moos RH. Work Environment Scale Manual. Palo Alto, CA: Consulting Psychologists Press; 1986.
- Feuerstein M, Papciak AS. Work Re-entry Questionnaire. Rochester, NY: Center for Occupational Rehabilitation, Universtiy of Rochester School of Medicine and Dentistry; 1988.
- Millon T. Manual for the MCMI-II. 2nd: National Computer Systems; 1987.
- Turner JA, Robinson J, McCreary CP. Chronic low back pain: predicting response to nonsurgical treatment. Arch Phys Med Rehabil 1983;64:560-3.
- Ransford A, Cairns D, Mooney V. The pain drawing as an aid to the psychologic evaluation of patients with low-back pain. Spine 1976;1:127-34. https://doi.org/10.1097/00007632-197606000-00007.
- Spangfort E, Wall PD, Melzack R. Textbook of Pain. Edinburgh: Churchill Livingstone; 1994.
- Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 1983;16:87-101. https://doi.org/10.1016/0304-3959(83)90088-x.
- Aaro L. Health Behaviours and Socioeconomic Status: A Study Among the Adult Population in Norway 1986.
- Ursin H, Endresen I, Ursin G. Psychological factors and self-reports of muscle pain. Eur J Appl Physiol Occup Physiol 1988;57:282-90. https://doi.org/10.1007/BF00635986.
- Spielberger CD. Manual for the State–Trait Anxiety Inventory STAI. Palo Alto, CA: Consulting Psychologists Press; 1983.
- Håseth K, Hagtvet KA, Spielberger CD. Psychometric properties and research with the Norwegian state-trait anxiety inventory. Cross Cult Anxiety 1990;4:169-81. https://doi.org/10.4324/9781315825724-14.
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci 1974;19:1-15. https://doi.org/10.1002/bs.3830190102.
- Central Bureau of Statistics of Norway . Health Survey 1985 1987.
- Eysenck HJ. Eysenck Personality Inventory. San Diego, CA: Educational and Industrial Testing Service; 1968.
- Håseth K. Manual for den norske versjon av Eysenck Personlighetsinventorium (Form A). Oslo: Gaustad Sykehus; 1969.
- Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy 1980;66:271-3.
- Matheson LN, Matheson ML. Spinal Function Sort. Wildwood, MO: Employment Potential Improvement Corporation; 1989.
- Mayer TG, Barnes D, Kishino ND, Nichols G, Gatchel RJ, Mayer H, et al. Progressive isoinertial lifting evaluation. I. A standardized protocol and normative database. Spine 1988;13:993-7. https://doi.org/10.1097/00007632-198809000-00005.
- Williams R, Binkley J, Bloch R, Goldsmith CH, Minuk T. Reliability of the modified-modified Schöber and double inclinometer methods for measuring lumbar flexion and extension. Phys Ther 1993;73:33-44. https://doi.org/10.1093/ptj/73.1.26.
- Perret C, Poiraudeau S, Fermanian J, Colau MM, Benhamou MA, Revel M. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch Phys Med Rehabil 2001;82:1566-70. https://doi.org/10.1053/apmr.2001.26064.
- Ito T, Shirado O, Suzuki H, Takahashi M, Kaneda K, Strax TE. Lumbar trunk muscle endurance testing: an inexpensive alternative to a machine for evaluation. Arch Phys Med Rehabil 1996;77:75-9. https://doi.org/10.1016/S0003-9993(96)90224-5.
- Latimer J, Maher CG, Refshauge K, Colaco I. The reliability and validity of the Biering-Sorensen test in asymptomatic subjects and subjects reporting current or previous nonspecific low back pain. Spine 1999;24:2085-9. https://doi.org/10.1097/00007632-199910150-00004.
- Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J 1973;85:546-62. https://doi.org/10.1016/0002-8703(73)90502-4.
- McInnis KJ, Balady GJ, Weiner DA, Ryan TJ. Comparison of ischemic and physiologic responses during exercise tests in men using the standard and modified Bruce protocols. Am J Cardiol 1992;69:84-9. https://doi.org/10.1016/0002-9149(92)90680-W.
- Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain 1983;17:33-44. https://doi.org/10.1016/0304-3959(83)90125-2.
- Jensen IB, Linton SJ. Coping Strategies Questionnaire (CSQ): Reliability of the Swedish version of the CSQ. Cogn Behav Ther 1993;22:139-45. https://doi.org/10.1080/16506079309455940.
- Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 1990;13:227-36. https://doi.org/10.1002/nur.4770130405.
- Huskisson EC. Measurement of pain. J Rheumatol 1982;9:768-9.
- Lawlis GF, Cuencas R, Selby D, McCoy CE. The development of the Dallas Pain Questionnaire. An assessment of the impact of spinal pain on behavior. Spine 1989;14:511-16. https://doi.org/10.1097/00007632-198905000-00007.
- Marty M, Blotman F, Avouac B, Rozenberg S, Valat J-P. Validation de la version française de l’échelle de Dallas chez les patients lombalgiques chroniques. Revu Rhumat 1998;65:139-47.
- Lamers LM, Stalmeier PF, McDonnell J, Krabbe PF, van Busschbach JJ. Measuring the quality of life in economic evaluations: the Dutch EQ-5D tariff. Ned Tijdschr Geneeskd 2005;149:1574-8.
- Salén BA, Spangfort EV, Nygren AL, Nordemar R. The Disability Rating Index: an instrument for the assessment of disability in clinical settings. J Clin Epidemiol 1994;47:1423-35. https://doi.org/10.1016/0895-4356(94)90086-8.
- Riley JF, Ahern DK, Follick MJ. Chronic pain and functional impairment: assessing beliefs about their relationship. Arch Phys Med Rehabil 1988;69:579-82.
- Beck AT. Cognitive Therapy of Depression. New York, NY: Guilford Press; 1979.
- Hudak PL, Amadio PC, Bombardier C, Beaton D, Cole D, Davis A, et al. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. Am J Ind Med 1996;29:602-8. https://doi.org/10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L.
- Boadella JM, Kuijer PP, Sluiter JK, Frings-Dresen MH. Effect of self-selected handgrip position on maximal handgrip strength. Arch Phys Med Rehabil 2005;86:328-31. https://doi.org/10.1016/j.apmr.2004.05.003.
- Kori S. Kinisophobia: a new view of chronic pain behavior. Pain Manage 1990:35-43.
- Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain 1995;62:363-72. https://doi.org/10.1016/0304-3959(94)00279-N.
- Aaronson NK, Muller M, Cohen PDA, Essink-Bot ML, Fekkes M, Sanderman R, et al. Translation, Validation, and Norming of the Dutch Language Version of the SF-36 Health Survey in Community and Chronic Disease Populations. J Clin Epidemiol 1998;51:1055-68. https://doi.org/10.1016/S0895-4356(98)00097-3.
- Matheson LN, Matheson ML, Grant J. Development of a measure of perceived functional ability. J Occup Rehabil 1993;3:15-30. https://doi.org/10.1007/BF01076739.
- Schochat T, Rehberg W, von Kempis J, Stucki G, Jäckel W. The North American Spine Society Lumbar Spine Outcome Assessment Instrument: Übersetzung und psychometrische Analyse der deutschen Version an einer Stichprobe von Rehabilitanden mit chronischen Rückenschmerzen. Z Rheumatol 2000;59:303-13. https://doi.org/10.1007/s003930070052.
- Scott J, Huskisson EC. Graphic representation of pain. Pain 1976;2:175-84. https://doi.org/10.1016/0304-3959(76)90113-5.
- Persson L, Moritz U. Pain-drawing: a quantitative and qualitative model for pain assessment in cervico-brachial pain syndrome. Pain Clinic 1994;7:13-22.
- Udén A, Aström M, Bergenudd H. Pain drawings in chronic back pain. Spine 1988;13:389-92. https://doi.org/10.1097/00007632-198804000-00002.
- Hunt SM, McKenna SP, McEwen J, Backett EM, Williams J, Papp E. A quantitative approach to perceived health status: a validation study. J Epidemiol Community Health 1980;34:281-6. https://doi.org/10.1136/jech.34.4.281.
- Hunt SM, McKenna SP, Williams J. Reliability of a population survey tool for measuring perceived health problems: a study of patients with osteoarthrosis. J Epidemiol Community Health 1981;35:297-300. https://doi.org/10.1136/jech.35.4.297.
- Wiklund I, Romanus B, Hunt SM. Self-assessed disability in patients with arthrosis of the hip joint. Reliability of the Swedish version of the Nottingham Health Profile. Int Disabil Stud 1988;10:159-63. https://doi.org/10.3109/09638288809164068.
- Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain 1986;27:117-26. https://doi.org/10.1016/0304-3959(86)90228-9.
- Gauvin MG, Riddle DL, Rothstein JM. Reliability of clinical measurements of forward bending using the modified fingertip-to-floor method. Phys Ther 1990;70:443-7. https://doi.org/10.1093/ptj/70.7.443.
- Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine 1984;9:106-19. https://doi.org/10.1097/00007632-198403000-00002.
- Strand LI, Wisnes AR. The development of a Norwegian pain questionnaire. Pain 1991;46:61-6. https://doi.org/10.1016/0304-3959(91)90034-U.
- Gracely RH, Wall PD, Melzack R. Textbook of Pain. Edinburgh: Churchill Livingstone; 1994.
- Strand LI, Ljunggren AE. The pick-up test for assessing performance of a daily activity in patients with back pain. Adv Physiother 2001;3:17-2. https://doi.org/10.1080/140381901300039288.
- Strand LI, Wie SL. The Sock Test for evaluating activity limitation in patients with musculoskeletal pain. Phys Ther 1999;79:136-45. https://doi.org/10.1093/ptj/79.2.136.
- Sundsvold M, Vaglum P, Denstad K. Comprehensive Physiotherapy Muscle Study. For Use in Clinical Work and Research. Oslo: Ullevål Hospital; 1982.
- Sundsvold M. Muscular pains and psychopathology: evaluation by GPM method. Pain Int Perspect Physi Ther 1985:18-47.
- Frost M, Stuckey S, Smalley LA, Dorman G. Reliability of measuring trunk motions in centimeters. Phys Ther 1982;62:1431-7. https://doi.org/10.1093/ptj/62.10.1431.
- Wie S. An Evaluation of Lifting Function in Persons With Low-Back Pain. An Assessment and Evaluation of the Reliability and Validity of the Dynamic Lift Test ‘Kystatesten Lifting-low’ 1996.
- Focus on research . Br J Occup Ther 1997;60:86-9. https://doi.org/10.1177/030802269706000211.
- Allen L. Embracing a new lifestyle after gastric bypass: a multidisciplinary approach to post-operative exercise program in acute care setting. Combined sections meeting: CSM2007: history repeats itself, Boston, February 14–18. Acute Care Perspect 2006;15:19-20.
- Aquilina R, Baldacchino D. An exploratory study of Maltese patients’ perceptions of their preparation for total joint replacement at the pre-admission clinic. J Orthop Nurs 2007;11:194-203. https://doi.org/10.1016/j.joon.2007.08.014.
- Arthur HM, Daniels C, McKelvie R, Hirsh J, Rush B. Effect of a preoperative intervention on preoperative and postoperative outcomes in low-risk patients awaiting elective coronary artery bypass graft surgery. A randomized, controlled trial. Ann Intern Med 2000;133:253-62. https://doi.org/10.7326/0003-4819-133-4-200008150-00007.
- Bitterli R, Sieben JM, Hartmann M, de Bruin ED. Pre-surgical sensorimotor training for patients undergoing total hip replacement: a randomised controlled trial. Int J Sports Med 2011;32:725-32. https://doi.org/10.1055/s-0031-1271696.
- Bondoc S. Rehabilitation of distal radius fractures: a primer for the OT generalist. OT Pract 2005;10:17-22.
- Bottomley M. An evidence based evaluation of the types and benefits of total hip replacement preoperative education programs used within Australian health districts. Aust Occup Ther J 2011;58.
- Budge G. An evaluation of the occupational therapy for spinal fusion hip spica patients. Br J Occup Ther 1997;60:365-9. https://doi.org/10.1177/030802269706000811.
- Burger H, Marincek C. Return to work after lower limb amputation. Disabil Rehabil 2007;29:1323-9. https://doi.org/10.1080/09638280701320797.
- Burton JH, Marshall JM, Munro P, Moule W, Snell GI, Westall GP. Rehabilitation and transition after lung transplantation in children. Transplant Proc 2009;41:296-9. https://doi.org/10.1016/j.transproceed.2008.10.047.
- Butler GS, Hurley CA, Buchanan KL, Smith-VanHorne J. Prehospital education: effectiveness with total hip replacement surgery patients. Patient Educ Couns 1996;29:189-97. https://doi.org/10.1016/0738-3991(96)00883-X.
- Chisholm DDC, Schreiber J. Creating occupation-based opportunities in a medical model clinical practice setting. OT Pract 2000;5.
- Cohen M, DiLeonardo M, Zaccariello J. Video education: a new approach to improving patient comprehension. OT Pract 2009;14:7-8.
- Conyers D, Prigge P. The first 12 months after upper-limb amputation. InMotion 2011;21:23-4.
- Coudeyre E, Jardin C, Givron P, Ribinik P, Revel M, Rannou F. Could preoperative rehabilitation modify postoperative outcomes after total hip and knee arthroplasty? Elaboration of French clinical practice guidelines. Ann Readapt Med Phys 2007;50:189-97. https://doi.org/10.1016/j.annrmp.2007.02.002.
- Criss M, Takacs S. Rehabilitation of hip fractures across the continuum of care. Top Geriatr Rehabil 2013;29:281-93. https://doi.org/10.1097/TGR.0b013e318292e904.
- Crowe J, Henderson J. Pre-arthroplasty rehabilitation is effective in reducing hospital stay. Can J Occup Ther 2003;70:88-96. https://doi.org/10.1177/000841740307000204.
- Crum KR. Readiness for discharge: occupation-based treatment in the orthopedic setting. OT Pract 2011;16:14-23.
- Dalury DF, Tucker KK, Kelley TC. When can I drive?: brake response times after contemporary total knee arthroplasty. Clin Orthop Relat Res 2011;469:82-6. https://doi.org/10.1007/s11999-010-1507-1.
- Davidson T. Total hip replacement: an audit of the provision and use of equipment. Br J Occup Ther 1999;62:283-7. https://doi.org/10.1177/030802269906200616.
- Dawson-Bowling SJ, Jha S, Chettiar KK, East DJ, Gould GC, Apthorp HD. A multidisciplinary enhanced recovery programme allows discharge within two days of total hip replacement; three- to five-year results of 100 patients. Hip Int 2014;24:167-74. https://doi.org/10.5301/hipint.5000100.
- Doe A. Hip replacement: what you really need to know. Br J Occup Ther 2004;67:234-5.
- Donohue K, Hoevenaars R, McEachern J, Zeman E, Mehta S. Home-based multidisciplinary rehabilitation following hip fracture surgery: what is the evidence?. Rehabil Res Pract 2013;2013:1-10. https://doi.org/10.1155/2013/875968.
- Dronkers JJ, Lamberts H, Reutelingsperger IM, Naber RH, Dronkers-Landman CM, Veldman A, et al. Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: a randomized controlled pilot study. Clin Rehabil 2010;24:614-22. https://doi.org/10.1177/0269215509358941.
- Drummond A, Coole C, Brewin C, Sinclair E. Hip precautions following primary total hip replacement: a national survey of current occupational therapy practice. Br J Occup Ther 2012;75:164-70. https://doi.org/10.4276/030802212X13336366278059.
- Drummond A, Edwards C, Coole C, Brewin C. What do we tell patients about elective total hip replacement in the UK? An analysis of patient literature. BMC Musculoskelet Disord 2013;14. https://doi.org/10.1186/1471-2474-14-152.
- Engblom E, Korpilahti K, Hämäläinen H, Rönnemaa T, Puukka P. Quality of life and return to work 5 years after coronary artery bypass surgery. Long-term results of cardiac rehabilitation. J Cardiopulm Rehabil 1997;17:29-36. https://doi.org/10.1097/00008483-199701000-00004.
- Filiz M, Cakmak A, Ozcan E. The effectiveness of exercise programmes after lumbar disc surgery: a randomized controlled study. Clin Rehabil 2005;19:4-11. https://doi.org/10.1191/0269215505cr836oa.
- Fletchall S. Occupational therapy from the onset: immediate therapeutic intervention accelerates recovery for new amputees. InMotion 2006;16:34-6.
- Fredericks S, Yau T. Educational intervention reduces complications and rehospitalizations after heart surgery. West J Nurs Res 2013;35:1251-65. https://doi.org/10.1177/0193945913490081.
- Ganjiwale D, Ganjiwale J. Occupational therapy rehabilitation of post operative hand injury cases using modified low cost splints and home based exercises: a rural Indian experience. Indian J Physiother Occup Ther 2014;8:208-13. https://doi.org/10.5958/0973-5674.2014.00383.9.
- Gaudry E, Booth J. Using Participatory Action Research (PAR) to develop a ‘my trip to hospital’ DVD with remote first Australian communities. Occupational Therapy Australia, 24th National Conference and Exhibition, 29 June – 1 July 2011. Aust Occup Ther J 2011;58.
- Gill SD, McBurney H. Does exercise reduce pain and improve physical function before hip or knee replacement surgery? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil 2013;94:164-76. https://doi.org/10.1016/j.apmr.2012.08.211.
- Gill SD, McBurney H, Schulz DL. Land-based versus pool-based exercise for people awaiting joint replacement surgery of the hip or knee: results of a randomized controlled trial. Arch Phys Med Rehabil 2009;90:388-94. https://doi.org/10.1016/j.apmr.2008.09.561.
- Gillen G, Berger SM, Lotia S, Morreale J, Siber MI, Trudo WJ. Improving community skills after lower extremity joint replacement. Phys Occup Ther Geriatr 2007;25:41-54. https://doi.org/10.1080/J148v25n04_03.
- Giraudet-Le Quintrec JS, Coste J, Vastel L, Pacault V, Jeanne L, Lamas JP, et al. Positive effect of patient education for hip surgery: a randomized trial. Clin Orthop Relat Res 2003;414:112-20. https://doi.org/10.1097/01.blo.0000079268.91782.bc.
- Grotle M, Garratt AM, Klokkerud M, Løchting I, Uhlig T, Hagen KB. What’s in team rehabilitation care after arthroplasty for osteoarthritis? Results from a multicenter, longitudinal study assessing structure, process, and outcome. Phys Ther 2010;90:121-31. https://doi.org/10.2522/ptj.20080295.
- Guo P. Preoperative education interventions to reduce anxiety and improve recovery among cardiac surgery patients: a review of randomised controlled trials. J Clin Nurs 2015;24:34-46. https://doi.org/10.1111/jocn.12618.
- Hagsten B, Svensson O, Gardulf A. Early individualized postoperative occupational therapy training in 100 patients improves ADL after hip fracture: a randomized trial. Acta Orthop Scand 2004;75:177-83. https://doi.org/10.1080/00016470412331294435.
- Hauer K, Specht N, Schuler M, Bärtsch P, Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age Ageing 2002;31:49-57. https://doi.org/10.1093/ageing/31.1.49.
- Heaton J, McMurray R, Sloper P, Nettleton S. Rehabilitation and total hip replacement: patients’ perspectives on provision. Int J Rehabil Res 2000;23:253-9. https://doi.org/10.1097/00004356-200023040-00001.
- Herbold JA, Bonistall K, Blackburn M. Effectiveness of continuous passive motion in an inpatient rehabilitation hospital after total knee replacement: a matched cohort study. PM&Amp;R 2012;4:719-25. https://doi.org/10.1016/j.pmrj.2012.07.004.
- Herbold JA, Bonistall K, Walsh MB. Rehabilitation following total knee replacement, total hip replacement, and hip fracture: a case-controlled comparison. J Geriatr Phys Ther 2011;34:155-60. https://doi.org/10.1519/JPT.0b013e318216db81.
- Hoffmann T, Russell T. Pre-admission orthopaedic occupational therapy home visits conducted using the internet. J Telemed Telecare 2008;14:83-7. https://doi.org/10.1258/jtt.2007.070808.
- Howell SM, Rogers SL. Method for quantifying patient expectations and early recovery after total knee arthroplasty. Orthopedics 2009;32. https://doi.org/10.3928/01477447-20091020-10.
- Ibrahim MS, Alazzawi S, Nizam I, Haddad FS. An evidence-based review of enhanced recovery interventions in knee replacement surgery. Ann R Coll Surg Engl 2013;95:386-9. https://doi.org/10.1308/003588413X13629960046435.
- Jame Bozorgi AA, Ghamkhar L, Kahlaee AH, Sabouri H. The effectiveness of occupational therapy supervised usage of adaptive devices on functional outcomes and independence after total hip replacement in Iranian elderly: a randomized controlled trial. Occup Ther Int 2016;23:143-53. https://doi.org/10.1002/oti.1419.
- Jepson P, Sands G, Beswick AD, Davis ET, Blom AW, Sackley CM. A feasibility randomised controlled trial of pre-operative occupational therapy to optimise recovery for patients undergoing primary total hip replacement for osteoarthritis (PROOF-THR). Clin Rehabil 2016;30:156-66. https://doi.org/10.1177/0269215515576811.
- Johanson MA, Cohen BA, Snyder KH, McKinley AJ, Scott ML. Outcomes for aging adults following total hip arthroplasty in an acute rehabilitation facility versus a subacute rehabilitation facility: a pilot study. J Geriatr Phys Ther 2009;32:29-34. https://doi.org/10.1519/00139143-200932020-00006.
- Kaiser GL, Bodell LS, Berger RA. Functional outcomes after arthroplasty of the distal radioulnar joint and hand therapy: a case series. J Hand Ther 2008;21:398-409. https://doi.org/10.1197/j.jht.2008.06.002.
- Kiefer DE, Emery LJ. Functional performance and grip strength after total hip replacement. Occup Ther Health Care 2005;18:41-56. https://doi.org/10.1080/J003v18n04_04.
- Kirk-Sanchez NJ, Roach KE. Relationship between duration of therapy services in a comprehensive rehabilitation program and mobility at discharge in patients with orthopedic problems. Phys Ther 2001;81:888-95. https://doi.org/10.1093/ptj/81.3.888.
- Koval KJ, Cooley MR. Clinical pathway after hip fracture. Disabil Rehabil 2005;27:1053-60. https://doi.org/10.1080/09638280500056618.
- Lenze EJ, Munin MC, Quear T, Dew MA, Rogers JC, Begley AE, et al. Significance of poor patient participation in physical and occupational therapy for functional outcome and length of stay. Arch Phys Med Rehabil 2004;85:1599-601. https://doi.org/10.1016/j.apmr.2004.03.027.
- Lucas B, Cox C, Perry L, Bridges J. Pre-operative preparation of patients for total knee replacement: an action research study. Int J Orthop Trauma Nurs 2013;17:79-90. https://doi.org/10.1016/j.ijotn.2012.08.005.
- MacKay C, Davis AM, Mahomed N, Badley EM. Expanding roles in orthopaedic care: a comparison of physiotherapist and orthopaedic surgeon recommendations for triage. J Eval Clin Pract 2009;15:178-83. https://doi.org/10.1111/j.1365-2753.2008.00979.x.
- Maillette PMCM, Gaudreault NG. Workers’ Perspectives on the Return to Work After Total Knee Arthroplasty n.d.
- Mallinson TR, Bateman J, Tseng HY, Manheim L, Almagor O, Deutsch A, et al. A comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after lower-extremity joint replacement surgery. Arch Phys Med Rehabil 2011;92:712-20. https://doi.org/10.1016/j.apmr.2010.12.007.
- Mata H, Mikkola A, Loveland J, Hallowell PT. Occupational therapy and bariatric surgery. OT Pract 2015;20:11-5.
- McCormick L. The role of occupational therapy in the adult bone marrow transplant process. Phys Disabil Spec Inter Sect Q 2014;37:1-4.
- McGregor AH, Probyn K, Cro S, Doré CJ, Burton AK, Balagué F, et al. Rehabilitation following surgery for lumbar spinal stenosis. A Cochrane review. Spine 2014;39:1044-54. https://doi.org/10.1097/BRS.0000000000000355.
- McMurray R, Heaton J, Sloper P, Nettleton S. Variations in the provision of occupational therapy for patients undergoing primary elective total hip replacement in the United Kingdom. Br J Occup Ther 2000;63:451-5. https://doi.org/10.1177/030802260006300909.
- McQuaid L, Cope J, Fenech A. Occupational therapy in orthopaedics: an alternative to hip precautions?. Int J Ther Rehabil 2014;21:508-10. https://doi.org/10.12968/ijtr.2014.21.11.508.
- McQueen J, Nivison C, Ballance F, Fairbairn P, Clyde D, Murray E. Hip precautions following hemiarthroplasty: a UK study of occupational therapists. Int J Ther Rehabil 2009;16:147-53. https://doi.org/10.12968/ijtr.2009.16.3.40068.
- Merle C, Brendle S, Wang H, Streit MR, Gotterbarm T, Schiltenwolf M. Multidisciplinary treatment in patients with persistent pain following total hip and knee arthroplasty. J Arthroplasty 2014;29:28-32. https://doi.org/10.1016/j.arth.2013.05.004.
- Messecar D. ‘Hospital at home’ care was generally as effective as routine hospital care for older adults. Evid Based Nurs 1999:50-1.
- Millet R. Occupational therapists set out their stall. Frontline 2012;18.
- Miró J, Raich RM. Effects of a brief and economical intervention in preparing patients for surgery: does coping style matter?. Pain 1999;83:471-5. https://doi.org/10.1016/S0304-3959(99)00151-7.
- Mirza SK, Deyo RA, Heagerty PJ, Turner JA, Martin BI, Comstock BA. One-year outcomes of surgical versus nonsurgical treatments for discogenic back pain: a community-based prospective cohort study. Spine J 2013;13:1421-33. https://doi.org/10.1016/j.spinee.2013.05.047.
- Moore SM. Effects of interventions to promote recovery in coronary artery bypass surgical patients. J Cardiovasc Nurs 1997;12:59-70. https://doi.org/10.1097/00005082-199710000-00007.
- Mulcahey MJ, Betz RR, Kozin SH, Smith BT, Hutchinson D, Lutz C. Implantation of the Freehand System during initial rehabilitation using minimally invasive techniques. Spinal Cord 2004;42:146-55. https://doi.org/10.1038/sj.sc.3101573.
- Munin MC, Putman K, Hsieh CH, Smout RJ, Tian W, DeJong G, et al. Analysis of rehabilitation activities within skilled nursing and inpatient rehabilitation facilities after hip replacement for acute hip fracture. Am J Phys Med Rehabil 2010;89:530-40. https://doi.org/10.1097/PHM.0b013e3181e29f54.
- Munin MC, Rudy TE, Glynn NW, Crossett LS, Rubash HE. Early inpatient rehabilitation after elective hip and knee arthroplasty. JAMA 1998;279:847-52. https://doi.org/10.1001/jama.279.11.847.
- Naglie G, Tansey C, Kirkland JL, Ogilvie-Harris DJ, Detsky AS, Etchells E, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ 2002;167:25-32.
- Naville J, Volz T, Curry J. A multidisciplinary approach to total joint replacement. Home Health Care Manage Pract 2009;21:415-8. https://doi.org/10.1177/1084822309335233.
- Nazzal MI, Bashaireh KH, Alomari MA, Nazzal MS, Maayah MF, Mesmar M. Relationship between improvements in physical measures and patient satisfaction in rehabilitation after total knee arthroplasty. Int J Rehabil Res 2012;35:94-101. https://doi.org/10.1097/MRR.0b013e32834df63c.
- Neville-Smith M, Trujillo L, Ammundson R. Special feature: consistency in postoperative education programs following total hip replacement. Top Geriatr Rehabil 2000;15:68-76. https://doi.org/10.1097/00013614-200006000-00008.
- Newport ML, Tucker RL. New perspectives on extensor tendon repair and implications for rehabilitation. J Hand Ther 2005;18:175-81. https://doi.org/10.1197/j.jht.2005.01.006.
- Nilsson I, Rogmark C. Hemiarthroplasty for displaced femoral neck fracture: good clinical outcome but uneven distribution of occupational therapy. Disabil Rehabil 2011;33:2329-32. https://doi.org/10.3109/09638288.2011.570412.
- Novalis SD, Messenger MF, Morris L. Occupational therapy benchmarks within orthopedic (hip) critical pathways. Am J Occup Ther 2000;54:155-8. https://doi.org/10.5014/ajot.54.2.155.
- Oberg T, Oberg U, Svidén G, Nordwall Persson A. Functional capacity after hip arthroplasty: a comparison between evaluation with three standard instruments and a personal interview. Scand J Occup Ther 2005;12:18-2. https://doi.org/10.1080/11038120510027153.
- O’Brien L, McKeough C, Abbasi R. Pre-surgery education for elective cardiac surgery patients: a survey from the patient’s perspective. Aust Occup Ther J 2013;60:404-9. https://doi.org/10.1111/1440-1630.12068.
- O’Donnell S, Kennedy D, MacLeod AM, Kilroy C, Gollish J. Achieving team consensus on best practice rehabilitation guidelines following primary total hip replacement (THR) surgery. Healthc Q 2006;9:60-4. https://doi.org/10.12927/hcq.2006.18354.
- Oldmeadow LB, Edwards ER, Kimmel LA, Kipen E, Robertson VJ, Bailey MJ. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg 2006;76:607-11. https://doi.org/10.1111/j.1445-2197.2006.03786.x.
- Orpen N, Harris J. Patients’ perceptions of preoperative home-based occupational therapy and/or physiotherapy interventions prior to total hip replacement. Br J Occup Ther 2010;73:461-9. https://doi.org/10.4276/030802210X12865330218267.
- Pace M, Maguire K. Hand and upper extremity transplantation: a rehabilitation process. OT Pract 2011;16:17-22.
- Peiris CL, Taylor NF, Shields N. Additional Saturday allied health services increase habitual physical activity among patients receiving inpatient rehabilitation for lower limb orthopedic conditions: a randomized controlled trial. Arch Phys Med Rehabil 2012;93:1365-70. https://doi.org/10.1016/j.apmr.2012.03.004.
- Pfund A, Pütz J, Wendland G, Theisson M, Aydin U, Hinzpeter B, et al. Coronary intervention and occupational rehabilitation – a prospective, randomized intervention study. Z Kardiol 2001;90:655-60. https://doi.org/10.1007/s003920170113.
- Piva SR, Moore CG, Schneider M, Gil AB, Almeida GJ, Irrgang JJ. A randomized trial to compare exercise treatment methods for patients after total knee replacement: protocol paper rehabilitation, physical therapy and occupational health. BMC Musculoskelet Disord 2015;16. https://doi.org/10.1186/s12891-015-0761-5.
- Pomerance J, Fine I. Outcomes of carpal tunnel surgery with and without supervised postoperative therapy. J Hand Surg Am 2007;32:1159-63. https://doi.org/10.1016/j.jhsa.2007.05.001.
- Poole JL, Walenta MH, Alonzo V, Coe A, Moneim M. A pilot study comparing of two therapy regimens following carpometacarpal joint arthroplasty. Phys Occup Ther Geriatr 2011;29:327-36. https://doi.org/10.3109/02703181.2011.613530.
- Prouty A, Cooper M, Thomas P, Christensen J, Strong C, Bowie L, et al. Multidisciplinary patient education for total joint replacement surgery patients. Orthop Nurs 2006;25:257-61. https://doi.org/10.1097/00006416-200607000-00007.
- Provinciali L, Giattini A, Splendiani G, Logullo F. Usefulness of hand rehabilitation after carpal tunnel surgery. Muscle Nerve 2000;23:211-16. https://doi.org/10.1002/(SICI)1097-4598(200002)23:2<211::AID-MUS11>3.0.CO;2-J.
- Rannou F, Coudeyre E, Ribinik P, Macé Y, Poiraudeau S, Revel M. Establishing recommendations for physical medicine and rehabilitation: the SOFMER methodology. Ann Readapt Med Phys 2007;50:100-10. https://doi.org/10.1016/j.annrmp.2007.01.003.
- Rapado A. General management of vertebral fractures. Bone 1996;18:191-6S. https://doi.org/10.1016/8756-3282(95)00501-3.
- Ribinik P, Le Moine F, de Korvin G, Coudeyre E, Genty M, Rannou F, et al. Physical and rehabilitation medicine (PRM) care pathways: ‘patients after total knee arthroplasty’. Ann Phys Rehabil Med 2012;55:533-9. https://doi.org/10.1016/j.rehab.2012.02.001.
- Riddell J. Occupational therapy for adults undergoing total hip replacement. Br J Occup Ther 2013;76.
- Rivard A, Warren S, Voaklander D, Jones A. The efficacy of pre-operative home visits for total hip replacement clients. Can J Occup Ther 2003;70:226-32. https://doi.org/10.1177/000841740307000406.
- Roberts K. Video review. Occupational therapy postoperative management: total hip joint replacement. Aust Occup Ther J 2003;50. https://doi.org/10.1046/j.1440-1630.2003.00390.x.
- Roddey TS, Olson SL, Gartsman GM, Hanten WP, Cook KF. A randomized controlled trial comparing 2 instructional approaches to home exercise instruction following arthroscopic full-thickness rotator cuff repair surgery. J Orthop Sports Phys Ther 2002;32:548-59. https://doi.org/10.2519/jospt.2002.32.11.548.
- Ronco M, Iona L, Fabbro C, Bulfone G, Palese A. Patient education outcomes in surgery: a systematic review from 2004 to 2010. Int J Evid Based Healthc 2012;10:309-23. https://doi.org/10.1111/j.1744-1609.2012.00286.x.
- Rucco V, Visentini A, Pellegrini E. The rehabilitation project in hip arthroplasty patients. Eur Medicophys 2003;39:45-57.
- Safdar S. Wide-awake flexor tendon repair. OT Pract 2015;20:7-16.
- Sameem M, Wood T, Ignacy T, Thoma A, Strumas N. A systematic review of rehabilitation protocols after surgical repair of the extensor tendons in zones V-VIII of the hand. J Hand Ther 2011;24:365-72. https://doi.org/10.1016/j.jht.2011.06.005.
- Sandell C. A multidisciplinary assessment and intervention for patients awaiting total hip replacement to improve their quality of life. J Orthop Nurs 2008;12:26-34. https://doi.org/10.1016/j.joon.2007.11.002.
- Sawatzky JA, Kehler DS, Ready AE, Lerner N, Boreskie S, Lamont D, et al. Prehabilitation program for elective coronary artery bypass graft surgery patients: a pilot randomized controlled study. Clin Rehabil 2014;28:648-57. https://doi.org/10.1177/0269215513516475.
- Schneider M, Kawahara I, Ballantyne G, McAuley C, Macgregor K, Garvie R, et al. Predictive factors influencing fast track rehabilitation following primary total hip and knee arthroplasty. Arch Orthop Trauma Surg 2009;129:1585-91. https://doi.org/10.1007/s00402-009-0825-9.
- Scott PJ. Occupational therapy services to enable liver patients to thrive following transplantation. Occup Ther Health Care 2011;25:240-56. https://doi.org/10.3109/07380577.2011.600427.
- Shahmansouri N, Janghorbani M, Salehi Omran A, Karimi AA, Noorbala AA, Arjmandi A, et al. Effects of a psychoeducation intervention on fear and anxiety about surgery: randomized trial in patients undergoing coronary artery bypass grafting. Psychol Health Med 2014;19:375-83. https://doi.org/10.1080/13548506.2013.841966.
- Sheehan MM, Wilson SF, Vaz AM. Ambulatory rehabilitation for hip and knee arthroplasty. Nurs Monogr 2007:16-9.
- Shuldham CM, Fleming S, Goodman H. The impact of pre-operative education on recovery following coronary artery bypass surgery. A randomized controlled clinical trial. Eur Heart J 2002;23:666-74. https://doi.org/10.1053/euhj.2001.2897.
- Siebens HC, Sharkey P, Aronow HU, Deutscher D, Roberts P, Munin MC, et al. Variation in rehabilitation treatment patterns for hip fracture treated with arthroplasty. PM&Amp;R 2016;8:191-207. https://doi.org/10.1016/j.pmrj.2015.07.005.
- Spalding N. Health promotion and the role of occupational therapy. Br J Ther Rehabil 1996;3:143-7. https://doi.org/10.12968/bjtr.1996.3.3.14855.
- Spalding NJ. Reducing anxiety by pre-operative education: make the future familiar. Occup Ther Int 2003;10:278-93. https://doi.org/10.1002/oti.191.
- Spalding NJ. Using vignettes to assist reflection within an action research study on a preoperative education programme. Br J Occup Ther 2004;67:388-95. https://doi.org/10.1177/030802260406700903.
- Spalevic MLM, Kocic M, Dimitrijevic L, Stankovic I, Savic D. The Effects of Preoperative Physical Therapy in Total Hip Replacement Surgery n.d. https://doi.org/10.1097/00004356-200908001-00133.
- Spiliotopoulou G, Atwal A. Is occupational therapy practice for older adults with lower limb amputations evidence-based? A systematic review. Prosthet Orthot Int 2012;36:7-14. https://doi.org/10.1177/0309364611428662.
- Stambough JB, Beaulé PE, Nunley RM, Clohisy J. Contemporary strategies for rapid recovery total hip arthroplasty. Instr Course Lect 2016;65:211-24.
- Stinnett KA. Occupational therapy intervention for the geriatric client receiving acute and subacute services following total hip replacement and femoral fracture repair. Top Geriatr Rehabil 1996:23-31. https://doi.org/10.1097/00013614-199609000-00005.
- Svendsen SW, Christiansen DH, Haahr JP, Andrea LC, Frost P. Shoulder function and work disability after decompression surgery for subacromial impingement syndrome: a randomised controlled trial of physiotherapy exercises and occupational medical assistance. BMC Musculoskelet Disord 2014;15. https://doi.org/10.1186/1471-2474-15-215.
- Szekeres M, King GJW. Total elbow arthroplasty. J Hand Ther 2006;19:245-54. https://doi.org/10.1197/j.jht.2006.02.010.
- Thien T, Becker J. Rehabilitation after surgery for flexor tendon injuries in the hand. Cochrane Database Syst Rev 2004;18. https://doi.org/10.1002/14651858.CD003979.pub2.
- Tian W, DeJong G, Munin MC, Smout R. Patterns of rehabilitation after hip arthroplasty and the association with outcomes: an episode of care view. Am J Phys Med Rehabil 2010;89:905-18. https://doi.org/10.1097/PHM.0b013e3181f1c6d8.
- Walker J. Care of patients undergoing joint replacement. Nurs Older People 2012;24:14-20. https://doi.org/10.7748/nop2012.02.24.1.14.c8898.
- Wang X, Emery LJ. Cognitive status after hip replacement. Phys Occup Ther Geriatr 2002;21:51-64. https://doi.org/10.1080/J148v21n01_04.
- Wasserman BR, Egol KA, Zuckerman JD. Managing hip fractures in older patients: perioperative decision making. J Musculoskelet Med 2008;25:326-34.
- Westby MD. Rehabilitation and total joint arthroplasty. Clin Geriatr Med 2012;28:489-508. https://doi.org/10.1016/j.cger.2012.05.005.
- Shyu YI, Liang J, Tseng MY, Li HJ, Wu CC, Cheng HS, et al. Comprehensive and subacute care interventions improve health-related quality of life for older patients after surgery for hip fracture: a randomised controlled trial. Int J Nurs Stud 2013;50:1013-24. https://doi.org/10.1016/j.ijnurstu.2012.11.020.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: University of Kent, PSSRU; 2015.
- Communities and Local Government . English Indices of Deprivation 2019 n.d. www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed 28 June 2020).
Appendix 1 Protocol version history
| Version | Date | Comments |
|---|---|---|
| 1.0 | 1 July 2016 | Project commenced with version 1.0 |
| 2.0 | 8 August 2016 | Minor changes to the protocol prior to final ethics submission. HRA approval issued on 4 October 2016 (6 October 2016 reissued) – see ethics approvals and HRA correspondence documents (www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/; accessed 2 May 2020) |
| 3.0 | 4 November 2016 |
Study protocol amendment relates to inclusion of nurses (involved in the care of the hip/knee replacement patient group) to be interviewed as part of the AHP group stakeholder interviews Amendment number/sponsor reference: NSA #2 – minor changes to protocol Amendment date: 31 January 2017 Amendment type: non-substantial |
| 4.0 | 4 April 2018 |
Protocol updated to include information relating to the Delphi process, adoption and implementation plans and feasibility testing. Change made to facilitate resubmission to HRA for approval of notified amendment prior to commencing patient recruitment for the feasibility element of the study (cohort 2) Amendment number/sponsor reference: 3 Amendment date: 26 April 2018 Amendment type: substantial non-CTIMP |
Appendix 2 Supporting information for the rapid evidence synthesis (IM stage 1)
Search strategies for the rapid evidence synthesis
Search strategies for systematic reviews
MEDLINE Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE
Date searched: 12 July 2016.
Date range searched: 1946 to present.
Search strategy
-
return to work/ (1009)
-
(return* adj2 (work* or employment)).tw. (9320)
-
(resum* adj2 (work* or employment)).tw. (885)
-
(back adj2 (work* or employment)).tw. (1474)
-
((back or return* or resum*) adj2 usual activit*).tw. (129)
-
((back or return* or resum*) adj2 normal activit*).tw. (2039)
-
(work or workplace* or worksite*).ti. (85,708)
-
Occupational Therapy/ (11,378)
-
Activities of Daily Living/ (55,286)
-
8 and 9 (1285)
-
(occupational adj2 (therapy or intervention$ or advice or information or guidance)).ti,ab. (8732)
-
(usual activit$ or daily activit$ or everyday activit$ or normal activit$).ti,ab. (20,849)
-
(everyday life or daily life).ti,ab. (18,856)
-
((social or community or family) adj2 participat$).ti,ab. (10,319)
-
12 or 13 or 14 (49,033)
-
11 and 15 (325)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 10 or 16 (97,766)
-
MEDLINE.tw. (79,537)
-
systematic review.tw. (78,220)
-
meta analysis.pt. (70,890)
-
18 or 19 or 20 (169,057)
-
17 and 21 (1452)
-
limit 22 to (english language and yr="2015 -Current") (229)
-
(systematic$ adj2 review$).ti,ab. (95,694)
-
meta-analysis as topic/ (15,169)
-
meta-analytic$.ti,ab. (4933)
-
meta-analysis.ti,ab,pt. (106,298)
-
metanalysis.ti,ab. (148)
-
metaanalysis.ti,ab. (1321)
-
meta analysis.ti,ab. (84,187)
-
meta-synthesis.ti,ab. (413)
-
metasynthesis.ti,ab. (194)
-
meta synthesis.ti,ab. (413)
-
meta-regression.ti,ab. (4024)
-
metaregression.ti,ab. (414)
-
meta regression.ti,ab. (4024)
-
(synthes$ adj3 literature).ti,ab. (1971)
-
(synthes$ adj3 evidence).ti,ab. (5745)
-
integrative review.ti,ab. (1434)
-
data synthesis.ti,ab. (8609)
-
(research synthesis or narrative synthesis).ti,ab. (1353)
-
(systematic study or systematic studies).ti,ab. (9268)
-
(systematic comparison$ or systematic overview$).ti,ab. (2428)
-
evidence based review.ti,ab. (1602)
-
comprehensive review.ti,ab. (9430)
-
critical review.ti,ab. (12,776)
-
quantitative review.ti,ab. (558)
-
structured review.ti,ab. (601)
-
realist review.ti,ab. (130)
-
realist synthesis.ti,ab. (101)
-
pooled analysis.ti,ab. (5483)
-
or/24-51 (224,199)
-
review.pt. (2,160,213)
-
medline.ab. (79,144)
-
pubmed.ab. (56,121)
-
cochrane.ab. (49,164)
-
embase.ab. (49,803)
-
cinahl.ab. (16,302)
-
psyc?lit.ab. (904)
-
psyc?info.ab. (13,963)
-
(literature adj3 search$).ab. (37,155)
-
(database$ adj3 search$).ab. (35,979)
-
(bibliographic adj3 search$).ab. (1686)
-
(electronic adj3 search$).ab. (13,608)
-
(electronic adj3 database$).ab. (16,767)
-
(computeri?ed adj3 search$).ab. (3066)
-
(internet adj3 search$).ab. (2284)
-
included studies.ab. (12,720)
-
(inclusion adj3 studies).ab. (10,033)
-
inclusion criteria.ab. (52,316)
-
selection criteria.ab. (27,264)
-
predefined criteria.ab. (1415)
-
predetermined criteria.ab. (846)
-
(assess$ adj3 (quality or validity)).ab. (54,589)
-
(select$ adj3 (study or studies)).ab. (48,320)
-
(data adj3 extract$).ab. (41,727)
-
extracted data.ab. (10,773)
-
(data adj2 abstracted).ab. (4065)
-
(data adj3 abstraction).ab. (1159)
-
published intervention$.ab. (137)
-
((study or studies) adj2 evaluat$).ab. (134,076)
-
(intervention$ adj2 evaluat$).ab. (7948)
-
confidence interval$.ab. (293,086)
-
heterogeneity.ab. (117,958)
-
pooled.ab. (60,403)
-
pooling.ab. (9358)
-
odds ratio$.ab. (192,922)
-
(Jadad or coding).ab. (143,477)
-
or/54-88 (1,028,147)
-
53 and 89 (163,451)
-
review.ti. (329,001)
-
91 and 89 (74,527)
-
(review$ adj4 (papers or trials or studies or evidence or intervention$ or evaluation$)).ti,ab. (133,651)
-
52 or 90 or 92 or 93 (389,132)
-
letter.pt. (932,159)
-
editorial.pt. (412,140)
-
comment.pt. (677,186)
-
95 or 96 or 97 (1,513,065)
-
94 not 98 (379,528)
-
exp animals/not humans/ (4,276,691)
-
99 not 100 (368,838)
-
17 and 101 (2468)
-
limit 102 to (english language and yr="2015 -Current") (366)
-
23 or 103 (375)
EMBASE
Date searched: 12 July 2016.
Date range searched: 1974 to 2016 week 28.
Search strategy
-
work resumption/ or return to work/ (5861)
-
((back or return* or resum*) adj2 normal activit*).tw. (2669)
-
((back or return* or resum*) adj2 usual activit*).tw. (164)
-
((back or return* or resum*) adj2 (work* or employment)).tw. (13,816)
-
(work or workplace* or worksite*).ti. (93,856)
-
Occupational Therapy/ (19,333)
-
daily life activity/ (65,541)
-
6 and 7 (2054)
-
(occupational adj2 (therapy or intervention$ or advice or information or guidance)).ti,ab. (12,270)
-
(usual activit$ or daily activit$ or everyday activit$ or normal activit$).ti,ab. (28,784)
-
(everyday life or daily life).ti,ab. (25,739)
-
((social or community or family) adj2 participat$).ti,ab. (11,513)
-
10 or 11 or 12 (64,544)
-
9 and 13 (529)
-
1 or 2 or 3 or 4 or 5 or 8 or 14 (111,455)
-
systematic$ review$.ti,ab. (106,926)
-
systematic$ literature review$.ti,ab. (7748)
-
“systematic review”/ (109,866)
-
“systematic review (topic)”/ (16,007)
-
meta analysis/ (111,622)
-
“meta analysis (topic)”/ (27,698)
-
meta-analytic$.ti,ab. (5491)
-
meta-analysis.ti,ab. (103,470)
-
metanalysis.ti,ab. (367)
-
metaanalysis.ti,ab. (4993)
-
meta analysis.ti,ab. (103,470)
-
meta-synthesis.ti,ab. (378)
-
metasynthesis.ti,ab. (182)
-
meta synthesis.ti,ab. (378)
-
meta-regression.ti,ab. (4754)
-
metaregression.ti,ab. (642)
-
meta regression.ti,ab. (4754)
-
(synthes$ adj3 literature).ti,ab. (2196)
-
(synthes$ adj3 evidence).ti,ab. (6216)
-
(synthes$ adj2 qualitative).ti,ab. (1079)
-
integrative review.ti,ab. (1173)
-
data synthesis.ti,ab. (10,472)
-
(research synthesis or narrative synthesis).ti,ab. (1275)
-
(systematic study or systematic studies).ti,ab. (9972)
-
(systematic comparison$ or systematic overview$).ti,ab. (2576)
-
(systematic adj2 search$).ti,ab. (16,572)
-
systematic$ literature research$.ti,ab. (189)
-
(review adj3 scientific literature).ti,ab. (1268)
-
(literature review adj2 side effect$).ti,ab. (12)
-
(literature review adj2 adverse effect$).ti,ab. (2)
-
(literature review adj2 adverse event$).ti,ab. (11)
-
(evidence-based adj2 review).ti,ab. (2732)
-
comprehensive review.ti,ab. (10,628)
-
critical review.ti,ab. (14,174)
-
critical analysis.ti,ab. (7020)
-
quantitative review.ti,ab. (617)
-
structured review.ti,ab. (752)
-
realist review.ti,ab. (119)
-
realist synthesis.ti,ab. (75)
-
(pooled adj2 analysis).ti,ab. (11,998)
-
(pooled data adj6 (studies or trials)).ti,ab. (1896)
-
(medline and (inclusion adj3 criteria)).ti,ab. (15,165)
-
(search adj (strateg$ or term$)).ti,ab. (24,858)
-
or/16-58 (341,191)
-
medline.ab. (89,743)
-
pubmed.ab. (68,036)
-
cochrane.ab. (55,437)
-
embase.ab. (56,000)
-
cinahl.ab. (16,308)
-
psyc?lit.ab. (965)
-
psyc?info.ab. (12,865)
-
lilacs.ab. (4553)
-
(literature adj3 search$).ab. (44,951)
-
(database$ adj3 search$).ab. (42,042)
-
(bibliographic adj3 search$).ab. (1882)
-
(electronic adj3 search$).ab. (14,783)
-
(electronic adj3 database$).ab. (20,773)
-
(computeri?ed adj3 search$).ab. (3486)
-
(internet adj3 search$).ab. (2935)
-
included studies.ab. (13,776)
-
(inclusion adj3 studies).ab. (11,147)
-
inclusion criteria.ab. (82,127)
-
selection criteria.ab. (25,286)
-
predefined criteria.ab. (1833)
-
predetermined criteria.ab. (1026)
-
(assess$ adj3 (quality or validity)).ab. (67,482)
-
(select$ adj3 (study or studies)).ab. (60,109)
-
(data adj3 extract$).ab. (50,271)
-
extracted data.ab. (10,865)
-
(data adj2 abstracted).ab. (6110)
-
(data adj3 abstraction).ab. (1567)
-
published intervention$.ab. (155)
-
((study or studies) adj2 evaluat$).ab. (180,324)
-
(intervention$ adj2 evaluat$).ab. (10,236)
-
confidence interval$.ab. (326,652)
-
heterogeneity.ab. (139,933)
-
pooled.ab. (78,503)
-
pooling.ab. (11,574)
-
odds ratio$.ab. (226,153)
-
(Jadad or coding).ab. (159,476)
-
evidence-based.ti,ab. (94,548)
-
or/60-96 (1,337,619)
-
review.pt. (2,180,899)
-
97 and 98 (164,450)
-
review.ti. (376,276)
-
97 and 100 (88,520)
-
(review$ adj10 (papers or trials or trial data or studies or evidence or intervention$ or evaluation$ or outcome$ or findings)).ti,ab. (372,964)
-
(retriev$ adj10 (papers or trials or studies or evidence or intervention$ or evaluation$ or outcome$ or findings)).ti,ab. (18,949)
-
59 or 99 or 101 or 102 or 103 (693,905)
-
letter.pt. (946,723)
-
editorial.pt. (513,729)
-
105 or 106 (1,460,452)
-
104 not 107 (680,968)
-
(animal/or nonhuman/) not exp human/ (5,063,625)
-
108 not 109 (654,903)
-
“cochrane database of systematic reviews$”.jn. (11,204)
-
110 not 111 (644,891)
-
conference abstract.pt. (2,296,758)
-
112 not 113 (561,003)
-
15 and 114 (3328)
-
limit 115 to (english language and yr="2015 -Current") (317)
Cochrane Database of Systematic Reviews and Database of Abstracts of Reviews of Effects
Date searched: 12 July 2016.
Date range searched: no restriction.
Search strategy
-
#1 MeSH descriptor: [Return to Work] explode all trees
-
#2 (return* near/2 (work* or employment)):ti,ab,kw (Word variations have been searched)
-
#3 (resum* near/2 (work* or employment)):ti,ab,kw (Word variations have been searched)
-
#4 (back* near/2 (work* or employment)):ti,ab,kw (Word variations have been searched)
-
#5 ((back or return* or resum*) near/2 usual activit*):ti,ab,kw (Word variations have been searched)
-
#6 ((back or return* or resum*) near/2 normal activit*):ti,ab,kw (Word variations have been searched)
-
#7 (work or workplace* or worksite*):ti (Word variations have been searched)
-
#8 MeSH descriptor: [Occupational Therapy] explode all trees
-
#9 MeSH descriptor: [Activities of Daily Living] this term only
-
#10 #8 and #9
-
#11 (occupational near/2 (therapy or intervention* or advice or information or guidance)):ti,ab,kw (Word variations have been searched)
-
#12 (usual activit* or daily activit* or everyday activit* or normal activit*):ti,ab,kw (Word variations have been searched)
-
#13 (everyday life or daily life):ti,ab,kw (Word variations have been searched)
-
#14 ((social or community or family) near/2 participat*):ti,ab,kw (Word variations have been searched)
-
#15 #12 or #13 or #14
-
#16 #11 and #15
-
#17 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #10 or #16
Search strategies for primary studies
Cumulative Index to Nursing and Allied Health Literature (via EBSCOhost)
Date searched: 19 August 2016.
Date range searched: 1996 to 19 August 2016.
Records identified: 484.
Search strategy
-
S1 (MH “Surgery, Operative+”) (426,382)
-
S2 elective N2 surgery OR elective N2 surgical OR plan* N2 surgery OR plan* N2 surgical (6,896)
-
S3 S1 OR S2 (428,083)
-
S4 (MH “Occupational Therapy+”) OR (MH “Occupational Therapy Practice, Research-Based”) OR (MH “Occupational Therapy Practice, Evidence-Based”) OR (MH “Occupational Therapy Assessment”) OR (MH “Occupational Therapy Service”) OR (MH “Occupational Therapy Practice”) OR (MH “Home Occupational Therapy”) (21,853)
-
S5 occupational N3 (advice or advis* or guidance or information or intervention* or therap*) (33,360)
-
S6 S4 OR S5 (34,139)
-
S7 S3 AND S6 (551)
-
S8 S3 AND S6 – English (543)
-
S9 S3 AND S6 - Published Date: 19960101-20161231 (484)
Cochrane Central Register of Controlled Trials (via the Cochrane Library)
Date searched: 23 August 2016.
Date range searched: no restriction.
Records identified: 24.
Search strategy
-
#1 MeSH descriptor: [Specialties, Surgical] explode all trees
-
#2 MeSH descriptor: [Colorectal Surgery] this term only
-
#3 MeSH descriptor: [General Surgery] explode all trees
-
#4 MeSH descriptor: [Gynecology] this term only
-
#5 MeSH descriptor: [Neurosurgery] this term only
-
#6 MeSH descriptor: [Obstetrics] this term only
-
#7 MeSH descriptor: [Ophthalmology] this term only
-
#8 MeSH descriptor: [Orthognathic Surgery] explode all trees
-
#9 MeSH descriptor: [Orthopedics] this term only
-
#10 MeSH descriptor: [Otolaryngology] this term only
-
#11 MeSH descriptor: [Surgery, Plastic] this term only
-
#12 MeSH descriptor: [Thoracic Surgery] this term only
-
#13 MeSH descriptor: [Traumatology] this term only
-
#14 MeSH descriptor: [Urology] this term only
-
#15 MeSH descriptor: [Sports Medicine] this term only
-
#16 MeSH descriptor: [Surgical Procedures, Operative] explode all trees
-
#17 MeSH descriptor: [Ablation Techniques] explode all trees
-
#18 MeSH descriptor: [Ambulatory Surgical Procedures] explode all trees
-
#19 MeSH descriptor: [Anastomosis, Surgical] explode all trees
-
#20 MeSH descriptor: [Assisted Circulation] explode all trees
-
#21 MeSH descriptor: [Bariatric Surgery] explode all trees
-
#22 MeSH descriptor: [Biopsy] explode all trees
-
#23 MeSH descriptor: [Bloodless Medical and Surgical Procedures] explode all trees
-
#24 MeSH descriptor: [Body Modification, Non-Therapeutic] explode all trees
-
#25 MeSH descriptor: [Cardiovascular Surgical Procedures] explode all trees
-
#26 MeSH descriptor: [Curettage] explode all trees
-
#27 MeSH descriptor: [Cytoreduction Surgical Procedures] explode all trees
-
#28 MeSH descriptor: [Debridement] explode all trees
-
#29 MeSH descriptor: [Decompression, Surgical] explode all trees
-
#30 MeSH descriptor: [Deep Brain Stimulation] explode all trees
-
#31 MeSH descriptor: [Device Removal] explode all trees
-
#32 MeSH descriptor: [Digestive System Surgical Procedures] explode all trees
-
#33 MeSH descriptor: [Dissection] explode all trees
-
#34 MeSH descriptor: [Drainage] explode all trees
-
#35 MeSH descriptor: [Elective Surgical Procedures] explode all trees
-
#36 MeSH descriptor: [Electrosurgery] explode all trees
-
#37 MeSH descriptor: [Endocrine Surgical Procedures] explode all trees
-
#38 MeSH descriptor: [Extracorporeal Circulation] explode all trees
-
#39 MeSH descriptor: [Hemostasis, Surgical] explode all trees
-
#40 MeSH descriptor: [Laparotomy] explode all trees
-
#41 MeSH descriptor: [Ligation] explode all trees
-
#42 MeSH descriptor: [Lymph Node Excision] explode all trees
-
#43 MeSH descriptor: [Mastectomy] explode all trees
-
#44 MeSH descriptor: [Metastasectomy] explode all trees
-
#45 MeSH descriptor: [Microsurgery] explode all trees
-
#46 MeSH descriptor: [Minimally Invasive Surgical Procedures] explode all trees
-
#47 MeSH descriptor: [Minor Surgical Procedures] explode all trees
-
#48 MeSH descriptor: [Monitoring, Intraoperative] explode all trees
-
#49 MeSH descriptor: [Obstetric Surgical Procedures] explode all trees
-
#50 MeSH descriptor: [Neurosurgical Procedures] explode all trees
-
#51 MeSH descriptor: [Ophthalmologic Surgical Procedures] explode all trees
-
#52 MeSH descriptor: [Filtering Surgery] explode all trees
-
#53 MeSH descriptor: [Light Coagulation] explode all trees
-
#54 MeSH descriptor: [Refractive Surgical Procedures] explode all trees
-
#55 MeSH descriptor: [Oral Surgical Procedures] explode all trees
-
#56 MeSH descriptor: [Orthopedic Procedures] explode all trees
-
#57 MeSH descriptor: [Ostomy] explode all trees
-
#58 MeSH descriptor: [Otorhinolaryngologic Surgical Procedures] explode all trees
-
#59 MeSH descriptor: [Pelvic Exenteration] explode all trees
-
#60 MeSH descriptor: [Perioperative Care] explode all trees
-
#61 MeSH descriptor: [Perioperative Period] explode all trees
-
#62 MeSH descriptor: [Prophylactic Surgical Procedures] explode all trees
-
#63 MeSH descriptor: [Prosthesis Implantation] explode all trees
-
#64 MeSH descriptor: [Punctures] explode all trees
-
#65 MeSH descriptor: [Reconstructive Surgical Procedures] explode all trees
-
#66 MeSH descriptor: [Reoperation] explode all trees
-
#67 MeSH descriptor: [Second-Look Surgery] explode all trees
-
#68 MeSH descriptor: [Splenectomy] explode all trees
-
#69 MeSH descriptor: [Surgery, Computer-Assisted] explode all trees
-
#70 MeSH descriptor: [Symphysiotomy] explode all trees
-
#71 MeSH descriptor: [Thoracic Surgical Procedures] explode all trees
-
#72 MeSH descriptor: [Transplantation] explode all trees
-
#73 MeSH descriptor: [Ultrasonic Surgical Procedures] explode all trees
-
#74 MeSH descriptor: [Urogenital Surgical Procedures] explode all trees
-
#75 MeSH descriptor: [Wound Closure Techniques] explode all trees
-
#76 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10
-
#77 #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20
-
#78 #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30
-
#79 #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40
-
#80 #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50
-
#81 #51 or #52 or #53 or #54 or #55 or #56 or #57 or #58 or #59 or #60
-
#82 #61 or #62 or #63 or #64 or #65 or #66 or #67 or #68 or #69 or #70
-
#83 #71 or #72 or #73 or #74 or #75
-
#84 #76 or #77 or #78 or #79 or #80 or #81 or #82 or #83
-
#85 (elective or plan*) near/2 (surgery or surgical):ti,ab,kw (Word variations have been searched)
-
#86 #84 or #85
-
#87 MeSH descriptor: [Occupational Therapy] explode all trees
-
#88 occupational near/3 (advice or advis* or guidance or information or intervention* or therap*):ti,ab,kw (Word variations have been searched)
-
#89 #87 or #88
-
#90 #86 and #88
EMBASE (via Ovid)
Date searched: 18 August 2016.
Date range searched: 1974 to 18 August 2016.
Records identified: 209.
Search strategy
-
*surgery/or exp *abdominal surgery/or exp *ambulatory surgery/or exp *breast surgery/or exp *cancer surgery/or exp *cardiovascular surgery/or exp *ear nose throat surgery/or exp *elective surgery/or exp *endocrine surgery/or exp *eye surgery/or exp *general surgery/or exp *”head and neck surgery”/or exp *major surgery/or exp *minimally invasive surgery/or exp *nanosurgery/or exp *neurosurgery/or exp *orthopedic surgery/or exp *pelvis surgery/or exp *plastic surgery/or exp *postoperative period/or exp *prophylactic surgical procedure/or exp *thorax surgery/or exp *transplantation/or exp *urologic surgery/ (1,842,495)
-
((elective or plan$) adj2 (surgery or surgical)).ti,ab. (36,275)
-
1 or 2 (1,864,768)
-
occupational therapy/or occupational therapist/ (22,937)
-
(occupational adj3 (advice or advis$ or guidance or information or intervention$ or therap$)).ti,ab. (18,412)
-
4 or 5 (28,298)
-
3 and 6 (651)
-
limit 7 to (english language and yr="1996 -Current") (432)
-
limit 8 to embase (384)
-
(conference or conference paper or conference proceeding or conference proceeding article or conference proceeding conference paper or conference proceeding editorial or conference proceeding note or “conference proceeding review” or journal conference abstract or journal conference paper or “journal conference review”).pt. (3,065,391)
-
9 not 10 (279)
-
(editorial or letter).pt. (1,471,286)
-
11 not 12 (269)
-
case report/ (2,125,490)
-
13 not 14 (209)
-
(animal or animals or cat or cats or dog or dogs or mouse or mice or rat or rats or pig or pigs or porcine or horse or horses or equine or sheep or goat or goats or ovine or cow or cows or cattle or bovine or rabbit$ or bird or birds).ti. (2,171,080)
-
15 not 16 (209)
MEDLINE (via Ovid) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE
Date searched: 23 August 2016.
Date range searched: 1946 to present.
Records identified: 319.
Search strategy
-
exp surgical procedures, operative/or ablation techniques/or exp ambulatory surgical procedures/or exp anastomosis, surgical/or exp assisted circulation/or exp bariatric surgery/or exp biopsy/or “bloodless medical and surgical procedures”/or exp body modification, non-therapeutic/or exp cardiovascular surgical procedures/or exp curettage/or cytoreduction surgical procedures/or debridement/or exp decompression, surgical/or deep brain stimulation/or device removal/or exp digestive system surgical procedures/or dissection/or exp drainage/or elective surgical procedures/or electrosurgery/or exp endocrine surgical procedures/or exp extracorporeal circulation/or exp hemostasis, surgical/or laparotomy/or ligation/or exp lymph node excision/or exp mastectomy/or metastasectomy/or exp microsurgery/or exp minimally invasive surgical procedures/or minor surgical procedures/or exp monitoring, intraoperative/or exp obstetric surgical procedures/or exp neurosurgical procedures/or exp ophthalmologic surgical procedures/or exp filtering surgery/or exp light coagulation/or exp refractive surgical procedures/or exp oral surgical procedures/or exp orthopedic procedures/or exp ostomy/or exp otorhinolaryngologic surgical procedures/or exp pelvic exenteration/or exp perioperative care/or exp perioperative period/or prophylactic surgical procedures/or exp prosthesis implantation/or exp punctures/or exp reconstructive surgical procedures/or reoperation/or second-look surgery/or splenectomy/or exp surgery, computer-assisted/or symphysiotomy/or exp thoracic surgical procedures/or exp transplantation/or exp ultrasonic surgical procedures/or exp urogenital surgical procedures/or exp wound closure techniques/ (2,723,809)
-
exp specialties, surgical/or exp colorectal surgery/or exp general surgery/or exp gynecology/or exp neurosurgery/or exp obstetrics/or exp ophthalmology/or exp orthognathic surgery/or exp orthopedics/or exp otolaryngology/or exp surgery, plastic/or exp thoracic surgery/or exp traumatology/or exp urology/or exp sports medicine/ (192,168)
-
((elective or plan$) adj2 (surgery or surgical)).ti,ab. (27,370)
-
1 or 2 or 3 (2,872,395)
-
Occupational Therapy/ (11,460)
-
(occupational adj3 (advice or advis$ or guidance or information or intervention$ or therap$)).ti,ab. (12,732)
-
5 or 6 (17,965)
-
4 and 7 (612)
-
limit 8 to (English language and yr="1996 -Current") (319)
OTseeker (via www.otseeker.com/)
Date searched: 23 August 2016.
Date range searched: 1996 to 23 August 2016.
Search strategy
Title/Abstract] like “surgery” OR [Title/Abstract] like “surgical” (162)
Records identified: 143 after limiting to 1996 onwards.
Data extraction form templates
Data extraction form: systematic reviews
Data extraction form: primary studies
Data extraction form: qualitative studies
List of the 50 full-text systematic reviews screened for eligibility
List of included systematic reviews
Oosterhuis T, Costa LO, Maher CG, de Vet HC, van Tulder MW, Ostelo RW. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev 2014;3:CD003007. https://doi.org/10.1002/14651858.CD003007.pub389
Aas RW, Tuntland H, Holte KA, Røe C, Lund T, Marklund S, Moller A. Workplace interventions for neck pain in workers. Cochrane Database Syst Rev 2011;4:CD008160. https://doi.org/10.1002/14651858.CD008160.pub290
Carroll C, Rick J, Pilgrim H, Cameron J, Hillage J. Workplace involvement improves return to work rates among employees with back pain on long-term sick leave: a systematic review of the effectiveness and cost-effectiveness of interventions. Disabil Rehabil 2010;32:607–21. 91
Désiron HA, de Rijk A, Van Hoof E, Donceel P. Occupational therapy and return to work: a systematic literature review. BMC Public Health 2011;11:615. https://doi.org/10.1186/1471-2458-11-61592
Elders LA, Beek AJ, Burdorf A. Return to work after sickness absence due to back disorders: a systematic review on intervention strategies. Int Arch Occup Environ Health 2000;73:339–48. 93
Franche RL, Cullen K, Clarke J, Irvin E, Sinclair S, Frank J. Workplace-based return-to-work interventions: a systematic review of the quantitative literature. J Occup Rehabil 2005;15:607–31. 94
Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, van Tulder MW. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst Rev 2014;9:CD000963. https://doi.org/10.1002/14651858.CD000963.pub395
Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, Koes B. Multidisciplinary rehabilitation for fibromyalgia and musculoskeletal pain in working age adults. Cochrane Database Syst Rev 1999;3:CD001984. 96
Karjalainen KA, Malmivaara AO, Tulder MW, Roine RP, Jauhiainen MS, Hurri HO, et al. Biopsychosocial rehabilitation for repetitive-strain injuries among working-age adults. Scand J Work Environ Health 2000;26:373–81. 97
Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, Koes B. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults. Cochrane Database Syst Rev 2003;2:CD002194. https://doi.org/10.1002/14651858.CD002194106
Meijer EM, Sluiter JK, Frings-Dresen MH. Evaluation of effective return-to-work treatment programs for sick-listed patients with non-specific musculoskeletal complaints: a systematic review. Int Arch Occup Environ Health 2005;78:523–32. 99
Nevala N, Pehkonen I, Koskela I, Ruusuvuori J, Anttila H. Workplace accommodation among persons with disabilities: a systematic review of its effectiveness and barriers or facilitators. J Occup Rehabil 2014;25:432–48. 100
Norlund A, Ropponen A, Alexanderson K. Multidisciplinary interventions: review of studies of return to work after rehabilitation for low back pain. J Rehabil Med 2009;41:115–21. 101
Palmer KT, Harris EC, Linaker C, Barker M, Lawrence W, Cooper C, et al. Effectiveness of community- and workplace-based interventions to manage musculoskeletal-related sickness absence and job loss: a systematic review. Rheumatology 2012;51:230–42. 102
Schaafsma FG, Whelan K, van der Beek AJ, van der Es-Lambeek LC, Ojajärvi A, Verbeek JH. Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database Syst Rev 2013;8:CD001822. https://doi.org/10.1002/14651858.CD001822.pub3103
Vargas-Prada S, Demou E, Lalloo D, Avila-Palencia I, Sanati KA, Sampere M, et al. Effectiveness of very early workplace interventions to reduce sickness absence: a systematic review of the literature and meta-analysis. Scand J Work Environ Health 2016;42:261–72. https://doi.org/10.5271/sjweh.3576104
Williams RM, Westmorland MG, Lin CA, Schmuck G, Creen M. Effectiveness of workplace rehabilitation interventions in the treatment of work-related low back pain: a systematic review. Disabil Rehabil 2007;29:607–24. 105
List of excluded systematic reviews with reason for exclusion
| Review | Reason for exclusion |
|---|---|
| Aas RW, Tuntland H, Holte KA, Røe C, Labriola M. Workplace interventions for low-back pain in workers. Cochrane Database Syst Rev 2009;4:CD008159. https://doi.org/10.1002/14651858.CD008159181 | Insufficient information (protocol only) |
| Åberg F. From prolonging life to prolonging working life: Tackling unemployment among liver-transplant recipients. World J Gastroenterol 2016;22:3701–11. https://doi.org/10.3748/wjg.v22.i14.3701182 | Not occupational advice |
| Bigos SJ, Holland J, Holland C, Webster JS, Battie M, Malmgren JA. High-quality controlled trials on preventing episodes of back problems: systematic literature review in working-age adults. Spine J 2009;9:147–68. https://doi.org/10.1016/j.spinee.2008.11.001183 | Not occupational advice |
| Bond-Smith G, Belgaumkar AP, Davidson BR, Gurusamy KS. Enhanced recovery protocols for major upper gastrointestinal, liver and pancreatic surgery. Cochrane Database Syst Rev 2016;2:CD011382. https://doi.org/10.1002/14651858.CD011382.pub2184 | Not occupational advice |
| Brown HE, Gilson ND, Burton NW, Brown WJ. Does physical activity impact on presenteeism and other indicators of workplace well-being? Sports Med 2011;41:249–62. https://doi.org/10.2165/11539180-000000000-00000185 | Not occupational advice |
| Corbiere MSJ. A Systematic Review of Psychological Return-to-Work Interventions for People with Mental Health Problems and/or Physical Injuries. Database of Abstracts of Reviews of Effects: Quality-assessed Reviews. York: Centre for Reviews and Dissemination; 2006186 | Not for relevant population |
| Ebrahim S, Malachowski C, Kamal El Din M, Mulla SM, Montoya L, Bance S, Busse JW. Measures of patients’ expectations about recovery: a systematic review. J Occup Rehabil 2015;25:240–55. https://doi.org/10.1007/s10926-014-9535-4187 | Not occupational advice |
| Ellis DJ, Mallozzi SS, Mathews JE, Moss IL, Ouellet JA, Jarzem P, Weber MH. The relationship between preoperative expectations and the short-term postoperative satisfaction and functional outcome in lumbar spine surgery: a systematic review. Global Spine J 2015;5:436–52. https://doi.org/10.1055/s-0035-1551650188 | Not occupational advice |
| Engers A, Jellema P, Wensing M, van der Windt DA, Grol R, van Tulder MW. Individual patient education for low back pain. Cochrane Database Syst Rev 2008;1:CD004057. https://doi.org/10.1002/14651858.CD004057.pub3189 | Not occupational advice |
| Euler U, Wegewitz UE, Schmitt J, Adams J, van Dijk JL, Seidler A. Interventions to support return-to-work for patients with coronary heart disease. Cochrane Database Syst Rev 2013;9:CD010748190 | Insufficient information (protocol only) |
| Faber E, Kuiper JI, Burdorf A, Miedema HS, Verhaar JA. Treatment of impingement syndrome: a systematic review of the effects on functional limitations and return to work. J Occup Rehabil 2006;16:7–25. https://doi.org/10.1007/s10926-005-9003-2191 | Not occupational advice |
| Handoll HH, Elliott J. Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev 2015;9:CD003324. https://doi.org/10.1002/14651858.CD003324.pub3192 | Not for relevant population |
| Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non-specific low-back pain. Cochrane Database Syst Rev 2004;4:CD000261. https://doi.org/10.1002/14651858.CD000261.pub2193 | Not occupational advice |
| Hlobil H, Staal JB, Spoelstra M, Ariëns GA, Smid T, van Mechelen W. Effectiveness of a return-to-work intervention for subacute low-back pain. Scand J Work Environ Health 2005;31:249–57194 | Not for relevant population |
| Hou WH, Chi CC, Lo HL, Kuo KN, Chuang HY. Vocational rehabilitation for enhancing return-to-work in workers with traumatic upper limb injuries. Cochrane Database Syst Rev 2013;10:CD010002. https://doi.org/10.1002/14651858.CD010002.pub2195 | Not for relevant population |
| Huda A, Newcomer R, Harrington C, Keeffe EB, Esquivel CO. Employment after liver transplantation: a review. Transplant Proc 2015;47:233–9. https://doi.org/10.1016/j.transproceed.2014.10.022196 | Not occupational advice |
| Karjalainen K, Malmivaara A, Tulder M, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2001;26:174–81107 | Superseded by a more updated version (Karjalainen et al. 200398) |
| Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, Koes B. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain in working-age adults: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2001;26:262–9. https://doi.org/10.1097/00007632-200102010-00011197 | Not for relevant population |
| Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, Koes B. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults. Cochrane Database Syst Rev 2003;2:CD002194. https://doi.org/10.1002/14651858.CD002194106 | Not for relevant population |
| Krause NDL, Neuhauser F. Modified Work and Return To Work: A Review of the Literature. Database of Abstracts of Reviews of Effects: Quality-assessed Reviews. York: Centre for Reviews and Dissemination; 1998198 | Not occupational advice |
| Kuijer PP, de Beer MJ, Houdijk JH, Frings-Dresen MH. Beneficial and limiting factors affecting return to work after total knee and hip arthroplasty: a systematic review. J Occup Rehabil 2009;19:375–81. https://doi.org/10.1007/s10926-009-9192-121 | Not occupational advice |
| Lin CW, Donkers NA, Refshauge KM, Beckenkamp PR, Khera K, Moseley AM. Rehabilitation for ankle fractures in adults. Cochrane Database Syst Rev 2012;11:CD005595. https://doi.org/10.1002/14651858.CD005595.pub3199 | Not for relevant population |
| Lurati AR. Management of acute lumbar injuries in the workplace. Orthop Nurs 2016;35:152–8. https://doi.org/10.1097/NOR.0000000000000244200 | Not occupational advice |
| Ostelo RW, de Vet HC, Waddell G, Kerckhoffs MR, Leffers P, van Tulder M. Rehabilitation following first-time lumbar disc surgery: a systematic review within the framework of the cochrane collaboration. Spine 2003;28:209–18. https://doi.org/10.1097/01.BRS.0000042520.62951.28201 | Superseded by an updated version (Oosterhuis et al. 201489) |
| Parreira P, Heymans MW, van Tulder MW, Esmail R, Koes BW, Poquet N, et al. Back Schools for chronic non-specific low back pain. Cochrane Database Syst Rev 2017;8:CD011674. https://doi.org/10.1002/14651858.CD011674.pub2202 | Not occupational advice |
| Petit A, Rozenberg S, Fassier JB, Rousseau S, Mairiaux P, Roquelaure Y. Pre-return-to-work medical consultation for low back pain workers. Good practice recommendations based on systematic review and expert consensus. Ann Phys Rehabil Med 2015;58:298–304. https://doi.org/10.1016/j.rehab.2015.08.001203 | Study type (not a systematic review) |
| Poquet N, Lin CW, Heymans MW, van Tulder MW, Esmail R, Koes BW, Maher CG. Back schools for acute and subacute non-specific low-back pain. Cochrane Database Syst Rev 2016;4:CD008325. https://doi.org/10.1002/14651858.CD008325.pub2204 | Not occupational advice |
| Schwarz B, Neuderth S, Gutenbrunner C, Bethge M. Multiprofessional teamwork in work-related medical rehabilitation for patients with chronic musculoskeletal disorders. J Rehabil Med 2015;47:58–65. https://doi.org/10.2340/16501977-1893205 | Not occupational advice |
| Smith TO, Jepson P, Beswick A, Sands G, Drummond A, Davis ET, Sackley CM. Assistive devices, hip precautions, environmental modifications and training to prevent dislocation and improve function after hip arthroplasty. Cochrane Database Syst Rev 2016;7:CD010815. https://doi.org/10.1002/14651858.CD010815.pub2206 | Not occupational advice |
| Tilbury C, Schaasberg W, Plevier JW, Fiocco M, Nelissen RG, Vliet Vlieland TP. Return to work after total hip and knee arthroplasty: a systematic review. Rheumatology 2014;53:512–25. https://doi.org/10.1093/rheumatology/ket38920 | Not occupational advice |
| Vogel N, Schandelmaier S, Zumbrunn T, Ebrahim S, de Boer WE, Busse JW, Kunz R. Return-to-work coordination programmes for improving return to work in workers on sick leave. Cochrane Database Syst Rev 2017;3:CD011618. https://doi.org/10.1002/14651858.CD011618.pub2207 | Insufficient information (protocol only) |
| Vooijs M, Leensen MC, Hoving JL, Wind H, Frings-Dresen MH. Interventions to enhance work participation of workers with a chronic disease: a systematic review of reviews. Occup Environ Med 2015;72:820–6. https://doi.org/10.1136/oemed-2015-103062208 | Study type (review of reviews) |
| Young AE, Besen E, Choi Y. The importance, measurement and practical implications of worker’s expectations for return to work. Disabil Rehabil 2015;37:1808–16. https://doi.org/10.3109/09638288.2014.979299209 | Not occupational advice |
Details of the 17 included systematic reviews
| Review (first author and year) | Population characteristics, total number of participants and intervention type | Work-related outcomes | Summary of results in relation to RTW (based on authors’ summaries) |
|---|---|---|---|
| Surgical | |||
|
Oosterhuis 201489 Search:a 2013 Number of included studies: 22 Number of relevant studies: 1 Meta-analysis: no AMSTAR score: 9 |
Population: adults aged 18–65 years who had first-time lumbar disc surgery due to lumbar disc prolapse Total number of participants: 2503 Intervention: active rehabilitation programmes, including exercise therapy, strength and mobility training, physiotherapy and multidisciplinary programmes |
RTW (RTW status, days off work) | The authors note that no firm conclusion can be drawn relating to the programme effectiveness owing to a lack of high- or moderate-quality evidence. No evidence was found to suggest that individuals need to restrict their activities following first-time lumbar disc surgery |
| Musculoskeletal | |||
|
Aas 201190 Search:a 2009 Number of included studies: 10 Number of relevant studies: 0 Meta-analysis: yes AMSTAR score: 9 |
Population: adults (aged 18–67 years) with neck pain (acute, subacute or chronic), at work or absent from work (on sick leave, early retirement or disability pension) but still connected to workplace by employment agreements Total number of participants: 2745 Intervention: group-based and individual interventions conducted at the workplace |
Work absenteeism: time on benefits, sick leave, proportion RTW, employment status, shift in employment status, disability pension, early retirement | Moderate-quality evidence of a reduction in sickness absence in the intermediate term from a multiple-component intervention, although not sustained over time. The review authors highlight the need for high-quality RCTs that feature well-designed workplace interventions |
|
Carroll 201091 Search:a 2009 Number of included studies: 13 Number of relevant studies: 1 Meta-analysis: no AMSTAR score: 6 |
Population: employees (full or part time) on long-term sick leave (≥ 2 weeks) with back pain Total number of participants: 3134 Intervention: workplace (full or partial involvement) |
RTW | Interventions encompassing consultation and consensus between stakeholders and subsequent work modifications ‘appear to be more effective’ in terms of RTW, compared with interventions that do not contain those elements |
|
Désiron 201192 Search:a 2010 Number of included studies: 6 Number of relevant studies: 4 Meta-analysis: no AMSTAR score: 6 |
Population: adults (aged 18–65 years) with non-congenital disorders who had participated in a rehabilitation programme Total number of participants: 899 Intervention: multidisciplinary rehabilitation programme aiming at RTW |
Work-related outcomes, such as RTW, sick leave or employment status | Sufficient evidence was found for rehabilitation programmes that included occupational therapy interventions contributing to RTW. However, it was noted that it is not clear which are the effective components, except for workplace interventions |
|
Elders 200093 Search:a 1999 Number of included studies: 12 Number of relevant studies: 0 Meta-analysis: no AMSTAR score: 3 |
Population: working adults with non-specific back pain or back disorders (acute, subacute or chronic) Total number of participants: 3939 Intervention: secondary type of non-medical prevention regarding non-specific back pain |
RTW, compliance, compliance sustainability, effect sustainability | Back school type interventions were more effective, irrespective of their programme and heterogeneity, after 60 days of sickness absence than other non-back school interventions |
|
Franche 200594 Search:a 2003 Number of included studies: 10 Number of relevant studies: 1 Meta-analysis: no AMSTAR score: 7 |
Population: working-age adults off work because of musculoskeletal and other pain-related conditions Total number of participants: 58,406 Intervention: planned intervention programmes aimed at reducing work disability burden |
Work disability duration: self-reported time to RTW, time on benefits, duration of lost time recurrences, point prevalence of status (back at work vs. not back at work) | Evidence was found to support workplace-based RTW interventions reducing work disability duration and associated cost. Strong evidence demonstrated work disability being significantly reduced via work accommodation offers and contact between health-care provider and workplace. There was moderate evidence that it reduced through interventions including early contact with worker by the workplace, ergonomic work site visits and presence of a RTWC |
|
Kamper 201495 Search:a 2014 Number of included studies: 41 Number of relevant studies: 13 Meta-analysis: yes AMSTAR score: 8 |
Population: adults aged > 18 years with non-specific chronic (≥ 12 weeks) low back pain Total number of participants: 6858 Intervention: multidisciplinary biopsychosocial rehabilitation |
Work status: RTW, sick leave | Multidisciplinary biopsychosocial rehabilitation positively influences work status when compared with physical treatment, although effects were found to be modest in size and should be balanced against the resource and time requirements of multidisciplinary biopsychosocial rehabilitation programmes |
|
Karjalainen 199996 Search:a 1998 Number of included studies: 7 Number of relevant studies: 1 Meta-analysis: no AMSTAR score: 7 |
Population: adults (aged 18–65 years) with fibromyalgia or widespread musculoskeletal pain Total number of participants: 1050 Intervention: multidisciplinary rehabilitation, either inpatient or outpatient |
Ability to work (e.g. sickness absence, RTW, number of days off work) | Little scientific evidence was found for the effectiveness of multidisciplinary rehabilitation for the musculoskeletal disorders under consideration |
|
Karjalainen 200097 Search:a 1998 Number of included studies: 2 Number of relevant studies: 0 Meta-analysis: no AMSTAR score: 8 |
Population: adults (aged 18–65 years) with upper extremity repetitive strain injuries Total number of participants: 80 Intervention: biopsychosocial rehabilitation programme, either inpatient or outpatient |
Ability to work (e.g. sickness absence, RTW, number of days off work) | The review found little scientific evidence for the effectiveness of biopsychosocial rehabilitation on repetitive strain injuries |
|
Karjalainen 2003106 Search:a 2002 Number of included studies: 2 Number of relevant studies: 0 Meta-analysis: no AMSTAR score: 8 |
Population: adults (aged 18–65 years) with neck or shoulder pain Total number of participants: 177 Intervention: multidisciplinary biopsychosocial rehabilitation programme, either inpatient or outpatient |
Ability to work (e.g. sickness absence, RTW, number of days off work) | There appeared to be little scientific evidence for the effectiveness of multidisciplinary biopsychosocial rehabilitation on neck and shoulder pain compared with other rehabilitation methods |
|
Meijer 200599 Search:a 2004 Number of included studies: 22 Number of relevant studies: 11 Meta-analysis: no AMSTAR score: 4 |
Population: sick listed adults (aged 18–65 years) with chronic non-specific musculoskeletal disorders Total number of participants: 3579 Intervention: RTW intervention focusing on five categories of conditioning – knowledge, physical, psychological, social or work |
RTW: defined as the difference in sick leave after treatment compared with sick leave preceding entry into treatment programme | Inconsistent findings regarding the effectiveness of treatment programmes in terms of RTW. With the exception of low back pain, no studies explicitly itemised the programme’s RTW effects according to regional musculoskeletal disorders (e.g. upper extremity musculoskeletal disorders) |
|
Nevala 2015100 Search:a 2012 Number of included studies: 11 Number of relevant studies: 1 plus qualitative studies Meta-analysis: no AMSTAR score: 5 |
Population: adults (aged 18–68 years) with permanent disability (physical cognitive or mental disability; visual or hearing impairment) Total number of participants: 1060 Intervention: workplace accommodation, occupational or vocational rehabilitation, assistive technology interventions |
Employment (getting and maintaining employment, RTW), work ability (functioning, sick leave) | Moderate evidence was found for specific forms of workplace accommodation promoting employment and reducing costs among those with physical disabilities. There was little evidence regarding workplace accommodation co-ordinated by case managers increasing RTW and being cost-effective among those with physical or cognitive disabilities |
|
Norlund 2009101 Search:a 2006 Number of included studies: 7 Number of relevant studies: 4 Meta-analysis: yes AMSTAR score: 6 |
Population: adults (aged 19–64 years) with low back pain (subacute or chronic) Total number of participants: 1450 Intervention: multidisciplinary interventions involving two or more health disciplines |
RTW, measured either directly or indirectly as sick leave days, with the opportunity to turn sick leave into RTW | Meta-analysis of all studies indicated limited effect, but with possible publication bias; therefore, the evidence is questionable. When limited to studies undertaken in similar Scandinavian settings for individuals with low back pain on sick leave for at least 4 weeks, evidence of multidisciplinary interventions having a significant effect on RTW was found |
|
Palmer 2012102 Search:a 2010 Number of included studies: 42 Number of relevant studies: 11 Meta-analysis: no AMSTAR score: 6 |
Population: working adults with musculoskeletal disorder and/or were on sick leave with a musculoskeletal disorder at entry, or taken sick leave in past 12 months Total number of participants: 10,547 Intervention: delivered in primary care or workplace setting, or conducted in collaboration with employers or primary care providers |
RTW, avoidance of health-related job loss and mean days of sick leave per month over follow-up | Most interventions appeared effective, although less benefit was shown by larger and better-quality studies, indicating publication bias. For the better-conducted studies, a median benefit of 10% improved chance of returning to work or avoidance of 0.3–0.5 days per month of sickness absence were demonstrated |
|
Schaafsma 2013103 Search:a 2012 Number of included studies: 25 Number of relevant studies: 12 Meta-analysis: yes AMSTAR score: 8 |
Population: adults (aged > 16 years) with work disability related to back pain (acute, subacute or chronic), involved in physical conditioning programmes Total number of participants: 4404 Intervention: physical conditioning programmes that comprised exercises designed for restoration of systemic, neurological, musculoskeletal or cardiopulmonary function; with an intended improvement in work status; the intervention is related to the job demands |
Work status outcomes: time between intervention and RTW; RTW status in terms of ‘at work’ or ‘off work’; time on light or modified duties | The effectiveness of physical conditioning compared with usual care or exercise therapy remains unclear. For individuals with chronic back pain, physical conditioning has a small effect on reducing sick leave when compared with usual care after 12 months’ follow-up. The extent to which physical conditioning as part of integrated care management might affect sick leave for workers with chronic back pain requires further research |
|
Vargas-Prada 2016104 Search:a 2014 Number of included studies: 3 Number of relevant studies: 0 Meta-analysis: yes AMSTAR score: 6 |
Population: workers on sick leave for ≤ 15 days Total number of participants: 419 Intervention: workplace interventions – carried out at workplace before day 15 of sickness absence, implemented by employer, including involvement from internal/external occupational health services |
Rates of and time until RTW, productivity loss and days lost, duration of sick leave, recurrences of sickness absence episodes (primary outcomes). Satisfaction with intervention, either of employees, line managers or employers (secondary outcomes) | There was limited evidence regarding the benefits of very early workplace interventions regarding RTW compared with usual care, with no significant differences in terms of productivity loss. The positive RTW impact of intervention within the first 2 weeks of sickness absence is stronger for workers with musculoskeletal disorders and less for those with mental health problems |
|
Williams 2007105 Search:a 2005 Number of included studies: 10 Number of relevant studies: 1 Meta-analysis: no AMSTAR score: 5 |
Population: injured workers with musculoskeletal work-related low back pain Total number of participants: 2909 Intervention: interventions conducted at the workplace, or secondary prevention interventions for the condition |
RTW status, duration of work absence/sick leave, time lost | The review identified that there is some evidence on the effectiveness of workplace rehabilitation interventions for injured workers with low back pain |
| AMSTAR criteria | Review (first author and year) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aas 201190 | Carroll 201091 | Désiron 201192 | Elders 200093 | Franche 200594 | Kamper 201495 | Karjalainen 199996 | Karjalainen 200097 | Karjalainen 2003106 | Meijer 200599 | Nevala 2015100 | Norlund 2009101 | Oosterhuis 201489 | Palmer 2012102 | Schaafsma 2013103 | Vargas-Prada 2016104 | Williams 2007105 | |
| 1. Was an ‘a priori’ design provided? | Yes | CA | CA | CA | CA | CAa | CAb | No | CA | CA | CA | CA | Yes | CA | CAb | CA | CA |
| 2. Was there duplicate study selection and data extraction? | Yes | No | No | CA | Yes | No | Yes | Yes | Yes | No | CA | CA | Yes | No | Yes | Yes | Yes |
| 3. Was a comprehensive literature search performed? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No |
| 4. Was the status of publication (i.e. grey literature) used as an inclusion criterion? | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | No | Yes | No | No |
| 5. Was a list of studies (included and excluded) provided? | Yes | No | No | No | No | Yes | CA | Yes | Yes | No | No | Yes | Yes | No | Yes | No | No |
| 6. Were the characteristics of the included studies provided? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 7. Was the scientific quality of the included studies assessed and documented? | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 8. Was the scientific quality of the included studies used appropriately in formulating conclusions? | Yes | Yes | Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9. Were the methods used to combine the findings of studies appropriate? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 10. Was the likelihood of publication bias assessed? | No | No | No | No | No | Yes | No | No | No | No | No | Yes | No | Yes | No | No | No |
| 11. Was the conflict of interest included? (For review and each of the included studies) | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| Total score (out of 11) | 9 | 6 | 6 | 3 | 7 | 8 | 7 | 8 | 8 | 4 | 5 | 6 | 9 | 6 | 8 | 6 | 5 |
Summary of relevant studies from included reviews, for work-related outcomes
| Study (first author and year) | Title of study | Population | Intervention details | Work-related findings |
|---|---|---|---|---|
| Surgical | ||||
|
Donceel 1999124 From review by Oosterhuis 201489 |
Cluster RCT comparing rehabilitation-oriented approach focused on early mobilisation and early resumption of professional activities for lumbar disc herniation surgery with usual claim-based practice | Workers who had surgery for herniated lumbar disc |
Medical advisors asked to base their medical practice on three rehabilitation guidelines: involving contact with patients, the treating physicians and fellow medical advisors Comparator: medical advisors asked to undertake medical practice as they did in the past, i.e. usual claim-based practice |
A statistically significant difference was found between the groups regarding RTW; the intervention group had a higher RTW rate (log-rank test: p < 0.001) |
| Musculoskeletal | ||||
|
Allaire 2003118 From review by Nevala 2014100 |
Reduction of job loss in persons with rheumatic diseases receiving vocational rehabilitation. a randomised controlled trial | Employed (aged 18–65 years), with a rheumatic disease and at risk of job loss |
Job retention vocational rehabilitation intervention consisting of job accommodation; vocational counselling and guidance; and education and self-advocacy Comparator: control group received same pamphlets/flyers on management of health-related employment problems and available resources as the intervention group |
Intervention was effective at preventing job loss when provided to those at risk of job loss but still employed: job loss was delayed and reduced in incidence |
|
Altmaier 1992210 |
The effectiveness of psychological interventions for the rehabilitation of low back pain: a randomized controlled trial evaluation | Patients with low back pain, not currently working due to pain (lasting between 3 and 30 months) |
Standard inpatient rehabilitation programme (multidisciplinary approach, involving physical therapy, education classes and vocational rehabilitation) with additional psychological components Comparator: control group received same standard treatment programme as intervention group |
Based on the conservative RTW measure, the difference between the control group (67%) and psychological group (48%) was not significant. Results were also non-significant when the liberal measure was used |
|
Arnetz 2003119 From reviews by Franche 2005,94 Meijer 2005,99 Palmer 2012102 and Kamper 201495 |
Early workplace intervention for employees with musculoskeletal-related absenteeism: a prospective controlled intervention study | Patients with physician-diagnosed musculoskeletal disorders |
Early workplace intervention comprising a more proactive role for insurance case managers and workplace ergonomic interventions (which involved employee, case manager, occupational therapist/ergonomist and employer). An interview was undertaken covering several topics/foci, a workplace visit and vocational training Comparator: traditional case management, i.e. received same study information and questionnaires as intervention group, but not the interview or worksite visits |
The number of sick days was significantly reduced in the intervention group compared with the comparator, for all three assessment periods (0–6 months, 6–12 months and 0–12 months) |
|
1998: A prospective, randomized 5-year follow-up study of functional restoration in chronic low back pain patients 1996: Multidisciplinary intensive treatment for chronic low back pain: a randomized, prospective study |
Chronic low back pain patients |
Functional restoration intervention: aerobics, weight training, work simulation, work hardening, relaxation, psychological group, stretching, theoretical class, recreation Comparator: participants were not treated by the study team but could go elsewhere for treatment |
There was a significant difference (p < 0.001) between the intervention and control groups in terms of the number of patients able to work at the 4-month follow-up | |
|
1995: Active treatment programmes for patients with chronic low back pain: a prospective, randomized, observer-blinded study 1998: A prospective, randomized 5-year follow-up study of functional restoration in chronic low back pain patients |
Chronic low back pain patients |
Functional restoration intervention: aerobics, weight training, work simulation, work hardening, relaxation, psychological group, stretching, theoretical class, recreation Comparator A: active physical training Comparator B: active combined with psychophysical programme |
Regarding sick leave days, a significant difference was found between comparator group B and the other two groups (p = 0.005). There was no difference between the intervention group and comparator group A (p = 0.5) | |
|
Bendix 2000212 From reviews by Kamper 2014,95 Norlund 2009101 and Schaafsma 2013103 |
Functional restoration versus outpatient physical training in chronic low back pain. A randomized comparative study | Chronic low back pain patients |
Functional restoration programme: focused on self-responsibility, activity and a multidisciplinary approach, including work hardening as part of occupational therapy Comparator: outpatient intensive physical training |
No difference in work-related variables was found between the two programmes |
|
Bethge 2011213 From review by Schaafsma 2013103 |
Work status and health-related quality of life following multimodal work hardening: a cluster randomised trial | Patients with musculoskeletal disorders (with at least 12 weeks of sick leave in the year before rehabilitation, or subjective expectation of long-term restrictions affecting occupational duties, or health-related unemployment) |
Multimodal work hardening: a work-related extension of conventional musculoskeletal rehabilitation programme. It comprised six modules: work and health; occupational competence; two exercise modules; functional capacity training; relaxation Comparator: conventional musculoskeletal rehabilitation |
The odds of having a positive work status (working with ≤ 6 weeks sick leave) were approximately 2.4 times higher in the multimodal work hardening group than in the control group, being statistically significant, at 6 months. At 12 months, however, the between-group effect (OR 1.914) was not significant |
|
Bültmann 2009120 From review by Palmer 2012102 |
Co-ordinated and tailored work rehabilitation: a randomized controlled trial with economic evaluation undertaken with workers on sick leave due to musculoskeletal disorders | Workers on sick leave for back pain or musculoskeletal disorders |
Co-ordinated and tailored work rehabilitation intervention comprising (1) work disability screening and (2) formulation and implementation of a co-ordinated, tailored and action-oriented work rehabilitation plan, developed in collaboration by an interdisciplinary team using a feedback-guided approach Comparator: conventional case management |
For all three follow-up points, a higher proportion of participants returned to work in the intervention group than in the control group |
|
Coole 2013128 From review by Kamper 201495 |
Individual work support for employed patients with low back pain: a randomized controlled pilot trial | Employed individuals who expressed concern over ability to work because of back pain |
Targeted vocational sessions in collaboration with group multidisciplinary rehabilitation for low back pain: group rehabilitation on self-management of back pain comprising education and physical conditioning; and individual work support from occupational therapist Comparator: the same group multidisciplinary back pain rehabilitation as the intervention group |
The effectiveness of the intervention on work ability was equivocal. According to the Work Ability Index, a better outcome was reported for the intervention group than for the control group. However, this was not the case according to the Graded Reduced Work Ability Scale |
|
Corey 1996123 |
A limited functional restoration programme for injured workers: a randomized trial | Soft-tissue injuries (majority related to back pain, and also shoulders, lower extremity, neck and thoracic); workers’ compensation board claimants |
Interdisciplinary programme emphasising a functional restoration approach to rehabilitation: focus on active physical therapy, work hardening, education in posture and body mechanics, group education and counselling, and active pain management strategies Comparator: referred back to family doctors for usual care |
A significant effect was found in terms of the number of individuals in the intervention group reporting that they were back at work (p = 0.02) |
|
Durand 2001116 From reviews by Carroll 2010,91 Palmer 2012102 and Williams 2007105 |
Therapeutic RTW: rehabilitation in the workplace | Work-related thoracic or lumbar pain (> 90 days) |
Therapeutic return to work: work rehabilitation programme is proposed; an agreement between occupational therapist and work supervisor on the expectations of worker; injured worker placed in a supplemental position and helps a co-worker do partial tasks of job; injured worker progressively increases duties Comparator 1: functional restoration therapy (no therapeutic return to work) Comparator 2: community services (excluded any rehabilitation) Comparator 3: no treatment (workers referred for programme but denied it by Compensation Board) |
The therapeutic return-to-work group had a significantly higher RTW rate only when compared with functional rehabilitation control and the no-treatment control group’s raw scores |
|
Feuerstein 1993117 From review by Palmer 2012102 |
Multidisciplinary rehabilitation of chronic work-related upper extremity disorders | Chronic work-related musculoskeletal disorders of the upper extremities; work-disabled for minimum of 3 months |
Multidisciplinary work re-entry rehabilitation programme: exercises, physical conditioning, work conditioning/simulation, job-related pain and stress management, ergonomic consultation, and vocational counselling/placement Comparator: usual care – did not receive the multidisciplinary rehabilitation |
The percentage who returned to work in the intervention group was significantly higher than in the usual-care control group |
|
Haldorsen 1998129 |
Multimodal cognitive behavioral treatment of patients sicklisted for musculoskeletal pain: a randomized controlled study | Patients sick-listed for musculoskeletal pain (for 8 weeks) |
Multidisciplinary rehabilitation programme: physical treatment, cognitive–behavioural modification, education, and workplace-based interventions Comparator: control group was followed up by GPs without any feedback or advice on therapy |
There were no significant differences in terms of RTW rates for the two groups However, improvements in the intervention group occurred in terms of ergonomic behaviour, work potential, life quality and psychological health |
|
Haldorsen 2002121 |
Is there a right treatment for a particular patient group? Comparison of ordinary treatment, light multidisciplinary treatment, and extensive multidisciplinary treatment for long-term sick-listed employees with musculoskeletal pain | Sick-listed workers with musculoskeletal pain |
Intervention A: light multidisciplinary treatment with follow-ups Intervention B: extensive multidisciplinary treatment programme with follow-ups Comparator: ordinary treatment – patients referred back to their GP after visit at outpatient spine clinic |
Both light and extensive multidisciplinary treatment is associated with an increase in the possibility of returning to work, with the effects found to be statistically significant For patients with a good prognosis, extensive multidisciplinary treatment does not result in higher RTW |
|
Henchoz 2010214 From review by Kamper 201495 |
Functional multidisciplinary rehabilitation versus outpatient physiotherapy for non-specific low back pain: randomised controlled trial | Low back pain (either subacute or chronic) |
Functional multidisciplinary rehabilitation in ambulatory setting, involving intensive physical and ergonomic training, psychological pain management, back school, instruction in social and work-related issues and a functional evaluation to increase self-responsibility. Each patient received individually tailored pharmacotherapy and regular follow-up by a medical doctor Comparator: outpatient physiotherapy |
Regarding the between-group difference for the functional multidisciplinary rehabilitation versus the comparator group in terms of return to full work, the difference was not significant at 6 months (p = 0.16), was significant at 9 months (p = 0.038) and ‘tended to be significant’ at 12 months (p = 0.087) |
|
Johansson 1998215 From review by Meijer 200599 |
Effects of a cognitive-behavioural pain-management programme | Chronic musculoskeletal pain that significantly disrupted patients’ lives |
Cognitive–behavioural inpatient programme: mostly in group format, involving multidisciplinary team delivering education sessions, goal-setting, graded activity training, exercise and individually tailored muscle training programmes, pacing of activities, relaxation, cognitive techniques, social skills training, drug-reduction methods, contingent management of pain behaviours and planning of the work return. A meeting with employer, work leader and insurance representative was organised for every patient, plus occupational training Comparator: waiting list control group. |
No significant differences were found regarding sick leave between the groups |
|
Jousset 2004110 From reviews by Désiron 2011,92 Kamper 201495 and Norlund 2009101 |
Effects of functional restoration versus 3 hours per week physical therapy: a randomized controlled study | Chronic low back pain |
Functional restoration programme: exercises/aerobic activities, occupational therapy including work simulation, endurance training, balneotherapy and individual interventions Comparator: active individual therapy |
A trend towards shorter sick leaves was demonstrated by the functional restoration programme; however, this difference (of 20 days) was not statistically significant |
|
Kool 2007111 From review by Kamper 201495 |
Function-centered rehabilitation increases work days in patients with nonacute nonspecific low back pain: 1-year results from a randomized controlled trial | Non-acute non-specific low back pain |
Function-centred treatment: work hardening and functional restoration programmes with a multidisciplinary team. Treatment was based on the patient’s job demands, revealed in a work-related assessment Comparator: pain-centred treatment |
The number of workdays accounting for time-reduced work was significantly higher in the function-centred rehabilitation group |
|
Lambeek 2010113 From reviews by Désiron 2011,92 Kamper 201495 and Palmer 2012102 |
Randomised controlled trial of integrated care to reduce disability from chronic low back pain in working and private life | Low back pain for > 12 weeks, and were absent or partially absent from work |
Integrated care: workplace intervention based on participatory ergonomics and a graded activity programme, given by a multidisciplinary team Comparator: usual care, from range of health professionals |
A significantly shorter RTW was found for the intervention group, with a beneficial effect on disability |
|
Lambeek 2010112 From reviews by Désiron 2011,92 Kamper 201495 and Schaafsma 2013103 |
Effect of integrated care for sick listed patients with chronic low back pain: economic evaluation alongside a randomised controlled trial | Low back pain for > 12 weeks, and were absent or partially absent from work | Same as above | In terms of RTW, the intervention was found to be cost-effective compared with usual care, and also effective for quality-adjusted life-years gained |
|
Lindh 1997216 |
A randomized prospective study of vocational outcome in rehabilitation of patients with non-specific musculoskeletal pain: a multidisciplinary approach to patients identified after 90 days of sick leave | ‘Non-specific’ diagnoses, i.e. chronic musculoskeletal pain, fibromyalgia, neck and shoulder pain, back pain and similar conditions; reaching a continuous sick leave of 90 days |
Outpatient multidisciplinary rehabilitation: physiotherapy sessions, psychologist sessions with a cognitive–behavioural approach, social worker involvement (e.g. family counselling, social support) and intervention from occupational therapist and vocational counseller to offer professional support in patients’ contact with employers/organisers of the work, preparations, outlines and follow-ups of vocational training in the workplace Comparator group description not provided; possibly treatment in primary care |
Note: study presented results according to ‘Swedes’ and ‘immigrants’ Among Swedes, the percentage of work-returners was similar in the long run (5 years) in the rehabilitation group and control group, although there was a faster initial rate of work return in the control group. This finding was similar for the ‘immigrants’ group, although there was a lower RTW rate at 5 years for the control group than for the rehabilitation group |
|
Marhold 2001217 |
A cognitive behavioral RTW programme: effects on pain patients with a history of long-term versus short-term sick leave | Women with musculoskeletal pain. One group of patients had a history of long-term sick leave (12 months) at the start of the programme and the other had a history of short-term sick leave (2–6 months) |
Cognitive–behavioural treatment: goal-setting (regarding work and leisure time), graded activity and training, pacing of activities; relaxation; cognitive techniques; social skills training; stress management; problem-solving; planning of the RTW; how to generalise coping skills to occupational risk factors; handling difficulties at the beginning of RTW; and individual maintenance programmes. The group also had free access to treatment as usual Comparator: treatment as usual, which did not include cognitive–behavioural interventions |
The number of sick days was reduced for the intervention group for those on short-term sick leave, but not for those on long-term sick leave |
|
Meijer 2006218 From review by Palmer 2012102 |
Cost-effectiveness of multidisciplinary treatment in sick-listed patients with upper extremity musculoskeletal disorders: a randomized, controlled trial with one-year follow-up | Non-specific upper extremity musculoskeletal disorders. Employment on a contract of at least 50% of full-time working hours and sick leave for over 50% of the contractual hours during a period between 4 and 20 weeks |
Multidisciplinary treatment programme: RTW sessions; physical sessions aimed at restoring muscle strength and endurance, as well as aerobic fitness, using graded activity training, education, sports activities; psychological sessions aimed at ‘demedicalising’, setting (and achieving) goals and improving coping strategies using cognitive techniques and education. The other psychological session prepared the participants to return to work, or to discuss work experiences. A workplace visit could be arranged Comparator: usual care |
There were no significant differences demonstrated for RTW over time |
|
Meyer 2005219 From review by Schaafsma 2013103 |
Feasibility and results of a randomised pilot-study of a work rehabilitation programme | Individuals with an inability to work owing to chronic non-specific pain of more than 3 months with musculoskeletal disorders |
Work rehabilitation programme: work-specific exercises, progressive exercise therapy with training devices, education in ergonomics, learning strategies to cope with pain and to increase self-efficacy, a group intervention with the psychologist, sports activities for recreation and a workplace visit to develop appropriate workload-related exercises for the programme Comparator: progressive exercise therapy |
Improvements overall were seen for the ability to work and work status; however, the differences were not found to be significant between the groups |
|
Mitchell 1994220 From reviews by Kamper 2014,95 Meijer 2005,99 Palmer 2012102 and Schaafsma 2013103 |
The functional restoration approach to the treatment of chronic pain in patients with soft-tissue and back injuries | Injured workers who were experiencing continuing chronic pain from soft-tissue or back injuries (who had not recovered within 90 days of injury and remained off work) |
Functional restoration programme: active exercise programme and functional simulation programme, with behavioural support; goal-setting; occupational gymnasium where undertook tasks commonly required in the workplace; behavioural or psychosocial support Comparator: control group referred to primary care provider for further treatment supervision |
In terms of the difference in percentage of injured workers in full-time work at 12-month follow-up for the intervention vs. control groups, no statistically significant findings were reported. The intervention group had fewer days off work after the injury, on average, than the control group |
|
Nordström-Björverud 1998122 From review by Meijer 200599 |
Interdisciplinary rehabilitation of hospital employees with musculoskeletal disorders | Musculoskeletal pain from the neck/shoulder region, elbow, thoracic/lumbar region or pelvic/hip region, age between 20 and 60 years and consecutive sick-listing for 2 months or repeated sick-listing during the previous 12 months |
Interdisciplinary rehabilitation programme: admission as day patients at rehabilitation clinic and contact with/visits to the workplace. Intervention involved the employee, physiotherapist, occupational therapist, workplace supervisors and sometimes workmates Comparator: received a questionnaire 2 years after referral to personnel department, and a request for a pain drawing |
A significant difference in RTW was demonstrated in favour of the intervention group |
|
Roche 2007114 From reviews by Kamper 201495 and Schaafsma 2013103 Roche 2011115 From review by Kamper 201495 |
2007: Comparison of a functional restoration programme with active individual physical therapy for patients with chronic low back pain: a randomized controlled trial (6-month results) 2011: Multidisciplinary intensive functional restoration versus outpatient active physio in chronic low back pain (12-month results) |
Chronic low back pain |
Functional restoration programme: exercises, work simulations during occupational therapy sessions, clinic visits with specialist in physical medicine and rehabilitation, dietary advice Comparator: active individual therapy |
RTW improved after treatment at 6-month follow-up At 12-month follow-up, the number of sick-leave days in the post-treatment year reduced significantly compared with the pre-treatment year. The reduction was higher in the intervention group than in the comparator group (p < 0.001) |
|
From reviews by Kamper 2014,95 Meijer 2005,99 Norlund 2009101 and Schaafsma 2013103 |
Relative cost-effectiveness of extensive and light multidisciplinary treatment programmes versus treatment as usual for patients with chronic low back pain on long-term sick leave | Chronic low back pain |
Intervention A: light multidisciplinary treatment Intervention B: extensive multidisciplinary treatment, including occasional workplace interventions and education sessions including mental coping strategies applied at work Comparator: treatment as usual |
Results split according to males and females: male patients return to work more often after light multidisciplinary treatment than the comparator. Female patients do not seem to benefit from either light or multidisciplinary treatment vs. the comparator |
|
Strand 2001222 From review by Kamper 201495 |
The impact of physical function and pain on work status at 1-year follow-up in patients with back pain | Patients on long-term sick leave (> 8 weeks) because of musculoskeletal pain |
Multidisciplinary rehabilitation programme: included physical treatment, education, cognitive and behavioural modification, and workplace-based interventions. Recommendations concerning RTW were not routine Comparator: treated in the community and did not follow a predefined treatment course |
Fewer participants returned to work fully after 1 year in the intervention group (47%) than in the control group (58%); this difference was not statistically significant |
Interventions with evidence of benefit from relevant studies (included systematic reviews)
| Study (first author and year) | Condition | Content of intervention | Duration and timing | Setting | Mode of delivery |
|---|---|---|---|---|---|
| Surgical | |||||
| Donceel 1999124 | Surgery for herniated lumbar disc |
Rehabilitation-oriented approach used by medical advisors to motivate patients and treating physicians towards social and professional reintegration Medical advisors asked to base medical practice on three rehabilitation guidelines:Guidelines that the intervention protocol is based on are referenced in the study |
Patients’ office visits: first visit at 6 weeks after operation, with monthly follow-up consultations | Office of medical advisors for a social security fund (Belgium) | Face to face |
| Musculoskeletal | |||||
| Allaire 2003118 | Rheumatic disease | Job-retention vocational rehabilitation intervention consisting of job accommodation; vocational counselling and guidance; and education and self-advocacy | Two 1.5-hour sessions of rehabilitation. Most participants completed the intervention within 5 months of randomisation, but took longer in a few cases (maximum 9 months) | Local office of state vocational rehabilitation programme at participant’s home, or in a public area (e.g. library) (Massachusetts, USA) | Face to face by rehabilitation counsellors |
| Arnetz 2003119 | Musculoskeletal disorders | Early workplace intervention comprising a more proactive role for insurance case managers and workplace ergonomic interventions (which involved employee, case manager, occupational therapist/ergonomist and employer). An interview was undertaken covering several topics/foci, a workplace visit and vocational training |
Within 1 week: visited local branch of Forsakringskassan for interview 1 week later: meeting with patient and professionals |
Local branch offices of Swedish National Insurance Agency Forsakringskassan (Sweden) | Face to face |
| Bendix 1996109/1998108 | Chronic low back pain patients | Functional restoration intervention: aerobics, weight training, work simulation, work hardening, relaxation, psychological group, stretching, theoretical class, recreation | All participants were on sick leave at entry to the programme. 39 hours per week (i.e. full time) for 3 successive weeks. After graduating from the programme, underwent a follow-up programme of 6 hours, once a week for 3 weeks | Copenhagen Back Centre (Denmark) |
Face to face (training provided in groups of seven or eight) Group structure essential: each week, two or three new patients enter the group, and can be inspired by the ‘third-weekers’ |
| Bültmann 2009120 | Musculoskeletal disorders | Co-ordinated and tailored work rehabilitation intervention, comprising (1) work disability screening and (2) formulation and implementation of a co-ordinated, tailored and action-oriented work rehabilitation plan, developed in collaboration by an interdisciplinary team using a feedback-guided approach |
The intervention began after 4–12 weeks of sick leave with a systematic work disability screening and identification of barriers to RTW Screening is 1 week after inclusion (takes 2.5 hours) plus interdisciplinary team conference (0.5 hours) Intervention is no longer than 3 months |
Department of Development and Labour Market (Denmark) | Face to face |
| Corey 1996123 | Soft-tissue injuries (majority related to back pain, and also shoulders, lower extremity, neck and thoracic) | Interdisciplinary programme emphasising a functional restoration approach to rehabilitation: focus on active physical therapy, work hardening, education in posture and body mechanics, group education and counselling, and active pain management strategies |
Participants were referred from 3 to 6 months post injury for the programme Treatment sessions were limited to 6.5 hours per day for a maximum of 35 days (average 32.9 days, median 35 days, range 3–35 days) |
Those receiving Worker’s Compensation Board (Toronto, ON, Canada) | Face to face |
| Durand 2001116 | Work-related thoracic or lumbar pain | Therapeutic return to work: work rehabilitation programme is proposed; an agreement between occupational therapist and work supervisor on the expectations of worker; injured worker placed in a supplemental position and helps a co-worker do partial tasks of job; injured worker progressively increases duties | Intervention was administered at a mean of 7.1 months after back injury | University hospital-based work rehabilitation facility (Québec, Canada) | Face to face |
| Feuerstein 1993117 | Chronic work-related musculoskeletal disorders of the upper extremities | Multidisciplinary work re-entry rehabilitation programme: exercises, physical conditioning, work conditioning/simulation, job-related pain and stress management, ergonomic consultation, and vocational counselling/placement | Daily treatment over a 4- to 6-week period, for those work disabled for more than 3 months | Centre for Occupational Rehabilitation, University of Rochester Medical Centre (USA) | Face to face (combination of group and individual sessions) |
| Haldorsen 2002121 | Sick-listed workers with musculoskeletal pain |
Intervention A: light multidisciplinary treatment with follow-ups Intervention B: extensive multidisciplinary treatment with follow-ups |
A: 1-hour session plus feedback provided after. A maximum of 12 additional sessions were recommended (on average, participants received three individual follow-ups) B: programme lasted for 4 weeks, with 6-hour sessions 5 days per week |
Outpatient clinic (Norway) | Face to face (combination of group and individual sessions) |
| Jousset 2004110 | Chronic low back pain | Functional restoration programme: exercises/aerobic activities, occupational therapy including work simulation, endurance training, balneotherapy and individual interventions | 6 hours per day, 5 days per week, for 5 weeks | Rehabilitation centres (France) | Face to face (group) |
| Kool 2007111 | Non-acute non-specific low back pain | Function-centred treatment: work hardening and functional restoration programmes with a multidisciplinary team. Treatment was based on the patient’s job demands, revealed in a work-related assessment | 4 hours per day for 3 weeks | Inpatient rehabilitation centre (Switzerland) | Face to face |
| Lambeek 2010113 | Low back pain | Integrated care: workplace intervention based on participatory ergonomics and a graded activity programme, given by a multidisciplinary team |
Integrated care management by clinical occupational physician: from week 1 to full sustainable RTW, or week 12 Workplace intervention: week 3 to week 12 Graded activity: week 2 to full sustainable RTW or after 26 sessions (within a maximum of 12 weeks) |
Primary care and secondary care (UK) | Face to face |
| Lambeek 2010112 | Low back pain | Same as above | Same as above | Same as above | Same as above |
| Nordström-Björverud 1998122 | Musculoskeletal pain from the neck/shoulder region, elbow, thoracic/lumbar region or pelvic/hip region | Interdisciplinary rehabilitation programme: admission as day patients at rehabilitation clinic and contact with/visits to the workplace. Intervention involved the employee, physiotherapist, occupational therapist, workplace supervisors and sometimes workmates | Six weeks of admission as ‘day patients’ at rehabilitation clinic, with activity 4 days per week (09.00–16.00). Contact with workplace recommended on fifth day. Rehabilitation physician saw patients within 2 weeks after referral and they were admitted within 6 weeks | Rehabilitation clinic and occupational health service unit, at Lund University Hospital (Sweden) | Face to face (groups of three people) |
| Roche 2007114 Roche 2011115 | Chronic low back pain | Functional restoration programme: exercises, work simulations during occupational therapy sessions, clinic visits with specialist in physical medicine and rehabilitation, dietary advice | For 5 weeks, involving 6 hours per day for 5 days per week | Rehabilitation centres and private ambulatory physiotherapy facilities (France) | Face to face (groups of six to eight people) |
Outcome measures in relevant studies from the systematic reviews
| Study (first author and year) | RTW (i.e. non-standardised measures) | Standardised scales for RTW or return to usual activities or social participation | Outcomes | |||
|---|---|---|---|---|---|---|
| Musculoskeletal symptoms | Quality of life | Psychological | Other | |||
| Surgical | ||||||
|
Donceel 1999124 From review by Oosterhuis 201489 |
RTW over 12-month follow-up period | Patterns of practice (study-specific questionnaire) | ||||
| Musculoskeletal | ||||||
|
Allaire 2003118 From review by Nevala 2014100 |
Time to first job loss (permanent or temporary); time to permanent job loss alone | |||||
|
Altmaier 1992210 |
Return to employment (conservative, i.e. full employment at same job; and liberal measures, i.e. if full time on light duties or part-time work or training) |
Low Back Pain Rating Scale (Lehmann 1983223) to assess disability McGill Pain Questionnaire (Melzack 1975224) for self-reported pain |
Confidence assessed using a 20-item self-efficacy measure and by the two-item self-control subscale of the West Haven–Yale Multidimensional Pain Inventory (Kerns 1985225) Negative Mood and Interference subscales of the West Haven–Yale Multidimensional Pain Inventory (Kerns 1985225) |
|||
|
Arnetz 2003119 From reviews by Franche 2005,94 Meijer 2005,99 Palmer 2012102 and Kamper 2014197 |
Number of sick days (at 6 and 12 months) Working hours of participant |
Self-rated health [using a five-graded response scale (Cott 1999226)] | Musculoskeletal symptoms [rated on four-point graded scale and Standardised Nordic Questionnaire (Kuorinka 1987227)] |
Cost of purchasing of vocational equipment Rehabilitation costs (costs for purchase of rehabilitation services) Medical diagnosis |
||
| Working or able to return to work/ability to work (five categories); Number of sick leave days (outcomes assessed at 12 months) | Function: 15 questions about how much the back problem interfered with activities of daily living (Manniche 1994125) |
Back pain (NRS scale of 0–10) Leg pain (NRS scale 0–10) (no reference provided; hence assume study-specific scales) |
Health-care utilisation (contacts with health-care system, admission to hospital because of low back pain, low back pain surgery) Medication (amount and type of prescription) |
|||
|
Working or able to return to work Days of sick leave |
Function: 15 questions about how much the back problem interfered with activities of daily living (Manniche 1994125) |
Back pain (NRS scale of 0–10) Leg pain (NRS scale 0–10) (no reference provided; hence assume study-specific scales) |
Utilisation (contacts with health-care system, admission to hospital because of low back pain, low back pain surgery) Medication (amount and type of prescription medication) |
|||
|
Bendix 2000212 From reviews by Kamper 2014,95 Norlund 2009101 and Schaafsma 2013103 |
Work capability (working or able to return to work) Number of sick leave days (Measurement at 1 year after treatment) |
Assessment for activities of daily living using the Manniche Rating Scale (15 questions) (Manniche 1994125) |
Back pain (NRS of 0–10) Leg pain (NRS of 0–10) (study specific) |
Overall assessment of quality of life (1–5) (study specific) | Utilisation (contacts with health-care system, admission to hospital because of low back pain, low back pain surgery) | |
|
Bethge 2011213 From review by Schaafsma 2013103 |
Work status at 6 and 12 months [defined as positive if patient was working and had < 6 or < 12 (after 12 months) weeks of sick leave] | Pain Management Questionnaire (Geissner 2001228) | SF-36 Health Survey of the Medical Outcomes Study (Ware 1992229) | Hospital Anxiety and Depression Scale (Snaith 2003230) | ||
|
Bültmann 2009120 From review by Palmer 2012102 |
Cumulative sickness absence hours (from Danish National Health Insurance Service Registry) Work status (RTW, full-time sick leave or part-time sick leave) |
Functional disability (using Danish version of Oswestry Low Back Pain Disability Questionnaire, with 10 sections referring to activities of daily living) [Lauridsen 2006 (part 1)231 and Lauridsen 2006 (part 2)232] | Pain intensity (by two items from Orebro Musculoskeletal Pain Screening Questionnaire on 10-point rating scale) (Linton 2003233) | Health-care costs | ||
|
Coole 2013128 From review by Kamper 201495 |
Perceived work ability: one question from Work Ability Index (Tuomi 1998234 and Ahlstrom 2010235), and the Graded Reduced Work Ability Scale (Haldorsen 1998130) Disability: Roland–Morris Disability Questionnaire (Roland 1983127) |
Self-efficacy: Pain Self-Efficacy Questionnaire (Nicholas 1989236) Pain VAS (Jensen 2001237) |
HADS to measure mood (Zigmond 1983238) Fear avoidance related to work: Fear Avoidance Beliefs Questionnaire – work (Waddell 1993239) |
|||
|
Corey 1996123 |
Self-reported work status (dichotomous, two versions, percentage) (Outcomes assessed at 18 months) |
Pain rating [scale 0–10 non-VAS (Murphy 1988240)] |
Medication use: mean reported narcotic intake (pills/week) Sleep quality rating (scale 1–3) (study specific) |
|||
|
Durand 2001116 From reviews by Carroll 2010,91 Palmer 2012102 and Williams 2007105 |
Work status (defined as working or not at regular job tasks, assessed using a questionnaire that was constructed) | Spitzer diagnostic scale for classification of workers |
Specific back disability (using Québec Back Pain Disability questionnaire) (Durand 1994241 and Kopec 1995242) Pain intensity (using VAS) (Durand 1998243 and Scott 1979244) |
Fear and Avoidance Beliefs questionnaire (Waddell 1993239) | ||
|
Feuerstein 1993117 From review by Palmer 2012102 |
Vocational outcome (employed full time/part time/actively enrolled in state-supported vocational training/retraining programme/currently unemployed) Duration of work disability (in months, from medical records) |
Perception of most recent work environment (using Work Environment Scale) (Moos 1986245) Expectation of RTW (VAS, 0–10 rating, completed as part of a work re-entry questionnaire) (Feuerstein 1998246) |
Pain severity (VAS, 0–10 rating) (study specific) |
Measures of anxiety Psychological state and personality style (using Millon Clinical Multiaxial Inventory-II) (Millon 1987247) Fear of reinjury (VAS, 0–10 rating) (study specific) |
||
|
Haldorsen 1998129 |
RTW |
Subjective work ability (Graded Work Ability scale, GRWA) Daily activities (Norwegian version of the Activity Discomfort Scale (Turner 1983248)] |
Pain drawing test (Ransford 1976249 and Spangfort 1994250) Pain VAS (Carlson 1983251) |
Health locus of control [measured by Multidimensional Health Locus of Control questionnaire – converted to Norwegian (Aaro 1986252)] |
Subjective health (Ursin’s Health Inventory, regarding common somatic and psychological complaints) (Ursin 1988253) Anxiety (Spielberger State Trait Anxiety Scale) (Spielberger 1983254) [Norwegian version – Haseth 1990255 and 1993 (unpublished manuscript)] Psychological distress (Hopkins Symptom Check List, HSCL-23) (Derogatis 1974256), Norwegian version – Central Bureau of Statistics of Norway 1987257) Personality [Eysenck Personality Inventory (EPI –Form A) (Eysenck 1968258)], Norwegian version (Haseth 1969259) |
|
|
Haldorsen 2002121 |
Percentage returned to work | Economic outcomes: costs and benefits of treatment | ||||
|
Henchoz 2010214 From review by Kamper 201495 |
Work status (percentage working) | Back-related functional disability: ODI (Fairbank 1980260 and Fairbank 2000126) | Physical assessments:
|
|||
|
Johansson 1998215 From review by Meijer 200599 |
Percentage sick leave Hours of occupational training per day |
Third section of multidimensional pain inventory used to measure ‘activity grade in the leisure time’ (Kerns 1985225) |
Ability to cope with pain (using Coping Strategies Questionnaire) (Rosenstiel 1983269 and Jenson 1993270) Daily ratings of pain intensity and interference (using VAS) (Wewers 1990271) |
|||
|
Jousset 2004110 From reviews by Désiron 2011,92 Kamper 201495 and Norlund 2009101 |
Percentage RTW, days of sick leave, ability to work | Back pain disability: Québec Disability Scale (Kopec 1995242) |
Pain (VAS) (Huskisson 1982272) Quality of life and functional indexes: French version of the Dallas Pain Questionnaire (Lawlis 1989273 and Marty 1998274) |
Anxiety/depression (HADS, Dallas Pain Questionnaire) | Use of prescription medication | |
|
Kool 2007111 From review by Kamper 201495 |
RTW, workdays (percentage at work), rate of patients receiving unemployment benefits or permanent disability allowances | Pain intensity (10-point NRS) |
Medication (percentage taking medication) Health-care utilisation |
|||
|
Lambeek 2010113 From reviews by Désiron 2011,92 Kamper 201495 and Palmer 2012102 |
RTW: duration of time off work (work disability) due to low back pain until full sustainable RTW | Functional status: Roland Disability Questionnaire (Roland 1983127) | Intensity of pain on VAS (Carlsson 1983251) | |||
|
Lambeek 2010112 From reviews by Désiron 2011,92 Kamper 201495 and Schaafsma 2013103 |
RTW (defined as duration of sick leave due to low back pain in calendar days from day of randomisation until full RTW in own or other work with equal earnings for at least 4 weeks without recurrence, partial or full) (measured at 3, 6, 9 and 12 months) | EQ-5D (Dutch tariff) to generate quality-adjusted life-years (Lamers 2005275) | Health-care resource use | |||
|
Lindh 1997216 |
RTW (i.e. the actual, part-time or full-time RTW during the follow-up period from 90th day of sick leave, regardless of work stability), working status | |||||
|
Marhold 2001217 |
Sick leave (number of days on sick leave over periods of 2 months) | Disability Rating Index (Salén 1994276) |
Multidimensional Pain Inventory (Kerns 1985225) Pain And Impairment Rating Scale (Riley 1988277) |
Coping Strategies Questionnaire (Rosenstiel 1983269) | Beck Depression Inventory (Beck 1979278) | |
|
Meijer 2006218 From review by Palmer 2012102 |
RTW (defined as mean percentage of RTW, where 100 was total return to regular work at the original number of hours. This was based on four questions regarding RTW information) |
Physical disability [using Dutch version of Disability Arm Shoulder Hand questionnaire (Hudak 1996279)] Hand grip strength (as measured using a Jamar hand dynamometer) [Sammons Preston Roylan Jamar Hand Dynamometer (Performance Health, IL, USA) and Boadella 2005280] Kinesiophobia (using the Dutch version of the Tampa Scale for Kinesiophobia) (Kori 1990281 and Vlaeyen 1995282) |
Physical functioning (using Dutch version of SF-36 Health Survey) (Ware 1992229 and Aaronson 1998283) |
Complaints assessed as pain and other complaints Also cost outcomes (e.g. costs of loss of free time, cost of productivity loss) |
||
|
Meyer 2005219 From review by Schaafsma 2013103 |
Ability to work in percentage of a full-time job, and the actual performed work status in percentage of a full-time job (Measured at 8 weeks post rehabilitation) |
Functional capacity, measured by three standardised lifting tests Self-estimation of physical performance using Performance Assessment of Capacity Testing (Matheson 1993284) Perceived pain using NRS Condition-specific questionnaire: Spinal Function Sort of the North American Spine Society (Schochat 2000285) |
SF-36 | |||
|
Mitchell 1994220 From reviews by Kamper 2014,95 Meijer 2005,99 Palmer 2012102 and Schaafsma 2013103 |
Return to full-time work Days lost from work (Measurement at 12 months after treatment) |
Cost per workers’ compensation claim | ||||
|
Nordström-Björverud 1998122 From review by Meijer 200599 |
Percentage RTW (work status, full-time working, part-time working, or not working, at follow-up) | Physical disability: using Disability Rating Index (Salén 1994276) |
Pain: using VAS (Scott 1976286) and pain drawing (Persson 1994287 and Udén 1998288) Questionnaire regarding working conditions |
Health-related quality of life: using the Nottingham Health Profile, (Hunt 1980,289 Hunt 1981290 and Wiklund 1988291) | Claims for work injury compensation, health insurance status and current health status | |
|
Roche 2007114 From reviews by Kamper 201495 and Schaafsma 2013103 Roche 2011115 From review by Kamper 201495 |
Percentage self-perceived ability to return to work Percentage RTW Percentage full-time RTW (Measurement directly after treatment) |
Severity of low back pain on VAS 0–10 (Jensen 1986292 and Huskisson 1982272) Dallas Pain Questionnaire – impact of pain on quality of life (Lawlis 1989273 and Marty 1998274) |
Trunk flexibility: fingertip-to-floor distance (Gauvin 1990293) Trunk muscle endurance: Sorensen test (Biering-Sorensen 1984294), Ito test (Ito 1996265) General endurance – by cycloergometer test Treatment costs |
|||
|
Skouen 2002221 From reviews by Kamper 2014,95 Meijer 2005,99 Norlund 2009101 and Schaafsma 2013103 |
Percentage RTW; information on sick leave status via National Health Insurance (Measurement after 12, 18 and 24 months after treatment |
|||||
|
Strand 2001222 From review by Kamper 201495 |
Work (percentage RTW) | Assessment of perceived functioning (Disability Rating Index) (Salén 1994276) | Pain: Norwegian Pain Questionnaire (Strand 1991295) and VAS (Gracely 1994296)Physical performance (five performance tests used): | |||
List of the 140 full-text primary studies screened for eligibility
List of included primary studies
Bardgett M, Lally J, Malviya A, Deehan D. Return to work after knee replacement: a qualitative study of patient experiences. BMJ Open 2016;6:e007912. https://doi.org/10.1136/bmjopen-2015-007912132
Donceel P, Du Bois M, Lahaye D. Return to work after surgery for lumbar disc herniation. A rehabilitation-oriented approach in insurance medicine. Spine 1999;24:872–6. https://doi.org/10.1097/00007632-199905010-00007124
Hinman MR. Factors influencing work disability for women who have undergone mastectomy. Women Health 2001;34:45–60. 133
Vonk Noordegraaf A, Anema JR, van Mechelen W, Knol DL, van Baal WM, van Kesteren PJ, et al. A personalised eHealth programme reduces the duration until return to work after gynaecological surgery: results of a multicentre randomised trial. BJOG 2014;121:1127–35. https://doi.org/10.1111/1471-0528.12661131
List of excluded primary studies
| Study | Reason for exclusion |
|---|---|
| Focus on research. Br J Occup Ther 1997;60:86–9303 | Not occupational advice intervention |
| Allen L. Embracing a new lifestyle after gastric bypass: a multidisciplinary approach to post-operative exercise program in acute care setting...Combined sections meeting: CSM2007: history repeats itself, Boston, February 14-18. Acute Care Perspect 2006;15:19–20304 | No comparator |
| Aquilina R, Baldacchino D. An exploratory study of Maltese patients’ perceptions of their preparation for total joint replacement at the pre-admission clinic. J Orthop Nurs 2007;11:194–203305 | No outcomes of interest |
| Arthur HM, Daniels C, McKelvie R, Hirsh J, Rush B. Effect of a preoperative intervention on preoperative and postoperative outcomes in low-risk patients awaiting elective coronary artery bypass graft surgery. A randomized, controlled trial. Ann Intern Med 2000;133:253–62306 | Not occupational advice intervention |
| Bitterli R, Sieben JM, Hartmann M, de Bruin ED. Pre-surgical sensorimotor training for patients undergoing total hip replacement: a randomised controlled trial. Int J Sports Med 2011;32:725–32. https://doi.org/10.1055/s-0031-1271696307 | Not occupational advice intervention |
| Bondoc S. Rehabilitation of distal radius fractures: a primer for the OT generalist. OT Pract 2005;10:17–22308 | Comparator |
| Bottomley M. An evidence based evaluation of the types and benefits of total hip replacement preoperative education programs used within Australian health districts. Aust Occup Ther J 2011;58:49309 | Full text unavailable |
| Budge G. An evaluation of the occupational therapy for spinal fusion hip spica patients. Br J Occup Ther 1997;60:365–9310 | Not occupational advice intervention |
| Burger H, Marincek C. Return to work after lower limb amputation. Disabil Rehabil 2007;29:1323–9311 | Not occupational advice intervention |
| Burton JH, Marshall JM, Munro P, Moule W, Snell GI, Westall GP. Rehabilitation and transition after lung transplantation in children. Transplant Proc 2009;41:296–9. https://doi.org/10.1016/j.transproceed.2008.10.047312 | Study type |
| Butler GS, Hurley CA, Buchanan KL, Smith-VanHorne J. Prehospital education: effectiveness with total hip replacement surgery patients. Patient Educ Couns 1996;29:189–97313 | No outcomes of interest |
| Chisholm DDC, Schreiber J. Creating occupation-based opportunities in a medical model clinical practice setting. OT Pract 2000;5:CE-1314 | No comparator |
| Clayton M, Verow P. Advice given to patients about return to work and driving following surgery. Occup Med 2007;57:488–9152 | No comparator |
| Cohen M, DiLeonardo M, Zaccariello J. Video education: a new approach to improving patient comprehension. OT Pract 2009;14:7–8315 | Not occupational advice intervention |
| Conyers D, Prigge P. The first 12 months after upper-limb amputation. inMotion 2011;21:23–4316 | Study type |
| Coudeyre E, Jardin C, Givron P, Ribinik P, Revel M, Rannou F. Could preoperative rehabilitation modify postoperative outcomes after total hip and knee arthroplasty? Elaboration of French clinical practice guidelines. Ann Readapt Med Phys 2007;50:189–97317 | Not occupational advice intervention |
| Cowie JG, Turnbull GS, Turnball GS, Ker AM, Breusch SJ. Return to work and sports after total hip replacement. Arch Orthop Trauma Surg 2013;133:695–700. https://doi.org/10.1007/s00402-013-1700-239 | Not occupational advice intervention |
| Criss M, Takacs S. Rehabilitation of hip fractures across the continuum of care. Top Geriatr Rehabil 2013;29:281–93. https://doi.org/10.1097/TGR.0b013e318292e904318 | Study type |
| Crowe J, Henderson J. Pre-arthroplasty rehabilitation is effective in reducing hospital stay. Can J Occup Ther 2003;70:88–96. https://doi.org/10.1177/000841740307000204319 | Not occupational advice intervention |
| Crum KR. Readiness for discharge: occupation-based treatment in the orthopedic setting. OT Practice 2011;16:14–23320 | Study type |
| Dalury DF, Tucker KK, Kelley TC. When can I drive?: brake response times after contemporary total knee arthroplasty. Clin Orthop Relat Res 2011;469:82–6. https://doi.org/10.1007/s11999-010-1507-1321 | No comparator |
| Davidson T. Total hip replacement: an audit of the provision and use of equipment. Br J Occup Ther 1999;62:283–7322 | No outcomes of interest |
| Dawson-Bowling SJ, Jha S, Chettiar KK, East DJ, Gould GC, Apthorp HD. A multidisciplinary enhanced recovery programme allows discharge within two days of total hip replacement; three- to five-year results of 100 patients. Hip Int 2014;24:167–74. https://doi.org/10.5301/hipint.5000100323 | No comparator |
| Doe A. Hip replacement: what you really need to know. Br J Occup Ther 2004;67:234–5324 | Study type |
| Donohue K, Hoevenaars R, McEachern J, Zeman E, Mehta S. Home-based multidisciplinary rehabilitation following hip fracture surgery: what is the evidence? Rehabil Res Pract 2013;2013:1–10325 | Not for relevant population |
| Dronkers JJ, Lamberts H, Reutelingsperger IM, Naber RH, Dronkers-Landman CM, Veldman A, van Meeteren NL. Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: a randomized controlled pilot study. Clin Rehabil 2010;24:614–22. https://doi.org/10.1177/0269215509358941326 | Not occupational advice intervention |
| Drummond A, Coole C, Brewin C, Sinclair E. Hip precautions following primary total hip replacement: a national survey of current occupational therapy practice. Br J Occup Ther 2012;75:164–70327 | No outcomes of interest |
| Drummond A, Edwards C, Coole C, Brewin C. What do we tell patients about elective total hip replacement in the UK? An analysis of patient literature. BMC Musculoskelet Disord 2013;14:152. https://doi.org/10.1186/1471-2474-14-1522328 | No outcomes of interest |
| Engblom E, Korpilahti K, Hämäläinen H, Rönnemaa T, Puukka P. Quality of life and return to work 5 years after coronary artery bypass surgery. Long-term results of cardiac rehabilitation. J Cardiopulm Rehabil 1997;17:29–36. https://doi.org/10.1097/00008483-199701000-00004329 | Not occupational advice intervention |
| Filiz M, Cakmak A, Ozcan E. The effectiveness of exercise programmes after lumbar disc surgery: a randomized controlled study. Clin Rehabil 2005;19:4–11. https://doi.org/10.1191/0269215505cr836oa330 | Not occupational advice intervention |
| Fletchall S. Occupational therapy from the onset: immediate therapeutic intervention accelerates recovery for new amputees. inMotion 2006;16:34–6331 | Full text not available |
| Foote JA, Smith HK, Jonas SC, Greenwood R, Weale AE. Return to work following knee arthroplasty. Knee 2010;17:19–22. https://doi.org/10.1016/j.knee.2009.06.00141 | Not occupational advice intervention |
| Fredericks S, Yau T. Educational intervention reduces complications and rehospitalizations after heart surgery. West J Nurs Res 2013;35:1251–65. https://doi.org/10.1177/0193945913490081332 | No outcomes of interest |
| Ganjiwale D, Ganjiwale J. Occupational therapy rehabilitation of post operative hand injury cases using modified low cost splints and home based exercises: a rural Indian experience. Indian J Physiother Occup Ther 2014;8:208–13333 | Comparator |
| Gaudry E, Booth J. Using Participatory Action Research (PAR) to develop a ‘my trip to hospital’ DVD with remote first Australian communities . . . Occupational Therapy Australia, 24th National Conference and Exhibition, 29 June – 1 July 2011. Aust Occup Ther J 2011;58:11334 | Not occupational advice intervention |
| Gignac MA, Badley EM, Lacaille D, Cott CC, Adam P, Anis AH. Managing arthritis and employment: making arthritis-related work changes as a means of adaptation. Arthritis Rheum 2004;51:909–16. https://doi.org/10.1002/art.2082210 | Not occupational advice intervention |
| Gill SD, McBurney H. Does exercise reduce pain and improve physical function before hip or knee replacement surgery? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil 2013;94:164–76. https://doi.org/10.1016/j.apmr.2012.08.211335 | Not occupational advice intervention |
| Gill SD, McBurney H, Schulz DL. Land-based versus pool-based exercise for people awaiting joint replacement surgery of the hip or knee: results of a randomized controlled trial. Arch Phys Med Rehabil 2009;90:388–94. https://doi.org/10.1016/j.apmr.2008.09.561336 | Not occupational advice intervention |
| Gillen G, Berger SM, Lotia S, Morreale J, Siber MI, Trudo WJ. Improving community skills after lower extremity joint replacement. Phys Occup Ther Geriatr 2007;25:41–54337 | Comparator |
| Giraudet-Le Quintrec JS, Coste J, Vastel L, Pacault V, Jeanne L, Lamas JP, et al. Positive effect of patient education for hip surgery: a randomized trial. Clin Orthop Relat Res 2003;414:112–20. https://doi.org/10.1097/01.blo.0000079268.91782.bc338 | Not occupational advice intervention |
| Grotle M, Garratt AM, Klokkerud M, Løchting I, Uhlig T, Hagen KB. What’s in team rehabilitation care after arthroplasty for osteoarthritis? Results from a multicenter, longitudinal study assessing structure, process, and outcome. Phys Ther 2010;90:121–31. https://doi.org/10.2522/ptj.20080295339 | Comparator |
| Guo P. Preoperative education interventions to reduce anxiety and improve recovery among cardiac surgery patients: a review of randomised controlled trials. J Clin Nurs 2015;24:34–46. https://doi.org/10.1111/jocn.12618340 | No outcomes of interest |
| Hagsten B, Svensson O, Gardulf A. Early individualized postoperative occupational therapy training in 100 patients improves ADL after hip fracture: a randomized trial. Acta Orthop Scand 2004;75:177–83. https://doi.org/10.1080/00016470412331294435341 | Not occupational advice intervention |
| Hauer K, Specht N, Schuler M, Bärtsch P, Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age Ageing 2002;31:49–57. https://doi.org/10.1093/ageing/31.1.49342 | Not occupational advice intervention |
| Heaton J, McMurray R, Sloper P, Nettleton S. Rehabilitation and total hip replacement: patients’ perspectives on provision. Int J Rehabil Res 2000;23:253–9. https://doi.org/10.1097/00004356-200023040-00001343 | Not occupational advice intervention |
| Herbold JA, Bonistall K, Blackburn M. Effectiveness of continuous passive motion in an inpatient rehabilitation hospital after total knee replacement: a matched cohort study. PM R 2012;4:719–25. https://doi.org/10.1016/j.pmrj.2012.07.004344 | Not occupational advice intervention |
| Herbold JA, Bonistall K, Walsh MB. Rehabilitation following total knee replacement, total hip replacement, and hip fracture: a case-controlled comparison. J Geriatr Phys Ther 2011;34:155–60. https://doi.org/10.1519/JPT.0b013e318216db81345 | Not occupational advice intervention |
| Hoffmann T, Russell T. Pre-admission orthopaedic occupational therapy home visits conducted using the internet. J Telemed Telecare 2008;14:83–7. https://doi.org/10.1258/jtt.2007.070808346 | Not occupational advice intervention |
| Howell SM, Rogers SL. Method for quantifying patient expectations and early recovery after total knee arthroplasty. Orthopedics 2009;32:884. https://doi.org/10.3928/01477447-20091020-10347 | Not occupational advice intervention |
| Ibrahim MS, Alazzawi S, Nizam I, Haddad FS. An evidence-based review of enhanced recovery interventions in knee replacement surgery. Ann R Coll Surg Engl 2013;95:386–9. https://doi.org/10.1308/003588413X13629960046435348 | Study type |
| Jame Bozorgi AA, Ghamkhar L, Kahlaee AH, Sabouri H. The effectiveness of occupational therapy supervised usage of adaptive devices on functional outcomes and independence after total hip replacement in Iranian elderly: a randomized controlled trial. Occup Ther Int 2016;23:143–53. https://doi.org/10.1002/oti.1419349 | Not occupational advice intervention |
| Jepson P, Sands G, Beswick AD, Davis ET, Blom AW, Sackley CM. A feasibility randomised controlled trial of pre-operative occupational therapy to optimise recovery for patients undergoing primary total hip replacement for osteoarthritis (PROOF-THR). Clin Rehabil 2016;30:156–66. https://doi.org/10.1177/0269215515576811350 | Not occupational advice intervention |
| Johanson MA, Cohen BA, Snyder KH, McKinley AJ, Scott ML. Outcomes for aging adults following total hip arthroplasty in an acute rehabilitation facility versus a subacute rehabilitation facility: a pilot study. J Geriatr Phys Ther 2009;32:29–34 [Erratum published in J Geriatr Phys Ther 2019;32:110.]351 | Not occupational advice intervention |
| Kaiser GL, Bodell LS, Berger RA. Functional outcomes after arthroplasty of the distal radioulnar joint and hand therapy: a case series. J Hand Ther 2008;21:398–409. https://doi.org/10.1197/j.jht.2008.06.002352 | Not occupational advice intervention |
| Kiefer DE, Emery LJ. Functional performance and grip strength after total hip replacement. Occup Ther Health Care 2005;18:41–56. https://doi.org/10.1080/J003v18n04_04353 | Comparator |
| Kirk-Sanchez NJ, Roach KE. Relationship between duration of therapy services in a comprehensive rehabilitation program and mobility at discharge in patients with orthopedic problems. Phys Ther 2001;81:888–95354 | Comparator |
| Koval KJ, Cooley MR. Clinical pathway after hip fracture. Disabil Rehabil 2005;27:1053–60355 | No outcomes of interest |
| Kuijer PP, de Beer MJ, Houdijk JH, Frings-Dresen MH. Beneficial and limiting factors affecting return to work after total knee and hip arthroplasty: a systematic review. J Occup Rehabil 2009;19:375–81. https://doi.org/10.1007/s10926-009-9192-121 | Not occupational advice intervention |
| Lenze EJ, Munin MC, Quear T, Dew MA, Rogers JC, Begley AE, Reynolds CF. Significance of poor patient participation in physical and occupational therapy for functional outcome and length of stay. Arch Phys Med Rehabil 2004;85:1599–601356 | Not for relevant population |
| Lucas B, Cox C, Perry L, Bridges J. Pre-operative preparation of patients for total knee replacement: an action research study. Int J Orthop Trauma Nurs 2013;17:79–90357 | Not occupational advice intervention |
| MacKay C, Davis AM, Mahomed N, Badley EM. Expanding roles in orthopaedic care: a comparison of physiotherapist and orthopaedic surgeon recommendations for triage. J Eval Clin Pract 2009;15:178–83. https://doi.org/10.1111/j.1365-2753.2008.00979.x358 | Not occupational advice intervention |
| Maillette PM CM, Gaudreault NG. Workers’ Perspectives on the Return to Work After Total Knee Arthroplasty. Conference: Work Disability Prevention and Integration, September 2016, Amsterdam, abstract no. 520359 | Not occupational advice intervention |
| Mallinson TR, Bateman J, Tseng HY, Manheim L, Almagor O, Deutsch A, Heinemann AW. A comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after lower-extremity joint replacement surgery. Arch Phys Med Rehabil 2011;92:712–20. https://doi.org/10.1016/j.apmr.2010.12.007360 | Not occupational advice intervention |
| Mata H, Mikkola A, Loveland J, Hallowell PT. Occupational therapy and bariatric surgery. OT Pract 2015;20:11–5361 | Not occupational advice intervention |
| McCormick L. The role of occupational therapy in the adult bone marrow transplant process. Phys Disabil Spec Inter Sect Q 2014;37:1–4362 | Not for relevant population |
| McGregor AH, Probyn K, Cro S, Doré CJ, Burton AK, Balagué F, et al. Rehabilitation following surgery for lumbar spinal stenosis. A Cochrane review. Spine 2014;39:1044–54. https://doi.org/10.1097/BRS.0000000000000355363 | Not occupational advice intervention |
| McMurray R, Heaton J, Sloper P, Nettleton S. Variations in the provision of occupational therapy for patients undergoing primary elective total hip replacement in the United Kingdom. Br J Occup Ther 2000;63:451–5364 | Study type |
| McQuaid L, Cope J, Fenech A. Occupational therapy in orthopaedics: an alternative to hip precautions? Int J Ther Rehabil 2014;21:508–10365 | No outcomes of interest |
| McQueen J, Nivison C, Ballance F, Fairbairn P, Clyde D, Murray E. Hip precautions following hemiarthroplasty: a UK study of occupational therapists. Int J Ther Rehabil 2009;16:147–53366 | Not occupational advice intervention |
| Merle C, Brendle S, Wang H, Streit MR, Gotterbarm T, Schiltenwolf M. Multidisciplinary treatment in patients with persistent pain following total hip and knee arthroplasty. J Arthroplasty 2014;29:28–32. https://doi.org/10.1016/j.arth.2013.05.004367 | Comparator |
| Messecar D. ‘Hospital at home’ care was generally as effective as routine hospital care for older adults [commentary on Shepperd S, Harwood D, Jenkinson C, Gray A, Vessey M, Morgan P. Randomised controlled trial comparing hospital at home care with inpatient hospital care. I: three month follow up of health outcomes. BMJ 1998;316:1786–91 and Shepperd S, Harwood D, Gray A, Vessey M, Morgan P. Randomised controlled trial comparing hospital at home care with inpatient hospital care. II: cost minimisation analysis. BMJ 1998;316:1791–6]. Evid Based Nurs 1999:50–1368 | Not occupational advice intervention |
| Millet R. Occupational therapists set out their stall. Frontline 2012;18:13369 | Study type |
| Miró J, Raich RM. Effects of a brief and economical intervention in preparing patients for surgery: does coping style matter? Pain 1999;83:471–5370 | Not occupational advice intervention |
| Mirza SK, Deyo RA, Heagerty PJ, Turner JA, Martin BI, Comstock BA. One-year outcomes of surgical versus nonsurgical treatments for discogenic back pain: a community-based prospective cohort study. Spine J 2013;13:1421–33. https://doi.org/10.1016/j.spinee.2013.05.047371 | Comparator |
| Moore SM. Effects of interventions to promote recovery in coronary artery bypass surgical patients. J Cardiovasc Nurs 1997;12:59–70. https://doi.org/10.1097/00005082-199710000-00007372 | Not occupational advice intervention |
| Mulcahey MJ, Betz RR, Kozin SH, Smith BT, Hutchinson D, Lutz C. Implantation of the Freehand System during initial rehabilitation using minimally invasive techniques. Spinal Cord 2004;42:146–55. https://doi.org/10.1038/sj.sc.3101573373 | Not occupational advice intervention |
| Munin MC, Putman K, Hsieh CH, Smout RJ, Tian W, DeJong G, Horn SD. Analysis of rehabilitation activities within skilled nursing and inpatient rehabilitation facilities after hip replacement for acute hip fracture. Am J Phys Med Rehabil 2010;89:530–40. https://doi.org/10.1097/PHM.0b013e3181e29f54374 | Not occupational advice intervention |
| Munin MC, Rudy TE, Glynn NW, Crossett LS, Rubash HE. Early inpatient rehabilitation after elective hip and knee arthroplasty. JAMA 1998;279:847–52375 | Comparator |
| Naglie G, Tansey C, Kirkland JL, Ogilvie-Harris DJ, Detsky AS, Etchells E, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ 2002;167:25–32376 | Not for relevant population |
| Naville J, Volz T, Curry J. A multidisciplinary approach to total joint replacement. Home Health Care Manage Pract 2009;21:415–8377 | Comparator |
| Nazzal MI, Bashaireh KH, Alomari MA, Nazzal MS, Maayah MF, Mesmar M. Relationship between improvements in physical measures and patient satisfaction in rehabilitation after total knee arthroplasty. Int J Rehabil Res 2012;35:94–101. https://doi.org/10.1097/MRR.0b013e32834df63c378 | Comparator |
| Neville-Smith M, Trujillo L, Ammundson R. Special feature: consistency in postoperative education programs following total hip replacement. Top Geriatr Rehabil 2000;15:68–76379 | No outcomes of interest |
| Newport ML, Tucker RL. New perspectives on extensor tendon repair and implications for rehabilitation. J Hand Ther 2005;18:175–81380 | Not for relevant population |
| Nilsson I, Rogmark C. Hemiarthroplasty for displaced femoral neck fracture: good clinical outcome but uneven distribution of occupational therapy. Disabil Rehabil 2011;33:2329–32. https://doi.org/10.3109/09638288.2011.570412381 | No outcomes of interest |
| Novalis SD, Messenger MF, Morris L. Occupational therapy benchmarks within orthopedic (hip) critical pathways. Am J Occup Ther 2000;54:155–8. https://doi.org/10.5014/ajot.54.2.155382 | No absence |
| Oberg T, Oberg U, Svidén G, Nordwall Persson A. Functional capacity after hip arthroplasty: a comparison between evaluation with three standard instruments and a personal interview. Scand J Occup Ther 2005;12:18–28. https://doi.org/10.1080/11038120510027153383 | Not occupational advice intervention |
| O’Brien L, McKeough C, Abbasi R. Pre-surgery education for elective cardiac surgery patients: a survey from the patient’s perspective. Aust Occup Ther J 2013;60:404–9. https://doi.org/10.1111/1440-1630.12068384 | No outcomes of interest |
| O’Donnell S, Kennedy D, MacLeod AM, Kilroy C, Gollish J. Achieving team consensus on best practice rehabilitation guidelines following primary total hip replacement (THR) surgery. Healthc Q 2006;9:60–4. https://doi.org/10.12927/hcq.2006.18354385 | Not occupational advice intervention |
| Oldmeadow LB, Edwards ER, Kimmel LA, Kipen E, Robertson VJ, Bailey MJ. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg 2006;76:607–11386 | Not occupational advice intervention |
| Oosterhuis T, Costa LO, Maher CG, de Vet HC, van Tulder MW, Ostelo RW. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev 2014;3:CD003007. https://doi.org/10.1002/14651858.CD003007.pub389 | Reviewed in systematic review library already |
| Orpen N, Harris J. Patients’ perceptions of preoperative home-based occupational therapy and/or physiotherapy interventions prior to total hip replacement. Br J Occup Ther 2010;73:461–9387 | No outcomes of interest |
| Ostelo RW, de Vet HC, Waddell G, Kerckhoffs MR, Leffers P, van Tulder M. Rehabilitation following first-time lumbar disc surgery: a systematic review within the framework of the cochrane collaboration. Spine 2003;28:209–18. https://doi.org/10.1097/01.BRS.0000042520.62951.28201 | Reviewed in systematic review library already |
| Pace M, Maguire K. Hand and upper extremity transplantation: a rehabilitation process. OT Practice 2011;16:17–22388 | Not occupational advice intervention |
| Peiris CL, Taylor NF, Shields N. Additional Saturday allied health services increase habitual physical activity among patients receiving inpatient rehabilitation for lower limb orthopedic conditions: a randomized controlled trial. Arch Phys Med Rehabil 2012;93:1365–70. https://doi.org/10.1016/j.apmr.2012.03.004389 | No outcomes of interest |
| Pfund A, Pütz J, Wendland G, Theisson M, Aydin U, Hinzpeter B, et al. [Coronary intervention and occupational rehabilitation – a prospective, randomized intervention study.] Z Kardiol 2001;90:655–60. https://doi.org/10.1007/s003920170113390 | Full text unavailable |
| Piva SR, Moore CG, Schneider M, Gil AB, Almeida GJ, Irrgang JJ. A randomized trial to compare exercise treatment methods for patients after total knee replacement: protocol paper rehabilitation, physical therapy and occupational health. BMC Musculoskelet Disord 2015;16391 | Not occupational advice intervention |
| Pomerance J, Fine I. Outcomes of carpal tunnel surgery with and without supervised postoperative therapy. J Hand Surg Am 2007;32:1159–63392 | Not occupational advice intervention |
| Poole JL, Walenta MH, Alonzo V, Coe A, Moneim M. A pilot study comparing of two therapy regimens following carpometacarpal joint arthroplasty. Phys Occup Ther Geriatr 2011;29:327–36393 | Not occupational advice intervention |
| Prouty A, Cooper M, Thomas P, Christensen J, Strong C, Bowie L, Oermann MH. Multidisciplinary patient education for total joint replacement surgery patients. Orthop Nurs 2006;25:257–61394 | No outcomes of interest |
| Provinciali L, Giattini A, Splendiani G, Logullo F. Usefulness of hand rehabilitation after carpal tunnel surgery. Muscle Nerve 2000;23:211–16395 | Not occupational advice intervention |
| Rannou F, Coudeyre E, Ribinik P, Macé Y, Poiraudeau S, Revel M. Establishing recommendations for physical medicine and rehabilitation: the SOFMER methodology. Ann Readapt Med Phys 2007;50:100–10396 | Study type |
| Rapado A. General management of vertebral fractures. Bone 1996;18(Suppl. 3):191–6S397 | Study type |
| Ribinik P, Le Moine F, de Korvin G, Coudeyre E, Genty M, Rannou F, et al. Physical and rehabilitation medicine (PRM) care pathways: ‘patients after total knee arthroplasty’. Ann Phys Rehabil Med 2012;55:533–9. https://doi.org/10.1016/j.rehab.2012.02.001398 | Study type |
| Riddell J. Occupational therapy for adults undergoing total hip replacement. Br J Occup Ther 2013;76:291399 | Study type |
| Rivard A, Warren S, Voaklander D, Jones A. The efficacy of pre-operative home visits for total hip replacement clients. Can J Occup Ther 2003;70:226–32400 | No outcomes of interest |
| Roberts K. Video review. Occupational therapy postoperative management: total hip joint replacement. Aust Occup Ther J 2003;50:191401 | Study type |
| Roddey TS, Olson SL, Gartsman GM, Hanten WP, Cook KF. A randomized controlled trial comparing 2 instructional approaches to home exercise instruction following arthroscopic full-thickness rotator cuff repair surgery. J Orthop Sports Phys Ther 2002;32:548–59. https://doi.org/10.2519/jospt.2002.32.11.548402 | Not occupational advice intervention |
| Ronco M, Iona L, Fabbro C, Bulfone G, Palese A. Patient education outcomes in surgery: a systematic review from 2004 to 2010. Int J Evid Based Healthc 2012;10:309–23. https://doi.org/10.1111/j.1744-1609.2012.00286.x403 | Not occupational advice intervention |
| Rucco V, Visentini A, Pellegrini E. The rehabilitation project in hip arthroplasty patients. Eur Medicophys 2003;39:45–57404 | Study type |
| Safdar S. Wide-awake flexor tendon repair. OT Pract 2015;20:7–16405 | Comparator |
| Sameem M, Wood T, Ignacy T, Thoma A, Strumas N. A systematic review of rehabilitation protocols after surgical repair of the extensor tendons in zones V-VIII of the hand. J Hand Ther 2011;24:365–72. https://doi.org/10.1016/j.jht.2011.06.005406 | Not for relevant population |
| Sandell C. A multidisciplinary assessment and intervention for patients awaiting total hip replacement to improve their quality of life. J Orthop Nurs 2008;12:26–34407 | Not occupational advice intervention |
| Sawatzky JA, Kehler DS, Ready AE, Lerner N, Boreskie S, Lamont D, et al. Prehabilitation program for elective coronary artery bypass graft surgery patients: a pilot randomized controlled study. Clin Rehabil 2014;28:648–57. https://doi.org/10.1177/0269215513516475408 | Not occupational advice intervention |
| Schneider M, Kawahara I, Ballantyne G, McAuley C, Macgregor K, Garvie R, et al. Predictive factors influencing fast track rehabilitation following primary total hip and knee arthroplasty. Arch Orthop Trauma Surg 2009;129:1585–91. https://doi.org/10.1007/s00402-009-0825-9409 | No outcomes of interest |
| Scott PJ. Occupational therapy services to enable liver patients to thrive following transplantation. Occup Ther Health Care 2011;25:240–56. https://doi.org/10.3109/07380577.2011.600427410 | Study type |
| Shahmansouri N, Janghorbani M, Salehi Omran A, Karimi AA, Noorbala AA, Arjmandi A, Nikfam S. Effects of a psychoeducation intervention on fear and anxiety about surgery: randomized trial in patients undergoing coronary artery bypass grafting. Psychol Health Med 2014;19:375–83. https://doi.org/10.1080/13548506.2013.841966411 | No outcomes of interest |
| Sheehan MM, Wilson SF, Vaz AM. Ambulatory rehabilitation for hip and knee arthroplasty. Nurs Monogr 2007:16–9412 | Not occupational advice intervention |
| Shuldham CM, Fleming S, Goodman H. The impact of pre-operative education on recovery following coronary artery bypass surgery. A randomized controlled clinical trial. Eur Heart J 2002;23:666–74. https://doi.org/10.1053/euhj.2001.2897413 | Not occupational advice intervention |
| Siebens HC, Sharkey P, Aronow HU, Deutscher D, Roberts P, Munin MC, et al. Variation in rehabilitation treatment patterns for hip fracture treated with arthroplasty. PM R 2016;8:191–207. https://doi.org/10.1016/j.pmrj.2015.07.005414 | Comparator |
| Smith TO, Jepson P, Beswick A, Sands G, Drummond A, Davis ET, Sackley CM. Assistive devices, hip precautions, environmental modifications and training to prevent dislocation and improve function after hip arthroplasty. Cochrane Database Syst Rev 2016;7:CD010815. https://doi.org/10.1002/14651858.CD010815.pub2206 | Study type; reviewed in systematic review library already |
| Spalding N. Health promotion and the role of occupational therapy. Br J Ther Rehabil 1996;3:143–7415 | No outcomes of interest |
| Spalding NJ. Reducing anxiety by pre-operative education: make the future familiar. Occup Ther Int 2003;10:278–93. https://doi.org/10.1002/oti.191416 | No outcomes of interest |
| Spalding NJ. Using vignettes to assist reflection within an action research study on a preoperative education programme. Br J Occup Ther 2004;67:388–95417 | No outcomes of interest |
| Spalevic M LM, Kocic M, Dimitrijevic L, Stankovic I, Savic D. The Effects of Preoperative Physical Therapy in Total Hip Replacement Surgery. Proceedings of the 10th Congress of the European Federation for Research in Rehabilitation, 9–12 September 2009, Riga, abstract no. 522418 | Full text not available |
| Spiliotopoulou G, Atwal A. Is occupational therapy practice for older adults with lower limb amputations evidence-based? A systematic review. Prosthet Orthot Int 2012;36:7–14. https://doi.org/10.1177/0309364611428662419 | No outcomes of interest |
| Stambough JB, Beaulé PE, Nunley RM, Clohisy J. Contemporary strategies for rapid recovery total hip arthroplasty. Instr Course Lect 2016;65:211–24420 | Study type |
| Stinnett KA. Occupational therapy intervention for the geriatric client receiving acute and subacute services following total hip replacement and femoral fracture repair. Top Geriatr Rehabil 1996:23–31421 | Study type |
| Svendsen SW, Christiansen DH, Haahr JP, Andrea LC, Frost P. Shoulder function and work disability after decompression surgery for subacromial impingement syndrome: a randomised controlled trial of physiotherapy exercises and occupational medical assistance. BMC Musculoskelet Disord 2014;15:215. https://doi.org/10.1186/1471-2474-15-215422 | Insufficient information available – protocol only |
| Szekeres M, King GJW. Total elbow arthroplasty. J Hand Ther 2006;19:245–54423 | Study type |
| Thien T, Becker J. Rehabilitation after surgery for flexor tendon injuries in the hand. Cochrane Database Syst Rev 2004;18:CD003979424 | Not occupational advice intervention |
| Tian W, DeJong G, Munin MC, Smout R. Patterns of rehabilitation after hip arthroplasty and the association with outcomes: an episode of care view. Am J Phys Med Rehabil 2010;89:905–18. https://doi.org/10.1097/PHM.0b013e3181f1c6d8425 | Full text unavailable |
| Walker J. Care of patients undergoing joint replacement. Nurs Older People 2012;24:14–20. https://doi.org/10.7748/nop2012.02.24.1.14.c8898426 | Study type |
| Wang X, Emery LJ. Cognitive status after hip replacement. Phys Occup Ther Geriatr 2002;21:51–64427 | Study type |
| Wasserman BR, Egol KA, Zuckerman JD. Managing hip fractures in older patients: perioperative decision making. J Musculoskelet Med 2008;25:326–34428 | Study type |
| Westby MD. Rehabilitation and total joint arthroplasty. Clin Geriatr Med 2012;28:489–508. https://doi.org/10.1016/j.cger.2012.05.005429 | Study type |
| Shyu YI, Liang J, Tseng MY, Li HJ, Wu CC, Cheng HS, et al. Comprehensive and subacute care interventions improve health-related quality of life for older patients after surgery for hip fracture: a randomised controlled trial. Int J Nurs Stud 2013;50:1013–24. https://doi.org/10.1016/j.ijnurstu.2012.11.020430 | Not occupational advice intervention |
Details of the four included primary studies
| Study (first author and year) | Country | Surgery | Design | Number of participants | Intervention(s) | Control |
|---|---|---|---|---|---|---|
| Quantitative | ||||||
| Donceel 1999124 | Belgium | Herniated lumbar disc | Cluster RCT | 345 vs. 365 | Rehabilitation-oriented approach focused on early mobilisation and resumption of professional activities | Usual claim-based practice: medical advisors performing their usual medical practice |
| Vonk Noordegraaf 2014131 | The Netherlands | Hysterectomy and/or laparoscopic adnexal surgery for benign indication | RCT | 110 vs. 105 | Personalised eHealth intervention comprising advice and instructions, online feedback from gynaecologist, videos, patient forum, website links and glossary. Involvement from health-care professionals and employer | Control eHealth intervention, plus usual care from gynaecologists, occupational physicians and GPs. Website provided hospital contact numbers and patient leaflets |
| Qualitative | ||||||
| Bardgett 2016132 | England | TKR | Qualitative: interviews | 10 patients | Exploration of factors affecting RTW from patient perspective following TKR | NA |
| Hinman 2001133 | Texas, USA | Modified radical mastectomy | Qualitative: surveys and interviews | 31 patients, 18 therapists, 5 employers | Exploration of factors influencing work disability following mastectomy, via experiences of advice or education or rehabilitation received regarding RTW | NA |
Risk-of-bias assessment for review of primary studies
| Question | Hinman (2001)133 | Bardgett et al. (2016)132 |
|---|---|---|
| 1. Was there a clear statement of the aims of the research? | Yes | Yes |
| 2. Is a qualitative methodology appropriate? | Yes | Yes |
| Is it worth continuing? | Yes | Yes |
| 3. Was the research design appropriate to address the aims of the research? | Yes | Yes |
| 4. Was the recruitment strategy appropriate to the aims of the research? | Yes | Yes |
| 5. Was the data collected in a way that addressed the research issue? | Can’t tell | Yes |
| 6. Has the relationship between researcher and participants been adequately considered? | Can’t tell | Can’t tell |
| 7. Have ethical issues been taken into consideration? | Can’t tell | Yes |
| 8. Was the data analysis sufficiently rigorous? | No | Yes |
| 9. Is there a clear statement of findings? | Yes | Yes |
| 10. How valuable is the research? | The study highlights the need for further research and states what the study adds to the existing knowledge on the topic | Discusses the study findings in relation to existing evidence, and also highlights where there is an absence of evidence in the literature. Suggests improvements in delivery of patient care via a future high-quality trial to evaluate the effect on work participation following joint replacement |
| Comments |
3. Yes, although no clear rationale as to why ‘employer group’ was interviewed and other groups surveyed 5. Methods and setting for data collection not justified, form of data is not clear, no discussion of saturation of data (for interviews) 8. No details of analysis of qualitative data provided |
| Question | Donceel et al. (1999)124 | Vonk Noordegraaf et al. (2014)131 |
|---|---|---|
| Adequate sequence generation? | ? | + |
| Allocation concealment? | ? | ? |
| Blinding of participants? | – | + |
| Blinding of providers? | – | – |
| Blinding of outcome assessors? | ? | – |
| Incomplete outcome data addressed? (All outcomes – dropouts?) | ? | + |
| Incomplete outcome data addressed? (All outcomes – ITT analysis?) | ? | + |
| Free of selective reporting? | ? | + |
| Similarity of at baseline characteristics? | + | + |
Criteria for Reporting the Development and Evaluation of Complex Interventions in Healthcare, for included primary studies82
| Criteria | Reported in publication (page number in publication)? |
|---|---|
| Donceel et al. (1999)124 | |
| First stage: development | |
| 1. Description of the intervention’s underlying theoretical basis | No |
| 2. Description of all intervention components, including the reasons for their selection as well as their aims/essential functions | No; p. 873 lists intervention components only; no additional detail |
| 3. Illustration of any intended interactions between different components | No |
| 4. Description and consideration of the context’s characteristics in intervention modelling | No |
| Second stage: feasibility and piloting | |
| 5. Description of the pilot test and its impact on the definite intervention | No |
| Third stage: evaluation | |
| 6. Description of the control condition (comparator) and reasons for the selection | Yes; p. 873 provides brief detail; no reason |
| 7. Description of the strategy for delivering the intervention within the study context | No |
| 8. Description of all materials or tools used to deliver the intervention | No |
| 9. Description of fidelity of the delivery process compared the study protocol | No |
| 10. Description of a process evaluation and its underlying theoretical basis | No |
| 11. Description of internal facilitators and barriers potentially influencing the delivery of the intervention as revealed by the process evaluation | No |
| 12. Description of external conditions or factors occurring during the study which might have influenced the delivery of the intervention or mode of action (how it works) | No |
| 13. Description of costs or required resources for the delivery of the intervention | No |
| Vonk Noordegraaf et al. (2014)131 | |
| First stage: development | |
| 1. Description of the intervention’s underlying theoretical basis | No |
| 2. Description of all intervention components, including the reasons for their selection as well as their aims/essential functions | Yes; pp. 1128–9 list/describe the intervention components. Detailed description of the intervention has been published elsewhere68 |
| 3. Illustration of any intended interactions between different components | No |
| 4. Description and consideration of the context’s characteristics in intervention modelling | No |
| Second stage: feasibility and piloting | |
| 5. Description of the pilot test and its impact on the definite intervention | No |
| Third stage: evaluation | |
| 6. Description of the control condition (comparator) and reasons for the selection | Yes; p. 1128; no reason |
| 7. Description of the strategy for delivering the intervention within the study context | Yes; p. 1129 |
| 8. Description of all materials or tools used to deliver the intervention | Yes; p. 1129 |
| 9. Description of fidelity of the delivery process compared the study protocol | Yes; pp. 1129–30 described compliance |
| 10. Description of a process evaluation and its underlying theoretical basis | No |
| 11. Description of internal facilitators and barriers potentially influencing the delivery of the intervention as revealed by the process evaluation | No |
| 12. Description of external conditions or factors occurring during the study which might have influenced the delivery of the intervention or mode of action (how it works) | Yes; p. 1133 |
| 13. Description of costs or required resources for the delivery of the intervention | No |
Intervention characteristics of the included primary studies
| Study (first author and year) | Surgery type | Content of intervention | Duration and timing | Setting | Mode of delivery |
|---|---|---|---|---|---|
| Donceel 1999124 | Lumbar disc herniation surgery |
Rehabilitation-oriented approach used by medical advisors to motivate patients and treating physicians towards social and professional reintegration Medical advisors asked to base medical practice on three rehabilitation guidelines:Guidelines that the intervention protocol is based on are referenced in the study |
Patients’ office visits: first visit at 6 weeks after operation, with monthly follow-up consultations | Medical advisors of a social security fund (Belgium) | Face to face |
| Vonk Noordegraaf 2014131 | Hysterectomy and/or laparoscopic adnexal surgery for a benign indication |
Personalised eHealth intervention Tailored preoperative and postoperative instructions regarding resumption of work and daily activities; advice for employer and employee about a successful work reintegration; evaluation of recovery and advice on which care provider(s) to approach in case of problems; evaluation of complications, with individualised online feedback if needed; instructional video for employer and employee to illustrate common pitfalls during perioperative and reintegration period; patient forum; website links and glossary; extensive list of answers to frequently asked questions about surgical procedure and practical issues with pictures; and involvement from health-care professionals and employer An intervention manual was not reported as being available, although a reference was provided for a more detailed description of the intervention |
Delivered from 4 weeks before surgery to 7 weeks after surgery | Home-based (the Netherlands) | Online, via logging onto website |
Data extraction for qualitative studies
| Source | |
|---|---|
| Author | Bardgett, Lally, Malviya and Deehan132 |
| Year | 2016 |
| Confirm eligibility for review | |
| Reason | Qualitative study exploring the patient’s perspective regarding RTW after knee replacement surgery |
| Participants | |
| Participants | 10 employed patients who had undergone TKR and who were all under the age of 60 years at the time of surgery |
| Country | England |
| Setting | Secondary care: large teaching hospital in the north of England |
| Percentage male | 50% |
| Study conducted during | December 2013 to March 2014 |
| Study objective | |
| Study objective | To gain a greater insight into the factors influencing RTW from the patient’s perspective, potential deficiencies in the delivery of care directly pertinent to RTW, and to identify key themes to inform future research in respect to optimising RTW outcomes. Focus was on the preoperative and early postoperative phases of the patient’s journey |
| Surgical procedure type | |
| TKR surgery | |
| Method of evaluation and underpinning methodology | |
|
Participants were selected from a cohort of 50 TKR patients recruited into a population-based postal questionnaire study investigating barriers to and facilitators of RTW after joint replacement carried out at the same institution. From the cohort of 50, 37 were in employment preoperatively and consented to be approached. From these, purposive sampling was used to select patients with a range of characteristics known to influence rates of RTW Using semistructured interviews, patients were asked to discuss the impact of their knee symptoms and surgery on work participation, incorporating both preoperative and postoperative experiences during the interview. Interviews were audio-recorded and transcribed verbatim The process used for analysis was based on thematic analysis as described by Braun and Clarke. 431 Researcher coding was checked by a second experienced qualitative researcher who verified initial codes and subsequent analytical themes to ensure internal validity in relation to the data set. Resulting themes and supporting data were also reported and discussed at regular meetings of the research team as a process of member validation |
|
| Views and experiences (related to return to work/normal activities/social participation) | |
|
Three themes influencing the patient’s experience of RTW following TKR were identified Theme 1: delays in surgical intervention (and the impact on work participation preoperatively) The majority of patients perceived age to be a barrier to referral for surgical intervention for knee osteoarthritis Patients described how they used coping mechanisms and adaption to counteract deteriorating physical function and mobility As symptoms persisted and increased in severity, patients discussed the subsequent impact on work participation in terms of reduced productivity in the workplace as well as patients reporting no choice but to take sick leave due to the inability to cope Patients perceived that their individual circumstances and the need to remain in employment were not given due consideration in the decision-making process Patients reported the physical and psychological impact of delayed intervention as well as the resulting lost working days, financial implications, and the negative impact on their sickness record and future employability Theme 2: limited and inconsistent advice between health-care providers to optimise RTW Advice received focused on the elderly, retired population and related to the inpatient episode and immediate postoperative recovery. Longer-term outcomes, such as RTW, were not routinely discussed Patients stated that preoperative education reinforced the perception of joint replacement surgery as a procedure for the older, retired population Returning to work was not routinely discussed preoperatively. Patients were therefore unsure of the processes involved. They often looked to health-care professionals postoperatively for guidance. Many patients waited until their routine postoperative hospital review for advice and permission to return to work When advice was given, it did not appear to be tailored to the individual. Generic advice sometimes delayed RTW even when patients felt able to return. Some patients reported their belief that they should not return to work until the clinician gave permission for insurance or health and safety reasons Patients acknowledged the potential benefits of tailored work-related advice or the involvement of an occupational health worker to discuss the individual’s requirements and facilitate the process of RTW Theme 3: the provision of rehabilitation to optimise recovery and RTW Patients described a large variation in the provision of postoperative rehabilitation. Rehabilitation goals were limited to general mobility and knee range of movement. Patients felt that they would have benefited from rehabilitation tailored to their individual needs Although the rehabilitation they did receive was not tailored to their RTW requirements, patients reported that the interaction and feedback they did receive from rehabilitation staff gave them the reassurance and confidence to progress in their physical and psychological recovery A small number of patients took the decision to seek additional rehabilitation, and reported the positive impact that the rehabilitation had on their physical function and ability to return to work |
|
| Process measures related to delivery of interventions | |
| Barriers and facilitators | Facilitators:
|
| Stakeholder perspectives (patients, health-care professionals, employers) | The patient’s perspectives are presented in the study; the study does not report the perspectives of the health-care professional or the employer but does identify their involvement in the process |
| Source | |
| Author | Hinman133 |
| Year | 2001 |
| Confirm eligibility for review | |
| Reason | Qualitative study exploring the work status, rehabilitation practices and barriers to work re-entry for mastectomy patients, from the perspective of the patient, occupational therapist and employer |
| Participants | |
| Participants | 31 patients who were post-modified radical mastectomy, 18 physical/occupational therapists working in cancer centres and 5 employers who represented a diverse group of businesses |
| Country | Texas, USA |
| Setting | Cancer centre at University of Texas (patients), rehabilitation medical centres specialising in cancer care (therapists), and public/private companies and businesses located in east and southeast Texas (employers) |
| Study conducted during | Data not available |
| Study objective | |
| Study objective | To describe and examine the relationship between the factors that interfere with women’s ability to return to work from the perspectives of patients, therapists and employers |
| Surgical procedure type | |
| MRM surgery | |
| Method of evaluation and underpinning methodology | |
|
Survey methods were used to solicit information from three independent sources:Quantitative and qualitative data were collected from each group of participants Patients: a survey of 10 items related to the patient’s cancer diagnosis, surgery and rehabilitation, preoperative and postoperative work status, was mailed out to patients. The survey included items related to patient demographics, preoperative and postoperative employment status, length of hospital stay, type and length of postoperative rehabilitation programme (if any) and whether or not the physical requirements of their job were addressed in their rehabilitation Physical and occupational therapists: a survey consisting of 10 items related to their own clinical experience, number of referrals received in previous year for post-MRM patients, types of physical impairments frequently demonstrated by these patients, work-related treatment goals, types of therapeutic interventions used and average length of rehabilitation programme Employers: personal interviews structured around an established list of seven open-ended questions addressing their past experiences with employees who had undergone mastectomy surgery Common factors that affect a woman’s ability to return to work following MRM surgery were identified and classified as physical limitations, psychological limitations or both |
|
| Views and experiences (related to return to work/normal activities/social participation) | |
|
The patients’ responses did not reference interventions relating to occupational advice. They referred more to information regarding exercises/physical job requirements. The only references to occupation were: Therapists’ responses covered topics such as the timing of referrals to therapy, descriptions of a typical treatment programme and the proportion achieving their treatment goals All interviewed employers reported having written policies or procedures that would allow employees to return to work following MRM surgery. The paper references accommodations such as changing work schedule, modifying job role, job reassignment, assistive devices and ergonomic changes to work stations |
|
| Process measures related to delivery of interventions | |
| Barriers and facilitators |
Facilitators: When asked what HCPs could do to facilitate an employee’s RTW following MRM surgery, employers’ requests included:Barriers: Only a small percentage of the women who had MRM surgery were referred to physical therapy or were visited by a recovery volunteer Barriers: perceived barriers to work re-entry and recommendations: There were three reasons for this: A further potential barrier is the timing of referrals to therapy. In some cases, referral was not routine and was instigated only ‘when patients got into trouble’ |
Appendix 3 Supporting information for the cohort study, health economic analysis and national survey of practice (intervention mapping stage 1)
Patient information sheet for OPAL cohort study (contact details removed)
Supplementary information for cohort study analyses
List of jobs given by participants in the cohort study (145 responses):
Petrol Station Operative.
Technical Sales Engineer.
Medical Secretary on a Neo Natal Unit.
Dog Walker, Pet Sitter.
I.T. Manager, manage I.T. Engineers.
Staff Nurse Trauma Orthopaedics - Rehab.
General Practitioner.
Mould tool maintenance. Toolmaker. Tooling engineer.
Non-professional fiction writer.
Volunteer Worker in my local Hospital Outpatient Receptionist.
Engine technician.
Mechanical Maintenance Fitter.
Hairdresser.
Volunteer- Arches Project Nottingham.
Train Cleaner.
Proprietor & Head Groomer at my Salon.
I am a teaching assistant in a special needs school covering a wide range of needs physically and mentally.
Tree surgery/groundsman.
Charity shop volunteer.
Admin or reception work on a temporary basis.
Tax manager in chartered accountants.
HCA [health-care assistant], NHS Medium Secure Unit.
work on Till, also self-scan.
I run a Headhunting company.
Carpenter.
Senior Supervisor in Production/Manufacturing supplements for human & animal welfare.
Social Worker in the community.
Assistant Practitioner.
Bindery guillotine operator.
I am a volunteer supervisor in a charity shop.
Builder: extensions, roofs, patios.
Work in family business.
I am a cleaner at our fun house.
porter nights.
shop fitter.
I do catering assistance in primary school serving pupils at lunch time.
admin/data input officer and telephone agent.
Administration officer with HMRC [Her Majesty’s Revenue and Customs].
teaching assistant.
Warranty administrator in car dealership.
Volunteer in church shop. General shop work duties.
GP receptionist. Admin work and support worker at homeless hostel.
Security consultant.
Assistant health visitor practitioner.
I have my own joinery business.
Social worker/best interests assessor.
admin team leader organising staff, computer work.
Manager curtain maker and designing and making curtains.
I work at the local council as a supervisor mechanic.
We have a farm and pony trekking centre.
Passenger assistant, a travel buddy to people young and old with complex needs.
I am a courier driver.
Pig farmer.
Company Director.
LGV [light goods vehicle] Driver - Farm work.
I work at bus depot, as a diesel fitter.
Lunchtime supervisor.
Construction manager.
Technical author.
Staff nurse.
Retired - But still working farmer.
Motor mechanic/Wagon driver.
Post man.
Plant operator, surface mines.
Taxi Driver, Long periods of sitting.
Minister of religion. Run children and youth clubs. Preach. Lead bible studies.
Cleaner.
Gamekeeper.
I am retired, I look after my grandma one day a week and i help my daughter with her homes 5 days a week.
Account work - Working part time at home, working from a desk or table.
Ordained curate.
Clean and take in main meal (career).
I work for council, as part of the reablement team.
Take orders; check stock, re plan units. Merchandise stock.
Primary School Teacher.
I worked as a Customer Service Officer.
Test & Development Engineer./Computer/desk and factory floor based.
Mechanical Engineer Building Services.
Warehouse Worker.
Motor Engineer.
Personnel Assistant.
Flooring Contractor.
Lecturer in business studies & accounting.
Civilian medical practitioner at RAF.
Sole trader of fruit and veg boxes.
I am a retired engineer, I now work as a hobby.
Street cleaner for council.
Post office counter clerk.
Chef.
2 voluntary jobs.
Postman.
Retired, but work a couple of days a week looking after a few properties I own.
Printer/pre-press.
Director of a plastering and property company.
I arrange busking groups to raise money for different charities.
Pall bearer.
partner in newspaper distribution business.
Litho Printer Operating Printing Press.
company director - managerial.
Floor porter.
Pick up furniture and delivering to homes.
Speech language and communications needs consultant.
delivery driver.
I am a transport officer working for council.
Joiner.
rigger off shore wind turbines and heavy lifting.
care worker.
manager.
NHS podiatrist.
sole proprietor of a 4 roomed b and b.
security guard.
police staff.
garage owner, car repairs and mot.
Parra planner.
bed and breakfast owner.
Monumental sculptor.
quality control inspector.
I’m a joiner by trade.
racecourse judges assistant.
Desk Job computer work.
heating engineer.
Electrician.
Butcher intake and outtake manager.
garage prop.
Practice Nurse.
Technical Assistant.
Teaching electrical commercial courses.
Bricklayer and building contractor.
Farmer.
Maintenance engineer.
Medical secretary/Medication dispenser in an NHS GP surgery.
Carer.
Retired/Self-employed architect.
Taxi driver/LGVI [light goods vehicle class 1] driver.
Maintenance Gearbox Oil/F.L.T. [forklift ruck]
Sales and market development director.
I am a farmer.
Assistant manager, cancer research shop.
Volunteer driver for ambulance service.
Clinical specialist nurse for discharges & palliative discharge.
Full time carer for wife at home.
Customer assistant.
Domestic cleaner.
Self-employed builder.
Reablement.
| Health measure | Operation type | Total (N = 154) | |
|---|---|---|---|
| Hip (N = 77) | Knee (N = 77) | ||
| PHQ-9, raw scores | n = 73 | n = 74 | n = 147 |
| Mean (SD) | 5.9 (5.5) | 4.9 (5.4) | 5.4 (5.5) |
| Median (Q1, Q3) | 5 (2, 9) | 3 (1, 7) | 4 (1, 8) |
| Minimum, maximum | 0, 24 | 0, 24 | 0, 24 |
| PHQ-9, categorised, n (%) | n = 77 | n = 77 | n = 154 |
| None (0–4) | 34 (44.2) | 44 (57.1) | 78 (50.7) |
| Mild (5–9) | 21 (27.3) | 18 (23.4) | 39 (25.3) |
| Moderate (10–14) | 13 (16.9) | 4 (5.2) | 17 (11.0) |
| Moderately severe (15–19) | 3 (3.9) | 7 (9.1) | 10 (6.5) |
| Severe (20–27) | 2 (2.6) | 1 (1.3) | 3 (2.0) |
| Missing | 4 (5.2) | 3 (3.9) | 7 (4.6) |
| GAD-2, n (%) | n = 77 | n = 77 | n = 154 |
| In the past 2 weeks how often have you been bothered by: | |||
| Feeling nervous, anxious or on edge? | |||
| Not at all | 40 (52.0) | 44 (57.1) | 84 (54.6) |
| Several days | 27 (35.1) | 25 (32.5) | 52 (33.8) |
| More than half the days | 6 (7.8) | 2 (2.6) | 8 (5.2) |
| Nearly every day | 1 (1.3) | 3 (3.9) | 4 (2.6) |
| Missing | 3 (3.9) | 3 (3.9) | 6 (3.9) |
| Not being able to stop or control worrying? | |||
| Not at all | 47 (61.0) | 50 (64.9) | 97 (63.0) |
| Several days | 20 (26.0) | 16 (20.8) | 36 (23.4) |
| More than half the days | 5 (6.5) | 5 (6.5) | 10 (6.5) |
| Nearly every day | 2 (2.6) | 3 (3.9) | 5 (3.3) |
| Missing | 3 (3.9) | 3 (3.9) | 6 (3.9) |
| BRS, raw score | n = 75 | n = 73 | n = 148 |
| Mean (SD) | 3.04 (0.38) | 3.03 (0.50) | 3.03 (0.44) |
| Median (Q1, Q3) | 3 (2.8, 3.2) | 3 (2.8, 3.2) | 3 (2.8, 3.2) |
| Minimum, maximum | 1, 4.3 | 1.3, 5 | 1, 5 |
| BRS, categorised, n (%) | n = 77 | n = 77 | n = 154 |
| Low (1.0–2.99) | 19 (24.7) | 21 (27.3) | 40 (26.0) |
| Normal (3.0–4.3) | 55 (71.4) | 51 (66.2) | 106 (68.8) |
| High (4.31–5) | 1 (1.3) | 0 (0.0) | 1 (0.7) |
| Missing | 2 (2.6) | 5 (6.5) | 7 (4.6) |
| OHS/OKS, raw score | n = 74 | n = 74 | n = 148 |
| Mean (SD) | 19.2 (7.3) | 20.9 (7.5) | 20.1 (7.4) |
| Median (Q1, Q3) | 18.5 (15, 23) | 20 (15, 27) | 19 (15, 25) |
| Minimum, maximum | 6, 44 | 8, 44 | 6, 44 |
| OHS/OKS, categorised, n (%) | n = 77 | n = 77 | n = 154 |
| Satisfactory (40–48) | 1 (1.3) | 1 (1.3) | 2 (1.3) |
| Mild to moderate (30–39) | 4 (5.2) | 8 (10.4) | 12 (7.8) |
| Moderate to severe (20–29) | 28 (36.4) | 30 (39.0) | 58 (37.7) |
| Severe (0–19) | 41 (53.3) | 35 (45.5) | 76 (49.4) |
| Missing | 3 (3.9) | 3 (3.9) | 6 (3.9) |
| Health measure | Hip (N = 77) | Knee (N = 77) | Total (N = 154) |
|---|---|---|---|
| Were you working in your usual role right up to your last day at work before your operation? | |||
| Yes, n (%) | 66 (85.7) | 66 (85.7) | 132 (85.7) |
| No, n (%) | 9 (11.7) | 9 (11.7) | 18 (11.7) |
| Missing, n (%) | 2 (2.6) | 2 (2.6) | 4 (2.6) |
| If no: which of the following options best describes how you have been working prior to your surgery? | N = 9 | N = 9 | N = 18 |
| Reduced hours, usual duties, n (%) | 2 (22.2) | 3 (33.3) | 5 (27.8) |
| Usual hours, amended duties, n (%) | 4 (44.4) | 5 (55.6) | 9 (0.5) |
| Reduced hours and amended duties, n (%) | 2 (22.2) | 0 (0.0) | 2 (11.1) |
| Missing, n (%) | 1 (11.1) | 1 (11.1) | 2 (11.1) |
| If no and you were working reduced hours: how many hours per week were you working? | N = 4 | N = 3 | N = 7 |
| Mean (SD) | 37.5 (10.4) | 20 (10) | 30 (13.2) |
| Median (Q1, Q3) | 37.5 (30, 45) | 20 (10, 30) | 30 (20, 40) |
| Minimum, maximum | 25, 50 | 10, 30 | 10, 50 |
| If no and you were working reduced hours: for how many weeks had you been working reduced hours? | N = 4 | N = 3 | N = 7 |
| Mean (SD) | 16.3 (26.5) | 19.3 (26.7) | 17.6 (24.3) |
| Median (Q1, Q3) | 3.5 (2.5, 30) | 7 (1, 50) | 4 (2, 50) |
| Minimum, maximum | 2, 56 | 1, 50 | 1, 56 |
| If no and you were working on amended duties before you left work: for how many weeks had you been working on amended duties? | N = 5 | N = 3 | N = 8 |
| Mean (SD) | 4 (4.7) | 10.7 (7.1) | 6.5 (6.2) |
| Median (Q1, Q3) | 2 (2, 4) | 12 (3, 17) | 3.5 (2, 12) |
| Minimum, maximum | 0, 12 | 3, 17 | 0, 17 |
| Have you had any periods of sick leave in the 6 months prior to your operation? | |||
| Yes, n (%) | 26 (33.8) | 15 (19.5) | 41 (26.6) |
| No, n (%) | 43 (55.8) | 46 (59.7) | 89 (57.8) |
| Missing, n (%) | 8 (10.4) | 16 (20.8) | 24 (15.6) |
| If yes: how many separate periods of sick leave have you had because of the joint that requires surgery? | N = 25 | N = 14 | N = 39 |
| Mean (SD) | 5.2 (15.7) | 2.6 (3.2) | 4.3 (12.7) |
| Median (Q1, Q3) | 2 (0, 3) | 2 (0. 4) | 2 (0, 3) |
| Minimum, maximum | 0, 80 | 0, 12 | 0, 80 |
| How many separate periods of sick leave have you had for other reasons? | N = 23 | N = 14 | N = 37 |
| Mean (SD) | 2.1 (4.5) | 1 (0.7) | 1.7 (3.6) |
| Median (Q1, Q3) | 1 (0, 2) | 1 (1, 1) | 1 (0, 2) |
| Minimum, maximum | 0, 20 | 0, 20 | 0, 20 |
| Approximately how many days work have you missed in the last 6 months because of the joint that requires replacement surgery? | N = 22 | N = 13 | N = 35 |
| Mean (SD) | 16.5 (24.9) | 7.3 (6.7) | 13.1 (20.4) |
| Median (Q1, Q3) | 6 (0, 28) | 6 (2, 13) | 6 (0, 15) |
| Minimum, maximum | 0, 90 | 0, 20 | 0, 90 |
| Approximately how many days work have you missed in the last 6 months because of other reasons? | N = 22 | N = 14 | N = 36 |
| Mean (SD) | 6.0 (13.8) | 2.2 (3.9) | 4.6 (11.1) |
| Median (Q1, Q3) | 1 (0, 3) | 0 (0, 3) | 0.5 (0, 3) |
| Minimum, maximum | 0, 60 | 0, 12 | 0, 60 |
| Is there a sickness absence policy in your place of work? | |||
| Yes, n (%) | 34 (44.2) | 38 (49.4) | 72 (46.8) |
| No, n (%) | 18 (23.4) | 16 (20.8) | 34 (22.1) |
| Unsure/do not know, n (%) | 13 (16.9) | 9 (11.7) | 22 (14.3) |
| Missing, n (%) | 12 (15.6) | 14 (18.2) | 26 (16.9) |
| Do you receive any of the following payments during periods of sick leave?a | |||
| Statutory sick pay, n (%) | 18 (23.4) | 20 (26.0) | 38 (24.7) |
| Employer-based sick pay, n (%) | 21 (27.3) | 18 (23.4) | 39 (25.3) |
| Do not know/unsure, n (%) | 15 (19.5) | 13 (16.9) | 28 (18.2) |
| If you do receive sickness payments, for how long do you receive them? | |||
| < 1 month, n (%) | 3 (3.9) | 2 (2.6) | 5 (3.3) |
| 1–3 months, n (%) | 2 (2.6) | 4 (5.2) | 6 (3.9) |
| 3–6 months, n (%) | 4 (5.2) | 10 (13.0) | 14 (9.1) |
| > 6 months, n (%) | 18 (23.4) | 13 (16.9) | 31 (20.1) |
| Don’t know/unsure, n (%) | 20 (26.0) | 16 (20.8) | 36 (23.4) |
| Missing, n (%) | 30 (39.0) | 32 (41.6) | 62 (40.3) |
| Were any changes made to your workplace to allow you to do your job in the 6 months before your operation? | |||
| Yes, n (%) | 14 (18.2) | 14 (18.2) | 28 (18.2) |
| No, n (%) | 59 (76.6) | 52 (67.5) | 111 (72.1) |
| Missing, n (%) | 4 (5.2) | 11 (14.3) | 15 (9.7) |
| Health measure | Hip (N = 77) | Knee (N = 77) | Total (N = 154) |
|---|---|---|---|
| Work scheduling autonomy | |||
| The job allows me to make my own decisions about how to schedule my work, n (%) | |||
| Strongly disagree | 4 (5.2) | 7 (9.1) | 11 (7.1) |
| Disagree | 7 (9.1) | 9 (11.7) | 16 (10.4) |
| Neither agree nor disagree | 7 (9.1) | 10 (13.0) | 17 (11.0) |
| Agree | 37 (48.1) | 24 (31.2) | 61 (39.6) |
| Strongly agree | 19 (24.7) | 26 (33.8) | 45 (29.2) |
| Missing | 3 (3.9) | 1 (1.3) | 4 (2.6) |
| The job allows me to decide on the order in which things are done on the job, n (%) | |||
| Strongly disagree | 4 (5.2) | 7 (9.1) | 11 (7.1) |
| Disagree | 7 (9.1) | 9 (11.7) | 16 (10.4) |
| Neither agree nor disagree | 5 (6.5) | 6 (7.8) | 11 (7.1) |
| Agree | 43 (55.8) | 28 (36.4) | 71 (46.1) |
| Strongly agree | 16 (20.8) | 24 (31.2) | 40 (26.0) |
| Missing | 2 (2.6) | 3 (3.9) | 5 (3.3) |
| The job allows me to plan how I do my work, n (%) | |||
| Strongly disagree | 4 (5.2) | 5 (6.5) | 9 (5.8) |
| Disagree | 6 (7.8) | 7 (9.1) | 13 (8.4) |
| Neither agree nor disagree | 7 (9.1) | 6 (7.8) | 13 (8.4) |
| Agree | 39 (50.7) | 32 (41.6) | 71 (46.1) |
| Strongly agree | 18 (23.4) | 23 (29.9) | 41 (26.6) |
| Missing | 3 (3.9) | 4 (5.2) | 7 (4.6) |
| Work scheduling autonomy average | N = 73 | N = 73 | N = 146 |
| Mean (SD) | 3.8 (0.9) | 3.8 (1.2) | 3.8 (1.1) |
| Median (Q1, Q3) | 4 (3.3, 4.3) | 4 (3, 5) | 4 (3.3, 4.7) |
| Minimum, maximum | 1, 5 | 1, 5 | 1, 5 |
| Work context: ergonomics | |||
| The seating arrangements on the job are adequate, n (%) | |||
| Strongly disagree | 10 (13.0) | 6 (7.8) | 16 (10.4) |
| Disagree | 6 (7.8) | 8 (10.4) | 14 (9.1) |
| Neither agree nor disagree | 13 (16.9) | 7 (9.1) | 20 (13.0) |
| Agree | 30 (39.0) | 26 (33.8) | 56 (36.4) |
| Strongly agree | 14 (18.2) | 23 (29.9) | 37 (24.0) |
| Missing | 4 (5.2) | 7 (9.1) | 11 (7.1) |
| The work place allows for all size differences between people in terms of clearance, reach, eye height, leg room, etc., n (%) | |||
| Strongly disagree | 5 (6.5) | 2 (2.6) | 7 (4.6) |
| Disagree | 7 (9.1) | 7 (9.1) | 14 (9.1) |
| Neither agree nor disagree | 12 (15.6) | 11 (14.3) | 23 (14.9) |
| Agree | 34 (44.2) | 28 (36.4) | 62 (40.3) |
| Strongly agree | 13 (16.9) | 19 (24.7) | 32 (20.8) |
| Missing | 6 (7.8) | 10 (13.0) | 16 (10.4) |
| The job involves excessive reaching, n (%) | |||
| Strongly disagree | 11 (14.3) | 9 (11.7) | 20 (13.0) |
| Disagree | 23 (29.9) | 22 (28.6) | 45 (29.2) |
| Neither agree nor disagree | 10 (13.0) | 18 (23.4) | 28 (18.2) |
| Agree | 16 (20.8) | 15 (19.5) | 31 (20.1) |
| Strongly agree | 11 (14.3) | 4 (5.2) | 15 (9.7) |
| Missing | 6 (7.8) | 9 (11.7) | 15 (9.7) |
| Ergonomics average | N = 69 | N = 65 | N = 134 |
| Mean (SD) | 3.3 (0.8) | 3.5 (0.7) | 3.4 (0.7) |
| Median (Q1, Q3) | 3.3 (3, 3.7) | 3.3 (3, 4) | 3.3 (3, 3.7) |
| Minimum, maximum | 1, 5 | 1, 5 | 1, 5 |
| Work context: physical demands | |||
| The job requires a great deal of muscular endurance, n (%) | |||
| Strongly disagree | 15 (19.5) | 9 (11.7) | 24 (15.6) |
| Disagree | 17 (22.1) | 17 (22.1) | 34 (22.1) |
| Neither agree nor disagree | 9 (11.7) | 10 (13.0) | 19 (12.3) |
| Agree | 16 (20.8) | 25 (32.5) | 41 (26.6) |
| Strongly agree | 13 (16.9) | 14 (18.2) | 27 (17.5) |
| Missing | 7 (9.1) | 2 (2.6) | 9 (5.8) |
| The job requires a great deal of muscular strength, n (%) | |||
| Strongly disagree | 16 (20.8) | 11 (14.3) | 27 (17.5) |
| Disagree | 18 (23.4) | 17 (22.1) | 35 (22.7) |
| Neither agree nor disagree | 11 (14.3) | 13 (16.9) | 24 (15.6) |
| Agree | 15 (19.5) | 18 (23.4) | 33 (21.4) |
| Strongly agree | 11 (14.3) | 13 (16.9) | 24 (15.6) |
| Missing | 6 (7.8) | 5 (6.5) | 11 (7.1) |
| The job requires a lot of physical effort, n (%) | |||
| Strongly disagree | 15 (19.5) | 7 (9.1) | 22 (14.3) |
| Disagree | 17 (22.1) | 16 (20.8) | 33 (21.4) |
| Neither agree nor disagree | 7 (9.1) | 7 (9.1) | 14 (9.1) |
| Agree | 19 (24.7) | 31 (40.3) | 50 (32.5) |
| Strongly agree | 16 (20.8) | 13 (16.9) | 29 (18.8) |
| Missing | 3 (3.9) | 3 (3.9) | 6 (3.9) |
| Physical demands average | N = 70 | N = 72 | N = 142 |
| Mean (SD) | 2.9 (1.4) | 3.2 (1.3) | 3.1 (1.3) |
| Median (Q1, Q3) | 2.7 (2, 4) | 3.3 (2, 4) | 3 (2, 4) |
| Minimum, maximum | 1, 5 | 1, 5 | 1, 5 |
| Social characteristics | |||
| I have the opportunity to develop close friendships in my job, n (%) | |||
| Strongly disagree | 5 (6.5) | 3 (3.9) | 8 (5.2) |
| Disagree | 3 (3.9) | 5 (6.5) | 8 (5.2) |
| Neither agree nor disagree | 8 (10.4) | 12 (15.6) | 20 (13.0) |
| Agree | 36 (46.8) | 29 (37.7) | 65 (42.2) |
| Strongly agree | 22 (28.6) | 24 (31.2) | 46 (29.9) |
| Missing | 3 (3.9) | 4 (5.2) | 7 (4.6) |
| I have the chance in my job to get to know other people, n (%) | |||
| Strongly disagree | 4 (5.2) | 2 (2.6) | 6 (3.9) |
| Disagree | 0 (0.0) | 2 (2.6) | 2 (1.3) |
| Neither agree nor disagree | 4 (5.2) | 4 (5.2) | 8 (5.2) |
| Agree | 40 (52.0) | 41 (53.3) | 81 (52.6) |
| Strongly agree | 27 (35.1) | 27 (35.1) | 54 (35.1) |
| Missing | 2 (2.6) | 1 (1.3) | 3 (2.0) |
| I have the opportunity to meet with others in my work, n (%) | |||
| Strongly disagree | 3 (3.9) | 1 (1.3) | 4 (2.6) |
| Disagree | 3 (3.9) | 2 (2.6) | 5 (3.3) |
| Neither agree nor disagree | 3 (3.9) | 2 (2.6) | 5 (3.3) |
| Agree | 39 (50.7) | 40 (52.0) | 79 (51.3) |
| Strongly agree | 26 (33.8) | 29 (37.7) | 55 (35.7) |
| Missing | 3 (3.9) | 3 (3.9) | 6 (3.9) |
| My supervisor is concerned about the welfare of the people who work for him/her, n (%) | |||
| Strongly disagree | 5 (6.5) | 3 (3.9) | 8 (5.2) |
| Disagree | 7 (9.1) | 3 (3.9) | 10 (6.5) |
| Neither agree nor disagree | 6 (7.8) | 17 (22.1) | 23 (14.9) |
| Agree | 29 (37.7) | 25 (32.5) | 54 (35.1) |
| Strongly agree | 15 (19.5) | 23 (29.9) | 38 (24.7) |
| Missing | 15 (19.5) | 6 (7.8) | 21 (13.6) |
| People I work with take a personal interest in me, n (%) | |||
| Strongly disagree | 3 (3.9) | 2 (2.6) | 5 (3.3) |
| Disagree | 4 (5.2) | 2 (2.6) | 6 (3.9) |
| Neither agree nor disagree | 9 (11.7) | 10 (13.0) | 19 (12.3) |
| Agree | 37 (48.1) | 32 (41.6) | 69 (44.8) |
| Strongly agree | 20 (26.0) | 26 (33.8) | 46 (29.9) |
| Missing | 4 (5.2) | 5 (6.5) | 9 (5.8) |
| People I work with are friendly, n (%) | |||
| Strongly disagree | 2 (2.6) | 1 (1.3) | 3 (2.0) |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neither agree nor disagree | 5 (6.5) | 3 (3.9) | 8 (5.2) |
| Agree | 39 (50.7) | 41 (53.3) | 80 (82.0) |
| Strongly agree | 27 (35.1) | 28 (36.4) | 55 (35.7) |
| Missing | 4 (5.2) | 4 (5.2) | 8 (5.2) |
| Social characteristics average | N = 62 | N = 70 | N = 132 |
| Mean (SD) | 4.0 (0.8) | 4.1 (0.8) | 4.1 (0.8) |
| Median (Q1, Q3) | 4 (3.8, 4.5) | 4 (3.7, 4.8) | 4 (3.8, 4.7) |
| Minimum, maximum | 1, 5 | 1.5, 5 | 1, 5 |
| Health measure | Hip (N = 77) | Knee (N = 77) | Total (N = 154) |
|---|---|---|---|
| Do you have access to an occupational health service through your employer? | |||
| Yes, n (%) | 25 (32.5) | 19 (24.7) | 44 (28.6) |
| No, n (%) | 41 (53.3) | 39 (50.7) | 80 (52.0) |
| Unsure/do not know, n (%) | 6 (7.8) | 13 (16.9) | 19 (12.3) |
| Missing, n (%) | 5 (6.5) | 6 (7.8) | 11 (7.1) |
| Have you received any advice from any individual or organisation about returning to work following your operation? | |||
| Yes, n (%) | 17 (22.1) | 22 (28.6) | 39 (25.3) |
| No, n (%) | 54 (70.1) | 49 (63.6) | 103 (66.9) |
| Unsure/don’t know, n (%) | 0 (0.0) | 1 (1.3) | 1 (0.7) |
| Missing, n (%) | 6 (7.8) | 5 (6.5) | 11 (7.1) |
| If you received advice about returning to work, whom did you receive it from?a | |||
| Surgeon, n (%) | 10 (13.0) | 10 (13.0) | 20 (13.0) |
| GP, n (%) | 2 (2.6) | 8 (10.4) | 10 (13.0) |
| Occupational health, n (%) | 4 (5.2) | 7 (9.1) | 11 (7.1) |
| Physiotherapist, n (%) | 3 (3.9) | 9 (11.7) | 12 (7.8) |
| Occupational therapist, n (%) | 0 (0.0) | 5 (3.3) | 5 (3.3) |
| Employer, n (%) | 3 (3.9) | 5 (3.3) | 8 (10.4) |
| Other, n (%) | 3 (3.9) | 2 (2.6) | 5 (3.3) |
| Have you received any advice about when it is safe to start driving after your operation? | |||
| Yes, n (%) | 51 (66.2) | 51 (66.2) | 102 (66.2) |
| No, n (%) | 15 (19.5) | 18 (23.4) | 33 (21.4) |
| Unsure/don’t know, n (%) | 4 (5.2) | 4 (5.2) | 8 (5.2) |
| Missing, n (%) | 7 (9.1) | 4 (5.2) | 11 (7.1) |
| How long (weeks) do you think it will be before you are ready to return to work after your operation? | N = 73 | N = 67 | N = 140 |
| Mean (SD) | 9.9 (8.2) | 8.9 (4.7) | 9.5 (6.8) |
| Median (Q1, Q3) | 8 (6, 12) | 8 (6, 12) | 8 (6, 12) |
| Minimum, maximum | 1, 68 | 1, 24 | 1, 68 |
| How long (weeks) do you think it will be before your employer is happy for you to return to work after your operation? | N = 59 | N = 52 | N = 111 |
| Mean (SD) | 9.7 (9.9) | 9.4 (4.4) | 9.6 (7.8) |
| Median (Q1, Q3) | 8 (6, 12) | 9 (7, 12) | 8 (6, 12) |
| Minimum, maximum | 0, 78 | 0, 24 | 0, 78 |
| How long (weeks) do you think it will be before you are ready to return to your usual daily activities after your operation? | N = 72 | N = 68 | N = 140 |
| Mean (SD) | 9.2 (10.5) | 9.3 (5.1) | 9.3 (8.3) |
| Median (Q1, Q3) | 6 (6, 12) | 8 (6, 12) | 8 (6, 12) |
| Minimum, maximum | 1, 78 | 1, 26 | 1, 78 |
| How long (weeks) do you think it will be before you are ready to drive after your operation? | N = 65 | N = 67 | N = 132 |
| Mean (SD) | 6.5 (2.1) | 6.1 (3.1) | 6.3 (2.7) |
| Median (Q1, Q3) | 6 (6, 6) | 6 (5, 6) | 6 (6, 6) |
| Minimum, maximum | 2, 16 | 1, 20 | 1, 20 |
| Health measure | Hip | Knee | Total |
|---|---|---|---|
| Baseline | N = 77 | N = 77 | N = 154 |
| Satisfactory (40–48), n (%) | 1 (1.3) | 1 (1.3) | 2 (1.3) |
| Mild to moderate (30–39), n (%) | 4 (5.2) | 8 (10.4) | 12 (7.8) |
| Moderate to severe (20–29), n (%) | 28 (36.4) | 30 (39.0) | 58 (37.7) |
| Severe (0–19), n (%) | 41 (53.3) | 35 (45.5) | 76 (49.4) |
| Missing, n (%) | 3 (3.9) | 3 (3.9) | 6 (3.9) |
| N = 74 | N = 74 | N = 148 | |
| Mean (SD) | 19.2 (7.3) | 20.9 (7.5) | 20.1 (7.4) |
| Median (Q1, Q3) | 18.5 (15, 23) | 20 (15, 27) | 19 (15, 25) |
| Minimum, maximum | 6, 44 | 8, 44 | 6, 44 |
| Week 8 | N = 50 | N = 43 | N = 93 |
| Satisfactory (40–48), n (%) | 15 (30.0) | 3 (7.0) | 18 (19.4) |
| Mild to moderate (30–39), n (%) | 19 (38.0) | 17 (39.5) | 36 (38.7) |
| Moderate to severe (20–29), n (%) | 11 (22.0) | 17 (39.5) | 28 (30.1) |
| Severe (0–19), n (%) | 5 (10.0) | 6 (14.0) | 11 (11.8) |
| Missing, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| N = 50 | N = 43 | N = 93 | |
| Mean (SD) | 33.6 (9.2) | 28.3 (8.4) | 31.1 (91) |
| Median (Q1, Q3) | 36.5 (26, 40) | 28 (22, 34) | 32 (24, 39) |
| Minimum, maximum | 16, 48 | 10, 45 | 10, 48 |
| Week 16 | N = 53 | N = 51 | N = 104 |
| Satisfactory (40–48), n (%) | 31 (58.5) | 16 (31.4) | 47 (45.2) |
| Mild to moderate (30–39), n (%) | 10 (18.9) | 18 (35.3) | 28 (26.9) |
| Moderate to severe (20–29), n (%) | 6 (11.3) | 9 (17.6) | 15 (14.4) |
| Severe (0–19), n (%) | 2 (3.8) | 4 (7.8) | 6 (5.8) |
| Missing, n (%) | 4 (7.5) | 4 (7.8) | 8 (7.7) |
| N = 49 | N = 47 | N = 96 | |
| Mean (SD) | 38.6 (9.2) | 34.1 (8.8) | 36.4 (9.2) |
| Median (Q1, Q3) | 42 (34, 45) | 35 (29, 41.5) | 39 (30, 44) |
| Minimum, maximum | 12, 48 | 14, 46 | 12, 48 |
| Week 24a | N = 23 | N = 18 | N = 41 |
| Satisfactory (40–48), n (%) | 11 (47.8) | 7 (38.9) | 18 (43.9) |
| Mild to moderate (30–39), n (%) | 3 (13.0) | 8 (44.4) | 11 (26.8) |
| Moderate to severe (20–29), n (%) | 5 (21.7) | 2 (11.1) | 7 (17.1) |
| Severe (0–19), n (%) | 2 (8.7) | 1 (5.6) | 3 (7.3) |
| Missing, n (%) | (8.7) | 0 (0.0) | 2 (4.9) |
| N = 21 | N = 18 | N = 39 | |
| Mean (SD) | 36.0 (13.2) | 35.7 (10.6) | 35.8 (11.9) |
| Median (Q1, Q3) | 43 (25, 47) | 37 (31, 43) | 38 (29, 46) |
| Minimum, maximum | 8, 48 | 2, 47 | 2, 48 |
| Health measure | Hip (N = 37) | Knee (N = 41) | Total (N = 78) |
|---|---|---|---|
| Did you return to work doing your usual hours and duties? | |||
| Yes, n (%) | 18 (48.7) | 20 (47.6) | 38 (48.1) |
| No, n (%) | 17 (46.0) | 20 (47.6) | 37 (47.4) |
| I have started a new job, n (%) | 2 (5.4) | 1 (2.4) | 3 (3.8) |
| Missing, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| If you did not return to work doing your usual hours and duties: how you were working on your first week at work following your operation? | N = 17 | N = 20 | N = 37 |
| Reduced hours, usual duties, n (%) | 6 (35.3) | 8 (40.0) | 14 (37.8) |
| Usual hours but with amended or altered duties, n (%) | 1 (5.8) | 2 (10.0) | 3 (8.1) |
| Reduced hours and amended or altered duties, n (%) | 9 (52.9) | 10 (50.0) | 19 (51.4) |
| Missing, n (%) | 1 (5.8) | 0 (0.0) | 1 (2.7) |
| If you returned to work on reduced hours: hours worked during first week back at work? | N = 15 | N = 18 | N = 33 |
| Mean (SD) | 14.4 (10.2) | 17.9 (10.2) | 16.3 (10.2) |
| Median (Q1, Q3) | 13 (7, 20) | 17.5 (9, 28) | 14 (8, 20) |
| Minimum, maximum | 3, 40 | 3, 37 | 3, 40 |
| If you returned to work on reduced hours: usual number of hours worked | N = 13 | N = 18 | N = 31 |
| Mean (SD) | 32.2 (15.2) | 35.4 (13.6) | 34 (14.1) |
| Median (Q1, Q3) | 37 (20, 38) | 36.5 (30, 40) | 36.5 (30, 40) |
| Minimum, maximum | 6, 60 | 8, 65 | 6, 65 |
| Were any adaptions or changes made to your workplace to help you return to work? | |||
| Yes, n (%) | 5 (13.5) | 8 (19.5) | 13 (16.7) |
| No, n (%) | 27 (73.0) | 30 (73.2) | 57 (73.1) |
| Don’t know/unsure, n (%) | 1 (2.7) | 0 (0.0) | 1 (1.3) |
| Missing, n (%) | 4 (10.8) | 3 (7.3) | 7 (9.0) |
| Were any adaptions or changes made your pattern of work to help you return to work? | |||
| Yes, n (%) | 10 (27.0) | 12 (29.3) | 22 (28.2) |
| No, n (%) | 22 (59.5) | 24 (58.5) | 46 (59.0) |
| Don’t know/unsure, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing, n (%) | 5 (13.5) | 5 (12.2) | 10 (12.8) |
| Health measure | Operation type | Total (N = 154) | |
|---|---|---|---|
| Hip (N = 77) | Knee (N = 77) | ||
| Have you been provided with a ‘fit note’ following your recent operation? | |||
| Week 8, n (%) | N = 50 | N = 43 | N = 93 |
| Yes | 30 (60.0) | 17 (39.5) | 47 (50.5) |
| No | 16 (32.0) | 16 (37.2) | 32 (34.4) |
| Missing | 4 (8.0) | 10 (23.3) | 14 (15.1) |
| Week 16, n (%) | N = 53 | N = 51 | N = 104 |
| Yes | 26 (49.1) | 25 (49.0) | 51 (49.0) |
| No | 18 (34.0) | 20 (39.2) | 38 (36.5) |
| Missing | 9 (17.0) | 6 (11.8) | 15 (14.4) |
| Week 24,a n (%) | N = 23 | N = 19 | N = 42 |
| Yes | 13 (56.5) | 10 (52.6) | 23 (54.8) |
| No | 3 (13.0) | 2 (10.5) | 5 (11.9) |
| Missing | 7 (30.4) | 7 (36.8) | 14 (33.3) |
| If yes, how many fit notes have you received since your operation? | |||
| Week 8 | N = 30 | N = 17 | N = 47 |
| Mean (SD) | 1.8 (0.7) | 2.3 (0.8) | 2.0 (0.8) |
| Median (Q1, Q3) | 2 (1, 2) | 2 (2, 3) | 2 (1, 2) |
| Minimum, maximum | 1, 3 | 1, 4 | 1, 4 |
| Week 16 | N = 25 | N = 23 | N = 48 |
| Mean (SD) | 2.3 (1.2) | 2.7 (1.2) | 2.5 (1.2) |
| Median (Q1, Q3) | 2 (1, 3) | 3 (2, 3) | 2 (1.5, 3) |
| Minimum, maximum | 1, 5 | 1, 6 | 1, 6 |
| Week 24a | N = 13 | N = 10 | N = 23 |
| Mean (SD) | 3 (1.7) | 2.8 (0.9) | 2.9 (1.4) |
| Median (Q1, Q3) | 2 (2, 5) | 2.5 (2, 3) | 2 (2, 4) |
| Minimum, maximum | 1, 6 | 2, 4 | 1, 6 |
| How many of the fit notes you were given advised that you were, n (%) | |||
| Week 8 | |||
| Not fit for work | N = 29 | N = 17 | N = 46 |
| Mean (SD) | 1.7 (0.8) | 2.2 (0.8) | 1.9 (0.8) |
| Median (Q1, Q3) | 2 (1, 2) | 2 (2, 3) | 2 (1, 2) |
| Minimum, maximum | 0, 3 | 1, 4 | 0, 4 |
| Don’t know, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing, n (%) | 1 (3.3) | 0 (0.0) | 1 (2.2) |
| May be fit for work | N = 24 | N = 16 | N = 40 |
| Mean (SD) | 0.1 (0.3) | 0.1 (0.3) | 0.1 (0.3) |
| Median (Q1, Q3) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Minimum, maximum | 0, 1 | 0, 1 | 0, 1 |
| Don’t know, n (%) | 2 (6.7) | 0 (0.0) | 2 (4.4) |
| Missing, n (%) | 4 (13.3) | 1 (6.3) | 5 (10.9) |
| Week 16 | |||
| Not fit for work | N = 29 | N = 26 | N = 55 |
| Mean (SD) | 1.9 (1.4) | 2.1 (1.6) | 2 (1.6) |
| Median (Q1, Q3) | 2 (1, 3) | 2 (0, 3) | 2 (1, 3) |
| Minimum, maximum | 0, 5 | 0, 6 | 0, 6 |
| Don’t know, n (%) | 2 (3.8) | 4 (7.8) | 6 (5.8) |
| Missing, n (%) | 22 (41.5) | 21 (41.2) | 43 (41.4) |
| May be fit for work | N = 28 | N = 26 | N = 54 |
| Mean (SD) | 0.1 (0.4) | 0.1 (0.3) | 0.1 (0.3) |
| Median (Q1, Q3) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Minimum, maximum | 0, 1 | 0, 1 | 0, 1 |
| Don’t know, n (%) | 3 (5.7) | 3 (5.9) | 6 (5.8) |
| Missing, n (%) | 22 (41.5) | 22 (41.5) | 44 (42.3) |
| Week 24a | N = 14 | N = 10 | N = 24 |
| Not fit for work | |||
| Mean (SD) | 2.4 (1.7) | 2.4 (1.2) | 2.4 (1.5) |
| Median (Q1, Q3) | 2 (1, 3) | 2 (2, 3) | 2 (2, 3) |
| Minimum, maximum | 0, 6 | 0, 4 | 0, 6 |
| Don’t know, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing, n (%) | 9 (39.1) | 8 (44.4) | 17 (41.5) |
| May be fit for work | N = 14 | N = 10 | N = 24 |
| Mean (SD) | 0.4 (0.9) | 0 (0.0) | 0.3 (0.7) |
| Median (Q1, Q3) | 0 (0, 1) | 0 (0, 0) | 0 (0, 0) |
| Minimum, maximum | 0, 3 | 0, 0 | 0, 3 |
| Don’t know, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing, n (%) | 9 (39.1) | 8 (44.4) | 17 (41.5) |
| The doctor who provided the note was | |||
| Week 8, n (%) | N = 30 | N = 16 | N = 46 |
| Hospital doctor | 9 (30.0) | 2 (12.5) | 11 (23.9) |
| GP | 21 (70.0) | 14 (87.5) | 35 (76.1) |
| Don’t know | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Week 16, n (%) | N = 26 | N = 26 | N = 52 |
| Hospital doctor | 8 (30.8) | 0 (0.0) | 8 (15.4) |
| GP | 16 (61.5) | 22 (84.6) | 38 (73.1) |
| Don’t know | 1 (3.9) | 2 (7.7) | 3 (5.8) |
| Missing | 1 (3.9) | 2 (7.7) | 3 (5.8) |
| Week 24, n (%) | N = 13 | N = 10 | N = 23 |
| Hospital doctor | 4 (30.8) | 0 (0.0) | 4 (17.4) |
| GP | 9 (69.2) | 10 (0.0) | 19 (82.6) |
| Don’t know | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| The length of the note (weeks) | |||
| Week 8 | N = 28 | N = 17 | N = 44 |
| Mean (SD) | 5.7 (2.2) | 5.4 (2.7) | 5.6 (2.4) |
| Median (Q1, Q3) | 6 (4, 7) | 4 (4, 8) | 6 (4, 8) |
| Minimum, maximum | 2, 10 | 2, 10 | 2, 10 |
| Week 16 | N = 24 | N = 16 | N = 40 |
| Mean (SD) | 6.4 (2.8) | 3.9 (1.5) | 5.4 (2.7) |
| Median (Q1, Q3) | 6 (4, 7) | 4 (3, 4) | 4 (4, 6) |
| Minimum, maximum | 2, 12 | 2, 8 | 2, 12 |
| Week 24a | N = 10 | N = 9 | N = 19 |
| Mean (SD) | 5.4 (3.0) | 3.6 (1.3) | 4.5 (2.5) |
| Median (Q1, Q3) | 6 (4, 8) | 4 (2, 4) | 4 (2, 6) |
| Minimum, maximum | 0, 10 | 2, 6 | 0, 10 |
| Which of the following options were selected?b | |||
| Week 8, n (%) | N = 30 | N = 16 | N = 46 |
| You are NOT fit for work | 26 (86.7) | 14 (87.5) | 40 (87.0) |
| You MAY be fit for work taking in to account – a phased return to work | 3 (10.0) | 1 (6.3) | 4 (8.7) |
| You MAY be fit for work taking in to account – amended duties | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| You MAY be fit for work taking in to account – altered hours | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| You MAY be fit for work taking in to account – workplace adaptions | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Don’t know/unsure | 1 (3.3) | 0 (0.0) | 1 (2.2) |
| Week 16, n (%) | N = 26 | N = 26 | N = 34 |
| You are NOT fit for work | 18 (69.2) | 16 (61.5) | 34 (65.4) |
| You MAY be fit for work taking in to account – a phased return to work | 3 (11.5) | 5 (19.2) | 8 (15.4) |
| You MAY be fit for work taking in to account – amended duties | 1 (3.9) | 3 (11.5) | 4 (7.7) |
| You MAY be fit for work taking in to account – altered hours | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| You MAY be fit for work taking in to account – workplace adaptions | 1 (3.9) | 0 (0.0) | 0 (0.0) |
| Don’t know/unsure | 1 (3.9) | 1 (3.9) | 2 (3.9) |
| Week 24,a n (%) | N = 13 | N = 10 | N = 23 |
| You are NOT fit for work | 9 (69.2) | 9 (90.0) | 18 (78.3) |
| You MAY be fit for work taking in to account – a phased return to work | 2 (15.4) | 1 (10.0) | 3 (13.0) |
| You MAY be fit for work taking in to account – amended duties | 1 (7.7) | 0 (0.0) | 1 (4.4) |
| You MAY be fit for work taking in to account – altered hours | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| You MAY be fit for work taking in to account – workplace adaptions | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Don’t know/unsure | 1 (7.7) | 0 (0.0) | 1 (4.4) |
| When (weeks post surgery) did you first drive following your operation? | |||
| Week 8 | N = 35 | N = 28 | N = 63 |
| Mean (SD) | 5.8 (1.9) | 5.6 (2.0) | 5.7 (1.9) |
| Median (Q1, Q3) | 6 (4, 7) | 6 (4.5, 7) | 6 (4, 7) |
| Minimum, maximum | 2, 10 | 0, 8 | 0, 10 |
| Don’t know, n (%) | 1 (2.0) | 1 (2.3) | 2 (2.2) |
| I don’t drive, n (%) | 3 (6.0) | 0 (0.0) | 3 (3.2) |
| Missing, n (%) | 11 (22.0) | 14 (32.6) | 25 (26.9) |
| Week 16 | N = 33 | N = 30 | N = 63 |
| Mean (SD) | 6.5 (1.9) | 6.5 (2.8) | 6.5 (2.3) |
| Median (Q1, Q3) | 6 (6, 7) | 6 (4.5, 8) | 6 (5, 8) |
| Minimum, maximum | 3, 12 | 1, 12 | 1, 12 |
| Don’t know, n (%) | 2 (3.8) | 0 (0.0) | 2 (1.9) |
| I don’t drive, n (%) | 5 (9.4) | 2 (3.9) | 7 (6.7) |
| Missing, n (%) | 13 (24.5) | 19 (37.3) | 32 (30.8) |
| Week 24 | N = 12 | N = 11 | N = 23 |
| Mean (SD) | 6.3 (3.3) | 5.9 (1.9) | 6.1 (2.6) |
| Median (Q1, Q3) | 6 (3.5, 9) | 6 (4, 7) | 6 (4, 8) |
| Minimum, maximum | 1, 12 | 4, 10 | 1, 12 |
| Don’t know, n (%) | 1 (4.4) | 0 (0.0) | 1 (2.4) |
| I don’t drive, n (%) | 3 (13.0) | 0 (0.0) | 3 (7.3) |
| Missing, n (%) | 7 (30.4) | 7 (38.9) | 14 (34.2) |
| In the last 2 weeks how much of the time: | Hip (N = 77) | Knee (N = 77) | Total (N = 154) |
|---|---|---|---|
| Did your physical health or emotional problems make it difficult for you to get going easily at the beginning of the day? | |||
| Baseline, n (%) | N = 77 | N = 77 | N = 154 |
| Difficult all of the time | 6 (7.8) | 4 (5.2) | 10 (6.5) |
| Difficult most of the time | 15 (19.5) | 21 (27.3) | 36 (23.4) |
| Difficult some of the time | 21 (27.3) | 19 (24.7) | 40 (26.0) |
| Difficult a slight bit of the time | 11 (14.3) | 13 (16.9) | 24 (15.6) |
| Difficult none of the time | 8 (10.4) | 3 (3.9) | 11 (7.1) |
| Does not apply to my job | 1 (1.3) | 1 (1.3) | 2 (1.3) |
| Missing | 15 (19.5) | 16 (20.8) | 31 (20.1) |
| Week 8, n (%) | N = 50 | N = 43 | N = 93 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult some of the time | 1 (2.0) | 2 (4.7) | 3 (3.2) |
| Difficult a slight bit of the time | 6 (12.0) | 10 (23.3) | 16 (17.2) |
| Difficult none of the time | 5 (10.0) | 6 (14.0) | 11 (11.8) |
| Does not apply to my job | 4 (8.0) | 0 (0.0) | 4 (4.3) |
| Missing | 34 (68.0) | 25 (58.1) | 59 (63.4) |
| Week 16, n (%) | N = 53 | N = 51 | N = 104 |
| Difficult all of the time | 1 (1.9) | 0 (0.0) | 1 (1.0) |
| Difficult most of the time | 1 (1.9) | 3 (5.9) | 4 (3.9) |
| Difficult some of the time | 6 (11.3) | 3 (5.9) | 9 (8.7) |
| Difficult a slight bit of the time | 7 (13.2) | 13 (25.5) | 20 (19.2) |
| Difficult none of the time | 21 (39.6) | 14 (27.5) | 35 (33.7) |
| Does not apply to my job | 2 (3.8) | 3 (5.9) | 5 (4.8) |
| Missing | 15 (28.3) | 15 (29.4) | 30 (28.9) |
| Week 24, n (%) | N = 23 | N = 18 | N = 41 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 3 (13.0) | 3 (16.7) | 6 (14.6) |
| Difficult some of the time | 0 (0.0) | 2 (11.1) | 2 (4.9) |
| Difficult a slight bit of the time | 3 (13.0) | 5 (27.8) | 8 (19.5) |
| Difficult none of the time | 9 (39.1) | 5 (27.8) | 14 (34.2) |
| Does not apply to my job | 1 (4.4) | 0 (0.0) | 1 (2.4) |
| Missing | 7 (30.4) | 3 (16.7) | 10 (24.4) |
| Did your physical health or emotional problems make it difficult for you to start your job on time as soon as you arrived at work? | |||
| Baseline, n (%) | N = 77 | N = 77 | N = 154 |
| Difficult all of the time | 4 (5.19) | 4 (5.19) | 8 (5.19) |
| Difficult most of the time | 9 (11.7) | 8 (10.4) | 17 (11.0) |
| Difficult some of the time | 12 (15.6) | 11 (14.3) | 23 (14.9) |
| Difficult a slight bit of the time | 12 (15.6) | 17 (22.1) | 29 (18.8) |
| Difficult none of the time | 18 (23.4) | 16 (20.8) | 34 (22.1) |
| Does not apply to my job | 6 (7.8) | 5 (6.5) | 11 (7.1) |
| Missing | 16 (20.8) | 16 (20.8) | 32 (20.8) |
| Week 8, n (%) | N = 50 | N = 43 | N = 93 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult some of the time | 0 (0.0) | 1 (2.3) | 1 (1.1) |
| Difficult a slight bit of the time | 4 (8.0) | 3 (7.0) | 7 (7.5) |
| Difficult none of the time | 5 (10.0) | 8 (18.6) | 13 (14.0) |
| Does not apply to my job | 4 (8.0) | 3 (7.0) | 7 (7.5) |
| Missing | 37 (74.0) | 28 (65.1) | 65 (6996) |
| Week 16, n (%) | N = 53 | N = 51 | N = 104 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 1 (1.9) | 0 (0.0) | 1 (1.0) |
| Difficult some of the time | 4 (7.6) | 6 (11.8) | 10 (9.6) |
| Difficult a slight bit of the time | 6 (11.3) | 3 (5.9) | 9 (8.7) |
| Difficult none of the time | 25 (47.2) | 20 (39.2) | 45 (43.3) |
| Does not apply to my job | 2 (3.8) | 6 (11.8) | 8 (7.7) |
| Missing | 15 (28.3) | 16 (31.4) | 31 (29.8) |
| Week 24, n (%) | N = 23 | N = 18 | N = 41 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 1 (4.4) | 0 (0.0) | 1 (2.4) |
| Difficult some of the time | 1 (4.4) | 1 (5.6) | 2 (4.9) |
| Difficult a slight bit of the time | 1 (4.4) | 5 (27.8) | 6 (14.6) |
| Difficult none of the time | 10 (43.5) | 7 (38.9) | 18 (41.5) |
| Does not apply to my job | 3 (13.0) | 2 (11.1) | 5 (12.2) |
| Missing | 7 (30.4) | 3 (16.7) | 10 (24.4) |
| Were you able to sit, stand, or stay in one position for longer than 15 minutes while working, without difficulty caused by physical health or emotional problems? | |||
| Baseline, n (%) | N = 77 | N = 77 | N = 154 |
| Able all of the time | 3 (3.9) | 6 (7.8) | 9 (5.8) |
| Able most of the time | 16 (20.8) | 19 (24.7) | 35 (22.7) |
| Able some of the time | 22 (28.6) | 16 (20.8) | 38 (24.7) |
| Able a slight bit of the time | 14 (18.2) | 12 (15.6) | 26 (16.9) |
| Able none of the time | 2 (2.6) | 4 (5.2) | 6 (3.9) |
| Does not apply to my job | 4 (5.2) | 3 (3.9) | 7 (4.6) |
| Missing | 16 (20.8) | 17 (22.1) | 33 (21.4) |
| Week 8, n (%) | N = 50 | N = 43 | N = 93 |
| Able all of the time | 3 (6.0) | 6 (14.0) | 9 (9.7) |
| Able most of the time | 2 (4.0) | 3 (7.0) | 5 (5.4) |
| Able some of the time | 2 (4.0) | 2 (4.7) | 4 (4.3) |
| Able a slight bit of the time | 2 (4.0) | 4 (9.3) | 6 (6.5) |
| Able none of the time | 0 (0.0) | 1 (2.3) | 1 (1.1) |
| Does not apply to my job | 4 (8.0) | 1 (2.3) | 5 (5.4) |
| Missing | 37 (74.0) | 26 (59.5) | 63 (67.7) |
| Week 16, n (%) | N = 53 | N = 51 | N = 104 |
| Able all of the time | 11 (20.8) | 9 (17.7) | 20 (19.2) |
| Able most of the time | 9 (17.0) | 11 (21.6) | 20 (19.2) |
| Able some of the time | 8 (15.1) | 6 (11.8) | 14 (13.5) |
| Able a slight bit of the time | 4 (7.6) | 4 (7.8) | 8 (7.7) |
| Able none of the time | 5 (9.4) | 2 (3.9) | 7 (6.7) |
| Does not apply to my job | 2 (3.8) | 3 (5.9) | 5 (4.8) |
| Missing | 4 (26.4) | 16 (31.4) | 30 (28.9) |
| Week 24, n (%) | N = 23 | N = 18 | N = 41 |
| Able all of the time | 2 (8.7) | 4 (22.2) | 6 (14.6) |
| Able most of the time | 6 (26.1) | 3 (16.7) | 9 (22.0) |
| Able some of the time | 3 (13.0) | 4 (22.2) | 7 (17.1) |
| Able a slight bit of the time | 2 (8.7) | 2 (11.1) | 4 (9.8) |
| Able none of the time | 1 (4.4) | 0 (0.0) | 1 (2.4) |
| Does not apply to my job | 2 (8.7) | 2 (11.1) | 4 (9.8) |
| Missing | 7 (30.4) | 3 (16.7) | 10 (24.4) |
| Were you able to repeat the same motions over and over again while working, without difficulty caused by physical health or emotional problems? | |||
| Baseline, n (%) | N = 77 | N = 77 | N = 154 |
| Able all of the time | 1 (1.3) | 5 (6.5) | 6 (3.9) |
| Able most of the time | 16 (20.8) | 18 (23.4) | 34 (22.1) |
| Able some of the time | 25 (32.5) | 16 (20.8) | 41 (26.6) |
| Able a slight bit of the time | 14 (18.2) | 13 (16.9) | 27 (17.5) |
| Able none of the time | 2 (2.6) | 3 (3.9) | 5 (3.3) |
| Does not apply to my job | 4 (5.2) | 4 (5.2) | 8 (5.2) |
| Missing | 15 (19.5) | 18 (23.4) | 33 (21.4) |
| Week 8, n (%) | N = 50 | N = 43 | N = 93 |
| Able all of the time | 2 (4.0) | 5 (11.6) | 7 (7.5) |
| Able most of the time | 5 (10.0) | 5 (11.6) | 10 (10.8) |
| Able some of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Able a slight bit of the time | 1 (2.0) | 4 (9.3) | 5 (5.4) |
| Able none of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Does not apply to my job | 5 (10.0) | 3 (7.0) | 8 (8.6) |
| Missing | 37 (74.0) | 26 (60.5) | 63 (67.7) |
| Week 16, n (%) | N = 53 | N = 51 | N = 104 |
| Able all of the time | 12 (22.6) | 9 (17.7) | 21 (20.2) |
| Able most of the time | 11 (20.8) | 11 (21.6) | 22 (21.2) |
| Able some of the time | 5 (9.4) | 5 (9.8) | 10 (9.6) |
| Able a slight bit of the time | 4 (7.6) | 2 (3.9) | 6 (5.8) |
| Able none of the time | 0 (0.0) | 2 (3.9) | 2 (1.9) |
| Does not apply to my job | 7 (13.2) | 5 (9.8) | 12 (11.5) |
| Missing | 14 (26.4) | 17 (33.3) | 31 (29.8) |
| Week 24, n (%) | N = 23 | N = 18 | N = 41 |
| Able all of the time | 6 (26.1) | 3 (16.7) | 9 (22.0) |
| Able most of the time | 3 (13.0) | 7 (38.9) | 10 (24.4) |
| Able some of the time | 3 (13.0) | 3 (16.7) | 6 (14.6) |
| Able a slight bit of the time | 1 (4.4) | 1 (5.6) | 2 (4.9) |
| Able none of the time | 1 (4.4) | 0 (0.0) | 1 (2.4) |
| Does not apply to | 2 (8.7) | 1 (5.6) | 3 (7.3) |
| Missing | 7 (30.4) | 3 (16.7) | 10 (24.4) |
| Did your physical health or emotional problems make it difficult for you to concentrate on your work? | |||
| Baseline, n (%) | N = 77 | N = 77 | N = 154 |
| Difficult all of the time | 1 (1.3) | 0 (0.0) | 1 (0.7) |
| Difficult most of the time | 10 (13.0) | 8 (10.4) | 18 (11.7) |
| Difficult some of the time | 16 (20.8) | 18 (23.4) | 34 (22.1) |
| Difficult a slight bit of the time | 15 (19.5) | 18 (23.4) | 33 (21.4) |
| Difficult none of the time | 14 (18.2) | 13 (16.9) | 27 (17.5) |
| Does not apply to my job | 8 (10.4) | 5 (6.5) | 13 (8.4) |
| Missing | 13 (16.9) | 15 (19.5) | 28 (18.2) |
| Week 8, n (%) | N = 50 | N = 43 | N = 93 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 1 (2.0) | 0 (0.0) | 1 (1.1) |
| Difficult some of the time | 2 (4.0) | 1 (2.3) | 3 (3.2) |
| Difficult a slight bit of the time | 3 (6.0) | 4 (9.3) | 7 (7.5) |
| Difficult none of the time | 8 (16.0) | 12 (27.9) | 20 (21.5) |
| Does not apply to my job | 2 (4.0) | 0 (0.0) | 2 (2.2) |
| Missing | 34 (68.0) | 26 (60.5) | 60 (64.5) |
| Week 16, n (%) | N = 53 | N = 51 | N = 104 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 1 (2.0) | 1 (1.0) |
| Difficult some of the time | 4 (7.6) | 1 (2.0) | 5 (4.8) |
| Difficult a slight bit of the time | 8 (15.1) | 8 (15.78) | 16 (15.4) |
| Difficult none of the time | 24 (45.3) | 19 (37.3) | 43 (41.4) |
| Does not apply to my job | 3 (5.7) | 6 (11.8) | 9 (8.7) |
| Missing | 14 (26.4) | 16 (31.4) | 30 (28.9) |
| Week 24, n (%) | N = 23 | N = 18 | N = 41 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 1 (5.6) | 1 (2.4) |
| Difficult some of the time | 3 (13.0) | 2 (11.1) | 5 (12.2) |
| Difficult a slight bit of the time | 3 (13.0) | 4 (22.2) | 7 (17.1) |
| Difficult none of the time | 9 (39.1) | 6 (33.3) | 15 (36.6) |
| Does not apply to my job | 1 (4.4) | 2 (11.1) | 3 (7.3) |
| Missing | 7 (30.4) | 3 (16.7) | 10 (24.4) |
| Did your physical health or emotional problems make it difficult for you to speak with people in-person, in meetings or on the phone? | |||
| Baseline, n (%) | N = 77 | N = 77 | N = 154 |
| Difficult all of the time | 1 (1.3) | 0 (0.0) | 1 (0.7) |
| Difficult most of the time | 4 (5.2) | 4 (5.2) | 8 (5.2) |
| Difficult some of the time | 9 (11.7) | 7 (9.1) | 16 (10.4) |
| Difficult a slight bit of the time | 15 (19.5) | 14 (18.2) | 29 (18.8) |
| Difficult none of the time | 27 (35.1) | 26 (33.8) | 53 (34.4) |
| Does not apply to my job | 9 (11.7) | 10 (13.0) | 19 (12.3) |
| Missing | 12 (15.6) | 16 (20.8) | 28 (18.2) |
| Week 8, n (%) | N = 50 | N = 43 | N = 93 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult some of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult a slight bit of the time | 4 (8.0) | 0 (0.0) | 4 (4.3) |
| Difficult none of the time | 9 (18.0) | 15 (34.9) | 24 (25.8) |
| Does not apply to my job | 4 (8.0) | 2 (4.7) | 6 (6.5) |
| Missing | 33 (66.0) | 26 (60.5) | 59 (63.4) |
| Week 16, n (%) | N = 53 | N = 51 | N = 104 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult some of the time | 2 (3.8) | 0 (0.0) | 2 (1.9) |
| Difficult a slight bit of the time | 7 (13.2) | 3 (5.9) | 10 (9.6) |
| Difficult none of the time | 27 (50.9) | 26 (51.0) | 553 (51.0) |
| Does not apply to my job | 3 (5.7) | 5 (9.8) | 8 (7.7) |
| Missing | 14 (26.4) | 17 (33.3) | 31 (29.8) |
| Week 24, n (%) | N = 23 | N = 18 | N = 41 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult some of the time | 1 (4.4) | 0 (0.0) | 1 (2.4) |
| Difficult a slight bit of the time | 2 (8.7) | 2 (11.1) | 4 (9.8) |
| Difficult none of the time | 11 (47.8) | 10 (55.6) | 21 (51.2) |
| Does not apply to my job | 2 (8.7) | 3 (16.7) | 5 (12.2) |
| Missing | 7 (30.4) | 3 (16.7) | 10 (24.4) |
| Did your physical health or emotional problems make it difficult for you handle your workload? | |||
| Baseline, n (%) | N = 77 | N = 77 | N = 154 |
| Difficult all of the time | 2 (2.6) | 2 (2.6) | 4 (2.6) |
| Difficult most of the time | 9 (11.7) | 14 (18.2) | 23 (14.9) |
| Difficult some of the time | 21 (27.3) | 13 (16.9) | 34 (22.1) |
| Difficult a slight bit of the time | 19 (24.7) | 12 (15.6) | 31 (20.1) |
| Difficult none of the time | 9 (11.7) | 15 (19.5) | 24 (15.6) |
| Does not apply to my job | 5 (6.5) | 5 (6.5) | 10 (6.5) |
| Missing | 12 (15.6) | 16 (20.8) | 28 (18.2) |
| Week 8, n (%) | N = 50 | N = 43 | N = 93 |
| Difficult all of the time | 1 (2.0) | 0 (0.0) | 1 (1.1) |
| Difficult most of the time | 1 (2.0) | 1 (2.3) | 2 (2.2) |
| Difficult some of the time | 0 (0.0) | 1 (2.3) | 1 (1.1) |
| Difficult a slight bit of the time | 6 (12.0) | 6 (14.0) | 12 (13.0) |
| Difficult none of the time | 5 (10.0) | 8 (18.6) | 13 (14.0) |
| Does not apply to my job | 2 (4.0) | 1 (2.3) | 3 (3.2) |
| Missing | 35 (70.0) | 26 (60.5) | 61 (65.6) |
| Week 16, n (%) | N = 53 | N = 51 | N = 104 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult some of the time | 3 (5.7) | 3 (5.9) | 6 (5.8) |
| Difficult a slight bit of the time | 7 (13.2) | 7 (13.7) | 14 (13.5) |
| Difficult none of the time | 24 (45.3) | 18 (35.3) | 42 (40.4) |
| Does not apply to my job | 5 (9.4) | 7 (13.7) | 12 (11.5) |
| Missing | 14 (26.4) | 16 (31.4) | 30 (28.9) |
| Week 24, n (%) | N = 23 | N = 18 | N = 41 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult some of the time | 1 (4.4) | 1 (5.6) | 2 (4.9) |
| Difficult a slight bit of the time | 4 (17.4) | 4 (22.2) | 8 (19.5) |
| Difficult none of the time | 9 (39.1) | 8 (44.4) | 17 (41.5) |
| Does not apply to my job | 2 (8.7) | 1 (5.6) | 3 (7.3) |
| Missing | 7 (30.4) | 4 (22.2) | 11 (26.8) |
| Did your physical health or emotional problems make it difficult for you to finish work on time? | |||
| Baseline, n (%) | N = 77 | N = 77 | N = 154 |
| Difficult all of the time | 5 (6.5) | 2 (2.6) | 7 (4.6) |
| Difficult most of the time | 9 (11.7) | 10 (13.0) | 19 (12.3) |
| Difficult some of the time | 10 (13.0) | 6 (7.8) | 16 (10.4) |
| Difficult a slight bit of the time | 9 (11.7) | 10 (13.0) | 19 (12.3) |
| Difficult none of the time | 17 (22.1) | 24 (31.2) | 41 (26.6) |
| Does not apply to my job | 13 (16.9) | 9 (11.7) | 22 (14.3) |
| Missing | 14 (18.2) | 16 (20.8) | 30 (19.5) |
| Week 8, n (%) | N = 50 | N = 43 | N = 93 |
| Difficult all of the time | 1 (2.0) | 1 (2.3) | 2 (2.2) |
| Difficult most of the time | 2 (4.0) | 0 (0.0) | 2 (2.2) |
| Difficult some of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult a slight bit of the time | 3 (6.0) | 2 (4.7) | 5 (5.4) |
| Difficult none of the time | 7 (14.0) | 9 (20.9) | 16 (17.2) |
| Does not apply to my job | 2 (4.0) | 4 (9.3) | 6 (6.5) |
| Missing | 35 (70.0) | 27 (62.8) | 62 (66.7) |
| Week 16, n (%) | N = 53 | N = 51 | N = 104 |
| Difficult all of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult most of the time | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Difficult some of the time | 2 (3.8) | 1 (2.0) | 3 (2.9) |
| Difficult a slight bit of the time | 4 (7.6) | 5 (9.8) | 9 (8.7) |
| Difficult none of the time | 24 (45.3) | 16 (31.4) | 40 (38.5) |
| Does not apply to my job | 9 (17.0) | 13 (25.5) | 22 (21.2) |
| Missing | 14 (26.4) | 16 (31.4) | 30 (28.9) |
| Week 24, n (%) | N = 23 | N = 18 | N = 41 |
| Difficult all of the time | 0 (0.0) | 1 (5.6) | 1 (2.4) |
| Difficult most of the time | 1 (4.4) | 0 (0.0) | 1 (2.4) |
| Difficult some of the time | 1 (4.4) | 0 (0.0) | 1 (2.4) |
| Difficult a slight bit of the time | 2 (8.7) | 2 (11.1) | 4 (9.8) |
| Difficult none of the time | 10 (43.5) | 7 (38.9) | 17 (41.5) |
| Does not apply to my job | 2 (8.7) | 4 (22.2) | 6 (14.6) |
| Missing | 7 (30.4) | 4 (22.2) | 11 (26.8) |
| Percentage of time lost | |||
| Baseline | N = 65 | N = 62 | N = 127 |
| Mean (SD) | 30.4 (34.1) | 24.2 (31.7) | 27.4 (32.9) |
| Median (Q1, Q3) | 25 (0, 50) | 0 (0, 50) | 0 (0, 50) |
| Minimum, maximum | 0, 100 | 0, 100 | 0, 100 |
| Week 8 | N = 19 | N = 18 | N = 37 |
| Mean (SD) | 19.7 (30.7) | 11.1 (26.0) | 15.5 (28.5) |
| Median (Q1, Q3) | 0 (0, 25) | 0 (0, 0) | 0 (0, 25) |
| Minimum, maximum | 0, 100 | 0, 100 | 0, 100 |
| Week 16 | N = 39 | N = 36 | N = 75 |
| Mean (SD) | 5.1 (13.1) | 5.6 (12.1) | 5.3 (12.1) |
| Median (Q1, Q3) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Minimum, maximum | 0, 50 | 0, 50 | 0, 50 |
| Week 24 | N = 16 | N = 15 | N = 31 |
| Mean (SD) | 10.9 (22.3) | 11.7 (26.5) | 11.3 (24.0) |
| Median (Q1, Q3) | 0 (0, 12.5) | 0 (0, 25) | 0 (0, 25) |
| Minimum, maximum | 0, 75 | 0, 100 | 0, 100 |
| Factors included | Coefficient | Standard error | p-value | Factor significant? |
|---|---|---|---|---|
| Patient characteristics | ||||
| Age | 0.01 | 0.02 | 0.65 | No |
| Sex | ||||
| Male | –0.65 | 0.50 | 0.45 | No |
| Female | 0.48 | 0.33 | 0.15 | No |
| BMI | –0.02 | 0.03 | 0.53 | No |
| Ethnicity | ||||
| White | –0.20 | 0.75 | 0.93 | No |
| Non-white | 0.21 | 0.69 | 0.76 | No |
| Type of employer | ||||
| Large (> 250 employees) | –0.21 | 0.25 | 0.39 | No |
| Median (50–250 employees) | 0.21 | 0.56 | 0.71 | No |
| Small (10–49 employees) | 0.50 | 0.59 | 0.40 | No |
| Micro (2–9 employees) | 1.15 | 0.51 | 0.02 | Yes |
| Self (1 employee) | 0.03 | 0.49 | 0.96 | No |
| Type of employment | ||||
| Full time | –0.03 | 0.26 | 0.90 | No |
| Part time | 0.14 | 0.42 | 0.74 | No |
| Self-employed | –0.02 | 0.42 | 0.96 | No |
| Unpaid | 0.73 | 0.61 | 0.23 | No |
| Other | –0.66 | 1.3 | 0.60 | No |
| Length of time with employer (years) | –0.01 | 0.02 | 0.53 | No |
| Replacement of | ||||
| Hip | –0.08 | 0.23 | 0.52 | No |
| Knee | 0.21 | 0.32 | 0.73 | No |
| Standardised measures at baseline | ||||
| OHS/OKS | –0.01 | 0.02 | 0.63 | No |
| BRS | –0.62 | 0.41 | 0.13 | No |
| Work Design Questionnaire | ||||
| Work scheduling autonomy | 0.06 | 0.16 | 0.71 | No |
| Ergonomics | 0.10 | 0.24 | 0.68 | No |
| Physical demands | –0.25 | 0.13 | 0.06 | No |
| Social support | 0.21 | 0.23 | 0.37 | No |
| PHQ-9 | 0.03 | 0.03 | 0.41 | No |
| Work Limitations Questionnaire | 0.01 | 0.01 | 0.22 | No |
Because only being a micro employer (n = 25 participants, 17.4% of the cohort) was considered a significant factor in predicting RTW time, it was determined that it would not be possible to create a model to predict RTW.
Supplementary information for the health economic analyses
| Item | Unit of measurement | Unit cost | Additional notes | Source |
|---|---|---|---|---|
| GP visit at GP’s practice | Per patient contact | £37.40 | Patient contact (surgery) lasting 9.22 minutes | Curtis and Burns140 |
| GP visit at home | Per home visit (11.4 minutes) plus 12 minutes of travel time | £93.60 | Cost per GP clinic visit minute sourced from PSSRU 2018.140 Durations sourced from PSSRU 2015432 | Curtis and Burns140,432 |
| Nurse visit at GP’s practice | Per 15.5-minute appointment | £10.85 | Based on £42 per hour | Curtis and Burns140 |
| Community nurse visit at home | Per consultation | £38.45 | Community health services sheet: consultation with district nurse, face to face (adult) | Department of Health and Social Care139 |
| Occupational therapist visit | Per hour | £47.00 | Community occupational therapist (local authority), including training | Curtis and Burns140 |
| Physiotherapist visit | Per visit | £57.25 | Community health services sheet: Physiotherapist, one to one (adult) | Department of Health and Social Care139 |
| Other health service visit | Per visit | £74.11 | Community health services sheet: other therapist, one to one (adult) | Department of Health and Social Care139 |
| Inpatient night in hospital (related to joint) | Per night | £405.34 | Total HRG sheet: sum of total expenditure on excess bed-days (elective and non-elective) divided by total activity for all HRG codes relating to knee/hip replacementa | Department of Health and Social Care139 |
| Inpatient night in hospital (related to another reason) | Per night | £345.76 | Total HRG sheet: sum of total expenditure on excess bed-days (elective and non-elective) divided by total activity | Department of Health and Social Care139 |
| Day-case visit to hospital (related to joint) | Per day-case admission | £1366.92 | Day-case sheet: sum of total cost divided by total activity for all HRG codes relating to knee/hip replacementa | Department of Health and Social Care139 |
| Day-case visit to hospital (related to another reason) | Per day-case admission | £742.09 | Total HRGs sheet: sum of total cost divided by total activity for all day cases | Department of Health and Social Care139 |
| Hospital outpatient visit (related to joint) | Per clinic visit | £145.52 | Total outpatient attendances sheet: rheumatology (code 410) | Department of Health and Social Care139 |
| Hospital outpatient visit (related to another reason) | Per clinic visit | £125.01 | Total outpatient attendances sheet: total cost for all outpatient attendances divided by total activity | Department of Health and Social Care139 |
| A&E visit | Per attendance | £160.32 | A&E sheet: sum of total cost divided by total attendances for all A&E service codes | Department of Health and Social Care139 |
| Hospital physiotherapy visit | Per attendance | £54.91 | Total outpatient attendances sheet, service code 650 (physiotherapy) | Department of Health and Social Care139 |
| Occupational health RTW advice | Assume 15 minutes | £4.30 | Based on average wage of a health and safety officer being £35,078 | Office for National Statistics145 |
| Employer RTW advice | Assume 15 minutes | £3.89 | Based on the average of annual pay for managers/supervisors across a range of employment sectors being £31,716b | Office for National Statistics145 |
| Type of resource use | Hip (n = 77) | Knee (n = 77) | ||
|---|---|---|---|---|
| Mean (SD) | Missing (%) | Mean (SD) | Missing (%) | |
| GP visits at GP’s practice | ||||
| Baselinea | 0.61 (1.12) | 21 (27.3) | 0.45 (0.92) | 22 (28.6) |
| 8 weeks | 0.29 (0.52) | 39 (50.6) | 0.53 (0.75) | 43 (55.8) |
| 16 weeks | 0.56 (0.64) | 38 (49.4) | 0.54 (1.17) | 42 (54.5) |
| 24 weeksb | 0.56 (0.86) | 21 (51.2) | 0.31 (0.48) | 30 (65.2) |
| GP visits at home | ||||
| Baseline | 0.00 (0.00) | 21 (27.3) | 0.00 (0.00) | 25 (32.5) |
| 8 weeks | 0.00 (0.00) | 40 (51.9) | 0.00 (0.00) | 43 (55.8) |
| 16 weeks | 0.06 (0.33) | 41 (53.2) | 0.18 (1.04) | 44 (57.1) |
| 24 weeks | 0.00 (0.00) | 24 (58.5) | 0.00 (0.00) | 31 (67.4) |
| Nurse visits at GP’s practice | ||||
| Baseline | 0.45 (0.99) | 21 (27.3) | 0.47 (1.07) | 24 (31.2) |
| 8 weeks | 0.24 (0.63) | 39 (50.6) | 0.33 (0.72) | 41 (53.2) |
| 16 weeks | 0.41 (0.76) | 40 (51.9) | 0.27 (0.57) | 44 (57.1) |
| 24 weeks | 0.41 (0.62) | 24 (58.5) | 0.40 (0.83) | 31 (67.4) |
| Community nurse visits at home | ||||
| Baseline | 0.00 (0.00) | 22 (28.6) | 0.11 (0.82) | 25 (32.5) |
| 8 weeks | 0.00 (0.00) | 40 (51.9) | 0.00 (0.00) | 44 (57.1) |
| 16 weeks | 0.76 (4.6) | 40 (51.9) | 0.00 (0.00) | 44 (57.1) |
| 24 weeks | 0.00 (0.00) | 24 (58.5) | 0.00 (0.00) | 31 (67.4) |
| Occupational therapist visits | ||||
| Baseline | 0.04 (0.19) | 22 (28.6) | 0.04 (0.20) | 26 (33.8) |
| 8 weeks | 0.00 (0.00) | 41 (53.2) | 0.00 (0.00) | 44 (57.1) |
| 16 weeks | 0.00 (0.00) | 42 (54.5) | 0.00 (0.00) | 44 (57.1) |
| 24 weeks | 0.00 (0.00) | 24 (58.5) | 0.00 (0.00) | 31 (67.4) |
| Physiotherapist visits | ||||
| Baseline | 0.18 (0.98) | 22 (28.6) | 0.04 (0.20) | 27 (35.1) |
| 8 weeks | 0.03 (0.17) | 41 (53.2) | 0.30 (1.24) | 44 (57.1) |
| 16 weeks | 0.00 (0.00) | 40 (51.9) | 0.24 (1.09) | 44 (57.1) |
| 24 weeks | 0.24 (0.56) | 24 (58.5) | 0.00 (0.00) | 31 (67.4) |
| Other health service visits | ||||
| Baseline | 0.14 (0.44) | 21 (27.3) | 0.08 (0.33) | 25 (32.5) |
| 8 weeks | 0.11 (0.66) | 40 (51.9) | 0.06 (0.25) | 45 (58.4) |
| 16 weeks | 0.41 (0.98) | 40 (51.9) | 0.09 (0.29) | 44 (57.1) |
| 24 weeks | 0.29 (0.99) | 24 (58.5) | 0.20 (0.41) | 31 (67.4) |
| Inpatient nights in hospital | ||||
| Baseline | 0.90 (5.89) | 25 (32.5) | 0.33 (1.10) | 37 (48.1) |
| 8 weeks | 0.03 (0.17) | 43 (55.8) | 0.00 (0.00) | 45 (58.4) |
| 16 weeks | 0.19 (0.71) | 41 (53.2) | 0.00 (0.00) | 44 (57.1) |
| 24 weeks | 0.00 (0.00) | 22 (53.7) | 0.00 (0.00) | 32 (69.6) |
| Day-case visits to hospital | ||||
| Baseline | 0.00 (0.00) | 23 (29.9) | 0.07 (0.26) | 35 (45.5) |
| 8 weeks | 0.00 (0.00) | 41 (53.2) | 0.00 (0.00) | 45 (58.4) |
| 16 weeks | 0.03 (0.17) | 41 (53.2) | 0.09 (0.38) | 44 (57.1) |
| 24 weeks | 0.00 (0.00) | 23 (56.1) | 0.07 (0.27) | 32 (69.6) |
| Outpatient attendances | ||||
| Baseline | 0.46 (1.53) | 25 (32.5) | 0.12 (0.40) | 36 (46.8) |
| 8 weeks | 0.12 (0.54) | 43 (55.8) | 0.07 (0.25) | 47 (61.0) |
| 16 weeks | 0.22 (0.71) | 40 (51.9) | 0.19 (0.59) | 45 (58.4) |
| 24 weeks | 0.33 (0.97) | 23 (56.1) | 0.29 (0.61) | 32 (69.6) |
| A&E visits | ||||
| Baseline | 0.04 (0.28) | 26 (33.8) | 0.05 (0.21) | 34 (44.2) |
| 8 weeks | 0.00 (0.00) | 42 (54.5) | 0.03 (0.18) | 45 (58.4) |
| 16 weeks | 0.03 (0.17) | 21 (27.3) | 0.00 (0.00) | 46 (59.7) |
| 24 weeks | 0.00 (0.00) | 23 (56.1) | 0.00 (0.00) | 32 (69.6) |
| Physiotherapy hospital attendances | ||||
| Baseline | 0.13 (0.97) | 25 (32.5) | 0.18 (0.96) | 37 (48.1) |
| 8 weeks | 0.00 (0.00) | 42 (54.5) | 0.14 (0.76) | 49 (63.6) |
| 16 weeks | 0.00 (0.00) | 41 (53.2) | 0.07 (0.37) | 47 (61.0) |
| 24 weeks | 0.56 (0.24) | 23 (56.1) | 0.00 (0.00) | 32 (69.6) |
| Cost item | Hip (N = 77) | Knee (N = 77) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline–8 weeks | 8–16 weeks | Baseline–8 weeks | 8–16 weeks | |||||
| Mean cost (£) (SD) | n | Mean cost (£) (SD) | n | Mean cost (£) (SD) | n | Mean cost (£) (SD) | n | |
| GP visits at GP’s practice | 10.83 (19.26) | 38 | 21.10 (23.96) | 39 | 19.80 (27.98) | 34 | 20.30 (43.83) | 35 |
| GP visits at home | 0.00 (0.00) | 37 | 5.20 (31.20) | 36 | 0.00 (0.00) | 34 | 17.02 (97.76) | 33 |
| Nurse visits at GP’s practice | 2.57 (6.88) | 38 | 4.40 (8.27) | 37 | 3.62 (7.78) | 36 | 2.96 (6.23) | 33 |
| Community nurse visits: home | 0.00 (0.00) | 37 | 29.10 (177.01) | 37 | 0.00 (0.00) | 33 | 0.00 (0.00) | 33 |
| Occupational therapist visits | 0.00 (0.00) | 36 | 0.00 (0.00) | 35 | 0.00 (0.00) | 33 | 0.00 (0.00) | 33 |
| Physiotherapist visits | 49.79 (82.41) | 46 | 0.00 (0.00) | 37 | 210.42 (139.88) | 40 | 13.88 (62.44) | 33 |
| Other health service visits | 8.01 (48.74) | 37 | 30.05 (72.99) | 37 | 4.63 (18.23) | 32 | 6.74 (21.64) | 33 |
| Inpatient nights in hospital | 10.17 (59.30) | 34 | 67.23 (245.45) | 36 | 0.00 (0.00) | 32 | 0.00 (0.00) | 33 |
| Day-case visits to hospital | 0.00 (0.00) | 36 | 20.61 (123.68) | 36 | 0.00 (0.00) | 32 | 67.46 (285.22) | 33 |
| Outpatient attendances | 14.71 (67.18) | 34 | 27.03 (89.06) | 37 | 8.33 (31.72) | 30 | 23.44 (74.04) | 32 |
| A&E visits | 0.00 (0.00) | 35 | 4.45 (26.72) | 36 | 5.01 (28.34) | 32 | 0.00 (0.00) | 31 |
| Physiotherapy hospital attendances | 0.00 (0.00) | 35 | 0.00 (0.00) | 36 | 7.84 (41.51) | 28 | 3.66 (20.05) | 30 |
| Total costs | 38.13 (93.73) | 29 | 163.95 (337.09) | 32 | 55.95 (118.36) | 25 | 170.69 (404.38) | 29 |
| Resource | Hip | Knee | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| GP visits at GP’s practice | 32 | 0.50 (0.95) | 24 | 0.46 (0.78) |
| GP visits at home | 31 | 0.00 (0.00) | 24 | 0.00 (0.00) |
| Nurse visits at GP’s practice | 32 | 0.56 (0.91) | 24 | 0.88 (1.36) |
| Community nurse visits at home | 31 | 1.13 (5.04) | 24 | 0.67 (2.35) |
| Occupational therapist visits | 32 | 0.34 (0.70) | 23 | 0.22 (0.60) |
| Physiotherapist visits | 30 | 1.43 (1.89) | 26 | 6.04 (4.49) |
| Other health service visits | 29 | 0.35 (0.81) | 23 | 0.22 (0.52) |
| Inpatient nights in hospital | 34 | 3.68 (3.42) | 26 | 3.31 (2.57) |
| Day-case visits to hospital | 32 | 0.00 (0.00) | 23 | 0.04 (0.21) |
| Outpatient attendances | 33 | 1.70 (1.42) | 24 | 1.38 (1.35) |
| A&E visits | 30 | 0.03 (0.18) | 23 | 0.17 (0.58) |
| Physiotherapy hospital attendances | 31 | 2.19 (2.65) | 24 | 4.38 (3.68) |
| Occupational health RTW advice | 33 | 0.15 (0.51) | 25 | 0.00 (0.00) |
| Employer RTW advice | 33 | 0.18 (0.39) | 25 | 0.16 (0.47) |
| Resource | Hip | Knee | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| GP visits at GP’s practice | 23 | 0.87 (0.92) | 17 | 0.94 (1.43) |
| GP visits at home | 21 | 0.95 (0.44) | 15 | 0.40 (1.55) |
| Nurse visits at GP’s practice | 22 | 0.64 (1.22) | 15 | 0.87 (1.55) |
| Community nurse visits at home | 21 | 0.00 (0.00) | 15 | 0.00 (0.00) |
| Occupational therapist visits | 20 | 0.00 (0.00) | 15 | 0.00 (0.00) |
| Physiotherapist visits | 20 | 0.05 (0.22) | 15 | 0.40 (1.55) |
| Other health service visits | 22 | 0.68 (1.86) | 16 | 0.13 (0.34) |
| Inpatient nights in hospital | 22 | 0.00 (0.00) | 16 | 0.00 (0.00) |
| Day-case visits to hospital | 23 | 0.04 (0.21) | 16 | 0.06 (0.25) |
| Outpatient attendances | 22 | 0.41 (1.50) | 15 | 0.33 (0.82) |
| A&E visits | 22 | 0.05 (0.21) | 16 | 0.00 (0.00) |
| Physiotherapy hospital attendances | 21 | 0.00 (0.00) | 15 | 0.00 (0.00) |
| Cost item | Hip | Knee | ||
|---|---|---|---|---|
| n | Total mean cost (£) (SD) | n | Total mean cost (£) (SD) | |
| GP visits at GP’s practice | 32 | 18.70 (35.54) | 24 | 17.14 (29.14) |
| GP visits at home | 31 | 0.00 (0.00) | 24 | 0.00 (0.00) |
| Nurse visits at GP’s practice | 32 | 6.10 (9.91) | 24 | 9.49 (14.77) |
| Community nurse visits at home | 31 | 43.42 (193.99) | 24 | 25.64 (90.48) |
| Occupational therapist visits | 32 | 16.16 (32.93) | 23 | 10.22 (28.19) |
| Physiotherapist visits | 30 | 82.07 (108.10) | 26 | 345.74 (257.32) |
| Other health service visits | 29 | 25.56 (60.33) | 23 | 16.11 (38.42) |
| Inpatient nights in hospital | 34 | 1490.20 (1385.28) | 26 | 1340.73 (1043.02) |
| Day-case visits to hospital | 32 | 0.00 (0.00) | 23 | 59.43 (285.02) |
| Outpatient attendances | 33 | 246.94 (207.34) | 24 | 200.08 (195.76) |
| A&E visits | 30 | 5.34 (29.27) | 23 | 27.88 (92.38) |
| Physiotherapy hospital attendances | 31 | 120.45 (145.57) | 24 | 240.23 (202.11) |
| Occupational health RTW advice | 33 | 0.65 (2.18) | 25 | 0.00 (0.00) |
| Employer RTW advice | 33 | 0.71 (1.52) | 25 | 0.62 (1.84) |
| Cost item | Hip | Knee | ||
|---|---|---|---|---|
| n | Total mean cost (£) (SD) | n | Total mean cost (£) (SD) | |
| GP visits at GP’s practice | 23 | 32.52 (34.40) | 17 | 35.20 (53.66) |
| GP visits at home | 21 | 8.91 (40.85) | 15 | 37.44 (145.00) |
| Nurse visits at GP’s practice | 22 | 6.90 (13.20) | 15 | 9.40 (16.84) |
| Community nurse visits at home | 21 | 0.00 (0.00) | 15 | 0.00 (0.00) |
| Occupational therapist visits | 20 | 0.00 (0.00) | 15 | 0.00 (0.00) |
| Physiotherapist visits | 20 | 2.86 (12.80) | 15 | 22.90 (88.70) |
| Other health service visits | 22 | 50.53 (137.96) | 16 | 9.26 (25.31) |
| Inpatient nights in hospital | 22 | 0.00 (0.00) | 16 | 0.00 (0.00) |
| Day-case visits to hospital | 23 | 32.26 (154.74) | 16 | 46.38 (185.52) |
| Outpatient attendances | 22 | 51.14 (187.65) | 15 | 41.67 (102.07) |
| A&E visits | 22 | 7.29 (34.18) | 16 | 0.00 (0.00) |
| Physiotherapy hospital attendances | 21 | 0.00 (0.00) | 15 | 0.00 (0.00) |
| Time point | Operation type | |||
|---|---|---|---|---|
| Hip (N = 77) | Knee (N = 77) | |||
| n | Mean score (SD) | n | Mean score (SD) | |
| Baseline (4 weeks pre surgery) | 71 | 0.312 (0.317) | 71 | 0.471 (0.220) |
| Baseline (today) | 72 | 0.359 (0.283) | 73 | 0.298 (0.301) |
| 8 weeks | 50 | 0.675 (0.215) | 42 | 0.693 (0.110) |
| 16 weeks | 47 | 0.771 (0.236) | 45 | 0.734 (0.196) |
| 24 weeks | 21 | 0.723 (0.321) | 18 | 0.762 (0.171) |
| Score | Hip | Knee | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (4 weeks pre surgery) | Baseline (today) | 8 weeks | 16 weeks | 24 weeks | Baseline (4 weeks pre surgery) | Baseline (today) | 8 weeks | 16 weeks | 24 weeks | |
| Mean EQ VAS score (SD) | 52.4 (26.0) | 60.0 (20.9) | 75.3 (17.6) | 79.7 (17.7) | 77.0 (21.3) | 64.9 (21.1) | 61.6 (20.9) | 73.6 (19.7) | 78.5 (15.7) | 80.2 (14.9) |
| Median EQ VAS score (IQR) | 50 (30–75) | 65 (50–75) | 78 (65–90) | 85 (70–90) | 87 (65–90) | 70 (50–80) | 65 (50–80) | 75 (70–85) | 85 (70–90) | 81 (70–95) |
| Time point | Completed EQ-5D, n (%) | Missing EQ-5D (one or more dimension missing), n (%) | ||
|---|---|---|---|---|
| Hip (N = 77) | Knee (N = 77) | Hip (N = 77) | Knee (N = 77) | |
| Baseline (4 weeks pre surgery) | 71 (92) | 71 (92) | 6 (8) | 6 (8) |
| Baseline (today) | 72 (94) | 73 (95) | 5 (7) | 4 (5) |
| 8 weeks | 50 (65) | 42 (55) | 27 (35) | 35 (46) |
| 16 weeks | 47 (61) | 45 (58) | 30 (39) | 32 (42) |
| N = 41 | N = 46 | N = 41 | N = 46 | |
| 24 weeks | 21 (51) | 18 (39) | 20 (49) | 28 (61) |
| Time point | Number of missing dimensions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hip | Knee | |||||||||
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |
| Baseline (4 weeks pre surgery) | 2 | 0 | 0 | 0 | 5 | 1 | 0 | 0 | 0 | 5 |
| Baseline (today) | 2 | 0 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 3 |
| 8 weeks | 0 | 0 | 0 | 0 | 27 | 1 | 0 | 0 | 0 | 34 |
| 16 weeks | 0 | 0 | 0 | 0 | 30 | 2 | 0 | 0 | 0 | 30 |
| 24 weeks | 0 | 0 | 0 | 0 | 20 | 0 | 0 | 0 | 0 | 28 |
| EQ-5D scale and health state severitya | Baseline (4 weeks pre surgery) | Baseline (today) | 8 weeks | 16 weeks | 24 weeks | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |
| Mobility | ||||||||||
| Level 1 | 1 | 1.3 | 2 | 2.6 | 16 | 20.8 | 25 | 32.5 | 12 | 29.3 |
| Level 2 | 6 | 7.8 | 11 | 14.3 | 17 | 22.1 | 9 | 11.7 | 2 | 4.9 |
| Level 3 | 27 | 35.1 | 30 | 39.0 | 17 | 22.1 | 11 | 14.3 | 4 | 9.8 |
| Level 4 | 37 | 48.1 | 27 | 35.1 | 0 | 0.0 | 2 | 2.6 | 3 | 7.3 |
| Level 5 | 2 | 2.6 | 4 | 5.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 4 | 5.2 | 3 | 3.9 | 27 | 35.1 | 30 | 39.0 | 20 | 48.8 |
| Number reporting any problems | 72 | 98.6 | 72 | 97.30 | 34 | 68.00 | 22 | 46.81 | 9 | 42.9 |
| Self-care | ||||||||||
| Level 1 | 10 | 13.0 | 11 | 14.3 | 30 | 39.0 | 36 | 46.8 | 15 | 36.6 |
| Level 2 | 25 | 32.5 | 19 | 24.7 | 12 | 15.6 | 7 | 9.1 | 3 | 7.3 |
| Level 3 | 27 | 35.1 | 29 | 37.7 | 6 | 7.8 | 3 | 3.9 | 2 | 4.9 |
| Level 4 | 10 | 13.0 | 14 | 18.2 | 2 | 2.6 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 1 | 1.3 | 2 | 2.6 | 0 | 0.0 | 1 | 1.3 | 1 | 2.4 |
| Missing | 4 | 5.2 | 2 | 2.6 | 27 | 35.1 | 30 | 39.0 | 20 | 48.8 |
| Number reporting any problems | 63 | 86.3 | 64 | 85.33 | 20 | 40.00 | 11 | 23.40 | 6 | 28.6 |
| Usual activities | ||||||||||
| Level 1 | 2 | 2.6 | 2 | 2.6 | 12 | 15.6 | 27 | 35.1 | 10 | 24.4 |
| Level 2 | 15 | 19.5 | 10 | 13.0 | 21 | 27.3 | 10 | 13.0 | 7 | 17.1 |
| Level 3 | 26 | 33.8 | 24 | 31.2 | 11 | 14.3 | 7 | 9.1 | 2 | 4.9 |
| Level 4 | 20 | 26.0 | 19 | 24.7 | 3 | 3.9 | 1 | 1.3 | 1 | 2.4 |
| Level 5 | 9 | 11.7 | 18 | 23.4 | 3 | 3.9 | 2 | 2.6 | 1 | 2.4 |
| Missing | 5 | 6.5 | 4 | 5.2 | 27 | 35.1 | 30 | 39.0 | 20 | 48.8 |
| Number reporting any problems | 70 | 97.2 | 71 | 97.26 | 38 | 76.00 | 20 | 42.55 | 11 | 52.4 |
| Pain/discomfort | ||||||||||
| Level 1 | 0 | 0.0 | 1 | 1.3 | 11 | 14.3 | 20 | 26.0 | 8 | 19.5 |
| Level 2 | 4 | 5.2 | 4 | 5.2 | 23 | 29.9 | 16 | 20.8 | 7 | 17.1 |
| Level 3 | 30 | 39.0 | 40 | 51.9 | 15 | 19.5 | 9 | 11.7 | 5 | 12.2 |
| Level 4 | 22 | 28.6 | 21 | 27.3 | 1 | 1.3 | 2 | 2.6 | 0 | 0.0 |
| Level 5 | 17 | 22.1 | 8 | 10.4 | 0 | 0.0 | 0 | 0.0 | 1 | 2.4 |
| Missing | 4 | 5.2 | 3 | 3.9 | 27 | 35.1 | 30 | 39.0 | 20 | 48.8 |
| Number reporting any problems | 73 | 100.0 | 73 | 98.65 | 39 | 78.00 | 27 | 57.45 | 13 | 61.9 |
| Anxiety/depression | ||||||||||
| Level 1 | 31 | 40.3 | 37 | 48.1 | 30 | 39.0 | 35 | 45.5 | 15 | 36.6 |
| Level 2 | 19 | 24.7 | 26 | 33.8 | 11 | 14.3 | 9 | 11.7 | 4 | 9.8 |
| Level 3 | 13 | 16.9 | 7 | 9.1 | 8 | 10.4 | 2 | 2.6 | 0 | 0.0 |
| Level 4 | 5 | 6.5 | 3 | 3.9 | 0 | 0.0 | 1 | 1.3 | 1 | 2.4 |
| Level 5 | 4 | 5.2 | 1 | 1.3 | 1 | 1.3 | 0 | 0.0 | 1 | 2.4 |
| Missing | 5 | 6.5 | 3 | 3.9 | 27 | 35.1 | 30 | 39.0 | 20 | 48.8 |
| Number reporting any problems | 41 | 57.0 | 37 | 50.00 | 20 | 40.00 | 12 | 25.53 | 6 | 28.6 |
| EQ-5D scale and health state severitya | Baseline (4 weeks pre surgery) | Baseline (today) | 8 weeks | 16 weeks | 24 weeks | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |
| Mobility | ||||||||||
| Level 1 | 1 | 1.3 | 1 | 1.3 | 9 | 11.7 | 19 | 24.7 | 8 | 17.4 |
| Level 2 | 9 | 11.7 | 10 | 13.0 | 21 | 27.3 | 20 | 26.0 | 5 | 10.9 |
| Level 3 | 31 | 40.3 | 17 | 22.1 | 10 | 13.0 | 6 | 7.8 | 5 | 10.9 |
| Level 4 | 31 | 40.3 | 34 | 44.2 | 3 | 3.9 | 2 | 2.6 | 0 | 0.0 |
| Level 5 | 0 | 0.0 | 11 | 14.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 5 | 6.5 | 4 | 5.2 | 34 | 44.2 | 30 | 39.0 | 28 | 60.9 |
| Number reporting any problems | 71 | 98.6 | 72 | 98.63 | 34 | 79.07 | 28 | 59.57 | 10 | 55.6 |
| Self-care | ||||||||||
| Level 1 | 37 | 48.1 | 18 | 23.4 | 32 | 41.6 | 35 | 45.5 | 16 | 34.8 |
| Level 2 | 14 | 18.2 | 16 | 20.8 | 8 | 10.4 | 9 | 11.7 | 2 | 4.3 |
| Level 3 | 18 | 23.4 | 29 | 37.7 | 3 | 3.9 | 3 | 3.9 | 0 | 0.0 |
| Level 4 | 2 | 2.6 | 9 | 11.7 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 1 | 1.3 | 2 | 2.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 5 | 6.5 | 3 | 3.9 | 34 | 44.2 | 30 | 39.0 | 28 | 60.9 |
| Number reporting any problems | 35 | 48.6 | 56 | 75.68 | 11 | 25.58 | 12 | 25.53 | 2 | 11.1 |
| Usual activities | ||||||||||
| Level 1 | 6 | 7.8 | 2 | 2.6 | 10 | 13.0 | 19 | 24.7 | 7 | 15.2 |
| Level 2 | 15 | 19.5 | 14 | 18.2 | 18 | 23.4 | 20 | 26.0 | 6 | 13.0 |
| Level 3 | 32 | 41.6 | 23 | 29.9 | 14 | 18.2 | 6 | 7.8 | 4 | 8.7 |
| Level 4 | 16 | 20.8 | 13 | 16.9 | 0 | 0.0 | 2 | 2.6 | 1 | 2.2 |
| Level 5 | 3 | 3.9 | 22 | 28.6 | 1 | 1.3 | 0 | 0.0 | 0 | 0.0 |
| Missing | 5 | 6.5 | 3 | 3.9 | 34 | 44.2 | 30 | 39.0 | 28 | 60.9 |
| Number reporting any problems | 66 | 91.7 | 72 | 97.30 | 33 | 76.74 | 28 | 59.57 | 11 | 61.1 |
| Pain/discomfort | ||||||||||
| Level 1 | 0 | 0.0 | 0 | 0.0 | 1 | 1.3 | 8 | 10.4 | 4 | 8.7 |
| Level 2 | 11 | 14.3 | 3 | 3.9 | 28 | 36.4 | 24 | 31.2 | 11 | 23.9 |
| Level 3 | 27 | 35.1 | 28 | 36.4 | 14 | 18.2 | 11 | 14.3 | 2 | 4.3 |
| Level 4 | 29 | 37.7 | 32 | 41.6 | 0 | 0.0 | 2 | 2.6 | 1 | 2.2 |
| Level 5 | 4 | 5.2 | 11 | 14.3 | 0 | 0.0 | 1 | 1.3 | 0 | 0.0 |
| Missing | 6 | 7.8 | 3 | 3.9 | 34 | 44.2 | 31 | 40.3 | 28 | 60.9 |
| Number reporting any problems | 71 | 100.0 | 73 | 100.0 | 42 | 97.67 | 38 | 82.61 | 14 | 77.8 |
| Anxiety/depression | ||||||||||
| Level 1 | 43 | 55.8 | 51 | 66.2 | 31 | 40.3 | 32 | 41.6 | 14 | 30.4 |
| Level 2 | 16 | 20.8 | 13 | 16.9 | 9 | 11.7 | 9 | 11.7 | 2 | 4.3 |
| Level 3 | 12 | 15.6 | 7 | 9.1 | 2 | 2.6 | 5 | 6.5 | 2 | 4.3 |
| Level 4 | 1 | 1.3 | 2 | 2.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 0 | 0.0 | 1 | 1.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 5 | 6.5 | 3 | 3.9 | 35 | 45.5 | 31 | 40.3 | 28 | 60.9 |
| Number reporting any problems | 29 | 40.3 | 23 | 31.08 | 11 | 26.19 | 14 | 30.43 | 4 | 22.2 |
Supplementary material for the survey of practice
| Question | Survey group | Yes | Sometimes | No | Don’t know/no response |
|---|---|---|---|---|---|
| Are patients in work and intending to return to work after surgery identified as a specific subset of patients for additional advice and information at any point during their care episode? | Orthopaedic surgeons | 8 | – | 59 | 11 |
| Physiotherapists | 5 | – | 13 | 2 | |
| Occupational therapists | 8 | – | 12 | 5 | |
| Nurse/specialist nurse/extended-scope practitioner | 9 | – | 8 | 8 | |
| Total (n = 148) | 30 (20%) | – | 92 (62%) | 26 (18%) | |
| Do patients in work and intending to return to work after surgery receive additional advice and support during their inpatient stay or after discharge? | Orthopaedic surgeons | 6 | – | 58 | 14 |
| Physiotherapists | 5 | – | 14 | 1 | |
| Occupational therapists | 5 | – | 15 | 5 | |
| Nurse/specialist nurse/extended-scope practitioner | 10 | – | 5 | 10 | |
| Total (n = 148) | 26 (18%) | – | 92 (62%) | 30 (20%) | |
| Do you feel an occupational advice intervention is needed? | Orthopaedic surgeons | 20 | 40 | 11 | 7 |
| Physiotherapists | 2 | 14 | 1 | 3 | |
| Occupational therapists | 9 | 12 | 0 | 4 | |
| Nurse/specialist nurse/extended-scope practitioner | 7 | 12 | 0 | 6 | |
| Total (n = 148) | 38 (26%) | 78 (52%) | 12 (8%) | 20 (14%) |
| Interviewee | Examples of advice |
|---|---|
| Orthopaedic surgeons | 3 months is the national agreed time off workAdvice is based on personal judgement onlyIf in doubt I suggest that they are assessed via their employer’s occupational health teamA lot depends on the job, sometimes it has to be left to the company’s occupational health department |
| Physiotherapists | Our hip school gives advice but not individualised to each patient’s occupationI would ask the patient to seek advice from their surgeon |
| Occupational therapist | If patient is in a heavy job, we advise that it is likely to be a total of 3 months before they can return to work unless they can moderate activities in a phased returnWe suggest 6–12 weeks before returning to work. Advice is given generically as part of class rather than on an individual basisAdvice is tailored for each individual as occupations and the work environment invariably differ |
| Nurse/specialist nurse/extended-scope practitioner | Patients are advised not to return to work until after their 6-week review appointment with their surgeonAdvice is given dependent upon the occupationWe usually reiterate what advice has been given by their consultantThey are advised that return to work is dependent on the job they do so length of time off work can vary from person to person |
Appendix 4 Supporting information for the patient interviews (intervention mapping stage 1)
Interview schedules
Patient interview schedule
-
Thank you for taking the time to meet with us today.
-
Have you read the information leaflet and informed consent form? Do you have any questions before we start? There are no right or wrong answers and you don’t have to answer any questions that you don’t feel comfortable talking about. If it’s OK with you, we will use a digital audio-recorder to ensure that the interview is accurately documented. Everything you say will be kept confidential and anonymous. Your name will not be mentioned on any published documents and, therefore, anything you say cannot be identified as coming from you. Any names of individuals or places that you might refer to during the interview will be anonymised when transcribed. The recording will be stored securely at the University of Nottingham.
-
You are welcome to request a copy of your interview transcript if you would like to review it for clarification, to add to it, or to indicate that all or part of it should not be used.
| Topic area | Question | Prompts |
|---|---|---|
| Personal information | Can you tell me about yourself? | Health, home, family, work, hobbies, interests. Usual work and other activities. Driving (may be relevant to work) |
| Relevant experience | What has been your experience of RTW/RUA following knee or hip replacement? |
Who else has been involved (e.g. GP, AHPs, occupational health, managers, HR, Fit for Work services, family) When and how are they involved – how effective are they? What has happened re RTW/RUA and when? |
| Perceived obstacles/facilitators |
What things make/could make it difficult for patients who have had knee or hip replacement to RTW/RUA? What things make/could make it easier for patients who have had knee or hip replacement to RTW/RUA? What helps/would help you and other patients to RTW/RUA? |
Information related Extent of sufficient/consistent/useful information/advice for patients/GPs/employers on RTW/RUA following surgery. What needed? How information/advice should be delivered/accessed? When? By whom? Patient related Motivation/attitude/beliefs/expectations re RTW/RUA including self-efficacy, anxiety Sick leave history/absence Extent of functional ability prior to surgery Life context – age, home circumstances, travel to work. Family roles and responsibilities. Work–life balance. Financial circumstances Transferable skills Comorbidities Adherence/compliance with advice/support Symptom management Workplace related Relationships Workplace/managerial support Workplace conditions – environment, pace, tasks, job demands, shifts/hours, travel, availability of adjustments/redeployment, culture, sick pay/absence policies Equipment Activity outside workplace Physical and mental demands of UA (including ADLs, hobbies, interests, family roles and responsibilities, social activities) RTW management Communication/transfer of information between key players. How conducted, by who, when? Extent of an agreed RTW plan Co-ordination of RTW Key players’ skill in RTW management Societal Economic factors/conditions – local, national Surgery related Waiting times/delays to surgery Surgical approach/type of operation/components used Experience/ability of surgeon Complications/consequences Restrictions/precautions Extent of focus on activity pre and post op Information about procedure/resumption of activity Certainty of time scales Extent of consistent/tailored advice and support re RTW/RUA provided by clinicians/AHPs Follow-up/postoperative rehabilitation |
| Occupational intervention | What would an occupational intervention for patients look like? |
Who would deliver? Individual/team/profession/expertise When, how? Where? Ward – outpatient clinic, community Format – paper, online, phone apps, one-to-one sessions Components – assessment, advice, information, liaison, signposting, workplace visits |
| Outcome measurement | We are developing an intervention to help people RTW/RUA after surgery. How do you think we might best measure the effectiveness of the intervention from your perspective? |
Functional performance Duration of sick leave Sustained RTW/RUA Well-being |
| Is there anything else that you would like to say that we haven’t already discussed? | ||
Characteristics of patient interviewees
Occupations of the patient participants
-
Petrol station operative.
-
Book keeper.
-
NHS secretary.
-
Curate.
-
Information technology manager.
-
Re-enablement officer.
-
Engine technician.
-
Test and development engineer.
-
Mechanical maintenance fitter.
-
Warehouse operative.
-
Teaching assistant.
-
Royal Air Force medic.
-
Tax manager.
-
Post Office clerk.
-
Health-care assistant.
-
Medical secretary.
-
Supermarket worker.
-
Litho printer.
-
Production supervisor.
-
Company director.
-
Social worker.
-
Speech and language consultant.
-
Social worker.
-
Transport manager.
-
Builder.
-
Offshore rigger.
-
Family business/education adviser.
-
Care worker.
-
Cleaner.
-
Stone mason.
-
Teaching assistant.
-
Bricklayer.
-
Social worker.
-
Maintenance engineer.
-
NHS ward clerk.
-
Family carer.
-
Shop manager.
-
Farmer.
-
Mechanic.
-
Volunteer ambulance driver.
-
School lunchtime supervisor.
-
Bank clerk.
-
Technical author.
-
Undertaker’s assistant.
-
Nurse.
Patient interview quotations
As described in Chapter 5, patient interviews produced the following six themes:
-
preoperative context
-
postoperative context
-
advice received
-
GP role and fit note
-
barriers to and facilitators of RTW
-
perceptions of an occupational advice intervention.
Direct quotations to supplement the narrative description in Chapter 5 are presented in the following sections.
Theme: the preoperative context
I was off 2 weeks before I had my operation on 6th of February because the cleaning was just too much for us with the pain in my leg, and I had stumbled a couple of times and had a fall before that. And the head was a bit too worried with working with small children as well, I didn’t want to be injuring myself before I had the operation.
1302
And before the operation I couldn’t bend down to put my work boots on, my wife was having to do that, and to put my socks on.
1204
I’d have let them chop my leg off. Because it just gets you down . . . I said to the boss before I had it done, when she came to see me when I was back at home, I said I was really at the end of my tether, I’d had enough.
1206
So it was just no good for work, so I thought I might as well just bite the bullet and get it done . . . they said well just take painkillers. I said that’s no good, because it doesn’t stop the pain. It just niggles all the time constantly. I couldn’t get any sleep because of it . . . I said well the way it is now I’ll not be able work within another 2 or 3 months anyway.
2301
I work as a tax manager and an accountant . . . so January tax return deadline I had to try and get it so that the appointment within the 8-week period fell preferably after the end of January . . . I just wouldn’t conceivably be able to have the time off work around November/December time . . . I just couldn’t afford to have 6 weeks off work at the time . . . so I’m the only person doing the tax.
1023
Theme: the postoperative context
I asked for it (fit note) and they didn’t get it organised and then on the day I was leaving they still hadn’t got it organised. So I then had to phone up the GP and get the GP to sort me one out . . . And it was the same with the medication, there was a mix up with the medication as well, so they just sent me home with paracetamol, which didn’t do anything . . . And it just amazed me, the test that they do to decide that you’re fit to go home, because one of the key things is whether you can get upstairs, well . . . they test you going up two steps. Well that in reality is totally different from getting up a whole flight of stairs.
1107
I have to say I was very disappointed with what the NHS physio service was like. My first appointment was at 4 weeks . . . So they looked at mobility rather than strength and stuff like that. My leg is still very weak and to my mind that’s keeping me from doing more stuff . . . But if I wasn’t paying physio to monitor what I was doing, I probably wouldn’t have ever done more strengthening exercises.
2009
I always knew that I would be working anyway. I had no intentions of not working totally. I always knew I was going to be on the telephone and talking to clients and things like that.
2201
I also tried to do bits and pieces of work at home because I got a laptop from work so I was at home for four weeks and I still wasn’t able to drive at that particular time but my mobility was pretty much OK for me to walk about. I had no issues with walking and climbing stairs or anything like that, so my manager actually at work would come and pick me up in the morning and bring me into work and then drop me home at night.
1105
Theme: advice received
. . . there wasn’t very much about going back to work.
2009
He actually said to me, are you driving? I’m like well, no, because I was told I had to get clearance from you to allow me to drive. He said well, look at you, you’re doing remarkably well, I’m delighted with your progress, you could have been driving.
1105
You get conflicting [advice], like I said with the running. The surgeon said you can run, the person I saw, and then the physios say whatever you do, you can’t run.
Well I sort of had a rough idea, they said like possibly 3 months. But basically that’s all I got told. You’ll be able to go back to work after 3 months really. That’s all I got told really to be honest.
1231
No, for me, it [information pack] answered all my questions and it was OK as a reference . . . it was quite nice having something to refer to.
2013
Theme: the general practitioner role and fit notes
I’m very pleased generally with my GP. He checked my knee all over, but obviously they’re not a specialist. So he referred me on, and he said he wasn’t very happy with it. But he did look at the X-ray as well. He looked at the X-ray and said that don’t look very good at all sort of thing. And said we need to look at seeing an orthopaedic surgeon basically. So yeah, I’m quite happy with the way they did things, they did it properly really.
2105
There’s very limited contact at all [with GP]. The only real contact was to request a sick note and pain relief.
2002
I think I was meant to get them [fit notes] from the hospital but I never ever got one. I had to go to my GP and get them from him.
1005
. . . she wanted to give me a longer one and I just said, we compromised. She said 8 weeks, I said oh no can you just give me it for 4 weeks? And she said well what about 6 weeks? I said no if we have 4 weeks, and then hopefully I might be able to go back. Anyway we compromised on the 4 weeks and she’d said to me when you go back you go back on phased return, I don’t want you working you know, and just discuss it your line manager. But at the end of the 4 weeks I found I was able to go back. So that was the end of her input.
1229
I didn’t have a sick note, no. They just said look, you’re off for 3 months. I’m self-employed, I didn’t require a sick note. Now, if I’d been employed, I would have asked for one, obviously. I would have said look, I need a sick note that says I’m off for 3 months to give to my gaffer, my boss. But because I didn’t require one, it wasn’t a problem really.
2201
Theme: workplace barriers to and facilitators of work
Prior to surgery
I didn’t tell him until I was actually on the waiting list. I didn’t think there was any point. I wasn’t having time off work with the hip, but I did need to let him know as soon as I went on the waiting list. I said I’ve got this problem and in 3 months’ time hopefully I shall be having the op and then I’ll be off for 6 weeks to give him notice.
1003
Well obviously I rang him up straightaway. And he was very understanding. He was more concerned that things had gone wrong for me than actually the implications at work, well that’s how he came across. Maybe what he said once I’d put the phone down, but actually no he was very good. So no, they were helpful. One of the things I suppose visually for my employer as well is that when I’d seen the consultant he actually said take some photographs of your X-rays. So I actually had them on my phone.
1005
I did say I was going to have another knee operation because it was so bad. And they were fine . . . They didn’t know I was going to have another one until the last minute, I never told them until it got so painful . . .
2101
Following surgery
I think they must have procedures. Once you’re off after 2 weeks or 3 weeks, then they must, or 12 weeks. Because I had someone from HR [human resources] come after my operation, after about 2 weeks you see to see me, to ask me questions and things like that.
1231
It was all me that was doing, that was telling them and advising them on how long I was going to be off.
1204
. . . I had open discussions with my boss about this, and his biggest concern was to keep the HR [human resources] people off his back and making sure that I could give him as much as possible to help him in that process. It was a joint effort against HR . . . Even though I had a sick note in place, and even though they had dates supported by that note and obviously health professionals, they were still chasing my boss’ boss every week . . . Again that’s because they’ve applied a blanket policy rather than considering individuals and the varying responsibilities.
2002
I did get a visit from the service manager and a lady from HR [human resources]. That was the week, 2 actually. It was probably 2 weeks before I was due to go back because that’s when I said I’ve got my sick notes. It runs out and I’m going to return to work on 13th and it was probably something like 9th, or something like that, and the HR lady said you can’t come back until we arrange for you to see the occupational [health] therapist.
1228
Job demands
It’s quite demanding, climbing on roofs and going down the voids underneath, and climbing ladders and climbing into the back of machinery and vents and everything like that . . . Eight until four Monday to Friday.
1012
. . . the job that I had with a lot of restraints, up and down from the floor and things quite a lot would also not do the hips a lot of good . . . As it was, I was getting by at work. If we ended up having a restraint, I’d be in quite a lot of pain afterwards, especially if it was one that went to the floor and then getting back up from the floor.
1101
I’m up and down on my seat, but I am in the banking hall as well as serving customers. And there’s a lot of coin and change involved, so lifting bags of change yeah . . .
2318
I think for work the reason might have been risk to myself of maybe falling or, you know, with working in a tight situation and like my first job’s with very small children in a dining room, in a playground and I’ve got to be able to move around fairly quickly.
1302
. . . walking across a [construction] site that can be quite uneven covered in bits, stones, you know, it’s very uneven ground it did make me very aware that it’s a quite a dangerous industry anyway and you do need to be fit.
2201
Line management
So I was very keen to get back, which the vicar knew, very keen to get back to some aspect of ministry that I could do. And he was aware that in the short term that there were things that I would be less likely to do, and then working towards as I progressed in mobility and so on working towards going back into doing anything that needed to be done within reason.
1319
I sorted it with my employer because I’m only part time and he’s very accommodating and I had no – if I’d had a different type of job, obviously I think I would have thought differently. But I went back to work knowing that if I couldn’t cope I could come home. I went back at the right time and I had lots of support from him.
2013
Probably being more around to talk to me, you know, it’s like I was told by my line manager that I couldn’t use a walking stick in school because of insurance reasons. And then I had the meeting with the head of the school and my line manager, and the head of the school said I can use my walking stick. So it’s things like that, it has got me a little bit annoyed, because then I wouldn’t have had been pushing myself and straining with walking without my stick.
1018
Policies and procedures
And obviously [employer name] are scared of litigation, simple as that. That’s why they won’t let me go back until I’m fit for work, until the doctor says you’re fit. Litigation, because if I fall, have an accident, all I’ve got to do is say well they made me come back and that’s it, I can sue them, job done.
1011
. . . It comes from management down unfortunately that’s the decision they’ve made, that they want it to be totally hot-desking. So it’s all down to work and work environment optimisation. And they don’t make any allowances.
. . . the manager there at that site was very helpful, his hands were tied because he isn’t, he is in charge of that plant, the directors are based somewhere else that say, no, we’re not employing anyone else and that’s a decision that he has to live with.
2303
Sick pay and sick leave
And the other good thing as well is the time off I had post surgery doesn’t go against my sickness record. Whereas some places it would go on your sickness record that you’ve been off for so many . . . No, they’ve got those 45 days down on my record, but it doesn’t trigger the sickness management procedure.
1107
Well, I wouldn’t, I won’t sign on the sick. I wouldn’t sign on because with us working before, my kind of work, now I can only work so long, we’re going to get tax money back, a rebate, so much. But if you sign on sick money or unemployment in the year you can’t get it back until the next month, because you have to tax to pay on your sick money. Now, I didn’t know until they told me – the tax office – so yes I was off for a few weeks. They would send me £3 a week, that’s all I got. And she says out of that it’s added up the end of the year on your wages, and you pay 20% tax on it, back to the government. Well I said it’s not worth, firstly it’s not worth then for £59 a week it worked out at, I said I just wouldn’t go to all the hassle and all the what goes on with it. So, you didn’t bother to do any of that? No, I never bothered. I lived off what I’d earned.
2209
I get 3 days sick pay from my employer and then I go on to statutory sick. I couldn’t afford to maintain myself on that because obviously I’ve got my overheads to pay. So I then had to allocate holiday and I also tried to do bits and pieces of work at home because I got a laptop from work so I was at home for 4 weeks and I still wasn’t able to drive at that particular time but my mobility was pretty much OK for me to walk about.
1105
. . . because in January I was fine. February I only got £800. March I only got . . . [unclear]. April I only got £400 I think, so I had to go back.
2004
Yes, well normally with working for the council you’re off for 6 months with full pay, and then after that you go on half pay. So I’m now on half pay until October.
1332
Colleagues
Yeah, they all like mucked in . . . they’re all saying I’ll take that out for you. I go no it’s all right, I can do it myself . . . I mean I know if I need help I’d only have to ask.
1206
Yeah, they’ve been OK, because they’ve had cover from the very beginning, so nobody’s doing outside, more than what they have to, they’ve covered it so everything’s just fine it’s been covered. Because I know when you’re off sometimes somebody else gets your workload, it cannot be very good, but it’s been all covered.
1307
Yeah they all say oh mind your leg and things like that. I say I’m all right, yeah. Oh yeah, people I work with yeah, yeah, they are very supportive but you know they’ll say I’ll go and do that, so, you know, at the end of the corridor and things like that.
2210
And so because my role changed a little bit. Instead of being a guy who puts engines together, I was a guy who was on the computer sorting out which bits had to go where, and they just saw that as lazy, because they saw me cycling into work . . . Everybody knew, it’s just that some people’s perception is skewed because in a workshop environment it can be quite aggressive shall we say. But it can be also on the bordering of bullying I would presume it would be.
1011
Work modifications
I’m fortunate in having the flexibility with regards to when and where I work. I suppose the best illustration of support at the moment is that I won’t drive for more than say 3 hours in a day. And I’ve been told, that was my decision and I’ve been told as a consequence of that if I need stay over at somewhere, get a hotel, then that is fine . . .
2002
I’m walking around a fair bit and I’m doing a 4-hour shift. I went back Monday 4 hours and I shall be doing 12 hours this week, just for a couple of weeks, and then I should go back to doing my full 15. I’m just phasing back gradually.
2013
Tuesday 4th January was the day I returned and what my manager had said was I think you should do restricted days, I think you should do 2 hours the first day, 4 hours the second day, 6 hours the third day, 8 hours the fourth day. Anyway, after the second day, I was back. I said no that’s not the answer, the answer is I need to do just a morning for the first week and maybe a little bit more on the second week, and that’s what I did . . . I know how I feel. I know what I can do and what I can’t do.
2206
I think they could have, yeah they could have said come back and see, why don’t you come back maybes and do a couple of hours and see how you feel. But they didn’t mention that to me, nothing . . . I thought, you know, but then I’m 56, and I think of my age, you know, what other professions, what could I do, will other people, you know, will I get another job at my age . . .
2210
Yeah I would have liked to have gone back part time, it wasn’t offered . . . if I hadn’t had the same job I would have been back at work, but not the job that I had been doing. You’re carrying motors around, you’re crawling under machines, you’re then climbing up through, up ladders, up into the roof space and things like that . . .
2303
Occupational health
I have to go to occupational health first for them to say yes I’m OK to return. And without a fit to return work note they won’t, they’ll say no, go and get one . . . And obviously [employers name] are scared of litigation, simple as that. That’s why they won’t let me go back until I’m fit for work, until the doctor says you’re fit. Litigation, because if I fall, have an accident, all I’ve got to do is say well they made me come back and that’s it, I can sue them, job done.
1011
The only time I’ve seen occupational health was when I was due to go back, which was about 3 months. That’s the only time I’ve seen, they’ve sent me to like your work’s doctors, occupational health . . .
1231
I had 2 months off, but when I did go back to work I had an occupational health review from work and well-being report. So two members of staff came out to see me at home . . . they came out and did a full report. And then when I did go back to work I went back on a phased return. But there was certain things that they wouldn’t let me do. I couldn’t lift any coins, they made sure I was up and down off my seat walking around every 20 minutes or so.
2318
Well there was occupational health involvement, and we have a, I had to have a risk assessment done. And they just, and in between occupational health, risk assessment officer and my manager, it was put in place for what I could and couldn’t do when I came back to work.
1229
I went there [occupational health] and she asked, previously I had to write down everything. How many stairs and so on, and how I feel going back to work, if I feel comfortable and so. And I wrote everything down, and then when I was there with this nurse she asked me the same questions, and I said the same what I wrote down. And then she said do you feel then, do you think you are ready to go to work? I said yeah what do you want really from me? I couldn’t get this. To be honest the whole thing was 10 minutes, and she, I think it was just a waste of time but it’s only what I think.
1106
Theme: perceptions of an occupational advice intervention
Perceived need
Yeah possibly, I wouldn’t say in my case that that was something that I was really crying out or really needed. I could see possibly cases where it would be useful.
1005
I would say no, nothing like that would have helped me. But I do feel that’s only because I’ve got a good insight.
1011
I never even thought about phoning them up for any information or support on getting back to work because I felt I was well supported by my own management. But if I’d felt that they’d been obstructive anyway or I was having problems I would have probably phoned the advice line. But I didn’t need to.
1107
Well yes and no. I mean I suppose it’s different for everybody. I mean I’ve got people at work I can raise issues with if I have concerns about things. So that for me wouldn’t be a problem. But it might be for somebody else.
1307
Format
I haven’t even got a computer, the wife has one, but . . . No, I’m one of these cave men when it comes to computers.
2103
. . . it maybe sounds a bit unusual for somebody who works in IT and is always looking at a screen. But yeah, I think I must admit I prefer the book and actually having something that you can handle sort of thing.
1005
I think if you’ve got it at hand you can carry it around with you, and you can get it out any time you need to.
2318
And perhaps the opportunity to talk to other people in similar circumstances, because we don’t tend to talk about these things, do we?
2002
I suppose if you hand them a leaflet and say look that’s what it’s going to involve, and that’s what I’m going to need off, etc. So they know what’s going on yeah, it would be a good idea for that.
2105
Content
I think just some more realistic time scales.
2002
Well that it’s beneficial to have an employee back for a limited amount of time on limited duties, rather than having somebody back straightaway who might regrettably have to go off again.
1001
I suppose everybody’s different but that would have been nice to have said, probably in a little leaflet or something, there is a chance you could be back at 8 weeks but don’t worry if you’re not, you know. It could take you longer and you’ve just go to sort of try and build that level of energy back up and your strength levels before you feel you should go back to work.
1102
. . . like an idiot’s guide to what’s going to happen because, like I say, it didn’t cross my mind about work.
1228
I mean just advice. I needed reassurance, am I doing the right thing? You know should I be standing in the tea bar from 8 until 4. Is that OK? If this hurts should I do . . . I just needed reassurance.
1205
Delivery
When you go to your GP or your surgeon shall we say, you maybe should get a booklet or a leaflet or something just to give you that bit more help and confidence.
1204
. . . a mentor or a physio person will be able to see you walk, can simulate what you do in your job, and then say yeah.
1011
Yeah it probably would have been quite useful, probably at the time that you actually put down that you do need a hip replacement and then you’ve got all the information there what you need instead of just like the information on the actual hip itself and the procedure.
1216
Obviously after the operation, and when I’ve, after a few weeks I’ve been obviously home after the operation. So once you’ve had a bit of a chance to recover a bit. To recover yeah, because obviously after the operation you don’t see anyone after that do you really?
1231
Appendix 5 Supporting information for the stakeholder interviews (intervention mapping stage 1)
Stakeholder interview schedules
| Topic area | Question | Prompts |
|---|---|---|
| Demographics | Can you tell me about your organisation? |
Size – small/medium/large or number of employees Sector – private, public, third Type of work – manufacturing, service Manual/non-manual work Environment – office/shopfloor/environment (in/outdoor), site work Special needs/statutory requirements of the jobs (e.g. HGV drivers/divers/pilots/food handlers/safety critical work/specialist equipment) Range of jobs RTW policies and procedures – availability of workplace adjustments, graded returns Occupational health provision – none/ad hoc, contracted out, on site |
| Individual role |
What is your position in the organisation? What role do you have in return-to-work/people management responsibilities? |
Duties, responsibilities, time in post Feelings/views about this role? Potential changes to/development of role |
| Relevant experience/knowledge |
What experience do you have of supporting people at work who have had knee or hip replacement? Details of any relevant training? |
Duties, hours of individual employee(s) How involved in providing support Who else involved – e.g. GP, AHPs, occupational health, managers, HR, Fit for Work services When and how were they involved – how effective were they? What happened, and when? |
|
Perceived obstacles/facilitators Needs of employer |
What things make/could make it difficult for employees who have had knee or hip replacement to return to work? What things make/could make it easier for employees who have had knee or hip replacement to return to work? What would help employers support people return to work following knee or hip replacement? |
Information related Extent of sufficient/consistent/useful information/advice for patients and employers on RTW following surgery. What needed? How information/advice should be delivered/accessed? When? By whom? Patient related Motivation/attitude/beliefs/expectations re RTW including self-efficacy, anxiety Sick leave history/absence Extent of functional ability prior to surgery Life context – age, home circumstances, travel to work. Family roles and responsibilities. Work–life balance. Financial circumstances Transferable skills Comorbidities Adherence/compliance with advice/support/RTW plan Symptom management Workplace related Relationships Workplace/managerial support Workplace conditions – environment, pace, tasks, job demands, shifts/hours, travel, equipment use, availability of adjustments/redeployment, culture, sick pay/absence policies Employer related Extent of time/resources/skills to support employee in RTW Experience/training Prior experiences (positive/negative) RTW management Communication/transfer of information between key players. How conducted, by who, when? Extent of an agreed RTW plan Co-ordination of RTW Key players’ skill in RTW management Societal Economic factors/conditions – local, national Surgery related Waiting times/delays to surgery Complications/consequences Restrictions/precautions Extent of focus on activity pre and post op Information about procedure/resumption of activity Certainty of time scales Extent of consistent/tailored advice and support re RTW provided by clinicians Follow-up/postoperative rehabilitation |
| Occupational intervention | What would an occupational intervention for employees look like? |
Who would deliver? Individual/team/profession/expertise When, how? Where? e.g. ward – outpatient clinic, community Format – paper, online, phone apps, one-to-one sessions Components – assessment, advice, information, liaison, signposting, workplace visits |
| Outcome measurement | We are developing an intervention to help people return to work after surgery. How do you think we might measure the effectiveness of the intervention? |
e.g. Days to RTW Subsequent sickness absence Duration of modified duties/hours Employer’s perception of work performance/productivity Time/resources required in supporting employee, e.g. occupational health referral, equipment needs |
| Is there anything else that you would like to say that we haven’t already discussed? | ||
| Topic area | Question | Prompts |
|---|---|---|
| Demographics | Can you tell me about your department? |
Number of surgeons Population served Specialism (general/specific) |
| Individual role |
What is your position in the department? What role do you have in patients’ return to work (RTW)/return to usual activity (RUA)? |
Duties, responsibilities, time in post. Occupational health training, full time/part time Consultant, registrar? individual specialism Whose role do you think RTW support is? Experiences/views about this role? Perceived future changes to/development of role |
| Relevant experience |
What experience do you have of supporting people RTW/RUA who have had knee or hip replacement? Any training? |
How have they been involved, actions taken? When? Pre-op post-op clinic? Who else involved – e.g. GP, AHPs, occupational health, managers, HR, Fit for Work services, family When and how are they involved – how effective are they? What happens and when? |
| Perceived obstacles/facilitators |
What things make/could make it difficult for patients who have had knee or hip replacement to RTW/RUA? What things make/could make it easier for patients who have had knee or hip replacement to RTW/RTUA? What would help you as a surgeon to support your patients to RTW/RUA? |
Information related Extent of sufficient/consistent/useful information/advice for patients/GPs on RTW/RUA following surgery. What needed? How information/advice should be delivered/accessed? When? By whom? Patient related Motivation/attitude/beliefs/expectations re RTW/RUA including self-efficacy, anxiety Sick leave history/absence Extent of functional ability prior to surgery Life context – age, home circumstances, travel to work. Family roles and responsibilities. Work–life balance. Financial circumstances Transferable skills Comorbidities (physical/psychological) Adherence/compliance with advice/support Symptom management Workplace related Relationships Workplace/managerial support Workplace conditions – environment, pace, tasks, job demands, shifts/hours, travel, availability of adjustments/redeployment, culture, sick pay/absence policies. Equipment Activity outside workplace Physical and mental demands of UA (including ADLs, hobbies, interests, family roles and responsibilities, social activities) Surgeon related Extent of time/resources/skills to support patient in RTW/RUA Experience/training Prior experiences (positive/negative) RTW management Communication/transfer of information between key players. How conducted, by who, when? Extent of an agreed RTW plan Co-ordination of RTW Key players’ skill in RTW management Societal Economic factors/conditions – local, national Surgery related Waiting times/delays to surgery Surgical approach/type of operation/components used Experience/ability of surgeon Complications/consequences Restrictions/precautions Extent of focus on activity pre and post op Information about procedure/resumption of activity Certainty of time scales Extent of consistent/tailored advice and support re RTW/RUA provided by clinicians/AHPs Follow-up/postoperative rehabilitation |
| Occupational intervention | What would an occupational intervention for these patients look like? |
Who would deliver? Individual/team/profession/expertise When, how? Where? Ward – outpatient clinic, community Format – paper, online, phone apps, one-to-one sessions Components – assessment, advice, information, liaison, signposting, workplace visits |
| Outcome measurement | We are developing an intervention to help people RTW/RUA after surgery. How do you think we might best measure the effectiveness of the intervention from your perspective? |
Patient’s functional performance Sustained RTW/RUA Specific outcome measures Well-being |
| Is there anything else that you would like to say that we haven’t already discussed? | ||
| Topic area | Question | Prompts |
|---|---|---|
| Demographics | Can you tell me about your GP practice? |
Indices of deprivation Size Population served |
| Individual role |
What is your position in the practice? What role do you have in patients’ RTW/RUA? |
Duties, responsibilities, time in post Partner, salaried, occupational health training, full time/part time Experiences/views about this role? Perceived future changes to/development of role |
| Relevant experience | What experience do you have of supporting people RTW/RUA who have had knee or hip replacement? |
How involved, actions taken. Use of fit notes, referral/signposting? Who else involved – e.g. AHPs, surgeon, occupational health, managers, HR, Fit for Work services, family When and how were they involved – how effective were they? What happened and when? |
|
Perceived obstacles/facilitators Needs of GP |
What things make/could make it difficult for people who have had knee or hip replacement to RTW/RUA? What things make/could make it easier for people who have had knee or hip replacement to RTW/RTUA? What would help you as a GP to support your patients to RTW/RUA? |
Information related Extent of sufficient/consistent/useful information/advice for patients/GPs on RTW/RUA following surgery. What needed? How information/advice should be delivered/accessed? When? By whom? Patient related Motivation/attitude/beliefs/expectations re RTW/RUA including self-efficacy, anxiety Sick leave history/absence Extent of functional ability prior to surgery Life context – age, home circumstances, travel to work. Family roles and responsibilities. Work–life balance. Financial circumstances Transferable skills Comorbidities Adherence/compliance with advice/support Symptom management Workplace related Relationships Workplace/managerial support Workplace conditions – environment, pace, tasks, job demands, shifts/hours, travel, availability of adjustments/redeployment, culture, sick pay/absence policies Activity outside workplace Physical and mental demands of UA (including ADLs, hobbies, interests, family roles and responsibilities, social activities) GP related Extent of time/resources/skills to support patient in RTW/RUA Experience/training Prior experiences (positive/negative) RTW management Communication/transfer of information between key players. How conducted, by who, when? Extent of an agreed RTW plan Co-ordination of RTW Key players’ skill in RTW management Societal Economic factors/conditions – local, national Surgery related Waiting times/delays to surgery Complications/consequences Restrictions/precautions Extent of focus on activity pre and post op Information about procedure/resumption of activity Certainty of time scales Extent of consistent/tailored advice and support re RTW/RUA provided by clinicians Follow-up/postoperative rehabilitation |
| Occupational intervention | What would an occupational intervention for these patients look like? |
Who would deliver? Individual/team/profession/expertise When, how? Where? Ward – outpatient clinic, community Format – paper, online, phone apps, one-to-one sessions Components – assessment, advice, information, liaison, signposting, workplace visits |
| Outcome measurement | We are developing an intervention to help people RTW/RUA after surgery. How do you think we might best measure the effectiveness of the intervention from your perspective? |
Amount and duration of sickness certification (not fit/may be fit) Frequency of GP consultations Resource implications of GP consultations – prescriptions, referral on, signposting Communication with other key players |
| Is there anything else that you would like to say that we haven’t already discussed? | ||
| Topic area | Question | Prompts |
|---|---|---|
| Demographics | Can you tell me about your department/unit/service? |
Number of therapists, qualified/support workers Population served/specialism |
| Individual role |
What is your position in the service? What role do you have in patients’ RTW/RUA? |
Duties, responsibilities, time in post Occupational health training, full time/part time Feelings/views about this role? Perceived future changes to/development of role |
| Relevant experience |
What experience do you have of supporting patients RTW/RUA who have had knee or hip replacement? Relevant training |
How have they been involved, actions taken? Pre-op, peri-op, post-op? Who else involved – e.g. GP, AHPs, occupational health, managers, HR, Fit for Work services, family When and how are they involved – how effective are they? What happens and when? |
| Perceived obstacles/facilitators |
What things make/could make it difficult for patients who have had knee or hip replacement to RTW/RUA? What things make/could make it easier for patients who have had knee or hip replacement to RTW/RTUA? What would help you as an AHP to support your patients to RTW/RUA? |
Information related Extent of sufficient/consistent/useful information/advice for patients/GPs/employers on RTW/RUA following surgery. What needed? How information/advice should be delivered/accessed? When? By whom? Patient related Motivation/attitude/beliefs/expectations re RTW/RUA including self-efficacy, anxiety Sick leave history/absence Extent of functional ability prior to surgery Life context – age, home circumstances, travel to work. Family roles and responsibilities. Work–life balance. Financial circumstances Transferable skills Comorbidities Adherence/compliance with advice/support Symptom management Low mood/well-being Workplace related Relationships Workplace/managerial support Workplace conditions – environment, pace, tasks, job demands, shifts/hours, travel, availability of adjustments/redeployment, culture, sick pay/absence policies. Equipment Activity outside workplace Physical and mental demands of UA (including ADLs, hobbies, interests, family roles and responsibilities, social activities) AHP related Extent of time/resources/skills to support patient in RTW/RUA Experience/training Prior experiences (positive/negative) Motivation to change practice/attitudes to AHP involvement in RTW issues Staffing structure and levels Organisational support/infrastructure RTW management Communication/transfer of information between key players. How conducted, by who, when? Extent of an agreed RTW plan Co-ordination of RTW Key players’ skill in RTW management Societal Economic factors/conditions/context – local, national Surgery related Waiting times/delays to surgery Surgical approach/type of operation/components used Experience/ability of surgeon Complications/consequences Restrictions/precautions Extent of focus on activity pre and post op Information about procedure/resumption of activity Certainty of time scales Extent of consistent/tailored advice and support re RTW/RUA provided by clinicians/AHPs Follow-up/postoperative rehabilitation |
| Occupational intervention | What would an occupational intervention for this patient group look like? |
Who would deliver? Individual/team/profession/expertise When, how? Where? Ward – outpatient clinic, community Format – paper, online, phone apps, one-to-one sessions Components – assessment, advice, information, liaison, signposting, workplace visits |
| Outcome measurement | We are developing an intervention to help people RTW/RUA after surgery. How do you think we might best measure the effectiveness of the intervention from your perspective? |
Patient’s functional performance Sustained RTW/RUA Specific outcome measures Well-being/QoL |
| Is there anything else that you would like to say that we haven’t already discussed? | ||
Characteristics of interviewees
| Workforce sizea | Relationship to employee | Sector |
|---|---|---|
| Small* | Colleague | Private health-care provider |
| Small* | Managing director | Manufacturing |
| Small | Manager | Hospitality |
| Medium | Manager | Manufacturing |
| Medium | Human resources | Service sector |
| Medium | Occupational health advisor | Manufacturing |
| Medium | Managing director | Service sector |
| Large | Manager | Central government |
| Large | Manager | Primary education |
| Large | Occupational health physiotherapist | Manufacturing |
| Large | Human resources | Transportation |
| Large | Occupational health nurse | Leisure/hospitality |
| Large | Human resources | Transportation |
| Large | Human resources | Leisure/hospitality |
| Large | Manager | Leisure/hospitality |
| Large | Manager | NHS trust |
| Large | Staff liaison manager | NHS trust |
| Large | Human resources manager | NHS trust |
| Large | Human resources | Further education |
| Large | Manager | Local government |
| Large* | Occupational health nurse | Local government |
| Large* | Employee relations | Higher education |
| Large* | Manager | Higher education |
| Large* | Human resources | Retail |
| Various | Occupational health physician | Various |
| Site | Method | THRa (number of replacements) | TKRa (number of replacements) | Number of years in post |
|---|---|---|---|---|
| A | Face to face | 165 | 230 | 11–15 |
| A | Face to face | 404 | 578 | 6–10 |
| A | Face to face | 207 | 179 | 21–30 |
| A | Face to face | 74 | 73 | 0–5 |
| B | Face to face | 376 | 337 | 11–15 |
| B | Face to face | 337 | 334 | 6–10 |
| B | Face to face | 102 | 145 | 0–5 |
| B | Telephone | 331 | 355 | 21–30 |
| C | Face to face | 264 | 102 | 11–15 |
| C | Face to face | 341 | 511 | 16–20 |
| C | Face to face | 189 | 328 | 11–15 |
| C | Face to face | 733 | 423 | 11–15 |
| Method | Clinical Research Network | Years in general practice | Practice population | aIndices of Multiple Deprivation433 |
|---|---|---|---|---|
| Telephone | B | 11–15 | 14,879 | 6 |
| Face to face | B | 16–20 | 14,244 | 9 |
| Face to face | B | 0–5 | 8838 | 4 |
| Telephone | B | 0–5 | 14,197 | 3 |
| Telephone | B | 6–10 | 14,197 | 3 |
| Telephone | C | 16–20 | 10,421 | 6 |
| Face to face | C | 21–30 | 8895 | 7 |
| Face to face | C | 21–30 | 8895 | 7 |
| Face to face | C | 21–30 | 8895 | 7 |
| Face to face | C | 0–5 | 8895 | 7 |
| Telephone | C | 6–10 | 5556 | 6 |
| Telephone | C | 0–5 | 13,334 | 5 |
| Telephone | A | 16–20 | 13,739 | 5 |
| Telephone | A | 21–30 | 15,477 | 6 |
| Telephone | A | 21–30 | 4262 | 8 |
| Telephone | A | 31–35 | 7887 | 3 |
| Profession | Band | Years in post | Hospital sitea |
|---|---|---|---|
| Physiotherapist | 7 | 6–10 | A |
| Physiotherapist | 7 | 16–25 | A |
| Occupational therapist | 6 | 0–5 | A |
| Occupational therapist | 5 | 0–5 | A |
| Nurse practitioner | 7 | 11–15 | A |
| Occupational therapist | 7 | 0–5 | B |
| Occupational therapist | 6 | 6–10 | B |
| Physiotherapist | 7 | 11–15 | B |
| Physiotherapist | 7 | 16–25 | B |
| Nurse practitioner | 7 | 0–5 | C |
| Nurse practitioner | 6 | 0–5 | C |
| Occupational therapist | 7 | 0–5 | C |
Interview quotations
Workplace representative interviews
As described in Chapter 6, interviews with workplace representatives produced the following three themes:
-
experiences of accommodating patients undergoing THR and TKR in the workplace
-
barriers to and facilitators of RTW
-
perceptions regarding an occupational advice intervention.
Direct quotations to supplement the narrative description in Chapter 6 are presented in the following sections.
Theme: experiences of accommodating patients undergoing total hip replacement and total knee replacement in the workplace
But my other lady, bless her, worked right up until she had it because she needed to work. So I made sure that she had a lot of support in place. A lot of our accommodation can be quite far out. I made sure she was close to base. And she found it a lot easier if she rode a bike instead of walking. So I made sure that she had her own bike to get to and from the accommodation. She struggled with making the beds side, so we had her beds made for her, just that extra support until she did go off and have it done.
15, manager
[Prior to surgery] The teacher wouldn’t let on that she was in pain, but you could see that she was getting tired and her hip was, you could see the way she walked was different . . . but you could see that she was in pain and at the end of a day that that fatigue crept in.
19, manager/headteacher
So what we had to do with him was look for alternative work. And we actually managed to get him alternative work within the engineering department that didn’t require him to do kneeling down.
3, head of human resources
I mean he’d been having problems with his knee for 18 months or so and then got advised from his doctor that he really needs to have the knee replaced and he shouldn’t be at work until such time as it’s done. So he’s been off basically sick awaiting the operation. Which he still hasn’t had and doesn’t expect to have until January . . . I would have thought he’d have been capable of doing, even if he was having this knee problem, but the advice from the doctor was no you should not be at work at all.
11, managing director
Theme: barriers to and facilitators of return to work
Occupational health
I think we’re probably in a better position than perhaps some smaller organisations or private organisations, and we’ve got access to an occupational health service which we purchase from a local hospital.
20, staff liaison manager
With anybody that’s coming back from any type of invasive surgery we would refer that person to occupational health just to make sure that we are doing everything with regards to the guidelines.
21, head of human resources
Our occupational health provider was so good at asking all the right questions and keeping us as informed as possible.
25, head of human resources
We sort of made it up as we went along. The person said oh I might be OK, my chair might be OK, I might not need anything. It was only when she came back and tried it and so there was a few days when she wasn’t comfortable and then there’s always a delay on OK so let’s get occupational health in now . . . I don’t think she [the employee] received anything automatically from our occupational health team. It wasn’t until we pulled them in. So there’s no policy to support a manager proactively prior to an operation, which would be helpful.
12, commissioning manager
We try to get them into the clinics before they come back as a whole anyway. I think it’s only the odd one that sometimes the clinics are just so full that that person is ready to come back; it’s just that we can’t get them in.
13, occupational health nurse
General practitioners
I know they only have 10 minutes at a time to have with each person, which is very limited, as to what the person’s job role is. Unless they volunteer the information, they just say well OK well when you go back to work I suggest work modifies your role and then they just tick the box. So I don’t think they’ve got to time to write things out a lot of the time.
17, occupational health adviser
Generally they’re [fit notes] not very good. I’ve got to be honest. They don’t put much information on there. They’re very vague. Just very . . . vague things, and just no, nothing that we can use. So that’s why we end up having to write to them asking them for more information.
6, occupational health adviser
. . . sometimes you get the impression that the doctors, I don’t know if rightly so, can be influenced by the individual . . . I don’t know if the GP’s up to spec with it [recovery from surgery]. And again I get the feeling that GPs can be influenced by how much the individual, what the individual says or expects.
18, manager
Other things that you asked are around a graded return, obviously known either by a phased return or more specifically in our department we call it part-time medical grounds. We can arrange that. We don’t need a GP’s consent or permission or approval for that. If we feel as management that it’s appropriate we can agree that directly with the individual.
16, manager
The employee
They’re ‘oh I’m really frustrated being at home, and I can’t go out and I really want to come back to work’. So I think it’s when they get to that stage it’s the right, well just because you’re feeling frustrated doesn’t mean that you’re fit enough to come back to work for example.
4, human resources employment relations manager
And sometimes we have staff members who say they feel fit to come back to work. And that might be because they actually do, or it might be because financially they’re worse off by not being at work.
11, managing director
. . . sometimes it’s quite daunting if somebody’s away for that length of them, you know, for them to feel a bit apprehensive about coming back into work. That individual, it took me 6 months to get them back to work and it was all to do with the fear side and the anxiety of it.
21, head of human resources
I suppose it’s down to how well they follow the instruction for their exercises and such to rehabilitate.
22, general manager
Because they’ve only either got a few months left or a couple of years left, and they just think do you know what, it’s not worth coming back and heaven forbid but doing any more damage.
3, human resources director
The workplace
So you have to adapt according to the number of staff that you have as well as to who can cover and who can help . . . it doesn’t always work that way if it’s a small company. That’s the difficulty as to how you can accommodate it accordingly and if other people are there to fill the shoes as well.
5, colleague
There wasn’t really the facility for her to come back on light duties or anything like that really because any administrative, we have admin staff for doing admin so, you know, and bookings where we get information off newly pregnant ladies and give them information, that would have involved a lot of sitting down which I don’t think would have been suitable for her. So you’ve got to hit that balance between activity and rest and I’m not sure we would have been able to provide activity and rest. It would have been a bit of a challenge for her I think.
23, ward manager
When they come back to work, we then continue the physiotherapy in-house. When we see them in-house then we carry out and do an assessment. We then provide them with an individualised strengthening programme and then we’ve got a rehabilitation gym. And then they complete their exercises down in our gym two to three times a day.
2, occupational health physiotherapist
Now obviously you can appreciate his return to work is very much more straightforward than somebody who’s out on the engineering shop floor.
3, human resources director
. . . it was difficult because we weren’t too sure how long he was going to be off for. He worked in a very specialised role so it was about training someone new to do that role and not knowing how long they were going to be able to be in that role for. It did make things really difficult.
25, head of human resources
Surgery
Her hip was fine, but she had a burn caused by whatever they use to cauterise the wound, caught the inside of her leg, which caused her quite a deep burn on the inside of her leg. So that was causing her more issue because that wasn’t healing very well. And that caused more issue than the actual hip in this case . . . that was the cause of her staying off longer.
19, manager/headteacher
. . . this particular case there was an added complication about soon after the operation she had DVT [deep-vein thrombosis] which extended that length of time that she couldn’t come back to work as well.
12, commissioning manager
And I suppose the difference then in NHS is that you may then have some people that are off for 6 weeks, some people are off for 8 weeks, maybe 10 weeks and it could potentially then cause problems.
2, occupational health physiotherapist
So anyway the operation was postponed several times over a period of about 2 years actually and of course the knee just deteriorated until he was struggling to walk . . . Well I think the postponement of the operations caused the problem to be exacerbated to the point where it was, it became a bigger and bigger operation if you like to do the work.
9, managing director
I think what delays them coming back to work is the length of time they have to wait for physiotherapy or stuff like that after their operation . . . Because I know that they want them to get up and get going, but then they have to wait a period of time before they’re having the physio or they’re checked . . .
14, human resources manager
Theme: perceptions regarding an occupational advice intervention
Perceived need
I think I would be very pleased to see it. Yeah to give us some kind of an idea, because an operation like that, I’ve got no idea how the recovery works and whether actually being physical and doing some work makes it better. I really don’t know. But I would be very interested to see something like that.
11, managing director
And therefore having guidance that lays out probably a best approach to return to work would be some phased return based around the advice from health-care professionals and the symptoms of the individual will lead to the person getting back to work and being an asset to the company or whatever . . . So I think from the employer having that sort of guidance. And I suppose at the moment, because that isn’t really in place it’s probably reliant on the individual having the surgery telling the employer well this is what’s going to happen.
7, manager/head of department
Timing
I mean getting the information as soon as we could would be helpful for us and presumably, I mean in [employee’s] case he had to finish work before he’d got a date for an operation or anything because it was so severe. What I would have thought with most people, they’re perhaps suffering and they would remain at work but perhaps have to be on restricted duties and you would then at least have a chance to say, you know, to timetable when the procedure’s going to be and what their recovery is going to be like.
11, managing director
I think it needs to be part of the consultation package to the employee, to the person who’s having the operation. So when the consultant’s talking about their operation and their recovery time and everything and you know, what work do you do and is that work feasible for you to go back to, I think it’s important that the consultant at that time finds out as much as possible and then probably gives it to them then. So that it’s sowing that seed right from the beginning that you will be able to return to work.
14, human resources manager
Because obviously if it’s, when you’ve gone for your appointment with the surgeon, being told about your operation, maybe that’s the point at which you should start thinking about it.
6, occupational health adviser
. . . but to me until the person has had their procedure and are therefore knowing whether there’s been any complications or whether the surgery went fine, that to me is when I personally would prefer it. Knowing that they’re going to be going off for a window of 6 to 12 weeks for example, that’s going to be the same. But obviously if then they’ve had complications and therefore it’s likely to extend past, or actually it’s been dead straightforward and it’s been easier than expected, that’s when personally I would feel that I would get the benefit out of it.
16, manager
Format
. . . when the employee has their surgery that as part of their pack maybe a leaflet with regards to advice for employers and the details of the website and the direction of where to go . . .
21, head of human resources
I think a leaflet kind of style rather than anything big and imposing. Again I can only really speak from this one person’s experience, but I know she doesn’t particularly like to read very much. So I guess things that have got illustrations in as much as useful words and things like that.
10, head of human resources
. . . if it was access online that would be great because every employer has got access for that. Because if it’s in a pamphlet or something, you know, I’m not being derogatory against people but you get a leaflet and it goes on the side and then it falls behind a cupboard and it’s gone; whereas I think everything that we look at now, as businesses, the first place that you do go for guidance is online.
21, head of human resources
And the other thing is, you see, we tend to – you’re not sitting in front of computer when you meet with them, so it would be nice to have something in your hand, you know, when you’re actually meeting with them that you can discuss.
24, senior human resources adviser
I mean I don’t know if there are advice lines or anything like that that people can contact if they’ve come back to work and they’re finding it a bit more difficult than they were anticipating to do so.
10, head of human resources
Delivery
. . . from the specialist or the doctor, so it’s specific to that person . . . I think probably his own GP, you know, because I mean there’s some, in the surgery I go to there’s some great nurses, nursing staff . . . and it could have been followed up, not going to hospital but attending as a patient at his own GP’s surgery. And that way you could probably go on a more frequent basis than going into hospital.
9, managing director
Well I mean I think from a functional perspective probably someone that’s at least got knowledge and skills related to that sort of post, well through rehabilitation I think . . . It does seem to me that folk like physios and occupational therapists would be well situated to take on that type of role – whether they’d want to or not . . .
7, manager/head of department
. . . if the site’s got an occupational health department, we would – either a 10-minute chat with the occupational health department and their line manager would probably be very good, to say we like to speak to the line managers directly and the occ [occupational] health department and have, and either give them this leaflet with guidelines and then they get to ask us any questions about the actual individual.
18, manager
I think it would be nice if you could have reports from people . . . But if the surgeon was to say well look, you know, you’ve chatted about what your job entails, then I would suggest that your work makes some modifications to, you shouldn’t really be doing this, this and this. And it actually has come our way in writing. I never get, we never hardly ever get anything, you know, it’s like scan results and X-ray results and physio updates. I mean they go off and have their physio and then they come back here and they say oh, oh, I say, how are you getting on with the physio? Oh I had my last one last week. Oh right, well how did it go? Oh not too bad. He said I don’t need to go anymore. Right, fine.
17, occupational health adviser
Content
So the booklet should turn round and say that if you have an occupational health centre, the best person to help you on any workplace adjustment is your occupational health centre, so please get in touch with them, because they’re the ones that have been out on the shop floor.
2, occupational health physiotherapist
I don’t know whether this is a barrier, but the fact that maybe if people have been off for 6 months, they may feel out of the loop so to speak, out of the loop of work . . . I think quite a lot of people seem, because the letter that we send out is quite a formal letter, and the meeting is called a formal attendance review meeting, so I think quite a lot of people get anxious and they’ve said that when they’ve turned up that they felt worried about it, because they weren’t sure what it was about. So I don’t know whether maybe as part of this manual thing maybe to give them an overview of what these meetings are, and the fact that they are a supportive method of helping to get, to find out what’s wrong with them and to help them and support them back to work . . . another thing to include in return to work is the rights of people coming back to work, that sort of thing.
10, head of human resources
Whether you’ve had one replacement or two replacements, and whether they’re done together or separately, and all of that sort of thing as well.
10, head of human resources
I suppose if it’s informative to all members of staff what to expect when they come back . . . be informative as to what they’ve been through and what to expect on their return . . . So that everybody can understand and well look, you can’t be expected to run up and down the stairs 10 times in the course of a day like you’d normally do.
5, colleague
And if the manual is also for HR [human resources], so if it’s about recommendations in terms of organisations, processes and procedures – one of my very key concerns is the sickness absence and how it’s recorded and how that could impact on the future career of that person . . . So I would guess a recommendation would be about identifying these situations where an employee may have to be in hospital and recovering and how is that recorded on your sickness processes and is it exempt from other types of sickness . . . So there’d be a bit of clarity for everybody about what the return to work would look like, who’s going to get involved and when.
12, commissioning manager
Measuring impact
That the person’s back in work, working at a level that is appropriate to where they should be and in comparison to the preoperative, how they worked pre operation really. And so you’re comparing that, in truth within a short period of time they should be working at an even better level than pre operation, because obviously the operation is there to fix them.
19, manager/headteacher
. . . has the employee made a successful return to work.
9, managing director
I suppose the success of somebody remaining in employment and feeling that they’ve been supported, so personal evaluation from the employee’s perspective and from the manager’s perspective.
20, staff liaison manager
. . . if there was further absences in the future related to that surgery . . .
8, human resources director
So if someone wasn’t coming back to work after 8 to 10 weeks, then what’s gone wrong? Is it infection?
2, occupational health physiotherapist
I mean to understand whether people read it and stuff it might be hits on the websites increases. Are people reading it and are people, your leaflet, are people picking up reading it and going to search for more information . . . are people taking it, is it hitting the right spot in terms of people going to look.
18, manager
Health-care team interviews (surgeons, general practitioners, allied health professionals and nurses)
As described in Chapter 6, interviews with the health-care team produced the following four themes:
-
decision to have surgery and expectations of recovery
-
advising patients about work and other activities
-
barriers to and facilitators of RTW
-
perceptions regarding an occupational advice intervention.
Direct quotations to supplement the narrative description in Chapter 6 are presented in the following sections.
Theme: the decision to have surgery and expectations of recovery
So you need to give people realistic expectations, and you’ve no idea preoperatively in terms of setting more realistic goals. You’ve no idea who’s going to be swellers and who aren’t, and who’s going to cope well with the pain and who isn’t, do you know what I mean?
AHP/N 3004-7a
But I guess there is the general idea of leave it as long as you can. That’s still very much what patients understand is being told to them all the time. And I don’t know whether that’s coming from the consultant necessarily or whether that’s, yeah.
GP 5013
If people fully understood what was involved, what the likelihood was that they could get back to work and how many months out, that really should probably be part of your decision-making process as to whether you’re going to have the surgery or not.
AHP/N 3001
I rarely see people that feel they’ve recovered within the time frame they say they’ve been advised, normally quite a lot longer . . . in general I think it would take a lot longer to recover than they anticipate before they go in.
GP 5004
The work aspects which drive people to surgery, I mean some would say – I can’t have surgery because I just can’t get the time off work. I can’t afford it – particularly if they’re self-employed. Some will say I can’t afford any more sick time, I need surgery. Or I’m self-employed, I’m getting to the point where I can’t work, and that’s why I need surgery . . .
S 4006
Theme: advising patients about work and other activities
Perception of roles
I think that the conversation is probably done by the consultant when they get listed for surgery and when obviously they go through all the surgery and all the recovery process . . . But during the inpatient stay, I don’t really recall that every single patient does have a concern or do ask us can I go back to work, when can I go back to work. But I don’t know if it’s something that they have already talked about before or if it’s something that they’re just assuming that I’ll have to wait until I come for my follow-up and then I can go back to work. So this is my thought, I don’t have a, I’m not hundred per cent sure.
AHP/N 3009
They don’t tend to ask us, but then I think that’s because we’re not asking them anything about work.
AHP/N 3004-7d
As a GP you kind of feel a bit uncomfortable sometimes interfering too much with the rehab process . . . in terms of encouraging people to get back to work, we’re more interested in making sure people feel well and that they’re getting better. And work is kind of secondary to that really.
GP 5002
I think we are often trying to give people advice about employment and we don’t necessarily know ourselves . . . We’re the people who end up keeping people off work because we’re the ones who are a bit scared. Even though we’re thinking surely with a bit more thought this could be OK.
GP 5013
We give them an information booklet at listing, which will have some information. But I’ve not been through that very carefully so I don’t know what it says about work to be honest.
S 4006
Differing management of total hip replacement/total knee replacement patients
The physio is the person mainly involved with seeing all the knee patients. So they’re kind of her patients . . . we did used to see knees years and years ago. And it actually came from one of the surgeons who advised us not to see the knees . . . And in terms of recovery evidence has shown that the knee recovers better when you’ve got the full bend etc. So – don’t raise toilets, don’t raise furniture, encourage the patient to bend their knee as much as possible really. It’s apparently all round enhancing the recovery. So at that point we were asked not to see people . . .
AHP/N 3002-3
Yeah, we don’t do a lot with hips these days to be honest with you. We stopped doing the exercises a few years ago because it was found that they weren’t of much benefit really . . . mostly they’ll go home and then they’ll get seen at the joint replacement clinic again in 2 weeks and then they’ll be seen by the consultant in a few weeks after that.
AHP/N 3012
I think that’s why it’s good that all of the knees at least get referred to physio now. Because at least that does give an opportunity for the physios, if they’re wired up and clued in and interested in knee replacements, to tailor their advice from 2 weeks post-op . . . definitely some of the patients that come back to clinic who have been and had physio out in the wilds say it’s very minimal the advice and information they’re given.
AHP/N 3004-7
. . . So not everyone who has a replacement done here at [name of main hospital] or within our trust boundaries has exactly that path because if the patient happens to live out in [another part of the region] then they might . . . they maybe actually rehabbed in a smaller centre as opposed to a main university hospital that we are, and so they don’t have the same facility for drop in clinics I think for that reason.
AHP/N 3001
Because recovery from knee replacements is very different from recovery from a hip replacement. It’s much more difficult, and you’ve got to educate the patients a bit on what to expect afterwards, and start them doing their exercises and start them doing some physio work beforehand to make it easier afterwards. So that’s why we target the knees because we know they might struggle.
S 4006
Advice currently provided
The key thing here really is this blanket bans and blanket time frames are very difficult to establish. The trust has adopted a rule that if you have a sedentary job you can’t return to work until 6 weeks post-op. If you have a heavy manual lifting carrying job . . . you can’t return until 3 months.
AHP/N 3004-7b
. . . the doctors will sign them off on the sick, obviously having had a knee replacement, but whether it’s 6 weeks, 8 weeks, 12 weeks . . .
AHP/N 3001
But we normally say because they all come back and see their consultant at 6 to 8 weeks, that’s when they’re given the sort of go ahead to get back to driving and sort of after 6 weeks and then we say at that point obviously as long as your consultant’s happy then it’s sort of a case of as long as you feel OK to go back to work.
AHP/N 3010
I follow the guidance really of the first post-op follow-up at the hospital. So I make sure that the consultant has reviewed them and hopefully there’s a decent letter that says, you know, they can now do whatever they like or they should be careful and carry on walking with crutches or, you know, whatever. So I’m very reliant on the specialist to tell me how well his work is progressing. I wouldn’t personally give an opinion without that. I mean it’s their hard work and if I tell the patient to do something that then upsets the whole thing I don’t think I’d be very popular.
GP 5003
Yeah, that’s the bit where we have to say look only you know your job. Most companies will have an occupational health person, so they can do it and they can do a return to work assessment.
S 4007
Communication with other stakeholders
I can’t think of a knee replacement where I’ve had much involvement or correspondence with an employer . . . I think that’s something I normally leave to the patient themselves to do.
AHP/N 3001
I do occasionally in clinic get asked if I can provide a, if I can send a copy of the clinic letter to an occupational health professional. But that’s only in the biggest best organised companies generally.
AHP/N 3004-7a
A lot of the first follow-ups are with the physios who are just more interested in the mobility and progressing them in that way. So in the letters to date they don’t really say anything about return to work in them normally. They’re just normally this person’s doing well. They can do this now. It’s that sort of level of information really.
GP 5002
Ours are pretty good. As I say, they’re putting on the discharge form how long a note they’ve given. And presumably in doing that they’ve discussed with the patient because we rarely get somebody coming in there afterwards. The physiotherapists usually either pass on messages via the patient – and that’s fine.
GP 5014
. . . it could help the GP if they do refer to those discharge letters, or they just get piled somewhere! If they are looking at them and they are looking at them, if a patient is in asking about work, if they thought well I’ll see what the discharge letter says. If there was some information there it could be useful. But then again the discharge letter is written by probably the most junior person, more often than not the most junior person in the team, because they tend to be done pretty much close to discharge by the junior staff on the ward.
S 4006
Fit notes
The sick note is better these days because you can specify to alter duties, phased return and workplace adaptations, and all those things are very useful and some people do ask for them when they’re returning to work, but they tend to be people who have decent-sized companies where there’s a good occupational health service available to them that they’ve utilised.
GP 5015
And I wouldn’t routinely see them unless something is flagged up for me to do that. And sometimes that’s a sick note that hasn’t been completed in the hospital, something as simple as that . . . And I think it is the hospital’s responsibility but they don’t always do it.
GP 5003
Yes it tends to be more the junior staff I suppose upon discharge. Then occasionally if they come to clinic and they’re needing a bit longer they’ll ask for an extension, so it’s on request really.
S 4001
I don’t write them. Well the nursing staff can sign a note covering their sick period whilst they’re in hospital. Beyond that it would generally go to the GP, and then the GPs do it. So it tends to be postoperative, post discharge tend to be all GPs.
S 4006
Often have that conversation with them. I’ll write you up for 6 weeks but you can go back when you want, when you feel free. And people sometimes ask for a note to go back to work.
I had to fill one in today actually because some employers require a safe to go back to work risk management thing which is a bit irritating but it is the way that they work.
4009-12
Advice about driving
But we normally say because they all come back and see their consultant at 6 to 8 weeks, that’s when they’re given the sort of go ahead to get back to driving and sort of after 6 weeks and then we say at that point obviously as long as your consultant’s happy then it’s sort of a case of as long as you feel OK to go back to work.
AHP/N 3010
. . . they get advised around not driving for 6 weeks, which is a historical thing which still I know is kind of fairly universally . . . By historical I think what I mean is I’ve never seen a paper which says it’s highly dangerous or illegal for anyone in less than 6 weeks to be driving a car. But it’s something which I know is still reinforced by so many different stages that I think we still do as well.
AHP/N 3001
I usually ask them, are you confident in driving? And I have got no means of assessing whether they are confident or not.
GP 5001
I think they do get advice on how to mobilise and when to start driving and when to start, you know, getting in and out of a car blah, blah, blah. But I assume they get that before they leave [the hospital] because we don’t give them that advice.
GP 5009-12
So for most people – ‘I can’t go to work because I can’t drive to work’.
S 4007
(A) You can’t assess somebody’s fitness to drive in clinic. (B) There’s no measure. (A) The only way you can really do that is to take someone out round a course in a car . . . (B) My rules on this, once they can put their full weight through the affected limb then they can probably balance and put power through it, so it’s safe to drive.
S 4002-5
Theme: barriers to and facilitators of return to work
Workplace
And they [employers] often think that it’s just a hip or a knee operation. They don’t class it as major surgery that will affect the whole body. And somebody I had I think a couple of weeks ago and said oh when I first told my employer I was going to have this operation they said oh well we can expect you back 2 weeks afterwards.
AHP/N 3008
I mean the more common ones within the UK now of course is the absence of sick pay, for the vast majority of people work in industry. So there will be a desire financially to return sooner for a lot of the people.
AHP/N 3004-7a
Some employers are quite good at finding work for people who have had a good track record in the company, others not so much. You ask them, can you do light duties, would that be helpful? No chance, I’m either there or I don’t have a job!
GP 5015
Public sector is much more forgiving and they want to get people back to work, and they’re happy to tolerate a phased return. I suspect those people in the private sector would just be back at work and doing their full job at the start of someone else’s phased return. So it just moves the pathway forwards a bit.
S 4002-5 B
I think a lot of companies and employers feel so risk averse with regards to people trying to sue them. ‘I went back on my crutches and I slipped and now this has happened’. And I think a lot of them are in that very risk-averse culture, which is complete nonsense because it’s probably not going to happen. But I think a lot of them try and prevent people getting back to work early because of that. Oh you might fall and you’ll sue us. I think that, there is a bit of a feeling that goes on around the place.
S 4006
Job demands
Teachers might be able to go back a little bit earlier, because they often can sit behind a desk and not really get involved in anything too active.
AHP/N 3008
We’ve obviously we do have patients that obviously do some office work and they can return to work earlier.
AHP/N 3009
But it does depend whether it’s a physically demanding job or whether they’ve got a desk job, how they get to work, you know, do they drive normally or do they get a lift or do they have to catch public transport . . . If it’s a physically demanding job then that’s going to take them a bit longer before they can get back.
AHP/N 3012
Yes well I think it does depend a bit what you’re doing, you know the difference between relaxing at a desk sipping coffee and resting at a computer is easier than wrestling with sacks of potatoes. So if it’s sedentary well it’s going back soon but if it’s hard manual you need to be able to cope with it. And so yeah . . .
S 4001
Manual workers, to be honest with you if you had a builder, yeah come on, they’re going to need to just take it easy. So anything that over-stresses it, puts too much stress on their joints you just want to let them settle really. Sat in an office chair is fine. Things like that.
S 4007
Occupational health
We’re in a different ballgame there, and that’s where individualised assessments come. Now obviously the big firms have their own occupational health service anyway. That’s fine. It is going to be a minutiae of people who work in, either for themselves or in small firms.
AHP/N 3004-b7
Because you quite often find that maybe they’re not very clued up really as to what hip and knee replacements should do for each individual trust or consultant . . . I think in occupational health circles as well, that doesn’t, they don’t understand the full work as well . . .
AHP/N 3008
. . . sometimes they’ll have an appointment with their occupational health practitioner before they go back to work. But that tends to be how are you getting along, is everything all right?
GP 5015
There is that, is it fit to work scheme or something you can refer, I have to confess I’ve never referred anybody to it. But there’s that you could refer if there was somebody who was having difficulty returning to work.
I don’t know quite what would happen to them if you referred but there you are.
Yes I don’t know either.
GP 5009-12
I know that in a lot of employers it’s very difficult to get occupational health advice. And it’s certainly difficult to get it on an ad hoc basis. I think too often you’ll end up with a sort of well this is the situation you are now in, can you do your job? Rather than planning.
S 4008
General practitioner
But outside agencies such as GPs, nurses at surgeries, they don’t understand the full whys and wherefores of joint replacement.
AHP/N 3008
I think another factor is the availability of the internet, and the fact that people these days are a lot better, are quite well read, again particularly the younger patients. And so actually there are, people are prepared to work a bit harder to persuade the GPs to refer them, because they know that there’s something that can be done.
AHP/N 3004-a7
I still think there’s probably that bit of a barrier too, and I think the GPs will stave them off as long as possible as well before they’ll even get to see a consultant.
AHP/N 3004-a7
So the GPs I think are vital in terms of identifying the patients and sending them to us. But they may well have to also speak to patients who are still in work and say you may well have to consider whether you will be able to continue your job, particularly the heavy manual type jobs, following surgery, and whether you would need to change career. But I appreciate that’s difficult for GPs as well, because a lot of them don’t have any occupational health training either. Some of them have an interest in occupational health but they’re very few I think.
S 4008
They might be under their GPs, and if the GP understands the GP will try other things and explain to them, or they might have been referred on, and I know people are referred on. And the consultant will say you are too young. And it’s not from any wrong reason, it’s just how long a prosthesis lasts for. So you have to factor that in.
3004-c7
Patient
And also you’ll find the self-employed cohort of patients are very much more keen to get back to work than the employed are. You’ll find the self-employed people are back sitting at their desks a week or 10 days afterwards to some degree or another, and there’s no way of persuading them that that’s not a sensible thing to do.
AHP/N 3004-7a
The thing that really affects the hip replacement – in the first 6 weeks – is the use of hip precautions. Which means their entry into the workplace is limited by their ability to travel to and from the workplace, and their ability to use the facilities within the workplace.
AHP/N 3004-7b
So the ones who, you tend to get people who err on the side of caution and they don’t do enough. And then you get the others who want to conquer the world within weeks, and they can often do too much. And by going back to work then they risk having to go off sick again because their hip is being asked, or knee, their joint is being asked too much of it. And they end up being in pain more at night time and more stiffness, more swelling. And then they might end up being off sick again.
AHP/N 3008
Or some patients have quite and black and white idea: I was told I’d be off for however long and that’s it. Their time’s up and they have to go back to work.
GP 5013
Well, we’re rural, so we’ve got lots of very stoic farmer types and they’re self-employed and they will not have time off work, so you know if you’re going to refer them for any surgery they’re going to be back at work within 2 or 3 weeks and that’s what they’ll do. And so that’s not to say they’ll necessarily be doing the full level, but they will be working.
GP 5013
Surgery
The hospital actually are quite kind and thoughtful about fitting them in around their work schedule, so one is a music teacher I’m thinking of and they allowed him to delay it to do it in summer holidays so that he didn’t need to have time off school. And another lady was a carer and had some family issues going on at the time and they allowed her to sort of be a bit flexible about the date that suited her caring duties.
GP 5003
There’s an ideal recovery time, but people are very variable and some people have complications. And some people deal with pain and physiotherapy much better than others.
GP 5015
They’re going to be at significant risk of getting a lot of swelling if they’re going to be on their feet all day long.
S 4006
Yes well I suppose it’s a whole separate channel of complications related to surgery. So obviously if you have the misfortune of a recurrently dislocating hip or infection requiring wash out, you know, anything that brings you back into hospital is obviously going to be a huge roadblock. And then things like stiff knees requiring a manipulation under anaesthetic. That would be a challenge for a chap who has to do stairs in his day-to-day work. But those are small, you know, a small subgroup of complications would obviously be a delay, but otherwise no.
S 4001
So if a lot of patients had their choice they would pick their times, and they would pick quiet times. So some teachers would pick a time post exams so they get rid of that busy time. People in the building trade will pick Christmas because the building trade closes down pretty much all over Christmas. If you work in the pub trade you’ll pick January because it’s your quietest time of the year . . . But then it becomes very difficult because of the logistics of the way the NHS works, and the issues of breaching times and this sort of thing . . .
S 4006
Resources
I think we’re quite fortunate here at this trust, and I’m sure it probably won’t be indefinite but as I speak there’s not huge pressures on you to review ratios, we are able to keep people on the books for quite a long period of time . . . I do think that a really high-quality outpatient sort of postoperative rehab plan to get someone back to a higher level is actually quite labour intensive . . . we haven’t got a pressure to discharge people quickly so we’re able to hang on to people for longer.
AHP/N 3001
So it’s that balance again between the resources, we’re offering that service to everybody as opposed to the very tiny proportion of people who might actually get back to work quicker. And that still isn’t going to benefit the NHS, but the resources would come out of the NHS to get them there.
AHP/N 3004-7a
I’ve seen quite a few cases in which I’ve been quite disappointed with the lack of physiotherapy, because patients are now being discharged early from the hospital because they need the beds.
GP 5001
Well, currently, with the CCG to restrict people going forward, they have to go through 6 months of conservative treatment before we’re allowed to refer them, which has to involve the physio appointment. And the physio appointments are pretty limited, they are sort of like, tend to be a single appointment with exercise advice rather than anything more.
GP 5009-12
But secondly there’s huge economic constraints on a very routine high throughput pathway that 5, 10 years ago people would be seen routinely up to about 10 years after the operation. Now if they’re doing well they get seen once by us and discharged at 8 weeks. And that’s it. So it’s trying to put this advice into the context of a very constrained health system working at the minute. Often people would be seen once in clinic to talk about the operation. They’d be put on the list. They’d be seen at pre-assessment, they’d get the operation, 2-weeks checks, 8-week check, goodbye.
S 4002-5 A
Theme: perceptions regarding an occupational advice intervention
Perceived need
I think there’s certainly, it does feel like it’s almost inevitable that we’re moving towards doing more and more knee replacements on people younger who are still working or older who are still working because as a result of kind of factors generally in society.
AHP/N 3001
I suppose the long and short of it is that we don’t tend to operate when people are under the age of 50 for knee replacement.
AHP/N 3004-7a
If they’re not discussing anything about work until they come back at 6 to 8 weeks post-op, some of them could feasibly already be back at work by then couldn’t they?
AHP/N 3004-7a
Not very many at all, I would say less than one in ten would be of working age. Most people will be in their 60s, 70s. But of course we’re all working longer now.
GP 5015
If you look at the average age of a joint replacement it’s in the 70s, so an awful lot of our patients aren’t working. So it’s pointless going on and telling them all about work when they’re not at work.
S 4006
Timing
Well probably it’s not the kind of thing that the surgeon will talk about when they first go to the appointment to be put on the waiting list. But equally I think that’s probably when it should be.
AHP/N 3008
. . . but it’s post [op], I think definitely people are just sent home, kind of left.
AHP/N 3011
At pre-op sort of time. Pre surgery, before they’ve got a date.
GP 5004
Well I would’ve thought as soon as they know they’re going to have one done really, the sooner the better. Because as soon as they’re going to start sharing that information with their employers and their employers have a better understanding of what’s likely to happen and how long they’re likely to be off and what’s likely to be needed afterwards, you know, they’re going to be, if there a half-decent employer anyway, you can then take that on board before they’ve actually gone off.
GP 5002
. . . so really the best time to start, the GP should talk to the patient to start with. But they’ve got less time. Before a GP refers a patient what they should say to the patient is that you realise you could be off work for 6 weeks to 3 months depending on what you do. And patients will go hang on, I can’t afford the time away from work. So that’s when it should start . . .
S 4007
Format
In social media now, they Google things, don’t they? They look up things. The younger generation, not so much obviously the older generation.
AHP/N 3011
We give away so much stuff and so many books and leaflets and whatever, sometimes it just gets thrown in a drawer and lost and whatever, that more paper might not be the way in.
AHP/N 3011
. . . a sort of thing that they could take away and sort of just show to their family, show to their employer. So they’ve got something written down to show people to say I can’t do this but I can do this, that sort of thing.
AHP/N 3010
. . . yeah I’m sure children still have ‘red books’. It’s something that’s given to the mum when the baby’s born and you take it with your baby to all health professionals involved and they sign off all their bits . . . that would allow physio and OT to sort of do their bit and make sure that everybody had optimised the care for the patient.
GP 5003
So I think predominantly written stuff is ideal, but there has to be the opportunity for some sort of either face-to-face or telephone interaction. Face to face probably better, so that they can be truly personalised, but we know from various studies that patients tend to forget everything that, 90% of what’s been said as soon as they leave the consulting room. So I think there has to be the backup of something written that they can go back to, and then the contact details so that when they think of the question 3 days later they can either phone or e-mail somebody just to ask that question.
S 4008
Content
. . . different jobs, so the patient could see which category they fitted into and by that whether their job was a particularly high demand job in terms of it was a very physical job, it was climbing ladders, it was being on their feet for long periods of the day.
AHP/N 3001
I think the main thing is having advice slightly specific to the type of work people are doing.
GP 5013
I think it would need to cover the guidance from the legal point of view in what you definitely can’t do, and then also about common complications and common pitfalls, and also giving people ideas of recovery times in general so people know what the impact is likely to be. I think a lot of this is covered by the orthopaedic team, whether it’s covered as in depth as possibly it could be but definitely making sure the patients are as well educated about the process as they can be before entering it . . .
GP 5016
I would assume you’d paint the scenario if you’re doing well you can do this and this would be your average and, you know, so I assume it would be common sense directed.
S 4001
What might be quite good is testimonials. These are my last 100 patients who work. Let’s just get them all to write a paragraph about what they did or what they thought, when did they go back to work? What was the reality, what was the hardest thing? And that might be, it’s something I always keep thinking that I should do at some stage. And then you just produce that and give it to the patients, and go look this is what my last 100 patients said about going back to work.
S 4007
Delivery
I’m sure if we’ve got the general consultant consensus and some guidance about the advice that we could provide that would be something that the [nurse] practitioner would be absolutely happy to help with and to give their guidance. And we’ve got a very cohesive team so we are direct contact as I said with our registrars but as well with our occupational therapists and physiotherapists so we all work on the same department and if there’s something that then is out of our range we’ve got ways of getting the advice straight away from other sources. But that would be something that it wouldn’t cause any problem for us to include that sort of advice.
AHP/N 3009
And then the person dealing with them needs to have a bit of an idea about the best advice, because advice will vary depending on the individual person’s work. And it needs to be tailored to that individual, all pre-op.
So people who would give advice, would they be, because I am just thinking would every doctor be able to do that to know that, they probably wouldn’t would they?
GP 5009-12
Specifically talking about occupation – I don’t know really, each and all of us I suppose.
S 4007
It’s difficult when you don’t see the patient until the clinic at 8 weeks after their surgery to make any recommendations on returning to work up until that point. You can from that point on. So someone like the physiotherapist who has perhaps seen them weekly at best or twice weekly for the first 6 weeks or so, they’re probably in a better position or have more time to judge recovery, achievements, expectations . . . as to when realistically they would be able to return to work.
S 4002-5
But it seems to me you’d need somebody who’s got some insight into occupational-type medicine or occupational therapy related to workplace, something like that, and somebody who’s got the time. I don’t think it’s me.
S 4006
Measuring the impact of the intervention
Well, you could look at simple: time to return to work. Because it might be actually that you get more rapid return to work by giving more information and more advice. You could look at their satisfaction with care throughout the procedure, whether that be encompassing everything from their experience from the general practice, the sick notes, their recovery, their physio and everything else. So actually, the patient’s satisfaction and actually recovery times are the important ones as well.
GP 5014
Well the most important would be getting people back to work earlier than they would do otherwise. But you’re going to find that’s difficult to get results. It’s going to be a bit muddy. People going back to work and then going back on the sick a little bit. So the failure rates of going back to work might be one. But that’s not going to be that often. And I suppose it’ll all be down to quality of life type stuff at the end of the day, and qualitative stuff. Because I think definite quantitative actions you’re going to need very large sample size.
GP 5016
Appropriate time for return to work. So probably, and that’s got to be patient-focused hasn’t it, that’s got to be the patient feeling they’re getting back to work at the time they feel they ought to be getting back to work. Not too early, not too late, just an appropriate and perhaps with feeling that they’ve been given support to help them achieve that.
S 4006
Well I suppose the most obvious one is a countrywide snapshot of the average mean return to work, subdivided by desk based or manual, and then try and improve it by 2 weeks and see if it happens or not. But to be honest it’s not a, you know, not to minimise it, but it’s not a prime focus of concern. Getting them through the hazards of ops to make it safely to the car to take them home is an excellent result and then getting them to work’s a bonus is a jaundiced view of it.
S 400
Appendix 6 Supporting information for intervention mapping stages 2 and 3
Parts of this appendix have been reproduced with permission from Coole et al. 149 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Change objectives for each of the performance objectives in the final OPAL intervention
Intervention mapping: patient matrix for performance objectives the developed occupational advice intervention tested in the feasibility assessment
Behaviour to be targeted: patient makes successful return to work following surgery.
| PO | Knowledge and awareness | Skills and self-efficacy | Attitudes/beliefs/emotions | Outcome expectations | Perceived norms |
|---|---|---|---|---|---|
| Pre surgery | |||||
| PO1. Patient completes occupational checklist prior to appointment with surgeon | Explains that completing the occupational checklist aims to inform the surgeon about their work activities and demands | Expresses confidence in completing the occupational checklist | States that completing an occupational checklist will help to inform the surgeon about their work activities and demands and facilitate an informed decision about surgery | States that completing an occupational checklist will facilitate an informed decision about surgery and positive RTW outcome | Recognises that nowadays patients are being encouraged to take an active part in their care. Recognises that RTW is now considered a health outcome |
| PO2. Patient makes informed decision about surgery with respect to work |
Appraises the general risks/benefits of surgery and RTW rates Appraises the likely impact of surgery on their ability to do their own job States that they have received sufficient information about surgery |
Expresses confidence in ability to make informed decision about surgery Demonstrates ability to process information about surgical procedure and make informed choice |
Expresses willingness to take responsibility for surgical decision Demonstrates appropriate emotional response with regard to their decision |
Describes a realistic expectation of RTW outcome following surgery |
Perceives that it is usual for patients to make an informed decision about surgery with respect to their work Recognises that nowadays patients are being encouraged to take an active part in their care Recognises that RTW is now considered a health outcome |
| PO3. Patient acquaints self with key information about recovery and RTW provided in the RTW workbook |
Describes the key advice and information concerning recovery and RTW, e.g. how work modifications (hours and duties) can facilitate RTW The risks of extended sickness absence The risks of returning to work too quickly |
Expresses confidence in their ability to acquaint themselves with key information about recovery and RTW provided in the RTW workbook |
States they have a responsibility to acquaint themselves with key information about recovery and RTW provided in the RTW workbook Expresses willingness to take this responsibility to acquaint themselves with key information? |
States that having a good understanding about recovery and RTW is likely to lead to a positive RTW outcome | Recognises that patients undergoing surgery acquaint themselves with key information about recovery and RTW provided by the HOT |
| PO4. Patient brings RTW workbook to each hospital appointment including hospital inpatient stay (and discusses with HOT) | Describes that the reason for bringing the RTW workbook to each appointment is to encourage patients and hospital staff to focus on RTW at each appointment | Expresses confidence in their ability to bring the RTW workbook to each hospital appointment |
States that it will help their recovery/RTW to bring the RTW workbook to each hospital appointment Expresses willingness to bring RTW workbook to each hospital appointment |
Expects that bringing the RTW workbook to each hospital appointment is likely to facilitate a positive RTW outcome | Recognises that nowadays patients are being encouraged to take an active part in their care |
|
PO5. Patient completes sections of RTW workbook that will help them understand the demands of their work and set an approximate RTW date With employera as required |
Explains that completing the workbook helps them understand the demands of their work and set an approximate RTW date Describes how to complete a RTW workbook and set an approximate RTW date, and how to do this with their employera if required |
Expresses confidence in their ability to complete the sections of the RTW workbook that will help them understand the demands of their work and set an approximate RTW date Expresses confidence in their ability to do this with their employera if required |
Expresses willingness to complete the sections of RTW workbook that will help them understand the demands of their work and set an approximate RTW date Expresses willingness to do this with their employera if required |
Expects that completing the sections of the RTW workbook (with their employer if required) that will help them understand the demands of their work and set an approximate RTW date is likely to lead to a positive RTW outcome |
Recognises that RTW is now considered a health outcome Recognises that nowadays patients are being encouraged to take an active part in their care Recognises that employersa are key stakeholders in RTW and involving them at an early stage can facilitate RTW |
|
PO6. Patient uses information resources provided in workbook to identify and prioritise potential barriers and solutions to a safe and appropriate RTW, and to develop a RTW plan With employera as required |
Lists the potential barriers and solutions to their own RTW and develops a RTW plan, with employer as required Explains how to identify and prioritise potential barriers and solutions to a safe and appropriate RTW and develop a RTW plan, with employer as required |
Expresses confidence in identifying barriers to/facilitators of their own safe and appropriate RTW, and to develop a RTW plan, with employer as required | States that identifying barriers/facilitators and the development of their RTW plan, with employer as required, will aid their own safe and appropriate RTW | Expects that identifying and prioritising potential barriers to and facilitators of RTW, and developing a RTW plan, with employer as required, will lead to a safe and appropriate RTW |
Recognises that nowadays patients are being encouraged to take an active part in their care Recognises that employersa are key stakeholders in RTW and involving them at an early stage can facilitate RTW |
| PO7. Patient discusses information within RTW workbook with RTWC (at hospital or by telephone) to help them further develop their RTW plan. This will include a minimum of one contact. The number and duration of further contacts will be governed by patient need based on progress and perceived level of ‘risk’ of prolonged sickness absence | Describes the process of engaging with their RTWC to further develop a RTW plan:
|
Expresses confidence in engaging with the RTWC to help them further develop their RTW plan Demonstrates how to negotiate a RTW plan with their employera |
States that engaging with the RTWC to help them further their RTW plan will aid their RTW Expresses acceptance that a RTW plan will aid their RTW |
Expects that engaging with the RTWC to help them further develop their RTW plan will lead to a positive RTW outcome | Recognises that the ideal RTW process relies on co-ordination and joint planning between health care, the patient and their employer |
| PO8. Patient provides employera with written information provided by the HOT about their planned surgery and recovery/RTW advice | Describes the information that they can provide to their employera/workplace, and who should receive it | Expresses confidence in their ability to provide this information to their employera/workplace | States that providing their employera with written information provided by the HOT about their planned surgery and recovery/RTW advice will facilitate their RTW | Employera is informed about the surgical process and RTW |
Recognises that employers do not necessarily know about this type of surgery and how best to facilitate RTW Recognises that employersa are key stakeholders in RTW and involving them at an early stage can facilitate RTW |
| Post surgery | |||||
| PO9. Patient meets with their employera to discuss their recovery and RTW plan |
Appraises the likely impact of surgery on their RTW, prior to their operation Describes how to discuss their RTW with their employera |
Expresses their ability to discuss their recovery and RTW plan with their employera/workplace Expresses confidence in their ability to discuss their recovery and RTW plan with their employera/workplace |
Expresses willingness to discuss their recovery and RTW plan with their employera | Employera is informed about patient’s recovery and RTW plan |
Recognises that nowadays patients are being encouraged to take an active part in their care Recognises that employersa are key stakeholders in RTW and involving them at an early stage can facilitate RTW |
| PO10. Patient communicates with employera regarding surgical outcome and progress/recovery | Appraises the likely impact of surgery on their RTW, post surgery | Expresses confidence in their ability to communicate with their employera regarding surgical outcomes and recovery (could be by telephone, in writing, in person) | States their willingness to communicate their surgical outcome and progress with their employera | Expects that communicating with their employera regarding surgical outcome and progress will lead to a positive RTW outcome | Recognises that communication with their employera is key to a successful RTW outcome |
| PO11. Patient revises RTW plan following surgery as necessary with their employera and hospital staff |
Explains why a RTW plan may need to be revised following surgery Describes how they will revise their RTW plan if necessary with their employera and hospital staff |
Expresses confidence in negotiating a revised RTW plan with their employera and hospital staff | States their willingness to revise their RTW plan following surgery | Expects that revising the RTW plan following surgery will provide a more positive RTW experience |
Recognises that nowadays patients are being encouraged to take an active part in their care Recognises that the ideal RTW process relies on co-ordination and joint planning between health care, the patient and their employer Recognise that RTW is an ongoing process that needs to monitored |
| PO12. Patient engages with RTWC via RTW helpline/answering service if having problems related to RTW for up to 16 weeks post surgery | Recalls the process of engaging with the RTWC:
|
Expresses confidence in their ability to engage with the RTWC if they are having problems post discharge |
States that engaging with the RTWC via the RTW helpline/answering service will potentially alleviate any RTW problems Expresses willingness to engage with this service if problems relating to RTW emerge |
Expects that engaging with the RTWC via RTW helpline/answering service if having problems related to RTW will help the patient to overcome the problem | Recognises that it is considered normal for patients to ask clinicians for help regarding problems at work, even after discharge from the service |
| PO13. Patient adheres to postoperative rehabilitation plan and advice | Describes their postoperative rehabilitation plan:
|
Expresses ability to attend/travel to postoperative rehabilitation sessions if required Expresses confidence about adhering to postoperative rehabilitation plan |
States that adhering to their postoperative rehabilitation plan is important for their recovery/RTW Expresses willingness to adhere to postoperative rehabilitation plan and advice |
Expects that adhering to their postoperative rehabilitation plan will have a positive impact on RTW |
Recognises that other patients undergoing surgery take an active part in postoperative rehabilitation Recognises that nowadays patients are being encouraged to take an active part in their care |
Intervention mapping: staff matrix for performance objectives the developed occupational advice intervention tested in the feasibility assessment
Behaviour to be targeted: work-focused advice and support is provided by the HOT.
| PO | Knowledge and awareness | Skills and self-efficacy | Attitudes/beliefs/expectations | Perceived norms |
|---|---|---|---|---|
| Pre surgery | ||||
PO1. The HOT:
|
Members of HOT describe role and responsibility of the RTWC and OPALCs Members of HOT state identity of the RTWC, their deputy, and OPALCs Members of HOT describe how to contact the RTWC, their deputy, and OPALCs Members of HOT describe how patients will use the telephone line/answerphone service to contact the RTWC |
Members of the HOT are confident that they are able to:
|
Members of the HOT state that the following actions will facilitate patients in RTW:
|
Members of the HOT recognise that the NHS now sees RTW as a measure of health and recovery from surgery Members of HOT recognise that patients undergoing THR and TKR are increasingly likely to RTW following surgery Members of the HOT recognise that HOTs have a role in supporting patients undergoing THR/TKR in RTW following surgery |
| PO2. The outpatient clinic team identifies RTW patients in clinic prior to consultation with surgical team | Members of the outpatient clinic team describe the process of identifying RTW patients:
|
Members of the outpatient clinic team express confidence in their ability to identify RTW patients in clinic | Members of the outpatient clinic team state that identifying RTW patients in clinic will help the surgeon/patient make an informed decision about surgery with regard to RTW | Members of the outpatient clinic team recognise that identifying RTW patients in clinic prior to appointment with surgeon is good practice |
|
PO3. The outpatient clinic team requests RTW patients to complete occupational checklist prior to consultation with surgeon and explain its purpose to the patient, model completion if necessary and give positive feedback on completion The outpatient clinic team gives completed occupational checklist to surgeon prior to patient’s appointment |
Members of the outpatient clinic team describe the process of asking RTW patients to complete an occupational checklist and giving it to the surgeon:
|
Members of the outpatient clinic team express confidence in their ability to ask RTW patients to complete an occupational checklist in clinic and giving it to the surgeon prior to patient’s appointment Members of the outpatient clinic team express confidence in modelling completion of the occupational checklist and giving positive feedback on its completion |
Members of the outpatient clinic team state that asking RTW patients to complete an occupational checklist in clinic will help the surgeon and patient make a more informed decision about surgery with regard to RTW Members of the outpatient clinic team state that modelling completion of the occupational checklist and giving positive feedback on its completion will help the patient to complete the checklist accurately and help the patient and surgeon make a more informed decision about surgery with regard to RTW |
Members of the outpatient clinic team recognise that preparing the patient and surgeon to discuss the patient’s RTW is good practice Members of the outpatient clinic team state that modelling completion of the occupational checklist and giving positive feedback on its completion is in accordance with good practice |
|
PO4. Surgeon discusses pros and cons of surgery with patient including expected time scales of surgery and recovery – in relation to the patient’s usual work and refers to/responds positively to the patient’s occupational checklist to enable patient to make informed decision about surgery; supports patient autonomy Provides patient with personal risk feedback on potential RTW outcomes Explores patient’s questions and concerns Informs listed patients that they will be given a RTW workbook to read and why, complete where possible, bring to each subsequent appointment, presenting positive message Informs listed patients that they will receive an employer workbook and why, that the patient will be contacted by a RTWC at least 4 weeks prior to surgery and why. Names them Explains that RTW plan may need to be revised and that RTWC will help with this Summarises and records patients’ RTW status/outcome in all clinic notes and following each appointment Communicates with GP at point patient is discharged from orthopaedic surgical care outlining current RTW status and progress and ongoing therapy received |
Surgeon describes current evidence regarding pros and cons of surgery in relation to work including expected time scales of surgery and recovery Surgeon describes the process by which they use occupational checklist Surgeon describes process of providing patient with personal risk feedback on potential RTW outcomes Surgeon describes process of enabling patient to make informed decision about surgery; supporting patient autonomy Surgeon describes the process of: |
Surgeon expresses confidence in discussing/answering patient’s questions about RTW and their decision to have surgery in relation to their work Surgeon expresses confidence in using the patient’s occupational checklist as a basis for their discussion with patient about surgery Surgeon expresses confidence in providing patient with personal risk feedback on potential RTW outcomes Surgeon expresses confidence in enabling patient to make informed decision about surgery; supporting patient autonomy Surgeon expresses confidence in: |
Surgeon states that surgeons should encourage patients to take an active role in the decision about surgery in relation to RTW Surgeon states that using the patient’s occupational checklist as a basis for their discussion about surgery will facilitate their discussion about surgery Surgeon states that providing patient with personal risk feedback on potential RTW outcomes and enabling patient to make informed decision about surgery – supporting patient autonomy – will facilitate their RTW Surgeon states that the patient’s RTW will be facilitated by: |
Surgeons recognise that discussing the pros and cons of surgery with patient including expected time scales of surgery and recovery – in relation to the patient’s usual work – is good practice Surgeon states that using the patient’s occupational checklist as a basis for their discussion about surgery is good practice Surgeon states that providing patient with personal risk feedback on potential RTW outcomes and enabling patient to make informed decision about surgery – supporting patient autonomy – is good practice Surgeon recognises that it is good practice to: |
|
PO5. The outpatient clinic team provides all RTW patients listed for surgery with written RTW workbook and gain contact details for RTWC to contact patient as completed in occupational checklist Outpatient clinic staff inform/encourage patient to bring RTW workbook to each hospital appointment, and draw attention to this instruction in the workbook Discuss potential reasons why this might not happen, and formulate solutions with patient Recommend patients read workbook and complete as much as they can (show relevant sections); present workbook positively and refer to coping model examples Recommend patient asks employer to assist patient in completion if wishes and suggests who this might include, and discuss possible difficulties and solutions re communicating with employer Outpatient clinic staff explain to patient that the RTWC will contact them at least 4 weeks prior to surgery about their RTW plan |
Members of the outpatient clinic team describe the process of giving patients a RTW workbook and gaining contact details for RTWC to contact patient: Outpatient clinic staff describe the process of: Outpatient clinic staff describe the process of recommending that patients read workbook and complete as much as they can (show relevant sections), presenting workbook positively and referring to coping model examples Outpatient clinic staff describe the process of recommending that patients asks employer to assist patient in completion if wishes and suggests who this might include, and discuss possible difficulties and solutions re communicating with employer Outpatient clinic staff describe the process of explaining to patient that the RTWC will contact them about their RTW plan |
Members of the outpatient clinic team express confidence in their ability to give patients a RTW workbook and gain contact details for RTWC to contact patient Outpatient clinic staff express confidence in their ability to: Outpatient clinic staff express confidence in their ability to recommend to patients that they read workbook and complete as much as they can (show relevant sections), presenting the workbook positively and referring to coping model examples Outpatient clinic staff express confidence in recommending that patient asks employer to assist patient in completion if wishes and suggests who this might include, and discuss possible difficulties and solutions re communicating with employer Outpatient clinic staff express confidence in their ability to explain to patient that the RTWC will contact them about their RTW plan |
Members of the outpatient clinic team state that giving patients a RTW workbook and RTWC contact telephone/e-mail will facilitate the patient’s RTW Outpatient clinic staff state that: Outpatient clinic states that recommending to patients that they read workbook and complete as much as they can (show relevant sections), presenting the workbook positively and referring to coping model examples will facilitate the patient’s RTW Outpatient clinic staff state that recommending that patients asks employer to assist patient in completion if wishes and suggesting who this might include, and discussing possible difficulties and solutions re communicating with employer will facilitate their RTW Outpatient clinic staff state that explaining to patient that the RTWC will contact them about their RTW plan will facilitate RTW |
Members of the outpatient clinic team recognise that it is good practice to give patients RTW information and support at an early stage Outpatient clinic staff recognise that informing/encouraging patient to bring RTW workbook to each hospital appointment, drawing attention to this instruction, and discussing potential reasons why this might not happen, and formulating solutions with the patient is good practice Outpatient clinic recognises that recommending to patients that they read workbook and complete as much as they can (show relevant sections), presenting the workbook positively and referring to coping model examples is good practice Outpatient clinic staff recognise that recommending that patients asks employer to assist patient in completion if wishes and suggesting who this might include, and discussing possible difficulties and solutions re communicating with employer is good practice Outpatient clinic staff recognise that explaining to patient that the RTWC will contact them about their RTW plan is good practice |
|
PO6. The outpatient clinic team provides all RTW patients listed for surgery with ‘employer RTW workbook’ to share with their employer/colleaguesa Outpatient clinic staff inform/encourage patient that giving the employer RTW workbook to employer/colleagues will help them understand surgery and prepare for patient’s RTW Suggests that patient might wish to meet with their employer to discuss RTW and who this might include Outpatient clinic staff suggest individuals in the workplace who might best receive the employer TRW workbook |
Members of the outpatient clinic team describe the process of giving patients the employer RTW workbook to share with their employer/colleagues:aOutpatient clinic staff describe process of informing/encouraging patient that giving an employer RTW workbook to their employer/colleagues will help them understand surgery and prepare for patient’s RTW Outpatient clinic staff describe the process of recommending that patients might wish to meet with their employer to discuss RTW and who this might include Outpatient clinic staff describe process of suggesting individuals in the workplace who might best receive the employer RTW workbook |
Members of the outpatient clinic team express confidence in their ability to provide patients with employer RTW workbook Outpatient clinic staff express confidence in their ability to inform/encourage patient that giving the ‘employer RTW workbook’ to employer/colleagues will help them understand surgery and prepare for patient’s RTW Outpatient clinic staff express confidence in recommending that patients might wish to meet with their employer to discuss RTW and who this might include Outpatient clinic staff express confidence in their ability to suggest individuals in the workplace who might best receive the employer information |
Members of the outpatient clinic team state that giving patients an employer RTW workbook to share with their employer/colleagues will facilitate the patient’s RTW Outpatient clinic staff state that informing/encouraging patient to give the ‘employer RTW workbook’ to employer/colleagues will help them understand surgery and prepare for patient’s RTW Outpatient clinic staff state that recommending that patients might wish to meet with their employer to discuss RTW and who this might include will facilitate their RTW Outpatient clinic staff state that suggesting individuals in the workplace who might best receive the employer information will facilitate the patient’s RTW |
Members of the outpatient clinic team recognise that it is good practice to educate/inform patients’ employers/colleaguesa about RTW information at an early stage Outpatient clinic staff recognise that it is good practice to inform/encourage patient to give the ‘employer RTW workbook’ to employer/colleagues Outpatient clinic staff recognise that recommending that patients might wish to meet with their employer to discuss RTW and who this might include is good practice Outpatient clinic staff recognise that it is good practice to suggest individuals in the workplace who might best receive the employer RTW workbook |
| PO7. The outpatient clinic team collects patient’s completed occupational checklist from surgeon and forwards to RTWC | Members of the outpatient clinic team describe the process of passing patients’ completed occupational checklists to RTWC:
|
Members of the outpatient clinic express confidence in their ability to pass patients’ completed occupational checklists to RTWC | Members of the outpatient clinic team state that passing patients’ completed occupational checklists to RTWC will help RTWC facilitate the patient’s RTW | Members of the outpatient clinic team recognise that it is good practice for HOTs to communicate patients’ occupational status to RTWC |
|
PO8. The preoperative assessment and education teams routinely include the topic of RTW in their clinics with examples of work demands, barriers to and facilitators of RTW, RTW plans, importance of adhering to postoperative rehabilitation plan/pacing up activities The preoperative assessment and education teams ask if patients have brought their RTW workbook to appointment, praise patients, refer positively to content and use of the workbooks, and promote engagement with the RTWC |
Members of the preoperative assessment and education teams describe how to routinely include the topic of RTW in their clinics with examples of work demands, barriers to and facilitators of RTW, RTW plans, importance of adhering to postoperative rehabilitation plan/pacing up activities Members of the preoperative assessment and education teams describe the process of asking if patients have brought their RTW workbook to appointment, praising patients and referring positively to content and use of the workbooks, and promoting engagement with the RTWC |
Members of preoperative assessment and education team express confidence in routinely including the topic of RTW in their clinics with examples of work demands, barriers to and facilitators of RTW, RTW plans, importance of adhering to postoperative rehabilitation plan/pacing up activities Members of the preoperative assessment and education teams express confidence in asking if patients have brought their RTW workbook to appointment, praising patients and referring positively to content and use of the workbooks, and promoting engagement with the RTWC |
Members of preoperative assessment and education team state that routinely including the topic of RTW in their clinics with examples of work demands, barriers to and facilitators of RTW, RTW plans, importance of adhering to postoperative rehabilitation plan/pacing up activities will facilitate the patient’s decision about surgery and their RTW Members of the preoperative assessment and education teams state that asking if patients have brought their RTW workbook to appointment, praising patients and referring positively to content and use of the workbooks, and promoting engagement with the RTWC will facilitate the patient’s RTW |
Members of preoperative assessment and education team recognise that routinely including the topic of RTW in their clinics with examples of work demands, barriers to and facilitators of RTW, RTW plans, importance of adhering to postoperative rehabilitation plan/pacing up activities is good practice Members of the preoperative assessment and education teams recognise that asking if patients have brought their RTW workbook to appointment, praising patients and referring positively to content and use of the workbooks, and promoting engagement with the RTWC is good practice |
|
PO9. RTWC contacts all RTW patients (telephone/meet-ups) at least 4 weeks prior to surgery to review:All patients receive at least one contact with the RTWC. This may be integrated within the pre-assessment/pre-admission process or done by telephone. The number and duration of additional contacts will be governed by patient need based on progress and perceived level of ‘risk’Refers positively to RTW workbook during discussions with patient:Encourages discussion about/coaches patient regarding communication with patient’s employer Refers on/signposts where appropriate Sets goals/steps with patient Discusses the possibility of needing to revise RTW plan following surgery Documents all consultations in RTWC workbook |
The RTWC describes the process of how, when and where they will:
|
The RTWC expresses confidence in their ability to:
|
The RTWC states that providing targeted individual RTW support and advice through contacting patients prior to surgery will facilitate their RTW | The RTWC recognises that providing targeted individual RTW support and advice through contacting patients prior to surgery is good practice |
| PO10. RTWC highlights RTW patients to teams managing preoperative education and assessment and records this action in RTWC workbook | The RTWC describes the process of highlighting RTW patients to the preoperative education and assessment team and recording this action in RTWC workbook:
|
The RTWC expresses confidence in their ability to highlight RTW patients to the preoperative education and assessment team and recording this action in RTWC workbook | The RTWC states that highlighting RTW patients to the preoperative education and assessment team and recording this action in RTWC workbook will facilitate the patient’s decision about surgery and their RTW | The RTWC recognises that highlighting RTW patients to the preoperative education and assessment team and recording this action in RTWC workbook is good practice |
| PO11. RTWC highlights RTW patients to the ward teams when admitted for surgery and records this action in the RTWC workbook | The RTWC describes the process of highlighting RTW patients to the ward team and recording this action in RTWC workbook when patient admitted:
|
The RTWC expresses confidence in their ability to highlight RTW patients to the ward team and recording this action in RTWC workbook | The RTWC states that highlighting RTW patients to the ward team and recording this action in RTWC workbook will facilitate the patient’s RTW | The RTWC states that highlighting RTW patients to the ward team and recording this action in RTWC workbook is good practice |
|
PO12. The ward team (nurse and doctor) checks RTW patients have brought workbook into hospital, and if not determine the reason for this. Give praise if workbook brought in Refer positively to RTW workbook |
The ward team (nurse and doctor) describes the process of checking that RTW patients have brought workbook into hospital, and if not determining the reason for this; giving praise if workbook brought in; referring positively to RTW workbook |
The ward team (nurse and doctor) describes the process of checking that RTW patients have brought workbook into hospital, and if not determining the reason for this. Give praise if workbook brought in Refer positively to RTW workbook |
The ward team (nurse and doctor) states that checking that RTW patients have brought workbook into hospital, and if not determining the reason for this, giving praise if workbook brought in and referring positively to RTW workbook will facilitate the patient’s RTW | The ward team (nurse and doctor) recognises that checking that RTW patients have brought workbook into hospital, and if not determining the reason for this, giving praise if workbook brought in and referring positively to RTW workbook is best practice |
| Post surgery | ||||
|
PO13. Ward therapists ask RTW patients if they have brought workbook into hospital, and if not determine the reason for this. Give praise if workbook brought in Refer positively to RTW workbook; enter notes as appropriate Liaise with RTWC to update them on the patient’s postoperative recovery prior to discharge |
Ward therapists describe the process of:
|
Ward therapists express confidence in:
|
Ward therapists state that:
|
Ward therapists recognise that it is good practice to:
|
|
PO14. The RTWC liaises with inpatient teams postoperatively to determine whether or not there are any issues with early recovery that may have an impact on the RTW plan The RTWC revises RTW plan with patient as required and ensures that plan is documented in patient’s RTW workbook The RTWC supports postoperative rehabilitation plans and problem-solves potential barriers to adherence with patient |
The RTWC describes the process of liaising with inpatient teams postoperatively to determine whether or not there are any issues with early recovery that may have an impact on the RTW plan: The RTWC describes the process of revising the RTW plan with patient as required and ensures that plan is documented in patient’s RTW workbookThe RTWC describes the process of supporting postoperative rehabilitation plans and problem-solving potential barriers to adherence with patient |
The RTWC expresses confidence in their ability to liaise with the inpatient therapy team regarding patient’s postoperative recovery The RTWC expresses confidence in revising the RTW plan with patient as required and ensuring that plan is documented in patient’s RTW workbook The RTWC expresses confidence in supporting postoperative rehabilitation plans and problem-solving potential barriers to adherence with patient |
The RTWC states that liaising with the inpatient therapy team regarding patient’s postoperative recovery will facilitate the patient’s RTW The RTWC states that revising the RTW plan with patient as required and ensuring that plan is documented in patient’s RTW workbook will facilitate the patient’s RTW The RTWC states that supporting postoperative rehabilitation plans and problem-solving potential barriers to adherence with patient will facilitate the patient’s RTW |
The RTWC recognises that liaising with the inpatient therapy regarding patient’s postoperative recovery is good practice The RTWC states that revising the RTW plan with patient as required and ensuring that plan is documented in patient’s RTW workbook is good practice The RTWC states that supporting postoperative rehabilitation plans and problem-solving potential barriers to adherence with patient is good practice |
|
PO15. The ward team (nurse/doctor) summarises patient’s expected RTW outcome and RTW plan in ward electronic discharge letter. A copy/copies will be given to the patient to share with employer, therapists, etc. The ward team (nurse/doctor) praise/refer to the RTW workbook and remind the patient to use the RTW helpline following discharge if they are having problems The ward team (nurse/doctor/therapist) highlights the importance of adhering to the postoperative rehabilitation plan |
The ward nurse and doctor describe how to summarise the patient’s expected RTW outcome and RTW plan in ward electronic discharge letter The ward nurse and doctor describe how a copy/copies will be given to the patient to share with employer, therapists The ward team (nurse/doctor) describes the process of praising/referring to the RTW workbook and reminding the patient to use the RTW helpline following discharge if they are having problems The ward team (nurse/doctor/therapist) describes the process of highlighting the importance of adhering to the postoperative rehabilitation plan |
The ward nurse and doctor express confidence in their ability to summarise the patient’s expected RTW outcome and RTW plan in ward electronic discharge letter The ward nurse expresses confidence in their ability to give a copy/copies of the discharge letter to the patient to share with employer, therapists The ward team (nurse/doctor) expresses confidence in praising/referring to the RTW workbook and reminding the patient to use the RTW helpline following discharge if they are having problems The ward team (nurse/doctor/therapist) expresses confidence in highlighting the importance of adhering to the postoperative rehabilitation plan |
The ward nurse and doctor state that summarising the patient’s expected RTW outcome and plan in the ward electronic discharge letter will facilitate the patient’s RTW The ward nurse and doctor state that giving the patient a copy/copies of the electronic discharge letter to share with their employer, therapists, etc., will facilitate the patient’s RTW The ward team (nurse/doctor) states that praising/referring to the RTW workbook and reminding the patient to use the RTW helpline following discharge if they are having problems will facilitate their RTW The ward team (nurse/doctor/therapist) states that highlighting the importance of adhering to the postoperative rehabilitation plan will facilitate their RTW |
The ward nurse and doctor recognise that summarising the patient’s expected RTW outcome and plan in the ward electronic discharge letter is good practice The ward nurse and doctor recognise that giving the patient a copy/copies of the electronic discharge letter to share with their employer, therapists, etc., is good practice The ward team (nurse/doctor) recognises that praising/referring to the RTW workbook and reminding the patient to use the RTW helpline following discharge if they are having problems is good practice The ward team (nurse/doctor/therapist) states that highlighting the importance of adhering to the postoperative rehabilitation plan is good practice |
| PO16. The specialist ward nurse/doctor asks each patient whether or not they require a fit note on discharge and completes the fit note in accordance with best-practice guidelines and the hospital contract, and with reference to the patient’s RTW plan in their workbook | The specialist ward nurse/doctor describes the process of asking each patient whether or not they require a fit note on discharge:
|
The specialist ward nurse/doctor express confidence in their ability to ask each patient whether or not they require a fit note on discharge The specialist ward nurse/doctor express confidence in their ability to complete the fit note in accordance with best-practice guidelines and the hospital contract, and with reference to the patient’s RTW plan in their workbook |
The specialist ward nurse/doctor state that asking each patient whether or not they require a fit note on discharge and completing the fit note in accordance with best-practice guidelines and the hospital contract, and with reference to the patient’s RTW plan in their workbook will facilitate the patient’s RTW | The specialist ward nurse/doctor recognise that asking each patient whether or not they require a fit note on discharge and completing the fit note in accordance with best-practice guidelines and the hospital contract, and with reference to the patient’s RTW plan is good practice |
| PO17. The RTWC checks the RTW helpline three times per week, and triages, advises (e.g. phone call) or refers back to therapy services (based on local service structure and availability) based on individual need | The RTWC describes the process of checking the helpline and the actions they are required to follow in response to the patient:
|
The RTWC expresses confidence in their ability to check the helpline and in taking the actions they are required to follow in response to the patient | The RTWC states that checking the helpline and taking the actions they are required to follow in response to the patient will facilitate the patient’s RTW | The RTWC recognises that checking the helpline and taking the actions they are required to follow in response to the patient is good practice |
| PO18. Surgeon, HOT and outpatient therapy teams summarise and record patient’s RTW status/outcome in all outpatient clinic notes and following each appointment | The surgeon, HOT and outpatient therapy teams describe the process of summarising and recording patient’s RTW status/outcome in all outpatient clinic notes and following each appointment:
|
The surgeon, HOT and outpatient therapy teams express confidence in their ability to summarise and record patients’ RTW status/outcome in all outpatient clinic notes and following each appointment | The surgeon, HOT and outpatient therapy teams state that summarising and recording patient’s RTW status/outcome in all outpatient clinic notes and following each appointment will facilitate the patient’s RTW | The surgeon, HOT and outpatient therapy teams recognise that summarising and recording patient’s RTW status/outcome in all outpatient clinic notes and following each appointment is good practice |
| PO19. Surgeon and HOT communicate with GP at point patient is discharged from orthopaedic surgical care, outlining current RTW status and progress and ongoing therapy received and encourage engagement with RTWC until 16 weeks post surgery (8 weeks for feasibility study) | Surgeon and HOT describe the process of communicating with the GP at the point that the patient is discharged from orthopaedic surgical care, outlining current RTW status and progress and ongoing therapy received | Surgeon and HOT express confidence in their ability to communicate with the GP at the point that the patient is discharged from orthopaedic surgical care, outlining current RTW status and progress and ongoing therapy received | Surgeon and HOT state that communicating with the GP at the point that the patient is discharged from orthopaedic surgical care, outlining current RTW status and progress and ongoing therapy received will facilitate the patient’s RTW | Surgeon and HOT state that communicating with the GP at the point that the patient is discharged from orthopaedic surgical care, outlining current RTW status and progress and ongoing therapy received is good practice |
|
PO20. RTWC continues to provide a point of access to RTW advice for patients following discharge from orthopaedic surgical care until 16 weeks post surgery (8 weeks for feasibility study) Records any changes to patient’s RTW progress/status/outcome in RTWC workbook |
RTWC describes the process of providing a point of access to RTW advice for patients following discharge from orthopaedic surgical care until 16 weeks post surgery (8 weeks for feasibility study) Describes the process of recording changes to patient’s RTW progress/status/outcome in RTWC workbook |
RTWC expresses confidence in their ability to provide a point of access to RTW advice for patients following discharge from orthopaedic surgical care until 16 weeks post surgery (8 weeks for feasibility study) Expresses confidence in recording changes to patient’s RTW progress/status/outcome in RTWC workbook |
RTWC states that providing a point of access to RTW advice for patients following discharge from orthopaedic surgical care until 16 weeks post surgery (8 weeks for feasibility study) will facilitate the patient’s RTW States that recording changes to patient’s RTW progress/status/outcome in RTWC workbook will facilitate the patient’s RTW |
RTWC recognises that providing a point of access to RTW advice for patients following discharge from orthopaedic surgical care until 16 weeks post surgery (8 weeks for feasibility study) is good practice Recognises that recording changes to patient’s RTW progress/status/outcome in RTWC workbook is good practice |
Patient methods and applications
Behaviour being targeted: patient makes safe and appropriate RTW.
| Determinant | Methods | Definition | Parameters | Applications |
|---|---|---|---|---|
| Knowledge/awareness | ||||
| Aware that completing an occupational checklist in clinic will inform the surgeon about their work activities and demands | Consciousness raising (HBM) | Providing information about the consequences for a problem behaviour | Raising awareness must be quickly followed by increase in problem-solving ability | Outpatient clinic staff explain that a completed checklist will help prompt the surgeon and the patient to discuss work issues in full otherwise they might not make the optimum decision about surgery |
| Knows the risks/benefits of surgery and RTW rates and likely impact of surgery on their ability to do their job | Personalise risk (PAPM) | Provide information about personal costs or risks of action or inaction with respect to target behaviour | Present messages as individual and undeniable | Individuals receive personal risk feedback from surgeon on potential RTW outcomes in relation to their work situation (surgeon prompted about potential risks by referring to patient’s occupational checklist) |
Knows key advice and information concerning recovery and RTW, for example:
|
Coherence and imagery (TIP) Discussion and elaboration (ELM) Reinforcement (LT) |
Encourage consideration of a topic in open informal debate Linking a behaviour to any consequence that increases it |
Listening to the learner to ensure that the correct schemas are activated |
A RTW workbook is provided to patient by outpatient clinic staff containing advice and information – sections of text have logical order and clearly related to each other; use graphical representations Contents and use of RTW workbook are referred to in discussions with all members of HOT: surgeon, RTWC, preoperative education/presentation, ward staff, outpatient therapy staff |
|
Aware that bringing the RTW workbook to each appointment is expected in order to encourage patients’ and staff focus on RTW Aware that discussing the content of the RTW workbook with hospital staff is expected to encourage patients and staff to focus on RTW |
Personalise risk (PAPM) Reinforcement (LT) |
Provide information about personal costs or risks of action or inaction with respect to target behaviour Linking a behaviour to any consequence that increases the behaviour’s rate, frequency or probability |
Present messages as individual and undeniable Needs to be tailored to the individual, group or organisation, follow the behaviour in time, and seen as a consequence of the behaviour |
Outpatient clinic staff inform patient that they are expected to bring the RTW workbook to enable the HOT to advise them on their individual RTW. Outpatient clinic staff draw attention to this instruction in the workbook Members of the HOT (preoperative assessment and education teams, RTWC, ward staff, therapy teams) ask patients if they have brought their RTW workbook to each appointment; praise patients for bringing their RTW workbook to each appointment; discuss the content of the patient’s RTW workbook at each appointment |
| Can describe how to assess the demands of their work and set an approximate RTW date, and how to do this with their employer if required |
Modelling (SCT) Variety of media (TIP) (repeated exposure) Elaboration (TIP) |
Providing an appropriate model Stimulating the learner to add meaning to the information that is processed |
Identification with the model, model receives positive reinforcement, coping vs. mastery model Messages that are personally relevant |
Examples of other patients’ work demands and setting approximate RTW dates included in workbook/on website and at preoperative presentations given by staff Discussions with RTWC and preoperative education and assessment teams |
| Can list the potential barriers and solutions to their own RTW and develop a RTW plan, with employer as required |
Modelling (SCT) Variety of media (TIP) Elaboration (TIP) |
Providing an appropriate model Stimulating the learner to add meaning to the information that is processed |
Identification with the model receives positive reinforcement, coping vs. mastery model Messages that are personally relevant |
Examples of other patients’ barriers and solutions and RTW plans included in workbook/on website and at preoperative presentations given by staff Discussions with RTWC and preoperative education and assessment team |
| Can describe the process of engaging with their RTWC by telephone or face to face at the hospital to further develop their RTW plan (how, when, where) |
Variety of media? Type of reinforcement? More/repeated exposure? (TIP) |
Information about engaging with the RTWC is given verbally by outpatient clinic staff, in the patient workbook and on website, on discharge letter – and posters on the ward | ||
| Know what information to provide to their employera/workplace, and who should receive it |
Modelling (SCT) Discussion |
Providing an appropriate model Encourage consideration of topic in open informal debate |
Identification with the model Listening to the learner to ensure that the correct schemas are activated |
Examples of other patients’ negotiation with employer Outpatient clinic staff explain that giving information to their employer will help the employer to understand their surgery and to help them plan the patient’s RTW Outpatient clinic staff will suggest the individuals in the workplace who might best receive the employer information |
| Know the likely impact of surgery on their RTW and how to discuss their RTW with their employera prior to surgery | Discussion (ELM) | Encourage consideration of topic in open informal debate | Listening to the learner to ensure that the correct schemas are activated | Discussion with/coaching by RTWC |
| Know why a RTW plan may need to be revised following surgery and how to do this | Scenario-based risk information (PAP model) | Providing information that may aid the construction of an image of the ways in which a future loss or accident might occur | Plausible scenario with a cause and scenario | Discussions with surgeon, RTWC, ward staff and outpatient therapy staff regarding unexpected outcomes of surgery and how these might have an impact on their RTW and RTW plan |
| Know the process of engaging with the RTWC via the RTW helpline following surgery (who, when, how, what to expect) |
Variety of media? Type of reinforcement? More/repeated exposure? (TIP) |
Information is provided verbally by RTWC, ward staff, outpatient clinic staff, in writing in the patient workbook and on website, on discharge letter – and posters on the ward and in clinic | ||
| Know their postoperative rehabilitation plan and the risks of not adhering to it | Scenario-based risk information (PAP model) | Providing information that may aid the construction of an image of the ways in which a future loss or accident might occur | Plausible scenario with a cause and scenario | Discussions with surgeon, RTWC, preoperative education/presentation, ward staff, outpatient therapy staff about the pros and cons of not adhering to their rehabilitation plan |
| Self-efficacy/skills | ||||
| Able to complete an occupational checklist prior to appointment with surgeon |
Verbal persuasion (SCT) Facilitation (SCT) |
Using messages that suggest that the participant possesses certain qualities Creating an environment that reduces barriers to action |
Credible source Requires identification and removal of barriers |
Outpatient clinic staff explain that this is an activity that they believe the patient can do Sufficient checklists available, clipboard, pens, time to complete, actual help provided by outpatient clinic staff |
| Able to process information about surgical procedure and make informed choice |
Motivational interviewing (SDT) Individualisation (TTM) |
Collaborative goal-orientated style of communication Provide opportunities for learners to have personal questions answered or paced according to progress |
Must recognise collaboration, exploration, autonomy Personal communication that responds to a learner’s needs |
Surgeon supports autonomy of patient in consultation by valuing patient perspective, offering choices, minimising pressures Surgeon facilitates communication at consultation RTWC, preoperative assessment and education teams provide further opportunities to discuss decision with RTW following consultation |
| Can acquaint themselves with key information about recovery and RTW provided in the RTW workbook |
Verbal persuasion (SCT) Goal-setting (GST, TSR) |
Using messages that suggest that the participant possesses certain qualities Prompting the patient to plan what they will do to reach the target behaviour |
Credible source Patient’s commitment to the goal |
Outpatient clinic staff and RTWC explain that the workbook has been designed for and approved by patients Outpatient clinic staff and RTWC discuss and agree the goal for the next appointment (e.g. to read/complete a particular section of workbook) |
|
Can bring the RTW workbook to each hospital appointment Can discuss their RTW workbook with hospital staff |
Verbal persuasion (SCT) Planning coping responses (TSR) Guided practice (SCT) |
Using messages that suggest that the participant possesses certain qualities Prompting patients to list potential barriers and ways to overcome these Prompting individuals to rehearse and repeat the behaviour various times, discuss the experience and provide feedback |
Credible source Identification of barriers and practise coping response Requires supervision by an experienced person |
Outpatient clinic staff and RTWC explain that this is an activity that they believe patients can do Outpatient clinic staff and RTWC discuss potential reasons why workbook might not be brought to appointment and formulate solutions with patient RTWC models target behaviour a number of times, then asks patient to do the same and gives comments, emphasising what has been done well |
| Can complete the sections of the RTW workbook that will help them understand the demands of their work and set an approximate RTW date (with employera if required) |
Modelling (SCT) Planning coping responses (TSR) |
Providing an appropriate model Prompting patients to list potential barriers and ways to overcome these |
Identification with the model Able to identify barriers and practise coping response |
Examples of other patients’ job demands in workbook/on website, also shared by RTWC and at preoperative presentations given by staff Outpatient clinic staff and RTWC discuss potential reasons why patients might struggle to discuss demands with employer, and formulate solutions with patient |
| Can identify barriers to/facilitators of their own safe and appropriate RTW and develop a RTW plan (with employer if required) |
Modelling (SCT) Planning coping responses (TSR) |
Providing an appropriate model Prompting patients to list potential barriers and ways to overcome these |
Identification with the model Able to identify barriers and practise coping response |
Examples of other patients’ barriers and solutions and RTW plans in workbook/on website, also shared by RTWC and at preoperative presentations given by staff Outpatient clinic staff and RTWC discuss potential reasons why patients might struggle to identify barriers/facilitators with employer, and formulate solutions with patient |
| Can engage with the RTWC to further develop their RTW plan – minimum of one contact | Individualisation | Providing opportunities to have personal questions answered or instructions paced according to individual progress | Personal communication that responds to an individual’s needs | RTWC contacts patient to help them develop their own individual RTW plan |
| Can provide written information provided by the HOT about their planned surgery and recovery/RTW advice to their employera/workplace | Verbal persuasion (SCT) | Using messages that suggest that the participant possesses certain qualities | Credible source |
Outpatient clinic staff and RTWC explain that this is an activity that they believe patients can do Outpatient clinic staff give each patient an information booklet to give to their employer |
| Can meet with their employera to discuss their recovery and RTW plan |
Verbal persuasion (SCT) Planning coping responses (TSR) Implementation intentions (GST) |
Using messages that suggest that the participant possesses certain qualities Prompting patients to list potential barriers and ways to overcome these Making plans for any obstacles that occur |
Credible source Identification of barriers and practise coping response |
Outpatient clinic staff and RTWC explain that this is an activity that they believe patients can do Outpatient clinic staff/RTWC discuss potential causes and formulate solutions with patient RTWC helps patient to prepare an if . . . then plan ready if they encounter any difficulties with their employer |
| Communicate with their employer regarding their surgical outcome and progress/recovery | Guided practice (SCT) | Prompting individuals to rehearse and repeat the behaviour various times, discuss the experience and provide feedback | Requires supervision by an experienced person | RTWC models target behaviour a number of times, then asks patient to do the same and gives comments, emphasising what has been done well |
| Negotiate a revised RTW plan with their employer and RTWC if necessary |
Verbal persuasion (SCT) Planning coping responses (TSR) Guided practice (SCT) Modelling could be good here too |
Using messages that suggest that the participant possesses certain qualities Prompting patients to list potential barriers and ways to overcome these Prompting individuals to rehearse and repeat the behaviour various times, discuss the experience and provide feedback |
Credible source Identification of barriers and practise coping response Requires supervision by an experienced person |
RTWC explains that this is an activity that they believe patients can do RTWC formulates solutions with patient RTWC models target behaviour a number of times, then asks patient to do the same and gives comments, emphasising what has been done well |
| Ability to engage with RTWC via helpline if they are having problems post discharge | Planning coping responses (TSR) | Prompting patients to list potential barriers and ways to overcome these | Identification of barriers and practise coping response | RTWC formulates solutions with patient to overcome any barriers they might experience in using the helpline |
| Adhere to their postoperative rehabilitation plan | Planning coping responses (TSR) | Prompting patients to list potential barriers and ways to overcome these | Identification of difficult situations and practise of coping response | RTWC formulates solutions with patient |
| Attend/travel to rehabilitation if required | Facilitation (SCT) | Creating an environment that makes the action easier or reduces barriers to action | Requires identification and removal of barriers | RTWC asks patient the optimum arrangements for any rehabilitation they require and liaises with outpatient therapy teams |
| Attitudes, beliefs, expectations | ||||
| Believes that completing an occupational checklist will facilitate RTW | Information about others’ approval | Providing information about what others think about the person’s behaviour | Positive expectations available in the environment | Outpatient clinic staff inform patient that the surgeon will approve of them completing the checklist |
| Is willing to take responsibility for surgical decision | Motivational interviewing | Explore person’s reasons for change within atmosphere of acceptance | Supportive relationship between client and professional | Surgeon supports autonomy of patient and offers choices about surgery where possible |
| Has realistic expectation of RTW outcome following surgery | Individualisation | Providing opportunities for learners to have personal questions answered | Personal communication that responds to a learner’s needs | Surgeon advises individual patient as to the likely outcome of RTW following surgery according to the patient’s characteristics and work demands |
| Believes that having a good understanding about recovery and RTW through RTW workbook is likely to lead to a positive RTW outcome |
Persuasive communication Repeated exposure |
Guiding individual towards adoption of action by using arguments and other means Making a stimulus repeatedly accessible to the individual’s sensory receptors |
Messages need to be relevant and not too discrepant to beliefs of individual |
HOT – especially surgeon, outpatient clinic staff, RTWC all present positive attitude to use of RTW workbook All members of the team consistently refer to intervention. Posters on ward |
|
Believes that bringing the RTW workbook to each hospital appointment is likely to facilitate a positive RTW outcome Believes that them discussing the RTW workbook at each hospital appointment is likely to facilitate a positive RTW outcome |
Persuasive communication Anticipated regret |
Guiding individual towards adoption of action by using arguments and other means Stimulate people to focus on their feelings after unintended risky behaviour |
Messages need to be relevant and not too discrepant to beliefs of individual Stimulation of imagery; assumes a positive intention to avoid the risky behaviour |
HOT – especially surgeon, outpatient clinic staff, RTWC refer to example of ‘red book’ given to new parents as an example of similar approach in health care, and importance of good communication Outpatient clinic staff, surgeon and RTWC asks individual to imagine what might happen if they did not bring the RTW workbook to each appointment |
| Expects that completing the sections of the workbook that will help them understand the demands of their work and set an approximate RTW date . . . with their employera if required is likely to lead to a positive RTW outcome |
Framing Modelling |
Using gain-framed messages emphasising the advantages of performing the healthy behaviour Or loss-framed messages Providing an appropriate model |
Requires high self-efficacy expectations Identification with the model |
Outpatient clinic staff, surgeon, RTWC and the RTW workbook emphasise the advantages of completing the workbook Outpatient clinic staff, surgeon, RTWC and the RTW workbook provide examples – coping models |
| Believes that identifying barriers/facilitators and developing a RTW plan will aid their own safe and appropriate RTW |
Modelling Framing |
Providing an appropriate model Using gain-framed messages emphasising the advantages of performing the healthy behaviour Or loss-framed messages |
Identification with the model Requires high self-efficacy expectations |
Outpatient clinic staff, surgeon, RTWC and the RTW workbook provide examples – coping models Outpatient clinic staff, surgeon, RTWC and the RTW workbook emphasise the advantages of completing the workbook |
| Believes that engaging with the RTWC and developing a RTW plan will lead to a positive RTW outcome |
Individualisation Elaboration |
Providing opportunities for learners to have personal questions answered Stimulating the learner to add meaning to information that is processed |
Personal communication that responds to a learner’s needs Messages that are personally relevant |
RTWC advises and supports individual patient with their RTW plan according to their individual characteristics and work demands RTWC discusses the RTW plan with the individual patient |
| Believes that providing their employer with written information about their forthcoming surgery and RTW will facilitate their RTW | Consciousness raising | Providing information about causes, consequences, alternatives | Can use feedback and confrontation, but raising awareness must be quickly followed by increase in self-efficacy | Key people in HOT (e.g. surgeon, outpatient clinic staff, RTWC) and workbook provide patient with feedback from phase 1 of the study in which employers stated that they would like more information about surgery and recovery to help employees RTW |
| Believes that meeting with their employer, informing their employera to discuss their recovery and RTW plan will facilitate their RTW | Belief selection (TPB, RAA) | Using messages designed to strengthen positive beliefs, weaken negative beliefs and introduce new beliefs | Requires investigation of the individual’s current beliefs | RTWC explores patient’s beliefs when engaging with patient |
| Believes that communicating with their employera regarding surgical outcome and progress will lead to a positive RTW outcome | Self re-evaluation | Encouraging combining both cognitive and affective assessments of one’s self-image with and without required behaviour | Needs stimulation of both cognitive and affective assessments of one’s self-image | RTWC encourages patient to compare his or her image as a person who does/does not communicate with their employer |
| Believes that revising the RTW plan following surgery will provide a more positive RTW experience |
Modelling Framing |
Providing an appropriate model Using gain-framed messages emphasising the advantages of performing the healthy behaviour Or loss-framed messages |
Identification with the model Requires high self-efficacy expectations |
RTWC and workbook/website provides examples of how patients have revised RTW plans following surgery |
| Believes that engaging with the RTWC via the RTW helpline/answering service will potentially alleviate any RTW problems | Modelling | Providing an appropriate model | Identification with the model | Workbook/website provides examples of how patients have contacted the RTWC via the helpline post surgery |
| Believes that adhering to their postoperative rehabilitation plan is important for their recovery/RTW | Persuasive communication | Guiding individuals towards the adoption of an idea by using arguments or other means | Messages need to be relevant and not too discrepant from beliefs of individual |
RTWC RTW workbook and website |
| Perceived norms | ||||
| Recognises that nowadays patients are being encouraged to take an active part in their care | Anticipated regret | Stimulate people to focus on their feelings after unintended risky behaviour | Stimulation of imagery; assumes a positive intention to avoid the risky behaviour | Outpatient clinic staff, surgeon, RTWC asks individual to imagine how they would feel/what might happen if they did not make an informed decision about surgery |
| Recognises that RTW is now considered a health outcome and that this is a good thing | Consciousness raising | Providing information about causes, consequences, alternatives | Can use feedback and confrontation, but raising awareness must be quickly followed by increase in self-efficacy |
Information in RTW workbook, website and members of HOT consistent in expressing their belief in work as a health outcome Evidence about relationship between work and good health in RTW workbook |
| Perceives that it is usual for patients to make an informed decision about surgery with respect to their work | Shifting perspectives (TSD) | Encourage taking the perspective of the other | Initiation from the perspective of the learner; needs imaginary competence | HOT enables patients to compare the potential result for patients who do vs. those who do not make informed decision |
|
Recognises that patients undergoing surgery acquaint themselves with key information about recovery and RTW provided by the HOT Recognises that discussing the RTW workbook with hospital staff is best practice |
Information about others’ approval Persuasive communication |
Providing information about what others think about the person’s behaviour Guiding individuals towards the adoption of an idea by using arguments or other means |
Positive expectations are available in the environment Messages need to be relevant and not too discrepant from beliefs of individual |
Patients are given information in their RTW workbook, and staff express approval of patients who acquaint themselves with key information about recovery and RTW provided by the HOT RTW workbook and website states that content informed by patients and other stakeholders and current evidence |
| Recognises that employersa are key stakeholders in RTW and involving them at an early stage can facilitate RTW | Consciousness raising | Providing information about causes, consequences, alternatives | Can use feedback and confrontation, but raising awareness must be quickly followed by increase in self-efficacy |
Information in RTW workbook, website and members of HOT consistent in expressing their belief in involving employers at an early stage Evidence about early involvement of employers in RTW workbook |
| Recognises that the ideal RTW process relies on co-ordination and joint planning between health care, the patient and their employer | Elaboration | Stimulating the learner to add information that is processed | Messages that are personally relevant, easily understandable | RTWC and HOT (e.g. pre-assessment education) encourage discussion of communication pathways |
| Recognises that employers do not necessarily know about this type of surgery and how best to facilitate RTW | Shifting perspectives (TSD) | Encourage taking the perspective of the other | Initiation from the perspective of the learner; needs imaginary competence | HOT helps patient to see RTW from the employer’s perspective – what they know and need |
| Recognises that communication with their employera is key to a successful RTW outcome | Modelling | Providing an appropriate model | Identification with the model | Information in RTW workbook, website and members of HOT consistent in expressing their belief in communication with employer |
| Recognises that RTW is an ongoing process that needs to monitored | Elaboration | Stimulating the learner to add information that is processed | Messages that are personally relevant, easily understandable | RTWC and HOT (e.g. pre-assessment education) encourage discussion of RTW monitoring |
Staff methods and applications
Behaviour to be targeted: HOTs to deliver work-focused support and advice.
Knowledge and awareness
| Methods | Definitions | Parameters | Applications |
|---|---|---|---|
| Discussion (elaboration likelihood model) | Stimulating the learner to add meaning to the information that is processed | Listening to the learner to ensure that the correct schemas are activated | OPAL staff training prior to implementation. Ideally group, face to face, interactive |
|
Elaboration (theories of information processing; elaboration likelihood model) Coherence and imagery (theories of information processing) |
Stimulating the learner to add meaning to the information that is processed | Messages personally relevant, easily understandable |
Each member of HOT has own OPAL study pack containing this information:Each work area has study pack available Computer-based version of training Study website Study newsletters |
| Individualisation/tailoring (transtheoretical model) | Matching to participant characteristics, opportunities for personal/paced learning | Tailoring to participant, personal communication responds to learner’s need, relevance |
Staff training tailored to specific profession/role/need One-to-one training/support from OPAL team as required |
| Modelling (social cognitive theory; theories of learning) | Providing an appropriate model |
Identification with model Coping vs. mastery model |
Coping models of staff ‘tasks’ used in training/study packs |
|
Consciousness raising (health belief model) Framing (protection motivation theory) |
Information about causes, and consequences of behaviour Emphasise pros and cons of behaviour |
Raising awareness should be quickly followed by increase in self-efficacy Frames are more readily accepted |
Staff training – consequences of providing RTW advice/support |
| Providing cues (theories of information processing) | Ensuring same cues are present at time of learning and time of retrieval | Work best when people select and provide own cues | Staff at each research study site to suggest cues to action
|
Skills and self-efficacy
| Methods | Definitions | Parameters | Applications |
|---|---|---|---|
| Verbal persuasion (social cognitive theory) | Use messages that suggest that the participants possess certain capabilities | Credible source | Research team explain through training that they believe that the HOT can do this; that OPAL study is informed by stakeholders and evidence |
| Facilitation (social cognitive theory) | Creating an environment that makes the action easier or reduces barriers | Required real changes in the environment | Staff training at optimal times/places/methods
|
|
Information about others’ approval Social comparison (theory of planned behaviour; social comparison theory) |
Providing information about whether others will approve or disapprove of any proposed behaviour change Observation of other non-experts to evaluate one’s own opinions and abilities |
Positive expectations available in environment Upwards comparison may help set better goals, downwards may increase sense of self-efficacy |
Staff training includes information on phase 1 stakeholder interviews, and increasing focus on work and health Comparison with other HOTs Comparison with support for other health conditions Study newsletters with updates from each site |
|
Feedback Reinforcement (theories of learning, goal-setting, social cognitive theory) |
Giving information as to the extent of impact of performance Lining behaviour to consequence that increases rate of behaviour |
Feedback needs to be individual, specific and follow the behaviour in time As above |
Regular contact maintained with HOT from OPAL team Study newsletters with updates from each site with positive feedback Praise from OPAL team for staff engagement with OPAL study |
|
Guided practice Modelling (social cognitive theory) |
Prompting individuals to rehearse and repeat behaviour various times, discuss experience and provide feedback Providing an appropriate model |
Requires supervision by an experienced person Identification with model Coping vs. mastery model |
OPAL team members model/role play/provide examples of target behaviours then ask staff to do the same and give feedback emphasising what has been done well |
| Planning coping responses (attribution theory; theories of self-regulation) | Prompting participants to list potential barriers and ways to overcome these | Identification of high-risk situations and practise of coping responses | OPAL team and HOT members discuss and problem-solve potential problems as part of training, e.g. patient avoids contact with RTWC, fails to bring RTW workbook |
Attitudes, beliefs, expectations
| Methods | Definitions | Parameters | Applications |
|---|---|---|---|
| Self re-evaluation (transtheoretical model) | Encourage combining both cognitive and affective assessments of one’s self-image with and without an ‘unhealthy’ behaviour | Raising awareness must be quickly followed by increase in problem-solving ability and self-efficacy | Training encourages staff to focus on what they think and how they feel about being a HCP who supports patients in returning to work |
| Shifting perspective (theories of stigma and discrimination) | Encouraging the perspective of another | Initiation from the perspective of the learner; needs imaginary competence | Encouraging staff to view a change in their clinical practice from the perspective of the patient returning to work and their employer, using examples from stakeholder interviews and cohort study in phase 1 of OPAL study as part of training programme |
| Persuasive communication (diffusion of innovations theory) | Guiding people towards the adoption of an idea or action by using arguments or other means | Messages need to be relevant and not too discrepant from the beliefs of the individual | Persuading staff that the delivery of work-focused advice and support at an early stage in the patient’s RTW process is possible |
| Belief selection (theory of planned behaviour) | Using messages to strengthen positive beliefs, weaken negative beliefs and introduce new beliefs | Requires investigation of current beliefs of individual before intervening | Using evidence-based data on RTW to change staff beliefs about the proportion of working patients undergoing surgery |
Perceived norms
| Method | Definition | Parameters | Applications |
|---|---|---|---|
|
Self re-evaluation (transtheoretical model) Belief selection Shifting perspective Persuasive communication |
See above examples | See above examples | Training to focus on encouraging staff to see it as good practice/in accordance with new thinking on work and health/feasible:
|
Training format: ideally group, face to face and interactive but backed up by online presentation, website and information pack.
Bespoke components for different professions/roles/needs are backed up by one-to-one support from the OPAL team.
Training content to include all or some of the following:
-
OPAL study/team overview
-
summary of phase 1 findings
-
overview of current evidence/guidance on work and health/RTW
-
overview of roles of different members of HOT in delivering OPAL
-
study documentation
-
use of the fit note
-
examples of work modifications, barriers and solutions, RTW plans
-
troubleshooting, problem-solving.
Appendix 7 Supporting information for the Delphi consensus process
Delphi consensus participants (n = 66)
| Role/occupation | Location (hospital/base) |
|---|---|
| Surgeons (n = 13) | |
| Surgeon | Middlesbrough |
| Surgeon | Exeter |
| Surgeon | Wrightington |
| Surgeon | Norwich |
| Surgeon | Exeter |
| Surgeon | Middlesbrough |
| Surgeon | Bristol |
| Surgeon | Norwich |
| Surgeon | Edinburgh |
| Surgeon | Aintree |
| Surgeon | West Suffolk |
| Surgeon | Golden Jubilee National Hospital |
| Surgeon | Northumbria |
| AHPs (n = 16) | |
| Research physiotherapist | Edinburgh |
| Physiotherapist | Middlesbrough |
| Research physiotherapist | Norwich |
| Physiotherapist | Bournemouth |
| Physiotherapist | Middlesbrough |
| Occupational therapist | Scunthorpe |
| Occupational therapist | Derby |
| Occupational therapist | Golden Jubilee National Hospital |
| Occupational therapist | Darlington |
| Occupational therapist | Burton |
| Occupational therapist | Northwich |
| Occupational therapist | Lancashire |
| Occupational therapist | St Helens |
| Nurse/research nurse | Edinburgh |
| Nurse practitioner | Middlesbrough |
| Joint replacement nurse | South Tees |
| GPs (n = 10) | |
| GP | South Tees |
| GP | Edinburgh |
| GP | Edinburgh |
| GP | Northumberland |
| GP | Teesside |
| Academic GP | Liverpool |
| Occupational health physician | Manchester |
| GP | Leicestershire |
| RCGP lead for chronic pain (currently in clinical research) | |
| GP | Nottingham |
| Employers (n = 13) | |
| Briar Chemicals | Norwich |
| Babcock International | Plymouth |
| East of England Co-operative Society | East of England |
| Center Parcs Sherwood Forest | Nottingham |
| Physiotherapist | Nottingham |
| Human resources manager | Schaeffler Group (Herzogenaurach, Germany) |
| – | Schaeffler Group |
| CMO/occupational health consultant | BAE Systems (Farnborough, UK) |
| – | Rolls-Royce Holdings (London, UK) |
| Head of safety, health and quality | Finning (Vancouver, BC, Canada) |
| Occupational health manager | Toyota (GB) plc (Burgh Heath, UK) |
| Physiotherapist, occupational health and training team | Rhondda Cynon Taf County Borough Council |
| Patients (n = 14) | |
| Patient lead NJR PLG | – |
| Patient | – |
| Patient/ambassador for global alliance for MSK health of the bone and joint decade | – |
| Patient | – |
| Patient | – |
| Patient | – |
| Service manager for arthritis care | – |
| Patient | – |
| Patient | – |
| Patient | – |
| Patient | – |
| Patient | – |
| Patient | – |
| Patient | – |
Delphi round 1
See OPAL Delphi questionnaires (www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/; accessed 2 May 2020).
| Question | N | Strongly agree | Agree | Disagree | Strongly disagree | Don’t know | Combined strongly agree and agree (%) | Combined strongly disagree and disagree (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||||
| Q3 | 43 | 33 | 76.7 | 9 | 20.9 | 1 | 2.3 | 0 | 0.0 | 0 | 0.0 | 97.7 | 2.3 |
| Q4 | 43 | 23 | 53.5 | 15 | 34.9 | 2 | 4.7 | 2 | 4.7 | 1 | 2.3 | 88.4 | 9.4 |
| Q5 | 43 | 33 | 76.7 | 8 | 18.6 | 2 | 4.7 | 0 | 0.0 | 0 | 0.0 | 95.3 | 4.7 |
| Q6 | 43 | 16 | 37.2 | 17 | 39.5 | 8 | 18.6 | 0 | 0.0 | 2 | 4.7 | 76.7 | 18.6 |
| Q7 | 43 | 11 | 25.6 | 17 | 39.5 | 11 | 25.6 | 1 | 2.3 | 3 | 7.0 | 65.1 | 27.9 |
| Q8 | 43 | 13 | 30.2 | 18 | 41.9 | 7 | 16.3 | 1 | 2.3 | 4 | 9.3 | 72.1 | 18.6 |
| Q9 | 43 | 33 | 76.7 | 10 | 23.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 100.0 | 0.0 |
| Q10 | 43 | 25 | 58.1 | 16 | 37.2 | 2 | 4.7 | 0 | 0.0 | 0 | 0.0 | 95.3 | 4.7 |
| Q11 | 43 | 7 | 16.3 | 28 | 65.1 | 6 | 14.0 | 0 | 0.0 | 2 | 4.7 | 81.4 | 14.0 |
| Q12 | 43 | 27 | 62.8 | 14 | 32.6 | 2 | 4.7 | 0 | 0.0 | 0 | 0.0 | 95.3 | 4.7 |
| Q13 | 43 | 24 | 55.8 | 19 | 44.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 100.0 | 0.0 |
| Q14 | 43 | 20 | 46.5 | 21 | 48.8 | 1 | 2.3 | 0 | 0.0 | 1 | 2.3 | 95.3 | 2.3 |
| Q15 | 43 | 31 | 72.1 | 11 | 25.6 | 0 | 0.0 | 0 | 0.0 | 1 | 2.3 | 97.7 | 0.0 |
| Q16 | 43 | 13 | 30.2 | 22 | 51.2 | 4 | 9.3 | 1 | 2.3 | 3 | 7.0 | 81.4 | 11.6 |
| Q17 | 43 | 14 | 32.6 | 19 | 44.2 | 8 | 18.6 | 1 | 2.3 | 1 | 2.3 | 76.7 | 20.9 |
| Q18 | 43 | 29 | 67.4 | 12 | 27.9 | 1 | 2.3 | 0 | 0.0 | 1 | 2.3 | 95.3 | 2.3 |
| Q19 | 43 | 12 | 27.9 | 26 | 60.5 | 3 | 7.0 | 1 | 2.3 | 1 | 2.3 | 88.4 | 9.3 |
| Q20 | 43 | 14 | 32.6 | 24 | 55.8 | 4 | 9.3 | 1 | 2.3 | 0 | 0.0 | 88.4 | 11.6 |
| Q21 | 43 | 18 | 41.9 | 20 | 46.5 | 3 | 7.0 | 0 | 0.0 | 2 | 4.7 | 88.4 | 7.0 |
| Q22 | 43 | 7 | 16.3 | 23 | 53.5 | 8 | 18.6 | 1 | 2.3 | 4 | 9.3 | 69.8 | 20.9 |
| Q23 | 43 | 14 | 32.6 | 26 | 60.5 | 2 | 4.7 | 0 | 0.0 | 1 | 2.3 | 93.0 | 4.7 |
| Q24 | 43 | 11 | 25.6 | 24 | 55.8 | 4 | 9.3 | 0 | 0.0 | 4 | 9.3 | 81.4 | 9.3 |
| Q25 | 43 | 10 | 23.3 | 19 | 44.2 | 9 | 20.9 | 2 | 4.7 | 3 | 7.0 | 67.4 | 25.6 |
| Q26 | 43 | 10 | 23.3 | 19 | 44.2 | 11 | 25.6 | 1 | 2.3 | 2 | 4.7 | 67.4 | 27.9 |
| Q27 | 43 | 10 | 23.3 | 26 | 60.5 | 4 | 9.3 | 0 | 0.0 | 3 | 7.0 | 83.7 | 9.3 |
| Q28 | 43 | 13 | 30.2 | 23 | 53.5 | 5 | 11.6 | 1 | 2.3 | 1 | 2.3 | 83.7 | 13.9 |
| Q29 | 43 | 20 | 46.5 | 18 | 41.9 | 4 | 9.3 | 1 | 2.3 | 0 | 0.0 | 88.4 | 11.6 |
| Q30 | 43 | 15 | 34.9 | 17 | 39.5 | 10 | 23.3 | 0 | 0.0 | 1 | 2.3 | 74.4 | 23.3 |
| Q31 | 43 | 17 | 39.5 | 18 | 41.9 | 7 | 16.3 | 0 | 0.0 | 1 | 2.3 | 81.4 | 16.3 |
| Q32 | 43 | 8 | 18.6 | 26 | 60.5 | 6 | 14.0 | 0 | 0.0 | 3 | 7.0 | 79.1 | 14.0 |
| Q33 | 43 | 8 | 18.6 | 21 | 48.8 | 10 | 23.3 | 0 | 0.0 | 4 | 9.3 | 67.4 | 23.3 |
| Q34 | 43 | 11 | 25.6 | 15 | 34.9 | 12 | 27.9 | 0 | 0.0 | 5 | 11.6 | 60.5 | 27.9 |
| Question | N | Strongly agree | Agree | Disagree | Strongly disagree | Don’t know | Combined strongly agree and agree (%) | Combined strongly disagree and disagree (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||||
| Q9 | 43 | 33 | 76.7 | 10 | 23.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 100.0 | 0.0 |
| Q13 | 43 | 24 | 55.8 | 19 | 44.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 100.0 | 0.0 |
| Q3 | 43 | 33 | 76.7 | 9 | 20.9 | 1 | 2.3 | 0 | 0.0 | 0 | 0.0 | 97.7 | 2.3 |
| Q15 | 43 | 31 | 72.1 | 11 | 25.6 | 0 | 0.0 | 0 | 0.0 | 1 | 2.3 | 97.7 | 0.0 |
| Q5 | 43 | 33 | 76.7 | 8 | 18.6 | 2 | 4.7 | 0 | 0.0 | 0 | 0.0 | 95.3 | 4.7 |
| Q18 | 43 | 29 | 67.4 | 12 | 27.9 | 1 | 2.3 | 0 | 0.0 | 1 | 2.3 | 95.3 | 2.3 |
| Q12 | 43 | 27 | 62.8 | 14 | 32.6 | 2 | 4.7 | 0 | 0.0 | 0 | 0.0 | 95.3 | 4.7 |
| Q10 | 43 | 25 | 58.1 | 16 | 37.2 | 2 | 4.7 | 0 | 0.0 | 0 | 0.0 | 95.3 | 4.7 |
| Q14 | 43 | 20 | 46.5 | 21 | 48.8 | 1 | 2.3 | 0 | 0.0 | 1 | 2.3 | 95.3 | 2.3 |
| Q23 | 43 | 14 | 32.6 | 26 | 60.5 | 2 | 4.7 | 0 | 0.0 | 1 | 2.3 | 93.0 | 4.7 |
| Q4 | 43 | 23 | 53.5 | 15 | 34.9 | 2 | 4.7 | 2 | 4.7 | 1 | 2.3 | 88.4 | 9.3 |
| Q29 | 43 | 20 | 46.5 | 18 | 41.9 | 4 | 9.3 | 1 | 2.3 | 0 | 0.0 | 88.4 | 11.6 |
| Q21 | 43 | 18 | 41.9 | 20 | 46.5 | 3 | 7.0 | 0 | 0.0 | 2 | 4.7 | 88.4 | 7.0 |
| Q20 | 43 | 14 | 32.6 | 24 | 55.8 | 4 | 9.3 | 1 | 2.3 | 0 | 0.0 | 88.4 | 11.6 |
| Q19 | 43 | 12 | 27.9 | 26 | 60.5 | 3 | 7.0 | 1 | 2.3 | 1 | 2.3 | 88.4 | 9.3 |
| Q28 | 43 | 13 | 30.2 | 23 | 53.5 | 5 | 11.6 | 1 | 2.3 | 1 | 2.3 | 83.7 | 14.0 |
| Q27 | 43 | 10 | 23.3 | 26 | 60.5 | 4 | 9.3 | 0 | 0.0 | 3 | 7.0 | 83.7 | 9.3 |
| Q31 | 43 | 17 | 39.5 | 18 | 41.9 | 7 | 16.3 | 0 | 0.0 | 1 | 2.3 | 81.4 | 16.3 |
| Q16 | 43 | 13 | 30.2 | 22 | 51.2 | 4 | 9.3 | 1 | 2.3 | 3 | 7.0 | 81.4 | 11.6 |
| Q24 | 43 | 11 | 25.6 | 24 | 55.8 | 4 | 9.3 | 0 | 0.0 | 4 | 9.3 | 81.4 | 9.3 |
| Q11 | 43 | 7 | 16.3 | 28 | 65.1 | 6 | 14.0 | 0 | 0.0 | 2 | 4.7 | 81.4 | 14.0 |
| Q32 | 43 | 8 | 18.6 | 26 | 60.5 | 6 | 14.0 | 0 | 0 | 3 | 7.0 | 79.1 | 14.0 |
| Q6 | 43 | 16 | 37.2 | 17 | 39.5 | 8 | 18.6 | 0 | 0.0 | 2 | 4.7 | 76.7 | 18.6 |
| Q17 | 43 | 14 | 32.6 | 19 | 44.2 | 8 | 18.6 | 1 | 2.3 | 1 | 2.3 | 76.7 | 20.9 |
| Q30 | 43 | 15 | 34.9 | 17 | 39.5 | 10 | 23.3 | 0 | 0.0 | 1 | 2.3 | 74.4 | 23.3 |
| Q8 | 43 | 13 | 30.2 | 18 | 41.9 | 7 | 16.3 | 1 | 2.3 | 4 | 9.3 | 72.1 | 18.6 |
| Q22 | 43 | 7 | 16.3 | 23 | 53.5 | 8 | 18.6 | 1 | 2.3 | 4 | 9.3 | 69.8 | 20.9 |
| Q25 | 43 | 10 | 23.3 | 19 | 44.2 | 9 | 20.9 | 2 | 4.7 | 3 | 7.0 | 67.4 | 25.6 |
| Q26 | 43 | 10 | 23.3 | 19 | 44.2 | 11 | 25.6 | 1 | 2.3 | 2 | 4.7 | 67.4 | 27.9 |
| Q33 | 43 | 8 | 18.6 | 21 | 48.8 | 10 | 23.3 | 0 | 0 | 4 | 9.3 | 67.4 | 23.3 |
| Q7 | 43 | 11 | 25.6 | 17 | 39.5 | 11 | 25.6 | 1 | 2.3 | 3 | 7.0 | 65.1 | 27.9 |
| Q34 | 43 | 11 | 25.6 | 15 | 34.9 | 12 | 27.9 | 0 | 0 | 5 | 11.6 | 60.5 | 27.9 |
Q9. Information about exercises and rehabilitation following surgery.
Q13. Information about returning to driving.
Q3. A broad overview written for all stakeholders of what to expect following surgery (rates and timing of expected recovery).
Q15. Information about managing pain, types of analgesia and side effects.
Q5. Information about postoperative precautions, restrictions and activities to avoid following surgery.
Q18. Information about symptom management in relation to return to work and specific occupations (e.g. expected levels of fatigue, pain and swelling).
Q12. Tips and tricks to help the patient manage around their home with day-to-day activities immediately following surgery.
Q10. Information regarding postoperative complications and their management.
Q14. Signposting to DVLA guidance.
Q23. Information for the patient about who to ask if they are having a problem returning to work.
Q4. Information about expected level of function at different time points following surgery.
Q29. Advice about adaptions to working patterns to assist return including the use of phased returns, modified hours and altered work schedules.
Q21. Information and resources to support self-advocacy and empowerment.
Q20. Information about when it might be appropriate for patients and employers to access occupational health services.
Q19. Information for patients and employers about how to access occupational health services.
Q28. A list of potential workplace modifications, aids and adjustments that could be used to assist with return to work, with examples.
Q27. Information for the patients about how to ask for help at work from their employer and colleagues.
Q31. Guidance on how to set an appropriate provisional return to work date based on the date and type of surgery.
Q16. Guidance for orthopaedic care teams and GPs on how to use and prescribe a fit note.
Q24. Signposts to national and local support services (e.g. Fit4Work, Citizens Advice and ACAS).
Q11. Information about how having surgery may impact on social relationships.
Q32. Advice about how psychosocial and emotional factors influence return to work.
Q6. Information about how long the hip and knee replacement prostheses will last.
Q17. Examples of the correct use of fit notes.
Q30. A list of potential return to work barriers for patients and employers to consider.
Q8. Information about managing more than one joint replacement in close succession.
Q22. Information about how to access resilience training courses and other resources aimed at helping people cope better during challenging times. Courses such as these improve the patient’s confidence in their ability to bounce back from the many pressures and adversities they encounter in today’s workplace.
Q25. Links to national workplace legislation and guidance (e.g. information on workers’ rights, employment law).
Q26. Testimonials and case studies of patients who have successfully returned to work after surgery.
Q33. Guidance and frameworks to facilitate meetings to discuss sickness and return to work between the patient and their employer.
Q7. Information about revision (redo) surgery.
Q34. Guidance for employers about how to perform a work capacity assessment.
ACAS, Advisory, Conciliation and Arbitration Service (London, UK).
Citizens Advice: London, UK.
Adapted with permission from Baker et al. 74 This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. This box includes minor additions and formatting changes to the original.
| Question | Percentage of respondents | Total groups SA/A | Total groups SD/D | Action | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgeon (n = 8) | AHP (n = 11) | GP (n = 6) | Employer (n = 4) | Patient (n = 14) | ||||||||||||||
| SA/A | SD/D | DK | SA/A | SD/D | DK | SA/A | SD/D | DK | SA/A | SD/D | DK | SA/A | SD/D | DK | ||||
| Q22 | 50 | 38 | 13 | 82 | 18 | 0 | 66 | 17 | 17 | 75 | 0 | 25 | 71 | 21 | 7 | 3 of 5 | 0 of 5 | Round 2 |
| Q25 | 50 | 38 | 13 | 73 | 9 | 18 | 66 | 33 | 0 | 100 | 0 | 0 | 64 | 36 | 0 | 2 of 5 | 0 of 5 | Round 2 |
| Q26 | 63 | 38 | 0 | 82 | 9 | 9 | 66 | 33 | 0 | 50 | 50 | 0 | 64 | 29 | 7 | 1 of 5 | 0 of 5 | Discarded |
| Q33 | 38 | 63 | 0 | 73 | 9 | 18 | 83 | 17 | 0 | 75 | 25 | 0 | 71 | 14 | 14 | 4 of 5 | 0 of 5 | Round 2 |
| Q7 | 50 | 50 | 0 | 64 | 27 | 9 | 50 | 33 | 17 | 75 | 0 | 25 | 79 | 21 | 0 | 2 of 5 | 0 of 5 | Round 2 |
| Q34 | 25 | 75 | 0 | 45 | 27 | 27 | 83 | 0 | 17 | 50 | 25 | 25 | 86 | 14 | 0 | 2 of 5 | 1 of 5 | Round 2 |
| Comment number | Comment |
|---|---|
| 1 | Some of the questions I may answer differently depending on the content and angle that the information is given. I feel adaptations at work have far more effect of disabling people and causing friction and ill feeling more than help in the long run. Phased return and temporarily modifying work would be much more successful in the long term. I feel questions/information around ‘expected’ time frames can be tricky for generic leaflets where so many variable factors exist and can again cause much pressure and friction with employers if not met |
| 2 | Qu 30 has wrong options |
| 3 | No mention thus far regarding type of work. What is reasonable and what is out of the question |
| 4 | I’ve found social media patient forums to be particularly useful |
| 5 | Crucial for patients to be given access to information about their condition and the range of health-care treatments/options, and self-management options, available to them (shared decision making) |
| 6 | Specific co-worker contact (volunteer) or case worker in larger organisation can help out with ‘tunnel vision’ situations |
| 7 | Surely the aim is to help employees & employers find a common ground. This section of points should be sufficient to facilitate this |
| 8 | All of my answers refer to NHS practitioners. Where I work, I have access to our own occupational health practitioners who were contacted and appropriate help and guidance was given from this source |
| 9 | All patients will vary in the recovery time due to healing process and managing pain. Physiotherapist sessions in groups help give an easy way to gudge [sic] progress. I found this most useful as I was slow at first |
| 10 | It would need to be clear that the adjustments, adaptations and aids would need to be specific to the individual. Information would need to reflect that there are many variations in the services offered by both NHS and employers |
| Question | N | Strongly agree | Agree | Disagree | Strongly disagree | Don’t know | Combined strongly agree and agree (%) | Combined strongly disagree and disagree (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||||
| Q36 | 43 | 18 | 41.9 | 19 | 44.2 | 1 | 2.3 | 0 | 0.0 | 5 | 11.6 | 86.0 | 2.3 |
| Q37 | 43 | 17 | 39.5 | 24 | 55.8 | 0 | 0.0 | 0 | 0.0 | 2 | 4.7 | 95.3 | 0.0 |
| Q38 | 43 | 15 | 34.9 | 17 | 39.5 | 9 | 20.9 | 0 | 0.0 | 2 | 4.7 | 74.4 | 20.9 |
| Q39 | 43 | 22 | 51.2 | 20 | 46.5 | 0 | 0.0 | 0 | 0.0 | 1 | 2.3 | 97.7 | 0.0 |
| Q40 | 43 | 15 | 34.9 | 21 | 48.8 | 4 | 9.3 | 0 | 0.0 | 3 | 7.0 | 83.7 | 9.3 |
| Q41 | 43 | 13 | 30.2 | 22 | 51.2 | 1 | 2.3 | 2 | 4.7 | 5 | 11.6 | 81.4 | 7.0 |
| Q42 | 43 | 14 | 32.6 | 24 | 55.8 | 2 | 4.7 | 0 | 0.0 | 3 | 7.0 | 88.4 | 4.7 |
| Q43 | 43 | 9 | 20.9 | 18 | 41.9 | 13 | 30.2 | 0 | 0.0 | 3 | 7.0 | 62.8 | 30.2 |
| Q44 | 43 | 9 | 20.9 | 21 | 48.8 | 7 | 16.3 | 1 | 2.3 | 5 | 11.6 | 69.8 | 18.6 |
| Q45 | 43 | 13 | 30.2 | 25 | 58.1 | 5 | 11.6 | 0 | 0.0 | 0 | 0.0 | 88.4 | 11.6 |
| Q46 | 43 | 13 | 30.2 | 22 | 51.2 | 6 | 14.0 | 0 | 0.0 | 2 | 4.7 | 81.4 | 14.0 |
| Q47 | 43 | 13 | 30.2 | 23 | 53.5 | 3 | 7.0 | 0 | 0.0 | 4 | 9.3 | 83.7 | 7.0 |
| Q48 | 43 | 14 | 32.6 | 22 | 51.2 | 6 | 14.0 | 0 | 0.0 | 1 | 2.3 | 83.7 | 14.0 |
| Q49 | 43 | 8 | 18.6 | 23 | 53.5 | 10 | 23.3 | 0 | 0.0 | 2 | 4.7 | 72.1 | 23.3 |
| Q50 | 43 | 9 | 20.9 | 16 | 37.2 | 15 | 34.9 | 0 | 0.0 | 3 | 7.0 | 58.1 | 34.9 |
| Q51 | 43 | 16 | 37.2 | 20 | 46.5 | 3 | 7.0 | 1 | 2.3 | 3 | 7.0 | 83.7 | 9.3 |
| Q52 | 43 | 22 | 51.2 | 18 | 41.9 | 2 | 4.7 | 0 | 0.0 | 1 | 2.3 | 93.0 | 4.7 |
| Q53 | 43 | 7 | 16.3 | 21 | 48.8 | 10 | 23.3 | 2 | 4.7 | 3 | 7.0 | 65.1 | 27.9 |
| Q54 | 43 | 8 | 18.6 | 28 | 65.1 | 6 | 14.0 | 1 | 2.3 | 0 | 0.0 | 83.7 | 16.3 |
| Q55 | 43 | 3 | 7.0 | 18 | 41.9 | 19 | 44.2 | 0 | 0.0 | 3 | 7.0 | 48.8 | 44.2 |
| Q56 | 42 | 12 | 28.6 | 22 | 52.4 | 5 | 11.9 | 0 | 0.0 | 3 | 7.1 | 81.0 | 11.9 |
| Q57 | 42 | 10 | 23.8 | 22 | 52.4 | 5 | 11.9 | 0 | 0.0 | 5 | 11.9 | 76.2 | 11.9 |
| Q58 | 42 | 11 | 26.2 | 22 | 52.4 | 5 | 11.9 | 0 | 0.0 | 4 | 9.5 | 78.6 | 11.9 |
| Q59 | 42 | 7 | 16.7 | 18 | 42.9 | 11 | 26.2 | 2 | 4.8 | 4 | 9.5 | 59.5 | 31.0 |
| Q60 | 42 | 8 | 19.0 | 19 | 45.2 | 8 | 19.0 | 3 | 7.1 | 4 | 9.5 | 64.3 | 26.2 |
| Q61 | 42 | 8 | 19.0 | 21 | 50.0 | 3 | 7.1 | 1 | 2.4 | 9 | 21.4 | 69.0 | 9.5 |
| Q62 | 42 | 11 | 26.2 | 22 | 52.4 | 3 | 7.1 | 0 | 0.0 | 6 | 14.3 | 78.6 | 7.1 |
| Q63 | 42 | 6 | 14.3 | 25 | 59.5 | 5 | 11.9 | 1 | 2.4 | 5 | 11.9 | 73.8 | 14.3 |
| Q64 | 42 | 9 | 21.4 | 27 | 64.3 | 3 | 7.1 | 0 | 0.0 | 3 | 7.1 | 85.7 | 7.1 |
| Q65 | 41 | 12 | 29.3 | 22 | 53.7 | 5 | 12.2 | 0 | 0.0 | 2 | 4.9 | 82.9 | 12.2 |
| Q66 | 41 | 9 | 22.0 | 21 | 51.2 | 3 | 7.3 | 0 | 0.0 | 8 | 19.5 | 73.2 | 7.3 |
| Q67 | 41 | 13 | 31.7 | 21 | 51.2 | 3 | 7.3 | 0 | 0.0 | 4 | 9.8 | 82.9 | 7.3 |
| Question | N | Strongly agree | Agree | Disagree | Strongly disagree | Don’t know | Unable to answer (n) | Combined strongly agree and agree (%) | Combined strongly disagree and disagree (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |||||
| Q36 | 39 | 10 | 25.6 | 19 | 48.7 | 5 | 12.8 | 0 | 0.0 | 5 | 12.8 | 4 | 74.4 | 12.8 |
| Q37 | 38 | 11 | 28.9 | 16 | 42.1 | 5 | 13.2 | 0 | 0.0 | 6 | 15.8 | 5 | 71.1 | 13.2 |
| Q38 | 37 | 11 | 29.7 | 12 | 32.4 | 9 | 24.3 | 0 | 0.0 | 5 | 13.5 | 6 | 62.2 | 24.3 |
| Q39 | 39 | 8 | 20.5 | 15 | 38.5 | 6 | 15.4 | 2 | 5.1 | 8 | 20.5 | 4 | 59.0 | 20.5 |
| Q40 | 38 | 9 | 23.7 | 21 | 55.3 | 4 | 10.5 | 0 | 0.0 | 4 | 10.5 | 5 | 78.9 | 10.5 |
| Q41 | 37 | 4 | 10.8 | 9 | 24.3 | 10 | 27.0 | 3 | 8.1 | 11 | 29.7 | 6 | 35.1 | 35.1 |
| Q42 | 37 | 4 | 10.8 | 22 | 59.5 | 3 | 8.1 | 0 | 0.0 | 8 | 21.6 | 6 | 70.3 | 8.1 |
| Q43 | 37 | 3 | 8.1 | 7 | 18.9 | 18 | 48.6 | 0 | 0.0 | 9 | 24.3 | 6 | 27.0 | 48.6 |
| Q44 | 40 | 7 | 17.5 | 24 | 60.0 | 4 | 10.0 | 0 | 0.0 | 5 | 12.5 | 3 | 77.5 | 10.0 |
| Q45 | 38 | 10 | 26.3 | 21 | 55.3 | 5 | 13.2 | 0 | 0.0 | 2 | 5.3 | 5 | 81.6 | 13.2 |
| Q46 | 39 | 5 | 12.8 | 14 | 35.9 | 9 | 23.1 | 4 | 10.3 | 7 | 17.9 | 4 | 48.7 | 33.3 |
| Q47 | 38 | 7 | 18.4 | 16 | 42.1 | 8 | 21.1 | 3 | 7.9 | 4 | 10.5 | 5 | 60.5 | 28.9 |
| Q48 | 38 | 9 | 23.7 | 15 | 39.5 | 7 | 18.4 | 5 | 13.2 | 2 | 5.3 | 5 | 63.2 | 31.6 |
| Q49 | 40 | 4 | 10.0 | 13 | 32.5 | 13 | 32.5 | 3 | 7.5 | 7 | 17.5 | 3 | 42.5 | 40.0 |
| Q50 | 38 | 6 | 15.8 | 12 | 31.6 | 15 | 39.5 | 0 | 0.0 | 5 | 13.2 | 5 | 47.4 | 39.5 |
| Q51 | 39 | 8 | 20.5 | 23 | 59.0 | 3 | 7.7 | 3 | 7.7 | 2 | 5.1 | 4 | 79.5 | 15.4 |
| Q52 | 39 | 14 | 35.9 | 18 | 46.2 | 2 | 5.1 | 0 | 0.0 | 5 | 12.8 | 4 | 82.1 | 5.1 |
| Q53 | 38 | 5 | 13.2 | 11 | 28.9 | 10 | 26.3 | 4 | 10.5 | 8 | 21.1 | 5 | 42.1 | 36.8 |
| Q54 | 40 | 4 | 10.0 | 17 | 42.5 | 8 | 20.0 | 2 | 5.0 | 9 | 22.5 | 3 | 52.5 | 25.0 |
| Q55 | 36 | 0 | 0.0 | 12 | 33.3 | 16 | 44.4 | 1 | 2.8 | 7 | 19.4 | 7 | 33.3 | 47.2 |
| Q56 | 38 | 7 | 18.4 | 18 | 47.4 | 2 | 5.3 | 2 | 5.3 | 9 | 23.7 | 4 | 65.8 | 10.5 |
| Q57 | 40 | 7 | 17.5 | 22 | 55.0 | 4 | 10.0 | 0 | 0.0 | 7 | 17.5 | 2 | 72.5 | 10.0 |
| Q58 | 41 | 9 | 22.0 | 19 | 46.3 | 6 | 14.6 | 0 | 0.0 | 7 | 17.1 | 1 | 68.3 | 14.6 |
| Q59 | 39 | 7 | 17.9 | 22 | 56.4 | 5 | 12.8 | 1 | 2.6 | 4 | 10.3 | 3 | 74.4 | 15.4 |
| Q60 | 35 | 4 | 11.4 | 13 | 37.1 | 8 | 22.9 | 3 | 8.6 | 7 | 20.0 | 7 | 48.6 | 31.4 |
| Q61 | 38 | 5 | 13.2 | 16 | 42.1 | 4 | 10.5 | 1 | 2.6 | 12 | 31.6 | 4 | 55.3 | 13.2 |
| Q62 | 38 | 8 | 21.1 | 22 | 57.9 | 1 | 2.6 | 0 | 0.0 | 7 | 18.4 | 4 | 78.9 | 2.6 |
| Q63 | 39 | 2 | 5.1 | 18 | 46.2 | 7 | 17.9 | 0 | 0.0 | 12 | 30.8 | 3 | 51.3 | 17.9 |
| Q64 | 39 | 6 | 15.4 | 25 | 64.1 | 2 | 5.1 | 0 | 0.0 | 6 | 15.4 | 3 | 79.5 | 5.1 |
| Q65 | 39 | 4 | 10.3 | 17 | 43.6 | 10 | 25.6 | 1 | 2.6 | 7 | 17.9 | 2 | 53.8 | 28.2 |
| Q66 | 38 | 7 | 18.4 | 17 | 44.7 | 3 | 7.9 | 0 | 0.0 | 11 | 28.9 | 3 | 63.2 | 7.9 |
| Q67 | 38 | 9 | 23.7 | 16 | 42.1 | 4 | 10.5 | 1 | 2.6 | 8 | 21.1 | 3 | 65.8 | 13.2 |
| Question | Combined strongly agree and agree (%) | Outcome | |
|---|---|---|---|
| Important | Deliverable | ||
| Q39 | 97.7 | 59.0 | Subgroup analysis |
| Q37 | 95.3 | 71.1 | Consensus reached |
| Q52 | 93.0 | 82.1 | Consensus reached |
| Q45 | 88.4 | 81.6 | Consensus reached |
| Q42 | 88.4 | 70.3 | Consensus reached |
| Q36 | 86.0 | 74.4 | Consensus reached |
| Q64 | 85.7 | 79.5 | Consensus reached |
| Q51 | 83.7 | 79.5 | Consensus reached |
| Q48 | 83.7 | 63.2 | Subgroup analysis |
| Q54 | 83.7 | 52.5 | Subgroup analysis |
| Q40 | 83.7 | 78.9 | Consensus reached |
| Q47 | 83.7 | 60.5 | Subgroup analysis |
| Q65 | 82.9 | 53.8 | Subgroup analysis |
| Q67 | 82.9 | 65.8 | Subgroup analysis |
| Q46 | 81.4 | 48.7 | Subgroup analysis |
| Q41 | 81.4 | 35.1 | Subgroup analysis |
| Q56 | 81.0 | 65.8 | Subgroup analysis |
| Q62 | 78.6 | 78.9 | Consensus reached |
| Q58 | 78.6 | 68.3 | Subgroup analysis |
| Q57 | 76.2 | 72.5 | Consensus reached |
| Q38 | 74.4 | 62.2 | Subgroup analysis |
| Q63 | 73.8 | 51.3 | Subgroup analysis |
| Q66 | 73.2 | 63.2 | Subgroup analysis |
| Q49 | 72.1 | 42.5 | Subgroup analysis |
| Q44 | 69.8 | 77.5 | Subgroup analysis |
| Q61 | 69.0 | 55.3 | Discarded |
| Q53 | 65.1 | 42.1 | Discarded |
| Q60 | 64.3 | 48.6 | Discarded |
| Q43 | 62.8 | 27.0 | Discarded |
| Q59 | 59.5 | 74.4 | Discarded |
| Q50 | 58.1 | 47.4 | Discarded |
| Q55 | 48.8 | 33.3 | Discarded |
Q37. A postoperative mechanism for the identification of patients who are not progressing towards return to work as planned.
Q52. Guidance for health services defining ‘best practice’ for patients returning to work after hip and knee replacement surgery.
Q45. Training for members of the hospital orthopaedic care team to increase awareness about return-to-work issues.
Q42. Interaction between the health-care team and patient by phone, e-mail or ‘online’ so that members of the care team can monitor progress and help the patient use the advice and information provided.
Q36. A mechanism for preoperative identification of patients at ‘high risk’ of prolonged sickness absence following surgery.
Q64. Guidance on when in the return-to-work process patients can safely be discharged back to primary care for continued management of their return to work.
Q51. Routine preoperative therapy assessment during which a return-to-work plan is developed between the patients and the hospital orthopaedic care team.
Q40. A separate intervention for hip and knee replacement patients who are not progressing towards return to work as planned.
Q62. A process by which work status can be included in referral information for all patients referred from primary care into secondary care for consideration of hip or knee replacement.
Q57. Information from patients who have experienced the process of returning to work after hip or knee replacement within the preoperative education process.
Fourteen statements that reached consensus for importance but failed to reach consensus for deliverabilityQ39. The ability to ‘step up’ the level of care and provide additional help and support for patients identified as ‘high risk’ of prolonged sickness absence or who that are not progressing towards return to work as planned.
Q48. A prescribed postoperative rehabilitation therapy programme including assessment at regularly defined intervals following surgery.
Q54. Specific preoperative, pre-assessment and educational classes for return-to-work patients to facilitate co-ordination of their care.
Q47. Specific therapy services/classes to oversee the rehabilitation of all patients aiming to return to work after hip and knee replacement.
Q65. A return-to-work plan that can be completed and agreed between the patient, their employer and relevant members of the health-care orthopaedic care team.
Q67. A screening checklist to help stratify work demands and provide a way of tailoring the expected time a patient will require to recover following their surgery before they return to work and the support they may need.
Q46. Greater access, over and above the standard care, to therapy services for all patients aiming to return to work following surgery.
Q41. A named return-to-work team that are members of the hospital orthopaedic care team and are responsible for communicating with patients and actively monitoring their progress and return to work after surgery.
Q56. The development of a local network for patients who have experienced the process of returning to work after hip or knee replacement to provide peer support and guidance.
Q58. Links to national and local online forums for peer support.
Q38. A standard pathway delivering the same level of care to all patients aiming to return to work following their surgery.
Q63. The ability to document and share information between stakeholders about whether workplace interventions/adaptions and changes to work schedules have been used.
Q66. The ability for patients to document and share the outcomes of the return-to-work meetings and discussions with their employer and members of the hospital orthopaedic care team.
Q49. Continued therapy involvement until the point at which the patient returns to work.
Two statements that reached consensus for deliverability but failed to reach consensus for importanceQ44. The ability for patients to be highlighted within the hip/knee replacement pathway documentation, e.g. ‘return to work patient’ in order to increase awareness among members of the hospital orthopaedic team.
Q59. The ability for copies of clinic letters to be sent to employers with patients’ consent.
Six statements that failed to reach consensus for either importance or deliverabilityQ61. The ability for the hospital orthopaedic care team to record information about the duration of and information provided in fit notes issued to individual patients.
Q53. Consideration of patients’ work schedules when listing for surgery.
Q60. A mechanism by which employers, GPs and surgeons could communicate directly with one another and share information about the care and progress of the patients (with the patient’s consent).
Q43. A specific return-to-work co-ordinator who liaises with the employer, GPs and hospital services on behalf of the patient (with the patient’s consent).
Q50. A progress chart to document recovery that could be completed by the patient and relevant members of the hospital orthopaedics care team and shared with the employer.
Q55. The ability for return-to-work patients to be seen by their surgeon at additional or alternative postoperative time points to those offered routinely.
Group statements are ordered based on level of consensus: the first level is based on the percentage of respondents answering strongly agree or agree to the ‘important’ question; the second level is based on the percentage of respondents answering strongly agree or agree to the ‘deliverable’ question.
Adapted with permission from Baker et al. 74 This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. This box includes minor additions and formatting changes to the original.
| Question | Combined strongly agree and agree (%) | Surgeons | AHP | GPs | Employers | Patients | Total | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| Importance | Deliverable | ||||||||
| Q39 | 97.7 | 59.0 | Yes | 1 | Discarded | ||||
| Q48 | 83.7 | 63.2 | Yes | Yes | Yes | 3 | Round 2 | ||
| Q54 | 83.7 | 52.5 | Yes | 1 | Discarded | ||||
| Q47 | 83.7 | 60.5 | Yes | Yes | 2 | Round 2 | |||
| Q65 | 82.9 | 53.8 | Yes | Yes | 2 | Round 2 | |||
| Q67 | 82.9 | 65.8 | Yes | Yes | Yes | 3 | Round 2 | ||
| Q46 | 81.4 | 48.7 | Yes | 1 | Discarded | ||||
| Q41 | 81.4 | 35.1 | Yes | 1 | Discarded | ||||
| Q56 | 81.0 | 65.8 | Yes | Yes | 2 | Round 2 | |||
| Q58 | 78.6 | 68.3 | Yes | Yes | 2 | Round 2 | |||
| Q38 | 74.4 | 62.2 | Yes | 1 | Discarded | ||||
| Q63 | 73.8 | 51.3 | Yes | 1 | Discarded | ||||
| Q66 | 73.2 | 63.2 | Yes | 1 | Discarded | ||||
| Q49 | 72.1 | 42.5 | 0 | Discarded | |||||
| Q44 | 69.8 | 77.5 | Yes | Yes | 2 | Round 2 | |||
| Q59 | 59.5 | 74.4 | Yes | 1 | Discarded | ||||
| Total | 6 | 2 | 6 | 8 | 2 | ||||
| Comment number | Comment |
|---|---|
| 1 | The constant reference to ‘return to work’ makes me, as a long term retired person, feel very much a second class of patient. In spite of being retired I do much volunteer work, some of it within the NHS umbrella |
| 2 | While identifying and supporting folk to return to work there can be no pre- and post-operation stratification between this group and those who do not work. They both merit the same intensity of management to enable them to achieve the best possible outcome |
| 3 | Employers will have their own risk assment [sic] programme for work planning according to their industry. Intervention in programming of work duties may cause difficulty |
| 4 | You are basing it all on those employed! Some of us are self-employed . . . so not helpful at all |
| 5 | Difficult to answer without considering all that we already do here for patients who are returning to work post joint replacement. We are an outpatient OT service advising and providing work simulation as part of rehab. Providing letters to GPs, employers and consultants with the required info re a patient’s potential to return to work. Completing workplace assessments and capacity assessments with reports. Interventions based on the therapist’s assessment of need and on a case by case basis |
Delphi round 2
| Question | N | Strongly agree | Agree | Disagree | Strongly disagree | Don’t know | Combined strongly agree and agree (%) | Combined strongly disagree and disagree (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||||
| Q2 | 26 | 4 | 15.4 | 13 | 50.0 | 6 | 23.1 | 2 | 7.7 | 1 | 3.9 | 65.4 | 30.8 |
| Q3 | 26 | 6 | 23.1 | 16 | 61.5 | 2 | 7.7 | 1 | 3.9 | 1 | 3.9 | 84.6 | 11.5 |
| Q4 | 26 | 4 | 15.4 | 17 | 65.4 | 2 | 7.7 | 0 | 0.0 | 2 | 7.7 | 80.7 | 7.7 |
| Q5 | 26 | 7 | 26.9 | 15 | 57.6 | 3 | 11.5 | 1 | 3.9 | 0 | 0.0 | 84.6 | 15.4 |
| Q6 | 26 | 5 | 19.2 | 13 | 50.0 | 3 | 11.5 | 1 | 3.9 | 4 | 15.4 | 69.2 | 15.4 |
| Q7 | 26 | 6 | 23.1 | 17 | 65.4 | 2 | 7.7 | 0 | 0.0 | 1 | 3.9 | 88.5 | 7.7 |
| Q8 | 26 | 12 | 46.2 | 10 | 38.5 | 3 | 11.5 | 0 | 0.0 | 1 | 3.9 | 84.6 | 11.5 |
| Q9 | 26 | 6 | 23.1 | 16 | 61.5 | 3 | 11.5 | 0 | 0.0 | 1 | 3.9 | 84.6 | 11.5 |
| Q10 | 26 | 8 | 30.8 | 16 | 61.5 | 2 | 7.7 | 0 | 0.0 | 0 | 0.0 | 92.3 | 7.7 |
| Q11 | 26 | 6 | 23.1 | 16 | 61.5 | 2 | 7.7 | 0 | 0.0 | 2 | 7.7 | 84.6 | 7.7 |
| Q12 | 26 | 12 | 46.2 | 7 | 26.9 | 3 | 11.5 | 1 | 3.9 | 3 | 11.5 | 73.2 | 15.4 |
| Q13 | 26 | 7 | 26.9 | 16 | 61.5 | 2 | 7.7 | 0 | 0.0 | 1 | 3.9 | 88.5 | 7.7 |
| Q14 | 26 | 5 | 19.2 | 12 | 46.2 | 4 | 15.4 | 0 | 0.0 | 5 | 19.3 | 65.4 | 15.4 |
| Question | N | Strongly agree | Agree | Disagree | Strongly disagree | Don’t know | Strongly agree and agree (%) | Disagree and strongly disagree (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||||
| Responsibility for delivery and co-ordination of the RTW intervention | |||||||||||||
| Q17 | 25 | 0 | 0.0 | 2 | 8.0 | 18 | 72.0 | 4 | 16.0 | 1 | 4.0 | 8.0 | 88.0 |
| Q18 | 25 | 5 | 20.0 | 10 | 40.0 | 6 | 24.0 | 2 | 8.0 | 2 | 8.0 | 60.0 | 32.0 |
| Q19 | 25 | 4 | 16.0 | 11 | 44.0 | 7 | 28.0 | 1 | 4.0 | 2 | 8.0 | 60.0 | 32.0 |
| Q20 | 25 | 8 | 32.0 | 5 | 20.0 | 9 | 36.0 | 2 | 8.0 | 1 | 4.0 | 52.0 | 44.0 |
| Q21 | 25 | 3 | 12.0 | 10 | 40.0 | 11 | 44.0 | 0 | 0.0 | 1 | 4.0 | 52.0 | 44.0 |
| Preoperative identification of patients at ‘higher risk’ of prolonged sickness absence following surgery who may require additional individualised help and support | |||||||||||||
| Q22 | 25 | 4 | 16.0 | 12 | 48.0 | 6 | 24.0 | 0 | 0.0 | 3 | 12.0 | 64.0 | 24.0 |
| Q23 | 25 | 7 | 28.0 | 13 | 52.0 | 3 | 12.0 | 0 | 0.0 | 2 | 8.0 | 80.0 | 12.0 |
| Q24 | 25 | 1 | 4.0 | 11 | 44.0 | 11 | 44.0 | 0 | 0.0 | 2 | 8.0 | 48.0 | 44.0 |
| Q25 | 25 | 1 | 4.0 | 9 | 36.0 | 9 | 36.0 | 1 | 4.0 | 5 | 20.0 | 40.0 | 40.0 |
| Q26 | 25 | 2 | 8.0 | 5 | 20.0 | 13 | 52.0 | 2 | 8.0 | 3 | 12.0 | 28.0 | 60.0 |
| Preoperative needs assessment | |||||||||||||
| Q27 | 25 | 7 | 28.0 | 8 | 32.0 | 5 | 20.0 | 3 | 12.0 | 2 | 8.0 | 60.0 | 32.0 |
| Q28 | 25 | 6 | 24.0 | 14 | 56.0 | 2 | 8.0 | 2 | 8.0 | 1 | 4.0 | 80.0 | 16.0 |
| Q29 | 25 | 11 | 44.0 | 11 | 44.0 | 2 | 8.0 | 0 | 0.0 | 1 | 4.0 | 88.0 | 8.0 |
| Q30 | 25 | 11 | 44.0 | 11 | 44.0 | 2 | 8.0 | 0 | 0.0 | 1 | 4.0 | 88.0 | 8.0 |
| Q31 | 25 | 5 | 20.0 | 15 | 60.0 | 4 | 16.0 | 0 | 0.0 | 1 | 4.0 | 80.0 | 16.0 |
| Q32 | 25 | 9 | 36.0 | 15 | 60.0 | 0 | 0.0 | 0 | 0.0 | 1 | 4.0 | 96.0 | 0.0 |
| Q33 | 25 | 10 | 40.0 | 12 | 48.0 | 3 | 12.0 | 0 | 0.0 | 0 | 0.0 | 88.0 | 12.0 |
| Q34 | 25 | 3 | 12.0 | 14 | 56.0 | 7 | 28.0 | 0 | 0.0 | 1 | 4.0 | 68.0 | 28.0 |
| Q35 | 25 | 17 | 68.0 | 8 | 32.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 100.0 | 0.0 |
| Postoperative identification of patients at risk of an extended period off work after surgery | |||||||||||||
| Q36 | 25 | 10 | 40.0 | 11 | 44.0 | 2 | 8.0 | 0 | 0.0 | 2 | 8.0 | 84.0 | 8.0 |
| Q37 | 25 | 8 | 32.0 | 8 | 32.0 | 5 | 20.0 | 0 | 0.0 | 4 | 16.0 | 64.0 | 20.0 |
| Q38 | 25 | 5 | 20.0 | 18 | 72.0 | 0 | 0.0 | 0 | 0.0 | 2 | 8.0 | 92.0 | 0.0 |
| Q39 | 25 | 3 | 12.0 | 6 | 24.0 | 10 | 40.0 | 4 | 16.0 | 2 | 8.0 | 36.0 | 56.0 |
| Q40 | 25 | 11 | 44.0 | 12 | 48.0 | 0 | 0.0 | 0 | 0.0 | 2 | 8.0 | 92.0 | 0.0 |
| Q41 | 25 | 6 | 24.0 | 12 | 48.0 | 6 | 24.0 | 0 | 0.0 | 1 | 4.0 | 72.0 | 24.0 |
| Additional care for patients identified as ‘higher risk’ of an extended period off work after surgery | |||||||||||||
| Q42 | 25 | 4 | 16.0 | 19 | 76.0 | 2 | 8.0 | 0 | 0.0 | 0 | 0.0 | 92.0 | 8.0 |
| Q43 | 25 | 3 | 12.0 | 16 | 64.0 | 3 | 12.0 | 0 | 0.0 | 3 | 12.0 | 76.0 | 12.0 |
| Q44 | 25 | 4 | 16.0 | 15 | 60.0 | 2 | 8.0 | 1 | 4.0 | 3 | 12.0 | 76.0 | 12.0 |
| Q45 | 25 | 2 | 8.0 | 21 | 84.0 | 2 | 8.0 | 0 | 0.0 | 0 | 0.0 | 92.0 | 8.0 |
| Q46 | 25 | 4 | 16.0 | 17 | 68.0 | 1 | 4.0 | 0 | 0.0 | 3 | 12.0 | 84.0 | 4.0 |
| Scope of training for staff | |||||||||||||
| Q48 | 25 | 7 | 28.0 | 12 | 48.0 | 4 | 16.0 | 1 | 4.0 | 1 | 4.0 | 76.0 | 20.0 |
| Q49 | 25 | 11 | 44.0 | 13 | 52.0 | 1 | 4.0 | 0 | 0.0 | 0 | 0.0 | 96.0 | 4.0 |
| Q50 | 25 | 7 | 28.0 | 15 | 60.0 | 2 | 8.0 | 0 | 0.0 | 1 | 4.0 | 88.0 | 8.0 |
| Q51 | 25 | 5 | 20.0 | 13 | 52.0 | 1 | 4.0 | 2 | 8.0 | 4 | 16.0 | 72.0 | 12.0 |
| Q52 | 25 | 6 | 24.0 | 10 | 40.0 | 1 | 4.0 | 0 | 0.0 | 8 | 32.0 | 64.0 | 4.0 |
| Communicating occupational status and progress between stakeholders | |||||||||||||
| Q53 | 25 | 12 | 48.0 | 12 | 48.0 | 1 | 4.0 | 0 | 0.0 | 0 | 0.0 | 96.0 | 4.0 |
| Q54 | 25 | 8 | 32.0 | 13 | 52.0 | 2 | 8.0 | 1 | 4.0 | 1 | 4.0 | 84.0 | 12.0 |
| Q55 | 25 | 16 | 64.0 | 8 | 32.0 | 0 | 0.0 | 0 | 0.0 | 1 | 4.0 | 96.0 | 0.0 |
| Q56 | 25 | 7 | 28.0 | 14 | 56.0 | 2 | 8.0 | 0 | 0.0 | 2 | 8.0 | 84.0 | 8.0 |
| Q57 | 25 | 9 | 36.0 | 10 | 40.0 | 4 | 16.0 | 1 | 4.0 | 1 | 4.0 | 76.0 | 20.0 |
| Q58 | 25 | 6 | 24.0 | 10 | 40.0 | 5 | 20.0 | 2 | 8.0 | 2 | 8.0 | 64.0 | 28.0 |
| Q59 | 25 | 6 | 24.0 | 15 | 60.0 | 2 | 8.0 | 0 | 0.0 | 2 | 8.0 | 84.0 | 8.0 |
| Q60 | 25 | 2 | 8.0 | 9 | 36.0 | 11 | 44.0 | 2 | 8.0 | 1 | 4.0 | 44.0 | 52.0 |
| Q61 | 25 | 8 | 32.0 | 8 | 32.0 | 6 | 24.0 | 2 | 8.0 | 1 | 4.0 | 64.0 | 32.0 |
| Fit notes | |||||||||||||
| Q62 | 25 | 11 | 44.0 | 13 | 52.0 | 1 | 4.0 | 0 | 0.0 | 0 | 0.0 | 96.0 | 4.0 |
| Q63 | 25 | 12 | 48.0 | 12 | 48.0 | 1 | 4.0 | 0 | 0.0 | 0 | 0.0 | 96.0 | 4.0 |
| Q64 | 25 | 3 | 12.0 | 1 | 4.0 | 13 | 52.0 | 5 | 20.0 | 3 | 12.0 | 16.0 | 72.0 |
| Q65 | 25 | 2 | 8.0 | 13 | 52.0 | 7 | 28.0 | 1 | 4.0 | 2 | 8.0 | 60.0 | 32.0 |
| Q66 | 25 | 6 | 24.0 | 13 | 52.0 | 4 | 16.0 | 1 | 4.0 | 1 | 4.0 | 76.0 | 20.0 |
| Q67 | 25 | 4 | 16.0 | 3 | 12.0 | 14 | 56.0 | 2 | 8.0 | 2 | 8.0 | 28.0 | 64.0 |
| Q68 | 25 | 2 | 8.0 | 10 | 40.0 | 8 | 32.0 | 1 | 4.0 | 4 | 16.0 | 48.0 | 36.0 |
| Format and delivery of patient information | |||||||||||||
| Q69 | 25 | 7 | 28.0 | 12 | 48.0 | 4 | 16.0 | 0 | 0.0 | 2 | 8.0 | 76.0 | 16.0 |
| Q70 | 25 | 6 | 24.0 | 14 | 56.0 | 5 | 20.0 | 0 | 0.0 | 0 | 0.0 | 80.0 | 20.0 |
| Q71 | 25 | 5 | 20.0 | 15 | 60.0 | 4 | 16.0 | 0 | 0.0 | 1 | 4.0 | 80.0 | 16.0 |
| Q72 | 25 | 3 | 12.0 | 20 | 80.0 | 1 | 4.0 | 0 | 0.0 | 1 | 4.0 | 92.0 | 4.0 |
| Q73 | 25 | 5 | 20.0 | 10 | 40.0 | 3 | 12.0 | 1 | 4.0 | 6 | 24.0 | 60.0 | 16.0 |
| Q74 | 25 | 4 | 16.0 | 12 | 48.0 | 7 | 28.0 | 0 | 0.0 | 2 | 8.0 | 64.0 | 28.0 |
| Q75 | 25 | 12 | 48.0 | 11 | 44.0 | 0 | 0.0 | 0 | 0.0 | 2 | 8.0 | 92.0 | 0.0 |
| Q76 | 25 | 1 | 4.0 | 22 | 88.0 | 0 | 0.0 | 0 | 0.0 | 2 | 8.0 | 92.0 | 0.0 |
| Q77 | 25 | 9 | 36.0 | 13 | 52.0 | 0 | 0.0 | 0 | 0.0 | 3 | 12.0 | 88.0 | 0.0 |
| When should the intervention commence? | |||||||||||||
| Q78 | 25 | 6 | 24.0 | 7 | 28.0 | 9 | 36.0 | 0 | 0.0 | 3 | 12.0 | 52.0 | 36.0 |
| Q79 | 25 | 4 | 16.0 | 9 | 36.0 | 10 | 40.0 | 0 | 0.0 | 2 | 8.0 | 52.0 | 40.0 |
| Q80 | 25 | 3 | 12.0 | 13 | 52.0 | 8 | 32.0 | 0 | 0.0 | 1 | 4.0 | 64.0 | 32.0 |
| Q81 | 25 | 0 | 0.0 | 2 | 8.0 | 20 | 80.0 | 2 | 8.0 | 1 | 4.0 | 8.0 | 88.0 |
| Defining RTW | |||||||||||||
| Q82 | 25 | 3 | 12.0 | 8 | 32.0 | 10 | 40.0 | 1 | 4.0 | 3 | 12.0 | 44.0 | 44.0 |
| Q83 | 25 | 2 | 8.0 | 11 | 44.0 | 9 | 36.0 | 1 | 4.0 | 2 | 8.0 | 52.0 | 40.0 |
| Q84 | 25 | 2 | 8.0 | 4 | 16.0 | 14 | 56.0 | 2 | 8.0 | 3 | 12.0 | 24.0 | 64.0 |
| Q85 | 25 | 1 | 4.0 | 2 | 8.0 | 16 | 64.0 | 2 | 8.0 | 4 | 16.0 | 12.0 | 72.0 |
| Q86 | 25 | 2 | 8.0 | 9 | 36.0 | 9 | 36.0 | 0 | 0.0 | 5 | 20.0 | 44.0 | 36.0 |
| The aim of the intervention | |||||||||||||
| Q87 | 25 | 6 | 24.0 | 13 | 52.0 | 2 | 8.0 | 0 | 0.0 | 4 | 16.0 | 76.0 | 8.0 |
| Q88 | 25 | 0 | 0.0 | 11 | 44.0 | 10 | 40.0 | 0 | 0.0 | 4 | 16.0 | 44.0 | 40.0 |
| Q89 | 25 | 1 | 4.0 | 2 | 8.0 | 16 | 64.0 | 0 | 0.0 | 6 | 24.0 | 12.0 | 64.0 |
| Measuring RTW | |||||||||||||
| Q90 | 25 | 5 | 20.0 | 18 | 72.0 | 2 | 8.0 | 0 | 0.0 | 0 | 0.0 | 92.0 | 8.0 |
| Q91 | 25 | 2 | 8.0 | 16 | 64.0 | 5 | 20.0 | 0 | 0.0 | 2 | 8.0 | 72.0 | 20.0 |
| Q92 | 25 | 0 | 0.0 | 3 | 12.0 | 15 | 60.0 | 5 | 20.0 | 2 | 8.0 | 12.0 | 80.0 |
| Q93 | 25 | 0 | 0.0 | 11 | 44.0 | 8 | 32.0 | 0 | 0.0 | 6 | 24.0 | 44.0 | 32.0 |
| Q94a | 25 | 5 | 20.0 | 10 | 40.0 | 8 | 32.0 | 2 | 8.0 | 0 | 0.0 | 60.0 | 40.0 |
| Q94b | 25 | 4 | 16.0 | 12 | 48.0 | 9 | 36.0 | 0 | 0.0 | 0 | 0.0 | 64.0 | 36.0 |
| Q94c | 25 | 3 | 12.0 | 10 | 40.0 | 7 | 28.0 | 3 | 12.0 | 2 | 8.0 | 52.0 | 40.0 |
| Q94d | 25 | 2 | 8.0 | 2 | 8.0 | 12 | 48.0 | 5 | 20.0 | 4 | 16.0 | 16.0 | 68.0 |
| Q95 | 25 | 5 | 20.0 | 15 | 60.0 | 3 | 12.0 | 1 | 4.0 | 1 | 4.0 | 80.0 | 16.0 |
| Q96 | 25 | 5 | 20.0 | 16 | 64.0 | 2 | 8.0 | 0 | 0.0 | 2 | 8.0 | 84.0 | 8.0 |
| Q97 | 25 | 8 | 32.0 | 16 | 64.0 | 0 | 0.0 | 0 | 0.0 | 1 | 4.0 | 96.0 | 0.0 |
| Q98 | 25 | 11 | 44.0 | 12 | 48.0 | 0 | 0.0 | 0 | 0.0 | 2 | 8.0 | 92.0 | 0.0 |
| Comment number | Comment |
|---|---|
| 1 | Patients should be encouraged to connect with organisations such as Arthritis Research UK/Arthritis Care who have excellent pre and post-surgery publications as well as access to self-management courses |
| 2 | Peer support in the workplace is useful & potentially important |
| 3 | Possibility of Self-employed patients being given specific information, as they may need to return to work earlier than others due to financial pressures |
| 4 | Original questions 47, 48, 56, 58, 65 and 67 were all green. Why are they being asked again? I should add that for 65 I put ‘Strongly disagree’ yet the table show zero for that item |
| 5 | Return to work process will vary depending on the physical demands of the work. There is no advice for those who may not be able to continue that previous type of work |
| 6 | Some of these questions are highly confusing asking only one answer for questions that originally had two answer options of important and deliverable |
| 7 | Too much personal information being shared with employer |
| 8 | Yes there are definitely 2 tiers of need |
| 9 | This is a good development. Some patients will feel enormous pressure to return to work but may need a range of interventions delivered at key stages of their recovery. Employers also need to be more involved in the process of work return |
| 10 | Seems reasonable providing the movement between groups is made flexible and easy to facilitate |
| 11 | Not yet clear how this dichotomy will be reached in a predictive framework? |
| 12 | Agree with stratifying into Gps A & B |
| 13 | All good ideas - I have concerns about who can deliver all the extra care. We have staffing shortages/overwork already |
| 14 | Sorry, this is all too complicated for me and I wish to withdraw from the scheme. Sorry, too much in-depth stuff |
| 15 | Agree that should access additional therapy if struggling, but this cannot be unrestricted pending return - the ability of the patient to actually return has not been defined and i am struggling to comment as to how one can predict which patients will need additional input - nor whether this will actually result in achieving return to work |
| 16 | ECONOMIC CASE FOR ALL OF THE ABOVE IS GOING TO BE CHALLENGING. ROUTINELY MOST THR PTS CURRENTLY GET NO PHYSIO IN THE NHS, AND TKR ARE SEEN IN GROUP SETTINGS. BUSINESS CASE FOR RETURNING TO WORK IS GOOD FOR UK PLC, BUT THIS DOES NOT HELP THE THERAPY MANAGER (CCG OR ACUTE) WHO HAS TO INCREASE SUPPORT TO THESE PTS WITH NO COST SAVING TO THEM |
| 17 | My unit already provides a 2 week postoperative review and physiotherapy and return to work issues are discussed |
Delphi round 3
| Role | Comments |
|---|---|
| Surgeon | I’ve been through the info and it all looks very good. Very thorough A lot for the patient to read but I guess there is a lot for them to go through. The employer booklet is good. The only bit I didn’t like was the pictures on the first page of the patient workbook do not really reflect the patients that we will be dealing with (40-60yr olds). The pictures show a very young man and a very old man in a wheelchair. While they are not completely unreasonable we probably would want the first page to have relevant pics (like most of the others on the other pages) |
| Surgeon (research lead for British Association for Surgery of the Knee) | Having been slightly sceptical about some of the outcomes from the project I think you have done a great job, it’s a superb resource. I am sure final printing will be high quality but the nice colours on the documents are likely to be printed locally on NHS black and White printers and therefore - white on grey isn’t great nor is grey on greyP13 7 in 10 should read 7 out of 10P13 personally I wouldn’t include the reference to return to work at 24 weeksP17 I would like to be monitored by the occupational . . . intervention summary doc typo p6/8 rtwc TOW should be to |
| Surgeon (past president for British Association for Surgery of the Knee) | Patient Workbook- Although strictly accurate it is unusual to place full stops when using ‘GP’- P6: Orange Bullet point 2: Start with ‘Of these 4 in 10’- P6 Blue Bullet 2 ‘adaptations’. We are not American- P8: Again an americanism ‘programme’. Program refers to computer software. Trust me the age-group you are aiming at may well be irritated by the Americanisms. Whilst I think about it, be careful not to use ‘surgery’ or worse ‘surgeries’ when you mean ‘operation’. Most of the time you use the word ‘surgery’ ‘operation’ would be more appropriate- P24 Second last Bullet point: ‘periods’- P25 L4: ‘3 out of 4 (75%)’ and then ‘4 in 10 (40%)’. You did this at the beginning!- P25: Braking reaction time is a poor surrogate for safe driving. There are driver simulator centres that do a proper assessment (for a fee) for those who want the assurance, and for those where they have an impairment- P25 Second column second paragraph: ‘At 4-6 weeks after your OPERATION’. See comments above!Employer booklet- P2: End: ‘adaptations’- P3 Second column second section: ‘programme’- P6 second column: In written texts numbers starting sentences are written as words e.g. One in four (25%)It is not clear if you tested patients’ and employers’ views on their respective booklets. At first glance they appear long and complicated. However, on reflection, the patients who want to return to work will read them religiously, and those employers who want to support their staff will do so as it gives detailed and practical advice |
| Patient (patient lead NJR PLG) | I have reviewed the materials and think they are excellentI am hopeful that the specified commitment required to support those of working age return to work after surgery is available. The level and range of contact and time required is considerable. Without that commitment this programme will not be so successfulI note on page 5 there is a suggestion to share the workbook knowledge with the patient’s GP. In fact the discharged patient may have a lot of contact post surgery with the GP for purpose of prescription pain relief and signing of ‘fit notes’ so I consider it vital to involve/inform the GP team about the Return To Work intervention programme at the earliest stageThe layout and explanation is clear. However, there is a lot to take in and consider so the patient needs to receive RTW booklet asap. This is indicated in the diagrammatic guide to the process on page 8The design with checklists and tickboxes makes the patient face the practical issues and really think about any obstacles on the journey back to work. This also has the effect of ‘setting the agenda’ for patients to move away from an entirely ‘medical’ model of surgery to fix a problem – to more about enabling them to continue to being active and independentSome patients will need more assistance and guidance than others as there is a lot of text. EG. Page 13 is suggesting that 10 weeks is a average target time for return to work, and that type of work had no real impact. These are key messages and could be at the top of the page followed by evidenceI am aware of Dame Carol Black’s review of the health of the working age population and its impact on the economy. This initiative will be valuable and could be rolled out for wider applicationOn a personal note, I am a patient with Rheumatoid Arthritis diagnosed in 1985. I managed to stay in work for 28 years, as opposed to the much shorter average of between 5-7 years at that time, because I worked for a large organisation with good commitment to occupational health who engaged with me from early in my diagnosis about how we would manage change and challengesLater, through Arthritis Care, I met many people with no such support who ‘dropped out’ of the workplace after flares and surgeries because of fear, lack of support and encouragement, and indeed their pain and medical perception of their situation became amplified. Where I live people with arthritis comprise the second largest PIP claimant group. They are perfectly entitled to it but it is not a successful outcome. I think the OPAL pathway to return to work identifies the vital role of taking the patient past the immediate recovery from surgery to the place where shared decision making, timely support and understanding gets them back into their life |
| Patient/ambassador for global alliance for MSK health of the bone and joint decade | I think the work that the OPAL Team have worked wondersThe patient and employer booklets are first class . . . I’d love to see the slides in due course, pleaseWhat is the time line to rolling out the work? When can I share these data with my colleagues at the BOA’s Patient Liaison group? will you be posting OPAL on LinkedIn? |
| Surgeon | The documents appear very professional with lots of information. Excellent job. My concern is that they are large and may be seen as a lot of extra work for already overworked staffLooks like it will require dedicated staff ? fundingSome patients may read it all – but I suspect a minority in [city of residence]?! |
| Research physiotherapist | Well done team . . . this looks a serious amount of work and it is great seeing it all together |
| GP [RCGP lead for chronic pain (currently in clinical research)] | Thank you for this information. I fully support the pathway that you have designed and the accompanying materials are superb - we just have to hope that the system is adequately resourced. I have been discussing the problem of return to work with a member of the House of Lords. They have a particular interest in pain and work and indeed chaired a focus group to feed back on the governments green paper on work. Could I send your documents to them, stressing that they are draft documents at present? |
| Employer (head of safety, health and quality) | Thank you for the documents they are very interesting and informative. Finning are already following the majority of the information for an employee returning to work after a Hip or Knee replacement. In our case the employee would return to work on a ‘phased return’ and ‘restricted duties’, we will also at this time adjust the start and working hours and if applicable, the work load. The checklist would be beneficial as it would probably provide more time to make the adjustments as the patient would read it on discharge and probably not leave it until they were due start back to work |
| Employer | I think I may have received this in error |
| Employer | Please could you remove me from the list as I will not be able to participate. Thank you |
Appendix 8 The OPAL study roles and responsibilities for hospital orthopaedic team members
Roles and responsibilities
Outpatient clinic staff
-
Complete tailored OPAL training.
-
Identify RTW patients prior to consultation with surgical team.
-
Ask RTW patients to complete occupational checklist prior to consultation with surgical team; explain:
-
Why this information is being collected.
-
That the surgeon will review this information and use it to assist the patient if they need to.
-
-
Model completion if necessary.
-
Give positive feedback to patient on completion.
-
Give surgeon the patient’s completed occupational checklist.
-
Give patients listed for surgery the RTW workbook; explain that patients have contributed to content and design.
-
Present workbook positively, why it is being used, similarity to ‘red book’.
-
Refer to coping model examples.
-
Recommend patient reads RTW workbook and completes as much as they can (shows them relevant sections).
-
Recommend patient asks employer to assist patient in completion if wishes and suggests who this might include; discuss possible difficulties and solutions re communicating with employer?
-
Informs patient that they are expected to bring the workbook to every hospital appointment – and why, and that HOT will use it. Draw patient’s attention to this instruction. Discuss potential reasons why this might not happen, and formulate solutions with patient.
-
Gives patient employer RTW workbook to pass on, and why, and suggests who this might include.
-
Present workbook positively.
-
Suggests that patient might wish to meet with their employer to discuss RTW, and who this might include.
-
Explains to patient that the RTWC will be contacting them at least 4 weeks before their operation to discuss their RTW plan. Shows them photo of RTWC and contact details.
-
Checks they have the patient’s chosen method of contact, contact details, and have recorded the optimum time to contact them within the occupational checklist.
-
Collects occupational checklist from surgeon and forwards to hospital RTWC.
Surgeon
-
Complete tailored OPAL training.
-
Refer to completed occupational checklist during consultation. Respond positively when the patient presents their completed checklist.
-
Give patient personal advice/information as to their potential RTW outcome.
-
Answer patient questions and concerns.
-
Support patient autonomy in decision about surgery.
-
Inform listed patients that they will be given a RTW workbook to read, and why, complete where possible, and bring to each subsequent appointment, presenting positive message.
-
Inform listed patients that they will receive an employer workbook to give to their employer and why.
-
Explain that patient will be contacted by a RTWC at least 4 weeks prior to surgery to help them with their RTW plan if they need it. Names them.
-
Explain that unexpected outcomes might result in the RTW plan being revised, and the RTWC will help them with this.
-
Summarise and record patient’s RTW status/outcome in all outpatient clinic notes and following each appointment.
-
Communicate with GP at point patient is discharged from orthopaedic surgical care, outlining current RTW status and progress and ongoing therapy received.
Preoperative assessment and education teams
-
Complete tailored OPAL training.
-
Refer to the RTW workbook positively and encourage the patient to read and use this resource.
-
Ask patients if they have brought workbook to appointment, praise patients who have, refer to it during appointment/presentation.
-
Examples of patient’s work demands, barriers and facilitators, work modifications and RTW plans referred to in discussions and presentations.
-
Highlight importance of recovery/rehabilitation in relation to work, pacing up activity.
-
Remind patient about role of RTWC.
Return-to-work co-ordinator/deputy
For additional information, see OPAL examples of developed materials at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/ (accessed 2 May 2020).
-
Complete tailored OPAL training.
-
Contacts patient at least 4 weeks prior to surgery (NB may have to do this out of office hours) to review/agree.
-
Information provided in occupational checklist.
-
Current job demands.
-
Provisional RTW date.
-
Perceived/potential barriers/facilitators.
-
Provisional RTW plan.
-
Refers on/signposts where appropriate.
-
Goals/steps.
-
-
This consultation should be documented in RTWC workbook for that individual patient.
-
Additional contact governed by patient need.
-
Refers positively to RTW workbook during discussions with patient.
-
Praises patient for bringing workbook to appointments.
-
Reminds patient to bring workbook when admitted to ward.
-
Refers to other patient examples/models of job demands/RTW plans, etc.
-
Encourages and supports/advises/problem-solves about contact with employer.
-
Advises patient that RTWC will assist with revised RTW plan if required.
-
Highlights RTW patients to teams managing preoperative education and assessment. Records this action in RTWC workbook.
-
Highlights RTW patients to ward teams when admitted for surgery. Records this action in RTWC workbook.
-
Liaises with inpatient teams postoperatively to determine whether or not there are any issues with early recovery that may impact on RTW plan.
-
Revises RTW plan with patient as required.
-
Ensures that RTW plan is documented in RTW workbook.
-
Supports postoperative rehabilitation plans and problem-solves potential barriers to adherence with patient based on individual need.
-
Checks helpline three times per week, triages, advises, refers on, based on individual need.
-
Continues to provide point of access following discharge until 16 weeks post surgery (8 weeks for feasibility study).
-
Records any changes to patient’s RTW progress/status/outcome in RTWC workbook.
Senior ward nurse and doctor
-
Complete tailored OPAL training.
-
Ask RTW patients if they have brought workbook into hospital, and if not determine the reason for this.
-
Give praise if workbook brought in.
-
Refer positively to RTW workbook.
-
Summarise patient’s expected RTW outcome and RTW plan in ward discharge letter.
-
Provide patient with copy/copies to give to significant others.
-
Ask each patient whether or not they require a fit note on discharge.
-
Complete fit note in accordance with best-practice guidelines and the hospital contract and with reference to the patient’s RTW plan in their workbook.
Ward therapists
-
Complete tailored OPAL training.
-
Ask RTW patients if they have brought workbook into hospital, and if not determine the reason for this.
-
Give praise if workbook brought in.
-
Refer positively to RTW workbook; enter notes as appropriate.
-
Liaise with RTWC to update them on the patient’s postoperative recovery prior to discharge.
-
Summarise and record patient’s RTW status/outcome in all outpatient clinic notes and following each appointment.
Appendix 9 Supporting information for the implementation strategy and feasibility assessment
Training logs for each of the OPAL feasibility sites
South Tees training log
| Role | Date of training |
|---|---|
| Physiotherapist – outpatients | 11 May 2018 |
| Physiotherapist – ward | 11 May 2018 |
| Physiotherapy assistant – ward | 11 May 2018 |
| Specialist nurse – pre-assessment and joint replacement clinic | 11 May 2018 |
| Pre-assessment sister | 11 May 2018 |
| Trauma outpatient department sister | 11 May 2018 |
| Physiotherapist | 11 May 2018 |
| Physiotherapist | 11 May 2018 |
| Research nurse | 11 May 2018 |
| Doctor – ward | 22 May 2018 |
| Physiotherapist – ward | 22 May 2018 |
| Physiotherapist – ward | 22 May 2018 |
| Doctor – ward | 22 May 2018 |
| Ward sister | 22 May 2018 |
| Nurse practitioner | 11 May 2018 |
| Community physiotherapist | 11 May 2018 |
| Physiotherapist – discharge team | 11 May 2018 |
| Nurse practitioner | 11 May 2018 |
| Occupational therapist | 11 May 2018 |
| Ward sister – ward 25 | 11 May 2018 |
| Surgical care practitionera | 11 May 2018 |
| Ward clerk | 11 May 2018 |
| Consultant surgeon | 16 May 2018 |
| Consultant surgeon | 16 May 2018 |
| Consultant surgeon | 25 May 2018 |
| Research nurse | 23 May 2018 |
| Research administrator | 23 May 2018 |
| Research nurse | 23 May 2018 |
Northumbria training log
| Role | Date of training |
|---|---|
| Physiotherapist | 25 May 2018 |
| Practice development leada | 25 May 2018 |
| Research nurse | 25 May 2018 |
| Senior research nurse | 25 May 2018 |
| Clinical trials practitioner | 25 May 2018 |
| Consultant surgeon | 25 May 2018 |
Nottingham training log
| Role | Date of training |
|---|---|
| Team lead physiotherapya | 23 May 2018 and 11 July 2018 |
| Consultant surgeon | 23 May 2018 |
| Consultant surgeon | 23 May 2018 |
| Consultant surgeon | 23 May 2018 |
| Outpatient assistant | 11 June 2018 |
| Outpatient assistant | 11 June 2018 |
| Outpatient assistant | 11 June 2018 |
| Outpatient assistant | 11 June 2018 |
| Deputy sister, outpatients | 11 June 2018 |
| Outpatient assistant | 11 June 2018 |
| Outpatient assistant | 11 June 2018 |
| Staff nurse, outpatients | 11 June 2018 |
| Registered nurse, outpatients | 11 June 2018 |
| Outpatient assistant | 11 June 2018 |
| Team lead occupational therapy | 12 June 2018 |
| Band 4 occupational therapist | 12 June 2018 |
| Research nurse | 12 June 2018 |
| Research facilitator | 12 June 2018 |
| Staff nurse, outpatients | 20 June 2018 |
| Staff nurse, outpatients | 20 June 2018 |
| HCA, outpatients | 20 June 2018 |
| TNA, outpatients | 20 June 2018 |
| HCA, outpatients | 20 June 2018 |
| Co-ordinator, outpatients | 20 June 2018 |
| Outpatient assistant | 20 June 2018 |
| HCA, outpatients | 20 June 2018 |
| Outpatient assistant | 20 June 2018 |
| Band 4 physiotherapista | 20 June 2018 |
| Ward occupational therapist | 9 July 2018 |
| Ward occupational therapist | 9 July 2018 |
| Ward sister | 9 July 2018 |
| Staff nurse – ward | 9 July 2018 |
| Deputy ward sister | 9 July 2018 |
| Ward sister | 9 July 2018 |
Lists of training materials created to supplement OPAL implementation
Examples of study paperwork (see OPAL examples of developed materials at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/; accessed 2 May 2020):
-
job demands examples
-
impact on work examples
-
RTW plan examples.
Training slides and documents (see OPAL examples of developed materials at www.journalslibrary.nihr.ac.uk/programmes/hta/152802/#/; accessed 2 May 2020):
-
slides: generic staff training slides version 1 and version 2
-
slides: ways of helping people to change behaviour
-
slides: occupational health
-
slides: fit notes
-
slides: work modifications
-
slides: performance objectives – all staff
-
slides: performance objectives – RTWC
-
slides: performance objectives – outpatient and pre-assessment teams
-
slides: performance objectives – surgeons
-
slides: performance objectives – ward staff and inpatient therapy teams
-
slides: research team slides
-
feasibility flow chart.
Checklist for intervention fidelity against performance objectives
| PO | Evidence of completion | Evidence source | How will this information be recorded? |
|---|---|---|---|
| PO1. Patient completes occupational checklist prior to appointment with surgeon |
|
|
|
| PO2. Patient makes informed decision about surgery with respect to work |
|
|
|
| PO3. Patient acquaints self with key information about recovery and RTW provided in the patient RTW workbook and associated online information resources |
|
|
|
|
PO4. Patient brings RTW workbook to each hospital appointment including hospital inpatient stay Patient shares/discusses workbook with hospital staff |
|
|
|
|
PO5. Patient completes sections of RTW workbook that will help them understand the demands of their work and set an approximate RTW date With employera as required |
|
|
|
|
PO6. Patient uses information resources provided to identify and prioritise potential barriers and solutions to a safe and appropriate RTW, and to develop a RTW plan With employera as required |
|
|
|
| PO7. Patient discusses information within RTW workbook with RTWC to help them further develop their RTW plan, during routine hospital preoperative appointment or by telephone. This will include a minimum of one contact. The number and duration of further contacts will be governed by patient need based on progress and perceived level of ‘risk’ of prolonged sickness absence |
|
|
|
| PO8. Patient provides employera with written information provided by the HOT about their planned surgery and recovery/RTW advice |
|
|
|
| PO9. Patient meets with their employera to discuss their recovery and RTW plan |
|
Patient workbook ‘step 5’ 8-week questionnaire ‘section 7’ |
Was patient workbook completed – was written information documented in section 5? Yes/no Did the patient state they discussed their RTW plan based on the question ‘Did you speak to someone you work with about the ‘return to work’ plan you developed in your patient “return to work” workbook?’? |
| PO10. Patient communicates with employera regarding surgical outcome and progress/recovery, by telephone, e-mail or face to face | No evidence collected | ||
| PO11. Patient revises RTW plan following surgery as necessary with their employera and hospital staff |
|
|
|
| PO12. Patient engages with RTWC via RTW helpline/answering service if having problems related to RTW for up to 16 weeks post surgery |
|
|
|
| PO13. Patient adheres to postoperative rehabilitation plan and advice | No evidence collected |
| PO | Evidence of completion | Evidence source | How will this information be recorded? |
|---|---|---|---|
PO1. The HOT:
|
|
|
|
| PO2. The outpatient clinic team identifies RTW patients in clinic prior to consultation with surgical team |
|
|
|
|
PO3. The outpatient clinic team requests RTW patients to complete occupational checklist prior to consultation with surgeon and explain its purpose to the patient, model completion if necessary and give positive feedback on completion The outpatient clinic team gives completed occupational checklist to surgeon prior to patient’s appointment |
|
|
|
|
PO4. Surgeon discusses pros and cons of surgery with patient including expected time scales of surgery and recovery – in relation to the patient’s usual work and refers to/responds positively to the patient’s occupational checklist to enable patient to make informed decision about surgery; supports patient autonomy Provides patient with personal risk feedback on potential RTW outcomes Explores patient’s questions and concerns Informs listed patients that they will be given a RTW workbook to read and why, complete where possible, bring to each subsequent appointment, presenting positive message Informs listed patients that they will receive an employer workbook and why, that the patient will be contacted by a RTWC at least 4 weeks prior to surgery and why. Names them Explains that RTW plan may need to be revised and that RTWC will help with this Summarises and records patients’ RTW status/outcome in all clinic notes and following each appointment Communicates with GP at point patient is discharged from orthopaedic surgical care outlining current RTW status and progress and ongoing therapy received |
|
|
|
|
PO5. The outpatient clinic team provides all RTW patients listed for surgery with written RTW workbook and gain contact details for RTWC to contact patient as completed in occupational checklist Outpatient clinic staff inform/encourage patient to bring RTW workbook to each hospital appointment, and draw attention to this instruction in the workbook Discuss potential reasons why this might not happen, and formulate solutions with patient Recommend that patients read workbook and complete as much as they can (show relevant sections); present workbook positively and refer to coping model examples Recommend that patient asks employer to assist patient in completion if wishes and suggests who this might include, and discuss possible difficulties and solutions re communicating with employer Outpatient clinic staff explain to patient that the RTWC will contact them at least 4 weeks prior to surgery about their RTW plan |
|
|
|
|
PO6. The outpatient clinic team provides all RTW patients listed for surgery with ‘employer RTW workbook’ to share with their employer/colleaguesa Outpatient clinic staff inform/encourage patient that giving the employer RTW workbook to employer/colleagues will help them understand surgery and prepare for patient’s RTW Suggests that patient might wish to meet with their employer to discuss RTW and who this might include Outpatient clinic staff suggest individuals in the workplace who might best receive the employer RTW workbook |
|
|
|
| PO7. The outpatient clinic team collects patient’s completed occupational checklist from surgeon and forwards to RTWC |
|
|
|
|
PO8. The preoperative assessment and education teams routinely include the topic of RTW in their clinics with examples of work demands, barriers to and facilitators of RTW, RTW plans, importance of adhering to postoperative rehabilitation plan/pacing up activities The preoperative assessment and education teams ask if patients have brought their RTW workbook to appointment, praise patients, refer positively to content and use of the workbooks, and promote engagement with the RTWC |
|
|
|
|
PO9. RTWC contacts all RTW patients (telephone/meet-ups) at least 4 weeks prior to surgery to review:All patients receive at least one contact with the RTWC. This may be integrated within the pre-assessment/pre-admission process or done by telephone. The number and duration of additional contacts will be governed by patient need based on progress and perceived level of ‘risk’ Refers positively to RTW workbook during discussions with patient:Encourages discussion about/coaches patient regarding communication with patient’s employer Refers on/signposts where appropriate Sets goals/steps with patient Discusses the possibility of needing to revise RTW plan following surgery Documents all consultations in RTWC workbook |
|
|
|
| PO10. RTWC highlights RTW patients to ward teams managing preoperative education and assessment and records this action in RTWC workbook |
|
|
|
| PO11. RTWC highlights RTW patients to the ward teams when admitted for surgery and records this action in the RTWC workbook |
|
|
|
|
PO12. The ward team (nurse and doctor) checks that RTW patients have brought workbook into hospital, and if not determine the reason for this. Give praise if workbook brought in Refer positively to RTW workbook |
|
|
|
|
PO13. Ward therapists ask RTW patients if they have brought workbook into hospital, and if not determine the reason for this. Give praise if workbook brought in Refer positively to RTW workbook, enter notes as appropriate Liaise with RTWC to update them on the patient’s postoperative recovery prior to discharge |
|
|
|
|
PO14. The RTWC liaises with inpatient teams postoperatively to determine whether or not there are any issues with early recovery that may have an impact on the RTW plan The RTWC revises RTW plan with patient as required and ensures that plan is documented in patient’s RTW workbook The RTWC supports postoperative rehabilitation plans and problem-solves potential barriers to adherence with patient |
|
|
|
|
PO15. The ward team (nurse/doctor) summarises patient’s expected RTW outcome and RTW plan in ward electronic discharge letter. A copy/copies will be given to the patient to share with employer, therapists, etc. The ward team (nurse/doctor) praises/refers to the RTW workbook and remind the patient to use the RTW helpline following discharge if they are having problems The ward team (nurse/doctor/therapist) highlights the importance of adhering to the postoperative rehabilitation plan |
|
|
|
| PO16. The specialist ward nurse/doctor asks each patient whether or not they require a fit note on discharge and completes the fit note in accordance with best-practice guidelines and the hospital contract, and with reference to the patient’s RTW plan in their workbook |
|
|
|
| PO17. The RTWC checks the RTW helpline three times per week, and triages, advises (e.g. telephone call) or refers back to therapy services (based on local service structure and availability) based on individual need |
|
|
|
| PO18. Surgeon, HOT and outpatient therapy teams summarise and record patient’s RTW status/outcome in all outpatient clinic notes and following each appointment |
|
|
|
| PO19. Surgeon and HOT communicate with GP at point patient is discharged from orthopaedic surgical care, outlining current RTW status and progress and ongoing therapy received and encourage engagement with RTWC until 16 weeks post surgery (8 weeks for feasibility study) |
|
|
|
| PO20. RTWC continues to provide a point of access to RTW advice for patients following discharge from orthopaedic surgical care until 16 weeks post surgery (8 weeks for feasibility study). Records any changes to patient’s RTW progress/status/outcome in RTWC workbook |
|
|
|
Feasibility patient interviews
Sampling
Fifteen of the 21 patients who had agreed to be approached for interview were recruited across three study sites. Of those not recruited, three were uncontactable, one did not respond to e-mail contact and two were not approached in order to achieve a balance in recruitment across the three study sites. Of the 15 participants, six had undergone THR and nine had a TKR. Six were employed in the private sector, four were employed in the public sector, two were self-employed, two were in voluntary roles and one was an out-of-contract contract worker. The aim had been to interview patients at 8 weeks post surgery; however, some were interviewed up to 13 weeks after surgery owing to holiday periods, difficulty in making contact and delays in obtaining agreement to take part in the interviews. All interviews were conducted by telephone between October 2018 and January 2019.
Interview quotations
As described in Chapter 10, patient interviews conducted in IM stage 6 (feasibility) produced the following three themes:
-
understanding of OPAL
-
opinion of OPAL
-
experience of OPAL.
Direct quotations to supplement the narrative description in Chapter 6 are presented in the following sections.
Theme: understanding of OPAL
Well I think it is about afterwards. It’s about getting back to normality if you like, getting back to work and that’s as I understood it. I mean that’s what to me it was all about, and encouraging returning to work, or returning to normal activity even or whatever.
2062
I guess it’s just getting back to work and having time off work to recover from the operation. And what is and isn’t possible, I guess, and what is and isn’t feasible following the surgery.
1060
Well basically my understanding was that it’s like kind of tailored individually. Instead of in the past you’ve seen the surgeon, you go into surgery, and then you get a sick note for, I don’t know, 6 or 8 weeks, everybody gets the same. My understanding was that it’s like tailored to you. What do you want out of it? When do you think you want, do you have a date that you want to get back to work, and how can we help you achieve that? And everybody gets involved in that. The doctor, the surgeon, your GP, everybody that you see.
2269
The other question that I have and I’ve still got it really is who is it designed to benefit? . . . Is it the employer or is it me? And I wasn’t clear about that really. Because if it’s designed to rush me back to work why the hell would I want to rush back to work.
1367
It’s just to research I think the benefits of people that have occupational health and help with going back to work and people that don’t I think. That’s what I think that it’s about.
2260
Theme: opinion of OPAL
. . . the idea of being able to actually have a discussion around going back to work and not just being off or being at work, having options, that has sort of pointed that out to me which I probably would have thought right I’ll have 6 weeks, 8 weeks, I’ll have a number of weeks off and then I’ll be going back to work full-time. So it was helpful inasmuch as knowing that that doesn’t have to be that way.
1061
I think it’s got to be given at quite an early stage and it fits in nicely with the preoperative stage process because not only does it give the patient, well the patient gets a bit of ownership in their own care don’t they?
2063
They should be helping them to recover; the return to work should be a consequence of that. Do you know what I mean? So the important thing for the NHS should be not to get the people back to work but to get them back to health, right. And coming back to work is irrelevant. So I think you should be establishing what it is that people want. Like me, I didn’t want a return to work, I wanted to return to sport. But for some people it might just simply be I want to be able to walk around the shops with my wife. And that might be what their expectation is. So that’s what you should be striving to do and helping them to manage that and achieve that. And if they express that they want that desire to return to work because it might be a self-employed guy or something like that, so he would want to return to work wouldn’t he?
1367
I already felt that I had the support and the plan already in place without the OPAL. But I mean I can imagine lots of people haven’t . . . it enabled the doctor to give me a longer fit note, which I found useful because I wasn’t having to then go to the GP and chase him every couple of weeks.
2260
Well probably because of the way I am. I was going to return to work in some form as soon as I could and I didn’t need a work co-ordinator to help me to get back to work. You know, because it’s common sense if you’ve just had a major knee operation, you’re not going to start moving kegs around or climbing ladders or whatever. So a lot of it was common sense and I didn’t need a works co-ordinator to help me get back to work.
2366
Theme: experience of OPAL
Return-to-work workbook
It was, well it was because it enabled the doctor to give me a longer fit note, which I found useful because I wasn’t having to then go to the GP and chase him every couple of weeks. In that respect it was useful. And it was good to write it all down, my plans, even before the surgery. And then I can look now and see where I’m at with those plans, and I think I’m on line with what I said, I’m on track with what I said before the surgery. So yes, it is a good reference, it’s like a diary for you to look back at and say oh yes, I am doing.
2260
Well I put things in, set a date for review, make contact with [RTWC]. Drive at 6 weeks, transfer to theatre [voluntary sector role]. So I just, this is things that she put down when she interviewed me.
1366
If I’m honest again, because I related it to my work situation rather than a general return to work, I thought it was absolutely helpful, really helpful, because it was a guide to recovery and getting back to work. To have, if you like, a proper plan in place to get back to work and my understanding is that’s what this is all about really.
2062
Well it’s just really putting it down on paper what’s already in my head really . . .
Neither useful nor not useful, not really anything, it’s in my mind anyway. But obviously as it was a study I did it . . . just because I know that that system is already in place with where I work. It would have been tremendously useful had I never been sick before.
2260
I took it [workbook] everywhere, every appointment I went to. I took it with me for the surgery, but it stayed in my bag because nobody mentioned it.
1061
Employer’s workbook
They weren’t interested, no. I think they looked upon it as another thing that they had to do.
1360
I know that she looked at it. I told her initially that I’d agreed to take part in it and she said well done, that’s really good. And I said is it? And she said yes, because if people don’t take part in these sort of projects then things don’t change, things aren’t learned, things don’t move forward, so well done for agreeing to do it. And she then happily took the employer handbook off me but we hadn’t sort of really discussed it any further than that.
1061
I tried to discuss it with occupational health, and she was a bit frightened, and she said she’d never seen it before and would have to speak to the consultant.
2260
She’d read the handbook and she’d made some notes, and she said that, obviously she said when do you think you’ll be coming back? I said well I don’t know, how long is a piece of string? . . . So financially it was finances that really decided me when I would go back.
2269
I know he’d got it next to him if we were going to discuss anything from it. But I think we’d already fully established the plan of action for the return a few week’s previous, because in effect it’s part of the policy and procedures within the organisation.
2063
OPAL helpline
Yeah I would never ring something like that. So I probably noticed it, but it’s just, me being the person I am I wouldn’t, I’m not really the kind of person that would ring something like that.
1367
But between leaving hospital and getting an 8-week review there’s nothing in between. I get that, but I just think you need to emphasise the importance of the helpline and I should have used it. So I take personal responsibility for that.
2262
Yeah definitely, because I mean the first time I met her she went through the things with us, and she’d emphasise this is my phone number, if you’ve got any questions don’t be frightened to ring. So again like I say you can’t fault her on that, she’s doing exactly what it says sort of thing. Because I think it’s down to the individual person. I have said this to [RTWC] as well after I saw her, when I had last seen the surgeon after I’d been discharged. I said for other people this is brilliant. It wasn’t, I’m not saying it wasn’t beneficial, it was beneficial based on me, but not as many benefits as there probably would have been for other people.
2364
. . . when I did phone the back-to-work co-ordinator, actually I think I phoned her a couple of times, and it’s always an answerphone. And so you have to leave a message . . . but they don’t always get back to you the same day, which is a bit frustrating. But then when they did get back to me it wasn’t her, it was somebody else.
2269
She did mention it but I did actually ring that a couple times while I was off just to query different things which I did . . . That wasn’t a helpline though; that was just a thing about sick notes and stuff like that because I didn’t know who to ring.
1363
The OPAL website
I didn’t actually realise there was a website if I’m honest. I might have been told there was, but I don’t remember anybody saying about a website, if that makes sense.
2269
No. I use a computer as little as possible. I’ve got a Tesco [Tesco PLC, Welwyn Garden City, UK] mobile, which I pay £7.50 a month for and that’s simple. No fancy phones. No computers. I don’t want to know.
2366
Interaction with OPAL team
Oh yes definitely. I thought she was very good, very, she was approachable. You could ask her stuff, which I’ve not being a person who’s been on the sick so I didn’t know about sick notes and stuff like that. And she’s helped me a lot with that, she found out about it. Also, I hadn’t got a follow-up appointment off the consultant and I queried that with her and she chased that up and got my appointment for us.
1363
Yeah, so she contacted me by e-mail. And I e-mailed her back and said that I’d got the booklet and what have you. And then nothing happened at all, I didn’t hear another thing from anybody.
2268
A lady called [research nurse]. I don’t remember her surname. And that’s the only person actually that I’ve seen. When I was in the hospital, they said somebody would come and see me in hospital and they didn’t actually. I didn’t see anybody.
1060
. . . guess my experience, this is just me personally, when I was asked about it I just said oh yeah, I’d help, not a problem. I didn’t see why I wouldn’t want to do it. But I got to be a bit fed up with it to be honest, because I just kept thinking well what is the point of this? Nobody’s really interested, nobody was interested, apart from Mr [surgeon]. I had a phone call to say oh you’ve got an appointment with Mr [surgeon] tomorrow, can you please make sure you bring your OPAL booklet. But apart from that I just felt that nobody was really interested in it, and maybe it’s because it wasn’t really, it’s not established and people are unaware of it.
2269
Yeah, but like I say I can’t, absolutely can’t fault Mr [surgeon] and his team, they’re outstanding . . . And that’s the thing, nobody’s spoke to me about actually getting back to work.
2268
Assessment of intervention effectiveness
| Characteristic | Hip (N = 10) | Knee (N = 16) | Total (N = 26) |
|---|---|---|---|
| Age (years) | n = 10 | n = 14 | n = 24 |
| Mean (SD) | 57.3 (14.3) | 55.4 (5.9) | 56.2 (10.0) |
| Median (Q1, Q3) | 57 (51, 64) | 54 (51, 59) | 54.5 (51, 63) |
| Minimum, maximum | 34, 84 | 46, 66 | 34, 84 |
| Sex, n (%) | |||
| Male | 3 (30.0) | 7 (43.8) | 10 (38.5) |
| Female | 7 (70.0) | 8 (50.0) | 15 (57.7) |
| Missing | 0 (0.0) | 1 (6.3) | 1 (3.9) |
| Employment,a n (%) | |||
| Full time | 4 (40.0) | 11 (68.8) | 15 (57.7) |
| Part time | 1 (10.0) | 3 (18.8) | 4 (15.4) |
| Self-employed | 1 (10.0) | 2 (12.5) | 3 (11.5) |
| Unpaid work | 4 (40.0) | 1 (6.3) | 5 (19.2) |
| Other | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Total time spent working in a week (hours) | n = 10 | n = 16 | n = 26 |
| Mean (SD) | 31.3 (12.5) | 40.1 (23.4) | 36.7 (20.1) |
| Median (Q1, Q3) | 33.8 (20, 40) | 37.5 (31.5, 45.5) | 37.5 (23, 44) |
| Minimum, maximum | 14, 50 | 8, 112 | 8, 112 |
| OHS/OKS | n = 10 | n = 16 | n = 26 |
| Mean (SD) | 17.4 (3.7) | 17.3 (6.3) | 17.3 (5.4) |
| Median (Q1, Q3) | 16.5 (15, 19) | 18 (11, 21.4) | 17 (14, 21) |
| Minimum, maximum | 14, 26 | 8, 29 | 8, 29 |
List of job titles given in the feasibility phase
Medical Sec/Receptionist.
Clinical Trials Data management & Trial Co-Ordination.
Volunteer with Sea Cadets.
Carer for grandchildren.
Carer for grandchildren/Help Girls Club on saturdays & 1 week holiday club for 11–16 year olds.
Plater involved in the fabrication of Heavy Engineering.
Activity Co-Ordinator in childrens Hospice.
Volunteer with Age UK North Tyne.
Distributer Manager UK & Ireland.
Lab Technician.
HCA [health-care assistant] – Working in Pre-Op.
Trade Counter Assistant/Clinical Hypnotherapist.
CSI Operations Manager.
Work with Special Needs Children.
District Nurse.
Operations Manager ‘Royal Mail’ Manage a Team of Managers operating units.
Kitchen Porter & Lifting Involved.
Health-care Assistant, Work at Friarage Hospital on Rutson Ward, Stroke Patients, Rehab, etc.
Intelligence Officer (Police Constable) at Cleveland Police.
Retail Wages Clerk, I work on a computer most of my shift. My work also involves walking.
SEN [special education needs] Teaching Assistant.
Receptionist Cardiology WGH [Western General Hospital].
Carer for Husband/Was also working in retail part time.
Publican.
Production Operator.
| Activity | Participants, n (%) | ||
|---|---|---|---|
| Hip (N = 10) | Knee (N = 16) | Total (N = 26) | |
| Are any of the following activities essential to your work? | |||
| Standing/walking for prolonged periods | |||
| Yes | 7 (70.0) | 14 (87.5) | 21 (80.8) |
| No | 3 (0.0) | 2 (12.5) | 5 (19.2) |
| Sitting for prolonged periods | |||
| Yes | 7 (70.0) | 11 (68.8) | 18 (69.2) |
| No | 3 (30.0) | 5 (31.3) | 8 (30.8) |
| Kneeling | |||
| Yes | 4 (40.0) | 5 (31.3) | 9 (34.6) |
| No | 6 (60.0) | 11 (68.8) | 17 (65.4) |
| Climbing, including stairs | |||
| Yes | 9 (90.0) | 11 (68.8) | 20 (76.9) |
| No | 1 (10.0) | 5 (31.3) | 6 (23.1) |
| Lifting/manual handling | |||
| Yes | 6 (60.0) | 9 (56.3) | 15 (57.7) |
| No | 4 (40.0) | 7 (43.8) | 11 (42.3) |
| Bending or crouching | |||
| Yes | 8 (80.0) | 13 (81.3) | 21 (80.8) |
| No | 2 (20.0) | 3 (18.8) | 5 (19.2) |
| Are you required to work rotating shifts at work? | |||
| Yes | 5 (50.0) | 7 (43.8) | 12 (46.2) |
| No | 5 (50.0) | 9 (56.3) | 14 (53.9) |
| Do you drive to work? | |||
| Yes | 9 (90.0) | 12 (75.0) | 21 (80.8) |
| No | 1 (10.0) | 4 (25.0) | 5 (19.2) |
| Do you drive while at work? | |||
| Yes | 5 (50.0) | 5 (31.3) | 10 (38.5) |
| No | 4 (40.0) | 10 (62.5) | 14 (53.9) |
| Missing | 1 (10.0) | 1 (6.3) | 2 (7.7) |
| Do you have access to occupational health services at work? | |||
| Yes | 3 (30.0) | 8 (50.0) | 11 (42.3) |
| No | 7 (70.0) | 5 (31.3) | 12 (46.2) |
| Don’t know | 0 (0.0) | 3 (18.8) | 3 (11.5) |
| Question | Hip (N = 10) | Knee (N = 16) | Total (N = 26) |
|---|---|---|---|
| Before the review with the surgical team | |||
| Were you given an occupational checklist to complete prior to your appointment with the surgical team? | |||
| Yes, n (%) | 5 (50.0) | 15 (93.8) | 20 (76.9) |
| No, n (%) | 4 (40.0) | 1 (6.3) | 5 (19.2) |
| Don’t know, n (%) | 1 (10.0) | 0 (0.0) | 1 (3.9) |
| Approximately how long did it take you to complete the occupational checklist (minutes)? | n = 8 | n = 14 | n = 22 |
| Mean (SD) | 5.4 (3.2) | 13.6 (15.4) | 10.7 (12.9) |
| Median (Q1, Q3) | 5 (3.5, 7.5) | 6.5 (2, 20) | 5 (2, 10) |
| Minimum, maximum | 1.5, 10 | 2, 55 | 1.5, 55 |
| During the review: did a member of the surgical team . . . | |||
| Refer to the information on the occupational checklist during your consultation? | |||
| Yes, n (%) | 5 (50.0) | 15 (93.8) | 20 (76.9) |
| No, n (%) | 4 (40.0) | 1 (6.3) | 5 (19.2) |
| Don’t know, n (%) | 1 (1.0) | 0 (0.0) | 1 (3.9) |
| Talk about your job when discussing the options for treatment? | |||
| Yes, n (%) | 9 (90.0) | 13 (81.3) | 22 (84.6) |
| No, n (%) | 1 (10.0) | 2 (12.5) | 3 (11.5) |
| Don’t know, n (%) | 0 (0.0) | 1 (6.3) | 1 (3.9) |
| Talk about how and when you might return to work after surgery? | |||
| Yes, n (%) | 7 (70.0) | 11 (68.8) | 18 (69.2) |
| No, n (%) | 3 (30.0) | 5 (31.3) | 8 (30.8) |
| Don’t know, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Refer to the OPAL return-to-work programme? | |||
| Yes, n (%) | 9 (90.0) | 14 (87.5) | 23 (88.5) |
| No, n (%) | 1 (10.0) | 2 (12.5) | 3 (11.5) |
| Don’t know, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| After the review | |||
| Did a member of staff explain the OPAL return-to-work programme to you? | |||
| Yes, n (%) | 10 (100.0) | 15 (93.8) | 25 (96.2) |
| No, n (%) | 0 (0.0) | 1 (6.3) | 1 (3.9) |
| Don’t know, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Baseline result | Hip (n = 10) | Knee (n = 16) | Total (n = 26) |
|---|---|---|---|
| Mean (SD) | 31.5 (4.1) | 33.4 (5.4) | 32.6 (4.9) |
| Median (Q1, Q3) | 30.5 (29, 35) | 35 (30.5, 37) | 33.5 (29, 37) |
| Minimum, maximum | 26, 38 | 22, 40 | 22, 40 |
| Time (weeks) | Hip (N = 10), n = 5 | Knee (N = 16), n = 5 | Total (N = 26), n = 10 |
|---|---|---|---|
| Mean (SD) | 5.2 (4.8) | 9.7 (5.7) | 7.4 (5.5) |
| Median (Q1, Q3) | 4.4 (3, 4.6) | 6.3 (5.9, 13.7) | 5.4 (4.4, 13.3) |
| Minimum, maximum | 0.6, 13.3 | 5, 17.7 | 0.6, 17.7 |
| Details | Hip (N = 10) | Knee (N = 16) | Total (N = 26) |
|---|---|---|---|
| Did you return to work following your surgery? | N = 10 | N = 16 | N = 26 |
| Yes, n (%) | 5 (50.0) | 5 (31.3) | 10 (38.5) |
| No, n (%) | 3 (30.0) | 6 (37.5) | 9 (34.6) |
| Missing,a n (%) | 2 (20.0) | 5 (31.3) | 7 (26.9) |
| If yes, did you return to your usual hours and duties? | N = 5 | N = 5 | N = 10 |
| Yes, n (%) | 2 (40.0) | 0 (0.0) | 2 (20.0) |
| No, n (%) | 3 (60.0) | 5 (100.0) | 8 (80.0) |
| Missing, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| If no, how did you return? | N = 3 | N = 5 | N = 8 |
| Reduced hours, usual duties, n (%) | 2 (66.7) | 1 (20.0) | 3 (37.5) |
| Usual hours, amended duties, n (%) | 0 (0.0) | 1 (20.0) | 1 (12.5) |
| Reduced hours and amended duties, n (%) | 0 (0.0) | 3 (60.0) | 3 (37.5) |
| Missing, n (%) | 1 (33.3) | 0 (0.0) | 1 (12.5) |
| If you returned on reduced hours, how many did you work in the first week? | N = 2 | N = 4 | N = 6 |
| Mean (SD) | 13 (9.9) | 14 (6.3) | 13.7 (6.6) |
| Median (Q1, Q3) | 13 (6, 20) | 15 (9, 19) | 15 (6, 20) |
| Minimum, maximum | 6, 20 | 6, 20 | 6, 20 |
| Were any adaptions made to your workplace? | |||
| Yes, n (%) | 1 (20.0) | 2 (40.0) | 3 (30.0) |
| No, n (%) | 4 (80.0) | 3 (60.0) | 7 (70.0) |
| Were any changes made to your pattern of work? | |||
| Yes, n (%) | 1 (20.0) | 3 (60.0) | 4 (40.0) |
| No, n (%) | 4 (80.0) | 2 (40.0) | 6 (60.0) |
| Details | Hip (N = 10) | Knee (N = 16) | Total (N = 26) |
|---|---|---|---|
| Have you been provided with a ‘fit note’ following your recent operation? | N = 8 | N = 13 | N = 21 |
| Week 8, n (%) | |||
| Yes | 3 (37.5) | 8 (61.5) | 11 (52.4) |
| No | 5 (62.5) | 2 (15.4) | 7 (33.3) |
| Missing | 0 (0.0) | 3 (23.1) | 3 (14.3) |
| Week 16, n (%) | |||
| Yes | 2 (25.0) | 4 (30.8) | 6 (28.6) |
| No | 4 (50.0) | 4 (30.8) | 8 (38.1) |
| Missing | 2 (25.0) | 5 (38.5) | 7 (33.3) |
| How many additional fit notes have you received after the one at discharge? | N = 1 | N = 4 | N = 5 |
| Mean (SD) | 3 (–) | 1.3 (0.5) | 1.6 (0.9) |
| Median (Q1, Q3) | – (–, –) | 1 (1, 1.5) | 1 (1, 2) |
| Minimum, maximum | –, – | 1, 2 | 1, 3 |
| How long was it for (weeks)? | |||
| Week 8 | N = 5 | N = 7 | N = 12 |
| Mean (SD) | 5.6 (5.5) | 6.4 (2.9) | 6.1 (4.0) |
| Median (Q1, Q3) | 6 (0, 10) | 6 (6, 7) | 6 (4, 8.5) |
| Minimum, maximum | 0, 12 | 2, 12 | 0, 12 |
| Week 16 | N = 6 | N = 8 | N = 14 |
| Mean (SD) | 2 (4.9) | 2.9 (3.4) | 2.5 (3.9) |
| Median (Q1, Q3) | 0 (0, 0) | 2 (0, 5.5) | 0 (0, 4) |
| Minimum, maximum | 0, 12 | 0, 8 | 0, 12 |
| Which of the following options were selected? | |||
| Week 8, n (%) | N = 8 | N = 13 | N = 21 |
| You are NOT fit for work | 2 (25.0) | 5 (38.5) | 7 (33.3) |
| You MAY be fit for work taking in to account – a phased return to work | 0 (0.0) | 2 (15.4) | 2 (9.5) |
| You MAY be fit for work taking in to account – amended duties | 0 (0.0) | 1 (6.7) | 1 (4.8) |
| You MAY be fit for work taking in to account – altered hours | 0 (0.0) | 1 (7.7) | 1 (4.8) |
| You MAY be fit for work taking in to account – workplace adaptions | 1 (12.5) | 0 (0.0) | 1 (4.8) |
| Do not know/unsure | 2 (25.0) | 0 (0.0) | 1 (4.8) |
| Week 16, n (%) | N = 8 | N = 16 | N = 26 |
| You are NOT fit for work | 0 (0.0) | 2 (15.4) | 2 (9.5) |
| You MAY be fit for work taking in to account – a phased return to work | 0 (0.0) | 2 (15.4) | 2 (9.5) |
| You MAY be fit for work taking in to account – amended duties | 0 (0.0) | 2 (15.4) | 2 (9.5) |
| You MAY be fit for work taking in to account – altered hours | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| You MAY be fit for work taking in to account – workplace adaptions | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Do not know/unsure | 2 (25.0) | 0 (0.0) | 2 (9.5) |
| When did you first driving following your operation? (weeks post surgery) | |||
| Week 8 | N = 6 | N = 8 | N = 14 |
| Mean (SD) | 5.7 (1.4) | 6.4 (1.1) | 6.1 (1.2) |
| Median (Q1, Q3) | 6 (6, 6) | 6.5 (5.5, 7) | 6 (6, 7) |
| Minimum, maximum | 3, 7 | 5, 8 | 3, 8 |
| Week 16 | N = 5 | N = 8 | N = 13 |
| Mean (SD) | 5 (1.2) | 6.6 (1.5) | 6 (1.6) |
| Median (Q1, Q3) | 5 (5, 6) | 6.5 (6, 7.5) | 6 (5, 7) |
| Minimum, maximum | 3, 6 | 4, 9 | 3, 9 |
| Statement | Participants, n (%) | ||
|---|---|---|---|
| Hip (N = 10) | Knee (N = 16) | Total (N = 26) | |
| For those not back in work yet | |||
| You don’t think you will ever be able to go back to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 3 (75.0) | 5 (71.4) | 8 (80.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 1 (25.0) | 1 (16.7) | 2 (20.0) |
| Mean (SD) | 1.5 (1.0) | 1.3 (0.8) | 1.4 (0.8) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 1 (100.0) | 3 (100.0) | 4 (100.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mean (SD) | 1.0 (–) | 1.0 (0.0) | 1 (0.0) |
| As far as you’re concerned, there is no point in thinking about returning to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 4 (100.0) | 5 (83.3) | 9 (90.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Mean (SD) | 1.3 (0.5) | 1.8 (1.2) | 1.6 (1.0) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 1 (100.0) | 3 (100.0) | 4 (100.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mean (SD) | 1.0 (–) | 1.3 (0.6) | 1.3 (0.5) |
| You are actively doing things now to get back to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 1 (25.0) | 1 (16.7) | 2 (20.0) |
| Agree | 3 (75.0) | 5 (83.3) | 8 (80.0) |
| Mean (SD) | 4.3 (1.0) | 4.2 (0.8) | 4.2 (0.8) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 1 (100.0) | 3 (100.0) | 4 (100.0) |
| Mean (SD) | 4.0 (–) | 4.3 (0.6) | 4.3 (0.5) |
| Physically, you are starting to feel ready to go back to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Neutral | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Agree | 4 (100.0) | 4 (66.7) | 8 (80.0) |
| Mean (SD) | 4.5 (0.6) | 3.5 (0.8) | 3.9 (0.9) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 1 (100.0) | 3 (100.0) | 4 (100.0) |
| Mean (SD) | 4.0 (–) | 4.3 (0.6) | 4.3 (0.5) |
| You have been increasing your activities at home in order to build up your strength to go back to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 4 (100.0) | 5 (83.3) | 9 (90.0) |
| Mean (SD) | 4.8 (0.5) | 3.8 (1.0) | 4.2 (0.9) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 1 (100.0) | 3 (100.0) | 4 (100.0) |
| Mean (SD) | 4.0 (–) | 4.3 (0.6) | 4.3 (0.5) |
| You are getting help from others to return to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Neutral | 1 (25.0) | 0 (0.0) | 1 (10.0) |
| Agree | 4.3 (1.0) | 3.5 (1.2) | 3.8 (1.1) |
| Mean (SD) | 3 (75.0) | 5 (83.3) | 8 (80.0) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 1 (100.0) | 1 (33.3) | 2 (50.0) |
| Agree | 0 (0.0) | 2 (66.7) | 2 (50.0) |
| Mean (SD) | 3.0 (–) | 4.0 (1.0) | 3.8 (1.0) |
| You are not ready to go back to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 1 (25.0) | 3 (50.0) | 4 (40.0) |
| Neutral | 1 (25.0) | 0 (0.0) | 1 (1.0) |
| Agree | 2 (50.0) | 3 (50.0) | 5 (50.0) |
| Mean (SD) | 3 (1.4) | 2.8 (1.3) | 2.9 (1.3) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 3 (100.0) | 3 (75.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 1 (100.0) | 0 (0.0) | 1 (25.0) |
| Mean (SD) | 4.0 (–) | 1.7 (0.6) | 2.3 (1.3) |
| You have found strategies to make your work manageable so you can return to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Neutral | 2 (50.0) | 2 (33.3) | 4 (40.0) |
| Agree | 2 (50.0) | 3 (50.0) | 5 (50.0) |
| Mean (SD) | 3.8 (1.0) | 3.5 (1.0) | 3.6 (1.0) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 1 (100.0) | 1 (33.3) | 2 (50.0) |
| Agree | 0 (0.0) | 2 (6.7) | 2 (50.0) |
| Mean (SD) | 3.0 (–) | 4.0 (1.0) | 3.8 (1.0) |
| You have been wondering if there is something you could do to return to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 1 (25.0) | 3 (50.0) | 4 (40.0) |
| Neutral | 1 (25.0) | 1 (16.7) | 2 (20.0) |
| Agree | 2 (50.0) | 1 (16.7) | 3 (30.0) |
| Missing | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Mean (SD) | 3.5 (1.3) | 2.6 (0.9) (n = 5) | 3 (1.1) (n = 9) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 1 (100.0) | 0 (0.0) | 1 (25.0) |
| Agree | 0 (0.0) | 3 (0.0) | 3 (75.0) |
| Mean (SD) | 3.0 (–) | 4.3 (0.6) | 4.0 (0.8) |
| You have a date for your return to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 2 (50.0) | 2 (33.3) | 4 (40.0) |
| Neutral | 1 (25.0) | 1 (16.7) | 2 (20.0) |
| Agree | 1 (25.0) | 2 (33.3) | 3 (30.0) |
| Missing | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Mean (SD) | 2.5 (1.3) | 3 (1.6) (n = 5) | 2.8 (1.4) (n = 9) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 1 (100.0) | 0 (0.0) | 1 (25.0) |
| Agree | 0 (0.0) | 3 (100.0) | 3 (75.0) |
| Mean (SD) | 3.0 (–) | 5.0 (0.0) | 4.5 (1.0) |
| You wish you had more ideas about how to get back to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 2 (50.0) | 4 (66.7) | 6 (60.0) |
| Neutral | 1 (25.0) | 0 (0.0) | 1 (10.0) |
| Agree | 1 (25.0) | 1 (16.7) | 2 (20.0) |
| Missing | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Mean (SD) | 2.3 (1.5) | 2.2 (1.1) (n = 5) | 2.2 (1.2) (n = 9) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 2 (66.7) | 2 (50.0) |
| Neutral | 0 (0.0) | 1 (33.3) | 1 (25.0) |
| Agree | 1 (100.0) | 0 (0.0) | 1 (25.0) |
| Mean (SD) | 4.0 (–) | 1.7 (1.2) | 2.3 (1.5) |
| You would like some advice about how to go back to work | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 1 (25.0) | 3 (50.0) | 4 (40.0) |
| Neutral | 2 (50.0) | 0 (0.0) | 2 (20.0) |
| Agree | 1 (25.0) | 2 (33.3) | 3 (30.0) |
| Missing | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Mean (SD) | 2.8 (1.3) | 2.8 (1.6) (n = 5) | 2.8 (1.4) (n = 9) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 0 (0.0) | 2 (66.7) | 2 (50.0) |
| Neutral | 0 (0.0) | 1 (33.3) | 1 (25.0) |
| Agree | 1 (100.0) | 0 (0.0) | 1 (25.0) |
| Mean (SD) | 4.0 (–) | 1.7 (1.2) | 2.3 (1.5) |
| As far as you are concerned, you don’t need to go back to work ever | |||
| Week 8 | N = 4 | N = 6 | N = 10 |
| Disagree | 4 (100.0) | 5 (83.3) | 9 (90.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 0 (0.0) | 1 (16.7) | 1 (10.0) |
| Mean (SD) | 1 (0) | 1.2 (0.4) (n = 5) | 1.1 (0.3) (n = 9) |
| Week 16 | N = 1 | N = 3 | N = 4 |
| Disagree | 1 (100.0) | 2 (66.7) | 3 (75.0) |
| Neutral | 0 (0.0) | 1 (33.3) | 1 (25.0) |
| Agree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mean (SD) | 1.0 (–) | 1.7 (1.2) | 1.5 (1.0) |
| For those back at work | |||
| You are doing everything you can to stay at work | |||
| Week 8 | N = 4 | N = 3 | N = 7 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 4 (100.0) | 3 (100.0) | 7 (100.0) |
| Mean (SD) | 4.8 (0.5) | 4.7 (0.6) | 4.7 (0.5) |
| Week 16 | N = 5 | N = 5 | N = 5 |
| Disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 5 (100.0) | 5 (100.0) | 10 (100.0) |
| Mean (SD) | 4.6 (0.5) | 4.8 (0.4) | 4.7 (0.5) |
| You have learnt different ways to cope with your pain so that you can stay at work | |||
| Week 8 | N = 4 | N = 3 | N = 7 |
| Disagree | 3 (75.0) | 0 (0.0) | 3 (42.9) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 1 (25.0) | 3 (100.0) | 4 (57.1) |
| Mean (SD) | 2.5 (1.7) | 4.7 (0.6) | 3.4 (1.7) |
| Week 16 | N = 5 | N = 5 | N = 10 |
| Disagree | 2 (40.0) | 0 (0.0) | 2 (20.0) |
| Neutral | 1 (20.0) | 0 (0.0) | 1 (1.0) |
| Agree | 2 (40.0) | 5 (100.0) | 7 (7.0) |
| Mean (SD) | 2.6 (1.5) | 4.8 (0.4) | 3.7 (1.6) |
| You are taking steps to prevent having to go off work again | |||
| Week 8 | N = 4 | N = 3 | N = 7 |
| Disagree | 1 (25.0) | 0 (0.0) | 1 (14.3) |
| Neutral | 1 (25.0) | 1 (33.3) | 2 (28.6) |
| Agree | 2 (50.0) | 2 (66.7) | 4 (57.1) |
| Mean (SD) | 3.5 (1.3) | 4.3 (1.2) | 3.9 (1.2) |
| Week 16 | N = 5 | N = 5 | N = 10 |
| Disagree | 2 (40.0) | 0 (0.0) | 2 (20.0) |
| Neutral | 1 (20.0) | 0 (0.0) | 1 (10.0) |
| Agree | 2 (40.0) | 5 (100.0) | 7 (70.0) |
| Mean (SD) | 2.8 (1.3) | 4.8 (0.4) | 3.8 (1.4) |
| You have found strategies to make your work manageable so you can stay at work | |||
| Week 8 | N = 4 | N = 3 | N = 7 |
| Disagree | 1 (25.0) | 0 (0.0) | 1 (14.3) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 3 (75.0) | 3 (100.0) | 6 (85.7) |
| Mean (SD) | 4.0 (1.4) | 4.7 (0.6) | 4.3 (1.1) |
| Week 16 | N = 5 | N = 5 | N = 10 |
| Disagree | 2 (40.0) | 0 (0.0) | 2 (20.0) |
| Neutral | 1 (20.0) | 0 (0.0) | 1 (10.0) |
| Agree | 2 (40.0) | 5 (100.0) | 7 (70.0) |
| Mean (SD) | 2.8 (1.3) | 4.8 (0.4) | 3.8 (1.4) |
| You are back at work but not sure you can keep up the effort | |||
| Week 8 | N = 4 | N = 3 | N = 7 |
| Disagree | 2 (50.0) | 2 (66.7) | 4 (57.1) |
| Neutral | 1 (25.0) | 1 (33.3) | 2 (28.6) |
| Agree | 1 (25.0) | 0 (0.0) | 1 (14.3) |
| Mean (SD) | 2.3 (1.5) | 2.0 (1.0) | 2.1 (1.2) |
| Week 16 | N = 5 | N = 5 | N = 10 |
| Disagree | 4 (80.0) | 3 (60.0) | 7 (70.0) |
| Neutral | 1 (20.0) | 2 (40.0) | 3 (30.0) |
| Agree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mean (SD) | 1.8 (0.8) | 2.0 (1.0) | 1.9 (0.9) |
| You worry about having to stop working again due to your injury | |||
| Week 8 | N = 4 | N = 5 | N = 10 |
| Disagree | 3 (75.0) | 3 (100.0) | 6 (85.7) |
| Neutral | 1 (25.0) | 0 (0.0) | 1 (14.3) |
| Agree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mean (SD) | 1.8 (1.0) | 1.7 (0.6) | 1.7 (0.8) |
| Week 16 | N = 5 | N = 5 | N = 10 |
| Disagree | 4 (80.0) | 3 (60.0) | 7 (7.0) |
| Neutral | 1 (20.0) | 0 (0.0) | 1 (10.0) |
| Agree | 0 (0.0) | 2 (40.0) | 2 (20.0) |
| Mean (SD) | 1.8 (0.8) | 2.6 (1.8) | 2.2 (1.4) |
| You still find yourself struggling to stay at work due to the effects of your injury | |||
| Week 8 | N = 4 | N = 3 | N = 7 |
| Disagree | 4 (100.0) | 3 (100.0) | 7 (100.0) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mean (SD) | 1.5 (0.6) | 1.7 (0.6) | 1.6 (0.5) |
| Week 16 | N = 5 | N = 5 | N = 10 |
| Disagree | 4 (80.0) | 2 (40.0) | 6 (60.0) |
| Neutral | 1 (20.0) | 1 (20.0) | 2 (20.0) |
| Agree | 0 (0.0) | 2 (40.0) | 2 (20.0) |
| Mean (SD) | 2.0 (0.7) | 3.0 (1.6) | 2.5 (1.3) |
| You are back at work and it is going well | |||
| Week 8 | N = 4 | N = 3 | N = 7 |
| Disagree | 0 (0.0) | 1 (33.3) | 1 (14.3) |
| Neutral | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Agree | 4 (100.0) | 2 (66.7) | 6 (85.7) |
| Mean (SD) | 4.8 (0.5) | 4.0 (1.7) | 4.4 (1.1) |
| Week 16 | N = 5 | N = 5 | N = 10 |
| Disagree | 0 (0.0) | 0 (0.0) | (0.0) |
| Neutral | 0 (0.0) | 1 (20.0) | 1 (10.0) |
| Agree | 5 (100.0) | 4 (80.0) | 9 (90.0) |
| Mean (SD) | 4.4 (0.5) | 4.6 (0.9) | 4.5 (0.7) |
| You feel you may need help in order to stay at work | |||
| Week 8 | N = 4 | N = 3 | N = 7 |
| Disagree | 2 (50.0) | 2 (66.7) | 4 (57.1) |
| Neutral | 2 (50.0) | 0 (0.0) | 2 (28.6) |
| Agree | 0 (0.0) | 1 (33.3) | 1 (14.3) |
| Mean (SD) | 2.0 (1.1) | 2.7 (2.1) | 2.3 (1.5) |
| Week 16 | N = 5 | N = 5 | N = 10 |
| Disagree | 5 (100.0) | 2 (40.0) | 7 (70.0) |
| Neutral | 0 (0.0) | 1 (20.0) | 1 (10.0) |
| Agree | 0 (0.0) | 2 (40.0) | 2 (20.0) |
| Mean (SD) | 1.4 (0.5) | 2.8 (1.8) | 2.1 (1.4) |
| Time point | Participants replying by time point, n (%) | ||
|---|---|---|---|
| Hip (N = 10) | Knee (N = 16) | Total (N = 26) | |
| Week 8 | 8 (88.9) | 10 (71.4) | 18 (78.3) |
| Week 16 | 6 (66.7) | 8 (57.1) | 14 (60.9) |
| Data | Percentage of time lost | ||
|---|---|---|---|
| Hip (N = 10) | Knee (N = 16) | Total (N = 26) | |
| Baseline | n = 9 | n = 13 | n = 22 |
| Mean (SD) | 36.4 (12.6) | 44.8 (18.8) | 41.4 (16.7) |
| Median (Q1, Q3) | 40.6 (25, 46.9) | 45.8 (28.1, 56.3) | 43.2 (25, 50) |
| Minimum, maximum | 21.9, 50 | 21.9, 71.9 | 21.9, 71.9 |
| Week 8 | n = 2 | n = 3 | n = 5 |
| Mean (SD) | 6.3 (0.0) | 34.4 (36.8) | 23.1 (30.3) |
| Median (Q1, Q3) | 6.3 (6.3, 6.3) | 25.0 (3.1, 75.0) | 6.3 (6.3, 25.0) |
| Minimum, maximum | 6.3, 6.3 | 3.1, 75.0 | 3.1, 75.0 |
| Week 16 | n = 3 | n = 5 | n = 8 |
| Mean (SD) | 10.4 (12.6) | 21.9 (13.4) | 17.6 (13.6) |
| Median (Q1, Q3) | 3.1 (3.1, 25) | 28.1 (18.8, 28.1) | 21.9 (3.1, 28.1) |
| Minimum, maximum | 3.1, 25 | 0, 34.4 | 0, 34.4 |
Assessment of economic data
Cost of return-to-work co-ordinator time
The average hourly cost of £53.24 was based on details of the four RTWCs involved in the feasibility work; the costs per working hour (including salary oncosts and overheads) of one band 4 RTWC (£29), two band 7 RTWCs (£53) and one band 8a RTWC (£63) were incorporated, with each having a qualifications cost added (of £3.38, based on recommendations from the PSSRU Unit Costs of Health and Social Care 2018140), to generate a cost per hour including qualifications.
Cost of return-to-work co-ordinator training
The hourly cost of the RTWC trainer was based on the average of the four RTWCs’ costs per working hour including qualifications (as above).
Cost of printing of the intervention
The £6.37 printing cost of the intervention materials consisted of:
-
£4.09 per participant for the patient and employer booklets [based on a printer’s cost of £409 for 100 patient booklets (24 pages) and 100 employer booklets (12 pages) in colour]
-
£2.28 per participant for the RTWC workbook/information resource (17 pages) and occupational checklist (13 pages) (based on a printer’s cost of £0.125 per single-sided page and £0.145 per double-sided page).
| Type of resource use | Hip (N = 10) | Knee (N = 16) | ||
|---|---|---|---|---|
| Mean (SD) | Missing, n (%) | Mean (SD) | Missing, n (%) | |
| GP visits at GP’s practice | ||||
| 8 weeksa | 0.13 (0.35) | 2 (20.0) | 1.11 (1.17) | 7 (43.8) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.58 (0.98) | 9 (56.3) |
| GP visits at home | ||||
| 8 weeks | 0.13 (0.35) | 2 (20.0) | 0.11 (0.33) | 7 (43.8) |
| 16 weeks | 0.17 (0.41) | 4 (40.0) | 0.00 (0.00) | 9 (56.3) |
| Nurse visits at GP’s practice | ||||
| 8 weeks | 0.57 (0.53) | 3 (30.0) | 0.22 (0.67) | 7 (43.8) |
| 16 weeks | 0.17 (0.41) | 4 (40.0) | 0.00 (0.00) | 9 (56.3) |
| Community nurse visits at home | ||||
| 8 weeks | 0.75 (1.04) | 2 (20.0) | 0.22 (0.44) | 7 (43.8) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 9 (56.3) |
| Occupational therapist visits | ||||
| 8 weeks | 0.00 (0.00) | 2 (20.0) | 0.13 (0.35) | 8 (50.0) |
| 16 weeks | 1.00 (2.45) | 4 (40.0) | 0.00 (0.00) | 9 (56.3) |
| Physiotherapist visits | ||||
| 8 weeks | 0.88 (1.13) | 2 (20.0) | 4.80 (3.71) | 6 (37.5) |
| 16 weeks | 0.17 (0.41) | 4 (40.0) | 3.71 (3.30) | 9 (56.3) |
| Other health service visits | ||||
| 8 weeks | 0.00 (0.00) | 2 (20.0) | 0.00 (0.00) | 7 (43.8) |
| 16 weeks | 0.00 (0.00) | 5 (50.0) | 0.71 (1.25) | 9 (56.3) |
| Inpatient nights in hospital | ||||
| 8 weeks | 2.25 (1.39) | 2 (20.0) | 3.00 (1.87) | 7 (43.8) |
| 16 weeks | 1.50 (2.07) | 4 (40.0) | 1.00 (1.41) | 8 (50.0) |
| Day-case visits to hospital | ||||
| 8 weeks | 0.00 (0.00) | 3 (30.0) | 0.50 (0.71) | 6 (37.5) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 8 (50.0) |
| Outpatient attendances | ||||
| 8 weeks | 0.50 (0.53) | 2 (20.0) | 1.00 (0.50) | 7 (43.8) |
| 16 weeks | 0.17 (0.41) | 4 (40.0) | 0.50 (0.76) | 8 (50.0) |
| A&E visits | ||||
| 8 weeks | 0.00 (0.00) | 2 (20.0) | 0.22 (0.67) | 7 (43.8) |
| 16 weeks | 0.33 (0.82) | 4 (40.0) | 0.38 (1.06) | 8 (50.0) |
| Physiotherapy hospital attendances | ||||
| 8 weeks | 0.63 (0.92) | 2 (20.0) | 4.22 (3.93) | 7 (43.8) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 2.88 (3.36) | 8 (50.0) |
| Type of resource use | Hip (N = 10) | Knee (N = 16) | ||
|---|---|---|---|---|
| Mean (SD) | Missing, n (%) | Mean (SD) | Missing, n (%) | |
| GP visits at GP’s practice | ||||
| 8 weeksa | 0.00 (0.00) | 4 (40.0) | 0.50 (0.58) | 12 (75.0) |
| 16 weeks | 0.17 (0.41) | 4 (40.0) | 0.86 (0.90) | 9 (56.3) |
| GP visits at home | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.20 (0.45) | 11 (68.8) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 8 (50.0) |
| Nurse visits at GP’s practice | ||||
| 8 weeks | 0.20 (0.45) | 5 (50.0) | 1.50 (2.38) | 12 (75.0) |
| 16 weeks | 1.00 (2.00) | 4 (40.0) | 0.25 (0.71) | 8 (50.0) |
| Community nurse visits at home | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 12 (75.0) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 8 (50.0) |
| Occupational therapist visits | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 12 (75.0) |
| 16 weeks | 1.00 (2.45) | 4 (40.0) | 0.00 (0.00) | 8 (50.0) |
| Physiotherapist visits | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 12 (75.0) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 8 (50.0) |
| Other health service visits | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 12 (75.0) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.43 (0.79) | 9 (56.3) |
| Inpatient nights in hospital | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 12 (75.0) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 9 (56.3) |
| Day-case visits to hospital | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 12 (75.0) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 9 (56.3) |
| Outpatient attendances | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 12 (75.0) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.43 (0.79) | 9 (56.3) |
| A&E visits | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 12 (75.0) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.14 (0.38) | 9 (56.3) |
| Physiotherapy hospital attendances | ||||
| 8 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 12 (75.0) |
| 16 weeks | 0.00 (0.00) | 4 (40.0) | 0.00 (0.00) | 9 (56.3) |
| Resource | Hip | Knee | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| GP visits at GP’s practice | 6 | 0.17 (0.41) | 5 | 2.20 (2.39) |
| GP visits at home | 6 | 0.33 (0.82) | 5 | 0.00 (0.00) |
| Nurse visits at GP’s practice | 6 | 0.67 (0.82) | 5 | 0.00 (0.00) |
| Community nurse visits at home | 6 | 1.00 (1.10) | 5 | 0.00 (0.00) |
| Occupational therapist visits | 6 | 1.00 (2.45) | 5 | 0.20 (0.45) |
| Physiotherapist visits | 6 | 0.67 (1.03) | 6 | 11.17 (4.36) |
| Other health service visits | 5 | 0.00 (0.00) | 5 | 0.60 (1.34) |
| Inpatient nights in hospital | 6 | 4.00 (2.97) | 6 | 4.17 (3.13) |
| Day-case visits to hospital | 5 | 0.00 (0.00) | 7 | 0.71 (0.76) |
| Outpatient attendances | 6 | 0.83 (0.75) | 6 | 1.33 (0.82) |
| A&E visits | 6 | 0.33 (0.82) | 6 | 0.83 (2.04) |
| Physiotherapy hospital attendances | 6 | 0.83 (0.98) | 6 | 7.83 (6.85) |
| Resource | Hip (N = 10) | Knee (N = 16) | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| GP visits at GP’s practice | 4 | 0.00 (0.00) | 2 | 0.50 (0.71) |
| GP visits at home | 4 | 0.00 (0.00) | 4 | 0.25 (0.50) |
| Nurse visits at GP’s practice | 4 | 0.50 (1.00) | 3 | 2.00 (2.65) |
| Community nurse visits at home | 4 | 0.00 (0.00) | 3 | 0.00 (0.00) |
| Occupational therapist visits | 4 | 1.50 (3.00) | 3 | 0.00 (0.00) |
| Physiotherapist visits | 4 | 0.00 (0.00) | 3 | 0.00 (0.00) |
| Other health service visits | 4 | 0.00 (0.00) | 2 | 0.50 (0.71) |
| Inpatient nights in hospital | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| Day-case visits to hospital | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| Outpatient attendances | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| A&E visits | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| Physiotherapy hospital attendances | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| Cost item | Hip (N = 10) | Knee (N = 16) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline–8 weeks | 8–16 weeks | Baseline–8 weeks | 8–16 weeks | |||||
| Mean cost (£) (SD) | n | Mean cost (£) (SD) | n | Mean cost (£) (SD) | n | Mean cost (£) (SD) | n | |
| GP visits at GP’s practice | 4.68 (13.22) | 8 | 0.00 (0.00) | 6 | 41.56 (43.63) | 9 | 21.37 (36.50) | 7 |
| GP visits at home | 11.70 (33.09) | 8 | 15.60 (38.21) | 7 | 10.40 (31.20) | 9 | 0.00 (0.00) | 7 |
| Nurse visits at GP’s practice | 6.20 (5.80) | 7 | 1.81 (4.42) | 6 | 2.41 (7.23) | 9 | 0.00 (0.00) | 7 |
| Community nurse visits at home | 28.84 (39.80) | 8 | 0.00 (0.00) | 6 | 8.54 (16.96) | 9 | 0.00 (0.00) | 7 |
| Occupational therapist visits | 0.00 (0.00) | 8 | 47.00 (115.13) | 6 | 5.88 (16.62) | 8 | 0.00 (0.00) | 7 |
| Physiotherapist visits | 50.10 (64.47) | 8 | 9.54 (23.37) | 6 | 274.83 (212.18) | 10 | 212.66 (189.07) | 7 |
| Other health service visits | 0.00 (0.00) | 8 | 0.00 (0.00) | 5 | 0.00 (0.00) | 9 | 52.94 (92.90) | 7 |
| Inpatient nights in hospital | 912.00 (562.90) | 8 | 608.00 (840.52) | 6 | 1216.00 (758.31) | 9 | 405.34 (573.23) | 8 |
| Day-case visits to hospital | 0.00 (0.00) | 7 | 0.00 (0.00) | 6 | 683.46 (966.55) | 10 | 0.00 (0.00) | 8 |
| Outpatient attendances | 72.76 (77.78) | 8 | 24.25 (59.41) | 6 | 145.52 (72.76) | 9 | 72.76 (110.00) | 8 |
| A&E visits | 0.00 (0.00) | 8 | 53.44 (130.90) | 6 | 35.63 (106.88) | 9 | 60.12 (170.04) | 8 |
| Physiotherapy hospital attendances | 34.32 (50.30) | 8 | 0.00 (0.00) | 6 | 231.84 (215.79) | 9 | 157.86 (184.32) | 8 |
| Total costs | 1341.54 (427.38) | 6 | 882.47 (1008.67) | 5 | 2582.49 (1679.46) | 7 | 1003.80 (405.34) | 7 |
| Cost item | Hip (N = 10) | Knee (N = 16) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline–8 weeks | 8–16 weeks | Baseline–8 weeks | 8–16 weeks | |||||
| Mean cost (£) (SD) | n | Mean cost (£) (SD) | n | Mean cost (£) (SD) | n | Mean cost (£) (SD) | n | |
| GP visits at GP’s practice | 0.00 (0.00) | 6 | 6.23 (15.27) | 6 | 18.70 (21.59) | 4 | 32.06 (33.65) | 7 |
| GP visits at home | 0.00 (0.00) | 6 | 0.00 (0.00) | 6 | 18.72 (41.86) | 5 | 0.00 (0.00) | 8 |
| Nurse visits at GP’s practice | 2.17 (4.85) | 5 | 10.85 (21.70) | 6 | 16.28 (25.83) | 4 | 2.71 (7.67) | 8 |
| Community nurse visits at home | 0.00 (0.00) | 6 | 0.00 (0.00) | 6 | 0.00 (0.00) | 4 | 0.00 (0.00) | 8 |
| Occupational therapist visits | 50.10 (64.47) | 8 | 47.00 (115.13) | 6 | 274.83 (212.18) | 10 | 0.00 (0.00) | 8 |
| Physiotherapist visits | 0.00 (0.00) | 6 | 0.00 (0.00) | 6 | 0.00 (0.00) | 4 | 0.00 (0.00) | 8 |
| Other health service visits | 0.00 (0.00) | 6 | 0.00 (0.00) | 6 | 0.00 (0.00) | 4 | 31.76 (58.31) | 7 |
| Inpatient nights in hospital | 0.00 (0.00) | 6 | 0.00 (0.00) | 6 | 0.00 (0.00) | 4 | 0.00 (0.00) | 7 |
| Day-case visits to hospital | 0.00 (0.00) | 6 | 0.00 (0.00) | 6 | 0.00 (0.00) | 4 | 0.00 (0.00) | 7 |
| Outpatient attendances | 0.00 (0.00) | 6 | 0.00 (0.00) | 6 | 0.00 (0.00) | 4 | 53.58 (98.36) | 7 |
| A&E visits | 0.00 (0.00) | 6 | 0.00 (0.00) | 6 | 0.00 (0.00) | 4 | 22.90 (60.59) | 7 |
| Physiotherapy hospital attendances | 0.00 (0.00) | 6 | 0.00 (0.00) | 6 | 0.00 (0.00) | 4 | 0.00 (0.00) | 7 |
| Total costs | 2.17 (4.85) | 5 | 64.08 (112.61) | 6 | 34.98 (24.34) | 4 | 167.30 (248.76) | 6 |
| Cost item | Hip (N = 10) | Knee (N = 16) | ||
|---|---|---|---|---|
| n | Total mean cost (£) (SD) | n | Total mean cost (£) (SD) | |
| GP visits at GP’s practice | 6 | 6.23 (15.27) | 5 | 82.28 (89.29) |
| GP visits at home | 6 | 31.20 (76.42) | 5 | 0.00 (0.00) |
| Nurse visits at GP’s practice | 6 | 7.23 (8.86) | 5 | 0.00 (0.00) |
| Community nurse visits at home | 6 | 38.45 (42.12) | 5 | 0.00 (0.00) |
| Occupational therapist visits | 6 | 47.00 (115.13) | 5 | 9.40 (21.02) |
| Physiotherapist visits | 6 | 38.17 (59.13) | 6 | 639.36 (249.35) |
| Other health service visits | 5 | 0.00 (0.00) | 5 | 44.47 (99.43) |
| Inpatient nights in hospital | 6 | 1621.34 (1202.42) | 6 | 1688.90 (1266.74) |
| Day-case visits to hospital | 5 | 0.00 (0.00) | 7 | 976.37 (1033.29) |
| Outpatient attendances | 6 | 121.26 (109.54) | 6 | 194.02 (118.81) |
| A&E visits | 6 | 53.44 (130.90) | 6 | 133.60 (327.25) |
| Physiotherapy hospital attendances | 6 | 45.76 (53.99) | 6 | 430.13 (376.31) |
| Occupational health RTW advice | 4 | 0.00 (0.00) | 2 | 18.70 (26.45) |
| Employer RTW advice | 4 | 0.00 (0.00) | 4 | 23.40 (46.80) |
| Cost item | Hip (N = 10) | Knee (N = 16) | ||
|---|---|---|---|---|
| n | Total mean cost (£) (SD) | n | Total mean cost (£) (SD) | |
| GP visits at GP’s practice | 4 | 0.00 (0.00) | 2 | 18.70 (26.45) |
| GP visits at home | 4 | 0.00 (0.00) | 4 | 23.40 (46.80) |
| Nurse visits at GP’s practice | 4 | 5.43 (10.85) | 3 | 21.70 (28.71) |
| Community nurse visits at home | 4 | 0.00 (0.00) | 3 | 0.00 (0.00) |
| Occupational therapist visits | 4 | 70.50 (141.00) | 3 | 0.00 (0.00) |
| Physiotherapist visits | 4 | 0.00 (0.00) | 3 | 0.00 (0.00) |
| Other health service visits | 4 | 0.00 (0.00) | 2 | 37.06 (52.40) |
| Inpatient nights in hospital | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| Day-case visits to hospital | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| Outpatient attendances | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| A&E visits | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| Physiotherapy hospital attendances | 4 | 0.00 (0.00) | 2 | 0.00 (0.00) |
| Time point | Completed EQ-5D, n (%) | Missing EQ-5D (one or more dimension missing), n (%) | ||
|---|---|---|---|---|
| Hip (N = 10) | Knee (N = 16) | Hip (N = 10) | Knee (N = 16) | |
| Baseline | 10 (100) | 16 (100) | 0 (0) | 0 (0) |
| 8 weeks | 7 (70) | 10 (62.5) | 3 (30) | 6 (37.5) |
| 16 weeks | 6 (60) | 8 (50) | 4 (40) | 8 (50) |
| Time point | Hip: number of missing dimensions (N = 10) | Knee: number of missing dimensions (N = 16) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |
| Baseline | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 8 weeks | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 6 |
| 16 weeks | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 8 |
| Time point | Hip (N = 10) | Knee (N = 16) | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| Baseline | 10 | 0.379 (0.226) | 16 | 0.347 (0.296) |
| 8 weeks | 7 | 0.749 (0.155) | 10 | 0.632 (0.238) |
| 16 weeks | 6 | 0.882 (0.144) | 8 | 0.691 (0.107) |
| EQ VAS score | Hip (N = 10) | Knee (N = 16) | ||||
|---|---|---|---|---|---|---|
| Baseline | 8 weeks | 16 weeks | Baseline | 8 weeks | 16 weeks | |
| Mean (SD) | 65.7 (24.7) | 81.4 (9.5) | 84.8 (13.0) | 51.6 (20.0) | 70.2 (30.7) | 72.5 (17.7) |
| Median (IQR) | 68.5 (55–90) | 80 (70–90) | 87 (75–95) | 52.5 (37.5–62.5) | 77.5 (60–90) | 75 (60–85) |
| EQ-5D scale and health state severitya | Hip (N = 10) | |||||
|---|---|---|---|---|---|---|
| Baseline | 8 weeks | 16 weeks | ||||
| n | % | n | % | n | % | |
| Mobility | ||||||
| Level 1 | 0 | 0.0 | 5 | 50.0 | 5 | 50.0 |
| Level 2 | 1 | 10.0 | 0 | 0.0 | 1 | 10.0 |
| Level 3 | 4 | 40.0 | 2 | 20.0 | 0 | 0.0 |
| Level 4 | 5 | 50.0 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 0 | 0.0 | 3 | 30.0 | 4 | 40.0 |
| Number reporting any problemsb | 10 | 100.00 | 2 | 28.57 | 1 | 16.67 |
| Self-care | ||||||
| Level 1 | 2 | 20.0 | 4 | 40.0 | 4 | 40.0 |
| Level 2 | 1 | 10.0 | 2 | 20.0 | 2 | 20.0 |
| Level 3 | 7 | 70.0 | 1 | 10.0 | 0 | 0.0 |
| Level 4 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 0 | 0.0 | 3 | 30.0 | 4 | 40.0 |
| Number reporting any problemsb | 8 | 80.00 | 3 | 42.86 | 2 | 33.33 |
| Usual activities | ||||||
| Level 1 | 0 | 0.0 | 3 | 30.0 | 4 | 40.0 |
| Level 2 | 1 | 10.0 | 1 | 10.0 | 2 | 20.0 |
| Level 3 | 6 | 60.0 | 3 | 30.0 | 0 | 0.0 |
| Level 4 | 2 | 20.0 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 1 | 10.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 0 | 0.0 | 3 | 30.0 | 4 | 40.0 |
| Number reporting any problemsb | 10 | 100.00 | 4 | 57.14 | 2 | 33.33 |
| Pain/discomfort | ||||||
| Level 1 | 0 | 0.0 | 1 | 10.0 | 4 | 40.0 |
| Level 2 | 1 | 10.0 | 4 | 40.0 | 2 | 20.0 |
| Level 3 | 4 | 40.0 | 2 | 20.0 | 0 | 0.0 |
| Level 4 | 4 | 40.0 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 1 | 10.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 0 | 0.0 | 3 | 30.0 | 4 | 40.0 |
| Number reporting any problemsb | 10 | 100.00 | 6 | 85.71 | 2 | 33.33 |
| Anxiety/depression | ||||||
| Level 1 | 4 | 40.0 | 5 | 50.0 | 6 | 60.0 |
| Level 2 | 4 | 40.0 | 2 | 20.0 | 0 | 0.0 |
| Level 3 | 2 | 20.0 | 0 | 0.0 | 0 | 0.0 |
| Level 4 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 0 | 0.0 | 3 | 30.0 | 4 | 40.0 |
| Number reporting any problemsb | 6 | 60.00 | 2 | 28.57 | 0 | 0.00 |
| EQ-5D scale and health state severitya | Time point (N = 16) | |||||
|---|---|---|---|---|---|---|
| Baseline | 8 weeks | 16 weeks | ||||
| n | % | n | % | n | % | |
| Mobility | ||||||
| Level 1 | 0 | 0.0 | 3 | 18.8 | 1 | 6.3 |
| Level 2 | 1 | 6.3 | 3 | 18.8 | 2 | 12.5 |
| Level 3 | 10 | 62.5 | 1 | 6.3 | 5 | 31.3 |
| Level 4 | 5 | 31.3 | 3 | 18.8 | 0 | 0.0 |
| Level 5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 0 | 0.0 | 6 | 37.5 | 8 | 50.0 |
| Number reporting any problems | 16 | 100.00 | 7 | 70.00 | 7 | 87.50 |
| Self-care | ||||||
| Level 1 | 7 | 43.8 | 8 | 50.0 | 6 | 37.5 |
| Level 2 | 6 | 37.5 | 2 | 12.5 | 2 | 12.5 |
| Level 3 | 2 | 12.5 | 0 | 0.0 | 0 | 0.0 |
| Level 4 | 1 | 6.3 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 0 | 0.0 | 6 | 37.5 | 8 | 50.0 |
| Number reporting any problems | 9 | 56.25 | 2 | 20.00 | 2 | 25.00 |
| Usual activities | ||||||
| Level 1 | 0 | 0.0 | 1 | 6.3 | 1 | 6.3 |
| Level 2 | 4 | 25.0 | 5 | 31.3 | 3 | 18.8 |
| Level 3 | 4 | 25.0 | 1 | 6.3 | 3 | 18.8 |
| Level 4 | 4 | 25.0 | 3 | 18.8 | 1 | 6.3 |
| Level 5 | 4 | 25.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 0 | 0.0 | 6 | 37.5 | 8 | 50.0 |
| Number reporting any problems | 16 | 100.00 | 9 | 90.00 | 7 | 87.50 |
| Pain/discomfort | ||||||
| Level 1 | 0 | 0.0 | 2 | 12.5 | 1 | 6.3 |
| Level 2 | 0 | 0.0 | 4 | 25.0 | 4 | 25.0 |
| Level 3 | 7 | 43.8 | 1 | 6.3 | 3 | 18.8 |
| Level 4 | 5 | 31.3 | 3 | 18.8 | 0 | 0.0 |
| Level 5 | 4 | 25.0 | 6 | 37.5 | 0 | 0.0 |
| Missing | 0 | 0.0 | 0 | 0.0 | 8 | 50.0 |
| Number reporting any problems | 16 | 100.00 | 14 | 87.50 | 7 | 87.50 |
| Anxiety/depression | ||||||
| Level 1 | 8 | 50.0 | 7 | 43.8 | 6 | 37.5 |
| Level 2 | 4 | 25.0 | 2 | 12.5 | 2 | 12.5 |
| Level 3 | 3 | 18.8 | 1 | 6.3 | 0 | 0.0 |
| Level 4 | 1 | 6.3 | 0 | 0.0 | 0 | 0.0 |
| Level 5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Missing | 0 | 0.0 | 6 | 37.5 | 8 | 50.0 |
| Number reporting any problems | 8 | 50.00 | 3 | 30.00 | 2 | 25.00 |
List of abbreviations
- A&E
- accident and emergency
- AHP
- allied health professional
- AMSTAR
- Assessing the Methodological Quality of Systematic Reviews
- BMI
- body mass index
- BOA
- British Orthopaedic Association
- BRS
- Brief Resilience Scale
- CASP
- Critical Appraisal Skills Programme
- DVLA
- Driver and Vehicle Licensing Agency
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQ VAS
- EuroQol visual analogue scale
- GAD-2
- Generalised Anxiety Disorder-2 item
- GCP
- good clinical practice
- GP
- general practitioner
- HOT
- hospital orthopaedic team
- HRA
- Health Research Authority
- IM
- intervention mapping
- ITT
- intention to treat
- NICE
- National Institute for Health and Care Excellence
- NJR
- National Joint Registry
- ODI
- Oswestry Disability Index
- OHS
- Oxford Hip Score
- OKS
- Oxford Knee Score
- OPAL
- Occupation advice for Patients undergoing Arthroplasty of the Lower limb
- PHQ-9
- Patient Health Questionnaire-9 items
- PI
- principal investigator
- PO
- performance objective
- PPI
- patient and public involvement
- PSSRU
- Personal Social Services Research Unit
- RCT
- randomised controlled trial
- RTW
- return to work
- RTWC
- return-to-work co-ordinator
- SD
- standard deviation
- THR
- total hip replacement
- TKR
- total knee replacement
