Notes
Article history
This themed issue of the Health Technology Assessment journal series contains a collection of research commissioned by the NIHR as part of the Department of Health’s (DH) response to the H1N1 swine flu pandemic. The NIHR through the NIHR Evaluation Trials and Studies Coordinating Centre (NETSCC) commissioned a number of research projects looking into the treatment and management of H1N1 influenza. NETSCC managed the pandemic flu research over a very short timescale in two ways. Firstly, it responded to urgent national research priority areas identified by the Scientific Advisory Group in Emergencies (SAGE). Secondly, a call for research proposals to inform policy and patient care in the current influenza pandemic was issued in June 2009. All research proposals went through a process of academic peer review by clinicians and methodologists as well as being reviewed by a specially convened NIHR Flu Commissioning Board.
Declared competing interests of authors
none
Permissions
Copyright statement
© 2010 Queen’s Printer and Controller of HMSO. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2010 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
The spread of infectious diseases is, in many cases, determined by patterns of mixing between individuals in a population. In the case of human-to-human transmission, social contact behaviour is the key to understanding the dynamics of a wide range of common infections, such as measles, influenza and the common cold. 1–15 The response to the 2009 H1N1 influenza (termed swine flu throughout) pandemic illustrated the requirement for well-parameterised mathematical models of the spread of infection. 5,9,16–17 Governments required modellers to provide guidance on likely scenarios, to aid planning and to give advice on vaccination strategies. 3,18–19 Over recent years, more and more research has been devoted to measuring and understanding human social contact patterns. Studies have ranged from detailed analyses of social networks within contained communities8,20–22 and small-scale detailed surveys,23 to large-scale population-based surveys of mixing patterns. 4,15,24 The most notable such study (POLYMOD), involving over 7000 individuals across Europe, consisted of self-completed contact diaries in which participants noted details of all the individuals with whom they came into contact over the course of a day. 15 The POLYMOD study allowed a quantitative comparison of contacts made, say, at home and at work, or of long- and short-duration contacts; it also allowed more complex quantities to be evaluated, such as the fraction of contacts made at home that lasted over 1 hour, and included skin-to-skin contact.
As a representation of normal social behaviour, the POLYMOD study is unsurpassed and its results have already been used to parameterise numerous models of infectious disease spread. 3,7,10,13,18 The flaw is that this and other studies are designed to measure only ‘normal’ behaviour; while this gives us important information, it does not tell us all that we need to know – in particular, it gives us little information about the behaviour of infectious individuals. If, as seems certain, social contact behaviour changes when we are sick, then models based on normal behaviour are in danger of reaching the wrong conclusions. Furthermore, ad hoc attempts to correct this by, for instance, assuming a halving of contacts when ill, are fraught with danger. Would home contacts and work contacts fall by the same amount? Would ill people reduce their interactions with people they normally meet only occasionally to the same extent as those with people whom they normally meet every day?
To shed light on these issues, therefore, in the study described here we aimed to measure changes in social contact behaviour that took place as a result of illness. Using methodology similar to that developed in the POLYMOD study,15 participants completed contact diaries to describe their contact patterns over the course of a day. In our study, however, participants completed two separate contact diaries: one when they were unwell and one when they had recovered.
The study took place during the 2009–10 swine flu pandemic. This new variant of influenza was first identified in April 2009 in the Americas, and was soon introduced into the UK. 3,19,25 Originally appearing as sporadic cases associated with travel to Mexico and the USA, swine flu soon established itself in the UK, with large numbers of cases occurring in July 2009. 3,25 Antiviral medication was made available in the UK to those with probable/suspected swine flu. Initially, prescriptions were generally issued by GPs, but in mid-July a telephone- and internet-based system [the National Pandemic Flu Service (NPFS)] was launched, whereby reporting a list of symptoms allowed individuals to be issued with an antiviral prescription. Ill individuals were encouraged to seek the assistance of a ‘flu friend’ to collect their prescription for them.
Cases were concentrated in children, and incidence fell once schools closed for their summer break. 25–31 However, it was expected, and indeed it came to pass, that a second wave of cases would be seen in the autumn once schools reopened.
In order to measure changes in social contact behaviour that took place as a result of illness, a questionnaire-based study was designed and carried out in the UK in autumn/winter 2009.
A second study was carried out to measure changes in school children’s contact behaviour as a result of school closure.
Chapter 2 Methods
Survey design
The questionnaire had two parts; the initial survey was designed to be filled in when participants were symptomatic with suspected swine flu; the follow-up survey was designed to be filled in once they had recovered. Each part was returned in a provided prepaid envelope.
Each part of the questionnaire had two sections: the first section collected information about the participant (age, sex, household size and composition), their health status (symptoms list, a measure of their current health, a measure of their health on the day that they were most unwell, date of symptom onset, antiviral use), their behaviour (work/school/college attendance, public transport use) and the impact of their illness on their activities (time off work, receiving care from others). This section also asked participants for their name and address so that the follow-up survey could be sent to them.
The second section was a contact diary in which participants were asked to list all of the people they met over the course of a day. A meeting was defined as ‘either talking face-to-face or skin to skin contact (e.g. a handshake, a kiss, contact sports)’. Participants were asked to give some information about each person whom they reported meeting:
-
age (or age range)
-
gender
-
whether there was skin-to-skin contact (such contacts will be referred to as ‘physical’ contacts below)
-
how long the encounter lasted (participants were asked to tick one of the following: under 5 minutes, 5–10 minutes, 10 minutes to 1 hour, 1–4 hours, over 4 hours)
-
where the encounter occurred (participants were asked to tick one or more of the following: home, work/school/college, travel, leisure activity, other)
-
how often they normally met this person (participants were asked to tick one of the following: daily or almost daily, once or twice weekly, once or twice monthly, less than monthly, never met before).
There was sufficient space on the contact diary to give this information about 33 different contacts. Participants were asked whether they had included everyone they met during the day and, if not, they were asked how many other people they met that day; these will be termed ‘additional contacts’.
The follow-up survey was posted to participants approximately 2 weeks after they completed and returned the initial survey; it was hoped that this time interval would be long enough to ensure that most participants would have recovered and resumed their normal activities, but not so long that they would have lost interest in taking part. Those participants who had not returned their follow-up survey within a further 2 weeks were sent a reminder. Survey forms were coded with a unique identification number that allowed us to match up an individual’s initial and follow-up surveys.
The intention was that each participant would record their social contact behaviour once when they were ill with swine flu and once when they had recovered.
A covering letter explaining the purpose of the study and instructions for filling in the forms was included with each survey. All questionnaire forms can be found in Appendix 1.
The study received ethical approval from the Riverside Research Ethics Committee.
It was intended that a similar study would be undertaken to measure the impact of swine flu-related school closures on the contact patterns of school pupils. 5,10–11,14 However, contrary to expectations, such closures did not occur in autumn 2009. Nevertheless, a small ‘half-term’ study was carried out in February/March 2010 – see Appendix 2 for further details.
Participant recruitment
Participants were recruited to the study through antiviral distribution centres (ADCs). ADCs (generally pharmacies) were sampled via a stratified random sampling design, in which two ADCs in each region of England were selected from a list of all ADCs. This allowed us to access individuals with probable swine flu and to achieve a wide geographical spread. It became apparent that many of the sampled ADCs were small and were handling very few cases by the time the survey was under way. Hence, it was decided to supplement the initial sample, by additionally sampling from among the busiest ADCs in each of the sampled regions. This resulted in a total of 31 ADCs being sampled. Questionnaire packs were distributed by ADCs along with antiviral prescriptions. Because of the abnormally heavy workload that these ADCs were experiencing, in many cases, due to the epidemic, and to reduce the demands placed on pharmacy staff, ADCs were not asked to screen potential participants (which would, in any case, have been made difficult by the fact that in many instances prescriptions were collected not by the potential participants themselves but on their behalf by their ‘flu friend’). No age restrictions were applied to participation; however, it was suggested in the covering letter that if the individual receiving antiviral medicine was under 16 years of age, then their parent/guardian might prefer to complete the survey on their behalf.
Each questionnaire pack contained a covering letter, instructions for filling in the forms, and the initial survey itself.
On the basis of a power calculation, using a conservative estimate of the expected change in number of social contacts (based on data collected in the POLYMOD study15) it was hoped to recruit 800 participants into the study.
Analysis
A database was designed using epidata 3.1, and data entry was carried out in March 2010, once all initial and follow-up surveys had been received.
Analyses were carried out to test whether changes in number of contacts took place, and to explore factors influencing the size of any such changes. Change in number of contacts was defined as ‘number of contacts reported in the follow-up survey minus number of contacts reported in the initial survey’, where ‘contacts’ could refer to a number of different measures of interactions – such as contacts at home, or contacts involving skin-to-skin contact.
To test whether the number of contacts changed, a non-parametric Wilcoxon signed-rank test was used. A backwards stepwise linear regression model was used to explore significant contributory factors, the factor with the largest non-significant p-value being removed at each step and the model rerun until all remaining factors were significant (p < 0.05).
Statistical analyses were carried out using stata 11.
Capping contacts
A few participants used the ‘additional contacts’ section of the contact diary to report that they had contact with many hundreds of people in a day (for instance, by working as teachers or in a busy shop); to avoid skewed results generated by such outliers a cap of 33 contacts (the number of rows on the contact diary) was applied to contacts listed, and a cap of 66 was applied to the total number of contacts (i.e. all listed on the contact diary plus the number reported as additional contacts).
The application of this cap affected only a small number of contact diaries (the option of reporting numbers of additional contacts without needing to record extra details about each of these contacts was not required by most participants – it was used three times in the initial contact diary and 12 times in the follow-up contact diary) and does not qualitatively alter our conclusions.
Study population
Participating ADCs
During mid-October 2009, 31 ADCs were recruited to take part in the study, distributing questionnaire packs along with antiviral prescriptions. Depending on their size, ADCs were given between 25 and 300 questionnaire packs to distribute, with some requesting additional packs.
In total, 4265 questionnaire packs were sent to ADCs, of which approximately 3795 were distributed along with antiviral prescriptions. Distribution of questionnaire packs by ADCs began on the 10 November 2009 and continued until approximately 9 January 2010. Details of the spatial distribution of ADCs can be found in Table 1.
| Region | ADCs recruited | Approximate no. of questionnaires distributed | Initial response (rate) (n, %) | Follow-up response (rate) (n, %) |
|---|---|---|---|---|
| East of England | 5 | 566 | 46 (8.1) | 30 (65.2) |
| East Midlands | 1 | 200 | 5 (2.5) | 2 (40.0) |
| London | 2 | 300 | 19 (6.3) | 11 (57.9) |
| North East | 3 | 619 | 73 (11.8) | 34 (46.8) |
| North West | 3 | 350 | 16 (4.6) | 10 (62.5) |
| South East Coast | 3 | 200 | 14 (7.0) | 9 (64.3) |
| South Central | 3 | 412 | 45 (10.9) | 26 (57.8) |
| South West | 4 | 252 | 32 (12.7) | 20 (62.5) |
| West Midlands | 4 | 384 | 41 (10.7) | 22 (53.7) |
| Yorkshire and the Humber | 3 | 512 | 26 (5.1) | 15 (57.7) |
| Total | 31 | 3795 | 317 (8.4) | 179 (56.5) |
Participants
Overall, 317 initial surveys were returned and 308 follow-up surveys were sent out (nine participants did not provide an address). A total of 179 follow-up surveys were eventually returned (45 of which had received a reminder). The interval between completing the initial and the follow-up surveys had a median of 19 days and an interquartile range (IQR) of 14 to 30 days. The overall response rate was disappointingly low – see below for further discussion (see Chapter 4 – Discussion). The rest of this report will describe the results provided by these 179 participants, which will be referred to as the ‘study population’.
The spatial distribution of participating ADCs and of participants is shown in Table 1. In some cases, participating ADCs were unable to confirm exactly how many initial surveys they distributed; in such cases we have assumed that all of the initial surveys that were sent to them were given out.
Population characteristics
The study population was not evenly split by gender (40.2% male, 59.8% female). The median age of the study population was 47 (IQR 27 to 56). The demographic characteristics of the sample are shown in Table 2. Within our sample, young adults are under-represented and older adults over-represented. It is not possible to calculate the response rates from different groups. Also included in Table 2 are the characteristics of those individuals who returned the initial survey but not the follow-up survey; those returning only the initial survey tend to be younger and to live in larger households.
| Completed initial survey only (n = 138) | Completed both surveys (n = 179) | UK population | |
|---|---|---|---|
| Female (%) | 62.9 | 59.8 | 50.9 |
| Age 0–14 (%) | 20.6 | 16.8 | 17.5 |
| Age 15–29 (%) | 22.8 | 11.2 | 20.0 |
| Age 30–44 (%) | 24.3 | 17.9 | 21.1 |
| Age 45–69 (%) | 20.6 | 34.6 | 19.2 |
| Age ≥ 60 (%) | 11.8 | 19.6 | 22.1 |
| Mean household size | 3.1 | 2.7 | 2.4 |
Within our sample of interest (those who returned both surveys), 117 (65%) reported that they would normally attend work/school/college on the day of their initial survey, while 22 (12%) respondents reported that they would normally use public transport on the day of their initial survey.
The mean household size in the study population was 2.7, with a median of 2 and an IQR of 2 to 4. As might be expected by the observed age distribution of the sample, a large fraction of households contained only one or two people.
Chapter 3 Results
Describing infection – initial survey
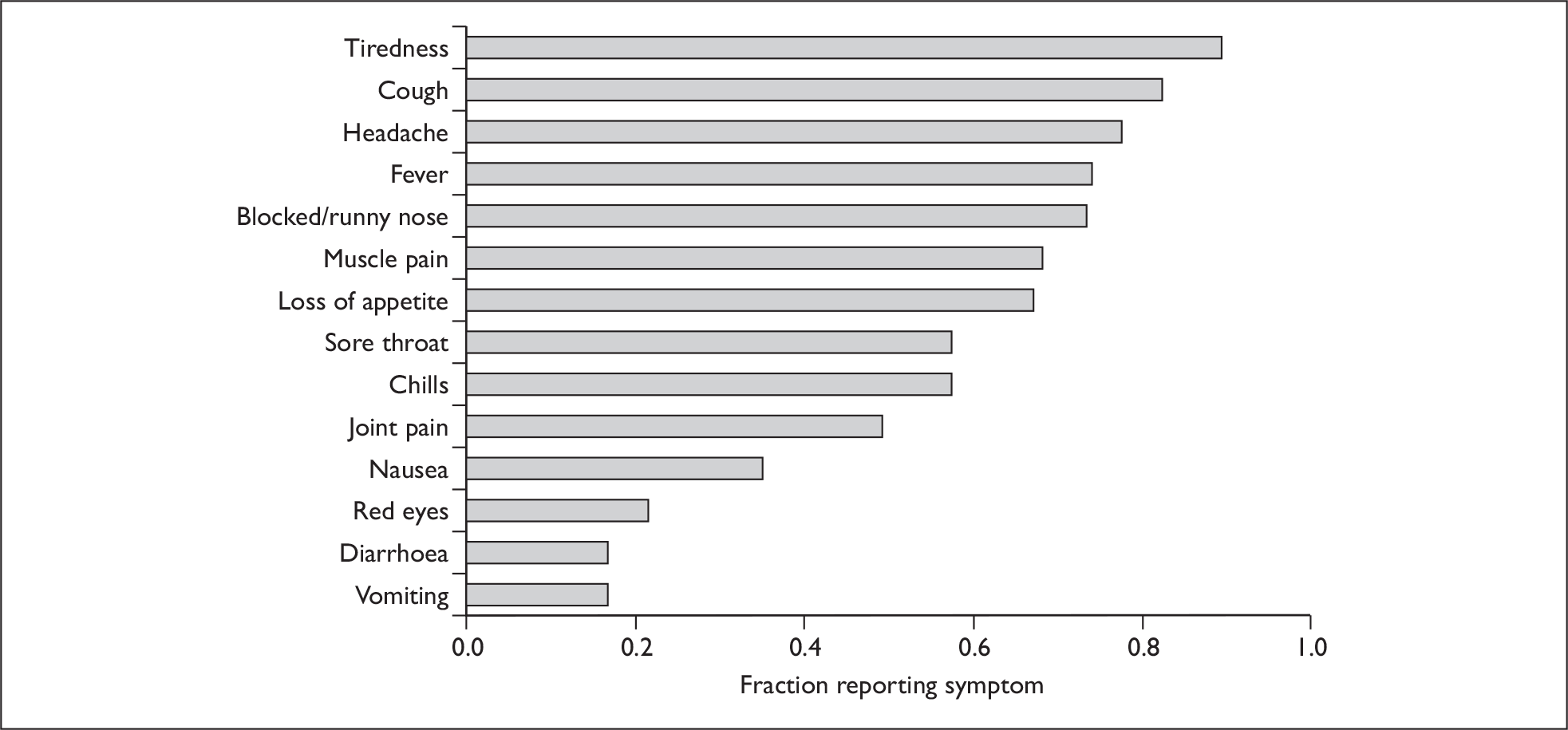
As anticipated, the vast majority [169 (94.4%)] of the study population reported that they were unwell with swine flu on the day that they completed the initial questionnaire. Ill individuals were asked to report which symptoms they had from a list of 14 possibilities. The fraction of individuals reporting each symptom is shown in Figure 1. On average, ill individuals reported 7.8 symptoms. Tiredness, cough, headache, fever and blocked/runny nose were the most common symptoms, being reported by over 70% of respondents.
FIGURE 1.
Fraction of individuals reporting each symptom from the symptoms list.
Individuals were also asked to record how ill they felt, on a scale of 0–10, with 0 being the ‘worst imaginable health state’ and 10 the ‘best imaginable health state’. The distribution of initial health states of those individuals who reported that they were unwell with swine flu when they completed the initial survey is shown in Figure 2. The mean reported health state was 3.38 [standard deviation (SD 1.66)]. For comparison, those individuals who completed only the initial survey had a mean reported health state of 3.61 (SD 1.95) – these two sets of reported health states were not significantly different.
FIGURE 2.
Distribution of initial health states reported by individuals unwell with swine flu (measured on a scale of 0 – the ‘worst imaginable health state’ – to 10 – the ‘best imaginable health state’).
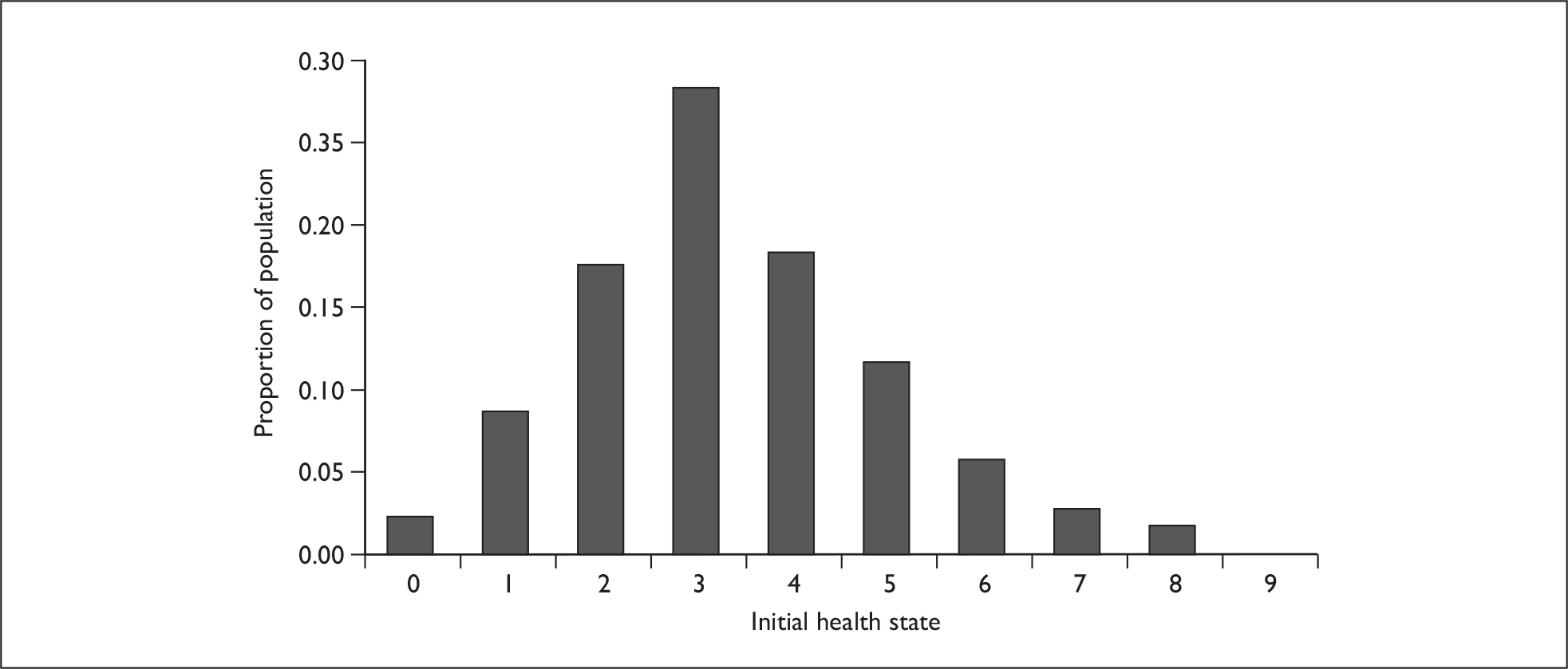
The mean reported health state of individuals on the day that they felt most ill was 1.98 (SD 1.23).
Describing recovery – comparing initial and follow-up questionnaires
Of those 169 individuals who were unwell with swine flu when they completed the initial questionnaire, 146 (86.4%) had recovered by the time they filled in the follow-up questionnaire. The median duration of infection of those who had recovered was 9 days (IQR 6 to 14 days), and 32 (21.9%) of participants reported that they were ill for over a fortnight.
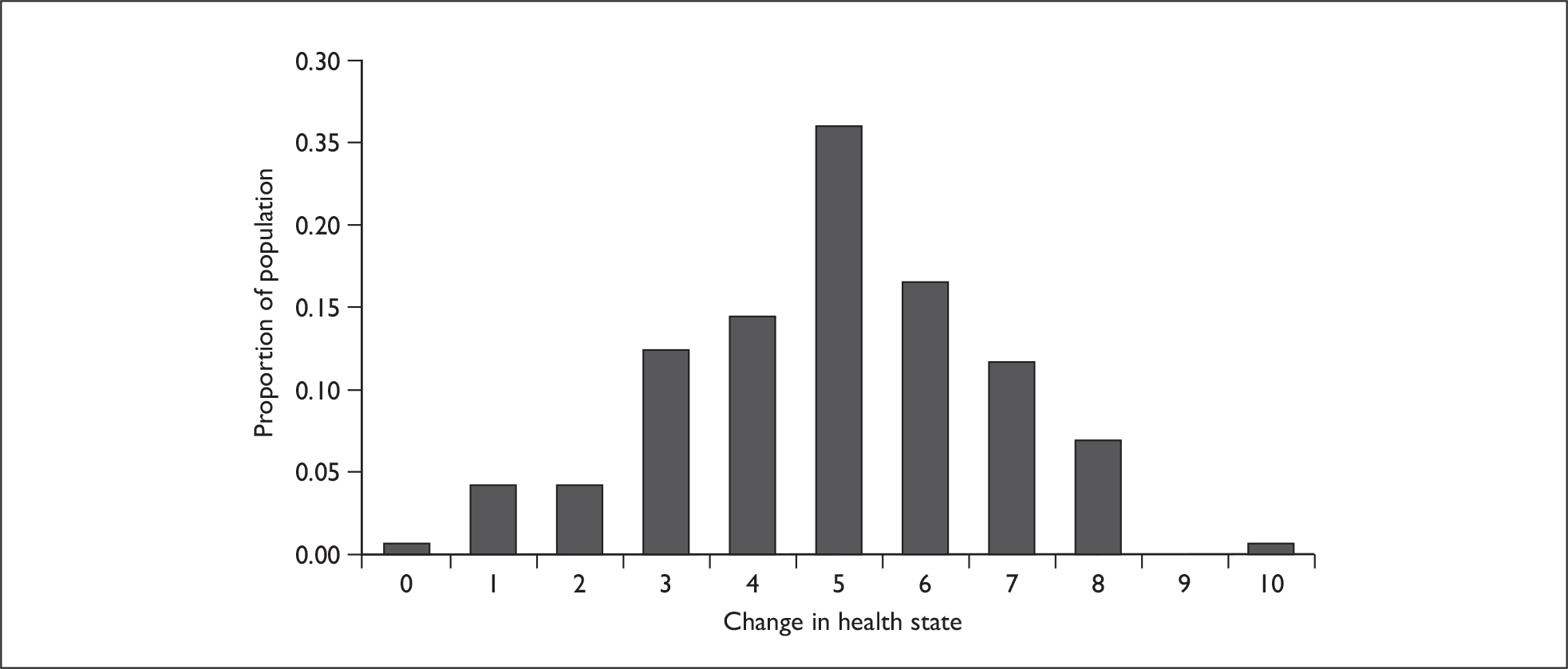
As anticipated, there were large changes in health state between the initial and follow-up survey reports of those who reported that they were no longer unwell when they completed the follow-up survey (Figure 3). We see, in most cases, that participants reported a substantial change in their health state (mean change 4.92, SD 1.83, p < 0.001, one-sample t-test).
FIGURE 3.
Change in health state of people who recorded that they were unwell when they filled in the initial survey but had recovered when they filled in the follow-up survey (n = 146).
Participants were asked whether they took time off work/school/college/child-care group/social activities because of their illness; 74.1% of the 162 participants who answered reported that they did take time off. The median length of time off was 6 days (IQR 4 to 8 days) and six (5.0%) respondents reported that they took over a fortnight away from work/school/college/child-care group/social activities.
Overall, 59 individuals (33.0%) reported that they did not attend work/school/college on the day that they completed the initial survey, but that they did attend work/school/college on the day that they completed the follow-up survey.
Contact patterns
Baseline behaviour – comparison with POLYMOD
The most extensive survey to date of normal contact patterns took place in the POLYMOD study in 2005–6. 15 The POLYMOD study sampled 7290 people around Europe, with 1012 in the UK; POLYMOD participants completed a contact diary very similar to that applied in this project. In order to check the reasonableness of our results, we will briefly compare them with those produced by POLYMOD.
POLYMOD sampled 1012 individuals from the UK, whose responses we compare with the 155 participants in our survey who reported that they were well on the day that they completed the follow-up survey; from these 155 individuals, 144 useable contact diaries were obtained.
POLYMOD reported that respondents from the UK named a mean of 11.74 contacts (SD 7.67); our results are broadly similar, with a mean of 10.30 contacts (SD 8.51); our study found that approximately 25% of contacts took place at home, while POLYMOD reported that 23% of contacts occurred at home. Our study found that approximately 40% of contacts involved skin-to-skin contact, which is consistent with POLYMOD (in which the proportion of contacts involving skin-to-skin contact ranges from about 35% in the workplace to 75% at home; our study found that approximately 25% of work/school/college contacts and 72% of home contacts involved skin-to-skin contact). Our study reported more contacts taking place at work/school/college (47% compared with 35%).
Our study and POLYMOD are therefore in broad agreement about ‘normal’ social contact behaviour. Differences, such as they are, may well be explained by differences in the sample population demographics – our study population contained more older adults – but seasonal differences may also have played a part (POLYMOD took place mainly in the spring, our study in the autumn/winter).
Changes in contact behaviour
The primary aim of this study was to measure the impact of illness on contact patterns. Here, therefore, we explore changes in each participant’s reported contact data. Because the methodology involved repeated sampling of participants, we have paired data (i.e. two completed contact diaries) from each participant.
The completed contact diaries contain a great deal of detail about contact behaviour, and there is therefore a multitude of different comparisons that could be attempted; for the sake of simplicity and clarity, and to avoid overanalysing a small database, we restricted ourselves to the following key measures:
-
all number of contacts listed on the contact diary
-
all plus additional contacts listed on the contact diary plus any ‘additional’ contacts
-
physical total number of physical (skin-to-skin) contacts reported
-
home total number of home contacts recorded
-
work total number of work/school/college contacts recorded
-
other total number of contacts recorded in travel/leisure/other settings
-
long duration total number of contacts recorded that lasted over 1 hour
-
short duration total number of contacts recorded that lasted less than 10 minutes
-
frequent total number of contacts recorded who were encountered once a week or more
-
infrequent total number of contacts recorded who were encountered less than once a month.
In each case, we seek to explore the extent to which the numbers of these different types of social contacts differed between the initial and the follow-up surveys.
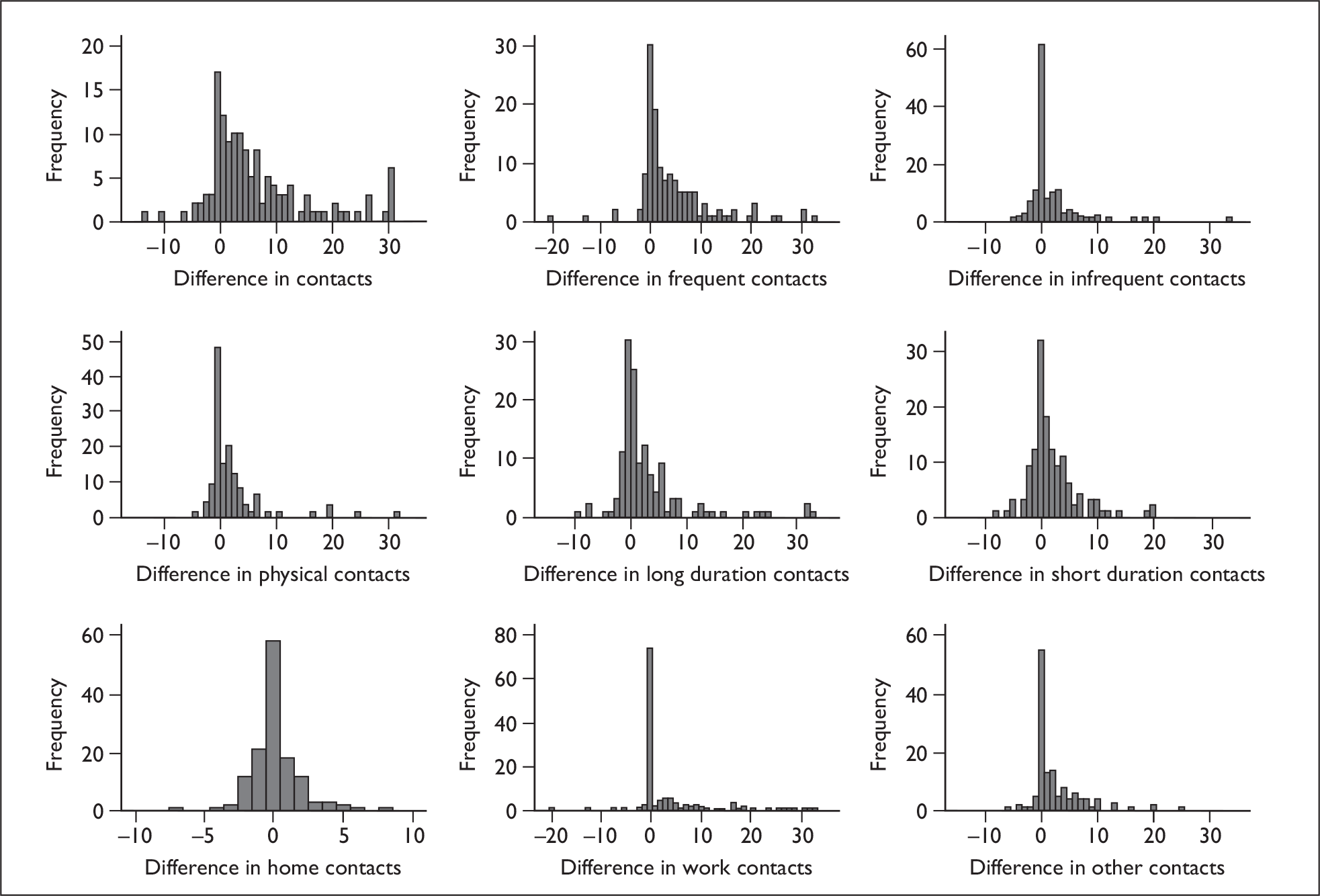
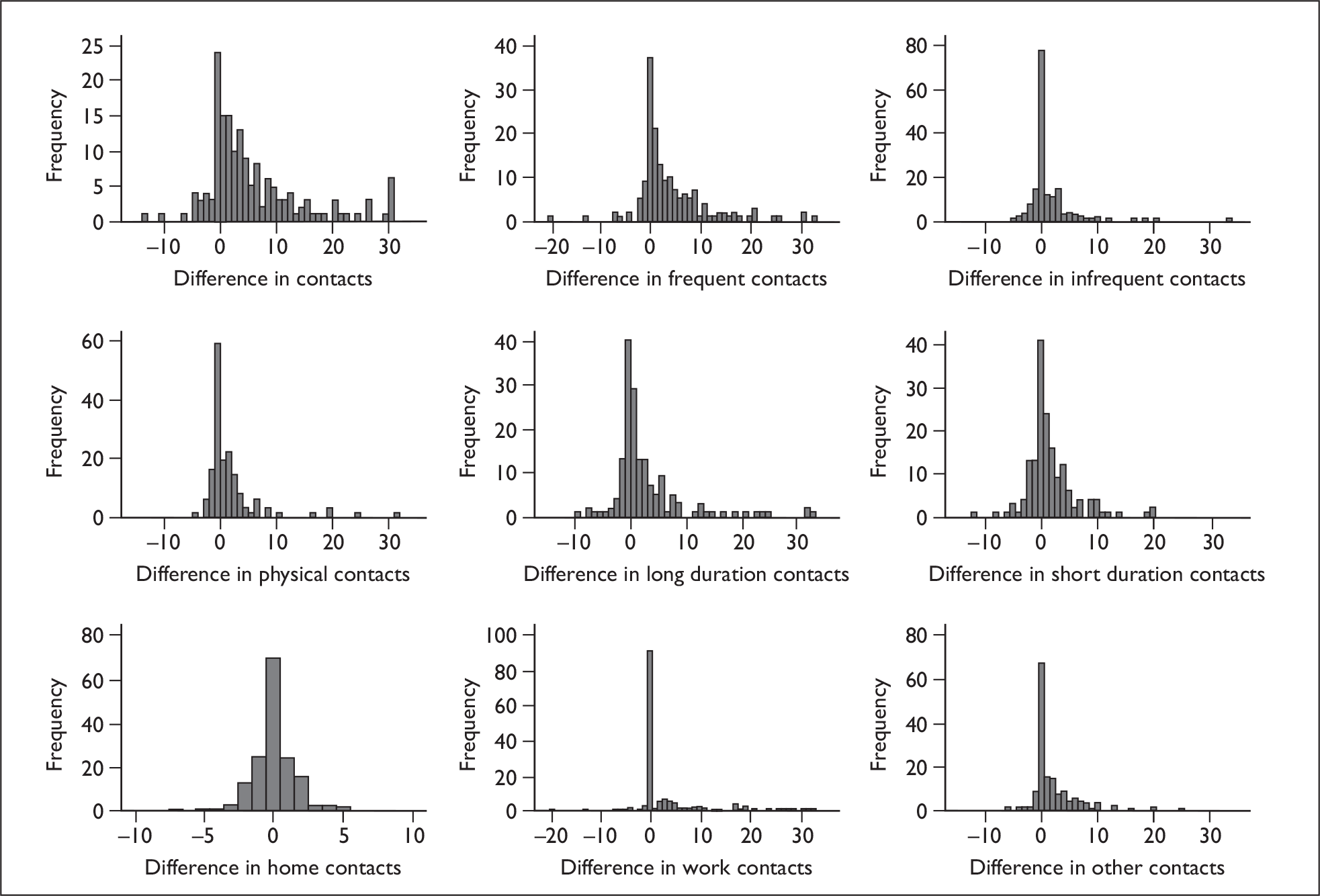
We expected the most marked behavioural changes in those people who were unwell at the time of the initial survey and had recovered by the time of the follow-up survey. When restricting our attention to this subsample (n = 146), we see that there were, indeed, noticeable changes in contact behaviour (Figure 4), although contacts taking place at home did not vary between the initial and follow-up surveys. The differences between the initial and follow-up surveys are shown in Table 3. For all types of a contact except contacts made at home the differences are highly significant (Wilcoxon signed-rank test, p < 0.001). There was no significant change in the number of home contacts.
FIGURE 4.
Change in number of contacts reported in the initial and follow-up surveys by those participants who reported that they were unwell on the day of the initial survey and had recovered by the time they completed the follow-up survey; for each of the participants who completed a useable contact diary for both the initial and the follow-up survey (n = 135), the change in number of contacts of the relevant type is defined as the number recorded in the follow-up survey minus the number recorded in the initial survey.
| Type of contact | Initial survey (n = 141): mean (SD) | Follow-up survey (n = 138): mean (SD) | Difference (n = 135) | |||
|---|---|---|---|---|---|---|
| Mean (SD) | Relative difference (percentage of follow-up mean) | Median (IQR) | p-value (median ≠ 0) | |||
| All | 3.58 (3.75) | 10.30 (8.51) | 6.82 (9.01) | 66 | 4 (1 to 10) | < 0.0001 |
| All plus additional | 3.58 (3.75) | 12.72 (14.80) | 9.30 (15.45) | 73 | 4 (1 to 11) | < 0.0001 |
| Frequent | 2.91 (3.48) | 7.33 (7.15) | 4.49 (7.63) | 61 | 2 (0 to 7) | < 0.0001 |
| Infrequent | 0.52 (0.11) | 2.08 (4.42) | 1.61 (4.74) | 77 | 0 (0 to 2) | 0.0003 |
| Physical | 1.77 (1.75) | 4.10 (5.10) | 2.36 (5.01) | 58 | 1 (0 to 3) | < 0.0001 |
| Long duration | 2.02 (2.29) | 5.42 (6.63) | 3.45 (6.86) | 64 | 1 (0 to 4) | < 0.0001 |
| Short duration | 1.01 (1.45) | 2.94 (4.18) | 1.99 (4.43) | 68 | 1 (0 to 4) | < 0.0001 |
| Home | 2.38 (1.54) | 2.58 (2.12) | 0.19 (1.81) | 7 | 0 (–1 to 1) | 0.5317 |
| Work/school/college | 0.73 (3.35) | 4.57 (7.92) | 3.90 (8.39) | 85 | 0 (0 to 5) | < 0.0001 |
| Other | 0.48 (1.16) | 3.01 (4.57) | 2.59 (4.62) | 86 | 1 (0 to 4) | < 0.0001 |
The bump on the right of some plots in Figure 4 is the result of the capping of the number of contacts permitted, as described above.
Very similar patterns are seen when the sample is not restricted to those who recovered between completing the initial and the follow-up surveys (see Figure 5 and Table 5, Appendix 3). The only notable difference between Figures 4 and 5 is that, as we would expect, there are more individuals in Figure 5 who reported no change in their contact behaviour.
However we view the sample, and whichever measure of contact we use, we can see that individuals made substantially fewer contacts when they were ill than when they were well. Contacts made by ill participants tended to take place at home (with very few in the workplace or in other settings); they were generally with people whom they met often and for long periods of time and they often included physical contact.
The distribution of social contacts changed when people were unwell; unwell people made approximately two-thirds of their social contacts at home, falling to one-quarter when they had recovered, although the reported absolute number of contacts made at home stayed almost constant. Not surprisingly, work/school/college contacts and contacts made in other settings (travel, leisure, other) fell dramatically when people were ill.
We note, for comparison, that individuals who completed only the initial survey reported 3.98 contacts on average when they were ill (SD 3.90); this is not significantly different from the number of contacts reported in the initial survey by those who completed both the initial and the follow-up survey (two sample t-test, p = 0.58).
We postulated that changes in social mixing patterns may be associated with age, gender, health status, attendance at work/school/college, household size and public transport use. However, because very few participants (6.7%) reported that their public transport use differed between the two questionnaires we exclude considerations of public transport use from the analysis that follows.
An initial simple regression analysis was carried out, suggesting that the following factors might have an influence on the observed changes in contact patterns:
-
age group (reference group: age 0–14)
-
gender
-
returning to work/school/college
-
change in health (measured as a binary unwell/well, or as change in number of symptoms reported, or as change in self-assessed health status recorded on a 10-point scale)
-
household size (the number of people in the participant’s household, not including the participant)
-
change in day of the week (from weekday to weekend or vice versa).
These factors were included in a backwards, stepwise regression model, with the factor with the largest non-significant p-value being removed at each step and the model rerun until all remaining factors were significant (p < 0.05). Results are shown in Table 4. The data set contains a small number of outliers, and therefore the confidence intervals should be treated with caution.
| Contact type | Factor | Coefficient | 95% confidence interval | p-value | r 2 |
|---|---|---|---|---|---|
| All plus additional | Returning to work | 11.00 | 5.91 to 16.09 | < 0.001 | 0.15 |
| All | Returning to work | 8.12 | 5.27 to 10.98 | < 0.001 | 0.24 |
| Change in no. of symptoms | 0.70 | 0.10 to 1.29 | 0.022 | ||
| Frequent | Returning to work | 6.76 | 4.31 to 9.21 | < 0.001 | 0.18 |
| Infrequent | Change in no. of symptoms | 0.66 | 0.33 to 1.00 | < 0.001 | 0.10 |
| House size | –0.57 | –1.12 to –0.02 | 0.041 | ||
| Age 15–29 | 2.05 | 0.09 to 4.02 | 0.041 | ||
| Physical | House size | –0.96 | –1.84 to –0.08 | 0.032 | 0.13 |
| Change in no. of symptoms | 0.47 | 0.09 to 0.84 | 0.015 | ||
| Age 45–59 | –3.21 | –5.83 to –0.59 | 0.017 | ||
| Age over 60 | –3.46 | –6.65 to –0.27 | 0.034 | ||
| Long duration | Returning to work | 3.70 | 1.32 to 6.07 | 0.003 | 0.15 |
| Age 30–44 | –4.85 | –8.29 to –1.42 | 0.006 | ||
| Age 45–59 | –4.96 | –8.10 to –1.81 | 0.002 | ||
| Age over 60 | –3.92 | –7.75 to –0.08 | 0.045 | ||
| Short duration | Returning to work | 2.06 | 0.56 to 3.56 | 0.007 | 0.10 |
| Change in no. of symptoms | 0.43 | 0.12 to 0.75 | 0.007 | ||
| Home | No significant factors | ||||
| Work | Returning to work | 9.09 | 6.55 to 11.63 | < 0.001 | 0.27 |
| Other | Returning to work | –2.04 | –3.64 to –0.44 | 0.013 | 0.05 |
As we can see, although there is a great deal of variation that is not explained by the model, several factors emerge as significant: returning to work/school/college, change in number of symptoms, age and household size.
Returning to work/school/college was associated with a large increased change in the number of contacts reported, being a significant factor in the change in all-plus-additional contacts (p < 0.001), all contacts (p < 0.001), frequent contacts (p < 0.001), long-duration contacts (p = 0.003), short-duration contacts (p = 0.007), contacts in ‘other settings’ (p = 0.013) and (unsurprisingly) work/school/college contacts (p < 0.001).
The change in the number of symptoms reported was also associated with an increased change in numbers of social contacts, being a significant factor in the change in all contacts (p = 0.022), infrequent contacts (p < 0.001), physical contacts (p = 0.015) and short contacts (p = 0.007).
Older age was associated with a reduced change in number of contacts: younger adults reported a larger change in their number of infrequent contacts (p = 0.041), whereas older adults reported a smaller change in their number of physical contacts (p = 0.017 for ages 45–59, p = 0.034 for ages over 60) and long-duration contacts (p = 0.006 for ages 30–44, p = 0.002 for ages 45–59, p = 0.045 for ages over 60).
A larger household was associated with a smaller change in the number of infrequent contacts (p = 0.041) and physical contacts (p = 0.032).
School closure
A similar paired survey carried out in schools to compare mixing patterns during the half-term holiday with those during school term observed large changes in social contact behaviour (see Appendix 2 for further details). Pupils who completed the survey reported, on average, 18.51 contacts (‘All’ contacts, in the terminology above) each day during term time and 9.24 during the half-term holiday, a reduction of over 50%. The change in number of contacts was highly significant (Wilcoxon signed-rank test, p < 0.0001).
Chapter 4 Discussion
Being infected with diagnosed swine flu had a considerable impact on the social contact patterns of those who participated in the study. Infected participants generally took time away from work/school/college and from social activities, and therefore made considerably fewer contacts when they were ill than when they had recovered. Participants made approximately two-thirds fewer contacts when they were unwell.
There was an observed tendency for the more transient contacts (infrequent contacts and contacts not involving physical contact) to be more influenced by illness than stronger contacts (frequent contacts and physical contacts). This again is unsurprising, as stronger contacts are more likely to be made in the home.
The regression analysis made clear the important role played by the workplace (or school, or college) on social contacts – returning to work was, by some distance, the most significant predictor of increased numbers of contacts.
The seriousness of infection also appeared to play a role, again confirming our intuition; the greater the change in the number of symptoms reported, the greater the change in the number of contacts.
Differences between age groups emerged, with those in younger age groups tending to have a greater change in their contact patterns; this can be explained by the differences in social mixing patterns between schools and workplaces, with older individuals appearing to mingle in smaller groups than younger individuals.
The results of the study were highly statistically significant, and the changes in measured contact behaviour were large. However, the study suffered from a number of limitations.
There was an apparently extremely low response rate; almost 3800 questionnaires were distributed along with antiviral prescriptions, and only slightly over 300 returned. Although we have no way of verifying that survey forms given to a potential participant’s ‘flu friend’ did in fact reach the potential participant, in the worst case this represents a response rate of only 8.4%. Furthermore, of the 308 follow-up surveys posted to participants who had completed the initial survey, only 179 were returned, of which 146 individuals reported that they were unwell when they completed the initial survey and had recovered by the time they completed the follow-up survey. Not only was this disappointing, but also it was some distance below the response rate obtained by a survey using very similar methodology: a two-part postal questionnaire survey (the EQ-5D study) carried out during the early stage of the 2009 swine flu pandemic received a response rate of 45%. 3 We postulate that, with hindsight, the low response rate was predictable; by the time the study was under way swine flu had been circulating in the UK for several months. After the initial media frenzy and the surge of attention that was generated by the launch of the NPFS, public interest had waned. By the time the sampling took place it was clear that the epidemic was in decline, and far fewer antiviral prescriptions were being distributed than at the epidemic’s peak. 25 For example, according to the Health Protection Agency weekly national influenza reports,26–31 there were an estimated 84,000 new cases in England in the peak week, the final week of October; by the middle of November, weekly incidence had fallen to 53,000 cases and to 22,000 by the end of November. Autumn weekly antiviral issues peaked in the penultimate week of October, had fallen by over 30% by the middle of November, and by over 40% by the end of November. With each passing week there were fewer cases, fewer potential participants, less media and public interest, and therefore a lower ability to sample and a lower likely response rate. Delays of a few weeks made a real difference. Had this study taken place earlier we believe that an improved response rate would have been achieved.
Unfortunately, the sluggish nature of the various stages of approval that the study was obliged to pass through meant that it was not possible to carry out the research in as timely a manner as had been anticipated. Because surveys were distributed at ADCs, some of which were NHS facilities, it was necessary to obtain local approval from each NHS trust within whose area questionnaires were distributed. Despite assurances that these local approvals would take 2–3 days, in practice, although some were indeed rapid, others took anything up to 2 months (and some never arrived). Clearly there is a need to reform the system of research governance to enable it to respond effectively to the urgent demands of real-time pandemic research if such research is to have a chance of success and of informing policy, as intended.
It is not clear whether or not there were non-response biases within our sample, although we would be surprised if there were not. When comparing individuals who returned both the initial and the follow-up survey with those who returned only the initial survey, we see that the latter group tends to be younger and to live in larger households. However, there was no significant difference between the groups in terms of either their reported severity of symptoms or their number of reported contacts when ill. Thus, though there are demographic differences, in key epidemiological and behavioural ways there is no significant difference between those who completed both surveys and those who completed only the initial survey. However, such comparisons tell us nothing about people who chose not to return the initial survey. What is almost certain is that the sample population was not a random sample of those who were infected with swine flu. Evidence collected from various sources and presented by the Health Protection Agency and other groups worldwide suggests that infection was concentrated in children. 25 Similarly, records collected by the NPFS show that antiviral distributions were also concentrated in younger age groups. 26–31 So, although our sample achieved a good coverage of age groups, it was not a random sample of the population of interest (i.e. those with swine flu).
At the time of the study, antiviral prescriptions were not issued to all individuals with swine flu, only to those who sought medication. Indeed, most participants received their diagnosis via a telephone line or a web page. Thus it may be that some, although reporting relevant symptoms, did not have swine flu. The participants probably ought, therefore, to be thought of as individuals with influenza-like illness rather than swine flu. It seems certain that those seeking antiviral medication were, in general, more ill than those who did not seek antiviral medication. Therefore, our sample is likely to be biased towards those with a more serious infection. This is supported by evidence from the EQ-5D study, carried out by the Health Protection Agency at the start of the pandemic and using similar methods to those used here, which aimed to recruit all cases of pandemic influenza; participants in the EQ-5D study reported an average health state (on a scale of 0–100) of 44 on their day of worst illness (AJ van Hoek, Health Protection Agency, 13 May 2010, personal communication), whereas participants in our study reported an average worst health state (on a scale of 0–10) of 1.98. More seriously ill people would be expected to be more likely to spend time away from their normal activities, and therefore to experience a greater change in their social contact behaviour than those with only mild infections. In this respect it is likely that our sample overestimates the extent of behavioural change. On the other hand, it might be that the principal difference between seriously ill individuals and those with less serious illness is the length of time taken away from work and other activities – the effect of taking time off may not depend on the seriousness of the infection, in which case our results may be more widely applicable.
However, it is not clear that our sample overestimates the behavioural change of those seeking antiviral medication. It might well be the case, for instance, that those who are most ill (and who therefore change their behaviour the most) would not feel in a fit state to fill in a survey. Furthermore, it is possible that those with the largest numbers of social contacts, when recovered, might decide that the contact diary would be too arduous to complete. These factors may lead to our data underestimating the effect of illness on social contact patterns.
Because the survey contains questions about participants’ symptoms and the extent to which participants take time off work, it is hoped that we will be able to compare our data with other data sources, when they become available, to assess the extent of biases by level of illness or of work-related behavioural change, thus to allow some corrections of any observed biases to be attempted.
The study took place in England (the only part of the UK in which the NPFS was in operation), therefore it was not possible to assess whether there were different behavioural changes in response to infection in other parts of the UK.
As with any self-reported questionnaire, we cannot be certain that participants answered the questions in the way that was intended. There may have been deliberate misreporting of behaviour, or there may have been misunderstanding of the questions. However, potential participants were provided with contact details (telephone number, e-mail address and postal address) for the research team and encouraged to make contact with any questions they had; only one query was received.
The brief school survey, although of limited size, gave the first survey-based quantitative measurements of the changes in contact patterns of school pupils occurring during school holiday periods. It is clear that school holidays have a large impact on social contacts, with children making about one-half of their number of term-time contacts during the holiday period. This observation helps explain the change in swine flu incidence that was seen during both the school summer holiday and, to a lesser extent, during the autumn half-term holiday. 25 Despite the low sample size, the measured behaviour change was highly significant. Although, as described, the study contained a range of biases and limitations, we are confident that the results obtained are a significant step forwards towards a more accurate understanding of the impact of illness on contact patterns. This understanding will facilitate more accurate mathematical modelling of epidemics, reduce the need for ad hoc approximations and aid future pandemic planning.
Chapter 5 Conclusions
The evidence from this study suggests that ill individuals make substantial changes to their social contact patterns. Participants in the study made approximately two-thirds fewer social contacts when they were ill compared with when they had recovered. The changes in contact patterns were strongly linked to absence from work and the severity of the reported illness, with age and household size also playing a role.
Epidemiological modellers should therefore be wary of using data about ‘normal’ contact patterns to parameterise mathematical models of disease spread, and should consider the implications of illness-related behavioural changes on model predictions. Of course, the changes measured here apply to symptomatic individuals, and care should be taken to use these data appropriately in cases when infected individuals may be asymptomatic or when infectiousness begins before symptom onset.
This study highlights areas for future research. Of particular value would be a more detailed study that aims to recruit a representative sample of cases; the study here, owing to its sampling methodology and the time constraints under which it took place, almost certainly ended up with a sample population that was experiencing relatively severe symptoms. Although such people are of interest, they may well display greater behavioural change than the average infected case. It would be of value, perhaps during forthcoming seasonal flu seasons, to carry out studies that measure the extent of behavioural change in a broader cross-section of infected cases.
The brief school study suggested that school children made approximately twice as many social contacts during school term as they do during the school holidays. As it was clear that children played a dominant role in the swine flu pandemic and might be expected to do so in future pandemics, and as it was apparent from the UK incidence data that normal patterns of school holidays had a significant impact on transmission, we advocate more detailed studies of the social contact patterns of school children, particularly focusing on differences between school terms and school holidays. Our experience, in this and other work (KTD Eames, unpublished), is that for school-based studies to be successful the research teams must be prepared to make a substantial investment of time and energy – such studies are therefore best conceived as long-term projects, achieving high levels of engagement with participating schools, rather than as rapid exercises. The presence of a pandemic cannot be taken as a guarantee of high participation.
Acknowledgements
We would like to thank all of the participating ADCs and schools for their willingness to assist with this study at a busy time. Also, we thank Fiona Marquet, Ellen Brookes Pollock and Rhian Daniel for their contributions.
Contributions of authors
Dr Ken Eames (mathematical epidemiologist) conceived and designed the study, carried out the analysis, and wrote the report.
Natasha Tilston (mathematical epidemiologist) assisted with the study and carried out the analysis.
Dr Peter White (mathematical epidemiologist) conceived the study and assisted with the study design.
Dr Elisabeth Adams (mathematical epidemiologist) carried out recruitment for the study.
Professor John Edmunds (mathematical epidemiologist) conceived the study and assisted with the study design.
Disclaimers
The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the Department of Health.
References
- Anderson RM, May RM. Infectious disease of humans. Oxford: Oxford Science Publications; 1991.
- Atchison C, Lopman B, Edmunds WJ. Modelling the seasonality of rotavirus disease and the impact of vaccination in England and Wales. Vaccine 2010;28:3118-26.
- Baguelin M, Hoek AJV, Jit M, Flasche S, White PJ, Edmunds WJ. Vaccination against pandemic influenza A/H1N1v in England: a real-time economic evaluation. Vaccine 2010;28:2370-84.
- Beutels P, Shkedy Z, Aerts M, Van Damme P. Social mixing patterns for transmission models of close contact infections: exploring self-evaluation and diary-based data collection through a web-based interface. Epidemiol Infect 2006;134:1158-66.
- Cauchemez S, Valleron AJ, Boelle PY, Flahault A, Ferguson NM. Estimating the impact of school closure on influenza transmission from sentinel data. Nature 2008;452:750-4.
- Conlan AJK, Rohani P, Lloyd AL, Keeling M, Grenfell BT. Resolving the impact of waiting time distributions on the persistence of measles. J R Soc Interface 2010;7:623-40.
- Edmunds W, Kafatos G, Wallinga J, Mossong J. Mixing patterns and the spread of close-contact infectious diseases. ETE 2006;3.
- Ford K, Sohn W, Lepkowski J. American adolescents: sexual mixing patterns, bridge partners, and concurrency. Sex Transm Dis 2002;29:13-9.
- Glass RJ, Glass LM, Beyeler WE, Min HJ. Targeted social distancing design for pandemic influenza. Emerg Infect Dis 2006;12:1671-81.
- Hens N, Ayele G, Goeyvaerts N, Aerts M, Mossong J, Edmunds J, et al. Estimating the impact of school closure on social mixing behaviour and the transmission of close contact infections in eight European countries. BMC Infect Dis 2009;9.
- Heymann AD, Hoch I, Valinsky L, Kokia E, Steinberg DM. School closure may be effective in reducing transmission of respiratory viruses in the community. Epidemiol Infect 2009;37:1369-76.
- Keeling MJ, Grenfell BT. Disease extinction and community size: modeling the persistence of measles. Science 1997;275:65-7.
- Kretzschmar M, Mikolajczyk RT. Contact profiles in eight European countries and implications for modelling the spread of airborne infectious diseases. PLoS ONE 2009;4.
- Mikolajczyk RT, Akmatov MK, Rastin S, Kretzschmar M. Social contacts of school children and the transmission of respiratory-spread pathogens. Epidemiol Infect 2007;135:1-10.
- Mossong J, Hens N, Jit M, Beutels P, Auranen K, Mikolajczyk R, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Medicine 2008;5:381-91.
- Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature 2006;442:448-52.
- Germann TC, Kadau K, Longini IM, Macken CA. Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci USA 2006;103:5935-40.
- Ghani AC, Baguelin M, Griffin J, Flasche S, Pebody R, van Hoek AJ, et al. The early transmission dynamics of H1N1pdm influenza in the United Kingdom. PLoS Curr Influenza 2009.
- Fraser C, Donnelly CA, Cauchemez S, Hanage WP, Van Kerkhove MD, Hollingsworth TD, et al. Pandemic potential of a strain of influenza A (H1N1): early findings. Science 2009;324:1557-61.
- Aral SO, Hughes JP, Stoner B, Whittington W, Handsfield HH, Anderson RM, et al. Sexual mixing patterns in the spread of gonococcal and chlamydial infections. Am J Public Health 1999;89:825-33.
- Bearman Peter S, Moody J, Stovel K. Chains of affection: the structure of adolescent romantic and sexual networks. Am J Sociol 2004;110:44-91.
- Read JM, Eames KT, Edmunds WJ. Dynamic social networks and the implications for the spread of infectious disease. J R Soc Interface 2008;5:1001-7.
- Edmunds W, O’Callaghan C, Nokes D. Who mixes with whom? A method to determine the contact patterns of adults that may lead to the spread of airborne infections. Proc R Soc Lond B Bio 1997;264:949-57.
- Mikolajczyk RT, Kretzschmar M. Collecting social contact data in the context of disease transmission: prospective and retrospective study designs. Soc Networks 2008;30:127-35.
- Donaldson LJ, Rutter PD, Ellis BM, Greaves FEC, Mytton OT, Pebody RG, et al. Mortality from pandemic A/H1N1 2009 influenza in England: public health surveillance study. BMJ 2009;339.
- Health Protection Agency . Weekly National Influenza Report (week 49) 2009.
- Health Protection Agency . Weekly National Influenza Report (week 48) 2009.
- Health Protection Agency . Weekly National Influenza Report (week 47) 2009.
- Health Protection Agency . Weekly National Influenza Report (week 46) 2009.
- Health Protection Agency . Weekly National Influenza Report (week 45) 2009.
- Health Protection Agency . Weekly National Influenza Report (week 44) 2009.
Appendix 1 Survey forms
Initial survey
The first part of the survey asks for general (background) information. Note: each form was marked with a two-letter code denoting the ADC at which the survey was distributed – each ADC had its own two-letter code. Each returned form had a three-digit code appended to this ADC code, and the resulting compound code was written on the follow-up forms sent to that participant, allowing a participant’s initial and follow-up data to be linked.
Contact diary
The same contact diary form was used for both the initial and the follow-up surveys.
Follow-up survey
The follow-up survey contained a shorter background questionnaire, and a second contact diary (identical to the first).
Appendix 2 School closure study
In summer 2009, in the early stages of the swine flu pandemic, several schools in the UK closed as a result of swine flu infections. It was expected that such closures would happen again in autumn 2009, either because of large numbers of cases in pupils or because of staff shortages owing to sickness. To help assess the impact of these closures on contact patterns, and therefore on transmission, it was planned to carry out a study similar to that described above, recruiting school children to complete a contact diary once when their school was closed as a result of swine flu and once when the school had reopened. Such a study would have helped us understand the impact of unplanned closures on children’s mixing patterns and informed us about the use of school closure as a control policy.
However, the UK swine flu epidemic in autumn 2009 was milder than expected, and school closures did not occur. The planned study could not, therefore, take place. Instead, as the study materials had already been developed, we took the opportunity to carry out a half-term study – asking pupils to complete a contact diary once during their spring half-term holiday and once during term time. This adapted study clearly does not inform us about the effects of unplanned closures, but instead quantifies the impact of school holidays.
Eight schools in London and Sussex were recruited to take part, and approximately 1100 study packs were distributed. All questionnaire forms were contained in the study pack, so participants (or their parents/guardians) needed to keep hold of the follow-up survey forms until the appropriate date. The initial and follow-up surveys were clearly distinguished within the study pack, and clear instructions given to ensure that forms were completed on the correct days (all forms were dated by participants, and forms filled in incorrectly could be excluded from the analysis). This approach enabled us to avoid having to ask for anyone’s name or address. In total, 134 forms were completed correctly (a response rate of approximately 12%) and, from these, a total of 119 paired contact diaries (response rate 10.9%) were obtained.
The results provided by those who participated are clear: during term time, participants reported an average of 18.51 contacts (95% confidence interval 17.03 to 20.00), whereas during the school holiday they reported an average of 9.24 contacts (95% confidence interval 8.15 to 10.32). There was a significant difference in the number of contacts reported in term time compared with during the half-term holiday (difference = 9.28; 95% confidence interval 7.77 to 10.79; p < 0.0001, Wilcoxon signed-rank test).
The sample is small and perhaps unrepresentative; however, within our sample children made approximately one-half of the number of social contacts during a day in the half-term holiday that they made during term time.
Appendix 3 Contact pattern changes – complete data set
In Chapter 3, Figure 4 and Table 3 show the changes in contacts recorded by participants who reported that they were unwell when they completed the initial survey but who reported that they had recovered by the time that they completed the follow-up survey. For completeness, Figure 5 and Table 5 show the equivalent data for all participants (i.e. including those who were still unwell when they completed the follow-up survey).
FIGURE 5.
Change in number of contacts reported in the initial and follow-up surveys; for each of the participants who completed a useable contact diary for both the initial and the follow-up survey (n = 165), the change in number of contacts is defined as the number recorded in the follow-up survey minus the number recorded in the initial survey.
| Type of contact | Initial survey (n = 172), mean (SD) | Follow-up survey (n = 168), mean (SD) | Difference (n = 165) | |||
|---|---|---|---|---|---|---|
| Mean (SD) | Relative difference (percentage of follow-up mean) | Median (IQR) | p-value (median ≠ 0) | |||
| All | 3.74 (3.76) | 9.76 (8.15) | 6.08 (8.67) | 62 | 4 (0 to 10) | < 0.0001 |
| All plus additional | 4.12 (6.10) | 12.10 (14.44) | 8.06 (16.04) | 67 | 4 (0 to 9) | < 0.0001 |
| Frequent | 3.05 (3.48) | 7.12 (6.90) | 4.11 (7.31) | 58 | 2 (0 to 7) | < 0.0001 |
| Infrequent | 0.49 (1.07) | 1.85 (4.06) | 1.39 (4.34) | 75 | 0 (0 to 2) | 0.0001 |
| Physical | 1.72 (1.70) | 3.76 (4.80) | 2.06 (4.70) | 55 | 1 (0 to 3) | < 0.0001 |
| Long duration | 2.07 (2.25) | 5.17 (6.38) | 3.13 (6.58) | 61 | 1 (0 to 4) | < 0.0001 |
| Short duration | 1.06 (1.72) | 2.71 (3.97) | 1.68 (4.34) | 62 | 1 (0 to 3) | < 0.0001 |
| Home | 2.41 (1.61) | 2.60 (2.09) | 0.16 (1.75) | 6 | 0 (–1 to 1) | 0.3740 |
| Work | 0.78 (3.20) | 4.36 (7.55) | 3.64 (7.96) | 83 | 0 (0 to 5) | < 0.0001 |
| Other | 0.57 (1.32) | 2.71 (4.25) | 2.18 (4.41) | 80 | 0 (0 to 3) | < 0.0001 |
List of abbreviations
- ADC
- antiviral distribution centre
- IQR
- interquartile range
- NPFS
- National Pandemic Flu Service
- SD
- standard deviation
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.