Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the HTA programme on behalf of NICE as project number 10/128/01. The protocol was agreed in October 2011. The assessment report began editorial review in May 2012 and was accepted for publication in August 2012. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Note
This monograph is based on the Technology Assessment Report produced for NICE. The full report contained a considerable number of data that were deemed commercial-in-confidence and/or academic-in-confidence. The full report was used by the Appraisal Committee at NICE in their deliberations. The full report with each piece of commercial-in-confidence and/or academic-in-confidence data removed and replaced by the statement ‘commercial-in-confidence and/or academic-in-confidence information (or data) removed’ is available on the NICE website: www.nice.org.uk.
The present monograph presents as full a version of the report as is possible while retaining readability, but some sections, sentences, tables and figures have been removed. Readers should bear in mind that the discussion, conclusions and implications for practice and research are based on all the data considered in the original full NICE report.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Norman et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
This health technology assessment was undertaken on behalf of the UK National Institute for Health and Care Excellence (NICE) as part of a NICE multiple technology appraisal (MTA) following two previous single technology appraisals (TA133 and TA201). These assessed omalizumab for severe persistent allergic asthma in adults and children respectively.
Description of health problem
Severe persistent allergic asthma
Asthma is a long-term disorder of the airways that results in ongoing inflammation associated with bronchial hyper-reactivity and variable airflow. 1 This leads to repeated episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night or in the early morning. Distinctions are made between allergic and non-allergic asthma. Allergic asthma results from the overexpression of immunoglobulin E (IgE) in response to environmental allergens such as house dust mite, pollen and moulds.
Asthma severity varies both between patients and within a patient over time. One commonly used pragmatic definition of asthma severity depends on the intensity of treatment required to achieve good asthma control. Good asthma control is characterised by the absence of asthma symptoms, normal lung function and no asthma exacerbations with the minimal amount of asthma treatment. Severe persistent allergic asthma is considered to be asthma which is poorly controlled despite the elimination of modifiable factors and the correct use of optimised standard therapy. 2 Patients with poorly controlled asthma are at risk of asthma exacerbations that may be serious and require unplanned medical intervention and sometimes hospitalisation, and have reduced quality of life (QoL) as a consequence of the day-to-day symptoms.
Aetiology, pathology and prognosis
The aetiology of asthma is complex, involving both genetic and environmental triggers.
Airflow obstruction and hyper-responsiveness are caused by inflammation and structural changes of the bronchial wall. Activated T lymphocytes, mast cells, eosinophils and neutrophils can infiltrate the airways thereby releasing cytokines, chemokines and growth factors. Structural changes are defined as airway remodelling, which includes shedding of bronchial epithelium, mucus gland hypertrophy, subepithelial fibrosis, myofibroblast hyperplasia, angiogenesis and increased smooth muscle mass. 3 These changes contribute to the progressive loss of lung function in asthma.
There is no cure for asthma. The aim of asthma therapy is therefore to achieve and maintain control of the condition while minimising the occurrence or severity of adverse effects from the treatments used. 4
Many patients with mild asthma are able to manage their disease using only short-acting β2-agonist (SABA) medication (reliever medication) when required. The majority of people with asthma who require additional treatment can be well controlled using moderate doses of inhaled corticosteroids (ICSs) with or without additional agents such as long-acting β2-agonists (LABAs). The next step in treatment involves high doses of ICS plus LABA and the possible addition of a third treatment such as a leukotriene receptor antagonist (LTRA). If control is still not achieved, additional treatment usually takes the form of the addition of continuous or frequent long-term oral corticosteroids (OCSs). These usually control asthma effectively but are associated with a number of serious side effects including reduced bone density in adults and growth restriction in children. However, a proportion of patients remain difficult to control despite multiple therapies including either maintenance OCSs or multiple courses of OCSs; approximately 5% of asthma patients have severe, persistent symptoms. 5 These patients use 50% of the resources available to the NHS for treatment of asthma. This group of patients is 20 times more likely to have a hospital admission and 15 times more likely to require emergency care. 6 It is these patients for whom omalizumab might be appropriate. 7 Omalizumab, an anti-IgE therapy licensed in the UK, is discussed in detail in Chapter 1, Description of technology under assessment, Summary of intervention.
Incidence and/or prevalence
The UK has one of the highest prevalence rates of asthma in the world. The Quality and Outcomes Framework (2008) estimated that 5.9% of the UK population have asthma, with estimates ranging from 3 to 5.4 million. 8 Asthma UK estimated that between 2008 and 2009 there were 79,794 emergency hospital admissions in England, of which 30,740 were of children aged up to 14 years. 9 According to Asthma UK, 75% of all hospital admissions for asthma are avoidable through good asthma management and routine care. 9
In the UK, deaths resulting from asthma have ranged between 1000 and 1200 per year since 2000. This is a low death rate given the high prevalence of asthma, and 60% of deaths occur in patients aged over 75 years. However, the figure for asthma-related premature deaths was 1.5 times higher in the UK than in the rest of Europe in 2008. Ninety per cent of these deaths are due to preventable factors. 10
There is considerable variation in outcomes across England; there may be a fivefold difference between primary care trust (PCT) areas in the number of emergency admissions in adults, and a sixfold difference for those under 18 years of age. 10
Impact of health problem
Significance for patients in terms of ill health (burden of disease)
Asthma affects the patients and their families, and also society in terms of days lost from work and school, reduced QoL, and avoidable health-care visits, hospitalisations and deaths. 11 Although severe uncontrolled asthma affects only a relatively small population, it accounts for a significant proportion of health-care resource use. 12 This group of patients remain at high risk of exacerbations that require additional treatment, health-care consultations and often hospitalisations. Severe exacerbations are also potentially life-threatening. 11
Psychological conditions such as anxiety and depression may be up to six times more common in people with asthma than in the general population. Depression may be present in between 14% and 41% of those with asthma. 13 It is particularly common in people with severe and difficult-to-control asthma, and this is emphasised in the British Asthma Guidelines. 13 Those with asthma who also have depression or anxiety experience more asthma symptoms and have worse outcomes in terms of higher use of health-care resources, increased health-care costs, less successful emergency treatment and increased hospitalisation. 10
Significance for the NHS
The costs of asthma are substantial and include both direct health costs (hospital admissions and cost of treatment) and indirect, non-medical costs (time lost from work, premature death). 1
Measurement of disease
Routine measures to assess asthma control include the following.
-
Monitoring of symptoms either through simple questioning or using questionnaires. Questionnaires in current use include those that focus on symptoms, rescue treatment use and lung function [forced expiratory volume in 1 second (FEV1)]. Examples are the Royal College of Physicians (RCP) 3 questions; Asthma Control Questionnaire (ACQ) and Asthma Control Test (ACT). The Mini Asthma Quality of Life Questionnaire (AQLQ) focuses on QoL. The questionnaire specifically developed for use in children with asthma [the Paediatric Asthma Quality of Life Questionnaire (PAQLQ)] covers symptoms, activity limitations, emotional function and environmental stimuli.
-
Monitoring of lung function by spirometry (FEV1) or peak expiratory flow (PEF).
-
Measurement of airway inflammation, which is responsive to ICS therapy by measuring, fractional exhaled nitric oxide (FeNO). This can be used in children. Adults may also be assessed using the eosinophil differential count in induced sputum. 13
These types of methods are usually used together to provide a complete assessment, although FeNO measurement may not be used on all occasions.
Current service provision
Treatment of asthma is based on a stepped approach to therapy: if asthma is not controlled on current treatment, then treatment is stepped up until control is achieved. 1 According to the Global Initiative for Asthma (GINA 2010)1 and British Thoracic Society/Scottish Intercollegiate Guidelines Network (BTS/SIGN),13 there are five treatment steps for adults, adolescents and children aged 5–12 years. Treatment at each step is summarised in Table 1 and, as can be seen, patients with severe persistent asthma are treated at BTS/SIGN steps 4 and 5. It should be noted that children under the age of 5 years are treated using a different stepwise approach not shown here.
| Step 1 | Step 2 | Step 3 | Step 4 | Step 5 |
|---|---|---|---|---|
| Mild intermittent asthma | Regular preventer therapy | Initial add-on therapy | Persistent poor control | Continuous or frequent use of oral steroids |
| Children aged 5–12 years | ||||
| Inhaled SABA as required | Add inhaled steroids 200–400 µg/daya (other preventer drug if inhaled steroid cannot be used) 200 µg is an appropriate starting dose for many patients |
|
Increase inhaled steroid up to 800 µg/day | Use daily steroid tablet in lowest dose providing adequate control |
| Start at dose of inhaled steroid appropriate to severity of disease | Maintain high dose of inhaled steroid at 800 µg/daya | |||
| Refer to respiratory paediatrician | ||||
| Adults | ||||
| Inhaled SABA as required | Add inhaled steroids 200–800 µg/day – 400 µg is an appropriate starting dose for many patients |
|
Consider trials of: | Use daily steroid tablet in lowest dose providing adequate control |
| Start at dose of inhaled steroid appropriate to severity of disease | Increasing inhaled steroid up to 2000 µg/daya | Maintain high dose of inhaled steroid at 2000 µg/daya | ||
| Addition of a fourth drug, e.g. LTRA, sustained-release theophylline, β2-agonist tablet | Consider the use of other treatments to minimise the use of steroid tablets | |||
| Refer patient for specialist care | ||||
At BTS/SIGN step 4, a small proportion of patients have inadequately controlled asthma despite treatment with a combination of high-dose ICS (800 µg/day in children aged 5–12 years, and 2000 µg/day in adults) and additional controller medication. The additional controller medication will include a combination of at least three of the following: LABA, LTRA, theophyllines and oral slow-release β2-agonists.
However, a small number of patients will continue to remain uncontrolled and will proceed to BTS/SIGN step 5, which is the addition of frequent or continuous OCSs. 13 The side effects of long term oral steroids are significant and include adrenal suppression, decreased bone mineral density, cataracts and glaucoma1 and growth failure in children. 14 Therefore, treatment at step 5 should use the lowest dose of OCS, with consideration given to the use of other treatments to minimise the use of OCSs. 13 Immunosuppressants (methotrexate, ciclosporin and oral gold) have been used in adults to decrease the long-term use of OCSs. However, their efficacy is very limited and they all have significant side effects. 13 The Clinical Advisors to this health technology appraisal commented that immunosuppressants are rarely used in practice (personal communications).
Current service cost
The costs of difficult-to-treat asthma to the NHS are estimated to be more than £680M per year. 9 The costs associated with standard care consist of the costs of standard therapy itself and the costs of routine secondary care. The costs for standard care were estimated at £1197 per year for adults and adolescents and £810 for children. 15 Patients with severe persistent allergic asthma have twice yearly appointments with their respiratory specialist, at a cost to the NHS of £160 per appointment for children and £190 for adults and adolescents. 16
Description of technology under assessment
Summary of intervention
Omalizumab (Xolair®, Novartis Pharmaceuticals) is a recombinant deoxyribonucleic acid (DNA)-derived humanised monoclonal antibody that blocks the binding of free serum human IgE to mast cells and basophils, thus inhibiting the release of various inflammatory mediators responsible for allergic asthma symptoms. 17
Omalizumab is licensed in the UK as add-on therapy to improve asthma control in adults and adolescents aged at least 12 years with severe persistent allergic asthma who have a positive skin test or in vitro reactivity to a perennial aeroallergen, who have reduced lung function (FEV1 < 80%) as well as frequent daytime symptoms or night-time awakenings and who have had multiple documented severe asthma exacerbations despite daily high-dose inhaled corticosteroids, plus a long-acting inhaled β2-agonist. 18 It is also indicated as add-on therapy to improve asthma control in children aged 6 to < 12 years with severe persistent allergic asthma who have a positive skin test or in vitro reactivity to a perennial aeroallergen and frequent daytime symptoms or night-time awakenings and who have had multiple documented severe asthma exacerbations despite daily high-dose inhaled corticosteroids, plus a LABA. 18
Omalizumab 75 mg (or 150 mg) solution for injection is given parenterally as a subcutaneous injection every 2–4 weeks, with the dose dependent on both weight and baseline IgE level. Doses should be adjusted for significant changes in body weight. Patients whose baseline IgE levels or body weights in kilograms are outside the stated limits should not be given omalizumab. 18 Omalizumab is intended for long-term treatment. Clinical trials have demonstrated that it takes at least 12–16 weeks for treatment to show effectiveness. Patients should be assessed after 16 weeks of treatment for treatment effectiveness before further injections are administered. In the UK, assessment is undertaken by a Specialist, usually a Consultant Respiratory Physician, Allergist, Immunologist or Paediatrician (personal communications). The decision to continue with omalizumab following the 16-week time point, or on subsequent occasions, is based on whether a significant improvement in overall asthma control is seen.
Relevant national guidelines, including National Service Frameworks
A number of guidelines on the management of asthma have been developed, including the GINA1 and the Expert Panel Report 311 developed by an expert panel commissioned by the National Asthma Education and Prevention Program (NAEPP) Coordinating Committee (CC), co-ordinated by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health. In the UK, the BTS and SIGN have jointly produced a comprehensive asthma guideline. 13 The guidelines provide recommendations based on current evidence for best practice in the management of asthma in adults, including pregnant women, adolescents and children, and include advice about the use of omalizumab.
Previous appraisals of omalizumab have been conducted in the UK to inform the NICE technology appraisals TA133 and TA201. Evidence on the clinical effectiveness of omalizumab for adults and adolescents was primarily based on the INvestigatioN of Omalizumab seVere Asthma Trial (INNOVATE), which examined the impact of omalizumab as add-on therapy in patients inadequately controlled despite high-dose ICS and LABAs (GINA step 4 treatment). 19 The evidence for children was primarily based on a preplanned subgroup of children from the IA-05 trial who received concomitant medication (high-dose ICS and LABA). 20
Current usage in the NHS
The manufacturer estimates that 1256 patients in England and Wales currently receive omalizumab, approximately 30 of whom are children aged 6 to < 12 years. It is estimated that in 2012 an additional 329 patients will commence therapy (eight aged 6 to < 12 years), and that this figure will rise to 653 patients in 2016 (16 aged 6 to < 12 years). A proportion of these patients will be non-responders to omalizumab, and will not, therefore, continue to receive omalizumab beyond 16 weeks.
NICE guidance currently recommends the use of omalizumab for adults and adolescents ≥ 12 years (TA133),2 but does not currently recommend the use of omalizumab in children aged 6–11 years (TA201). 14 In contrast, the Scottish Medicines Consortium (September 2007 and March 2010) advise that omalizumab can be used in NHS Scotland as add-on therapy to improve asthma control in children aged 6–11 years who are prescribed chronic systemic corticosteroids and in whom all other treatments have failed. 21
Anticipated costs of intervention
Costs associated with omalizumab therapy include the costs of the drug itself and the costs of administration and monitoring. Omalizumab is administered as a subcutaneous injection every 2–4 weeks and the exact dose depends on the patient's serum IgE and weight. It is available as 75 mg and 150 mg prefilled syringes at prices of £128.07 and £256.15 respectively. 22 In addition to the acquisition costs of omalizumab, the costs associated with omalizumab therapy include administration and monitoring for anaphylaxis.
Chapter 2 Definition of decision problem
Decision problem
The decision problem relates to the effectiveness and cost-effectiveness of omalizumab as add-on therapy in patients whose asthma is poorly controlled by optimised standard BTS/SIGN step 4 or step 5 therapy. The decision problem differs depending on whether patients at step 4 or step 5 treatment are considered. For patients at step 4, omalizumab is an alternative to the addition of frequent or continuous OCSs; in patients at step 5 it is given in addition to frequent or continuous OCS, but it may nevertheless allow a reduction in dose of OCS. Avoidance of, or reduction in, OCS is desirable because of the adverse effects associated with long-term systemic corticosteroid use.
Overall aims and objectives of assessment
We undertook this health technology assessment as a multiple technology appraisal (MTA) on behalf of NICE as part of its appraisal of omalizumab for the treatment of severe persistent allergic asthma in children aged 6 and over and adults. The appraisal was a review of two previous single technology appraisals (STAs) – TA133 and TA201. The assessment stage of the MTA process involves an independently conducted review of the clinical effectiveness and cost-effectiveness of omalizumab, together with the development of a de novo economic model. As part of the NICE appraisal process the manufacturer of the technology of interest provides a submission, which we considered as an additional source of information for our independent assessment.
The aim of our assessment was to determine the clinical effectiveness, safety and cost-effectiveness of omalizumab, within its licensed indication, in addition to standard therapy, compared with standard therapy without omalizumab, for the treatment of severe persistent allergic asthma in (1) adults and adolescents aged at least 12 years and (2) children aged 6–11 years.
In the context of the decision problem, the assessment addressed the efficacy of omalizumab in addition to standard BTS/SIGN step 4 treatment compared with standard step 4 therapy alone; and in addition to standard BTS/SIGN step 5 treatment compared with standard step 5 therapy alone. This included an evaluation of the long-term efficacy of omalizumab at both step 4 and step 5 and an evaluation of the adverse effects of omalizumab. In addition, the safety of OCSs in asthma patients including long-term adverse events (and therefore the benefits of steroid-sparing) has been assessed. The additional areas of uncertainty relating to the relationships between outcome variables and health-related quality of life (HRQoL) identified as arising from TA133 and TA201 will also be considered.
Chapter 3 Assessment of clinical effectiveness
Methods for reviewing clinical effectiveness
The review of clinical effectiveness addressed five distinct questions which arose from the decision problem (see Chapter 2, Definition of decision problem, Decision problem): the efficacy of omalizumab; the long-term efficacy of omalizumab; the steroid-sparing effect of omalizumab; the safety of omalizumab; and the adverse effects of OCSs. The review of clinical effectiveness was conducted following the general principles published in the Centre for Reviews and Dissemination (CRD)'s guidance for conducting systematic reviews23 and the PRISMA statement. 24 However, the conduct of full systematic reviews of the evidence to address all five questions was neither warranted nor possible within the limited time available for the review: the methods used are detailed by question below.
Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing)
This review of the efficacy of omalizumab comprised a full systematic review.
Search strategy
Studies relevant to an assessment of the therapeutic effect of omalizumab were identified by searching the following databases: MEDLINE, MEDLINE In-Process & Other Non-Indexed Citations, EMBASE, Cochrane Database of Systematic Reviews (CDSR), Cochrane Central Register of Controlled Trials (CENTRAL), Database of Abstracts of Reviews of Effects (DARE) and Health Technology Assessment (HTA) Database, National Institutes for Health (NIH) ClinicalTrials.gov Register, Current Controlled Trials, Conference Proceedings Citation Index (CPCI-S), and EconLit. Searches were run in September 2011 and rerun in October 2011 following the identification of an additional search term at the screening stage of the review. Full details of the search strategy are provided in Appendix 1. Additional searches of trial registers, journals and reference lists of relevant published systematic reviews were conducted to identify any further studies of relevance. No limits on date, language or study design were applied. EndNote software (Thomson Reuters, CA, USA) was used to download and import references and remove duplicates. The submissions were provided to NICE by Novartis Pharmaceuticals and the associated documents were also used as sources of relevant studies for the review.
Study selection
Abstracts of identified studies and potentially relevant full papers were independently assessed for inclusion in the review by two reviewers using the criteria outlined below. Disagreements were resolved through discussion and, where necessary, by consultation with a third reviewer. In cases where it was unclear if a study met inclusion criteria, attempts were made to contact authors for further information.
Intervention
The intervention of interest was omalizumab given parenterally as a subcutaneous injection every 2–4 weeks, depending on dose, in addition to best standard therapy at step 4 or step 5 of the BTS/SIGN treatment guideline (the dose and frequency of administration of omalizumab are determined by baseline IgE measured before the start of treatment, and body weight).
Comparators
The direct comparator considered was optimised standard therapy. Standard therapy was step 4 or step 5 (BTS/SIGN guideline) treatment. Optimisation of standard therapy was considered to include the elimination of modifiable factors in addition to treatment compliance. The following comparators were considered:
In adults and children:
-
daily high-dose ICS plus a LABA with the possible addition of LTRA, theophyllines, or slow-releasing β2-agonist tablets (BTS/SIGN step 4)
-
daily high-dose ICS plus a LABA with the possible addition of LTRA, theophyllines, or slow-releasing β2-agonist tablets plus frequent or continuous OCSs (BTS/SIGN step 5).
While optimised standard therapy was an inclusion criterion, a pragmatic approach was adopted. Where optimisation was reported by study investigators but it was unclear if therapy was in fact optimised at recruitment, this concern is discussed.
After finalisation of the review protocol it was established that methotrexate, ciclosporin and gold were not considered appropriate treatment for adults or children at step 4 or step 5 (BTS/SIGN guideline), and therefore these treatments were not included as comparators in the review.
Participants
Studies in which the whole population, or a clearly defined subgroup of the population, or a large proportion of the population, met the following criteria (which reflect the UK licence for omalizumab) were eligible for inclusion in the review: adults and adolescents aged at least 12 years with severe persistent allergic asthma and:
-
a positive skin test or in vitro reactivity to a perennial aeroallergen
-
reduced lung function (FEV1 < 80%)
-
frequent daytime symptoms or night-time awakenings
-
multiple documented severe asthma exacerbations despite daily high-dose ICS plus a long-acting inhaled β2-agonist
or children aged between ≥ 6 and 12 years with severe persistent allergic asthma and:
-
a positive skin test or in vitro reactivity to a perennial aeroallergen
-
frequent daytime symptoms or night-time awakenings
-
multiple documented severe asthma exacerbations despite daily high-dose ICS plus a long-acting inhaled β2-agonist.
To address the question of the steroid-sparing effect of omalizumab, for which it was anticipated evidence would be sparse, studies whose populations did not meet these criteria were also included.
Outcomes
The primary outcome was clinically significant exacerbations. Studies that reported this or the following secondary outcomes were eligible for the review: asthma symptoms, incidence of clinically significant severe exacerbations, hospitalisations resulting from asthma-related incidents, mortality, use of OCSs (reduction in dose or frequency or withdrawal), time to discontinuation of omalizumab treatment, adverse effects of treatment and HRQoL.
Study designs
Randomised controlled trials with a comparator of placebo, standard care or another active intervention were eligible for the review. Data from quasi-randomised controlled trials (RCTs) and observational studies were also considered in order to provide supporting evidence and, in particular, data on longer-term response and adherence to treatment and steroid-sparing. These included open-label continuation studies, non-comparative cohort studies and postmarketing studies [to include ≥ 30 patients or long-term data (≥ 2 years)].
Data extraction
Data relating to both study design and quality were extracted by one reviewer using a standardised data extraction form and independently checked for accuracy by a second reviewer. Disagreements were resolved through consensus, and, if necessary, a third reviewer was consulted. Attempts were made, where possible, to contact authors and study sponsors when a potentially relevant study was reported in abstract form only or could not be fully identified. Authors were also contacted when it was unclear whether multiple publications referred to the same study. Data from studies with multiple publications were extracted and reported as a single study. Additional data were also extracted from the manufacturer's submission (MS); where this is the case the fact is noted and the trial publications are not referenced.
Intention-to-treat (ITT) data were used where possible; where this was not possible, the fact was noted. Rate ratios were reported for the outcomes of exacerbations and hospitalisation and other unscheduled care use. Mean differences were reported where possible for outcomes of QoL and asthma symptoms.
Where rate ratios or other summary measures were reported in the source documents, these were used. The majority of rate ratios reported in the published papers and in the MS were calculated using a Poisson regression. Where reported, this included factors such as dosing schedule, country grouping and asthma medication strata. Where these summary measures were not reported, they were calculated by the review team using numbers of exacerbations and patient time, where possible, and this is noted. When only very limited data were reported which precluded calculation of a summary measure, or where only the result of a statistical test (with or without a p-value) were reported, then these were presented.
Quality assessment
In all cases, quality assessment was performed by one reviewer, and independently checked by a second. All disagreements were resolved through consensus, and, if necessary, a third reviewer was consulted.
The quality of RCTs was assessed using standard checklists following the principles of CRD. 23 The following criteria were assessed: randomisation (were details of an appropriate method reported?); allocation concealment (were details of an appropriate method reported?); blinding of outcome assessors; baseline comparability of groups and equal treatment of groups (with the exception of the intervention); use of appropriate analysis including use of a sample size calculation and selective outcome reporting; treatment of withdrawals and dropouts. Full details are given in Appendix 7.
The original protocol was amended to also include the assessment of risk of bias following the principles of the Cochrane Collaboration. 25 This assessment was conducted by using the answers to the original quality assessment to give a risk of bias score. The overall risk of bias was considered to be the highest risk scored for any single criterion. For example, if a trial was considered at low risk of bias on all criteria except one where the risk was unclear, then the overall risk of bias was recorded as unclear; where the risk was low or unclear on all criteria except one which was scored as high then the overall risk of bias was recorded as high. All outcomes were considered to be subjective. Because there was therefore no reason to believe risk of bias differed between outcomes, a risk of bias was calculated for the study as a whole rather than for each outcome. This is because even seemingly objective outcomes, such as exacerbations, are influenced by (for example) compliance with concomitant medication and symptom perception. Criteria not included in the risk of bias assessment (such as reporting of a power calculation) did not contribute to the overall risk of bias for the study. Criteria such as comparability of baseline characteristics and use of an appropriate analysis were independently assessed by the review team; if authors reported tests of statistical significance for potential baseline imbalances, these were used to inform the assessment.
For non-randomised studies, tools based on CRD guidance23 were used. The criteria assessed were: recruitment of a representative sample from a relevant population; use of explicit criteria for inclusion; baseline comparability of groups (where applicable), blinding of outcome assessors (where applicable); completeness of follow-up; adequate reporting of outcomes, including sufficient follow-up. No overall quality score was calculated but aspects of the quality assessment were used to inform the consideration of observational study results.
Details of the methods used in the quality assessment are provided in Appendix 7.
Data analysis
Outcomes
Data were presented separately for each outcome reported. Some trials divided the primary review outcome of clinically significant exacerbations into clinically significant severe (CSS) exacerbations and clinically significant non-severe (CSNS) exacerbations. Therefore an outcome of ‘total exacerbations’ is reported which includes all exacerbations reported as clinically significant from all trials. CSS and CSNS exacerbations, where reported, were also analysed separately. Where possible, data on each component of unscheduled health-care use [hospitalisation, emergency room (ER) attendance and unscheduled doctor appointments] were analysed separately; in cases where only composite outcomes were reported this was noted. Asthma symptom scores, QoL and incidence of particular symptom measures were summarised where possible, given the heterogeneity in assessment methods. Where appropriate and where data were available, study estimates of the effect of omalizumab relative risks, risk ratios, mean differences, with 95% CI were calculated.
Efficacy of omalizumab: randomised controlled trials
Data from RCTs were considered separately from those from observational studies. RCTs enrolling adults and children were considered separately throughout. In both adults and children a distinction was drawn between included trials which included only patients who met the licence criteria, those in which a defined subgroup met or closely approximated the licence criteria and those which were included as supportive evidence only, in which an undefined proportion of the trial population (not a defined subgroup) met the licence criteria. In all analyses data are reported for the whole trial population where this corresponded to the licensed population; where a defined subgroup of the trial population met the licence criteria, the analyses used the data for that subgroup. For supportive trials, data for the whole trial were reported with the caveat that patients outside the licensed population contributed to the estimates of effect.
Efficacy of omalizumab: observational studies
No quasi-randomised studies were identified. Observational studies were included in a narrative synthesis. No quantitative pooling of data from these studies was undertaken. Data from observational studies were reported for all outcomes. These data were sought in order to support the limited RCT data, to investigate the generalisability of the RCT and to provide data where RCT data were lacking, and were considered to provide supportive evidence to that provided by RCTs.
Approach to synthesis
Although a statistical synthesis (meta-analysis) of the results of the identified RCT was planned, in practice this was not appropriate for any analysis. The trials of adult patients were subject to significant methodological and, to a lesser degree, clinical, heterogeneity identified by the quality assessment (see Validity assessment and risk of bias of RCTs). There was clear clinical heterogeneity between trials in the licensed population and those included as supportive evidence. Methodological heterogeneity prevented meaningful pooling of the trials in the adult licensed population. In the case of children there was only one trial in which a defined subgroup met the licence criteria and one further trial was included as supportive evidence.
Responder analyses
Efficacy in the responder population (patients showing improvements in asthma symptoms with omalizumab treatment at 16 weeks) is of key importance to the assessment of both clinical and cost-effectiveness. Therefore, in addition to an ITT analysis, detailed consideration was given to the analyses comparing omalizumab responders with control patients where these were reported. As this was not an a priori subgroup, the analyses were underpowered. As with the ITT analyses, meta-analysis was not appropriate and a narrative synthesis, supported by detailed evidence tables, was conducted.
Subgroups
The subgroups of patients who met licence criteria in included trials with broader inclusion criteria were discussed above. In addition, analyses of the following subgroups were undertaken where sufficient data were available. These subgroups were prespecified in the review protocol. These included:
-
subgroups defined by the degree of poor asthma control in terms of number, type and severity of exacerbations, including hospitalisation for an asthma exacerbation (adults and children)
-
subgroups defined according to concomitant treatment received such as maintenance OCS (adults only).
These subgroups were explored in the ITT analyses and the responder analyses. The subgroup data were derived from the MS and from additional information supplied by the manufacturer in response to a request from the assessment group, and represented subgroups which comprised small numbers of patients. These were post hoc analyses by the trial investigators. The methodological heterogeneity between the trials identified for the ITT populations was reflected in these subgroups, and therefore statistical pooling of subgroup data was not undertaken for either the ITT or the responder analyses.
Tests for interaction were undertaken to explore the relationship of hospitalisation or maintenance OCS use to treatment effect for the primary outcome. These analyses assess the validity of any differential subgroup effect.
Observational studies
Observational studies were combined in a narrative synthesis supported by evidence tables for each outcome. These data were at all times considered to represent supportive evidence of efficacy in clinical practice.
Long-term (≥ 52 weeks' data)
There was limited reporting of long-term data and persistence of response; the available data which were reported from RCTs and observational studies were summarised narratively.
Oral corticosteroid-sparing
Where appropriate and where data were available, study estimates of the effect of omalizumab (relative risks, risk ratios, mean differences, with 95% CI) were calculated. The limited evidence from RCTs showed high levels of clinical heterogeneity, which meant that statistical pooling was not appropriate.
Methods for reviewing the safety of omalizumab
The review of the safety of omalizumab was a pragmatic review that utilised the reviews of the adverse effects of omalizumab submitted to, and conducted by, regulatory agencies [European Medicines Agency (EMA) and US Food and Drug Administration (FDA)] and to NICE and existing relevant reviews identified by the searches undertaken for the review of efficacy. A review of adverse effects data reported in the studies considered in the review of the efficacy of omalizumab was also conducted.
Search strategy
In addition to the searches conducted for the review of the efficacy of omalizumab (see Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Search strategy), information on adverse events of omalizumab was identified from searching resources of the US and European drug regulatory agencies (FDA and EMA). No language or date restrictions were applied to the search strategy. In addition, reference lists of all included studies and industry submissions made to NICE in this and previous appraisals (TA133 and TA201) were hand-searched to identify further relevant studies.
Inclusion and exclusion criteria
The FDA, EMA and NICE documents and efficacy studies that reported information on the adverse effects of omalizumab were relevant for the review. The lists of titles/abstracts generated by the electronic searches and all full paper manuscripts and documents of possible relevance to the review of safety of omalizumab were obtained, where possible, and the relevance of each study was assessed by two reviewers; any discrepancies were resolved by consensus. Potentially relevant studies that did not meet all of the criteria were excluded and their bibliographic details listed with reasons for exclusion.
Study design
Randomised controlled trials (including any open-label extensions of these RCTs) and observational studies (including postmarketing surveillance) were included in the evaluation of safety. Information on the rate of adverse events was sought from regulatory sources (FDA, EMA). Previously published reviews were also included where their main aim was to assess the safety of omalizumab. Ongoing long-term safety studies were also identified and are briefly discussed in Adverse events and serious adverse events of omalizumab from review of primary studies, Ongoing studies.
Outcomes
A general overview of the adverse effects of omalizumab was obtained from previous reviews and regulatory agency documents. Our review of primary studies specifically focused on the adverse events of particular concern associated with omalizumab, identified in the Summary of Product Characteristics for omalizumab26 and by clinical advisors, namely: malignancies, anaphylaxis, arterial thrombotic events and mortality. In addition, data relating to the most commonly reported adverse events were also considered.
Data extraction, quality assessment and data analysis
Data relating to adverse and serious adverse events were extracted using a standardised data extraction form and the quality of RCTs and other study designs were assessed using standard checklists as detailed in Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Quality assessment. Reviews and regulatory documents were not formally quality assessed, but the reliability of the data were discussed where relevant. Data extraction and quality assessment was performed by one reviewer and independently checked for accuracy by a second reviewer. Disagreements were resolved through consensus. No formal analysis of the data was performed; the adverse effects of omalizumab were presented as a narrative synthesis.
Methods for reviewing the adverse effects of oral corticosteroids
The review of the adverse effects of OCSs comprised a review of existing systematic reviews.
Search strategy
The review team were given access to an existing internal CRD database of systematic reviews of adverse events as previously used by Golder et al. 27 This database was searched using the terms steroid, corticosteroid, glucocorticoid and all individual steroid names (see Appendix 1). This search was supplemented by a search of The Cochrane library and DARE using terms for steroids coupled with terms for asthma. A further supplementary search was conducted on PubMed to try to identify any very recent relevant systematic reviews (SR).
As for the other review questions, information provided in the MS to NICE was also considered
Inclusion and exclusion criteria
Any systematic review of the adverse effects of OCSs was considered for inclusion in the review. The steroid-related adverse events of particular interest included: bone outcomes (such as fracture), incidence of infectious disease, hypertension, ocular outcomes including cataracts and glaucoma and, in children and adolescents, growth retardation.
Data extraction, quality assessment and data analysis
Relevant data were extracted by one reviewer and checked by a second. The quality of the included reviews was discussed in terms of accepted criteria for systematic reviews as used for the DARE database (clear review question and inclusion criteria, adequate literature searches, quality assessment of included studies, appropriate synthesis), but a formal checklist was not used. The findings of the included reviews were combined in a narrative synthesis.
Results of review of clinical effectiveness: overview
Quantity and quality of research available
The review of clinical effectiveness addressed multiple questions and these are addressed in separate sections Results of review of clinical effectiveness: efficacy of omalizumab to Results of assessment of safety of omalizumab. The quantity and quality of research included to address each question is summarised separately for each question. The studies included in each section of the review are summarised in Figure 1.
FIGURE 1.
Flow chart showing number of studies identified and included in the review of omalizumab efficacy. AE, adverse event.
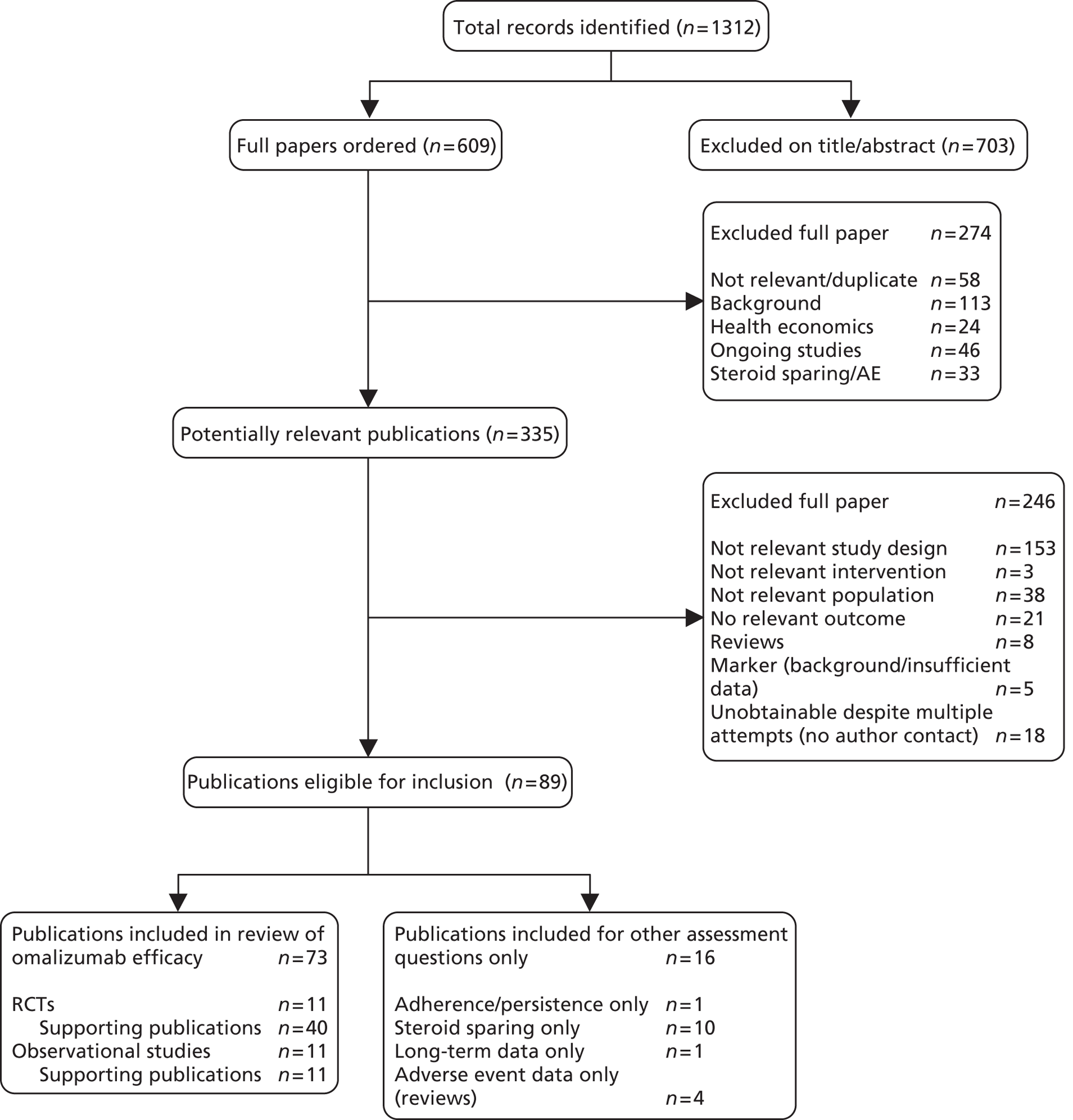
A total of 1312 records were identified from the clinical effectiveness searches (see Figure 1). These searches also identified records relevant to other assessment questions for which separate searches were undertaken (see Figure 2 for the flow chart for the review of the adverse effects of omalizumab). Details of studies excluded at the full publication stage are provided in Appendix 2. All identified records were reported in English.
Results of review of clinical effectiveness: efficacy of omalizumab
Quantity and quality of evidence
Seventy-three publications, representing multiple publications of 11 RCTs and their extensions,19,20,28–36 and 11 observational studies met the inclusion criteria. 37–47 Baseline characteristics from all 11 RCTs and 11 observational studies are presented in Appendices 3–6. The ALTO (a study to evaluate the safety of Xolair in moderate to severe persistent asthma patients) trial was excluded from the review on the basis that the population was not required to have uncontrolled asthma, however defined. Two further large RCTs were excluded because the population was required to be taking ICSs alone and therefore could not meet the omalizumab licence criteria. 48,49 A full list of excluded studies is provided in Appendix 2. The trial of Holgate et al. 2004 (Trial 011)50 was excluded from the main review of efficacy because the patients were required to have well-controlled asthma; however, a subgroup of the trial was included in the review of the steroid-sparing effect of omalizumab.
Quantity and quality of evidence: randomised controlled trials
Of the 11 RCTs included in the review of effectiveness, 10 were relevant to the adult licence (age ≥ 12 years),19,28–36 one was relevant to the children's licence, (age < 12 years)20 and one was relevant to both licences (age 6–20 years). 28 The criteria for the licence and their relationship to the inclusion criteria of included trials and their specified subgroups are shown in Table 2. Full details of the inclusion criteria and population characteristics of these trials are given in Appendices 3 and 4. The MS provided additional information on four RCTs and two observational studies, all of which were identified in the systematic review process. These data were used to supplement those obtained from the published papers. In particular the manufacturer provided data on the omalizumab responder population and on subgroups within the INNOVATE, Evaluate Xolair for Asthma as Leading Treatment (EXALT) and IA-05-EUP (European Union population) trials. Where data are derived from the MS this is explicitly stated. In all other instances the source was a publicly available (published or otherwise) document identified during the systematic review process.
| Trial | Baseline medication | ≥ 2 documented exacerbations | FEV < 80% | Frequent symptoms including required severe uncontrolled asthma | Licence met by inclusion criteria | |
|---|---|---|---|---|---|---|
| High-dose ICS required | LABA required | |||||
| Adults | ||||||
| INNOVATE19 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| EXALT31 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| IA-0430 | ✓ | – | ✓ | – | ✓ | – |
| EUP subgroup | ✓ | ✓ | ✓ | – | ✓ | ✓ |
| Chanez 201029 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Hanania 201133 | ✓ | ✓ | – | ✓ | ✓ | ✓ |
| SOLAR36 | – | – | ✓ | – | ✓ | – |
| Bardelas 201232 | – | –a | – | –b | ✓ | – |
| Hoshino 201234 | ✓ | ✓ | – | – | ✓ | – |
| Ohta 200935 | ✓ | –a | – | –b | ✓ | – |
| Children | ||||||
| IA-0520 | – | – | ✓ | NA | ✓ | – |
| EU subgroup | ✓ | ✓ | ✓ | NA | ✓ | ✓ |
| Busse 201128 | – | – | – | –/NA | ✓ | – |
In the case of studies in which the inclusion criteria did not determine that the trial population or a defined subgroup would correspond with the licence criteria, the reasons for concluding that a substantial, although undifferentiated, proportion of patients met these criteria are documented in Table 3.
| Trial | Baseline medication | Documented exacerbations or other relevant outcome | Mean FEV% predicted | Frequent symptoms including required severe uncontrolled asthma | |
|---|---|---|---|---|---|
| High-dose ICS | LABA or other medication additional to ICSs | ||||
| Adults | |||||
| Hanania 201133 | All patients | All patients | Mean exacerbation rate 1.95/year; subgroup on OCSs or with ≥ 4 exacerbations/year | All patients < 80% | All patients |
| SOLAR36 | Range 200–2400 μg BDP equivalent | 39% LABA | All patients ≥ 2 exacerbations | Mean 78% | All patients |
| Bardelas 201232 | ≥ Fluticasone 250/BDP 360 μg equivalent | 63% LABA | NR | Mean 76% | All patients |
| Alternative to LABA 6% | |||||
| Hoshino 201234 | Mean 829 μg | 30% OCS | NR | Mean 67% | All patients |
| LTRA 73% | |||||
| Theophylline 43%a | |||||
| Ohta 200948 | Mean 1169 μg | 50% LABA | 10% hospitalised in past year; 19% attended ER in past year | Mean 75% | All patients |
| LTRA 54% | |||||
| Theophylline 39% | |||||
| OCS 9%a | |||||
| Children | |||||
| Busse 200148 | 54% receiving 360 μg BDP equivalent | 54% LABA | 25% hospitalised in past year; 78% with unscheduled doctor visit | NA | All patients |
Included randomised controlled trials in which the whole trial population met the omalizumab licence criteria
Three RCTs were included in which the whole trial population met or closely approximated the licence criteria. These were the INNOVATE study (n = 419),19 the EXALT study (n = 404)31 and the study by Chanez et al. (n = 31). 29 All pertained to the adult licence.
Included randomised controlled trials in which a named subgroup of the population met the omalizumab licence criteria
An additional group of RCTs had populations broader than the licence but contained identified subgroups which conformed or approximated to the licence criteria, and for which at least some outcome data were reported. These were the IA-04 study (n = 312)30 in adults and the IA-05 trial in children (n = 628). These both contained an EU population subgroup which met the licence criteria. This subgroup was specified a priori in the IA-05 study, but was post hoc in the IA-04 study. In the case of IA-05, this subgroup provides the only data for the licensed paediatric population.
Included randomised controlled trials in which an undifferentiated proportion of the population met the omalizumab licence criteria
A final group of studies in which it appeared that a proportion of the population met the licence criteria, but where these individuals were not an identified subgroup, was included. These were the studies in adults by Hanania et al. 33 Bardelas et al.,32 the SOLAR (study of omalizumab in comorbid asthma and rhinitis) trial,36 Hoshino et al.,34 and Ohta et al. 35 and the trial by Busse et al. (n = 419)28 for children and young adults. In the absence of defined subgroup or individual patient data (IPD) these trials were included as evidence supportive of the assessment of efficacy in the licensed population.
The Hanania et al. (2011) trial identified three subgroups of patients: those on ICS plus LABA only (M1), those taking ICS plus LABA plus other concomitant medication but not maintenance OCS (M2) and those either taking maintenance OCS or with ≥ 4 exacerbations/past year requiring OCSs (M3). 33 It is considered that the M3 subgroup closely approximates the licensed population, whereas the M2 subgroup is likely to contain a substantial majority of patients who meet the licence criteria. However, as very limited published data were reported for these subgroups and further data were not provided by the manufacturer, this trial could not be used to directly address the review question or be combined with INNOVATE. It is therefore included as supportive evidence only but is considered to be highly relevant to the efficacy of omalizumab in the population of patients with severe uncontrolled allergic asthma (although not as relevant as those trials whose populations reflect the licence).
The trial by Busse et al. is considered to provide supportive evidence for efficacy in children, with 60% of the individuals included aged < 12 years; the population is acknowledged to include a significant proportion of children who do not meet the licence requirements as they are not on maintenance therapy. 28 Nevertheless, in view of the limited evidence pertaining to the licensed paediatric population it is included as supportive evidence.
Validity assessment and risk of bias of randomised controlled trials
The results of the validity assessment and the Cochrane risk of bias assessment for the RCTs are shown in Table 4, with full details in Appendix 7. Overall risk of bias was calculated as outlined in Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Quality assessment. In some cases trials conducted by the manufacturer had unclear reporting of randomisation, allocation concealment and blinded outcome assessment, but it was indicated that the procedures had in fact been conducted using the manufacturer's standard approach. In these cases, the risk of bias from these measures was assumed to be low as the standard process documented in other manufacturer's trial reports represented a low risk of bias. This process was used for the following trials: SOLAR36 and the trials by Hoshino et al.,34 Ohta et al. 35 and Bardelas et al.,32 all of which were included as supportive trials. This materially affected the overall risk of bias judgement only for SOLAR and the trial by Ohta; in both cases the effect was to make the judgement ‘low’ rather than ‘unclear’.
Trials of patients in licensed population
The quality assessment demonstrated that the majority of trials were well conducted. All those in the licensed population or with defined subgroups of patients in the licensed population (INNOVATE, EXALT, and IA-05 EUP and Chanez et al.) had adequate allocation concealment and randomisation. Blinded outcome assessment was reported for INNOVATE,19 Chanez et al. 29 and IA-0520 but not for IA-04 or EXALT;30,31 INNOVATE had an imbalance in baseline characteristics (which was adjusted for in the analyses); other trials reported that baseline characteristics were comparable. Analyses were considered to be appropriate in all trials. Power calculations were reported for all the trials. These related to the primary outcomes of the trials which varied considerably. INNOVATE and IA-05 had clinically significant exacerbations as the primary outcome,19,20 but in EXALT persistence of response was the primary outcome31 and in IA-04 it was asthma deterioration-related incidents. 30 Chanez et al. had a primary outcome related to the expression of an IgE receptor. 29 In IA-04 and IA-05 the defined subgroups which met the licence criteria were not powered to detect the difference identified in the power calculation. 20,30
The INNOVATE and IA-05 studies and the study by Chanez et al. were considered to be at low risk of bias. 19,20,29 The EXALT trial and the IA-04 trial with the EU subgroup of licensed population in adults were considered to be at high risk of bias as a result of their open-label designs. 30,31
Supportive trials
Hanania et al. and Ohta et al. reported adequate allocation concealment, and in Hanania et al. true randomisation procedures were clearly reported as was blinded outcome assessment. 33,35 There was unclear reporting in a number of instances. Power calculations were reported for all trials except the small trial by Hoshino et al. 34 Hanania et al. had clinically significant exacerbations as a primary outcome;33 in SOLAR it was one of two designated primary outcomes. 36 In other trials the power calculation related to ACT score, and other measures of symptoms and lung function.
Of the supportive trials in adults three were considered to be at low risk of bias, including that of Hanania et al. (2011) which was considered highly relevant to the licensed population,33 one at high risk of bias34 and one to have unclear bias. 32 The supportive trial in children had an unclear risk of bias. 28
| Study | Concealed treatment allocation | True randomisation | Outcome assessment blind | Power calculationb | Baseline comparability | Patients accounted for | Appropriate analysis | Risk of bias |
|---|---|---|---|---|---|---|---|---|
| Adults: licensed population | ||||||||
| Ayres 200430 | Yes | Yes | No | Yes | Yes | Yes (partly) | Yes | |
| IA-04 | Low | Low | High | Low | UC | Low | High | |
| Bousquet 201031 | Yes | Yes | No | Yes | Yes | Yes | Yes | |
| EXALT | Low | Low | High | Low | Low | Low | High | |
| Humbert 200519 | Yes | Yes | Yes | Yes | Noc | Yesd | Yes | |
| INNOVATE | Low | Low | Low | Low | Low | Low | Low | |
| Chanez 200429 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Low | Low | Low | Low | Low | Low | Low | ||
| Adults: supportive trials | ||||||||
| Hanania 201133 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Low | Low | Low | Low | Low | Low | Low | ||
| Vignola 200436 | UC | UC | UC | Yes | Yes | Yes | Yes | |
| SOLAR | Low | Low | Low | Low | Low | Low | Low | |
| Hoshino 201234 | UC | UC | No | No | Yes | Yes | No | |
| UC | UC | High | Low | Low | High | High | ||
| Ohta 200935 | Yes | UC | UC | Yes | Yes | Yes | Yes | |
| Low | Low | Low | Low | Low | Low | Low | ||
| Bardelas 201232 | UC | UC | UC | Yes | UC | Yes | Yes | |
| Low | Low | Low | UC | Low | Low | UC | ||
| eHolgate 2004 (011)50 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Low | Low | Low | Low | Low | Low | Low | ||
| Children: licensed population | ||||||||
| Lanier 200920 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| IA-05 | Low | Low | Low | Low | Low | Low | Low | Low |
| Children: supportive trials | ||||||||
| Busse 201128 | UC | UC | Yes | Yes | Yes | Yes | Yes | |
| UC | UC | Low | Low | Low | Low | UC | ||
Randomised controlled trial study and population characteristics
Inclusion criteria for the included RCTs are shown in Appendix 3, population characteristics in Appendix 4 and trial characteristics in Table 5, from which it can be seen that EXALT, IA-04 and the trial of Hoshino et al. were open-label trials with a comparator of standard care. 30,31,34 All other trials were double blind and placebo controlled.
Duration ranged from 16 to 52 weeks overall in adult trials. Trials in which the entire population met licence criteria had durations ranging from 16 weeks (Chanez et al. 29) to 32 weeks (EXALT31); the duration of INNOVATE was 28 weeks. 19 In trials in children the total duration of IA-05 was 52 weeks, of which the final 28 weeks constituted a steroid-sparing phase,20 while Busse et al. had a duration of 60 weeks. 28 Data for IA-05 EUP are reported for the 24-week primary outcome, the 28-week steroid-sparing phase and the total 52-week trial duration, where possible due to the limited data available in this population. Repeated measures data were not available for any adult trial except EXALT, in which treatment protocols did not change over the course of the trial.
| Study | n | Duration (weeks) | Funding | Population | Licencea | Location | Multicentre | Design | Comparator | Randomisation ratio (omalizumab : comparator) | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ayres 2004 | 312 | 52 | Novartis | Adult | 2 | Multinational – five European countries | Yes | Open label | No additional treatment | 2 : 1 | High |
| IA-0430 | |||||||||||
| EU population subgroup | 164 | 1 | |||||||||
| Bousquet 2010 EXALT31 | 404 | 32 | Novartis | Adult | 1 | Multinational –14 countries | Yes | Open label | No additional treatment | 2 : 1 | High |
| Humbert 2005 | 419 | 28 | Novartis | Adult | 1 | Multinational –14 countries | Yes | Double blind | Placebo | 1 : 1 | Low |
| INNOVATE19 | |||||||||||
| Chanez 201029 | 31 | 16 | Novartis | Adult | 1 | France | No | Double blind | Placebo | 2 : 1 | Low |
| bHanania 201133 | 850 | 48 | Novartis | Adult | 3b | USA and Canada | Yes | Double blind | Placebo | 1 : 1 | Low |
| M2 subgroup | |||||||||||
| M3 subgroup | |||||||||||
| Vignola 2004 | 405 | 28 | Novartis | Adult | 3 | NR | Yes | Double blind | Placebo | 1 : 1 | Low |
| SOLAR36 | |||||||||||
| Hoshino 201234 | 30 | 16 | NR | Adult | 3 | Japan | NR | Open label | No additional treatment | 1 : 1 | High |
| Ohta 200935 | 327 | 16 | Novartis | Adult | 3 | Japan | Yes | Double blind | Placebo | 1 : 1 | Low |
| Bardelas 201232 | 271 | 24 | Novartis | Adult | 3 | NR | Yes | Double blind | Placebo | 1 : 1 | Unclear |
| Lanier 2009 | 628 | 24 + 28 steroid reduction | Novartis | Children | 2 | Multinational – seven countries | Yes | Double blind | Placebo | 2 : 1 | Low |
| IA-0520 | 235 | ||||||||||
| EU population subgroup | |||||||||||
| Busse 201128 | 419 | 60 | National Institute of Allergy and Infectious Diseases/Novartis | Children and adolescents | 3 | USA | Yes | Double blind | Placebo | 1 : 1 | Unclear |
Baseline medication
Trials of patients in licensed population
There was some variation in the inclusion criteria and actual medication regimen, even among trials in which the whole population or a defined subgroup met licence criteria (high-dose ICS plus LABA).
The EXALT trial permits the inclusion of patients taking a lower dose of ICSs (≥ 800 μg BDP equivalent) than the IA-04 subgroup or INNOVATE (both ≥ 1000 μg BDP equivalent) and the mean dose for included patients reflects this at approximately 2000 μg compared with 2300 μg for INNOVATE and 2850 μg for IA-04 (see table for exact figures). All of these trials required the use of a LABA, as did the EUP subgroup of IA-04. 19,31,51
The EXALT trial did not report the use of concomitant medications such as LTRA or theophyllines, although these were permitted. 31 Rates of LTRA were comparable between the IA-04 EU subgroup and INNOVATE, although there were differences in other medications reported, for example only INNOVATE reported the use of theophyllines. 19,52 The proportion of patients on OCSs was comparable between EXALT and INNOVATE; their use was not reported in IA-04. Use of rescue medication in IA-04 (mean 4.8 puffs/day) was slightly higher than in EXALT (mean 4 puffs/day), but was lower than use in INNOVATE (mean 6 puffs/day). In the small Chanez et al. (2010) trial, most patients were taking an additional medication and just over 20% were on OCSs. 29
In the IA-05 EU subgroup, children were required to be taking ≥ 500 μg fluticasone or equivalent plus a LABA. The mean dose of fluticasone was 743 μg and 58% were taking an additional medication of which the overwhelming majority were receiving an LTRA. Only six patients were on maintenance OCS. 20
Supportive trials
There was considerably greater variation in inclusion criteria and actual medication regimes for patients in trials which are included as supportive evidence because a proportion of patients met the licence criteria. Notably, the trial by Hanania et al., considered highly relevant to the licensed population, required a dose of ≥ 500 μg fluticasone twice a day or equivalent plus LABA; rescue medication use was 4 puffs/day and 7% of the patients were on OCSs, with 86% of those taking additional concomitant medication (but not OCSs) using an LTRA. 33 A brief summary of data for supportive trials is given in Table 3 above; full details are given in Appendices 3 and 4.
Optimisation of treatment at baseline
The MS stated that INNOVATE, EXALT, IA-04-EUP and IA-05-EUP patients received optimised standard therapy. However, the IA-04 EU subgroup patients were not reported as taking maintenance OCS, despite having an inferred mean exacerbation rate substantially higher than that of patients in EXALT or INNOVATE (in which > 20% of patients were on maintenance OCS) and a requirement to have received treatment in an ER or hospital. It therefore seems possible that they were not receiving optimised standard care at baseline and that the comparison between omalizumab and standard care in the trial may not be conservative. Actual approaches to the optimisation of therapy varied between trials, with different run-in periods reported; variations were also seen in the supportive trials.
Exacerbation and treatment histories
The baseline exacerbation rate reported in the main adult trials was 2.5/14 months for INNOVATE and 2.1/year for EXALT. 19,29,31 It was not reported for EU IA-04, but over 99% of this subgroup had received ≥ 1 OCS course and the mean number of OCS courses in the past year was 4.1. 51 As OCSs are usually prescribed for clinically significant exacerbations, this is an indicator of the probable baseline exacerbation rate. The exacerbation rate in the IA-05 EUP subgroup (which meets the paediatric licence) was 2.8 per year. 20
Only INNOVATE reported the baseline severe exacerbation rate.
In line with the high baseline exacerbation rate, IA-04 EUP subgroup patients had higher rates of both hospitalisation (47%) and ER visits (92%) in the past year than patients in INNOVATE (39% and 56% respectively). 19,51 This also reflects the fact that the inclusion criteria required that one of the two qualifying exacerbations in the past year have resulted in hospitalisation or ER attendance. EXALT patients, by contrast, had substantially lower rates of both hospitalisation (22%) and ER visits (30%) compared with INNOVATE. 31 This is likely to be reflective of the less strict inclusion criteria with respect to exacerbation history.
Baseline exacerbation rates in the supportive adult trials were only reported in Hanania (1.95/year)33 and SOLAR (2.1/year);36 hospitalisation rates were reported only by the Ohta trial (9.8%). 35
The IA-05 EU subgroup had a hospitalisation rate of 12%;20 that in the supportive Busse et al. (2011) trial was substantially higher at 25%, reflecting the fact that this trial included a group of children and adolescents who were not receiving appropriate maintenance treatment. 28
Other parameters
Baseline FEV1 was comparable between studies in the licensed adult population, ranging from 61% to 65% expected, although IA-04 did not use FEV1 as an inclusion criterion. In supportive trials, FEV1 ranged from 65% to 78% expected value. Mean age was also comparable between the adult trials, ranging from 39 to 47 years in the licensed populations and 38 to 55 years in supportive trials. FEV1 was substantially higher in the children's trials at 82% for the IA-05 EUP group and 92% in the Busse trial.
Summary
There were four RCTs that met the adult licence criteria. Two of these were double blind and placebo controlled and were judged to be at low risk of bias; one of these was very small. The remaining two were well conducted but had a high risk of bias because of their open-label design; in one of these only a subgroup of patients met licence criteria. These open-label trials were not placebo-controlled but had a comparator of standard care without omalizumab. There were some differences in the baseline characteristics of these trial and subgroup populations, which are discussed above, but these were not sufficient to make comparisons between trials unreasonable.
One trial with a subgroup in the licensed paediatric population was identified; this was a good-quality double-blind placebo-controlled RCT with a low risk of bias.
Five RCTs were identified as providing supportive evidence for adults and one for the paediatric licence. Of these, only one large trial in adults was considered to be at low overall risk of bias. There were higher levels of clinical heterogeneity between the populations in these trials.
Quantity and quality of evidence: observational studies
The 13 observational studies included in the main review as supporting evidence of the effect of omalizumab in ‘real-world’ clinical situations are summarised in Table 6; full details of the inclusion criteria and population characteristics are in Appendices 5 and 6. Eleven of these studies related to the adult licence and two assessed efficacy in children. It had been anticipated that the observational studies would provide data on the longer-term efficacy of omalizumab but, in the event, this was relatively limited. One study (PERSIST) reported very limited data at 120 weeks follow-up, and only for about a third of the original patients. 39,60 Two relevant studies not identified by our systematic selection process were identified by the manufacturer: those by Britton et al. 61 and Tzortzaki et al. 62 (Two additional studies identified by the manufacturer as potentially relevant did not meet the inclusion criteria for population and were excluded. Chung et al. reported an extension study related to trial 011, in which patients were well controlled at baseline. 63 Storms et al. reported a study in which it was unclear how many patients were using a LABA at baseline and in which high attrition rates made it difficult to determine if outcome data were reported for any patients who met the license criteria. 64)
Tzortzaki et al. provided data on a number of relevant outcomes including clinically relevant exacerbations at 4 years,62 whereas Britton et al. reported mean follow-up of 982 days. These studies provided useful additional data on the longer-term efficacy of omalizumab but were small: Tzortzaki reported on 60 patients and Britton on 52.
Several studies reported data on only a small number of outcomes. Five additional studies were included only for the outcomes of persistence of response, OCS-sparing and safety of omalizumab; these studies are discussed in sections Results of review of clinical effectiveness: efficacy of omalizumab, Evidence of long-term-efficacy and persistence of response to Results of assessment of safety of omalizumab.
The results of the quality assessment for all observational studies, including those included in the assessments of safety and steroid-sparing are shown in Appendix 7. The quality of the observational studies was generally poor. Only one of the observational studies included for the main review, the PAX-LASER cohort, had a control group and in this study it was unclear whether outcome assessment was blinded. 47 The majority of studies reported eligibility criteria, but in most there was poor reporting of losses to follow-up or these losses were substantial (20% or greater). Few studies reported using reliable outcome measures. Six of the studies had sufficient follow-up for long-term assessment but in only three cases was this over 52 weeks (see above). Data derived from these observational studies are included as supportive data; these have relevance to real-world clinical practice but issues of uncertainty or low quality should be borne in mind throughout.
| Study | n | Follow-up duration | Population (licence) | Design | Review questions addressed |
|---|---|---|---|---|---|
| APEX (AIC)37 | 136 | 12 months | Adult (3) | Retrospective one-group | 1 and 3 |
| eXpeRience53 | 876 | 8 months | Adult (3) | Postmarketing surveillance | 1 and 3 |
| Brodlie 201254 | 34 | 16 weeks | Children and adolescents (3) | Prospective one-group | 1 and 3 |
| aKirk 201055 | 18 | 16 weeks | Children (3) | Retrospective one-group | 3 |
| PERSIST39 | 158 analysed (53 retrospective follow-up) | 52 weeks (120 weeks) | Adult (1) | Prospective one-group | 1, 2 and 3 |
| Cazzola 201040 | 142 | 12 months | Adult (2) | Prospective one-group | 1, 2 and 3 |
| Costello 201141 | 93 analysed | 6 months | Adult (2) | Retrospective one-group | 1 and 3 |
| Deschildre 201042 | 104 | 4–6 months | Children and adolescents (3) | Non-comparative cohort | 1 |
| Domingo 201156 | 31 analysed | Mean 17 months | Adult (3) | Prospective one-group | 3 |
| Gutierrez 200757 | 284 | 18 months | Adult (3) | Retrospective comparative | 2 |
| Korn 200944 | 280 (102 maintenance OCS subgroup) | 6 months (> 16 weeks) | Adult (1) | Postmarketing surveillance | 1 and 3 |
| Molimard 200845 | 146 analysed (64 maintenance OCS subgroup) | > 5 months (> 16 weeks) | Adult (2) | Prospective one-group | 3 |
| Ohta 201046 | 133 (37 severe uncontrolled subgroup) | 48 weeks | Adult (3) | Prospective one-group | 1 |
| Randolph 201058 | 29 analysed | 6 years, mean 2.1 years | Adults and children (3) | Prospective one-group | 1 and 2 |
| Stukus 200859 | 45 analysed | NR | Adult (3) | Retrospective one-group | 3 |
| PAX-LASER47 | 767 (486 allergic patients) | ≥ 12 months | Adult (3) | Prospective controlled | 1 and 2 |
| Britton 201161 | 52 | 982 days (median) | Adult | Retrospective one-group | 1, 2 and 3 |
| Tzortzaki 201262 | 60 | 4 years | Adult | Retrospective one-group | 1 and 2 |
Treatment effects of omalizumab: response to treatment
Response to treatment is not the primary outcome of the review, but is presented here first because the derivation of the responder population is key to some of the analyses presented for the primary outcome of clinically significant exacerbations and for unscheduled health-care utilisation.
Response to treatment: global evaluation of treatment effectiveness
The global evaluation of treatment effectiveness (GETE) measures response to asthma treatment on a five-point scale: excellent (complete control of asthma), good (marked improvement of asthma), moderate (discernible, but limited improvement in asthma), poor (no appreciable change in asthma) to worsening of asthma.
GETE ratings were reported by four RCTs in adults (INNOVATE, EXALT, SOLAR and the trial by Bardelas et al. ) and by IA-05-EUP in children. The proportion of omalizumab and standard care patients with physician-rated GETE scores of good or excellent are shown in Table 7.
| Trial | Time point | Omalizumab | Comparator | RR (95% CI) | ||
|---|---|---|---|---|---|---|
| n | % of patients with good/excellent GETE rating | n | % of patients with good/excellent GETE rating | |||
| Adults: licensed population | ||||||
| INNOVATEa | 28 weeks | 209 | 56.5b | 210 | 41.0b | 1.38 (1.13 to 1.69) |
| EXALTa | 16 weeks | 271 | 70.0b | 133 | 28.2b | 2.24 (1.71 to 2.92) |
| Adults: supportive trials | ||||||
| Bardelas 201232 | 24 weeks | 136 | 55.1 | 135 | 48.1 | 1.15 (0.91 to 1.44) |
| SOLAR36 | 28 weeks | 209 | 59.3 | 196 | 41.3 | 1.44 (1.17 to 1.76) |
| Children: licensed population | ||||||
| IA-05a | 52 weeks | 166 | 76.7 | 80 | 64.5 | 1.15 (0.95 to 1.39) |
| EU subgroupa | ||||||
Response to treatment: Asthma Quality of Life Questionnaire change ≥ 0.5 points
IA-04 EUP and SOLAR reported the proportion of patients with a change from baseline in total AQLQ score ≥ 0.5 points, which represents the minimally important difference and is sometimes used as an alternative measure of response (Table 8). Data on this outcome were also reported for INNOVATE, EXALT and IA-05EUP, but these were not used to assess response to treatment by the study authors. There were no data from observational studies on response rate assessed using this criterion. The AQLQ criterion, representing as it does a minimally important difference, may result in an overestimation of the percentage of responders compared with evaluation using GETE. 20 This is supported by comparison of the two measures of response using data from the SOLAR trial.
| Trial | Time point | Omalizumab | Comparator | RR (95% CI) | ||
|---|---|---|---|---|---|---|
| n | % of patients with AQLQ change ≥ 0.5 points | n | % of patients with AQLQ change ≥ 0.5 points | |||
| Adults: licensed population | ||||||
| IA-04 EUP51 | 27 weeks | 115 | 62a | 49 | 42b | NA |
| Adults: supportive trials | ||||||
| SOLAR36 | 28 weeks | 209 | 79 | 196 | 70 | 1.40 (1.06 to 1.85)c |
Response rates from observational studies
Response rates were reported in six observational studies (Table 9): five measured by the GETE and one study in children by a combination of prednisolone dose, lung function and overall clinical status. 54 At 16 weeks the GETE response rate ranged from 69.6% to 86.4% and at 1 year it was reported as 72.3% or 77%.
| Study | n at baseline | n at follow-up | Duration (assessment time point) | Percentage of patients assessed who were responders |
|---|---|---|---|---|
| APEX37 | 136 | 136 | 16 weeks | 82 |
| eXpeRience38 | NR | 523 | 16 weeks | 69.6 |
| PERSIST39 | 158 | 153 | 16 weeks | 82.4 |
| 158 | 130 | 52 weeks | 72.3 | |
| Cazzola 201040 | NR | NR | 12 months | 77 |
| Britton 201161 | 52 | 52 | 16 weeks | 86.4 |
| Brodlie 201254 | 34 | 34 | 16 weeks | 85 |
Response rates: summary of omalizumab treatment effect
The omalizumab GETE response rate in adults reported in the double-blind RCT was around 55% with a RR of around 1.2. The open-label EXALT trial had a substantially higher proportion of omalizumab responders than INNOVATE (70% compared with 56.5%) and a much larger RR (2.24 vs. 1.38). This appears highly likely to be the result of the open-label design of the trial, as the proportion of patients classified as responders is likely to be elevated by the patients' and assessors' knowledge of their treatment allocation. The impact of these differential response rates is discussed in relation to the treatment effects observed in the responder analysis in sections Treatment effects of omalizumab: exacerbations and Hospitalisation and other unscheduled medical care requirements. It is worth noting that the response rate derived from EXALT is likely to be more representative of that seen in clinical practice, partly because of patients' knowledge of their treatment and partly because the assessment was conducted at 16 weeks, as it is in clinical practice. The EXALT omalizumab GETE response rate approaches, but is still lower than, those reported in observational studies.
In children the proportion of omalizumab responders in the IA-05 EUP subgroup was high at 74%, but a high proportion of the placebo group were also classified as responders (RR 1.15; 95% CI 0.95 to 1.39).
Treatment effects of omalizumab: exacerbations
Total clinically significant exacerbations
All the included RCTs reported data on the primary outcome of clinically significant (CS) exacerbations, with the exceptions of Bardelas et al. 32 and Hoshino et al. 34 There was some degree of heterogeneity in the definition of clinically significant exacerbations within trials (see Appendix 8); however, this was not considered sufficient to preclude comparability. CS exacerbations are sometimes reported as total exacerbations, as exacerbations which are not clinically significant are not considered. A number of trials reported data on (or enabled the calculation of) the number of patients experiencing no CS exacerbations.
Results from trials providing data on total exacerbations are presented in Table 10. As can be seen, there is a consistent finding of benefit with omalizumab for both the incidence rate and proportion of patients with no exacerbations in the follow-up period, with the exception of the small trial of Chanez et al. 29 These benefits were statistically significant in all studies except SOLAR, in which a relatively low proportion of patients were taking a LABA. 36 A full report of the data reported for each trial is presented in Appendix 8.
| Trial | Omalizumab | Comparator | Rate ratio (95% CI)a | Patients with zero exacerbations n (%) | Relative risk (95% CI)b | |||
|---|---|---|---|---|---|---|---|---|
| n | Incidence rate | n | Incidence rate | Omalizumab | Comparator | |||
| Adults: licensed population | ||||||||
| cINNOVATE19 | 209 | 0.68c | 210 | 0.91 | 0.738 (0.552 to 0.998) | NR | NR | NA |
| EXALT31 | 271 | 0.55 | 133 | 0.98 | 0.570 (0.417 to 0.778) | 183 (67) | 64 (50) | 1.35 (1.11 to 1.63) |
| IA-04 | 115 | 1.26 | 49 | 3.06 | 0.41 (0.288 to 0.583) | NR | NR | NA |
| EU subgroup51 | ||||||||
| Chanez 201029 | 20 | NR | 11 | NR | NA | 9 (45) | 7 (64) | 0.71 (0.37 to 1.37) |
| Adults: supportive trials | ||||||||
| dHanania 201133 | ||||||||
| ITT | 427 | 0.66 | 423 | 0.88 | 0.75 (0.61 to 0.92) | 275 (64) | 234 (55) | 1.16 (1.04 to 1.30) |
| M2 group | 203 | NR | 191 | NR | 0.72 (0.53 to 0.98) | NR | NR | |
| M3 group | 73 | NR | 71 | NR | 0.95 (0.63 to 1.43) | NR | NR | |
| SOLAR | 209 | NR | 196 | NR | NA | 171 (82) | 146 (75) | 1.10 (0.99 to 1.22) |
| Ohta | 158 | NR | 169 | NR | NA | 145 (96) | 146 (89) | 1.08 (1.01 to 1.15) |
| Children: licensed population | ||||||||
| IA-05 EU subgroup20 | 166 | 80 | NR | NR | NA | |||
| Over 24 weeks | 0.42 | 0.63 | 0.662 (0.441 to 0.995) | |||||
| 24–52 weeks (steroid-sparing phase) | 0.43 | 1.09 | 0.394 (0.27 to 0.57) | |||||
| Over 52 weeks | 0.73 | 1.44 | 0.504 (0.350 to 0.725) | |||||
| Children: supportive trials | ||||||||
| eBusse 201128 | 208 | NR | 211 | NR | NA | 145 (70) | 110 (52) | 1.16 (1.06 to 1.28) |
There was some heterogeneity in the estimates of efficacy for rates of CS exacerbation for the individual trials. This appears to be primarily because of the trial design, with the open-label trials EXALT and IA-04 EUP showing larger estimates of effect than those that were double blind. It is notable that the overall estimate of effect for the Hanania trial was comparable to that for INNOVATE, with the M2 subgroup mirroring this effect. The lack of a treatment benefit in the M3 subgroup is notable but the subgroup was relatively small and underpowered. This cannot, therefore, be considered as evidence for a lower treatment effect in patients using OCSs as maintenance or repeat therapy.
There was considerable clinical heterogeneity across the main and supportive trials in terms of trial design and population. In the main trials, IA-05 was undertaken in children and could not therefore be combined with adult data. IA-04 EUP was a post hoc subgroup of a larger trial. EXALT was an open-label trial with a comparator of optimised standard care which provided consistently higher estimates of the omalizumab treatment effect compared with the double-blind placebo-controlled INNOVATE. Therefore, combining results in a meta-analysis was not considered appropriate.
Apart from the trial by Hanania, supportive trials did not report rates of exacerbations, but SOLAR and the trial by Ohta did report numbers of patients with zero exacerbations in adults. This was statistically significant in the Ohta trial but not the SOLAR trial. 35,36
In children the IA-05-EUP data for the 24-week constant treatment phase (the primary outcome) showed a statistically significant treatment benefit for omalizumab in terms of a reduced CS exacerbations rate. This benefit was seen for the total 52-week period of the trial; despite a steroid-sparing phase between weeks of the trial, it appeared that substantial benefit was accrued in the omalizumab group. The Busse trial also reported a statistically significant benefit of omalizumab in the number of patients with zero exacerbations in children and adolescents. 28
Clinically significant severe exacerbations and clinically significant non-severe exacerbations
Only three of the included trials reported the incidence of CSS exacerbations (Table 11); separate data on CSNS exacerbations in these trials were provided by the manufacturer. All of these were trials in which the inclusion criteria closely approximated the terms of the licence(s): INNOVATE19 and EXALT31 trials in adults and the IA-05 trial (EUP)20 in children.
| CSS exacerbations | ||||||||
|---|---|---|---|---|---|---|---|---|
| Trial | Omalizumab | Comparator | Rate ratio (95% CI)a | Patients with zero exacerbations n (%) | Relative risk (95% CI)b | |||
| n | Incidence rate | n | Incidence rate | Omalizumab | Comparator | |||
| Adults: licensed population | ||||||||
| INNOVATE19 | 209 | 0.24 | 210 | 0.48 | 0.499 (0.321 to 0.777) | 174 (83.2) | 155 (73.8) | 1.13 (1.02 to 1.25) |
| EXALT31 | 271 | 0.24 | 133 | 0.42 | 0.562 (0.341 to 0.924) | NR | NR | NA |
| Children: licensed population | ||||||||
| IA-05 EUP51 | 166 | 80 | NR | NR | NA | |||
| 24 weeks | 0.14 | 0.22 | 0.655 (0.302 to 1.421) | |||||
| 24–52 weeks (steroid-sparing phase)c | 0.11 | 0.25 | 0.44 (0.30 to 0.83)b | |||||
| 52 weeks | 0.27 | 0.50 | 0.545 (0.274 to 1.084) | |||||
| CSNS exacerbations (data from MS)c | ||||||||
| Trial | Omalizumab | Comparator | Rate ratio (95% CI) | NR | NR | NA | ||
| n | Incidence rate | n | Incidence rate | |||||
| Adults: licensed population | ||||||||
| INNOVATE | 209 | 0.44 | 210 | 0.43 | 1.027 (0.77 to 1.372) | NR | NR | NA |
| EXALT | 271 | 0.32 | 133 | 0.58 | 0.56 (0.45 to 0.76) | NR | NR | NA |
| Children: licensed population | ||||||||
| IA-05 (EU subgroup) | 166 | 80 | NR | NR | NA | |||
| 24 weeks | 0.48 | 0.68 | 0.71 (0.50 to 1.00) | |||||
| 24–52 weeks | 0.32 | 0.84 | 0.38 (0.27 to 5.44) | |||||
| 52 weeks | 0.81 | 1.52 | 0.53 (0.41 to 0.68) | |||||
Both INNOVATE and IA-05 EUP defined a CSS exacerbation as a clinically significant exacerbation with an FEV1 (or PEF in the case of INNOVATE) of < 60% of personal best; EXALT used a slightly broader definition, having multiple additional options for meeting the criterion (see Appendix 9). 19,31 This may have resulted in more exacerbations being classified as severe in EXALT compared with INNOVATE or IA-05 EUP. Whether this might have favoured omalizumab in EXALT more than in the other main trials is unclear.
The two adult trials both found a statistically significant treatment benefit of omalizumab. As a result of clinical heterogeneity across the main and supportive trials in terms of trial design and population, combining results in a meta-analysis was not considered appropriate.
IA-05 EUP also reported relative risks in favour of omalizumab in children at 24 weeks, and at 52 weeks despite the steroid-sparing phase from week 28, but they were not statistically significant.
The result from INNOVATE suggests that omalizumab has no treatment benefit in terms of reducing CSNS: its benefit comes through reducing the rate of CSS exacerbations. In contrast, the results from both EXALT and IA-05 EUP suggest that omalizumab has an equally beneficial effect on CSS and CSNS exacerbations. A difference between INNOVATE and EXALT could be explained by the different definitions of CSS exacerbation adopted in these two trials or because one trial is double blind whereas the other is open label, but this cannot hold for the difference between INNOVATE and IA-05 EUP.
Exacerbations: subgroup analyses
Results for post hoc subgroups for INNOVATE and EXALT and IA-05-EUP were provided by the manufacturer (Novartis Pharmaceuticals) (in their submission to NICE or additionally to the assessment group). The subgroups were:
-
patients with a history of hospitalisation
-
patients on OCSs at baseline (not for IA-05-EUP because of the very small number of patients).
Data on patients not on OCSs at baseline and on those with an exacerbation history of ≤ 2 and ≥ 3 exacerbations per year at baseline were also provided to the assessment group and were used in regression analyses.
Data on total exacerbations, CSS exacerbations and CSNS exacerbations were reported. These are shown in Tables 12 and 13 for patients on OCSs or with a history of hospitalisation. Rate ratios were calculated by the AG using an approximation of the standard error (SE) to derive confidence intervals. 25 These data are presented with the caveat that they are derived from small post hoc subgroup analyses and confidence intervals are wide, representing the high uncertainty around the estimate. This is particularly the case with the IA-05 trial, in which we are considering post hoc subgroups of an a priori subgroup.
| Trial | Omalizumab | Control | Rate ratio (95% CI)a | ||||
|---|---|---|---|---|---|---|---|
| n | Exacerbations | Rate | n | Exacerbations | Rate | ||
| Total exacerbations | |||||||
| INNOVATE | 83 | 69 | 0.95 | 79 | 89 | 1.33 | 0.71 (0.52 to 0.97) |
| EXALT | 58 | 52 | 0.99 | 32 | 43 | 1.40 | 0.71 (0.47 to 1.06) |
| IA-05 EU subgroup | 37 | 13 | |||||
| Over 24 weeks | 40 | 1.07 | 16 | 1.23 | 0.87 (0.49 to 1.55) | ||
| 24–52 (28) weeks | 27 | 0.84 | 24 | 1.60 | 0.53 (0.31 to 0.92) | ||
| Over 52 weeks | 67 | 1.94 | 40 | 2.61 | 0.74 (0.50 to 1.09) | ||
| CSS exacerbations | |||||||
| INNOVATE | 83 | 30 | 0.37 | 79 | 52 | 0.66 | 0.56 (0.36 to 0.88) |
| EXALT | 58 | 26 | 0.49 | 32 | 25 | 0.82 | 0.60 (0.35 to 1.04) |
| IA-05 EU subgroup | 37 | 13 | |||||
| Over 24 weeks | 15 | 0.41 | 6 | 0.44 | 0.93 (0.36 to 2.40) | ||
| 24–52 (28) weeks | 10 | 0.33 | 9 | 0.71 | 0.46 (0.19 to 1.13) | ||
| Over 52 weeks | 25 | 0.75 | 15 | 1.15 | 0.65 (0.34 to 1.23) | ||
| CSNS exacerbations | |||||||
| INNOVATE | 83 | 39 | 0.47 | 79 | 37 | 0.47 | 1.00 (0.64 to 1.57) |
| EXALT | 58 | 26 | 0.45 | 32 | 18 | 0.56 | 0.80 (0.44 to 1.46) |
| IA-05 EU subgroup | 37 | 13 | |||||
| Over 24 weeks | 25 | 0.68 | 10 | 0.77 | 0.88 (0.42 to 1.83) | ||
| 24–52 (28) weeks | 17 | 0.46 | 15 | 1.15 | 0.40 (0.20 to 0.80) | ||
| Over 52 weeks | 42 | 1.14 | 25 | 1.92 | 0.59 (0.36 to 0.97) | ||
| Trial | Omalizumab | Control | Rate ratio (95% CI)a | ||||
|---|---|---|---|---|---|---|---|
| n | Exacerbations | Rate | n | Exacerbations | Rate | ||
| Total exacerbations | |||||||
| INNOVATE | 49 | 43 | 0.88 | 42 | 56 | 1.33 | 0.66 (0.44 to 0.99) |
| EXALT | 59 | 56 | 0.98 | 23 | 41 | 1.91 | 0.51 (0.34 to 0.76) |
| CSS exacerbations | |||||||
| INNOVATE | 49 | 14 | 0.29 | 42 | 34 | 0.81 | 0.36 (0.19 to 0.67) |
| EXALT | 59 | 29 | 0.51 | 23 | 20 | 0.93 | 0.55 (0.31 to 0.97) |
| CSNS exacerbationsa | |||||||
| INNOVATE | 49 | 29 | 0.59 | 42 | 22 | 0.52 | 1.13 (0.65 to 1.97) |
| EXALT | 59 | 27 | 0.46 | 23 | 21 | 0.91 | 0.51 (0.29 to 0.90) |
The rate ratios of the subgroup data indicated that there may be an increased treatment effect in patients on OCS maintenance therapy in the INNOVATE trial; however, this was not confirmed by a test for interaction for total exacerbations (OCS interaction with treatment: RR 0.85; 95% CI 0.44 to 1.66). Results of tests for interaction in the hospitalisation group of INNOVATE and in both subgroups in the EXALT trial data also did not show evidence of a significant interactions. Data on subgroups of patients with ≤ 2 exacerbations/year and ≥ 3 exacerbations/year at baseline did not suggest evidence of differential effectiveness in these groups. These data are not presented because they are commercial-in-confidence (CiC). For all outcomes there was considerable overlap of confidence intervals between all subgroups and the ITT population. For all of the subgroups it appeared that the treatment effect on total exacerbations was driven by the impact on CSS exacerbations to a greater degree in INNOVATE than in EXALT; this mirrors the pattern of observed effects in the ITT population.
Exacerbations: responder analyses
The manufacturer also supplied analyses based on patients who responded to omalizumab. For three trials (INNOVATE, EXALT and IA-05 EU subgroup): the responder subgroups were defined using a GETE rating of good or excellent (see section Treatment effects of omalizumab: response to treatment) at 28, 16 and 52 weeks respectively. 19,30,31 For the IA-04 EUP trial, responder status was defined using the criterion of an improvement in mini-AQLQ score of ≥ 0.5 points at 27.
| Trial | n omalizumab/comparator | CSNS exacerbations | CSS exacerbations | Total exacerbations (CS) |
|---|---|---|---|---|
| Rate ratio (95% CI)a | Rate ratio (95% CI)a | Rate ratio (95% CI)a | ||
| Adults: licensed population | ||||
| INNOVATE | 118/210 | 0.51 (0.33 to 0.79) | 0.25 (0.14 to 0.44) | 0.37 (0.27 to 0.52) |
| EXALT | 190/133 | 0.40 (0.28 to 0.58) | 0.42 (0.27 to 0.66) | 0.41 (0.31 to 0.55) |
| IA-04 EU subgroupb | 71/49 | – | – | 0.365 (0.244 to 0.546) |
| Children: licensed population | ||||
| IA-05 EU subgroup | 118/80 | 0.36 (0.32 to 1.03) | 0.35 (0.22 to 0.55) | 0.38 (0.15 to 0.91) |
In the responder analyses both INNOVATE and EXALT demonstrated statistically significant benefits of omalizumab for CS exacerbations and CSS exacerbations (Table 14); the differential estimate of benefit between these trials seen in the ITT analyses was not present. The responder analysis in the EU population subgroup of the double-blind children's trial IA-05 also showed a statistically significant benefit for CSS and CS exacerbations.
Although the open-label design of EXALT is likely to have inflated the response rate compared with that seen in the double-blind INNOVATE, this bias will have been moderated in the responder analysis as the responder population in EXALT probably contained a proportion of people who may be classed as false-positives in terms of response status.
Further responder analyses by subgroup were provided by the manufacturer. These are given in Appendix 10. The concerns about post hoc subgroups discussed in the case of the ITT analysis apply to an even greater extent in the responder analyses where the overall numbers are even smaller. Briefly, although the rate ratios appeared to show larger estimates of treatment effect in patients on maintenance OCS or with at least one hospitalisation in the previous year, confidence intervals were wide, overlapping those for the whole population of omalizumab responders. The subgroup data also appeared to show that response rates in EXALT were close to those of INNOVATE for the subgroups of patients with a history of hospitalisation, patients on maintenance OCS and patients with ≥ 3 exacerbations at baseline (data not presented because they are CiC). This suggests that the much higher response rate in the ITT population of EXALT may be driven by patients outside these groups who had less severe disease at baseline.
Exacerbation rates: data from observational studies
Data on total exacerbations were reported by nine observational studies (Table 15). As can be seen, the data indicate substantial reductions in the exacerbation rate from baseline, and where a treatment effect was reported this showed statistical significance. Studies which are of particular relevance to the appraisal are the Asthma Patient Experience on Xolair (APEX) study, which has high clinical relevance to UK clinical practice, and the Tzortzaki study, which showed sustained benefit over a 4-year period. However, the methodological problems with these studies, including their lack of control groups, should be borne in mind.
| Study | n | Duration (assessment time point) | Exacerbation rate at baseline | Exacerbation rate at follow-up | Difference from baseline |
|---|---|---|---|---|---|
| APEX37 | 136 | 12 months | 3.67/year | 1.73/year | p < 0.001 |
| eXpeRience53 | 876 | 8 months | NRa | 0.4/8 months | NA |
| PERSIST39 | 160 | 16 weeks | NR | 0.95 | 66.5% reduction |
| Cazzola 201040 | 142 | 12 months | 4.87/year | 1.00/year | NR |
| Korn 200944 | 280 | 6 months | NRb | 44/182 had ≥ 1 | NR |
| OCS subgroup | 95 | 0.7/year | −5.0 | ||
| Costello 201141 | 93 | 6 months | 3.18/6 months | 1.24/6 months | p < 0.0001 |
| Molimard 200845 | 154 | > 5 months | 5.5/year | 2.3/yearc | NR |
| Randolph 201058 | 50 (29 assessed) | Mean 2.1 years | NR | NR | No exacerbations 12/29 |
| Reduced exacerbations 7/29 | |||||
| Exacerbations unchanged 10/29 | |||||
| Tzortzaki 201262 | 60 | 4 years | 2.27/year | 0.66/year at 4 years | p < 0.0001 |
Data on severe exacerbations were reported by five observational studies (Table 16). Where reported the data indicated substantial reductions in incidence of severe exacerbations relative to baseline; in Korn et al. this was reported as being statistically significant. 44 However, the comparative PAX-LASER cohort showed statistically significant reductions in severe exacerbation rates in both the omalizumab and control arms, although the reduction was larger in the omalizumab arm (between-group comparisons were not reported). 47 The data from Deschildre et al. indicated substantial reductions in children (mean age 11.8 years). 42
| Study | n | Duration (assessment time point) | Exacerbation rate at baseline | Exacerbation rate at follow-up | Difference from baseline |
|---|---|---|---|---|---|
| eXpeRience53 | 876 | 8 months | 2.1/year | 0.1/8 months | NR |
| PERSIST 200939 | 160 | 16 weeks | 2.67/year | NR, but 84/128 free from severe exacerbation | NR |
| PAX-LASER Zureik 201047 | 767 | ≥ 12 months | NR | HR from baseline | |
| 374 omalizumab | 20.8/100 patient/year | 0.40 (0.28 to 0.58) | |||
| 393 control | 33.4/100 patient/year | 0.56 (0.43 to 0.74) | |||
| Korn 200944 | 280 | 6 months | 4.5/year | 0.3/year | p < 0.001 |
| aDeschildre 201042 | 104 | 4–6 months | 4.4/year | 0.51/year | NR |
Exacerbation rates: summary of omalizumab treatment effect
There was clear evidence of efficacy of omalizumab in RCTs and RCT subgroups in the adult licensed populations, with statistically significant benefits for the outcomes of total (CS) exacerbations; CSS exacerbations and CSNS exacerbations (where reported). 19,30,31 There was evidence of a larger treatment effect in the open-label trials than in the double-blind placebo-controlled trials.
There was also evidence of treatment benefit in wider populations in trials included as supportive evidence; in particular in the large (n = 850) trial of Hanania et al., which showed statistically significant benefits in the whole trial population and in the M2 subgroup of patients taking medication additional to ICS plus LABA. 33 Although the M3 subgroup of patients on maintenance OCS or with four or more exacerbations in the previous year did not show such a benefit, this group was underpowered. All adult trials except SOLAR (which has a low proportion of patients who potentially meet the licence criteria) and the small study of Chanez et al. showed a statistically significant benefit of omalizumab, with the SOLAR result close to statistical significance.
As the only two trials in adults that reported on CSS, both INNOVATE and EXALT found statistically significant reductions in CSS exacerbations with similar effect sizes, but only EXALT showed a statistically significant benefit for CSNS exacerbations. This may indicate that in the double-blind placebo-controlled trial much of the benefit in total exacerbation reduction was driven by reductions in severe exacerbations.
Responder analyses from INNOVATE and EXALT comparing omalizumab responders with all comparator patients showed a similar pattern to the ITT analyses with a statistically significant benefit for all licensed populations for total exacerbations and CSS and CSNS exacerbations. In contrast to the ITT analyses, there was little difference between the estimates of effect from the trials in total; as discussed above, this may be a consequence of the impact of trial design on the proportion of responders. However, it remained the case that INNOVATE showed a larger treatment benefit for CSS exacerbations than for CSNS exacerbations, whereas EXALT showed a similar effect size for both types of exacerbation.
There was limited evidence from observational studies but the available data reflected that from the RCTs, indicating substantial reductions from baseline and, where statistical tests were reported, these indicated that significant benefit was obtained for both total exacerbations and CSS exacerbations.
In children there was a statistically significant benefit of omalizumab on total exacerbation rate in the IA-05 EUP subgroup but not on the CSS or CSNS exacerbation rates. It is probable that this was a consequence of lack of power in the subgroup. The responder population showed a statistically significant benefit for both total and CSS exacerbations. The Busse et al. trial, which was included as supportive evidence, also showed a statistically significant benefit for the number of children and adolescents with zero exacerbations. 28 The limited evidence from a single uncontrolled observational study indicated a substantial reduction in severe exacerbations in children. 42 The value of this supportive evidence is limited by quality and issues of generalisability to UK clinical practice.
Hospitalisation and other unscheduled medical care requirements
A range of outcomes were recorded, from admissions to intensive care units to unscheduled general practitioner (GP) appointments. The most relevant outcomes for the purposes of the review were hospitalisation, attendance at emergency department and unscheduled/urgent medical appointments. Five trials reported at least one of these outcomes.
Hospitalisation
Hospitalisation data for adult populations were reported by the IA-04-EUP, EXALT and INNOVATE trials19,30,31 and the small study by Chanez et al. (which reported zero events)29 (Table 17). The relative treatment effect for hospitalisation rate favoured omalizumab in both INNOVATE and EXALT, but was statistically significant only in EXALT. No trial found a treatment effect of omalizumab in terms of the number of patients avoiding hospitalisation (zero hospitalisation), although EXALT did find a benefit when hospitalisation and ER visits were counted together (RR 1.24; 95% CI 1.08 to 1.41). In EXALT and IA-04 EUP the number of days in hospital was also reported but statistical comparisons were not reported.
In children, the IA-05 EUP showed no evidence of a difference in hospitalisation rates between the groups or in the number of patients with zero hospitalisations (see Table 21). The supporting Busse et al. trial,28 which did not report data separately for those aged < 12 years, reported a very small but statistically significant benefit of omalizumab. This may reflect the inclusion of patients not receiving appropriate maintenance therapy at baseline. 28
| Trial | Omalizumab | Comparator | Rate ratio (95% CI)a | Patients with zero hospitalisations n (%) | Relative risk (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| n | Rate of hospitalisations/treatment period | n | Rate of hospitalisations/treatment period | Omalizumab | Comparator | |||
| Adults: licensed population | ||||||||
| INNOVATE | 209 | 0.06 | 210 | 0.12 | 0.540 (0.250 to 1.166) | 198 (95) | 192 (91) | 1.04 (0.98 to 1.09) |
| EXALTb | 271 | 0.05 | 133 | 0.14 | 0.332 (0.118 to 0.937) | 249 (92)c | 112 (88)c | 1.05c (0.97 to 1.13) |
| IA-04, EU subgroupd | 115 | NR | 49 | NR | NA | 103 (89) | 44 (90) | 1.00 (0.89 to 1.12) |
| Chanez 201029 | 20 | 0 | 11 | 0 | N/A | 20 (100) | 11 (100) | N/A |
| Children: licensed population | ||||||||
| IA-05, EU subgroup | 166 | 0.06 | 80 | 0.06 | 1.002 (0.268 to 3.743) | 151 (95) | 72 (95) | 1.00 (0.94 to 1.06) |
| Children: supportive trials | ||||||||
| eBusse 201128 | 208 | NR | 211 | NR | NA | 205 (99) | 198 (94) | 1.05 (1.01 to 1.09) |
Data on hospitalisation rates from INNOVATE and EXALT were also reported in the MS for the subgroups of patients who had been hospitalised in the previous year and for patients on maintenance OCS (Table 18). The rate ratios are suggestive of a greater effect in these subgroups. However, CI calculated using an approximation of the standard error were wide and these are subgroup results, so great reliance should not be placed on them, particularly given the lack of a statistically significant interaction in the primary outcome of CS exacerbations.
| Trial | Rate of hospitalisations/treatment period | Rate ratio (95% CI)a | |||
|---|---|---|---|---|---|
| Omalizumab | Comparator | ||||
| n | Rate | n | Rate | ||
| Hospitalisation subgroup | |||||
| INNOVATE | 83 | 0.15 | 79 | 0.25 | 0.60 (0.29 to 1.22) |
| EXALT | 58 | 0.17 | 32 | 0.29 | 0.59 (0.24 to 1.45) |
| Maintenance OCS subgroup | |||||
| INNOVATE | 49 | 0.13 | 42 | 0.28 | 0.46 (0.17 to 1.22) |
| EXALT | 59 | 0.09 | 23 | 0.28 | 0.32 (0.10 to 1.05) |
Emergency care use: emergency department visits and unscheduled doctor visits
The results are presented in Table 19. A statistically significant reduction in total emergency visits was seen in all three of these adult trials. The small Chanez trial reported a non-significant difference in median change from baseline for emergency department and doctor visits combined. 29 Emergency department treatment and unscheduled doctor visits were reported separately by the INNOVATE, EXALT and IA-04 –EUP trials. 19,30,31 As with hospitalisation rates, the only study to show a statistically significant benefit of omalizumab for emergency department visits was EXALT; the INNOVATE and IA-04 EUP trials showed non-significant results favouring omalizumab. Unscheduled doctor visits showed a corresponding pattern, with only EXALT showing a statistically significant benefit of omalizumab in event rate. A statistically significant reduction in total emergency visits was seen in all three of these trials.
| Trial | n omalizumab | n comparator | ER attendance | Unscheduled doctor visits | Total emergency visitsa |
|---|---|---|---|---|---|
| Rate ratio (95% CI)b | Rate ratio (95% CI)b | Rate ratio (95% CI)b | |||
| Adults: licensed population | |||||
| INNOVATE19 | 209 | 210 | 0.659 (0.208 to 2.094) | 0.546 (0.271 to 1.100) | 0.561 (0.325 to 0.968) |
| EXALT31 | 271 | 133 | 0.186 (0.057 to 0.613) | 0.452 (0.268 to 0.760) | 0.400 (0.244 to 0.654) |
| IA-04 EUP51 | 115 | 49 | 0.67 (0.34 to 1.33) | 0.77 (0.53 to 1.11) | 0.76 (0.64 to 0.89) |
| Chanez 201029 | 20 | 11 | Omalizumab: change from baseline 0.0 (−2 to 1) | NR | |
| Comparator: change from baseline 0.0 (−1 to 1) | |||||
| Children: licensed population | |||||
| IA-05 EUP20 | 166 | 80 | 1.467 (0.767 to 2.62) | 1.417 (0.767 to 2.620) | 1.347 (0.751 to 2.416) |
For children the IA-05 EUP subgroup showed no statistically significant difference between omalizumab and placebo at either 24 or 52 weeks for the incidence of emergency department attendance, unscheduled doctor visits and total emergency (Table 19), but the direction of effect favoured placebo, in contrast to the result in adults. Busse et al. 28 did not report data for these outcomes.
Data on emergency care use from INNOVATE, EXALT and IA-05 EUP were also reported in the MS for the subgroups of patients who had been hospitalised in the previous year or who were on maintenance OCS (Table 20), and the effects look favourable. However, CIs calculated using an approximation of the standard error were wide so great reliance should not be placed on them, particularly given the lack of a statistically significant interaction on the primary outcome of CS exacerbations.
| Trial | Rate of attendance/treatment period | Rate ratioa | |||
|---|---|---|---|---|---|
| Omalizumab | Comparator | ||||
| n | Rate | n | Rate | ||
| Hospitalisation subgroup | |||||
| ER attendance | |||||
| INNOVATE | 83 | 0.06 | 79 | 0.09 | 0.67 (0.21 to 2.11) |
| EXALT | 58 | 0.06 | 32 | 0.16 | 0.38 (0.09 to 1.59) |
| Unscheduled doctor visits | |||||
| INNOVATE | 83 | 0.11 | 79 | 0.38 | 0.29 (0.14 to 0.61) |
| EXALT | 58 | 0.40 | 32 | 0.85 | 0.47 (0.27 to 0.82) |
| Total emergency visits | |||||
| INNOVATE | 83 | 0.33 | 79 | 0.75 | 0.44 (0.28 to 0.69) |
| EXALT | 58 | 0.63 | 32 | 1.31 | 0.48 (0.31 to 0.75) |
| Maintenance OCS subgroup | |||||
| ER attendance | |||||
| INNOVATE | 49 | 0.10 | 42 | 0.10 | 1.00 (0.27 to 3.72) |
| EXALT | 59 | 0.03 | 23 | 0.09 | 0.33 (0.05 to 2.34) |
| Unscheduled doctor visits | |||||
| INNOVATE | 49 | 0.12 | 42 | 0.14 | 0.86 (0.28 to 2.67) |
| EXALT | 59 | 0.59 | 23 | 0.98 | 0.60 (0.35 to 1.01) |
| Total emergency visits | |||||
| INNOVATE | 49 | 0.28 | 42 | 0.41 | 0.68 (0.34 to 1.38) |
| EXALT | 59 | 0.71 | 23 | 1.35 | 0.53 (0.33 to 0.84) |
Emergency care use: responder analysis
In the responder analyses of emergency care use, INNOVATE and EXALT showed a benefit of omalizumab although it was not always statistically significant, but in IA-04 EUP this was much less pronounced with very wide non-significant confidence intervals (Table 21). The differential estimate of benefit between INNOVATE and EXALT seen in the ITT analyses was not present. In children in the IA-05 EUP subgroup there was a statistically significant benefit in hospitalisation rates but non-significant benefits for other emergency care use measures.
| Trial | Hospitalisation | ER attendance | Unscheduled doctor visits | Total emergency visits |
|---|---|---|---|---|
| Rate ratio (95% CI)a | Rate ratio (95% CI)a | Rate ratio (95% CI)a | Rate ratio (95% CI)a | |
| Adults: licensed population | ||||
| INNOVATE | 0.28 (0.10 to 0.80) | 0.27 (0.06 to 1.19) | 0.25 (0.12 to 0.53) | 0.24 (0.14 to 0.41) |
| EXALT | 0.15 (0.05 to 0.43) | 0.21 (0.07 to 0.62) | 0.32 (0.23 to 0.44) | 0.27 (0.20 to 0.35) |
| IA-04, EU subgroupb | 0.83 (0.27 to 2.56) | 0.62 (0.27 to 1.42) | 0.92 (0.60 to 1.42) | NR |
| Children: licensed population | ||||
| IA-05,c EU subgroup | 0.25 (0.09 to 0.67) | 0.69 (0.35 to 1.39) | 0.76 (0.50 to 1.17) | 0.79 (0.56 to 1.10) |
Subgroup responder analyses for adult patients on OCS maintenance or hospitalisation in the previous year were presented by the manufacturer (see Appendix 10). These were suggestive of a greater magnitude of treatment effect on hospitalisation rates in both subgroups and on total unscheduled care in the OCS maintenance subgroup. As before, the small numbers, multiple subgroups and lack of variance estimates should be borne in mind in interpreting this evidence.
Emergency care use: data from observational studies
Hospital visits, ER attendance and unscheduled doctor visits were reported by nine observational studies; data are shown in Table 22. The APEX study reported statistically significant benefits of omalizumab for all three measures of unscheduled care, whereas Korn et al. reported such benefits for hospitalisation and a combined measure of emergency visits and PAX-LASER for combined hospitalisation and ER visits. 37,44,47 PAX-LASER also reported a statistically significant benefit over the comparator group for this outcome. Although other studies did not report statistical tests of difference from baseline, the data which were reported did support the pattern of a reduction in incidence of unscheduled care of all kinds associated with omalizumab treatment. In particular, Britton et al. reported numerical reductions in all forms of unscheduled care. The results of the APEX and Britton et al. studies are of particular relevance to UK clinical practice, representing data from UK severe asthma centres over periods of 12 months and 2.7 years respectively. 61,65 The controlled PAX-LASER study is also of importance in showing significant benefits over usual care. 47 The observational studies showed a consistent pattern of statistical significance which corresponds to that seen in the EXALT trial;31 benefits in the double-blind RCT did not reach statistical significance. This may reflect weaker methodology or may be indicative of the fact that in many of the studies (e.g. Britton et al. 61) it is unclear whether only data for responders are reported.
| Study | n | Duration (assessment time point) | Hospital admission | ER attendance | Unscheduled doctor visits |
|---|---|---|---|---|---|
| APEX37 | 136 | Baseline | 1.30/year | 1.52/year | 4.54/yeara |
| 12 months | 0.51/year | 0.46/year | 3.82 | ||
| Difference from baseline | p < 0.001 | p < 0.001 | p < 0.001 | ||
| eXpeRience53 | 876 | Baseline | 6.2/year | ||
| 8 months | 0.3/8 months | ||||
| Difference from baseline | NR | ||||
| PERSIST39 | 160 | Baseline | 64 (40.5%) | 22 (13.9%) | NR |
| 120 weeks | 1/53 (1.9%) | 0/53 (0%) | NR | ||
| Difference from baseline | NR | NR | NA | ||
| PAX-LASER47 | 767 | Baseline | NR | NR | |
| 8 months | NR | NR | |||
| Difference from baseline | RR 0.40 (95% CI 0.28 to 0.58) | NA | |||
| RR 0.56 (95% CI 0.43 to 0.74) compared with standard care | |||||
| Korn 200944 OCS subgroup | 280 | Baseline | 67 (23.9%) | 238 (85% 4.4/year) | |
| 6 months | 12 (5%) | 48 (19.9%) | |||
| Difference from baseline | p < 0.001 | p < 0.001 | |||
| 95 | Baseline | NR | NR | ||
| 6 months | 0.1/year | NR | |||
| Difference from baseline | −0.5/year | NA | |||
| Cazzola 201040 | 142 | Baseline | 4.45/year | 1.53/year | |
| 12 months | 1.23/year | NR | |||
| Difference from baseline | NR | NR | |||
| Costello 201141 | 93 | Baseline | 2.4/6 months | NR | NR |
| 6 months | 0.8/6 months | NR | NR | ||
| Difference from baseline | p < 0.001 | NA | NA | ||
| Molimard 200845 | 154 | Baseline | 1.5/year | 3.0/year | NR |
| > 5 months | 1.2/year | 1.1/year | NR | ||
| Difference from baseline | NR | NR | NR | ||
| Britton 201161 | 52 | Baseline | 165/2 years | 164/2 years | 474/2 years |
| Mean 982 days (range 112–3839) | 12 | 27 | 115 | ||
| Difference from baseline | NR | NR | NR | ||
Hospitalisation and unscheduled care: summary of omalizumab treatment effect
There was limited evidence of benefit in the adult ITT populations: of the trials which reported data for these outcomes only EXALT showed statistically significant benefits. There was some indication of greater benefit in subgroups of patients taking maintenance OCS or with a history of hospitalisation in the previous year for the outcome of hospitalisation, but confidence intervals calculated using an approximation of the standard error were wide and a post hoc subgroup effect was not supported by tests for interaction on the outcomes of CS exacerbations.
Analyses comparing omalizumab responders with placebo/standard care patients showed evidence of statistically significant benefit for both INNOVATE and EXALT across the outcomes assessed with the exception of ER attendance in INNOVATE. This pattern of results is similar to that seen for exacerbations.
Only limited data on emergency care use were available from observational studies but they showed evidence of substantial reductions across all types of care; where statistical tests were reported these showed significant benefits of omalizumab treatment relative to baseline or standard care.
In children the IA-05 EUP group showed no significant differences between the groups for any emergency care use outcome in the ITT analysis. Supportive evidence from the trial by Busse et al. 28 indicated a statistically significant benefit of reduced hospitalisation, but this result may be driven by children/adolescents not on appropriate maintenance therapy.
Responder analysis results from IA-05-EUP indicated a statistically significant benefit in reduced hospitalisation rates in omalizumab responders, but only non-significant effects on other unscheduled care.
Asthma symptoms
Symptom scores
A number of different scales were used to assess symptom control in the included trials (Table 23): the Wasserfallen asthma symptom score; ACT; ACQ; the Total Asthma Symptom Severity score; and an unspecified asthma symptom score. Full data on changes from baseline in total asthma clinical symptom scores were reported for INNOVATE, IA-04 EUP and IA-05 EUP in the MS, together with changes in the nocturnal symptom score, morning symptom score and daytime symptom score. These supplemented the more limited data reported in trial publications. Different measurement tools were used to assess change in asthma symptoms over time. The ACT scores symptoms on a scale of 1 (worst) to 5 (best), with a higher overall score denoting greater improvement. By contrast, a higher overall score using the ACQ, Total Asthma Symptom score and Wasserfallen symptom denotes a worsening in symptoms; a lower score represents better asthma control.
There were statistically significant benefits of omalizumab on change from baseline in the total symptom score in the INNOVATE trial. The IA-04 EU subgroup showed a statistically significant benefit of omalizumab on the Wasserfallen symptom score, whereas the EXALT trial showed a similar benefit on the ACQ.
In supportive trials in adults the SOLAR and Hanania et al. trials found statistically significant benefits on the Total Asthma Symptom Severity score and the Wasserfallen symptom score respectively. 33,36
In the IA-05 EU subgroup there were no statistically significant changes from baseline in total asthma clinical symptom score in children at either 24 or 52 weeks; similar results were found using the Wasserfallen symptom score. Busse et al. found a statistically significant benefit on ACT score in children aged ≤ 11 years but not in older children and adolescents. 28
| Trial | Outcome reported | Time point (weeks) | Omalizumab | Comparator | Treatment effect | ||
|---|---|---|---|---|---|---|---|
| n | Difference | n | Difference | ||||
| Adults: licensed population | |||||||
| INNOVATEa | Total asthma clinical symptom score | 28 | 172 | −0.66 | 177 | −0.40 | p = 0.039 |
| EXALTa | ACQ | 32b | 238 | −0.91 | 104 | −0.04 | RR −0.87 (95% CI −1.09 to −0.65) |
| IA-04 EU subgroupa | Wasserfallen symptom score | 52 | 115 | −6.7 | 49 | 0.5 | p < 0.05 |
| Adults: supportive trials | |||||||
| Hanania (2011)28 | Total Asthma Symptom Severity score | 48 | 427 | −1.58 | 421 | −1.31 | −0.26 (95%CI −0.42 to −0.10) |
| SOLAR31 | Wasserfallen symptom score | 28 | 204 | NR | 181 | NR | −1.8 (p = 0.023) |
| Bardelas (2012)27 | ACT | 24 | 136 | 5.01 | 135 | 4.36 | 0.61 (95% CI −0.30 to 1.59) |
| Ohta (2009)30 | Unspecified | 16 | 151 | NR | 164 | NR | NS favoured omalizumab |
| Children: licensed population | |||||||
| IA-05, EU subgroupa | Total asthma clinical symptom score | 24 | 158 | −1.41 | 75 | −1.12 | p = 0.434 |
| 52 | 158 | −1.81 | 75 | −1.67 | p = 0.494 | ||
| Wasserfallen symptom score | 24 | 155 | −6.99 | 155 | −6.68 | p = 0.781 | |
| 52 | 74 | −8.57 | 74 | −8.16 | p = 0.695 | ||
| Children: supportive trials | |||||||
| Busse (2011)28 | ACT | 60 | 195 | 191 | |||
| Age 4–11 yearsc | 2.5d | 1.8d | 0.78 (95% CI 0.21 to 1.35) | ||||
| Age ≥ 12 yearsc | 2.2d | 2.0d | 0.19 (95% CI −0.42 to 0.79) | ||||
Individual symptoms
INNOVATE and EXALT and the small Chanez et al. trial reported data on at least one individual asthma symptom for the licensed population in adults; in children data were reported for the IA-05 EU subgroup. Supportive trials reporting data were those of Bardelas and Ohta in adults and Busse et al. in children (Table 24). 28,32,35 Outcomes reported were night awakenings, days with/without symptoms and activity impairment. Individual components of the asthma symptom score reported above also addressed night-time, morning and daytime symptoms. The results were variable but there was some evidence of impact on disturbed sleep, with statistically significant results reported by EXALT and the Bardelas et al. trial, as well as the Busse et al. trial in children and adolescents; the Ohta trial and the small Chanez trial reported non-significant results.
| Trial | Outcome reported | Time point (weeks) | Omalizumab | Comparator | Treatment effect | ||
|---|---|---|---|---|---|---|---|
| n | Difference | n | Difference | ||||
| Adults: licensed population | |||||||
| aINNOVATE19 | Days symptom free/2 weeks (%) | 28 | 172 | 37.2b | 177 | 22.6 | NR |
| aEXALT31 | Days disturbed sleep/2 weeks | 32b | 238 | −4.05c | 104 | −2.71c | p = 0.039 |
| Chanez 201029 | Median (range) days disturbed sleep | 16 | 20 | −0.6 (−6 to 1)c | 11 | 0.3 (−4 to 2)c | p = 0.405 |
| Median (range) days with symptoms | −1.4 (−7 to 3)c | (−4 to 2)c | p = 0.140 | ||||
| Median (range) days with activity impairment | −0.4 (−7 to 2)c | −0.3 (−7 to 2)c | p = 0.740 | ||||
| Adults: supportive trials | |||||||
| Bardelas 201232 | Days/week symptoms | 24 | 136 | −2.16c | 135 | −1.77c | p = 0.202 |
| Night wakening/week | −1.45c | −1.06c | p = 0.019 | ||||
| Ohta 200935 | No days disturbed sleep | 16 | 151 | NR | 164 | NR | NS improvement favouring omalizumab |
| Children: licensed population | |||||||
| cIA-05 EUP20 | Days sleep disturbed mean (SD) | 24 | 158 | −0.63c | 75 | −0.50c | p = 0.114 |
| Children: supportive trials | |||||||
| dBusse 201128 | Mean (SE) days/week with symptoms | 60 | 195 | 1.32 | 191 | 1.76 | 0.44 (95% CI −0.70 to −0.17) |
| Mean (SE) days sleep disturbed | 0.42 | 0.59 | −0.17 (95% CI −0.31 to −0.03) | ||||
| Mean (SE) days with activity impairment | 0.70 | 0.98 | −0.28 (95% CI −0.47 to −0.09) | ||||
Asthma symptoms data from observational studies
Six small observational studies reported on asthma symptoms (Table 25). Five of the studies reported ACT scores (four in adults and one in children) and one ACQ scores over 8 months in adults. Where adult studies reported difference from baseline these indicated statistical significance, in other studies it was unclear. The Brodlie et al. study54 found statistically significant increases in the ACT, providing some useful evidence of the impact of omalizumab on day-to-day asthma symptoms in UK children with severe OCS-dependent asthma.
| Study | n at baseline | n at follow-up | Duration (assessment time point) | Score at baseline | Score at follow-up | Difference from baseline |
|---|---|---|---|---|---|---|
| ACT | ||||||
| APEX37 | 54 | 54 | 16 weeks | 10 | 16 | Reported to be statistically significant |
| 15 | 15 | ≤ 12 months | 11 | 20 | Reported to be statistically significant | |
| Brodlie et al. 201254 | 23 | 23 | 16 weeks | 12 (6 to 24) | 20 (12 to 26) | p = 0.0001 |
| • ≤ 12 years subgroup | 8 | 8 | 16 weeks | 11 (6 to 15) | 18 (12 to 26) | p = 0.0027 |
| • 12–16 years subgroup | 15 | 15 | 16 weeks | 16 (6 to 24) | 21 (15 to 25) | p = 0.0075 |
| Randolph 201058 | 50 | 29 | Mean 2.1 years | NR | 25/29 (86%) scored ≥ 20 | NR |
| Britton 201061 | 52 | 52 | Mean 982 days | NR | NR | + 7.29 (SD 4.64) points |
| Tzortzaki 201262 | 60 | 60 | 4 years | 17.28 | 21.50 | p < 0.0001 |
| ACQ | ||||||
| eXpeRience53 | NR | NR | 8 months | 2.7 | 1.83 | −0.74 (1.17) |
Data on the percentage of patients experiencing daily asthma symptoms and night-time awakenings was also reported by Korn et al. who found statistically significant reductions (p < 0.001) in both measures at both 4 and 6 months. 44
Asthma symptoms: summary of omalizumab treatment effect
There was considerable heterogeneity in the assessment of asthma symptoms in the included studies:19,31–33,35,36,61,62,65 a wide range of scales and individual symptom measures were used to assess response to therapy. In RCTs there was evidence of a statistically significant benefit of omalizumab on symptom scales in the three licensed population groups in adults (INNOVATE, EXALT and IA-04-EUP) and also in the supportive SOLAR and Hanania et al. trials; the studies of Bardelas et al. and Ohta et al. showed non-significant benefits. The observational studies APEX and eXpeRience showed evidence of benefit on symptom scores but did not report statistical test results, although APEX reported that there were significant differences compared with baseline. Additional studies by Tzortzaki and Britton also showed evidence of benefit with Tzortzaki showing statistical significance at 4 years. Although these studies were small and uncontrolled, they showed evidence of sustained benefit of omalizumab treatment over a relatively long period of time in patients relevant to UK clinical practice.
There was mixed evidence of impact on individual symptom measures, with most evidence of a treatment benefit for outcomes related to disturbed sleep for which benefits were reported in EXALT and the trial by Bardelas et al. as well as the observational study of Korn et al.
There was limited evidence of efficacy in children. The IA-05-EUP showed a non-significant benefit of omalizumab on both the total asthma symptom score and disturbed sleep assessment. Supportive evidence from the Busse et al. trial indicated a significant benefit in ACT score in children aged > 12 years, but a non-significant effect in those aged < 12 years; individual symptom scores showed significant benefit for the whole trial population of children and adolescents. The small study by Brodlie et al. indicated highly statistically significant gains in asthma control in OCS-dependent children aged < 12 years as well as in older adolescents;54 these children correspond closely to those treated in severe asthma clinics in the UK.
Symptom control is one of the key aims of asthma therapy but evaluation of symptom outcomes is complicated by the wide range of measures used to assess day-to-day symptoms. A number of different scales were employed in the studies, including in the key trials, making comparisons, even within the licensed population, difficult. Different methods were used to appraise individual symptom occurrence, with few symptoms reported consistently across trials and observational studies.
Use of rescue medication
Use of rescue medication: results from randomised controlled trials
A majority of trials reported some data on rescue medication use (Table 26). This was reported as either puffs required or number of days on which the medication was required. In the licensed population, INNOVATE, the IA-04 EU subgroup and the Chanez et al. trials reported data for adults and the IA-05 EU subgroup reported data for children. For INNOVATE and the IA-04 EU subgroup these data were drawn from the review by King et al., which was an appendix to the MS;66 data for the whole trial population were reported for slightly different outcomes (data not shown). Supportive trials reporting data in adults were SOLAR and the trials by Hanania, Bardelas and Ohta. With the exception of the IA-04 EUP and Hanania et al. trials, the differences between the groups favoured omalizumab but were not statistically significant; King et al. suggested that the IA-04 EUP result was anomalous with respect to repeated measures data throughout the trial. 66
| Trial | Outcome reported | Time point (weeks) | Omalizumab | Comparator | Treatment effect | ||
|---|---|---|---|---|---|---|---|
| n | Difference | n | Difference | ||||
| Adults: licensed population | |||||||
| INNOVATE19 | SABA mean puffs/day, change from baseline | 28 | 179 | −1.03 | 179 | −0.79 | p = 0.409 |
| Number rescue-free days, change from baseline | 28 | 179 | 0.9 | 179 | 0.6 | p = 0.679 | |
| IA-04 EU subgroup51 | Salbutamol mean puffs/day over 14 days | 52 | 102 | 3.91 | 40 | 5.33 | p = 0.008 |
| Chanez 201029 | Median (range) puffs SABA, change from baseline | 16 | 20 | 1.0 (−45 to 17) | 11 | 0.0 (−22 to 4) | p = 0.477 |
| Adults: supportive trials | |||||||
| Hanania 201133 | Albuterol mean puffs day, change from baseline | 48 | 427 | −1.58 | 421 | −1.31 | 0.27 (95% CI −0.49 to −0.04) |
| SOLAR31 | SABA mean puffs/day | 28 | 28 | 1.8 (−1.0 from baseline) | 181 | 2.4 (−0.4 from baseline) | NR (described as similar) |
| Bardelas 201232 | Days/week SABA use, change from baseline | 24 | 24 | −1.74 | 135 | −1.49 | p = 0.374 |
| Ohta 200935 | Mean puffs (medication NR), changes from baseline | 16 | 151 | NR | 164 | NR | NS favoured omalizumab |
| Children: licensed population | |||||||
| IA-05 EU20 | SABA puffs rescue med/day mean (SD) at 24 weeks, change from baseline | 24 | 367 | −1.3 | 182 | −1.0 | p = 0.047, but NS after correction for multiple testing |
Data on use of rescue mediation from observational studies
Only two observational studies41,59 reported on changes in rescue inhaler use. Both reported substantial reductions following omalizumab treatment (Table 27). Costello41 found a 56% reduction in the number of puffs for a group of omalizumab responders 6 months after treatment initiation. Another study59 showed that approximately 66% of its participants had either reduced or stopped using a rescue inhaler. Neither study specified which inhalers were used.
| Study | n baseline | n follow-up | Duration (assessment time point) | Use at baseline | Use at follow-up | Difference from baseline |
|---|---|---|---|---|---|---|
| Costello 201141 | NR (≤ 63) | NR (≤ 63) | 6 months | Mean 41.0 (SD 43.0) puffs per month | Mean 18.0 (SD 18.0) puffs per month | 56% reduction in number of puffs |
| Stukus 200859 | 45 | 45 | NR | NR | NR | 66% reduction in frequency of use; 31% stopping |
Summary of treatment effect on use of rescue medication
There was limited evidence of efficacy of omalizumab in reducing requirement for rescue medication. Of the trials in the adult licensed populations only the IA-04-EUP found a statistically significant benefit. Hanania et al. also found a statistically significant benefit. 33 There was extremely limited evidence from observational studies, with two studies reporting reduced use but no results of statistical tests.
In children, the IA-05-EUP initially showed a statistically significant benefit which lost significance following adjustment for multiple testing. There was no additional evidence from supporting RCTs or observational studies.
Forced expiratory volume in 1 second
Forced expiratory volume in 1 second results from randomised controlled trials
All trials in adults except Hanania et al. 33 and Ohta et al. 35 reported change from baseline in percentage of predicted FEV1 (Table 28): Ohta et al. reported changes in volume (ml). 35
All of the main adult RCTs showed a statistically significant impact of omalizumab on FEV1% predicted, although the between-group differences in INNOVATE and EXALT were small in absolute terms at 2.8% and 4.4% respectively. The supportive SOLAR trial and Ohta trial reported a significant effect in the increase in FEV1 in ml). 35,36 The small Chanez et al. trial, and the supportive trials by Bardelas et al. and Hoshino et al. did not find a statistically significant benefit. 29,32,34
FEV1 was not reported for the paediatric IA-05 EUP subgroup, but the supportive Busse et al. trial found no difference between the treatment groups in children and adolescents. 28
| Trial | Time point (weeks) | Omalizumab | Comparator | Treatment effect | ||
|---|---|---|---|---|---|---|
| n | FEV1 (% predicted) | n | FEV1 (% predicted) | |||
| Adults: licensed population | ||||||
| INNOVATE | 28 | 209 | 67.01 | 210 | 64.18 | p = 0.043 |
| EXALT | 32a | 271 | 68.1 | 133 | 63.7 | p = 0.007 |
| IA-04 EUP subgroup | 52 | 115 | 71 | 49 | 60 | p < 0.01 |
| Chanez 201029 | 16 | 20 | 2.6a (median) | 11 | 1.7a (median) | p = 0.312 |
| Adults: supportive trials | ||||||
| SOLAR36 | 28 | 209 | NR | 196 | NR | p = 0.065b |
| Bardelas 201232 | 24 | 136 | 0.08a | 135 | 0.16a | p = 0.123 |
| Hoshino 201234 | 16 | 14 | 73.5 change from baseline p < 0.01 | 16 | 68.6 change from baseline p = NS | 4.90 (95% CI −2.91 to 12.71)c |
| Ohta 200935 | 16 | 158 | NR | 169 | NR | NRd |
| Children: supportive trials | ||||||
| Busse 201128 | 60 | 208 | 92.6 | 211 | 91.7 | 0.92 (95% CI −0.81 to 2.64) |
Forced expiratory volume in 1 second from observational studies
Five observational studies37,39,41,58,62 reported changes in FEV1% predicted following omalizumab treatment (Table 29). Of those, four37,39,41,62 showed statistically significant improvements in FEV1% from baseline, and one58 reported no improvement in the longer term (mean 2.1 years).
| Study | n at baseline | n at follow-up | Duration (assessment time point) | Mean % at baseline | Mean % at follow-up | % difference from baseline |
|---|---|---|---|---|---|---|
| APEX37 | 111 | 111 | 16 weeks | 62.94 | 70.98 | 8.04, p < 0.001 |
| 32 | 32 | ≤12 months | 69.90 | 78.60 | 8.70, p = 0.002 | |
| PERSIST39 | 158 | 134 | 16 weeks | 56.54 | 68.69 | 12.15, p < 0.001 |
| 158 | NR | 52 weeks | 56.54 | 68.77 | 12.23, p < 0.001 | |
| Costello 201141 | 61 | 61 | 6 months | 66.3 (19) | 71.0 (21) | 4.7, p = 0.002 |
| Randolph 201058 | 29 | 29 | Mean 2.1 years (median 1.8 years, from 6 months to 6 years) | 76 | NR | No improvement (p-value NR) |
| Tzortzaki 201262 | 60 | 60 | 4 years | 60.13 (18) | 71.76 (17) | p < 0.0001 |
The PERSIST39 study found a clinically and statistically significant increase of about 12 points in FEV1% at 16 weeks (p < 0.001). This improvement was maintained after 1 year of treatment (p < 0.001). The APEX study, which retrospectively analysed patient data from 10 UK centres, reported a significant increase of about 8% at 16 weeks (p < 0.001, n = 111) and at up to 12 months treatment (p = 0.002, n = 32). Although it is unclear which proportion of patients included in this analysis strictly met the EU licence, these results are likely to reflect outcomes observed in UK practice. Ohta 201046 showed no significant change in a group of 133 moderate-to-severe asthma persistent patients after 48 weeks of treatment, but found a statistically significant improvement in a subgroup of 37 severe patients (from 1.76 to 1.89 l; p = 0.031). However, the subgroup in Ohta 201046 was classed as severe uncontrolled according to the Japanese label, which includes patients with less severe asthma than the EU licence. The Tzortzaki study showed evidence of sustained benefit over 4 years in patients who met licence criteria.
The study by Brodlie,54 which included children and adolescents treated in the UK on step 5 therapy, showed an increase in median FEV1 from 2.10 to 2.25 l that was not statistically significant (p = 0.1) following 16 weeks of treatment. Similar results were reported for children aged ≤ 12 and adolescents between 12 and 16 years.
Three observational studies37,43,46,54 reported on changes in FEV1 (l). The APEX study found an improvement that was significant at 12 months follow-up (from 1.99 to 2.22 l; n = 70, p < 0.001) but not at 16 weeks (from 1.99 to 2.10 l; n = 88, p = 0.22).
Forced expiratory volume in 1 second: summary of omalizumab treatment effect
Randomised controlled trial data indicated statistically significant benefits of omalizumab on FEV1 as a percentage of the predicted value in the licensed population, although the absolute benefits were small. Supportive trials did not indicate a statistically significant benefit, but these were undertaken in populations with higher mean baseline FEV1 values than the main trials. One supportive trial showed a benefit in FEV1 measured in ml. Observational studies provided additional evidence that omalizumab leads to significant improvements in lung function in adults with uncontrolled severe asthma.
In children there was no evidence from the licensed population as IA-05-EUP did not assess FEV1. The supportive Busse et al. trial found no evidence of an effect of treatment in children and adolescents. 28 Some improvements were reported in children and adolescents treated in severe asthma UK centres, although these results were not statistically significant and drawn from a single small observational study. 54
Quality of life
Quality-of-life results from randomised controlled trials
Some measure of asthma-related QoL was reported by six adult trials (INNOVATE, EXALT and IA-04 EU subgroup in the licensed population and the supportive trials SOLAR and the trials of Hanania and Hoshino) and by the IA-05 EUP subgroup in children. 19,20,31,33,34,36,51 The AQLQ or, in the case of IA-05 EUP, the paediatric AQLQ, was employed in all except the Ohta trial, which reported daily activity scores as a measure of QoL. EXALT reported EQ-5D scores in addition to AQLQ scores.
Data were reported on the mean difference in AQLQ score from baseline and/or on the proportion of patients who improved by ≥ 0.5 points, ≥ 1 point and ≥ 1.5 points from baseline; ≥ 0.5 points is defined as the minimally important difference (Table 30).
| Trial | Time point assessed (weeks) | Omalizumab | Comparator | Treatment difference | Omalizumab | Comparator | Treatment difference | ||
|---|---|---|---|---|---|---|---|---|---|
| n | Change from baseline | n | Change from baseline | n (%) with ≥ 0.5 point increase from baseline | n (%) with ≥ 0.5 point increase from baseline | ||||
| Adults: licensed population | |||||||||
| INNOVATEa | 28 | 209 | 0.91 | 210 | 0.46 | p < 0.001 | 124 (61) | 98 (48) | p = 0.008 |
| EXALTa | |||||||||
| AQLQ | 31 | 271 | 1.06 (95% CI 0.88 to 1.24) | 133 | −0.07 (95% CI −0.31 to 0.17) | p < 0.001 | 165 (74) | 25 (26) | p < 0.001 |
| EQ-5D utility index | 194 | 0.091(95% CI 0.051 to 0.132) | 81 | 0.064 (95%CI 0.008 to 0.121) | p = 0.350 | ||||
| EQ-5D Health Assessment | 194 | 9.3 (95% CI 5.2 to 13.4) | 80 | −2.8 (95% CI −8.5 to 3.0) | p < 0.001 | ||||
| IA-04 | 52 | 115 | 1.32 | 49 | 0.17 | p < 0.001 | 88 (77) | 21 (42)b | p < 0.001 |
| EU subgroupa | |||||||||
| Adults: supportive trials | |||||||||
| Hanania (2011)33 | 48 | 427 | 1.15 | 423 | 0.92 | 0.29 (95% CI 0.15 to 0.43) | NR | NR | NA |
| SOLAR36 | 28 | 209 | NR | 196 | NR | NA | 164 (79) | 134 (70) | RR 1.15 (95% CI 1.02 to 1.29)c |
| Hoshino (2012)34 | 16 | 14 | 1.47 (p < 0.001) | 16 | 0.28 (p = NS) | NR | NR | NR | NA |
| Children: licensed population | |||||||||
| IA-05d | 24 weeks | 166 | 0.78 | 80 | 0.70 | p = 0.566 | 96 (62) | 42 (58) | p = 0.654 |
| EU subgroupa | |||||||||
The treatment effect (Table 30) on both the main change from baseline and the number of patients reaching a minimally important difference in AQLQ was statistically significant in all cases in main and supportive trials (where reported), although the size of effect was substantially larger in the open-label EXALT and IA-04 (EU subgroup) trials than in INNOVATE. The supporting Hanania trial, which was double blind, also gave a more conservative estimate of treatment effect for mean change from baseline score. 33 The difference between the treatment groups in SOLAR just reached significance, because of a very high treatment response in the placebo arm. 36 The small open-label Hoshino trial did not calculate the between-group difference. 34 The trial by Ohta et al. found no significant difference from baseline in either group in daily activity scores. 35
In children, the IA-05 EU population subgroup showed no difference between groups in either measure of QoL, with very high response rate in the placebo arm.
EXALT showed no difference in change from baseline on the EQ-5D utility index score, but a statistically significant benefit of omalizumab on the EQ-5D health state assessment (p < 0.001).
Quality-of-life data from observational studies
In observational studies the reporting of changes in quality of life was variable; seven observational studies reported some measure of QoL (see Table 31). APEX reported a mean increase ≥ 2 points in the AQLQ at assessment at 16 weeks; a minority of participants were assessed after at least 12 months and reported comparable gains from baseline. 37 In eXpeRience 58.2% of patients reported the minimally important increase of ≥ 0.5 points, whereas in PERSIST this was higher at 84.4% although only 56.7% registered an improvement in utility on the EQ-5D scale. 39
Importantly, the Brodlie et al. study documented evidence of a statistically significant increase in mini-AQLQ scores in children aged both < 12 years and in those aged > 12 years. The numbers involved were very small but these data are valuable as there is very limited evidence on QoL impact associated with omalizumab treatment in children. As this study enrolled OCS-dependent children with very severe asthma attending UK clinics, it may be considered a useful indicator of the potential treatment effect of omalizumab on QoL in children. 54
| Study | Baseline no. | Follow-up no. | Duration (assessment time point) | Score at baseline | Score at follow-up | Difference from baseline |
|---|---|---|---|---|---|---|
| AQLQ | ||||||
| APEX37 | 83 | 83 | 16 weeks | 2.8 | 5.2 | 2.4 points increase |
| 21 | 21 | ≤ 12 months | 2.8 | 5.7 | 2.3 points increase | |
| eXpeRience53 | 294 | NR | 8 months | 4.22 | 5.58 | 1.04 points (1.34) increase |
| 58.2% with ≥ 0.5 points increase | ||||||
| PERSIST39 | 157 | 122 | 52 weeks | 3.24 (1.21) | NR | 1.79 (1.13) mean difference |
| 84.4% with ≥ 0.5 points increase | ||||||
| 68.9% with ≥ 1.0 points increase | ||||||
| 53.3% with ≥ 1.5 points increase | ||||||
| 157 | 147 | 16 weeks | 3.24 (1.21) | NR | Mean absolute change: 1.37 (NR) | |
| Britton 2011 | 52 | 52 | Mean 982 days | NR | NR | Mean change + 1.39 (SD 1.80) |
| Mini-AQLQ | ||||||
| Brodlie et al. 201254 | 24 | 24 | 16 weeks | 3.5 (1 to 8.4) | 5.9 (3.2 to 9.9) | p < 0.0001 |
| 92% with increase | ||||||
| ≥ 12 years subgroup | 8 | 8 | 16 weeks | 2.3 (1.7 to 4.2) | 5.2 (3.5 to 6.9) | p = 0.0078 |
| 12–16 years subgroup | 16 | 16 | 16 weeks | 3.8 (1.0 to 8.4) | 6.1 (3.2 to 9.9) | p = 0.0013 |
| Korn44 | NR | NR | 6 months | 2.9 (0.9) | 4.5 (1.2) | p < 0.001 |
| EQ-5D index/utility | ||||||
| PERSIST39 | 126 | 67 | 52 weeks | 0.54 (0.24) | NR | 56.7% improving utility (≥ 0.074) |
| EQ-5D (VAS) | ||||||
| PERSIST39 | 124 | 67 | 52 weeks | 52.29 (17.34) | NR | Mean (SD) improvement 0.14 (0.23) p < 0.001 |
Quality of life: summary of omalizumab treatment effect
Studies in the adult licensed population showed statistically significant evidence of benefit on the AQLQ. Supporting this, the Hanania et al. trial also showed a statistically significant benefit. 33 This benefit was not seen in the SOLAR trial where there was a substantial placebo response. 36 In children, the IA-05-EUP also demonstrated a substantial placebo response and showed no significant evidence of treatment benefit. 20 In the observational study by Brodlie et al. there was evidence of statistically and clinically significant increases in mini-AQLQ scores in OCS-dependent children in the UK, including those aged under 12 years. Although this population is small, it represents the only evidence on children with OCS-dependent asthma. 54
Withdrawals rates
Withdrawals rates results from randomised controlled trials
Nine RCTs reported omalizumab discontinuation rates (see Table 32). Discontinuation rates varied across the trials, both in the omalizumab and comparator arms. The double-blind RCTs in adults reported withdrawal rates in the omalizumab arm of between 2.4% and 19.4%, compared with 7.7% and 22.2% on placebo. In the open-label trials the withdrawal rates were much higher in the comparator compared with the omalizumab arm. In the one trial in children (IA-05 EU subgroup) the rate of withdrawal was around 20% in both arms.
Three studies reported rates of discontinuation because of lack of treatment efficacy. 19,20,31 Rates were generally low and not dissimilar between treatment groups in two of these RCTs. 19,20 The open-label EXALT trial showed a marked difference between treatment groups, with a higher rate of withdrawals because of lack of treatment efficacy reported in comparator patients.
| Study | Duration | Total discontinuations | Discontinued because of lack of efficacy | ||
|---|---|---|---|---|---|
| Omalizumab | Comparator | Omalizumab | Comparator | ||
| Adult | |||||
| Double blind | |||||
| INNOVATE19 | 28 weeks | 30/209 (14.4%) | 22/210 (10.5%) | 2 | 2 |
| Hanania 201133 | 48 weeks | 83/427 (19.4%)a | 94/423 (22.2%)a | NR | NR |
| SOLAR36 | 28 weeks | 5/209 (2.4%) | 15/196 (7.7%) | NR | NR |
| Ohta 200935 | 16 weeks treatment + 12 week follow-up | 13/151 (8.6%) | 28/164 (17.1%) | NR | NR |
| Chanez 201029 | 16 weeks | 3/20 (15.0%) | 3/11 (27.3%) | NA | NR |
| Bardelas 201232 | 24 weeks | 16/136 (11.8%) | 13/135 (9.6%) | NR | NR |
| Open label | |||||
| IA-04 EU subgroup30 | 52 weeks | 20/115 (17.4%) | 15/49 (30.6%) | NR | NR |
| Bousquet 201031 EXALT | 32 weeks | 22/273 (8.1%) | 25/131 (19.1%) | 1 | 6 |
| Children | |||||
| Double blind | |||||
| IA-05 EU subgroup20 | 52 weeks (24-week fixed steroid, 28-week adjustable steroid) | 32/166 (19.3%) | 16/80 (20%) | 1 | 2 |
Withdrawal rates data from observational studies
The observational studies that reported data on withdrawals over a reported period of follow-up are listed in Table 33. The reporting of withdrawals was inconsistent, with a lack of clarity regarding the follow-up duration, timing of withdrawal and, in many cases, the reason for withdrawal. No withdrawals data were found for cohorts on OCS maintenance.
In clinical practice, response to omalizumab is checked at 16 weeks. Four observational studies reported withdrawal rates at this 16-week timepoint. 37,41,43,44,54 Rates ranged from 14.4% to 17.6%. Rates for withdrawal because of lack of efficacy at various time points were consistent at around 15–20% (Table 33). Withdrawal rates reported for longer periods of follow-up were variable: although four studies39,41,44,45 reported a rate around 30% at 6 months or 12 months, two others,40,54 including the largest study (postmarketing surveillance),53 reported lower rates of around 8.5%.
| Study | Study design | Duration | n | Total discontinuations | Discontinued because of lack of treatment efficacy |
|---|---|---|---|---|---|
| APEX37 | Retrospective one-group | 12 months | 136 | NR | 24/136 (17.6%) at 16 weeks (non-responders) |
| eXpeRience38,53 | Postmarketing surveillance | 8 months | 876 | 11 (8.8%) | NR |
| Brodlie 201254 (children) | Prospective one-group | 16 weeks | 34 | 4 (11.8%) | 4 |
| PERSIST39 | Prospective one-group | 52 weeks | 158 | 55/158 (34.8%) (at 52 weeks), subgroup with 120 weeks follow-up: 8/53 (15.1%) | 21/158 (13.3%) at 52 weeks |
| Cazzola 201040 | Prospective one-group | 12 months | 142 | 12/142 (8.5%) | 2 |
| Costello 201141 | Retrospective one-group | 6 months | 93 | 31/93 (33.3%) | 13/93 (14.3%) (at 4 months) |
| Domingo 201156 | Prospective one-group | ≥ 1 year; mean 17.2 ± 8.5 months (range 4–34) | 32 (31) | 1 | 0 |
| Korn 200944 | Postmarketing surveillance | Mean 195 ± 60 days | 280 | At 4 months: 47/280 (16.8%) | After 4 months 23/280 (8.2%) |
| Total 91/280 (32.5%) | Total 40/280 (14.3%) | ||||
| Molimard 200845 | Prospective one-group | > 5 months | 154 (146) | 45/147 (30.6%) | 28/147 (19.0%) |
| 18 of 33 underdosed patients discontinued |
Withdrawal rates: summary
There were considerable variations in withdrawal rates between studies. The key INNOVATE study showed lower withdrawal rates than other trials, with a lower disparity between trial arms than the open-label trials EXALT and IA-04-EUP in which comparator arms showed a higher withdrawal rate than omalizumab arms. Withdrawal rates in observational studies did not appear markedly different to RCT data, although there was greater variation. The withdrawal rate in the APEX study, which might be considered most reflective of UK clinical practice was around 18% at 16 weeks. The IA-05 EUP trial in children had a withdrawal rate of 20%, which was at the upper end of the range for adult RCTs; there was no imbalance between the trial arms.
Evidence of long-term efficacy and persistence of response
Of the 11 RCTs and 11 observational studies identified from the search for studies on the efficacy of omalizumab, three RCTs20,28,30 and six observational studies40,47,58,60 reported follow-up data at 52 weeks or longer. This includes the two additional observational studies identified by the manufacturer. 61,62 These nine studies are presented in Table 34. The study by Randolph et al. 58 was available only in abstract form, with very limited data reported for patient history and medication use at baseline. It was also unclear whether or not the population fully met the licence criteria. The findings from this study should, therefore, be interpreted with caution.
| Study | Duration | Population |
|---|---|---|
| RCTs | ||
| IA-04 EUP51 | 52 weeks | Adults, subgroup licensed population |
| IA-05 EUP20 | 52 weeks | Children, subgroup licensed population |
| Busse 201128 | 60 weeks | Children and adolescents, supportive study |
| Observational studies | ||
| APEXa | 1 year | Adults supportive study |
| PERSIST39 | 52 weeks + 120 weeks follow-up of single arm | Adults licensed population |
| Cazzola 201040 | 52 weeks + 52 weeks follow-up | Adults licensed population |
| Randolph 201058 | Up to 6 years | Adults supportive study |
| PAX-LASER47 | ≥ 12 months | Adults licensed population |
| Britton 201161 | Mean 982 days (range 112–3839) | Adults licensed population |
| Tzortzaki 201262 | 4 years | Adults licensed population |
These studies, although providing some longer-term information, provide relatively limited data on the persistence of response in individual patients. The data from the PERSIST study indicated continuing high response rates at 12 months and at over 2 years in those patients who were subsequently followed up in the extension of the original study. The longest follow-up (at mean durations of 2.7 and 4 years respectively) was available from the additional studies identified by the manufacturer. 61,62 The study by Tzortzaki indicated that response at 4 months was sustained at assessment at 1 and 4 years' follow-up across a range of efficacy measures. Although this study reported zero dropouts, it is difficult to determine if all treated patients were included in the report. The small numbers of patients included (n = 60) should be noted.
Studies not included in evaluation of long-term response
A small number of studies appeared to be long term but were not included in this section for the following reasons. Braunstahl53 reported a follow-up duration up to 2 years, but reported outcome data up to 8 months only. Gutierrez57 reported follow-up data at 18 months, but did not report data on the outcomes of interest. These two observational studies were therefore not included in the overview of long-term data. Domingo56 reported data at a mean follow-up of 17 months, but only reported data on OCS use. 56,67 To avoid duplication, this is discussed in the OCS-sparing review and is not reported in this section.
Results of assessment of steroid-sparing effect of omalizumab
Quantity and quality of evidence
One RCT subgroup68 and nine observational studies37–41,43–45,47,54 included in the review of omalizumab efficacy studies also reported sufficient information on the steroid-sparing effects of omalizumab.
Ten additional publications were identified from the search for omalizumab efficacy studies. Three provided data on the steroid-sparing effect of omalizumab: one RCT subgroup50 and two observational studies. 56,59
All studies provided rates of OCS withdrawal or reduction, or data allowing calculation of at least one of these outcomes. Eight reported on OCS dose change or reported data allowing calculation of this outcome.
Steroid-sparing effect of omalizumab: randomised controlled trials
| Study | Mean age (years) | ICS dose (mean) | LABA n (%) | OCS, n (%) | Other medications | Clinically significant exacerbations/year | Hospitalisations in past year | Emergency room visits in past year | FEV1 (% predicted) |
|---|---|---|---|---|---|---|---|---|---|
| EXALT31 | 45 | NR | 82 (100%) | 82 (100) | Theophylline and LTRA permitted. SABA allowed as needed | 3.0 | 0.6 (mean number of events/pt) | 0.9 (mean number of events)/pt | 61 |
| Trial number 01169 | NR | 1453 µg/day | NR (permitted) | 95 (100) | Theophylline and LTRA not permitted. SABA allowed as needed | NR | 21 (22.6%) (n) | 1.14 (mean number of events/pt) | 59 |
Two RCTs (01150,69 and EXALT31) provided substantive data on changes in oral steroid use (Table 35). EXALT was an open-label comparison with Best Supportive Care; trial 011 was double blind and placebo controlled. Both reported data on stratified subgroups of adults on OCS maintenance at baseline. The main report of the trial 011 published by Holgate et al. 50 was excluded from the other sections of our review because patients were required to have well-controlled asthma. However, the OCS maintenance subgroup of this study (011 OCS)69 was included in this analysis for two reasons: other than EXALT, no RCTs reported substantive data on the effect of omalizumab on changes in OCS use; and as in the EXALT subgroup, all patients were on OCS maintenance at baseline. As a result of limited reporting of patient characteristics, the extent to which these subgroups are comparable is unclear. In particular, there is a question regarding to what extent the (011 OCS)69 subgroup is representative of the licensed population on BTS/SIGN step 5 treatment. As Table 35 shows, the report of this OCS subgroup study did not give the rates of patients receiving a LABA or the rates of exacerbations in the year preceding baseline. Only 22.6% of the OCS subgroup in this study had been hospitalised during the year before baseline and the mean number of emergency room visits per patient was 1.14, suggesting that although this population was to some degree uncontrolled on best supportive care (step 5 in this case), it does not match the licence requirements. 69 In comparison with the EXALT OCS subgroup, theophylline and LTRA were not permitted for patients in the 011 OCS subgroup, suggesting that the 011 OCS subgroup may have less severe asthma than the EXALT subgroup, or that their therapy had not been optimised prior to the introduction of OCSs.
The results from these two RCTs were very different from each other (Table 36). In the EXALT trial at both 16 and 32 weeks, omalizumab patients stopped or reduced the use of OCSs around twice as often as those on best supportive care alone and this difference was statistically significant at 32 weeks. EXALT also found that omalizumab statistically significantly reduced OCS dose at 32 weeks ([mean difference (MD) −6.70 mg/day; 95% CI −12.93 to −0.47 mg/day]). In contrast, in 011 OCS there was no treatment benefit with omalizumab: rates of patients reducing or stopping OCSs were high at 32 weeks follow-up (over 70%) in both the omalizumab and the placebo groups (RR 1.01; 95% CI 0.79 to 1.28) and the mean dose reduction was smaller with omalizumab than with placebo at both 32 weeks (36.0% vs. 55.6% reduction; MD 1.70; 95% CI −2.17 to 5.57) and at 44 weeks (39.0% vs. 64.2% reduction; MD 2.30; 95% CI −1.75 to 6.35).
The large overall reduction in rates of patients who stopped or reduced OCS treatment in 011 OCS69 may be because of an overestimation of OCS need for a significant proportion of participants at baseline: during the run-in phase of the trial, the authors reported that steroid doses were not adequately adjusted according to protocol for 39% of patients on OCSs. In such a population no clear difference could be demonstrated between the active and placebo in terms of a steroid-sparing effect. In addition to overuse of OCSs, as mentioned above, the OCS subgroup in 011 OCS69 is not representative of an uncontrolled severe population on step 5 treatment because patients were not required to be on LABA, nor were they experiencing exacerbations. Therefore, it is unclear the extent to which the study conclusions apply to the UK licence population. The divergent results of the two trials may be further explained by differences in study designs. In the open-label EXALT trial, the assessment of OCS dosage at follow-up may have been affected by the prescribers' and patients' knowledge of treatment allocation, thereby artificially increasing differences between treatment and control, whereas in the Holgate study there appears to have been a strong placebo effect.
| Study | Follow-up duration | Change of maintenance, n/N (%) | Change in dose from baseline [mg/day (SD), prednisolone equivalents] | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stopped | Reduced | Stopped or reduced | |||||||||||
| Omalizumab | Control | RR (95% CI) | Omalizumab | Control | RR (95% CI) | Omalizumab | Control | RR (95% CI) | Omalizumab | Control | MD (95% CI) | ||
| EXALT31 | 16 weeks | 17.9% (10/56) | 10.5% (2/19) | 1.70 (0.41 to 7.06) | 25% (14/56) | 10.5% (2/19) | 2.38 (0.59 to 9.51) | 42.9% (24/56) | 21.1% (4/19) | 2.04 (0.81 to 5.12) | Mean 20.1% reduction (63.08) | Mean 36.8% increase (212.03) | NA |
| 32 weeks | 32.2% (19/59) | 13.0% (3/23) | 2.47 (0.81 to 7.55) | 30.5% (18/59) | 17.4% (4/23) | 1.75 (0.66 to 4.63) | 62.7% (37/59) | 30.4% (7/23) | 2.06 (1.08 to 3.94) | Mean 45.0% reduction (50.22), from 13.1 (9.20) to 8.4 (12.08) | Mean 18.3% increase (85.13), from 12.8 (10.71) to 15.1 (13.26) | −6.70 (−12.93 to −0.47) | |
| Trial number 01169 | 32 weeks | 42.0% (21/50) | 42.0% (19/45) | 0.99 (0.62 to 1.59) | 32.0% (16/50) | 31.1% (14/45) | 1.03 (0.57 to 1.86) | 74.0% (37/50) | 73.3% (33/45) | 1.01 (0.79 to 1.28) | Mean 36.0% reduction, from 10.0 (6.3) to 6.4 (12.3) | Mean 55.6% reduction, from mean 10.6 (6.7) to 4.7 (6.3) | 1.70 (−2.17 to 5.57) |
| 44 weeks | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mean 39.0% reduction, from 10.0 (6.3) to 6.1 (12.7) | Mean 64.2% reduction, from 10.6 (6.7) to 3.8 (4.7) | 2.30 (−1.75 to 6.35) | |
Steroid-sparing effect of omalizumab: observational studies
Ten uncontrolled observational studies reported data on OCS-sparing following omalizumab treatment. All studies provided rates of OCS withdrawal or reduction, or data allowing calculation of at least one of these outcomes. Eight reported on OCS dose change or data allowing calculation of this outcome. All 10 studies were of patients who took OCSs at baseline: seven studies37,40,41,43,53–55,70 (297+ patients) reported outcomes for patients on OCS maintenance at baseline (Table 37), whereas four37,39,56,59 (206 patients) reported outcomes for mixed populations (with or without OCSs at baseline, see Table 38). Where reported, follow-up time ranged from 16 weeks to 17 months.
As a result of limited reporting of patient characteristics, it is unclear the extent to which the groups and subgroups included in this analysis meet the omalizumab licence specification. In the studies with mixed groups (with or without maintenance), the proportion of patients taking OCSs and the frequency of treatment intake in the year preceding baseline are unclear because of gaps in reporting. Where reported, mean baseline OCS doses varied from 14.3 mg (SD 11.86)70 to 26.5 mg (SD 19.36) prednisolone per day70 in the OCS maintenance subgroups, and from 7.19 mg (SD 11.1)56 to 21.35 mg37 for the cohorts combining patients with and without OCSs.
The results of the effect of omalizumab use on OCS use from observational studies are presented in Tables 37 and 38. For adults on OCS maintenance, OCS withdrawal rates ranged from 25.9% to 71.2%, and data from three studies37,53,70 showed that between 49.0% and 65.6% had reduced or stopped taking OCSs following omalizumab treatment. These rates are comparable to the ones observed in the omalizumab arms of the RCT.
| Study | Follow-up duration | Withdrawal rate (n/N) | Reduction rate (n/N) | Withdrawal + reduction rate (n/N) | Reduction in daily dose (mg/day, prednisolone equivalents) |
|---|---|---|---|---|---|
| APEX37 OCS maintenance subgroup | 12 months | 38.9% (35/90) | 26.7% (24/90) | 65.6% (59/90) | NR |
| eXpeRience53 | 8 months | NR | NR | 55.6% (NR) | 40.4% (NR)a |
| Brodlie 201254 | 16 weeks | 20.6% (7/34) | 64.7% (22/34) | 85.3% (29/34)b | From median 20 (range 2.5 to 50) to 5 (range 0 to 40)c |
| Brodlie 13–16 years subgroup | 26.3% (5/19) | NR | NR | From median 10 (2.5 to 40) to 5 (0 to 20)d | |
| Brodlie 5–12 years subgroup | 13.3% (2/15) | NR | NR | From median 20 (range 5 to 50) to 5 (0 to 40)c | |
| Kirk 201155 (linked to Brodlie) (6–11 years)b | 16 weeks | 22.2% (4/18) | 77.8% (14/18) | 100% (18/18) | 73.3%, from 19.1 to 5.1a |
| Cazzola 201040 | 12 months | 71.2% (37/52) | NR | NR | NR |
| Costello 201141 | 6 months | 25.9% (7/27) | NR | NR | Median 10 at baseline and follow-upa |
| Molimard 201070 French maintenance OCS subgroup | > 16 weeks | NR | NR | 53.1% (34/64)e | 30.3% (SD 47.06), from 26.5 (SD 19.36) to 17.8 (SD 17.75)a |
| Molimard 201070 German maintenance OCS subgroup | > 16 weeks | NR | NR | 49.0% (50/102) | 29.2% (SD 83.35), from 14.3 (SD 11.86) to 8.3 (SD 9.92)a |
| Study | Follow-up duration | Withdrawal rate (n/N) | Reduction rate (n/N) | Withdrawal + reduction rate (n/N) | Reduction in daily dose (mg/day, prednisolone equivalents) |
|---|---|---|---|---|---|
| APEX37 | 12 months | 48.5% (66/136) | 15.4% (21/136) | 64.0% (87/136) | 25.6%, from 21.35 to 15.88a |
| PERSIST39 | 52 weeks | 18.5% (24/130) | NR | NR | 39.4% (7.31, SD 13.86), from 18.55 to 11.24 (n = 130)a |
| Domingo 201156 | Mean 17 months | 74.2% (23/31) | NR | NR | 54.2%, from 7.19 (SD 11.1) to 3.29 (SD 11.03)b |
| Stukus 200859 | NR | 26.7% (12/45) | NR | NR | NR |
| Britton 201161 | Mean 982 days | NR | NR | NR | 54.8% from 12.6 to 5.7 (n = 43)c |
Outcomes for children on OCS maintenance were reported in two UK studies. 43,54,55 Both studies reported on a small number of children (15 patients aged 5–12 years54 and 18 omalizumab responders aged 6–11 years55) and the study populations in these two studies may overlap, although the extent to which this may be the case is unclear. Brodlie et al. 54 reported that all patients were receiving optimised OCS doses at baseline. Both studies showed a significant decrease in OCS burden after 16 weeks of treatment. Withdrawal rates were 13.3%55 and 22.2%,55 and all patients recruited in Kirk et al. had either reduced or stopped OCS treatment at follow-up. The reductions in mean daily dose reported were 14 mg,55 and from median 20 mg (range 5–50 mg) to 5 mg (range 0–40 mg)54 (see Table 38).
From the studies where the patient cohorts comprised patients using OCSs as maintenance or occasional or intermittent use, OCS doses were reduced in all adult studies reporting on this outcome except one. 41 Unpublished results from the APEX study, which involved 136 patients from 10 specialist UK centres, showed a statistically significant decrease in mean daily dose of 5.47 mg at 12 months. 37
Summary of steroid-sparing effect of omalizumab
There is limited evidence from RCTs on the oral steroid-sparing effect of omalizumab and the results were mixed. Only two RCTs were identified, and both reported data from small adult subgroups. The results were heterogeneous and limited by design flaws (EXALT) and insufficient OCS dose adjustment during the run-in phase of the trial (011 OCS). 31,69
Ten observational studies provided data on a larger number of patients than the RCTs. They suggest that omalizumab is effective in reducing OCS use, including for children on OCS maintenance in a real-life UK setting. 54 However, these studies had significant design flaws (all were uncontrolled and relatively small), and none provided relevant data beyond 12 months except for one small study. 56
Overall, the evidence for a clear and clinically significant OCS-sparing effect of omalizumab is limited.
Results of assessment of safety of omalizumab
Quantity and quality of research
As stated in Methods for reviewing the safety of omalizumab, within the context and time constraints of this health technology assessment it was not possible to fully systematically review the adverse events of omalizumab and therefore the findings presented here are of a pragmatic review of the available sources of relevant evidence. Of the 89 publications identified as potentially relevant for the review of omalizumab efficacy, 11 RCTs,19,20,28–33,35,36,50 and 11 observational studies38–41,43–46,54,56,59,71 reported adverse event data for omalizumab. These publications reported adverse event rates directly or provided sufficient information to calculate these rates. Details of these studies and their quality assessment have been reported earlier in the section Quantity and quality of evidence.
Separate searches identified 31 potentially relevant data sources (including 15 reviews which were also identified by the efficacy searches) in addition to those primary studies included in the review of efficacy. Ten of these additional sources were included in the review of omalizumab safety18,72–79 (Figure 2). An additional review (Busse et al. 81) was subsequently identified by the manufacturer.
FIGURE 2.
Flow chart showing number of additional omalizumab safety publications identified and included.
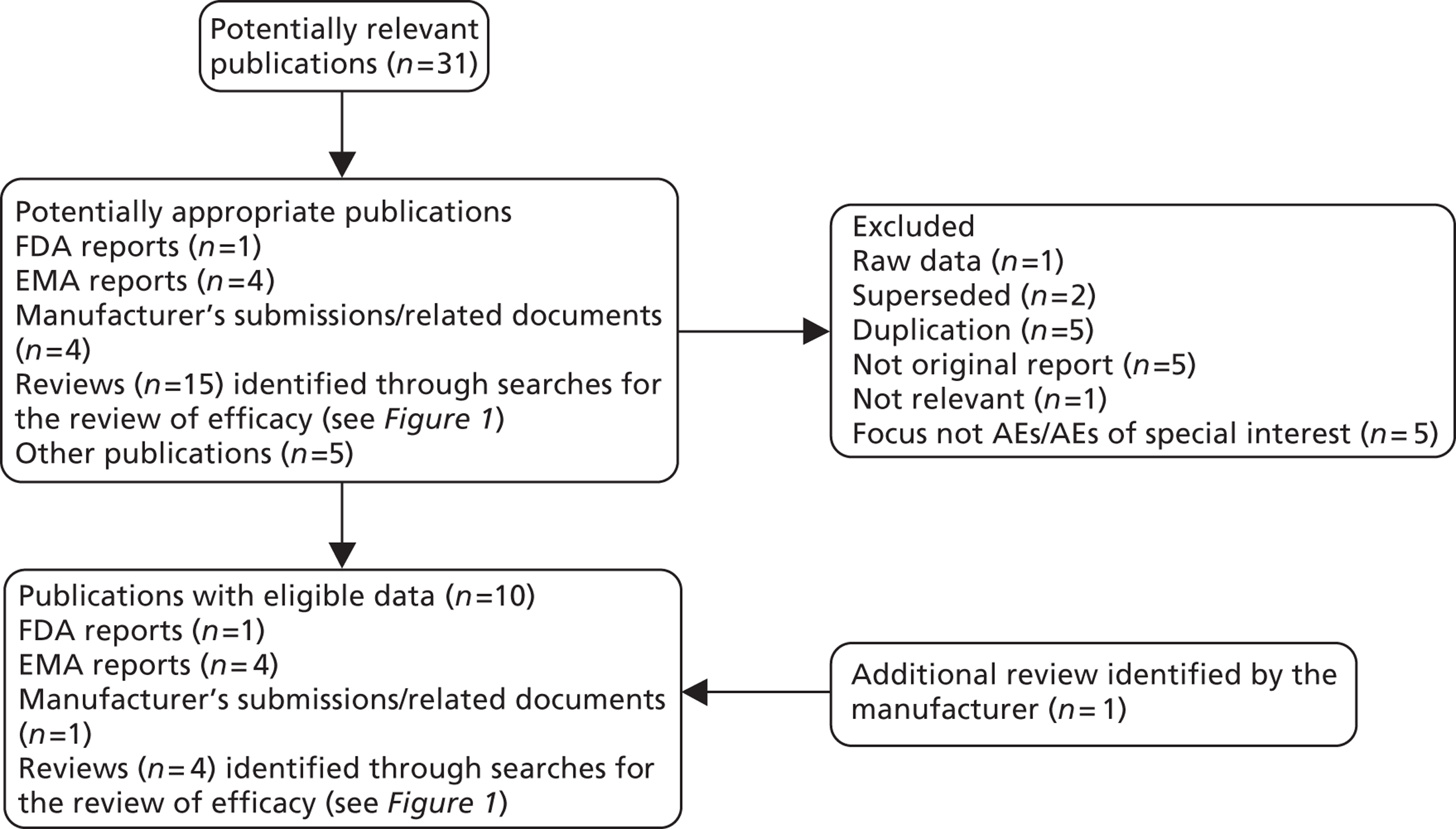
The included sources of adverse effects information are summarised in Table 39. The FDA data are sourced from the Adverse Event Reporting System (AERS) which supports the FDA's postmarketing safety surveillance programme for all approved drug and therapeutic biologic products. Similarly, the EMA data are derived from that agency's monitoring of the safety of authorised medicines in close co-operation with health-care professionals and pharmaceutical companies. The adverse drug reactions reported are received from manufacturers, health-care professionals and patients. The reporting of adverse events is voluntary and the figures provided may therefore underestimate the incidence of adverse events. The quality of these reports is therefore uncertain, although the work conducted by regulatory authorities may be assumed to meet appropriate professional standards.
Adverse event data reported in the MS were collected from the RCTs included in the submission (INNOVATE, EXALT, IA-04 and IA-05). 19,20,30,31 Supplementary data from an observational study (PERSIST),40 the summary of product characteristics (SPC),18 and a recent review by Tan and Corren80 were also discussed in the MS. Information sourced from the MS can be more complete than that from journal articles but may be presented to favour the technology of interest.
The four existing reviews of adverse events associated with omalizumab were published between 2007 and 2011. 76–79 The sample size of included reviews ranged from 3429 to 57,300 patients. Two reviews included RCTs76,78 and one included both RCTs and open-label studies. 77 One review included only patients with severe persistent allergic asthma,77 one included patients with moderate-to-severe persistent allergic asthma78 and the third included patients exposed to omalizumab in whom the indication was unclear. 76 The remaining review assessed the incidence of anaphylaxis in patients with asthma exposed to omalizumab. 79 These data were voluntarily reported to the AERS and may therefore underestimate the incidence of anaphylaxis.
Three of these reviews were not undertaken systematically, which means that the findings may be vulnerable to error and bias. These publications combined adverse event data using a narrative synthesis, which seems appropriate. There appears to be an overlap of patient populations and data in some of these publications, and with the primary studies summarised in Adverse events and serious adverse events of omalizumab for review of primary studies. This should be taken into account when interpreting the overall evidence. Only one review78 used systematic review methodology and combined rates of adverse events using meta-analysis to calculate pooled relative risks and 95% CI. This was a good-quality systematic review apart from the fact that it was unclear whether or not any language restrictions were made, and abstracts were excluded; these factors may have introduced the possibility of language and publication bias.
Adverse events and serious adverse events of omalizumab from existing summaries and reviews
The existing publications on the overall rates of adverse and serious adverse events are summarised in Table 39. Overall, high incidence rates of adverse events are reported in both patients exposed to omalizumab and those exposed to placebo. Rates were generally similar between treatment groups. The MS did, however, report a statistically significant reduction in serious adverse events in patients treated with omalizumab (RR 0.49; 95% CI 0.26 to 0.94) in one of the four double-blind RCTs that were described. Assessment of specific adverse events showed a trend towards higher levels of adverse events such as injection site reactions in patients exposed to omalizumab. One publication assessed safety in children72,74 and reported serum sickness in children, but symptoms were generally mild. A second publication reported higher levels of circulating immune complex in children receiving the highest doses of omalizumab, as compared with adults. The implications associated with this are unknown.
Specific serious adverse events
Concerns also exist suggesting that omalizumab may be associated with an increased risk of specific serious adverse events. The SPC18 highlights immune system disorders, including anaphylaxis, a numerical imbalance in malignancies arising in patients taking omalizumab and arterial thromboembolic events (such as stroke, myocardial infarction, and cardiovascular death). Clinical advisors to the assessment group highlighted anaphylaxis, malignancy and acute thrombotic events as important potential adverse effects to consider in this assessment. Mortality rates associated with treatment and withdrawals because of adverse events are also potentially important drivers for the economic model. The data on these adverse events from the existing reviews are summarised in Table 40. Reporting on adverse events of special interest was generally limited and where events were reported incidence was generally low.
Mortality
Five publications reported mortality rates, which were generally low (< 1%) and similar between treatment groups. 72–74,78
Anaphylaxis
Anaphylaxis was generally reported as a rare occurrence and the estimated risks were similar between omalizumab- and placebo-treated patients.
Malignancy
Numerically higher rates of malignancy were reported in the SPC,18 EMA European Public Assessment Report (EPAR)73 and by Corren (2009);77 all documents stated that malignant neoplasms were reported in 25 of 5015 (0.50%) patients receiving omalizumab compared with five of 2854 patients (0.18%) receiving controls (see Table 44). The EMA EPAR suggests against a causal link between omalizumab and malignancy, but further investigations are needed.
The assessment group calculated the relative risk using the above data: RR 2.85; 95% CI 1.09 to 7.42).
Four additional publications72,76,78 and Busse et al. 81 [see reference 60] assessed malignancy rates, none of which reported significant differences between treatment arms. A review published after the assessment group report submission date (Busse 2012) was considered to include relevant additional evidence on malignancies to support the suggestion that a causal link between omalizumab and malignancy is unlikely. No systematic review methods were reported. The data reported in Busse et al. 81 showed numerically higher rates of malignancy with omalizumab in certain study groups, but the differences were not statistically significant (see Table 44).
Arterial thrombotic events
Interim data from the EXCELS study71 reported an imbalance in the number of arterial thrombotic events, although the difference was not statistically significant. Long-term follow-up data from this study is awaited. No other publications reported a significant difference between treatment groups.
Withdrawals
Withdrawals because of adverse events were not often reported. Corren77 identified a statistically significantly higher proportion of withdrawals by patients receiving omalizumab (RR 1.94; 95% CI 1.20 to 3.14) compared with patients in control groups. One RCT included in the MS also identified a higher rate of withdrawals because of adverse events in the omalizumab group30 RR 8.23 (95% CI 1.11 to 61.24), but no significant differences as a result of serious adverse events. The 95% CI reported by the studies included in the submission were generally wide, which affects the reliability of the findings. No other publications reported significant differences.
Data from our systematic review of RCTs and observational studies are summarised in Appendix 14 and Appendix 15 and discussed in the section Adverse events and serious adverse events of omalizumab from review of primary studies.
| Publication | Quality assessment by assessment group | Nature of document | Evidence summarised | General findings on adverse effects |
|---|---|---|---|---|
| FDA reports | ||||
| Starke P. FDA Clinical Review Omalizumab (Xolair) (Paediatric supplement) 200972 | Overview/discussion on clinical data submitted by manufacturer | Review of clinical data relating to safety in children. The report also includes a summary (and update) of safety data in adults and adolescents | Children: data from a safety database of 1217 children aged 6–11 years. Of these, 624 were exposed to omalizumab in the context of a RCT (1A-05 and 10 core): 583 for 6 months and 360 for 1 year or longer. Two placebo-controlled trials in children | The review of safety in children revealed no new or unusual safety trends or trends for severe or common adverse events beyond those already identified in adults; those being malignancy and anaphylaxis |
| No systematic review methods used | Adults/adolescents: three premarketing studies in adults and adolescents; one postmarketing study (EXCELS); FDA AERS | One new safety issue is that higher levels of circulating immune complex than those seen in adults are likely in children who receive the highest doses of omalizumab. The risks associated with this, particularly over many years, are unknown | ||
| Postmarketing study (EXCELS) interim data (June 2004–November 2008) showed a statistically significant higher rate of serious adverse events with omalizumab (RR 1.47; 95% CI 1.31 to 1.64) | ||||
| EMEA reports | ||||
| EMA EPAR Xolair (omalizumab) (adult licence) 200573 | Discussion on clinical data submitted by manufacturer | The EMEA assessment report for omalizumab73 documents the safety data in the adult population | Data from a safety database of over 5300 patients | 82% of patients in both treatment arms of placebo-controlled studies experienced an adverse event. Compared with placebo or standard therapy, injection site reactions, exanthema/urticaria, gastrointestinal disorders and sinusitis were observed more frequently in omalizumab-treated patients |
| No systematic review methods used | ||||
| EMA EPAR Xolair (omalizumab) (licence variation for paediatric use) 200974 | Discussion on clinical data submitted by manufacturer | The EMEA assessment report for omalizumab74 documents safety data in the paediatric population | Data provided by two double-blind RCTs (Novartis trials IA-05 and 010), and 10 open-label controlled and uncontrolled studies in children aged 6 to < 12 years with allergic asthma or any indication (total n = 1217). The mean duration of exposure to omalizumab ranged from 42.0 weeks to 121.6 weeks | Approximately 90% of patients in both treatment arms of placebo-controlled studies experienced an adverse event. The most frequently reported adverse event was respiratory infections, with a slightly higher incidence in placebo patients. The rates of other adverse events were generally similar between treatment groups. Two anaphylactic reactions were reported but not considered to be treatment-related. Two severe cases of thrombocytopenia were reported; one in the omalizumab arm and one in the placebo arm. ‘Serum sickness’ was experienced by the paediatric population, but symptoms were mild in the majority of children. Local reactions were not considered a cause for concern |
| No systematic review methods used | ||||
| SPC (Xolair). London: EMA 201118 | Discussion on clinical data submitted by manufacturer | The SPC18 is published by the EMEA as part of the product licence | Data from clinical trials including 4400 allergic asthma patients (adults and children) (number of trials not specified) | The most commonly reported adverse events in adult and adolescent patients (≥ 12 years) were injection site reactions, including injection site pain, swelling, erythema and pruritus, and headaches. In clinical trials in children 6 to < 12 years, the most frequently reported adverse events considered to be treatment-related were headache, pyrexia and upper abdominal pain. Most cases were mild or moderate in severity |
| No systematic review methods used | ||||
| Medicines and Healthcare Products Regulatory Agency (MHRA) Drug Safety Update75 | Document produced by regulatory authority: assumed to be appropriate quality | A drug safety update on an imbalance of arterial thrombotic events (ATE) associated with omalizumab. ATE include stroke, transient ischaemic attack, myocardial infarction, unstable angina and cardiovascular death (including death from unknown cause) | Data from controlled trials (number of trials and number of patients not specified) and an ongoing observational study (EXCELS) (n = 7500; 5000 omalizumab, 2500 standard care) | A numerical imbalance of ATE was reported |
| Vigilance for possible thrombotic adverse events recommended | ||||
| MS and related documents | ||||
| Novartis MS for MTA | Document produced by regulatory authority: assumed to be appropriate quality | Analysis of adverse effects of omalizumab from the safety populations of the four RCTs specific to the licensed population (INNOVATE, EXALT, 1A-04 and 1A-05) | A total of 1824 (1146 omalizumab and 678 placebo) were included in the analysis. Data were not pooled across the trials | Any adverse events |
| Only one RCT (an open-label trial) showed a statistically significant difference between omalizumab and control groups (RR 1.25; 95% CI 1.04 to 1.49)31 | ||||
| Serious adverse events | ||||
| Only one RCT showed statistically significant difference (reduction) in omalizumab-treated patients (RR 0.49; 95% CI 0.26 to 0.94). | ||||
| The MS also referred to the SPC (see above) | ||||
| Reviews | ||||
| Buhl 201176 | No systematic review methods reported; very limited information on which to base quality assessment (abstract only) | Abstract only | Data from 32 randomised, double-blind, placebo-controlled trials in patients with unknown indications; n = 7432 | Malignancy data only, see Table 40 |
| Pooled data to examine incidence of primary malignancy in omalizumab-treated patients | Observation times censored at first malignancy 3382 patient-years for omalizumab and 2473 patient-years for placebo-treated patients. Treatment exposure durations of 2143.9 in omalizumab patients and 1689.1 in placebo patients | |||
| Busse 201281 (additional review data incorporated; identified by the manufacturer, but published after assessment group report submission date) | Pooled analysis; no systematic review methods reported | Pooled Novartis/Genentech data to examine incidence of primary malignancy in omalizumab-treated patients | Data from 32 randomised, double-blind, placebo-controlled trials in patients with unknown indications; n = 7432 (Buhl et al.76 ). Plus data from 35 controlled clinical trials, plus events occurring in patients after clinical trial termination captured by the ARGUS safety database (Novartis safety and pharmacovigilance database) | Malignancy data only, see Table 40 |
| Treatment exposure durations for omalizumab- and placebo-treated patients: 5800 and 2168 patient-years, respectively, in all clinical trials; 2978 and 2168 patient-years, respectively, in controlled clinical trials; and 2144 and 1689 patient-years, respectively, in randomised, double-blind, placebo-controlled trials | ||||
| Corren 200977 | Pooled analysis; no systematic review methods reported | Three large data sets (the omalizumab development programme ‘safety analysable population’) | The data set was derived from six placebo-controlled trials (plus two extension studies) and two open-labelled standard therapy controlled trials in severe persistent allergic asthma, and seven trials in other indications; n = 6130 | Any adverse events |
| One study (011) collected data for up to 4 years | Omalizumab: 2752/3678 (74.8%) | |||
| The findings relate to overall 2484 patients exposed to omalizumab ≥ 24 weeks, with 555 ≥ 52 weeks. The omalizumab dose in the majority of patients was 150 or 300 mg/4 weeks | Control: 1844/2452 (75.2%) | |||
| 35 Phase I, II and III trials were included in an analysis of malignancy only) | RR: 0.99 (95% CI 0.97 to 1.02) | |||
| Serious adverse events | ||||
| Omalizumab: 153/3678 (4.2%) | ||||
| Control: 92/2452 (3.8%) | ||||
| RR: 1.11 (95% CI 0.86 to 1.43) | ||||
| Long-term data: patient exposure was 191.4 (SD 21.3) weeks. The most common AE (> 3%) were bronchitis (4.2%), acute bronchitis (3.4%), lower respiratory tract infection (3.4%) and headache (3.4%) | ||||
| Rodrigo 201178 | Good-quality review based on literature searches of MEDLINE, EMBASE, CENTRAL, FDA and Novartis databases. Each stage of the review process performed in duplicate, including quality assessment | A systematic review of eight placebo-controlled trials of omalizumab | Data were derived from eight company sponsored trials (n = 3429, 1883 omalizumab). Study durations were less than 1 year | Any adverse events |
| Appropriate statistical analysis methods used | Trials were included if omalizumab was used in addition to corticosteroids | Omalizumab 84.9%, placebo 82.4% RR 1.01 (95% CI 0.97 to 1.05; p = 0.80) | ||
| Adult and children studies included | Serious adverse events | |||
| Omalizumab 3.8%, placebo 5.3% (RR 0.75; 95% CI 0.52 to 1.10; p = 0.14) | ||||
| Treatment-related AEs were more common with omalizumab (RR 1.61; 95% CI 1.05 to 2.47; n = 2112) | ||||
| Injection site reactions were more common with omalizumab (RR 1.43; 95% CI 1.15 to 1.79; n = 2853) | ||||
| Limb 200779 | Not a systematic review; incidence data only | A review and analysis of the incidence of anaphylaxis associated with omalizumab | 124 cases of anaphylaxis were identified from an estimated 57,300 omalizumab patients | Omalizumab-induced anaphylaxis may be characterised by a delayed onset and a protracted progression of symptoms. The unusual timing challenges the understanding of anaphylaxis |
| All spontaneous adverse event reports of anaphylaxis submitted to the FDA and to manufacturers of omalizumab June 2003–December 2006 and cases reported in the literature were reviewed | ||||
| Study details | Mortality | Anaphylaxis | Malignancy | Thrombotic/thrombotic-related events | Withdrawals because of AEs |
|---|---|---|---|---|---|
| FDA review 200972 | Children | Children | Children | Children | Children |
| 0 | Two (one patient was on placebo). Three further possible cases, although no temporal link with omalizumab | Two (both in the placebo arm of a trial) | Seven patients, three of whom were treated with omalizumab, experienced low platelet counts | NR | |
| Adults/adolescents | Adults/adolescents | Adults/adolescents | Adults/adolescents (cardiac disorders) | Adults/adolescents | |
| Omalizumab: 45/5041 (0.9%) | Four cases in preapproval safety database and a further 124 events between 2003 and 2006 (AERS) (estimated risk of 0.2%) | (events per 1000 patient-years) | Interim data from the EXCELs study report a RR of 1.5 (95% CI 0.9 to 3.0) for embolic, thrombotic and thrombophlebitis events | NR | |
| Non-omalizumab: 26/2886 (0.9%) | Omalizumab: 4.8 (20/4127) | ||||
| Non-omalizumab: (5/2236) | |||||
| RR 2.2 (95% CI 0.82 to 5.77) | |||||
| 96 malignancy events (AERS, 2003 to 2009) | |||||
| EMA EPAR Xolair (omalizumab) (adult licence) 200573 | Five (in clinical trials, three on omalizumab, two on placebo. None were considered treatment-related | ‘. . .a large number of listed anaphylactic reactions, urticaria and allergic reactions’ were reported as part of the international postmarketing experience prior to the UK licence | Across all completed studies malignant neoplasms occurred in 25/5015 (0.5%) omalizumab patients and 5/2854 (0.18%) placebo patients.a 0% of the cancers in omalizumab patients occurred within 1 year of starting treatment which would suggest against a causal link. Further investigation needed | Nothing reported | In placebo-controlled trials > 2% of patients in both groups withdrew because of AE |
| EMA EPAR Xolair (omalizumab) (licence variation for paediatric use) 200974 | 0 | Total: 3/926 (0.32%) | Total: 1/1217 (0.08%) | Nothing reported | 4/926 (0.43%) |
| Omalizumab: two | Omalizumab: 0 | ||||
| Placebo: one | Placebo: one | ||||
| SPC18 | NR | Reported as occurring rarely (≥ 1/10,000 to < 1/1000 | Clinical trials (≥ 12 years) | Controlled clinical trials | NR |
| Omalizumab: 25/5015 (0.5%) | Omalizumab: 6.29 (17/2703 patient-years) | ||||
| Control: 5/2854 (0.18%) | Control: 3.42 (6/1755 patient-years) HR 1.86; 95% CI 0.73 to 4.72 | ||||
| Observational studies | |||||
| Omalizumab: 5.59 (79/14,140 patient-years) | |||||
| Control: 3.71 (31/8366 patient-years) HR 1.11; 95% CI 0.70 to 1.76 | |||||
| MHRA Drug Safety Update 201175 | NR | NR | NR | Arterial thrombotic events per 1000 patient-years of treatment (patient-years) | NR |
| Data from EXCELS | |||||
| Omalizumab: 5.59 (79/14,140) | |||||
| Control: 3.71 (31/8366) | |||||
| Adjusted HR 1.11 (95% CI 0.70 to 1.76) | |||||
| Data from controlled trials | |||||
| Omalizumab: 6.29 (17/2703) | |||||
| Control: 3.42 (6/1755) | |||||
| Unadjusted HR 1.86 (95% CI 0.73 to 4.72) | |||||
| MS and related documents | |||||
| Novartis MS for MTA | Omalizumab: one | NR | NR | NR | INNOVATE |
| Placebo: five | RR: 2.42 (95% CI 0.77 to 7.60) | ||||
| EXALT | |||||
| RR: 8.91 (95% CI 0.52 to 151.96) | |||||
| IA-04 | |||||
| RR: 8.23 (95% CI 1.11 to 61.24) | |||||
| IA-05 | |||||
| RR: 0.98 (95% CI 0.09 to 10.78) | |||||
| Reviews | |||||
| Buhl 201176 | NR | NR | 2003 | NR | NR |
| Omalizumab: 5.86 (9/1536)a | |||||
| Placebo: 3.56 (4/1124)a | |||||
| RR: 1.65 (95% CI 0.46 to 7.31) | |||||
| 2006 | |||||
| Omalizumab: 4.21 (9/2136)a | |||||
| Placebo: 3.50 (6/1715)a | |||||
| RR: 1.20 (95% CI 0.43 to 3.38) | |||||
| 2010 | |||||
| Omalizumab: 4.14 (14/3382)a | |||||
| Placebo: 4.45 (11/2473)a | |||||
| RR: 0.93 (95% CI 0.39, to 2.27) | |||||
| Busse 201281 | NR | NR | 67 clinical trials + ARGUS safety database | NR | NR |
| 177 patients (209 malignancies) | |||||
| After blinded assessment, 47 judged as non-malignant | |||||
| Of the remaining 162 events, 56 patients identified with malignancies (62 in total): | |||||
| Omalizumab: 43/56 | |||||
| Placebo: 13/56 | |||||
| Incidence of primary malignancy | |||||
| All clinical trials | |||||
| Omalizumab: 39/7789a | |||||
| Placebo: 12/4252a | |||||
| RR: 1.35 (95% CI 0.69 to 2.85) | |||||
| Controlled clinical trials (including ARGUS data) | |||||
| Omalizumab: 20/6246a | |||||
| Placebo: 12/4252a | |||||
| RR: 1.13 (95% CI 0.52 to 2.54) | |||||
| Randomised double-blind placebo-controlled trials (excluding ARGUS data) | |||||
| Omalizumab: 11/4254a | |||||
| Placebo:11/3178a | |||||
| RR: 0.73 (95% CI 0.29 to 1.86)b | |||||
| Corren 200977 | NR | Omalizumab: 5/3678 (0.14%) | Omalizumab: 25/5015 (0.50%) | Nothing reported | Omalizumab: 64/3678 (1.7%) |
| Control: 2/2452 (0.07%) | Control: 5/2854 (0.18%) | Control: 22/2452 (0.9%) | |||
| RR: 1.67 (95% CI 0.32 to 8.58) | Assessment group calculated RR: 2.85 (95% CI 1.09 to 7.42) | RR: 1.94 (95% CI 1.20 to 3.14) | |||
| Limb 200779 | NR | 124 cases | NR | NR | NR |
| Time to onset | |||||
| < 30 minutes: 43/124 (35%) | |||||
| 30–60 minutes: 20/124 (16%) | |||||
| > 60–90 minutes: 3/124 (2%) | |||||
| < 90–120 minutes: 8/124 (6%) | |||||
| 2–6 hours: 6/124 (5%) | |||||
| 6–12 hours: 17/124 (14%) | |||||
| 12–24 hours: 10/124 (8%) | |||||
| > 24 hours up to 4 days: 11/124 (9%) | |||||
| Rodrigo 201178 | Omalizumab: 0/1883 | Omalizumab: two (0.33%) | Omalizumab: one | Cardiovascular adverse events | Omalizumab: 25/1883 (1.3%) |
| Placebo: 1/1546 (0.06%) | Placebo: one (0.24%) | Placebo: one | Omalizumab: 0 | Placebo: 23/1546 (1.5%) | |
| RR: 1.08 (95% CI 0.13 to 8.74) | Placebo: three | RR 0.97 (95% CI 0.43 to 2.20) | |||
Adverse events and serious adverse events of omalizumab from review of primary studies
Adverse effect data were extracted from the primary studies (11 RCTs and 12 observational studies) included in the clinical review (Appendices 14 and 15). There appears to be an overlap of patient populations and data in some of the studies. No attempt has therefore been made to pool values across studies, rather the rates of adverse events and individual study risk ratios have been summarised as a narrative synthesis.
Ongoing studies
A number of publications refer to an ongoing long-term safety study in patients with moderate-to severe asthma (EXCELS). Interim data (to November 2010)71 reports on malignancy rates in patients aged at least 12 years from US centres. The report comprises 18,860 person-years in the omalizumab cohort and 10,947 person-years in the non-omalizumab cohort. No statistically significant differences were shown in the incidence of study-emergent primary malignancy: risk difference (RD) −1.70 per 1000 person-years (95% CI −6.43 to 2.21 per 1000 person-years; see also Adverse events and serious adverse events of omalizumab from existing summaries and reviews). Twenty-four other ongoing studies were identified from the ClinicalTrials.gov website. There were insufficient data available to determine whether these studies met the criteria for inclusion in the review, and attempts to obtain further data or links to publications were unsuccessful.
Attempts were made to access data from a national audit of asthma deaths that is being led by Dr Nasser from Cambridge University Hospital. Unfortunately, data collection only commenced at the beginning of 2012 and data are therefore not yet available. However, Dr Nasser has been running a regional confidential enquiry into asthma deaths for many years and reported that the number of deaths is very small locally (approximately 20) (personal communication, 30 August 2011).
Any adverse event and serious adverse events
Adverse event data in adults and adolescents were reported in nine RCTs (see Appendix 14). Adverse event rates and serious adverse events were generally similar between treatment groups. Two RCTs in adults and adolescents31,36 showed statistically significant higher rates of adverse events in patients exposed to omalizumab (RR 1.25; 95% CI 1.05 to 1.50; and RR 1.14; 95% CI 1.01 to 1.28).
Adverse event data in children were reported in two RCTs (see Appendix 14). 20,28 The proportion of patients experiencing one or more adverse events in the two RCTs including children was similar between treatment groups. Serious adverse event rates, however, were statistically significantly higher in the placebo-treated groups in both RCTs (RR 0.45; 95% CI 0.24 to 0.85 and RR 0.49; 95% CI 0.26 to 0.94). A subgroup of 155 patients with severe asthma were assessed in the children-only trial and the rates of serious adverse events were no longer significantly different (six patients receiving omalizumab and eight receiving placebo). 21
Nine observational studies reported the number of patients experiencing one or more adverse events and eight reported on serious adverse events (see Appendix 15). The rates of adverse and serious adverse events ranged from 6.5% to 98.5%, and 0% to 24.4% respectively. The proportion of patients experiencing adverse events in the observational studies varied more than in patients receiving omalizumab in the RCT. Most RCTs reported more than 50% omalizumab patients experiencing adverse events compared with observational studies, which mainly reported figures < 50%. Serious adverse events generally occurred in < 20% of the population in both the RCTs and the observational studies. Follow-up durations for the majority of observational studies ranged from 4 months up to 2 years. In comparison, follow-up for the majority of RCTs was 48 weeks or less.
Specific serious adverse events
Serious adverse events of special interest (anaphylaxis, malignancy and thrombotic events) were rarely reported.
Mortality
Six RCTs assessed mortality;20,30–33,36 three of these (including IA-05 trial in children only20) reported no deaths,20,32,36 whereas the remaining three reported a total of six deaths (one in the omalizumab group and five in the comparator group). 30–32 RRs were calculated for three RCTs, none of which showed statistically significant treatment differences. It should be borne in mind that these RCTs were not powered to investigate mortality rates and the incidence of death in asthma patients, and especially in paediatric patients is low. Six observational studies reported mortality rates; there were a total of 13 deaths, with all-cause mortality rates ranging from 0% to 2.5% in the individual studies. 38,39,41,45,46,62 These rates were slightly higher than those for the omalizumab arms of the RCTs (0% to 0.71%).
Anaphylaxis
Two RCTs in adults reported three anaphylactic events, with no statistically significant differences between treatment groups. 32,33 Nine cases were reported in two RCTs enrolling children (two patients receiving omalizumab, seven receiving comparator), but neither RCT reported a statistically significant difference between treatment groups. 20,28 One observational study reported the rate of anaphylaxis, which was 0%. 46 No study was powered to investigate the rate of anaphylaxis, and its association with omalizumab use based on these studies remains unclear.
Malignancy
Malignancy was reported in two RCTs on adults and adolescents and was evident in six patients; three patients in each treatment group. 32,33 The RCTs including children reported one case of malignancy in a patient receiving placebo. 20,22 Rates were also low in the observational studies. One observational study reported malignancy in one patient, but this was not considered treatment-related. Neither study was sufficiently powered to investigate the rate of malignancy. 41,71
Arterial thrombotic events
Thrombotic/thrombotic related events were reported in three adult RCTs. 30,32,33 The types of events varied among studies and the data were not particularly clear. There were no statistically significant differences in the number of events between treatment groups. The RCTs in children only reported a significantly higher rate of thrombotic events/thrombotic-related events in children receiving placebo (RR 0.08; 95% CI 0.01 to 0.64). 28
As for the other serious adverse effects, none of the studies identified were sufficiently powered to investigate the association with omalizumab.
Two non-comparative studies reported > 5% frequency of vascular events in patients exposed to omalizumab. 39,46
Other adverse events
The most commonly reported adverse events in adults and adolescents in the RCTs were pain at site of injection, and infections and infestations (including respiratory tract infections). One trial reported a significantly higher rate of gastrointestinal disorders in patients exposed to omalizumab compared with comparator (25% vs. 9.1% respectively). 20
In children, significantly fewer haematological events were reported in the omalizumab group compared with placebo group, but significantly more gastrointestinal disorders were reported (see Appendix 14). 20 The most frequently occurring adverse events reported in the children and adolescent trial were nasopharyngitis, sinusitis, upper respiratory tract infection, pyrexia, headache, influenza, cough, bronchitis, viral upper respiratory tract infection and vomiting. 28 Rates were generally slightly higher in the placebo group.
Similar to other frequently reported adverse events in the RCTs, five observational studies reported pain at site of injection as occurring frequently; ranging from 1.4% to 35.3%. 40,41,46,59,70 Two observational studies reported rate of infection and infestation; 5% and 76.7%. 44,46
Withdrawals because of adverse events
Rates of withdrawals because of adverse events were similar between treatment groups in adults and adolescents. Three children withdrew from the children only trial because of adverse events; two (0.5%) in the omalizumab group (one of whom had severe asthma) and one in the placebo group, but the difference was not statistically significant. 20
Rates of withdrawals because adverse events were generally similar in the nine observational studies38–41,45,46,59,62,70 reporting this outcome compared with rates reported in the RCTs. Rates ranged from 1% to 12% in the observational and between 0% and 7.2% in the RCTs. 19,20,28–33,35,50
Results of assessment of adverse effects of oral corticosteroids
Relevant publications on adverse effects of oral corticosteroids
The following published systematic reviews were identified as relevant to this review question: Hoes et al. ,82 Sarnes et al. 83 and Manson et al. 84 Information was also taken from the Novartis submission to the MTA process. One additional review was the only source of information on the effects of OCSs on growth (Allen et al. 199485). The information provided by each source is summarised by section below.
Hoes et al.82
This paper describes a systematic review of the adverse effects of low to medium low doses of OCSs (doses of ≤ 30 mg, with some flexibility). The literature searches included MEDLINE, EMBASE and CINAHL using appropriate search terms. The criteria for studies to be included in this review were: the study was of adults with inflammatory diseases treated with corticosteroids (glucocorticoids); dose of corticosteroids ≤ 30 mg (one study that used a higher dose for the first month was included); dichotomous adverse events data had to be reported; the study was reported in a full paper. Studies that included patients with previous long-term or recent experience of OCSs were excluded. We note that there is some ambiguity about whether or not the paper was purely about OCSs.
A potential limitation of this systematic review is that only papers that reported dichotomous data were included, with the risk that some potentially relevant data might be missing. In addition, the actual duration of each trial's follow-up is not reported, ignoring the possibility that event rates may change with time. For the purposes of the present appraisal, the results of this review are further limited by the fact that there were no included trials of asthma or chronic obstructive pulmonary disease (COPD). The results were reported overall and by diagnosis [rheumatoid arthritis (RA), polymyalgia rheumatica (PMR) and inflammatory bowel disease (IBD)] and rates were found to vary between indications, raising the question of the generalisability to asthma patients. Finally, the data from the IBD trials included in the review were different from those from other trials; however, this may reflect the fact that they are short-term trials: short-term trial results are more heterogeneous and with higher event rates than those of longer-term trials.
The Hoes et al. review calculated and reported rates of adverse events based on single-arm or uncontrolled data: all adverse events and also categories (by body systems) of adverse events. However, it did not report rates of individual adverse events, for example it reported ‘cardiovascular’ but not acute myocardial infarction (AMI). All results were reported as dichotomous data (events/patient-years) with calculated event rates (rate/100 patient-years) and 95% CI. The latter are given in Table 41. The paper stated that ‘comparison of low and medium dosages did not show dose dependency of any of the adverse events’. This could be a reflection of some flaw in the analysis, as it does not reflect other findings related to adverse events of OCSs: it could be that the dose range studied is too narrow, or the dichotomy between low and medium too crude, to reveal a dose-dependent effect.
| Adverse event | AE rate (95% CI) |
|---|---|
| Psychological and behavioural disturbances | 25 (15 to 34) |
| Gastrointestinal | 19 (14 to 24) |
| Dermatological | 15 (10 to 20) |
| Neurological | 12 (6 to 19) |
| Musculoskeletal | 12 (7 to 17) |
| Infectious | 12 (8 to 16) |
| Endocrine and metabolic | 11 (7 to 14) |
| Cardiovascular | 8 (5 to 11) |
| Ophthalmological | 3 (2 to 4) |
| Other | 8 (5 to 11) |
In summary, although the Hoes et al. paper described a good-quality systematic review, unfortunately it included only single-arm or uncontrolled data and only presented data for the number of patients experiencing any adverse event or rates of classes of adverse events, for example the rate for ‘gastrointestinal’ events. This information was not useful for the purposes of the economic model.
Sarnes et al.83
This study was a semi-systematic review of the adverse events associated with oral and parenteral corticosteroids. It is, in part, an update of the review by Manson et al. 84 and so there is much overlap between these two publications. The study included appropriate literature searches of databases including MEDLINE, EMBASE and The Cochrane Library, with dates reported (up to 2009) and the inclusion criteria were reported. However, the synthesis was not systematic nor transparent. Some relevant data were presented together with costs in the US context.
The review included 47 studies, but four were excluded for being of too poor quality. Twenty-four of the studies were of OCSs: 19 were of parenteral corticosteroids or parenteral and oral mixed. Six studies were in paediatric patients, but results for adverse events in children were not presented separately. The results of this study were presented as risk ratios for specified adverse events associated with certain dose levels of corticosteroids, although some incidences are also reported. However, the sources of results are not reported consistently: sometimes the source is an individual primary study, or a narrative synthesis of primary studies, sometimes it is the results of another review article or articles. One additional problem was that the results for OCSs were not separated from parenteral corticosteroid use.
Unfortunately, this review did not use adequate systematic review methods and it is not possible to be certain that the results are reliable.
Manson et al.84
This was a semi-systematic review that involved literature searches of key databases including MEDLINE, EMBASE and The Cochrane Library, covering the period January 1990–March 2007. This aim of the review was to identify studies that considered adverse events because of OCS treatment. It specified criteria for inclusion of studies in the review: that studies reported on adverse effects/events of OCSs (prevalence of OCS adverse effects, relationship between OCS adverse effects and patient characteristics or duration of steroid use, dose–response relationship for OCSs and adverse effects, or threshold effect for OCS adverse events). Studies that investigated non- (or sub-)clinical adverse effects, e.g. effects on bone markers, were not included. Non-English-language papers were not included. However, the synthesis was poor, such that, although all studies were presented there was no clarity regarding the method of synthesis: the data synthesis was essentially narrative and not transparent.
The paper reported individual trial results and also reported relative risks for certain adverse effects, but only those where relative risks were reported in the primary publication. Unfortunately, the review did not report the variance. Importantly, the relative risks reported are just from individual studies with no explanation why synthesis was not attempted, or how studies or data were selected.
The Novartis submission to the multiple technology appraisal
The review of the adverse effects of OCSs presented in the MS was based on the paper by Manson et al. (2009). 84 Given that this published systematic review was relatively recent, the manufacturer did not undertake a separate or updated systematic review to inform this analysis. However, a bibliography search of Manson et al. (2009)84 and further investigation identified the source data for establishing the excess risk of the following disease outcomes:
-
type 2 diabetes
-
myocardial infarction
-
glaucoma
-
cataracts
-
ulcer
-
osteoporosis
-
stroke.
The bibliography search identified glaucoma as an additional disease outcome with quantified excess risk that was not included in Manson et al. 84 Also, the impact of OCS use on the incidence of non-Hodgkin's lymphoma was excluded from this analysis because of its rarity and very small cost impact (£0.41 per patient per year) in Manson et al. 84
Allen et al.85
This study was a meta-analysis of data on the effects of corticosteroids on height attained by children. This meta-analysis was not based on a systematic review. Although the source data were reported as having been identified through an ‘exhaustive literature search of “leading medical journals” up to January 1993’, further details were not given. It was unclear what study designs were included and there was no attempt at quality assessment of the included studies.
It was a meta-analysis of studies comparing attained height with expected height. The analysis included 21 studies including 810 patients (395 of whom were on OCSs). It is unclear how representative the included studies are of all studies on the effects of OCSs on growth, given that only those that reported the precise numbers of children at or above their expected height were included. The use of meta-analysis appears appropriate. However, the results of the meta-analysis are presented only as a Z-value, p-value and mean correlation coefficient (r).
The results found that prednisone (and separately other OCSs) is associated with a statistically significant tendency to not attain expected height (Table 42). However, there was no information on how short of expected height these children were.
| Steroid | Tendency to be shorter than expected |
|---|---|
| Oral prednisone (n = 196) | Z = 2.137, p = 0.0164, mean r = −0.295 |
| Other OCSs (n = 299) | Z = 9.107, p = 2.44, mean r = −0.260 |
Although growth retardation is a known and concerning adverse effect of OCS use in children, an estimate of the size and clinical significance of this effect has not been identified from the literature.
Synthesis
The most useful and appropriate source of information on the adverse effects of OCSs was the semi-systematic review by Manson et al. 84 This was because it focused on OCSs, whereas the updated review by Sarnes et al. 83 included oral and i.v. administration. The Manson et al. 84 publication also presented relative risks or odds ratios which are required for the economic model. The analysis presented in the Novartis submission was also considered a good source of evidence, especially as the effect sizes reported in the Novartis submission were, in the most part, derived from the Manson et al. study. However, there were some inconsistencies between the information provided in the MS and the Manson et al. paper, and therefore the primary studies were checked and data used from those primary sources where necessary. The summarised estimates are listed in Table 43. These were taken, in most cases from Manson et al., and the primary study authors and citation number from Manson et al. are reported in the table. Where an estimate was taken directly from a primary source, that source is cited directly.
| AE | RR from Manson et al.84 | RR/OR from single studies | Study (citation number in Manson et al.84) |
|---|---|---|---|
| Fracture | 1.95 | ||
| Fracture (hip/femur) | OR 1.66 (95% CI 1.46 to 1.90) | De Vries 2007 (55) (n = 6763) | |
| Fracture | RR 1.90 (95% CI 1.68 to 2.16) | Donnan 2005 (6) (n = 20,266) | |
| Osteoporotic fracture (short-term use of high dose ≥ 30 mg) | RR 1.21 (95% CI 1.04 to 1.42) | Van Staa 2005 (20) (n = 191,752) | |
| Osteoporotic fracture (cumulative dose of > 1 g and current use 15–29.9 mg/day) | RR 2.84 (95% CI 2.45 to 3.30) | Van Staa 2005 (20) (n = 191,752) | |
| Osteoporotic fracture (related to doses of > 60 mg/day) | RR 2.5 (95% CI 1.70 to 3.70) | Zonana-Nacach 2000 (19) (n = 539) | |
| Fracture | RR 1.75 (95% CI 1.6–1.9) | Steinbuch 2004 (14) (n=17,957) | |
| Vertebral fracture | RR 2.92 (95% CI 2.0 to 4.3) | Steinbuch 2004 (14) (n = 17,957) | |
| Vertebral fracture | RR 2.60 (95% CI 2.31 to 2.92) | Van Staa 2000 (71) (n = 244,235) | |
| Fractures in children taking ≥ 30 mg/day | RR 1.24 | Van Staa 2003 (16) (n = 37,562) | |
| Fractures in children taking more than four courses | RR 1.32 | ||
| Diabetes | 2.31 | ||
| Hyperglycaemia requiring treatment | RR 2.23 (95% CI 1.92 to 2.59) [current (or within 45 days) use of OCSs] | Gurwitz 1994 (21) (n = 11,855) | |
| Peptic ulcer | 2.00 | ||
| Peptic ulcer in patients with gastric/duodenal ulcer | RR 2.0 (95% CI 1.3 to 3.0) | Piper 1991 (30) (n = 1415) | |
| Stroke | 1.20 | ||
| Stroke (related to doses of > 60 mg/day) | RR 1.2 (95% CI 1.0 to 1.5) | Zonana-Nacach 2000 (19) (n = 539) | |
| Cataract | 1.90 | ||
| Cataract (related to doses of > 60 mg/day) | RR 1.9 (95% CI 1.4 to 2.5) | Zonana-Nacach 2000 (19) (n = 539) | |
| Cataract (in patients aged 50 years or more with asthma, COPD or fibrosing alveolitis) | Unadjusted OR 2.6 (95% CI 1.8 to 3.9) | Walsh 2001 (5) (n = 367) | |
| Cataract high cumulative usage (18 months of 10 mg/day) vs. low cumulative usage (6 months of 10 mg/day) | Adjusted OR 1.83 (95% CI 1.25 to 2.69) | Curtis 2006 (27) (n = 1869) | |
| Myocardial infarction | 1.42 | ||
| Myocardial infarction (in current users of OCSs, all doses) | Adjusted RR 1.71 (95% CI 1.44 to 2.02), Multivariate adjusted 1.42 (95% CI 1.17 to 1.72) | Varas-Lorenzo 2007 (24) (n = 4795) | |
| Myocardial infarction (in current users of OCSs, > 10 mg/day) | Adjusted RR 2.50 (95% CI 1.77 to 3.53), multivariate adjusted 2.15 (95% CI 1.45 to 3.14) | Varas-Lorenzo 2007 (24) (n = 4795) | |
| Myocardial infarction (in current users of OCSs) | Adjusted RR 2.01 (95% CI 1.13 to 3.58) | Huiart 2006 (25) (n = 371)a | |
| Non-Hodgkin's lymphoma [standardised incidence ratio (observed to expected)] | 1.30 | SIR 1.30 (95% CI 1.06 to 1.58) | Sorensen 2004 (32) (n = 333,733 person-years) |
| Adrenal insufficiency | -- | OR 2.0 (95% CI 1.6 to 2.5) | Mortimer 2006 (56) (n = 154)b |
| Heart failure (in patients with ischaemic heart disease) | Adjusted OR 2.66 (95% CI 2.46 to 2.87) | Souverein 2004 (26) (n = 50,656) | |
| Avascular necrosis (related to doses of > 60 mg/day) | RR 1.2 (95% CI 1.1 to 1.4) | Zonana-Nacach 2000 (19) (n = 539) | |
| Glaucoma | |||
| Ocular hypertension (glaucoma) all doses including > 20 mg/day | Adjusted OR 1.41 (95% CI 1.22 to 1.63) | Garbe 1997 (22) (n = 9793) | |
| Ocular hypertension (glaucoma) <10mg/day | Adjusted OR 1.26 (95% CI 1.01 to 1.56) | Garbe 1997 (22) (n = 9793) | |
| Sleep disturbance [high cumulative usage (18 months of 10 mg/day) vs. low cumulative usage (6 months of 10 mg/day) (calculated as 5.5 g vs. 1.8 g)] – high dose equals APEX study mean value for 12 months | Adjusted OR 2.77 (95% CI 2.14 to 3.59) | Curtis 2006 (27) (n = 2146) | |
| Mood problems [high cumulative usage (18 months of 10 mg/day) vs. low cumulative usage (6 months of 10 mg/day)] | Adjusted OR 2.39 (95% CI 1.83 to 3.12) | Curtis 2006 (27) (n = 2025) | |
| Weight gain [high cumulative usage (18 months of 10 mg/day) vs. low cumulative usage (6 months of 10 mg/day)] | Adjusted OR 2.20 (95% CI 1.65 to 2.95) | Curtis 2006 (27) (n = 2040) | |
| Growth | Tendency to be shorter than expected | Allen et al. 1994 (subgroups of prednisone and ‘other OCS’ patients)84 | |
| Oral prednisone (n = 196) | |||
| Z = 2.137, p = 0.0164, mean r = −0.295 | |||
| Other OCSs (n = 299) | |||
| Z = 9.107, p = 2.44 mean r = −0.260 |
Discussion of clinical effectiveness
Issues arising from the licensing restriction
The assessment of clinical effectiveness has been constrained by the requirements of the licence criteria in two important ways. Firstly, the licence requirements differ between adults and adolescents aged ≥ 12 years and children aged < 12 years, and NICE has always considered these populations separately. Discussion with the clinical advisors to the assessment group has indicated that the distinction is, in some respects, artificial, and that severe allergic asthma in the two groups does not differ in a meaningful way in its characteristics or response to treatment. Although children are clearly a separate population from adults, the value of a cut-off at age 12 between paediatric and adult populations is unclear. This view is supported by the similarity of the estimates of effect for the primary outcome of total exacerbations in the key double-blind placebo-controlled trials in the licensed population in adults (INNOVATE) and children (IA-05-EUP) respectively. Given that the randomised data in children who meet the licence criteria is so restricted, limited as it is to this single subgroup, it may be reasonable to extrapolate supportive evidence from the data in adults and older children. This is particularly the case in considering children who are dependent on maintenance OCS, of whom only six were included in IA-05-EUP.
The licence in both children and adults imposes multiple requirements. In addition to a positive skin test or in vitro reactivity to a perennial aeroallergen, these comprise frequent daytime symptoms or night-time awakenings and multiple documented severe asthma exacerbations despite daily high-dose ICS plus LABA. Adults are also required to have reduced lung function, with FEV1 < 80% predicted.
In our assessment we have included several trials as supportive evidence in which it was clear that a substantial proportion of the trial population met licence criteria, but for which outcome data for these patients could not be separated from those who did not meet the licence criteria. In the case of the large placebo-controlled double-blind (n = 850) trial by Hanania et al., it appeared probable that a very large majority of the patients did in fact meet licence criteria and that almost the whole of two of the subgroups for which exacerbation data were reported would meet the criteria. However, because the patients were not required to have experienced multiple exacerbations it was not possible to statistically combine data from this trial with data from INNOVATE or to use these data to inform the economic model. The same problem was encountered with other trials in which a lower, although still significant, proportion of patients were known to meet the licence criteria but for which for the relevant subgroup data were not available.
In clinical practice this criterion of multiple exacerbations for treatment eligibility is problematic. Firstly, because it applies equally to patients on BTS/SIGN treatment step 4 and step 5, patients at step 4 who should be on step 5 treatment, or who are not fully compliant are eligible, whereas those who are well-managed and have high treatment compliance on step 5 therapy are not. Secondly, it has the potential to provide a perverse incentive for patients at both step 4 and step 5 to reduce their compliance with standard therapy. It could also be considered that it might provide such an incentive for clinicians to undermanage patients at both steps. Thirdly, if one of the key benefits of omalizumab is its steroid-sparing effect then this is clearly anomalous. If it were assumed that patients who were at BTS/SIGN step 5 would be uncontrolled at BTS/SIGN step 4, then patients on maintenance OCS would be eligible for omalizumab therapy whether or not they experienced multiple exacerbations. The SMC guidance which restricts omalizumab to patients who are on maintenance OCS therapy, but does not impose a restriction based on exacerbation incidence appears more pragmatic in this respect; this guidance also applies to children aged < 12 years.
It is evident from the submissions made by consultees in the NICE process that day-to-day symptoms of poorly controlled asthma impose a substantial health burden on patients (both adults and children), which may be present in the absence of repeated exacerbations. Such patients cannot be considered to be eligible for omalizumab although they may experience considerable disease-related impairments in QoL despite optimised standard therapy.
Nature of the evidence
There is a considerable body of randomised controlled evidence addressing the efficacy of omalizumab in adults and adolescents aged ≥ 12 years who met the licence criteria. In part, this comprises the licence-specific trials and subgroups (one large double-blind placebo-controlled trial, one large open-label trial and an a priori subgroup of a second open-label trial), but also includes additional evidence drawn from a number of placebo-controlled trials in which a proportion of patients met the licence criteria. This included one large high-quality trial in which it appeared that a substantial majority of patients met the licence criteria. Some evidence from a number of observational studies was also identified but this was limited by poor reporting and heterogeneity.
Although it is clear that there is a significant quantity of data relating to the efficacy of omalizumab in the licensed population, a substantial amount of this data relates to patients outside of trials whose inclusion criteria conform to those of the omalizumab licence. As there was little or no reporting of subgroup data for these patients, this review has been forced to adduce the data from the whole trial populations as supportive evidence rather than being able to fully include the licensed patient data. However, given that this was the only way in which such data could be included without benefit of subgroup analyses or IPD, the effect has been to demonstrate efficacy of omalizumab in populations wider than that defined by the licence.
As outlined in Assessment of clinical effectiveness, Treatment effectiveness of omalizumab, the impact of trial design on response rate and exacerbation rates was considerable. A higher proportion of patients in the open-label EXALT trial were responders and there was a larger treatment effect on total exacerbations in the ITT population of EXALT compared with the double-blind INNOVATE trial. It is the combination of this methodological heterogeneity together with the issue of licence criteria which has prevented statistical pooling of trials in this review.
Limited evidence addressing the efficacy of omalizumab in children under 12 meeting the licence criteria was identified. Randomised data were limited to an a priori subgroup of a single double-blind placebo-controlled RCT. Additional evidence was drawn from a large RCT with a mixed population of inner-city children and adolescents conducted in the USA. As only half of the participants were receiving appropriate maintenance therapy and no subgroup data were presented, the relevance of this evidence to the UK population is likely to be limited. Two observational studies were identified which reported some useful data on children with severe uncontrolled allergic asthma in the UK and France respectively. Neither of these studies was limited to children aged < 12 years.
The evidence on the important question of OCS-sparing was limited to two RCTs subgroups (only one of which was in the licensed population) and a number of observational studies. There was almost no evidence to address this question in children: only two small linked observational studies were identified.
Benefit of omalizumab: main review of clinical effectiveness
The primary outcome of the review was clinically significant exacerbations. Based on total exacerbations and CSS exacerbations, there was clear evidence of benefit in both licensed populations and in supportive trials with slightly wider populations in adults; this benefit was seen in both double-blind and open-label trials. Not surprisingly, these benefits were reflected in the responder populations. There was also evidence of significantly reduced exacerbations in the double-blind RCT subgroup of children who met the licence criteria; this benefit was also present in the responder analysis. The results from the RCTs were reflected in the observational studies, including those conducted in the UK providing some support for the generalisability to use by the NHS.
Because of clinical and methodological heterogeneity, estimates of effect more precise than those from single trials could not be obtained and therefore the effect size in terms of omalizumab's impact on clinically significant or severe exacerbations is somewhat uncertain.
Benefits in terms of hospitalisation and other forms of unscheduled care were also identified for omalizumab therapy. However, although treatment effects showed a pattern comparable to that for exacerbations in adults, they were not present in the ITT analysis in children. The responder analysis showed a benefit of reduced hospitalisation for paediatric patients but no other benefits in terms of reduced health-care use.
Subgroup analyses suggested that there may be a greater benefit in patients on maintenance OCS at baseline and, in the responder analyses, in patients with a history of hospitalisation in the previous year, but CI were wide and this was not confirmed by tests of interaction. Furthermore, caution should be exercised in the use of data from these post hoc subgroups, which in some cases represent subgroups of subgroups.
Although measures of exacerbation and unscheduled health-care utilisation are clearly of key importance, not least to the question of cost-effectiveness, they do not fully capture the treatment benefit of omalizumab. Reductions in day-to-day symptoms and steroid requirements are likely to be of key importance to QoL and there is clear evidence of an omalizumab treatment benefit in adults assessed, both in the licensed populations and more widely. However, symptom relief was not the primary outcome in the majority of trials and was assessed using a variety of measures. Both of these factors made it difficult to quantify the treatment effect on this outcome. Evidence of symptom reduction was supported by small but statistically significant benefits in increased FEV1. Evidence of reductions in individual symptoms was more mixed, as was evidence of reduced requirements for reliever medication where most results were not statistically significant. There was a clear benefit in QoL, with increased scores on the AQLQ in omalizumab groups across the trials assessing the licensed population. This was also seen in some of the supportive trials including that of Hanania et al. 33 In other trials where a benefit was not seen this appeared to be because of large placebo effects in the comparator arm.
There was limited data on the benefits of omalizumab in children across secondary outcomes. The IA-05-EUP subgroup showed no statistically significant results across outcomes related to symptoms or QoL, but was underpowered to assess this outcome. Although the supportive trial by Busse et al. (2011) did show evidence of benefit in ACT score, this effect was not present in children aged < 12 years; equally the reductions in individual symptoms may have been driven by older children and/or children not on maintenance therapy. 28 Limited additional evidence is drawn from small numbers of children with OCS-dependent asthma in the UK-based observational study by Brodlie et al. 54 This demonstrated statistically and clinically significant benefits of reduced ACT and increased mini-AQLQ scores.
Lower than expected event rates in comparator arms across a range of outcomes (including in open-label trials), appear likely to be a consequence of the closer clinical management of patients in clinical trials.
There was some evidence from observational studies on the effectiveness of omalizumab beyond 12 months duration in either adults or children. Three studies (the PERSIST study and those of Britton et al. and Tzortzaki et al. ) reported some follow-up data at 120 weeks, 2.5 years and 4 years respectively. 39,61,62 In PERSIST, these were limited and related to only one-third of the patients in the original study; other studies which appeared to assess longer-term treatment reported only interim results. However, where data were available, they indicated continued effectiveness of omalizumab at the later time points.
Benefit of omalizumab: oral corticosteroid-sparing
For both patients on maintenance OCS and those who require frequent OCS courses to treat exacerbations, a significant benefit of omalizumab is thought to come from the reduced steroid burden which treatment permits. However, there were limited RCT data on the steroid-sparing effect of omalizumab in adults and none in children, with only two subgroups identified, only one of which was in the licensed population (EXALT). 31 The OCS-dependent patients in EXALT stopped or reduced maintenance OCS at a significantly higher rate in the omalizumab arm than in the standard care arm, but the open-label design may have influenced this finding. This benefit was not found in the second RCT subgroup,50 but this trial had been conducted in patients with controlled asthma and a very substantial reduction in the placebo arm (as well as the omalizumab arm) indicated potential overtreatment at baseline. 50 Therefore, much of the evidence for any steroid-sparing effect of omalizumab is drawn from observational studies. 31 It was unclear in many instances to what extent the populations of the observational studies conformed to the licence criteria, particularly in respect of optimised standard care at baseline. However, the evidence of benefit was consistent both across observational studies and with the single open-label RCT subgroup from the licensed population. In view of the limited RCT evidence, the evidence of a reduction in the cumulative dose of OCS and in the proportion of patients requiring maintenance OCS should be considered as supportive evidence. There is, however, a clear need for a further RCT to explore the OCS-sparing effect of omalizumab in step 5 patients.
Whereas the evidence for OCS-sparing in adults is limited, that for children is almost totally lacking. There were a tiny number of children on maintenance OCS in the one RCT (subgroup) (IA-05-EUP) and no comparative data were available from them (all were treated with omalizumab). A single small uncontrolled observational study conducted in UK children with OCS-dependent severe allergic asthma and optimised baseline treatment reported statistically and clinically significant benefits of reduced median daily doses of OCSs in children aged 5–12 years at a single centre with no losses to follow-up; the linked multicentre study reported similar reductions in dose. 54 All patients in this study were reported to have reduced or stopped OCSs. As with the majority of the included observational studies, study quality was unclear on a number of criteria. Clearly, evidence from small observational studies of this kind can only be regarded as suggestive of an effect and any RCT of omalizumab in OCS-dependent patients should enrol children who meet the paediatric licence.
Adverse events of oral corticosteroids
The translation of any steroid-sparing effects of omalizumab into patient benefit is dependent on the avoidance of the adverse events associated with OCSs. Although OCS adverse events are widely recognised, there has been limited systematic appraisal of the level of risk associated with maintenance use of OCSs. All the evidence syntheses identified in our review were subject to limitations, and the reliability of the data were unclear. The most reliable source of evidence provided quantitative evidence for the known adverse events of fracture, diabetes, peptic ulcer, cardiovascular events including myocardial infarction and stroke, cataract and glaucoma, sleep and mood disturbance, and weight gain. 84 Increased fracture risk remains a long-term consequence even when OCS is discontinued as a consequence of irreversible osteoporosis. Weight gain has also been identified, both by consultee submissions to NICE for the appraisal of omalizumab and by the clinical advisors to this technology assessment, as being of key importance and as leading to a cycle of reduced asthma control, increased OCS requirement and further weight gain. There is some evidence of a relationship between childhood OCS treatment and failure to achieve expected adult height. 85
Safety of omalizumab
The review of safety identified no evidence of serious adverse events beyond those identified in the SPC. Although the levels of adverse events reported in the included primary studies were high, there were few differences between treatment groups. Key adverse events that should be considered are anaphylaxis, for which patients are monitored at initiation of treatment, and arterial thrombotic events where there is a need for further, longer-term data. Both of these are rare and have not been conclusively linked to omalizumab. The evidence on the relationship between omalizumab and the incidence of malignancy is also subject to some uncertainty and an area in which further data are required. Although there is reasonable evidence for the short-term safety profile of omalizumab, long-term safety data were generally limited either because of a lack of published data on the safety of long-term treatment, or infrequent reporting on some of the adverse events of interest.
Summary
Omalizumab for the treatment of severe persistent asthma has been studied in a number of RCTs and observational studies. Overall, the evidence base indicates a clear treatment benefit in adults and children on the primary outcome of clinically significant exacerbations. There is also evidence of benefit in reducing hospitalisations and other unscheduled health-care use, symptoms and lung function, and improved QoL in adults. However, evidence for these secondary outcomes is limited or lacking in children. There is some evidence that omalizumab reduces requirements for OCSs in patients who are treated at step 5, but this is also considerably more robust for adults than for children.
Chapter 4 Assessment of existing cost-effectiveness evidence
Systematic review of existing cost-effectiveness evidence
The following sections provide an overview of the cost-effectiveness evidence and an assessment of the quality and relevance of the data from the perspective of the UK NHS. Summary data extraction tables (all studies) and quality assessment checklists applied to the most relevant studies are presented in Appendix 16. The differences in the approaches and assumptions used across the studies were examined in order to explain any discrepancies in the findings and to identify key areas of remaining uncertainty. The findings from the review provide the basis for the development of a new decision-analytic model reported in the section Assessment of cost-effectiveness: York Economic Assessment. An overall summary of the cost-effectiveness evidence and the key issues is provided at the end of the section.
Methods
Systematic searches of the literature were conducted to identify potentially relevant studies for inclusion in the assessment of cost-effectiveness of omalizumab against any comparator. Full economic evaluations that compared two or more options and considered both costs and consequences (including cost-effectiveness, cost–utility and cost–benefit analyses) were included. Full details of the search strategies are reported in Appendix 1. Titles and abstracts were assessed independently by two reviewers for inclusion and any discrepancies were resolved by consensus. Data were extracted by one reviewer using a standardised data extraction form and checked for accuracy by a second reviewer. The quality of these studies was assessed according to a general checklist based on that developed by Drummond86 together with a more specific checklist for decision models from Philips. 87 This information is summarised within the text of the report, alongside a detailed critique of the main studies and their relevance to the UK NHS. The findings from the review provide the basis for the development of a new model reported in Assessment of cost-effectiveness: York Economic Assessment.
Omalizumab has been the subject of two previous NICE STAs, TA133 for adults and adolescents aged ≥ 12 years88 and TA201 for children aged 6–11 years. 89 The submissions by the manufacturer for these appraisals and the evidence review group (ERG) critique are reviewed and summarised below (see section Previous NICE single technology appraisals).
The manufacturer (Novartis UK) also submitted de novo evidence on the cost-effectiveness of omalizumab for severe persistent allergic asthma for the present evaluation of omalizumab. The MS is reviewed below, alongside a detailed critique. A review of existing cost-effectiveness evidence was also undertaken by the manufacturer. Their aim was to identify full economic evaluations of omalizumab in the specific patient population corresponding to the UK/EU marketing authorisation of omalizumab. The manufacturer's review excluded studies of patients aged < 6 years, and studies including patients with mild, moderate, acute or intermittent asthma, or conditions other than asthma. Therefore, the inclusion criteria for the manufacturer's systematic review were stricter than the review presented here. The studies included in the manufacturer's review were examined and compared with those found in the review presented here.
Results
A total of 130 unique records were identified from the systematic literature search of existing cost-effectiveness evidence, of which six studies subsequently met the inclusion criteria. 90–95 In addition, two previous NICE STA (TA13388 and TA20189) were identified and a de novo cost-effectiveness analysis and electronic model was submitted by Novartis; however, these were excluded from the systematic review but were summarised and discussed separately (see following sections). Figure 3 presents a flow diagram summarising the identification and selection of studies. A brief summary of the six studies is reported in Table 44. More detailed data extraction summary tables are presented in Appendix 16.
All studies evaluated the cost-effectiveness of omalizumab from a health-care or payer perspective and compared omalizumab add-on therapy with standard asthma therapy. The patient population differed across studies, reflecting the different marketing authorisation in the US compared with Europe. Studies reporting a US setting focused on patients with moderate to severe persistent allergic asthma, who are inadequately controlled with ICSs: Oba and Salzman,90 Wu et al. 91 and Campbell et al. 92 Dewilde et al. ,93 Brown et al. 94 and Dal Negro et al. 96 focused on a patient population consistent with the UK/EU marketing authorisation: patients with severe persistent allergic asthma, inadequately controlled at GINA step 4 (high-dose ICS and LABA). Although all studies reported ‘usual care’ or ‘standard therapy’ as the comparator, its definition depends on the patient population and the relevant marketing authorisation. Oba and Salzman,90 Wu et al. 91 and Campbell et al. 92 considered ICS plus additional rescue medication as required as standard therapy, whereas Dewilde et al. ,93 Brown et al. 94 and Dal Negro et al. 96 considered GINA step 4, that is high-dose ICS and LABA, as standard therapy.
FIGURE 3.
Flow chart showing number of studies identified and included in the review of cost-effectiveness of omalizumab.
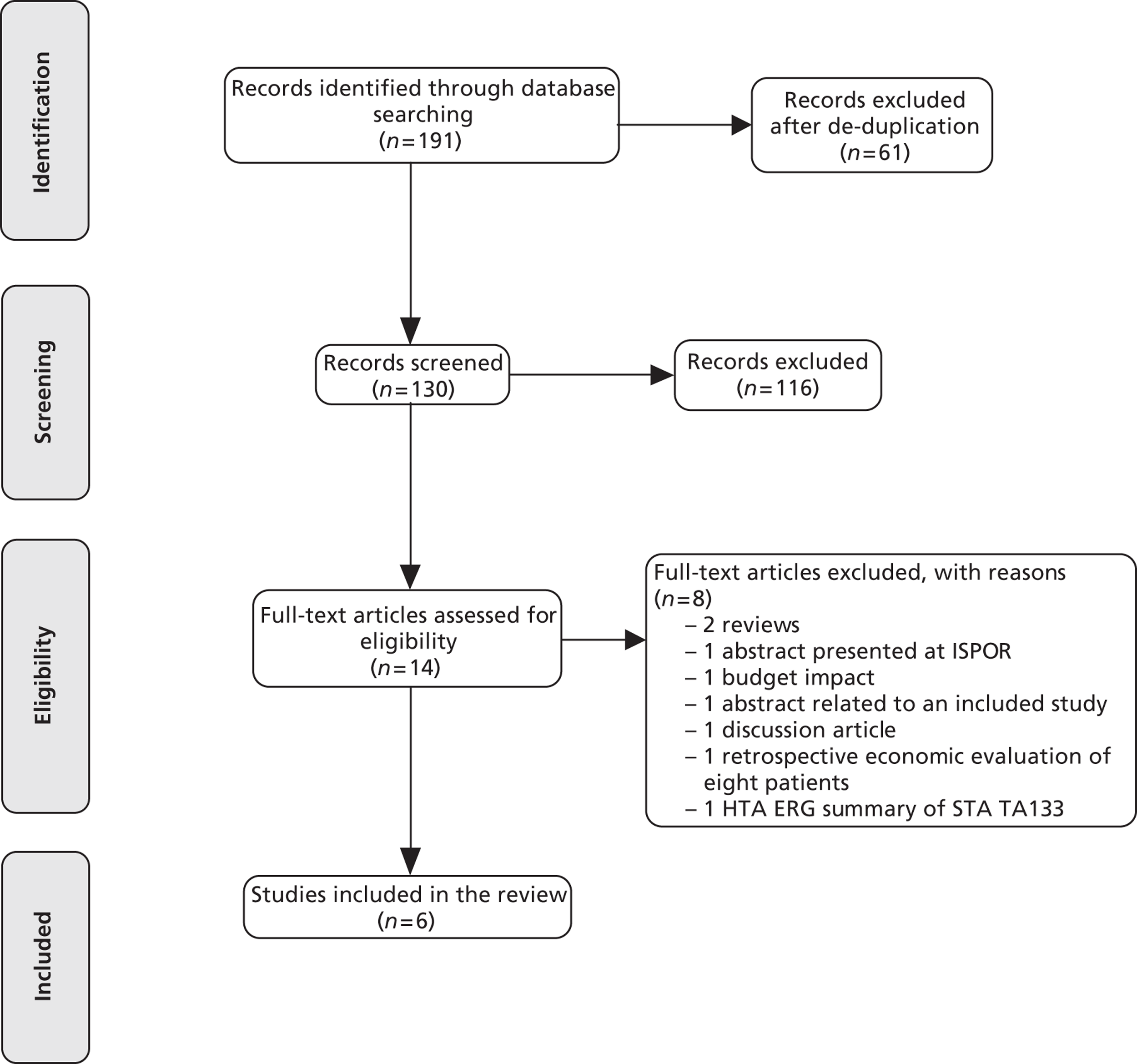
Two studies90,96 used individual patient data to assess the cost-effectiveness of omalizumab. Oba and Salzman90 was based on data collected in RCT 00848 and 009,97 which examined the clinical effectiveness of omalizumab compared with usual care (ICS plus rescue medication), whereas Dal Negro et al. 96 used before-and-after data from 23 patients who had been on omalizumab for 12 months. The other four studies91–94 used decision-analytic models to estimate the cost-effectiveness of omalizumab. Dewilde et al. 93 and Brown et al. 94 used a Markov state transition model similar to the model used in the previous STA and the manufacturer's new submission. In brief, this model comprises five health states: day-to-day asthma symptoms, CSNS exacerbation, CSS exacerbation, asthma-related death and death from all causes. A detailed discussion of this model is presented in the section TA133: omalizumab for severe persistent allergic asthma in adults and adolescents ≥ 12 years, alongside the summary and critique of the manufacturer's new submission. The decision-analytic model in Wu et al. 91 was also a Markov model but with different health states. It comprised three health states according to disease status: chronic/stable asthma, acute/hospitalisation and death (as a result of asthma or other causes), whereas Campbell et al. 92 used a Markov model with five heath states: chronic asthma, oral steroid burst, emergency room visit, hospitalisation and death. The oral steroid burst state in the Campbell et al. 92 model was equivalent to CSNS exacerbation in Dewilde et al. 93 and Brown et al. ,94 whereas hospitalisation was equivalent to CSS exacerbation.
Despite the differences in the labelling of health states, all models typically assumed that the benefits of omalizumab, compared with standard care, were conferred to patients through a reduction in clinically significant exacerbations. The transitions between health states were largely based on the exacerbation rates observed in the RCTs of omalizumab. Dewilde et al. 93 used data on exacerbation rates data from INNOVATE,19 Brown et al. used exacerbation rates reported in the severe subgroup of the IA-04 trial30 and Campbell et al. used data from a published meta-analysis of RCTs of omalizumab compared with standard care. 98 In contrast to the direct use of exacerbation rates from the RCTs, the transitions between states in Wu et al. 91 were based on the relationship between FEV1% predicted and exacerbations observed in a published retrospective study.
Treatment duration with omalizumab varied across the six studies. Oba and Salzman90 and Dal Negro et al. 96 assumed 1-year treatment duration, which reflected the length of follow-up of the studies. For the model-based studies, treatment duration varied between 5 years92–94 and 10 years. 91 Three studies92–94 incorporated the assessment of response to omalizumab at 16 weeks. Wu et al. 91 assumed that all patients were responders. Oba and Salzman90 and Dal Negro96 do not mention assessment of response.
| Study | Country (perspective) | Population | Comparators | Outcomes | Results |
|---|---|---|---|---|---|
| Oba and Salzman 200490 | USA (health-care payer) | Adults and adolescents (≥ 12 years) with uncontrolled asthma despite ICSs | Usual care: ICS plus rescue medication | Cost per 0.5-point increase in the AQLQ score | $378 (£237a) per 0.5-point AQLQ increase |
| Cost per successfully controlled day | $525 (£330a) per successfully controlled day | ||||
| Dewilde 200693 | Sweden (health-care payer) | Adults and adolescents (≥ 12 years) with uncontrolled severe persistent asthma despite high-dose ICS and LABA | Optimised standard therapy at GINA step 4: high-dose ICS plus LABA and additional rescue medication | Incremental cost per QALY (ICER) | ICER = €56,091/QALY (£46,800/QALYa) |
| Brown 200794 | Canada (health-care payer) | Adults and adolescents (≥ 12 years) with uncontrolled severe persistent asthma despite high-dose ICS and LABA | Standard therapy: high-dose ICS plus LABA and additional rescue medication | Incremental cost per QALY (ICER) | ICER = €31,209/QALY (£26,000/QALYa) |
| Wu 200789 | USA (societal) | Adults with severe uncontrolled asthma | Standard therapy: ICS plus rescue medication | Incremental cost per QALY (ICER) | ICER = $821,000/QALY (£516,500/QALYa) |
| Incremental cost per symptom-free day | Incremental cost = $120 | ||||
| Campbell 201092 | USA (health-care payer) | Adults with moderate to severe persistent asthma uncontrolled with ICSs | Standard therapy: ICS + rescue and additional medication as required | Incremental cost per QALY (ICER) for base-case (and responders subgroup) | ICER = $287,200/QALY (£180,700/QALYa) |
| Responders: $172,320/QALY (£108,400/QALYa) | |||||
| Dal Negro et al. 201196 | Italy (health-care payer) | Adults on omalizumab in addition to optimised standard therapy | Optimised standard therapy | Incremental cost per QALY (ICER) | ICER=€26,000/QALY (£21,700/QALYa) |
There was marked variation across the studies in the results of the cost-effectiveness (Table 44). Five studies used quality-adjusted life-years (QALYs) to estimate incremental cost-effectiveness ratios (ICERs) for omalizumab compared with standard therapy. 91–94,96 The ICERs ranged from €26,000 to $821,000/QALY (approximately £21,700 to £516,500/QALY). The studies, which used a model similar to the manufacturer's, reported ICERs between €31,209 and €56,091/QALY (approximately £26,000 to £46,800/QALY). Campbell et al. reported an ICER of $287,200/QALY for all patients (responders and non-responders to omalizumab) and $172,320/QALY (approximately £108,400/QALY) for responders only. 92 As a result, conclusions based on the cost-effectiveness of omalizumab differed across the studies. Oba and Salzman90 and Dewilde et al. 93 concluded that omalizumab may be cost-effective for patients with severe asthma. Brown et al. concluded that omalizumab is a cost-effective use of health-care resources. 94 Wu et al. concluded that omalizumab is not cost-effective unless its acquisition price is reduced substantially. 91 Campbell et al. 92 and Dal Negro et al. 96 concluded that omalizumab improves HRQoL but also increases costs substantially.
The difference in ICERs across studies is because of the different approaches used for asthma-related mortality, HRQoL improvement as a result of omalizumab, assessment of response and the patient populations considered. Studies that considered more severe patient populations (patients with severe persistent allergic asthma uncontrolled with high-dose ICS)93,94,96 presented lower ICERs than studies looking at patients with moderate to severe persistent asthma. 91,92 This suggests that severity of asthma, and consequently the risk of exacerbations, should be considered in the cost-effectiveness of omalizumab.
The approach used for modelling asthma-related mortality varied between the studies. Oba and Salzman90 and Dal Negro et al. 96 did not consider asthma-related death. Dewilde et al. 93 used an asthma-related mortality risk following CSS exacerbations of 2.082%. This rate was calculated as a weighted average of 67% of patients at high risk of an exacerbation in INNOVATE being at a 3.108% risk of death following an exacerbation and 33% being at no risk. The ICER more than doubled from €56,091 per QALY in the base-case analysis to €131,130 per QALY when asthma-related mortality was reduced from 2.082% to 0%, whereas it reduced by around 20% to €46,268 when asthma-related mortality was increased to 3.108%. Brown et al. 94 used a mortality risk of 3.108% following an exacerbation, also based on Lowhagen et al. 99 The ICER increased from €31,209/QALY to €66,443/QALY when a 0% asthma-related mortality rate was used instead of the base-case value of 3.108%, and to €33,578 when the mortality rate was reduced to 2.48%. Campbell et al. (2010)91 assumed that asthma-related mortality occurred following a hospitalisation for asthma at a risk of 1.1%, obtained from Sullivan et al. (2009). 100 Wu et al. (2007) applied a monthly age-dependent risk of asthma death of 0.0001% for patients 18–35 years of age, and 0.0002% for patients > 35 years. This is equivalent to annual mortality risks of 0.0012% and 0.0024% respectively. These results indicate that asthma-related mortality is a key driver of the cost-effectiveness of omalizumab.
HRQoL improvement as a result of omalizumab was incorporated differently across the studies. Dewilde et al. ,93 Brown et al. 94 and Campbell et al. 92 used EQ-5D utility values mapped from AQLQ scores collected during INNOVATE; the placebo arm of the trial informed the HRQoL of the cohort on standard care, whereas the scores from the omalizumab responders informed the HRQoL of responders in the model. Brown et al. 94 applied the same approach but used EQ-5D mapped from mini-AQLQ collected during ETOPA. In Wu et al. ,91 HRQoL was dependent on FEV1% predicted. Omalizumab was assumed to improve FEV1% predicted by 2.9%, and therefore improve HRQoL. Dal Negro et al. 96 used EQ-5D scores mapped from the St George Respiratory Questionnaire before (for standard care group) and after (for omalizumab group) treatment with omalizumab. Campbell et al. 92 examined the impact on the ICER of reducing the difference between HRQoL on standard care and on omalizumab. The ICERs increased from $287,200/QALY to $690,800/QALY when the difference in HRQoL between omalizumab and standard therapy was reduced from 0.06 to 0.02. Therefore, the HRQoL improvement as a result of omalizumab therapy appears to have a major impact on the cost-effectiveness of omalizumab.
Some studies incorporated assessment of response to omalizumab and assumed that non-responders reverted back to standard therapy. 93,94 Assessment of response to omalizumab was not included in the analysis in Oba and Salzman90 and Wu et al. ,91 and was considered only in a scenario for Campbell et al. 92 The base-case ICER for Campbell et al. 92 was $287,200 (£187,700) and reduced to $172,320 (£108,400) per QALY gained when patients on omalizumab were assessed for response and non-responders discontinued omalizumab therapy. Therefore, including the assessment of response and discontinuation of omalizumab therapy for non-responders is likely to have had an influence on the cost-effectiveness results.
In the systematic review of existing cost-effectiveness evidence conducted by the manufacturer, five studies were identified as relevant: Dewilde et al.,93 Brown et al. ,94 Lecomte et al. ,101 and the two previous STA submissions on omalizumab. 88,89 All these studies were identified in the independent review, but Lecomte et al. 101 was excluded because it was only available as an abstract. According to the manufacturer's review, Lecomte et al. 101 used the same model structure as Dewilde et al. 93 and Brown et al. 94 with data from the PERSIST study, a prospective cohort study of patients on omalizumab. 39 Lecomte et al. reported an ICER of €29,187 per QALY, which was sensitive to the discount rate and time horizon applied. 101 The previous STA submissions are discussed in TA133: omalizumab for severe persistent allergic asthma in adults and adolescents ≥ 12 years).
Across the full range of studies considered a number of common issues and limitations were identified, which preclude reliable conclusions to be drawn on the cost-effectiveness of omalizumab.
These include:
-
Variability in the patient population used across studies. The patient population depended on the setting and the relevant marketing authorisation. Patients with moderate to severe persistent allergic asthma were defined variously as uncontrolled by regular-dose ICS, high-dose ICS, maintenance OCS or a combination of ICS and OCSs.
-
A lack of consideration of additional risk factors/higher-risk subgroups that might be important issues for cost-effectiveness. None of the studies directly examined the cost-effectiveness of omalizumab in higher-risk subgroups within the main population considered. However, Oba and Salzman90 hypothesised that omalizumab may be associated with cost-savings in a more severe population composed of patients hospitalised five or more times per year, 20 days or longer per year or who require emergency department care seven or more times per month.
-
The relative efficacy and safety of omalizumab compared with OCSs was not addressed in any of the studies.
-
None of the models considered the adverse effects of omalizumab or standard therapy. As part of standard therapy, some patients were receiving OCSs, which is widely acknowledged to have long-term adverse consequences.
-
A lack of robust data for asthma-related mortality rates and HRQoL improvements from omalizumab. Both were key drivers of cost-effectiveness but systematic searches of the literature were not conducted to identify the values used in the models.
-
A lack of consensus on treatment duration and persistence of effect of omalizumab. The implications on the cost-effectiveness results have not been explored.
Previous National Institute for Health Care Excellence single technology appraisals
As discussed in Chapter 1, omalizumab has been the subject of two STAs for NICE; TA133 in adults and adolescents (≥ 12 years)88 and TA201 in children aged 6–11 years. 89 As part of these previous STAs, evidence was submitted by the manufacturer and a review of the submission was undertaken by a separate ERG. In this section, each STA is briefly reviewed separately, and an overall critique is presented at the end.
Technology appraisal number 133: omalizumab for severe persistent allergic asthma in adults and adolescents (≥ 12 years)
Technology appraisal number 133 assessed whether omalizumab as an add-on therapy to optimised standard care was an effective technology and a cost-effective use of NHS resources for patients aged ≥ 12 years with severe persistent allergic asthma. 88 The MS and the critique by the previous ERG102 are briefly summarised below.
Manufacturer's submission for technology appraisal number 13388
The manufacturer approached the decision problem by looking at adults and adolescents with severe persistent allergic asthma in accordance with the EU/UK marketing authorisation. Omalizumab as an add-on therapy to standard care was compared with standard care alone. Standard care included high-dose ICS, long- and short-acting β2-agonists, OCSs, leukotriene antagonists and, where appropriate, theophylline. The MS presented evidence on the clinical effectiveness of add-on therapy with omalizumab based on the results of the INNOVATE trial. The primary outcomes from this trial were the rate of CS asthma exacerbations, the rate of CSS exacerbations and the rate of emergency visits for asthma. The input parameters in the economic analysis were largely based on the INNOVATE study. 19
The Markov transition model had a lifetime of 40 years and consisted of five health states: day-to-day symptoms, CSNS exacerbation, CSS exacerbation, asthma-related death and death from other causes. In the model, it was assumed that patients on omalizumab were assessed for response to treatment at 16 weeks. The proportion of patients on omalizumab who were responders at 16 weeks was based on the proportion of responders observed in the INNOVATE study at 28 weeks. Non-responders were assumed to revert back to standard therapy and receive the same exacerbation rates and HRQoL as patients on standard care. Responders to omalizumab continued on omalizumab treatment for 5 years. During the period of treatment, responders to omalizumab were assumed to experience the exacerbation rates and HRQoL improvements observed in the omalizumab responders of the INNOVATE study. After treatment discontinuation (5 years), patients who were on omalizumab were assumed to experience the exacerbation rates and HRQoL of patients on standard care. HRQoL for day-to-day symptoms with omalizumab and standard care were estimated by mapping the AQLQ scores collected during INNOVATE for each treatment arm to EQ-5D utility scores using a published mapping function. 103 The loss of HRQoL associated with CSNS and CSS exacerbations were based on a published study by Lloyd et al. (2007). 104 Asthma-related mortality was assumed to occur only from a CSS exacerbation. As no deaths were observed in INNOVATE, an asthma-related mortality risk of 3.108% was obtained from a Swedish observational study on data collected between 1988 and 1990. 99 Costs were based on health-care resources consumed in INNOVATE with UK unit prices applied. The acquisition cost of omalizumab was based on the distribution of doses observed in INNOVATE, and assuming no vial wastage and re-use of unused vial portions. Appendix 16 presents the input parameters used in the MS for TA133.
The base-case analysis for the patient characteristics of the INNOVATE population produced an ICER of £30,647 per QALY gained. Two subgroup populations were also presented: (1) a high-risk hospitalisation subgroup, consisting of 39% of patients in INNOVATE, who had asthma exacerbations requiring hospital admission in the year prior to enrolling in the trial, and (2) a severe subgroup of patients from the IA-04 study who met the EU/UK marketing authorisation requirements for omalizumab. 30 The ICERs for the hospitalisation subgroup were £26,500 per QALY gained, whereas the ICERs for the IA-04 subgroup were £21,700 per QALY gained. Table 45 presents the results of the manufacturer's one-way sensitivity analysis. These suggested that the cost-effectiveness results were most sensitive to the asthma-related mortality risk, treatment duration and time horizon. Reducing the asthma-related mortality rate from 3.109% to 2.478% increased the ICERs from £30,647 to £33,468 per QALY gained, whereas a 0% mortality rate increased the ICER to £73,177.
| Parameter | Range or alternative | Results |
|---|---|---|
| Base case | £30,647 | |
| Discount rates | 0–6% | £24,101–£41,776 |
| Time horizon | 5 years | £58,040 |
| 10 years | £44,201 | |
| 20 years | £34,602 | |
| Treatment duration (base case = 5 years) | 2 years | £68,402 |
| 10 years | £30,672 | |
| Asthma-related mortality (base case = 3.109%) | 0% | £73,177 |
| 2.478% | £33,468 | |
| HRQoL for day-to-day symptom state for standard therapy | 0.594 | £26,270 |
| HRQoL values for CSNS and CSS exacerbations | 0.556, 0.526 | £30,994 |
| Omalizumab drug cost | Based on vial cost | £33,865 |
| Omalizumab drug dose distribution | All INNOVATE | £33,253 |
| CSNS and CSS exacerbation costs | Doubled | £30,084 |
The previous Evidence Review Group's critique102
The MS was considered to be of good quality and to meet the requirements of the NICE reference case. 105 The modelling approach, health states and structural assumptions were considered reasonable. However, the ERG identified a number of issues with the parameters used in the economic model and uncertainties relating to the cost-effectiveness analysis. Some data sources were not adequately justified, for example, the source used to inform asthma-related mortality. The one-way sensitivity analysis conducted by the manufacturer did not capture uncertainty adequately, as it was performed on a limited number of parameters and using inappropriate ranges of parameter values.
The ERG considered that the asthma-related mortality applied in the model may not be reflective of the mortality risk faced by patients in the UK. The asthma-related mortality used in the base-case analysis was obtained from a Swedish observational study that evaluated the impact of training ambulance crews on the management of acute asthma. Data on the number of calls concerning acute asthma and on the number of deaths following ambulance arrival were collected between 1988 and 1990. 99 It was unclear whether the results were generalisable to the UK setting or appropriate for the year of the appraisal (2006). In addition, the mortality rate observed in the Swedish study was for an average age of 62.3 years but the manufacturer applied the rate to a patient cohort starting in the model at 43 years of age. Furthermore, the definition of CSS exacerbations used in the model and INNOVATE, where the mortality is applied, may not correspond to the same definition of an acute asthma attack that prompted patients to call an ambulance as used in Lowhagen et al. 99
The ERG noted uncertainties surrounding the utility values assigned to CSNS and CSS exacerbations, and the cost of omalizumab on a per milligram basis. Therefore, the ERG performed an exploratory scenario analysis on alternative assumptions for these parameters. The ICERs for these scenarios ranged from £33,320 to £40,889 per additional QALY for the base-case population (base-case ICER = £30,647), between £29,849 and £34,303 per additional QALY for the hospitalisation subgroup (base-case ICER = £26,509) and between £24,698 and £30,715 for the IA-04 subgroup (base-case ICER = £21,660). The ERG also performed an amended probabilistic sensitivity analysis and estimated a mean probabilistic ICER of £38,900 per QALY gained, and a probability that omalizumab is cost-effective of 0.236 at the £30,000 per QALY threshold. The ERG concluded that, in addition to asthma-related mortality, the improvement in HRQoL from omalizumab and the assumptions used to calculate the cost of omalizumab were the key drivers of cost-effectiveness.
Technology appraisal number 201: omalizumab for severe persistent allergic asthma in children aged 6–11 years89
Technology appraisal number 201 assessed whether omalizumab as an add-on therapy to optimised standard care was an effective technology and a cost-effective use of NHS resources for patients aged 6–11 years with severe persistent allergic asthma. The MS and the critique by the previous ERG are briefly summarised below.
Manufacturer's submission for technology appraisal number 20189
The manufacturer approached the decision problem by looking at children aged 6–11 years with severe persistent allergic asthma in accordance with the EU/UK marketing authorisation. Omalizumab as an add-on therapy to standard care was compared with standard care alone from the UK NHS perspective over a lifetime horizon. Standard care included high-dose ICS, LABAs and, where appropriate, OCSs. The manufacturer undertook a systematic review of previously published economic evaluations relevant to the decision problem but no studies were found. Therefore, the manufacturer submitted a de novo economic model. The model had the same structure as that used for TA133. The exacerbation rates and resource use data were drawn largely from the preplanned subgroup IA-05 EUP of the IA-05 trial in children, corresponding to the EU/UK marketing authorisation.
Patients on omalizumab should be assessed for response at 16 weeks. The MS included a post hoc ‘responder’ subgroup of the EUP population. Responders were defined as children who were rated as excellent or good on the GETE scale at 52 weeks of treatment. The manufacturer used the response rate at 52 weeks as a proxy for the proportion of patients on omalizumab who were responders at 16 weeks. Non-responders were assumed to revert back to standard therapy and receive the same exacerbation rates, costs and HRQoL as patients on standard therapy alone. Responders to omalizumab and patients on standard therapy (or non-responders) were assumed to experience the exacerbation rates and resource use observed in the respective treatment arms of the IA-05 EUP study. No deaths were observed in the IA-05 EUP study; therefore, asthma-related mortality was obtained from an alternative published source (Watson et al. 106). Watson et al. 106 examined the rate of all-cause mortality following hospital admissions for asthma and acute severe asthma in the UK. Similar to the adult and adolescent's model, asthma-related mortality was assumed to occur only from a CSS exacerbation. The authors estimated an asthma-related mortality rate following hospital admission for acute severe asthma of 0.097% for children aged < 12 years, 0.319% for ages 12–16 years, 0.383% for ages 17–44 years and 2.48% for ages ≥ 45 years. No HRQoL values for children were available from the IA-05 EUP study. IA-05 EUP used the paediatric-AQLQ, but a non-significant difference was observed between treatment groups. Therefore, the base-case analysis assumed that there was no HRQoL improvement in day-to-day symptoms for omalizumab compared with standard therapy until patients reached the age of 12 years. After age 12 years, children were assumed to receive the HRQoL improvements observed in INNOVATE, based on the AQLQ improvement which was mapped onto EQ-5D (the same as the MS for TA133). The HRQoL values for CSNS and CSS exacerbations were based on values reported in Lloyd et al. (2007)104 (the same as for adults and adolescents in TA133). Costs were based on the resource use observed in IA-05 EUP with UK unit prices applied. For the acquisition costs of omalizumab, the same assumptions of no vial wastage and re-use of vials were employed as in the adults and adolescents model. More importantly, children were assumed to remain on the same baseline dose schedule throughout the entire treatment duration. Appendix 16 presents the input parameters used in the MS for TA201.
The base-case analysis corresponded to the patient characteristics observed in the IA-05 EUP population. The MS also presented a post hoc subgroup analysis for a high-risk population, the EUP hospitalisation subgroup, consisting of patients who experienced at least one hospitalisation for an asthma exacerbation in the year prior to study entry. The ICER for the base-case analysis was £91,188 per QALY gained, which was reduced to £91,169 followed a slight amendment to the model noted by the ERG. The ICER for the hospitalisation subgroup was £65,911 per QALY gained. The manufacturer conducted extensive one-way sensitivity analyses. Table 46 presents the results of the manufacturer's sensitivity analysis. Despite some scenarios having a substantial impact on the ICER, none reduced the ICER to below £68,029 per QALY gained (achieved by assuming that children aged < 12 years experience the same HRQoL improvement with omalizumab as adults). An ICER of £69,603 per QALY gained was achieved by doubling the asthma-related mortality rate for all ages. The ICER was most sensitive to the length of treatment duration, the HRQoL improvement assumed for omalizumab compared with standard therapy and the asthma-related mortality, suggesting that these parameters were the main drivers of cost-effectiveness. Probabilistic sensitivity analyses suggested that if maximum acceptable thresholds of £20,000 and £30,000, respectively, for an additional QALY gained were used, omalizumab had a 0% probability of being considered cost-effective.
| Parameter | TA201 (patients between 6 and 11 years old) | |
|---|---|---|
| Range or alternative | Results | |
| Base case | – | £91,188 |
| Discount rates | 0–6% | £56,350–£74,305 |
| Time horizon | 10 years | £102,452 |
| 45 years | £92,769 | |
| Treatment duration | 2 years | £684,665 |
| 5 years | £137,902 | |
| 20 years | £77,589 | |
| Asthma-related mortality | 0% | £104,854 |
| Mortality rate increased 100% | £81,836 | |
| Mortality rate increased 200% | £69,603 | |
| HRQoL for day-to-day symptom state for standard therapy | No difference in day-to-day symptoms | £379,893 |
| Same HRQoL for responders regardless of age = 0.779 | £68,029 | |
| HRQoL values for CSNS and CSS exacerbations | No decrease for CSNS exacerbations | £96,245 |
| No decrease in for CSS exacerbations | £96,049 | |
| No decrease in for CSNS and CSS exacerbations | £101,677 | |
| Omalizumab drug cost | Based on vial cost | £105,480 |
| Drug costs ± 20% | £108,777; £73,598 | |
| Omalizumab administration costs | Anaphylaxis monitoring costs = £0 | £90,474 |
| Anaphylaxis monitoring costs increased by 100% | £91,902 | |
| Time per administration reduced to 10 minutes | £88,237 | |
| CSNS and CSS exacerbation costs | Doubled | £89,167 |
| Exploring different assumptions in exacerbation costs | £75,754–£92,028 | |
| Starting age in the model | 6 years old | £146,372 |
| 11 years old | £71,529 | |
| Exacerbation rates | Both treatment arms ± 50% | £90,768; £91,610 |
| 52-week data after year 1 | £95,682 | |
| Proportion of omalizumab responders | Proportion of responders + 10% | £90,711 |
| Proportion of responders – 10% | £91,770 | |
The previous Evidence Review Group's critique for technology appraisal number 201107
As with TA133, the ERG considered the economic submission to be of good quality, meeting most of the requirements of the NICE reference case, and that the structure of the Markov model was appropriate for the decision problem. Many of the key uncertainties, such as asthma-related mortality and treatment duration were explored through one-way sensitivity analysis for the base-case population but not for the hospitalisation subgroup.
The ERG undertook exploratory analysis to identify the factors underlying the cost-effectiveness results in children aged 6–11 years using alternative parameter values which matched those used in TA133 for adults and adolescents. The exploratory analysis focused on the hospitalisation subgroup and the parameter values for exacerbation rates, proportion of responders, asthma-related mortality and HRQoL. The exploratory analysis showed that applying the efficacy rates for CSNS and CSS exacerbations from INNOVATE (as used in TA133) to patients aged ≥ 12 years in the hospitalisation subgroup resulted in an increase in the ICER from £65,911 to £73,779. Applying an improvement in HRQoL associated with omalizumab relative to standard care for day-to-day symptoms for children < 12 years decreased the ICER to £53,133. The exploratory analysis demonstrated that asthma-related mortality was the key driver of cost-effectiveness. The asthma-related mortality used in the children's submission was substantially lower than that applied in the submission for TA133. The model for adults and adolescents (aged ≥ 12 years) considered a cohort with an average age of 45 years and an asthma mortality risk of 3.109%. Applying the higher mortality of 3.109% from TA133 to the children's model (average age 9 years) once patients reach the age of 12 years, reduced the ICER to £31,737. The ERG expressed the view that the higher mortality rate may be appropriate for patients aged > 45 years but it was unlikely to be appropriate for younger populations.
The previous ERG identified a number of potential weaknesses and remaining uncertainties in the economic submission for TA201. These included: (1) the use of 52-week data as a proxy for 16-week assessment of response to treatment (the period specified in the marketing authorisation); (2) the assumption that exacerbation rates remain constant over time in children and adolescents, especially as adolescent growth can have an impact on asthma; (3) no systematic literature searches were undertaken to identify key parameters such as asthma-related mortality; (4) no uncertainty was considered in the cost estimates as part of the probabilistic sensitivity analysis; (5) the cost of an exacerbation was not differentiated according to severity; (6) a treatment duration of 10 years was assumed without providing justification; (7) HRQoL values for children were informed by studies in adults; and (8) other more severe subgroup populations were not considered in the economic analysis, for example, patients with more than three exacerbations per year.
Remaining uncertainties
A number of key areas of uncertainty and potential limitations were identified from the previous appraisals. These include:
-
Patient subgroups for whom omalizumab is potentially more cost-effective were defined according to hospitalisations as a result of asthma. As a result, the NICE Committee recommended omalizumab only in patients who have been hospitalised for asthma in the previous year. However, restricting omalizumab to patients with previous hospitalisations may incentivise patients to present at hospital rather than at the primary care services. Alternative definitions of severity, such as number of exacerbations or medication, could be used to define more severe patient subgroups.
-
Omalizumab may potentially reduce the dose of maintenance OCS or eliminate the need for maintenance OCS in patients at step 5 of BTS/SIGN guideline. The long-term use of OCSs is associated with adverse effects. The steroid-sparing potential of omalizumab has not been addressed nor have adverse effects from long-term use of OCSs been incorporated into the analysis.
-
Asthma-related mortality as a result of CSS exacerbations is a key driver of cost-effectiveness. However, evidence on the link between mortality, age, asthma severity, and number and severity of exacerbations has not been identified systematically in the previous appraisals.
-
The cost-effectiveness of omalizumab was highly sensitive to estimates of the improvement in HRQoL because of omalizumab. The estimates of HRQoL improvement were obtained from EQ-5D mapped from AQLQ at week 28 of INNOVATE and were applied at a constant rate for the duration of treatment. Patients < 12 years of age were assumed not to experience HRQoL improvement because of omalizumab.
-
Adverse effects of omalizumab and standard therapy have not been considered in the previous submissions.
-
Treatment duration with omalizumab and long-term persistence of response to treatment is unknown. Treatment duration was assumed to be 10 years for children (TA201) and 5 years for adults and adolescents (TA133).
Summary and critique of manufacturer's de novo submission15
Overview
The manufacturer approached the decision problem in accordance with the EU/UK marketing authorisation, that is children aged 6–11 years and adults and adolescents aged ≥ 12 years with severe persistent allergic asthma uncontrolled despite daily high-dose ICS plus a LABA uncontrolled at BTS/SIGN step 4 or above. The manufacturer submitted a de novo economic evaluation which compared the costs and health outcomes of omalizumab as an add-on therapy to standard care compared with standard care alone in two separate base-case populations; one for adults and adolescents (≥ 12 years) and the other for children aged 6–11 years. The model evaluated costs from the perspective of the NHS and Personal Social Services (NHS and PSS), expressed in UK £ sterling at a 2010 price base. Outcomes in the model were expressed in terms of QALYs. Both costs and health outcomes were discounted at a rate of 3.5% per annum.
The base case for adults and adolescents was primarily based on evidence on the clinical effectiveness of omalizumab add-on therapy from the INNOVATE study,19 whereas the base case for children was primarily based on evidence from the IA-05 EUP study. 20 EXALT,31 an open-label RCT, and APEX,37 a non-RCT (before-and-after) study, were used to provide separate estimates of cost-effectiveness. Separate ICERs were presented based on analysis largely informed by either INNOVATE, EXALT or APEX. Given that APEX was an observational study, the assessment group considers that APEX is less relevant for the decision problem and population of the economic model. No additional studies were used to inform the base case of children.
In considering the relevance and appropriateness of INNOVATE, EXALT and APEX as a basis for populating the economic model, the assessment group considered a number of factors, namely: (1) their relevance in terms of defining the natural history of UK patients with severe persistent asthma; (2) issues around the impact of study design in terms of providing an unbiased estimate of relative treatment effect; and (3) reporting of data that allows for the estimation of QALYs and costs in a way which is concordant with the requirements of the NICE reference case and appropriate to the NHS setting. As INNOVATE was a double-blind RCT conducted in the EU/UK licensed population using GETE to assess response to omalizumab, the assessment group considered it as the best available evidence to populate the base case. However, EQ-5D was not directly measured in INNOVATE. EXALT, on the other hand, did measure EQ-5D directly in patients. However, and as discussed in the section Quantity and quality of research available, EXALT may be affected by bias because of its open-label design. APEX could be viewed as an appropriate source of data on exacerbation rates experienced by patients in the UK but not for treatment effectiveness, because of the risk of bias inherent to its observational non-randomised design. Table 47 summarises the patient populations included in the MS.
| Adults and adolescents | Children | |||
|---|---|---|---|---|
| Base case | Scenarios | Subgroups | Base case | Subgroup |
| INNOVATE | EXALT | Hospitalisationa | IA-05 EUP | Hospitalisationa |
| APEX | Maintenance OCSb | |||
Subgroup analysis was presented for two subgroup populations; (1) hospitalisation subgroup for patients from INNOVATE, EXALT, APEX and IA-05 EUP, and (2) maintenance OCS for patients from INNOVATE, EXALT and APEX (data for this subgroup were not available from IA-05 EUP as only six patients were on maintenance OCS at baseline and these were all in the omalizumab treatment group). The hospitalisation subgroup consisted of patients who were hospitalised in the year prior to trial entry, corresponding to 38.4% of the total INNOVATE trial population, 20.4% of EXALT, 59.7% of APEX and 17% of IA-05 EUP. The maintenance OCS subgroup consisted of patients who were receiving maintenance OCS at trial baseline, corresponding to 19.8% of the INNOVATE population, 17% of EXALT and 65.9% of APEX. A maintenance OCS subgroup population had not been considered in the previous STAs (TA133 and TA201).
The health outcomes considered in the economic analysis were the rate of CSNS exacerbations, CSS exacerbations, asthma-related mortality, response to treatment, HRQoL and use of OCSs. The cost and health impact of long-term adverse effects were not modelled, except in a scenario analysis for the maintenance OCS subgroup population. Evidence on the clinical effectiveness of add-on therapy with omalizumab based on the results of the individual studies (52-, 28- and 32-week follow-up for IA-05 EUP, INNOVATE and EXALT respectively) was extrapolated over the period of treatment duration, which was assumed to be 10 years in both base-case populations. Adherence to omalizumab and standard therapy was assumed to be 100% with no withdrawals from treatment. In the children's base-case population (average age 9 years), patients were assumed to receive the efficacy estimates observed in IA-05 EUP up to the age of 11 years only. After this age (≥ 12 years), patients switch to the efficacy estimates based on INNOVATE. The implication of applying the switch in this manner in the children's model is that on reaching the age of 12, patients are assumed to immediately experience the same exacerbation rates and HRQoL observed in the adult/adolescent trials, which are based on an average patient age of approximately 40 years.
Table 48 summarises the assumptions and Appendix 17 presents the parameter inputs employed in the manufacturer's model for the base-case populations, alternative scenarios and patient subgroups. The following sections discuss the different aspects of the economic analysis in more detail.
| Input | Assumption |
|---|---|
| Transitions between health states | Constant exacerbation rates through time and treatment duration |
| Exacerbation rates sourced from studies on omalizumab: INNOVATE and IA-05 EUP for the base case; EXALT and APEX for scenarios (adult/adolescent only) | |
| Exacerbations classified into CSNS and CSS | |
| Asthma-related mortality | Asthma-related mortality can only occur because of CSS exacerbation |
| Cycle length | The first cycle lasts 16 weeks, at which point patients on omalizumab are assessed for response to treatment |
| For children < 12 years of age, the second cycle lasts 8 weeks to match with the data collection points in the IA-05 EUP study, at 24 and 52 weeks. | |
| For patients entering the model aged ≥ 12 years, the second cycle lasts 10 weeks. Subsequent cycles have 3-month duration. A half-cycle correction was employed | |
| Response to omalizumab | After the first 16-week cycle, the omalizumab cohort is divided into omalizumab responders and non-responders |
| Omalizumab non-responders revert to standard therapy | |
| Omalizumab responders are assumed to remain responders for the duration of treatment | |
| Adverse effects | Not considered |
| Non-compliance/withdrawals are assumed to occur during the first 16 weeks of therapy | |
| Long-term effects of OCSs | Not considered in the base case. Incorporated in scenario analysis for maintenance OCS subgroup |
| Treatment duration and time horizon | A lifetime horizon was considered |
| Treatment duration was assumed to be 10 years | |
| Treatment effect | The results of INNOVATE and IA-05 EUP are generalisable to the UK NHS |
| Omalizumab improves HRQoL in patients ≥ 12 years | |
| Omalizumab reduces exacerbation rates | |
| HRQoL | Omalizumab patients ≥ 12 years experience higher HRQoL in day-to-day symptoms than patients on standard care only |
| Exacerbations are associated with lower HRQoL, independent of treatment |
Model structure
The economic evaluation employed a model structure identical to that used in the previous STA (TA13388 and TA20189), Dewilde et al. 93 and Brown et al. 94 based on five health states: day-to-day asthma symptoms, CSNS exacerbations, CSS exacerbations, asthma-related death and all-cause death. The structure of the Markov model was considered appropriate by the assessment group. Patients start in the day-to-day asthma symptoms state on either omalizumab add-on therapy or standard therapy alone. At 16 weeks, patients on omalizumab are assessed for response to treatment, at which point omalizumab responders are separated from non-responders. Responders remain on omalizumab for the period of treatment duration and are assumed to experience the exacerbation rates observed for responders in the clinical trials. Non-responders are assumed to discontinue omalizumab, revert to standard care alone and experience the same exacerbation rates as patients randomised to the standard care arm of the trials. During each subsequent cycle of the model, patients may remain in the day-to-day symptom state or may experience an exacerbation (CSNS or CSS). Asthma-related death is assumed to occur only through a CSS exacerbation. However, patients may die as a result of all other causes from any state of the model. Following a non-fatal exacerbation, the patient returns to the day-to-day asthma symptoms state.
The model follows patients through a lifetime horizon (up to age 100 years). The first cycle lasts 16 weeks, at which point omalizumab responders are identified. The second cycle differs in the base-case populations according to the data collection time point in the trials; for children the second cycle lasts 8 weeks to match the 24-week data collected in IA-05 EUP, whereas for adults and adolescents, the second cycle lasts 10 weeks. Subsequent cycles have 3-month duration. A half-cycle correction was correctly employed.
Effectiveness data: response and exacerbations
The evidence on the clinical effectiveness of omalizumab add-on therapy was based on the results of INNOVATE and IA-05 EUP for the base-case populations of adults and adolescents and children, respectively, and EXALT and APEX for additional scenario analysis in adults and adolescents. Treatment effectiveness was based on two key components: response rates to omalizumab and CSNS and CSS exacerbation rates. The outcome of asthma-related mortality was not directly affected by treatment but indirectly through a reduction in CSS exacerbations.
Responders to omalizumab therapy
The proportion of patients responding to omalizumab treatment observed in the trials was used to inform the probability of being an omalizumab responder at 16 weeks. For the base case of adults and adolescents, the proportion of responders observed at 28 weeks in INNOVATE was used as a proxy for response at 16 weeks. For children, the proportion of responders observed at 52 weeks in IA-05 EUP was used as a proxy for response at 16 weeks. For the EXALT and APEX scenarios, the 16-week response rates reported in these studies were used. For the subgroup analyses, the response rate observed in each of the subgroups was used. Once patients were identified as responders, they were assumed to receive the exacerbation rates of responders over the entire duration of treatment.
Table 49 presents the proportion of responders to omalizumab therapy used in the economic model for the base-case populations, alternative scenarios and patient subgroups. The proportion of responders observed differed in the two double-blind RCTs: 56.5% in INNOVATE and 74.2% in IA-05 EUP. The proportion of responders in EXALT was greater than in INNOVATE at 69.9%. However, the assessment of response in EXALT may have been influenced by the open-label design of the trial. The proportion of responders in APEX was the highest at around 80%. This may reflect not only the selection of the most suitable patients for omalizumab in clinical practice but also the influence of knowing the treatment status of the patient when assessing for response. The proportion of responders in the patient subgroups was generally lower than in the overall population.
| Analysis | Proportion of responders (%) |
|---|---|
| Base case | |
| Adults and adolescents: INNOVATE | 56.5 |
| Children: IA-05 EUP | 74.2 |
| Alternative scenarios | |
| Adults and adolescents: EXALT | 69.9 |
| Adults and adolescents: APEX | 82.4 |
| Patient subgroups: hospitalisation | |
| Adults and adolescents: INNOVATE | 56.6 |
| Adults and adolescents: EXALT | 56.9 |
| Adults and adolescents: APEX | 82.7 |
| Children: IA-05 EUP | 54.1 |
| Patient subgroups: maintenance OCS | |
| Adults and adolescents: INNOVATE | 46.9 |
| Adults and adolescents: EXALT | 52.5 |
| Adults and adolescents: APEX | 78.9 |
The approach assumes that the response to omalizumab treatment remains unchanged over time. However, evidence from EXALT suggests that this may not be the case; around 8.6% of responders at 16 weeks in EXALT were not considered responders at 32 weeks. Although these results may have been influenced by the open-label design of the trial, they indicate that response may not persist through time. Therefore, there may be patients who discontinue treatment after 16 weeks or patients who remain on treatment but experience a reduced treatment effect. The potential impact of this was not considered in the MS.
Exacerbation rates
The exacerbation rates observed during the trials were used to inform the probability of experiencing an exacerbation in the model. The exacerbation rates from the trial follow-up period were annualised and assumed constant throughout the model. Patients on standard care were assumed to experience the exacerbation rates observed in the standard care arm of the trials. During the first 16-week cycle, patients on omalizumab experience the exacerbation rates observed for all patients who were randomised to receive omalizumab in the trials, regardless of response rate. From 16 weeks onwards, omalizumab responders were identified and received the exacerbation rates observed by the responders in the trial. Non-responders were assumed to revert back to standard therapy and experience the exacerbation rates in the standard care arm of the trials. Similarly, once omalizumab treatment is discontinued omalizumab responders revert to standard care.
Table 50 summarises the values for the key parameters on treatment effectiveness used in the model.
| Analysis | Standard care | Omalizumab responders | RR | ||
|---|---|---|---|---|---|
| Annual CS exacerbation rate | % CSS | Annual CS exacerbation rate | % CSS | ||
| Base case | |||||
| Adults and adolescents: INNOVATE | 1.689 | 52.4 | 0.630 | 35.0 | 0.373 |
| Children: IA-05 EUP | 2.028 | 22.9 | 0.519 | 27.3 | 0.256 |
| Alternative scenarios | |||||
| Adults and adolescents: EXALT | 1.587 | 40.8 | 0.650 | 42.1 | 0.410 |
| Adults and adolescents: APEX | 3.67 | 52.4 | 1.52 | 35.0 | 0.414 |
| Patient subgroups: hospitalisation | |||||
| Adults and adolescents: INNOVATE | 2.092 | 58.4 | 0.869 | 42.9 | 0.415 |
| Adults and adolescents: EXALT | 2.184 | 41.9 | 0.985 | 45.0 | 0.451 |
| Adults and adolescents: APEX | 3.400 | 58.4 | 1.630 | 42.9 | 0.479 |
| Children: IA-05 EUP | 3.429 | 37.5 | 0.743 | 25.0 | 0.217 |
| Patient subgroups: maintenance OCS | |||||
| Adults and adolescents: INNOVATE | 2.476 | 60.7 | 0.727 | 44.4 | 0.293 |
| Adults and adolescents: EXALT | 2.897 | 48.8 | 1.468 | 46.4 | 0.507 |
| Adults and adolescents: APEX | 3.700 | 60.7 | 1.440 | 44.4 | 0.389 |
The approach taken by the manufacturer seems appropriate in light of the available evidence. However, the exacerbation rates observed for patients in the placebo group may be lower than those experienced by patients on standard care in clinical practice, because of the increased contact with health-care professionals inherent to any RCT. If patients on standard care experience exacerbations more frequently than in INNOVATE, omalizumab may be more cost-effective than the base-case results suggest. In addition, some observational studies suggest that the likelihood of a future exacerbation is dependent on number of past exacerbations, that is exacerbation rates are not necessarily constant over time. 108–110
Asthma-related mortality
No deaths attributable to asthma were observed in the clinical trials during follow-up. Therefore, asthma-related mortality was obtained from alternative published sources. The manufacturer undertook a systematic review of the literature to identify any studies that reported mortality from CSS or hospitalisations for asthma. The inclusion criteria for the review were clinical trials, epidemiological studies and routine data that report mortality rates from severe asthma exacerbations or mortality rates from asthma exacerbations in patients aged ≥ 6 years. Studies which included participants with conditions other than asthma were excluded, as well as studies where deaths could not be reasonably associated with an exacerbation episode because of a follow-up time longer than 1 month post an exacerbation-related event. Studies using data from the Office for National Statistics and equivalent organisations were excluded as they could not provide a rate of death per exacerbation episode. The systematic review identified 22 studies meeting the inclusion criteria, of which five were conducted in the UK. 106,111–114 Watson et al. 106 report all-cause mortality for acute severe asthma hospitalisations [International Classification of Diseases (ICD) code J46] and asthma hospitalisations (ICS code J45). Gupta et al. 113 and Wildman et al. 114 report mortality following admission to the intensive care unit (ICU). Kearney et al. ,112 Seddon and Heaf111 and Gupta et al. 113 report mortality in patients who required mechanical ventilation. Mortality risks reported in these studies varied from 0.097% (0–11 years in Watson et al. 106) to 25.8% (ventilated children aged 0–15 years in Seddon and Heaf111).
Based on the results of the review, the manufacturer concluded that Watson et al. 106 provide the only UK-specific data on the mortality risk from exacerbations resulting in non-ICU related hospitalisations. This was the same study used to inform TA201 in children. Table 51 presents the mortality per admission code reported in Watson et al. 106 The risk of asthma-related death following a CSS exacerbation in the model was informed by the risk of death following hospitalisation for acute severe asthma (ICD code J46) for both base-case populations. Therefore, the model assumes that each CSS exacerbation is associated with a mortality risk of 0.097% for children < 12 years, 0.319% for ages 12–16 years, 0.383% for ages 17–44 years and 2.478% for ages ≥ 45 years.
| Age (years) | Mortality following hospitalisation for asthma (95% CI) | Mortality following CSS exacerbation used in the model | ||
|---|---|---|---|---|
| ICD J45 | ICD J46 | Children | Adults and adolescents | |
| Hospitalisation for asthma | Hospitalisation for acute severe asthma | Age at treatment initiation = 9 years | Age at treatment initiation = 43 years | |
| 0–11 | 0.004% (0.001 to 0.011) | 0.097% (0.042 to 0.191) | 0.097% | NA |
| 12–16 | 0.034% (0.009 to 0.086) | 0.319% (0.104 to 0.742) | 0.319% | NA |
| 17–44 | 0.052% (0.035 to 0.073) | 0.383% (0.267 to 0.529) | 0.383% | 2.478% |
| ≥ 45 | 1.190% (1.109 to 1.275) | 2.478% (2.129 to 2.865) | 2.478% | 2.478% |
| Total | 0.374% (0.349 to 0.400) | 0.858% (0.750 to 0.977) | 2.478% | 2.478% |
It is important to note that the base-case population for adults and adolescents (average age of 43 years) incorporates the mortality risk of 2.478% (age ≥ 45 years). Although the model assumes a mean age of 43, there is variation in the ages of patients within this population. As age affects the asthma-related mortality risk, the impact of age at treatment initiation should be considered, either by presenting subgroups based on age, or, if age is not considered an appropriate basis for subgroups, by combining estimates for different ages into the final ICER estimates.
The manufacturer acknowledged that all asthma-related deaths ultimately occur because of a CSS asthma exacerbation, but that the definition of CSS exacerbations used in the omalizumab trials differs from the definition used in the studies included in the mortality review. Although only a proportion of CSS exacerbations observed in the omalizumab trials resulted in hospitalisation, hospitalisation was considered to be the only available proxy for CSS exacerbation available in the literature. For example, in INNOVATE only 7% of CSS exacerbations involved the accident and emergency unit, and 13% involved hospitalisation. In IA-05 EUP, 63% of CSS exacerbations involved the accident and emergency unit and 40% involved hospitalisation. Consequently, the model assumes that mortality risk for patients following a hospitalisation for severe asthma can be applied to all patients experiencing a CSS exacerbation regardless of whether this resulted in a hospitalisation. In the manufacturer's review, the need to establish a clear link between CSS exacerbations and death may have resulted in the exclusion of potentially relevant studies which report on asthma-related mortality. These additional studies may have provided a way to assess the external validity of a key assumption applied in the model; namely the generalisability of mortality data from hospitalised to non-hospitalised patients experiencing a CSS exacerbation.
All-cause mortality
All-cause mortality was based on interim life-tables for England and Wales for the years 2007–2009 from the Office for National Statistics. 115 However, asthma-related deaths were not removed from the life-tables and so there is some element of double counting of mortality in the model. However, because of the small number of asthma deaths in the general population, this is unlikely to be a significant issue.
Resource utilisation and cost data
Data on resource utilisation was primarily based on resource use in the trials, which related to medications and cost of clinically significant exacerbations. Unit costs were sourced from NHS Reference costs 2009–10 and the Personal Social Services Research Unit (PSSRU). 116 Table 52 summarises the costs used in the MS.
Omalizumab therapy costs
Costs associated with omalizumab therapy include the costs of the drug itself and the costs of administration and monitoring. Omalizumab is administered as a subcutaneous injection every 2–4 weeks, and the exact dose depends on the patient's serum IgE and weight.
The dosing distribution of omalizumab used in the economic analysis refers to the ‘standard dose’ of treatment rather than the ‘expanded dose’. An expanded dose above 375 mg per administration and/or dosing for some lower weight patients with IgE of greater than 700–1500 international units (IU)/ml was included in the EU SPC in a January 2010 update. 26 However, the standard dose was applied in the earlier studies of INNOVATE, EXALT, APEX and IA-05 EUP.
Omalizumab is currently available as 75 mg and 150 mg prefilled syringes. 22 At the time of the previous STAs, omalizumab was only available as a 150-mg vial. Consequently, the assumptions regarding vial wastage and re-use in the previous appraisals are no longer relevant. For the base-case populations, the model assumes an average dose of omalizumab corresponding to the dose-distribution of the patient population in INNOVATE, EXALT, APEX and IA-05. Although children would be expected to increase in weight during the period of treatment duration, the model does not adjust for an increase in weight. However, the average cost per patient is similar across populations; therefore, the increase in weight is unlikely to change the results significantly.
Costs of administration and monitoring
The costs of administration were estimated by assuming 10 minutes of administration time and using the hourly cost of a specialist asthma nurse at £47/hour. 116 Monitoring costs for anaphylaxis were included up to and including the 16-week responder assessment. For the first three administrations, the monitoring was assumed to take 2 hours, while from the fourth administration up to the 16-week assessment, monitoring was assumed to take only 1 hour, with each hour costing 15 minutes of specialist asthma nurse time. The costs of administration and monitoring were considered appropriate by our clinical advisors.
| Analysis | Omalizumab therapy | Standard care | Exacerbations | |||||
|---|---|---|---|---|---|---|---|---|
| Omalizumab costs per annum (with administration)a | Monitoring | Initiation | 16-week response assessment | Medication (per year) | Routine visits (two per year) | CSNS | CSS | |
| Base case | ||||||||
| Adults and adolescents: INNOVATE | £8200.73 | £11.75 per hour of monitoring | £245 | £160 | £1196.81 | £160 | £87.70 | £124.32 |
| Children: IA-05 | £8606.73 | £11.75 per hour of monitoring | £247 | £190 | £810.07 | £190 | £213.89b | £213.89b |
| Alternative scenarios | ||||||||
| Adults and adolescents: EXALT | £9226.86 | £11.75 per hour of monitoring | £245 | £160 | £1153.75 | £160 | £179.56b | £179.56b |
| Adults and adolescents: APEX | £10,547.04 | £11.75 per hour of monitoring | £245 | £160 | £1196.81 | £160 | £304.51b | £304.51b |
| Patient subgroup: hospitalisation | ||||||||
| Adults and adolescents: INNOVATE | £8200.73 | £11.75 per hour of monitoring | £245 | £160 | £1196.81 | £160 | £154.70 | £178.87 |
| Adults and adolescents: EXALT | £9226.86 | £11.75 per hour of monitoring | £245 | £160 | £1153.75 | £160 | £267.44b | £267.44b |
| Adults and adolescents: APEX | £10,547.04 | £11.75 per hour of monitoring | £245 | £160 | £1196.81c | £160 | £487.66b | £487.66b |
| Children: IA-05 EUP | £8606.73 | £11.75 per hour of monitoring | £247 | £190 | £810.07 | £190 | £213.89d | £213.89d |
| Patient subgroup: maintenance OCS | ||||||||
| Adults and adolescents: INNOVATE | £8200.73 | £11.75 per hour of monitoring | £245 | £160 | £1196.81 | £160 | £86.51 | £136.04 |
| Adults and adolescents: EXALT | £9226.86 | £11.75 per hour of monitoring | £245 | £160 | £1153.75 | £160 | £147.37b | £147.37b |
| Adults and adolescents: APEX | £10,547.04 | £11.75 per hour of monitoring | £245 | £190 | £1196.81d | £160 | £308.46b | £308.46b |
Standard care costs: standard therapy and routine secondary care
Routine secondary care visits
All patients were assumed to have two routine outpatient appointments per year with a hospital specialist. In addition, patients on omalizumab have two extra visits: an initiation appointment and a follow-up appointment at 16 weeks to assess response to treatment. These assumptions were considered appropriate by our clinical advisors.
Standard therapy costs
Data on medication use was collected during INNOVATE, EXALT, APEX and IA-05 EUP. The cost of standard therapy in the model corresponds to the standard therapy medication used by all patients in the relevant trial, regardless of treatment group. As patients on omalizumab add-on therapy and standard care alone accrue the costs of therapy, these costs will not affect the ICER of omalizumab.
Costs of exacerbations
Resource use associated with clinically significant exacerbations were collected during INNOVATE, EXALT, APEX and IA-05. The costs of exacerbations include GP consultations, outpatient appointments, emergency admissions, rehab appointments, general ward stay and ICU stay. For the base case of adults and adolescents, resource use in INNOVATE was reported separately for CSNS and CSS exacerbations. However, for the base case of children, and for EXALT and APEX scenarios, the manufacturer was unable to separate the data into type of exacerbation so the average cost was calculated across all exacerbations and applied to both types. Unit costs for resource use were obtained from UK cost information. 16
Health-related quality of life
HRQoL was expressed in terms of QALYs by quality-adjusting the period of time the average patient was alive within the model using an appropriate utility score. Two key elements of HRQoL were considered: the QoL associated with day-to-day asthma symptoms and clinically significant non-severe and severe exacerbations. Table 53 summarises the HRQoL values used in the economic model.
| Analysis | HRQoL day-to-day symptoms | HRQoL for exacerbations | |||
|---|---|---|---|---|---|
| Standard care | Omalizumab responders | CSNSa | CSSb | Mean duration | |
| Base case | |||||
| Adults and adolescents: INNOVATE | 0.669 | 0.779 | 0.572 | 0.326 | 12.8 |
| Children: IA-05 EUP | 0.669 | 0.779/0.669c | 0.572 | 0.326 | 17.1 |
| Alternative scenarios | |||||
| Adults and adolescents: EXALT | 0.719 | 0.767 | 0.572 | 0.326 | 14.6 |
| Adults and adolescents: APEX | 0.669a | 0.779a | 0.572 | 0.326 | As per INNOVATE |
| Patient subgroups: hospitalisation | |||||
| Adults and adolescents: INNOVATE | 0.634 | 0.772 | 0.572 | 0.326 | 12.8 |
| Adults and adolescents: EXALT | 0.631 | 0.761 | 0.572 | 0.326 | 14.6 |
| Adults and adolescents: APEX | 0.634a | 0.772a | 0.572 | 0.326 | As per INNOVATE |
| Children: IA-05 EUP | 0.634 | 0.767/0.634c | 0.572 | 0.326 | 17.1 |
| Patient subgroups: maintenance OCS | |||||
| Adults and adolescents: INNOVATE | 0.639 | 0.745 | 0.572 | 0.326 | 12.8 |
| Adults and adolescents: EXALT | 0.686 | 0.791 | 0.572 | 0.326 | 14.6 |
| Adults and adolescents: APEX | 0.639a | 0.745a | 0.572 | 0.326 | As per INNOVATE |
Day-to-day symptoms
Health utilities for day-to-day symptoms applied in the base-case analysis for the adult/adolescent population were derived from AQLQ data collected at 28 weeks in the INNOVATE trial and mapped onto EQ-5D using a published mapping function. 103 Data on daily symptoms and functioning were collected in IA-05 EUP using the paediatric AQLQ (PAQLQ). As the PAQLQ results found no difference in QoL between omalizumab and standard care, the manufacturer conservatively assumed that there was no HRQoL gain associated with omalizumab for patients < 12 years of age. Once patients reached 12 years, it was assumed that the population of patients that informed INNOVATE was a relevant source of HRQoL for day-to-day symptoms in the children's base case. The EXALT scenario used EQ-5D values directly collected during EXALT, whereas the APEX scenario used the EQ-5D values mapped from AQLQ collected at INNOVATE.
Exacerbations
Utility decrements for clinically significant non-severe and severe exacerbations were obtained from Lloyd et al. ,104 a prospective study conducted in the UK in four specialist asthma centres. In this study, patients (n = 112) with moderate to severe asthma (step 4 or 5 of BTS/SIGN guidelines) completed the EQ-5D questionnaire at baseline and 4-week follow-up. Patients were classified by type of exacerbation experienced during the 4-week period: no exacerbation (n = 85), exacerbation requiring OCS use (n = 22) or asthma-related hospitalisation (n = 5). The EQ-5D value for an exacerbation requiring OCS use was used as a proxy for CSNS exacerbation, whereas the value for asthma-related hospitalisation was used for CSS exacerbation. However, as previously stated when discussing the mortality data, the definition of clinically significant severe exacerbations used in the model may not reflect an asthma-related hospitalisation. In INNOVATE, only 20% of CSS exacerbations involved hospitalisation or an emergency room visit, 21% involved a GP or hospital outpatient visit and 59% were managed without any primary or secondary use of services. Therefore, it is unclear whether or not the HRQoL loss for asthma-related hospitalisation from Lloyd et al. 104 can be applied to all for a CSS exacerbation.
Table 54 summarises the EQ-5D values reported in Lloyd et al. 104 and the EQ-5D values applied in the economic model. The manufacturer uses the absolute HRQoL value at end of follow-up for an exacerbation requiring OCS use and asthma-related hospitalisation reported in Lloyd et al. (2007)104 instead of the difference in HRQoL between baseline and follow-up (mean change from baseline in Table 54). This appears particularly important as it is the decrement in HRQoL because of these events that should be incorporated in the model. In addition, there also appears to be a marked difference in the baseline HRQoL estimates across the groups of patients in the Lloyd study, suggesting that the patients requiring OCSs or hospitalisation had a worse HRQoL prior to the event (i.e. patients experiencing an event were not a random subset of the total sample).
| Lloyd et al. (2007)103 | Manufacturer's model | ||||
|---|---|---|---|---|---|
| Type of exacerbation | Mean | Mean change from baseline | Event | HRQoL during exacerbation | Implied change from day-to-day symptoms |
| Exacerbation with OCSs | 0.57 | −0.10 | CSNS exacerbation | 0.57 | −0.097 |
| Exacerbation with hospitalisation | 0.33 | −0.20 | CSS exacerbation | 0.33 | −0.343 |
Exacerbations were assumed to last for an average of 12.8 days (INNOVATE) and 17.1 days (IA-05 EUP) in adults and adolescents and children respectively. The appropriate HRQoL for CSNS and CSS exacerbations is further complicated by the issue of timing and duration of the exacerbations in Lloyd et al. 104 If the exacerbation occurred close to the 4-week follow-up time point, the value may appropriately reflect the utility associated with an exacerbation. However, if the exacerbation occurred close to baseline, the patient may have recovered by the 4-week follow-up assessment. Consequently, although the use of absolute HRQoL estimates are likely to overestimate the impact of an event on HRQoL, the timing of administration of EQ-5D may also underestimate the extent of the decrement during the exacerbation period. The combined impact of these alternative factors is unclear in terms of assessing whether the approach used by the manufacturer results in an over- or underestimate of the HRQoL impact of CSNS and CSS events.
Cost-effectiveness results
The results of the economic evaluation were presented for the two base-case populations, two alternative scenarios for adults and adolescents using data from EXALT and APEX, and for the subgroup populations. One-way sensitivity analysis and probabilistic sensitivity analysis (PSA) were conducted for the base-case populations.
Base-case populations
Table 55 presents the cost-effectiveness results for the base-case populations, alongside the ICER from TA133 and TA201 for comparison. The deterministic ICER for the base-case of adults and adolescents aged ≥ 12 years is £32,076 per QALY gained, and the probabilistic ICER is £33,268. The deterministic ICER for children aged 6–11 years is £80,747 per QALY gained and the probabilistic ICER is £88,998. The probabilities that omalizumab is cost-effective at thresholds of £20,000 and £30,000 per QALY gained for the adult and adolescent population are 0.005 and 0.267 respectively.
| Population | Trial | Incremental costs (£) | Incremental QALY | Deterministic ICER (£/QALY) | Probabilistic ICER (£/QALY) |
|---|---|---|---|---|---|
| ≥ 12 years | INNOVATE | 40,748 | 1.27 | 32,076 | £33,268 |
| 6–11 years | IA-05 EUPa | 54,432 | 0.67 | 80,747 | £88,998 |
Table 56 presents the cost-effectiveness results for the alternative scenarios based on data from EXALT and APEX. The ICER of £61,687 for the EXALT scenario is approximately double the value for the base-case population, whereas the ICER of £29,773 for the APEX scenario is slightly lower than the base-case population. The difference in ICER between the INNOVATE base case and the EXALT scenario is largely because of two factors: (1) the lower treatment effect observed in omalizumab responders in EXALT compared with INNOVATE, and (2) the magnitude of the HRQoL improvement for day-to-day symptoms estimated in INNOVATE (based on a mapping between AQLQ and EQ-5D) and EXALT (based on directly observed EQ-5D data). The reduction in the rate of total exacerbations was more pronounced in INNOVATE (RR 0.373) than in EXALT (RR 0.410). Similarly, the health utility improvement in day-to-day symptoms in omalizumab responders in INNOVATE was greater than in EXALT (0.110 vs. 00.048). APEX represents a before-and-after study based on a small number of patients; therefore the results based on APEX are considered less reliable than those based on RCTs such as INNOVATE and EXALT.
| Population | Trial | Incremental costs (£) | Incremental QALY | ICER (£/QALY) |
|---|---|---|---|---|
| ≥ 12 years | EXALT | 53,983 | 0.88 | 61,687 |
| APEX | 72,071 | 2.42 | 29,773 |
Subgroup analysis
Table 57 presents the results of the hospitalisation and maintenance OCS subgroup populations. The ICER for the hospitalisation subgroup for adults and adolescents based on INNOVATE was £27,928 per QALY gained, which is £4148 (13%) lower than the base-case population. The ICER for the maintenance OCS subgroup for adults and adolescents was £26,320 per QALY gained, which is £5756 (18%) lower than the base case. The ICER for the hospitalisation subgroup for children based on IA-05 EUP was £65,100 per QALY gained, which is a reduction of £15,647 (19%) from the base-case in children.
| Patient population | Trial | Incremental costs (£) | Incremental QALY | Deterministic ICER (£/QALY) | Probabilistic ICER (£/QALY) |
|---|---|---|---|---|---|
| Hospitalisation subgroup | |||||
| ≥ 12 years | INNOVATE | 40,248 | 1.44 | 27,928 | NR |
| ≥ 12 years | EXALT | 43,613 | 1.24 | 35,198 | NR |
| ≥ 12 years | APEX | 70,251 | 2.31 | 30,407 | NR |
| 6–11 years | IA-05 EUP | 39,999 | 0.61 | 65,100 | NR |
| Maintenance OCS subgroup | |||||
| ≥ 12 years | INNOVATE | 34,615 | 1.32 | 26,320 | NR |
| ≥ 12 years | EXALT | 40,181 | 1.07 | 37,604 | NR |
| ≥ 12 years | APEX | 68,670 | 2.31 | 29,685 | NR |
Impact on the incremental cost-effectiveness ratio of alternative scenarios
Deterministic sensitivity analysis
A large number of deterministic sensitivity analyses were conducted on the base-case populations (INNOVATE and IA-05 EUP). Table 4.23 (pp. 99–100 of the MS) presented the results of the manufacturer's sensitivity analysis. The manufacturer concluded that the ICER is most sensitive to changes in the following parameters: time horizon, exacerbation rates, asthma-related mortality, HRQoL values for day-to-day asthma symptoms, omalizumab drug costs and discount rate.
From the results in table 4.23 (pp. 99–100 of the MS), the major cost-effectiveness drivers are the asthma-related mortality and the HRQoL improvement with omalizumab, which is in line with the findings in the previous submissions. The ICER for the adults and adolescent population increases from £32,076 to £72,113 per QALY gained when the asthma-related mortality risk is set to zero. The effect on the ICER for the children's population is not as pronounced, as the asthma-related mortality risk used for this population is much lower than in the adult and adolescent population.
For the child population, treatment duration and age at treatment initiation have a considerable impact on the cost-effectiveness of omalizumab. Assuming a 2-year treatment duration increases the ICER from £80,747 to £662,893 per QALY gained. If treatment duration is halved from 10 years to 5 years, the ICER increases to £122,429 per QALY gained. Similarly, reducing the age at treatment initiation from 9 to 6 years increases the ICER to £130,475 per QALY gained. If age at initiation of treatment is 11 years old, the ICER is reduced by 21.5% to £63,365 per QALY. These results reflect the assumption of no HRQoL improvement in day-to-day symptoms with omalizumab therapy until patients reach age 12. The younger patients initiate omalizumab therapy or the shorter the treatment duration, the lower the HRQoL benefits accrued with omalizumab therapy; hence, the less cost-effective omalizumab appears.
Incorporation of long-term consequences of oral corticosteroids
Overview
The manufacturer conducted an exploratory sensitivity analysis incorporating the adverse effects of maintenance OCS use. This ‘OCS-sparing’ analysis was conducted for the maintenance OCS subgroup of EXALT and APEX, as the protocol of INNOVATE did not allow for changes in concomitant medication during the study period. In EXALT, 41.9% of omalizumab responders discontinued maintenance OCS after 32 weeks, whereas in APEX 45.1% of omalizumab responders discontinued maintenance OCS at follow-up. The annual burden of OCSs was applied in the model as a reduction in costs and an improvement in QALYs for omalizumab responders who discontinued maintenance OCS.
Table 58 summarises the parameter inputs used in the ‘OCS-sparing’ sensitivity analysis. The annual burden of OCS use was estimated in terms of direct costs to the NHS and HRQoL losses, which were expressed in disability-adjusted life-years (DALYs). DALYs measure years of life lost as a result of premature death and years of ‘healthy’ life lost as a result of illness. The costs to the NHS consisted of the drug costs associated with OCS use (based on data collected in EXALT and APEX) and the costs associated with OCS-related adverse effects. At baseline in EXALT, patients on omalizumab were taking a mean OCS dose of 13.1 mg per day costing £99.45 per patient per year, whereas patients in APEX were taking 18.56 mg per day at a cost of £140.93 per patient per year. The average daily dose of OCS in APEX and EXALT is similar to that reported for the BTS Difficult Asthma cohort of 15 mg per day. 67
| Parameter | EXALT | APEX |
|---|---|---|
| Average daily dose of OCS | 13.1 mg | 18.56 mg |
| Cost of OCS per patient per year | £99.45 | £140.93 |
| % of omalizumab responders who stopped OCS at follow-up | 41.9 | 45.1 |
The analysis assumed that:
-
Infrequent OCS bursts as a result of clinically significant exacerbations do not increase the risk of OCS-related adverse effects and have negligible cost.
-
The excess risk attributable to OCSs is based solely on current exposure to OCSs, and once patients discontinue OCSs the excess relative risk becomes negligible.
-
Patients who discontinue OCSs will not restart on OCSs if omalizumab treatment is discontinued.
-
Patients who do not receive omalizumab receive maintenance OCS for the remainder of their life.
-
Health utility losses estimated in DALYs are equivalent to QALYs.
The following sections discuss the manufacturer's ‘OCS-sparing’ analysis in more detail.
Adverse effects of oral corticosteroids
Estimates of relative risk associated with OCS use for a range of conditions were obtained from the study by Manson et al. ,84 which is discussed in detail in Chapter 3, Other adverse events. The excess relative risk associated with OCS use was identified for the following conditions: type 2 diabetes, myocardial infarction, glaucoma, cataracts, ulcer, osteoporosis and stroke. Other conditions for which risk because of OCS use is available are non-Hodgkin's lymphoma, sleep disturbance, acne, skin bruising and thinning, weight gain, mood problems and muscle weakness. These latter conditions were not included in the economic analysis because of insufficient data on the associated costs and health losses. Non-Hodgkin's lymphoma was excluded because of its rarity and the small associated cost estimated in Manson et al. of £0.41 per patient per year on OCSs. 84
Table 59 summarises the risks used in the ‘OCS-sparing’ analysis, alongside the alternative sources considered by the manufacturer. When more than one source of risk was available, the manufacturer considered the study design and the OCS dose examined in the study. Studies with larger sample sizes and reporting OCS doses similar to those used in UK clinical practice were favoured over smaller studies and those which did not report or stratify by OCS dose, or which used OCS doses much greater or smaller than those reported in APEX.
| Condition | Applied in the ‘OCS-sparing’ analysis | Other potential sources for the condition | ||||
|---|---|---|---|---|---|---|
| RR/OR | OCS dosea | Source | RR/OR | OCS dosea | Source | |
| Diabetes | 3.02 | 10–19.75 mg | Gurwitz et al. (1994)117 | 2.31 | NR | Blackburn et al. (2002)118 |
| 1.40 | All doses | Walsh et al. (2001)119 | ||||
| Myocardial infarction | 2.50 | > 10 mg | Varas-Lorenzo et al. (2007)120 | 2.01 | < 25 mg | Huiart et al. (2006)121 |
| Osteoporosis | 2.84 | 15–29.9 mg | Van Staa et al. (2005)122 | 1.90 | NR | Donnan (2005)123 |
| 2.07 | All doses | Steinbuch (2004)124 | ||||
| 1.80 | All doses | Walsh et al. (2001)119 | ||||
| Glaucoma | 1.37 | 10–20 mg | Garbe et al. (1997)125 | NA | NA | NA |
| Ulcer | 2.00 | All doses | Piper et al. (1991)126 | NA | NA | NA |
| Cataract | 1.83 | > 6.5 mg | Curtis et al. (2006)127 | 2.60 | All doses | Walsh et al. (2001)119 |
| 4.76 | NR | Wang et al. (2009)128 | ||||
| Stroke | NA | NA | NA | 1.20 | > 60 mg | Zonana-Nacach et al. (2000)129 |
The sources chosen to inform the relative risks appear appropriate except for ulcer. The relative risk for ulcer refers to patients with pre-existing gastric/duodenal ulcer and, therefore, may be an overestimate of the effects of OCS use in the general asthma population. As acknowledged by the manufacturer, the exclusion of a number of conditions because of insufficient data may have led to the underestimation of the adverse impact of OCS use. Nevertheless, the approach taken by the manufacturer appears to be a reasonable approximation of the risks associated with maintenance OCS use.
Costs and health losses because of oral corticosteroid-related adverse effects
The costs incurred and health losses because of OCS-related adverse effects were estimated by applying the excess relative risk to the costs and health losses associated with each condition.
Table 60 presents the estimates of costs and health losses because of OCS-related adverse effects and the data used in the calculations. The excess relative risk is the additional risk attributable to the exposure of interest (i.e. maintenance OCS use) after removing the background relative risk. 130 Therefore, the excess relative risk associated with OCS use corresponds to the relative risk (or odds ratio) minus one, where the background relative risk = 1. The average cost per patient for OCS-related adverse effects is the aggregate sum of the costs per patient for each condition multiplied by the excess relative risk. The average cost per patient for each condition corresponds to the total NHS cost for the condition divided by the relevant population (England or UK, depending on the condition and source for costs). The NHS cost for each condition was obtained from published sources (see table 3 in appendix G, p. 144 of the MS for further details). 15 The resulting cost of OCS-related adverse effects was estimated at £205.61 per year per patient on maintenance OCS. The health losses because of OCS-related adverse effects are the aggregate sum of the average health loss for each condition multiplied by the excess relative risk because of OCS use. The average health loss for each condition corresponds to the annual DALY burden in the UK divided by the UK population. The annual DALY burden was informed by the World Health Organization (WHO) study on global burden of disease. 131 The resulting health loss because of OCS-related adverse effects was estimated at 0.02331 DALY per patient per year on maintenance OCS. Therefore, the economic analysis includes an annual cost reduction of £205.61 and an annual QALY benefit of 0.02331 (under the assumption that DALYs are equivalent to QALYs) for the proportion of omalizumab responders assumed to stop OCSs.
| Condition | RR of OCS use | Current cost (£M) | Average cost per person (£) | Additional average cost per patient on OCS per year (£) | Annual DALY burden in UK (‘000) | Annual DALY burden per individual | DALYs as a result of OCS use per patient on OCS per year |
|---|---|---|---|---|---|---|---|
| Diabetes | 3.02 | 1,550 | 29.67 | 59.94 | 139.173 | 0.00232 | 0.00469 |
| MI | 2.50 | 2,240 | 42.88 | 64.33 | 637.470 | 0.01063 | 0.01595 |
| Osteoporosis | 2.84 | 2,390 | 38.39 | 70.64 | 62.257 | 0.00104 | 0.00191 |
| Glaucoma | 1.37 | 140 | 2.25 | 0.83 | 22.702 | 0.00038 | 0.00014 |
| Ulcer | 2.00 | 361 | 6.91 | 6.91 | 32.055 | 0.00053 | 0.00053 |
| Cataract | 1.83 | 222 | 3.57 | 2.96 | 6.881 | 0.00011 | 0.00010 |
| Total | 205.61 | 0.02331 |
The approach used by the manufacturer to estimate the costs because of OCS-related adverse effects is considered reasonable and appropriate to the decision problem. However, the method used to estimate health utility losses because of OCS-related adverse effects is based on the assumption that DALYs are equivalent to QALYs, which may not be appropriate.
Table 61 summarises the different elements of health corresponding to a DALY and compares these with the QALYs. DALYs measure the gap between current health status and ‘healthy life’, where everyone lives to an advanced age free of disease and disability. 132 The DALY incorporates four key elements: years of life lost as a result of disease, QoL lost as a result of disease, age-weights, which reflect the differential social value of age, and a discount rate of 3% per annum, which reflects society's preference for valuing present health more than future health. 132,133 The major differences between DALYs and QALYs are in the measurement of life-years and weights used to quality-adjust life-years. DALYs measure years of life lost compared with an ideal life expectancy of 82.5 years for women and 80 years for men,132 whereas QALYs measure years of life gained and, therefore, do not require knowledge of the life expectancy of the general population. DALYs use disability weights obtained from expert deliberation for specific diseases, whereas QALYs use HRQoL weights obtained from a sample of the general population based on the desirability of particular health states. The number of DALYs saved are equivalent to the number of QALYs gained under the following conditions: (1) the HRQoL weight is equivalent to one minus the corresponding disability weight; (2) both the HRQoL weight and the disability weight are constant throughout the disease duration; (3) the same discount rate is used for both calculations; and (4) DALYs are not weighted according to age. 134
| DALY = (YLL + YLD) | QALY = YLG × utility weight |
|---|---|
| DALYs measure number of lost healthy life-years | QALYs measure number of gained healthy life-years |
| YLL: years of life lost | YLG: years of life gained. |
| Corresponds to the number of deaths multiplied by the standard life expectancy at the age at which death occurs | Corresponds to the number of years gained from the age at which the intervention is introduced |
| The standard life expectancy is taken to be the life expectancy of an average Japanese woman of 82.5 years, and an average Japanese man of 80 years | |
| YLD: years of life lost as a result of disability | The utility weight reflects the QoL associated with different health states. Utility weights were obtained from a sample of the general population |
| Corresponds to the number of incident cases of each disease multiplied by the average duration of the disease until remission or death and the disability weight attributed to the disease | The utility weight reflects the HRQoL associated with the health state on a scale of 1 (perfect health) to 0 (equivalent to death), but states worse than death are also allowed (negative values) |
| The disability weight reflects the severity of the disease on a scale of 0 (perfect health) to 1 (equivalent to death) | |
| Optional factors | |
| Age weighting reflects the differential social value of people of different ages (greater weight for young adults and smaller weights for young children and elderly) | QALYs are not age-weighted |
| A discount rate of 3% per annum is applied to reflect society's time preference for benefits delivered sooner rather than benefits delivered later | A discount rate of 3.5% per annum is applied to reflect society's time preference for benefits delivered sooner rather than benefits delivered later |
| Schematic representation | |
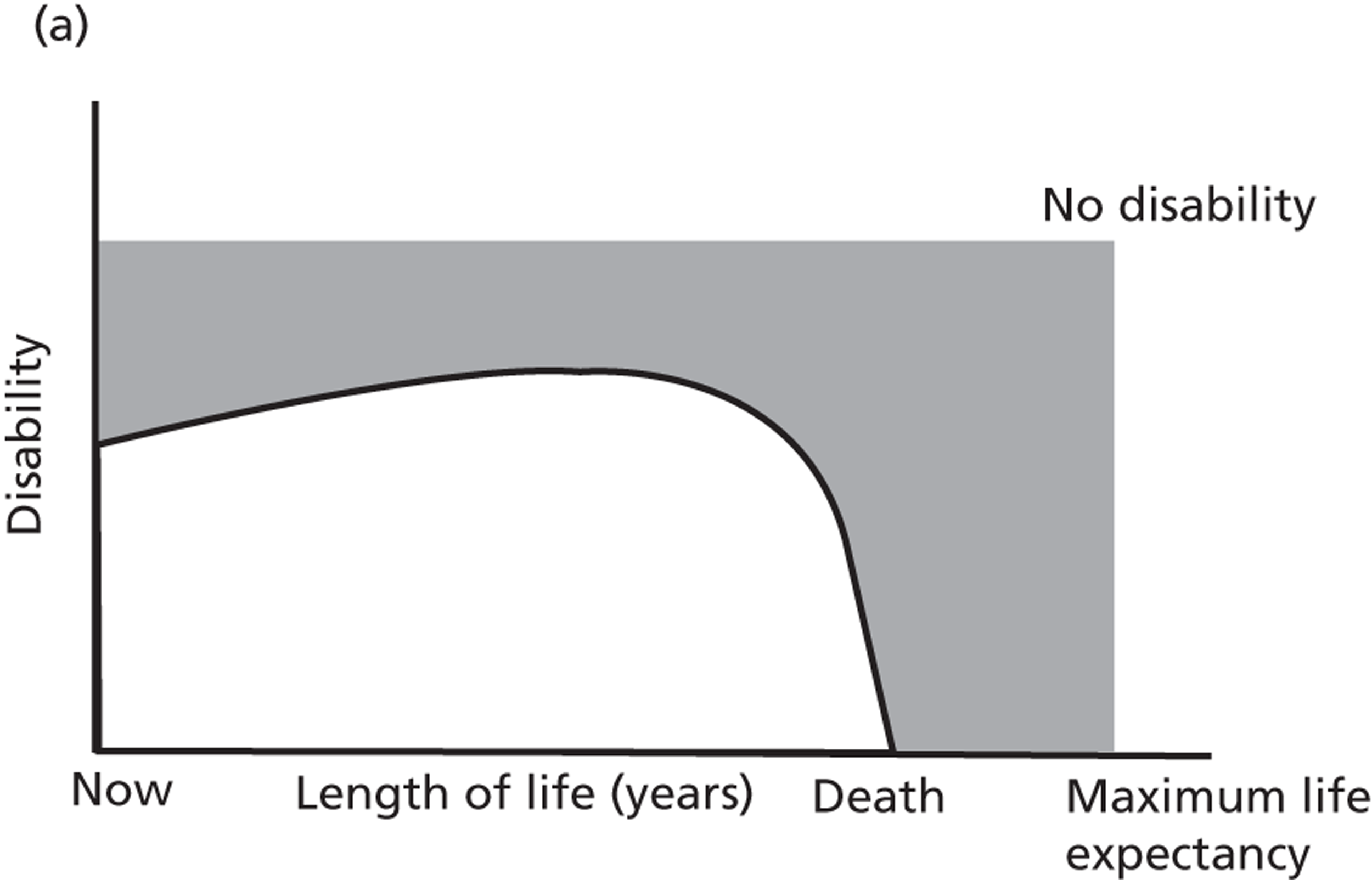
|
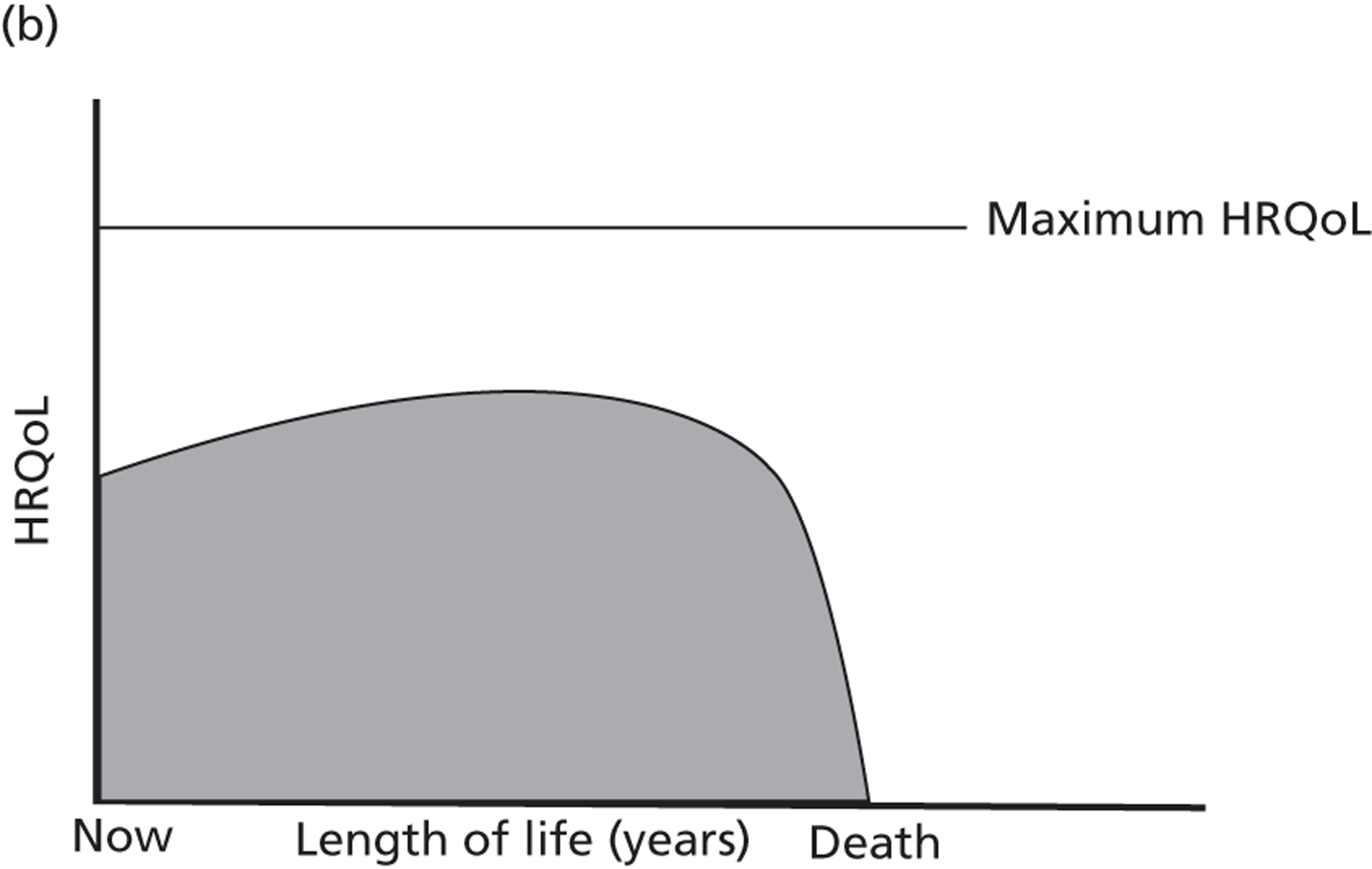
|
| The area highlighted in grey corresponds to the disease burden in DALYs | The area highlighted in grey corresponds to the quality-adjusted life expectancy in QALYs |
The manufacturer's approach is reasonable in terms of quantifying the risk, costs and DALYs. In the absence of a systematic review of QALY losses because of OCS adverse events, the use of DALYs, as an approximation for QALYs lost, is a pragmatic approach for estimating the health loss as a result of OCS-related adverse effects. However, it should be noted that QALYs are not weighted by age. Furthermore, the model applies a 3.5% discount rate per year to the approximate QALY estimates, which already incorporate a 3% discount rate in the DALY calculation. The process used to estimate the annual cost and QALY burden is less appropriate because of a number of assumptions which appear relatively favourable to omalizumab: (1) patients who discontinue on omalizumab will not restart OCSs, despite treatment not being continued throughout their lifetime; and (2) all patients receiving standard care continue to receive maintenance OCS for the remainder of their lifetime. For the former assumption to be appropriate, omalizumab would need to demonstrate a long-term disease-modifying effect, which has not been established. The latter is also unlikely, given that in both EXALT and trial number 011, patients on standard care discontinued omalizumab (13%, 3/23 in EXALT at 32 weeks;68 42.0%, 19/45 in 011 at 32 weeks69) (see Chapter 3, Results of assessment of safety of omalizumab: other adverse events for more details). For these reasons, the ‘steroid-sparing’ benefits of omalizumab may have been overestimated.
Results of ‘oral corticosteroid-sparing’ sensitivity analysis
Table 62 presents the results of the ‘OCS-sparing’ analysis, which incorporates the long-term consequences of OCS use. The ICER for the maintenance OCS subgroup of EXALT was reduced from £37,604 to £28,319 per additional QALY, whereas the ICER for the maintenance OCS subgroup of APEX was reduced from £28,685 to £25,099 per QALY gained.
| Analysis | Deterministic ICER (/QALY)a | % change in ICER |
|---|---|---|
| EXALT ‘maintenance OCS’ subgroup | £37,604 | – |
| + estimate of OCS-sparing effect | £28,319 | −24.7% |
| APEX ‘maintenance OCS’ subgroup | £29,685 | – |
| + estimate of OCS-sparing effect | £25,099 | −15.4% |
The analysis was only conducted for adults and adolescents ≥ 12 years and older as IA-05 EUP did not provide data on the potential OCS-sparing effect of omalizumab in children. The manufacturer suggested that a further 0.061 QALY gain could be assumed for children who discontinue OCSs because of omalizumab. The value of 0.061 QALY per patient per year relates to the effects of OCSs on impaired growth, which was taken from the NICE appraisal TA188135 based on a study evaluating the relationship between height and health utility in the adult UK population. The results suggest that an improvement of 1 height standard deviation score (HSDS) is associated with a significant change in EQ-5D of 0.061 for individuals shorter than −2.0 HSDS, whereas for individuals between −2 and 0 HSDS the improvement of 1 HSDS is associated with a significant change in EQ-5D score of 0.010. The meta-analysis of Allen et al. 84 suggests that OCS use is associated with growth impairment in children. However, it is unclear whether any costs can be attributed to OCS-related growth impairment and whether the costs and health losses associated with OCS-related adverse effects for adults are appropriate for children.
Discussion of existing cost-effectiveness evidence
A number of key areas of uncertainty and potential limitations are identified from the previous STA. These include: (1) the relative efficacy and safety of omalizumab compared with OCSs has not been addressed; (2) markers of poor asthma control have not been adequately captured; (3) the mortality risk associated with asthma exacerbations remains unclear; (4) improvements in HRQoL with omalizumab have not been addressed in children; (5) the duration of treatment with omalizumab is unknown; and (6) adverse effects of omalizumab and/or OCSs have not been considered. The MS (2012) has attempted to address some of these issues. The relative efficacy and safety of omalizumab compared with OCSs has been examined by defining a post hoc maintenance OCS subgroup population. An exploratory analysis which incorporates the costs and health losses associated with maintenance OCS use has also been undertaken. An additional subgroup population consisting of patients who were hospitalised for asthma in the previous year was also conducted for the base-case and alternative scenarios. Systematic reviews have been conducted to identify studies used to inform the asthma-related mortality risk associated with CSS exacerbations and the HRQoL associated with omalizumab and clinically significant exacerbations. The impact of treatment duration on the cost-effectiveness results has been explored through sensitivity analysis.
A number of key uncertainties remain: (1) the mortality risk associated with asthma and the relationship between mortality, age and severity of exacerbations; (2) the HRQoL improvement with omalizumab in both adults and adolescents and children; (3) the influence of age on the cost-effectiveness results; and (4) the overall positioning of omalizumab in the stepwise therapy. The asthma-related mortality risk applied in the model may have resulted in an overestimation of asthma deaths because the mortality risk following a hospitalisation for acute severe asthma was applied to the CSS exacerbation state, whereas only about 20% of CSS exacerbations in INNOVATE involved hospital admissions. In addition, the starting age used in the model masks the distribution of different ages at treatment initiation both in the trials and in clinical practice. As age affects the asthma-related mortality risk, the impact of age at treatment initiation should be considered, either by presenting subgroups based on age or, if age is not considered an appropriate basis for subgroups, by combining estimates for different ages into a final ‘weighted’ ICER estimate.
The HRQoL improvement because of omalizumab was informed by mapping AQLQ scores collected in INNOVATE onto EQ-5D, although EQ-5D was directly collected in EXALT. The direct estimates of EQ-5D would seem a more appropriate choice for informing the HRQoL improvement with omalizumab. Patients < 12 years of age were assumed not to experience any HRQoL improvement with omalizumab up until they reached age 12 years. Without further trial evidence, it remains unclear whether or not younger children receive HRQoL benefits from omalizumab. The short duration of the trials (< 1-year of follow-up) provides limited information about the sustained effect of treatment over the long term.
The differences in ICERs for the base-case populations, subgroups and scenarios make the assessment of the overall positioning of omalizumab within the stepwise therapy difficult. For the adult and adolescent population, the ICERs ranged from £27,928 per QALY (INNOVATE hospitalisation subgroup) to £61,687 per QALY (EXALT scenario). For the children's population, the ICER was £65,100 per QALY for the hospitalisation subgroup and £80,747 per QALY for the overall IA-05 EUP population. A number of issues arise from these results. Firstly, whether it is appropriate to address the cost-effectiveness of omalizumab separately according to whether a patient cohort is older or younger than 12 years of age, given that there is no reason to believe that asthma is fundamentally different under and above this cut-off age. If age is not considered an appropriate marker for risk stratification in asthma, then the cost-effectiveness estimates for different ages should be combined into a ‘weighted’ ICER for the overall population. Secondly, the ICERs using EXALT (£61,687 per QALY) and INNOVATE (32,076 per QALY) data are substantially different; therefore, it remains unclear which scenario provides the most reliable base to inform the cost-effectiveness of omalizumab. Thirdly, whether previous hospitalisations or asthma therapy are robust indicators of asthma severity and appropriate for the definition of patient subgroups. Patients controlled on step 5 therapy may not have experienced a hospitalisation for asthma because of the asthma control conferred by maintenance OCS, whereas patients who experienced previous hospitalisations could arguably have their therapy stepped up to maintenance OCS in order to ensure asthma control. These aspects are considered in more detail as part of a new decision-analytic model developed to evaluate the cost-effectiveness of omalizumab.
Chapter 5 Assessment of cost-effectiveness: York Economic Assessment
Overview
A decision-analytic model was developed to formally assess the cost-effectiveness of omalizumab as an add-on therapy to optimised standard care compared with optimised standard care alone from the perspective of the UK NHS. Outcomes are expressed in terms of QALYs. Costs are expressed in UK pounds sterling at a 2009–10 price base. Both costs and outcomes are evaluated over a lifetime and discounted using a 3.5% annual discounted rate, according to the NICE reference case.
Decision problem and populations
The decision problem addresses the cost-effectiveness of the addition of omalizumab to optimised standard step 4 or step 5 therapy in patients whose asthma is poorly controlled by therapy. The decision problem differs depending on whether patients are at step 4 or step 5 treatment. Omalizumab treatment has the potential to improve asthma control and reduce the need for maintenance OCS use, which is associated with long-term adverse effects. The EU/UK marketing authorisation reserves omalizumab add-on therapy for patients with severe persistent allergic asthma uncontrolled at BTS/SIGN step 4. Therefore, omalizumab has a potential dual role in the stepwise management of severe persistent allergic asthma: (1) at step 4, omalizumab can act as an alternative to maintenance OCS for patients in the process of being stepped up to step 5 or, at step 5, omalizumab can act as a replacement to frequent or continuous OCS; or (2) omalizumab can be used in conjunction with OCSs, with a view to reducing the maintenance dose of OCSs in patients at step 5. The appropriate comparators depend on the positioning of omalizumab as either an addition to step 4 optimised therapy or as an alternative to step 5.
The population corresponds to patients uncontrolled at step 4, and in the process of moving up to step 5 (maintenance OCS), and patients controlled at step 5 whose asthma would be uncontrolled if they were on step 4 therapy. The population reflects the EU/UK product licence and corresponds to the patient populations enrolled in the clinical trials assessing the clinical effectiveness of omalizumab. The overall patient population corresponds to the population in INNOVATE for adults and adolescents ≥ 12 years, and IA-05 EUP for children aged 6–11 years. Given the heterogeneity in the population enrolled in the trials and the concomitant medication used at baseline, subgroup populations are defined. These subgroups stratify patients according to different indicators of asthma severity: (1) number of hospitalisations in the past year because of an exacerbation (hospitalisation subgroup); (2) maintenance OCS use (maintenance OCS subgroup); and (3) number of exacerbations in the past year (≥ 3 exacerbations subgroup, based on patients experiencing three or more exacerbations in the year prior to trial enrolment). The subgroups are presented for the base case of adults and adolescents and children separately, with the exception of the maintenance OCS subgroup, which is not presented for the children as only six patients in IA-05 EUP were on maintenance OCS at baseline.
The cost-effectiveness of omalizumab is separately examined as an addition to standard step 4 treatment compared with standard step 4 therapy alone, and in addition to standard step 5 treatment compared with standard step 5 therapy alone. The former is evaluated by examining the efficacy and safety of omalizumab add-on therapy compared with standard therapy alone based on evidence from the clinical trials, whereas the latter is evaluated using the maintenance OCS subgroup population from the trials. In the absence of trials directly comparing omalizumab with OCSs, the ‘optimal’ position of omalizumab within the overall stepwise treatment approach to asthma cannot be assessed. The steroid-sparing potential of omalizumab is considered by examining the efficacy and safety of long-term OCS use.
Model structure
The model structure is identical to that employed by the manufacturer in their submission. However, the input parameters and some of the assumptions employed, particularly for asthma-related mortality and HRQoL, differ. Unlike the manufacturer's model, where all asthma-related deaths are linked directly to a CSS exacerbation event, the model assumes that patients in the day-to-day asthma symptoms state have an elevated risk of asthma-related death at each cycle. All asthma-related deaths are assumed to occur because of a CSS exacerbation; therefore, both approaches are equivalent. However, the latter approach does not restrict the use of input parameter estimates for asthma-related mortality to only those which can be directly associated with an exacerbation episode or event as in the MS (see Natural history: mortality, below, for further details). For HRQoL, no direct measure of utility has been estimated in a paediatric population on omalizumab. However, an improvement in asthma-related QoL was observed in IA-05 EUP, although not statistically significant. Therefore, the model assumes that children aged 6–11 years experience the same improvement from omalizumab treatment as adults and adolescents based on EQ-5D data collected in EXALT. All other assumptions described in table 48, p. 154 (as employed in the MS) are also used in the independent assessment. Scenario analyses are used to explore the impact of alternative assumptions on the results.
Model input parameters
Natural history: baseline rate of exacerbations
Baseline exacerbation rates are informed by the number of CSNS and CSS exacerbations observed in the standard care arm of INNOVATE for adults and adolescents (≥ 12 years) and IA-05 EUP for children (6–11 years). The rates for children differ in the first two cycles of the model: up to week 24, the exacerbation rates correspond to those observed in the first 24-week constant treatment phase, whereas from week 24 onwards, the exacerbation rates correspond to those observed between weeks 24 and 52. Once patients reach age 12 years, the exacerbation rates in the children's population are switched to those observed in INNOVATE for adults and adolescents. Annual exacerbation rates were calculated using the number of exacerbations (CSNS, CSNS or total exacerbations) divided by the person-years of exposure.
| Patient population | CSNS exacerbations | CSS exacerbations | Total exacerbations | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | LCI | UCI | Mean | LCI | UCI | Mean | LCI | UCI | |
| Base-case populations | |||||||||
| INNOVATE all | 0.8046 | 0.6552 | 0.9881 | 0.8842 | 0.7268 | 1.0756 | 1.6888 | 1.4655 | 1.9461 |
| IA-05 EUP first 24 weeks | 1.4815 | 1.1289 | 1.9442 | 0.4558 | 0.2793 | 0.7441 | 1.9373 | 1.5275 | 2.4571 |
| IA-05 EUP from 24 weeks onwards | 1.5648 | 1.2248 | 1.9992 | 0.4645 | 0.2963 | 0.7283 | 2.0293 | 1.6365 | 2.5164 |
| Subgroup populations | |||||||||
| INNOVATE hospitalisation | 0.8706 | 0.6308 | 1.2016 | 1.2235 | 0.9323 | 1.6057 | 2.0941 | 1.7013 | 2.5777 |
| INNOVATE maintenance OCS | 0.9735 | 0.6410 | 1.4784 | 1.5044 | 1.0749 | 2.1055 | 2.4779 | 1.9069 | 3.2198 |
| IA-05 EUP hospitalisation, first 24 weeks | 1.6667 | 0.8967 | 3.0976 | 1.0000 | 0.4493 | 2.2259 | 2.6667 | 1.6337 | 4.3528 |
| IA-05 EUP hospitalisation from 24 weeks onwards | 2.1429 | 3.5545 | 1.2918 | 1.2857 | 0.6690 | 2.4711 | 3.4286 | 2.2980 | 5.1153 |
Table 63 presents the baseline annual rate of exacerbations for the base-case populations and subgroups. The baseline rates for CSNS exacerbations are greater in children than in adults and adolescents, whereas the baseline rates for CSS exacerbations are lower in children than in adults and adolescents. For both subgroup populations, the baseline exacerbation rates are greater than for the overall base-case population, particularly for the hospitalisation subgroup in children where the rate of CSS exacerbations is about double that of the overall patient population. The hospitalisation and maintenance OCS subgroups represent patients with more severe persistent asthma than those in the overall population. Therefore, the greater baseline exacerbation rates observed in these subgroups is consistent with the increased severity of the disease in these patients.
The exacerbation rates observed in patients in the 12 months prior to omalizumab treatment in APEX are used in a scenario analysis for patients aged ≥ 12 years. APEX was a UK-based retrospective observational study comparing OCS use and frequency of exacerbations in the 12 months before and 12 months after initiation with omalizumab treatment in patients with severe persistent allergic asthma. APEX reports the exacerbation rates experienced by patients who match the marketing authorisation in the UK-NHS clinical setting. However, the use of data from APEX has several limitations. Firstly, CSS exacerbations were not differentiated from CSNS exacerbations. The MS presents a scenario using data from APEX by assuming the same split observed in INNOVATE to apportion exacerbations between CSS and CSNS. Secondly, the eligibility criteria for omalizumab treatment under current NICE guidance may have resulted in the exacerbation rates in the 12 months prior to omalizumab treatment being biased upwards. The current NICE guidance restricts omalizumab to patients who required two hospital admissions or one admission and two accident and emergency (A&E) attendances for asthma in the previous 12 months. Therefore, patients may have had a perverse incentive to present at hospital or A&E more frequently than they would have otherwise.
The National Difficult Asthma Registry established by the BTS Difficult Asthma Network is a potential source of baseline exacerbation rates in the UK patient population. 137 There are currently seven UK dedicated Specialist Difficult Asthma Centres submitting data to the National Difficult Asthma Registry. Patients in this registry have difficult asthma defined as persistent symptoms and/or frequent exacerbations despite treatment at step 4/5 of the BTS/SIGN guidelines. (Academic-in-confidence information has been removed.)136 Although patient demographics, lung function, medication use and health-care contacts have been reported,67,137 rates of exacerbation have not, which precludes use of the National Difficult Asthma Registry for this appraisal.
Natural history: mortality
Asthma-related mortality
In the previous STA, asthma-related mortality was identified as one of the key drivers of the cost-effectiveness of omalizumab. Therefore, a systematic review on asthma-related mortality was conducted to identify studies reporting mortality rates as a result of severe persistent asthma, or risk factors for asthma-related death in the UK. The searches were restricted to the year 2000 onwards in order to find estimates that accurately reflect the mortality risk in current patients. The inclusion criteria were wider than the manufacturer's review, which was restricted to studies reporting mortality rates associated with an asthma exacerbation event. Appendix 18 discusses the systematic review on asthma-related mortality in detail. Two studies emerged from the review as potential sources to inform asthma-related mortality rates used in the model: those by de Vries et al. 138 and Watson et al. 106
de Vries et al. 138 used data from the General Practice Research Database (GPRD). The GPRD is a computerised database of anonymised data from patient records in GP practices, including demographic information, prescription details, hospital admissions and major outcomes. In de Vries et al. , all permanently registered patients aged ≥ 18 years who received a prescription for inhaled SABA or LABA after 1 January 1993, were followed up to the latest GPRD data collection, the patient's transfer out of the practice, or the patient's death, whichever came first. Patients with codes for COPD were excluded. Exposure was classified according to medication received in the previous 3-month period, using the BTS/SIGN guidelines of 2005. Patients were also stratified according to the latest PEF measurement, where available. Cause of death was evaluated from the free text entries at the date of death, as well as a review of the clinical record for appropriate medical codes within 21 days of the date of death. Overall, 507,966 UK patients were followed for an average of 5.0 years (median 4.2 years). Mean age was 42.7 years and 58.7% were female. Asthma-related mortality rates varied between 0.01 per 100 person-years for those on high-dose ICS only and 0.4 per 100 person-years for those on maintenance OCS. For those with PEF above median, the asthma-related mortality rate was 0.02 per 100 person-years, whereas for those with PEF below median, the rate was 0.1. The median PEF was not reported.
de Vries et al. 138 represents an important source of UK asthma-related mortality rates. However, there are a number of challenges associated with the application of the mortality data from de Vries et al. 138 to the economic model. Omalizumab is licensed for patients uncontrolled at step 4 or above of the BTS/SIGN guidelines. However, in de Vries et al. , patients are classified according to their treatment step, independent of asthma control. The patients at each treatment step are therefore a mixture of both controlled and uncontrolled patients. Consequently, the mortality rates represent the risk faced on average by controlled and uncontrolled patients at each treatment step. This does not present an issue for patients at step 5 (who can be assumed to be uncontrolled at step 4) as these patients are eligible for omalizumab regardless of control with maintenance OCS. Therefore, the asthma-related mortality rates reported for patients at step 5 can be used for the maintenance OCS subgroup. However, for the overall population and the other subgroups it is less clear whether we can use the mortality rates reported for patients at step 4 as they may not reflect the risk faced by uncontrolled patients. Patients uncontrolled at step 4 should be, or are, in the process of being stepped up to step 5, and hence the relevant mortality risk may be those of patients at step 5 rather than uncontrolled at step 4. Furthermore, the study only includes patients aged ≥ 18 years and, hence, may not be generalisable to younger patients.
The study by Watson et al. 106 reports mortality risk for patients hospitalised for asthma and acute severe asthma by age category (< 12, 12–16, 17–44 and ≥ 45 years). Although it reports mortality for patients across all age ranges, it requires a number of assumptions in order to be used in the model. Firstly, the mortality risk refers to death following a hospitalisation for asthma or acute severe asthma. Asthma deaths occurring in the community are not included, which may underestimate mortality. Secondly, patients may have been admitted to hospital because of asthma but died from other causes, such as hospital-acquired pneumonia. Thirdly, hospitalisations because of respiratory conditions other than asthma may have been misclassified under the ICD asthma codes (J45 and J46). Fourthly, the age category of ≥ 45 years may mask the influence of age on mortality as the median age of survivors (25 years) was much lower than the median age of those who died (77 years). Lastly, but most importantly, the mortality risk reported by Watson et al. is a conditional probability, that is it represents the probability of death given a hospitalisation for asthma. In order to obtain the asthma-related mortality risk, the mortality risk following hospitalisation needs to be multiplied by the risk of hospitalisation for asthma. The manufacturer applied the risks from Watson et al. 106 directly to the CSS exacerbation state, which implies that CSS exacerbations are equivalent to hospitalisations for acute severe asthma. However, given that only 20% of CSS exacerbations in INNOVATE involved hospitalisation or an ER visit, it is highly likely that the assumption that CSS exacerbations are equivalent to hospitalisations will overestimate the asthma-related mortality risk.
Table 64 compares the asthma-related mortality rates reported in de Vries et al. 138 and Watson et al. 106 In order to make this comparison, the rate of 0.04 per 100 person-years for patients at step 5 in de Vries et al. 138 was converted into a probability of death of 0.001 over 3 months (the cycle length used in the model). The mortality risk following a hospitalisation reported in Watson et al. 106 was converted into a probability of asthma death assuming that CSS exacerbation rates observed in IA-05 EUP and INNOVATE are equivalent to hospitalisation rates. The resulting probability of death over 3 months is 0.0001 for < 12 years, 0.0006 for 12–16 years, 0.0008 for 17–44 years and 0.0049 for 45 + years. The probability of death derived from de Vries et al. 138 was divided by the probability obtained from Watson et al. 106 to obtain a ratio shown in Table 64. Assuming that the mortality of patients aged ≥ 18 years and older from de Vries et al. 138 can be used for patients < 12 years (in the absence of data), the risks reported by de Vries are higher than those reported by Watson by a factor of 9.6 in children. For patients aged 12–44 years, the risks are similar across both sources. For patients aged ≥ 45 years, the risk of asthma-related death reported in de Vries et al. is about one-fifth of the risk reported in Watson et al. 106 However, given that around 20% of CSS exacerbations in INNOVATE involved hospitalisation or an ER visit, the mortality risk reported in de Vries et al. 138 is consistent with Watson et al. 106
| Age | Data from Watson et al. (2007)106 | Data from de Vries et al. (2010)137 | Ratio de Vries : Watson | ||
|---|---|---|---|---|---|
| Probability of death following J46 admission | Probability of death in 3-month cyclea | Mortality rate (per 100 person-years) | Probability of death in 3-month cycle | ||
| 0–11 years | 0.0009 | 0.0001 | NR | NR | 9.6b |
| 12–16 years | 0.0031 | 0.0006 | NR | NR | 1.6b |
| 17–44 years | 0.0038 | 0.0008 | 0.4 | 0.0010 | 1.3 |
| ≥ 45 years | 0.02478 | 0.0049 | 0.4 | 0.0010 | 0.2 |
The paper by de Vries et al. 138 has the advantage that it reports mortality rates based on GPRD data and stratifies patients by severity. Given that the asthma-related mortality rate for patients at BTS/SIGN step 5 (regular OCS) is the highest rate of death in de Vries, and it also represents patients who are uncontrolled at step 4, this rate was considered the most appropriate to be used for the base-case populations and subgroups. Watson et al. 106 is used in a sensitivity analysis to explore the sensitivity of the results to alternative assumptions on asthma mortality.
All-cause mortality
The model includes a competing risk of non-asthma related mortality. The age-dependent risk of other cause mortality was estimated using UK age- and sex-specific mortality rates based on interim life-tables for England and Wales for the years 2008–10. 115 These rates were adjusted to exclude those deaths pertaining to asthma using a cause elimination approach.
Effectiveness evidence
Treatment effectiveness has two key components: response to omalizumab treatment and reduction in number of CSNS and CSS exacerbations. The evidence for omalizumab add-on therapy compared with standard therapy alone is based on the results of INNOVATE19 and IA-05 EUP20 for the base cases of adults and adolescents and children respectively.
Responders
The proportion of patients responding to omalizumab treatment observed in the trials is used to inform the probability of being an omalizumab responder at 16 weeks. As response was only assessed at 28 weeks in INNOVATE and 52 weeks in IA-05 EUP, the response rates at these time points are used as a proxy for response at 16 weeks. This is in line with the MS.
Table 65 presents the proportion of responders to omalizumab treatment applied in the model. The response rate was greater in IA-05 EUP (74%) than in INNOVATE (56.5%) for the base-case population but similar for the hospitalisation subgroup.
| Patient population | Proportion of responders | LCI | UCI |
|---|---|---|---|
| Base case | |||
| INNOVATE: all | 0.5646 | 0.4974 | 0.6318 |
| IA-05 EUP: all | 0.7421 | 0.6741 | 0.8101 |
| Subgroups | |||
| INNOVATE: hospitalisation | 0.5663 | 0.4596 | 0.6729 |
| INNOVATE: OCS | 0.4694 | 0.3297 | 0.6091 |
| IA-05 EUP: hospitalisation | 0.5405 | 0.3800 | 0.7011 |
Evidence from observational studies suggests that the proportion of responders in clinical practice can be higher than in placebo-controlled trials. For example, the proportion of responders at 16 weeks in the APEX65 study and the PERSIST39 study was 82.0 and 82.4% respectively.
Treatment effect on exacerbations
The effect of omalizumab on exacerbations is applied as a risk ratio of the rate of exacerbations observed in the omalizumab group to the rate observed in the standard care group of the relevant trials. Treatment effect is assumed constant over time, that is the risk ratio observed in the trials is used throughout the treatment duration.
For the first 16-week cycle in the model, all patients on omalizumab experience the treatment effect observed for all patients randomised to omalizumab in the trials. At 16 weeks, omalizumab responders are identified and the cohort is separated into responders and non-responders. Omalizumab responders experience the exacerbation rates of responders in the trials. Non-responders revert back to standard therapy alone and experience the exacerbation rates of the standard care group. In the base case for children, the exacerbation rates observed in IA-05 EUP are applied up to the age of 12 years. After this age, patients are assumed to experience the exacerbation rates observed in INNOVATE.
Table 66 presents the risk ratio and corresponding 95% CI for CSNS, CSS and total CS exacerbations for the base-case populations and subgroups. Risk ratios were calculated by dividing the annual rate of exacerbations in omalizumab responders (or omalizumab all) by the annual rate of exacerbations in the standard care group. In INNOVATE the effect of omalizumab is more pronounced for CSS exacerbations than for CSNS exacerbations. The results for the INNOVATE hospitalisation subgroup are similar to those in the overall patient population. A higher reduction in exacerbations is observed in the INNOVATE maintenance OCS subgroup, although the difference is not statistically significant. In the first 24 weeks of the IA-05 EUP study, omalizumab approximately halves the rate of total exacerbations, and from week 24 onwards the treatment effect is increased further (risk ratio 0.256). A similar trend is also observed for the hospitalisation subgroup. However, the CI in the IA-05 EUP hospitalisation subgroup are much wider than the other populations, which may be because of low patient numbers and lack of power to significantly detect differences between treatment groups.
| Patient population | CSNS exacerbations | CSS exacerbations | Total CS exacerbations | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Risk ratio | LCI | UCI | Risk ratio | LCI | UCI | Risk ratio | LCI | UCI | |
| Omalizumab: responders | |||||||||
| Base case | |||||||||
| INNOVATE: all | 0.5089 | 0.3291 | 0.7869 | 0.2494 | 0.1425 | 0.4362 | 0.3730 | 0.2653 | 0.5245 |
| IA-05 EUP: first 24 weeks | 0.5078 | 0.3372 | 0.7647 | 0.5233 | 0.2517 | 1.0879 | 0.5114 | 0.3578 | 0.7311 |
| IA-05 EUP: from 24 weeks onwards | 0.2415 | 0.1511 | 0.3861 | 0.3051 | 0.1380 | 0.6743 | 0.2561 | 0.1711 | 0.3833 |
| Subgroups | |||||||||
| INNOVATE: hospitalisation | 0.5902 | 0.3137 | 1.1103 | 0.2907 | 0.1433 | 0.5900 | 0.4152 | 0.2604 | 0.6622 |
| INNOVATE: OCS | 0.4142 | 0.1569 | 1.0938 | 0.2144 | 0.0761 | 0.6042 | 0.2929 | 0.1449 | 0.5921 |
| IA-05 EUP: hospitalisation first 24 weeks | 0.3913 | 0.1422 | 1.0767 | 0.5435 | 0.1659 | 1.7808 | 0.4484 | 0.2081 | 0.9661 |
| IA-05 EUP: hospitalisation from 24 weeks onwards | 0.2593 | 0.1006 | 0.6682 | 0.1440 | 0.0311 | 0.6666 | 0.2160 | 0.0971 | 0.4809 |
| Omalizumab: all | |||||||||
| Base case | |||||||||
| INNOVATE: all | 1.0274 | 0.7696 | 1.3717 | 0.4926 | 0.3500 | 0.6933 | 0.7474 | 0.6015 | 0.9287 |
| IA-05 EUP: first 24 weeks | 0.7081 | 0.4981 | 1.0067 | 0.6874 | 0.3632 | 1.3011 | 0.7032 | 0.5168 | 0.9570 |
| IA-05 EUP: from 24 weeks onwards | 0.3807 | 0.2635 | 0.5501 | 0.4527 | 0.2376 | 0.8625 | 0.3972 | 0.2886 | 0.5466 |
| Subgroups | |||||||||
| INNOVATE: hospitalisation | 1.0022 | 0.6391 | 1.5714 | 0.5485 | 0.3500 | 0.8597 | 0.7371 | 0.5383 | 1.0094 |
| INNOVATE: OCS | 1.1284 | 0.6484 | 1.9640 | 0.3525 | 0.1892 | 0.6568 | 0.6573 | 0.4418 | 0.9781 |
| IA-05 EUP: hospitalisation first 24 weeks | 0.8772 | 0.4213 | 1.8264 | 0.8772 | 0.3403 | 2.2609 | 0.8772 | 0.4912 | 1.5663 |
| IA-05 EUP hospitalisation: from 24 weeks onwards | 0.3987 | 0.1991 | 0.7983 | 0.3908 | 0.1588 | 0.9619 | 0.3957 | 0.2283 | 0.6858 |
INNOVATE is chosen for the base-case population of adults and adolescents as it is the only double-blind RCT in which the GETE has been used to assess response to treatment and where a responder analysis is available. Treatment effectiveness by response status was available from EXALT; however, the open-label design of EXALT makes the trial more susceptible to a number of potential biases. Knowing the patient's treatment allocation may have affected the investigator's assessment of response to omalizumab and the patient's reporting of exacerbations. Nevertheless, as EXALT provides a plausible alternative estimate of treatment effect, an alternative option would be to pool the results across EXALT and INNOVATE in a meta-analysis and use the pooled estimate of treatment effect in the model. However, as discussed in the section Quantity and quality of evidence, there is evidence of clinical heterogeneity between EXALT and INNOVATE; in addition to the different trial design, patients in INNOVATE appear to have received more concomitant medication than those in EXALT. A scenario analysis is used to explore the sensitivity of the cost-effectiveness results to different efficacy estimates by using the treatment effect observed in EXALT and the pooled estimate from EXALT and INNOVATE.
Long-term effectiveness
The trials evaluating the clinical effectiveness of omalizumab had a relatively short follow-up. INNOVATE had a follow-up of 28 weeks, EXALT of 32 weeks and IA-05 EUP of 52 weeks. These short-term effectiveness estimates are extrapolated over a longer period of treatment duration.
Treatment duration
Treatment duration is assumed to be 10 years, in line with the MS and considered appropriate by our clinical advisors. As omalizumab is a long-term treatment for a chronic condition, lifetime treatment duration is explored in a scenario analysis.
Persistence of response
Persistence of response refers to whether omalizumab responders continue to respond to treatment over the entire treatment duration of 10 years. For the base-case analysis, response is assumed to remain constant over the treatment duration. However, there is some evidence suggesting that response may decline over time. In EXALT, 8.7% of responders at 16 weeks were considered non-responders at 32 weeks. In the observational study of PERSIST, 82.4% of the ITT population (n = 153) were considered responders at 16 weeks, whereas only 72.3% of the ITT population (n = 130) were considered responders at 52 weeks. 39 If patients experience declining response to omalizumab, they may either withdraw from treatment or continue to remain on treatment but not experience the benefits of therapy. In a worst case scenario, patients would continue to receive omalizumab but no longer respond to the treatment, which could arise if patients are not continually assessed after the 16-week responder assessment using the GETE. In this case, these patients would accrue the costs of therapy but not the health benefits of omalizumab.
Withdrawals from treatment
The base-case analysis assumes that there are no withdrawals from treatment after the 16-week responder assessment. However, in clinical practice patients may discontinue omalizumab for a variety of reasons: decrease in perceived effectiveness, adverse effects of treatment, or other compliance issues unrelated to the treatment itself, for example difficulty in attending the clinic for administration of omalizumab.
Results of assessment of safety of omalizumab discusses the evidence on the safety of omalizumab treatment. Rates of adverse events in the RCT are generally low and similar between treatment groups (omalizumab add-on therapy and standard therapy alone), including serious adverse events such as death and anaphylaxis. Therefore, no adverse events are included in the model. From the section Evidence of long-term efficacy and persistence of response, six observational studies provided data on withdrawals from treatment. The proportion of patients on omalizumab who discontinue treatment ranged from 8.5% in Cazzola et al. 40 to 34% in Brusselle et al. 39 Only one patient in Cazzolla et al. 40 (n = 142) withdrew as a result of adverse events compared with 12% (19/158) of patients in Brusselle et al. 39 A sensitivity analysis is used to examine the impact of treatment withdrawal on the cost-effectiveness results of omalizumab.
Resource utilisation and costs
Resource use can be split into three components: (1) resource use relating to omalizumab therapy; (2) standard care (standard therapy and routine secondary care visits); and (3) CSNS and CSS exacerbations. Resource use is based on the resources consumed in INNOVATE and IA-05 EUP for the base case of adults and adolescents and children, respectively, and primarily drawn from the MS. Unit costs are based on the year 2009–10.
Omalizumab therapy costs
Costs associated with omalizumab therapy include the costs of the drug itself and the costs of administration and monitoring.
Omalizumab is administered as a subcutaneous injection every 2–4 weeks and the exact dose depends on the patient's serum IgE and weight. It is available as 75- and 150-mg prefilled syringes at prices of £128.07 and £256.15 respectively. 22 The unit price of the 75-mg syringe was used to estimate the average omalizumab cost per patient. Similar to the MS, the model uses an average annual cost of omalizumab per patient. The average annual cost of omalizumab was based on the distribution of doses used by patients in the trials. 138 Data on the dosage distribution were obtained from the MS. For adults and adolescents, the base case uses the dose distribution from INNOVATE, whereas for children the dose distribution corresponds to IA-05.
In addition to the acquisition costs of omalizumab, the costs associated with omalizumab therapy include administration and monitoring for anaphylaxis. The administration and monitoring costs follow the methods and assumptions used in the MS. Administration is assumed to take 10 minutes of specialist asthma nurse time at £47 per hour. 115 For the first three administrations, monitoring is assumed to take 2 hours at a cost of 15 minutes of nurse time at £47 per hour. From the fourth administration up to the 16-week responder assessment, monitoring takes 1 hour. From 16 weeks onwards, no monitoring costs are incurred.
Table 67 presents the costs of omalizumab therapy used in the model for the base-case analysis. The average cost per patient using INNOVATE is similar to IA-05 EUP.
| Patient population | Average cost of omalizumab | Administration and monitoring costs | |
|---|---|---|---|
| First year | Thereafter | ||
| Base case | |||
| INNOVATE: all | £8056 | £260 | £146 |
| IA-05 EUP | £8455 | £268 | £151 |
Patients on omalizumab are assumed to have an extra appointment to initiate omalizumab therapy; £245 for adults and adolescents from NHS reference costs 2009–10 (service code 340 Respiratory Medicine, Consultant Led: First attendance multi-professional non-admitted face to face),16 and £247 for children (service code 258 Paediatric Respiratory Medicine, Consultant Led: First attendance multi-professional non-admitted face to face16). The 16-week assessment of response is assumed to take place in one of the routine appointments. This is slightly different from the MS, where it is assumed that the 16-week responder assessment requires an additional follow-up appointment.
Standard care costs: standard therapy and routine secondary care
The costs associated with standard care consist of the costs of standard therapy itself and the costs of routine secondary care. The costs used in the MS were used in the model (Table 68). 15 As these costs are incurred by both treatment groups, omalizumab add-on therapy to standard care and standard care alone, they will not influence the cost-effectiveness results.
Costs of exacerbations
The costs of exacerbations are based on data from the trials as reported in the MS. 15 Table 69 presents the costs of CSNS and CSS exacerbations for the base-case populations and subgroups. For adults and adolescents, CSS exacerbations have a cost of £124.32 and CSNS exacerbations of £87.70. For children, the cost of CSS exacerbations is equal to the cost of CSNS exacerbations because it was not possible to separate resource use by type of exacerbation in IA-05 EUP. Therefore, a single cost of £213.89 is used for any exacerbation. The cost of exacerbations for the maintenance OCS subgroup is similar to the overall INNOVATE population, whereas the cost for the INNOVATE hospitalisation subgroup is greater than the overall population and the maintenance OCS subgroup.
| Patient population | Cost of exacerbations | |
|---|---|---|
| CSNS | CSS | |
| Base case | ||
| INNOVATE: all | £87.70 | £124.32 |
| IA-05 EUP | £213.89a | £213.89a |
| Subgroups | ||
| INNOVATE: hospitalisation | £154.70 | £178.87 |
| INNOVATE: OCS | £86.51 | £136.04 |
| IA-05 EUP: hospitalisation | £213.89b | £213.89b |
It should be noted that data on resource use was only reported for 59% of the exacerbations in INNOVATE. It is unclear whether the other 41% of exacerbations did not involve any health-care resource use or whether the data was inefficiently reported. Considering that the average cost of a hospitalisation for asthma was estimated in the MS at £785 (weighted average of all asthma inpatient Healthcare Resource Group codes DZ15A-f and PA12Z)16 and that the average cost of a CS exacerbation in APEX is £304.51 (as reported in the MS15), it is possible that the costs of exacerbations have been underestimated. A sensitivity analysis is used to explore the impact of higher exacerbation costs on the cost-effectiveness of omalizumab.
Health-related quality of life
Health-related quality of life is expressed in terms of QALYs by quality-adjusting the period of time for which the average patient is alive within the model using an appropriate utility value. HRQoL associated with day-to-day asthma symptoms on standard therapy and omalizumab add-on therapy, and HRQoL associated with exacerbations is considered. In the previous STA, HRQoL was identified as a key driver of cost-effectiveness of omalizumab. Therefore, a systematic review was conducted to identify utility values for day-to-day asthma symptoms and clinically significant exacerbations. Only studies measuring EQ-5D were included; however, as EQ-5D is not commonly used in children, any utility measurement was included in the review for children. Appendix 18 provides full details of the systematic review and the studies identified.
Day-to-day symptoms
Health-related quality of life for day-to-day asthma symptoms for omalizumab compared with standard therapy is informed by EQ-5D data collected at 32 weeks in EXALT. EXALT is the only RCT to directly measure the utility of patients using the EQ-5D. 15 The manufacturer used indirect data of INNOVATE by mapping AQLQ scores onto EQ-5D in their base-case analysis. The systematic review identified a prospective cohort study, Brusselle et al. ,39 which measured EQ-5D directly in patients at baseline and 52 weeks. Responders to omalizumab reported an improvement in utility of 0.15 (standard deviation, 0.24) from baseline to 52 weeks. However, the observational design of this study may have introduced potential bias. Therefore, the direct EQ-5D data collected in EXALT is the preferred estimate to inform the base-case analysis.
No utility index score could be derived from the PAQLQ in children; however, there is evidence of an improvement in asthma symptoms for omalizumab compared with standard therapy. 89 Therefore, an assumption is made whereby children (aged 6–11 years) experience the same HRQoL improvements with omalizumab compared with standard therapy as adults and adolescents.
Table 70 presents the utility values applied in the model for the base-case populations and subgroups. The difference in EQ-5D between omalizumab responders and patients on standard care in the overall EXALT population was 0.048, whereas the difference in the subgroup populations was considerably greater at 0.13 for the hospitalisation subgroup and 0.105 for the maintenance OCS subgroup. 15 These results suggest that more severe patient populations experience a greater HRQoL improvement with omalizumab.
| Patient population | Data source | Day-to-day asthma symptoms | Difference | |
|---|---|---|---|---|
| Standard care | Omalizumab responders | |||
| Base case | ||||
| Adult and adolescent | EXALT | 0.719 (0.026) | 0.767 (0.02) | 0.048 |
| Children | EXALTa | 0.719 (0.026) | 0.767 (0.02) | 0.048 |
| Subgroups | ||||
| Adult and adolescent: hospitalisation | EXALT: hospitalisation | 0.631 (0.061) | 0.761 (0.046) | 0.130 |
| Adult and adolescent: maintenance OCS | EXALT: maintenance OCS | 0.686 (0.07) | 0.791 (0.032) | 0.105 |
| Children: hospitalisation | EXALTa: hospitalisation | 0.631 (0.061) | 0.761 (0.046) | 0.130 |
Exacerbations
The systematic review identified two studies reporting utility values associated with exacerbations, Lloyd et al. 104 and Steuten et al. 140 Given that the study by Lloyd et al. 104 was conducted in UK patients (Steuten et al. was based in the Netherlands), it is used to inform the utility estimates for CSNS and CSS exacerbations in the model. Lloyd et al. 104 collected EQ-5D data at baseline and 4-week follow-up for 112 patients with moderate to severe asthma (step 4 or 5 of BTS/SIGN guideline). This section discusses Lloyd et al. 104 in detail. The difference in utility between follow-up and baseline is taken as a decrement in HRQoL because of an exacerbation. The manufacturer uses the absolute HRQoL value at end of follow-up for an exacerbation requiring OCS use and asthma-related hospitalisation reported in Lloyd et al. (2007) instead of the difference in HRQoL between baseline and follow-up. Table 71 presents the decrements in EQ-5D for CSNS and CSS exacerbations. The loss in utility because of an exacerbation is applied in the model for duration of 4 weeks (28 days). However, it should be noted that the impact of an exacerbation on the HRQoL score may not be fully captured if the exacerbation occurred several days or weeks before the data collection time point.
| Patient population | Decrement as a result of CS exacerbations | Duration in weeks | |
|---|---|---|---|
| CSNS | CSS | Used in the model | |
| Base-case and subgroup populations | |||
| Adults and adolescents | −0.10 | −0.20 | 4 |
| Children | −0.10 | −0.20 | 4 |
Furthermore, the definitions of CSNS and CSS exacerbations used in the model do not link directly to the definitions used by Lloyd et al. 104 For adults and adolescents, a CS exacerbation was defined in INNOVATE as an episode of worsening of asthma symptoms requiring treatment with systemic corticosteroids, and a CSS exacerbation was one in which PEF or FEV1 was < 60% of personal best. Therefore, a CSNS exacerbation was defined as PEF or FEV1 > 60% of personal best. For children, a CS exacerbation in IA-05 EUP was defined similar to INNOVATE as worsening of asthma symptoms judged clinically by the investigator requiring doubling of baseline ICS dose and/or treatment with systemic corticosteroids for at least 3 days. A CSS exacerbation was one in which PEF or FEV1 were < 60% of personal best. Lloyd et al. 104 classified exacerbations according to whether or not the patient was receiving OCSs or whether or not the exacerbation involved hospitalisation. Only 20% of exacerbations in INNOVATE required hospitalisation or a visit to the A&E. Therefore, the exacerbations requiring hospitalisation in Lloyd et al. 104 may be more severe than the CSS exacerbations in INNOVATE. This implies that the utility loss from Lloyd et al. 104 may overestimate the HRQoL loss because of an exacerbation. A sensitivity analysis will examine the impact of the utility decrement applied to exacerbations on the cost-effectiveness of omalizumab.
Adverse effects because of maintenance oral corticosteroids
A systematic review of economic evaluations comparing steroids against any comparator for the treatment of asthma was conducted to identify studies quantifying the costs and health losses associated with long-term OCS use. Full details of the search strategies and the systematic review are presented in Appendices 1 and 18 respectively. Briefly, 830 records were identified, of which 88 full-text records were assessed for eligibility. Only one study was included in the systematic review: Fuhlbrigge et al. 41 which evaluated the increased costs and health losses associated with fracture following long-term use of ICSs. However, Fuhlbrigge et al. 141 is of limited relevance for the economic analysis as it focuses on a patient population of mild to moderate asthma in women, examines the consequences of ICSs instead of OCSs and considers the effect of ICSs on bone mineral density and risk of fracture only. As discussed in Adverse and serious adverse events of omalizumab from existing summaries, a comprehensive search was also undertaken to identify previously published systematic reviews on adverse effects of OCSs. The most useful review identified was that of Manson et al. ,84 which examined the cumulative burden of OCS adverse effects.
A scenario incorporating the adverse effects of OCSs use follows the same approach taken by the manufacturer based on Manson et al. The patient population considered is the maintenance OCS subgroup. The proportion of omalizumab responders who discontinue maintenance OCS is assumed to be 41.9% based on EXALT. Table 72 summarises the assumptions used for the scenario analysis and compares them with the manufacturer's ‘OCS-sparing’ analysis. In general, the same assumptions as the manufacturer are employed but it is assumed that patients return to maintenance OCS once treatment with omalizumab is discontinued. As discussed in the section Incorporation of long-term consequences of oral corticosteroids, these assumptions may favour the results towards omalizumab.
| Manufacturer's ‘OCS-sparing’ analysis | Independent assessment scenario analysis |
|---|---|
|
|
The excess relative risk associated with OCS use is considered for the following disease outcomes: type 2 diabetes, myocardial infarction, osteoporotic fracture, glaucoma, ulcer, cataracts and stroke. For each disease outcome, the aggregate QoL burden is based on the WHO global burden of disease,131 whereas the aggregate cost burden is based on average annual costs of each outcome weighted by its excess relative risk plus costs of OCS drugs. The acquisition cost of OCSs is based on the average prednisolone dose recorded at baseline in EXALT; 13.1 mg of prednisolone per day at £99.45 per patient per year. 68 Alternative scenarios are used to assess the impact of OCS-related adverse effects.
Analytic methods
Base-case analysis
The cost-effectiveness of omalizumab is evaluated by comparing the additional costs of omalizumab add-on therapy to its additional benefits in terms of improvement in HRQoL and reduction in exacerbations compared with standard care alone. The costs and health outcomes of both responders and non-responders to omalizumab therapy are included in the total costs and outcomes of treatment.
The cost-effectiveness of omalizumab is estimated using conventional decision rules and reported as an ICER. 142 The ICER represents the additional cost of omalizumab over standard care for each additional QALY gained. All results, unless otherwise stated, are presented using probabilistic analysis. The model is probabilistic in that input parameters are entered as probability distributions to reflect uncertainty in the mean estimates. 143 Monte Carlo simulation is used to propagate the uncertainty in the input parameters over 10,000 draws. Mean costs and QALYs are obtained by averaging over the 10,000 simulations. Cost-effectiveness acceptability curves (CEAC) are used to represent the probability that omalizumab is a more cost-effective use of NHS resources than standard care over a range of threshold values, which represent the maximum willingness to pay for an additional QALY gained with omalizumab. 143
Two base-case populations are presented: (1) adults and adolescents (age ≥ 12 years) and (2) children aged 6–11 years. Table 73 summarises the assumptions used for the base-case populations and compares them with the manufacturers. Appendix 18 presents the parameter inputs and respective sources for the base-case and subgroup populations.
| Parameter | York independent assessment | MS |
|---|---|---|
| Overview | ||
| Base case | Adults and adolescents (≥ 12 years): INNOVATE | Same |
| Children (< 12 years): IA-05 EUP | ||
| Alternative base case | MS presented two alternative scenarios based on the EXALT trial and on the APEX study | |
| Subgroups | Hospitalisation, maintenance OCS, ≥ 3 exacerbations at baseline, < 3 exacerbations at baseline | MS presents hospitalisation and maintenance OCS subgroups for base case and scenarios |
| Age at model entry | Adults and adolescents (≥ 12 years): 43 years of age | Same |
| Children (< 12 years): 9 years of age | ||
| Effect of age at model entry evaluated in the sensitivity analysis | ||
| Treatment duration | Assumed 10 years | Same |
| Cycle length | 3 months | Same |
| Time horizon | Lifetime (age 100 years) | Same |
| Natural history | ||
| Baseline rate of exacerbations | Assumption: the exacerbation rates observed in the clinical trials are constant throughout time and can be annualised
|
Same |
| Scenarios use rates observed in each study (EXALT and APEX) | ||
| Any-cause mortality | UK life-tables based on years 2008–10 adjusted by asthma death (based on year 2010) | UK life-tables based on years 2007–09 unadjusted for asthma deaths |
| Asthma-related mortality | Base case: de Vries et al. (2010)138 death because of asthma using GPRD data | Assumption: asthma-related death can only occur following a severe exacerbation |
| Sensitivity analysis: | Base case: Watson et al. (2007)105 mortality from any cause following hospitalisation for acute severe asthma | |
| Sensitivity analysis: | ||
| Clinical effectiveness | ||
| Proportion of responders | Proportion of responders observed in the clinical trials:
|
Same |
| Scenarios use proportion of responders observed in each study at 16 weeks (EXALT and APEX) | ||
| Persistence of response | Treatment effect and proportion of responders is assumed constant throughout treatment duration | Same |
| Omalizumab effect on exacerbations | Omalizumab reduces the rate of exacerbations as observed in the clinical trials
|
Same |
| Scenarios use exacerbation rates observed in each study (EXALT and APEX) | ||
| Adverse events | Not considered | Same |
| Withdrawals from treatment | Not considered in the base case | Same |
| Tested in the sensitivity analysis | ||
| Resource use and costs | ||
| Costs associated with omalizumab add-on therapy | Costs of omalizumab estimated using the dose distribution observed in:
|
Same |
| Initiation of omalizumab requires one initiation appointment with respiratory consultant | Scenarios use dosing distributions observed in each study (EXALT and APEX) | |
| Administration by specialist asthma nurse assumed to take 10 minutes | Initiation of omalizumab AND assessment of response require additional appointments with respiratory consultants | |
Monitoring by specialist asthma nurse assumed to take 15 minutes per hour of monitoring. The duration of monitoring varies as follows:
|
||
| Costs associated with standard care | Costs of standard care include costs of standard therapy and the costs of routine secondary visits
|
Same |
| Scenarios use standard therapy observed in each study (EXALT and APEX) | ||
| Costs of exacerbations | Resource use due to exacerbations obtained from the INNOVATE and IA-05 EUP trials
|
Same |
| Unit costs used in the MS confirmed and used to cost exacerbations | Scenarios use resource use observed in each study (EXALT and APEX) | |
| HRQoL | ||
| Day-to-day symptoms | Based on the EQ-5D data collected during the EXALT trial | Same |
Base case uses INNOVATE data:
|
||
| Exacerbations | Decrement from baseline reported by Lloyd et al. (2007)103 in:
|
Same |
| HRQoL observed at follow-up in patients who experienced exacerbations was subtracted to the HRQoL of day-to-day symptoms on standard care to obtain HRQoL decrement associated with exacerbations | ||
| Duration of exacerbations | HRQoL loss associated with an exacerbation assumed to last 4 weeks, corresponding to the follow-up period of Lloyd et al. (2007)104 | Average duration of an exacerbation as observed in the clinical trials |
| Children | Children experience the same HRQoL improvement from omalizumab therapy as adults and adolescents | No |
| Assumed no improvement as a result of omalizumab until 12 years of age | ||
Subgroup analysis
The aim of the subgroup analysis is to identify patient subgroups where the intervention is potentially more or less cost-effective than in the overall patient population. Subgroup analysis is presented for two populations: (1) hospitalisation subgroup for adults and adolescents and children, and (2) maintenance OCSs for adults and adolescents (data for children were not available from IA-05 EUP). As discussed in the section Summary and critique of manufacturer's de novo submission (2012), Overview, the hospitalisation subgroup consists of patients who were hospitalised in the year prior to trial entry, corresponding to 38.4% of the total INNOVATE population and 17% of IA-05 EUP. The maintenance OCS subgroup consists of patients who were receiving maintenance OCS at trial baseline, corresponding to 19.8% of the INNOVATE population. The results for these subgroups are presented alongside the base-case populations.
In addition, one further subgroup was identified according to baseline number of exacerbations at trial entry. Data on number of CSNS and CSS exacerbations and HRQoL were requested from the manufacturer for patients who experienced three or more exacerbations in the year before commencing the trial (≥ 3 exacerbations) from INNOVATE, EXALT and IA-05 EUP. The results for the additional subgroup (≥ 3 exacerbations) are presented in the section Additional subgroup analysis: ≥ 3 exacerbations at baseline.
Scenario analysis
A number of alternative scenarios are considered in which the assumptions used as part of the base-case results are varied. These analyses are undertaken to assess the robustness of the base-case results to variation in the sources of data used to populate the model and alternative assumptions.
Table 74 summarises the alternative scenarios considered. For each element, the position in the base-case analysis is outlined, alongside the alternative assumption applied. The cost-effectiveness of omalizumab is considered under each of the scenarios for the base-case and subgroup populations.
| Scenario | Element | Position in base-case analysis | Variation in scenario analysis |
|---|---|---|---|
| 1 | Baseline exacerbation rates | Baseline rates from INNOVATE for adults and adolescents | Baseline rates from APEX for adults and adolescents |
| 2 | Treatment effectiveness | Effectiveness estimates from INNOVATE for adults and adolescents | Effectiveness estimates from EXALT |
| 3 | Pooled effectiveness estimate from INNOVATE and EXALT | ||
| 4 | Asthma-related mortality | Data from de Vries et al. (2010)138 | Data from Watson et al. (2007)106 |
| 5 | HRQoL in day-to-day asthma symptoms state | EQ-5D directly collected in EXALT at 32 weeks | EQ-5D mapped from AQLQ collected in INNOVATE at 28 weeks |
| 6 | Patients < 12 years of age experience HRQoL improvement from omalizumab therapy equivalent to patients ≥ 12 years | Patient < 12 years experience no HRQoL improvement from omalizumab therapy | |
| 7 | Treatment duration | 10 years treatment duration | Lifetime treatment duration |
| 8 | Costs of omalizumab | Based on the dose distribution in INNOVATE, corresponding to the standard dosing table | Based on the dose distribution for the eligible patients in the UK Difficult Asthma Registry, corresponding to the expanded dosing table135 |
| 9 | Adverse effects of OCSs | Adverse effects of OCSs not considered | Incorporates the health and cost consequences from adverse effects of OCSs in the maintenance OCS subgroup |
Model validation
The structure and assumptions of the model largely follow those employed in the MS, the previous STA and published peer-reviewed cost-effectiveness studies of omalizumab. The model was developed in EXCEL by one analyst and independently checked by another. As part of an overall quality assurance process, the internal validity of the model was assessed by extensively exploring logical consistency in the model results. In addition, all parameter inputs used in the manufacturer's base-case analysis were applied in the model to replicate the results of the manufacturer.
Results of independent economic assessment
Results of the base-case analysis
Table 75 presents the cost-effectiveness results for the base-case populations. For both populations, omalizumab add-on therapy is more costly but also more effective than standard therapy alone. The ICER for adults and adolescents (≥ 12 years of age) is £83,822 per QALY gained, whereas the ICER for children aged 6–11 years is £78,009 per QALY gained. The probability that omalizumab is cost-effective at a threshold of £30,000 per QALY is zero in both populations.
| Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|
| Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 33,218 | 13.66 | |
| Omalizumab | 72,938 | 14.13 | 83,822 |
| Children (6–11 years of age) – age at model entry: 9 years | |||
| Standard care | 40,218 | 16.72 | |
| Omalizumab | 92,497 | 17.39 | 78,009 |
Table 76 presents the cost-effectiveness results for the hospitalisation and maintenance OCS subgroups. Omalizumab add-on therapy is more costly and more effective than standard therapy but the ICER for the subgroup populations is considerably lower than the ICER for the overall population. For the hospitalisation subgroup, the ICER of £46,431 per additional QALY for adults and adolescents and £44,142 per QALY for children is about half the ICER of the overall population. The ICER for the maintenance OCS subgroup in adults and adolescents of £50,181 per additional QALY is slightly higher than the hospitalisation subgroup but considerably lower than the overall population. The probability that omalizumab is cost-effective at a threshold of £30,000 per QALY is zero in all subgroups.
| Subgroup | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Hospitalisation | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 36,449 | 11.83 | ||
| Omalizumab | 75,826 | 12.68 | 46,431 | |
| Children (6–11 years of age) – age at model entry: 9 years | ||||
| Standard care | 44,718 | 14.45 | ||
| Omalizumab | 83,145 | 15.32 | 44,142 | |
| Maintenance OCS | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 35,902 | 12.78 | ||
| Omalizumab | 68,995 | 13.44 | 50,181 | |
The degree of decision uncertainty is illustrated in Figures 4 and 5, which present the CEAC for the base-case and subgroup populations respectively. The probability that omalizumab is cost-effective in the base-case populations remains close to zero up to a threshold of £70,000 per QALY. For the hospitalisation and maintenance OCS subgroups, the probability that omalizumab is cost-effective starts to depart from zero at a threshold around £35,000. At very high thresholds of > £70,000 per QALY, the probability that omalizumab is cost-effective is > 0.9 for all subgroup populations.
FIGURE 4.
Cost-effectiveness acceptability curves for base-case populations.
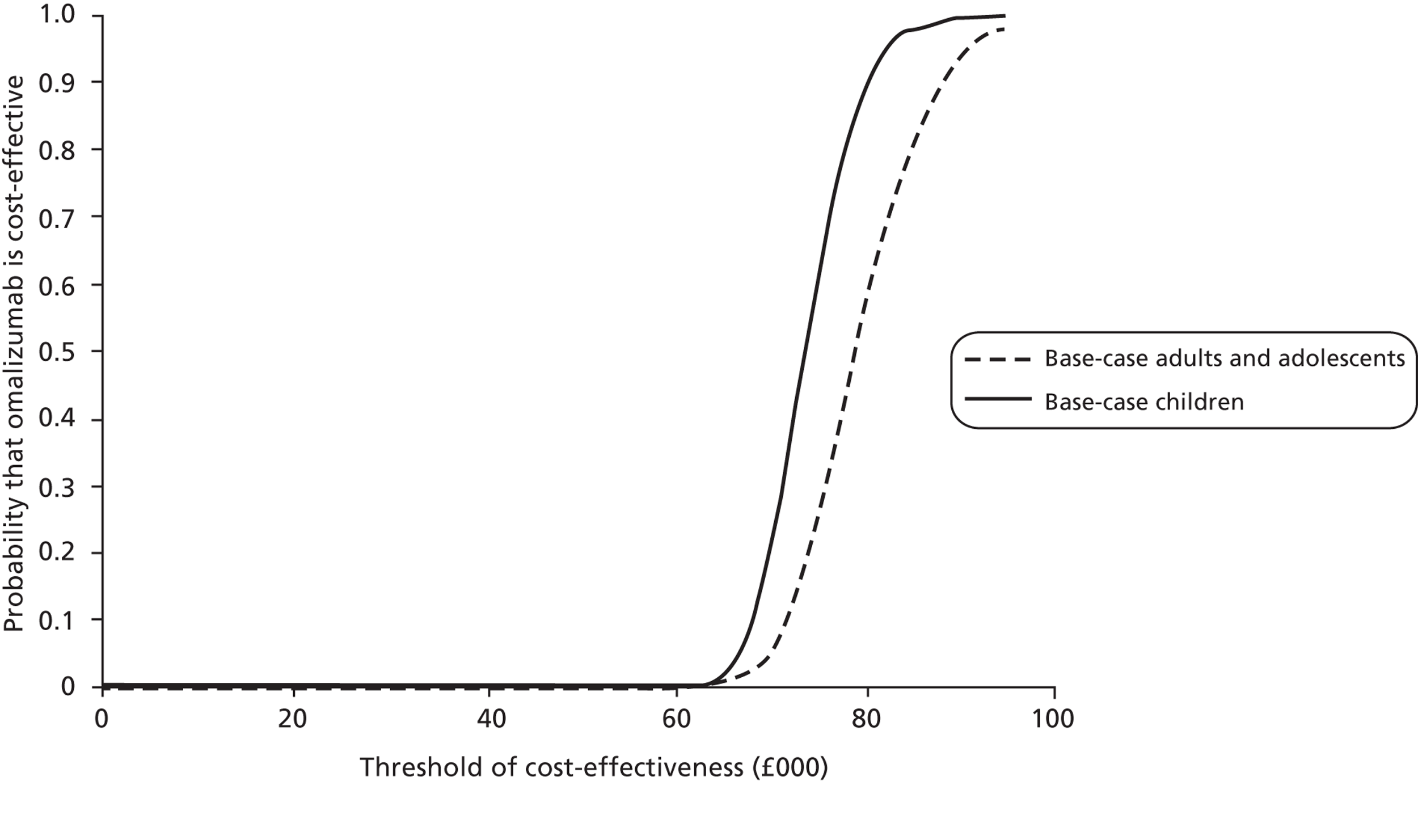
FIGURE 5.
Cost-effectiveness acceptability curves for subgroup populations: hospitalisation and maintenance OCS.
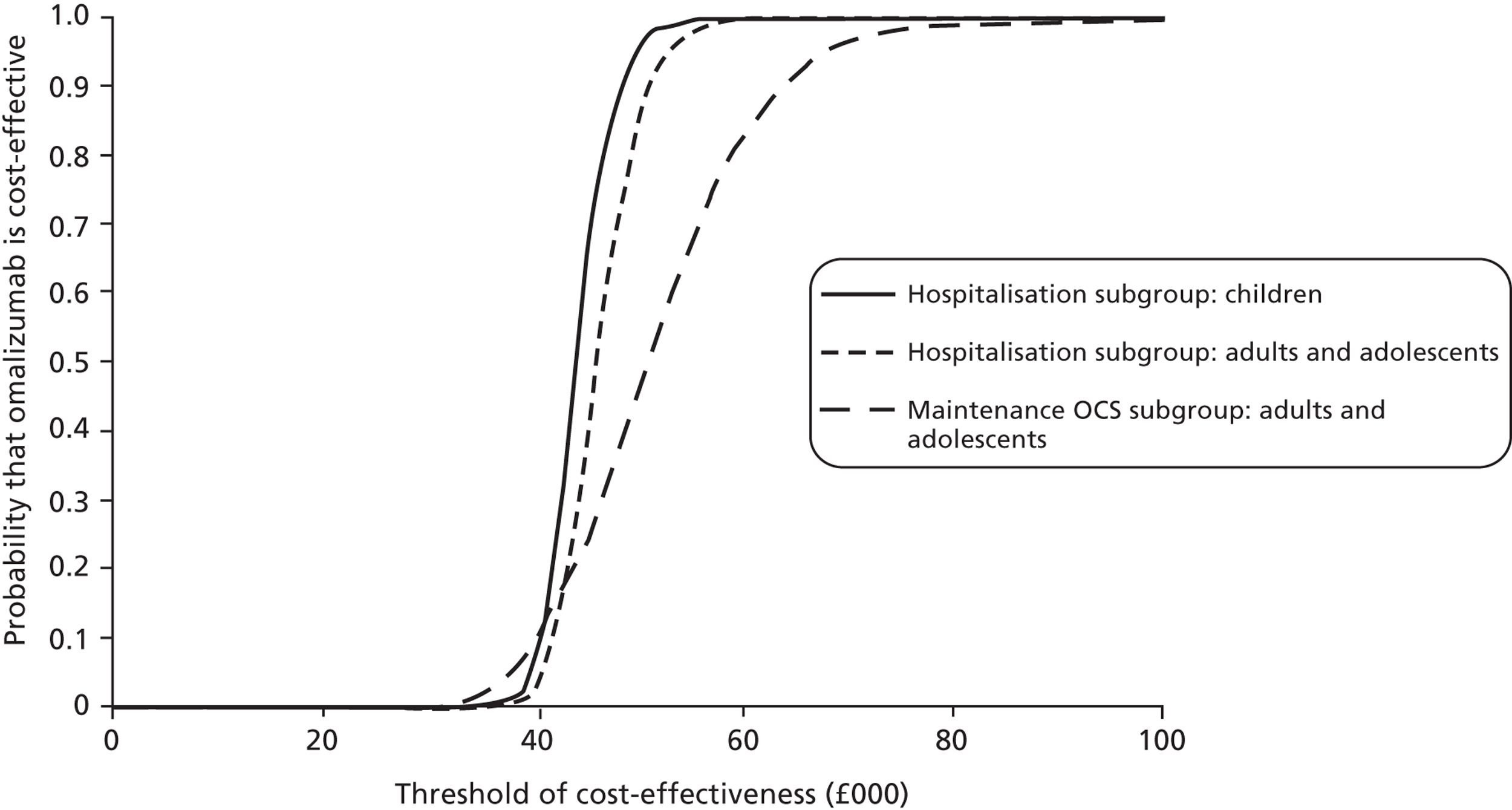
The cost-effectiveness results for the base-case and subgroup populations are different from the manufacturer's results. The manufacturer's probabilistic ICER for adults and adolescents is £33,268 per QALY gained, which is less than half the ICER of £83,822 above. For children, the manufacturer's probabilistic ICER is £88,998 per QALY gained, which is about 14% greater than the ICER of £78,009 above. For the hospitalisation subgroup, the manufacturer reported an ICER of £27,928 for adults and adolescents and £65,100 for children, whereas the ICER above is in the region of £45,000 for both age groups. The ICER for the maintenance OCS subgroup is £26,320 in the MS compared with £50,181 above.
In order to understand the reasons for the differences in results between the MS and the independent economic assessment, the following section uses a series of alternative scenarios to compare and contrast the different assumptions and parameter inputs used in both models. In addition, sensitivity analysis over a range of alternative parameter values is used to explore any remaining areas of uncertainty.
Impact on the incremental cost-effectiveness ratio of alternative scenarios
Baseline exacerbation rates
Scenario 1: using baseline exacerbation rates from APEX65
The MS presented an alternative base-case analysis using data from APEX to inform the baseline exacerbation rates, treatment effectiveness and costs. APEX is an observational before-and-after study; therefore, the estimate of treatment effectiveness is likely to be subject to potential bias. However, APEX provides an alternative source for baseline rates of exacerbation in UK clinical practice.
Table 77 compares the exacerbation rates observed in the standard care arm of INNOVATE19 with those observed in APEX in the 12-month period prior to treatment with omalizumab for the base-case and subgroup populations. The exacerbation rates from APEX are considerably higher than the baseline rates from INNOVATE. The data suggest that patients in UK clinical practice may experience exacerbations more frequently than observed in a clinical trial. Patients enrolled in INNOVATE had their therapy optimised before the trial commenced, whereas some patients in clinical practice may not be fully optimised before receiving omalizumab. In addition, patients in clinical trials such as INNOVATE have regular contact with health-care professionals, which can increase compliance with therapy.
| Patient population | CSNS exacerbations | CSS exacerbations | Total exacerbations | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | LCI | UCI | Mean | LCI | UCI | Mean | LCI | UCI | |
| Base-case and patient subgroups: INNOVATE | |||||||||
| Overall population | 0.8046 | 0.6552 | 0.9881 | 0.8842 | 0.7268 | 1.0756 | 1.6888 | 1.4655 | 1.9461 |
| Hospitalisation | 0.8706 | 0.6308 | 1.2016 | 1.2235 | 0.9323 | 1.6057 | 2.0941 | 1.7013 | 2.5777 |
| Maintenance OCS | 0.9735 | 0.6410 | 1.4784 | 1.5044 | 1.0749 | 2.1055 | 2.4779 | 1.9069 | 3.2198 |
| Scenario 1: APEX | |||||||||
| Overall population | 1.7500 | 1.5412 | 1.9871 | 1.9191 | 1.6999 | 2.1667 | 3.6691 | 3.3609 | 4.0056 |
| Hospitalisation | 1.4074 | 1.1714 | 1.6910 | 1.9877 | 1.7032 | 2.3197 | 3.3951 | 3.0166 | 3.8210 |
| Maintenance OCS | 1.4556 | 1.2265 | 1.7274 | 2.2444 | 1.9553 | 2.5763 | 3.7000 | 3.3232 | 4.1195 |
Table 78 presents the cost-effectiveness results using the exacerbation rates observed in the 12-month period prior to omalizumab treatment in APEX as the source of baseline exacerbation rates. Note that as APEX recruited patients aged ≥ 12 years, the analysis is conducted for the population of adults and adolescents only. The ICER for the base-case population reduced from £83,822 to £72,009 per additional QALY, £46,432 to £43,627 in the hospitalisation subgroup and £50,181 to £47,252 in the maintenance OCS subgroup. The probability that omalizumab is cost-effective at a threshold of £30,000 per QALY is zero for all populations. Although the ICER using data from APEX is lower than using data from INNOVATE, it is still considerably higher than the ICER reported in the MS of £29,773 for the overall population using APEX data. The difference occurs because of the use of alternative sources for informing asthma-related mortality rates, HRQoL improvement from omalizumab and treatment effectiveness estimates.
| Patient population | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Overall population | Standard care | 37,638 | 12.21 | |
| Omalizumab | 76,761 | 13.75 | 72,484 | |
| Hospitalisation | Standard care | 40,563 | 11.52 | |
| Omalizumab | 79,358 | 12.41 | 43,627 | |
| Maintenance OCS | Standard care | 37,803 | 12.53 | |
| Omalizumab | 70,637 | 13.22 | 47,252 |
Effectiveness data
Scenario 2: using effectiveness estimates from EXALT31
The MS also presented an alternative base-case analysis using data from EXALT to inform the baseline exacerbation rates, estimates of treatment effectiveness, HRQoL and costs. For the reasons discussed previously (see section Model input parameters, Effectiveness evidence), estimates of treatment effect from INNOVATE are preferable over EXALT because of the double-blind nature of INNOVATE compared with the open-label design of EXALT. However, EXALT is a relevant RCT in the population of interest, which used GETE to assess response to omalizumab treatment and for which a responder analysis is available. Therefore, an alternative scenario is considered which uses the estimate of treatment effect from EXALT to inform the cost-effectiveness of omalizumab. Table 79 compares the estimate of risk ratio for exacerbations in the base-case and subgroup populations from INNOVATE and EXALT. For all exacerbations and CSS exacerbations, the treatment effect observed in INNOVATE is greater than the effect observed in EXALT. In contrast, the treatment effect for CSNS exacerbations observed in EXALT is greater than in INNOVATE. These results reflect the different proportion of CSNS and CSS exacerbations observed between treatment arms; in INNOVATE, 35% of exacerbations were classified as CSS in omalizumab responders and 52% in standard care, whereas in EXALT 42.1% of exacerbations were classified as CSS in omalizumab responders and 40.8% in standard care. Although the definition of total exacerbations was the same in EXALT and INNOVATE, the classification of exacerbations into CSS was different in the studies. CSS exacerbations in INNOVATE were defined as an episode of worsening of asthma symptoms requiring treatment with systemic corticosteroids in which PEF or FEV1 were < 60% of personal best. 19 CSS exacerbations in EXALT were defined as an episode of worsening of asthma symptoms requiring treatment with systemic corticosteroids and one of the following: (1) hospital admission and/or intubation; (2) A&E visit, (3) breathlessness at rest or PEF/FEV1 < 60% predicted or personal best, (4) a > 30% fall from personal best PEF in two successive days. 32
| Patient population | CSNS exacerbations | CSS exacerbations | Total exacerbations | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Risk ratio | LCI | UCI | Risk ratio | LCI | UCI | Risk ratio | LCI | UCI | |
| Base-case and subgroup populations: INNOVATE | |||||||||
| Overall population | 0.5089 | 0.3291 | 0.7869 | 0.2494 | 0.1425 | 0.4362 | 0.3730 | 0.2653 | 0.5245 |
| Hospitalisation | 0.5902 | 0.3137 | 1.1103 | 0.2907 | 0.1433 | 0.5900 | 0.4152 | 0.2604 | 0.6622 |
| Maintenance OCS | 0.4142 | 0.1569 | 1.0938 | 0.2144 | 0.0761 | 0.6042 | 0.2929 | 0.1449 | 0.5921 |
| Scenario 2: EXALT | |||||||||
| Overall population | 0.4008 | 0.2760 | 0.5821 | 0.4230 | 0.2718 | 0.6580 | 0.4098 | 0.3082 | 0.5450 |
| Hospitalisation | 0.4852 | 0.2180 | 1.0801 | 0.4270 | 0.2101 | 0.8678 | 0.4514 | 0.2655 | 0.7672 |
| Maintenance OCS | 0.5310 | 0.2738 | 1.0301 | 0.4832 | 0.2404 | 0.9715 | 0.5077 | 0.3140 | 0.8209 |
| Patient population | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Overall population | Standard care | 33,351 | 13.66 | |
| Omalizumab | 81,537 | 14.18 | 92,235 | |
| Hospitalisation | Standard care | 36,800 | 11.82 | |
| Omalizumab | 76,175 | 12.62 | 48,892 | |
| Maintenance OCS | Standard care | 35,108 | 12.79 | |
| Omalizumab | 71,784 | 13.43 | 57,639 |
Table 80 presents the cost-effectiveness results using the treatment effect observed in EXALT. The ICER for the overall population and subgroups are 5–10% greater than the base-case results. The manufacturer also presented a scenario using data from EXALT, which resulted in an ICER of £61,687 per QALY for the overall population, almost double the base-case results using data from INNOVATE. However, for the hospitalisation and maintenance OCS subgroups, the manufacturer's ICER was close to the results of the INNOVATE subgroup at £35,198 and £37,604 per QALY respectively.
Scenario 3: using a pooled estimate of effect from INNOVATE and EXALT
In principle, the treatment effect observed in INNOVATE and EXALT can be combined using a meta-analysis to provide a pooled estimate of effect. However, as discussed above, different definitions were used in the trials to classify exacerbations into CSS and CSNS. Therefore, a pooled estimate of effect on the number of CSS and CSNS exacerbations separately would result in considerable heterogeneity [see section Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing) Data analysis] between the trials. Instead, the total number of exacerbations is combined to provide a pooled estimate of risk ratio and 95% CI. This pooled estimate is then applied to the baseline rates of CSS and CSNS exacerbations separately, that is the scenario assumes that omalizumab reduces the rate of CSS and CSNS exacerbations equally. Table 81 compares the risk ratios used in the model for the base-case populations informed by INNOVATE only with the pooled estimate from EXALT and INNOVATE. As noted above, the treatment effect estimate from EXALT is of a lower magnitude than INNOVATE, therefore, the combined EXALT and INNOVATE estimate lies between the estimates from the individual trials.
| Patient population | Total exacerbations | |||
|---|---|---|---|---|
| Risk ratio | LCI | UCI | I 2 | |
| Base-case and subgroup populations: INNOVATE | ||||
| Overall population | 0.3730 | 0.2653 | 0.5245 | NA |
| Hospitalisation | 0.4152 | 0.2604 | 0.6622 | NA |
| Maintenance OCS | 0.2929 | 0.1449 | 0.5921 | NA |
| Scenario 3: pooled estimates INNOVATE and EXALT | ||||
| Overall population | 0.394 | 0.317 | 0.491 | 0.0% |
| Hospitalisation | 0.431 | 0.303 | 0.611 | 0.0% |
| Maintenance OCS | 0.426 | 0.287 | 0.634 | 37.5% |
Table 82 presents the cost-effectiveness results using the pooled estimate of risk ratio for total exacerbations from INNOVATE and EXALT. For the overall population, the ICER increased from £83,822 to £88,281, whereas for the hospitalisation and maintenance OCS subgroups, the ICER also increased from £46,431 to £47,235 and £50,181 to £53,454 respectively. Although the pooled estimate of treatment effects for total exacerbations in the overall population and hospitalisation subgroup is less favourable than the effect from INNOVATE alone, the estimate of cost-effectiveness of omalizumab is also determined by the split in CSNS and CSS exacerbations. In this scenario, the treatment effect is applied equally to both types of exacerbation, which results in a slight increase in the ICER results. With the alternative estimates of treatment effect in scenarios 2 and 3, the ICERs remain well above conventional thresholds of cost-effectiveness, suggesting that the clinical effectiveness estimates alone are not a key driver of cost-effectiveness.
| Patient population | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Overall population | Standard care | 33,506 | 13.67 | |
| Omalizumab | 73,065 | 14.11 | 88,281 | |
| Hospitalisation | Standard care | 36,670 | 11.80 | |
| Omalizumab | 75,924 | 12.64 | 47,235 | |
| Maintenance OCS | Standard care | 35,417 | 12.80 | |
| Omalizumab | 68,456 | 13.42 | 53,454 |
Asthma-related mortality
Scenario 4: estimates from Watson et al.106
As discussed in the section Natural history: mortality, Asthma-related mortality, the risk of asthma-related mortality reported in Watson et al. provides an alternative source of mortality rates. However, it is confounded by a number of factors; most notably the definition of a hospitalisation in Watson et al. does not match the definition of a CSS exacerbation as used in the trials. Table 83 presents the cost-effectiveness results using asthma-related mortality risks from Watson et al. 106 For adults and adolescents, who enter the model at an average age of 43 years, the ICER is almost halved from £83,822 to £46,029 per QALY in the base-case population, £46,431 to £31,576 in the hospitalisation subgroup and £50,181 to £29,657 in the maintenance OCS subgroup. The probability that omalizumab is cost-effective at a threshold of £30,000 per QALY increases from zero to 0.34 for the hospitalisation subgroup and to 0.55 for the maintenance OCS subgroup. In contrast, the ICER for children, who enter the model at an average age of 9 years, increases from £78,009 to £98,688 in the base case and £44,142 to £47,430 in the hospitalisation subgroup. As discussed in Model input parameters, the mortality risk for adults > 45 years in Watson et al. is about five times greater than the risk in de Vries et al. ;138 therefore the ICER falls as expected. For children < 11 years, the mortality risk in Watson et al. is much lower than the assumed mortality risk from de Vries et al. ; therefore, the ICER increases. These results suggest that asthma-related mortality risk is a key driver of cost-effectiveness of omalizumab. In addition, the age at treatment initiation has a major impact on the cost-effectiveness as the mortality risk is very much age-dependent according to the estimates from Watson et al.
| Patient population | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Overall population | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 27,415 | 11.24 | ||
| Omalizumab | 67,675 | 12.11 | 46,029 | |
| Children (6–11 years of age) – age at model entry: 9 years | ||||
| Standard care | 39,487 | 16.51 | ||
| Omalizumab | 91,697 | 17.04 | 98,688 | |
| Hospitalisation | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 28,159 | 9.04 | ||
| Omalizumab | 68,055 | 10.30 | 31,576 | |
| Children (6–11 years of age) – age at model entry: 9 years | ||||
| Standard care | 42,993 | 13.86 | ||
| Omalizumab | 81,166 | 14.66 | 47,430 | |
| Maintenance OCS | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 25,387 | 9.28 | ||
| Omalizumab | 59,145 | 10.41 | 29,657 | |
Figure 6 illustrates the effect of age at treatment initiation on the ICER for the base-case population using the estimate of mortality from de Vries et al. 138 and using the age-dependent asthma-related mortality from Watson et al. in the manufacturer's model. In the base case using estimates from de Vries et al. ,138 the ICER increases with age at treatment initiation; the older the patient cohort initiates treatment, the shorter the period of time the patient can benefit from treatment because of decreased life expectancy. There is a small discontinuity at age 12 years when the exacerbation rates from IA-05 EUP switch to those from INNOVATE. In contrast, the relationship between age at treatment initiation and ICER changes using the age-dependent mortality risks from Watson et al. 106 At a model starting age of 6 years, the ICER is £130,475. As the starting age is increased from 6 to 12 years, the ICER falls sharply. Two factors are responsible for the sharp decline in the ICER: (1) the asthma-related mortality risk for age 12 years increases threefold from 0.097% (0–11 years) to 0.319% (12–16 years); and (2) the manufacturer assumes that children < 12 years do not experience any HRQoL improvement from omalizumab. Therefore, if the cohort enters the model at age 6 years, it experiences 6 years with no HRQoL improvement and 4 years with HRQoL improvement. The higher asthma-related mortality risk and HRQoL improvement at age 12 years drives the ICER down to its first minimum of £56,386 for treatment initiation at age 12. From age 12–35 years, the ICER remains fairly constant at around £56,000 per QALY. From age 35–45 years, the ICER decreases sharply to a minimum of £32,437 for treatment initiation at age 45. This sharp decrease occurs because of another discontinuity in the asthma-related mortality risk at age 45 years. At this age, the mortality rate of 2.478% is more than six times greater than the mortality risk of 0.38% for patients aged 17–44 years. Treatment duration is assumed to be 10 years; therefore a patient cohort initiating treatment at age 35 experiences 9 years at the lower mortality risk and 1 year at the higher risk of 2.478%. As the age at treatment initiation increases, the number of years experiencing the higher asthma-related mortality risk of 2.478% also increases. From age 45 years, the asthma-related mortality risk remains constant. The increased ICER from this age onwards is because of the progressively lower life expectancy from all-cause mortality.
FIGURE 6.
Effect of age at treatment initiation on the ICER.
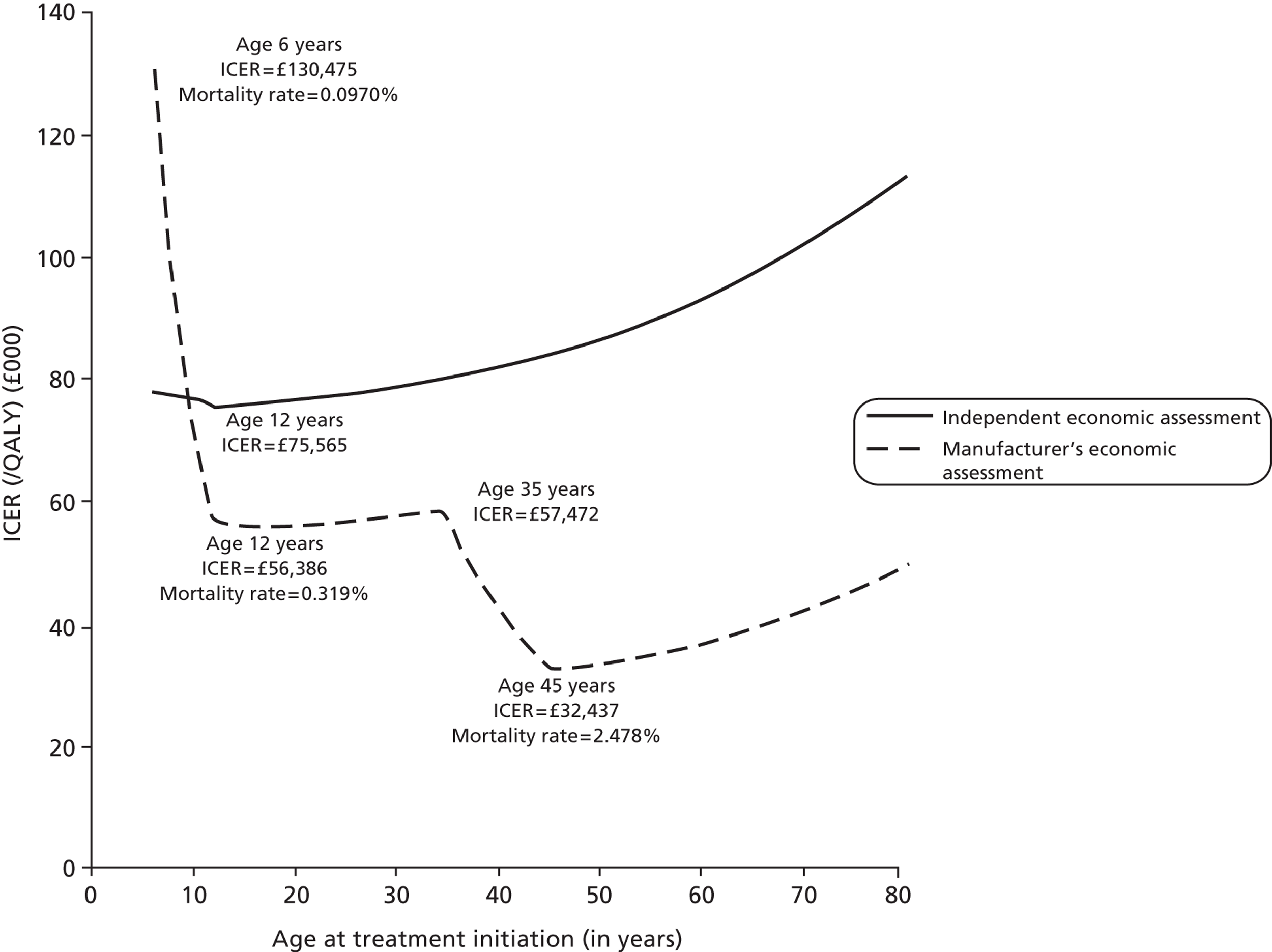
The cost-effectiveness results for the base-case population of adults and adolescents assume an average starting age of 43 years, reflecting the average age of the population in INNOVATE. The results for the base-case population of children aged 6–11 years assume an average starting age of 9 years, reflecting the average age of the population in IA-05 EUP. It is easy to see, on the basis of Figure 6, why the manufacturer's cost-effectiveness results differ substantially between the base-case populations. The starting age used in the model for the base-case population of adults and adolescents (aged ≥ 12 years) masks the age distribution of patients likely to receive omalizumab in clinical practice. Therefore, the assessment group requested information from the manufacturer on the proportion of patients on omalizumab in the UK stratified by age or age category. The manufacturer provided the age distribution of patients recruited into APEX, which represents approximately one-eighth of the population receiving omalizumab in the UK (Table 84).
| Age (years) | Number of patients | % of patients | Source |
|---|---|---|---|
| 6–11a | 3 | 2.2 | Estimateb |
| 12a–14 | 6 | 4.3 | APEX study |
| 15–19 | 9 | 6.5 | APEX study |
| 20–24 | 9 | 6.5 | APEX study |
| 25–29 | 6 | 4.3 | APEX study |
| 30–34 | 9 | 6.5 | APEX study |
| 35–39 | 18 | 12.9 | APEX study |
| 40–44 | 20 | 14.4 | APEX study |
| 45–49 | 21 | 15.1 | APEX study |
| 50–54 | 16 | 11.5 | APEX study |
| 55–59 | 10 | 7.2 | APEX study |
| 60–64 | 8 | 5.8 | APEX study |
| 65–69 | 2 | 1.4 | APEX study |
| 70–74 | 0 | 0.0 | APEX study |
| 75–79 | 1 | 0.7 | APEX study |
| 80–84 | 1 | 0.7 | APEX study |
| Total | 139 | 100 |
Table 85 presents the cost-effectiveness results using an average ICER weighted by the age distribution of patients in APEX for the base-case population of adults and adolescents and the hospitalisation and maintenance OCS subgroups. The average ICER in the independent assessment does not change very much from the base-case analysis (£83,710 vs. £83,222 per QALY) as the mortality risk is assumed constant across all ages from de Vries et al. In contrast, the average weighted ICER using the manufacturer's model of £44,444 is greater than the base-case results reported in the MS of £32,076 for the overall population. Similarly, the average weighted ICER for the hospitalisation and maintenance OCS subgroups is higher than that reported in the MS; £37,300 (weighted ICER) compared with £27,928 (age 43 years) for the hospitalisation subgroup and £36,687 (weighted ICER) compared with £26,320 (age 43 years) for the maintenance OCS subgroup.
| ICER | Overall population | Hospitalisation subgroup | Maintenance OCS subgroup | |||
|---|---|---|---|---|---|---|
| Independent assessment | Manufacturer | Independent assessment | Manufacturer | Independent assessment | Manufacturer | |
| Average ICER (£/QALY) | 83,710 | 44,444 | 46,132 | 37,300 | 48,630 | 36,687 |
Health-related quality of life
Scenario 5: using EQ-5D utility values mapped from Asthma Quality of Life Questionnaire scores from INNOVATE16
The base-case analysis uses utility values for day-to-day asthma symptoms informed by EQ-5D data collected in EXALT at 32 weeks, in line with the NICE reference case. In contrast, the manufacturer's base case uses AQLQ data collected in INNOVATE and mapped onto EQ-5D values. Table 86 provides a comparison of the utility values from EXALT and INNOVATE for the base-case and subgroup populations. The difference in utility between omalizumab responders and patients on standard care in the overall EXALT population (0.048) is less than half of the INNOVATE population (0.110). This may reflect differences in the study design (open-label vs. double-blind RCT) or it may be an artefact of using an indirect method of mapping from a condition-specific QoL instrument to a generic measure of HRQoL. The difference in utility between omalizumab and standard therapy estimated from the direct and indirect measure is similar in the subgroup populations; for the hospitalisation subgroup, the improvement in HRQoL observed for omalizumab is 0.130 from EXALT and 0.138 from INNOVATE, whereas for the maintenance OCS subgroup, the improvement is 0.105 from EXALT and 0.106 from INNOVATE.
| Patient population | Data source | Day-to-day asthma symptoms | Difference | |
|---|---|---|---|---|
| Standard care | Omalizumab responders | |||
| Base-case populations | ||||
| Adult and adolescent | EXALT | 0.719 (0.026) | 0.767 (0.02) | 0.048 |
| Children | EXALTa | 0.719 (0.026) | 0.767 (0.02) | 0.048 |
| Subgroup populations | ||||
| Adult and adolescent: hospitalisation | EXALT: hospitalisation | 0.631 (0.061) | 0.761 (0.046) | 0.130 |
| Adult and adolescent: maintenance OCS | EXALT: maintenance OCS | 0.686 (0.07) | 0.791 (0.032) | 0.105 |
| Children: hospitalisation | EXALTa: hospitalisation | 0.631 (0.061) | 0.761 (0.046) | 0.130 |
| Scenario 5 | ||||
| INNOVATE: all | INNOVATE | 0.669 (0.011) | 0.779 (0.013) | 0.110 |
| INNOVATE: hospitalisation | INNOVATE | 0.634 (0.019) | 0.772 (0.023) | 0.138 |
| INNOVATE: maintenance OCS | INNOVATE | 0.639 (0.026) | 0.745 (0.03) | 0.106 |
Table 87 presents the cost-effectiveness results using EQ-5D utility values mapped from AQLQ scores from INNOVATE. For the base-case population of adults and adolescents, the ICER is reduced from £83,822 to £52,236, whereas for children the ICER is reduced from £78,009 to £50,319 per QALY. The large decrease in ICER reflects the higher HRQoL improvement with omalizumab of 0.110 using the indirect estimate of EQ-5D compared with the base-case improvement of 0.048 using EQ-5D utility values collected in EXALT. The impact on the ICER in the hospitalisation and maintenance OCS subgroups is less marked as the HRQoL improvement with omalizumab is similar between the base-case analysis and scenario 5. The results suggest that HRQoL improvement in day-to-day asthma symptoms is a key driver of the cost-effectiveness of omalizumab.
| Patient population | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Overall population | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 32,982 | 12.68 | ||
| Omalizumab | 72,710 | 13.45 | 52,236 | |
| Children (6–11 years of age) – age at model entry: 9 years | ||||
| Standard care | 40,504 | 15.52 | ||
| Omalizumab | 92,796 | 16.56 | 50,319 | |
| Hospitalisation | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 36,405 | 11.88 | ||
| Omalizumab | 75,814 | 12.77 | 44,430 | |
| Children (6–11 years of age) – age at model entry: 9 years | ||||
| Standard care | 45,004 | 14.52 | ||
| Omalizumab | 83,389 | 15.43 | 42,296 | |
| Maintenance OCS | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 35,345 | 11.89 | ||
| Omalizumab | 68,499 | 12.55 | 50,068 | |
Scenario 6: assuming no health-related quality-of-life improvement in children up until age 12 years
An assumption in the base-case analysis is that children up until age 12 years experience the same HRQoL improvement with omalizumab as adults and adolescents > 12 years. The MS conservatively assumed that children do not experience any HRQoL improvement up until the age of 12 years, when they then experience the improvement observed in INNOVATE. Scenario 6 employs the same assumption as the manufacturer, but once patients reach age 12 years the HRQoL improvement is the same as adults and adolescents from the EQ-5D values observed in EXALT.
Table 88 presents the cost-effectiveness results assuming no HRQoL improvement in children up until age 12 years. The ICER increases from £78,009 to £95,177 in the overall population and from £44,141 to £63,908 in the hospitalisation subgroup. The resulting ICERs suggest that this assumption has a major impact on the cost-effectiveness of omalizumab, although the ICERs are well above conventional thresholds of cost-effectiveness.
| Patient population | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Overall population | Children (6–11 years of age) – age at model entry: 9 years | |||
| Standard care | 40,126 | 16.77 | ||
| Omalizumab | 92,447 | 17.32 | 95,177 | |
| Hospitalisation | Children (6–11 years of age) – age at model entry: 9 years | |||
| Standard care | 43,575 | 15.74 | ||
| Omalizumab | 82,055 | 16.34 | 63,908 | |
Treatment duration
Scenario 7: lifetime treatment duration
The base-case analysis assumes a 10-year treatment duration, after which treatment with omalizumab is discontinued. In the absence of long-term follow-up data, the effectiveness of continuing to treat patients with omalizumab over a longer time horizon remains highly uncertain. As asthma is a chronic condition, patients may continue to face a risk of clinically significant exacerbations for the remainder of their lifetime. Therefore, a scenario is explored which examines the potential cost-effectiveness of maintaining patients on omalizumab over a lifetime duration. Table 89 presents the cost-effectiveness results assuming lifetime treatment duration. The ICER increases slightly from £83,822 to £89,230 in the base-case population of adults and adolescents and from £78,009 to £79,923 in the base case of children. A similar increase in the ICER is observed for the subgroup populations. Although the benefits from treatment are experienced for longer, the increased costs because of omalizumab are also accrued for longer and are therefore greater. The results suggest that treatment duration does not have much impact on the cost-effectiveness of omalizumab.
| Patient population | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Overall population | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 32,628 | 13.66 | ||
| Omalizumab | 128,286 | 14.74 | 89,230 | |
| Children (6–11 years of age) – age at model entry: 9 years | ||||
| Standard care | 40,701 | 16.72 | ||
| Omalizumab | 196,900 | 18.67 | 79,923 | |
| Hospitalisation | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 36,536 | 11.83 | ||
| Omalizumab | 131,131 | 13.81 | 47,590 | |
| Children (6–11 years of age) – age at model entry: 9 years | ||||
| Standard care | 44,549 | 14.42 | ||
| Omalizumab | 157,167 | 16.92 | 45,025 | |
| Maintenance OCS | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 35,298 | 12.78 | ||
| Omalizumab | 114,479 | 14.31 | 51,862 | |
Costs
Scenario 8: using dosing table expansion
As discussed in the section Omalizumab therapy costs, the dosing table for omalizumab was expanded in January 2010, which raised the maximum doses from 375 mg four times a week to 600 mg twice a week and permitted dosing in patients with higher IgE levels. The dose distribution observed in the clinical trials refers to the ‘standard dose’ of treatment rather than the ‘expanded dose’, which is now used in clinical practice. Heaney et al. have examined the impact of the dosing table expansion on the size of the patient population potentially eligible for omalizumab in the UK. (Academic-in-confidence information has been removed.)136 The supplementary information provided by Heaney et al. permits the calculation of average cost per patient for ‘standard dose’ and ‘expanded dose’. Table 90 presents the average cost of omalizumab based on data from INNOVATE, APEX and the BTS ‘expanded-dose’ population. (Academic-in-confidence information has been removed.)
| Patient population | Average cost of omalizumab | Administration and monitoring costs | |
|---|---|---|---|
| First year | Thereafter | ||
| Base case | |||
| INNOVATE: all | £8056 | £260 | £146 |
| Scenario analysis | |||
| APEX | £10,381 | £289 | £165 |
| Academic-in-confidence information has been removed | Academic-in-confidence information has been removed | Academic-in-confidence information has been removed | Academic-in-confidence information has been removed |
Scenario analysis is used to explore the impact of the increased average cost on the cost-effectiveness of omalizumab. Table 91 presents the cost-effectiveness results using the average cost from the BTS ‘expanded dose’ for adults and adolescents. The ICER increases from £83,822 to £112,033 in the overall population, £46,431 to £62,339 in the hospitalisation subgroup and £50,181 to £67,363 in the maintenance OCS subgroup. The results suggest that the expansion of the dosing table has a major impact on the cost-effectiveness of omalizumab.
| Patient population | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Overall population | ||||
| Standard care | 32,986 | 13.66 | ||
| Omalizumab | 86,141 | 14.14 | 112,033 | |
| Hospitalisation | ||||
| Standard care | 36,753 | 11.82 | ||
| Omalizumab | 89,600 | 12.67 | 62,339 | |
| Maintenance OCS | ||||
| Standard care | 35,443 | 12.80 | ||
| Omalizumab | 79,984 | 13.46 | 67,363 | |
Incorporation of adverse effects of oral corticosteroids
Scenario 9: adverse effects of oral corticosteroids
A number of alternative scenarios are used to assess the impact of OCS-related adverse effects on the cost-effectiveness of omalizumab:
-
Scenario 9A: Adapts the same approach as the manufacturer. The total annual quality-of-life burden expressed in terms of DALYs is estimated to be 0.02331 per patient and the total annual cost is £205.60 per patient on maintenance OCS.
-
Scenario 9B: Uses the same costs as scenario 9A, but uses undiscounted and non-age-weighted DALYs. As discussed in Incorporation of long-term consequences of OCS, the DALY burden used by the manufacturer incorporated an adjusted age-weight factor, which gives less weight to diseases in the young and elderly. In addition, a 3% per annum discount rate was used in the DALY calculation and then a further 3.5% discount rate per year applied in the model. As NICE recommends that all health gains receive the same weight regardless of who benefits,105 the non-age-weighted DALY are used in this scenario. 144 A 3.5% per annum discount rate is applied to the DALYs in the model. The resulting annual quality-of-life burden is estimated to be 0.04507 DALY, almost double that of scenario 9A.
-
Scenario 9C: Same approach as scenario 9B but includes an additional health loss for non-Hodgkin's lymphoma, adrenal insufficiency and sleep disturbance. The DALY burden for non-Hodgkin's lymphoma is based on the WHO burden of disease for lymphomas and multiple myeloma (0.00126 DALY). 143 The DALY burden for adrenal insufficiency is based on nutritional and endocrine disorders (0.00340 DALY), whereas the burden for sleep disturbance is based on primary insomnia (0.00053 DALY). Other conditions not related with OCS use may be included in these estimates; therefore the DALY burden associated with these conditions is likely to be an overestimate. The resulting annual DALY burden for this scenario is estimated to be 0.04978 DALY, slightly greater than scenario 9B.
Table 92 summarises the costs and health losses associated with OCS-related adverse effects in each scenario.
| Conditions | Relative risk | Annual DALY loss per patient | Annual cost per person (£) |
|---|---|---|---|
| Scenario 9A: using the manufacturer's estimates | |||
| Diabetes | 3.02 | 0.00232 | 29.67 |
| Myocardial infarction | 2.5 | 0.01063 | 42.88 |
| Osteoporotic fracture | 2.84 | 0.00104 | 38.39 |
| Glaucoma | 1.37 | 0.00038 | 2.25 |
| Ulcer | 2 | 0.00053 | 6.91 |
| Cataract | 1.83 | 0.00011 | 3.57 |
| Annual burden | 0.02331 | 205.60 | |
| Scenario 9B: using undiscounted and non-age-weighted DALY144 | |||
| Diabetes | 3.02 | 0.00514 | 29.67 |
| Myocardial infarction | 2.5 | 0.01861 | 42.88 |
| Osteoporotic fracture | 2.84 | 0.00096 | 38.39 |
| Glaucoma | 1.37 | 0.00111 | 2.25 |
| Ulcer | 2 | 0.00122 | 6.91 |
| Cataract | 1.83 | 0.00408 | 3.57 |
| Annual burden | 0.04507 | 205.60 | |
| Scenario 9C: incorporating DALY burden from non-Hodgkin's lymphoma, adrenal insufficiency and sleep disturbance144 | |||
| Non-Hodgkin's lymphoma | 1.30 | 0.00126 | Not included |
| Adrenal insufficiency | 2.00 | 0.00340 | Not included |
| Sleep disturbance | 2.77 | 0.00053 | Not included |
| Annual burden (includes those of scenario 9B) | 0.04978 | 205.60 | |
Table 93 presents the cost-effectiveness results incorporating OCS-related adverse effects in the maintenance OCS subgroup. Under base-case assumptions, the ICER for the maintenance OCS subgroup is £50,181 per QALY gained in adults and adolescents. Incorporating the adverse effects of OCS use reduces the ICER to £46,634 under scenario 9A, £44,692 under scenario 9B and £44,292 per additional QALY under scenario 9C. The results suggest that the incorporation of OCS-related adverse effects has a major impact on the cost-effectiveness of omalizumab.
| Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY)a |
|---|---|---|---|
| Base case: maintenance OCS subgroup | |||
| Standard care | 35,902 | 12.78 | |
| Omalizumab | 68,995 | 13.44 | 50,181 |
| Scenario 9A: using the manufacturer's estimates | |||
| Standard care | 41,315 | 12.35 | |
| Omalizumab | 74,042 | 13.05 | 46,634 |
| Scenario 9B: using undiscounted and non-age-weighted DALYs | |||
| Standard care | 41,315 | 11.92 | |
| Omalizumab | 74,042 | 12.66 | 44,692 |
| Scenario 9C: incorporating DALY burden for non-Hodgkin's lymphoma, adrenal insufficiency and sleep disturbance | |||
| Standard care | 41,315 | 11.83 | |
| Omalizumab | 74,042 | 12.57 | 44,292 |
A major limitation of this analysis is that the number of DALYs saved is assumed equivalent to the number of QALYs gained. As discussed in Adverse effects because of maintenance oral corticosteroids, this assumption holds only if: (1) the HRQoL weight is equal to one minus the disability weight; (2) both the HRQoL and disability weights are constant throughout the disease duration; and (3) DALYs are not age-weighted. An exploratory analysis is used to assess the equivalence between HRQoL weights and disability weights in order to infer whether the health losses as a result of OCS-related adverse effects, estimated with DALYs, would be greater or smaller than the anticipated health losses estimated with QALY. Table 94 presents a comparison between the disability and HRQoL weights for the disease outcomes. The disability weights are based on the global burden of disease 2004 calculations145 and the HRQoL weights are UK-based catalogue EQ-5D index scores from Sullivan et al. 146 Sullivan et al. used the responses to the EQ-5D from the Medical Expenditure Panel Survey conducted in the USA to derive a catalogue of EQ-5D scores using the UK tariff of the HRQoL loss (marginal disutility) associated with a range of conditions. The HRQoL loss represents the decrement in EQ-5D for each condition after controlling for age, comorbidities, gender, race, ethnicity, income and education. In general, the HRQoL weights are smaller than the disability weights, with the exception of gastric ulcer, suggesting that the health losses as a result of OCS-related adverse effects estimated with QALYs may be smaller than those estimated with DALYs.
| Conditions | Disability weight | HRQoL loss attributable to the condition | HRQoL loss/DALY weight |
|---|---|---|---|
| Diabetes | 0.066–0.595 | 0.0565–0.0621 | 0.1–0.9 |
| Myocardial infarction | 0.405–0.477 | 0.0557 | 0.1 |
| Osteoporotic fracture | 0.185–0.221 | 0.1017–0.0418 | 0.2–0.5 |
| Glaucoma | 0.170–0.600 | 0.0278 | 0.05–0.2 |
| Ulcer | 0.003–0.092 | 0.05552 | 0.6–18.5 |
| Cataract | 0.170–0.595 | 0.0217 | 0.04–0.1 |
Sensitivity analysis
A large number of one-way sensitivity analyses were performed to explore the additional impact of changing particular input parameter values on the cost-effectiveness results. Table 95 presents the results of the sensitivity analysis. The ICER is most sensitive to assumptions regarding treatment withdrawal and HRQoL loss because of exacerbations. A 10% withdrawal rate from omalizumab per year increases the ICER by 20% from £83,822 to £100,535 in adults and adolescents, and from £78,009 to £94,218 in children. The largest decrease in the ICER is under the extreme assumption that the absolute utility associated with an exacerbation is zero; however, the resulting ICER of £59,428 in adults and adolescents and £54,210 in children remain well above conventional thresholds of cost-effectiveness.
| Analysis description | Adult and adolescent (≥ 12 years) | Children (6–11 years) | ||
|---|---|---|---|---|
| ICERa (£/QALY) | % change from base case | ICER (£/QALY) | % change from base case | |
| Base case | ||||
| 83,822 | – | 78,009 | – | |
| Baseline exacerbation rates | ||||
| +50% | 78,017 | −6.9 | 72,423 | −7.2 |
| −50% | 88,998 | 6.2 | 82,276 | 5.5 |
| Proportion of responders | ||||
| +50% | 82,762 | −1.3 | 76,694 | −1.7 |
| −50% | 84,354 | 0.6 | 78,526 | 0.7 |
| Treatment effect on exacerbations | ||||
| +50% | 76,036 | −9.3 | 69,558 | −10.8 |
| −50% | 91,772 | 9.5 | 86,390 | 10.7 |
| Withdrawals from treatment | ||||
| 10% per annum | 100,535 | 19.9 | 94,218 | 20.8 |
| 20% per annum | 117,247 | 39.9 | 110,664 | 41.9 |
| HRQoL for exacerbations | ||||
| No decrease in utility for exacerbations | 94,414 | 12.6 | 86,449 | 10.8 |
| Utility for exacerbations = 0 | 59,428 | −29.1 | 54,210 | −30.5 |
| Costs of exacerbations | ||||
| +50% | 82,658 | −1.4 | 76,346 | −2.0 |
| −50% | 83,703 | −0.1 | 77,819 | −0.2 |
Additional subgroup analysis: ≥ 3 exacerbations at baseline
An additional subgroup population consisting of patients experiencing ≥ 3 exacerbations in a year is considered. The rationale for considering this subgroup is based on data reported in the previous STA TA201, which suggested that patients who had experienced ≥ 3 exacerbations in the year prior to trial enrolment benefited significantly from omalizumab. 89 In response to a request from the assessment group, the manufacturer provided data on the clinical effectiveness of omalizumab in a subgroup of patients who had experienced ≥ 3 exacerbations in the year prior to enrolment in INNOVATE and IA-05 EUP. In this subgroup of patients, HRQoL associated with day-to-day asthma symptoms for omalizumab and standard care was obtained from EXALT, as EQ-5D utility values were measured directly in this study. However, the manufacturer also provided the mapped EQ-5D utility values from INNOVATE for this subgroup population. Table 96 presents the subgroup data used in the model for patients with ≥ 3 exacerbations at baseline.
| Patient population | CSNS exacerbations | CSS exacerbations | Total exacerbations | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | LCI | UCI | Mean | LCI | UCI | Mean | LCI | UCI | |
| Baseline exacerbation rates: annualised rate and 95% CI | |||||||||
| Adults and adolescents: INNOVATE | 0.9524 | 0.6986 | 1.2984 | 1.2619 | 0.9641 | 1.6518 | 2.2143 | 1.8070 | 2.7133 |
| Children: IA-05 EUPa | 2.1460 | 1.6353 | 2.8163 | 0.6190 | 0.3732 | 1.0269 | 2.7651 | 2.1763 | 3.5132 |
| Omalizumab effect on exacerbations for responders: risk ratio and 95% CI | |||||||||
| Adults and adolescents: INNOVATE | 0.5850 | 0.3069 | 1.1151 | 0.1840 | 0.0735 | 0.4602 | 0.3565 | 0.2126 | 0.5978 |
| Children: IA-05 EUPa | 0.2105 | 0.1232 | 0.3598 | 0.2838 | 0.1157 | 0.6960 | 0.2269 | 0.1433 | 0.3592 |
| Proportion of responders | |||||||||
| Adults and adolescents: INNOVATE | 0.4651 (0.3597 to 0.5705) | ||||||||
| Children: IA-05 EUP | 0.7708 (0.6868 to 0.85449) | ||||||||
| Omalizumab effect on HRQoLb | |||||||||
| Adults and adolescents, children | EXALT subgroup ≥ 3 exacerbations at baseline | ||||||||
| Standard care = 0.698; omalizumab responders = 0.7400; difference = 0.0420 | |||||||||
| INNOVATE subgroup ≥ 3 exacerbations at baseline | |||||||||
| Standard care = 0.651; omalizumab responders = 0.7870; difference = 0.136 | |||||||||
The baseline exacerbation rates are higher than those in the overall patient population but not statistically significant. In the overall population of INNOVATE, the baseline exacerbation rate for total exacerbations is 0.1688 (1.4655 to 1.9461), whereas for the subgroup of ≥ 3 exacerbations it is 2.2143 (1.8070 to 2.7133). Similarly, the rate for the overall population of IA-05 EUP is 2.0293 (1.6365 to 2.5164), whereas for the subgroup of ≥ 3 exacerbations it is 2.7651 (2.1763 to 3.5132). The effect of omalizumab is comparable between the subgroup and the overall populations; the risk ratio for total exacerbations in the overall population of INNOVATE is 0.3730 (0.2653 to 0.5245), whereas for the subgroup of ≥ 3 exacerbations it is 0.3565 (0.2126 to 0.5978). For the overall population of IA-05 EUP, the risk ratio for total exacerbations is 0.2561 (0.1711 to 0.3833), whereas for the subgroup of ≥ 3 exacerbations it is 0.2269 (0.1433 to 0.3592). Although patients are at a higher risk of an exacerbation, the results suggest that the effect of omalizumab on exacerbations is similar to the effect on the overall population. The HRQoL improvement observed in EXALT is lower in the subgroup population than the HRQoL improvement observed in INNOVATE. This is similar to the HRQoL data for the overall population, where the improvement observed in INNOVATE was greater than that observed in EXALT. Given that HRQoL improvement with omalizumab is a key driver of cost-effectiveness, the improvement observed in INNOVATE is used in an alternative scenario.
Table 97 presents the cost-effectiveness results for the subgroup of ≥ 3 exacerbations at baseline. The ICERs for this subgroup are slightly higher than the ICERs for the base-case population of adults and adolescents (£84,332 vs. £83,822) and children (£76,149 vs. £78,009). However, the ICERs are still well above conventional cost-effectiveness thresholds of £20,000 and £30,000 per additional QALY used by NICE. 105 Using the HRQoL data from INNOVATE (EQ-5D mapped from AQLQ scores), reduces the ICER considerably to £41,523 in adults and adolescents and £41,429 in children.
| Data source | Intervention | Mean costs (£) | Mean QALY | ICER (£/QALY) |
|---|---|---|---|---|
| Using HRQoL data from EXALT | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | 36,582 | 12.92 | ||
| Omalizumab | 69,317 | 13.34 | 77,868 | |
| Children (6–11 years of age) – age at model entry: 9 years | ||||
| Standard care | 42,704 | 16.04 | ||
| Omalizumab | 96,611 | 16.74 | 76,149 | |
| Using HRQoL data from INNOVATE | Adults and adolescents (≥ 12 years of age) – age at model entry: 43 years | |||
| Standard care | £34,421 | 12.19 | ||
| Omalizumab | £67,545 | 12.95 | £43,523 | |
| Children (6–11 years of age) – age at model entry: 9 years | ||||
| Standard care | 42,560 | 14.92 | ||
| Omalizumab | 96,514 | 16.23 | 41,429 | |
Discussion of cost-effectiveness analysis
The results from the base-case analysis demonstrate important variation across the separate populations in terms of the cost-effectiveness results. The ICER estimates are lower (and therefore more favourable towards omalizumab) in more severe populations compared with the overall severe persistent allergic asthma population. This finding reflects the greater exacerbation risk faced by more severe populations and the greater HRQoL improvement in day-to-day symptoms conferred by omalizumab. Nevertheless, the ICER estimates are above conventional thresholds of cost-effectiveness used by NICE across all populations.
Independent economic assessment versus manufacturer's assessment
The cost-effectiveness results from the independent assessment are noticeably different from those of the manufacturer. Table 98 summarises the ICER results for the base-case and subgroup populations for both the independent and manufacturer's assessment. The ICER for the base case of adults and adolescents is about 2.5 times greater than the manufacturer's probabilistic ICER of £33,268, whereas the ICER for the base case of children is about £10,000 less than the manufacturer's ICER but still remains well above conventional thresholds of cost-effectiveness at £78,009 per additional QALY. A range of scenarios were considered to explore the robustness of the cost-effectiveness results to alternative parameter inputs and assumptions, and to identify the key parameters which result in the differences between the assessments.
| Parameter | ICER (£/QALY) | |
|---|---|---|
| Adults and adolescents (≥ 12 years) | Children (6–11 years) | |
| Independent assessment | 83,822 | 78,009 |
| Manufacturer's assessment | 35,972 | 80,747 |
| Alternative parameter estimates varied individually in the independent assessment model | ||
| Using Watson et al. (2007)106 for asthma-related mortality | 46,029 | 98,688 |
| Using EQ-5D utility values mapped from AQLQ scores | 52,236 | 50,139 |
| Assuming no HRQoL improvement up until age 12 years | NA | 95,177 |
| Using the estimates of absolute HRQoL for exacerbations from Lloyd et al.104 and the duration of an exacerbation from the trials | 84,690 | 77,904 |
| Cumulative effect of altering the parameters above simultaneously in the independent assessment model | ||
| 35,972 | £80,540 | |
The difference in the cost-effectiveness results is largely as a result of two key parameter inputs: (1) asthma-related mortality risk and (2) HRQoL improvement with omalizumab. Using the asthma-related mortality risk from Watson et al. ,106 instead of de Vries et al. ,138 reduces the ICER from £83,822 to £46,029 per QALY in adults and adolescents, and increases the ICER from £78,009 to £98,688 in children. Using the HRQoL improvement with omalizumab from the indirect mapping of AQLQ scores onto EQ-5D, instead of the EQ-5D values collected in EXALT, reduces the ICER from £83,822 to £52,236 in adults and adolescents and from £78,009 to £50,139 in children. The conservative assumption that patients < 12 years of age do not experience any HRQoL improvement with omalizumab increases the ICER from £78,009 to £95,177. Using the estimates of absolute HRQoL for exacerbations from Lloyd et al. and the duration of an exacerbation as reported in the trials, instead of the decrement in utility for exacerbations reported over a 4-week period in Lloyd et al. ,104 has only a marginal effect on the ICER, reducing it by £105. The cumulative effect of altering the parameters above simultaneously results in an ICER of £35,972 per additional QALY for adults and adolescents, and £80,540 per additional QALY for children.
Key drivers of cost-effectiveness
A number of scenarios explored the impact of alternative assumptions and parameter inputs on the cost-effectiveness of omalizumab. Table 99 summarises the cost-effectiveness results for the base-case and subgroup populations and the scenario analysis. The base-case ICER for the subgroup populations is smaller than the overall population but still well above conventional thresholds of cost-effectiveness; the ICER for the hospitalisation subgroup, which consists of patients who were hospitalised at least once in the year prior to trial enrolment, is £46,431 for adults and adolescents and £44,142 for children, whereas the ICER for the maintenance OCS subgroup, which consists of patients on maintenance OCS (step 5 of BTS/SIGN guidelines), is £50,181 for adults and adolescents.
The key drivers of cost-effectiveness are: (1) asthma-related mortality rates; (2) HRQoL improvement associated with omalizumab treatment; and (3) the incorporation of adverse effects of OCSs. As discussed previously, the high asthma-related mortality rate reported in Watson et al. (2007) reduces the ICER substantially; however, it only brings the ICER under a threshold of £30,000 per additional QALY in the maintenance OCS subgroup, at £29,657 in adults and adolescents. The HRQoL improvement with omalizumab (scenarios 5 and 6) has a substantial impact on the ICER; however, the ICER does not fall below £30,000 per QALY in any population (smallest ICER is £42,296 in the hospitalisation subgroup in children). The incorporation of adverse effects of OCSs in the maintenance OCS subgroup (scenario 9) also reduces the ICER but not much closer to conventional thresholds of cost-effectiveness. The ICER is reduced from £50,181 to £44,292 under scenario 9C (using undiscounted non-age-weighted DALYs including non-Hodgkin's lymphoma, adrenal insufficiency and sleep disturbances). However, this result should be interpreted with caution given the assumptions required to incorporate adverse effects of OCSs in the model.
| Analysis | ICER (£/QALY) | |
|---|---|---|
| Adult and adolescents | Children | |
| Overall population | ||
| Base case | 83,822 | 78,009 |
| Scenario 1: using baseline exacerbation rates from APEX | 78,484 | – |
| Scenario 2: using effectiveness estimates from EXALT | 92,235 | – |
| Scenario 3: using pooled effectiveness estimates INNOVATE and EXALT | 89,473 | – |
| Scenario 4: asthma-related mortality from Watson et al. (2007) | 46,029 | 98,688 |
| Scenario 5: using EQ-5D mapped from AQLQ collected during INNOVATE | 52,236 | 50,319 |
| Scenario 6: assuming no HRQoL improvement until patients reach age 12 | – | 95,177 |
| Scenario 7: lifetime treatment duration | 89,230 | 79,923 |
| Scenario 8: using expanded dosing table | 112,033 | – |
| Hospitalisation | ||
| Base case | 46,431 | 44,142 |
| Scenario 1: using baseline exacerbation rates from APEX | 43,627 | – |
| Scenario 2: using effectiveness estimates from EXALT | 48,892 | – |
| Scenario 3: using pooled effectiveness estimates INNOVATE and EXALT | 47,235 | – |
| Scenario 4: asthma-related mortality from Watson et al. (2007) | 31,576 | 47,430 |
| Scenario 5: using EQ-5D mapped from AQLQ collected during INNOVATE | 44,430 | 42,296 |
| Scenario 6: assuming no HRQoL improvement until patients reach age 12 | – | 63,908 |
| Scenario 7: lifetime treatment duration | 47,590 | 45,025 |
| Scenario 8: using expanded dosing table | 62,339 | – |
| Maintenance OCS | ||
| Base case | 50,181 | – |
| Scenario 1: using baseline exacerbation rates from APEX | 47,252 | – |
| Scenario 2: using effectiveness estimates from EXALT | 57,639 | – |
| Scenario 3: using pooled effectiveness estimates INNOVATE and EXALT | 53,454 | – |
| Scenario 4: asthma-related mortality from Watson et al. (2007) | 29,657 | – |
| Scenario 5: using EQ-5D mapped from AQLQ collected during INNOVATE | 50,068 | – |
| Scenario 6: assuming no HRQoL improvement until patients reach age 12 | – | – |
| Scenario 7: lifetime treatment duration | 51,862 | – |
| Scenario 8: using expanded dosing table | 67,363 | – |
| Scenario 9: incorporation of long-term effects of OCSs | £46,634 to £44,292 | – |
Chapter 6 Assessment of factors relevant to the NHS and other parties
Patients with severe uncontrolled allergic asthma are well recognised to be relatively high users of NHS resources. They are currently managed in severe asthma clinics. Before omalizumab therapy is initiated, existing treatment regimens are optimised and patients are fully assessed and treated for comorbidities. This may substantively reduce the number of eligible patients. 147 Therefore, the population of adults in whom NHS omalizumab treatment is started is highly selected. If omalizumab were to be recommended by NICE for children aged < 12 years, a similar process would be used to identify paediatric patients for whom omalizumab was an appropriate treatment option. The impact on clinic resources is likely to be low, as eligible children would already be managed in these settings. Current procedure also ensures that only adult patients with objective evidence of response on review at 16 weeks continue to long-term therapy with omalizumab, and children would follow the same clinical pathway were omalizumab approved for this population. Therefore, omalizumab would not be started in children for whom it was not an appropriate option and would not be continued in those who did not respond; this would represent a continuation of current best practice in adults. As only omalizumab responders will incur significant resource costs related to omalizumab, it is legitimate to employ responder population data in assessing the implications for the NHS. It may be appropriate to establish, in collaboration with the consultee organisations, a registry of patients treated with omalizumab therapy, in order to explore characteristics of patients who show greatest treatment benefit and to evaluate persistence of response.
There is clear evidence that reductions in exacerbations and improved symptom control and quality of life with omalizumab treatment are linked to reduced unscheduled health-care use across a range of outcomes in adults in the licensed population who respond to omalizumab therapy, and to reduced hospitalisations in children aged < 12 years who are responders. These reductions in unscheduled health-care use, and particularly in hospitalisations, represent benefits to the NHS in terms of reduced emergency resource requirement. Based on current practice in adults, and evidence from the use of omalizumab in a highly selected population of children in Scotland, there may also be reductions in requirements for maintenance therapy, including but not limited to OCSs, and decreased scheduled attendance for medical review. There is evidence that omalizumab reduces the use of OCSs; this evidence is considerably stronger for adults than for children but the documented risks associated with steroid use are arguably even greater in children than in adults. Reductions in OCS-related harms such as fracture risk, which persist beyond the duration of OCS therapy, are likely to make omalizumab more favourable.
Chapter 7 Discussion
Statement of principal findings
Adults and adolescents aged ≥ 12 years
There is evidence from RCTs, one of which had a low risk of bias, that omalizumab reduces the total rate of CS exacerbations, including CSS exacerbations, in the licensed adult population. Comparable but larger treatment effects were also observed in those patients who were considered to be omalizumab responders. Trials which were included as supportive evidence also showed evidence of benefit on the outcome of total exacerbations in wider populations. As a result of clinical and statistical heterogeneity, estimates of effect more precise than those from single trials could not be obtained and therefore the effect size in terms of omalizumab's impact on CS or severe exacerbations is somewhat uncertain. The reductions in total and severe exacerbations were reflected in significantly reduced total unscheduled health-care usage in both main trials. Low event rates in comparator arms appear likely to be a consequence of the closer clinical management of patients in clinical trials.
The main RCT also found that omalizumab treatment significantly reduced day-to-day asthma symptoms and improved QoL in the licensed adult population. These treatment effects were also observed in the trials with populations broader than those covered by the licence, although the effect was not statistically significant in all trials. Statistically significant but small increases in lung capacity measured by percentage of predicted FEV1 were also observed across the licensed populations.
In general, data from observational studies reflected the findings of the RCTs, indicating that the results should be generalisable to clinical practice.
The evidence for a steroid-sparing impact of omalizumab treatment was limited but largely consistent. A statistically significant benefit in terms of reduced OCS dose and proportion of patients stopping or reducing maintenance OCS was seen in the OCS maintenance subgroup of a RCT in the licensed population, but the open-label design of this trial may have influenced the findings. In addition, a number of observational studies showed substantive reductions in OCS use.
The review of safety did not identify any adverse events associated with omalizumab which were not documented in the SPC. Data on serious adverse events of special interest (anaphylaxis, malignancy and thrombotic events) were rarely reported; their relationship to omalizumab treatment remains unclear.
There was a lack of any randomised evidence relating to long-term efficacy and safety beyond 52 weeks, and evidence from observational studies was limited by relatively low numbers of patients and uncontrolled study designs. However, this evidence suggested that the effect of omalizumab may not diminish over time when assessed at treatment durations of up to 4 years.
Children aged < 12 years
The evidence of efficacy in the licensed paediatric population came from a single a priori but underpowered subgroup of a good-quality double-blind RCT. This showed that omalizumab significantly reduced total exacerbations, a benefit sustained during a subsequent steroid-sparing phase of the trial. Health-care utilisation showed no evidence of a treatment effect, with the exception of reduced hospitalisations, in the responder population. There was no evidence of significant treatment effects on measures of symptom control and QoL in the randomised study in the licensed population. There was very limited evidence of the OCS-sparing benefit of omalizumab in children: two small linked observational studies relevant to the UK context showed clinically and statistically significant benefits. There was also very limited evidence pertaining to the safety of omalizumab in children; the FDA documentation did not indicate any differences from the adult safety profile. There was no evidence on the efficacy of omalizumab beyond 60 weeks' treatment duration and no evidence in the licensed population beyond 52 weeks.
Adverse effects of oral corticosteroids
The identified reviews provided quantitative evidence for the known adverse events of fracture, diabetes, peptic ulcer, cardiovascular events including myocardial infarction and stroke, cataract and glaucoma, sleep and mood disturbance, and weight gain. All of these syntheses were subject to limitations. There was some very limited evidence for the impact of OCSs on growth in children.
Cost-effectiveness of omalizumab
The cost-effectiveness of omalizumab was evaluated by comparing the additional costs of omalizumab add-on therapy with its additional benefits in terms of improvement in HRQoL and reduction in exacerbations compared with standard care alone, over a lifetime horizon. The costs and health outcomes of both responders and non-responders to omalizumab therapy were included in the total costs and outcomes of treatment. Health outcomes were expressed in QALY and costs were expressed in UK pounds sterling at a 2010 price base from the perspective of the NHS. A new decision-analytic model was developed to provide a framework for the synthesis of data from the systematic reviews on clinical effectiveness of omalizumab, asthma-related mortality risk, HRQoL in asthma patients, and costs and health outcomes from OCS-related adverse effects. Cost-effectiveness estimates were presented for two base-case populations of adults and adolescents (patients ≥ 12 years) and children (6–11 years), and five separate subgroup populations: (1) adults and adolescents hospitalised for asthma in the previous year, (2) children hospitalised for asthma in the previous year, (3) adults and adolescents on maintenance OCS, (4) adults and adolescents who experienced ≥ 3 or more exacerbations in the previous year, and (5) children who experienced ≥ 3 or more exacerbations in the previous year. The base-case population for adults and adolescents corresponded to the INNOVATE population, whereas the population for children corresponded to IA-05 EUP. The subgroup analysis corresponded to the post hoc subgroups from INNOVATE (for adults and adolescents) and IA-05 EUP (for children). The base-case and subgroup analyses were conducted according to a set of assumptions used as part of the base-case analysis. The impact of alternative assumptions and parameter inputs was explored with scenario and one-way sensitivity analyses. Probabilistic results were presented for the base-case analysis, subgroup populations and scenario analysis.
The base-case and subgroup populations attempted to address the positioning of omalizumab within the overall stepwise treatment approach to asthma on the basis of the clinical evidence available. Omalizumab has a potential dual role in the stepwise management of severe persistent allergic asthma: (1) as a replacement for OCSs in patients on maintenance OCS (step 5) or for patients at step 4 in the process of stepping up to step 5 maintenance OCS; or (2) used in conjunction with OCSs, with a view to reducing the maintenance dose of OCS in patients at step 5. The clinical trials enrolled a mixture of patients uncontrolled at step 4 and step 5. Given the heterogeneity in the patient population and the concomitant medication used at baseline, patient subgroups were defined post hoc by stratifying patients according to different indicators of asthma severity: hospitalisations, number of exacerbations in the past year and maintenance OCS use. However, the subgroup analyses may have been underpowered to detect differences in treatments, which in turn may have reduced the comparative effectiveness and cost-effectiveness of omalizumab.
The cost-effectiveness results from the base-case analysis demonstrated variation across the separate populations. The ICER estimates were lower (and therefore more favourable towards omalizumab) in the more severe subgroup populations compared with the overall severe persistent allergic asthma population. The findings reflect the greater risk of exacerbations faced by more severe populations and the greater HRQoL improvement in day-to-day asthma symptoms conferred by omalizumab. Nonetheless, the ICER was above conventional thresholds of cost-effectiveness used by NICE in all populations, including the severe subgroup populations. The key drivers of cost-effectiveness were: (1) asthma-related mortality rates; (2) HRQoL improvement associated with omalizumab treatment; and (3) adverse effects associated with OCS use. The cost-effectiveness results were more favourable towards omalizumab using a very high asthma-related mortality risk, assuming greater HRQoL improvement with omalizumab compared with standard therapy, and incorporating large costs and health losses associated with OCS-related adverse effects. The ICER for omalizumab across all populations and scenarios were above £30,000 per additional QALY gained, except for the adult and adolescent maintenance OCS subgroup population when the higher asthma-related mortality risk of 2.478% is used.
The cost-effectiveness results from the independent assessment were noticeably different from those of the manufacturer. The ICER for the base case of adults and adolescents (£83,822) was about 2.5 times greater than the manufacturer's ICER (£35,972), whereas the ICER for the base case of children (£78,009) was closer to the manufacturer's ICER (£80,747), but well above conventional thresholds of cost-effectiveness. The difference in the cost-effectiveness results was largely as a result of differences in two key parameter inputs: (1) asthma-related mortality risk and (2) HRQoL improvement with omalizumab. The asthma-related mortality risk used by the manufacturer of 2.478% in adults and adolescents suggests that two to three asthma deaths would be expected in INNOVATE for the 100 CSS exacerbations observed in INNOVATE, and six to seven asthma deaths would be expected in APEX for the 261 CSS exacerbations observed in APEX, but no deaths attributable to asthma were observed in the trials. Therefore, the asthma-related mortality risk used in the MS for adults and adolescents is likely to be an overestimate of mortality. For children, the asthma-related mortality risk is much lower, resulting in similar ICER estimates for the assessments. In terms of HRQoL improvement with omalizumab, the manufacturer's analysis differed from the independent assessment in two aspects. Firstly, the manufacturer assumed that patients under < 12 years do not experience any HRQoL improvement with omalizumab, whereas the independent assessment assumed that they experience the same improvement as patients ≥ 12 years. Secondly, the HRQoL in the MS was informed by AQLQ scores mapped onto EQ-5D values collected in INNOVATE, whereas the independent assessment used the EQ-5D values directly collected in EXALT. The difference in utility between omalizumab responders and patients on standard care in the overall EXALT population was less than half of the INNOVATE population, but similar in the hospitalisation and maintenance OCS subgroups. Therefore, the manufacturer presented two base-case analyses providing very different results: an ICER slightly above the threshold of £30,000/QALY for patients ≥ 12 years, who were assumed to initiate treatment at an average age of 43 years, and an ICER well above the NICE threshold for children aged 6–11 years, who were assumed to initiate treatment at an average age of 9 years. As age affected the asthma-related mortality risk used in the MS, the impact of age at treatment initiation should have been considered. The manufacturer failed to provide a ‘weighted’ ICER by the age distribution of patients expected to be seen in clinical practice.
In conclusion, omalizumab is shown to improve the health outcomes of patients with uncontrolled severe persistent allergic asthma but it also substantially increases the costs. The ICER estimates are more favourable in the severe subgroup population of maintenance OCS compared with the overall population. However, the ICERs remain above conventional NICE thresholds of cost-effectiveness. The cost-effectiveness of omalizumab depends on the asthma-related mortality risk, whether HRQoL improvements with omalizumab are sustained throughout the entire treatment duration, and whether the assumptions used to estimate costs and health losses associated with OCS-related adverse effects are plausible.
Strengths and limitations of the assessment
The review of clinical effectiveness addressed five distinct questions which arose from the decision problem: the efficacy of omalizumab; the long-term efficacy of omalizumab; the steroid-sparing effect of omalizumab; the safety of omalizumab; and the adverse effects of OCSs. Although it was not possible within the constraints of a NICE MTA to conduct full systematic reviews for all of these questions, the reviews do represent a valuable appraisal of the available information required by any decision-maker considering the place of omalizumab in asthma therapy.
There is RCT-based evidence for the short- to medium-term efficacy of omalizumab in adults and adolescents aged > 12 years across a range of outcomes. This included two appropriately powered RCTs and a RCT subgroup in the licensed population. However, only one of the RCTs was a double-blind placebo-controlled trial considered to be at low risk of bias. This evidence is supported by data from a number of trials in patient populations which are slightly broader than the licensed population and by evidence of efficacy in uncontrolled observational studies.
There is less evidence available for the assessment of omalizumab in children. However, the single subgroup which conformed to the licensed criteria was an a priori subgroup from a placebo-controlled double-blind trial with a low risk of bias.
There were several limitations of the assessment of clinical evidence. Regarding the main efficacy outcome of CS exacerbations, meta-analysis of the results from primary studies could not be conducted because of the clinical and methodological heterogeneity. Thus, despite there being a good number of trials, a precise estimate of effect could not be generated. Furthermore, data from those patients who met the licence criteria but were enrolled in trials with broader populations could not be fully utilised in the assessment as relevant subgroup data could not be identified. Regarding patients on OCSs (step 5 patients), there is a lack of robust data on the effect of omalizumab on exacerbation rates and on the OCS-sparing effect of omalizumab, particularly for the paediatric population. There is also a lack of robust data on efficacy of omalizumab beyond 52 weeks in the licensed populations of both adults and children, although data from small observational studies suggested continuing efficacy. Finally, no trials that compared the use of OCSs with omalizumab at step 5 of therapy were found.
Although the adverse events of OCSs are widely known, the syntheses identified were all subject to limitations and the reliability of the data was unclear. There was a particular lack of evidence pertaining to the safety of OCS treatment in children.
For the evaluation of the cost-effectiveness of omalizumab for severe persistent allergic asthma, the areas of uncertainty identified from the previous STAs have been addressed with a series of systematic reviews, subgroup and scenario analyses. Systematic reviews were conducted to identify evidence on (1) the cost-effectiveness of omalizumab, (2) the mortality risk associated with asthma and the relationship between mortality, age and severity of exacerbations, (3) the HRQoL improvement with omalizumab in both adults and adolescents and children, and (4) the costs and health losses associated with OCS-related adverse effects. The relative efficacy and safety of omalizumab compared with OCSs have been examined by defining a post hoc maintenance OCS subgroup population. The hospitalisation and ≥ 3 exacerbation subgroups evaluated the cost-effectiveness of omalizumab in patients with severely uncontrolled asthma. The costs and health losses associated with maintenance OCS use were estimated and their impact on the cost-effectiveness results explored. The impact of uncertainty in the cost-effectiveness results have been assessed with probabilistic sensitivity analysis, scenario and additional one-way sensitivity analyses. Scenario analyses assessed the robustness of the base case results to variation in the data sources used to populate the model and alternative assumptions. One-way sensitivity analyses were used to evaluate the impact of varying particular parameter inputs on the cost-effectiveness results.
A limitation of this appraisal is the assessment of costs and health losses associated with maintenance OCS use. Within the time limits of this appraisal, it would be impossible to purposely build an economic model to assess the costs and health outcomes associated with maintenance use of OCSs. A systematic review of economic evaluations comparing steroids against any comparator for the treatment of asthma did not identify studies quantifying the costs and health losses associated with long-term OCS use. Therefore, a scenario incorporating the adverse effects of OCSs was used. This scenario required a number of assumptions to be made, which may underpin the validity of the estimates obtained. These include: (1) patients who do not receive omalizumab will continue to receive maintenance OCS for the remainder of their lifetime; (2) the excess relative risk attributable to OCSs is based solely on current exposure to OCSs, and once patients discontinue OCSs the excess relative risk becomes negligible; and (3) that health losses expressed in DALYs are equivalent to health losses expressed in QALYs.
Uncertainties
Although the efficacy of omalizumab across a range of outcomes in adults is clear, the impact of treatment on daily symptoms and QoL in children is unclear. The RCT subgroup in the licensed population did not show clear evidence of efficacy on these outcomes but was underpowered. A supportive trial indicated some efficacy but it was not clear whether this was driven by patients not on maintenance therapy. There is some uncertainty as to the OCS-sparing benefits of omalizumab; the RCT evidence in the licensed population was limited but supportive of such a benefit, but this represents an underpowered post hoc subgroup of an open-label trial. There is no randomised evidence on the efficacy of omalizumab in children on maintenance OCS or OCS-sparing potential in children.
There is a lack of evidence on the long-term safety and efficacy of omalizumab in both adults and children; although several observational studies appeared to assess longer-term outcomes, most only reported interim data. The medium-term adverse event profile of omalizumab indicates some uncertainty as to the relationship between omalizumab therapy and the incidences of arterial thrombotic events and malignancies.
The cost-effectiveness of omalizumab hinges on three main issues: (1) the mortality risk associated with asthma and the relationship between mortality, age and severity of exacerbations, (2) the HRQoL improvement with omalizumab in both adults and adolescents and children, and (3) the costs and health losses associated with OCS-related adverse effects. The asthma-related mortality risk is a major driver of cost-effectiveness and is the main reason for the difference in ICER estimates between the independent assessment presented in this report and that in the MS for adults and adolescents, and for the difference between the manufacturer's estimates between the adult and adolescent and children populations. Importantly, although the mortality risk was subject to two independent systematic reviews by the manufacturer and the assessment group, the most appropriate value remains unclear.
In addition to the asthma-related mortality risk, the HRQoL improvement with omalizumab in both adults and adolescents and children drives the differences in results between the independent and the manufacturer's assessments. In the independent assessment, patients aged < 12 years were assumed to experience the same HRQoL improvement as patients aged ≥ 12 years, whereas in the MS, patients aged < 12 years were assumed not to experience any HRQoL improvement with omalizumab up until they reached the age of 12 years. The PAQLQ scores collected during IA-05 EUP suggest that children experience some benefit from omalizumab treatment, but the difference between treatment groups did not reach statistical significance. A further source of uncertainty is whether the HRQoL improvement observed during the trials (< 1 year of follow-up) is sustained over the longer treatment durations.
The estimation of costs and health losses because of OCS-related adverse effects used in the model required a number of assumptions to be made, which may have overestimated the impact of maintenance OCS use. It is assumed that, without omalizumab, patients on maintenance OCS will continue to receive OCSs for the remainder of their lifetime, and that health losses expressed in DALYs are equivalent to health losses expressed in QALYs. If patients on standard care can discontinue maintenance OCS without omalizumab, or if health losses expressed in QALYs are lower than those expressed in DALYs, the ‘steroid-sparing’ effect of omalizumab may not be enough to drive down the ICER towards conventional cost-effectiveness thresholds.
Other relevant factors
From the MS, age at treatment initiation appears to have a major impact on the cost-effectiveness of omalizumab. The effect of age in the MS occurs because of the age-dependent asthma mortality risk used and the assumption that children do not experience HRQoL improvement with omalizumab. The independent assessment used the same asthma-related mortality rate for children and adults and adolescents, and assumed that children experience the same HRQoL improvement with omalizumab as adults and adolescents. As a result, the ICER estimates for children are similar to those for adults and adolescents. Given that there is little reason to believe that asthma is fundamentally different under and above the cut-off age of 12 years, consideration should be given to which set of assumptions are most relevant to the UK patient population.
Chapter 8 Conclusions
The decision problem relating to the use of omalizumab in clinical practice in the NHS differs depending on whether patients at step 4 or step 5 treatment are considered. For patients at step 4, omalizumab is an alternative to the addition of frequent or continuous OCSs; in patients at step 5 it is given in addition to frequent or continuous OCSs, but it may nevertheless allow a reduction in dose of OCS.
The conclusions from our review of clinical effectiveness and safety were:
Although a considerable amount of clinical research into omalizumab in the treatment of asthma in adults has been conducted, precise estimates of treatment effect cannot be calculated because of clinical and methodological heterogeneity among the studies. The value of some of the evidence was limited by the lack of data on subgroups which conformed to the licence requirements. The amount of efficacy and safety data in children was very limited.
There is limited, underpowered subgroup evidence that omalizumab reduces the incidence of CS and CSS exacerbations in the most severe patients who are uncontrolled at step 5. There is only very limited evidence for any OCS-sparing effect of omalizumab. Evidence is even more limited in children being restricted to small observational studies. There is no direct evidence comparing the effect of omalizumab with OCSs as add-on therapy.
There is evidence that at step 4, omalizumab reduces the incidence of CS and CSS exacerbations in the short to medium term. There is uncertainty around the precise size of the treatment effect, and the effects of omalizumab in the long term. The precision of individual trial estimates could not be improved on as a result of an inability to combine trials in a meta-analysis because of clinical and methodological heterogeneity. There is also uncertainty around whether the effect of omalizumab is through an effect in reducing all CS exacerbations or only CSS exacerbations. The evidence base in children regarding omalizumab's impact on exacerbations is weak, being based on a single underpowered RCT subgroup.
There is evidence of a beneficial effect of omalizumab in terms of other relevant outcomes: asthma symptoms, emergency care use, HRQoL and FEV1. Again, the evidence is limited, particularly in children in whom the evidence is much weaker and more uncertain.
The conclusions from the cost-effectiveness assessment are:
Omalizumab appears to improve the health outcomes of patients with uncontrolled severe persistent allergic asthma but it also substantially increases the costs to the NHS.
For both patient populations (adults and adolescents ≥ 12 years; children 6–11 years) and the subgroup populations (hospitalised in the year prior to treatment, maintenance OCS at treatment initiation, experiencing ≥ 3 exacerbations in the year prior to treatment), the ICER are above conventional NICE thresholds of cost-effectiveness.
The key drivers of cost-effectiveness are the asthma-related mortality risk and, to a lower extent, the HRQoL improvement with omalizumab, and the costs and health burden associated with OCS-related adverse effects.
Implications for service provision
Omalizumab reduces exacerbations and severe exacerbations. These reductions are associated with reduced unscheduled health-care use across a range of outcomes in adults, including hospitalisations. These reductions in emergency resource use by patients with severe allergic asthma represent a potential benefit to the NHS. In particular, extension of treatment to children as well as adults with severe uncontrolled allergic asthma may be expected to reduce hospitalisations in those children who respond to treatment. In addition, omalizumab enables a proportion of patients to reduce or stop their use of OCSs. Although this evidence is stronger in adults than in children, the documented risks for OCS use in children are high. OCS-related adverse events represent a cost to the NHS which may persist beyond the duration of OCS treatment (e.g. increased fracture risk as a result of bone loss). Reduction of OCS use in some patients treated with omalizumab is likely to reduce both routine and emergency service use across a range of specialties. However, despite these benefits, omalizumab does not appear to be cost-effective in the base-case model or in the scenarios explored.
Suggested research priorities
A number of research priorities were identified. These are presented below in order of their priority.
-
There is some evidence that omalizumab reduces requirements for OCSs in patients at step 5. Further research is required to establish that this effect is robust in both adult and paediatric patients. An adequately powered double-blind placebo-controlled RCT enrolling adults and children on maintenance OCS, optimised at baseline is warranted. An a priori subgroup analysis of children versus adults should be conducted. This should be a pragmatic RCT with as few exclusion criteria as possible so that patients with comorbidities are included to increase the clinical relevance of the trial. In addition to OCS-sparing, this should assess also clinical efficacy across a range of outcomes, including QoL and symptom alleviation. Both the EQ-5D and the AQLQ should be used to assess QoL, whereas the ACT should be used to assess symptoms.
-
As has been noted, one of the principal limitations of this review has been the inability fully to incorporate data from trials where the inclusion criteria did not match those of the licence. As a considerable number of patients who do meet the licence requirements have participated in such trials, it would be appropriate for an IPD meta-analysis of good-quality double-blind RCTs to be conducted which could fully explore the characteristics of patients, both within and without the licence, who derive the greatest benefit from omalizumab treatment. This should assess symptom reduction and improvements in QoL, as well as reduced exacerbations and unscheduled care.
-
The costs and health losses associated with OCS-related adverse effects were a major source of uncertainty in the assessment of the cost-effectiveness of omalizumab. Although maintenance use of OCSs is widely acknowledged to result in long-term adverse effects, such as adrenal suppression and increased risk of fracture, there is little evidence on their impact of costs and health. Given that OCSs are used for a wide range of conditions in addition to asthma, it is important to quantify the costs and health losses resulting from their long-term use.
-
It may be appropriate to establish, potentially in collaboration with the manufacturer and the NICE consultee organisations, a registry of patients treated with omalizumab therapy. This would help to address the following four issues:
-
(a) Further research is required to establish treatment effects of omalizumab on symptom and QoL improvement in children. There is a lack of randomised evidence for this, which may be a consequence of the licensed subgroup being underpowered, although limited observational evidence suggested a significant benefit.
-
(b) There is scope for further research on the efficacy of omalizumab for day-to-day symptom reduction in both adults and children, particularly as this has been identified as being of key importance by consultee submissions. Information on subgroups who meet licence criteria from existing trials which assessed primary outcomes of symptom reduction would be valuable in this respect. This would be addressed were an IPD meta-analysis (see 2 above) to be conducted. As identified above, further RCT evidence appears particularly important in paediatric licensed populations (see 1 above).
-
(c) Postmarketing surveillance and ongoing cohort studies should continue to accrue and report data in order to increase the evidence relating to the long-term safety and efficacy of omalizumab. Where possible children should also be enrolled in these studies, in order to increase the very limited evidence base in paediatric populations. Such studies should also contribute data on the persistence of treatment effect over time.
-
(d) Asthma-related mortality risk in patients with severe allergic asthma and its relationship with exacerbations. Asthma-related mortality risk is the major driver of cost-effectiveness, and, although both the manufacturer and the assessment group conducted systematic reviews of the published literature, there is still considerable uncertainty on the mortality risk associated with severe persistent allergic asthma. A registry of patients on omalizumab could record frequency of CSS exacerbations and whether a fatality occurred, which would then inform future appraisals of omalizumab and related drugs.
-
Acknowledgements
We would like to thank Belen Corbacho for providing assistance with the economic review.
Contribution of authors
Dr Gill Norman led on all stages of the clinical review from development of the protocol, through screening studies and data extraction to analysis and synthesis and production of the final report.
Ms Rita Faria led on all stages of the economic review from development of the protocol, study selection, development of the economic model and production of the final report
Ms Fiona Paton was involved in all stages of the clinical review from development of the protocol, through screening studies and data extraction to analysis and synthesis and production of the final report.
Mr Alexis Llewellyn was involved in screening studies and data extraction, analysis and synthesis and the production of the final report.
Mr Dave Fox devised the search strategy, carried out the literature searches and wrote the search methodology sections of the report.
Professor Stephen Palmer provided input at all stages of the economic review and commented on drafts of the report.
Dr Ian Clifton provided clinical advice throughout the review process and commented on the draft report.
Dr James Paton provided clinical advice throughout the review process and commented on the draft report.
Dr Nerys Woolacott provided input at all stages of the review, commented on drafts of the report and took overall responsibility for the clinical review.
Dr Claire McKenna was involved in all stages of the economic review from development of the protocol, study selection, development of the economic model and production of the final report, and took overall responsibility for the economic section.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Global Initiative for Asthma (GINA) . Global Strategy for Asthma Management and Prevention 2010. www.ginasthma.org/pdf/GINA_Report_2010.pdf.
- National Institute for Health and Clinical Excellence . NICE Technology Appraisal Guidance 133: Omalizumab for Severe Persistent Allergic Asthma 2007. www.nice.org.uk/guidance/TA133.
- Pascual RM, Peters SP. Airway remodeling contributes to the progressive loss of lung function in asthma: An overview. J Allergy Clin Immunol 2005;116:477-86. http://dx.doi.org/10.1016/j.jaci.2005.07.011.
- Baumel MJ, Du Buske L, Szefler SJ, Rosenwasser L, Nash DB. National guidelines for a novel therapy: Update on clinical trials and experience using consensus panel recommendations for incorporating omalizumab into asthma management. Pharm Ther 2006;31:276-82.
- Gibeon DS, Campbell DA, Menzies-Gow AN. The systematic assessment of difficult-to-treat asthma: Why do it?. Clin Pulm Med 2010;17:255-9. http://dx.doi.org/10.1097/CPM.0b013e3181f9d80c.
- Robinson DS, Campbell DA, Durham SR, Pfeffer J, Barnes PJ, Chung KF, et al. Systematic assessment of difficult-to-treat asthma. Eur Respir J 2003;22:478-83. http://dx.doi.org/10.1183/09031936.03.00017003.
- Heaney LG, Robinson DS. Severe asthma treatment: need for characterising patients. Lancet 2005;365:974-6. http://dx.doi.org/10.1016/S0140-6736(05)71087-4.
- NHS Information Centre for Health and Social Care . Quality and Outcomes Framework 2008 2009 Prevalence Data Tables n.d. http://data.gov.uk/dataset/quality-and-outcomes-framework-2008-2009-prevalence-data-tables (accessed 23 August 2012).
- Asthma UK. ‘Facts for journalists’ Webpage n.d. www.asthma.org.uk/news-centre/facts-for-journalists/ (accessed 23 August 2012).
- Department of Health . An Outcomes Strategy for Chronic Obstructive Pulmonary Disease (COPD) and Asthma in England 2011. www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_128428.pdf.
- National Asthma Education Prevention Program . Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol 2007;120:S94-138. http://dx.doi.org/10.1016/j.jaci.2007.09.029.
- Kelly HW. Rationale for the major changes in the pharmacotherapy section of the National Asthma Education and Prevention Program guidelines. J Allergy Clin Immunol 2007;120:989-94. http://dx.doi.org/10.1016/j.jaci.2007.01.035.
- British Thoracic Society, Scottish Intercollegiate Guidelines Network . British Guideline on the Management of Asthma: A National Clinical Guideline 2012. www.sign.ac.uk/pdf/sign101.pdf.
- National Institute for Health and Clinical Excellence . NICE Technology Appraisal Guidance 201: Omalizumab for Severe Persistent Allergic Asthma in Children Aged 6 to 11 Years 2010. www.nice.org.uk/guidance/TA201.
- Manufacturer Submission of Evidence to the National Institute of Health and Clinical Excellence: Multiple Technology Appraisal (MTA) Xolair (omalizumab) for the Treatment of Severe Persistent Allergic Asthma (review of TA133 and TA201). Camberley: Novartis Pharmaceuticals UK Ltd; 2012.
- NHS Reference Costs 2009–2010 n.d. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_123459 (accessed 24 April 2012).
- NHS collaboration of the United Kingdom Medicines Information Pharmacists’ Group and The National Prescribing Centre . New Drugs in Clinical Development: Omalizumab 2001. www.ukmi.nhs.uk/Newmaterial/html/docs/OMALIZUMAB%20FINAL.pdf.
- European Medicines Agency . Summary of Product Characteristics (Xolair) 2011. www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000606/WC500057298.pdf.
- Humbert M, Beasley R, Ayres J, Slavin R, Hebert J, Bousquet J, et al. Benefits of omalizumab as add-on therapy in patients with severe persistent asthma who are inadequately controlled despite best available therapy (GINA 2002 step 4 treatment): INNOVATE. Allergy 2005;60:309-16. http://dx.doi.org/10.1111/j.1398-9995.2004.00772.x.
- Lanier B, Bridges T, Kulus M, Taylor AF, Berhane I, Vidaurre CF. Omalizumab for the treatment of exacerbations in children with inadequately controlled allergic (IgE-mediated) asthma. J Allergy Clin Immunol 2009;124:1210-16. http://dx.doi.org/10.1016/j.jaci.2009.09.021.
- Scottish Medicines Consortium . Product Update: Omalizumab (Xolair®) 75mg, 150mg Solution for Injection As Prefilled Syringe (No: 708 11) 2011. www.scottishmedicines.org.uk/files/advice/omalizumab_Xolair_ABBREVIATE_FINAL_May_2011_for_website.pdf.
- British Medical Association and Royal Pharmaceutical Society of Great Britain . British National Formulary 2012. www.medicinescomplete.com/mc/bnf/current/129493.htm#_129493.
- Systematic reviews: CRD’s guidance for undertaking reviews in healthcare. 2009.
- Moher D, Liberati A, Tetzlaff J, Altman D. The PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009;6. https://doi.org/10.1371/journal.pmed.97.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration; n.d.
- Novartis Pharmaceuticals UK Ltd . Summary of Product Characteristics (SPC) for Xolair® (omalizumab) 2011. www.medicines.org.uk/EMC/medicine/24912/SPC/Xolair+Solution+for+Injection/ (accessed 28 December 2011).
- Golder S, Loke Y, McIntosh HM. Poor reporting and inadequate searches were apparent in systematic reviews of adverse effects. J Clin Epidemiol 2008;61:440-8. http://dx.doi.org/10.1016/j.jclinepi.2007.06.005.
- Busse WW, Morgan WJ, Gergen PJ, Mitchell HE, Gern JE, Liu AH, et al. Randomized trial of omalizumab (anti-IgE) for asthma in inner-city children. N Engl J Med 2011;364:1005-15. http://dx.doi.org/10.1056/NEJMoa1009705.
- Chanez P, Contin-Bordes C, Garcia G, Verkindre C, Didier A, De Blay F, et al. Omalizumab-induced decrease of FcRI expression in patients with severe allergic asthma. Respir Med 2010;104:1608-17. http://dx.doi.org/10.1016/j.rmed.2010.07.011.
- Ayres JG, Higgins B, Chilvers ER, Ayre G, Blogg M, Fox H. Efficacy and tolerability of anti-immunoglobulin E therapy with omalizumab in patients with poorly controlled (moderate-to-severe) allergic asthma. Allergy 2004;59:701-8. http://dx.doi.org/10.1111/j.1398-9995.2004.00533.x.
- Bousquet J, Siergiejko Z, Swiebocka E, Humbert M, Rabe KF, Smith N, et al. Persistency of response to omalizumab therapy in severe allergic (IgE-mediated) asthma. Allergy 2011;66:671-8. http://dx.doi.org/10.1111/j.1398-9995.2010.02522.x.
- Bardelas J, Figliomeni M, Kianifard F, Meng X. A 26-week, randomized, double-blind placebo-controlled, multicenter study to evaluate the effect of omalizumab on asthma control in patients with persistent allergic asthma. J Asthma 2012;49:144-52. http://dx.doi.org/10.3109/02770903.2011.648296.
- Hanania NA, Alpan O, Hamilos DL, Condemi JJ, Reyes-Rivera I, Zhu J, et al. Omalizumab in severe allergic asthma inadequately controlled with standard therapy: a randomized trial. Ann Intern Med 2011;154:573-82.
- Hoshino M, Ohtawa J. Effects of adding omalizumab, an anti-immunoglobulin E antibody, on airway wall thickening in asthma. Respiration 2012;83:520-8. http://dx.doi.org/10.1159/000334701.
- Ohta K, Miyamoto T, Amagasaki T, Yamamoto M. Efficacy and safety of omalizumab in an Asian population with moderate-to-severe persistent asthma. Respirology 2009;14:1156-65. http://dx.doi.org/10.1111/j.1440-1843.2009.01633.x.
- Vignola AM, Humbert M, Bousquet J, Boulet LP, Hedgecock S, Blogg M, et al. Efficacy and tolerability of anti-immunoglobulin E therapy with omalizumab in patients with concomitant allergic asthma and persistent allergic rhinitis: SOLAR. Allergy 2004;59:709-17. http://dx.doi.org/10.1111/j.1398-9995.2004.00550.x.
- Barnes N, Menzies-Gow A, Mansur A, Spencer D, Percival F, Niven R, et al. Effectiveness of omalizumab in severe allergic asthma: a retrospective real world study in 10 UK centres. J Asthma 2013;50:529-36.
- Braunstahl G-J, Leo J, Chien-Wei C, Maykut R, Panayiotis G, Peachey G. The eXpeRience registry: monitoring the ‘real-world’ effectiveness of omalizumab in allergic asthma n.d. www.ers-education.org/ersMade/abstract_print_11/search/3284.htm.
- Brusselle G, Michils A, Louis R, Dupont L, Van de Maele B, Delobbe A, et al. “Real-life” effectiveness of omalizumab in patients with severe persistent allergic asthma: The PERSIST study. Respir Med 2009;103:1633-42. http://dx.doi.org/10.1016/j.rmed.2009.06.014.
- Cazzola M, Camiciottoli G, Bonavia M, Gulotta C, Ravazzi A, Alessandrini A, et al. Italian real-life experience of omalizumab. Respir Med 2010;104:1410-16. http://dx.doi.org/10.1016/j.rmed.2010.04.013.
- Costello RW, Long DA, Gaine S, McDonnell T, Gilmartin JJ, Lane SJ. Therapy with omalizumab for patients with severe allergic asthma improves asthma control and reduces overall healthcare costs. Ir J Med Sci 2011;180:637-41. http://dx.doi.org/10.1007/s11845-011-0716-2.
- Deschildre A, Just J, Marguet C, Rittie JL, Derelle J, Pin I, et al. Short term improvement of asthma control by omalizumab in difficult-to-treat asthmatic children: A French national survey n.d. www.ersnet.org/learning_resources_player/abstract_print_10/main_frameset.htm.
- Brodlie M. Effect of Omalizumab on Oral Corticosteroid Requirements of Young Children With Severe Asthma; Data Relating to North East England n.d.
- Korn S, Thielen A, Seyfried S, Taube C, Kornmann O, Buhl R. Omalizumab in patients with severe persistent allergic asthma in a real-life setting in Germany. Respir Med 2009;103:1725-31. http://dx.doi.org/10.1016/j.rmed.2009.05.002.
- Molimard M, de Blay F, Didier A, Le Gros V. Effectiveness of omalizumab (Xolair) in the first patients treated in real-life practice in France. Respir Med 2008;102:71-6. http://dx.doi.org/10.1016/j.rmed.2007.08.006.
- Ohta K, Yamamoto M, Sato N, Ikeda K, Miyamoto T. One year treatment with omalizumab is effective and well tolerated in Japanese patients with moderate-to-severe persistent asthma. Allergol Int 2010;59:167-74. http://dx.doi.org/10.2332/allergolint.09-OA-0137.
- Zureik M, Molimard M, Aubier M, Levy J, Humbert M, Grimaldi-Bensouda L. Effect of omalizumab on the risk of hospitalisation in patients with uncontrolled severe asthma in real life. The PAX-LASER cohort n.d. www.ers-education.org/media/2010/ePosters/150305.html.
- Busse W, Corren J, Lanier BQ, McAlary M, Fowler-Taylor A, Cioppa GD, et al. Omalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthma. J Allergy Clin Immunol 2001;108:184-90. http://dx.doi.org/10.1067/mai.2001.117880.
- Buhl R, Hanf G, Solèr M, Bensch G, Wolfe J, Everhard F, et al. The anti-IgE antibody omalizumab improves asthma-related quality of life in patients with allergic asthma. Eur Respir J 2002;20:1088-94. http://dx.doi.org/10.1183/09031936.02.00016502.
- Holgate ST, Chuchalin AG, Hébert J, Lötvall J, Persson GB, Chung KF, et al. Efficacy and safety of a recombinant anti-immunoglobulin E antibody (omalizumab) in severe allergic asthma. Clin Exp Allergy 2004;34:632-8. http://dx.doi.org/10.1111/j.1365-2222.2004.1916.x.
- Niven R, Chung KF, Panahloo Z, Blogg M, Ayre G. Efficacy of omalizumab in patients with inadequately controlled severe persistent allergic (IgE-mediated) asthma: a subgroup analysis of an open label trial n.d.
- Buhl R, Soler M, Fox H, Ashby M, McAlary M, Cooper J, et al. Omalizumab (Xolair®, rhumab-e25) decreases hospitalization due to serious asthma exacerbations. Am J Respir Crit Care Med 2001;163.
- Braunstahl G-J, Leo J, Thirlwell J, Peachey G, Maykut R. Uncontrolled persistent allergic asthma in practice: eXpeRience registry baseline characteristics. Curr Med Res Opin 2011;27:761-7. http://dx.doi.org/10.1185/03007995.2011.557717.
- Brodlie M, McKean MM, Moss S, Spencer DA. The oral corticosteroid-sparing effect of omalizumab in children with severe asthma. Arch Dis Child 2012;97:604-9. http://dx.doi.org/10.1136/archdischild-2011-301570.
- Kirk A, Spencer D, Radwan A. Effect of omalizumab on oral corticosteroid requirements of young children with severe asthma; results of a UK survey. Thorax 2010;65.
- Domingo C, Moreno A, Jose Amengual M, Monton C, Suarez D, Pomares X. Omalizumab in the management of oral corticosteroid-dependent IGE-mediated asthma patients. Curr Med Res Opin 2011;27:45-53. http://dx.doi.org/10.1185/03007995.2010.536208.
- Gutierrez B. Persistence and compliance with omalizumab in a managed-care population. J Allergy Clin Immunol 2007;119. http://dx.doi.org/10.1016/j.jaci.2006.11.565.
- Randolph CC, Kearney D. Omalizumab therapy for moderate to severe asthma in private allergy practice: A six year experience. J Allergy Clin Immunol 2010;125.
- Stukus DR, Lang DM. A retrospective evaluation of outcomes in asthmatic patients receiving omalizumab, including patients with IgE levels > 700 IU/L n.d.
- Michils A, Vandenplas O, Brusselle G, Lee C, Van Schoor J, Gurdain S, et al. Real-life persistence beyond the first year of omalizumab treatment in patients with severe allergic asthma: The R-Pixel study n.d. www.ers-education.org/ersMade/abstract_print_11/search/3290.htm.
- Britton M, Howes T, Boland A, Saralaya D, Hepburn D, Nordstrom M, et al. Real-life effectiveness of omalizumab in patients with severe persistent allergic (IgE-mediated) asthma: Pooled data from 3 UK centres n.d. www.ers-education.org/ersMade/abstract_print_11/search/0108.htm.
- Tzortzaki EG, Georgiou A, Kampas D, Lemessios M, Markatos M, Adamidi T, et al. Long-term omalizumab treatment in severe allergic asthma: The South-Eastern Mediterranean “real-life” experience. Pulm Pharmacol Ther 2012;25:77-82. http://dx.doi.org/10.1016/j.pupt.2011.11.004.
- Chung K, Ankerst J, Rolli M, Gao J, Reisner C. Long-term asthma control with omalizumab, an anti-IgE monoclonal antibody, in patients with severe allergic asthma n.d. https://www.ersnetsecure.org/public/prg_congres.abstract?ww_i_presentation=18266.
- Storms W, Bowdish MS, Farrar JR. Omalizumab and asthma control in patients with moderate-to-severe allergic asthma: A 6-year pragmatic data review. Allergy Asthma Proc 2012;33:172-7. http://dx.doi.org/10.2500/aap.2012.33.3527.
- Barnes N, Radwan A. The APEX study: Retrospective review of oral corticosteroid use in omalizumab-treated severe allergic asthma patients in UK clinical practice n.d. www.ers-education.org/ersMade/abstract_print_11/search/0104.htm.
- King S, Patterson J, West S, McCool R, Duffy S, Glanville J, et al. A report on asthma-related mortality rates from severe exacerbations. York: York Health Economics Consortium (YHEC) for Novartis AG; 2011.
- Sweeney J, Brightling CE, Menzies-Gow A, Niven RM, Patterson CC, Heaney LG, et al. Clinical management and outcome of refractory asthma in the UK from the British Thoracic Society Difficult Asthma Registry. Thorax 2012;67:754-6. http://dx.doi.org/10.1136/thoraxjnl-2012-201869.
- Siergiejko Z, Świebocka E, Smith N, Peckitt C, Leo J, Peachey G, et al. Oral corticosteroid sparing with omalizumab in severe allergic (IgE-mediated) asthma patients. Curr Med Res Opin 2011;27:1-6. http://dx.doi.org/10.1185/03007995.2011.620950.
- Kaiser J. Medical Officer’s Efficacy Review, Genentech, Omalizumab BLA STN 103976/0. Food and Drug Administration (FDA); 2003.
- Molimard M, Buhl R, Niven R, Le Gros V, Thielen A, Thirlwell J, et al. Omalizumab reduces oral corticosteroid use in patients with severe allergic asthma: real-life data. Respir Med 2010;104:1381-5. http://dx.doi.org/10.1016/j.rmed.2010.06.001.
- Eisner M, Miller M, Chou W, Rahmaoui A, Bradley M. Omalizumab and malignancy: Interim results from the EXCELS study 2011. www.ers-education.org/ersMade/abstract_print_11/search/3285.htm.
- Starke P. FDA Clinical Review: BLA STN 103976/5149: Xolair® (omalizumab): Pediatric supplement for 6–11 years of age. Food and Drug Administration (FDA); 2009.
- European Medicines Agency (EMA) . Xolair: EPAR – Scientific Discussion 2005. www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Scientific_Discussion/human/000606/WC500057295.pdf (accessed 30 March 2012).
- European Medicines Agency (EMA) . Xolair-H-C-606-II-18: EPAR – Assessment Report – Variation 2009. www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Assessment_Report_-_Variation/human/000606/WC500057307.pdf (accessed 30 March 2012).
- Medicines and Healthcare Products Regulatory Agency (MHRA) . Omalizumab: potential risk of arterial thrombotic events. Drug Safety Update 2011;4. www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON108685 (accessed 30 March 2012).
- Buhl R, Fernandez Vidaurre C, Blogg M, Zhu J, Eisner MD, Canvin J, et al. No difference observed in the risk of malignancy in patients exposed to omalizumab compared with controls n.d. www.ers-education.org/ersMade/abstract_print_11/search/3335.htm.
- Corren J, Casale TB, Lanier B, Buhl R, Holgate S, Jimenez P. Safety and tolerability of omalizumab. Clin Exp Allergy 2009;39:788-97. http://dx.doi.org/10.1111/j.1365-2222.2009.03214.x.
- Rodrigo GJ, Neffen H, Castro-Rodriguez JA. Efficacy and safety of subcutaneous omalizumab vs. placebo as add-on therapy to corticosteroids for children and adults with asthma: a systematic review. Chest 2011;139:28-35. http://dx.doi.org/10.1378/chest.10-1194.
- Limb SL, Starke PR, Lee CE, Chowdhury BA. Delayed onset and protracted progression of anaphylaxis after omalizumab administration in patients with asthma. J Allergy Clin Immunol 2007;120:1378-81. http://dx.doi.org/10.1016/j.jaci.2007.09.022.
- Tan RA, Corren J. Safety of omalizumab in asthma. Expert Opin Drug Saf 2011;10:463-71. http://dx.doi.org/10.1517/14740338.2011.563840.
- Busse W, Buhl R, Vidaurre CF, Blogg M, Zhu J, Eisner MD, et al. Omalizumab and the risk of malignancy: results from a pooled analysis. J Allergy Clin Immunol 2012;129:983-9.
- Hoes JN, Jacobs JWG, Verstappen SMM, Bijlsma JWJ, Van der Heijden GJMG. Adverse events of low- to medium-dose oral glucocorticoids in inflammatory diseases: a meta-analysis. Ann Rheum Dis 2009;68:1833-8. http://dx.doi.org/10.1136/ard.2008.100008.
- Sarnes E, Crofford L, Watson M, Dennis G, Kan H, Bass D. Incidence and US Costs of Corticosteroid-Associated Adverse Events: A Systematic Literature Review. Clin Ther 2011;33:1413-32. http://dx.doi.org/10.1016/j.clinthera.2011.09.009.
- Manson SC, Brown RE, Cerulli A, Vidaurre CF. The cumulative burden of oral corticosteroid side effects and the economic implications of steroid use. Respir Med 2009;103:975-94. http://dx.doi.org/10.1016/j.rmed.2009.01.003.
- Allen DB, Mullen M, Mullen B. A meta-analysis of the effect of oral and inhaled corticosteroids on growth. J Allergy Clin Immunol 1994;93:967-76. http://dx.doi.org/10.1016/S0091-6749(94)70043-5.
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. BMJ 1996;313:275-83. http://dx.doi.org/10.1136/bmj.313.7052.275.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess 2004;8:1-158.
- Novartis Pharmaceuticals UK Ltd . Xolair® (omalizumab). Single Technology Appraisal (STA). Manufacturer Submission of Evidence 2007. www.nice.org.uk/nicemedia/live/11686/37589/37589.pdf (accessed 30 March 2012).
- Novartis Pharmaceuticals UK Ltd . Xolair® (omalizumab) for Severe Persistent Allergic Asthma in Children Aged 6–≪12 Years. Single Technology Appraisal (STA). Manufacturer Submission of Evidence 2007. www.nice.org.uk/nicemedia/live/12266/48874/48874.pdf (accessed 30 March 2012).
- Oba Y, Salzman GA. Cost-effectiveness analysis of omalizumab in adults and adolescents with moderate-to-severe allergic asthma. J Allergy Clin Immunol 2004;114:265-9. http://dx.doi.org/10.1016/j.jaci.2004.05.049.
- Wu AC, Paltiel AD, Kuntz KM, Weiss ST, Fuhlbrigge AL. Cost-effectiveness of omalizumab in adults with severe asthma: results from the Asthma Policy Model. J Allergy Clin Immunol 2007;120:1146-52. http://dx.doi.org/10.1016/j.jaci.2007.07.055.
- Campbell JD, Spackman DE, Sullivan SD. The costs and consequences of omalizumab in uncontrolled asthma from a USA payer perspective. Allergy 2010;65:1141-8.
- Dewilde S, Turk F, Tambour M, Sandstrom T. The economic value of anti-IgE in severe persistent, IgE-mediated (allergic) asthma patients: adaptation of INNOVATE to Sweden. Curr Med Res Opin 2006;22:1765-76. http://dx.doi.org/10.1185/030079906X132389.
- Brown R, Turk F, Dale P, Bousquet J. Cost-effectiveness of omalizumab in patients with severe persistent allergic asthma. Allergy 2007;62:149-53. http://dx.doi.org/10.1111/j.1398-9995.2006.01310.x.
- Dal Negro RW, Guerriero M, Micheletto C, Tognella S, Visconti M. Changes in total IgE plasma concentration measured at the third month during anti-IgE treatment predict future exacerbation rates in difficult-to-treat atopic asthma: a pilot study. J Asthma 2011;48:437-41. http://dx.doi.org/10.3109/02770903.2011.578316.
- Dal Negro RW, Pradelli L, Tognella S, Micheletto C, Iannazzo S. Cost-utility of add-on omalizumab in difficult-to-treat allergic asthma in Italy. Eur Ann Allergy Clin Immunol 2011;43:45-53.
- Soler M. Omalizumab, a monoclonal antibody against IgE for the treatment of allergic diseases. Int J Clin Pract 2001;55:480-3.
- Bousquet J, Cabrera P, Berkman N, Buhl R, Holgate S, Wenzel S, et al. The effect of treatment with omalizumab, an anti-IgE antibody, on asthma exacerbations and emergency medical visits in patients with severe persistent asthma. Allergy 2005;60:302-8. http://dx.doi.org/10.1111/j.1398-9995.2004.00770.x.
- Lowhagen O, Ekstrom L, Holmberg S, Wennerblom B, Rosenfeldt M. Experience of an emergency mobile asthma treatment programme. Resuscitation 1997;35:243-7. http://dx.doi.org/10.1016/S0300-9572(97)00059-2.
- Sullivan S, Eisner MC, JD, Omachi T. Risk of mortality associated with asthma exacerbation n.d. http://ajrccm.atsjournals.org/cgi/reprint/179/1_MeetingAbstracts/A4770.
- Lecomte P, Lee CS, Van Nooten FE, Thompson CL. Cost-effectiveness analysis of xolair under real life conditions in Belgian patients with severe allergic asthma. Value Health 2009;12.
- Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al. Omalizumab for the treatment of severe persistent allergic asthma. Health Technol Assess 2009;13:31-9.
- Tsuchiya A, Brazier J, McColl E, Parkin D. Deriving preference-based single indices from non-preference-based condition-specific instruments: Converting AQLQ into EQ-5D indices. Sheffield: ScHARR; 2002.
- Lloyd A, Price D, Brown R. The impact of asthma exacerbations on health-related quality of life in moderate to severe asthma patients in the UK. Prim Care Respir J 2007;16:22-7. http://dx.doi.org/10.3132/pcrj.2007.00002.
- Guide to the methods of technology appraisal. London: NICE; 2008.
- Watson L, Turk F, James P, Holgate ST. Factors associated with mortality after an asthma admission: a national United Kingdom database analysis. Respir Med 2007;101:1659-64. http://dx.doi.org/10.1016/j.rmed.2007.03.006.
- Walker S, Burch J, McKenna C, Wright K, Griffin S, Woolacott N. Omalizumab for the treatment of severe persistent allergic asthma in children aged 6–11 years. Health Technol Assess 2011;15:13-21.
- Miller MK, Lee JH, Miller DP, Wenzel SE, Tenor Study G. Recent asthma exacerbations: A key predictor of future exacerbations. Respir Med 2007;101:481-9. http://dx.doi.org/10.1016/j.rmed.2006.07.005.
- Sullivan SD, Wenzel SE, Bresnahan BW, Zheng B, Lee JH, Pritchard M, et al. Association of control and risk of severe asthma-related events in severe or difficult-to-treat asthma patients. Allergy 2007;62:655-60. http://dx.doi.org/10.1111/j.1398-9995.2007.01383.x.
- Haselkorn T, Fish JE, Zeiger RS, Szefler SJ, Miller DP, Chipps BE, et al. Consistently very poorly controlled asthma, as defined by the impairment domain of the Expert Panel Report 3 guidelines, increases risk for future severe asthma exacerbations in The Epidemiology and Natural History of Asthma: Outcomes and Treatment Regimens (TENOR) study. J Allergy Clin Immunol 2009;124:895-902. http://dx.doi.org/10.1016/j.jaci.2009.07.035.
- Seddon PC, Heaf DP. Long term outcome of ventilated asthmatics. Arch Dis Child 1990;65:1324-7. http://dx.doi.org/10.1136/adc.65.12.1324.
- Kearney SE, Graham DR, Atherton ST. Acute severe asthma treated by mechanical ventilation: a comparison of the changing characteristics over a 17 yr period. Respir Med 1998;92:716-21. http://dx.doi.org/10.1016/S0954-6111(98)90001-4.
- Gupta D, Keogh B, Chung KF, Ayres JG, Harrison DA, Goldfrad C, et al. Characteristics and outcome for admissions to adult, general critical care units with acute severe asthma: a secondary analysis of the ICNARC Case Mix Programme Database. Crit Care 2004;8:R112-21. http://dx.doi.org/10.1186/cc2835.
- Wildman MJ, Sanderson CFB, Groves J, Reeves BC, Ayres JG, Harrison D, et al. Survival and quality of life for patients with COPD or asthma admitted to intensive care in a UK multicentre cohort: the COPD and Asthma Outcome Study (CAOS). Thorax 2009;64:128-32. http://dx.doi.org/10.1136/thx.2007.091249.
- United Kingdom, Interim Life Tables, 1980–82 to 2008–10 (EXCEL Sheet 858Kb) 2011. www.ons.gov.uk/ons/rel/lifetables/interim-life-tables/2008-2010/sum-ilt-2008-10.html (accessed 26 April 2012).
- Curtis L. Unit Costs of Health and Social Care 2010 2010. www.pssru.ac.uk/uc/uc2010contents.htm (accessed 12 December 2011).
- Gurwitz JH, Bohn RL, Glynn RJ, Monane M, Mogun H, Avorn J. Glucocorticoids and the risk for initiation of hypoglycemic therapy. Arch Intern Med 1994;154:97-101. http://dx.doi.org/10.1001/archinte.1994.00420010131015.
- Blackburn D, Hux J, Mamdani M. Quantification of the risk of corticosteroid-induced diabetes mellitus among the elderly. J Gen Intern Med 2002;17:717-20. http://dx.doi.org/10.1046/j.1525-1497.2002.10649.x.
- Walsh LJ, Wong CA, Oborne J, Cooper S, Lewis SA, Pringle M, et al. Adverse effects of oral corticosteroids in relation to dose in patients with lung disease. Thorax 2001;56:279-84. http://dx.doi.org/10.1136/thorax.56.4.279.
- Varas-Lorenzo C, Alberto Garcia Rodriguez L, Maguire A, Castellsague J, Perez-Gutthann S. Use of oral corticosteroids and the risk of acute myocardial infarction. Atherosclerosis 2007;192:376-83. http://dx.doi.org/10.1016/j.atherosclerosis.2006.05.019.
- Huiart L, Ernst P, Ranouil X, Suissa S. Oral corticosteroid use and the risk of acute myocardial infarction in chronic obstructive pulmonary disease. Can Respir J 2006;13:134-8.
- van Staa TP, Geusens P, Pols HAP, de Laet C, Leufkens HGM, Cooper C. A simple score for estimating the long-term risk of fracture in patients using oral glucocorticoids. QJM 2005;98:191-8. http://dx.doi.org/10.1093/qjmed/hci029.
- Donnan PT, Libby G, Boyter AC, Thompson P. The population risk of fractures attributable to oral corticosteroids. Pharmacoepidemiol Drug Saf 2005;14:177-86. http://dx.doi.org/10.1002/pds.1075.
- Steinbuch M, Youket TE, Cohen S. Oral glucocorticoid use is associated with an increased risk of fracture. Osteoporos Int 2004;15:323-8. http://dx.doi.org/10.1007/s00198-003-1548-3.
- Garbe E, LeLorier J, Boivin JF, Suissa S. Risk of ocular hypertension or open-angle glaucoma in elderly patients on oral glucocorticoids. Lancet 1997;350:979-82. http://dx.doi.org/10.1016/S0140-6736(97)03392-8.
- Piper JM, Ray WA, Daugherty JR, Griffin MR. Corticosteroid use and peptic ulcer disease: Role of nonsteroidal anti-inflammatory drugs. Ann Intern Med 1991;114:735-40.
- Curtis JR, Westfall AO, Allison J, Bijlsma JW, Freeman A, George V, et al. Population-based assessment of adverse events associated with long-term glucocorticoid use. Arthritis Rheum 2006;55:420-6. http://dx.doi.org/10.1002/art.21984.
- Wang JJ, Rochtchina E, Tan AG, Cumming RG, Leeder SR, Mitchell P. Use of inhaled and oral corticosteroids and the long-term risk of cataract. Ophthalmology 2009;116:652-7. http://dx.doi.org/10.1016/j.ophtha.2008.12.001.
- Zonana-Nacach A, Barr SG, Magder LS, Petri M. Damage in systemic lupus erythematosus and its association with corticosteroids. Arthritis Rheum 2000;43:1801-8. http://dx.doi.org/10.1002/1529-0131(200008)43:8<1801::AID-ANR16>3.0.CO;2-O.
- Suissa S. Relative excess risk: An alternative measure of comparative risk. Am J Epidemiol 1999;150:279-82. http://dx.doi.org/10.1093/oxfordjournals.aje.a009999.
- WHO Disease and Injury Country Estimates; Burden of Disease; Table 2. Estimated DALYs per 100,000 population by cause, and Member State, United Kingdom. World Health Organization; 2004.
- Murray CJL, Acharya AK. Understanding DALYs. J Health Econ 1997;16:703-30. http://dx.doi.org/10.1016/S0167-6296(97)00004-0.
- Williams A . Calculating the global burden of disease: Time for a strategic reappraisal?. Health Econ 1999;8:1-8. http://dx.doi.org/10.1002/(SICI)1099-1050(199902)8:1<1::AID-HEC399>3.0.CO;2-B.
- Sassi F. Calculating QALYs, comparing QALY and DALY calculations. Health Policy Plan 2006;21:402-08. http://dx.doi.org/10.1093/heapol/czl018.
- National Institute for Health and Clinical Excellence (NICE) . Human Growth Hormone (somatropin) for the Treatment of Growth Failure in Children 2010. www.nice.org.uk/guidance/TA188 (accessed 30 March 2012).
- Heaney LG. The effect of the Omalizumab dosing table expansion on the size of the population of severe persistent allergic asthma patients potentially eligible for omalizumab therapy: analysis of data from the BTS Difficult Asthma Registry. Centre for Infection and Immunity, Queen’s University of Belfast, on behalf of the British Thoracic Society Difficult Asthma Network; n.d.
- Heaney LG, Brightling CE, Menzies-Gow A, Stevenson M, Niven RM. British Thoracic Society Difficult Asthma Network . Refractory asthma in the UK: cross-sectional findings from a UK multicentre registry. Thorax 2010;65:787-94. http://dx.doi.org/10.1136/thx.2010.137414.
- de Vries F, Setakis E, Zhang B, van Staa TP. Long-acting beta2-agonists in adult asthma and the pattern of risk of death and severe asthma outcomes: a study using the GPRD. Eur Respir J 2010;36:494-502. http://dx.doi.org/10.1183/09031936.00124209.
- Aburuz S, Gamble J, Heaney LG. Assessment of impairment in health-related quality of life in patients with difficult asthma: psychometric performance of the Asthma Quality of Life Questionnaire. Respirology 2007;12:227-33. http://dx.doi.org/10.1111/j.1440-1843.2006.01020.x.
- Steuten L, Palmer S, Vrijhoef B, van Merode F, Spreeuwenberg C, Severens H. Cost-utility of a disease management program for patients with asthma. Int J Technol Assess Health Care 2007;23:184-91. http://dx.doi.org/10.1017/S0266462307070298.
- Fuhlbrigge AL, Bae SJ, Weiss ST, Kuntz KM, Paltiel AD. Cost-effectiveness of inhaled steroids in asthma: impact of effect on bone mineral density. J Allergy Clin Immunol 2006;117:359-66. http://dx.doi.org/10.1016/j.jaci.2005.10.036.
- Johannesson M, Weinstein S. On the decision rules of cost-effectiveness analysis. J Health Econ 1993;12:459-67. http://dx.doi.org/10.1016/0167-6296(93)90005-Y.
- Briggs A, Claxton K, Sculpher M. Decision Modelling for Health Economic Evaluation 2005.
- World Health Organization . Global Burden of Disease 2004 Summary Tables n.d. www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0CEsQFjAA&url=http%3A%2F%2Fwww.who.int%2Fentity%2Fhealthinfo%2Fglobal_burden_disease%2FDALYMDG_00_2004.xls&ei=zVnkT5nCIuag0QWLp8n0CA&usg=AFQjCNH2XdlwuILXVa2qemtubIl-J_qovw (accessed 6 March 2012).
- World Health Organization . Global Burden of Disease 2004 Update: Disability Weights for Diseases and Conditions 2004. www.who.int/healthinfo/global_burden_disease/GBD2004_DisabilityWeights.pdf (accessed 30 March 2012).
- Sullivan PW, Slejko JF, Sculpher MJ, Ghushchyan V. Catalogue of EQ-5D Scores for the United Kingdom. Med Decis Making 2011;31:800-4. http://dx.doi.org/10.1177/0272989X11401031.
- McLoughlin H, Hart-Thomas A, Slough J, Capstick T. Use of a protocol to select patients for omalizumab treatment n.d. www.ersnet.org/learning_resources_player/abstract_print_08/search/1648.htm.
- Lanes SF, Garcia Rodriguez LA, Huerta C. Respiratory medications and risk of asthma death. Thorax 2002;57:683-6. http://dx.doi.org/10.1136/thorax.57.8.683.
- Sturdy PM, Victor CR, Anderson HR, Bland JM, Butland BK, Harrison BDW, et al. Psychological, social and health behaviour risk factors for deaths certified as asthma: a national case–control study. Thorax 2002;57:1034-9. http://dx.doi.org/10.1136/thorax.57.12.1034.
- Hansell A, Hollowell J, McNiece R, Nichols T, Strachan D. Validity and interpretation of mortality, health service and survey data on COPD and asthma in England. Eur Respir J 2003;21:279-86. http://dx.doi.org/10.1183/09031936.03.00006102.
- Anderson HR, Ayres JG, Sturdy PM, Bland JM, Butland BK, Peckitt C, et al. Bronchodilator treatment and deaths from asthma: case–control study. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.38316.729907.8F.
- Harrison B, Stephenson P, Mohan G, Nasser S. An ongoing Confidential Enquiry into asthma deaths in the Eastern Region of the UK, 2001–2003. Prim Care Respir J 2005;14:303-13. http://dx.doi.org/10.1016/j.pcrj.2005.08.004.
- Panickar JR, Dodd SR, Smyth RL, Couriel JM. Trends in deaths from respiratory illness in children in England and Wales from 1968 to 2000. Thorax 2005;60:1035-8. http://dx.doi.org/10.1136/thx.2005.044750.
- Sturdy PM, Butland BK, Anderson HR, Ayres JG, Bland JM, Harrison BDW, et al. Deaths certified as asthma and use of medical services: a national case–control study. Thorax 2005;60:909-15. http://dx.doi.org/10.1136/thx.2004.025593.
- Fleming DM, Cross KW, Sunderland R, Ross AM. Comparison of the seasonal patterns of asthma identified in general practitioner episodes, hospital admissions, and deaths. Thorax 2000;55:662-5. http://dx.doi.org/10.1136/thorax.55.8.662.
- Tarride J-E, Burke N, Bischof M, Hopkins RB, Goeree L, Campbell K, et al. A review of health utilities across conditions common in paediatric and adult populations. Health Qual Life Outcomes 2010;8. http://dx.doi.org/10.1186/1477-7525-8-12.
- Willems DCM, Joore MA, Hendriks JJE, Wouters EFM, Severens JL. Cost-effectiveness of a nurse-led telemonitoring intervention based on peak expiratory flow measurements in asthmatics: results of a randomised controlled trial. Cost Eff Resour Alloc 2007;5. http://dx.doi.org/10.1186/1478-7547-5-10.
- Burstrom K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res 2001;10:621-35. http://dx.doi.org/10.1023/A:1013171831202.
- Ko Y, Coons SJ. Self-reported chronic conditions and EQ-5D index scores in the US adult population. Curr Med Res Opin 2006;22:2065-71. http://dx.doi.org/10.1185/030079906X132622.
- Lubetkin EI, Jia H, Franks P, Gold MR. Relationship among sociodemographic factors, clinical conditions, and health-related quality of life: Examining the EQ-5D in the U.S. general population. Qual Life Res 2005;14:2187-96. http://dx.doi.org/10.1007/s11136-005-8028-5.
- Polley L, Yaman N, Heaney L, Cardwell C, Murtagh E, Ramsey J, et al. Impact of cough across different chronic respiratory diseases: comparison of two cough-specific health-related quality of life questionnaires. Chest 2008;134:295-302. http://dx.doi.org/10.1378/chest.07-0141.
- Saarni SI, Härkänen T, Sintonen H, Suvisaari J, Koskinen S, Aromaa A, et al. The impact of 29 chronic conditions on health-related quality of life: a general population survey in Finland using 15D and EQ-5D. Qual Life Res 2006;15:1403-14. http://dx.doi.org/10.1007/s11136-006-0020-1.
- Garratt AM, Hutchinson A, Russell I. Patient-assessed measures of health outcome in asthma: a comparison of four approaches. Respir Med 2000;94:597-606. http://dx.doi.org/10.1053/rmed.2000.0787.
- Sullivan P, Lawrence W, Ghushchyan V. A national catalog of preference-based scores for chronic conditions in the United States. Med Care 2005;43:736-49. http://dx.doi.org/10.1097/01.mlr.0000172050.67085.4f.
- Szende A, Leidy NK, Stahl E, Svensson K. Estimating health utilities in patients with asthma and COPD: evidence on the performance of EQ-5D and SF-6D. Qual Life Res 2009;18:267-72. http://dx.doi.org/10.1007/s11136-008-9429-z.
- McTaggart-Cowan HM, Marra CA, Yang Y, Brazier JE, Kopec JA, FitzGerald JM, et al. The validity of generic and condition-specific preference-based instruments: the ability to discriminate asthma control status. Qual Life Res 2008;17:453-62. http://dx.doi.org/10.1007/s11136-008-9309-6.
- Szende A, Svensson K, Stahl E, Meszaros A, Berta GY. Psychometric and utility-based measures of health status of asthmatic patients with different disease control level. Pharmacoeconomics 2004;22:537-47. http://dx.doi.org/10.2165/00019053-200422080-00005.
- Ferreira LN, Brito U, Ferreira PL. Quality of life in asthma patients. Rev Port Pneumol 2010;16:23-55.
- Kardos P, Wittchen HU, Muhlig S, Ritz T, Buhl R, Rabe K, et al. Controlled and uncontrolled allergic asthma in routine respiratory specialist care – a clinical-epidemiological study in Germany. Curr Med Res Opin 2011;27:1835-47. http://dx.doi.org/10.1185/03007995.2011.606805.
- Chen H, Gould MK, Blanc PD, Miller DP, Kamath TV, Lee JH, et al. Asthma control, severity, and quality of life: quantifying the effect of uncontrolled disease. J Allergy Clin Immunol 2007;120:396-402. http://dx.doi.org/10.1016/j.jaci.2007.04.040.
- Carroll AE, Downs SM. Improving decision analyses: parent preferences (utility values) for pediatric health outcomes. J Pediatr 2009;155:21-5. http://dx.doi.org/10.1016/j.jpeds.2009.01.040.
- Oga T, Nishimura K, Tsukino M, Sato S, Hajiro T, Mishima M. A comparison of the responsiveness of different generic health status measures in patients with asthma. Qual Life Res 2003;12:555-63. http://dx.doi.org/10.1023/A:1025051829223.
Appendix 1 Literature search strategies
Searches for clinical review
Searches for omalizumab and all asthma, no date, language, study design limits applied
The Cochrane Library (includes CDSR, DARE, HTA, NHS Economic Evaluation Database and CENTRAL)
Searched 14 September 2011 via http://onlinelibrary.wiley.com/o/cochrane/cochrane_search_fs.html.
Strategy
(asthma*:ti,ab or exp asthma/) and (omalizumab or xolair):ti,ab
One hundred and eighty-one total results comprising:
-
CDSR (Cochrane Reviews) – 1
-
DARE (Other systematic reviews) – 2
-
HTA (Health Technology Assessments) – 6
-
NHS Economic Evaluation Database (NHS EED; economic evaluations) – 4
-
CENTRAL (Trials) –168
MEDLINE and MEDLINE In-Process and Other Non-Indexed Citations
Database: Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations and Ovid MEDLINE(R) 1948–present.
Searched 14 September 2011 via OVID interface.
Strategy
(asthma$.ti,ab. or exp asthma/) and (omalizumab or xolair).ti,ab.
Four hundred and forty-nine results.
EMBASE
Database: EMBASE 1974 to 2011 September 13
Searched 14 September 2011 via OVID interface
Strategy
(asthma$.ti,ab. or exp asthma/) and (omalizumab or xolair).ti,ab.
Seven hundred and fifty-nine results.
NIH ClinicalTrials.gov Register
Searched 15 September 2011 via http://clinicaltrials.gov/ct2/search.
Strategy
(omalizumab or xolair) AND asthma
Ninety-two results.
Current Controlled Trials
Searched 15 September 2011 via www.controlled-trials.com/mrct/searchform. Searched all registers except NIH ClinicalTrials.gov Register (as searched above)
Strategy
(omalizumab or xolair) AND asthma
One result.
Conference Proceedings Citation Index (CPCI-S)
Searched 15 September 2011 via Wiley Web of Science interface.
Strategy
Topic=(omalizumab or xolair) AND Topic=(asthma)
Seventy-six results.
EconLit
Database: Econlit 1961 to August 2011.
Searched 16 September 2011 via OVID interface.
Strategy
(omalizumab or xolair).ti,ab.
No results.
Rhumab-e25 additional search 12 October 2011
Rhumab-e25 was identified from papers screened as a potential search term for omalizumab so all searches above were rerun with this additional term to identify any potential papers that had not been identified by the original searches. After de-duplication 22 results (13 MEDLINE, five from EMBASE and four from CENTRAL) were identified.
Searches for oral steroids and asthma, no date, language, study design limits applied
Adverse events search 31 October 2011
Searched an internal CRD database of studies of adverse events, for any relating to steroids in any condition.
Searched 31 October 2011 – 25 results, 20 from DARE and five from CDSR.
Journal of Allergy and Clinical Immunology search 9 November 2011
Searched 9 November 2011 via ScienceDirect interface.
Strategy
TITLE-ABSTR-KEY((omalizumab or xolair or rhumab-e25)) and SRCTITLEPLUS(journal of allergy and clinical immunology)
Two hundred and one results.
Search of The Cochrane Library (CDSR and DARE) 21 November 2011
Search undertaken for systematic reviews of oral steroids and asthma, ideally excluding steroid-sparing.
http://onlinelibrary.wiley.com/o/cochrane/cochrane_search_fs.html.
(asthma*:ti,ab or exp asthma/) and (steroid*:ti,ab or exp steroids/)
Searched online for systematic reviews in CDSR and DARE of any steroid AND asthma.
#1 MeSH descriptor Asthma explode all trees 8619
#2 asthma*:ti,ab 18191
#3 (#1 OR #2) 18776
#4 steroid*:ti,ab 9956
#5 MeSH descriptor Steroids explode all trees 34459
#6 (#4 OR #5) 40339
#7 (#3 AND #6) 3132
Of the 3132 total results found in The Cochrane Library, 77 were from CDSR and 32 were from DARE.
Searches for economic review
Two initial search strategies used, one narrow search for omalizumab and asthma and economics, and a broader search for all steroids and asthma and economics.
No date, language, study design limits applied
NHS Economic Evaluation Database
Searched 29 September 2011 via http://onlinelibrary.wiley.com/o/cochrane/cochrane_search_fs.html
Strategy
#1 (asthma*:ti,ab or exp asthma/) and (omalizumab or xolair):ti,ab (181)
#2 (asthma*:ti,ab or exp asthma/) (18,056)
#3 (exp steroids/ or exp adrenal cortex hormones/ or exp glucocorticoids/) (523)
#4 (steroid* or glucocorticoid* or corticosteroid* or glucosteroid* or cyclocosteroid*):ti,ab (16,791)
#5 (beclomethasone or beclometasone or beclamet or beclocort or becotide or betamethasone or betadexamethasone or flubenisolone or celeston* or cellestoderm or betnelan or oradexon or dexamethasone or dexameth or dexone or dexam-etasone or decadron or dexasone or hexadecadron or hexadrol or methylfluorprednisolone or millicorten or flunisolide or fluticasone or hydrocortisone or cortisol or cortifair or cortril or hyrocortone or cortef or epicortisol or efcortesol or methylprednisolone or medrol or metripred or urbason or mometasone or prednisolone or precortisyl or deltacortril or deltastab or prednesol or deltasone or prednisone or cortan or paramethasone or triamcinolone or aristocort or volon or atolone or kenacort or orasone or panasol or prednicen or azathioprine or imuran or "oral gold" or terbutaline or brethine or bricanyl or ciclosporin or neoral or sandimmune or methotrexate or maxtrex or panafcortelone or prednisolone or ciclesonide or alvesco or budesonide or budelin or pulmicort or qvar or "clenil modulite" or asmabec or becodisks or flixotide or asmanex):ti,ab (26,881)
#6 (#3 OR #4 OR #5) (36,782)
#7 (#2 AND #6) (6367)
Of the 181 omalizumab results in The Cochrane Library, four were from NHS EED.
Of the 6367 all-steroid results in The Cochrane Library, 50 were from NHS EED.
MEDLINE and MEDLINE In-Process and Other Non-Indexed Citations
Database: Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations and Ovid MEDLINE(R) 1948–present.
Searched 29 September 2011 via OVID interface.
Strategy
-
economics/ (26,174)
-
exp "costs and cost analysis"/ (160,106)
-
economics, dental/ (1851)
-
exp "economics, hospital"/ (17,442)
-
economics, medical/ (8506)
-
economics, nursing/ (3854)
-
economics, pharmaceutical/ (2279)
-
(econom$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. (380,928)
-
(expenditure$ not energy).ti,ab. (15,315)
-
(value adj1 money).ti,ab. (22)
-
budget$.ti,ab. (16,128)
-
or/1-11 (494,639)
-
((energy or oxygen) adj cost).ti,ab. (2506)
-
(metabolic adj cost).ti,ab. (659)
-
((energy or oxygen) adj expenditure).ti,ab. (14,101)
-
or/13-15 (16,619)
-
12 not 16 (490,742)
-
letter.pt. (743,411)
-
editorial.pt. (294,309)
-
historical-article.pt. (280,230)
-
or/18-20 (1,304,841)
-
17 not 21 (465,114)
-
animals/ (4,883,931)
-
human/ (12,102,907)
-
23 not (23 and 24) (3,590,774)
-
22 not 25 (439,448)
-
asthma$.ti,ab. or exp asthma/ (123,197)
-
(omalizumab or xolair).ti,ab. (627)
-
exp Steroids/ (654,804)
-
exp Adrenal Cortex Hormones/ (314,120)
-
exp Glucocorticoids/ (150,323)
-
(steroid$ or glucocorticoid$ or corticosteroid$ or glucosteroid$ or cyclocosteroid$).ti,ab. (256,020)
-
(beclomethasone or beclometasone or beclamet or beclocort or becotide or betamethasone or betadexamethasone or flubenisolone or celeston$ or cellestoderm or betnelan or oradexon or dexamethasone or dexameth or dexone or dexam-etasone or decadron or dexasone or hexadecadron or hexadrol or methylfluorprednisolone or millicorten or flunisolide or fluticasone or hydrocortisone or cortisol or cortifair or cortril or hyrocortone or cortef or epicortisol or efcortesol or methylprednisolone or medrol or metripred or urbason or mometasone or prednisolone or precortisyl or deltacortril or deltastab or prednesol or deltasone or prednisone or cortan or paramethasone or triamcinolone or aristocort or volon or atolone or kenacort or orasone or panasol or prednicen or azathioprine or imuran or "oral gold" or terbutaline or brethine or bricanyl or ciclosporin or neoral or sandimmune or methotrexate or maxtrex or panafcortelone or prednisolone or ciclesonide or alvesco or budesonide or budelin or pulmicort or qvar or "clenil modulite" or asmabec or becodisks or flixotide or asmanex).ti,ab. (180,136)
-
29 or 30 or 31 or 32 or 33 (875,878)
-
26 and 27 and 28 (63)
-
26 and 27 and 34 (764)
Sixty-three omalizumab and 764 all-steroid results.
EMBASE
Database: EMBASE 1974 to 2011 September 28.
Searched 29 September 2011 via OVID interface.
Strategy
-
health-economics/ (31,139)
-
exp economic-evaluation/ (172,147)
-
exp health-care-cost/ (166,241)
-
exp pharmacoeconomics/ (139,298)
-
1 or 2 or 3 or 4 (395,048)
-
(econom$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. (463,082)
-
(expenditure$ not energy).ti,ab. (18,613)
-
(value adj2 money).ti,ab. (978)
-
budget$.ti,ab. (19,534)
-
6 or 7 or 8 or 9 (482,922)
-
5 or 10 (715,320)
-
letter.pt. (747,429)
-
editorial.pt. (383,393)
-
note.pt. (447,454)
-
12 or 13 or 14 (1,578,276)
-
11 not 15 (643,388)
-
(metabolic adj cost).ti,ab. (697)
-
((energy or oxygen) adj cost).ti,ab. (2724)
-
((energy or oxygen) adj expenditure).ti,ab. (15,683)
-
17 or 18 or 19 (18,399)
-
16 not 20 (639,144)
-
exp animal/ (1,641,339)
-
exp animal-experiment/ (1,571,551)
-
nonhuman/ (3,713,974)
-
(rat or rats or mouse or mice or hamster or hamsters or animal or animals or dog or dogs or cat or cats or bovine or sheep).ti,ab,sh. (4,389,242)
-
22 or 23 or 24 or 25 (6,258,120)
-
exp human/ (12,644,651)
-
exp human-experiment/ (293,559)
-
27 or 28 (12,646,076)
-
26 not (26 and 29) (4,993,698)
-
21 not 30 (594,258)
-
asthma$.ti,ab. or exp asthma/ (175,586)
-
(omalizumab or xolair).ti,ab. (951)
-
exp steroid/ (1,006,945)
-
exp corticosteroid/ (623,162)
-
exp glucocorticoid/ (475,942)
-
(steroid$ or glucocorticoid$ or corticosteroid$ or glucosteroid$ or cyclocosteroid$).ti,ab. (309,300)
-
(beclomethasone or beclometasone or beclamet or beclocort or becotide or betamethasone or betadexamethasone or flubenisolone or celeston$ or cellestoderm or betnelan or oradexon or dexamethasone or dexameth or dexone or dexam-etasone or decadron or dexasone or hexadecadron or hexadrol or methylfluorprednisolone or millicorten or flunisolide or fluticasone or hydrocortisone or cortisol or cortifair or cortril or hyrocortone or cortef or epicortisol or efcortesol or methylprednisolone or medrol or metripred or urbason or mometasone or prednisolone or precortisyl or deltacortril or deltastab or prednesol or deltasone or prednisone or cortan or paramethasone or triamcinolone or aristocort or volon or atolone or kenacort or orasone or panasol or prednicen or azathioprine or imuran or "oral gold" or terbutaline or brethine or bricanyl or ciclosporin or neoral or sandimmune or methotrexate or maxtrex or panafcortelone or prednisolone or ciclesonide or alvesco or budesonide or budelin or pulmicort or qvar or "clenil modulite" or asmabec or becodisks or flixotide or asmanex).ti,ab. (216,195)
-
34 or 35 or 36 or 37 or 38 (1,135,863)
-
31 and 32 and 33 (124)
-
31 and 32 and 39 (2519)
One hundred and twenty-four omalizumab results.
Two thousand, five hundred and nineteen all-steroid results.
EconLit
Database: Econlit 1961 to August 2011
Searched 29 September 2011 via OVID interface
Strategy
-
asthma$.ti,ab. or exp asthma/ (135)
-
(omalizumab or xolair).ti,ab. (0)
-
(steroid$ or glucocorticoid$ or corticosteroid$ or glucosteroid$ or cyclocosteroid$).ti,ab. (36)
-
(beclomethasone or beclometasone or beclamet or beclocort or becotide or betamethasone or betadexamethasone or flubenisolone or celeston$ or cellestoderm or betnelan or oradexon or dexamethasone or dexameth or dexone or dexam-etasone or decadron or dexasone or hexadecadron or hexadrol or methylfluorprednisolone or millicorten or flunisolide or fluticasone or hydrocortisone or cortisol or cortifair or cortril or hyrocortone or cortef or epicortisol or efcortesol or methylprednisolone or medrol or metripred or urbason or mometasone or prednisolone or precortisyl or deltacortril or deltastab or prednesol or deltasone or prednisone or cortan or paramethasone or triamcinolone or aristocort or volon or atolone or kenacort or orasone or panasol or prednicen or azathioprine or imuran or "oral gold" or terbutaline or brethine or bricanyl or ciclosporin or neoral or sandimmune or methotrexate or maxtrex or panafcortelone or prednisolone or ciclesonide or alvesco or budesonide or budelin or pulmicort or qvar or "clenil modulite" or asmabec or becodisks or flixotide or asmanex).ti,ab. (21)
-
3 or 4 (53)
-
1 and 2 (0)
-
1 and 5 (16)
No results for omalizumab.
Sixteen all-steroid results.
Searches for quality of life in asthma and omalizumab, and mortality in asthma and omalizumab, no date, language, study design limits applied
Quality of Life MEDLINE and MEDLINE In-Process and Other Non-Indexed Citations
Database: Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations and Ovid MEDLINE(R) 1948–present.
Searched 7 November 2011 via OVID interface.
Strategy
-
(asthma$.ti,ab. or exp asthma/) and (omalizumab or xolair).ti,ab. (456)
-
exp life tables/ (11,127)
-
"quality of life"/ (96,456)
-
health status/ (50,314)
-
exp health status indicators/ (162,916)
-
(utilit$ approach$ or health gain or hui or hui2 or hui 2 or hui3 or hui 3).ti,ab. (1165)
-
(health measurement$ scale$ or health measurement$ questionnaire$).ti,ab. (32)
-
(standard gamble$ or categor$ scal$ or linear scal$ or linear analog$ or visual scal$ or magnitude estimat$).ti,ab. (3901)
-
(time trade off$ or rosser$ classif$ or rosser$ matrix or rosser$ distress$ or hrqol).ti,ab. (5752)
-
(index of wellbeing or quality of wellbeing or qwb).ti,ab. (158)
-
(rating scale$ or multiattribute$ health ind$ or multi attribute$ health ind$).ti,ab. (28,346)
-
(health utilit$ index or health utilit$ indices).ti,ab. (523)
-
(multiattribute$ theor$ or multi attribute$ theor$ or multiattribute$ analys$ or multi attribute$ analys$).ti,ab. (9)
-
(health utilit$ scale$ or classification of illness state$ or 15d or 15 d or 15 dimension).ti,ab. (3063)
-
(health state$ utilit$ or 12d or 12 d or 12 dimension).ti,ab. (2111)
-
well year$.ti,ab. (22)
-
(multiattribute$ utilit$ or multi attribute$ utilit$).ti,ab. (161)
-
health utilit$ scale$.ti,ab. (7)
-
(qol or 5d or 5-d or 5 dimension or quality of life or eq-5d or eq5d or eq 5d or euroqol).ti,ab. (124,856)
-
(qualy or qaly or qualys or qalys or quality adjusted life year$).ti,ab. (5080)
-
life year$ gain$.ti,ab. (1393)
-
willingness to pay.ti,ab. (1667)
-
(hye or hyes or health$ year$ equivalent$).ti,ab. (59)
-
(person trade off$ or person tradeoff$ or time tradeoff$ or time trade off$).ti,ab. (823)
-
theory utilit$.ti,ab. (6)
-
life table$.ti,ab. (6862)
-
health state$.ti,ab. (3024)
-
(sf36 or sf 36).ti,ab. (10,501)
-
(short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirtysix or shortform thirty six or short form thirtysix or short form thirty six).ti,ab. (4841)
-
(6d or 6-d or 6 dimension).ti,ab. (4857)
-
or/2-30 (394,966)
-
1 and 31 (139)
One hundred and thirty-nine results.
EMBASE
Database: EMBASE 1974 to 2011 Week 44.
Searched 7 November 2011 via OVID interface.
Strategy
-
(asthma$.ti,ab. or exp asthma/) and (omalizumab or xolair).ti,ab. (772)
-
life tables/ (3065)
-
exp "quality of life"/ (187,078)
-
health status/ (67,024)
-
health survey/ (127,969)
-
(utilit$ approach$ or health gain or hui or hui2 or hui 2 or hui3 or hui 3).ti,ab. (1392)
-
(health measurement$ scale$ or health measurement$ questionnaire$).ti,ab. (44)
-
(standard gamble$ or categor$ scal$ or linear scal$ or linear analog$ or visual scal$ or magnitude estimat$).ti,ab. (4344)
-
(time trade off$ or rosser$ classif$ or rosser$ matrix or rosser$ distress$ or hrqol).ti,ab. (7247)
-
(index of wellbeing or quality of wellbeing or qwb).ti,ab. (174)
-
(rating scale$ or multiattribute$ health ind$ or multi attribute$ health ind$).ti,ab. (35,328)
-
(health utilit$ index or health utilit$ indices).ti,ab. (591)
-
(multiattribute$ theor$ or multi attribute$ theor$ or multiattribute$ analys$ or multi attribute$ analys$).ti,ab. (14)
-
(health utilit$ scale$ or classification of illness state$ or 15d or 15 d or 15 dimension).ti,ab. (3472)
-
(health state$ utilit$ or 12d or 12 d or 12 dimension).ti,ab. (2338)
-
well year$.ti,ab. (24)
-
(multiattribute$ utilit$ or multi attribute$ utilit$).ti,ab. (198)
-
health utilit$ scale$.ti,ab. (9)
-
(qol or 5d or 5-d or 5 dimension or quality of life or eq-5d or eq5d or eq 5d or euroqol).ti,ab. (159,155)
-
(qualy or qaly or qualys or qalys or quality adjusted life year$).ti,ab. (6473)
-
life year$ gain$.ti,ab. (1694)
-
willingness to pay.ti,ab. (2093)
-
(hye or hyes or health$ year$ equivalent$).ti,ab. (74)
-
(person trade off$ or person tradeoff$ or time tradeoff$ or time trade off$).ti,ab. (929)
-
theory utilit$.ti,ab. (7)
-
life table$.ti,ab. (7138)
-
health state$.ti,ab. (3892)
-
(sf36 or sf 36).ti,ab. (13,485)
-
(short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirtysix or shortform thirty six or short form thirtysix or short form thirty six).ti,ab. (5445)
-
(6d or 6-d or 6 dimension).ti,ab. (4976)
-
or/2-30 (457,207)
-
1 and 31 (208)
Two hundred and eight results.
Mortality
MEDLINE and MEDLINE In-Process and Other Non-Indexed Citations
Database: Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations and Ovid MEDLINE(R) 1948–present.
Searched 7 November 2011 via OVID interface.
Strategy saved as omalizumab and asthma and mortality MEDLINE.
Strategy
-
exp asthma/mo (1699)
-
asthma$.ti,ab. or exp asthma/ (124,556)
-
exp Mortality/ (244,643)
-
(mortalit$ or death$).ti,ab. (753,792)
-
3 or 4 (890,229)
-
2 and 5 (4992)
-
1 or 6 (5499)
-
(omalizumab or xolair).ti,ab. (635)
-
7 and 8 (23)
Twenty-three results.
EMBASE
Database: EMBASE 1974 to 2011 Week 44.
Searched 7 November 2011 via OVID interface.
Strategy saved as omalizumab and asthma and mortality EMBASE.
Strategy
-
asthma$.ti,ab. or exp asthma/ (177,096)
-
exp Mortality/ (495,938)
-
(mortalit$ or death$).ti,ab. (890,210)
-
2 or 3 (1,079,314)
-
1 and 4 (8280)
-
(omalizumab or xolair).ti,ab. (967)
-
5 and 6 (36)
Thirty-six results.
Searches for quality of life in asthma, no date, language, study design limits applied
MEDLINE and MEDLINE In-Process In-Process and Other Non-Indexed Citations
Database: Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations and Ovid MEDLINE(R) 1948–present.
Searched 10 November 2011 via OVID interface.
Strategy
-
asthma$.ti,ab. or exp asthma/ (124,770)
-
quality adjusted life year/ (5343)
-
quality adjusted life.tw. (4537)
-
(qaly$ or qald$ or qale$ or qtime$).tw. (3805)
-
disability adjusted life.tw. (875)
-
daly$.tw. (895)
-
(sf6 or sf 6 or short form 6 or shortform 6 or sf six or sfsix or shortform six or short form six).tw. (1167)
-
(sf12 or sf 12 or short form 12 or shortform 12 or sf twelve or sftwelve or shortform twelve or short form twelve).tw. (1931)
-
(sf36 or sf 36).tw. (10,533)
-
(short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirtysix or shortform thirty six or short form thirtysix or shortform thirty six).tw. (4851)
-
(sf20 or sf 20 or short form 20 or shortform 20 or sf twenty or sftwenty or shortform twenty or short form twenty).tw. (311)
-
(qol or 5d or 5-d or 5 dimension or eq-5d or eq5d or eq 5d or euroqol or euro qol).tw. (25,543)
-
(hql or hqol or h qol or hrqol or hr qol).tw. (5632)
-
(hye or hyes).tw. (51)
-
health$ year$ equivalent$.tw. (37)
-
health utilit$.tw. (825)
-
(hui or hui1 or hui2 or hui3).tw. (725)
-
disutili$.tw. (166)
-
willingness to pay.tw. (1673)
-
standard gamble$.tw. (593)
-
time trade off.tw. (602)
-
time tradeoff.tw. (190)
-
tto.tw. (463)
-
or/2-23 (52,108)
-
1 and 24 (805)
Eight hundred and five results.
EMBASE
Database: EMBASE 1974 to 2011 Week 44.
Searched 10 November 2011 via OVID interface.
Strategy
-
asthma$.ti,ab. or exp asthma/ (177,096)
-
quality adjusted life year/ (7903)
-
quality adjusted life.tw. (5398)
-
(qaly$ or qald$ or qale$ or qtime$).tw. (5090)
-
disability adjusted life.tw. (998)
-
daly$.tw. (1104)
-
(sf6 or sf 6 or short form 6 or shortform 6 or sf six or sfsix or shortform six or short form six).tw. (1331)
-
(sf12 or sf 12 or short form 12 or shortform 12 or sf twelve or sftwelve or shortform twelve or short form twelve).tw. (2421)
-
(sf36 or sf 36).tw. (13,485)
-
(short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirtysix or shortform thirty six or short form thirtysix or shortform thirty six).tw. (5445)
-
(sf20 or sf 20 or short form 20 or shortform 20 or sf twenty or sftwenty or shortform twenty or short form twenty).tw. (277)
-
(qol or 5d or 5-d or 5 dimension or eq-5d or eq5d or eq 5d or euroqol or euro qol).tw. (32,270)
-
(hql or hqol or h qol or hrqol or hr qol).tw. (7133)
-
(hye or hyes).tw. (61)
-
health$ year$ equivalent$.tw. (41)
-
health utilit$.tw. (1001)
-
(hui or hui1 or hui2 or hui3).tw. (851)
-
disutili$.tw. (214)
-
willingness to pay.tw. (2093)
-
standard gamble$.tw. (638)
-
time trade off.tw. (698)
-
time tradeoff.tw. (196)
-
tto.tw. (585)
-
or/2-23 (65,346)
-
1 and 24 (1222)
One thousand, two hundred and twenty-two results.
Searches for mortality in asthma, no date, language, study design limits applied
MEDLINE and MEDLINE In-Process and Other Non-Indexed Citations
Database: Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations and Ovid MEDLINE(R) 1948–present.
Searched 10 November 2011 via OVID interface. Search was limited to UK only.
Strategy
-
exp asthma/mo (1701)
-
asthma$.ti,ab. or exp asthma/ (124,770)
-
exp Mortality/ (245,578)
-
(mortalit$ or death$).ti,ab. (755,946)
-
3 or 4 (892,955)
-
2 and 5 (5004)
-
1 or 6 (5511)
-
exp Great Britain/ (271,012)
-
((britain or british or uk or "united kingdom" or england or english or wales or welsh or scotland or scottish or "northern ireland" or "northern irish" or "channel islands" or "National Health Service" or NHS or "Primary Care Trust" or PCT) not ("new england" or "new south wales")).ti,ab. (208,089)
-
8 or 9 (395,197)
-
7 and 10 (433)
Four hundred and thirty-three results.
EMBASE
Database: EMBASE 1974 to 2011 Week 44.
Searched 10 November 2011 via OVID interface. Search was limited to UK only.
Strategy
-
asthma$.ti,ab. or exp asthma/ (177,096)
-
exp Mortality/ (495,938)
-
(mortalit$ or death$).ti,ab. (890,210)
-
2 or 3 (1,079,314)
-
exp United Kingdom/ (274,625)
-
((britain or british or uk or "united kingdom" or england or english or wales or welsh or scotland or scottish or "northern ireland" or "northern irish" or "channel islands" or "National Health Service" or NHS or "Primary Care Trust" or PCT) not ("new england" or "new south wales")).ti,ab. (303,111)
-
5 or 6 (474,952)
-
1 and 4 and 7 (573)
Five hundred and seventy-three results.
Appendix 2 Table of excluded studies with rationale
Not relevant study design
Ahn CJ, Baumann BM, Kysia RF, Radeos MS, Stiffler K, Camargo CA. Stability of IgE levels during acute asthma: Implications for initiation of omalizumab therapy after the emergency department visit. J Allergy Clin Immunol 2007;119:S250(977).
Anonymous. Omalizumab appears effective in patients with poorly controlled allergic asthma. Formulary 2003;197.
Anonymous. Omalizumab for allergy-related asthma. WHO Drug Information 2003:169–70.
Anti-immunoglobulin E (omalizumab) for the treatment of allergic asthma in adults. Copenhagen: Danish Centre for Evaluation and Health Technology Assessment (DACEHTA); 2003. URL: www.sst.dk/publ/Publ2004/Tidlig_varsling_05_UK.pdf (last accessed 30 March 2012).
Ayre G, Fox H, Reisner C. Evaluating Response to Omalizumab Therapy in Clinical Practice. J Allergy Clin Immunol 2006;117:S10.
Bargagli E, Rottoli P. Omalizumab treatment associated with Churg–Strauss vasculitis. Int Arch Allergy Immunol 2008;145:268.
Barry PJ, O'Mahony A, Finnegan C, O'Connor TM. Delayed allergic reactions to omalizumab: are patients reporting all cases? J Allergy Clin Immunol 2008;121:785–86.
Battisti A, Brussino L, Bucca C, Badiu I, Heffler E, Cadario G, et al. Clinical and functional monitoring, and assessment of the inflammation (with expired NO) in asthmatics treated with an anti-IgE antibody. [Italian]. GIMT – Giornale Italiano delle Malattie del Torace 2007;61:47–51.
Beeh KM, Pereno R, Chen H, Jimenez P. Adding omalizumab to high dose ICS and LABA significantly improves quality of life in patients with severe persistent allergic asthma. Eur Respir J 2006;28:440s(P2566).
Belliveau PP. Omalizumab: a monoclonal anti-IgE antibody. Medscape General Medicine 2005;7:27.
Berger W, Fox H, Ayre G, Blogg M, Massanari M, Reisner C. Add-on omalizumab improves asthma control across multiple measures of response in patients with severe persistent allergic asthma. J Allergy Clin Immunol 2006;117:S8(32).
Berger W, Ostrom N, Soler M, Hedgecock S, Fox H, Blogg M. Omalizumab significantly reduces asthma exacerbations in patients with severe persistent asthma: A pooled analysis. J Allergy Clin Immunol 2005;115:S75.
Berger WE. Monoclonal anti-IgE antibody: a novel therapy for allergic airways disease. Ann Allergy Asthma Immunol 2002;88:152–62.
Bousquet J, Cabrera P, Berkman N, Buhl R, Holgate S, Wenzel S, et al. The effect of treatment with omalizumab, an anti-IgE antibody, on asthma exacerbations and emergency medical visits in patients with severe persistent asthma. Allergy 2005;60:302–8.
Bousquet J, Holgate S, Fox H, Liu J, Castellsague J. Efficacy of omalizumab in allergic asthma patients at high risk for asthma related death. J Allergy Asthma Immunol 2002;109:Abstract 460.
Bousquet J, Holgate S, Wenzel S, Fox H, Gupta N. Omalizumab is well tolerated in patients at high risk of serious asthma-related morbidity and mortality. Allergy 2002;57:322–3.
Bousquet J, Rabe K, Humbert M, Chung KF, Berger W, Fox H, et al. Predicting and evaluating response to omalizumab in patients with severe allergic asthma. Respir Med 2007;101:1483–92.
Bousquet J, Wenzel S, Holgate S, Lumry W, Freeman P, Fox H. Predicting response to omalizumab, an anti-IgE antibody, in patients with allergic asthma. Chest 2004;125:1378–86.
Britton M, Howes T, Boland A, Saralaya D, Hepburn D, Nordstrom M, et al. Real-life effectiveness of omalizumab in patients with severe persistent allergic (IgE-mediated) asthma: Pooled data from 3 UK centres. European Respiratory Society Annual Conference. Amsterdam, 2011. Session 51 P273. URL: www.ers-education.org/ersMade/abstract_print_11/search/0108.htm (last accessed 30 March 2012).
Brunori M, Pierro R, Pignataro FS, Onelli G. Long-term treatment with monoclonal antibodies anti-IgE in severe asthma: Follow-up of ten patients. European Respiratory Society Annual Conference. Amsterdam, 2011. Session 51 P275. URL: www.ers-education.org/ersMade/abstract_print_11/search/0110.htm (last accessed 30 March 2012).
Buhl R, Soler M, Fox H, Ashby M, McAlary M, Cooper J, et al. Omalizumab (Xolair®, rhumab-e25) decreases hospitalisation due to serious asthma exacerbations. Am J Respir Crit Care Med 2001;163:A858.
Busse W, Fox H, Surrey K, Maykut R, Reisner C. Clinically relevant improvements in asthma-related quality of life in patients receiving omalizumab as add-on therapy. J Allergy Clin Immunol 2006;117:S8(30).
Busse WW, Corren J, Lanier BQ, Everhard F, Surrey K, Kirchdoerfer L. Omalizumab improves asthma specific quality of life (QoL): An analysis of data from 1071 patients. J Allergy Asthma Immunol 2002;109:Abstract 891.
Busse WW, Massanari M, Kianifard F, Geba GP. Effect of omalizumab on the need for rescue systemic corticosteroid treatment in patients with moderate-to-severe persistent IgE-mediated allergic asthma: a pooled analysis. Curr Med Res Opin 2007;23:2379–86.
Campbell JM, Wofford JD, Knutsen AP. Omalizumab treatment in children 6 to 18 years old with severe asthma at a children's medical centre. Paediatr Asthma Allergy Immunol 2008;21:129–35.
Chipps B, Buhl R, Beeh K-M, Fox H, Thomas K, Reisner C. Improvement in quality of life with omalizumab in patients with severe allergic asthma. Curr Med Res Opin 2006;22:2201–8.
Chipps B, Corren J, Finn A, Hedgecock S, Fox H, Blogg M. Omalizumab significantly improves quality of life in patients with severe persistent asthma. J Allergy Clin Immunol 2005;115:S5.
Chipps B. Systemic reaction to omalizumab. Ann Allergy Asthma Immunol 2006;97:267.
Clark J, Chiang D, Casale TB. Omalizumab in the treatment of allergic respiratory disease. J Asthma 2006;43:87–93.
Corren J, Busse W, Buhl R, Solèr M, Fox H, Fowler Taylor A, et al. Omalizumab (Xolair) decreases the risk of serious asthma exacerbations requiring hospitalisation in patients with moderate-to-severe allergic asthma. J Allergy Clin Immunol 2001;107:932.
Corren J, Casale T, Deniz Y, Ashby M. Omalizumab, a recombinant humanised anti-IgE antibody, reduces asthma-related emergency room visits and hospitalizations in patients with allergic asthma. J Allergy Clin Immunol 2003;111:87–90.
Corren J, Casale T, Lanier BQ, Blogg M, Reisner C, Gupta N. Omalizumab is well tolerated in adolescent/adult patients (≥ 12 Years) with moderate-to-severe persistent asthma. J Allergy Clin Immunol 2005;115:S75. URL: www.sciencedirect.com/science/article/pii/S0091674904035705 (last accessed 30 March 2012).
Cox L, Platts-Mills TAE, Finegold I, Schwartz LB, Simons FER, Wallace DV, et al. American Academy of Allergy, Asthma & Immunology/American College of Allergy, Asthma and Immunology Joint Task Force Report on omalizumab-associated anaphylaxis. J Allergy Clin Immunol 2007;120:1373–7.
Currie GP, Saha S, Lee DKC. Omalizumab and changes in airway hyperresponsiveness. Am J Respir Crit Care Med 2005;171:88–9.
Dal Negro RW, Guerriero M, Micheletto C, Tognella S, Visconti M. Changes in total IgE plasma concentration measured at the third month during anti-IgE treatment predict future exacerbation rates in difficult-to-treat atopic asthma: a pilot study. J Asthma 2011;48:437–41.
Deniz YM, Gupta N. Safety and tolerability of omalizumab (Xolair), a recombinant humanised monoclonal anti-IgE antibody. Clin Rev Allergy Immunol 2005;29:31–48.
Di Domenico M, Polverino M, De Rosa C, Ricci V, Bisogno A, Capasso A. Xolair: A new monoclonal drug anti-IgE antibody for the treatment of allergic asthma. Biomed Res 2011;22:111–19.
Diaz M, Hernandez M, Lis A, Reyes J, Almero R, Giner A. Effect of omalizumab on skin reactivity in seven patients with allergic severe asthma. Allergy 2008;63:561(1554).
Drug approval extension: Omalizumab for asthmatic patients with high IgE values. [German]. Deutsche Apotheker Zeitung 2010;150:32–4.
Emerging Drug List: Omalizumab for adult asthma. Ottawa: Canadian Coordinating Office for Health Technology Assessment; 2003 September. URL: www.cadth.ca/media/pdf/108_No49_omalizumab_edrug_e.pdf (last accessed 30 March 2012).
Frew AJ. Effects of anti-IgE in asthmatic subjects. Thorax 1998;53(Suppl. 2):S52–7.
Greenberger PA. Persistent severe asthma and ageing: step-up therapy with omalizumab to improve control. Ann Allergy Asthma Immunol 2010;105:408–10.
Grossman HL, Schlender A, Alperin P, Stanley EL, Zhang J. Modelling the effects of omalizumab over 5 years among patients with moderate-to-severe persistent allergic asthma. Curr Med Res Opin 2010;26:2779–93.
Hadj Tahar A. Omalizumab as add-on therapy to inhaled steroids for asthma. Issues in Emerging Health Technologies 2004;58. URL: http://cadth.ca/media/pdf/282_omalizumab_cetap_e.pdf (last accessed 30 March 2012).
Hahn E, Vo M, Hussain I. Omalizumab does not improve pulmonary function or Lessen medical therapy in patients with mild to severe persistent asthma after 6 months of treatment. J Allergy Clin Immunol 2005;115:S76.
Hanssen HP. Asthma: Omalizumab attenuates seasonal asthma attacks. [German]. Deutsche Apotheker Zeitung 2011;151:43–4.
Harris JM, Wong DA, Kapp AV. Development of the Asthma Control Composite outcome measure to predict omalizumab response. Ann Allergy Asthma Immunol 2011;107:273–80.
Hirdt AP. Effectiveness of Omalizumab in Patients with IgE Greater Than 700. J Allergy Clin Immunol 2008;121:S219.
Holgate S, Buhl R, Bousquet J, Smith N, Panahloo Z, Jimenez P. Corrigendum to “The use of omalizumab in the treatment of severe allergic asthma: A clinical experience update” [Respir Med 2009;103:1098–113] (DOI:10.1016/j.rmed.2009.03.008). Respir Med 2010;104:924.
Holgate ST, Bousquet J, Wenzel S, Fox H, Liu J, Castellsague J. Efficacy of omalizumab, an anti-immunoglobulin E antibody, in patients with allergic asthma at high risk of serious asthma-related morbidity and mortality. Curr Med Res Opin 2001;17:233–40.
Johansson SGO, Haahtela T, O'Byrne PM. Omalizumab and the immune system: an overview of preclinical and clinical data. Ann Allergy Asthma Immunol 2002;89:132–38.
Joyce DP, Jackevicius C, Chapman KR, McIvor RA, Kesten S. The placebo effect in asthma drug therapy trials: a meta-analysis. J Asthma 2000;37:303–18.
Kanemitsu Y, Kita H, Fuseya Y, Tanimura K, Katayama Y, Nisihara Y. [Therapeutic effect of omalizumab on 10 patients with severe persistent asthma]. Arerugi – Japan J Allergol 2010;59:965–73.
Kardos P, Wittchen HU, Mhlig S, Ritz T, Buhl R, Rabe K, et al. Controlled and uncontrolled allergic asthma in routine respiratory specialist care- a clinical-epidemiological study in Germany. Curr Med Res Opin 2011;27:1835–47.
Karpel J, Massanari M, Geba GP, Kianifard F, Inhaber N, Zeldin RK. Effectiveness of omalizumab in reducing corticosteroid burden in patients with moderate to severe persistent allergic asthma. Ann Allergy Asthma Immunol 2010;105:465–70.
Korenblat P, Meltzer E, Busse W, Hedgecock S, Fox H, Blogg M. Omalizumab, an anti-IgE antibody, significantly reduces emergency visits in patients with severe persistent asthma: A pooled analysis. J Allergy Clin Immunol 2005;115:S76.
Korn S, Schumann C, Kropf C, Stoiber K, Thielen A, Taube C, et al. Effectiveness of omalizumab in patients 50 years and older with severe persistent allergic asthma. Ann Allergy Asthma Immunol 2010;105:313–19.
Kourtidou-Papadeli C, Papadelis C, Perantoni E, Panagiotopoulou E, Sichletidis L. Pattern of IgE complex with omalizumab in patients treated for uncontrolled allergic asthma with initial IgE levels higher than 700 IU/mL. Allergy 2008;63:561(1553).
Kourtis G, De Serio A, Rucco A, Lotti A, Loconte F, Caiaffa M, et al. Omalizumab and retrospective symptom score and PEF monitoring in severe asthma. Allergy 2008;63:559(1548).
Kourtis G, Rucco AS, Loconte F, Caiaffa MF, Macchia L. Omalizumab in severe allergic asthma: efficacy assessment by comparison of symptom score and peak expiratory flow values before and after therapy. J Invest Allergol Clin Immunol 2010;20:451–2.
Krishnan JA, Gould M. Omalizumab for severe allergic asthma: dollars and sense. J Allergy Clin Immunol 2007;120:1015–17.
Kusnick C. Drug approval expansion: Omalizumab for children with severe asthma. [German]. Deutsche Apotheker Zeitung 2009;149:37.
Kusnick C. Severe asthma: Anaphylaxis due to the monoclonal antibody omalizumab. [German]. Deutsche Apotheker Zeitung 2007;147:32–4.
Lanier B, Marshall GD, Jr. Unanswered questions on omalizumab (Xolair) patient selection and follow-up.[Erratum appears in Ann Allergy Asthma Immunol 2004;92:581]. Ann Allergy Asthma Immunol 2004;92:198–200.
Lanier BQ, Chang TW. Will anti-IgE therapy compromise normal immune functions? Allergy Clin Immunol Int 2004;16:237–40.
Lanier BQ. Newer aspects in the treatment of paediatric and adult asthma: monoclonal anti-IgE. Ann Allergy Asthma Immunol 2003;90:13–15.
Lanier BQ. Unanswered questions and warnings involving anti-immunoglobulin E therapy based on 2-year observation of clinical experience. Allergy Asthma Proc 2005;26:435–9.
Lecomte P, Lee CS, Van Nooten FE, Rentz AM. Xolair quality of life results as measured in a Belgian observational study in patients with severe allergic asthma. Value Health 2009;12:A305(PRS36).
Ledford DK. Omalizumab: overview of pharmacology and efficacy in asthma. Expert Opin Biol Ther 2009;9:933–43.
Lemke MP, Henson MR, Fahrenholz JM. Efficacy of omalizumab in a university allergy practice. J Allergy Clin Immunol 2009;123:S79(294).
Li Bianchi E, Lucantoni G, Patrizi A. Usefulness of the treatment with Omalizumab as been confirmed in allergic patients suffering from uncontrolled asthma. [Italian]. GIMT – Giornale Italiano delle Malattie del Torace 2007;61:291–3.
Liebhaber M, Dyer Z. Home therapy with subcutaneous anti-immunoglobulin-E antibody omalizumab in 25 patients with immunoglobulin-E-mediated (allergic) asthma. J Asthma 2007;44:195–6.
Liebhaber MI, Dyer Z. The safety of home therapy with subcutaneous anti-immunoglobulin E antibody omalizumab in twenty-five patients with allergic asthma. J Allergy Clin Immunol 2007;119:S247(967).
Limb SL, Starke PR, Lee CE, Chowdhury BA. Delayed onset and protracted progression of anaphylaxis after omalizumab administration in patients with asthma. J Allergy Clin Immunol 2007;120:1378–81.
Lin RY, Rodriguez-Baez G, Bhargave GA. Omalizumab-associated anaphylactic reactions reported between January 2007 and June 2008. Ann Allergy Asthma Immunol 2009;103:442–5.
Lowe P, Tannenbaum S, Gautier A, Jimenez P, Panahloo Z. Relationship between omalizumab pharmacokinetics, immunoglobulin E pharmacodynamics and clinical symptoms in patients with severe persistent allergic (immunoglobulin E-mediated) asthma. Allergy 2008;63:561(1552).
Lowe PJ, Renard D. Omalizumab decreases IgE production in patients with allergic (IgE-mediated) asthma; PKPD analysis of a biomarker, total IgE. Br J Clin Pharmacol 2011;72:306–20.
Luskin AT, Kosinski M, Bresnahan BW, Ashby M, Wong DA. Symptom control and improved functioning: the effect of omalizumab on asthma-related quality of life (ARQL). J Asthma 2005;42:823–37.
MacGlashan D, Jr. Therapeutic efficacy of omalizumab. J Allergy Clin Immunol 2009;123:114–15.
Maek ANW, Silachamroon U. Asthma control and patient satisfaction after treatment of omalizumab among moderate to severe asthma: 1 year observation. J Allergy Clin Immunol 2009;123:S158(605).
Maselli D, Diaz J, Peters J. Omalizumab in asthmatics with IgE levels > 700 IU/ml. European Respiratory Society Annual Conference. Amsterdam, 2011. Session 51 P266. URL: www.ers-education.org/ersMade/abstract_print_11/search/0101.htm (last accessed 30 March 2012).
Massanari A, Deniz Y, Maykut R, Reisner C, Geba G. Omalizumab improves asthma outcomes irrespective of GET (LTRA) use. Clin Immunol 2005;115:S51(F1.19).
Massanari M, Kianifard F, Zeldin RK, Geba GP. Efficacy of omalizumab in cat-allergic patients with moderate-to-severe persistent asthma. Allergy Asthma Proc 2009;30:534–9.
Massanari M, Maykut R, Zeldin R, Kianifard F. Effect of omalizumab on pulmonary function and asthma-related outcome measures in patients allergic to cat dander. Clin Immunol 2007;123:S75(Sa.5).
Massanari M, Milgrom H, Pollard S, Maykut RJ, Kianifard F, Fowler-Taylor A, et al. Adding omalizumab to the therapy of adolescents with persistent uncontrolled moderate--severe allergic asthma. Clin Pediatr 2009;48:859–65.
Massanari M, Sacco P, Kianifard F, Maykut R, Zeldin R. Addition of omalizumab improved functional health status in patients with impaired quality of life associated with moderate to severe persistent allergic asthma. J Allergy Clin Immunol 2008;121:S154(592).
Maykut R, Massanari M, Kianifard F, Zeldin R. Effect of Omalizumab on asthma control and quality of life in patients with moderate severe persistent IgE-mediated asthma and allergy to house dust mite. J Allergy Clin Immunol 2008;121:S157(603).
Maykut R, Massanari M, Zeldin R, Kianifard F, Deniz Y, Reisner C, et al. In moderate-severe asthma, omalizumab reduced the need for rescue systemic steroid bursts and improved ratings of treatment effectiveness: A pooled analysis. J Allergy Clin Immunol 2006;117:S10(39).
Maykut RJ, Deniz Y, Massanari M, Reisner C, Kianifard F, Geba GP. Response of older patients with asthma to omalizumab: A pooled analysis across 5 clinical trials. Clin Immunol 2005;115:S589(F1.39).
Maykut RJ, Kianifard F, Geba GP. Response of older patients with IgE-mediated asthma to omalizumab: a pooled analysis. J Asthma 2008;45:173–81.
Maykut RJ, Massanari M, Kianifard F, Zeldin R, Geba GP. Omalizumab improves symptoms and reduces rescue beta-agonist use in older patients with uncontrolled asthma. Chest 2005;128:243S.
Mazer B. Omalizumab reduced inhaled corticosteroid use and exacerbations in childhood allergic asthma. ACP J Club 2002;136:16.
McFeeters M, Clayton S, Murphy A. Are children with severe persistent allergic asthma receiving omalizumab routinely prescribed an adrenaline auto-injector for use in the event of anaphylaxis? Thorax 2009;64(Suppl. IV):A101–A02.
Milgrom H, Anderson A. Add-on omalizumab (xolair) for moderate-to-severe, allergic asthma in children. P and T 2009;34:688–9.
Milgrom H, Fink J, Fowler-Taylor A, Fernandez Vidaurre C, Blogg M. Safety and tolerability of omalizumab in children with inadequately controlled moderate-to-severe allergic (IgE-mediated) asthma. Thorax 2009;64:A18(S31).
Milgrom H, Fowler-Taylor A, Fernandez-Vidaurre C, Jayawardene S. Safety of omalizumab therapy in children with allergic asthma. European Respiratory Society Annual Congress, 12–16 September 2009, Vienna, Austria: 471s P1214.
Milgrom H, Fowler-Taylor A, Vidaurre CF, Jayawardene S. Safety and tolerability of omalizumab in children with allergic (IgE-mediated) asthma. Curr Med Res Opin 2011;27:163–9.
Milgrom H, Magssanari M, Maykut R, Kianifard F, Zeldin R, Geba G. Omalizumab improves treatment effectiveness of children and adolescents with moderate-severe persistent IgE-mediated asthma and reduces school absenteeism. Chest 2007;132:483S.
Milgrom H, Massanari M, Maykut RJ, Kianifard F, Zeldin RK, Geba GP. Addition of omalizumab reduces school absenteeism in children with moderate to severe persistent asthma. J Allergy Clin Immunol 2007:S150(590).
Molimard M, Niven R, Buhl R, Le Gros V, Thielen A, Thirlwell J. Omalizumab therapy reduces oral corticosteroid use in patients with severe allergic (IgE-mediated) asthma: European real-life experience. European Respiratory Society Annual Congress 2009:E-communication: E1867. URL: www.ers-education.org/media/2009/eposters/1524.html (last accessed 30 March 2012).
Molimard M, Niven R, Le Gros V, McBryan D, Panahloo Z, Thirlwell J. The Anglo-French real-life experience of maintenance OCS use in omalizumab-treated patients with severe persistent allergic asthma. European Respiratory Society Annual Congress. Berlin, 2008. 345s (Poster P2011). URL: www.ersnet.org/learning_resources_player/abstract_print_08/files/226.pdf (last accessed 30 March 2012).
Namazy J, Miller MK, Wang V, Gershman A, Andrews E. The Xolair pregnancy registry (EXPECT): Design of an observational study of safety of (Omalizumab) during pregnancy in women with asthma. Birth Defects Research Part A – Clinical and Molecular Teratology 2011;91:387 Workshop W3.
Nicolini A, Campodonico C. Efficacy of omalizumab in the treatment of severe allergic asthma. [Italian]. GIMT – Giornale Italiano delle Malattie del Torace 2007;61:459–61.
Niven R, Molimard M, Buhl R, Le Gros V, Thielen A, Thirlwell J, et al. Omalizumab reduces maintenance oral corticosteroid use in patients with severe persistent allergic asthma. Thorax 2009;64(Suppl. IV):A130(P29).
Nopp A, Johansson SGO. Persistent beneficial effect after six years with Xolair. Allergy 2010;65:529–30.
Omalizumab (asthma): Too many unknowns for an anti-lgE. Prescrire Int 2007;16:179–82.
Omalizumab (Xolair) for severe persistent allergic asthma in children. Birmingham: National Horizon Scanning Centre (NHSC); 2009 February. URL: www.nhsc-healthhorizons.org.uk/files/downloads/1431/1936.44ba4c9c14edacee243338b71739fe1a.pdf.
Omalizumab (Xolair) for the treatment of severe allergic asthma. [Dutch]. Geneesmiddelenbulletin 2007;41:9–10.
Omalizumab in children: a negative risk-benefit balance in severe persistent asthma. Prescrire Int 2011;20:92.
Omalizumab Safety data from the EXCELS study. [German]. Gynakologische Praxis 2009;33:768–9.
Omalizumab: Cardiac adverse effects. Prescrire Int 2010;19:75.
Pace E, Ferraro M, Bruno A, Bousquet J, Gjomarkaj M. Anti-inflammatory effects of seven years treatment with Omalizumab in severe uncontrolled asthmatics. Allergy 2010;65:1495–6.
Pace E, Ferraro M, Bruno A, Chiappara G, Bousquet J, Gjomarkaj M. Clinical benefits of 7 years of treatment with omalizumab in severe uncontrolled asthmatics. J Asthma 2011;48:387–92.
Pacheco-Galvan A, Hinojosa-Macias M, Hurtado-Barbudo B, Gonzalez-Cervera J, Sueiro-Bendito A. [Analysis of asthma control and quality of life in severe allergic asthmatics under treatment with anti-IgE, omalizumab]. Med Clin 2009;133:460–3.
Pilette C, Coppens N, Houssiau FA, Rodenstein DO. Severe serum sickness-like syndrome after omalizumab therapy for asthma. J Allergy Clin Immunol 2007;120:972–3.
Pitts J, Sheikh S, McCoy K. Safety and efficacy of omalizumab in children with allergic asthma. European Respiratory Society Annual Conference. Amsterdam, 2011. Session 495 P4826. URL: www.ers-education.org/ersMade/abstract_print_11/search/4049.htm.
Polk B. Approval of the anti-IgE antibody omalizumab for the treatment of severe persistent bronchial asthma. [German]. Med Monatsschr Pharm 2006;29:74–5.
Pollard SJ, Maykut RJ, Massanari M, Kianifard F, Zeldin RK, Geba GP. Effect of Omalizumab on measures of control in adolescents with moderate-severe persistent asthma. J Allergy Clin Immunol 2007;119:S10(36).
Poto S, Perillo G. Efficacy of omalizumab in adolescents with severe asthma uncontrollable by conventional therapies. [Italian]. GIMT – Giornale Italiano delle Malattie del Torace 2007;61:123–5.
Price KS, Woodard L, Pingle L, Larson M, Galloway K, Graves D. Anaphylaxis to Omalizumab after 14 Months of Successful Therapy. J Allergy Clin Immunol 2006;117:S10.
Probst M, Gogolka A, Krull M, Noga O. In search of clinically relevant parameters to monitor successful Omalizumab therapy in allergic asthma. [German]. Allergologie 2011;34:299–306.
Pruzinec P, Benedik R, Helbich M. Biological treatment of persistent asthma. [Slovak]. Klinicka Imunologia a Alergologia 2009;19:31–34.
Randhawa I, Klaustermeyer WB. Oral corticosteroid-dependent asthma: a 30-year review. Ann Allergy Asthma Immunol 2007;99:291–303.
Rees PJ. Review: omalizumab reduces exacerbation and steroid use in chronic asthma. Arch Dis Child Educ Pract 2007;92:ep127.
Ruppert A-M, Averous G, Stanciu D, Deroide N, Riehm S, Poindron V, et al. Development of Churg–Strauss syndrome with controlled asthma during omalizumab treatment. J Allergy Clin Immunol 2008;121:253–4.
Schultze-Werninghaus G. Anti-IgE in respiratory diseases: Clinical evidence of efficacy and safety in allergic asthma. [German]. Allergologie 2007;30:326–33.
Schumann C, Merk T, Hundack L, Stoiber K, Thielen A, Kroegel C, et al. Efficacy of Omalizumab in the therapy of severe persistent bronchial asthma – Exclusive – Compliance and utilisation investigation under real-life conditions. Allergy 2009;64:308 P787.
Sheinkopf LE, Rafi AW, Do LT, Klaustermeyer WB, Katz RM. Reasons for discontinuation of Omalizumab therapy in the treatment of patients with moderate to severe persistent asthma. J Allergy Clin Immunol 2008;121:S139(537).
Shimizu Y, Dobashi K, Fueki N, Fueki M, Okada T, Tomioka S, et al. Changes of immunomodulatory cytokines associated with omalizumab therapy for severe persistent asthma. J Biol Regul Homeos Agents 2011;25:177–86.
Skiepko R, Zietkowski Z, Tomasiak M, Bodzenta-Lukaszyk A, Lenczewska D. Clinical efficacy and anti-inflammatory activity of anti-immunoglobulin E therapy with omalizumab in patients with severe persistent allergic asthma. Allergy 2008;63:559(1547).
Slavin RG, Ferioli C, Tannenbaum SJ, Martin C, Blogg M, Lowe PJ, et al. Asthma symptom re-emergence after omalizumab withdrawal correlates well with increasing IgE and decreasing pharmacokinetic concentrations: Commentary. [Portuguese]. Rev Port Imunoalergol 2009;17:195–6.
Slavin RG, Ferioli C, Tannenbaum SJ, Martin C, Blogg M, Lowe PJ. Asthma symptom re-emergence after omalizumab withdrawal correlates well with increasing IgE and decreasing pharmacokinetic concentrations. J Allergy Clin Immunol 2009;123:107–13.
Slavin RG, Jimenez P. Reduction of the total IgE Level by omalizumab in children and adolescents. J Asthma 2009;46:102–3.
Sorkness CA, Curry MD, Massanari M, Wildfire J. Eligibility for omalizumab dosing in children and young adults based on IgE and body weight. J Allergy Clin Immunol 2009;123:S80(298).
Stanziola AA, Battiloro G, Cianciulli F, Corbo R, Di Spirito V, Pisano V, et al. Omalizumab in the treatment of severe steroid-dependent asthma. [Italian]. GIMT – Giornale Italiano delle Malattie del Torace 2007;61:128–30.
Steiff J-O, Rudloff S, Lindemann H, Zimmer K-P. Reduction of the total immunoglobulin E level by omalizumab in children and adolescents. J Asthma 2010;47:832–3.
Steiss JO, Schmidt A, Lindemann H, Rudloff S, Staatz A, Strohner P, et al. Monitoring of omalizumab therapy in children and adolescents. [German]. Atemwegs- und Lungenkrankheiten 2011;37:131–8.
Steiss JO, Strohner P, Zimmer KP, Lindemann H. Reduction of the total IgE level by omalizumab in children and adolescents. J Asthma 2008;45:233–6.
Stute A. Bronchial asthma – Omalizumab improves disease control. [German]. Pneumologie 2011;65:399.
Tan RA, Corren J. Safety of omalizumab in asthma. Expert Opin Drug Saf 2011;10:463–71.
Tarantini F, Braido F, Baiardini I, Fumagalli F, Passalacqua G, Canonica GW. Targeted therapy for allergic asthma: predicting and evaluating response to omalizumab. Exp Rev Clin Immunol 2007;3:463–7.
Thien F. ACP journal club. Review: Omalizumab added to corticosteroids reduces exacerbations and corticosteroid use in adults and children with asthma. Ann Intern Med 2011;154:JC5–11.
Thien F. Review: omalizumab reduces asthma exacerbations and daily steroid use. ACP J Club 2004;140:13.
Verma P, Randhawa I, Klaustermeyer WB. Severe geriatric asthma: Efficacy of omalizumab in a VA population. J Allergy Clin Immunol 2011;127:AB160(607).
Walker S, Monteil M, Phelan K, Thien F. Review: Omalizumab reduces asthma exacerbations and daily steroid use. Evid Based Med 2004;9:17.
Walker S. Omalizumab reduces frequency of asthma exacerbations in children. J Pediatr 2011;159:512–13.
Warner JO. Omalizumab for childhood asthma. Expert Rev Respir Med 2010;4:5–7.
Wolfe JD, Fox H, Thirlwell J. Omalizumab demonstrates inhaled corticosteroids (ICS) sparing in asthma across a range of disease severities. J Allergy Clin Immunol 2001;107:S107(357).
Zeldin R, Massanari M, Blogg M, Jimenez P, Geba G. Treatment of moderate severe asthma with omalizumab is associated with a decrease in peripheral blood eosinophils. Eur Respir J 2007:353s (P2132).
Zeldin R, Massanari M, Maykut R, Kianifard F, Deniz Y, Reisner C, et al. Omalizumab Reduced Need for Steroid Bursts in Asthmatics Concomitantly Using Leukotrine Receptor Antagonists (LTRAs). J Allergy Clin Immunol 2006;117:S280.
Zietkowski Z, Skiepko R, Tomasiak-Lozowska MM, Bodzenta-Lukaszyk A. Anti-IgE therapy with omalizumab decreases endothelin-1 in exhaled breath condensate of patients with severe persistent allergic asthma. Respiration 2010;80:534–42.
Zietkowski Z, Tomasiak M, Lenczewska D, Bodzenta-Lukaszyk A, Skiepko R. Effectiveness of 52 weeks of omalizumab therapy in patients with severe persistent allergic asthma. Allergy 2010;65:552–3.
Not relevant intervention
Korzh O, Krasnokutskiy S, Lavrova E. Effect of Anti-IgE antibody omalizumab on airway remodelling and the expression of interleukins in asthma. J Allergy Clin Immunol 2007;119:S155(608).
Nopp A, Johansson SG, Adedoyin J, Ankerst J, Palmqvist M, Oman H. After 6 years with Xolair; a 3-year withdrawal follow-up. Allergy 2010;65:56–60.
Slavin R, Lowe P, Ferioli C, Fox H, Carpenter L, Martin C, et al. Exploring the effect on asthma control of omalizumab reduction after 28 weeks treatment. J Allergy Clin Immunol 2007;119:S308(1201).
Not relevant population
Berger W, Gupta N, McAlary M, Fowler-Taylor A. Evaluation of long-term safety of the anti-IgE antibody, omalizumab, in children with allergic asthma. Ann Allergy Asthma Immunol 2003;91:182–8.
Boulet LP, Chapman KR, Cote J, Kalra S, Bhagat R, Swystun VA, et al. Inhibitory effects of an anti-IgE antibody E25 on allergen-induced early asthmatic response. Am J Respir Crit Care Med 1997;155:1835–40.
Bradley M. A prospective, randomised, double-blind study of the efficacy of Xolair in atopic asthmatics with good lung capacity who remain difficult to treat (Exact). ClinicalTrials.gov[serial online] 2005. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/672/CN-00507672/frame.html (last accessed 30 March 2012).
Buhl R, Beeh KM, Bensch G, Noga O, O'Brien JA, Solèr M, et al. Rhumab-E25 (omalizumab, Xolair®) treatment allows sustained reduction of the need for inhaled corticosteroids in moderate/severe allergic asthma. J Allergy Clin Immunol 2001:S106(356).
Buhl R, Hanf G, Solèr M, Bensch G, Wolfe J, Everhard F, et al. The anti-IgE antibody omalizumab improves asthma-related quality of life in patients with allergic asthma. Eur Respir J 2002;20:1088–94.
Buhl R, Solèr M, Matz J, Townley R, O'Brien J, Noga O, et al. Omalizumab provides long-term control in patients with moderate-to-severe allergic asthma. Eur Respir J 2002;20:73–78.
Bush R, Watrous M, Miller D, Fick R, Kirchdoerfer L. rhuMAb-E25 improves quality of life (QoL) in adult patients with moderate-severe asthma. Am J Respir Crit Care Med 1998;157:A751.
Busse W, Corren J, Lanier BQ, McAlary M, Fowler-Taylor A, Cioppa GD, et al. Omalizumab, anti-IgE recombinant humanised monoclonal antibody, for the treatment of severe allergic asthma. J Allergy Clin Immunol 2001;108:184–90.
Chipps B, Kim K, Korenblat P, Deniz Y, Zberg B, Caroll A. Effect of omalizumab on healthcare utilisation in patients with moderate to severe allergic asthma. J Allergy Clin Immunol 2003;2:S144.
Chivato T, Prieto L, Ancochea J, Casan P, Picado C, Casafont J. Clinical profile and evolution of the patients treated with omalizumab in Spain. Allergy 2009;64:307(785).
Chung F, Fox H, Thirwell J. Omalizumab (Xolair®) increases the number of asthma controlled days in moderate-to-severe asthma patients compared to placebo. J Allergy Clin Immunol 2001:S112(373).
Cooper PJ, Lima F, Sarinho EC, Ayre G, Martin C, Fox H, et al. Safety of Anti-IgE therapy with omalizumab in allergic patients at risk of geohelminth infection. J Allergy Clin Immunol 2006;117:S9(33).
Corren J, Wood RA, Patel D, Zhu J, Fish JE. A randomised, double-blind, placebo-controlled, parallel- group study of the efficacy of omalizumab in prevention of bronchoconstriction following environmental aeroallergen exposure. J Allergy Clin Immunol 2010;125:AB72(283).
Corren J, Wood RA, Patel D, Zhu J, Yegin A, Dhillon G, et al. Effects of omalizumab on changes in pulmonary function induced by controlled cat room challenge. J Allergy Clin Immunol 2011;127:398–405.
Cruz AA, Lima F, Sarinho E, Ayre G, Martin C, Fox H, et al. Safety of anti-immunoglobulin E therapy with omalizumab in allergic patients at risk of geohelminth infection. Clin Exp Allergy 2007;37:197–207.
Djukanovi R, Wilson SJ, Kraft M, Jarjour NN, Steel M, Chung KF, et al. Effects of treatment with anti-immunoglobulin E antibody omalizumab on airway inflammation in allergic asthma. Am J Respir Crit Care Med 2004;170:583–93.
Fahy JV, Fleming HE, Wong HH, Liu JT, Su JQ, Reimann J, et al. The effect of an anti-IgE monoclonal antibody on the early- and late- phase responses to allergen inhalation in asthmatic subjects. Am J Respir Crit Care Med 1997;155:1828–34.
Finn A, Gross G, van Bavel J, Lee T, Windom H, Everhard F, et al. Omalizumab improves asthma-related quality of life in patients with severe allergic asthma. J Allergy Clin Immunol 2003;111:278–84.
Hendeles L. The effect of omalizumab on airway responsiveness to adenosine in patients with poorly controlled asthma. ClinicalTrials.gov[serial online] 2005. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/241/CN-00592241/frame.html (last accessed 30 March 2012).
Kopp M, Seyfried S, Sieder C, Stenglein S, Klimek L, Brehler R, et al. Add-on omalizumab significantly improves Global Evaluation of Treatment Effectiveness (GETE) in adult and adolescent patients with seasonal allergic asthma and comorbid seasonal allergic rhinoconjunctivitis. Allergy 2007;62:12(26).
Kopp MV, Hamelmann E, Zielen S, Kamin W, Bergmann KC, Sieder C, et al. Combination of omalizumab and specific immunotherapy is superior to immunotherapy in patients with seasonal allergic rhinoconjunctivitis and co-morbid seasonal allergic asthma. Clin Exp Allergy 2009;39:271–9.
Kroegel C, Merk T, Hundack L, Stoiber KM, Kropf C, Rüdiger S, et al. Practice-related treatment of severe persistent bronchial asthma using omalizumab in Germany: the compliance and utilisation investigation under real-life-study (XCLUSIVE). European Respiratory Society 19th Annual Congress Vienna 2009:Poster E1872. URL: www.ers-education.org/media/2009/eposters/1529.html (last accessed 30 March 2012).
Lanier R, Busse W, Corren J, Chervinsky P, Bernstein J, McAlary M, et al. Long-term improvement in asthma control and exacerbation frequency is achieved with omalizumab (xolair®) in patients with moderate-to-severe asthma. Am J Respir Crit Care Med 2001;163:A858.
Lanier B, Fowler Taylor A, Vidaurre CF, Blogg M. Number needed to treat (NNT) to prevent one exacerbation per year with omalizumab (OMA) In children with inadequately controlled allergic (IgE-mediated) asthma. European Respiratory Society Annual Congress, 18–22 September, Barcelona, Spain, 2010:472s P2640.
Massanari M, Nelson H, Casale T, Busse W, Kianifard F, Geba GP, et al. Effect of pretreatment with omalizumab on the tolerability of specific immunotherapy in allergic asthma. J Allergy Clin Immunol 2010;125:383–9.
Matz J, Fox H, Thirlwell J. Omalizumab (Xolair ®) increased FEV1 in asthma patients compared to placebo. J Allergy Clin Immunol 2001;107:S315(1028).
Milgrom H, Fick RB, Jr., Su JQ, Reimann JD, Bush RK, Watrous ML, et al. Treatment of allergic asthma with monoclonal anti-IgE antibody. rhuMAb-E25 Study Group. N Engl J Med 1999;341:1966–73.
Milgrom H, Berger W, Nayak A, Gupta N, Pollard S, McAlary M, et al. Treatment of childhood asthma with anti-immunoglobulin E antibody (omalizumab). Pediatrics 2001;108:E36.
Nayak A, Milgrom H, Berger W, Pollard S, Watrous M, Doyle J, et al. Rhumab-E25 (E25) improves quality of life (QOL) in children with allergic asthma. Am J Respir Crit Care Med 2000;161:A504.
Nelson H, Fick R, Fowler Taylor A, Ashby M, Busse W, Chervinsky P, et al. Increased time to first asthma exacerbation seen in xolair® treated patients compared with placebo. Ann Allergy Asthma Immunol 2001;98. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/295/CN-00385295/frame.html (last accessed 30 March 2012).
Noah TL. Effect of ozone on airways inflammation in allergic asthmatics treated with omalizumab. ClinicalTrials.gov[serial online] 2006. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/542/CN-00591542/frame.html (last accessed 30 March 2012).
Noga O, Hanf G, Kunkel G. Immunological and clinical changes in allergic asthmatics following treatment with omalizumab. Int Arch Allergy Immunol 2003;131:46–52.
Novartis. A 26-week, randomised, double-blind, parallel-group, placebo-controlled, multi-centre study to evaluate the effect of omalizumab on improving the tolerability of specific immunotherapy in patients with persistent allergic asthma. ClinicalTrials.gov[serial online] 2005. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/932/CN-00591932/frame.html (last accessed 30 March 2012).
O'Brien JA, Fox H, Thirlwell J. Omalizumab (Xolair®) increased the time to first exacerbations in patients with moderate-to-severe asthma compared with placebo. J Allergy Clin Immunol 2001;107:S107 [358].
Patel BM, Chiang DT, Clark JP, Romero FA, Casale TB. Effects of Omalizumab (Xolair®) on Airway Hyperresponsiveness. J Allergy Clin Immunol 2009:S263(1022).
Silkoff PE, Romero FA, Gupta N, Townley RG, Milgrom H. Exhaled nitric oxide in children with asthma receiving Xolair (omalizumab), a monoclonal anti-immunoglobulin E antibody. Pediatrics 2004;113:e308–12.
Soler M, Buhl R, Bensch G, Noga O, O'Brian J, Champain K, et al. Omalizumab (xolair, ® rhumab-e25) treatment reduces inhaled corticosteroid use in moderate/severe allergic asthma. Am J Respir Crit Care Med 2001;163:A858.
Soler M, Matz J, Townley R, Buhl R, O'Brien J, Fox H, et al. Erratum: The anti-IgE antibody omalizumab reduces exacerbations and steroid requirement in allergic asthmatics. Eur Respir J 2001;18:739–40.
No relevant outcome
Boulet L, Panahloo Z, Blogg M, Ayre G. Exploring the relationship between asthma and rhinitis response following omalizumab therapy: Patients who achieve greatest benefit for their asthma experience greatest benefit for rhinitis. J Allergy Clin Immunol 2007;119:S308(1202).
Boulet LP, Niven R. Examining the relation between asthma and rhinitis response following omalizumab therapy. Thorax 2007;62:A6(S8).
Chung KF, Holgate S, O'Brien J, Fox H, Thirlwell J. Inhaled corticosteroid dose-reducing effect of omalizumab in patients with controlled, severe asthma according to usage of inhaled long-acting beta-agonists. J Allergy Clin Immunol 2002;109:S239.
Corren J, Froehlich J, Schoenhoff M, Spector S, Rachelefsky G, Schanker H, et al. 251 Phase I study of anti-IgE recombinant humanised monoclonal antibody rhuMAB-E25 (E25) in adults with moderate to severe asthma. J Allergy Clin Immunol 1996;97:245.
Eisner MD, Yegin A, Trzaskoma B. Severity of Asthma score prospectively predicts clinical outcomes. Chest 2010;138:Supplement 823A.
Hanf G, Brachmann I, Kleine-Tebbe J, Seybold J, Kunkel G, Suttorp N, et al. Omalizumab decreased IgE-release and induced changes in cellular immunity in patients with allergic asthma. Allergy 2006;61:1141–44.
Humbert M, Boulet LP, Niven RM, Panahloo Z, Blogg M, Ayre G. Omalizumab therapy: patients who achieve greatest benefit for their asthma experience greatest benefit for rhinitis. Allergy 2009;64:81–4.
Israel E, Cohn J, Meltzer E, McCarty J, Zheng B, Carroll A. Omalizumab does not induce thrombocytropenia in treatment of asthma. J Allergy Clin Immunol 2003:S146(310).
Johansson SG, Nopp A, Oman H, Ankerst J, Cardell LO, Grönneberg R, et al. The size of the disease relevant IgE antibody fraction in relation to ‘total-IgE’ predicts the efficacy of anti-IgE (Xolair) treatment. Allergy 2009;64:1472–7.
Lowe P, Jaffe J, Martin C, Brookman L, Fox H. The effect of discontinuing omalizumab therapy on free lgE concentration. J Allergy Clin Immunol 2007:S6(22).
Martin-Rebollo M, Padilla Galo A, Alfonso MP, Alberto LN. ROMA (registry omalizumab in Malaga): Study of 84 patients. European Respiratory Society Annual Conference. Amsterdam, 2011. Session 51 P274. URL: www.ers-education.org/ersMade/abstract_print_11/search/0109.htm (last accessed 30 March 2012).
Miller DP, Tom G, Rasouliyan L, Chipps B. Patient-reported outcomes among omalizumab and salmeterol/fluticasone combination therapy patients. J Asthma 2009;46:179–85.
Noga O, Hanf G, Brachmann I, Klucken AC, Kleine-Tebbe J, Rosseau S, et al. Effect of omalizumab treatment on peripheral eosinophil and T-lymphocyte function in patients with allergic asthma. J Allergy Clin Immunol 2006;117:1493–9.
Noga O, Hanf G, Kunkel G, Kleine-Tebbe J. Basophil histamine release decreases during omalizumab therapy in allergic asthmatics. Int Arch Allergy Immunol 2008;146:66–70.
Nopp A, Johansson SG, Ankerst J, Palmqvist M, Oman H. CD-sens and clinical changes during withdrawal of Xolair after 6 years of treatment. Allergy 2007;62:1175–81.
Vennera M, Valero A, Bartra J, Muoz R, Mora R, Picado C. Omalizumab in severe uncontrolled asthma: A 2-year clinical experience. Allergy 2009;64:306(782).
Wahn U, Martin C, Freeman P, Blogg M, Jimenez P. Relationship between pretreatment specific IgE and the response to omalizumab therapy. Allergy 2009;64:1780–7.
Wechsler ME, Wong DA, Miller MK, Lawrence-Miyasaki L. Churg-strauss syndrome in patients treated with omalizumab. Chest 2009;136:507–18.
Zaidi AK, Saini SS, MacGlashan Jr DW. Changes in the Fc-epsilonRI-Beta: Fc-epsilonRI-alpha Ratio During Treatment with Omalizumab. J Allergy Clin Immunol 2009;123:S193(739).
Zielen S, Lieb A, De Monchy J, De la Motte S, Wagner F, Fuhr R, et al. Omalizumab protects against allergen-induced bronchoconstriction in patients with allergic (IgE-mediated) asthma and high baseline IgE levels. European Respiratory Society Annual Congress, 12–16 September 2009, Vienna, Austria; E1869.
Zietkowski Z, Skiepko R, Tomasiak-Lozowska MM, Lenczewska D, Bodzenta-Lukaszyk A. RANTES in exhaled breath condensate of patients with severe persistent allergic asthma during omalizumab therapy. Int Arch Allergy Immunol 2011;154:25–32.
Background/insufficient data
U.S. Food and Drug Administration (FDA). FDA Alert: Information for Healthcare Professionals: Omalizumab (marketed as Xolair). Silver Spring, MD: U.S. Food and Drug Administration (FDA); 2007 February, updated July. URL: www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm162905.htm (last accessed 30 March 2012).
Noga O, Gogolka A, Glaser S, Kunkel G, Suttorp N, Hanf G. Airway resistance as a parameter for monitoring the efficacy of omalizumab treatment in patients with allergic asthma. Allergy 2007;62:215(591).
Novartis P. The efficacy and safety of omalizumab in patients with severe persistent asthma. ClinicalTrials.gov 2003. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/364/CN-00462364/frame.html (last accessed 30 March 2012).
Heaney LG, Brightling CE, Menzies-Gow A, Stevenson M, Niven RM, British Thoracic Society Difficult Asthma Network. Refractory asthma in the UK: cross-sectional findings from a UK multicentre registry. Thorax 2010;65:787–94.
Sweeney J, Brightling CE, Menzies-Gow A, Niven RM, Patterson CC, Heaney LG, et al. Clinical management and outcome of refractory asthma in the UK: follow-up data from the British Thoracic Society Difficult Asthma Registry. Thorax 2012;67:754–6.
Unobtainable
Anonymous. Anti-IgE antibody reduces need for glucocorticosteroids [Anti–IgE Antikörper: Bedarf an Glucocorticoiden sinkt]. Deutsche Apotheker Zeitung 2000;140:1289–92.
Bush A, Pedersen S, Hedlin G, Baraldi E, Barbato A, de Benedictis F, et al. Pharmacological treatment of severe, therapy-resistant asthma in children: what can we learn from where? Eur Respir J 2011;38:947–58.
Berger W, Humbert M, Leighton T, Turk F, Hedgecock S, Ayre G, et al. Asthma patients judged by the physician to have responded to add-on omalizumab therapy have a greater percentage of symptom-free days. Proceedings of the American Thoracic Society 2006:A591 [Poster L67]. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/399/CN-00591399/frame.html (last accessed 30 March 2012).
Bousquet J, Holgate S, Wenzel S, Fox H, Liu J. Omalizumab reduces the incidence and frequency of exacerbations in patients at high-risk of serious asthma-related morbidity and mortality. Am J Respir Crit Care Med 2002:A187. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/352/CN-00400352/frame.html (last accessed 30 March 2012).
Buhl R, Soler M, Fox H, Ashby M, McAlary M, Cooper J, et al. Recombinant humanised monoclonal antibody (rhuMAb) E25 in the prevention of serious asthma exacerbations. Eur Respir J 2000;16:277s.
Chung KF, Britton M, Harnest U, Ayre G, Blogg M, Fox H. Omalizumab, an anti-IgE antibody, decreases the rate of asthma deterioration-related incidents in patients with poorly controlled allergic asthma. Allergy Clin Immunol Int 2003:Abstract 0–17–4. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/668/CN-00486668/frame.html (last accessed 30 March 2012).
Holgate S, Bousquet J, Wenzel S, Fox H, Liu J. Omalizumab improves disease control in patients at high-risk of serious asthma-related morbidity and mortality. Am J Respir Crit Care Med 2002;165:A187. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/310/CN-00401310/frame.html (last accessed 30 March 2012).
Holgate S, Chuchalin A, Herbert J, Lotvall J, Chung F, Bousquet J, et al. Omalizumab improves asthma-specific quality of life in patients with severe allergic asthma. Eur Respir J 2001:37s. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/822/CN-00429822/frame.html (last accessed 30 March 2012).
Howes T, Izquierdo JL, Chilvers E, Blogg M, Oshinyemi K, Ayre G, et al. Omalizumab, an anti-IgE antibody, decreases exacerbations in patients with poorly controlled allergic asthma. American Thoracic Society 99th International Conference 2003:C104 Poster D39. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/780/CN-00445780/frame.html (last accessed 30 March 2012).
Massanari M, Deniz Y, Lee J, Kianifard F, Blogg M, Reisner C, et al. Omalizumab improved asthma control and reduced rescue steroid bursts in moderate to severe allergic asthma. XIX World Allergy Organisation Congress, 26 June–1 July 2005, Munich, Germany:Abstract 308. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/145/CN-00548145/frame.html (last accessed 30 March 2012).
Massanari M, Zeldin R, Maykut R, Kianifard F, Geba G. Omalizumab improves lung function and treatment effectiveness in patients with moderate-severe asthma receiving fluticasone 500mcg/salmeterol 50mcg. Proceedings of the American Thoracic Society 2006: A590 [Poster L65]. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/374/CN-00591374/frame.html (last accessed 30 March 2012).
Matz J, Melamed I, Ledford D, Hedgecock S, Fox H, Surrey K, et al. Add-on omalizumab therapy significantly improves quality of life in patients with inadequately controlled severe persistent asthma despite GINA 2002 step 4 treatment, INNOVATE. American Thoracic Society 2005 International Conference; 20–25 May, San Diego, CA, USA: B36 [Poster: G47]. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/328/CN-00525328/frame.html (last accessed 30 March 2012).
Milgrom H, Miller SD, Lanier BQ, Fowler-Taylor A, Chen H, Gupta N. Long-term omalizumab therapy is well tolerated in children with moderate-to-severe IgE-medicated asthma. American Thoracic Society 2005 International Conference; 20–25 May, San Diego, CA, USA: B36. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/372/CN-00525372/frame.html (last accessed 30 March 2012).
Niven R, Chung KF, Panahloo Z, Blogg M, Ayre G. Efficacy of omalizumab in patients with inadequately controlled severe persistent allergic (IgE-mediated) asthma: a subgroup analysis of an open label trial. American Thoracic Society International Conference, 18–23 May 2007, San Francisco, CA, USA 2007:Poster #414. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/686/CN-00651686/frame.html (last accessed 30 March 2012).
Noga O, Hanf G, Kirchhof E, Buettner C, Kunkel G. Treatment with omalizumab (rhuMAb-E25), a monoclonal anti-IgE antibody induces effective changes in subjects with allergic asthma. Eur Respir J 2001:37s. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/793/CN-00429793/frame.html (last accessed 30 March 2012).
Scripps C. Double blind study to determine effect of omalizumab treatment in patients with the co-morbid conditions of aspirin exacerbated respiratory disease(AERD) and allergic asthma and rhinitis [completed]. ClinicalTrials.gov [serial online] 2009:ClinicalTrials.gov ID: NCT00286416. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/026/CN-00725026/frame.html (last accessed 31 October 2009).
Siergiejko Z, Swiebocka E, Peckitt C, Maykut R, Peachey G. Omalizumab Improves Quality Of Life In Adults And Adolescents (e12 Years) With Uncontrolled Severe Allergic Asthma. Am J Respir Crit Care Med 2010;181:A6651. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/394/CN-00757394/frame.html (last accessed 30 March 2012).
Williams G. Effect of omalizumab (Xolair) in treatment of patients with AERD and allergy asthma. ClinicalTrials.gov[serial online] 2006. URL: www.mrw.interscience.wiley.com/cochrane/clcentral/articles/540/CN-00591540/frame.html (last accessed 30 March 2012).
Appendix 3 Inclusion criteria of included randomised controlled trials
| Study | Age in years | Baseline medication | Clinically significant exacerbations/severe exacerbationsa | Definition clinically significant exacerbations/severe exacerbations | Hospitalisations/unscheduled care | FEV1 | Other | Met licence criteriab | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICS | LABA | OCS | Other | ||||||||
| Ayres 2004 (IA-04)30 | 12–75 | ≥ 400 µg/day (12–18 years), ≥ 800 µg/day (> 18 years) BDP equivalent | NR | NR | NR | ≥ 1 course of OCS in the last year in addition to ≥ 1 hospitalisation event | Requiring treatment with OCS | ≥ 1 emergency room visit/hospitalisation in past year | ≥ 12% within 30 minutes of taking inhaled salbutamol | NA | 2 |
| EU population subgroup | > 1000 µg BDP equivalent | Required | As above | ||||||||
| Bardelas (AIC)32 | ≥ 12 | Fluticasone 250 µg/day or budesonide 160 µg b.i.d. | ≥ salmeterol 50 µg or formeterol 4.5 µg x 2 b.i.d. one of additional required treatments (see other) | Permitted if stable for > 3 months | LTRA OR theophylline or zileuton permitted alternatives to LABA | NR | NR | NR | See Other (4) | ACT ≤ 19 PLUS one of: (1) symptoms > 2 days/week, (2) night wakening ≥ 1 week, (3) SABA use > 2 days/week, (4) FEV1≤ 80%/predicted/personal best | 3 |
| Bousquet 2010 (EXALT)31 | 12–75 | ≥ 800 µg BDP equivalent | Required | Permitted | SABA permitted as rescue medication | ≥ 2 severe asthma exacerbations (requiring treatment with OCS); ≥ 1 severe exacerbation within the previous year | Requiring treatment with OCS | NR | ≥ 12% reversibility within 30 minutes of taking 2–4 × 100 µg salbutamol between 40% and 80% predicted | NA | 1 |
| Theophyllines, cromones, antileukotrienes permitted | Severe exacerbation also required one of (1) hospital admission/intubation, (2) emergency care visit, (3) breathlessness at rest, (4) PEF or FEV1 < 60% predicted/personal best, (5) >30% fall from personal best PEF on 2 successive days | ||||||||||
| Humbert 2005 (INNOVATE)19 | 12–75 | > 1000 µg BDP or equivalent | Required | Permitted (≤ 20 mg/day) if ≥ 1 qualifying exacerbation occurred on OCS | Theophyllines, SABA, oral β2-agonists and LTRA permitted | ≥ 2 requiring OCS OR ≥ 1 severe exacerbation requiring hospital treatment in past year | Requiring treatment with OCSs | ≥ 1 unless ≥ 2 clinically significant exacerbations | 40–80% predicted | NA | 1 |
| Severe exacerbation also PEF or FEV1 < 60% personal best | |||||||||||
| Hanania 201133 | 12–75 | ≥ 500 µg fluticasone dry powder b.i.d. | Salmeterol 50 µg b.i.d. or formeterol 12 µg b.i.d. | Permitted | SABA albuterol (rescue medication), LTRA; zileuton; oral, nasal or inhaled anticholinergic therapy; mast cell stabilisers; specific immunotherapy; theophylline permitted | ≥ 1 clinically significant in past year | Requiring treatment with OCSs for ≥ 3 days; for patients receiving long-term OCSs, ≥ 20 mg increase in average daily dose of oral prednisone or comparable | NR | 40–80% predicted | Average ≥ 1 night wakening/week and daytime asthma symptoms requiring rescue medication for ≥ 2 days/week in 4 weeks before screening and for 2 consecutive weeks of ≤ 4 weeks before randomisation | 2 |
| Vignola 2004 (SOLAR)36 | 12–75 | ≥ 400 µg/day BDP | Permitted | Not permitted | Other asthma medications not permitted, nasal steroids permitted for rhinitis | NR | Requiring treatment with OCSs or doubling of the baseline inhaled budesonide dosec | ≥ 2 unscheduled visits in past year or ≥ 3 in past 2 years | ≥ 12% increase after 400 µg salbutamol | Score of > 64/192 on AQLQ | 3 |
| Vignola 2004 (SOLAR)36 | 20–75 | ≥ 400 µg fluticasone propionate or equivalent | Required | Permitted if ≥ exacerbation in past year (≤ 20 mg/day prednisolone) | Theophylline or LTRA permitted | NR | NR | NR | Reversibility of > 12% after 200 µg salbutamol | Average ≥ 1 night-time awakenings/week and daytime symptoms requiring rescue medication ≥ 2 days per week | 3 |
| Ohta 200935 | 20–75 | ≥ 800 g/day | One of required additional treatments (see OCSs/other for permitted alternatives) | Permitted alternative to LABA (≤ 10 mg/day) | Theophylline or LTRA permitted alternatives to LABA | Not required | Requiring treatment with OCSsd | NR | See Other (5) | One of (1) symptoms interfere with sleep ≥ 1 night/week, (2) symptoms restrict daily activities ≥ 1 day/week, (3) rescue medication needed ≥ 1 day/week, (4) PEF diurnal variation ≥ 20% ≥ 1 day/week, (5) FEV1 40–80% predicted value, (6) mean PEF 40–80% predicted value | 3 |
| Chanez 200429 | ≥ 18 | > 1000 µg beclometasone diproprionate or equivalent | Required | NR | NR | ≥ 2 or ≥ 1 severe exacerbation in past year | Requiring treatment with systemic corticosteroids | See severe exacerbations | < 80% predicted | Symptoms ≥ 4 days/week or nocturnal awakening ≥ 1/week | 1 |
| Severe exacerbations required hospitalisation/emergency room treatment | |||||||||||
| Busse 201128 | 6–20 (inner city children) | NR | NR | Not permitted for > 30/60 days before recruitment | NR | NR | NR | Hospitalisation/unscheduled urgent care in previous 6–12 months for patients on long-term control therapy. Persistent symptoms and uncontrolled asthma for other patientse | NR | See hospitalisation | 3 |
| Lanier 2009 (IA-05)20 | 6 to < 12 | Permitted | Permitted | Permitted | Anticholinergics and beta-adrenergics not permitted | ≥ 2 within 1 year or ≥ 3 within 2 years, or ≥ 1 severe exacerbation requiring hospitalisation within 1 year | Requiring doubling of baseline ICS and/or treatment with rescue OCS for ≥ 3 days | NR | NR | Daytime or night-time symptoms | 2 |
| EU population subgroup | ≥ 500 µg fluticasone equivalent | Required | Severe exacerbations required OCSs plus peak FEV1 < 60% personal best | ||||||||
Appendix 4 Population characteristics of included randomised controlled trials
| Study | n | Age in years, mean | Baseline medication | Clinically significant exacerbations/year | Hospitalised in past year n (%) | Received unscheduled care/year n (%) | FEV1 (% predicted) | Trial pop meets licence criteria | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICS dose (µg/day) | LABA n (%) | OCS n (%) | Other asthma medication n (%) | ||||||||
| Ayres 2004 (IA-04)30 | 312 | 38 | 0–500: 7 (2.2) | 243 (77.9) | 66 (21.2) | NR | NR | 135 (43.3) | 283 (90.7) (ER) | 71 | 2 |
| > 500–1000: 99 (31.7) | |||||||||||
| > 1000–10,000: 206 (66.0) | |||||||||||
| BDP equivalent | |||||||||||
| EU population subgroup (GINA step 4) | 164 | 39 | 2852.7 BDP equivalent | 161 (98.2) | NR | LTRA 60 (36.6) | NRa | 77 (47.0) | 151 (92.1) (ER) | 65 | 1 |
| Anticholinergics 24 (14.6) | |||||||||||
| Xanthines 44 (26.8) | |||||||||||
| Antihistamines 7 (4.3) | |||||||||||
| Bardelas (AIC)32 | 271 | 41 | NR but ≥ fluticasone 250 µg/day or BDP 160 µg b.i.d. (see Appendix 3) | 170 (63) | NR | ICS + LABA + other 50 (18.5) | NR | NR | NR | 76 | 3 |
| ICS + other 16 (5.9) | |||||||||||
| Bousquet 2010 (EXALT)31 | 404 | 46 | 1999 BDP equivalent | 399 (99.8) | 88 (22.0) | SABA 371 (92.8) | 2.1 | 90 (22.4) | 120 (29.8) (ER) | 62 | 1 |
| 327 (81) (Dr visits) | |||||||||||
| OCS at baseline | 82 | 45 | NR | 82 (100) | 82 (100) | NR | 3.0b | NRc | NRd | 61 | 1 |
| Humbert 2005 (INNOVATE)19 | 419 | 43 | 2330 BDP or equivalent | 419 (100) | 91 (21.7) | LTRA 146 (35) | 2.52/14 mo | 162 (38.7) | 234 (55.8) (ER) | 61 | 1 |
| Theophyllines 115 (27) | 41 (9.8) ICU | ||||||||||
| β2-agonists 4 (1%) | |||||||||||
| Hanania 201133 | 850 | 44 | NR but ≥ 500 µg fluticasone dry powder b.i.d. (see Appendix 3) | 850 (100) | 60 (7.1) | 1.95 | NR | NR | 65 | 2 | |
| M1 subgroup (ICS + LABA only) | 310 | 100 | 0 | 0 | 2 | ||||||
| M2 subgroup (ICS + LABA + other non-OCSs) | 394 | 100 | 0 | LTRA (86%) | 2 | ||||||
| M3 subgroup (OCS or ≥ 4 exacerbations requiring OCS/year) | 144 | 100 | 60 (7.1%) plus 84 (9.8%) with ≥ 4 exacerbations requiring OCS | Tiotropium bromide 6% | 1 | ||||||
| Theophylline 6%; ipratropium bromide (4%) | |||||||||||
| Cromolyn sodium, nedocromil sodium and aminophylline all ≤ 1% | |||||||||||
| Vignola 2004 (SOLAR)36 | 405 | 38 | 400–2400 µg/day BDP equivalent | 157 (38.8) | N/A | Nasal steroids 67 (16.5%) | 2.1 | NR | NR | 78 | 3 |
| Receiving LABA | 157 | ||||||||||
| Not receiving LABA | 248 | ||||||||||
| Hoshino 201234 | 30 | 55 | 829 fluticasone equivalent | 30 (100) | 9 (30%) | LTRA 22 (73.3) | NR | NR | NR | 67 | 3 |
| Theophylline 13 (43.3) | |||||||||||
| Ohta 200935 | 327 | 49 | 1169 | 162 (49.5) | 30 (9.2)e | LTRA 176 (53.8) | NR | 32 (9.8) | 62 (19) (ER) | 75 | 3 |
| Theophylline 126 (38.5) | |||||||||||
| Chanez 200429 | 31 | 47 | 3556 beclometasone equivalent | 31 (100) | 7 (22.6) | Theophylline 2 (6.5) | 4.4 | NRf | NR | 63 | 1 |
| Montelukast 12 (38.7) | |||||||||||
| Anticholinergics 12 (38.7) | |||||||||||
| Busse 201128 | 419 | 10.8 | 54% receiving BDP 360 µg | 54% receiving Advair 250/50 µg or 500/50 µg b.i.d | Not permitted | LTRA | NR | 104 (25) | 328 (78) (unscheduled visit) | 92 | 3 |
| 60% aged < 12 | Montelukast | ||||||||||
| Ns not reported | |||||||||||
| Lanier 2009 (IA-05)20 | 628 | 8.6 | NR | 423 (67.4) | 8 (1.3) | LTRA 230 (36.6) | 2.6 | NR | NR | 86 | 2 |
| SABA 549 (87.4) | |||||||||||
| EU population subgroup | 235 | 9.0 | 743 mg fluticasone equivalent | 412 (100) | 6 (1.5) | LTRA 236 (57.4) | 2.8 | 50g | NR | 82.1 | 1 |
| Theophylline 1 (0.2) | |||||||||||
Appendix 5 Study design and inclusion criteria of observational studies
| Study | Design | Age in years | Baseline medication | Clinically significant exacerbations/severe exacerbations? | Definition clinically significant exacerbations/severe exacerbations/exacerbations | Hospitalisations/unscheduled care | FEV1 (% predicted) | Other | Uncontrolled asthma? | Multicentre? | Funding | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ICS | LABA | OCS | Other | |||||||||||
| Barnes (APEX) (AIC)37 | Retrospective one-group | ≥ 12 years | NR | NR | Permitted | ≥ 1 omalizumab course ≥ 12 months before data collection | NR/NR | NR/NR/Increase in symptoms requiring treatment with SCS | NR | NR | Severe persistent | NRa | Yes (10 centres) | Novartis UK |
| Braunstahl 2011 (eXpeRience)58 | Postmarketing surveillance | ≥ 12 years | > 1000 µg/day BDP or equivalent | Required | NR | NA | NR/NR | Worsening of asthma judged clinically significant by physician requiring rescue SCS/Clinically significant exacerbation with a reduction in PEF to < 60% of predicted/personal best/NR | NR | NR | NRb | Yesc | Yes | Novartis Pharma AG |
| Brodlie 201259 | Prospective one-group | Children | Required step 5 (BTS/SIGN) | Required step 5 (BTS/SIGN) | Maintenance ≥ 3 months | NR | NR/NR | NR | NR | NR | NR | No | Yes (seven centres) | NR |
| Brusselle 2009 (PERSIST)39 | Prospective one-group | ≥ 12 years | Required | Required | NR | NR | NR/≥ 2 in the past 2 years | NR/requiring OCSs or an emergency room visit or hospitalisation/NR | NR | < 80 | Severe asthma treatment (GINA 2005) | Yes | Yes (35 centres) | Novartis |
| Positive radioallergosorbent test | ||||||||||||||
| Regular day or night-time asthma symptoms | ||||||||||||||
| IgE ≥ 76 IU/ml | ||||||||||||||
| Cazzola 201040 | Prospective one-group | ≥ 12 years | High dose | Permitted | NR | NR | NR/NR | NR/NR/NR | NR | NR | Positive reaction to at least one perennial allergen | Yes | Yes (12 centres) | NA |
| Moderate-severe (GINA) | ||||||||||||||
| IgE 30–700 IU/ml | ||||||||||||||
| Costello 201141 | Retrospective one-group | NR | Required | Required | Permitted | NR | NR/NR | NR/NR/Patients requiring an increase in, or commencement on OCS medication or antibiotics for a chest infection/pneumonia and/or a visit to A&E or hospital admission | NR | NR | Severe persistent despite ICS+LABA | Yes | Yes (six centres) | Novartis |
| Omalizumab treatment for ≥ 6 months | ||||||||||||||
| Deschildre 201042 | Non-comparative cohort | Children (school age) | As maintenance therapy | As maintenance therapy | NR | NR | NR | NR | NR | NR | NR | NR | Yes | Novartis – France |
| Domingo 201161 | Prospective one-group | ≥ 18 years | NR | NR | ≥ 7.5 mg/day prednisolone or 6 mg/day methyl prednisolone; ≥ 6 courses/year for ≥ 2 weeks | None | NR/NR | NR/NR/NR | NR | ≥ 60; ≥ 12 reversibility; ≥ 200 ml | IgE 30–700 IU/ml | NR | No | Fundació Catalana de Pneumologia |
| Obstructive airway disease with an FEV1 reversibility ≥ 12% and 200 ml | ||||||||||||||
| Receiving steroids in addition to BSC (GINA 2010) | ||||||||||||||
| Positive reaction to ≥ 1 perennial allergen | ||||||||||||||
| 25–150 kgd | ||||||||||||||
| Eisner 2011 (EXCELS)71 | Prospective comparative (FDA postmarketing) | ≥ 12 years | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Yes (448 centres) | Genentech and Novartis |
| Gutierrez 200762 | Retrospective comparative | 12–64 years | Permitted | Permitted | NR | Fluticasone/salmeterol, LTRA permitted | NR | NR | NR | NR | NR | NR | NR | Genentech |
| Kirk 201060 | Retrospective one group | 6–11 years | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Yes (seven centres) | NR |
| Korn 200944 | Postmarketing surveillance | ≥ 12 years | Required high doses | Required | Permitted as maintenance therapy | Slow-release theophyllines, LTRA permitted | NR/≥ 2 | NR/NR/FEV1 < 60% of personal best, intermittent OCS, unscheduled health-care visits, emergency treatments, hospitalisations because of asthma | NR | < 80 | IgE 30–700 IU/ml | Yes | Yes | Novartis Pharma GmbH |
| 20–150 kg | ||||||||||||||
| Severe exacerbations despite high ICS + LABA | ||||||||||||||
| Positive reaction to perennial aeroallergen | ||||||||||||||
| Frequent daily symptoms or nocturnal awakenings | ||||||||||||||
| Molimard 200845 | Prospective one-group | NR | NR | NR | NR | NR | NR/NR | NR/NR/FEV1< 60% of personal best, requiring an OCS burst and unscheduled doctor/emergency visit or hospitalisation | NR | NR | NR | Yes | Multiple | Novartis Pharma AG |
| Ohta 201046 | Prospective one-group | 20–75 years | ≥ 400 µg/day BDP-CFC or equivalent 1 month prior to screening | NR | NR | NR | NR/NR | NR/NR/NR | NR | 40–80 of predicted normal value for the patient per week | 30–150 kg | Yesf | Yes (24 centres) | Novartis Pharma KK |
| IgE 30–700 IU/ml | ||||||||||||||
| Moderate-severe diagnosis using equivalent to GINA (2002)e | ||||||||||||||
| Positive reaction to perennial aeroallergen | ||||||||||||||
| Exclude immunosuppressants 3 months prior to first visit | ||||||||||||||
| Randolph 201063 | Prospective one-group | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | No | NR |
| Stukus 200864 | Retrospective uncontrolled | Adults | NR | NR | NR | NR | NR/NR | NR/NR/NR | NR | NR | IgE > 700 IU/ml permitted | NR | No | William Wagner Research and Education |
| Zureik 2010 (PAX-LASER)47 | Prospective controlled | NR | > 1000 µg beclometasone-equivalent | Required | 5 mg prednisone equivalent for ≥ 6 months, or ≥ 3 OCS courses in 1 year (or predicted FEV1 < 80%) | NR | NR/NR | NR/Hospitalisation/emergency room visit, recorded for the year before and during the prospective follow-up period/NR | NR | < 80 (or OCS) | NR | Yes | Yes (163 centres) | NR |
| Britton 201154 | Retrospective one-group | NR | NR | NR | NR | NR | NR | NR | NR | NR | Yes | Yes | Not reported | |
| Tzortzaki 201255 | Retrospective one-group | ≥ 12 years | High dose required | Required | NR | NR | ≥ 2/year | Required OCS or ER visit or hospitalisation | See exacerbations | < 80% OR night-time asthma symptoms | IgE 30–1000 IU/ml | Yes | Yes | Not reported |
Appendix 6 Population characteristics of included observational studies
| Study | n at baseline | Mean age, years | Follow-up duration | Baseline medication | Clinically significant exacerbations/year, mean (SD) | Hospitalisations in past year, mean (SD) | ED visits in past year, mean (SD) | Other unscheduled care/year, mean (SD) | FEV1 (% predicted) | Trial pop meets licence criteriab | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ICS dose (µg/day), mean (SD)a | LABA n (%) | OCS n (%) | Other asthma medication n (%) | ||||||||||
| Barnes (APEX) (AIC)37 | 136 | NR (median 43) | 12 months | NR ('maximum inhaled therapy') | NR | 90 (66.2) | NR | 3.67 (NR) | 1.30 (1.73) (81 (59.6) with ≥ 1 events) | 1.52 (2.19) | NR | 68 | 3 |
| Braunstahl 2011 (eXpeRience)58 | 294 (876 at follow-up) | 46 | 8 months | 1590 (803) | 282 (95.9) (combined and monotherapy) | 83 (28.2) | LTRA 181 (61.6); SABA 20 (6.8); anticholinergics 63 (21.4); SABA + anticholinergics 22 (7.5); other 71 (24.1) | 4.8 (5.12) | 0.8 (1.47) | 1.3 (2.22) | 3.7 (5.6) (doctor visit) | 62.4 | 3 |
| Brodlie 201259 | 34 | NR (range 5–16 years) | 16 weeks | NR (step 5 BTS/SIGN) | NR(step 5 BTS/SIGN) | 34 (100) | NR | NR | NR | NR | NR | NR | 3 |
| Brusselle 2009 (PERSIST)39 | 160 (158 analysed) | 48 | 52 weeks + 120 weeks (retrospective follow-up, n = 53) | NR (158 (100) 'high- dose') | 158 (100) | 45 (28.5) | Theophylline/derivatives 61 (38.6); anticholinergics 63 (39.9) | 2.67 (1.28) severe events (158 (100) with ≥ 1 severe events) | NR (64 (40.5) with ≥ 1 events) | NR (22 (13.9) with ≥ 1 events) | NR (69 (43.7) GP; 149 (94.3) asthma specialist) | 57 | 1 |
| Cazzola 201040 | 142 | 50 | 12 months | 2225 (1837) | 140 (98.6) | 52 (36.6) | LTRA 99 (69.7); slow-release theophylline 21 (14.8) | 4.87(4.00) (123 (88.5) with ≥ 1 events) | 4.45 (4.31) (89 (63.6) with ≥ 1 events) | 1.53 (0.71)c | See ED visits | 65 | 2 |
| Costello 201141 | 93 (63 analysed) | 48 | 6 months | NR | NR | 27 (43) | NR | NR (3.18 (2.3) in past 6 months) | 2.4 (3.0) | NR | NR | 66 | 2 (no reporting of ICS dosage) |
| Deschildre 201042 | 104 | 11.8 | 4–6 months | NR (698) | 104 (100) | NR | NR | Severe rate per year: 0.51 | NR | NR | NR | NR | 3 |
| Domingo 201161 | 32 (31 analysed) | 51 | Mean 17 months | 1000 (NR) fluticasone | 32 (100) | 21 (67.8) | Methotrexate 3 (9) | NR | NR | NR | NR | 64 | 3 (uncontrolled?) |
| Eisner 2011 (EXCELS)71 | 7951 | 45 | ≤ 5 years | NR | NR | 1534 (19.3) | NR | NR (15% frequent, 17% may affect activity and sleep, 20% brief, 16% rare, 32% none) | NR | NR | NR | 79 | 3 |
| Gutierrez 200762 | 92,192 | NR | 18 months | NR | NR | NR | NR | NR | NR | NR | NR | NR | 3 |
| Kirk 201061 | 18 | NR | Mean 14.6 weeks | NR | NR | 18 (100) | NR | NR | NR | NR | NR | NR | 3 |
| Korn 200944 | 280 | 44 | 6 months | NR (100% 'high doses') | 280 (100) | 129 (46.1) | Slow-release theophylline 122 (43.6); LTRA 136 (48.6) | 4.5 (7.5) severe events, 252 (90.0%)with frequent severe events | NR (167 (23.9) with ≥ 1 events) | 4.4 (4.6)d | See ED visits | NR | 1 |
| Maintenance OCS subgroup | 102 | 45 | > 16 wks | NR | 96 (94.1) | 102 (100) | NR | 5.5 (8.82) | 0.6 (1.11) | NR | NR | NR | 1 |
| Molimard 200845 | 154 (146 analysed) | 47 | > 5 months | 3071 (1580) | 147 (100) | 54(62) | NR | 5.5 (NR) | 1.5 (NR) (146 (100) with ≥ 1 events) | 3 (NR) (146 (100) with ≥ 1 events) | NR | NR | 2 |
| Maintenance OCS subgroup | 64 | 48 | > 16 weeks | NR | 63 (98.4) | 64 (100) | NR | NR | 1.5 (2.32) | NR | NR | NR | 2 |
| Ohta 201046 | 133 | 48 | 48 weeks | 1026 (568.3) | 54 (40.6) | 14 (10.5) | Slow-release theophylline 79 (59.4), LTRA 51 (38.3) | NR | NR (10 (7.5) with ≥ 1 events) | NR (24 (18.0) with ≥ 1 events) | NR | 77 | 3 |
| Severe uncontrolled subgroup | 37 | 54 | 1487 (657.1) | 29 (78.4) | 13 (35.1) | Slow-release theophylline 30 (81.1), LTRA 27 (73.0) | NR | NR (11 (29.7) patients with ≥ 1 events) | NR (5 (13.5) patients with ≥ 1 events) | NR | 66 | 3 | |
| Randolph 201063 | 50 (29 analysed) | 31 | ≤ 6 years | NR | NR | NR | NR | NR | NR | NR | NR | 76 | 3 |
| Stukus 200864 | 63 (45 analysed) | 46 | NR | 1090 (NR) (drug unspecified) | NR | 13 (28.9) | NR | NR | NR | NR | NR | 63 | 3 |
| Zureik 2010 (PAX-LASER)47 | 767 | 54 | ≥ 12 months | NR | 97% | 195 (25.4) | LTRA 351 (45.8) | NR | NR | NR | NR | NR | 3 |
| Allergic patients subgroup | 486 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 3 (no data on exacerbations and symptoms) | |
| Britton et al 201154 | 52 | NR | Mean 982 days (112–3839 | NR | NR | 29 (55.8%) | NR | NR | 165/2 years | 164/2 years | 474/2 years | NR | 3 but UK severe asthma clinic |
| Tzortzaki 2012 55 | 60 | 54 | 4 years | 1021.62 (188.02) | 55/60 (91.6%) | 16 (26.6%) | LTRA 26 (43.4%) | 2.27 (2.82) | NR | NR | NR | 60.13 | 1 |
Appendix 7 Quality assessment
Methods used in the quality assessment
Quality Assessment Checklist for randomised controlled trials
-
Was assignment to the treatment groups really random?
-
Were adequate approaches to sequence generation reported (e.g. computer-generated random numbers or random numbers tables)?
-
-
Was the treatment allocation adequately concealed?
-
Were adequate approaches to concealment of randomisation reported (e.g. serially number identical containers)?
-
-
Were the treatment groups similar in terms of baseline characteristics?
-
Were groups similar at baseline in terms of important confounding variables? If not was the analysis adjusted to account for the imbalance?
-
-
Were outcome assessors blinded to the treatment allocation?
-
Was knowledge of the allocated intervention to outcome assessors adequately prevented during the study?
-
-
Were incomplete outcome data adequately addressed?
-
Were any outcome data missing?
-
Were reasons for missing outcome data reported?
-
Were missing data imputed using appropriate methods?
-
-
Was the RCT sufficiently powered to detect treatment effect?
-
Was a power calculation reported? If so, did it show sufficient power? If not, code as UNCLEAR.
-
-
Were statistical analysis methods appropriate?
-
Were intention-to-treat (ITT) analyses undertaken? If not was this justified?
-
Was a modified ITT analysis done instead? Was this appropriate?
-
Were per protocol (PP) analyses undertaken (inappropriate in this case)?
-
Were only comparisons from baseline reported (no between-group measure)? If so, code as NO.
-
All criteria were judged as YES (i.e. low risk of bias), NO (i.e. high risk of bias) or UNCLEAR (i.e. uncertain risk of bias).
Quality Assessment/Risk of Bias Checklist for randomised controlled trials23,25
-
Randomisation
-
Were details on methods of randomisation reported? If yes, was the method adequate?
-
-
Concealment
-
Were details on the method of allocation concealment reported? If described, was the method adequate?
-
-
Blinding
-
Were details on blinding of outcome assessors reported?
-
-
Comparability of groups
-
Were treatment groups comparable at baseline in terms of baseline scores and demographics?
-
Were groups treated the same throughout the trial, with the exception of the intervention?
-
-
Analysis
-
Were all trial participants accounted for throughout the trial?
-
Was loss to follow-up < 20%?
-
Was it stated that an ITT analysis was performed?
-
Was a sample size calculation performed?
-
Was there selective reporting of outcome measures?
-
Where adequate details were provided on each criterion, this indicated low risk of bias. Where no details were provided, this indicated high risk of bias. Where insufficient or unclear details were reported, this indicated unclear risk of bias.
An overall risk of bias judgement was made for each trial based on the highest risk scored for any single criterion. For example, if a trial was considered at low risk of bias on all criteria except one where the risk was unclear, then the overall risk of bias was recorded as unclear; where the risk was low or unclear on all criteria except one which was scored as high then the overall risk of bias was recorded as high.
Quality Assessment Checklist for observational studies
-
Were eligibility criteria/recruitment methods reported?
-
Is the population based on a representative sample selected from a relevant population?
-
Are the criteria for inclusion explicit?
-
-
Where applicable, were the treatment groups similar in terms of baseline characteristics?
-
Were groups similar at baseline in terms of important confounding variables? If not, was the analysis adjusted to account for the imbalance?
-
-
Were outcome assessors blinded to the treatment allocation?
-
Was knowledge of the allocated intervention to outcome assessors adequately prevented during the study?
-
-
Was completeness to follow-up sufficient?
-
Were losses to follow-up > 20%?
-
Were all patients accounted for at the end of study follow-up?
-
-
Was outcome reporting sufficient?
-
Were reliable methods used to measure outcomes?
-
Was the study sufficiently powered to detect treatment effect?
-
Was study follow-up duration sufficient to detect long-term treatment effect?
-
All criteria were judged as YES (indicating low risk of bias), NO (indicating high risk of bias) or UNCLEAR (indicating uncertain risk of bias).
Results of quality assessment of randomised controlled trials
| Study | Concealed treatment allocation | True randomisation | Outcome assessment blind | Power calculationa | Baseline comparability | Patients accounted for | Appropriate analysis |
|---|---|---|---|---|---|---|---|
| Adults: licensed population | |||||||
| Ayres 200430 | Yes | Yes | No | Yes | Yes | Yes (partly) | Yes |
| IA-04 | |||||||
| Bousquet 201031 | Yes | Yes | No | Yes | Yes | Yes | Yes |
| EXALT | |||||||
| Humbert 200519 | Yes | Yes | Yes | Yes | Nob | Yesc | Yes |
| INNOVATE | |||||||
| Chanez 200429 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Adults: supportive trials | |||||||
| Hanania 201133 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Vignola 200436 | UC | UC | UC | Yes | Yes | Yes | Yes |
| SOLAR | |||||||
| Hoshino 201234 | UC | UC | No | No | Yes | Yes | No |
| Ohta 200935 | Yes | UC | UC | Yes | Yes | Yes | Yes |
| Bardelas 201232 | UC | UC | UC | Yes | UC | Yes | Yes |
| dHolgate (011)50 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Children: licensed population | |||||||
| Lanier 200920 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| IA-05 | |||||||
| Children: supportive trials | |||||||
| Busse 201128 | UC | UC | Yes | Yes | Yes | Yes | Yes |
Results of risk of bias assessmenta for randomised controlled trials
| Study | Concealed treatment allocation | True randomisation | Outcome assessment blind | Baseline comparability | Patients accounted for | Appropriate analysis | Risk of bias |
|---|---|---|---|---|---|---|---|
| Adults: licensed population | |||||||
| Ayres 200430 | Low | Low | High | Low | UC | Low | High |
| IA-04 | |||||||
| Bousquet 201031 | Low | Low | High | Low | Low | Low | High |
| EXALT | |||||||
| Humbert 200519 | Low | Low | Low | Lowb | Lowc | Low | Low |
| INNOVATE | |||||||
| Chanez 200429 | Low | Low | Low | Low | Low | Low | Low |
| Adults: supportive trials | |||||||
| Hanania 201133 | Low | Low | Low | Low | Low | Low | Low |
| Vignola 200436 | Low | Low | Low | Low | Low | Low | Low |
| SOLAR | |||||||
| Hoshino 201234 | UC | UC | High | Low | Low | High | High |
| Ohta 200935 | Low | Low | Low | Low | Low | Low | Low |
| Bardelas 201232 | Low | Low | Low | UC | Low | Low | UC |
| dHolgate (011)50 | Low | Low | Low | Low | Low | Low | Low |
| Children: licensed population | |||||||
| Lanier 200920 | Low | Low | Low | Low | Low | Low | Low |
| IA-05 | |||||||
| Children: supportive trials | |||||||
| Busse 201128 | UC | UC | Low | Low | Low | Low | UC |
Results of quality assessment results for observational studies
| Study | Similar baseline characteristics between groups (if not, adjusted) | Eligibility/recruitment criteria reported | Blinding of outcome assessor | Sufficient follow-up for long-term effect assessment | Losses to follow-up reported and included in analysis | Losses to follow-up > 20% | Sufficiently powered to detect an effect | Reliable outcome measures | All patients accounted for at follow-up |
|---|---|---|---|---|---|---|---|---|---|
| Barnes (APEX)37 | NA | Yes | NA | Yes | No | Unclear | Unclear | Partly | Unclear |
| Braunstahl 2011 (eXpeRience)53 | NA | Yes | NA | No | No | No | Unclear | Unclear | Yes |
| Brodlie 201254 | NA | Yes | NA | No | No | NA | Unclear | Unclear | Yes |
| Brusselle 2009 (PERSIST)39 | NA | Yes | NA | Yes | Yes | No | Yes | Partly | No |
| Cazzola 201040 | NA | Yes | NA | Yes | Yes | Yes | Unclear | Unclear | Yes |
| Costello 201141 | NA | No | NA | No | Yes | Yes | Unclear | No | Yes |
| Deschildre 201042 | NA | Yes | NA | No | No | Unclear | No | Unclear | Unclear |
| Domingo 201156 | NA | Yes | NA | No | Yes | No | NA | Yes | Yes |
| Eisner 2011 (EXCELS)71 | No | Yes | Unclear | Yes | No | Unclear | Unclear | Unclear | Unclear |
| Gutierrez 200757 | Unclear | Yes | Unclear | NA | No | Unclear | NA | No | Unclear |
| Kirk 201055 | NA | Yes | NA | No | NA | NA | Unclear | Unclear | NA |
| Korn 200944 | NA | Yes | NA | No | No | Unclear | Unclear | No | Yes |
| Molimard 200845 | NA | No | No | Yes | No | No | Unclear | No | No |
| Ohta 201046 | NA | Yes | NA | No | Yes | No | Unclear | Partly | Yes |
| Randolph 201058 | NA | No | NA | Yes | Yes | Yes | No | Unclear | Yes |
| Stukus 200859 | No | No | NA | Unclear | Unclear | No | NA | No | Unclear |
| Zureik 2010 (PAX-LASER)47 | Yes | Yes | Unclear | Unclear | No | Unclear | Unclear | Unclear | Unclear |
| Britton 201161 | NA | Yes | NA | Yes | No | Unclear (outcome-dependent) | Unclear | Unclear | Unclear (outcome-dependent) |
| Tzortzaki 201262 | NA | Yes | NA | Yes | Yes | No | Unclear | Unclear | Yes |
Appendix 8 Clinically significant exacerbations (randomised controlled trial data)
| Study ID | n (subgroups) | Duration | Definition | Outcome measure | Data (Omal vs. Comp) | Conversion |
|---|---|---|---|---|---|---|
| Ayres 2004 (IA-04)30 | 312 | 52 weeks | Requiring systemic CS | Mean annualised number | 1.12 vs. 2.86 | Annualised incidence rate |
| EU population subgroup | 164 | 1.26 vs. 3.06 | ||||
| Bardelas (AIC)32 | 271 | 24 weeks | NR | NR | NA | NA |
| Bousquet 2010 (EXALT)31 | 404 | 32 weeks | Requiring systemic CS | Mean event rate at 32 weeks | 0.55 vs. 0.98 | Annualised incidence rate possible to extrapolate? |
| Rate ratio | 0.57 (95% CI 0.417 to 0.778)a | 0.89 vs. 1.59 | ||||
| Numbers with 0,1,2,3 or ≥ 4 | Numbers with ≥ 1 calculable: | |||||
| 89/272 vs. 64/128 | ||||||
| = 33% vs. 50% | ||||||
| Humbert 2005 (INNOVATE)19 | 419 | 28 weeks | Requiring systemic CS | Rate | 0.68 vs. 0.91 | Annualised incidence rate possible to extrapolate? |
| Rate ratio | 0.738 (95% CI 0.552 to 0.998)a | 1.26 vs. 1.69 | ||||
| NNT | 2.2 | |||||
| Hanania 201133 | 850 | 48 weeks | Requiring OCS ≥ 3 days; or increase in average daily dose for long-term OCS ≥ 20 mg | Incidence rate/patient/48 weeks | 0.66 vs. 0.88 | Annualised incidence rate possible to extrapolate? |
| Treatment difference IRR for subgroups | M1 0.66 (95% CI 0.44 to 0.97) | 0.72 vs. 0.95 | ||||
| Numbers with 0, 1,2,3 or ≥ 4 | M2 0.72 (95% CI 0.53 to 0.98) | Numbers with ≥ 1 calculable | ||||
| M3 0.95 (95% CI 0.63 to 1.43) | 152/427 vs. 189/423 | |||||
| 36% vs. 45% | ||||||
| Vignola 2004 (SOLAR)36 | 405 | 28 weeks | Doubling ICSs or OCS burst | Number with ≥ 1 exacerbation | 38/209 vs. 50/196 | Number with ≥1 |
| 157 on LABA | 18/86 vs. 25/71 | |||||
| Hoshino 201234 | 30 | 16 weeks | NR | NR | NR | NA |
| Ohta 200935 | 327 | 16 weeks treatment + 12-week follow-up | Requiring OCSs | Number experiencing exacerbation | 6/151 vs. 18/164 | Numbers with ≥ 1 |
| Chanez 200429 | 31 | 16 weeks | Not defined beyond inclusion criteria | % with no exacerbations | 45% vs. 63.6% | Numbers with ≥ 1 calculable |
| 55% vs. 36% | ||||||
| 11/20 vs. 4/11 | ||||||
| bBusse 201128 | 419 | 60 weeks | Need for SCS and/or hospitalisation | % with ≥ 1 exacerbations | 30.3%(3.3) vs. 48.8%(3.7) | Number with ≥ 1 calculable |
| 226 high ICS + LABA | 63/208 vs. 101/211 | |||||
| cLanier 2009 (IA-05)20 (EU population subgroup) | 628 | 52 weeks (24-week fixed steroid, 28-week adjustable steroid) | Doubling of baseline ICS dose and/or treatment with rescue systemic corticosteroids for ≥ 3 days | Rates at 52 weeks | 0.73 vs. 1.44 | Annualised incidence rate |
| [246 severe (LABA, 57% LTR)] | RR at 52 weeks | 0.504 (95% CI 0.350 to 0.725)a | ||||
| Rates at 24 weeks | 0.42 vs. 0.63 | |||||
| RR at 24 weeks | 0.662 (95% CI 0.441 to 0.995)a |
Appendix 9 Clinically significant severe exacerbations (randomised controlled trial data)
| Study ID | n (subgroups) | Duration | Definition | Outcome measure | Data (omalizumab vs. comparator) |
|---|---|---|---|---|---|
| Bousquet 2010 (EXALT)31 | 404 | 32 weeks | Requiring treatment with OCSs plus one of (1) hospital admission/intubation, (2) emergency care visit, (3) breathlessness at rest, (4) PEF or FEV1 < 60% predicted/personal best, (5) > 30% fall from personal best PEF on 2 successive days | Mean event rate at 32 weeks | 0.24 vs. 0.42 |
| RR 0.56 (95% CI 0.341 to 0.924)a | |||||
| Humbert 2005 (INNOVATE)19 | 419 | 44 weeks (28 weeks = 16 f/u) | Requiring treatment with OCSs plus PEF or FEV1 < 60% personal best | Number of severe exacerbations | 49 in 35/209 (16.8%) vs. 100 in 55/210 (26.2%) |
| Number of patients with ≥ 1 severe exacerbations | Rate 0.24 vs. rate 0.48 | ||||
| Rate in 28 weeks | |||||
| 49 in 35/209 (16.8%) rate 0.24 | |||||
| Comparator 100 in 55/210 (26.2%) rate 0.48 | |||||
| bLanier 2009 (IA-05)20 | 628 | 52 weeks (24-week fixed steroid, 28-week adjustable steroid) | OCS plus peak FEV1 < 60% personal best | Severe exacerbation rate at 24 and 52 weeks with RR | 24 weeks 0.10 vs. 0.18 |
| EU population subgroup | [246 severe (LABA, 57% LTR)] | RR 0.55 (95% CI 0.32 to 0.95)a | |||
| 412 | 52 weeks 0.12 vs. 0.24 | ||||
| RR 0.49 (95% CI 0.30 to 0.80)a | |||||
| 24 weeks: 0.14 vs. 0.22 | |||||
| RR 0.656 (0.302 to 1.421)a |
Appendix 10 Exacerbation rates: responder analyses (data from the manufacturer's submission)
As with the ITT subgroup data, exacerbation rates (where not reported by the manufacturer) and rate ratios have been calculated and CI have been calculated using an approximation of the standard error. The data are presented with the caveat that these are small post hoc subgroup analyses in which CI would be expected to be very wide, representing the high uncertainty around the estimate. As with the main analyses data from INNOVATE, refer to assessment for response at 28 weeks, whereas data from EXALT refer to assessment for response at 16 weeks. Data from patients with ≤ 2 or ≥ 3 exacerbations in the previous year were also considered.
Exacerbation data for patients with a history of hospitalisation: responder analysis
| Trial | Omalizumab responders | Control | RR (95% CI)a | ||||
|---|---|---|---|---|---|---|---|
| n (% ITT) | Exacerbations | Rate | n | Exacerbations | Rate | ||
| Total exacerbations | |||||||
| INNOVATE | 47 (56.6) | 22 | 0.49 | 79 | 89 | 1.33 | 0.37 (0.14 to 0.59) |
| EXALT | 33 (56.9) | 20 | 0.63 | 32 | 43 | 1.40 | 0.45 (0.26 to 0.76) |
| IA-05 EU subgroup | 20 (54.1) | 13 | |||||
| > 24 weeks | 11 | 0.52 | 16 | 1.00 | 0.52 (0.24 to 1.12) | ||
| 24–52 (28) weeks | 8 | 0.38 | 24 | 1.60 | 0.24 (0.11 to 0.53) | ||
| > 52 weeks | 19 | 0.91 | 40 | 2.61 | 0.35 (0.20 to 0.60) | ||
| CSS exacerbations | |||||||
| INNOVATE | 47 (56.6) | 9 | 0.18 | 79 | 52 | 0.66 | 0.27 (0.13 to 0.55) |
| EXALT | 33 (56.9) | 11 | 0.34 | 32 | 25 | 0.82 | 0.41 (0.20 to 0.83) |
| IA-05 EU subgroup | 20 (54.1) | 13 | |||||
| > 24 weeks | 5 | 0.19 | 6 | 0.44 | 0.43 (0.13 to 1.41) | ||
| 24–52 (28) weeks | 2 | 0.10 | 9 | 0.71 | 0.14 (0.03 to 0.65) | ||
| > 52 weeks | 7 | 0.32 | 15 | 1.15 | 0.28 (0.11 to 0.69) | ||
| CSNS exacerbations | |||||||
| INNOVATE | 47 (56.6) | 13 | 0.28 | 79 | 37 | 0.47 | 0.60 (0.32 to 1.13) |
| EXALT | 33 (56.9) | 9 | 0.27 | 32 | 18 | 0.56 | 0.48 (0.22 to 1.07) |
| IA-05 EU subgroup | 20 (54.1) | 13 | |||||
| > 24 weeks | 6 | 0.30 | 10 | 0.77 | 0.39 (0.14 to 1.07) | ||
| 24–52 (28) weeks | 6 | 0.30 | 15 | 1.15 | 0.26 (0.10 to 0.67) | ||
| > 52 weeks | 12 | 0.60 | 25 | 1.92 | 0.31 (0.16 to 0.62) | ||
Exacerbation data for patients on maintenance oral corticosteroids: responder analysis
| Trial | Omalizumab responders | Control | RRa | ||||
|---|---|---|---|---|---|---|---|
| n (% ITT) | Exacerbations | Rate | n | Exacerbations | Rate | ||
| Total exacerbations | |||||||
| INNOVATE | 23 (46.9) | 9 | 0.39 | 42 | 56 | 1.33 | 0.29 (0.14 to 0.59) |
| EXALT | 31 (52.5) | 28 | 0.89 | 23 | 41 | 1.91 | 0.51 (0.31 to 0.82) |
| CSS exacerbations | |||||||
| INNOVATE | 23 (46.9) | 5 | 0.17 | 42 | 34 | 0.81 | 0.21 (0.08 to 0.54) |
| EXALT | 31 (52.5) | 13 | 0.41 | 23 | 20 | 0.93 | 0.44 (0.22 to 0.88) |
| CSNS exacerbations | |||||||
| INNOVATE | 23 (46.9) | 4 | 0.17 | 42 | 22 | 0.52 | 0.33 (0.11 to 0.96) |
| EXALT | 31 (52.5) | 15 | 0.48 | 23 | 21 | 0.91 | 0.53 (0.27 to 1.03) |
Health-care use by subgroups: responder analysis
| Hospitalisation subgroup | Maintenance OCS subgroup | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Trial | Rate of attendance/treatment period | Rate ratio (95% CI)a | Rate of attendance/treatment period | Rate ratio (95% CI)a | ||||||
| Omalizumab responder | Comparator | Omalizumab responder | Comparator | |||||||
| n (% ITT subgroup) | Rate | n | Rate | n (% ITT subgroup) | Rate | n | Rate | |||
| Adults: licensed population | ||||||||||
| Hospitalisation | ||||||||||
| INNOVATE | 47 (56.6) | 0.07 | 79 | 0.25 | 0.28 (0.09 to 0.90) | 23 (46.9) | 0.04 | 42 | 0.28 | 0.14 (0.02 to 1.17) |
| EXALT | 33 (56.9) | 0.06 | 32 | 0.29 | 0.21 (0.06 to 0.80) | 31 (52.5) | 0.06 | 23 | 0.28 | 0.21 (0.04 to 1.09) |
| ER attendance | ||||||||||
| INNOVATE | 47 (56.6) | 0.00 | 79 | 0.09 | – | 23 (46.9) | 0.00 | 42 | 0.10 | – |
| EXALT | 33 (56.9) | 0.06 | 32 | 0.16 | 0.38 (0.07 to 1.97) | 31 (52.5) | 0.03 | 23 | 0.09 | 0.33 (0.02 to 3.86) |
| Unscheduled doctor visits | ||||||||||
| INNOVATE | 47 (56.6) | 0.05 | 79 | 0.38 | 0.13 (0.03 to 0.49) | 23 (46.9) | 0.13 | 42 | 0.14 | 0.93 (0.23 to 3.7) |
| EXALT | 33 (56.9) | 0.09 | 32 | 0.85 | 0.11 (0.03 to 0.36) | 31 (52.5) | 0.63 | 23 | 0.98 | 0.64 (0.35 to 1.17) |
| Total emergency visits | ||||||||||
| INNOVATE | 47 (56.6) | 0.03 | 79 | 0.75 | 0.04 (0.01 to 0.21) | 23 (46.9) | 0.17 | 42 | 0.41 | 0.41 (0.14 to 1.23) |
| EXALT | 33 (56.9) | 0.22 | 32 | 1.31 | 0.17 (0.08 to 0.37) | 31 (52.5) | 0.73 | 23 | 1.35 | 0.54 (0.31 to 0.93) |
Appendix 11 Unscheduled health-care use (randomised controlled trials)
| Study ID | n (subgroups) | Duration | Hospitalisation | Emergency room treatment | Unscheduled medical care | |||
|---|---|---|---|---|---|---|---|---|
| Outcome | Data: omalizumab vs. comparator | Outcome | Data: omalizumab vs. comparator | Outcome | Data: omalizumab vs. comparator | |||
| Ayres 2004 (IA-04)30 | 312 | 52 weeks | n/N (%) | 16/191 (8.4%) vs. 8/89 (9.0%) | n/N (%) | 24/191 (12.6%) vs. 17/89 (19.1%) | n/N (%) | 64/191 (33.5%) vs. 45/89 (50.6%) |
| EU population subgroup | n/N (%) | N with 0 hospitalisation | Rate | N with 0 ER visits | Rate | 43/107 vs. 21/40 | ||
| 12/115 (11.2%) vs. 5/49 (12.5%) | 18/107 vs. 10/40a | |||||||
| Bardelas (AIC)32 | 271 | 24 weeks | NR | NR | NR | |||
| Bousquet 2010 (EXALT)31 | 404 | 32 weeks | Mean rate at 16 and 32 weeks, RR for 16 and 32 weeks | 0.05 vs. 0.14 at 32 weeks | Mean rate at 16 and 32 weeks | 0.02 vs. 0.10 at 32 weeks | Mean rate at 32 weeks | 0.28 vs. 0.59 at 32 weeks |
| Number with 0, 1, 2, 3, ≥ 4 hospitalisations OR emergency visits | N with 0 hospitalisation/emergency visits: 226/272 vs. 86/128 | RR for 16 and 32 weeksb | RR 0.19 (0.06 to 0.61) | RR 0.45 (0.27 to 0.76) | ||||
| Humbert 2005 (INNOVATE)19 | 419 | 44 weeks (28 weeks = 16 f/u) | Number | 13 vs. 25 total hospitalisation | Number | 9 vs. 14 | Number | 28 vs. 54 |
| Rate/28 weeks | 0.06 vs. 0.12 | Rate/28 weeks | 0.04 vs. 0.06 | Rate/28 weeks | 0.13 vs. 0.24 | |||
| Rate ratio | 0.54 (95% CI 0.25 to 1.170 | Rate ratio | 0.66 (95% CI 0.21 to 2.09) | Rate ratio | 0.55 (95% CI 0.27 to 1.10) | |||
| N with 0 hospitalisationa | 11/209 vs. 18/211 | |||||||
| Hanania 201133 | 850 | 48 weeks | NR | NR | NR | |||
| Vignola 2004 (SOLAR)36 | 405 | 28 weeks | NR | NR | NR | |||
| 157 on LABA | ||||||||
| Holgate 200450 | 246 | 32 weeks (16 + 16 steroid reduction phase) | NR | NR | NR | |||
| Hoshino 201234 | 30 | 16 weeks | NR | NR | NR | |||
| Ohta 200935 | 327 | 16 weeks treatment +12-week follow-up | NR | NR | NR | |||
| Chanez 200429 | 31 | 16 weeks | Number | 0 vs. 0 | Change from baseline [median (range)]b | 0 (−2 to 1) vs. 0 (−1 to1) | See Emergency room treatment | |
| cBusse 201128 | 419 | 60 weeks | % with ≥ 1 hospitalisation | 1.5 (SE 0.9) vs. 6.3 (SE 1.8) | NR | NR | ||
| 226 high ICS + LABA | Treatment difference | –4.7 (95% CI –8.6 to –0.9) | ||||||
| N with ≥ 1 | ||||||||
| dLanier 2009 (IA-05)20 | 628 | 52 weeks (24-week fixed steroid, 28-week adjustable steroid) | Number with 1, 2, 3, ≥ 4 hospitalisations at 24 and 52 weeksa | |||||
| EU population subgroup | [246 severe (LABA, 57% LTRA)] | Number with 0 and mean number calculable (and hence rate) | 0.06 vs. 0.06 at 24 weeks | Rate at 24 and 52 weeks | 0.32 vs. 0.24 at 24 weeks | Rate at 24 and 52 weeks | 0.27 vs. 0.19e at 24 weeks | |
| Rate at 24 and 52 weeks | 8/159 vs. 4/76 | RR | RR | |||||
| RR | ||||||||
| n/N | ||||||||
Appendix 12 Quality of life and asthma symptoms (randomised controlled trials)
| Study ID | n subgroups | Duration (weeks) | AQLQ or other measure of QoL | ACT or other asthma symptom score | Asthma symptoms | GETE excellent/good | FEV1% predicted | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Data | Outcome | Data | Outcome | Data | Physician rating | ||||
| Ayres 2004 (IA-04)30 (EU population subgroup) | 312 | 52 | n with ≥ 0.5 increase from baseline in omalizumab group only | 71/115 (62%)a | Wasserfallen asthma symptom score; mean reduction from baseline | 6.7 vs. 0.5 | % requiring rescue meds ≥ 1 day/week | 75 (41.4%) vs. 18 (20.7%) | NR | 75 vs. 69 |
| Median puffs | 0.60 vs. 3.00 | (p < 0.05) | ||||||||
| Change from baseline calculable | ||||||||||
| Bardelas (AIC)32 | 271 | 24 | NR | ACT change from baseline mean | 5.01 vs. 4.36 | Changes from baseline | 55.1% vs. 48.1 | Change from baseline 0.08 vs. 0.16 | ||
| LSM difference | 0.64 (95% CI 0.30 to 1.59) | Days/week SABA use | −1.74 vs. −1.49 | Treatment difference −0.08 −0.19 to 0.02) | ||||||
| Days/week symptoms | −2.16 vs. −1.77 | |||||||||
| Night wakening/week | −1.45 vs. 1.06 | |||||||||
| Bousquet 2010 (EXALT)31 | 404 | 32 | AQLQ LSM change from baseline at weeks 15 and 31 | At 31 weeks | ACQ LSM change from baseline (SE) at 16 and 32 weeks | At 32 weeks | Days disturbed sleep in last 2 weeks change from baseline (SD) | −4.05 (5.45) vs. −2.71 (5.38) | 70% vs. 28.2%1 | 68.1 vs. 63.7 |
| EQ-5D LSM change from baseline at weeks 15 and 31; utility index | 1.06 (95% CI 0.88 to 1.24) vs. −0.07 (95% CI −0.31 to 0.17) | RR | −0.91 (0.081) vs. −0.04 (0.110) | |||||||
| Health state assessment | At 31 weeks | −0.87 (95% CI −1.09 to −0.65) | ||||||||
| 0.09 (95% CI 0.05 to 0.13) vs. 0.06 (95% CI 0.01 to 0.12) | ||||||||||
| 9.3 (95% CI 5.2 to 13.4) vs. −2.8 (−8.5 to 3.0) | ||||||||||
| Humbert 2005 (INNOVATE)19 | 419 | 44 (28 + 16 f/u) | AQLQ LSM change from baseline | 0.91 vs. 0.46 | NR | Days symptom-free in last 2 weeks (%) | 37.2 vs. 22.6 | 56.5% vs. 41.0%1 | NRb | |
| p-value | < 0.001 | |||||||||
| n with ≥ 0.5, ≥ 1.0 and ≥ 1.5 improvement also reported | ||||||||||
| Hanania 201133 | 850 | 48 | AQLQ change from baseline | 1.15 vs. 0.92 | Total asthma severity score change from baseline | −1.56 vs. −1.31 | Puffs rescue med/day change from baseline | −1.58 vs. −1.31 | NR | NR |
| Treatment difference | 0.29 (95% CI 0.15 to 0.43) | Treatment difference | −0.26 (95% CI −0.43 to −0.10) | Treatment difference | −0.27 (95% CI −0.49 to −0.04) | |||||
| Vignola 2004 (SOLAR)36 | 405 | 28 | AQLQ N(%) with ≥ 0.5, ≥ 1.0 and ≥ 1.5 point improvement | 0.5 point improvement | Wasserfallen asthma symptom score treatment difference | −1.8 (p = 0.023) | Patient and investigator assessment of control of asthma symptoms: Good or excellent n/N | Patient: 137/209 vs. 127/196 | NR | p = 0.065 |
| 157 on LABA | 164 (78.8%) vs. 134 (69.8%) | Puffs rescue med/day | Investigator 124/209 vs. 81/196 | |||||||
| ≥ 1 point improvement | 1.8 vs. 2.4 | |||||||||
| 140 (67.3) vs. 96 (50.0) | ||||||||||
| Hoshino 201234 | 30 | 16 | AQLQ change from baseline | 1.47 (p < 0.001) vs. 0.28 (NS) | NR | NR | NR | 73.5 vs. 68.6 | ||
| Change from baseline calculable | ||||||||||
| Ohta 200935 | 327 | 16 treatment + 12-week follow-up | Daily activity score | No sig change from baseline | Asthma symptom score | Non-significant improvement favouring omalizumab | Changes from baseline | NR | NRc | |
| Mean puffs rescue med | NS improvement favouring omalizumab | |||||||||
| Mean no. days sleep disturbed | NS improvement favouring omalizumab | |||||||||
| Chanez 200429 | 31 | 16 | NR | NR | Changes from baseline | NR | Median (range) change from baseline 2.6% (−10 to 60) vs. 1.7% (−19 to 7) | |||
| Median (range) puffs rescue med | 1.00 (−45 to 17) vs. 0.0 (−22 to 4) | |||||||||
| Median (range) days disturbed sleep | −0.6 (−6 to 1) vs. 1.0 (−4 to 2) | |||||||||
| Median (range) days with symptoms | −1.4 (−7 to 3) vs. 0.0 (−4 to 2) | |||||||||
| Median (range) days with activity impairment | −0.4 (−7 to 2) vs. –0.3 (−7 to 2) | |||||||||
| dBusse 201128 | 419 | 60 | NR | ACT score mean (SE) | ≥ 4 to ≤ 11 years | Mean (SE) days/2 weeks with symptoms | 1.32 (0.09) vs. 1.76 (0.09) | NR | 92.6 (SE 0.64) vs. 91.7 (0.64) | |
| ≥ 4 to ≤ 11 years | 226 high ICS + LABA | Treatment difference | 23.0 (0.21) vs. 22.2 (0.21) | Treatment difference | −0.44 (95% CI −0.70 to −0.17) | Change from baseline calculable | ||||
| ≥ 12 years | Change from baseline calculable | 0.78 (95% CI 0.21 to 1.35) | Mean (SE) days sleep disturbed | 0.42 (0.05) vs. 0.59 (0.05) | ||||||
| ≥ 12 years | Treatment difference | −0.17 (95% CI −0.31 to −0.03) | ||||||||
| 22.5 (0.22) vs. 22.3 (0.22) | Mean (SE) days with activity impairment | 0.70 (0.07) vs. 0.98 (0.07) | ||||||||
| 0.19 (95% CI −0.42 to 0.79) | Treatment difference | −0.28 (95% CI −0.47 to −0.09) | ||||||||
| eLanier 2009 (IA-05)20 | 628 | 52 (24 fixed steroid, 28 adjustable steroid) | Paediatric AQLQ | 0.04 in favour of omalizumab (NS) | NR | Puffs rescue med/day mean (SD) at 24 weeks | −1.3 (2.84) vs. −1.0 (2.50) | 79% vs. 56% | NR | |
| EU population subgroup | [246 severe (LABA, 57% LTR)] | LSM difference at 24 weeks | Days sleep disturbed mean (SD) at 24 weeks | −0.63 (0.72) vs. 0.50 (0.71) | ||||||
| 412 | ||||||||||
Appendix 13 Long-term effectiveness data
| Study ID | Study design | n | Population characteristics/inclusion criteria | Duration | Exacerbations (omal vs. comp) | Definitiona | Asthma symptoms (omal vs. comp) | Unscheduled health-care visits (omal vs. comp) | Controller medication use (omal vs. comp) | QoL (omal vs. comp) |
|---|---|---|---|---|---|---|---|---|---|---|
| Ayres 2004 (IA-04)30 | Open-label RCT | 312 | ≥ 1 emergency room visit/hospitalisation and ≥ 1 additional course of OCSs in the last year | 52 weeks | 1.12 vs. 2.86 | Requiring systemic CS | NR | Hospitalisations: | OCSs increased: | Mini-AQLQ change from baseline for step 4 subgroup: 1.32 vs. 0.17, p < 0.001 |
| EU population subgroup | −60.8 (95% CI 46.9 to 71.0%), p < 0.001 (mean annualised number) | 16/191 vs. 8/89, p = NS | 99 (51.8) vs. 58 (65.2) | Step 4 subgroup, mini-AQLQ patients with: | ||||||
| Subgroup step 4 | Subgroup GINA 4: | p = 0.037 | ≥ 0.5 improvements: | |||||||
| Mean annual rate: 1.26 vs. 3.06 (ITT) | 12/115 vs. 5/49 | 76.5% vs. 41.7%, p < 0.001 | ||||||||
| ED: 24/191 vs. 17/89, p = NS | ≥ 1.0 improvements: | |||||||||
| Subgroup GINA 4: | 55.1% vs. 25.0%, p = 0.003 | |||||||||
| 18/115 vs. 10/49 | (≥ 1.5) improvements: | |||||||||
| Doctors: 64/191 vs. 45/89 (PP), p = 0.007 | 45.9% vs. 13.9%, p < 0.001 | |||||||||
| Subgroup step 4: | Wasserfallen score mean reduction (ITT): 6.2 vs. 0.7, p < 0.001 | |||||||||
| 43/115 vs. 21/49, p = NR | ||||||||||
| Busse 201128,b | Double-blind RCT | 419 | Hospitalisation or unscheduled urgent care in the 6–12 months prior to study entry for patients receiving long-term therapy for disease control. Persistent symptoms and uncontrolled asthma for patients not receiving long-term control therapy | 60 weeks | 63/208 (30.3%, SE 3.3) vs. 103/211 (48.8%, SE 3.7) | Need for SCS and/or hospitalisation | Mean (SE) days sleep disturbed because of asthma: | Hospitalisations: | NR | ACT (4–11 years) Mean (SE): 23.0 (0.21) vs. 22.2 (0.21). |
| 226 high ICS + LABA | Difference: −18.5 (95% CI −28.2 to −8.8) | 0.42 (SE 0.05) vs. 0.59 (SE 0.05) | Adjusted% with ≥ 1: 1.5 (SE 0.9) vs. 6.3 (SE 1.8) | Difference: 0.78 (95% CI 0.21 to 1.35) | ||||||
| Difference: −18.5 (95% CI −28.2 to −8.8) | Difference: −4.7 (95% CI −8.6 to −0.9) | ACT (≥ 12 years): 22.5 (0.22) vs. 22.3 (0.22) | ||||||||
| ED: NR | Difference: 0.19 (95% CI −0.42 to 0.79) | |||||||||
| Doctors: NR | ||||||||||
| Brusselle 2009 (PERSIST)39 | Prospective single group | 160 (158 evaluable) | ≥ 2 documented asthma exacerbations requiring OCSs, emergency services or hospitalisation in the past 2 years. Severe asthma treatment (GINA 2005), positive radioallergosorbent test, regularly occurring day or night-time asthma symptoms | 52 weeks | Rate: 0.95 (1.78 points (66.5% reduction from baseline) | Severe exacerbation: requiring OCSs or an emergency room visit or hospitalisation | Percentage of patients with a reduction in frequency of daytime | NR | Methylprednisolone | AQLQ (no improving by ≥ 0.5 at 52 weeks (ITT): |
| at 52 weeks | discontinued: 24/130 (18.45%) (ITT) | 103/122 (84.4%) | ||||||||
| ITT: 63.8% (p < 0.001) | Reduction in average daily dose: 39.4%, mean (SD) 7.31 [13.86] mg, p < 0.001 | GETE excellent or good: | ||||||||
| PP: 72.4% (p < 0.001) | budesonide | at 52 weeks (ITT): 94/130 (72.3%) | ||||||||
| Percentage of patients with a reduction in frequency of night-time symptoms | Reduction in average daily dose: 10.1%, mean (SD) 94.14 [352.48] µg, p = 0.047 | |||||||||
| at 52 weeks | formoterol | |||||||||
| ITT: 49.2% (p = NS) | Reduction in average daily dose: 9.6%, mean (SD) 3.03 [11.16] mg, p = 0.038 | |||||||||
| PP: 54.3% (p = 0.009) | leukotriene antagonists | |||||||||
| discontinued: 9 (p = NS) | ||||||||||
| Anticholinergic | ||||||||||
| Discontinued: 11 (p = 0.013) | ||||||||||
| Antihistamines | ||||||||||
| discontinued: 6 (p = NS) | ||||||||||
| theophylline/derivatives | ||||||||||
| discontinued: 5 (p = NS) | ||||||||||
| Retrospective single-arm | 53 | + 120 weeks retrospective follow-up | NR | N/A | NR | Hospitalisations: 1/53 (1.9%) | % requiring OCSs: 18.9% (n = NR) | AQLQ (no improving by ≥ 0.5: at follow-up: | ||
| ED: 0/53 | > 90% (n not reported) | |||||||||
| Doctor: NR | GETE excellent or good at follow-up > 85% (n = not reported) | |||||||||
| Cazzola 201040 | Prospective single-arm | 93 | Moderate to severe according to GINA guidelines. Persistence of symptoms, emergency room visits, hospitalisations the previous year, despite ongoing treatment with high-dose ICS and LABAs | 12 months duration, 12 months follow-up | Pre-12 months treatment: 123/139 (88.5%) | NR | NR | Hospitalisations: pre-12 months treatment: 89/140 (63.6%) | NR | NR |
| Mean (SD) exacerbations/patient/year pre-12 months treatment: 4.87 (4.00) | Mean (SD) number visits/year pre-12 months treatment: 4.45 (4.31) | |||||||||
| Post-12 months treatment: 17/93 (18.3%) | Post-12 months treatment: 7/92 (7.6%) | |||||||||
| Mean (SD) exacerbations/patient/year post-12 months treatment: 1 (1.29) | Mean (SD) number visits/year post-12 months treatment: 1.23 (0.49) | |||||||||
| ED Visits: NR | ||||||||||
| Doctor visits: Pre-12 months treatment (health-care contact/emergency visits): 33/141 (23%) | ||||||||||
| Post-12 months treatment (health care contact/emergency visits): 1/93 (1.1%) | ||||||||||
| Lanier 2009 (IA-05)20 | Double-blind RCT | 628 | ≥ 2 exacerbations within 1 year, ≥ 3 within 2 years or ≥ 1 severe exacerbation requiring hospitalisation within 1 year before study entry) | 52 weeks (24-week fixed steroid, 28-week adjustable steroid) | Rate at 52 weeks: 0.12 vs. 0.24 | Severe exacerbations: doubling of baseline ICS dose and/or treatment with rescue systemic corticosteroids for ≥ 3 days | NR | NR | SCS mean reduction (mg/day) at 52 weeks (n = 576: O: 384; C: 192) | GETE excellent/good (physician rated) at 52 weeks: 118/159 vs. 42/76, p < 0.001 |
| EU population subgroup | [246 severe (LABA, 57% LTR)] | RR 0.49 (95% CI 0.30 to 0.80) | 233.5 vs. 316.7 | GETE excellent/good (patient rated) at 52 weeks: 80% vs. 72%, p < 0.001 | ||||||
| p = 0.006 | ||||||||||
| (post hoc analysis) | ||||||||||
| Randolph 201063 | Prospective observation and chart review | Omalizumab: 29 patients with moderate to severe allergic asthma | Age: mean 31 years; median 22 years (range 10 66) | 6 years | Reduced: 7/29 (24%) | NR | Optimal/good control (ACT ≥ 20): 25/29 (86%) | NR | Declined: 4/29 (14%) | ACT ≥ 20 (good control): 25/29 (86%) |
| Abstract | Inclusion criteria: NR | Treatment exposure: 6 months to 6 years (mean 2.1 years; median 1.8 years) | Unchanged: 10/29 (35%) | Less than optimal/poor control (ACT ≤ 19): 4/29 (14%) | Unchanged: 22/29 (76%) | ACT ≤ 19 (less than optimal/poor control): 4/29 (14%) | ||||
| No exacerbations: 12/29 (41%) | None use: 3/29 (10%) | |||||||||
| Zureik 201047 PAX-LASER | Prospective controlled observational study | 486 | > 1000 µg beclometasone or equivalent; 5 mg prednisone equivalent for ≥ 6 months or ≥ 3 courses of OCSs in 1 year | ≥ 12 months | Rates per 100 patient-years | Severe exacerbation: hospitalisation/emergency room visit, recorded for the year before and during the prospective follow-up | NR | As per exacerbations | NR | NR |
| Abstract | Adjusted RR 0.56 (95% CI 0.43 to 0.74) | |||||||||
| Allergic patients subgroup | Omalizumab pre–post: adjusted RR 0.40 (95% CI 0.28 to 0.58) |
Appendix 14 Randomised controlled trial adverse event data: number of patients reporting events (%)
| Study details | Study duration/ follow-up | Population age | Patients with any AE | No. patients with serious AE | Mortality | Anaphylaxis | Malignancy | ATE | Withdrawals because of AE |
|---|---|---|---|---|---|---|---|---|---|
| Ayres (2004)30 | 12 months | 12–75 years | Omalizumab: 175/206 (85.0%) | Omalizumab: 34/206 (16.5%) (excludes death) | Omalizumab: 1/206 (0.49%) | NR | NR | Omalizumab: NR (1 withdrawn) | Omalizumab: 15 |
| Open-label RCT | BSC: 82/106 (77.4%) | BSC: 14/106 (13.2%) | BSC: 0/106 | BSC: NR | BSC: NR | ||||
| RR: 1.10 (95% CI 0.98 to 1.24) | RR: 1.25 (95% CI 0.70 to 2.22) | RR: 1.55 (95% CI 0.06 to 37.74 | N/A | N/A | N/A | N/A | |||
| Bardelas (2012)32 | 24 weeks | ≥ 12 years | Omalizumab: 90/136 (66.2%) | NR | 0 | 0 | Omalizumab: 2/136 (1.47%) | Omalizumab: 1/136 (0.74%) | Omalizumab: 3/136 (2.2%) |
| Double-blind RCT | Placebo: 93/135 (68.9%) | Placebo: 0/135 | Placebo: 0/135 | Placebo: 3/135 (2.2%) | |||||
| RR: 0.96 (95% CI 0.81 to 1.13) | N/A | N/A | N/A | RR: 4.96 (95% CI 0.24 to 102.43) | RR: 2.98 (95% CI 0.12 to 72.46) | RR: 0.99 (95% CI 0.20 to 4.83) | |||
| Bousquet (2010)31 | 32 weeks | 12–75 years | Omalizumab: 184/272 (67.2%) | Omalizumab: 24/272 (8.8%) | Omalizumab: 0/272 | NR | NR | NR | Omalizumab: 7/274 (2.5%) |
| EXALT study | OAT: 69/128 (53.9%) | OAT: 11/128 (8.6%) | OAT: 1/128 (0.8%) | OAT: 2/128 (1.5%) | |||||
| Open-label RCT | |||||||||
| RR: 1.25 (95% CI 1.05, 1.50) | RR: 1.03 (95% CI 0.52 to 2.03) | RR: 0.16 (95% CI 0.01, 3.84) | N/A | N/A | N/A | RR: 1.64 (95% CI 0.34 to 7.76) | |||
| Busse (2011)28 | 60 weeks treatment | 6–20 years | Omalizumab: 82/208 (39.4%) 39.4% | Omalizumab: 13/208 (6.3%) 39.4% | NR | Omalizumab: 1/208 (0.48%) | NR | Omalizumab: 1/208 (0.48%) | NR |
| ICATA study | Placebo: 100/211 (47.4%) | Placebo: 29/211 (13.7%) | Placebo: 6/211 (2.84%) | Placebo: 12/211 (5.69%) | |||||
| Double-blind RCT | |||||||||
| RR: 0.83 (95% CI 0.67 to 1.04) | RR: 0.45 (95% CI 0.24 to 0.85) | N/A | RR: 0.17 (95% CI 0.02 to 1.39) | N/A | RR: 0.08 (95% CI 0.01 to 0.64) | N/A | |||
| Chanez (2010)29 | 16 weeks | ≥ 18 years | Omalizumab: 11/20 (55%) | Omalizumab: 0/20 | NR | NR | NR | NR | Omalizumab: 1/20 (5.0%) |
| Double-blind RCT | Placebo: 7/11 (63.6%) | Placebo: 1/11 (9.1%) | Placebo: 2/11 (18.2%) | ||||||
| RR: 0.86 (95% CI 0.48 to 1.57) | RR: 0.19 (95% CI 0.01 to 4.32) | N/A | N/A | N/A | N/A | RR: 0.28 (95% CI 0.03 to 2.70) | |||
| Hanania (2011)33 | 48 weeks | 12–75 years | Omalizumab: 344/428 (80.4%) | Omalizumab: 40/428 (9.3%) | Omalizumab: 0/428 | Omalizumab: 1/428 (0.23%) | Omalizumab: 1/428 (0.23%) | Omalizumab: 2/428 (0.47%) | Omalizumab: 16/428 (3.7%) |
| Double-blind RCT | Placebo: 334/420 (79.5%) | Placebo: 44/420 (10.5%) | Placebo: 3/420 (0.71%) | Placebo: 2/420 (0.48%) | Placebo: 3/420 (0.71%) | Placebo: 2/420 (0.48%) | Placebo: 10/420 (2.4%) | ||
| RR: 1.01 (95% CI 0.94 to 1.08) | RR: 0.89 (95% CI 0.59 to 1.34) | RR: 0.14 (95% CI 0.01 to 2.71) | RR: 0.49 (95% CI 0.04 to 5.39) | RR: 0.33 (95% CI 0.03 to 3.13) | RR: 0.98 (955 CI 0.14 to 6.93) | RR: 1.57 (95% CI 0.72 to 3.42) | |||
| Holgate (2004)50 | 16 weeks + 16 weeks steroid reduction | 12–75 years | Omalizumab: 96/126 (76.2%) | Omalizumab | NR | NR | NR | NR | Omalizumab: 0/126 |
| RCT | Placebo: 99/120 (82.5) | 1/126 (0.8%) | Placebo: 2/120 | ||||||
| Placebo: 5/120 (4.2%) | |||||||||
| RR: 0.92 (95% CI 0.81 to 1.05) | RR: 0.19 (95% CI 0.02 to 1.61) | N/A | N/A | N/A | N/A | RR: 0.19 (0.01 to 3.93) | |||
| Humbert (2005)19 | 28 weeks + 16 week follow-up | 12–75 years | Omalizumab: 177/245 (72.2%) | Omalizumab: 29/245 (11.8%) | NR | NR | NR | NR | Omalizumab: 11/245 (4.49%) |
| INNOVATE study | Placebo: 179/237 (75.5%) | Placebo: 37/237 (15.6%) | Placebo: 4/237 (1.69%) | ||||||
| Double-blind RCT | |||||||||
| RR: 0.96 (95% CI 0.86 to 1.06) | RR: 0.76 (95% CI 0.48 to 1.19) | N/A | N/A | N/A | N/A | RR: 2.66 (95% CI 0.86 to 8.24) | |||
| Lanier (2009)20 (severe asthma) | 52 weeks | 6 to < 12 years | Omalizumab: 380/421 (90.3%) | Omalizumab: 17/421 (4.0%) | 0 | Omalizumab: 1/421 (0.24%) | Omalizumab: 0/421 | NR | Omalizumab: 2/421 (0.5%) |
| Double-blind RCT | Placebo: 194/207 (93.7%) | Placebo: 17/207 (8.2%) | Placebo: 1/207 (0.48%) | Placebo: 1/207 (0.48%) | Placebo: 1/207 (0.5%) | ||||
| RR: 0.96 (95% CI 0.92 to 1.01) | RR: 0.49 (95% CI 0.26 to 0.94) | N/A | RR: 0.49 (95% CI 0.03 to 7.82) | RR: 0.16 (95% CI 0.01 to 4.02) | N/A | RR: 0.98 (95% CI 0.09 to 10.78) | |||
| Severe subgroup | Omalizumab: 155/166 (93.4%) | Omalizumab: 6/166 (3.6%) | NR | NR | NR | NR | Omalizumab: 1/421 (1.2%) | ||
| Omalizumab: 166 | Placebo: 76/80 (95.0%) | Placebo: 8/80 (10.0%) | Placebo: 0/207 | ||||||
| Placebo: 80 | |||||||||
| RR: 0.98 (95% CI 0.92 to 1.05) | RR: 0.36 (95% CI 0.13 to 1.01) | N/A | N/A | N/A | N/A | RR: 1.48 (95% CI 0.06 to 36.14) | |||
| Ohta (2009)35 | 16 week treatment + 12 weeks follow-up | 20–75 years | Omalizumab: 136/151 (90.1%) | NR | NR | NR | NR | NR | Omalizumab: 6/151 (4.0%) |
| Double-blind RCT | Placebo: 142/164 (86.6%) | Placebo: 7/164 (4.3%) | |||||||
| RR: 1.04 (95% CI 0.96 to 1.13) | N/A | N/A | N/A | N/A | N/A | RR: 0.93 (95% CI 0.32 to 2.71) | |||
| Vignola (2004)36 | 28 weeks treatment | 12–75 years | Omalizumab: 164/209 (78.5%) | NR | 0 | NR | NR | NR | NR |
| SOLAR study | Placebo:135/196 (68.9%) | ||||||||
| Double-blind RCT | |||||||||
| RR: 1.14 (95% CI 1.01 to 1.28) | N/A | N/A | N/A | N/A | N/A | N/A | |||
Appendix 15 Observational studies: adverse event data: number of patients reporting events (%)
| Study details | Study duration/follow-up | Population age | Patients with any AE | No. patients with serious AE | Mortality | Anaphylaxis | Malignancy | ATE | Withdrawals because of AE |
|---|---|---|---|---|---|---|---|---|---|
| Cazzolla (2010)40 | 12 months | Total no. patients: 142 | 9 (6.7%) | 1 | NR | NR | NR | NR | 1 |
| Design: prospective observational before-and-after study | ≥ 12 years | ||||||||
| Braunstahl (2011)38 | Up to 2 years | ≥ 12 years | NR | 41/876 (4.7%) | 6/876 (0.68%) | NR | NR | NR | 12/876 (1.4%) |
| Design: postmarketing surveillance | |||||||||
| Brusselle (2009)39 | 52 weeks | ≥ 12 years | Overall: 89/160 (55.6%) | 39/160 (24.4%) | 4/160 (2.5%) | NR | NR | Vascular disorders (not otherwise specified) ≥ 5% frequency | 19/158 (12.0%) |
| Design: non-comparative prospective cohort | |||||||||
| Costello (2011)41 | 6 months | Mean (SD) 48 (21) | 6/93 (6.5%) | NR | 1/93 (1.1%) | NR | 1/93 (1.1%) | NR | 6/93 (6.5%) |
| Design: non-comparative cohort (retrospective observational) | |||||||||
| Domingo (2011)56 | ≥ 1 year; mean 17.2 ± 8.5 months (range 4–34) | ≥ 18 years | 5/32 (15.6%) | NR | NR | NR | NR | NR | 1/32 (3.1%) |
| Design: non-comparative cohort | |||||||||
| Brodlie 201254 | 16 weeks | 5–16 years | NR | 0/34 | NR | NA | NR | NR | NA |
| Design: non-comparative cohort | |||||||||
| Eisner 201171 | Average follow-up of 3.8 person-years | NR | NR | NR | NR | NR | Omalizumab: 12.78/1000 person-years | NR | NR |
| EXCELS study | Control:14.48/1000 person-years | ||||||||
| Design: ongoing controlled postmarketing study | Rate difference: −1.70/1000 person-years (95% CI −6.43 to 2.21) | ||||||||
| Korn (2009)44 | 4 and 6 months, mean 195 ± 60 days | ≥ 12 years | 100/280 (35.7%) | 67/280 (23.9%) | NR | NR | NR | NR | NR |
| Design: postmarketing surveillance | |||||||||
| Molimard (2008)45 | ≥ 5 months | Mean (SD) overall age | 39/147 (26.5%) | 5/147 (3.4%) | 1/147 (0.68%) | NR | NR | NR | 8/147 (5.4%) |
| Design: non-comparative cohort | 46.5 ± 13.55 | ||||||||
| Ohta (2010)46 | 48-week treatment period, 12-week follow-up | 20–75 years | 131/133 (98.5%) | Serious AE | 1/133 (0.75%) | 0/133 | NR | Vascular disorders (not otherwise specified): 7/133 (5.3%) | 2/133 (1.5%) |
| Design: non-comparative extension study (open-label) | Severe Japanese label population (n = 37): AE data not reported separately | 6/133 (4.5%) | |||||||
| Severe AE | |||||||||
| 3/133 (2.3%) | |||||||||
| Stukus (2008)59 | NR | Mean 46.1 years | Group 1 (IgE > 700 IU/l): 2/10 (20%) | NR | NR | NR | NR | NR | 3/45 (6.7%) |
| Design: Uncontrolled retrospective cohort | Group 2 (IgE 30–700 IU/l): 4/35 (11.4%) | ||||||||
| Tzortzaki 201262 | 4 years | Mean 54 years ± 14 | 7/60 (11.6%) | 0/60 (0%) | 0/60 | NR | NR | NR | 0/60 (0%) |
Appendix 16 Systematic review on cost-effectiveness studies on omalizumab
Summary table of cost-effectiveness studies on omalizumab
| Study details | Oba and Salzman (2004)90 | Dewilde et al. (2006)93 |
|---|---|---|
| Economic evaluation type | Cost-effectiveness analysis | Cost–utility analysis |
| Currency (year) | 2003 | 2005? |
| Study design | Trial-based (pooled analysis of RCT 008 and 009) | Markov model (same as MS for TA133 and TA201) |
| Perspective | Third-party (health-care) payer | Third party (health-care) payer |
| Setting | USA | Sweden |
| Patient population | Based on the RCT 008 and 009: adolescents (≥ 12 years) and adults suffering from asthma, uncontrolled despite ICSs. Average age of 39 years, 54% female, mean BDP dose of 670 µg/day | Based on the INNOVATE trial: severe persistent asthma patients, 68% female, average age of 43 years, on ICSs > 2300 µg/day |
| Inclusion criteria: positive prick test response to more than one common allergen (mites, cockroach, cat, dog), total serum IgE levels of > 30 to < 700 IU/ml, and FEV1 values between 40% and 80% of predicted values. | Inclusion criteria: FEV1 ≥ 40 to < 80% of predicted value, continuing asthma symptoms, at least two asthma exacerbations requiring systemic corticosteroids (or one severe exacerbation PEV/FEV < 60% of personal best requiring systemic corticosteroids) resulting in hospital admission or emergency treatment in the past 12 months despite high-dose ICS and LABA | |
| Exclusion criteria: patients taking other controller medication other than ICSs and current smokers | ||
| Time horizon | Unclear. As per RCT? | Lifetime |
| Comparators | Usual care: ICSs | Optimised standard therapy at GINA step 4 (high-dose ICS and LABA) |
| Resources used and costs | Medication: omalizumab, rescue medication, ICSs | Medication: drug and dose distribution found in INNOVATE |
| Health-care use: treatment for drug-related adverse events, unscheduled physician visits, emergency department visits and hospitalisations | Administration costs of omalizumab (cost of GP visit) | |
| Cost of assessment of response at 16 weeks | ||
| Health-care use because of exacerbations | ||
| Costs in added years of life (difference between annual consumption and production of surviving individuals) | ||
| Source of resources used | Trial data – 008 and 009 RCT | INNOVATE trial |
| Source of costs | Omalizumab: personal communication with Novartism $433 for one 150-mg vial | Medication costs were derived from the Swedish price database for reimbursed medicines (omalizumab €394.34 per vial) |
| Rescue medication and ICSs: average wholesale price | Unit costs for health-care use were taken from published studies | |
| Emergency visit, hospitalisation: published economic study | Costs in added years of life from published economic study | |
| Physician visit: average reimbursement for a visit, according to published economic study | ||
| Clinical outcomes | Treatment success: increase of 0.5 points or greater in the AQLQ score from baseline values | Response to omalizumab treatment, evaluated based on the physician global evaluation of treatment effectiveness scale (GETE) scale |
| Successfully controlled days (SCD): day on which morning peak expiratory flow rate of 90% or greater than baseline value (mean of 14 days before exacerbation) AND daytime asthma score of 1 or less (on a scale of 0–4) AND night-time asthma score of 0 (on a scale of 0–4) AND rescue medication use of two puffs or fewer | CS and CSS exacerbations rates (standard therapy exacerbation rate: 6.3%, of which 47.7% CS and 52.3% CSS; RR of omalizumab vs. standard therapy was 0.36). CS exacerbation was defined as a worsening of asthma symptoms requiring treatment with systemic corticosteroids. CSS is a CS exacerbation in which the patient's PEF/FEV1 were less than 60% of personal best | |
| Severe exacerbation-related death (2.082% for the base case, 3.108% and 0% for sensitivity analyses) | ||
| Death from all causes | ||
| Source of clinical outcomes | Trial data: two published RCT | INNOVATE trial for response to omalizumab treatment, and CS and CSS exacerbations |
| Severe exacerbation-related mortality derived from published observational study set in Sweden | ||
| Death from all causes taken from Swedish life tables | ||
| HRQoL | Not included | QALYs |
| Source of HRQoL | Not applicable | Utilities for day-to-day asthma state were obtained from the AQLQ values collected during INNOVATE and mapped onto EQ-5D (omalizumab: 0.779, standard therapy: 0.669) |
| Utilities for CS and CSS states were obtained from a published study conducted in the UK using self-administered EQ-5D (CS: 0.572, CSS: 0.326) | ||
| Adverse events | Not included | Not included |
| Subgroup analysis | Not analysed explicitly but discussed potential cost-savings if omalizumab is given to a more severe population defined as those who are hospitalised five or more times or 20 days or longer per year, or for those who require emergency department visits seven or more times per month | None |
| Discounting | Not applied | 3% for costs and benefits |
| CEA results | Mean daily cost of treatment for each patient achieving at least a 0.5 point increase in the AQLQ score was $378 | ICER = €56,091 per additional QALY for treatment duration of 5 years (additional lifetime cost of €42,754 for 0.762 QALY) |
| Mean daily cost for each patient achieving a SCD was $523 | Probability of omalizumab being cost-effective at willingness to pay for an additional QALY of €60,000 is 0.50 | |
| Probabilistic ICER of €57,961 per additional QALY, non-parametric 95% CI of €31,328; €120,552 | ||
| Assessment of uncertainty | Threshold analysis: | Scenario sensitivity analysis: |
| Costs required to achieve a 0.5-point and 1.5-point increase in the AQLQ scale | Severe exacerbation-related death: 3.108% and 0% | |
| Scenario sensitivity analysis: | Discounting: no discounting, 5% discounting, no discounting of outcomes and 3% of costs | |
| Best-case scenario: lowest acquisition cost of omalizumab, lowest hospitalisation cost of omalizumab, highest hospitalisation cost for placebo group | Utilities based on direct health state evaluation (omalizumab: 0.857, standard therapy: 0.784) | |
| Worst-case scenario: highest acquisition cost of omalizumab | Utility of day-to-day asthma on standard therapy of 0.594 (based on pooled baseline data) | |
| Federal supply schedule cost of omalizumab of $323.29 for one 150-mg vial | Age-dependent utility function | |
| Exclusion of costs with added years of life | ||
| Time horizon: 3 and 5 years. | ||
| Probabilistic sensitivity analysis, including distributions on costs, efficacy and utilities | ||
| Conclusions | Omalizumab is more expensive than other controller medications in patients with moderate allergic asthma. Omalizumab could be cost-saving in a restricted group of patients with severe asthma | Omalizumab may be cost-effective for patients suffering from severe IgE-mediated asthma, who are symptomatic despite best available care, have an increased risk of asthma-related mortality and are at high risk of needing emergency health care during severe asthma exacerbations |
| Key CE drivers | Cost of omalizumab | The key CE driver is severe exacerbation-related death: ICER = €131,130 per QALY gained if mortality is 0%; ICER = €46,268 per QALY gained if mortality is 3.108% |
| Authors also mention patient adherence to treatment and time-independence assumption as having great impact on the CE | ||
| Conflicts of interest | None | Study funded by Novartis |
| Study details | Brown et al. (2007)94 | Wu et al. (2007)91 |
|---|---|---|
| Economic evaluation type | Cost-utility analysis | Cost-utility analysis, cost-effectiveness analysis |
| Currency (year) | 2005 | 2005 |
| Study design | Markov model (same as MS for TA133, TA201 and Dewilde et al. 2006) | Markov model (asthma policy model) |
| Three health states: chronic asthma, acute asthma and death | ||
| Perspective | Third party (health-care) payer | Third party (health-care) payer |
| Setting | Canada | USA |
| Patient population | Based on IA-04 study, a 1-year randomised open-label trial of omalizumab in the subgroup of patients who were receiving high-dose ICS plus a LABA (and additional controller medication if required) | Adult patients with severe uncontrolled asthma |
| Time horizon | Lifetime | 10 years |
| Comparators | Standard therapy (high-dose ICS plus LABA and additional controller medication if required) | ICS therapy in addition to rescue medication |
| Resources used and costs | Costs of exacerbations (cost of CS exacerbation = €177.40; cost of CSS exacerbation = €260.90) | Baseline chronic costs include medication, routine medical visits, laboratory testing ($77 per month) |
| Medication costs (annual omalizumab cost = €11,634; annual standard therapy cost = €1,938) | Acute event costs include non-emergency department urgent visits ($75 each), emergency department visits ($290 each) and hospitalisations ($3800 each) | |
| Routine visits (cost = €153) | Omalizumab cost: estimated from the average IgE levels reported in two clinical trials (197 IU/ml) and assuming patient weights 70 kg, resulting in $15,000 per year (sensitivity analysis varied costs by 10% to 200% of their baseline value) | |
| Source of resources used | IA-04 trial: resource use associated with CS exacerbation and medication use | Published resource use studies |
| INNOVATE trial: CSS exacerbation resource use | ||
| Source of costs | Unit costs taken from Ontario Schedule of Benefits and Fees for 2005 | Published sources |
| Hospitalisation costs determined according to the Canadian Institute of Health Information | ||
| Clinical outcomes | Responders to omalizumab treatment, defined as those who experienced ≥ 0.5-point improvement in the MiniAQLQ | Change in FEV1 as a percentage of predicted normal value relative to baseline |
| CS and CSS exacerbations rates (standard therapy exacerbation rate: 2.22, of which 42.4% CS and 57.6% CSS; omalizumab exacerbation rate: 1.00, of which 89.2% CS and 10.8% CSS). Same definition as INNOVATE | ICS therapy improved FEV1 by 17% for the base case (sensitivity analysis tested from 9% to 17%) | |
| Severe exacerbation-related death (3.108% as base case and 2.48% for SA) | Omalizumab therapy improved FEV1 by 2.9% | |
| Death from all causes (0.12%) | Exacerbation rates | |
| Omalizumab achieved 46% reduction in the rate of exacerbations (sensitivity analysis explored a range of 33% to 92%) | ||
| Duration of hospitalisation because of exacerbations | ||
| 12.7 days for standard therapy vs. 7.8 days for omalizumab add-on therapy | ||
| Source of clinical outcomes | Exacerbation rates: IA-04 study data | ICS effect on FEV1: published economic study |
| Proportion of CSS exacerbations: INNOVATE study data | Omalizumab effect on FEV1, and omalizumab effect on exacerbations: published Cochrane review | |
| Severe-exacerbation related death: Novartis analysis of asthma deaths among patients hospitalised in the UK for acute, severe asthma, aged 45 and over (unpublished) | Omalizumab effect on hospitalisations: published effectiveness study (RCT) | |
| Death from all causes: Statistics Canada | ||
| HRQoL | QALYs | QALYs |
| Source of HRQoL | Utilities for day-to-day asthma state were obtained from the Mini AQLQ values collected during IA-04 and mapped onto EQ-5D (omalizumab: 0.82, standard therapy: 0.65) | Published study reporting direct utility values obtained with TTO and relating them with FEV1 per cent predicted through OLS. Assuming an improvement in FEV1 per cent predicted of 2.9% with omalizumab, the corresponding utility increase would be 0.9% |
| Utilities for CS and CSS states were obtained from a published study conducted in the UK using self-administered EQ-5D (CS: 0.572, CSS: 0.326) | Sensitivity analysis tested an increase between 0 and 7.2%, corresponding to the improvement reported in another published study | |
| Adverse events | Not included | Not included |
| Subgroup analysis | None | None |
| Discounting | 5% for costs and outcomes | 3% for costs |
| CEA results | ICER = €31,209 per additional QALY for treatment duration of 5 years (additional lifetime cost of €33,854 for 1.08 QALY) | ICER = $821,000 per QALY gained (treatment duration not discussed) |
| Probability of omalizumab being cost-effective at willingness to pay for an additional QALY of €35,000 is 0.697 | ICER = $120 per free-symptom day achieved | |
| Non-parametric 95% CI around the ICER of €27,379; €40,840 | ||
| Assessment of uncertainty | Scenario sensitivity analysis: | Univariate sensitivity analysis: |
| Discounting: no discounting, 3% for costs and outcomes | Annual cost of omalizumab | |
| Time horizon of 5 years | HRQoL improvement achieved with omalizumab (varied between 0% and 7.2%) | |
| Administration costs included | Baseline acute event rate (multiplied by a factor of 5) | |
| Severe exacerbation-related death: 0% and 2.48% | Reduction in exacerbations from 33% to 92% | |
| Probabilistic sensitivity analysis. Parameters included and respective distributions not provided | ||
| Conclusions | Omalizumab is cost-effective as an add-on therapy for the treatment of severe persistent allergic asthma | Omalizumab does not provide sufficient clinical benefit and resource savings to provide good value for money, unless its price falls significantly |
| Key CE drivers | Severe exacerbation-related death: ICER increases to €66,443 per QALY gained if mortality reduced to 0%, and to €33,578 if mortality is reduced to 2.48% | Cost of omalizumab: monthly drug costs of $100 and $200 per month (from $1300 for base case) would be required to lower ICER to $50,000 and $100,000 per QALY gained respectively |
| Time horizon: ICER increases to €52,394 if time horizon is reduced to 5 years | Improvement in HRQoL with omalizumab | |
| Conflicts of interest | Study funded by Novartis | Study funded by National Heart, Lung, and Blood Institute grant. Some authors disclosed potential conflicts of interest |
| Study details | Campbell et al. (2010)92 | Dal Negro et al. (2011)96 |
|---|---|---|
| Economic evaluation type | Cost–utility analysis | Cost–utility analysis |
| Currency (year) | 2008 US dollar | 2008 Euro |
| Study design | Markov model similar to MS for TA133 and TA201 | Before-and-after study: |
| Health states: | Using data from 23 patients who had 12 months follow-up previous to omalizumab treatment | |
| Chronic asthma | Lung Department of the Orlandi General Hospital database | |
| Oral-steroid burst exacerbation | Statistical analysis: | |
| Emergency room exacerbation | t-test comparison of means for resource use and HRQoL | |
| Hospitalisation exacerbation | ICER | |
| Asthma-related mortality (from hospitalisation only) | ||
| Other cause mortality | ||
| Perspective | Third party (health-care) payer (cost of omalizumab was adjusted by subtracting the average patients co-payment) | Third-party payer (Regional Health System) |
| Setting | USA | Italy |
| Patient population | Patients with moderate to severe persistent asthma, a positive skin test or in vitro reactivity to a perennial aeroallergen, and symptoms inadequately controlled with ICSs. Average age of 40 and 60% women | Patients sensitised to perennial antigens with severe difficult to treat asthma, who have been using omalizumab in addition to optimised therapy |
| Time horizon | Life time with 5 years of treatment with omalizumab | 2 years (1 year pre-omalizumab, 1 year with omalizumab) |
| Comparators | Usual care: ICS + SABA as needed +additional medication if required | Standard therapy ICS + LABAs (GINA 2002 step 4) |
| Resources used and costs | Medication costs: | Medication costs |
| Omalizumab: based on the IPD meta-analysis of RCT (average of 35.9 vials per year, including vial wastage). Patient co-payment subtracted to omalizumab costs. Average 1st year cost=$19,800 per patient | Omalizumab (€526.68 per patient per month) | |
| Standard care: mediation used by usual care arm of open-label trial (Ayres et al. 2004).30 $2410 per patient per year for both treatment groups | ST (€0.97 per patient per month) | |
| Exacerbation costs: | Costs of hospitalisation (€1759.20) | |
| Oral steroid burst:1 GP visit ($120) | Costs of emergency visit (€200) | |
| Emergency room exacerbation ($548) | Costs of specialist visits (€14.25) | |
| Hospitalisation exacerbation ($9132) | Costs of GP visits (€12.32) | |
| Source of resources used | Omalizumab utilisation plus administration: published IPD meta-analysis | Database of Lung Department of the Orlandi General Hospital |
| Usual pharmacotherapy: published RCT | ||
| Source of costs | MarketScan (medical and pharmacy claims database | Hospitalisations: DRG-based remuneration tariff |
| Omalizumab: wholesale acquisition cost ($561.96) | Specialist visits: regional specialists tariff | |
| GP visits: published economic study | ||
| Clinical outcomes | Omalizumab responders (SA only): 60.5% as per INNOVATE | Improvement on asthma control as measured by: |
| Exacerbations (rate per year): | FEV1 (Δ = 17.85) and maximal mid-expiratory flow | |
| Oral steroid burst (ST 1.346, OMAL RR 0.634, OMALR RR 0.360) | Reversibility of airway obstruction | |
| Emergency room (ST 0.066, OMAL RR 0.397, OMALR RR 0.360) | IgE serum levels | |
| Hospitalisation (ST 0.062, OMAL RR 0.732, OMALR RR 0.360) | Asthma control test (Δ = 7.53) | |
| Asthma-related mortality: 0.011, SE 0.004 | St. George Respiratory Questionnaire | |
| Source of clinical outcomes | Omalizumab responders: INNOVATE | Database of Lung Department of the Orlandi General Hospital |
| Exacerbation rates: published IPD meta-analysis (Bousquet et al. 2005;31 Humbert et al., 200520) | ||
| Asthma-related mortality rates: Sullivan et al. (2009)100 | ||
| HRQoL | QALYs | QALYs |
| Source of HRQoL | Obtained from published sources: | St. George Respiratory Questionnaire (SGRQ) data mapped to EQ-5D |
| Chronic asthma (ST 0.669, omalizumab 0.732, omalizumab responders 0.779), which mapped AQLQ to EQ-5D | SGRQ administered immediately before (T0) and every 6 months following omalizumab initiation | |
| Oral steroids burst: 0.572 | T0 assumed representative of the previous year on standard therapy | |
| Emergency room visit: 0.449 | Last SGRQ measurement assumed representative of 12 months on omalizumab | |
| Hospitalisation: 0.326 | ||
| Adverse events | Not included | None recorded |
| Subgroup analysis | Omalizumab responders (60.5% of treated): | None |
| Non-responders reverted to ST after 16 weeks of omalizumab treatment | ||
| Discounting | Costs and outcomes discounted at 3% per annum | None |
| CEA results | ICER base case: | Omalizumab improved asthma control as measured by: |
| For the 1st year of treatment: $306,200/QALY (95% CI $237,500 to $636,900) | Lung function measures (improvement) | |
| ICER for lifetime:$287,200/QALY (95% CI$219,300 to $557,900) | Use of rescue medication (decrease) | |
| ICER responders subgroup | ACT (improvement) | |
| $172,300,200/QALY (95% CI $121,800 to $511,300) | Exacerbations (decrease) | |
| CEAC: probability of being cost-effective is below 0.10 up to threshold of $250,000/QALY | Days of inactivity (improvement) | |
| SGRQ (improvement) | ||
| ICER = €26,000/QALY | ||
| Assessment of uncertainty | Exacerbation rates from the model at 1 year were estimated and calibrated to that of the IPD meta-analysis | None |
| Univariate sensitivity analysis varied one input parameter at a time using the lower and upper bound of the 95% CI; price of omalizumab varied by 20% | ||
| Varying utility weights for omalizumab chronic state had the greatest impact: ICER ranged from $245,200 to $690,800/QALY | ||
| Results also sensitive to asthma-related mortality rate ($261,600–$301,000), cost of omalizumab ($257,500–$287,200) and proportion of severe exacerbations ($273,800–$299,600) | ||
| Probabilistic sensitivity analysis | ||
| Conclusions | Omalizumab as an add-on therapy to usual care improves health outcomes but also increases costs | Omalizumab leads to a substantial improvement in clinical outcomes and HRQoL. Its acquisition cost is not offset by the reduction in health-care resource use (less exacerbations, rescue medication, hospitalisations) |
| Key CE drivers | Utility difference between ST and omalizumab for the chronic asthma state | Acquisition cost of omalizumab |
| Conflicts of interest | Research supported by unrestricted grant from Novartis | None |
Checklist for the economic evaluations submitted for Technology Appraisal No. 133,88 Technology Appraisal No. 20189 and for the current manufacturer's submission15
| MS for TA133/TA201 | Novartis submission | |
|---|---|---|
| Study question | Grade | Grade |
| 1. Costs and effects examined | ✓ | ✓ |
| 2. Alternatives compared | ✓ | ✓ |
| 3. The viewpoint(s)/perspective of the analysis is clearly stated (e.g. NHS, society) | ✓ | ✓ |
| Selection of alternatives | ||
| 4. All relevant alternatives are compared (including do-nothing if applicable) | ✓ | ✓ |
| 5. The alternatives being compared are clearly described (who did what, to whom, where and how often) | ✓ | ✓ |
| 6. The rationale for choosing the alternative programmes or interventions compared is stated | ✓ | ✓ |
| Form of evaluation | ||
| 7. The choice of form of economic evaluation is justified in relation to the questions addressed | ✓ | ✓ |
| 8. If a cost-minimisation design is chosen, have equivalent outcomes been adequately demonstrated? | NA | NA |
| Effectiveness data | ||
| 9. The source(s) of effectiveness estimates used are stated (e.g. single study, selection of studies, systematic review, expert opinion) | ✓ | ✓ |
| 10. Effectiveness data from RCT or review of RCT | ✓ | ✓ |
| 11. Potential biases identified (especially if data not from RCT) | ✗ | ✗ |
| 12. Details of the method of synthesis or meta-analysis of estimates are given (if based on an overview of a number of effectiveness studies) | NA | NA |
| Costs | ||
| 13. All the important and relevant resource use included | ✓ | ✓ |
| 14. All the important and relevant resource use measured accurately (with methodology) | ✓ | ✓ |
| 15. Appropriate unit costs estimated (with methodology) | ✓ | ✓ |
| 16. Unit costs reported separately from resource use data | ✓ | ✓ |
| 17. Productivity costs treated separately from other costs | NA | NA |
| 18. The year and country to which unit costs apply is stated with appropriate adjustments for inflation and/or currency conversion | ✓ | ✓ |
| Benefit measurement and valuation | ||
| 19. The primary outcome measure(s) for the economic evaluation are clearly stated | ✓ | ✓ |
| 20. Methods to value health states and other benefits are stated | ✓ | ✓ |
| 21. Details of the individuals from whom valuations were obtained are given | ✓ | ✓ |
| Decision modelling | ||
| 22. Details of any decision model used are given (e.g. decision tree, Markov model) | ✓ | ✓ |
| 23. The choice of model used and the key input parameters on which it is based are adequately detailed and justified | ✓ | ✓ |
| 24. All model outputs described adequately | ✓ | ✓ |
| Discounting | ||
| 25. Discount rate used for both costs and benefits | ✓ | ✓ |
| 26. Do discount rates accord with NHS guidance? | ✓ | ✓ |
| Allowance for uncertainty | ||
| Stochastic analysis of patient-level data | NA | NA |
| 27. Details of statistical tests and CI are given for stochastic data | NA | NA |
| 28. Uncertainty around cost-effectiveness expressed (e.g. CIs around ICERs, cost-effectiveness acceptability curves) | ✓ | ✓ |
| 29. Sensitivity analysis used to assess uncertainty in non-stochastic variables (e.g. unit costs, discount rates) and analytic decisions (e.g. methods to handle missing data) | ✓ | ✓ |
| Stochastic analysis of decision models | ||
| 30. Are all appropriate input parameters included with uncertainty? | ✗ (costs not included in PSA) | ✓ |
| 31. Is second-order uncertainty (uncertainty in means) included rather than first-order (uncertainty between patients)? | ✓ | ✓ |
| 32. Are the probability distributions adequately detailed and appropriate? | ✓ | ✓ |
| 33. Sensitivity analysis used to assess uncertainty in non-stochastic variables (e.g. unit costs, discount rates) and analytic decisions (e.g. methods to handle missing data) | ✗ (see 30) | ✓ |
| Deterministic analysis | ||
| 34. The approach to sensitivity analysis is given (e.g. univariate, threshold analysis, etc.) | ✓ | ✓ |
| 35. The choice of variables for sensitivity analysis is justified | ✓ | ✓ |
| 36. The ranges over which the variables are varied are stated | ✓ | ✓ |
| Presentation of results | ||
| 37. Incremental analysis is reported using appropriate decision rules | ✓ | ✓ |
| 38. Major outcomes are presented in a disaggregated as well as aggregated form | ✓ | ✓ |
| 39. Applicable to the NHS setting | ✓ | ✓ |
Input parameters used in the manufacturer's submission for Technology Appraisal No. 13388 and Technology Appraisal No. 20189
| Submission for TA133 (patients ≥ 12 years) | Submission for TA201 (patients 6–11 years) | |||
|---|---|---|---|---|
| Overview | ||||
| Treatment duration | 5 years | 10 years | ||
| Data sources | Exacerbation rates, resource use and HRQoL for day-to-day symptom state based on INNOVATE | Exacerbation rates and resource use are based on IA-05 EUP | ||
| HRQoL loss because of exacerbations and mortality obtained from published sources | HRQoL for day-to-day symptom state based on INNOVATE | |||
| HRQoL loss because of exacerbations and mortality obtained from published sources | ||||
| Assessment of response | Response to treatment is determined at 16 weeks | Response to treatment is determined at 16 weeks | ||
| 28-week responder rate is a proxy for the 16-week response rate | 52-week responder rate is a proxy for the 16-week response rate | |||
| Exacerbations rates | 28-week exacerbation rates annualised and used throughout model | 24-week exacerbation rates used for first 24 weeks | ||
| 28-week exacerbation rates annualised and used throughout model | ||||
| Treatment effect on exacerbations | The relative risk (RR) of exacerbations applied in the model related to the comparison of omalizumab responders vs. total placebo group | The relative risk (RR) of exacerbations applied in the model related to the comparison of omalizumab responders vs. total placebo group | ||
| Variables | Value | Source | Value | Source |
| Annual exacerbation rates | ||||
| Standard care | 1.689 | INNOVATE | 2.028 | IA-05 EUP |
| % CSS on standard care | 52.4% | INNOVATE | 22.9% | IA-05 EUP |
| Omalizumab responders | 0.598 (RR = 0.354) | INNOVATE | 0.519 (RR = 0.256) | IA-05 EUP |
| % CSS for omalizumab responders | 34.2% | INNOVATE | 27.2% | IA-05 EUP |
| Proportion of responders | 60.5% | INNOVATE | 74.2% | IA-05 EUP |
| Mortality | ||||
| All-cause mortality | UK life-tables not adjusted for asthma-related deaths | ONS | UK life-tables not adjusted for asthma-related deaths | ONS |
| Asthma-related deaths | Severe exacerbations lead to asthma death | Lowhagen et al. (1997)99 | Severe exacerbations lead to asthma death | Watson et al. (2007)106 |
| Mortality risk = 3.109% | Mortality risk for age 0–11 = 0.097%; 12–16 = 0.319%; 17–44 = 0.383%; 45+ = 2.478% | |||
| HRQoL | ||||
| Omalizumab effect on HRQoL | HRQoL difference observed in the trial | INNOVATE | No HRQoL difference between treatments up to age 12 | IA-05 EUP |
| 0.779 (omalizumab) vs. 0.669 (standard care) | From age 12, HRQoL difference as in TA133 | INNOVATE | ||
| HRQoL loss due to exacerbations | CSNS = 0.572 | Lloyd et al. (2007)104 | CSNS = 0.572 | Lloyd et al. (2007)104 |
| CSS = 0.326 | CSS = 0.326 | |||
| Duration of exacerbation | 12.7 days | INNOVATE | 17.1 days | |
| Resource use and costs | ||||
| Cost of exacerbations | CSNS = £186 | INNOVATE | CSNS = CSS = £175 | IA-05 EUP |
| CSS = £275 | ||||
| Routine visits | 4 per year | Two per year at a cost of £128 each | NHS reference costs | |
| Cost not reported | ||||
| Responder assessment appointment | Cost not stated | £128 | ||
| Standard therapy costs (per year) | £1525 | INNOVATE | £1175 | IA-05 EUP |
| Omalizumab costs (per year) | £8520 (cost per mg) | INNOVATE | £8881 (cost per mg) | IA-05 EUP |
| £10,255 (cost per vial) | ||||
Appendix 17 Input parameters used in the manufacturer's submission for the base-case populations: adult and adolescents (patients ≥ 12 years of age) and children (6–11 years)15
| Variables | Adults and adolescents (patients ≥ 12 years) | Children (patients 6–11 years) | ||
|---|---|---|---|---|
| Value | Source | Value | Source | |
| Annual exacerbation rates | ||||
| Standard care | 1.689 | INNOVATE | 2.028 | IA-05 EUP |
| % CSS on standard care | 52.4% | INNOVATE | 22.9% | IA-05 EUP |
| Omalizumab responders | 0.630 | INNOVATE | 0.519 | IA-05 EUP |
| % CSS for omalizumab responders | 35.0% | INNOVATE | 27.3% | IA-05 EUP |
| Proportion of responders | 56.5% | INNOVATE | 74.2% | IA-05 EUP |
| Mortality | ||||
| All-cause mortality | UK life-tables not adjusted for asthma-related deaths | ONS | UK life-tables not adjusted for asthma-related deaths | ONS |
| Asthma-related deaths | Severe exacerbations lead to asthma death | Watson et al. (2007)107 | Severe exacerbations lead to asthma death | Watson et al. (2007)106 |
| Mortality risk = 2.478% | Mortality risk for: | |||
| age 0–11 = 0.097%; 12–16 = 0.319%; | ||||
| 17–44 = 0.383%; | ||||
| 45+ = 2.478% | ||||
| HRQoL | ||||
| Omalizumab effect on HRQoL | HRQoL difference observed in the trial | INNOVATE | No HRQoL difference between treatments up to age 12 | IA-05 EUP |
| 0.779 (omalizumab) vs. 0.669 (standard care) | From age 12, HRQoL difference as in INNOVATE | INNOVATE | ||
| HRQoL loss because of exacerbations | CSNS = 0.572 | Lloyd et al. (2007)104 | CSNS = 0.572 | Lloyd et al. (2007)104 |
| CSS = 0.326 | CSS = 0.326 | |||
| Duration of exacerbation | 12.7 days | INNOVATE | 17.1 days | IA-05 EUP |
| Resource use and costs | ||||
| Cost of exacerbations | CSNS = £87.7 | INNOVATE | CSNS = CSS = £213.89 | IA-05 EUP |
| CSS = £124.32 | ||||
| Routine visits | Two per year, £160 each | NHS reference costs16 | Two per year, £190 each | NHS reference costs16 |
| Initiation of therapy | £245 | £247 | ||
| Responder assessment appointment | £160 | £190 | ||
| Standard therapy costs (per year) | £1197 | INNOVATE | £810 | IA-05 EUP |
| Omalizumab costs (per year) | £8201 | INNOVATE | £8607 | IA-05 EUP |
Input parameters used in the manufacturer's submission for the EXALT and APEX scenarios: adult and adolescents (patients ≥ 12 years of age)
| Variables | EXALT | APEX | ||
|---|---|---|---|---|
| Value | Source | Value | Source | |
| Annual exacerbation rates | ||||
| Standard care | 1.587 | EXALT | 3.67 | APEX |
| % CSS on standard care | 40.8% | EXALT | 52.4% | APEX |
| Omalizumab responders | 0.650 | EXALT | 1.52 | APEX |
| % CSS for omalizumab responders | 42.1% | EXALT | 35.0% | APEX |
| Proportion of responders | 69.9% | EXALT | 82.4% | APEX |
| Mortality | ||||
| All-cause mortality | UK life-tables not adjusted for asthma-related deaths | ONS | UK life-tables not adjusted for asthma-related deaths. | ONS |
| Asthma-related deaths | Severe exacerbations lead to asthma death | Watson et al. (2007)106 | Severe exacerbations lead to asthma death | Watson et al. (2007)106 |
| Mortality risk = 2.478% | Mortality risk = 2.478% | |||
| HRQoL | ||||
| Omalizumab effect on HRQoL | HRQoL difference observed in the trial | EXALT | HRQoL difference observed in the trial | INNOVATE |
| 0.767 (omalizumab) vs. 0.719 (standard care) | 0.779 (omalizumab) vs. 0.669 (standard care) | |||
| HRQoL loss because of exacerbations | CSNS = 0.572 | Lloyd et al. (2007)104 | CSNS = 0.572 | Lloyd et al. (2007)104 |
| CSS = 0.326 | CSS = 0.326 | |||
| Duration of exacerbation | 14.6 days | EXALT | 12.8 days | INNOVATE |
| Resource use and costs | ||||
| Cost of exacerbations | CSNS = CSS = £179.56 | EXALT | CSNS = CSS = £304.51 | APEX |
| Routine visits | Two per year, £160 each | NHS reference costs16 | Two per year, £160 each | NHS reference costs16 |
| Initiation of therapy | £245 | £245 | ||
| Responder assessment appointment | £160 | £190 | ||
| Standard therapy costs (per year) | £1154 | EXALT | £1197 | INNOVATE |
| Omalizumab costs (per year) | £9227 | EXALT | £10,547 | APEX |
Input parameters used in the manufacturer's submission for the hospitalisation subgroup: adult and adolescents (patients ≥ 12 years of age) and children (6–11 years)
| Variables | INNOVATE | EXALT | APEX | IA-05 EUP | ||||
|---|---|---|---|---|---|---|---|---|
| Value | Source | Value | Source | Value | Source | Value | Source | |
| Annual exacerbation rates | ||||||||
| Standard care | 2.092 | INNOVATE hospitalisation | 2.184 | EXALT hospitalisation | 3.400 | APEX hospitalisation | 3.429 | IA-05 EUP hospitalisation |
| % CSS on standard care | 58.4% | INNOVATE hospitalisation | 41.9% | EXALT hospitalisation | 58.4% | APEX hospitalisation | 37.5% | IA-05 EUP hospitalisation |
| Omalizumab responders | 0.869 | INNOVATE hospitalisation | 0.985 | EXALT hospitalisation | 1.630 | APEX hospitalisation | 0.743 | IA-05 EUP hospitalisation |
| % CSS for omalizumab responders | 42.9% | INNOVATE hospitalisation | 45.0% | EXALT hospitalisation | 42.9% | APEX hospitalisation | 25.0% | IA-05 EUP hospitalisation |
| Proportion of responders | 56.6% | INNOVATE hospitalisation | 56.9% | EXALT hospitalisation | 82.4% | APEX hospitalisation | 54.1% | IA-05 EUP hospitalisation |
| Mortality | ||||||||
| All-cause mortality | UK life-tables not adjusted for asthma-related deaths | ONS | UK life-tables not adjusted for asthma-related deaths | ONS | UK life-tables not adjusted for asthma-related deaths | ONS | UK life-tables not adjusted for asthma-related deaths | ONS |
| Asthma-related deaths | Severe exacerbations lead to asthma death | Watson et al. (2007)106 | Severe exacerbations lead to asthma death | Watson et al. (2007)106 | Severe exacerbations lead to asthma death | Watson et al. (2007)106 | Severe exacerbations lead to asthma death | Watson et al. (2007)106 |
| Mortality risk = 2.478% | Mortality risk = 2.478% | Mortality risk = 2.478% | Mortality risk for: | |||||
| Age (years) 0–11 = 0.097%; 12–16 = 0.319%; | ||||||||
| 17–44 = 0.383%; | ||||||||
| 45+ = 2.478% | ||||||||
| HRQoL | ||||||||
| Omalizumab effect on HRQoL | HRQoL difference observed in the trial | INNOVATE hospitalisation | HRQoL difference observed in the trial | EXALT hospitalisation | HRQoL difference observed in the trial | INNOVATE hospitalisation | No HRQoL difference between treatments up to age 12 years | INNOVATE hospitalisation |
| 0.772 (omalizumab) vs. 0.634 (standard care) | 0.761 (omalizumab) vs. 0.631 (standard care) | 0.772 (omalizumab) vs. 0.634 (standard care) | From age 12 years, HRQoL difference as in INNOVATE | |||||
| HRQoL loss because of exacerbations | CSNS = 0.572 | Lloyd et al. (2007)104 | CSNS = 0.572 | Lloyd et al. (2007)104 | CSNS = 0.572 | Lloyd et al. (2007)104 | CSNS = 0.572 | Lloyd et al. (2007)104 |
| CSS = 0.326 | CSS = 0.326 | CSS = 0.326 | CSS = 0.326 | |||||
| Duration of exacerbation | 12.7 days | INNOVATE | 12.8 days | EXALT | 12.8 days | INNOVATE | 12.8 days | INNOVATE |
| Resource use and costs | ||||||||
| Cost of exacerbations | CSNS = £154.7 | INNOVATE hospitalisation | CSNS = CSS = £267.44 | EXALT hospitalisation | CSNS = CSS = £487.66 | APEX hospitalisation | CSNS = CSS = £213.89 | IA-05 EUP |
| CSS = £178.87 | ||||||||
| Routine visits | Two per year, £160 each | NHS reference costs16 | Two per year, £160 each | NHS reference costs16 | Two per year, £160 each | NHS reference costs16 | Two per year, £190 each | NHS reference costs16 |
| Initiation of therapy | £245 | £245 | £245 | £247 | ||||
| Responder assessment appointment | £160 | £160 | £160 | £160 | ||||
| Standard therapy costs (per year) | £1196.81 | INNOVATE | £1154 | EXALT | £1197 | INNOVATE | £810 | IA-05 |
| Omalizumab costs (per year) | £8201 | INNOVATE | £9227 | EXALT | £10,547 | APEX | £8607 | IA-05 |
Input parameters used in the manufacturer's submission for the maintenance oral corticosteroids subgroup: adult and adolescents (patients ≥ 12 years of age)
| Variables | INNOVATE | EXALT | APEX | |||
|---|---|---|---|---|---|---|
| Value | Source | Value | Source | Value | Source | |
| Annual exacerbation rates | ||||||
| Standard care | 2.476 | INNOVATE maintenance OCS | 2.897 | EXALT maintenance OCS | 3.700 | APEX maintenance OCS |
| % CSS on standard care | 60.7% | INNOVATE maintenance OCS | 48.8% | EXALT maintenance OCS | 60.7% | APEX maintenance OCS |
| Omalizumab responders | 0.727 | INNOVATE maintenance OCS | 1.468 | EXALT maintenance OCS | 1.440 | APEX maintenance OCS |
| % CSS for omalizumab responders | 44.4% | INNOVATE maintenance OCS | 46.4% | EXALT maintenance OCS | 44.4% | APEX maintenance OCS |
| Proportion of responders | 46.9% | INNOVATE maintenance OCS | 52.5% | EXALT maintenance OCS | 78.9% | APEX maintenance OCS |
| Mortality | ||||||
| All-cause mortality | UK life-tables not adjusted for asthma-related deaths | ONS | UK life-tables not adjusted for asthma-related deaths | ONS | UK life-tables not adjusted for asthma-related deaths | ONS |
| Asthma-related deaths | Severe exacerbations lead to asthma death | Watson et al. (2007)106 | Severe exacerbations lead to asthma death | Watson et al. (2007)106 | Severe exacerbations lead to asthma death | Watson et al. (2007)106 |
| Mortality risk = 2.478% | Mortality risk = 2.478% | Mortality risk = 2.478% | ||||
| HRQoL | ||||||
| Omalizumab effect on HRQoL | HRQoL difference observed in the trial | INNOVATE maintenance OCS | HRQoL difference observed in the trial | EXALT maintenance OCS | HRQoL difference observed in the trial | INNOVATE maintenance OCS |
| 0.745 (omalizumab) vs. 0.639 (standard care) | 0.791 (omalizumab) vs. 0.686 (standard care) | 0.745 (omalizumab) vs. 0.639 (standard care) | ||||
| HRQoL loss because of exacerbations | CSNS = 0.572 | Lloyd et al. (2007)104 | CSNS = 0.572 | Lloyd et al. (2007)104 | CSNS = 0.572 | Lloyd et al. (2007)104 |
| CSS = 0.326 | CSS = 0.326 | CSS = 0.326 | ||||
| Duration of exacerbation | 12.7 days | INNOVATE | 14.6 days | EXALT | 12.7 days | INNOVATE |
| Resource use and costs | ||||||
| Cost of exacerbations | CSNS = £86.51 | INNOVATE maintenance OCS | CSNS = CSS = £147.37 | EXALT maintenance OCS | CSNS = CSS = £308.46 | APEX maintenance OCS |
| CSS = £136.04 | ||||||
| Routine visits | Two per year, £160 each | NHS reference costs16 | Two per year, £160 each | NHS reference costs16 | Two per year, £160 each | NHS reference costs16 |
| Initiation of therapy | £245 | £245 | £245 | |||
| Responder assessment appointment | £160 | £160 | £160 | |||
| Standard therapy costs (per year) | £1197 | INNOVATE | £1154 | EXALT | £1197 | INNOVATE |
| Omalizumab costs (per year) | £8201 | INNOVATE | £9227 | EXALT | £10,547 | APEX |
Modelling checklist for the Novartis submission15,89
| Quality criterion | Question(s) | Response (✓, ✗ or NA) | Comments |
|---|---|---|---|
| S1 | Is there a clear statement of the decision problem? | ✓ | 'An economic evaluation was conducted using a combined and updated version of the health economic model submitted to NICE for TA133 and TA201. Clinical trial data were used to estimate the cost effectiveness of “standard dose” omalizumab as add-on therapy to standard therapy (ST) alone.' (p. 7 of MS) |
| Is the objective of the evaluation and model specified consistent with the stated decision problem? | ✓ | ||
| Is the primary decision-maker specified? | ✓ | Not explicitly, although it is a submission to NICE | |
| S2 | Is the perspective of the model stated clearly? | ✓ | |
| Are the model inputs consistent with the stated perspective? | ✓ | NHS costs and QALYs | |
| Has the scope of the model been stated and justified? | ✓ | Patient groups and options under evaluation are specified clearly. Each structural assumption is discussed and (in some cases) justified | |
| Are the outcomes of the model consistent with the perspective, scope and overall objective of the model? | ✓ | Main results are reported in terms of incremental cost per QALY gained, incremental cost per avoided exacerbation and incremental cost per avoided severe exacerbation | |
| S3 | Is the structure of the model consistent with a coherent theory of the health condition under evaluation? | ✓ | 'The model reflects the chronic day-to-asthma symptoms that patients experience and the observation that patients experience intermittent asthma exacerbations that can vary in severity. (. . .) Markov models are well suited to chronic conditions like asthma, which is characterised by recurring symptomatic events (i.e. exacerbations) in all patients and condition-specific mortality in a small proportion of patients.' (p. 80–81 of MS) |
| Are the sources of data used to develop the structure of the model specified? | ✓ | ||
| Are the causal relationships described by the model structure justified appropriately? | ✓ | ||
| S4 | Are the structural assumptions transparent and justified? | ✓ | Assumptions were detailed in p. 88 of MS |
| Are the structural assumptions reasonable given the overall objective, perspective and scope of the model? | ✓ | ||
| S5 | Is there a clear definition of the options under evaluation? | ✓ | |
| Have all feasible and practical options been evaluated? | ✓ | ||
| Is there justification for the exclusion of feasible options? | NA | ||
| S6 | Is the chosen model type appropriate given the decision problem and specified causal relationships within the model? | ✓ | The Markov model is appropriate to the natural course of asthma |
| S7 | Is the time horizon of the model sufficient to reflect all important differences between options? | ✓ | A lifetime time horizon was employed |
| Are the time horizon of the model, the duration of treatment and the duration of treatment effect described and justified? | ✗ | Duration of treatment and duration of treatment effect are not justified but presented as assumptions because of lack of data | |
| S8 | Do the disease states (state transition model) or the pathways (decision tree model) reflect the underlying biological process of the disease in question and the impact of interventions? | ✓ | The disease states represent the symptoms patients experience throughout the course of the disease |
| S9 | Is the cycle length defined and justified in terms of the natural history of disease? | ✓/✗ | The cycle length is defined but not justified in terms of the natural history of the disease |
| D1 | Are the data identification methods transparent and appropriate given the objectives of the model? | ✓ | Systematic reviews were conducted when appropriate |
| Where choices have been made between data sources, are these justified appropriately? | ✓ | ||
| Has particular attention been paid to identifying data for the important parameters in the model? | ✓ | ||
| Has the quality of the data been assessed appropriately? | ✓ | ||
| Where expert opinion has been used, are the methods described and justified? | NA | ||
| D2 | Is the data modelling methodology based on justifiable statistical and epidemiological techniques? | NA | |
| D2a | Is the choice of baseline data described and justified? | ✓ | Baseline data were derived from the control or standard care arm in each of the trials used for model inputs |
| Are transition probabilities calculated appropriately? | ✓ | ||
| Has a half-cycle correction been applied to both cost and outcome? | ✓ | ||
| If not, has this omission been justified? | NA | ||
| D2b | If relative treatment effects have been derived from trial data, have they been synthesised using appropriate techniques? | NA | No evidence synthesis was used |
| Have the methods and assumptions used to extrapolate short-term results to final outcomes been documented and justified? | ✓/✗ | The methods and assumptions have been documented but not all have been justified | |
| Have alternative extrapolation assumptions been explored through sensitivity analysis? | ✓/✗ | Some assumptions were explored in the sensitivity analysis | |
| Have assumptions regarding the continuing effect of treatment once treatment is complete been documented and justified? | NA | Treatment effect is assumed not to continue beyond treatment duration | |
| Have alternative assumptions regarding the continuing effect of treatment been explored through sensitivity analysis? | ✗ | No alternative assumptions regarding continuing effect of treatment have been explored | |
| D2c | Are the costs incorporated into the model justified? | ✓ | |
| Has the source for all costs been described? | ✓ | ||
| Have discount rates been described and justified given the target decision-maker? | ✓ | ||
| D2d | Are the utilities incorporated into the model appropriate? | ✓ | |
| Is the source for the utility weights referenced? | ✓ | ||
| Are the methods of derivation for the utility weights justified? | ✓ | ||
| D3 | Have all data incorporated into the model been described and referenced in sufficient detail? | ✓ | All sources are referenced |
| Has the use of mutually inconsistent data been justified (i.e. are assumptions and choices appropriate)? | NA | ||
| Is the process of data incorporation transparent? | ✓ | Data were incorporated as distributions and as point estimates | |
| If data have been incorporated as distributions, has the choice of distribution for each parameter been described and justified? | ✗ | The distributions are stated but not justified (p. 100 of MS) | |
| If data have been incorporated as distributions, is it clear that second order uncertainty is reflected? | ✓ | Monte Carlo simulation used to reflect second order uncertainty | |
| D4 | Have the four principal types of uncertainty been addressed? | ✗ | No |
| If not, has the omission of particular forms of uncertainty been justified? | ✗ | No | |
| D4a | Have methodological uncertainties been addressed by running alternative versions of the model with different methodological assumptions? | ✓ | Effect of different discount rates assessed (p. 99 of MS) |
| D4b | Is there evidence that structural uncertainties have been addressed via sensitivity analysis? | ✗ | No |
| D4c | Has heterogeneity been dealt with by running the model separately for different subgroups? | ✓ | Two subgroups were studied for the base case and each scenario: hospitalisation subgroup and maintenance OCS subgroup |
| D4d | Are the methods of assessment of parameter uncertainty appropriate? | ✓ | Probabilistic sensitivity analysis and one-way sensitivity analysis |
| If data are incorporated as point estimates, are the ranges used for sensitivity analysis stated clearly and justified? | ✓ | Mean value used for the deterministic analysis. The use of the mean was not justified but is standard practice | |
| C1 | Is there evidence that the mathematical logic of the model has been tested thoroughly before use? | ✓ | Model has been validated by two ERG |
| C2 | Are any counterintuitive results from the model explained and justified? | NA | The results do not appear to be counterintuitive |
| If the model has been calibrated against independent data, have any differences been explained and justified? | NA | ||
| Have the results of the model been compared with those of previous models and any differences in results explained? | ✗ |
Appendix 18 Model inputs
Systematic review of asthma-related mortality
Methods
A broad search strategy was employed using terms relating to asthma and to mortality. No date, language, study design limits were applied. The inclusion criteria were clinical trials, epidemiological studies and routine data analysis reporting asthma-related mortality or risk factors for asthma death for people ≥ 6 years of age with severe persistent allergic asthma, in the UK setting and published from the year 2000 onwards. The date limit was applied to more accurately reflect the mortality risk faced by patients in current UK practice. Studies including patients with conditions other than asthma and studies providing trends in mortality over time, but not mortality risks or rates were excluded. Titles and abstracts were assessed independently by two reviewers for inclusion and any discrepancies were resolved by consensus. Data were extracted by one reviewer using a standardised data extraction form and checked for accuracy by a second reviewer.
Results
Figure 7 presents the flow diagram of identification and selection of studies. Briefly, 337 records were found, of which 294 were rejected at title screening. Thirty-one full papers were assessed, of which 21 were rejected.
FIGURE 7.
Flow diagram of the systematic review on asthma-related mortality.
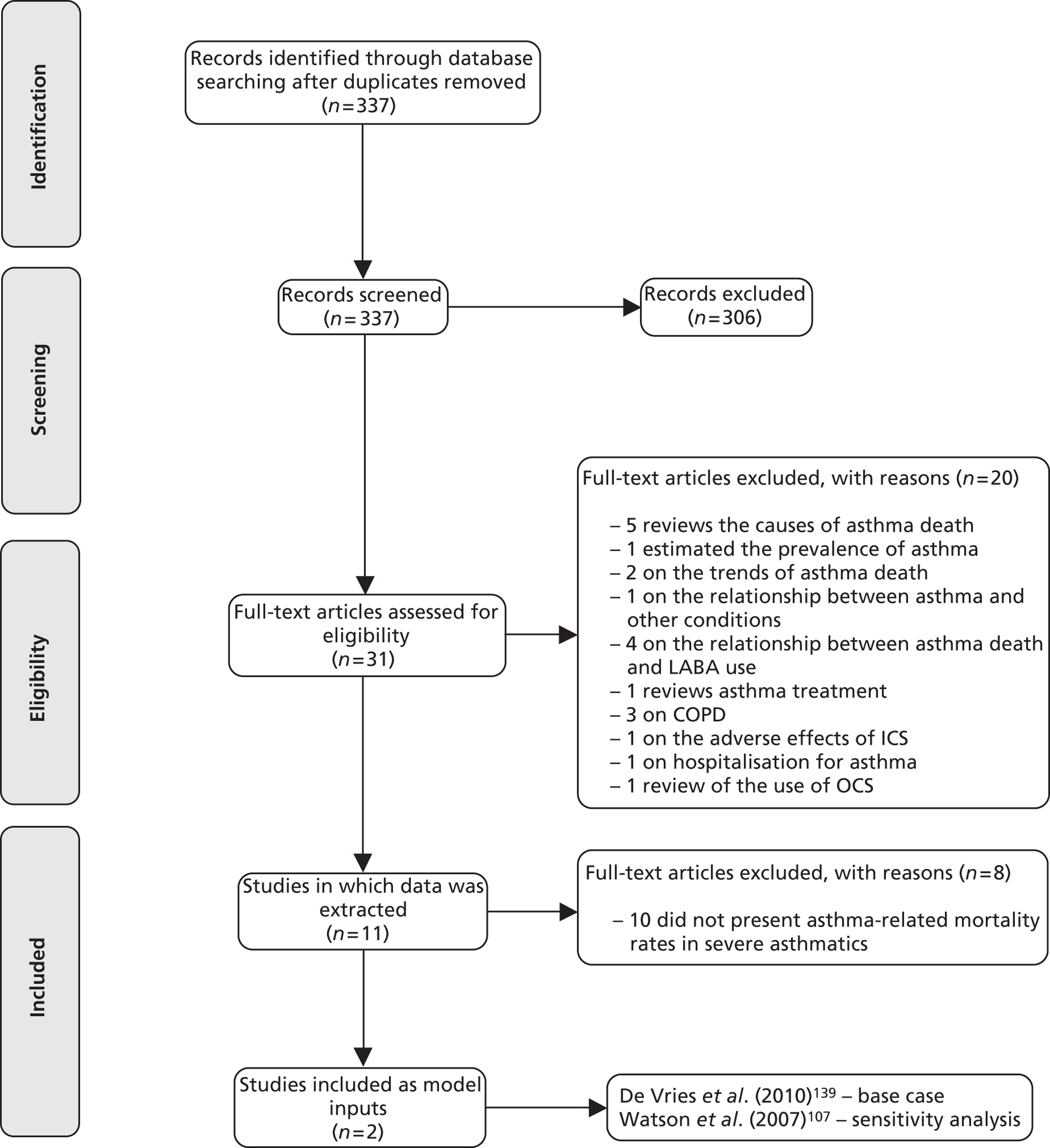
Data were extracted for 10 studies (see Table 100 for data extraction tables). Two studies were selected as potentially appropriate to inform asthma-related mortality risks experienced by severe asthma patients in the UK.
Flemming (2000)155
| First author (year) | Flemming (2000)155 |
|---|---|
| Title | Comparison of the seasonal patterns of asthma in general practitioner episodes, hospital admissions and deaths |
| Objective | Investigate the seasonal patterns of asthma attacks in the community and their relationship with hospital admissions and deaths |
| Methods | Data were collected between 1990 and 1997 from GPRD, hospital episode statistics for England, and ONS. Mortality rates were estimated by age bands: 0–4, 5–14, 14–44, 45–64 and 65+ years |
| Decomposition method was used to analyse the data | |
| Results | In 1994, there were 15,708 GP episodes, 90,864 admissions and 1514 deaths from asthma |
| Results for the remaining years were presented in graphical form | |
| Comments | Not included |
| Does not provide mortality rate for severe asthmatics |
Lanes (2000)148
| First author (year) | Lanes (2000)148 | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Title | Comparison of the seasonal patterns of asthma in general practitioner episodes, hospital admissions and deaths | |||||||||||||||||||||||||||||||
| Objective | Evaluate the relationship between each of the major classes of therapeutic drugs and asthma death | |||||||||||||||||||||||||||||||
| Methods | Analysis of the GPRD database between 1994 and 1998 | |||||||||||||||||||||||||||||||
| Cohort consistent of patients 10–79 years old who were permanently registered with a GP for at least 2 years between 1994 and 1998 with a diagnosis of asthma, and free from any cancer diagnosis on entry into the study | ||||||||||||||||||||||||||||||||
| Cohort followed until death, date of cancer diagnosis or October 1998 | ||||||||||||||||||||||||||||||||
| Asthma deaths identified from patient records, and confirmed with GP | ||||||||||||||||||||||||||||||||
| The 43 asthma deaths were analysed further in a nested case–control analysis, by sampling 860 controls from the study cohort, and matched to cases by year and sex | ||||||||||||||||||||||||||||||||
| Results | Incidence of asthma death by age and gender: | |||||||||||||||||||||||||||||||
| ParameterPerson-yearsAsthma deathsIncidence per 100,000 person-years (95% CI)Age (years)10–49239,60683.3 (1.7 to 6.6)50–79105,8243533.1 (23.8 to 46.0)GenderMale170,3642011.7 (7.6 to 18.1)Female175,0662313.1 (8.8 to 19.7)Total375,4304312.5 (9.2 to 16.8) | Parameter | Person-years | Asthma deaths | Incidence per 100,000 person-years (95% CI) | Age (years) | 10–49 | 239,606 | 8 | 3.3 (1.7 to 6.6) | 50–79 | 105,824 | 35 | 33.1 (23.8 to 46.0) | Gender | Male | 170,364 | 20 | 11.7 (7.6 to 18.1) | Female | 175,066 | 23 | 13.1 (8.8 to 19.7) | Total | 375,430 | 43 | 12.5 (9.2 to 16.8) | ||||||
| Parameter | Person-years | Asthma deaths | Incidence per 100,000 person-years (95% CI) | |||||||||||||||||||||||||||||
| Age (years) | ||||||||||||||||||||||||||||||||
| 10–49 | 239,606 | 8 | 3.3 (1.7 to 6.6) | |||||||||||||||||||||||||||||
| 50–79 | 105,824 | 35 | 33.1 (23.8 to 46.0) | |||||||||||||||||||||||||||||
| Gender | ||||||||||||||||||||||||||||||||
| Male | 170,364 | 20 | 11.7 (7.6 to 18.1) | |||||||||||||||||||||||||||||
| Female | 175,066 | 23 | 13.1 (8.8 to 19.7) | |||||||||||||||||||||||||||||
| Total | 375,430 | 43 | 12.5 (9.2 to 16.8) | |||||||||||||||||||||||||||||
Statistical significant risk factors for asthma death include:
|
||||||||||||||||||||||||||||||||
| Comments | Not included | |||||||||||||||||||||||||||||||
| Does not provide mortality rate for severe asthmatics | ||||||||||||||||||||||||||||||||
Sturdy et al. (2002)149
| First author (year) | Sturdy et al. (2002)149 |
|---|---|
| Title | Psychological, social and health behaviour risk factors for deaths certified as asthma: a national case–control study |
| Objective | Estimate the relationship between asthma death and psychosocial and health behaviour factors |
| Methods | A community based case–control study of 533 cases, comprising 78% of all asthma deaths under age 65 years and 533 hospital controls individually matched for age, district and asthma admission date corresponding to date of death was undertaken in seven regions of Britain (1994–8) |
| Data were extracted blind from anonymised copies of primary care records for the previous 5 years and non-blind for the earlier period | |
| Results | Asthma death is significantly associated with the following health behaviour and psychosocial factors (data presented for odds ratio adjusted for sex, other psychosocial factors, COPD, obesity and age of onset):
|
| Comments | Not included |
| Does not provide mortality rate for severe asthmatics |
Hansell (2003)150
| First author (year) | Hansell (2003)150 |
|---|---|
| Title | Validity and interpretation of mortality, health service and survey data |
| Objective | Comparison of the epidemiological patterns seen for asthma and COPD in England in 1991–5 across four routine data sources, as part of a project to investigate the validity of using such data to examine environmental influences on respiratory health |
| Methods | The data sources were ONS for mortality, hospital episode statistics for emergency hospital admissions, GPRD for primary care and the Health Survey for England of 1995 for symptoms |
| Asthmatics were those who reported wheezing or whistling in the chest in the previous 12 months. People with COPD were defined as those reporting cough or phlegm for at least 3 months in the winter | |
| Results | According to ONS data, 7729 people died of asthma among 242,731,000 person-years at risk. Mortality rates increase with age |
| Comments | Not included |
| Does not provide mortality rate for severe asthmatics |
Gupta et al. (2004)113
| First author (year) | Gupta et al. (2004)113 | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Title | Characteristics and outcome for admissions to adult, general critical care units with acute severe asthma: a secondary analysis of the ICNARC Case Mix Programme Database | |||||||||||||||||||
| Objective | To describe the case mix, outcome and activity for admissions to ICU for acute severe asthma, and to investigate the case mix on outcomes | |||||||||||||||||||
| Methods | Secondary analysis of the Intensive Care National Audit and Research Centre Case Mix Programme Database of 128 general critical care units across England, Wales and Northern Ireland over 1995–2001 | |||||||||||||||||||
| Data were extracted for those admissions to ICU was ‘asthma attack in new or know asthmatic’ | ||||||||||||||||||||
| Results | The use of systemic steroids in the previous 6 months to hospitalisation is not significantly associated with death: OR 0.83 (0.53 to 1.29) | |||||||||||||||||||
| Age is associated with increased risk of death: OR 1.68 (1.54 to 1.85) per 10-year increase in age | ||||||||||||||||||||
| Table 1 (PR115) presents the case mix, outcome and activity for admissions with primary or secondary reason for admission to ICU of asthma. The table below presents the section on mortality | ||||||||||||||||||||
| ParametersAll (n = 2152)Mechanically ventilated (n = 1223)Not mechanically ventilated (n = 929)Age (years)43.6(19.2)47.4 (18.6)38.6 (18.8)Sex (%male)33.234.831.0Death in CMP unit133 (6.3%)123 (10.3%)10 (1.1%)Death in any hospital199 (9.8%)177 (15.4%)22 (2.5%) | Parameters | All (n = 2152) | Mechanically ventilated (n = 1223) | Not mechanically ventilated (n = 929) | Age (years) | 43.6(19.2) | 47.4 (18.6) | 38.6 (18.8) | Sex (%male) | 33.2 | 34.8 | 31.0 | Death in CMP unit | 133 (6.3%) | 123 (10.3%) | 10 (1.1%) | Death in any hospital | 199 (9.8%) | 177 (15.4%) | 22 (2.5%) |
| Parameters | All (n = 2152) | Mechanically ventilated (n = 1223) | Not mechanically ventilated (n = 929) | |||||||||||||||||
| Age (years) | 43.6(19.2) | 47.4 (18.6) | 38.6 (18.8) | |||||||||||||||||
| Sex (%male) | 33.2 | 34.8 | 31.0 | |||||||||||||||||
| Death in CMP unit | 133 (6.3%) | 123 (10.3%) | 10 (1.1%) | |||||||||||||||||
| Death in any hospital | 199 (9.8%) | 177 (15.4%) | 22 (2.5%) | |||||||||||||||||
| Comments | Not included | |||||||||||||||||||
| Does not provide mortality rate for severe asthmatics |
Anderson (2005)151
| First author (year) | Anderson (2005)151 |
|---|---|
| Title | Bronchodilator treatment and deaths from asthma: case–control study |
| Objective | Investigate the association between bronchodilator treatment and death from asthma |
| Methods | Case–control study similar to Sturdy et al. (2002)149 |
| The main outcome measures were odds ratios for deaths from asthma associated with prescription of bronchodilators and other treatment, with sensitivity analyses adjusting for age at onset, previous hospital admissions, associated COPD and a number of other drug categories | |
| Results | Odds ratio and 95% CI were presented for death associated with prescription of asthma drugs in 3 months, 4–12 months and 1–5 years before index date |
| There was no significant association between medication prescribed in the past 3 months and asthma death, except OCSs [OR 0.75 (0.59 to 0.96)], all corticosteroids [OR 0.72 (0.55 to 0.95)] and all antibiotics [OR 0.75 (0.58 to 0.96)]. | |
| For drugs prescribed 4–12 months before death, there was no statistically significant association for asthma death except for all anti-muscarinics [OR 1.29 (1.01 to 1.65)] | |
| For drugs prescribed in the past 1–5 years, a statistically significant association was found for inhaled beta-adrenoceptor [OR 1.52 (1.04 to 2.22)], inhaled SABA [OR 1.54 (1.06 to 2.24)], all routes beta-adrenoceptor [OR 1.53 (1.05 to 2.23)] and all antibiotics [OR 0.67 (0.46 to 0.97)] | |
| Comments | Not included |
| Does not provide mortality rate for severe asthmatics |
Harrison (2005)152
| First author (year) | Harrison (2005)152 |
|---|---|
| Title | An ongoing Confidential Enquiry into asthma deaths in the Eastern Region of the UK, 2001–3 |
| Objective | Analyse retrospectively all asthma deaths in patients under the age of 65 in the region over the three-year period (2001–3) |
| Methods | Analysis of ONS data on all deaths registered under the age of 65 in the region for the previous year with asthma recorded in the first part of the death certificate |
| Eastern regions include: Norfolk, Suffolk, Cambridgeshire, Bedfordshire, Essex and Hertfordshire (excluding the areas within the M25 London orbital motorway), as well as the Unitary Authorities (Districts) of Peterborough, Luton and Southend-on-Sea | |
| Patient details analysed by chest physician and GP | |
| Results | Among the total study population of 5,245,012 individuals, there were 95 asthma deaths between 2001 and 2003 |
| Only 57 deaths (60%) were confirmed as asthma deaths, of which 30 (53%) were in severe asthmatics, 12 (21%) were in moderately severe asthmatics, nine (16%) in mild asthmatics and six (11%) in patients whose asthma severity was unknown | |
| Eleven deaths (20.4%) were because of sudden severe asthma attacks. In the other 43 cases, the final fatal attack was not sudden | |
| In 21 of the 30 patients with severe asthma there was evidence of poor compliance | |
| Comments | Not included |
| Does not provide mortality rate for severe asthmatics |
Panickar (2005)153
| First author (year) | Panickar (2005)153 |
|---|---|
| Title | Trends in deaths from respiratory illness in children in England and Wales from 1968 to 2000 |
| Objective | Investigate the trends in all respiratory causes of death in children in England and Wales from 1968 to 2000 |
| Methods | ONS data analysed in per age group: postnatal infants, 1–5 years, 6–10 years and 11–16 years |
| Results expressed by 100,000 people using the ONS mid-year population estimates | |
| Results | Age-specific mortality rates because of asthma have decreased: |
| 1–5-year-olds: from 0.58 to 0.13. | |
| 6–10-years-old: from 0.53 to 0.23 | |
| 11–16-years-old: 1.38–0.37 | |
| Comments | Not included |
| Does not provide mortality rate for severe asthmatics |
Sturdy (2005)154
| First author (year) | Sturdy (2005)154 | |||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Title | Deaths certified as asthma and use of medical services: a national case–control study | |||||||||||||||||||||||||||||||||||||||||||||||
| Objective | Estimate the relationship between asthma death and use of medical services | |||||||||||||||||||||||||||||||||||||||||||||||
| Methods | As per Sturdy et al. (2002)149 | |||||||||||||||||||||||||||||||||||||||||||||||
| Results | Table 4 presents the association between asthma death and use of medical services factors. Results are presented for mutually adjusted odds ratio and 95% CI, adjusted for sex, drugs, COPD and psychosocial factors:
|
|||||||||||||||||||||||||||||||||||||||||||||||
| Comments | Not included | |||||||||||||||||||||||||||||||||||||||||||||||
| Does not provide mortality rate for severe asthmatics | ||||||||||||||||||||||||||||||||||||||||||||||||
| First author (year) | Watson et al. (2007)105 | |||||||||||||||||||||||||||||||||||||||||||||||
| Title | Factors associated with mortality after an asthma admission: a national UK database analysis. | |||||||||||||||||||||||||||||||||||||||||||||||
| Objective | Evaluate the mortality rate in UK patients hospitalised for asthma between 2000 and 2005 | |||||||||||||||||||||||||||||||||||||||||||||||
| Methods | Data from NHS Acute Trusts which have A&E departments with admission beds or short stay inpatient beds, 70% of inpatient coverage for 1992–2005 | |||||||||||||||||||||||||||||||||||||||||||||||
| Patients hospitalised for J45 (asthma) and J46 acute severe asthma between April 2000 and March 2005 | ||||||||||||||||||||||||||||||||||||||||||||||||
| Results | DiagnosisAge band (years)Asthma admissions (n)Deaths post asthma admissions (n)Deaths post 100,000 admissions (95% CI)J450–1182,62434 (1 to 11)12–1611,917434 (9 to 86)17–4462,1023252 (35 to 73)≥ 4567,060781190 (119 to 1275Total223,703837374 (349 to 400J460–118222897 (42 to 191)12–1615685319 (104 to 742)17–44940736383 (267 to 529)≥ 4571431772478 (2129 to 2865)Total26,340226858 (750 to 977) | Diagnosis | Age band (years) | Asthma admissions (n) | Deaths post asthma admissions (n) | Deaths post 100,000 admissions (95% CI) | J45 | 0–11 | 82,624 | 3 | 4 (1 to 11) | 12–16 | 11,917 | 4 | 34 (9 to 86) | 17–44 | 62,102 | 32 | 52 (35 to 73) | ≥ 45 | 67,060 | 78 | 1190 (119 to 1275 | Total | 223,703 | 837 | 374 (349 to 400 | J46 | 0–11 | 8222 | 8 | 97 (42 to 191) | 12–16 | 1568 | 5 | 319 (104 to 742) | 17–44 | 9407 | 36 | 383 (267 to 529) | ≥ 45 | 7143 | 177 | 2478 (2129 to 2865) | Total | 26,340 | 226 | 858 (750 to 977) |
| Diagnosis | Age band (years) | Asthma admissions (n) | Deaths post asthma admissions (n) | Deaths post 100,000 admissions (95% CI) | ||||||||||||||||||||||||||||||||||||||||||||
| J45 | 0–11 | 82,624 | 3 | 4 (1 to 11) | ||||||||||||||||||||||||||||||||||||||||||||
| 12–16 | 11,917 | 4 | 34 (9 to 86) | |||||||||||||||||||||||||||||||||||||||||||||
| 17–44 | 62,102 | 32 | 52 (35 to 73) | |||||||||||||||||||||||||||||||||||||||||||||
| ≥ 45 | 67,060 | 78 | 1190 (119 to 1275 | |||||||||||||||||||||||||||||||||||||||||||||
| Total | 223,703 | 837 | 374 (349 to 400 | |||||||||||||||||||||||||||||||||||||||||||||
| J46 | 0–11 | 8222 | 8 | 97 (42 to 191) | ||||||||||||||||||||||||||||||||||||||||||||
| 12–16 | 1568 | 5 | 319 (104 to 742) | |||||||||||||||||||||||||||||||||||||||||||||
| 17–44 | 9407 | 36 | 383 (267 to 529) | |||||||||||||||||||||||||||||||||||||||||||||
| ≥ 45 | 7143 | 177 | 2478 (2129 to 2865) | |||||||||||||||||||||||||||||||||||||||||||||
| Total | 26,340 | 226 | 858 (750 to 977) | |||||||||||||||||||||||||||||||||||||||||||||
| Comments | Not included | |||||||||||||||||||||||||||||||||||||||||||||||
| Does not provide mortality rate for severe asthmatics |
de Vries (2010)138
| First author (year) | de Vries (2010)138 | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Title | Long-acting beta2-agonists in adult asthma and the pattern of risk of death and severe asthma outcomes: a study using the GPRD | ||||||||||||||||||
| Objective | Describe risks of death and asthma outcomes with prescription of LABAs, SABAs or ICSs in general practice | ||||||||||||||||||
| Methods | Data was collected from GPRD on permanently registered patients > 18 years of age who received a prescription for inhaled SABA or LABA after 1 January 1993. Patients coded as COPD were excluded | ||||||||||||||||||
| Patients were followed from the index data up to the latest GPRD data collection, the patient's transfer out of the practice or the patient's death, whichever first | |||||||||||||||||||
| Outcomes of interest were death, asthma death, hospitalisation for J46 – acute severe asthma and visit to the GP | |||||||||||||||||||
| Exposure was classified according to the BTS/SIGN step guidelines | |||||||||||||||||||
| The rate of outcomes was estimated during current exposure, that is the time within 3 months of a prescription for the asthma medication. | |||||||||||||||||||
| Results | 507,966 patients followed up for an average 5.0 years (median 4.2) | ||||||||||||||||||
| Mean age was 42.7 years and 58.7% were female. Table 2, p. 467, provides the incidence rates of death, asthma death, J46 hospitalisations and GP visits for asthma during current exposure to asthma medication. Death rates are presented below | |||||||||||||||||||
| StepHigh-dose ICS + SABAHigh-dose ICS + otherHigh-dose ICS + SABA, no LABAHigh-dose ICS onlyRegular OCSsNo SABA, no LABACases56354157Rate0.070.30.10.010.4 | Step | High-dose ICS + SABA | High-dose ICS + other | High-dose ICS + SABA, no LABA | High-dose ICS only | Regular OCSs | No SABA, no LABA | Cases | 56 | 3 | 54 | 1 | 57 | Rate | 0.07 | 0.3 | 0.1 | 0.01 | 0.4 |
| Step | High-dose ICS + SABA | High-dose ICS + other | High-dose ICS + SABA, no LABA | High-dose ICS only | Regular OCSs | ||||||||||||||
| No SABA, no LABA | |||||||||||||||||||
| Cases | 56 | 3 | 54 | 1 | 57 | ||||||||||||||
| Rate | 0.07 | 0.3 | 0.1 | 0.01 | 0.4 | ||||||||||||||
| Comments | Included |
Table 101 presents a summary of the studies. All studies examined asthma mortality in patients with asthma. Only one study stratified patients according to severity. 138 Two studies focused on patients hospitalised for asthma: Gupta et al. 113 on those admitted to the ICU, and Watson et al. 106 on those hospitalised for asthma [international diagnostic code (International Classification of Diseases) J45] or for acute severe asthma (International Classification of Diseases code J46). The methodology varied between the studies: five studies analysed registry,106,113,150,153,155 two followed a cohort of asthma patients retrospectively,138,147 two used a case–control methodology to estimate odds ratio for asthma deaths149,154 and one152 reported on an ongoing confidential inquiry into the asthma-related deaths which occurred in the eastern region of England.
| First author (year) | Population | Methodology | Data sources for mortality | Potentially relevant results | Included? Yes/no |
|---|---|---|---|---|---|
| Fleming (2000)155 | Asthma patients | Analysis of registry data. | ONS | Number of asthma deaths in 1994 | No |
| Trends in asthma deaths | |||||
| Lanes (2002)148 | Asthma patients | Retrospective cohort | GPRD | Number of asthma deaths 1994–8 | No |
| Death-rates in general population | |||||
| Sturdy (2002)149 | Asthma patients | Case–control | ONS | OR for asthma death | No |
| GP case notes | |||||
| Hansell (2003)150 | Asthma patients | Analysis of registry data | ONS | Number of asthma deaths | No |
| Number of person-years at risk | |||||
| Gupta (2004)112 | Asthma patients in ICU | Analysis of registry data | ICNARC-CMPD | Number of deaths | No |
| Number of patients in ICU for asthma | |||||
| Anderson (2005)151 | Asthma patients | Case–control | ONS | OR for asthma death | No |
| GP case notes | |||||
| Harrison (2005)152 | Asthma patients | Inquiry into asthma deaths | ONS | Number of deaths by severity | No |
| GP case notes | |||||
| Panickar (2005)153 | Asthma patients | Analysis of registry data | ONS | Age-specific asthma-mortality rates in the general population | No |
| Sturdy (2005)154 | Asthma patients | Case–control | ONS | OR for asthma death | No |
| GP case notes | |||||
| Watson (2007)106 | Asthma patients hospitalised for asthma (J45) and acute severe asthma (J46). | Analysis of registry data | CHKS (hospitalisation) database | Number of all-cause deaths in patients hospitalised by age | Yes |
| Number of patients hospitalised by age | Sensitivity analysis | ||||
| Age-specific all-cause mortality rates | |||||
| de Vries (2010)138 | Asthma patients stratified by BTS/SIGN treatment step | Retrospective cohort | GPRD | Number of asthma deaths by treatment step | Yes. Used for the base case |
| Asthma-related annual mortality rate by treatment step |
Most studies used data from the Office for National Statistics (ONS) to inform mortality because of asthma. 148–154 Four of these subsequently confirmed the cause of death using GP case notes. 149,151,152,154 In the study by Harrison et al.,152 only 60% of deaths whose cause had been registered as asthma were confirmed as asthma deaths. Lanes et al. 148 and de Vries et al. 138 used GPRD data. Two used registry data from hospitals. Gupta et al. 113 conducted a secondary analysis of the Intensive Care National Audit and Research Centre Case Mix Programme Database of 128 general critical care units across England, Wales and Northern Ireland over 1995–2001. Watson et al. 106 used data from the Camper Healthcare Knowledge Systems (CHKS) database, which provides 70% of inpatient coverage in the UK.
The results presented differed across the 10 studies. Fleming et al. ,155 Lanes et al.,148 Hansell et al. 150 and Harrison et al. 152 reported the number of asthma deaths in a particular period of time. Lanes et al. 148 and Panickar et al. 153 reported the asthma-related mortality rates by 100,000 person-years of the general population. Three studies reported the odds ratio of risk factors for asthma death related with health behaviour, such as poor inhaler technique,149 number of GP contacts,154 medication use,151 or BTS/SIGN treatment step. 138 Only de Vries et al. 138 reported the asthma-related mortality rate in asthma patients stratified by severity, defined as the treatment step in the BTS/SIGN guidelines of 2005.
Discussion
On the basis of the review, two studies emerged as potentially appropriate to inform the asthma-related mortality risk experienced by patients with severe persistent allergic asthma, Watson et al. 106 and de Vries et al. 138 de Vries et al. report asthma-related mortality rate for patients according to BTS/SIGN treatment step. As long as the BTS/SIGN treatment steps are accepted as sufficiently robust markers of severity, the mortality rates reported in de Vries et al. for patients at step 4 and 5 could be used as an appropriate proxy for mortality rates for patients with severe persistent asthma. However, the mortality reported by de Vries et al. refers solely to patients 18 years and older. Asthma-related mortality in adults may not be applicable to children and adolescents.
Watson et al. 106 report the mortality risk for patients hospitalised for asthma and acute severe asthma by age category (< 12, 12–16, 17–44 and ≥ 45 years of age). Although they report mortality for patients across all age ranges, this requires a number of assumptions in order to be used as asthma-related mortality risk for patients with severe persistent allergic asthma. Firstly, the mortality risk refers to death following a hospitalisation for asthma or acute severe asthma. Asthma deaths occurring in the community would not be included, which could underestimate mortality. Secondly, patients may have been admitted because of asthma but died as a result of other causes, such as hospital acquired-pneumonia. Thirdly, hospitalisations may have been misclassified under asthma. Fourthly, the age category of ≥ 45 years may mask the influence of age in mortality, as the median age of survivors was much lower than the median age of those deceased (25 vs. 77 years of age). Finally, the mortality risk reported by Watson et al. 106 is a conditional probability, that is the probability of death given a hospitalisation for asthma. In order to obtain the asthma-related mortality risk, the mortality risk following hospitalisation needs to be divided by the risk of hospitalisations for asthma.
Systematic review of health-related quality of life in asthma
Methods
A broad search strategy was employed using terms relating to asthma and to HRQoL. No date, language, study design limits were applied. The inclusion criteria were clinical trials, cross-sectional or cohort studies reporting HRQoL in asthma patients, directly measured with EQ-5D in the case of adult and adolescents (≥ 12 years of age) and using any utility instrument or technique for children (≤ 11 years). Titles and abstracts were assessed independently by two reviewers for inclusion and any discrepancies were resolved by consensus. Data were extracted by one reviewer using a standardised data extraction form and checked for accuracy by a second reviewer.
Results
Figure 8 presents the flow diagram of identification and selection of studies. Briefly, 1351 records were found, of which 1229 were rejected at title screening. Of these, 121 full-text articles were assessed. A review of health utilities was identified and its references examined. 156 One additional study was included: HRQoL data from EXALT was presented in the MS for omalizumab. EXALT was a RCT where EQ-5D was directly collected from patients. Data were extracted from 21 studies, presented in Table 102.
Nine studies reported HRQoL for asthma patients. 157–165 Ten other studies presented results stratified by severity140,165–169 or focused exclusively on patients with severe persistent15,104 or difficult asthma. 139,170 Two studies reported the HRQoL improvement from omalizumab treatment. 15,39 Two studies reported HRQoL for exacerbations. 104,140
FIGURE 8.
Flow diagram of the systematic review on HRQoL.
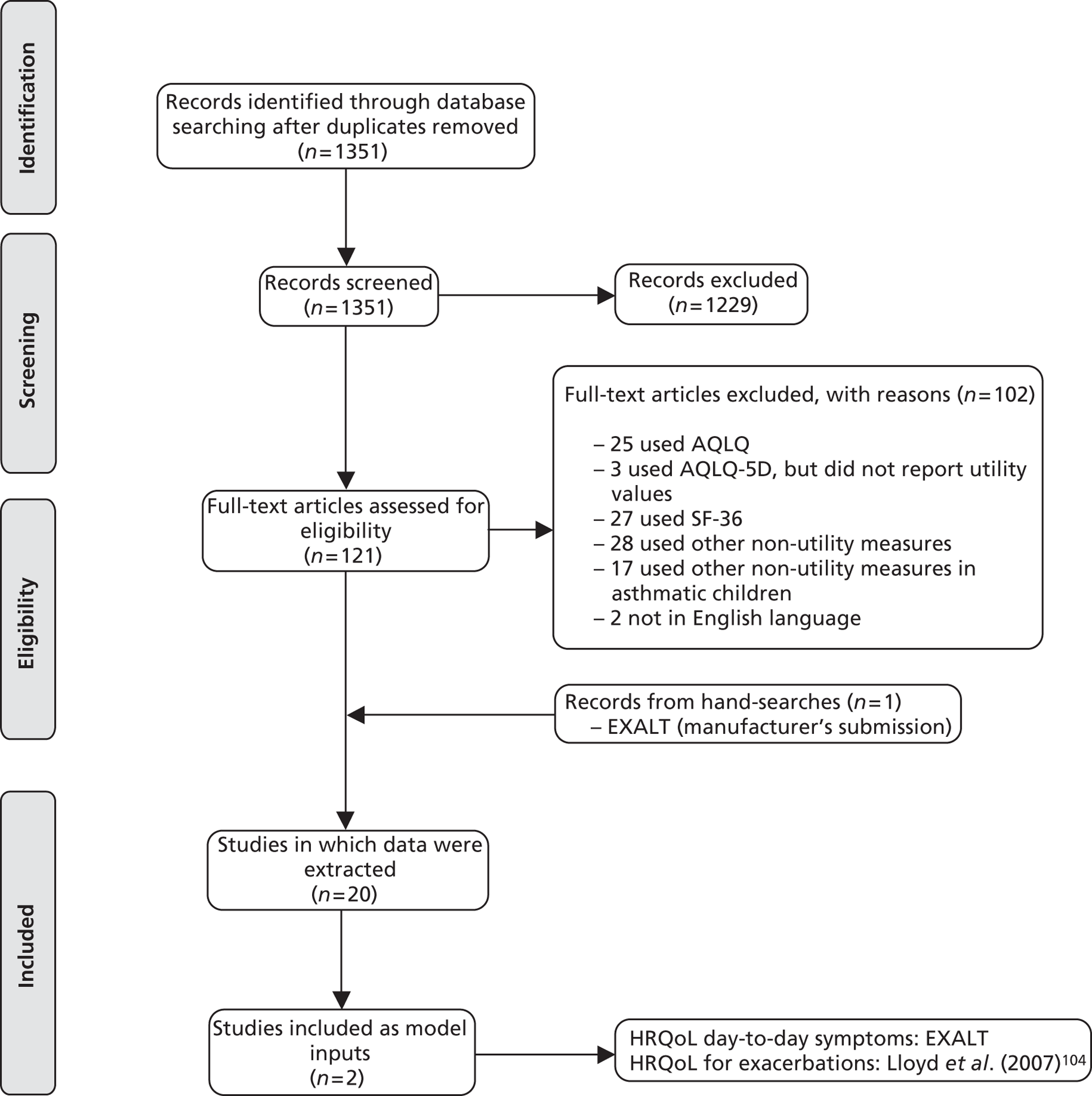
Three studies were based in the UK. 104,139,163 Aburuz et al. reported a mean EQ-5D value of 0.47 (standard deviation 0.33) from adult patients with difficult asthma. Garratt et al. (2000) reported EQ-5D values for a cohort of asthma patients, stratified by smoking status. Mean EQ-5D for non-smokers was 0.80 (standard deviation 0.27) and for smokers was 0.76 (standard deviation 0.25). Lloyd et al. obtained EQ-5D values from moderate to severe asthmatics at baseline and at 4 weeks. At 4 weeks, patients who had no exacerbations during the follow-up period reported a mean EQ-5D of 0.89 (standard deviation 0.15), patients who had an exacerbation involving OCS reported a mean EQ-5D of 0.57 (standard deviation 0.36) and patients who were hospitalised for asthma reported a mean EQ-5D of 0.33 (standard deviation 0.39). Baseline values were not reported but change from baseline was. Patients without exacerbations experienced a non-statistically significant improvement of 0.05, patients who had an exacerbation requiring OCSs experienced a non-statistically significant improvement of 0.10 and patients who were hospitalised experienced a statistically significant decrement of 0.20. Ten studies were in Europe. 139,140,157–159,161,165,167–169 Five were based in the USA. 159,160,164,170,171 One was based in Japan172 and another in Canada. 166 Finally, one study, EXALT, was a multicentre RCT. 15
Only two studies presented HRQoL values for children, Willems et al. 157 and Carroll et al. 171 In Willems et al.,157 parents or caregivers completed the child proxy version of EQ-5D. Carroll et al. 171 used time trade-off and standard gamble techniques to obtain HRQoL values from parents for conditions hypothetically experienced by their children.
The systematic review identified two studies reporting health utility values associated with exacerbations, Lloyd et al. 104 and Steuten et al. 140 Lloyd et al. 104 examined the impact of exacerbations on HRQoL in patients with moderate to severe asthma (BTS steps 4 and 5) in the UK. EQ-5D, as well as other QoL instruments, were administered at baseline and at 4 weeks. Only the 4-week data and change from baseline are reported. The data collected may not reflect the HRQoL loss associated with an exacerbation if the exacerbations occurred shortly after baseline assessment. Only if the exacerbation occurred shortly before or during the follow-up assessment would the values collected reflect the HRQoL loss as a result of an exacerbation. Therefore, the health utility losses reported by Lloyd et al. 104 could be interpreted as the average decrement because of an exacerbation over 4 weeks.
Steuten et al. 140 reports the cost–utility analysis of a disease management programme for adults with asthma in comparison with standard care. A Markov model with four health states, in addition to death, was used to estimate the 5-year impact of the programme beyond the 15-month follow-up of the RCT. The patient population was classified into three levels of severity: managed by the GP, managed by the respiratory nurse specialist and managed by the pulmonologist (respiratory consultant). Health utility values were collected during the RCT and used in the Markov model for successful control, suboptimal control, primary care-managed exacerbation and hospital-managed exacerbation.
| First author (year) | Country and population | Study design (follow-up) | Setting | Mean age (SD) | Baseline: number of individuals (n), mean EQ-5D and (SD) | Follow-up: number of individuals (n), mean EQ-5D and (SD) | Comments |
|---|---|---|---|---|---|---|---|
| Willems (2007)157 | Netherlands | RCT (12 m) | Outpatient clinic | Adults control: 45.9 (15.9) | n = 27; 0.78 (0.17) | n = 27; 0.79 (0.21) | |
| Children and adults suffering from asthma | Adults intervention: 45.7 (11.3) | n = 26; 0.89 (0.13) | n = 26; 0.90 (0.11) | ||||
| Children control: 10.9 (2.3) | n = 27; 0.96 (0.07) | n = 27; 0.97 (0.05) | |||||
| Children intervention: 10.6 (2.1) | n = 29; 0.92 (0.20) | n = 29; 0.98 (0.04) | |||||
| Aburuz (2007)139 | UK | CS | Asthma specialist care | 42.3 (15.0) | n = 86; 0.47 (0.33) | NA | 79.1% on maintenance OCSs |
| Difficult asthma | |||||||
| Burstrom (2001)159 | Sweden | CS | National health survey (n = 3112) | Men: 48.7, women: 49.0 | n = 253; overall: 0.79 (0.015); male: 0.80 (0.027); female: 0.78 (0.017) | NA | |
| Asthma | |||||||
| Chen (2007)170 | USA | CS data from prospective cohort | National cohort | 52.8 | NR | 987; 0.86 (0.16) | US population values |
| TENOR study | 0 ATAQ problems n = 357; 0.91 (0.13) | ||||||
| 1 ATAP problems n = 223; 0.88 (0.13) | |||||||
| 2 ATAQ problems n = 229; 0.83 (0.15) | |||||||
| 3 ATAQ problems n = 129; 0.80 (0.18) | |||||||
| 4 ATAQ problems n = 49; 0.73 (0.21) | |||||||
| Ko and Coons (2006)159 | USA | CS | General population survey (n = 4048) | 44.7 (17.4) | n = 68; 0.924 (0.0117) | ||
| Asthma | |||||||
| Lloyd (2007)104 | UK | Prospective cohort (4 weeks) | Outpatient clinic and GP clinics | No exacerbation: 40.5 (11.6) | NR | n = 85; 0.89 (0.15) | UK population values |
| Moderate to severe asthmatics (BTS steps 4 or 5) | Exacerbation: 41.4 (12.0) | NR | n = 22; 0.57 (0.36) | Mean change from baseline: | |||
| Exacerbation with hospitalisation: 48.4 (11.0) | NR | n = 5; 0.33 (0.39) | No exacerbation: 0.05 | ||||
| Exacerbation week/OCS: −0.10 | |||||||
| Exacerbation week/hospitalisation: −0.20 | |||||||
| Lubetkin (2005)160 | USA | CS | General population survey (n = 13,646) | NR | n = 1202; 0.82 (0.0069) | NA | |
| Asthma | |||||||
| Oga (2003)172 | Japan | Prospective cohort (6 m) | Outpatient | 46.8 (19.3) | n = 54; 0.808 (0.187) | n = 54; 0.879 (0.146) | Japanese population values |
| Asthma (step 3 or above) | |||||||
| Polley (2008)161 | Ireland | CS | Respiratory outpatient clinic | 51.6 (17.5) | n = 20; 0.63 (0.38) | NA | |
| Stable asthma | |||||||
| Saarni (2006)162 | Finland | CS | General population survey (n = 6681) | 52.6 | n = 534; 0.766 (0.011) | NA | UK population values |
| Asthma | |||||||
| McTaggart-Cowan (2008)166 | Canada | CS | Self-reported asthma patients recruited from poster advertisement | 35.0 (7.9) | n = 157; 0.84 (0.23) | NA | UK population values |
| Asthma stratified by severity and control | Very mild asthma n = 21; 0.84 (0.29) | ||||||
| Mild asthma n = 59; 0.89 (0.18) | |||||||
| Moderate asthma, n = 51; 0.81 (0.21) | |||||||
| Severe asthma, n = 20; 0.76 (0.27) | |||||||
| Very well controlled; n = 37; 0.90 (0.22) | |||||||
| Well controlled, n = 43; 0.84 (0.20) | |||||||
| Adequately controlled, n = 54; 0.81 (0.22) | |||||||
| Not well controlled, n = 19; 0.80 (0.21) | |||||||
| Szende (2004)167 | Hungary | CS | Outpatients and inpatients | 49 | Good control, n = 36; 0.93 | NA | |
| Asthma stratified by severity | Mildly reduced control, n = 64; 0.76 | ||||||
| Moderate reduced control, n = 82; 0.65 | |||||||
| Poor control, n = 46; 0.52 | |||||||
| Ferreira (2010)168 | Portugal | CS | Asthma specialist care | 49 (16.9) | n = 115; 0.85 (0.16) | NA | UK population values |
| Stratified by severity and FEV1 | Stage I 17%; 0.91 (0.12) | ||||||
| Stage II and III 76%; 0.85 (0.14) | |||||||
| Stage III 0.82 (0.18) | |||||||
| Stage IV 0.75 (0.23) | |||||||
| FEV1% < 50%; 0.88 (0.16) | |||||||
| 74 < FEV1 < 50; 0.83 (0.17) | |||||||
| 99 < FEV1 < 75; 0.84 (0.16) | |||||||
| FEV1 > 99; 0.82 (0.16) | |||||||
| Garratt (2000)163 | England | Prospective cohort (6 m) | Primary care | NR | Non-smoker n = 177; 0.80 (0.27) | NR | UK population values |
| Asthma | Smoker, n = 36; 0.76 (0.25) | ||||||
| Sullivan (2005)164 | USA | CS | National health survey (38,678) | 45 | n = 3504; 0.802 (0.77–0.83) | NA | |
| Asthma | |||||||
| Szende (2009)165 | Hungary | CS | Outpatients and inpatients | 47.8 (15.3) | n = 228; 0.68 (0.23) | NA | UK population values |
| Asthma stratified by severity | Intermittent n = 36; 0.89 (0.16) | ||||||
| Mild, n = 62; 0.70 (0.20) | |||||||
| Moderate, n = 80; 0.63 (0.23) | |||||||
| Severe, n = 43; 0.51 (0.16) | |||||||
| Steuten (2007)140 | Netherlands | RCT (12 m) | Primary and specialist care | NR | All results for severe persistent asthma | NR | |
| Stratified by severity | 658 participants, 10% severe persistent asthma | Successful control; 0.70 (0.03) | |||||
| Suboptimal control; 0.69 (0.04) | |||||||
| GP exacerbation; 0.62 (0.03) | |||||||
| Hospital exacerbation; 0.60 (0.05) | |||||||
| Kardos (2011)169 | Germany | CS | Outpatient care | 47.5 (16.3) | Controlled: n = 313; 0.83(0.17) | NA | |
| Stratified by severity and asthma control | Partially controlled n = 21; 10.75(0.19) | ||||||
| Uncontrolled n = 48; 0.57 (0.18) | |||||||
| Children | |||||||
| Carroll (2009)171 | USA | CS | Primary care and specialist care – convenience sample | NR | 10-day hospitalisation (n = 434) | NA | Parent values using time trade off and standard gamble for hypothetical health states |
| Asthma | SG: 0.94 (0.14); TTO: 0.95 (0.15) | ||||||
| 10-day intensive care unit (n = 403) | |||||||
| SG: 0.87 (0.20); TTO: 0.91 (0.18) | |||||||
| Mild intermittent asthma (n = 324) | |||||||
| SG: 0.91 (0.18); TTO: 0.91 (0.17) | |||||||
| Mild persistent asthma (n = 383) | |||||||
| SG: 0.90 (0.18); TTO: 0.91 (0.17) | |||||||
| Moderate persistent asthma (n = 329) | |||||||
| SG: 0.88 (0.18); TTO: 0.91 (00.15) | |||||||
| Severe persistent asthma (n = 350) | |||||||
| SG: 0.83 (0.21); TTO: 0.85 (0.20) | |||||||
| Omalizumab effect on HRQoL as measured by EQ-5D | |||||||
| Brusselle (2009)39 | Belgium | Prospective cohort (52 weeks) | Specialist care | 48.17 (17.18) | Started on treatment: 158 | Improvement from baseline: ITT = 0.14(0.23), PP = 0.15(0.24) | 28.5% on maintenance OCS |
| ≥ 12 years of age, poorly controlled severe persistent asthma, as per UK/EU PL for omalizumab | Omalizumab real-life setting | 0.54 | |||||
| EXALT15 | Multiple countries | Open-label RCT (32 weeks) | Specialist care | 41 (range:14–73) | Baseline utility: 0.653 (0.025) | Standard care: 128, 0.719 (0.026) | |
| ≥ 12 years of age, poorly controlled severe persistent asthma, as per UK/EU PL for omalizumab | Omalizumab responders: 190, 0.767 (0.020) | ||||||
Parameter inputs used for the independent assessment
Base-case populations: adult and adolescents (patients ≥ 12 years of age) and children (6–11 years)
| Variables | Adults and adolescents (patients ≥ 12 years) | Children (patients 6–11 years) | ||
|---|---|---|---|---|
| Value | Source | Value | Source | |
| Baseline rate of exacerbations | ||||
| CSNS exacerbations | 0.8046 (0.6552 to 0.9881) | INNOVATE | 1.5648 (1.2248 to 1.9992) | IA-05 EUP |
| CSS exacerbations | 0.8842 (0.7268 to 1.0756) | INNOVATE | 1.2235 (0.9323 to 1.6057) | IA-05 EUP |
| Treatment effectiveness | ||||
| Proportion of responders | 56.5% (49.74% to 63.18%) | INNOVATE | 74.2% (67.41% to 81.01%) | IA-05 EUP |
| Risk ratio for CSNS exacerbations (responders) | 0.5089 (0.3291 to 0.7869) | INNOVATE | 0.2415 (0.1511 to 0.3861) | IA-05 EUP |
| Risk ratio for CSS exacerbations (responders) | 0.2494 (0.1425 to 0.4362) | INNOVATE | 0.3051 (0.1380 to 0.6743) | IA-05 EUP |
| Mortality | ||||
| All-cause mortality | UK life-tables adjusted for asthma-related deaths | ONS | UK life-tables adjusted for asthma-related deaths | ONS |
| Asthma-related deaths | Asthma-related mortality rate = 0.4 per 100 person-years | de Vries et al. (2010)138 | Asthma-related mortality rate = 0.4 per 100 person-years | de Vries et al. (2010)138 |
| HRQoL | ||||
| Omalizumab effect on HRQoL | HRQoL difference observed in the trial | EXALT | No HRQoL difference between treatments up to age 12 | EXALT |
| 0.767 (omalizumab) vs. 0.719 (standard care) | From age 12, HRQoL difference as adults and adolescents | |||
| HRQoL loss because of exacerbations | CSNS = −0.10 | Lloyd et al. (2007)104 | CSNS = −0.10 | Lloyd et al. (2007)104 |
| CSS = −0.20 | CSS = −0.20 | |||
| Duration of exacerbation | 4 weeks | 4 weeks | ||
| Resource use and costs | ||||
| Cost of exacerbations | CSNS = £87.7 | INNOVATE | CSNS = CSS = £213.89 | IA-05 EUP |
| CSS = £124.32 | ||||
| Routine visits | Two per year, £160 each | NHS reference costs16 | Two per year, £190 each | NHS reference costs16 |
| Initiation of therapy | £245 | £247 | ||
| Standard therapy costs (per year) | £1197 | INNOVATE | £810 | IA-05 EUP |
| Omalizumab costs (per year) | £8056 | INNOVATE | £8455 | IA-05 EUP |
| Administration and monitoring costs | First year: £260 | INNOVATE | First year: £268 | IA-05 EUP |
| Thereafter: £146 | Thereafter: £151 | |||
Model inputs for subgroup populations: hospitalisation, maintenance oral corticosteroids and ≥ 3 exacerbations
| Variables | Hospitalisation subgroup | |||
|---|---|---|---|---|
| Adults and adolescents (patients ≥ 12 years) | Children (patients 6–11 years) | |||
| Value | Source | Value | Source | |
| Baseline annual rate of exacerbations | ||||
| CSNS exacerbations | 0.8706 (0.6308 to 1.2016) | INNOVATE hospitalisation | 2.1429 (3.5545 to 1.2918) | IA-05 EUP hospitalisation |
| CSS exacerbations | 1.2235 (0.9323 to 1.6057) | INNOVATE hospitalisation | 1.2857 (0.6690 to 2.4711) | IA-05 EUP hospitalisation |
| Treatment effectiveness | ||||
| Proportion of responders | 56.63% (45.96% to 67.29%) | INNOVATE hospitalisation | 54.05% (38.00% to 70.11%) | IA-05 EUP hospitalisation |
| Risk ratio for CSNS exacerbations (responders) | 0.5902 (0.3137 to 1.1103) | INNOVATE hospitalisation | 0.2593 (0.1006 to 0.6682) | IA-05 EUP hospitalisation |
| Risk ratio for CSS exacerbations (responders) | 0.2907 (0.1433 to 0.5900) | INNOVATE hospitalisation | 0.1440 (0.0311 to 0.6666) | IA-05 EUP hospitalisation |
| Mortality | ||||
| All-cause mortality | UK life-tables adjusted for asthma-related deaths | ONS | UK life-tables adjusted for asthma-related deaths | ONS |
| Asthma-related deaths | Asthma-related mortality rate = 0.4 per 100 person-years | de Vries et al. (2010)138 | Asthma-related mortality rate = 0.4 per 100 person-years | de Vries et al. (2010)138 |
| HRQoL | ||||
| Omalizumab effect on HRQoL | HRQoL difference observed in the trial | EXALT hospitalisation | No HRQoL difference between treatments up to age 12 | EXALT hospitalisation |
| 0.761 (omalizumab) vs. 0.631 (standard care) | From age 12, HRQoL difference as adults and adolescents | |||
| HRQoL loss because of exacerbations | CSNS = −0.10 | Lloyd et al. (2007)104 | CSNS = −0.10 | Lloyd et al. (2007)104 |
| CSS = −0.20 | CSS = −0.20 | |||
| Duration of exacerbation | 4 weeks | Lloyd et al. (2007)104 | 4 weeks | Lloyd et al. (2007)104 |
| Resource use and costs | ||||
| Cost of exacerbations | CSNS = £154.70 | INNOVATE hospitalisation | CSNS = CSS = £213.89 | IA-05 EUP hospitalisation |
| CSS = £178.87 | ||||
| Routine visits | Two per year, £160 each | NHS reference costs16 | Two per year, £190 each | NHS reference costs16 |
| Initiation of therapy | £245 | £247 | ||
| Standard therapy costs (per year) | £1197 | INNOVATE | £810 | IA-05 EUP |
| Omalizumab costs (per year) | £8056 | INNOVATE | £8455 | IA-05 EUP |
| Administration and monitoring costs | First year: £260 | INNOVATE | First year: £268 | IA-05 EUP |
| Thereafter: £146 | Thereafter: £151 | |||
| Baseline annual rate of exacerbations | ||||
| CSNS exacerbations | 0.9735 (0.6410 to 1.4784) | INNOVATE maintenance OCS | ||
| CSS exacerbations | 1.000 (0.4493 to 2.2259) | INNOVATE maintenance OCS | ||
| Proportion of responders | 46.94% (32.97% to 60.91%) | INNOVATE maintenance OCS | ||
| Risk ratio for CSNS exacerbations (responders) | 0.4142 (0.1569 to 1.0938) | INNOVATE maintenance OCS | ||
| Risk ratio for CSS exacerbations (responders) | 0.2144 (0.0761 to 0.6042) | INNOVATE maintenance OCS | ||
| Mortality | ||||
| All-cause mortality | UK life-tables adjusted for asthma-related deaths | ONS | ||
| Asthma-related deaths | Asthma-related mortality rate = 0.4 per 100 person-years | de Vries et al. (2010)138 | ||
| HRQoL | ||||
| Omalizumab effect on HRQoL | HRQoL difference observed in the trial | EXALT maintenance OCS | ||
| 0.791 (omalizumab) vs. 0.686 (standard care) | ||||
| HRQoL loss because of exacerbations | CSNS = −0.10 | Lloyd et al. (2007)104 | ||
| CSS = −0.20 | ||||
| Duration of exacerbation | 4 weeks | Lloyd et al. (2007)104 | ||
| Resource use and costs | ||||
| Cost of exacerbations | CSNS = £86.51 | INNOVATE maintenance OCS | ||
| CSS = £136.04 | ||||
| Routine visits | Two per year, £160 each | NHS reference costs16 | ||
| Initiation of therapy | £245 | |||
| Standard therapy costs (per year) | £1197 | INNOVATE | ||
| Omalizumab costs (per year) | £8056 | INNOVATE | ||
| Administration and monitoring costs | First year: £260 | INNOVATE | ||
| Thereafter: £146 | ||||
| Incorporation of OCS-related adverse effects | ||||
| Proportion of omalizumab responders who discontinue OCSs | 41.9% | EXALT maintenance OCS | ||
| Annual acquisition costs of OCSs | £99.45 per patient | EXALT | ||
| Costs because of adverse effects of OCSs | £205.60 | See Appendix G of MS | ||
| Health losses because of adverse effects of OCSs | Scenario A: 0.02331 DALY | WHO Global burden of disease 2004 | ||
| Scenario B: 0.04507 DALY | ||||
| Scenario C: 0.04978 DALY | ||||
| Baseline annual rate of exacerbations | ||||
| CSNS exacerbations | 2.2143 (1.8070 to 2.7133) | INNOVATE ≥ 3 exacerbations | 2.7651 (2.1763 to 3.5132) | IA-05 EUP ≥ 3 exacerbations |
| CSS exacerbations | 1.2619 (0.9618 to 1.6518) | INNOVATE ≥ 3 exacerbations | 0.6190 (0.3732 to 1.0269) | IA-05 EUP ≥ 3 exacerbations |
| Treatment effectiveness | ||||
| Proportion of responders | 46.51% (35.97% to 57.05%) | INNOVATE ≥ 3 exacerbations | 77.08% (68.68% to 85.45%) | IA-05 EUP ≥ 3 exacerbations |
| Risk ratio for CSNS exacerbations (responders) | 0.3565 (0.2126 to 0.5978) | INNOVATE ≥ 3 exacerbations | 0.2269 (0.1433 to 0.3592) | IA-05 EUP ≥3 exacerbations |
| Risk ratio for CSS exacerbations (responders) | 0.1840 (0.0735 to 0.4602) | INNOVATE ≥ 3 exacerbations | 0.2838 (0.1157 to 0.6960) | IA-05 EUP ≥3 exacerbations |
| Mortality | ||||
| All-cause mortality | UK life-tables adjusted for asthma-related deaths | ONS | UK life-tables adjusted for asthma-related deaths | ONS |
| Asthma-related deaths | Asthma-related mortality rate = 0.4 per 100 person-years | de Vries et al. (2010)138 | Asthma-related mortality rate = 0.4 per 100 person-years | de Vries et al. (2010)138 |
| HRQoL | ||||
| Omalizumab effect on HRQoL | HRQoL difference observed in the trial | EXALT ≥ 3 exacerbations | No HRQoL difference between treatments up to age 12 | EXALT ≥ 3 exacerbations |
| 0.740 (omalizumab) vs. 0.698 (standard care) | INNOVATE ≥ 3 exacerbations | From age 12, HRQoL difference as adults and adolescents | INNOVATE ≥ 3 exacerbations | |
| INNOVATE: 0.787 vs. 0.651 | ||||
| HRQoL loss because of exacerbations | CSNS = −0.10 | Lloyd et al. (2007)104 | CSNS = −0.10 | Lloyd et al. (2007)104 |
| CSS = −0.20 | CSS = −0.20 | |||
| Duration of exacerbation | 4 weeks | Lloyd et al. (2007)104 | 4 weeks | Lloyd et al. (2007)104 |
| Resource use and costs | ||||
| Cost of exacerbations | CSNS = £154.70 | INNOVATE | CSNS = CSS = £213.89 | IA-05 EUP |
| CSS = £178.87 | ||||
| Routine visits | Two per year, £160 each | NHS reference costs16 | Two per year, £190 each | NHS reference costs16 |
| Initiation of therapy | £245 | £247 | ||
| Standard therapy costs (per year) | £1,197 | INNOVATE | £810 | IA-05 EUP |
| Omalizumab costs (per year) | £8056 | INNOVATE | £8455 | IA-05 EUP |
| Administration and monitoring costs | First year: £260 | INNOVATE | First year: £268 | IA-05 EUP |
| Thereafter: £146 | Thereafter: £151 | |||
Systematic review of economic evaluations of economic evaluations of steroids in asthma
Methods
A broad search strategy was employed using terms relating with asthma, steroids and economic evaluations. No date, language, study design limits were applied. Full economic evaluations that compared two or more options and considered both costs and consequences (including cost-effectiveness, cost–utility and cost–benefit analyses) were included. Full details of the search strategies are reported in Appendix 1. Titles and abstracts were assessed independently by two reviewers for inclusion and any discrepancies were resolved by consensus. Data were extracted by one reviewer using a standardised data extraction form and checked for accuracy by a second reviewer.
Results
Figure 9 presents the flow diagram of identification and selection of studies. Briefly, 830 records were found, of which 105 were duplicates and 637 were rejected at title screening. Overall, 88 full-text records were assessed for eligibility: 63 were within-trial economic evaluations, 18 used observational or routine data, one was a review on the economic consequences of steroids and six were model-based economic evaluations. None included long-term consequences of steroids except Fuhlbrigge et al. ,141 which included the increased costs and health losses as a result of fracture associated with long-term use of ICSs. Therefore, only one study was included in the systematic review. Table 103 presents the data extracted from Fuhlbrigge et al. 141
FIGURE 9.
Flow diagram of the systematic review of economic evaluations of steroids in asthma.
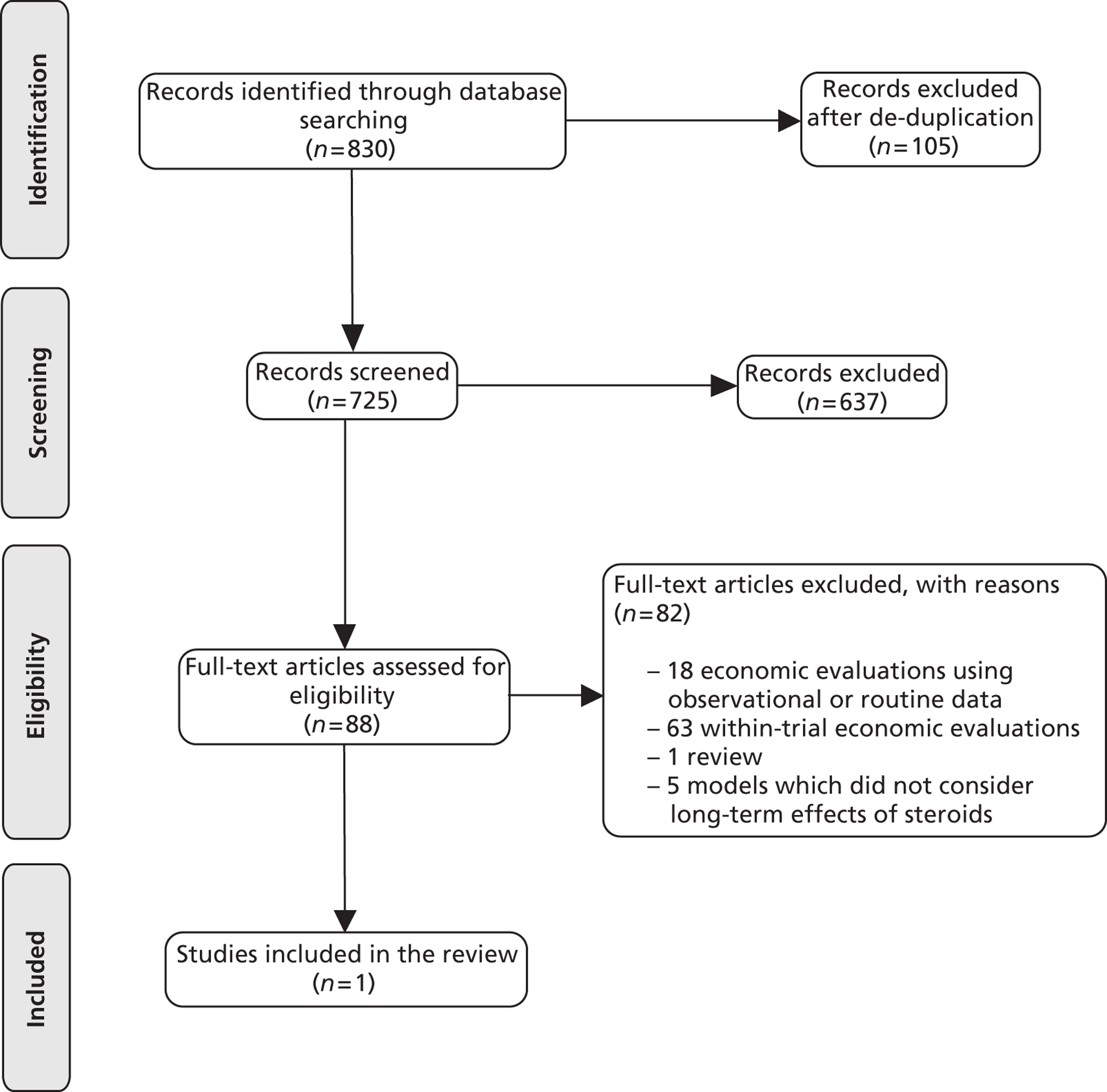
| Study details | Fuhlbrigge et al. (2006)140 |
|---|---|
| Decision problem | Cost-effectiveness of ICSs vs. SABA as required, including bone mineral density (BMD) loss as a result of systemic effects from ICSs |
| Patient population | Women, 35 years old, with mild-to-moderate asthma |
| Model structure | Markov model with five health states according to disease status:
|
Transitions depend on:
|
|
| Assumptions | FEV1% predicted is a predictor of transition between health states and of the HRQoL experienced by patients |
| The only adverse effects considered in the base case are those of ICSs on BMD. For SA, adverse effects from ICS therapy incorporated as disutility. SABA is assumed to be free of adverse effects | |
| ICS effect on FEV1% and on BMD is linear and equivalent across all preparations | |
| The consequence of loss of BMD is fracture as predicted by Melton et al. (1988) equations. All patients who suffer fracture move to nursing home placement and suffer disutility from living in nursing home | |
| How was severity addressed | Severity was classified according to lung function
|
| How were exacerbations addressed | Acute event incidence was derived from the relationship between FEV1% predicted and ED visits observed in a retrospective study31 |
| EDrate = logit(2.1872 – 0.56 FEV1%) | |
| The estimated rate of ED visits was adjusted upwards or downwards depending on the number of prior hospitalisations32,33 | |
| Same database was used to estimate the proportion of all asthma-related ED visits that results in hospitalisation | |
| How was mortality addressed | Monthly probability of asthma-related death:48
|
| Treatment effectiveness | ICS increases FEV1% by 7.6% in mild disease and by 11.6% in moderate disease |
| Inhalation of 100 µg of ICS/year is equivalent to a BMD loss of 0.00028 g/cm2 | |
| Effect of BMD on fracture risk was estimated using equations developed by Melton et al. (1988) | |
| HRQoL | Asthma: utility study using TTO and mapped to FEV1%: utility = 0.521 + 0.0003958 × FEV1% |
Hip fracture:
|
|
| Adverse effects from medication | Incorporated as utility decrement due to ICS therapy → assumed 0% for base case, values up to 3% in the sensitivity analysis |
| Long-term consequences | None besides ICSs on BMD |
| CE drivers | Efficacy of ICS therapy |
| HRQoL | |
| Effect of ICSs on BMD | |
| Uncertainties | Relationship between FEV1% predicted and transition between health states |
| Relationship between FEV1% predicted and utilities | |
| Relationship between ICSs and FEV1% predicted and BMD | |
| Relationship between BMD and fracture risk | |
| Impact of OCSs via exacerbations |
Discussion
No economic evaluations were found quantifying the costs and health losses because of adverse effects from long-term use of OCSs in asthma. Only one economic evaluation was found that considered the long-term consequences of ICSs in terms of increased risk of fracture in adult women. Although the adverse effects of long-term use of OCSs by severe asthma patients are thought to have a significant impact on health outcomes and costs, no study has so far quantified their economic and health burden.
Appendix 19 The Preferred Reporting Items for Systematic Reviews and Meta-analyses
| Section/topic | # | Checklist item | Reported on page # |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both | Title page |
| ABSTRACT | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number | Executive summary |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known | Chapter 1 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS) | Chapter 2 |
| METHODS | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g. web address), and, if available, provide registration information including registration number | PROSPERO: Reg No. CRD42011001625 |
| Eligibility criteria | 6 | Specify study characteristics (e.g. PICOS, length of follow-up) and report characteristics (e.g. years considered, language, publication status) used as criteria for eligibility, giving rationale | Methods for reviewing clinical effectiveness |
| Information sources | 7 | Describe all information sources (e.g. databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched | Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Search strategy |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated | Appendix 1 |
| Study selection | 9 | State the process for selecting studies (i.e. screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis) | Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Study selection |
| Data collection process | 10 | Describe method of data extraction from reports (e.g. piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators | Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Data extraction |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made | Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Study selection |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis | Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Quality assessment |
| Summary measures | 13 | State the principal summary measures (e.g. risk ratio, difference in means) | Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Data analysis |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g. I2) for each meta-analysis | Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Data analysis |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g. publication bias, selective reporting within studies) | Validity assessment and risk of bias of randomised controlled trials and Quantity and quality of evidence: observational studies |
| Additional analyses | 16 | Describe methods of additional analyses (e.g. sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified | Methods for reviewing the efficacy of omalizumab (including long-term outcomes and steroid-sparing), Data analysis |
| RESULTS | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram | Figures 1 and 2 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g. study size, PICOS, follow-up period) and provide the citations | Appendices 3–6 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12) | Table 4 and Appendix 7 |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot | Chapter 3 |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency | NA |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see item 15) | Validity assessment and risk of bias of randomised controlled trials |
| Additional analysis | 23 | Give results of additional analyses, if done (e.g. sensitivity or subgroup analyses, meta-regression [see item 16]) | Chapter 3 |
| DISCUSSION | |||
| Summary of evidence | 24 | Summarise the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g. health-care providers, users, and policy-makers) | Chapter 3 summary sections |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g. risk of bias), and at review-level (e.g. incomplete retrieval of identified research, reporting bias) | Results of assessment of adverse effects of oral corticosteroids |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research | Chapters 7 and 8 |
| FUNDING | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g. supply of data); role of funders for the systematic review | Title page |
Appendix 20 Protocol
Glossary
- Adverse event
- An abnormal or harmful effect caused by, and attributable to, exposure to a chemical (e.g. a drug), which is indicated by some result such as death, a physical symptom or visible illness. An effect may be classed as adverse if it causes functional or anatomical damage, causes irreversible change in the homeostasis of the organism or increases the susceptibility of the organism to other chemical or biological stress.
- Anaphylactic shock
- When an abnormal response of the body to a foreign substance is so severe that it leads to profound shock and collapse, and which, unless treated urgently, can cause death.
- Arterial thrombotic event
- Occurs under conditions of rapid blood flow and involves a defect in the number of platelets that help blood to coagulate.
- Asthma Control Questionnaire (ACQ)
- Self-completion questionnaire relating to asthma symptoms during the past week including night-time waking, symptoms on waking, activity limitation, shortness of breath, wheeze, and rescue short-acting medication use. Clinicians measure per cent predicted prebronchodilator forced expiratory volume in 1 second (FEV1).
- Asthma Control Test (ACT)
- A self-completed questionnaire relating to asthma symptoms during the past 4 weeks; including frequency of shortness of breath, frequency of awakening during the night or early morning as a result of symptoms, frequency of reliever medication use, frequency of symptoms impacting on work, school or home.
- Asthma Quality of Life Questionnaire (AQLQ)
- Self-completion questionnaire relating to asthma symptoms, activity limitation, emotional function and environmental stimuli.
- Clinically significant non-severe exacerbation (CSNS)
- An exacerbation in which peak expiratory flow (PEF) or forced expiratory volume in 1 second (FEV1) is greater than 60% of personal best.
- Clinically significant severe exacerbation (CSS)
- A clinically significant exacerbation in which peak expiratory flow (PEF) or forced expiratory volume in 1 second (FEV1) is lower than 60% of personal best.
- Confidence interval (CI)
- Quantifies the uncertainty in a measurement. Wider intervals indicate greater uncertainty, and narrower intervals indicate greater precision. Formally, if the experiment were repeated many times, it provides the range of values which would include the true value of a measurement 95% of the time.
- Controller medication
- Medicines aimed at preventing asthma symptoms and asthma exacerbations (or asthma attacks) from occurring. These include anti-inflammatory medicines (e.g. inhaled corticosteroids) and airway openers (e.g. long-acting β2-agonists, sustained-release theophylline or sustained-release β2-agonist).
- Corticosteroids
- Medicine used to relieve and prevent inflammation of the airways. Corticosteroids can be inhaled, taken orally or injected depending on the severity of the symptoms.
- Cost-effectiveness analysis
- An economic evaluation that expresses the effects or consequences of interventions on a single dimension. This would normally be expressed in units of effectiveness, usually the same as those clinical outcomes used to measure effectiveness in clinical trials or practice (e.g. cases cured, life-years gained, additional strokes prevented). The difference in cost and effectiveness between the two interventions is expressed as an incremental cost-effectiveness ratio (e.g. the incremental cost per life-year gained).
- Cost–utility analysis
- The same as a cost-effectiveness analysis but the effects or consequences of interventions are expressed in generic units of health gain, usually quality-adjusted life-years (QALYs).
- Disability-adjusted life-years (DALYs)
- A measure of overall disease burden.
- Effect size
- A generic term for the estimate of treatment effect for a study.
- EQ-5D
- A self-completed questionnaire relating to mobility, self-care, usual activities, pain/discomfort and anxiety/depression.
- Fixed-effect model
- A statistical model that stipulates that the units under analysis (e.g. people in a trial or study in a meta-analysis) are the ones of interest, and thus constitute the entire population of units. Only within-study variation is taken to influence the uncertainty of results (as reflected in the confidence interval) of a meta-analysis using a fixed-effect model.
- Forced expiratory volume (FEV1)
- The volume of air exhaled in 1 second of forced blowing into a spirometer.
- Forced vital capacity (FVC)
- The total amount of air that a person can forcibly blow out after full inspiration, measured in litres.
- Global Evaluation of Treatment Effectiveness (GETE)
- Self-completion or physician-completed questionnaire to assess how much improvement in asthma control has been experienced compared with baseline. Should be graded as excellent (complete control of asthma); good (marked improvement of asthma); moderate (discernible, but limited improvement in asthma); poor (no appreciable change in asthma); or worsening (of asthma). A score of excellent/good indicates patients classified as responders to omalizumab.
- Heterogeneity
- The variability or differences between studies in the estimates of effects. A distinction is sometimes made between ‘statistical heterogeneity’ (differences in the reported effects), ‘methodological heterogeneity’ (differences in study design) and ‘clinical heterogeneity’ (differences between studies in key characteristics of the participants, interventions or outcome measures).
- Immunoglobin E (IgE)
- A class of antibody associated with allergic reactions.
- Incremental cost-effectiveness analysis
- An analysis where estimates are made of the additional cost per year of life saved or gained. This type of analysis is often carried out to provide a more meaningful comparison of costs and consequences between different interventions.
- Intention-to-treat analysis
- An intention-to-treat analysis is one in which all participants in a trial are analysed according to the intervention to which they were allocated, whether they received it or not.
- Leukotriene-receptor antagonist (LTRA)
- A drug that inhibits leukotrienes (fatty signalling molecules), which trigger inflammation in asthma and allergic rhinitis.
- Long-acting β2-agonists (LABA)
- A bronchodilator that relaxes the smooth muscles and functionally enlarges the size of the airways of the lung. The effects last for 12 hours or more.
- Meta-analysis
- The statistical pooling of the results of a collection of related individual studies, primarily used to increase statistical power and synthesise the findings of the studies.
- Odds ratio (OR)
- The odds ratio is similar to relative risk, except that the denominator takes into account the number of individuals within the population that experienced the event of interest. The results of relative risk and odds ratio calculations are very similar for rare events, but diverge as events become more common.
- Peak expiratory flow (PEF) rate
- The maximum rate at which air is expired from the lungs when blowing into a peak flow meter or spirometer.
- Perennial aeroallergen
- Any airborne particulate matter that can induce allergic responses in sensitive persons throughout the year (as opposed to seasonally). These typically include pet dander or dust mites.
- PRISMA statement
- A set of items to help improve the reporting of systematic reviews and meta-analyses.
- Quality-adjusted life-year (QALY)
- An index of survival that is weighted or adjusted by the patient's quality of life during the survival period. QALYs have the advantage of incorporating changes in both quantity (mortality) and quality (morbidity) of life.
- Quality of life
- A concept incorporating factors that might impact on an individual's life, including factors such as the absence of disease or infirmity, as well as other factors which might affect the individual's physical, mental and social well-being.
- Random effects model
- A statistical model sometimes used in meta-analysis in which both within-study sampling error (variance) and between-studies variation are included in the assessment of the uncertainty (confidence interval) of the results of a meta-analysis.
- Randomised controlled trial
- A study in which people are allocated at random (by chance alone) to receive or not receive one or more interventions that are being compared.
- Relative risk (synonym: risk ratio; RR)
- The ratio of risk in the intervention group to the risk in the control group.
- Rescue medication
- Medicines that provide rapid relief from an asthma attack by quickly opening up the narrowed airways, also known as relievers, airway openers or bronchodilators. The most widely used short and quick-acting airway openers are salbutamol (also known as albuterol) and terbutaline.
- Responder analysis
- The proportion of patients responding to omalizumab treatment observed in the trials is used to inform the probability of being an omalizumab responder at 16 weeks.
- Sensitivity analysis
- An analysis used to determine how sensitive the results of a study or systematic review are to changes in how it was done. Sensitivity analyses are used to assess how robust the results are to uncertain decisions or assumptions about the data and the methods that were used.
- Slow-release (short-acting) β2-agonists (SABAs)
- A bronchodilator that provides relief of acute asthma symptoms (e.g. salbutamol).
- Statistical significance
- An estimate of the probability of an association (effect) as large or larger than what is observed in a study occurring by chance.
- Subgroup analysis
- Use of meta-analysis to compare the mean effect for different subgroups of studies.
- Uncontrolled study
- A trial or study that does not have an intervention against which the intervention of interest is compared.
- Utility
- A measure of the strength of an individual's preference for a given health state or outcome. Utilities assign numerical values on a scale from 0 (death) to 1 (optimal or ‘perfect’ health), and provide a single number that summarises all the health-related qualities of life. Hence, utility has been described as a global measure of health-related quality of life.
- Values
- A measure of the strength of an individual's preference for a given health state or outcome. In contrast to utilities, values reflect preferences without risk (or uncertainty).
- Wasserfallen symptom score
- Self-completed assessment of the severity of asthma symptoms during the night and day, measured on a scale of none to extremely severe.
List of abbreviations
- ACQ
- Asthma Control Questionnaire
- ACT
- Asthma Control Test
- A&E
- accident and emergency
- AE
- adverse event
- AERS
- adverse event reporting system
- AIC
- academic-in-confidence
- AMI
- acute myocardial infarction
- APEX
- Asthma Patient Experience on Xolair study
- AQLQ
- Asthma Quality of Life Questionnaire
- ATE
- arterial thrombotic event
- BDP
- beclomethasone dipropionate
- BSC
- best supportive care
- BTS
- British Thoracic Society
- CDSR
- Cochrane Database of Systematic Reviews
- CEAC
- cost-effectiveness acceptability curve
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CHE
- Centre for Health Economics
- CHKS
- Camper Healthcare Knowledge Systems
- CiC
- commercial-in-confidence
- COPD
- chronic obstructive pulmonary disease
- CPCI-S
- Conference Proceedings Citation Index
- CRD
- Centre for Reviews and Dissemination
- CS
- clinically significant
- CSNS
- clinically significant non-severe
- CSS
- clinically significant and severe
- DALY
- disability-adjusted life-year
- DARE
- Database of Abstracts of Reviews of Effects
- DNA
- deoxyribonucleic acid
- EMA
- European Medicines Agency
- EPAR
- European Public Assessment Report
- ER
- emergency room
- ERG
- Evidence Review Group
- EU/EUP
- European Union/European Union population
- EXALT
- Evaluate Xolair for Asthma as Leading Treatment trial
- FDA
- US Food and Drug Administration
- FeNO
- fractional exhaled nitric oxide
- FEV1
- forced expiratory volume in 1 second
- GETE
- global evaluation of treatment effectiveness
- GINA
- Global Initiative for Asthma
- GP
- general practitioner
- GPRD
- General Practice Research Database
- HRQoL
- health-related quality of life
- HSDS
- Height Standard Deviation Scores
- HTA
- Health Technology Assessment
- IBD
- inflammatory bowel disease
- ICD
- International Classification of Diseases
- ICER
- incremental cost-effectiveness ratio
- ICNARC-CMPD
- Intensive Care National Audit and Research Centre Case Mix Programme Database
- ICS
- inhaled corticosteroid
- ICU
- intensive care unit
- IgE
- immunoglobulin E
- INNOVATE
- INvestigatioN of Omalizumab seVere Asthma Trial
- IPD
- individual patient data
- ITT
- intention to treat
- LABA
- long-acting β2-agonist
- LCI
- lower confidence interval
- LTRA
- leukotriene-receptor antagonist
- MD
- mean difference
- MHRA
- Medicines and Healthcare Products Regulatory Agency
- MS
- manufacturer's submission
- MTA
- multiple technology appraisal
- NA
- not applicable
- NAEPP
- National Asthma Education and Prevention Program
- NHLBI
- National Heart, Lung and Blood Institute
- NHS EED
- National Health Services Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NIH
- National Institutes for Health
- NR
- not reported
- OAT
- optimised asthma therapy
- OCS
- oral corticosteroid
- ONS
- Office for National Statistics
- PAQLQ
- Paediatric Asthma Quality of Life Questionnaire
- PCT
- primary care trust
- PEF
- peak expiratory flow
- PMR
- polymyalgia rheumatica
- PSA
- probabilistic sensitivity analysis
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RA
- rheumatoid arthritis
- RCP
- Royal College of Physicians
- RCT
- randomised controlled trial
- RD
- risk difference
- RR
- relative risk
- Rx
- prescription
- SABA
- short-acting β2-agonist
- SD
- standard deviation
- SE
- standard error
- SIGN
- Scottish Intercollegiate Guidelines Network
- SOLAR
- study of omalizumab in comorbid asthma and rhinitis
- SPC
- summary of product characteristics
- SR
- systematic review
- ST
- standard therapy
- STA
- single technology appraisal
- UC
- unclear
- UCI
- upper confidence interval
- VAS
- visual analogue scale
- WHO
- World Health Organization