Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 10/57/22. The contractual start date was in February 2012. The draft report began editorial review in July 2013 and was accepted for publication in February 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Andrew Lotery has received honoraria from Bayer, Novartis and Alcon and his institution has received educational grants from Novartis Pharmaceuticals. Winfried Amoaku has received personal fees from Alcon, Alimera Sciences, Allergan, Bayer, Novartis and ThromboGenics, grants from Allergan and Novartis, non-financial support from CenterVue SpA and Novartis, and other support from Pfizer.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Mowatt et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Description of health problem
Brief statement describing the health problem
Neovascular age-related macular degeneration (nAMD) causes severe visual loss and is the most common cause of blindness in persons aged > 50 years in the Western world. In recent years, there have been significant advances in the clinical management of patients with nAMD. For example, there are now effective treatments, specifically antivascular endothelial growth factor (antiVEGF), and novel diagnostic technologies, including both imaging and functional tests. Patients who are being treated for nAMD with antiVEGF require frequent and long-term follow-up for treatment to be most effective.
The current reference standard for diagnosis of nAMD is fundus fluorescein angiography (FFA)1 which may also be used to monitor the activity of the disease after treatment. However, FFA is time-consuming, invasive and requires expert interpretation. Optical coherence tomography (OCT) is now widely used for the diagnosis and management of nAMD. OCT is non-invasive, safer and more straightforward to do and interpret than FFA. OCT may help clinicians to provide a more cost-effective service for people with nAMD by potentially replacing the current reference standard of FFA and helping to distinguish between those patients with active disease requiring treatment and those whose disease is not active at a particular point in time and who do not require treatment. OCT might also lead to efficiencies by allowing other categories of health professionals to become involved in the diagnosis and monitoring of patients.
Aetiology, pathology and prognosis
Neovascular age-related macular degeneration is a pathological process in which new blood vessels arising from the choroid breach the normal tissue barriers and come to lie within the subretinal pigment epithelium (subRPE) and/or subretinal spaces. These new vessels, commonly referred to as choroidal neovascularisation (CNV) or choroidal neovascular membrane (CNVM), leak fluid, lipids and blood, elicit an inflammatory response and, as part of their natural history, undergo a scarring process, all of which has a deleterious effect on the visual cells of the retina (photoreceptors), leading to central loss of vision. Besides CNV, there are two other recognised phenotypes of nAMD: (1) retinal angiomatous proliferation (RAP) in which vascular complex seems to arise de novo from the retinal circulation, or results from CNV anastomosing with the retinal circulation; and (2) intrachoroidal/subRPE aneurysmal dilatation(s) of the choroidal vasculature, known as idiopathic polypoidal choroidal vasculopathy (IPCV). 2 These phenotypes may occur in isolation or be mixed with other phenotypes. 3
The onset of nAMD results in progressive and unremitting loss of central vision in the affected eye, with rare exceptions in cases of IPCV in which spontaneous improvement may be observed. A number of studies have shown that extrafoveal CNV will grow towards the fovea. Once foveal involvement has occurred, CNV will expand and involve ever-increasing areas of the macula. Thus, the majority of eyes will experience acute visual loss, either moderate [defined as a doubling of the visual angle which equates to a three-line worsening on the Early Treatment Diabetic Retinopathy Study (ETDRS) visual acuity (VA) chart] or severe (defined as a quadrupling of the visual angle and which equates to a six-line worsening on the ETDRS VA chart). However, some patients with a fellow eye with good vision will not notice any such changes despite the onset of neovascularisation.
Neovascular age-related macular degeneration is now treated with repeated intraocular injections of drugs designed to antagonise vascular endothelial growth factor (antiVEGF). This will stabilise sight in most patients (≈90%) and will improve vision in a smaller group (≈30%) during the first 2 years of treatment. 1 Long-term (beyond 3–4 years) outcomes from randomised controlled trials (RCTs) using antiVEGF are, however, not available. These drugs are administered monthly (often with a mandated minimum of three injections for the first 3 months, and thereafter depending on whether or not active nAMD is present) as intraocular injections until the macula is rendered fluid free. When the disease becomes quiescent, treatment is stopped and patients are monitored for relapse, with treatment being restarted if needed, by monthly intraocular injections based on findings of VA checks, clinical examination and OCT. FFA is typically used to confirm the diagnosis of nAMD prior to initiating antiVEGF therapy, but it is used only in selected circumstances for monitoring activity of nAMD after treatment. Relapse of nAMD is unpredictable and can occur within weeks, months or even years after stopping treatment.
Epidemiology, incidence and prevalence
The prevalence of all forms of age-related macular degeneration (AMD) (including neovascular and atrophic AMD), which affects more than 600,000 people in the UK, is expected to rise by a quarter to nearly 756,000 by 2020. The estimated number of individuals with nAMD in the UK for 2011 is 368,000 and will increase substantially due to the ageing population. 4–6 Estimates of incidence of nAMD in the UK suggest that there are between 13,000 and 37,000 new cases annually. 5 The National Institute for Health and Care Excellence (NICE) guidance on ranibizumab [Lucentis®, Genentech Inc. (USA)/Novartis Pharmaceutical Ltd] and pegaptanib (Macugen®, Pfizer Ltd) for the treatment of age-related macular degeneration (AMD) (issued 2008 and modified 2012) estimated that there were about 26,000 new cases of nAMD in the UK each year. 7 Many of these individuals will require monthly monitoring and treatment for several years. Relevant risk factors include age, cigarette smoking, nutritional factors, cardiovascular diseases and genetic markers, including genes regulating complement, lipid, angiogenic and extracellular matrix pathways.
Impact of health problem
Significance for patients in terms of ill-health (burden of disease); significance for the NHS
Age-related macular degeneration is the most common cause of blindness and partial sighted registration in the UK. 1 As the incidence of AMD increases with age, the burden of disease to the NHS and society is expected to increase with an ageing population. Furthermore, loss of vision contributes to a psychological ill-health (depression, emotional distress) and reduced quality of life.
Ophthalmology accounts for 10% (5 million per year) of all outpatient attendances to the NHS and AMD accounts for 15% of all ophthalmology outpatient attendances. 1 Loss of VA is associated with a profound impairment of quality of life. Visual loss increases the risk of frequent falls. Depression and visual hallucinations (Charles Bonnet syndrome) are frequent accompaniments of severe central vision loss. Patients with Charles Bonnet syndrome (associated with visual loss) and their family members should be informed that visual symptoms are not unusual and are not a sign of psychosis or mental deterioration.
Measurement of disease
The spectrum of disease may be classified according to the reduction of VA (e.g. mild, moderate or severe). In addition to this spectrum of disease, during monitoring of patients undergoing treatment with antiVEGF drugs, it is important to determine whether or not the disease is active. Disease activity is typically determined with imaging technologies, mainly FFA and OCT.
Current service provision
Management of disease
Diagnosis of neovascular age-related macular degeneration and care pathway
Typically, patients with possible AMD present to primary care (optometrists or general practitioners) with non-specific symptoms (such as reduced, blurred and distorted vision). Some patients do not report symptoms and are diagnosed at routine eye examination. Clinical examination of the retina reveals typical changes associated with AMD such as drusen and irregularities in the appearance of the retinal pigment epithelium (RPE), most commonly in both eyes. However, the presence of a neovascular component may be difficult to detect clinically, especially early on in the course of its development. The diagnostic pathway for nAMD and the management of patients with known disease include imaging technologies (Figure 1).
FIGURE 1.
Current diagnostic pathway of nAMD.
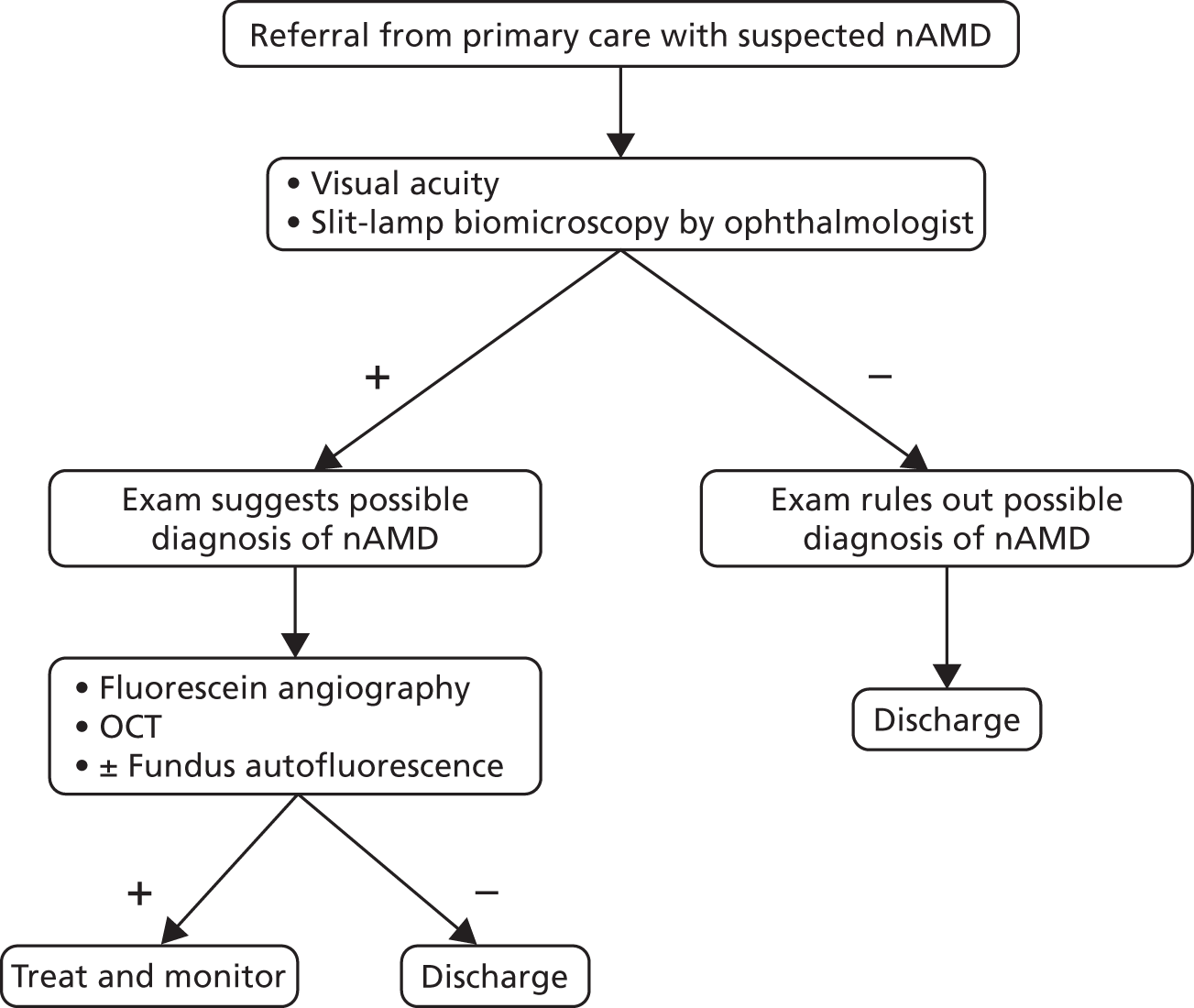
According to current guidelines from the Royal College of Ophthalmologists (RCO),1 FFA interpreted by an ophthalmologist is the method of choice and reference standard test to diagnose nAMD. Occasionally, indocyanine green angiography (ICGA) is associated with FFA as part of the reference standard when particular phenotypes of nAMD are suspected, including RAP and IPCV (see above). FFA is an invasive and time-consuming procedure, entailing the injection of a dye into a peripheral vein by a nurse and a trained photographer to undertake the test (obtain the images of the CNV, RAP, IPCV lesions). In addition to FFA, current guidelines recommend using OCT at diagnosis. Owing to recent developments in technology, it is possible that in some cases OCT might be superior to FFA in detecting nAMD (Table 1).
| Features | OCT (index test) | FFA (reference standard) |
|---|---|---|
| Accuracy | High? | Reference standard |
| Invasiveness | Non-invasive | Invasive |
| Knowledge and skills needed to interpret | Moderate | High |
| Interpretable | Most tests | Nearly all tests |
| Cost | Low to moderate | Moderate |
| Side effects | None | Allergy (rarely anaphylactic shock) |
Treatment and monitoring of neovascular age-related macular degeneration
When active nAMD is confirmed, treatment with antiVEGF therapy is initiated. 8,9 For all patients with nAMD it is common practice to use three consecutive (monthly) intravitreal injections of antiVEGF therapy, and then the patient is reassessed to evaluate whether or not the disease is active (i.e., neovascularisation leaking fluid/blood at the macula) or inactive (Figure 2). For this purpose, both FFA and OCT may be used, although the latter more often than the former, according to the guidelines of the RCO. 1 Studies that have a large influence in current practice used VA and OCT at monthly intervals and FFA at quarterly intervals to decide on the need for retreatment. In some units, OCT is the only test performed to determine activity of the neovascular process in clinical practice; in some centres FFA is performed in selected cases during the monitoring phase. Other technologies such as fundus autofluorescence (FAF) may also be used at baseline and at variable intervals during the follow-up of these patients as areas of atrophy in the RPE (difficult to detect clinically but easily observed on autofluorescence images) could be associated with fluid in the retina in the absence of active nAMD.
FIGURE 2.
Current monitoring pathway of nAMD.
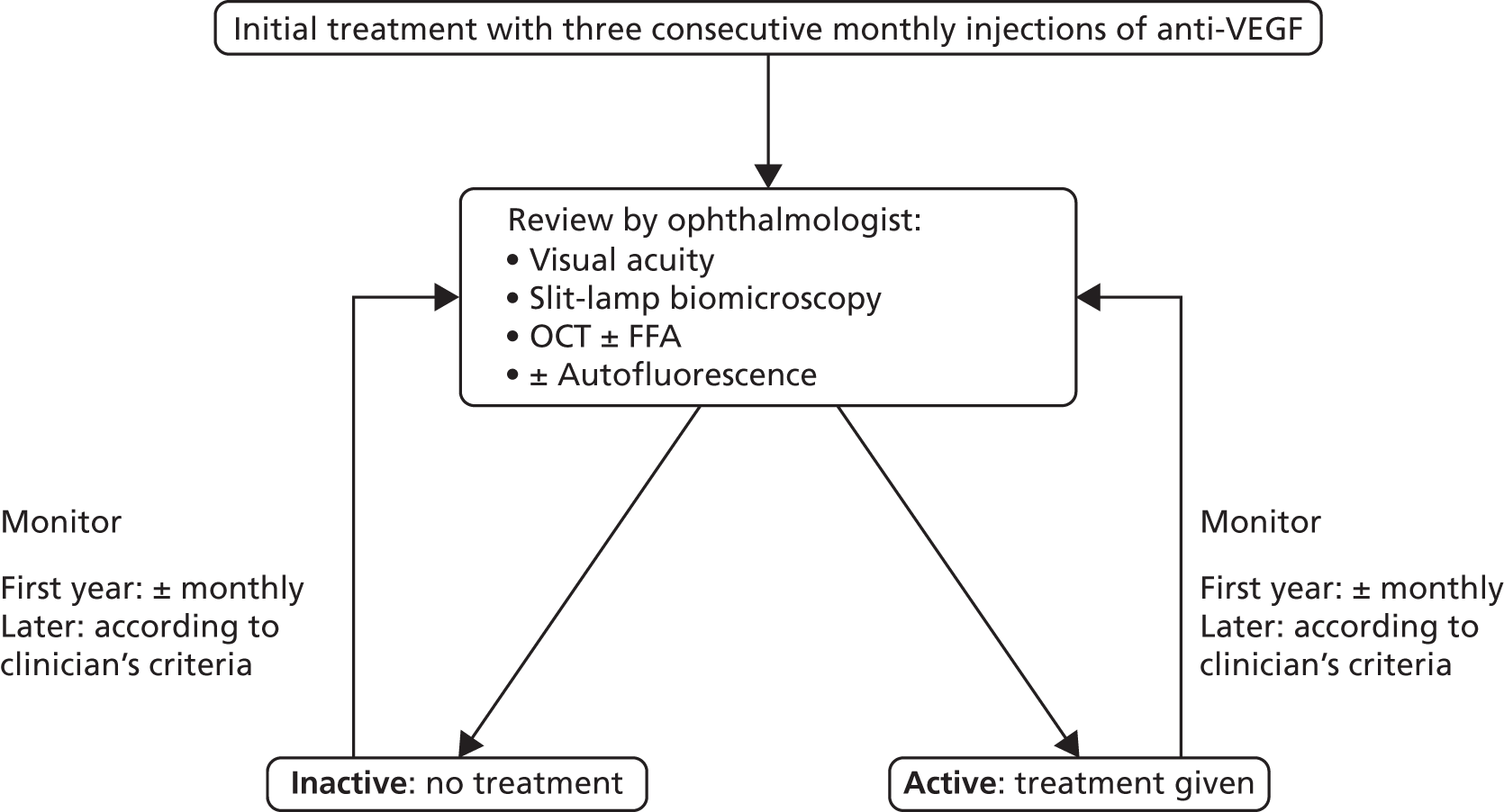
If fluid is not seen intraretinally or subretinally, further treatment is not given and the patient is followed thereafter regularly. The timing of follow-up visits is variable, typically every 4 weeks for the first year, extending the intervals after the second year. Varying intervals have been proposed, such as ‘treat and extend’ strategy, where if there is no active disease, no treatment is given and the monitoring intervals are progressively extended. If the disease is judged to be active, further injections of antiVEGF are given. Either a single injection or three injections are administered if activity is detected on follow-up and then the patient returns to the monthly monitoring scheme. The possibility of using VA (without imaging tests) as the only test to guide treatment during monitoring (i.e. treatment would be given if there is a loss of five or more letters from best previously observed VA) has been modelled using data from published trials for nAMD. 10 The authors concluded that an individualised VA-guided regimen could sustain visual outcomes and improve cost-effectiveness compared with current regimes.
Current service cost
Table 2 shows an estimation of unit costs associated with current diagnosis and monitoring care pathways. A first referral visit to a hospital eye service will involve an eye examination and is costed at £106. In addition, OCT and FFA tests can be indicated, with the overall cost for the first visits ascending to £274.71. A follow-up monitoring visit can involve a face-to-face attendance with an ophthalmologist and an OCT test only (£131). However, if a FFA is indicated, the monitoring visit will cost £248.27. Without doubt, the major cost category is given by the treatment cost. There are two possible antiVEGF treatments: ranibizumab and bevacizumab (Avastin®, Roche) at £742.17 and £50 per injection respectively. NICE guidelines advocate for the use of ranibizumab unless individual sight is heavily deteriorated. It should be noted that special cost arrangements are in place and a reduced cost for ranibizumab is agreed under a Patient Access Scheme negotiated between the manufacturer and the Department of Health. Under this agreement, the cost of ranibizumab to the UK NHS (confidential) is significantly lower than the list price given above. The cost of bevacizumab is based on that of a compounded product as supplied by different compounding pharmacies in the UK.
| Intervention | Unit costs (£, 2011–12) | Source | |
|---|---|---|---|
| Diagnosis | Monitoring | ||
| Ophthalmologist visit | £106.18 | £79.74 | NHS Reference Costs 2011–1211 (Ophthalmology – consultant led: first attendance or follow-up non-admitted face to face) |
| FFA | £117.26 | £117.26 | NHS Reference Costs 2011–1211 (HRG BZ23Z minor vitreous retinal procedures) |
| OCT | £51.27 | £51.27 | NHS Reference Costs 2011–1211 (HRG RA23Z ultrasound scan, less than 20 minutes) |
| Medication ranibizumab | £742.17 | Ranibizumab. Source: BNF12 (accessed 9 May 2013) [Lucentis® (Novartis) solution for intravitreal injection, ranibizumab 10 mg/ml, net price 0.23-ml vial = £742.17] | |
| Medication bevacizumab | £50.00 | As supplied by compounding pharmacies. Manufacturer’s list price not applicable | |
Variation in service and/or uncertainty about best practice
Once nAMD has been diagnosed, monotherapy with an antiVEGF drug (administered into the vitreous) is the current standard of care. Ranibizumab is highly effective and recommended by current guidelines. Bevacizumab remains unlicensed in the UK although its use worldwide reflects the fact that it is much cheaper than ranibizumab (as currently supplied for intravitreal administration) with similar efficacy. 8,9
Retinal imaging with OCT before and after intravitreal administration of antiVEGF therapy is regularly used. 13 Following antiVEGF therapy a reduction of intraretinal and subretinal fluid is typically observed, often with rapid unification of the retinal layers and improvement/restoration of the anatomical contours. This anatomical improvement is often accompanied by improvements in VA.
The ultimate treatment goal when nAMD has already developed is to achieve restoration of central vision and prevent visual loss with normal or near normal foveal and macular anatomy. Complete cessation of exudation can result in good unification of the tissue layers, but most patients report difficulty with reading small print and other visually demanding tasks, even when tissue contours have been apparently restored. High-resolution OCT scans obtained after antiVEGF treatment show persistent abnormalities of the outer retina even though the tissues appear to be fluid free. In cases where localised atrophy and fibrosis have already occurred, considerable impairment of central visual function can remain, despite the achievement of a fluid free macula.
Patients who have been treated with antiVEGF therapy should be examined at regular intervals. Although most clinicians will use OCT for monitoring patients with nAMD, there is probably large variability on the tests used (e.g. biomicroscopy of the fundus, FFA and fundus photography).
As explained above, patients treated with antiVEGF injection should receive injections monthly for the first 3 months and, thereafter, should be monitored monthly. If active nAMD is present, treatment should be continued, and if there is no active exudative AMD, observation at monthly intervals is recommended. The use of technologies, including OCT, FFA and FAF during the follow-up of these patients is variable as it depends on clinical findings, the judgement of the treating ophthalmologist and the clinical pathways established at different centres. The workload associated with such contemporary AMD services is significant and is expected to increase, as the best outcomes are achieved with monthly follow-up visits. It is expected that these follow-up visits may continue for as long as 4 years or longer. The pressure on resources and service delivery in the AMD clinics is expected to become even more intense as many patients cannot be discharged, and there is a need to accommodate new incident cases. The regular monthly follow-up for AMD patients under treatment, in order to maintain efficacy, is demanding. This situation is likely to be further aggravated by the impending treatments with intravitreal therapies of macular oedema secondary to diabetic retinopathy and retinal vein occlusion. As such, the problem seems more acute than was originally envisaged, and is expected to get worse. It has been suggested engaging non-medical staff (optometrists, nurses, technicians) to undertake some of the duties in the AMD clinic in order to increase capacity. Such roles include clinical assessments, especially retreatment decision-making.
Relevant national guidelines, including National Service Frameworks
Subsequent to the technology appraisal and issuing of guidance by NICE, ranibizumab has been widely adopted as the treatment of choice for subfoveal nAMD in the UK. 7 However, the high cost of ranibizumab, along with the positive clinical experience with bevacizumab, has stimulated a debate on whether or not bevacizumab could be used in practice.
In the UK, guidelines for the management and treatment of nAMD were published by the RCO in 2009 (and in 2013 were undergoing revision). 1 According to the RCO guidelines, FFA interpreted by an ophthalmologist is the method of choice and reference standard test to diagnose nAMD. Occasionally, ICGA is associated with FFA as part of the reference standard when particular phenotypes of nAMD are suspected, including RAP and IPCV. In addition to FFA, current guidelines recommend using OCT at diagnosis. During follow-up and monitoring of disease activity, after treatment the current guidelines recommend the use of OCT mainly, and FFA at the discretion of the clinician.
Description of technologies under assessment
Reference standard: fundus fluorescein angiography
Fundus fluorescein angiography is currently the reference standard for diagnosing CNV in AMD. A fluorescein angiogram is a sequence of images captured of the fundus over a 10-minute period after injection of the non-toxic dye fluorescein isothiocyanate into a suitable peripheral vein.
Neovascular lesions are classified by their location with reference to the foveal avascular zone – extrafoveal, juxtafoveal or subfoveal. Lesions lying more than 200 μm from fixation are defined as extrafoveal and may also be described as juxtafoveal or subfoveal when immediately adjacent to or involving the geometric centre of the fovea respectively. Neovascular lesions located away from the macula are termed peripheral and those around the optic nerve juxtapapillary. A more refined classification of the neovascular lesion is obtained by describing the composition of the exudative lesion after stereoscopic review of the entire sequence of the angiogram. The exudative lesion is defined as the area occupied by the neovascular complex, any associated blood, thick exudate and pigment epithelial detachments (PEDs) that are contiguous to the neovascular complex and obscure its margins. The neovascular complex can, therefore, consist of RAP, CNV and IPCV.
The classification of nAMD lesions is based on the temporal and spatial features of the patterns of fluorescence as observed on the FFA. CNV lesions are classified according to their location relative to the fovea (see above), and pattern of fluorescein angiographic leakage. The majority of CNVs occur subfoveally.
Classic choroidal neovascularisation
Classic CNV is said to be present when an area of well-delineated hyperfluorescence appears in the early phases of the FFA, usually before seconds have elapsed following injection of the fluorescent dye into a peripheral vein. Most commonly, classic CNV represents new vessels that have breached the RPE and lie in the subretinal space. Sometimes a typical lacy pattern of hyperfluorescence is observed in the very early phase of the angiogram which corresponds to the vascular profiles before the fluorescein has leaked out of these vessels and obscured the margins. Classic CNV also leaks aggressively and hence there is considerable pooling of fluorescein dye in the subretinal space in late frames of the angiogram.
Occult choroidal neovascularisation
Occult CNV, as its name suggests, refers to the presence of leakage without clear evidence of neovascular profiles in the early angiographic images. Two types of occult leakage are recognised. The first is a characteristic stippled hyperfluorescence which occurs early and is located at the level of the RPE. The RPE layer is elevated and in the later phases of the angiogram there is increasing hyperfluorescence and pooling of dye in the subretinal pigment epithelial space. The pattern of leakage suggests new vessels between Bruch’s membrane and the RPE and it is therefore considered to be a fibrovascular PED. The second pattern of occult leakage is a more diffuse hyperfluorescence with poorly demarcated boundaries which occurs late in the angiographic phase, generally after 2 minutes have elapsed since injection of dye. There is no corresponding hyperfluorescence in the early frames and there is shallow elevation of the RPE. This type of leakage is referred to as late leakage of indeterminate origin. Many lesions are mixed showing combinations of classic and occult features. It is now common practice to classify lesions by presence or absence of classic and/or occult CNV. In the absence of any occult CNV, lesions are termed classic with no occult (100% classic) and conversely occult with no classic (0% classic).
When CNV is mixed, the lesion is classified by the proportion of classic. When the lesion is composed primarily of classic CNV (i.e. classic > 50%), it is termed predominantly classic. When there is 1–49% classic, the lesions are termed minimally classic.
Retinal angiomatous proliferation
One type of neovascularisation that has been well recognised by the use of high-speed video angiography using the scanning laser ophthalmoscope (SLO) is the RAP lesion. RAP is seen commonly as a round area of intraretinal telangiectatic, dilated blood vessels located juxta- or extrafoveally. On viewing stereo pairs of images, the vessels are often seen to turn sharply from the inner retina towards the choroidal interface. Except in early stages, RAPs are associated with PEDs. They leak and hence the adjacent retina is usually disrupted with cystoid spaces. ICGA is a helpful test to determine the presence of RAP.
Idiopathic polypoidal choroidal vasculopathy
Polyps are seen as focal, round areas of abnormal dilated choroidal vessels, often associated with large areas of lipid deposition and haemorrhage. The presence of haemorrhagic PED is highly suggestive of the presence of this phenotype. These are best visualised by ICGA.
Optical coherence tomography
Optical coherence tomography was developed at the Michigan Institute of Technology, MI, USA in 1991. It is a light-wave-based technology producing cross-sectional images of the retina with scan rates and resolution parameters that have greatly improved over the last 10 years. OCT is a non-invasive, non-contact visual test that requires around 5–10 minutes to assess both eyes. 14 From the investigator’s point of view, it is user friendly (e.g. OCT is easier to do than FFA), typically undertaken by trained medical photographers or ophthalmic imaging technicians, and interpreted by ophthalmologists. Automated analysis can also be used.
There are two main types of OCT system. The earlier time domain optical coherence tomography (TD-OCT) system, available from 1995, had an image rate of 100–400 scans per second and provided information for a limited view of the retina by taking six scans radially-oriented 30 degrees from each other with a resolution in the range of 10 to 20 µm. 14 The newer system, spectral domain optical coherence tomography (SD-OCT), has been available since 2006. Improvements with this system include (i) a faster scan speed of approximately 27,000 scans per second, (ii) the ability to scan larger areas of the retina by taking several horizontal line scans such that there are no ‘missed areas’, (iii) increased resolution at 5 µm, and (iv) ‘real time registration’, which was not previously available with TD-OCT. 14 The real-time registration feature enables the identification of specific anatomical locations on the retina, against which subsequent tests may be evaluated, which is of particular importance in the monitoring of patients. 14 Compared with TD-OCT, the faster scan speed of SD-OCT enables the collection of additional information on larger regions of the retina and eliminates image distortion arising from patient movement, while the improved resolution allows for a clearer and more distinguishable view of retinal layers, with the possibility of detecting earlier signs of disease. 14
Identification of important subgroups
There are different subgroups of patients with nAMD. They are diagnosed according to FFA findings and are described above. Subgroup classification depends on the location (extra-, juxta- and subfoveal) and type of neovascularisation (classic and occult CNV, RAP, and IPCV), which could be mixed in different combinations. Although the initial treatment is similar for all subgroups (with antiVEGF therapy), the natural history and progression after treatment are different. It is also possible that the performance of diagnostic technologies may be different among subtypes of nAMD. OCT is not currently used in isolation to identify subgroups.
Current usage in the NHS
Both FFA and OCT are currently used in the NHS to diagnose and monitor patients with nAMD. They are recommended technologies to provide standard care. FFA is essential for diagnosis of the condition. Regarding monitoring, FFA is less commonly used than OCT.
Anticipated costs associated with intervention
Table 3 presents an estimation of the number of visits in a lifetime of the population. Based on census, nAMD prevalence and Interim Life Table data, it is possible to estimate the number of visits for the population lifetime. Calculations in Table 3 are for England and Wales, based on 2011 data and assumed that every individual with nAMD would contact NHS services. This estimation resulted in 33.7 million visits. If OCT was conducted at every monitoring visit, this would result in an undiscounted lifetime cost of above £1.7B [i.e. £51.27 (see Table 2) multiplied by 33.7 million people].
| Population by gender and age | Population for England and Wales, 2011 census-based estimates15 | nAMD prevalence rates, %6 | nAMD cases, n | Life expectancy (years)16 | Total number of monthly monitoring visits (lifetime) |
|---|---|---|---|---|---|
| Men (age, years) | |||||
| 65–69 | 1,096,335 | 0.38 | 4166 | 16.64 | 833,215 |
| 70–74 | 1,027,959 | 1.40 | 14,391 | 13.06 | 2,259,454 |
| 75–79 | 810,590 | 2.63 | 21,319 | 9.87 | 2,515,585 |
| 80–84 | 557,203 | 5.56 | 30,980 | 7.16 | 2,664,322 |
| 85–89 | 295,680 | 5.56 | 16,440 | 5.07 | 1,002,828 |
| 90–99 | 333,448 | 5.56 | 18,540 | 3.00 | 667,430 |
| Total males | 9,942,833 | ||||
| Women (age, years) | |||||
| 65–69 | 1,154,292 | 0.92 | 10,619 | 19.15 | 2,442,482 |
| 70–74 | 1,140,959 | 1.42 | 16,202 | 15.20 | 2,948,694 |
| 75–79 | 976,657 | 2.17 | 21,193 | 11.59 | 2,945,891 |
| 80–84 | 788,087 | 10.50 | 82,749 | 8.46 | 8,440,412 |
| 85–89 | 532,677 | 10.50 | 55,931 | 5.95 | 3,971,107 |
| 90–99 | 717,989 | 10.50 | 75,389 | 3.36 | 3,015,554 |
| Total females | 23,764,139 | ||||
| Total overall population | 33,706,973 | ||||
Alternative tests
Clinical evaluation (with slit-lamp biomicroscopy with or without use of diagnostic contact lens and evaluation of patients’ symptoms)
The onset of exudative AMD is heralded by the appearance of central visual blurring and distortion. Most patients will complain that straight lines appear crooked or wavy. Sometimes patients do not notice visual symptoms when the first eye is affected. When nAMD occurs in the second eye, patients suddenly become limited in their daily activities, for example reading, driving and seeing fine detail such as facial expressions.
Examination of the macula usually reveals fluid and/or lipid (yellow deposition) and/or blood. Other features of AMD such as drusen and pigmentary irregularities are most often present. Sometimes these latter features are not observed once exudative AMD has supervened or in certain phenotypes such as IPCV. However, the fellow eye would usually exhibit some or all of these AMD early clinical signs (drusen and RPE changes) and their presence is helpful in confirming that the neovascular lesion is due to AMD (again with the exception of IPCV where the fellow eye may also be normal). Following slit-lamp biomicroscopy (SLB) the presence or absence of the following signs should be noted:
-
Subretinal or subRPE neovascularisation which may be visible as a dark grey lesion. Occasionally the lesion will have a dark pigmented edge which is thought to be due to proliferation of the RPE at the edge of the membrane.
-
Serous detachment of the neurosensory retina.
-
RPE detachment.
-
Haemorrhages: subretinal pigment epithelial, subretinal, intraretinal or preretinal. Breakthrough bleeding into the vitreous may also occur, indicating most often the presence of IPCV.
-
Hard exudates (lipids) within the macular area related to any of the above and not related to other retinal vascular disease.
-
Epiretinal, intraretinal, subretinal or subpigment epithelial scar/glial tissue or fibrin-like deposits.
-
RAPs: red, round, extra- or juxtafoveal lesions located within the retina.
-
Polyps: red, round lesions located underneath the RPE or protruding through the RPE layer.
Visual acuity (for monitoring)
Visual acuity is a measure of the spatial resolution of the visual processing system. VA is tested by requiring the person whose vision is being tested to identify characters (like letters and numbers) on a chart from a set distance. Chart characters are typically represented as black symbols against a white background (for maximum contrast). The distance between the person’s eyes and the testing chart is set at a sufficient distance to approximate infinity in the way the lens attempts to focus.
Amsler grid
The Amsler grid is a grid of horizontal and vertical lines used to monitor a person’s central visual field. It is a diagnostic tool that aids in the detection of visual disturbances caused by changes in the retina, particularly the macula (e.g. macular degeneration). In the test, the person looks with each eye separately at the small dot in the centre of the grid. Patients with macular disease may see wavy lines or some lines may be missing. Amsler grids are supplied by ophthalmologists, optometrists or from websites, and may be used to test one’s vision at home.
Colour fundus photographs
Colour fundus photography provides a record of the appearance of the macular retina. Stereoscopic images of the macula viewed appropriately can help localise pathology to the different tissue layers. For the purposes of recording macular pathology, stereoscopic pairs of images taken at 35 degrees centred on the macula are recommended. Red-free images (RFs) can help detect some features of the fundus associated with nAMD, such as haemorrhages.
Infrared reflectance
Confocal near-infrared fundus reflectance is a non-invasive en-face imaging technique using an 830-nm diode laser capable of visualising subretinal pathology. In contrast to visible wavelength illumination, fundus reflectance may be up to 10 times higher in the near-infrared wavelength and is then largely independent of melanin content, which advances the visibility of deep fundus structures.
Red-free images or blue reflectance
See Colour fundus photographs, above.
Fundus autofluorescence imaging or blue reflectance
This test can give an indication of the health of the RPE. The conventional FAF signal (obtained with 488 nm) originates, predominantly, from lipofuscin in RPE cells. The near-infrared autofluorescence (NIA) signal originates, predominantly, from melanin in the RPE, with some contribution from choroidal melanin. Increased FAF represents accumulation of lipofuscin and suggests that the RPE cells are beginning to fail. Absence of a FAF and NIA signal, which appears as black areas in FAF and NIA images, is due to loss of RPE cells. The finding of patches of absent autofluorescence may explain central scotoma patterns. Although different patterns have been described in early and late AMD, the exact diagnostic performance of autofluorescence is yet to be determined. The role of FAF may be more important in monitoring patients undergoing antiVEGF therapy to evaluate atrophy (e.g. for potential discontinuation of treatment).
Indocyanine green angiography, dynamic high speed or digital subtraction indocyanine green angiography
Indocyanine green (ICG) is an alternative dye to fluorescein which is used to visualise the choroidal circulation. This dye binds to plasma protein and hence does not egress easily through the fenestrae of the choroidal vessels, remaining within the vascular compartment. ICGA is obtained using longer wavelengths than FFA and, thus, can penetrate through areas of fluid/blood, permitting visualisation of pathology in circumstances where fluorescein may not. ICG also has some limitations and very thick blood or pigment can reduce or block transmission of the ICG infra-red wavelength and the emitted light is of lower intensity compared with that of fluorescein. The use of the SLO with video capture can, however, yield images of high resolution. Video ICGA also allows better imaging of RAP. As ICG dye does not leak into the subretinal and subpigment epithelial spaces to the same extent as fluorescein, the enhanced definition of the vascularised tissue as a hotspot is possible and a combination of FFA and ICGA can produce complementary information. A dose of 25 mg of ICG in aqueous solution is usually injected intravenously and images acquired for up to 30 minutes.
Preferential hyperacuity perimetry
Preferential hyperacuity perimetry (PHP) is a psychophysical test of macular function that exploits the ability of the human visual system to perceive even minute differences in the relative localisation of two objects in space; a phenomenon termed hyperacuity. When there is separation of the retinal layers through breakdown of the blood–retinal barrier or blood–RPE barrier, distorted vision is the consequence. Through presentation of lines with artificial distortions of different intensities on the PHP, the presence of a real distortion in the patient’s central visual field can be detected as the brain ignores the smaller deviation when a larger one is introduced.
In a PHP test, the macula is scanned with a succession of stimuli, each stimulus consisting of a series of dots arranged along a vertical or horizontal axis. In each stimulus, a small number of dots are misaligned, thereby creating an artificial distortion (bump or wave). The examinee’s task is to perceive these artificial distortions and mark their locations on the visual field. When a stimulus is projected on a healthy portion of the retina, the examinee identifies the artificial distortion and is likely to mark a correct location. If the stimulus is projected on a damaged region of the retina, a pathological distortion may be perceived instead of the artificial distortion, especially if the pathological distortion is more prominent than the artificial distortion. The examinee may then mark a location that is distant from the artificial distortion, indicating that a pathological distortion may have been perceived. By manipulating the amplitude of artificial distortions, the amplitude of the pathology in the area of interest can be quantified. At the end of the test, comparison of the set of erroneous responses against a normative data base is used to determine if test results are within normal limits.
Microperimetry
One conventional measure of vision is subjective visibility thresholds of small, short-duration stimuli as performed by conventional automated static perimetry. In conventional perimetry, retinal localisation of a stimulus is implied indirectly from the assumed retinal location of fixation. This approach can work well when fixation is stable and foveal. However, loss of fixation stability or foveal vision, such as occurs commonly in nAMD, complicates the measurement of macular function with conventional perimetry. Accurate correspondence between retinal structures and visual function requires simultaneous imaging of the fundus. Microperimetry includes real-time automated tracking of the fundus and appropriate compensation of the location of stimulus presentation at predefined retinal loci.
Care pathway
See Diagnosis of neovascular age-related macular degeneration and care pathway, above.
Currently, patients with suspected nAMD seen by optometrists or other health professionals will be referred to secondary care where ophthalmologists with expertise on AMD will perform the following tests: VA measurement, SLB and, if the diagnosis of nAMD remains a possibility, FFA and OCT. The FFA and OCT imaging tests are used to confirm the diagnosis and they also provide a baseline reference for future comparisons during the follow-up of the patient. Alternative technologies are used at presentation in some units (e.g. FAF imaging), to evaluate the status of the RPE which may have prognostic implications.
Chapter 2 Definition of the decision problem
Decision problem
New treatments for nAMD have been approved by NICE for use in the NHS. These treatments often require repeated injections of antiVEGF over a period of years, with frequent monitoring greatly increasing the demand on secondary care AMD services.
Fundus fluorescein angiography, an invasive test, is the reference standard recommended for detecting nAMD at initial presentation and also for detecting recurrent activity at some monitoring visits (e.g. quarterly, or according to clinician criteria). OCT is a non-invasive test now widely used for detecting nAMD both at initial presentation and for detecting recurrent activity during monitoring visits. Two OCT systems are in use. The more recently introduced SD-OCT incorporates a number of improvements over the earlier TD-OCT. Depending on the performance of OCT, in some situations its use could possibly replace that of FFA. Also, as the interpretation of OCT images is more straightforward than that of FFA, it could potentially be interpreted by other health professionals (e.g. medical photographers, nurses).
However, the value of OCT has not been well-defined and given the burden of monthly lifelong monitoring by ophthalmologists, involving multiple tests, an assessment of the role of OCT in the diagnosis, monitoring and guiding of treatment for nAMD is needed.
Index test(s)
The index test considered was OCT, either alone or in combination with alternative tests as described below. Both TD-OCT and SD-OCT were considered.
Population
The population considered was people with newly suspected nAMD or those previously diagnosed with the disease and under surveillance monitoring.
The setting considered was secondary care.
Relevant comparators
The alternative tests considered included the following examinations:
-
clinical evaluation (with SLB, with or without use of diagnostic contact lens and evaluation of patients’ symptoms)
-
VA (for monitoring)
-
Amsler grid
-
colour fundus photographs
-
infrared reflectance (IR)
-
RFs or blue reflectance
-
FAF imaging
-
ICGA, dynamic high-speed or digital subtraction indocyanine green angiography (DS-ICGA)
-
PHP
-
microperimetry.
Reference standard
The reference standard considered was ophthalmologist-interpreted FFA. FFA is generally acknowledged as being the recognised reference standard for detecting nAMD. The RCO states in its guidelines for management of AMD that FFA is currently the reference standard for diagnosing exudative disease. 1 However, as few studies reported individual ophthalmologist-interpreted FFA (rather than reading centre-interpreted FFA), studies using FFA as the reference standard but with unclear information about which type of health-care professionals interpreted the images were also considered.
Outcomes
The following outcomes were considered for the use of OCT at presentation and during follow-up of patients with nAMD:
-
diagnostic accuracy [e.g. sensitivity, specificity, likelihood ratios (LRs), diagnostic odds ratio (DOR)]
-
clinical effectiveness (e.g. VA, anatomical control of the disease, patient-reported outcomes)
-
interpretability of the test – to be defined as in included studies, considering the ability to acquire a quality image that can be interpreted or analysed
-
acceptability of the test – to be defined as in included studies, considering users and health-care providers’ perspective
-
proportion of participants not able to receive the diagnostic test [due to an eye condition (e.g. lens or other media opacity), or personal circumstances (e.g. wheelchair bound)].
The evidence for the use of OCT was considered separately for the purposes of diagnosis and monitoring.
Key issues
The key issues to be addressed are:
-
How good a test is OCT, when used either alone or in combination with alternative tests, in the diagnosis of people newly presenting with a suspicion of nAMD?
-
How good a test is OCT, when used either alone or in combination with alternative tests, in detecting recurrent nAMD activity during surveillance monitoring of people previously diagnosed with the disease?
-
Is SD-OCT a better test than TD-OCT?
-
Could OCT images be interpreted by other health professionals in addition to ophthalmologists?
-
Could OCT replace FFA in some situations in the diagnostic and/or monitoring pathways?
-
How cost-effective are strategies involving OCT, both in the diagnostic and monitoring pathways?
Overall aims and objectives of assessment
The overall aim of the review was to determine the optimal role of OCT in (i) the diagnosis of people newly presenting with suspected nAMD and (ii) monitoring those previously diagnosed with the disease.
Specific research objectives were:
-
to determine the diagnostic performance of OCT, alone or in combination with alternative tests, in detecting nAMD, including accuracy, interpretability and acceptability
-
to determine the performance of OCT and/or other alternative tests in the monitoring of the disease post diagnosis, specifically in detecting activity of the disease and the need for further treatment
-
to determine the performance of other health professionals (e.g. medical photographers, nurses) compared with ophthalmologists in interpreting OCT findings
-
to model the effects of using OCT and/or other alternative tests in the diagnosis and management of the disease and estimate the relative cost-effectiveness of alternative diagnostic and monitoring strategies, including determination of an optimal cut-off point for sensitivity and specificity for use in practice, and the alternative timing between tests during monitoring
-
to identify future research needs.
Chapter 3 Methods for reviewing test performance
Methods were in accordance with the protocol.
Identification of studies
Published, unpublished and ongoing studies were identified from literature searches of electronic databases (from 1995 onwards) and appropriate websites. The search strategies were designed to be highly sensitive, including appropriate subject headings and text word terms that reflected both the clinical condition and diagnostic tests under review. There were no language restrictions. Databases searched included MEDLINE, MEDLINE In-Process & Other Non-Indexed Citations, EMBASE, Bioscience Information Services and Science Citation Index for all reviews. The Cochrane Central Register of Controlled Trials was searched for additional reports of RCTs for the effectiveness review and PsycINFO and Applied Social Sciences Index and Abstracts for patient acceptability data. The Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, Medion and Health Technology Assessment (HTA) database were searched for relevant systematic reviews and HTA reports. Abstracts and presentations from recent conferences (2009 onwards) of the American Academy of Ophthalmology, the Association for Research in Vision and Ophthalmology (ARVO) and the European Association for Vision and Eye Research (EVER) were also searched. The World Health Organization International Clinical Trials Registry Platform, ClinicalTrials.gov and European Union Clinical Trials Registry were searched for ongoing studies. Websites of professional organisations and manufacturers of OCT equipment were also consulted. Reference lists of all included studies were scanned and experts contacted for details of additional potentially relevant reports. The date of the final searches was March 2013. Full details of the search strategies used are provided in Appendix 1.
Inclusion and exclusion criteria
Types of studies
The following types of studies were considered.
-
Diagnostic studies:
-
Direct (head-to head) comparisons in which the index test and comparator test(s) are evaluated in the same study population. These could be fully paired [all study participants receive the index test, comparator test(s) and the reference standard] or not fully paired (participants receive only a subset of the tests, e.g. a randomised direct comparison in which study participants are randomly allocated to receive the index test or the comparator and all receive the reference standard.
-
Indirect comparisons in which estimates of the accuracy of the respective tests are obtained in different study groups, for example two-gate or ‘case–control’ type studies where different sets of criteria are used for those with and without the target condition. Indirect comparisons were to be considered if there was insufficient evidence from direct comparisons.
-
-
Studies reporting clinical effectiveness:
-
RCTs evaluating outcomes when treatment was based on OCT compared with FFA findings.
-
-
Qualitative studies evaluating patients’ and/or clinicians’/health-care professionals’ acceptability and/or interpretability of the OCT tests.
Types of participants
The types of participants considered were people with newly suspected nAMD or those previously diagnosed with the disease and under surveillance monitoring.
The setting considered was secondary care.
Index tests
The index test considered was OCT, either alone or in combination with alternative tests as described below. Both TD-OCT and SD-OCT were considered.
Comparator tests
The alternative tests considered included the following examinations:
-
clinical evaluation (with SLB, with or without use of diagnostic contact lens and evaluation of patients’ symptoms)
-
VA (for monitoring)
-
Amsler grid
-
colour fundus photographs
-
IR
-
RFs or blue reflectance
-
FAF imaging
-
ICGA, dynamic high-speed or DS-ICGA
-
PHP
-
microperimetry.
Reference standard
The reference standard considered was ophthalmologist-interpreted FFA. FFA is generally acknowledged as being the recognised reference standard for detecting nAMD. The RCO states in its guidelines for management of AMD that FFA is currently the reference standard for diagnosing exudative (neovascular) AMD. 1 However, as few studies reported individual ophthalmologist-interpreted FFA (rather than reading centre interpreted FFA), studies using FFA as the reference standard but with unclear information about which type of health-care professionals interpreted the images were also considered.
Types of outcomes
The following outcomes were considered for the use of OCT at presentation and during follow-up of patients with nAMD:
-
diagnostic accuracy (e.g. sensitivity, specificity, LRs, DOR)
-
clinical effectiveness (e.g. VA, anatomical control of the disease, patient-reported outcomes)
-
interpretability of the test – defined as in the included studies, considering the ability to acquire a quality image that can be interpreted or analysed
-
acceptability of the test – defined as in the included studies, considering users and healthcare providers’ perspective;
-
proportion of participants not able to receive the diagnostic test [due to an eye condition (e.g. lens or other media opacity), or personal circumstances (e.g. wheelchair bound)].
The evidence for the use of OCT was considered separately for the purposes of diagnosis and monitoring.
Data extraction strategy
Two reviewers (MC plus GM or AAB) screened the titles (and abstracts if available) of all reports identified by the search strategy. Full-text copies of all studies deemed to be potentially relevant were obtained and two reviewers (MC plus GM or AAB) independently assessed them for inclusion. Disagreements were resolved by consensus or arbitration by a third reviewer.
A data extraction form was developed and piloted. One reviewer (MC) extracted details of study design, participants, index, comparator and reference standard tests and outcome data, and a second reviewer (AAB or GM) checked the data extraction. Disagreements were resolved by consensus or arbitration by a third reviewer.
Critical appraisal strategy
Two reviewers (MC plus GM or AAB) independently assessed the risk of bias and applicability concerns of all included full-text diagnostic and monitoring studies using the updated quality assessment of diagnostic accuracy studies, version 2 (QUADAS-2) checklist. 17 Any disagreements were resolved by consensus or arbitration by a third party. The original QUADAS checklist was developed for use in systematic reviews of diagnostic studies through a formal consensus method and was based on empirical evidence. Following anecdotal reports and feedback which suggested problems with QUADAS, the QUADAS-2 tool was developed. QUADAS-2 consists of four key domains covering (1) patient selection, (2) index test, (3) reference standard, and (4) flow of patients through the study, and timing of the index test(s) and reference standard. Each domain is assessed in terms of the risk of bias. The first three domains are also assessed for concerns regarding their applicability in terms of whether (i) the participants and setting, (ii) the index test, its conduct or interpretation, and (iii) the target condition, as defined by the reference standard, match the question being addressed by the review. Within each domain signalling questions are included to assist in making a judgement about the risk of bias, with the standard tool containing 11 such questions across the four domains.
Both the original and updated checklists were designed to be adapted to be more applicable to a specific review topic. For this review, QUADAS-2 was modified by adding an additional signalling question to domain 1 (patient selection) to assess whether or not participant pre-selection had been avoided. Domains 2 (index test), 3 (reference standard) and 4 (flow and timing) were retained in their entirety. Therefore the modified tool contained 12 signalling questions, with each worded so that a rating of ‘Yes’ was always optimal in terms of methodological quality. If any signalling questions within a domain were rated ‘No’ then that domain was judged to be at high risk of bias. With regard to question 9 in the modified tool (appropriateness of the time interval between the index test and the reference standard), it was agreed that to be considered appropriate, the time interval between the index test and reference standard should be no longer than 1 week. An example of the QUADAS-2 checklist used in this review is shown at the end of the protocol (www.nets.nihr.ac.uk/__data/assets/pdf_file/0010/81685/PRO-10-57-22.pdf).
We planned to assess the methodological quality of any RCTs reporting effectiveness outcomes that met our inclusion criteria using the Cochrane risk of bias tool. 18 This tool addresses six specific domains relating to methodological quality (sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and ‘other issues’). However, no RCTs reporting effectiveness outcomes were identified that met our inclusion criteria.
Methods of data synthesis
The results of the individual diagnostic studies were tabulated and, where data allowed, sensitivity, specificity, predictive values, LRs and DORs were calculated.
Summary receiver operating characteristic (SROC) curves were produced for each test where two or more diagnostic studies reported sufficient data. In the event of studies reporting 2 × 2 data [true positives (TPs), false positives (FPs), false negatives (FNs), true negatives (TNs)] for a number of different cut-off values we planned to select the most frequently used cut-off value across studies. However, this situation did not arise. Meta-analysis models were fitted using the hierarchical summary receiver operating characteristic (HSROC) model19 in SAS version 9.1 (SAS Institute Inc., Cary, NC, USA). A symmetric SROC model was used, which takes proper account of the diseased and non-diseased sample sizes in each study, and allows estimation of random effects for the threshold and accuracy effects. The SROC curves from the HSROC models were produced on the corresponding SROC plots. Summary sensitivity, specificity, positive and negative LRs and DORs for each model were reported as point estimate and 95% confidence interval (CI).
If numerical difficulties were encountered with the HSROC model and there was no evidence of a threshold effect then we planned to pool sensitivity and specificity using the weighted average method. 20 Pooled LRs and DOR were to be calculated using the DerSimonian and Laird random-effects method. 21 These analyses were to be carried out using Metadisc software (version 1.4, Unit of Clinical Biostatistics team of the Ramón y Cajal Hospital, Madrid), with heterogeneity assessed using the I2 statistic, which describes the percentage of the variability in effect estimates that is due to heterogeneity rather than sampling error. 22
For relevant clinical outcomes reported based on use of the tests, where appropriate, we planned to use meta-analysis to estimate a summary measure of effect. Dichotomous outcome data were to be combined using the Mantel–Haenszel relative risk method and continuous outcomes were to be combined using the inverse-variance weighted mean difference method. For the estimates of relative risk and weighted mean difference, 95% CIs and p-values were to be calculated. Chi-squared tests and I2 statistics were to be used to explore statistical heterogeneity across studies, with possible reasons for heterogeneity being investigated using sensitivity analysis. Heterogeneity is to be expected in diagnostic test accuracy studies, and random-effects models were to be used to describe the variability across studies. However, no studies reporting clinical outcomes based on use of the tests were identified that met our inclusion criteria.
Where a quantitative synthesis was considered inappropriate (e.g. studies reporting acceptability of tests), or not feasible, a narrative synthesis of results was provided.
Chapter 4 Assessment of diagnostic and monitoring studies
This chapter is structured as follows: Quantity of research available describes the quantity of research available for both diagnostic and monitoring studies together; Assessment of diagnostic studies and Assessment of monitoring studies report the results for the diagnostic and monitoring studies, respectively; and Summary of the reviews of diagnostic and monitoring studies provides a summary of the chapter. Within each of the sections on diagnostic and monitoring studies there are subsections on the characteristics of the included studies, their risk of bias, diagnostic accuracy results (single tests; studies directly comparing tests; studies reporting combinations of tests) and other outcomes of interest.
Quantity of research available
Number and type of studies included
Appendix 2 lists the 29 studies, published in 31 reports, that met the inclusion criteria for the review of diagnostic and monitoring studies. 23–53 There were two reports of the studies by Cachulo et al. 25,47 and Torron et al. 50,51 Figure 3 shows a flow diagram outlining the screening process, with reasons for exclusion of full-text papers.
FIGURE 3.
Flow diagram outlining the screening process.
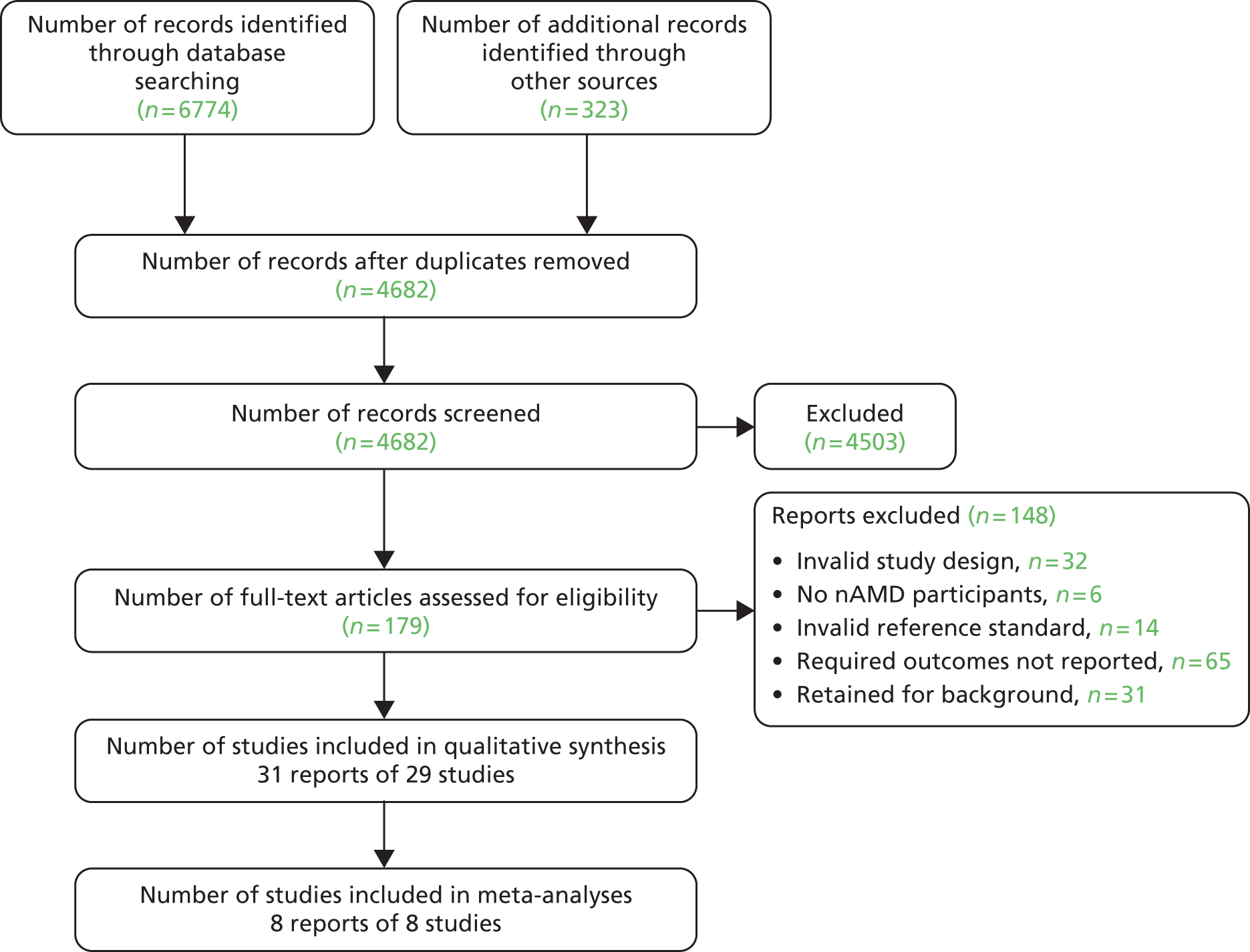
Twenty-seven studies (29 reports in total as two studies each had two associated reports) were full-text papers and two studies were only available as abstracts. 34,42 Four studies (five reports) were non-English language, with one each in Japanese,29 Chinese,26 German37 and Spanish. 50,51 Of the 29 included studies, 22 (24 reports)24–27,29,31,33–42,44–51 were diagnostic studies involving people with suspected nAMD and eight23,28,30,32,43,45,52,53 were monitoring studies involving people previously diagnosed with nAMD and under follow-up surveillance. One study, by Salinas-Alaman et al. ,45 reported results for both diagnosis and monitoring.
Number and type of studies excluded
A list of full-text papers that were excluded along with the reasons for their exclusion is given in Appendix 3. These reports were excluded because they failed to meet one or more of the inclusion criteria in terms of the type of study, participants, test, reference standard or outcomes reported.
Assessment of diagnostic studies
Characteristics of the included diagnostic studies
Appendix 4 (see Table 42) provides details of the individual study characteristics for the 22 diagnostic studies. Table 4 provides summary information for these studies. Of the 22 studies, nine were prospective24,25,27,33,39–41,45,46 and seven were retrospective. 34–36,38,39,49,51 Seven studies did not provide this information. 26,29,31,37,42,44,48 (The study by Loewenstein et al. 39 reported both a prospective and retrospective component.) In 10 studies, participant recruitment was consecutive. 33,34,38,39,42,44–46,48,49 The studies enrolled more than 2000 participants. Twenty-one studies reported eye as the unit of analysis (1754 eyes), whereas one42 reported patient as the unit of analysis (155 patients).
| Characteristic | Number | Number of studies |
|---|---|---|
| Participants enrolleda | 2124 | 22 |
| Analysed (eyes) | 1754 | 21 |
| Analysed (patients) | 155 | 1 |
| Age: median (range) of means/medians | 76.0 (51.4–84.6) | 15 |
| Gender: male : female, n (%) | 742 (45.4) : 891 (54.6) | 14 |
| Median (range) prevalence of nAMDb | 80.0% (17.2–100.0%) | 13 |
| Tests reported (number enrolled) | ||
| OCT | 1335 | 13 |
| TD-OCT | 1316 | 12 |
| SD-OCT | 19 | 1 |
| ICGA | 458 | 8 |
| PHP | 491 | 3 |
| Colour fundus photography | 185 | 1 |
| Amsler grid | 98 | 1 |
| FAF | 62 | 1 |
Seven studies were undertaken in the USA,27,34,36,38,40,41,44 three in the UK,33,46,49 two each in Japan,29,31 Austria37,48 and Spain,45,51 and one each in Portugal,25 Italy (involving eight centres),42 the Republic of Korea35 and China. 26 The remaining two studies were international, taking place in (a) seven centres in the USA, Germany, Israel, Austria and Portugal24 and (b) 15 centres in Israel and the USA. 39 Of the three UK-based studies, two took place at the Royal Victoria Infirmary, Newcastle upon Tyne,46,49 while the third took place at King’s College Hospital, London. 33 One of the UK-based studies, by Talks et al. , involved a nurse-led, fast-track screening clinic. 49
The largest study was by Kozak et al. ,36 which reported TD-OCT, was set in the USA and analysed 541 eyes, whereas the smallest was by Sulzbacher et al. ,48 reporting ICGA and included only 13 eyes.
Across 15 studies reporting the mean or median age of the participants,24–27,29,31,35–37,39,40,45,46,49,51 the median (range) of these values was 76 years (51.4–84.6 years). Fourteen studies involving 1633 participants provided information on gender, in which 742 (45.4%) participants were men and 891 (54.6%) were women. 24,25,27,29,31,35,36,39–41,45,46,49,51 The median (range) prevalence of nAMD across 13 studies where this information was available at participant level was 80.0% (17.2–100.0%). 24,25,27,33,35,38–41,44,45,49,51
In three studies, by Cachulo et al. ,25 Do et al. 27 and Padnick-Silver et al. ,40 the inclusion criteria specified that participants were required to have previously diagnosed nAMD in the non-study eye.
Thirteen studies reported OCT (12 TD-OCT;25,27,33–38,40,45,46,49 one SD-OCT). 41 The study by Kozak et al. ,36 reporting TD-OCT, included a subset of patients who underwent additional examination with SD-OCT. 36
Of the other tests reported, three studies reported PHP,24,27,39 one reported colour fundus photography,24 one Amsler grid,27 one FAF imaging25 and eight ICGA. 25,26,29,31,42,44,48,51 Of the studies reporting more than one test, Cachulo et al. 25 reported TD-OCT, ICGA and FAF, Do et al. 27 TD-OCT, Amsler grid and PHP, and Alster et al. 24 reported PHP and colour fundus photography. Two studies reported combinations of tests: Alster et al. 24 reported colour fundus photography plus VA, whereas Sandhu and Talks46 reported TD-OCT plus colour fundus photography.
The 13 studies reporting OCT analysed 1262 eyes; in eight studies one eye per patient was analysed (n = 479 eyes) (all TD-OCT). 25,27,33–35,38,40,49 Eight studies reported detection of nAMD phenotypes (predominantly classic, minimally classic, occult CNV). 25,33,34,37,38,41,46,49 Four of these studies also reported detection of RAP. 25,34,37,38
Of the eight studies reporting ICGA, seven used the eye as the unit of analysis (number of eyes analysed = 291). 25,26,29,31,44,48,51 In three of these studies, one eye per patient was analysed (n = 109 eyes). 25,31,44 Three studies only reported detection of nAMD phenotypes: IPCV;31 occult CNV;26 and type 2 CNV without an occult component. 48 The study by Parravano et al. ,42 with patient as the unit of analysis (n = 155 patients), also only reported detection of an nAMD phenotype – RAP.
The three studies reporting PHP analysed one eye per patient (n = 302 eyes),24,27,39 as did the studies reporting colour fundus photography (n = 120 eyes),24 Amsler grid (n = 46 eyes)27 and FAF (n = 50 eyes). 25
Risk of bias of the included diagnostic studies
All 20 full-text papers were assessed using a modified version of the QUADAS-2 tool containing 12 items. QUADAS-2 consists of four key domains covering (1) patient selection, (2) index test, (3) reference standard, and (4) flow of patients through the study and timing of the index test(s) and reference standard. Each domain is assessed in terms of the risk of bias and the first three domains are also assessed for concerns regarding their applicability in terms of whether or not they match the question being addressed by the review. Figure 4 presents a summary of the results for the QUADAS-2 risk of bias and applicability domains across the full-text diagnostic papers. Appendix 5 (see Table 44) presents the results of the risk of bias and applicability concerns for the individual studies.
FIGURE 4.
Summary of risk of bias and applicability domains (diagnostic studies).
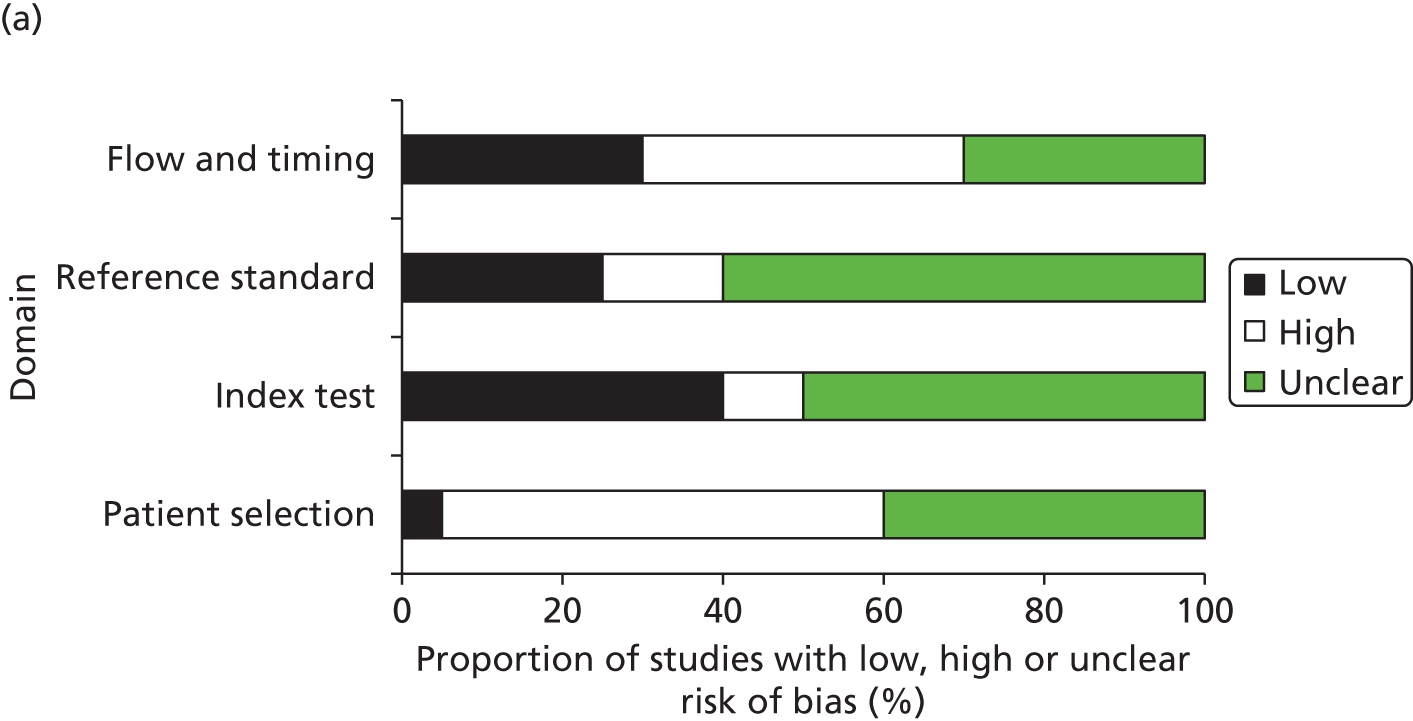
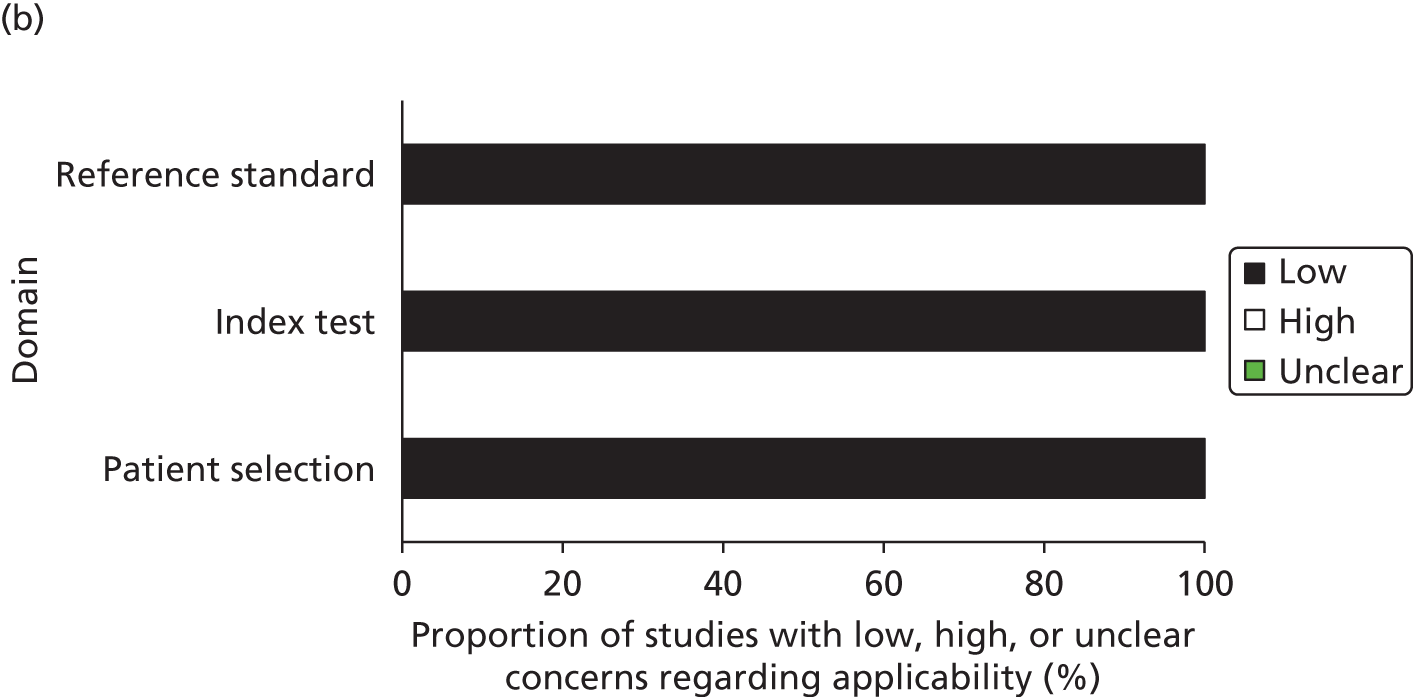
No study was judged to have a low risk of bias across all domains; in three studies the risk of bias was judged to be unclear across all domains. 29,35,48 The domains in which the greatest number of studies were judged to be at high risk of bias were the patient selection domain (n = 11, 55%) and flow and timing domain (n = 8, 40%).
In the patient selection domain, only one study36 was judged to be at low risk of bias, whereas the majority were considered to have either a high (n = 11, 55%)24,27,31,37–41,44,45,49 or unclear (n = 8, 40%)25,26,29,33,35,46,48,51 risk of bias. Reasons for studies being judged to be at high risk of bias included not enrolling a consecutive sample of participants,27,37 not avoiding inappropriate exclusions24,31,38–41,44 and not avoiding pre-selection of participants. 24,27,31,39,40,44,45,49
In the index/comparator test domain, eight studies (40%) were judged to be at low risk of bias,24,27,33,37,38,41,46,49 two (10%) were considered high risk of bias44,51 and in half (n = 10, 50%) the risk of bias was considered to be unclear. 25,26,29,31,35,36,39,40,45,48 The reasons for the two studies being judged to be at high risk of bias were that the test (ICGA in both cases) was interpreted with knowledge of the results of the reference standard.
In the reference standard domain, five studies (25%) were judged to be at low risk of bias,24,27,33,37,46 three (15%) were considered high risk of bias44,49,51 and in the majority (n = 12, 60%) the risk of bias was considered to be unclear. 25,26,29,31,35,36,38–41,45,48 The reasons for the three studies being judged to be at high risk of bias were that the reference standard test was interpreted with knowledge of the results of the index test (TD-OCT)49 or comparator test (ICGA). 44,51
In the flow and timing domain, six studies (30%) were judged to be at low risk of bias,26,31,37,38,41,44 and the majority were considered to have either a high (n = 8, 40%)24,25,27,36,39,40,46,49 or unclear (n = 6, 30%)29,33,35,45,48,51 risk of bias. Reasons for studies being judged to be at high risk of bias included an interval of more than 1 week between the index/comparator test and reference standard,24,39 not all patients receiving the reference standard test,39 or not all patients being included in the analysis. 24,25,27,36,37,40,46,49
All 20 diagnostic studies were judged to have low concerns for applicability regarding the patient selection, index/comparator test and reference standard domains, in that the participants and setting, index/comparator test and target condition as defined by the reference standard were considered to match the question being addressed by the review.
Results: diagnostic accuracy
Individual study results are presented in Appendix 6 (see Table 46).
Single tests
Optical coherence test
Thirteen studies, analysing 1262 eyes, reported the diagnostic accuracy of OCT in detecting nAMD (12 TD-OCT;25,27,33–38,40,45,46,49 one SD-OCT41). In eight studies, one eye per patient was analysed (n = 479 eyes) (all TD-OCT). 25,27,33–35,38,40,49 Eight studies reported detection of nAMD phenotypes. 25,33,34,37,38,41,46,49
The median (range) prevalence of nAMD across nine OCT studies where this information was available at participant level was 100.0% (17.2–100.0%). 25,27,33,35,38,40,41,45,49
Figure 5 shows a forest plot of the sensitivity and specificity of the individual studies (excluding three where information was only available at phenotype level). 34,37,38 Across these 10 studies, the median (range) sensitivity and specificity values reported were 94.5% (36.0–100.0%) and 73.5% (66.0–94.0%) respectively. Only four studies (all TD-OCT) reported specificity. For TD-OCT, across the studies, the median (range) sensitivity values reported were 92.0% (36.0–100.0%) whereas the only SD-OCT study reported sensitivity of 100%.
FIGURE 5.
Individual study results for all OCT diagnostic studies reporting sensitivity and/or specificity.
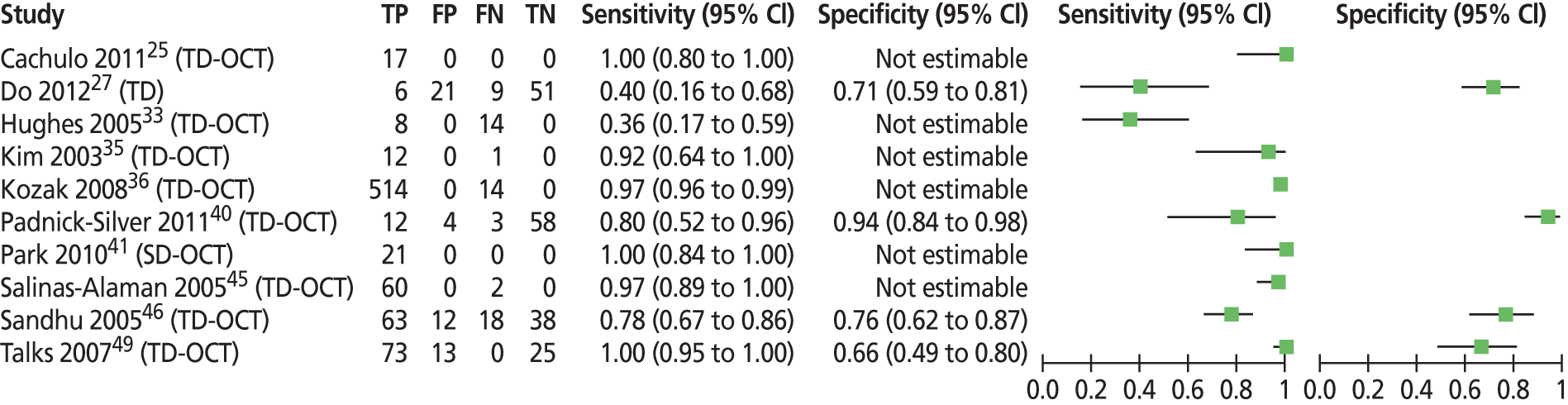
The studies shown in Figure 5 demonstrate heterogeneity across the sensitivities reported. The lowest sensitivity reported was by Hughes et al. 33 (36%) and Do et al. 27 (40%). In the study by Hughes et al. ,33 set in the UK, 22 individuals were classed as nAMD by FFA, seven with classic and 15 with occult CNV. TD-OCT detected six of the seven classic CNVs but only 2 of the 15 occult CNVs, hence the low overall sensitivity. The overall prevalence of nAMD in this study was 100%. Do et al. ,27 using TD-OCT in a study set in the USA, reported two separate sets of results, one for when the reference standard was FFA graded as positive by the reading centre irrespective of treatment decision (sensitivity 40.0%, specificity 70.8%), and one for when the reference standard was FFA graded as positive by the reading centre and the clinician recommended treatment (sensitivity 69.2%, specificity 66.2%) (see also Appendix 6, Table 46). The former reference standard was considered closer to the one used in this review and therefore it was these results that were taken to represent the study. Of 87 eyes analysed by Do et al. ,27 15 were classed as nAMD by FFA, with 13 of the 15 CNVs described as occult with no classic. The overall prevalence of nAMD in this study was low at 17.2%. In theory, prevalence should not affect sensitivity, but if the low prevalence contained more people with phenotypes that were difficult to diagnose compared with studies with a higher prevalence of disease, then this might reduce the sensitivity of the test.
By far, the largest study was that by Kozak et al. 36 This retrospective study was set in the USA and involved the analysis of 1272 eyes of 654 participants with a diagnosis of confirmed or suspected macular oedema of various aetiologies; in 541 eyes (number of participants not reported) the aetiology was nAMD. In this study, no data were presented for TNs for the nAMD group and the total number of suspected nAMD classed by FFA as without disease was not reported; as such it was not possible to calculate specificity. The study stated that TD-OCT had detected nAMD in 13 eyes that had not been detected by FFA. As the reference standard of FFA, for the purposes of this review, was considered to have perfect sensitivity and specificity, these 13 cases were classed as TD-OCT FP (although not shown in Figure 5 in order to prevent a spurious specificity value of 0% being calculated based on 13 FPs and zero TNs).
Pigment epithelial detachments can be classified as serous (non-specific) or vascularised. The latter are characteristic of nAMD. A serous PED can occur as a result of retinal conditions other than nAMD, such as central serous chorioretinopathy, angioid streaks or others. The study by Sandhu and Talks,46 considered a serous PED to constitute presence of nAMD and on this basis reported sensitivity of 96.4% and specificity of 66.0%. However, as a serous PED did not fall within our definition of nAMD for diagnostic studies, cases with serous PED were classed as non-nAMD and the data from the study were recalculated accordingly, resulting in alternative values for sensitivity of 77.8% and specificity of 76.0% and it was these values that were taken to represent this study.
Four studies, all TD-OCT,27,40,46,49 reported both sensitivity and specificity, providing sufficient data for inclusion in a meta-analysis. One of the studies, by Talks et al. 49 was a retrospective audit on new patients referred with nAMD to a nurse-led, fast-track screening clinic. Figure 6 shows a forest plot of the sensitivity and specificity of the individual studies and a SROC curve for the four OCT studies. Table 5 shows the pooled estimates for the OCT studies. For all OCT studies, the pooled sensitivity and specificity (95% CI) was 88% (46% to 98%) and 78% (64% to 88%) respectively.
FIGURE 6.
All OCT diagnostic studies reporting sensitivity and specificity. (a) Individual study results; and (b) SROC curve.
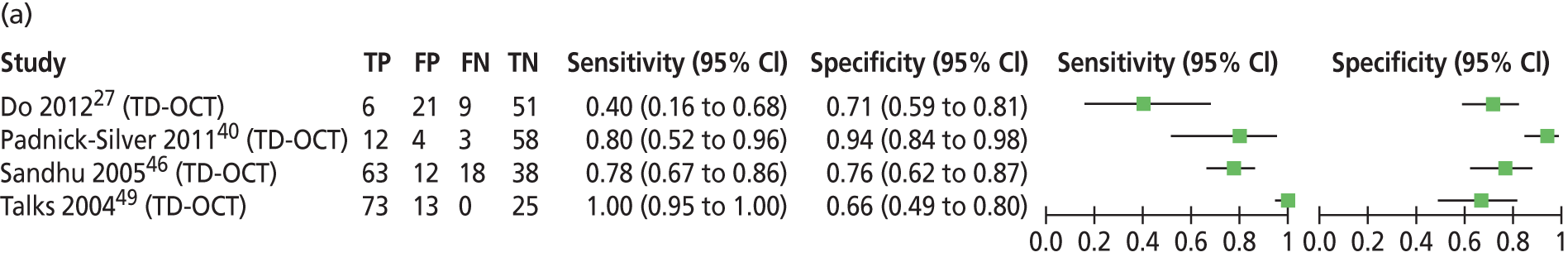
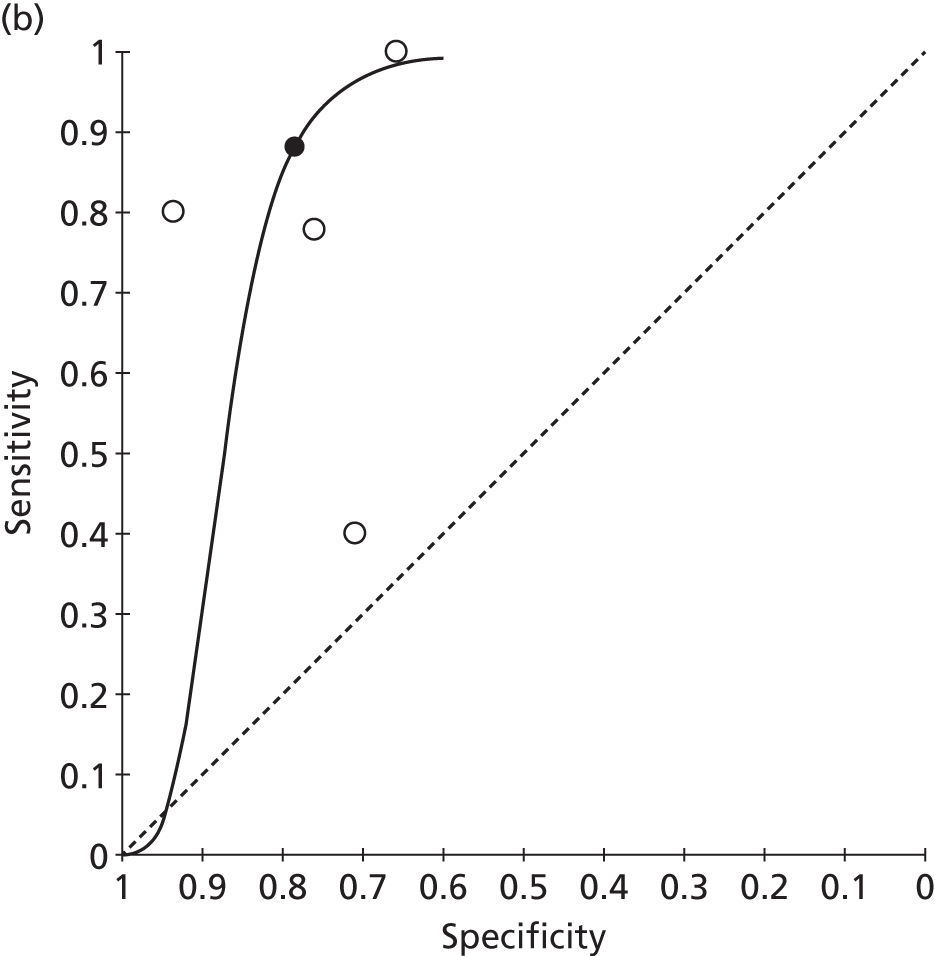
| Test | Number of studies | Number of eyes analysed | Pooled estimates (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Sensitivity, % | Specificity, % | LR+ | LR– | DOR | |||
| All OCT | 4 | 406 | 88 (46 to 98) | 78 (64 to 88) | 4.08 (2.37 to 7.04) | 0.15 (0.02 to 0.98) | 26.86 (3.36 to 214.81) |
A LR describes how many times a person with disease is more likely to receive a positive (LR+) or negative (LR–) test result than a person without disease. It has been suggested that LR+s > 10 or LR−s < 0.1 can provide convincing diagnostic evidence, whereas those > 5 and < 0.2 demonstrate strong diagnostic evidence. 54 The LR+ did not exceed 5 for OCT.
The DOR is a single summary of diagnostic performance and describes the ratio of the odds of a positive test result in an individual with disease compared with someone without disease. It has been suggested that a DOR of 25 could provide strong diagnostic evidence and that a DOR of 100 could provide convincing diagnostic evidence. 20
The risk of bias assessment of the four OCT studies included in the meta-analysis is shown in Table 6. The domains in which most studies were judged to be at high risk of bias were the patient selection domain, for reasons such as not enrolling a consecutive sample of participants,27 not avoiding inappropriate exclusions40 and not avoiding pre-selection of participants,27,40,49 and the flow and timing domain, due to all patients not being included in the analysis (all four studies).
| Study | Risk of bias domain | |||
|---|---|---|---|---|
| Patient selection | Index/comparator test | Reference standard | Flow and timing | |
| Do 201227 | High | Low | Low | High |
| Padnick-Silver 201240 | High | Unclear | Unclear | High |
| Sandhu 200546 | Unclear | Low | Low | High |
| Talks 200749 | High | Low | High | High |
Eight studies25,33,34,37,38,41,46,49 reported the sensitivity of OCT in the detection of nAMD phenotypes (Table 7). The studies by Cachulo et al. 25 and Khondkaryan et al. ,34 and Talks et al. ,49 using TD-OCT, and Park et al. 41 using SD-OCT showed equally high sensitivity for the detection of classic CNV compared with occult CNV. On the other hand, the studies by Hughes et al. 33 (TD-OCT), Krebs et al. 37 (TD-OCT), Liakopoulos et al. 38 (TD-OCT), and Sandhu and Talks46 (TD-OCT) reported higher sensitivity for OCT in the detection of classic CNV compared with occult CNV.
| Study ID | Test | Unit of analysis | nAMD phenotype | Number by FFA | OCT sensitivity, % |
|---|---|---|---|---|---|
| Cachulo 201125 | TD-OCT | Eye | Predominantly classic | 2 | 100.0 |
| Minimally classic | 4 | 100.0 | |||
| Occult | 6 | 100.0 | |||
| RAP | 5 | 100.0 | |||
| Hughes 200533 | TD-OCT | Eye | Classic | 7 | 85.7 |
| Occult | 15 | 13.3 | |||
| Khondkaryan 200934 | TD-OCT | Eye | Classic | Not reported | 80.9 |
| Occult | 81.1 | ||||
| RAP | 57.1 | ||||
| Krebs 200737 | TD-OCT | Eye | Primarily classic | 5 | 100.0 |
| RAP | 11 | 72.7 | |||
| Liakopoulos 200838 | TD-OCT | Eye | Subretinal fluid | ||
| Predominantly classic | 11 | 100.0 | |||
| Minimally classic | 23 | 91.3 | |||
| Occult with no classic | 24 | 79.2 | |||
| RAP stage III | 8 | 50.0 | |||
| Cystoid oedema | |||||
| Predominantly classic | 11 | 81.8 | |||
| Minimally classic | 23 | 73.9 | |||
| Occult with no classic | 24 | 58.3 | |||
| RAP stage III | 8 | 100.0 | |||
| Park 201041 | SD-OCT | Eye | Classic | 7 | 100.0 |
| Minimally classic | 3 | 100.0 | |||
| Occult | 11 | 100.0 | |||
| Sandhu 200546 | TD-OCT | Eye | Classic | 56 | 78.6 |
| Occult | 25 | 20.0 | |||
| TD-OCT + fundus photo | Eye | Classic | 56 | 82.1 | |
| Occult | 25 | 12.0 | |||
| Talks 200749 | TD-OCT | Eye | Predominantly classic | 22 | 100.0 |
| Minimally classic | 6 | 100.0 | |||
| Occult | 45 | 100.0 |
Amsler grid
One study, by Do et al. ,27 in an analysis of 46 eyes of 46 patients, reported sensitivity of 41.7% for the Amsler grid in detecting nAMD (specificity not reported and insufficient information to calculate prevalence of nAMD in this group). As this study also reported OCT, information on risk of bias is presented in that section. 27
Fundus autofluorescence imaging
One study, by Cachulo et al. ,25 in an analysis of 50 eyes of 50 patients, reported sensitivity of 93.3% and specificity of 37.1% for FAF in detecting nAMD. The prevalence of nAMD in this group was 30.0%. As this study also reported ICGA, information on risk of bias is presented in that section. 25
Colour fundus photography
One study, by Alster et al. ,24 in an analysis of 120 eyes of 120 patients, reported sensitivity of 70.0% and specificity of 95.0% for colour fundus photography in detecting nAMD. The prevalence of nAMD in this study was 53.3%. As this study also reported PHP, information on risk of bias is presented in that section. 24
Preferential hyperacuity perimetry
Three studies analysing 302 eyes of 302 patients reported the diagnostic accuracy of the PHP test in detecting nAMD. 24,27,39 Figure 7 shows a forest plot with the individual study results for sensitivity and specificity. The studies by Alster et al. 24 and Loewenstein et al. 39 reported similarly high sensitivity and specificity. However, it was not possible to calculate pooled estimates using HSROC methodology due to insufficient data. The study by Do et al. 27 reported lower sensitivity and did not report specificity. Across the studies the median (range) of sensitivity values reported was 82% (50–85%). The specificity values reported by Alster et al. 24 and Loewenstein et al. 39 were 88% and 85% respectively.
FIGURE 7.
Preferential hyperacuity perimetry studies: individual study results for sensitivity and specificity.
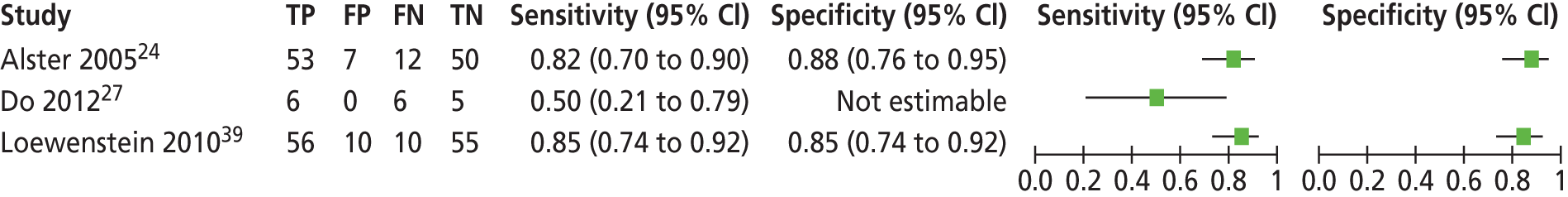
Across the three studies, the median (range) prevalence of nAMD was 50.4% (17.2–53.3%).
The risk of bias assessment of the three PHP studies is shown in Table 8. The domains in which most studies were judged to be at high risk of bias were the patient selection domain, for reasons such as inappropriate exclusions24,39 and pre-selection of participants,24,27,39 and the flow and timing domain, for reasons such as an interval of more than 1 week between the index test and reference standard,24,39 not all patients receiving the reference standard test39 and not all patients included in the analysis. 24,39
| Study | Risk of bias domain | |||
|---|---|---|---|---|
| Patient selection | Index/comparator test | Reference standard | Flow and timing | |
| Alster 200524 | High | Low | Low | High |
| Do 201227 | High | Low | Low | High |
| Loewenstein 201039 | High | Unclear | Unclear | High |
Loewenstein et al. 39 also reported the ability of PHP in detecting nAMD phenotypes, with 90% (18/20) sensitivity for minimally or predominantly classic CNV and 82.6% (38/46) sensitivity for occult CNV.
Indocyanine green angiography
Eight studies reported the diagnostic accuracy of ICGA in detecting nAMD, of which seven25,26,29,31,44,48,51 reported the eye as the unit of analysis and one42 reported the patient as the unit of analysis. Four of these studies only reported detection of nAMD phenotypes: IPCV;31 occult CNV;26 type 2 CNV without an occult component;48 and RAP. 42
The median (range) prevalence of nAMD across three studies where this information was available at participant level (and excluding studies reporting results only at phenotype level) was 80.0% (32.7–100.0%). 25,44,51
Figure 8 shows a forest plot of the sensitivity and specificity of the individual studies (excluding the four that only reported detection of phenotypes). Across the studies, the median (range) sensitivity reported was high at 93% (85–100%). Only the study by Fujii et al. 29 reported specificity, which was low at 37%.
FIGURE 8.
Indocyanine green angiography sensitivity and specificity: individual study results.
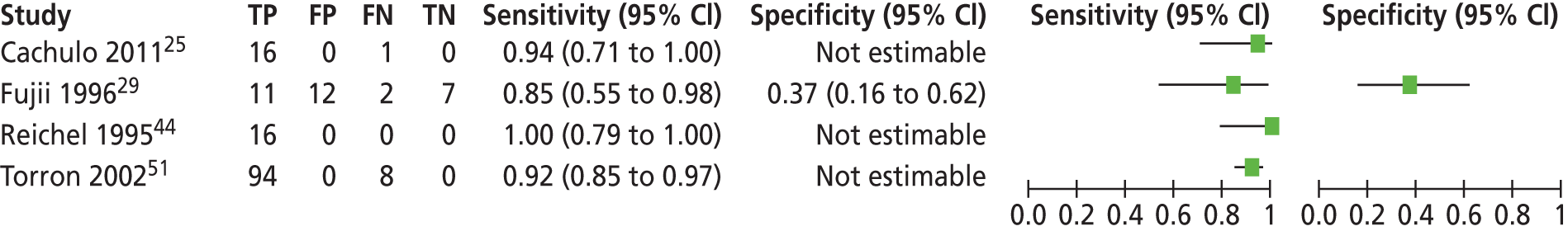
In the study by Reichel et al. ,44 all participants were deemed to have nAMD (therefore there could be no TNs and it was not possible to calculate specificity). Only participants who were suspected to have a CNV obscured by haemorrhage were included in this study. The authors stated that ICGA had detected nAMD in four eyes that had not been detected by FFA. As the reference standard of FFA, for the purposes of this review, was considered to have perfect sensitivity and specificity, these four cases were classed as ICGA FPs (although not shown in Figure 8 in order to prevent a spurious specificity value of 0% being calculated based on four FPs and zero TNs).
The risk of bias assessment of the four ICGA studies is shown in Table 9. The domains in which most studies were judged to be at high risk of bias were the index/comparator test domain, due to the ICGA test being interpreted with knowledge of the FFA results, and the reference standard domain, due to FFA being interpreted with knowledge of the ICGA results. 44,51
| Study | Risk of bias domain | |||
|---|---|---|---|---|
| Patient selection | Index/comparator test | Reference standard | Flow and timing | |
| Cachulo 201125 | Unclear | Unclear | Unclear | High |
| Fujii 199629 | Unclear | Unclear | Unclear | Unclear |
| Reichel 199544 | High | High | High | Low |
| Torron 200251 | Unclear | High | High | Unclear |
Four studies26,31,42,48 reported the sensitivity of ICGA in the detection of nAMD phenotypes, with each study reporting detection of a different phenotype (Table 10). Sensitivity was 100% for detection of IPCV31 and type 2 CNV without an occult component,48 high (85.1%) for detection of RAP42 but lower (62.9%) for detection of occult CNV. 26
Studies directly comparing tests
Preferential hyperacuity perimetry versus colour fundus photography versus colour fundus photography plus visual acuity
One study, by Alster et al. ,24 analysing one eye per patient, reported PHP (n = 122 eyes) compared with colour fundus photography (n = 120 eyes) and colour fundus photography plus VA (n = 66 eyes). Sensitivity was highest for PHP (81.5%), followed by colour fundus photography (70.0%) and lowest for colour fundus photography plus VA (53.0%). Specificity was similarly high for colour fundus photography (95.0%) and colour fundus photography plus VA (94.0%), followed by PHP (87.7%).
Time domain optical coherence tomography versus indocyanine green angiography versus fundus autofluorescence imaging
One study, by Cachulo et al. ,25 analysing one eye per patient, reported TD-OCT (n = 52 eyes) compared with ICGA (n = 52 eyes) and FAF (n = 50 eyes). Sensitivity was high for all three tests (TD-OCT 100.0%, ICGA 94.1%, FAF 93.3%). Specificity was only reported for FAF, which was low at 37.1%.
Time domain optical coherence tomography versus Amsler grid versus preferential hyperacuity perimetry
One study, by Do et al. ,27 analysing one eye per patient, reported TD-OCT (n = 87 eyes) compared with Amsler grid (n = 46 eyes) and PHP (n = 49 eyes). Based on the set of results for CNV defined as positive by FFA irrespective of the treatment decision, the sensitivity for all three tests was fairly low (PHP 50.0%, Amsler grid 41.7%, TD-OCT 40.0%). Specificity was only reported for TD-OCT, which was moderate at 70.8%. As previously stated, the overall prevalence of nAMD in this study was low at 17.2%, the majority of which were occult CNV, which might at least partly explain the low sensitivity reported by this study for TD-OCT.
Time domain optical coherence tomography versus time domain optical coherence tomography plus stereo colour fundus photography
One study, by Sandhu and Talks,46 reported TD-OCT compared with TD-OCT plus stereo colour fundus photography (both n = 131 eyes of 118 participants). As previously stated, serous PED did not fall within this review’s definition of nAMD for diagnostic studies and the study data were recalculated accordingly. Based on the recalculated data, sensitivity was similar and moderately high for both tests (TD-OCT 77.8%, TD-OCT plus stereo colour fundus photography 74.1%), whereas specificity was higher for the combination (92.0%) than for TD-OCT alone (76.0%).
Studies reporting combinations of tests
Two studies reported combinations of tests. Sandhu and Talks46 reported TD-OCT combined with stereo colour fundus photography. Alster et al. 24 reported colour fundus photography combined with VA. As both studies also reported other tests, the results for the test combinations are included in the preceding section on studies directly comparing tests.
Assessment of other outcomes of interest
Clinical effectiveness
No studies were identified that met our inclusion criteria of providing information on clinical effectiveness outcomes (e.g. VA) when treatment was based on OCT compared with FFA findings.
Interpretability of the tests
Six diagnostic studies24,25,27,36,39,46 provided information relating to the interpretability of the tests, in as much as they reported on the numbers excluded from analysis due to poor image quality (Table 11). In the TD-OCT study by Do et al. ,27 166 individuals were screened and 98 were enrolled; in 6 of the 68 individuals screened but not enrolled, the reason given was poor image quality. However, it was unclear whether the excluded images related to OCT, colour fundus photography or FFA. In the TD-OCT study by Sandhu and Talks,46 10/128 individuals (7.8%) were excluded from the analysis due to poor image quality. It was also unclear in this study whether the excluded images related to OCT or FFA.
| Study | Test | Excluded from analysis, n (%) | Reason |
|---|---|---|---|
| Alster 200524 | PHP | 11/185 (5.9) individuals/eyes | Results judged to be unreliable |
| Colour fundus photography | 17/185 (9.2) individuals/eyes | Inadequate or poor-quality photographs | |
| Cachulo 201125 | FAF | 2/52 (3.8) individuals/eyes | Pattern of autofluorescence could not be determined |
| Do 201227 | TD-OCT, PHP, Amsler grid, colour fundus photography | 6/104 (5.8) individuals/eyesa | Poor image quality that was insufficient to permit successful participation |
| Kozak 200836 | TD-OCT | 35/1307 (2.7) eyesb | Poor quality or image decentration |
| Loewenstein 201039 | PHP, colour fundus photography | 40/208 (19.2) individuals/eyesc | Geographic atrophy, early AMD, pattern dystrophy, no or poor-quality photographs |
| Sandhu 200546 | TD-OCT | 10/128 (7.8) individuals | Poor quality of the images |
Acceptability of the tests
No studies were identified meeting our inclusion criteria that reported the acceptability of the tests, either to those providing the tests or to those receiving them.
Proportion of participants unable to receive the diagnostic test
Ten studies reported exclusion criteria relating to eye conditions (see Appendix 7, Table 48). 24,25,27,31,39–41,44,48,49 The studies detailed various eye-related exclusion criteria, for example evidence of macular disease other than AMD, previous surgical or laser treatment within the macular area, presence of any significant media opacity that precluded a clear view of the fundus, subretinal or subpigment epithelial haemorrhages that obscured lesions, and recent ocular surgery in the study eye.
A few non-ophthalmic exclusion criteria were reported, including current or past history of a medical condition that would preclude scheduled study visits or completion of the study,25 allergy to fluorescein dye27 and allergy to iodine-based dye. 44 In the PHP study by Loewenstein et al. ,39 individuals with no experience of using a computer mouse were taught how to use the mouse and participation in the study was conditional on passing an in-house computer mouse tutorial. The authors reported that 15 people did not pass the tutorial and were excluded from the study.
Other health professionals compared with ophthalmologists interpreting optical coherence tomography findings
No studies were identified meeting our inclusion criteria that reported the performance of other health professionals compared with ophthalmologists in interpreting OCT findings. The setting for the TD-OCT study by Talks et al. 49 was a nurse-led, fast-track screening clinic in the UK for new nAMD referrals, but did not involve a comparison with other health professionals in interpreting OCT findings. Trained nurses and an ophthalmic photographer, who consulted an ophthalmologist when in doubt, conducted the screening visit. If the VA was ≥ 6/60 an OCT was performed. If dry AMD or other retinal pathology was seen, the patient was referred for management appropriate to their condition but no further imaging was performed. The remaining patients underwent simultaneous FFA and ICGA. The images were taken, using standard protocols, by an ophthalmic photographer. The ophthalmologist reviewed the images the following day. 49
Assessment of monitoring studies
Characteristics of the included monitoring studies
Appendix 4 (see Table 43) provides details of the individual study characteristics for the eight monitoring studies. 23,28,30,32,43,45,52,53 Table 12 provides summary information for the studies. Of the eight monitoring studies, four were prospective,32,43,45,53 three were retrospective,23,28,30 and in the study by van de Moere et al. 52 this information was not reported. In five studies, the participants were a consecutive sample. 28,30,43,45,53 The eight studies enrolled 463 participants.
| Characteristic | Number | Number of studies |
|---|---|---|
| Participants enrolled | 463 | 8 |
| Analysed (eyes) | 363 | 5 |
| Analysed (examinations, pairs) | 291 | 3 |
| Age: median (range) of means/medians | 76.5 (73.9–78.1) | 7 |
| Gender: male : female, n (%) | 177 (46.8) : 201 (53.2) | 6 |
| Median (range) prevalence of active nAMDa | 57.9% (49.2–83.3%) | 5 |
| Tests reported (number enrolled)b | ||
| OCT | 442 | 7 |
| TD-OCT | 349 | 6 |
| SD-OCT | 152 | 2 |
| ICGA | 21 | 1 |
| Type of treatment received | ||
| AntiVEGF | 149 | 2 |
| PDT | 293 | 5 |
| Laser photocoagulation | 21 | 1 |
Five studies used the eye as the unit of analysis (363 eyes),23,28,30,52,53 whereas three used test examination as the unit of analysis (61 pairs of OCT and FFA examinations,32 176 pairs of OCT and FFA examinations45 and 54 pairs of ICGA and FFA examinations). 43
Two studies were undertaken in the USA23,43 and one each in Italy,30 Germany,32 the Netherlands,53 Spain45 and the UK (Royal Victoria Infirmary, Newcastle upon Tyne). 52 One study was international, taking place in two centres in the USA and Germany. 28
The largest study was by van de Moere et al. ,52 which reported TD-OCT, was set in the UK and analysed 121 eyes, while the smallest was by van Velthoven et al. ,53 reporting TD-OCT and analysing 30 eyes.
Across seven studies23,28,30,43,45,52,53 reporting the mean or median age of the participants, the median (range) of these values was 76.5 years (73.9–78.1 years). Six studies involving 378 participants provided information on gender,28,30,43,45,52,53 in which 177 (46.8%) participants were men and 201 (53.2%) women. The median (range) prevalence of active nAMD across five studies where this information was available at participant level was 57.9% (49.2–83.3%). 23,28,30,52,53
Seven studies reported OCT (six TD-OCT;23,28,32,45,52,53 and two SD-OCT). 23,30 (The study by Khurana et al. 23 reported both TD-OCT and SD-OCT.) One study, by Regillo et al. ,43 reported ICGA.
Of the seven studies reporting OCT, five used the eye as the unit of analysis (number of eyes analysed = 363). 23,28,30,52,53 In four of these studies, one eye per patient was analysed (n = 304 eyes). 28,30,52,53 Two studies reported examination as the unit of analysis (both TD-OCT). 32,45 Two studies reported detection of nAMD phenotype activity: classic and occult CNV;30 and PED and cystoid macular oedema. 52 The studies by Henschel et al. 32 and van de Moere et al. 52 also reported the performance of OCT in detecting intraretinal and subretinal fluid.
In two OCT monitoring studies,23,30 the participants had received antiVEGF therapy and in five28,32,45,52,53 the treatment was photodynamic therapy (PDT). In the study reporting ICGA,43 the participants had received laser photocoagulation treatment.
Risk of bias of the included monitoring studies
Figure 9 presents a summary of the results for the QUADAS-2 risk of bias and applicability domains across the eight full-text monitoring papers. Appendix 5 (see Table 45) presents the results of the risk of bias and applicability concerns for the individual studies.
FIGURE 9.
Summary of risk of bias and applicability domains (monitoring studies).
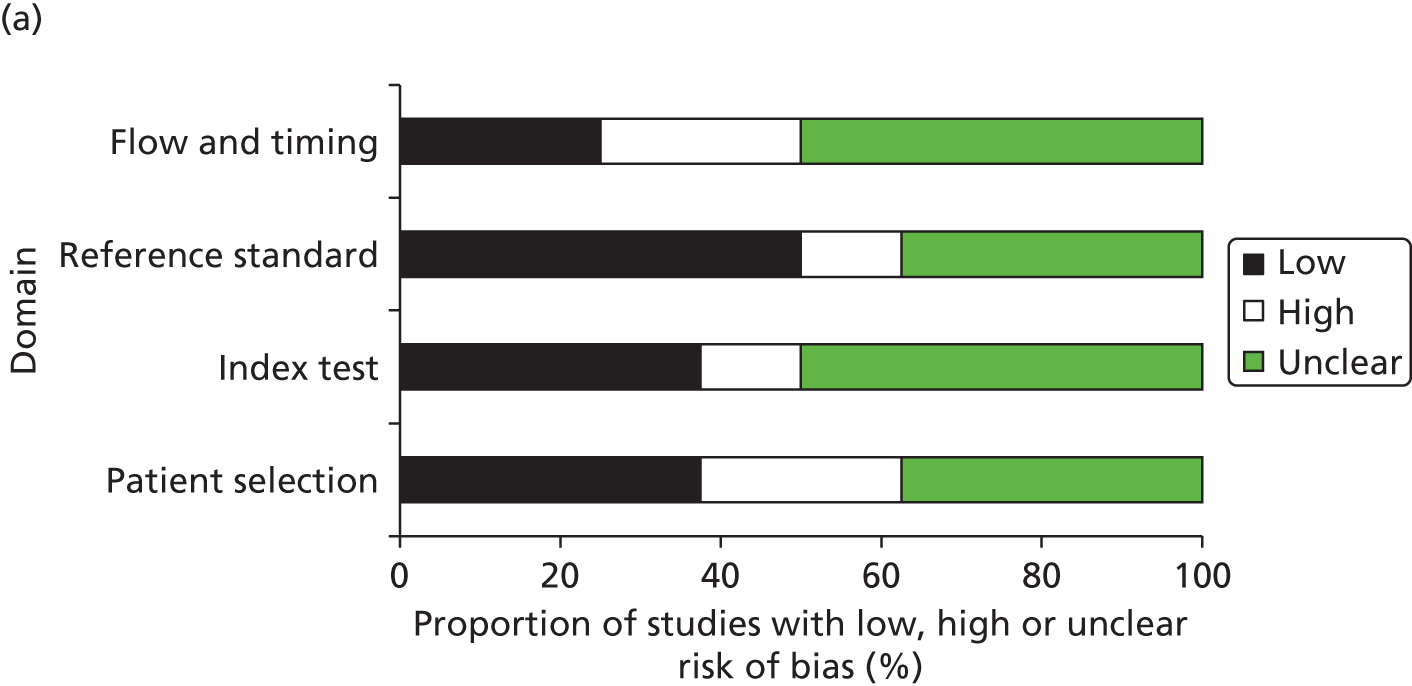
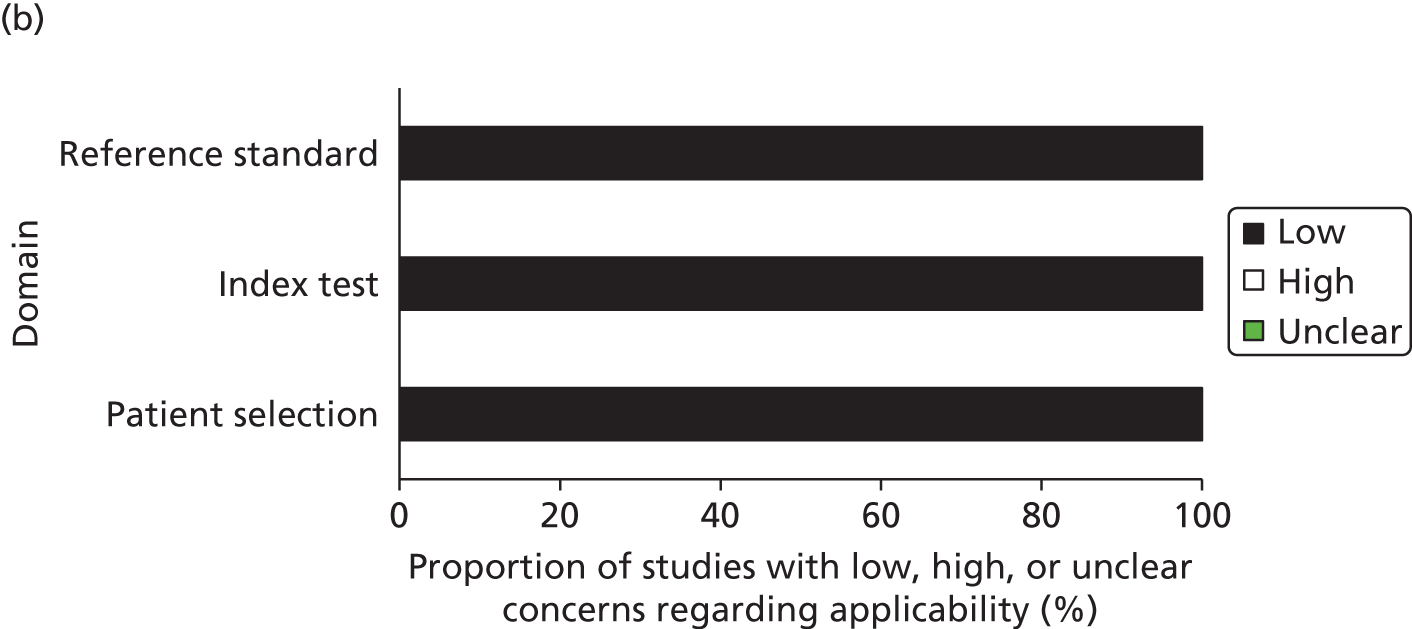
No study was judged to have a low risk of bias across all domains. More studies in the patient selection domain (n = 2, 25%) and the flow and timing domain (n = 2, 25%) were judged to be at high risk of bias than in the index/comparator test domain (n = 1, 12.5%) and reference standard domain (n = 1, 12.5%).
In the patient selection domain, three studies43,52,53 (37.5%) were judged to be at low risk of bias, two30,45 (25%) were considered to have a high risk of bias and in three23,28,32 (37.5%) the risk of bias was unclear. The study by Giani et al. 30 was judged to be at high risk of bias due to not avoiding inappropriate exclusions and pre-selection of participants, whereas the study by Salinas-Alaman et al. 45 was judged to be at high risk of bias due to not avoiding pre-selection of participants.
In the index/comparator test domain, three studies (37.5%) were judged to be at low risk of bias,28,30,32 one (12.5%) was considered high risk of bias43 and in the remaining four (50%) the risk of bias was considered to be unclear. 23,45,52,53 The reasons for the study by Regillo et al. 43 being judged to be at high risk of bias was that the test (ICGA) was interpreted with knowledge of the results of the reference standard.
In the reference standard domain, four studies (50%) were judged to be at low risk of bias,28,30,32,53 one (12.5%) was considered high risk of bias43 and in the remaining three (37.5%) the risk of bias was considered to be unclear. 23,45,52 The Regillo et al. 43 study was judged to be at high risk of bias as the reference standard test was interpreted with knowledge of the results of the comparator test (ICGA).
In the flow and timing domain, two studies (25%) were judged to be at low risk of bias,23,43 two45,52 (25%) were considered to have a high risk of bias and in the remaining four28,30,32,53 (50%) the risk of bias was considered to be unclear. The studies by Khurana et al. 23 and Regillo et al. 43 were judged to be at high risk of bias as not all patients were included in the analysis.
All eight studies were judged to have low concerns for applicability on the patient selection, index/comparator test and reference standard domains.
Results: detection of active neovascular age-related macular degeneration
Individual study results are presented in Appendix 6 (see Table 47).
Single tests
Optical coherence tomography
Seven studies reported the accuracy of OCT in detecting active nAMD, of which five reported TD-OCT,28,32,45,52,53 one reported SD-OCT30 and one reported both TD-OCT and SD-OCT. 23 In five studies the unit of analysis was the eye23,28,30,52,53 and in two the unit of analysis was pairs of OCT and FFA examinations. 32,45
The median (range) prevalence of active nAMD across five studies where this information was available at participant level was 57.9% (49.2–83.3%). 23,28,30,52,53
Three TD-OCT studies23,28,53 and two SD-OCT studies,23,30 with eye as the unit of analysis, reported both sensitivity and specificity, providing sufficient data for inclusion in a meta-analysis. Figure 10 shows forest plots of the sensitivity and specificity of the individual studies and SROC curves for (a) all of the OCT studies, (b) the three TD-OCT studies and (c) the two SD-OCT studies respectively. Table 13 shows the pooled estimates for these studies. As the study by Khurana et al. 23 reported both TD-OCT and SD-OCT for the same 59 eyes, we chose to display only the data for SD-OCT from this study in the forest plot of all OCT studies and to include only the SD-OCT data from this study in the pooled estimates for all OCT studies, in order to avoid double counting and on the basis that the SD-OCT data were the more appropriate to include in the pooled estimates for all OCT. The TD-OCT data from Khurana et al. 23 are included in the forest plot and SROC curve for TD-OCT in Figure 10 and were included in the pooled estimates for TD-OCT shown in Table 13. For all OCT studies, the pooled sensitivity and specificity (95% CI) was 85% (72% to 93%) and 48% (30% to 67%) respectively. For TD-OCT, the pooled sensitivity and specificity (95% CI) was 70% (56% to 80%) and 65% (48% to 79%) respectively. For both TD-OCT and the group of all four OCT studies, the LR and DOR values reported were below the level suggestive of strong diagnostic evidence.
FIGURE 10.
Optical coherence tomography monitoring studies reporting sensitivity and specificity for detection of nAMD activity: individual study results and SROC curves. (a) Sensitivity and specificity – individual study results – all OCT; (b) sensitivity and specificity – individual study results – TD-OCT; (c) sensitivity and specificity – individual study results – SD-OCT; (d) SROC curve – all OCT; (e) SROC curve – TD-OCT; and (f) SROC curve – SD-OCT.
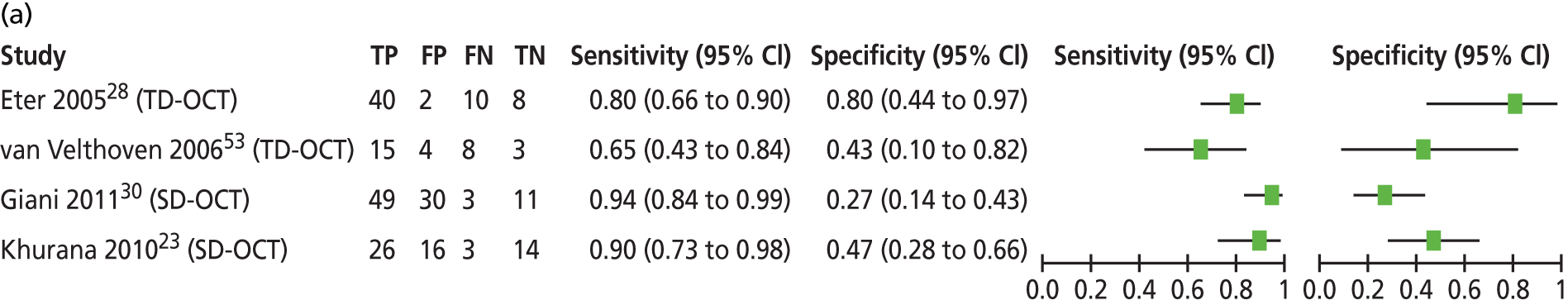
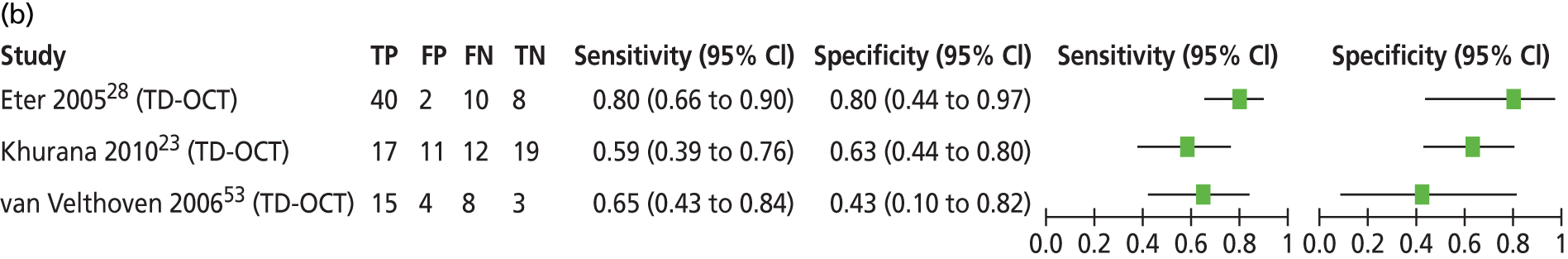
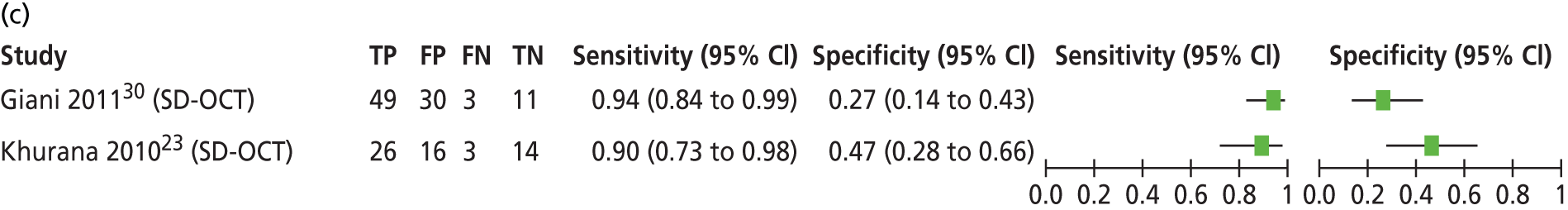
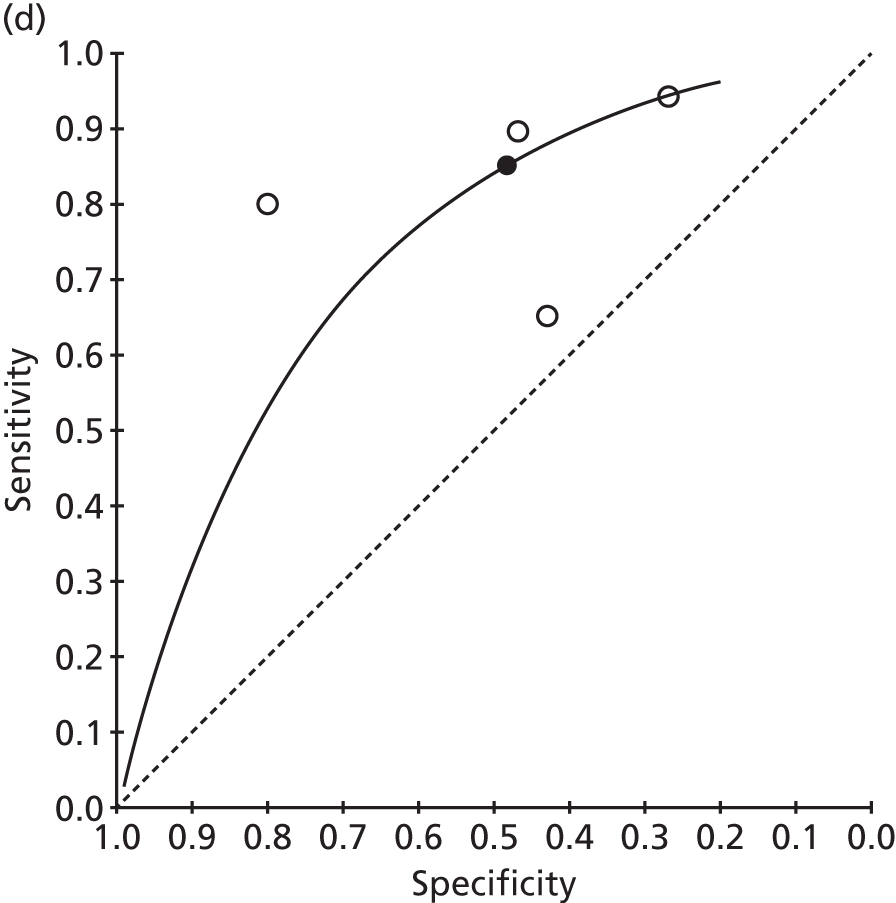
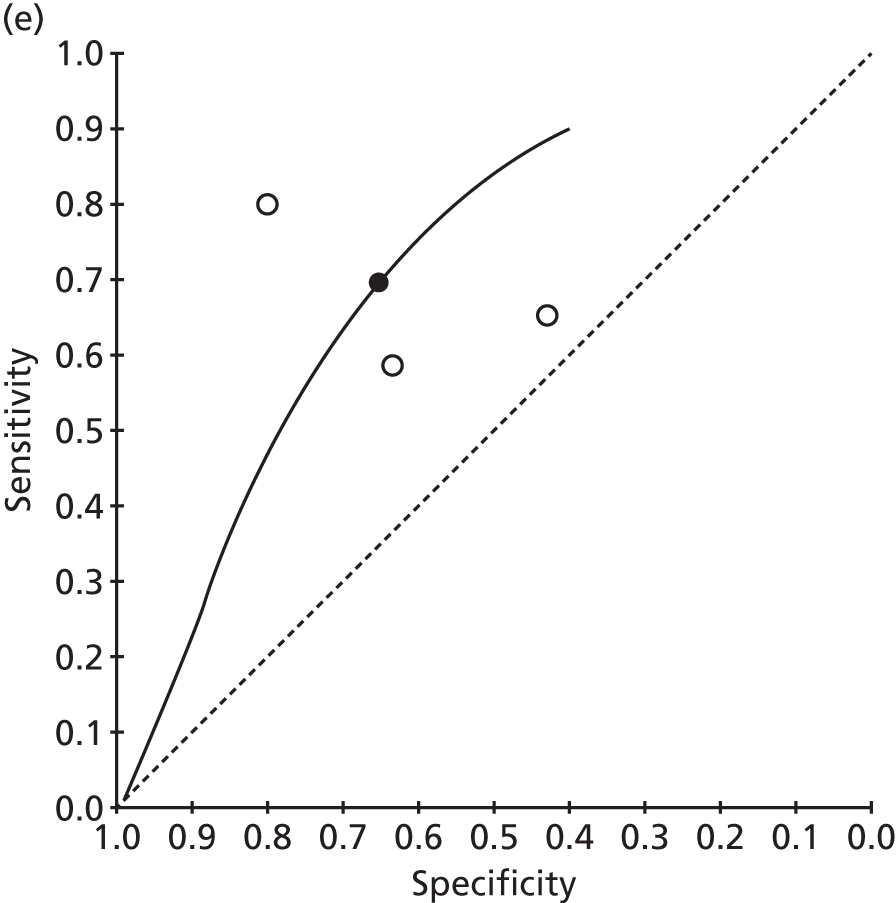
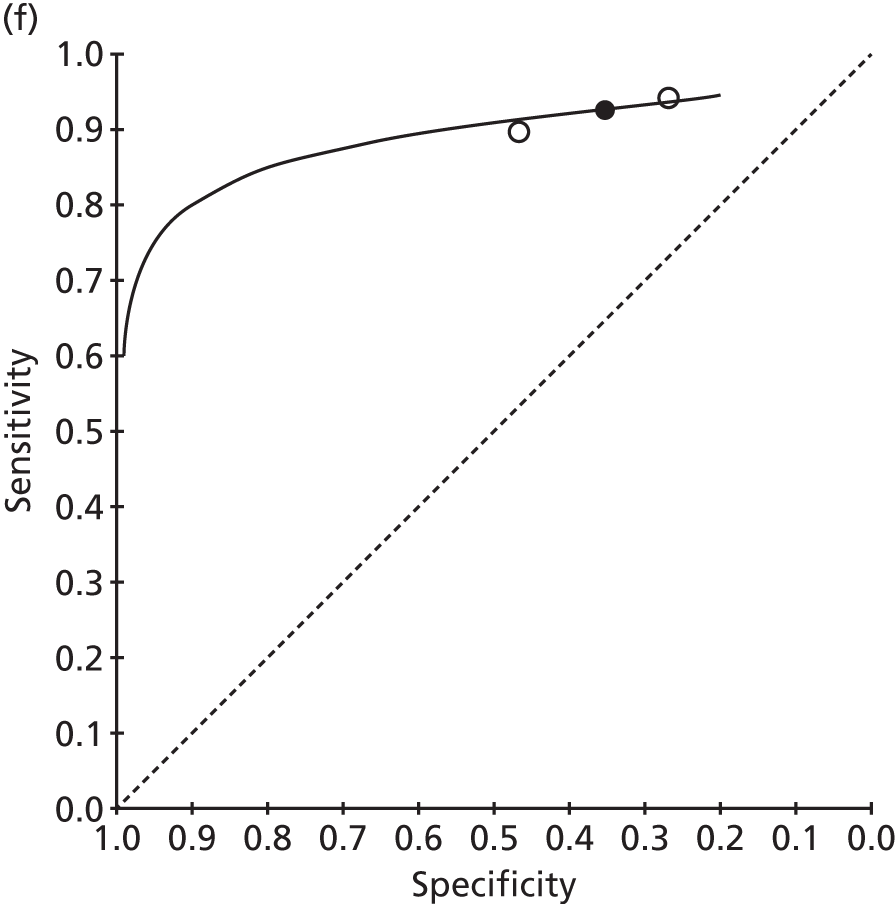
| Test | Number of studies | Number of eyes analysed | Pooled estimates (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Sensitivity, % | Specificity, % | LR+ | LR– | DOR | |||
| All OCTa | 4 | 242 | 85 (72 to 93) | 48 (30 to 67) | 1.64 (1.19 to 2.26) | 0.31 (0.18 to 0.54) | 5.33 (2.57 to 11.06) |
| TD-OCT | 3 | 149 | 70 (56 to 80) | 65 (48 to 79) | 2.00 (1.19 to 3.36) | 0.47 (0.28 to 0.78) | 4.27 (1.58 to 11.53) |
| SD-OCT | 2 | 152 | Not calculable using HSROC methodology | ||||
It was not possible to calculate pooled estimates using HSROC methodology for the two SD-OCT studies due to insufficient data. These studies reported sensitivities of 94%30 and 90%23 and specificities of 27%30 and 47%,23 which suggests that SD-OCT has higher sensitivity than TD-OCT but lower specificity.
The risk of bias assessment of the four OCT studies included in the meta-analysis is shown in Table 14. The only judgement of high risk of bias was for the study by Giani et al. 30 for the patient selection domain (inappropriate exclusions and pre-selection of participants).
| Study | Risk of bias domain | |||
|---|---|---|---|---|
| Patient selection | Index/comparator test | Reference standard | Flow and timing | |
| Eter 200528 | Unclear | Low | Low | Unclear |
| Giani 201130 | High | Low | Low | Unclear |
| Khurana 201023 | Unclear | Unclear | Unclear | Low |
| van Velthoven 200653 | Low | Unclear | Low | Unclear |
Two studies used examination as the unit of analysis. Henschel et al. ,32 in an analysis of 61 pairs of TD-OCT and FFA examinations from 14 patients, reported sensitivity of 96.8% and specificity of 36.7% for CNV based on detection of intraretinal and/or subretinal fluid. Salinas-Alaman et al. ,45 in an analysis of 176 pairs of TD-OCT and FFA examinations (number of patients not stated), reported sensitivity of 95.7% and specificity of 59.0% based on detection of intraretinal or subretinal fluid.
Four studies23,30,32,52 reported the sensitivity of OCT in detecting active nAMD phenotypes or active nAMD based on detection of intraretinal/subretinal fluid (Table 15). The study by Giani et al. 30 reported high sensitivity for the detection by SD-OCT of both classic and occult CNV activity (90.9% and 100% respectively). In the studies by Henschel et al. 32 (unit of analysis: examination) and van de Moere et al. 52 (unit of analysis: eye) sensitivity was higher for nAMD activity based on detection of intraretinal fluid (90.3% and 82.9% respectively) compared with subretinal fluid (71.0% and 47.1% respectively). van de Moere et al. 52 also reported sensitivity of TD-OCT for detection of cystoid macular oedema and PED, both low at 22.9% and 5.7% respectively. In the study by Khurana et al. ,23 the sensitivity of SD-OCT was higher than that of TD-OCT for nAMD activity based on the detection of intraretinal fluid, retinal cystoid abnormalities or subretinal fluid.
| Study | Unit of analysis | Detection of | Number by FFA | OCT sensitivity, % |
|---|---|---|---|---|
| Giani 201130 (SD-OCT) | Eye | Classic CNV | 57 | 90.9 |
| Occult CNV | 36 | 100.0 | ||
| Khurana 201023 (TD-OCT) | Eye | Intraretinal fluid | 29 | 37.9 |
| Retinal cystoid abnormalities | 29 | 34.5 | ||
| Subretinal fluid | 29 | 48.3 | ||
| Khurana 201023 (SD-OCT) | Eye | Intraretinal fluid | 29 | 65.5 |
| Retinal cystoid abnormalities | 29 | 58.6 | ||
| Subretinal fluid | 29 | 69.0 | ||
| van de Moere 200652 (TD-OCT) | Eye | Intraretinal fluid | Not reported | 82.9 |
| Subretinal fluid | Not reported | 47.1 | ||
| CMO | Not reported | 22.9 | ||
| PED | Not reported | 5.7 | ||
| Henschel 200932 (TD-OCT) | Exam | Intraretinal fluid | 31 | 90.3 |
| Subretinal fluid | 31 | 71.0 |
Indocyanine green angiography
One study, by Regillo et al. ,43 in an analysis of 54 pairs of ICG angiograms compared with fluorescein angiograms, obtained from 24 eyes of 21 patients, reported sensitivity of 75.9% and specificity of 88.0% in detecting nAMD activity. It was not possible to ascertain (at participant-level) the prevalence of nAMD. This study was judged as high risk of bias for the index/comparator test and reference standard domains, due to the ICGA–FFA pairs being analysed directly from the computer monitor (ICGA test results interpreted with knowledge of the FFA results, and vice versa) and low risk of bias for the other domains.
Studies directly comparing tests
Time domain optical coherence tomography versus spectral domain optical coherence tomography
One study, by Khurana et al. ,23 compared TD-OCT with SD-OCT in an analysis of 59 eyes of 56 participants. Although sensitivity was considerably higher for SD-OCT than for TD-OCT (89.7% vs. 58.6%), specificity was lower (46.7% vs. 63.3%).
Assessment of other outcomes of interest
Clinical effectiveness
No studies were identified that met our inclusion criteria providing information on clinical effectiveness outcomes (e.g. VA) when treatment was based on OCT compared with FFA findings.
Interpretability of the tests
Only one monitoring study, by van de Moere et al. ,52 reported information relating to the interpretability of the tests. This TD-OCT study reported that, of 136 participants enrolled, 17 (12.5%) were excluded from the analysis due to the poor quality of the OCT or FFA images. The study did not specify how many of these poor quality images were OCT images and how many were FFA.
Acceptability of the tests
No studies were identified that met our inclusion criteria reporting the acceptability of the tests, either to those providing the tests or to those receiving them.
Proportion of participants unable to receive the monitoring test
Two studies reported exclusion criteria relating to eye conditions (see Appendix 7, see Table 49). 23,30 The study by Giani et al. 30 contained the following exclusion criteria: any previous laser treatment, PDT or vitreoretinal surgery on the study eye; significant macular haemorrhage that obscured the lesion; and a spherical refractive error > 6 diopters. The study by Khurana et al. 23 excluded patients with CNV resulting from causes other than AMD.
Other health professionals compared with ophthalmologists interpreting optical coherence tomography findings
No studies were identified meeting our inclusion criteria that reported the performance of other health professionals compared with ophthalmologists in interpreting OCT findings.
Summary of the reviews of diagnostic and monitoring studies
Diagnostic studies
Twenty-two diagnostic studies were included (20 full-text papers, two abstracts). 24–27,29,31,33–42,44–46,48,49,51 The full-text papers were assessed for risk of bias using the QUADAS-2 checklist. The domains in which the greatest number were judged to be at high risk of bias were the patient selection domain (55%, 11/20), for reasons such as inappropriate exclusions and pre-selection of participants, and flow and timing domain (40%, 8/20), for reasons such as the length of time between the index test and the reference standard, and not all participants being included in the analysis. The risk of bias in the index/comparator test and reference standard domains was judged to be unclear in 50% (10/20) and 60% (12/20) of studies respectively. All of the studies were judged to have low concerns in terms of their applicability to the question being addressed by the review.
A descriptive summary of the results of the diagnostic studies with eye as the unit of analysis is shown in Table 16 (excluding studies that only reported detection at phenotype level). Across the studies the median (range) sensitivity was high for OCT (94.5%, range 36.0–100.0%; 10 studies25,27,33,35,36,40,41,45,46,49). Sensitivity was also high for ICGA (93.2%, range 84.6%–100.0%; four studies25,29,44,51) and FAF (93.3%; one study25), followed by PHP (81.5%, range 50.0–84.8%; three studies24,27,29), colour fundus photography (70.0%; one study24) and lowest for Amsler grid (41.7%; one study27). The median (range) specificity for OCT was moderate (73.5%, range 66.0–94.0%; four studies27,40,46,49). Specificity was highest for colour fundus photography (95%; one study24), followed by PHP (84.6% and 87.7%; two studies24,39), and was low for FAF (37.1%; one study25) and ICGA (36.8%; one study29).
| Test | Number of studies | Number of eyes analysed | Median (range) sensitivity, % | Median (range) specificity, % |
|---|---|---|---|---|
| All OCT | 10 | 1117 | 94.5 (36.0–100.0) | 73.5 (66.0–94.0) |
| TD-OCT | 9 | 1096 | 92.3 (36.0–100.0) | 73.5 (66.0–94.0) |
| SD-OCT | 1 | 21 | 100.0 | Not reported |
| Amsler grid | 1 | 46 | 41.7 | Not reported |
| PHP | 3 | 302 | 81.5 (50.0–84.8) | (84.6, 87.7)a |
| Colour fundus photography | 1 | 120 | 70.0 | 95.0 |
| FAF | 1 | 50 | 93.3 | 37.1 |
| ICGA | 4 | 167 | 93.2 (84.6–100.0) | 36.8 |
| TD-OCT + colour fundus photography | 1 | 131 | 74.1 | 92.0 |
| Colour fundus photography + VA | 1 | 66 | 53.0 | 94.0 |
Two studies reported the diagnostic accuracy of combinations of tests. Sensitivity and specificity for TD-OCT plus colour fundus photography46 was 74.1% and 92.0%, respectively, whereas for colour fundus photography plus VA,24 sensitivity was lower at 53.0% but with similarly high specificity at 94.0%.
Four OCT diagnostic studies (all TD-OCT) provided sufficient data for inclusion in a meta-analysis (Table 17). 27,40,46,49 The pooled sensitivity and specificity (95% CI) for all four OCT studies was 88% (46% to 98%) and 78% (64% to 88%) respectively.
| Test | Number of studies | Number of eyes analysed | Pooled estimates (95% CI) | |
|---|---|---|---|---|
| Sensitivity, % | Specificity, % | |||
| All OCT | 4 | 406 | 88 (46 to 98) | 78 (64 to 88) |
Eight diagnostic studies reported the sensitivity of OCT in the detection of specific nAMD phenotypes. 25,33,34,37,38,41,46,49 Four showed equally high sensitivity for the detection of classic CNV compared with occult CNV. 25,34,41,49 In four others, sensitivity for OCT was higher in the detection of classic CNV (range 79–100%) compared with occult CNV (range 13–79%). 33,37,38,46 Four studies reported the sensitivity of ICGA in the detection of specific nAMD phenotypes. 25,29,44,51 Each study reported detection of a different phenotype, with 100% sensitivity for detection of IPCV and type 2 CNV without an occult component, high sensitivity (85.1%) for detection of RAP but lower sensitivity (62.9%) for detection of occult CNV. 25,29,44,51
Monitoring studies
Eight monitoring studies were included (all full-text papers). 23,28,30,32,43,45,52,53 Seven reported OCT,23,28,30,32,45,52,53 five with eye as the unit of analysis23,28,30,52,53 (one of which only reported detection at phenotype level30) and two with test examination as the unit of analysis. 32,45 One study reported ICGA. 43 As with the diagnostic studies, the QUADAS-2 domains in which the greatest number of monitoring studies were judged to be at high risk of bias were the patient selection domain (25%, 2/8),30,45 for reasons such as inappropriate exclusions and pre-selection of participants, and flow and timing domain (25%, 2/8),30,45 for reasons such as the length of time between the index test and the reference standard, and not all participants being included in the analysis. The risk of bias in the index/comparator test and reference standard domains was judged to be unclear in 50% (4/8)23,45,52,53 and 37.5% (3/8)23,45,52 of studies respectively. All of the monitoring studies were judged to have low concerns in terms of their applicability to the question being addressed by the review.
Four OCT monitoring studies, with eye as the unit of analysis, provided sufficient data for inclusion in a meta-analysis (Table 18). The pooled sensitivity and specificity (95% CI) for all four OCT studies was 85% (72% to 93%) and 48% (30% to 67%) respectively. For TD-OCT, the pooled sensitivity and specificity was 70% (56% to 80%) and 65% (48% to 79%). It was not possible to calculate pooled estimates using HSROC methodology for the two SD-OCT studies due to insufficient data. These two studies reported sensitivities of 94% and 90% and specificities of 27% and 47%, which suggests that SD-OCT has higher sensitivity than TD-OCT but lower specificity.
| Test | Number of studies | Number of eyes analysed | Pooled estimates (95% CI) | |
|---|---|---|---|---|
| Sensitivity, % | Specificity, % | |||
| All OCTa | 4 | 242 | 85 (72 to 93) | 48 (30 to 67) |
| TD-OCT | 3 | 149 | 70 (56 to 80) | 65 (48 to 79) |
| SD-OCT | 2 | 152 | Not calculable using HSROC methods | |
Two OCT monitoring studies used test examination as the unit of analysis. The first, in an analysis of 61 pairs of TD-OCT and FFA examinations from 14 patients, reported high sensitivity of 96.8% but low specificity of 36.7%, for CNV based on detection of intraretinal and/or subretinal fluid. The second, in an analysis of 176 pairs of TD-OCT and FFA examinations (number of patients not stated), reported similarly high sensitivity of 95.7% and moderate specificity of 59.0% based on detection of intraretinal or subretinal fluid.
One ICGA monitoring study used test examination as the unit of analysis. In an analysis of 54 pairs of ICGAs compared with fluorescein angiograms, obtained from 24 eyes of 21 patients, sensitivity of 75.9% and specificity of 88.0% was reported for detecting nAMD activity.
Three studies reported OCT sensitivity in detecting activity of specific nAMD phenotypes or nAMD activity based on detection of intraretinal/subretinal fluid. SD-OCT sensitivity was high for the detection of both classic and occult CNV activity (90.9% and 100% respectively) (one study). 30 Sensitivity of TD-OCT for detection of cystoid macular oedema and PED was low (22.9% and 5.7% respectively) (one study). 52 In two studies, sensitivity was higher for detection of nAMD activity based on intraretinal fluid (90.3% and 82.9% respectively) compared with subretinal fluid (71.0% and 47.1% respectively). 32,52
Chapter 5 Assessment of cost-effectiveness
The health economic component of this study explored the evidence for the cost-effectiveness of using OCT for diagnosis and/or monitoring of individuals with nAMD. For this, a two-step approach was used, with (1) a systematic review of economic evaluations to retrieve any readily available evidence on cost-effectiveness, followed by (2) a de novo decision-analytic model to synthesise the available evidence on effectiveness, health-care resources used and costs. Systematic review of economic evaluations reports the systematic review of cost-effectiveness studies and Economic evaluation modelling exercise focuses on the economic model exercise.
Systematic review of economic evaluations
The aim of this review was to retrieve evidence, from the perspective of the UK NHS, on the cost-effectiveness of the use of OCT in the diagnosis and/or monitoring of individuals with nAMD. This was attempted by systematically identifying and quality assessing all economic evaluations comparing strategies that included OCT for diagnosing and/or monitoring of individuals with nAMD.
Inclusion and exclusion criteria
Inclusion criteria required the studies to be full economic evaluations,55 that is, to consider cost and effects for more than one strategy, in order to be included in the review. No restrictions were imposed in the way cost and/or effects were calculated. In addition, at least one of the compared strategies for diagnosis or monitoring of nAMD had to include OCT. Finally, the studies were required to be performed in adults with nAMD.
Search strategy
Studies that reported both costs and outcomes in diagnosing nAMD using OCT were sought from a systematic review of the literature. No language restrictions or limitations to searches were imposed.
Databases searched were MEDLINE (1996–November Week 2 2012), EMBASE (1980–Week 45 2012), MEDLINE In-Process & Other Non-Indexed Citations (14 November 2012), NHS Economic Evaluation Database (inception to October 2012), HTA database (inception to October 2012), Health Management Information Consortium (1979–September 2012), Research Papers in Economics (September 2012) and ARVO meeting abstracts from April 2009. In addition, reference lists of all included studies were scanned to identify additional potentially relevant studies. Full details of the search strategies used are documented in Appendix 1.
Results
From the database searches, 473 hits (titles and abstracts) were retrieved; from these 44 studies were selected for full-text assessment. No studies fulfilled the inclusion criteria as none of these were diagnosis or monitoring interventions for individuals with nAMD.
Economic evaluation modelling exercise
The aim of the economic model was to determine the relative efficiency of strategies for diagnosis and monitoring of individuals with nAMD. Care pathways were developed within the project management group and the project advisory group meetings. The groups initially considered all possible tests (see Chapter 1) and several combinations of these. After subsequent discussions, a number of these options were excluded. For instance, FFA only was originally considered as one of the (monthly) monitoring pathways. However, this option was deemed unfeasible (i.e. FFA is an invasive test) and consequently dropped. Three different strategies were finally selected for the nAMD diagnosis and monitoring stages, respectively, giving a total of nine diagnosis–monitoring combinations.
Diagnosis strategies
-
(Stereoscopic) FFA interpreted by an ophthalmologist. If positive, treat and monitor; if negative, discharge.
-
OCT alone interpreted by an ophthalmologist. If positive, treat and monitor; if negative, discharge.
-
VA, OCT and SLB in all. If positive or unclear, then arrange for stereoscopic FFA. If negative, discharge. This is the strategy for diagnosis that best reflects standard practice.
Monitoring strategies
-
OCT alone (interpreted by an ophthalmologist). If positive, treat; if negative or unclear, review in 1 month’s time.
-
VA, SLB and OCT interpreted together by an ophthalmologist. If positive, treat; if negative, review in 1 month’s time. If unclear, then the ophthalmologist will arrange for a stereoscopic FFA. This is the monitoring strategy that best reflects standard practice.
-
VA and OCT interpreted by a technician or nurse. If negative, review in 1 month’s time. If positive or unclear, refer for ophthalmologist assessment (e.g. SLB and ophthalmologist’s own interpretation of VA and OCT test results). The ophthalmologist will make a decision: if positive, treat; if negative, review in 1 month’s time; if unclear, arrange for stereoscopic FFA.
Monitoring strategy c has been included in the monitoring stage in order to explore the cost-effectiveness of the option, for example, of virtual clinics involving other health-care professionals (e.g. nurses, technicians). Virtual clinics are increasingly used in NHS services for monitoring patients with nAMD. 56
Table 19 shows the final nine combined strategies incorporated into the decision model. All strategies considered monitoring on a monthly basis with a decision to treat when the disease was deemed active (i.e. retinal fluid on OCT). All monitoring strategies that relied on stereoscopic FFA as a final assessment step (e.g. monitoring strategies b and c) would treat if FFA positive, or review in a month’s time if FFA negative. Treatment consisted of one injection only (i.e. 0.5 mg ranibizumab) with review in 1 month’s time.
| Strategy | Strategy label | Diagnostic pathway | Monitoring pathway | Treatment |
|---|---|---|---|---|
| 1 | FFA & OCT | FFA interpreted by an ophthalmologist. If positive, treat and monitor; if negative, discharge | OCT alone (interpreted by an ophthalmologist). If positive, treat. If negative or unclear review in 1 month | One monthly injection if disease deemed active |
| 2 | FFA & Ophthalmologist | FFA interpreted by an ophthalmologist. If positive, treat and monitor; if negative, discharge | VA, SLB and OCT interpreted together by an ophthalmologist. If positive, treat; if negative, review in a month’s time. If unclear, then the ophthalmologist will arrange for stereoscopic FFA | One monthly injection if disease deemed active |
| 3 | FFA & Nurse | FFA interpreted by an ophthalmologist. If positive, treat and monitor; if negative, discharge | VA and OCT interpreted by a technician or nurse. If negative, review in a month. If positive or unclear, referral for an ophthalmologist assessment (e.g. SLB and own interpretation of VA and OCT test results). If assessment positive, treat; if negative, review in a month time; if unclear, arrange for stereoscopic FFA | One monthly injection if disease deemed active |
| 4 | OCT & OCT | OCT alone interpreted by an ophthalmologist. If positive, treat and monitor; if negative, discharge | OCT alone (interpreted by an ophthalmologists). If positive, treat. If negative or unclear review in 1 month | One monthly injection if disease deemed active |
| 5 | OCT & Ophthalmologist | OCT alone interpreted by an ophthalmologist. If positive, treat and monitor; if negative, discharge | VA, SLB and OCT interpreted together by an ophthalmologist. If positive, treat; if negative, review in a month’s time. If unclear, then the ophthalmologist will arrange for stereoscopic FFA | One monthly injection if disease deemed active |
| 6 | OCT & Nurse | OCT alone interpreted by an ophthalmologist. If positive, treat and monitor; if negative, discharge | VA and OCT interpreted by a technician or nurse. If negative, review in a month. If positive or unclear, referral for an ophthalmologist assessment (e.g. SLB and own interpretation of VA and OCT test results). If assessment positive, treat; if negative, review in a month’s time; if unclear, arrange for stereoscopic FFA | One monthly injection if disease deemed active |
| 7 | Ophthalmologist & OCT | VA, OCT and SLB in all interpreted by an ophthalmologist. If negative, discharge. If positive or unclear, then arrange for stereoscopic FFA. If FFA positive, treat and monitor; if negative, discharge | OCT alone (interpreted by an ophthalmologist). If positive, treat. If negative or unclear review in 1 month | One monthly injection if disease deemed active |
| 8 | Ophthalmologist & Ophthalmologist | VA, OCT and SLB in all interpreted by an ophthalmologist. If negative, discharge. If positive or unclear, then arrange for stereoscopic FFA. If FFA positive, treat and monitor; if negative, discharge | VA, SLB and OCT interpreted together by an ophthalmologist. If positive, treat; if negative, review in a month’s time. If unclear, then the ophthalmologist will arrange for stereoscopic FFA | One monthly injection if disease deemed active |
| 9 | Ophthalmologist & Nurse | VA, OCT and SLB in all interpreted by an ophthalmologist. If negative, discharge. If positive or unclear, then arrange for stereoscopic FFA. If FFA positive, treat and monitor; if negative, discharge | VA and OCT interpreted by a technician or nurse. If negative, review in a month. If positive or unclear, referral for an ophthalmologist assessment (e.g. SLB and own interpretation of VA and OCT test results). If assessment positive, treat; if negative, review in 1 month; if unclear, arrange for stereoscopic FFA | One monthly injection if disease deemed active |
The economic model
A Markov model approach was selected for the decision-analytic model exercise. 57–60 Markov models have Markov states where individuals spend a period of time, named a ‘cycle’. At the end of each cycle the individuals can remain in their current Markov state or move to another state. The probabilities of moving to other Markov states or remaining in the current state are named ‘transition probabilities’. Individuals in the model would accrue costs and benefits (e.g. ‘life-years’) depending on the time spent in each Markov state and the interventions and/or events modelled within each Markov state. Markov models are particularly suitable to model recurrent issues and chronic diseases. They allow incorporating health states to reflect the movement of the patients during diagnosis and monitoring. In the current study, model states reflect the underlying condition (e.g. nAMD active or inactive) together with the decision on treatment (e.g. treated or untreated nAMD) and VA states of the individuals (Table 20). In all these models, an absorbing state is included where all individuals would end up if the model was run for a sufficiently long period of time (e.g. death state).
| Visual health states (Snellen fractions) | Visual health status | |
|---|---|---|
| 1 | > 6/12 | Normal VA |
| 2 | ≤ 6/12 to > 6/24 | Mild VA loss |
| 3 | ≤ 6/24 to > 6/60 | Moderate VA loss |
| 4 | ≤ 6/60 to > 3/60 | Severe VA loss |
| 5 | ≤ 3/60 | Profound visual loss/blindness |
The present model incorporates a first diagnosis stage combined with a recurrent (monthly) monitoring phase.
The Markov models
This section presents a stepwise introduction to the Markov models used to compare the alternative strategies. Individuals’ VA status is set aside for the moment to focus on the other two issues and assumptions underpinning the movement of individuals throughout the model: (1) the underlying disease condition (e.g. if the disease is present or not and, if present, its active or inactive status) as well as (2) the diagnosis or monitoring test results on which the treatment decision will depend (i.e. a positive result will trigger a decision to treat and a negative results will trigger a decision not to treat). Figure 11 shows the schematic diagram of the final model used for the economic evaluation for this study.
FIGURE 11.
Markov model schematic diagram assuming imperfect information at diagnosis and monitoring stages. ‘Inactive’ = underlying condition regarded as inactive nAMD when the disease was actually not present.
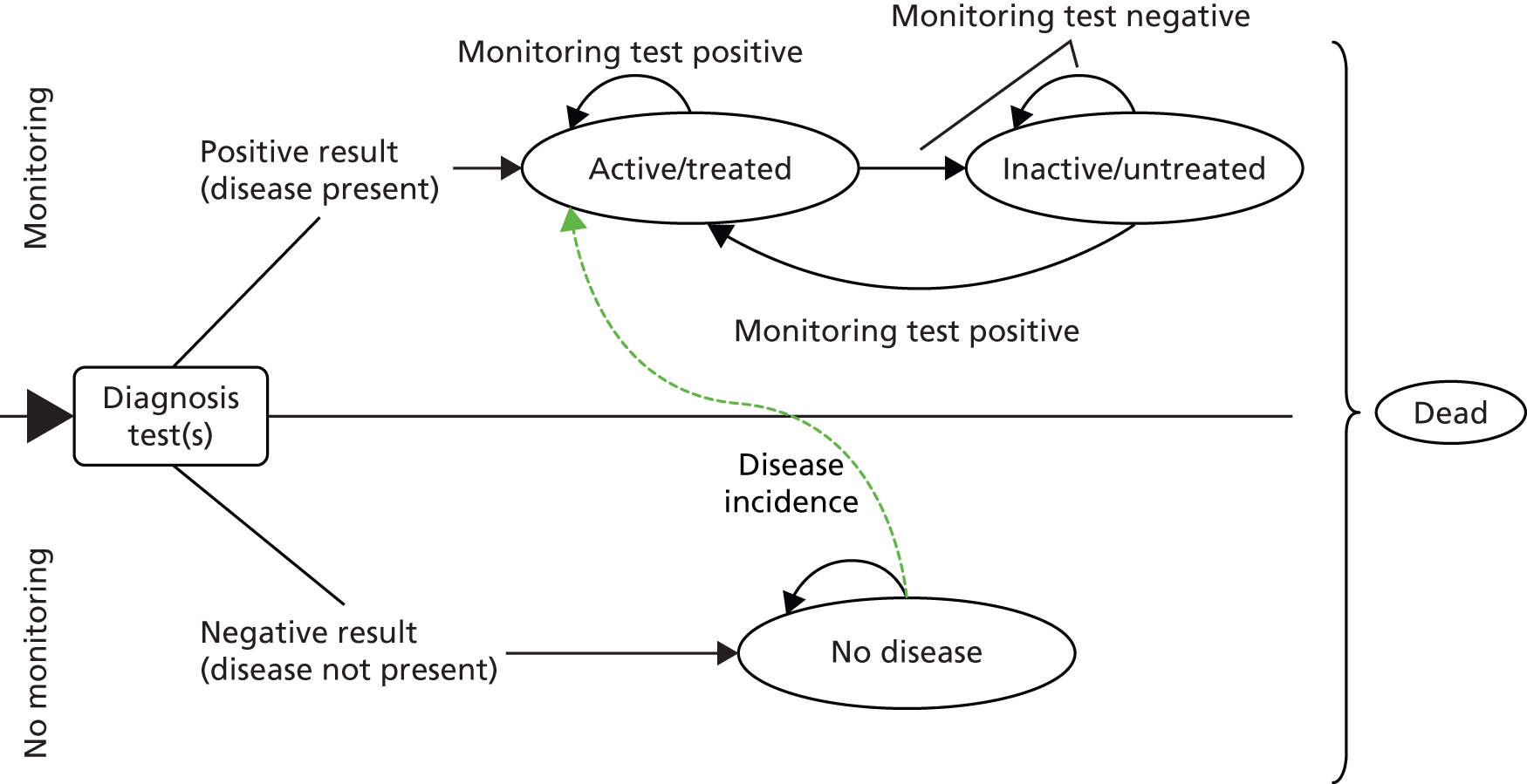
This section presents three schematic diagrams for this model. The figures differ in the assumptions made with respect to the information retrieved from the diagnosis and/or monitoring test or assessments. Namely, if perfect information from the tests or assessments is assumed, then there would be no FP or FN results (i.e. equivalent to assuming that sensitivity and specificity are equal to 1). That is, the underlying condition is detected with certainty. When this assumption is relaxed, then the possibility of incorrect assessments appears.
Perfect information from diagnosis and monitoring tests
Figure 12 assumes perfect information at diagnosis and monitoring stages in the model. The whole modelled cohort starts at the black arrow on the left hand side of the figure (corresponding to an initial Markov model stage). The assumption of perfect information means that, at diagnosis stage, all individuals with the disease will have a positive result while all those without the disease will obtain a negative result. Individuals with a positive result will go to a monitoring scheme while those with a negative result will be discharged. Those individuals with the disease and positive results will start within a Markov model state with an ‘active disease and under treatment’ (e.g. ‘active/treated’ state). Note that ‘active’ refers to the underlying condition while ‘treated’ or not depends on the test or assessment result.
FIGURE 12.
Markov model schematic diagram assuming perfect information at diagnosis and monitoring stages.

Assuming monthly monitoring visits and assessments, a positive result at a monitoring visit means the individual’s disease is active (assuming, again, perfect information and no possibility of FP or FN results) and will therefore mean that the person remains in the ‘active/treated’ Markov state. If a negative result from the monitoring assessment is obtained, then it would mean that the individual’s disease has become inactive and the decision not to administer treatment will follow. In this case, the individual will move to the ‘inactive/untreated’ Markov state. At each Markov cycle (monthly) individuals can become active or inactive; this status would be detected at the next monitoring visit with a positive or negative result, and the individual will either move from or stay in the corresponding Markov model state with a consistent treatment decision.
Individuals without the disease at the moment of first diagnosis could develop the disease in the future (i.e. incident cases among the population). In the model (see Figures 11–13), it was assumed that these individuals would be correctly diagnosed within a second visit and eventually moved to be monitored within the ‘active/treated’ state. Finally, the ‘dead’ state is the absorbing state in this model (i.e. a state that individuals cannot move out of); individuals can move from any other Markov state into the ‘dead’ absorbing state.
Imperfect information from diagnosis test combined with perfect information from monitoring tests
Figure 13 shows a similar schematic diagram but in this case there is imperfect information at the moment of first diagnosis. After this initial diagnostic intervention, further diagnosis and/or monitoring assessments will be done with certainty (e.g. assuming perfect information). This opens the possibility of obtaining TP, TN as well as FP and FN results from the initial diagnosis test/s. Individuals with positive results, therefore, might not have nAMD whereas individuals with negative diagnostic test results might actually have the disease. This situation will have an effect on the Markov states the individuals will start at after diagnosis. Those with a TP result will start with their active disease being treated and eventually move to an inactive state (e.g. ‘inactive/untreated’) depending on the treatment effect. Individuals with a FP result will not have nAMD but will be treated and monitored. However, this treatment cannot be effective as these people did not have the disease. As this schematic diagram assumes perfect information at the monitoring phase, these individuals would be correctly assessed in their subsequent monitoring visits, moving to the ‘inactive/untreated’ state.
FIGURE 13.
Markov model schematic diagram assuming imperfect information at diagnosis and perfect information at monitoring stage. ’Inactive’ = underlying condition regarded as inactive nAMD when the disease was actually not present.
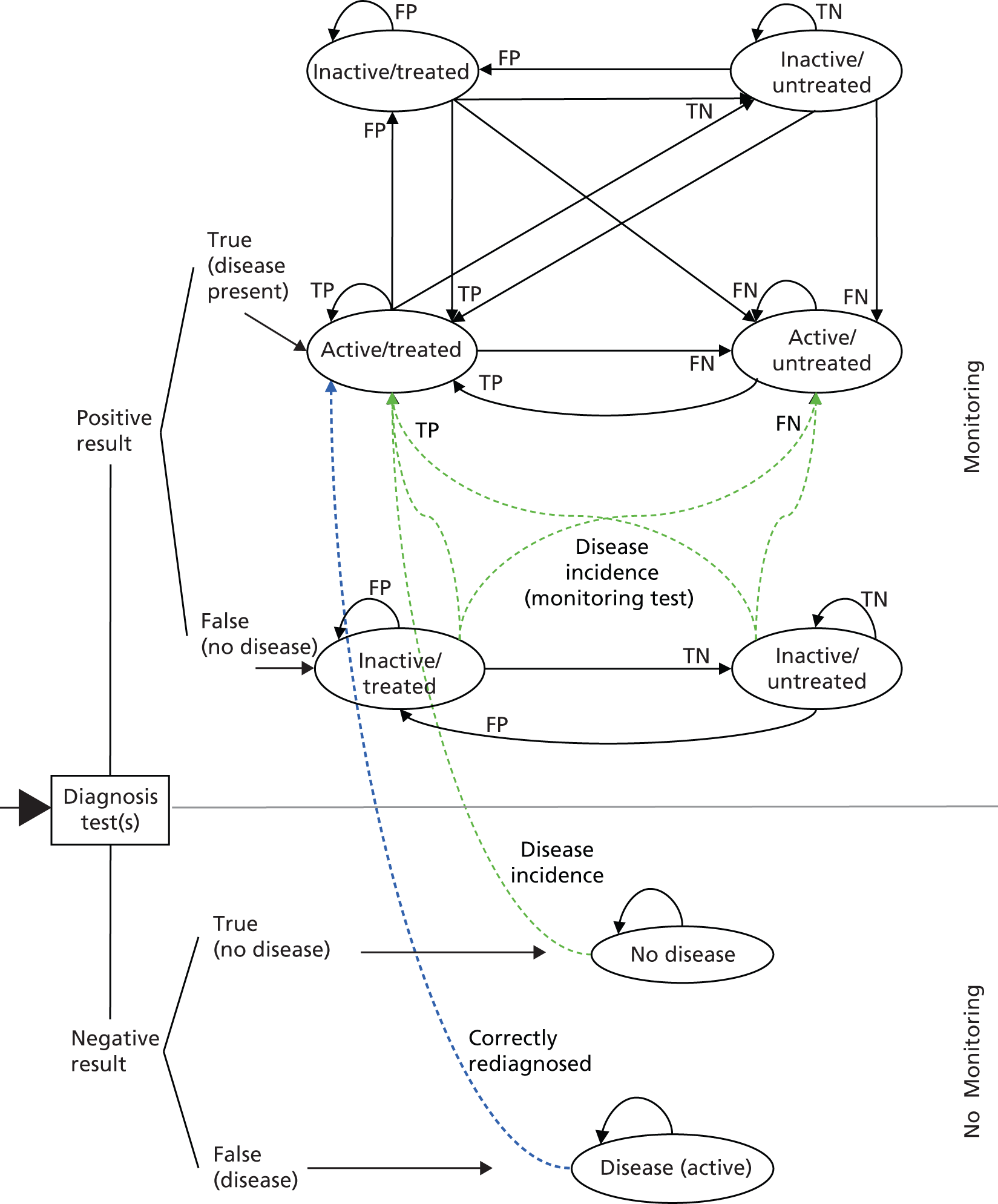
In addition, if the person has a negative result at diagnosis, this could be a TN or a FN result. In either case the individual would be discharged under the belief that nAMD was not present. If TN, meaning that the disease was not present, the individual will start at the ‘no disease’ state and will remain at that stage unless they develop nAMD. If FN (patients with the disease and negative test), the person will start within the ‘disease (active)’ state.
Finally, an identical assumption of using FFA for diagnosis for those presenting for a second time (rediagnosis) is followed for those with FN results at first diagnosis. These people will start to be monitored and moved to the ‘active/treated’ state after second presentation for diagnosis. A further assumption is used for this subgroup: based on expert opinion, these nAMD individuals that have been missed at first diagnosis will present for rediagnosis within 3 months. The rationale behind this was the natural history of the disease and the belief that nAMD would advance with VA deterioration making the individual return for a further eye check.
Imperfect information from diagnosis and monitoring tests
Figure 11 shows the schematic diagram for the actual Markov model used. In this case, imperfect information at diagnosis as well as monitoring phases was assumed. The cases for those with first diagnosis negative results are identical to those in Figure 13 (lower part of Figure 11). However, the diagram for those with positive results at first diagnosis will differ.
Individuals with TP results at first diagnosis will start as before within the ‘active/treated’ state. After this, depending on the underlying condition (e.g. active or inactive) and the monitoring assessment result (e.g. positive or negative, with a positive result reflecting the presence of disease activity), individuals will move to alternative Markov states (e.g. ‘inactive/untreated’; ‘inactive/treated’; ‘active/untreated’). The arrows in the figure show the direction in which individuals can move due to their underlying condition and assessment while the arrow labels refer to the result of the assessment (e.g. TN, TP, FN, FP).
A further assumption in the model is that those individuals under monitoring who do not have nAMD (i.e. ‘Inactive’ states) that subsequently become nAMD would be detected by the monitoring strategy test/s. This monitoring strategy could include FFA (perfect information test) or other non-perfect information test (e.g. OCT alone). Therefore, these individuals that now have nAMD could move to ‘active/treated’ or ‘active/untreated’ depending on positive or negative monitoring assessment respectively.
Markov model states and health status valuation link
The former diagrams show how individuals can move in the model according to their underlying condition and the result of the test/s or assessments. However, it is not possible to attach utility weights to these Markov states. In essence, individuals can experience alternative active or inactive disease but no difference in their reported health status. The economic model attaches utility weights according to, mainly, VA. Therefore, the effect on health status will come through the deterioration in VA, whereas VA deterioration will result from the fact of individuals being misdiagnosed (e.g. no nAMD when actually the disease was present) or misclassified as inactive when their true condition was active nAMD.
In terms of the presented diagrams, the number of Markov states is multiplied by the number of VA ranges considered by the model. Therefore, there is a trade-off between the number of VA ranges in order to reflect differences in VA – and patient-reported health status – and the model complexity. Utility differences between the alternative model strategies result from the different periods of time individuals are misclassified within each strategy. It was considered that five VA states (see Table 20) would give sufficient refinement for utility differences to be reflected. This approach has been used in other models in this area of health care. 61 Therefore, each strategy (i.e. each Markov model) has 32 Markov model states [e.g. four VA states multiplied by six monitoring states, plus four VA states multiplied by one nAMD undiagnosed state, plus profound visual loss/blindness, a ‘no disease’ state (normal VA only), the absorbing state ‘dead’, and an initial state for first diagnosis].
Figure 14 shows a Markov model schematic diagram for the VA states considered in the model. Arrows in the figure show the possible movements in the model in one cycle (e.g. 1 month). Individuals’ VA can remain the same, improve or deteriorate in one particular cycle. Individuals can have their VA improved and move one level up at the end of a cycle; however, their VA can deteriorate and move one or two levels down from their current VA state. Finally, the model considered that a VA deterioration of ≤ 3/60 (i.e. profound visual loss/blindness) was not reversible and the individual was referred to supportive care.
FIGURE 14.
Markov model schematic diagram for VA states.
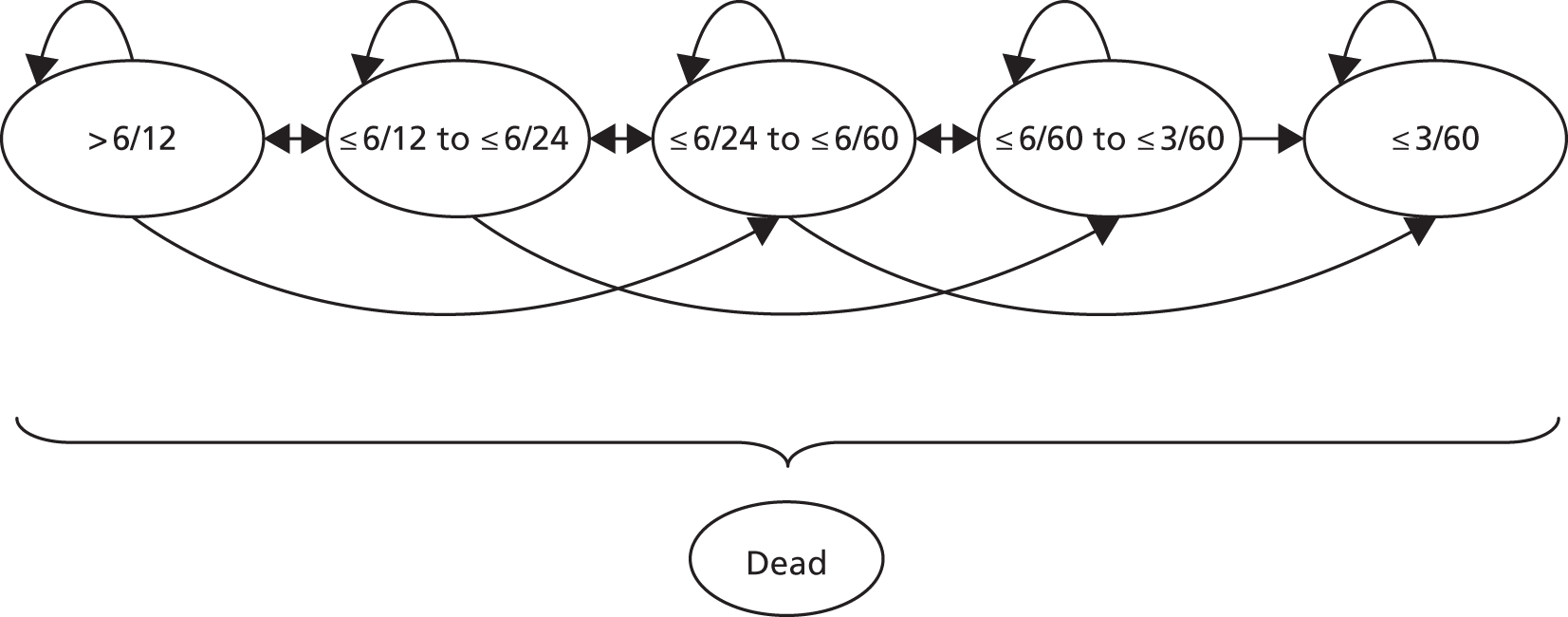
Parameter estimates used in the economic model
The parameter estimates required to populate the economic model were obtained from the systematic review of diagnostic and monitoring studies (see Chapter 4) as well as structured and focused literature searches. When no suitable data resulted from these searches, expert opinion was sought. The next section gives details of the probabilities, unit costs and utility weights used in the model. The section also provides details of the probability distributions used for the probabilistic sensitivity analysis. 62 Probabilistic sensitivity analysis involves attaching probability distributions to model parameters and conducting a number of Monte Carlo simulations (e.g. 1000). In each of these simulations a set of parameter values will be drawn from the attached distributions, the model is run and results calculated. It is possible then to obtain a distribution of the model cost-effectiveness results that reflects the overall parameter uncertainty in the economic evaluation model. 63,64
Probabilities
Table 21 shows data on nAMD prevalence, incidence and VA at the start of the model run. Colquitt et al. 61 reviewed studies assessing the prevalence and incidence of AMD and nAMD. The setting for this economic evaluation was secondary care; therefore, the prevalence rate to inform the model should be that corresponding to the group of individuals referred to hospital eye services with a suspected nAMD diagnosis. The prevalence rate used was obtained from the literature retrieved by the systematic review of test accuracy and agreed within the project management and advisory groups. An overall incidence of 1% per year was used based on Mitchell et al. 65 These incidence figures, presented for Australia, were similar to the results by van Leeuwen et al. 66 for the Rotterdam study but were reported in a form that could be readily incorporated into the economic model. Mortality data were obtained from Interim Life Tables for England and Wales (2009–11). 16 No difference in mortality rates were found when comparing age-specific mortality rates form the Interim Life Tables and those from the Comparison of Age-Related Macular Degeneration Treatments Trials (CATT)8 and the Inhibit VEGF in Age-related choroidal Neovascularisation (IVAN)9 studies. Therefore, no excess mortality was included due to nAMD. 67,68 However, excess mortality risk was incorporated for the last disease VA stage (profound visual loss/blindness – VA ≤ 3/60).
| Variable | Value | Probability distribution | Source | |
|---|---|---|---|---|
| Epidemiological data | ||||
| Prevalence for nAMD | 70% | Uniform (0.6; 0.8) | Expert opinion and articles from SR test accuracy | |
| Incidence rate of nAMD (monthly) | 0.084% | Gamma (1; 1190) | Mitchell et al.65 | |
| Mortality | Various | Interim Life Tables, England and Wales (2009–11)16 | ||
| Profound visual loss/blindness excess mortality | 17% | Uniform (0.1; 0.5) | Assumption | |
| Cohort details at start | ||||
| Age (years) | 65 | n/a | n/a | Assumption based on expert opinion |
| Mean VA | ||||
| Individuals with nAMD | ||||
| ≤ 6/12 to > 6/24 state | 100% | n/a | n/a | Assumption based on expert opinion and CATT and IVAN RCTs mean VA at start |
| Individuals without nAMD | ||||
| > 6/12 | 100% | n/a | n/a | Assumption based on expert opinion |
Table 21 also shows probability distributions defined for the probabilistic sensitivity analysis. Uninformative uniform distributions were used for nAMD prevalence and profound visual loss/blindness excess mortality. Ranges for defining these were assumptions based on data from the literature if available (e.g. from the review of test accuracy). A gamma distribution was defined for nAMD incidence based on mean and standard deviation (e.g. 1/10 of the mean) using the tool provided by TreeAge (TreeAge Software, Inc., Williamstown, MA, 2013).
The cohort start age was set at 65 years as this is the age where particular changes are observed in the retina and macula (Dr Noemi Lois and Project Advisory Group, NHS Grampian, 2012, personal communication). In addition, mean VA at the start was set at between ≤ 6/12 to > 6/24 for those individuals with nAMD. This was agreed to be the most common VA at presentation by experts and also the mean VA at baseline in the CATT and IVAN studies. 8,9
Table 22 presents diagnostic test performance data. As mentioned above, three strategies were defined for diagnosis within the economic model. For each of these strategies, sensitivity and specificity data were needed, specifically for FFA, OCT, and ophthalmologist assessment (i.e. with VA test, SLB, and the results from the OCT). FFA interpreted by an ophthalmologist was stated as the reference standard for the diagnosis of nAMD; therefore, perfect information was assumed from this test, with sensitivity and specificity equal to 1. OCT sensitivity and specificity were obtained from the systematic review of diagnostic studies. These data correspond to OCT pooled estimates (four studies, number of eyes 406). 27,40,46,49 No studies were identified on the ophthalmologist assessment diagnostic performance. Hence, sensitivity and specificity estimates were derived from expert opinion.
| Variable | Value | Range | Probability distribution | Source |
|---|---|---|---|---|
| FFA | ||||
| Sensitivity | 1 | n/a | n/a | Assumption |
| Specificity | 1 | n/a | n/a | Assumption |
| OCT | ||||
| Sensitivity | 0.88 | 0.46–0.98 | Beta(36.3; 4.9) | Systematic review of diagnostic studies |
| Specificity | 0.78 | 0.64–0.88 | Beta(82.9; 23.4) | Systematic review of diagnostic studies |
| Ophthalmologist assessment (with VA, OCT and SLB) | ||||
| Sensitivity | 0.99 | Beta(0.22; 0.002) | Assumption based on expert opinion, using the systematic review results as a starting point | |
| Specificity | 0.9 | Beta(9.1; 1) | Assumption based on expert opinion, using the systematic review results as a starting point | |
| Unclear | 0.1 | 0.0–0.5 | Beta(89.9; 809.1) | Assumption based on expert opinion |
Sensitivity and specificity data are bounded between 0 and 1. Therefore, beta distributions were defined for probabilistic sensitivity analysis. For OCT, these were obtained using mean values and standard deviation in order to obtain values within the 95% CI provided by the systematic review of diagnostic studies (see Chapter 4, Table 17). Probability distributions for ophthalmologist diagnosis assessment were obtained using the approximation tool provided by TreeAge, based on mean and standard deviation (e.g. 1/10 of mean).
Table 23 shows similar data to Table 22 but for monitoring of individuals with nAMD. FFA was also stated as the reference standard to detect disease activity; therefore, perfect information was assumed, with sensitivity and specificity defined as equal to 1. OCT monitoring sensitivity and specificity data were obtained from the systematic review of test performance (see Chapter 4). Pooled estimates (e.g. four studies, n = 242), were used. 23,28,30,53 No studies were identified reporting the diagnostic performance of nurse or technician assessment, or for ophthalmologist assessment. Therefore, estimates for the sensitivity and specificity of these strategies were derived from expert opinion.
| Variable | Value | Range | Probability distribution | Source |
|---|---|---|---|---|
| FFA | ||||
| Sensitivity | 1 | n/a | n/a | Assumption |
| Specificity | 1 | n/a | n/a | Assumption |
| OCT | ||||
| Sensitivity | 0.85 | 0.72–0.93 | Beta(105; 18.5) | Systematic review of monitoring studies |
| Specificity | 0.48 | 0.30–0.67 | Beta(32.8; 35.5) | Systematic review of monitoring studies |
| Technician/nurse assessment (VA and OCT) | ||||
| Sensitivity | 0.9 | Beta(108.9; 12.1) | Assumption based on expert opinion, using the systematic review results as a starting point | |
| Specificity | 0.6 | Beta(72.6; 48.4) | Assumption based on expert opinion, using the systematic review results as a starting point | |
| Unclear | 0.1 | Beta(89.9; 809.1) | Assumption based on expert opinion | |
| Ophthalmologist assessment (VA, OCT and SLB) | ||||
| Sensitivity | 0.97 | Beta(2.51; 0.08) | Assumption based on expert opinion, using the systematic review results as a starting point | |
| Specificity | 0.8 | Beta(19.2; 4.8) | Assumption based on expert opinion, using the systematic review results as a starting point | |
| Unclear | 0.1 | Beta(89.9; 809.1) | Assumption based on expert opinion | |
A similar approach to the one used for the sensitivity and specificity of diagnostic tests was used for this information for monitoring tests. Beta probability distributions were approximated and defined using mean and standard deviation (e.g. 1/10 of the mean) values. The range of values of OCT used in the model did not exceed the 95% CI values obtained from the systematic review of monitoring studies (i.e. OCT range data in Table 23).
Disease progression in the model was defined in terms of VA changes. Gaining or losing three lines in the Snellen chart (approximately 15 letters in the ETDRS chart) was assumed to make individuals move from their current Markov model state to the next level (see Table 20 and Figure 14). Data for this were obtained from Rosenfeld et al. 69 [i.e. the Minimally Classic/Occult Trial of the Anti-VEGF Antibody Ranibizumab in the Treatment of Neovascular Age-Related Macular Degeneration (MARINA) study]. This study was based in the USA, involved 716 participants and compared monthly treatment with ranibizumab (0.3 mg, n = 238 or 0.5 mg, n = 240) against sham injection (n = 238). Data from treatment (0.5 mg) and control groups were used to calculate monthly progression probabilities for active treated and non-treated individuals respectively. No VA progression was assumed for nAMD inactive individuals as well as non-AMD individuals.
Beta distributions were attached to VA progression data for probabilistic sensitivity analysis (Table 24). Unfortunately, there were no data available to construct CIs around mean values used in the model. As such, probability distributions parameter values were developed using mean values and assuming 1/10 of mean values for standard errors.
| Variable | Year 1 | Year 2 onwards | ||
|---|---|---|---|---|
| Value | Probability distribution | Value | Probability distribution | |
| Treatment | ||||
| Gain at least three lines | 0.0338 | Beta(96.6; 2761.9) | 0.0167 | Beta(98.3; 5777) |
| Gain or lose less than three lines | Default | Default | ||
| Lose between three and six lines | 0.0036 | Beta(99.6; 27817) | 0.0032 | Beta(99.7; 30634) |
| Lose six lines or more | 0.0010 | Beta(99.9; 99252) | 0.0011 | Beta(99.9; 94640) |
| No treatment | ||||
| Gain at least three lines | 0.0043 | Beta(99.6; 23244) | 0.0016 | Beta(99.8; 61799) |
| Gain or lose less than three lines | Default | Default | ||
| Lose between three and six lines | 0.0221 | Beta(97.8; 4331) | 0.0116 | Beta(98.8; 8431) |
| Lose six lines or more | 0.0128 | Beta(98.7; 7627) | 0.0107 | Beta(98.9; 9171) |
Additional data were required on disease status, namely the probability of becoming active when the individual’s disease was inactive and under no treatment, as well as the probability of becoming inactive when the individual’s disease was active and under treatment. First year data for these were developed using data from the IVAN study (Dr Chris Rogers, University of Bristol, 12 June 2013, personal communication). The IVAN study was a 2 × 2 factorial design and adults with untreated nAMD were randomised into four groups: ranibizumab or bevacizumab, given either every month (continuous) or as needed (discontinuous). All individuals were reviewed on a monthly basis. Survival data for participants’ first treatment failure (e.g. subretinal fluid, increasing intraretinal fluid, or fresh blood) for the discontinuous arm (n = 302) were used to develop mean probability values. All individuals were active at baseline and 95% of these did not fail the retreatment criteria (i.e. did not need to be treated) at 3 months. This rate was used to obtain the monthly probability of becoming inactive when active and under treatment. 62 At month 6, 54% of individuals were still inactive. The difference between the proportion of inactive individuals at months 3 and 6 was used to develop the probability of becoming active when inactive and under no treatment (Table 25). Probability distributions were developed using the 95% CI from the IVAN study survivor function using Crystal Ball software (release 11.1.2.0.00, 2010, Oracle Corporation, Redwood Shores, CA, USA) (see Table 25).
| Variable | Value | Probability distribution | Source |
|---|---|---|---|
| Probability of becoming | |||
| Inactive when active and under treatment | |||
| Year 1 | 0.616 | Beta(176.6; 110) | Based on data from IVAN study9 |
| Year 2 onwards | 0.365 | Beta(63.1; 110) | Based on data from CATT study8 |
| Active when inactive and under no treatment | |||
| Year 1 | 0.306 | Beta(148; 335) | Based on data from IVAN study9 |
| Year 2 onwards | 0.097 | Gamma(100; 1029) | Based on Horster et al.70 |
| Active when inactive and under treatment | 0.5 × active when inactive and under no treatment | ||
Second year data for the probability of becoming inactive were developed using data from the CATT study. The inclusion criteria and the treatment group for the CATT study were similar to that of the IVAN study. However, within the IVAN study three monthly injections were administered when participants failed the disease inactive criteria. The CATT study administered one injection only and reviewed participants in 1 month’s time before making a further treatment decision. A monthly probability was sought in order to obtain the CATT study mean number of injections within the as needed arm at 2 years. A beta distribution was attached based on mean value and 1/10 of the mean value as standard error (TreeAge software).
Second year data for the probability of becoming active when participants were inactive and under no treatment was developed using data reported by Horster et al. 70 The authors reviewed data on all patients receiving intravitreal ranibizumab injections for nAMD at the University of Cologne, Germany. Eyes with at least two recurrences (i.e. reappearance of intraretinal or subretinal fluid on OCT, and/or leakage on angiography) were selected. The mean follow-up time (months) and number of recurrences were 28.8 and 2.8 respectively.
A number of individuals that were inactive at 3 months within the monthly treatment group in the IVAN study9 failed the no retreatment criteria (e.g. subretinal fluid, increasing intraretinal fluid, or fresh blood) in subsequent months. This means that, even under monthly treatment, inactive individuals could become active again. Based on this, half the probability of becoming active when inactive and under no treatment was assumed for the probability of becoming active when inactive and under treatment.
Diagnosis or monitoring strategies could result in over- or undertreatment; therefore, it was believed important to include adverse events as a result of treatment. Two recent studies8,9 report systemic and ocular adverse event rates. It was not clear from inspection of these data that systemic adverse events could be due to treatment of nAMD. Therefore, only ocular adverse events were included in the model. Table 26 shows monthly estimates for the proportion of individuals that were under treatment that experienced cataract, endophthalmitis, glaucoma, retinal detachment and uveitis.
Costs
Table 27 shows cost estimates used in the model. Prices are expressed in 2011–12 pounds sterling (£). Strategy assessment costs were a combination of the cost of a visit (e.g. ophthalmologist, nurse or technician) and the cost of a particular test used for the assessment (e.g. FFA or OCT). For instance, the diagnosis cost for strategies where diagnosis was conducted using FFA only was calculated adding up the cost of an ophthalmologist visit and the cost for an FFA (e.g. £79.74 + £117.26 = £197.00). NHS reference costs were used for all but the ranibizumab unit costs in Table 27, for which British National Formulary (BNF) data were used (£742.17). 12 The unit cost for face-to-face consultant-led follow-up attendance that resulted in non-admission for the ophthalmology service was used for the cost of a diagnosis or monitoring visit to the ophthalmologist (£79.74). Likewise, non-consultant led was used for the cost of a nurse or technician monitoring visit (£58.53). Minor vitreous retinal procedures cost category [Healthcare Resource Group (HRG) BZ23Z code] was used to cost FFA (£117.26). Finally, after consultation with clinical experts, an ultrasound scan (HRG RA23Z Ultrasound scan, less than 20 minutes) was deemed more likely to reflect the cost of an OCT test (£51.27).
| Variable | £ (2011–12) | Range | Probability distribution | Source |
|---|---|---|---|---|
| Ophthalmologist visit | 79.74 | 68–86 | Gamma(309.9; 3.9) | NHS Reference Costs 2011–12 (consultant led: follow-up attendance non-admitted face to face. 130: ophthalmology)11 |
| Nurse/technician visit | 58.53 | 42–71 | Gamma(34.3; 0.59) | NHS Reference Costs 2011–12 (non-consultant led: follow-up attendance non-admitted face to face. 130: ophthalmology)11 |
| FFA | 117.26 | Gamma(25; 0.21) | NHS Reference Costs 2011–12 (HRG BZ23Z minor vitreous retinal procedures)11 | |
| OCT | 51.27 | 32–62 | Gamma(48.8; 0.95) | NHS Reference Costs 2011–12 (HRG RA23Z Ultrasound scan, less than 20 minutes)11 |
| Treatment | ||||
| Medication ranibizumab | 742.17 | Gamma(4; 0.01) | BNF12 | |
Gamma probability distributions were defined for unit cost data for probabilistic sensitivity analysis as these are defined non-negative and provide a possibility of a right tail that could account for few very high unit cost cases. Ranges for reference cost based data are also reported in Table 27; these are lower and upper quartiles. These were used to tailor cost probability distributions.
The cost of profound visual loss/blindness from the NHS and Personal Social Services perspective was calculated following Colquitt et al. 61 The authors used proportion for service utilisation developed by Meads and Hyde71 (Table 28). The unit costs reported by Colquitt et al. 61 were updated using Hospital and Community Health Service specific price inflation index (base 2005 = 100) for March 2012 (e.g. £121.85). Using an alternative weekly cost figure of £497 for residential care (the item in the list with higher unit cost) reported by Curtis,72 results in an annual cost of £556 and £537 for the first and subsequent years, respectively, and these were used as the basis for deterministic sensitivity analysis.
| Variable | Requiring (%) | Cost (£, 2005) | Cost (£, 2012) | Annual cost (£) | Monthly cost (£) |
|---|---|---|---|---|---|
| Severe sight impairment registration | 95 | 115 | 140 | 133 | 11.09 |
| Low-vision aids | 33 | 150 | 183 | 60 | 5.03 |
| Low-vision rehabilitation | 11 | 259 | 316 | 35 | 2.89 |
| Community care | 6 | 6552 | 7984 | 479 | 39.92 |
| Residential care | 30 | 13,577 | 16,544 | 4963 | 413.59 |
| Depression | 39 | 431 | 525 | 205 | 17.07 |
| Hip replacement | 5 | 5379 | 6554 | 328 | 27.31 |
| Total year 1 | 6203 | 517.00 | |||
| Total year 2+ | 5975 | 498.00 |
Utility weights
Guidelines for economic evaluation of health-care technologies in the UK advocate the use of a preference-based measure of utility. 73 We conducted a focused search for these data for AMD individuals. It was confirmed that one group had the majority of studies in this area74,75 and data from Brown et al. 74 were included in the economic model. The study by Brown et al. 75 used the time trade-off approach on 72 consecutive patients seen at the Retina Vascular Unit at Wills Eye Hospital, Philadelphia, USA, to obtain utility weights for alternative VA scores. Table 29 presents utility weights used in the economic model according to the Markov model health state. CIs were also obtained from Brown et al. 74 Mean utility weights and CIs were used to define beta distributions (see Table 29) for probabilistic sensitivity analysis.
| Health state | Mean | 95% CI | Probability distribution | Source |
|---|---|---|---|---|
| > 6/12 | 0.89 | 0.82 to 0.96 | Beta(12.7; 1.6) | Colquitt et al.61 based on Brown et al.74 |
| ≤ 6/12 to > 6/24 | 0.81 | 0.73 to 0.89 | Beta(18.7; 4.4) | |
| ≤ 6/24 to > 6/60 | 0.57 | 0.47 to 0.67 | Beta(42.4; 32) | |
| ≤ 6/60 to > 3/60 | 0.52 | 0.38 to 0.66 | Beta(51.4; 47.4) | |
| ≤ 3/60 | 0.4 | 0.29 to 0.50 | Beta(59.6; 89.4) | |
| Utility decrements (monthly) due to adverse events | ||||
| Cataract | 0.012 | Brown et al.75 | ||
| Endophthalmitis | 0.025 | |||
| Retinal detachment | 0.023 | |||
| Uveitis | 0.025 | Assumed equal to endophthalmitis | ||
Utility decrements due to adverse events were retrieved from Brown et al. 75 The authors derived utility values from 233 patients with AMD and decrement values were obtained from individuals who experienced alternative adverse events. Table 29 shows the (monthly) utility decrements used within the model. These were applied to the proportion of individuals who experienced an adverse event from within those that were under treatment (see Table 26). Searches were conducted to retrieve information on the effect of treatment injections on the quality of life of patients with nAMD; however, no evidence was found. Moreover, from discussions within the project advisory group and clinical experts, anxiety seemed to be associated with the uncertainty of the disease condition (i.e. active or inactive) rather than the treatment itself. Adding a utility decrement for each monthly monitoring visit for all strategies would have had no effect on the final results. As such, no utility adjustments were conducted due to treatment injections.
Base-case and sensitivity analyses
The UK NICE guidelines of methods for technology appraisals were followed. 73 The model base-case analysis was run for a cohort of 65-year-old men for a time horizon of 35 years (lifetime). A 1-month cycle length was defined. The analysis was conducted from the NHS and Personal Social Services perspective. Costs were expressed in 2011–12 pounds sterling and effectiveness in quality-adjusted life-years (QALYs). Costs and QALYs were discounted at 3.5%. 73 Cost-effectiveness analysis results are reported using incremental cost-effectiveness ratios (ICERs). 55 ICERs are calculated as the ratio between the difference in average cost between two alternative strategies and the difference in average QALYs. This ratio measures the additional cost that would have to be paid in order to obtain an extra unit of effectiveness (i.e. an extra QALY). Probabilistic analysis results are reported using cost-effectiveness acceptability curves (CEACs). 76,77 CEACs show the probability of a particular strategy to be cost-effective at alternative values of willingness to pay for an extra QALY.
Sensitivity analysis
Uncertainty in the economic model was explored conducting one-way sensitivity analysis, scenario analysis and probabilistic sensitivity analysis. As mentioned above, the base-case analysis was run for a male cohort. Gender-specific data were not available and the only different data for men and women were mortality rates. Female mortality data show longer life expectancy. These could result in longer time for benefits, but also costs. A further analysis was conducted using mortality data for women to observe the effect of longer life expectancy in the model results.
One-way sensitivity analyses were conducted on test diagnosis sensitivity and specificity, the probability of ophthalmologist diagnosis or monitoring results being unclear, tests and assessment monitoring sensitivity and specificity, probability of the nurse or technician assessment being unclear, and unit costs for OCT, FFA and ranibizumab.
Further deterministic sensitivity analyses were conducted using alternative discount rates for costs and QALYs, as well as prevalence rates for nAMD. In addition, population utility weights were retrieved from Czoski-Murray et al. 78 The authors elicited time trade-off-based utility values from 108 healthy individuals for AMD states simulated using contact lenses.
Given base-case and sensitivity analyses results, three scenario analyses were tested. All of these incorporated data that favoured OCT (Table 30). Scenario 1 used the upper limit for the 95% CI for OCT sensitivity and specificity for diagnosis and monitoring obtained from the systematic review of diagnostic and monitoring studies, together with £20.90 and £139 unit costs for OCT and FFA respectively. Scenario 2 used the same data as for scenario 1 but assuming a cost per treatment injection of £50 instead of £742. Finally, scenario 3 assumed the same input data as for scenario 1 but monitoring pathways that based their decisions on OCT only considered the unit cost of the OCT test for the monitoring visit as that of the OCT test for an optometry community service (£20.90). 80 The cost of an ophthalmologist visit was not considered in every monitoring visit but added only if the patient needed to be treated. This scenario explored the effect of monitoring patients within the community and only referred them to secondary care for treatment.
| Variable | Diagnosis | Monitoring | Source |
|---|---|---|---|
| FFA | |||
| Sensitivity | 0.99 | 0.99 | Assumption |
| Specificity | 0.99 | 0.99 | Assumption |
| OCT | |||
| Sensitivity | 0.98 | 0.93 | Systematic review of diagnostic and monitoring studies |
| Specificity | 0.88 | 0.67 | Systematic review of diagnostic and monitoring studies |
| Unit costs (£, 2011–12) | |||
| FFA | 139 | NHS Reference Costs 2011–12 (HRG BZ23Z minor vitreous retinal procedures)11 | |
| OCT | 20.9 | General Ophthalmic Services: Increases to NHS Sight Test Fee 79 | |
Base-case and selected sensitivity analyses are presented in the next section. Full sensitivity analysis results are reported in Appendix 8.
Results
Table 31 reports base-case analysis results for men for the nine compared strategies. Model strategies are ordered in terms of average cost in an ascending order. Diagnosis with FFA combined with the nurse or technician-led monitoring strategy (e.g. nurse or technician as first monitoring contact conducting a VA examination and interpreting OCT test results; if negative, discharge, if positive or unclear, refer to an ophthalmologist for further assessment) was the strategy with the lowest average total cost. The next non-dominated strategy (i.e. dominated strategy meaning a strategy with higher expected costs and lower expected QALYs) is diagnosis based on FFA only, followed by ophthalmologist-led monitoring. This strategy has higher total expected cost but also produces higher total expected QALYs. However, the incremental cost for an extra QALY (i.e. ICER) to adopt this strategy is above the often accepted cost-effectiveness threshold (i.e. £30,000). 73 All other strategies are dominated by either of the strategies that based diagnosis in FFA only followed by nurse-led or ophthalmologist-led monitoring. Diagnosis based only on OCT appears in third place combined with nurse-led monitoring. In terms of costs, the strategies’ order is driven mainly by the monitoring pathway, with the lowest average total costs coming from the nurse-led monitoring pathway (first to third places), then the ophthalmologist-led (fourth to sixth) and OCT only-based (seventh to ninth) monitoring pathways respectively. It should be noted, then, that the three model strategies that used OCT only as the basis for monitoring criteria were the strategies with higher average costs (see Table 31). This is due to the cost of treatment, that represents 76% of the total average cost within these strategies, the highest proportion for all compared strategies (e.g. average 65% and minimum 55%).
| Strategy | Cost (£) | Incremental cost (£) | QALYs | Incremental QALYs | ICER (£)a |
|---|---|---|---|---|---|
| (3) FFA & Nurse | 39,769 | – | 10.473 | 0.000 | 0 |
| (9) Ophthalmologist & Nurse | 39,790 | 21 | 10.472 | –0.001 | –33,237 |
| (6) OCT & Nurse | 41,607 | 1838 | 10.465 | –0.008 | –224,403 |
| (2) FFA & Ophthalmologist | 44,649 | 4880 | 10.575 | 0.102 | 47,768 |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 20 | 10.574 | –0.001 | –31,094 |
| (5) OCT & Ophthalmologist | 47,131 | 2482 | 10.567 | –0.008 | –293,938 |
| (1) FFA & OCT | 62,759 | 18,110 | 10.449 | –0.126 | –144,229 |
| (7) Ophthalmologist & OCT | 62,778 | 18,129 | 10.449 | –0.126 | –143,662 |
| (4) OCT & OCT | 67,421 | 22,772 | 10.442 | –0.133 | –170,859 |
Figure 15 shows the cost-effectiveness plane for the base-case analysis and the nine diagnosis–monitoring combination strategies. For easier interpretation, data marker shapes relate to the diagnosis strategy and marker filling/colour relates to the monitoring strategy. Namely, square, circle and triangle shapes are used for FFA only, OCT only, and ophthalmologist stepwise diagnosis respectively. In addition, blue, green and none marker fillings correspond to ophthalmologist-led, nurse- or technician-led and OCT only-based monitoring respectively.
FIGURE 15.
Base-case cost-effectiveness results: men.
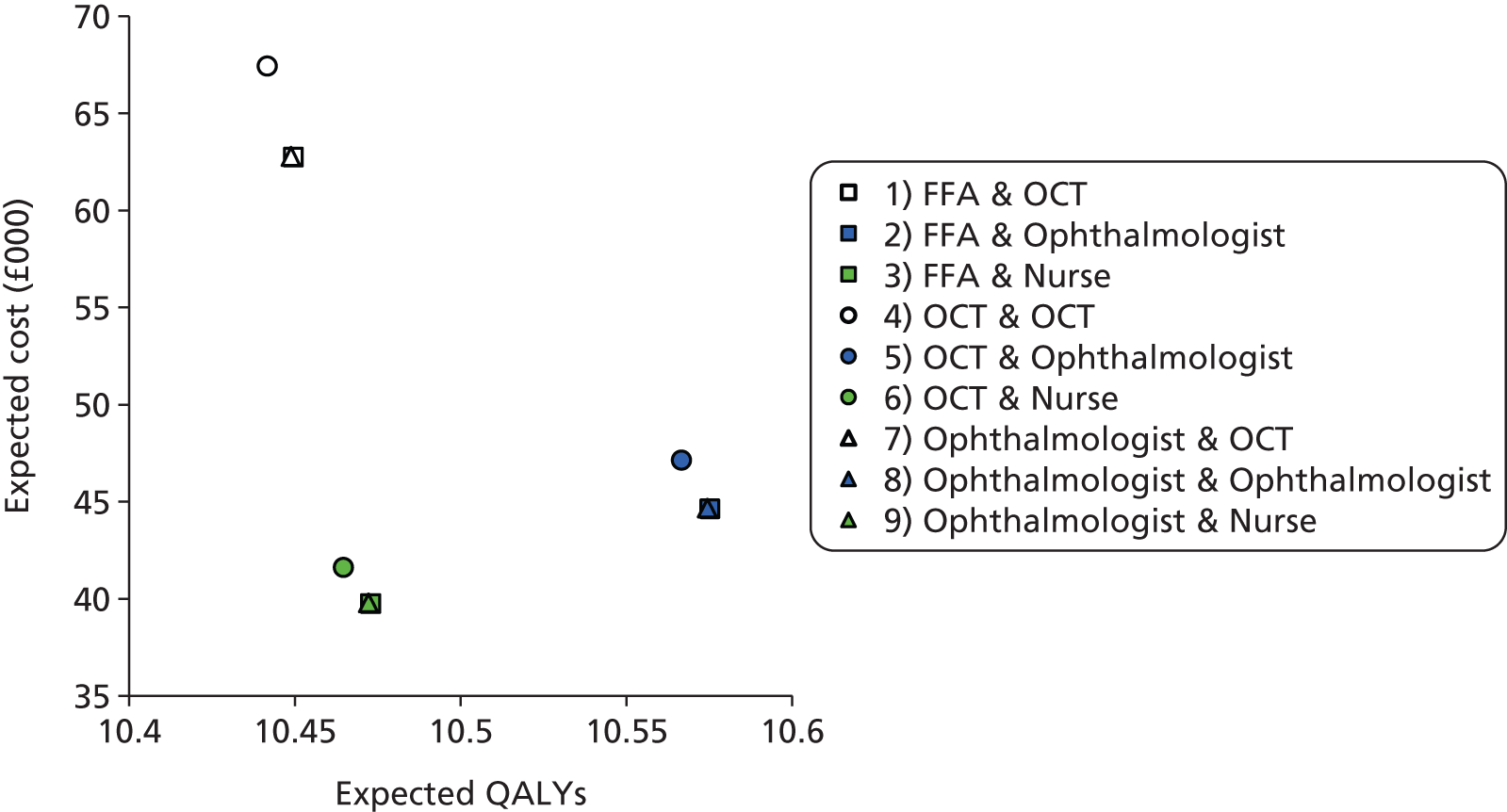
Three clusters can be seen in Figure 15 according to the monitoring strategy. As such, the ophthalmologist-led monitoring strategy cluster seems to produce higher expected QALYs and slightly higher expected costs than the nurse- or technician-led monitoring strategy. The OCT only monitoring strategy cluster results in a higher expected cost and lower expected QALYs than the other two monitoring strategies.
Within each of these clusters, the FFA diagnosis strategy dominates OCT only as well as the ophthalmologist stepwise diagnosis strategy (e.g. VA, OCT and SLB in all, followed by FFA if positive or unclear results). Also, to note is that the ophthalmologist diagnostic and FFA diagnostic pathways have very similar expected cost and QALYs within each cluster and, as such, data markers seem to overlap. This is due to the close values assumed for diagnosis sensitivity and specificity in these two diagnostic pathways.
Table 32 and Figure 16 show probabilistic sensitivity analysis for the base case. Diagnosing with FFA only followed by nurse- or technician-led monitoring has the highest probability of being cost-effective for up to £40,000 willingness to pay for an extra QALY. At higher threshold values (e.g. £50,000) diagnosing with FFA only followed by ophthalmologist-based monitoring has a higher probability of being cost-effective. Overall, diagnosis with FFA with either nurse- or ophthalmologist-led monitoring has more than a 70% chance of being cost-effective at willingness-to-pay values for an extra QALY of between £10,000 and £50,000. These strategies lose some ground against ophthalmologist-based diagnosis (e.g. ‘Ophthalmologist & Ophthalmologist’ and ‘Ophthalmologist & Nurse’) at high levels of willingness to pay for extra QALY threshold values (see Table 32 and Figure 16). At £30,000 willingness to pay for a QALY threshold value and regardless of the diagnosis pathways (e.g. FFA only, OCT only or ophthalmologist), nurse- or technician-led monitoring has a 61% probability of being cost-effective.
| Strategy | Probability of strategy being cost-effective at alternative threshold values for society’s willingness to pay for a QALY (%) | ||||
|---|---|---|---|---|---|
| £10,000 | £20,000 | £30,000 | £40,000 | £50,000 | |
| (1) FFA & OCT | 0.6 | 0.9 | 1.2 | 1.2 | 1.7 |
| (2) FFA & Ophthalmologist | 12.2 | 21.8 | 31.3 | 36.7 | 42.6 |
| (3) FFA & Nurse | 67.7 | 57.4 | 46.4 | 39.0 | 29.9 |
| (4) OCT & OCT | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| (5) OCT & Ophthalmologist | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| (6) OCT & Nurse | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| (7) Ophthalmologist & OCT | 0.0 | 0.1 | 0.1 | 0.3 | 0.5 |
| (8) Ophthalmologist & Ophthalmologist | 1.5 | 3.3 | 7.2 | 10.3 | 13.8 |
| (9) Ophthalmologist & Nurse | 18.0 | 16.5 | 13.8 | 12.5 | 11.5 |
FIGURE 16.
Base case cost-effectiveness acceptability curves: men.
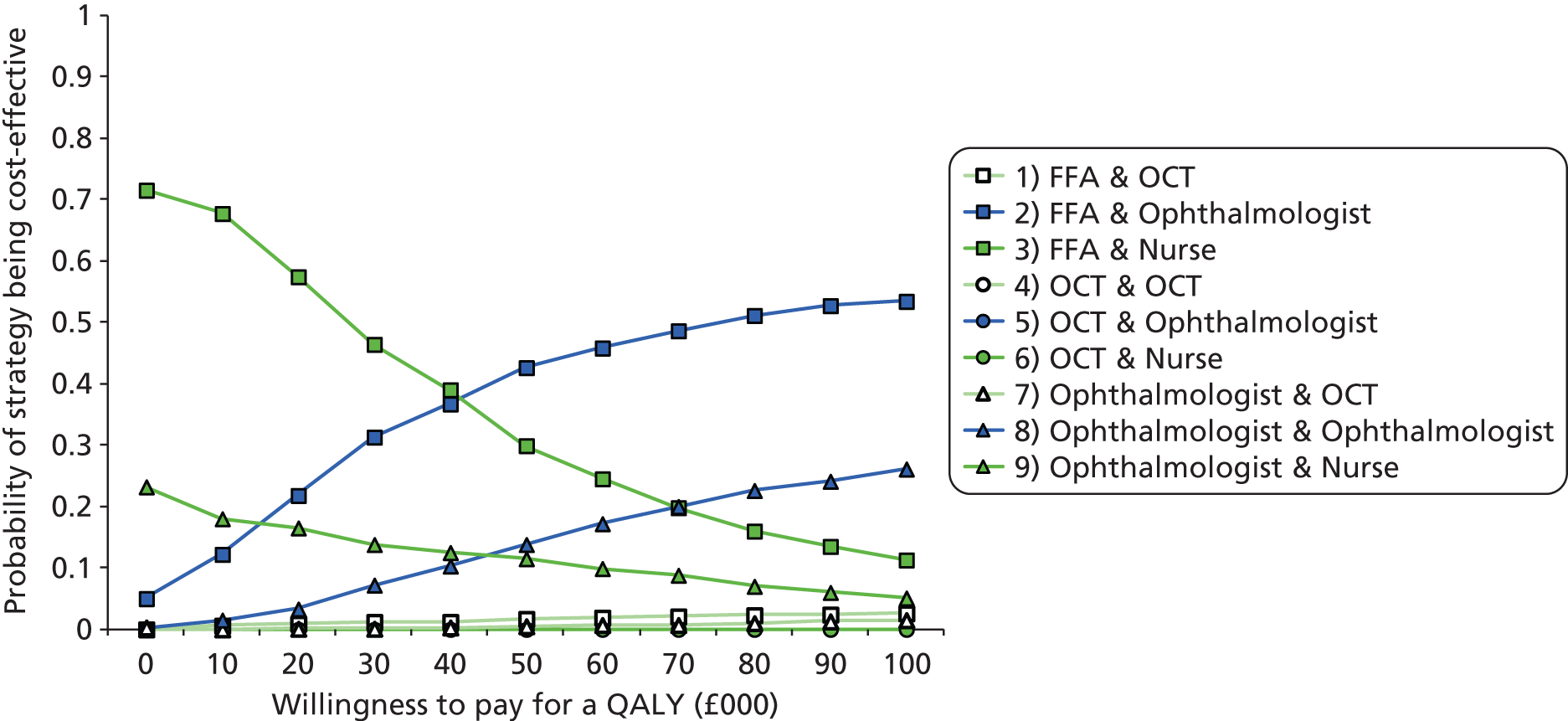
Figure 16 shows that when expanding this range up to £100,000, diagnosing with FFA only followed by the ophthalmologist-based monitoring strategy will have more than a 50% chance of being cost-effective. In addition, FFA only-based diagnosis strategies lose some ground against ophthalmologist-based diagnosis strategies (i.e. ‘Ophthalmologist & Ophthalmologist’ and ‘Ophthalmologist & Nurse’) at high levels of willingness to pay threshold values (see Table 32 and Figure 16).
Sensitivity analysis
Using mortality rate data for women
Table 33 and Figure 17 present cost-effectiveness results for women. As expected, all strategies produce more QALYs, incurring higher average costs. This is because of the longer life expectancy for women. This affects all of the model strategies in a similar manner. As such, there are no differences in the (average cost) order of the strategies or the general results compared with those for the base-case analysis for men (see Table 31). Diagnosing with FFA followed by nurse- or technician-led monitoring is still the strategy with the lowest average cost and dominates all other compared strategies, apart from diagnosis with FFA followed by ophthalmologist-led monitoring. However, the ICER for moving to the latter strategy is above the usually accepted cost-effectiveness threshold (i.e. £30,000). 73
| Strategy | Cost (£) | Incremental cost (£) | QALYs | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|
| (3) FFA & Nurse | 44,099 | 0 | 11.604 | 0.000 | 0 |
| (9) Ophthalmologist & Nurse | 44,119 | 21 | 11.603 | –0.001 | –30,521 |
| (6) OCT & Nurse | 46,125 | 2026 | 11.595 | –0.009 | –226,433 |
| (2) FFA & Ophthalmologist | 49,527 | 5428 | 11.725 | 0.121 | 44,959 |
| (8) Ophthalmologist & Ophthalmologist | 49,547 | 20 | 11.724 | –0.001 | –28,491 |
| (5) OCT & Ophthalmologist | 52,262 | 2735 | 11.715 | –0.009 | –296,276 |
| (1) FFA & OCT | 69,712 | 20,185 | 11.576 | –0.148 | –136,016 |
| (7) Ophthalmologist & OCT | 69,731 | 20,204 | 11.576 | –0.149 | –135,517 |
| (4) OCT & OCT | 74,847 | 25,321 | 11.568 | –0.157 | –161,433 |
FIGURE 17.
Cost-effectiveness results: women.
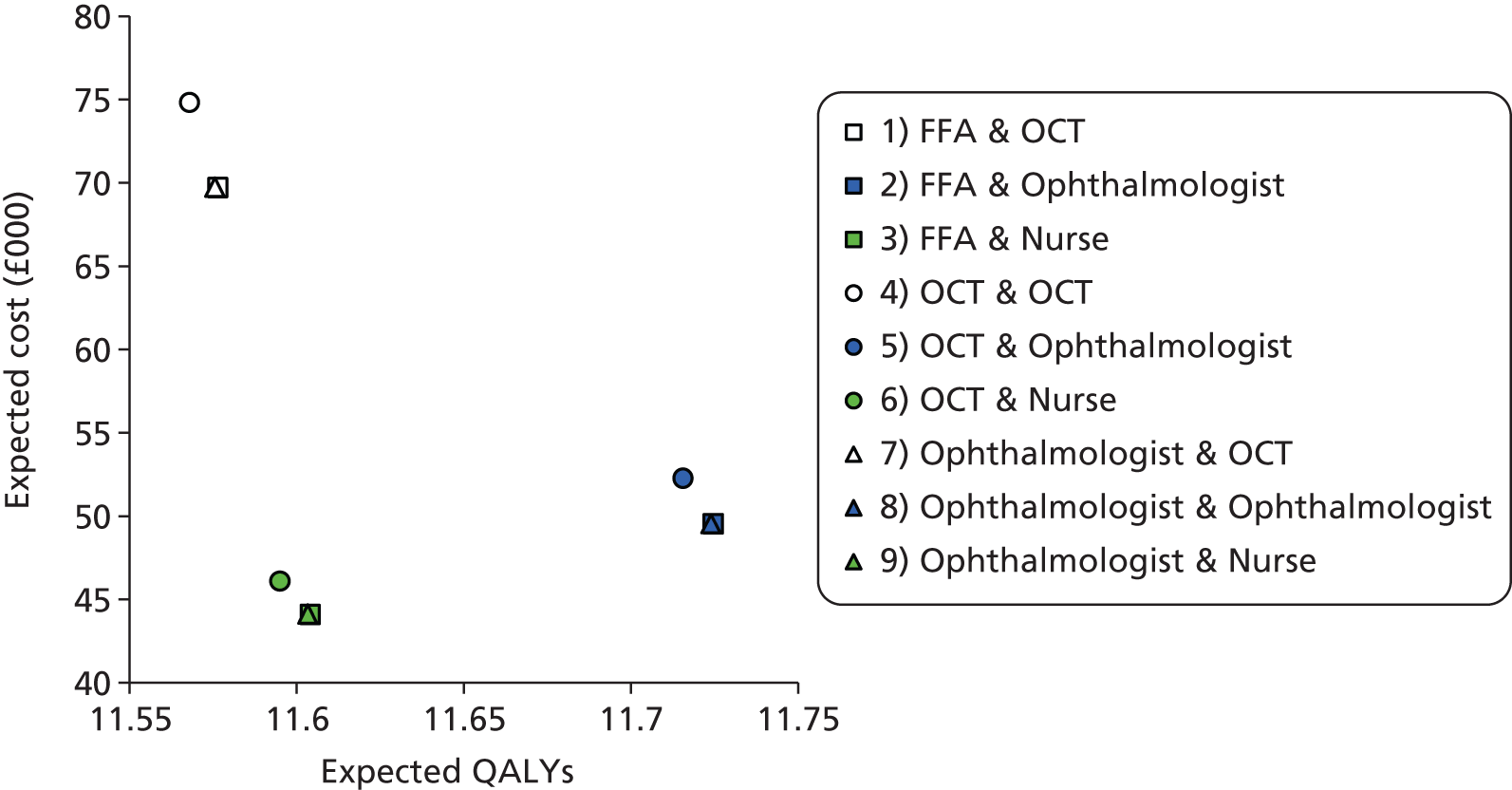
Similar clusters can be observed in the cost-effectiveness results for men (see Figure 15) and women (see Figure 17), with the three clusters depending on the monitoring care pathway (i.e. OCT only, nurse-, technician-, or ophthalmologist-led monitoring). As was the case with Figure 15, the ophthalmologist diagnostic and FFA diagnostic pathways have very similar expected cost and QALYs within each cluster and, as such, data markers seem to overlap. The Table 33 and Figure 17 results indicate that no dramatic differences can be expected for the women and men model run results. Therefore, further sensitivity analyses were conducted only for the male cohort.
One-way sensitivity analyses
Extensive one-way sensitivity analyses were undertaken. This section reports a selected number of these, with full results presented in Appendix 8. All one-way sensitivity analyses show results moving in the expected direction (i.e. lower sensitivity or specificity for OCT would result in OCT-based strategies being less cost-effective). Tables 34–38 show one-way sensitivity analysis for OCT diagnostic sensitivity and specificity, OCT monitoring sensitivity and specificity and OCT unit cost respectively. The base-case analysis results seem robust. In all reported sensitivity analyses, diagnosis with FFA combined with nurse- or technician-led monitoring (based on VA and OCT with a referral to the ophthalmologist if positive or unclear) has the lowest total expected costs and dominates all others, apart from FFA for diagnosis with ophthalmologist-led monitoring. In a limited number of model runs, alternative strategies stop being dominated by diagnosis with FFA followed by nurse- or technician-led monitoring. However, in many of these cases the variable values used to run the analysis were extreme (see Tables 34 and 36 for OCT diagnostic and monitoring sensitivities equal to 1 respectively). Results are sensitive to the value of monitoring specificity for OCT. Table 37 suggests that OCT monitoring specificity above 80% could make diagnosis with FFA combined with monitoring with OCT only, a cost-effective strategy. However, this is to almost double the specificity values reported for monitoring in Chapter 4.
| OCT diagnostic sensitivity | Strategy | Cost | QALYs | Incremental cost | Incremental QALYs | ICER |
|---|---|---|---|---|---|---|
| 0.8 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,594 | 10.459 | 1824 | –0.014 | –133,258 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,114 | 10.561 | 2465 | –0.014 | –173,407 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 67,394 | 10.436 | 22,745 | –0.139 | –163,795 | |
| 0.9 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,611 | 10.466 | 1841 | –0.007 | –270,172 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,135 | 10.568 | 2486 | –0.007 | –355,119 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 67,428 | 10.443 | 22,779 | –0.132 | –172,719 | |
| 1.0 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,628 | 10.473 | 1859 | 0.000 | 31,635,704 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 3021 | 0.102 | 29,593 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,157 | 10.575 | 2507 | 0.000 | 11,797,675 | |
| (1) FFA & OCT | 62,759 | 10.449 | 15,602 | –0.126 | –124,050 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 15,621 | –0.126 | –123,584 | |
| (4) OCT & OCT | 67,462 | 10.450 | 20,306 | –0.125 | –162,290 |
| OCT diagnostic sensitivity | Strategy | Cost | QALYs | Incremental cost | Incremental QALYs | ICER |
|---|---|---|---|---|---|---|
| 0.55 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 43,619 | 10.465 | 3850 | –0.008 | –473,564 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 49,821 | 10.567 | 5172 | –0.008 | –629,095 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 72,407 | 10.442 | 27,758 | –0.133 | –209,343 | |
| 0.60 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 43,182 | 10.465 | 3412 | –0.008 | –419,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 49,236 | 10.567 | 4587 | –0.008 | –554,702 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 71,324 | 10.442 | 26,674 | –0.133 | –200,943 | |
| 0.65 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 42,744 | 10.465 | 2975 | –0.008 | –364,772 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 48,651 | 10.567 | 4002 | –0.008 | –481,174 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 70,240 | 10.442 | 25,590 | –0.133 | –192,562 | |
| 0.70 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 42,307 | 10.465 | 2538 | –0.008 | –310,643 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 48,067 | 10.567 | 3418 | –0.008 | –408,495 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 69,156 | 10.442 | 24,507 | –0.133 | –184,200 | |
| 0.75 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,870 | 10.465 | 2100 | –0.008 | –256,690 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,482 | 10.567 | 2833 | –0.008 | –336,651 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 68,072 | 10.442 | 23,423 | –0.133 | –175,856 | |
| 0.80 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,432 | 10.465 | 1663 | –0.008 | –202,914 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 46,897 | 10.567 | 2248 | –0.008 | –265,626 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 66,988 | 10.442 | 22,339 | –0.133 | –167,531 | |
| 0.85 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 40,995 | 10.465 | 1226 | –0.008 | –149,312 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 46,312 | 10.567 | 1663 | –0.009 | –195,408 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 65,904 | 10.442 | 21,255 | –0.133 | –159,225 | |
| 0.90 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 40,558 | 10.465 | 788 | –0.008 | –95,884 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 45,727 | 10.566 | 1078 | –0.009 | –125,982 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 64,820 | 10.441 | 20,171 | –0.134 | –150,937 | |
| 0.95 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 40,120 | 10.465 | 351 | –0.008 | –42,629 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 45,143 | 10.566 | 494 | –0.009 | –57,335 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | |
| (4) OCT & OCT | 63,736 | 10.441 | 19,087 | –0.134 | –142,667 | |
| 1.0 | (6) OCT & Nurse | 39,683 | 10.465 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 86 | 0.008 | 10,453 | |
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (5) OCT & Ophthalmologist | 44,558 | 10.566 | 4789 | 0.094 | 51,214 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 91 | 0.009 | 10,545 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| 4) OCT & OCT | 62,652 | 10.441 | 18,003 | –0.134 | –134,416 | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 |
| Monitoring sensitivity OCT | Strategy | Cost | QALYs | Incremental cost | Incremental QALYs | ICER |
|---|---|---|---|---|---|---|
| 0.9 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | |
| (1) FFA & OCT | 63,312 | 10.503 | 18,663 | –0.072 | –260,619 | |
| (7) Ophthalmologist & OCT | 63,331 | 10.503 | 18,682 | –0.072 | –258,561 | |
| (4) OCT & OCT | 67,974 | 10.495 | 23,325 | –0.080 | –293,337 | |
| 1.0 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | |
| (1) FFA & OCT | 64,277 | 10.600 | 19,628 | 0.025 | 788,482 | |
| (7) Ophthalmologist & OCT | 64,296 | 10.599 | 19 | –0.001 | –28,229 | |
| (4) OCT & OCT | 68,939 | 10.592 | 4662 | –0.008 | –565,643 |
| Monitoring specificity OCT | Strategy | Cost | QALYs | Incremental cost | Incremental effectiveness | ICER |
|---|---|---|---|---|---|---|
| 0.3 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | |
| (1) FFA & OCT | 74,212 | 10.459 | 29,563 | –0.116 | –255,643 | |
| (7) Ophthalmologist & OCT | 74,230 | 10.459 | 29,581 | –0.116 | –254,397 | |
| (4) OCT & OCT | 80,083 | 10.452 | 35,434 | –0.123 | –287,514 | |
| 0.4 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | |
| (1) FFA & OCT | 67,780 | 10.454 | 23,130 | –0.121 | –190,790 | |
| (7) Ophthalmologist & OCT | 67,798 | 10.453 | 23,149 | –0.122 | –189,953 | |
| (4) OCT & OCT | 72,979 | 10.446 | 28,330 | –0.129 | –219,784 | |
| 0.5 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | |
| (1) FFA & OCT | 61,521 | 10.448 | 16,872 | –0.127 | –133,240 | |
| (7) Ophthalmologist & OCT | 61,540 | 10.448 | 16,891 | –0.127 | –132,734 | |
| (4) OCT & OCT | 66,049 | 10.441 | 21,400 | –0.134 | –159,275 | |
| 0.6 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | |
| (1) FFA & OCT | 55,429 | 10.443 | 10,780 | –0.132 | –81,774 | |
| (7) Ophthalmologist & OCT | 55,449 | 10.443 | 10,800 | –0.132 | –81,537 | |
| (4) OCT & OCT | 59,286 | 10.435 | 14,636 | –0.140 | –104,824 | |
| 0.7 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | |
| (1) FFA & OCT | 49,498 | 10.438 | 4849 | –0.137 | –35,432 | |
| (7) Ophthalmologist & OCT | 49,518 | 10.438 | 4869 | –0.137 | –35,418 | |
| (4) OCT & OCT | 52,683 | 10.430 | 8033 | –0.145 | –55,508 | |
| 0.8 | (3) FFA & Nurse | 39,769 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (1) FFA & OCT | 43,721 | 10.433 | 3952 | –0.040 | –99,944 | |
| (7) Ophthalmologist & OCT | 43,742 | 10.433 | 3973 | –0.040 | –98,928 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (4) OCT & OCT | 46,234 | 10.425 | 1585 | –0.150 | –10,589 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | |
| 0.9 | (1) FFA & OCT | 38,093 | 10.429 | |||
| (7) Ophthalmologist & OCT | 38,114 | 10.428 | 21 | –0.001 | –34,221 | |
| (3) FFA & Nurse | 39,769 | 10.473 | 1676 | 0.044 | 37,884 | |
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (4) OCT & OCT | 39,934 | 10.421 | 164 | –0.052 | –3,146 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | |
| 1.0 | (1) FFA & OCT | 32,608 | 10.424 | |||
| (7) Ophthalmologist & OCT | 32,629 | 10.423 | 21 | –0.001 | –35,125 | |
| (4) OCT & OCT | 33,776 | 10.416 | 1168 | –0.008 | –144,031 | |
| (3) FFA & Nurse | 39,769 | 10.473 | 7161 | 0.049 | 146,783 | |
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 |
| Unit Cost OCT | Strategy | Cost | QALYs | Incremental cost | Incremental QALYs | ICER |
|---|---|---|---|---|---|---|
| 30 | (9) Ophthalmologist & Nurse | 37,446 | 10.472 | |||
| (3) FFA & Nurse | 37,446 | 10.473 | 1 | 0.001 | 835 | |
| (6) OCT & Nurse | 39,071 | 10.465 | 1625 | –0.008 | –198,353 | |
| (8) Ophthalmologist & Ophthalmologist | 42,317 | 10.574 | 4870 | 0.102 | 47,980 | |
| (2) FFA & Ophthalmologist | 42,318 | 10.575 | 1 | 0.001 | 1398 | |
| (5) OCT & Ophthalmologist | 44,586 | 10.567 | 2268 | –0.008 | –268,648 | |
| (7) Ophthalmologist & OCT | 60,434 | 10.449 | 18,116 | –0.126 | –143,560 | |
| (1) FFA & OCT | 60,436 | 10.449 | 18,118 | –0.126 | –144,295 | |
| (4) OCT & OCT | 64,885 | 10.442 | 22,567 | –0.133 | –169,320 | |
| 40 | (3) FFA & Nurse | 38,538 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 38,548 | 10.472 | 9 | –0.001 | –15,184 | |
| (6) OCT & Nurse | 40,263 | 10.465 | 1725 | –0.008 | –210,601 | |
| (2) FFA & Ophthalmologist | 43,414 | 10.575 | 4875 | 0.102 | 47,723 | |
| (8) Ophthalmologist & Ophthalmologist | 43,423 | 10.574 | 9 | –0.001 | –13,878 | |
| (5) OCT & Ophthalmologist | 45,783 | 10.567 | 2369 | –0.008 | –280,538 | |
| (1) FFA & OCT | 61,528 | 10.449 | 18,114 | –0.126 | –144,264 | |
| (7) Ophthalmologist & OCT | 61,536 | 10.449 | 18,122 | –0.126 | –143,608 | |
| (4) OCT & OCT | 66,078 | 10.442 | 22,664 | –0.133 | –170,044 | |
| 50 | (3) FFA & Nurse | 39,630 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 39,650 | 10.472 | 19 | –0.001 | –31,202 | |
| (6) OCT & Nurse | 41,456 | 10.465 | 1825 | –0.008 | –222,848 | |
| (2) FFA & Ophthalmologist | 44,510 | 10.575 | 4879 | 0.102 | 47,763 | |
| (8) Ophthalmologist & Ophthalmologist | 44,529 | 10.574 | 19 | –0.001 | –29,154 | |
| (5) OCT & Ophthalmologist | 46,979 | 10.567 | 2469 | –0.008 | –292,428 | |
| (1) FFA & OCT | 62,620 | 10.449 | 18,110 | –0.126 | –144,233 | |
| (7) Ophthalmologist & OCT | 62,638 | 10.449 | 18,128 | –0.126 | –143,656 | |
| (4) OCT & OCT | 67,270 | 10.442 | 22,760 | –0.133 | –170,767 | |
| 60 | (3) FFA & Nurse | 40,722 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 40,752 | 10.472 | 29 | –0.001 | –47,221 | |
| (6) OCT & Nurse | 42,648 | 10.465 | 1926 | –0.008 | –235,095 | |
| (2) FFA & Ophthalmologist | 45,606 | 10.575 | 4884 | 0.102 | 47,803 | |
| (8) Ophthalmologist & Ophthalmologist | 45,635 | 10.574 | 29 | –0.001 | –44,429 | |
| (5) OCT & Ophthalmologist | 48,176 | 10.567 | 2569 | –0.008 | –304,319 | |
| (1) FFA & OCT | 63,712 | 10.449 | 18,106 | –0.126 | –144,201 | |
| (7) Ophthalmologist & OCT | 63,740 | 10.449 | 18,134 | –0.126 | –143,703 | |
| (4) OCT & OCT | 68,462 | 10.442 | 22,856 | –0.133 | –171,491 | |
| 70 | (3) FFA & Nurse | 41,814 | 10.473 | |||
| (9) Ophthalmologist & Nurse | 41,854 | 10.472 | 39 | –0.001 | –63,240 | |
| (6) OCT & Nurse | 43,840 | 10.465 | 2026 | –0.008 | –247,342 | |
| (2) FFA & Ophthalmologist | 46,702 | 10.575 | 4888 | 0.102 | 47,842 | |
| (8) Ophthalmologist & Ophthalmologist | 46,741 | 10.574 | 39 | –0.001 | –59,705 | |
| (5) OCT & Ophthalmologist | 49,372 | 10.567 | 2670 | –0.008 | –316,209 | |
| (1) FFA & OCT | 64,805 | 10.449 | 18,102 | –0.126 | –144,170 | |
| (7) Ophthalmologist & OCT | 64,842 | 10.449 | 18,140 | –0.126 | –143,751 | |
| (4) OCT & OCT | 69,655 | 10.442 | 22,953 | –0.133 | –172,214 |
Scenario analysis
Scenario analysis favouring the OCT test was conducted to explore conditions under which OCT only-based strategies could become cost-effective. The scenarios are described in Base-case and sensitivity analyses and the input data used reported in Table 30. Best possible OCT test sensitivity and specificity were incorporated into the model. In addition, the lowest possible unit cost for OCT and a higher assumed unit cost value for FFA were used. Scenario 2 differs in the unit cost assumed for each treatment injection (£50) and scenario 3 explores community monitoring (e.g. unit cost for OCT as for community optometrist and an ophthalmologist visit cost added only when treatment was needed). Tables 39–41 show the scenario analysis results. For scenario 1 (see Table 39) and scenario 3 (see Table 41) strategies that based their diagnosis or monitoring decisions on OCT test results only are dominated (i.e. have higher expected costs and lower expected QALYs). It should be noted that, due to the lower unit cost for the OCT test, the strategy with the lower expected cost is diagnosis by an ophthalmologist combined with nurse- or technician-led monitoring.
| Strategy | Cost (£) | Incremental cost (£) | QALYs | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|
| (9) Ophthalmologist & Nurse | 36,320 | – | 10.478 | ||
| (3) FFA & Nurse | 36,707 | 387 | 10.471 | –0.007 | –54,280 |
| (6) OCT & Nurse | 37,417 | 1097 | 10.470 | –0.008 | –140,873 |
| (8) Ophthalmologist & Ophthalmologist | 41,284 | 4964 | 10.579 | 0.101 | 49,012 |
| (2) FFA & Ophthalmologist | 41,740 | 456 | 10.573 | –0.006 | –73,232 |
| (5) OCT & Ophthalmologist | 42,781 | 1497 | 10.573 | –0.007 | –218,869 |
| (7) Ophthalmologist & OCT | 48,24 | 6957 | 10.536 | –0.043 | –161,687 |
| (1) FFA & OCT | 48,791 | 7507 | 10.530 | –0.050 | –151,253 |
| (4) OCT & OCT | 50,273 | 8989 | 10.529 | –0.050 | –179,277 |
| Strategy | Cost (£) | Incremental cost (£) | QALYs | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|
| (7) Ophthalmologist & OCT | 13,983 | – | 10.536 | ||
| (1) FFA & OCT | 14,158 | 175 | 10.530 | –0.007 | –26,423 |
| (4) OCT & OCT | 14,583 | 600 | 10.529 | –0.007 | –84,256 |
| (8) Ophthalmologist & Ophthalmologist | 14,840 | 857 | 10.579 | 0.043 | 19,917 |
| (2) FFA & Ophthalmologist | 15,024 | 184 | 10.573 | –0.006 | –29,567 |
| (5) OCT & Ophthalmologist | 15,477 | 636 | 10.573 | –0.007 | –93,000 |
| (9) Ophthalmologist & Nurse | 15,601 | 761 | 10.478 | –0.101 | –7,511 |
| (3) FFA & Nurse | 15,790 | 949 | 10.471 | –0.108 | –8,757 |
| (6) OCT & Nurse | 16,218 | 1377 | 10.470 | –0.109 | –12,627 |
| Strategy | Cost (£) | Incremental cost (£) | QALYs | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|
| (9) Ophthalmologist & Nurse | 36,320 | – | 10.478 | 0.000 | 0 |
| (3) FFA & Nurse | 36,707 | 387 | 10.471 | –0.007 | –54,280 |
| (6) OCT & Nurse | 37,417 | 1097 | 10.470 | –0.008 | –140,873 |
| (8) Ophthalmologist & Ophthalmologist | 41,284 | 4964 | 10.579 | 0.101 | 49,012 |
| (2) FFA & Ophthalmologist | 41,740 | 456 | 10.573 | –0.006 | –73,232 |
| (5) OCT & Ophthalmologist | 42,781 | 1497 | 10.573 | –0.007 | –218,869 |
| (7) Ophthalmologist & OCT | 43,527 | 2243 | 10.536 | –0.043 | –52,132 |
| (1) FFA & OCT | 44,018 | 2734 | 10.530 | –0.050 | –55,084 |
| (4) OCT & OCT | 45,257 | 3974 | 10.529 | –0.050 | –79,247 |
Table 40 shows results for scenario 2 (i.e. the same input data as for scenario 1 but assuming cost of treatment of £50 per injection). The pathway strategy with the lowest cost is the ophthalmologist stepwise diagnosis followed by monitoring decisions based on OCT only. The next costly strategy is the one that based the diagnosis decision on FFA only and the monitoring treatment decision on OCT test results only. However, this strategy is dominated by the former. The next non-dominated strategy was diagnosis by an ophthalmologist followed by ophthalmologist-led monitoring (e.g. ‘Ophthalmologist & Ophthalmologist’) with an ICERs of £19,917. This is within the usual £30,00073 threshold and potentially worthwhile to adopt. The results in Table 40 indicate that OCT strategies could become cost-effective if the cost of treatment was lower. In terms of the economic model, this would be a lower penalisation for those strategies that treat individuals who do not need to be treated (i.e. those tests or strategies that result in lower specificity and therefore a higher number of FP results).
Summary and discussion
This chapter reported on a systematic review of economic evaluations and a model-based economic evaluation of alternative strategies for the diagnosis and monitoring of individuals with nAMD. No studies identified in the literature met the inclusion criteria for the systematic review.
Nine strategies (combinations of three different diagnostic and monitoring pathways) were considered within the economic model. The strategies used OCT for diagnosis and/or monitoring of nAMD individuals to a different extent. Extensive deterministic and probabilistic sensitivity analyses were conducted. The strategy that based its diagnosis decision on the results of FFA only, combined with VA and OCT interpreted together by a nurse or technician as the first monitoring step, with a referral to an ophthalmologist if the first monitoring assessment was positive or unclear (‘FFA & Nurse’), had the lowest expected total cost. This strategy dominated (i.e. lower expected costs and higher expected QALYs) all others apart from one: diagnosis with FFA only, combined with monitoring by an ophthalmologist (‘FFA & Ophthalmologist’). The ‘FFA & Nurse’ and ‘FFA & Ophthalmologist’ strategies had, respectively, a 46.5% and 29.8% probability of being cost-effective at the £30,000 threshold value of willingness to pay for an extra QALY. In addition, the ‘FFA & Nurse’ strategy dominated all others in the great majority of sensitivity analyses.
The strategies that used OCT only for their monitoring decisions were in almost every model run ordered last in terms of total expected cost and were often dominated by others. The strategy that used OCT only for both diagnosis and monitoring decisions was in almost every model run, the most costly strategy.
Scenario analysis was conducted in order to explore the conditions under which an OCT only strategy would become cost-effective. Three scenarios were developed using the best test performance data for OCT combined with a lower cost for OCT (£20.90) and a higher cost for FFA (£137). Scenario 2 added to this a lower unit cost for treatment (e.g. equivalent to the cost of bevacizumab, £50, instead of the £742 cost of ranibizumab considered for the base-case analysis). This scenario showed the ophthalmologist stepwise pathway for diagnosis combined with OCT only for monitoring, to be, on average, the least costly strategy. Alternative strategies were either dominated (i.e. more costly and produced fewer QALYs) or the resulted ICER was well above the usual threshold accepted for policy decisions. 73 This was an expected result. The low OCT specificity for monitoring in these scenarios and in the base case (0.61 and 0.44, respectively) meant that a high number of positive results would actually be FPs. The lower cost of treating individuals who do not need to be treated reduced the model penalisation for the OCT only-based strategies and therefore improved their cost-effectiveness.
Best practice guidelines were followed for this model-based economic evaluation exercise. 73,81 In spite of this, these results should be interpreted with caution. A considerable effort was made to retrieve the best available test or assessment performance data by conducting a systematic review of the literature. Other data were obtained from focused but reproducible searches. Nevertheless, there is an inherent problem with model-based economic evaluations that incorporate evidence from several sources, even when these data have been obtained systematically. The limitations of the SD-OCT performance data incorporated into the economic model have been mentioned in Chapter 4, with no SD-OCT studies contributing to the diagnosis performance data and only two SD-OCT studies23,30 contributing to the monitoring performance data. Moreover, although OCT diagnosis and monitoring performance data were retrieved from a systematic review of the literature, no such data were available for the strategies involving diagnosis or monitoring assessment by an ophthalmologist or monitoring assessment by a nurse or technician. Therefore, these data for the model were obtained from expert opinion. This constitutes a major caveat of the analysis and further research in this area is needed.
This economic model needed to consider individuals’ disease status (i.e. active or inactive nAMD) as well as test results on a monthly basis. In addition, these had to be combined with alternative VA states in order to incorporate utility weights into the model. It was felt that considering the effect of a fellow eye status (VA and nAMD status) would add major complexity to the model without a great deal of benefit from such incorporation. This is the most common approach used among economic models in this health area but constitutes a limitation of the current study. Utility weights used were obtained from nAMD individuals and grouped according to VA in the better-seeing eye. It is believed that this would better reflect individuals’ health status. However, the clear limitation of ‘one eye models’ is the underestimation of resources used. A proportion of monitored nAMD individuals will have this condition in both eyes instead of one, and, had the disease been active, would be receiving treatment injections in each eye. Intuitively, this would increase the treatment cost for those strategies with a higher number of TP and FP results (i.e. higher sensitivity and lower specificity) and hence would be unlikely to modify the overall conclusions of this economic evaluation.
The model did not consider effects on utility due to treatment injections. Anxiety in nAMD individuals was believed to occur at each monitoring visit mainly due to the uncertainty of the underlying condition (i.e. whether or not nAMD was active) and not the effects of the treatment injections. No evidence was obtained on this issue in spite of focused searches. Further research in this area is needed. Utility weight decrements from treatment adverse effects were included and this might partially overcome the above-mentioned potential limitation.
Limited evidence was available on the probability of nAMD active individuals becoming inactive when under treatment or inactive nAMD individuals becoming active. Data were retrieved from the literature and also from a UK-based RCT. 9 Survival data were received from the IVAN study (Dr Chris Rogers, personal communication) on first retreatment failure criteria (i.e. inactive individuals who needed to be retreated). These were used to develop model parameter values for the first year of the model run. There were no such data available for further failures and we had to rely on the available limited data from the literature70 or on expert opinion for year 2 onwards. In addition, progression data on VA were based on the 2-year follow-up MARINA study. 69 All of these were relatively short-term follow-up studies (around 2 years) but used to inform model parameters for a lifetime time horizon. These are clear limitations of the model and therefore its results should be interpreted with caution. Further research investigating individuals’ nAMD active/inactive status (e.g. probability of disease changing from inactive to active) would be desirable.
Conclusions
A strategy that based its diagnostic decision on the results of FFA only, combined with VA and OCT interpreted together by a nurse or technician as a first monitoring step, with a referral to an ophthalmologist if this first monitoring assessment was positive or unclear, had the lowest expected total cost. This strategy had a 46.5% probability of being cost-effective at a £30,000 threshold value of willingness to pay for an extra QALY. In addition, this strategy dominated all others apart from one (i.e. diagnosis with FFA combined with ophthalmologist-led monitoring) in the great majority of sensitivity analyses. Strategies that used OCT test results alone to make diagnosis or monitoring treatment decisions were unlikely to be a cost-effective use of resources. This result seemed to be driven by the OCT low specificity that resulted in a high number of FP results. The present analysis indicated that a further refinement of monitoring (i.e. a further monitoring step other than OCT alone) seemed desirable.
These results should be interpreted with caution. The economic model would benefit from further research to better inform a number of model parameter values. Studies that investigate the likelihood of nAMD individuals becoming active or inactive after subsequent treatments are desirable. In addition, a preference-based health status and process of care valuation study to explore the effects of treatment injections on individuals’ utility weights is needed. Finally, a comparative study to establish the performance of the ophthalmologist-based strategy compared with the nurse- or technician-based strategy for monitoring individuals with nAMD is required to inform future economic models in this area.
Chapter 6 Assessment of factors relevant to the NHS and other parties
The introduction of OCT and other diagnostic technologies for the diagnosis and monitoring of patients with nAMD has a range of implications for the NHS, patients and other parties. There has already been a shift in the diagnostic pathway for this group of patients caused by the adoption of OCT, rather than the previously used FFA, as a method of establishing the diagnosis and of evaluating disease activity. There are consequential effects not only on patient outcomes but also on service delivery, health-care professionals and wider society of this change in preferred diagnostic technologies used.
Factors relevant to the NHS
Estimating the numbers of patients with neovascular age-related macular degeneration
A summary of the epidemiology of nAMD has been described in this study. In brief, the prevalence and incidence of nAMD and the consequent burden to the NHS will increase over the next few decades because of the ageing population. By 2060, mean life expectancy will grow by 8.5 years for men (to 84.5 years) and 6.9 years for women (to 89.0 years). 82
Implications for service provision
The clinical workload associated with the frequent follow-up required for patients with nAMD is substantial. As more new patients are diagnosed and the population continues to age, the patient population will continue to increase. It is thus vital that clinical services continue to adapt so that they can provide a fast and efficient service for patients with nAMD.
There are still challenges and questions about whether or not ophthalmology departments have sufficient capacity and the means to offer relevant testing and treatments within adequate time scales. Local diagnostic pathways require updating and assessment to ensure compliance with national guidelines (e.g. to detect recurrence of active disease in these subjects). Occasional local disruptions may occur if OCT equipment suffers technical failures.
In 2012, Amoaku et al. 56 published a document entitled ‘Action on AMD’ that was developed by eye health-care professionals and patient representatives with the intention of highlighting the urgent and continuing need for change within nAMD services. This document also provided examples of good practice and service development, including the possibility of involving other health professionals and using OCT in the community.
Considerations regarding the performance of optical coherence tomography for diagnosis and monitoring
At the diagnostic stage, OCT is currently used in addition to FFA to provide a baseline that will be used for comparisons during the monitoring stage.
For monitoring, OCT has virtually replaced FFA in most NHS units. 83 During follow-up, monitoring also includes VA testing. There is larger variability in the adoption of other tests and perceived need for FFA during follow-up. The replacement of FFA is probably due to the convenience of OCT (e.g. non-invasive, user friendly, quick, efficient). However, expert clinicians recognise the difficulty of interpreting FFA and OCT in patients with previously treated nAMD who often develop atrophic changes. The low specificity of OCT observed in this study would suggest that OCT alone should not be used for monitoring.
Another consideration is the evolving technology. For example, theoretically an increased sensitivity and specificity of new versions or novel technologies (SD-OCT) would lead to more patients being correctly diagnosed with active nAMD, and fewer wrongly diagnosed as having no active disease. This review did not find sufficient evidence on the performance of SD-OCT and it is unclear if it is superior to TD-OCT.
Regarding cost implications, there will be little cost implications for procuring and maintaining OCT equipment because most centres already use this technology. Although many units will already have access to the new SD-OCT equipment, other centres may have to upgrade the current TD-OCT (e.g. purchase or lease new SD-OCT equipment).
There may be a need for training ophthalmology staff to ensure adequate technical skills to interpret the OCT scans. There is a learning curve to interpreting OCT images, especially in relation to those patients who are being monitored after treatment. Adequate quality control and quality assurance programmes would be needed in order to maintain high standards of interpretation.
Factors relevant to patients and other parties
A highly specific test may reduce the number of patients undergoing unnecessarily treatment with antiVEGF injections, avoiding the associated discomfort, side effects and possible complications. Using OCT alone for diagnosis or monitoring would be associated with a number of FPs and unnecessary treatments. From the efficiency point of view, a specificity of at least 80% would be required for a monitoring strategy using OCT alone to be cost-effective.
From a patient preference point of view, if the diagnostic performance were adequate, it is likely that patients would prefer OCT when compared with FFA because of the unpleasantness of the latter procedure.
Monitoring in the community would be a positive development for patients and carers, who would have less distance to travel to access OCT testing. This may be possible as OCT is becoming increasingly used by community optometrists but would need to be associated with another test (e.g. VA). Local arrangements and financial support would need to be put in place as community optometrists would need to be trained and reimbursed for their services. Community optometrists should also be able to communicate their findings in a timely and efficient way to clinicians in secondary care. However, inequalities in access may arise as people from disadvantaged socioeconomic backgrounds may be reluctant to attend private community optometrists.
Chapter 7 Discussion
Diagnostic accuracy
Statement of principal findings
Diagnostic studies
Twenty-two diagnostic studies were included (20 full-text papers,24–27,29,31,33,35–41,44–51 two abstracts34,42) involving over 2000 participants. The studies reported the performance of OCT (13 studies25,27,33–38,40,41,45,46,49), ICGA (eight studies25,26,29,31,42,44,48,51), PHP (three studies24,27,39), colour fundus photography, Amsler grid27 and FAF25 (one study each) in the detection of nAMD. Studies that reported true and false positive and true and false negative or provided information that allowed these data to be calculated were considered for inclusion in pooled estimates (meta-analyses), which were performed with eye as the unit of analysis.
Full-text papers were assessed for risk of bias using the QUADAS-2 tool. The domains with the greatest number of studies judged to be at high risk of bias were the patient selection domain (55%, 11/20), for reasons such as inappropriate exclusions and pre-selection of participants, and the flow and timing domain (40%, 8/20), for reasons such as the length of time between the index test and the reference standard being longer than 1 week, and not all participants being included in the analysis. In the index/comparator test domain and reference standard domain, the risk of bias was judged to be unclear in around half of the studies [50% (10/20) and 60% (12/20) respectively]. However, all of the studies were judged to be of low concern in terms of their applicability to the review question.
Only four OCT diagnostic studies (all TD-OCT)27,40,46,49 provided sufficient data for inclusion in a meta-analysis. The pooled sensitivity and specificity (95% CI) for all OCT was moderately high at 88% (46% to 98%) and 78% (64% to 88%) respectively.
Of the other tests of interest, median sensitivity (range) was similarly high for ICGA [93.2% (84.6–100%); four studies25,29,44,51] and FAF (93.3%; one study25), followed by PHP [81.5% (50.0–84.8%); three studies24,27,39] and colour fundus photography (70.0%; one study24) and was lowest for Amsler grid (41.7%; one study27). Specificity was highest for colour fundus photography (95%; one study24), followed by PHP (84.6% and 87.7%; two studies24,39), and was similarly low for FAF (37.1%; one study25) and ICGA (36.8%; one study29).
Two studies reported test combinations. For OCT plus colour fundus photography,46 sensitivity was moderate at 74.1%, with specificity high at 92.0%. For colour fundus photography plus VA,24 sensitivity was low at 53.0% but again specificity was high at 94.0%.
Monitoring studies
Eight monitoring studies23,28,30,32,43,45,52,53 were included (all full-text) involving over 400 participants. Seven reported the performance of OCT (five TD-OCT,28,32,45,52,53 one SD-OCT,30 one both types23) and one the performance of ICGA in the detection of nAMD activity. 43 As with the diagnostic studies, the QUADAS-2 domains with the greatest number of monitoring studies judged to be at high risk of bias were the patient selection domain (25%, 2/8)30,45 and flow and timing domain (25%, 2/8),45,52 for similar reasons to those reported above. In the index/comparator test domain and reference standard domain the risk of bias was judged to be unclear in 50% (4/8)23,45,52,53 and 37.5% (3/8)23,45,52 of studies respectively. Similar to the diagnostic studies, all of the monitoring studies were judged to be of low concern in terms of their applicability to the review question.
Four of the OCT studies provided sufficient data for inclusion in a meta-analysis. 23,28,30,53 The pooled sensitivity (95% CI) for all OCT was moderately high at 85% (72% to 93%) but with low specificity at 48% (30% to 67%). For TD-OCT,23,28,53 the pooled sensitivity and specificity was moderate at 70% (56% to 80%) and 65% (48% to 79%) respectively. It was not possible to calculate pooled estimates for the two SD-OCT studies23,30 using HSROC methodology due to insufficient data. These studies reported sensitivities of 94%30 and 90%23 and specificities of 27%30 and 47%. 23 These results suggest that SD-OCT has higher sensitivity but lower specificity than TD-OCT. In particular, the specificity of the SD-OCT monitoring studies was quite low.
Other than OCT, one study reported ICGA,43 with sensitivity of 75.9% and specificity of 88.0% for the detection of active nAMD.
Strengths and limitations of the assessment
In terms of strengths, a comprehensive literature search was undertaken and non-English-language studies were included. Risk of bias was assessed using a modified QUADAS-2 questionnaire, tailored to the needs of this review. A HSROC model was used for the analysis, which takes account of the trade-off between TPs/FPs and models between-study heterogeneity. 84 The evidence for diagnosis and monitoring was considered separately. In addition to the pooled estimates for all OCT, separate pooled estimates were undertaken for TD-OCT (monitoring studies). It was not possible to undertake separate pooled estimates for SD-OCT as no SD-OCT studies were included in the diagnosis meta-analysis, and, in the monitoring meta-analysis, there were insufficient data from the two SD-OCT studies to use HSROC methods.
There was a very limited amount of evidence available for evaluating the performance of SD-OCT, both for diagnosis (one study) and for surveillance monitoring of those previous diagnosed with nAMD. There was also limited evidence for the performance of TD-OCT for surveillance monitoring. Although this review considered a number of alternative tests, only a few of these were reported by studies that met our inclusion criteria. There was insufficient information to address the questions of (1) the clinical effectiveness of OCT compared with FFA; (2) the acceptability of the tests; and (3) the performance of other health professionals compared with ophthalmologists in interpreting OCT findings.
Uncertainties
Reference standard
Fundus fluorescein angiography interpreted by an ophthalmologist was our reference standard test and as such was assumed to have perfect sensitivity and specificity for the detection of active nAMD. Therefore, it was not possible to address the question of whether or not OCT might actually have better sensitivity or specificity than FFA; the optimal judgement that could have been made about OCT was that it had equally high sensitivity and specificity as FFA. In fact, although OCT did have very high sensitivity, the specificity for diagnosis and monitoring was suboptimal.
Glasziou et al. 85 considered the question of when a new test should replace the existing reference standard. They suggested that this might be determined by a ‘fair umpire’ test applied to the cases where the new test and reference standard differed. This third test, although potentially less accurate than either the new test or reference standard, could be considered a fair umpire, if its errors were considered to be independent of the other tests, although it was acknowledged that this would usually be difficult to demonstrate. Possible umpires suggested included causal exposures, concurrent testing, prognosis, or response to treatment. Glasziou et al. 85 argued that using this approach, the umpire test might be able to distinguish which test was the better reference standard. An example given was that of a new test for tuberculosis, with the tuberculin skin test as the reference standard, interferon-γ enzyme-linked immunospot (ELISpot) assays as the new test and tuberculosis exposure as the fair umpire. 85 However, none of the studies included in our review provided a sufficient level of information to allow such a ‘fair umpire’ approach to be applied.
False positives
Excluding studies where information was only available for detection of phenotypes,34,37,38,52 specificity for OCT was reported by six23,28,30,32,45,53 of seven monitoring studies, but only 427,40,46,49 of 10 diagnostic studies.
As already reported, specificity for OCT for diagnosis was only moderate and for monitoring was lower, with a large number of FP results. A few studies provided some additional information on their FP results, with suggested reasons for these including the presence of a disciform scar with persistent cystic cavities,45 an increase in the central subfield measurement,27 drusen/atrophy,46,49 cystoid abnormalities,23 subretinal fluid being detected before FFA leakage was observed,40 and the detection of remnants of intraretinal fluid that had not yet been resorbed even though the underlying CNV was no longer actively leaking fluid. 32 Do et al. 27 suggested that SD-OCT may have lower specificity for the detection of CNV than TD-OCT because it is more likely to detect structural changes in the retina, which may be a normal anatomic variant and not necessarily representative of secondary changes in the retina owing to CNV.
Sandhu and Talks46 noted that the OCT FP rate was reduced with the addition of stereo colour images (separate test). In current practice OCT is typically associated with VA data which may improve the specificity of the test.
In two of the monitoring studies,23,30 participants had been treated with antiVEGF therapy and in five28,32,45,52,53 they were treated with PDT. For all OCT, median sensitivity was similar across the antiVEGF (90%) and PDT (88%) groups of studies, whereas median specificity was slightly higher across the PDT studies (51%) compared with the antiVEGF studies (43%). It is possible that following treatment with PDT there is less likelihood of having fluid in the retina than following therapy with antiVEGF, as fluid is a common feature in eyes treated with antiVEGF, even after many sessions of treatment. Currently PDT is rarely used for nAMD, but the reviewed literature reflects this older modality of treatment. OCT (especially the newer version with the highest resolution, SD-OCT) may detect fluid, even when only a small amount is present and it does not necessarily relate to CNV activity (e.g. fluid may be present if there is RPE dysfunction/damage as a result of the disease or its treatment, as in normal circumstances RPE pumps fluid out of the retina). Therefore, it is possible that there might be more OCT FPs resulting in lower specificity for detecting active nAMD following antiVEGF compared with PDT treatment.
In two diagnostic studies, by Kozak et al. 36 and Reichel et al. ,44 some patients were classed as having nAMD who were negative on FFA but positive on one of the other tests being assessed (13/541 eyes by TD-OCT in the Kozak et al. study36 and 4/20 participants by ICGA in the Reichel et al. 44 study). For the purposes of this review, these cases were considered to be test FPs (as the reference standard of FFA was considered to have perfect sensitivity and specificity). However, in some cases (e.g. with retinal haemorrhage), it is possible that ICGA may be better than FFA in detecting nAMD.
Heterogeneity across the studies
Other than the fact that one group of studies was concerned with initial diagnosis of nAMD and another with monitoring of those previously diagnosed, there were a number of other differences across the studies. In terms of differences across the participant groups, the prevalence of nAMD in the diagnostic studies ranged from 17.2% to 100% (median 80.0%) and of active nAMD in the monitoring studies from 49.2% to 83.3% (median 57.9%). The proportion of participants classed as having specific nAMD phenotpyes (e.g. classic CNV, occult CNV) varied across the studies. In eight diagnostic studies24,27,31,39,40,44,45,49 and one monitoring study30 participants were judged to have been pre-selected.
Detection of phenotypes
Twelve studies (eight diagnostic,25,33,34,37,38,41,46,49 four monitoring23,30,32,52) reported the sensitivity of OCT in the detection of nAMD phenotypes (predominantly classic, minimally classic, occult or RAP). None of the studies reported detection of IPCV. Results were mixed and overall there was insufficient evidence to understand whether or not the performance of OCT differs among the different phenotypes. The monitoring study by Giani et al. 30 (SD-OCT) reported high sensitivity for the detection of both classic and occult CNV activity (90.9% and 100% respectively).
Across four (TD-OCT) diagnostic studies25,34,37,38 reporting detection of RAP the median (range) sensitivity was 65% (50–100%). Of the monitoring studies, Khurana et al. 23 reported higher sensitivity for SD-OCT (59%) compared with TD-OCT (35%) for detecting retinal cystoid abnormalities, whereas van de Moere et al. 52 reported poor sensitivity for TD-OCT for detecting cystoid macular oedema (23%) and PED (6%).
Unit of analysis issues
Twelve OCT studies used one eye per patient in the analysis. 25,27,28,30,33–35,38,40,49,52,53 In three of these studies25,27,40 the inclusion criteria stipulation for the fellow eye meant that only one (study) eye per subject was eligible for analysis. In the remaining studies, the inclusion criteria were such that both eyes of some subjects might have been potentially eligible. 23,36,37,41,45,46 Of these, however, only the study by van de Moere et al. 52 reported the method used for selecting the study eye in the event of such a situation, stating that if both eyes were eligible one eye was randomly chosen for analysis. It was unclear from the other studies whether only one eye per subject had met the inclusion criteria or whether for some subjects both eyes were eligible but only one was selected.
In six OCT studies, both eyes of some participants met the inclusion criteria and were included in the analysis;23,36,37,41,45,46 however, none of these studies mentioned the issue of the possible influence that the non-independence of the fellow eye might have on the analysis.
All studies included in the meta-analyses used one eye per subject, apart from the study by Sandhu and Talks46 (meta-analysis of diagnostic studies) and the study by Khurana et al. 23 (meta-analysis of monitoring studies). In the study by Sandhu and Talks,46 131 eyes of 118 patients were included in the analysis, as 13 patients had bilateral activity. In the study by Khurana et al. ,23 59 eyes of 56 patients were included in the analysis, as three patients had received antiVEGF treatment for nAMD in both eyes. These studies did not report whether or not any adjustment had been made to take account of the non-independence of the fellow eye and contained an insufficient level of detail to allow for an exploration of this issue. However, the potential impact of fellow eye non-independence would probably be minor, at most, given the small number of subjects in the two studies for whom both eyes were included in the analysis.
Other relevant factors
Ongoing studies
No ongoing studies were identified of OCT or alternative tests of interest compared with a reference standard of FFA for the diagnosis, monitoring and guiding of treatment for nAMD.
Comparison of our results with other systematic reviews/health technology assessments
Our searches identified four HTA reports that included an assessment of OCT in the detection of nAMD. 14,86–88 The German HTA report by Stürzlinger et al. 87 (report summary in English, full text in German), published in 2007, considered head-to-head comparisons between OCT and FFA for newly presenting patients. Eight studies were included, of which three were included in our review. 33,35,46 The other five studies did not meet our inclusion criteria (assessment of RPE tear,89 retinal PED,90 drusen,91 geographic atrophy,92 and no diagnostic outcomes reported). 93 The report’s conclusions were that although OCT yielded diagnostic findings in addition to FFA results, OCT could not replace FFA during the primary diagnostic procedure.
The Belgian Health Care Knowledge Centre report by Van den Bruel et al. ,88 published in 2008, considered five ophthalmic tests in clinical practice, including OCT. The assessment identified the German HTA report and included an additional three studies,28,37,45 all three of which were included in our review. The review considered FFA as the reference standard for neovascular AMD, and, similar to our review, reported high sensitivity (96–97%) and moderate specificity (66%) of OCT in detecting CNV.
In the Australian Medical Services Advisory Committee (MSAC) report,86 published in 2009, OCT was compared (a) with FFA or clinical observation in the diagnosis of macular diseases; (b) in addition to FFA and clinical examination in the monitoring of patients with macular diseases; (c) in addition to computerised perimetry and clinical examination in the diagnosis of glaucoma; and (d) in addition to computerised perimetry and clinical examination in the monitoring of patients with glaucoma. Regarding the diagnostic accuracy of OCT for AMD, the MSAC report concluded that due to the absence of a valid reference standard, the diagnostic accuracy of OCT for the detection of macular abnormalities could not be assessed. This approach contradicted our study, the German and Belgian HTA reports and also current practice in the UK where FFA is considered the reference standard for the diagnosis of nAMD.
In the evidence-based analysis by the Medical Advisory Secretariat, Ontario, Canada,14 published in 2009, OCT was compared with the reference standard of FFA for AMD and diabetic macular oedema. The evaluation summarised the German HTA report and the study by Sandhu and Talks46 that was also included in our review. This report also questioned the validity of FFA as a reference standard and presented conclusions that were based on expert consultations.
Aflibercept
In May 2013, NICE published final draft guidance recommending aflibercept solution for injection as an option for treating nAMD (www.nice.org.uk/guidance/ta294). Full guidance was published in July 2013 (www.nice.org.uk/guidance/ta294/resources/guidance-aflibercept-solution-for-injection-for-treating-wet-agerelated-macular-degeneration-pdf). The treatment and monitoring schedule for this drug differs from that of ranibizumab. According to the summary of product characteristics for aflibercept, treatment should be given monthly for three consecutive 2-mg doses, followed by one injection every 2 months, with no need for monitoring between injections. After the first 12 months of treatment, the treatment interval may be extended based on visual and anatomic outcomes, with the schedule for monitoring determined by the treating doctor. In terms of the economic model, extending the length of time between monitoring visits would reduce the cost associated with monitoring as well as the number of treatment courses needed. However, this would be expected to affect all model strategies in a similar manner and therefore would be unlikely to modify the general conclusions from the economic analysis. This might nevertheless reduce the cost associated with treatment and monitoring of nAMD patients for the NHS.
Future technological developments
It is likely that future technological developments in OCT will be introduced. Most OCT devices create cross-sectional images of the retina. En-face OCT technology is an emerging imaging technique derived from SD-OCT that creates images of frontal sections of retinal layers that are compatible with conventional fundus images.
Another emerging technique is OCT angiography, which uses high-speed Fourier-domain OCT for non-invasive three-dimensional imaging of the vasculature and blood flow at the posterior part of the eye.
Cost-effectiveness
Statement of principal findings
No studies met the inclusion criteria for the systematic review of economic evaluations as none compared diagnostic or monitoring strategies for individuals with nAMD.
Nine strategies that used to a different extent OCT for diagnosis and/or monitoring of nAMD individuals were considered within the Markov cohort economic evaluation model. The strategy that based its diagnosis decision on the results of FFA only, combined with VA and OCT interpreted together by a nurse or technician as the first monitoring step, with a referral to an ophthalmologist if the first monitoring assessment was positive or unclear (‘FFA & Nurse’), had the lowest expected total cost. This strategy dominated (i.e. lower expected costs and higher expected QALYs) all others apart from one: diagnosis with FFA only, combined with monitoring by an ophthalmologist (‘FFA & Ophthalmologist’). The ‘FFA & Nurse’ and ‘FFA & Ophthalmologist’ strategies had, respectively, a 46.5% and 29.8% probability of being cost-effective at the £30,000 threshold value of willingness to pay for an extra QALY. In addition, the ‘FFA & Nurse’ strategy dominated all others in the great majority of sensitivity analyses.
The strategies that used OCT only for their monitoring decisions were, in almost every model run, ordered last in terms of ascending total expected cost and were often dominated by others. The strategy that used OCT as its only criteria for diagnosis and monitoring decisions was in almost every model run the most costly strategy.
Results were sensitive to the unit cost of treatment injections. A scenario with a lower unit cost for treatment (e.g. £50, equivalent to the cost of bevacizumab, instead of £742 considered for the base-case analysis) resulted in the FFA only for diagnosis combined with OCT only for monitoring strategy having the lowest total expected cost. Alternative strategies were either dominated or had an ICER well above the usual threshold stated for cost-effectiveness (i.e. £30,000).
Strengths and limitations of the economic assessment
The major strength of the economic evaluation is that it attempted to use the best available evidence with the compared strategies developed from extensive discussions within the project team and advisory group. Best practice guidelines were followed for this economic evaluation exercise. 73 For instance, test performance data were obtained from the systematic review of the literature with other data retrieved from focused but reproducible searches. There is, however, an inherent problem with model-based economic evaluations that incorporate evidence from several sources, even when these data have been retrieved systematically.
The economic model needed to consider individuals’ disease status (i.e. active or inactive nAMD) as well as test results on a monthly basis. In addition, these had to be combined with alternative VA states in order to incorporate utility weights into the model. It was felt that considering the effect of fellow eye status (VA and nAMD status) would add major complexity to the model without much benefit from this incorporation. A clear limitation of the so-called ‘one eye models’ is the underestimation of resources used. A proportion of nAMD individuals will have this condition in both eyes instead of one eye and would need treatment injections in each eye should the disease be active. In the current model this would increase the cost for those strategies with higher numbers of FPs (i.e. lower specificity) and therefore would be unlikely to modify the general conclusions of this study. A ‘one eye model’ has also been adopted by other teams involved in economic evaluations in this health area. 61
The model did not consider effects on utility due to treatment injections. Anxiety in nAMD individuals was believed to occur at each monitoring visit mainly due to the uncertainty of the underlying condition (i.e. active or inactive nAMD) and not the effects of the treatment injections. No evidence was obtained on this from the utility weight searches. However, utility weight decrements from adverse effects as a result of the treatment were included and this might partially overcome the above-mentioned potential limitation. The model did not consider factors relating to patient experience of alternative monitoring schemes. As such, there was no consideration of the process of care on patient preferences and only the effect of VA and the adverse effects of treatment on individual utility were incorporated into the model.
Limited evidence was available on the probability of nAMD active individuals becoming inactive when under treatment or inactive nAMD individuals becoming active. Data were retrieved from the literature, from a UK-based RCT (Dr Chris Rogers, personal communication) and expert opinion. In addition, progression data on VA were based on the 2-year follow-up MARINA study. 69 All these data were based on short follow-up but in a number of cases extrapolated to a lifetime time horizon. These clear limitations of the analysis indicate that its results should be interpreted with caution. Further research looking at the individual’s nAMD active/inactive status is desirable. A conditional or a retrospective analysis of existing data sets would be helpful in order to obtain data to inform future economic models.
The analysis was conducted from the NHS and Personal Social Services perspective, incorporating cost of visual impairment that considered, for instance, cost for community care and residential care. The model, however, did not take into account the cost for patients or their carers. For instance, as this is likely to be an elderly population, someone might accompany the patient for their monitoring visits. These costs have not been considered in the model.
Uncertainties of the economic analysis
Undoubtedly, the limitations of the data together with the assembly of key data of varied quality are of most concern. No SD-OCT studies contributed to the diagnosis performance data and only two SD-OCT studies23,30 contributed to the monitoring performance data in the economic model. Moreover, although OCT diagnosis and monitoring sensitivity and specificity data were retrieved from a systematic review of the literature, no such data were available for other tests proposed in alternative diagnosis or monitoring pathways (e.g. examination by the ophthalmologist or the monitoring assessment by a nurse or technician). Therefore, data for the model were obtained from expert opinion. These constitute major limitations of the analysis and further research in these areas is needed.
Chapter 8 Conclusions
Implications for service provision
In terms of OCT test performance, the evidence, which was limited in quantity, especially for monitoring studies, and variable in quality, suggests that:
-
For diagnosis of newly suspected nAMD, OCT has high sensitivity (88%) and moderate specificity (78%) (meta-analysis)
-
For monitoring of those previously diagnosed with nAMD, OCT has relatively high sensitivity (85%) but low specificity (48%) (meta-analysis)
-
SD-OCT had higher sensitivity than TD-OCT but lower specificity (monitoring studies).
The strategy that based its diagnostic decision on the results of FFA only, combined with a nurse- or technician-led stepwise approach for monitoring, had the lowest expected total cost and a 47% probability of being cost-effective at a £30,000 threshold value of willingness to pay for an extra QALY. In addition, this strategy dominated all others apart from one (i.e. diagnosis with FFA combined with stepwise ophthalmologist-led monitoring) in the great majority of sensitivity analyses. The economic evaluation results suggest that strategies that used OCT test results alone to make diagnosis or monitoring treatment decisions were unlikely to be a cost-effective use of resources. This seems to be driven by the OCT low specificity inducing a high number of individuals with FP test results being treated.
There has already been a shift in the diagnostic and monitoring pathways for nAMD caused by the adoption of OCT. At the diagnostic stage, OCT is currently used in addition to FFA (reference standard), whereas for monitoring it has largely replaced FFA, which is only used in selected circumstances. The evidence suggests that using OCT as the only test for monitoring patients with nAMD and detecting activity would, potentially, result in a substantial proportion of patients receiving treatment unnecessarily with intraocular injections of antiVEGF.
The continuing rise in the ageing population, with increasing numbers of people being diagnosed with nAMD and moving on to monitoring for renewed disease activity, will continue to present challenges for ophthalmology departments to have sufficient capacity to provide timely testing, and treatment.
Suggested research priorities
-
Regarding monitoring of nAMD, in current practice OCT is routinely used and FFA is used only in particular scenarios. There is a substantial disagreement between OCT and FFA. There is a need to research if OCT (without FFA) is an acceptable way of detecting active nAMD and guiding treatment. As there is the theoretical possibility of OCT being better in some cases than the current reference standard, such studies might be designed to include a ‘fair umpire’ test, if available, to examine differences between OCT and FFA, or should be designed to incorporate a period of follow-up to assess the consequences of the tests in terms of clinical effectiveness outcomes (e.g. VA). Currently used SD-OCT models should be evaluated, rather than TD-OCT.
-
Regarding diagnosis of nAMD, current practice consists of FFA (as reference standard) associated with OCT. Further research should be considered to establish the added value of OCT, and whether or not OCT (associated with SLB and VA) can fully replace FFA. As above, such studies might be designed to include a ‘fair umpire’ test, or the evaluation of the consequences of the diagnostic intervention. Currently used SD-OCT models should be evaluated, rather than TD-OCT.
-
Regarding the different phenotypes of nAMD, further evidence on the natural history, efficacy of treatment and diagnostic performance of OCT according to phenotype of nAMD is required.
-
For both diagnosis and monitoring of nAMD, prospective studies are required to assess the diagnostic accuracy and clinical effectiveness of strategies involving possible different combinations and sequences of tests (e.g. VA, SLB, FAF imaging, OCT), including a comparison of their interpretation by ophthalmologists compared with other health professionals.
-
To strengthen the evidence base used to develop the economic model, it would be important to explore the likelihood of active and inactive nAMD individuals becoming inactive or active respectively. In addition, a preference-based study to assess utility weights (e.g. decrements) associated with treatment and frequent monitoring is needed.
-
Further research is needed to evaluate health status (utilities) in patients with nAMD, taking into consideration the visual function and spectrum of disease in both eyes and exploring the value added by inclusion of fellow eye information.
Acknowledgements
We thank David Findlay Clark (service user with the condition), Graham Findlay (Chief Executive, North East Sensory Services) and Helen Jackman (Chief Executive, Macular Society) for providing valuable consumer insight and advice, and for commenting on the Plain English summary, and Malcolm McPherson (Community Optometrist) for providing a community optometrist perspective, through their participation as members of the study’s project advisory group; Usha Chakravarthy, Chris Rogers and colleagues for providing data from the IVAN trial; Mari Imamura and Xueli Jia for translating non-English language papers; and Lara Kemp for secretarial support.
The economic model developed for the analysis was informed by an existing economic model developed by the Southampton Health Technology Assessments Centre (SHTAC), University of Southampton, UK. The intellectual property rights associated with the SHTAC economic model are owned by the University of Southampton (UK) – all rights reserved. We thank Andrew Clegg and Jeremy Jones for providing access to the SHTAC AMD economic evaluation model (see www.southampton.ac.uk/shtac/research/published/eyediseases.page?).
This report was commissioned by the National Institute for Health Research (NIHR) HTA Programme as project number 10/57/22. The Health Services Research Unit and Health Economics Research Unit, Institute of Applied Health Sciences, University of Aberdeen, are core-funded by the Chief Scientist Office of the Scottish Government Health and Social Care Directorates. The views and opinions expressed are those of the authors and do not necessarily reflect those of the funders.
Rider on responsibility for report
The views expressed in this report are those of the authors and not necessarily those of the NIHR HTA Programme. Any errors are the responsibility of the authors.
Contributions of authors
Graham Mowatt (coprincipal investigator, Senior Research Fellow) co-ordinated the study and wrote the decision problem, methods and assessment of diagnostic and monitoring studies chapters and sections of the scientific summary, discussion and conclusions chapters.
Rodolfo Hernández (Research Fellow) conducted the economic evaluation and wrote the cost-effectiveness chapter and sections of the scientific summary, discussion and conclusions chapters.
Mayret Castillo (Research Assistant) led the day-to-day running of the study and reviewed the evidence on test performance with assistance from Graham Mowatt and Augusto Azuara-Blanco.
Noemi Lois (Professor of Ophthalmology) wrote sections of the background and factors relevant to the NHS and other parties chapters.
Andrew Elders (Statistician) provided statistical support.
Cynthia Fraser (Information Specialist) developed and ran the search strategies, managed the reference database and formatted references.
Olatunde Aremu (Research Fellow) was involved with the initial development of the economic model (model conceptualisation), with supervision from Rodolfo Hernández.
Noemi Lois, Augusto-Azuara-Blanco, Winfried Amoaku (Clinical Associate Professor and Reader in Ophthalmology and Visual Sciences), Jennifer Burr (Reader) and Andrew Lotery (Professor of Ophthalmology) provided expert advice on clinical aspects of the study.
Craig Ramsay (Health Care Assessment Programme Director) and Jennifer Burr provided advice on methodological aspects of the study.
Augusto Azuara-Blanco (coprincipal investigator, Professor of Ophthalmology) jointly co-ordinated the study with Graham Mowatt, wrote the background and factors relevant to the NHS and other parties chapters, sections of the scientific summary, discussion and conclusions chapters, and was responsible for the final editing.
All authors commented on drafts of the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Age-Related Macular Degeneration – Guidelines for Management. London: Royal College of Ophthalmologists; 2013.
- Imamura Y, Engelbert M, Iida T, Freund KB, Yannuzzi LA. Polypoidal choroidal vasculopathy: a review. Surv Ophthalmol 2010;55:501-15. http://dx.doi.org/10.1016/j.survophthal.2010.03.004.
- Obata R, Yanagi Y, Kami J, Takahashi H, Inoue Y, Tamaki Y. Polypoidal choroidal vasculopathy and retinochoroidal anastomosis in Japanese patients eligible for photodynamic therapy for exudative age-related macular degeneration. Jpn J Ophthalmol 2006;50:354-60. http://dx.doi.org/10.1007/s10384-005-0337-2.
- Minassian DC, Reidy A, Lightstone A, Desai P. Modelling the prevalence of age-related macular degeneration (2010–2020) in the UK: expected impact of anti-vascular endothelial growth factor (VEGF) therapy. Br J Ophthalmol 2011;95:1433-6. http://dx.doi.org/10.1136/bjo.2010.195370.
- Owen CG, Jarrar Z, Wormald R, Cook DG, Fletcher AE, Rudnicka AR. The estimated prevalence and incidence of late stage age related macular degeneration in the UK. Br J Ophthalmol 2012;96:752-6. http://dx.doi.org/10.1136/bjophthalmol-2011-301109.
- Augood CA, Vingerling JR, de Jong PT, Chakravarthy U, Seland J, Soubrane G, et al. Prevalence of age-related maculopathy in older Europeans: the European Eye Study (EUREYE). Arch Ophthalmol 2006;124:529-35. http://dx.doi.org/10.1001/archopht.124.4.529.
- Pegaptanib and Ranibizumab for the Treatment of Age-Related Macular Degeneration. NICE Technology Appraisal Guidance TA155. London: NICE; 2008.
- Martin DF, Maguire MG, Fine SL, Ying GS, Jaffe GJ, . Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group . Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology 2012;119:1388-98. http://dx.doi.org/10.1016/j.ophtha.2012.03.053.
- Ivan SI, Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, et al. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology 2012;119:1399-411. http://dx.doi.org/10.1016/j.ophtha.2012.04.015.
- Holz FG, Korobelnik JF, Lanzetta P, Mitchell P, Schmidt-Erfurth U, Wolf S, et al. The effects of a flexible visual acuity-driven ranibizumab treatment regimen in age-related macular degeneration: outcomes of a drug and disease model. Invest Ophthalmol Vis Sci 2010;51:405-12. http://dx.doi.org/10.1167/iovs.09-3813.
- NHS Reference Costs 2011–12. London: Department of Health; 2012.
- British National Formulary. London: BMA and RPS; 2013.
- Gupta OP, Shienbaum G, Patel AH, Fecarotta C, Kaiser RS, Regillo CD. A treat and extend regimen using ranibizumab for neovascular age-related macular degeneration clinical and economic impact. Ophthalmology 2010;117:2134-40. http://dx.doi.org/10.1016/j.ophtha.2010.02.032.
- Medical Advisory Secretariat . Optical Coherence Tomography for Age-Related Macular Degeneration and Diabetic Macular Edema: An Evidence-Based Analysis. Ont Health Technol Assess Ser 2009;9. www.health.gov.on.ca/english/providers/program/mas/tech/reviews/pdf/rev_oct_20090925.pdf (accessed June 2013).
- Office for National Statistics . Statistical Bulletin: 2011 Census – Population and Household Estimates for England and Wales, March 2011 2011. www.ons.gov.uk/ons/rel/census/2011-census/population-and-household-estimates-for-england-and-wales/stb-e-w.html (accessed June 2013).
- Interim Life Tables. London: UK Government Actuary’s Department; 2013.
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529-36. http://dx.doi.org/10.7326/0003-4819-155-8-201110180-00009.
- Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 2011. www.cochrane-handbook.org/ (accessed April 2013).
- Rutter CM, Gatsonis CA. A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med 2001;20:2865-84. http://dx.doi.org/10.1002/sim.942.
- Deeks J. Systematic reviews in health care: systematic reviews of evaluations of diagnostic and screening tests. BMJ 2001;323:157-62. http://dx.doi.org/10.1136/bmj.323.7305.157.
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. http://dx.doi.org/10.1016/0197-2456(86)90046-2.
- Glossary of Cochrane Terms. Oxford: The Cochrane Collaboration; 2013.
- Khurana RN, Dupas B, Bressler NM. Agreement of time-domain and spectral-domain optical coherence tomography with fluorescein leakage from choroidal neovascularization. Ophthalmology 2010;117:1376-80. http://dx.doi.org/10.1016/j.ophtha.2009.11.039.
- Alster Y, Bressler NM, Bressler SB, Brimacombe JA, Crompton RM, Duh YJ, et al. Preferential hyperacuity perimeter (PreView PHP) for detecting choroidal neovascularization study. Ophthalmology 2005;112:1758-65. http://dx.doi.org/10.1016/j.ophtha.2005.06.008.
- Cachulo L, Silva R, Fonseca P, Pires I, Carvajal-Gonzalez S, Bernardes R, et al. Early markers of choroidal neovascularization in the fellow eye of patients with unilateral exudative age-related macular degeneration. Ophthalmologica 2011;225:144-9. http://dx.doi.org/10.1159/000321064.
- Chen S, Han M, Wang L. Indocyanine green angiography of exudative age-related macular degeneration. Chin Ophthalmic Res 2003;21:428-30.
- Do DV, Gower EW, Cassard SD, Boyer D, Bressler NM, Bressler SB, et al. Detection of new-onset choroidal neovascularization using optical coherence tomography: the AMD DOC Study. Ophthalmology 2012;119:771-8. http://dx.doi.org/10.1016/j.ophtha.2011.10.019.
- Eter N, Spaide RF. Comparison of fluorescein angiography and optical coherence tomography for patients with choroidal neovascularization after photodynamic therapy. Retina 2005;25:691-6. http://dx.doi.org/10.1097/00006982-200509000-00002.
- Fujii C, Inobe K, Sugimoto Y, Sugimoto A, Takahashi Y, Akagi Y. Indocyanine green angiographic findings in eyes with age-related macular degeneration. Folia Ophthalmol Japonica 1996;47:300-5.
- Giani A, Luiselli C, Esmaili DD, Salvetti P, Cigada M, Miller JW, et al. Spectral-domain optical coherence tomography as an indicator of fluorescein angiography leakage from choroidal neovascularization. Invest Ophthalmol Vis Sci 2011;52:5579-86. http://dx.doi.org/10.1167/iovs.10-6617.
- Gomi F, Sawa M, Mitarai K, Tsujikawa M, Tano Y. Angiographic lesion of polypoidal choroidal vasculopathy on indocyanine green and fluorescein angiography. Graefes Arch Clin Exp Ophthalmol 2007;245:1421-7. http://dx.doi.org/10.1007/s00417-007-0564-y.
- Henschel A, Spital G, Lommatzsch A, Pauleikhoff D. Optical coherence tomography in neovascular age related macular degeneration compared to fluorescein angiography and visual acuity. Eur J Ophthalmol 2009;19:831-5.
- Hughes EH, Khan J, Patel N, Kashani S, Chong NV. In vivo demonstration of the anatomic differences between classic and occult choroidal neovascularization using optical coherence tomography. Am J Ophthalmol 2005;139:344-6. http://dx.doi.org/10.1016/j.ajo.2004.07.058.
- Khondkaryan A, Keane PA, Liakopoulos S, Walsh AC, Sadda SR. Comparison of optical coherence tomography and fluorescein angiography for the classification of neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2009;50.
- Kim SG, Lee SC, Seong YS, Kim SW, Kwon OW. Choroidal neovascularization characteristics and its size in optical coherence tomography. Yonsei Med J 2003;44:821-7.
- Kozak I, Morrison VL, Clark TM, Bartsch DU, Lee BR, Falkenstein I, et al. Discrepancy between fluorescein angiography and optical coherence tomography in detection of macular disease. Retina 2008;28:538-44. http://dx.doi.org/10.1097/IAE.0b013e318167270b.
- Krebs I, Binder S, Stolba U, Krepler K, Zeiler F, Glittenberg C. The value of optical coherence tomography in diagnosis and therapy of age-related macular degeneration. Spektrum Der Augenheilkunde 2007;21:33-8. http://dx.doi.org/10.1007/s00717-006-0169-6.
- Liakopoulos S, Ongchin S, Bansal A, Msutta S, Walsh AC, Updike PG, et al. Quantitative optical coherence tomography findings in various subtypes of neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2008;49:5048-54. http://dx.doi.org/10.1167/iovs.08-1877.
- Loewenstein A, Ferencz JR, Lang Y, Yeshurun I, Pollack A, Siegal R, et al. Toward earlier detection of choroidal neovascularization secondary to age-related macular degeneration: multicenter evaluation of a preferential hyperacuity perimeter designed as a home device. Retina 2010;30:1058-64. http://dx.doi.org/10.1097/IAE.0b013e3181d1a75e.
- Padnick-Silver L, Weinberg AB, Lafranco FP, MacSai MS. Pilot study for the detection of early exudative age-related macular degeneration with optical coherence tomography. Retina 2012;32:1045-56. http://dx.doi.org/10.1097/IAE.0b03e31823fb82b.
- Park SS, Truong SN, Zawadzki RJ, Alam S, Choi SS, Telander DG, et al. High-resolution Fourier-domain optical coherence tomography of choroidal neovascular membranes associated with age-related macular degeneration. Invest Ophthalmol Vis Sci 2010;51:4200-6. http://dx.doi.org/10.1167/iovs.09-4256.
- Parravano M, Varano M, Virgili G. Integrated imaging approach in RAP diagnosis. Acta Ophthalmol (Copenh) 2012;90.
- Regillo CD, Blade KA, Custis PH, O’Connell SR. Evaluating persistent and recurrent choroidal neovascularization. The role of indocyanine green angiography. Ophthalmology 1998;105:1821-6. http://dx.doi.org/10.1016/S0161-6420(98)91022-3.
- Reichel E, Duker JS, Puliafito CA. Indocyanine green angiography and choroidal neovascularization obscured by hemorrhage. Ophthalmology 1995;102:1871-6. http://dx.doi.org/10.1016/S0161-6420(95)30781-6.
- Salinas-Alaman A, Garcia-Layana A, Maldonado MJ, Sainz-Gomez C, Alvarez-Vidal A. Using optical coherence tomography to monitor photodynamic therapy in age related macular degeneration. Am J Ophthalmol 2005;140:23-8. http://dx.doi.org/10.1016/j.ajo.2005.01.044.
- Sandhu SS, Talks SJ. Correlation of optical coherence tomography, with or without additional colour fundus photography, with stereo fundus fluorescein angiography in diagnosing choroidal neovascular membranes. Br J Ophthalmol 2005;89:967-70. http://dx.doi.org/10.1136/bjo.2004.060863.
- Silva R, Cachulo ML, Fonseca P, Bernardes R, Nunes S, Vilhena N, et al. Age-related macular degeneration and risk factors for the development of choroidal neovascularisation in the fellow eye: a 3-year follow-up study. Ophthalmologica 2011;226:110-18. http://dx.doi.org/10.1159/000329473.
- Sulzbacher F, Kiss C, Munk M, Deak G, Sacu S, Schmidt-Erfurth U. Diagnostic evaluation of type 2 (classic) choroidal neovascularization: optical coherence tomography, indocyanine green angiography, and fluorescein angiography. Am J Ophthalmol 2011;152:799-806e1. http://dx.doi.org/10.1016/j.ajo.2011.04.011.
- Talks J, Koshy Z, Chatzinikolas K. Use of optical coherence tomography, fluorescein angiography and indocyanine green angiography in a screening clinic for wet age-related macular degeneration. Br J Ophthalmol 2007;91:600-1. http://dx.doi.org/10.1136/bjo.2006.108043.
- Torron FB, Melcon SF, Ferrer N, Ruiz M, Honrubia L. Indocyanine green angiography and subretinal neovascularization. Patterns in age related macular degeneration. Arch Soc Esp Oftalmol 2001;76:221-8.
- Torron FB, Perez O, Melcon SF, Ferrer N, Ruiz-Moreno O, Honrubia L. Dynamic angiography in age related macular degeneration. Arch Soc Esp Oftalmol 2002;77:353-9.
- van de Moere A, Sandhu SS, Talks SJ. Correlation of optical coherence tomography and fundus fluorescein angiography following photodynamic therapy for choroidal neovascular membranes. Br J Ophthalmol 2006;90:304-6. http://dx.doi.org/10.1136/bjo.2005.079947.
- van Velthoven ME, de Smet MD, Schlingemann RO, Magnani M, Verbraak FD. Added value of OCT in evaluating the presence of leakage in patients with age-related macular degeneration treated with PDT. Graefes Arch Clin Exp Ophthalmol 2006;244:1119-23. http://dx.doi.org/10.1007/s00417-005-0209-y.
- Jaeschke R, Guyatt G, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA 1994;271:389-91. http://dx.doi.org/10.1001/jama.1994.03510290071040.
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Amoaku W, Blakeney S, Freeman M, Gale R, Johnston R, Kelly SP, et al. Action on AMD. Optimising patient management: act now to ensure current and continual delivery of best possible patient care. Eye 2012;26:S2-21. http://dx.doi.org/10.1038/eye.2011.343.
- Barton P, Bryan S, Robinson S. Modelling in the economic evaluation of health care: selecting the appropriate approach. J Health Serv Res Policy 2004;9:110-18. http://dx.doi.org/10.1258/135581904322987535.
- Brennan A, Chick SE, Davies R. A taxonomy of model structures for economic evaluation of health technologies. Health Econ 2006;15:1295-310. http://dx.doi.org/10.1002/hec.1148.
- Siebert U, Alagoz O, Bayoumi AM, Jahn B, Owens DK, Cohen DJ, et al. State-transition modeling: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-3. Value Health 2012;15:812-20. http://dx.doi.org/10.1016/j.jval.2012.06.014.
- Sonnenberg FA, Beck JR. Markov models in medical decision making: a practical guide. Med Decis Making 1993;13:322-38. http://dx.doi.org/10.1177/0272989X9301300409.
- Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A. Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation. Health Technol Assess 2008;12.
- Briggs A, Sculpher M, Claxton K. Decision Modelling for Health Economic Evaluation. Oxford: Oxford University Press; 2006.
- Briggs A, Drummond M, McGuire A. Economic Evaluation in Health Care: Merging Theory with Practice. Oxford: Oxford University Press; 2001.
- Briggs AH, Weinstein MC, Fenwick EA, Karnon J, Sculpher MJ, Paltiel AD, et al. Model parameter estimation and uncertainty: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-6. Value Health 2012;15:835-42. http://dx.doi.org/10.1016/j.jval.2012.04.014.
- Mitchell P, Wang JJ, Foran S, Smith W. Five-year incidence of age-related maculopathy lesions: the Blue Mountains Eye Study. Ophthalmology 2002;109:1092-7. http://dx.doi.org/10.1016/S0161-6420(02)01055-2.
- van Leeuwen R, Klaver CC, Vingerling JR, Hofman A, de Jong PT. The risk and natural course of age-related maculopathy: follow-up at 6 1/2 years in the Rotterdam study. Arch Ophthalmol 2003;121:519-26. http://dx.doi.org/10.1001/archopht.121.4.519.
- Thiagarajan M, Evans JR, Smeeth L, Wormald RP, Fletcher AE. Cause-specific visual impairment and mortality: results from a population-based study of older people in the United Kingdom. Arch Ophthalmol 2005;123:1397-403. http://dx.doi.org/10.1001/archopht.123.10.1397.
- Xu L, Wang YX, Wang J, Jonas JJ. Mortality and ocular diseases: the Beijing Eye Study. Ophthalmology 2009;116:732-8. http://dx.doi.org/10.1016/j.ophtha.2008.11.003.
- Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006;355:1419-31. http://dx.doi.org/10.1056/NEJMoa054481.
- Horster R, Ristau T, Sadda SR, Liakopoulos S. Individual recurrence intervals after anti-VEGF therapy for age-related macular degeneration. Graefes Arch Clin Exp Ophthal 2011;249:645-52. http://dx.doi.org/10.1007/s00417-010-1588-2.
- Meads C, Hyde C. What is the cost of blindness?. Br J Ophthalmol 2003;87:1201-4. http://dx.doi.org/10.1136/bjo.87.10.1201.
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: Personal Social Services Research Unit; 2012.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Brown GC, Sharma S, Brown MM, Kistler J. Utility values and age-related macular degeneration. Arch Ophthalmol 2000;118:47-51. http://dx.doi.org/10.1001/archopht.118.1.47.
- Brown GC, Brown MM, Brown HC, Kindermann S, Sharma S. A value-based medicine comparison of interventions for subfoveal neovascular macular degeneration. Ophthalmology 2007;114:1170-8. http://dx.doi.org/10.1016/j.ophtha.2006.09.019.
- Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves – facts, fallacies and frequently asked questions. Health Econ 2004;13:405-15. http://dx.doi.org/10.1002/hec.903.
- van Hout BA, Al MJ, Gordon GS, Rutten FF. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ 1994;3:309-19. http://dx.doi.org/10.1002/hec.4730030505.
- Czoski-Murray C, Carlton J, Brazier J, Young T, Papo NL, Kang HK. Valuing condition-specific health states using simulation contact lenses. Value Health 2009;12:793-9. http://dx.doi.org/10.1111/j.1524-4733.2009.00527.x.
- General Ophthalmic Services: Increases to NHS Sight Test Fee. Redditch: NHS England; 2013.
- The General Ophthalmic Services Contracts (Payments) Directions 2013. Redditch: NHS, England; 2013.
- Petrou S, Gray A. Economic evaluation using decision analytical modelling: design, conduct, analysis, and reporting. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d1766.
- Rechel B, Grundy E, Robine JM, Cylus J, Mackenbach JP, Knai C, et al. Ageing in the European Union. Lancet 2013;381:1312-22. http://dx.doi.org/10.1016/S0140-6736(12)62087-X.
- Chakravarthy U, Evans J, Rosenfeld PJ. Age related macular degeneration. BMJ 2010;340:526-30.
- Leeflang MM, Deeks JJ, Gatsonis C, Bossuyt PM. Systematic reviews of diagnostic test accuracy. Ann Intern Med 2008;149:889-97. http://dx.doi.org/10.7326/0003-4819-149-12-200812160-00008.
- Glasziou P, Irwig L, Deeks JJ. When should a new test become the current reference standard?. Ann Intern Med 2008;149:816-22. http://dx.doi.org/10.7326/0003-4819-149-11-200812020-00009.
- Optical Coherence Tomography MSAC Application 1116. Canberra: Medical Services Advisory Committee (MSAC); 2009.
- Stürzlinger H, Fröschl B, Genser D. Evaluation of Optical Coherence Tomography in the Diagnosis of Age Related Macular Degeneration Compared with Fluorescence Angiography. Cologne: The German Agency for Health Technology Assessment (DAHTA); 2007.
- Van den Bruel A, Gailly J, Vijens F, Devriese S. Guidance for the Use of Five Ophthalmic Tests in Clinical Practice KCE reports 71C. Brussels: The Belgian Health Care Knowledge Centre (KCE); 2008.
- Giovannini A, Amato G, Mariotti C, Scassellati-Sforzolini B. Optical coherence tomography in the assessment of retinae pigment epithelial tear. Retina 2000;20:37-40. http://dx.doi.org/10.1097/00006982-200001000-00007.
- Sato T, Iida T, Hagimura N, Kishi S. Correlation of optical coherence tomography with angiography in retinal pigment epithelial detachment associated with age-related macular degeneration. Retina 2004;24:910-14. http://dx.doi.org/10.1097/00006982-200412000-00011.
- Hassenstein A, Ruhl R, Richard G. OCT in age related macular degeneration and differential diagnosis. Spektrum Der Augenheilkunde 2000;14:209-13. http://dx.doi.org/10.1007/BF03162805.
- Hassenstein A, Ruhl R, Richard G. Optical coherence tomography in geographic atrophy – a clinicopathologic correlation. Klin Monatsbl Augenheilkd 2001;218:503-9. http://dx.doi.org/10.1055/s-2001-16293.
- Ting TD, Oh M, Cox TA, Meyer CH, Toth CA. Decreased visual acuity associated with cystoid macular edema in neovascular age-related macular degeneration. Arch Ophthalmol 2002;120:731-7. http://dx.doi.org/10.1001/archopht.120.6.731.
Appendix 1 Search strategies
Clinical effectiveness and diagnostic accuracy of optical coherence tomography for age-related macular degeneration
EMBASE, Ovid MEDLINE(R) and Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations
Searched: 1988 to 2013 Week 12 (EMBASE), 1946 to March Week 2 2013 [Ovid MEDLINE(R)] and 25 March 2013 [Ovid MEDLINE(R)] (In-Process & Other Non-Indexed Citations).
Ovid multifile search. URL: https://shibboleth.ovid.com/.
Date of search: 25 March 2013.
Search strategy
-
( *macular degeneration/ or wet macular degeneration/) use mesz
-
macular edema/ not (diabetic or diabetes).hw.
-
( *retina macula age related degeneration/ or exudative macular degeneration/) use emed
-
retinal hemorrhage/ use mesz or choroid hemorrhage/ use mesz
-
retina haemorrhage/ use emed or choroid haemorrhage/ use emed
-
choroidal neovascularization/ use mesz
-
subretinal neovascularization/ use emed
-
retinal neovascularization/ use mesz not (diabetes or diabetic).hw.
-
retina neovascularization/ use emed not (diabetes or diabetic).hw.
-
((exudative or wet or neovascular) and amd).tw.
-
((exudative or wet or neovascular) adj3 age related).tw.
-
((exudative or wet or neovascular) adj3 degenerat$).tw.
-
((exudative or wet or neovascular) adj3 macula$).tw.
-
or/1-13
-
Tomography, Optical Coherence/ use mesz
-
optical coherence tomography/ use emed
-
oct.tw.
-
(stratus or cirrus or spectralis or rtvue or soct).tw.
-
or/15-18
-
autofluorescence.tw.
-
autofluorescence/ use emed
-
(fund$ adj3 (photograph$ or imag$)).tw.
-
photography/ use mesz
-
eye photography/ use emed
-
(microperimetry or micro perimetry).tw.
-
(visual acuity adj3 (test$ or assess$ or measure$ or value$ or exam$)).tw.
-
(dva or nva or bcva).tw
-
icga.tw.
-
indocyanine green angiograph$.tw
-
(dynamic adj3 angiograph$).tw
-
digital subtraction angiograph$.tw
-
preferential hyperacuity perimet$.tw
-
amsler$.tw.
-
clinical exam$.tw.
-
(ophthalmol$ adj1 (exam$ or assess$ or evaluat$)).tw.
-
or/20-35
-
14 and (19 or 36)
-
nonhuman/ not human/
-
animals/ not humans/
-
37 not (38 or 39)
-
40 not (letter or editorial or comment).pt.
-
41 not case report/
-
("2008" or “2007”).yr. and conference abstract.pt.
-
42 not 43 (4803)
-
remove duplicates from 44
-
limit 45 to yr=“1995 –Current”
Science Citation Index and Bioscience Information Services
Searched: 1995–22 March 2013 (Science Citation Index) and 1995–22 March 2013 (Bioscience Information Services).
ISI Web of Knowledge. URL: http://wok.mimas.ac.uk/.
Date of search: 22 March 2013.
Search strategy
#1 ((TS=(AMD and (exudative or wet or neovascular*))))
#2 ((TS=((exudative or wet or neovascular) NEAR/3 “age related”)))
#3 (((TS=((exudative or wet or neovascular) NEAR/3 degenerat*))
#4 (((TS=((exudative or wet or neovascular) NEAR/3 macula*))))
#5 ((TS=(choroid* NEAR/1 neovascular*)))
#6 (TS= (macular NEAR/1 (edema or oedema))
#7 (((TS=(retina* NEAR/1 neovascular*))))
#8 #1 or #2 or #3 or #4 or #5 or #6 or #7
#9 (((TS=optical coherence tomography)))
#10 (((TS=(stratus or cirrus or spectralis or rtvue or soct))))
#11 ((TS=autofluorescence)))
#12 (((TS=(fundus NEAR/3 (photograph* or imag*)))))
#13 (((TS=(microperimetry or “micro perimetry”))))
#14 TS=(dva or nva or bcva)
#15 TS=icga
#16 TS= indocyanine green angiograph*
#17 TS=(dynamic NEAR/3 angiograph*)
#18 TS= digital subtraction angiograph*
#19 TS= preferential hyperacuity perimet*
#20 TS=amsler*
#21 TS=clinical exam*
#22 TS=(ophthalmol* NEAR/1 (exam* or assess* or evaluat*))
#23 #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22
#24 #8 and #23
The Cochrane Library
Searched: Cochrane Database of Systematic Reviews Issue 2 2013; Cochrane Central Register of Controlled Trials Issue 1 2013.
URL: www3.interscience.wiley.com/.
Date of search: 22 March 2013.
Search strategy
#1 MeSH descriptor Macular Degeneration, this term only
#2 MeSH descriptor Macular Edema, this term only
#3 MeSH descriptor Wet Macular Degeneration explode all trees
#4 MeSH descriptor Retinal Hemorrhage, this term only
#5 MeSH descriptor Choroid Hemorrhage, this term only
#6 MeSH descriptor Choroidal Neovascularization, this term only
#7 MeSH descriptor Retinal Neovascularization, this term only
#8 (exudative or wet or neovascular) and amd:ti,ab,kw or (exudative or wet or neovascular) NEAR/3 age related:ti,ab,kw and (exudative or wet or neovascular) NEAR/3 degenerat*:ti,ab,kw and (exudative or wet or neovascular) NEAR/3 macula*:ti,ab,kw
#9 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8)
#10 MeSH descriptor Tomography, Optical Coherence, this term only
#11 (stratus or cirrus or spectralis or rtvue or soct or oct):ti,ab,kw
#12 (#10 OR #11)
#13 (autofluorescence):ti,ab,kw or (fund* NEAR/3 (photograph* or imag*)):ti,ab,kw or (microperimetry or micro perimetry):ti,ab,kw or (visual acuity NEAR/3 (test* or assess* or measure* or value* or exam*)):ti,ab,kw or (dva or nva or bcva):ti,ab,kw
#14 (clinical exam*):ti,ab,kw or (ophthalmol* NEAR/1 (exam* or assess* or evaluat*)).:ti,ab,kw
#15 (#13 OR #14)
#16 (#9 AND #12)
#17 (#9 AND #15)
#18 (#16 OR #17)
#19 (diabetes):ti,ab,kw or (diabetic):ti,ab,kw
#20 (#18 AND NOT #19)
#21 (#20), from 1995 to 2012
Health Technology Assessment database/Database of Abstracts of Reviews of Effects
Searched: inception until March 2013.
Centre for Reviews and Dissemination. URL: www.york.ac.uk/inst/crd/index.htm.
Date of search: March 2013.
Search strategy
#1 MeSH macular degeneration EXPLODE 1
#2 Amd or macular degeneration
#3 MeSH Tomography, Optical Coherence EXPLODE 1
#4 # 1 or #2 or #3
Medion
Searched: inception until March 2013.
URL: www.mediondatabase.nl/.
Date of search: March 2013.
Search strategy
Textword=Macular degeneration
ClinicalTrials.gov
Searched: inception until March 2013.
URL: http://clinicaltrials.gov/ct/gui/c/r.
Date of search: October 2014.
Search strategy
Condition=macular degeneration AND tomograph*
International Clinical Trials Registry Platform
Searched: inception until March 2013.
World Health Organization. URL: www.who.int/ictrp/en/.
Date of search: October 2012.
Search strategy
Condition=macular degeneration AND Intervention=tomography
Conference proceedings
Association for Research In Vision and Ophthalmology
Searched: 2009–12.
URL: www.iovs.org/search?arvomtgsearch=true.
Date of search: March 2013.
Search strategy
macular degeneration (as phrase) in title and wet exudative neovascular (any words) in title or abstract, from January 2009 through January 2012.
American Association of Ophthalmology
Searched: 2009–12.
URL: http://aao.scientificposters.com/.
Date of search: October 2012.
Search strategy
Macular degeneration and tomography
European Association for Vision and Eye Research
Searched: 2009–12.
URL: www.ever.be/.
Date of search: October 2012.
EVER 2009, September 30–3 October 2009 Portoroz, Slovenia.
EVER 2010, October 6–9, Crete, Greece.
EVER 2011, October 5–8, Crete, Greece.
EVER 2012, October 10–13, Nice, France.
Search strategy
Manufacturers’ websites
Date of search: March 2013
Carl Zeiss Meditec: www.meditec.zeiss.com/.
Optovue: www.optovue.com/.
Heidelberg Engineering: http://www.heidelbergengineering.co.uk/.
Patient acceptability of optical coherence tomography
EMBASE Ovid MEDLINE(R), Ovid MEDLINE(R) and In-Process & Other Non-Indexed Citations
Searched: 1988 to 2013 Week 12 [EMBASED Ovid MEDLINE(R)], 1946 to March Week 2 2013 [Ovid MEDLINE(R)] and 25 March 2013 (In-Process & Other Non-Indexed Citations).
Ovid multifile search. URL: https://shibboleth.ovid.com/.
Date of search: 25 March 2013.
Search strategy
-
*macular degeneration/ or wet macular degeneration/ use mesz
-
macular edema/
-
*retina macula age related degeneration/ or exudative macular degeneration/ use emed
-
retinal hemorrhage/ use mesz or choroid hemorrhage/ use mesz
-
retina haemorrhage/ use emed or choroid haemorrhage/ use emed
-
choroidal neovascularization/ use mesz
-
subretinal neovascularization/ use emed
-
retinal neovascularization/ use mesz
-
retina neovascularization/ use emed
-
((exudative or wet or neovascular) and amd).tw.
-
((exudative or wet or neovascular) adj3 age related).tw.
-
((exudative or wet or neovascular) adj3 degenerat$).tw.
-
((exudative or wet or neovascular) adj3 macula$).tw.
-
or/1-13
-
Tomography, Optical Coherence/ use mesz
-
optical coherence tomography/ use emed
-
oct.tw.
-
(stratus or cirrus or spectralis or rtvue or soct).tw.
-
or/15-18
-
14 and 19
-
exp patient acceptance of health care/ use mesz
-
exp patient attitude/ use emed
-
consumer satisfaction/ use mesz
-
patient dropouts/ use mesz
-
attitude of health personnel/ use mesz
-
health personnel attitude/ use emed
-
(patient? adj3 (compliance or participat$ or accept$ or refus$)).tw.
-
((patient? or ophthalmolog$ or optometr$ or clinician?) adj3 (attitide? or prefer$ or perception? or satisfaction)).tw.
-
qualitative research/
-
questionnaires/
-
(qualitative or interview$ or focus group? or questionnaire$ or survey$).tw.
-
(ethno$ or grounded or thematic or interpretive or narrative).tw.
-
or/21-32
-
20 and 33
-
exp eye diseases/
-
*Tomography, Optical Coherence/ use mesz
-
*optical coherence tomography/ use emed
-
oct.ti.
-
(stratus or cirrus or spectralis or rtvue or soct).ti.
-
35 and (36 or 37 or 38 or 39)
-
33 and 40 (124)
-
34 or 41 (212)
-
remove duplicates from 42
-
limit 43 to yr=“1995 -Current”
Applied Social Science Index and Abstracts (1995–23 March 2013)
Searched: 1995–23 March 2013.
ProQuest. URL: http://search.proquest.com/assia/.
Date of search: 23 March 2013.
Search strategy
KW=(OCT or optical coherence tomograph*)
PsycINFO
Searched: 1995–26 March 2013.
EBSCOhost. URL: http://web.ebscohost.com/ehost/.
Date of search: 26 March 2013.
Search strategy
Optical coherence tomograph* AND macular degeneration (ALL TEXT)
Cost-effectiveness for coherence tomography for age-related macular degeneration
EMBASE, Ovid MEDLINE(R) and Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations
Searched: 1980–2012 week 45 (EMBASE), 1996–November week 2 2012 [Ovid MEDLINE(R)] and 14 November 2012 (Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations)
Ovid Multifile Search URL: https://shibboleth.ovid.com/
Date searched: November 2012.
Search strategy
-
*macular degeneration/ or wet macular degeneration/ use mesz
-
macular edema/
-
*retina macula age related degeneration/ or exudative macular degeneration/ use emez
-
retinal hemorrhage/ use mesz or choroid hemorrhage/ use mesz
-
retina haemorrhage/ use emez or choroid haemorrhage/ use emez
-
choroidal neovascularization/ use mesz
-
subretinal neovascularization/ use emez
-
retinal neovascularization/ use mesz
-
[retina neovascularization/ use emez
-
((exudative or wet or neovascular) and amd).tw.
-
((exudative or wet or neovascular) adj3 age related).tw.
-
((exudative or wet or neovascular) adj3 degenerat$).tw.
-
((exudative or wet or neovascular) adj3 macula$).tw.
-
or/1-13
-
Tomography, Optical Coherence/ use mesz
-
optical coherence tomography/ use emed
-
(stratus or cirrus or spectralis or rtvue or soct).tw.
-
or/14-18
-
exp "costs and cost analysis"/ use mesz
-
exp economic evaluation/ use emez
-
economics/
-
health economics/ use emez
-
exp economics,hospital/ use mesz
-
exp economics,medical/ use mesz
-
economics,pharmaceutical/ use mesz
-
exp budgets/
-
exp models, economic/ use mesz
-
exp decision theory/
-
monte carlo method/
-
markov chains/
-
exp technology assessment, biomedical/
-
cost$.ti.
-
(cost$ adj2 (effective$ or utilit$ or benefit$ or minimis$)).ab.
-
economics model$.tw
-
(economic$ or pharmacoeconomic$).tw.
-
(price or prices or pricing).tw.
-
(value adj1 money).tw.
-
markov$.tw
-
monte carlo.tw.
-
(decision$ adj2 (tree? or analy$ or model$)).tw.
-
or/15-36
-
14 and 37
-
remove duplicates from 38
-
39 not (letter or editorial or comment).pt.
Health Technology Assessment/NHS Economic Evaluation Databases
Searched: inception until October 2012.
Centre for Reviews & Dissemination. URL: http://nhscrd.york.ac.uk/welcome.htm
Date searched: October 2012.
Search strategy
#1 MeSH macular degeneration EXPLODE 1
#2 Amd or macular degeneration
#3 MeSH Tomography, Optical Coherence EXPLODE 1
#4 # 1 or #2 or #3
Health Management Information Consortium
Searched: 1979 September 2012.
Ovid URL: https://shibboleth.ovid.com/
Date of search: November 2012.
Search strategy
-
macular degeneration/
-
retinal diseases/
-
((exudative or wet or neovascular) and amd).tw.
-
((exudative or wet or neovascular) adj3 age related).tw.
-
((exudative or wet or neovascular) adj3 degenerat$).tw.
-
((exudative or wet or neovascular) adj3 macula$).tw.
-
or/1-6
Research Papers in Economics
Searched: inception until September 2012.
URL: http://repec.org/
Date of search: September 2012.
Search strategy
macula or macular
Association for Research In Vision and Ophthalmology
Searched: January 2009 to January 2012.
URL: www.iovs.org/search?arvomtgsearch=true.
Date searched: January 2012.
Search strategy
macular degeneration (as phrase) in title and wet exudative neovascular (any words) in title or abstract.
Quality of life and neovascular age-related macular degeneration
EMBASE, Ovid MEDLINE(R) and Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations
Searched: 1980–2012 week 45 (Embase), 1946–November week 2 2012 [Ovid MEDLINE(R)], 14 November 2012 [Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations].
Ovid Multifile Search URL: https://shibboleth.ovid.com/
Date searched: November 2012.
Search strategy
-
*macular degeneration/ or wet macular degeneration/
-
macular edema/ not (diabetic or diabetes).hw
-
*retina macula age related degeneration/ or exudative macular degeneration/
-
retinal hemorrhage/ use mesz or choroid hemorrhage/
-
retina haemorrhage/ use emez or choroid haemorrhage/
-
choroidal neovascularization/
-
subretinal neovascularization/
-
retinal neovascularization/ use mesz not (diabetes or diabetic).hw.
-
retina neovascularization/ use emed not (diabetes or diabetic).hw.
-
((exudative or wet or neovascular) and amd).tw.
-
((exudative or wet or neovascular) adj3 age related).tw.
-
((exudative or wet or neovascular) adj3 degenerat$).tw.
-
((exudative or wet or neovascular) adj3 macula$).tw.
-
or/1-13
-
quality of life/
-
quality adjusted life year/
-
"Value of Life"/ use mesz
-
health status indicators/ use mesz
-
health status/ use emez
-
sickness impact profile/ use mesz
-
disability evaluation/ use mesz
-
disability/ use emez
-
activities of daily living/ use mesz
-
exp daily life activity/ use emez
-
cost utility analysis/ use emez
-
rating scale/
-
questionnaires
-
(quality adj1 life).tw.
-
quality adjusted life.tw.
-
disability adjusted life.tw.
-
(qaly? or qald? or qale? or qtime? or daly?).tw
-
(euroqol or euro qol or eq5d or eq 5d).tw.
-
(hql or hqol or h qol or hrqol or hr qol).tw.
-
(hye or hyes).tw.
-
health$ year$ equivalent$.tw.
-
(hui or hui1 or hui2 or hui3).tw
-
(health adj3 (utilit$ or disutili$)).tw.
-
(health adj3 (state or status)).tw.
-
(sf36 or sf 36 or short form 36 or shortform 36).tw.
-
(sf6 or sf 6 or short form 6 or shortform 6).tw.
-
(sf12 or sf 12 or short form 12 or shortform 12).tw.
-
(sf16 or sf 16 or short form 16 or shortform 16).tw.
-
(sf20 or sf 20 or short form 20 or shortform 20).tw.
-
willingness to pay.tw.
-
standard gamble.tw
-
trade off.tw.
-
conjoint analys?s.tw.
-
discrete choice.tw.
-
(case report or editorial or letter).pt.
-
case report/
-
(VQOL or NEI-VFQ-25 or MACDQOL or ADVS or VF-14 or SIPV).tw.
-
or/15-48,51
-
14 and 52
-
53 not (49 or 50)
-
remove duplicates from 54
Appendix 2 List of included studies
Diagnostic studies
Alster 2005
Alster Y, Bressler NM, Bressler SB, Brimacombe JA, Crompton RM, Duh YJ, et al. Preferential hyperacuity perimeter (PreView PHP) for detecting choroidal neovascularization study. Ophthalmology 2005;112:1758–65.
Cachulo 2011
Cachulo L, Silva R, Fonseca P, Pires I, Carvajal-Gonzalez S, Bernardes R, et al. Early markers of choroidal neovascularization in the fellow eye of patients with unilateral exudative age-related macular degeneration. Ophthalmologica 2011;225:144–9.
Silva R, Cachulo ML, Fonseca P, Bernardes R, Nunes S, Vilhena N, et al. Age-related macular degeneration and risk factors for the development of choroidal neovascularisation in the fellow eye: a 3-year follow-up study. Ophthalmologica 2011;226:110–18. (Secondary to Cachulo 2011.)
Chen 2003
Chen S, Han M, Wang L. Indocyanine green angiography of exudative age-related macular degeneration. Chin Ophthalmol Res 2003;21:428–30.
Do 2012
Do DV, Gower EW, Cassard SD, Boyer D, Bressler NM, Bressler SB, et al. Detection of new-onset choroidal neovascularization using optical coherence tomography: the AMD DOC Study. Ophthalmology 2012;119:771–8.
Fujii 1996
Fujii C, Inobe K, Sugimoto Y, Sugimoto A, Takahashi Y, Akagi Y. Indocyanine green angiographic findings in eyes with age-related macular degeneration. Folia Ophthalmol Jpn 1996;47:300–5.
Gomi 2007
Gomi F, Sawa M, Mitarai K, Tsujikawa M, Tano Y. Angiographic lesion of polypoidal choroidal vasculopathy on indocyanine green and fluorescein angiography. Graefes Arch Clin Exp Ophthalmol 2007;245:1421–7.
Hughes 2005
Hughes EH, Khan J, Patel N, Kashani S, Chong NV. In vivo demonstration of the anatomic differences between classic and occult choroidal neovascularization using optical coherence tomography. Am J Ophthalmol 2005;139:344–6.
Khondkaryan 2009
Khondkaryan A, Keane PA, Liakopoulos S, Walsh AC, Sadda SR. Comparison of optical coherence tomography and fluorescein angiography for the classification of neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2009;50:E-abstract 5259.
Kim 2003
Kim SG, Lee SC, Seong YS, Kim SW, Kwon OW. Choroidal neovascularization characteristics and its size in optical coherence tomography. Yonsei Med J 2003;44:821–7.
Kozak 2008
Kozak I, Morrison VL, Clark TM, Bartsch DU, Lee BR, Falkenstein I, et al. Discrepancy between fluorescein angiography and optical coherence tomography in detection of macular disease. Retina 2008;28:538–44.
Krebs 2007
Krebs I, Binder S, Stolba U, Krepler K, Zeiler F, Glittenberg C. The value of optical coherence tomography in diagnosis and therapy of age-related macular degeneration. Spektrum der Augenheilkunde 2007;21:33–8.
Liakopoulos 2008
Liakopoulos S, Ongchin S, Bansal A, Msutta S, Walsh AC, Updike PG, et al. Quantitative optical coherence tomography findings in various subtypes of neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2008;49:5048–54.
Loewenstein 2010
Loewenstein A, Ferencz JR, Lang Y, Yeshurun I, Pollack A, Siegal R, et al. Toward earlier detection of choroidal neovascularization secondary to age-related macular degeneration: multicenter evaluation of a preferential hyperacuity perimeter designed as a home device. Retina 2010;30:1058–64.
Padnick-Silver 2012
Padnick-Silver L, Weinberg AB, Lafranco FP, MacSai MS. Pilot study for the detection of early exudative age-related macular degeneration with optical coherence tomography. Retina 2012;32:1045–56.
Park 2010
Park SS, Truong SN, Zawadzki RJ, Alam S, Choi SS, Telander DG, et al. High-resolution Fourier-domain optical coherence tomography of choroidal neovascular membranes associated with age-related macular degeneration. Invest Ophthalmol Vis Sci 2010;51:4200–6.
Parravano 2012
Parravano M, Varano M, Virgili G. Integrated imaging approach in RAP diagnosis. Acta Ophthalmol 2012;90:abstract 4426.
Reichel 1995
Reichel E, Duker JS, Puliafito CA. Indocyanine green angiography and choroidal neovascularization obscured by hemorrhage. Ophthalmology 1995;102:1871–6.
Salinas-Alaman 2005
Salinas-Alaman A, Garcia-Layana A, Maldonado MJ, Sainz-Gomez C, Alvarez-Vidal A. Using optical coherence tomography to monitor photodynamic therapy in age related macular degeneration. Am J Ophthalmol 2005;140:23–8.
Sandhu 2005
Sandhu SS, Talks SJ. Correlation of optical coherence tomography, with or without additional colour fundus photography, with stereo fundus fluorescein angiography in diagnosing choroidal neovascular membranes. Br J Ophthalmol 2005;89:967–70.
Sulzbacher 2011
Sulzbacher F, Kiss C, Munk M, Deak G, Sacu S, Schmidt-Erfurth U. Diagnostic evaluation of type 2 (classic) choroidal neovascularization: optical coherence tomography, indocyanine green angiography, and fluorescein angiography. Am J Ophthalmol 2011;152:799–806e1.
Talks 2007
Talks J, Koshy Z, Chatzinikolas K. Use of optical coherence tomography, fluorescein angiography and indocyanine green angiography in a screening clinic for wet age-related macular degeneration. Br J Ophthalmol 2007;91:600–1.
Torron 2002
Torron FB, Perez O, Melcon SF, Ferrer N, Ruiz-Moreno O, Honrubia L. Dynamic angiography in age related macular degeneration. Arch Soc Esp Oftalmol 2002;77:353–9.
Torron FB, Melcon SF, Ferrer N, Ruiz M, Honrubia L. Indocyanine green angiography and subretinal neovascularization. Patterns in age related macular degeneration. Archiv Soc Esp Oftalmol 2001;76:221–8. (Secondary to Torron 2002.)
Monitoring studies
Eter 2005
Eter N, Spaide RF. Comparison of fluorescein angiography and optical coherence tomography for patients with choroidal neovascularization after photodynamic therapy. Retina 2005;25:691–6.
Giani 2011
Giani A, Luiselli C, Esmaili DD, Salvetti P, Cigada M, Miller JW, et al. Spectral-domain optical coherence tomography as an indicator of fluorescein angiography leakage from choroidal neovascularization. Invest Ophthalmol Vis Sci 2011;52:5579–86.
Henschel 2009
Henschel A, Spital G, Lommatzsch A, Pauleikhoff D. Optical coherence tomography in neovascular age related macular degeneration compared to fluorescein angiography and visual acuity. Eur J Ophthalmol 2009;19:831–5.
Khurana 2010
Khurana RN, Dupas B, Bressler NM. Agreement of time-domain and spectral-domain optical coherence tomography with fluorescein leakage from choroidal neovascularization. Ophthalmology 2010;117:1376–80.
Regillo 1998
Regillo CD, Blade KA, Custis PH, O’Connell SR. Evaluating persistent and recurrent choroidal neovascularization. The role of indocyanine green angiography. Ophthalmology 1998;105:1821–6.
Salinas-Alaman 2005
Salinas-Alaman A, Garcia-Layana A, Maldonado MJ, Sainz-Gomez C, Alvarez-Vidal A. Using optical coherence tomography to monitor photodynamic therapy in age related macular degeneration. Am J Ophthalmol 2005;140:23–8.
van de Moere 2006
van de Moere A, Sandhu SS, Talks SJ. Correlation of optical coherence tomography and fundus fluorescein angiography following photodynamic therapy for choroidal neovascular membranes. Br J Ophthalmol 2006;90:304–6.
van Velthoven 2006
van Velthoven ME, de Smet MD, Schlingemann RO, Magnani M, Verbraak FD. Added value of OCT in evaluating the presence of leakage in patients with age-related macular degeneration treated with PDT. Graefes Arch Clin Exp Ophthalmol 2006;244:1119–23.
Appendix 3 List of excluded studies
Study design (n = 30)
Arias L, Garcia-Arumi J, Ramon JM, Badia M, Rubio M, Pujol O. Optical coherence tomography analysis of a randomized study combining photodynamic therapy with intravitreal triamcinolone. Graefes Arch Clin Exp Ophthalmol 2008;246:245–54.
Baranano AE, Keane PA, Ruiz-Garcia H, Walsh AC, Sadda SR. Impact of scanning density on spectral domain optical coherence tomography assessments in neovascular age-related macular degeneration. Acta Opthalmol 2012;90:e274–80.
Bojke L, Claxton K, Sculpher MJ, Palmer S. Identifying research priorities: the value of information associated with repeat screening for age-related macular degeneration. Med Decis Making 2008;28:33–43.
Cruess AF, Zlateva G, Pleil AM, Wirostko B. Photodynamic therapy with verteporfin in age-related macular degeneration: a systematic review of efficacy, safety, treatment modifications and pharmacoeconomic properties. Acta Ophthalmol 2009;87:118–32.
Dunavoelgyi R, Sacu S, Simader C, Pruente C, Schmidt-Erfurth U. Changes in macular sensitivity after reduced fluence photodynamic therapy combined with intravitreal triamcinolone. Acta Opthalmol 2011;89:166–71.
Elsner H, Barbazetto I, Schmidt-Erfurth U. Natural course of events in subfoveal choroidal neovascularisation by age-linked macular degeneration. Ophthalmologe 2001;98:665–70.
Freund KB, Ho IV, Barbazetto IA, Koizumi H, Laud K, Ferrara D, et al. Type 3 neovascularization – the expanded spectrum of retinal angiomatous proliferation. Retina 2008;28:201–11.
Gupta B, Adewoyin T, Patel SK, Sivaprasad S. Comparison of two intravitreal ranibizumab treatment schedules for neovascular age-related macular degeneration. Br J Ophthalmol 2011;95:386–90.
Heimes B, Lommatzsch A, Zeimer M, Gutfleisch M, Spital G, Dietzel M, et al. Long-term visual course after anti-VEGF therapy for exudative AMD in clinical practice evaluation of the German reinjection scheme. Graefes Arch Clin Exp Ophthalmol 2011;249:639–44.
Hernandez-Pastor LJ, Ortega A, Garcia-Layana A, Giraldez J. Cost-effectiveness of ranibizumab compared with pegaptanib in neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2010;248:467–76.
Holz FG, Jorzik J, Schutt F, Flach U, Unnebrink K. Agreement among ophthalmologists in evaluating fluorescein angiograms in patients with neovascular age-related macular degeneration for photodynamic therapy eligibility (FLAP-Study). Ophthalmology 2003;110:400–5.
Horster R, Ristau T, Sadda SR, Liakopoulos S. Individual recurrence intervals after anti-VEGF therapy for age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2011;249:645–52.
Javier Hernandez-Pastor Lle, Ortega A, Garcia-Layana A, Giraldez J. Cost-effectiveness of ranibizumab compared with photodynamic treatment of neovascular age-related macular degeneration. Clin Ther 2008;30:2436–51.
Kaiser RS, Berger JW, Williams GA, Tolentino MJ, Maguire AM, Alexander J, et al. Variability in fluorescein angiography interpretation for photodynamic therapy in age-related macular degeneration. Retina 2002;22:683–90.
Katz G, Giavedoni L, Muni R, Evans T, Pezda M, Wong D, et al. Effectiveness at 1 year of monthly versus variable-dosing intravitreal ranibizumab in the treatment of choroidal neovascularization secondary to age-related macular degeneration. Retina 2012;32:293–8.
Kubicka-Trzaska A. The differential diagnosis of exudative age-related macular degeneration with posterior pole choroidal tumours. Klinika Oczna 2005;107:147–55.
Loewenstein A. Use of home device for early detection of neovascular age-related macular degeneration. Ophthalmic Res 2012;48(Suppl. 1):11–15.
Maier MM, Feucht N, Fegert C, Fiore B, Winkler V, Lohmann C. [Intravitreal Ranibizumab Injection for the Treatment of Occult and Classic CNV in Exsudative AMD.] Klin Monatsbl Augenheilkd 2011;228:161–7.
Mekjavic PJ, Kraut A, Urbancic M, Lenassi E, Hawlina M. Efficacy of 12-month treatment of neovascular age-related macular degeneration with intravitreal bevacizumab based on individually determined injection strategies after three consecutive monthly injections. Acta Opthalmol 2011;89:647–53.
Mookhtiar M, Downey L. Combined OCT and colour fundus photography in virtual clinic assessments of wet AMD patients. Eye 2012;26:619.
Neubauer AS, Holz FG, Sauer S, Wasmuth T, Hirneiss C, Kampik A, et al. Cost-effectiveness of ranibizumab for the treatment of neovascular age-related macular degeneration in Germany: model analysis from the perspective of Germany’s statutory health insurance system. Clin Ther 2010;32:1343–56.
Nischler C, Oberkofler H, Ortner C, Paikl D, Riha W, Lang N, et al. Complement factor H Y402H gene polymorphism and response to intravitreal bevacizumab in exudative age-related macular degeneration. Acta Opthalmol 2011;89:e344–9.
Patel PJ, Browning AC, Chen FK, Da C, Tufail A. Interobserver agreement for the detection of optical coherence tomography features of neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2009;50:5405–10.
Pieniazek M, Sobaszek A, Nowak W, Hachol A, Misiuk-Hojlo M. Pupil reactivity in infrared pupillometry in patients with varied stages of age related macular degeneration. 10th European Neuro-Ophthalmology Society, EUNOS Meeting Barcelona, Spain, 2011.
Pumariega NM, Smith RT, Sohrab MA, Letien V, Souied EH. A prospective study of reticular macular disease. Ophthalmology 2011;118:1619–25.
Rosenfeld PJ, Shapiro H, Tuomi L, Webster M, Elledge J, Blodi B, et al. Characteristics of patients losing vision after 2 years of monthly dosing in the phase III ranibizumab clinical trials. Ophthalmology 2011;118:523–30.
Scholl HP, Peto T, Dandekar S, Bunce C, Xing W, Jenkins S, et al. Inter- and intra-observer variability in grading lesions of age-related maculopathy and macular degeneration. Graefes Arch Clin Exp Ophthalmol 2003;241:39–47.
Smiddy WE. Economic implications of current age-related macular degeneration treatments. Ophthalmology 2009;116:481–7.
Trikha R, Morse LS, Zawadzki RJ, Werner JS, Park SS. Ten-year follow-up of eyes treated with stereotactic fractionated external beam radiation for neovascular age-related macular degeneration. Retina 2011;31:1303–15.
van Zeeburg EJ, Cereda MG, van der Schoot J, Pertile G, van Meurs JC. Early perfusion of a free RPE-choroid graft in patients with exudative macular degeneration can be imaged with spectral domain-OCT. Invest Ophthalmol Vi Sci 2011;52:5881–6.
Not age-related macular degeneration (n = 6)
Helb HM, Charbel I, Fleckenstein M, Schmitz-Valckenberg S, Scholl HP, Meyer CH, et al. Clinical evaluation of simultaneous confocal scanning laser ophthalmoscopy imaging combined with high-resolution, spectral-domain optical coherence tomography. Acta Opthalmol 2010;88:842–9.
Krebs I, Binder S, Stolba U. Value of the optical coherence tomography (OCT) for follow up examinations after photodynamic therapy (PDT). Spek Augenheilkd 2003;17:164–9.
Kuerzinger GR, Lang GK, Lang GE. [Retinal angiomatous proliferation in age-related macular degeneration.] Klin Monatsbl Augenheilkd 2006;223:691–5.
Sikorski BL, Bukowska D, Kaluzny JJ, Szkulmowski M, Kowalczyk A, Wojtkowski M. Drusen with accompanying fluid underneath the sensory retina. Ophthalmol 2011;118:82–92.
Spraul CW, Lang GE, Lang GK. Optical coherence tomography of age-related macular degeneration. Correlation of diagnostic techniques of fluorescence angiography and OCT. Klin Monatsbl Augenheilkd 1998;212:141–8.
Toju R, Iida T, Sekiryu T, Saito M, Maruko I, Kano M. Near-infrared autofluorescence in patients with idiopathic submacular choroidal neovascularization. Am J Ophthalmol 2012;153:314–19.
Reference standard (n = 13)
Brancato R, Introini U, Pierro L, Setaccioli M, Forti M, Bolognesi G, et al. Optical coherence tomography (OCT) in retinal angiomatous proliferation (RAP). Eur J Ophthalmol 2002;12:467–72.
Coscas G, De Benedetto U, Coscas F, Li Calzi CI, Vismara S, Roudot-Thoraval F, et al. Hyperreflective dots: a new spectral-domain optical coherence tomography entity for follow-up and prognosis in exudative age-related macular degeneration. Ophthalmologica 2013:229:32–7.
El-Mollayess GM, Mahfoud Z, Schakal AR, Salti HI, Jaafar D, Bashshur ZF. Fixed-interval versus OCT-guided variable dosing of intravitreal bevacizumab in the management of neovascular age-related macular degeneration: a 12-month randomized prospective study. Am J Ophthalmol 2012;153:481–9.
Giacomelli G, Volpe R, Scrivanti M, Mencucci R, Salvi G. Fluorangiography and indocyanine green angiography by SLO in detecting choroidal neovessels in age related macular degeneration. Anna Ottalmol Clin Oculist 1996;122:97–106.
Hoerster R, Muether PS, Hermann MM, Koch K, Kirchhof B, Fauser S. Subjective and functional deterioration in recurrences of neovascular AMD are often preceded by morphologic changes in optic coherence tomography. Br J Ophthalmol 2011;95:1424–6.
Jain S, Hamada S, Membrey WL, Chong V. Screening for age-related macular degeneration using nonstereo digital fundus photographs. Eye 2006;20:471–5.
Khan S, Engelbert M, Imamura Y, Freund KB. Polypoidal choroidal vasculopathy: simultaneous indocyanine green angiography and eye-tracked spectral domain optical coherence tomography findings. Retina 2012;32:1057–68.
Mantel I, Deli A, Iglesias K, Ambresin A. Prospective study evaluating the predictability of need for retreatment with intravitreal ranibizumab for age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2013;251:697–704.
Pece A, Sannace C, Menchini U, Virgili G, Galli L, Isola V, et al. Fluorescein angiography and indocyanine green angiography for identifying occult choroidal neovascularization in age-related macular degeneration. Eur J Ophthalmol 2005;15:759–63.
Pirbhai A, Sheidow T, Hooper P. Prospective evaluation of digital non-stereo color fundus photography as a screening tool in age-related macular degeneration. Am J Ophthalmol 2005;139:455–61.
Querques G, Querques L, Rafaeli O, Canoui-Poitrine F, Bandello F, Souied EH. Preferential hyperacuity perimeter as a functional tool for monitoring exudative age-related macular degeneration in patients treated by intravitreal ranibizumab. Invest Ophthalmol Vis Sci 2011;52:7012–18.
Vujosevic S, Vaclavik V, Bird AC, Leung I, Dandekar S, Peto T. Combined grading for choroidal neovascularisation: colour, fluorescein angiography and autofluorescence images. Graefes Arch Clin Exp Ophthalmol 2007;245:1453–60.
Yannuzzi LA, Negrao S, Iida T, Carvalho C, Rodriguez-Coleman H, Slakter J, et al. Retinal angiomatous proliferation in age-related macular degeneration. Retina 2001;21(Suppl. 1):416–34.
Outcomes (n = 63)
Ahlers C, Michels S, Elsner H, Birngruber R, Pruente C, Schmidt-Erfurth U. Topographic angiography and optical coherence tomography: a correlation of imaging characteristics. Eur J Ophthalmol 2005;15:774–81.
Almony A, Mansouri A, Shah GK, Blinder KJ. Efficacy of intravitreal bevacizumab after unresponsive treatment with intravitreal ranibizumab. Can J Ophthalmol 2011;46:182–5.
Amaro MH, Amaro FAH, Roller AB, Motta CT, Motta MMD. Treatment of nonsubfoveal choroidal neovascularization in age-related macular degeneration. Analysis of a cases series and revision paper. Rev Bras Oftalmol 2011;70:261–7.
Ampornpruet A, Ruamviboonsuk P, Kokekhuntod S. The fundoscopic features for differentiation between polypoidal choroidal vasculopathy and choroidal neovascularization from age-related macular degeneration. J Med Assoc Thai 2005;88:S51–6.
Atmaca L, Batioglu F, Atmaca P. Detection of subretinal neovascular membranes with idiocynanine green videoangiography. J Fr Ophtalmol 1997;20:189–94.
Bearelly S, Espinosa-Heidmann DG, Cousins SW. The role of dynamic indocyanine green angiography in the diagnosis and treatment of retinal angiomatous proliferation. Br J Ophthalmol 2008;92:191–6.
Bermig J, Tylla H, Jochmann C, Nestler A, Wolf S. Angiographic findings in patients with exudative age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2002;240:169–75.
Bernardes R, Santos T, Serranho P, Lobo C, Cunha-Vaz J. Noninvasive evaluation of retinal leakage using optical coherence tomography. Ophthalmologica 2011;226:29–36.
Bidot ML, Malvitte L, Bidot S, Bron A, Creuzot-Garcher C. [Efficacy of three intravitreal injections of bevacizumab in the treatment of exudative age-related macular degeneration.] J Fr Opthalmol 2011;34:376–81.
Byun YJ, Lee SJ, Koh HJ. Predictors of response after intravitreal bevacizumab injection for neovascular age-related macular degeneration. Jpn J Ophthalmol 2010;54:571–7.
Campa C, Hagan R, Sahni JN, Brown MC, Beare NA, Heimann H, et al. Early multifocal electroretinogram findings during intravitreal ranibizumab treatment for neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2011;52:3446–51.
Campa C, Harding SP, Pearce IA, Beare NA, Briggs MC, Heimann H. Incidence of neovascularization in the fellow eye of patients with unilateral retinal angiomatous proliferation. Eye 2010;24:1585–9.
Coscas G, Coscas F, Vismara S, Souied E, Soubrane G. [Spectral Domain OCT in age-related macular degeneration: preliminary results with Spectralis HRA-OCT.] J Fr Opthalmol 2008;31:353–61.
Coscas F, Querques G, Forte R, Terrada C, Coscas G, Souied EH. Combined fluorescein angiography and spectral-domain optical coherence tomography imaging of classic choroidal neovascularization secondary to age-related macular degeneration before and after intravitreal ranibizumab injections. Retina 2012;32:1069–76.
Coscas F, Coscas G, Querques G, Massamba N, Querques L, Bandello F, et al. En face enhanced depth imaging optical coherence tomography of fibrovascular pigment epithelium detachment. Invest Ophthalmol Vis Sci 2012;53:4147–51.
Dandekar SS, Jenkins SA, Peto T, Scholl HP, Sehmi KS, Fitzke FW, et al. Autofluorescence imaging of choroidal neovascularization due to age-related macular degeneration. Arch Ophthalmol 2005;123:1507–13.
de Bruin DM, Burnes DL, Loewenstein J, Chen YL, Chang S, Chen TC, et al. In vivo three-dimensional imaging of neovascular age-related macular degeneration using optical frequency domain imaging at 1050 nm. Invest Ophthalmol Vis Sci 2008;49:4545–52.
Giani A, Esmaili DD, Luiselli C, Cigada M, Salvetti P, Miller JW, et al. Displayed reflectivity of choroidal neovascular membranes by optical coherence tomography correlates with presence of leakage by fluorescein angiography. Retina 2011;31:942–8.
Grunwald JE, Daniel E, Ying GS, Pistilli M, Maguire MG, Alexander J, et al. Photographic assessment of baseline fundus morphologic features in the Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology 2012;119:1634–41.
Gutfleisch M, Heimes B, Schumacher M, Dietzel M, Lommatzsch A, Bird A, et al. Long-term visual outcome of pigment epithelial tears in association with anti-VEGF therapy of pigment epithelial detachment in AMD. Eye 2011;25:1181–6.
Haddad WM, Coscas G, Soubrane G. Eligibility for treatment and angiographic features at the early stage of exudative age related macular degeneration. Br J Ophthalmol 2002;86:663–9.
He S, Wang W, Li X, Tang R. [Characteristics of optical coherence tomography for exudative age-related macular degeneration.] Chin J Ophthalmol 2002;38:543–5.
Hee MR, Baumal CR, Puliafito CA, Duker JS, Reichel E, Wilkins JR, et al. Optical coherence tomography of age-related macular degeneration and choroidal neovascularization. Ophthalmology 1996;103:1260–70.
Helbig H, Niederberger H, Valmaggia C, Bischoff P. Simultaneous fluorescein and indocyanine green angiography for exudative macular degeneration. Klin Monatsbl Augenheilkd 2005;222:202–5.
Kang SW, Chung SE, Shin WJ, Lee JH. Polypoidal choroidal vasculopathy and late geographic hyperfluorescence on indocyanine green angiography. Br J Ophthalmol 2009;93:759–64.
Krebs I, Ansari-Shahrezaei S, Goll A, Binder S. Activity of neovascular lesions treated with bevacizumab: comparison between optical coherence tomography and fluorescein angiography. Graefes Arch Clin Exp Ophthalmol 2008;246:811–15.
Krebs I, Binder S, Stolba U, Schmid K, Glittenberg C, Brannath W, et al. Optical coherence tomography guided retreatment of photodynamic therapy. Br J Ophthalmol 2005;89:1184–7.
Li X, Tang Y. The application of fundus angiography and OCT in the classification of choroidal neovascularization complicated in central exudative choretinopathy. Chin Ophthalmic Res 2009;27:490–3.
Malamos P, Sacu S, Georgopoulos M, Kiss C, Pruente C, Schmidt-Erfurth U. Correlation of high-definition optical coherence tomography and fluorescein angiography imaging in neovascular macular degeneration. Invest Ophthalmol Vis Sci 2009;50:4926–33.
Maruko I, Iida T, Saito M, Nagayama D. Combined cases of polypoidal choroidal vasculopathy and typical age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2010;248:361–8.
McBain VA, Townend J, Lois N. Fundus autofluorescence in exudative age-related macular degeneration. Br J Ophthalmol 2007;91:491–6.
Mendrinos E, Petropoulos IK, Pournaras CJ. Retinal angiomatous proliferations: when should we suspect them and how should we detect them? Klin Monatsbl Augenheilkd 2009;226:284–8.
Miura M, Elsner AE, Beausencourt E, Kunze C, Hartnett ME, Lashkari K, et al. Grading of infrared confocal scanning laser tomography and video displays of digitized color slides in exudative age-related macular degeneration. Retina 2002;22:300–8.
Moutray T, Alarbi M, Mahon G, Stevenson M, Chakravarthy U. Relationships between clinical measures of visual function, fluorescein angiographic and optical coherence tomography features in patients with subfoveal choroidal neovascularisation. Br J Ophthalmol 2008;92:361–4.
Nazemi PP, Fink W, Lim JI, Sadun AA. Scotomas of age-related macular degeneration detected and characterized by means of a novel three-dimensional computer-automated visual field test. Retina 2005;25:446–53.
Okubo A, Hirakawa M, Ito M, Sameshima M, Sakamoto T. Clinical features of early and late stage polypoidal choroidal vasculopathy characterized by lesion size and disease duration. Graefes Arch Clin Exp Ophthalmol 2008;246:491–9.
Otsuji Tokaj, Tsumura A, Takahashi K, Sho K, Nagai Y, Fukuchi T, et al. Evaluation of cases of polypoidal choroidal vasculopathy showing classic choroidal neovascularization in their natural course. Nippon Ganka Gakkai Zasshi 2006;110:454–61.
Parravano M, Pilotto E, Musicco I, Varano M, Introini U, Staurenghi G, et al. Reproducibility of fluorescein and indocyanine green angiographic assessment for RAP diagnosis: a multicenter study. Eur J Ophthalmol 2012;22:598–606.
Pauleikhoff D, Kirchhof B. Retreatment criteria in anti-VEGF therapy of exudative AMD: critical analysis of present regimes and new morphological definition of ‘lesion activity’. Graefes Arch Clin Exp Ophthalmol 2011;249:631–2.
Petropoulos IK, Matter MA, Katsimpris JM, Desmangles PM. The role of spectral-domain optical coherence tomography in the diagnosis of retinal angiomatous proliferation. Klin Monatsbl Augenheilkd 2010;227:309–11.
Reichel E, Pollock DA, Duker JS, Puliafito CA. Indocyanine green angiography for recurrent choroidal neovascularization in age-related macular degeneration. Ophthalmic Surg Lasers 1995;26:513–18.
Rouvas AA, Papakostas TD, Ntouraki A, Douvali M, Vergados I, Ladas ID. Angiographic and OCT features of retinal angiomatous proliferation. Eye 2010;24:1633–42.
Rouvas AA, Ladas ID, Georgalas I, Vergados I, Papakonstantinou D, Kotsolis AI. Ranibizumab for the treatment of exudative age-related macular degeneration associated with retinal pigment epithelial tear. Retina 2011;31:1083–8.
Sadda SR, Liakopoulos S, Keane PA, Ongchin SC, Msutta S, Chang KT, et al. Relationship between angiographic and optical coherence tomographic (OCT) parameters for quantifying choroidal neovascular lesions. Graefes Arch Clin Exp Ophthalmol 2010;248:175–84.
Sahni J, Stanga P, Wong D, Harding S. Optical coherence tomography in photodynamic therapy for subfoveal choroidal neovascularisation secondary to age related macular degeneration: a cross sectional study. Br J Ophthalmol 2005;89:316–20.
Sarks J, Arnold J, Ho IV, Sarks S, Killingsworth M. Evolution of reticular pseudodrusen. Br J Ophthalmol 2011;95:979–85.
Sato T, Iida T, Hagimura N, Kishi S. Correlation of optical coherence tomography with angiography in retinal pigment epithelial detachment associated with age-related macular degeneration. Retina 2004;24:910–14.
Semoun O, Guigui B, Tick S, Coscas G, Soubrane G, Souied EH. Infrared features of classic choroidal neovascularisation in exudative age-related macular degeneration. Br J Ophthalmol 2009;93:182–5.
Spaide RF. Enhanced depth imaging optical coherence tomography of retinal pigment epithelial detachment in age-related macular degeneration. Am J Ophthalmol 2009;147:644–52.
Squirrell DM, Bacon JF, Brand CS. To investigate the prevalence of polypoidal choroidal vasculopathy in presumed age-related peripapillary subretinal neovascular membranes. Clin Exp Ophthalmol 2009;37:368–72.
Strauss RW, Rombold F, Kampik A, Neubauer AS. Fluorescein angiography compared to three-dimensional measurements by the retinal thickness analyzer in classic choroidal neovascularization. Ophthalmic Res 2007;39:98–102.
Suren E, Batioglu F, Ozmert E. Autofluorescence characteristics of choroidal neovascular membranes in age related macular degeneration before and after treatment. Retina Vitreus 2009;17:120–4.
Tamura H, Tsujikawa A, Otani A, Gotoh N, Sasahara M, Kameda T, et al. Polypoidal choroidal vasculopathy appearing as classic choroidal neovascularisation on fluorescein angiography. Br J Ophthalmol 2007;91:1152–9.
Tang KC, Liu HA. Scanning laser ophthalmoscopy of choroidal neovascularisation using indocyanine green. Aust NZ J Ophthalmol 1995;23:195–202.
Theelen T, Berendschot TTJM, Hoyng CB, Boon CJF, Klevering BJ. Near-infrared reflectance imaging of neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2009;247:1625–33.
Vaclavik V, Vujosevic S, Dandekar SS, Bunce C, Peto T, Bird AC. Autofluorescence imaging in age-related macular degeneration complicated by choroidal neovascularization: a prospective study. Ophthalmology 2008;115:342–6.
Vandelli G, Giacomotti E, Nozza F. Fluorescein and indocyanine green angiography in the diagnosis of coroideal neovascolarization. Ann Ottalmol Clin Oculist 2000;126:201–15.
Watzke RC, Klein ML, Hiner CJ, Chan BK, Kraemer DF. A comparison of stereoscopic fluorescein angiography with indocyanine green videoangiography in age-related macular degeneration. Ophthalmology 2000;107:1601–6.
Windisch R, Windisch BK, Cruess AF. Use of fluorescein and indocyanine green angiography in polypoidal choroidal vasculopathy patients following photodynamic therapy. Can J Ophthalmol 2008;43:678–82.
Xiao M. Analysis on fundus fluorescein angiography in patients with age related macular degeneration. Int J Ophthalmol 2010;10:962–3.
Yaylali SA, Akcakaya AA, Erbil HH, Candemir B, Mesci C, Acar H. The relationship between optical coherence tomography patterns, angiographic parameters and visual acuity in age-related macular degeneration. Int Ophthalmol 2012;32:25–30.
Zahlava J, Karel I, Dubska Z, Lestak J. [Optical coherence tomography in age-related macular degeneration.] Ceska Slov Oftalmol 2002;58:98–104.
Zuo CG, Wen F, Huang SZ, Luo GW, Yan H, Wu WJ, et al. Angiographic leakage of polypoidal choroidal vasculopathy on indocyanine angiography. Chin Med J 2010;123:1548–52.
Appendix 4 Characteristics of the included studies
| Study | Participants | Tests | Outcomes reported |
|---|---|---|---|
| Alster 200524 Full text: Yes Study type: Comparative, concurrent, non-randomised Prospective: Yes Multicentre: Yes (seven centres) Country: USA Study start/end dates: 15 October 2003/23 August 2004 Duration of study: 10 months, 1 week |
Enrolled: 185 Analysed: 122 patients (65 CNV; 57 intermediate AMD) Consecutive: Yes Age (years) median: 77 Gender M : F: 26 : 39 Baseline BCVA: 20/63 (Snellen equivalent) Inclusion criteria: Age ≥ 50 years, BCVA 220/160 or better, newly diagnosed (≤ 60 days) non-treated neovascular lesion from AMD, mental and physical ability to perform PHP test, ability to tolerate intravenous fluorescein angiography, subject able and willing to sign consent form and participate in study Exclusion criteria: Evidence of macular disease other than AMD, previous surgical or laser treatment within the macular area, presence of any significant media opacity that precludes a clear view of the macular area as identified by biomicroscopy, fundus photography, or fluorescein angiography, any non-macular-related ocular surgery performed within 3 months before the study |
Index test(s): N/R Definition of positive test result: n/a Interpreted by: N/R Comparator test(s): PHP Definition of positive test result: N/R Interpreted by: N/R Reference standard: Stereoscopic FFA Interpreted by: Experienced photograph reading centre |
Unit of analysis (n): Patient (one eye per patient) If both eyes per subject eligible, how was study eye selected: The enrolling ophthalmologist and the participant made a joint decision regarding which eye would be the study eye Diagnostic accuracy: Yes Sensitivity: PHP 82% (95% CI 70% to 90%) Colour fundus photography 70% Colour fundus photography + VA 53% (95% CI 30% to 76%) Specificity: PHP 88% (95% CI 76% to 95%) Colour fundus photography 95% Colour fundus photography + VA 94% (95% CI 83% to 99%) Clinical effectiveness: N/R Interpretability of the test: 11 patients (5.9%) were excluded from analysis as PHP results were judged to be unreliable Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Cachulo 201125 (Silva 2011 – 3 years secondary report to Cachulo 2011)47 Full text: Yes Study type: Observational, longitudinal 2 years plus 1-year extension study Prospective: Yes Multicentre: No Country: Portugal Study start/end dates: N/R Duration of study: 3 years |
Enrolled: 62 patients Analysed: 52 patients Consecutive: Unclear Age (years) mean (range/SD): 76 (56–92/6) Gender M : F: 26 : 26 Baseline BCVA: N/R Inclusion criteria: Patients aged ≥ 50 years, any race and either sex, early age-related maculopathy in the study eye (at least ≥ 5 intermediate drusen, ≥ 1 large soft drusen or confluent drusen within 3000 µm of the foveal centre; with or without pigmentary changes), nAMD in the fellow eye, signed inform consent, able to returned to the required visits Exclusion criteria: Other fundus disease (e.g. vascular retinopathy, central serous chorioretinopathy, inflammation or non-AMD CNV), current or past history of intraocular surgery within 60 days prior to enrolling in the study, evidence of past or present CNV in the study eye |
Index test: TD-OCT (Stratus OCT™, Carl Zeiss Meditec, Dublin, CA) Definition of positive test result: N/R Interpreted by: N/R Comparator test(s): ICGA, FAF Definition of positive test result: N/R Interpreted by: N/R Reference standard: Non-stereoscopic FFA Interpreted by: N/R (assumed interpreted by ophthalmologist) |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: n/a Diagnostic accuracy: Yes Sensitivity – Cachulo 2011:25 TD-OCT 100% ICGA 94.1% FAF 93.3% Sensitivity – Silva 2011:47 100% Specificity – Cachulo 2011:25 TD-OCT N/R ICGA N/R FAF 37% Specificity – Silva 201147 N/R Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Chen 200326 Full text: Yes Study type: Direct head-to-head comparison Prospective/retrospective: N/R Multicentre: Unclear Country: China Study start/end dates: November 1999/December 2000 Duration of study: 1 year |
Enrolled: 52 patients Analysed: 52 patients Consecutive: Unclear Age (years) mean (range/SD): 64.12 (51–80/8.59) Gender M : F: N/R Baseline BCVA: ≈0.7 (index/30 cm) Inclusion criteria: Patients with diagnosis of exudative AMD following the diagnostic criteria in Chinese ophthalmology diagnosing guidance Exclusion criteria: N/R |
Index test: N/R Definition of positive test result: N/R Interpreted by: N/R Comparator test: ICGA Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (unclear if stereoscopic or not)a Interpreted by: N/R |
Unit of analysis (n): Eye (one eye per patient, except in 13 patients with both eyes assessed) Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: 62.90% Specificity: N/R Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Do 201227 Full text: Yes Study type: Direct head-to-head observational Prospective: Yes Multicentre: Yes (four centres) Country: USA Study start/end dates: N/R Duration of study: 2 years |
Enrolled: 98 patients Analysed: 87 patients Consecutive: No Age (years) median (range): 79 (58–91) Gender M : F: 31 : 56 Baseline BCVA: Median 20/25 (Snellen equivalent), range (66–95) Inclusion criteria: Minimum age 50 years, nAMD in the non-study eye, BCVA (ETDRS) of ≥ 65 (Snellen of approximately 20/50), no evidence of CNV or foveal geographic atrophy in the fellow eye (candidate study eye), ≥ 1 large druse (> 125 μm) and focal RPE hyperpigmentation within 3600 µm of the macula centre, visible on colour or red-free fundus photographs or FFA Exclusion criteria: Allergy to fluorescein dye, advanced AMD with CNV in both eyes confirmed on FFA, geographic atrophy extending through the centre of the macula in the candidate study eye, positive OCT for the candidate eye, evidence of macular disease other than AMD in the candidate study eye, prior surgical or laser treatment to the macula in the study eye |
Index test: TD-OCT (Stratus OCT™) Definition of positive test result: 10% increase in the central subfield thickness measurement relative to baseline, subretinal fluid questioned or graded as definitely present, intraretinal cystoid abnormalities questioned or graded as definitely present Interpreted by: trained masked graders at the reading centre Comparator test(s): Amsler grid (supervised) PHP Definition of positive test result: Any defect perceived by the subject Interpreted by: N/R Reference standard: Stereoscopic FFA Interpreted by: two trained masked graders at the reading centre |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: n/a Diagnostic accuracy: Yes Sensitivity: CNV defined by the reading centre only Irrespective of treatment decision TD-OCT 40% (95% CI 16% to 68%) Amsler grid 41.7% (95% CI 15% to 72%) PHP 50% Specificity: TD-OCT 70.8% Amsler grid N/R PHP N/R Clinical effectiveness: N/R Interpretability of the test: 6/68 (8.8%) screened but not enrolled as ineligible and excluded cases due to poor image quality that was insufficient to permit successful study participation Acceptability of the test: n/a Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Fujii 199629 Full text: Yes Study type: Direct head-to-head [all participants receive index and comparator test(s) and reference standard] Prospective/retrospective: Unclear Multicentre: No Country: Japan Study start/end dates: N/R Duration of study: N/R |
Enrolled: 24 patients (32 eyes) Analysed: 24 patients (32 eyes) Consecutive: Unclear Age (years) mean (range): 68.6 (61–86) Gender M : F: 17 : 7 Baseline BCVA: N/R Inclusion criteria: Patients with diagnosis of AMD with CNV not detected by FFA, or unlikely to be the subject of photocoagulation (e.g. CNV located in the fovea) Exclusion criteria: N/R |
Index test: N/R Definition of positive test result: N/R Interpreted by: N/R Comparator test: ICGA Definition of positive test result: Four stages: stage I neovascularisation of RPE without injury of palisade tissue; stage II bleeding (leakage) – subretinal haemorrhage injury of RPE, exudates subretinal space; stage III subretinal fibrosis and membranes proliferation plus stage II; and stage IV scar tissue Interpreted by: N/R Reference standard: Non-stereoscopic FFA interpreted by ophthalmologist Interpreted by: N/R |
Unit of analysis (n): Eye Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: 84.61% Specificity: 36.84% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Gomi 200731 Full text: Yes Study type: Direct head-to-head comparison Prospective/retrospective: Unclear Multicentre: No Country: Japan Study start/end dates: July 2005/January 2006 Duration of study: 6 months |
Enrolled: 37 patients Analysed: 37 patients Consecutive: Unclear Age (years) mean (range): 71.6 (54–83) Gender M : F: 27 : 10 Baseline BCVA: N/R Inclusion criteria: Patients diagnosed with PCV in the macular region; informed consent provided Exclusion criteria: Eyes with subretinal or subpigment epithelial haemorrhages that obscured lesions; eyes with a history of any previous treatment and any other macular pathologies such as CNV or central serous chorioretinopathy |
Index test: N/R Definition of positive test result: N/R Interpreted by: N/R Comparator test: ICGA Definition of positive test result: N/R Interpreted by: N/R Reference standard: Non-stereoscopic FFA Interpreted by: Images were traced by two readers. When no agreement was reached by the readers on the location of the lesion borders, another author arbitrated |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: 100% Specificity: N/R Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Hughes 200533 Full text: Yes Study type: Direct head-to-head comparison Prospective: Yes Multicentre: No Country: UK Study start/end dates: N/R Duration of study: N/R |
Enrolled: 22 patients Analysed: 22 patients Consecutive: Yes Age (years) mean/median (range/SD): N/R Gender M : F: N/R Baseline BCVA: N/R Inclusion criteria: Patients with acute CNV Exclusion criteria: N/R |
Index test(s): TD-OCT (OCT 3000™, Carl Zeiss Ophthalmic Systems Inc., Dublin, CA) Definition of positive test result: Presence of a discreet subretinal lesion indicating a CNV membrane Interpreted by: N/R Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (unclear if stereoscopic or not)a Interpreted by: N/R |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: 36.36% Specificity: n/a Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Khondkaryan 200934 Abstract: Yes Study type: Direct head-to-head [all participants receive index and comparator test(s) and reference standard] Retrospective: Yes Multicentre: N/R Country: USA Study start/end dates: N/R Duration of study: N/R |
Enrolled: 51 patients (51 eyes) Analysed: 51 patients (51 eyes) Consecutive: Yes Age (years) mean/median (range/SD): N/R Gender M : F: N/R Baseline BCVA: N/R Inclusion criteria: Newly diagnosed patients with nAMD who underwent stratus OCT imaging and FFA at the time of diagnosis Exclusion criteria: N/R |
Index test: TD-OCT (Stratus OCT™) Definition of positive test result: N/R Interpreted by: N/R Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (not specified whether stereoscopic or not)a Interpreted by: N/R |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: Classic CNV 80.90% RAP 57.10% Occult CNV 81.10% Specificity: Classic CNV 56.70% RAP 81.80% Occult CNV 42.90% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Kim 200335 Full text: Yes Study type: Direct head-to-head comparison Retrospective: Yes Multicentre: No Country: the Republic of Korea Study start/end dates: N/R Duration of study: N/R |
Enrolled: 32 patients (32 eyes) Analysed: 13 eyes Consecutive: Unclear Age (years) mean (SD): 51.38 (20.68) Gender M : F: 16 : 16 Baseline BCVA: N/R Inclusion criteria: Patients with diagnosis of CNV Exclusion criteria: N/R |
Index test: TD-OCT (manufacturer N/R) Definition of positive test result: Lesion classed as well defined, poorly defined, fibrovascular PED, haemorrhagic PED and serous PED (not considered as this is a diagnostic study) Interpreted by: N/R Comparator test: ICGA Definition of positive test result: Hyperfluorescent lesion by ICGA was confined as the leaking on late phase, and measured relative to the diameter of the optic disc Interpreted by: N/R Reference standard: FFA (not specified whether or not stereoscopic) Interpreted by: N/R |
Unit of analysis (n): Eye If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: 92.30% Specificity: N/R Clinical effectiveness: No Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Kozak 200836 Full text: Yes Study type: Direct head-to-head comparison Retrospective: Yes Multicentre: No Country: USA Study start/end dates: 1 October 2005/1 October 2006 Duration of study: 12 months |
Enrolled: Unclear (541 eyes) Analysed: 541 eyes Consecutive: Yes Age (years) mean/median (range/SD): 54 ± 12.1 years Gender M : F: N/R Baseline BCVA: N/R Inclusion criteria: Patients with diagnosis of macular oedema (confirmed or suspected) Exclusion criteria: N/R |
Index test(s): TD-OCT (Stratus OCT™) although a subset of patients received SD-OCT (SLO, OTI Ophthalmic Technologies, Inc., Toronto, ON, Canada) Definition of positive test result: Macular oedema defined as loss of central contour, intraretinal cysts, subretinal fluid, retinal thickening > 250 μm (foveal and perifoveal) Interpreted by: Ophthalmologists Comparator test(s): Colour fundus photograph (TRC-50 VT, Topcon, Tokyo, Japan) Definition of positive test result: N/R Interpreted by: N/R Reference standard: Stereoscopic FFA Interpreted by: Ophthalmologists (retina specialists) |
Unit of analysis (n): Eye Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: 97.3% Specificity: n/a Clinical effectiveness: N/R Interpretability of the test: 35 eyes (6.5%) were excluded from the analysis due to poor quality or image decentration Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Krebs 200737 Full text: Yes Study type: Direct head-to-head comparison Retrospective: Yes Multicentre: No Country: Austria Study start/end dates: N/R Duration of study: N/R |
Enrolled: 50 patients Analysed: 50 patients Consecutive: No Age (years) mean/median (range/SD): 77.8 ± 6.4 years Gender M : F: N/R Baseline BCVA: N/R Inclusion criteria: N/R Exclusion criteria: N/R |
Index test(s): TD-OCT (OCT 3000™) Definition of positive test result: Increase retinal thickness compared with healthy retina of the study eye or fellow eye, neurosensory detachment, PED Interpreted by: N/R Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: N/R |
Unit of analysis (n): Eye Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: CNV primarily classic 100% RAP 72.7% Specificity: 100% for dry AMD (as negative diagnosis) Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Liakopoulos 200838 Full text: Yes Study type: Direct head-to-head comparison Retrospective: Yes Multicentre: No Country: USA Studystart/end dates: N/R Duration of study: N/R |
Enrolled: 66 patients (eyes) Analysed: 66 patients (eyes) Consecutive: Y/N Age (years) mean/median (range/SD): N/R Gender M : F: N/R Baseline BCVA: N/R Inclusion criteria: Previously untreated, active subfoveal CNV due to AMD, stratus OCT and FFA imaging performed on the same date, the entire CNV lesion had to fall within a 6 mm-diameter circle centred on the fovea Exclusion criteria: N/R |
Index test(s): TD-OCT (Stratus OCT™) Definition of positive test result: Active CNV defined as the presence of haemorrhage or evidence of lesion growth within the prior 3 months Interpreted by: Certified graders Comparator test(s): Colour fundus photographs (TOPCON 50 I X, Topcon, Tokyo, Japan) Definition of positive test result: N/R Interpreted by: N/R Reference standard: Stereoscopic FFA Interpreted by: Ophthalmologists (certified graders) |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity based on subretinal fluid: Occult with no classic 79.2% Minimally classic 91.3% Predominantly classic 100% RAP stage III 50% All subtypes 83.3% Specificity: n/a Sensitivity based on cystoid oedema: Occult with no classic 79.2% Minimally classic 91.3% Predominantly classic 81.8% RAP stage III 100% All subtypes 72.7% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Loewenstein 201039 Full text: Yes Study type: Prospective and retrospective Prospective/retrospective: Yes Multicentre: Yes Country: Israel, USA (for the prospective part only) Study start/end dates: Retrospective part: January–September 2007 Prospective part: April–September 2008 Duration of study: Retrospective part: 8 months Prospective part: 5 months |
Enrolled: Retrospective: 109 patients Prospective: 99 patients Analysed: Retrospective part: 77 patients Prospective part: 54 patients Consecutive: Retrospective part: Unclear Prospective part: Yes Age (years) mean/median (range/SD): Retrospective part: 76 years Prospective part: 78 years Gender M : F: Retrospective part: 41 : 35 (one unknown) Prospective part: 17 : 34 (three unknown) Baseline BCVA: Retrospective part: 20/33 (iAMD group); 20/63 (CNV group) Prospective part: 20/30 (iAMD group); 20/63 (CNV group) Inclusion criteria: Retrospective part: Passing an in-house tutorial Prospective part: Mouse experience, willingness and ability to sign a written informed consent, intermediate AMD (using the definition from Age-Related Eye Disease study), recent onset CNV within 3000 μm of the fovea in the study eye, aged > 50 years, CVA > 20/200 on Snellen charts Exclusion criteria: Macular disease other than AMD, geographic atrophy, media opacity precluding a clear view of the fundus, no or poor-quality photographs that prevented unambiguous grading, ocular surgery in the study eye within the previous 3 months |
Index test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Comparator test(s): PHP Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: N/R |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: Retrospective part: 85.3% Prospective part: 84.4% All: 84.8% Specificity: Prospective part: 83.7% Retrospective part: 86.4% All: 84.6% Clinical effectiveness: N/R Interpretability of the test: 40 patients (19.2%) were excluded from the analysis due to geographic atrophy, early AMD, pattern dystrophy, no or poor-quality photographs Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Padnick-Silver 201240 Full text: Yes Study type: Observational, non-randomised Prospective: Yes Multicentre: No Country: USA Study start/end dates: N/R Duration of study: N/R |
Enrolled: 79 patients Analysed: 77 patients Consecutive: Unclear Age (years) mean/median (range/SD): 79.7 ± 6.3 years Gender M : F: 24 : 55 Baseline BCVA: 0.27 ± 0.21 (≈20/40) in the study eye, 1.42 ± 0.74 (< 20/400) in the fellow eye Inclusion criteria: Patients with bilateral AMD who had developed unilateral exudative changes Exclusion criteria: Presence of other retinal disease in the eye with non-exudative AMD,for example, significant diabetic retinopathy, glaucomatous retinal atrophy, retinal detachment |
Index test(s): TD-OCT (Stratus OCT™) Definition of positive test result: Subretinal pigment epithelial or subretinal fluid Interpreted by: Retinal physician Comparator test(s): N/R Definition of positive test result: n/a Interpreted by: N/R Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: N/R |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: n/a Diagnostic accuracy: Yes Sensitivity: 80% Specificity: 93.5% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Park 201041 Full text: Yes Study type: Direct head-to-head comparison Prospective: Yes Multicentre: No Country: USA Study start/end dates: September 2005/June 2006 Duration of study: 9 months |
Enrolled: 19 patients (21 eyes) Analysed: 21 eyes Consecutive: Unclear Age (years) Mean/median (range/SD): 78 (48–92) years Gender M : F: 8 : 11 Baseline BCVA: N/R Inclusion criteria: Patients newly diagnosed with exudative AMD Exclusion criteria: Eyes diagnosed with RAP or concurrent macular haemorrhage that may obscure part of the CNM on FFA |
Index test(s): SD-OCT (Fourier domain) (constructed at the University of California, Davis Medical Centre) Definition of positive test result: CNVM images as a highly reflective lesion in the subretinal space, subretinal pigment epithelial space or both Interpreted by: Ophthalmologists (retinal specialists) Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: Ophthalmologists (retinal specialists) |
Unit of analysis (n): Eye Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: 100% Specificity: N/R Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Parravano 201242 Abstract: Yes Study type: Diagnostic cross-sectional Prospective: Yes Multicentre: Yes (eight centres) Country: Italy Study start/end dates: N/R Duration of study: N/R |
Enrolled: 155 patients (201 eyes) Analysed: 155 patients Consecutive: Yes Age (years) mean/median (range/SD): 76 ± 8 years Gender M : F: N/R Baseline BCVA: N/R Inclusion criteria: Patients with newly diagnosed neovascular AMD Exclusion criteria: N/R |
Index test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Comparator test(s): ICGA Definition of positive test result: N/R Interpreted by: All images were graded by two observers from different institutions Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: All images were graded by two observers from different institutions |
Unit of analysis (n): Patient Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: 85.1% Specificity: N/R Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Reichel 199544 Full text: Yes Study type: Direct head-to-head comparison Prospective/retrospective: N/R Multicentre: No Country: USA Study start/end dates: September 1991/January 1993 Duration of study: 16 months |
Enrolled: 200 patients Analysed: 20 patients Consecutive: Yes Age (years) mean/median (range/SD): N/R Gender M : F: N/R Baseline BCVA: N/R Inclusion criteria: Patients with central visual symptoms with clinical suspicious for CNV due to the presence of a retinal PED, exudates, subretinal fluid, macular oedema and/or subretinal or intraretinal haemorrhage, patients suspected to have a CNV obscured by haemorrhage Exclusion criteria: Patients with small amounts of intraretinal or subretinal haemorrhage (no significant thickening on slit lamp biomicroscopy), known allergy to iodine-base dye, previous laser photocoagulation in the study eye |
Index test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Comparator test(s): ICGA Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: N/R |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: 100% Specificity: N/R Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Salinas-Alaman 200545 Full text: Yes Study type: Direct head-to-head comparison, observational Prospective: Yes Multicentre: No Country: Spain Study start/end dates: N/R Duration of study: N/R |
Enrolled: 53 patients Analysed: 62 eyes (53 patients) Consecutive: Yes Age (years) mean/median (range/SD): 76.50 ± 7.5 years Gender M : F: 26 : 27 Baseline BCVA: 20/80 Inclusion criteria: Patients presenting with signs of exudative AMD with predominantly classic CNV Exclusion criteria: N/R |
Index test(s): TD-OCT (OCT 2000™, Humphrey Instruments, San Leonardo, CA) Definition of positive test result: Presence of subretinal or intraretinal fluid Interpreted by: Unclear (independent observers) Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: Unclear (independent observers) |
Unit of analysis (n): Eye Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: 96.8% Specificity: n/a Clinical effectiveness: N/R Interpretability of the test: 20 cases (9.6%) were excluded from the analysis as OCT tests were performed by a less experienced technician Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Sandhu 200546 Full text: Yes Study type: Direct head-to-head comparison Prospective: Yes Multicentre: No Country: UK Study start/end dates: N/R Duration of study: 6 months |
Enrolled: 128 patients Analysed: 118 patients (131 eyes) Consecutive: Yes Age (years) mean/median (range/SD): 73.2 ± 13.7 (30–97) years Gender M : F: 42.4% : 57.6% Baseline BCVA: N/R Inclusion criteria: First time presentation of suspected CNV with potentially treatable lesion; predominantly classic CNV with no PED Exclusion criteria: N/R |
Index test(s): TD-OCT (OCT 3™, Zeiss, Dublin, CA) Definition of positive test result: (a) classic CNV – subretinal band (RPE) with choriocapilaris thickened and disrupted-fusiform shape with/without intraretinal or subretinal fluid; (b) occult CNV – less well-defined band than ‘(a)’ but more subRPE with more disorganisation of the retina and intraretinal fluid (cystoid)/subretinal fluid; (c) serous PED – dome shape elevation of the reflective band (RPE) with area of low reflectivity underneath Interpreted by: Ophthalmologists Comparator test(s): SD-OCT + stereo colour fundus photography Definition of positive test result: N/R Interpreted by: N/R Reference standard: Stereoscopic FFA Interpreted by: Ophthalmologists |
Unit of analysis (n): Eye Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: SD-OCT: 77.8% SD-OCT + stereo colour fundus photograph: 74.1% Specificity: SD-OCT: 76% SD-OCT + stereo colour fundus photograph): 92.0% Clinical effectiveness: N/R Interpretability of the test: 10 patients (7.8%) were excluded from the analysis due to poor quality of images Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Sulzbacher 201148 Full text: Yes Study type: Direct head-to-head comparison Prospective/retrospective: Unclear Multicentre: No Country: Austria (Vienna) Study start/end dates: July 2008/August 2009 Duration of study: 12 months |
Enrolled: 13 eyes Analysed: 13 eyes Consecutive: Yes Age (years) mean/median (range/SD): N/R Gender M : F: N/R Baseline BCVA: N/R Inclusion criteria: CNV type 2 treatment-naive eyes without an occult component Exclusion criteria: Occult component (CNV), neovascular maculopathy from pathologic myopia, angioid streaks, infectious inflammatory chorioretinal disease, tumours, hereditary disorders or trauma |
Index test(s): SD-OCT (Spectralis™, Heidelberg Engineering, Heidelberg, Germany) Definition of positive test result: N/R Interpreted by: Certified reader at the Vienna reading centre (non-ophthalmologist technician, optometrist, nurse, or other) Comparator test(s): ICGA Definition of positive test result: Detection of type 2 CNV (without an occult component): area of choroidal hyperfluorescence with well-demarcated boundaries, with progressive leakage beyond the initial boundaries of the CNV and an area of hypercyanescence without marked leakage activity on ICGA (early phase – neovascular complex; late phase – retinal leakage) Interpreted by: Certified reader at the Vienna reading centre (non-ophthalmologist technician, optometrist, nurse, or other) Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: Ophthalmologists (experienced readers) |
Unit of analysis (n): Eye Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: 100% Specificity: N/R Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Talks 200749 Full text: Yes Study type: Retrospective audit Retrospective: Yes Multicentre: No Country: UK Study start/end dates: N/R Duration of study: N/R |
Enrolled: 134 patients Analysed: 111 patients Consecutive: Yes Age (years) mean/median (range/SD): 84.6 (58–97) years Gender M : F: 53:81 Baseline BCVA: N/R Inclusion criteria: Patients referred with suspected wet AMD Exclusion criteria: N/R |
Index test(s): TD-OCT (OCT 3™, Zeiss) Definition of positive test result: N/R Interpreted by: N/R Comparator test(s): ICGA Definition of positive test result: N/R Interpreted by: Ophthalmologists Reference standard: Stereoscopic FFA Interpreted by: Ophthalmologists |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: 100% Specificity: 65.8% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Torron 200251 (and 2-year interim study – Torron 2001)50 Full text: Yes Study type: Direct head-to-head comparison Retrospective: Yes Multicentre: No Country: Spain Study start/end dates: April 1998/April 2001 Duration of study: 3 years |
Enrolled: Torron 200251 – 95 patients (102 eyes) Torron 200150 – 55 patients (56 eyes) Analysed: Torron 200251 – 102 eyes Torron 200150 – 56 eyes Consecutive: Unclear Age (years) mean/median (range/SD): 75.3 (60–85) years Gender M : F: 44 : 51 Baseline BCVA: ≤ 0.1 (42 eyes), 0.1–0.3 (28 eyes), > 0.3 (30 eyes) Inclusion criteria: N/R Exclusion criteria: N/R |
Index test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Comparator test(s): ICGA (SLO 101, Rodenstock, Germany) Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: N/R |
Unit of analysis (n): Eye Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: Torron 2002:51 92.2% Torron 2001:50 89.3% Specificity: Torron 200251/2001:50 N/R Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Study | Participants | Tests | Outcomes reported |
|---|---|---|---|
| Eter 200528 Full text: Yes Study type: Direct head-to head comparison Retrospective: Yes Multicentre: Yes (two centres) Country: Germany Study start/end dates: N/R Duration of study: N/R |
Enrolled: 60 patients (60 eyes) Analysed: 60 patients (60 eyes) Consecutive: Yes Age (years) median: 78 years Gender M : F: 31 : 29 Baseline BCVA: 20/100 Inclusion criteria: Patients with predominantly classic CNV secondary to AMD treated with PDT with verteporfin Exclusion criteria: N/R |
Index test(s): TD-OCT (Zeiss, Humphrey Instruments) Definition of positive test result: Subretinal fluid or cystoid spaces within the retina. Subretinal fluid defined as hyporeflective, black zone between retinal pigment epithelial layer and outer neuro-sensory retinal surface. Cystoid spaces defined as hyporeflective black area of at least 2 × 2 pixels within the neuro-retina Interpreted by: Ophthalmologists Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (unclear if stereoscopic or not)a Interpreted by: N/R |
Unit of analysis (n): Eye (one eye per patient)
If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: 80% Specificity: 80% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Giani 201130 Full text: Yes Study type: Direct head-to-head comparison, cross-sectional Retrospective: Yes Multicentre: No Country: Italy (Milan) Study start/end dates: N/R Duration of study: N/R |
Enrolled: 93 patients (93 eyes) Analysed: 93 patients (93 eyes) Consecutive: Yes Age (years) mean (range/SD): 77 years Gender M : F: 41 : 52 BCVA: Mean 0.40 (SD 0.25) Inclusion criteria: Clinical history of AMD, FFA diagnosis of subfoveal CNV, previous treatment with antiVEGF agents for CNV Exclusion criteria: Any previous laser treatment, PDT, vitreo-retinal surgery, macular haemorrhage (significant) that obscured the lesion, spherical refractive error > 6 diopters |
Index test(s): SD-OCT (HRA + OCT Spectralis™) Definition of positive test result: At least one of the following parameters: intraretinal cystic spaces, without differentiation in retinal layer localisation, content, or number/density; RPE detachment (PED), defined as a localised elevation of RPE due to fluid or fibrovascular tissue; and neurosensory retinal detachment, defined as a fluid detachment of the retinal layers from the RPE Interpreted by: N/R (two different examiners) Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: Dynamic video FFA (unclear if stereoscopic or not)a Interpreted by: N/R |
Unit of analysis (n): Eye (1 eye per patient) If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: Overall: 94.2% Classic: 90.9% Occult: 100% Specificity: Overall: 26.8% Classic: 37.5% Occult: 11.8% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Henschel 200932 Full text: Yes Study type: Direct head-to-head comparison Prospective: Yes Multicentre: No Country: Germany Study start/end dates: N/R Duration of study: N/R |
Enrolled: 14 patients (61 examinations) Analysed: 61 pair of examinations (OCT and FFA) Consecutive: Unclear Age (years) mean/median (range/SD): N/R Gender M : F: N/R BCVA: 20/32 – 20/200 (range) Inclusion criteria: Patients with CNV for AMD (different types as predominantly classic and occult) Exclusion criteria: N/R |
Index test(s): TD-OCT (Stratus OCT™) Definition of positive test result: Presence of intraretinal or subretinal fluid present when loculated hyporeflective cystoid spaces were visible in one of the acquired scans; subretinal fluid was rated as present if a hyporeflective space was definable between the outer retinal surface and the hyporeflective RPE/choriocapilary complex in one of the OCT scans Interpreted by: N/R Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (unclear if stereoscopic or not)a Interpreted by: Ophthalmologists |
Unit of analysis (n): Examination Diagnostic accuracy: Yes Sensitivity: CNV based in detection of intraretinal fluid: 90.3% CNV based on detection of subretinal fluid: 71% CNV based on detection of intraretinal and/or subretinal fluid: 96.8% Specificity: CNV based in detection of intraretinal fluid: 40% CNV based on detection of subretinal fluid: 73.3% CNV based on detection of intraretinal and/or subretinal fluid: 36.7% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Khurana 201023 Full text: Yes Study type: Direct head-to-head comparison Retrospective: Yes Multicentre: No Country: USA Study start/end dates: November 2007/June 2008 Duration of study: 8 months |
Enrolled: 56 patients (59 eyes) Analysed: 59 eyes Consecutive: Yes Age (years) mean/median (range/SD): 78.1 (7.8) Gender M : F: N/R BCVA: 0.64 ± 0.35 (mean, log-MAR); Snellen equivalent 20/80 (median) Inclusion criteria: Age ≥ 50 years, CNV secondary to AMD, FFA, TD-OCT and SD-OCT performed at the same visit Exclusion criteria: Patients with CNV resulting from other causes |
Index test(s): TD-OCT (Stratus OCT™) and SD-OCT (Cirrus™, Carl Zeiss Meditec, Dublin, CA) Definition of positive test result: Presence of intersticial retinal fluid, retinal cystoid abnormalities, and subretinal fluid (subretinal pigment epithelial abnormalities were not evaluated) Interpreted by: Trained grader (non-ophthalmologist technician, optometrist, nurse, or other) Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: Stereoscopic FFA Interpreted by: Trained grader (non-ophthalmologist technician, optometrist, nurse, or other) |
Unit of analysis (n): Eye Was adjustment made for non-independence of fellow eyes for cases where both eyes per subject included: N/R Diagnostic accuracy: Yes Sensitivity: TD-OCT: 58.6% SD-OCT: 89.7% Specificity: TD-OCT: 63.3% SD-OCT: 46.7% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Regillo 199843 Full text: Yes Study type: Direct head-to-head comparison Prospective: Yes Multicentre: No Country: USA Study start/end dates: April 1995/December 1996 Duration of study: 20 months |
Enrolled: 21 patients (24 eyes) Analysed: 54 examinations Consecutive: Yes Age (years) mean/median (range/SD): 75 (59–91) years Gender M : F: 11 : 10 BCVA: N/R Inclusion criteria: patients with eAMD that had conventional laser treatment for CNV, first post-treatment visit and all subsequent follow-up Exclusion criteria: N/R |
Index test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Comparator test(s): ICGA (H1024, Topcon, Tokyo, Japan) Definition of positive test result: N/R Interpreted by: N/R Reference standard: Unclear if FFA stereoscopic or not [as macular stereoscopic colour fundus photographs were taken at the beginning of all angiogram (or FFA) pairs] Interpreted by: Ophthalmologists |
Unit of analysis (n): Examination Diagnostic accuracy: Yes Sensitivity: 75.9% Specificity: 88% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| Salinas-Alaman 200545 Full text: Yes Study type: Direct head-to-head comparison, observational Prospective: Yes Multicentre: No Country: Spain Study start/end dates: N/R Duration of study: N/R |
Enrolled: N/R Analysed: Follow-up at 6 months 62 eyes Follow-up at 12 months 42 eyes Consecutive: Yes Age (years) mean/median (range/SD): 76.5 ± 7.5 years at 6 months (N/R at 12 months) Gender M : F: 26 : 27 at 6 months (N/R at 12 months) BCVA: N/R Improvement of BCVA reported: At 6 months: 40 eyes same VA; 7 eyes improved VA; 15 eyes with worse VA At 12 months: 25 eyes same VA; 5 eyes improved VA; 12 eyes with worse VA Inclusion criteria: Patients presenting with signs of exudative AMD with predominantly classic CNV Exclusion criteria: N/R |
Index test(s): TD-OCT (OCT 2000™, Humphrey Instruments) Definition of positive test result: Presence of subretinal or intraretinal fluid Interpreted by: Unclear (independent observers) Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: FFA (not specified whether or not stereoscopic)a Interpreted by: Unclear (independent observers) |
Unit of analysis (n): Remarks (= examination) Diagnostic accuracy: Yes (CNV activity after PDT treatment) Sensitivity: 95.7% Specificity: 59% Clinical effectiveness: N/R Interpretability of the test: 20 cases (9.6%) were excluded from the analysis as OCT tests were performed by a less experienced technician Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| van de Moere 200652 Full text: Yes Study type: Direct head-to-head comparison Retrospective: Yes Multicentre: No Country: UK Study start/end dates: July 2001/October 2004 Duration of study: 3 years, 3 months |
Enrolled: 136 patients Analysed: 121 eyes (121 patients) Consecutive: Yes Age (years) mean/median (range/SD): 73.9 (30–94) years Gender M : F: 55 : 66 BCVA: N/R Inclusion criteria: Patients who had all received initial PDT with verteporfin (Visudyne®, Novartis AG) for a classic or predominantly classic subfoveal CNV secondary to AMD Exclusion criteria: Poor quality of the OCT or FFA images |
Index test(s): TD-OCT (OCT 3™, Zeiss) Definition of positive test result: PED (not specified if vascular component present or not), subretinal fluid, intraretinal fluid (solitary foveal cyst, sponge-like retinal thickening, intraretinal cysts or cystoid macular oedema), vitreomacular tractions Interpreted by: N/R Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: Stereoscopic FFA Interpreted by: Ophthalmologists |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: If both eyes were eligible, one eye was randomly chosen for analysis Diagnostic accuracy: Yes Sensitivity: PED: 5.7% Subretinal fluid: 47.1% Intraretinal fluid: 82.9% Cystoid macular oedema: 98% Specificity: PED: 100% Subretinal fluid: 84.3% Intraretinal fluid: 52.9% Cystoid macular oedema: 22.9% Clinical effectiveness: N/R Interpretability of the test: 17 cases (12.5%) were excluded from analysis due to poor quality of OCT or FFA Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
| van Velthoven 200653 Full text: Yes Study type: Direct head-to-head comparison Retrospective: Yes Multicentre: No Country: Netherlands Study start/end dates: July 2003/October 2003 Duration of study: 3 months |
Enrolled: 30 patients (30 eyes) Analysed: 30 patients (30 eyes) Consecutive: Yes Age (years) mean/median (range/SD): 75.5 ± 9.0 years Gender M : F: 13 : 17 BCVA: Mean 45 ± 14 (SD) Inclusion criteria: Patients with AMD and subfoveal CNV who had received at least one prior PDT treatment Exclusion criteria: N/R |
Index test(s): TD-OCT (Stratus OCT™) Definition of positive test result: OCT activity score – positive if any sign of leakage, that is cystoid macular oedema and/or subretinal fluid and/or retinal thickening Interpreted by: N/R Comparator test(s): N/R Definition of positive test result: N/R Interpreted by: N/R Reference standard: Stereoscopic FFA Interpreted by: N/R |
Unit of analysis (n): Eye (one eye per patient) If both eyes per subject eligible, how was study eye selected: N/R Diagnostic accuracy: Yes Sensitivity: 65.2% Specificity: 42.9% Clinical effectiveness: N/R Interpretability of the test: N/R Acceptability of the test: N/R Proportion of participants not able to receive the test due to an eye condition/personal circumstances: N/R |
Appendix 5 Results of the risk of bias and applicability concerns for the individual full-text studies
| Study | Risk of bias | Applicability concerns | |||||
|---|---|---|---|---|---|---|---|
| Patient selection | Index test | Reference standard | Flow and timing | Patient selection | Index test | Reference standard | |
| Alster 200524 | – | + | + | – | + | + | + |
| Cachulo 201125 | ? | ? | ? | – | + | + | + |
| Chen 200326 | ? | ? | ? | + | + | + | + |
| Do 201227 | – | + | + | – | + | + | + |
| Fujii 199629 | ? | ? | ? | ? | + | + | + |
| Gomi 200731 | – | ? | ? | + | + | + | + |
| Hughes 200533 | ? | + | + | ? | + | + | + |
| Kim 200335 | ? | ? | ? | ? | + | + | + |
| Kozak 200836 | + | ? | ? | – | + | + | + |
| Krebs 200737 | – | + | + | + | + | + | + |
| Liakopoulos 200838 | – | + | ? | + | + | + | + |
| Loewenstein 201039 | – | ? | ? | – | + | + | + |
| Padnick-Silver 201140 | – | ? | ? | – | + | + | + |
| Park 201041 | – | + | ? | + | + | + | + |
| Reichel 199544 | – | – | – | + | + | + | + |
| Salinas-Alaman 200545 | – | ? | ? | ? | + | + | + |
| Sandhu 200546 | ? | + | + | – | + | + | + |
| Silva 201147 | ? | ? | ? | – | + | + | + |
| Sulzbacher 201148 | ? | ? | ? | ? | + | + | + |
| Talks 200749 | – | + | – | – | + | + | + |
| Torron 200150 | ? | – | – | + | + | + | + |
| Torron 200251 | ? | – | – | ? | + | + | + |
| Study | Risk of bias | Applicability concerns | |||||
|---|---|---|---|---|---|---|---|
| Patient selection | Index test | Reference standard | Flow and timing | Patient selection | Index test | Reference standard | |
| Eter 200528 | ? | + | + | ? | + | + | + |
| Giani 201130 | – | + | + | ? | – | + | + |
| Henschel 200932 | ? | + | + | ? | + | + | + |
| Khurana 201023 | ? | ? | ? | + | + | + | + |
| Regillo 199843 | + | – | – | + | + | + | + |
| Salinas-Alaman 200545 | – | ? | ? | – | + | + | + |
| van de Moere 200652 | + | ? | ? | – | + | + | + |
| van Velthoven 200653 | + | ? | + | ? | + | + | + |
Appendix 6 Individual study results
| Study ID | Test | Unit of analysis | Number analysed | TP | FP | FN | TN | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|---|---|---|
| Alster 200524 | PHP | Eye/patient | 122 | 53 | 7 | 12 | 50 | 81.5 | 87.7 |
| Colour fundus photography | Eye/patient | 120 | 45 | 3 | 19 | 53 | 70.0 | 95.0 | |
| Colour fundus photography plus VA | Eye/patient | 66 | 10 | 3 | 9 | 44 | 53.0 | 94.0 | |
| Cachulo 201125 | TD-OCT | Eye/patient | 52 | 17 | 0 | 100.0 | NC | ||
| ICGA | Eye/patient | 52 | 16 | 1 | 94.1 | NC | |||
| FAF (but not clear whether before conversion or at time of conversion so may not be usable) | Eye/patient | 50 | 14 | 22 | 1 | 13 | 93.3 | 37.1 | |
| Silva 201147 (secondary report to Cachulo 201125) | TD-OCT | Eye/patient | 52 | 24 | 0 | 100.0 | NC | ||
| Chen 200326 | ICGA | Eye | |||||||
| Occult CNV detection | 35 | 22 | 13 | 62.9 | NC | ||||
| Do 201227 | CNV defined as FFA positive by the Reading Centre irrespective of treatment decision (n = 15) | ||||||||
| TD-OCT | Eye/patient | 87 | 6 | 21 | 9 | 51 | 40.0 | 70.8 | |
| Amsler grid | Eye/patient | 46 | 5 | NC | 7 | 34 | 41.7 | N/R | |
| PHP | Eye/patient | 49 | 6 | NC | 6 | 37 | 50.0 | N/R | |
| CNV defined as FFA positive by the Reading Centre and the clinician recommended treatment (n = 13) | |||||||||
| TD-OCT | Eye/patient | 87 | 9 | 25 | 4 | 49 | 69.2 | 66.2 | |
| Amsler grid | Eye/patient | 47 | 5 | NC | 5 | 37 | 50.0 | N/R | |
| PHP | Eye/patient | 45 | 7 | NC | 3 | 35 | 70.0 | N/R | |
| Fujii 199629 | ICGA/DH/DS | Eye | 32 | 11 | 12 | 2 | 7 | 84.6 | 36.8 |
| Gomi 200731 | ICGA/DH/DS | Eye/patient | |||||||
| PCV detection | 37 | 37 | NC | 0 | NC | 100.0 | NC | ||
| Hughes 200533 | TD-OCT | Eye/patient | 22 | 8 | 14 | 36.4 | NC | ||
| Khondkaryan 200934 | TD-OCT | Eye/patient | |||||||
| Detection of occult | 51 | 30 | 8 | 7 | 6 | 81.1 | 42.9 | ||
| Detection of classic | 51 | 17 | 13 | 4 | 17 | 80.9 | 56.7 | ||
| Detection of RAP | 51 | 4 | 8 | 3 | 36 | 57.1 | 81.8 | ||
| Kim 200335 | TD-OCT | Eye/patient | 13 | 12 | 1 | 92.3 | NC | ||
| Kozak 200836 | TD-OCT (although subset of patients received SD-OCT) | Eye | 541 | 514 | 13 | 14 | NC | 97.3 | NC |
| Krebs 200737 | TD-OCT | Eye | |||||||
| Primarily classic | 5 | 5 | 0 | 100.0 | |||||
| RAP | 11 | 8 | 3 | 72.7 | |||||
| Dry AMD as negative diagnosis | 12 | 0 | 12 | 100.0 | |||||
| Liakopoulos 200838 | TD-OCT | Eye/patient (n = 66 for both) | |||||||
| Subretinal fluid | |||||||||
| Occult with no classic | 24 | 19 | 5 | 79.2 | NC | ||||
| Minimally classic | 23 | 21 | 2 | 91.3 | NC | ||||
| Predominantly classic | 11 | 11 | 0 | 100.0 | NC | ||||
| RAP stage III | 8 | 4 | 4 | 50.0 | NC | ||||
| All | 66 | 55 | 11 | 83.3 | NC | ||||
| Cystoid oedema | |||||||||
| Occult with no classic | 24 | 14 | 10 | 58.3 | NC | ||||
| Minimally classic | 23 | 17 | 6 | 73.9 | NC | ||||
| Predominantly classic | 11 | 9 | 2 | 81.8 | NC | ||||
| RAP stage III | 8 | 8 | 0 | 100.0 | NC | ||||
| All | 66 | 48 | 18 | 72.7 | NC | ||||
| Loewenstein 201039 | PHP | Eye/patient | |||||||
| Retrospective part | 77 | 29 | 7 | 5 | 36 | 85.3 | 83.7 | ||
| Prospective part | 54 | 27 | 3 | 5 | 19 | 84.4 | 86.4 | ||
| All | 131 | 56 | 10 | 10 | 55 | 84.8 | 84.6 | ||
| Padnick-Silver 201240 | TD-OCT | Eye/patient | 77 | 12 | 4 | 3 | 58 | 80.0 | 93.5 |
| Park 201041 | SD-OCT | Eye | 21 | 21 | 0 | 100.0 | NC | ||
| Parravano 201242 | ICGA | Patient | |||||||
| Detection of RAP | 155 | 40 | 7 | 85.1 | NC | ||||
| Reichel 199544 | ICGA | Eye/patient | 20 | 16 | 4 | 0 | NC | 100.0 | NC |
| Salinas-Alaman 200545 | TD-OCT | Eye | 62 | 60 | 2 | 96.8 | NC | ||
| Sandhu 200546 | TD-OCT | Eye | 131 | 63 | 12 | 18 | 38 | 77.8a | 76.0a |
| SD-OCT + stereo colour fundus photography | Eye | 131 | 60 | 4 | 21 | 46 | 74.1a | 92.0a | |
| Sulzbacher 201148 | ICGA | Eye | |||||||
| Detection of type 2 CNV without an occult component | 13 | 13 | 0 | 100.0 | NC | ||||
| Talks 200749 | TD-OCT | Eye/patient | 111 | 73 | 13 | 0 | 25 | 100.0 | 65.8 |
| Torron 200251 | ICGA | Eye | 102 | 94 | 8 | 92.2 | NC | ||
| Torron 200150 (secondary report to Torron 200251) | ICGA | Eye | 56 | 50 | 6 | 89.3 | NC | ||
| Study ID | Test | Unit of analysis | Number analysed | TP | FP | FN | TN | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|---|---|---|
| Eter 200528 | TD-OCT | Eye/patient | 60 | 40 | 2 | 10 | 8 | 80.0 | 80.0 |
| Giani 201130 | SD-OCT | Eye/patient | |||||||
| Classic CNV | 57 | 30 | 15 | 3 | 9 | 90.9 | 37.5 | ||
| Occult CNV | 36 | 19 | 15 | 0 | 2 | 100.0 | 11.8 | ||
| Overall CNV | 93 | 49 | 30 | 3 | 11 | 94.2 | 26.8 | ||
| Henschel 200932 (14 patients; 61 pairs of OCT and FFA examinations) | TD-OCT | Examination | |||||||
| CNV based on detection of intraretinal fluid | 61 | 28 | 18 | 3 | 12 | 90.3 | 40.0 | ||
| CNV based on detection of subretinal fluid | 61 | 22 | 8 | 9 | 22 | 71.0 | 73.3 | ||
| CNV based on detection of intraretinal and/or subretinal fluid | 61 | 30 | 19 | 1 | 11 | 96.8 | 36.7 | ||
| Khurana 201023 | TD-OCT | Eye | 59 | 17 | 11 | 12 | 19 | 58.6 | 63.3 |
| SD-OCT | Eye | 59 | 26 | 16 | 3 | 14 | 89.7 | 46.7 | |
| Regillo 199843 (54 angiogram pairs obtained from 24 eyes of 21 patients) | ICGA/DH/DS | Examination | 54 | 22 | 3 | 7 | 22 | 75.9 | 88.0 |
| Salinas-Alaman 200545 | TD-OCT | Remark (= examination) | 176 | 110 | 25 | 5 | 36 | 95.7 | 59.0 |
| van de Moere 200652 | TD-OCT | Eye/patient | |||||||
| Detection of PED as criteria for positive test result | 121 | 4 | 0 | 66 | 51 | 5.7 | 100.0 | ||
| Detection of subretinal fluid as positive test result | 121 | 33 | 8 | 37 | 43 | 47.1 | 84.3 | ||
| Detection of intraretinal fluid as positive test result | 121 | 58 | 24 | 12 | 27 | 82.9 | 52.9 | ||
| Detection of CMO as a positive test result | 121 | 16 | 1 | 54 | 50 | 22.9 | 98.0 | ||
| van Velthoven 200653 | TD-OCT | Eye/patient | 30 | 15 | 4 | 8 | 3 | 65.2 | 42.9 |
Appendix 7 Studies reporting eye-related exclusion criteria
| Study | Eye-related exclusion criteria |
|---|---|
| Alster 200524 |
|
| Cachulo 201125 |
|
| Do 201227 |
|
| Gomi 200731 |
|
| Loewenstein 201039 |
|
| Padnick-Silver 201240 |
|
| Park 201041 |
|
| Reichel 199544 |
|
| Sulzbacher 201148 |
|
| Talks 200749 |
|
Appendix 8 Sensitivity analysis results
One-way sensitivity analysis
All analyses show results moving in the expected direction (e.g. lower sensitivity or specificity for OCT would result in OCT-based strategies being less cost-effective). Briefly, base-case analysis results seem robust. In a limited number of model runs, alternative OCT-based strategies stopped being dominated or became cost-effective. However, in these cases the variable values used to run the analysis were extreme. For instance, diagnosing with OCT combined with nurse-/technician-led monitoring seemed worthwhile when OCT diagnosis sensitivity and specificity was equal to 1. It should be noted that it is unlikely that the other strategies’ diagnostic assessment that were also based on OCT and other tests would result in a lower sensitivity and specificity than using OCT only (interpreted by the same ophthalmologist) (Tables 50–74).
| Diagnosis sensitivity OCT | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.1 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,474 | 10.411 | 1705 | –0.062 | –27,580 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 46,965 | 10.510 | 2316 | –0.065 | –35,789 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,155 | 10.387 | 22,506 | –0.188 | –119,903 | Dominated | |
| 0.2 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,491 | 10.418 | 1722 | –0.055 | –31,342 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4,880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 46,986 | 10.518 | 2337 | –0.057 | –40,649 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,189 | 10.394 | 22,540 | –0.181 | –124,721 | Dominated | |
| 0.3 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,508 | 10.425 | 1739 | –0.048 | –36,180 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,008 | 10.525 | 2358 | –0.050 | –46,904 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,223 | 10.401 | 22,574 | –0.174 | –129,926 | Dominated | |
| 0.4 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,525 | 10.432 | 1756 | –0.041 | –42,633 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,029 | 10.532 | 2380 | –0.043 | –55,254 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,257 | 10.408 | 22,608 | –0.167 | –135,566 | Dominated | |
| 0.5 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,542 | 10.439 | 1773 | –0.034 | –51,673 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,050 | 10.539 | 2401 | –0.036 | –66,965 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,292 | 10.415 | 22,642 | –0.160 | –141,699 | Dominated | |
| 0.6 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,559 | 10.445 | 1790 | –0.027 | –65,241 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,071 | 10.546 | 2422 | –0.029 | –84,573 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,326 | 10.422 | 22,677 | –0.153 | –148,392 | Dominated | |
| 0.7 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,576 | 10.452 | 1807 | –0.021 | –87,881 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,093 | 10.554 | 2444 | –0.021 | –114,038 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,360 | 10.429 | 22,711 | –0.146 | –155,725 | Dominated | |
| 0.8 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,594 | 10.459 | 1824 | –0.014 | –133,258 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,114 | 10.561 | 2465 | –0.014 | –173,407 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,394 | 10.436 | 22,745 | –0.139 | –163,795 | Dominated | |
| 0.9 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,611 | 10.466 | 1841 | –0.007 | –270,172 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,135 | 10.568 | 2486 | –0.007 | –355,119 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,428 | 10.443 | 22,779 | –0.132 | –172,719 | Dominated | |
| 1.0 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,628 | 10.473 | 1859 | 0.000 | 31,635,704 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 3021 | 0.102 | 29,593 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,157 | 10.575 | 2507 | 0.000 | 11,797,675 | ||
| (1) FFA & OCT | 62,759 | 10.449 | 15,602 | –0.126 | –124,050 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 15,621 | –0.126 | –123,584 | Dominated | |
| (4) OCT & OCT | 67,462 | 10.450 | 20,306 | –0.125 | –162,290 | Dominated |
| Diagnosis specificity OCT | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.55 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 43,619 | 10.465 | 3850 | –0.008 | –473,564 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 49,821 | 10.567 | 5172 | –0.008 | –629,095 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 72,407 | 10.442 | 27,758 | –0.133 | –209,343 | Dominated | |
| 0.60 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 43,182 | 10.465 | 3412 | –0.008 | –419,079 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 49,236 | 10.567 | 4587 | –0.008 | –554,702 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 71,324 | 10.442 | 26,674 | –0.133 | –200,943 | Dominated | |
| 0.65 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 42,744 | 10.465 | 2975 | –0.008 | –364,772 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 48,651 | 10.567 | 4002 | –0.008 | –481,174 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 70,240 | 10.442 | 25,590 | –0.133 | –192,562 | Dominated | |
| 0.70 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 42,307 | 10.465 | 2538 | –0.008 | –310,643 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 48,067 | 10.567 | 3418 | –0.008 | –408,495 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 69,156 | 10.442 | 24,507 | –0.133 | –184,200 | Dominated | |
| 0.75 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,870 | 10.465 | 2100 | –0.008 | –256,690 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,482 | 10.567 | 2833 | –0.008 | –336,651 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 68,072 | 10.442 | 23,423 | –0.133 | –175,856 | Dominated | |
| 0.80 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,432 | 10.465 | 1663 | –0.008 | –202,914 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 46,897 | 10.567 | 2248 | –0.008 | –265,626 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 66,988 | 10.442 | 22,339 | –0.133 | –167,531 | Dominated | |
| 0.85 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 40,995 | 10.465 | 1226 | –0.008 | –149,312 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 46,312 | 10.567 | 1663 | –0.009 | –195,408 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 65,904 | 10.442 | 21,255 | –0.133 | –159,225 | Dominated | |
| 0.90 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 40,558 | 10.465 | 788 | –0.008 | –95,884 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 45,727 | 10.566 | 1078 | –0.009 | –125,982 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 64,820 | 10.441 | 20,171 | –0.134 | –150,937 | Dominated | |
| 0.95 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 40,120 | 10.465 | 351 | –0.008 | –42,629 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 45,143 | 10.566 | 494 | –0.009 | –57,335 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 63,736 | 10.441 | 19,087 | –0.134 | –142,667 | Dominated | |
| 1.00 | (6) OCT & Nurse | 39,683 | 10.465 | ||||
| (3) FFA & Nurse | 39,769 | 10.473 | 86 | 0.008 | 10,453 | ||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (5) OCT & Ophthalmologist | 44,558 | 10.566 | 4789 | 0.094 | 51,214 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 91 | 0.009 | 10,545 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (4) OCT & OCT | 62,652 | 10.441 | 18,003 | –0.134 | –134,416 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated |
| OCT diagnosis | Strategy | Expected Cost (£) | Expected QALYs | NMB (£) | Maximum NMB | |
|---|---|---|---|---|---|---|
| Sensitivity | Specificity | |||||
| 0.60 | 0.55 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,312 | 10.4229 | 240,374 | |||
| (5) OCT & Ophthalmologist | 49,761 | 10.5466 | 266,636 | |||
| (6) OCT & Nurse | 43,571 | 10.4455 | 269,793 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.60 | 0.60 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 71,228 | 10.4227 | 241,454 | |||
| (5) OCT & Ophthalmologist | 49,177 | 10.5465 | 267,220 | |||
| (6) OCT & Nurse | 43,134 | 10.4455 | 270,230 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.60 | 0.65 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 70,144 | 10.4226 | 242,533 | |||
| (5) OCT & Ophthalmologist | 48,592 | 10.5465 | 267,803 | |||
| (6) OCT & Nurse | 42,696 | 10.4454 | 270,667 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.60 | 0.70 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 69,060 | 10.4224 | 243,613 | |||
| (5) OCT & Ophthalmologist | 48,007 | 10.5464 | 268,386 | |||
| (6) OCT & Nurse | 42,259 | 10.4454 | 271,104 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.60 | 0.75 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 67,976 | 10.4223 | 244,692 | |||
| (5) OCT & Ophthalmologist | 47,422 | 10.5464 | 268,970 | |||
| (6) OCT & Nurse | 41,822 | 10.4454 | 271,541 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.60 | 0.80 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 66,892 | 10.4221 | 245,772 | |||
| (5) OCT & Ophthalmologist | 46,837 | 10.5463 | 269,553 | |||
| (6) OCT & Nurse | 41,384 | 10.4454 | 271,978 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.60 | 0.85 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 65,808 | 10.4220 | 246,851 | |||
| (5) OCT & Ophthalmologist | 46,253 | 10.5463 | 270,136 | |||
| (6) OCT & Nurse | 40,947 | 10.4454 | 272,415 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.60 | 0.90 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 64,724 | 10.4218 | 247,931 | |||
| (5) OCT & Ophthalmologist | 45,668 | 10.5462 | 270,720 | |||
| (6) OCT & Nurse | 40,510 | 10.4454 | 272,851 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.60 | 0.95 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 63,641 | 10.4217 | 249,010 | |||
| (5) OCT & Ophthalmologist | 45,083 | 10.5462 | 271,303 | |||
| (6) OCT & Nurse | 40,072 | 10.4454 | 273,288 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.60 | 1.00 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 62,557 | 10.4215 | 250,089 | |||
| (5) OCT & Ophthalmologist | 44,498 | 10.5462 | 271,886 | |||
| (6) OCT & Nurse | 39,635 | 10.4453 | 273,725 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 0.55 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,346 | 10.4299 | 240,550 | |||
| (5) OCT & Ophthalmologist | 49,783 | 10.5538 | 266,831 | |||
| (6) OCT & Nurse | 43,588 | 10.4523 | 269,982 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 0.60 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 71,262 | 10.4297 | 241,629 | |||
| (5) OCT & Ophthalmologist | 49,198 | 10.5538 | 267,415 | |||
| (6) OCT & Nurse | 43,151 | 10.4523 | 270,419 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 0.65 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 70,178 | 10.4296 | 242,708 | |||
| (5) OCT & Ophthalmologist | 48,613 | 10.5537 | 267,998 | |||
| (6) OCT & Nurse | 42,714 | 10.4523 | 270,856 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 0.70 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 69,094 | 10.4294 | 243,788 | |||
| (5) OCT & Ophthalmologist | 48,028 | 10.5537 | 268,581 | |||
| (6) OCT & Nurse | 42,276 | 10.4523 | 271,293 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 0.75 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 68,010 | 10.4293 | 244,867 | |||
| (5) OCT & Ophthalmologist | 47,444 | 10.5536 | 269,165 | |||
| (6) OCT & Nurse | 41,839 | 10.4523 | 271,730 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 0.80 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 66,926 | 10.4291 | 245,947 | |||
| (5) OCT & Ophthalmologist | 46,859 | 10.5536 | 269,748 | |||
| (6) OCT & Nurse | 41,402 | 10.4523 | 272,167 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 0.85 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 65,842 | 10.4290 | 247,026 | |||
| (5) OCT & Ophthalmologist | 46,274 | 10.5535 | 270,331 | |||
| (6) OCT & Nurse | 40,964 | 10.4523 | 272,604 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 0.90 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 64,759 | 10.4288 | 248,106 | |||
| (5) OCT & Ophthalmologist | 45,689 | 10.5535 | 270,915 | |||
| (6) OCT & Nurse | 40,527 | 10.4522 | 273,041 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 0.95 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 63,675 | 10.4287 | 249,185 | |||
| (5) OCT & Ophthalmologist | 45,104 | 10.5534 | 271,498 | |||
| (6) OCT & Nurse | 40,090 | 10.4522 | 273,478 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.70 | 1.00 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 62,591 | 10.4285 | 250,265 | |||
| (5) OCT & Ophthalmologist | 44,520 | 10.5534 | 272,081 | |||
| (6) OCT & Nurse | 39,652 | 10.4522 | 273,914 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 0.55 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,380 | 10.4368 | 240,725 | |||
| (5) OCT & Ophthalmologist | 49,804 | 10.5610 | 267,026 | |||
| (6) OCT & Nurse | 43,605 | 10.4592 | 270,171 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 0.60 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 71,296 | 10.4367 | 241,804 | |||
| (5) OCT & Ophthalmologist | 49,219 | 10.5610 | 267,610 | |||
| (6) OCT & Nurse | 43,168 | 10.4592 | 270,608 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 0.65 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 70,212 | 10.4365 | 242,884 | |||
| (5) OCT & Ophthalmologist | 48,634 | 10.5609 | 268,193 | |||
| (6) OCT & Nurse | 42,731 | 10.4592 | 271,045 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 0.70 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 69,128 | 10.4364 | 243,963 | |||
| (5) OCT & Ophthalmologist | 48,050 | 10.5609 | 268,776 | |||
| (6) OCT & Nurse | 42,293 | 10.4592 | 271,482 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 0.75 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 68,044 | 10.4362 | 245,043 | |||
| (5) OCT & Ophthalmologist | 47,465 | 10.5608 | 269,360 | |||
| (6) OCT & Nurse | 41,856 | 10.4592 | 271,919 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 0.80 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 66,961 | 10.4361 | 246,122 | |||
| (5) OCT & Ophthalmologist | 46,880 | 10.5608 | 269,943 | |||
| (6) OCT & Nurse | 41,419 | 10.4592 | 272,356 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 0.85 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 65,877 | 10.4359 | 247,201 | |||
| (5) OCT & Ophthalmologist | 46,295 | 10.5607 | 270,526 | |||
| (6) OCT & Nurse | 40,981 | 10.4591 | 272,793 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 0.90 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 64,793 | 10.4358 | 248,281 | |||
| (5) OCT & Ophthalmologist | 45,710 | 10.5607 | 271,110 | |||
| (6) OCT & Nurse | 40,544 | 10.4591 | 273,230 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 0.95 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 63,709 | 10.4356 | 249,360 | |||
| (5) OCT & Ophthalmologist | 45,126 | 10.5606 | 271,693 | |||
| (6) OCT & Nurse | 40,107 | 10.4591 | 273,667 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.80 | 1.00 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 62,625 | 10.4355 | 250,440 | |||
| (5) OCT & Ophthalmologist | 44,541 | 10.5606 | 272,277 | |||
| (6) OCT & Nurse | 39,669 | 10.4591 | 274,104 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 0.55 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,414 | 10.4438 | 240,900 | |||
| (5) OCT & Ophthalmologist | 49,825 | 10.5682 | 267,222 | |||
| (6) OCT & Nurse | 43,622 | 10.4661 | 270,360 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 0.60 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 71,330 | 10.4437 | 241,979 | |||
| (5) OCT & Ophthalmologist | 49,241 | 10.5682 | 267,805 | |||
| (6) OCT & Nurse | 43,185 | 10.4661 | 270,797 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 0.65 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 70,246 | 10.4435 | 243,059 | |||
| (5) OCT & Ophthalmologist | 48,656 | 10.5681 | 268,388 | |||
| (6) OCT & Nurse | 42,748 | 10.4661 | 271,234 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 0.70 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 69,163 | 10.4434 | 244,138 | |||
| (5) OCT & Ophthalmologist | 48,071 | 10.5681 | 268,972 | |||
| (6) OCT & Nurse | 42,310 | 10.4661 | 271,671 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 0.75 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 68,079 | 10.4432 | 245,218 | |||
| (5) OCT & Ophthalmologist | 47,486 | 10.5680 | 269,555 | |||
| (6) OCT & Nurse | 41,873 | 10.4660 | 272,108 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 0.80 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 66,995 | 10.4431 | 246,297 | |||
| (5) OCT & Ophthalmologist | 46,901 | 10.5680 | 270,138 | |||
| (6) OCT & Nurse | 41,436 | 10.4660 | 272,545 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 0.85 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 65,911 | 10.4429 | 247,377 | |||
| (5) OCT & Ophthalmologist | 46,317 | 10.5679 | 270,722 | |||
| (6) OCT & Nurse | 40,998 | 10.4660 | 272,982 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 0.90 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 64,827 | 10.4428 | 248,456 | |||
| (5) OCT & Ophthalmologist | 45,732 | 10.5679 | 271,305 | |||
| (6) OCT & Nurse | 40,561 | 10.4660 | 273,419 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 0.95 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 63,743 | 10.4426 | 249,535 | |||
| (5) OCT & Ophthalmologist | 45,147 | 10.5678 | 271,888 | |||
| (6) OCT & Nurse | 40,124 | 10.4660 | 273,856 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.90 | 1.00 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 62,659 | 10.4425 | 250,615 | |||
| (5) OCT & Ophthalmologist | 44,562 | 10.5678 | 272,472 | |||
| (6) OCT & Nurse | 39,686 | 10.4660 | 274,293 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 0.55 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,448 | 10.4508 | 241,075 | |||
| (5) OCT & Ophthalmologist | 49,847 | 10.5754 | 267,417 | |||
| (6) OCT & Nurse | 43,639 | 10.4730 | 270,550 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 0.60 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 71,365 | 10.4506 | 242,154 | |||
| (5) OCT & Ophthalmologist | 49,262 | 10.5754 | 268,000 | |||
| (6) OCT & Nurse | 43,202 | 10.4730 | 270,986 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 0.65 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 70,281 | 10.4505 | 243,234 | |||
| (5) OCT & Ophthalmologist | 48,677 | 10.5753 | 268,583 | |||
| (6) OCT & Nurse | 42,765 | 10.4729 | 271,423 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 0.70 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 69,197 | 10.4503 | 244,313 | |||
| (5) OCT & Ophthalmologist | 48,092 | 10.5753 | 269,167 | |||
| (6) OCT & Nurse | 42,327 | 10.4729 | 271,860 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 0.75 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 68,113 | 10.4502 | 245,393 | |||
| (5) OCT & Ophthalmologist | 47,507 | 10.5752 | 269,750 | |||
| (6) OCT & Nurse | 41,890 | 10.4729 | 272,297 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 0.80 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 67,029 | 10.4500 | 246,472 | |||
| (5) OCT & Ophthalmologist | 46,923 | 10.5752 | 270,333 | |||
| (6) OCT & Nurse | 41,453 | 10.4729 | 272,734 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 0.85 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 65,945 | 10.4499 | 247,552 | |||
| (5) OCT & Ophthalmologist | 46,338 | 10.5752 | 270,917 | |||
| (6) OCT & Nurse | 41,015 | 10.4729 | 273,171 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 0.90 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 64,861 | 10.4497 | 248,631 | |||
| (5) OCT & Ophthalmologist | 45,753 | 10.5751 | 271,500 | |||
| (6) OCT & Nurse | 40,578 | 10.4729 | 273,608 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 0.95 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 63,777 | 10.4496 | 249,711 | |||
| (5) OCT & Ophthalmologist | 45,168 | 10.5751 | 272,083 | |||
| (6) OCT & Nurse | 40,141 | 10.4729 | 274,045 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.00 | 1.00 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | |||
| (4) OCT & OCT | 62,693 | 10.4494 | 250,790 | |||
| (5) OCT & Ophthalmologist | 44,583 | 10.5750 | 272,667 | |||
| (6) OCT & Nurse | 39,703 | 10.4728 | 274,482 | ✓ | ||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| Diagnosis sensitivity ophthalmologist assessment | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.1 | (9) Ophthalmologist & Nurse | 39,587 | 10.417 | ||||
| (3) FFA & Nurse | 39,769 | 10.473 | 182 | 0.056 | 3267 | ||
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 44,433 | 10.517 | 4664 | 0.044 | 106,648 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 216 | 0.058 | 3696 | ||
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (7) Ophthalmologist & OCT | 62,439 | 10.393 | 17,790 | –0.182 | –97,705 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.2 | (9) Ophthalmologist & Nurse | 39,610 | 10.423 | ||||
| (3) FFA & Nurse | 39,769 | 10.473 | 159 | 0.050 | 3215 | ||
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 44,460 | 10.523 | 4691 | 0.050 | 93,392 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 189 | 0.052 | 3647 | ||
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (7) Ophthalmologist & OCT | 62,477 | 10.399 | 17,828 | –0.176 | –101,411 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.3 | (9) Ophthalmologist & Nurse | 39,633 | 10.430 | ||||
| (3) FFA & Nurse | 39,769 | 10.473 | 136 | 0.043 | 3149 | ||
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 44,486 | 10.530 | 4717 | 0.057 | 83,170 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 163 | 0.045 | 3584 | ||
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (7) Ophthalmologist & OCT | 62,515 | 10.405 | 17,866 | –0.170 | –105,393 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.4 | (9) Ophthalmologist & Nurse | 39,656 | 10.436 | ||||
| (3) FFA & Nurse | 39,769 | 10.473 | 114 | 0.037 | 3061 | ||
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 44,513 | 10.536 | 4744 | 0.063 | 75,047 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 136 | 0.039 | 3501 | ||
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (7) Ophthalmologist & OCT | 62,553 | 10.412 | 17,904 | –0.163 | –109,680 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.5 | (9) Ophthalmologist & Nurse | 39,678 | 10.442 | ||||
| (3) FFA & Nurse | 39,769 | 10.473 | 91 | 0.031 | 2938 | ||
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 44,539 | 10.543 | 4770 | 0.070 | 68,438 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 110 | 0.032 | 3383 | ||
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (7) Ophthalmologist & OCT | 62,591 | 10.418 | 17,942 | –0.157 | –114,311 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.6 | (9) Ophthalmologist & Nurse | 39,701 | 10.448 | ||||
| (3) FFA & Nurse | 39,769 | 10.473 | 68 | 0.025 | 2754 | ||
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 44,566 | 10.549 | 4797 | 0.076 | 62,955 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 83 | 0.026 | 3207 | ||
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (7) Ophthalmologist & OCT | 62,629 | 10.424 | 17,980 | –0.151 | –119,327 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.7 | (9) Ophthalmologist & Nurse | 39,724 | 10.454 | ||||
| (3) FFA & Nurse | 39,769 | 10.473 | 45 | 0.019 | 2446 | ||
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 44,592 | 10.556 | 4823 | 0.083 | 58,333 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 57 | 0.019 | 2914 | ||
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (7) Ophthalmologist & OCT | 62,667 | 10.431 | 18,018 | –0.144 | –124,780 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.8 | (9) Ophthalmologist & Nurse | 39,746 | 10.460 | ||||
| (3) FFA & Nurse | 39,769 | 10.473 | 23 | 0.012 | 1831 | ||
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 44,619 | 10.562 | 4850 | 0.089 | 54,384 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 30 | 0.013 | 2328 | ||
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (7) Ophthalmologist & OCT | 62,706 | 10.437 | 18,056 | –0.138 | –130,729 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.9 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,769 | 10.467 | 0 | –0.006 | –15 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 44,645 | 10.569 | 4876 | 0.096 | 50,971 | ||
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4 | 0.006 | 569 | ||
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (7) Ophthalmologist & OCT | 62,744 | 10.443 | 18,095 | –0.132 | –137,244 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 1.0 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,792 | 10.473 | 23 | 0.000 | 0 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,672 | 10.575 | 23 | 0.000 | 0 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,782 | 10.449 | 18,133 | –0.126 | –144,410 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated |
| Diagnosis sensitivity ophthalmologist assessment | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.1 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,815 | 10.472 | 46 | –0.001 | –74,082 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,695 | 10.574 | 45 | –0.001 | –70,022 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,803 | 10.449 | 18,154 | –0.126 | –143,862 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.2 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,812 | 10.472 | 43 | –0.001 | –68,977 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,691 | 10.574 | 42 | –0.001 | –65,156 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,800 | 10.449 | 18,151 | –0.126 | –143,837 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.3 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,809 | 10.472 | 40 | –0.001 | –63,871 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,688 | 10.574 | 39 | –0.001 | –60,290 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,797 | 10.449 | 18,148 | –0.126 | –143,812 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.4 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,806 | 10.472 | 36 | –0.001 | –58,765 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,685 | 10.574 | 36 | –0.001 | –55,424 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,794 | 10.449 | 18,145 | –0.126 | –143,787 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.5 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,802 | 10.472 | 33 | –0.001 | –53,659 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,682 | 10.574 | 33 | –0.001 | –50,558 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,791 | 10.449 | 18,141 | –0.126 | –143,762 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.6 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,799 | 10.472 | 30 | –0.001 | –48,554 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,679 | 10.574 | 30 | –0.001 | –45,692 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2,482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,787 | 10.449 | 18,138 | –0.126 | –143,737 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.7 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,796 | 10.472 | 27 | –0.001 | –43,448 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,676 | 10.574 | 27 | –0.001 | –40,826 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,784 | 10.449 | 18,135 | –0.126 | –143,712 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.8 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,793 | 10.472 | 24 | –0.001 | –38,342 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,673 | 10.574 | 23 | –0.001 | –35,960 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,781 | 10.449 | 18,132 | –0.126 | –143,687 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.9 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 1.0 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,787 | 10.472 | 17 | –0.001 | –28,131 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,666 | 10.574 | 17 | –0.001 | –26,228 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,775 | 10.449 | 18,126 | –0.126 | –143,637 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated |
| Ophthalmologist diagnosis | Strategy | Expected cost (£) | Expected QALYs | NMB (£) | Maximum NMB | |
|---|---|---|---|---|---|---|
| Sensitivity | Specificity | |||||
| 0.8 | 0.5 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,204 | 10.531 | 249,730 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,632 | 10.562 | 272,229 | |||
| (9) Ophthalmologist & Nurse | 39,759 | 10.460 | 274,055 | |||
| 0.8 | 0.6 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,201 | 10.531 | 249,733 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,628 | 10.562 | 272,232 | |||
| (9) Ophthalmologist & Nurse | 39,756 | 10.460 | 274,058 | |||
| 0.8 | 0.7 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,197 | 10.531 | 249,736 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,625 | 10.562 | 272,235 | |||
| (9) Ophthalmologist & Nurse | 39,753 | 10.460 | 274,061 | |||
| 0.8 | 0.8 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,194 | 10.531 | 249,739 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,622 | 10.562 | 272,239 | |||
| (9) Ophthalmologist & Nurse | 39,750 | 10.460 | 274,064 | |||
| 0.8 | 0.9 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,191 | 10.531 | 249,743 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,619 | 10.562 | 272,242 | |||
| (9) Ophthalmologist & Nurse | 39,746 | 10.460 | 274,068 | |||
| 0.8 | 1.0 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,188 | 10.531 | 249,746 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,616 | 10.562 | 272,245 | |||
| (9) Ophthalmologist & Nurse | 39,743 | 10.460 | 274,071 | |||
| 0.9 | 0.5 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,244 | 10.538 | 249,886 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,658 | 10.569 | 272,397 | |||
| (9) Ophthalmologist & Nurse | 39,782 | 10.467 | 274,218 | |||
| 0.9 | 0.6 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,241 | 10.538 | 249,890 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,655 | 10.569 | 272,400 | |||
| (9) Ophthalmologist & Nurse | 39,779 | 10.467 | 274,221 | |||
| 0.9 | 0.7 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,238 | 10.538 | 249,893 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,652 | 10.569 | 272,404 | |||
| (9) Ophthalmologist & Nurse | 39,776 | 10.467 | 274,224 | |||
| 0.9 | 0.8 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,235 | 10.538 | 249,896 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,649 | 10.569 | 272,407 | |||
| (9) Ophthalmologist & Nurse | 39,772 | 10.467 | 274,227 | |||
| 0.9 | 0.9 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,232 | 10.538 | 249,899 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,645 | 10.569 | 272,410 | |||
| (9) Ophthalmologist & Nurse | 39,769 | 10.467 | 274,231 | |||
| 0.9 | 1.0 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,228 | 10.538 | 249,902 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,642 | 10.569 | 272,413 | |||
| (9) Ophthalmologist & Nurse | 39,766 | 10.467 | 274,234 | |||
| 1.0 | 0.5 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,285 | 10.544 | 250,043 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,685 | 10.575 | 272,566 | |||
| (9) Ophthalmologist & Nurse | 39,805 | 10.473 | 274,381 | |||
| 1.0 | 0.6 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,281 | 10.544 | 250,046 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,681 | 10.575 | 272,569 | |||
| (9) Ophthalmologist & Nurse | 39,801 | 10.473 | 274,384 | |||
| 1.0 | 0.7 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,278 | 10.544 | 250,049 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,678 | 10.575 | 272,572 | |||
| (9) Ophthalmologist & Nurse | 39,798 | 10.473 | 274,387 | |||
| 1.0 | 0.8 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| 1.0 | 0.8 | (7) Ophthalmologist & OCT | 66,275 | 10.544 | 250,053 | |
| (8) Ophthalmologist & Ophthalmologist | 44,675 | 10.575 | 272,575 | |||
| (9) Ophthalmologist & Nurse | 39,795 | 10.473 | 274,390 | |||
| 1.0 | 0.9 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,272 | 10.544 | 250,056 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,672 | 10.575 | 272,578 | |||
| (9) Ophthalmologist & Nurse | 39,792 | 10.473 | 274,393 | |||
| 1.0 | 1.0 | (1) FFA & OCT | 66,249 | 10.544 | 250,079 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.473 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,821 | 10.544 | 243,493 | |||
| (5) OCT & Ophthalmologist | 47,971 | 10.574 | 269,244 | |||
| (6) OCT & Nurse | 42,237 | 10.472 | 271,910 | |||
| (7) Ophthalmologist & OCT | 66,269 | 10.544 | 250,059 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.575 | 272,581 | |||
| (9) Ophthalmologist & Nurse | 39,789 | 10.473 | 274,397 | |||
| Ophthalmologist diagnoses unclear results (%) | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,786 | 10.472 | 17 | –0.001 | –24,950 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,666 | 10.574 | 17 | –0.001 | –23,196 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,774 | 10.449 | 18,125 | –0.126 | –143,554 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.1 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.2 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,793 | 10.472 | 24 | –0.001 | –43,595 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,673 | 10.574 | 24 | –0.001 | –40,966 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,782 | 10.449 | 18,132 | –0.126 | –143,770 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.3 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,797 | 10.472 | 27 | 0.000 | –56,912 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,676 | 10.575 | 27 | –0.001 | –53,658 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,785 | 10.449 | 18,136 | –0.126 | –143,878 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.4 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,800 | 10.472 | 31 | 0.000 | –74,669 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,680 | 10.575 | 31 | 0.000 | –70,581 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,789 | 10.449 | 18,140 | –0.126 | –143,986 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.5 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,803 | 10.473 | 34 | 0.000 | –99,528 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,683 | 10.575 | 34 | 0.000 | –94,274 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,792 | 10.449 | 18,143 | –0.126 | –144,094 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated |
| OCT monitoring sensitivity | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.4 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 54,070 | 9.686 | 9421 | –0.889 | –10,596 | Dominated | |
| (7) Ophthalmologist & OCT | 54,090 | 9.686 | 9441 | –0.890 | –10,614 | Dominated | |
| (4) OCT & OCT | 58,742 | 9.681 | 14,093 | –0.894 | –15,761 | Dominated | |
| 0.5 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 56,826 | 9.915 | 12,177 | –0.661 | –18,436 | Dominated | |
| (7) Ophthalmologist & OCT | 56,846 | 9.914 | 12,197 | –0.661 | –18,453 | Dominated | |
| (4) OCT & OCT | 61,495 | 9.909 | 16,845 | –0.666 | –25,281 | Dominated | |
| 0.6 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 59,000 | 10.103 | 14,351 | –0.472 | –30,377 | Dominated | |
| (7) Ophthalmologist & OCT | 59,019 | 10.102 | 14,370 | –0.473 | –30,384 | Dominated | |
| (4) OCT & OCT | 63,666 | 10.096 | 19,017 | –0.479 | –39,707 | Dominated | |
| 0.7 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 60,740 | 10.259 | 16,090 | –0.316 | –50,949 | Dominated | |
| (7) Ophthalmologist & OCT | 60,759 | 10.259 | 16,110 | –0.316 | –50,918 | Dominated | |
| (4) OCT & OCT | 65,404 | 10.252 | 20,754 | –0.323 | –64,283 | Dominated | |
| 0.8 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,151 | 10.391 | 17,502 | –0.184 | –95,174 | Dominated | |
| (7) Ophthalmologist & OCT | 62,170 | 10.391 | 17,521 | –0.185 | –94,962 | Dominated | |
| (4) OCT & OCT | 66,814 | 10.384 | 22,165 | –0.191 | –115,799 | Dominated | |
| 0.9 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 63,312 | 10.503 | 18,663 | –0.072 | –260,619 | Dominated | |
| (7) Ophthalmologist & OCT | 63,331 | 10.503 | 18,682 | –0.072 | –258,561 | Dominated | |
| (4) OCT & OCT | 67,974 | 10.495 | 23,325 | –0.080 | –293,337 | Dominated | |
| 1.0 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2,482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 64,277 | 10.600 | 19,628 | 0.025 | 788,482 | ||
| (7) Ophthalmologist & OCT | 64,296 | 10.599 | 19 | –0.001 | –28,229 | Dominated | |
| (4) OCT & OCT | 68,939 | 10.592 | 4662 | –0.008 | –565,643 | Dominated |
| OCT monitoring specificity | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.3 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 74,212 | 10.459 | 29,563 | –0.116 | –255,643 | Dominated | |
| (7) Ophthalmologist & OCT | 74,230 | 10.459 | 29,581 | –0.116 | –254,397 | Dominated | |
| (4) OCT & OCT | 80,083 | 10.452 | 35,434 | –0.123 | –287,514 | Dominated | |
| 0.4 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 67,780 | 10.454 | 23,130 | –0.121 | –190,790 | Dominated | |
| (7) Ophthalmologist & OCT | 67,798 | 10.453 | 23,149 | –0.122 | –189,953 | Dominated | |
| (4) OCT & OCT | 72,979 | 10.446 | 28,330 | –0.129 | –219,784 | Dominated | |
| 0.5 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 61,521 | 10.448 | 16,872 | –0.127 | –133,240 | Dominated | |
| (7) Ophthalmologist & OCT | 61,540 | 10.448 | 16,891 | –0.127 | –132,734 | Dominated | |
| (4) OCT & OCT | 66,049 | 10.441 | 21,400 | –0.134 | –159,275 | Dominated | |
| 0.6 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 55,429 | 10.443 | 10,780 | –0.132 | –81,774 | Dominated | |
| (7) Ophthalmologist & OCT | 55,449 | 10.443 | 10,800 | –0.132 | –81,537 | Dominated | |
| (4) OCT & OCT | 59,286 | 10.435 | 14,636 | –0.140 | –104,824 | Dominated | |
| 0.7 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 49,498 | 10.438 | 4849 | –0.137 | –35,432 | Dominated | |
| (7) Ophthalmologist & OCT | 49,518 | 10.438 | 4869 | –0.137 | –35,418 | Dominated | |
| (4) OCT & OCT | 52,683 | 10.430 | 8033 | –0.145 | –55,508 | Dominated | |
| 0.8 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (1) FFA & OCT | 43,721 | 10.433 | 3952 | –0.040 | –99,944 | Dominated | |
| (7) Ophthalmologist & OCT | 43,742 | 10.433 | 3973 | –0.040 | –98,928 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (4) OCT & OCT | 46,234 | 10.425 | 1585 | –0.150 | –10,589 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| 0.9 | (1) FFA & OCT | 38,093 | 10.429 | ||||
| (7) Ophthalmologist & OCT | 38,114 | 10.428 | 21 | –0.001 | –34,221 | Dominated | |
| (3) FFA & Nurse | 39,769 | 10.473 | 1676 | 0.044 | 37,884 | ||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (4) OCT & OCT | 39,934 | 10.421 | 164 | –0.052 | –3,146 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| 1.0 | (1) FFA & OCT | 32,608 | 10.424 | ||||
| (7) Ophthalmologist & OCT | 32,629 | 10.423 | 21 | –0.001 | –35,125 | Dominated | |
| (4) OCT & OCT | 33,776 | 10.416 | 1168 | –0.008 | –144,031 | Dominated | |
| (3) FFA & Nurse | 39,769 | 10.473 | 7161 | 0.049 | 146,783 | ||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated |
| OCT monitoring | Strategy | Expected cost (£) | Expected QALYs | NMB (£) | Maximum NMB | |
|---|---|---|---|---|---|---|
| Sensitivity | Specificity | |||||
| 0.8 | 0.3 | (1) FFA & OCT | 73,512 | 10.4055 | 238,652 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 79,384 | 10.3981 | 232,558 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 73,531 | 10.4048 | 238,615 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.8 | 0.4 | (1) FFA & OCT | 67,127 | 10.3974 | 244,794 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 72,327 | 10.3899 | 239,370 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 67,146 | 10.3967 | 244,757 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.8 | 0.5 | (1) FFA & OCT | 60,925 | 10.3896 | 250,762 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 65,454 | 10.3821 | 246,008 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 60,944 | 10.3890 | 250,725 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.8 | 0.6 | (1) FFA & OCT | 54,899 | 10.3821 | 256,564 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 58,756 | 10.3745 | 252,480 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 54,918 | 10.3815 | 256,527 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.8 | 0.7 | (1) FFA & OCT | 49,041 | 10.3749 | 262,206 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 52,226 | 10.3672 | 258,791 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 49,061 | 10.3743 | 262,168 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.8 | 0.8 | (1) FFA & OCT | 43,344 | 10.3680 | 267,695 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 45,858 | 10.3602 | 264,949 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 43,365 | 10.3674 | 267,656 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.8 | 0.9 | (1) FFA & OCT | 37,803 | 10.3613 | 273,035 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 39,645 | 10.3535 | 270,960 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 37,824 | 10.3607 | 272,997 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.8 | 1.0 | (1) FFA & OCT | 32,411 | 10.3548 | 278,234 | ✓ |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | |||
| (4) OCT & OCT | 33,581 | 10.3469 | 276,828 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 32,432 | 10.3542 | 278,195 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.9 | 0.3 | (1) FFA & OCT | 74,844 | 10.5091 | 240,429 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 80,715 | 10.5013 | 234,324 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 74,862 | 10.5084 | 240,391 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.9 | 0.4 | (1) FFA & OCT | 68,371 | 10.5059 | 246,806 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 73,570 | 10.4980 | 241,371 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 68,389 | 10.5052 | 246,768 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.9 | 0.5 | (1) FFA & OCT | 62,063 | 10.5028 | 253,020 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 66,591 | 10.4949 | 248,255 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 62,082 | 10.5021 | 252,982 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.9 | 0.6 | (1) FFA & OCT | 55,915 | 10.4998 | 259,078 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 59,770 | 10.4918 | 254,982 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 55,934 | 10.4991 | 259,040 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.9 | 0.7 | (1) FFA & OCT | 49,920 | 10.4968 | 264,985 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 53,103 | 10.4887 | 261,559 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 49,939 | 10.4962 | 264,946 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.9 | 0.8 | (1) FFA & OCT | 44,072 | 10.4940 | 270,747 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 46,584 | 10.4858 | 267,990 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 44,093 | 10.4933 | 270,707 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.9 | 0.9 | (1) FFA & OCT | 38,367 | 10.4912 | 276,368 | ✓ |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | |||
| (4) OCT & OCT | 40,207 | 10.4829 | 274,282 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 38,388 | 10.4906 | 276,329 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.9 | 1.0 | (1) FFA & OCT | 32,800 | 10.4885 | 281,854 | ✓ |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | |||
| (4) OCT & OCT | 33,967 | 10.4801 | 280,438 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 32,821 | 10.4878 | 281,815 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.0 | 0.3 | (1) FFA & OCT | 75,937 | 10.5978 | 241,996 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 81,809 | 10.5897 | 235,882 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 75,955 | 10.5971 | 241,958 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.0 | 0.4 | (1) FFA & OCT | 69,399 | 10.5990 | 248,571 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 74,598 | 10.5908 | 243,126 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 69,417 | 10.5983 | 248,532 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.0 | 0.5 | (1) FFA & OCT | 63,011 | 10.6001 | 254,992 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 67,539 | 10.5919 | 250,217 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 63,030 | 10.5994 | 254,953 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.0 | 0.6 | (1) FFA & OCT | 56,770 | 10.6011 | 261,265 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 60,625 | 10.5928 | 257,159 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 56,789 | 10.6005 | 261,225 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.0 | 0.7 | (1) FFA & OCT | 50,669 | 10.6021 | 267,394 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 53,852 | 10.5937 | 263,958 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 50,689 | 10.6014 | 267,354 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.0 | 0.8 | (1) FFA & OCT | 44,705 | 10.6030 | 273,384 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 47,215 | 10.5945 | 270,619 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 44,725 | 10.6023 | 273,344 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.0 | 0.9 | (1) FFA & OCT | 38,872 | 10.6038 | 279,241 | ✓ |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | |||
| (4) OCT & OCT | 40,710 | 10.5952 | 277,145 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 38,893 | 10.6031 | 279,201 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 1.0 | 1.0 | (1) FFA & OCT | 33,167 | 10.6045 | 284,968 | ✓ |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | |||
| (4) OCT & OCT | 34,331 | 10.5958 | 283,543 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 33,188 | 10.6038 | 284,928 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| Ophthalmologist monitoring assessment sensitivity | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.1 | (3) FFA & Nurse | 35,469 | 8.830 | ||||
| (9) Ophthalmologist & Nurse | 35,491 | 8.830 | 22 | 0.000 | –121,961 | Dominated | |
| (2) FFA & Ophthalmologist | 35,931 | 8.920 | 462 | 0.089 | 5167 | ||
| (8) Ophthalmologist & Ophthalmologist | 35,953 | 8.920 | 22 | 0.000 | –108,940 | Dominated | |
| (6) OCT & Nurse | 37,324 | 8.828 | 1392 | –0.092 | –15,092 | Dominated | |
| (5) OCT & Ophthalmologist | 38,432 | 8.917 | 2501 | –0.003 | –810,442 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 26,828 | 1.530 | 17,539 | ||
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 19 | –0.001 | –30,303 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 4662 | –0.008 | –604,118 | Dominated | |
| 0.2 | (3) FFA & Nurse | 36,017 | 9.133 | ||||
| (9) Ophthalmologist & Nurse | 36,039 | 9.133 | 22 | 0.000 | –84,837 | Dominated | |
| (2) FFA & Ophthalmologist | 37,512 | 9.243 | 1495 | 0.109 | 13,708 | ||
| (8) Ophthalmologist & Ophthalmologist | 37,534 | 9.242 | 22 | 0.000 | –76,050 | Dominated | |
| (6) OCT & Nurse | 37,869 | 9.130 | 358 | –0.113 | –3,169 | Dominated | |
| (5) OCT & Ophthalmologist | 40,010 | 9.238 | 2498 | –0.004 | –609,285 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 25,247 | 1.207 | 20,919 | ||
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 19 | –0.001 | –30,303 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 4662 | –0.008 | –604,118 | Dominated | |
| 0.3 | (3) FFA & Nurse | 36,593 | 9.397 | ||||
| (9) Ophthalmologist & Nurse | 36,615 | 9.397 | 22 | 0.000 | –66,222 | Dominated | |
| (6) OCT & Nurse | 38,444 | 9.392 | 1851 | –0.005 | –402,106 | Dominated | |
| (2) FFA & Ophthalmologist | 38,913 | 9.517 | 2320 | 0.120 | 19,394 | ||
| (8) Ophthalmologist & Ophthalmologist | 38,934 | 9.516 | 21 | 0.000 | –59,673 | Dominated | |
| (5) OCT & Ophthalmologist | 41,408 | 9.512 | 2495 | –0.005 | –499,702 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 23,846 | 0.933 | 25,560 | ||
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 19 | –0.001 | –30,303 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 4662 | –0.008 | –604,118 | Dominated | |
| 0.4 | (3) FFA & Nurse | 37,161 | 9.625 | ||||
| (9) Ophthalmologist & Nurse | 37,183 | 9.625 | 21 | 0.000 | –55,221 | Dominated | |
| (6) OCT & Nurse | 39,010 | 9.620 | 1849 | –0.005 | –345,207 | Dominated | |
| (2) FFA & Ophthalmologist | 40,137 | 9.749 | 2976 | 0.124 | 24,018 | ||
| (8) Ophthalmologist & Ophthalmologist | 40,159 | 9.749 | 21 | 0.000 | –50,052 | Dominated | |
| (5) OCT & Ophthalmologist | 42,630 | 9.744 | 2492 | –0.006 | –432,284 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 22,621 | 0.700 | 32,314 | ||
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 19 | –0.001 | –30,303 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 4662 | –0.008 | –604,118 | Dominated | |
| 0.5 | (3) FFA & Nurse | 37,703 | 9.824 | ||||
| (9) Ophthalmologist & Nurse | 37,725 | 9.824 | 21 | 0.000 | –48,047 | Dominated | |
| (6) OCT & Nurse | 39,550 | 9.818 | 1847 | –0.006 | –306,735 | Dominated | |
| (2) FFA & Ophthalmologist | 41,202 | 9.948 | 3499 | 0.124 | 28,209 | ||
| (8) Ophthalmologist & Ophthalmologist | 41,223 | 9.948 | 21 | 0.000 | –43,812 | Dominated | |
| (5) OCT & Ophthalmologist | 43,692 | 9.942 | 2490 | –0.006 | –387,406 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 21,557 | 0.501 | 43,001 | ||
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 19 | –0.001 | –30,303 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 4662 | –0.008 | –604,118 | Dominated | |
| 0.6 | (3) FFA & Nurse | 38,211 | 9.997 | ||||
| (9) Ophthalmologist & Nurse | 38,232 | 9.997 | 21 | 0.000 | –43,049 | Dominated | |
| (6) OCT & Nurse | 40,055 | 9.991 | 1845 | –0.007 | –279,334 | Dominated | |
| (2) FFA & Ophthalmologist | 42,128 | 10.119 | 3917 | 0.121 | 32,250 | ||
| (8) Ophthalmologist & Ophthalmologist | 42,148 | 10.118 | 21 | –0.001 | –39,488 | Dominated | |
| (5) OCT & Ophthalmologist | 44,615 | 10.112 | 2488 | –0.007 | –355,836 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 20,631 | 0.331 | 62,364 | ||
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 19 | –0.001 | –30,303 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 4662 | –0.008 | –604,118 | Dominated | |
| 0.7 | (3) FFA & Nurse | 38,680 | 10.149 | ||||
| (9) Ophthalmologist & Nurse | 38,701 | 10.148 | 21 | –0.001 | –39,397 | Dominated | |
| (6) OCT & Nurse | 40,523 | 10.141 | 1843 | –0.007 | –259,036 | Dominated | |
| (2) FFA & Ophthalmologist | 42,934 | 10.266 | 4254 | 0.117 | 36,287 | ||
| (8) Ophthalmologist & Ophthalmologist | 42,955 | 10.265 | 21 | –0.001 | –36,346 | Dominated | |
| (5) OCT & Ophthalmologist | 45,420 | 10.258 | 2486 | –0.007 | –332,704 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 19,825 | 0.184 | 107,925 | ||
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 19 | –0.001 | –30,303 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 4662 | –0.008 | –604,118 | Dominated | |
| 0.8 | (3) FFA & Nurse | 39,113 | 10.281 | ||||
| (9) Ophthalmologist & Nurse | 39,134 | 10.281 | 21 | –0.001 | –36,631 | Dominated | |
| (6) OCT & Nurse | 40,954 | 10.274 | 1841 | –0.008 | –243,534 | Dominated | |
| (2) FFA & Ophthalmologist | 43,639 | 10.394 | 4526 | 0.112 | 40,409 | ||
| (1) FFA & OCT | 62,759 | 10.449 | 19,119 | 0.056 | 341,760 | ||
| (8) Ophthalmologist & Ophthalmologist | 43,660 | 10.393 | 20 | –0.001 | –33,978 | Dominated | |
| (5) OCT & Ophthalmologist | 46,124 | 10.386 | 2484 | –0.008 | –315,219 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 19 | –0.001 | –30,303 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 4662 | –0.008 | –604,118 | Dominated | |
| 0.9 | (3) FFA & Nurse | 39,511 | 10.399 | ||||
| (9) Ophthalmologist & Nurse | 39,531 | 10.398 | 21 | –0.001 | –34,477 | Dominated | |
| (6) OCT & Nurse | 41,350 | 10.391 | 1839 | –0.008 | –231,400 | Dominated | |
| (2) FFA & Ophthalmologist | 44,259 | 10.505 | 4749 | 0.106 | 44,674 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,280 | 10.504 | 20 | –0.001 | –32,144 | Dominated | |
| (5) OCT & Ophthalmologist | 46,742 | 10.497 | 2483 | –0.008 | –301,676 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,500 | –0.056 | –332,463 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,519 | –0.056 | –329,091 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 23,162 | –0.063 | –365,551 | Dominated | |
| 1.0 | (3) FFA & Nurse | 39,875 | 10.503 | ||||
| (9) Ophthalmologist & Nurse | 39,896 | 10.502 | 21 | –0.001 | –32,760 | Dominated | |
| (6) OCT & Nurse | 41,713 | 10.494 | 1838 | –0.008 | –221,712 | Dominated | |
| (2) FFA & Ophthalmologist | 44,806 | 10.603 | 4931 | 0.100 | 49,125 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,827 | 10.602 | 20 | –0.001 | –30,691 | Dominated | |
| (5) OCT & Ophthalmologist | 47,288 | 10.595 | 2481 | –0.009 | –290,979 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 17,953 | –0.154 | –116,811 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 17,972 | –0.154 | –116,459 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,615 | –0.161 | –140,112 | Dominated |
| Ophthalmologist monitoring assessment specificity | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.1 | (3) FFA & Nurse | 56,447 | 10.483 | ||||
| (9) Ophthalmologist & Nurse | 56,467 | 10.482 | 19 | –0.001 | –30,720 | Dominated | |
| (6) OCT & Nurse | 60,233 | 10.475 | 3786 | –0.008 | –475,573 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 6312 | –0.033 | –189,611 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 6331 | –0.034 | –186,661 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 10,974 | –0.041 | –267,627 | Dominated | |
| (2) FFA & Ophthalmologist | 84,302 | 10.575 | 27,854 | 0.092 | 301,922 | ||
| (8) Ophthalmologist & Ophthalmologist | 84,319 | 10.574 | 18 | –0.001 | –26,020 | Dominated | |
| (5) OCT & Ophthalmologist | 91,018 | 10.567 | 6716 | –0.008 | –845,509 | Dominated | |
| 0.2 | (3) FFA & Nurse | 53,989 | 10.481 | ||||
| (9) Ophthalmologist & Nurse | 54,009 | 10.481 | 20 | –0.001 | –31,085 | Dominated | |
| (6) OCT & Nurse | 57,497 | 10.473 | 3508 | –0.008 | –438,888 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 8770 | –0.032 | –275,574 | Dominated | |
| 0.2 | (7) Ophthalmologist & OCT | 62,778 | 10.449 | 8789 | –0.032 | –270,828 | Dominated |
| (4) OCT & OCT | 67,421 | 10.442 | 13,432 | –0.040 | –339,701 | Dominated | |
| (2) FFA & Ophthalmologist | 78,264 | 10.575 | 24,275 | 0.094 | 258,685 | ||
| (8) Ophthalmologist & Ophthalmologist | 78,282 | 10.574 | 18 | –0.001 | –26,767 | Dominated | |
| (5) OCT & Ophthalmologist | 84,376 | 10.567 | 6112 | –0.008 | –763,048 | Dominated | |
| 0.3 | (3) FFA & Nurse | 51,557 | 10.480 | ||||
| (9) Ophthalmologist & Nurse | 51,577 | 10.479 | 20 | –0.001 | –31,448 | Dominated | |
| (6) OCT & Nurse | 54,787 | 10.472 | 3230 | –0.008 | –402,465 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 11,202 | –0.030 | –368,763 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 11,221 | –0.031 | –361,908 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 15,864 | –0.038 | –416,445 | Dominated | |
| (2) FFA & Ophthalmologist | 72,358 | 10.575 | 20,801 | 0.095 | 218,127 | ||
| (8) Ophthalmologist & Ophthalmologist | 72,377 | 10.575 | 18 | –0.001 | –27,506 | Dominated | |
| (5) OCT & Ophthalmologist | 77,865 | 10.567 | 5507 | –0.008 | –681,762 | Dominated | |
| 0.4 | (3) FFA & Nurse | 49,150 | 10.478 | ||||
| (9) Ophthalmologist & Nurse | 49,170 | 10.478 | 20 | –0.001 | –31,809 | Dominated | |
| (6) OCT & Nurse | 52,102 | 10.470 | 2951 | –0.008 | –366,309 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 13,609 | –0.029 | –470,106 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 13,628 | –0.030 | –460,768 | Dominated | |
| (2) FFA & Ophthalmologist | 66,579 | 10.575 | 17,428 | 0.097 | 179,997 | ||
| (8) Ophthalmologist & Ophthalmologist | 66,597 | 10.575 | 19 | –0.001 | –28,239 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 843 | –0.133 | –6313 | Dominated | |
| (5) OCT & Ophthalmologist | 71,481 | 10.567 | 4902 | –0.008 | –601,684 | Dominated | |
| 0.5 | (3) FFA & Nurse | 46,769 | 10.477 | ||||
| (9) Ophthalmologist & Nurse | 46,789 | 10.476 | 20 | –0.001 | –32,169 | Dominated | |
| (6) OCT & Nurse | 49,442 | 10.469 | 2673 | –0.008 | –330,421 | Dominated | |
| (2) FFA & Ophthalmologist | 60,922 | 10.575 | 14,153 | 0.098 | 144,077 | ||
| (8) Ophthalmologist & Ophthalmologist | 60,941 | 10.575 | 19 | –0.001 | –28,964 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 1837 | –0.126 | –14,607 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 1856 | –0.126 | –14,685 | Dominated | |
| (5) OCT & Ophthalmologist | 65,219 | 10.567 | 4297 | –0.008 | –522,843 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 6500 | –0.133 | –48,691 | Dominated | |
| 0.6 | (3) FFA & Nurse | 44,411 | 10.476 | ||||
| (9) Ophthalmologist & Nurse | 44,432 | 10.475 | 20 | –0.001 | –32,527 | Dominated | |
| (6) OCT & Nurse | 46,806 | 10.467 | 2395 | –0.008 | –294,806 | Dominated | |
| (2) FFA & Ophthalmologist | 55,384 | 10.575 | 10,972 | 0.100 | 110,175 | ||
| (8) Ophthalmologist & Ophthalmologist | 55,403 | 10.575 | 19 | –0.001 | –29,681 | Dominated | |
| (5) OCT & Ophthalmologist | 59,076 | 10.567 | 3692 | –0.008 | –445,261 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 7375 | –0.126 | –58,658 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 7394 | –0.126 | –58,517 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 12,038 | –0.133 | –90,204 | Dominated | |
| 0.7 | (3) FFA & Nurse | 42,078 | 10.474 | ||||
| (9) Ophthalmologist & Nurse | 42,099 | 10.474 | 20 | –0.001 | –32,882 | Dominated | |
| (6) OCT & Nurse | 44,195 | 10.466 | 2116 | –0.008 | –259,466 | Dominated | |
| (2) FFA & Ophthalmologist | 49,961 | 10.575 | 7882 | 0.101 | 78,122 | ||
| (8) Ophthalmologist & Ophthalmologist | 49,981 | 10.574 | 20 | –0.001 | –30,391 | Dominated | |
| (5) OCT & Ophthalmologist | 53,048 | 10.567 | 3087 | –0.008 | –368,955 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 12,798 | –0.126 | –101,847 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 12,817 | –0.126 | –101,491 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 17,461 | –0.133 | –130,910 | Dominated | |
| 0.8 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.9 | (3) FFA & Nurse | 37,483 | 10.472 | ||||
| (9) Ophthalmologist & Nurse | 37,504 | 10.471 | 21 | –0.001 | –33,589 | Dominated | |
| (6) OCT & Nurse | 39,043 | 10.463 | 1560 | –0.008 | –189,620 | Dominated | |
| (2) FFA & Ophthalmologist | 39,446 | 10.575 | 1962 | 0.103 | 18,981 | ||
| (8) Ophthalmologist & Ophthalmologist | 39,466 | 10.574 | 21 | –0.001 | –31,789 | Dominated | |
| (5) OCT & Ophthalmologist | 41,322 | 10.566 | 1877 | –0.009 | –220,218 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 23,313 | –0.125 | –185,856 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 23,332 | –0.126 | –185,082 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 27,976 | –0.133 | –210,099 | Dominated | |
| 1.0 | (2) FFA & Ophthalmologist | 34,347 | 10.575 | ||||
| (8) Ophthalmologist & Ophthalmologist | 34,368 | 10.574 | 21 | –0.001 | –32,476 | Dominated | |
| (3) FFA & Nurse | 35,221 | 10.470 | 874 | –0.105 | –8357 | Dominated | |
| (9) Ophthalmologist & Nurse | 35,242 | 10.470 | 895 | –0.105 | –8507 | Dominated | |
| (5) OCT & Ophthalmologist | 35,618 | 10.566 | 1271 | –0.009 | –147,799 | Dominated | |
| (6) OCT & Nurse | 36,502 | 10.462 | 2155 | –0.113 | –19,102 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 28,412 | –0.125 | –226,777 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 28,431 | –0.126 | –225,797 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 33,074 | –0.133 | –248,673 | Dominated |
| Ophthalmologist monitoring | Strategy | Expected cost (£) | Expected QALYs | NMB (£) | Maximum NMB | |
|---|---|---|---|---|---|---|
| Sensitivity | Specificity | |||||
| 0.8 | 0.5 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 59,393 | 10.4103 | 252,918 | |||
| (3) FFA & Nurse | 45,800 | 10.2925 | 262,976 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 63,691 | 10.4027 | 248,389 | |||
| (6) OCT & Nurse | 48,475 | 10.2850 | 260,076 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 59,412 | 10.4097 | 252,880 | |||
| (9) Ophthalmologist & Nurse | 45,820 | 10.2919 | 262,938 | |||
| 0.8 | 0.6 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 54,012 | 10.4045 | 258,125 | |||
| (3) FFA & Nurse | 43,544 | 10.2888 | 265,120 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 57,705 | 10.3968 | 254,199 | |||
| (6) OCT & Nurse | 45,941 | 10.2813 | 262,498 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 54,031 | 10.4039 | 258,087 | |||
| (9) Ophthalmologist & Nurse | 43,564 | 10.2882 | 265,082 | |||
| 0.8 | 0.7 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 48,762 | 10.3989 | 263,206 | |||
| (3) FFA & Nurse | 41,315 | 10.2851 | 267,238 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 51,851 | 10.3911 | 259,883 | |||
| (6) OCT & Nurse | 43,434 | 10.2776 | 264,893 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 48,782 | 10.3983 | 263,168 | |||
| (9) Ophthalmologist & Nurse | 41,336 | 10.2845 | 267,200 | |||
| 0.8 | 0.8 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 43,639 | 10.3935 | 268,166 | |||
| (3) FFA & Nurse | 39,113 | 10.2815 | 269,331 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 46,124 | 10.3856 | 265,445 | |||
| (6) OCT & Nurse | 40,954 | 10.2739 | 267,264 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 43,660 | 10.3929 | 268,127 | |||
| (9) Ophthalmologist & Nurse | 39,134 | 10.2809 | 269,294 | |||
| 0.8 | 0.9 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 38,639 | 10.3882 | 273,008 | ✓ | ||
| (3) FFA & Nurse | 36,938 | 10.2779 | 271,400 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 40,519 | 10.3803 | 270,890 | |||
| (6) OCT & Nurse | 38,500 | 10.2703 | 269,610 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 38,660 | 10.3876 | 272,969 | |||
| (9) Ophthalmologist & Nurse | 36,959 | 10.2774 | 271,362 | |||
| 0.8 | 1.0 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 33,758 | 10.3831 | 277,736 | ✓ | ||
| (3) FFA & Nurse | 34,788 | 10.2744 | 273,445 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 35,032 | 10.3751 | 276,221 | |||
| (6) OCT & Nurse | 36,072 | 10.2668 | 271,932 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 33,779 | 10.3825 | 277,697 | |||
| (9) Ophthalmologist & Nurse | 34,809 | 10.2739 | 273,407 | |||
| 0.9 | 0.5 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 60,343 | 10.5119 | 255,013 | |||
| (3) FFA & Nurse | 46,394 | 10.4057 | 265,776 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 64,640 | 10.5039 | 250,476 | |||
| (6) OCT & Nurse | 49,068 | 10.3978 | 262,867 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 60,362 | 10.5112 | 254,975 | |||
| (9) Ophthalmologist & Nurse | 46,414 | 10.4051 | 265,738 | |||
| 0.9 | 0.6 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 54,861 | 10.5096 | 260,425 | |||
| (3) FFA & Nurse | 44,074 | 10.4034 | 268,026 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 58,554 | 10.5015 | 256,490 | |||
| (6) OCT & Nurse | 46,470 | 10.3955 | 265,394 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 54,881 | 10.5089 | 260,387 | |||
| (9) Ophthalmologist & Nurse | 44,095 | 10.4028 | 267,988 | |||
| 0.9 | 0.7 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 49,502 | 10.5073 | 265,717 | |||
| (3) FFA & Nurse | 41,780 | 10.4011 | 270,252 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 52,589 | 10.4991 | 262,385 | |||
| (6) OCT & Nurse | 43,897 | 10.3931 | 267,897 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 49,522 | 10.5067 | 265,678 | |||
| (9) Ophthalmologist & Nurse | 41,800 | 10.4005 | 270,213 | |||
| 0.9 | 0.8 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,259 | 10.5051 | 270,893 | |||
| (3) FFA & Nurse | 39,511 | 10.3988 | 272,453 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 46,742 | 10.4969 | 268,164 | |||
| (6) OCT & Nurse | 41,350 | 10.3908 | 270,376 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,280 | 10.5045 | 270,854 | |||
| (9) Ophthalmologist & Nurse | 39,531 | 10.3982 | 272,415 | |||
| 0.9 | 0.9 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 39,130 | 10.5029 | 275,957 | ✓ | ||
| (3) FFA & Nurse | 37,266 | 10.3966 | 274,631 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 41,008 | 10.4946 | 273,831 | |||
| (6) OCT & Nurse | 38,827 | 10.3886 | 272,831 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 39,151 | 10.5023 | 275,918 | |||
| (9) Ophthalmologist & Nurse | 37,287 | 10.3960 | 274,592 | |||
| 0.9 | 1.0 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 34,111 | 10.5008 | 280,913 | ✓ | ||
| (3) FFA & Nurse | 35,045 | 10.3944 | 276,786 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 35,384 | 10.4924 | 279,389 | |||
| (6) OCT & Nurse | 36,328 | 10.3863 | 275,263 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 34,132 | 10.5002 | 280,873 | |||
| (9) Ophthalmologist & Nurse | 35,066 | 10.3938 | 276,747 | |||
| 1.0 | 0.5 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 61,151 | 10.6006 | 256,868 | |||
| (3) FFA & Nurse | 46,920 | 10.5057 | 268,253 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 65,449 | 10.5923 | 252,322 | |||
| (6) OCT & Nurse | 49,592 | 10.4976 | 265,334 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 61,170 | 10.6000 | 256,829 | |||
| (9) Ophthalmologist & Nurse | 46,940 | 10.5051 | 268,214 | |||
| 1.0 | 0.6 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 55,592 | 10.6015 | 262,455 | |||
| (3) FFA & Nurse | 44,548 | 10.5047 | 270,594 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 59,284 | 10.5932 | 258,511 | |||
| (6) OCT & Nurse | 46,942 | 10.4965 | 267,953 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 55,611 | 10.6009 | 262,415 | |||
| (9) Ophthalmologist & Nurse | 44,568 | 10.5041 | 270,555 | |||
| 1.0 | 0.7 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 50,144 | 10.6024 | 267,927 | |||
| (3) FFA & Nurse | 42,200 | 10.5037 | 272,912 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 53,231 | 10.5939 | 264,586 | |||
| (6) OCT & Nurse | 44,316 | 10.4955 | 270,549 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 50,164 | 10.6017 | 267,887 | |||
| (9) Ophthalmologist & Nurse | 42,220 | 10.5031 | 272,873 | |||
| 1.0 | 0.8 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,806 | 10.6031 | 273,288 | |||
| (3) FFA & Nurse | 39,875 | 10.5028 | 275,207 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,288 | 10.5946 | 270,550 | |||
| (6) OCT & Nurse | 41,713 | 10.4945 | 273,121 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,827 | 10.6025 | 273,248 | |||
| (9) Ophthalmologist & Nurse | 39,896 | 10.5021 | 275,168 | |||
| 1.0 | 0.9 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 39,574 | 10.6038 | 278,541 | ✓ | ||
| (3) FFA & Nurse | 37,574 | 10.5018 | 277,480 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 41,450 | 10.5952 | 276,407 | |||
| (6) OCT & Nurse | 39,133 | 10.4935 | 275,671 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 39,595 | 10.6032 | 278,501 | |||
| (9) Ophthalmologist & Nurse | 37,594 | 10.5012 | 277,440 | |||
| 1.0 | 1.0 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 34,445 | 10.6045 | 283,690 | ✓ | ||
| (3) FFA & Nurse | 35,295 | 10.5008 | 279,730 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 35,716 | 10.5958 | 282,159 | |||
| (6) OCT & Nurse | 36,576 | 10.4925 | 278,198 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 34,466 | 10.6038 | 283,650 | |||
| (9) Ophthalmologist & Nurse | 35,316 | 10.5002 | 279,690 | |||
| Ophthalmologist monitoring assessment unclear results (%) | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0 | (3) FFA & Nurse | 39,548 | 10.470 | ||||
| (9) Ophthalmologist & Nurse | 39,569 | 10.469 | 21 | –0.001 | –33,315 | Dominated | |
| (6) OCT & Nurse | 41,400 | 10.462 | 1852 | –0.008 | –226,583 | Dominated | |
| (2) FFA & Ophthalmologist | 44,524 | 10.572 | 4976 | 0.102 | 48,739 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,544 | 10.571 | 20 | –0.001 | –31,134 | Dominated | |
| (5) OCT & Ophthalmologist | 47,035 | 10.563 | 2511 | –0.008 | –298,363 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,235 | –0.122 | –148,955 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,254 | –0.123 | –148,350 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,897 | –0.130 | –175,949 | Dominated | |
| 0.1 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.2 | (3) FFA & Nurse | 39,991 | 10.476 | ||||
| (9) Ophthalmologist & Nurse | 40,012 | 10.475 | 21 | –0.001 | –33,159 | Dominated | |
| (6) OCT & Nurse | 41,815 | 10.468 | 1824 | –0.008 | –222,233 | Dominated | |
| (2) FFA & Ophthalmologist | 44,778 | 10.578 | 4787 | 0.102 | 46,820 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,798 | 10.578 | 20 | –0.001 | –31,053 | Dominated | |
| (5) OCT & Ophthalmologist | 47,231 | 10.570 | 2453 | –0.008 | –289,539 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 17,981 | –0.129 | –139,671 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,000 | –0.129 | –139,140 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,643 | –0.136 | –165,940 | Dominated | |
| 0.3 | (3) FFA & Nurse | 40,214 | 10.479 | ||||
| (9) Ophthalmologist & Nurse | 40,234 | 10.478 | 21 | –0.001 | –33,081 | Dominated | |
| (6) OCT & Nurse | 42,024 | 10.471 | 1811 | –0.008 | –220,072 | Dominated | |
| (2) FFA & Ophthalmologist | 44,911 | 10.581 | 4698 | 0.102 | 45,894 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,931 | 10.581 | 20 | –0.001 | –31,011 | Dominated | |
| (5) OCT & Ophthalmologist | 47,335 | 10.573 | 2423 | –0.009 | –285,164 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 17,848 | –0.132 | –135,275 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 17,867 | –0.133 | –134,778 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,510 | –0.140 | –161,186 | Dominated | |
| 0.4 | 3) FFA & Nurse | 40,437 | 10.482 | ||||
| 9) Ophthalmologist & Nurse | 40,458 | 10.482 | 20 | –0.001 | –33,003 | Dominated | |
| 6) OCT & Nurse | 42,234 | 10.474 | 1797 | –0.008 | –217,921 | Dominated | |
| 2) FFA & Ophthalmologist | 45,048 | 10.585 | 4611 | 0.102 | 44,991 | ||
| 8) Ophthalmologist & Ophthalmologist | 45,068 | 10.584 | 20 | –0.001 | –30,969 | Dominated | |
| 5) OCT & Ophthalmologist | 47,443 | 10.576 | 2394 | –0.009 | –280,815 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 17,711 | –0.135 | –131,033 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 17,730 | –0.136 | –130,567 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,373 | –0.143 | –156,587 | Dominated | |
| 0.5 | (3) FFA & Nurse | 40,661 | 10.485 | ||||
| (9) Ophthalmologist & Nurse | 40,682 | 10.485 | 20 | –0.001 | –32,926 | Dominated | |
| (6) OCT & Nurse | 42,445 | 10.477 | 1784 | –0.008 | –215,780 | Dominated | |
| (2) FFA & Ophthalmologist | 45,189 | 10.588 | 4528 | 0.103 | 44,111 | ||
| (8) Ophthalmologist & Ophthalmologist | 45,209 | 10.587 | 20 | –0.001 | –30,925 | Dominated | |
| (5) OCT & Ophthalmologist | 47,554 | 10.579 | 2365 | –0.009 | –276,491 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 17,570 | –0.138 | –126,936 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 17,589 | –0.139 | –126,500 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,233 | –0.146 | –152,138 | Dominated |
| Nurse monitoring assessment sensitivity | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.1 | (3) FFA & Nurse | 32,207 | 8.877 | ||||
| (9) Ophthalmologist & Nurse | 32,229 | 8.877 | 22 | 0.000 | –116,739 | Dominated | |
| (6) OCT & Nurse | 34,065 | 8.874 | 1859 | –0.003 | –623,825 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 12,443 | 1.698 | 7329 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.2 | (3) FFA & Nurse | 33,490 | 9.193 | ||||
| (9) Ophthalmologist & Nurse | 33,512 | 9.193 | 22 | 0.000 | –81,140 | Dominated | |
| (6) OCT & Nurse | 35,346 | 9.189 | 1856 | –0.004 | –469,932 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 11,159 | 1.382 | 8077 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.3 | (3) FFA & Nurse | 34,692 | 9.465 | ||||
| (9) Ophthalmologist & Nurse | 34,714 | 9.465 | 22 | 0.000 | –63,348 | Dominated | |
| (6) OCT & Nurse | 36,545 | 9.460 | 1853 | –0.005 | –383,994 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 9957 | 1.110 | 8973 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.4 | (3) FFA & Nurse | 35,788 | 9.699 | ||||
| (9) Ophthalmologist & Nurse | 35,809 | 9.699 | 22 | 0.000 | –52,864 | Dominated | |
| (6) OCT & Nurse | 37,638 | 9.693 | 1850 | –0.006 | –330,369 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 8862 | 0.876 | 10,115 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.5 | (3) FFA & Nurse | 36,773 | 9.900 | ||||
| (9) Ophthalmologist & Nurse | 36,794 | 9.900 | 21 | 0.000 | –46,047 | Dominated | |
| (6) OCT & Nurse | 38,620 | 9.894 | 1847 | –0.006 | –294,327 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 7876 | 0.675 | 11,672 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.6 | (3) FFA & Nurse | 37,654 | 10.074 | ||||
| (9) Ophthalmologist & Nurse | 37,675 | 10.074 | 21 | –0.001 | –41,312 | Dominated | |
| (6) OCT & Nurse | 39,499 | 10.067 | 1845 | –0.007 | –268,779 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 6995 | 0.501 | 13,967 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.7 | (3) FFA & Nurse | 38,440 | 10.225 | ||||
| (9) Ophthalmologist & Nurse | 38,461 | 10.225 | 21 | –0.001 | –37,863 | Dominated | |
| (6) OCT & Nurse | 40,282 | 10.218 | 1842 | –0.007 | –249,932 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 6209 | 0.350 | 17,753 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.8 | (3) FFA & Nurse | 39,142 | 10.357 | ||||
| (9) Ophthalmologist & Nurse | 39,162 | 10.357 | 21 | –0.001 | –35,259 | Dominated | |
| (6) OCT & Nurse | 40,982 | 10.349 | 1840 | –0.008 | –235,590 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 5507 | 0.218 | 25,280 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.9 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 1.0 | (3) FFA & Nurse | 40,332 | 10.575 | ||||
| (9) Ophthalmologist & Nurse | 40,352 | 10.574 | 20 | –0.001 | –31,631 | Dominated | |
| (6) OCT & Nurse | 42,168 | 10.566 | 1836 | –0.009 | –215,499 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4318 | 0.000 | 31,416,455 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated |
| Nurse monitoring assessment specificity | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0.1 | (2) FFA & Ophthalmologist | 44,649 | 10.575 | ||||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (3) FFA & Nurse | 47,769 | 10.476 | 3120 | –0.099 | –31,362 | Dominated | |
| (9) Ophthalmologist & Nurse | 47,789 | 10.475 | 3140 | –0.100 | –31,367 | Dominated | |
| (6) OCT & Nurse | 50,523 | 10.467 | 5874 | –0.108 | –54,589 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.2 | (2) FFA & Ophthalmologist | 44,649 | 10.575 | ||||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (3) FFA & Nurse | 46,156 | 10.475 | 1507 | –0.100 | –15,067 | Dominated | |
| (9) Ophthalmologist & Nurse | 46,176 | 10.474 | 1527 | –0.101 | –15,174 | Dominated | |
| 0.2 | (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated |
| (6) OCT & Nurse | 48,727 | 10.467 | 4078 | –0.108 | –37,703 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.3 | (3) FFA & Nurse | 44,550 | 10.474 | ||||
| (9) Ophthalmologist & Nurse | 44,570 | 10.474 | 20 | –0.001 | –32,581 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 99 | 0.101 | 988 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (6) OCT & Nurse | 46,938 | 10.466 | 2288 | –0.109 | –21,050 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.4 | (3) FFA & Nurse | 42,950 | 10.474 | ||||
| (9) Ophthalmologist & Nurse | 42,970 | 10.473 | 20 | –0.001 | –32,800 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 1699 | 0.101 | 16,809 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (6) OCT & Nurse | 45,154 | 10.466 | 505 | –0.109 | –4624 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.5 | (3) FFA & Nurse | 41,356 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 41,377 | 10.473 | 20 | –0.001 | –33,019 | Dominated | |
| (6) OCT & Nurse | 43,378 | 10.465 | 2021 | –0.008 | –247,178 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 3293 | 0.102 | 32,401 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.6 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.7 | (3) FFA & Nurse | 38,188 | 10.472 | ||||
| (9) Ophthalmologist & Nurse | 38,209 | 10.472 | 21 | –0.001 | –33,454 | Dominated | |
| (6) OCT & Nurse | 39,843 | 10.464 | 1655 | –0.008 | –201,701 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 6461 | 0.103 | 62,917 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.8 | (3) FFA & Nurse | 36,614 | 10.472 | ||||
| (9) Ophthalmologist & Nurse | 36,635 | 10.471 | 21 | –0.001 | –33,672 | Dominated | |
| (6) OCT & Nurse | 38,085 | 10.464 | 1472 | –0.008 | –179,071 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 8035 | 0.103 | 77,851 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.9 | (3) FFA & Nurse | 35,046 | 10.471 | ||||
| (9) Ophthalmologist & Nurse | 35,066 | 10.471 | 21 | –0.001 | –33,888 | Dominated | |
| (6) OCT & Nurse | 36,334 | 10.463 | 1288 | –0.008 | –156,514 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 9604 | 0.104 | 92,575 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 1.0 | (3) FFA & Nurse | 33,484 | 10.471 | ||||
| (9) Ophthalmologist & Nurse | 33,505 | 10.470 | 21 | –0.001 | –34,105 | Dominated | |
| (6) OCT & Nurse | 34,589 | 10.463 | 1105 | –0.008 | –134,030 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 11,166 | 0.104 | 107,095 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated |
| Nurse monitoring | Strategy | Expected cost (£) | Expected QALYs | NMB (£) | Maximum NMB | |
|---|---|---|---|---|---|---|
| Sensitivity | Specificity | |||||
| 0.6 | 0.4 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 40,503 | 10.0787 | 261,857 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 42,714 | 10.0718 | 259,441 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 40,524 | 10.0782 | 261,821 | |||
| 0.6 | 0.5 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 39,074 | 10.0764 | 263,218 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,102 | 10.0696 | 260,985 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,095 | 10.0759 | 263,182 | |||
| 0.6 | 0.6 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 37,654 | 10.0742 | 264,571 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 39,499 | 10.0673 | 262,521 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 37,675 | 10.0737 | 264,535 | |||
| 0.6 | 0.7 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 36,242 | 10.0720 | 265,917 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 37,903 | 10.0651 | 264,049 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 36,263 | 10.0714 | 265,881 | |||
| 0.6 | 0.8 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 34,837 | 10.0698 | 267,256 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 36,316 | 10.0629 | 265,571 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 34,858 | 10.0692 | 267,219 | |||
| 0.6 | 0.9 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 33,440 | 10.0676 | 268,587 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 34,736 | 10.0607 | 267,084 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 33,462 | 10.0671 | 268,550 | |||
| 0.6 | 1.0 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 32,051 | 10.0654 | 269,911 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 33,163 | 10.0585 | 268,591 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 32,073 | 10.0649 | 269,874 | |||
| 0.7 | 0.4 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 41,424 | 10.2286 | 265,433 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 43,633 | 10.2212 | 263,004 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 41,445 | 10.2280 | 265,396 | |||
| 0.6 | 0.5 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 39,928 | 10.2269 | 266,879 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,954 | 10.2196 | 264,633 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,949 | 10.2264 | 266,842 | |||
| 0.6 | 0.6 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 38,440 | 10.2253 | 268,318 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 40,282 | 10.2179 | 266,255 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 38,461 | 10.2247 | 268,280 | |||
| 0.6 | 0.7 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 36,959 | 10.2236 | 269,750 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 38,618 | 10.2163 | 267,869 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 36,980 | 10.2231 | 269,712 | |||
| 0.6 | 0.8 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 35,485 | 10.2220 | 271,175 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 36,961 | 10.2146 | 269,477 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 35,507 | 10.2215 | 271,137 | |||
| 0.6 | 0.9 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 34,019 | 10.2204 | 272,593 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 35,312 | 10.2130 | 271,078 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 34,040 | 10.2198 | 272,555 | |||
| 0.6 | 1.0 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 32,560 | 10.2188 | 274,004 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 33,669 | 10.2114 | 272,672 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 32,581 | 10.2182 | 273,966 | |||
| 0.8 | 0.4 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 42,235 | 10.3593 | 268,545 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 44,441 | 10.3515 | 266,105 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 42,255 | 10.3587 | 268,506 | |||
| 0.8 | 0.5 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 40,685 | 10.3582 | 270,062 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 42,708 | 10.3504 | 267,805 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 40,705 | 10.3576 | 270,024 | |||
| 0.8 | 0.6 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 39,142 | 10.3571 | 271,573 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 40,982 | 10.3493 | 269,498 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,162 | 10.3566 | 271,534 | |||
| 0.8 | 0.7 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 37,606 | 10.3561 | 273,077 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 39,263 | 10.3483 | 271,185 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 37,626 | 10.3555 | 273,038 | |||
| 0.8 | 0.8 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 36,076 | 10.3550 | 274,574 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 37,550 | 10.3472 | 272,866 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 36,097 | 10.3544 | 274,536 | |||
| 0.8 | 0.9 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 34,554 | 10.3540 | 276,065 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 35,844 | 10.3461 | 274,539 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 34,575 | 10.3534 | 276,027 | |||
| 0.8 | 1.0 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 33,038 | 10.3529 | 277,550 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 34,145 | 10.3451 | 276,207 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 33,059 | 10.3523 | 277,511 | |||
| 0.9 | 0.4 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | ✓ | ||
| (3) FFA & Nurse | 42,950 | 10.4739 | 271,267 | |||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 45,154 | 10.4657 | 268,818 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 42,970 | 10.4733 | 271,229 | |||
| 0.9 | 0.5 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 41,356 | 10.4734 | 272,845 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 43,378 | 10.4652 | 270,578 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 41,377 | 10.4728 | 272,806 | |||
| 0.9 | 0.6 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 39,769 | 10.4728 | 274,416 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 41,607 | 10.4647 | 272,332 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 39,790 | 10.4722 | 274,377 | |||
| 0.9 | 0.7 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 38,188 | 10.4723 | 275,981 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 39,843 | 10.4641 | 274,080 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 38,209 | 10.4717 | 275,942 | |||
| 0.9 | 0.8 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 36,614 | 10.4718 | 277,540 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 38,085 | 10.4636 | 275,822 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 36,635 | 10.4712 | 277,501 | |||
| 0.9 | 0.9 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 35,046 | 10.4713 | 279,092 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 36,334 | 10.4630 | 277,557 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 35,066 | 10.4707 | 279,053 | |||
| 0.9 | 1.0 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 33,484 | 10.4707 | 280,639 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 34,589 | 10.4625 | 279,286 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 33,505 | 10.4701 | 280,599 | |||
| 1.0 | 0.4 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 43,584 | 10.5749 | 273,664 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 45,787 | 10.5664 | 271,206 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 43,604 | 10.5743 | 273,624 | |||
| 1.0. | 0.5 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 41,955 | 10.5749 | 275,292 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 43,974 | 10.5664 | 273,017 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 41,975 | 10.5742 | 275,252 | |||
| 1.0 | 0.6 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 40,332 | 10.5749 | 276,914 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 42,168 | 10.5663 | 274,823 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 40,352 | 10.5742 | 276,875 | |||
| 1.0 | 0.7 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 38,714 | 10.5748 | 278,531 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 40,367 | 10.5663 | 276,622 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 38,735 | 10.5742 | 278,491 | |||
| 1.0 | 0.8 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 37,103 | 10.5748 | 280,141 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 38,573 | 10.5663 | 278,415 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 37,124 | 10.5742 | 280,101 | |||
| 1.0 | 0.9 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 35,498 | 10.5748 | 281,746 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 36,784 | 10.5662 | 280,203 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 35,518 | 10.5741 | 281,706 | |||
| 1.0 | 1.0 | (1) FFA & OCT | 62,759 | 10.4494 | 250,724 | |
| (2) FFA & Ophthalmologist | 44,649 | 10.5750 | 272,601 | |||
| (3) FFA & Nurse | 33,898 | 10.5748 | 283,345 | ✓ | ||
| (4) OCT & OCT | 67,421 | 10.4417 | 245,830 | |||
| (5) OCT & Ophthalmologist | 47,131 | 10.5666 | 269,866 | |||
| (6) OCT & Nurse | 35,001 | 10.5662 | 281,984 | |||
| (7) Ophthalmologist & OCT | 62,778 | 10.4488 | 250,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.5744 | 272,561 | |||
| (9) Ophthalmologist & Nurse | 33,919 | 10.5741 | 283,305 | |||
| Nurse monitoring assessment unclear (%) | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0 | (3) FFA & Nurse | 39,518 | 10.460 | ||||
| (9) Ophthalmologist & Nurse | 39,539 | 10.460 | 21 | –0.001 | –33,469 | Dominated | |
| (6) OCT & Nurse | 41,306 | 10.452 | 1788 | –0.008 | –219,099 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 5131 | 0.115 | 44,737 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,919 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.1 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.2 | (3) FFA & Nurse | 40,027 | 10.485 | ||||
| (9) Ophthalmologist & Nurse | 40,048 | 10.485 | 21 | –0.001 | –33,009 | Dominated | |
| (6) OCT & Nurse | 41,915 | 10.477 | 1888 | –0.008 | –229,688 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4622 | 0.090 | 51,428 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,958 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.3 | (3) FFA & Nurse | 40,292 | 10.497 | ||||
| (9) Ophthalmologist & Nurse | 40,312 | 10.497 | 21 | –0.001 | –32,787 | Dominated | |
| (6) OCT & Nurse | 42,230 | 10.489 | 1938 | –0.008 | –234,954 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4357 | 0.078 | 55,983 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,978 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.4 | (3) FFA & Nurse | 40,563 | 10.509 | ||||
| (9) Ophthalmologist & Nurse | 40,584 | 10.508 | 20 | –0.001 | –32,570 | Dominated | |
| (6) OCT & Nurse | 42,552 | 10.501 | 1989 | –0.008 | –240,202 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4086 | 0.066 | 61,882 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,998 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.5 | (3) FFA & Nurse | 40,841 | 10.521 | ||||
| (9) Ophthalmologist & Nurse | 40,862 | 10.520 | 20 | –0.001 | –32,358 | Dominated | |
| (6) OCT & Nurse | 42,880 | 10.512 | 2039 | –0.008 | –245,435 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 3808 | 0.054 | 69,925 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –294,018 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated |
| OCT unit cost (£) | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 30 | (9) Ophthalmologist & Nurse | 37,446 | 10.472 | ||||
| (3) FFA & Nurse | 37,446 | 10.473 | 1 | 0.001 | 835 | ||
| (6) OCT & Nurse | 39,071 | 10.465 | 1625 | –0.008 | –198,353 | Dominated | |
| (8) Ophthalmologist & Ophthalmologist | 42,317 | 10.574 | 4870 | 0.102 | 47,980 | ||
| (2) FFA & Ophthalmologist | 42,318 | 10.575 | 1 | 0.001 | 1398 | ||
| (5) OCT & Ophthalmologist | 44,586 | 10.567 | 2268 | –0.008 | –268,648 | Dominated | |
| (7) Ophthalmologist & OCT | 60,434 | 10.449 | 18,116 | –0.126 | –143,560 | Dominated | |
| (1) FFA & OCT | 60,436 | 10.449 | 18,118 | –0.126 | –144,295 | Dominated | |
| (4) OCT & OCT | 64,885 | 10.442 | 22,567 | –0.133 | –169,320 | Dominated | |
| 40 | (3) FFA & Nurse | 38,538 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 38,548 | 10.472 | 9 | –0.001 | –15,184 | Dominated | |
| (6) OCT & Nurse | 40,263 | 10.465 | 1725 | –0.008 | –210,601 | Dominated | |
| (2) FFA & Ophthalmologist | 43,414 | 10.575 | 4875 | 0.102 | 47,723 | ||
| (8) Ophthalmologist & Ophthalmologist | 43,423 | 10.574 | 9 | –0.001 | –13,878 | Dominated | |
| (5) OCT & Ophthalmologist | 45,783 | 10.567 | 2369 | –0.008 | –280,538 | Dominated | |
| (1) FFA & OCT | 61,528 | 10.449 | 18,114 | –0.126 | –144,264 | Dominated | |
| (7) Ophthalmologist & OCT | 61,536 | 10.449 | 18,122 | –0.126 | –143,608 | Dominated | |
| (4) OCT & OCT | 66,078 | 10.442 | 22,664 | –0.133 | –170,044 | Dominated | |
| 50 | (3) FFA & Nurse | 39,630 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,650 | 10.472 | 19 | –0.001 | –31,202 | Dominated | |
| (6) OCT & Nurse | 41,456 | 10.465 | 1825 | –0.008 | –222,848 | Dominated | |
| (2) FFA & Ophthalmologist | 44,510 | 10.575 | 4879 | 0.102 | 47,763 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,529 | 10.574 | 19 | –0.001 | –29,154 | Dominated | |
| (5) OCT & Ophthalmologist | 46,979 | 10.567 | 2469 | –0.008 | –292,428 | Dominated | |
| (1) FFA & OCT | 62,620 | 10.449 | 18,110 | –0.126 | –144,233 | Dominated | |
| (7) Ophthalmologist & OCT | 62,638 | 10.449 | 18,128 | –0.126 | –143,656 | Dominated | |
| (4) OCT & OCT | 67,270 | 10.442 | 22,760 | –0.133 | –170,767 | Dominated | |
| 60 | (3) FFA & Nurse | 40,722 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 40,752 | 10.472 | 29 | –0.001 | –47,221 | Dominated | |
| (6) OCT & Nurse | 42,648 | 10.465 | 1926 | –0.008 | –235,095 | Dominated | |
| (2) FFA & Ophthalmologist | 45,606 | 10.575 | 4884 | 0.102 | 47,803 | ||
| (8) Ophthalmologist & Ophthalmologist | 45,635 | 10.574 | 29 | –0.001 | –44,429 | Dominated | |
| (5) OCT & Ophthalmologist | 48,176 | 10.567 | 2569 | –0.008 | –304,319 | Dominated | |
| (1) FFA & OCT | 63,712 | 10.449 | 18,106 | –0.126 | –144,201 | Dominated | |
| (7) Ophthalmologist & OCT | 63,740 | 10.449 | 18,134 | –0.126 | –143,703 | Dominated | |
| (4) OCT & OCT | 68,462 | 10.442 | 22,856 | –0.133 | –171,491 | Dominated | |
| 70 | (3) FFA & Nurse | 41,814 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 41,854 | 10.472 | 39 | –0.001 | –63,240 | Dominated | |
| (6) OCT & Nurse | 43,840 | 10.465 | 2026 | –0.008 | –247,342 | Dominated | |
| (2) FFA & Ophthalmologist | 46,702 | 10.575 | 4888 | 0.102 | 47,842 | ||
| (8) Ophthalmologist & Ophthalmologist | 46,741 | 10.574 | 39 | –0.001 | –59,705 | Dominated | |
| (5) OCT & Ophthalmologist | 49,372 | 10.567 | 2670 | –0.008 | –316,209 | Dominated | |
| (1) FFA & OCT | 64,805 | 10.449 | 18,102 | –0.126 | –144,170 | Dominated | |
| (7) Ophthalmologist & OCT | 64,842 | 10.449 | 18,140 | –0.126 | –143,751 | Dominated | |
| (4) OCT & OCT | 69,655 | 10.442 | 22,953 | –0.133 | –172,214 | Dominated |
| FFA unit cost (£) | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 80 | (3) FFA & Nurse | 39,503 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,533 | 10.472 | 30 | –0.001 | –47,802 | Dominated | |
| (6) OCT & Nurse | 41,360 | 10.465 | 1857 | –0.008 | –226,713 | Dominated | |
| (2) FFA & Ophthalmologist | 44,207 | 10.575 | 4704 | 0.102 | 46,042 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,236 | 10.574 | 29 | –0.001 | –44,992 | Dominated | |
| (5) OCT & Ophthalmologist | 46,690 | 10.567 | 2483 | –0.008 | –294,041 | Dominated | |
| (1) FFA & OCT | 62,721 | 10.449 | 18,514 | –0.126 | –147,446 | Dominated | |
| (7) Ophthalmologist & OCT | 62,749 | 10.449 | 18,542 | –0.126 | –146,934 | Dominated | |
| (4) OCT & OCT | 67,417 | 10.442 | 23,210 | –0.133 | –174,147 | Dominated | |
| 90 | (3) FFA & Nurse | 39,575 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,602 | 10.472 | 27 | –0.001 | –43,865 | Dominated | |
| (6) OCT & Nurse | 41,427 | 10.465 | 1852 | –0.008 | –226,089 | Dominated | |
| (2) FFA & Ophthalmologist | 44,326 | 10.575 | 4751 | 0.102 | 46,509 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,353 | 10.574 | 27 | –0.001 | –41,236 | Dominated | |
| (5) OCT & Ophthalmologist | 46,809 | 10.567 | 2482 | –0.008 | –294,013 | Dominated | |
| (1) FFA & OCT | 62,731 | 10.449 | 18,405 | –0.126 | –146,577 | Dominated | |
| (7) Ophthalmologist & OCT | 62,757 | 10.449 | 18,430 | –0.126 | –146,050 | Dominated | |
| (4) OCT & OCT | 67,418 | 10.442 | 23,092 | –0.133 | –173,258 | Dominated | |
| 100 | (3) FFA & Nurse | 39,647 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,672 | 10.472 | 25 | –0.001 | –39,929 | Dominated | |
| (6) OCT & Nurse | 41,494 | 10.465 | 1847 | –0.008 | –225,465 | Dominated | |
| (2) FFA & Ophthalmologist | 44,446 | 10.575 | 4799 | 0.102 | 46,975 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,470 | 10.574 | 24 | –0.001 | –37,479 | Dominated | |
| (5) OCT & Ophthalmologist | 46,928 | 10.567 | 2482 | –0.008 | –293,985 | Dominated | |
| (1) FFA & OCT | 62,741 | 10.449 | 18,295 | –0.126 | –145,707 | Dominated | |
| (7) Ophthalmologist & OCT | 62,765 | 10.449 | 18,319 | –0.126 | –145,165 | Dominated | |
| (4) OCT & OCT | 67,420 | 10.442 | 22,974 | –0.133 | –172,370 | Dominated | |
| 110 | (3) FFA & Nurse | 39,719 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,741 | 10.472 | 22 | –0.001 | –35,992 | Dominated | |
| (6) OCT & Nurse | 41,560 | 10.465 | 1842 | –0.008 | –224,840 | Dominated | |
| (2) FFA & Ophthalmologist | 44,565 | 10.575 | 4847 | 0.102 | 47,442 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,587 | 10.574 | 22 | –0.001 | –33,723 | Dominated | |
| (5) OCT & Ophthalmologist | 47,047 | 10.567 | 2482 | –0.008 | –293,958 | Dominated | |
| (1) FFA & OCT | 62,752 | 10.449 | 18,186 | –0.126 | –144,837 | Dominated | |
| (7) Ophthalmologist & OCT | 62,772 | 10.449 | 18,207 | –0.126 | –144,281 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,855 | –0.133 | –171,481 | Dominated | |
| 120 | (3) FFA & Nurse | 39,791 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,811 | 10.472 | 20 | –0.001 | –32,056 | Dominated | |
| (6) OCT & Nurse | 41,627 | 10.465 | 1837 | –0.008 | –224,216 | Dominated | |
| (2) FFA & Ophthalmologist | 44,685 | 10.575 | 4894 | 0.102 | 47,908 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,704 | 10.574 | 19 | –0.001 | –29,967 | Dominated | |
| (5) OCT & Ophthalmologist | 47,167 | 10.567 | 2482 | –0.008 | –293,930 | Dominated | |
| (1) FFA & OCT | 62,762 | 10.449 | 18,077 | –0.126 | –143,968 | Dominated | |
| (7) Ophthalmologist & OCT | 62,780 | 10.449 | 18,095 | –0.126 | –143,396 | Dominated | |
| (4) OCT & OCT | 67,422 | 10.442 | 22,737 | –0.133 | –170,593 | Dominated | |
| 130 | (3) FFA & Nurse | 39,863 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,880 | 10.472 | 17 | –0.001 | –28,119 | Dominated | |
| (6) OCT & Nurse | 41,694 | 10.465 | 1831 | –0.008 | –223,592 | Dominated | |
| (2) FFA & Ophthalmologist | 44,805 | 10.575 | 4942 | 0.102 | 48,374 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,822 | 10.574 | 17 | –0.001 | –26,211 | Dominated | |
| (5) OCT & Ophthalmologist | 47,286 | 10.567 | 2482 | –0.008 | –293,903 | Dominated | |
| (1) FFA & OCT | 62,772 | 10.449 | 17,968 | –0.126 | –143,098 | Dominated | |
| (7) Ophthalmologist & OCT | 62,788 | 10.449 | 17,984 | –0.126 | –142,512 | Dominated | |
| (4) OCT & OCT | 67,423 | 10.442 | 22,618 | –0.133 | –169,704 | Dominated | |
| 140 | (3) FFA & Nurse | 39,934 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,949 | 10.472 | 15 | –0.001 | –24,182 | Dominated | |
| (6) OCT & Nurse | 41,761 | 10.465 | 1826 | –0.008 | –222,967 | Dominated | |
| (2) FFA & Ophthalmologist | 44,924 | 10.575 | 4990 | 0.102 | 48,841 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,939 | 10.574 | 15 | –0.001 | –22,454 | Dominated | |
| (5) OCT & Ophthalmologist | 47,405 | 10.567 | 2481 | –0.008 | –293,875 | Dominated | |
| (1) FFA & OCT | 62,783 | 10.449 | 17,859 | –0.126 | –142,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,796 | 10.449 | 17,872 | –0.126 | –141,627 | Dominated | |
| (4) OCT & OCT | 67,424 | 10.442 | 22,500 | –0.133 | –168,815 | Dominated |
| Unit cost for ranibizumab (£) | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | ICER | Dominated |
|---|---|---|---|---|---|---|---|
| 0 | (1) FFA & OCT | 15,064 | 10.449 | ||||
| (7) Ophthalmologist & OCT | 15,087 | 10.449 | 23 | –0.001 | –36,724 | Dominated | |
| (2) FFA & Ophthalmologist | 16,110 | 10.575 | 1047 | 0.126 | 8335 | ||
| (8) Ophthalmologist & Ophthalmologist | 16,133 | 10.574 | 23 | –0.001 | –35,089 | Dominated | |
| (4) OCT & OCT | 16,226 | 10.442 | 116 | –0.133 | –867 | Dominated | |
| (5) OCT & Ophthalmologist | 17,364 | 10.567 | 1254 | –0.008 | –148,531 | Dominated | |
| (3) FFA & Nurse | 17,386 | 10.473 | 1276 | –0.102 | –12,486 | Dominated | |
| (9) Ophthalmologist & Nurse | 17,409 | 10.472 | 1298 | –0.103 | –12,633 | Dominated | |
| (6) OCT & Nurse | 18,647 | 10.465 | 2537 | –0.110 | –22,993 | Dominated | |
| 50 | (2) FFA & Ophthalmologist | 18,033 | 10.575 | ||||
| (8) Ophthalmologist & Ophthalmologist | 18,055 | 10.574 | 23 | –0.001 | –34,820 | Dominated | |
| (1) FFA & OCT | 18,277 | 10.449 | 244 | –0.126 | –1944 | Dominated | |
| (7) Ophthalmologist & OCT | 18,300 | 10.449 | 267 | –0.126 | –2114 | Dominated | |
| (3) FFA & Nurse | 18,894 | 10.473 | 861 | –0.102 | –8427 | Dominated | |
| (9) Ophthalmologist & Nurse | 18,916 | 10.472 | 884 | –0.103 | –8597 | Dominated | |
| (5) OCT & Ophthalmologist | 19,370 | 10.567 | 1337 | –0.008 | –158,327 | Dominated | |
| (4) OCT & OCT | 19,675 | 10.442 | 1642 | –0.133 | –12,320 | Dominated | |
| (6) OCT & Nurse | 20,194 | 10.465 | 2161 | –0.110 | –19,586 | Dominated | |
| 100 | (2) FFA & Ophthalmologist | 19,955 | 10.575 | ||||
| (8) Ophthalmologist & Ophthalmologist | 19,978 | 10.574 | 22 | –0.001 | –34,551 | Dominated | |
| (3) FFA & Nurse | 20,402 | 10.473 | 446 | –0.102 | –4368 | Dominated | |
| (9) Ophthalmologist & Nurse | 20,424 | 10.472 | 469 | –0.103 | –4561 | Dominated | |
| (5) OCT & Ophthalmologist | 21,375 | 10.567 | 1420 | –0.008 | –168,123 | Dominated | |
| (1) FFA & OCT | 21,490 | 10.449 | 1535 | –0.126 | –12,222 | Dominated | |
| (7) Ophthalmologist & OCT | 21,513 | 10.449 | 1557 | –0.126 | –12,339 | Dominated | |
| (6) OCT & Nurse | 21,741 | 10.465 | 1786 | –0.110 | –16,180 | Dominated | |
| (4) OCT & OCT | 23,124 | 10.442 | 3168 | –0.133 | –23,772 | Dominated | |
| 250 | (3) FFA & Nurse | 24,926 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 24,948 | 10.472 | 22 | –0.001 | –35,686 | Dominated | |
| (2) FFA & Ophthalmologist | 25,723 | 10.575 | 798 | 0.102 | 7810 | ||
| (8) Ophthalmologist & Ophthalmologist | 25,745 | 10.574 | 22 | –0.001 | –33,743 | Dominated | |
| (6) OCT & Nurse | 26,381 | 10.465 | 658 | –0.110 | –5962 | Dominated | |
| (5) OCT & Ophthalmologist | 27,391 | 10.567 | 1668 | –0.008 | –197,512 | Dominated | |
| (1) FFA & OCT | 31,130 | 10.449 | 5406 | –0.126 | –43,056 | Dominated | |
| (7) Ophthalmologist & OCT | 31,151 | 10.449 | 5428 | –0.126 | –43,014 | Dominated | |
| (4) OCT & OCT | 33,471 | 10.442 | 7748 | –0.133 | –58,129 | Dominated | |
| 500 | (3) FFA & Nurse | 32,465 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 32,487 | 10.472 | 21 | –0.001 | –34,442 | Dominated | |
| (6) OCT & Nurse | 34,115 | 10.465 | 1650 | –0.008 | –201,441 | Dominated | |
| (2) FFA & Ophthalmologist | 35,337 | 10.575 | 2871 | 0.102 | 28,107 | ||
| (8) Ophthalmologist & Ophthalmologist | 35,358 | 10.574 | 21 | –0.001 | –32,397 | Dominated | |
| (5) OCT & Ophthalmologist | 37,418 | 10.567 | 2081 | –0.008 | –246,492 | Dominated | |
| (1) FFA & OCT | 47,196 | 10.449 | 11,859 | –0.126 | –94,447 | Dominated | |
| (7) Ophthalmologist & OCT | 47,216 | 10.449 | 11,879 | –0.126 | –94,138 | Dominated | |
| (4) OCT & OCT | 50,716 | 10.442 | 15,379 | –0.133 | –115,391 | Dominated | |
| 750 | (3) FFA & Nurse | 40,005 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 40,026 | 10.472 | 21 | –0.001 | –33,198 | Dominated | |
| (6) OCT & Nurse | 41,849 | 10.465 | 1844 | –0.008 | –225,146 | Dominated | |
| (2) FFA & Ophthalmologist | 44,950 | 10.575 | 4945 | 0.102 | 48,404 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,970 | 10.574 | 20 | –0.001 | –31,052 | Dominated | |
| (5) OCT & Ophthalmologist | 47,445 | 10.567 | 2495 | –0.008 | –295,472 | Dominated | |
| (1) FFA & OCT | 63,262 | 10.449 | 18,312 | –0.126 | –145,838 | Dominated | |
| (7) Ophthalmologist & OCT | 63,281 | 10.449 | 18,331 | –0.126 | –145,263 | Dominated | |
| (4) OCT & OCT | 67,962 | 10.442 | 23,011 | –0.133 | –172,653 | Dominated | |
| 1000 | (3) FFA & Nurse | 47,545 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 47,565 | 10.472 | 20 | –0.001 | –31,954 | Dominated | |
| (6) OCT & Nurse | 49,583 | 10.465 | 2038 | –0.008 | –248,850 | Dominated | |
| (2) FFA & Ophthalmologist | 54,564 | 10.575 | 7018 | 0.102 | 68,701 | ||
| (8) Ophthalmologist & Ophthalmologist | 54,583 | 10.574 | 19 | –0.001 | –29,706 | Dominated | |
| (5) OCT & Ophthalmologist | 57,472 | 10.567 | 2908 | –0.008 | –344,453 | Dominated | |
| (1) FFA & OCT | 79,328 | 10.449 | 24,765 | –0.126 | –197,229 | Dominated | |
| (7) Ophthalmologist & OCT | 79,346 | 10.449 | 24,782 | –0.126 | –196,387 | Dominated | |
| (4) OCT & OCT | 85,207 | 10.442 | 30,643 | –0.133 | –229,914 | Dominated | |
| 1500 | (3) FFA & Nurse | 62,625 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 62,643 | 10.472 | 18 | –0.001 | –29,466 | Dominated | |
| (6) OCT & Nurse | 65,052 | 10.465 | 2427 | –0.008 | –296,260 | Dominated | |
| (2) FFA & Ophthalmologist | 73,790 | 10.575 | 11,166 | 0.102 | 109,294 | ||
| (8) Ophthalmologist & Ophthalmologist | 73,808 | 10.574 | 18 | –0.001 | –27,014 | Dominated | |
| (5) OCT & Ophthalmologist | 77,526 | 10.567 | 3735 | –0.008 | –442,414 | Dominated | |
| (1) FFA & OCT | 111,461 | 10.449 | 37,670 | –0.126 | –300,011 | Dominated | |
| (7) Ophthalmologist & OCT | 111,476 | 10.449 | 37,685 | –0.126 | –298,636 | Dominated | |
| (4) OCT & OCT | 119,697 | 10.442 | 45,907 | –0.133 | –344,438 | Dominated |
| Cycle number (month) | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs |
|---|---|---|---|---|---|
| 20 | (2) FFA & Ophthalmologist | 20,496 | 10.575 | ||
| (8) Ophthalmologist & Ophthalmologist | 20,516 | 10.574 | –31,610 | Dominated | |
| (3) FFA & Nurse | 21,096 | 10.473 | –5877 | Dominated | |
| (9) Ophthalmologist & Nurse | 21,117 | 10.472 | –6046 | Dominated | |
| (1) FFA & OCT | 21,383 | 10.449 | –7064 | Dominated | |
| (7) Ophthalmologist & OCT | 21,403 | 10.449 | –7186 | Dominated | |
| (5) OCT & Ophthalmologist | 21,928 | 10.567 | –169,602 | Dominated | |
| (6) OCT & Nurse | 22,455 | 10.465 | –17,749 | Dominated | |
| (4) OCT & OCT | 23,010 | 10.442 | –18,867 | Dominated | |
| 30 | (2) FFA & Ophthalmologist | 22,099 | 10.575 | ||
| (8) Ophthalmologist & Ophthalmologist | 22,119 | 10.574 | –31,597 | Dominated | |
| (3) FFA & Nurse | 22,341 | 10.473 | –2374 | Dominated | |
| (9) Ophthalmologist & Nurse | 22,362 | 10.472 | –2563 | Dominated | |
| (5) OCT & Ophthalmologist | 23,608 | 10.567 | –178,823 | Dominated | |
| (6) OCT & Nurse | 23,735 | 10.465 | –14,830 | Dominated | |
| (1) FFA & OCT | 24,137 | 10.449 | –16,237 | Dominated | |
| (7) Ophthalmologist & OCT | 24,157 | 10.449 | –16,313 | Dominated | |
| (4) OCT & OCT | 25,990 | 10.442 | –29,197 | Dominated | |
| 40 | (3) FFA & Nurse | 23,536 | 10.473 | ||
| (9) Ophthalmologist & Nurse | 23,557 | 10.472 | –33,809 | Dominated | |
| (2) FFA & Ophthalmologist | 23,639 | 10.575 | 1004 | ||
| (8) Ophthalmologist & Ophthalmologist | 23,659 | 10.574 | –31,582 | Dominated | |
| (6) OCT & Nurse | 24,964 | 10.465 | –12,010 | Dominated | |
| (5) OCT & Ophthalmologist | 25,223 | 10.567 | –187,585 | Dominated | |
| (1) FFA & OCT | 26,785 | 10.449 | –25,054 | Dominated | |
| (7) Ophthalmologist & OCT | 26,805 | 10.449 | –25,086 | Dominated | |
| (4) OCT & OCT | 28,851 | 10.442 | –39,107 | Dominated | |
| 50 | (3) FFA & Nurse | 24,684 | 10.473 | ||
| (9) Ophthalmologist & Nurse | 24,705 | 10.472 | –33,789 | Dominated | |
| (2) FFA & Ophthalmologist | 25,118 | 10.575 | 4251 | ||
| (8) Ophthalmologist & Ophthalmologist | 25,139 | 10.574 | –31,565 | Dominated | |
| (6) OCT & Nurse | 26,144 | 10.465 | –9296 | Dominated | |
| (5) OCT & Ophthalmologist | 26,772 | 10.567 | –195,899 | Dominated | |
| (1) FFA & OCT | 29,327 | 10.449 | –33,518 | Dominated | |
| (7) Ophthalmologist & OCT | 29,347 | 10.449 | –33,507 | Dominated | |
| (4) OCT & OCT | 31,596 | 10.442 | –48,603 | Dominated | |
| 60 | (3) FFA & Nurse | 25,784 | 10.473 | ||
| (9) Ophthalmologist & Nurse | 25,805 | 10.472 | –33,766 | Dominated | |
| (2) FFA & Ophthalmologist | 26,537 | 10.575 | 7368 | ||
| (8) Ophthalmologist & Ophthalmologist | 26,557 | 10.574 | –31,546 | Dominated | |
| (6) OCT & Nurse | 27,275 | 10.465 | –6686 | Dominated | |
| (5) OCT & Ophthalmologist | 28,258 | 10.567 | –203,778 | Dominated | |
| (1) FFA & OCT | 31,764 | 10.449 | –41,629 | Dominated | |
| (7) Ophthalmologist & OCT | 31,784 | 10.449 | –41,578 | Dominated | |
| (4) OCT & OCT | 34,226 | 10.442 | –57,687 | Dominated | |
| 70 | (3) FFA & Nurse | 26,837 | 10.473 | ||
| (9) Ophthalmologist & Nurse | 26,858 | 10.472 | –33,742 | Dominated | |
| (2) FFA & Ophthalmologist | 27,895 | 10.575 | 10,356 | ||
| (8) Ophthalmologist & Ophthalmologist | 27,916 | 10.574 | –31,526 | Dominated | |
| (6) OCT & Nurse | 28,357 | 10.465 | –4181 | Dominated | |
| (5) OCT & Ophthalmologist | 29,679 | 10.567 | –211,234 | Dominated | |
| (1) FFA & OCT | 34,097 | 10.449 | –49,392 | Dominated | |
| (7) Ophthalmologist & OCT | 34,117 | 10.449 | –49,302 | Dominated | |
| (4) OCT & OCT | 36,741 | 10.442 | –66,365 | Dominated | |
| 80 | (3) FFA & Nurse | 27,844 | 10.473 | ||
| (9) Ophthalmologist & Nurse | 27,865 | 10.472 | –33,717 | Dominated | |
| (2) FFA & Ophthalmologist | 29,194 | 10.575 | 13,217 | ||
| (8) Ophthalmologist & Ophthalmologist | 29,215 | 10.574 | –31,506 | Dominated | |
| (6) OCT & Nurse | 29,391 | 10.465 | –1780 | Dominated | |
| (5) OCT & Ophthalmologist | 31,037 | 10.567 | –218,279 | Dominated | |
| (1) FFA & OCT | 36,327 | 10.449 | –56,808 | Dominated | |
| (7) Ophthalmologist & OCT | 36,347 | 10.449 | –56,682 | Dominated | |
| (4) OCT & OCT | 39,143 | 10.442 | –74,642 | Dominated | |
| 90 | (3) FFA & Nurse | 28,805 | 10.473 | ||
| (9) Ophthalmologist & Nurse | 28,825 | 10.472 | –33,691 | Dominated | |
| (6) OCT & Nurse | 30,377 | 10.465 | –191,957 | Dominated | |
| (2) FFA & Ophthalmologist | 30,434 | 10.575 | 15,951 | ||
| (8) Ophthalmologist & Ophthalmologist | 30,454 | 10.574 | –31,484 | Dominated | |
| (5) OCT & Ophthalmologist | 32,333 | 10.567 | –224,925 | Dominated | |
| (1) FFA & OCT | 38,455 | 10.449 | –63,882 | Dominated | |
| (7) Ophthalmologist & OCT | 38,475 | 10.449 | –63,720 | Dominated | |
| (4) OCT & OCT | 41,433 | 10.442 | –82,523 | Dominated | |
| 100 | (3) FFA & Nurse | 29,719 | 10.473 | ||
| (9) Ophthalmologist & Nurse | 29,740 | 10.472 | –33,665 | Dominated | |
| (6) OCT & Nurse | 31,316 | 10.465 | –194,908 | Dominated | |
| (2) FFA & Ophthalmologist | 31,615 | 10.575 | 18,559 | ||
| (8) Ophthalmologist & Ophthalmologist | 31,636 | 10.574 | –31,462 | Dominated | |
| (5) OCT & Ophthalmologist | 33,567 | 10.567 | –231,184 | Dominated | |
| (1) FFA & OCT | 40,482 | 10.449 | –70,616 | Dominated | |
| (7) Ophthalmologist & OCT | 40,502 | 10.449 | –70,420 | Dominated | |
| (4) OCT & OCT | 43,612 | 10.442 | –90,013 | Dominated | |
| 110 | (3) FFA & Nurse | 30,589 | 10.473 | ||
| (9) Ophthalmologist & Nurse | 30,610 | 10.472 | –33,638 | Dominated | |
| (6) OCT & Nurse | 32,208 | 10.465 | –197,680 | Dominated | |
| (2) FFA & Ophthalmologist | 32,739 | 10.575 | 21,043 | ||
| (8) Ophthalmologist & Ophthalmologist | 32,759 | 10.574 | –31,439 | Dominated | |
| (5) OCT & Ophthalmologist | 34,740 | 10.567 | –237,067 | Dominated | |
| (1) FFA & OCT | 42,409 | 10.449 | –77,015 | Dominated | |
| (7) Ophthalmologist & OCT | 42,428 | 10.449 | –76,787 | Dominated | |
| (4) OCT & OCT | 45,683 | 10.442 | –97,119 | Dominated | |
| 120 | (3) FFA & Nurse | 31,413 | 10.473 | ||
| (9) Ophthalmologist & Nurse | 31,434 | 10.472 | –33,611 | Dominated | |
| (6) OCT & Nurse | 33,054 | 10.465 | –200,280 | Dominated | |
| (2) FFA & Ophthalmologist | 33,804 | 10.575 | 23,404 | ||
| (8) Ophthalmologist & Ophthalmologist | 33,825 | 10.574 | –31,416 | Dominated | |
| (5) OCT & Ophthalmologist | 35,853 | 10.567 | –242,585 | Dominated | |
| (1) FFA & OCT | 44,236 | 10.449 | –83,080 | Dominated | |
| (7) Ophthalmologist & OCT | 44,256 | 10.449 | –82,822 | Dominated | |
| (4) OCT & OCT | 47,645 | 10.442 | –103,844 | Dominated | |
| (2) FFA & Ophthalmologist | 20,496 | 10.575 |
| Discount rate | Strategy | Expected cost (£) | Expected QALYs | NMB (£) | Maximum NMB | |
|---|---|---|---|---|---|---|
| Costs (%) | QALYs (%) | |||||
| 0 | 0 | (1) FFA & OCT | 88,482 | 14.665 | 351,465 | |
| (2) FFA & Ophthalmologist | 62,690 | 14.867 | 383,317 | |||
| (3) FFA & Nurse | 55,747 | 14.702 | 385,326 | ✓ | ||
| (4) OCT & OCT | 94,956 | 14.654 | 344,673 | |||
| (5) OCT & Ophthalmologist | 66,141 | 14.855 | 379,520 | |||
| (6) OCT & Nurse | 58,304 | 14.691 | 382,433 | |||
| (7) Ophthalmologist & OCT | 88,501 | 14.664 | 351,420 | |||
| (8) Ophthalmologist & Ophthalmologist | 62,711 | 14.866 | 383,270 | |||
| (9) Ophthalmologist & Nurse | 55,767 | 14.702 | 385,280 | |||
| 0.01 | 0.01 | (1) FFA & OCT | 79,586 | 13.211 | 316,729 | |
| (2) FFA & Ophthalmologist | 56,451 | 13.385 | 345,109 | |||
| (3) FFA & Nurse | 50,221 | 13.243 | 347,070 | ✓ | ||
| (4) OCT & OCT | 85,439 | 13.201 | 310,588 | |||
| (5) OCT & Ophthalmologist | 59,569 | 13.375 | 341,676 | |||
| (6) OCT & Nurse | 52,532 | 13.233 | 344,454 | |||
| (7) Ophthalmologist & OCT | 79,605 | 13.210 | 316,686 | |||
| (8) Ophthalmologist & Ophthalmologist | 56,471 | 13.385 | 345,065 | |||
| (9) Ophthalmologist & Nurse | 50,242 | 13.242 | 347,026 | |||
| 0.02 | 0.02 | (1) FFA & OCT | 72,037 | 11.974 | 287,173 | |
| (2) FFA & Ophthalmologist | 51,156 | 12.126 | 312,623 | |||
| (3) FFA & Nurse | 45,532 | 12.002 | 314,529 | ✓ | ||
| (4) OCT & OCT | 77,358 | 11.965 | 281,589 | |||
| (5) OCT & Ophthalmologist | 53,990 | 12.116 | 309,502 | |||
| (6) OCT & Nurse | 47,631 | 11.993 | 312,151 | |||
| (7) Ophthalmologist & OCT | 72,056 | 11.973 | 287,133 | |||
| (8) Ophthalmologist & Ophthalmologist | 51,176 | 12.125 | 312,581 | |||
| (9) Ophthalmologist & Nurse | 45,552 | 12.001 | 314,487 | |||
| 0.03 | 0.03 | (1) FFA & OCT | 65,588 | 10.915 | 261,863 | |
| (2) FFA & Ophthalmologist | 46,633 | 11.049 | 284,824 | |||
| (3) FFA & Nurse | 41,526 | 10.940 | 286,671 | ✓ | ||
| (4) OCT & OCT | 70,452 | 10.907 | 256,757 | |||
| (5) OCT & Ophthalmologist | 49,223 | 11.040 | 281,970 | |||
| (6) OCT & Nurse | 43,444 | 10.931 | 284,497 | |||
| (7) Ophthalmologist & OCT | 65,607 | 10.914 | 261,824 | |||
| (8) Ophthalmologist & Ophthalmologist | 46,653 | 11.048 | 284,784 | |||
| (9) Ophthalmologist & Nurse | 41,547 | 10.939 | 286,631 | |||
| 0.04 | 0.04 | (1) FFA & OCT | 60,045 | 10.003 | 240,053 | |
| (2) FFA & Ophthalmologist | 42,746 | 10.121 | 260,886 | |||
| (3) FFA & Nurse | 38,083 | 10.025 | 262,674 | ✓ | ||
| (4) OCT & OCT | 64,514 | 9.996 | 235,362 | |||
| (5) OCT & Ophthalmologist | 45,124 | 10.113 | 258,265 | |||
| (6) OCT & Nurse | 39,845 | 10.017 | 260,676 | |||
| (7) Ophthalmologist & OCT | 60,064 | 10.003 | 240,016 | |||
| (8) Ophthalmologist & Ophthalmologist | 42,766 | 10.120 | 260,848 | |||
| (9) Ophthalmologist & Nurse | 38,104 | 10.025 | 262,635 | |||
| 0.05 | 0.05 | (1) FFA & OCT | 55,252 | 9.213 | 221,149 | |
| (2) FFA & Ophthalmologist | 39,384 | 9.318 | 240,151 | |||
| (3) FFA & Nurse | 35,106 | 9.233 | 241,879 | ✓ | ||
| (4) OCT & OCT | 59,377 | 9.206 | 216,817 | |||
| (5) OCT & Ophthalmologist | 41,579 | 9.310 | 237,731 | |||
| (6) OCT & Nurse | 36,731 | 9.226 | 240,035 | |||
| (7) Ophthalmologist & OCT | 55,271 | 9.213 | 221,113 | |||
| (8) Ophthalmologist & Ophthalmologist | 39,404 | 9.317 | 240,114 | |||
| (9) Ophthalmologist & Nurse | 35,127 | 9.232 | 241,842 | |||
| 0.06 | 0.06 | (1) FFA & OCT | 51,083 | 8.525 | 204,668 | |
| (2) FFA & Ophthalmologist | 36,460 | 8.618 | 222,087 | |||
| (3) FFA & Nurse | 32,517 | 8.542 | 223,756 | ✓ | ||
| (4) OCT & OCT | 54,908 | 8.519 | 200,652 | |||
| (5) OCT & Ophthalmologist | 38,495 | 8.611 | 219,843 | |||
| (6) OCT & Nurse | 34,023 | 8.536 | 222,047 | |||
| (7) Ophthalmologist & OCT | 51,102 | 8.525 | 204,634 | |||
| (8) Ophthalmologist & Ophthalmologist | 36,481 | 8.618 | 222,051 | |||
| (9) Ophthalmologist & Nurse | 32,538 | 8.542 | 223,720 | |||
| nAMD prevalence | Strategy | Expected cost (£) | Expected QALYs | Incremental cost (£) | Incremental QALYs | Strategy | Expected cost (£) |
|---|---|---|---|---|---|---|---|
| 0.1 | (9) Ophthalmologist & Nurse | 9785 | 11.109 | ||||
| (3) FFA & Nurse | 9820 | 11.109 | 34 | 0.000 | 388,603 | ||
| (8) Ophthalmologist & Ophthalmologist | 10,979 | 11.130 | 1159 | 0.021 | 55,404 | ||
| (2) FFA & Ophthalmologist | 11,013 | 11.130 | 34 | 0.000 | 370,944 | ||
| (7) Ophthalmologist & OCT | 15,389 | 11.106 | 4376 | –0.024 | –184,037 | Dominated | |
| (1) FFA & OCT | 15,424 | 11.107 | 4411 | –0.024 | –186,193 | Dominated | |
| (6) OCT & Nurse | 15,524 | 11.108 | 4511 | –0.022 | –204,863 | Dominated | |
| (5) OCT & Ophthalmologist | 18,663 | 11.130 | 7650 | –0.001 | –12,771,991 | Dominated | |
| (4) OCT & OCT | 29,660 | 11.107 | 18,647 | –0.023 | –813,472 | Dominated | |
| 0.2 | (9) Ophthalmologist & Nurse | 14,786 | 11.003 | ||||
| (3) FFA & Nurse | 14,811 | 11.003 | 25 | 0.000 | 142,530 | ||
| (8) Ophthalmologist & Ophthalmologist | 16,594 | 11.038 | 1783 | 0.034 | 51,892 | ||
| (2) FFA & Ophthalmologist | 16,619 | 11.038 | 25 | 0.000 | 136,422 | ||
| (6) OCT & Nurse | 19,871 | 11.001 | 3252 | –0.037 | –88,510 | Dominated | |
| (7) Ophthalmologist & OCT | 23,288 | 10.997 | 6668 | –0.041 | –163,248 | Dominated | |
| (1) FFA & OCT | 23,313 | 10.997 | 6694 | –0.041 | –164,599 | Dominated | |
| (5) OCT & Ophthalmologist | 23,408 | 11.036 | 6789 | –0.002 | –3,561,016 | Dominated | |
| (4) OCT & OCT | 35,954 | 10.996 | 19,334 | –0.041 | –467,969 | Dominated | |
| 0.3 | (9) Ophthalmologist & Nurse | 19,787 | 10.897 | ||||
| (3) FFA & Nurse | 19,803 | 10.897 | 16 | 0.000 | 60,505 | ||
| (8) Ophthalmologist & Ophthalmologist | 22,209 | 10.945 | 2406 | 0.048 | 50,354 | ||
| (2) FFA & Ophthalmologist | 22,225 | 10.945 | 16 | 0.000 | 58,248 | ||
| (6) OCT & Nurse | 24,218 | 10.894 | 1993 | –0.051 | –38,729 | Dominated | |
| (5) OCT & Ophthalmologist | 28,152 | 10.942 | 5927 | –0.003 | –1,844,329 | Dominated | |
| (7) Ophthalmologist & OCT | 31,186 | 10.887 | 8960 | –0.058 | –154,713 | Dominated | |
| (1) FFA & OCT | 31,202 | 10.888 | 8977 | –0.058 | –155,725 | Dominated | |
| (4) OCT & OCT | 42,247 | 10.885 | 20,022 | –0.060 | –335,328 | Dominated | |
| 0.4 | (9) Ophthalmologist & Nurse | 24,787 | 10.791 | ||||
| (3) FFA & Nurse | 24,794 | 10.791 | 7 | 0.000 | 19,493 | ||
| (8) Ophthalmologist & Ophthalmologist | 27,824 | 10.852 | 3030 | 0.061 | 49,491 | ||
| (2) FFA & Ophthalmologist | 27,831 | 10.853 | 7 | 0.000 | 19,161 | ||
| (6) OCT & Nurse | 28,565 | 10.786 | 734 | –0.066 | –11,095 | Dominated | |
| (5) OCT & Ophthalmologist | 32,897 | 10.848 | 5066 | –0.005 | –1,120,483 | Dominated | |
| (7) Ophthalmologist & OCT | 39,084 | 10.778 | 11,253 | –0.075 | –150,064 | Dominated | |
| (1) FFA & OCT | 39,091 | 10.778 | 11,260 | –0.075 | –150,889 | Dominated | |
| (4) OCT & OCT | 48,541 | 10.775 | 20,710 | –0.078 | –265,161 | Dominated | |
| 0.5 | (3) FFA & Nurse | 29,786 | 10.685 | ||||
| (9) Ophthalmologist & Nurse | 29,788 | 10.685 | 2 | 0.000 | –5,114 | Dominated | |
| (6) OCT & Nurse | 32,913 | 10.679 | 3127 | –0.006 | –539,595 | Dominated | |
| (2) FFA & Ophthalmologist | 33,437 | 10.760 | 3651 | 0.075 | 48,610 | ||
| (8) Ophthalmologist & Ophthalmologist | 33,439 | 10.760 | 2 | 0.000 | –4,291 | Dominated | |
| (5) OCT & Ophthalmologist | 37,642 | 10.754 | 4205 | –0.006 | –721,367 | Dominated | |
| (1) FFA & OCT | 46,981 | 10.668 | 13,543 | –0.092 | –147,846 | Dominated | |
| (7) Ophthalmologist & OCT | 46,982 | 10.668 | 13,545 | –0.092 | –147,138 | Dominated | |
| (4) OCT & OCT | 54,834 | 10.664 | 21,397 | –0.096 | –221,744 | Dominated | |
| 0.6 | (3) FFA & Nurse | 34,778 | 10.579 | ||||
| (9) Ophthalmologist & Nurse | 34,789 | 10.578 | 11 | –0.001 | –21,519 | Dominated | |
| (6) OCT & Nurse | 37,260 | 10.572 | 2482 | –0.007 | –354,998 | Dominated | |
| (2) FFA & Ophthalmologist | 39,043 | 10.668 | 4266 | 0.089 | 48,125 | ||
| (8) Ophthalmologist & Ophthalmologist | 39,054 | 10.667 | 11 | –0.001 | –19,926 | Dominated | |
| (5) OCT & Ophthalmologist | 42,386 | 10.660 | 3343 | –0.007 | –468,497 | Dominated | |
| (1) FFA & OCT | 54,870 | 10.559 | 15,827 | –0.109 | –145,754 | Dominated | |
| (7) Ophthalmologist & OCT | 54,880 | 10.558 | 15,837 | –0.109 | –145,128 | Dominated | |
| (4) OCT & OCT | 61,128 | 10.553 | 22,085 | –0.115 | –192,228 | Dominated | |
| 0.7 | (3) FFA & Nurse | 39,769 | 10.473 | ||||
| (9) Ophthalmologist & Nurse | 39,790 | 10.472 | 21 | –0.001 | –33,237 | Dominated | |
| (6) OCT & Nurse | 41,607 | 10.465 | 1838 | –0.008 | –224,403 | Dominated | |
| (2) FFA & Ophthalmologist | 44,649 | 10.575 | 4880 | 0.102 | 47,768 | ||
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 10.574 | 20 | –0.001 | –31,094 | Dominated | |
| (5) OCT & Ophthalmologist | 47,131 | 10.567 | 2482 | –0.008 | –293,938 | Dominated | |
| (1) FFA & OCT | 62,759 | 10.449 | 18,110 | –0.126 | –144,229 | Dominated | |
| (7) Ophthalmologist & OCT | 62,778 | 10.449 | 18,129 | –0.126 | –143,662 | Dominated | |
| (4) OCT & OCT | 67,421 | 10.442 | 22,772 | –0.133 | –170,859 | Dominated | |
| 0.8 | (3) FFA & Nurse | 44,761 | 10.367 | ||||
| (9) Ophthalmologist & Nurse | 44,790 | 10.366 | 30 | –0.001 | –42,025 | Dominated | |
| (6) OCT & Nurse | 45,954 | 10.357 | 1194 | –0.009 | –127,138 | Dominated | |
| (2) FFA & Ophthalmologist | 50,255 | 10.482 | 5494 | 0.116 | 47,495 | ||
| (8) Ophthalmologist & Ophthalmologist | 50,284 | 10.482 | 29 | –0.001 | –39,470 | Dominated | |
| (5) OCT & Ophthalmologist | 51,876 | 10.473 | 1620 | –0.010 | –166,190 | Dominated | |
| (1) FFA & OCT | 70,648 | 10.340 | 20,393 | –0.143 | –143,066 | Dominated | |
| (7) Ophthalmologist & OCT | 70,676 | 10.339 | 20,421 | –0.143 | –142,545 | Dominated | |
| (4) OCT & OCT | 73,715 | 10.331 | 23,460 | –0.152 | –154,673 | Dominated | |
| 0.9 | (3) FFA & Nurse | 49,752 | 10.261 | ||||
| (9) Ophthalmologist & Nurse | 49,791 | 10.260 | 39 | –0.001 | –48,860 | Dominated | |
| (6) OCT & Nurse | 50,302 | 10.250 | 549 | –0.011 | –51,888 | Dominated | |
| (2) FFA & Ophthalmologist | 55,861 | 10.390 | 6109 | 0.129 | 47,279 | ||
| (8) Ophthalmologist & Ophthalmologist | 55,900 | 10.389 | 38 | –0.001 | –45,984 | Dominated | |
| (5) OCT & Ophthalmologist | 56,620 | 10.379 | 759 | –0.011 | –68,648 | Dominated | |
| (1) FFA & OCT | 78,537 | 10.230 | 22,676 | –0.160 | –142,151 | Dominated | |
| (7) Ophthalmologist & OCT | 78,574 | 10.230 | 22,713 | –0.160 | –141,666 | Dominated | |
| (4) OCT & OCT | 80,009 | 10.220 | 24,147 | –0.170 | –141,988 | Dominated |
| Strategy | Cost (£) | Incremental cost (£) | QALYs | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|
| (3) FFA & Nurse | 39,769 | – | 8.582 | 0.000 | 0 |
| (9) Ophthalmologist & Nurse | 39,790 | 21 | 8.582 | 0.000 | –51,961 |
| (6) OCT & Nurse | 41,607 | 1838 | 8.577 | –0.005 | –354,384 |
| (2) FFA & Ophthalmologist | 44,649 | 4880 | 8.649 | 0.067 | 72,717 |
| (8) Ophthalmologist & Ophthalmologist | 44,669 | 20 | 8.649 | 0.000 | –49,222 |
| (5) OCT & Ophthalmologist | 47,131 | 2482 | 8.644 | –0.005 | –474,382 |
| (1) FFA & OCT | 62,759 | 18,110 | 8.578 | –0.071 | –255,538 |
| (7) Ophthalmologist & OCT | 62,778 | 18,129 | 8.578 | –0.071 | –254,352 |
| (4) OCT & OCT | 67,421 | 22,772 | 8.574 | –0.076 | –301,288 |
Glossary
- Case–control study
- This type of study compares a group of people who have the disease and a group who do not have the disease.
- Choroidal neovascularisation
- New blood vessels originating from the choroid. The choroid is a thin layer of connective tissue that lies between the retina and the sclera and supplies blood to the outer layers of the retina.
- Diagnostic odds ratio
- The ratio of the odds of testing positive in those with the disease relative to the odds of testing positive in those without the disease.
- Direct head-to-head study
- A study in which people receive both index and comparator tests (i.e. tests are evaluated in the same participants).
- False negative/true negative/false positive/true positive
- In terms of diagnostic accuracy, indicators of index test results as compared with the reference standard: negative index test, positive reference standard/negative index test, negative reference standard/positive index test, negative reference standard/positive index test, positive reference standard.
- Fundus fluorescein angiography
- An invasive imaging test that examines the circulation of the retina and choroid. A fluorescein dye is injected into a vein in the arm and a specialised camera photographs the dye as it passes through the blood vessels in the eye.
- Index test
- The diagnostic test which is being evaluated.
- Likelihood ratio
- A description of how many times more likely it is that a person with the disease will receive a particular test result than a person without the disease.
- Macula
- The central part of the retina containing the xanthophyll pigment and two or more layers of ganglion cells. Damage to the centre of the macula, the so-called fovea, often results in loss of central vision.
- Meta-analysis
- The quantitative pooling of data from two or more studies.
- Negative predictive value
- The proportion of those with negative test results who do not have the disease.
- Neovascular age-related macular degeneration
- In neovascular or ‘wet’ age-related macular degeneration, abnormal blood vessels grow into the macula and leak blood or fluid, leading to scarring of the macula and rapid loss of central vision.
- Optical coherence tomography
- A non-invasive imaging technology used to obtain high resolution cross-sectional images of the retina.
- Positive predictive value
- The proportion of those with positive test results who actually have the disease.
- Randomised controlled trial
- A study in which people are randomly allocated to receive – or not receive – a particular treatment or intervention. This is said to be the best study type to determine effectiveness of a treatment.
- Reference standard
- The best available test for establishing the presence or absence of the disease.
- Retina
- The light-sensitive layer of tissue located in the back of the eye. The retina receives images via the eye’s lens, converts them to electric signals and transmits them to the brain.
- Sensitivity
- The proportion of those who actually have the disease and who are correctly identified with positive test results.
- Specificity
- The proportion of those who actually do not have the disease and who are correctly identified with negative test results.
- Visual acuity
- Sharpness of vision, which is tested by identifying characters on a chart from a set distance. Normal visual acuity is usually referred to as 20/20 vision, meaning the detail that a person with normal eyesight would see from 20 feet away.
- Visual impairment
- ≤ 6/60 to > 3/60, severe visual impairment; ≤ 3/60, profound visual impairment/blindness.
List of abbreviations
- AMD
- age-related macular degeneration
- antiVEGF
- antivascular endothelial growth factor
- ARVO
- Association for Research in Vision and Ophthalmology
- BNF
- British National Formulary
- CATT
- Comparison of Age-related Macular Degeneration Treatments Trials
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CNV
- choroidal neovascularisation
- CNVM
- choroidal neovascular membrane
- DOR
- diagnostic odds ratio
- DS-ICGA
- digital subtraction indocyanine green angiography
- ETDRS
- Early Treatment Diabetic Retinopathy Study
- EVER
- European Association for Vision and Eye Research
- FAF
- fundus autofluorescence
- FFA
- fundus fluorescein angiography
- FN
- false negative
- FP
- false positive
- HRG
- Healthcare Resource Group
- HSROC
- hierarchical summary receiver operating characteristic
- HTA
- Health Technology Assessment
- ICER
- incremental cost-effectiveness ratio
- ICG
- indocyanine green
- ICGA
- indocyanine green angiography
- IPCV
- idiopathic polypoidal choroidal vasculopathy
- IR
- infrared reflectance
- IVAN
- Inhibit VEGF in Age-related choroidal Neovascularisation
- LR
- likelihood ratio
- MARINA
- Minimally Classic/Occult Trial of the Anti-VEGF Antibody Ranibizumab in the treatment of Neovascular Age-Related Macular Degeneration
- MSAC
- Medical Services Advisory Committee
- nAMD
- neovascular age-related macular degeneration
- NIA
- near-infrared autofluorescence
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OCT
- optical coherence tomography
- PDT
- photodynamic therapy
- PED
- pigment epithelial detachment
- PHP
- preferential hyperacuity perimetry
- QALY
- quality-adjusted life-year
- QUADAS-2
- quality assessment of diagnostic accuracy studies, version 2
- RAP
- retinal angiomatous proliferation
- RCO
- Royal College of Ophthalmologists
- RCT
- randomised controlled trial
- RF
- red-free image
- RPE
- retinal pigment epithelium
- SD-OCT
- spectral domain optical coherence tomography
- SHTAC
- Southampton Health Technology Assessments Centre
- SLB
- slit-lamp biomicroscopy
- SLO
- scanning laser ophthalmoscope
- SROC
- summary receiver operating characteristic
- subRPE
- subretinal pigment epithelium
- TD-OCT
- time domain optical coherence tomography
- TN
- true negative
- TP
- true positive
- VA
- visual acuity
- VEGF
- vascular endothelial growth factor