Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0606-1066. The contractual start date was in August 2007. The final report began editorial review in April 2012 and was accepted for publication in May 2013. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Gary Ford has received honoraria for consultancy and educational activities (Lundbeck Ltd; Boehringer Ingelheim Ltd UK). Tom Quinn is a member of the steering group for the Strategic Reperfusion Early After Myocardial Infarction (STREAM) trial (Boehringer Ingelheim Ltd UK); Medicines Company for the European Ambulance Acute Coronary Syndrome Angiography (EUROMAX) trial and is a local collaborator/principal investigator for the 30 Day Study to Evaluate Efficacy and Safety of Pre-hospital vs. In-hospital Initiation of Ticagrelor Therapy in STEMI Patients Planned for Percutaneous Coronary Intervention (ATLANTIC) trial (AstraZeneca).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Watkins et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Stroke is a leading cause of mortality and disability worldwide. 1 Stroke is increasingly recognised as a time-dependent medical emergency in which rapid access to specialist care reduces death and dependency. 1 For every minute that a large-vessel ischaemic stroke is untreated, the average patient loses 1.9 million neurons. 2 Rapid access to emergency stroke care can reduce death or disability by enabling immediate provision of interventions such as physiological monitoring, stabilisation and thrombolysis. 3 In the UK, stroke is the third most common cause of death and the largest single cause of severe disability. 4 More than 140,000 people per annum will have a stroke, which will cost the NHS over £2.8B annually. 4 A key feature of effective stroke care is rapid access to specialised acute stroke services, including timely brain scanning. 4
Recombinant tissue plasminogen activator (rtPA) has also been shown to improve neurological outcome for patients with ischaemic strokes if given within 4.5 hours of onset. 5 Around 5% of stroke patients currently receive rtPA each year in England. 6 The cost of providing rtPA to 9% of all stroke patients has been calculated to give a potential net saving of > £16M a year. 4 However, delays in presentation and specialist assessment frequently prevent patients from receiving rtPA. Emergency medical dispatch sensitivity and positive predictive value (PPV) for identifying stroke is < 50%,7–9 and this is compounded by long delays in patients accessing emergency medical services (EMSs). 10 Studies have shown that activation of the EMSs is the single most important factor in the rapid triage and treatment of acute stroke patients. Stroke patients who access emergency health care via the EMSs, rather than by other routes, arrive at emergency departments (EDs) earlier and are more rapidly evaluated. 11–15 Between 12% and 70% of all stroke patients obtain first medical contact from the EMSs. 16–19
In the UK, people seeking urgent medical assistance call a universal number (999) and are connected to the EMS dispatch centre in closest proximity. All calls to the EMSs in the UK are digitally recorded for training and governance purposes. Once the call is logged and patient location established, an emergency medical dispatcher (EMD) will dispatch the closest ambulance. Calls to EMSs are triaged using the Advanced Medical Priority Dispatch System (AMPDS), a system also used widely in Europe and North America. EMD classification and prioritisation directly impact speed of ambulance response and the level of medical care (e.g. paramedic) sent. If the EMD suspects a time-critical condition such as stroke, an ambulance can be dispatched as a high priority (category A: currently up to a 19-minute response). The categories for response prioritisation are pre-determined by the Department of Health (DoH). However, identifying ‘true stroke’ from an EMS call is challenging. A recent Australian study reported that stroke was spontaneously identified by the caller in only 44% of EMS patients in whom the final ED diagnosis was confirmed as stroke. 20
The communication between the caller and emergency call handler is crucial in identifying suspected stroke in order to minimise delays and improve outcomes. Published reports on EMDs’ accuracy in recognition of acute stroke symptoms from callers’ descriptions are few. 21–23 Although problems with communication between callers and EMDs have been previously identified,23 no studies have explored the caller’s experience of making a 999 call at the onset of stroke symptoms. Further exploration of the words used by callers and the response this prompts from EMDs may lead to ways of improving emergency services for suspected stroke patients.
In this programme of research, we explored the interaction between the public and the EMSs during emergency calls for stroke in order to inform the content of stroke-specific online training for EMDs. Exploratory work included a retrospective records review; exploring callers’ experiences; and identifying the key words used by the public to describe stroke. 24 We developed the stroke-specific online training package for EMDs in order to increase their ability to recognise stroke (i.e. improve their sensitivity). Subsequently, we evaluated the impact of the training on the EMDs’ ability to recognise stroke. The programme consists of eight phases. The overall aim of the programme was to facilitate recognition of stroke by EMDs who play a key role in facilitating the public’s access to the emergency services. Objectives for each phase involved:
Phase 1: identifying a cohort of patients in hospital with a final diagnosis of stroke and exploring the identification and diagnosis of stroke in this cohort by ambulance dispatchers and ED staff.
Phase 2: exploring communication between the public and EMDs to explore the features that expedited or delayed people’s initial decision to contact EMSs.
Phase 3: exploring communication of the patients in phase 1 with EMDs to identify the ‘key indicator’ words for suspected stroke, and to compare these with the final diagnosis in hospital.
Phase 3a: identifying how patients’ consciousness level was questioned, described and interpreted by callers and EMDs.
Phase 4: comparing the words used by the public making 999 calls to the EMSs, the subsequent ambulance dispatch codes and final diagnosis in hospital, for stroke and non-stroke calls.
Phase 5: developing algorithms and protocols for ambulance and NHS Direct staff to assist in the identification of those with suspected stroke.
Phase 6: developing an online stroke-specific training package for EMDs informed by the previous phases.
Phase 7: implementing the training package and evaluating the content within one EMD control centre.
Phase 8: evaluating the impact of the training package on the recognition of stroke by EMDs.
Chapter 2 ESCORTT phase 1: the relationship between stroke symptoms and diagnosis at different points on the stroke pathway – a cohort study
Background
Stroke is a leading cause of mortality and disability worldwide. 1 In England, 110,000 strokes and a further 20,000 transient ischaemic attacks (TIAs) occur every year. 4 Stroke is increasingly recognised as a medical emergency for which rapid access to specialist care reduces death and dependency4 through the delivery of thrombolysis and other medical, nursing and therapy interventions. 3
Rapid access to specialist care relies on a layperson’s recognition of symptoms and an understanding of the need for an emergency response. The time from symptom onset to the first point of contact for any help accounts for much of the pre-hospital delay. 25 Raising public awareness and encouraging people to contact the EMSs when they suspect a stroke is difficult. 26 A more modifiable aspect of pre-hospital delays may be to raise awareness of stroke among EMS staff, particularly as up to 70% of patients (or someone on their behalf) who seek help from a health professional make their first medical contact with the EMSs. 16–18
The interaction of EMDs with callers is likely to play a key role in the early identification of stroke and initiation of a rapid EMS response. Published reports on the ability of EMDs to recognise stroke from callers’ descriptions suggest that EMD sensitivity and PPV for identifying stroke are < 50%. 7–9 Therefore, improving the communication between EMDs and callers to increase the likelihood that stroke is recognised would promote the initiation of the pre-hospital pathways that are known to expedite patients’ access to specialist assessment and treatment. 27
There is evidence to suggest that the EMSs are more likely to be contacted by the public for suspected stroke if the person’s symptoms include speech problems, weakness, decreased level of consciousness and dizziness/loss of co-ordination. 28 There is less evidence of an association between the different types of stroke symptoms and the response of the EMSs.
We have undertaken a programme of work with the aim of increasing the ability of EMDs to identify stroke. The study described here is the first phase of this programme, in which we describe the associations between patient characteristics, stroke symptoms and diagnoses at different points on the stroke pathway.
Methods
Aim
To explore how patient and stroke characteristics are associated with dispatch code; accuracy of dispatch code; ambulance diagnosis and how dispatch code was associated with time to arrival at hospital.
Setting
An ambulance service and three hospitals in the north-west of England.
Subjects and sampling
The subjects were patients arriving at hospital by ambulance during a 12-month period (1 October 2006 to 30 September 2007).
Inclusion criteria
Patients who had a diagnosis of suspected stroke by the EMS call handler and/or a final diagnosis of stroke in hospital.
Exclusion criteria
Patients whose general practitioner (GP) contacted the EMSs on their behalf and patients who had a stroke while already a hospital inpatient were excluded.
Sampling strategy
The sample was identified through a retrospective audit of hospital and EMS records. Hospital and EMS records were linked by patient name and date of birth. Stroke patients were identified from the hospital stroke register or the hospital coding system at the three sites with no register. Additional patients were identified by searching through ED records. Case notes were ordered for any patients identified from these records with stroke-like symptoms who were not on the register or the coding system; the case notes were reviewed and the diagnosis checked by an experienced stroke research nurse. We obtained EMS data for all patients identified in hospital. Independent of the data gathered in hospital, the EMSs also identified patients who had been dispatched as a stroke. Not all patients who were identified from hospital records arrived at hospital via the EMSs. However, all patients selected for the analysis had arrived at hospital via the EMSs. The hospital case notes were obtained for all patients identified through the EMSs. Patients were considered to have a final diagnosis of stroke if they were discharged from the ED and the ED records stated stroke; they were still on the stroke register at the time of discharge from hospital; or, where there was no register, their discharge letter stated a diagnosis of stroke.
This sampling strategy allowed calculation of the sensitivity and to some extent the PPV of the dispatch diagnosis.
Procedure
Data were recorded from the electronic patient report forms used by EMS staff, and from patients’ hospital case notes. EMS report forms provided data on dispatch code (dichotomised into stroke or not stroke and subsequently referred to as dispatch diagnosis); whether or not the Face Arm Speech Test (FAST)29 was performed in the ambulance (and the result); ambulance crew diagnosis (dichotomised into stroke or not stroke and subsequently referred to as ambulance diagnosis); and the times of call made to ambulance service, call passed to ambulance, ambulance arrival at the scene, ambulance leaving the scene and ambulance arrival at hospital. The time variables used in the analysis and how they were calculated are shown in Table 1 . From the case notes we recorded patient characteristics (age, sex); stroke history; pre-stroke status [Rankin scale score, dichotomised (0–2) vs. (3–5)]; consciousness level (alert vs. drowsy/stupor/comatose); neurological impairment; and final diagnosis (dichotomised into stroke or not stroke).
| Time variable | Method of calculation |
|---|---|
| Call to call passed | Time call passed to ambulance minus time call made to ambulance service |
| Call passed to arrival at scene | Time ambulance arrived at scene minus time call passed to ambulance |
| Arrival at to departure from scene | Time ambulance left scene minus time ambulance arrived at scene |
| Departure from scene to arrival at hospital | Time ambulance arrived at hospital minus time ambulance left scene |
| Call to arrival at hospital | Time ambulance arrived at hospital minus time call made |
Statistical analysis
Univariate analyses explored the association between diagnosis of stroke or not stroke (separately for dispatch and the ambulance) and patient characteristics, stroke characteristics, and time, using Mann–Whitney U-tests (ordinal and continuous variables) and chi-squared tests (dichotomous categorical variables). Multivariate analyses were made using multiple logistic regression, in which diagnosis of stroke or not stroke was the dependent variable, and characteristics (patient and stroke) were the independent variables. Separate models were developed for dispatch and ambulance diagnoses. Initially, all variables were entered into the models and removed using backward elimination (variables were removed if p < 0.10) until no further variables could be removed. The data reported are from the final iteration of the models. A range of approaches was taken for the modelling. The first model included only those independent variables that were significant in the univariate analysis (p < 0.10). Subsequent models included all variables regardless of whether or not they were significant in the univariate analysis; missing values included as a valid category. Missing values were included as a valid category only if they contributed > 5% of the data for a variable (see Tables 2 and 4 ). When modelling with the ambulance diagnosis as the dependent variable, a model was created first without the inclusion of dispatch diagnosis as an independent variable. Then, because the ambulance staff would have been aware of the dispatch diagnosis, this variable was added to the model. The effect of the inclusion of the dispatch diagnosis on the estimates of the patient and stroke characteristics effects provided an indication of whether observation or collection of these characteristics by the ambulance personnel provided additional diagnostic information beyond that obtained from the dispatch diagnosis. Variables in the final models were considered to have a significant association with diagnosis when p < 0.05. Data reported for the models included number of cases, p-values, odds ratios (ORs) and 95% confidence intervals (CIs). Analysis was performed using SPSS (versions 19 and 20; SPSS Inc., Chicago, IL, USA).
Ethical approval
Approval for this phase was granted by the Patient Information Advisory Group (now the National Information Governance Board for Health and Social Care), the Local Research Ethics Committee and by the Faculty of Health Ethics Committee at the University of Central Lancashire.
Results
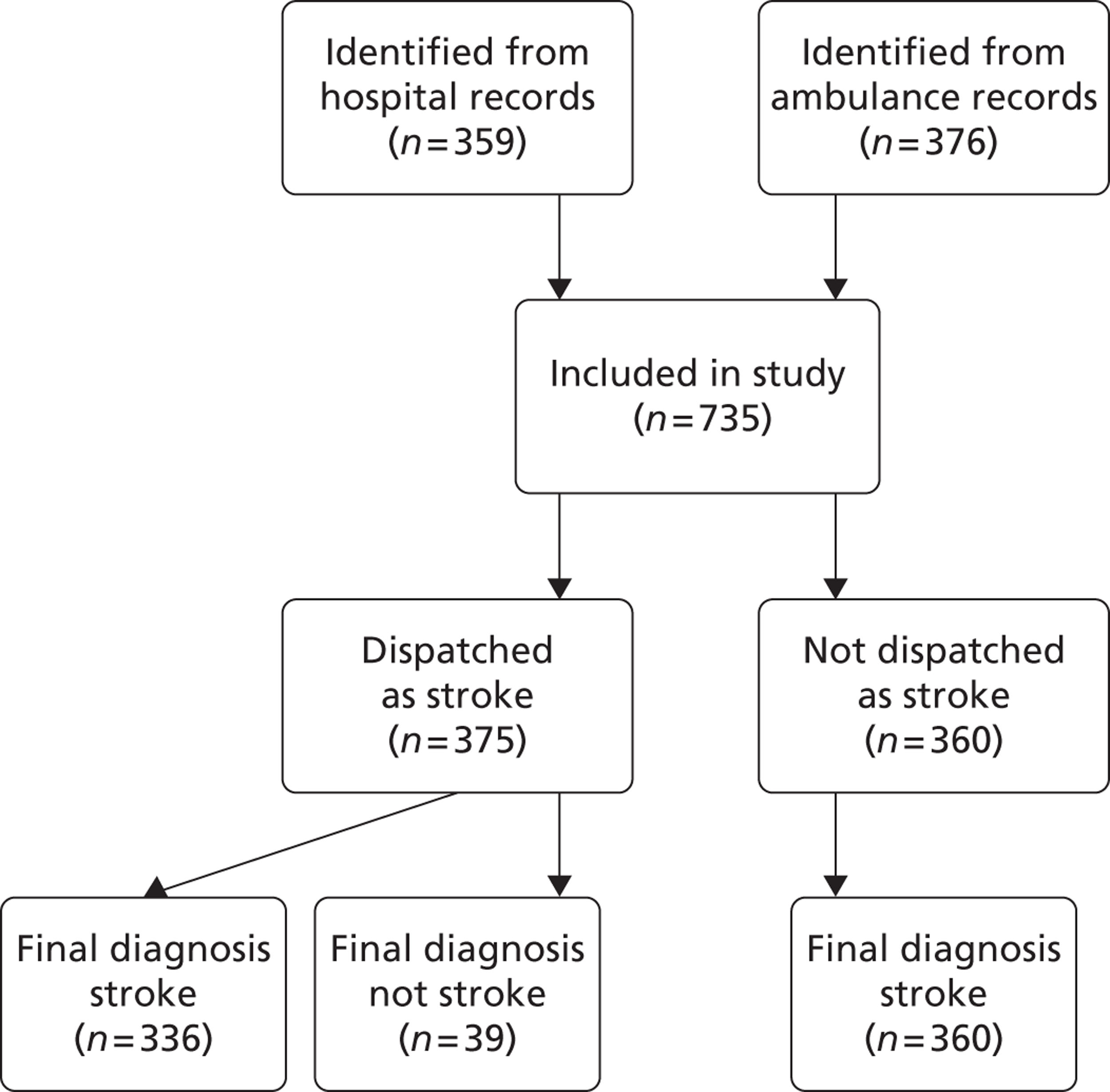
Seven hundred and thirty-five patients were included in this phase, of whom 359 (48.8%) were identified through hospital records ( Figure 1 ). The median age of the included patients was 78 years [interquartile range (IQR) 68–84 years]; 394 (53.6%) were male. Two hundred and forty (32.7%) patients had experienced a previous stroke and 178 (24.2%) patients had moderate to severe disability before the incident that led to the call to the EMSs ( Table 2 ). Six hundred and ninety-six (94.7%) patients had a final diagnosis of stroke and 166 (22.6%) patients died in hospital.
FIGURE 1.
Flow diagram of patients.
| Characteristic | Dispatched as stroke | Dispatched as not stroke | p-valuea | ||
|---|---|---|---|---|---|
| All patients (n = 375) | Final diagnosis not stroke (n = 39) | Final diagnosis stroke (n = 336) | Final diagnosis stroke (n = 360) | ||
| Median age (years) (IQR) | 77 (68–84) | 80 (69–87) | 77 (68–83) | 78 (68.25–84) | p = 0.50 |
| Sex | |||||
| Male (%) | 167 (44.5) | 10 (25.6) | 157 (46.7) | 171 (47.5) | p = 0.87 |
| Female (%) | 207 (55.2) | 29 (74.4) | 178 (53.0) | 187 (51.9) | |
| Missing (%) | 1 (0.3) | 0 (0) | 1 (0.3) | 2 (0.6) | |
| Previous stroke | |||||
| Yes (%) | 138 (36.8) | 18 (46.2) | 120 (35.7) | 102 (28.3) | p = 0.087 |
| No (%) | 197 (52.5) | 18 (46.2) | 179 (53.3) | 206 (57.2) | |
| Missing (%) | 40 (10.7) | 3 (7.7) | 37 (11.0) | 52 (14.4) | |
| Pre-incident Rankin scale score | |||||
| No symptoms to slight disability (0–2) (%) | 277 (73.9) | 22 (56.4) | 255 (75.9) | 262 (72.8) | p = 0.52 |
| Moderate to severe disability (3–5) (%) | 90 (24.0) | 15 (38.5) | 75 (22.3) | 88 (24.4) | |
| Missing (%) | 8 (2.1) | 2 (5.1) | 6 (1.8) | 10 (2.8) | |
| Consciousness level | |||||
| Alert (%) | 353 (94.1) | 35 (89.7) | 295 (87.8) | 244 (67.8) | p < 0.001 |
| Drowsy/stupor/coma (%) | 13 (3.5) | 3 (7.7) | 33 (9.8) | 108 (30.0) | |
| Missing (%) | 9 (2.4) | 1 (2.6) | 8 (2.4) | 8 (2.2) | |
| Unilateral face weakness at 24 hours | |||||
| Yes (%) | 226 (60.3) | 16 (41.0) | 210 (62.4) | 155 (43.1) | p = 0.003 |
| No (%) | 114 (30.4) | 18 (46.1) | 96 (28.6) | 120 (33.3) | |
| Missing (%) | 35 (9.4) | 5 (12.9) | 30 (9.0) | 85 (23.6) | |
| Unilateral arm/hand weakness at 24 hours | |||||
| Yes (%) | 257 (68.5) | 22 (56.4) | 235 (69.9) | 221 (61.4) | p = 0.79 |
| No (%) | 103 (27.5) | 12 (30.8) | 91 (27.1) | 91 (25.3) | |
| Missing (%) | 15 (4.0) | 5 (12.8) | 10 (3.0) | 48 (13.3) | |
| Unilateral leg/foot weakness at 24 hours | |||||
| Yes (%) | 230 (61.3) | 18 (46.1) | 212 (63.1) | 213 (59.2) | p = 0.50 |
| No (%) | 126 (33.6) | 15 (38.5) | 111 (33.0) | 98 (27.2) | |
| Missing (%) | 19 (5.0) | 6 (15.4) | 13 (3.9) | 49 (13.6) | |
| Speech problem at 24 hours | |||||
| Yes (%) | 236 (62.9) | 16 (41.0) | 220 (65.5) | 167 (46.4) | p = 0.005 |
| No (%) | 52 (13.9) | 9 (23.1) | 43 (12.8) | 62 (17.2) | |
| Missing (%) | 87 (23.2) | 14 (35.9) | 73 (21.7) | 131 (36.4) | |
| Mental impairment at 24 hours | |||||
| Yes (%) | 73 (19.5) | 14 (35.9) | 59 (17.6) | 77 (21.4) | p = 0.011 |
| No (%) | 156 (41.6) | 14 (35.9) | 142 (42.2) | 105 (29.2) | |
| Missing (%) | 146 (38.9) | 11 (28.2) | 135 (40.2) | 178 (49.4) | |
Pre-hospital pathway
Dispatch diagnosis
Three hundred and seventy-five (51.0%) incident calls to the EMSs were recorded as having been dispatched as a potential stroke or TIA (see Table 2 ). The sensitivity of the dispatch diagnosis was 48.3% (336/696) and the PPV was 89.6% (336/375). For the 696 with a final diagnosis of stroke, in the univariate analyses, those dispatched as stroke, compared with those not dispatched as stroke, were similar in age (p = 0.50) and sex (p = 0.87). Those dispatched as stroke were more likely to have had a previous stroke (p = 0.087), have a higher consciousness level (p < 0.001), have facial weakness (p = 0.003) or speech problems (p = 0.005) and have no mental impairment (p = 0.011). Pre-stroke disability (p = 0.52), arm/hand weakness (p = 0.79) or leg/foot weakness (p = 0.50) were not significantly associated with dispatch code.
When considered jointly in a multiple logistic regression model (260 cases in analysis), previous stroke (p = 0.009; OR 2.22, 95% CI 1.22 to 4.04), higher consciousness level (p = 0.001; OR 0.17, 95% CI 0.06 to 0.46), facial weakness (p = 0.001; OR 2.86, 95% CI 1.57 to 5.21), speech problems (p = 0.001; OR 3.07, 95% CI 1.59 to 5.93) and no mental impairment (p = 0.001; OR 0.35, 95% CI 0.19 to 0.65) were significantly associated with dispatch diagnosis and retained in the final model ( Table 3 ).
| Characteristic | Variables significant in the univariate analysis (n = 260) | All variables entered into the model (n = 249) | Missing data analysed as a valid category (n = 664) | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Previous stroke | 2.22 (1.22 to 4.04) | 0.009 | 2.09 (1.13 to 3.87) | 0.018 | 1.55 (1.07 to 2.23) | 0.019a |
| 0.98 (0.58 to 1.66) | 0.94b | |||||
| Lower consciousness level | 0.17 (0.06 to 0.46) | 0.001 | 0.19 (0.07 to 0.55) | 0.002 | 0.26 (0.16 to 0.41) | 0.001a |
| Unilateral face weakness | 2.86 (1.57 to 5.21) | 0.001 | 3.60 (1.86 to 6.97) | 0.001 | 1.72 (1.17 to 2.52) | 0.006a |
| 0.68 (0.38 to 1.20) | 0.18b | |||||
| Unilateral leg/foot weakness | 0.57 (0.30 to 1.08) | 0.085c | ||||
| Speech problems | 3.07 (1.59 to 5.93) | 0.001 | 3.09 (1.59 to 6.02) | 0.001 | 2.39 (1.46 to 3.93) | 0.001a |
| 1.59 (0.90 to 2.82) | 0.11b | |||||
| Mental impairment | 0.35 (0.19 to 0.65) | 0.001 | 0.42 (0.22 to 0.78) | 0.006 | 0.54 (0.34 to 0.87) | 0.011a |
| 0.72 (0.49 to 1.08) | 0.11b | |||||
In the alternative modelling, the association between dispatch diagnosis and both patient and stroke characteristics were similar (see Table 3 ). When all variables were initially entered into the model (249 cases in analysis), previous stroke (p = 0.018; OR 2.09, 95% CI 1.13 to 3.87), higher consciousness level (p = 0.002; OR 0.19, 95% CI 0.07 to 0.55), facial weakness (p < 0.001; OR 3.60, 95% CI 1.86 to 6.97), speech problems (p = 0.001; OR 3.09, 95% CI 1.59 to 6.02) and no mental impairment (p = 0.006; OR 0.42, 95% CI 0.22 to 0.78) were significantly associated with a dispatch diagnosis of stroke in the final model; leg weakness, although in the final model, was non-significant (p = 0.085; OR 0.57, 95% CI 0.30 to 1.08).
In the modelling where missing values were included as a valid category, a similar pattern of results was seen (664 cases in analysis). A higher level of consciousness (p < 0.001; OR 0.26, 95% CI 0.16 to 0.41) was associated with a dispatch diagnosis of stroke. Presence of a previous stroke (p = 0.019; OR 1.55, 95% CI 1.07 to 2.23) was significantly associated with a dispatch diagnosis of stroke, while, if this information was missing, the association was non-significant (p = 0.9; OR 0.98, 95% CI 0.58 to 1.66). Presence of facial weakness had a significant association with dispatch diagnosis (p < 0.001; OR 1.90, 95% CI 1.35 to 2.68); having missing facial weakness information had no significant association with dispatch diagnosis (p = 0.18; OR 0.68, 95% CI 0.38 to 1.20). Speech problems (p = 0.001; OR 2.39, 95% CI 1.46 to 3.93) were associated with an increased chance and mental impairment (p = 0.011; OR 0.54, 95% CI 0.34 to 0.87) was associated with a decreased chance of a dispatch diagnosis of stroke, and, where information on these characteristics was missing, the associations were marginally non-significant [p = 0.11 (OR 1.59, 95% CI 0.90 to 2.82) and p = 0.11 (OR 0.72, 95% CI 0.49 to 1.08) for speech problems and mental impairment respectively] (see Table 3 ). The variables age, sex, pre-stroke disability, arm/hand weakness and leg/foot weakness were not significant in any of the models.
Ambulance diagnosis
An ambulance diagnosis was available for 674 (96.8%) of the 696 patients with a final diagnosis of stroke ( Table 4 ). Overall, a FAST result was obtained and recorded for 314 (46.6%) patients, with a positive test result recorded for 295 of these (93.9%). There were 397 patients with an ambulance diagnosis of stroke: 280 (70.5%) patients had a FAST performed, with 269 (96.1%) cases being FAST positive. Of the remaining 277 patients with a non-stroke ambulance diagnosis, 34 (12.3%) patients had a FAST performed, with 26 (76.5%) cases being FAST positive.
| Characteristic | Ambulance diagnosis of stroke (n = 397) | Ambulance diagnosis of not stroke (n = 277) | p-valuea |
|---|---|---|---|
| Median age (years) (IQR) | 78 (69–83.5) | 76 (68–84) | p = 0.26 |
| Sex | |||
| Male (%) | 190 (47.9) | 133 (48.0) | p = 1.0 |
| Female (%) | 205 (51.6) | 143 (51.6) | |
| Missing (%) | 2 (0.5) | 1 (0.4) | |
| Previous stroke | |||
| Yes (%) | 125 (31.5) | 94 (33.9) | p = 0.64 |
| No (%) | 221 (55.7) | 151 (54.5) | |
| Missing (%) | 51 (12.8) | 32 (11.6) | |
| Pre-incident Rankin scale score | |||
| No symptoms to slight disability (0–2) (%) | 297 (74.8) | 199 (71.8) | p = 0.64 |
| Moderate to severe disability (3–5) (%) | 93 (23.4) | 69 (24.9) | |
| Missing (%) | 7 (1.8) | 9 (3.2) | |
| Dispatched as stroke | |||
| Yes (%) | 245 (61.7) | 82 (29.6) | p < 0.001 |
| No (%) | 152 (38.3) | 195 (70.4) | |
| Missing (%) | 0 (0) | 0 (0) | |
| Consciousness level | |||
| Alert (%) | 312 (78.6) | 211 (76.2) | p = 0.54 |
| Drowsy/stupor/coma (%) | 76 (19.1) | 59 (21.3) | |
| Missing (%) | 9 (2.3) | 7 (2.5) | |
| Unilateral face weakness at 24 hours | |||
| Yes (%) | 260 (65.5) | 94 (33.9) | p < 0.001 |
| No (%) | 88 (22.2) | 119 (43.0) | |
| Missing (%) | 49 (12.3) | 64 (23.1) | |
| Unilateral arm/hand weakness at 24 hours | |||
| Yes (%) | 307 (77.3) | 136 (49.1) | p < 0.001 |
| No (%) | 70 (17.6) | 105 (37.9) | |
| Missing (%) | 20 (5.0) | 36 (13.0) | |
| Unilateral leg/foot weakness at 24 hours | |||
| Yes (%) | 285 (71.8) | 128 (46.2) | p < 0.001 |
| No (%) | 89 (22.4) | 112 (40.4) | |
| Missing (%) | 23 (5.8) | 37 (13.4) | |
| Speech problem at 24 hours | |||
| Yes (%) | 258 (65.0) | 115 (41.5) | p < 0.001 |
| No (%) | 47 (11.8) | 55 (19.9) | |
| Missing (%) | 92 (23.2) | 107 (38.6) | |
| Mental impairment at 24 hours | |||
| Yes (%) | 68 (17.1) | 61 (22.0) | p = 0.10 |
| No (%) | 148 (37.3) | 90 (32.5) | |
| Missing (%) | 181 (45.6) | 126 (45.5) | |
Univariate analyses revealed that patients with an ambulance diagnosis of stroke were more likely to have facial weakness (p < 0.001), arm/hand weakness (p < 0.001), leg/foot weakness (p < 0.001), speech problems (p < 0.001) or no mental impairment (p = 0.10). Age (p = 0.26), sex (p = 1.0), previous stroke (p = 0.64) and having less pre-stroke disability (p = 0.64) or a higher consciousness level (p = 0.54) were not significantly associated with ambulance diagnosis (see Table 4 ).
When considered jointly in a multiple logistic regression model (277 cases in analysis), facial weakness (p < 0.001; OR 3.77, 95% CI 2.06 to 6.92), leg/foot weakness (p = 0.007; OR 2.26, 95% CI 1.25 to 4.09), speech problems (p = 0.008; OR 2.35, 95% CI 1.24 to 4.42) and no mental impairment (p = 0.017; OR 0.47, 95% CI 0.25 to 0.87) still had a significant association with an ambulance diagnosis of stroke and were retained in the model; arm/hand weakness was not included in the final model ( Table 5 ).
| Characteristic | Variables significant in the univariate analysis (n = 277) | All variables entered into the model (n = 239) | Missing data analysed as a valid category (n = 642) | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age | 1.02 (1.00 to 1.05) | 0.09a | ||||
| Unilateral face weakness | 3.77 (2.06 to 6.92) | 0.001 | 3.14 (1.64 to 6.01) | 0.001 | 2.46 (1.62 to 3.73) | 0.001b |
| 1.19 (0.66 to 2.13) | 0.57c | |||||
| Unilateral arm/hand weakness | 2.10 (1.38 to 3.18) | 0.001b | ||||
| 0.89 (0.42 to 1.92) | 0.77c | |||||
| Unilateral leg/foot weakness | 2.26 (1.25 to 4.09) | 0.007 | 2.80 (1.47 to 5.33) | 0.002 | ||
| Speech problems | 2.35 (1.24 to 4.42) | 0.008 | 2.35 (1.18 to 4.66) | 0.015 | 2.07 (1.24 to 3.46) | 0.006a , b |
| 1.16 (0.64 to 2.07) | 0.63a , c | |||||
| Mental impairment | 0.47 (0.25 to 0.87) | 0.017 | 0.54 (0.27 to 1.06) | 0.073a | 0.53 (0.32 to 0.87) | 0.013 |
| 0.82 (0.53 to 1.25) | 0.35 | |||||
In the alternative modelling, the association between patient and stroke characteristics and ambulance diagnosis varied slightly when all variables were initially entered into the model (239 cases in analysis). Facial weakness (p = 0.001; OR 3.14, 95% CI 1.64 to 6.01), leg/foot weakness (p = 0.002; OR 2.80, 95% CI 1.47 to 5.33) and speech problems (p = 0.015; OR 2.35, 95% CI 1.18 to 4.66) were still significant, whereas age (p = 0.090; OR 1.02, 95% CI 1.00 to 1.05) and mental impairment (p = 0.073; OR 0.54, 95% CI 0.27 to 1.06), although retained in the model, were non-significant (see Table 5 ).
In the modelling in which missing values were included as a valid category (642 cases in analysis; see Table 5 ), presence of facial weakness (p < 0.001; OR 2.46, 95% CI 1.62 to 3.73), arm/hand weakness (p < 0.001; OR 2.10, 95% CI 1.38 to 3.18), speech problems (p = 0.006; OR 2.07, 95% CI 1.24 to 3.46) and no mental impairment (p = 0.013; OR 0.53, 95% CI 0.32 to 0.87) were significantly associated with an ambulance diagnosis of stroke, and included in the final model. For all these variables, a missing value was not significantly associated with an ambulance diagnosis of stroke: facial weakness (p = 0.57; OR 1.19, 95% CI 0.66 to 2.13), arm/hand weakness (p = 0.77; OR 0.89, 95% CI 0.42 to 1.92), speech problems (p = 0.63; OR 1.16, 95% CI 0.64 to 2.07) and no mental impairment (p = 0.35; OR 0.82, 95% CI 0.53 to 1.25). The variables age, sex, previous stroke, pre-stroke disability, consciousness level, or leg/foot weakness were not significant in the model where missing values were included as a valid category.
The inclusion of dispatch diagnosis as an independent variable led to the exclusion of some variables from some of the final models ( Table 6 ). In the modelling that initially included only those variables significant in the univariate analyses (277 cases in analysis), the final model contained dispatched as stroke (p < 0.001; OR 4.82, 95% CI 2.63 to 8.81), facial weakness (p < 0.001; OR 3.29, 95% CI 1.79 to 6.06) and leg/foot weakness (p = 0.001; OR 3.01, 95% CI 1.58 to 5.75). Both speech problems and mental impairment were no longer included in the final model. Where missing values were included as valid categories for the independent variables (642 cases in analysis), dispatched as stroke was significant and included in the final model (p < 0.001; OR 3.71, 95% CI 2.56 to 5.37). Presence of facial weakness (p < 0.001; OR 2.27, 95% CI 1.48 to 3.50) and arm/hand weakness (p < 0.001; OR 2.55, 95% CI 1.65 to 3.96) were significantly associated with ambulance diagnosis of stroke and included in the final model. Speech problems (p = 0.008; OR 1.60, 95% CI 0.95 to 2.69), although not having a significant association with ambulance diagnosis, was also included in the final model. Mental impairment dropped out of the final model when dispatch diagnosis was included. Missing data for facial weakness (p = 0.43; OR 1.27, 95% CI 0.70 to 2.33), arm/hand weakness (p = 0.50; OR 1.31, 95% CI 0.60 to 2.90) and speech problems (p = 0.92; OR 1.03, 95% CI 0.58 to 1.83) were not significantly associated with ambulance diagnosis.
| Characteristic | Variables significant in the univariate analysis (n = 277) | All variables entered into the model (n = 239) | Missing data analysed as a valid category (n = 642) | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Unilateral face weakness | 3.29 (1.79 to 6.06) | 0.001 | 2.62 (1.34 to 5.11) | 0.005 | 2.27 (1.48 to 3.50) | 0.001b |
| 1.27 (0.70 to 2.33) | 0.43c | |||||
| Unilateral arm/hand weakness | 2.55 (1.65 to 3.96) | 0.001b | ||||
| 1.31 (0.60 to 2.90) | 0.50c | |||||
| Unilateral leg/foot weakness | 3.01 (1.58 to 5.75) | 0.001 | 3.95 (1.91 to 8.16) | 0.001 | ||
| Speech problems | 1.60 (0.95 to 2.69) | 0.08a , b | ||||
| 1.03 (0.58 to 1.83) | 0.92a , c | |||||
| Dispatched as stroke | 4.82 (2.63 to 8.81) | 0.001 | 6.48 (3.26 to 12.89) | 0.001 | 3.71 (2.56 to 5.37) | 0.001 |
Emergency department diagnosis
Of the 735 patients, an ED diagnosis was available for 666 (90.6%) patients, of whom a large majority 593 (89.0%) had a final diagnosis of stroke. This meant that comparisons between ED diagnosis (of stroke and not stroke) and patient and stroke characteristics had limited value, and so were not performed.
Sensitivity of patient and stroke characteristics
Given the sampling strategy we were able to properly explore only the sensitivity of the patient and stroke characteristics, and not the specificity, PPV or negative predictive value. The sensitivity of the characteristics can be seen in Table 7 . The characteristics with the highest sensitivities were ‘being alert’ and having no or only slight disability prior to the incident. The lowest sensitivities were seen for ‘previous stroke’ and ‘no mental impairment’.
| Characteristic | Sensitivity (%) | 95% CI (%) |
|---|---|---|
| Being female | 52.4 | 48.7 to 56.1 |
| Previous stroke | 31.9 | 28.4 to 35.4 |
| Having a pre-incident Rankin scale score of between 0 and 2 (no symptoms to slight disability) | 74.3 | 71.1 to 77.5 |
| Being alert | 77.4 | 74.3 to 80.5 |
| Unilateral facial weakness | 52.4 | 48.7 to 56.1 |
| Unilateral arm/hand weakness | 65.5 | 62.0 to 69.0 |
| Unilateral leg/foot weakness | 61.1 | 57.5 to 64.7 |
| Speech problem | 55.6 | 51.9 to 59.3 |
| No mental impairment | 35.5 | 31.9 to 39.1 |
Effect of diagnosis on time variables from emergency medical services call to emergency department arrival
Of the 735 patients with a final diagnosis of stroke, data were available for each of the time points in Table 8 for 688 (93.6%) patients. For those with a final diagnosis of stroke, the time variables were compared between those dispatched as stroke with those dispatched as not stroke (see Table 8 ). Relative to the initial call, patients dispatched as stroke arrived at hospital earlier than those not dispatched as stroke.
| Time intervals | All patients (IQR) (n = 688) | Patients dispatched as stroke (IQR) (n = 332) | Patients dispatched as not stroke (IQR) (n = 356) | Difference in medians (95% CI) |
|---|---|---|---|---|
| Call, to call passed Time from 999 call to call information passed to the ambulance crew |
0 (0–2) | 0 (0–2) | 0 (0–2) | 0 (0 to 0) |
| Call passed, to arrival at scene Time from call information passed to the ambulance crew to arrival of the ambulance at the scene |
8 (5–12) | 8 (5–11) | 8 (5–12) | −1 (−1 to 0) |
| Arrival at, to departure from scene Time from arrival of the ambulance at the scene to departure of the ambulance from the scene |
19 (13–25) | 17 (12–23) | 20 (14–26) | −3 (−4 to −1)a |
| Departure from scene, to arrival at hospital Time from departure of the ambulance from the scene to arrival of the ambulance at hospital |
11 (8–15) | 11.5 (8–16) | 11 (7–14) | 1 (0 to 2) |
| Call, to arrival at hospital Time from 999 call to arrival at the ambulance at hospital |
41 (34–51) | 40 (33–48) | 43 (35–53) | −3 (−5 to −1)a |
Discussion
This is the largest study reported to date to describe how the characteristics of suspected stroke patients are associated with a diagnosis of stroke at different points on the acute stroke pathway. We found that for people with a final diagnosis of stroke, the characteristics most consistently associated with a dispatch diagnosis of stroke were previous stroke, consciousness level, facial weakness, speech problems and lack of mental impairment. Therefore, if a caller describes any of these characteristics, there is an increased likelihood that the person has had a stroke. When patients are correctly dispatched as stroke, time from call to arrival at hospital is reduced.
The clear association between speech problems and a stroke diagnosis is consistent with other studies. Speech problems have been found to be one of the symptoms likely to prompt the public to contact the EMSs. 15,28 During calls to the EMSs for suspected stroke, speech problems have been the most frequently reported symptoms. 30 Similar to the findings of this phase, it has also been reported that speech problems were associated with a correct ambulance diagnosis of stroke. 20 Speech problems also affect the speed of response by the public: a rapid call (within 1 hour) to the EMSs was found to be more likely when speech problems were present. 20 The association between speech problems and stroke would clearly be important to include in any training package.
One of the other stroke symptoms we found to be associated with a dispatch diagnosis of stroke was facial weakness. This is consistent with the symptoms included in the FAST29 and Recognition of Stroke in the Emergency Room (ROSIER)31 assessments. Facial weakness has also been associated with unprompted stroke recognition by EMDs. 20
We found only a weak association between lower limb weakness and a dispatch diagnosis of stroke. This was unexpected because unilateral weakness is one of the main symptoms of stroke and lower limb weakness is included in the ROSIER assessment. Moreover, in other studies, the onset of limb weakness has been found to precipitate a call to the EMSs. 28 This finding may be explained by the way in which callers described symptoms to the EMDs. We have found previously that leg and arm weakness are rarely reported (< 5% of cases) as such during a call to the EMSs. 24 Instead, motor problems are often reported by their consequences, such as a person collapsing, falling to the floor or being found on the floor, or dropping or not being able to hold an object. 24
The patient and stroke characteristics most often associated with an ambulance diagnosis of stroke were facial weakness, speech problems, no mental impairment and either leg/foot or arm/hand weakness. This fits in with previous research, which found that ambulance personnel are more likely to identify total anterior circulation strokes,32 whose symptoms include speech problems and motor and/or sensory deficit of at least two areas of face, arm or leg. This finding could suggest that speech problems, facial and arm/hand weakness are key stroke symptoms; these symptoms are usually assessed using the FAST. This does not mean that leg and foot weakness are not useful symptoms when diagnosing stroke. The FAST was not always undertaken in the ambulance, and the reasons for this lack of assessment were not documented in the EMS records. However, the high proportion of FAST-positive results suggests that ambulance staff tended to perform the FAST when they suspected stroke. A dispatch diagnosis of stroke was associated with facial weakness, and yet both dispatch diagnosis of stroke and facial weakness were independently associated with an ambulance diagnosis of stroke. This gives further support to the value of facial weakness when diagnosing stroke over the telephone or in the ambulance.
The modelling of the ambulance diagnosis initially included only patient and stroke characteristics as independent variables (as for the dispatch diagnosis). However, because ambulance staff would have been aware of the dispatch diagnosis, it was felt that modelling should be extended to include dispatch diagnosis in the modelling of ambulance diagnosis. When dispatch diagnosis was included as an explanatory variable in the modelling of ambulance diagnosis, the ORs for speech problems and mental impairment were attenuated, resulting in the terms no longer being significant, independent, explanatory variables for ambulance diagnosis. Both facial and leg/foot weakness remained in the models, but with differing effects on their ORs. The ORs for facial weakness were attenuated slightly, whereas that for leg/foot weakness increased slightly. The dispatch diagnosis demonstrated associations with both facial and leg/foot weakness as well as speech problems and mental impairment. The association between these last two variables and dispatch diagnosis may explain why they were not included in all of the ambulance diagnosis models when dispatch diagnosis was included. This may also reflect differences around the reporting of characteristics. Speech and mental impairment may be more likely or more clearly reported over the telephone. This contrasts with weakness, which may be described by its consequences. 24 For example, someone with leg/foot weakness, will often describe a fall, which is a consequence of leg weakness rather than reporting the actual leg/foot weakness. Facial weakness may be described over the telephone but it may be more observable in person by, for example, ambulance staff, which may explain some attenuation of the ORs.
The inclusion of missing data as a valid category in the models attenuated the ORs for the presence or absence of the characteristic. The characteristics were still present in the final models, meaning that the interpretation of the association between the characteristics and diagnosis was not greatly affected by missing data. The OR for the missing values of any of the characteristics tended towards unity (compared with presence of the characteristic), suggesting that the ‘true’ values of the missing data are likely to be a mixture of the presence or absence of that characteristic. There were some exceptions to this pattern. When previous stroke was modelled with dispatch diagnosis the OR was 0.98, suggesting that the ‘true’ value for missing data for this characteristic is likely to be absence of this characteristic. If someone has had a previous stroke it is highly likely that this would be known, whereas if there was no knowledge of a previous stroke, this is likely to mean that a person has not had stroke. There was a similar pattern with the association between arm/hand weakness and ambulance diagnosis. It is possible that if this characteristic is absent it is more likely to be not recorded than if it was present. For facial weakness, the OR for the missing value category was smaller than unity, albeit non-significantly smaller; this also suggests that those with missing data were typically those without facial weakness, and that the reason data were missing was non-assessment, probably because ambulance personnel did not suspect stroke.
The sensitivity of the dispatch diagnosis was just under 50%, which is similar to that reported in other studies. 7–9 If this is to be increased, it is necessary to identify those symptoms likely to have a high sensitivity in relation to a final diagnosis of stroke. The characteristics with the highest sensitivities were having no to only slight pre-stroke disability, and being alert. The latter characteristic is consistent with reduced consciousness being scored as a negative sign for stroke in the ROSIER assessment. In terms of positive signs, the sensitivity of unilateral weakness in the arm/hand or leg/foot was over 60% and these signs should be assessed. The sensitivity of the other signs consistent with a diagnosis of stroke, facial weakness and speech problems, was only just over 50%. This contrasts with the results of the modelling in which facial weakness and speech problems were consistently associated with stroke diagnoses. This may indicate the need to consider multiple symptoms when diagnosing stroke.
In our sample, 29.5% were identified as having a suspected stroke by ambulance personnel, despite having no record of a positive FAST. A possible explanation for this is the lower sensitivity of FAST to identify posterior circulation strokes. If non-FAST symptoms such as diplopia or visual field defect were present, ambulance personnel might reasonably have suspected stroke despite the absence of a positive FAST.
It is known that EMD dispatch classification and prioritisation directly impact the speed of ambulance response and the level of medical care sent. If the EMD suspects a time-critical condition such as stroke, an ambulance can be dispatched as a high priority; this is currently category A and up to a 19-minute response. The results of this phase showed that the times from the EMS call through to arrival of the ambulance at hospital were significantly shorter (except for time from departure at scene to arrival at hospital) for those patients with a final diagnosis of stroke who were dispatched as stroke. The median time from call to arrival at hospital was 3 minutes shorter for those dispatched as stroke than for those dispatched as not stroke. This gain appeared to be mainly attributable to reduced time at the scene, which could be because of ambulance staff expecting to deal with a stroke. The CI indicated that this difference was likely to be between 1 and 5 minutes. This potential reduction of up to 5 minutes in the time for a stroke patient to reach hospital if correctly dispatched highlights the potential importance of an accurate dispatch diagnosis so that an ambulance is dispatched with an appropriate level of priority. This would therefore facilitate early presentation and rapid specialist treatment, particularly thrombolysis, the benefits of which are highly time dependent. 3
Our findings are therefore consistent with those of other studies, which have shown that activation of the EMSs is the single most important factor in the rapid triage and treatment of acute stroke patients. Stroke patients (or those who act on their behalf) who activate the EMSs arrive at EDs earlier and are more rapidly evaluated. 11–15
Limitations
The retrospective nature of this phase has given rise to some limitations. In terms of the sampling, it would have been ideal if we could have prospectively studied every person making a call to the EMSs and determined their subsequent diagnosis. Clearly this was impractical, so instead we designed a sampling strategy utilising data from EMSs, EDs, hospital records and stroke registers. This was intended to maximise capture of records of patients going to hospital via the EMSs and in whom there was a suspected or confirmed diagnosis of acute stroke. One disadvantage of this strategy is that our sample was biased towards confirmed stroke patients. Also, the diagnosis of stroke was based on information recorded in the case notes. Although there is no reason to suspect that a high proportion of cases had been misdiagnosed, the findings would have been more robust if there had been a mechanism in place for verification of a sample of the diagnoses by an independent examination. The retrospective audit of hospital and EMS records included patients arriving at hospital by ambulance during a 12-month period (1 October 2006 to 30 September 2007). During this time AMPDS version 11.3 was used by EMDs across England. Therefore, the findings from this phase may apply only to EMDs using this version of AMPDS. Finally, the symptoms used in the analyses of dispatch diagnoses were not necessarily what the callers had reported.
Logistic regression is one of a number of techniques that could have been applied to investigate how patient characteristics and symptoms were related to diagnosis. The approach used did not consider how these clustered together, so the resulting model might not have been optimal for predictive purposes. Consideration of the use of alternative classification approaches, such as classification and regression trees and neural networks, would be recommended if the aim were to develop an algorithm predicting diagnosis. However, the purpose of this phase was simply to investigate which patient and stroke characteristics are associated with dispatch code, accuracy of dispatch code and ambulance diagnosis, for which logistic regression was the most appropriate and simple approach.
This study is the first phase of a programme of work with the ultimate aim of improving recognition of stroke by EMDs. This phase has contributed to the programme by identifying those symptoms that are strongly associated with a diagnosis of stroke.
Conclusion
Of all the symptoms of stroke that may be described to EMDs, facial weakness and speech problems are highly likely to indicate that the caller is describing a stroke. Although individual symptoms can indicate a stroke, the likelihood of a stroke is higher when more than one symptom is present. These findings will be synthesised with the findings from subsequent phases and included in training described later in this report aimed at developing EMDs’ awareness and recognition of stroke symptoms.
Summary
The findings from phase 1 have suggested that facial weakness and speech problems are highly likely to indicate that the caller is describing a stroke. Although these problems were present, it is unknown whether or not they were communicated to the EMD. The communication between the caller and the EMD is crucial in identifying suspected stroke and minimising delays. 33 Although problems with communication have been previously identified,23 no studies have explored callers’ experience of making a 999 call at the onset of stroke symptoms. Therefore, the next phase (phase 2) will aim to identify the features that expedited or delayed people’s initial decision to contact EMSs at the onset of acute stroke, and to explore callers’ experiences of the call.
Chapter 3 ESCORTT phase 2: callers’ experiences of making emergency calls at the onset of acute stroke – a qualitative study
Background
In the UK, EMDs currently use the AMPDS to categorise ambulance response and decide on the level of medical care sent. The system is effective at ruling out acute stroke in people with other conditions. However, it is poor at correctly identifying acute stroke, with > 50% of people subsequently confirmed as having had a stroke being misclassified as presenting with another condition by the EMD. 9 During a 999 call, the communication that takes place between the caller and the emergency call handler is crucial in the identification of suspected stroke. Correct identification of acute stroke by the EMD minimises delays and improves patient outcomes. Problems with communication have been identified previously. 23 However, callers’ experiences of making a 999 call at the onset of stroke symptoms have not been previously explored. The purpose of this phase was to explore callers’ experiences of the 999 call including the factors that influence their decisions to contact EMSs at the onset of stroke.
Methods
Aim
The aim of this phase was to identify the features that expedited or delayed people’s initial decision to contact EMSs at the onset of acute stroke, and to explore callers’ experiences of the call.
Study design
In order to fulfil the aim of the study to explore people’s experiences in depth, a qualitative methodology was used. Semi-structured interviews were undertaken to identify perceptions, behaviour, practice and process. Content analysis was performed to identify themes.
Setting
Two hospitals in the north-west of England (total population approximately 810,000) serving approximately 1600 new stroke patients each year.
Selection of participants
A criterion-based purposive sample was identified to select informants who would enable us to study issues of central importance to the purpose of the research34 (i.e. why and how people call 999 following stroke). Using the stroke register at the hospital and medical notes, subjects were selected if they had a confirmed diagnosis of acute stroke and arrived via ambulance after contacting EMSs, during a 3-month period (10 October 2008 to 22 January 2009). Subjects were excluded if their admission was arranged by their GP, they attended the ED directly (not via the ambulance service), the diagnosis of stroke was not confirmed by the stroke physician, or they had a stroke while in hospital. Relatives or carers of patients who had died or remained critically ill were not approached. The person who had made the initial call to the EMSs (999 call), after the onset of stroke symptoms, was identified as the potential participant in the study. This could be the patient, a relative or another person.
Procedure
A member of the clinical team confirmed that the patient met the inclusion criteria for the study (arrived at hospital by ambulance; diagnosis of stroke confirmed by a stroke physician; patient not critically ill or deceased). Patients (or a consultee for those who had significant cognitive impairment) were then approached about the study by a member of the clinical team during their inpatient stay, within a maximum of 2 weeks after admission. The person who had made the initial call to EMSs (the patient, their relative or another person) was then invited to take part in the study and was given at least 24 hours to decide if he or she would like to participate. At this point, a researcher would approach the participant to confirm participation and obtain written informed consent. Anonymity and confidentiality of data generated by participants were discussed, and participants gave written consent only once informed and satisfied that any questions they had were answered. The interviews were conducted face to face using a semi-structured interview guide, either in a quiet, private room on the hospital stroke unit or at the caller’s home. Interviews were digitally recorded.
Data collection
An interview schedule was developed by the authors and was piloted with input from patient representatives to ensure clarity and validity. Subsequent to the piloting, a final interview guide of 19 questions was developed. This consisted of explorative open-ended questions such as ‘How did you explain to the person answering the 999 call about what was happening?’ Brief details about the caller were also collected at the time of the interview (age, sex and relationship to the patient).
Primary data analysis
Interview recordings were initially transcribed verbatim. Analysis was undertaken using a constant comparative method in order to identify patterns and relationships within the data. 35 Open codes were created for each interview, and were then clustered with each other in order to create broader categories. These categories were then grouped to develop themes inductively. Each interview was analysed independently by two of three researchers; discrepancies were resolved by discussion with the third researcher. The researchers also met regularly to discuss emerging themes in order to ensure a consistent approach to data collection and coding. The themes were reviewed by patient representatives. Themes were supported by reporting the most relevant and significant participant quotes.
Ethical approval
Approval for this phase was granted by the Local NHS Research Ethics Committee.
Results
Table 9 outlines the characteristics of the callers who participated, their relationship to the patient, and action taken.
| Characteristic | Participants (n = 50) |
|---|---|
| Median age (years) | 62 |
| Age range (years) | 24–83 |
| Female (%) | 68 |
| Caller (n) | |
| Patient | 1 |
| Relative/friend/neighbour (n) | 41 |
| Other bystander (n) | 6 |
| Personal medical alert system (n) | 2 |
| Actiona | |
| Called EMSs immediately (n) | 30 |
| Delayed contacting EMSs (n) | 20 |
Over half of the participants called the EMSs immediately (see Table 9 ). Of the 20 who did not seek help from the EMSs immediately, initial help was sought from family or friends (n = 9), GP (n = 8), NHS Direct (n = 1) or by calling EMSs but after a delay of > 2 hours (n = 2).
Four central themes were identified. Two of these related to the initial decision to contact EMSs at the onset of stroke: perceived seriousness, and seeking and receiving lay or professional advice. Two themes related to communication between the caller and the call handler: description of stroke symptoms by the caller and emotional response to acute stroke symptoms. Verbatim quotes in the following section are followed by the caller’s relationship to the patient, and the caller’s gender and age.
Perceived seriousness
Twenty-five (50%) callers recognised that the symptoms were stroke related and serious, and contacted EMSs immediately. They based this on previous experience of stroke (n = 13), stroke knowledge (n = 6) or a combination of both (n = 6).
Because, well, there’s nothing else can be done you know, I could see how, you know, serious it was.
Neighbour, male, age 45 years
You know it’s something quite serious when you can’t feel that right side or left side.
Daughter-in-law, age 43 years
I just thought it’s got to be 999. I mean I’m one of these who wouldn’t call an ambulance cause I think, you know, for little things, but I thought, just to look at him I thought, no it’s got to be 999.
Daughter, age 59 years
I said, told him straight, I said you’ve had a stroke and you’ll have to go into hospital.
Friend, male, age 50 years
So I got the ambulance because me mother used to have mini strokes.
Wife, age 50 years
A further nine (18%) callers, although they recognised that the symptoms were stroke related, were unsure of the seriousness of the symptoms and sought further advice before contacting EMSs. These callers either contacted a family member (n = 4) or the GP (n = 5) for support and advice before calling 999:
I rung the (GP) surgery and the doctor said, ‘ambulance’ straightaway.
Friend, male, age 69 years
So first of all I rang actually primary care, and once I gave them the symptoms, they said just ring 999 immediately, which I did.
Wife, age 70 years
Well I decided right away to ring the doctor. He always said if ever we needed him, to ring him you see. But it was a bad time . . . I rang the health centre up and the lady answered it, and she said the doctor really was busy at the time, he had a surgery that morning . . . He (the GP) didn’t phone me back for about 45 minutes.
Wife, age 83 years
I knew it was an emergency ish but kind of wanted a second opinion.
Husband, age 66 years
The remaining 16 (32%) callers stated that they did not recognise the symptoms as stroke. Five (10%) of these callers did, however, recognise that the problem was sufficiently serious to warrant calling 999 immediately. Their concerns included suspected heart attack, hypoglycaemic attack or lack of movement. Nine (18%) callers were unsure of the seriousness of the situation, and either delayed calling 999 (n = 2) or sought further lay advice (n = 4) or professional advice from the GP (n = 3) before calling 999:
I thought at first his leg had gone to sleep, you know, when you lie in a funny position.
Wife, age 80 years
I told them (EMD) what’d happened, I’d collapsed and I said in my opinion I was having a heart attack. I said I’m just having some kind of a funny do like a heart attack and can you get me an ambulance.
Patient, age 67 years
She was on the floor and . . . I knew she wasn’t well because she is an independent woman.
Daughter, age 51 years
I thought it was the same as a diabetic’s hypo. It was the same symptoms really.
Husband, age 66 years
Two callers (4%) recognised that the situation was serious but still sought further advice before calling 999. One of these callers contacted NHS Direct (a nurse-led telephone helpline) because they did not want to waste the emergency services’ time, and the other contacted a relative and subsequently their GP.
I rang them (NHS Direct) . . . and said she’s had a funny turn . . . and they said right well we’re going to put you straight through to an ambulance.
Wife, age 45 years
Seeking and receiving lay or professional advice
Eighteen (36%) callers were unsure about the significance of the symptoms and sought advice and clarification from others before dialling 999. Sources of advice included friends or relatives (n = 9), of whom two went on to ask for further advice from the GP or the ED, primary care services (n = 8), and NHS Direct (n = 1). Two or three additional steps were taken before the 999 call was eventually made (see Appendix 1 ), with each extra step having the potential to introduce further delay.
We phoned the doctor to find out if it was a stroke or not because obviously the advert that is running at the moment doesn’t really highlight what my husband was having, apart from the slurred speech.
Daughter-in-law, age 43 years
I said mum don’t wait for the doctor, I said I think we had better ring for the ambulance.
Daughter, age 61 years
Although participants recognised that they were delaying emergency help by seeking advice from sources other than EMSs they often tried to justify this delay:
Rather than calling the emergency services out I just wanted to wait that few minutes or get somebody else to tell me that was, you know, get a second opinion.
Husband, age 66 years
I don’t like wasting anyone’s time, you always think people are always busy; you don’t want to waste people’s time . . . So I thought if I rang NHS Direct first and I’ll tell them the symptoms and see if they can give me their advice.
Daughter-in-law, age 43 years
Of the eight (16%) callers who sought help from primary care, seven received telephone advice to contact EMSs immediately:
So first of all I rang actually Primary Care (GP), and once I gave them the symptoms, they said just ring 999 immediately, which I did.
Wife, age 45 years
So the lady (GP receptionist) said that she’d put me through to another doctor and so I spoke to the doctor, and he was quite nice with me, and he said, well the best thing really you can do is to dial 999 and get the ambulance.
Wife, age 83 years
I phoned our own doctor and when I got through to the receptionist she said oh you better phone 999.
Wife, age 64 years
One caller initially made an appointment for the patient to see the GP. Following deterioration of the patient’s condition, and then making a second phone call to primary care, she was advised to call 999 immediately.
I phoned the GP and made an appointment . . . and then she (the patient) seemed to pick up a bit and I spoke to the GP and she said oh I’ll just come out and see her. Ten minutes later she went bad again, you know she seemed to deteriorate so I phoned the GP back and she said phone an ambulance now so I phoned the ambulance and they came out.
Carer, female, age 32 years
Description of stroke symptoms by the caller
Thirty-four (68%) callers stated during the interview that they had suspected that the person was having a stroke, but only 27 (54%) recalled mentioning the word ‘stroke’ to the call handler:
I had been told to ring you straight away, my wife’s having a stroke.
Husband, age 54 years
I said I think it’s a stroke I’m not 100% sure but this is what happened, he’s sat with me now, he’s not talking.
Carer, female, age 45 years
Of the 27 callers who mentioned ‘stroke’ to the call handler, 24 also reported that they had described other stroke-specific symptoms. These included movement problems or numbness on one side (n = 19), altered speech (n = 16), facial droop (n = 11) and a fall (n = 6):
I think he’s had a stroke . . . his mouth’s drooped to one side, he’s slurring his speech and he can’t move one side of his body.
Neighbour, male, age 45 years
I said I was ringing on behalf of my husband who’s complaining of a terrific headache and lost numbness, that feeling such like in his right arm and leg and that his head ache was on the left hand side.
Wife, age 71 years
No matter how many times I’ve rung 999 . . . I still end up getting tongue tied and jumbled up. Its nerves isn’t it? Do you know what I mean? So I probably just explained what (patient’s name) was displaying . . . The lean on to one side, unresponsive to voices, distinctly dropped mouth, very--, hard to describe it.
Carer, 47, age female years
So I said that she has fallen but it looks a bit, her mouth’s funny, I said her mouth’s funny and her arm’s weird.
Daughter, age 51 years
Participants also recalled mentioning symptoms which were less stroke-specific, such as headache, collapse, funny turn, unable to get out of bed and unresponsive. Five (10%) callers had reported suspected diagnoses other than stroke such as heart attack. Eighteen (36%) callers were unsure of what they had reported to the call handler.
Callers’ emotional response to acute stroke symptoms
Twenty-six (52%) callers described their emotional response to the onset of stroke. This included feelings of panic (n = 7), nervousness (n = 4) and fear (n = 3). Nine callers described feelings of frustration, worry and upset. Three callers described the need to overcome their emotions and to stay calm:
You know nothing about it, you start panicking.
Husband, age 76 years
The fact that they (ambulance) came so quickly was great on our part really because like I say she (wife) was struggling . . . and I was starting to panic a bit.
Husband, age 66 years
I tend to get a bit panicky and I get a bit out of breath and, the gentleman, the men (ambulance crew) that came first he sat me down on the settee . . . and said you sit there you’re having a panic attack and I don’t want to take two of you in.
Wife, age 68 years
We were both frightened.
Wife, age 68 years
Callers recognised that there was a potential conflict for the EMS call handler between dealing efficiently with the call and with acknowledging the caller’s emotional distress:
You have to explain everything, you know, what’s going on, her age, date of birth, address, name . . . but you’re panicking thinking please don’t just ask these questions, get here straight away.
Daughter-in-law, age 45 years
However, the call handler’s efficient manner was in itself supportive, and helped the caller to stay calm. Some callers also felt that the call handler gave emotional support in addition to practical advice:
Yeah she was very reassuring with her tone of voice . . . you know, managed to keep me calm because normally I start panicking a bit.
Wife, age 50 years
Just sort of reassuring us and saying if you need us come straight back to us, but the ambulance will be with you in a few minutes sort of thing.
Daughter, age 51 years
She said just reassure him that he’s alright.
Wife, age 50 years
It was also identified that once the call was made, the call handler took responsibility for the situation:
She does calm you down and help you cope with the situation, you feel like you’re just going with the flow.
Wife, age 69 years
I handed the phone over to my husband while I went to see to my mum and the chap in the other end of the phone stayed on the line the whole time and told my husband to tell me what to do.
Daughter, age 42 years
Callers found it helpful to be assured that the ambulance was on its way throughout the call:
They were speaking to me all the time, telling me the emergency people were on their way now . . . it gives you confidence, it does really.
Husband, age 76 years
However, it was also felt that the call handler’s assurance that the ambulance was en route was not always clear:
I don’t recall her actually saying an ambulance is on the way . . . they ask you all these questions and you’re thinking . . . have you decided yet, are you sending one?
District nurse, female, age 33 years
Discussion
Thirty participants sought first medical contact from the EMSs, with the remainder initially contacting primary medical services or a relative or friend. Only one patient (2%) called for an ambulance themselves, consistent with previous studies. 21,22 Patients who were alone often contacted a family member, who then sought further help. 36 Nine participants (18%) contacted a family member or friend for help.
People’s emotional response to the onset of stroke symptoms was a theme that emerged during data collection, with 52% of callers describing feelings such as panic, nervousness and fear. Participants contacted primary care, family or friends in order to receive advice or support about the course of action that should be taken. This was a common cause of delay in contacting EMSs.
The efficiency of the call handler was found to be reassuring. Emotional support and practical advice were both important to callers. However, some callers were unsure whether or not an ambulance had actually been dispatched during the call.
Although 68% of the callers suspected stroke, only 54% of the sample reported this to the call handler, consistent with previous findings that stroke is reported as the presenting problem in 44% of ambulance calls leading to a final diagnosis of acute stroke. 20 Currently, AMPDS algorithms require the call handler to ask questions about ‘what has happened’ to the patient, rather than asking what the caller suspects may be the diagnosis. This may make it more difficult for callers to report their suspicion of stroke.
Previous research into decision-making processes in people with symptoms of myocardial infarction has identified that prior knowledge of symptoms alone is not enough to initiate prompt action. 37 A recent review of the public’s awareness of stroke found that although between 27% and 100% of participants stated that they would call the EMSs, only 18% had actually done so. 26 Emotional response and context appear to be influential in deciding to seek emergency help. 38
Limitations
This design of this phase does have some limitations. This phase did not set out to identify and measure time delays between onset of symptoms and making an EMS call, as it was intended instead to study the caller’s experience of the process of seeking emergency help for acute stroke. Although participants were interviewed soon after the event, the effects of recall bias may have influenced the findings. Participants were representative in terms of the age and sex distribution of people who call 999 for suspected stroke. However, it was particularly difficult to contact and recruit callers who were unrelated to the patient, and this group is likely to be under-represented. Furthermore, relatives or carers of critically ill or deceased patients were not approached to take part. Therefore, the most serious strokes were not included and are under-represented. This phase was concerned only with patients who accessed EMSs via a 999 call in response to stroke symptoms. Further work would be needed to examine the experiences of patients who accessed health care by other routes such as direct presentation to ED, accessing other primary care services, or who did not seek health advice.
Conclusion
This is the first study to examine in detail the factors that influence the initial decision to contact EMSs at the onset of stroke symptoms, and to explore the stroke-specific factors that facilitate or misdirect effective communication between the caller and EMSs. Many callers seek lay or professional advice prior to contacting EMSs, and some believe that the onset of acute stroke symptoms does not warrant an immediate 999 call. The findings also underline the need for ongoing public education to raise public awareness of stroke symptoms and the appropriate response, in order to reduce delays in accessing emergency treatment.
Summary
At the onset of stroke, the callers’ ability to convey their suspected diagnosis is limited by a lack of stroke symptom recognition, often as a result of the diverse presentation of stroke symptoms. Many callers believe that the onset of acute stroke symptoms does not necessarily warrant an immediate call to EMSs. Delays often arise because the caller feels it necessary to seek other lay or professional advice prior to calling EMSs.
Even when callers recognise stroke and call EMSs, often they do not convey this impression to the call handler. The form of structured questioning used by the call handler does not always enable the caller to convey their full impression of what the problem is, or allow the call handler to assure callers that an ambulance has been arranged. In order to improve outcomes in hyperacute stroke care, more public education is needed to improve awareness of a wider range of stroke symptoms and the need for an urgent response.
If members of the public can recognise stroke symptoms but do not always convey this to call handlers, how do they describe their symptoms? The next phase (phase 3) aims to identify ‘key indicator’ words used by people making emergency calls for suspected stroke and to compare these with the final diagnosis in hospital. It entails a retrospective review of digitally recorded EMS calls for patients who had a diagnosis of suspected stroke by the EMS call handler and/or a final diagnosis of stroke.
Chapter 4 ESCORTT phase 3: the identification of acute stroke – an analysis of emergency calls
Background
Stroke is a time-dependent medical emergency in which rapid access to specialist care reduces death and dependency. 1 The interaction of EMDs with callers is potentially important in early identification of symptoms suggestive of stroke and the initiation of a rapid EMS response. However, published reports on EMDs’ accuracy in recognition of stroke from callers’ descriptions are very few. Identifying ‘true stroke’ from an EMS call is challenging. This can be partly attributed to callers’ lack of use of the term ‘stroke’ when stroke symptoms are present. A recent study reported that stroke was spontaneously identified by the caller in only 44% of EMS patients in whom the final ED diagnosis was stroke. 4 Similarly, EMD sensitivity and PPV for identifying stroke using AMPDS software have been estimated at < 50%. 7–9 Detailed investigation of the terms used during EMS calls for suspected or subsequently confirmed stroke has not been previously undertaken. We wished to explore the terms which were used by callers and what response these prompted from the EMD, in order to identify the stroke- and non-specific terms used and EMDs’ response to them. We planned to use these findings in order to better inform training and service development for emergency services, for suspected stroke patients.
The aim of this phase was to identify ‘key indicator’ words used by people making emergency calls for suspected stroke.
Methods
Setting
Regional EMSs and two acute hospital trusts in the north-west of England serving a diverse urban/rural population of 810,000.
Subjects and sampling
Patients with suspected acute stroke who arrived at a participating hospital through telephoning the EMSs, during a 12-month period (1 October 2006 to 30 September 2007).
Patients were identified through retrospective review of the stroke register, hospital coding system, case notes and electronic EMS documentation forms. Once patients were identified we checked with the EMSs for presence of an emergency call; the study design precluded inclusion of patients who presented via other routes such as GP referral, self-presentation at the ED or stroke onset as an inpatient. Demographic and dispatch data were collected, including: the relationship of the caller to the patient; location of the patient; dispatch code and category of response (e.g. A is up to a 19-minute response).
Inclusion criteria
Patients who had a diagnosis of suspected stroke made by the EMS call handler and/or a final diagnosis of stroke. A patient was considered to have a final diagnosis of stroke if the ED records stated a stroke (for those patients discharged from the ED), they were still on the stroke register at the time of discharge or their discharge letter stated a diagnosis of stroke (where there was no register).
Exclusion criteria
Patients who did not arrive at hospital through EMSs, patients who had a stroke as an inpatient, patients who received a diagnosis of subarachnoid haemorrhage, patients for whom the call was made by their primary care physician (GP) or GP staff on behalf of the patient and patients for whom we did not have data for final medical diagnosis.
Ethical approval
Approval for this phase was granted by the National Patient Information Advisory Group, the Local Research Ethics Committee, the Faculty of Health Ethics Committee at the University of Central Lancashire, and NHS Research and Development at the EMSs and acute hospitals.
Data collection and analysis
Every call recording for our sample was listened to in full by a researcher trained in qualitative research methods. At the beginning of a call to the EMSs, the caller is asked the open question ‘What’s the problem, tell me exactly what happened?’ by an EMD to establish the chief presenting complaint. We focused the analysis on the caller’s response to this first question, which we termed ‘the first story’. The first story was deemed to have come to an end when the EMD asked the closed question about consciousness: ‘Are they conscious?’ The first story typically involves the description of a number of presenting problems; we selected the problems reported in the first story. The words used by the caller to describe the problem were termed ‘key indicator’ words. For any call a problem might be reported multiple times, but for the purpose of the analysis each problem was only counted once per call.
Analysis was undertaken by coding the terms used by the caller to describe the presenting issue, diagnosis or condition. To ensure inter-rater reliability, 100 consecutive calls were coded by at least two researchers and any discrepancies were resolved by discussion. Analysis was undertaken using a constant comparative method in order to identify key indicator words and relationships within the data. 35,38 Open coding of the data was undertaken using content analysis (facilitated by ATLAS.ti software; ATLAS.ti, Berlin, Germany). The research team met regularly to discuss the coding categories in order to ensure a consistent approach to analysis of the data. New categories were considered and added to the list of key indicator words at weekly intervals. Key indicator words identified were grouped to form categories.
Further data were collected from EMSs and patient medical records regarding dispatch code (e.g. stroke, unconscious, faint) and diagnosis information recorded by each of the following sources: attending EMS personnel, ED, medical admissions unit, stroke unit or other clinical area, and final medical diagnosis from ED or discharge letter.
Results
Six hundred and forty-three calls were received by the EMSs where patients were either dispatched as stroke and/or had a final diagnosis of stroke, of which 592 (92.1%) had complete EMS and hospital data. From the 592 calls, 473 (79.9%) patients had a final medical diagnosis of stroke or TIA and 119 (20.1%) patients had non-stroke diagnoses.
Three hundred and sixty-six (62%) of the callers were female. The majority 323 (55%) of the callers were family members ( Table 10 ). Of these, daughters (30%) and wives (28%) were the most likely to call EMSs on behalf of the patient. Median duration of calls was 2 minutes 40 seconds.
| Caller | Final diagnosis of stroke (n = 473) | Final diagnosis was not stroke (n = 119) | All patients (n = 592) |
|---|---|---|---|
| Patient, n (%) | 10 (2.1) | 2 (1.7) | 12 (2.0) |
| Family member, n (%) | 262 (55.4) | 61 (51.3) | 323 (54.6) |
| Neighbour, n (%) | 19 (4.0) | 5 (4.2) | 24 (4.1) |
| Friend, n (%) | 16 (3.4) | 8 (6.7) | 24 (4.1) |
| Carer, n (%) | 1 (0.2) | 0 (0) | 1 (0.2) |
| Care/nursing home staff, n (%) | 58 (12.3) | 20 (16.8) | 78 (13.2) |
| Police, n (%) | 10 (2.1) | 4 (3.4) | 14 (2.4) |
| Careline staff, n (%) | 7 (1.5) | 3 (2.5) | 10 (1.7) |
| NHS staff, n (%) | 18 (3.8) | 9 (7.6) | 27 (4.6) |
| Leisure industry (i.e. sports arena staff), n (%) | 20 (4.2) | 1 (0.8) | 21 (3.5) |
| Worker (i.e. bus driver, shop assistant), n (%) | 16 (3.4) | 2 (1.7) | 18 (3.0) |
| Other, n (%) | 35 (7.4) | 4 (3.4) | 39 (6.6) |
| Missing, n (%) | 1 (0.2) | 0 (0) | 1 (0.2) |
Most patients (n = 425; 72%) were in their own home at the time of the call to the EMSs. The next prevalent locations were public places (n = 76; 13%), and nursing and residential care settings (n = 82; 14%).
The patients’ characteristics can be seen in Table 11 . The average age, gender distribution and levels of consciousness were similar in those with and without a final diagnosis of stroke.
| Patient characteristics | Final diagnosis of stroke (n = 473) | Final diagnosis not stroke (n = 119) | All patients (n = 592) |
|---|---|---|---|
| Median age (years) (IQR) | 77 (69–84) | 76 (65–83) | 75 (13) |
| Female, n (%) | 244 (52) | 67 (56) | 311 (53) |
| AVPU level on admission | |||
| Alert | 387 (82) | 97 (81) | 484 (81) |
| Responds to voice, n (%) | 39 (8) | 12 (10) | 51 (9) |
| Responds to painful stimulus, n (%) | 18 (4) | 4 (3) | 22 (4) |
| Unresponsive, n (%) | 19 (4) | 3 (3) | 22 (4) |
| Missing data, n (%) | 10 (2) | 3 (3) | 13 (2) |
Of the participants with a final diagnosis of stroke and where scan results were available, 85.9% had a cerebral infarction.
Reporting of problems
The frequency of the number of problems reported in the first stories can be seen in Table 12 . The modal number of problems was three, occurring in just over 62% of calls. Four or more problems were reported in < 7% of calls. The pattern of number of problems reported was similar, regardless of whether or not the final diagnosis was stroke, although none of the non-stroke calls described more than four problems. In total, 1352 problems were mentioned for the 592 patients.
| Number of problems | All patients |
|---|---|
| Number with: | |
| One problem | 88 |
| Two problems | 97 |
| Three problems | 369 |
| Four problems | 16 |
| Five problems | 14 |
| Six problems | 0 |
| Seven problems | 4 |
| Eight problems | 4 |
| Total | 592 |
The more common problems reported in the first story can be seen in Table 13 . Overall, collapse or fall was the most commonly reported problem (39.9%), with stroke the second most common (37.2%).
| Problem | Number reported (n = 592) |
|---|---|
| Collapse or fall, n (%) | 236 (39.9) |
| Stroke/TIA, n (%) | 220 (37.2) |
| Consciousness level, n (%) | 99 (16.7) |
| Limb weakness, n (%) | 86 (14.5) |
| Speech problems, n (%) | 80 (13.5) |
| Generally unwell, n (%) | 62 (10.5) |
| Previous medical history (e.g. atrial fibrillation, dizzy spells, catheter), n (%) | 54 (9.1) |
| Confused, n (%) | 49 (8.3) |
| Previous medical history of stroke, n (%) | 45 (7.6) |
| Pain, n (%) | 30 (5.1) |
| Dizzy, n (%) | 26 (4.4) |
| Breathing problems, n (%) | 30 (5.1) |
| Fitting, n (%) | 25 (4.2) |
| Temperature changes, n (%) | 28 (4.7) |
| Facial weakness, n (%) | 24 (4.1) |
Table 14 shows the number of problems described during the call for those with and without a final diagnosis of stroke. For those patients that had a final diagnosis of stroke, stroke was the most commonly reported problem (39.7%), whereas for patients that did not have a final diagnosis of stroke, fall or collapse was the most common problem (45.4%).
| Problem | Number of people that mentioned problem in their first story | |
|---|---|---|
| Final diagnosis of stroke (n = 473) | Final diagnosis of not stroke (n = 119) | |
| Stroke/TIA, n (%) | 188 (39.7) | 32 (26.9) |
| Collapse or fall, n (%) | 182 (38.5) | 54 (45.4) |
| Consciousness level, n (%) | 77 (16.3) | 22 (18.5) |
| Limb weakness, n (%) | 70 (14.8) | 16 (13.4) |
| Speech problems, n (%) | 72 (15.2) | 8 (6.7) |
| Generally unwell, n (%) | 49 (10.4) | 13 (10.9) |
| Previous medical history (e.g. atrial fibrillation, dizzy spells, catheter), n (%) | 44 (9.3) | 10 (8.4) |
| Confused, n (%) | 42 (8.9) | 7 (5.9) |
| Previous medical history of stroke, n (%) | 31 (6.6) | 14 (11.8) |
| Pain, n (%) | 23 (4.9) | 7 (5.9) |
| Dizzy, n (%) | 23 (4.9) | 3 (2.5) |
| Breathing problems, n (%) | 22 (4.7) | 8 (6.7) |
| Fitting, n (%) | 19 (4) | 6 (5) |
| Temperature changes, n (%) | 21 (4.4) | 7 (5.9) |
| Facial weakness | 17 (3.6) | 7 (5.9) |
Of the 220 calls where stroke or TIA was mentioned, 188 (85.5%) had a final diagnosis of stroke or TIA confirmed in hospital. Of the 173 calls where one or more of the FAST symptoms was mentioned, 145 (83.8%) had a final diagnosis of stroke. Of the 236 calls where fall or collapse was mentioned, 182 (77.1%) had a final diagnosis of stroke.
For the patients with a final diagnosis of stroke, one or more of the individual items of the FAST were reported in 145 (30.7%) patients. Limb weakness and speech problems were mentioned in 70 (14.8%) and 72 (15.2%) calls, respectively, with only a small number of calls mentioning facial weakness (n = 17; 3.6%). None of the calls included mention of all three of the FAST symptoms, but 17 calls included two FAST symptoms, with limb weakness and speech problems occurring in 13 (76.5%) of these calls.
Mentioning stroke had moderate sensitivity of 39.7% and high PPV of 85.5%. Further exploration of the sensitivity of the different words used will take place in phase 4, along with estimates of specificity. Of the 188 patients who had a final diagnosis of stroke and where stroke was mentioned, 163 (86.7%) were dispatched as stroke. The EMSs used a stroke dispatch code in 269 (45.4%) of cases, and of these 223 (82.9%) patients had a final diagnosis of stroke.
Discussion
There is evidence to suggest that the public are more likely to contact the EMSs for suspected stroke if their symptoms include speech problems, weakness, decreased level of consciousness, and dizziness/loss of co-ordination. 28
In this phase, the problem reported most frequently by callers to the EMSs was collapse or fall (39.9%). Motor problems were often reported by their consequences, which resulted in a person collapsing, falling to the floor, or being found on the floor. The terms fall or collapse have previously been reported by 17% and 21% of callers respectively. 20,22 The term stroke was used with similar frequency to collapse or fall, but is, at 37.2%, lower than the 45–51% reported in smaller series. 20,23 However, this phase is much larger than previous studies and focuses on the first reported problems between the caller and EMD when callers are most likely to report their initial interpretation of the problem. Following these first reported problems, the conversation becomes a series of closed questions as the EMD follows a specific AMPDS algorithm. Stroke was not mentioned in around 60% of the calls when the final diagnosis was stroke. This figure may not be too surprising given that the public is asked to describe what is wrong, which may lead them to state symptoms such as speech problems or limb weakness, rather than to provide a diagnosis.
We have found that the use of any of the terms ‘collapse or fall’, or ‘stroke’ by the caller tend to be associated with a final diagnosis of stroke, and have moderate sensitivity. These terms were also used by callers when the final diagnosis was not stroke. Stroke was mentioned nearly half as often in calls where the final diagnosis was not stroke compared with calls where the final diagnosis was stroke. For fall or collapse, a similar proportion of calls included mention of this term whether or not the final diagnosis was stroke. However, these data only provide part of the story around how terms mentioned in the call are indicative of final diagnosis. The sample in this phase had a diagnosis of stroke at either dispatch or as the final diagnosis. This means that we cannot draw any conclusions about the specificity of the terms. To properly gain an understanding of the specificity of these terms we needed to identify a sample of patients that have a non-stroke final diagnosis: this will be reported in Chapter 6 .
An important finding of this phase was that the common warning signs and symptoms of stroke (face weakness, limb weakness and speech disturbance) were stated in around 30% of cases. One of the FAST symptoms most frequently reported was speech problems. This finding is reflected in a recent Australian study, which found that speech problems were the most commonly reported FAST symptom by bystanders. 39 The same study39 found that facial weakness was reported in around 1% of cases, which is similar, although lower, to our finding of 4%. They found that arm weakness was reported in as few as 1% of cases in contrast to our findings where 14.5% stated arm weakness. However, this was still less than half of the number of cases that used the word stroke. The low numbers stating limb weakness may be due to callers having a tendency to describe the consequences of the weakness, such as being unable to grip or hold objects, rather than using such terms as arm weakness itself. These calls were made to the EMSs prior to the public FAST campaign. 40
Of calls where the EMS response was to dispatch as a stroke, the proportion of patients with a final medical diagnosis of stroke or TIA was 83%. EMDs used an AMPDS code of stroke in only 45% of all calls. Generic codes such as sick person and fall were often used, with the potential to delay appropriate assessment and treatment for stroke.
The callers to EMSs in our study were predominantly family members, the patient’s daughter being most likely, consistent with previously published Australian data. 20 The patient was rarely the caller (2% of all calls), consistent with other series12,20,41 and phase 2 of our research (reported earlier).
Patients with a final non-stroke-specific medical diagnosis were found to have both neurological and non-neurological conditions such as seizure, respiratory conditions and infections. Common stroke mimics such as seizure, syncope, space-occupying lesions, hypoglycaemia and sepsis have been reported elsewhere. 31
Pre-hospital notification of a patient with suspected stroke is known to be strongly associated with rapid admission to hospital,42 and is perhaps especially important in expediting assessment and delivery of thrombolytic therapy for eligible patients. It is possible that this opportunity is missed when non-stroke categories are used by EMDs.
Limitations
Detailed analysis of recorded calls to the EMSs has enabled us to study what was actually said by callers, rather than relying on abstracting data from patient records alone. However, this limited the number of data that we were able to collect about the caller, as we were only able to record those details discussed during the call, which were generally confined to the caller’s relationship to the patient. We also had to rely on the accuracy of the final medical diagnosis as recorded in the case notes and did not conduct any independent verification of this.
Conclusion
This is the largest study to look at the content of calls to the EMSs for suspected stroke. Within our sample, when callers contacted the EMSs and reported stroke as part of the first story they were correct in 85.5% of cases. This suggests that members of the public who use the word ‘stroke’ during the call are playing a vital role in initiating an immediate and appropriate response as outlined in the ‘stroke chain of survival’. 43
Summary
Detailed analysis of actual calls to the EMSs has enabled us to study what was said by callers during 999 calls for acute stroke. The problems reported most frequently by callers to the EMSs were collapse or fall, and stroke. Collapse or fall was most likely used by callers to describe motor problems, which resulted in a person collapsing, falling to the floor, or being found on the floor. When the term ‘stroke’ was used by the caller, the proportion of patients with a confirmed diagnosis of stroke or TIA was high. If stroke is suspected, members of the public should be encouraged to say the word stroke. However, findings of phase 2 of this programme suggest that even when callers suspect stroke, they may not always convey this to the EMD.
Within the sample selected, of those who said stroke, the majority of patients had a final diagnosis of stroke. However, it is not known if the word stroke is used by callers contacting the EMSs with other conditions. By listening to further calls in phase 4 we will identify any similarities or distinguishing key words that are said for other (non-stroke-related) conditions.
During analysis of the phase 3 EMS calls, it became apparent that misunderstanding of consciousness level was an important theme. Impaired consciousness level is an important, adverse prognostic sign in acute stroke, but is often also associated with stroke mimics such as epilepsy. Although not an intended phase of this programme of research, further investigation was thought to be necessary in order to explore this unexpected finding. We therefore undertook a secondary analysis of EMS recordings relating to discussion of consciousness level in patients with symptoms suggestive of acute stroke, which is reported in the next phase (phase 3a).
Chapter 5 ESCORTT phase 3a: ‘Is he awake?’ – dialogues between callers and call handlers about consciousness during emergency calls for suspected acute stroke
Background
Acute stroke is a medical emergency, in which timely access to emergency medical treatment, notably thrombolytic therapy, is vital to reduce mortality and morbidity. 3 However, symptoms of acute stroke are not always easy for bystanders to recognise. 26 Public information campaigns about common symptoms, such as the FAST, have been implemented in many countries including the UK, USA and Australia to expedite help-seeking behaviour. 39,44,45 Prompt access to emergency stroke services also depends on a bystander’s (usually not the patient themselves) identification and interpretation of the symptoms as requiring EMS response, callers’ ability to communicate with the EMS call handler about the patient’s symptoms, and the call handler’s questioning and listening skills. 33,46
Clinical presentation of acute stroke often includes an altered state of consciousness. This is an important sign of stroke severity and a prognostic indicator. Consciousness is defined as ‘the state of being aware of physical events or mental concepts. Conscious patients are awake and responsive to their surroundings’. 47
The question ‘Is he/she conscious?’ is routinely asked by EMS call handlers to determine the presence of life-threatening conditions, and is included as a standard question in computer-aided systems such as the AMPDS (v11.3) used by over 3000 agencies worldwide. Currently in the UK, EMS calls are prioritised as ‘red’ (attendance at the scene within 9 minutes), ‘amber’ (up to 19 minutes) or ‘green’ (up to 60 minutes). Assessment of the patient’s consciousness level is an important factor in correctly coding and prioritising calls to ensure the appropriate level of response. However, lay persons’ understanding of the term ‘conscious’ is known to be poor. 48 Although health-care professionals utilise tools such as the Glasgow Coma Scale (GCS), the Alert, Voice, Pain, Unconscious (AVPU) score and the National Institutes of Health Stroke Scale (NIHSS) stroke assessment framework, to assess patients’ responses to stimuli and thus identify patients with reduced or fluctuating levels of consciousness, these are not generally available to untrained bystanders and do not feature in media campaigns.
During analysis of the phase 3 EMS calls, the theme of misunderstanding of consciousness level emerged. Impaired consciousness level is an important adverse prognostic sign in acute stroke, but is often also associated with stroke mimics such as epilepsy and metabolic causes. Patients with an altered level of consciousness need to receive the highest priority of ambulance dispatch to enable urgent medical assessment, irrespective of the cause. We therefore undertook a secondary analysis of EMS recordings relating to discussion of consciousness level in patients with symptoms suggestive of acute stroke. The aim of this phase was to identify how patients’ consciousness level was questioned, described and interpreted by callers and EMDs during calls to the EMSs for suspected stroke.
Methods
Design
Retrospective audit.
Setting
Regional EMSs and two acute hospital trusts in the north-west of England serving a diverse urban/rural population of 810,000.
Subjects and sampling
Patients with suspected acute stroke who arrived at a participating hospital through telephoning the EMSs, during a 12-month period (1 October 2006 to 30 September 2007).
Inclusion criteria
Patients who were admitted to hospital with symptoms suggestive of stroke, a subsequent in-hospital diagnosis of acute stroke, or both. Calls were included in the secondary analysis if misinterpretation or protracted dialogue (or both) about the patient’s level of consciousness were apparent.
Exclusion criteria
Patients aged < 18 years. Calls made by a GP (or receptionist) on behalf of the patient.
Approval for this phase was granted by the Patient Information Advisory Group, the Local Research Ethics Committee and by the Faculty of Health Ethics Committee at the host university.
Data collection and analysis
Through a retrospective audit of patient case notes and ambulance report forms, patients’ records were identified and the corresponding EMS calls were analysed. Demographic and dispatch information were also collected, including the relationship of the caller to the patient, location of the patient, dispatch code and prioritisation category. The level of consciousness documented by EMS staff following clinical assessment was also ascertained.
Audio recordings of EMS calls were listened to in full by one of three researchers (SJ, JMc, JG). Calls were analysed by coding the key words used to describe the consciousness level of the patient. This analysis focused on the caller’s response to the two standard questions asked by the call handler about consciousness level: ‘Is the patient conscious?’ and ‘Is he/she completely awake?’ Any other dialogue during the call which related to consciousness level or alertness was also included in the analysis. Responses from the caller which suggested misinterpretation of terms such as conscious, awake, responsive or alert, or where the call handler had to use additional questions to clarify the patient’s level of consciousness, were analysed in detail.
A second researcher independently followed the same procedure and any discrepancies were resolved by discussion between the researchers. Relationships between the responses to the two standard questions were mapped.
Results
There were 592 calls in the data set, of which 109 (18%) patients had been noted to have an altered level of consciousness documented by attending EMS personnel. Of these, 44 (40%) calls had required further clarification of the patient’s level of consciousness by the call handler. Of these calls, 30 (68%) were dispatched as red, 5 (11%) as amber, 2 (5%) as green and no category of dispatch was recorded for 7 (16%). All 44 calls were made by a bystander (e.g. a family member), not by the patient themselves. Demographic information for patients and callers is summarised in Table 15 .
| Characteristic | n |
|---|---|
| Patient | |
| Median age (years) (IQR) | 78 (65–85) |
| Female (%) | 21 (47) |
| Location | |
| At home (%) | 35 (80) |
| Nursing/care home (%) | 6 (14) |
| Public place (%) | 2 (5) |
| Other: primary care centre (%) | 1 (2) |
| Caller | |
| Age (mean) | Unavailable |
| Female (%) | 19 (43) |
| Caller relationship | |
| Male family member (%) | 13 (29) |
| Female family member (%) | 13 (29) |
| Nursing or care home staff (%) | 8 (18) |
| Neighbour (%) | 2 (5) |
| Friend (%) | 2 (5) |
| Other (e.g. landlord, sheltered accommodation staff) (%) | 6 (14) |
In the 44 calls included in this analysis, responses to the initial standard question ‘Is he/she conscious?’ were as follows: 14 callers replied that the patient was conscious, 5 callers replied that the patient was unconscious, 9 stated that they were ‘semi-conscious’ or used a similar term, and 16 callers were unable to state whether or not the patient was conscious.
In many calls there was apparent misunderstanding or clarification needed about the patient’s level of consciousness. This entailed unscripted or protracted dialogue between the caller and call handler. In response to an equivocal statement by the caller, the call handler would repeat, paraphrase or reverse the standard questions, usually until a ‘yes’ or ‘no’ response was received. Even then, the final response itself might be qualified by the caller with some additional information. An example is shown in Table 16 . In this case, the call handler repeatedly asks if the patient is ‘conscious’ or ‘awake’, but receives equivocal responses. The question is then reversed to ask ‘Is he unconscious?’, yet still fails to elicit a clear ‘yes/no’ response from the caller.
| Caller or call handler | Dialogue |
|---|---|
| Caller | He’s not quite with it; he can’t speak properly or anything. |
| Call handler | Is he conscious? |
| Caller | Well not really. |
| Call handler | Is he awake? |
| Caller | Not properly no. |
| Call handler | Is he awake at all, is he . . . |
| Caller | No, no, no. |
| Call handler | Is he unconscious? |
| Caller | Yes, we just keep, if you speak to him he sort of mutters. |
Questions asked by call handlers to clarify patients’ consciousness level included variations on the standard questions ‘Is he/she conscious?’ and ‘Is he/she completely awake?’ There were also variations on a further question, ‘Is he/she able to talk normally?’ which was prompted by the AMPDS algorithm if the call had been identified as suspected stroke by the call handler. This question was not prompted, for calls that were coded as another presenting problem such as fall.
Clarifying questions used by call handlers fell into four categories: consciousness level; level of awakeness, awareness or alertness; patient’s ability to talk and patient’s response to stimuli (usually verbal) ( Table 17 ).
| Type of question | Questions asked |
|---|---|
| Questions about consciousness level | At the moment, is he conscious? Is he unconscious? Is she still unconscious? So she’s not conscious? She’s not unconscious? |
| Questions about awakeness, awareness or alertness | Is he awake at all? Sorry, is he? Is he completely awake? So you can’t wake him? Are her eyes open? Did she open her eyes or? Is she aware of her surroundings? Is she alert? Is he alert to what’s going on? Would you say she was alert? |
| Questions about patient’s ability to talk | Is she able to talk? Is he able to talk normally? So he’s not able to talk to you? Can she breathe or talk at all? |
| Questions about patient’s responsiveness to stimuli | Is she responding to you? Is he responding? Will he respond? So she’s not responding? Right, she’s not responding? Does she respond at all? So (she’s) not responding if you call her name out or try to talk to her? |
In contrast to the semi-scripted line of questioning from the call handler, callers engaged in protracted and discursive descriptions of the patient’s consciousness level. Three themes were identified within the dialogues:
-
caller’s difficulty in determining consciousness level
-
miscommunication and need for clarification of stated consciousness level
-
association of consciousness level with breathing.
Difficulty in determining consciousness level
Some callers were unable to clearly assess or describe the patient’s consciousness level. This occurred when the patient was not obviously fully conscious nor completely unconscious, or when the level of consciousness appeared to be fluctuating, when terms such as ‘semi-conscious’ were used. There was also misunderstanding owing to the presence of other acute stroke symptoms such as speech difficulty or cognitive impairment, when the patient was not fully responsive despite being clearly ‘awake’.
Example 1:
Example 2:
Where the caller was unable to determine clearly whether the patient was ‘conscious’ or ‘not conscious’, they often used other colloquial terms to describe the patient’s condition.
Example 3:
Example 4:
Miscommunication and need for clarification of consciousness level
When asked by the call handler if the patient was conscious, of the 14 callers who gave a clear response of ‘yes’, six gave additional and often contradictory information when questioned further. Sixteen other callers were unsure when initially questioned by the call handler. Of five callers who initially answered ‘no’, all but one changed their assessment (two to ‘conscious’, one to ‘semi-conscious’ and one patient regained consciousness).
In some cases, the caller initially gave a clear response of ‘yes’ to the question of whether the patient was conscious, but then gave additional information during the call (often in response to the standard question ‘Is he/she awake?’). This additional dialogue served either to give a more detailed assessment of the patient’s consciousness level, or to convey additional information that contradicted the original response.
Similarly, there were instances where the caller initially gave a clear response of ‘no’ when asked if the patient was conscious, but then contradicted this, or gave a more detailed description ( Table 18 ).
| Original response | Original response qualified with additional dialogue | Original response contradicted |
|---|---|---|
| Yes | Call handler: Is she conscious? Caller: Yes Call handler: Is she awake? Caller: She is sort of but she keeps sort of going asleep | Call handler: Is she conscious? Caller: Yes but when I say she’s conscious, but I can’t seem to rouse her, do you know what I mean |
| Yes | Call handler: Is she conscious? Caller: Yes she’s conscious . . . she’s completely awake but she’s very, very drowsy | Call handler: Is he conscious? Caller: Yes . . . no, I can’t, no he’s not conscious. He won’t wake up |
| No | Call handler: Is she conscious? Caller: No, come on quickly Call handler: Is she still unconscious? Caller: She’s half way, more or less unconscious | Call handler: Is he conscious? Caller: No Call handler: Is he awake? Caller: He is awake, yes |
Association of consciousness level with breathing difficulties
The AMPDS protocol prompts call handlers to ask firstly ‘Is he/she conscious?’, and then ‘Is he/she breathing?’ However, some callers’ responses suggested that they equated ‘conscious’ with ‘breathing’, or suggested that the patient was conscious yet not breathing:
Example 5:
Example 6:
Discussion
This is the first study that has explored the public’s understanding and communication of consciousness level during EMS calls for patients with symptoms suggestive of acute stroke.
Emergency medical services calls are one example of ‘institutional talk’. 49 Such interactions are partly or wholly scripted, or follow additional rules to those in everyday conversation, in order to achieve a specific outcome. In the case of EMS calls, the intended outcome is the classification of the urgency and nature of the patient’s presenting problem in order to facilitate the provision of appropriate and timely emergency medical care. However, the highly structured format of the caller–call handler dialogue, and the nature of the medical emergency situation, may make it difficult for callers to ask for clarification of medical terms used by the call handler, and to convey uncertainty about their interpretation of the patients’ symptoms.
Despite poor public understanding, the term ‘conscious’ is used routinely in both the AMPDS system, and in the NHS Pathways programme which is being implemented across EMSs in the UK. Further to this, the call handler’s standard question ‘Is he/she conscious?’ implies that a dichotomous ‘yes/no’ answer is expected from the caller. This is unhelpful and potentially misleading in stroke, where more subtle changes in consciousness level may be present. Therefore, it is unsurprising that some callers make partial, equivocal and sometimes contradictory statements about the patient’s consciousness level. Call handlers are then obliged to resort to the use of rephrased questions and other terms such as awake, alert, responsive and speech/communication, in order to more fully elicit the patient’s level of consciousness. This can lead to protracted, time-consuming and often somewhat confusing dialogue as the caller attempts to convey the nuances of the patient’s level of consciousness.
The widely used GCS50 comprises three responses (motor, eye opening and speech) to assess consciousness level. Its use is problematic in stroke patients as those with aphasia may be unable to speak and yet may be fully conscious and alert. The NIHSS utilises a four-point scale which enables a more accurate delineation of the patient’s consciousness level in stroke. In contrast, the dichotomous nature of questioning about consciousness level in EMS protocols does not allow for recognition of gradations of consciousness level, other than a simple ‘yes/no’ response.
Many acute stroke patients experience symptoms of aphasia or cognitive impairment. 51 Such presentations may make it more difficult for a bystander to distinguish ‘true’ changes in consciousness level,52 and adds to the challenge of conveying the patient’s actual level of consciousness to the call handler. It can therefore be difficult for callers to swiftly and accurately assess the consciousness level of a patient with acute stroke symptoms and to communicate this information with the call handler.
In this phase, attending EMS personnel documented that 17% (109/643) of patients had an altered consciousness level, within the range of previously reported prevalence rates of 16–41% in stroke. 52 Although some patients’ consciousness level may have deteriorated or improved between the initial call and ambulance arrival, it is also possible that impaired consciousness level was under-reported during the emergency calls.
Although GP-initiated calls were excluded from this phase, we included calls from nursing and residential care home settings. Some of these did not provide an unequivocal description of the patient’s consciousness level, but tended to describe altered consciousness level using subjective terms such as ‘drowsy’ and ‘unresponsive’, rather than giving a ‘yes/no’ answer to the call handler.
Our findings suggest that, despite its wide use in medical practice and specifically in EMS dispatch protocols, the term ‘conscious’ is not widely understood and is poorly communicated by bystanders when making EMS calls about patients with symptoms suggestive of acute stroke. This phenomenon may lead to imprecise, contradictory and lengthy information exchange which may be time wasting, misleading and potentially dangerous. Our findings suggest that a structured assessment by ambulance dispatchers of consciousness level, with categories encompassing drowsiness and the separate assessment of speech and breathing problems might assist in obtaining a more accurate assessment of consciousness level in patients with suspected stroke.
Limitations
We were unable to verify patients’ actual level of consciousness at the time the EMS call was made. We used data recorded by attending EMS personnel on or shortly after arrival at the scene as a proxy for this. However, the patient’s consciousness level could have improved or deteriorated since the time the call was made. We were limited in the number of data we were able to collect about caller characteristics, as such information is not routinely obtained during EMS calls. Our findings were restricted to calls relating to patients with suspected or confirmed stroke, but there are, of course, many other emergency conditions that affect level of consciousness.
Conclusion
Routine questioning of EMS callers about a patient’s consciousness level is important to help prioritise the EMS response, but is characterised by ambiguities or contradictions in statements made by callers. When there is a reduced or fluctuating level of consciousness, or cognitive or speech impairment, a dichotomous ‘yes/no’ answer does not capture nuances of the patient’s condition. The closed nature of routine questioning does not necessarily elicit the necessary information and is therefore supplemented by both call handlers and callers with additional unscripted questions and colloquial responses. Although our study relates only to patients with acute stroke, our findings have implications for other EMS calls. It is possible that the issues described in this phase are also found in emergency calls about patients with other conditions associated with acute changes in consciousness level. Further research is needed to explore this, and to inform EMS call handler education and future public awareness campaigns. Further work is also needed with members of the public to identify which term or terms are best understood in conveying altered levels of consciousness in emergency situations.
Summary
This secondary analysis of EMS recordings relating to discussion of consciousness level was not an intended phase of this programme of research. This analysis revealed that although routine questioning of EMS callers about a patient’s consciousness level is important to help prioritise the EMS response, the discussion is characterised by ambiguities or contradictions in statements made by callers. Establishing a patient’s consciousness level during an EMS call is potentially more difficult in stroke patients with cognitive or speech impairment, where a dichotomous ‘yes/no’ answer does not capture the nuances of the patient’s condition. Further research would be required to explore if these findings have implications for patients with conditions other than stroke. The training package to be developed later in this programme of research will include issues around establishing consciousness level during EMS calls for patients with stroke.
In the previous phase (phase 3) the majority of callers to the EMSs who said ‘stroke’ had a confirmed final diagnosis of stroke in hospital. However, it is not known if the word stroke is used by callers contacting the EMSs with other conditions. By listening to further calls in the next phase (phase 4) we will identify any similarities or distinguishing key words that are said for other non-stroke conditions, illnesses and injuries.
Chapter 6 ESCORTT phase 4: exploring the words used by callers for non-stroke-related calls to the emergency medical services and a comparison with the words used describing stroke-related calls
Background
Stroke is increasingly recognised as a medical emergency for which rapid access to specialist care can reduce death and dependency. 4 Rapid access therefore has the potential to reduce severity of stroke, health services input and length of stay. In the longer term, the burden of stroke could be reduced for individuals, carers and society as a whole. It is therefore vitally important that the public and front-line staff such as EMSs are able to recognise the symptoms of suspected stroke and initiate a rapid response. People with suspected stroke should be taken immediately to hospital. Early presentation at hospital provides greater opportunity for time-dependent stroke treatment, such as thrombolysis. 53 Subsequently, patients will have more immediate access to organised stroke care, which is known to have a positive impact on survival and dependency. 54 Furthermore, early neurological attention is related to improved functional outcome and shorter hospitalisation. 55
One way of facilitating a patient’s transfer to hospital and therefore improving the chance for early presentation is through enhancing communication between the general public and the EMSs. Although problems with communication have been identified,23 no studies to date have explored the content of these verbal interactions. If we had a better understanding of how patients or those acting on their behalf interact with emergency services, this may lead to ways of improving emergency service utilisation among suspected stroke patients. 23 Furthermore, if we explore the interaction between people and the EMSs and identify how this communication can be enhanced, we can use this information to inform the content of the stroke-specific training provided for EMS personnel.
In a previous phase of this programme of research (phase 3) we listened to 999 calls and recorded the key indicator words said by people describing a suspected stroke. By listening to further calls we will identify any similarities or distinguishing key words that are said for non-stroke-related conditions, illnesses and injuries.
Methods
Aim
To compare the words used by the public making calls to the EMSs, the subsequent ambulance dispatch codes and final diagnosis in hospital, for stroke and non-stroke calls.
Study design
A retrospective mixed-methods study.
Setting
A regional EMS and an acute hospital trust.
Sample and sampling
The calls between the public and the EMSs that led to an EMS vehicle being dispatched were identified over a 1-week period (8–14 March 2010). Figure 2 shows the flow diagram for the study.
FIGURE 2.
Flow diagram of inclusion and exclusion in study. Reproduced with permission from Leathley MJ, Jones SP, Gibson JME, Ford GA, McAdam JJ, Quinn T, et al. ‘Can you send an ambulance please?’: a comparison of callers’ requests for emergency medical dispatch in non-stroke and stroke calls [published online ahead of print 13 July 2013]. Emerg Med J 2014.
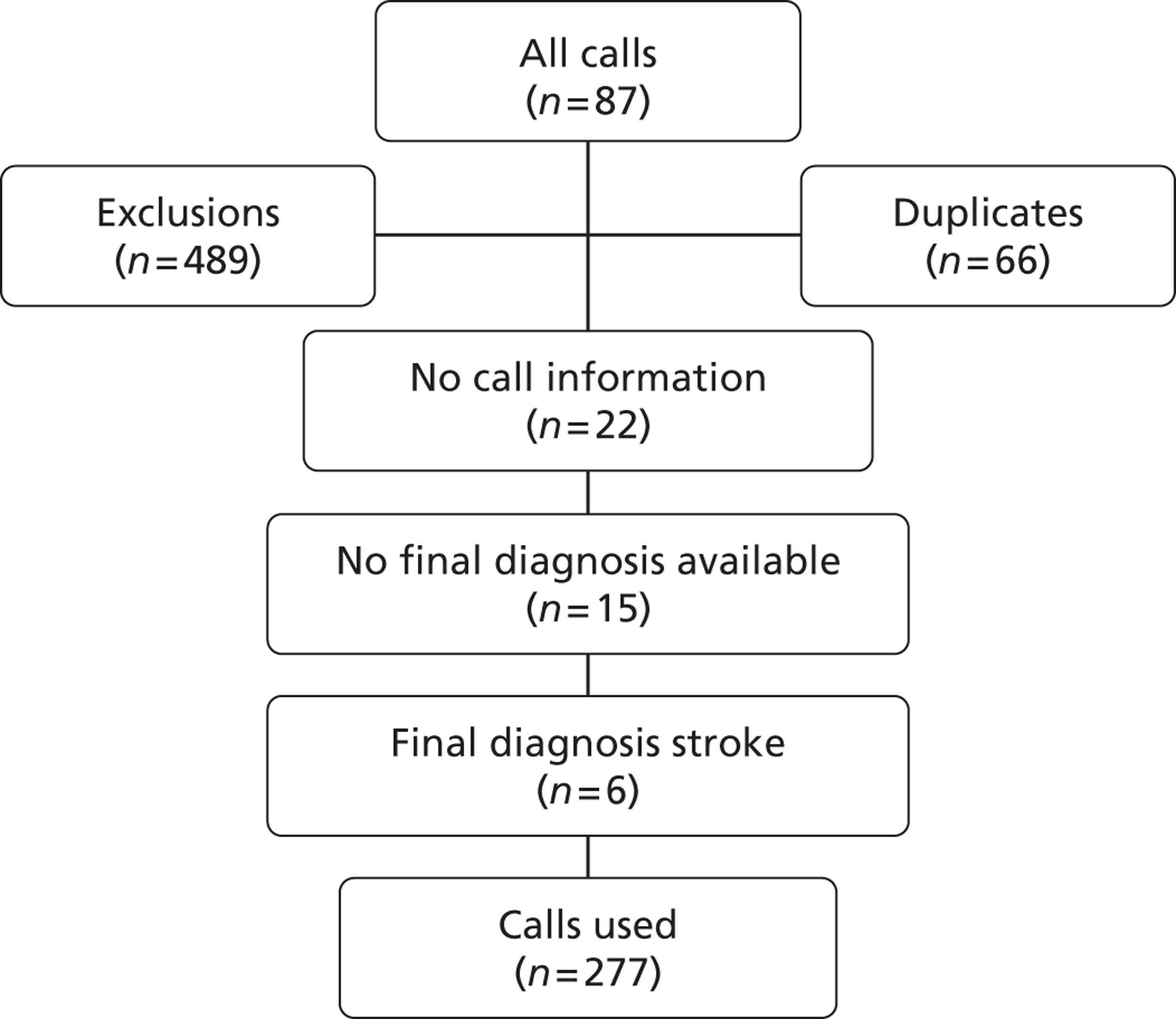
Inclusion criteria
The 999 call was made by a member of the public; patients arrived at hospital through EMSs; patients presented to the study hospital ED (whether admitted, or discharged after ED attendance).
Exclusion criteria
Calls relating to patients aged < 18 years. Calls which were likely to contain highly distressing or sensitive material were also excluded from the analysis; these included traumatic injury (i.e. laceration) (n = 70), poisoning (n = 40), physical or sexual assault-related injuries (n = 28), suicide (n = 27), road traffic accident (n = 24), choking (n = 4); women in labour (n = 3), and animal attack (n = 1). Calls were excluded if a medical practitioner had already seen the patient [i.e. interhospital transfers; patients referred by their primary care physician (GP) or GP staff on behalf of the patient) (n = 293)]. Sixty-six duplicate calls were excluded. For 22 people dispatched by the EMSs, no call data were available. Calls in which the final diagnosis was missing or the final diagnosis was stroke were also excluded.
Call data from phase 3 were also included in the analysis (a description of the sampling for these data can be found in Chapter 4 ).
Ethical approval
Approval for this phase was granted by the Patient Information Advisory Group (now the National Information Governance Board for Health and Social Care Ethics and Confidentiality Committee), the Local Research Ethics Committee, the Faculty of Health Ethics Committee at the University of Central Lancashire, and NHS Research and Development at the EMSs and acute hospital.
Procedure
All call recordings for the sample were listened to in full by a researcher trained in qualitative research methods. At the beginning of a call to EMSs, the caller is routinely asked the open question ‘What’s the problem, tell me exactly what happened?’ by an EMD to establish the chief complaint. We focused the analysis on the callers’ response to this first question, which we termed ‘the first story’. The first story typically involves the description of one or more presenting problems by the caller.
Calls were analysed by coding the first story by the caller to describe the presenting problem. Open coding of the data was undertaken using content analysis (facilitated by ATLAS.ti software). Analysis was undertaken using the constant comparative method in order to identify key indicator words (subsequently referred to as problem) and relationships within the data. 35 The research team met regularly to discuss the coding categories in order to ensure a consistent approach to analysis of the data. New categories were considered and added to the list of indicator words at weekly intervals. Key indicator words identified were grouped to form categories based on the Medical Dictionary for Regulatory Activities (MedDRA) coding system. 56 This stage of analysis was performed ‘blind’ to the final diagnoses for this sample.
The final diagnosis was obtained by an experienced research nurse from patients’ medical records. Where patients were discharged from the ED, the ED diagnosis was used. For all other patients the discharge letter was used.
Results
Analysis focused on the calls made to the EMSs for the 277 patients for whom we had complete call data and a final medical diagnosis. One hundred and seventy-three (62.5%) of the callers were female. Family members accounted for a large proportion of the callers (40.1%) ( Table 19 ). Of these, wives (10.8%), daughters (8.7%) and sons (8.3%) were the most likely to call EMSs on behalf of the patient.
| Patient characteristics | n (%) |
|---|---|
| n | 277 |
| Other (bystander, police, buzzer helpline, staff in public place) | 116 (41.9) |
| Family | 111 (40.1) |
| Patient | 35 (12.6) |
| Friend | 8 (2.9) |
| Care home staff | 4 (1.4) |
| Neighbour | 3 (1.1) |
Most patients (79.1%) were in their own home at the time of the call to the EMSs; others were in public places (10.8%) or in nursing and residential care settings (6.5%). The remainder were unknown (3.5%). Patient characteristics can be seen in Table 20 .
| Patient characteristics | n (%) |
|---|---|
| n | 277 |
| Median age (years) (IQR) | 65 (46–80) |
| Female | 147 (53) |
| Final medical diagnosis | |
| Infection | 44 (15.9) |
| Nervous system disorders | 31 (11.2) |
| Gastrointestinal disorders | 26 (9.4) |
| Injury | 28 (10.1) |
| Cardiac disorders | 24 (8.7) |
| Musculoskeletal disorders | 24 (8.7) |
| Respiratory disorders | 14 (5.1) |
| Metabolism and nutrition disorders | 9 (3.2) |
| Psychiatric disorders | 11 (4) |
| Pain | 10 (3.6) |
| Other (e.g. renal, blood, immune disorders) | 56 (20.2) |
The frequency of the number of problems reported in the first stories can be seen in Table 21 . The modal number of problems was one, occurring in just under 30% of calls. Similarly, four or more problems were reported in around 30% of calls, with < 5% reporting six problems. In total, 738 problems were mentioned for the 277 patients.
| Number with | All patients |
|---|---|
| One problem | 78 |
| Two problems | 70 |
| Three problems | 48 |
| Four problems | 41 |
| Five problems | 28 |
| Six problems | 12 |
| Total | 277 |
Of the 277 calls that were identified, stroke or TIA were mentioned in eight calls (2.9%). One or more of the individual FAST items were mentioned in 24 calls (8.7%). The most often reported FAST items were limb weakness in 12 (4.3%) calls, speech problems in 11 (4.0%) calls, with only one (0.4%) call including facial weakness. None of the calls included mention more than one of the FAST items.
We explored the relationship between the most common problems mentioned in the first story from phase 3 and whether the final diagnosis in hospital was stroke or not stroke ( Table 22 ). Within the table, the data pertaining to calls with a final diagnosis of stroke come from phase 3, and the data pertaining to calls with a non-stroke final diagnosis come from this phase (phase 4).
| Problems in first story | Final diagnosis of stroke from phase 3 calls (n = 473) | Final diagnosis not stroke from phase 4 calls (n = 277) |
|---|---|---|
| Stroke (%) | 188 (39.7) | 8 (2.9) |
| Fall (%) | 182 (38.5) | 72 (26.0) |
| Speech problems (%) | 72 (15.2) | 11 (4.0) |
| Limb weakness (%) | 70 (14.8) | 12 (4.3) |
| Consciousness level (%) | 77 (13.0) | 29 (10.5) |
| Generally unwell (%) | 49 (8.3) | 15 (5.4) |
| Facial weakness (%) | 17 (3.6) | 1 (0.4) |
| More than one FAST symptom (%) | 14 (3.0) | 0 (0) |
Table 22 shows that when the final diagnosis was stroke, nearly 40% of the callers mentioned stroke. In contrast, when the final diagnosis was not stroke, only 2.9% of callers mentioned stroke. The mention of fall or collapse was common in calls where the final diagnosis was stroke (around 40%), and it was also used in one-quarter of calls where the final diagnosis was not stroke. Both speech problems and limb weakness were mentioned in around 15% of calls where the final diagnosis was stroke, whereas these two problems were each mentioned in < 5% of calls relating to a non-stroke diagnosis. Consciousness level was mentioned a similar number of times for final diagnosis stroke or not stroke, as was mention of being ‘generally unwell’. Facial weakness was mentioned in < 4% of calls relating to a final diagnosis of stroke, but was only mentioned once in calls where there was a non-stroke final diagnosis. Describing more than one of the FAST items occurred in only 3% of calls where the final diagnosis was stroke, but where the final diagnosis was not stroke, none of the callers mentioned more than one FAST item.
Because of the sampling strategy adopted in phases 3 and 4 we are only able to describe for the word ‘stroke’ the sensitivity from phase 3 and the specificity from phase 4 data; these data can be extracted from Table 22 . In phase 3, the sensitivity of ‘stroke’ was 39.7% and in phase 4 specificity is 97.1%. The sensitivity of the individual FAST items in identifying stroke was low for speech (15.2%), limb weakness (14.8%) and very low for facial weakness (3.6%). However, the specificity of the individual items was very high: 96%, 95.7% and 99.6% for speech problems, limb weakness and facial weakness respectively. If more than one item of the FAST was used, this had low sensitivity (3.0%) but 100% specificity.
Discussion
Detailed analysis of actual calls to the EMSs has enabled us to study what was said by callers during stroke and non-stroke calls, rather than relying on abstracting data from patient records alone. The callers to EMSs in this phase were more often bystanders, the police or through buzzer helplines, compared with the stroke calls, where family members were the most likely people to call the EMSs. 20,46 In the non-stroke calls the patient was also more likely to be the caller (12.6%) than in calls for patients with suspected stroke (2.1%). The non-stroke calls tended to be based on patients who were younger: the average age of the non-stroke patients was 65 years, compared with the 77 years for stroke patients. However, around one-quarter of all stroke patients are aged < 65 years, so this is not a definitive marker of stroke or not.
The data from this phase have shown that the word ‘stroke’ is rarely used by callers when describing a problem where the final diagnosis is not stroke. In phase 3 it was identified that use of the word ‘stroke’ was associated with a final diagnosis of stroke in around 40% of cases. Taken together, these findings suggest that if a caller mentions the word ‘stroke’ during the first story, there is some probability that they are describing a stroke, but if they do not use the word ‘stroke’, there is a very high probability that they are describing something other than stroke.
The individual items of the FAST show similar patterns in relation to how frequently they are used in stroke compared with non-stroke calls. Both speech problems and limb weakness were reported in < 5% of the calls where the final diagnosis was not stroke, but were reported in around 15% of calls where the final diagnosis was stroke. Although facial weakness was mentioned in < 4% of calls where the final diagnosis was stroke, it was mentioned in well under 1% of the calls where the final diagnosis was not stroke. This suggests that absence of facial weakness may be useful to indicate a non-stroke diagnosis. In addition, although more than one item of the FAST was mentioned in only a small number of cases of stroke, multiple items were never mentioned when the diagnosis was not stroke. Similar to the absence of facial weakness, a lack of multiple FAST items may be useful to indicate a non-stroke diagnosis.
Describing a collapse or fall occurred in 26% of the non-stroke calls; this was less than in the stroke calls (38.5%). These are much higher values than reported elsewhere for terms such as ‘collapse’ or ‘fall’, which have previously been reported as presenting stroke symptoms by 17% and 21% of callers respectively. 20,22 Despite the common occurrence of ‘fall’ as the key presenting symptom in calls where stroke is subsequently diagnosed,46 it has little discriminatory value if as many as one-quarter of the non-stroke calls also mention collapse or fall. It is, however, important that EMDs are able to distinguish between ‘mechanical’ falls where there is a clear external cause, and fall/collapse where an underlying medical condition has led to the presentation as ‘fall’. The AMPDS algorithm for ‘fall’ includes the question ‘What caused the fall?’, which could be held to imply that a mechanical, rather than medical, cause is the precipitating factor. In the non-stroke calls, despite a high proportion of callers reporting a fall, only 2% had a final diagnosis of fall in hospital.
Limitations
The samples of calls for phases 3 and 4 were based within the catchment area of the same regional ambulance trust, but utilised different acute hospital trusts, and also covered different time periods. This means that the populations studied in these phases are not directly comparable, but they do allow separate estimates of sensitivity (phase 3) and specificity (phase 4). The nature of the sampling in phase 3 meant that the stroke population was over sampled, which meant that it was harder to explore the relationship between the words used and the final diagnosis when the final diagnosis was non-stroke. In order to address this, in phase 4 we identified all calls to the EMSs over a 1-week period, thereby allowing us to identify all the calls related to a non-stroke final diagnosis and subsequently explore the words used by the callers in such calls. Within the calls identified, only six had a final diagnosis of stroke, demonstrating that stroke accounts for < 1% of calls to the EMSs. This sample of all calls could have allowed us to more fully explore sensitivity, specificity, PPV and negative predictive value; however, the small sample of true stroke patients would have led to very imprecise estimates of these values. Rather than over analyse or over interpret these data it was felt that a more cautious approach should be taken and so we only analysed calls associated with a non-stroke final diagnosis.
There were very limited data available about the callers as we were only able to record details discussed during the call itself. This generally included the caller’s relationship to the patient. Callers’ genders were attributed according to relationship with the patient, or voice, if it was not apparent from the content of the call. It was not possible to identify the callers’ ages. Patients’ final medical diagnoses were taken from the case notes, but there was no mechanism to verify these independently.
A large proportion of the calls to the EMSs were excluded from the analysis, but it is unlikely that the problems described for these excluded cases are likely to overlap to a great extent with the problems we identified (e.g. calls relating to women in labour or assault injury). In addition, the context of many of the excluded calls is likely to indicate that the problem is due to extrinsic rather than intrinsic factors, such as road traffic accident.
Conclusion
The non-stroke calls were more likely to be made by someone other than the patient themselves and the patients tended to be younger. Less than 5% of callers in the non-stroke calls mentioned either ‘stroke’ or any of the FAST items and none of the calls included more than one FAST item. This compares with the mention of ‘stroke’ in around 40% and FAST items in around 15% of the stroke calls. Mention of ‘stroke’ or ‘FAST’ items in the first story was much more common in stroke than in non-stroke calls and not mentioning these terms occurred frequently in the non-stroke calls. Fall was a common presenting complaint in both the stroke and non-stroke calls, meaning that whether or not it is mentioned is not indicative of a stroke or non-stroke diagnosis.
Summary
In previous phases of this programme of work we identified that the majority of calls made to the EMSs on behalf of someone with suspected stroke were made by a female relative: stroke patients rarely made the EMS call themselves. Callers tended to talk in terms of the consequences of loss of function (e.g. unable to grip, cannot stand) rather than describing symptoms themselves, such as weakness. Nevertheless, findings from the earlier phases indicate that if the patient has, or the caller mentions, one or more of facial weakness, limb weakness, or speech problems (or even uses the word ‘stroke’), there is an increased probability that the person has had a stroke. This phase has added to these data by showing that callers very rarely mention the word ‘stroke’ or any of the FAST items for non-stroke calls. This programme of work is therefore building a picture of the relationship between problems described, or not, and whether the call relates to a stroke or non-stroke diagnosis. There is no one definitive indicator word for a diagnosis of stroke, but a call made by a third party, describing an older patient and mentioning the word ‘stroke’ or one or more of limb or facial weakness, or speech problems has a higher probability of being associated with a final diagnosis of stroke. In contrast, a call made by the patient, who is of a younger age and does not mention the word ‘stroke’, or describe limb or facial weakness, or speech problems has a high probability of having a diagnosis of not stroke. The findings from phases 1–4 of this programme of research will be used in phases 5 and 6 to inform the development of algorithms, protocols and a training package aimed at improving recognition of stroke. Although the aim of the next phase (phase 5) was to develop algorithms and protocols for EMSs and NHS Direct staff to assist in the identification of those with suspected stroke, this was not possible, reasons for this will be now be explained further.
Chapter 7 ESCORTT phase 5: developing algorithms and protocols for ambulance and NHS Direct staff to assist in the identification of those with suspected stroke
Background
In the UK, people seeking urgent medical assistance call a universal number (999) and are connected to the EMS dispatch centre in closest proximity. All calls to the EMSs in the UK are digitally recorded for training and governance purposes. Once the call is logged and patient location established, an EMD will dispatch the closest ambulance. Calls to EMSs are triaged using AMPDS,57 an algorithm-based system which is also used widely in Europe and North America. In 2007, the AMPDS system was used by more than 3000 public safety agencies in over 23 countries. 58 The design and publishing licence for AMPDS is owned by Priority Dispatch Corp. EMD classification within AMPDS and prioritisation directly impact the speed of ambulance response and the level of medical care (e.g. paramedic) sent.
The AMPDS protocol is designed to standardise and codify the operation of EMDs while optimising safe and effective patient care through dispatch life support and EMS system response. AMPDS provides EMDs with software that supports decision making during a 999 call. The EMD firstly establishes the patient’s address and contact details and then asks specific questions about the patient’s condition. EMDs must follow the questions that are scripted within AMPDS. AMPDS also provides EMDs with information about specific conditions/problems, as well as online pre-arrival and post-dispatch instructions, appropriate response and referral recommendations. The aim of this phase of the programme was to develop algorithms and protocols for ambulance and NHS Direct staff, informed by earlier phases to assist in the identification of those with suspected stroke.
Methods
Aim
To develop algorithms and protocols for ambulance and NHS Direct staff, informed by earlier phases to assist in the identification of those with suspected stroke.
Study design
Although a specific change methodology approach was not utilised at the time of the study, the steps taken to identify and explore a process of revising current algorithms and scripted questions within the EMSs and NHS Direct have been mapped to Kotter’s eight-step change model. 59
Results
Step 1: create urgency
Support and collaboration was sought from key stakeholders including North West Ambulance Service, Yorkshire Ambulance Service, London Ambulance Service, NHS Direct, the National Academies of Emergency Dispatch, and NHS Pathways. Discussions took place with key stakeholders to explore the findings from phases 1–4 and how those findings could be used to change current AMPDS and NHS algorithms.
Potential barriers to changing current algorithms were identified and included:
-
evidence generated from the data collected in only one regional ambulance trust
-
a limited number of data from NHS Direct due to difficulties in obtaining NHS Direct calls
-
AMPDS being based on published standards from a wide range of international institutions including the National Association of EMS Physicians (NAEMSP), the American Society for Testing and Materials (ASTM), the American College of Emergency Physicians (ACEP), the United States Department of Transportation (USDOT), the National Institutes of Health (NIH) and the American Medical Association (AMA)
-
the intended replacement of AMPDS and NHS Direct with NHS Pathways.
The project team worked with NHS Direct, the National Academies of Emergency Dispatch and NHS Pathways to work through a number of different scenarios using the findings of phases 1–4. Publication of the National Stroke Strategy in 2007 highlighted that stroke should be treated as a medical emergency. 44 Nationally, there was a sense of urgency around the need for change and that stroke patients should be identified and transported to hospital as quickly as possible.
Step 2: form a powerful coalition
The Emergency Stroke Calls: Obtaining Rapid Telephone Triage (ESCORTT) project steering team included a number of influential stakeholders and the project also had support from key stakeholders within a range of ambulance services, NHS Direct, the National Academies of Emergency Dispatch and NHS Pathways, bringing together a team of influential people varying in status and expertise. Although key stakeholders were in agreement about suggested changes to AMPDS, a number of external factors had a major influence over the change process.
Between phases 1 and 4 (October 2006 to March 2010) the versions of AMPDS changed from v11.3 to v12.2. The latter version includes the FAST, an addition that would have been recommended based on the findings from phases 1, 3 and 4. In phase 1 facial weakness and speech problems were consistently associated with dispatch (face p < 0.001; speech p < 0.002) and ambulance (face p < 0.001; speech p < 0.01) diagnosis of stroke. In phase 3 at least one of the FAST items was reported in 145 (30.7%) of the calls, where the final diagnosis was stroke: speech being the most common (n = 72, 15.2%). Whereas in phase 4, people who contacted the EMSs about non-stroke conditions rarely said stroke (n = 12, 4.3%), limb weakness (n = 12, 4.3%), speech problems (n = 11, 4.0%) or facial weakness (n = 1, 0.4%).
Step 3: create a vision
The proposed changes were aligned with the strategic aims of the key stakeholder organisations as outlined below:
Staff
Any changes to algorithms could be supported by providing evidence-based training for staff, thus contributing towards continuing professional development.
Value for money
The evidence had already been generated and the training packages had been developed as part of this programme of research, the training had already been endorsed through the UK Stroke Forum Education and Training.
Quality of care
Stroke is a leading cause of mortality and disability worldwide and is increasingly recognised as a time-dependent medical emergency in which early presentation to specialist care reduces death and dependency. It is important that stroke is recognised at the earliest opportunity to ensure that an ambulance is dispatched with an appropriate level of priority, therefore facilitating early presentation and rapid specialist treatment.
Communities
Any changes to algorithms and protocols would be based on research that explored patient and public experiences of contacting the ambulance service and NHS Direct for suspected stroke.
Step 4: communicate the vision
Meetings and presentations took place with all key stakeholder organisations over a period of 9 months. Meetings involved presentations of the ESCORTT research findings, the use of different scenarios within NHS Direct, AMPDS and NHS Pathway algorithms and discussions about the facilitators and barriers to change.
Step 5: remove obstacles
The stakeholder group identified a number of potential processes and structures that would be obstacles to the change process as outlined in step 2. However, the stakeholder group also identified that these obstacles could not be removed mainly due to large external organisational changes that were already occurring such as the move from AMPDS to NHS Pathways.
Step 6: create short-term wins
Although it was not possible to change the AMPDS or NHS Direct algorithms, stakeholders felt that the project findings could be used to inform NHS Pathways algorithms in the future. Based on the findings from phase 3a discussions have already taken place with NHS Pathways regarding the use of the term consciousness in all algorithms.
Step 7: build on the change
With the continuing roll-out of NHS Pathways there may be a number of opportunities in the near future to use the findings from ESCORTT to underpin new and existing algorithms. The ESCORTT group have continued to maintain links with key stakeholder organisations and are currently exploring ways in which to take the findings from ESCORTT forward.
Step 8: anchor the change in the culture
By presenting the results of ESCORTT at a range of local, national and international meetings and conferences, the project has maintained a presence among key stakeholder organisations and the ESCORTT group will continue to work with key stakeholders in the future.
Discussion
It was not possible to change the AMPDS algorithm for stroke within the ambulance service or NHS Direct, based on the findings from ESCORTT. Further evidence would be required as AMPDS is based on published standards from a wide range of international institutions including the NAEMSP, the ASTM, the ACEP, the USDOT, the NIH and the AMA. 58
Similarly, NHS Direct algorithms are aligned to DoH, NHS and National Institute for Health and Care Excellence (NICE) policies and are reviewed annually. Too few calls relating to patients who had contacted NHS Direct for suspected stroke could be identified to suggest any changes to the NHS Direct algorithm for stroke.
A new system, NHS Pathways, has recently been developed with the intention of replacing AMPDS. This development took place during the same period as the ESCORTT programme of research. NHS Pathways is a suite of clinical content assessment for triaging telephone calls from the public, based on the symptoms they report when they call. NHS Pathways sets out to deliver a single clinical assessment tool that provides effective triage over the telephone in any setting which takes calls from the public. This includes calls to 999, NHS Direct, GP out-of-hours, NHS 111 and any other Single Point of Access number in place. 60 NHS Pathways was developed and is maintained by a group of NHS clinicians with extensive experience of urgent and emergency care provision, and clinical decision support tools. The system is currently being used by five ambulance trusts in the UK and many ambulance trusts have expressed an interest in using NHS Pathways as their primary clinical assessment tool for incoming 999 calls. The switch over to NHS Pathways from AMPDS will require extensive training of EMDs and changes to information technology (IT) systems, and so the roll-out of NHS Pathways has taken longer than expected. The Ambulance Trust within which the ESCORTT programme of research took place had a service delivery plan in place to move from AMPDS to the NHS Pathways system in 2011. However, at the time of writing this process is yet to take place.
Limitations
Although a specific change methodology approach was not utilised at the time of the study, the steps taken to identify and explore a process of revising current algorithms and scripted questions with the EMSs and NHS Direct have been mapped to Kotter’s eight-step change model. 59 It is not envisaged that using an alternative change model would have provided any additional benefits or would have better facilitated the change process.
Conclusion
It was not possible to change the AMPDS algorithm for stroke based purely on the findings from ESCORTT, and within Ambulance Trusts across the UK AMPDS is to be replaced by NHS Pathways. Future research could evaluate the impact of NHS Pathways in terms of dispatch/prioritisation for suspected stroke, as little is known about the impact of NHS Pathways.
Summary
The aim of this phase of the programme was to develop algorithms and protocols for ambulance and NHS Direct staff, informed by earlier phases, to assist in the identification of those with suspected stroke. It was not possible to change the AMPDS algorithm for stroke within the ambulance service or NHS Direct, based on the findings from ESCORTT. AMPDS is gradually being replaced by NHS Pathways. The findings of the ESCORTT programme may contribute to the development of effective stroke algorithms in this new system.
Chapter 8 ESCORTT phase 6: developing an online training package for emergency medical dispatchers to assist in the identification of those with suspected stroke
Background
Stroke outcomes can be improved by timely care. It is therefore vital that EMS personnel are able to recognise the symptoms of suspected stroke and initiate a rapid response. People with suspected stroke should be taken immediately to a hospital ED which offers hyperacute stroke care. Early presentation at hospital provides greater opportunity for time-dependent treatments, such as thrombolysis, and for early admission to specialist stroke care. 3
A training package will need to be developed for use by EMDs informed by the results of phases 1–4. The aim of the training package will be to improve education and increase awareness of staff in recognising the symptoms of stroke and the importance of treating stroke as a medical emergency. The training package will consider the ability of EMDs to identify key words and phrases that might indicate acute stroke. Development of the package will include input from the EMSs, other health-care professionals, academics, and users and carers. The course will be accessible via the internet, completed and evaluated online.
Online delivery allows flexibility of access by allowing participants to collapse time and space. 61 However, online materials must be appropriately designed to promote learning and engage the learner. 62 This training package was intended to complement an existing training package for EMSs – Rapid Emergency Stroke Pathways: OrgaNised Systems and Education (RESPONSE). The RESPONSE course is an interactive online acute stroke course that has been completed by over 2000 health professionals worldwide and is endorsed by the UK Stroke Forum Education and Training.
Methods
Aim
To develop an online training package to improve the recognition of stroke by EMDs, informed by phases 1–4.
Study design
Development of a training package informed by phases 1–4 of the ESCORTT programme of research and the views of an expert committee.
Setting
One EMD control centre within a large regional EMS in England, providing services to a population of 7 million people across a geographical area of approximately 5400 square miles.
Selection of participants
We recruited a convenience sample of 12 people from the project steering group or individuals who were identified by members of the steering group as having specific expertise in relation to stroke and/or the development of online learning materials. These participants formed an expert committee comprising academics, health professionals and patients.
Ethical approval
As this phase involved the development of an online training package only, ethics approval was not required.
Procedure
The findings from phases 1–4 were used to inform the development of a training package. The main content of the training package in relation to general information about stroke was based on the previously developed and endorsed RESPONSE acute stroke online course. An expert committee was convened to provide advice on which aspects of the ESCORTT programme of research should be included in the training package, to identify the most important findings and to determine how these should be included within the training package. The content of the online training package was then circulated to members of the steering group for feedback.
Results
The expert committee comprised four academics, six health professionals and two stroke survivors. The committee reviewed the content of the existing RESPONSE acute stroke online course and identified sections that could also be incorporated into the training package. These sections included:
-
risk factors for stroke
-
‘what is a stroke?’
-
different types of stroke
-
suspected stroke and dialling 999
-
the signs and symptoms of stroke
-
TIA
-
other signs and symptoms
-
stroke mimics
-
thrombolysis.
The expert committee also felt that it was important to include general information about ESCORTT and the purpose of the research programme.
The findings from phases 1–4 were used to inform the sections of the training package. Table 23 gives details of how and where the findings of each phase of the ESCORTT programme were incorporated into the training package. The full training package content can be found in Appendix 2 .
| Content | Phase | Form within the training package |
|---|---|---|
| What influences the public’s initial decision to contact the EMSs at the onset of stroke symptoms? | 2 | Text describing what influences someone to contact the EMSs at the onset of stroke symptoms |
| Suspected stroke – describing the symptoms | 3 | Text describing the words used by the public for describing stroke symptoms. Audio recordings (anonymised and re-recorded by the research team) of calls to the EMSs for suspected stroke |
| The proportion of patients (or someone on their behalf) who obtain first medical contact from the EMSs for suspected stroke | 3 | Text describing the proportion of patients (or someone on their behalf) who obtain first medical help from the EMSs for suspected stroke |
| Who is most likely to dial 999 for suspected stroke? | 3 | Test describing who is most likely to dial 999 for suspected stroke |
| How stroke symptoms may be described by the public? | 3 | Text and audio recordings of how stroke symptoms may be described by the public |
| Communication between the EMD and caller | 2 | Text describing the experiences of patients and those who act on their behalf, of their communication with EMDs during calls for suspected stroke |
| How often is suspected stroke confirmed as a stroke in hospital? | 1 | Text describing how often suspected stroke is confirmed as stroke in hospital |
| Do non-stroke callers mention ‘stroke’ and/or the FAST symptoms? | 4 | Text describing that ‘stroke’ and/or the FAST symptoms are rarely used in calls to the EMSs in non-stroke-related calls |
| Understanding the term consciousness | 3a | Card-sort interactive activity, sorting the words that the public do and do not use to describe different levels of consciousness |
Once the initial training package content had been developed this was circulated to the ESCORTT steering group for members to review. The training package was also discussed at project steering groups.
Members of the expert committee with specific expertise in developing online educational materials emphasised the importance of developing interactive activities that would aid learning. The course therefore also included interactive animations that allowed the EMDs to alter physiological parameters in order to visualise their effects on the post-stroke brain ( Figure 3 ), and a multiple choice quiz ( Figure 4 ).
FIGURE 3.
An interactive animation showing perfusion and oxygen saturation.

FIGURE 4.
Multiple-choice quiz.
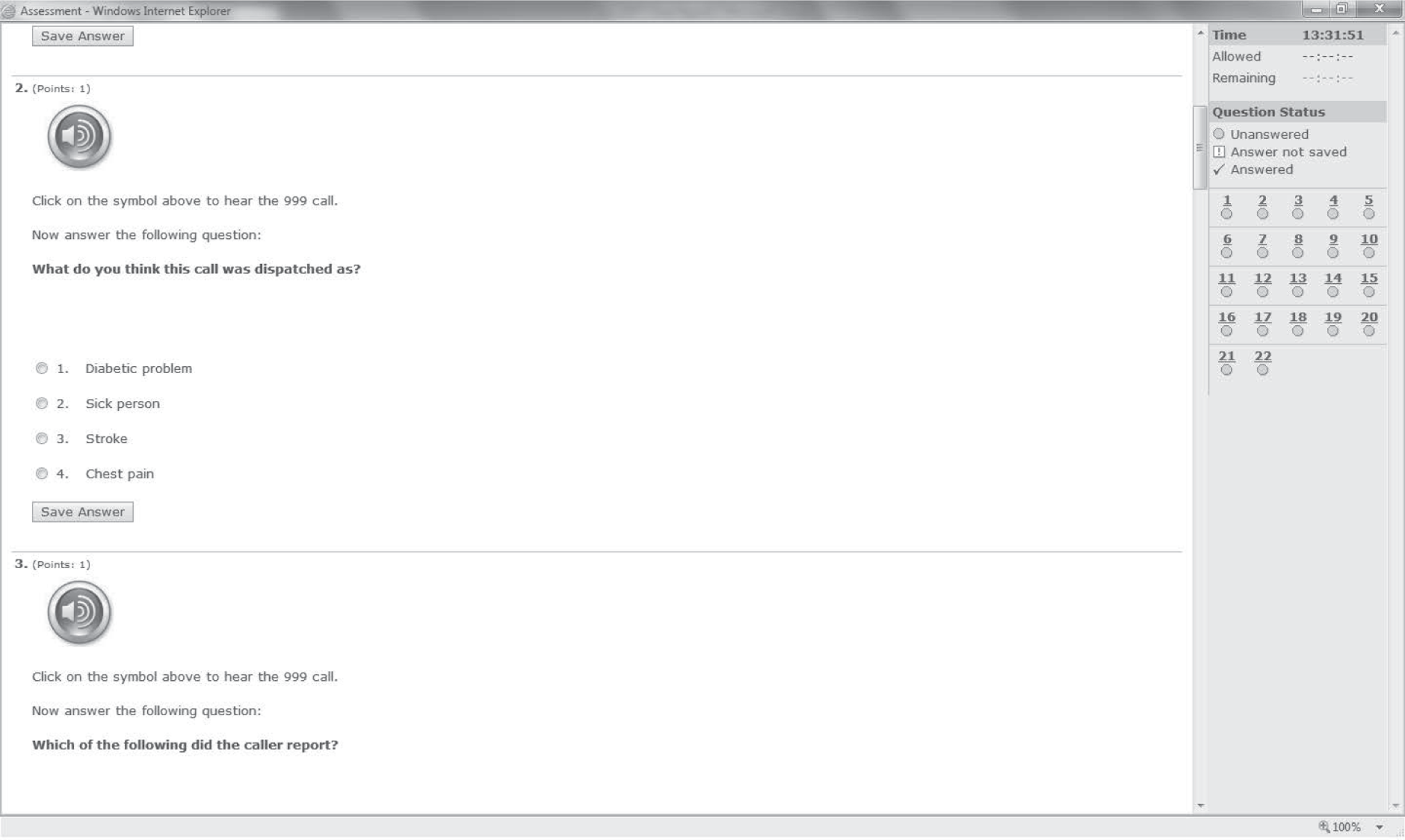
Interactive activities also included an online card-sort game in which EMDs had to put cards onto two piles according to the words they thought that the public used to describe the term ‘consciousness’ ( Figure 5 ).
FIGURE 5.
Interactive card-sort game for words that the public use to describe the term ‘consciousness’.
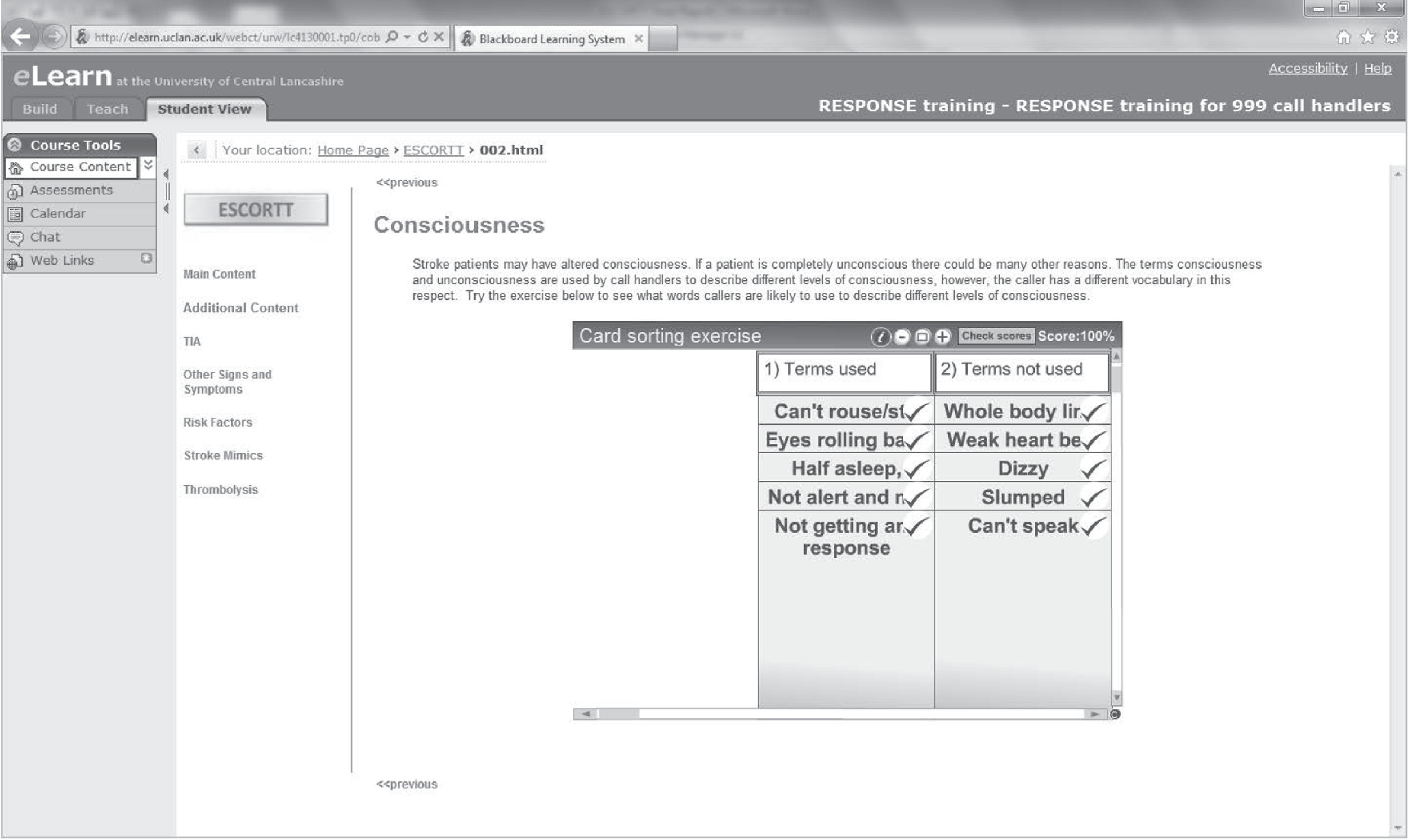
The course also included audio simulations of 999 calls in which miscommunication or poor stroke symptom recognition had resulted in incorrect categorisation, to add context and impact. These calls were based on transcripts of actual calls from phase 3. They were anonymised, with all identifying material removed, before being audio-recorded by members of the research team.
Discussion
This is the first stroke-specific training package to be developed for EMDs with the aim of improving their recognition of stroke. The training package includes stroke-specific information relating to risk factors; what a stroke is; different types of stroke; suspected stroke and dialling 999; TIA; stroke mimics and thrombolysis.
Underpinned by the findings from phases 1–4 of the ESCORTT programme of research, the training package also provides detailed information about what influences people in their initial decision to contact the EMSs at the onset of stroke symptoms; how the public describe the symptoms of stroke during a 999 call; the proportion of patients (or someone on their behalf) who obtain first medical contact from the EMSs for suspected stroke; who is most likely to dial 999 for suspected stroke; important communication issues between EMDs and callers; how often suspected stroke is confirmed as a stroke by ambulance crews and in hospital; details of the words that are used to describe non-stroke-related conditions; and the public’s understanding of different levels of ‘consciousness’ and how these are described during 999 calls.
A range of interactive activities have also been developed to assist learning including interactive animations; a multiple-choice quiz; card-sort activity and re-enactments of anonymised 999 calls.
Based on the previous success of the RESPONSE acute stroke online course,63 the training package was developed in a similar format for delivery online. Online delivery allows flexibility of access61 and the development of a range of interactive activities (e.g. listening to re-enactments of 999 calls and deciding which dispatch code to assign to that call). Interactive activities are designed to promote learning through enabling the learner to engage with the training material. However, it was acknowledged that online learning may be new to some and might not suit the learning style of others. The EMD evaluation of the training package, including its delivery mode and content, will be explored in the next phase (phase 7).
Conclusion
This is the first stroke-specific training package to be developed for EMDs, and is underpinned by the findings from each phase of the ESCORTT programme of research. A range of interactive activities have also been developed to assist learning including interactive animations; a multiple-choice quiz; card-sort activity; and re-enactments of anonymised 999 calls. The development of a stroke-specific training package will provide an exceptional learning opportunity for EMDs in improving their awareness of the key words and phrases that can indicate acute stroke during calls to the EMSs. Online delivery promotes flexibility of access by allowing participants to complete the training at the times most convenient for them.
Summary
The next phase (phase 7) of this programme of research involved the implementation of a training package in one EMD control centre. The next phase will outline an evaluation of EMDs’ satisfaction with the training package, including the method of assessment, usability, level of content, self-perception of increased knowledge and understanding of emergency stroke issues, and any changes that they felt should be made to the training package.
Chapter 9 ESCORTT phase 7: implementation and evaluation of an online stroke-specific training package for emergency medical dispatchers
Background
It is important that stroke is recognised at the earliest opportunity to ensure that an ambulance is dispatched with an appropriate level of priority, therefore facilitating early presentation and rapid specialist treatment. Informed by the results from phases 1–4 a training package was developed for use by EMDs. The findings from phases 1–4 were used to inform the sections of the training package that specifically relate to:
-
How often is suspected stroke confirmed as a stroke by ambulance crews and in hospital? (Phase 1.)
-
What influences the public’s initial decision to contact EMSs at the onset of stroke symptoms? (Phase 2.)
-
Communication between the EMD and caller. (Phase 2.)
-
Suspected stroke – describing the symptoms. (Phase 3.)
-
The proportion of callers who obtain first medical contact from the EMSs for suspected stroke. (Phase 3.)
-
Who is most likely to dial 999 for suspected stroke? (Phase 3.)
-
How stroke symptoms may be described by the public? (Phase 3.)
-
Callers’ understanding the term ‘conscious’. (Phase 3a.)
-
Do non-stroke callers mention ‘stroke’ and/or the FAST symptoms? (Phase 4.)
Phase 7 explores the implementation of the training package in one EMD control centre. It outlines an evaluation of EMDs’ satisfaction with the training package overall, the method of assessment, usability and level of content. EMDs were also asked about any increases in knowledge of the anatomy and physiology in relation to stroke, knowledge of the signs and symptoms of stroke, any increases in understanding that stroke should be treated as a medical emergency, and about any changes that they felt should be made to the training package. The impact of the training package on the recognition of stroke by EMDs will be evaluated in phase 8.
Methods
Aim
To implement and evaluate the online training package.
Setting
One EMD control centre within the north-west of England.
Subjects and sampling
All EMDs who were employed at one EMD control centre between September 2009 and January 2010.
Procedure
Emergency medical dispatcher trainers were identified at one EMD control centre. ESCORTT project staff who had been involved in the development of the training package met with the trainers to discuss the content, how to access the training, how to deliver the training and complete the evaluation. Two EMD trainers then took over the roll-out and completion of the training package and evaluations.
Data collection and analysis
Once the training package had been developed, an evaluation questionnaire was designed. The online evaluation was made up of 12 questions, which is within the optimum range (10–15) for ensuring good completion rates. 64 The questions covered satisfaction with the course; increase in knowledge and understanding; usefulness of the course and suggested changes.
The first section of the evaluation questionnaire related to satisfaction with the course. It consisted of five closed questions that asked participants to rate their satisfaction with the course overall, the method of assessment, the animations, usability and level of content. The second section concerned increased knowledge. It contained three closed questions asking if the course had increased participants’ knowledge of the anatomy and physiology in relation to stroke; increased knowledge of the signs and symptoms of stroke; increased understanding that stroke should be treated as a medical emergency. The final section concerned suggestions for changes to the course. It consisted of four open-ended questions. These asked participants if there were any topics in relation to acute stroke that they did not feel had been covered adequately; if there were any topics that they did not find useful; to identify the most useful features of the course and to suggest changes to the course.
Analysis of the closed questions was undertaken by describing the overall proportions of participants’ scores for each question. The responses to the open-ended questions were collated and grouped into categories relating to each open-ended question.
Results
The training package was undertaken by two educational and training managers who in turn rolled it out to 67 call handlers, 76% of whom were female.
Results of course evaluation
The first question within the evaluation was ‘How satisfied were you with the training package?’
Overall 65 (97%) of the call handlers were either very satisfied or satisfied with the training package as a whole. Comments included:
I am very impressed with the training package and cannot think of any changes I would make. It is also a valuable piece of CPD [continuing professional development] evidence.
Very informative, I wish there were other courses like this.
I enjoyed the course and the certificate of completion is in my CPD folder.
Completion of the training package was assessed with a 20-question multiple-choice test. Sixty-three (94.0%) were also either very satisfied or satisfied with the multiple-choice test as the method of assessment:
After passing the test I received a certificate of completion. This is very useful in terms of my continuing professional development.
The quiz wasn’t too difficult and it was useful to assess what I have learned.
The assessment reflected what we covered in the course and I knew more than I thought.
Sixty-three (94.0%) EMDs were either very satisfied or satisfied with the usability of the training package:
An interesting course, the content was easy to use.
The content was easy to follow and was divided into sections which helped keep it (the content) clear.
Easy to use and follow.
As the course was aimed at all EMDs, the degree of difficulty of the training package may have been an issue as the training package has been completed by a range of staff from trainees to managers. Sixty-three (94.0%) were either very satisfied or satisfied with the level of the course:
I was happy with the package in terms of content and the content level.
I feel I have learnt a lot without it (the course) being too much, it wasn’t at too high a level.
Just right, if it’s too difficult it can be off putting but it was just right I would say.
During the development of the training package it was decided by the project steering group that the course content should include information that may be of interest to EMDs but may have been more in-depth than required by some participants. Sixty-four (95.5%) participants reported an increase in stroke symptom knowledge, 63 (94.0%) participants reported an increased knowledge in the management of acute stroke, and 64 (95.5%) participants reported an increase in their awareness of stroke as a medical emergency.
The best features of the training package were found to be the content:
Clear, simple and easy to follow.
Symptoms, what people say, how people describe stroke.
Knowing what people actually say for stroke, you suspect it might be that (stroke) during a call but you don’t know if it actually is.
Some minor suggestions of how the training package could be changed or improved were received, including more information on potential stroke mimics, what to do if the patient has had a previous stroke and handling urgent calls from GPs:
More on stroke mimics.
What happens if it’s an old stroke?
GP urgents, GPs still book ambulances for 2 hours.
No, covered all relevant topics.
Discussion
The training package was successfully undertaken and completed by EMD call handlers in one EMD control centre. The majority of respondents found the training package to be informative, generally raising knowledge of stroke, its symptoms and the importance of stroke as a medical emergency. To our knowledge, no previous studies have evaluated stroke-specific EMD training with the aim of improving EMD recognition of stroke. Although the majority of participants reported an increase in knowledge of stroke symptoms, the management of acute stroke and stroke as a medical emergency, we did not formally test knowledge before the training package was completed and so this is a subjective outcome.
In health care, as in many other educational fields, there have been recent advances in the use of technology as a tool for facilitating student learning, particularly for those accessing courses from the practice setting. 65 There is also a demand for continuing professional development and updating of knowledge and skills. 65 As in previous studies66 this evaluation has highlighted a demand for stroke-specific training. The training package takes only 2 hours to complete and is free to access, both features known to facilitate the uptake of learning opportunities. 66 The training package can be accessed via any computer with internet access, at home or work. Staff reported that they had enjoyed completing the course, but also stressed the importance of accessibility of suitable training opportunities in relation to their continuing professional development.
Limitations
The training package was implemented and evaluated in only one EMD control centre and so the generalisability of the findings of this phase is limited. Although the uptake of the training package has been encouraging, e-learning is an approach that does not suit everybody’s learning style or technological abilities. Other barriers to the use of e-learning may also include a lack of personal discipline65 and out-of-date computer equipment which may be inadequate for the use of some elements of an e-learning training package, such as the use of interactive animations.
Emergency medical dispatchers were asked to rate their own improvements in stroke knowledge and so this is a subjective outcome. Stroke knowledge was assessed only following implementation of the training package and so no baseline comparisons can be made.
Conclusion
We believe that this is the first study to (develop and) evaluate stroke training for EMDs with the aim of improving recognition of stroke. We have also shown that online learning for EMDs is well received and can increase self-reported stroke knowledge and that EMDs welcome the opportunity for continuing professional development. Further information about the course can be found at http://ukfst.org/courses/50/.
Summary
Following the successful development and implementation of a stroke-specific training package for EMDs, the impact of this newly-developed, stroke-specific, online training package on the recognition of stroke by EMDs will be evaluated in phase 8. In phase 7, two trainers and 67 EMDs completed the training package. Phase 8 will evaluate the accuracy of dispatch diagnosis of EMDs using an interrupted time series design.
Chapter 10 ESCORTT phase 8: training emergency services’ dispatchers to recognise stroke – the evaluation and impact of a training package
Background
Stroke is a leading cause of mortality and disability worldwide1 and is increasingly recognised as a time-dependent medical emergency in which early presentation to specialist care reduces death and dependency. 3
Up to 70% of all stroke patients obtain first medical contact from the EMSs. 3,7,24 Calls to the EMSs are triaged using AMPDS,8 a system also used widely in Europe and North America. EMDs use this system to categorise ambulance response and decide on the level of medical care sent. If the EMD suspects a time critical condition such as stroke, an ambulance can be dispatched as a high priority (category A, currently up to a 19-minute response). In the UK the categories for response prioritisation are pre-determined by the DoH.
Identifying ‘true stroke’ from an EMS call is challenging. Although AMPDS is effective at ruling out acute stroke in people with other conditions, it is poor at correctly identifying acute stroke, with > 50% of strokes being misclassified. 9–11 It is important that stroke is recognised at the earliest opportunity to ensure that an ambulance is dispatched with an appropriate level of priority, therefore facilitating early presentation and rapid specialist treatment.
One way of facilitating rapid EMS transport to hospital, thereby improving the chance for early presentation is through enhancing communication between the general public and the EMSs. As part of a programme of research, we explored the interaction between the public and the EMSs during emergency calls for stroke, in order to inform the content of stroke-specific, online training for EMDs; this included exploring callers’ experiences12 and identifying the key words used by the public, to describe and that are indicative of stroke. 13 The aim of this study was to evaluate the impact of this newly-developed, stroke-specific, online training package on the recognition of stroke by EMDs, and on the impact of stroke recognition on the time between the call to EMSs and stroke patients reaching hospital.
Methods
Design
Interrupted time series.
Setting
An ambulance service and a hospital trust in the north-west of England.
Subjects and sampling
Subjects were patients with suspected stroke arriving at hospital by ambulance during an 18-month period (16 March 2009 to 29 August 2010). For every 3-week period, we identified 1 week of consecutive patients (arrival at hospital between 0000 hours on the Monday through to 1159 hours the following Sunday). Each sampled week was deemed an observation.
Inclusion criteria
Patients who had a diagnosis of suspected stroke by the EMS call handler and/or a final diagnosis of stroke in hospital.
Exclusion criteria
Patients whose GP contacted the EMSs on their behalf and patients who had a stroke while already an inpatient.
The sample was identified through a retrospective audit of hospital and EMS records. Hospital and EMS records were linked by patient name and date of birth. Stroke patients were identified in hospital from a comprehensive stroke register, which is regularly reviewed and updated during a patient’s stay to ensure that only ‘true’ stroke patients stay on the register. Additional patients were identified from hospital by searching the hospital coding system and the ED records. Case notes were ordered for any patients recorded as stroke in the coding system or with stroke-like symptoms in the ED records who were not on the register; the case notes were reviewed and the diagnosis checked by an experienced stroke research nurse. For all patients identified in hospital we obtained their EMS data. Independent from the data gathered in hospital, the EMSs identified patients who had been dispatched as a stroke. The hospital case notes were obtained for all patients identified through the EMSs. A patient was considered to have a final diagnosis of stroke if they were discharged from the ED and the ED records stated stroke, or if they were still on the stroke register at the time of discharge from hospital.
Approval for this study was granted by the Patient Information Advisory Group (now the National Information Governance Board for Health and Social Care), the Local Research Ethics Committee and by the Faculty of Health Ethics Committee at the University of Central Lancashire.
Procedure
Data were recorded from the electronic patient report forms used by EMS staff, and the patient’s hospital case notes. EMS report forms provided data on dispatch code, ambulance diagnosis and the following event times: call made to EMSs; ambulance arrived at scene and ambulance arrived at hospital. From the case notes and stroke register we recorded time of admission; time of triage; demographics; side affected by the stroke; limbs affected by stroke; facial weakness; speech problems; consciousness level and final diagnosis.
Study data were divided into three periods: (1) pre-implementation, prior to training the EMS call handlers; (2) during-implementation, during which 69 EMDs (2 trainers and 67 EMDs) completed the training; and (3) post implementation, following completion of the training. There were nine, seven and 10 1-week blocks in the three periods, respectively, giving a total of 26 observations. We dichotomised patient diagnosis as stroke or not stroke at the point of dispatch and for the final diagnosis. Time intervals from call to EMSs and other key events (arrival at scene, arrival at hospital) were calculated (as described in Table 24 ). For each observation (i = 1, . . . , 26) we produced the following outcome summary statistics for analysis:
-
Proportion with final diagnosis stroke (n i ) dispatched as stroke (y i ).
-
Mean time interval between call and ambulance arrival at scene.
-
Mean time interval between call and arrival at hospital.
| Time interval | Method of calculation |
|---|---|
| Call to arrival at scene | Time ambulance arrived at scene minus time call made to EMSs |
| Call to arrival at hospital | Time ambulance arrived at hospital minus time call made to EMSs If time arrived at hospital was missing, time of admission to hospital was used instead. If both these were missing, time of triage was used |
Data analysis
Patient demographics, stroke characteristics and diagnosis data are presented overall and for each period. Time series plots are presented to illustrate trends for each outcome.
The effect of the intervention on:
-
accuracy of dispatch diagnosis was investigated using binomial (grouped) logistic regression, with the number of subjects with a dispatch diagnosis of stroke as the numerator and the number of subjects with a final diagnosis of stroke as denominator for each observation
-
call to arrival at scene and call to arrival at hospital were investigated using linear modelling, with observations weighted by that week’s number admitted with a final diagnosis of stroke.
Analysis was performed using complete cases (i.e. those with data available for both dispatch and final diagnosis). It was suspected that, given the non-contiguous nature of the observation periods, serial autocorrelation would be absent or weak. However, potential autocorrelation [due to the time of the weekly diagnosis rates and clustering (overdispersion) of the accuracy within observations] was investigated; standard errors would be adjusted for any observed lack of independence or overdispersion.
Regression models included the intervention factor ‘pre’, ‘during’, ‘post’: this segments the regression model and allows a ‘jump’ in outcome on transition from one period to the next. An overall linear trend over the period of data collection and an interaction between the intervention factor and the linear trend (to allow the intervention to influence any underlying trend and to allow a gradual impact of the introduction of the intervention) were also included. Where there was no evidence of either an overall trend or difference in trend between periods (p > 0.15), the corresponding term was removed. Findings from the more parsimonious model are presented. Sensitivity analysis was performed to assess the potential impact of missing dispatch and/or final diagnosis by imputing possible diagnoses, including extreme imputations (dispatch diagnosis as ‘not stroke’ and final diagnosis as ‘stroke’, and vice-versa). For the time intervals, sensitivity analyses was performed by repeating the modelling on geometric rather than arithmetic means for each observation (to reduce the potential influence of outlying times). Analysis was performed using SPSS (versions 19 and 20) and Intercooled Stata (version 11.0; StataCorp LP, College Station, TX, USA). Unless otherwise stated, inferential analyses used a 5% significance level; 95% CIs are presented.
Results
Over the 26 observation weeks, 464 patients met the study’s inclusion criteria. Sixty-six patients were included due to a final diagnosis of stroke only, 251 patients were included due to having a stroke dispatch code only, and 147 patients met both these inclusion criteria. Their median (IQR) age was 75 (62–83) years; 241 (51.9%) were female. Data were collected on 174 (mean 19.3 per week), 116 (mean 16.6 per week) and 174 (mean 17.4 per week) patients over the pre-, during- and post-implementation periods respectively. Dispatch data were available for 450 patients and, of these, 398 (88.4%) were dispatched as stroke. A final confirmed diagnosis was recorded for 424 patients and, of these, 213 (50.2%) had a final diagnosis of stroke ( Table 25 ).
| Patient characteristics | Pre (n = 174) | During (n = 116) | Post (n = 174) | Overall (n = 464) |
|---|---|---|---|---|
| Median age (years) (IQR) | 76 (65–82) | 74.5 (61–83.75) | 75 (61.75–83.25) | 75 (62–83) |
| Female (%) | 81/174 (46.6) | 63/116 (54.3) | 97/174 (55.7) | 241/464 (51.9) |
| Dispatched as stroke (all diagnoses) (%) | 134/168 (79.8) | 105/111 (94.6) | 159/171 (93.0) | 398/450 (88.4) |
| Final diagnosis of stroke (%) | 98/162 (60.5) | 53/106 (50.0) | 62/159 (39.0) | 213/427 (49.9) |
The characteristics of the stroke patients are shown in Table 26 . Of the 213 patients with a final diagnosis of stroke, dispatch data were available for 199, of whom 147 (73.9%) had been dispatched as stroke.
| Patient characteristics | Pre (n = 92) | During (n = 48) | Post (n = 59) | Overall (n = 199) |
|---|---|---|---|---|
| Median age (years) (IQR) | 76 (65–83) | 75 (64–83) | 75 (66–82) | 76 (65–83) |
| Female (%) | 38/92 (41.3) | 21/48 (43,8) | 25/59 (42.4) | 84/199 (42.2) |
| Side affected by stroke | ||||
| No clear lateralisation (%) | 23/88 (26.1) | 11/46 (23.9) | 10/58 (17.2) | 44/192 (22.9) |
| Right side (%) | 31/88 (35.2) | 20/46 (43.5) | 21/58 (36.2) | 72/192 (37.5) |
| Left side (%) | 34/88 (38.6) | 15/46 (32.6) | 27/58 (46.6) | 76/192 (39.6) |
| Arm weakness (%) | 47/87 (54.0) | 25/46 (54.3) | 24/53 (45.3) | 96/186 (51.6) |
| Leg weakness (%) | 39/85 (45.9) | 21/46 (45.7) | 20/53 (37.7) | 80/184 (43.5) |
| Facial weakness (%) | 43/81 (53.1) | 27/46 (58.7) | 23/53 (43.4) | 93/180 (51.7) |
| Speech problems (%) | 50/76 (65.8) | 29/42 (69.0) | 23/50 (46.0) | 102/168 (60.7) |
| Consciousness level | ||||
| Alert (%) | 74/88 (84.1) | 42/48 (87.5) | 57/59 (96.6) | 173/195 (88.7) |
| Drowsy (%) | 9/88 (10.2) | 5/48 (10.4) | 2/59 (3.4) | 16/195 (8.2) |
| Stupor (%) | 3/88 (3.4) | 0/48 (0) | 0/59 (0) | 3/195 (1.5) |
| Coma (%) | 2/88 (2.3) | 1/48 (2.1) | 0/59 (0) | 3/195 (1.5) |
For the patients with a final diagnosis of stroke, the proportions dispatched as ‘stroke’ or ‘not stroke’ (dispatch accuracy) for each of the three periods, and for each of the 26 observation weeks are given in Table 27 .
| Period of study | Week | Observation | Number with final diagnosis of stroke | Number dispatched as stroke | Percentage dispatched as stroke |
|---|---|---|---|---|---|
| Pre | 1 | 1 | 16 | 12 | 75 |
| 4 | 2 | 11 | 7 | 64 | |
| 7 | 3 | 11 | 5 | 45 | |
| 10 | 4 | 10 | 6 | 60 | |
| 13 | 5 | 17 | 10 | 59 | |
| 16 | 6 | 3 | 3 | 100 | |
| 19 | 7 | 8 | 6 | 75 | |
| 22 | 8 | 11 | 6 | 55 | |
| 25 | 9 | 5 | 3 | 60 | |
| Total | 92 | 58 | 63 | ||
| During | 28 | 10 | 3 | 1 | 33 |
| 31 | 11 | 8 | 6 | 75 | |
| 34 | 12 | 7 | 7 | 100 | |
| 37 | 13 | 10 | 10 | 100 | |
| 40 | 14 | 7 | 6 | 86 | |
| 43 | 15 | 8 | 8 | 100 | |
| 46 | 16 | 5 | 4 | 80 | |
| Total | 48 | 42 | 88 | ||
| Post | 49 | 17 | 3 | 2 | 67 |
| 52 | 18 | 4 | 4 | 100 | |
| 55 | 19 | 6 | 4 | 67 | |
| 58 | 20 | 5 | 4 | 80 | |
| 61 | 21 | 8 | 8 | 100 | |
| 64 | 22 | 7 | 5 | 71 | |
| 67 | 23 | 4 | 4 | 100 | |
| 70 | 24 | 8 | 6 | 75 | |
| 73 | 25 | 7 | 6 | 86 | |
| 76 | 26 | 7 | 4 | 57 | |
| Total | 59 | 47 | 80 | ||
| Overall | 199 | 147 | 74 |
Trends in the number dispatched as stroke and the number dispatched as not stroke are illustrated in Figure 6 and the corresponding diagnostic accuracy is shown in Figure 7 . Logistic regression showed no significant change in trend in diagnostic accuracy across the observation weeks (p = 0.18), nor an overall trend in diagnostic accuracy across the observation weeks (p = 0.85). However, a significant change in dispatch diagnosis accuracy between periods was detected (p = 0.003), reflecting an improvement in dispatch accuracy relative to the pre-implementation period for both the during-implementation (OR 4.10, 95% CI 1.58 to 10.66) and post-implementation (OR 2.30, 95% CI 1.07 to 4.92) periods; the difference in dispatch accuracy between during- and post-implementation periods was not significant (p = 0.29). There was no evidence of (first-order) autocorrelation of residuals (r = −0.0123, p = 0.95), so no adjustment of standard errors was necessary. These findings were robust to the various imputations applied: the difference between periods in proportions correctly dispatched as stroke was significant for all imputations, with p-values ranging from 0.001 to 0.017. When data from the during- and post-implementation periods were combined and compared with the pre-implementation data the overall effect of training was significant (p = 0.002; OR 2.90, 95% CI 1.50 to 5.61).
FIGURE 6.
Weekly numbers of patients with final diagnosis of stroke dispatched as stroke and not stroke.
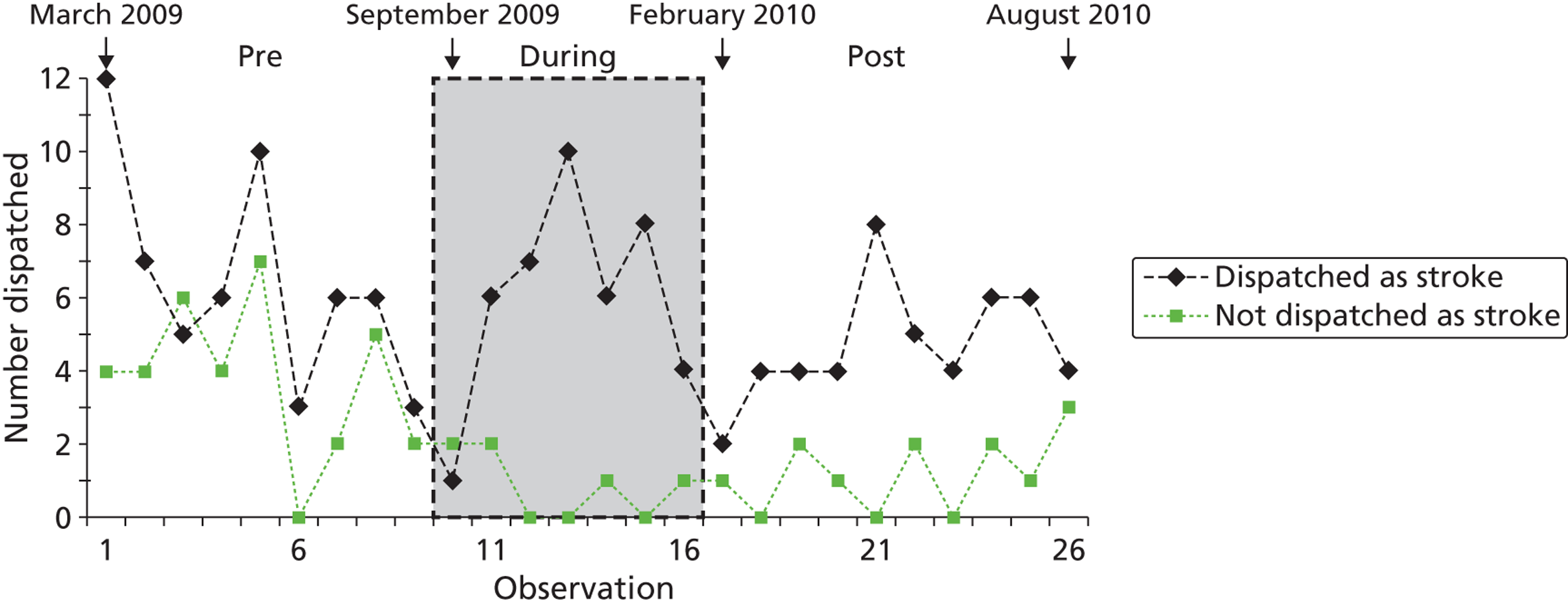
FIGURE 7.
Weekly percentages of patients dispatched as stroke (denominators are patients with a final diagnosis of stroke).
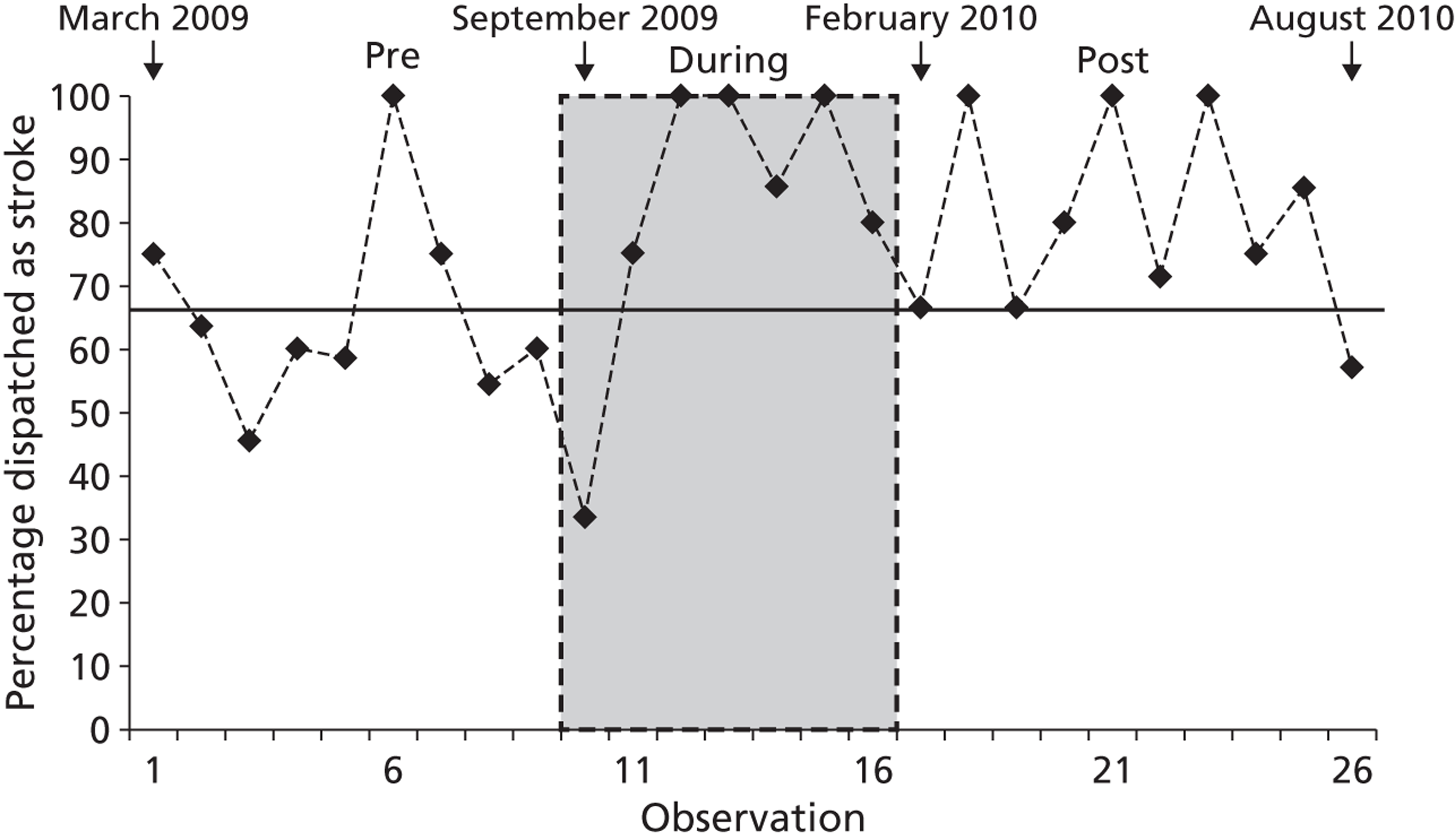
For the 199 patients with a final diagnosis of stroke and dispatch data, time of call was missing for three (1.5%). Of the remainder, 25 had missing arrival at hospital time. Twenty-two of these patients had admission to hospital time recorded and one further patient had triage time recorded, so these were used for the time of arrival at hospital. One hundred and ninety-four patients had mean (standard deviation; SD) call to arrival at scene 13.1 (12.0) minutes (median 9, IQR 7–15, range 3–99 minutes) and mean (SD) call to arrival at hospital 47.0 (16.3) minutes (median 44, IQR 36–53, range 22–124 minutes).
There was a marginally non-significant reduction in mean time from the EMS call to arrival of the ambulance at the scene of 2.8 minutes (95% CI −0.2 to 5.9 minutes; p = 0.068) between pre- and post-implementation periods ( Table 28 ). However, these mean times increased significantly overall during implementation (7.0 minutes, 95% CI 3.8 to 10.3 minutes; p < 0.001). There was no evidence of autocorrelation of residuals (r = −0.16; p = 0.40), so adjustment of standard errors was not deemed necessary. Overall, there was no significant underlying trend in mean time from the EMS call to arrival of the ambulance at the scene (p = 0.18), but potentially appeared to decline over the during-implementation period (p = 0.081). Findings were similar when geometric rather than arithmetic means were modelled.
| Implementation period (n) | Mean call to arrival at scene (SD) | Median call to arrival at scene (IQR) | Mean call to arrival at hospital (SD) | Median call to arrival at hospital (IQR) |
|---|---|---|---|---|
| Pre (88) | 12.2 (8.0) | 10 (8–14.8) | 45.0 (13.5) | 43.5 (37–50) |
| During (48) | 19.2 (19.3) | 12.5 (7–21.8) | 52.9 (22.7) | 48.0 (35.3–61.5) |
| Post (58) | 9.4 (6.2) | 8 (6–10.3) | 44.9 (12.5) | 43 (36.0–52.0) |
The mean call to arrival at hospital time was unchanged between pre- and post-implementation periods (difference −0.1 minutes, 95% CI −5.5 to 5.3 minutes; p = 0.23) ( Figure 8 ). However, there was a significant short-term increase during implementation of 7.9 minutes (95% CI 2.2 to 13.6 minutes; p = 0.009). There was no evidence of autocorrelation of residuals (r = −0.26, p = 0.16), so adjustment of standard errors was not deemed necessary. Overall, there was a significant underlying trend in mean time from the EMS call to arrival of the ambulance at the scene (p = 0.028), but no evidence that this underlying trend varied between periods (p = 0.55). Findings were similar when geometric rather than arithmetic means were modelled.
FIGURE 8.
Weekly mean times from call to arrival at scene and times from call to arrival at hospital.
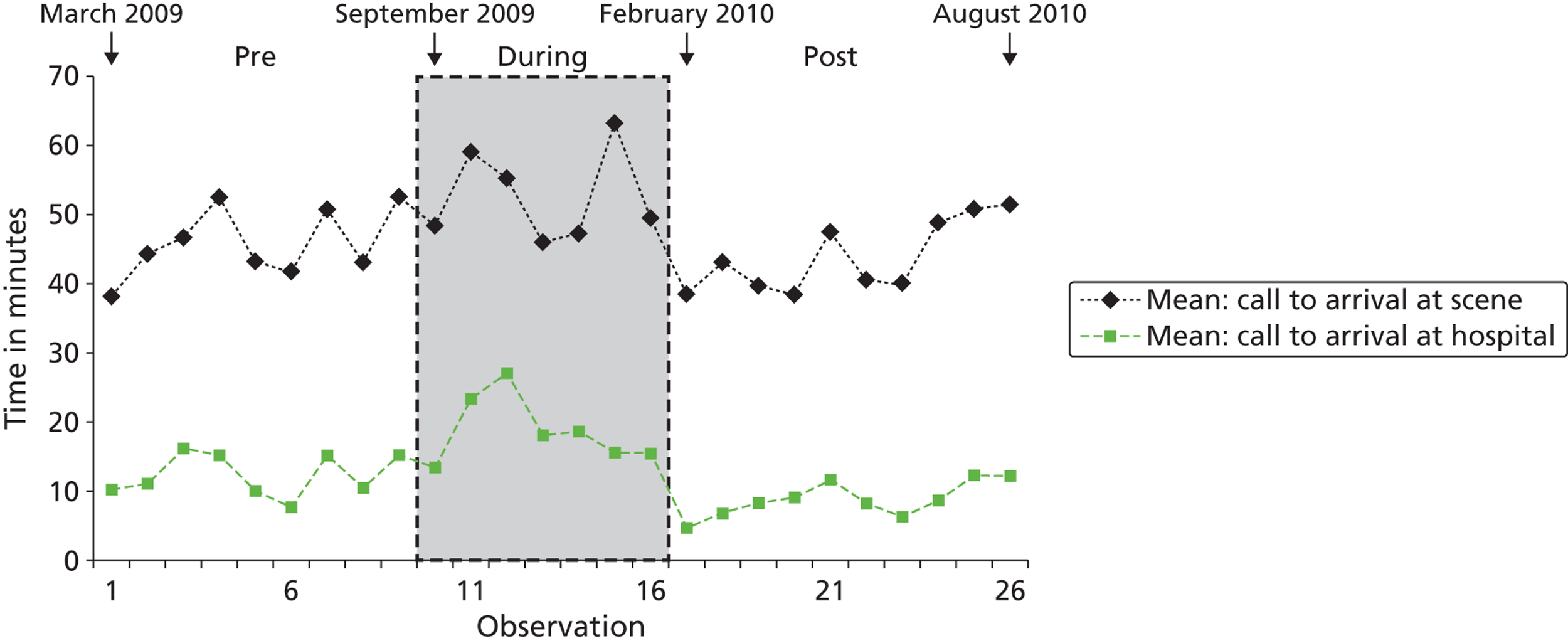
Discussion
Implementation of stroke-specific online training resulted in an increased recognition of stroke by EMDs and a modest reduction in the time from the call to the ambulance’s arrival at the scene.
Prior to training, for every 10 stroke calls made, approximately six were correctly identified by the EMDs. This increased to 8 out of 10 after training was implemented and was just short of 9 out of 10 in the during-implementation period. The recognition of stroke even at baseline was much higher in comparison with previous reports in the literature, where studies have shown that EMD sensitivity for identifying stroke is < 50%,7–9 and the findings in phase 1. One explanation for this may be the FAST campaign, which was coming to an end when phase 8 started; the FAST may have raised awareness of stroke in both the public and EMDs. Despite the relatively high proportion correctly recognised as stroke by EMDs at baseline, the difference between periods in proportions of strokes, correctly dispatched as such, was both clinically and statistically significant. This effect was robust to assumptions made about missing dispatch and final diagnosis, and there was no evidence of non-independence. The effect of the training was observed quickly, with a steep rise in the proportion of strokes being dispatched as such during implementation. These proportions were similar or better during implementation than post implementation. The difference between pre- and during-implementation periods was seen as a step change close to the time that the training package was introduced, rather than a trend, evidence of which would have been visible through the use of an interrupted time series design. This step change strengthens the evidence for the effectiveness of the intervention because it suggests that the cause of the change happened close to the time of the introduction of the training. Further evidence to support the introduction of the training as the cause of the improvement in correctly dispatching strokes as such comes from the expected rate of effect. The training reached maximal effect at the time of the third observation week in the during-implementation period, which would be consistent with increasing numbers of EMDs having received the training and being able to implement it in practice: the critical mass of EMDs needed to bring about a demonstrable effect.
One method of improving recognition of stroke would be to alter the algorithm used by EMDs. At the outset of our programme of work it had been identified that it would not be possible to change the AMPDS system and so we opted to develop training that would complement existing knowledge and skills of the EMDs. In addition, the versions of AMPDS changed between phases 1 and 8 (from v11.3 to v12.2). The latter version includes the FAST, which could also have contributed to the higher level of stroke recognition during the pre-implementation period. However, the inclusion of the FAST within the AMPDS system does not negate the value of the training. Our training is aimed at aiding EMDs recognise stroke, primarily during what we termed in phase 3, the first story. The idea being that the training will guide and support the EMDs in their recognition of the call as being one relating to stroke, resulting in the EMD choosing the stroke algorithm (and using a dispatch code, priority level, and emergency vehicle commensurate with stroke). As the FAST is only included in the stroke algorithm, the value of the training is that it will guide EMDs to that algorithm and thereby allow use of the FAST.
As a result of this approach we believe that this is the first study to (develop and) evaluate stroke training for EMDs and subsequently demonstrate an improvement in the recognition of stroke by EMDs. To our knowledge, no previous studies have evaluated EMD training in relation to the recognition of stroke; therefore, this is the first study to improve the recognition of stroke by EMDs. Previous studies have evaluated educational programmes aimed at improving paramedic, hospital and community awareness. 53 This training increased paramedic diagnosis of stroke from 61% to 79%53 and demonstrated that stroke-specific training for EMS personnel can be effective in improving stroke recognition. This suggests that there is a potential for increasing pre-hospital recognition of stroke further by including training for ambulance staff. We have shown that online learning for EMS staff can increase stroke knowledge and provides the opportunity for continuing professional development,63 although we did not study the impact on diagnostic accuracy or timeliness of service.
There was a significant difference in the number of stroke patients correctly dispatched as such between periods, but there was no significant overall trend in observation week. This may be due partly to the wide variation in the number of stroke patients who accessed the EMSs over the study period, which ranged from 3 to 17 patients per week. In addition, there were differences in the average number of patients identified in the observation weeks between periods. In the pre-implementation period there was an average of nine patients per observation week, but in both of the subsequent periods there was an average of six patients per week. However, prior to the beginning of the study the national FAST mass media campaign40 had just ended. This may explain the larger numbers of patients accessing hospital via the EMSs in the pre-implementation period. As the impact of the FAST campaign dwindled, more patients in the during- and post-implementation periods may have accessed emergency help by other means such as direct attendance at the ED, and therefore would not have been included in our study.
As well as increasing recognition of stroke by EMDs, the training package reduced pre-hospital delay in terms of call to arrival at scene time (although this failed to reach traditional levels of significance), but did not affect call to arrival at hospital time. One previous study reported that following the implementation of a training package for paramedics the time from dispatch to arrival at hospital increased from 42.2 minutes to 45.8 minutes. 53 Our study shows that EMD training not only improves recognition of stroke but may have the potential to contribute towards reducing pre-hospital delays, at least in terms of call to arrival at scene time. There are potentially many factors that can influence the time between a call being made and a patient arriving at hospital, from the dispatch code and priority through to road conditions. An improvement in the correct identification of stroke patients has the greatest probability of influencing the time between call and arrival at scene through ensuring the correct dispatch code, vehicle, and priority are used. Our findings are consistent with such an effect. The reason that the effect on time from call to arrival at scene was not reflected in a reduced time from call to arrival at hospital is unclear. Also unclear is the reason for the pattern of times during implementation, in particular the number of sharp increases and decreases. Potential explanations outside of the influence of the EMSs include presence of road works, shorter daylight hours and the recording of data in December and early January. It is difficult to provide explanations for these patterns, but sampling over longer time frames, to include the same annual periods, and/or increasing the frequency of observations may have helped with interpreting the data.
This modest reduction in time may assist in expediting assessment and delivery of thrombolytic therapy for eligible patients. It is possible that this opportunity to deliver thrombolysis may be missed when non-stroke categories are used by EMDs. However, the delay in contacting the EMSs continues to be one of the main causes of patient exclusion, in receiving thrombolysis, with around 5% of stroke patients currently receiving thrombolysis each year in England. 6 Reasons for pre-hospital delay often include poor awareness of stroke symptoms, reluctance to seek medical help and stroke not being viewed as a medical emergency. 67,68
Limitations
The nature of the intervention meant it could not be evaluated as a single centre randomised controlled trial and so we used an interrupted time series design. Although this design is not as robust as randomised controlled trial methodology, it is more robust than a simple before and after study. Alternatively, the intervention could have been evaluated using a cluster randomised controlled trial, or even a stepped-wedge cluster randomised controlled trial, but this would have meant a much larger-scale study, which would have been beyond the limit of the resources available.
We tried to ensure that data capture was over a long period in order to obtain a large enough sample to demonstrate the impact of the intervention. By sampling over 18 months we can be reasonably certain the sample was representative of the annual intake of stroke patients at the centre, and that there was unlikely to be an impact of seasonal variation. In contrast, an 18-month period was a relatively short time series and so has limited the potential for investigation and explanation of underlying trends in the data, for example, in the time from call to arrival at scene and hospital. However, this does not invalidate the findings of improved recognition of stroke by the EMDs and the modest reduction in times from pre- to post-implementation.
The intervention was implemented in one ambulance service, which may limit generalisability. Also, the EMD recognition of stroke at baseline was high compared with other studies, so it could be argued that the EMDs’ prior awareness of stroke facilitated further learning. The sample was identified through a retrospective audit of hospital and EMS records, meaning that the data collected for the study was dependent on previously documented information, and so it was not possible to verify the information through independent assessment. Given the nature of the data that were used, this is unlikely to have affected the results of the study: dispatch data are an objective measure of the code used by EMDs; the stroke register is comprehensive, has been in place over 17 years and is managed by an experienced team.
Conclusion
This is the first study to develop, implement and evaluate the impact of a training package for EMDs with the aim of improving the recognition of stroke. The findings suggest that in addition to improving the recognition of stroke by EMDs, the training has the potential to contribute to a reduction in pre-hospital delays.
Summary
Phase 8 is the culmination of a programme of research, which explored stroke symptoms and how they are used in the communication between the public and EMDs in order to develop online training aimed at raising awareness of stroke for EMDs. This is the first study to develop and evaluate the impact of such an intervention. We have shown that our stroke-specific online training package can improve the recognition of stroke by EMDs.
Chapter 11 Overall conclusion
This report is the culmination of a programme of research, the first of its kind, to explore the communication between the public and EMDs in order to develop and evaluate the impact of a new intervention aimed at raising EMDs’ awareness of stroke. We have shown that a stroke-specific online training package can improve the recognition of stroke by EMDs, and may be able to contribute towards reducing pre-hospital delays.
In phase 1 approximately 50% of calls to the EMSs were dispatched as stroke. The dispatch diagnosis was correct in just over 50% of cases. A correct diagnosis of stroke by EMDs resulted in a rapid journey to hospital. There was evidence to suggest that if a caller describes one or more of the symptoms (facial weakness, speech problems, and to some extent limb weakness) then there is a high probability that they are describing a stroke.
In phase 2 we discovered that pre-hospital delays often arose because the caller felt it necessary to seek other lay or professional advice prior to calling the EMSs. Many callers believed that the onset of acute stroke symptoms did not necessarily warrant an immediate call to the EMSs. Even when callers recognised stroke and called the EMSs, they did not always convey this impression to the call handler. The form of structured questioning used by the call handler did not always enable the caller to convey their full impression of what the problem was, or allow the call handler to assure the caller that an ambulance had been arranged. In order to improve outcomes in hyperacute stroke care, more public education is needed to improve awareness of a wider range of stroke symptoms, how to report these and the need for an urgent response.
In phase 3 we found that callers to the EMSs for suspected stroke were predominantly family members, the patient’s daughter being the most likely individual. When the term ‘stroke’ was spontaneously used by the caller, the proportion of patients with a confirmed diagnosis of stroke or TIA was high, at around 85%. The ‘FAST’ warning signs and symptoms of stroke (face weakness, arm weakness and speech problems) were rarely reported as the first problem: speech was the most common FAST symptom reported. However, phase 3 was conducted using calls made to the EMSs prior to the FAST media campaign in England and Wales. Pre-hospital notification to the ED of a patient with suspected stroke is known to be strongly associated with rapid admission to hospital. Although this is important in order to expedite assessment and treatment by a specialist stroke team, which itself is known to improve outcomes, rapid admission is perhaps especially important in expediting assessment and delivery of thrombolytic therapy for eligible patients. It is possible that this opportunity is missed or delayed when non-stroke categories are used by EMDs. If stroke is suspected, members of the public should be encouraged to say the word ‘stroke’ when contacting the EMSs in order to initiate an immediate and appropriate response as outlined in the ‘stroke chain of survival’. 43 Training for EMDs should include who is most likely to make an emergency call for suspected stroke, and how the public describe stroke symptoms.
Phase 3a was the first study that has explored the public’s understanding and communication of consciousness level during EMS calls for patients with symptoms suggestive of acute stroke. Despite poor public understanding, the term ‘conscious’ is used routinely in both the AMPDS system, and in the NHS Pathways programme which is being implemented across EMSs in the UK. The highly structured format of the caller–call handler dialogue, and the nature of stroke in a medical emergency situation, may make it difficult for callers to ask for clarification of medical terms used by the call handler, and to convey uncertainty about their interpretation of the patients’ symptoms.
Our findings suggest that, despite its wide use in medical practice and specifically in EMS dispatch protocols, the term ‘conscious’ is not widely understood and is poorly communicated by bystanders when making EMS calls about patients with symptoms suggestive of acute stroke. This phenomenon may lead to imprecise, contradictory and lengthy information exchange which may be time wasting, misleading and potentially dangerous. Our findings suggest that a structured assessment by ambulance dispatchers of consciousness level, with categories encompassing drowsiness and the separate assessment of speech and breathing problems might assist in obtaining a more accurate assessment of consciousness level in patients with suspected stroke.
The findings from phase 3 indicated that if the patient has, or the caller mentions, one or more of facial weakness, limb weakness, or speech problems (or even uses the word ‘stroke’), there is an increased probability that the person has had a stroke. Phase 4 has added to these data by showing that callers very rarely mention the word ‘stroke’ or any of the FAST items for non-stroke calls. These words are more frequently used when people contact the EMSs about stroke. The word ‘fall’ is commonly used in both stroke and non-stroke calls.
The AMPDS protocol is designed to standardise and codify the operation of EMDs while optimising safe and effective patient care through dispatch life support and EMS system response. Within phase 5, it was not possible to change the AMPDS algorithm for stroke within the ambulance service or NHS Direct, based on the findings from ESCORTT. Further evidence would be required because AMPDS is based on published standards from a wide range of international institutions including the NIH and the AMA. Similarly, NHS Direct algorithms are aligned to DoH, NHS and NICE policies.
Underpinned by the findings from phases 1–4, an online training package was developed in phase 6. The training package provided detailed information about what influences people in their initial decision to contact the EMSs at the onset of stroke symptoms; how the public describe the symptoms of stroke during a 999 call; the proportion of patients (or someone on their behalf) who obtain first medical contact from the EMSs for suspected stroke; who is most likely to dial 999 for suspected stroke; how stroke symptoms may be described by the public; important communication issues between EMDs and callers; how often suspected stroke is confirmed as a stroke by ambulance crews and in hospital; details of the words that are used to describe non-stroke-related conditions and the public’s understanding of different levels of ‘consciousness’ and how these are described during 999 calls. The development of a stroke-specific training package provided a unique learning opportunity for EMDs in improving their awareness of the key words and phrases that might indicate acute stroke during calls to the EMSs. In phase 7, an evaluation of the training package showed that online learning for EMDs is well received and can increase self-reported stroke knowledge and that EMDs welcome the opportunity for continuing professional development.
In phase 8 the recognition of stroke by EMDs increased from 63% in the pre-implementation period to 88% during implementation, and was maintained at 80% in the post-implementation period. The recognition of stroke even at baseline was much higher (63%) in comparison with previous studies, which have typically reported EMDs as recognising stroke in around 50% of cases. Despite the high proportion of calls correctly recognised as stroke by EMDs at baseline, the difference between implementation periods in proportions correctly dispatched as stroke was significant. To date, no previous studies have evaluated EMD training in relation to the recognition of stroke, and to our knowledge this is the first study to demonstrate a significant improvement in recognition of stroke by EMDs.
When this programme was conducted, the universal emergency number in the UK was 999. Recently, an alternative number (111) for urgent but non-emergency health advice has been introduced in the NHS in some areas. Our findings demonstrated that people often incurred significant delays before phoning 999 for acute stroke symptoms. In the future, the availability of the 111 service might encourage some callers to seek help sooner than they would otherwise have done, for example if they are uncertain about whether the patient’s condition is a true emergency. In this case, the responder can arrange an emergency ambulance response. However, the development also adds another layer of complexity to the provision of urgent and emergency care. The availability of the 111 service could compound lay-people’s uncertainty over whether the call is an emergency or non-emergency matter. In some cases this could lead to potential further delay in seeking help for acute stroke.
The overall findings of this programme of research suggest that if a caller to the EMSs mentions one or more of facial weakness, arm/hand weakness, or speech problems, there is an increased likelihood that the patient has had a stroke. If stroke is suspected, use of the word stroke by the public during the call to the EMSs should increase the likelihood that an immediate and appropriate response is initiated, as outlined in the stroke chain of survival. The majority of calls made to the EMSs on behalf of someone with suspected stroke were made by a female relative. The public’s awareness of the symptoms of stroke and how to report this when contacting the EMSs are important. Callers tended to talk in terms of the consequences of loss of function (e.g. unable to grip, cannot stand) rather than describing symptoms themselves, such as weakness. EMDs should be made more aware of the terminology used by callers describing suspected stroke and should probe for specific symptoms when stroke is suspected. Callers very rarely mention stroke or FAST symptoms for non-stroke calls; mention of ‘stroke’ or ‘FAST’ symptoms is over 10 times more common in stroke than in non-stroke calls. This is the first study to develop, implement and evaluate the impact of a training package for EMDs with the aim of improving the recognition of stroke. The findings suggest that in addition to improving the recognition of stroke, training also leads to a reduction in pre-hospital delays, allowing initiation of emergency treatments and specialist stroke care, which can prevent death and reduce disability.
Chapter 12 Implications for practice
The following section will list and integrate the applied learning from all the phases within this programme of research, identifying key actions, agencies and roles required for implementation where appropriate.
From phases 1–4 there are a number of key findings which could be incorporated and emphasised in future EMD stroke training.
Phase 1: if a caller describes one or more of the symptoms: facial weakness, speech problems, and to some extent limb weakness, then there is a high probability that they are describing a stroke.
Phase 2: even when callers recognised stroke and called the EMSs, they did not always convey this impression to the EMDs. The form of structured questioning used by the call handler did not always enable the caller to convey their full impression of what the problem was, or allow the call handler to assure the caller that an ambulance had been arranged.
Phase 3: callers to the EMSs for suspected stroke were predominantly family members, the patient’s daughter being the most likely individual. When the term ‘stroke’ was spontaneously used by the caller, the proportion of patients with a confirmed diagnosis of stroke or TIA was high, at around 85%.
Phase 3a: our findings suggest that despite its wide use in medical practice and specifically in EMS dispatch protocols, the term ‘conscious’ is not widely understood and is poorly communicated by bystanders when making EMS calls about patients with symptoms suggestive of acute stroke. Our findings suggest that a structured checklist for EMDs, with categories of consciousness encompassing drowsiness and separate questioning around speech and breathing problems, might assist in obtaining a more accurate assessment of consciousness level in patients with suspected stroke.
Phase 4: callers very rarely mention the word ‘stroke’ or any of the FAST items for non-stroke calls. These words are more frequently used when people contact the EMSs about stroke.
Phase 7: the development of a stroke-specific training package provided an exceptional learning opportunity for EMDs, which can improve their awareness of the key words and phrases that might indicate acute stroke during calls to the EMSs. An evaluation of the training package showed that online learning for EMDs was well received, increased self-reported stroke knowledge, and was welcomed as an opportunity for continuing professional development.
Phase 8: the recognition of stroke by EMDs increased from 63% in the pre-implementation period to 88% during implementation, and was maintained at 80% in the post-implementation period.
The key findings may have implications for the future stroke training of EMDs. Findings from the individual phases have important implications in their own right. Phase 8 demonstrated the impact of the training package that synthesised the key findings. The results from phase 8 suggest that implementation of the training into routine practice could improve recognition of stroke by EMDs.
Dissemination of the findings within key organisations has already taken place locally through presentations at medical senior management team meetings within the ambulance service and nationally through the National Ambulance Research Steering Group. Further engagement with the International Academies of Emergency Dispatch, Ambulance Trusts, and NHS Pathways is required for implementation of the findings into training opportunities for EMDs. Engagement with these bodies will continue in order to promote staff awareness of the online training package, which is now freely accessible.
Chapter 13 Recommendations for future research
This programme of research makes these recommendations for future research.
Current practice in EMS dispatch varies across the country and not all call handlers have stroke-specific training. There is therefore scope to test the effectiveness of the training package developed within this programme on the recognition of stroke across other EMSs in England.
Accurate recognition of stroke means that people could arrive at hospital quickly and benefit from access to specialist assessment and treatment, including thrombolysis which is highly time-dependent. This has the potential to reduce prevalence of post-stroke dependency. The impact of the early identification of stroke by call handlers on specialist assessment and treatment, and on thrombolysis rates has yet to be explored.
The training led to increased correct identification of stroke patients in an ambulance service that used AMPDS. There is now scope to test the effectiveness of the training in services that have recently adopted the NHS Pathways triage system. NHS Pathways sets out to deliver a single clinical assessment tool that provides effective triage over the telephone in any setting taking calls from the public. The system encompasses EMSs, NHS Direct, Primary Care Physician out-of-hours services and the non-urgent NHS 111 telephone number.
Many callers seek lay or professional advice prior to contacting EMSs and some believe that the onset of acute stroke symptoms does not warrant an immediate 999 call. The findings underline the need for further research into effective methods of raising the public’s awareness of stroke symptoms, the importance of contacting the EMSs, and what to convey to the EMD during the call in order to reduce delays in accessing emergency treatment.
Ambiguities and contradictions in dialogue about consciousness level arise during ambulance calls for suspected and confirmed stroke. Further research is needed to identify whether or not these issues also arise in non-stroke calls, and which term or terms are best understood in conveying altered levels of consciousness in emergency situations.
If accuracy and speed of EMS diagnosis are improved, then the EMSs can send one correct vehicle to the incident rather than potentially two vehicles (e.g. paramedic car followed by ambulance), or at least enable recall of a second vehicle. Further research could explore the financial implications of this within the EMSs.
Further research could also explore the effectiveness of the training programme on improving longer-term stroke outcomes (e.g. reduced length of stay and disability) resulting from earlier and more accurate diagnoses.
Longer-term follow up of the impact of the training package could usefully explore such issues as timing, frequency and mode of delivery or refresher sessions.
Acknowledgements
We would like to thank the stroke survivors who contributed to the development and management of this programme of research. We would also like to thank the stroke survivors and carers who took the time to take part in interviews and who shared their experiences and views.
This report presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research scheme (RP-PG-0606–1066). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the DoH.
Contributions of authors
Professor Caroline L Watkins (Professor of Stroke and Older People’s Care, University of Central Lancashire): substantial contributions to the design and methodology, advised on the data collection and data analysis for all phases. Contributed to the writing, revision and approval of the final report.
Dr Stephanie P Jones (Research Fellow, University of Central Lancashire): substantial contributions to the design and methodology, data collection and data analysis for all phases. Contributed to the writing, revision and approval of the final report.
Dr Michael J Leathley (Principal Lecturer, University of Central Lancashire): substantial contributions to the design and methodology, advised on the data collection and data analysis for all phases. Contributed to the writing, revision and approval of the final report.
Professor Gary A Ford (Jacobson Chair of Clinical Pharmacology, Newcastle University): substantial contributions to the design and methodology, advised on the data collection and data analysis for all phases. Contributed to the writing, revision and approval of the final report.
Professor Tom Quinn (Professor of Clinical Practice, University of Surrey): substantial contributions to the design and methodology, advised on the data collection and data analysis for all phases. Contributed to the writing, revision and approval of the final report.
Miss Joanna J McAdam (Research Associate, University of Central Lancashire): substantial contributions to the design and methodology, data collection and data analysis for all phases. Contributed to the writing, revision and approval of the final report.
Dr Josephine ME Gibson (Senior Lecturer, University of Central Lancashire): substantial contributions to the design and methodology, data collection and data analysis for all phases. Contributed to the writing, revision and approval of the final report.
Professor Kevin C Mackway-Jones (Medical Director, North West Ambulance Service): contributed to the design and methodology, the revision and approval of the final report.
Mr Stuart Durham (Consultant in Emergency Medicine, Royal Preston Hospital): substantial contributions to the design and methodology. Contributed to the revision and approval of the final report.
Dr David Britt (Honorary Research Fellow and Patient Adviser, University of Liverpool): substantial contributions to the design and methodology. Contributed to the revision and approval of the final report.
Dr Sara Morris (Senior Research Associate, University of Lancaster): substantial contributions to the design and methodology. Contributed to the revision and approval of the final report.
Dr Mark O’Donnell (Consultant Stroke Physician, Blackpool Victoria Hospital): contributed to the interpretation of the data, the revision and approval of the final report.
Dr Hedley CA Emsley (Consultant Neurologist, Royal Preston Hospital): contributed to the interpretation of the data, the revision and approval of the final report.
Dr Shuja Punekar (Consultant Physician, Royal Preston Hospital): contributed to the interpretation of the data, the revision and approval of the final report.
Dr Anil Sharma (Consultant Physician, Aintree Hospital): contributed to the interpretation of the data, the revision and approval of the final report.
Dr Chris J Sutton (Principal Lecturer, University of Central Lancashire): substantial contributions to the design, methodology and data analysis. Contributed to the writing, revision and approval of the final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health.
References
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006;367:1747-57. http://dx.doi.org/10.1016/S0140-6736(06)68770-9.
- Saver JL. Time is brain-quantified. Stroke 2006;37:263-6. http://dx.doi.org/10.1161/01.STR.0000196957.55928.ab.
- European Stroke Organisation (ESO) . Executive Committee and the ESO Writing Committee. Guidelines for Management of Ischaemic Stroke and Transient Ischaemic Attack 2008 n.d. http://www.eso-stroke.org/pdf/ESO08_Guidelines_Original_english.pdf (accessed 15 June 2010).
- Reducing Brain Damage: Faster Access to Better Stroke Care. Report by the Comptroller and Auditor General. London: The Stationery Office; 2005.
- Bluhmki E, Chamorro A, Dávalos A, Machnig T, Sauce C, Wahlgren N, et al. Stroke treatment with alteplase given 3.0-4.5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol 2009;8:1095-102. http://dx.doi.org/10.1016/S1474-4422(09)70264-9.
- The National Sentinel Stroke Audit 2010 Round 7. London: Royal College of Physicians; 2011.
- Ramanujam P, Guluma KZ, Castillo EM, Chacon M, Jensen MB, Patel E, et al. Accuracy of stroke recognition by emergency medical dispatchers and paramedics – San Diego experience. Prehosp Emerg Care 2008;12:307-13.
- Buck BH, Starkman S, Eckstein M, Kidwell CS, Haines J, Huang R, et al. Dispatcher recognition of stroke using the national academy medical priority dispatch system. Stroke 2009;40:2027-30. http://dx.doi.org/10.1161/STROKEAHA.108.545574.
- Deakin CD, Alasaad M, King P, Thompson F. Is ambulance telephone triage using advanced medical priority dispatch protocols able to identify patients with acute stroke correctly?. EMJ 2009;26:442-5. http://dx.doi.org/10.1136/emj.2008.059733.
- Kothari R, Jauch E, Broderick J, Brott T, Sauerbeck L, Khoury J, et al. Acute stroke: delays to presentation and emergency department evaluation. Ann Emerg Med 1999;33:3-8. http://dx.doi.org/10.1016/S0196-0644(99)70431-2.
- Kothari R, Sauerbeck L, Jauch E. Patients awareness of stroke, signs, symptoms and risk factors. Stroke 1997;28:1871-5. http://dx.doi.org/10.1161/01.STR.28.10.1871.
- Williams LS, Bruno A, Rouch D, Marriott DJ. Stroke patients’ knowledge of stroke. Influence on time to presentation. Stroke 1997;28:912-15.
- Menon SC, Pandey DK, Morganstern LB. Critical factors in determining access to acute stroke care. Neurology 1998;51:427-32. http://dx.doi.org/10.1212/WNL.51.2.427.
- Rosamond W, Gorton R, Hinn A, Hohenhaus S, Morris D. Rapid response to stroke symptoms: the Delay in Accessing Stroke Healthcare (DASH) study. Acad Emerg Med 1998;5:45-51. http://dx.doi.org/10.1111/j.1553-2712.1998.tb02574.x.
- Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Pre-hospital and emergency department delays. The Genetech stroke presentation survey. Stroke 2000;31:2585-90.
- Barsan WG, Brott TG, Broderick JP, Haley EC, Levy DE, Marler JR. Time of hospital presentation in patients with acute stroke. Arch Intern Med 1993;153:2558-61. http://dx.doi.org/10.1001/archinte.153.22.2558.
- Bratina P, Greenberg L, Pasteur W, Grotta JC. Current emergency department management of stroke in Houston, Texas. Stroke 1995;26:409-14. http://dx.doi.org/10.1161/01.STR.26.3.409.
- Zweifler R, York D, U TT, Mendizabal JE, Rothrock JF. Accuracy of paramedic diagnosis of stroke. J Stroke Cerebrovasc Dis 1998;7:446-8. http://dx.doi.org/10.1016/S1052-3057(98)80130-4.
- Hsia AW, Castle A, Wing JJ, Edwards DF, Brown NC, Higgins TM, et al. Understanding reasons for delay in seeking acute stroke care in an underserved urban population. Stroke 2011;42:1697-701. http://dx.doi.org/10.1161/STROKEAHA.110.604736.
- Mosley I, Nicol M, Donnan G, Patrick I, Dewey H. Stroke symptoms and the decision to call for an ambulance. Stroke 2007;38:361-6. http://dx.doi.org/10.1161/01.STR.0000254528.17405.cc.
- Porteous GH, Corry MD, Smith WS. Emergency medical services dispatcher identification of stroke and transient ischemic attack. Prehosp Emerg Care 1999;3:211-16. http://dx.doi.org/10.1080/10903129908958939.
- Handschu R, Poppe R, Rauß J, Neundörfer B, Erbguth F. Emergency calls in acute stroke. Stroke 2003;34:1005-9. http://dx.doi.org/10.1161/01.STR.0000063366.98459.1F.
- Rosamond WD, Evenson KR, Schroeder EB, Morris DL, Johnson AM, Brice JH. Calling emergency medical services for acute stroke: a study of 911 tapes. Prehosp Emerg Care 2005;9:19-23.
- The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group . Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333:1581-7.
- Lacy CR, Suh D-C, Bueno M, Kostis JB. S.T.R.O.K.E. Collaborative Study Group . Delay in presentation and evaluation for acute stroke: Stroke Time Registry for Outcomes Knowledge and Epidemiology (S.T.R.O.K.E.). Stroke 2001;32:63-9.
- Jones SP, Jenkinson AJ, Leathley MJ, Watkins CL. Stroke knowledge and awareness: an integrative review of the evidence. Age Ageing Adv Access 2009;39:11-22. http://dx.doi.org/10.1093/ageing/afp196.
- De Luca A, Toni D, Lauria L, Sacchetti ML, Rossi PG, Ferri M. IMPLementazione Percorso Clinico Assistenziale ICtus Acuto (IMPLICA) study group . An emergency clinical pathway for stroke patients – results of a cluster randomised trial. BMC Health Serv Res 2009;9. http://dx.doi.org/10.1186/1472-6963-9-14.
- Kleindorfer D, Khoury J, Broderick JP, Rademacher E, Woo D, Flaherty ML, et al. Temporal trends in public awareness of stroke. Warning signs, risk factors and treatment. Stroke 2009;40:2502-6. http://dx.doi.org/10.1161/STROKEAHA.109.551861.
- Nor AM, McAllister C, Louw SJ, Dyker AG, Davis M, Jenkinson D. Agreement between ambulance paramedic and physician recorded neurological signs with face arm and speech test (FAST) in acute stroke patients. Stroke 2004;35:1355-9. http://dx.doi.org/10.1161/01.STR.0000128529.63156.c5.
- Krebes S, Ebinger M, Baumann AM, Kellner PA, Rozanski M, Doepp F, et al. Development and validation of a dispatcher identification algorithm for stroke emergencies. Stroke 2012;43:776-81. http://dx.doi.org/10.1161/STROKEAHA.111.634980.
- Nor AM, Davis J, Sen B, Shipsey D, Louw SJ, Dyker AG, et al. The Recognition of Stroke in the Emergency Room (ROSIER) scale: development and validation of a stroke recognition instrument. Lancet 2005;4:727-34.
- Harbison J, Hossain O, Jenkinson D, Davis J, Louw S, Ford G. Diagnostic accuracy of stroke primary care, emergency room physicians and ambulance staff using the face arm speech test. Stroke 2003;34:71-6. http://dx.doi.org/10.1161/01.STR.0000044170.46643.5E.
- Jones SP, Dickinson HA, Ford GA, Gibson JME, Leathley MJ, McAdam JJ, et al. Obtaining Rapid Telephone Triage Group. Callers’ experiences of making emergency calls at the onset of acute stroke: a qualitative study. Emerg Med J 2012;29:502-5.
- Patton MQ. Qualitative Evaluation and Research Methods. Newbury Park, CA: Sage Publications; 1990.
- Glaser BG. Basics of Grounded Theory Analysis. Emergence vs Forcing. Mill Valley, CA: Sociology Press; 1992.
- Carroll C, Hobart J, Fox C, Teare L, Gibson J. Stroke in Devon: knowledge was good, but action was poor. J Neurol Neurosurg Psychiatr 2004;75:567-71. http://dx.doi.org/10.1136/jnnp.2003.018382.
- Pattenden Watt I, Lewin R, Stanford N. Decision making processes in people with symptoms of acute myocardial infarction: qualitative study. BMJ 2002;324:1006-11. http://dx.doi.org/10.1136/bmj.324.7344.1006.
- Glaser BG. Theoretical Sensitivity: Advances in the Methodology of Grounded Theory. Mill Valley, CA: Sociology Press; 1978.
- Bray JE, O’Connell BO, Gilligan A, Livingston PM, Bladin C. Is FAST stroke smart? Do the content and language used in awareness campaigns describe the experience of stroke symptoms?. Int J Stroke 2010;5:440-6. http://dx.doi.org/10.1111/j.1747-4949.2010.00484.x.
- Department of Health . Stroke: Act F.A.S.T. Awareness Campaign 2011. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_094239 (accessed December 2011).
- Wein TH, Staub L, Felberg R, Hickenbottom SL, Chan W, Grotta JC, et al. Activation of emergency medical services for acute stroke in a nonurban population: the T.L.L. Temple Foundation Stroke Project. Stroke 2000;3:1925-8. http://dx.doi.org/10.1161/01.STR.31.8.1925.
- Mosley I, Nicol M, Donnan G, Patrick I, Kerr F, Dewey H. The impact of ambulance practice on acute stroke care. Stroke 2007;38:2765-70. http://dx.doi.org/10.1161/STROKEAHA.107.483446.
- Adams HP, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups. Circulation 2007;115:e478-534.
- National Stroke Strategy. London: DoH; 2007.
- Wall HK, Beagon BM, O’Neill HJ, Foell KM, Boddie-Willis CL. Addressing Stroke Signs and Symptoms Through Public Education: The Stroke Heroes Act FAST Campaign 2008. www.cdc.gov/pcd/issues/2008/apr/07_0214.htm (accessed May 2007).
- Jones SP, Carter B, Ford GA, Gibson JM, Leathley MJ, McAdam JJ, et al. Obtaining Rapid Telephone Triage Group. The identification of acute stroke: an analysis of emergency calls. Int J Stroke 2013;8:408-12.
- Marcovitch H. Black's Medical Dictionary. London: Black; 2005.
- Cooke MW, Wilson S, Cox P, Roalfe A. Public understanding of medical terminology: non-English speakers may not receive optimal care. J Accid Emerg Med 2000;17:119-31. http://dx.doi.org/10.1136/emj.17.2.119.
- Fitch AL, Sanders RE. Handbook of Language and Social Interaction. New Jersey, NJ: Lawrence Erlbaum Associates; 2005.
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974;2:81-4.
- Lawrence ES, Coshall C, Dundas R, Stewart J, Rudd AG, Howard R, et al. Estimates of the prevalence of acute stroke impairments and disability in a multiethnic population. Stroke 2001;32:1279-84. http://dx.doi.org/10.1161/01.STR.32.6.1279.
- Warlow CP, Dennis MS, Van Gijn J, Hankey GJ, Sandercock PAG, Bamford JM, et al. Stroke: A Practical Guide to Management. London: Blackwell Sciences; 1996.
- Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Houston paramedic and emergency stroke treatment and outcomes study (HoPSTO). Stroke 2005;36:1512-18. http://dx.doi.org/10.1161/01.STR.0000170700.45340.39.
- Stroke Unit Trialists’ Collaboration . Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2007;4. http://dx.doi.org/10.1002/14651858.CD000197.
- Davalos A, Castillo J, Martinez-Vila E. Cerebrovascular Diseases Study Group of the Spanish Society of Neurology . Delay in Neurological Attention and Stroke Outcome. Stroke 1995;26:2233-7.
- Introductory Guide to MedDRA Version 13.1. Chantilly, VA: MedDRA Maintenance and Support Organisation; 2010.
- National Academies of Emergency Dispatch . Resources, Emergency Dispatch Systems, Medical Priority Dispatch Systems 2013. www.emergencydispatch.org/ResourcesEDS (accessed February 2013).
- National Academies of Emergency Dispatch . Resources, Emergency Dispatch Systems, The System Takes Off 2013. www.emergencydispatch.org/ResourcesEDS (accessed February 2013).
- Kotter JP, Cohen DS. The Heart of Change. Boston, MA: Harvard Business School Press; 2002.
- NHS Connecting for Health . About NHS Pathways 2013. www.connectingforhealth.nhs.uk/systemsandservices/pathways/about (accessed February 2013).
- Cole R. Issues in Web-Based Pedagogy: A Critical Primer. Westport, CT: Greenwood Press; 2000.
- Anderson T. The Theory and Practice of Online Learning. Athabasca, AB: Athabasca University, AU Press; 2008.
- Jones SP, McLoughlin ASR, Watkins CL. Acute stroke management: an online course. J Paramedic Practice 2011;3:322-7.
- Harris C. Developing Online Market Research Methods and Tools n.d.
- Blake H. Staff perceptions of e-learning for teaching delivery in healthcare. Learn Health Soc Care 2009;8:223-34. http://dx.doi.org/10.1111/j.1473-6861.2009.00213.x.
- Dames D, Handscomb A. A pilot study to assess the case for e-learning in the NHS. J Research Nursing 2002;7:428-43. http://dx.doi.org/10.1177/136140960200700605.
- Becker KJ, Fruin MS, Gooding TD, Tirschwell DL, Love PJ, Mankowski TM. Community based education improves stroke knowledge. Cerebrovasc Dis 2001;11:34-43. http://dx.doi.org/10.1159/000047609.
- Evenson KR, Rosamond WD, Morris D. Pre-hospital and in-hospital delays in acute stroke care. Neuroepidemiology 2001;20:65-76.
- Pancioli AM, Broderick J, Kothari R. Public perception of stroke warning signs and knowledge of potential risk factors. J Am Med Assoc 1998;279:1288-92. http://dx.doi.org/10.1001/jama.279.16.1288.
- Saver JL, Lutsep MD. Thrombolytic Therapy in Stroke 2007. http://emedicine.medscape.com/article/1160840-overview (accessed 3 February 2012).
Appendix 1 Routes taken to calling 999 at the onset of stroke-like symptoms
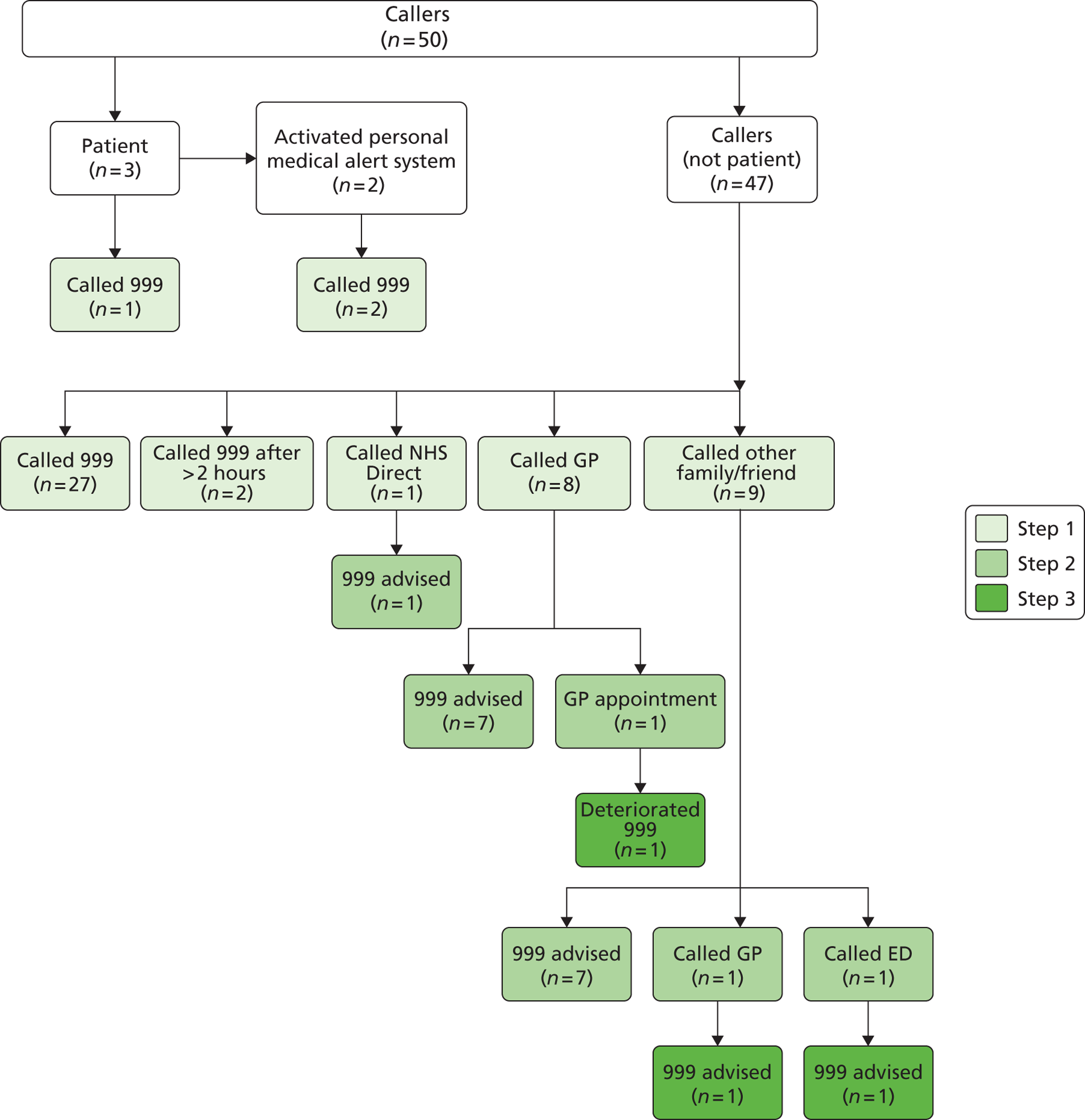
Appendix 2 Training package content
About the course
The aim of this course is to improve the knowledge and skills of emergency medical call handlers in the identification of patients with acute stroke.
This course will help you to:
-
understand why stroke is a medical emergency
-
appreciate the importance of early identification
-
recognise the symptoms of stroke and how the symptoms are reported by members of the general public.
Background
Stroke is the third most common cause of death in the UK and the leading cause of adult neurological disability.
The National Stroke Strategy (2007) recommends that all patients with suspected acute stroke are immediately transferred by ambulance to hospital.
The National Stroke Strategy also recommends that public and professional awareness of the risk factors and symptoms of stroke should be improved and that stroke should be treated as a medical emergency.
This content of this course has been informed by a large research project called ESCORTT (Emergency Stroke Calls: Obtaining Rapid Telephone Triage). ESCORTT has involved reviewing patient records, interviewing patients and other people who have contacted the emergency services for suspected stroke, as well as listening to actual 999 calls for stroke and other conditions.
Public awareness
The symptoms and severity of stroke can vary from person to person. Because of this, members of the public may have difficulty recognising that they have the symptoms of a stroke (Panicoli et al. 69).
From 2009 onwards, a national campaign led by the Department of Health aimed to raise public awareness. By helping members of the public and health professionals to identify stroke symptoms and to ensure that stroke is treated as a medical emergency by dialling 999.
Routes into hospital
When a person has dialled 999 with a suspected stroke, they will receive a category A (currently up to a 19-minute response) and should be transported as quickly as possible to the nearest Trust with an Acute Stroke Unit. Some patients (e.g. those suitable for thrombolysis) may need to be transported to specialist centres in accordance with local agreements.
Local agreements may also require ambulance personnel to contact the stroke team as the patient is transported to hospital. Depending on local agreements the patient will need to be taken to the Accident and Emergency (A&E) Department or directly to the Acute Stroke Unit. Receiving clinicians must be made aware that stroke is a medical emergency.
Stroke is a medical emergency
It is imperative to seek immediate medical treatment at the first sign of stroke, by calling 999.
The quicker a person is treated, the more brain will be saved and the better the chance of a complete recovery. 1.9 million neurons are lost for each minute that a stroke is left untreated.
Time is brain!
What is a stroke?
A stroke is a disruption of blood flow to the brain or part of the brain due to a blood clot (blockage) or bleed (haemorrhage).
Symptoms of stroke may vary from problems such as difficulties speaking or inability to use the arm or leg to loss of consciousness.
There are different types of stroke
Ischaemic infarction
80–85% of all strokes are caused by an ischaemic infarction.
An ischaemic stroke is the result of a blockage in an artery leading to part of the brain. Some arteries contain fatty material called plaque, which can build up over a number of years. If the arteries become too narrow, blood cells may collect and form blood clots.
These blood clots can block the artery where they are formed (thrombosis), or can dislodge and become trapped in arteries closer to the brain (embolism). In either, these blockages will prevent blood reaching a particular part of the brain, causing a loss of brain function.
Primary intracerebral haemorrhage (PICH)
10–15% of all strokes are caused by a bleed (PICH). This type of stroke occurs when a blood vessel ruptures, bleeding into the surrounding brain tissue. The pressure on adjacent brain tissue from the sudden outflow of blood, along with a deficit in blood supply, causes rapid and severe damage.
Transient ischaemic attack (TIA)
What if the symptoms of stroke go away quickly? An ischaemic stroke event that resolves quickly is called a transient ischaemic attack or TIA.
Most TIAs only last between 5–30 minutes and present with the symptoms of stroke. A person who has had a TIA has a 7–10% risk of having a stroke in the next 7 days.
Those with TIA are more likely to go on to have a stroke within 24 hours of onset of symptoms, than a person with chest pain going on to have a heart attack.
TIA is a medical emergency, particularly for those who have more than one TIA in a week.
Any patient with a suspected TIA requires an urgent full neurological assessment. All TIA patients should be taken to A&E even if though their symptoms may have resolved. If the patient does not want to go to hospital, they should be informed of the risk of having a stroke and that they need a neurological assessment.
Animation
The following animations demonstrate how the obstruction of different arteries in the brain results in a range of symptoms.
Stroke is a medical emergency. If people suspect that they have had a stroke they should dial 999 immediately. This is because 1.9 million neurons (nerve cells) are lost for every minute in which stroke is left untreated (Saver and Lutsep70).
The following animations demonstrate how the obstruction of different arteries in the brain results in a range of symptoms.
Use the sliders to alter the physiological parameters, to see the effects on the post-stroke brain.
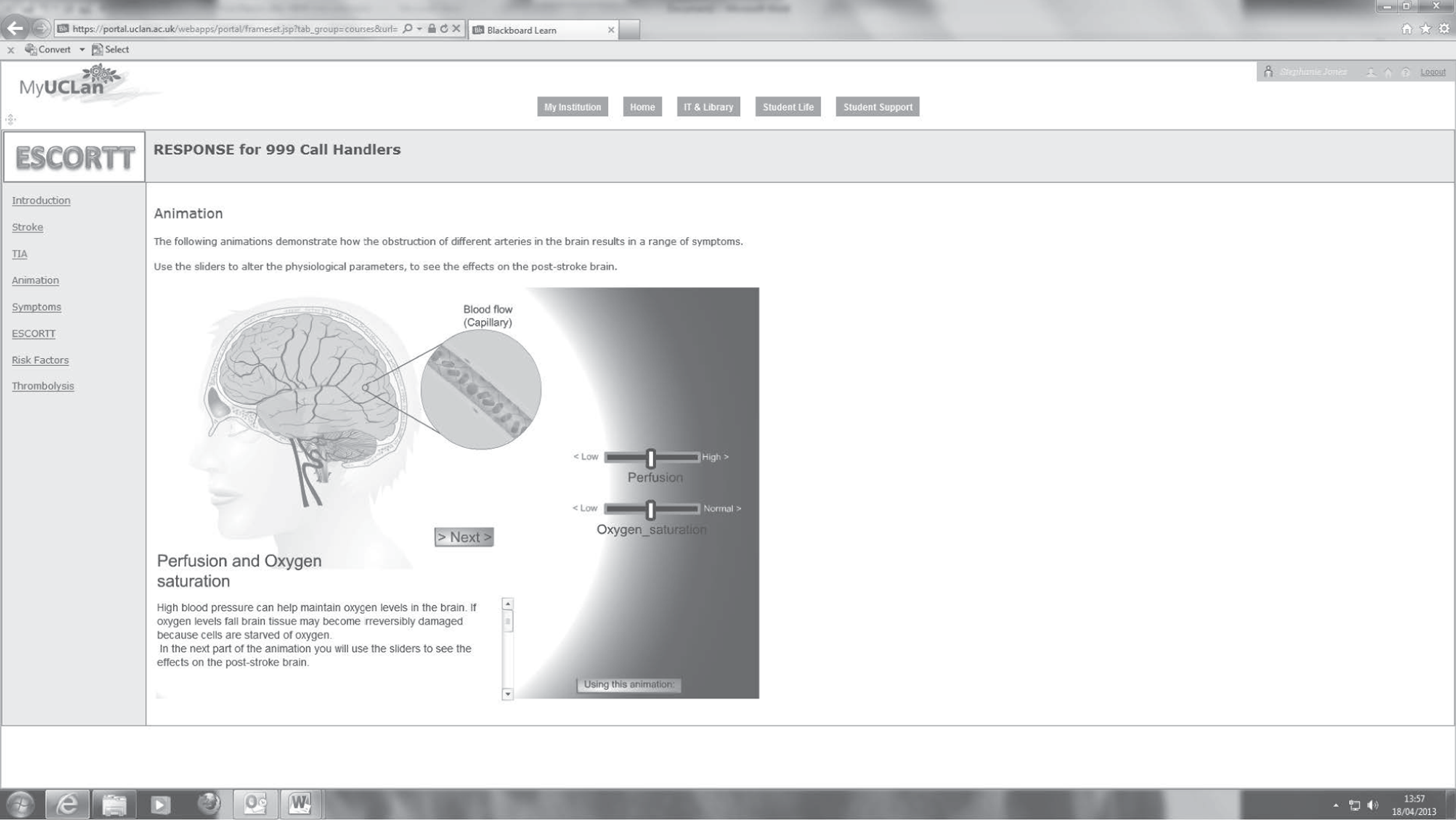
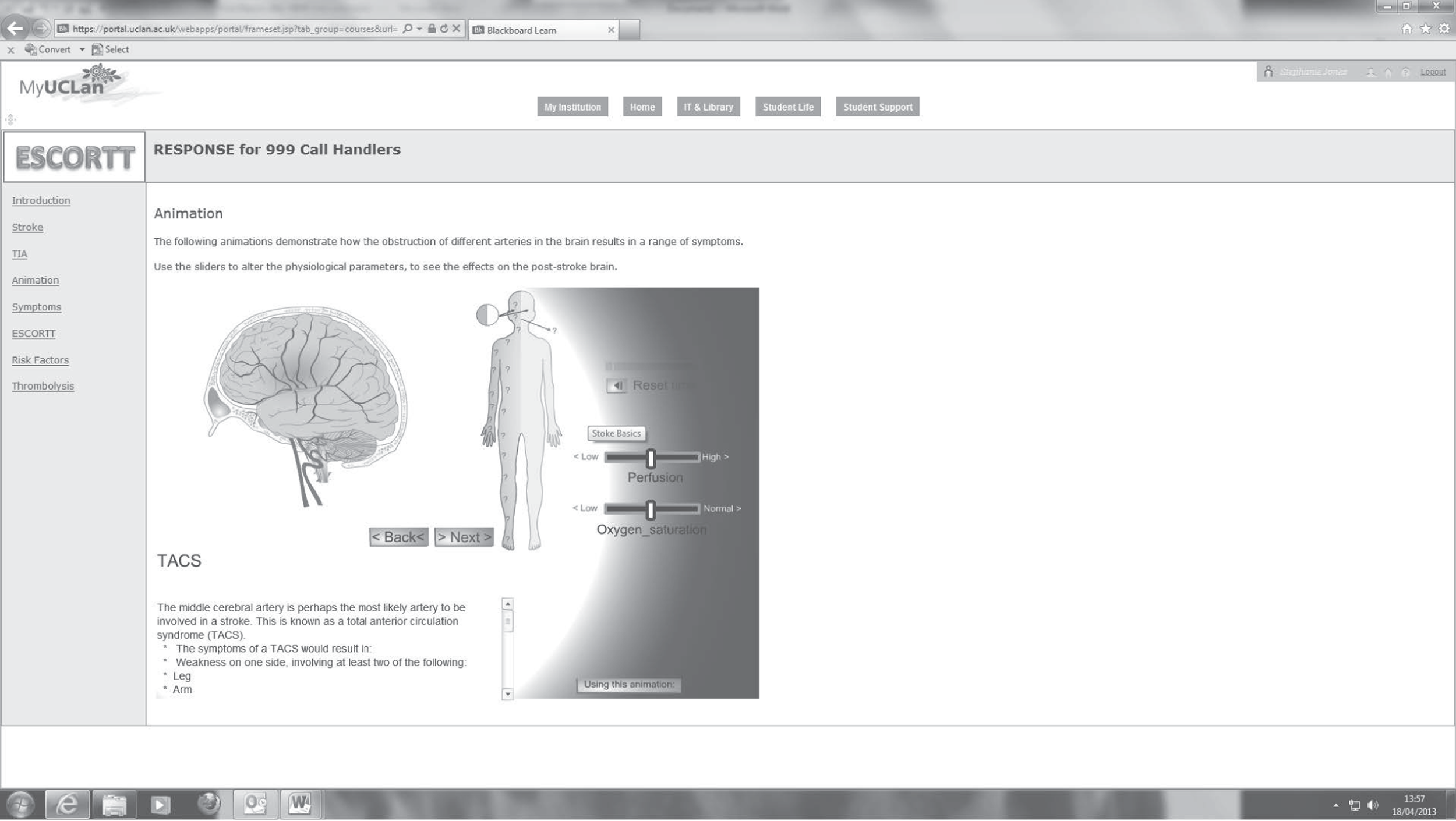
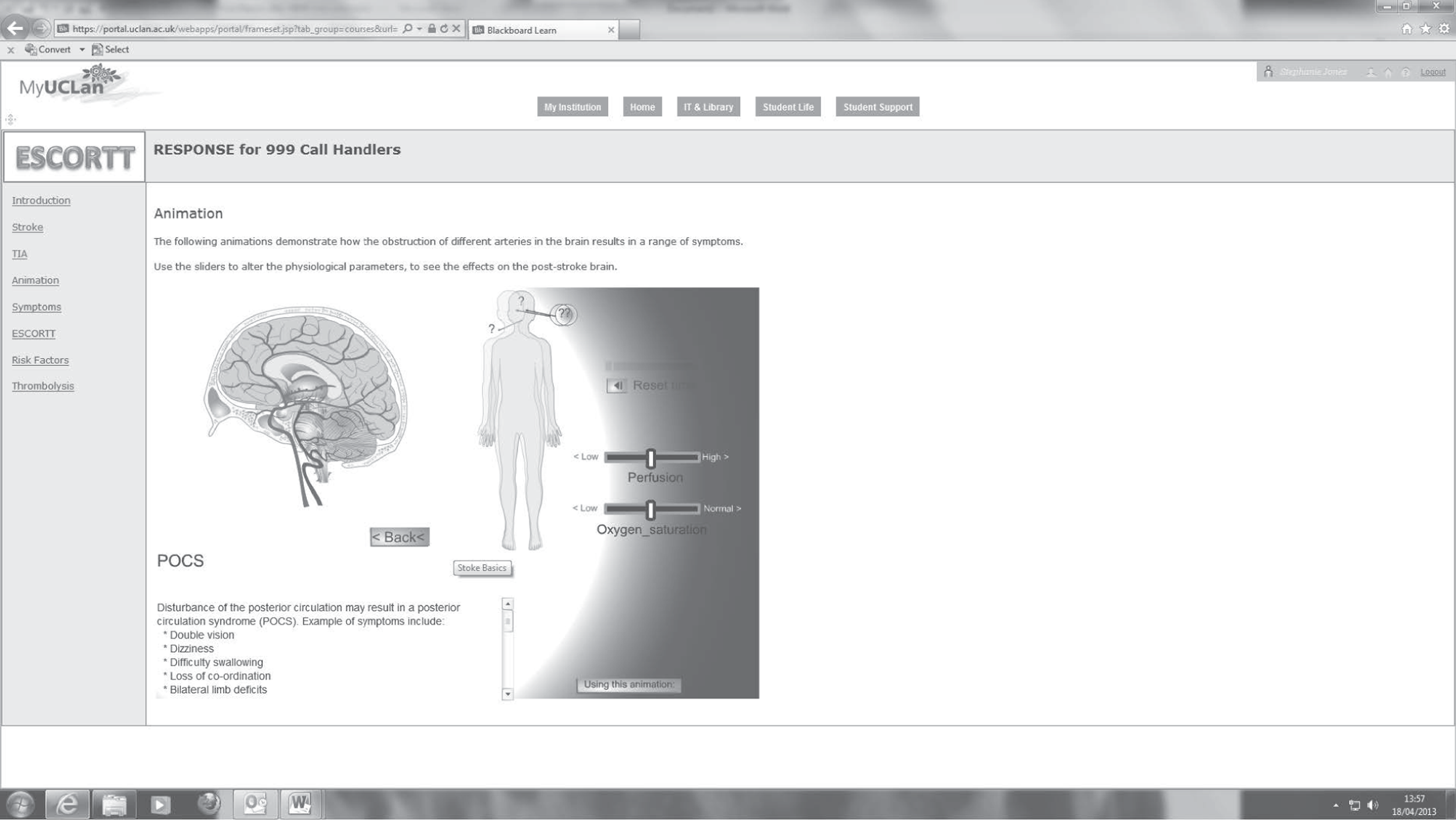
Suspected stroke and dialling 999
On the onset of symptoms two-thirds of stroke patients obtain first medical contact from the emergency medical services (EMSs).
In nearly all cases of suspected stroke, people who call 999 are family members, friends, neighbours or unrelated bystanders.
Only 3% of calls are made by the patients themselves.
The symptoms and severity of stroke can vary from person to person and because of this, members of the public may have difficulty recognising the symptoms of a stroke.
Around one-third of callers recognise the problem as a stroke.
How can I recognise a stroke? – The signs and symptoms
The signs and symptoms of stroke can vary from person to person depending on what part of the brain has been affected. A person may present with one, or a combination of the symptoms listed below.
The symptoms of stroke are usually:
-
sudden weakness, numbness, or paralysis of the face, arm, or leg, on one side of the body
-
sudden difficulty walking, loss of balance or co-ordination, known as ataxia
-
sudden, severe headache with no known cause
-
sudden trouble seeing in one or both eyes.
Visual disturbance may include blurred or double vision or hemianopia, whereby blindness in the visual field of both eyes means that the patient can see left with one eye and right with the other. Other visuospatial problems may include inattention where the person does not recognise one side of their body as being part of them or are unable to acknowledge left/right visual-space.
Other symptoms
The following symptoms may occur in combination with those listed above or they may occur alone. These symptoms may also arise from other acute illness:
-
confusion, which may be as a result of the event or related to the patient’s prior medical history
-
some patients will be agitated and may be aggressive, this could be as a result of hypoxia (lack of oxygen)
-
patients are likely to feel frightened, anxious and are unable to make sense of what is happening to them
-
patients and their carers will require reassurance
-
body temperature often rises in the acute phase of stroke and so patients may have a warm flushed appearance
-
vomiting
-
incontinence.
Stroke mimics
Hypoglycaemia – blood glucose monitoring should be carried out on any patient that is neurologically compromised.
Bell’s palsy – a condition in which one side of the face becomes paralysed, the symptoms are usually temporary.
Previous stroke – this may have left the person with a residual deficit.
Hemiplegic migraine – symptoms can include sudden hemiplegia (paralysis on one side of the body) fever, the symptoms of meningitis without the actual illness.
Consciousness – ranging from confusion to profound coma.
Intoxication – caused by alcohol or drugs.
Acute confusional state – may be a posterior circulation episode. Commonly, particularly with the older patient, an acute confusional state is due to sepsis.
Emergency Stroke Calls: Obtaining Rapid Telephone Triage (ESCORTT)
What is ESCORTT?
ESCORTT is a research project funded by the National Institutes of Health Research Programme Grant. The aim of ESCORTT is to facilitate the recognition of stroke by ambulance call handlers.
Why is the ESCORTT research programme important?
In order to achieve rapid access to specialised stroke services through early identification it is imperative that frontline staff can recognise the symptoms of stroke and initiate a rapid response. This will intensify in the future because NHS Direct and primary care are being targeted to pass on those with stroke-like symptoms to ambulance call handlers and dispatchers.
What did we do?
Through interviewing people who had dialled 999 and by listening to 999 calls we have identified factors that can improve the accuracy of early diagnosis of stroke. Using this information, this course has been developed for call handlers.
The impact of the training package was assessed to see if stroke patients can be identified and diagnosed more quickly by call handlers who have completed this training. An evaluation of the training package took place in one EMS regional control centre. Sixty-nine call handlers completed the training.
The evaluation showed that before implementation of the training package call handlers correctly identified 63% of stroke patients; this increased to 80% following completion of the training.
Suspected stroke: describing the symptoms
We listened to 592 calls to the EMSs for patients who went on to have a confirmed diagnosis of stroke in hospital. Overall, collapse or fall was the most commonly reported problem (40%), with stroke the second most common (37%).
Other common reported problems included:
-
17% said change in consciousness level
-
15% said limb weakness
-
8% said previous history of stroke
-
4% said facial weakness.
Stroke patients who have facial weakness and speech problems are more likely to be given a correct diagnosis of stroke by call handlers. A correct diagnosis of stroke by the EMSs results in a quicker journey to hospital.
People who dial 999 about non-stroke conditions rarely say stroke, limb weakness, speech problems, or facial weakness. However, the word fall is commonly used in both stroke and non-stroke calls.
Other descriptions included:
-
funny turn
-
confused
-
unable to move
-
dizzy
-
unresponsive
-
cannot speak
-
seizure.
What have we found?
If a person has had a stroke, they or someone calling on their behalf are more likely to dial 999 if they perceive their symptoms to be serious.
In nearly all cases of suspected stroke, people who call 999 are family members, friends, neighbours or unrelated bystanders. Only 3% of calls are made by the patients themselves.
After someone has had a stroke, the person ringing 999 may also use the terms or descriptions: fall, collapse and problems speaking. The likelihood of it being stroke is increased if the caller uses two or more of the following descriptors together:
-
stroke
-
fall
-
collapse
-
problems speaking.
Callers often feel reassured by the advice given by the EMSs during the 999 call, but some can be uncertain about whether an ambulance had been dispatched or not.
When reviewing EMS patient report forms, a diagnosis of stroke was most likely to be made by call handlers and ambulance personnel when stroke patients had facial weakness and/or speech problems.
Levels of consciousness
The terms consciousness and unconsciousness are used by call handlers but callers have difficulty understanding different levels of consciousness.
For example, callers often describe levels of consciousness in the following ways:
-
not awake
-
unresponsive
-
asleep
-
cannot wake them up
-
not with it
-
keep drifting in and out
-
semi-coma
-
delirious
-
disorientated
-
cannot seem to recognise me
-
consciousness.
Stroke patients may have altered consciousness. If a patient is completely unconscious there could be many other reasons. The terms consciousness and unconsciousness are used by call handlers to describe different levels of consciousness, however, the caller has a different vocabulary in this respect.
Levels of consciousness activity
Try the exercise below to see what words callers are likely to use to describe different levels of consciousness.
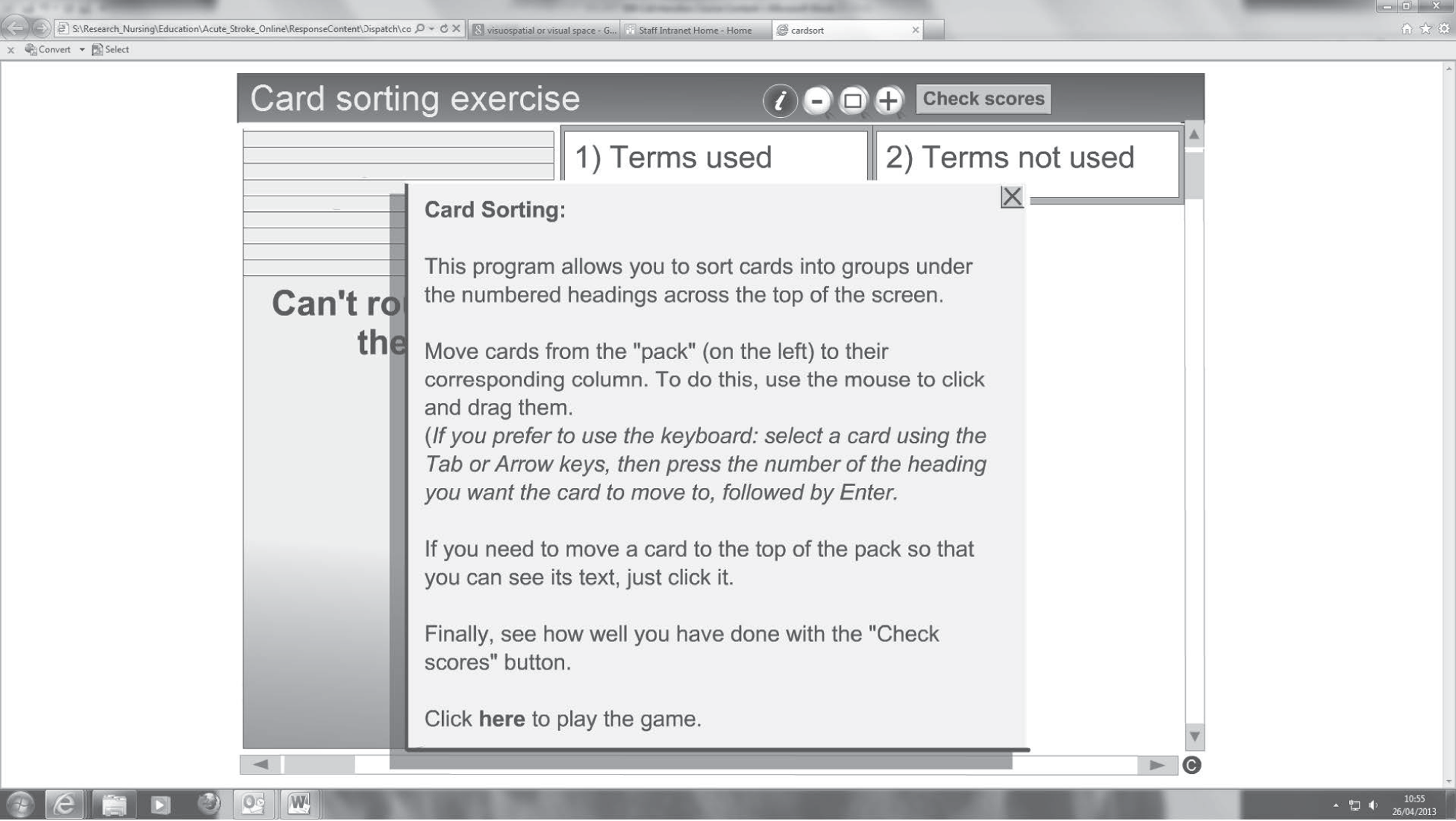
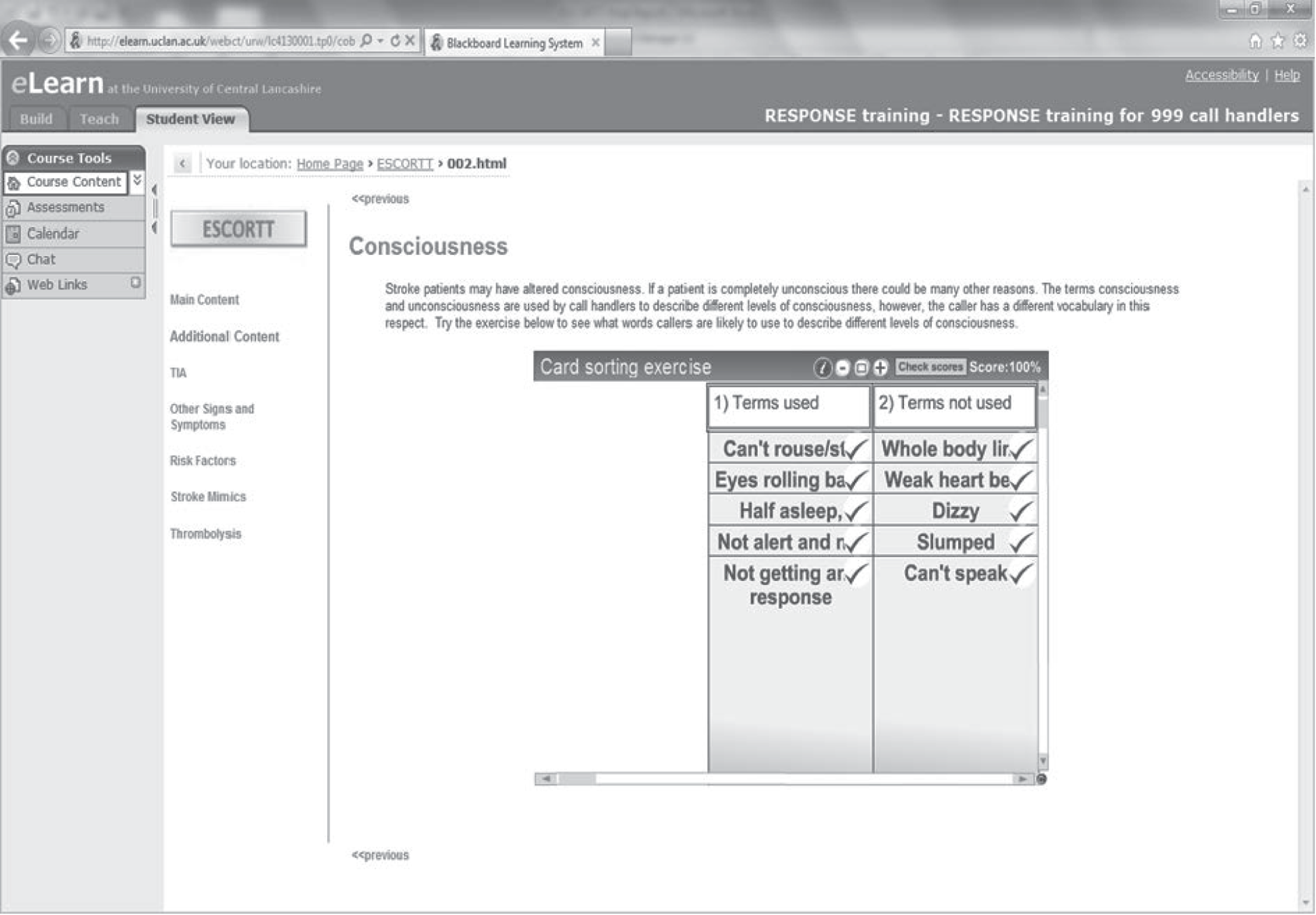
Risk factors
A patient’s past medical history may include some of the risk factors for stroke. There are a number of factors that increase the risk of stroke. Risk factors can be divided into three categories:
Non-modifiable: Those the patient cannot change.
Treatable: Those that can be treated.
Modifiable: Those that can be improved through positive changes in lifestyle.
Non-modifiable risk factors
Age: 1 in 4 men and 1 in 5 women over the age of 45 will have a stroke. The risk of stroke increases with age.
Family history: Stroke is more common in people whose close relatives have suffered a stroke.
Ethnicity: Stroke is more prevalent in some ethnic minority groups.
Treatable risk factors
Hypertension: High blood pressure is the greatest risk factor for stroke. Medication can be prescribed to lower blood pressure.
Previous stroke or Transient Ischaemic Attack (TIA): Greatly increases the risk of a recurrent event. Medication is required, and in some cases surgery.
Diabetes: Blood glucose levels need to be carefully monitored and controlled.
Heart disease: Atrial fibrillation in particular increases the risk of stroke. Medication to thin the blood (for example warfarin) or to reduce cholesterol (for example statins) may be prescribed.
High cholesterol: Cholesterol levels need to be carefully monitored and controlled.
Modifiable risk factors (lifestyle)
Smoking.
Obesity.
Physical inactivity.
Excessive alcohol consumption.
Drug use.
Thrombolysis
For those who do experience a stroke or TIA, rapid access to effective stroke care and treatment can reduce death and dependency by enabling the immediate provision of interventions such as thrombolysis. Access to organised stroke care is also important, as it has been shown to save lives and reduce disability.
Thrombolysis is a ‘clot-busting’ medicine that can dissolve blood clots following acute ischaemic stroke.
Thrombolysis for ischaemic stroke is becoming widely available across the UK. Recent research from the IST3 trial and a systematic review have provided more detailed information about which patients may benefit from thrombolysis and at what time-points.
The following must be answered yes if a patient is to be considered eligible for thrombolysis.
Does the patient have the symptoms and signs of acute stroke?
Is there a clear time of onset within the last 6 hours?
Is the patient over 18 years old?
Not all patients with ischaemic stroke are eligible for thrombolysis and eligibility will be assessed further by the ambulance crew and by hospital staff on arrival at hospital.
Multiple-choice quiz
To access the multiple-choice quiz, click on assessments on the tool bar on the left of your screen. When you have completed the quiz click submit, your submission will be graded immediately.
To pass the quiz you must achieve 60%. If you successfully complete the quiz you will receive a certificate of completion, an electronic certificate will be sent to you.
Your certificate of completion will only be sent out when you have completed the online module evaluation form. This can be accessed by clicking on assessments and then module evaluation.
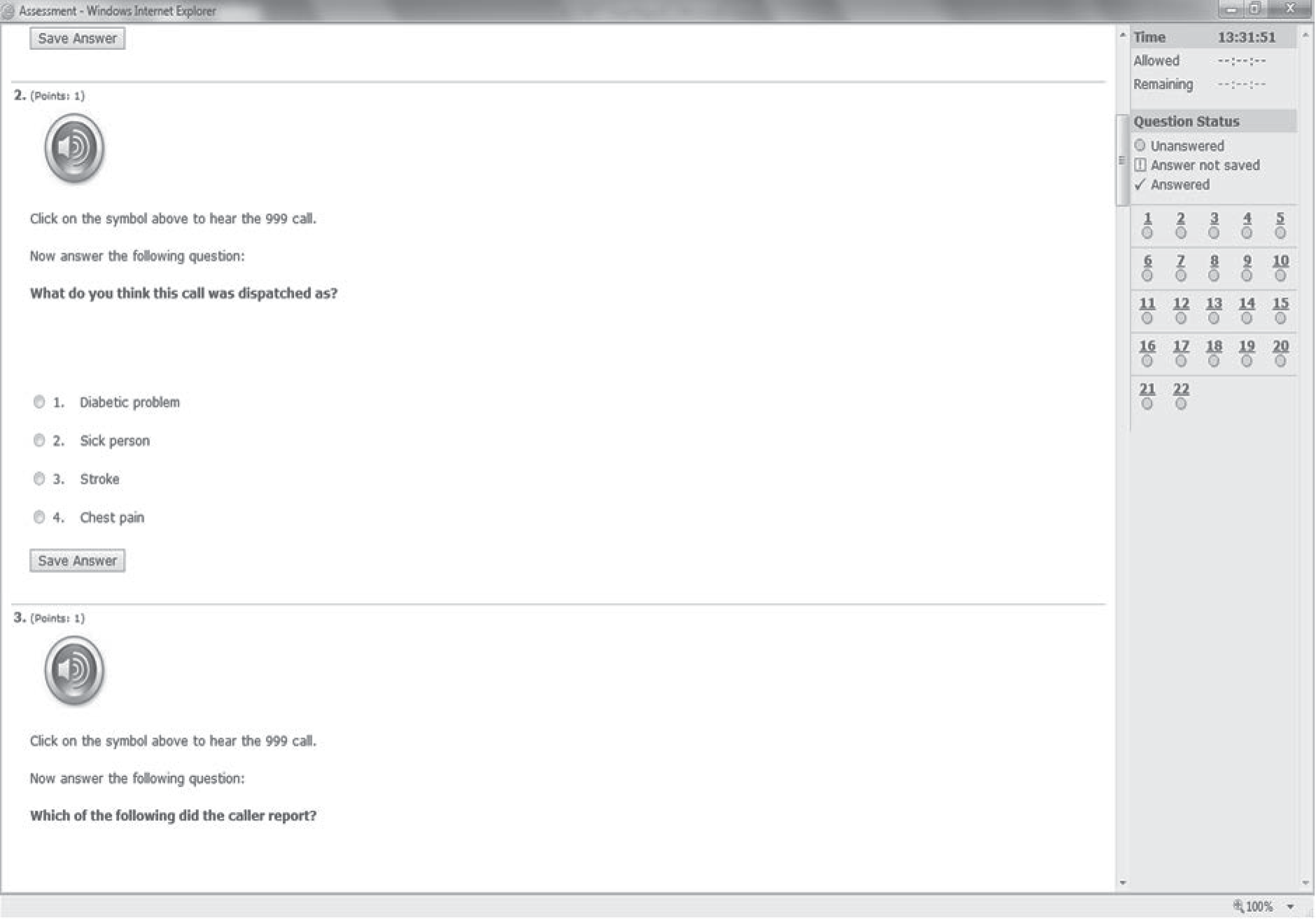
Appendix 3 Overall programme protocol
ESCORTT phase 1: identifying stroke: the association between patient characteristics and stroke symptoms with pre-hospital diagnosis and time to admission
Aim
To explore how patient and stroke characteristics are associated with: dispatch code; accuracy of dispatch code; ambulance diagnosis; and how dispatch code was associated with time to arrival at hospital.
Design
Retrospective audit of hospital and EMS records.
Methods
Setting
An ambulance service and three hospitals in the north-west of England.
Subjects and sampling
The subjects will be patients arriving at hospital by ambulance during a 12-month period (1st October 2006 to 30th September 2007). The sample will be identified through a retrospective audit of hospital and EMS records. Stroke patients will be identified in hospital from the stroke register or the hospital coding system at the two sites with no register. Additional patients will be identified from hospital by searching through the Emergency Department (ED) records. Case notes will be ordered for any patients identified from these records with stroke-like symptoms who were not on the register or the coding system; the case notes were reviewed and the diagnosis checked by an experienced stroke research nurse. For all patients identified in hospital we will obtain their EMS data. Independent from the data gathered in hospital, patients will be identified from EMS records who had either been dispatched as a stroke or who had been diagnosed in the ambulance as having had a stroke. The hospital case notes will be obtained for all patients identified through the EMSs. A patient will be considered to have had a stroke if they were discharged from the ED and the ED records stated stroke; they were still on the stroke register at the time of discharge from hospital, or, where there was no register, their discharge letter stated a diagnosis of stroke.
Inclusion criteria: patients who had a diagnosis of suspected stroke by the EMS call handler and/or a final diagnosis of stroke in hospital.
Exclusion criteria: patients whose General Practitioner contacted the EMSs on their behalf; patients who had a stroke in hospital.
Procedure
The sample will be identified through a retrospective audit of hospital and EMS records. Stroke patients will be identified from the hospital stroke register or the hospital coding system at the three sites with no register. Additional patients will be identified by searching through ED records. Case notes will be ordered for any patients identified from these records with stroke-like symptoms who were not on the register or the coding system; the case notes will be reviewed and the diagnosis checked by an experienced stroke research nurse. For all patients identified in hospital we will obtain their EMS data. Independent from the data gathered in hospital, the EMSs will also identify patients who had either been dispatched as a stroke or who had been diagnosed in the ambulance as having had a stroke. The hospital case notes will be obtained for all patients identified through the EMSs. A patient will be considered to have a final diagnosis of stroke if: they were discharged from the ED and the ED records stated stroke; they were still on the stroke register at the time of discharge from hospital, or, where there was no register, their discharge letter stated a diagnosis of stroke.
Data collection
Data will be recorded from the electronic patient report forms used by EMS staff, and the patient’s hospital case notes. EMS report forms will provide data on dispatch code (dichotomised into stroke or not-stroke), whether the Face Arm Speech Test (FAST) was completed in the ambulance and the results, and the following times: call made to Ambulance Service; call passed to ambulance; ambulance arrived at scene; ambulance left scene; ambulance arrived at hospital. From the case notes we will record: demographics; stroke history; pre-stroke status; type of stroke (due to ischaemia or haemorrhage); side affected by the stroke; consciousconsciousness level; neurological impairment; status at discharge; diagnosis at different stages of the care pathway, e.g. Emergency Department, Medical Assessment Unit, Stroke Unit; final diagnosis.
Data analysis
Univariate analyses will explore the association between diagnosis of stroke or not stroke (separately for dispatch and the ambulance) and patient characteristics, stroke characteristics, and time, using Mann-Whitney U-tests (continuous and ordinal variables) and χ2-tests (dichotomous categorical variables). Multivariate analyses will be made using multiple logistic regression, where diagnosis of stroke or not was the dependent variable, and characteristics (patient and stroke) were the independent variables. Separate models will be developed for dispatch and ambulance diagnoses.
Storage of data
Any patient identifiable information that is collected will removed before the data are stored. Data will be stored in Brook 417 at the University of Central Lancashire. This is a locked room with locked data storage cupboards. Data collection sheets will also be scanned and stored as electronic files. All electronic files will be password protected. All written data will be stored for ten years.
Ethical issues
This audit requires accessing patient case notes without individual consent. Although approval from the Local Research Ethics Committee is not required, Faculty of Health Ethics Committee at the University of Central Lancashire and R&D approval at the relevant Trusts will be sought.
Outputs
The findings of this research will contribute to a programme of work to increase the timeliness and accuracy of the identification and diagnosis of acute stroke.
Costings
Researchers will be reimbursed for any travel expenses. No other costs are anticipated.
Dissemination
Public output will include publication in peer reviewed journals and presentations at conferences.
Project milestones
| November 2007 to December 2007 | Faculty of Health Ethics and R&D approval |
| January 2008 | Identify case notes and EMS patient report forms |
| January 2008 to December 2008 | Collect data |
| June 2008 to February 2009 | Analyse data |
| March 2009 to May 2009 | Final Report |
| March 2009 to July 2009 | Prepare presentations and publications |
ESCORTT phase 2: callers’ experiences of making emergency calls at the onset of acute stroke: a qualitative study
Aim
To identify the features that expedited or delayed people’s initial decision to contact EMSs at the onset of acute stroke, and to explore callers’ experiences of the call.
Design
A qualitative study using semi-structured interviews.
Methods
Setting
Two acute trusts in the north-west of England.
Subjects and sampling
Patients or their carers will be identified from a criterion based purposive sample of patients with a final diagnosis of stroke from two acute trusts, over a 12-month period. We will identify up to 50 patients or their carers (25 per trust), from the hospital stroke registers. We will identify patients, or carers of patients who have been admitted with an acute stroke, and who arrived at hospital via the ambulance service. This purposive sample will be representative of the stroke patients admitted to hospital during this 12-month period, in terms of age, sex, ethnic group, and speed of response by the ambulance.
Inclusion criteria: patient, or carer of a patient who received final diagnosis of acute stroke made by a physician; arrived at hospital via the ambulance service; recruited to this phase within one month of stroke onset; 18 years or older; and medically stable (as determined by the stroke team).
Exclusion criteria: patient or carer who has severe communication or cognitive difficulties as diagnosed by a clinician. Patient, or carer of a patient who had a stroke in hospital as an inpatient; who received a diagnosis of subarachnoid haemorrhage. Subjects were also excluded if their admission was arranged by primary care (GP), they attended ED directly or they had a stroke while in hospital.
Procedure
A member of the clinical team will confirm that the patient meets the inclusion criteria for the study (arrived at hospital by ambulance; diagnosis of stroke confirmed by a stroke physician; patient not critically ill or deceased). Patients (or a consultee for those who had significant cognitive impairment) will then be approached about the study by a member of the clinical team during their inpatient stay, within a maximum of two weeks after admission. The person who had made the initial call to EMSs (the patient, their relative, or other person) will then be invited to take part in the study and will be given at least 24 hours to decide if they would like to participate. At this point a researcher will approach the participant to confirm participation and obtain written informed consent. Anonymity and confidentiality of data generated by participants will be discussed with participants and participants then written informed consent will be obtained. The interviews will be conducted face to face using a semi-structured interview guide, either in a quiet, private room on the hospital stroke unit or at the caller’s home. Interviews will be digitally recorded.
For patients or carers who speak Urdu or Punjabi, a researcher who can speak these languages is available to conduct the interview.
The term ‘carer’ in this instance is used to denote the person who contacted the emergency services on behalf of the patient. The carer may be a relative, close friend or neighbour. All carers will be approached through the patient, with the patients’ permission.
The interview schedule will be devised by members of the research team and will use open-ended questions to explore the feelings and views of the participants.
Data collection
Brief details about the caller will be collected at the time of the interview (age, sex and relationship to the patient).
Data analysis
All interviews will be digitally recorded and transcribed verbatim by an established transcription company who are familiar with the issues surrounding patient or carer interviews. The transcriptions will be analysed using content analysis (facilitated by Atlas.ti software) to identify themes and sub themes. Independent analysis of the interviews by another researcher will check the reliability and validity of the identified themes. Respondent validity will be addressed by asking the interviewees if they agree with the themes identified.
Storage of data
To ensure confidentiality any personal data collected will only be accessible by the research team. Data will be stored in Brook 417 at the University of Central Lancashire. This is a locked room with locked data storage cupboards. Any electronic files will be password protected. Voice recordings will be destroyed after 12-months. All written data will be stored for five years.
Ethical issues
Patients or carers will not be approached directly by the research team; the patient or carer will be introduced to the researcher by a member of clinical team. Informed consent will be gained for all participants taking part in the interviews by a member of the research team. Should the interviews raise any issues that cause emotional distress to the participant, the interview will be suspended until the participant feels able to continue. Alternatively, the interview may be halted at that time and the participant will be given the opportunity to complete the interview at a later date or decline further contact. The interviewers will be experienced in dealing with stroke patients and carers and will know how to manage such situations either through talking to or advising a healthcare professional.
Outputs
The findings of this research will be used as part of a programme of work to increase the timeliness and accuracy of the identification and diagnosis of acute stroke.
Costings
Each participant will be reimbursed for any travel expenses.
Dissemination
Public output will include publication in peer reviewed journals and presentations at conferences. Patients or carers will not be identified in any public outputs.
Project milestones
| September 2008 | Finalise interview schedule |
| October 2008 to January 2009 | Identify potential participants |
| October 2008 to January 2009 | Conduct 50 interviews |
| January 2009 to March 2009 | Transcribe interviews |
| March 2009 to December 2009 | Analyse data |
| March 2009 to December 2009 | Final Report |
| January 2010 to December 2010 | Prepare presentations and publications |
ESCORTT phase 3: The Identification of Acute Stroke: An Analysis of Emergency Calls
Aim
To identify ‘key indicator’ words used by people making emergency calls for suspected stroke.
Design
A retrospective qualitative study.
Methods
Setting
An ambulance service in the north-west of England.
Subjects and sampling
Patients with suspected acute stroke who arrived at a participating hospital through calling the EMSs, during a 12-month period (1st October 2006 to 30th September 2007).
Patients will be identified through a retrospective review of the stroke register, hospital coding system, case notes and EMS documentation forms. Once patients have been identified we will check for the EMSs for presence of an emergency call. Demographic and dispatch data will also be collected. These data will include: the relationship of the caller to the patient, location of the patient, dispatch code and category of response (e.g. A is an eight minute response).
Inclusion criteria: patients who had a diagnosis of suspected stroke by the EMS call handler and/or a final diagnosis of stroke. A patient was considered to have had a stroke if: ED records stated a stroke (for those patients discharged from the ED); they were still on the stroke register at the time of discharge; their discharge letter stated a diagnosis of stroke (where there was no register).
Exclusion criteria: Patients who did not arrive at hospital through EMSs, patients who had a stroke as an inpatient, patients who received a diagnosis of subarachnoid haemorrhage, patients for whom the call was made by their primary care physician (GP) or GP staff on behalf of the patient, and patients for whom we did not have data for final medical diagnosis.
Procedure
For all patients, we will identify the tape recorded dispatch conversations that resulted in an ambulance being dispatched. There are 4 categories of ambulance response, A (8 minutes), B (19 minutes), C (30 minutes), and GP urgent (where the GP speaks directly to Dispatch, an ambulance is dispatched anytime the same day). From previous experience it is estimated there will be approximately 700 calls. It is anticipated that some of the calls will not be in English. Therefore, we will utilise community researchers from a variety of ethnic groups, with whom we have worked previously, who are able to translate from Urdu, Gujurati, Bengali, Punjabi, Kokani, and Pushto into English. Other languages will be translated where possible.
A researcher (with an NHS honorary contract) will listen to and transcribe each call. During the recording of each call, the caller (patient or their representative) will have been asked by the dispatcher for their name and address. This part of the call will have to be listened to so we can ensure we are listening to the correct call but will not be transcribed. We will annotate the transcription of the call with a patient registration number (a unique identifier, which does not include personal details). The call will be transcribed verbatim from when the dispatcher asks the caller the first health-related question (i.e. what is the problem, tell me exactly what happened). No identifiable patient information will be transcribed.
Data collection
All calls will be listened to in full by a researcher trained in qualitative research methods. At the beginning of a call to the EMSs, the caller is asked the open question, “What’s the problem, tell me exactly what happened?” by an EMD to establish the chief presenting complaint. We will focus the analysis on the caller’s response to this first question, which will term ‘the first story’. The end of the first story comes when the EMD asks the closed question about consciousness, “Are they conscious?” The first story typically involves the description of a number of presenting problems; we will select the problems reported in the first story. The words used by the caller to describe the problem will be termed ‘key indicator’ words.
Data analysis
Calls will be analysed by coding the problems used by the caller to describe the presenting issue, diagnosis or condition. To ensure inter-rater reliability, 100 consecutive calls will be coded by at least two researchers and any discrepancies will be resolved by discussion. Analysis will be undertaken using a constant comparative method in order to identify key indicator words and relationships within the data. Open coding of the data will be undertaken using content analysis (facilitated by Atlas.ti software). The research team will meet regularly to discuss the coding categories in order to ensure a consistent approach to analysis of the data. New categories will be considered and added to the list of key indicator words at weekly intervals. Key indicator words identified will be grouped to form categories.
Further data will be collected from EMSs and patient medical records regarding dispatch code (e.g. stroke, unconscious, faint) and diagnosis information from each of the following: attending EMS personnel, emergency department, medical admissions unit, stroke unit or other clinical area and final medical diagnosis from ED or discharge letter.
Storage of data
If we provide the ambulance service with an incident number they can access the call and download it to a password protected CD. They will do this for all 700 calls. The CD will be collected from the ambulance service by a member of the research team, in person. The audio files will be also be transferred into a password protected folder on a computer at the University of Central Lancashire. When the audio files have been transcribed by a member of the research team, the transcriptions will only be accessible by members of the research team. Data will be stored in Brook 417 at the University of Central Lancashire. This is a locked room with locked data storage cupboards. Any electronic files will be password protected. All written data will be stored for five years.
Ethical issues
The ambulance service do not have the resources/technology to anonymise each of the calls. However, we have established that not all of the calls would contain patient identifiable information. For example, the call could be made by a third party (including the GP), or from an address that is not the patients. Thus the CD would contain a mixture of identifiable and non identifiable patient data.
There would be difficulty in obtaining consent when identifiable information has been given by the caller, whether it be the patient or a third-party caller. There are likely to be a minimum of 250 calls that have identifiable data.
Due to the way that data are captured for this phase it is not possible to obtain informed consent for each of the callers to dispatch. The callers will be unaware that their call is being listened to as part of this research project.
In order to gain consent it would be necessary to find each patient's address. This may not be easy to find if the call is made from somewhere other the patient's home, as the patient’s address would not be recorded. Another problem exists if the call is made by a third party; in such circumstances it would seem inappropriate to contact the caller to ask them details about the patient in order to facilitate contacting the patient to obtain their consent. In addition, before any contact is made, patient status (alive or dead) would need to be checked. The necessary steps and safeguards that we would have to take in order to approach patients in an appropriate manner would make gaining consent impractical.
Should any calls raise any issues that cause emotional distress to the researcher, de-briefing and counselling will be made available by the University of Central Lancashire.
PIAG application
Section 60 of the Health and Social Care Act 2001 relates to using patient identifiable information for medical purposes in circumstances where patient consent has not been obtained. Due to the ethical issues outlined above and following discussions with PIAG, we have been advised to submit a PIAG application.
Following PIAG approval, an application will also be made to the Local Research Ethics Committee, the Faculty of Health Ethics Committee at the University of Central Lancashire and NHS Research and Development at the EMSs and acute hospital trusts.
Outputs
The findings of this research will contribute to a programme of work to increase the timeliness and accuracy of the identification and diagnosis of acute stroke.
Costings
Researchers will be reimbursed for any travel expenses.
Dissemination
Public output will include publication in peer reviewed journals and presentations at conferences.
Project milestones
| January 2008 to June 2008 | PIAG, ethics and R&D applications |
| June 2008 to October 2008 | Identify participants |
| March 2008 to March 2009 | Listen to calls and transcribe calls |
| March 2008 to July 2009 | Analyse data |
| July 2009 to December 2009 | Final Report |
| July 2009 to December 2009 | Prepare presentations and publications |
ESCORTT phase 3a: “Is he awake?”: Dialogues between callers and call handlers about consciousness during emergency calls for suspected acute stroke
Aim
To identify how patients’ consciousness level was questioned, described and interpreted by callers and EMDs during calls to the EMSs for suspected stroke.
Design
A retrospective audit.
Methods
Setting
Regional EMSs and two acute hospital trusts in the north-west of England.
Participants and sampling
Audio recordings of EMS calls for patients with symptoms suggestive of acute stroke, a subsequent in-hospital diagnosis of stroke, or both, admitted to one hospital in the north-west of England over a 12-month period (1st October 2006 to 30th September 2007) were retrieved.
Inclusion criteria: patients who were admitted to hospital with symptoms suggestive of stroke, a subsequent in-hospital diagnosis of acute stroke, or both. Calls were included in the secondary analysis if misinterpretation or protracted dialogue (or both) about the patient’s level of consciousness were apparent.
Exclusion criteria: Patients under 18 years. Calls made by a GP (or receptionist) on behalf of the patient.
Data collection
Demographic and dispatch information will be collected, including the relationship of the caller to the patient, location of the patient, dispatch code and prioritisation category. The level of consciousness documented by EMS staff following clinical assessment will be ascertained. Audio recordings of EMS calls will be listened to in full by one of three researchers.
Data analysis
Calls will be analysed by coding the key words used to describe the consciousness level of the patient. This analysis will focus on the caller’s response to the two standard questions asked by the call handler about consciousness level: ‘Is the patient conscious?’ and ‘Is he/she completely awake?’ Any other dialogue during the call which related to consciousness level or alertness will also be included in the analysis. Responses from the caller which suggest misinterpretation of terms such as conscious, awake, responsive or alert, and where the call handler had to use additional questions to clarify the patient’s level of consciousness, will be analysed in detail. A second researcher will independently follow the same procedure and any discrepancies were resolved by discussion between the researchers.
Ethical issues
The ambulance service do not have the resources/technology to anonymise each of the calls. However, we have established that not all of the calls would contain patient identifiable information. For example, the call could be made by a third party (including the GP), or from an address that is not the patients. Thus the CD would contain a mixture of identifiable and non-identifiable patient data.
There would be difficulty in obtaining consent when identifiable information has been given by the caller, whether it be the patient or a third party caller. Due to the way that data are captured for this phase it is not possible to obtain informed consent for each of the callers to dispatch. The callers will be unaware that their call is being listened to as part of this research project.
In order to gain consent it would be necessary to find each patient's address. This may not be easy to find if the call is made from somewhere other the patient's home, as the patient’s address would not be recorded. Another problem exists if the call is made by a third party; in such circumstances it would seem inappropriate to contact the caller to ask them details about the patient in order to facilitate contacting the patient to obtain their consent. In addition, before any contact is made, patient status (alive or dead) would need to be checked. The necessary steps and safeguards that we would have to take in order to approach patients in an appropriate manner would make gaining consent impractical.
Should any calls raise any issues that cause emotional distress to the researcher, de-briefing and counselling will be made available by the University of Central Lancashire.
PIAG application
Section 60 of the Health and Social Care Act 2001 relates to using patient identifiable information for medical purposes in circumstances where patient consent has not been obtained. Due to the ethical issues outlined above and following discussions with PIAG, we submitted a PIAG application for phase 3, which was approved.
Costings
No costs are anticipated as salary is supported by programme grant.
Dissemination
Public output will include publication in peer reviewed journals and presentations at conferences. Callers will not be identified in any public outputs.
Project milestones
| January 2010 to February 2010 | Identify participants |
| January 2010 to April 2010 | Listen to calls and transcribe calls |
| April 2010 to September 2010 | Analyse data |
| October 2010 to March 2011 | Final report |
| October 2010 to December 2011 | Prepare presentations and publications |
ESCORTT phase 4: exploring the words used by callers for non-stroke-related calls to the emergency medical services and a comparison with the words used describing stroke-related calls
Aim
To compare the words used by the public making calls to the EMSs, the subsequent ambulance dispatch codes and final diagnosis in hospital, for stroke and non-stroke calls.
Design
A retrospective mixed-methods study.
Methods
Setting
An ambulance service and an acute trust in the north-west of England.
Subjects and sampling
We will identify calls made to the EMSs that led to an EMS vehicle being dispatched during a one-week period (8th March 2010 to 14th March 2010).
Inclusion: the 999 call was made by a member of the public; patients arrived at hospital through the EMSs; patients presented to the study hospital ED (whether admitted, or discharged after ED attendance).
Exclusion: Calls relating to patients under 18 years of age, and those with a final diagnosis of stroke. Calls which were likely to contain highly distressing or sensitive material including: traumatic injury e.g. laceration; poisoning; physical or sexual assault-related injuries; suicide; road traffic accident; choking (n = 4); women in labour; and animal attack. Calls will be excluded if a medical practitioner had already seen the patient (i.e. inter-hospital transfers; patients referred by their primary care physician (GP) or GP staff on behalf of the patient) and/or if final diagnosis data are not available.
Procedure
All call recordings to the EMSs over a one week period will be requested from the EMSs. The calls will be listened to in full by a researcher trained in qualitative research methods. Further data will be collected from EMSs and patient medical records regarding dispatch code (e.g. fall, stroke, unconscious, faint) and final diagnosis from ED or discharge letter.
Data collection
At the beginning of a call to EMSs, the caller is routinely asked the open question: “What’s the problem, tell me exactly what happened?” by an EMD to establish the chief complaint. We will focus the analysis on the callers’ response to this first question, which we termed ‘the first story’. The first story typically involves the description of up to three presenting problems by the caller.
Data analysis
Calls will be analysed by coding the first story by the caller to describe the presenting problem, suspected diagnosis or condition. Open coding of the data will be undertaken using content analysis (facilitated by Atlas.ti software). Analysis will be undertaken using the constant comparative method in order to identify key indicator words and relationships within the data. 35 The research team will meet regularly to discuss the coding categories in order to ensure a consistent approach to analysis of the data. New categories will be considered and added to the list of indicator words at weekly intervals. Key indicator words identified will be grouped to form categories based on the MedDRA Coding system.
Storage of data
The ambulance service will access and download the calls to a password protected CD. They will do this for all 800 calls. The CD will be collected from the ambulance service by a member of the research team, in person. The audio files will be transferred into a password protected folder on a computer at the University of Central Lancashire. When the audio files have been coded by a member of the research team, the transcriptions will only be accessible by members of the research team. The CDs will be stored in Brook Building at the University of Central Lancashire. They will be in a lockable room with lockable data storage cupboards. Any electronic files will be password protected. All electronic data will be stored for five years in line with the University of Central Lancashire data protection policy.
Ethical issues
Approval for this phase will be sought from: the Patient Information Advisory Group (now the National Information Governance Board for Health and Social Care Ethics and Confidentiality Committee), the Local Research Ethics Committee, the Faculty of Health Ethics Committee at the University of Central Lancashire and NHS Research and Development at the EMSs and acute hospital.
The ambulance service does not have the resources or technology to anonymise each of the calls. This would mean that the calls supplied may have identifiable information. However, there would be great difficulty in obtaining consent when identifiable information has been given by the caller, whether it is the patient or a third party caller. In order to gain consent it would be necessary to find each patient's address. This may not be easy to find if the call is made from somewhere other the patient's home, because the patient’s address would not be recorded. Another problem exists if the call is made by a third party; in such circumstances it likely to be inappropriate to contact the caller to ask them for details about the patient – in order to facilitate us contacting the patient to obtain their consent. In addition, before any contact is made, patient status (alive or dead) would need to be checked, which would mean identifying and approaching the patient’s GP. The necessary steps and safeguards that we would have to take in order to approach patients in an appropriate manner makes gaining consent impractical.
In terms of listening to the calls, if a researcher is distressed by the content of the calls, they will be offered de-briefing and counselling through the Clinical Practice Research Unit.
PIAG application
Section 60 of the Health and Social Care Act 2001 relates to using patient identifiable information for medical purposes in circumstances where patient consent has not been obtained. Due to the ethical issues outlined above and following discussions with PIAG, we have been advised to submit a PIAG application.
Following PIAG approval, an application will also be made to the Local Research Ethics Committee, the Faculty of Health Ethics Committee at the University of Central Lancashire and NHS Research and Development at the EMSs and acute hospital trusts.
Outputs
The findings of this research will contribute to a programme of work to increase the timeliness and accuracy of the identification and diagnosis of acute stroke.
Costings
Researchers will be reimbursed for any travel expenses. No other costs are anticipated as salary is supported by programme grant.
Dissemination
Public output will include publication in peer reviewed journals and presentations at conferences. Callers will not be identifiable in any public outputs.
Project milestones
| August 2010 to December 2010 | Identify participants |
| August 2010 to December 2010 | Listen to and code calls |
| August 2010 to December 2010 | Identify final diagnosis |
| August 2010 to March 2011 | Analyse data |
| March 2011 to May 2011 | Final Report |
| May 2011 to December 2011 | Prepare presentations and publications |
ESCORTT phase 5: Developing algorithms and protocols for ambulance and NHS Direct staff to assist in the identification of those with suspected stroke
Aim
To develop algorithms and protocols for ambulance and NHS Direct staff to assist in the identification of those with suspected stroke.
Design
Development of algorithms and protocols.
Methods
Procedure
Identify changes to be made to AMPDS and NHS Direct algorithms informed by the results of phases 1 to 4 and contact AMPDS and NHS Direct. AMPDS is based on published standards from a wide range of international institutions including: the National Association of EMS Physicians (NAEMSP), the American Society for Testing and Materials (ASTM), the American College of Emergency Physicians (ACEP), the U.S. Department of Transportation (USDOT), the National Institutes of Health (NIH) and the American Medical Association (AMA). NHS Direct algorithms are aligned to Department of Health, NHS and NICE policies and are reviewed annually.
Ethical issues
There are no ethical issues associated with this phase.
Storage of data
Data will be stored in Brook 417 at the University of Central Lancashire. This is a locked room with locked data storage cupboards. Any electronic files will be password protected. All written data will be stored for five years.
Outputs
Changes to AMPDS and NHS Direct protocols.
Costings
Researchers will be reimbursed for any travel expenses. No other costs are anticipated.
Project milestones
| January 2009 to April 2009 | Identify changes to be made to AMPDS and NHS Direct algorithms informed by phases 1 to 4 |
| April 2009 to September 2009 | Contact AMPDS and NHS Direct |
ESCORTT phase 6: Developing an on-line training package for Emergency Medical Dispatchers to assist in the identification of those with suspected stroke
Aim
To develop an on-line training package to improve the recognition of stroke by EMDs, informed by the results from phases 1 through 4.
Design
Development of a training package.
Methods
Setting
One EMD control centre within a large regional EMS.
Subjects and sampling
A convenience sample of twelve people from the project steering group or people who are identified by members of the steering group as having specific expertise in relation to stroke and/or the development of on-line learning materials, will be invited to take part in the development of the training package. These participants will form an expert committee comprising academics, health professionals and patients/carers.
Procedure
The findings from phases 1, 2, 3, 3a and 4 will be used to inform the development of a training package. The main content of the training package in relation to general information about stroke will be based on the previously developed and endorsed RESPONSE acute stroke on-line course. An expert committee will be convened to provide advice on which aspects of the ESCORTT programme of research should be included in the training package, what are the most important findings and how these should be included within the training package. The content of the on-line training package will then be circulated to members of the steering group for feedback before the training package is implemented within one EMD control centre.
Ethical issues
As this phase involves only the development of an on-line training package, ethical approval will not be required.
Storage of data
Data will be stored in Brook 417 at the University of Central Lancashire. This is a locked room with locked data storage cupboards. Any electronic files will be password protected. All written data will be stored for five years.
Outputs
Development of an on-line training package.
Costings
Researchers will be reimbursed for any travel expenses. No other costs are anticipated.
Project milestones
| November 2008 | Form expert committee |
| December 2008 to March 2009 | Develop on-line training package |
| March 2009 to June 2009 | Pilot and make any final changes |
ESCORTT phase 7: Implementation and evaluation of an on-line stroke-specific training package for Emergency Medical Dispatchers
Aim
To implement and evaluate the on-line training package.
Design
Evaluation of an on-line training package.
Methods
Setting
One EMD control centre within a large regional EMS.
Subjects and sampling
All EMDs who were employed at one EMD control centre in March 2009.
Procedure
All EMDs at one EMD control centre will complete the on-line training package and will then complete an evaluation questionnaire consisting of open and closed questions.
Data collection
The on-line evaluation will be made up of 12 questions in total, covering: satisfaction with the course; increase in knowledge and understanding; usefulness of the course and suggested changes.
Data analysis
Analysis of the closed questions will be undertaken by describing the overall proportions of participants’ scores for each question. The responses to the open ended questions will be collated and grouped into categories relating to each open ended question.
Ethical issues
As this phase involves completion of a questionnaire by EMDs ethical approval will not be required.
Storage of data
All data will be anonymised. Data will be stored in Brook 417 at the University of Central Lancashire. This is a locked room with locked data storage cupboards. Any electronic files will be password protected. All written data will be stored for five years.
Costings
Researchers will be reimbursed for any travel expenses. No other costs are anticipated.
Dissemination
Public output will include oral presentations for EMS staff.
Project milestones
| February 2009 to June 2009 | Train the trainers |
| September 2009 to January 2010 | Roll out training and complete evaluation questionnaires |
| December 2009 to April 2010 | Analyse data |
ESCORTT phase 8: Training Emergency Services’ Dispatchers to recognise stroke: The evaluation and impact of a training package
Aim
To evaluate the impact of this newly developed stroke-specific, on-line training package on the recognition of stroke by EMDs.
Design
An interrupted time-series analysis.
Methods
Setting
An ambulance trust and an acute trust in the north-west of England.
Subjects and sampling
Subjects will be patients with suspected stroke arriving at hospital by ambulance during an 18 month period (16th March 2009 to 29th August 2010). For every three week period, we identified one week of consecutive patients (arrival at hospital between 0000 hours on the Monday through to 1159 hours the following Sunday). Each sampled week was deemed an observation.
Inclusion criteria: patients who had a diagnosis of suspected stroke by the EMS call handler and/or a final diagnosis of stroke in hospital.
Exclusion criteria: patients whose General Practitioner contacted the EMSs on their behalf; patients who had a stroke while already an inpatient.
Procedure
The sample will be identified through a retrospective audit of hospital and EMS records. Stroke patients will be identified in hospital from the stroke register. Additional patients will be identified from hospital by searching the hospital coding system and the ED records. Case notes will be ordered for any patients recorded as stroke in the coding system or with stroke-like symptoms in the ED records who were not on the register; the case notes will be reviewed and the diagnosis checked by an experienced stroke research nurse. For all patients identified in hospital we will obtain their EMS data. Independent from the data gathered in hospital, the EMSs will identify patients who had either been dispatched as a stroke or who had been diagnosed in the ambulance as having had a stroke. The hospital case notes will be obtained for all patients identified through the EMSs. A patient will be considered to have had a stroke if they were discharged from the ED and the ED records stated stroke or if they were still on the stroke register at the time of discharge from hospital.
Data collection
Data will be recorded from the electronic patient report forms used by EMS staff, and the patient’s hospital case notes. EMS report forms provided data on dispatch code, ambulance diagnosis and the following event times: call made to EMSs; ambulance arrived at scene; ambulance arrived at hospital. From the case notes and stroke register we will record: demographics; side affected by the stroke; limbs affected by stroke; facial weakness; speech problems; consciousconsciousness level. EMS report forms will provide data on dispatch code, ambulance diagnosis and event times including: time call to the EMSs was made; arrival of ambulance at scene; and time ambulance arrived at hospital.
Study data will be divided into three periods: Pre-implementation – prior to training the EMS call handlers; During-implementation – when 69 EMDs (2 trainers and 67 EMDs) completed the training; Post-implementation – following completion of the training.
Data analysis
Patient demographics, stroke characteristics and diagnosis data will be presented overall and for each period. The effect of the intervention on the accuracy of dispatch diagnosis will be investigated using binomial (grouped) logistic regression, with the number of subjects with a dispatch diagnosis of stroke as the numerator and the number of subject with a final diagnosis of stroke as denominator for each observation. The regression model will include the intervention factor (pre; during; post), an overall linear trend over the period of data collection and an interaction between the intervention factor and the linear trend (to allow the intervention to influence any underlying trend / to allow a gradual impact of the introduction of the intervention).
Analysis will be performed using complete cases, i.e. data available for both dispatch and final diagnosis. Potential autocorrelation (due to the time series nature of the design) of the weekly diagnosis rates and clustering (over-dispersion) of the accuracy within observations will be investigated.
Sensitivity analysis will performed to assess the potential impact of missing dispatch and/or final diagnosis by imputing possible diagnoses, including extreme imputations (dispatch diagnosis as ‘not stroke’ and final diagnosis as ‘stroke’, and vice-versa).
Ethical issues
We will submit an ethics application to the LREC however we envisage that as only anonymised patient data is required, section 251 support will not be required to carry out this evaluation.
Storage of data
To ensure confidentiality any personal data collected will only be accessible by the research team. Data will be stored in Brook 417 at the University of Central Lancashire. This is a locked room with locked data storage cupboards. Any electronic files will be password protected. All written data will be stored for five years.
Costings
Researchers will be reimbursed for any travel expenses. No other costs are anticipated.
Dissemination
Public output will include publication in peer reviewed journals, and presentations at conferences, and with user groups.
Project milestones
| April 2009 to September 2010 | Identify participants |
| April 2009 to September 2010 | Collect data |
| October 2010 to December 2010 | Analyse data |
| November 2010 to January 2011 | Report for phase 8 |
| January 2011 to March 2011 | Prepare presentations and publications |
Appendix 4 Publications and presentations by phase
Phase 1
Leathley MJ, Jones SP, Sutton CJ, McLoughlin ASR, Emsley HCA, Punekar S, et al. The relationship between stroke symptoms and diagnosis: a cohort study. Emerg Med J submitted. Outcome awaited.
Jones S, Leathley M, McDonald K, Watkins C, on behalf of the ESCORTT Group. Pre-hospital Identification of Stroke. Third UK Stroke Forum Conference Book of Abstracts. 2008:22–3.
Sutton CJ, Dickinson H, Jones SP, Leathley MJ, McLoughlin A, Watkins CL, on behalf of the ESCORTT Group. Emergency Stroke Calls Obtaining Rapid Telephone Triage (ESCORTT) Phase 1: how and when are patients diagnosed with stroke? Int J Stroke 2010;5(Suppl. 3):15. [Presented as poster at the Fifth UK Stroke Forum Conference, 30 November to 2 December 2010, Glasgow, UK.]
Phase 2
Jones SP, Dickinson HA, Ford GA, Gibson JME, Leathley MJ, McAdam JJ, on behalf of the ESCORTT Group. Callers’ experiences of making emergency calls at the onset of acute stroke: a qualitative study. Emerg Med J 2012;29:502–5.
Jones S, Dickinson H, Gibson JME, Leathley M, McAdam J, McDonald K, on behalf of the ESCORTT Group. Caller experiences of dialling 999 for suspected stroke. Int J Stroke 2009;4(Suppl. 2):13. [Presented as poster at the Fourth UK Stroke Forum Conference, 1–3 December 2009, Glasgow, UK.]
Phase 3
Jones SP, Carter B, Ford GA, Gibson JME, Leathley MJ, McAdam JJ, on behalf of the ESCORTT group. The identification of acute stroke: an analysis of emergency calls. Int J Stroke 2013;8:408–12.
Jones SP, McAdam JJ, Gibson JME, Leathley MJ, Dodd A, Watkins CL, on behalf of the ESCORTT Group. How do callers describe symptoms when contacting emergency services at the onset of acute stroke? A study of the ‘first story’ given by callers. Int J Stroke 2010;5(Suppl. 3):14. [Presented as poster at the Fifth UK Stroke Forum Conference, 30 November to 2 December 2010, Glasgow, UK.]
Phase 3a
Gibson JME, Bullock M, Ford GA, Jones SP, Leathley MJ, McAdam JJ, et al., on behalf of the ESCORTT Group. ‘Is he awake?’: dialogues between callers and call handlers about consciousness during emergency calls for suspected acute stroke. Emerg Med J 2012;30:414–18.
Jones SP, McAdam JJ, McLoughlin ASR, Gibson JM, Leathley MJ, Watkins CL, on behalf of ESCORTT Group. Understanding of the term conscious when used during emergency calls for suspected stroke. Cerebrovasc Dis 2011;31(Suppl. 2):234. [Presented as poster by Jones SP at the 10th European Stroke Conference, 24–27 May 2011, Hamburg, Germany.]
Phase 4
Jones SP, Gibson JME, McAdam JJ, Leathley MJ, Ford GA, Quinn T, et al., on behalf of the ESCORTT Group. ‘Can you send an ambulance please?’: a comparison of callers’ requests for emergency medical dispatch in stroke and non-stroke calls. Emerg Med J 2013. doi: emermed-2013-202752.
Phase 7
Jones SP, Ford GA, Leathley MJ, McAdam JJ, McLoughlin AS, Quinn T, et al., on behalf of the ESCORTT Group. An evaluation of stroke-specific training for emergency medical dispatchers. Cerebrovasc Dis 2012;33(Suppl. 2):616–17. [Presented as poster at the 11th European Stroke Conference, 22–25 May 2012, Lisbon, Portugal.]
Jones SP, Leathley MJ. Emergency Stroke Calls: Obtaining Rapid Telephone Triage: An Evaluation of Stroke-specific Training for Emergency Medical Dispatchers. North West Ambulance Service NHS Trust paramedic training event, 15 August 2012. North West Ambulance Service NHS Trust Head Quarters, Bolton, UK.
Phase 8
Watkins CL, Leathley MJ, Jones SP, Ford GA, Quinn CJ, Sutton CJ, on behalf of the ESCORTT Group. Training emergency services’ dispatchers to recognise stroke: the evaluation and impact of a training package. BMC Health Serv Res 2013;13:318.
Jones SP, Sharma A, Dodd A, Leathley MJ, McAdam JJ, Quinn T, et al., on behalf of the ESCORTT Group. Training call handlers to recognise stroke: the evaluation and impact of a training package. Int J Stroke 2011;6(Suppl. 2):5. [Oral presentation by Jones SP at the Sixth UK Stroke Forum Conference, 30 November 2011, Glasgow, UK.]
All phases
Jones SP, Watkins C. Emergency stroke calls: obtaining rapid telephone triage. Stroke Matters 2009;2:14.
McAdam JJ, Jones SP. Emergency Stroke Calls: Obtaining Rapid Telephone Triage (ESCORTT): An Overview. World Stroke Day Conference – Advancing Stroke Care Through Research, 28 October 2011, Wigan, UK.
Jones SP. Emergency Stroke Calls: Obtaining Rapid Telephone Triage. National Ambulance Research Group Meeting, 31 January 2012, London, UK.
Watkins CL, Jones SP, Leathley MJ. Emergency Stroke Calls: Obtaining Rapid Telephone Triage: An Overview of the Results. North West Ambulance Service NHS Trust, Medical Senior Management Team Meeting, 11 July 2012. North West Ambulance Service NHS Trust, Bolton, UK.
Watkins CL. Emergency Stroke Calls: Obtaining Rapid Telephone Triage (ESCORTT): The Results. World Stroke Day Conference, 29 October 2012, Wigan, UK.
List of abbreviations
- ACEP
- American College of Emergency Physicians
- AMA
- American Medical Association
- AMPDS
- Advanced Medical Priority Dispatch System
- ASTM
- American Society for Testing and Materials
- CI
- confidence interval
- DoH
- Department of Health
- ED
- emergency department
- EMD
- emergency medical dispatcher
- EMS
- emergency medical service
- ESCORTT
- Emergency Stroke Calls: Obtaining Rapid Telephone Triage programme of research
- FAST
- Face Arm Speech Test
- GCS
- Glasgow Coma Scale
- GP
- general practitioner
- IQR
- interquartile range
- NAEMSP
- National Association of EMS Physicians
- NICE
- National Institute for Health and Care Excellence
- NIH
- National Institutes of Health
- NIHSS
- National Institutes of Health Stroke Scale
- OR
- odds ratio
- PPV
- positive predictive value
- RESPONSE
- Rapid Emergency Stroke Pathways: OrgaNised Systems and Education course
- ROSIER
- Recognition of Stroke in the Emergency Room assessment
- rtPA
- recombinant tissue plasminogen activator
- SD
- standard deviation
- TIA
- transient ischaemic attack
- USDOT
- Unites States Department of Transportation