Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0606-1109. The contractual start date was in August 2007. The final report began editorial review in September 2012 and was accepted for publication in March 2013. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Challis et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
This chapter provides an introduction to the programme of work contained in this report and sets the current provision of specialist mental health services for older people in the context of their development from the late 1960s to the present day. It also highlights the marked lack of evidence currently available to inform service planning for this client group.
ObjectivesIn this context, the chapter sets out the three fundamental concerns the programme sought to address. These were the best combination of inpatient, residential and community services to provide for older people with mental health problems; the factors that make for the effective working of community mental health teams for older people (CMHTsOP); and the quality and quantity of mental health support provided to older care home residents. A trial of depression management in care homes as part of the third objective was removed at review by National Institute for Health Research (NIHR) prior to the award of funding.
Background
This study addresses the urgent need for better evidence to inform the provision of care for older people with mental health problems, a significant and growing group whose care costs constitute a substantial proportion of the health and social care budget. Entitled National Trends and Local Delivery in Old Age Mental Health Services, the research explores the most appropriate and cost-effective ways of organising and delivering care for this client group at the macro (strategic planning) and mezzo (provider unit) levels, locally and nationally.
The rising number of older people in the UK presents a considerable challenge to policy-makers, commissioners and service providers nationwide. More than 10 million people in the UK are aged ≥ 65 years, and this figure is anticipated to rise by almost two-thirds in the next 20 years. Moreover, the fastest growth in numbers will be among the ‘oldest old’, the biggest users of care services. Population projections suggest that by 2033 the number of people aged ≥ 85 years will have doubled. 1,2
Although many older people will lead healthy, fulfilling lives, increasingly involving work or roles as volunteers or carers,3,4 this demographic change will have a significant impact on the ability of services to meet the needs of older people with mental health problems, not least because the prevalence of dementia increases exponentially with age. Some 5% of the population aged > 65 years and 20% of those aged > 80 years have dementia, while approximately 15% of all older adults have depression. Others are affected by anxiety, schizophrenia, paranoid states and substance misuse. 5–7
Such disorders carry very high costs, both personal and economic, for many are subject to relapse or of long duration. Mental health problems can affect every aspect of a person’s functioning, exacerbate physical ill health and cause significant personal and family distress. 7,8 They are also associated with increased service use. 9,10 Relatively conservative estimates suggest that 40% of older adults visiting their general practitioner (GP), 50% of general hospital inpatients and 60% of care home residents have a mental health problem,11 and older people with mental illness make greater demands on home care services than the older population as a whole. 12–14 Indeed, the total economic costs of dementia have been put at £23B per year,15 more than the annual cost for stroke, cancer and heart disease combined. 16 This provides a marked incentive to make the best use of resources, particularly in a climate of economic constraint. 17
Although old age psychiatry was not formally recognised as a specialty within the NHS until 1989, the need for specialist services for older people with mental health problems was first recognised in the 1940s, prompted by the already increasing number of older people, the differentiation of clearly demarcated syndromes of psychiatric disorder in later life and the inadequacies of care in long-stay institutions. 18–21 Until then older people with mental health problems had generally been cared for by general psychiatrists, but in the late 1960s and early 1970s the first consultant psychogeriatricians were appointed and reports of specialist services began to emerge. 20,22,23 Steady service development followed, and by 1980 there were approximately 120 consultant psychiatrists with a substantial time commitment to the care of older people. Many of these staff were based in hospitals, with beds in long-stay wards and a high proportion of chronically ill patients. 24
The pattern of service development over subsequent decades reflects a move away from the medical assessment of patients in largely hospital-based services towards the multidisciplinary assessment, treatment and support of patients in predominantly community-orientated services. 25 This shift was in keeping with the growing policy imperative for community care,26–28 and was stimulated by a variety of considerations including costs and cost-effectiveness,10,29 with institutional care generally perceived to be more expensive than care in the community. 30 There was also a growing belief that most older people, including those with complex needs could, and would rather be, cared for in their own homes. 10,31 However, such preferences are themselves likely to be influenced by the relative availability and quality of care in different settings, the availability of informal care, and cultural expectations about family obligations and personal cost. 32
As the number of NHS hospital beds fell throughout the 1980s, the care home sector grew, boosted by a paradoxical financial incentive whereby people eligible for supplementary benefit could have their care in private and voluntary sector homes funded through income maintenance support with no medical or social work assessment required. 33–35 The resulting concerns about service funding and organisation led to the 1990 NHS and Community Care Act,36 which stressed the role of local authorities as arrangers/purchasers rather than providers of care and highlighted the need for a comprehensive review of individuals’ health and social care needs before admission to long-term care. Mechanisms to increase choice and flexibility, match services with need, and promote accountability and quality were described, and a special transitional grant was made available to fund community care packages as well as care home placements. 33,35,37–39 Designed as a corrective to the institutional bias of the previous decade, by the mid-1990s dependency levels in residential settings were considerably greater than in the mid-1980s40 and have risen further since. 41,42
Despite little government guidance on the role of mental health services for older people, specialist services continued to grow rapidly throughout the 1980s and 1990s. 43,44 The dominance of ‘the medical model’ declined further, and an increasing emphasis was placed on the need for health and social services to work together. 3 By the end of the twentieth century, localities aimed to offer mental health services that were ‘comprehensive, accessible, responsive, individualised, multidisciplinary, accountable and systematic’. 44 However, many areas could not live up to such aspirations, and variation in service practice was deemed likely to have a negative impact on equity, efficiency and patient outcomes. 43,45–47
The publication of the National Service Framework for Older People (NSFOP) in 200131 and a string of linked initiatives11,48,49 were widely welcomed as an attempt to address these inconsistencies and improve the quality of care. Outlining a 10-year programme of reform, the NSFOP aimed to deliver fair, integrated and high-quality services based on eight national standards, one of which concerned the provision of care for older people with mental health problems and their carers. Integrated health and social care services, including a broad range of hospital- and community-based facilities, were to deliver effective diagnosis, treatment and support. 31 Multidisciplinary community mental health teams for older people (CMHTsOP) were given a key role in the provision of specialist care for people with severe or complex mental health problems at home, as well as providing support and advice to staff working in primary, care home and general hospital services. In comparison with the previously published framework for adults of working age, however, the framework contained less prescriptive models of service and no dedicated resources. 50
Despite such high ambitions, recent years have witnessed several reports expressing profound criticism of the care received by older people with mental health problems, including the ongoing difficulties of getting services to work together. 50–53 Although specialist mental health services have continued to grow, there remains significant disquiet about the degree of variation in practice and investment, whereas the ongoing efficiency savings demanded from local authorities have led to tighter eligibility criteria and fewer people receiving services. 2,54–56 The National Dementia Strategy was designed to address at least some of these concerns, and early priority has been given to the need to provide good quality diagnosis and intervention for all; improve the quality of care in general hospitals and care homes; and reduce the use of antipsychotic medication (a particular concern in care homes). 57–59 Although it has been argued that the primary function of long-stay facilities is to provide care for people with advanced dementia60 and the proportion of residents with depressive symptoms is also high,61–63 evidence suggests that care home staff are often ill equipped to meet such needs and that many mental health problems go undetected and undertreated. 63,64
The need for new research
Although a consensus exists on the need to improve mental health care for older people, and on its underlying principles, evidence on the relative clinical effectiveness and/or cost-effectiveness of different service models is sparse. 7,65,66 Relatively few studies have made useful service comparisons enabling inferences to be drawn about the best ways of delivering care, and evidence from other countries with different service arrangements is not always transferable to the UK. 7,49 In the absence of clear evidence, local service development and commissioning have reflected both historical funding patterns and individual enthusiasm and commitment. 66,67 There is then an obvious need to help health and social care commissioners and providers make informed decisions about resource allocation and address any unwarranted variation in supply. 68,69 The programme of work detailed in this publication seeks to contribute to that process focused on three fundamental concerns at different levels of the health delivery system in England:
-
to refine and apply ‘the balance of care (BoC) approach’ (a systematic framework for choosing between alternative patterns of support by identifying people whose care needs could be met in more than one setting, and comparing their costs and outcomes) to the care of older people with mental health problems
-
to identify whether, how and at what cost the mix of services provided for this client group might be more optimally developed in a particular locality
-
to enable other health and social care decision-makers to apply the BoC framework independently
-
to identify core features of national variation in the structure, organisation and processes of community mental health teams (CMHTs)
-
to examine whether or not different CMHT models are associated with different costs and outcomes
-
to identify core features of national variation in the nature and extent of specialist mental health outreach services for older care home residents
-
to scope the evidence on the association between different models of outreach and resident outcomes; and
-
to disseminate the findings and service development tools from the work to NHS trusts, commissioners, local authorities and national policy-makers.
First, at the macro level, the programme examines the combination or mix of inpatient, residential and community services, health and social care, provided for older people with mental health problems, and whether or not the balance between them can be altered beneficially (workstream 1). As noted earlier, the configuration of supply and investment in localities varies and is subject to debate. However, there is relatively little evidence about the characteristics of those people who benefit most from different services or the relative cost-effectiveness of institutional and non-institutional care. 7,65,70 Against this background, Chapter 2 reports the findings of a systematic review of the past use of ‘the balance of care’ approach, which offers a systematic framework for choosing between alternative patterns of support by identifying people whose care needs can be met in more than one setting and comparing the costs and outcomes of different options. 71,72 Building on this, Chapters 3–5 outline the results of a new development to this approach and demonstrate its utility in planning care for older people with mental health problems through a detailed evaluation of the mix of services needed in three areas of north-west England.
Second, at the mezzo level, the programme explores the factors which make for the effective working of CMHTs for older people (workstream 2). The provision of integrated, multidisciplinary CMHTs has formed a central plank of mental health policy for older people with mental health problems. 11,31,48,57 However, although there is a modest evidence base to support a range of individual-level interventions undertaken by staff in such teams,7,65 comparatively little is known about the service design features or models of teams associated with better outcomes, or their relative costs. 49,70 To this end, Chapter 6 details the findings of a systematic literature review to establish the known nature and extent of variation in teams’ structures and processes over time, and the strength of the evidence-base linking variations in team approaches to service user, staff and service outcomes. This is complemented by the results of a national survey of the composition and working practices of contemporary CMHTs, and the findings of an evaluation of the relative costs and outcomes of different team models using a multiple case study approach (see Chapters 7–11).
Lastly, the programme provides a detailed picture of the support available to meet the mental health needs of older care home residents (workstream 3). Improving access to specialist care and advice for this population has recently become a prominent concern11,57 and many specialist services already provide support for care home staff. 73 However, relatively little is known about the quality and availability of the services they offer. This work seeks to address that gap and reports the findings of a systematic literature review that examined how the structure, organisation and activities of specialist mental health services vary in their provision of outreach to older care home residents, as well as the impact of such services on resident outcomes (see Chapter 12). This is augmented by the results of two national surveys, one of CMHTs outreach services, and one of care home managers (see Chapters 13 and 14). Although a proposed trial of depression management for older care home residents was not funded, this work provides a valuable scoping of a critically important area in old age mental health services.
In summary, the programme presents both national data that will act as a benchmark for future service development and monitoring, and new information on the most cost-effective ways of organising and providing services to facilitate evidence-based development. As befits complex evaluations, it displays a concern for both measurement and meaning, process and outcomes,66,74 and draws on a combination of quantitative and qualitative approaches. Given the breadth and depth of this programme, the material presented necessarily covers only a proportion of the work undertaken and forms just one element of a comprehensive dissemination strategy. Nevertheless, the findings will be useful to a range of different stakeholders, including service providers, commissioners, policy-makers, carers and older people themselves.
Chapter 2 The balance of care approach to health and social care planning: a systematic review of the literature
The ‘balance of care’ model, a framework for estimating the local economic consequences of adjusting the supply of health and social care services for specified client groups, has been widely used but with variations in methodology and application.
ObjectivesTo synthesise existing applications of the BoC model since its inception 40 years ago, and to highlight methodological lessons for future research.
MethodA systematic literature review adopted a bibliographic database search [MEDLINE, PsycINFO, Applied Social Sciences Index and Abstracts (ASSIA), EMBASE, Health Management Information Consortium (HMIC), Web of Science] for empirical applications of the BoC model, supplemented by hand searches and expert knowledge, with no restriction to jurisdiction, time or provenance.
ResultsForty-two papers were identified encompassing 33 separate studies, concentrated in the UK but showing an even spread over the past four decades. Most studies focused on older people’s services and on the margins between hospital, residential and community care. The review revealed a narrow approach to service costing: few studies considered the impact of changing the BoC on wider public agencies (e.g. housing/benefit costs) or informal carers. Furthermore, just eight studies made use of data on service user outcomes and there was a lack of clarity as to how this was incorporated into the BoC approach. More generally, the review found variation in reporting standards.
ConclusionsFuture studies should widen their scope, to incorporate a broader range of cost implications; more alternative care scenarios; and the potential benefits to service users/carers. Local practitioners and service users could be involved in developing alternative care options and establishing preferences for these.
Introduction, background and aims
The growing demand for public services alongside resource scarcity make the efficient use of available resources an increasing imperative. 75,76 Against this background, one longstanding issue has been the concern to provide the most cost-effective mix of hospital-based, residential and community-based services and to this end, the policies of many developed countries have converged, with each designed to reduce the growth of institutional care and promote the use of community support. 77 However, despite policy initiatives dating back to the 1960s, there remains considerable variation in the balance of resources invested in different services in different areas, and relatively few tools with which to evaluate the options for improvement. 26,27,78,79 The ‘balance of care approach’, a specific application of marginal analysis, which provides a systematic framework for exploring the potential costs and outcomes of changes in the provision of community and institutional services, offers the potential to examine service efficiency. 71,72
Although the origins of the BoC model have been attributed to a national policy analysis tool developed by the then Department for Health and Social Security (DHSS) in the early 1970s,80 over time the approach has taken on a number of manifestations, some more sophisticated than others. However, all are predicated on the belief that although resources are scarce, there are significant amounts of money that can be moved from one client group/service to another81 and are grounded in the principles of cost–benefit analysis. 82 Thus, they do not try to identify total need but instead ask whether or not any redeployment of available resources could increase total benefit. 71,80
At the heart of this approach is the identification of those people whose care needs could be met in more than one setting. Although it is generally accepted that there are some people for whom a particular location, say residential care, is the only appropriate one, the approach is particularly concerned with those individuals who could be supported in more than one setting, say residential care or extra care housing (ECH) (people ‘on the margins of care’). It then examines the costs and consequences of the possible alternatives with a view to informing the strategic planning process. The defining features of BoC studies are thus:
-
the identification and measurement of those client characteristics that affect decisions about where best to care for them (e.g. dependency and cognition)
-
the specification of resources and service inputs required
-
some means of allocating clients to the most appropriate setting; and
-
a determination of the relative costs (and ideally outcomes) of care in different settings. 71,72
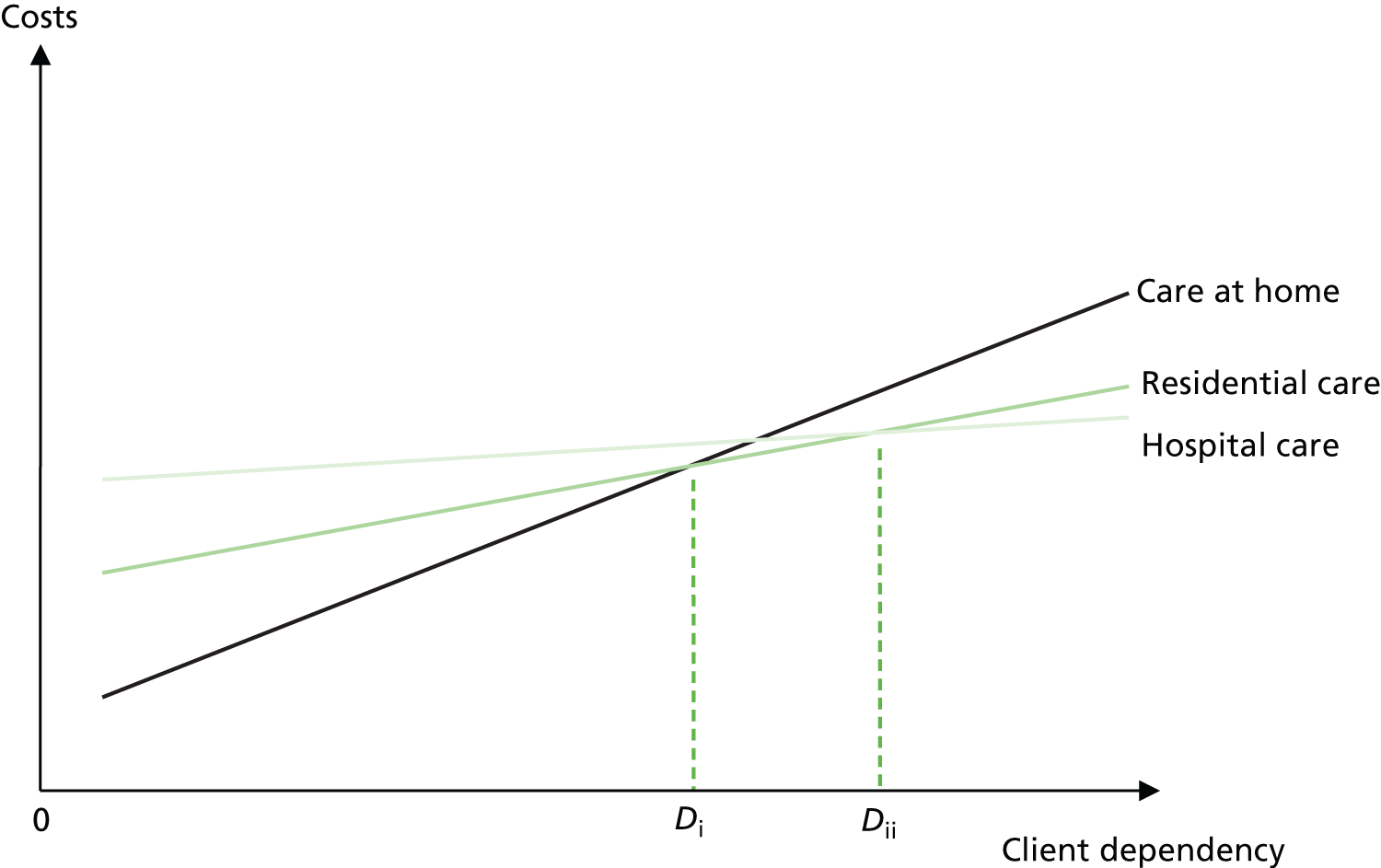
The central premises of the model are formally illustrated in Figure 1, in which the three upwards-sloping lines represent the association between the costs and characteristics of people supported at home, in residential care and in hospital. Each assumes that costs and dependency are positively correlated. However, their position and gradient differ, indicating that for people with low dependency, care at home is cheaper than residential care, which in turn is cheaper than hospital care, whereas for people with high dependency, this hierarchy reverses. Indeed, if the outcomes for people in all three settings were equally acceptable, the most cost-effective place to support people with low levels of dependency (between 0 and Di) would be their own homes, whereas for people with moderate dependency levels (between Di and Dii) it would be residential care, and for people with dependency levels greater than Dii, hospital.
FIGURE 1.
Costs by dependency for people at home, in residential care and in hospital.
This is the BoC approach at its most basic. However, in reality people’s preferences for different modes of care vary and, following Knapp,83 Figure 2 thus considers marginal costs and benefits. In order to keep the diagram relatively clear, just two alternatives are shown.
FIGURE 2.
Costs and benefits by dependency for people at home and in residential care.
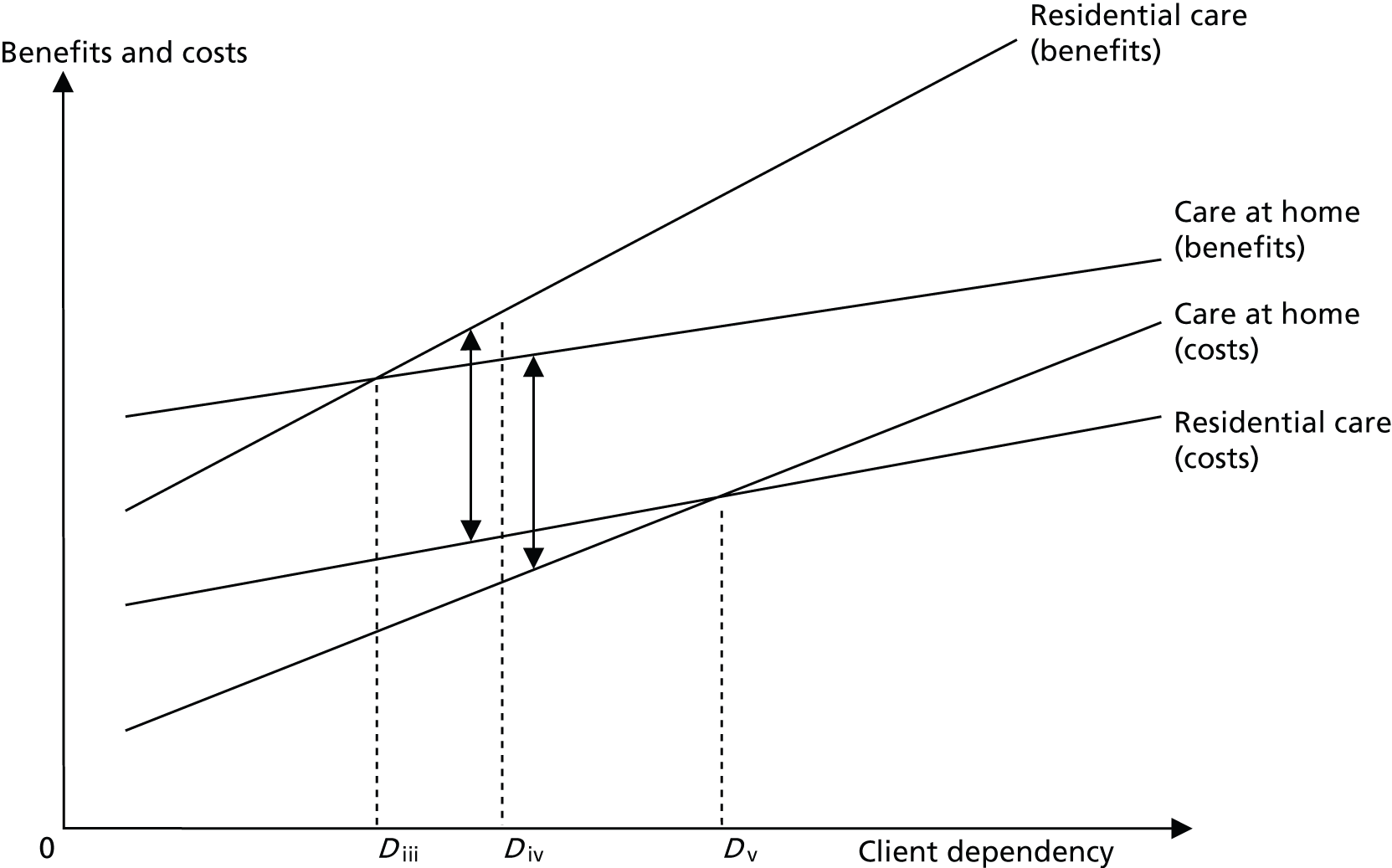
Although the lines representing the relationship between cost and dependency are the same in Figure 2 as in Figure 1, two new lines representing the relationship between benefit and dependency have been added. These are again assumed to be positively correlated, and, as with the cost-dependency lines, cross. Thus people with dependency between 0 and Diii gain more benefit from community services, whereas people with dependency higher than Diii gain more from residential care.
When considering both costs and benefits the situation becomes more complicated. Nevertheless, the most cost-efficient placement for people with dependency levels beneath Diii is clearly home, where the benefits are greater and costs lower than residential placement, whereas the most cost-efficient placement for people with dependency above Dv is residential care, where these arguments reverse. For people with dependency between Diii and Dv, however, residential care is more beneficial and more expensive, and it is the point at which marginal social cost equals marginal social benefit (Div) that determines the most cost-effective placement. For people with dependency below Div, this is care at home, whereas for people with dependency above Div, residential care is optimal.
Although not all applications have explicitly applied the above framework, over the years a number of BoC studies have been reported in the literature. This work is, however, not easy to access, for studies have been generated by a variety of organisations and span several decades. Moreover, no systematic review of the model’s use has been conducted, so an overall picture of past research that can inform its future application and development is lacking. This chapter was designed to fill this gap by identifying how key elements of the BoC approach have been operationalised and illuminating its strengths and weaknesses. The principal research question was ‘How has the BoC approach to health and social care planning been used over the past 40 years?’
Method
Search strategy
A systematic literature review was undertaken following established guidance. 84,85 An initial search for existing reviews was executed in the Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effectiveness, Health Technology Assessment database, National Health Service Economic Evaluation Database and Social Care Online in June 2008. The following databases were then searched for individual studies on 22 and 23 October 2008, from the earliest to the most recent dates available: MEDLINE, PsycINFO, Applied Social Sciences Index and Abstracts (ASSIA), HEMBASE, Health Management Information Consortium (HMIC) and Web of Science. No attempt was made to limit the searches by language (although the search terms were in English), nor to a particular geographical location or time period.
The search strategy aimed to capture not only those studies that explicitly employed the BoC approach, but applications based on the same principles, and an iterative approach was taken to the identification of potential search terms to identify that combination yielding the greatest number of relevant publications. The final strategy sought references containing any of the following phrases:
-
‘balance of care’
-
‘margin(s) of care’
-
‘marginal analysis’ or ‘marginal analyses’,
in their title or abstract, as well as work citing Mooney, an early key exponent of the approach. 71,82,86 The Web of Science search also contained terms to limit the topic area to health/social care. An example is given in Appendix 1.
Additional searches for the term ‘balance of care’ were subsequently undertaken in the System for Information on Grey Literature in Europe; the websites of a number of specialist research centres and Google; the reference lists of relevant publications were scrutinised for further studies; and experts were asked to identify missing studies.
Study selection and data extraction process
The process of selecting studies had two stages. First, one researcher screened the titles and abstracts of all citations against the initial inclusion criteria (Box 1), while a second researcher confirmed the exclusion of each rejected reference. Where decisions were not clear, the full text was reviewed, and, if uncertainty persisted, this was resolved through discussion. One researcher then read the full text of the retained references and extracted data about the key characteristics of studies meeting the full inclusion criteria (in summary, empirical studies providing data about client characteristics, service use and costs). A second researcher confirmed the inclusion of, and independently extracted data from, approximately one-third of these references, and double-checked the inclusion of, and data extracted from, all other retained publications. They also confirmed the screening-out of each excluded reference, with any inconsistencies/disagreements again resolved by discussion.
Include: peer and non-peer-reviewed journal articles, books/book chapters, reports, discussion papers.
Exclude: other grey literature.
Study designInclude: all studies, empirical and non-empirical designs.
Focus of interventionInclude: references focusing on the prospective strategic planning of health and/or social care (including reports of implementation issues).
Exclude: references not concerned with any aspect of health or social care; descriptive accounts of past or current services; references concerned with a particular type of clinical care/treatment; references with a policy focus; references with a managerial/financial focus.
ParticipantsInclude: references concerned with the planning of care for any health or social care client group.
Exclude: references concerned with individual care planning for specific patients.
Outcomes: no outcome criteria will be applied.
Second screen Study designInclude: empirical studies and other applications.
Exclude: non-empirical work, including descriptive accounts of planning models, their development, limitations and assumptions.
Focus of interventionInclude: studies that can contribute to planning decisions by simulating resource allocation options AND draw on data about client dependency AND draw on data about service receipt AND provide information about the relative costs of care in different settings.
Exclude: studies utilising other approaches to health and social care planning.
A standardised electronic form based on guidance from the Centre for Reviews and Dissemination85 was used to extract all data. This was tested and refined on a sample of five studies before full data extraction began. It contained 15 domains covering studies’ aims, settings, populations, data collection processes, analyses and conclusions (see Appendix 2).
Quality assessment
Two researchers working independently and then together determined the extent that the reported studies exhibited a number of features of good practice. These were drawn from established criteria for systematic reviews and economic evaluations, reporting standards for economic submissions to major health and social science journals and expert opinion85,87,88 (Box 2) and included questions about studies’ design, conduct and analysis. Clear coding guidance was given (see Appendix 3). Where two or more publications related to a single study, these were considered both separately and together, resulting in two sets of codes, by reference and by study.
-
Was the purpose of the study clear?
-
Was the number of cases the analysis was based on large enough to instil confidence in the results?
-
Were the cases the analysis was based on broadly typical of the population of interest?
-
Where decisions about care were based on case types, did these have face validity?
-
Were those service user characteristics most likely to be important in determining individuals’ placements/care packages considered?
-
Was the approach to costing comprehensive?
-
Were the cost data used valid?
-
Was the approach to costing fit for purpose?
-
Were the dates to which resources and prices referred reported?
-
Were appropriate adjustments made for inflation?
-
Was there any attempt to investigate cost shifting?
-
Were any outcomes measured/considered?
-
Where decisions about alternative care packages were not based on research or policy, were they made by appropriate personnel?
-
Was there an attempt to optimise the care provided?
-
Were sensitivity analyses conducted to investigate uncertainty in estimates (of costs or consequences) and test the robustness of the results?
-
Were key assumptions noted?
Lastly, four summary measures were constructed to depict the proportion of good practice indicators
-
exhibited by
-
not applicable to
-
not clearly described in, or
-
not exhibited by,
for each study. In essence, these counted the number of responses in each category and expressed them as a percentage of the total.
Results
Included/excluded literature
The search for systematic reviews identified no relevant publications. However, a small selective review of past BoC studies undertaken by one of the authors helped conceptualise the current review. 72
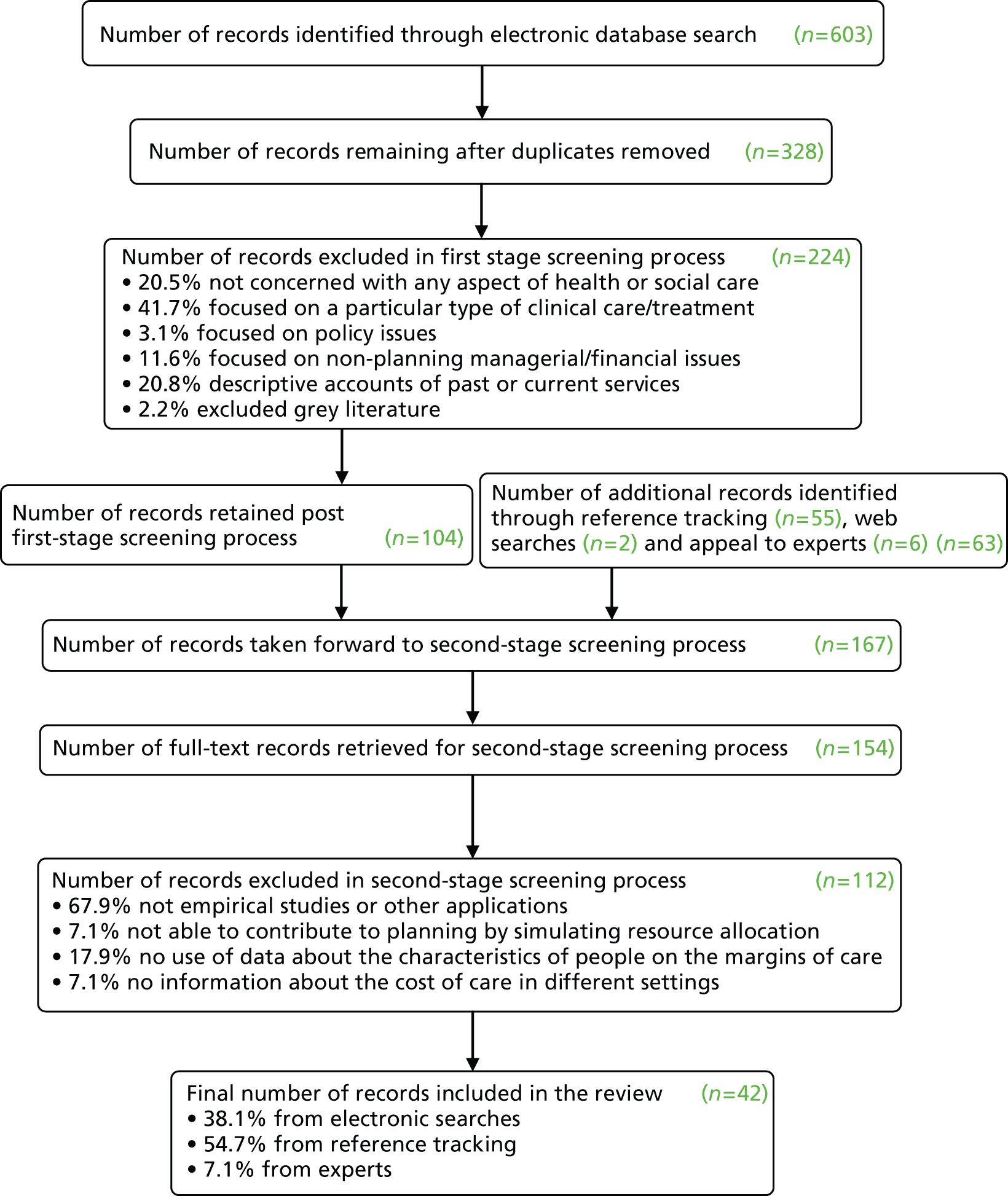
The electronic database search identified 328 references, of which 16 met the inclusion criteria. A further 26 citations were identified by reference tracking and experts, giving 42 citations in the final review (Figure 3). Of these, 22 were published in 22 different journals, whereas the remainder constituted a disparate mix of monographs, book chapters, discussion papers and reports. Slightly more references were identified from the 1980s and 1990s than from previous or subsequent decades. However, given the potential delay in recent reports reaching electronic databases, the general picture was suggestive of a steady flow of publications (Table 1).
FIGURE 3.
Flow diagram of the study selection process.
| Decade of publication | Number | Number by publication type | Percentage | |
|---|---|---|---|---|
| 1970s | 9 | Journal article | 5 | 21.4 |
| Book chapter | 0 | |||
| Report | 2 | |||
| Other | 2 | |||
| 1980s | 13 | Journal article | 5 | 31.0 |
| Book chapter | 2 | |||
| Report | 5 | |||
| Other | 1 | |||
| 1990s | 12 | Journal article | 7 | 28.6 |
| Book chapter | 3 | |||
| Report | 0 | |||
| Other | 2 | |||
| 2000+ | 8 | Journal article | 5 | 19.0 |
| Book chapter | 0 | |||
| Report | 1 | |||
| Other | 2 | |||
Thirty-three discrete studies were described in this data set, which included multiple reports of the same study and single publications describing multiple studies. Given that the review sought to elucidate the BoC methodology, it was the studies per se that were of interest, and this is the unit of analysis reported in the rest of this chapter. As there was too much information to present everything, the following material and references have been chosen to illustrate important points. Additional information is given in Appendices 4 and 5, and in Tucker et al. 89
Coverage of included studies
Table 2 confirms the longevity of the BoC approach and highlights its limited geographical employment. The origins of the BoC model have been attributed to the British government,81,90 and the vast majority of subsequent studies have been undertaken in the British Isles. 91–96 Nothing in the approach, however, limits its use to this policy context, as demonstrated by studies from Italy97 and Canada,98 nor to the national level, with local studies predominating. 71,97–101
| Study | Decadea | Location | Main population | Settings explored | References |
|---|---|---|---|---|---|
| 1 | 1970s | Essex | Older people | Residential, community | Wager 197291 |
| 2 | 1970s | UK | Multiple patient groups | Hospital, residential, community | McDonald et al. 1974;80 Gibbs 197890 |
| 3 | 1970s | London (multiple sites) | Older people | Residential, community | Plank 197799 |
| 4 | 1970s | Birmingham | Older people | Hospital, residential, community | Opit 197792 |
| 5 | 1970s | Essex | Older people | Residential, community | Whitfield and Symonds 1976109 |
| 6 | 1970s | Devon | Multiple patient groups | Hospital, residential, community | Canvin et al. 1978;119 Boldy et al. 1981,120 1982121 |
| 7 | 1970s | Aberdeen | Older people | Hospital, residential, community | Mooney 1977,115 1978;71 Fordyce et al. 1981;116 Mooney et al. 198686 |
| 8 | 1970s | England (multiple sites) | Older people | Hospital, residential, community | Wright et al. 1981102 |
| 9 | 1970s | Devon | Older people | Hospital, residential, community | DHSS 1981124 |
| 10 | 1970s | Avon | Older people | Residential, community | Avon County Council SSD 1980110 |
| 11 | 1980s | East Sussex | Older people | Hospital, residential, community | Klemperer and McClenahan 1981105 |
| 12 | 1980s | Wiltshire | Older people | Hospital, residential, community | Klemperer and McClenahan 1981105 |
| 13 | 1980s | England (multiple sites) | Older people | Hospital, residential, community | Audit Inspectorate 198393 |
| 14 | 1980s | England and Wales (multiple sites) | Children/adults with learning difficulties | Hospital, residential, community | Audit Inspectorate 198394 |
| 15 | 1980s | England and Wales (multiple sites) | Children | Residential, community | District Auditors 1981127 |
| 16 | 1980s | Kent | Adults with learning difficulties | Long-term hospital, residential, community | Challis and Shepherd 1983106 |
| 17 | 1980s | Ireland | Older people | Residential (two options) | O’Shea and Costello 199195 |
| 18 | 1980s | Ireland | Older people | Hospital, community | O’Shea and Corcoran 1989,113 1990114 |
| 19 | 1980s | London | People with HIV/AIDS | Hospital, community | Rizakou et al. 1991;126 Rosenhead et al. 1990125 |
| 20 | 1990s | Oxfordshire | Older people | Residential, community | Bebbington et al. 1990103 |
| 21 | 1990s | South Belfast | Older people | Hospital, residential, community | McCallion 1993107 |
| 22 | 1990s | England | Older people with cognitive impairment | Hospital, residential, community | Kavanagh et al. 1993,122 1995123 |
| 23 | 1990s | North London | Older people | Hospital, residential, community | Forte and Bowen 1994108 |
| 24 | 1990s | Sandwell | Older people | Hospital, residential, community | Forte and Bowen 1997100 |
| 25 | 1990s | North Midlands | Older people | Hospital, residential, community | Forte and Bowen 1997100 |
| 26 | 1990s | England and Wales (multiple sites) | Functional mental illness | Acute hospital, residential | Knapp et al. 1997112 |
| 27 | 1990s | North-east Italy | People with HIV/AIDS | Acute hospital, residential, community | Tramarin et al. 199797 |
| 28 | 1990s | Gateshead | Older people | Residential, community | Challis et al. 2000;101 Challis and Hughes 2002104 |
| 29 | 2000s | UK, but not clear where | People using dialysis services | Acute hospital (three options) | Rutherford and Forte 2003111 |
| 30 | 2000s | England (multiple sites) | Older people | Residential, community | Clarkson et al. 200596 |
| 31 | 2000s | England | Older people | Residential, community | Wanless et al. 200610 |
| 32 | 2000s | Cumbria | Older people with mental health problems | Acute hospital, residential, community | Tucker et al. 2005,117 2008118 |
| 33 | 2000s | Toronto, Canada | Older people | Residential, community | Williams et al. 200998 |
The original model’s applicability across multiple client groups was not found in later studies, with all but two focusing on just one population, older people. 10,102–104 Again, however, there seems nothing to restrict the model’s use to this group (as illustrated by the diversity of groups represented in Table 2), nor to a particular setting. Thus, while more than half of studies echoed the then DHSS’s interest in shifts between hospital, residential and community services,105–108 almost one-third focused simply on the residential/domiciliary margin. 96,99,109,110 The remainder included studies of the potential to locate renal dialysis services in three alternative hospital settings111 and divert acute psychiatric inpatients to supported hostels. 112 Furthermore, although most studies focused only on downward shifts from supposedly more costly, institutional settings to cheaper, community provision,91,97,98 a handful considered moves in both directions. 71,113,114
Approaches to profiling clients
One key feature of BoC studies is their depiction of the needs of people supported in different settings, and in the majority of studies (n = 20) this information was collected via some form of local survey, typically completed by practitioners110,115–118 and/or researchers. 119–121 Those studies that employed secondary data generally obtained this from national data sets or surveys in other areas. 96,122,123
Although all bar two studies provided information about their data sources, only just over a half provided enough detail to judge whether or not the cases forming the basis of their analyses were (a) sufficient in number to instil confidence in the results and (b) broadly typical of the population of interest (n = 18 in each instance). In the vast majority of studies where this information was provided, cases seemed valid and representative. Nevertheless, one study’s sample was judged too small (13 people in each setting),95 and another failed to address an important subsection of the target group. 109
Detailing the original BoC philosophy, Arthur Andersen and Company81 state that when considering alternative care options it is preferable to look at groups of clients, not individuals. In practice, this means dividing the population into categories of clients (case types) with similar needs for support on the basis of those characteristics deemed most significant in determining the locus of and/or costs of their care. Of the 33 studies in this review, 23 took this approach. Table 3 lists the variables most frequently used, with the person’s ability to undertake daily activities of living,103–105,120,121 the extent of their informal care93,96,101 and the impact of their mental state/behaviour108,117,118,124 commonly thought important. Those studies concerned with the location for a specific treatment (as opposed to where different groups of people might reside) also considered such factors as the distance a person would have to travel97,111 and the severity of their illness. 97,125,126 Less frequently mentioned variables included age, gender and level of risk.
| Attribute | Number of studies employing this attribute (maximum n = 23) | Percentage of studies employing this attribute |
|---|---|---|
| Dependency/disability | 18 | 78 |
| Informal support | 16 | 70 |
| Mental state/behaviour | 13 | 57 |
| Incontinence | 7 | 30 |
| Housing/place of residence | 6 | 26 |
Most studies used between three and five attributes, each with two or three levels (e.g. the presence or absence of cognitive impairment), resulting in between 16 and 48 possible case types. The subgroups used in four studies were, however, considered too broad to identify clinically recognisable groups. For example one broke the population into just three ‘standard’ groups of children,127 which would not be clinically recognisable groups.
Approaches to profiling services
Although a comparison of the services people currently receive and alternative ways of meeting their needs is central to the BoC approach, the very first DHSS studies assumed that the total amount of resources available would be curbed by limits on the overall supply of services. 90,119 By contrast, later adaptations of the DHSS model ran both with and without resource constraints,128 whereas other studies tended not to restrict resources to pre-specified levels,98,122,123 though sometimes suggested that account be taken of likely financial constraints. 101,117 In order to estimate the total resource requirements of the various options, the aggregate resources proposed for the care of different individuals/case types were then compared with the resources actually used by the same population.
The range of resources considered varied according to studies’ aims, populations and margins of interest, but generally included those public services likely to account for a significant proportion of total client group spending. Hospital and care home beds, as well as commonly utilised community services, therefore featured frequently. 10,80,113,114,124 The sources of service receipt data were generally poorly detailed. However, some studies employed aggregate measures of available resources taken from routinely collected statistics,80,93,94 whereas others undertook individual-level data collections similar to those above. 71,92,99
Approaches to identifying alternative care arrangements
In the original DHSS studies, alternative care services were identified by modellers after consultation with a team of medical, nursing and social work advisors and ‘mathematical programming’ was used to estimate how practitioners might allocate these based on existing patterns of resource allocation. 80,105 Subsequent BoC studies have, however, generally taken a simpler approach. Many asked practitioners (individuals, monodisciplinary or multidisciplinary groups) to identify the most appropriate form of care for particular case types/individuals (facilitating the incorporation of new services),101,117,118,120,121 whereas others asked practitioners to identify those people in location A who could be cared for in location B. 71,91,113,114 An alternative was to draw on policy documents,103 research recommendations10,121,122 or comparative provision elsewhere. 93,94
Approaches to costing
A comparison of the costs of current and alternative care forms a key element of BoC studies. Few studies provided detailed descriptions, and it was not always clear what costs were included. Furthermore, there is not necessarily one single ‘right’ concept of costs. 129 Thus, in studies exploring how public expenditure might be reduced, it could be argued that only public costs are relevant, whereas this is inadequate when valuing wider social opportunity costs. 130 The consideration of costs undertaken in this review therefore addressed a number of different questions (Table 4).
| Question | Insufficient data to judge | Yes | No |
|---|---|---|---|
| 1. Was the approach to costing comprehensive? | 1 | 5 | 27 |
| 2. Were the cost data used valid? | 11 | 21 | 1 |
| 3. Was the approach to costing fit for purpose? | 21 | 11 | 1 |
| 4. Were the dates to which resources and prices referred reported? | 0 | 20 | 13 |
| 5. Were appropriate adjustments made for inflation? | 20 | 13 | 0 |
| 6. Was there any attempt to investigate cost shifting? | 5 | 4 | 24 |
Less than one-sixth of studies undertook a comprehensive costings approach encompassing not only those costs incurred by public agencies, but also the costs of housing, personal consumption/living expenses and informal care. 92,95,112,122,123 A further fifth incorporated some of these elements. 71,91,110 The remainder considered only public expenditure which, depending on their foci, covered the costs incurred by health and/or social services. 103,106,118,120,121 Interestingly, although many aspired to a comprehensive costing approach, there was little evidence that one framework had come to dominate the field. However, there appeared to be an order in which non-public costs were considered with more studies including housing than living expenses, and informal care costs least likely to be examined.
In all except one study the data used appeared valid, that is related to costs drawn from empirical sources in keeping with the study’s coverage. The costs of local public services were typically supplied by the relevant agencies’ finance departments, whereas national costs were calculated from statistics provided by the Chartered Institute of Public Finance and Accountancy131 or the average local costs in the studied sites. Living costs were generally taken from the Family Expenditure Survey,132 whereas housing cost sources included the estimates of an experienced valuer, national survey data and rateable values. Just two studies described the valuation of informal care costs, with one basing these on the replacement costs of formal care services,10 and the other considering the costs of foregone paid work, non-market work and leisure time. 113,114
Where costs were valid and in keeping with studies’ aims they were deemed ‘fit for purpose’. Thus, studies undertaken from a provider/commissioner perspective (interested in public expenditure) that included the most important health and/or social care costs and used valid data were scored positively, as were those that sought to calculate comprehensive costs and included the four elements detailed above. In almost two-thirds of cases, however, there was insufficient information to make this judgement. Furthermore, a substantial number of studies failed to report the year to which costs referred, whether appropriate adjustments were made for inflation or the extent to which any reallocation of resources would change the distribution of the cost burden between health and social care/the public and private sector. There were no reports of the transaction costs that might be incurred in reallocating resources between care locations or creating new services.
Approaches to the inclusion of outcomes
Consideration of the relative benefits of alternative care options was widely advocated, although only four studies reported collecting any outcome information. 97,99,101,127 A further four demonstrated awareness of existing outcome data. 10,91,102,122,123 Not all of those studies that collected outcome information explained how it was used. However, one used data on fostering breakdown to explore concerns that greater use of fostering might increase placement failure,127 whereas another used information on (among other things) the extent to which people’s needs were met and how satisfied they were to indicate care quality. 99
Most of those studies that drew on existing evidence were more explicit. One cited research on the relative benefits of community and institutional care to support its plans to increase domiciliary support,91 whereas another discussed possible changes to the support of older people with cognitive impairment based on evidence of the quality and effectiveness of each option. 122,123 More recently still, Wanless et al. 10 created an outcomes-led estimate of the costs of addressing the social care needs of vulnerable older people. This work aside, several studies used practitioners to make explicit judgements of best placements, on the assumption that ‘best interests’ evaluations of outcome were included,96,117,118 whereas others simply presented decision makers with the relevant cost data alongside a description of the individuals likely to be affected by any reallocation of resources, leaving them to judge the relative benefits of any proposed transition in terms of, say, equity, continuity, normalisation and/or effectiveness.
Good practice indicators
The preceding sections have summarised the extent to which studies exhibited the criteria of good practice identified in Box 2 and demonstrated how key elements of the BoC framework have been operationalised, but have not addressed the overall design or reporting of individual studies.
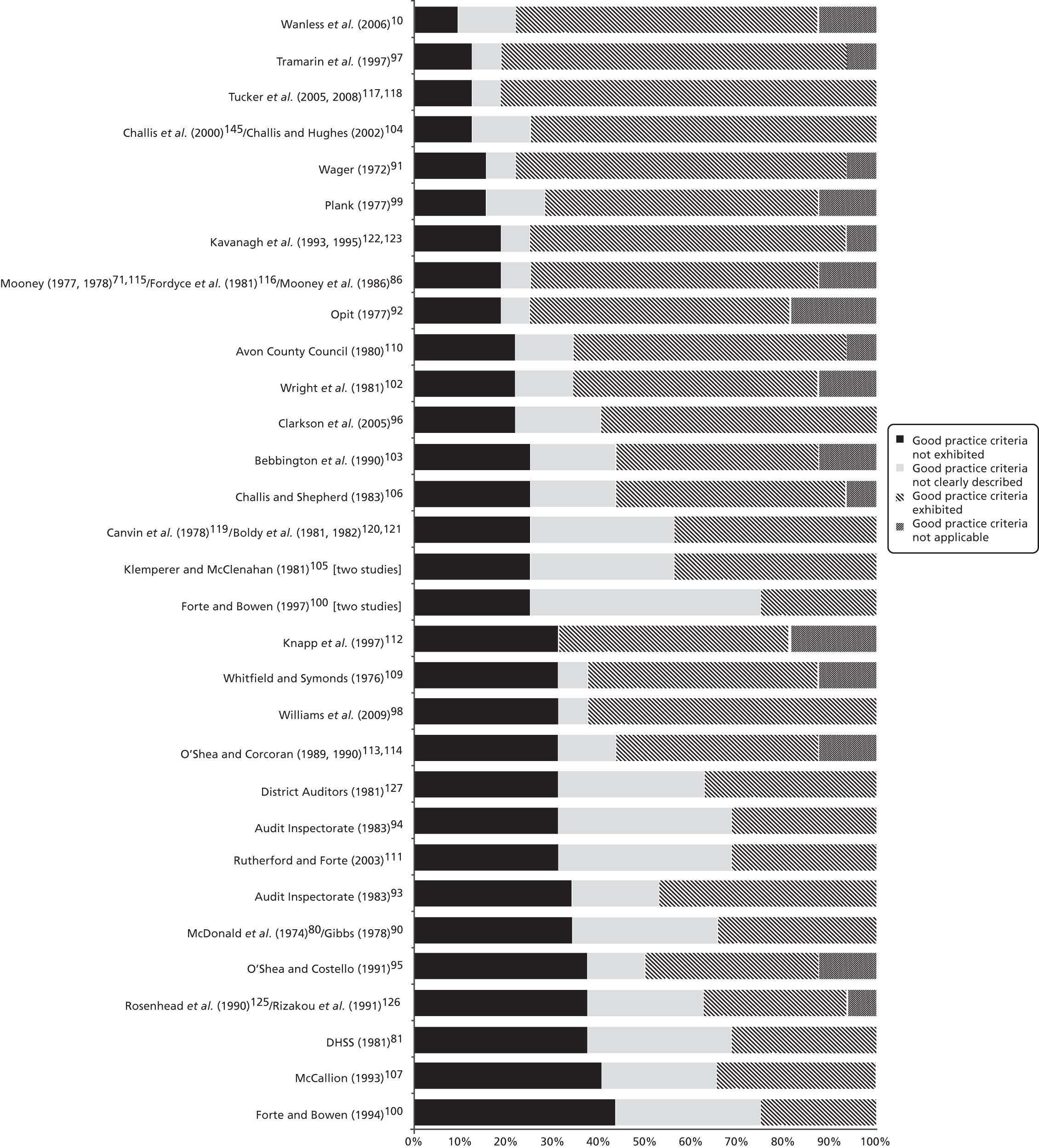
To assist such a comparison, Figure 4 ranks the studies by the number of good practice indicators exhibited (most to least). As can be seen, not one study exhibited all 16 components, whereas approaching half (n = 15) exhibited < 50%. As one moves down the figure, however, the proportion of items not reported increases more than the proportion definitely not exhibited, suggesting that study designs may be less variable than reporting standards. This distinction is reinforced by Figure 5, which ranks the studies from least to most good practice indicators not exhibited, and although the upper sections of Figures 4 and 5 are similar, the ordering of those studies in the middle and lower sections changes considerably. Interestingly, there is no indication that studies with multiple publications or described at more length performed systematically better than studies described in single publications or at less length. Moreover, there is no straightforward association with year of publication, since most of the more recent studies are in the upper half, as are some of the earliest.
FIGURE 4.
Ranking of studies by good practice criteria exhibited (most to least).
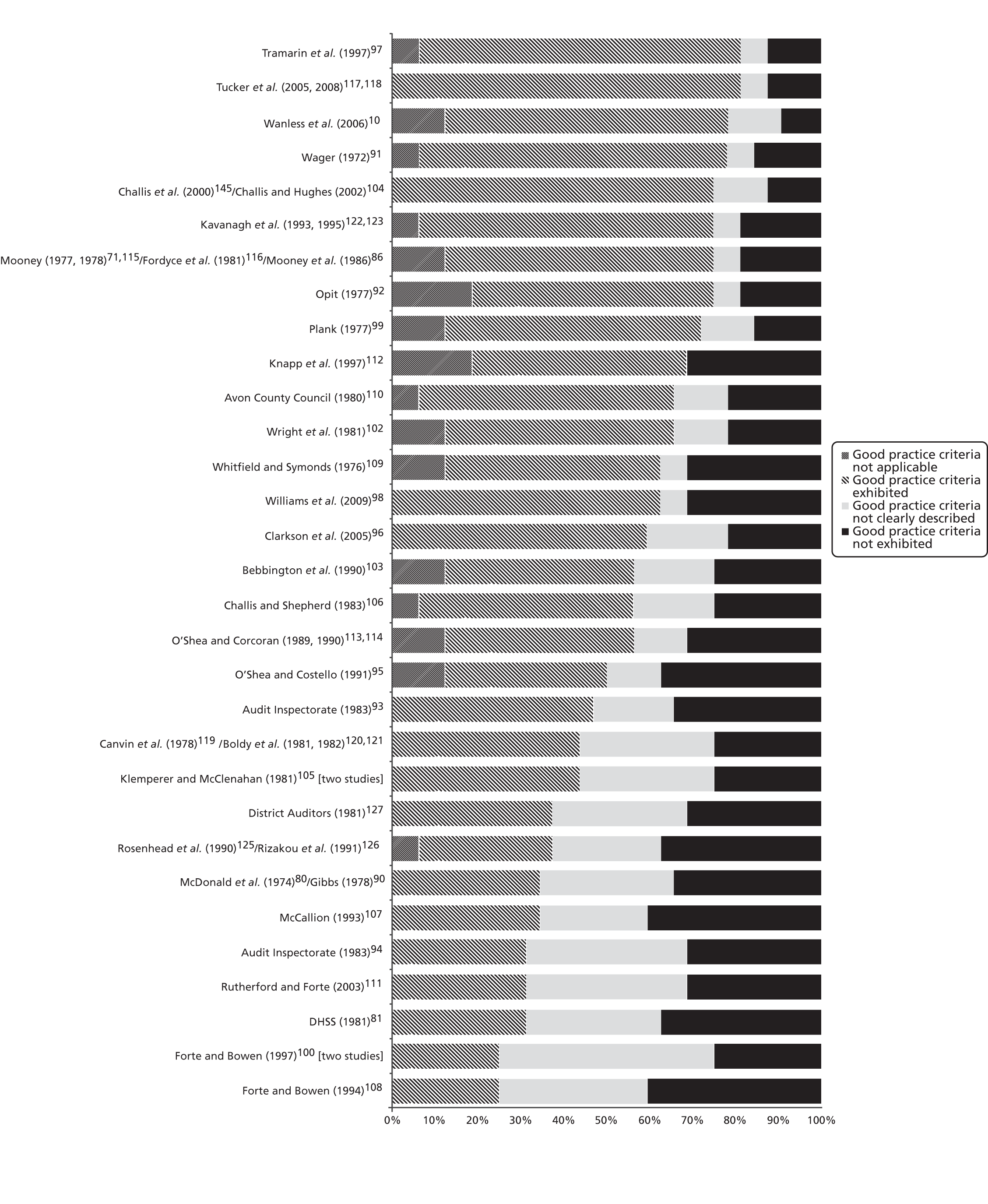
FIGURE 5.
Ranking of studies by good practice criteria not exhibited (least to most).
Discussion
The strategic allocation of resources has been described as one the most difficult tasks facing health and social care decision-makers. The NHS and local authorities deliver a complex range of services, with benefits that are imperfectly understood, to a population that is heterogeneous in its needs and expectations. 133 The enduring appeal of the BoC approach, which offers service commissioners and providers a formal structure for exploring potential changes in service mix, is thus unsurprising. However, it is clear that there is not one standard approach. The studies included in this review spanned an array of programme areas/services at local, regional and national levels. Although some were large in scale and ambition, others had more modest aims. Nonetheless, in identifying service users on the margins of care, articulating costs and identifying the values placed on different care settings, each exposed its key assumptions to critical debate. Furthermore, there is some suggestion that, despite certain shortcomings, the most recent studies were among the more robust.
Methodological considerations
This review faced a number of methodological challenges, not least of which was the desire to examine not only that work that explicitly used the BoC model, but that sharing the same approach. Although the selected search terms may not have captured all relevant studies, experts highlighted only a handful of additional publications suggesting the final list was relatively complete, and just two unsourced references related to studies not captured elsewhere. The lack of methodological detail given in many publications was also problematic, and no suitable validated quality assessment tool was identified. The components of the constructed checklist were, however, selected with due consideration for the scope and purpose of the exercise (if not necessarily all of equal importance), and highlighted a number of areas in need of methodological refinement.
Lessons for future applications
Key lessons arising from this review focus on the need to minimise bespoke data collections, the formation of case types, the choice of margins, the delineation of care alternatives, the measurement of costs and the inclusion of outcome data.
Data collection
Past studies have relied mainly on local data collections. Such exercises can be time-consuming and expensive. It is thus suggested that future studies ascertain precisely what routinely collected data is available before undertaking additional collection, and limit this to that information essential to the planning exercise.
Case types
The use of case types has been widely adopted and reduces demands on busy practitioners. Nonetheless, the formation of case types requires careful thought, given the trade-off to be made between the number of characteristics taken into account and the number of people captured by each type. Attention should also be given to whether or not the selected attributes form single scales. Thus, although some commonly used variables (e.g. physical dependency) lend themselves to this, others (e.g. behavioural problems) can encompass a number of different dimensions needing different care. 102 Furthermore, some way must be found of incorporating those less objectively measurable characteristics (e.g. clients’/carers’ preferences) that affect placement decisions and surely influence the relationship between resources and outcomes. 130
Margins
Although a number of past studies have focused on services administered by either health or social services, in today’s more complex planning environment the viability of many people’s care depends on both. Future applications should thus consider taking a cross-agency approach. Similarly, whereas previous applications tended to focus on just one or two settings, in light of the increasing development of new forms of support, a careful determination is needed of both the choices available and the widest margins of care. 130,134,135
Care alternatives
The engagement of local practitioners in generating care options is widely acknowledged as a strength of past BoC studies. However, thought should be given to the selection of staff involved, for different professional groups hold different values and opinions,136 while the extent to which staff can think beyond current practice is fundamental to the method. Some studies have addressed this using multidisciplinary groups of professionals,97,117,118 encouraging participants to be more explicit about the rationale for their choices, and, through consensus decision-making processes, facilitating peer review. Such approaches could be widened to include other stakeholders, including the public.
Costs
Although most past studies examined only public expenditure, few saw this as ideal, acknowledging it significantly underestimated the burden of community care. As other studies illustrated, however, there are a number of ways of incorporating housing, living and informal care costs into the methodology. Future studies should also give thought to the practical problems of reallocating resources between care settings/providers, for although it is often assumed the monies released from one service can be used to pay for another, in practice this may be difficult, particularly if it involves a transfer between agencies. 137 In addition, capacity cannot always be reduced/increased in a linear fashion and there may be a need for new and old services to run in parallel, at least in the short-term. Hence, the transaction costs of shifting resources should be considered.
Outcomes
Despite widespread support for including outcome data in the model, few past studies have attempted to do this. This is potentially the biggest challenge facing future applications, for without this information the approach risks being perceived as a cost-minimisation tool. With adequate benefit information, it could become a much more sophisticated and flexible toolset. Decisions to be made include whose perspective to consider, which outcomes are important, and how best to measure them. 71
Conclusions
Some 40 years after the development of the BoC approach, its utility appears as high as ever. A number of factors account for this. First, the search for the most appropriate and efficient ways of caring for different client groups is an enduring one, and is of relevance to service providers/planners at many levels within the health and social care system. Second, the approach is pragmatic, incorporating a mixture of local data, research, practitioners’ and clients’ views, yet based on sound economic principles. It accepts service planning is not fully informed, but provides a systematic and explicit framework to guide the exploration of alternative actions. Third, the approach both involves and cedes control to local stakeholders, who inform the study’s scope, suggest alternatives and choose solutions, engendering the support of the people who will need to implement change. Fourth, precisely because the approach is applied within a particular geographical area/service, and is based on local data, the findings are of immediate and specific relevance to local decision-makers. Indeed, as demographic profiles and relative marginal service costs vary, decisions made in one area/service will, and should, differ from those in another.
There is, however, undoubtedly the potential to improve the methodology, as specified above, providing important pointers for future studies. There are, in addition, a number of gaps in the research, including the need for future qualitative studies on current decision-making and resource allocation processes and a follow-up evaluation of past BoC studies to determine their success in facilitating change.
Chapter 3 Services for older people with mental health problems. The North-West Balance of Care Study: method
Introduction, aims and objectives
Following on from Chapter 2, the research detailed in the next three chapters employs a BoC approach to explore a more appropriate and efficient mix of services for older people with mental health problems in three areas of north-west England. The BoC approach was described in Chapter 2, and will not be repeated here. It identifies groups of people whose needs can be met in more than one setting (marginal cases), and examines the costs and consequences of these alternatives. Although 33 studies have employed variants of the BoC model over the last 40 years, only two have considered the services needed by older people with mental health problems. Moreover, several methodological shortcomings were evident in previous use of the framework.
This study was designed to build on past applications and had three main aims:
-
to demonstrate the potential of the BoC approach to inform strategic service planning for this client group
-
to develop and refine the methodology and
-
to enable other health and social care decision-makers to apply the framework independently.
In order to achieve these aims the research sought to:
-
apply the BoC framework to the care of older people with mental health problems, examining whether, how and with what consequences the mix of institutional and community services provided by health and local authorities could be improved
-
expand the number of settings considered
-
further investigate the potential for diverting older people from acute mental health inpatient care
-
examine the implications of taking a comprehensive, as opposed to a public, expenditure costing approach
-
explore different ways of incorporating final outcome data into the analysis
-
improve understanding of the determinants of the BoC in the main study site; and
-
inform the production of a BoC workbook.
Overview
The research was undertaken in three areas of north-west England – sites X, Y and Z – and explored the support needed by older people with mental health problems in five key settings in which this client group receive support from specialist secondary mental health and local authority (LA) social care services:
-
acute mental health inpatient wards
-
care homes (with and without nursing)
-
ECH
-
home with specialist mental health support from a CMHT; and
-
home with social services but no specialist mental health support.
The approach drew on both quantitative and qualitative methods in a sequential mixed-methods design and was grounded in the experience and knowledge of local practitioners and service users. It contained seven work packages encompassing 17 interlinked activities, described below. The work packages are numbered 1 to 7 and the activities within work packages are numbered to reflect their work packages (e.g. activity 3.1). Although one locality, site X, served as an exemplar for the use of the BoC methodology across the entire spectrum of services, facilitating a whole systems analysis, data about ECH tenants and care home and hospital inpatient admissions were sought in all three sites to increase sample sizes and permit between-area comparisons. This was only partially successful, for the council in site Z, which had originally intended to participate in the study, was subsequently unable to do so, and substantial delays in obtaining research governance approval from the mental health trust in site Z reduced the amount of data it could provide.
Ethical approval was granted by Cambridgeshire 3 Research Ethics Committee (reference number 10/H0306/51) and research governance procedures in each participating organisation were fulfilled.
Work package 1: profiling service provision and service users
Activity 1.1
Multiple, secondary data sources were used to develop an overview of the existing distribution of resources for older people with mental health problems, providing a baseline against which future changes in service provision could be considered. These data were compared with published national findings in order to benchmark service provision in the study sites against other areas, providing a wider context for the research.
Activity 1.2
Front-line practitioners completed bespoke surveys providing information about the sociodemographic, functional, clinical and service receipt characteristics of service users in each setting (the baseline data collection) drawing on routinely collected data (Box 3). In the ECH, care home and inpatient samples, they also indicated which of a list of factors identified from the literature contributed to the admission. The questionnaires (see Appendices 6 and 7) were designed to collect the minimum amount of information necessary to profile the populations of interest, including standardised measures such as the modified Barthel Index,138–140 the Cognitive Performance Scale (CPS)141 and, where available, the Mini Mental State Examination (MMSE),142 Geriatric Depression Scale (GDS)143 and Hospital Anxiety and Depression Scale (HADS). 144
| Setting | Population of interest | Approach to sampling | Information domains | Site |
|---|---|---|---|---|
| Acute mental health inpatient wards | All older people (aged ≥ 65 years) admitted to an acute mental health assessment ward excepting admissions for planned respite Target sample: 300 |
Consecutive admissions in the following time periods: Site X: October 2010–March 2011 Site Y: November 2010–April 2011 Site Z: April–September 2011 Discharge information collected until December 2011 (Information provided by nominated nursing staff shortly after admission) |
Sociodemographic information Admission details Daily functioning Clinical characteristics Informal care Formal service receipt Discharge arrangements |
Site X, two wards Site Y, two wards Site Z, three wards |
| Care homes | All older people (aged ≥ 65 years) with mental health problems admitted to a care home with the approval of Social Services’ Older People’s Resource Allocation Panels and/or known to CMHTs excepting admissions for planned respite and people moving from one care home to another Target sample: 350 |
Consecutive admissions approved/known about in the following time periods: Site X: October 2010–April 2011 Site Y: January–May 2011 Site Z: February–May 2011 (Information provided by service users’ care co-ordinators shortly after admission. Forms completed by staff in social services. Older people’s teams contained a preliminary mental health screen to exclude service users with no indication of mental health problems) |
Sociodemographic information Admission details Daily functioning Clinical characteristics Informal care Formal service receipt Funding arrangements |
Site X LA Site Y LA Site X CMHT Site Y CMHT Site Z six CMHTs |
| ECH | All older people (aged ≥ 65 years) with mental health problems on the caseloads of the Social Services Older People’s Teams or CMHTs resident in (specialist or non-specialist) ECH Target sample: 30 |
The population known to CMHTs on a nominated day in June 2011; plus the population of site X’s LA ECH schemes who took up tenancies in the year preceding June 2011. (Note: Local staff advised that contemporary information was unlikely to be available about longer-term residents) (Information provided by service users’ care co-ordinators in June/July 2011. Forms relating to site X LA tenants contained a preliminary mental health screen to exclude service users with no indication of mental health problems) |
Sociodemographic information Admission details Daily functioning Clinical characteristics Informal care Formal service receipt |
Site X LA Site X CMHT Site Y CMHT Site Z six CMHTs |
| Home with specialist mental health support | All older people (aged ≥ 65 years) on the caseloads of the trusts’ CMHTsOP who were not long-term residents of care homes or ECH Target sample: 900 |
All clients with an organic mental illness plus a one in four systematic random sample from a clinician-generated list of clients with functional mental health problems stratified by practitioner Samples selected on nominated days in: Site X: November 2010 Site Y: December 2010 Site Z: June 2011 (Information provided by service users’ care co-ordinators in the month following sample selection) |
Sociodemographic information Daily functioning Clinical characteristics Informal care Formal service receipt |
Site X CMHT Site Y CMHT Site Z six CMHTs |
| Home with social services support (but no specialist mental health input) | All older people (aged ≥ 65 years) with mental health problems on the caseloads of the older people’s locality teams who were not currently receiving specialist mental health care or living in care homes or ECH Target sample: 100 |
A random sample of 199 active cases stratified by care co-ordinator were selected in July 2011 (Note: Local staff advised that contemporary information was unlikely to be available about inactive cases) (Information provided by service users’ care co-ordinators in the 2 months following sample selection) Forms contained a preliminary mental health screen to exclude service users with no indication of mental health problems |
Sociodemographic information Daily functioning Clinical characteristics (partial) Informal care Formal service receipt |
Site X LA |
All information supplied to the research team was provided in a fully anonymised form. However, in order to facilitate the identification of people for whom outcome data would be sought in Activity 4.4, each proforma included a unique study or non-sensitive agency number. As the participating social services’ documentation did not reliably distinguish older people with mental health problems from other older people, the relevant forms also contained a brief screen to identify the study population for whom the full data set was then collected.
The sampling strategy aimed to identify individuals at a point on the care pathway where real life choices are made between settings, while simultaneously generating sufficient numbers for the formation of case types (see Activity 2.1) and the power required by the planned outcome analysis (see Activity 4.4). The focus on people with an organic mental illness in the CMHT sample was also influenced by the need to match CMHT clients with care home admissions (see Activity 4.4), whereas the small size of the ECH sampling frame necessitated a whole population approach.
Data were initially entered onto SPSS for Windows (version 19; SPSS Inc., Chicago, IL, USA) and checked for errors, while subsequent analyses were conducted with Stata (versions 10 to 12; StataCorp LP, College Station, TX, USA). Where data permitted, critical gaps were filled by model-based imputation routines and scores for summary measures were calculated from their constituent elements (see Appendices 8 and 9). Differences between groups were explored using appropriate statistical tests.
Work package 2: developing case types and formulating vignettes
Activity 2.1
The study samples were divided into relatively homogeneous subgroups (case types) on the basis of those client characteristics deemed likely to be important in determining the locus of/and/or costs of their care. The attributes employed (Box 4), were informed by the literature review (see Chapter 2), the wider literature on care home and inpatient admission predictors and exploratory analyses of the empirical data. Further details are given in Appendix 10. As each of the three variables used in the domiciliary, ECH and care home settings had three levels, this gave 27 possible different combinations or case types, whereas the four variables used in the inpatient classification generated 72 possible subgroups.
| Setting of interest | Attributes | Number of case types |
|---|---|---|
| Home, ECH, care home entrants | A three-level rating of dependency based on a modified version of the Barthel ADL Index:
|
27 |
| Inpatient admissions | A three-way grouping of primary diagnosis:
|
72 |
Activity 2.2
Vignettes were formulated to exemplify the most prevalent case types for care home admissions in site X (see Appendix 11). Based on real individuals, they took the form of brief case histories which systematically incorporated information about the three key variables as well as individuals’ falls risk, physical health, living situation, service receipt, location immediately prior to admission and preferences. A few control vignettes were also constructed to depict two of the same case types in the CMHT sample as well as the most commonly populated CMHT case type, and the homeogeneity of the needs of the people represented by each vignette was checked.
A similar process was used to formulate vignettes representing the inpatient sample, but depicting the most prevalent case types across the three sites to facilitate wider exploration of the appropriateness of inpatient admission. They also included information about individuals’ mental health history (see Appendix 12). In one instance, where the needs of the individuals represented by a particular case type appeared too heterogeneous, the relevant case type was divided according to the individuals’ usual place of residence (i.e. home or care home).
To adhere to the study timeline, this exercise was started approximately half-way through the baseline data collection exercise.
Work package 3: identifying marginal case types and alternative care arrangements
Two different approaches to the identification of people on the margins of care were explored.
Activity 3.1
First, an empirical analysis was undertaken of the extent to which the same case types were found in the two domiciliary, ECH and care home samples.
Activity 3.2
Second, local staff attending a series of practitioner workshops identified those commonly populated care home and inpatient case types whose needs could be met by other services, scoping the potential for downwards substitution from the two most intensive settings. Box 5 sets out the workshops’ key characteristics.
| Primary case types of interest | Practitioners involved | Locality |
|---|---|---|
| Care home residents | Mental health nursing, support worker, managerial, social care and housing staff | Site X only |
| Acute mental health inpatients | Mental health community and inpatient nursing, medical, occupational therapy, counselling, managerial, commissioning and social care staff | Sites X, Y and Z (three separate exercises) |
Participants in the care home workshop worked in five small groups, with each group pseudo-randomly allocated a set of pre-selected care home and domiciliary control vignettes.
Working alone, practitioners first indicated where they believed the depicted ‘client’ would be most appropriately cared for and, where care home placement was felt preferable, recorded the main reason for their decision. They also indicated if their decision would be different if (a) the service user lived with or without a coresident carer and (b) was at home or in hospital at the point of assessment. Working collectively, each group then identified between two and four cases that could appropriately be diverted from care home admission (‘marginal care home cases’) and compiled care plans specifying the alternative community resources required.
In this exercise participants were asked to put aside short-term constraints in current services and be creative, while remembering that all services inevitably have funding implications. To help practitioners to think creatively, they were given a care planning sheet containing a list of services already available in other areas.
Employing a similar process, participants at the inpatient workshops first individually indicated whether it was ‘completely’, ‘possibly’ or ‘not’ appropriate to admit the ‘client’ to a mental health bed. To construct a hierarchy of appropriateness, case types were then scored: two points were given for each respondent stating ‘completely’; one point for each respondent stating ‘possibly’; the points were totalled; and totals expressed as a percentage of the maximum possible. Working in small groups, practitioners then formulated care plans to enable the four to six lowest scoring admissions in each workshop (‘marginal inpatient cases’) to be diverted from hospital care.
Activity 3.3
Statistical modelling was undertaken to illuminate the decision-making process. The individual decisions made during workshops (clustered by rater) formed the analysis data set, and a series of logistic regression analyses were undertaken to explore the factors associated with those care home and inpatient case types that were definitely not divertible, as well as rater characteristics that may have influenced these decisions.
Work package 4: identifying the costs and outcomes of alternative packages of care
This study component sought to estimate the costs of alternative support for marginal care home and inpatient cases and to identify different potential outcome evidence for inclusion in the BoC analysis.
Activity 4.1
A comprehensive approach was employed in the costing exercise for the marginal care home case types. This covered the most important (expensive or commonly incurred) public sector and service user costs that might be expected to vary between settings.
The main health and social care costs stemmed from the receipt of services, information on which was drawn from the baseline data collection exercise (see Activity 1.2) and practitioner workshops (see Activity 3.2), with any gaps filled by estimates from published evidence. Wherever possible, service-related costs were calculated from data provided by the participating agencies in the main research site. Where local costs were unavailable, however, figures were based on national sources. Information on the receipt of benefits (including attendance allowance, housing benefit and council tax benefit) were similarly obtained from external sources, whereas data on expenditure retrieved through charging for formal social care services was obtained from the LA.
The estimation of private costs (i.e. costs to service users and their carers) was similarly derived from information collected in the baseline data collection exercise, including where service users lived, with whom they lived, and the extent of their informal support. The living expenses of people residing at home were informed by data from the Family Expenditure Survey, and figures for the opportunity costs of owner-occupied housing were calculated by imputing a rent from comparable market values. Informal carers’ time was also costed using an equivalent market value approach.
Costs were adjusted to take account of the real distribution of service receipt within case types; confidence intervals were calculated to reflect uncertainty about the quantity and cost of resources used in the alternative planning scenarios; and a range of sensitivity analyses were undertaken to explore the effects of different costing assumptions. The potential for cost-shifting between health and social services, the public sector and private individuals was also explored. Further details of the specific costs and general approach used in this exercise are given in Appendices 13 and 14.
A similar approach was taken to the costing of the marginal inpatient case types. However, in the absence of good information on the general health care, private and other government costs for these service users, this focused mainly on the potential trade-offs between mental health inpatient, mental health community and social services costs.
Activity 4.2
Three approaches were employed in the identification of outcomes of people with similar needs for care supported in different settings. The first was a selective literature review that focused on the outcomes of older people with mental health problems supported in ECH as compared with domiciliary or care home settings. This involved interrogating several electronic databases [including PubMed, PsycINFO and Cumulative Index to Nursing and Allied Health Literature (CINAHL)] using search terms such as ‘care home’, ‘extra care housing’, ‘dementia’, ‘older persons’, ‘outcomes’ and ‘effects’, with similar search terms used to identify relevant grey literature. Studies that examined the effects of ECH on residents’ outcomes or investigated the margins between ECH and domiciliary or care home placements were included, and data was extracted on all reported outcomes, including social engagement, activities of daily living (ADL) and cognitive status.
Activity 4.3
The second approach involved a search for secondary national data sets that contained the study target populations, such as the English Longitudinal Study of Ageing. Relevant publications and sources such as the UK Data Archive were also considered.
Activity 4.4
The third approach explored the feasibility of collecting primary outcome data. It was designed as a matched cohort study, and aimed to compare the 4-month outcomes of 120 marginal care home cases, represented by a small number of case types, with those of a matched sample of 120 service users who received CMHT support at home. Examples in Box 6 illustrate how the sample size was determined.
| Information from the literature | Implications for cohort study |
|---|---|
| Challis et al.145 reported that the mean Barthel score (0–20 scale) for new care home residents was 11.4 (SD 5.5), i.e. in the low–medium dependency range | If a particular case type is characterised by medium dependency, a much reduced SD (say 2.3) would be expected to accompany the same mean value. If the care home and domiciliary groups were then compared, and one group deteriorated to a Barthel score of 10.2 while the other remained unchanged, a group size of 58 cases would be needed in order to detect that difference with 80% power at the 95% confidence level |
| Fletcher and Mant146 reported that 31% of a sample of vulnerable older people living at home experienced more than two emergency admissions in a 3-month period | If the corresponding figure in the care home sample is 15% (as might be conceivable in a more protective environment), a group size of 62 cases would be needed to detect that difference with 60% power at the 90% confidence level |
To be eligible for inclusion in the cohort study, service users were required to:
-
have remained in their respective care setting for the 4-month period since baseline data collection
-
be physically well enough to participate in an interview
-
be mentally well enough to participate in an interview (e.g. not unduly anxious or agitated) and
-
be able to meaningfully answer questions about their care experience as judged by their keyworker/care co-ordinator.
These staff also judged service users’ capacity to participate in the study, identifying a family member/informal carer possibly willing to act as personal consultee where capacity was lacking.
Potentially eligible service users (or consultees) were first approached about the study by their key worker/care co-ordinator and, if interested, were sent a study information sheet and invitation to participate by the research team. A Personal Social Services Research Unit (PSSRU) interviewer subsequently telephoned to provide further details and, subject to verbal agreement, arranged to visit. Written consent or a written record of consultation was gained prior to the formal interview. A summary of the measures this encompassed is given in Box 7 and the full interview schedule forms are in Appendices 15 and 16.
| Outcome | Coverage | Respondent | Collected at baseline |
|---|---|---|---|
| Change in daily functioning | Ten ADL measured by the modified Barthel ADL Index,139,140,147 a widely used scale measuring functional independence in personal care and mobility. The version used had a simple scoring system in which each item was rated 0–5, 0–10 or 0–15 depending on the amount of help the person received. Individual item scores were then summed to provide a total of between 0 and 100. Lower scores represent higher dependency | Service user and carer | Yes |
| Change in daily functioning | Five instrumental ADL taken from the Nottingham Extended ADL Scale148 covering the person’s ability to make a hot snack, shop, use the phone, travel by car/public transport and manage their medication using a four-point scale: not at all; with help; on their own with difficulty; on their own easily | Service user and carer | Yes |
| Change in cognitive functioning | A range of cognitive functions affected in dementia, including orientation, memory and attention as measured by the MMSE,142 a well-known and widely used test of cognitive function. There is a maximum score of 30, with scores of 0–10 commonly described as severe dementia, 11–20 moderate dementia and 21–24/25 mild dementia | Service user only | Yes |
| Change in mood | Ten simple yes/no questions about non-somatic symptoms of depression as covered by the GDS-10.149 This scale has been validated in primary care patients and recommended for use with care home residents.150 Individual items are summed to provide a total of between 0 and 10 with scores of 4–10 indicative of a high probability of depression. Although its validity with people with severe cognitive impairment remains uncertain, adequate sensitivity has been reported in people with MMSE scores of ≥ 15151 | Service user only | Yes |
| QoL | Thirteen items covering aspects of the person’s physical and mental health, relationships, finances and overall life quality as given in the QoL-AD scale152 which can be satisfactorily completed by people with MMSE scores as low as 3153,154 and has been validated in people without dementia.155 Each item is rated 1–4 (poor, fair, good or excellent) giving a total possible score of between 13 and 52. Higher scores indicate better QoL | Service user only | No |
| Service satisfaction | A short (six-item) questionnaire about people’s satisfaction with their service setting developed by the PSSRU | Service user and carer | No |
| Service receipt | A modified version of the Client Service Receipt Inventory,156 collecting information about the use of health and social care services over the previous 4 months | Service user and carer | No |
Work package 5: incorporating the cost and outcome data into the balance of care analysis
Activity 5.1
Details of the marginal care home case types were presented at a specially convened meeting of the site X Resource Allocation Management (RAM) Panel which, in effect, acts as gatekeeper for access to care home placement. These utilised local proformas and included information on service users’:
-
situation, presentation and needs
-
original care home placements (including their cost to social services) and
-
alternative care plans (including their cost to social services) as devised by local practitioners in Activity 3.2.
The RAM Panel then decided whether or not the alternative support was appropriate; sufficient to enable the people represented by each case type to stay in the community; and fundable, mirroring local decision-making processes.
Activity 5.2
The RAM Panel was next given further information about two case types and asked whether or not this would affect their placement decisions. In essence, the additional information explored the weight the RAM Panel gave to service users’ preferences, carers’ preferences and carers’ stress levels and evidence about service user outcomes.
These exercises were recorded and the discussion transcripts were subjected to a thematic analysis using a framework approach to identify both the manifest and latent content of the conversation. Three researchers from different professional backgrounds independently coded the entire script to give greater reliability to the development of themes and increase the trustworthiness of the analysis. 157
Work package 6: validating alternative packages of care
Activity 6.1
The acceptability of the RAM Panel’s decisions was reviewed at two workshops attended by a mix of older people who either had, or supported someone with, dementia. Participants first read a small random selection of (appropriately modified) vignettes about recent care home entrants for whom the Panel had approved an alternative community care package. Working in small groups they decided whether or not the original care placement or the suggested alternative was preferable, noted the main reason for their decision and listed any other support they felt was needed.
Activity 6.2
In a similar exercise, a number of acknowledged experts in the care of older people with mental health problems reviewed a sample of the marginal care home cases by examining details of actual care placements and proposed alternatives. Participants were asked to identify their preferred care option, the main reason for their decision, and to specify any further support they deemed necessary.
An equivalent exercise was undertaken for marginal inpatient case types, with respondents also asked to indicate how appropriate they felt inpatient admission was.
Work package 7: exploring the potential implications of changes in the balance of care
Activity 7.1
The final stage of the study consisted of an analysis of the potential for local agencies to shift the BoC provided for older people with mental health problems. In essence this explored the resource implications of caring for different combinations of those care home entrant and inpatient case types thought to have the most potential for diversion from institutional to community care and the effects of any change on the wider care system. Although the care home analysis related to site X alone, the inpatient exploration encompassed all three sites.
In order to understand the full cost implications of different BoC scenarios, deterministic sensitivity analyses were used to explore the impact on the results of changing a number of structural aspects of the model. For the care home analysis, these included the proportion of service users in each case type that might realistically be cared for in alternative settings and the length of time it might be possible to divert them from care home entry. This latter factor had important implications for the attribution of so-called ‘one-off’ costs (e.g. an expensive inpatient stay for assessment purposes). In order to standardise cost components all costs were annualised. First, the likely annual prevalence of potentially divertible care home entrants was estimated from the baseline data collection, assuming current conditions prevailed. Second, total annual costs were calculated for all cost components by combining the alternative costs incurred during the chosen diversion period with the ‘original’ costs incurred during the remainder of the year. For example, where it was thought a case type could be diverted for 12 months, only alternative costs were incurred, whereas where it was thought a case type could be diverted for only 6 months, 6 months’ worth of alternative and 6 months’ worth of original expenditure were incurred. Third, the linear cost trade-offs associated with increasing diversion ‘success rates’ were illustrated by means of cost tables and charts.
The inpatient analysis followed a similar approach, albeit this considered only those costs directly associated with the inpatient stay and/or the alternative packages provided to prevent admission. An adjustment was also made for the possibility that service users in any marginal inpatient case type may have more than one admission per year based on information from the baseline data collection, whereas estimates of the likely length of inpatient stay for each case type were informed by the discharge data collection.
The aggregate costs associated with the inappropriate admission of service users in each case type were then calculated: N × weekly costs × time on ward × repeat admission multiplier. In order to calcuate the costs of the alternative care needed to prevent such admissions, however, it was necessary to make a number of assumptions about the likely duration of the proposed care packages. The aim was to include only those inputs that acted as direct substitutes for inpatient admission. Thus if, for example, a social care package was recommended to prevent an inpatient spell of 50 days and it seemed likely that the patient would have received the same or a very similar package on discharge from hospital anyway (based on their obvious lack of critically needed formal support prior to admission), then only the ‘extra’ cost of the 50 days diverted from hospital was considered as an alternative social service cost. Following a similar principle, the alternative community mental health-care package was costed exactly as specified at the beginning, but assumed to reduce over time to a point at which it would not differ from the ‘normal’ level of support that might be expected after discharge from hospital anyway.
Activity 7.2
A range of key stakeholders from the participating sites, including service commissioners, managers, providers, front-line staff, older people and carers were invited to a presentation and discussion of the study’s main findings. This acted as a form of respondent validation and provided further understanding of the main issues. Attendees were also invited to comment on the impediments to health and social care staff participating in research and ways of enhancing service user recruitment.
Chapter 4 Services for older people with mental health problems. The North-West Balance of Care Study: findings I
The work described in the following two chapters sought to refine the BoC approach and to demonstrate its utility to the planning of services for older people with mental health problem in three areas of north-west England. This chapter aims to identify the number and characteristics of this client group in five different settings, and to identify those care home and inpatient admissions whose needs could be more appropriately met elsewhere.
MethodData collection exercises permitted the development of the most prevalent inpatient and care home entrant ‘case types’. Groups of practitioners subsequently identified what alternative care arrangements might be viable.
ResultsOf the 14 most prevalent care home entrant case types, nine (representing 53% of placements) could have been more appropriately supported at home or in ECH. Those case types judged most appropriate for care home placement tended to be older, male, and have a combination of high physical dependency, cognitive and/or behavioural difficulties. Of the 17 most prevalent inpatient case types, three (representing more than 10% of admissions) were considered ‘not appropriate’ by most practitioners, while a further two might potentially be better supported in the community. Those case types most likely to be rated as appropriate for inpatient admission tended to be at risk of self-harm, to live alone and to be unknown to mental health services.
ConclusionsThe analysis identified a number of care home entrants and inpatient admissions which might potentially have been avoided through the provision of community care. Whether or not these would be preferable, however, would depend on their costs and consequences.
Introduction
The first part of this chapter explores the current BoC in the study sites and the extent to which people with different profiles receive different services. This information then informs the identification of those people whose combination of needs suggest that they could potentially be met in more than one setting. These are people on the margins of care. Although this material forms only a proportion of that collected, it is designed to provide an understanding of those older people with mental health problems who are in contact with LA and specialist health services, and the potential to improve service provision. In the text, for ease of reference, links are made to the relevant sections of Chapter 3.
A profile of current service provision (see Chapter 3, Activity 3.1)
As previously noted, the study was undertaken in three sites in north-west England: site X (the main research site), site Y and site Z. According to the Office for National Statistics (ONS)158 site X (the main research site) is a ‘prospering smaller town’, site Y an ‘industrial hinterland’ and site Z a ‘centre with industry’. All three are predominantly urban.
Table 5 summarises relevant characteristics of their populations. In combination, they closely match the sociodemographic profile of England as a whole, covering a mix of relatively affluent as well as poor areas. In terms of health needs, the population of site X most closely resembles the England average, if rather older and less ethnically diverse. Although it has areas of significant deprivation, it also has a better average socioeconomic profile.
| Variable | Site X | Site Y | Site Z | England | Source |
|---|---|---|---|---|---|
| Population size (all adults aged ≥ 16 years) | 230,900 | 173,300 | 398,500 | 42,105,300 | ONS 2009159 estimates |
| Population size (adults aged ≥ 65 years) | 48,000 | 32,000 | 51,000 | 8,434,600 | ONS 2009159 estimates |
| Adults aged ≥ 65 years as a percentage of all adults | 21.7 | 19.3 | 12.6 | 20.0 | ONS 2009159 estimates |
| % pensioners living alone | 35.2 | 38.2 | 43.1 | 35.2 | ONS 2001160 |
| Age-standardised limiting long-term illness rate among people aged ≥ 65 years | 99 | 113 | 119 | 100 | aCSCI 2007161 |
| Pensioner income support rate per 1000 | 170 | 250 | 332 | 227 | aCSCI 2007161 |
| % ethnic minority population (% of population aged ≥ 65 years) | 4.3 (1.3) | 5.4 (1.9) | 19.0 (7.1) | 9.1 (2.9) | ONS 2001160 |
| % residents living in rural area | 8.6 | 1.1 | 0 | 19.5 | ONS 2001160 (DEFRA) |
| Standardised mortality ratio | 97 | 120 | 125 | 100 | aCSCI 2007161 |
As shown in Table 6, the levels of social care provided for older people in site X are also close to England averages, although a greater proportion of people in sites Y and Z receive intensive community and residential care. Indeed, compared with other areas in north-west England, site X appears to lack care home beds, including beds for people with dementia. Despite this, a relatively high proportion of older hospital patients are discharged to care homes. There is, in addition, no specialist ECH for older people with mental health problems, although the Council are committed to the principle of ECH and have upgraded a number of sheltered complexes into generic ECH facilities.
| Variable | Site X | Site Y | Site Z | England | Source |
|---|---|---|---|---|---|
| % of households in which care is provided (not age specific) | 10.4 | 10.6 | 8.9 | 9.7 | ONS 2001160 |
| Number of older people helped to live at home per 1000 aged ≥ 65 years | 91.4 | 97.0 | 107.3 | 80.2 | aCSCI 2007161 |
| Number of households receiving intensive home care per 1000 aged ≥ 65 years | 11.2 | 18.8 | 27.5 | 14.3 | aCSCI 2007161 |
| Number of people in long-stay residential care per 1000 aged ≥ 65 years | 15.1 | 23.4 | 21.2 | 14.1 | aCSCI 2007161 |
| Proportion of people aged ≥ 65 years discharged directly to residential care | 2.4 | 3.5 | 2.5 | Not known | ADASS/AQuA 2011162 |
| Percentage of per capita social services spending for people aged ≥ 75 years spent on residential care (gross) | 49 | 57 | 52 | 54 | aCSCI 2007161 |
In the 2008/9 performance assessment exercise, adult social care services provided by site X’s Council were considered to be ‘performing well’, and particular note was made of the Council’s rapid response and reablement services, use of technology and preventative interventions. Progress in providing services for carers and reducing long-term admissions was also commended.
Specialist mental health services for older people in site X are provided by site X NHS Foundation Trust, and were considered ‘excellent’ in the 2008/9 NHS performance rating exercise. Twenty-two acute mental health inpatient beds for people with functional mental health problems are provided at the district general hospital, with a 10-bedded ward for people with organic disorders in a small community hospital, where the large, multidisciplinary CMHT is also based. An earlier national survey suggested that the main barriers to providing good care for people with dementia in the area included problems arranging appropriate discharges for general hospital patients and inappropriate admissions to psychiatric wards. 163
Comparable services in site Y are managed by the same trust, though on another district general hospital site. These include two separate wards for people with organic and functional mental health problems (10 and 15 beds, respectively) and a CMHT with a specialist care home outreach function.
In site Z these services are delivered by site Z Integrated Trust, which has 61 acute mental health beds on three joint wards for people with functional and organic disorders located across the city. There are six CMHTs, which are of smaller size than those in sites X and Y, but contain a similar mix of staff. Although there have been concerns about aspects of the trust’s performance in recent years, the 2008/9 NHS performance rating exercise rated service quality as ‘good’.
Current service users (see Chapter 3, Activity 1.2)
Older people living at home with social services support but no specialist mental health input (site X)
Local authority information indicated that, in June 2011, there were 2375 older people (aged ≥ 65 years) recorded on the locality teams’ caseloads, of whom over three-quarters lived at home. Of the latter, almost 4 in 10 were open to a named practitioner. The original target sample size was 100, and baseline information was sought for 199, which although considerably less than originally requested, represented the maximum number of cases local managers deemed acceptable at a time of great organisational change given the lack of financial incentives for local authorities to participate in research.
Completed forms were returned for 128 service users, of whom 38 were excluded because they had no indication of mental health problems; a further 37 received specialist mental health input; and three no longer lived at home. This gave a study sample of 50 (i.e. approximately 64% of the maximum achievable number of eligible cases).
The first column of Table 7 details the sociodemographic characteristics, dependency and general health of this service user group. Mirroring the sampling frame, females outnumbered males by roughly two to one, while more than four-tenths were in the oldest age category, over one-quarter were very/totally dependent and a similar proportion had poor health. Over half lived on their own compared with some 35% of older people in site X generally.
| Attribute | Social services clients | CMHT clients | ECH tenants | Care home entrants | Acute inpatient admissions | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Site X (%) | Site X (%)a | Site Y (%)a | Site Z (%)a | All areas (%) | Site X (%) | Site Y (%) | Site Z (%) | Site X (%) | Site Y (%) | Site Z (%) | ||
| Gender | Female | 66.7 | 63.0 | 66.8 | 61.5 | 59.4 | 68.9 | 67.7 | 64.7 | 66.7 | 54.7 | 58.3 |
| Male | 33.3 | 37.0 | 33.2 | 38.5 | 40.6 | 31.1 | 32.3 | 35.3 | 33.3 | 45.3 | 41.7 | |
| Age (years) | 65–74 | 8.7b | 34.1 | 45.0 | 29.6 | 31.3 | 9.0 | 10.7 | 6.7b | 37.3 | 44.9 | 44.8 |
| 75–84 | 47.8 | 57.0 | 30.6 | 49.8 | 50.0 | 33.7 | 50.0 | 46.7 | 44.8 | 38.8 | 39.6 | |
| ≥ 85 | 43.5 | 8.9 | 24.4 | 20.7 | 18.8 | 57.3 | 39.3 | 46.7 | 17.9 | 16.3 | 15.6 | |
| Ethnicity | White | 89.1 | 95.7 | 95.3 | 92.5 | 100.0 | 100.0 | 100.0 | 94.1 | 100.0 | 96.2 | 92.6 |
| Non-white | 10.9 | 4.3 | 4.7b | 7.5 | – | – | – | 5.9b | – | 3.8b | 7.4 | |
| Usual or former place of residence | Home: alone | 56.0 | 47.8 | 51.1 | 46.1 | 50.0 | 58.4 | 41.0 | 29.4 | 28.4 | 40.4 | 42.6 |
| Home: with other | 40.0 | 51.8 | 46.3 | 44.2 | 32.2 | 39.3 | 32.8 | 17.7b | 53.8 | 32.7 | 35.1 | |
| Home: unclear | 2.0b | 0.4b | 2.6b | 9.8 | 3.6b | 1.1b | 14.8 | 17.7b | 1.5b | – | 3.2b | |
| Care home | N/A | N/A | N/A | N/A | 3.6b | N/A | N/A | N/A | 16.4 | 19.2 | 17.0 | |
| Other institution (e.g. ECH) | 2.0b | N/A | N/A | N/A | 10.7b | 1.1b | 11.5 | 35.3 | – | 7.7b | 2.1b | |
| ADLc | Independent | 18.8 | 87.2 | 68.3 | 67.9 | 48.4 | 5.6 | 10.7 | 41.2 | 56.7 | 50.9 | 70.8 |
| Minimal help needed | 33.3 | 7.9 | 20.2 | 18.0 | 32.3 | 23.6 | 19.6 | 23.5b | 25.4 | 32.1 | 21.9 | |
| Partially dependent | 20.8 | 3.8 | 6.1 | 7.9 | 16.1 | 38.2 | 30.4 | 23.5b | 7.5 | 11.3 | 4.2b | |
| Very dependent | 16.7 | 0.4b | 4.0b | 2.7 | – | 16.9 | 21.4 | 11.8b | 7.5 | 3.8b | 3.1b | |
| Totally dependent | 10.4 | 0.8b | 1.4b | 3.6 | 3.2b | 15.7 | 17.9 | – | 3.0b | 1.9b | – | |
| General health status | Very good/excellent | 4.4b | 19.3 | 10.5 | 18.6 | 3.5b | 10.7 | 9.8 | 6.3b | 12.1 | 17.7 | 6.5 |
| Good | 15.6 | 33.5 | 33.2 | 25.7 | 27.6 | 14.3 | 21.6 | 37.5 | 13.6 | 19.6 | 46.2 | |
| Fair | 57.8 | 29.4 | 38.0 | 36.1 | 37.9 | 38.1 | 33.3 | 31.3 | 34.9 | 41.2 | 36.6 | |
| Poor | 22.2 | 17.8 | 18.3 | 19.6 | 31.0 | 36.9 | 35.3 | 25.0b | 39.4 | 21.6 | 10.8 | |
| n (minimum–maximum) | 45–50 | 136–141 | 72–75 | 227–241 | 28–32 | 84–90 | 51–62 | 15–17 | 66–67 | 49–53 | 93–96 | |
As shown in Table 8, just under half had a known diagnosis of dementia. However, given their lack of contact with specialist mental health services (who often make such diagnoses), this may well be an underestimate. Indeed, Table 9 indicates that over three-quarters had at least mild cognitive impairment. Furthermore, although we lack data on severity, approximately half (53%) displayed indicators of low mood or anxiety. Similarly, over half had moderately or highly challenging behaviour.
| Diagnosis | Social services users | CMHT clients | ECH tenants | Care home entrants | Acute inpatient admissions | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Site X (%) | Site X (%)a | Site Y (%)a | Site Z (%)a | All areas (%) | Site X (%) | Site Y (%) | Site Z (%) | Site X (%) | Site Y (%) | Site Z (%) | ||
| Psychiatric diagnosis | Alzheimer’s disease | 18.0 | 5.6 | 4.2 | 13.2 | 9.4b | 21.1 | 8.1 | 5.9b | 3.0b | 15.1 | 8.3 |
| Vascular dementia | 22.0 | 13.7 | 7.7 | 8.4 | 6.3b | 24.4 | 8.1 | 23.5b | 10.5 | 15.1 | 8.3 | |
| Other unspecified dementia | 8.0 | 4.4 | 3.5 | 9.8 | 12.5b | 12.2 | 24.2 | 23.5b | 11.9 | 13.2 | 8.3 | |
| Other/multiple organic | 6.0b | 4.1 | 1.4b | 6.7 | 6.3b | 1.1b | 3.2 | 5.9b | 1.5b | 5.7b | 2.1b | |
| Depression/anxiety | 12.0 | 41.9 | 29.0 | 20.8 | 6.3b | 5.6a | – | 11.8b | 37.3 | 32.1 | 37.5 | |
| Other affective disorder | 2.0a | 10.4 | 5.9b | 6.6 | 6.3b | – | – | – | 16.4 | 7.6b | 6.3 | |
| Schizophrenia | – | 6.3 | 11.1 | 5.6 | 18.8 | – | 1.6b | 11.8b | 4.5b | 1.9b | 5.2 | |
| Other/multiple functional | – | 3.7b | 21.5 | 10.9 | 9.4b | – | – | 5.9b | 9.0 | 3.8b | 12.5 | |
| Mixed organic/functional | – | 7.4 | 8.7 | 7.4 | 6.3b | 6.7 | 4.8b | 5.9b | 4.5b | 5.7b | 7.3 | |
| No formal diagnosis reported | 32.0 | 2.6b | 7.0 | 10.7 | 18.8 | 28.9 | 50.0 | 5.9b | 1.5b | – | 4.2b | |
| n | 50 | 141 | 75 | 241 | 32 | 90 | 62 | 17 | 67 | 53 | 96 | |
| Mental health needs | Social services clients | CMHT clients | ECH tenants | Care home entrants | Acute inpatient admissions | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Site X (%) | Site X (%)a | Site Y (%)a | Site Z (%) | All areas (%) | Site X (%) | Site Y (%) | Site Z (%) | Site X (%) | Site Y (%) | Site Z (%) | ||
| Indicators of low mood (any) | Yes | 47.9 | 54.6 | 60.8 | 46.6 | 60.0 | 41.3 | 52.2 | 64.3 | 74.6 | 57.5 | 67.1 |
| No | 52.1 | 45.4 | 39.2 | 53.4 | 40.0 | 58.8 | 47.8 | 35.7 | 25.4 | 42.6 | 33.0 | |
| Indicators of anxiety | Yes | 23.4 | 37.3 | 48.7 | 35.2 | 54.8 | 47.4 | 52.3 | 40.0 | 39.7 | 62.5 | 42.9 |
| No | 76.6 | 62.8 | 51.3 | 64.8 | 45.2 | 52.6 | 47.7 | 60.0 | 60.3 | 37.5 | 57.1 | |
| Challenging behaviourb | Low | 43.8 | 56.3 | 31.8 | 37.2 | 25.0 | 21.1 | 3.7c | 5.9c | 10.5 | 17.0 | 10.4 |
| Medium | 47.9 | 41.5 | 62.3 | 59.9 | 62.5 | 48.9 | 59.3 | 76.5 | 73.1 | 52.8 | 61.5 | |
| High | 8.3c | 2.2 | 5.9c | 3.0 | 12.5c | 30.0 | 37.0 | 17.7c | 16.4 | 30.2 | 28.1 | |
| Cognitiond | Intact | 8.0c | 40.0 | 26.2 | 23.5 | 15.6 | 5.6 | 1.8c | – | 56.7 | 30.2 | 30.5 |
| Borderline intact | 14.0 | 22.6 | 31.6 | 24.0 | 18.8 | 6.7 | – | 5.9c | 14.9 | 13.2 | 26.3 | |
| Mild impairment | 20.0 | 11.1 | 16.2 | 24.7 | 31.3 | 10.0 | 7.1c | 5.9c | 4.5c | 15.1 | 14.7 | |
| Moderate impairment | 30.0 | 18.5 | 11.0 | 20.3 | 9.4c | 36.7 | 25.0 | 47.1 | 10.5 | 17.0 | 12.6 | |
| Moderate–severe impairment | 12.0 | 1.5c | 0.7c | 2.1 | 12.5c | 5.6 | 21.4 | 29.4 | 1.5c | 5.7c | 7.4 | |
| Severe impairment | 14.0 | 5.9 | 14.3 | 4.6 | 12.5c | 28.9 | 44.6 | 11.8c | 11.9 | 18.9 | 7.4 | |
| Very severe impairment | 2.0c | 0.4c | – | 0.8c | – | 6.7 | – | – | – | – | 1.1c | |
| MMSE score (categorisation) | Normal (25–30) | – | 45.7 | 39.9 | 37.0 | 22.2c | – | – | – | 41.7 | 50.0 | 28.6 |
| Mild (21–24) | – | 34.8 | 16.1 | 27.3 | 44.4c | 6.7c | 14.3c | 11.1c | 25.0c | 16.7c | 32.1 | |
| Moderate (10–20) | – | 15.2 | 40.8 | 32.2 | 33.3c | 73.3 | 42.9c | 55.6 | 33.3c | 27.8 | 39.3 | |
| Severe (<10) | – | 4.4c | 3.2c | 3.5 | – | 20.0c | 42.9c | 33.3c | – | 5.6c | – | |
| n (minimum–maximum) | 47–50 | 132–141 | 66–75 | 221–241 | 30–32 | 76–90 | 44–56 | 14–17 | 63–67 | 47–53 | 84–96 | |
| n (MMSE score) | – | 40 | 23 | 135 | 9 | 15 | 7 | 9 | 12 | 18 | 28 | |
Given this picture of general frailty plus cognitive impairment, the high proportion of people considered at risk of falls or self-neglect in Table 10 is perhaps not surprising. Almost one-quarter were reported to be of medium or high risk of accidental self-harm, with a similar proportion considered at risk of abuse by others, illustrating the vulnerability of this group.
| Risk type | Social services clients | CMHT clients | |||
|---|---|---|---|---|---|
| Site X (%) | Site X (%)a | Site Y (%)a | Site Z (%)a | ||
| Risk of falls | Low | 30.6 | 67.3 | 56.0 | 48.3 |
| Medium | 28.6 | 19.7 | 36.7 | 37.8 | |
| High | 40.8 | 13.0 | 7.3 | 14.0 | |
| Risk of self-neglect | Low | 39.6 | 66.9 | 43.3 | 49.6 |
| Medium | 29.2 | 24.9 | 48.5 | 36.1 | |
| High | 31.3 | 8.2 | 8.2 | 14.4 | |
| Risk of deliberate self-harm | Low | 100.0 | 86.2 | 87.2 | 90.6 |
| Medium | – | 13.8 | 7.5 | 8.4 | |
| High | – | – | 5.3b | 1.1b | |
| Risk of accidental self-harm | Low | 76.1 | 91.3 | 79.5 | 76.8 |
| Medium | 19.6 | 7.9 | 17.2 | 18.8 | |
| High | 4.4b | 0.8b | 3.3b | 4.4 | |
| Risk of abuse by others | Low | 69.8 | 94.8 | 81.9 | 81.9 |
| Medium | 25.6 | 4.5 | 14.8 | 16.0 | |
| High | 4.7b | 0.7b | 3.3b | 2.0 | |
| Risk of harm to others | Low | 95.2 | 97.0 | 95.1 | 97.1 |
| Medium | 2.4b | 2.6 | 4.2 | 2.6 | |
| High | 2.4b | 0.4b | 0.7b | 0.3b | |
| n (minimum–maximum) | 42–49 | 139–140 | 74–75 | 214–217 | |
Although the vast majority of service users had at least some informal care, and approximately two-thirds received ≥ 8 hours per week (Table 11), the nature of this help varied. Around half of carers (typically service users’ children) provided assistance with general tasks (e.g. shopping, housework) and emotional and social support, whereas the other half also undertook personal care. As expected, the overwhelming majority received formal social care, though only just over one-quarter received an intensive care package.
| Service receipt | Social services clients | CMHT clients | ECH tenants | Care home entrants | Acute inpatient admissionsa | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Site X (%) | Site X (%)b | Site Y (%)b | Site Z (%)b | All areas (%) | Site X (%) | Site Y (%) | Site Z (%) | Site X (%) | Site Y (%) | Site Z (%) | ||
| Informal care (at home) (hours) | None | 14.0 | 52.8 | 27.3 | 33.4 | 29.0 | 13.8 | 8.8 | 23.5c | 33.3 | 47.5 | 45.3 |
| 1–7 | 20.0 | 24.9 | 38.0 | 26.4 | 51.6 | 28.7 | 21.1 | 11.8c | 7.4c | 22.5 | 18.7 | |
| 8–20 | 34.0 | 8.3 | 17.3 | 19.5 | 19.4 | 31.0 | 33.3 | 41.2 | 9.3 | 10.0c | 24.0 | |
| ≥ 21 | 32.0 | 14.0 | 17.5 | 20.6 | – | 26.4 | 36.8 | 23.5c | 50.0 | 20.0 | 12.0 | |
| Main informal carerd | Spouse | 32.6 | 54.0 | 38.7 | 22.9 | 20.0c | 31.2 | 30.6 | 15.4c | 72.2 | 57.1 | 40.0 |
| Child (including in-laws) | 51.2 | 34.9 | 31.6 | 52.3 | 65.0 | 59.7 | 51.0 | 46.2 | 27.8 | 28.6 | 46.7 | |
| Someone else | 16.3 | 11.1 | 29.7 | 24.8 | 15.0c | 9.1 | 18.4 | 38.5 | – | 14.3c | 13.3 | |
| Lives with main informal carerd | Yes | 39.5 | 62.7 | 47.4 | 41.2 | 4.6c | 37.2 | 38.5 | 30.8c | 80.6 | 59.1 | 53.7 |
| No | 60.5 | 37.3 | 52.7 | 58.8 | 95.5 | 62.8 | 61.5 | 69.2 | 19.4 | 40.9 | 46.3 | |
| Nature of informal supportd | Personal and/or physical | 48.7 | 32.2 | 35.8 | 40.6 | – | 47.1 | 37.5 | 63.6 | 20.0 | 53.3 | 54.3 |
| Other practical help | 51.3 | 67.8 | 64.2 | 59.4 | 100.0 | 52.9 | 62.5 | 36.4c | 80.0 | 46.7 | 45.7 | |
| Formal social support (at home) | None or very minor | 8.2 | 64.5 | 37.0 | 50.0 | 3.5c | 20.2 | 5.8c | 42.9 | 85.1 | 55.6 | 67.8 |
| Intermittent support | 6.1 | 5.7 | 11.3 | 6.0 | – | 2.4c | 3.9c | – | 8.5c | 22.2 | 5.1c | |
| Limited care package | 51.0 | 20.0 | 37.6 | 28.8 | 65.5 | 28.6 | 25.0 | 28.6c | 4.3c | 8.3c | 22.0 | |
| Intensive care package | 34.7 | 9.8 | 14.1 | 15.2 | 31.0 | 48.8 | 65.4 | 28.6c | 2.1c | 13.9 | 5.1c | |
| CMHT input | Yes | N/A | 98.8 | 100.0 | 100.0 | 96.8 | 44.8 | 54.4 | 94.1 | 69.7 | 73.6 | 75.0 |
| No | 100.0 | 1.2c | – | – | 3.2c | 55.2 | 45.7 | 5.9c | 30.3 | 26.4 | 25.0 | |
| Recent mental health admission | Yes | 5.1c | 16.2 | 10.1 | 15.1 | 4.4c | 5.3c | 13.3c | 36.4c | 16.1 | 19.2 | 17.6 |
| No | 94.1 | 83.8 | 89.9 | 84.9 | 95.6 | 94.7 | 86.7 | 63.6 | 83.9 | 80.9 | 82.4 | |
| n (informal/formal care) | 50, 49 | 139, 139 | 74, 71 | 237, 215 | 31, 29 | 87, 84 | 57, 52 | 17, 14 | 54, 47 | 40, 36 | 75, 59 | |
| n (minimum–maximum)d | 39–43 | 85–90 | 54–58 | 168–180 | 20–22 | 68–78 | 32–52 | 11–13 | 35–36 | 15–22 | 35–45 | |
| n (mental health input) | 50, 40 | 140, 121 | 72, 56 | 237, 202 | 31, 23 | 87, 75 | 46, 30 | 17, 11 | 66, 62 | 53, 47 | 92, 91 | |
Older people living at home with community mental health team support (sites X, Y and Z)
The original target sample size was 900 and, based on information supplied by practitioners, at the point of sampling there were 1277 people on the CMHT caseloads. However, of these, only 926 (73%) were aged ≥ 65 years and lived at home [significantly less than the number indicated by the participating trusts’ information technology (IT) systems at the study design stage].
Baseline information was sought for 542 cases and completed forms returned for 501. Of these, 14 were excluded because they no longer lived at home/had moved out of area, 10 were duplicates, eight had not been assessed/seen in the past 3 months, seven were in hospital and five had died. This gave a study sample of 457 (i.e. approximately 93% of the maximum achievable number of eligible cases).
Of the 141 who were from site X, the proportion of women on the CMHT caseload (see column 2, Table 7) was similar to that in the social services sample. However, the CMHT clients were significantly more likely to be physically independent (design-based chi-squared: 95.34, F = 1,187, p < 0.001) and were in better physical health (design-based chi-squared: 8.41, F = 1,190, p = 0.004). They also appeared more likely to live with others, although this was not statistically significant (design-based chi-squared: 0.87, F = 1,190, p = 0.351).
Such differences are, at least in part, likely to be age related, for the CMHT sample were significantly younger (mean age of 77.3 years) than the social services caseload [mean age of 83.6 years; t-test/weighted regression: t = –5.09, degrees of freedom (df) = 186, p < 0.001]. However, they may also be influenced by the different referral criteria the two agencies operate. Thus, while over a third of the CMHT caseload had a known organic disorder (including people with co-existent functional mental health problems), more than four-tenths had a primary diagnosis of anxiety and/or depression (see Table 8).
Table 9 confirms that the CMHT caseload were significantly less likely than the social services sample to be cognitively impaired (design-based chi-squared: 16.78, F = 1,190, p < 0.001) and displayed significantly lower levels of challenging behaviour (design-based chi-squared: 4.89, F = 1,189, p = 0.028). However, they did not have more indicators of low mood or anxiety (design-based chi-squared: 0.60, F = 1,183, p = 0.439). This variation is again likely to be related to their respective diagnostic profiles. Indeed, further analysis of just cases with dementia showed that, although the CMHT clients had a younger, more independent profile than their social services counterparts, their affect and behaviour were very similar.
Given these differences, the significantly smaller proportion of the CMHT than of the social services caseload considered at high risk from falls or self-neglect is understandable, for both are likely to be frailty/dependency related, whereas the CMHT caseload contained a greater proportion of people considered at moderate risk of deliberate self-harm (see Table 10). The caseloads’ differing sociodemographic and clinicial profiles are also likely to explain the different patterns of support shown in Table 11, with a significantly higher proportion of the CMHT caseload receiving no informal (design-based chi-squared: 22.0, F = 1,188, p < 0.001) or formal social care (design-based chi-squared: 48.63, F = 1,187, p < 0.001). Not surprisingly, however, the vast majority of the CMHT caseload had received CMHT input in the previous month, and approaching one-sixth had a mental health inpatient admission in the previous 6 months.
In comparison with the site X CMHT sample, the sites Y and Z caseloads had a somewhat older, more dependent profile. The site Z sample also contained a higher proportion of people with dementia.
Extra care housing residents (sites X, Y and Z)
Information was collected about 32 older people with mental health problems living in ECH (original target sample size n = 30). Of these, nine were generic ECH tenants known to site X’s council, whereas the remainder were tenants of specialist mental health facilities identified by sites Y and Z’s CMHTs. Although not a random sample, these arguably represent the range of older people with mental health problems for whom ECH was provided in the study area.
Given their small number and mixed provenance, no statistical analysis was undertaken on these data. Nevertheless, the fifth column of Table 7 suggests that although this group had a similar age profile to the site X CMHT caseload, they were in poorer health and more dependent, if not as dependent as the social services sample. As might be expected, the vast majority of tenants (87%), about whom CMHTs provided information, but fewer site X cases (67%), about whom generic social care teams provided data, had a formal psychiatric disorder. Moreover, whereas most of the site X tenants had dementia, the majority in site Y had a functional mental illness and the site Z sample had a more mixed profile (see Table 8). Understandably, then, the site X tenants were rather less likely to display indicators of anxiety or depression and rather more likely to be cognitively impaired than tenants in other areas (see Tables 9 and 10). However, levels of challenging behaviour (which were somewhat higher than in the previous samples) and risk were simliar in all sites.
In terms of their level of support, Table 11 shows that, although the majority of ECH tenants (all in site X) received informal care, the level of this was generally lower than that in the social services or CMHT samples, while in no instance were family or friends providing personal care. On the other hand, all bar one tenant received formal social support, and roughly one-third received an intensive care package (similar to the social services sample), with the risk of self-neglect said to have contributed to approximately four-tenths of moves to ECH (Table 12).
| Risk | Reasona | ECH tenants | Care home entrants | Acute inpatient admissions | ||||
|---|---|---|---|---|---|---|---|---|
| All areas (%) | Site X (%) | Site Y (%) | Site Z (%) | Site X (%) | Site Y (%) | Site Z (%) | ||
| Risk of falls | No | 78.1 | 47.8 | 58.1 | 58.8 | 85.1 | 100.0 | 94.8 |
| Yes | 21.9 | 52.2 | 41.9 | 41.2 | 14.9 | – | 5.2 | |
| Risk of self-neglect | No | 59.4 | 46.7 | 56.5 | 64.7 | 53.7 | 79.3 | 55.2 |
| Yes | 40.6 | 53.3 | 43.6 | 35.3 | 46.3 | 20.8 | 44.8 | |
| Risk of deliberate self-harm | No | 96.9 | 97.8 | 96.8 | 100.0 | 74.6 | 79.3 | 67.7 |
| Yes | 3.1b | 2.2b | 3.2b | – | 25.4 | 20.8 | 32.3 | |
| Risk of accidental self-harm | No | 93.8 | 64.4 | 72.6 | 64.7 | 89.6 | 98.1 | 78.1 |
| Yes | 6.3b | 35.6 | 27.4 | 35.3 | 10.5 | 1.9b | 21.9 | |
| Risk of abuse by others | No | 81.3 | 95.6 | 93.6 | 88.2 | 91.0 | 98.1 | 92.7 |
| Yes | 18.8 | 4.4b | 6.5b | 11.8b | 9.0 | 1.9b | 7.3 | |
| Risk of harm to others | No | 100.0 | 92.2 | 87.1 | 94.1 | 77.6 | 79.3 | 81.3 |
| Yes | – | 7.8 | 12.9 | 5.9b | 22.4 | 20.8 | 18.8 | |
| n | 32 | 90 | 62 | 17 | 67 | 53 | 96 | |
Perhaps not surprisingly given the nature of the sampling frame, the most frequently reported reason for moving into ECH was the person’s mental health. Indeed, this was the main reason in approximately one-quarter of cases (Tables 13 and 14). Physical health problems and an inability to perform daily activities of living were also commonly given reasons for moving into ECH, although these were rarely the main reason, with other, often related, factors such as the risk of self-neglect or breakdown of care, carrying more weight. Service users’ preferences were said to have contributed to the move in four-tenths of cases.
| Reason for admission | ECH tenants | Care home entrants | ||
|---|---|---|---|---|
| All areas (%) | Site X (%) | Site Y (%) | Site Z (%) | |
| Physical health problems | 41 | 62 | 46 | 35 |
| Mental health problems | 66 | 72 | 77 | 76 |
| Inability to perform daily activities of living | 63 | 84 | 81 | 65 |
| Need for rehabilitation | 13a | 2a | 8 | 6a |
| At unacceptable risk of deliberate self-harm | 3a | 2a | 3a | – |
| At unacceptable risk of accidental self-harm | 6a | 36 | 27 | 35 |
| At unacceptable risk of falls | 22 | 52 | 42 | 41 |
| At unacceptable risk of harming others | – | 8 | 13 | 6a |
| At unacceptable risk of self-neglect | 41 | 53 | 44 | 35 |
| At unacceptable risk of abuse/exploitation | 19 | 4a | 6a | 12a |
| Presenting with disruptive behaviours | 13a | 24 | 32 | 24a |
| Lack of motivation to care for self | 38 | 32 | 29 | 24a |
| Usual place of residence physically unsuitable | 22 | 10 | 16 | 24a |
| Homelessness | 6a | 2a | 2a | – |
| Recent catastrophic event (e.g. acute illness) | 9a | 18 | 10 | 12a |
| Loneliness/isolation | 16 | 26 | 10 | 29a |
| Anxiety/fear | 28 | 30 | 16 | 24a |
| Joining spouse or partner | 3a | 1a | – | – |
| Carer stress | 19 | 40 | 35 | 29a |
| Other breakdown of care | 16 | 13 | 13 | 18a |
| Service user’s preference | 41 | 12 | 8 | 12a |
| n | 32 | 90 | 62 | 17 |
| Main reason for admission | ECH tenants | Care home entrants | ||
|---|---|---|---|---|
| All areas (%) | Site X (%) | Site Y (%) | Site Z (%) | |
| Physical health problems | – | 25.6 | 25.0 | 12.5a |
| Mental health problems | 25.9 | 29.3 | 31.8 | 25.0a |
| Inability to perform daily activities of living | 7.4a | 1.2a | 11.4 | 18.8a |
| Need for rehabilitation | – | – | 2.3a | – |
| At unacceptable risk of deliberate self-harm | – | – | – | – |
| At unacceptable risk of accidental self-harm | – | 2.4a | 6.8a | – |
| At unacceptable risk of falls | – | 4.9a | – | 12.5a |
| At unacceptable risk of harming others | – | – | 2.3a | – |
| At unacceptable risk of self-neglect | 18.5 | 8.5 | 6.8a | 12.5a |
| At unacceptable risk of abuse/exploitation | – | – | – | – |
| Presenting with disruptive behaviours | – | 4.9a | 2.3a | 12.5a |
| Lack of motivation to care for self | 3.7a | – | – | 6.3a |
| Usual place of residence physically unsuitable | 3.7a | – | 2.3a | – |
| Homelessness | – | – | – | – |
| Recent catastrophic event (e.g. acute illness) | – | 2.4a | – | – |
| Loneliness/isolation | – | – | – | – |
| Anxiety/fear | 7.4a | 4.9a | – | – |
| Joining spouse or partner | 3.7a | – | – | – |
| Carer stress | 3.7a | 8.5 | 4.6a | – |
| Other breakdown of care | 14.8 | 7.3 | 4.6a | – |
| Service user’s preference | 11.1a | – | – | – |
| n | 27 | 82 | 44 | 16 |
Care home entrants (sites X, Y and Z)
The original target sample size was 350, but recruitment to this strand of the study was severely affected by the unexpected decision of the Council in site Z not to participate in the research, despite prior commitment. Nevertheless, information was collected about 197 care home entrants (including 104 from site X out of a possible 150 in the data collection period). Of these, 28 (14%) were excluded because they had no identified mental health problems. This gave a study sample of 169 (i.e. approximately 69% of the maximum achievable number of eligible cases).
In contrast to the domiciliary and ECH samples, all of whom were resident in their settings, these individuals were described as they presented just before care home entry. Most did not move into a care home directly from home. Indeed, of the 164 people for whom this information was available, 81 (49%) were transferred from a general hospital ward and 15 (9%) from a mental health ward.
The sociodemographic, functional and general health characteristics of the site X care home entrants are detailed in Table 7 (sixth column). Women again outnumbered men by roughly two to one and the mix of people living alone/with others was also similar to the social services sample. The mean age (84.8 years) of the care home entrants was, however, significantly higher than in previous settings (mean of 78.2 years; t-test/weighted regression: t = 6.97, df = 275, p < 0.001). Accordingly, they were more likely to need help with daily activities (design-based chi-squared: 140.46, F = 1,276, p < 0.001) and experienced worse physical health (only 30% reported to be in a least good health; design-based chi-squared: 7.84, F = 1,280, p = 0.006).
As might be expected, approaching nine-tenths had at least mild cognitive impairment, and a similar proportion of those with formal psychiatric diagnoses had an organic mental health problem (predominantly dementia) (see Tables 8 and 9). Indeed, over one-third had severe/very severe impairment, and nearly four-fifths presented moderate or worse levels of challenging behaviour, which typically included agitation, aggression and/or wandering, setting them apart from previous samples. Anxiety was more evident in this group, while the fact that more than half were considered at risk of falls (see Table 12) indicates their physical as well as mental frailty.
This group received similar levels of informal support before admission to that of the social services domiciliary sample, the vast majority having had some help, typically from their children (see Table 11). However, although just under half had an intensive formal social care package, approximately one-fifth received no/minor social care input. Furthermore, less than half had received recent mental health support.
Consistent with this profile, the most commonly cited reason for care home admission was the service user’s inability to undertake daily activities of living (see Table 13), although this was never the only factor implicated, and very rarely the main one (see Table 14). As with the ECH sample, mental health problems were the most important driver for admission, while physical health problems also featured highly as both ‘a’ and ‘the main’ reason for admission. Other factors cited in at least one-third of cases included carer stress and the risk of falls, self-neglect and accidental self-harm.
Compared with site X, site Y entrants were slightly younger and rather less likely to have been living alone, but had similar health and dependency profiles. Reported levels of cognitive impairment and challenging behaviour, and formal and informal care inputs were, however, all higher in this site. Site Z cases, all identified by CMHTs, presented a rather different subgroup, with a higher proportion experiencing functional mental health problems, while remaining relatively independent. Nonetheless, nearly all presented with at least moderately challenging behaviour and over one-third with a recent mental health admission.
Acute mental health inpatient admissions (sites X, Y and Z)
The original target sample size was 300, but recruitment to this strand of the research was affected by a number of issues, including the closure to admissions of one of the participating wards. However information was collected about 216 admissions to acute mental health beds (67 in site X) of which the vast majority (96%) related to people who had a single admission episode in the 6-month data collection period.
Within the site X sample (see ninth column, Table 7) the gender ratio was very similar to that in other settings, though a significantly lower proportion of women had an organic rather than a functional diagnosis (chi-squared: 4.13, df = 1, p = 0.042). Although the whole sample’s age profile was relatively young and independent, the mean age of the organic cases (80.0 years) was somewhat older than that of the functional ones (mean of 77.1 years; one-sided t-test: t = 1.33, df = 64, p = 0.094; note, the effect is highly significant in a two-sided t-test when pooling all three locations). Organic cases appeared to be in better health (chi-squared: 3.39, df = 1, p = 0.066) with 48% of functional cases (as opposed to 24%) reportedly suffering poor health.
Although these findings were not unexpected, the very low proportion of inpatients who lived alone prior to admission was more surprising, possibly arising by chance. An alternative explanation is that the one-sixth of admissions from care homes previously lived alone. Certainly, the admissions from care homes formed a distinct subgroup, with more than one-third being very or totally dependent.
Diagnostic and clinical profiles (see Tables 8 and 9) suggest that people with a functional disorder outnumbered people with organic problems by roughly two to one. A very high percentage of inpatients exhibited indicators of low mood, while the proportion who exhibited at least moderately challenging behaviour was also greater than in any other setting, highlighting the severity of this sample’s presentation. Almost half were described as often agitated/restless; a similar proportion displayed at least occasional delusions/hallucinations/paranoia; still more were sometimes or often disturbed at night; and almost four-fifths were considered at unacceptable risk of deliberate self-harm, harming others or self-neglect (see Table 12).
Approximately two-thirds of the inpatients who normally lived at home received some informal care before their admission, most commonly from their spouse (see Table 11). Indeed, half received more than 20 hours of help per week. However, less than one-quarter were said to have had any formal social support, and only one had an intensive care package. Interestingly, most (over seven-tenths) were receiving community mental health input, and approximately one-sixth had undergone a recent inpatient admission.
Table 15 shows the two most frequent reasons for inpatient admission as behavioural management and medication review, whereas other factors contributing to at least one-third of cases were the risk of self-neglect, the need for general diagnostic assessment and carer stress. As in the care home admission sample, these were not necessarily the main reasons for admission. Although behavioural management was the most frequently cited main driver for admission, this was closely followed by the risk of harm to others for the organic and care home subgroups, and the risk of deliberate self-harm for the functional subgroup (Table 16).
| Diagnostic group | Site X | Site Y | Site Z | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| O (%) | F (%) | All (%) | O (%) | F (%) | All (%) | O (%) | F (%) | All (%) | O (%) | F (%) | All (%) | |
| At unacceptable risk of deliberate self-harm | 14a | 31 | 26 | 3a | 42 | 21 | 12a | 44 | 33 | 10 | 39 | 27 |
| At unacceptable risk of accidental self-harm | 14a | 9a | 11 | 3a | – | 2a | 27 | 17 | 21 | 16 | 11 | 13 |
| At unacceptable risk of self-neglect | 24 | 58 | 47 | 24 | 17a | 21 | 30 | 51 | 43 | 27 | 47 | 39 |
| At unacceptable risk of falls | 24 | 11 | 15 | – | – | – | 9a | 3a | 5a | 10 | 5 | 7 |
| At unacceptable risk of harming others | 43 | 13 | 23 | 38 | – | 21 | 30 | 12 | 18 | 36 | 10 | 20 |
| At unacceptable risk of abuse/exploitation | 5a | 11 | 9 | 3a | – | 2a | 6a | 7a | 7 | 5a | 7 | 6 |
| For general diagnostic assessment | 38 | 40 | 39 | 17 | 29 | 23 | 67 | 41 | 50 | 42 | 38 | 40 |
| For behavioural management | 62 | 69 | 67 | 52 | 8a | 32 | 52 | 27 | 36 | 54 | 38 | 45 |
| For review of medication | 67 | 62 | 64 | 52 | 8a | 32 | 88 | 81 | 84 | 70 | 61 | 64 |
| For other treatment | – | 9a | 6a | 10a | 4a | 8a | 6a | 10 | 9 | 6 | 9 | 8 |
| For assessment of future care needs/placement | 19a | 9a | 12 | 62 | 8a | 38 | 67 | 39 | 49 | 53 | 23 | 35 |
| To relieve carer stress | 38 | 49 | 45 | 21 | 4a | 13 | 42 | 22 | 29 | 34 | 28 | 30 |
| Other breakdown of care | – | 7a | 5a | 24 | – | 13 | 9a | 8a | 9 | 12 | 6 | 9 |
| n | 21 | 45 | 66 | 29 | 24 | 53 | 33 | 59 | 92 | 83 | 128 | 211 |
| Diagnostic group | Site X | Site Y | Site Z | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| O (%) | F (%) | All (%) | O (%) | F (%) | All (%) | O (%) | F (%) | All (%) | O (%) | F (%) | All (%) | |
| At unacceptable risk of deliberate self-harm | 4.8a | 28.9 | 21.2 | – | 40.0 | 16.7 | 6.1a | 32.8 | 23.1 | 3.7a | 32.5 | 21.0 |
| At unacceptable risk of accidental self-harm | – | 6.7a | 4.6a | – | – | – | 9.1a | 1.7a | 4.4a | 3.7a | 3.3a | 3.4 |
| At unacceptable risk of self-neglect | 9.5a | 11.1 | 10.6 | 17.9 | 10.0a | 14.6 | 15.2 | 29.3 | 24.2 | 14.6 | 19.5 | 17.6 |
| At unacceptable risk of falls | – | – | – | – | – | – | – | – | – | – | – | – |
| At unacceptable risk of harming others | 23.8 | 8.9a | 13.6 | 21.4 | – | 12.5 | 15.2 | – | 5.5 | 19.5 | 3.3a | 9.8 |
| At unacceptable risk of abuse/exploitation | – | 2.2a | 1.5a | 3.6a | – | 2.1a | 3.0a | 1.7a | 2.2a | 2.4a | 1.6a | 2.0a |
| For general diagnostic assessment | 14.3a | 6.7a | 9.1 | 10.7a | 35.0 | 20.8 | 6.1a | 5.2a | 5.5 | 9.8 | 10.6 | 10.2 |
| For behavioural management | 33.3 | 22.2 | 25.8 | 32.1 | 5.0a | 20.8 | 18.2 | 13.8 | 15.4 | 26.8 | 15.5 | 20.0 |
| For review of medication | 4.8a | – | 1.5a | 3.6a | 5.0a | 4.2a | 6.1a | 10.3 | 8.8 | 4.9a | 5.7a | 5.4 |
| For other treatment | – | 4.4a | 3.0a | 3.6a | – | 2.1a | 3.0a | 1.7a | 2.2a | 2.4a | 2.4a | 2.4 |
| For assessment of future care needs/placement | – | – | – | – | 5.0a | 2.1a | 9.1a | – | 3.3a | 3.7a | 0.8a | 2.0a |
| To relieve carer stress | 9.5a | 6.7a | 7.6 | 7.1a | – | 4.2a | 3.0a | – | 1.1a | 6.1 | 2.4a | 3.9 |
| Other breakdown of care | – | 2.2a | 1.5a | – | – | – | 6.1a | 3.5a | 4.4a | 2.4a | 2.4a | 2.4 |
| n | 21 | 45 | 66 | 28 | 20 | 48 | 33 | 58 | 91 | 82 | 123 | 205 |
Compared with their site X counterparts, the site Y and site Z samples were younger and more likely to live alone. They also had a higher proportion of men, but a similar proportion of care home residents. The site Y sample included a higher percentage of people with an organic mental health problem (chi-squared: 7.28, df = 2, p = 0.026), whereas the site Z cohort seemed to be in better physical health (chi-squared: 34.52, df = 6, p < 0.001) and more independent. Levels of challenging behaviour were high throughout, and the need for behavioural management and an unacceptable risk of deliberate self-harm featured among the top three reasons for admission in all sites. The proportion of admissions with previous CMHT support or inpatient admissions were also almost identical.
Although the previous four settings may be perceived as people’s permanent residence, an inpatient ward is generally a short-term placement. In resource terms, this raises questions about the appropriateness of admission, the timing of discharge and the extent to which certain inpatients stay longer than necessary. To investigate this, discharge data was obtained for approximately two-thirds of the sample (Table 17). This covered around four-fifths of admissions in sites X and Y, but less than half in site Z where baseline data collection started later.
| Inpatient status at follow-up | Site X | Site Y | Site Z | Total |
|---|---|---|---|---|
| Number of patients for whom baseline information was available | 67 | 53 | 96 | 216 |
| Number of patients who died in hospital | 1 | 1 | 1 | 3 |
| Number of patients transferred to general hospital wards and lost to follow-up | 2 | 5 | 1 | 8 |
| Number of patients transferred to other mental health wards and lost to follow-up | 3 | 2 | 4 | 9 |
| Number of patients not ready for discharge at end of follow-up | 3 | 1 | 44 | 48 |
| Number of patients for whom at least some discharge data was provided at follow-upa | 56 | 44 | 46 | 146 |
The mean length of stay (LOS) for completed inpatient episodes was nearly 68 days (Table 18). However, people with organic mental health problems typically stayed longer than people with functional disorders (Mann–Whitney: z = –2.50, p = 0.012), and inpatient stays in site Y were longer than elsewhere (84 days compared with 64 and 57 days) (Mann–Whitney: z = –1.81, p = 0.070).
| Diagnostic group | Site X | Site Y | Site Z | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| O | F | All | O | F | All | O | F | All | O | F | All | |
| Mean LOS of completed cases (days) | 78.1 | 58.2 | 63.6 | 100.4 | 67.9 | 83.8 | 75.4 | 47.4 | 57.0 | 86.5 | 57.1 | 67.6 |
| Median LOS of completed cases (days) | 49 | 50.5 | 50.5 | 91 | 58.5 | 74 | 80 | 48 | 56 | 77 | 49 | 57 |
| n (LOS) | 15 | 40 | 56 | 21 | 22 | 43 | 15 | 29 | 44 | 51 | 91 | 143 |
| Percentage of inpatients with delayed discharge | 73.3 | 17.9 | 33.3 | 77.7 | 36.8 | 56.7 | 93.3 | 81.4 | 85.7 | 81.3 | 42.3 | 56.4 |
| Mean length of delay (days) | 13.8 | 5.4 | 10.6 | 9.2 | 3.9 | 7.4 | 22.5 | 8.9 | 13.9 | 15.1 | 7.3 | 11.3 |
| Median length of delay (days) | 7 | 6 | 7 | 2 | 4 | 2 | 11 | 5 | 7 | 7 | 5 | 6 |
| n (delayed discharge) | 11 | 7 | 18 | 14 | 7 | 21 | 13 | 22 | 35 | 38 | 36 | 74 |
Of 100 patients admitted from their own home (either directly or via another ward/service), most (81) returned there, while one person was discharged to ECH and 16 others (12 with organic disorders) entered a care home, including four in site X. In the great majority of cases (123/129, 95%), the discharge setting was deemed optimal in which to meet their needs, with four of the remaining six entering a care home when a less intensive care setting was judged preferable.
Only a minority (58 of 132 admissions, 43.9%) were discharged on the date they were deemed medically fit for discharge, with the remainder experiencing some delay. Although in 22 cases (29.7%) this was just 1 or 2 days, while discharge arrangements were confirmed (medications obtained, transport arranged, etc.), 34 discharges (46.0%) were delayed by at least a week, and 12 (16.2%) by more than a fortnight. The most commonly given reason for longer delays was the need to organise a suitable care home placement, including the identification of an appropriate home, funding and assessment by care home staff.
People on the margins of care (see Chapter 3, Activities 2.1, 2.2, 3.1, 3.2 and 3.3)
An empirical analysis of the overlap between the domiciliary, extra care housing and care home samples
As seen in Table 19, of the 27 case types used to characterise the domiciliary, ECH and care home samples, 26 were populated. Together they captured 94% of the social services sample, 99% of the CMHT sample, 97% of the ECH sample and 94% of the care home sample. However, some case types were more prevalent than others and their distribution varied across settings.
| Case type number | Case type profile | Social services clients | CMHT clients | ECH tenants | Care home entrants | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physical dependency | Cognitive impairment | Challenging behaviour | Site X (%) | Site X (%) | Site Y (%)a | Site Z (%)a | All (%) | All areas (%) | Site X (%) | Site Y (%) | Site Z (%) | All (%) | |
| 1 | Low | Low | Low | 17.0 | 48.1 | 29.0 | 31.4 | 36.6 | 19.4 | 1.1b | – | 5.9b | 1.3b |
| 2 | Low | Low | Medium | 12.8 | 24.4 | 37.7 | 32.1 | 30.5 | 32.3 | 5.6 | 3.8b | – | 4.4 |
| 3 | Low | Low | High | – | – | 0.7b | 0.8b | 0.5b | 6.5b | – | – | – | – |
| 4 | Low | Medium | Low | 4.3b | 5.6 | 0.7b | 4.0 | 3.9 | – | – | – | – | – |
| 5 | Low | Medium | Medium | 8.5b | 10.5 | 6.3 | 13.4 | 11.1 | 6.5b | 6.7 | 5.7b | 35.3 | 9.4 |
| 6 | Low | Medium | High | – | 0.8b | 2.6b | – | 0.7b | – | 4.5b | 5.7b | 5.9b | 5.0 |
| 7 | Low | High | Low | 2.1b | 1.1b | – | 0.3b | 0.5b | 3.2b | – | – | – | – |
| 8 | Low | High | Medium | 6.4b | 3.4 | 8.9 | 4.0 | 4.7 | 6.5b | 2.3b | 9.4 | 11.8b | 5.7 |
| 9 | Low | High | High | – | 1.1b | 2.6b | 0.3b | 1.0 | 6.5b | 9.0 | 7.6b | 5.9b | 8.2 |
| 10 | Medium | Low | Low | 4.3b | 0.4b | 0.7b | – | 0.3b | 3.2b | 3.4b | – | – | 1.9b |
| 11 | Medium | Low | Medium | 2.1b | 0.4b | 2.6b | 5.6 | 3.3 | 3.2b | 4.5b | 1.9b | 5.9b | 3.8 |
| 12 | Medium | Low | High | – | – | – | 0.3b | 0.1b | – | 1.1b | – | – | 0.6b |
| 13 | Medium | Medium | Low | 4.3b | 0.4b | 1.4b | 0.5b | 0.6 | – | 4.5b | – | – | 2.5b |
| 14 | Medium | Medium | Medium | 2.1b | 1.5b | – | 0.8b | 0.9 | 3.2b | 9.0 | 5.7b | – | 6.9 |
| 15 | Medium | Medium | High | – | – | – | – | – | – | 2.3b | – | 5.9b | 1.9b |
| 16 | Medium | High | Low | – | – | – | – | – | – | 1.1b | – | – | 0.6b |
| 17 | Medium | High | Medium | 6.4b | 1.1b | 1.4b | 0.3b | 0.8 | 6.5b | 5.6 | 11.3 | 11.8b | 8.2 |
| 18 | Medium | High | High | 2.1b | – | – | 0.3b | 0.1b | – | 6.7 | 13.2 | – | 8.2 |
| 19 | High | Low | Low | 2.1b | – | – | 1.0b | 0.5b | – | 2.3b | – | – | 1.3b |
| 20 | High | Low | Medium | 2.1b | – | 3.3b | 1.0b | 1.1b | – | 4.5b | 1.9b | – | 3.1 |
| 21 | High | Low | High | – | – | – | – | – | – | – | – | – | – |
| 22 | High | Medium | Low | 8.5b | – | – | 0.3b | 0.1b | – | 4.5b | 1.9b | – | 3.1 |
| 23 | High | Medium | Medium | – | – | – | 1.4b | 0.7b | – | 4.5b | 5.7b | – | 4.4 |
| 24 | High | Medium | High | 2.1b | – | – | – | – | – | 1.1b | 1.9b | – | 1.3b |
| 25 | High | High | Low | – | – | – | – | – | – | 4.5b | 1.9b | – | 3.1 |
| 26 | High | High | Medium | 8.5b | 0.8b | 2.1b | 1.3 | 1.3 | 3.2b | 6.7 | 13.2 | 11.8b | 9.4 |
| 27 | High | High | High | 4.3b | 0.4b | – | 1.1b | 0.6 | – | 4.5b | 9.4 | – | 5.7 |
| n | 47 | 140 | 75 | 236 | 451 | 31 | 89 | 53 | 17 | 159 | |||
The most common case types were case type 1 in the two domiciliary settings (low dependency, low cognitive impairment, low challenging behaviour), case type 2 (low dependency, low cognitive impairment, medium challenging behaviour) in the ECH sample and case type 5 (low dependency, medium cognitive impairment, medium challenging behaviour) for the care home entrants. In order to render the text more readable, in the remainder of this report these have been abbreviated to LLL, LLM and LMM, with all other combinations of the three defining characteristics following the same pattern.
Case types commonly found in more than one setting (i.e. containing at least 5% of two or more samples) might theoretically represent people on the margins of care, although given the small numbers in some of these cells, it clearly is not possible to say definitively these are the boundaries offering the biggest scope for service substitution. The emerging distribution (Table 20) nevertheless gives some indication of the likely spread of cases, and the potential for both upward (more intensive) and downward (less intensive) service substitution across settings.
| Case type | Social services users | CMHT clients | ECH tenants | Care home entrants | |
|---|---|---|---|---|---|
| 1 | LLL | ✓ | ✓ | ✓ | |
| 2 | LLM | ✓ | ✓ | ✓ | ✓ |
| 5 | LMM | ✓ | ✓ | ✓ | ✓ |
| 8 | LHM | ✓ | ✓ | ||
| 9 | LHH | ✓ | ✓ | ||
| 17 | MHM | ✓ | ✓ | ✓ | |
| 26 | HHM | ✓ | ✓ | ||
The identification of potentially marginal care home entrants by practitioners
By contrast, Table 21 identifies which of 14 commonly populated care home case types (those representing at least four site X admissions at the point of analysis) local practitioners believed could be more appropriately cared for in other settings. Seventeen staff members participated in this exercise, and each case type was considered by at least six individuals.
| Case type | Profile | Number in site X sample | Most appropriate placement as identified by individual practitioners | Most appropriate placement as identified by small groups of practitioners | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Own home | ECH | Specialist ECH | Care home | Specialist care home | Care home with nursing | Specialist care home with nursing | ||||
| 2 | LLM | 5 | 2 | 5 | – | 1 | – | – | – | Specialist ECH |
| 5 | LMM | 6 | 8 | 1 | – | – | – | – | – | Own home |
| 6 | LMH | 4 | 2 | – | 4 | – | 2 | – | – | Own home |
| 9 | LHH | 8 | 3 | – | 2 | – | 1 | – | – | Specialist ECH |
| 13 | MML | 4 | 3 | 4 | – | – | – | – | – | Own home or ECH |
| 14 | MMM | 8 | 6 | 1 | 1 | – | – | – | – | Own home |
| 17 | MHM | 5 | 2 | 1 | 3 | – | – | – | – | ECH or specialist ECH |
| 18 | MHH | 6 | 1 | – | 2 | – | 7 | – | 1 | Some form of care homea |
| 20 | HLM | 4 | – | 2 | – | 2 | – | 2 | – | Some form of care homea |
| 22 | HML | 4 | – | 6 | – | 1 | – | – | – | ECH |
| 23 | HMM | 4 | 2 | 3 | 1 | – | – | – | – | ECH |
| 25 | HHL | 4 | – | – | 1 | 1 | – | 3 | 2 | Some form of care homea |
| 26 | HHM | 6 | 2 | – | – | – | – | 2 | 3 | Some form of care homea |
| 27 | HHH | 4 | – | – | – | – | 2 | – | 4 | Some form of care homea |
| 2 | LLM | 26 | 4 | – | – | – | – | – | – | Own home |
| 5 | LMM | 25 | 3 | – | 3 | – | – | – | – | Own home or specialist ECH |
| 8 | LHM | 9 | 1 | – | 2 | – | 3 | – | – | Own home |
Although the degree of consensus between practitioners varied across case types, staff working in small groups concluded that nine case types could appropriately be diverted from care home admission. However, they did not necessarily believe they should remain at home, with ECH often seen as a better option.
As might be expected, the needs of those case types considered suitable for diversion were generally less complex than those for whom care home placement was deemed the best option. For example, the people represented by just two of the nine case types for whom an alternative community setting was preferred were highly dependent, compared with four of the five for whom care home placement was supported. The logistic regression model presented in Tables 22 and 23 shows that case types with high physical dependency were almost five times more likely to be deemed in need of care home placement than those with moderate or low levels of dependency. Case types displaying high levels of two or more of the key variables (physical dependency, cognitive impairment and challenging behaviour) were approximately 10 times more likely to be considered best placed in a care home over and above this. A case type’s age and gender had additional positive impacts on the perceived need for care home placement.
| Variable | Categories (n case types)a | Values (%)b | Status in model |
|---|---|---|---|
| Practitioner decision | Own home | 49 (36.0) | |
| ECH | 50 (36.8) | ||
| Care home | 37 (27.2) | Dependent variable (binary/’care home’) | |
| Case type’s physical dependency | Low (7) | 48 (40.3) | Independent variable (binary) |
| Medium (4) | 32 (26.9) | ||
| High (6) | 39 (32.8) | ||
| Case type’s level of cognitive impairment | Low (3) | 18 (15.1) | Not a significant predictor on its own |
| Medium (7) | 51 (42.9) | ||
| High (7) | 50 (42.0) | ||
| Case type’s level of behaviour problems | Low (3) | 21 (17.7) | Not a significant predictor on its own |
| Medium (10) | 67 (56.3) | ||
| High (4) | 31 (26.1) | ||
| Case type had at least two ‘high’ ratings | Yes (5) | 37 (31.1) | Independent variable (binary) |
| No (12) | 82 (68.9) | ||
| Case type’s gender | Female (12) | 80 (67.2) | Independent variable (binary) |
| Male (5) | 39 (32.8) | ||
| Case type’s living status | Lives with others (6) | 41 (34.5) | Associated with other predictors |
| Lives alone (11) | 78 (65.6) | ||
| Case type’s physical health | Described as poor (9) | 61 (51.3) | Associated with other predictors |
| Described as good (8) | 58 (48.7) | ||
| Case type’s prior social care status | Had care package (9) | 66 (55.5) | Associated with other predictors |
| Had no prior input (8) | 55 (44.5) | ||
| Case type’s setting prior to admission | Was inpatient (10) | 73 (61.3) | Associated with other predictors |
| Was at home (7) | 46 (38.7) | ||
| Case type’s age | Mean (SD) | 83.6 (6.0) | Independent variable (continuous; centred: mean = 0) |
| Median | 83 | ||
| Minimum–maximum | 69–96 | ||
| n | 119 |
| Predictorsa | Coefficients (OR) | z-value | Robust SEb (p-value)c |
|---|---|---|---|
| Case type’s physical dependency rating is high | 4.87 | 2.83 | 2.72 (0.005) |
| Case type has at least two high ratings (physical dependency, cognition or behaviour score) | 10.20 | 5.51 | 4.30 (< 0.001) |
| Case type’s reported age | 1.08 | 2.34 | 0.035 (0.019) |
| Case type’s reported gender is male | 4.00 | 2.22 | 2.50 (0.027) |
| Model fit | Wald χ2(4) = 54.40 (p < 0.001) Pseudo-R2 = 0.35 Linktest p(_hat) < 0.001, p(_hatsq) = 0.503 n = 118 |
||
Interestingly, living situation appeared to have a less clear effect. For no case type was it suggested that, had their living situation been different from that depicted, staff would have been more likely to advocate care home placement. Indeed, in one instance where care home placement was felt to be the best option (case type 18, MHH) there was a suggestion that, had the individual lived alone, staff might have been more inclined to try to maintain him at home (the need for care home admission at least partly driven by carer stress). Whether or not the depicted ‘client’ was at home or in hospital also appeared to make litttle difference to staff recommendations.
Although more will be said about the alternative care options suggested for the nine case types discussed in Chapter 5, it is noteworthy that together they constitute more than half (53%) of the site X sample. Of the four group decisions relating to people from the domiciliary samples (i.e. the controls), three confirmed that home was the most appropriate placement, whereas one advocated specialist ECH as a more appropriate setting for people in case type 5 (LMM). Furthermore, although there was some discrepancy between the recommendations made for the vignettes representing the care home entrants in case types 2 and 5 and their counterparts in the community, care home placement was never the preferred option.
The identification of potentially marginal inpatient admissions by practitioners
Of 72 case types used to characterise the inpatient sample, 46 were populated, which between them captured 98% of admissions overall (100% in site X, Table 24). Again, some combinations of characteristics were more prevalent than others and only those 16 case types that contained four or more admissions at the point of analysis were considered for further exploration. However, as one of these contained two slightly different subgroups relating to individuals’ place of residence (home or care home), these were subsequently treated separately and 17 case types were used in the subsequent analysis.
| Case type | Broad diagnosis | Main reason for admission | Challenging behaviour | Lives alone | Number in site X | Number in site Y | Number in site Z | Number in sample |
|---|---|---|---|---|---|---|---|---|
| 1 | Depression/anxiety | Risk of deliberate self-harm | Low | No | 2 | 1 | 3 | 6 |
| 2 | Depression/anxiety | Risk of deliberate self-harm | Low | Yes | 2 | 4 | 0 | 6 |
| 3 | Depression/anxiety | Risk of deliberate self-harm | Medium | No | 5 | 1 | 7 | 13 |
| 4 | Depression/anxiety | Risk of deliberate self-harm | Medium | Yes | 4 | 1 | 6 | 11 |
| 5 | Depression/anxiety | Other risksa | Low | Yes | 1 | 0 | 3 | 4 |
| 6 | Depression/anxiety | Other risksa | Medium | No | 2 | 3 | 7 | 12 |
| 7 | Depression/anxiety | Other risksa | Medium | Yes | 2 | 0 | 6 | 8 |
| 8 | Depression/anxiety | Other risksa | High | No | 1 | 0 | 0 | 1 |
| 9 | Depression/anxiety | Behaviour management relatedb | Medium | No | 7 | 0 | 2 | 9 |
| 10 | Depression/anxiety | Behaviour management relatedb | Medium | Yes | 3 | 0 | 1 | 4 |
| 11 | Depression/anxiety | Behaviour management relatedb | High | No | 0 | 1 | 0 | 1 |
| 12 | Depression/anxiety | Behaviour management relatedb | High | Yes | 0 | 0 | 2 | 2 |
| 13 | Depression/anxiety | Assessment/treatment/medication review | Low | No | 1 | 0 | 1 | 2 |
| 14 | Depression/anxiety | Assessment/treatment/medication review | Low | Yes | 0 | 3 | 0 | 3 |
| 15 | Depression/anxiety | Assessment/treatment/medication review | Medium | No | 0 | 3 | 0 | 3 |
| 16 | Depression/anxiety | Assessment/treatment/medication review | Medium | Yes | 0 | 5 | 3 | 8 |
| 17 | Depression/anxiety | Assessment/treatment/medication review | High | No | 1 | 0 | 2 | 3 |
| 18 | Depression/anxiety | Assessment/treatment/medication review | High | Yes | 1 | 0 | 0 | 1 |
| 19 | Organic | Risk of deliberate self-harm | Medium | No | 1 | 0 | 2 | 3 |
| 20 | Organic | Other risksa | Low | Yes | 1 | 1 | 0 | 2 |
| 21 | Organic | Other risksa | Medium | No | 2 | 2 | 3 | 7 |
| 22 | Organic | Other risksa | Medium | Yes | 1 | 2 | 4 | 7 |
| 23 | Organic | Other risksa | High | No | 0 | 0 | 2 | 2 |
| 24 | Organic | Other risksa | High | Yes | 0 | 2 | 0 | 2 |
| 25 | Organic | Behaviour management relatedb | Low | No | 0 | 0 | 1 | 1 |
| 26 | Organic | Behaviour management relatedb | Medium | No | 7 | 4 | 4 | 15 |
| 27 | Organic | Behaviour management relatedb | Medium | Yes | 1 | 1 | 0 | 2 |
| c28a | Organic | Behaviour management relatedb | High | No | 3 | 6 | 5 | 14 |
| c28b | Organic | Behaviour management relatedb | High | No | 2 | 4 | 3 | 9 |
| 29 | Organic | Assessment/treatment/medication review | Medium | No | 4 | 3 | 2 | 9 |
| 30 | Organic | Assessment/treatment/medication review | Medium | Yes | 0 | 1 | 1 | 2 |
| 31 | Organic | Assessment/treatment/medication review | High | No | 0 | 2 | 4 | 6 |
| 32 | Organic | Assessment/treatment/medication review | High | Yes | 0 | 0 | 1 | 1 |
| 33 | Other | Risk of deliberate self-harm | Low | No | 0 | 0 | 1 | 1 |
| 34 | Other | Risk of deliberate self-harm | Low | Yes | 0 | 0 | 1 | 1 |
| 35 | Other | Risk of deliberate self-harm | Medium | No | 0 | 1 | 1 | 2 |
| 36 | Other | Other risksa | Medium | No | 3 | 0 | 0 | 3 |
| 37 | Other | Other risksa | Medium | Yes | 2 | 0 | 0 | 2 |
| 38 | Other | Other risksa | High | No | 1 | 0 | 1 | 2 |
| 39 | Other | Other risksa | High | Yes | 0 | 0 | 3 | 3 |
| 40 | Other | Behaviour management relatedb | Medium | No | 4 | 0 | 1 | 5 |
| 41 | Other | Behaviour management relatedb | Medium | Yes | 0 | 0 | 1 | 1 |
| 42 | Other | Behaviour management relatedb | High | No | 1 | 0 | 1 | 2 |
| 43 | Other | Behaviour management relatedb | High | Yes | 0 | 0 | 2 | 2 |
| 44 | Other | Assessment/treatment/medication review | Medium | No | 0 | 0 | 3 | 3 |
| 45 | Other | Assessment/treatment/medication review | Medium | Yes | 1 | 1 | 2 | 4 |
| 46 | Other | Assessment/treatment/medication review | High | No | 1 | 1 | 0 | 2 |
In Table 25 these 17 case types are ranked in order of appropriateness for admission (from most to least) as judged by groups of local staff. Thirty-eight staff members participated in this exercise, and each case type was considered by at least 17 individuals. Thus, of 22 practitioners who rated case type 2 (which was considered most suitable for admission), 20 believed the ‘client’ depicted was completely appropriate for admission, whereas no-one considered the admissions represented by case types 26 or 31 to be definitely suitable for admission.
| Case type | Broad diagnosis | Main reason for admission | Challenging behaviour | Lives alone | Completely appropriate | Possibly appropriate | Not appropriate | % appropriate scorea |
|---|---|---|---|---|---|---|---|---|
| 2 | Depression/anxiety | Risk of deliberate self-harm | Low | Yes | 20 | 2 | 0 | 95.4 |
| 4 | Depression/anxiety | Risk of deliberate self-harm | Medium | Yes | 15 | 11 | 0 | 78.9 |
| 1 | Depression/anxiety | Risk of deliberate self-harm | Low | No | 11 | 9 | 1 | 73.8 |
| 3 | Depression/anxiety | Risk of deliberate self-harm | Medium | No | 7 | 14 | 4 | 56.0 |
| 7 | Depression/anxiety | Other risksb | Medium | Yes | 7 | 11 | 5 | 54.4 |
| c28b | Organic | Behaviour management relatedd | High | No | 6 | 16 | 4 | 53.8 |
| 29 | Organic | Assessment/treatment/check medication | Medium | No | 6 | 14 | 6 | 50.0 |
| 9 | Depression/anxiety | Behaviour management relatedd | Medium | No | 2 | 20 | 3 | 48.0 |
| 40 | Other | Behaviour management relatedd | Medium | No | 4 | 8 | 6 | 44.4 |
| 22 | Organic | Other risksb | Medium | Yes | 5 | 9 | 9 | 41.3 |
| 21 | Organic | Other risksb | Medium | No | 2 | 11 | 8 | 35.7 |
| 16 | Depression/anxiety | Assessment/treatment/check medication | Medium | Yes | 2 | 8 | 8 | 33.3 |
| c28a | Organic | Behaviour management relatedc | High | No | 0 | 12 | 9 | 28.6 |
| 10 | Depression/anxiety | Behaviour management relatedd | Medium | Yes | 1 | 11 | 11 | 28.3 |
| 6 | Depression/anxiety | Other risksb | Medium | No | 1 | 9 | 11 | 26.2 |
| 26 | Organic | Behaviour management relatedd | Medium | No | 0 | 10 | 11 | 23.8 |
| 31 | Organic | Assessment/treatment/check medication | High | No | 0 | 4 | 13 | 11.8 |
Logistic regression suggested that a variety of intrinsic and extrinsic factors played a role in predicting those case types considered definitely suitable for admission. Where the main risk of admission was deliberate self-harm (as opposed to any other reason), the likelihood of admission being seen as definitely appropriate increased more than fivefold (Tables 26 and 27). Living alone or lack of any previous contact with mental health services were also positively associated with the probability of being considered an appropriate admission. Other tested intrinsic factors either had no effect (e.g. age and gender) or were already explained by the main predictors (e.g. diagnosis and whether or not the person was admitted in normal working hours). However, certain rater characteristics did affect decisions. Compared with clinical staff, managers and commissioners were only half as likely to perceive inpatient admission as definitely appropriate, while staff who worked all or some of the time in community settings were less likely to fully endorse inpatient care than staff who worked solely in inpatient settings.
| Variable | Categories (n case types or staff)a | Values (%)b | Status in model |
|---|---|---|---|
| Practitioner decision | Placement not appropriate | 109 (28.9) | |
| Placement maybe appropriate | 179 (47.5) | ||
| Placement completely appropriate | 89 (23.6) | Dependent variable (binary/’appropriate’) | |
| Case type’s diagnosis | Organic (7) | 155 (41.1) | Associated with other predictors |
| Depression/anxiety (9) | 204 (54.1) | ||
| Other diagnosis (1) | 18 (4.8) | ||
| Case type’s reason for admission | Risk of deliberate self-harm (4) | 94 (24.9) | Independent variable (binary) |
| Behaviour management (6) | 134 (35.5) | ||
| Assessment/treatment (3) | 61 (16.2) | ||
| Other risks (4) | 88 (23.3) | ||
| Case type’s level of behaviour problems | Low (2) | 43 (11.4) | Associated with other predictors |
| Medium (12) | 270 (71.6) | ||
| High (3) | 64 (17.0) | ||
| Case type’s living status | Lives with others (11) | 242 (64.2) | Independent variable (binary) |
| Lives alone (6) | 135 (35.8) | ||
| Case type’s gender | Female (13) | 288 (76.4) | Not a significant predictor |
| Male (4) | 89 (23.6) | ||
| Case type’s time of admission | During regular hours (15) | 334 (88.6) | Associated with other predictors |
| Outside regular hours (2) | 43 (11.4) | ||
| Case type’s previous access | Already known to service (15) | 334 (88.6) | Independent variable (binary) |
| New to service (2) | 43 (11.4) | ||
| Case type’s place before admission | At home (11) | 249 (66.1) | Not a significant predictor |
| Care home (3) | 64 (17.0) | ||
| Hospital (3) | 64 (17.0) | ||
| Role of rater | Nurse (12) | 117 (31.0) | Independent variable (binary) |
| Consultant/physician (7) | 70 (18.6) | ||
| Managerc (16) | 160 (42.4) | ||
| Other front-line staff (3) | 30 (8.0) | ||
| Rater is involved in liaison work | Yes (3) | 30 (9.2) | Not a significant predictor |
| No (30) | 297 (90.8) | ||
| Rater is involved in community work | Yes (20) | 199 (60.9) | Independent variable (binary) |
| No (13) | 128 (39.1) | ||
| Rater is involved in inpatient work | Yes (18) | 178 (54.4) | Not a significant predictor |
| No (15) | 149 (45.6) | ||
| Case type’s age (years) | Mean (SD) | 74.5 (6.9) | Not a significant predictor |
| Median | 74 | ||
| Minimum–maximum | 65–88 | ||
| n | 377 |
| Predictorsa | Coefficients (OR) | z-value | Robust SEb (p-value)c |
|---|---|---|---|
| Case type’s stated reason for admission is risk of deliberate self-harm | 5.73 | 4.44 | 2.25 (< 0.001) |
| Case type is described as living alone | 2.96 | 3.60 | 0.89 (< 0.001) |
| Case type is reported to be unknown to mental health services | 3.85 | 2.84 | 1.83 (0.005) |
| Rater is a manager | 0.41 | −2.46 | 0.15 (0.014) |
| Rater works in a community setting | 0.46 | −2.44 | 0.15 (0.015) |
| Model fit | Wald χ2(5) = 68.08 (p < 0.001) Pseudo-R2 = 0.27 Linktest p(_hat) < 0.001, p(_hatsq) = 0.997 n = 327 |
||
As any attempt to change the BoC might logically be expected to focus on those case types considered least appropriate for admission, the potential implications for admission can be estimated. Depending on the level of ambition, diversion of the three case types at the bottom of the distribution (6, 26 and 31) to community care might reduce inpatient admissions in site X by over 10%. If it was also possible to support case types 10 and 28a in the community, a reduction of more than 20% might be feasible. However, whether or not this would be a better option than the status quo would depend on the relative costs and consequences of the alternative options. These issues are the subject of Chapter 5.
Chapter 5 Services for older people with mental health problems. The North-West Balance of Care Study: findings II
This chapter presents estimates of the likely care costs and consequences of alternative care services for marginal case types presented in Chapter 4; and assesses the viability and preferences for these according to older people and experts.
MethodA comprehensive costs approach incorporated public agency and service user/carer consequences of alternative care scenarios. The acceptability of proposed alternatives was assessed by a panel of national experts and local older people/carers.
ResultsThe alternative care plans for all nine marginal care home entrant case types were found to be more expensive than the status quo using comprehensive costings. Care at home was generally less expensive to social services, but more expensive for the NHS, compared with care home entry. Older people and experts tended to prefer the community-based alternatives, but for some case types advocated even more intensive support. Carers were more likely to recommend care home placements. By contrast, the alternative care arrangements for all five marginal inpatient admissions were cheaper, although an expert panel validated only three as being appropriately diverted from hospital care. Extrapolating across the three localities, up to £1.5M per annum could potentially be released for other uses, mostly within the NHS. Sensitivity analysis confirmed that these estimates depend on whether a critical mass of service users can be diverted from inpatient facilities.
ConclusionsThe study illustrates the utility of the BoC, and the merits of new methodological developments. In this application, cost savings could be achieved by avoiding some inpatient admissions, but not by replacing care home entry with expanded community support.
Introduction
This chapter presents further detail of the alternative care packages formulated for the marginal care home and inpatient case types identified by practitioners in Chapter 4, and explores their relative costs and benefits. It also examines the packages’ wider validity as assessed by local older people and national experts. The findings are then tested in a series of sensitivity analyses and lessons for future research and service planning explored. As in the previous chapter, for ease of understanding, links are made to the description of methods in Chapter 3.
The costs and outcomes of alternative care packages for current care home entrants
Costs of alternative care options (see Chapter 3, Activity 4.1)
The estimated costs of the community care arrangements deemed most appropriate by local practitioners to meet the needs of the nine marginal care home case types identified in Chapter 4 are detailed in Table 28, alongside those of their actual residential care placement. Further information about their constituent elements is given in Box 8. A number of the alternatives involved moves to ECH (variously specialist or generic). Other commonly employed resources included home care (again both specialist and generic) and support from specialist mental health services [predominantly community mental health nurse (CMHN) and psychiatrist input]. Considerable use was also made of telecare, including pendant alarms and smoke, gas and fall detectors. Where more than one alternative was provided these are presented in the table.
| Care plan | Original option (care home placement) | Alternative option (home or ECH) | Difference/sensitivity | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case type | Option | SSD costs | NHS mental health costs | NHS general health costs | Other government costs | Private costs | Total costs | SSD costs | NHS mental health costs | NHS general health costs | Other government costs | Private costs | Total costs | Total cost differenceb | Lower bound | Upper bound |
| 2 (LLM) | A | 231 | 9 | 175 | 13 | 152 | 580 | 162 | 52 | 232 | 70 | 445 | 959 | 380 | −77 | 807 |
| 5 (LMM) | A | 268 | 9 | 175 | 13 | 177 | 643 | 222 | 41 | 175 | 65 | 348 | 851 | 208 | −156 | 592 |
| B | 268 | 9 | 175 | 13 | 177 | 643 | 105 | 41 | 175 | 65 | 288 | 674 | 31 | −333 | 415 | |
| C | 268 | 9 | 175 | 13 | 177 | 643 | 293 | 131 | 175 | 65 | 338c | 1002 | 359 | −11 | 719 | |
| 6 (LMH) | A | 268 | 9 | 175 | 13 | 184 | 649 | 29 | 1092 | 175 | 65 | 203 | 1565 | 915 | 465 | 1383 |
| 9 (LHH) | A | 268 | 9 | 175 | 13 | 190 | 656 | 942 | 33 | 175 | 70 | 623 | 1843 | 1188 | 754 | 1558 |
| 13 (MML) | A | 231 | 9 | 175 | 13 | 165 | 593 | 137 | 7 | 252 | 70 | 329 | 795 | 202 | −206 | 601 |
| B | 231 | 9 | 175 | 13 | 165 | 593 | 266 | 12 | 218 | 65 | 323 | 885 | 292 | −83 | 658 | |
| 14 (MMM) | A | 231 | 9 | 175 | 13 | 165 | 593 | 152 | 7 | 175 | 65 | 313 | 712 | 119 | −284 | 494 |
| B | 231 | 9 | 175 | 13 | 165 | 593 | 124 | 31 | 175 | 65 | 343c | 739 | 145 | −269 | 539 | |
| 17 (MHM) | A | 268 | 9 | 175 | 13 | 190 | 656 | 131 | 7 | 175 | 70 | 486 | 869 | 213 | −213 | 666 |
| B | 268 | 9 | 175 | 13 | 190 | 656 | 189 | 7 | 175 | 70 | 356 | 796 | 140 | −228 | 536 | |
| 22 (HML) | A | 268 | 9 | 284 | 13 | 177 | 751 | 307 | 7 | 187 | 70 | 416 | 987 | 236 | −130 | 609 |
| 23 (HMM) | A | 268 | 9 | 284 | 13 | 190 | 765 | 159 | 10 | 175 | 70 | 383 | 796 | 31 | −361 | 456 |
| Case type | Summary of practioners’ plans | Summary of RAM Panel’s plan |
|---|---|---|
| 2 (LLM) | Option A: Move to specialist ECH with specialist home care input four times a day; case manager, CMHN and psychiatrist input | Return home with direct payment to employ own carers; ≥ 2 days day care per week; respiratory nurse and mental health input |
| 5 (LMM) | Option A: Stay at home with specialist home care input four times a day; twice weekly social input from a personal assistant; CMHN input; telecare Option B: Stay at home with specialist home care input twice a day; CMHN input; telecare Option C: Stay at home with home care input four times a day; three times weekly social input from a mental health support worker and befriender; 1 day a week day care; CMHN, SW and GP input; telecare |
Start with option B with a view to moving to a hybrid of A and C in the longer term |
| 6 (LMH) | Option A: Further assessment on a mental health ward with a view to returning home with three times daily input from a mental health support worker; CMHN and psychiatrist input; telecare | Further assessment in a short-term residential care placement with a view to returning home |
| 9 (LHH) | Option A: Move to specialist ECH with specialist home care input twice a day; 3 days a week specialist day care; nightly night sitter; residential respite 1 week in 6; CMHN, social work and psychiatrist input; lifeline | Further assessment on a mental health ward with a view to returning home |
| 13 (MML) | Option A: Move to non-specialist ECH with home care input four times a day; DN and GP input Option B: Return home with home care input four times a day; weekly domestic help; social work, OT, GP, dietitian; Macmillan nurse; psychiatrist, CMHN and welfare rights input; carer support; lifeline |
Option B plus the option of some day care |
| 14 (MMM) | Option A: Stay at home with home care input four times a day; input from a GP; telecare Option B: Stay at home with home care input three times a day; daily input from a befriender; GP, consultant psychiatrist, OT and physiotherapist input; carer support |
Option B but with four home care visits per day |
| 17 (MHM) | Option A: Move to specialist ECH with specialist home care input three times a day; daily visit from family; telecare Option B: Move to non-specialist ECH with home care input four times day; 2 days a week specialist day care |
Stay at home with home care input three times a day; 2 days a week day care; support for carers; telecare. Fall-back position move to ECH |
| 22 (HML) | Option A: Move to non-specialist ECH with home care input five times day (two workers); DN input; telecare | Option A |
| 23 (HMM) | Option A: Move to non-specialist ECH with home care input four times day; daily meal at lunchtime; on-site social activity; CMHN input; telecare | Stay at home with home care input up to four times a day |
Taking a comprehensive costings approach, the total predicted costs of the alternative plans exceeded those of care home placement in every case. However, some were relatively more expensive than others. Additional expenditure per service user ranged from £31 to £1188 per week, with a mean difference of almost £320 per week. Much of this can be attributed to the increased private (personal) costs associated with the alternative packages, which averaged £195 per week more than for residential care placement. In comparison, public expenditure varied less. Seven community packages increased public costs and seven decreased them. There was also a clear shift in the distribution of public expenditure, with NHS and other government costs typically higher for alternative options and social services costs generally higher for care home options.
Although these figures are best or central estimates, the upper and lower bounds in Table 28 represent the possible extremes of any cost differences, allowing for uncertainty in the quantity and cost of resources and the representativeness of vignettes. These, understandably, introduce much more variation into the model. Nevertheless, even after such adjustments, the alternative care packages for case types 6 and 9 remain considerably more expensive than their original care home placements.
Outcomes of alternative care options (see Chapter 3, Activities 4.2–4.4)
A marked lack of relevant literature comparing the relative outcomes of people with similar needs supported at home, in care homes or ECH was identified. Furthermore, although a number of publications addressed the outcomes of older people with mental health problems cared for in particular settings, none provided enough detail about their samples to match them to this study’s case types. Although mostly originating from small, descriptive studies, there is, however, a growing body of evidence to suggest that social well-being and quality of life (QoL) in ECH are generally good. 164–166 In one recent study, people who moved into ECH reported significantly improved levels of QoL and decreased levels of unmet need compared with people living at home. 167
The search for secondary data sets containing comparative information about the outcomes of older people supported in different settings similarly proved unfruitful. Even the English Longitudinal Study of Ageing included relatively few older people who received formal mental health support, and fewer still who had entered a care home. This may reflect the relatively young age of the study’s participants. However, even if the numbers had been larger, the data would have required considerable manipulation to be suitable for our purposes.
The attempt to collect primary data (matched cohort study) about the relative outcomes of care home entrants and older people living at home with CMHT support also encountered difficulties. Not least of these was the Council in site Z’s unexpected late decision not to participate in the study. Both the achieved care home sample and the number of people represented by the care home case types were considerably smaller than anticipated, and the degree of empirical overlap between the two samples was also less than expected.
The plan to investigate the outcomes of people in one or two matched case types was thus abandoned and a broader approach taken in which all potentially marginal care home entrants (i.e. all case types commonly found in both samples) were considered for follow-up. In effect, this amounted to all care home entrants who were less than ‘very dependent’ (Barthel > 40) and less than ‘severely cognitively impaired’ (CPS score < 4) so long as they did not have complex challenging behaviour (behaviour score < 9) and were appropriate for interview (e.g. could express their basic needs). Comparable CMHT clients were then chosen using a manual ‘nearest neighbour’ approach that took into account individuals’ age, gender and diagnostic group as well as case type. As the study progressed, however, additional individuals just outside the margins of care were included in an attempt to boost numbers.
Despite these actions, the number of achieved interviews remained disappointingly small (Figure 6). Only 16% of the care home entrants and 13% of the CMHT clients the study attempted to recruit participated in this exercise. Forty-four per cent of the selected care home entrants and 58% of the CMHT clients were deemed ineligible by their keyworkers, while no response was received for a further 22% and 14% respectively. Of those service users who were considered eligible, however, 73% were happy to be approached by the research team, and 66% were interviewed (11 care home entrants and 12 CMHT clients).
FIGURE 6.
Flow diagram of matched cohort study recruitment. (a) Care home arm; and (b) CMHT arm.
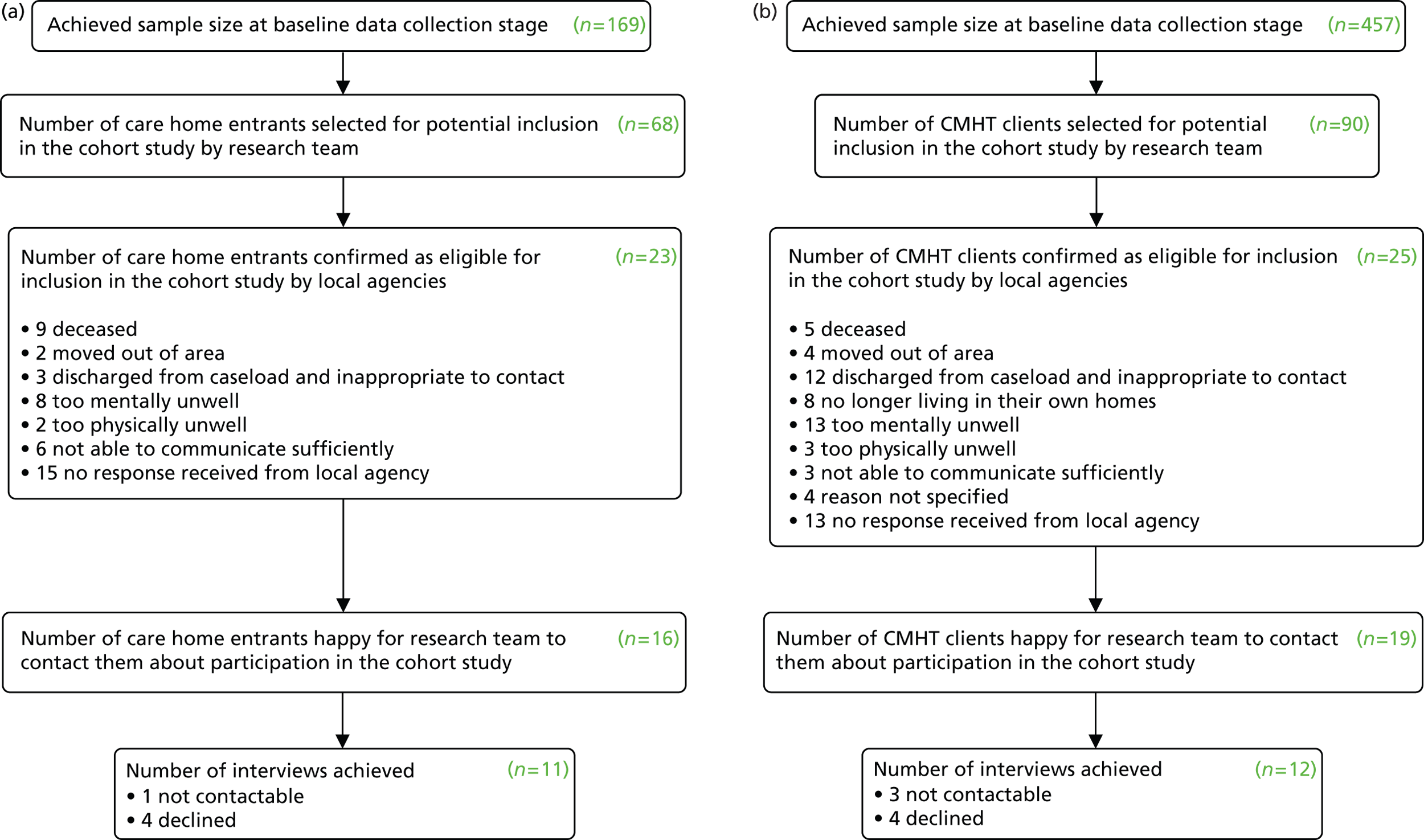
Bearing in mind the small numbers and our intention to capture people with similar needs, the interviewed care home entrants were significantly older than the CMHT clients (mean age 87.8 years compared with 78.8 years, t-test: 3.41, df = 21, p = 0.003). They also needed more help with activities of living, with 9 of 11 care home entrants compared with just 1 of 12 CMHT clients unable to manage stairs (chi-squared: 12.68, df = 2, p = 0.002). Consequently, though matches were achieved for six of the care home entrants, the study lacked community clients to match those admissions with more dependent profiles.
Perhaps unsurprisingly, no statistically significant differences were found in the two samples’ outcomes with regard to QoL or satisfaction, which were generally said to be good. However, when asked if they were basically satisfied with their lives, two CMHT clients but no care home entrants said ‘no’, and the same number indicated that they were not getting enough help. Asked to name the best thing about their current situation, care home entrants typically spoke about security and food, while the worst aspects of care home life were the lack of stimulation and the manner of certain carers. Correspondingly, those interviewees supported at home most frequently praised the help they received from different agencies, whereas any negative comments were particular to individual circumstances.
The incorporation of the cost and outcome data into the balance of care analysis (see Chapter 3, Activities 5.1 and 5.2)
When presented with the details of the marginal care home case types identified by practitioners, their original care home placements and suggested alternative care packages, the site X RAM Panel opted to support all nine cases in the community. As shown in Box 8, however, they did not necessarily agree with the proposed care plans, particularly where these involved moves to ECH. Indeed, the only situation in which this was endorsed concerned a case type whose home was described as physically unsuitable to meet their needs, such that a change of residence was, at least in the short-term, inevitable. They were also inclined to make more use of day care and considerable use of telecare, including the ‘Just Checking’ system.
Although typically lower than the costs of the practitioners’ plans, the estimated costs of the packages of care the Panel recommended exceeded those of care home placement for eight of the nine case types (Table 29). Furthermore, even using the most extreme plausible values, the costs of the alternative care packages for case types 6 and 9 exceeded those of residential care.
| Case type | Original option (care home placement) | Alternative option (home or ECH) | Difference/sensitivity | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SSD costs | NHS mental health costs | NHS general health costs | Other government costs | Private costs | Total costs | SSD costs | NHS mental health costs | NHS general health costs | Other government costs | Private costs | Total costs | Total cost differenceb | Lower bound | Upper bound | |
| 2 (LLM) | 231 | 9 | 175 | 13 | 152 | 580 | 236 | 52 | 232 | 65 | 308 | 893 | 313 | −93 | 680 |
| 5 (LMM) | 268 | 9 | 175 | 13 | 177 | 643 | 166 | 56 | 175 | 65 | 301 | 763 | 120 | −231 | 484 |
| 6 (LMH) | 268 | 9 | 175 | 13 | 184 | 649 | 127 | 477 | 175 | 65 | 206 | 1051 | 401 | 53 | 770 |
| 9 (LHH) | 268 | 9 | 175 | 13 | 190 | 656 | 272 | 667 | 175 | 65 | 456 | 1635 | 980 | 372 | 1528 |
| 13 (MML) | 231 | 9 | 175 | 13 | 165 | 593 | 296 | 28 | 218 | 65 | 338 | 945 | 352 | −26 | 727 |
| 14 (MM) | 231 | 9 | 175 | 13 | 165 | 593 | 158 | 31 | 175 | 65 | 313 | 743 | 150 | −243 | 535 |
| 17 (MHM) | 268 | 9 | 175 | 13 | 190 | 656 | 159 | 7 | 175 | 65 | 313 | 719 | 63 | −311 | 462 |
| 22 (HML) | 268 | 9 | 284 | 13 | 177 | 751 | 307 | 7 | 187 | 70 | 417 | 988 | 236 | −129 | 610 |
| 23 (HM) | 268 | 9 | 284 | 13 | 190 | 765 | 169 | 10 | 175 | 65 | 321 | 740 | −24 | −399 | 377 |
As shown in Table 30, much of this difference was again attributable to the greater private costs associated with the enhanced packages, which averaged £153 more per week than those of care home placement. However, even taking a purely public expenditure approach, the alternative package costs for seven case types were similar to, or higher than, those of a care home. Nevertheless, a clear financial incentive remained for the Social Services Department (SSD) to maintain certain groups of service users in the community, as direct savings were predicted for five of the nine case types.
| Case type | SSD costs | NHS mental health costs | NHS general health costs | All NHS costs | Other government costs | All public expenditure | Private costs |
|---|---|---|---|---|---|---|---|
| 2 (LLM) | 5 | 43 | 57 | 100 | 52 | 157 | 156 |
| 5 (LMM) | −102 | 47 | – | 47 | 52 | −3 | 124 |
| 6 (LMH) | −141 | 468 | – | 468 | 52 | 379 | 22 |
| 9 (LHH) | 4 | 658 | – | 658 | 52 | 714 | 266 |
| 13 (MML) | 65 | 19 | 43 | 61 | 52 | 179 | 173 |
| 14 (MMM) | −72 | 22 | – | 22 | 52 | 2 | 148 |
| 17 (MHM) | −110 | −2 | – | −2 | 52 | −60 | 123 |
| 22 (HML) | 39 | −2 | −97 | −99 | 57 | −3 | 239 |
| 23 (HMM) | −99 | 1 | −109 | −108 | 52 | −155 | 131 |
Qualitative analysis of the panels’ decision-making process identified six main themes (Box 9), of which perhaps the most pervasive was their strong desire to maintain people at home. Their explanation to the research team was:
. . . and our key brief and our key principle is that we will always try and support someone in their own home, taking into account the risks that they would actually face in doing that, before we would agree any form of residential care . . .
| Main theme | Coverage | Number of case types related to | Quotes |
|---|---|---|---|
| The desire to support the service user at home |
|
9 | Why can she not return home? Because that’s what we’d be looking to do . . .There was no care package, at all, going in to support this lady and this couple before she went into hospital . . . I think what we are saying is that there is still work to do to explore what can be provided in the current home environmentHe’s quite clear he wants to go home. That’s what he’s stated although he doesn’t have capacity, but that is his overriding wishes . . . |
| Risks |
|
6 | The fire risk seems to be the one that comes out in terms of activity relating to food preparation, doesn’t it? I suppose it’s how we deal with thatI guess the risks are beginning to really sort of be significant, in terms of clearly life and limb aren’t they, in that sense? |
| Arguments against moving the service user from their home |
|
6 | Let’s start the other way. Do we feel that he needs some form of residential care or not? Does he need 24-hour supervision?What would extra care housing give her that we couldn’t provide by enhancing her care package?. . . presumably she might not want another change of accommodation |
| The likelihood of the home situation improving |
|
5 | There’s too many issues not bottomed out . . . We’d want to know about what the dizzy spells are linked to. I think that needs fuller investigation . . . understand whether this is, is this a continuation of a deterioration of his vascular dementia . . . or is it something that can be addressed? |
| The service user’s concerns/best interests |
|
5 | I think anxiety is going to be a key issue to overcome . . .My worry would be she’s resisted it up to now. If you go in with four calls a day of 45 minutes, I wouldn’t have thought straight away that’s necessarily going to be an option. I would have thought if you go in top heavy rather than build it up slowly, build it back upI wonder as she’s taken a dislike to particular carers, perhaps we could encourage her to take a direct payment and perhaps employ her own . . . |
| Carers’ concerns |
|
3 | What are we going to do to actually try and prevent the, or reduce the volume of calls that Mrs F is making to her daughter, because that appears to be a key pressure area . . .I suppose we are looking to see what additional support can we provide within the home to support the husband |
Indeed, the other five domains could be interpreted as adjuncts to this. The minimisation of risks, for example, seems a necessary step in making home care viable, while the possibility of the service user improving over time may be viewed as strengthening the case for maintaining them at home.
There was surprisingly little discussion of costs, which were only mentioned in relation to one case type. Potential outcomes were also only discussed at a very general level (that staying at home would be in the service user’s ‘best interests’). There was, however, some debate about the best time to enter ECH, acknowledging that for certain individuals it might be better to move while they were still able to adjust to a new environment (although, in only one instance did they opt for such care). Furthermore, the provision of specific evidence about the likely social benefits of ECH compared with care at home, and the advantages of care home placement over ECH for people with advanced dementia, made no difference to the Panel’s decisions. Thus, in the first instance they reiterated that:
Our decision-making will always be, if the person can be supported where they are in their own home and that’s where they would like to be, then that will be our starting point.
They were also inclined to feel that the evidence would not apply to the case type in question, thus relying on maintenance at home as the priority.
Athough the last quote suggests that account was taken of service users’ preferences, the weight given to these appeared dependent on setting. Thus, where service users expressed a positive desire to remain at home, this was seen as justification for maintaining them in the community, whereas if they or their family expressed concerns about staying at home, the Panel tried to find ways of alleviating/overcoming these. Indeed, as one member of the panel put it, although they always tried to:
. . . consider somebody’s wishes . . . in terms of making a decision as to whether or not we can use the public purse to support someone in residential care . . . (we would) differentiate between want and need.
The panel did, however, acknowledge that it could be very difficult for front-line staff to promote the case for home care in the face of strong family opposition, and that for many carers the admission of their relative to hospital served as a ‘tipping point’. The pressure to discharge people from hospital before they had reached their full potential also increased pressure on staff to arrange short-term care home placements, a proportion of which inevitably became long-term. This was particularly true if their stay became protracted, they lost skills or confidence, they or their carers did not engage with plans to return home, and/or the care home wished to keep them.
The validation of local practitioners’ decisions (see Chapter 3, Activities 6.1 and 6.2)
The majority of older people’s groups (34 participants) who reviewed the plans proposed by the RAM Panel favoured the suggested community care packages over care home placement (Table 31). Indeed, the sole exception to this concerned case type 14 (MMM), where opinion was divided. However, complete consensus was only achieved for one case type (9, LHH), while in a number of instances it was felt that the depicted ‘clients’ would need a higher level of community support than had been recommended, including more day care, carer support and telecare services.
| Case type | Number of older people’s groups who felt original care home placement was preferable | Number of older people’s groups who felt suggested alternative care package was preferable | Number of experts who felt original care home placement was preferable | Number of experts who felt suggested alternative care package was preferable |
|---|---|---|---|---|
| 2 (LLM) | 1 | 2 | 0 | 6 |
| 5 (LMM) | 1 | 3 | 1 | 4 |
| 6 (LMH) | 1 | 2 | 2 | 3 |
| 9 (LHH) | 0 | 4 | 1 | 5 |
| 13 (MML) | 1 | 3 | 1 | 3 |
| 14 (MMM) | 2 | 2 | 1 | 5 |
| 17 (MHM) | 1 | 2 | 2 | 3 |
| 22 (HML) | 1 | 2 | 2 | 4 |
| 23 (HMM) | 1 | 3 | 1 | 4 |
Expert opinion was similarly divided among the seven participants. Although for every case type the majority of experts favoured the alternative option, six of the seven experts advocated residential care in at least one instance. As with the older people, many proposed additional resources, echoing the call for more carer support and stressing the value of experienced social work input, the importance of meeting people’s social care needs, and the benefits of short-term placement in a dedicated assessment and rehabilitation unit. When the decisions made by the older people, carers and national experts were included in the logisitic regression analysis presented in Chapter 4 (see Tables 22 and 23), the model suggested older people and carers were considerably more likely than local staff to favour care home placement, whereas experts were also somewhat more likely to support residential care (albeit each individual looked only at a subset of cases).
When asked to state the main reason for preferring community care, both older people and experts stressed their desire to respect service users’ wishes, and a belief that community services could meet people’s needs. The experts also highlighted the need for further assessment at home before care home entry and the desire to avoid potentially debilitating moves, whereas the older people were more likely to point to the potential financial implications of care home entry for service users. Conversely, care home entry was typically predicated on the need for more care than could be provided at home (particularly at night) and the risks service users posed to themselves and others.
The costs and outcomes of alternative care packages for current inpatient admissions
Costs of alternative care options (see Chapter 3, Activity 4.1)
Box 10 details the packages of care local practitioners’ believed would meet the needs of the five most marginal inpatient case types. Interestingly, all three plans for care home residents involved input from a specialist care home support team (CHST), whereas those for people admitted from home drew on an intensive mix of primary care and mental health expertise, including frequent mental health support worker input to assist people with their diet, medication, personal and social care needs.
| Case type | Profile | Summary of practioners’ plans |
|---|---|---|
| 28a | Organic disorder; admission behaviour management related;a high level of challenging behaviour; lives with spouse | Option A: Stay at home; twice daily visits from mental health support worker; day care; occupational therapy input; referral to social services, continence service and the memory clinic; carer’s assessment and possible attendance at a carer’s support group for service user’s wife Option B: Stay at home; daily visit from home carer; psychiatric day hospital assessment; twice weekly specialist mental health day care; weekly mental health support worker input; occupational therapy assessment; consultant psychiatrist medication review; CMHN input |
| 10 | Depression/anxiety; admission behaviour management related;a medium level of challenging behaviour; lives alone | Option A: Stay at home; weekly CBT from psychologist; one-off dietician assessment; one-off DN input; community equipment assessment; social services referral with a view to individual budget; fortnightly CMHT input Option B: Stay at home; twice daily mental health support worker visits; physical assessment and review; fortnightly pain management; stoma care; dietician assessment; weekly CMHN input including anxiety management; occupational therapy input; access to 24-hour crisis line; advocacy |
| 6 | Depression/anxiety; admission for other risks;b medium level of challenging behaviour; lives with spouse | Option A: Stay at home; at least twice daily visits from support worker to assist with personal care, diet, medication and social activity; CMHN assessment/review; social services referral; carer’s assessment; DN input Option B: Stay at home; at least daily visits from intensive homecare support team; daily home care; meals; three times weekly district nursing assistant input; twice weekly CMHN input; weekly consultant psychiatrist visit; referral to memory clinic; carer’s assessment Option C: Stay at home; twice daily visits from mental health support worker; weekly consultant psychiatrist visit; weekly CMHN input |
| 26 | Organic disorder; admission behaviour management related;a medium level of challenging behaviour; care home resident | Option A: Stay in care home; weekly CMHN input to initiate/review ABC and sleep charts; twice weekly community support worker input; dementia care mapping; care home staff training; weekly care home intervention team input; one-off physical screen by GP; one-off consultant psychiatrist review Option B: Stay in care home; weekly care home service input to initiate and review ABC chart, establish activities programme and help staff manage aggression; three times weekly psychologist input; one-off review of physical health by GP; medication review by consultant psychiatrist; input from OT and SW |
| 31 | Organic disorder; admitted for assessment/treatment/check medication; high level of challenging behaviour; care home resident | Option A: Stay in care home with daily input from the CHST for a 2-week period; physical review by the GP; assessment and advice from a speech and language therapist; referral to the continence service if remains incontinent at 2 weeks; referral to a psychiatrist if remains challenging at 2 weeks |
The estimated mental health and social care costs of the alternative arrangements are set out in Table 32, suggesting that in every case the predicted costs of the proposed community care packages were lower than those of hospital admission. Indeed, the mean weekly difference was £1873. Even allowing for considerable uncertainty in the quantity and cost of resources and the representativeness of vignettes, the general picture remained unchanged. The vast majority of this difference was attributable to the relatively low costs of providing community as opposed to inpatient mental health care, even where this involved multiple staff and frequent input. Furthermore, in contrast to the care home entrants modelling, there was no obvious trade-off between health and social care costs.
| Care plan | Original option (inpatient admission) | Alternative option (home or care home) | Difference/sensitivity | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Case type | Option | NHS mental health costs | SSD costs | Total costs | NHS mental health costs | SSD costs | Total costs | Total cost differenceb | Lower bound | Upper bound |
| 28a | A | 2193 | 73 | 2265 | 249 | 103 | 352 | –1913 | –2408 | –1527 |
| B | 2193 | 73 | 2265 | 155 | 115 | 269 | –1996 | –2444 | –1657 | |
| 10 | A | 2193 | 73 | 2265 | 131 | 96 | 227 | –2038 | –2517 | –1668 |
| B | 2193 | 73 | 2265 | 260 | 0 | 260 | –2005 | –2441 | –1678 | |
| 6 | A | 2193 | 73 | 2265 | 394 | 61 | 455 | –1810 | –2246 | –1483 |
| B | 2193 | 73 | 2265 | 442 | 118 | 561 | –1705 | –2177 | –1342 | |
| C | 2193 | 73 | 2265 | 876 | 0 | 876 | –1389 | –1825 | –1062 | |
| 26 | A | 2193 | 73 | 2265 | 284 | 9 | 293 | –1972 | –2453 | –1600 |
| B | 2193 | 73 | 2265 | 159 | 24 | 184 | –2082 | –2530 | –1742 | |
| 31 | A | 2193 | 146 | 2341 | 508 | 9 | 517 | –1821 | –2552 | –1199 |
The validation of local practitioners’ decisions (see Chapter 3, Activities 6.1 and 6.2)
As shown in Table 33, although national experts tended to support the commuity care of three of the above case types (26, 28a and 31), including both those representing care home residents (26 and 31), they were less inclined to support the alternative community care arrangements suggested for case types 6 and 10. Indeed, although the local appropriateness ratings for these two case types were 26.2% and 28.3%, respectively, the corresponding experts’ scores were 56.2% and 43.8%, with some perceiving them as entirely appropriate for admission, and others completely inappropriate. This may in part reflect the necessarily limited amount of information it was possible to include in the vignettes, for a number of experts commented that it was sometimes difficult to make such judgements without knowing more about the people’s circumstances, including their life and medical history; current and past medication; and wider informal network.
| Case type | Completely appropriate | Possibly appropriate | Not appropriate | % appropriate scorea |
|---|---|---|---|---|
| 28a | 0 | 3 | 5 | 16.7 |
| 10 | 2 | 3 | 3 | 43.8 |
| 6 | 3 | 3 | 2 | 56.2 |
| 26 | 0 | 4 | 4 | 25.0 |
| 31 | 0 | 2 | 6 | 12.5 |
When asked to indicate the most appropriate care packages for case types 6, 10, 26 and 28a (see Box 10), the majority of experts favoured option B in every case. However, almost without exception, additional, different, or more timely resource inputs were proposed. Recurrent themes included the desirability of experienced social work and primary care support; the need for earlier consultant psychiatrist involvement; the importance of ruling out physical causes for changes in presentation; the need for detailed behavioural and functional analyses of individuals’ behaviour as the basis for person-centred intervention strategies; and the relative advantages of intensive home treatment/CHSTs over multiple professionals from different organisations. The main reasons for favouring community care were the potentially negative effects of inpatient admission and the limited chance of acquiring any new insights in hospital. Correspondingly, where inpatient admission was advocated, this was typically predicated on the need to provide a place of safety and/or more intensive care than was available at home.
The potential implications of changes in the balance of care
Marginal care home cases (see Chapter 3, Activity 7.1)
In Table 34 the aggregate annual costs of providing the alternative care arrangements proposed by the RAM Panel have been compared with the costs of their original care home placement (site X only). The key variables in this table are the number of service users represented by each case type (projected over a 12-month period assuming those admissions for whom no baseline data was obtained had the same case type distribution as the achieved sample) and the anticipated number of months it might prove possible to divert each case type (based on experts’ degree of confidence in the alternative care packages as reported in Table 31). Thus, although Table 29 shows that the additional estimated weekly costs of supporting case type 2 (LLM) in the community were less than those for case type 6 (LMH), in view of the higher number of service users represented by case type 2 and the longer expected diversion period, the aggregate cost implications are greater.
| Case type | Expected n per year | Expected average months of diversionb | Total difference in SSD costs | Total difference in NHS costs | Total difference in other government costs | Total difference in private costs | Total difference in total costs |
|---|---|---|---|---|---|---|---|
| 2 (LLM) | 14 | 12 | 3809 | 68,748 | 37,900 | 113,983 | 224,440 |
| 5 (LMM) | 17 | 6 | –44,777 | 20,657 | 22,740 | 54,041 | 52,661 |
| 6 (LMH) | 11 | 3 | –6226 | 49,188 | 7580 | 728 | 51,270 |
| 9 (LHH) | 22 | 6 | 2125 | 383,789 | 30,320 | 155,126 | 571,360 |
| 13 (MML) | 11 | 6 | 18,990 | 17,917 | 15,160 | 50,470 | 102,536 |
| 14 (MMM) | 22 | 6 | –42,060 | 13,099 | 30,320 | 86,054 | 87,412 |
| 17 (MHM) | 14 | 3 | –18,887 | –365 | 9475 | 22,335 | 12,558 |
| 22 (HML) | 11 | 3 | 5675 | –14,393 | 8255 | 34,903 | 34,440 |
| 23 (HMM) | 11 | 6 | –28,841 | –31,523 | 15,160 | 38,069 | –7135 |
| Total | 134 | –110,193 | 507,117 | 176,909 | 555,709 | 1,129,542 |
Focusing solely on costs to social services, the biggest potential savings (albeit modest) would seem to come from supporting case types 5 (LMM) and 14 (MMM) in the community, where savings of approximately £45,000 and £42,000 per year might be made. Indeed, the maximum annual saving that social services could make is predicted to be just over £140,000 (achieved by maintaining all service users in case types 5, 6, 14, 17 and 23 in the community for the specified period), while the corresponding increase in private and total costs is in the order of £201,000 and £197,000 respectively. If it proved possible to divert all 134 marginal care home entrants, the corresponding figures would be around £110,000, £556,000 and £1,130,000 respectively.
It is, of course, unlikely that even with the benefit of enhanced community services, it would be possible to maintain 100% of marginal care home entrants in the community for the full diversion periods. This population has changing needs and with increasing mental or physical incapacity, some would inevitably need earlier care home placement. In light of this, Figures 7 and 8 show the effect of different diversion success rates on total costs (e.g. the effect of maintaining 10%, 20%, 30%, etc., of each case type in the community). These illustrate the almost equal trade-off between health and social care costs as agencies divert more care home entrants. For case types without significant one-off costs, they may also be viewed as proxy indicators of the costs of diverting 100% of service users for 10%, 20%, 30%, etc., of the specified time period.
FIGURE 7.
Marginal care home analysis. The effect on different cost types of different diversion rates: site X only (£s per year). NGO, non-governmental organisation.
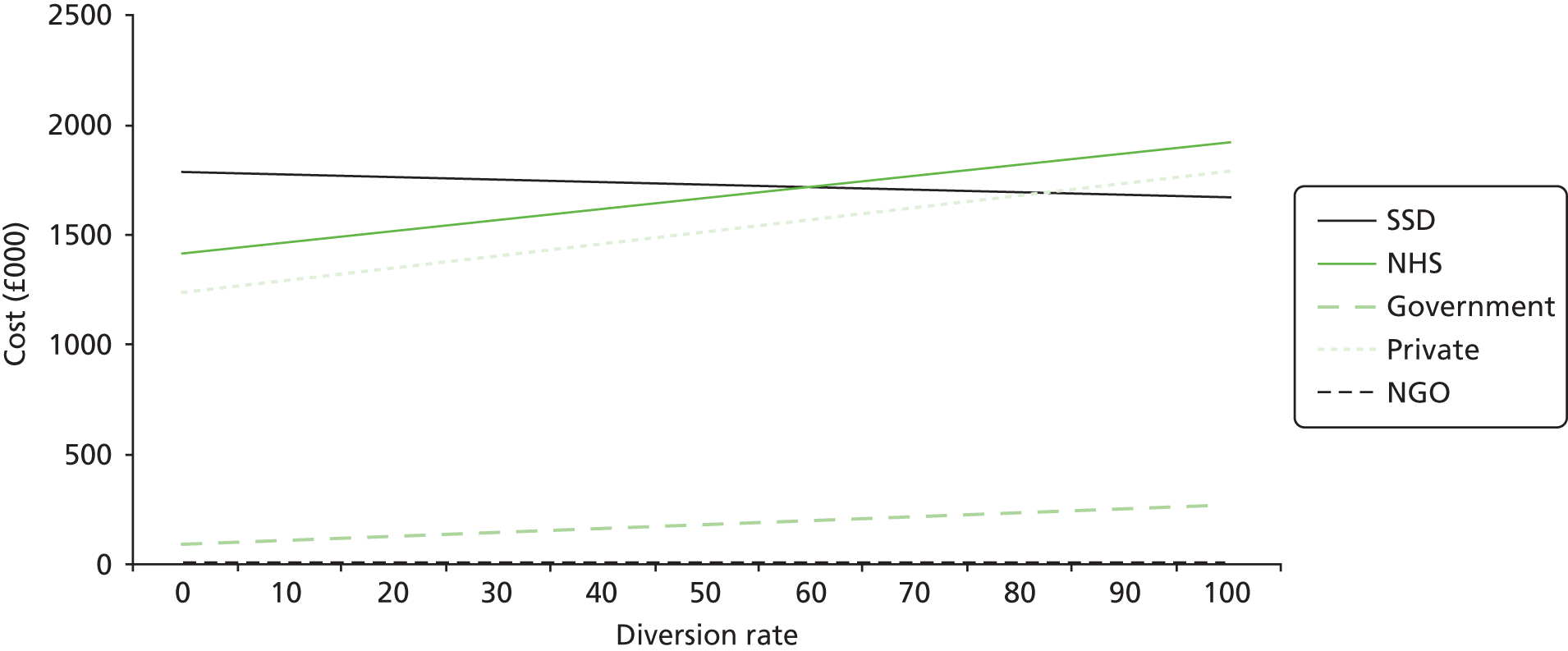
FIGURE 8.
Marginal care home analysis. The effect on public and private costs of different diversion rates: site X only (£s per year).
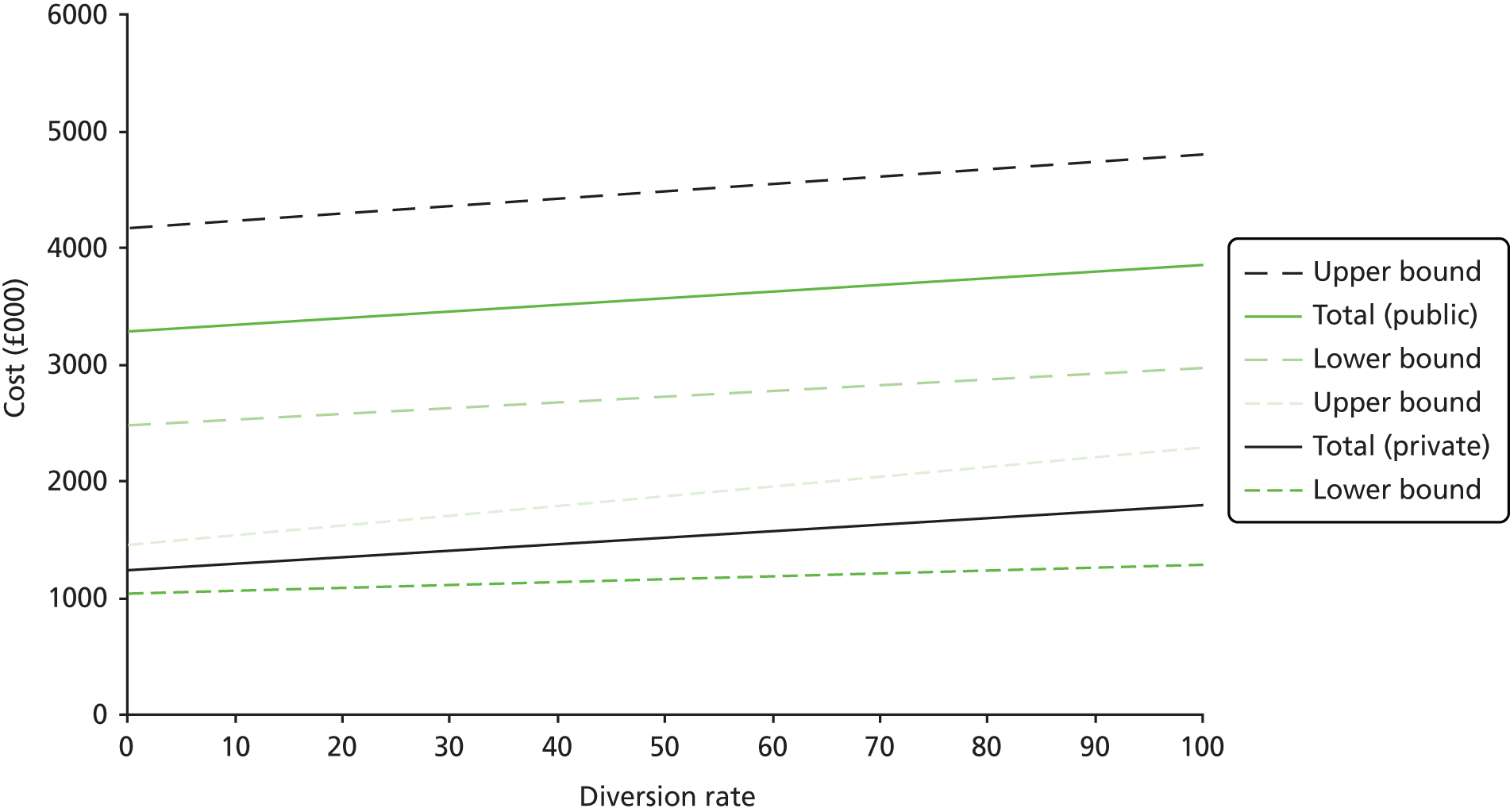
There are several reasons why the overall cost implications of the above analysis are likely to be more complicated. As shown in Chapter 4 (see Table 8), 42.6% of service users on the active social services caseload who lived at home, and were not known to the specialist mental health service, were in one of the nine marginal care home case types. In addition, 39.8% of the site X CMHT caseload who lived at home were similarly in one of the nine case types. Furthermore, another 17% of the active social services sample who lived at home were in one of the five non-marginal (i.e. most appropriately placed in a care home) case types. At any time, there are thus substantial numbers of older people with mental health problems living in the community who are on the verge of care home entry, but who (again based on information from Chapter 4) are unlikely to receive the substantial care packages necessary to maintain them at home. There are also a number of older people living at home for whom care home placement may be a more appropriate option.
Marginal inpatient cases (see Chapter 3, Activity 7.1)
Echoing the approach described above, Tables 35 (all sites) and 36 (site X only) detail the estimated annual aggregate costs of providing enhanced community care packages for the five most marginal inpatient case types compared with those of inpatient admission. These are based on the locally formulated care packages preferred by the experts, and focus solely on costs incurred by mental health and social services. The key variables are the expected number of patients represented by each case type (projected over a 12-month period), the estimated number of inappropriate admissions each individual might experience a year (based on information from the baseline data collection), the anticipated length of inpatient stay (based on the inpatient discharge data collection), and the number of days the intensive community care package might need to be employed (based on information from the practitioner care planning exercise). If it were possible to divert all of these five case types, local agencies might expect savings in the region of £2M. Even focussing only on the three case types which experts concurred were inappropriate (i.e. case types 26, 28a and 31), savings of more than £1.5M might still be achieved.
| Case type | Expected n per year | Estimated average number of inappropriate admissions per year | Median LOS (days) | Days alternative intensive community mental health support per prevented admission episode | Days additional SSD care package per prevented admission episode | Total difference in NHS costs | Total difference in SSD costs | Total difference in total costs |
|---|---|---|---|---|---|---|---|---|
| 28a | 25 | 1.14 | 56 | 42 | 56 | –460,989 | 9363 | –451,626 |
| 10 | 6 | 1.25 | 104 | 63 | 0 | –241,694 | –8641 | –250,335 |
| 6 | 17 | 1.45 | 36 | 36 | 52 | –216,025 | 10,461 | –205,564 |
| 26 | 23 | 1.29 | 91 | 28 | 28 | –820,472 | –25,449 | –845,921 |
| 31 | 10 | 1.17 | 77 | 42 | 42 | –252,876 | –18,551 | –271,427 |
| Total | 81 | –1,992,056 | –32,817 | –2,024,872 |
| Case type | Expected n per year | Estimated average number of inappropriate admissions per year | Median LOS (days) | Days alternative intensive community mental health support per prevented admission episode | Days additional SSD care package per prevented admission episode | Total difference in NHS costs | Total difference in SSD costs | Total difference in total costs |
|---|---|---|---|---|---|---|---|---|
| 28a | 5 | 1.14 | 56 | 42 | 56 | –99,475 | 2020 | –97,454 |
| 10 | 5 | 1.25 | 104 | 63 | 0 | –181,271 | –6481 | –187,751 |
| 6 | 3 | 1.45 | 36 | 36 | 52 | –36,544 | 1770 | –34,775 |
| 26 | 11 | 1.29 | 91 | 28 | 28 | –384,555 | –11,928 | –396,483 |
| 31 | 0 | N/A | N/A | N/A | N/A | 0 | 0 | 0 |
| Total | 24 | –701,845 | –14,619 | –716,463 |
As with the marginal care home case types, however, it is not realistic to believe that it would be possible to keep all 81 people out of hospital and Figure 9 shows the effect of increasing diversion success rates on the different cost elements. There is, furthermore, a difference between the funds that would accrue to the SSD on diverting people from care homes and those that might be realised by trusts in preventing admissions. If, for example, just one or two care home placements a year were prevented, local authorities might expect to make modest savings. By contrast, the avoidance of a few inpatient admissions would only release very limited resources. Although small reductions in admissions might enable higher quality of care for other patients (e.g. by staff spending more time with each patient), the number of hospital admissions prevented would need to reach a critical mass before fixed costs could be reduced to allow any transfer of monies.
FIGURE 9.
Marginal inpatient analysis. The effect on different cost types of different diversion rates: all sites (£s per year).
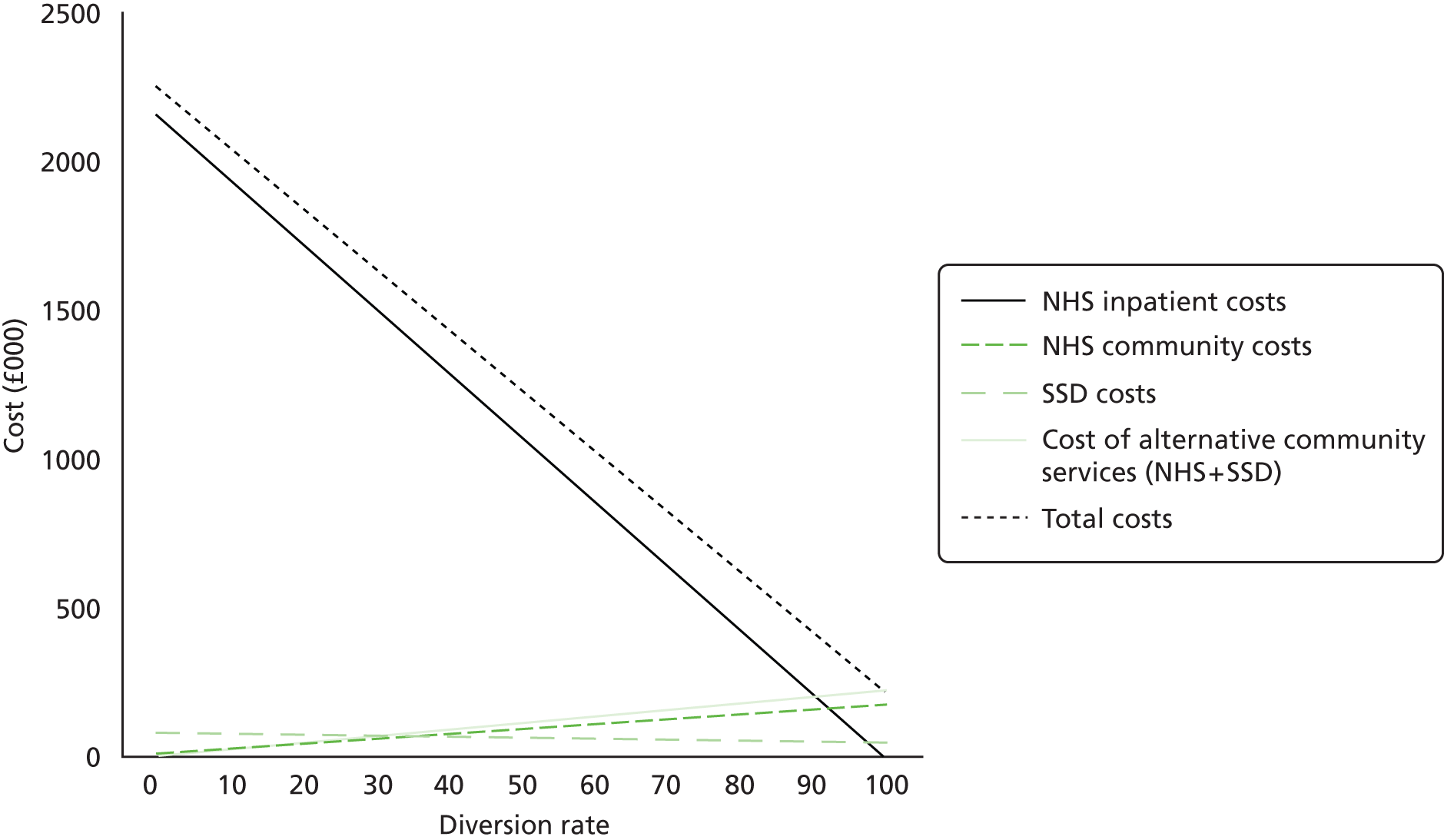
Taking the implications for site X as an example, if it only proved possible to keep half of the people in case types 5, 10, 26 and 28a at home, the trust would divert just 12 individuals a year, probably below the critical threshold noted earlier. If, however, they were able to divert all cases, potential savings might approach £700,000.
Discussion
Although the BoC approach has often been used to estimate the resource implications of caring for frail older people in alternative settings, the work described here demonstrates its potential to inform service planning for older people with mental health problems, a particularly complex and vulnerable client group. Based on the findings of the systematic literature review (see Chapter 2), the approach was refined to: expand the number of settings considered in the model; investigate the implications of comprehensive costing as opposed to a public expenditure approach; explore the potential for incorporating outcome data; and improve understanding of the factors underpinning the present BoC. In contrast to some other BoC analyses, the study was firmly grounded in the knowledge and experience of local practitioners, older people and carers, ensuring the results would be relevant to local agencies and of practical utility to commissioners and other decision-makers.
The findings offer an overall picture of the needs and number of older people receiving different types of service across the current spectrum of care, from informal support at home to acute mental health inpatient admission, providing a starting point for any joint planning process. 46,47 They also reveal the potential to change the current pattern of service delivery. Thus, despite a policy of community care dating back more than 50 years,26,27,78,79 the study suggests that front line staff and managers still believe that if enhanced community services were available, a significant proportion of those people currently admitted to a care home or acute mental health inpatient bed could be successfully and appropriately supported in alternative settings. Moreover, their views are broadly shared by older people, carers and outside experts. However, as opposed to nearly all past BoC studies,89 the analyses suggest that there is no longer the potential to generate significant savings for the public purse by diverting more older people from care home admission. Indeed, service planners seeking to support a higher proportion of care home entrants in their own homes or supported housing will need to invest significantly in community services. This is perhaps not surprising, as many of the marginal care home entrants had multiple and complex needs which would be expensive to meet in any setting. By contrast, it would appear that there remain strong economic arguments for replacing the current hospital care of certain inpatient groups with intensive community-based arrangements.
Methodological considerations/lessons for future studies
A number of assumptions were built into this work. Perhaps the most significant of these was that the overall level of health and social services expenditure on older people with mental health problems was unlikely to vary a great deal from year to year, and that the age structure and associated needs for care of the local population would change little in the short-term. Inevitably, there was also a degree of uncertainty about service costs, such that the results constitute estimates of expenditure. The main findings, however, appear robust, and sensitivity analysis helped understand how different factors might influence future costs and their distribution. Furthermore, in taking account of the empirical variability of costs within case types (rather than simply average costs) the study was able to test out the implications of group-based placement decisions. Like previous published analyses, however, no account was taken of the transaction costs that might be incurred in reallocating resources between settings or the creation of new services.
Although the achieved study samples at the baseline data collection stage fell short of expectations, compared with related studies89,117,118 they were still large. Furthermore, the data suggested that the study had reached saturation in the development of case types. The smaller than expected CMHT and care home samples did, however, have consequences in reducing the pool of people from which individuals could be recruited for the matched cohort study.
Other limitations include the pragmatic identification of older people with mental health problems within the social services samples. This may have captured some people without a formal mental illness, including those with cognitive impairment attributable to other causes and people with subthreshold depression. However, mild depressive symptoms are often clinically significant,168,169 and feedback from practitioners suggested the study did accurately identify those older people with mental health problems who commonly present to social services. An unavoidable weakness of the sampling process was that it only captured those older care home entrants known to social or specialist mental health services. As such, the findings take no account of the potential for diverting those self-funded care home entrants who currently have no such contact with services.
A key lesson concerns the importance of the vignettes. These were based on real individuals (see Chapter 3) and (although limited to one side of A4, so as to not overload the reader) contained a wealth of information about factors known to be significant in determining the most appropriate locus of care. Furthermore, participants were told to assume anything not mentioned was non-problematic. However, although feedback on the vignettes was overwhelmingly positive, suggesting participants could easily picture the service users depicted, some staff would have liked more detail and a few commented that this impaired their ability to make informed judgements about optimal care settings.
Perhaps the most important limitation of the study, however, was its failure to identify or collect sufficient data on the relative merits of different service options for specific groups of people on the margins of care. The research programme aimed to generate objective evidence of absolute and relative benefits of alternative care options. This would have been invaluable in making decisions on the cost-effectiveness of alternative care packages for marginal cases. It is simple to assess cost-effectiveness where benefits are greater and costs lower than alternatives. Where, however, both costs and benefits are greater, sound knowledge of the magnitude of the difference in benefits becomes critical to sound resource allocation. Lacking this intelligence, the reader is thus left to assume that in determining where service users were best placed, participants will have made some form of normative judgement about their best interests. 30,97,102
Given this, the presentation of more general evidence to the RAM Panel should be viewed as a simulation/pilot of one way of exploring whether knowledge of likely outcomes makes a difference to service manager decision-making. One cannot, however, conclude from this exercise that it has little effect, for more account may have been taken of evidence that specifically related to the relevant case types. Furthermore, the real situation is likely to be much more complicated than this study was able to model, with any one particular setting delivering relative improvement in some outcomes, but worse performance in others.
If this study found that robust information on the relative outcomes of specific groups of older people with mental health problems supported in different settings is urgently needed, it also suggested that this will not be easy to generate. To obtain the target numbers for the planned cohort outcome study, this exercise would have had to run for 12 times longer than the allotted period, or included 12 times the number of teams. Other possibilities to improve recruitment might have included further relaxing the inclusion criteria to encompass service users with higher needs levels (albeit this may have decreased the overall recruitment rate further); undertaking proxy interviews with informal carers; and/or expanding the recruitment process to people living at home in the social services sample (although this was of itself a small sample). In retrospect, however, the main problem with this element of the study was the requirement to recruit service users via practitioners, which led to a complicated process, outside the research team’s control.
Feedback from practitioners identified a number of disincentives to participation in recruitment, including concerns that they would be seen as responsible if users had negative experiences, damaging trust; their already heavy workloads; and the lack of any direct benefit to themselves, while other studies have faced similar problems. 170 Thus, despite the suggestion that those practitioners who participated in this study would be more receptive to future research involvement, we would echo calls to test new ways of quantifying staff impact on the recruitment process and the possibility of linking this to tangible rewards. 170,171
Implications for local service providers
This study suggests that services for older people with mental health problems in site X do not always correspond with their needs and preferences, and identifies a shared aspiration to shift care towards the community. It also identifies a number of building blocks that might need to be put in place to achieve this. These include the growth of a range of community services; a clarification of the role of ECH; a more timely response to the needs of people on the cusp of acute mental health inpatient admission; and improvements in hospital discharge planning. None of these proposals are radical. They are not concerned with new or novel ideas, but rather concentrate on doing important things well, on increasing efficiency and on strengthening existing arrangements.
When asked to identify appropriate services for marginal care home case types, local practitioners recommended a mix of generic and specialist home care, community mental health staff input and telecare. Managers, older people and experts also advocated the use of more day care, carer support services and dedicated assessment/rehabilitation beds. Packages of care deemed best for marginal inpatient case types similarly relied substantially on community mental health services (including mental health support worker input), primary care and specialist CHSTs. Indeed, an important point about care home support services, whatever form they take, is that the resources invested in preventing one admission, might arguably also prevent future admissions as care home staff gain skills in caring for this client group.
Although most, if not all, of these services were theoretically available in the catchment area, feedback from staff and service users raised doubts about the quality of some (including certain home care services) and the quantity of others. The input of mental health support workers, for example, was said to be time-limited, while traditional day care services were seen as closing consequent on the introduction of personal budgets and the deconstruction of block contracts. This raises questions about how to stimulate markets to meet individual need. A need for 24-hour, rather than 9–5 community services was also identified, with the suggestion that workforce flexibility had not kept pace with changes in care requirements and settings. There was a general recognition of the need for more mental health training for staff and the development of funding arrangements able to support more flexible services.
The specific roles that generic and specialist ECH might play in any future service configuration perhaps needs particular thought. Although practitioners identified this as a more appropriate option for many marginal care home entrants, in practice relatively few vacancies arise each year. Moreover, at present there is no facility for potential tenants to try ECH on a short-term basis, as is possible with care home placements. These factors suggest a move to ECH is more likely to be a planned change than a response to immediate needs, and perhaps explain why RAM Panel members failed to sanction many such proposals. However, the question of exactly when in the care trajectory ECH is the best option did not appear to have been resolved. The place of capital resources in a context of revenue resource dominated community care is complex. 172,173
If adequate capacity of community services for the needs of older people with mental health problems is clearly vital, the study also suggests the timeliness of such provision may be equally important. This was particularly evident with regard to the marginal inpatient case types, where the data suggested approximately four-fifths of patients had some involvement with the mental health service before their admission. Although some appeared to be relatively new referrals at a point of crisis, others were longer-term clients, with existing care packages. In both situations, however, what was striking was the large discrepancy between the intensity of the enhanced community support felt necessary to keep them out of hospital and the amount of support they were actually receiving before their admission, suggesting higher levels of input may be needed sooner.
Similarly, the data suggest that some three-quarters of marginal care home entrants were already known to social services (although in many cases data on this aspect of the study were missing). There was once again a large discrepancy between the packages of care many actually received and those thought necessary to divert them from care home placement. As with the inpatient sample, there may be many reasons for this, including a sudden change in circumstances (resulting from say a fall or stroke) and service refusal. That said, the data from the social services domiciliary sample would seem to suggest that at any one time there are a number of people in the community with considerable ongoing care needs who receive relatively little formal support. In the light of evidence that specialist integrated assessment may potentially defer the care home admission of older people at risk,174 the fact that more than half of care home entrants had not been seen by specialist mental health services was also noteworthy.
Finally, perhaps one of the most striking findings from this study was the very high proportion of marginal care home entrants admitted from general hospital wards or at unacceptable risk of falls. This illustrates the complex morbidity of this client group, and also highlights the number of placements arranged in the context of crises, as identified elsewhere in the literature. 175 This made assessment of individuals’ potential functioning more difficult, and gave little time to organise home care packages or garner support from informal carers. In recognition of this, the SSD has recently commissioned a number of beds in the local community hospital for assessment purposes, as suggested by the experts in this study. As seen with the mental health inpatient data, however, it is important to ensure that any such beds are used only for those people who really need them, and also that the efficiencies to be gained in the discharge planning process to prevent delayed discharge are achieved. Indeed, the data suggest that as many as 834 inpatient bed-days may have been lost across the three sites over the 6-month data collection period.
Wider implications
Although one of the perceived strengths of the BoC approach is the particular relevance of its results to local decision-makers, it is anticipated that many of the challenges facing care providers in this study will be echoed across the country. Indeed, the settings investigated are both generic and ubiquitous. The findings also raise some important issues for national policy-makers.
One obvious question is how the continuing promotion of community care fits with drives to reduce public expenditure, for the study suggests that diverting greater numbers of older people from care home admission will actually raise total public costs. Although there was some potential for site X LA to achieve modest cost savings through the reduction of long-term placements, these would be more than offset by increases in other public expenditure. Indeed, the current system of parallel services (and budgets) would seem to encourage the continuation of such cost shifting. The common perception of a hierarchy of costs (in which community care is cheapest) running in parallel with one of choice (in which care at home is the preferred option) may now need revising, although it would still seem to hold compared against hospital admission.
Another question in light of the above is ‘What is now driving the desire among staff to keep people at home?’. Older people themselves were markedly more likely to favour residential care than were practitioners, with the latter expressing a lack of confidence that care homes can meet the needs of this client group, an issue explored further in Chapters 12–14. Indeed, if there were to be a shift towards the greater use of care homes, local practitioners suggested it would be necessary to increase the amount of funding attached to care home placements, so facilitating improvements in the quality of care provided.
One final lesson concerns the potential utility of the BoC approach as a way of capturing uncertainty in the service planning process. As well as facilitating communication between diverse stakeholders by creating a shared representation of the whole system at a time of considerable change in the provision of health and social care services, the application reported here has the advantage of ‘tempering perspectives that overestimate the reliability of prediction’ and ‘bringing uncertainty into the open’. 176 Based on this work, the research team are thus currently developing a BoC workbook complete with cost modelling templates that will enable other health and social care decision-makers to apply the framework independently.
Chapter 6 Community mental health teams for older people: a systematic review of the literature
Community mental health teams for older people have been described as the ‘cornerstone’ of mental health care for older people, yet little is known about how such teams operate or the efficacy of different ways of working.
ObjectivesObjective 1: to synthesise existing descriptions of team structures and processes. Objective 2: to review whether these team features are shown to influence service user outcomes.
MethodA systematic literature review adopting a bibliographic database search (EMBASE, MEDLINE, PsycINFO, Web of Science) restricted to UK materials published since 1998 for objective 1, and peer-reviewed papers from any jurisdiction since 1989 for objective 2.
ResultsForty-four references met the inclusion criteria for objective 1, and seven for objective 2. All but one reference related to UK teams. Only a minority of teams included the full recommended range of professional disciplines, although there was evidence of improvement over time. Initial assessments were normally undertaken at home by an old age psychiatrist, with multidisciplinary assessment rate. No evidence was found to support many of the recommended core attributes, including the multidisciplinary composition of team membership; flexible professional roles that blur generic and specialist duties; and multiprofessional assessment at home. Limited evidence supported open referral systems, the use of shared standardised assessment documentation and the conduct of initial assessments by other (non-consultant) qualified staff. The most rigorous studies were, however, conducted in a narrow range of ‘exemplar’ CMHTsOP.
ConclusionsAlthough some evidence gaps can be filled from related fields (e.g. working-age adult services) further research is required that moves beyond description to evaluation of the impact of team design on service user outcomes.
Background: history of the development of community mental health teams for older people
Community mental health teams for older people emerged in an ad hoc manner during the 1980s, as part of old age psychiatry services which had evolved following the rundown of mental hospitals from the 1960s. 177,178 A key issue for psychiatrists was to widen access to specialist mental health provision for older people alongside the need to utilise their own profession effectively. The former was supported by open referral systems and the latter by enabling other professions to conduct initial assessments. These features remain at the heart of CMHTsOP, while debate continues about the nature and extent of integrated services that will produce the most effective outcomes.
Although widespread by the mid-1990s43,73,179,180 it was not until 2000 that CMHTsOP were recognised in national policy as central to the delivery of specialist mental health services for older people. 31,46 The following decade cemented this position, emphasised in a range of reports/policy documents. 11,47,48,50,57,163,181 The policy context was also shifting, becoming both more prescriptive [e.g. National Service Frameworks (NSFs) were established with the explicit aim of reducing variations in care31] and dominated by the wider health and social services integration agenda. 182 In contrast to the 1980s and 1990s, when CMHTsOP development appeared highly idiosyncratic, driven largely by local practitioners, managers and other personnel within individual services, the early 2000s saw a shift to a more top-down approach, with CMHTsOP increasingly expected to conform to a set of externally derived ‘best practice’ guidelines. Although these guidelines were fairly broad, designed to accommodate existing variations in organisation and function, they identified key characteristics that an effective CMHTOP should encompass, many mirroring those of the early CMHTsOP set up in south-east London. These included multidisciplinary teams (MDTs);31,181 operating a single point of access (SPA)183 with open referral systems. 31 All professional disciplines within the team were expected to conduct initial assessments (jointly if appropriate) at the patient’s home, using standardised documentation stored in a single case file11,31,181 while consultant old age psychiatrists were to become fully integrated team members. 184
Aims of the review
It has been suggested that much of this guidance is predicated on ‘good practice, not good evidence’ (p. 116). 183 A systematic literature review was consequently undertaken to explore these issues. 185 Its aims were to identify the variety of team structures and processes in existence (objective 1), and to evaluate the evidence of the impact of the range of approaches found on service user and staff outcomes (objective 2).
Review methods
Four electronic databases (EMBASE, MEDLINE, PsycINFO and Web of Science) were searched in October 2008 for relevant English-language articles, using search terms which described the service (e.g. ‘geriatric psychiatry’, ‘mental health team’, ‘community mental health’), the user group (e.g. ‘old*’, ‘aged’, ‘elder*’) or team characteristics and processes (e.g. ‘professional relation*’, ‘multidisciplin*’, ‘interprofession*’, ‘interdisciplin*’). An example of the search strategy can be found in Appendix 17. Hand-searches were undertaken of the bibliographies and reference lists of all included literature; of the three journals most frequently cited in the initial searches; and of generic search engines and individual organisation websites to identify grey literature. The authors also consulted recognised experts to identify additional studies.
Inclusion criteria
Inclusion criteria are detailed in Box 11. Only empirical studies were included. Objective 1 references were restricted to the UK. For objective 2, literature had to measure at least one service user, staff or process outcome, and compare different CMHTOP approaches. The last of these criteria excluded studies which compared the work of CMHTsOP with other service models (e.g. single-discipline nurse interventions).
| Objective 1 | |
|---|---|
| To describe variations in team structures and processes | Include:
|
| Objective 2 | |
| To evaluate linkage between team approaches and service user outcomes | Include:
|
| Adapted from figure 1, Abendstern M, Harrington V, Brand C, Tucker S, Wilberforce M, Challis D. Variations in structure, processes and outcomes of community mental health teams for older people: a systematic review of the literature. Aging Ment Health 2012;16:861–73. | |
Two reviewers undertook the data extraction process using a standardised electronic form. The first 10 were completed together to ensure reliability. Data were extracted on team attributes indicative of structures and processes and, where available, outcomes and relevant findings (see Appendix 18). A full list of data items can be found in Appendix 19. Studies were subjected to a three-stage screening process (Figure 10). Retained references were read in full by one of two reviewers with the final decision on inclusion being made via discussion between them. The main reasons for excluding references can be found in Appendix 20. The extent to which publications provided detailed and relevant information about how teams were organised, as well as evaluations of their effectiveness, were captured in a bespoke centrality tool (see Appendices 21 and 22). An existing quality appraisal tool,186 covering sampling, measurement, analysis and the interpretation of results, was used to assess the quality of studies addressing objective 2 (see Appendix 23).
FIGURE 10.
Study selection process. Adapted from figure 2, Abendstern M, Harrington V, Brand C, Tucker S, Wilberforce M, Challis D. Variations in structure, processes and outcomes of community mental health teams for older people: a systematic review of the literature. Aging Ment Health 2012;16:861–73. O, objective.
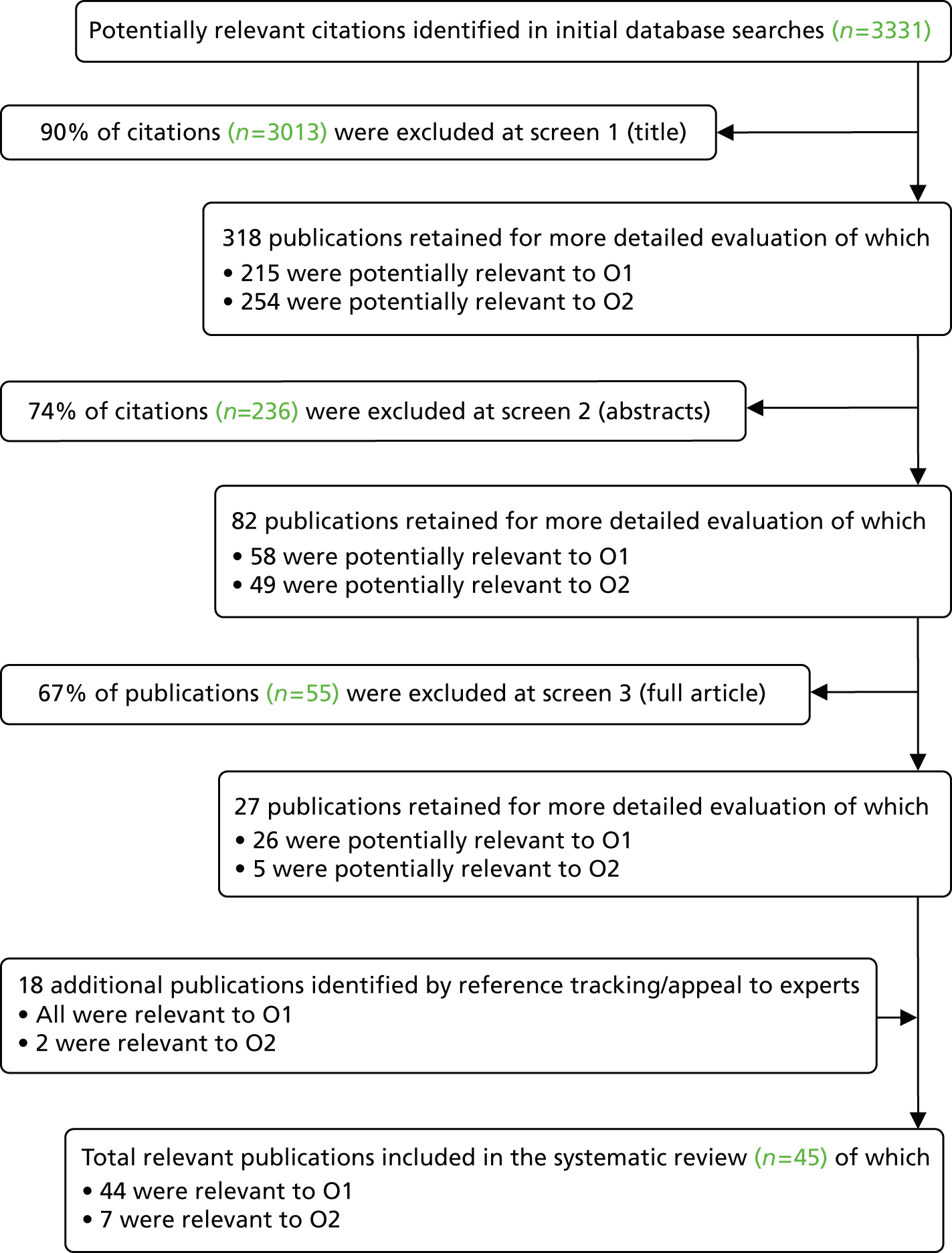
The review follows a narrative synthesis style84,187 with findings divided into key areas of the research questions relating to structure, process and outcomes, as well as service user characteristics. Data from individual teams identified within the studies were compared to explore characteristics across teams. Where possible, results were compared with national level data reported in other studies. Consideration was given to the heterogeneous nature of the literature in assessing possible bias when synthesising results.
Results
Details of included and excluded literature
Forty-five studies were included in the review: just over 1% of those initially identified. Most references were excluded from objective 1 because they were not UK based and from objective 2 because they did not relate to older people or did not contain comparisons to determine the impact of a CMHTOP process on user outcomes.
Included studies were heterogeneous in relation to both publication type and the nature of what was reported with a shift visible in the latter over time. Pre-2000 publications, for example, were predominantly reports of local teams with a focus on their aims, philosophy and key features. In comparison, almost half (10 of 24) of post-2000 publications were large-scale surveys or audits which documented and compared the range and variation of provision across the country, implicitly or explicitly determining overall progress towards pre-determined indicators of good practice. Over 75% of studies had a local focus, covering 57 teams. Ten publications25,188–196 related to just three of these teams which can be regarded as ‘exemplars’: early well-resourced teams, established by research active consultants, wanting to test new service delivery approaches. Local studies offered a level of detail not available in the broader national/regional literature. Depth and breadth of reporting overall was highly variable whereas data were geographically skewed towards London. A description of the studies included in objective 1 alone can be found in Table 37; those included in both objective 1 and objective 2 in Table 38; and the study only included in objective 2 in Table 39.
| Reference | Study level (local or regional/national) | Design and data collection summary | Main focus | Findings |
|---|---|---|---|---|
| Abendstern et al. 2006197 | Regional | Observational (cross-sectional) study using a primary survey completed by team leaders (59% response rate) to collect quantitative data An evaluative study but descriptive for current review |
Integration of processes within teams providing services for people with dementia. Compares multidisciplinary (n = 35) and single discipline (n = 17) teams | MDTs had greater levels of integrated processes |
| Arthur et al. 2002198 | Local | Experimental (RCT) study using both primary (survey) and secondary (case notes) data. Forty-seven people in study though only 34 agreed to assessment An evaluative study but descriptive for current review |
Primary/secondary divide – case finding issues. Comparison of CMHTOP assessment/intervention with usual GP care for people with depression | CMHTOP assessment/intervention made little difference to outcomes |
| Audit Commission 200046 | National (12 health authority areas) with one local case study | National service audit. Descriptive study using primary (survey) and secondary (administrative and case notes) tools to collect quantitative data in 12 areas | Audit of mental health services for older people. Describes a range of CMHTOP processes including staffing and integration | Wide variation in practice and provision |
| Audit Commission England 200247 | National (all health authority areas) | National service audit. Descriptive study using primary (survey) and secondary (administrative and case notes) tools to collect quantitative data in 70 areas | Audit of mental health services for older people. Describes a range of CMHTOP processes including staffing and integration | Wide variation in practice and provision |
| Audit Commission Wales 2002199 | National (10 multiagency sites) | National service audit. Descriptive study using primary (survey) and secondary (administrative and case notes) tools to collect quantitative data in 10 areas | Audit of mental health services for older people. Describes a range of CMHTOP processes including staffing and integration | Wide variation in practice and provision |
| Baillon et al. 1996200 | Local | Descriptive study using quantitative primary survey data from CMHT staff (68% response), care home managers (100% response) and GPs (36% response) | Views of CMHTOP members, care home managers and GPs regarding CMHT liaison with care homes | General support for regular contact and direct referrals |
| Banerjee et al. 1996194 | Local | Experimental (RCT) study, appropriately powered using both primary (interview) and secondary (case note) data. Sixty-nine people in total, 36 in control group. Three standardised/validated measures used | Primary/secondary divide – case finding issues. Comparison of CMHTOP intervention with usual GP care for frail elderly people with depression | Positive outcome (higher rates of recovery) in CMHTOP group |
| Barlow 2006201 | Local | Descriptive study using primary data collected via a survey. Nine respondents. Qualitative data | Perceived roles of CPNs by CMHTOP staff | No consensus between staff groups |
| Bedford et al. 1996202 | Local | Observational (panel/cohort) study using both primary and secondary data collection. Data collected at baseline and at 6-month follow-up | Comparison of outcomes between people with dementia and those with functional disorders following intervention by CMHTOP | Significant differences between the two groups |
| Brown et al. 1996189 | Local | Observational (retrospective panel) study using secondary case notes of 120 randomly selected service users to collect quantitative data | Comparison between referral and ongoing caseload population of CMHTOP, and destinational outcomes of service users | Lower proportion of people with dementia on ongoing caseloads compared with referral population, and higher proportion entering care homes compared with functional service users |
| Challis et al. 2002179 | National (318 COAPs) | Observational (cross-sectional) survey of COAPs. Collected primary quantitative data. 73% response rate (n = 318) | Professional autonomy, community orientation and integration between health and social care provision within old age psychiatry services in England | Substantial variation across all domains |
| Coles et al. 1991203 | Local | Observational (before and after) study using secondary case notes of 193 service users to collect quantitative data An evaluative study but descriptive for current review |
Describes setting up of CMHTOP, main reasons for its establishment, and compares processes and outcomes with former traditional model of service delivery | |
| Dare and Benbow 1997204 | Local | Description of service development by the service manager and COAP | Impact of secondment of COAP to service which had been without one for 10 years. Includes impact on CMHTOP | CMHTOP provided more active and timely community support with better access to consultant |
| Das and Bouman 2008205 | Local | Observational (before and after) study using secondary case notes of 40 service users to collect quantitative data | Evaluation of introduction of direct referral system from SSD | No overall increase in referral levels, almost all social services referrals deemed appropriate |
| Dening 199219 | Local (multiple case study – seven old age psychiatry services) | Descriptive study using survey of seven COAPs and interviews with a range of CMHTOP staff to collect qualitative primary data | Description of author’s visits to a small number of old age psychiatry services, focussing on main issues in providing community-oriented services. In relation to CMHTsOP emphasis is on referral and assessment processes and the role of medics within teams | A lot of variation between services |
| Eastley and Nowers 1997206 | Local | A descriptive mixed-methods study using a primary survey of 105 GPs (77% response rate) | Reports views of GPs in one NHS trust on newly set up CMHTOP | Most GPs felt the service had improved since introduction of team (faster and easier access) |
| Gupta et al. 1996207 | Local | Largely descriptive study with small evaluative component using quantitative data collected via both primary survey of 109 service users and all GPs in area and secondary administrative and case notes from 971 service users. Survey response rate was 28% from service users and 50% from GPs | Review of new community mental health service with particular emphasis on impact of open-access system. Also considers assessment and outcomes | Open access did not lead to inappropriate referrals. Majority of assessments at home |
| Healthcare Commission 200950 | National (though only six specialist mental health trusts) | Largely descriptive study with small evaluative component using primary survey and interviews with service users and carers, trust staff, LA care and commissioning staff to collect qualitative data | Broad focus on four issues of old age psychiatry services: age discrimination, quality of inpatient care, comprehensiveness of services, working with other organisations. Includes discussion of integration of CMHTs | Huge variation of provision and levels of integration |
| Hoskins et al. 2005208 | Local | An uncontrolled evaluation study (observational time series) using validated tool to collect primary quantitative data from carers assessment interview and questionnaire An evaluative study but descriptive for current review |
Impact of CMHTOP support on carer stress | Reduced stress over time Interventions included carers group run by team |
| Jenkins and Macdonald 1994195 | Local | Experimental (RCT) study using primary interviews with 65 service users (39 in control group) to collect quantitative data. Standardised/validated measures used An evaluative study but descriptive for current review |
Primary/secondary divide – case finding issues. Compares outcomes of intervention by CMHTOP with usual GP care for people with depression | No difference overall between two services in relation to level of depression. Both groups improved |
| Jolley et al. 1997209 | Local | A description of service development by COAPs | Description of secondment of COAP with aim of developing the OAP service. Minor reference to setting up of CMHTOP (doctors and nurses only) as part of this service | |
| Junaid and Bruce 1994210 | Local | A small-scale descriptive study using primary survey method (four respondents) to collect quantitative data | Comparison of four CMHTsOP (doctors and nurses only), particularly in relation to work of CPNs | Wide variation but little evidence of strategic planning |
| Lawley et al. 2005211 | Local | A description of service development by COAPs | Role of two COAPs in service and impact of reorganisation of their workload and responsibilities. Includes brief reference to impact on CMHT | Improved job satisfaction for COAPs and perceived improvement in engagement with CMHTsOP |
| Lingard and Milne 200448 | National (32 ‘English Health Communities’) with two local case studies | A resource document/good practice guide which combines a literature review and primary survey providing quantitative data on 32 mental health services in England | Integration of CMHTsOP | Wide variation with only 47% respondents stating that they had fully integrated teams |
| MacDonald et al. 2007193 | Local | A descriptive study of service user characteristics using secondary administrative and case notes of 10,000 service users to capture quantitative data on change over time | Compares referral patterns over time (17 years) | Open access did not lead to inappropriate referrals. Provides stronger (longitudinal) evidence to counter arguments against open access |
| Mander 2007212 | Local | Description of service development by the service manager | Describes development and introduction of a new model designed to ensure fair access to services Argue that new model promoted improved communication between health and social care. Stresses importance of collaboration with a range of stakeholders in model development |
|
| McCrae et al. 2007213 | Local | Observational (cross-sectional) study using a primary survey of staff to collect quantitative data. One standardised measure used. One hundred and sixty-two respondents of which 13% were CMHTOP staff An evaluative study but descriptive for current review |
Comparison of workplace satisfaction in three OAP settings (CMHTOP, day hospital and inpatient) | CMHTOP staff reported higher levels of autonomy and supervisory support than inpatient staff but lower than day hospitals |
| McCrae et al. 2008214 | Local | Mixed-method case study design using primary survey, interviews and focus group data. Data collected in three time periods but no comparison over time. One standardised/validated measure used An evaluative study but descriptive for current review |
Evaluation of introduction of support workers into CMHTOP | Perceived improvement to service quality but significant levels of staff dissatisfaction due to role ambiguity and disparity between intended and actual roles |
| Melzer et al. 1996215 | Local | Observational (cross-sectional) study using a primary survey of 34 carers capturing both qualitative and quantitative data. One standardised/validated measure used An evaluative study but descriptive for current review |
Considers use of carers’ views to inform service development and compares CMHTOP staff perceptions of carer stress with GHQ scores | High levels of carer dissatisfaction with services and discrepancies between CMHTOP views and GHQ scores |
| NAO 200752 | National | National audit/census collecting quantitative data via online survey. Responses from 371 teams | National audit of services for people with dementia including national survey of CMHTs | Significant variability in integration and services provided by CMHTs |
| O’Connor et al. 1991216 | Local | Experimental (‘controlled trial’) using primary interviews to collect quantitative data. One hundred and fifty-nine service users in study (86 in experimental group). Standardised/validated measures used. Main outcome measure was permanent admission to long-term care An evaluative study but descriptive for current review |
Primary/secondary divide – case finding issues Comparison of intervention by new CMHTOP with usual GP care for people with dementia |
Intervention led to increased admissions |
| Philpot et al. 2000196 | Local | Observational (retrospective panel) study using secondary case notes of a total of 131 service users (59 in CMHTOP group) to collect quantitative data An evaluative study but descriptive for current review |
Comparison between traditional and CMHTOP models of support for people with depression following discharge from hospital | Better outcomes for those seen by CMHTOP |
| Sheard and Cox 1998217 | Local (multiple case study) | Descriptive report of teams operating in different parts of Britain. Qualitative data derived from development and consultancy work with teams and service networks | Description of development, philosophy and characteristics of a range of CMHTsOP with emphasis on integration and interprofessional working | |
| Simpson and De Silva 2003218 | Local | Descriptive study of two teams using quantitative primary survey data from a postal questionnaire. Team 1 response rate: 78% of CMHTOP members, 83% of patients and carers, 93% of GPs. Team 2 response rate: 79% of GPs | Describes an ‘adapted team’ approach to the referral and assessment of older people in CMHTsOP. Two approaches described | Broad satisfaction by GPs for both |
| Stevenson et al. 2006219 | Local | Naturalistic evaluation (before–after observation) using mixed methods to obtain primary data on 65 service users (22 referred to new service) and views of eight carers (randomly selected for interview) and 18 workers (survey with 64% response rate). Standardised/validated measures used An evaluative study but descriptive for current review |
Evaluation of an EAST for people with dementia compared with usual service (day hospital or admission ward) | Work of EAST shortened assessment time and improved outcomes at 1 year (reduced admissions) |
| Tucker et al. 200773 | National (318 COAPs) | Descriptive study using a primary survey of COAPs with a 60% response rate (n = 318) to collect quantitative data. Eighty-nine per cent of England’s trusts covered An evaluative study but descriptive for current review |
National survey describing OAP services, including CMHTs 3 years after the introduction of the NSFOP | Continued variation across country despite NSF aims to address inconsistencies |
| Tucker et al. 2009180 | National (318 COAPs) | Descriptive study using a primary survey of COAPs with a 60% response rate (n = 318) to collect quantitative data. Eighty-nine per cent of England’s trusts covered An evaluative study but descriptive for current review |
National survey examining how integrated OAP services, including CMHTsOP, are 3 years after the introduction of the NSFOP. Focus on requirements for effective integration | |
| Von Abendorff et al. 199425 | Local | Observational (cross-sectional) study using specially designed staff activity record capturing quantitative data from 16 staff in two teams An evaluative study but descriptive for current review |
Comparison of work activities of core and extended team members | Core members had more people with dementia on caseloads and spent more time in direct contact with service users than did extended role members |
| Wattis 199943 | National (231 COAPs) | Descriptive study using a primary survey of 242 COAPs (representing a 51% response rate) to capture quantitative data | National survey of COAPs and the services they work in. Includes some CMHT data | Found wide variation |
| Reference | Focus | Design | Comparison | Outcomes measured and how | Limitations | Findings |
|---|---|---|---|---|---|---|
| Challis et al. 2002192 | The effects of intensive case management within a CMHTOP for people with dementia | Experimental (non-randomised trial) using primary qualitative data. Forty-three matched pairs interviewed at 6 and 12 months. One standardised/validated measure used | Compares two CMHTsOP, one with and one without intensive care management input | Destinational outcomes Costs Service user QoL (including CAPE, CARE) Carer QoL (including the Malaise scale) Service utilisation |
Assessors not blind to whether service users and carers were in intervention or control group | Found improved outcomes of intensive support for people with dementia and their carers. Greater difference between groups at 12 months than at 6 months |
| Collighan et al. 1993190 | Whether medics only or any professional member of the CMHTOP should conduct initial assessments | Observational (cross-sectional) study using both primary interviews and secondary case notes of 100 service users to collect quantitative data | Comparison of two models of assessment – MD or consultant only Although evaluation is of the two approaches within one team it is an evaluation of two CMHTOP models |
One standardised/validated measure used: GMS Full medical, psychiatric history Physical examination with routine blood tests |
Small-scale study, limited generalisabilty | Overall conclusion – high degree of diagnostic accuracy when CMHTOP members conduct initial assessments. Very high level of agreement between team and research psychiatrist (complete in 86% of cases, partial in 3%). Highest misclassification was for dementia. Level of agreement significantly higher in professionals with greater experience (> 1 year) |
| Das and Bouman 2008205 | To evaluate an open referral system from social services to a CMHTOP and whether or not it resulted in changes in numbers of referrals | Observational (before-and-after) study of numbers of referrals | Compares two models of referral with one CMHTOP in two different time periods | Reason for referral Whether assessed for cognition, total number of referrals and whether or not fulfilled eligibility criteria |
Crude outcome measures. Possible bias as case notes of 25% of original sample could not be found and were therefore excluded Only social services referrals were examined – no comparisons with medical referrals group. Small-scale study. No background information about existing relationships between social services and CMHTOP |
No increase in number of referrals following new system (in fact a slight decrease from 476 to 450) |
| Lindesay et al. 1996188 | Compares multidisciplinary treatment decisions by CMHTOP with consultant-only decisions | Observational (cross-sectional) study using both primary interviews and secondary case notes of 100 service users to collect quantitative data | Compares two models of post assessment decision making – MD or consultant only Although evaluation is of the two approaches within one team it is an evaluation of two CMHTOP models |
Psychiatrist researcher assessment and care plan is compared with CMHTOP assessment and care plan Researcher interview included a GMS, a full medical and psychiatric history, a physical examination and routine blood test Measured hospital admission, antidepressant treatment and use of neuroleptics, psychological treatments |
Found satisfactory agreement between groups regarding most decisions: good agreement (87%) regarding antidepressant use. Satisfactory agreement regarding use of neuroleptic medication. Less agreement regarding psychological interventions – to same extent but to different groups. Authors noted that disagreement did not mean poor practice. Overall, teams biased in favour of physical treatments – perhaps because psychological ones are less available than in the ideal service imagined by the researchers. Overall, no evidence that assessments conducted by teams resulted in substantial under-use or inappropriate use of psychiatric interventions | |
| MacDonald et al. 1994191 | Compares characteristics of referrals between traditional GP and open-access sources | Audit of service user characteristics using secondary case notes from 1477 service users to capture quantitative data | Comparison is between different sources of referral (traditional vs. open) to one team during same period teams | Compares numbers and characteristics of referrals from traditional sources (GPs, receptionists, district nurses and hospital wards) and via new open-access (SWs home care organisers, housing officers, care home, relatives, voluntary organisations) to community psychogeriatric service Measured referral source, diagnosis, age and gender |
Traditional sources might have been affected by open-access system – refer less. Diagnoses categories broad which do not conform to ‘standard classifications’ due to 30% of referrals -not being generated by medics – easily used by CMHTOP ‘No statistics are presented as no reliable assumptions can be made about the expected distribution of diagnoses’ (p. 710) |
Overall, significant numbers referred via new route. No evidence of inappropriate referrals from open access route. Low numbers of people with depression referred by SWs is raised as a concern. Sixty-five per cent of referrals came from traditional sources. GPs referred disproportionately more people with delirium (53% of all within this category) and depression (49% with this diagnosis). SWs referred few people with depression (10% of all with this diagnosis) and more with alcohol (38%) and paranoid (34%) problems |
| Treloar 1996220 | Evaluates introduction and use of a new structured assessment tool | Observational (before-and-after) study using secondary case notes of 60 randomly selected people (30 in each group) | Compares two approaches to assessment, structured vs. unstructured | Quality of information on history, clinical examination and correspondence with GP | No information about service users. Although randomly selected, we do not know if they were comparable groups. Not sure how much this matters as it is the extent of information collected which is being measured | Found that quality of recording of some domains and communication with GPs was statistically significantly improved Most of the improvement in communication with GPs was in the form of improved documentation of clinical information. Improvements were larger than those reported from straight forward case note reviews |
| Reference | Focus | Design | Comparison | Outcomes measured and how | Limitations | Findings |
|---|---|---|---|---|---|---|
| George and MacDonald 2005221 | Describes new triage model of accessing one community team in Australia using a ‘triage officer’ | Primarily a description and audit of new process in one team with observational (before-and-after) component. Uses quantitative method and secondary data (administrative records) | Compares two models of access to a CMHTOP in two time periods | Monthly referral figures and monthly figures of cases accepted by team | Fairly crude outcome measures and limited data | Over 50% increase in number of referrals (1884 to 2918) but only 16% increase in number of cases accepted by team (703 to 818). Fifty per cent of referrals did not require any further action from service. Authors argue this suggest the new system is more accessible and responsive. An alternative interpretation is that the service was poorly targeted |
Findings/descriptive synthesis
Team membership was available from 30 studies. Less than one-third (n = 13) of teams described contained staff from each of the five disciplines commonly recommended, although there was some evidence this was increasing over time. 47,48,73,209,210 The nature of the work of core team members was considered by 11 publications, in particular, how profession-specific or blurred these roles were. A range of practices were reported, ranging from strict adherence to discrete professional roles to far greater flexibility in the range of responsibilities across team members. Role blurring was particularly indicated where assessment and care planning was open to community psychiatric nurses (CPNs), occupational therapists (OTs) and social services personnel, and where health professionals could commission social care services.
Ten papers reported on team management, with the most common arrangements being (a) one overall manager, accountable for all core team members, irrespective of discipline;48 (b) two team managers; one for health staff and one for social care staff;179,219 and (c) those without a formal team manager217 (cited only in the pre-2000 literature). Three national surveys suggested an increase in joint management arrangements (type a) over time, from just under one-third to 47%. 50,163,179 The changing role of consultants within teams is considered by 11 studies. 19,46–48,180,190,202–204,209,210 They suggested a shift from leadership to membership over time, ranging from 40% at the turn of the century to 93% more recently46,47,73 reflecting policy guidance. 11
Consultant engagement with teams through support and supervision and involvement in team meetings was a second aspect of their role considered in the literature which indicated a variety of input, although attendance at multidisciplinary meetings was found to be the norm. Finally, the question of whether some of the work traditionally undertaken by consultants could be competently done by others was considered by a number of articles, particularly those reporting on teams in Lewisham and Cambridge. 48,188,203,204,209 This related particularly to initial assessments, one of the few aspects to have been evaluated, and, as such, is considered further in the next section.
Other aspects of assessment were its setting, with general agreement that domiciliary assessments were vital to gathering accurate information on people’s needs;19,46,47,179,189,190,199,217 and the extent of multidisciplinary involvement. 19,46,47,179,208,218 National reports suggested that such practice occurred in only a minority of teams, varied greatly, and most frequently involved doctors and nurses only. 46,47,179 It was harder to draw conclusions from local team data which did not always provide such information. Only two local studies reported that initial assessments were conducted by two or more professionals,208,218 in one case a social worker and a nurse. 208
A range of practices in referral and access arrangements were identified. Although the majority described open referral systems, half represented exemplar teams, whereas the most recent publication,205 claimed that most UK CMHTsOP only accepted referrals from doctors. Evidence on how teams were accessed, in particular the prevalence of a SPA, proved inconclusive. 19,179,197,211 Reference to the importance of sharing information was common in the literature. However, reports of the type of record system used, and whether or not shared, were rare and only present in the post 2000 literature. 46,47,50,73,197,199 Electronic systems were the exception. 73 Nowhere were information systems fully compatible between health and social care agencies. A recent study found that social workers within CMHTs often had to enter data twice. 50
Core staff location was reported by seven papers43,47,197,211,216,217,219 with a minority reporting colocation of all core members. Joint funding was reported in seven papers; either in the form of pooled budgets for individual care packages, or whether or not health and social care staff had easy access to each others’ services. 46,48,50,163,210,216,217 Pooled budgets were rare in 200046 whereas ‘some’ instances were reported by 2009. 46
Evidence of effectiveness
Seven papers43,47,197,211,216,217,219 reported outcome data that compared different CMHTOP approaches. All were local studies, four188,190–192 referring to exemplar teams. Three examined referral/access arrangements, three others considered assessment or immediate post-assessment issues, and one focused on longer term support. Measures were largely process related, for example the number, appropriateness and timeliness of referrals or the content and accuracy of assessments, diagnoses and post-assessment decisions. Only one study considered outcomes from the perspective of the service user,179 measuring QoL following intensive care management. None considered consequences for staff.
Three papers described work aiming to widen access for new referrals to CMHTsOP. 191,205,221 Two191,205 were set in the UK. The third represented the only study outside the UK in this review. 221 The earliest191 assessed whether or not open-access systems improved the accessibility of the team to people who might not otherwise have been referred to them without leading to inappropriate referrals. It concluded that such concerns were not realised and that had there only been a traditional referral route available, many people would have faced delays and some may not have been referred at all. It did not, however, consider how operating the two systems simultaneously might change how they worked. The second paper considered the characteristics of social services referrals to a CMHTOP 1 year after the introduction of an ‘open’ referral system as well as the total number of referrals with those of the previous year. They found that 90% of referrals from social workers (n = 36) had a mental illness, demonstrating that social services referred appropriately. No increase in the overall number of referrals following the introduction of the new system was found. 205 The non-UK study compared the numbers and characteristics of new referrals, following the introduction of a triage system; finding this led to a large increase in referrals although only a minority appeared to need specialist mental health input. These articles provide conflicting evidence on whether systems introduced to widen access result in more inappropriate referrals.
In relation to assessment, one article evaluated the introduction of a new structured tool, comparing the quality of recording and communication with GPs before and after its introduction. Significant improvements were reported in the collection of medical and social history, and documentation of clinical information from GPs. Two other papers were closely linked, relating to the same service (Lewisham) and the same sample of service users. The first compared the psychiatric diagnoses of 100 service users made by MDT members against an assessment and diagnosis undertaken by research psychiatrists, revealing a high degree of diagnostic accuracy by CMHT members and a very high level of agreement between the team and research psychiatrist assessments. 190 Length of community experience was more significant than the profession of the assessor. The second considered post-assessment decision-making and reported a high degree of agreement in relation to antidepressant use; satisfactory agreement regarding the use of neuroleptic drugs; but less agreement with regard to psychological interventions. 188 The authors concluded that this did not suggest that assessments by non-doctors resulted in either ‘substantial under-use or inappropriate use of psychiatric interventions’ (p. 80). A possible weakness of these two studies, acknowledged by the authors, was that where psychiatric assessment and diagnosis was conducted by a non-clinician, recognised medical classifications could not be used. Non-medical staff used broad classifications which were not comparable with other studies of diagnoses, limiting the comparability of these data. Use of research psychiatrists as proxies for real decision makers, also potentially limited generalisability. 188,190
One paper evaluated the impact of intensive care management (involving a designated case manager with a flexible budget) for older people with dementia and their carers in comparison with those provided with ‘usual’ support from the CMHT. 192 Findings after 2 years revealed that, at an increased cost to social care budgets, just over half of those receiving the intensive service remained at home compared with 35% of the control group.
Table 40 summarises the studies on team attributes and evidence of their effectiveness, listing potential design features of a CMHTOP.
| Key attributes identified in policy and practice guidance | No. of publications | Summary description of attribute development in included literature | Evidence of effectiveness in included literature | |
|---|---|---|---|---|
| 1 | Multidisciplinary membership | 30 | Thirty per cent of 43 teams represented included five or more disciplines | No evidence found |
| 2 | Single management structure | 7 | Direct line management and clinical supervision most frequently provided by different staff | No evidence found |
| 3 | Colocation (of core members) | 6 | Limited colocation found | No evidence found |
| 4 | Regular multidisciplinary meetings | 16 | Multidisciplinary case discussion meetings including consultant held weekly in majority | No evidence found |
| 5 | Professional role flexibility | 11 | Care co-ordination conducted by a range of professional groups common | No evidence found |
| 6 | Consultant fully integrated into team | 11 | Evidence of shift from management to membership. Contested opinion on nature of consultant role | No evidence found |
| 7 | Flexible support | 11 | People with dementia represented the largest single diagnostic group on team caseloads. Short-term input the norm with evidence that those with dementia received shorter-term input than others | Improved carer support and prolonged service user community tenure resulting from focused long-term input192 |
| 8 | Control of resources/joint funding | 7 | Joint funding increasing but still minority | No evidence found |
| 9 | Open referral systems and SPA | 17 | Ambiguity as to proportion of teams operating open systems or SPA. GP referrals dominate | Improved access without loss of accuracy.191,205,221 Dedicated referral role improved access221 |
| 10 | Domiciliary assessment | 13 | Initial assessment at home was the norm. Variation in follow-up | No evidence found |
| 11 | Multidisciplinary assessment | 7 | Multidisciplinary assessment rare. Where found, frequently limited to doctor and nurse | No evidence found |
| 12 | Common standardised assessment | 7 | Increased standardisation and use of common assessment documents over time | Structured tool improved quality of recording and communication with GPs220 |
| 13 | All professionals conduct initial assessments | 7 | Involvement of professionals other than OAPs largely limited to exemplar teams | High-quality assessment and decision-making retained188,190 |
| 14 | Outreach to non-specialist services | 8 | Support to care homes most evident | No evidence found |
Discussion
This review faced challenges, born from its broad scope and the nature of the literature, requiring a degree of methodological compromise. First and foremost was the breadth of potentially relevant literature relating to the first objective. To manage the volume, and to ensure a focus on those with the highest quality, this review included only publications from peer-reviewed journals, or national reports or studies. It is, however, possible that the review inadvertently excluded high-quality local reports that were not subject to peer review. For objective 1, the review included only UK studies. Studies from outside the UK were sought for objective 2 though only one relevant study was found. Perhaps the search might have captured more had it included more equivalent non-UK care system terms. The initial search did, however, find a large number of non-UK papers, all of which, except for the single included study, were excluded on similar grounds to the domestic literature, validating the strategy used. The review did not appraise evidence comparing the effectiveness of CMHTsOP against alternative forms of care (for which there are many more relevant studies), but the relative merits of different aspects of CMHTs’ operation. This evidence base was very limited.
The results must be considered in relation to whether or not the sample as a whole was sufficiently comprehensive to adequately capture variations across time and place (range and spread), and the relevance of each individual study to the review questions. The literature varied on a number of dimensions adding breadth and richness to the data set, but resulting in a number of limitations. First, little national evidence was found relating to the early period of CMHT development, while the local studies comprised only a small proportion of UK teams. Second, many of the local data came from ‘exemplar’ rather than typical teams. The authors of these studies acknowledged that their findings should be taken in the context of two mature and well managed teams. Third, there was a lack of transparency about study site selection in some national studies; and, fourth, despite the multidisciplinary nature of CMHTs, it was the consultants’ perspectives which were most commonly sought in the postal surveys. Finally, the relevance of each individual publication to the review questions varied. Although a solid core (55.5%) was highly relevant to the review, almost half of the publications were of more limited value (see Appendices 21 and 22). For the small number of papers that included evaluations of different CMHT practices, limitations were also evident. Five papers contained enough information about the study methods to be able to evaluate their quality. These studies scored highly overall (see Appendix 23), with weaknesses mainly recognised by the authors. In only one was there potential selection bias which the authors had not considered. 193
Integration was one of the driving forces behind the development of CMHTsOP217 and was integral to this review, relating to many specific issues. There is broad agreement across the policy and professional literature on those key attributes which an integrated CMHTOP should possess – highlighted in Table 40. Studies emphasised different aspects of this list with none including every item. The disparate nature of the literature impaired comparisons across studies, hampering the ability to assess the extent and level of integration achieved by CMHTsOP. Overall, the findings suggested that progress towards integration had been uneven. There was also a lack of consensus whether some of these attributes represented the most effective way of delivering a service. The opening of initial assessments to a range of professionals, and of referrals from a range of agencies, were particularly contested. However, the use of standard common approaches to assessment appeared to have increased. Related to this is the issue of professional roles and how to make the best use of different expertise within the MDT. Most commentators advocate a flexible approach to multidisciplinary working, warning against team members either sticking too rigidly to their traditional professional roles, or roles becoming too blurred, with a subsequent loss of professional skill and expertise. In general, the literature provided few examples of exactly how teams implement this in practice, and little consideration of interdisciplinary conflict. The literature on roles focused on two related themes: the role of the consultant within the team; and whether non-medical members should carry out initial assessments. Consultants have adopted a range of positions in relation to CMHTsOP, from external advisor through attachment, full membership and team leadership. Over time, however, there appears to have been a broad shift from leadership to membership43,46,210 coinciding, perhaps, with the advent of formal team managers. This raises the issue of clinical responsibility: the degree to which teams should work under the clinical guidance of medical staff or operate semi-independently; and whether or not it is necessary for all service users to be seen by a doctor. Again, no evaluations have been carried out and the Department of Health (DH) and Care Services Improvement Partnership11 guidelines did not address the issue. Government guidance has, however, stated clearly that any team member should be able to carry out an initial assessment on behalf of the team – a practice which the descriptive literature suggests was already widespread by this point, although only one evaluation of its impact was found. 190
Conclusions
This review addressed two important questions: first, how the organisation, structures and processes of CMHTsOP in the UK vary; and second, how these variations affect the outcomes of service users, staff and services. Overall, although a number of studies provided data to illuminate the first issue, detail and coverage was uneven, both chronologically and geographically. Evidence of the impact of various approaches was also limited. Although a solid evidence base might be expected for recent guidance, the review demonstrates just how little evidence exists. Research is needed not only on how teams currently operate and vary, but also on the impact of these variations on users, staff and services.
Chapter 7 Community mental health teams for older people: aims and methods
Although a modest evidence base exists to support the benefits of specialist CMHTsOP relative to other care options,65 there is scant evidence to assist service managers in designing team structures and processes. 183 Where these questions have been addressed, the literature review in Chapter 6 identified a broad range of team features perceived as important for the successful delivery of CMHTOP services. There is, however, a remarkable lack of evaluation, limited to a narrow range of team processes (e.g. assessment and case finding) and to exemplar teams in England (e.g. Lewisham). Given the substantial resources expended through CMHTsOP56,222 and their importance in delivering NHS priorities, in particular to older people with dementia, the relevance of this evidence gap is apparent.
An exercise was undertaken to prioritise the workstream aims. This was informed by the literature review (see Chapter 6) and included a consultation with old age psychiatrists, service managers and other CMHTOP practitioners via a local conference convened by the research team specifically to debate future research objectives. Two priority themes emerged. First, service integration, broadly defined to reflect aspects of joint working across both professional and agency boundaries, was identified as a critical avenue for future research. The literature review found numerous descriptive assessments of integrated CMHTOP practices across recent decades, but little evidence demonstrating its consequences for service users, nor any systematic investigations of which components of integration appear most important. This priority was also supported by the repeated emphasis given to integration across old age care services from successive governments, professional bodies, charitable organisations and regulators11,31,46–48,52,181,183 in addition to receiving high priority within the National Dementia Strategy. 57
Second, insufficient research has investigated the evolving role of the psychiatrist within CMHTsOP. A broad-based consensus has given impetus for reform of traditional consultant approaches,223 in particular the presumption that psychiatrists take lead clinical responsibility for all service users referred to a service. Team leadership has also evolved, as management responsibilities shifted gradually from consultants to other senior practitioners in dedicated roles. 43,46,47,73 These new ways of working have not been universally welcomed224 and the implications for both staff and service users have not been adequately evaluated.
Research aims
The workstream aims were thus:
-
to investigate national variation in ways of working across CMHTsOP in England; and
-
to evaluate service user, carer and staff outcomes across a purposive sample of CMHTsOP, representing different approaches to (i) integrated working and (ii) the role of the consultant psychiatrist.
To meet these aims, a multimethods research design was constructed featuring three discrete work packages: (i) a national survey; (ii) detailed local case studies with an observational study of service user outcomes; and (iii) a survey of CMHTOP staff working in nine mental health trusts. Box 12 presents more detailed individual research questions for each work package, and indicates the chapters in which the corresponding findings are presented.
-
1. What are the similarities and differences in CMHTs’ structures, processes and functions across England?
-
2. What team and trust characteristics are associated with variations in integrated working practices?
-
3. Are different approaches to (i) integrated working and (ii) the role of the consultant psychiatrist associated with variations in:
-
Ways of working, including:
-
team composition and management
-
team processes, roles and responsibilities
-
caseload profiles and
-
service provision?
-
-
Service user and carer outcomes and resource use?
-
-
4. Are integrated working practices associated with different staff outcomes and job characteristics?
-
5. What aspects of integrated working facilitate/hinder positive staff outcomes?
Work package 1: a national survey of community mental health teams for older people
To address Research questions 1 and 2, a national survey of all CMHTsOP in England was conducted.
Design and measures
A paper questionnaire was developed to collect information on general team characteristics (location, type of community served, age of service); team composition (size and professional groups represented, and management arrangements); referral characteristics (use of the SPA, numbers of referrals received and primary sources of referrals); features of care co-ordination (including assessment processes and record-keeping); aspects of the consultant role (including proportion of caseload seen, role in decision-making) and outreach and liaison work (services provided and settings served). To enable comparisons over time, the schedule adapted existing question-sets from previous CMHT surveys where possible, including previous work by study team members. 73,225 The questionnaire was designed with closed response options for most questions, but with open text boxes for elaboration and clarification.
Particular focus in the design was given to collecting objective indicators of integrated working practices across CMHTsOPs. Potential indicators were identified from the literature review, as well as published policy documents;31,57 service development guides;11,48 national audit reports and parliamentary inquiries;51,226 performance measures227 guidance from the National Institute for Health and Care Excellence (NICE)183 and standards of professional practice. 181 Indicators were chosen for inclusion based on the degree of consensus across these documents and the extent to which they could be objectively reported by respondents. Box 13 presents the final nine chosen standards of integrated practice, which represent aspects of team composition and management; care co-ordination; data sharing and record-keeping; and co-ordination and sharing of resources. 228
-
A multidisciplinary core team. a
-
All core staff directly line-managed within the team.
-
SPA used for all or most referrals.
-
All staff groups use the same structured assessment documentation.
-
All/most service users have a single care co-ordinator.
-
All/most service users have a single care plan containing details of their health and social care.
-
At least one health professional within the team can authorise social care services.
-
The team and LA can access relevant service user records from each other.
-
All core team members share the same office base.
a Defined as teams including a social worker and at least two health disciplines, in addition to any consultants and team managers.
The draft schedule was piloted with six teams from three mental health trusts and the final questionnaire was posted to the team managers of 457 CMHTsOP in England, identified by the Combined Mapping Framework,229 and then audited by the research team to identify changes since that exercise was conducted. Questionnaires were sent in November 2008, with a follow-up of non-responders both by post and subsequently by telephone, and with fieldwork closing in March 2009. The final questionnaire is included in Appendix 24.
Analysis
Analysis was predominantly by means of descriptive tables. In addition, the nine standards of integration were combined into a simple integration ‘score’, permitting further exploration of those team characteristics associated with variations in integration (research question 2), using ordinary least squares (OLS) regression.
Work package 2: local case studies including an observational study of outcomes
A second study aimed to address research questions 3a and 3b in Box 12, through a series of local case studies including an observational study of outcomes.
Settings
The national survey data were used as a sampling frame to select teams representing different ways of working with respect to service integration and the role of the consultant psychiatrist. A broad team typology was developed, in consultation with experts both within and outside the study’s management group. Consequently, the initial selection process aimed to identify:
-
teams exhibiting evidence of (i) extensive and (ii) limited service integration and
-
teams in which clinical responsibility for the team’s work (i) predominantly rested with consultant psychiatrists, and (ii) was shared across practitioners.
A total of eight teams (two per team model) were sought to enable a robust inquiry of CMHT approaches across teams and team models, while remaining within the resource constraints of a case study approach. Potential teams were identified through a two-stage screening process, outlined in Box 14. Final team selection was based on the perceived fit of each team to the typology, drawing on the range of objective and subjective data collected from interviews with managers of shortlisted teams at the second stage of screening, while also ensuring a spread across England and across rural/urban areas.
| First stage screen | |
|---|---|
| Data source | National survey |
| Information used | Nine indicators of integration |
| Team composition | |
| Proportion of team caseload seen by a consultant psychiatrist | |
| How classified | Low integration: maximum of four indicators of integration, and without a social worker in the team |
| High integration: minimum of seven indicators of integration, and with a social worker in the team | |
| Consultant-led responsibility: ‘all or most’ of team caseload had been seen by a consultant psychiatrist | |
| Shared responsibility: only ‘some’ or ‘few’ of team caseload had been seen by a consultant psychiatrist | |
| Exclusion criteria | Specialist teams supporting service users with only organic (or functional) illness |
| Exceptionally large/small teams | |
| Second stage screen | |
| Data source | Telephone interviews with 28 shortlisted team managers |
| Information used | Updated indicators of integration and data on the proportion of team caseload seen by a consultant |
| Responses to brief open-ended questions on: | |
| (i) the nature and effectiveness of multiprofessional and multiagency working | |
| (ii) the nature, scope and depth of the consultant’s influence within the team | |
| Exclusion criteria | Updated data used in first stage screen indicates the team would no longer meet classification |
The final team selection is portrayed in Figure 11. As can be seen, an additional team was recruited in quadrant C, in response to a substantial delay in achieving local governance approval for another participating team. Further, it should be noted that team G comprised two small locality teams covering separate geographical patches, and which were too small individually to fulfil the requirements of the research. However, both teams operated identical policies and processes; covered similar catchment areas; shared consultant staff; and were overseen by the same service manager (the researchers thus designated these as a single team for the purposes of the study, in agreement with local managers). A favourable ethical opinion was obtained from Cambridgeshire 3 Research Ethics Committee in August 2010 (Reference: 10/H0306/43).
FIGURE 11.
Team typology.
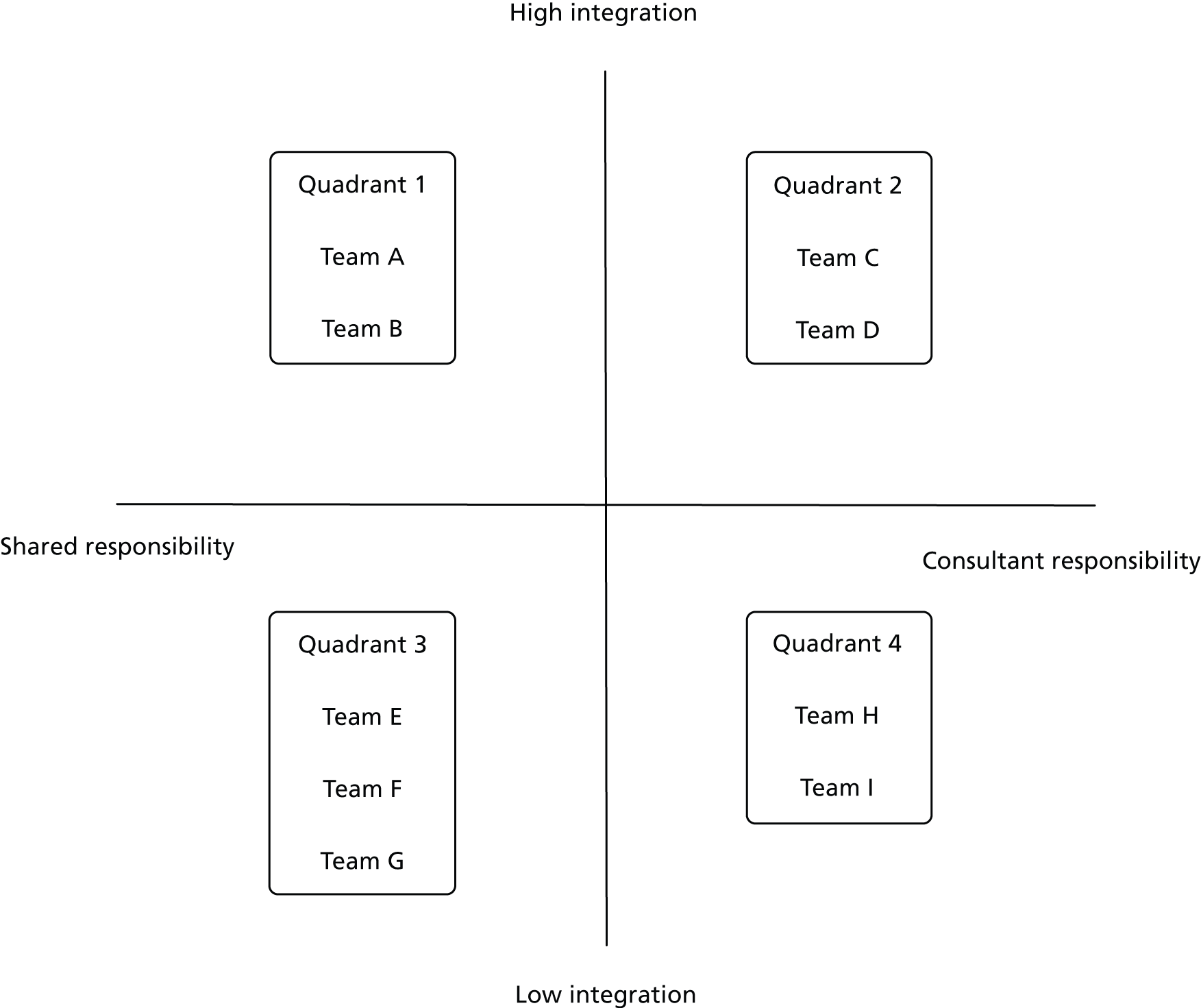
Study design
The breadth of the research questions demanded a mixed-methods data collection approach, comprising (i) qualitative interviews with staff and (ii) an observational study of service user and carer outcomes.
Qualitative study
The qualitative components of data collection concentrated on the various ways of working across the individual case study sites, to enable contrasting views of important features of team design and process to emerge. In doing so, the interviews also sought to provide an assessment of the utility and meaning of the proposed typology, including an exploration and elucidation of its key components, and the fidelity of chosen teams within it. Consequently, the interviews shaped the subsequent analysis of the observational study of outcomes and also highlighted additional contextual factors that gave greater clarity in the interpretation of results.
Semi-structured interviews were conducted individually with a broad selection of staff with questions tailored to reflect their position within the team (see Appendices 25–28). A broad thematic framework was developed to provide a structure for the interviews while also allowing other topics of importance to interviewees to emerge. Interviews were undertaken by four members of the research team between January and August 2011. Each interview was recorded and professionally transcribed.
Data analysis adopted a grounded theory approach,230 using a systematic approach to ensure that subjective interpretations were visible and thus open to challenge and refinement by the research team. 231 Basic codes were initially produced from a priori concepts used to frame the interview guides. Close reading of a small number of transcripts led to the identification of further themes which were then used to categorise the full set of transcripts, with additional codes being added throughout this process, involving some recoding of earlier transcripts. Individual codes were organised into ‘families’ as a tool for making links between concepts and of moving between empirical description and a more theoretical understanding of the data. 232 Three members of the research team were involved in coding and analysis to ensure the reliability of decisions. 157
Observational study of service user and carer outcomes
An observational study was designed to address research question 3b, by comparing service user outcomes across team types. Table 41 summarises key features of the study data collection which had three discrete stages. A detailed overview of all the standardised measures used within the study can be found in Box 15. Data collection proformas can be found in Appendices 29–32.
| Data collection | Baseline stage | Interview stage | Follow-up stage |
|---|---|---|---|
| Target sample size | 960 | 320 | 960 |
| Participants | Random selection of caseload, excluding service users:
|
Matched sample across team models, excluding service users:
|
All service users at baseline stage |
| Method | Form completed by care co-ordinator | Face-to-face interview by researchers | Form completed by care co-ordinator |
| Timing | October 2010 to April 2011 | March 2011 to July 2011 | 6 months after baseline stage |
| Outcome measures | N/A | QoL (QoL-AD) | Inpatient admissions (primary outcome) |
| Satisfaction (bespoke items) | Care home admissions | ||
| Service user, characteristics and clinical presentation | Sociodemographic information | Dependency (modified Barthel Index) | |
| Informal care receipt | Depression (GDS-15) | ||
| Dependency (Barthel Index) | Cognition (MMSE) | ||
| Instrumental ADL (six items) | General health (single item) | ||
| Psychiatric diagnosis | |||
| Depression screen (PHQ-2) | |||
| Cognition (MMSE) | |||
| Behavioural problems (seven items) | |||
| Risk (six items) | |||
| Service receipt | Team contacts in last month | Inpatient admissions | Discharge from service |
| Duration on caseload | Outpatient appointments | ||
| Inpatient admissions in last 6 months | Ambulance use | ||
| Other mental health service receipt | GP visits | ||
| Personal social care | DN visits | ||
| Day care | SW visits | ||
| Other social care services | Other health-care worker visits |
| Outcome | Coverage | When collected |
|---|---|---|
| Change in daily functioning | Ten ADL measured by the modified Barthel ADL Index139,140,147 a widely used scale measuring functional independence in personal care and mobility. The version used had a simple scoring system in which each item was rated 0–5 or 0–10 or 0–15 depending on the amount of help the person received. Individual item scores were then summed to provide a total of between 0 and 100. Lower scores represent higher dependency | Baseline and service user interview |
| Change in daily functioning | Five instrumental ADL taken from the Nottingham Extended ADL Scale148 covering the person’s ability to make a hot snack, shop, use the phone, travel by car/public transport and manage their medication using a four-point scale: not at all; with help; on their own with difficulty; on their own easily | Baseline and service user interview |
| Change in cognitive functioning | A range of cognitive functions affected in dementia, including orientation, memory and attention as measured by the MMSE,142 a well known and widely used test of cognitive function. There is a maximum score of 30, with scores of 0–10 commonly described as severe dementia, 11–20 moderate dementia, and 21–24/25 mild dementia | Baseline and service user interview |
| Change in mood | Fifteen simple yes/no questions about non-somatic symptoms of depression as covered by the GDS-15.233 This scale has been validated in primary care patients and recommended for use with older people living in their own homes234 and with care home residents.150 Individual items are summed to provide a total of between 0 and 15 with scores between 5 and 9 indicating mild, and 10 or more, moderate to severe depression. Although its validity with people with severe cognitive impairment remains uncertain, adequate sensitivity has been reported in people with MMSE scores of ≥ 15151) | Baseline and service user interview |
| QoL | Thirteen items covering aspects of the person’s physical and mental health, relationships, finances and overall life quality as given in the QoL-AD152 which can be satisfactorily completed by people with MMSE scores as low as three153,154 and has been validated in people without dementia.155 Each item is rated 1–4 (poor, fair, good or excellent) giving a total possible score of between 13 and 52. Higher scores indicate better QoL | Service user interview |
| Service satisfaction | A questionnaire about people’s satisfaction with services was developed by the PSSRU using domains highlighted in the literature and a consultation with service users and carers | Service user interview |
| Service receipt | A modified version of the Client Service Receipt Inventory,156 collecting information about service user’s use of health and social care services over the previous 4 months | Service user interview |
| Carer affect | The HADS144 containing 14 questions with four response options on a Likert scale, coded 0–3. Responses are summed to provide separate scores for anxiety and depression, each taking possible values of 0–21, with higher scores indicative of greater anxiety/depression. Scores in excess of eight or nine have been widely used to indicate clinical anxiety/depression,235 although no thresholds unique to older people have been identified236 | Carer questionnaire |
| Carer strain | The Modified Caregiver Strain Index237 containing 13 questions with three response options, coded 0–2. Responses are summed to provide a single measure taking possible values 0–26, with higher scores indicating greater carer strain | Carer questionnaire |
Baseline stage
Detailed information was sought on a random selection of eligible community-dwelling service users open to the team, comprising service users who had been on the caseload for at least 6 weeks; who were living in their own home; and who were receiving regular and active input from the team (specifically, those who had been seen by a team member in the previous month, and for a primary reason other than reviewing medication). Proformas aimed to collect sociodemographic details, health status and service receipt (see Table 41), and were designed to collate data already known as part of assessment and care co-ordination arrangements.
The proforma collected information under the following headings:
-
background characteristics
-
informal care
-
specialist mental health support (amount and type)
-
community support (amount and type).
The standardised measures of physical functioning and mental health status included within the proforma are adapted forms of the Barthel Index139 and Nottingham Extended ADL Scale148 (five items only), the Patient Health Questionnaire for Major Depressive Disorder (two items);239 the GDS;143,150 the HADS144 (teams participating in the study were most commonly found to use either the GDS or the HADS as measures of depression, and so each team was expected to only complete one of these scores per service user); and the MMSE. 142
Interview stage
At the interview stage, the research team aimed to interview a sample of 320 service users (40 per team), chosen according to a stratified matching process designed to select similar service users across each team model. A simple ‘case type’ approach was adopted, in which the most prevalent combinations of age group (under/over 75 years), living arrangements (living alone/not alone), dependency (independent/some dependency) and diagnosis (organic/functional illness) were populated with potential interviewees. In the initial design, sampled cases which did not proceed to a completed interview were replaced by another service user of the same case type.
Potential participants were excluded where MMSE scores were below 10, as adopted in comparable research investigating care outcomes. 152,240 Care co-ordinators were also asked to exclude service users where the individual was in a ‘crisis’ situation; or where their cognitive capacity had declined to a point such that they could not meaningfully participate in an interview. Service users were subsequently invited to participate in an interview, via a letter with an information sheet, with signed consent achieved on the day. Interviews were conducted directly with service users in their own homes, accompanied by carers in some instances. The interviews collected information on dependency levels via the Barthel Index of physical functioning and mobility;139,140,147,148 non-somatic symptoms of depression via the GDS;143,149–151 and cognition levels via the MMSE. 142 Service receipt was collected via an adapted version of the Client Service Receipt Inventory156 and QoL via the Quality of Life-Alzheimer’s Disease (QoL-AD) tool. 152,155 Satisfaction with services was collected via a bespoke scale adapted from several sources.
To capture informal carer outcomes, a questionnaire was left at each household where the interviewed service user reported that they were supported by an unpaid carer. Where the service user had more than one carer, a single questionnaire was left for the main carer, as designated by the service user. The questionnaire was designed for self-completion and a freepost envelope was provided for ease of return. The questionnaire collected basic sociodemographic information; a brief carer service receipt inventory; and measures of carer strain (Modified Caregiver Strain Index)237 and mood (HADS). 144
Follow-up stage
The follow-up stage sought data for all service users included at the baseline stage and 6 months later. The one-page proforma collected discharge information (date and primary reason for discharge, where applicable); admissions to mental health beds (including dates of admission and discharge); and last known residence type (own home/residential home/nursing home/other) including relevant dates of all entries to care homes.
Outcomes
The primary outcome was the proportion of service users admitted to a mental health bed between baseline and follow-up stages, supplemented by analysis of the length of time from baseline to first admission. Secondary outcomes were (i) the proportion of service users placed in a care home in the follow-up period; (ii) differences in QoL; and (iii) satisfaction with services.
Target sample sizes
Target sample sizes were based on power calculations, with adjustments to reflect the context of the current study (in particular the capacity of local services). For the primary outcome, a small effect size was cautiously predicted, in the absence of prior evidence of the likely impact of team design on inpatient admissions; the relatively low number of likely admissions over a 6-month period on average; and the importance of including regression-based controls, given a non-experimental design. A total sample size of 960 service users would have 80% power to detect close to a ‘small’ effect size241 in a 2 × 4 contingency table. For the secondary outcome measures collected at the interview stage, an analysis of variance (ANOVA) test with four groups would have 80% power to detect a small-to-moderate effect size with a sample size of 320.
Analysis
Data were initially entered onto SPSS for Windows (version 19) and checked for errors, while subsequent analyses were conducted with Stata (version 11). Where data permitted, critical gaps were filled by model-based imputation routines and scores for summary measures were calculated from their constituent elements (see Appendices 8 and 9). Differences between groups were explored using appropriate statistical tests.
Regression models were used to test for systematic differences in service user outcomes between team types, controlling for variations in case mix. A similar approach was taken to the analysis of costs, which focused on the provision of those community services (both health and social care) that might potentially be under the control of a fully integrated CMHTOP and drew on a combination of service receipt information from the baseline stage and national unit cost data. 242 The extent to which team types differed in the pattern of services they provided and/or the costs of supporting service users with particular need profiles were also examined. The findings from these two exercises were then brought together in a cost-effectiveness analysis. Further detail about this is provided in Chapter 10.
Work package 3: community mental health teams for older people staff survey
A staff survey was designed to investigate variations in practitioner status, well-being and job characteristics across different CMHTsOP (research questions 4 and 5).
Settings
The survey was distributed across all 38 CMHTsOP within the nine mental health trusts selected for the local case study research (above) as an extension to the initial research design. To enable comparisons to be made across team type, the research team first completed short telephone interviews with team managers in each CMHTOP prior to the survey. These interviews collected factual data about team composition and management, in addition to the nine standards of integration used in the national survey above.
Design and measures
The self-administered questionnaire was designed to collect information on job outcomes and psychosocial characteristics of work. Two job outcomes were measured: job satisfaction, derived from a single-item question using a six-point Likert scale; and intention to quit, derived from two items on a four-point Likert scale, capturing thoughts about quitting and actual job search under way.
With respect to psychosocial job characteristics, the study adopted the Job Content Questionnaire243 for measures of:
-
job demands (psychological demands – five items measuring perceptions of the degree of work-related pressure)
-
job control (decision latitude – nine items measuring perceptions of control over key decisions affecting respondents’ work environment, and the variety of skills that they can develop and deploy in the job)
-
coworker support [six items, measuring perceptions of (instrumental and emotional) support from colleagues]
-
supervisory support (five items, measuring satisfaction with support from managers).
Two other subscales developed from the questionnaire have not been fully validated and were not employed in the analysis.
The questionnaire (see Appendix 33) also collected information on a range of personal and job characteristics, including age, gender, job title, length of time within the team, length of time in mental health services and caseload size. The questionnaire was piloted with two members of staff from one team, before being distributed to all participating teams in September 2011. A second mail-out was conducted in October/November, with fieldwork closing in December 2011.
Analysis
The analysis aimed to investigate the personal, professional and team characteristics associated with job outcomes and psychosocial job content. In keeping with the research questions, particular focus was paid to the correspondence between team integration and these key variables.
The study used the job demand–control (JDC) model as a framework for analysis. The JDC model proposes that job demands and controls are critical components in determining a wide range of job and personal outcomes, including aspects of physical and psychological health. Specifically, the combination of high demands with low control is believed to be particularly detrimental to well-being. 244 One review of 63 empirical applications of the JDC model concluded that workers reporting simultaneous high demands and low controls consistently reported lower general psychological well-being, lower job satisfaction, and greater levels of burnout. 245 Consequently, the present study focused on the balance reported between demands and controls within the sample. For further details of the approach see Box 16.
Job stress has profound implications for the health and social care workforce; their employing organisations; and ultimately service users. Exposure to prolonged stress has been linked to a range of mental health problems, including ‘burnout’ which is characterised by emotional exhaustion; depersonalisation/cynicism; and low perceptions of personal accomplishment. 246 Physiological responses to stress include damage to cardiovascular, respiratory, gastro-intestinal and immune systems. 247 These combined effects lead to increased absenteeism, reduced productivity and job turnover, with stress being the largest occupational health problem in the UK (recently overtaking musculoskeletal disorders such as back pain248).
Contemporary theories of stress explore the structural characteristics of how a person interacts with their work environment. 249 Chief among these is the JDC model243 which hypothesises that psychosocial work characteristics interact. Specifically, high pressure work is not, in itself, a major source of risk. However, where high pressures coincide with low discretion over the work environment (such as feeling unable to control resources, decisions or the nature of the work) there is an elevated risk of stress. Empirically, this has been used to explain why some high status medical professionals are able to tolerate acute work pressures, whereas lower status professionals report more burnout. 244 The JDC model has since been extended to incorporate the ‘buffering’ effects of social support in the workplace. 250 Social support is hypothesised to moderate potentially stressful work environments through emotional support (e.g. providing sources of motivation or compassion) and instrumental support (e.g. providing advice, guidance or direct assistance relevant to specific tasks). Social support includes assistance from both coworkers and supervisors.
The Job Content Questionnaire is adopted within the present study to provide measures of demands, controls and support. 251 A range of analytical frameworks exist to inform subsequent data exploration. Most commonly, researchers explore those workers who report combinations of high demands/low controls in a logistical regression framework. In the absence of recent UK benchmarks at a sufficiently detailed level of occupation, analysts tend to use sample means as a reference point. An alternative approach, giving improved model fit in empirical tests,252 is to create a new continuous variable representing the arithmetic difference between measures of controls and demands. Respondents reporting low scores on this variable face an imbalance between demands and controls (relative to other respondents) are thus most at risk from stress and burnout.
The quantitative results were augmented by findings from the qualitative interviews with staff from the local case study teams. In addition to questions about how their teams worked, the interviews explored a number of the themes measured by the quantitative survey including staff views regarding: the pressures and rewards of working in their particular team; the extent of autonomy experienced; the quality of the support they received both from colleagues and managers; and the nature of their professional identity. These qualitative data provided a deeper insight into these issues than the quantitative findings, albeit for a smaller number of respondents. The method used to conceptualise and code the qualitative data mirrored that outlined in work package 2 above.
Chapter 8 Community mental health teams for older people: a national survey of structure and process
The national survey aimed to (i) describe variations in team structures, processes and functions across England; and (ii) establish the team characteristics associated with integrated working practices.
MethodA self-administered postal questionnaire was sent to the managers of all 457 CMHTsOP in England during 2008/9.
ResultsA total of 376 teams responded, representing a response rate of 87.7%. The study found that progress was being made against a number of key national standards of multiprofessional and multiagency working. Team membership was typically more multidisciplinary than found in a comparable 2004 study, with particular growth in OT and support worker numbers, albeit with some continued difficulties integrating psychologists and social workers. Most teams used a SPA; were colocated with other team members; and used the same assessment documentation. However, the study also found that most teams could not access LA service user records, nor were any health staff within most teams able to arrange social care services. Regression analysis concluded that teams with the lowest levels of integration tended to work across multiple LAs were managed by a nurse; had high referral rates and were, paradoxically, located in formally integrated care trusts.
ConclusionsTeams had typically incorporated a wider range of professional disciplines than a previous study, but improved information sharing across agencies was still required. Formally integrating health and social care functions at an agency level was not linked to improved integration.
Introduction
It will be remembered from the previous chapter that there were two broad aims to this stream of work. These involved the investigation of patterns of variation in CMHTsOP and the examination of variations in outcomes associated with different patterns of working, reflecting degrees of integration and different consultant roles within teams. This chapter outlines the findings from a national survey, which identified the prevalence of different ways of working and provided a national sampling frame from which to select the sites for more detailed investigation.
Findings
Questionnaires were received from 376 teams, a response rate of 87.7%. At least one response was received from 67 trusts, representing just over 93% of organisations providing CMHTOP services as reported on the 2008 Mapping Framework. 226 Almost three-quarters (74%) of questionnaires were completed by team managers, 15% by service or locality managers, and the remainder by team members. As not all questions were applicable to, or answered by, all respondents, figures are given as a percentage of those participants who responded to each individual question.
Team characteristics and composition
The data collected on CMHT characteristics revealed variation in what, exactly, constituted ‘a team’. Although the majority of respondents reported that their CMHT was a single and distinct team, just under 10% reported that the team was amalgamated with a memory clinic, home treatment team, a specialist outreach service, or had other broader remits than would be expected of a CMHTOP. Just over a half of teams (56%) organised their staff around geographical patches or GP practices, with only around 3% organised according to type of illness. Most teams (71%) worked within a single LA; 17% worked with two LAs; and 12% operated across three or more LA boundaries. Just under half (47%) of teams described the community they served as ‘mixed urban/rural’, with 38% being mainly urban and the remainder (15%) being rural. Most CMHTs (72%) had been in operation for more than 5 years, with just 9% being new teams (operating for under 2 years). However, this does not mean that CMHTs were stable: almost two-thirds (63%) of teams reported major changes to the structure and organisation of the team within the preceding year.
Table 42 depicts the reported location of the team base. The most common team base was a community mental health centre, followed by psychiatric or general hospital sites. The remaining teams were situated in a diverse range of locations, including GP surgeries; LA settings (ranging from social services offices to day centres); community hospitals; and other buildings such as high street offices and business parks. Just over 10% of teams had more than one office base.
| Location | n | % |
|---|---|---|
| Community mental health centre | 125 | 33.4 |
| Psychiatric hospital | 69 | 18.5 |
| Psychiatric unit on a general hospital site | 66 | 17.7 |
| Multiple sites | 43 | 11.5 |
| Other location | 28 | 7.5 |
| LA site | 20 | 5.4 |
| Community hospital | 13 | 3.5 |
| Primary care site | 10 | 2.7 |
| n = 374 |
The survey collected detailed information with respect to team composition. Particular attention was paid to the ‘type’ of team membership, by distinguishing between ‘core’ and ‘sessional’ team membership. 253,254 Core team members were defined as devoting a substantial proportion of their working week to the CMHT, contrasted against sessional members who dedicated a regular but more limited input. The data revealed substantial variation in team size, with a median of 16 core members (excluding administrative staff) and a range of 1–47, with 26% of teams comprising 10 or fewer core staff members, and a similar proportion again (24%) having 20 or more.
Table 43 shows team membership by staff group from the present survey alongside comparable data from 2004. 73 Professional disciplines that were not formally part of the team (the first two columns) were recorded either as being accessed separately (e.g. via referral to another service – column 3), or as unavailable in the area (column 4). The table shows evidence of a greater representation of all staff groups within CMHTsOP between the two surveys, with greater ‘core’ membership, and reduced proportions being accessed outside the team or entirely absent. However, by contrast, it was noteworthy that consultants appeared less likely to be core team members in 2009. Social work and psychology continue to be the most challenging professions to integrate within teams, with around one-third and one-quarter of CMHTs reporting that they did not have social workers and psychologists respectively as team members. Just under 1 in 10 teams were unable to access psychology services at all. The data also revealed that 75% of team managers had a nursing background, 20% a social work background, with the remainder being OTs.
| Core team member | Associate team member | Accessed outside team | No access | |||||
|---|---|---|---|---|---|---|---|---|
| Year | 2009 | 2004 | 2009 | 2004 | 2009 | 2004 | 2009 | 2004 |
| Consultant | 82.7 | 74.3 | 14.6 | 18.8 | 2.7 | 6.9 | 0.0 | 0.0 |
| CPN | 98.9 | 96.7 | 0.5 | 0.3 | 0.5 | 3.0 | 0.0 | 0.0 |
| OT | 84.0 | 64.8 | 4.3 | 12.2 | 7.4 | 14.5 | 4.3 | 8.6 |
| Psychology | 50.3 | 31.0 | 23.4 | 21.5 | 17.0 | 29.4 | 9.3 | 18.2 |
| SW | 66.8 | 53.5 | 6.4 | 12.3 | 23.7 | 28.8 | 3.2 | 5.6 |
| Support worker | 87.0 | 58.8 | 0.8 | 4.1 | 7.7 | 6.9 | 4.5 | 24.8 |
Referrals, assessment and outreach
Community mental health teams for older people received, on average, 36 new referrals per month, with significant variation between teams as depicted in Figure 12. High referral numbers were particularly associated with larger teams, and teams combining CMHT functions with other services (e.g. memory services). Almost all teams used a SPA and 80% of teams had formal referral criteria. Table 44 presents the source of referrals, as reported by respondents. As expected, GPs were the primary source of referrals, although psychiatrists, social workers and care homes provided a ‘large proportion’ of referrals for 20%, 15% and 13% of teams respectively. Self-referrals were accepted by about half the teams, contributing relatively small numbers in almost all cases. ‘Other’ sources of referrals included general hospitals and other health services.
FIGURE 12.
Distribution of referrals received per month.
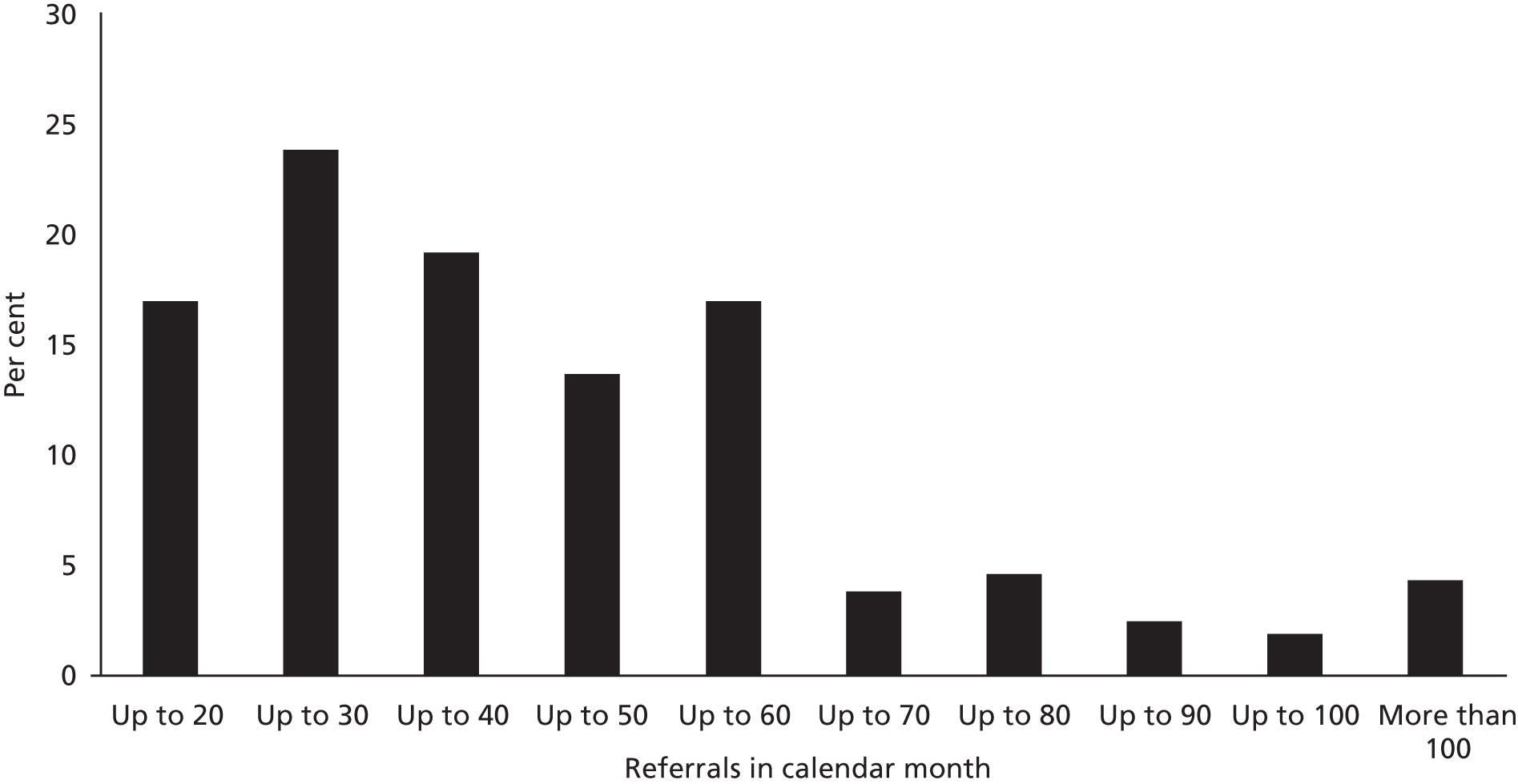
| Source of referral | A large proportion, % | A small proportion, % | Not accepted, % |
|---|---|---|---|
| GPs | 96.0 | 2.7 | 1.3 |
| Psychiatrists | 19.7 | 73.6 | 6.7 |
| Other mental health practitioners | 4.6 | 87.2 | 8.2 |
| SWs | 15.4 | 67.8 | 16.9 |
| Voluntary organisations | 0.0 | 43.8 | 56.3 |
| Self-referrals | 1.6 | 48.0 | 50.5 |
| Care homes | 12.8 | 46.8 | 40.4 |
| Other | 14.6 | 58.3 | 27.1 |
| n = 373 |
Just under two-thirds (63%) of teams made their first contact with service users within 2 weeks of the date of referral (for routine cases), on average. For just under one-third (31%) this took up to a month, and for 6% even longer. For almost all teams (93%), the initial assessment was conducted in the service user’s home. Consultants and CMHNs conducted assessments in almost all teams. In addition, OTs conducted assessments in 81% of teams; social workers in 79% of teams; and psychologists in 62% of teams that had these professionals within them. All teams used some form of a key worker/case co-ordinator system, though only 60% used this for all or most clients, and for co-ordinating care between agencies. CMHNs, OTs and social workers were the most common professional disciplines acting as key workers. In 69% of teams the consultant also acted as a key worker; and in 58% of teams psychologists performed this task. Over half of respondents (58%) reported that a consultant psychiatrist would have seen ‘all or most’ patients on the team caseload, while 42% reported that they would have seen only ‘some’.
Almost all teams (97%) reported being involved in at least some liaison and outreach work. One-third of teams (34%) reported having a link worker system in care homes, and just under two-thirds (61%) reported that they provided education or training to care home workers. Just under one-quarter of teams reported that they had a link worker system in GP surgeries and general hospitals, whereas 18% conducted education and training in these settings. Other forms of outreach work, such as open clinics and case finding and screening, were rare.
Team integration and joint working
Table 45 summarises the data collected on the nine indicators of integration, introduced in Chapter 7. It shows that some aspects of integration (a SPA, colocation, single joint care plans) were features of over 80% of CMHTs. Over two-thirds of teams also used the same assessment documentation between all professional disciplines, a marked increase from a little over one-third of teams in 2004. 73 Sixty per cent of teams were regarded as multidisciplinary (defined as having at least a social worker and two health workers as core team members). 25,52,181 Half of CMHTs also reported that all core members were directly line managed within the team. Fewer than one-third of teams (32%) reported that their CMHTOP and social services teams shared service user records, and just 57 teams (15%) stated that health staff within the CMHTOP were able to commission social care services directly.
| Indicator | n | % |
|---|---|---|
| Multidisciplinary core teama | 227 | 60.4 |
| All core staff are directly line-managed within the team | 179 | 49.9 |
| A SPA is used for all or most referrals | 321 | 88.0 |
| All core team members share the same office base | 326 | 86.9 |
| All staff groups use the same structured assessment documentation | 263 | 70.1 |
| All/most clients have a single care co-ordinator | 219 | 59.7 |
| All/most clients have a single care plan with the details of both health and social services provided | 293 | 80.0 |
| At least one health professional within the team can authorise services funded by the LA | 57 | 15.2 |
| The team and local social services can access each other’s service user records | 118 | 31.6 |
A composite integration score was constructed as a simple count of the number of the nine indicators (see Table 45) present in each team (following Reilly et al. ;255 Tucker et al. 180). The mean score across all teams was 5.45, ranging from 1 to 9. Regression analysis explored the association between the integration score and a range of team characteristics (Table 46). Teams managed by nurses were less well integrated than teams led by managers from other professional disciplines, and teams with larger numbers of referrals per team member had lower integration scores (although this relationship weakened as referrals per team member increased, as demonstrated by the positive coefficient on the squared term). CMHTs in rural communities were found to be less well integrated than teams that served urban or ‘mixed’ populations, although this was on the very fringes of significance even at the 10% level. Further investigation showed that this was largely driven by the fact that rural teams were the least likely to have had all their staff sharing a single base, as might well be expected. Finally, the results showed that teams working with just one LA were more integrated, on average. However, a subset of these teams, those that operated in formally integrated health and social care trusts, was found to have particularly low scores.
| Variable | Coefficient | SE | p-value |
|---|---|---|---|
| TM is a nurse | –0.426 | 0.189 | 0.025 |
| Referral per team member per month | –0.387 | 0.131 | 0.003 |
| Referral per team member per month squared | 0.022 | 0.012 | 0.062 |
| Team is based in a social service building | 0.633 | 0.388 | 0.104 |
| Team serves a rural area | –0.431 | 0.260 | 0.099 |
| Works with one LA | 0.432 | 0.196 | 0.028 |
| Works with one LA and in a care trust | –0.619 | 0.332 | 0.063 |
| Constant | 6.535 | 0.359 | 0.000 |
Conclusions
These findings offer a unique and timely investigation of the breadth and depth of integration in CMHTOPs, and, importantly, a high response rate (88%) gives confidence both in the representativeness of the findings and in the robustness of the statistical tests performed. However the results need to be interpreted in the context of the survey’s design and implementation. First, this study sought the views of team leaders which provides just one interpretation of the team’s working; in particular they may differ from the perspectives of consultants that have responded to previous team surveys. 73,179 Second, it is possible that some respondents may have been less circumspect than others in saying they had particular practices in place. For example, although nearly one-third of respondents reported that they could access LA service user records, contextual information provided in freetext form sometimes suggested that this was only after formal requests had been made. This contrasts with other teams that said they had direct electronic access from their desktops. It is also important to reflect on how this study conceptualised and measured ‘integration’. First, the analysis focused on a relatively narrow concept of operational integration, primarily across health and social care boundaries and professional disciplines, and at team level. As will be clear from the literature outlined above, this is distinct from broader concepts of joint working that may consider cultural aspects or integration at a ‘macro’ organisational level. Second, although the nine indicators of integration are found in key policy documentation and supported by professional consensus, there is nonetheless little evidence from the literature to validate each as critical to patient outcomes. 183 Third, the composite integration score gives equal weight to each indicator, but an alternative approach could impose differential weighting based on perceptions of each indicator’s relative importance (see, for example, Healthcare Commission50). However without evidence linking these to service user outcomes such an approach remains highly subjective. A recent international review concluded that 24 different approaches to measuring health-care integration have been formulated, but a well-established technique has yet to emerge. 256
One aim of this study was to assess the extent of service integration using a set of key indicators. Although past research has highlighted access to social workers and psychologists as of particular concern, our survey suggests that some progress has been made. For example, whereas surveys undertaken in 2000 and 2004 reported that approximately half of teams contained core social workers, and about one-third had core psychologists,73,179 our data suggest these proportions had increased to two-thirds and a half, respectively, by the time of the survey. Moreover, the proportions of teams reporting that they had no access to psychology services stood at just 10%, down from a reported 18% in 2004. 73 However, as the National Audit Office (NAO) note, having access to specific staff groups is not equivalent to having access in sufficient numbers. 52 Nonetheless, it appeared that a lower proportion of consultant psychiatrists were core members of teams than had been the case previously. Whether this reflects differing degrees of engagement of consultants in CMHTsOP or in part reflects the different questionnaire respondents is unclear. Nonetheless, there is some suggestion that team processes and procedures in this study were more integrated than they were in earlier research. Eighty-eight per cent of teams in this study had a SPA, up from 60% in 2004; while 70% used the same assessment documentation, compared to a little over one-third previously. 73 The proportion of teams that reported using single care plans is also higher than the earlier studies discussed. However the presence of some standards of integration was more infrequent, especially those that require greater degrees of co-operation and trust between health and social services at the agency (as opposed to practitioner) level. Indeed, just 32% of CMHTsOP reported that they, and social service teams, were able to access each other’s service user records. Furthermore, health staff could directly commission LA services in only 15% of teams. This latter finding chimes with a recent study of six mental health trusts which found only one example of a CMHTOP able to commission social care. 50 This is perhaps disappointing given the repeated policy efforts in England to encourage interagency commissioning as noted above, including measures such as pooled budgets and other partnership arrangements. 257
Although it would seem that joint working has increased since 2000, it is helpful to consider the characteristics of teams that did not score well on integration. The analysis shows that teams that worked with more than one LA tended to be less integrated, echoing the Healthcare Commission findings that it is easier to make joint working arrangements with one authority than multiple arrangements with several. 50 However, contrary to their suggestions, the length of time that the team had existed was not found to be a key determinant of closer joint working in this study. The finding that teams operating in a formally integrated care trust had lower levels of integration, after controlling for other factors, is particularly noteworthy. It may be that the initial decision to form closer structural ties across trust and LA boundaries was itself influenced by previous difficulties in joint working, as has been reported elsewhere. 258 If so, these results would support suggestions that organisational restructuring alone is not a sufficient condition for overcoming barriers to developing integrated practice. 179,255,257,259
A wide range of studies on service integration have suggested that organisational change and instability can hinder joint working,50,225,260 but this is not supported by our analysis which found that teams that had faced major organisational change in the preceding 12 months were no more or less integrated than other teams. Features that seemed to be more important included the location of the team base and the discipline of the team manager, although, interestingly, no previous work seems to have considered these. Our study found that teams based in psychiatric hospitals tended to be less well integrated than those in community mental health centres or in social service buildings. Furthermore, teams managed by nurses had lower scores than teams led by an OT or social worker. Together, these findings suggest that traditional models of CMHTs (nurse-led, hospital-based) seem less likely to incorporate joint working practices.
The negative association between the level of referrals per core team member and integration is harder to explain. It may be that such teams were understaffed (teams with high referrals also had particularly high numbers of vacancies) or were particularly busy and so had less time to devote to collaborative work, as has been suggested elsewhere. 253,260 An alternative explanation is that more integrated teams had clearer operational policies and eligibility criteria which limited referral numbers. Further work is needed to validate and better understand this finding, and also to investigate the other factors associated with effective joint working across professional disciplines and organisational boundaries; including less tangible contextual, cultural and political factors. Perhaps more importantly still, we do not yet know what particular features, or combinations of features, of integration are associated with better outcomes for older people with mental health problems.
Chapter 9 Community mental health teams for older people: local models of service delivery
A multimethods research study was designed to evaluate service user outcomes across CMHTOP case studies, representing different approaches to integrated working and the role of the consultant psychiatrist. This chapter aims to (i) describe the case study teams with respect to structure, process and practice; caseload characteristics; and service delivery; and (ii) to evaluate the typologies used for team selection.
MethodThis chapter utilises data from the in-depth interviews with team managers and consultant psychiatrists, supplemented by information on 948 sampled service users on team caseloads.
ResultsTeam structures varied considerably, but had some common features. All teams had consultants, nurses, OTs and support workers as members (with social workers, by definition, only present in the integrated teams). Care co-ordination was universally undertaken by nurses and social workers, but was less consistently undertaken by other professional groups. Consultant roles differed across teams, with complex and sometimes contradictory perspectives of their responsibilities and influence. Variation was found in teams’ caseload characteristics: for example, the proportion of the sample with a diagnosis of an organic disease ranged from 27% to 78% across teams, and the proportion recorded as ‘high risk’ ranged from 9% to 26%. The typology was broadly supported, but only with respect to integration and with a more refined grouping apparent.
ConclusionsA new team typology was formed reflecting different aspects of integrated working, comprising ‘network’, ‘low-integration’, ‘nominal integration’ and ‘high-integration’ teams. This typology was adopted in subsequent outcomes analyses (see Chapter 10).
Introduction
This chapter describes the individual teams involved in the study in relation to important attributes of structure and practice, caseload characteristics, and service use. It has two key aims: first to describe the teams and the similarities and variations found between them; and second to test whether or not the original classification of teams is supported by more detailed examination and consequently if the ‘typologies’ are an appropriate basis on which to compare service outcomes. Teams were categorised on two dimensions: the extent of integration with social services (based on data from the national survey) and the degree to which clinical responsibility for the team’s work was shared across the team or rested predominantly with the consultant (based on survey data and discussions with team managers). Information for this chapter is drawn primarily from qualitative interviews with team managers and consultants. Interview schedules can be found in Appendices 25–28. Following a brief overview, team characteristics are reported in relation to one or both dimensions, reflecting their relevance to the particular attribute. Subsequently, variation in team caseload characteristics and service receipt is reported, based on quantitative data collection.
Team overview and context
It will be remembered from Chapter 7 that the teams involved in the detailed case study were identified from the national survey and interviews with team managers. They were initially divided into four groupings based on information about the degree of integration and the role of the consultant. This created four quadrants each containing two or three teams: quadrant 1 = high integration and shared responsibility; quadrant 2 = high integration and consultant responsibility; quadrant 3 = low integration and shared responsibility; quadrant 4 = low integration and consultant responsibility as summarised in Tables 47 to 50. This categorisation was further developed based on the work described in this chapter and summarised in Box 18 and Appendix 34.
| Quadrant | Quadrant 1a | Quadrant 2a | Quadrant 3a | Quadrant 4a | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Team | A | B | C | D | E | F | G | H | I | ||
| Team members | TM | 2b | 2 | 1 | 1 | 1 | 1 | 2 | 1 | 2b | 14 |
| Consultant psychiatrist | 2 | 1 | 1 | 1 | 3 | 2 | 1 | 1 | 1 | 14 | |
| Other doctor | 1 | 0 | 0 | 1 | 0 | 2 | 1 | 1 | 1 | 7 | |
| Nurse | 9 | 5 | 4 | 4 | 2 | 5 | 9 | 5 | 9 | 54 | |
| OT | 3 | 1 | 1 | 1 | 2 | 1 | 3 | 1 | 2 | 17 | |
| Clinical psychologist | 0 | 1 | 1 | 0 | 0 | 1 | 0c | 0 | 1 | 5 | |
| SW | 2 | 5 | 3 | 3 | 0 | 0 | 0 | 0 | 0 | 13 | |
| Support worker/equivalent | 3 | 2 | 2 | 2 | 1 | 2 | 5 | 2 | 2 | 22 | |
| Other professional | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 2 | |
| Total team size (headcount) | 24 | 17 | 13 | 13 | 9 | 14 | 22 | 12 | 19 | 147 | |
| Total team size (WTE) | 17 | 15 | 12 | 12 | 8 | – | – | 9.5 | 14.5 | 83 | |
| Experience | Mean years in team | 6 | 5 | 8 | 4 | 8 | 6 | – | – | 7 | |
| Mean years experience | 13 | 9 | 14 | 12 | 18 | 14 | – | – | 19 | ||
The nine participating teams, selected for the presence of different characteristics, were from nine separate mental health trusts spanning the south-east, south-west, Midlands, Yorkshire, north-west and north-east England. Teams included a variety of urban/rural/mixed communities, represented a mix of affluent and deprived populations and included a number of inner-city teams from large urban centres. Further details of the characteristics of the areas in which teams were situated are described in Chapter 10.
At the start of the research period, four teams were based on hospital sites (A, D, E and H); one was situated in a health centre (C) and four were based in trust office buildings with some public access. Two teams moved premises during the research period, one from a hospital site to a town centre building which included public access (A) and another to an office-only location some distance from its patch (C).
Six teams had access to a separate memory clinic within their area (all four integrated and two non-integrated – I and E). The CMHT consultant had responsibility for this service in one integrated team (C), whereas in two, one integrated and one not, it was operated either by a different directorate (B) or trust (E). Three non-integrated teams operated a memory monitoring service (something described as falling short of a full memory clinic) within the team (F, H, G). Other related services were in a state of flux. Hospital beds had recently been centralised in two areas (A and F), LA day care was reported to be reducing in others (B and E). The range of specialist services for older people was limited with only two teams reporting that they had access to a rapid response team (B and I), a shortfall confounded by the lack of eligibility or ease of access to generic services noted by at least one other (A). Comments about the availability of wider support services highlighted increased pressure on CMHTs to manage more people in the community and to do this with reduced day services. Some managers felt that this left either the CMHT or the inpatient service with nothing in between.
All teams operated within a level of uncertainty about their future. Four faced imminent mergers with working-age adult teams (C, D, G and I). Two of the integrated teams also faced restructuring within their respective social service departments and were unsure of the future of their own social workers (B and D).
Team structures
Team organisation
Teams served defined geographic areas. In four, two integrated (A and B) and two not (E and F), these were further broken down into ‘sectors’. This arrangement was considered an efficiency measure to cut down on travel time. In non-integrated teams it also related to the catchment areas of individual consultants. Although most consultants operated across community and inpatient sectors within a geographic area, a minority, one integrated (A) and two non-integrated (F and I) had ‘only’ community responsibility. In all teams health and medical staff were employed by mental health trusts whereas social workers were employed by local authorities. In one non-integrated team (E) CPNs and OTs were employed by separate trusts. Core team members, apart from consultants and psychologists, were colocated in the same room in all teams.
Management and membership
Overall, only one team (H), the smallest numerically, did not have a full-time management post. Team managers were themselves managed by older people’s services leads from their respective trusts in all but two teams (B and E). In team B management of the two managers from the health and social care ‘subteams’ was separately undertaken by the trust and SSD head of service respectively. The nurse lead in team E was managed by a ‘modern matron’ whereas the senior OT was managed by a lead clinician from this service. In neither case were these managers colocated. Six teams had a single management structure whereby the same manager had both line management and clinical responsibility across disciplines/agencies (including three operating with job-share partners) for all core staff. Two teams, one integrated and one not, had a dual structure. In the former the division was between health and social care staff (B) while in the latter it was between nurses and OTs (E). A second non-integrated team (I) referred to OTs being ‘double managed’ by the team manager within the team and by their professional lead outside. Psychologists were managed separately in all teams. The majority of teams were managed by nurses (7 of 10), with social workers managing the remaining three. Within the integrated teams, social workers were managed by nurses in two (A and C) and nurses by a social worker in one (D), whereas in the non-integrated teams nurses were managed by a social worker in one team (H). One nurse manager of an integrated team carried a caseload (C) compared with three from non-integrated teams (E, F and I). The team manager role in one team (E) stood out as complex, with the ‘manager’ carrying a full caseload and regarding him/herself more as a senior practitioner and leader, rather than having a managerial role.
Teams ranged in size from 8 to 17 whole-time equivalent staff (see Table 47). All teams had at least three CPNs, with a maximum of nine. All teams also contained at least one OT and support worker, with a maximum of four and five respectively. Four teams had between two and five social workers each (A–D) and four had a psychologist (plus one vacant post) although only two had both (B and C). Psychologists appeared to have the least clear positions within the teams. Of those that currently had them, two were new and not fully integrated (B and C), and one was about to leave and their post potentially not filled (F). One team currently without a psychologist, did have one in the recent past, the post having been cut when the psychologist left (A). In another the post was vacant (G). Team members were almost all described as having ‘core’ status although psychologists did not appear to operate as such.
All teams had one or more consultant psychiatrists who were considered to be core members of all but two teams (G and I), where they were described as providing ‘sessional’ input. The number of ‘sessions’ (half-days) that consultants were available to teams varied between five and eight per week, though for some there seemed to be considerable flexibility; they were there for ‘whatever needs to happen’ (C).
Formal supervision arrangements
Staff had regular, formal supervision in all teams, although the frequency, content and supervisor varied. ‘Managerial’ as opposed to ‘clinical’ supervision tended to be regularly timetabled (monthly or bi-monthly) and undertaken by team managers, although within health disciplines, particularly in the larger teams, this role was often ‘cascaded’ down to senior nurses and OTs who supervised more junior nurses, OTs and support workers. In two examples (B and D), senior social workers supervised junior social care staff.
Where a manager and team member came from different disciplines, professional supervision arrangements varied. There were no examples of formal, regular supervision of this kind for either nurses or social workers from outside the team. Where it occurred, it tended to be arranged on an ad hoc basis and to be left to the individual worker to seek out. OTs and psychologists frequently received regular external professional supervision. In most teams consultants provided formal supervision to junior medical staff and advice and guidance to other team members when sought and within team meetings. The exception to this was in team F where the consultant supervised the nurse prescriber in relation to her work in the memory clinic.
Care pathways
Access and referral processes
Six teams only accepted referrals from GPs or other doctors. Two integrated teams (A and C) operated ‘open’ systems whereas one (B) accepted referrals from social services into its social care subteam. All but two teams overall described having a SPA where new referrals were gathered together on a weekly basis (unless they required an urgent response) for discussion and allocation. The two exceptions either had separate access points for health and social care referrals (B, integrated) or accepted direct referrals from GPs to individual nurses or to the consultant (E, non-integrated).
Most teams (all integrated and two non-integrated) used duty systems to take new referrals. Non-urgent cases were passed from ‘duty’ to the manager to collate for consideration at the weekly multidisciplinary meeting. Urgent cases were passed to ‘daily responders’ and/or the consultant to pursue. In three of the integrated teams (A, B and D) post-referral decisions were made largely by the whole team during regular MDT meetings (although managers and consultants reported they might also hold prior discussions). In the remaining integrated and all non-integrated teams, these decisions were generally made by team managers and consultants, prior to team meetings.
Initial assessments
Initial assessments were undertaken by a range of professional staff in three of the four integrated teams, including psychiatrists, although this only included the OT in one team (D). In the fourth, a ‘subteam’ of two nurses undertook this work, although the manager stated that this work had been offered to anyone in the team. In the non-integrated teams initial assessments were undertaken by nurses in all teams, by psychiatrists in four (E, F, H and I), and by OTs in two (H and I). OTs were regarded in most teams as having a specialist role. They were also less numerous than either nurses or social workers in the integrated teams. Psychologists were not involved in initial assessments in any team. Initial assessments were reported across all teams to be undertaken jointly by either a nurse and doctor, nurse and social worker, or social worker and doctor only where complex circumstances were indicated.
Case management practices
In three of the four integrated teams it was the norm to allocate a case to a single ‘care co-ordinator’, described by one manager (A) as ‘running a team’ for that case – drawing in other professionals as and when needed. In the fourth (B) it was common to have two allocated workers, one from health and one from social care. Social workers in this team employed the single assessment process (SAP) framework whereas their health colleagues used the care programme approach (CPA). All professional groups used the CPA in the other integrated teams. Team B’s model mirrored the practice within the non-integrated teams where a single care co-ordinator within the team would be joined by an allocated care manager from social services, if the latter were involved in the case.
A number of practices were found in relation to the closure or discharge of cases. In two teams, one integrated and one not (A and E), cases were closed without reference to the views of the consultant if the latter were not involved. In all other teams, consultants sanctioned the decision of the key worker. Secondly, a number of managers and consultants reported a change in practice in recent years from long- to short-term involvement.
Working with social services outside and within teams
For the five non-integrated teams without social workers, referral to the SSD was required when social care support was indicated. Working relationships between individual staff were invariably reported to be good. Systems, often beyond the teams’ control, sometimes appeared to hinder rather than help effective referral, communication and co-ordination. In two teams, longstanding relationships had been tested by the recent reorganisation of the SSD, which had changed the nature of communication and joint working (E and H). This was exacerbated in one by a change of location for the CMHT away from the building that also housed a small specialist mental health social work team with whom they had worked closely (H). Ongoing joint working was hampered by these systems and a sense of ‘referring on’ rather than working together was reported, perhaps reflecting differing priorities of the two organisations and a lack of clarity about the specific input sought. Two teams reported regular meetings with social workers involved in individual cases to support communication (F and G).
In contrast, in the integrated teams social work input could be accessed quickly and informally. In some teams ‘internal referrals’ were recorded for workload monitoring (B, C and H). Social workers in three of the four integrated teams could not always take on every case with social care needs referred to the team, nor was this always considered to be appropriate. The demarcation between a case that should be referred to the generic older person’s social work team and one that needed the involvement of a social worker within the CMHTOP was based on mental health complexity and whether or not a generic social worker was already involved. Teams with social workers all spoke of trying to limit their work with generic social work teams and of the benefits of having social workers within the team, to the extent that in one team all cases with a social care component, accepted by the team, were dealt with by a CMHTOP social worker. These issues are discussed further in the next chapter.
Record keeping
Record keeping and information sharing, particularly between health and social care were a challenge for all teams. Health records were accessible across disciplines in all but one non-integrated team (E). In contrast, social care records were not accessible to any of the non-integrated teams. In integrated teams practice varied. One team had separate health and social care systems with ‘read only’ access between the two (B). Two operated separate systems where only social workers could access the social services system (A and D), though social workers were also required to enter data onto the health system. Finally, one team operated a new integrated system for both health and social care (C).
Roles and responsibilities
The consultant old age psychiatrist
The original research typology regarding the role of the consultant focused on the extent to which responsibility for the mental health of service users was shared between the consultant and the team. Five teams within the study were originally described by managers as sharing responsibility and four operating a more consultant-led service. Data from the interviews, however, suggested a more complex picture.
Most consultants had a range of clinical responsibilities within and beyond the CMHTs, including the oversight of inpatient wards and memory clinics. They often had additional non-clinical commitments outside the teams. Consultants did not have a team management role in any of the teams. Typically, they saw themselves and were viewed by others as team members with a clinical leadership role (Box 17, quote 1). The latter, however, encompassed a variety of attributes that were executed differently by the various teams. Key differences related first to whether consultants saw most or every patient referred to the CMHT; second, whether or not their responsibility extended to people they did not see themselves; and third, their influence within the team beyond individual cases.
| Attribute/theme | Example | Team and profession | |
|---|---|---|---|
| 1 | Consultant as team member rather than manager | . . . the concept of the consultant’s role within a multi-disciplinary team is actually that we are an equal part of the team . . . a degree of leadership is expected but I think the idea of a multi-disciplinary team is just to work together to achieve certain goals . . . I think that this is more like teamwork and I’m not a line manager | Team H, consultant |
| We are not Consultant led. We all have roles within the team and we . . . function together as a team | Team H, team manager | ||
| 2 | Consultant has ultimate responsibility for all | . . . the ultimate responsibility has to be . . . with the consultant . . . , though . . . , this . . . , model, the ‘New Ways of Working’223 . . . , I do like it . . . It . . . gives credit to the multi-disciplinary component of the team . . . , but there has to be accountability and yes, accountability has to be shared, but at the same time I think . . . , it should be the Consultant who is responsible . . . | Team D, consultant |
| 3 | Team share responsibility | Any professional person going to see somebody has a responsibility for their assessment and their management there and then. You have your own professional responsibility. Obviously a lot of these patients are with CPA care co-ordinators and they have their responsibilities which I think are greater than they initially thought, and then obviously as a consultant and a senior clinician, I have the responsibility there. So you have to be working together and communicating. So it is not either/or . . . , it is all of those really | Team C, consultant |
| For example, a patient is referred in . . . they may be seen by the community nurse . . . and they will present that patient, and they will say ‘we have done this, this and this . . . , they need a diagnosis . . . you had better go and see the patient’. I say, ‘well I can give you a diagnosis, you have done the memory test, you have got the history, it is vascular dementia’ . . . ’Oh? You don’t have to see the patient?’ ‘No, I don’t really, because you have done everything’ . . . I don’t have to see the patient . . . , if they have done a good assessment . . . If there is any doubt, then I will go out . . . but every new patient is seen by the CPN and the social workers first, it is then discussed in our team meeting . . . they present . . . their management plan . . . so I think it is trying to build them up . . . because we are all . . . multi-skilled professionals . . . If they have the confidence to say, – I know this . . . , you know . . . , I will check with you, but I know this | Team C, consultant | ||
| 4 | Consultant only has responsibility for those s/he sees | I am responsible for the things that I do . . . if somebody hasn’t crossed my path . . . , then the person hasn’t felt the need to . . . , sort of . . . , take them up with me . . . , then it remains their responsibility . . . it is quite different from when I started out | Team A, consultant |
| 5 | Consultant influence is of an equal nature to other team members | I am sure she has as much influence . . . , as anybody else . . . when it is a medical thing, she has a lot of influence, because that is her area of expertise, but it is also recognised that an OT, a nurse and a psychologist have the same level of respect and influence | Team B, health manager |
| 6 | Consultant influence is of an equal nature to other team members | It’s an equal influence, and what he says doesn’t always go, because we don’t work like that . . . We don’t see him as being anything other than equal . . . | Team D, team manager |
Only a minority of interviewees stated that a doctor was likely to see every person referred to the CMHT. More often, managers and consultants agreed that the latter would only see a proportion of team cases, and that this was appropriate given the range of cases referred and the skills of other team members. Consultants were most frequently reported as only seeing complex cases. Five consultants nevertheless saw themselves as having a higher level of clinical responsibility than others in the team, regardless of the degree of their personal involvement (quote 2). For example, one consultant commented that it was the responsibility of the consultant to ‘oversee everything’ (B) including cases not seen by them. Two consultants commented that they wanted their teams to take on more and recognised that responsibility was already shared with each professional having responsibility for their own work input (C and I) (quote 3). In contrast, in two other teams both managers and consultants reported that the latter were only responsible for the cases that they saw (A and E) (quote 4). These examples highlight the complexity and elusiveness of this issue – something mirrored in the policy guidance referred to by one consultant quoted in Box 17.
The nature of the work undertaken by consultants also varied. In seven teams they were frequently involved in initial assessments, particularly where referrals suggested complex issues (B, C, D, E, F, H and I). In two teams, one integrated and one not, they were not involved at all (A and G). In only one team was the consultant described as a care co-ordinator (D).
Influence, like responsibility, is not a straightforward concept and was interpreted in a variety of ways by interviewees including the provision of support and guidance; the extent to which the work of the teams was organised around consultants’ timetables; the nature of the relationships between managers and consultants; and the extent to which others deferred to consultants’ opinions. All consultants interviewed described the provision of guidance and support to other team members as being at the core of their work, achieved through participation in regular multidisciplinary meetings and the operation of an ‘open door’ policy whereby staff could access them whenever necessary. In all but two teams, consultants attended MDT meetings where new referrals, complex cases and possible discharges were discussed and advice sought. In the remaining two, meetings were run by the consultants to discuss ‘their’ caseloads. These occurred in teams that had either only recently acquired a team manager (F) and still operated as they had done prior to their employment, or where the service was acknowledged to be ‘consultant-led’ (E) – both non-integrated teams. Most managers and consultants described the team working around the consultants’ external commitments to ensure that they could attend team meetings. In only one team was this not the case (D). Nevertheless, within three of these teams the consultants appeared to have little involvement or influence in day-to-day matters (A, E and G). One of these was an integrated team, where consultant and manager both commented on the limitations of the consultant’s influence and involvement. Interestingly, the other two teams were those having consultant-led meetings, highlighting the complexity of this issue. In five others, influence was regarded as being on an equal standing with the rest of the team (B, D, F, H and I) (quotes 5 and 6). In the remaining team (C) the consultant appeared to have greater influence, something which both the team manager and the consultant commented on and which appeared to be related to the manager’s more traditional view of the consultant role. Deference to consultants’ views varied across teams and in relation to different issues. In most, however, consultants were seen as having greater authority in relation to issues of medication but to be on an equal footing with other team members when other aspects of care were considered. Team members’ views of how consultants operated and the impact of this on their work are considered further in the next chapter. All quotations referred to above can be found in Box 17.
Other professional roles
The extent to which the professional groups represented in the teams performed discrete and overlapping roles varied both by team type and profession. A slightly greater extent of role blurring was seen in integrated compared with non-integrated teams. Three of the former were described by managers as operating a blend where individual expertise was acknowledged and valued alongside a degree of genericism. In two (A and D), staff from different professionals had attended joint training courses designed to develop generic skills. Team B was the outlier within the integrated group with separate roles and functions across the two subteams. The most generic model was seen in team D where initial assessments and care co-ordination were undertaken by all core staff, including nurses, OTs, social workers and psychiatrists. Of the five teams that did not have social workers, one (H) described itself in a similar way to the integrated teams, with nurses and OTs having a similar set of core functions.
Some professions were seen as more ‘generic’ than others with scarcity appearing to impact on this view. Nurses, as the most numerous profession, tended to be seen as the least specialist – although their key role in relation to administering and monitoring medication was acknowledged. Nurses undertook most initial assessments, an activity seen as ‘core’ rather than ‘specialist’, and were care co-ordinators in all teams. Three non-integrated teams highlighted specialist roles undertaken by nurses: those working only with people with a particular diagnosis (H); non-medical prescribers (F); and dedicated care home liaison nurses (I). Both the latter were seen as an asset to their team, whereas the former were regarded by managers as limiting flexibility and cohesion within the teams (F and H). In one team (F), nurse prescribers were responsible for the day-to-day operation of the team’s memory monitoring service.
Social workers were also seen as combining generic and specialist functions, the latter relating to arranging care packages and care home placements, conducting financial assessments, and having expert knowledge of mental health legislation and safeguarding issues. They were also frequently involved in both initial assessments and care co-ordination/management. Social workers in three of the four integrated teams were reported to carry smaller caseloads than nurses. This appeared to be related to their need to enter data onto two systems. In one of these teams (C), this issue was changing with the introduction of an integrated record system.
Occupational therapists occupied a mid-point between the more generic nurse and specialist psychologist, appearing to move in one or other direction largely in relation to their numbers within the team and the other professions represented. In teams with only one OT, for example, they rarely acted as care co-ordinator, to maximise their availability for specialist short-term input (B and F). One manager commented that she expected OTs (and psychologists) to ‘dig deeper’ in their assessments than nurses.
No differences were discerned in relation to the work of psychologists in integrated and non-integrated teams. In all the teams where represented, they were seen as slightly separate to other core members. As well as offering specific therapies, they worked closely with the consultants, particularly in relation to neuro-psychological assessments for people with possible dementia, and, in some teams, provided an educational and supervisory role (F). Psychologists acted as care co-ordinators in only one team (F), then only in exceptional cases. They appeared to have more autonomy than other members and to have a dual identity as members of both their teams and their psychology departments.
The role of the support worker
All interviewees saw support workers as vital to good-quality support for service users. One consultant commented that ‘ . . . if you look at it as a vehicle I would say they are the tyres’ (D). They performed a variety of roles ranging from short-term intensive support to prevent hospital admission to long-term monitoring, including escorting service users to appointments, encouraging community engagement, supporting self-care, mental health monitoring, anxiety management and general support visits. Job titles included ‘support time and recovery’ worker, ‘community support worker’, ‘mental health support worker’, ‘community health-care assistant’, and ‘occupational therapy assistant’. Some operated as generic workers although others, as their titles suggest, were more closely aligned to particular professions. Only one was employed by social services (D), the others by health trusts.
Support workers generally did not carry independent caseloads – working alongside and reporting back to a qualified member of staff, undertaking time consuming tasks that were judged not to need a qualified worker. Staff shortages in two teams, however, one integrated and one not, resulted in support workers holding independent caseloads and reporting directly to the consultant (B) and the manager (H).
Team caseload characteristics
Routine data collection was conducted across all nine teams, as shown in Table 48. Data on 948 service users was collected (target sample, 960). Data collection was not evenly spread across all teams, and varied from 71 service users (H) to 121 cases (G). Approximately two-thirds were female, varying between 55% and 74%. The overall sample had a median age of 78 years, varying modestly across teams from 76 to 81 years. Just under 5% were from black and minority ethnic groups, ranging from 0% to 17% across teams, broadly representing the characteristics of local populations. Clients’ living arrangements varied only marginally across teams, except in team H where substantially fewer lived alone in their own home. The proportion of the sample with informal care also varied across teams, from 38.3% to 74.8%. Just under three-quarters (73.8%) of the sample were ‘independent’, as measured by ADL,140 ranging from 59.6% to 91.3%.
| Quadrant | Quadrant 1a | Quadrant 2a | Quadrant 3a | Quadrant 4a | Total, % | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Team | A, % | B, % | C, % | D, % | E, % | F, % | G, % | H, % | I, % | ||
| Gender | Female | 73.7 | 72.4 | 54.6 | 68.1 | 66.7 | 69.2 | 69.4 | 57.1 | 57.8 | 65.8 |
| Male | 26.3 | 27.6 | 45.4 | 31.9 | 33.3 | 30.8 | 30.6 | 42.9 | 42.2 | 34.2 | |
| Age (years) | 65–74 | 44.7 | 23.8 | 35.5 | 24.5 | 37.7 | 37.9 | 29.9 | 32.8 | 18.1 | 31.7 |
| 75–84 | 38.6 | 46.7 | 45.8 | 53.2 | 46.5 | 37.9 | 47.9 | 46.3 | 43.1 | 44.9 | |
| ≥ 85 | 16.7 | 29.5 | 18.7 | 22.3 | 15.8 | 24.3 | 22.2 | 20.9 | 38.8 | 23.4 | |
| Ethnicity | White British | 83.3 | 97.1 | 94.4 | 94.7 | 100.0 | 94.2 | 96.7 | 98.6 | 98.3 | 95.1 |
| BME groups and othersb | 16.7 | 2.9c | 5.6 | 5.3 | – | 5.8 | 3.3c | 1.4c | 1.7c | 4.9 | |
| Usual place of residence | Own home: lives alone | 54.9 | 47.6 | 47.2 | 33.3 | 48.2 | 53.8 | 40.8 | 26.2 | 43.1 | 44.9 |
| Own home: lives with other | 35.4 | 47.6 | 37.8 | 46.2 | 48.2 | 40.2 | 53.0 | 72.3 | 53.4 | 47.3 | |
| Other including ECH | 9.8 | 4.8 | 15.1 | 20.4 | 3.6 | 5.8 | 5.8 | 1.5 | 3.4 | 7.9 | |
| Informal care (hours per week) | None | 35.8 | 30.0 | 29.4 | 43.9 | 52.7 | 61.7 | 27.0 | 35.3 | 25.2 | 37.6 |
| 1–7 | 40.4 | 33.0 | 35.3 | 12.2 | 13.4 | 17.9 | 24.5 | 14.7 | 20.7 | 24.2 | |
| 8–20 | 11.0 | 19.0 | 14.7 | 12.2 | 8.9 | 11.6 | 24.5 | 20.6 | 27.0 | 16.6 | |
| ≥ 21 | 12.8 | 18.0 | 20.6 | 31.7 | 25.0 | 9.5 | 23.6 | 29.4 | 27.0 | 21.6 | |
| ADL | Independent | 77.2 | 69.5 | 72.4 | 59.6 | 85.1 | 91.3 | 66.2 | 62.0 | 63.0 | 73.8 |
| Minimal help needed | 15.8 | 19.0 | 18.1 | 18.1 | 7.9 | 5.8 | 16.2 | 19.7 | 20.4 | 14.9 | |
| Partially dependent | 2.6 | 9.5 | 5.7 | 16.0 | 3.5 | 2.9 | 12.3 | 11.3 | 10.2 | 7.3 | |
| Very/totally dependent | 4.4 | 2.0c | 3.9c | 6.4 | 3.5c | – | 5.2c | 7.0 | 6.5 | 4.0 | |
| Physical health affecting ADL | Great extent | 29.3 | 29.6 | 33.9 | 27.3 | 23.8 | 48.0 | 26.2 | 40.9 | 33.8 | 31.5 |
| Moderate extent | 34.7 | 28.2 | 35.6 | 45.5 | 52.4 | 26.0 | 49.2 | 36.4 | 47.3 | 39.9 | |
| Little extent | 36.0 | 42.3 | 30.5 | 27.3 | 23.8 | 26.0 | 24.6 | 22.7 | 18.9 | 28.7 | |
| n (minimum–maximum) | 109–114 | 100–105 | 102–108 | 82–94 | 112–114 | 95–104 | 110–121 | 65–71 | 108–117 | 889–946 | |
| Physical health affecting ADL, n | 75 | 71 | 59 | 55 | 63 | 50 | 65 | 22 | 74 | 534 | |
Table 49 shows the diagnostic profile of the caseloads sampled. In total, 37.5% of all service users had an organic disorder, 45.3% a functional disorder, 6.8% a mixed diagnosis and 10.4% no diagnosis. Diagnosis again varied substantially across teams, with three-quarters (77.5%) of service users in team H having an organic disorder (including mixed diagnosis) compared with just 26.9% in team F. Two teams (B and G) had in excess of one-quarter of all cases without a probable diagnosis recorded. As anticipated, the proportion of a team’s caseload with an organic diagnosis was directly proportional to cognitive impairment. Just 5.8% exhibited ‘high’ levels of behavioural difficulties (see Table 49), using a broad-rating scale described earlier in Box 4. This proportion varied, from a minimal level (fewer than five cases) in teams F, G and H to 12.8% in team D. Similar variation was found with respect to risks, with just 8.7% in team F exhibiting at least one high risk, as compared with over one-quarter (25.7%) in team H.
| Quadrant | Quadrant 1a | Quadrant 2a | Quadrant 3a | Quadrant 4a | Total, % | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Team | A, % | B, % | C, % | D, % | E, % | F, % | G, % | H, % | I, % | ||
| Diagnosis | Alzheimer’s disease | 6.1 | 11.4 | 6.5 | 1.1b | 6.1 | 3.8 | 19.0 | 42.3 | 14.5 | 11.4 |
| Vascular dementia | 4.4 | 3.8b | 14.8 | 6.4 | 1.8b | 1.0b | 5.8b | 11.3 | 18.8 | 7.5 | |
| Other unspecified dementia | 7.9 | 11.5 | 11.2 | 33.0 | 12.3 | 9.6 | 11.6 | 14.1 | 21.4 | 14.4 | |
| Other/multiple organic | 0.9 | 3.9b | 3.8 | 3.2b | 5.3 | 5.8 | 6.6 | 4.2b | 3.5b | 4.2 | |
| Depression/anxiety | 28.9 | 24.8 | 25.0 | 44.7 | 51.8 | 55.8 | 17.4 | 11.3 | 7.7 | 29.9 | |
| Other affective disorder | 12.3 | 6.7 | 6.5 | 4.3b | 5.3 | 6.7 | 3.3 | 4.2b | 2.6b | 5.8 | |
| Schizophrenia | 21.1 | 2.9b | 6.5 | 2.1b | 1.8b | 2.9b | 1.7b | 2.8b | 1.7b | 5.0 | |
| Other/multiple functional | 8.8 | 1.0b | 7.4 | 3.2b | 6.1 | 6.8 | 1.7b | 2.8b | 3.4b | 4.6 | |
| Mixed organic/functional | 5.3 | 8.6 | 8.3 | 2.1b | 7.0 | 6.7 | 6.6 | 5.6b | 9.4 | 6.8 | |
| No recorded diagnosis | 4.4 | 25.7 | 9.3 | – | 2.6b | 1.0b | 26.4 | 1.4b | 17.1 | 10.4 | |
| Indicators of low mood | Yes | 57.7 | 42.2 | 41.3 | 61.1 | 52.6 | 46.2 | 43.8 | 35.3 | 38.7 | 46.8 |
| No | 42.3 | 57.8 | 58.7 | 38.9 | 47.4 | 53.8 | 56.3 | 64.7 | 61.3 | 53.2 | |
| Cognitionc | No impairment | 38.1 | 23.2 | 27.8 | 36.0 | 38.1 | 40.3 | 26.8 | 18.5 | 16.0 | 29.7 |
| Mild impairment | 37.9 | 36.9 | 37.3 | 25.1 | 36.3 | 42.4 | 36.9 | 34.3 | 32.4 | 36.7 | |
| Moderate impairment | 19.3 | 34.4 | 26.1 | 19.7 | 22.1 | 15.7 | 34.3 | 38.0 | 41.7 | 27.8 | |
| Severe impairment | 4.7 | 5.5 | 8.9 | 19.2 | 3.5 | 1.6 | 1.9 | 9.1 | 9.9 | 6.9 | |
| Challenging behaviour | Low | 28.9 | 40.0 | 33.3 | 41.5 | 64.0 | 72.1 | 42.0 | 58.6 | 31.9 | 45.2 |
| Medium | 67.5 | 56.2 | 59.0 | 45.7 | 31.6 | 26.0 | 56.3 | 35.7 | 56.6 | 49.0 | |
| High | 3.5b | 3.8b | 7.6 | 12.8 | 4.4 | 1.9b | 1.7b | 5.7b | 11.5 | 5.8 | |
| Risks | Low risk | 36.3 | 37.9 | 38.1 | 41.7 | 36.3 | 60.2 | 41.6 | 32.9 | 46.1 | 41.5 |
| At least one medium risk | 39.8 | 43.7 | 38.1 | 39.6 | 42.5 | 31.1 | 41.5 | 41.4 | 40.9 | 39.8 | |
| At least one high risk | 23.9 | 18.4 | 23.8 | 18.7 | 21.2 | 8.7 | 16.9 | 25.7 | 13.0 | 18.7 | |
| n (minimum–maximum) | 111–114 | 102–105 | 104–108 | 90–94 | 114–114 | 103–104 | 114–121 | 68–71 | 112–117 | 918–948 | |
Services received
Four aspects of service receipt were collected (Table 50). The median LOS on the caseload at the point of data collection was 12 months, with evidence of a substantial ‘tail’ in the distribution. Over one-quarter (27.8%) of the total had been on the caseload longer than 2 years, and this proportion varied from 18.3% to 47.8% across teams. In addition, one-third (33.8%) of all service users were known to the CMHTOP prior to the current episode. Table 50 also provides data on contact between team members and service users. Most service users (68.7%) had seen a CMHTOP doctor in the previous 6 months, though this proportion was markedly lower than average in two teams (B and G). Nearly two-thirds (65.6%) of service users had seen a CMHN in the preceding month, varying from less than a half (H and I) to all service users (E). OTs formed a smaller proportion of contacts with service users, although 38% of service users in team H had seen an OT in the previous month. Social worker input was significant within highly integrated teams, and ‘other’ professional workers provided smaller contributions except in teams C and F where psychologists provided a substantial input. Support workers visited 20.4% of all service users in the sample in the preceding month, although this varied from a nominal level (fewer than five cases) in team E, to 40.7% in team D.
| Quadrant | Quadrant 1a | Quadrant 2a | Quadrant 3a | Quadrant 4a | Total, % | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Team | A, % | B, % | C, % | D, % | E, % | F, % | G, % | H, % | I, % | ||
| Duration on caseload (months) | < 6 | 28.3 | 21.0 | 34.6 | 27.7 | 38.1 | 40.4 | 40.5 | 13.4 | 17.4 | 29.8 |
| 6–12 | 19.5 | 24.8 | 20.2 | 22.3 | 16.8 | 15.4 | 12.4 | 13.4 | 33.0 | 20.0 | |
| 12–24 | 21.2 | 29.5 | 26.9 | 27.7 | 23.9 | 14.4 | 14.9 | 25.4 | 21.7 | 22.5 | |
| ≥ 24 | 31.0 | 24.8 | 18.3 | 22.3 | 21.2 | 29.8 | 32.2 | 47.8 | 27.8 | 27.7 | |
| Contact with CMHTOP memberb | Doctor | 74.6 | 47.6 | 83.0 | 76.9 | 74.6 | 76.9 | 33.3 | 79.7 | 78.6 | 68.7 |
| Nurse | 72.8 | 58.3 | 69.4 | 74.7 | 100.0 | 58.7 | 58.3 | 42.3 | 48.7 | 65.6 | |
| OT | 18.4 | 7.6 | 9.3 | 12.2 | 9.6 | 1.9c | 15.8 | 38.0 | 15.4 | 13.5 | |
| SW | 21.1 | 25.0 | 28.7 | 31.8 | – | – | – | – | – | 12.3 | |
| Other qualified worker | 1.8 | 1.9 | 7.4 | 4.0 | – | 22.1 | 5.2 | – | |||
| Support worker | 23.7 | 26.9 | 19.4 | 40.7 | 3.5c | 23.1 | 22.5 | 17.1 | 10.3 | 20.4 | |
| Mean contacts by doctors | 1.3 | 0.9 | 1.8 | 3.5 | 1.3 | 1.2 | 0.5 | 1.1 | 1.1 | 1.4 | |
| Mean contacts by others | 3.6 | 3.3 | 3.3 | 4.3 | 3.2 | 2.1 | 2.0 | 2.3 | 1.3 | 2.8 | |
| Inpatient admissions | Yes | 11.5 | 2.9c | 10.2 | 16.3 | 9.6 | 7.7 | 3.4c | 1.4 | 7.7 | 8.0c |
| No | 88.5 | 97.1 | 89.8 | 83.7 | 90.4 | 92.3 | 96.6 | 98.6 | 92.3 | 92.0 | |
| Other mental health service | Yes | 2.7c | 18.4 | 13.8 | 18.5 | 11.4 | 1.0c | – | – | 4.3 | 7.8c |
| No | 97.3 | 81.6 | 86.2 | 81.5 | 88.6 | 99.0 | – | 94.7 | 91.2 | ||
| Social care services | No/minor support | 53.3 | 49.0 | 48.0 | 54.7 | 62.7 | 68.9 | 72.3 | 61.5 | 47.2 | 57.3 |
| Intermittent support | 11.4 | 6.0 | 6.9 | 4.7c | 9.1 | 4.9 | 6.4 | 13.8 | 13.0 | 8.4c | |
| Limited regular support | 30.5 | 31.0 | 33.3 | 23.3 | 16.4 | 19.4 | 12.8 | 20.0 | 28.7 | 24.2 | |
| Intensive regular support | 4.8 | 14.0 | 11.8 | 17.4 | 11.8 | 6.8 | 8.5 | 4.6b | 11.1 | 10.2 | |
| n (minimum–maximum) | 65–59 | 103–104 | 108–117 | 94–121 | 110–114 | 94–105 | 102–108 | 105–114 | 86–94 | 873–942 | |
Overall, 8% of service users had been admitted to a mental health ward in the 6 months preceding the baseline stage. This varied from a negligible proportion (H) to 16.3% (D). Other specialist mental health service use similarly varied, from zero reported contacts in teams G and H, to 18.5% of service users in team D. The most commonly used other services were day hospitals, used by 50 service users across the sample. Surprisingly, very few service users were recorded as having used other psychological therapies outside the CMHTsOP. With respect to social care, nine services (and associated frequency of use) have been collapsed into four categories displayed in Table 50, mirroring the approach detailed in Appendix 9. Over half (57.3%) of service users within the sample received no/minor social care support, with this proportion rising to 72.3% in team G. More service users in team D received intensive regular support (17.4%), reflecting their above-average ADL and behavioural difficulties noted above.
Discussion
This chapter demonstrates the complex and varied patterns of practice within individual teams (key attributes are summarised in Appendix 34). The main similarities between the teams were that they had colocated core members (apart from two consultants) consisting of nurses, OTs, support workers and consultant psychiatrists, and that nurses conducted initial assessments and took on the role of care co-ordinator in all teams. In all other respects one or more teams differed significantly from the majority in aspects of organisation or operation.
Seven teams had a single-line management structure although only two of these, both integrated, provided both line management and clinical supervision to all staff within their team. Social workers were present in four teams. Five teams had psychologists although the extent to which they were used appeared to vary. All but two teams operated a SPA, newly introduced in one case (F). Six teams accepted referrals only from medical sources. Although in most teams initial assessments could be undertaken by a range of staff including nurses, OTs, social workers and consultants, in one team this was restricted to nurses. Care co-ordination was undertaken by social workers in all teams where present, although one team did not use this term (B). OTs were cited as being care co-ordinators in some teams though in others they were used as specialists, brought in to work alongside a care co-ordinator on a short-term basis. Psychologists and psychiatrists were each reported to take on the role of care co-ordinators in only one team (F and D respectively). In seven teams consultants were described as carrying ultimate clinical responsibility for all the patients seen by members of the CMHT, regardless of whether seen by them or not (B, C, D, F, G, H and I), although this was not clear cut.
Our data suggest a broad fidelity to the intentions of the initial typology on team integration. Four teams had social workers. Of these more integrated teams, three also had a single manager and operated a SPA. Three accepted referrals from a range of agencies and could all access the other agency’s records or had a unified system. Four of the five teams classified as non-integrated also had a single manager and a SPA. However, none were able to access social services records and they only accepted referrals from medical professionals. Two teams nevertheless, stand out from the typology. Team E, one of the less integrated teams, more closely conforms to the definition of a ‘network team’,253 as a group of quasi-autonomous professionals, working on related cases with professional groups from other teams as required. Although nurses and OTs were colocated, unlike other teams they remained separately managed and employed. Team B was another anomaly, achieving all of the ‘objective’ standards of integration identified within the National Survey (see Chapter 8), and yet operating more like two colocated subteams, one for health and one for social care, each with its own manager, albeit with good communication channels between them. This was the only ‘integrated’ team where it was common for there to be two allocated workers, one from health and one from social care, acting as care co-ordinators/managers, a similar approach to the non-integrated teams where external social care input was required. Thus, the typology has been extended to incorporate what might be perceived to be a hierarchy of integration ranging from a health only network team to a fully integrated health and social care team. The four team types are summarised in Box 18.
| Team type | Team characteristics | Team(s) |
|---|---|---|
| Network | Colocated multidisciplinary health team with separate managers for different professions located outside the team | E |
| Low integration | Colocated multidisciplinary health team with single manager located within the team | F, G, H, I |
| Nominal integration | Colocated health and social care team with separate managers for health and social care professionals located within the team | B |
| High integration | Colocated health and social care team with single manager located within the team | A, C, D |
The consultants’ role did not appear strongly related to whether or not teams were integrated, although the examples of consultant-led meetings were in two non-integrated teams (E and F). The qualitative evidence suggests that the teams did not adhere well to the original typology on this dimension. The concepts of ‘responsibility’ and ‘influence’ were found to be less clear-cut, while the patterns of working found were more complex and cross cutting than originally identified. The extent to which practices were in flux in some teams also made the original typology elusive. The closeness of the working relationships between consultants and other staff within the teams did not correlate with the description of how responsibility was shared. Team E again stands out because it was perceived to be a consultant-led team and yet exhibited aspects of shared responsibility – with the consultant only responsible for the clients they saw, and having little influence on the day-to-day work of the team. Teams B, C and I also appeared to be incorrectly positioned within the original typology: the former due to the consultant stating she had the responsibility to oversee everything and the latter two because the consultants thought that team members ought to take on more responsibility for decision-making.
The impact of these variations on service users and staff – in particular in relation to whether teams were more or less integrated with social care services is the subject of the next two chapters.
Chapter 10 Community mental health teams for older people: the outcomes and costs of different ways of working
This chapter explores the impact of different ways of working on service user and carer outcomes.
MethodA mixed-methods study comprising in-depth interviews with practitioners and an observational study of service user and carer outcomes, using the refined typology identified in Chapter 9.
ResultsStaff interviews indicated the perceived value of integrated care, characterised as having a social worker as a core member of the team. Identified benefits included better access to a wide range of skills and services, easier access to information and avoidance of duplication of effort. Other valued indicators of integration between health and social care services included a single team manager and a SPA. The continuity of care across mental health services provided when consultants had both inpatient and community responsibilities was also highly valued.
No evidence was found that well integrated CMHTsOP (as identified in this study) were more effective than less integrated teams with regard to preventing admissions to hospitals or care homes, or in improving service users’ QoL and satisfaction. No significant differences in carer outcomes were identified. However, marked within team type variation clouded definitive conclusion.
ConclusionsThe study identified the need for greater clarity as to what constitutes ‘integration’, beyond formal structures to shared cultures and understanding, as well as the role of leadership. Given the degree of interest in developing integrated approaches to care, it will be important to further discern the goals of integration and the particular components of an integrated care approach which produce beneficial outcomes.
Introduction
Following on from Chapter 9, this chapter starts with an exploration of the nature of the relationship between teams’ working practices and service user outcomes as perceived by staff themselves, drawing on data from the qualitative interviews. Using information from baseline and follow-up data collections, it then examines whether or not different approaches to integrated working were associated with variations in service user and carer outcomes (including admissions to inpatient wards and care homes, satisfaction and QoL) and costs. It also outlines some of the key difficulties of this work, and explores the lessons learned for future evaluations.
Findings
Staff views on the relationship between teams’ working practices and service user outcomes
When describing the impact of different aspects of their working practice on user outcomes, interviewees tended to focus on the extent to which the services they provided were holistic in character, timely, and delivered in a seamless manner across time and settings. Although all of these features relate directly to the issue of integration, the latter was also perceived to relate to the role of the consultant. Example quotations from interviews illustrating the points made below can be found in Boxes 19 and 20.
| No. | Attribute/theme | Example | Team and professional |
|---|---|---|---|
| 1 | Multidisciplinary improves efficiency:informal coworking | I think that the advantages are that . . . we provide a more seamless service so . . . if . . . I had identified that . . . an OT could . . . have a more enabling role . . . I could actually have a conversation with that OT, discuss co-working with them for maybe a short period, maybe a long period . . . I can dip into my colleagues case load where there’s a social care need identified without them having to . . . go through the process of referring to . . . [social services] | Team A, social worker |
| 2 | Multidisciplinary working enhances skills of all | Everybody learns so much and when you go out to someone . . . years ago, perhaps a nurse would go out and somebody would ask them about benefits . . . So it’s not like . . . ’this is nothing to do with me’ . . . they don’t do that anymore . . . They can come back to the team, speak to somebody who knows a little bit more and they’ll go straight out . . . It widens your knowledge and we’re not there for anybody else other than the client, so it is beneficial . . . | Team D, team manager |
| 3 | Integrated team work offers a more efficient and holistic service | Because the other person you want to refer to . . . , you are sitting alongside them, you can have a chat and discussion about the patients beforehand . . . So you are not referring them blind . . . the patient never actually realises that there is any change to anything because, we all work together in the same team and you are referring to a colleague, which is a lot quicker because you are not sending it out of the office, onto a waiting list . . . | Team B, health team manager |
| you’ve got the social workers understanding and knowing the patient prior to so you’re not fighting for service . . . you’re not having to state your case and really having to fluff it up . . . just to get them to respond . . . | Team I, nurse | ||
| 4 | Importance of having mental health social workers in team | It is a huge benefit . . . They are . . . very skilled and they have a good knowledge of the Mental Health Act and they have good knowledge of safeguarding . . . they just bring a different dimension really. They are very good at risk assessments . . . they take on the more complex patients . . . I think it is imperative to have mental health social workers in the teams. We do bring in other social workers for less complex clients, but the communication isn’t as good certainly . . . I just don’t think that the patients get as good an assessment really | Team C, consultant |
| 5 | Impact of lack of shared records | [We]’ve got like five IT systems. None of which talk to each other . . . we’ve got social services who have got their own, we’ve got the OTs who use SAP, we’re using MHIS, the consultants use hand written things yes, and the wards use hand written things . . . I can’t get on to SAP, I can’t get on to the social workers site . . . I don’t know what that the OTs are doing unless I physically go and ask an OT . . . So I think that if you just opened those lines of communication a little, if you could open the IT systems . . . That would be a huge improvement | Team E, team leader |
| 6 | Non-integrated team: duplication, slow response | At the moment we call what’s called the Adult Help Desk which is a central number . . . we make the referral to the[m] . . . and then that tends to sit on a waiting list until it’s assigned and then, we don’t even know when it happens unless we actually keep checking and finding out so there is a lack of communication . . . | Team I, nurse |
| 7 | Non-integrated team: lack of shared goals and pressures | . . . I don’t know where they sit . . . they are interested, but . . . just . . . in their bit and . . . they are just thinking, well if it is open to that CPN, and they want to look for a care provision then as quick as possible get it sorted . . . I don’t want to sit here and say we don’t get on well with social services on a grass roots levels. It’s an organisational thing, it is about each of us trying to deal with our own pressures . . . it’s about how their systems have changed . . . , and it is about our changes as well, just they are not changing together at all. We are changing much further apart . . . | Team H, team manager |
| 8 | Impact of lack of understanding of mental health needs by generic social workers | It used to be that we could contact the individual (social worker) . . . but now . . . what we have to do for anyone who needs a social worker is to go through ‘Adult Social Care Direct’ . . . they’ve got a phone number . . . and then request that it would be the mental health social worker, because in the past when that system was first set up, it could go to any social worker and there were a few kinks in the armour in that they action it and ring the person and then say, – I’ve had a referral from the OT, I’m coming out to see you. Well I might have had a discussion with that person and taken a long time to get them to agree, and because of the dementia they might have already forgotten. They would get a phone call and then say, – “no I didn’t ask for anybody”, so then . . . [the social worker] wouldn’t go out. So what we tend to do is, [say] they need a mental health social worker and . . . can you contact us before you make any contact with the client or the family so we can clarify what it’s about . . . | Team E, OT |
| 9 | Relationships can overcome lack of integration | we have a really good working relationship with a social worker who used to be part of our team and . . . A few years ago, yes it was a few years ago but she tends to get all of the [area name] referrals from the ward, so we do tend to work well with her simply because she does know the score really . . . | Team I, nurse |
| 10 | Difficulties of separate managers | what one organisation sees as the higher priority . . . , the other might not, so then you have two managers who are then saying, – “what we need to do is to do this”, and you say well, – “that will have a knock on effect on this”, and if you had one who has an understanding of our service then that might be better . . . | Team E, OT |
| 11 | Strengths of having a SPA | If we compare it to the other model . . . which is you have some referrals come to the consultants, some . . . to the team . . . , the nurse or the social worker of the team, the problem with that is that …you are not bringing all the skills together to work for the patient. . . . By single point of access, what happens is all the referrals are going to one place, and now we have a duty system here which enhances it further because . . . the duty worker will respond straight away and find out what the situation is, . . . if it is a high risk situation, that gets immediately passed onto the respective team, and then as a team, they will discuss the medical/social component and respond together . . . Otherwise . . . , I feel the multidisciplinary part of the work will take place, but in stages | Team D, consultant |
| 12 | Internal referrals would improve efficiency | Classically we used to get things off the GP saying, – ‘please can you go and see this lady who has got an MMSE of 12 I think she may have some memory problems’, and we’ll go, – ‘well, yeah’ (laughs) . . . we just have to kick them back to the GP . . . , and the GP has to write back and what not. That’s ridiculous . . . if you could . . . open the referral systems. That would be a huge improvement | Team E, team leader |
| 13 | Direct re-referral by public to improve access | We actually give them a card to say that they actually can . . . self refer back to our service. So it used to be in the old days that they had to go round the consultant and the GP to get back, . . . So now we discharge and their significant other, carer, whoever . . . , you know . . . , if there is a problem they can ring up and ask our advice and we would just pick them back up on our caseload. One of the big factors for ourselves was that we were quite nervous to discharge if people had to go via various routes to come back, so if we agreed within our service that this would do that, they could fast track back to ourselves | Team E, OT |
| 14 | Difficulties of co-ordinating care across services | The time when the Rapid Response Team might withdraw and we might need to sort of engage more . . . it is not as good as it could be, whereas, if they were within . . . , people could talk to each other, – what are you doing?, and all of that sort of stuff, then you know, just the barrier gets in the way | Team B, team manager |
| 15 | Advantages to having a range of services colocated | It is an excellent model with the multidisciplinary integrated team with its own independent memory services, and its own in-patient unit and its own day hospital . . . everything in . . . one place. Some of the service I was with previously . . . things [were] in different places, . . . your functional ward in one place and ten/fifteen miles away will be your organic ward, and your office will be somewhere else and your team’s office somewhere else, so you can imagine working in an environment like that . . . but in an environment like this here . . . the physical integration is very much there, so that itself brings in integration | Team D, consultant |
| No. | Attribute | Example | Team and professional |
|---|---|---|---|
| 16 | Strengths of sectorised model for staff and service users | I cannot see any disadvantage for the patient, and I cannot stress that strongly enough . . . there is a massive advantage in knowing them right from the start and supporting the family right the way through, because boy, do they need support and that familiar face, so they don’t have to go through everything again, information doesn’t get lost, with the best will in the world all the information doesn’t get translated, the finer points, the subtle nuances don’t get translated on when you are handing over from one person to another, or in the form of a letter . . . For me continuity of care is everything, I know my patients really well and when they come into hospital and I look after them, I already know the family . . . I think as a consultant body, we feel quite strongly about maintaining the continuity regardless of systems . . . | Team E, consultant |
| 17 | Difficulties of operating a sectorised system in a large trust and challenges of the functionalised system for consultants | At that time we had six consultants in older adults and it just became really challenging to have ward rounds, to have six consultants, the nurses just could not cope with having six consultants coming to do ward rounds every day of the week and junior doctors coming in all the time, so it made sense to say . . . “why don’t we just have two consultants doing in-patient work?”, that is easier for the nurses and everything else to manage, . . . It’s had mixed results I think. The immediate challenge that we had was the continuity of care . . . we in the community look after people in their homes in the community and if they need to be admitted then we’ll arrange for them to go to the in-patient unit and at that point your responsibility is handed over to someone else . . . you have a care plan and you hope that they’ll follow your care plan but if they don’t agree with your care plan then they could change things, manage this patient on the ward, discharge them back into your care and again, are you happy with what they have done?, have they made any changes?, that was a bit of a challenge . . ., but again you know we’ve been using that model now for close on three years and after the initial blips . . . , I think it’s working fairly well . . . | Team F, consultant |
| Well I mean . . . , everyone is different and everyone had their own way of doing things, I think that people will be used to my little whims and foibles . . . I think we all knew what we were working towards. . . . I think it is difficult . . . I think there have been some transition problems with . . . reporting to a different consultant . . . So I think that has put a bit of a strain on the CMHTOP . . . You know . . . , when you are just down the corridor from the ward, you can bob in and see somebody that you are involved with . . . you may only be bobbing in for ten minutes and it is literally like that, but to bob in for ten minutes . . . , is [now] a half day experience | Team A, consultant | ||
| 18 | Strengths of functionalised model | Sometimes it’s positive because it’s someone else who doesn’t know the patient looking at them in a sort of . . . , in a different way very often, and they may change the approach and, you know . . . , sometimes it works. So it hasn’t been all negative by any means . . . | Team F, consultant |
| 19 | Weaknesses of functionalised model | The thing I am concerned about it that I . . . have established a relationship . . . I have got an idea of their sort of, preferences. They have got an idea of how I work and we are sort of used to each other, and perhaps when they are at their most vulnerable, and they are suddenly confronted by a different consultant, who works in a slightly different way . . . It is just that it is somebody different . . . It is another face . . . So I think the system lacks a bit of continuity | Team A, conslutant |
| 20 | Difficulties for consultants of operating within a sectorised model | It is obviously better for the patients because you get that continuity of care, and it really helps having that . . . , having me as a point of contact between all the different services . . . , but in terms of managing the work load . . . , it is pretty hard em . . . , because there is just never enough time for anything, and that is why the adult services went on to community and in-patient | Team B, consultant |
| 21 | Strengths of combination of integrated team and sectorised model of consultant working | I have done quite a bit of research looking at different models . . . looking at trying to work efficiently and modernise the service . . . but I have to say, for me, from our patients point of view, that works best, having that continuity of care. Having a healthy, robust, community model and then when people are needing that input, being able to follow that through with the care co-ordinator and back out again. I think if you have got a good functioning team, and good medical staff, it works . . . it is not about being old fashioned and not wanting to modernise but you do feel the patients do like that way of working | Team C, consultant |
| 22 | Fractures in system where there is a non-integrated team and a sectorised model | If they’ve been an in-patient without a social worker prior to them coming in, if they are not known to social services . . . Then they get a hospital social worker, and that’s really to sort of make it quick so that they can get seen. So that works quite well, you know, we can discharge them sort of fairly soon, and I don’t have a huge issue with that except that there needs to be a robust communication process at the point where the hospital team want to either hand over or discharge, or whatever. I think that’s probably the stumbling block sometimes . . . I don’t have an issue with the system . . . , it’s just that little bit of it in the middle, where a potential changeover may happen. They need to recognise that that person is managed by a multidisciplinary team | Team E, consultant |
| 23 | Fractures in system where there is a non-integrated team and a functionalised model | Now we have an in-patient consultant, obviously his viewpoint might be different to what [the community consultant’s] might be, sometimes patients have come out with no knowledge, sometimes that patients are in there . . . The communication thing, it can break down sometimes . . . , communication . . . , sometimes they have not referred patients and the patients have slipped through the net, for want of a better word . . . and I think the expectation sometimes . . . what they are expecting us to do is what we shouldn’t be doing . . . they think that sometimes at in-patients . . ., we should do everything, without understanding that actually the patient is sort of in hospital . . . I think what they expect us to do is see every single patient that comes out of hospital and I don’t always think that is appropriate | Team F, nurse |
Features of integration across health and social care were regarded as crucial. Most evidence related to the extent of multidisciplinarity and in particular to having social workers represented in the team or not. Working within a MDT was regarded positively by all staff interviewed, including team managers and consultants. They described this model as providing a wider range of easily accessible skills and expertise to support service users than would have been possible in single discipline teams. This was thought to create a more seamless approach to casework with the informal input of different professions across a range of perspectives (quote 1). As one nurse commented ‘the main advantage . . . [is] getting other views . . . from different disciplines’ (H). Recruiting a wider range of staff was also regarded as having the potential to enhance the skills of all individual members by fostering informal learning between colleagues (quote 2). Members of only one team did not welcome further multidisciplinarity (E), regarding it as a threat to their current model which was thought to work well.
Although multidisciplinarity is but one attribute of integration, it represented the crux of this model where it encompassed both social care and health professionals. Having one or more social workers in a CMHTOP meant that other attributes of integration were more likely, including having a single manager across all disciplines, a shared record system and assessment documents, a single care co-ordinator responsible for both health and social care input and the ability for health professionals to access social care resources. 228
There was almost unanimous support for having social workers within CMHTsOP, both from staff in teams who currently had them and from those that did not. The reasons given were similar in many ways to those relating to multidisciplinarity; more generally, wider expertise, role enhancement, and faster and more holistic service delivery (quote 3). Social workers were described as bringing into the team specific mental health expertise, knowledge of social services procedures and funding, and the ability to access social care resources directly, all core aspects of the work of a CMHTOP (quote 4). This was described as easing transfers to social services teams when required. Only with social workers as core members were teams able to gain access to social care records, seen as improving efficiency and reducing duplication. The team leader of the least formally integrated team in the study (E) described five separate systems used by professionals working with older people with mental ill health ‘none of which talk to each other’ (quote 5). However, efficiency within integrated teams was hampered where social workers were expected to complete two sets of records, one for health and one for social care.
Members of teams that did not have their own social workers identified consequent difficulties. These ranged from duplication of effort, slow response and the limited understanding of mental health work by generic social workers (quote 6), to a lack of shared goals and of understanding of each others’ pressures resulting in limited joint working (quote 7). The loss of information acquired by CMHTOP staff in transferring cases to social services, particularly where a central referral system was in place was an additional concern. Together these issues were thought to result in an inefficient service where either the work undertaken by one team was repeated by another or services recommended by one were withdrawn due to limited understanding of the service user’s needs by the other (quote 8). There were examples of teams without social workers where joint working was reported to be effective as a result of strong informal arrangements based on stable long-standing relationships as well as where the local social services team comprised of specialist mental health workers. These instances were in the minority however and their fragility was also recognised (quote 9).
The impact of other integration attributes on the effectiveness of service delivery suggests that working for the same organisation and having a single manager across disciplines was thought by respondents to aid efficiency. In team E, for example, the OT commented that they did not share a manager with the nurses and, despite colocation, this could result in different priorities being placed on them, limiting the effectiveness of their joint practice (quote 10). Incomplete integration in team B was also reported by the social worker to lead to misunderstandings sometimes causing delays. An example arose where the lack of shared assessment documentation and processes (CPA by health staff and SAP by social care staff) resulted in duplication and a lack of shared understanding.
The availability of a SPA was viewed positively by most staff members, with the suggestion that it streamlined referrals and ensured a more appropriate response, utilising the skills of the whole team (quote 11). Interestingly, intrareferring between health and social care was reported by the social care manager of team B to be one of the ‘best things’ to come out of integration. Where previously they had to refer via the GP to obtain a CMHN opinion, they could now access colocated nurses, seen as improving efficiency and reducing duplication. As one team manager put it, it meant that you were ‘not referring blind’ (B, health). Team C also operated the SPA slightly differently from the others, an extra level of ‘screening’ by a team member occurring before an initial assessment took place. This was thought by some staff to be inefficient and a duplication of work. The only other team to criticise this approach did not themselves use it (E), accepting referrals from GPs directly to nurses or consultants and viewing a SPA as cumbersome and unnecessary. However, the team leader of this team was equally critical of their current system which did not allow them to inter-refer, with consequent additional delays (quote 12). Accessibility to the public was an issue of concern for some staff, particularly for teams that did not accept open referrals. Trying to address this, OTs in one team (E) had developed a system that enabled service users to re-refer directly to individual occupational therapy staff post discharge (quote 13).
Teams did not work in isolation and required positive working relationships with other services to be effective. Co-ordination of care across settings was regarded by many team members as key to the delivery of an effective service. Structural integration with social services was one dimension of this. Another was the nature of linkage with primary care, with related teams and services such as memory clinics, rapid response teams, and the support and liaison provided to care homes and general hospitals. Several staff considered the service provided to people with dementia to be rather disjointed as the various teams involved did not liaise effectively, leading to duplication on the one hand and people potentially falling through the net on the other (quote 14). In contrast, where a range of services were colocated, staff reported advantages in terms of communication and co-ordination. One consultant noted the positive impact of having memory clinic and care home liaison nurses colocated with the CMHTOP (I), whereas another commented on the value of having a range of services under one roof (D) (quote 15). Team managers of three teams reported positive relations with primary care, with nurses attending regular meetings in two (C and E). In the third, relationships with GPs and consequently the quality of referrals and communication between them and the CMHTOP had improved enormously as a result of the work of the consultant (I).
The importance of ‘continuity of care’ between community and inpatient wards was a phrase and concept used repeatedly by consultants in relation to the delivery of a good service that they felt benefited service users. Six of the consultants in this study operated within a ‘sectorised’ model, having clinical responsibility for the geographic ‘patch’ covered by the team. In the three other teams consultant responsibility was either in community or inpatient settings (‘functionalised model’). All consultants operating within the ‘sectorised’ framework felt that it was vital to the provision of good-quality care, providing reassurance for the patient that they would see a familiar face in hospital, and ensuring that detailed information and knowledge of the individual was not lost in transfer (quote 16). Other staff also commented on its strengths, noting, for example, that it eased the process of finding a bed for a patient.
The three consultants who did not operate within this system were all based in very large trusts where the ‘sectorised’ model had proved unworkable. Team F, for example, prior to the introduction of the ‘functionalised’ model 3 years ago, had six consultants attending ward rounds, some travelling long distances to do so, leaving them less time to see patients in the community (quote 17). The consultant from team F commented that she had misgivings about the change in relation to continuity of care. On the other hand she also noted that another consultant with a different approach might be just what some patients needed (quote 18). This was a minority view, however, with other consultants expressing concern about the change in personnel (quote 19). Generally, the ‘functionalised’ model was regarded as worse for patients, though more manageable for consultants (quote 20).
A sectorised model of consultant working was reported to improve service delivery; as was integration between health and social care above, particularly in the form of having social workers in CMHTsOP. The most beneficial model was believed to be where these approaches operated together. Three of the nine teams operated in this way (B, C and D), although in one case this only related to patients with functional mental disorders. Staff from team C described how this ensured that the same consultant was aware of the needs of their patients across settings and that a social worker from the team was allocated at hospital discharge, reducing the possibility of breakdown in arrangements post discharge and providing a high level of continuity for service users (quote 21). Where teams operated a sectorised model but did not have social workers within the team (E and H), although hospital discharges were usually straightforward, transfer of cases from hospital social workers initially, to community social work staff after a few weeks of responsibility, sometimes led to a breakdown in communication (quote 22). Where teams had neither social workers as core staff nor consultants whose responsibility included both community and hospital (F and I), access to hospital beds and discharge arrangements were both seen as problematic. In one team (F), for example, staff felt misunderstood by hospital staff who they thought expected too much of them while their team manager and the team consultant interviewed were concerned about the limited engagement of their community nurses with the inpatient wards (quote 23).
Service user outcomes
Integration was clearly perceived by staff to be a necessary factor in the delivery of better service user outcomes. The second part of this chapter explores the relationship between the costs and outcomes of the four team types identified in Chapter 9 (i.e. high integration, nominal integration, low-integration and network teams), drawing on information from the baseline and follow-up data collections. However, as any such analysis must take account of differences in service user profiles, this section starts with a summary of the baseline and follow-up samples.
As described in Chapter 9, 948 service users were captured in the stage 1 baseline data collection and much has already been said about their specific characteristics. Table 51 categorises this sample by a number of key variables, summarising the distribution of individuals according to 16 case types (i.e. groups of people with similar clinical profiles).
| Key characteristics | Network | Low integration | Nominal | High integration | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case type | Broad diagnostic group | Physically dependent | Challenging behaviour | At least one medium risk | E | H | F | I | G | B | C | A | D | |
| 1 | Organic | No | No | No | 3.6 | 22.1 | 10.7 | 14.9 | 18.6 | 2.6 | 8.2 | 2.8 | 4.3 | 9.2 |
| 2 | Organic | No | No | Yes | 4.6 | 10.3 | 3.9 | 8.0 | 11.6 | 7.8 | 5.1 | 1.8 | 1.1 | 5.7 |
| 3 | Organic | No | Yes | No | 4.6 | 4.4 | 6.8 | 10.3 | 10.5 | 6.5 | 5.1 | 1.8 | – | 5.4 |
| 4 | Organic | No | Yes | Yes | 10.0 | 7.4 | 1.9 | 12.6 | 9.3 | 14.3 | 11.2 | 8.3 | 5.4 | 8.8 |
| 5 | Organic | Yes | No | No | – | – | – | 2.3 | – | – | – | – | 1.1 | 0.4 |
| 6 | Organic | Yes | No | Yes | 0.9 | 14.7 | – | 3.4 | 3.5 | 3.9 | 1.0 | 1.8 | – | 2.8 |
| 7 | Organic | Yes | Yes | No | 0.9 | 1.5 | 1.9 | 9.2 | 2.3 | 5.2 | 2.0 | – | 6.4 | 3.1 |
| 8 | Organic | Yes | Yes | Yes | 9.1 | 19.1 | 1.9 | 18.4 | 10.5 | 11.7 | 17.4 | 9.3 | 26.9 | 13.4 |
| 9 | Functional | No | No | No | 23.6 | 4.4 | 33.0 | 4.6 | 8.1 | 18.2 | 13.3 | 14.8 | 21.5 | 16.5 |
| 10 | Functional | No | No | Yes | 29.1 | 4.4 | 21.4 | 1.2 | 4.6 | 7.8 | 5.1 | 6.5 | 10.8 | 10.8 |
| 11 | Functional | No | Yes | No | 2.7 | 1.5 | 6.8 | 6.9 | 8.1 | 5.2 | 7.1 | 17.6 | 7.5 | 7.4 |
| 12 | Functional | No | Yes | Yes | 6.4 | 5.9 | 6.8 | 5.8 | 9.3 | 9.1 | 17.4 | 23.2 | 9.7 | 10.7 |
| 13 | Functional | Yes | No | No | – | – | 1.0 | – | – | 2.6 | 1.0 | – | – | 0.5 |
| 14 | Functional | Yes | No | Yes | 1.8 | 2.9 | 1.9 | – | – | 1.3 | – | 1.8 | 2.2 | 1.3 |
| 15 | Functional | Yes | Yes | No | – | – | – | 1.2 | – | – | – | – | – | 0.1 |
| 16 | Functional | Yes | Yes | Yes | 2.7 | 1.5 | 1.9 | 1.2 | 3.5 | 3.9 | 6.1 | 10.2 | 3.2 | 4.0 |
| n (valid) | 110 | 68 | 103 | 87 | 86 | 77 | 98 | 108 | 93 | 830 | ||||
| n (not classified)a | 4 | 3 | 1 | 30 | 35 | 28 | 10 | 6 | 1 | 118 | ||||
Caution is needed in interpreting this table, as in three teams a lack of information (most typically about diagnosis) prevented the classification of more than one-quarter of service users (B, G and I). Nevertheless, differences can be seen in the teams’ case mix. For example, approaching four-fifths of the service users in team H, but only one-third or less of those in teams A, E and F had an organic diagnosis (including people with co-existent functional mental health problems). Furthermore, even if one looks only at those service users with an organic or a functional mental health problem, it is clear their profiles varied. Thus, although the majority of people with an organic mental health problem in team D were in the highest needs category (i.e. physically dependent, with challenging behaviour and at least one medium-level risk), the largest proportion in team F were in the lowest needs category. Although the low-integration teams appeared to support a greater proportion of people with an organic mental health problem in the lowest needs category than the high-integration teams (noting the gaps in diagnostic information), there was very little evidence of any other systematic differences in the case mix supported by these two team types. The picture was one of variation between individual teams rather than systematic variation between team types, and may reflect different referral criteria the teams operated and the availability of other services (Table 52).
| Case type | Broad diagnostic group | Physically dependent | Challenging behaviour | At least one medium risk | Network | Low integration | Nominal | High integration |
|---|---|---|---|---|---|---|---|---|
| 1 | Organic | No | No | No | 3.6 | 16.0 | 2.6 | 5.0 |
| 2 | Organic | No | No | Yes | 4.6 | 8.1 | 7.8 | 2.7 |
| 3 | Organic | No | Yes | No | 4.6 | 8.1 | 6.5 | 2.3 |
| 4 | Organic | No | Yes | Yes | 10.0 | 7.6 | 14.3 | 8.4 |
| 5 | Organic | Yes | No | No | – | 0.6 | – | 0.3 |
| 6 | Organic | Yes | No | Yes | 0.9 | 4.7 | 3.9 | 1.0 |
| 7 | Organic | Yes | Yes | No | 0.9 | 3.8 | 5.2 | 2.7 |
| 8 | Organic | Yes | Yes | Yes | 9.1 | 11.6 | 11.7 | 17.4 |
| 9 | Functional | No | No | No | 23.6 | 14.0 | 18.2 | 16.4 |
| 10 | Functional | No | No | Yes | 29.1 | 8.7 | 7.8 | 7.4 |
| 11 | Functional | No | Yes | No | 2.7 | 6.1 | 5.2 | 11.0 |
| 12 | Functional | No | Yes | Yes | 6.4 | 7.0 | 9.1 | 17.1 |
| 13 | Functional | Yes | No | No | – | 0.3 | 2.6 | 0.3 |
| 14 | Functional | Yes | No | Yes | 1.8 | 1.2 | 1.3 | 1.3 |
| 15 | Functional | Yes | Yes | No | – | 0.3 | – | – |
| 16 | Functional | Yes | Yes | Yes | 2.7 | 2.0 | 3.9 | 6.7 |
| n (valid) | 110 | 344 | 77 | 299 | ||||
| n (not classified)a | 4 | 69 | 28 | 17 | ||||
Although it had been intended to obtain outcome data, including QoL and satisfaction, from interviews with a matched sample of 320 of service users at stage 2 (40 per team), early attrition was much higher than expected. Consequently, this plan was adapted and a broader approach taken which sought to include all potentially interviewable service users. This included any service user with a MMSE score of 10 or more deemed eligible for inclusion by their care co-ordinator.
Despite amended plans and the concerted efforts of the research team, the number of interviews remained short of target (Table 53). Only 308 (38.7%) of 796 service users for whom contact details were sought were both considered eligible by their care co-ordinators and consented to receive information about the study. Approximately one-third of these subsequently declined to participate. The resultant sample (n = 193) thus represented just 24% of those for whom an approach had been made and the actual number of interviews achieved ranged from 10 to 36 per team. Equivalent numbers for the four team types ranged from 22 to 68 (Table 54).
| Stage of recruitment process | Network | Low integration | Nominal | High integration | Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| E | H | F | I | G | B | C | A | D | ||
| Number of service users for whom have baseline information | 114 | 71 | 104 | 117 | 121 | 105 | 108 | 114 | 94 | 948 |
| Number of service users selected for interview | 108 | 36 | 90 | 99 | 91 | 100 | 97 | 85 | 90 | 796 |
| Number of service users for whom contact details received | 53 | 17 | 42 | 27 | 14 | 37 | 48 | 42 | 28 | 308 |
| Number of interviews achieved | 36 | 12 | 27 | 19 | 10 | 22 | 27 | 26 | 14 | 193 |
| % of baseline cases selected for interview | 94.7 | 50.7 | 86.5 | 84.6 | 75.2 | 95.2 | 89.8 | 74.6 | 95.7 | 84.0 |
| % of selected users for whom received contact details | 49.1 | 47.2 | 46.7 | 27.3 | 15.4 | 37.0 | 49.9 | 49.4 | 31.1 | 38.7 |
| % of people for whom had contact details interviewed | 68.0 | 70.6 | 64.3 | 70.4 | 71.4 | 59.5 | 56.2 | 61.9 | 50.0 | 62.7 |
| % of selected cases interviewed | 33.3 | 33.3 | 30.0 | 19.2 | 11.0 | 22.0 | 27.8 | 30.6 | 15.6 | 24.2 |
| Stage of recruitment process | Network | Low integration | Nominal | High integration |
|---|---|---|---|---|
| Number of service users for whom have baseline information | 114 | 413 | 105 | 316 |
| Number of service users selected | 108 | 316 | 100 | 272 |
| Number of service users for whom contact details received | 53 | 100 | 37 | 119 |
| Number of interviews achieved | 36 | 68 | 22 | 67 |
| % of baseline cases selected for interview | 94.7 | 76.5 | 95.2 | 86.1 |
| % of selected users for whom received contact details | 49.1 | 31.6 | 37.0 | 43.8 |
| % of people for whom had contact details interviewed | 68.0 | 68.0 | 59.5 | 56.3 |
| % of selected cases interviewed | 33.3 | 21.5 | 22.0 | 24.6 |
In light of the above, it is perhaps not surprising that those service users who participated in the stage 2 interview exercise had a somewhat different profile from those identified at baseline. In comparison with Table 51, service users in case type 8 were under-represented at interview (making up 8.3% as compared with 13.4% of the sample), whereas those in case types 9 and 10 were over-represented (constituting 25.6% and 15.6% of the interview sample compared with 16.5% and 10.8% of the baseline sample). Furthermore, although the other case types were fairly well represented in the total sample, in no single team was a fully representative subsample achieved.
Additional information on the number of psychiatric inpatient and permanent care home admissions experienced by the stage 1 sample was sought from eight of the nine teams approximately 7 months post baseline. The exception was team H, where local delays in starting the baseline data collection precluded their participation in this element of the study. All teams provided information on the number and timing of hospital admissions – the main outcome variable. They were, however, less confident about accurately identifying all care home admissions and their precise timing, particularly where individuals had been discharged from the CMHTOP caseload and/or the team could not access social services records (i.e. in less integrated teams) as this information was often derived from last known address details. Hence it is likely that at least some transitions were missed, while dates of admission were frequently unknown.
With these caveats, Table 55 presents information on the six outcome variables explored in this study, which as can be seen, varied considerably between teams. For example, the percentage of mental health inpatient admissions over the follow-up period ranged from 1.7 in team I to 13.8 in team D, while the percentage of care home admissions ranged from 5.1 in team G to 21.9 in team C. Similar variations were seen for other measures, with service users in team G reporting particularly high QoL and service satisfaction levels, and those in teams C and F among the lowest scoring samples.
| Outcome | Network | Low integration | Nominal | High integration | Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| E | Ha | F | I | G | B | C | A | D | ||
| % of mental health inpatient admissions since baseline | 8.0 | N/A | 1.9 | 1.7 | 2.5 | 2.9 | 9.4 | 7.0 | 13.8 | 5.8 |
| (n of mental health inpatient admissions since baseline) | (9) | N/A | (2) | (2) | (3) | (3) | (10) | (8) | (13) | (50) |
| Mean number of days to first hospital admission | 90 | N/A | 79 | 109 | 91 | 114 | 83 | 116 | 132 | 105 |
| Median number of days to first hospital admission | 100 | N/A | 79 | 109 | 84 | 150 | 58 | 148 | 140 | 105 |
| Minimum number of days to first hospital admission | 4 | N/A | 9 | 72 | 48 | 6 | 12 | 15 | 31 | 4 |
| Maximum number of days to first hospital admission | 177 | N/A | 149 | 146 | 141 | 187 | 200 | 198 | 204 | 204 |
| % of care home admissions since baseline | 5.4 | N/A | 5.8 | 9.4 | 5.1 | 8.6 | 21.9 | 6.1 | 13.8 | 9.3 |
| (n of care home admissions since baseline) | (6) | N/A | (6) | (11) | (6) | (9) | (23) | (7) | (13) | (81) |
| Mean QoL-AD score | 33.4 | 33.3 | 33.1 | 35.9 | 38.6 | 33.8 | 33.6 | 33.7 | 30.6 | 33.8 |
| Median QoL-AD | 34 | 33 | 34 | 37 | 39.5 | 36 | 33 | 32.5 | 32 | 34 |
| Minimum QoL-AD | 19 | 18 | 18 | 27 | 25 | 21 | 20 | 22 | 19 | 18 |
| Maximum QoL-AD | 45 | 48 | 45 | 45 | 48 | 45 | 47 | 46 | 47 | 48 |
| Mean satisfaction with services score | 14.7 | 13.9 | 12.5 | 14.2 | 16.9 | 14.0 | 13.5 | 12.8 | 14.1 | 13.8 |
| Median satisfaction with services score | 14.5 | 14 | 13 | 14 | 17 | 14 | 14 | 13.5 | 14 | 14 |
| Minimum satisfaction with services score | 7 | 8 | 5 | 9 | 10 | 12 | 6 | 3 | 7 | 3 |
| Maximum satisfaction with services score | 19 | 19 | 18 | 18 | 21 | 17 | 19 | 17 | 21 | 21 |
| Mean satisfaction with key mental health worker | 14.4 | 15.4 | 12.8 | 12.8 | 17.6 | 13.0 | 12.6 | 13.9 | 13.9 | 13.8 |
| Median satisfaction with key mental health worker | 15 | 15.5 | 12.5 | 13 | 18 | 12 | 12 | 14.5 | 14.5 | 14 |
| Minimum satisfaction with key mental health worker | 9 | 12 | 5 | 11 | 16 | 9 | 3 | 8 | 7 | 3 |
| Maximum satisfaction with key mental health worker | 18 | 18 | 18 | 15 | 18 | 18 | 18 | 17 | 18 | 18 |
| n (minimum–maximum) for QoL-AD and the two satisfaction scoresb | 32–34 | 11–12 | 20–27 | 9–19 | 8–10 | 21–21 | 22–25 | 24–26 | 13–14 | 164–185 |
As shown in Table 56, there were also some substantial differences between the outcomes of service users in low- and high-integration teams, particularly with regard to inpatient and care home admissions. Service users supported by high-integration teams appeared considerably more likely to be admitted to inpatient beds and care homes than those in the low-integration teams. However, it should be noted that these tables take no account of differences in case mix – this is explored in the following regression analyses.
| Outcome | Network | Low integration | Nominal | High integration |
|---|---|---|---|---|
| % of mental health inpatient admissions since baseline | 8.0 | 2.1 | 2.9 | 9.8 |
| (n of mental health inpatient admissions since baseline) | (9) | (7) | (3) | (31) |
| Mean number of days to first hospital admission | 90 | 93 | 114 | 112 |
| Median number of days to first hospital admission | 100 | 84 | 150 | 122 |
| Minimum number of days to first hospital admission | 4 | 9 | 6 | 12 |
| Maximum number of days to first hospital admission | 177 | 149 | 187 | 204 |
| % of care home admissions since baseline | 5.4 | 6.8 | 8.6 | 13.7 |
| (n of care home admissions) | (6) | (23) | (9) | (43) |
| Mean QoL-AD score | 33.4 | 34.8 | 33.8 | 33.0 |
| Median QoL-AD | 34 | 36 | 36 | 32 |
| Minimum QoL-AD | 19 | 18 | 21 | 19 |
| Maximum QoL-AD | 45 | 48 | 45 | 47 |
| Mean satisfaction with services score | 14.7 | 13.8 | 14.0 | 13.3 |
| Median satisfaction with services score | 14.5 | 14 | 14 | 14 |
| Minimum satisfaction with services score | 7 | 5 | 12 | 3 |
| Maximum satisfaction with services score | 19 | 21 | 17 | 21 |
| Mean satisfaction with key mental health worker | 14.4 | 14.2 | 13.0 | 13.4 |
| Median satisfaction with key mental health worker | 15 | 15 | 12 | 14 |
| Minimum satisfaction with key mental health worker | 9 | 5 | 9 | 3 |
| Maximum satisfaction with key mental health worker | 18 | 18 | 18 | 18 |
| n (minimum–maximum) for QoL-AD and the two satisfaction scoresa | 32–34 | 49–67 | 21–21 | 60–64 |
In Table 57, the first logistic regression model demonstrates the relationship between the risk of inpatient admission in the 7-month follow-up period and a range of service user characteristics. Although the total sample was large (> 800), the predictive power of the model was restricted by the limited number of events of interest (i.e. hospital admissions). Furthermore, the service user information was taken from the stage 1 baseline data collection (i.e. up to 7 months before admission). It is perhaps not surprising, therefore, that the model’s explanatory power is fairly low (approximately 15%). Nevertheless, certain clinical profiles were clearly associated with a higher risk of inpatient admission, if mostly at borderline significance levels. For example, service users with depressive symptomatology were more than twice as likely to be admitted as those without. There was also a positive relationship between the amount of medical input service users received (perhaps a proxy for case complexity) and their likelihood of hospital admission. The presence of regular informal support, on the other hand, had a protective effect.
| Predictors (at baseline) | Y = inpatient admission (logit) | Y = inpatient admission (logit) | Y = inpatient admission (time to first inpatient admission – Cox modela) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient (odds ratio) | z-value | SE (p-value)b | Coefficient (odds ratio) | z-value | SE (p-value)b | Coefficient (hazard ratio) | z-value | SE (p-value)b | |
| Aged ≥ 85 years | 0.29 | –2.00 | 0.18 (0.045) | 0.32 | –1.81 | 0.20 (0.070) | 0.36 | –1.66 | 0.22 (0.098) |
| Indication of depression | 2.64 | 2.68 | 0.96 (0.007) | 2.42 | 2.40 | 0.89 (0.016) | 2.17 | 2.23 | 0.75 (0.026) |
| Diagnostic groups | Reference group: all other combinations | Reference group: all other combinations | Reference group: all other combinations | ||||||
| Depression and no challenging behaviour | 2.38 | 1.78 | 1.15 (0.074) | 2.27 | 1.64 | 1.14 (0.101) | 2.12 | 1.58 | 1.01 (0.114) |
| Other functional and challenging behaviour | 3.21 | 2.04 | 1.84 (0.042) | 2.64 | 1.69 | 1.52 (0.092) | 2.58 | 1.75 | 1.40 (0.08) |
| Organic and challenging behaviour | 2.42 | 1.83 | 1.17 (0.068) | 2.15 | 1.55 | 1.06 (0.122) | 2.03 | 1.53 | 0.94 (0.127) |
| Mixed and challenging behaviour | 3.08 | 1.77 | 1.95 (0.076) | 2.78 | 1.54 | 1.84 (0.123) | 2.36 | 1.43 | 1.42 (0.154) |
| ≥ 8 hours/week personal/physical informal care | 2.33 | 2.11 | 0.94 (0.035) | 2.76 | 2.39 | 1.18 (0.017) | 2.54 | 2.39 | 0.99 (0.017) |
| Time since referral (months) | 0.98 | –1.81 | 0.01 (0.071) | 0.98 | –1.71 | 0.01 (0.088) | 0.98 | –1.75 | 0.01 (0.081) |
| Number of medical visits (up to five) | 1.44 | 3.38 | 0.15 (0.001) | 1.28 | 2.14 | 0.15 (0.032) | 1.26 | 2.20 | 0.13 (0.028) |
| Team type | Reference group: low integration | Reference group: low integration | |||||||
| Network | – | – | – | 4.54 | 2.40 | 2.87 (0.016) | 4.47 | 2.45 | 2.73 (0.014) |
| Nominally integrated | – | – | – | 2.33 | 1.08 | 1.83 (0.282) | 2.36 | 1.12 | 1.80 (0.263) |
| Highly integrated | – | – | – | 5.18 | 2.83 | 3.01 (0.005) | 4.66 | 2.72 | 2.64 (0.006) |
| Constant | 0.01 | –8.56 | 0.01 (< 0.001) | 0.00 | –7.72 | 0.00 (< 0.001) | – | – | – |
| Model fit | LR χ2(9) = 48.34 (p < 0.001) Pseudo-R2 = 0.15 Linktest p(_hat) = 0.008 p(_hatsq) = 0.466 Hosmer–Lemeshow χ2(8) = 11.83 (p = 0.159) |
LR χ2(12) = 59.64 (p < 0.001) Pseudo-R2 = 0.18 Linktest p(_hat) = 0.015 p(_hatsq) = 0.744 Hosmer–Lemeshow χ2(8) = 11.80 (p = 0.160) |
LR χ2(12) = 58.73 (p < 0.001) Linktest p(_hat) = 0.058 p(_hatsq) = 0.953 Proportional hazards global test (12): 11.67 (p = 0.473)c |
||||||
| n (excluding one team) | 800 | 800 | 802 | ||||||
Contrary to expectations, when the four team types were added to the model, the analysis suggested that service users supported by high-integration or network teams were considerably more likely to be admitted to hospital than service users from other team types. Indeed, although the presence of depressive symptoms and frequent medical input were still positively associated with inpatient admission, service users from high-integration teams were approximately five times more likely to be admitted independently of this.
An examination of the influence of individual teams (not shown) confirmed the group effect (e.g. all high-integration teams were associated with a higher risk of admission), as did the Cox survival model. The inclusion of the team types influenced the precision of the other coefficients, suggesting that the model had reached the limits of its capacity to control for the already large number of covariates. Furthermore, given the direct association between the number of hospital beds in each area and the individual teams, it was not possible to include such a supply variable in the model (the problem of multicollinearity). Important contextual information is therefore presented in Table 58. These factors did not, however, appear to explain the findings, there being no obvious systematic differences between team types.
| Contextual variable | Network | Low integration | Nominal | High integration | Primary source | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| E | H | F | I | G | B | C | A | D | ||
| Estimated size of population covered by trust (adults aged ≥ 65 years) | 33,900 | 172,600 | 419,000 | 109,000 | 234,100 | 84,700 | 109,500 | 144,600 | 100,900 | ONS 2009157 estimates |
| Type of area covered by CMHTOP (predominantly rural/urban/mixed) | Rural | Mixed | Mixed | Rural | Mixed | Mixed | Mixed | Mixed | Urban | National survey data, current study |
| Percentage of CMHTOP baseline sample in professional/managerial occupationsa | 26.0 | 18.8 | 51.0 | 34.8 | 26.9 | 25.0 | 19.3 | 30.6 | 14.5 | Baseline data collection, current study |
| CMHTOP team size (WTE core team members) | 8 | 9.5 | 14 | 14.5 | Not knownb | 15 | 12 | 17 | 12 | Qualitative interview data, current study |
| Typical caseload size per core CMHTOP member | 33 | 25 | 30 | 35–40 | Not known | 30–35 | 40 | 35 | 30 | Qualitative interview data, current study |
| Number of old age psychiatry inpatient beds per 10,000 population covered by trust (adults aged ≥ 65 years) | 14 | 8 | 3 | 4 | 4 | 8 | 5 | 5 | 8 | Qualitative interview data, current study |
| CMHTOP consultant psychiatrist works across inpatient and community services | Yes | Yes | No | No | Yes | Yes | Yes | No | Yes | Qualitative interview data, current study |
| Number of care home beds per 10,000 population covered by CMHTOP (adults aged ≥ 65 years) | 59 | 52 | 57 | 44 | 47 | 47 | 41 | 51 | 32 | Care Quality Commission, 2012, personal communication |
| Level at which FACS bands were set in the CMHTOP area | Critical and substantial | Critical and substantial | Critical and substantial | Not known | Critical and substantial | Critical and substantial | Critical and substantial | Critical and substantial | Critical and substantial | Qualitative interview data, current study |
Following a similar approach, a complementary log-log model was used to explore the association between service user characteristics, team type and risk of care home entry over the 7–10-month follow-up period. In addition to the challenges on sample size and representativeness, this analysis was further constrained by the fact that the admissions were observed over varying amounts of time and that specific dates of admission were frequently unavailable. The outcome variable was thus modelled as a rate occurring within a discrete time frame.
As shown in Table 59, the resulting model identified a number of service user characteristics predicting care home entry. These included increasing age (the risk of care home entry rising by roughly 4% for each additional year), a need for help with daily activities of living, presence of severe cognitive impairment and presence of medium or (in particular) high levels of challenging behaviour. The availability of appropriate help from family and friends again had a preventative effect.
| Predictors (at baseline) | Y = care home entry (cloglog) | Y = care home entry (cloglog) | Y = care home entry (cloglog) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient (exponential) | t-value | SE (p-value)a | Coefficient (exponential) | t-value | SE (p-value)a | Coefficient (exponential) | t-value | SE (p-value)a | |
| Age (centred) | 1.04 | 2.32 | 0.02 (0.020) | 1.05 | 2.66 | 0.02 (0.008) | 1.04 | 2.53 | 0.02 (0.011) |
| Physical dependency | Reference group: independent | Reference group: independent | Reference group: independent | ||||||
| Minor help needed | 2.03 | 2.32 | 0.62 (0.021) | 1.82 | 1.94 | 0.56 (0.052) | 1.98 | 2.28 | 0.60 (0.023) |
| Major help needed | 1.84 | 1.72 | 0.65 (0.085) | 1.68 | 1.46 | 0.60 (0.144) | 2.00 | 1.93 | 0.72 (0.054) |
| Cognitive impairment (MMSE) | Reference group: normal (27–30) | Reference group: normal (27–30) | Reference group: normal (27–30) | ||||||
| Mild (21–26) | 1.36 | 0.68 | 0.62 (0.495) | 1.42 | 0.78 | 0.64 (0.434) | 1.36 | 0.69 | 0.62 (0.493) |
| Moderate (10–20) | 1.81 | 1.40 | 0.77 (0.162) | 2.03 | 1.69 | 0.85 (0.092) | 1.86 | 1.50 | 0.77 (0.135) |
| Severe (0–9) | 3.43 | 2.47 | 1.71 (0.014) | 3.34 | 2.48 | 1.62 (0.013) | 3.44 | 2.58 | 1.65 (0.010) |
| Problematic behaviours | Reference group: low | Reference group: low | Reference group: low | ||||||
| Medium | 1.74 | 1.82 | 0.53 (0.069) | 1.67 | 1.68 | 0.51 (0.093) | 1.64 | 1.63 | 0.50 (0.102) |
| High | 7.29 | 4.75 | 3.05 (< 0.001) | 7.28 | 4.73 | 3.06 (< 0.001) | 7.41 | 4.79 | 3.10 (< 0.001) |
| Service user lives alone | 1.56 | 1.72 | 0.40 (0.086) | 1.66 | 1.93 | 0.44 (0.054) | 1.57 | 1.73 | 0.41 (0.084) |
| ≥ 8 hours/week personal/physical informal care | 0.46 | –2.27 | 0.16 (0.023) | 0.52 | –1.91 | 0.18 (0.056) | 0.44 | –2.33 | 0.15 (0.020) |
| Team type | Reference group: low integration | ||||||||
| Network | – | – | – | 1.11 | 0.23 | 0.53 (0.818) | – | – | – |
| Nominally integrated | – | – | – | 0.96 | –0.11 | 0.38 (0.913) | – | – | – |
| High integration | – | – | – | 1.81 | 2.10 | 0.51 (0.036) | – | – | – |
| Alternative: team C | – | – | – | – | – | – | 2.71 | 3.68 | 0.73 (< 0.001) |
| Constant | 0.00 | –13.96 | 0.00 (< 0.001) | 0.00 | –12.79 | 0.00 (< 0.001) | 0.00 | –14.03 | 0.00 (< 0.001) |
| log (time at risk)b | 1 | (offset) | 1 | (offset) | 1 | (offset) | |||
| Model fitc | F (10,30220.0) = 7.78 ( p < 0.001) | F (13,81290.4) = 6.27 ( p < 0.001) | F (11,43143.3) = 7.77 ( p < 0.001) | ||||||
| n (excluding one team) | 812 | 812 | 812 | ||||||
When the four team types were added in the second iteration, the model again suggested that service users supported by high-integration teams were considerably more likely to be admitted to care homes than those supported by other team types – almost twice as likely. However, individual team level analysis indicated this was almost certainly an artefact of the very high admission rate in just one high-integration team – team C.
The remaining outcome measures were also analysed with multiple regression models, following similar modelling strategies. Variables considered as controls included age, gender, diagnostic profile, service receipt (exploratory, as service receipt differences were also encapsulated in team and team-type differences) and, in particular, GDS scores. However, the GDS could not be used in combination with the QoL-AD outcome variable as these were highly correlated (r = –0.73).
Although considerable variability existed in both of the satisfaction indicators and the QoL scores between individual teams (see Table 55), no systematic effects were associated with team type and these models are not presented. It is, nevertheless, worth noting that service user satisfaction with their mental health key worker could not be predicted by any combination of covariates except individual teams, which were also the strongest predictors of satisfaction with service receipt and QoL. Team G was the only team consistently associated with more positive outcomes than average: on satisfaction with service receipt (coefficient = 2.57, t-value = 2.26, p = 0.025), satisfaction with key mental health worker (coefficient = 4.03, t-test = 3.47, p = 0.001), and QoL-AD (coefficient = 3.64, t-test = 1.69, p = 0.092). All other teams had more mixed results profiles, although team F scored consistently below the average on both satisfaction measures (coefficient = –1.64, t-test = –2.6, p = 0.010 and coefficient = –1.48, t-test = –1.85, p = 0.066).
Carer outcomes
Of 193 service users interviewed, 118 reported being supported by an unpaid carer each of whom was subsequently left a postal questionnaire to complete and return by post. Seventy-seven questionnaires were returned to the research team representing a response rate of 65%, although not all respondents answered all questions. Approximately two-thirds (n = 48, 63%) of respondents were female with a mean age of 70 years. Forty-two carers were the husband/wife/partner of the main service user; 24 were the son or daughter; five were another relative; and four were friends or neighbours. Most carers (n = 55, 72%) had been supporting the service user in excess of 3 years. Sixty-one carers (80%) reported that the service user they supported had memory problems while forty-eight (62%) reported low mood or anxiety problems (36 reported both memory and mood problems). Just 14 carers indicated that they had received formal carer support services themselves.
Table 60 presents key outcome statistics. For the full sample, the mean HADS anxiety score was 8.60, and over half (52%) scored ≥ 9 (a conventional threshold representing anxiety of clinical significance236). The incidence of depression was lower, with a mean HADS depression score of 6.63% and 34% of the sample scoring ≥ 9. Contrasts between integrated and non-integrated teams are also shown, although further disaggregation into the (four category) team typology was not possible due to small cell sizes. None of the outcome differences between integrated and non-integrated teams reached statistical significance. The point-estimate of the HADS depression score provided a tentative indication of lower mood among carers in non-integrated teams, although this difference was confounded by age effects: on average, carers in non-integrated teams were older than their counterparts in integrated teams, with age and depression being positively, albeit weakly, correlated in the sample.
| Outcome | All teams | Integrated teams (A–D) | Non-integrated teams (E–I) | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| HADS: anxiety | 72 | 8.60 (4.59) | 32 | 8.19 (4.09) | 40 | 8.93 (4.98) |
| HADS: depression | 76 | 6.63 (4.19) | 32 | 5.72 (3.64) | 44 | 7.30 (4.47) |
| Modified Carer Strain Index | 63 | 10.00 (5.79) | 26 | 10.54 (6.59) | 37 | 9.62 (5.22) |
Cost-effectiveness analysis
To assess the cost-effectiveness of different team types, detailed service receipt information was sought at the baseline and follow-up stages. Unfortunately, however, a high level of missing information in the follow-up data collections, leading to inaccuracy, precluded the planned analysis of comparative total costs over the follow-up period. Tables 61 and 62 thus present the average costs of the mental health and social care input received by each team’s and team type’s baseline sample, offering a cross-sectional view of the expenditure on services that might potentially be under the control of a fully integrated CMHTOP for users living at home.
| Care component | Network | Low integration | Nominal | High integration | All teams | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| E | H | F | I | G | B | C | A | D | ||
| Specialist mental health costs (£) CMHT contacts | 237 | 204 | 205 | 138 | 125 | 220 | 307 | 318 | 443 | 240 |
| Other mental health costs (£)a | 45 | 21 | 37 | 49 | 15 | 91 | 90 | 66 | 50 | 55 |
| Total mental health-care costs (£) | 305 | 210 | 223 | 189 | 141 | 320 | 397 | 392 | 496 | 306 |
| n (minimum–maximum) | 87–114 | 50–68 | 63–104 | 111–117 | 57–119 | 67–96 | 101–108 | 91–114 | 77–87 | 704–927 |
| Social care package costs (£)b | ||||||||||
| Personal care (generic) | 363 | 273 | 414 | 319 | 345 | 89 | 237 | 194 | 626 | 303 |
| Personal care (specialist) | 163 | 26 | 0 | 42 | 0 | 479 | 124 | 4 | 28 | 113 |
| Domestic help | 127 | 42 | 128 | 140 | 131 | 63 | 131 | 96 | 62 | 105 |
| Meals | 48 | 9 | 25 | 64 | 71 | 45 | 67 | 79 | 46 | 53 |
| Day care (generic) | 30 | 37 | 112 | 45 | 138 | 22 | 54 | 33 | 41 | 51 |
| Day care (specialist) | 80 | 126 | 59 | 53 | 63 | 75 | 79 | 119 | 43 | 77 |
| Sitting service | 34 | 39 | 0 | 84 | 20 | 89 | 17 | 0 | 44 | 40 |
| Respite | 28 | 42 | 18 | 9 | 18 | 30 | 20 | 44 | 12 | 24 |
| Total social care costs | 888 | 564 | 723 | 709 | 639 | 920 | 724 | 575 | 790 | 733 |
| n (care package) | 41 (36%) | 26 (37%) | 32 (31%) | 57 (49%) | 26 (21%) | 51 (49%) | 53 (49%) | 49 (43%) | 38 (41%) | 373 (39%) |
| Total care costs (£) | 616 | 454 | 523 | 512 | 284 | 842 | 729 | 691 | 830 | 625 |
| Care component | Network | Low integration | Nominal | High integration | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | Maximum | Mean | Median | Maximum | Mean | Median | Maximum | Mean | Median | Maximum | |
| Specialist mental health costs | ||||||||||||
| CMHT contacts (£) | 237 | 189 | 1405 | 162 | 124 | 913 | 220 | 181 | 806 | 349 | 254 | 1939 |
| Other mental health costs (£)a | 45 | 5 | 434 | 34 | 0 | 663 | 91 | 5 | 357 | 70 | 5 | 663 |
| Total mental health-care costs (£) | 316 | 253 | 1609 | 191b | 130 | 913 | 320 | 252 | 1140 | 423 | 326 | 1944 |
| n (minimum–maximum) | 87–114 | 281 (other mental health service costs), 405 (CMHTOP) | 67–96 | 269–309 | ||||||||
| Social care package costsc | ||||||||||||
| Personal care (generic) (£) | 363 | 0 | 2184 | 337 | 0 | 3276 | 89 | 0 | 936 | 328 | 156 | 3120 |
| Personal care (specialist) (£) | 163 | 0 | 2669 | 22 | 0 | 667 | 479 | 286 | 2860 | 56 | 0 | 2002 |
| Domestic help (£) | 127 | 0 | 1092 | 117 | 0 | 1092 | 63 | 0 | 780 | 100 | 0 | 1638 |
| Meals (£) | 48 | 0 | 364 | 45 | 0 | 364 | 45 | 0 | 364 | 66 | 0 | 364 |
| Day care (generic) (£) | 30 | 0 | 312 | 76 | 0 | 1092 | 22 | 0 | 468 | 43 | 0 | 1092 |
| Day care (specialist) (£) | 80 | 0 | 702 | 70 | 0 | 1638 | 75 | 0 | 702 | 84 | 0 | 1638 |
| Sitting service (£) | 34 | 0 | 624 | 45 | 0 | 936 | 89 | 0 | 2730 | 18 | 0 | 468 |
| Respite (£) | 28 | 0 | 348 | 18 | 0 | 566 | 30 | 0 | 392 | 26 | 0 | 1392 |
| Total social care costs (£) | 888 | 468 | 3562 | 675 | 546 | 3510 | 920 | 667 | 3382 | 685 | 511 | 2817 |
| n (care package) | 41 (36%) | 141 (34%) | 51 (49%) | 140 (44%) | ||||||||
| Total care costs (£) | 640 | 285 | 4388 | 464 | 239 | 3575 | 842 | 443 | 3842 | 743 | 562 | 3391 |
As can be seen in Table 61, individual team’s mental health costs varied considerably. Thus, the monthly average costs of CMHTOP contact ranged from £125 to £443 per month, while total monthly mental health costs (including the costs of LA social work input in non-integrated teams which offers a truer comparison), ranged from £141 to £496. The monthly costs of average social care packages, and total costs, also differed greatly.
Substantial differences were also found between the costs of the mental health services provided to service users in low- and high-integration teams (see Table 62). Indeed, the latter averaged £232 per month more than the former, whereas the mental health costs of the other two team types were also greater than those of the low-integration teams. Average social care expenditure (of course conditional on receiving social care) was, however, similar in both low- and high-integration teams, despite a higher proportion of the latter’s caseload receiving such support.
These findings must be considered in the context of data imputation procedures deemed necessary to maximise the number of valid cases, particularly for the low-integration teams, for the observed group effects clearly coincided with missing value patterns. That is, although low-integration teams tended to report lower levels of service receipt (in particular for input outside the CMHTOP), they were also less likely to complete these questions in the first place. This raises the possibility that, even after imputation, a non-random missing effect may have occurred if the low-integration teams were simply less able to retrieve this information for certain client groups. However, analysis of data from the stage 2 interview data suggested this might not be the case, and verified the pattern seen in the baseline data collection. This included the suggestion that levels of CMHTOP and social work input, as well as social care, were lower in the low- than in the high-integration teams. Furthermore, it also suggested that the latter was attributable to relatively independent clients being more likely to have a formal social care package in the high-integration teams. For example, 25% of physically independent interviewees in high-integration compared with 13% in low-integration teams reported receiving a home care package. Other generic health inputs [including contact with district nurses (DNs), GPs and accident and emergency (A&E)] which are arguably less likely to be related to CMHTOP activity differed little between team types.
The comparisons in Tables 61 and 62 are also only valid once account is taken of case-mix. A range of covariates were, therefore, included in subsequent regression analyses to isolate any team effects. As the cost data displayed typical distributional effects (i.e. a strong positive skew), this employed generalised linear models from the gamma family, with log-links. The resultant statistical models offered a better reflection of the data than standard regression models. However, it still proved difficult to reliably predict the very high expenditure on some service users. Furthermore, as social care expenditure only applied to approximately 40% of service users, modelling used a two-stage approach whereby the probability of receiving social care was modelled separately from the amount of services received. The two results were then combined for average cost prediction purposes.
Table 63 presents the prediction models for all three cost accounts (i.e. total, mental health and social care package costs) and a standard set of covariates. To aid comparison, all predictors (including insignificant ones) have been retained in each model. The interpretation of these log-linked models is as follows: the constant is the monthly cost of an average service user (centred predictor) belonging to each of the designated reference categories (e.g. organic diagnosis, no challenging behaviours), while the coefficients represent the relative cost differences.
| Predictors (at baseline) | Y = mental health costs (GLM: gamma/log-link) | Y = cost of social care packages if receiving (GLM: gamma/log-link) | Y = total cost of services (GLM: gamma/log-link) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient (exponential) | t-test | SE (p-value)a | Coefficient (exponential) | t-test | SE (p-value)a | Coefficient (exponential) | t-test | SE (p-value)a | |
| Age (centred) | 0.99 | –2.54 | 0.00 (0.011) | 1.01 | 1.20 | 0.01 (p = 0.231) | 1.01 | 1.50 | 0.01 (p = 0.133) |
| Physical dependency | Reference group: independent | Reference group: independent | Reference group: independent | ||||||
| Minor help needed | 1.17 | 1.75 | 0.11 (0.080) | 1.55 | 3.55 | 0.19 (< 0.001) | 2.09 | 6.76 | 0.23 (< 0.001) |
| Major help needed | 0.97 | –0.30 | 0.11 (0.766) | 1.77 | 3.84 | 0.26 (< 0.001) | 2.32 | 6.25 | 0.31 (< 0.001) |
| Cognitive impairment (MMSE) | Reference group: normal (27–30) | Reference group: normal (27–30) | Reference group: normal (27–30) | ||||||
| Mild (21–26) | 1.06 | 0.61 | 0.10 (0.541) | 1.02 | 0.14 | 0.18 (0.888) | 1.07 | 0.63 | 0.11 (0.532) |
| Moderate (10–20) | 1.02 | 0.20 | 0.12 (0.838) | 1.17 | 0.78 | 0.24 (0.436) | 1.33 | 2.10 | 0.18 (0.037) |
| Severe (0–9) | 1.25 | 1.28 | 0.22 (0.201) | 1.32 | 0.98 | 0.38 (0.329) | 1.88 | 3.03 | 0.39 (0.003) |
| Challenging behaviours | Reference group: low | Reference group: low | Reference group: low | ||||||
| Medium | 1.16 | 2.28 | 0.08 (0.023) | 1.41 | 3.08 | 0.16 (0.002) | 1.31 | 3.39 | 0.11 (0.001) |
| High | 1.56 | 3.04 | 0.23 (0.002) | 1.34 | 1.48 | 0.27 (0.138) | 1.55 | 2.44 | 0.28 (0.015) |
| Diagnosis | Reference group: organic mental illness | Reference group: organic mental illness | Reference group: organic mental illness | ||||||
| Depression/anxiety | 1.04 | 0.45 | 0.10 (0.653) | 0.81 | –1.39 | 0.12 (0.165) | 0.90 | –0.98 | 0.10 (0.328) |
| Other functional | 0.94 | –0.60 | 0.10 (0.546) | 0.94 | –0.33 | 0.17 (0.740) | 0.94 | –0.49 | 0.12 (0.628) |
| No formal diagnosis | 0.69 | –3.29 | 0.08 (0.001) | 0.82 | –1.15 | 0.14 (0.248) | 0.68 | –2.95 | 0.09 (0.003) |
| Mixed organic/functional | 1.02 | 0.13 | 0.13 (0.855) | 0.88 | –0.77 | 0.15 (0.443) | 1.02 | 0.15 | 0.15 (0.878) |
| Indication of depression | 1.16 | 2.35 | 0.07 (0.019) | 1.04 | 0.37 | 0.11 (0.712) | 1.22 | 2.64 | 0.09 (0.008) |
| Service user lives alone | 1.17 | 2.45 | 0.07 (0.014) | 1.04 | 0.31 | 0.12 (0.757) | 1.42 | 4.52 | 0.11 (< 0.001) |
| Personal and physical informal care ≥ 8 hours | 0.86 | –1.60 | 0.08 (0.109) | 0.71 | –2.38 | 0.10 (0.017) | 0.66 | –3.69 | 0.07 (< 0.001) |
| Time on caseload (months) | 0.996 | –2.87 | 0.002 (0.004) | 1.001 | 0.27 | 0.002 (0.791) | 0.998 | –1.53 | 0.002 (0.126) |
| Team type | Reference group: low integration | Reference group: low integration | Reference group: low integration | ||||||
| Network | 1.30 | 2.75 | 0.12 (0.006) | 1.36 | 1.87 | 0.22 (0.062) | 1.37 | 2.84 | 0.15 (0.005) |
| Nominally integrated | 1.66 | 4.32 | 0.16 (< 0.001) | 1.21 | 1.24 | 0.19 (0.214) | 1.66 | 4.03 | 0.21 (< 0.001) |
| High integration | 1.84 | 8.46 | 0.13 (< 0.001) | 0.91 | –0.85 | 0.11 (0.398) | 1.53 | 4.92 | 0.13 (< 0.001) |
| Constant | 175.28 | 47.36 | 19.12 (< 0.001) | 450.21 | 27.59 | 99.70 (< 0.001) | 245.77 | 41.76 | 32.39 (< 0.001) |
| Model fitb | F(19,20903.0) = 9.28 (p < 0.001) Estimated R2: 0.20 |
F(19,41391.5) = 3.28 (p < 0.001) Estimated R2: 0.22 |
F(19,27469.4) = 12.64 (p < 0.001) Estimated R2: 0.20 |
||||||
| n | 854 | 339 | 854 | ||||||
Predictor variables did not impact equally on the three cost categories. For example, although physical dependency was a major driver of social care expenditure, and by implication, total expenditure, it had little bearing on mental health costs. Interestingly, this was also true for cognitive impairment when the effect of the ‘moderate’ and ‘severe’ categories were combined. Challenging behaviours were associated with higher expenditure although the likelihood of receiving a social care package was less clearly associated (Table 64). Broad diagnosis seemed to have little influence on service user costs, although people without a formal diagnosis received less mental health input, and those with a mixed organic and functional disorder were more likely to receive a social care package than the organic reference category. Not surprisingly, the availability of a high level of informal care had a negative influence on costs.
| Predictors (at baseline) | Y = presence of social care package (logit) | ||
|---|---|---|---|
| Coefficient (OR) | t-test | SE (p-value)a | |
| Age (centred) | 1.06 | 4.50 | 0.01 (< 0.001) |
| Physical dependency | Ref: independent | ||
| Minor help needed | 5.20 | 6.09 | 1.41 (< 0.001) |
| Major help needed | 8.77 | 6.11 | 3.12 (< 0.001) |
| Cognitive impairment (MMSE) | Ref: normal (27–30) | ||
| Mild (21–26) | 1.22 | 0.78 | 0.31 (0.436) |
| Moderate (10–20) | 1.75 | 1.78 | 0.55 (0.077) |
| Severe (0–9) | 2.28 | 1.62 | 1.16 (0.107) |
| Challenging behaviours | Ref: low | ||
| Medium | 1.26 | 1.23 | 0.23 (0.219) |
| High | 1.96 | 1.56 | 0.84 (0.118) |
| Diagnosis | Ref: organic mental illness | ||
| Depression/anxiety | 0.73 | –1.21 | 0.19 (0.228) |
| Other functional | 1.01 | 0.02 | 0.30 (0.986) |
| No formal diagnosis | 0.86 | –0.49 | 0.27 (0.624) |
| Mixed organic/functional | 2.15 | 2.12 | 0.78 (0.034) |
| Indication of depression | 1.20 | 1.01 | 0.22 (0.314) |
| Service user lives alone | 3.17 | 6.05 | 0.60 (< 0.001) |
| Personal and physical informal care ≥ 8 hours | 0.63 | –1.60 | 0.18 (0.111) |
| Time on caseload (months) | 0.999 | –0.39 | 0.004 (0.693) |
| Team type | Ref: low integration | ||
| Network | 1.39 | 1.22 | 0.38 (0.223) |
| Nominally integrated | 1.62 | 1.76 | 0.45 (0.078) |
| High integration | 1.59 | 2.24 | 0.33 (0.025) |
| Constant | 0.14 | –6.00 | 0.05 (< 0.001) |
| Model fitb | F(19,28727.3) = 7.86 (p < 0.001) Estimated linktest p(_hat) = 0.001 p(_hatsq) = 0.836 |
||
| n | 854 | ||
The total costs associated with the high-integration teams (and the network and nominally integrated teams) were approximately 50% higher than those of the low-integration teams. Indeed, looking solely at mental health expenditure, high-integration teams were predicted to cost approximately 80% more than low-integration teams. By contrast, with regard to social care support, no statistically significant differences were seen between team types. That is, given a certain needs profile, service users in all team types received not dissimilar amounts of social care, at least in terms of cost. However, service users in high-integration teams were approximately 1.6 times more likely to receive a social care package than those in low-integration teams, reinforcing the earlier suggestion that high-integration teams were providing social care packages for a broader mix of clients.
Multiplying the probability of care package receipt by the predicted costs of the social care packages revealed that social care costs in high-integration teams were approximately £63 per service user per month higher than those in low-integration teams, while the equivalent additional sum in the nominally integrated team was £160. In contrast the network team costs were broadly similar to low-integration teams.
It is important to note that these seem to be genuine group differences and thus not attributable to individual teams. However, as the strength of these effects varied between teams, their relative influence on the group effect is likely to have differed considerably.
Finally, the main results of both the outcome and cost regression models were brought together in simple cost-effectiveness planes. Given that the analyses lacked clear-cut markers for ‘good’ or ‘bad’ outcomes, ‘more’ or ‘less’ economical services, these focused on the actual regression coefficients, i.e. teams’ deviation from the sample average after accounting for the effects of covariates.
To this effect, Figure 13 plots mental health costs (i.e. those costs considered most under the control of CMHTsOP) against satisfaction with services, whereas Figure 14 plots the same costs against inpatient service use during follow-up.
FIGURE 13.
Cost-effectiveness evaluation (mental health costs and satisfaction with services received). H, high-integration team; L, low-integration team; Ne, network team; No, nominally integrated team.
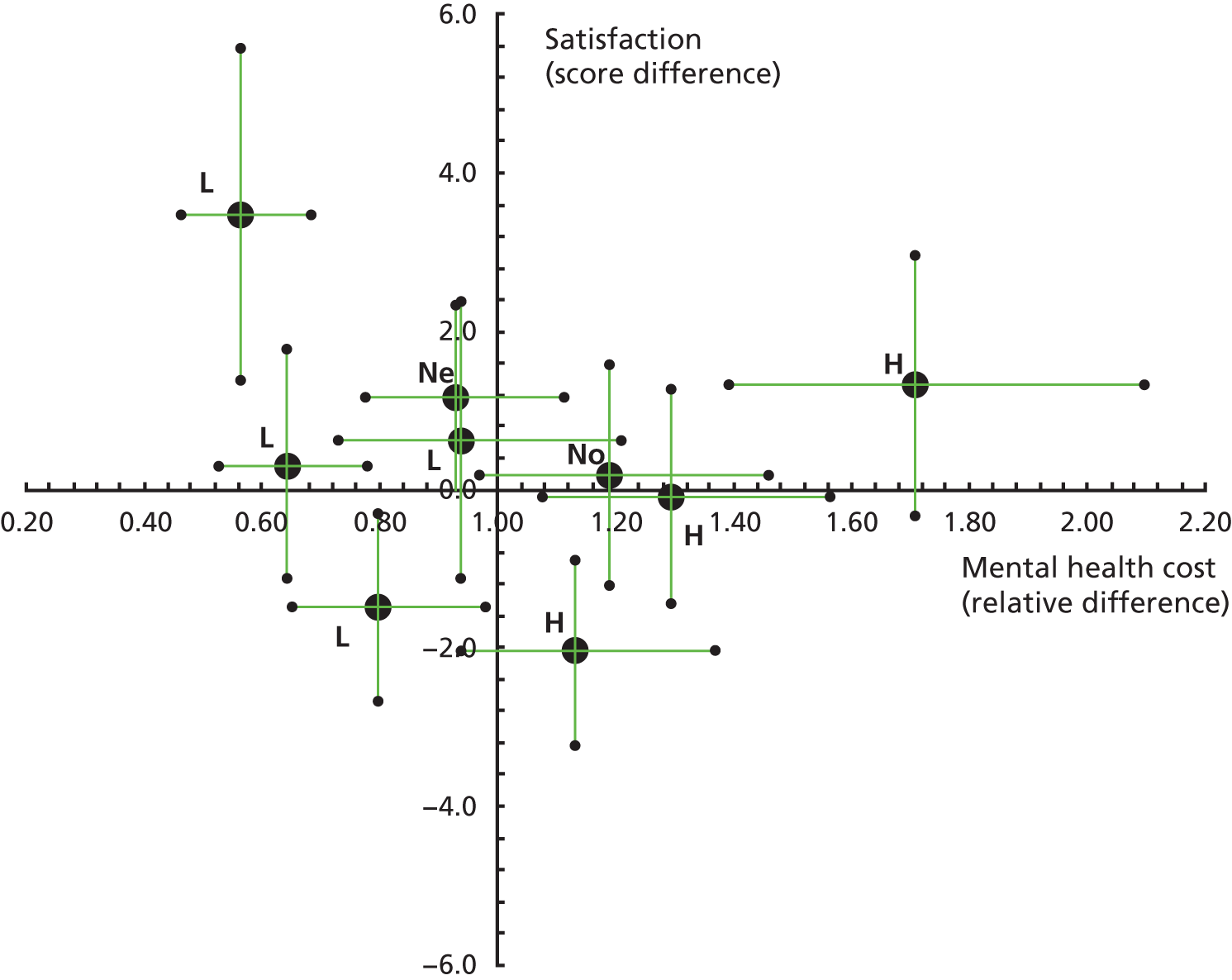
FIGURE 14.
Cost-effectiveness evaluation (mental health costs and admission to hospital). H, high-integration team; L, low-integration team; Ne, network team; No, nominally integrated team.
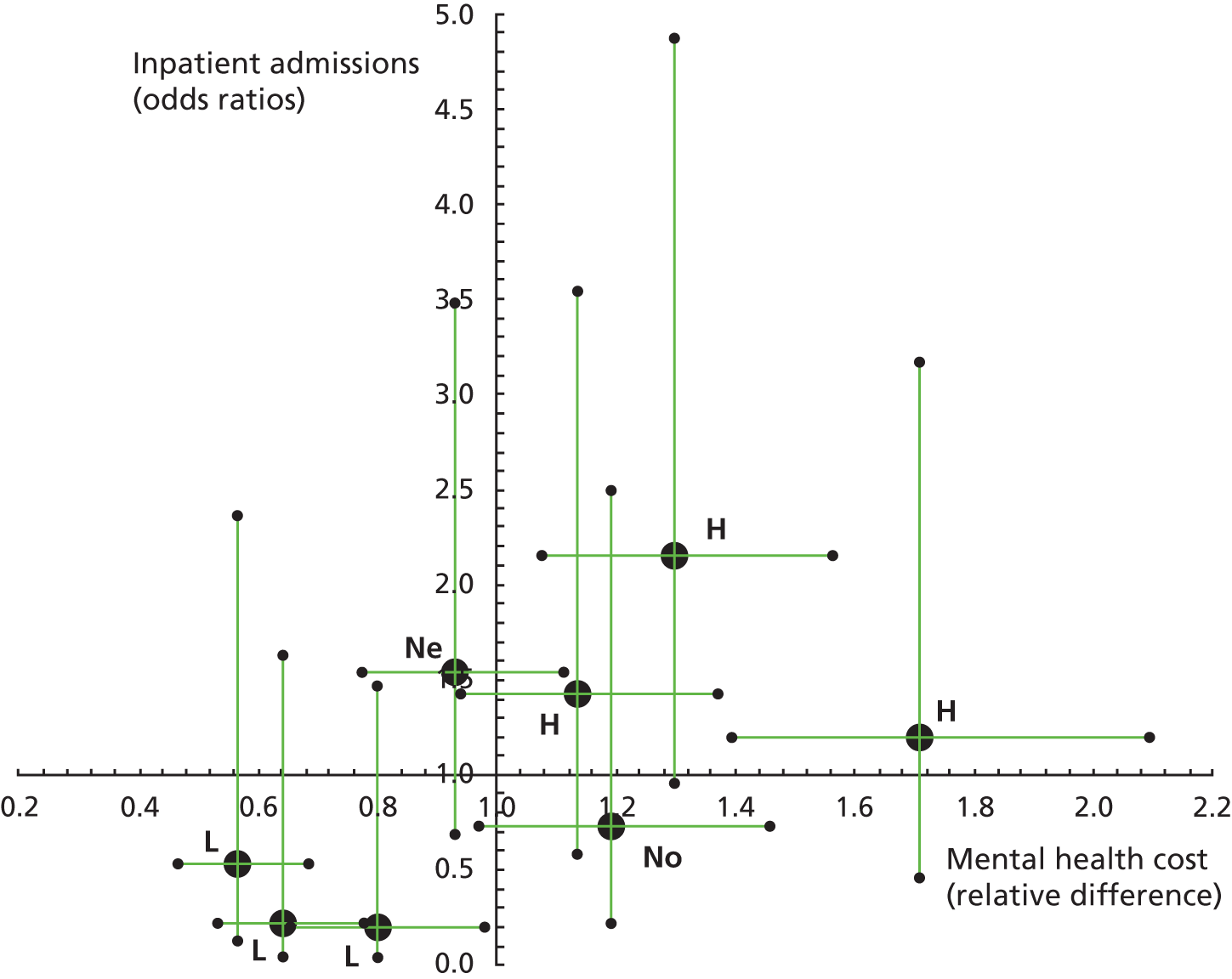
In order to highlight the full complexity of the analytical picture, individual teams rather than team types have been displayed. This presentation, however, also reveals the considerable statistical uncertainty involved in these analyses, indicated in the form of 95% confidence intervals for all estimates. Furthermore, the chosen perspective (i.e. comparing each team against all others, including those of the same team type, and crossing the two confidence intervals) is rather conservative, making it difficult to definitively locate any one team in a particular quadrant.
Figure 13 illustrates both an apparent systematic difference in team types’ costs and the lack of a consistent pattern in their satisfaction scores. In contrast, Figure 14 presents a more coherent picture, although the confidence intervals surrounding the likelihood of admission are very wide. Thus, if one were to combine all low and all high-integration teams, the former would be clearly located in the more ‘cost-effective’ bottom-left quadrant, whereas the latter would be situated in the less ‘cost-effective’ upper-right quadrant.
Discussion
In recent years, the desire to deliver more integrated services for older people has formed the focus of numerous policy initiatives around the world. 261–263 This includes services for older people with mental health problems. 11,31,264 Indeed, it has been argued that the provision of joined-up, co-ordinated care is particularly important for this client group, whose complicated and changing needs often require a response spanning health and social care, specialist and mainstream services. 7,11
The consequences for service users of a lack of integration have been well documented, and include difficulties accessing services and subjection to the overlapping assessment and case management arrangements of health and social care services. 48,52,226,265 However, the evidence base to support integration is just that – supportive not definitive. 10,77,260 On the one hand, for example, the Healthcare Commission50 found integration had a significant impact on how older people with mental health problems and their carers got the help they needed and service satisfaction. On the other hand, a systematic review of home and community services for frail older people, including people with dementia, concluded that although evidence from non-randomised trials showed integrated care increased service use, evidence from randomised trials indicated it did not improve clinical outcomes. 266
A major difficulty with this literature is that the term integration is not always defined, yet appears to have taken on a wide range of meanings ranging from the closer co-ordination of an individual’s clinical care to the formation of joint health and social care organisations. 257,262 This has reflected the fact that integration can take place at different levels in the care system from performance of care tasks to care systems. 267 Furthermore, a distinction is often made between horizontal integration, in which links are made within a single level of care (e.g. MDTs), and vertical integration, where different levels of care are linked (e.g. primary, secondary and tertiary services). 257,267,268 Where CMHTsOP are considered, however, Evans et al. 269 have noted that ‘integration is generally understood in policy and practice terms as, at a minimum, the presence of social workers or social care support workers in the team’ (p. 25).
The work described in this chapter employed a similar definition of integration at the team level, focused on the presence of social workers in teams, and set out to examine whether or not certain associated features of CMHTsOP’ practices affected a range of outcomes for older people with mental health problems. The study found almost unanimous support for the belief that integration facilitated better outcomes from staff working in both highly and less integrated teams. In particular, integrated teams were perceived to offer a greater breadth of skills and knowledge, to work more efficiently (with less duplication, improved communication and shared priorities), and to have access to a wider range of services. The co-ordination of care across settings (both within mental health services and with primary and generic services, including care homes) was also seen as crucial, as was the continuity of care across time. However, empirical analysis found no evidence that highly integrated teams were more effective than less integrated ones with regard to the prevention of hospital and care home admissions, promoting service users’ QoL and satisfaction or improving carer outcomes. Furthermore, although the costs of high-integration teams were greater than those of low-integration ones, at least in part because they provided social care services to a broader mix of clients, service users supported by the former were more likely to be admitted to a mental health ward. However, these conclusions were subject to marked within team type variability, suggesting the influence of other factors such as leadership on outcomes.
Methodological considerations
The most important weakness in this study’s design was its unavoidable reliance on observational data. In order to understand the causal mechanisms that determine the costs and outcomes of CMHTsOP, one would ideally want to randomise service users into different team types at baseline and then observe various changes over time. Needless to say, given the many complexities involved in such a design, such an approach seems unlikely, at least in the foreseeable future.
In the absence of service user randomisation, the study as outlined here and in Chapter 7 was a pragmatic attempt to approximate the features of a randomised controlled trial (RCT) within limited resources. However, despite careful checks with the participating teams at the study design stage, difficulties were experienced obtaining data of sufficient quantity and quality, hampering effectiveness. Although the target baseline sample was very nearly achieved, the planned recruitment of matched subsamples of service users at stage 2 suffered from the same recruitment problems discussed in Chapter 5. Analysis of carer outcomes was particularly hampered by low sample sizes, despite a reasonable response rate to the self-completed questionnaire. Furthermore, the utility of the secondary outcome data collected at stage 3 was limited by problems with missing information and delays in data return, resulting in varying follow-up periods. The refinement of the original classification of team types (as derived from the national survey) to the four-level categorisation employed in this chapter also necessitated various changes to the analysis. However, the very ability of the qualitative data to reveal such subtleties must be viewed as a strength of the mixed-methods approach employed.
In light of such shortcomings, certain aspects of the planned analysis were necessarily not pursued. The aforementioned gaps in follow-up data, for example, precluded an examination of changes in outcomes over time, as trajectories of cognition, affect and dependency could not be described for sufficient numbers of service users. Plans to calculate resource use over the follow-up period could similarly not be implemented, as costs could only be meaningfully estimated at the baseline stage. Indeed, the successful implementation of both these strands (i.e. the measurement of differences in costs and outcomes) would have facilitated a less ambiguous cost-effectiveness analysis.
However, even if the design had been implemented in full, at least one other generic limitation would have remained. Namely, this was in essence a multiple case study approach, whereby the representativeness of any grouping of teams could not be guaranteed (or even statistically evaluated). It may be assumed that the selected teams were a fair, if approximate, representation of all teams with similar characteristics in England given the very high response rate to the national survey described in Chapter 8. Nevertheless, further studies in this area might wish to consider recruiting a wider random sample of teams, enabling multilevel analysis of service costs and outcomes, while retaining many of the original features of this work.
Broader implications
General design issues aside, a more substantive challenge for future researchers, commissioners, service providers and policy-makers wishing to understand CMHTsOP effectiveness is the selection of suitable outcome domains. Although this study was based on the premise that integration is a desirable feature of CMHTsOP,11,31,48 and it is difficult to argue against something that has come to stand for co-operation and collaboration,263 integration is not an end in itself. 270 While the outcomes investigated reflected government policy objectives,31,57,271,272 it is important to consider further how operationalisable these were, and to specify precisely the myriad of aims of CMHTsOP.
As already noted in Chapter 1, the history of service provision for older people with mental health problems reflects the long-standing desire of policy-makers in all health systems to reduce hospital beds, on grounds of costs and user preferences. 25,273 Not only does inpatient care account for the vast majority of specialist mental health expenditure,56 hospital admission can be a traumatic event. 274,275 In this situation it is essential that only those people for whom hospital care is the most appropriate way of meeting their needs should be admitted, but there is some suggestion that this is not always the case. 118,276 Indeed, despite long-standing attempts to shift the BoC in the direction of the community, the BoC study described earlier in this report found both professionals and older people believed that if sufficient and appropriately configured community support were available, the needs of a number of older adults with mental health problems currently admitted to inpatient beds might be more appropriately met in alternative community settings (see Chapters 4 and 5).
Although there is every incentive to reduce inappropriate admissions and to ensure that hospital stays are no longer than really necessary, this is not to say that reducing hospital admissions is an absolute good, for there will always be a significant minority of people for whom hospital care is the most appropriate and best option. Indeed, national service guidelines suggest that inpatient care is indicated for those older people with the most complex and severe mental illness, especially if there is a risk to their own or others’ safety, and for intensive assessment and treatment. 31 One favourable interpretation of this study’s findings, therefore, albeit a very speculative one, might be that higher integration teams were better at identifying those service users who needed hospital treatment, and at facilitating their admission. Furthermore, while the Royal College of Psychiatrists181 have previously recommended that one to two acute beds be provided for every 1000 older people, the figures provided by the trusts participating in this study were all considerably lower than this, suggesting thresholds for admission would probably have been high.
Although no systematic differences were found between team types and care home admissions, many of the same questions may be asked about the utility of this as a measure of effectiveness. Thus, although the policy of governments in many countries is predicated on the belief that most older people can, and would, prefer to live in their own homes, care home admission per se is not always an undesirable event. 216,277 Inappropriate admissions are a more sensitive target, albeit more complex to adjudge.
In light of evidence that older people with mental health problems use fewer mental health services than their needs justify,278 the finding that high-integration teams provided services to a wider range of clients is particularly interesting, especially given that CMHTsOP are typically less integrated than those for working-age adults. 50 Indeed, it is important to note that although this study found that high-integration teams cost more than other team types, in effect this simply means they provided more resources, which could arguably be viewed as a positive outcome itself. These findings are in keeping with the systematic review mentioned above266 and might tend to suggest that more integrated teams are better at accessing and/or targeting resources for a particular subsection of their caseload with less obvious dependency, perhaps with a view to maintaining their independence. Such provision would fit well with concerns about the concentration of resources on people with high-level needs, at the expense of those for whom relatively small inputs might prevent or delay deterioration. 279–281 Furthermore, it is interesting to note from the qualitative analysis that what other staff appeared to value about social workers was at least as much about access to services and systems as it was about professional skills.
Finally, although we would support the use of QoL and satisfaction outcomes, which are commonly seen as essential to the development of good health and social care services,79,282–284 it must be acknowledged that there are a number of problems with these measures. QoL, for example, may be affected by many external factors outside CMHTsOP sphere of influence,285 while the known reluctance of older people to express dissatisfaction with services may undermine the utility of satisfaction measures. 286–288 Furthermore, assuming CMHTsOP main aims include the resolution, improvement and minimisation of mental health problems, future studies will also need to include measures of clinical change.
Conclusions
Despite the limitations discussed, this study is believed to constitute the most comprehensive examination of the costs and outcomes of CMHTsOP conducted to date, and sheds light on a very complex area. If its findings are inconclusive – and at times counterintuitive – it may be that at a time of reduction in provision and service change, the effects of integration, however defined, were simply obscured by bigger issues, including access to resources. 52
In the absence of further evidence to the contrary, the study suggests that service commissioners and providers need to develop a very clear focus on the goals and outcomes of integrating care provision, whether at the team level through the inclusion of social workers in teams, or more macro level changes (see Chapter 8). It appears that other factors, often less tangible or subject to change, such as leadership, shape outcomes. The decision to prefer one service model over another needs to reflect this since integration is not a costless exercise. 263 Indeed, as identified in the qualitative evidence, the presence of social care staff is only one of a number of aspects of integration perceived to be of benefit to service users, and further research is needed to investigate whether other features, or combination of features, prove more influential.
Chapter 11 Practitioner study
Community mental health teams for older people team structures and processes, in particular with respect to integrated working practices, are anticipated to impact on practitioner job satisfaction and well-being.
ObjectivesTo explore what personal and team characteristics, including the degree of integrated working, are associated with better/worse job outcomes.
MethodA self-administered postal survey and 24 in-depth interviews with team practitioners in nine mental health trusts.
ResultsMost survey respondents (n = 295, 59% response rate) reported that they were satisfied with their job, with support workers enjoying high job satisfaction, and social workers and OTs the lowest. Social workers reported particularly low job controls, suggesting they perceived difficulty in influencing the nature of their work and the skills they could develop. Regression analysis found that working in a ‘high-integration’ team was associated with poor job characteristics, although this effect dissipated with the inclusion of other explanatory factors, including staff mix, job insecurity and (among nurses) being managed outside of one’s own profession. Interview data found that social workers and OTs were most vocal about both the benefits and pitfalls of generic (vs. specialist) working. Support workers enjoyed their direct work with service users, but had some concerns about career prospects and role definition.
ConclusionsThe finding that support workers enjoyed such high job satisfaction is in contrast to some earlier research, implying that the role is becoming better established within teams. Integrated working practices have a complex relationship with job outcomes, with the balance between generic/specialist working, and appropriate line management arrangements, remaining causes for concern and debate.
Introduction
Many studies have explored job satisfaction and stress in community mental health care, but with a focus on working-age adult services. The evidence shows that CMHT practitioners experience significant levels of burnout compared with population norms, other NHS workers, and mental health practitioners in hospital settings. 289–295 Studies focusing on old age mental health workers are rare, but find broadly similar levels of stress and job satisfaction. 213,296,297 One study of CMHNs working in a broad range of CMHTs in Wales found evidence of greater burnout among those with an elderly caseload. 298 Existing evidence identifies a range of personal and organisational characteristics associated with high stress including job pressures, such as high caseloads and conflicting demands; limited discretion over the work environment, including insufficient resources and skill development; and problematic team working and supervision. 293 However, few studies have addressed the importance of CMHT structures, especially in old age services, despite evidence linking team design to staff well-being299,300 and patient outcomes301 in mental health-care settings.
The practitioner study reported in this chapter aimed to explore the personal and team characteristics associated with positive job outcomes, and to identify which aspects of integrated working facilitate and/or hinder a positive working environment. As detailed in Chapter 7, a postal survey was conducted with 38 teams operating in the nine mental health trusts that participated in the CMHTsOP workstream. The survey was supplemented with in-depth face-to-face interviews with a sample of practitioners restricted to the nine case study teams reported in Chapters 9 and 10.
Quantitative findings
Respondent characteristics
Questionnaires were given to an estimated 500 practitioners, either direct or via administrative sources, making the exact number difficult to specify, and by close of fieldwork in December 2011 a total of 295 questionnaires were returned, a response rate of 59%. Table 65 presents an overview of key personal and team-related characteristics. Nurses comprised the largest single professional group within the sample (40%), while SWs and OTs comprised the smallest (7.8% and 8.5% respectively). Estimated response rates varied across the 38 teams from 40% to 100%. Contrasts with both the original sampling frame for the nine trusts, and the national survey reported in Chapter 8, suggest a slight over-representation of nurses and TMs but an under-representation of doctors. Excluding doctors, the sample mean caseload size was 28.3, varying by staff group from 16.6 (support workers) to 35.7 (nurses). Most respondents (68.9%) worked in moderately sized teams with between 11 and 20 members and one-fifth of respondents (17.3%) worked in ‘high’ integration teams (having at least seven indicators of integration noted in Chapter 8).
| Characteristic | Category | n | % |
|---|---|---|---|
| Professional group | TM | 27 | 9.2 |
| Doctors | 27 | 9.2 | |
| Nurses | 118 | 40.0 | |
| OTs | 25 | 8.5 | |
| SW | 23 | 7.8 | |
| Support worker | 43 | 14.6 | |
| Other disciplinesa | 32 | 10.8 | |
| Gender | Male | 64 | 21.7 |
| Female | 231 | 78.3 | |
| Age (years) | < 35 | 37 | 12.6 |
| 35–44 | 80 | 27.3 | |
| 45–54 | 129 | 44.0 | |
| ≥ 55 | 47 | 16.0 | |
| Employment status | Full time | 218 | 75.2 |
| Part time | 72 | 24.8 | |
| Active caseload size | < 15 | 53 | 19.5 |
| 15–24 | 76 | 27.9 | |
| 25–34 | 57 | 21.0 | |
| 35–44 | 40 | 14.7 | |
| ≥ 45 | 46 | 16.9 | |
| Years employed in team | < 2 | 44 | 25.3 |
| 2–5 | 71 | 40.8 | |
| 6–9 | 29 | 16.7 | |
| ≥ 10 | 30 | 17.2 | |
| Team size | ≤ 10 | 41 | 13.9 |
| 11–15 | 112 | 38.0 | |
| 16–20 | 85 | 28.8 | |
| ≥ 21 | 57 | 19.3 | |
| Integration categoryb | Low | 66 | 22.4 |
| Medium | 178 | 60.3 | |
| High | 51 | 17.3 |
Job satisfaction, intention-to-quit and the psychosocial characteristics of work
As noted in Chapter 7, the practitioner survey collected measures of job satisfaction, intent to quit, and a range of key psychosocial characteristics of work known to be key determinants of stress (job demands, controls and two components of social support – see Box 16). Table 66 presents summary information. In total, 73% of respondents reported that they were at least ‘quite satisfied’ with their job, with a mean score of 3.98 on a 1–6 (extremely dissatisfied–extremely satisfied) Likert scale. Just over one-third (35.4%) of respondents agreed or strongly agreed that they often thought about quitting their job, with this proportion falling to 16% indicating active job searching. An ‘intent-to-quit’ score was constructed by combining these two questions (ranging from 2 to 8, with higher scores indicating a greater intent to quit) with a mean of 4.2. Cronbach’s alpha statistics for all variables met standard thresholds for internal consistency. 302 Pearson correlation coefficients confirmed expected associations: job satisfaction was negatively associated with intent to quit and psychological demands, and positively associated with job controls and both measures of social support in the workplace.
| Job satisfaction | Intent to quit | Job demands | Job controls | Supervisory support | Coworker support | |
|---|---|---|---|---|---|---|
| Summary statistics | ||||||
| Mean | 3.98 | 4.19 | 35.66 | 71.81 | 12.08 | 13.13 |
| SD | 1.05 | 1.43 | 5.83 | 8.04 | 2.35 | 1.67 |
| Minimum | 1.00 | 2.00 | 22.00 | 48.00 | 4.00 | 10.00 |
| Maximum | 6.00 | 8.00 | 48.00 | 94.00 | 16.00 | 16.00 |
| Cronbach’s alpha | N/A | 0.77 | 0.79 | 0.71 | 0.93 | 0.81 |
| n | 288 | 288 | 282 | 281 | 281 | 288 |
| Correlation coefficientsa | ||||||
| Intent to quit | –0.485 (0.000) | |||||
| Job demands | –0.329 (0.000) | 0.349 (0.000) | ||||
| Job controls | 0.334 (0.000) | –0.306 (0.000) | 0.049 (0.422) | |||
| Supervisory support | 0.387 (0.000) | –0.390 (0.000) | –0.109 (0.090) | 0.272 (0.000) | ||
| Coworker support | 0.189 (0.001) | –0.174 (0.003) | –0.066 (0.273) | 0.173 (0.004) | 0.357 (0.000) | – |
Table 67 presents mean values for job satisfaction, intent to quit and the psychosocial characteristics of work across a range of personal characteristics. The data revealed significant variation in job satisfaction by professional group (ANOVA: F = 2.96, df = 6, p = 0.008) with social workers reporting lower satisfaction than support workers (Bonferroni: p = 0.030) and ‘other disciplines’ (Bonferroni: p = 0.026). Similar results were found with intent to quit (ANOVA: F = 3.02, df = 6, p = 0.007), with social workers reporting greater intent to quit than support workers (Bonferroni: p = 0.007). Psychological demands also varied (ANOVA: F = 10.911, df = 6, p < 0.000), with support workers reporting lower psychological demands than all other staff groups (Bonferroni: p < 0.000 in all cases, except doctors p = 0.035) and team managers reporting higher demands than doctors (Bonferroni: p = 0.026). Job controls varied significantly (ANOVA: F = 5.977, df = 6, p < 0.000), with team managers reporting higher job controls than nurses (Bonferroni: p = 0.011), social workers (Bonferroni: p < 0.000), support workers (Bonferroni: p = 0.003) and OTs (Bonferroni: p = 0.002). Social workers reported lower job control than nurses (Bonferroni: p = 0.032) and other staff (Bonferroni: p = 0.002). There were few staff group differences with respect to supervisory and coworker support, with none reaching statistical significance.
| Characteristic | Category | Job satisfaction (mean) | Intent to quit (mean) | Job demands (mean) | Job controls (mean) | Supervisory support (mean) | Coworker support (mean) |
|---|---|---|---|---|---|---|---|
| Professional group | TM | 4.15 | 4.00 | 39.28 | 77.76 | 11.92 | 12.92 |
| Doctors | 4.00 | 3.92 | 34.33 | 72.00 | 11.33 | 13.17 | |
| Nurses | 3.90 | 4.32 | 36.59 | 71.83 | 12.27 | 13.00 | |
| OTs | 3.68 | 4.57 | 37.46 | 69.17 | 11.92 | 13.12 | |
| SW | 3.41 | 4.91 | 36.68 | 65.90 | 11.43 | 12.68 | |
| Support worker | 4.29 | 3.57 | 29.97 | 70.34 | 12.37 | 13.60 | |
| Other disciplinesa | 4.34 | 4.13 | 35.34 | 74.73 | 12.28 | 13.45 | |
| Gender | Male | 3.73 | 4.30 | 35.50 | 68.83 | 11.54 | 12.81 |
| Female | 4.05 | 4.16 | 35.71 | 72.62 | 12.23 | 13.22 | |
| Age (years) | < 35 | 3.94 | 4.49 | 34.68 | 71.58 | 12.42 | 13.26 |
| 35–44 | 4.12 | 4.05 | 35.38 | 71.31 | 12.30 | 13.19 | |
| 45–54 | 3.96 | 4.20 | 36.39 | 72.34 | 12.02 | 13.04 | |
| ≥ 55 | 3.87 | 4.13 | 34.98 | 71.78 | 11.70 | 13.19 | |
| Employment status | Full time | 3.99 | 4.19 | 35.84 | 71.94 | 12.11 | 13.20 |
| Part time | 3.97 | 4.16 | 35.16 | 71.57 | 12.07 | 13.00 |
With respect to gender, age and employment status, very few differences were evident within the data. Women tended to report better job characteristics than men as evidenced by slightly higher job satisfaction (two-tailed t-test: t = 2.150, df = 286, p = 0.032), job controls (two-tailed t-test: t = 3.294, df = 279, p = 0.001) and supervisory support (two-tailed t-test: t = 2.031, df = 279, p = 0.043).
Table 68 presents mean values for job satisfaction, intent to quit and psychosocial characteristics of work for a range of team-related variables. The data suggest that there is a negative association between caseload size and job outcomes, with mean job satisfaction ranging from 4.15 to 3.71 between those with the lowest and highest caseloads. This association only reached significance when excluding doctors from the analysis (two-tailed Pearson correlation: r = –0.153, p = 0.017). Few associations were evident with respect to the length of time respondents had worked for the team. There was some suggestion that job controls increase with time spent within the team, but this did not reach statistical significance. Furthermore, team size was not associated with any job outcome variables, despite the possibility that larger teams may have inferior supervisory support.
| Characteristic | Job satisfaction (mean) | Intent to quit (mean) | Job demands (mean) | Job controls (mean) | Supervisory support (mean) | Coworker support (mean) | |
|---|---|---|---|---|---|---|---|
| Active caseload | < 15 | 4.15 | 3.98 | 34.84 | 73.91 | 12.16 | 13.16 |
| 15–24 | 4.12 | 4.08 | 34.46 | 71.65 | 11.99 | 13.25 | |
| 25–34 | 4.06 | 4.18 | 37.28 | 70.11 | 12.25 | 13.25 | |
| 35–44 | 3.79 | 4.60 | 37.18 | 71.50 | 12.81 | 12.97 | |
| ≥ 45 | 3.71 | 4.23 | 35.74 | 73.09 | 11.73 | 12.91 | |
| Time in team (years) | < 2 | 4.21 | 4.03 | 35.10 | 70.78 | 12.20 | 13.22 |
| 2–5 | 3.74 | 4.40 | 36.40 | 71.36 | 12.16 | 12.94 | |
| 6–9 | 4.11 | 4.34 | 35.45 | 72.00 | 11.59 | 13.07 | |
| ≥ 10 | 4.00 | 3.93 | 36.38 | 73.17 | 12.17 | 13.23 | |
| Team size | ≤ 10 | 4.03 | 4.10 | 35.65 | 73.13 | 12.16 | 13.22 |
| 11–15 | 3.86 | 4.40 | 35.71 | 70.76 | 11.99 | 13.00 | |
| 16–20 | 3.99 | 4.08 | 35.52 | 72.12 | 12.10 | 13.25 | |
| ≥ 21 | 4.18 | 4.02 | 35.80 | 72.44 | 12.16 | 13.12 | |
| All time spent in team? | Yes | 3.98 | 4.19 | 35.68 | 71.72 | 12.15 | 13.14 |
| No | 4.10 | 4.31 | 35.96 | 71.61 | 11.67 | 12.96 | |
| TM same disciplinea | Yes | 4.02 | 4.20 | 36.59 | 72.39 | 12.32 | 13.13 |
| No | 3.52 | 4.75 | 36.93 | 68.43 | 11.83 | 12.78 | |
| Integrationb | Low | 4.18 | 3.78 | 34.83 | 72.87 | 11.81 | 13.20 |
| Medium | 3.94 | 4.30 | 35.87 | 72.02 | 12.25 | 13.12 | |
| High | 3.86 | 4.35 | 36.09 | 69.70 | 11.81 | 13.06 | |
The questionnaire also asked respondents whether they worked only for the CMHTOP in question, or had additional responsibilities elsewhere (closely related to the issues of ‘core’ and ‘sessional’ membership, outlined in Chapter 8). The raw data indicated slightly improved supervisory and coworker support for respondents who worked solely for the team, although, again, this did not reach statistical significance. For a subset of respondents (nurses, social workers and OTs, n = 166) separate analysis explored the implications of having a team manager from the same (vs. different) professional discipline: the results suggest higher job outcomes with respect to job satisfaction (two-tailed t-test: t = 3.220, df = 159, p = 0.002), intent to quit (two-tailed t-test: t = 2.572, df = 161, p = 0.011) and job controls (two-tailed t-test: t = 3.183, df = 159, p = 0.002).
Finally, the analysis investigated outcomes for respondents who worked in teams with different levels of service integration. Table 68 illustrates that respondents who worked in ‘high’ integration teams tended to have slightly inferior job outcomes, with lower job satisfaction, higher intent to quit, increased job demands and reduced job controls. However, these differences were relatively small, with only intent-to-quit reaching statistical significance at conventional levels (Bonferroni: p = 0.032).
Job demand–control regression analysis
There is a well-established association (see Chapter 7) between the balance of job demands and controls, and a range of physical and psychological health outcomes, especially stress and burnout. Several approaches are available to measure the imbalance between demands and controls (see Box 16), with the present analysis adopting the ‘subtraction’ method. 252 Consequently, a new variable was constructed as the arithmetic difference between job controls and demands [mean = 36.2, standard deviation (SD) = 9.75; minimum–maximum = 8–62], with larger values indicating a better balance between demands and controls.
Stepwise OLS regression investigated the estimated contribution of team integration to the balance between job demands and controls (Table 69). Without adjusting for confounding factors, Block A indicates that working in a high (vs. low) integration team was associated with a poorer balance of demands and controls. Block B includes gender and professional group in the regression, and suggests that women exhibited improved balance between demands and controls relative to men, and OTs and social workers reported a poorer balance relative to all other professional groups. Controlling for gender and professional group reduced the effect of working in a high-integration team. Block C suggests that respondents who had worked within their team longer reported a superior demand/control balance than staff who had joined more recently. Caseload size for the full sample was not found to be significant, in particular because doctors, support workers and team managers did not show the conventional association between caseload size and job demands. However, an interaction between caseload size and being a nurse, social worker or OT (who most commonly acted as community key workers) demonstrated a slight negative association with demand–control balance.
| Model | Block A | Block B | Block C | Block D | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | p-value | Coefficient | SE | p-value | Coefficient | SE | p-value | Coefficient | SE | p-value | ||
| Integration | Low | Reference group | Reference group | Reference group | Reference group | ||||||||
| Medium | –1.960 | 1.45 | 0.179 | –1.760 | 1.41 | 0.212 | –1.077 | 1.46 | 0.461 | 0.230 | 1.43 | 0.872 | |
| High | –4.558 | 1.90 | 0.017 | –3.334 | 1.86 | 0.074 | –0.286 | 1.99 | 0.886 | 0.740 | 1.95 | 0.705 | |
| Gender | Male | Reference group | Reference group | Reference group | |||||||||
| Female | 3.404 | 1.37 | 0.014 | 2.472 | 1.45 | 0.076 | 2.452 | 1.39 | 0.080 | ||||
| Professional group | SW | –7.142 | 2.21 | 0.001 | –7.977 | 2.41 | 0.001 | –6.956 | 2.34 | 0.003 | |||
| OT | –5.817 | 2.01 | 0.004 | –5.908 | 1.93 | 0.003 | –6.036 | 1.88 | 0.002 | ||||
| Time in team | 0.261 | 0.11 | 0.015 | 0.229 | 0.10 | 0.029 | |||||||
| Caseload size | 0.010 | 0.01 | 0.471 | –0.002 | 0.01 | 0.881 | |||||||
| Interaction: caseload size × (nurse/OT/SW) | –0.055 | 0.03 | 0.045 | –0.047 | 0.03 | 0.073 | |||||||
| Nurse managed by non-nurse | –5.225 | 1.82 | 0.005 | –6.126 | 1.76 | 0.001 | |||||||
| Job security | 3.245 | 0.76 | < 0.000 | ||||||||||
| Constant | 38.167 | 1.25 | < 0.000 | 36.206 | 1.655 | < 0.000 | 35.877 | 2.03 | < 0.000 | 27.793 | 2.65 | < 0.000 | |
| n | 275 | 275 | 229 | 223 | |||||||||
| Diagnostics | |||||||||||||
| R2 | 0.021 | 0.098 | 0.165 | 0.249 | |||||||||
| Adjusted R2 | 0.014 | 0.082 | 0.130 | 0.214 | |||||||||
| Shapiro–Wilk (residuals) | W = 0.992, p = 0.130 | W = 0.995, p = 0.518 | W = 0.994, p = 0.449 | W = 0.992, p = 0.315 | |||||||||
| Breusch–Pagan (residuals) | χ2(1) = 0.12, p = 0.730 | χ2(1) = 0.02, p = 0.883 | χ2(1) = 1.20, p = 0.274 | χ2(1) = 0.42, p = 0.517 | |||||||||
| RESET test (specification) | N/A | F(3,266) = 0.220, p = 0.882 | F(3,216) = 0.500, p = 0.680 | F(3,209) = 0.270, p = 0.848 | |||||||||
The final model (Block D) includes an interaction term indicating nurses who were managed by a non-nurse, and suggests that this group, with professionally dissimilar managers, faced a significantly inferior demand–control balance to other staff. This interaction could not be extended to other staff groups due to small cell sizes. Further, job security was positively correlated with improved demand–control balance, with a substantial effect size and associated increase in the model fit. Following the inclusion of all significant correlates, the impact of team integration on demand–control balance was negligible.
Factors influencing staff well-being: views from interviews
Introduction
Interviews with a subsample of nurses, social workers, OTs and support workers from the nine case-study teams focused on the association between different organisational approaches and service delivery, including an exploration of the impact of team arrangements on staff well-being. Specifically, the interviews explored the extent and nature of autonomy; professional identity and generic working; the nature and quality of the support received from peers, consultants and managers; whether or not they felt that their contribution was valued; and the pressures and frustrations they faced. Respondents were also asked to state what they found most rewarding about their work. Quotations illustrating the findings can be found in Box 21.
| Attribute/theme | Example | Team and professional | |
|---|---|---|---|
| 1 | A high level of autonomy in CMHTs compared with other settings | . . . there is so much more flexible . . . If it is within the ward you have an admission, an assessment, you have . . . got . . . a pathway . . . whereas there are so many things that can change within the community . . . very enjoyable | Team D, nurse |
| 2 | . . . that is one of the huge bonuses of working at the CMHT . . . I do feel that I have quite substantial autonomy | Team A, social worker | |
| 3 | Less autonomy than in the past due to cut backs | Sometimes you get the feeling that you are not really trusted, that your professional judgement isn’t perhaps trusted . . . I think things have got worse recently, because of cut backs and spending restrictions, I’m not . . . , certainly my feeling is that it’s a lot more tense about things, and there’s a lot more making sure that, not only we’re doing our jobs properly, but that we all gets seen by the “powers that be”, to be doing our jobs properly | Team C, nurse |
| 4 | Autonomy balanced with support from team manager | Yes you can (make decisions), and that’s good, but the thing is that if you’re worried about it you’ve always got the team backup and the support of your managers as well to discuss with them | Team I, nurse |
| 5 | Strengths and weaknesses of having a lot of autonomy | It does kind of set me apart from the rest of the team in some ways. So I am sort of protected from some of the stresses and pressures that other team members have . . . but there are disadvantages . . . sometimes I am seen as being a bit separate from the team, and perhaps not understanding the pressure that they are under . . . | Team F, psychologist |
| 6 | Joint professional and team identity | My main focus is this team . . . When I am doing generic work I am always an OT as some level. I’m quite comfortable with that | Team H, OT |
| 7 | I’m very proud of being an OT. I would say OT first, team second . . . | Team I, OT | |
| 8 | Dual identity and role | I’ve always had a dual role . . . as a mental health professional and as a social worker . . . | Team A, social worker |
| 9 | Blurred role with health | Where initially it was about procurement and care management, now it’s much more inclusive, much more . . . monitoring through peoples mental health, looking at medications, so the role has expanded and taken it away from traditional social worker role and it is much more blurry now with health . . . Though there are these blurrings around the edges . . . people still have certain specialisms | Team C, social worker |
| 10 | Positive aspects of role blurring: role expansion | When cases are being allocated you can lend yourself to a lot more problems than maybe you would initially have thought you would . . . | Team A, OT |
| 11 | Negative aspects of role blurring: loss of specialists | . . . the OT and Nurse [role] overlap . . . maybe the OT skills don’t get used as specifically as they could be | Team I, psychologist |
| 12 | I sort of feel that we’ve got different skills and we should use them and, perhaps for the patient, it’s the best person for the job depending on their problems | Team B, OT | |
| 13 | Lack of understanding of social work role | Our role is to go in and set up services and monitor the services, not to provide the ongoing support, and I think that there is a bit of confusion around that because some of the grumbles if you like have been, – “well I’ve been to see this person and social worker hasn’t had any contact with them”, but when you unpick it … there’s actually no need for the social worker to have any contact, but the CPN hasn’t . . . understood that that is not what we do | Team B, social worker |
| 14 | Envying the support worker role | I quite envy their role really . . . it is quite an enviable role, it is very . . . hands on . . . as a professional I do an initial assessment and then you are sending other people out . . . | Team D, social worker |
| 15 | Positive view of support worker role: valued by other staff and feeling they are helping people | I think I have got a real good role, I work among all these professional people, that treat me equally, and that is a good feeling | Team C, support worker |
| 16 | [I know] that I’m making a difference to their lives. I know that sounds big headed, but I know I am. I couldn’t do it if I wasn’t. I never finish the day thinking that I haven’t helped them people | Team F, support worker | |
| 17 | Support workers feeling undervalued and misused | I am told I can’t do assessments . . . [The team manager] asked if I could go out and see these two people and I said no . . . that is not my responsibility . . . I refused . . . I am told I can’t do things on one hand, but then again when it suits . . . it is all right to bring me in | Team H, support worker |
| 18 | Working as a team | . . . this is an excellent team, and we really do work together. The thing I like about our team is that we discuss every person. It isn’t a case of she has her ten patients, she has hers, she has hers, and she has hers . . . , everybody talks about them, and we value each other’s opinions, so it really is, we pull together everyone | Team D, support worker |
| 19 | Lack of case discussion | One of the things I would like to do is . . . facilitate kind of case discussion groups where it’s not about people necessarily passing the work on to someone else but just being able to just brainstorm and think together and draw on each others’ experience and skills. I think that would be really valuable . . . | Team F, psychologist |
| 20 | Profession of team manager and impact | I think it’s the understanding of what the job actually is. If it was a Nurse Manager they would have the similar background training and things to yourself, and they would have probably different expectations or an understanding of a problem that you are discussing | Team H, nurse |
| 21 | Pressures and frustrations caused by not having easy access to social workers | They’ve put everything down to one number where people take referrals . . . We have to refer everything through this central control . . . Sometimes they will then phone the . . . patient, say they’ve been referred . . . I’ve gone out and seen the lady . . . I’ve just done this, this week, . . . she has dementia . . . So I put in a referral, which she was agreeable, . . . Now if they ring her and say “we’ve had a referral from [the CPN]” she’ll say “no I don’t want it” because she would have forgotten and then they’ve just closed the case and then you have to go through the whole process again | Team H, nurse |
| 22 | Difficulties resulting from centralisation of inpatient beds | . . . it’s the time factor. Things have to change on how we do the ward rounds . . . I mean, I’ve got a couple over in [place name], and I need to go over three times a week for [each] review it’s like three or four hours taken out of my working day, three times a week. You can’t sustain that | Team A, nurse |
| 23 | The rewards of the job: seeing people get better or improve their circumstances | When . . . you’re in this situation, you take obviously the small victories, because for some people particularly with a dementia diagnosis . . . , then obviously the future is very bleak, so in those situations you get joy from the small victories like getting an extra day at day care so that the carer has got an extra day to recharge their batteries, or you manage to get a particular home care service in which means the client’s dignity is protected . . . Obviously with functional illnesses you can have complete turnaround . . . someone can be suicidal, then six months later they can be up and about and doing what they have always been doing. Without a doubt, that’s the best type and you do, you get quite emotional . . . it’s quite journey that you take with someone emotionally so when they do improve . . . it’s a massive source of joy and fulfilment so that’s definitely the best bit | Team C, nurse |
Autonomy and its impact
Interviewees mostly reported a high level of autonomy. Its level and nature varied, the greatest being among psychologists and the least (although still felt to be substantial) among support workers. Among nurses an example was given of autonomy being greater than on hospital wards, something described as both rewarding and challenging (quote 1). Social workers all reported experiencing greater autonomy within their CMHT compared with working in social services teams (quote 2). Staff tended to distinguish between autonomy that took the form of flexibility to ‘run their own diary’ (E, support worker) and that which related to having authority to make decisions. Most staff reported the former to be the norm in their teams although there were examples of this practice being undermined by the pressures of increased workloads and the use of electronic diaries which resulted in staff feeling ‘watched’ and ‘not trusted’ by senior management (C, staff). Staff reported that they had less authority to take decisions than in the past, and a perceived increase in pressure to improve speed and ‘throughput’ of cases (quote 3). Achieving an appropriate balance of independent working and support was vital to how staff felt (quote 4) and varied between professional groups. Too little guidance and oversight from supervisors and managers – particularly for support workers – could lead to feelings of isolation and anxiety. Psychologists noted that their relative autonomy created a divide between them and the rest of the team (quote 5).
Professional identity and generic working
The expressed desire to retain one’s professional identity varied between interviewees and did not relate to any specific team type. OTs and psychologists appeared to have the strongest sense of professional identity, although among OTs this was not seen to conflict with also having a strong team identity (quotes 6 and 7). Social workers referred to having a dual or blurred identity, as both social workers and mental health workers (quotes 8 and 9) (apart from team B where work was less generic). Nurses tended to refer to working as part of a team, and to getting the job done. Most interviewees were comfortable with the level of generic working in their team although some were clear that they did not want this to go further.
Social workers and OTs were the most vocal about both the strengths and weaknesses of generic working. Some found working in this way a positive experience which enhanced their role and fostered effective team working (quote 10). Others, including psychologists, were concerned that this practice resulted in the loss of valuable specialist expertise with staff not being able to use their skills effectively (quotes 11 and 12). Concerns were expressed in particular about the expectation to monitor medication. Most staff described feeling that their contribution was valued by their colleagues; although some psychologists and social workers felt that their role was misunderstood, resulting in the under-use of their skills (quote 13).
Support workers were described by many interviewees as having an enviable role within the team, having taken on all the most fulfilling aspects of direct work with service users that professional staff no longer had time to do (quote 14). Support workers recognised this, describing their work positively in terms of both its value and their own satisfaction (quotes 15 and 16). There were two examples of support workers who thought that they were sometimes used inappropriately, for example as a transport service (E) or as a substitute for qualified nurses (H). In the latter example, the individual’s anxiety and stress were compounded by not feeling appropriately supported in this role. These feelings were heightened by the view that they were only allowed to take on this level of work when it suited management, at other times being told that they did not have the expertise required (quote 17). This issue was a source of frustration for another support worker who felt that while her team recognised her abilities and treated her as their equal, she was not regarded as such by the organisation which offered no formal structure through which she could develop her career.
Team climate and support
Most staff portrayed multidisciplinary working in CMHTs positively, particularly the support received from other disciplines. Staff mostly reported being part of a team that worked well together: having knowledge and understanding of each others’ caseloads and pressures, commonly joint working, and making decisions as a team (quote 18). Although team members tended to support each other informally, formal forums for case discussions were reported to be lacking in a small number of teams. This was reported as detracting from effective teamwork leading to poorer understanding between disciplines and team members working in isolation (quote 19).
Team managers and consultants both played an important role in influencing team climate. Having an accessible and approachable consultant was important in enabling staff to make decisions safely. Many interviewees described their consultants treating team members as equals and valuing their expertise. A minority found their consultant more difficult to approach and did not feel their views were listened to, resulting in both frustration and anxiety. Most interviewees also reported good support from their team managers. Two factors appeared to influence this: whether or not the team manager had the same professional background as the interviewee; and whether or not they carried a caseload. Views on the effect of carrying a caseload were equivocal. Some thought it helped the team manager to understand the clinical work of their staff and the pressures they faced. Others thought it resulted in managers not having enough time for team management. Views also varied in relation to the professional background of the team manager, with some suggesting that characteristics such as empathy were more important, whereas others thought that better support would, or did, come from a manager who shared their professional background (quote 20).
Pressures and frustrations
Many of the pressures faced by CMHT staff were similar across team types: increased workloads, lack of resources, bureaucratic demands, and uncertainty about the future. There were, however, two organisational features that resulted in particular frustrations. First, members of non-integrated teams frequently reported difficulties when trying to contact social workers in local authorities, including wasted time and lost information resulting from the centralised access systems increasingly used by SSDs. The lack of understanding of mental health issues they encountered when working with generic social workers was an additional frustration (quote 21). Second, staff in CMHTs where consultants did not have inpatient responsibilities, felt that this resulted in ward staff placing unreasonable demands on CMHT staff. Centralisation of beds within one hospital in geographically large trusts was also noted (quote 22).
Rewards
Every interviewee stated that they gained immense satisfaction from the role they played in helping people – service users and carers – to get better or improve their circumstances. Most spoke with enthusiasm for their work and about their team. In particular, working in MDTs was described as being interesting and rewarding, providing opportunities to learn from others and to impart their own knowledge and skills to colleagues (quote 23).
Discussion
The present study revealed a stark contrast in job outcomes for different professional disciplines. Social workers reporting low job satisfaction and poorer job characteristics relative to other practitioners is consistent with comparable studies. 289,292,294,303 However, the negative outcomes and job characteristics reported by OTs is, arguably, more surprising. Social workers and (to a lesser extent) OTs have reported significant difficulties with professional identification, role ambiguity and role conflict in CMHT settings290,292,303–305 and dissatisfaction with the genericism that characterises some multidisciplinary approaches, preferring more specialist roles to be maintained. 306 Some studies have linked role ambiguity to the legislative framework in mental health, with no statutory role for OTs, and the replacement of the exclusive ‘approved social worker’ with the more generic ‘approved mental health practitioner’ open to all disciplines. 304,307 Interview data is equivocal on this issue with some OTs operating comfortably within a generic framework while others expressed a strong desire to retain their discrete role. Role ambiguity was a concern for some but not all social workers. It is noteworthy, however, that social workers tended to express a preference for specialist multidisciplinary working compared with generic LA teams.
The analysis shows that support workers enjoyed particularly positive work characteristics, with the lowest demands, highest controls and highest social support. Existing studies of support worker job satisfaction are complicated by the heterogeneous nature of roles undertaken, and overlapping boundaries between support workers and other practitioners, making contrasts difficult. 308 This lack of role clarity has been suggested as a significant factor reducing job satisfaction. 214,303 In a recent mixed-methods study of (newly appointed) support workers in four CMHTsOP, support workers also reported reduced innovation, problematic supervision, and a lack of control over their work compared with other CMHTsOP practitioners. 214 This contrasts with the present survey, perhaps suggesting that the support worker role is becoming more established in teams. The qualitative data supports some of the current survey findings with high levels of satisfaction reported by those support workers interviewed and a feeling of being valued by colleagues. There were, however, also less positive examples including poor support from managers and lack of a clear career structure.
Integration and job characteristics
A key research question concerned the association between team integration and job outcomes. Relatively few studies have considered the impact of team integration in its broadest sense, instead focusing on the narrow aspect of multidisciplinarity. Previous evidence is equivocal. One longitudinal study, investigating the introduction of an integrated mental health and social care trust found reduced job satisfaction and increased stress within newly formed teams,300 although whether this was due to organisational form or recent change is unclear. By contrast, a cross-sectional comparison of community mental health care in four English areas found that respondents in integrated teams reported less role conflict and greater perceptions of team innovation than those in non-integrated teams. 303
Within the present study, practitioners in ‘high’ (vs. ‘low’) integration teams had greater ‘intent-to-quit’ scores, and were more likely to face an imbalance between job demands and controls. However, stepwise regression revealed that this effect was reduced and statistically insignificant when controlling for other team features. In particular, much of the apparent integration effect could be explained by staff mix, job insecurity and (among nurses) the difficulties of being managed from outside one’s own profession, posing an interesting challenge for the management and supervision of practitioners in a multidisciplinary environment. The qualitative data also suggested improved understanding between professional groups resulting from MDT membership, and almost unanimous support for multidisciplinary working, despite the many challenges this also brings. Among non-integrated teams there were reports of frustrations in accessing social services support, which were not reflected in the quantitative survey.
Limitations
Important qualifications should be considered in interpreting these results. First, the study was restricted to CMHTOP practitioners in nine mental health trusts, and undertaken at a time of organisational upheaval associated with concern over public sector finances. Although team restructuring is an occupational hazard throughout the NHS and local authorities,309,310 this issue was a dominant factor at the time of the study. It is possible that highly-integrated teams, with social worker members employed by local authorities with acute financial reductions, may have felt greater instability than non-integrated teams. Second, although the survey achieved a reasonable response rate (a recent review noting that many practitioner surveys do not exceed 50%293), it is possible that non-respondents would differ from respondents. Third, the study adopted a measure of integration (outlined in Chapter 8) based on a simple count of team features with the resultant limitations outlined. Although not a unique approach,303 it is open to debate. Additionally, this study did not measure stress directly due to space constraints within the questionnaire. The study instead relied on measures of job satisfaction, intent to quit, and, most importantly, the balance between job demands and controls that have been consistently correlated with stress and burnout. 293,311 Finally, due to space and time constraints, the qualitative data utilised for this study did not include the views of team managers or consultants, who may have held alternative views.
Conclusions
This new evidence suggests that OTs and social workers continue to face difficulty in finding optimal roles within MDTs. Support workers appear to be becoming more established, but with residual concerns about career structure and progression. These are persistent issues for consideration by professional bodies, Skills for Care and other stakeholders in addition to local managers. Integration, in a broader sense than has been considered hitherto in the literature, appears to bring both rewards and challenges. Practitioners enjoy working in a multidisciplinary environment, and integrated teams facilitate access to social care services. However concerns remain, especially where team managers and practitioners are from different professional disciplines, implying the need for improved peer mentoring and support in CMHTsOP. Further research to understand ‘what works’ in the formation of well integrated teams is warranted.
Chapter 12 Specialist mental health outreach to older residents of care homes: a systematic review of the literature
Specialist mental health support to older people in care homes is now regarded as an NHS priority, yet little is known about existing models of delivery and their efficacy.
ObjectivesTo review the literature so as to (question 1) describe patterns of specialist mental health care home outreach service delivery and organisation in the UK; and (question 2) review the impact of these on resident outcomes.
MethodA systematic literature review adopting a bibliographic database search (EMBASE, MEDLINE, PsycINFO, Web of Science) for relevant English-language materials published since 2000 (question 1) and 1989 (question 2), supplemented by hand-searching of references. The review excluded studies focused on short-term training interventions.
ResultsFifteen references were identified (7 and 12 relevant to questions 1 and 2, respectively), all from either the UK or Australia. Six restricted their interest to residents with dementia and three to those with depression. All except one investigated a specific service model, featuring a MDT and involving regular meetings with care home staff and/or GPs; the preparation of tailored resident care plans; and/or training of care home staff. The quality of outcome studies varied with respect to whether or not they used an experimental design; the length of follow-up; the outcome measures used; and sample size. Although all three studies of depressed residents found evidence of positive outcomes following the outreach intervention, each lacked an appropriate control group. The impact of services for residents with dementia was mixed, although there was tentative evidence that outreach services can reduce the use of neuroleptics without an associated deterioration in resident behaviour.
ConclusionsThere is insufficient evidence with respect to existing outreach service configurations and their (cost-) effectiveness. Given current efforts to expand such service provision, filling this evidence gap should be afforded high research priority.
Background
It has been recognised that the mental health needs of care home residents are generally not well met, with input from mental health services usually occurring on an ad-hoc basis and referrals to specialist services usually made at times of crisis. 57 Up to three-quarters of residents in non-specialist care homes have dementia312 and there is considerable concern regarding the overuse of antipsychotic medication to manage the associated behavioural and psychological symptoms. 313 There is evidence that these drugs are prescribed freely, not always reviewed appropriately and not withdrawn as soon as they could be. 59 Clinically significant levels of depression affect between 30% and 40% of UK care home residents,62 with one study reporting ‘case’ level depression in 45% of new care home admissions. 314 Furthermore, care home staff find this hard to detect. 64 Recent recommendations for improving quality of care for residents with dementia include commissioning specialist in-reach services from CMHTs; appropriate use of antipsychotic medication for people with dementia; and readily available guidance for care home staff on best practice in dementia care. 57
Reviews of mental health outreach to care home residents have mainly focused on dealing with the challenging behaviours associated with dementia,315 including alternatives to pharmacological interventions. 316,317 Earlier reviews have identified MDT models as being the most beneficial,318,319 with the least effective model consisting of traditional consultation-liaison services with a clinician providing treatment recommendations on an as-needed basis. 318 The lack of rigorously designed studies has also been noted. 318,319
Review questions
A systematic literature review was undertaken to address two questions. First, how do the structure, organisation and activities of specialist mental health services in the UK in the twenty-first century vary in the provision of outreach support for older people in care homes? Second, what is the impact of these outreach services on service user outcomes? The literature review was also used to inform two subsequent surveys: one of outreach provided by CMHTs for older people in care homes and the other of care homes’ perspective of outreach services.
Review methods
A systematic review of the literature commenced in 2010 with discussions with experts in the field to focus on areas of investigation for this part of the study. A search was made of four electronic databases (EMBASE, MEDLINE, PsycINFO and Web of Science) from 1989 to the current date on the 15 June 2010. The search terms included those describing the service user, the care setting and components of outreach in terms of who does it and what they do. The search strategy is included in Appendix 35. Subsequent hand searches were made of relevant journals in the field and references from papers selected for the review.
All potential studies were assessed against inclusion criteria, which were different for the two questions (Box 22). Question 1 focused on more recent papers, since 2000, to provide a contemporary picture of services in the UK. Question 2 focused on outcomes and included papers since 1989, when old age psychiatry was recognised as a specialty within the NHS. It was originally intended to only include studies of existing service models and not studies specifically set up for research. This was subsequently widened to include the latter to increase the number of studies included in the review.
| Question 1 | |
|---|---|
| How do the structure, organisation and activities of specialist mental health services in the UK in the twenty-first century vary in the provision of outreach to support older people in care homes? | Type of literature Include: UK literature published in peer-reviewed journal articles; books/book chapters; reports in English in or after 2000 Exclude: International literature; discussion papers; other grey literature Study design Include: Empirical and non-empirical studies Focus of intervention Include: Describe at least one aspect of structure, organisation or activities (including training alone only if regular and not one-off/short-term) relating to the provision of specialist mental health outreach to care homes Exclude: One-off, short-term training studies; services focusing on physical health; intermediate care services; primary care services Participants Include: Older people with mental health problems Exclude: Not mental health; not older people |
| Question 2 | |
| What is the impact of these outreach services on service user outcomes? | Type of literature Include: International literature published in peer-reviewed journal articles, books/book chapters, reports in English in or after 1989 Exclude: Discussion papers and other grey literature Study design Include: Empirical studies Focus of intervention Include: Evaluate at least one aspect of structure, organisation or activities (including training alone only if regular and not one-off/short-term) relating to the provision of specialist mental health outreach to care homes Exclude: One-off, short-term training studies; services focusing on physical health; intermediate care services; primary care services Participants Include: Older people with mental health problems Exclude: Not mental health; not older people Outcomes Include: Must include one or more service user outcomes, including change/reduction in antipsychotic/antidepressant drug use, mortality, cognitive function, behaviour problems, depression and well-being Exclude: No outcome measures; physical functioning alone |
Initial screening of titles and abstracts was undertaken by one reviewer. A second reviewer undertook a random check of 10% of the 1241 papers to ensure consistency. Full copies of the considered papers were retrieved and were assessed by both reviewers independently and agreement was reached regarding their inclusion. Both reviewers were involved in the preparation of data extraction forms, which are included as Appendix 36. The forms were used to extract the data from each paper summarising the key elements of the intervention. For question 1, this included aims of the study; study design; scale of the intervention; information about staff undertaking the intervention; what the intervention consisted of; how it was undertaken; details of residents taking part; and study findings. The same information was collected from papers addressing question 2, with additional information on any comparison intervention; outcomes for service users; use of services; cost measures; limitations of the study; and a measure of study quality. The latter used an existing instrument, which described and measured key characteristics of the studies across a range of categories including descriptions, sampling, measurement, analysis and interpretation of results. 186 Each paper was assigned a score of nine possible limitations, which was collapsed to three categories: good quality (0–1), fair quality (2–4) and limited quality (≥ 5) to decide on inclusion. 320 For consistency, the first two studies were discussed and extracted by both reviewers together. The remainder were extracted by one reviewer. The data were then entered onto an Excel™ spreadsheet (version 2007; Microsoft Corporation, Redmond, WA, USA). A narrative synthesis approach was used to explore the relationship between the studies. 187 Findings are presented regarding care home settings, the residents who receive the service followed by the research questions to provide information on the structure, organisation and activities of outreach and outcomes for residents.
Results
The literature
The electronic database search yielded 1241 references (Figure 15), of which 12321–332 met the inclusion criteria. A further three papers333–335 were identified from reference tracking, giving a total of 15 papers, of which seven321–325,333,334 were relevant to question 1 and 12323–332,334,335 were relevant to question 2. All were papers published in peer-reviewed journals and each represented a different study. The earliest paper332 was published in 1992, followed by two papers326,332 published in 1999, eight papers321,323,325,327–329,331,333 between 2001 and 2005 and four322,324,334,335 published between 2006 and 2011. The main reasons for rejection were first, that they focused solely on short-term training initiatives set up for research and second, that their focus was not on mental health support or outreach. The latter category included papers about prevalence and activities provided in the home for residents with no specialist professional input.
FIGURE 15.
Study selection process. N/A, not applicable.
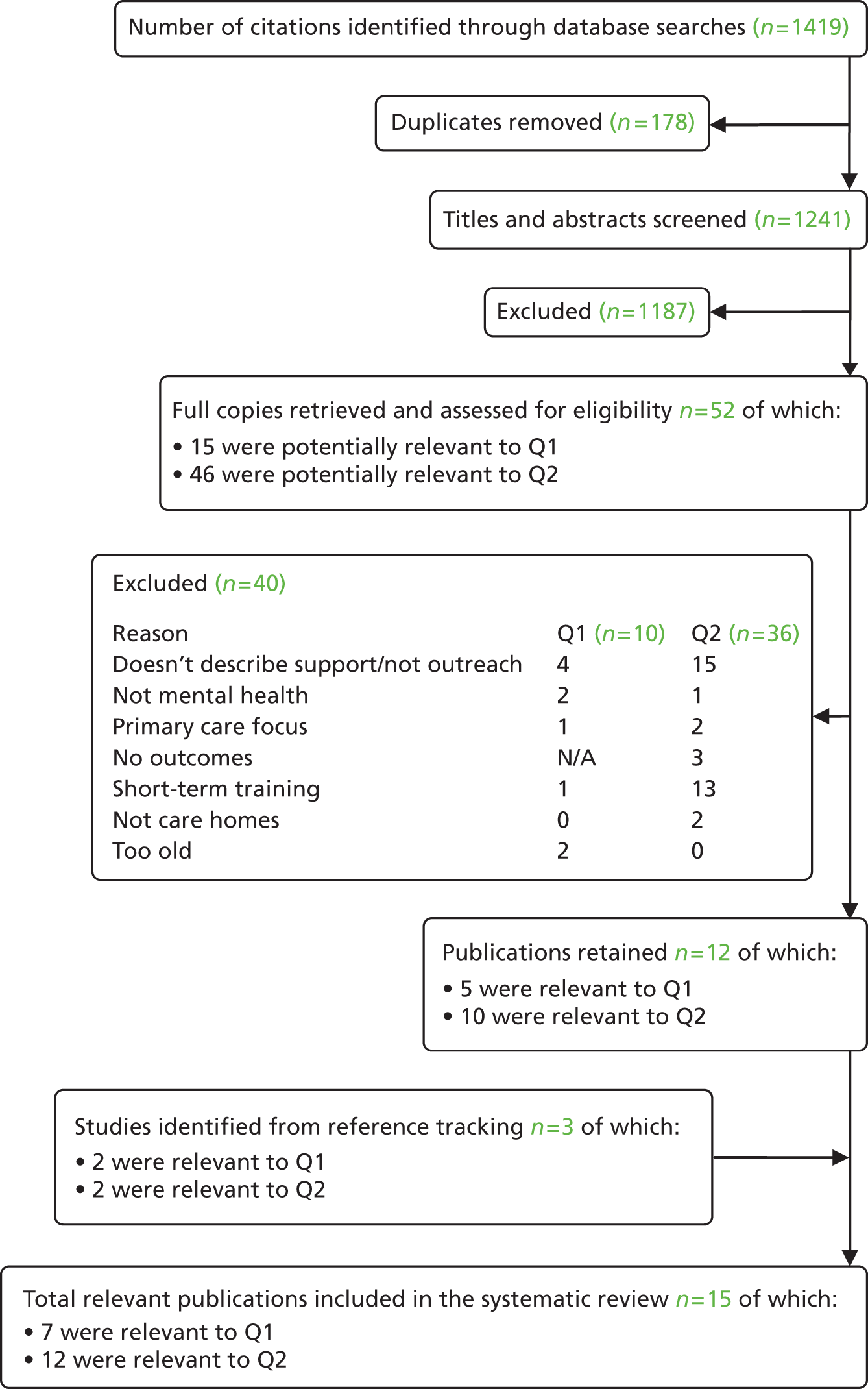
The studies
Summary descriptions of the studies are shown in Table 70. These included one survey. Eight of the studies were based in the UK, including a survey of care home managers. 321–326,333,334 One study was too old to be included for question 1. 326 Seven studies were undertaken in Australia. 327–332,335 Five of the studies described existing service models, three in the UK322,333,334 and two in Australia,327,332 while nine studies had been specifically set up for research of which four were UK-based323–326 and five were Australian-based327–331 studies.
| Authors and location | Target population | Study aims | Outreach activity | Outcomes, limitations and conclusions |
|---|---|---|---|---|
| Studies addressing question 1 only | ||||
| Hayes and Martin 2004333 UK |
Mental health (56 nursing homes) |
Describes a multidisciplinary CHST model | Specialist nurse undertook assessment, held caseload, advised on care planning, referred to specialist services and monitored care Training programme for staff Medication review by pharmacist |
The model facilitated effective working between primary care services, the CHST and the independent sector and care staff The role of the specialist nurse has proven to be feasible and popular with the homes and GPs |
| Purandare et al. 2004321 UK |
Mental health and behaviour problems | A survey of care home managers focused on the extent of service provision by old age psychiatrists and the type and adequacy of support given | Various | Perception that needs were not met to satisfaction of care home managers Variation across UK in visits from old age psychiatrists and only half felt the frequency was adequate Only one-fifth received help with staff training Little SW or psychologist input Over half perceived non-pharmacological advice as inadequate |
| Rands et al. 2009322 UK |
Mental health and behaviour problems (1 care home) |
Describes the evolution of a multidisciplinary group | Consultation liaison meetings involving care staff, manager, link GP and psychiatrist followed by further assessment and investigations | Eleven care staff completed a questionnaire: led to a better management of patients, increased knowledge, effective multiprofessional work and improved communications |
| Studies addressing question 1 and question 2 | ||||
| Ballard et al. 2002323 UK |
Dementia (208 intervention and 125 control residents) |
Evaluates use of a multidisciplinary psychiatric liaison service in reducing neuroleptic drugs use, improve quality of care and decrease health service utilisation | Residents reviewed within 24 hours by CPN following referral CPN helped to develop care plans for residents discontinued from neuroleptic drugs. ABC diaries used Psychological interventions were first-line approach Each resident received a psychiatric evaluation, including medication review |
Neuroleptics discontinued in 41% of residents with no significant exacerbation of symptoms Significant overall reduction in neuroleptics in liaison homes but not in controls. No significant difference between proportions discontinuing over 9 months between the two Significantly fewer GP contacts in liaison homes No significant improvement in resident well-being in liaison homes Limitations: Provision of support for staff over weeks rather than longer |
| Hirst and Oldknow 2009334 UK |
Mental health (460 residents) |
Describes a care home liaison service involving psychiatrist and mental health nurses | Assessment, formulation of person-centred care plans Support, education and training for staff |
Reductions in hospital admissions from care homes Less antipsychotic drug use Reduced LOS on mental health wards for those discharged to a care home Empowered care home workforce New links with primary care and specialist services Limitations: No information on how outcomes obtained |
| aLyne et al. 2006324 UK |
Depression (156 residents) |
Evaluates a training and care planning approach to reducing depression by a CMHT for older people | Staff training programme – four 3-hour weekly sessions CPNs and OT acted as mentors to care staff working with intervention group – weekly one-to-one No contact with resident |
Clinically significant improvements in depression scores associated with the care planning interventions Intervention less effective in reducing depression in residents with more severe dementia Improvements not accounted for by changes in psychotropic medication Limitations: No control group. Not all depressed residents received intervention due to lack of care staff. Delays due to staffing problems in the care homes |
| aMoxon et al. 2001325 UK |
Depression (36 residents for first part, 8 for second part) |
Assesses feasibility of involving care staff in reducing prevalence of depression by a CMHT for older people | Staff training programme – four 3-hour weekly sessions on recognising and dealing with depression Care planning intervention – mental health staff acted as mentors to support care staff in implementing care planning interventions |
Reduction in depression to below case-level in seven out of eight residents Limitations: No control group. Low sample size |
| Studies addressing question 2 only | ||||
| Borbasi et al. 2011335 Australia |
Dementia (behavioural and psychological symptoms) (7 intervention and 13 control homes) |
Describes the implementation and evaluation of a multidisciplinary dementia outreach service | Specialist nurse undertakes assessment, provides advice and refers to service Nurses work with staff to manage behaviour and implement tailored interventions Training on one-to-one and group basis |
Inconclusive findings on resident QoL improvements Mean level of resident feelings had slightly greater increase for intervention group Staff improved knowledge and confidence Fewer acute admissions Facility-level satisfaction with service Limitations: High staff turnover affected the study |
| Brodaty et al. 2003327 Australia |
Dementia complicated by depression or psychosis (28 case management, 27 consultation and 31 control residents) |
Compares outcomes of multidisciplinary psychogeriatric case management model with GP consultative model and standard care | Case managers allocated to individual residents Treatment plans provided for homes and GPs Behavioural management programmes Interventions for depression including individual therapy Staff education on psychosis Drug review |
All three groups improved on either depression or psychosis scales. Mode of management made no difference in rate or amount of improvement Use of antidepressant or antipsychotic drugs did not predict outcomes Trend towards greater improvement in behaviours in case management group Limitations: Complex study design and multiple entry criteria. Residents selected on preset criteria. Possible leakage of treatment techniques as residents fully randomised |
| Crotty et al. 2004328 Australia |
Dementia (behaviour problems) (50 intervention, 54 and 50 controls) |
Evaluates the impact of multidisciplinary case conferences | Medication review Identification of problems Two multidisciplinary case conferences 6–12 weeks apart Half-day workshop on managing challenging behaviours |
Improved medication appropriateness in intervention group Significant reduction in inappropriate prescribing of benzodiazepines in intervention group No impact on resident behaviours Limitations: Low level of behaviour problems among participants at baseline. Possible change in staff perceptions of behaviours |
| Kotynia-English et al. 2005329 Australia |
Mental health (depression or behaviour symptoms associated with dementia) (53 intervention, 53 control residents) |
Assesses the effect of early multidisciplinary psychiatric intervention | Assessment of referrals by case manager and psychiatrist Management plan drawn up Review by other team members if required |
Early screening of behavioural problems did not significantly change mortality, number of medical contacts or mental health outcomes. Both groups had poor outcomes Limitations: Screening following random allocation to group meant that clinical intervention was not necessarily the same for all |
| Llewellyn Jones et al. 1999330 Australia |
Depression (109 intervention, 111 control residents) |
Evaluates the effectiveness of a multifaceted shared care intervention | Regular multidisciplinary meetings Education for GPs and care staff on managing depression Health education and activity programmes for residents, the latter assisted by volunteers to enable elderly residents to participate |
Significantly greater improvement in depression in intervention group Evidence that the intervention helped prevent mild depression from becoming worse No greater use of antidepressants or reduction in depressogenic drugs Limitations: Groups were studied over different time periods |
| Opie et al. 2002331 Australia |
Dementia (challenging behaviours) (48 intervention, 51 control residents) |
Evaluates the use of individually tailored care planning interventions by a MDT | Psychiatrist assessment at baseline Team met weekly to discuss new referrals and formulate care plans Individual behaviour management plans presented to staff and reviewed a week later |
Observation showed behaviours lessened in both groups but occurred uncommonly anyway Behaviour scores decreased for both groups prior to introduction of strategies Staff ratings showed modest but significant improvement in target behaviours Limitations: Short follow-up period of 4 weeks |
| Proctor et al. 1999326 UK |
Dementia (behaviour problems) (60 intervention, 60 control residents) |
Evaluates a behavioural intervention by multidisciplinary hospital outreach team | Staff attended seven 1-hour seminars CPN visited homes weekly to advise and support staff in developing care planning skills using a goal planning strategy |
Intervention group residents had significantly improved scores for depression and cognitive impairment but not for behaviour rating or ability to undertake ADL Intervention homes had fewer GP visits at follow-up, otherwise little variation in service use Limitations: Staff who received training were aware of the intervention. Longer follow-up to assess how long positive effects continued after intervention ceased |
| Seidel et al. 1992332 Australia |
Mental health (behaviour problems) (66 intervention residents) |
Assesses the usefulness of a small psychogeriatric outreach team | Assessment on referral by psychiatrist and CPN Management plan included diagnostic investigations, psychotropic medication, services and financial advice and implemented by allocated case manager in consultation with GP, care workers and family Emphasis on involving GP. Small team and high referral rate so other professionals carry out recommendations Team involved in follow-up |
Reduction in behavioural disturbances Patients with dementia and psychotic disorders showed clinically and statistically significant improvement No significant improvement for patients with major depression Limitations: No control group |
The recipients
Six studies addressed outreach to residents with mental health problems more generally, of which four were based in the UK. 321,322,333,334 including a survey. 321 One of these was based in a nursing home providing psychiatric nursing care. 322 These also included two Australian studies, which targeted services on residents with both dementia and depression. 329,332 Four of the five studies of existing services were also in this group. 322,332–334 Six papers examined outreach for older people with dementia and all were mainly concerned with reducing behavioural problems. This included two UK studies both undertaken in care homes323,326 and four papers based on studies undertaken in Australia, three of which were undertaken in nursing homes327,328,331 and one in aged care facilities335 in different Australian states. Only three of the studies focused solely on older people with depression: two were UK based324,325 and the other Australian. 330 Of the UK studies, one was a pilot study undertaken in two homes324 while the second involved 14 homes in a single area with a mix of LA, private and voluntary homes. 325
Team structure
All studies, except the survey,321 reported outreach activities undertaken by some form of MDT. The composition of the teams varied. All teams included psychiatric nurses who performed a central role in undertaking outreach activities across the studies. It was not always clear exactly which professional staff groups were involved in all the studies reviewed here, though all included input from a psychiatrist, either direct or in a supervisory role. Psychologist input appeared common, with some input also from other physicians. OTs appeared to be involved to a lesser extent with little social work input described. The survey focused on the extent of outreach provided by old age psychiatrists. 321 The findings revealed large variation across the UK. Only half of the survey respondents felt the frequency of visits by old age psychiatrists to care homes was adequate.
Organisation of outreach
Variation was evident across the studies in how outreach services were delivered. Three studies reported holding multidisciplinary meetings within the care homes. 322,328,330 In the study of an existing service by Rands et al. 322 this involved a 3-hour meeting every 3 months in the care home involving care staff and manager, a link GP and psychiatrist and included a general update; review of concerns; and discussion of up to 16 residents at each meeting looking at problems and management options. In two studies this involved weekly visits to care homes by a CPN. 323,326 Another study reported regular visits with the allocated time of an older people’s specialist nurse. 333
Outreach activities
Referral, assessment and review
Direct referral of residents to mental health services has been associated with a speedier response and the perception of a better service by care homes. 336 In only two of the studies were care home staff able to directly refer residents to the outreach service. 323,332 In one of these, residents were then assessed within 24 hours. 323 Systematic case finding or screening occurred in three of the studies,322,323,329 while six reported the use of standardised tools and measures to assess resident need. 322,323,327,329,331,333 The intervention in eight of the studies included reviews of medication and the mental health of residents (following an initial assessment). 322,323,327,328,331–334 Only one study stated that medication review was undertaken by a pharmacist. 333
Care planning
Almost all studies involved mental health staff in the preparation of individually-tailored care plans for residents. This frequently included giving advice on behaviour management, and activities and individual therapy interventions for residents with depression. 327 Different care planning strategies were used including antecedent, behaviour, consequences (ABC) diaries323,337 and the use of goal planning strategy. 326 In the study by Ballard et al. 323 the aim was to use psychological interventions in the first instance. The study by Opie et al. 331 involved the team formulating care plans, presenting these to care home staff and reviewing them a week later. In one study332 this involved the allocation of a case manager, who implemented the plan in consultation with the GP, care staff and the resident’s family. In two studies, psychiatric nurses and the OT acted as mentors to care staff and met weekly on a one-to-one basis to do so. 324,325
Training
Although the review did not include studies that focused solely on short-term training interventions, nine of the studies included training of care home staff as part of the service. 324–328,330,333–335 This ranged from small-scale one-off training or workshops for care home staff on areas such as managing challenging behaviours328 and depression330 to the provision of training programmes to staff. 324–326,333 In the studies by Lyne et al. 324 and Moxon et al. 325 staff participated in a training programme consisting of four 3-hour weekly sessions, focussing on problem recognition, identification of depression, strategies of responding and the use of a checklist to assess the presence and degree of depression. One study included training on recognition and management of depression for GPs as part of the intervention. 330 The survey found that only one-fifth of the care home managers reported receiving some help with staff training and about 80% wanted more input in this area. 321
Outcomes for residents
Twelve studies examined the impact of outreach services on service user outcomes. 323–332,334,335 The resident outcomes measured by the studies included reduction in depression scores; reduction in drug use and more appropriate use of medications; improved clinical outcomes; improvement in behaviour problems; and QoL.
Three of these studies examined the effect of mental health services on residents more generally. 329,332,334 An assessment of an existing small psychogeriatric outreach team involving assessment, care planning and involvement in follow-up had mixed results with a reduction in challenging behaviours and statistically significant improvement for patients with dementia, but no significant improvement for patients with major depression. 332 This study did not have a control group. A second study found that early screening of behavioural problems did not significantly impact on mental health outcomes,329 although in this study residents were screened following random allocation to the intervention group. The final study reported a reduction in antipsychotic drug use, but no information was given on how this was measured. 334
Six studies focused on the impact of mental health services on residents with a primary diagnosis of dementia. 323,326–328,331,335 A study aiming to reduce drug use with a review by a CPN and assistance with developing care plans found that this led to a discontinuation of neuroleptics in 41% of residents with no significant exacerbation of symptoms and a significant overall reduction in neuroleptics in intervention homes. 323 Another study evaluating the impact of two multidisciplinary case conferences 6–12 weeks apart found improved medication appropriateness in the intervention group, but no impact on resident behaviours, possibly explained by the low level of behaviour problems at baseline. 328 Similarly, a further study of care planning interventions showed a reduction in behaviours in both intervention and control residents, but again from a low level at the start. 331 Proctor et al. 326 found significantly improved scores for depression and cognitive impairment, but no improvement for behaviours as a result of their care planning intervention. However, a study by Brodaty et al. ,327 evaluating a multidisciplinary dementia outreach service involving nurses working with staff to manage behaviour and implement a tailored intervention, found a trend towards greater improvement in behaviours in their case management group. Their findings on changes to resident QoL were inconclusive. 327
Only three studies focused on residents with depression324,325,330 and all reported positive outcomes for residents. Two studies which involved a staff training programme and then support with care planning found a reduction in depression scores,324,325 although this was less effective in reducing depression in residents with more severe dementia. 325 However, there were no control groups in these studies and in that by Moxon et al. 325 the sample was very small. The third study, involving education for care staff and GPs and health education and activity programmes for residents, found a significantly greater improvement in depression in the intervention group and evidence that the intervention helped prevent mild depression from worsening with no greater use of antidepressants. 330
There was much variation in the follow-up periods of the studies, ranging from just 4 weeks331 to 12 months,329 with only four studies having a follow-up period of between 6 and 12 months. 323,326,329,330
Methodological quality
The methodological quality of the papers addressing outcomes was assessed. 320 Three of the 12 studies were rated as ‘good’,326,329,332 eight were rated as ‘fair’323–325,327,328,330,331,335 and only one of the studies was rated as ‘limited’. 334 All of the outcomes papers had some form of limitation associated with the methodology. Several studies had no control group. 324,325,332,334 A relatively short-lasting intervention and follow-up period were limitations in two studies. 323,331 Other limitations included the effect of staffing problems within the care homes,324,335 a complex study design327 and low sample size. 325 Furthermore, different measures were used to measure resident outcomes across the studies.
Discussion
This review has several possible limitations. First, only two of the papers were discussed and extracted by two researchers, the remainder were examined by one researcher alone and the information extracted was not checked by a second researcher. Second, the information extracted for the review was restricted to that available in the publications. It is possible that other relevant material was not identified. In particular, the quality of the information in the papers that only addressed the first question on the variation in specialist mental health services in the UK in the twenty-first century was somewhat variable. It had been anticipated that these papers would be important in providing a comprehensive understanding of outreach arrangements in a UK setting. Third, differences between countries in terms of culture and how outreach is undertaken must be taken into consideration. This review included studies from the UK and Australia with different care home organisational arrangements and policies, although the studies’ findings were similar.
The review brings together different types of studies: existing service descriptions and evaluations, evaluations of studies set up for research and a survey of care homes to look at the variation in the provision of outreach in the UK and the impact of outreach services on service user outcomes internationally. The review found very few studies of existing ‘real-life’ services, five in all, with only published evaluations of two Australian studies. The outreach services reported were predominantly multidisciplinary in nature and involved primarily care planning interventions targeted at behaviour problems for residents with dementia and activities for residents with depression, with some degree of training for care staff in recognising and dealing with problems in about half the studies. This was reflected across both the UK and international studies. The study findings showed improvements for residents with depression, although based on few studies, whereas the impact of outreach services on residents with dementia was less clear.
Few studies included a screening element, which has been suggested to have an important role to play in improving outcomes for residents with depression by intervening at an early stage before the illness becomes more severe. 338 In view of the lack of evidence found for screening for depression in care homes, work such as the proposed trial originally planned for this study, but not funded, could be particularly useful. The importance of early diagnosis and treatment is also an objective in recent policy on caring for older people with dementia. 57 Although the studies were mainly multidisciplinary interventions, the main input appeared to be provided by a psychiatric nurse and psychiatrist with little occupational therapy input. The latter may reflect the fact that few of the studies focused on residents with depression, where their input with activities may be more expected. There was a clear positive effect across studies of staff education and training, and the survey of care homes identified a low level of training provision for staff.
Conclusions
The review examined two questions. In relation to the first, the UK studies included here showed similarities in the structure, organisation and activities of specialist mental health services for care home residents. They all involved multidisciplinary input, care planning interventions and all except one included a support and training element for staff. Regarding the second, the impact of outreach services was not clear from the evidence currently available. Information from subsequent surveys will identify the national pattern of variation in mental health services for this group and it will be interesting to see if, and to what extent, the above elements are included. To address the inconclusive evidence on the impact of services, particularly in the UK, an evaluation of which aspects of outreach, undertaken by whom are the most appropriate for residents with different mental health problems in different types of care home settings would be very beneficial.
Chapter 13 Specialist mental health outreach to older residents of care homes: methods
Introduction
The aim of this part of the study was to identify the national pattern of specialist mental health outreach services for older people living in care homes. The original intention was to focus on services for older people with depression; this was later extended to include older people suffering from other mental health problems, including dementia. The study was informed by a literature review, previous surveys undertaken by the PSSRU on old age mental health73,339 and consultation with old age psychiatrists in the local area. It involved two national surveys, one of CMHTsOP and one of care home managers, which are described below.
Community mental health team survey
Questionnaire development
A questionnaire was developed by the research team to provide an overview of the nature and extent of the mental health support provided by CMHTsOP to care homes (see Appendix 37). It was piloted in three CMHTsOP and revised. The questionnaire was designed with mainly fixed-response fields with some open-text fields for elaboration. The broad domains covered by the questionnaire were:
-
background information on staff numbers and qualifications
-
extent of staff input into care homes
-
the referral of residents to the team
-
case finding and screening
-
assessment of residents
-
mental health and medication review
-
involvement in care planning
-
the provision of training to care staff
-
the availability of other services in the locality
-
views on the sufficiency and quality of the mental health service.
Data collection
A national survey of all CMHTsOP in England was undertaken in 2011. A database of these was created based on the one used by the earlier CMHTsOP study presented in this report (see Chapter 8), with thorough checking to identify changes. A paper questionnaire was sent to the team managers of the 421 CMHTsOP identified in England in July. This was followed in August by a second mailing to non-respondents and subsequently by telephone calls. Fieldwork ended in January 2012.
Care homes survey
Questionnaire development
A short questionnaire (see Appendix 38) was developed by the research team to ascertain the amount and adequacy of mental health support received by care homes from external health-care services. The main domains included in the questionnaire were:
-
information on the mental health of residents
-
staff numbers and qualifications
-
frequency of visits by health service professionals
-
referral procedures
-
quality of mental health support
-
sufficiency of mental health support.
Data collection
A database of all active care homes England was provided by the Care Quality Commission in September 2011. A stratified sample of 1000 homes was created for homes with and without nursing and with provision for older people and/or dementia. A paper questionnaire was sent to 1000 care home managers in late 2011, with a second mailing to non-respondents in January 2012. Fieldwork ended in March 2012.
Data management and analysis
Data were analysed using SPSS for Windows (version 19). The analyses were predominantly descriptive. Coding frames were prepared for the open-ended questions from the responses provided. Differences between groups were explored using appropriate statistical tests. Regression models were used to explore factors influencing perceived quality of care.
Chapter 14 Specialist mental health outreach to older residents of care homes: national surveys
To describe existing patterns of specialist mental health outreach for older care home residents, and perspectives of the quality and sufficiency of these services.
MethodTwo national self-administered postal surveys of CMHTsOP’ managers and a representative sample of care home managers.
ResultsMembers of 231 (55%) CMHTsOP returned a questionnaire, almost all (97%) reporting that their team offered support to care home residents. One-third of teams reported that they dedicated ring-fenced staff time to these activities. Systematic case finding, and open clinics were not commonplace, but regular visits to care homes and telephone advice were provided by most teams. Seventy per cent of teams reported that they had processes in place for the initiation, review and cessation of antipsychotics for residents with dementia. Most (85%) teams felt that care home staff were not appropriately skilled for the care of residents with dementia, but only 41% of teams reported that they provided formal training.
In addition, questionnaires were received from 391 (40%) of invited care homes. Respondents reported that more mental health support to care homes was provided by GPs and community nurses than by specialist mental health practitioners. Most (85%) respondents rated the quality of mental health support as at least ‘fair’, but fewer than one-third of respondents were confident that their staff were appropriately trained to care for residents with mental health needs.
ConclusionsBoth surveys revealed a lack of confidence about the capacity of care home staff to meet the mental health needs of older residents, suggesting specialist outreach support could refocus on building their skills and confidence.
Introduction
The aim of this part of the study was to identify the national pattern of specialist mental health outreach services for older people living in care homes. This chapter presents the findings from two national surveys: one on CMHTsOP outreach to care homes and the other on the external services received by care homes to support the mental health needs of residents.
Community mental health team survey
Questionnaires were received from 231 CMHTsOP, a response rate of 55%. At least one questionnaire was returned from all except one of the then current NHS mental health trusts across England. Six of the included CMHTsOP were specifically care home liaison teams. The average number of staff in the sample of CMHTsOP was 19 per team. The numbers of staff ranged from 2 to 61, with just under one-third of teams having 21 or more members of staff and one-fifth of teams having 10 or fewer. On average, one-third of the team members were not professionally qualified. This included support workers and administrative staff. Almost all CMHTsOP (97%) supported residents in care homes, whether or not the home had nursing staff.
Outreach activities in care homes
Information was obtained about the outreach activities of CMHT members in care homes. These included case finding, assessment, medication and mental health reviews, care planning and staff training. These are described below.
Nearly three-quarters (72%) of CMHTsOP reported that they did not undertake any systematic case-finding in care home settings. Of those who did, about one-fifth (59 in total) focused on identifying dementia, depression and mental health problems in general. Four-fifths of these CMHTs reported using standard tools for screening. The majority of teams used cognitive measures, such as the MMSE142 and Addenbrooke’s Cognitive Examination-Revised340 (ACE-R). Some use was also made of tools to identify depression, such as the GDS143 and Cornell Scale for Depression Inventory. 341 Such case-finding was generally undertaken on request (87% of the time in 58 teams), with few reporting case-finding to be done routinely, or following admission to a care home. In the majority of CMHTsOP, clinical staff undertook this activity, with nurses and consultants recorded most frequently. Other members of the CMHTsOP such as SWs, OTs and psychologists were reported much less frequently.
The use of standardised assessment tools was reported by almost all teams (98%). The tools most commonly used were MMSE142 and ACE-R,340 which were used by about twice as many teams as used tools to measure depression. The sources of information for assessments of residents are shown in Table 71. Discussions with the care home staff and the resident, alongside a review of records were reported as being the main means of information gathering, followed by consultation with the resident’s family and finally the GP (78%). In terms of the staff undertaking assessment, greater variation was evident than for screening. Medical staff, such as consultants and nurses, formed the majority, but it was reported frequently that all team members could undertake initial assessments, including OTs, social workers and psychologists.
| Information source | Regularly | Sometimes | Rarely/never | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Assessment (n = 219) | ||||||
| Discussion/liaison with GP | 171 | 78.1 | 41 | 18.7 | 7 | 3.2 |
| Discussion with care home staff | 215 | 98.2 | 4 | 1.8 | – | – |
| Review of records | 203 | 92.7 | 12 | 5.5 | 4 | 1.8 |
| Consultation with resident | 214 | 97.7 | 5 | 2.3 | – | – |
| Consultation with resident’s family | 183 | 83.6 | 34 | 15.5 | 2 | 0.9 |
| Medication review (n = 153) | ||||||
| Discussion/liaison with GP | 135 | 88.2 | 15 | 9.8 | 3 | 2.0 |
| Discussion/liaison with a pharmacist | 43 | 28.1 | 59 | 38.6 | 51 | 33.3 |
| Discussion with care home staff | 144 | 94.1 | 7 | 4.6 | 2 | 1.3 |
| Review of records | 137 | 89.5 | 8 | 5.2 | 8 | 5.2 |
| Consultation with resident | 128 | 83.7 | 17 | 11.1 | 8 | 5.2 |
| Consultation with resident’s family | 105 | 68.6 | 35 | 22.9 | 13 | 8.5 |
| Mental health review (n = 209) | ||||||
| Discussion/liaison with GP | 152 | 72.7 | 50 | 23.9 | 7 | 3.3 |
| Discussion with care home staff | 207 | 99.0 | 2 | 1.0 | – | – |
| Review of records | 199 | 95.2 | 9 | 4.3 | 1 | 0.5 |
| Consultation with resident | 202 | 96.7 | 6 | 2.9 | 1 | 0.5 |
| Consultation with resident’s family | 172 | 82.3 | 35 | 16.7 | 2 | 1.0 |
The majority (70%) of CMHTs reported a systematic process in place for the initiation, review and/or cessation of antipsychotics for care home residents with dementia. A high proportion of teams reported that medication reviews regularly involved consultation with GPs, care home staff, the resident and review of residents’ records (see Table 71). Regular pharmacist input was reported by 28% of CMHTsOP. The majority of medication reviews were undertaken by medical or nursing staff. Ninety-four per cent of CMHTs reported that they undertook mental health reviews of residents. In response to when residents were reviewed, over three-quarters reported that this was on request, with over half also reporting both routine reviews and reviews following changes in resident care. Mental health reviews also regularly involved consultation with care home staff and the resident with a record review (see Table 71). These assessments were again carried out predominantly by medical and nursing staff, with much less input from OT and social workers as might be expected.
The provision of regular care planning advice on individual residents to care home staff was reported by almost all teams (98%). Over three-quarters of CMHTsOP reported visiting homes both on a regular and an as-required basis to see specific residents. The provision of regular advice by telephone was reported by two-thirds of the teams. However, the regular provision of open clinics within homes was uncommon (12%). The majority of staff involved were, again, consultants and nurses. However, input by care co-ordinators, OTs and social workers was also reported.
Fewer than half (41%) of CMHTsOP reported that they provided formal training to care home staff. Where this occurred it was mainly undertaken by CPNs. Teams described training as focusing on dementia awareness with behaviour management a large part of this. Risk assessment training and a small amount of medication training were also reported, but to lesser extents. Four fifths of teams targeted training at care staff, followed by regular training for nursing staff (62%) and care home managers (44%). About one-third of teams reported that training was regularly undertaken by means of one-off sessions within the care homes. Regular ongoing training within homes was reported by just under one-fifth of teams. Training external to homes was reported to occur less commonly.
Structure and organisation of outreach services
This section reports team arrangements for working with care homes, including team structures, clinical responsibility for residents and referral procedures.
Community mental health teams for older people were asked about the extent to which staff had ring-fenced time to work with care homes. Only 20% of CMHTsOP reported having a team member fully committed to this work and fewer (12%) had a member partially committed. When asked if the CMHTsOP had identified staff members linked to specific homes, 44% of CMHTsOP responded that this was the case for at least some, if not all, homes. Additionally, about two-fifths, reported having an identified senior staff member who took the lead for dementia care within the homes. Clinical responsibility for the mental health of residents was unclear. Under half of teams stated that this was held by the consultant psychiatrist or by other team members whereas just over one-quarter, reported that this was held by the GP.
Table 72 shows the sources of referrals from care homes to CMHTsOP. Most were through GPs, with 92% of CMHTs regularly receiving such referrals. One-third of teams reported regularly receiving referrals from social services staff, whereas one-quarter of teams regularly received referrals from care home staff. Referrals from community nurses were reported less frequently. Although almost all CMHTs reported that they saw residents within the care homes, 59% of teams reported regularly or occasionally seeing residents in memory clinics, and half in hospital outpatient departments.
| Source of referral | Regularly | Sometimes | Rarely/never | Total | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | |
| GP | 206 | 92.0 | 16 | 7.1 | 2 | 0.9 | 224 |
| Community nurses | 25 | 11.3 | 101 | 45.5 | 96 | 43.2 | 220 |
| SSD staff | 75 | 33.5 | 99 | 44.2 | 50 | 22.3 | 224 |
| Care home staff | 55 | 24.6 | 64 | 28.6 | 105 | 46.9 | 224 |
| Relatives/friends | 3 | 1.3 | 37 | 16.5 | 184 | 82.1 | 224 |
| Other specialist mental health staff | 50 | 22.3 | 99 | 44.2 | 75 | 33.5 | 224 |
The sufficiency and quality of the mental health service
Community mental health teams were asked how strongly they agreed with a list of statements relating to the sufficiency and quality of the mental health services provided by their trust. The responses are shown in Table 73. The quality of support in the area was rated as good by a large majority of CMHTs (87%). Responses relating to whether or not care homes received enough support for their needs were evenly split as were the ratings on senior managers placing a high priority on providing care home support. This was also the case for views on improvements as a result of the implementation of the National Dementia Strategy. Just under two-thirds of CMHTs felt that specialist care home support was not well resourced in the trust. Approximately two-fifths felt that when resources were tight care home support was one of the first areas that suffered. A large majority (85%) of CMHTs felt that care home staff did not have adequate skills to care for older people with mental health problems. Although 90% strongly agreed that they wanted to provide more support, the same proportion indicated that they lacked the capacity to provide this.
| Statement | Completely agree | Tend to agree | Tend to disagree | Completely disagree | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| The quality of the specialist mental health support provided to care homes in our area is good (n = 228) | 80 | 35.1 | 118 | 51.8 | 26 | 11.4 | 4 | 1.8 |
| Care homes receive enough specialist mental health support for their needs (n = 228) | 19 | 8.3 | 91 | 39.9 | 102 | 44.7 | 16 | 7.0 |
| Specialist care home support is well resourced in our trust (n = 225) | 11 | 4.9 | 68 | 30.2 | 108 | 48.0 | 38 | 16.9 |
| When resources are tight care home support is one of the first areas that suffers (n = 226) | 24 | 10.6 | 68 | 30.1 | 83 | 36.7 | 51 | 22.6 |
| Senior managers in our trust place a high priority on providing care home support (n = 221) | 17 | 7.7 | 93 | 42.1 | 89 | 40.3 | 22 | 10.0 |
| Care home staff have the skills they need to care for older people with mental health problems (n = 226) | 3 | 1.3 | 30 | 13.3 | 138 | 61.1 | 55 | 24.3 |
| The implementation of the National Dementia Strategy has improved the mental health support our trust provides to care homes (n = 224) | 16 | 7.1 | 92 | 41.1 | 91 | 40.6 | 25 | 11.2 |
| Our CMHT would like to provide more care home support (n = 227) | 108 | 47.6 | 95 | 41.9 | 22 | 9.7 | 2 | 0.9 |
| Our CMHT has the capacity to provide more care home support (n = 226) | 8 | 3.5 | 15 | 6.6 | 95 | 42.0 | 108 | 47.8 |
Factor and reliability analyses exploring the quality of the mental health service were undertaken. Analyses led to the exclusion of the questions relating to restrictions to the care home support activities when resources were constrained in the trust and the questions relating to CMHTsOP capacity to increase support to care homes. The remaining questions and team caseload characteristics were then analysed using backward stepwise regression (R2 = 0.137 and an adjusted R2 = 0.122). This indicated that not having at least one team member’s time fully committed to care home work had a negative influence on the perceived quality of mental health-care outreach (beta = –0.216; p < 0.004). The absence of a systematic process for the management of antipsychotics for care home residents with dementia was negatively associated with the perceived quality of mental health-care outreach (beta = –0.179; p = 0.016). These findings are preliminary, though they suggest that such factors can interact and may impact on the quality of mental health outreach to care homes.
Care homes survey
Questionnaires were received from 391 of the 1000 care homes selected. Eleven homes had closed, resulting in a response rate of 40%. Table 74 shows the percentage of questionnaires returned by the different categories of care home: homes with nursing provision and not registered for dementia (Nur/NoDem), homes with nursing provision and registered for dementia (Nur/Dem), homes without nursing provision and not registered for dementia (NoNur/NoDem) and homes without nursing provision and registered for dementia (NoNur/Dem).
| Care home category | Definition | n | % |
|---|---|---|---|
| Nur/NoDem | With nursing, no dementia | 77 | 44.8 |
| Nur/Dem | With nursing, dementia | 99 | 37.2 |
| NoNur/NoDem | Without nursing, no dementia | 78 | 39.8 |
| NoNur/Dem | Without nursing, dementia | 137 | 38.6 |
| All | 391 | 39.5 |
Care home residents and staffing
Care home managers were asked about the proportions of residents with dementia or confusion, challenging behaviour and depressive symptoms. Overall, 29% of homes reported that more than three-quarters of residents suffered from dementia or confusion (Table 75). This was highest for Nur/Dem and NoNur/Dem homes, which had provision for older people with dementia. This was, however, higher for homes without nursing provision (45%) than for homes with this provision (37%). At the other end of the scale, 40% of NoNur/NoDem homes reported that less than one-quarter of residents suffered from dementia or confusion. This represented a statistically significant difference overall (p < 0.001). Challenging behaviours, were less prevalent, with 83% overall reporting that less than one-quarter of residents presented with challenging behaviours. The highest proportion was among residents of Nur/Dem homes, where 10% reported that over three-quarters of residents had challenging behaviours. The proportions of residents with depressive symptoms was reported to be less than one-quarter by about two-thirds of homes. Fifteen per cent of Nur/Dem homes reported that more than half of their residents had depressive symptoms. This information was missing for 13% of homes overall; slightly higher for care homes without nursing.
| Mental health problem | ≤ 25% | 26–50% | 51–75% | ≥ 76% | Total, n | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Dementia/confusion | |||||||||
| Nur/NoDem | 22 | 28.9 | 30 | 39.5 | 16 | 21.1 | 8 | 10.5 | 76 |
| Nur/Dem | 9 | 9.3 | 25 | 25.8 | 27 | 27.8 | 36 | 37.1 | 97 |
| NoNur/NoDem | 31 | 40.3 | 27 | 35.1 | 13 | 16.9 | 6 | 7.8 | 77 |
| NoNur/Dem | 6 | 4.4 | 21 | 15.3 | 48 | 35.0 | 62 | 45.3 | 137 |
| All | 68 | 17.6 | 103 | 26.6 | 104 | 26.9 | 112 | 28.9 | 387 |
| Challenging behaviour | |||||||||
| Nur/NoDem | 67 | 95.7 | 2 | 2.9 | 1 | 1.4 | – | – | 70 |
| Nur/Dem | 59 | 65.6 | 12 | 13.3 | 10 | 11.1 | 9 | 10.0 | 90 |
| NoNur/NoDem | 63 | 92.6 | 3 | 4.4 | 2 | 2.9 | – | – | 68 |
| NoNur/Dem | 103 | 82.4 | 13 | 10.4 | 7 | 5.6 | 2 | 1.6 | 125 |
| All | 292 | 82.7 | 30 | 8.5 | 20 | 5.7 | 11 | 3.1 | 353 |
| Depressive symptoms | |||||||||
| Nur/NoDem | 49 | 71.0 | 15 | 21.7 | 4 | 5.8 | 1 | 1.4 | 69 |
| Nur/Dem | 49 | 56.3 | 25 | 28.7 | 10 | 11.5 | 3 | 3.4 | 87 |
| NoNur/NoDem | 46 | 69.7 | 14 | 21.2 | 6 | 9.1 | – | – | 66 |
| NoNur/Dem | 78 | 66.1 | 29 | 24.6 | 10 | 8.5 | 1 | 0.8 | 118 |
| All | 222 | 65.3 | 83 | 24.4 | 30 | 8.8 | 5 | 1.5 | 340 |
Information was obtained from the homes about the staff providing direct care. Table 76 shows mean numbers of staff by the different categories of homes. The mean numbers of staff ranged from 26 for NoNur/NoDem homes to 56 for Nur/Dem homes, the latter providing nursing care and services for older people with dementia. The two categories with nursing provision employed registered nurses representing just over one-fifth of the home staff group. In homes without nursing provision, four-fifths of the care staff were working towards National Vocational Qualification (NVQ) 2 or above, exceeding the national recommendation of at least 50%. The mean proportion of staff leaving the home within the last year was highest for Nur/Dem homes.
| Care home category | Total number of staff (mean) | Proportion registered nurses (mean) | Proportion working to NVQ2 or above (mean) | Proportion left within year (mean) |
|---|---|---|---|---|
| Nur/NoDem | 37.92 | 23.84 | 53.24 | 11.83 |
| Nur/Dem | 56.45 | 20.09 | 57.59 | 16.60 |
| NoNur/NoDem | 26.18 | 0.58 | 80.41 | 11.17 |
| NoNur/Dem | 30.21 | 1.79 | 79.87 | 11.91 |
| All | 37.47 | 10.46 | 69.31 | 12.88 |
Specialist mental health support
Only 18% of homes were able to refer a resident directly to mental health services, rather than through the GP. This was more common for Nur/Dem homes at 28%, compared with around 15% for the other categories (borderline statistical significant, p = 0.052). This may reflect the more frequent referrals made by this category of home for people with dementia and better links with nursing staff in these homes.
Care homes were asked to provide information on how frequently different professional groups visited the home in connection with the mental health of residents. The list of professional groups included mental health specialists as well as other groups who might provide this support. The groups reported most frequently are shown in Table 77. Homes reported very low weekly input from mental health services. More regular visits by old age psychiatrists were reported by the homes with dementia residents. CPN visits were less frequent to Nur/NoDem homes and most frequent to NoNur/Dem homes without nursing provision for residents with dementia. More frequent input overall was reported for other health professionals. GPs were reported by two-fifths of care homes overall as visiting at least on a weekly basis. This was highest for homes with nursing provision and residents with dementia. Community nurse input was also reported to be at least weekly by about one-third of homes overall and was highest for the categories of homes without nursing provision and especially for homes identified as providing a service for people with dementia. Overall, homes reported a low level of weekly input from social workers, but this was reported as more frequent by Nur/Dem homes. Pharmacist input was reported more frequently by homes with dementia residents, with about one-quarter reporting visits at least on a monthly basis. Very little other input was reported by care homes and only 6% of homes overall reported at least monthly visits by a geriatrician.
| Professional | At least weekly | At least monthly | Rarely/never | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| CPN | ||||||
| Nur/NoDem | 2 | 2.6 | 14 | 18.2 | 61 | 79.2 |
| Nur/Dem | 8 | 8.1 | 34 | 34.3 | 57 | 57.6 |
| NoNur/NoDem | 6 | 7.7 | 26 | 33.3 | 46 | 59.0 |
| NoNur/Dem | 10 | 7.3 | 64 | 46.7 | 63 | 46.0 |
| All | 26 | 6.6 | 138 | 35.3 | 227 | 58.1 |
| Old age psychiatrist | ||||||
| Nur/NoDem | 1 | 1.3 | 8 | 10.4 | 68 | 88.3 |
| Nur/Dem | 1 | 1.0 | 17 | 17.2 | 81 | 81.8 |
| NoNur/NoDem | – | – | 7 | 9.0 | 71 | 91.0 |
| NoNur/Dem | – | – | 23 | 16.8 | 114 | 83.2 |
| All | 2 | 0.5 | 55 | 14.1 | 334 | 85.4 |
| GP | ||||||
| Nur/NoDem | 33 | 42.9 | 23 | 29.9 | 21 | 27.3 |
| Nur/Dem | 61 | 61.6 | 20 | 20.2 | 18 | 18.2 |
| NoNur/NoDem | 30 | 38.5 | 14 | 17.9 | 34 | 43.6 |
| NoNur/Dem | 49 | 35.8 | 52 | 38.0 | 36 | 26.3 |
| All | 173 | 44.2 | 109 | 27.9 | 109 | 27.9 |
| Community nurse | ||||||
| Nur/NoDem | 13 | 16.9 | 6 | 7.8 | 58 | 75.3 |
| Nur/Dem | 21 | 21.2 | 12 | 12.1 | 66 | 66.7 |
| NoNur/NoDem | 32 | 41.0 | 7 | 9.0 | 39 | 50.0 |
| NoNur/Dem | 60 | 43.8 | 22 | 16.1 | 55 | 40.1 |
| All | 126 | 32.2 | 47 | 12.0 | 218 | 55.8 |
| SW | ||||||
| Nur/NoDem | 5 | 6.5 | 24 | 31.2 | 48 | 62.3 |
| Nur/Dem | 17 | 17.2 | 46 | 46.5 | 36 | 36.4 |
| NoNur/NoDem | 3 | 3.8 | 19 | 24.4 | 56 | 71.8 |
| NoNur/Dem | 5 | 3.6 | 51 | 37.2 | 81 | 59.1 |
| All | 30 | 7.7 | 140 | 35.8 | 221 | 56.5 |
| Pharmacist | ||||||
| Nur/NoDem | 3 | 3.9 | 5 | 6.5 | 69 | 89.6 |
| Nur/Dem | 5 | 5.1 | 19 | 19.2 | 75 | 75.8 |
| NoNur/NoDem | 6 | 7.7 | 6 | 7.7 | 66 | 84.6 |
| NoNur/Dem | 9 | 6.6 | 25 | 18.2 | 103 | 75.2 |
| All | 23 | 5.9 | 55 | 14.1 | 313 | 80.1 |
Care homes were asked to rate the mental health support provided to their home, including support from both mental health and non mental health specialists. Table 78 shows that just under one-third of homes overall rated the support they received as excellent or very good, whereas just under 15% felt the support was poor. The two categories of homes without nursing provision reported higher ratings. One-fifth of Nur/NoDem homes rated the support as poor. This latter group reported less frequent input from both psychiatric and community nursing professionals.
| Care home category | Excellent/very good | Good/fair | Poor | Total, n | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Nur/NoDem | 14 | 18.2 | 46 | 59.8 | 17 | 22.1 | 77 |
| Nur/Dem | 25 | 25.5 | 58 | 59.2 | 15 | 15.3 | 98 |
| NoNur/NoDem | 31 | 39.7 | 38 | 48.8 | 9 | 11.5 | 78 |
| NoNur/Dem | 47 | 34.3 | 74 | 54.0 | 16 | 11.7 | 137 |
| All | 117 | 30.0 | 216 | 55.4 | 57 | 14.6 | 390 |
The sufficiency and quality of mental health services
Care homes were asked how strongly they agreed with a list of statements relating to normal practice within their home and the provision of services by external mental health professionals. Table 79 shows the ratings for the provision of assessment and review services. Just over one-fifth of homes overall reported complete agreement with the statement that their residents were appropriately assessed on admission to the home by external health professionals. There were significant differences between the categories of homes in their levels of agreement over the presence of a systematic process in respect to antipsychotic medication. Although about one-fifth of homes completely agreed that there were regular reviews of residents’ mental health status, for Nur/NoDem homes almost one-third completely disagreed.
| Statement | Completely agree | Tend to agree | Tend to disagree | Completely disagree | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| The mental health status of residents is appropriately assessed on admission by external health professionals | ||||||||
| Nur/NoDem | 16 | 21.3 | 24 | 32.0 | 23 | 30.7 | 12 | 16.0 |
| Nur/Dem | 23 | 23.7 | 32 | 33.0 | 29 | 29.9 | 13 | 13.4 |
| NoNur/NoDem | 18 | 23.7 | 27 | 35.5 | 19 | 25.0 | 12 | 15.8 |
| NoNur/Dem | 26 | 19.4 | 60 | 44.8 | 36 | 26.9 | 12 | 9.0 |
| All | 83 | 21.7 | 143 | 37.4 | 107 | 28.0 | 49 | 12.8 |
| Significance of home category differences: NS | ||||||||
| Home has a systematic process in place for the initiation, review and cessation of antipsychotics for residents with dementia | ||||||||
| Nur/NoDem | 22 | 29.7 | 16 | 21.6 | 24 | 32.4 | 12 | 16.2 |
| Nur/Dem | 47 | 48.0 | 31 | 31.6 | 10 | 10.2 | 10 | 10.2 |
| NoNur/NoDem | 21 | 27.6 | 24 | 31.6 | 15 | 19.7 | 16 | 21.1 |
| NoNur/Dem | 57 | 42.9 | 43 | 32.3 | 26 | 19.5 | 7 | 5.3 |
| All | 147 | 38.6 | 114 | 29.9 | 75 | 19.7 | 45 | 11.8 |
| Significance of home category differences: p < 0.001 | ||||||||
| Care home residents’ mental health status is reviewed on a regular basis by external health professionals | ||||||||
| Nur/NoDem | 4 | 5.4 | 28 | 37.8 | 21 | 28.4 | 21 | 28.4 |
| Nur/Dem | 18 | 18.4 | 42 | 42.9 | 22 | 22.4 | 16 | 16.3 |
| NoNur/NoDem | 19 | 25.0 | 26 | 34.2 | 20 | 26.3 | 11 | 14.5 |
| NoNur/Dem | 36 | 26.9 | 52 | 38.8 | 32 | 23.9 | 14 | 10.4 |
| All | 77 | 20.2 | 148 | 38.7 | 95 | 24.9 | 62 | 16.1 |
| Significance of home category differences: p < 0.001 | ||||||||
Table 80 shows care home ratings for the availability of external services. Less than one-fifth of homes felt (completely or tended to agree) that outreach visits were made at regular set times. Agreement on the availability of telephone support was higher for the two categories of homes without nursing provision, perhaps reflecting their greater need for such support. More NoNur/NoDem homes reported that external health professionals responded quickly to their needs compared to other home types. This finding may be a result of the lower level of mental health need of their residents. The provision of training for care staff is shown in Table 81. Overall, very few homes either completely or tended to agree that training was provided within the care home, most agreeing that staff attended external education and training sessions. Over one-quarter of NoNur/NoDem homes completely agreed that this was the case, whereas a similar proportion of Nur/NoDem homes completely disagreed. A high proportion of homes overall, either completely or tended to agree that care home staff were appropriately trained (ranging from 73% to 86%). Greater disagreement with confidence in care staff ability was reported by homes who did not provide a service for people with dementia. Table 82 shows the response of care homes in respect of the overall sufficiency of the mental health support they receive. Only 14% of homes completely agreed that they received enough support. A higher proportion of Nur/NoDem homes felt this was the case.
| Statement | Completely agree | Tend to agree | Tend to disagree | Completely disagree | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| External health professionals have regular set times when they visit home | ||||||||
| Nur/NoDem | 10 | 13.5 | 4 | 5.4 | 7 | 9.5 | 53 | 71.6 |
| Nur/Dem | 16 | 16.3 | 6 | 6.1 | 17 | 17.3 | 59 | 60.2 |
| NoNur/NoDem | 9 | 11.8 | 5 | 6.6 | 18 | 23.7 | 44 | 57.9 |
| NoNur/Dem | 9 | 6.7 | 8 | 6.0 | 27 | 20.1 | 90 | 67.2 |
| All | 44 | 11.5 | 23 | 6.0 | 69 | 18.1 | 246 | 64.4 |
| Significance of home category differences: NS | ||||||||
| External health professionals are readily available to provide telephone support on mental health issues | ||||||||
| Nur/NoDem | 8 | 10.8 | 27 | 36.5 | 23 | 31.1 | 16 | 21.6 |
| Nur/Dem | 16 | 16.3 | 29 | 29.6 | 35 | 35.7 | 18 | 18.4 |
| NoNur/NoDem | 23 | 30.3 | 25 | 32.9 | 13 | 17.1 | 15 | 19.7 |
| NoNur/Dem | 37 | 27.6 | 48 | 35.8 | 29 | 21.6 | 20 | 14.9 |
| All | 84 | 22.0 | 129 | 33.8 | 100 | 26.2 | 69 | 18.1 |
| Significance of home category differences: p < 0.05 | ||||||||
| External health professionals respond quickly to our needs | ||||||||
| Nur/NoDem | 7 | 9.3 | 37 | 49.3 | 24 | 32.0 | 7 | 9.3 |
| Nur/Dem | 10 | 10.2 | 39 | 39.8 | 38 | 38.8 | 11 | 11.2 |
| NoNur/NoDem | 18 | 23.7 | 35 | 46.1 | 14 | 18.4 | 9 | 11.8 |
| NoNur/Dem | 22 | 16.4 | 53 | 39.6 | 50 | 37.3 | 9 | 6.7 |
| All | 57 | 14.9 | 164 | 42.8 | 126 | 32.9 | 36 | 9.4 |
| Significance of home category differences: p < 0.05 | ||||||||
| Statement | Completely agree | Tend to agree | Tend to disagree | Completely disagree | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| External health professionals provide regular education and training sessions on mental health issues within the home | ||||||||
| Nur/NoDem | 1 | 1.4 | 8 | 10.8 | 20 | 27.0 | 45 | 60.8 |
| Nur/Dem | 2 | 2.0 | 8 | 8.2 | 30 | 30.6 | 58 | 59.2 |
| NoNur/NoDem | 5 | 6.6 | 11 | 14.5 | 18 | 23.7 | 42 | 55.3 |
| NoNur/Dem | 5 | 3.8 | 14 | 10.5 | 38 | 28.6 | 76 | 75.1 |
| All | 13 | 3.4 | 41 | 10.8 | 106 | 27.8 | 221 | 58.0 |
| Significance of home category differences: NS | ||||||||
| Home staff regularly attend external education and training sessions on mental health issues | ||||||||
| Nur/NoDem | 8 | 10.8 | 28 | 37.8 | 18 | 24.3 | 20 | 27.0 |
| Nur/Dem | 8 | 8.2 | 42 | 42.9 | 34 | 34.7 | 14 | 14.3 |
| NoNur/NoDem | 21 | 27.6 | 24 | 31.6 | 18 | 23.7 | 13 | 17.1 |
| NoNur/Dem | 24 | 17.9 | 46 | 34.4 | 36 | 26.9 | 28 | 20.9 |
| All | 61 | 16.0 | 140 | 36.6 | 106 | 27.7 | 75 | 19.6 |
| Significance of home category differences: p < 0.05 | ||||||||
| Confident that the care staff within the home are appropriately trained to care for residents’ mental health needs | ||||||||
| Nur/NoDem | 12 | 16.0 | 43 | 57.3 | 17 | 22.7 | 3 | 4.0 |
| Nur/Dem | 26 | 26.5 | 58 | 59.2 | 11 | 11.2 | 3 | 3.1 |
| NoNur/NoDem | 29 | 38.2 | 28 | 36.8 | 16 | 21.1 | 3 | 3.9 |
| NoNur/Dem | 50 | 37.3 | 65 | 48.5 | 18 | 13.4 | 1 | 0.7 |
| All | 117 | 30.5 | 194 | 50.7 | 62 | 16.2 | 10 | 2.6 |
| Significance of home category differences: p < 0.001 | ||||||||
| Statement | Completely agree | Tend to agree | Tend to disagree | Completely disagree | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Home receives enough external health support for residents’ mental health needs | ||||||||
| Nur/NoDem | 5 | 6.7 | 18 | 24.0 | 31 | 41.3 | 21 | 28.0 |
| Nur/Dem | 9 | 9.2 | 37 | 37.8 | 33 | 33.7 | 19 | 19.4 |
| NoNur/NoDem | 20 | 26.7 | 24 | 32.0 | 20 | 26.7 | 11 | 14.7 |
| NoNur/Dem | 19 | 14.2 | 43 | 32.1 | 51 | 38.1 | 21 | 15.7 |
| All | 53 | 13.9 | 122 | 31.9 | 135 | 35.3 | 72 | 18.8 |
| Significance of home category differences: p < 0.01 | ||||||||
Finally, homes were asked what was the one thing that would most improve the services they receive to support the mental health needs of residents. Three-quarters of homes responded. Most frequently they wanted to be able to refer residents directly to mental health services and have quicker access to this support (28% of those who responded). This was reported most frequently by NoNur/Dem homes. More staff training was the second most important area of concern (25%), again a comment most frequently made by NoNur/Dem homes. This was followed by more regular visits from mental health professionals, including the provision of regular clinics and reviews for residents, not just in response to a crisis (22%), an area of concern identified by more Nur/Dem homes than the other categories. Sixteen per cent of homes wanted to be able to access advice more easily. This was a particular priority for NoNur/Dem homes.
Discussion
These two national surveys, with information collected both from CMHTsOP and care homes, provide a unique overview of mental health support to older people in care homes. Response rates of 55% for the CMHTOP survey and 40% for the care home survey are acceptable and enable us to draw reliable conclusions from the data. However, the findings should be interpreted in the context of the design of the study. Although the CMHTsOP survey was sent to team managers and was mainly factual in relation to the services the team provided, there was an element of personal judgement on the quality and sufficiency of the services. The same applies to the care home survey, sent to care homes managers. Information was obtained from CMHTsOP only about the services they provide directly. However, there was evidence that in some localities other services were also providing mental health support to care homes. These included dementia care teams and in-reach care home teams.
Different levels of CMHTOP outreach activities were evident. A low proportion of teams undertook case finding, which reflects the findings of both the CMHTOP survey described earlier in this report and a survey of old age psychiatrists. 73 A relatively high proportion of CMHTsOP reported undertaking reviews both of mental health and medication use. Old age psychiatrists and CPNs were the main professional staff groups undertaking these activities. In addition, greater input from OTs, psychologists and social workers was evident in care planning activities. The provision of training for care homes was relatively low, slightly lower than in the earlier CMHTOP survey and the study by Tucker et al. 73 However, this study focused on the provision of formal training to staff so might be expected to be lower than other studies. This formal training was mainly undertaken by CPNs. Team structures varied and one-fifth of teams reported having a member of staff’s time fully committed to working with care homes and a further 12% had staff partially committed to this activity. Link workers with at least some of the homes in their area were reported by 44% of teams, higher than for the earlier CMHTOP survey. Although few teams reported regularly holding open clinics in care homes, this was nevertheless twice as high than the figure provided in the earlier CMHTOP survey. Notably, a high proportion felt that care home staff did not have the skills to care for older people with mental health problems, and while a high majority wanted to provide more support to care homes, the same proportion indicated no capacity for this.
In the survey of care homes, a low proportion reported being able to refer residents directly to mental health services, largely having to go through the GP. This was a priority area for service improvement. The findings reveal that more regular visits to care homes in respect of residents’ mental health were made by GPs and community nurses, with fewer visits by specialist mental health staff. There was low overall provision of education and training within care homes from external health professionals and only one-third of homes were confident that their staff were appropriately trained to care for residents with mental health needs. Again, more staff training was noted as a priority area for many homes. Differences between the categories of homes were evident throughout the findings; mainly these were as might be expected, although interestingly, more Nur/NoDem homes rated the support they received as poor and also reported that overall they did not receive enough support for residents’ mental health needs.
These two surveys provide a comprehensive overview of mental health support for older people in care homes and suggest areas for further investigation. Regular training for care staff has been shown to have a beneficial effect on staff. 326 However, the surveys revealed that training for care home staff was viewed as insufficient, mainly provided by means of one-off events. Difficulties in accessing mental health services were noted by care homes, largely due to their inability to refer residents directly to CMHTsOP. This finding may be reflected in the greater input from GPs and community nurses rather than specialist mental health services. The importance of early diagnosis and treatment for older people with dementia has been emphasised in recent policy. 57 The surveys revealed that case-finding was uncommon. The importance of screening for depression has been seen as vital to improving outcomes by intervening at an early stage. 338 Care homes were, however, less able to provide prevalence figures for depression than for dementia and there was generally less use of standardised screening tools compared with those used to assess cognition.
Chapter 15 Lessons, conclusions and synthesis
This chapter reviews some of the main findings of the programme of work, details plans for their dissemination, and identifies some possible research questions emerging. The potential value of the BoC approach for commissioning mental health services, the largest Clinical Commissioning Groups’ (CCGs) spend category, was noted. Although the opportunity to provide more care in settings other than care homes and hospitals was identified, it appeared that the redistribution of costs involved could be problematic and would need to be addressed.
The impact of integration on the performance of care services appeared to be highly complex and no simple relationship between more integrated care systems and enhanced community tenure was found. Nonetheless, there was a strongly held view in the workforce that integration provides the capacity to deliver a more efficient service – a necessary but not sufficient condition.
Care homes appeared to require enhanced support from CMHTsOP to effectively support older people in care homes and minimise avoidable hospital admissions. However, current levels of this support appeared, on average, to be insufficient to achieve these goals.
Several research questions emerged from the study, of which one concerned the research process and the critically important task of how to enhance recruitment rates without overburdening front-line staff. Two of the most prominent research questions were the need to unravel the impact of age inclusive mental health services on the provision of care to older people; and identification of the most cost-effective approach to provide specialist mental health support to older people living in care homes.
Introduction
Old age mental health services have grown and developed substantially from their emergence in the late 1970s and 1980s with committed leaders in mental health care. As these services have developed there have been substantial debates as to the range of services needed, the ways in which staff should work, the mix of staff required for an effective and efficient service, the roles of staff within the service, how the service should be accessed and the balance and extent of their contribution to care at home, in care homes and in hospital.
This study sought to address a number of these questions through three main areas of activity or workstreams (see Appendix 39). These were the BoC workstream, focusing on service mix between predominantly community based and residential/hospital based provision; the CMHT workstream, examining the impact of different ways of working; and the care home workstream, which scoped the roles and contribution of specialist mental health services in meeting the mental health needs of residents in care homes.
In this chapter we briefly review the evidence from each of the workstreams before identifying the broader messages which emerge from the study which may have utility for research, practice, commissioning and policy.
Main findings
Balance of care (see Chapters 2–5)
The literature indicated that the use of the BoC approach had been relatively limited in scope. In particular there was a need for studies to employ more comprehensive approaches to costing and to explore more complex care options or margins. These would not just lie between community and hospital but also between distinctly different levels of community-based care. There was also relatively little consideration of outcomes in the literature, with costs the main variable, a point made many years previously. 134
In the BoC consultations, it was interesting that, following the simulation exercises, staff perceived additional opportunities to reduce the use of hospital beds and care home places by substituting these for community-based support. Of course, the proposed community-based support was more costly, more substantial and more intensive than the norms of care at home in the localities. Older people and carers themselves tended to concur with these views although they were less likely to perceive care homes as an inappropriate option than staff. Older people and carers voiced concerns about the reliability and quality of community-based care, the management of risk in community settings, the quality of care homes and financial issues of funding their long-term care. Indeed, the very concerns at the core of the Dilnot Report342 regarding funding of long-term care reflected substantially their concerns.
In the analysis of substitution opportunities, the limited extent to which senior managers perceived ECH as a viable alternative to care home admission was notable. It was not clear whether this was a local effect or whether staff were cognisant of the length of time required to set up a new tenancy or purchase, and that this was therefore not planned as a relatively short-term solution. Nonetheless, there were still opportunities identified to substitute institutional forms of care by home support. The findings suggested that approximately one-fifth of inpatient admissions might be substitutable and a reduction in delayed discharge was also possible. Furthermore, it was suggested that some 50% of care home admissions might be avoided or delayed with sufficient quality and intensity of home support services available. This was surprisingly high. Linked to this was the observation that some of the most inappropriate hospital admissions appeared to come from care homes.
Community mental health teams for older people (see Chapters 6–10)
The literature review demonstrated the dominance of a particular approach to CMHTsOP emerging from one centre. Studies exploring the impact of different ways of working offered evidence of achieving improved processes such as better access to services or enhanced multidisciplinary assessment. Other areas addressed related to staff efficiencies such as substituting the roles of more expensive and rarer staff members. Indeed, there appeared to be a focus on the concerns of Mental Health: New Ways of Working for Everyone343 well before its publication. However, there were no studies making a clear link between certain team components and improved final outcomes for patients and carers.
The survey data indicated the extent to which, like many NHS services, CMHTsOP were in flux; changing their scale and organisational components in response to exogenous factors such as staff turnover rather than focusing on promoting optimal performance. There was a tendency for teams to be increasing in size, through mechanisms such as team mergers and incorporation of memory services. As this occurred, it could be argued that the distinction between a team and the service as a whole was becoming blurred. Operationally, it appeared that, despite the longstanding debate about improving patient access, provision of open access had not increased, with most referrals proceeding through the traditional route, via GPs. Most teams were found to be providing a service to care homes, with around one-third providing this though a link worker, with the remainder offering education in recognition and management of mental health problems.
In terms of service development, certain facets of service integration that were within the teams’ control had often been implemented, such as shared assessment tools and certain aspects of role blurring. However, features beyond the teams’ control had not been implemented, such as integrated budgets and shared commissioning of services. These depended on wider interagency agreements for their implementation.
Within the teams selected for the detailed case study, the focus was predominantly on the impact of integration between health and social care. This was due to the difficulty of applying a valid and reliable classification to the role of consultants within teams. The subtleties of categorising integration led to a graded typology based on the extent of integration. There was marked variation in diagnosis mix, with perhaps unsurprisingly more social work input from integrated teams with social workers. Different CMHTOP staff saw direct access to nurses, social workers and OTs as one of key benefits of integrated team work, leading to more timely responses and access to resources for patients. However, there was widespread concern that integration should not mean complete role blurring and generic working. The consultant role was seen as most effective when spanning community and inpatient settings. Staff perceived the most effective service model to be an integrated team with the consultant working on a sectorised basis. 344
Considering staff experience working in teams, as might be expected, psychologists and psychiatrists had greater role control and autonomy. Conversely, social workers perceived themselves as low on these domains although in integrated teams they saw this as higher than within a social services team. A theme of potential conflict in teams was that of staff being managed across professions (such as a nurse managed by a non-nurse), which was associated with lower indicators of well-being.
With regard to service outcomes, no association was found between more integrated services and reduced hospital or care home admissions. There was also no positive association between more integrated services and QoL, patient satisfaction or carer outcomes. Costs generally appeared higher in integrated teams. However, there was some cost data uncertainty due to variation in reporting between team types, leading to more complete cost recordings in integrated teams.
Care homes: scoping the need (see Chapters 12–14)
The care homes workstream was primarily designed to scope the issues in relation to old age mental health. An earlier plan to test an intervention designed to identify depression in older people in care homes was not funded. From the literature review it appeared that most interventions identified were focused on providing multidisciplinary care planning and staff training. By contrast, there was much less evidence of screening of the care home residents as a whole, but rather opportunistic case finding where home staff identified individuals needing further investigation. With regard to outreach services, those which focused on dementia alone demonstrated limited impact. However, where depression was a target, studies suggested that there were improvements. In general, where CMHTsOP offered training to care home staff, this appeared to have a positive impact.
The surveys of teams and of care homes suggested that, as with open access more generally, there was limited direct access for homes to teams, with only 20% able to do this. There was little evidence of genuine screening of care home populations, rather frequent evidence of opportunistic case finding. As indicated in the literature, it appeared that homes were unaware of the levels or extent of depression among residents. The service to care homes was mainly on a crisis and informal basis whereas homes wanted more formal arrangements. Fewer than one-third of homes were confident that their staff were appropriately trained to care for residents with mental health needs. Both surveys revealed a lack of confidence about the capacity of care home staff to meet the mental health needs of older residents, suggesting specialist outreach support could valuably refocus on building their skills and confidence. In general, it appeared that the level of input to care homes, while valued, was insufficient to prevent hospital admissions or identify and manage disorders.
Dissemination activities and plans
Dissemination of the findings is an ongoing process and is necessarily at an early stage at the time of writing. Nevertheless, as detailed in Appendix 40, a number of workshops reported early findings to staff, service users and carers as a means of sharing these data and of engaging them in shaping subsequent stages of the research. Members of the research team have also given various conference papers, presented seminars and participated in academic and professional workshops. Publications achieved so far include articles in peer-reviewed journals as well as a suite of accessible reports and summaries designed to maximise impact with service managers, commissioners and practitioners. Further dissemination is planned consisting of a broad series of peer-reviewed publications; a BoC workbook to support health and social care decision-makers to apply this framework independently; and further feedback designed for trusts and local authorities, older people and carers.
Research recommendations
From the three distinct work streams in this study emerge a number of areas for further research. Some of these questions relate to the research process itself and more efficient means of recruitment of participants. We have listed these in terms of our perception of their relative order of priority:
-
What are the costs and benefits for older people with mental health needs of integrating mental health services by means of the development of age inclusive services?
-
What is the relative cost-effectiveness of different approaches to the provision of specialist mental health support for older people in care homes?
-
How might it be possible to collect data on the outcomes of people with similar needs in different care settings so as to identify the impact of care setting on outcomes for marginal individuals?
-
(a) What mechanisms can be employed to incentivise social care organisations and their practitioners to participate in research? (b) What new methods could be employed to access potential research participants without making too great a demand on increasingly pressured front line staff to facilitate contact?
-
(a) What are the critical components of an effective and efficient CMHTOP? (b) What are the critical components, or combination thereof, which make for an effective and efficient integrated community mental health service?
-
What has been the impact of previous BoC studies on service planning and commissioning, and how might this evidence be employed to assist effective commissioning?
Study findings, service development and practice
For Clinical Commissioning Groups (CCGs) the largest programme of expenditure is mental health. 222 It remains, however, an area that is perhaps given less attention than other areas of spend, such as cancer or cardiovascular disease. It may be that in old age a clearer focus is being given to services for people with dementia through the National Dementia Strategy57 and related activities but other aspects of old age mental health such as depression may be less visible. However, the findings suggest that the BoC offers a framework within which CCGs can evaluate more carefully the different potential strategies for delivering mental health care. BoC is essentially a clinically intuitive, straightforward approach focused on marginal patients in different modes of care, and the data underlying it is not contentious. Essential for the BoC approach is marshalling and organising basic intelligence to understand who is where, who gets what and at what cost. The development of more effective commissioning requires this basic evidence and structures to collect and focus its analysis. It is for this important purpose that the team are producing a tool to facilitate commissioners’ work.
In workstream 1, BoC, potentially inappropriate hospital and care home admissions were identified. The mechanism identified to address these was more intensive forms of community support than are routinely available. An interesting approach at the hospital care margin, building on this approach, would be the kind of reviews currently taking place in primary care trusts (PCTs) with a view to providing a sounder clinical evidence base for identifying the drivers of readmissions, including those which are not within the immediate control of the acute provider. 345 From the proposed alternative care packages, a critical issue is the degree to which a community care strategy involves cost shifting. At the care home margin social care is provided with an incentive not to admit people as, with community support, other parties incur additional costs. These costs appear to be borne by the NHS, older people and their carers. Furthermore, outcomes, a key component of enhanced decision-making, proved very complicated to integrate into the model. Presenting likely future outcomes to day-to-day decision-makers lacked resonance. If this is so, what mechanisms might align these policy and practice issues better? One possible forum might be Health and Wellbeing Boards, offering settings where these issues of cost and outcome could be required to be addressed. The identified hospital readmissions might also benefit from oversight at this level. In this context, BoC is probably the most valid and practicable conceptual and analytical framework.
Not only has the BoC workstream clearly demonstrated the potential for cost shifting and served to reveal the complexity of outcomes, it has also identified the prevalence of certain belief systems shaping the micro level decisions of front-line staff. For example, staff were much more likely to propose maintaining older people in the community than carers and older people. By contrast, older people and carers were more positive about care homes. Staff appeared to have internalised a perception of a need to rebalance care towards a reduction in use of institutional settings. Inevitably, today this is much more complex than when the reforms of community care were undertaken in the 1990s,346 given the differences of perspective between staff and carers and the differences in the populations now supported in these different settings. With a greater degree of subtlety in community care, BoC will need to look not just at the distinction between care home and living at home but also subtle variations between levels of community care and support. It was also surprising to see the relatively low priority given to ECH by social services managers. Nonetheless, the BoC analyses suggest there is a professional perspective within social care and also the NHS to tend to place people in community settings where greater costs are incurred, either by families and carers or by the NHS.
An important finding in workstream 2 was the variability in staff well-being and satisfaction according to individual professions and by team type. The lower levels of satisfaction of staff in integrated teams were not predicted and the data suggest that some of these variations may be more attributable to factors such as leadership processes within teams than the nature of teams themselves. This will require managers who are sophisticated people managers who can address the complex relationships within teams. Hence, it is possible that investment in management might also contribute to delivering better outcomes from CMHTsOP. In this context, it is interesting that a team with coherent sets of relationships and a vision of effective working may continue with that culture after initial leaders have moved on. 347
Workstream 2 also indicated that integration is a complex and multifaceted phenomenon. Since integration is a means of reducing the impact of boundaries in provision, clearly boundary management is important. In the present study these boundaries involved both access to social care and access to clinical care for care home residents. Of course the housing boundary also remains important, but is difficult to manage in the short-term, as emerged in workstream 1. Part of the development of integrated care may be in facilitating environments where more effective boundary spanning can be facilitated as the role of particular actors – ‘reticulists’348–350 – as well as the more commonly identified structural solutions.
Interviews with practitioners revealed strong support for the presence of social workers in CMHTsOP, yet the survey also found that social workers did not feel as able to utilise or develop their skills and shape their work environment compared with other professional groups. One interpretation of these findings would be that social workers are valued in teams not so much for their unique skills, but for the access they provide about social services and their governing structures. A recent study by Evans et al. 269 found that access to services was reported to be an important reason for social worker team membership, according to service managers in mental health trusts. Furthermore, where social worker skills were explicitly mentioned, these included reference to the statutory role of Approved Social Workers, which have now been replaced by the generic Approved Mental Health Professional. 351 Consequently, the rationale for social worker membership of CMHTsOP needs revisiting if the causes of poor job satisfaction are to be addressed. It is likely to impact not just on staff but turnover, and perhaps performance and service quality. Integrated teams may provide a better service, but this is by no means clear from the data. Workstream 2 provides evidence that staff want to work together in MDTs in order to achieve what they perceive as important goals. However, in the survey in Chapter 8 it was evident that integrated organisations appear sometimes to have been created to rectify what have been particularly non-integrated services. This may also have confounded the relationships that were investigated in the study, where some integrated settings were perhaps ‘less than willing partnerships’.
In workstreams 1–3 the contribution made and required from old age mental health services to care homes was very clear. Many inappropriate admissions to hospital appeared to come from care homes, and significant inputs by CMHTsOP were made to training and case finding in homes. However, the perspective of care home managers was that the level of support they received remained insufficient to enable them to manage the care of certain residents. Given the prevalance of depression among older people in care homes, a trial of systematic screening and intervention, as it had been hoped to undertake, would appear to be of significant value. It is a source of interest whether or not a tendency to develop more generic age-inclusive services would dilute the core elements identified in the study as being performed by CMHTsOP. With such arrangements, the needs of care homes might be perceived as less pressing, leading to the loss of the training role performed by specialist staff. There could also be a clash between the sectorised approach valued in old age services344 with the predominant approach in adult mental health services. This is one of a number of challenges and opportunities in determining the provision of best quality care for older people with mental health problems. Old age mental health services emerged as a discipline within psychiatry driven by a need to provide care to a group of patients who were eschewed by general psychiatric services, including older people in long-stay care, many of whom had dementia. This approach is now under review, as a discipline predicated on reaching a specific age, rather than having a set of particular clinical needs, may sit less than comfortably with current age discrimination legislation. 352,353 The rise of dementia as a clinical challenge, embraced by government in its broadest sense,354 has served to focus attention on that disorder, to the possible exclusion of affective, psychotic and personality disorders arising out of, or being carried into, old age.
Some of the key implications for practice are summarised in Box 23.
Staff support for integrated CMHTs was almost universal. Nevertheless, the lack of evidence that integrated teams are more effective than non-integrated ones at improving outcomes or satisfaction has implications for staff and managers. The findings suggest that certain frequently recommended features of integrated services – primarily relating to CMHT structures and processes – may not be as important as anticipated. Service standards often define ‘integrated’ CMHTs by whether or not they contain both health and social care practitioners (a sufficient condition for multidisciplinary working). However, practitioners identified broader facets of integration that effect service delivery, including the extent and quality of joint-working between different specialists (interdisciplinary working) and the blurring of traditional boundaries via role substitution and skills transfer (transdisciplinary working). The ability and authority of practitioners to undertake certain activities (e.g. commissioning social care, arranging hospital admissions and organising medication reviews) was also seen to impact on service quality and efficiency. Teams may thus benefit from looking beyond their organisational structures at team-working and responsibilities.
The future role of support workers was highlighted in two strands of the research. Support worker input formed a key component of the alternative care recommended for four marginal inpatient case types in the BoC study, which identified the potential for significant savings through reduced hospital admissions. However, the CMHT workstream raised concerns about support workers’ roles, with some reportedly used as substitutes for qualified staff (holding independent caseloads) and another used as a transport service. Support workers themselves were also frustrated by the lack of a career structure. Service managers might therefore want to consider the pivotal position such staff can play, while ensuring that their jobs are appropriately and clearly defined.
Finally, the value of specialist mental health outreach to care homes was highlighted repeatedly throughout the research, providing a persuasive, if not definitive, case for improving and expanding CMHT provision to care homes in keeping with the aspirations of the National Dementia Strategy. The care home manager survey found relatively high levels of satisfaction with the quality of specialist mental health support. However, over half of respondents felt outreach services were not sufficiently available and several CMHT managers acknowledged that such services were among the first to suffer from budget cutbacks. In the BoC study, local practitioners suggested that a significant minority of inappropriate inpatient admissions could be avoided with additional specialist mental health-care home support, while national experts further noted the benefits of dedicated, specialist CHSTs over fragmented services from multiple organisations.
Conclusions
The results of this programme provide an opportunity to help refocus and refresh the consideration of how best to provide for older people with mental health problems spanning health and social care, away from the self-interest of any professional or managerial group, to deliver the best evidence-based practice. The findings will be available just prior to the 25th anniversary of old age psychiatry as a clinical discipline (2014) giving the ideal opportunity to empower patients, their carers and professionals to engage in an informed debate about future provision of care.
Acknowledgements
Contributions of authors
Professor David Challis (Director of PSSRU at the University of Manchester) was Chief Investigator and contributed to planning the study; was responsible for management of staff, oversight of the programme and interpretation of data and writing the manuscript.
Sue Tucker (Research Fellow at PSSRU at the University of Manchester) was a Co-Applicant, planned the study; conducted the review of BoC; undertook the data collection for the BoC workstream; undertook analyses; and contributed to writing the manuscript.
Mark Wilberforce (Research Fellow at PSSRU at the University of Manchester) was responsible for the CMHTsOP workstream; was responsible for planning and undertaking data collection and analysis; liaison with sites; and contributing to the manuscript.
Dr Christian Brand (Research Associate at PSSRU at the University of Manchester) contributed to design of workstreams 1 and 2; was responsible for data collection and analysis in workstreams 1 and 2; and contributed to the manuscript.
Dr Michele Abendstern (Research Associate at PSSRU at the University of Manchester) was responsible for qualitative work and the literature review in workstream 2; and contributed to the manuscript.
Karen Stewart (Research Fellow at PSSRU at the University of Manchester) was responsible for the literature review on care homes; the care home data collection and analysis and contributed to writing the manuscript.
Rowan Jasper (Research Assistant at PSSRU at the University of Manchester) worked on the CMHTsOP workstream; contributed to data collection and analysis and contributed to the manuscript.
Dr Val Harrington (Research Associate at PSSRU at the University of Manchester) contributed to the design and collection of data, the literature review in the CMHTOP workstream; and the manuscript.
Dr Hilde Verbeek (Research Fellow at CAPHRI School for Public Health and Primary Care, Department of Health Services Research, Maastricht University and Hon Research Associate at PSSRU at the University of Manchester) contributed to the BoC, CMHTsOP and care homes outreach workstreams, qualitative and quantitative data analysis; and contributed to the preparation of the manuscript.
Dr David Jolley (Hon Reader at PSSRU at the University of Manchester) was a Co-Applicant and contributed to planning the study; the interpretation and analysis of data in the BoC and CMHTsOP workstreams; and to preparing the manuscript.
Dr Jose-Luis Fernandez (Principal Research Fellow, PSSRU, London School of Economics) contributed to the BoC literature review in workstream 2; health economics input; the data analysis in workstreams 1 and 2; and to the manuscript.
Professor Graham Dunn (Professor of Biomedical Statistics, University of Manchester) was a Co-Applicant; contributed to planning the study; provided statistical and data analytic guidance; and contributed to the manuscript.
Professor Martin Knapp (Professor of Social Policy at London School of Economics) was a Co-Applicant; contributed to planning the study, the BoC literature review, health economics input; the analysis of the CHMTOPs workstream and the manuscript.
Dr Ian Bowns (Hon Research Fellow at PSSRU at Manchester and Director, Public Health Priorities) contributed to interpretation and synthesis of findings; and writing the manuscript.
Other contributions
The older people and their carers in the study who generously gave of their time in interviews.
Health and social care staff in all of the trusts and LAs where the studies took place for their good humour and assistance.
Members of Older People’s groups in Greater Manchester who advised and assisted us during the study.
The team of sessional interviewers who carried out interviews with older people.
Sue Martin and Asha Myers at PSSRU at Manchester who provided secretarial support, including producing questionnaires, data entry, organised consultation groups and other organisation of the study.
Angela Worden at PSSRU at Manchester undertook management of finance, administrative staff, staff recruitment and made significant inputs into the initial design and planning of the study.
Clarissa Giebel at PSSRU at Manchester assisted with data entry and undertook interviews for the study.
Anthony Crook at PSSRU at Manchester assisted with data entry.
Fiona Holland, Biomedical Statistics at the University of Manchester assisted with data analysis.
Dr Sean Lennon facilitated access to NHS colleagues.
Professor Robert Baldwin was a Co-Applicant and valuable source of advice in planning and undertaking the CMHTsOP study.
Ahmed Lambat provided an invaluable patient and public involvement perspective at advisory groups and at other times during the study.
Finally, we thank all our colleagues at PSSRU Manchester for their support in this study.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- Age UK . Later Life in the United Kingdom 2013. www.ageuk.org.uk/Documents/EN-GB/Factsheets/Later_Life_UK_factsheet.pdf?dtrk=true (accessed 22 January 2014).
- Care in Crisis 2012. London: Age UK; 2012.
- Manthorpe J, Iliffe S. The mental health of older people: taking a long view. J Integr Care 2008;16:4-13. http://dx.doi.org/10.1108/14769018200800034.
- Office for National Statistics . Older Workers in the Labour Market 2012. www.ons.gov.uk/ons/dcp171776_267809.pdf (accessed 30 June 2012).
- Hofman A, Rocca WA, Brayne C, Breteler MMB, Clarke M, Cooper B, et al. The prevalence of dementia in Europe: a collaborative study of 1980–1990 findings. Int J Epidemiol 1991;20:736-48. http://dx.doi.org/10.1093/ije/20.3.736.
- Beekman ATF, Copeland JRM, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry 1999;174:307-11. http://dx.doi.org/10.1192/bjp.174.4.307.
- Draper B, Low L. What Is the Effectiveness of Old Age Mental Health Services? 2004. www.euro.who.int/document/E83685.pdf (accessed 30 June 2012).
- Moriarty J, Webb S. Part of their lives: Community Care for Older People with Dementia. Bristol: Policy Press; 2000.
- Wimo A, Karlsson G, Winblad B, Burns A, O’Brien J, Ames D. Dementia. London: Hodder Arnold; 2005.
- Wanless D, Forder J, Fernandez J, Poole T, Beesley L, Henwood M. Securing Good Care for Older People: Taking a Long-Term View. London: King’s Fund; 2006.
- Everybody’s Business. Integrated Mental Health Services for Older Adults: A Service Development Guide. London: Department of Health; 2005.
- Burholt V, Wenger GC, Scott A. Dementia, disability and contact with formal services: a comparison of dementia sufferers and non-sufferers in rural and urban settings. Health Soc Care Community 1997;5:384-97. http://dx.doi.org/10.1111/j.1365-2524.1997.tb00136.x.
- Livingston G, Manela M, Katona C. Cost of community care for older people. Br J Psychiatry 1997;171:56-69. http://dx.doi.org/10.1192/bjp.171.1.56.
- Moriarty JM. Use of community and long-term care by people with dementia in the UK: a review of some issues in service provision and carer and user preferences. Aging Ment Health 1999;3:311-19. http://dx.doi.org/10.1080/13607869956082.
- Luengo-Fernandez R, Leal J, Gray A. Dementia 2010: The Economic Burden of Dementia and Associated Research Funding in the United Kingdom. Cambridge: Alzheimer’s Research Trust; 2010.
- Lowin A, Knapp M, McCrone. Alzheimer’s disease in the UK: comparative evidence on the cost of illness and volume of health services research funding. Int J Geriatr Psychiatry 2001;16:1143-8. http://dx.doi.org/10.1002/gps.499.
- The Operating Framework for the NHS in England 2011/12. London: Department of Health; 2010.
- Jolley DJ, Arie T. Organisation of psychogeriatric services. Br J Psychiatry 1978;132:1-11.
- Dening T. Community psychiatry of old age: a UK perspective. Int J Geriatr Psychiatry 1992;7:757-66. http://dx.doi.org/10.1002/gps.930071012.
- Philpot M, Banerjee S, Johnson S, Ramsay R, Thornicroft G, Brooks L, et al. London’s Mental Health. The Report to the King’s Fund London Commission. London: King’s Fund Publishing; 1997.
- Hilton C. The origins of old age psychiatry in Britain in the 1940s. Hist Psychiatry 2005;16:267-89. http://dx.doi.org/10.1177/0957154X05050075.
- Arie T. The first year of the Goodmayes psychiatric service for old people. Lancet 1970;2:1179-82. http://dx.doi.org/10.1016/S0140-6736(70)90357-0.
- Wattis JP. Geographical variations in the provision of psychiatric services for old people. Age Ageing 1988;17:171-80. http://dx.doi.org/10.1093/ageing/17.3.171.
- Wattis J, Wattis L, Arie T. Psychogeriatrics: a national survey of a new branch of psychiatry. Br Med J 1981;282:1529-33. http://dx.doi.org/10.1136/bmj.282.6275.1529.
- Von Abendorff R, Challis D, Netten A. Staff activity patterns in a community mental health team for older people. Int J Geriatr Psychiatry 1994;9:897-906. http://dx.doi.org/10.1002/gps.930091106.
- A Hospital Plan for England and Wales. London: Her Majesty’s Stationery Office (HMSO); 1962.
- Priorities for Health and Personal Social Services in England: A Consultative Document. London: Her Majesty’s Stationery Office (HMSO); 1976.
- Growing Older. London: Her Majesty’s Stationery Office (HMSO); 1981.
- Knapp M. Money talks: Nine things to remember about mental health financing. J Ment Health 2005;14:89-93. http://dx.doi.org/10.1080/09638230500086073.
- Harvey S, McMahon L. Shifting the Balance of Care to Local Settings: The SeeSaw Report. London: King’s Fund; 2008.
- National Service Framework for Older People. London: Department of Health; 2001.
- Knapp M, Prince M, Albanese E, Banerjee S, Dhanasiri S, Fernandez JL, et al. Dementia UK. London: Alzheimer’s Society; 2007.
- Challis D. The effectiveness of community care. Rev Clin Gerontol 1993;3:97-104. http://dx.doi.org/10.1017/S0959259800003300.
- The Coming of Age: Improving Care Services for Older People. London: Audit Commission; 1997.
- Cotter A, Meyer J, Roberts S. Humanity or bureaucracy? The transition from hospital to long-term continuing institutional care. NT Res 1998;3:247-56. http://dx.doi.org/10.1177/174498719800300403.
- National Health Service and Community Care Act 1990. London: Her Majesty’s Stationery Office (HMSO); 1990.
- Care Management and Assessment: Managers’ Guide. London: Her Majesty’s Stationery Office (HMSO); 1991.
- Care Management and Assessment: Practitioners’ Guide. London: Her Majesty’s Stationery Office (HMSO); 1991.
- Norman IJ, Redfern SJ, Bodley D, Holroyd S, Smith C, White E. The Changing Educational Needs of Mental Health and Learning Disability Nurses. London: English National Board for Nursing, Midwifery and Health Visiting; 1996.
- Darton R, Miles K. Cross-Sectional Survey of Residential and Nursing Homes for Elderly People. Comparisons of Residents in Residential and Nursing Homes for Elderly People, 1981–1996. Canterbury: Personal Social Services Research Unit, University of Kent; 1997.
- Netten A, Forder J, Shapiro J. Measuring Personal Social Services Outputs for National Accounts: Services for Older People. Canterbury: Personal Social Services Research Unit, University of Kent; 2006.
- Care Homes Under Pressure – An England Report. London: RCN; 2010.
- Wattis J, MacDonald A, Newton P. Old age psychiatry: a speciality in transition. Results of the 1996 survey. Psychiatr Bull 1999;23:331-5. http://dx.doi.org/10.1192/pb.23.6.331.
- Burns A, Dening T, Baldwin R. Care of older people: mental health problems. BMJ 2001;322:789-91. http://dx.doi.org/10.1136/bmj.322.7289.789.
- No Accounting for Health: Health Commissioning for Dementia. London: ADS; 1997.
- Forget Me Not: Mental Health Services for Older People. London: Audit Commission; 2000.
- Forget Me Not 2002: Developing Mental Health Services for Older People in England. London: Audit Commission; 2002.
- Lingard J, Milne A. Integrating Older People’s Mental Health Services: Community Mental Health Teams for Older People. London: Department of Health; 2004.
- Dementia: Supporting People with Dementia and their Carers in Health and Social Care. London: The Stationery Office (TSO); 2006.
- Equality in Later Life. A National Study of Older People’s Mental Health Services. London: Healthcare Commission; 2009.
- Promoting Mental Health and Wellbeing in Later Life. London: Age Concern and Mental Health Foundation; 2006.
- Improving Services and Support for People with Dementia: Report by the Comptroller and Auditor General. London: The Stationery Office (TSO); 2007.
- Always a Last Resort: Inquiry into the Prescription of Antipsychotic Drugs to People with Dementia in Care Homes. London: Alzheimer’s Society; 2008.
- No Health Without Mental Health. A Cross-Government Mental Health Outcomes Strategy for People of All Ages. London: Department of Health/HM Government; 2011.
- Improving Value for Money in Adult Social Care. London: Audit Commission; 2011.
- 2020/11 National Survey of Investment in Mental Health Services for Older People. London: Department of Health; 2011.
- Living Well with Dementia: A National Dementia Strategy. London: Department of Health; 2009.
- Quality Outcomes for People with Dementia: Building on the Work of the National Dementia Strategy. London: Department of Health; 2010.
- Banerjee S. The Use of Antipsychotic Medication for People with Dementia: Time for Action. London: Department of Health; 2009.
- Macdonald A, Cooper B. Long-term care and dementia services: an impending crisis. Age Aging 2007;36:16-22. http://dx.doi.org/10.1093/ageing/afl126.
- Ames D. Epidemiological studies of depression among the elderly in residential and nursing homes. Int J Geriatr Psychiatry 1991;6:347-54. http://dx.doi.org/10.1002/gps.930060604.
- Mann AH, Schneider J, Mozley CG, Levin E, Blizard R, Netten A, et al. Depression and the response of residential homes to physical health needs. Int J Geriatr Psychiatry 2000;15:1105-12. http://dx.doi.org/10.1002/1099-1166(200012)15:12%3C1105::AID-GPS252%3E3.0.CO;2-W.
- Dening T, Bains J. Mental health services for residents of care homes. Age Ageing 2004;33:1-2. http://dx.doi.org/10.1093/ageing/afh004.
- Bagley H, Cordingley L, Burns A, Godlove Mozeley C, Sutcliffe C, Challis D, et al. Recognition of depression by staff in nursing and residential homes. J Clin Nurs 2000;9:445-50. http://dx.doi.org/10.1046/j.1365-2702.2000.00390.x.
- Draper B. The effectiveness of old age psychiatry services. Int J Geriatr Psychiatry 2000;15:687-703. http://dx.doi.org/10.1002/1099-1166(200008)15:8%3C687::AID-GPS181%3E3.0.CO;2-K.
- McCrae N, Banerjee S. The challenge of evaluating mental health services for older people. Int J Geriatr Psychiatry 2010;26:551-7. http://dx.doi.org/10.1002/gps.2576.
- Macdonald A, Draper BM. Psychogeriatric Service Delivery: An International Perspective. Oxford: Oxford University Press; 2005.
- Medical Research Council . Final Report From the MAGDR Subgroup 1 on Priority Topics in Dementia Research 2011. www.mrc.ac.uk/consumption/groups/public/documents/content/mrc007843.pdf (accessed 4 July 2012).
- Appleby J, Raleigh V, Frosini F, Bevan G, Gao H, Lyscom T. Variations in Health Care. London: The King’s Fund; 2011.
- Banerjee S. Organisation of old age psychiatry services. Rev Clin Gerontol 1998;8:217-25.
- Mooney GH. Planning for balance of care of the elderly. Scott J Political Economy 1978;25:149-64. http://dx.doi.org/10.1111/j.1467-9485.1978.tb00242.x.
- Hughes J, Challis DJ. Frail older people – margins of care. Rev Clin Gerontol 2004;14:155-64. http://dx.doi.org/10.1017/S0959259804001364.
- Tucker S, Baldwin R, Hughes J, Benbow S, Barker A, Burns A, et al. Old age mental health services in England: implementing the National Service Framework for Older People. Int J Geriatr Psychiatry 2007;22:211-17. http://dx.doi.org/10.1002/gps.1662.
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321:694-6. http://dx.doi.org/10.1136/bmj.321.7262.694.
- High Quality Care For All: NHS Next Stage Review Final Report. London: Department of Health; 2008.
- Appleby J, Crawford R, Emmerson C. How Cold Will It Be? Prospects for NHS Funding: 2011–17. London: The King’s Fund; 2009.
- Johri M, Beland F, Bergman H. International experiments in integrated care for the elderly: a synthesis of the evidence. Int J Geriatr Psychiatry 2003;18:222-35. http://dx.doi.org/10.1002/gps.819.
- Keeping the NHS Local – A New Direction of Travel. London: Department of Health; 2003.
- Our Health, Our Care, Our Say: A New Direction for Community Services. London: The Stationery Office (TSO); 2006.
- McDonald AG, Cuddeford GC, Beale EML. Balance of care: some mathematical models of the National Health Service. Br Med Bull 1974;30:262-71.
- A User’s Guide to the Balance of Care Report: Volume One: Non-Technical User Manual. London: Department of Health and Social Security (DHSS); 1981.
- Mooney GH, Drummond MF. Developing health care policies. Part III (continued). Br Med J 1982;285:1329-31. http://dx.doi.org/10.1136/bmj.285.6351.1329.
- Knapp M. The Economics of Social Care. Basingstoke: Macmillan; 1984.
- Coren E, Fisher M. The Conduct of Systematic Research Reviews for SCIE Knowledge Reviews. London: Social Care Institute for Excellence; 2006.
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York: Centre for Reviews and Dissemination, University of York; 2009.
- Mooney GH, Russell EM, Weir RD. Choices for Health Care. A Practical Introduction to the Economics of Health Provision. Basingstoke: Macmillan; 1986.
- Nixon J, Stoykova B, Glanville J, Christie J, Drummond M, Kleijnen J. The U.K. NHS Economic Evaluation Database. Economic issues in evaluations of health technology. Int J Technol Assess Health Care 2000;16:731-42. http://dx.doi.org/10.1017/S0266462300102016.
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ (British Medical Journal). BMJ 1996;313:275-83.
- Tucker S, Brand C, Wilberforce M, Challis D. The Balance of Care Approach to Health and Social Care Planning: A Systematic Review of the Literature. Manchester: Personal Social Services Research Unit, The University of Manchester; 2011.
- Gibbs RJ. The use of a strategic planning model for health and personal social services. J Operational Res Soc 1978;29:875-83. http://dx.doi.org/10.2307/3009560.
- Wager R. Care of the Elderly: An Exercise in Cost Benefit Analysis Commissioned by Essex County Council. London: Institute of Municipal Treasurers and Accountants; 1972.
- Opit LJ. Domiciliary care for the elderly sick – economy or neglect?. Br Med J 1977;1:30-3. http://dx.doi.org/10.1136/bmj.1.6052.30.
- Social Services: Provision of Care to the Elderly. London: Her Majesty’s Stationery Office (HMSO); 1983.
- Social Services: Care of Mentally Handicapped People. London: Her Majesty’s Stationery Office (HMSO); 1983.
- O’Shea E, Costello J. Boarding out as an option for the care of elderly people. Age Ageing 1991;20:95-9. http://dx.doi.org/10.1093/ageing/20.2.95.
- Clarkson P, Hughes J, Challis D. The potential impact of changes in public funding for residential and nursing home care in the United Kingdom: the residential allowance. Ageing Soc 2005;25:159-80. http://dx.doi.org/10.1017/S0144686X04002582.
- Tramarin A, Tolley K, Campostrini S, de Lalla F. Efficiency and rationality in the planning of health care for people with AIDS: an application of the balance of care approach. AIDS 1997;11:809-16. http://dx.doi.org/10.1097/00002030-199706000-00014.
- Williams P, Challis D, Deber R, Watkins J, Kuluski K, Lum JM, et al. Balancing institutional and community-based care: why some older persons can age successfully at home while others require residential long-term care. Healthc Q 2009;12:95-105. http://dx.doi.org/10.12927/hcq.2009.3974.
- Plank D. Caring for the Elderly: Report of a Study of Various Means of Caring for Dependent Elderly People in Eight London Boroughs. London: Greater London Council; 1977.
- Forte P, Bowen T, Cropper S, Forte P. Enhancing Health Services Management. Buckingham: Open University Press; 1997.
- Challis D, McNiven F, Hughes J, Darton R, Stewart K, Evans S. Estimating the Balance of Care in Gateshead. Manchester: Personal Social Services Research Unit, The University of Manchester; 2000.
- Wright KG, Cairns JA, Snell MC. Costing Care: The Cost of Alternative Patterns of Care for the Elderly. Sheffield: University of Sheffield Joint Unit for Social Services Research; 1981.
- Bebbington A, Charnley H, Fitzpatrick A. Balance and Allocation of Services to Elderly People in Oxfordshire. Canterbury: Personal Social Services Research Unit, University of Kent; 1990.
- Challis D, Hughes J. Frail old people at the margins of care: some recent research findings. Br J Psychiatry 2002;180:126-30. http://dx.doi.org/10.1192/bjp.180.2.126.
- Klemperer PD, McClenahan JW. Joint strategic planning between health and local authorities. Omega 1981;9:481-91. http://dx.doi.org/10.1016/0305-0483(81)90004-9.
- Challis D, Shepherd R. An assessment of the potential for community living of mentally handicapped patients in hospital. Br J Soc Work 1983;13:501-20.
- McCallion G. Planning care for elderly people using the balance of care model. Health Serv Manag Res 1993;6:218-28.
- Forte P, Bowen T, Rey J, Tilquin C. SYSTED94: Dependency, the Challenge for the Year 2000. Lausanne: Swiss Institute of Public Health; 1994.
- Whitfield J, Symonds J. Alternatives to Residential Provision for the Elderly. Essex: Essex County Council Social Services Department; 1976.
- Admissions to Homes for the Elderly. A Survey and Assessment of Alternatives. Bristol: County of Avon Social Services Department; 1980.
- Rutherford P, Forte P. Successful development and application of a strategic dialysis planning model (RENPLAN). Adv Perit Dial 2003;19:106-10.
- Knapp M, Chisholm D, Astin J, Lelliott P, Audini B. The cost consequences of changing the hospital-community balance: the mental health residential care study. Psychol Med 1997;27:681-92. http://dx.doi.org/10.1017/S0033291796004667.
- O’Shea E, Corcoran R. The placement of elderly persons: a logit estimation and cost analysis. Econ Soc Rev 1989;20:219-41.
- O’Shea E, Corcoran R. Balance of care considerations for elderly persons: dependency, placement and opportunity costs. Appl Econ 1990;22:1167-80. http://dx.doi.org/10.1080/00036849000000037.
- Mooney GH. Planning for Balance of Care of the Elderly. Health Economics Research Unit Discussion Papers. Aberdeen: University of Aberdeen; 1977.
- Fordyce JD, Mooney GH, Russell EM. Economic analysis in health care. Health Bull 1981;39:29-38.
- Tucker S, Hughes J, Challis D, Burns A. Services for Older People with Mental Health Problems: The Balance of Care in Cumbria. Manchester: Personal Social Services Research Unit, The University of Manchester; 2005.
- Tucker S, Hughes J, Burns A, Challis D. The balance of care: reconfiguring services for older people with mental health problems. Aging Ment Health 2008;12:81-9. http://dx.doi.org/10.1080/13607860701366038.
- Canvin R, Hamson J, Lyons J, Russell JC. Balance of care in Devon: joint strategic planning of health and social services at AHA and county level. Health Soc Serv J 1978;88:17-20.
- Boldy D, Canvin R, Russell J, Royston G, Boldy D. Operational Research Applied to Health Services. London: Croom Helm; 1981.
- Boldy D, Russell J, Royston G. Planning the balance of health and social services in the United Kingdom. Manag Sci 1982;28:1258-69. http://dx.doi.org/10.1287/mnsc.28.11.1258.
- Kavanagh S, Schneider J, Knapp M, Beecham J, Netten A. Elderly people with cognitive impairment: costing possible changes in the balance of care. Health Soc Care Community 1993;1:69-80. http://dx.doi.org/10.1111/j.1365-2524.1993.tb00199.x.
- Kavanagh S, Schneider J, Knapp M, Beecham J, Netten A, Knapp M. The Economic Evaluation of Mental Health Care. Aldershot: Arena; 1995.
- Report of a Study on Community Care. Stanmore: Department of Health and Social Security Information Division; 1981.
- Rosenhead J, Reddington K, Rizakou E, Dangerfield B, Roberts. OR Work in HIV/AIDS. Birmingham: Operational Research Society; 1990.
- Rizakou E, Rosenhead J, Reddington K. AIDSPLAN: a decision support model for planning the provision of HIV/AIDS-related services. Interfaces 1991;21:117-29. http://dx.doi.org/10.1287/inte.21.3.117.
- The Provision of Child Care: A Study at Eight Local Authorities in England and Wales. Final Report. Bristol: District Auditors; 1981.
- Rosenhead J, Midgley J, Piachaud D. The Fields and Methods of Social Planning. London: Heinemann Educational Books; 1984.
- Culyer AJ, Birch S. Caring for the elderly: a European perspective on today and tomorrow. J Health Politics Policy Law 1985;10:469-87. http://dx.doi.org/10.1215/03616878-10-3-469.
- Davies B, Challis D. Matching Resources to Needs in Community Care. Aldershot: Gower; 1986.
- Chartered Institute of Public Finance and Accountancy n.d. www.cipfa.org/.
- Family Expenditure Survey, 1961–2001. Essex: UK Data Archive; 2002.
- Smith P. Large scale models and large scale thinking – the case of the health services. Omega 1995;23:145-57. http://dx.doi.org/10.1016/0305-0483(95)00001-5.
- Knapp M. Planning for balance of care of the elderly: a comment. Scott J Political Econ 1980;27:288-94. http://dx.doi.org/10.1111/j.1467-9485.1980.tb00933.x.
- Davies B, Knapp M, Sinclair I. Residential Care. The Research Reviewed. Literature Surveys Commissioned by the Independent Review of Residential Care. London: Her Majesty’s Stationery Office (HMSO); 1988.
- Duncan IB, Curnow RN. Operational research in the health and social services. J R Stat Soc 1978;141:153-94. http://dx.doi.org/10.2307/2344452.
- Eddama O, Coast J. A systematic review of the use of economic evaluation in local decision-making. Health Policy 2008;86:129-41. http://dx.doi.org/10.1016/j.healthpol.2007.11.010.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index: a simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Rehabilitation 1965;4:61-5.
- Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud 1988;10:61-3. http://dx.doi.org/10.3109/09638288809164103.
- Sinoff G, Ore L. The Barthel Activities of Daily Living Index: self-reporting versus actual performance in the old-old (≥75 years). J Am Geriatr Soc 1997;45:832-6.
- Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V, et al. MDS Cognitive Performance Scale. J Gerontol 1994;49:M174-82. http://dx.doi.org/10.1093/geronj/49.4.M174.
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey MB, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1983;17:37-49. http://dx.doi.org/10.1016/0022-3956(82)90033-4.
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361-70. http://dx.doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Challis D, Mozley C, Sutcliffe C, Bagley H, Price L, Burns A, et al. Dependency in older people recently admitted to care homes. Age Ageing 2000;29:255-60. http://dx.doi.org/10.1093/ageing/29.3.255.
- Fletcher K, Mant J. A before and after study of the impact of specialist workers for older people. J Eval Clin Pract 2009;15:335-40. http://dx.doi.org/10.1111/j.1365-2753.2008.01008.x.
- Mahoney FI, Wood OH, Barthel DW. Rehabilitation of chronically ill patients: the influence of complications on the final goal. South Med J 1958;51:605-9. http://dx.doi.org/10.1097/00007611-195805000-00011.
- Nouri FM, Lincoln NB. An extended activities of daily living index for stroke patients. Clin Rehabil 1987;1:301-5.
- D’Ath P, Katona P, Mullan E, Evans S, Katona C. Screening, detection and management of depression in elderly primary care attenders. 1: the acceptability and performance of the 15-item Geriatric Depression Scale (GDS-15) and the development of short versions. Fam Prac 1994;11:260-6.
- Jongenelis K, Pot AM, Eisses AMH, Gerritsen DL, Derksen M, Beekman ATF, et al. Diagnostic accuracy of the original 3-item and shortened versions of the Geriatric Depression Scale in nursing home patients. Int J Geriatr Psychiatry 2005;20:1067-74.
- McGivney SA, Mulvihill MM, Taylor B. Validating the GDS depression screen in a nursing home. J Am Geriatr Soc 1994;42:490-2.
- Logsdon RG, Gibbons LE, McCurry SM, Teri L. Assessing quality of life in older adults with cognitive impairment. Psychosom Med 2002;64:510-19.
- Thorgrimsen L, Selwood A, Spector A, Royan L, de Madariaga Lopez M, Woods RT, et al. Whose quality of life is it anyway? The validity and reliability of the quality of Life-Alzheimer’s Disease (QOL-AD) scale. Alzheimer Dis Assoc Disord 2003;17:201-8. http://dx.doi.org/10.1097/00002093-200310000-00002.
- Hoe J, Katona C, Roch B, Livingston G. Use of the QOL-AD for measuring quality of life in people with severe dementia – The LASER-AD study. Age Ageing 2005;34:130-5. http://dx.doi.org/10.1093/ageing/afi030.
- Galvin JE, Fu Q, Scharff DP. Assessing the quality of life – Alzheimer’s disease scale in a community sample of nondemented older people. J Alzheimer’s Assoc 2008;4.
- Beecham J, Knapp M, Thornicroft G, Brewin C, Wing JK. Measuring Mental Health Needs. London: Gaskill; 1992.
- Henwood KL, Pidgeon NF. Qualitative research and psychological theorizing. Br J Psychol 1992;83:97-111. http://dx.doi.org/10.1111/j.2044-8295.1992.tb02426.x.
- Office for National Statistics . Census: Area Classifications 2001. www.ons.gov.uk/ons/guide-method/geography/products/area-classifications/ns-area-classifications/index/datasets/local-authorities/index.html (accessed 20 August 2012).
- Office for National Statistics . Updated Mid-2009 Population Estimates 2009. www.statistics.gov.uk (accessed 17 August 2012).
- Office for National Statistics . Census: Standard Area Statistics (England and Wales) 2001. http://census.ukdataservice.ac.uk/get-data.aspx (accessed 23 January 2014).
- Performance Assessment Framework. Dr Foster Intelligence; 2007.
- Association of Directors of Adult Social Services and Advancing Quality Alliance . NHS &Amp; Local Government. Quality and Efficiency Scorecard for Frail Elderly 2011. www.transitionalliance.co.uk/phocadownload/ScorecardDec/aqua_adass_locality_scorecard_dec11.pdf (accessed 17 August 2012).
- National Audit Office Census of Community Mental Health Teams for Older People. Dementia Services Feedback Report: Stockport CMHT. London: National Audit Office; 2007.
- Croucher K, Hicks L, Jackson K. Housing with Care for Later Life: A Literature Review. York: Joseph Rowntree Foundation; 2006.
- Callaghan L, Netten A, Darton R. The Development of Social Well-being in New Extra Care Housing Schemes. York: Joseph Rowntree Foundation; 2009.
- Dutton R. Extra Care Housing and People with Dementia. A Scoping Review of the Literature 1998–2008. Beaconsfield: Housing and Dementia Research Consortium; 2009.
- Bäumker T, Netten A, Darton R. Costs and outcomes of an extra care housing scheme in England. J Housing Elder 2010;24:151-70. http://dx.doi.org/10.1080/02763891003757098.
- Rovner BW, Katz IR. Psychiatric disorders in the home: a selective review of nursing studies related to clinical care. Int J Geriatr Psychiatry 1993;8:75-87. http://dx.doi.org/10.1002/gps.930080112.
- Slater SL, Katz IR. Prevalence of depression in the aged: formal calculations versus clinical facts. J Am Geriatr Soc 1995;43:78-9.
- Lowery DP, Warner J, Cerga-Pashoja A, Thuné-Boyle I, Iliffe S. Clinicians as recruiters to dementia trials: lessons from the EVIDEM-E project. Int J Geriatr Psychiatry 2011;26:765-69. http://dx.doi.org/10.1002/gps.2671.
- Rendell JM, Merritt RK, Geddes J. Incentives and Disincentives to Participation by Clinicians in Randomised Controlled Trials (Review) 2007. www.onlinelibrary.wiley.com/doi/10.1002/14651858.MR000021.pub3/pdf (accessed 19 August 2012).
- Glendinning C, Challis DJ, Fernandez JL, Jacobs SR, Jones K, Knapp M, et al. Evaluation of the Individual Budgets Pilot Programme. York: Social Policy Research Unit, University of York; 2008.
- Richardson A, Higgins A. The Limits of Case Management: Lessons from the Wakefield Case Management Project. Leeds: Nuffield Institute for Health Services Studies, The University of Leeds; 1992.
- Clarkson P, Venables D, Hughes J, Burns A, Challis D. Integrated specialist assessment of older people and predictors of care-home admission. Psychol Med 2006;36:1011-21. http://dx.doi.org/10.1017/S0033291706007434.
- Taylor BJ, Donnelly M. Professional perspectives on decision making about the long-term care of older people. Br J Soc Work 2006;36:807-26. http://dx.doi.org/10.1093/bjsw/bch322.
- Barlow J, Bayer S. Raising the profile of simulation and modelling in health services planning and implementation. J Health Serv Res Policy 2011;16:129-30. http://dx.doi.org/10.1258/jhsrp.2011.011018.
- A Hospital Plan for England and Wales. London: Her Majesty’s Stationery Office (HMSO); 1962.
- Hilton C. The provision of mental health services in England for people over 65 years of age, 1970-1978. Hist Psychiatry 2008;19:297-320.
- Challis D, Reilly S, Hughes J, Burns A, Gilchrist H, Wlison K. Policy, organisation and practice of specialist old age psychiatry in England. Int J Geriatr Psychiatry 2002;17:1018-26. http://dx.doi.org/10.1002/gps.741.
- Tucker S, Baldwin R, Hughes J, Benbow S, Barker A, Burns A, et al. Integrating mental health services for older people in England – from rhetoric to reality. J Interprof Care 2009;23:341-54. http://dx.doi.org/10.1080/13561820902739833.
- Raising the Standard: Specialist Services for Older People with Mental Illness. Report of the Faculty of Old Age Psychiatry. London: Royal College of Psychiatry; 2006.
- Means R, Richards S, Smith R. Community Care. Basingstoke: Palgrave Macmillan; 2008.
- Dementia: The NICE/SCIE guideline on Supporting People with Dementia and their Carers in Health and Social Care. London: British Psychological Society; 2007.
- Who cares Wins. Improving the Outcome for Older People Admitted to the General Hospital: Guidelines for the Development of Liaison Mental Health Services for Older People. London: Royal College of Psychiatrists; 2005.
- Abendstern M, Harrington V, Brand C, Tucker S, Wilberforce M, Challis D. Variations in structures, processes and outcomes of community mental health teams for older people: a systematic review of the literature. Aging Ment Health 2012;16:861-73. http://dx.doi.org/10.1080/13607863.2011.651431.
- Zaza S, Wright-De Aguero L, Briss P, Truman B, Hopkins D, Hennessy M, et al. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Am J Prevent Med 2000;18:44-7.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Final Report. Lancaster: ESRC Methods Programme, Institute of Health Research; 2006.
- Lindesay J, Herzberg J, Collighan G, Macdonald A, Philpot M. Treatment decisions following assessment by multidisciplinary psychogeriatric teams. Psychiatric Bull 1996;20:78-81. http://dx.doi.org/10.1192/pb.20.2.78.
- Brown P, Challis D, von Abendorff R. The work of a community mental health team for the elderly: referrals, caseloads, contact history and outcomes. Int J Geriatr Psychiatry 1996;11:29-3. http://dx.doi.org/10.1002/(SICI)1099-1166(199601)11:1%3C29::AID-GPS265%3E3.0.CO;2-K.
- Collighan G, Macdonald A, Herzberg J, Philpot M, Lindesay J. An evaluation of the multidisciplinary approach to psychiatric diagnosis in elderly people. BMJ 1993;306:821-4. http://dx.doi.org/10.1136/bmj.306.6881.821.
- MacDonald A, Goddard C, Poynton A. Impact of ‘open access’ to specialist services the case of community psychogeriatrics. Int J Geriatr Psychiatry 1994;9:709-14. http://dx.doi.org/10.1002/gps.930090905.
- Challis D, von Abendorff R, Brown P, Chesterman J, Hughes J. Care management, dementia care and specialist mental health services: an evaluation. Int J Geriatr Psychiatry 2002;17:315-25. http://dx.doi.org/10.1002/gps.595.
- Macdonald A, Ball C, Burton S, Herzberg J, Murphy E, Philpot M, et al. The birth of a specialty: the first ten thousand patients of an old age psychiatry service. Int Psychogeriatr 2007;19:53-6. http://dx.doi.org/10.1017/S1041610206003759.
- Banerjee S, Shamash K, Macdonald A, Mann A. Randomised controlled trial of effect of intervention by psychogeriatric team on depression in frail elderly at home. BMJ 1996;313:1058-61. http://dx.doi.org/10.1136/bmj.313.7064.1058.
- Jenkins D, MacDonald D. Should GPs refer more of their elderly depressed patients to psychiatric services?. Int J Geriatr Psychiatry 1994;9:461-5.
- Philpot M, Drahman B, Ball C, MacDonald A. The prognosis of late-life depression in two contiguous old age psychiatry services: an exploratory study. Aging Ment Health 2000;1:72-8. http://dx.doi.org/10.1080/13607860056008.
- Abendstern M, Reilly S, Hughes J, Venables D, Challis D. Levels of integration and specialisation within professional community teams for people with dementia. Int J Geriatr Psychiatry 2006;21:77-85. http://dx.doi.org/10.1002/gps.1427.
- Arthur A, Jagger C, Lindesay J, Matthews R. Evaluating a mental health assessment for older people with depressive symptoms in general practice: a randomised controlled trial. Br J Gen Pract 2002;52:202-7.
- Losing Time: Developing Mental Health Services for Older People in Wales. London: Audit Commission; 2002.
- Baillon S, Neville P, Broome C. A survey of the relationship between CMHTs and residential homes for the elderly. Int J Geriatr Psychiatry 1996;11:807-11.
- Barlow K. Perceptions of the role of the community psychiatric nurse. Nurs Times 2006;102:34-8.
- Bedford S, Melzer D, Dening T, Lawton C, Todd C, Badger G, et al. What becomes of people with dementia referred to community psychogeriatric teams?. Int J Geriatr Psychiatry 1996;11:1051-6. http://dx.doi.org/10.1002/(SICI)1099-1166(199612)11:12%3C1051::AID-GPS567%3E3.0.CO;2-R.
- Coles R, von Abendorff R, Herzberg J. The impact of a new community mental health team on an inner city psychogeriatric service. Int J Geriatr Psychiatry 1991;6:31-9. http://dx.doi.org/10.1002/gps.930060106.
- Dare S, Benbow S. Sharing caring service: one trust’s response to the problem of recruiting a consultant in old-age psychiatry. Total Qual Manag 1997;8:211-16. http://dx.doi.org/10.1080/0954412979460.
- Das S, Bouman W. Direct referrals from social services to community teams for older people with mental illness. Psychiatric Bull 2008;32:164-5. http://dx.doi.org/10.1192/pb.bp.107.015883.
- Eastley R, Nowers M. A community mental health team for the elderly: a survey of GPs’ views on the service. Psychiatric Bull 1997;21:88-90. http://dx.doi.org/10.1192/pb.21.2.88.
- Gupta K, Coupland L, Fottrell E. A two-year review of an ‘open access’ multidisciplinary community psychiatric service for the elderly. Int J Geriatr Psychiatry 1996;11:795-9. http://dx.doi.org/10.1002/(SICI)1099-1166(199609)11:9%3C795::AID-GPS377%3E3.0.CO;2-5.
- Hoskins S, Coleman M, McNeely D. Stress in carers of individuals with dementia and CMHTs: an uncontrolled evaluation study. J Adv Nurs 2005;50:325-33.
- Jolley D, Jenkins R, Dixey S. First light: old age psychiatry in Wolverhampton 1995-1996. Psychiatric Bull 1997;21:503-5. http://dx.doi.org/10.1192/pb.21.8.503.
- Junaid O, Bruce J. Providing a community psychogeriatric service – models of community psychiatric nursing provision in a single health district. Int J Geriatr Psychiatry 1994;9:715-20. http://dx.doi.org/10.1002/gps.930090906.
- Lawley D, Bestley J, Talbot A, Hostick G. Service innovations: the role of a consultant in old age psychiatry. Psychiatric Bull 2005;29:101-3. http://dx.doi.org/10.1192/pb.29.3.101.
- Mander P. A needs-based model for older people’s mental health. Int J Older People Nurs 2007;2:141-7. http://dx.doi.org/10.1111/j.1748-3743.2007.00065.x.
- McCrae N, Prior S, Silverman M, Banerjee S. Workplace satisfaction in a mental health service for older adults: an analysis of the effects of setting and professional status. Arch Psychiatr Nurs 2007;21:17-24. http://dx.doi.org/10.1016/j.apnu.2006.09.002.
- McCrae N, Banerjee S, Murray J, Prior S, Silverman M. An extra pair of hands? A case of the introduction of support workers in community mental health teams for older adults. J Nurs Manag 2008;16:734-43. http://dx.doi.org/10.1111/j.1365-2834.2008.00929.x.
- Melzer D, Bedford S, Dening T, Lawton C. Carers and the monitoring of psychogeriatric community teams. Int J Geriatr Psychiatry 1996;11:1057-61. http://dx.doi.org/10.1002/(SICI)1099-1166(199612)11:12%3C1057::AID-GPS568%3E3.3.CO;2-Y.
- O’Connor D, Pollitt P, Brook C, Reiss B, Roth M. Does early intervention reduce the number of elderly people with dementia admitted to institutions for long term care?. BMJ 1991;302:871-5. http://dx.doi.org/10.1136/bmj.302.6781.871.
- Sheard D, Cox S. Teams, Multidisciplinary and Interprofessional Working and Dementia. Stirling: The Dementia Services Development Centre, University of Stirling; 1998.
- Simpson C, De Silva P. Multidisciplinary team assessments: a method of improving the quality and accessibility of old age psychiatry services. Psychiatric Bull 2003;27:346-8.
- Stevenson G, Ewing H, Herschell J, Keith D. An enhanced assessment and support team (EAST) for dementing elders – review of a Scottish regional initiative. J Ment Health 2006;2:251-8. http://dx.doi.org/10.1080/09638230600609006.
- Treloar A. Improving methods of assessment in a community mental health team. Psychiatr Bull 1996;20:30-2. http://dx.doi.org/10.1192/pb.20.1.30.
- George K, MacDonald G. A new model of triage in an aged persons mental health service. Australas Psychiatry 2005;13:60-3. http://dx.doi.org/10.1111/j.1440-1665.2004.02151.x.
- Yorkshire and Humber Public Health Observatory . PCT Spend and Outcome Factsheet (SPOT) 2012. www.yhpho.org.uk/default.aspx?RID=49488 (accessed July 2012).
- New Ways of Working for Psychiatrists: Enhancing Effective, Person-Centred Services through New Ways of Working in Multidisciplinary and Multiagency Contexts: Final Report. London: Department of Health; 2005.
- Clark A. New ways of working is dead, long live new ways of working! Revised joint guidance on the employment of consultant psychiatrists. Psychiatrist 2010;34:149-50. http://dx.doi.org/10.1192/pb.bp.109.025551.
- Onyett S, Heppleston T, Bushnell D. A national survey of community mental health teams: team structure and process. J Ment Health 1994;3:175-94. http://dx.doi.org/10.3109/09638239409003798.
- Improving Services and Support for People with Dementia, 6th Report of Session 2007-8 of the Committee of Public Accounts. London: Her Majesty’s Stationery Office (HMSO); 2008.
- The Annual Health Check 2007/08, A National Overview of the Performance of the NHS Trusts in England. London: Commission for Health Care Audit and Inspection; 2008.
- Wilberforce M, Harrington V, Brand C, Tucker S, Abendstern M, Challis D. Towards integrated community mental health teams for older people in England: progress and new insights. Int J Geriatr Psychiatry 2011;26:221-8. http://dx.doi.org/10.1002/gps.2517.
- National Equalities in Mental Health . Finance and Service Mapping 2008. www.mentalhealthequalities.org.uk/our-work/later-life/everybodys-business/finance-and-service-mapping (accessed September 2009).
- Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York, NY: Aldine de Gruyter; 1967.
- Ritchie J, Spencer L. Analysing Qualitative Data. London: Routledge; 1994.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Sheikh JI, Yesavage J, Jerome A. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clinical Gerontologist. J Aging Ment Health 1986;5:165-73.
- Arthur A, Jagger C, Lindesay L, Graham C, Clarke M. Using an annual over-75 health check to screen for depression: Validation of the Short Depression Scale (GDS15) within general practice. Int J Geriatr Psychiatry 1999;14:431-9. http://dx.doi.org/10.1002/(SICI)1099-1166(199906)14:6%3C431::AID-GPS937%3E3.3.CO;2-9.
- McDowell I. Measuring Health: A Guide to Rating Scales and Questionnaires. Oxford: OUP; 2006.
- Therrien Z, Hunsley J. Assessment of anxiety in older adults: a systematic review of commonly used measures. Aging Ment Health 2012;16:1-16. http://dx.doi.org/10.1080/13607863.2011.602960.
- Thornton M, Travis S. Analysis of the reliability of the modified Caregiver Strain Index. J Gerontol B 2003;58:S127-32. http://dx.doi.org/10.1093/geronb/58.2.S127.
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69-77.
- Kroenke K, Spitzer RL, Williams J. The Patient Health Questionnaire-2: validity of a two-Item depression screener. Med Care 2003;41:1284-92. http://dx.doi.org/10.1097/01.MLR.0000093487.78664.3C.
- Mozley C, Huxley P, Sutcliffe C, Bagley H, Burns A, Challis D, et al. ‘Not knowing where I am doesn’t mean I don’t know what I like!’: cognitive impairment and quality of life responses in elderly people. Int J Geriatr Psychiatry 1999;14:776-83.
- Cohen J. A power primer. Psychol Bull 1992;112:155-9. http://dx.doi.org/10.1037//0033-2909.112.1.155.
- Curtis L. Unit Costs of Health and Social Care 2011. Canterbury: Personal Social Services Research Unit, University of Kent; 2011.
- Karasek R. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q 1979;24:285-308. http://dx.doi.org/10.2307/2392498.
- Karasek R, Theorell T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life. New York, NY: Basic Books; 1990.
- van der Doef M, Maes S. The Job Demand-Control (-Support) Model and psychological well-being: a review of 20 years of empirical research. Work Stress 1999;13:87-114. http://dx.doi.org/10.1080/026783799296084.
- Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behav 1981;2:99-113. http://dx.doi.org/10.1002/job.4030020205.
- Cox T. Stress Research and Stress Management: Putting Theory to Work. London: Health and Safety Executive; 1993.
- Morris L. The process of decision making by stressed social workers: to stay or leave the workplace. Int Rev Psychiatry 2005;17:345-54. http://dx.doi.org/10.1080/09540260500238488.
- Cox T, Griffiths A, Leka S, Houdmont J. A Textbook of Occupational Health Psychology. Chichester: Wiley-Blackwell; 2010.
- Johnson JV, Hall EM. Job strain, work place social support, and cardiovascular disease: a cross-sectional study of a random sample of the Swedish working population. Am J Public Health 1988;78:1336-42. http://dx.doi.org/10.2105/AJPH.78.10.1336.
- Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The job content questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol 1998;3:322-55. http://dx.doi.org/10.1037//1076-8998.3.4.322.
- Courvoisier D, Perneger T. Validation of alternative formulations of job strain. J Occup Health 2010;1:5-13. http://dx.doi.org/10.1539/joh.L9084.
- Ovretveit J. Coordinating Community Care: Multidisciplinary Teams and Care Management. London: Open University Press; 1993.
- Miller C, Freeman M, Ross N. Interprofessional Practice in Health and Social Care: Challenging the Shared Learning Agenda. London: Hodder Arnold; 2001.
- Reilly S, Challis D, Burns A, Hughes J. Does integration really make a difference? A comparison of old age psychiatry services in England and Northern Ireland. Int J Geriatr Psychiatry 2003;18:887-93. http://dx.doi.org/10.1002/gps.942.
- Strandberg-Larson M, Krasnik A. Measurement of integrated healthcare delivery: a systematic review of methods and future research directions. Int J Integr Care 2009;9:1-10.
- Glendinning C. Breaking down barriers: integrating health and care services for older people in England. Health Policy 2003;65:139-51. http://dx.doi.org/10.1016/S0168-8510(02)00205-1.
- Glendinning C, Hudson B, Hardy B, Young R. National Evaluation of Notifications for use of the Section 31 Partnership Flexibilities in the Health Act 1999. Manchester: National Primary Care Research and Development Centre; 2002.
- Hudson B. Interprofessionality in health and social care: the Achilles’ heel of partnership?. J Interprof Care 2002;16:7-17. http://dx.doi.org/10.1080/13561820220104122.
- Cameron A, Lart R. Factors promoting and obstacles hindering joint working: a systematic review of the research evidence. J Integr Care 2003;11:9-17. http://dx.doi.org/10.1108/14769018200300013.
- Integration of Health Care Delivery. Report of a WHO Study Group. Geneva: WHO; 1996.
- Leutz WN. Five laws for integrating medical and social services: lessons from the United States and the United Kingdom. Milbank Q 1999;77:77-110. http://dx.doi.org/10.1111/1468-0009.00125.
- Glendinning C, Coleman A, Rummery K. Partnerships, performance and primary care: developing integrated services for older people in England. Ageing Soc 2002;22:185-208. http://dx.doi.org/10.1017/S0144686X02008565.
- Organisation of Care in Psychiatry of the Elderly: A Technical Consensus Statement. Geneva: WHO and WPA; 1997.
- Kodner DL, Knapp M, Challis D, Fernandez J-L, Netten A. Long-Term Care: Matching Resources and Needs. Aldershot: Ashgate; 2004.
- Low L-F, Yap M, Brodaty H. A Systematic Review of Different Models of Home and Community Care Services for Older Persons 2011. www.biomedcentral.com/content/pdf/1472-6963-11-93.pdf (accessed 20 August 2012).
- Challis D, Darton R, Johnson L, Stone M, Traske K. Care Management and Health Care of Older People. Aldershot: Ashgate; 1995.
- Leichsenring K. Developing Integrated Health and Social Care Services for Older Persons in Europe 2004. www.ncbi.nlm.nih.gov/pmc/articles/PMC1393267/pdf/ijic2004-200410.pdf (accessed 21 August, 2012).
- Evans S, Huxley P, Baker C, White J, Madge S, Onyett S. The social care component of multidisciplinary mental health teams: a review and national survey. J Health Serv Res Policy 2012;17:23-9. http://dx.doi.org/10.1258/jhsrp.2012.011117.
- Kodner DL, Spreeuwenberg C. Integrated Care: Meaning, Logic, Applications and Implications – A Discussion Paper 2002. www.ijic.org/index.php/ijic/article/view/URN%3ANBN%3ANL%3AUI%3A10-1-100309/133 (accessed 21 August 2012).
- Independence, Well-being and Choice: Our Vision for the Future of Social Care for Adults in England. London: The Stationery Office (TSO); 2005.
- Putting People First. A Shared Vision and Commitment to the Transformation of Adult Social Care. London: Department of Health; 2007.
- McDonagh MS, Smith DH, Goddard M. Measuring appropriate use of acute beds. A systematic review of methods and results. Health Policy 2000;53:157-84.
- Sorensen L, Tybjerg J, Lund H, Andersen F, Jensen J, Gulmann NC. The admission and discharge patterns of patients with dementia in psychiatric hospitals (Danish). Ugeskr Laeger 1992;154:65-7.
- Fottrell E. Acute psychogeriatric assessment wards: the case against. Geriatr Med 1996;26:19-21.
- Fulop N, Koffman J, Hudson M. Challenging bed behaviours: the use of acute psychiatric beds in an inner-London District Health Authority. J Ment Health 1992;1:335-41. http://dx.doi.org/10.3109/09638239208991563.
- Woods RT, Wills W, Higginson IJ, Hobbins J, Whitby M. Support in the community for people with dementia and their carers: a comparative outcome study of specialist mental health service interventions. Int J Geriatr Psychiatry 2003;18:298-307. http://dx.doi.org/10.1002/gps.822.
- Beecham J, Knapp, M, Fernández J-L, Huxley P, Mangalore R, McCrone PR, et al. Age Discrimination in Mental Health Services. London: Personal Social Services Research Unit; 2008.
- The Importance of ‘Low Level’ Preventive Services to Older People. York: Joseph Rowntree Foundation; 1998.
- Fair Access to Care Services: Guidance on Eligibility Criteria for Adult Social Care. London: Department of Health; 2002.
- Partnerships for Older People Programme (POPP). London: Department of Health; 2006.
- Barnes M, Wistow G, Barnes M, Wistow G. Researching User Involvement. Leeds: Nuffield Institute for Health Services Studies; 1992.
- A Vision for Adult Social Care: Capable Communities and Active Citizens. London: Department of Health; 2010.
- Banerjee S, Samsi K, Petrie CD, Alvir J, Treglia M, Schwam EM, et al. What do we know about quality of life in dementia? A review of the emerging evidence on the predictive and explanatory value of disease specific measures of health related quality of life in people with dementia. Int J Geriatr Psychiatry 2009;24:15-24. http://dx.doi.org/10.1002/gps.2090.
- Okun M, Stock W. Correlates and components of subjective well-being among the elderly. J Appl Gerontol 1987;6:95-112. http://dx.doi.org/10.1177/073346488700600108.
- Bauld L, Chesterman J, Judge K. Measuring satisfaction with social care amongst older service users: issues from the literature. Health Soc Care Community 2000;8:316-24. http://dx.doi.org/10.1046/j.1365-2524.2000.00256.x.
- Williams B, Coyle J, Healy D. The meaning of patient satisfaction: an explanation of high reported levels. Soc Sci Med 1998;47:1351-9. http://dx.doi.org/10.1016/S0277-9536(98)00213-5.
- Edwards C, Staniszewska S. Accessing the user’s perspective. Health Soc Care Community 2000;8:417-24. http://dx.doi.org/10.1046/j.1365-2524.2000.00267.x.
- Evans S, Huxley P, Gately C, Webber M, Mears A, Pajak S, et al. Mental health, burnout and job satisfaction among mental health social workers in England and Wales. Br J Psychiatry 2006;188:75-80. http://dx.doi.org/10.1192/bjp.188.1.75.
- Mistral W, Velleman R. CMHTs: the professionals’ choice?. J Ment Health 1997;6:125-40.
- Norman I, Peck E. Working together in adult community mental health services: an inter-professional dialogue. J Ment Health 1999;8:217-30.
- Onyett S, Pillinger T, Muijen M. Job satisfaction and burnout among members of community mental health teams. J Ment Health 1997;6:55-66.
- Onyett S. Revisiting job satisfaction and burnout in community mental health teams. J Ment Health 2011;20:198-209. http://dx.doi.org/10.3109/09638237.2011.556170.
- Prosser D, Johnson S, Kuipers E, Szmukler G, Bebbington P, Thornicroft G. Mental health, ‘burnout’ and job satisfaction among hospital and community-based mental health staff. Br J Psychiatry 1996;169:334-7. http://dx.doi.org/10.1192/bjp.169.3.334.
- Wykes T, Stevens W, Everitt B. Stress in community care teams: will it affect the sustainability of community care?. Soc Psychiatry Psychiatr Epidemiol 1997;32:398-407.
- Benbow S, Jolley D. Burnout and stress amongst old age psychiatrists. Int J Geriatr Psychiatry 2002;17:710-14. http://dx.doi.org/10.1002/gps.647.
- Spear J, Wood L, Chawla S, Devis A, Nelson J. Job satisfaction and burnout in mental health services for older people. Australas Psychiatry 2004;12:58-61. http://dx.doi.org/10.1046/j.1039-8562.2003.02061.x.
- Hannigan B, Edwards D, Coyle D, Fothergill A, Burnard P. Burnout in community mental health nurses: findings from the all-Wales stress study. J Psychiatric Ment Health Nurs 2000;7:127-34. http://dx.doi.org/10.1046/j.1365-2850.2000.00279.x.
- Buttrieg S, West M, Dawson J. Well-structured teams and the buffering of hospital employees from stress. Health Serv Manag Res 2011;24:203-12.
- Gulliver P, Towell D, Peck E. Staff morale in the merger of mental health and social care organisations in England. J Psychiatric Ment Health Nurs 2003;10:101-7.
- Borrill C, Carletta J, Carter A, Dawson J, Garrod S, Rees A, et al. The effectiveness of health care teams in the National Health Service. Birmingham: Aston Centre for Health Service Organization Research; 2000.
- Streiner D, Norman G. Health Measurement Scales: A Practical Guide to their Development and Use. Oxford: Oxford University Press; 2008.
- Carpenter J, Schneider J, Brandon T, Wooff D. Working in multidisciplinary community mental health teams: the impact on social workers and health professionals of integrated mental health care. Br J Soc Work 2003;33:1081-103. http://dx.doi.org/10.1093/bjsw/33.8.1081.
- Hughes J. Occupational therapy in community mental health teams: a continuing dilemma? Role theory offers an explanation. Br J Occup Ther 2001;64:34-40.
- Reid Y, Johnson S, Morant N, Kuipers E, Szmukler G, Thornicroft G, et al. Explanations for stress and satisfaction in mental health professionals: a qualitative study. Soc Psychiatry Psychiatr Epidemiol 1999;34:301-8. http://dx.doi.org/10.1007/s001270050148.
- Lloyd C, McKenna K, King R. Is discrepancy between actual and preferred work activities a factor in work-related stress for mental health occupational therapists and social workers?. Br J Occup Ther 2004;67:353-60.
- Bailey D, Liyanage L. The role of the mental health social worker: political pawns in the reconfiguration of adult health and social care. Br J Soc Work 2012;42:1113-31. http://dx.doi.org/10.1093/bjsw/bcs069.
- Manthorpe J, Martineau S. Support workers: their role and tasks. A scoping review. London: Social Care Workforce Research Unit, King’s College London; 2008.
- Coffey M. Stress and coping in forensic community mental health nurses: demographic information and qualitative findings. Nurs Times Res 2000;4:100-14. http://dx.doi.org/10.1177/136140960000500205.
- Edwards D, Burnard P, Coyle D, Fothergill A, Hannigan B. A stepwise multivariate analysis of factors that contribute to stress for mental health nurses in the community. J Adv Nurs 2001;36:805-13. http://dx.doi.org/10.1046/j.1365-2648.2001.02035.x.
- Lloyd C, King R, Chenoweth L. Social work, stress and burnout: a review. J Ment Health 2002;11:255-65. http://dx.doi.org/10.1080/09638230020023642.
- Macdonald AJ, Carpenter GI, Box O, Roberts A, Sahu S. Dementia and use of psychotropic medication in non-‘Elderly Mentally Infirm’ nursing homes in South East England. Age Ageing 2002;31:58-64. http://dx.doi.org/10.1093/ageing/31.1.58.
- Home from Home: A report highlighting opportunities for improving standards of dementia care in care homes. London: Alzheimer’s Society; 2007.
- Mozley CG, Challis D, Sutcliffe C, Bagley H, Burns A, Huxley P, et al. Psychiatric symptomatology in elderly people admitted to nursing and residential homes. Ageing Ment Health 2000;4:136-41. http://dx.doi.org/10.1080/13607860050008655.
- Kuske B, Hanns S, Luck T, Angermeyer MC, Behrens J, Riedel-Heller SG. Nursing home staff training in dementia care: a systematic review of evaluated programs. Int Psychogeriatr 2007;19:818-41. http://dx.doi.org/10.1017/S1041610206004352.
- Cohen-Mansfield J. Non-pharmacologic interventions for inappropriate behaviours in dementia. Am J Geriatr Psychiatry 2001;9:361-81.
- Turner S. Behavioural symptoms of dementia in residential settings: a selective review of non-pharmacological interventions. Aging Ment Health 2005;9:93-104. http://dx.doi.org/10.1080/13607860512331339090.
- Bartels SJ, Moak GS, Dums AR. Models of mental health services in nursing homes: a review of the literature. Psychiatr Serv 2002;53:1390-6. http://dx.doi.org/10.1176/appi.ps.53.11.1390.
- Collett J, de Vugt ME, Verhey FRJ, Schols JMGA. Efficacy of integrated interventions combining psychiatric care and nursing home care for nursing home residents: a review of the literature. Int J Geriatr Psychiatry 2009;25:3-13. http://dx.doi.org/10.1002/gps.2307.
- Briss P, Zaza S, Pappaioanou M, Fielding J, Wright-De Aguero L, Truman B, et al. Developing an evidence-based guide to community preventive services – methods. Am J Prev Med 2000;18:35-43.
- Purandare N, Burns A, Challis D, Morris J. Perceived mental health needs and adequacy of service provision to older people in care homes in the UK: a national survey. Int J Geriatr Psychiatry 2004;19:549-53. http://dx.doi.org/10.1002/gps.1126.
- Rands G, Ford M, Okeowo A, Matthew-Bernard C, Kapfumvuti J, Skinner A. How consultation liaison meetings improved staff knowledge, communication and care. Nurs Times 2009;105:18-20.
- Ballard C, Powell I, James I, Reichelt K, Myint P, Potkins D, et al. Can psychiatric liaison reduce neuroleptic use and reduce health service utilization for dementia patients residing in care facilities. Int J Geriatr Psychiatry 2002;17:140-5. http://dx.doi.org/10.1002/gps.543.
- Lyne KJ, Moxon S, Sinclair I, Young P, Kirk C, Ellison S. Analysis of a care planning intervention for reducing depression in older people in residential care. Aging Ment Health 2006;10:394-403. http://dx.doi.org/10.1080/13607860600638347.
- Moxon S, Lyne K, Sinclair I, Young P, Kirk C. Mental health in residential homes: a role for care staff. Ageing Soc 2001;21:71-93. http://dx.doi.org/10.1017/S0144686X01008054.
- Proctor R, Burns A, Stratton Powell H, Tarrier N, Faragher B, . Behavioural management in nursing and residential homes: a randomised controlled trial. Lancet 1999;345:25-9.
- Brodaty H, Draper BM, Millar J, Low L-F, Lie D, Sharah S, et al. Randomized controlled trial of different models of care for nursing home residents with dementia complicated by depression or psychosis. J Clin Psychiatry 2003;64:63-72.
- Crotty M, Halbert J, Rowett D, Giles L, Birks R, Williams H, et al. An outreach geriatric medication advisory service in residential aged care: a randomised controlled trial of case conferencing. Age Ageing 2004;33:612-17. http://dx.doi.org/10.1093/ageing/afh213.
- Kotynia-English R, McGowan H, Almeida OP. A randomized trial of early psychiatric intervention in residential care: impact on health outcomes. Int Psychogeriatr 2005;17:475-85. http://dx.doi.org/10.1017/S1041610205001572.
- Llewellyn-Jones RH, Baikie KA, Smithers H, Cohen J, Snowdon J, Tennant CC. Multifaceted shared care intervention for late life depression in residential care: randomised controlled trial. BMJ 1999;319:676-82. http://dx.doi.org/10.1136/bmj.319.7211.676.
- Opie J, Doyle C, O’Connor DW. Challenging behaviours in nursing home residents with dementia: a randomized controlled trial of multidisciplinary interventions. Int J Geriatr Psychiatry 2002;17:6-13. http://dx.doi.org/10.1002/gps.493.
- Seidel G, Smith C, Hafner RJ, Holme G. A psychogeriatric community outreach service: description and evaluation. Int J Geriatr Psychiatry 1992;7:347-50. http://dx.doi.org/10.1002/gps.930070507.
- Hayes N, Martin F. Supporting care homes: the older people’s specialist nurse. Br J Nurs 2004;13:1250-7.
- Hirst J, Oldknow H. Rapid access for older people to specialist mental health service. Nurs Times 2009;105:12-3.
- Borbasi S, Emmanuel E, Farrelly B, Ashcroft J. Report of an evaluation of a nurse-led dementia outreach service for people with behavioural and psychological symptoms of dementia living in residential aged care facilities. Perspect Public Health 2011;131:124-30. http://dx.doi.org/10.1177/1757913911400143.
- Glendinning C, Jacobs S, Alborz A, Hann M. A survey of access to medical services in nursing and residential homes in England. Br J Gen Prac 2002;52:545-8.
- Holden U, Chapman A. Wait a Minute!: A Practice Guide on Challenging Behaviour and Aggression for Staff Working with Individuals who have Dementia. Dementia Services Development Centre. Stirling: University of Stirling; 1994.
- Soon JA, Levine M. Screening for depression in patients in long-term care facilities: a randomized controlled trial of physician response. J Am Geriatr Soc 2002;50:1092-9. http://dx.doi.org/10.1046/j.1532-5415.2002.50266.x.
- Reilly S, Abendstern M, Hughes J, Challis D, Venables D, Pedersen I. Quality in long term care homes for people with dementia: an assessment of specialist provision. Ageing Soc 2006;26:649-68. http://dx.doi.org/10.1017/S0144686X06004909.
- Mioshi E, Dawson K, Mitchell J, Arnold R, Hodges J. The Addenbrooks Cognitive Examination Revised (ACE-R): a brief cognitive test battery for dementia screening. Int J Geriatr Psychiatry 2006;21:1078-85. http://dx.doi.org/10.1002/gps.1610.
- Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Cornell Scale for Depression in Dementia. Biol Psychiatry 1988;23:271-84. http://dx.doi.org/10.1016/0006-3223(88)90038-8.
- Fairer Care Funding: The Report of the Commission on Funding of Care and Support. London: The Stationery Office (TSO); 2011.
- Mental Health: New Ways of Working for Everyone. London: Department of Health; 2007.
- Pinner G, Hillam J, Branton T, Ramakrishnan A. In-patient Care for Older People within Mental Health Services. London: Faculty of the Psychiatry of Old Age of the Royal College of Psychiatrists; 2011.
- Payment by Results Guidance for 2012–13. London: Department of Health; 2012.
- Caring for People. London: The Stationery Office (TSO); 1989.
- Challis D, Sutcliffe C, Hughes J, von Abendorff R, Brown P, Chesterman J. Supporting People with Dementia at Home. Farnham: Ashgate; 2009.
- Webb A. Co-ordination: a problem in public sector management. Policy Politics 1991;19:229-41.
- Wenger E. Communities of practice and social learning systems. Organization 2000;7:225-46.
- Williams P. The competent boundary spanner. Public Adm 2002;80:103-24. http://dx.doi.org/10.1111/1467-9299.00296.
- Mental Health Act 2007. London: Her Majesty’s Stationery Office; 2007.
- Age Discrimination in Mental Health Services: Making Equality a reality: Royal College of Psychiatrists’ position statement. London: Royal College of Psychiatrists; 2009.
- The Need to Tackle Age Discrimination in Mental Health: A Compendium of Evidence. London: Royal College of Psychiatrists; 2009.
- Prime Ministers Challenge on Dementia – Delivering Major Improvements in Dementia Care and Research by 2015. London: Department of Health; 2012.
- Curtis L. Unit Costs of Health and Social Care 2010. Canterbury: Personal Social Services Research Unit; 2010.
- Age UK. Paying for Permanent Residential Care 2012. www.ageuk.org.uk/home-and-care/care-homes/paying-for-permanent-residential-care/ (accessed 24 August 2012).
- Furniss L, Burns A, Lloyd Craig SK, Scobie S, Cooke J, Faragher B. Effects of a pharmacist’s medication review in nursing homes. Br J Psychiatry 2000;176:563-7. http://dx.doi.org/10.1192/bjp.176.6.563.
- Griffiths P, Harris R, Richardson G, Hallett N, Heard S, Wilson-Barnett J. Substitution of a nursing-led inpatient unit for acute services: randomized controlled trial of outcomes and cost of nursing-led intermediate care. Age Ageing 2001;30:483-8. http://dx.doi.org/10.1093/ageing/30.6.483.
- National Institute for Health and Care Excellence . Costing Statement. Diagnosis, Prevention and Management of Delirium 2010. www.nice.org.uk/nicemedia/live/13060/49998/49998.pdf (accessed 24 August 2012).
- Challis D, Clarkson P, Hughes J, Chester H, Davies S, Sutcliffe C, et al. Community Support Services for People with Dementia: The Relative Costs and Benefits of Specialist and Generic Domiciliary Care Services. Manchester: Personal Social Services Research Unit; 2010.
- Zermansky AG, Alldred DP, Petty DR, Raynor DK, Freemantle N, Eastaugh J, et al. Clinical medication review by a pharmacist of elderly people living in care homes – randomised controlled trial. Age Ageing 2006;35:586-91. http://dx.doi.org/10.1093/ageing/afl075.
- Organisation for Economic Co-operation and Development . What Are Equivalence Scales? 2012. www.oecd.org/eco/growth/OECD-Note-EquivalenceScales.pdf (accessed 22 January 2014).
- Guide to Local Rents 2009: Part 1: Cross Tenure Rents. Cambridge Centre for Housing and Planning Research. University of Cambridge; 2010.
- Housing Needs Study. 2008.
- Department for Work and Pensions . Housing Benefit and Council Tax Benefit Caseload 2012. www.gov.uk/government/publications/housing-benefit-and-council-tax-benefit-summary-statistics-december-2012 (accessed 22 January 2014).
- Philp I, Appleby L. Securing Better Mental Health for Older Adults. London: Department of Health; 2005.
- Philp I. A New Ambition for Old Age: Next Steps in Implementing the National Service Framework for Older People. London: Department of Health; 2006.
- Clarkson P, Hughes J, Challis D. Public funding for residential and nursing home care: projection of the potential impact of proposals to change the residential allowance in services for older people. Int J Geriatr Psychiatry 2003;18:211-16. http://dx.doi.org/10.1002/gps.814.
- Palmore E. Physical, mental and social factors in predicting longevity. Gerontologist 1969;9:103-8.
Appendix 1 Balance of care literature review: example of search strategy
Appendix 2 Balance of care literature review: data extraction form
Appendix 3 Balance of care literature review: good practice guidelines
| Question | Guidance |
|---|---|
| 1. Was the purpose of the study clear? (Score ✗ or ✓) |
The aims of the study, or question being addressed, should be clearly stated |
| 2. Was the number of cases the analysis was based on large enough to instil confidence in the results? (Score ✗, ✓ or not stated) |
Were specific tests used? Were the minimum requirements met? Where specific tests were not used, were there enough cases for the study to have face validity? |
| 3. Were the cases the analysis was based on broadly typical of the population of interest? (Score ✗, ✓ or not stated) |
Was the description of the case selection clear? Were the cases used in the analysis representative of the wider population from which they were drawn? Were the cases used in the analysis typical of the population about whom conclusions are drawn? |
| 4. Where decisions about care were based on case types, did these have face validity? (Score ✗, ✓, not stated or not applicable) |
Categories should be such that the people within each group have similar needs for care, while the people in different groups should have different needs for care |
| 5. Were those service user characteristics most likely to be important in determining individuals’ placements/care packages considered? (Score ✗, ✓ or not stated) |
One might normally expect these to reflect both the service user’s need for care and their home circumstances. When thinking about the care needed by an older person, for example, one might consider their need for help with ADL, their degree of cognitive impairment, their home circumstances and the availability of any informal support |
| 6. Was the approach to costing comprehensive? (Score ✗, ✓, ½ or not stated) |
Was a broad, societal perspective taken? Were non-market and non-public sector costs explicitly included (i.e. housing costs, living expenses and informal care costs)? Possible codings include: ✗ (public expenditure approach only); ✓ (social costing approach including costs to the public sector, housing costs, personal consumption costs/living expenses AND informal care costs); and ½ (moves towards a social costings approach, but does not have all three other elements necessary for a full social costings approach) |
| 7. Were the cost data used valid? (Score ✗, ✓ or not stated) |
Were costs measured accurately? Were the sources used reliable? Possible codings include: ✓ (costs are local/national in accordance with local/national study AND costs not charges/fees AND taken from empirical, not imputed, data); and ✗ (at least one of these criteria is not met) |
| 8. Was the approach to costing fit for purpose? (Score ✗, ✓, not stated or not clear) |
Were the reported costs in keeping with the study’s perspective (e.g. those of the commissioner, provider institution or society)? For example, if a societal perspective is chosen, the author should include all direct medical and non-medical costs as well as indirect costs such as travel and productivity costs due to loss of earnings for the patient and other informal carers Possible codings include: ✓ (no big concerns identified); not clear (where either not enough detail was given to judge, or studies combined public expenditure and some, but not all, wider costs); and ✗ (where the cost data sources were not valid) |
| 9. Were the dates to which resources and prices referred reported? (Score ✗ or ✓) |
|
| 10. Were appropriate adjustments made for inflation? (Score ✗, ✓, not stated or not applicable) |
|
| 11. Was there any attempt to investigate cost shifting? (Score ✗, ✓ or not stated) |
|
| 12. Were any outcomes measured or was any evidence on outcomes considered? (Score ✗ or ✓) |
|
| 13. Where decisions about alternative care packages were not based on research or policy, were they made by appropriate personnel? (Score ✗, ✓, not stated, not clear or not applicable) |
Would ideally want to involve a number of individuals who have experience of making these decisions in reality |
| 14. Was there an attempt to optimise the care provided? (Score ✗, ✓, ½, not stated or not applicable) |
Possible codings include: ✗ (service users received existing levels of care received by individuals in other, usually homogeneous, groups); ½ (care packages were limited to currently available services); and ✓ (care packages allowed for an increase in the range of services provided and/or quantities of services provided to individuals) |
| 15. Were sensitivity analyses conducted to investigate uncertainty in estimates (of costs or consequences) and test the robustness of the results? (Score ✗ or ✓) |
|
| 16. Were key assumptions noted? (Score ✗ or ✓) |
Appendix 4 Balance of care literature review: rating of good practice indicators by reference
| Indicator | aAudit Inspectorate93 | bAuditInspectorate94 | AvonCountyCouncil110 | Bebbington et al.103 | Boldy et al.120 | Boldy et al.121 | Canvin et al.119 | Challis and Hughes104 | Challis et al.101 | Challis and Shepherd106 | Clarkson et al.96 | DHSS124 | District Auditors127 | Forte and Bowen108 | cForte and Bowen100 | Gibbs90 | McDonald et al.80 | Kavanagh et al.122 | Kavanagh et al.123 | cKlemperer and McClenahan105 | Knapp et al.112 | McCallion107 | Fordyce et al.116 | Mooney et al.86 | Mooney71 | Mooney115 | O’Shea and Corcoran113 | O’Shea and Corcoran114 | O’Shea and Costello95 | Opit92 | Plank99 | Rizakou et al.126 | Rosenhead et al.125 | Rutherford and Forte111 | Tramarin et al.97 | Tucker et al.118 | Tucker et al.117 | Wager91 | Wanless et al.10 | Whitfield and Symonds109 | Williams et al.98 | Wright et al.102 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was the purpose of the study clear? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 2. Was the number of cases the analysis was based on large enough to instil confidence in the results? | NS | NS | ✓ | NS | NS | NS | NS | ✓ | ✓ | ✓ | ✓ | NS | NS | NS | NS | NS | NS | NS | NS | NS | ✓ | ✓ | NS | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | NS | NS | NS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 3. Were the cases the analysis was based on broadly typical of the population of interest? | NS | NS | ✓ | NS | NS | NS | NS | ✓ | ✓ | ✓ | ✓ | NS | NS | NS | NS | NS | NS | ✓ | ✓ | NS | ✓ | ✓ | NS | ✓ | ✓ | ✓ | NS | NS | ✗ | ✓ | ✓ | NS | NS | NS | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ |
| 4. Where decisions about care were based on case types, did these have face validity? | ✓ | NS | N/A | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | ✓ | ✗ | ✓ | ✓ | NS | ✓ | ✗ | ✗ | ✓ | N/A | ✗ | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | N/A | ✓ | ✗ |
| 5. Were those service user characteristics most likely to be important in determining individuals’ placements/care packages considered? | ✓ | NS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | NS | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | NS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | NS | ✓ | ✗ |
| 6. Was the approach to costing comprehensive? | ✗ | ✗ | ½ | ✗ | ✗ | ✗ | ✗ | NS | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✗ | ✓ | ½ | ½ | ½ | ½ | ½ | ½ | ✓ | ✓ | ✓ | ½ | ✗ | NS | NS | ✗ | ✗ | ✗ | ½ | ½ | ✗ | ✗ | ½ |
| 7. Were the cost data used valid? | ✓ | ✓ | ✓ | ✓ | NS | NS | NS | NS | ✓ | ✓ | NS | ✓ | ✓ | NS | NS | NS | NS | ✓ | ✓ | NS | ✓ | ✓ | NS | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | NS | ✓ | NS | NS | ✓ | ✓ | ✓ | ✓ | NS | ✓ | ✓ | ✓ |
| 8. Was the approach to costing fit for purpose? | NC | NC | NC | ✓ | NC | NC | NC | NS | NC | ✓ | NC | NC | ✓ | NC | NC | NC | NC | ✓ | ✓ | NS | ✓ | NC | NC | NC | NC | NC | ✗ | ✗ | ✓ | ✓ | NC | NC | NS | NS | ✓ | ✓ | ✓ | NC | NC | ✓ | ✓ | NC |
| 9. Were the dates to which resources and prices referred reported? | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ |
| 10. Were appropriate adjustments made for inflation? | ✓ | ✓ | NS | N/A | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | ✓ | ✓ | NS | N/A | NS | NS | N/A | N/A | N/A | N/A | N/A | N/A | NS | N/A | NS | NS | NS | N/A | NS | NS | ✓ | N/A | N/A | NS | NS |
| 11. Was there any attempt to investigate cost shifting? | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | NS | ✗ | ✗ | ✗ | ✗ | NS | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | NS | ✗ | ✗ | ✗ | ✗ | ✗ | NS | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ |
| 12a. Were any outcomes measured? | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| 12b. Was any evidence on outcomes considered? | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | N/A | ✗ | ✗ | ✗ | N/A | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | N/A | ✗ | ✗ | ✗ | N/A | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ✓ |
| 13. Where decisions about alternative care packages were not based on research or policy, were they made by appropriate personnel? | ✗ | ✗ | ✓ | N/A | ✓ | ✓ | ✓ | ✓ | ✓ | NS | ✓ | ✓ | NS | ✗ | ✓ | ✗ | ✗ | N/A | N/A | ✓ | N/A | NS | ✓ | ✓ | ✓ | ✓ | NC | NC | NC | N/A | ✓ | N/A | N/A | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | ✓ | N/A |
| 14. Was there an attempt to optimise the care provided? | ½ | NS | ✓ | NS | ✓ | ✓ | ✓ | NS | ✓ | ✓ | ½ | NS | NS | ✓ | NS | ½ | ½ | ✓ | ✓ | ✓ | ✗ | NS | ½ | ½ | ½ | ½ | ✗ | ✗ | ✗ | N/A | ✓ | NS | NS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A |
| 15. Were sensitivity analyses conducted to investigate uncertainty in estimates (of costs or consequences) and test the robustness of the results? | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | ✗ | ✗ | NS | ✗ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 16. Were key assumptions noted? | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | ✓ |
Appendix 5 Balance of care literature review: rating of good practice indicators by study
| Indicator | aAudit Inspectorate93 | bAudit Inspectorate94 | Avon County Council110 | Bebbington et al.103 | Boldy et al.119–121 | Chalis et al.101,104 | Challis and Shepherd106 | Clarkson et al.96 | DHSS124 | District Auditors127 | Forte and Bowen108 | cForte and Bowen100 | Gibbs90/McDonald et al.80 | Kavanagh et al.122,123 | cKlemperer and McClenahan105 | Knapp et al.112 | McCallion107 | Mooney et al.71,86,115,116 | O’Shea and Corcoran113,114 | O’Shea and Corcoran95 | Opit92 | Plank99 | Rizakou et al.126/Rosenhead et al.125 | Rutherford and Forte111 | Tramarin et al.97 | Tucker et al.117,118 | Wager91 | Wanless et al.10 | Whitfield and Symonds109 | Williams et al.98 | Wright et al.102 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was the purpose of the study clear? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 2. Was the number of cases the analysis was based on large enough to instil confidence in the results? | NS | NS | ✓ | NS | NS | ✓ | ✓ | ✓ | NS | NS | NS | NS | NS | NS | NS | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | NS | NS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 3. Were the cases the analysis was based on broadly typical of the population of interest? | NS | NS | ✓ | NS | NS | ✓ | ✓ | ✓ | NS | NS | NS | NS | NS | ✓ | NS | ✓ | ✓ | ✓ | NS | ✗ | ✓ | ✓ | NS | NS | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ |
| 4. Where decisions about care were based on case types, did these have face validity? | ✓ | NS | N/A | ✓ | ✓ | ✓ | N/A | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | ✓ | N/A | ✗ | N/A | N/A | N/A | N/A | N/A | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | N/A | ✓ | ✗ |
| 5. Were those service user characteristics most likely to be important in determining individuals’ placements/care packages considered? | ✓ | NS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | NS | ✓ | ✗ |
| 6. Was the approach to costing comprehensive? | ✗ | ✗ | ½ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ½ | ½ | ✓ | ✓ | ✓ | ½ | ✗ | NS | ✗ | ✗ | ½ | ½ | ✗ | ✗ | ½ |
| 7. Were the cost data used valid? | ✓ | ✓ | ✓ | ✓ | NS | ✓ | ✓ | NS | ✓ | ✓ | NS | NS | NS | ✓ | NS | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | NS | ✓ | NS | ✓ | ✓ | ✓ | NS | ✓ | ✓ | ✓ |
| 8. Was the approach to costing fit for purpose? | NC | NC | NC | ✓ | NC | NC | ✓ | NC | NC | ✓ | NC | NC | NC | ✓ | NS | ✓ | NC | NC | ✗ | ✓ | ✓ | NC | NC | NS | ✓ | ✓ | NC | NC | ✓ | ✓ | NC |
| 9. Were the dates to which resources and prices referred reported? | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ |
| 10. Were appropriate adjustments made for inflation? | ✓ | ✓ | NS | N/A | NS | NS | NS | NS | NS | NS | NS | NS | NS | ✓ | NS | N/A | NS | N/A | N/A | N/A | NS | N/A | NS | NS | N/A | NS | ✓ | N/A | N/A | NS | NS |
| 11. Was there any attempt to investigate cost shifting? | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | NS | ✗ | ✗ | ✗ | ✗ | NS | ✗ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | NS | ✗ | ✗ | ✗ | ✗ | NS | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ |
| 12a. Were any outcomes measured? | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| 12b. Was any evidence on outcomes considered? | ✗ | ✗ | ✗ | ✗ | ✗ | N/A | ✗ | ✗ | ✗ | N/A | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | N/A | ✗ | ✗ | N/A | ✗ | ✓ | ✓ | ✗ | ✗ | ✓ |
| 13. Where decisions about alternative care packages were not based on research or policy, were they made by appropriate personnel? | ✗ | ✗ | ✓ | N/A | ✓ | ✓ | NS | ✓ | ✓ | NS | ✗ | ✓ | ✗ | N/A | ✓ | N/A | NS | ✓ | NC | NC | N/A | ✓ | N/A | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | ✓ | N/A |
| 14. Was there an attempt to optimise the care provided? | ½ | NS | ✓ | NS | ✓ | ✓ | ✓ | ½ | NS | NS | ✓ | NS | ½ | ✓ | ✓ | ✗ | NS | ½ | ✗ | ✗ | N/A | ✓ | NS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A |
| 15. Were sensitivity analyses conducted to investigate uncertainty in estimates (of costs or consequences) and test the robustness of the results? | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | ✗ | NS | ✓ | ✗ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 16. Were key assumptions noted? | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | ✓ |
Appendix 6 Social services team survey data collection form
Appendix 7 Care home survey data collection form
Appendix 8 Balance of care and community mental health team for older people study methods: overview of imputed variables
| Variable | Average proportion missing in data setsa | Approachb | Reason |
|---|---|---|---|
| Behaviour score (both studies) | 6% | Single model-based imputation using known items from question battery (restricted to up to two of seven items missing) | Bias when describing data: higher severity items more likely to be missing (listwise deletion) |
| Barthel score (both studies) | 11% | Single model-based imputation using known items from question battery (restricted to up to 2 of 10 items missing) | Bias when describing data: higher severity items more likely to be missing (listwise deletion) |
| Cognitive performance scale score (BoC study only) | 5% | Single ‘manual’ imputation based on most likely combinations in variable’s coding instruction; mixture introduced when imputed case could be on either side of a category (e.g. case can be either borderline or intact; selected every third one as borderline if probability was 33%) | Bias when describing data: higher severity items more likely to be missing (listwise deletion) |
| Cognitive impairment/recent MMSE score (CMHT study only) | 48% | Multiple imputation: truncated regression model drawing on client’s clinical profile | Bias when describing data: lower severity scores more likely to be missing (less likely to be reported/available) |
| Cost of CMHT input (CMHT study only) | 2% | Multiple imputation: predictive mean matching drawing on client’s clinical profile and CMHT | No bias, but aim was to maximise number of cases used in analyses |
| Cost of other mental health input (CMHT study only) | 24% | Multiple imputation: predictive mean matching drawing on client’s clinical profile and CMHT | No observable bias within groups, although pattern of missingness clearly varying by groups. Aim was to maximise number of cases used in analyses |
| Cost of social care packages (CMHT study only) | 13% (combined effect of all components) | Multiple imputation of each social care cost component: predictive mean matching drawing on client’s clinical profile and CMHT | No observable bias within groups, although pattern of missingness clearly varying by groups. Aim was to maximise number of cases used in analyses |
| Satisfaction scores (CMHT study only) | 22% | Single model-based imputation using known items from question battery (restricted to up to two of six items missing) | Bias when describing data: lower satisfaction items more likely to be missing (listwise deletion) |
| QoL-AD score (CMHT study only) | 25% | Single model-based imputation using known items from question battery (restricted to up to 4 of 13 items missing) | Bias when describing data: lower QoL items more likely to be missing (listwise deletion) |
| GDS score (CMHT study only) | 36% | Single model-based imputation using known items from question battery (restricted to up to 5 of 15 items missing) | Bias when describing data: higher severity items more likely to be missing (listwise deletion) |
Appendix 9 Balance of care and community mental health team for older people study methods: compilation of summary measures
Modified Barthel Index (both studies)
| Activity | No help | Minor help | Major help | Full help |
|---|---|---|---|---|
| Grooming | 5 | 0 | 0 | 0 |
| Bathing | 5 | 0 | 0 | 0 |
| Dressing | 10 | 5 | 5 | 0 |
| Use of toilet | 10 | 5 | 5 | 0 |
| Transfers | 15 | 10 | 5 | 0 |
| Stairs | 10 | 5 | 5 | 0 |
| Activity | Continent | Occasional accidents | Incontinent |
|---|---|---|---|
| Continence (urinary) | 10 | 5 | 0 |
| Continence (faecal) | 10 | 5 | 0 |
| Activity | Independent | Walks with help | Wheelchair independent | Immobile |
|---|---|---|---|---|
| Mobility | 15 | 10 | 5 | 0 |
| Activity | Independent | Needs supervision | Needs limited help | Needs major help | Needs full help |
|---|---|---|---|---|---|
| Eating | 10 | 5 | 5 | 5 | 0 |
Categories:
-
80–100, independent
-
60–79, needs minimal help with ADL
-
40–59, partially dependent
-
20–39, very dependent
-
< 20, totally dependent.
Cognitive performance scale score (Balance of Care Study only)
| Level (score) | Impairment count (decision-making not independent, not fully understood, memory problems) | Severe impairment count (decision-making moderately impaired, sometimes/never understood) | Decision-making: severe impairment | Total dependent eating |
|---|---|---|---|---|
| Intact (0) | 0 | N/A | No | N/A |
| Borderline intact (1) | 1 | N/A | No | N/A |
| Mild impairment (2) | 2–3 | 0 | No | N/A |
| Moderate impairment (3) | 2–3 | 1 | No | N/A |
| Moderate/severe impairment (4) | 2–3 | 2 | No | N/A |
| Severe impairment (5) | N/A | N/A | Yes | No |
| Very severe impairment (6) | N/A | N/A | Yes | Yes |
Behaviour scale
| Range | Label | Description |
|---|---|---|
| 0–1 | No challenging behaviour pattern | None or only one occasional behaviour listed (36% overall). Some service users in this group are on occasion either agitated or passive, or (less likely) show other challenging behaviours with the exception of wandering away from the caregiver or being physically aggressive towards people or objects |
| 2–7 | Limited challenging behaviour pattern | Typical service users in this broad category have a tendency to be at least occasionally agitated as well as disturbed at night, but may also be either unco-operative, passive or delusional at times (rarely a combination of these behaviours). They are relatively unlikely to wander away from the caregiver or to be physically aggressive towards objects or people (52% overall) |
| 8–14 | Complex challenging behaviour pattern | Typical service users in this category are frequently agitated as well as disturbed at night and delusional. In addition, they are rather likely to show at least some degree of wandering away from caregivers, lack of co-operation or physical aggression. On occasion, they may also be passive in addition to the aforementioned behaviour patterns (12% overall) |
Formal support (both studies)
| Code | Label | Remark |
|---|---|---|
| 0 | No or minor input (e.g. SW input only) | Social work input not available in inpatient data collection |
| 1 | Intermittent input (not daily and mainly outside home) | Everyone with some limited input who was not already placed in categories 0, 2 or 3 |
| 2 | Limited care package (1–9 hours personal care/domestic help/sitting service combined or seven or more meals per week) | |
| 3 | Intensive care package (≥ 10 hours personal care/domestic help/sitting service combined) | |
| 4 | Amount of support unclear | Mainly due to respondents not reporting figures but merely confirming provision of support |
| 5 | Is in care home (N/A) | Only applicable in inpatients sample |
Appendix 10 Balance of care and community mental health team for older people methods: further information on the distribution of the Barthel and behaviour scores
Barthel scores. (a) Totally dependent; (b) very dependent; (c) partially dependent; (d) minimal help needed; and (e) independent.
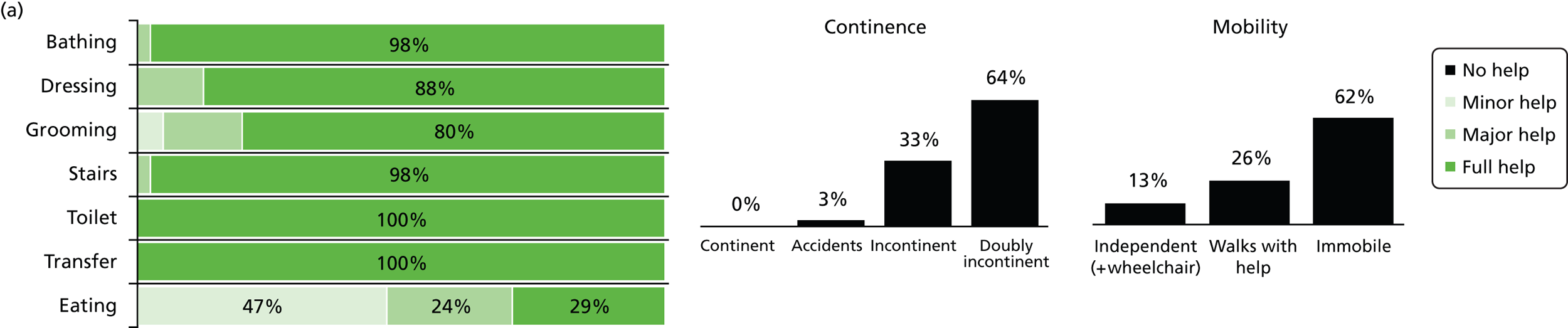
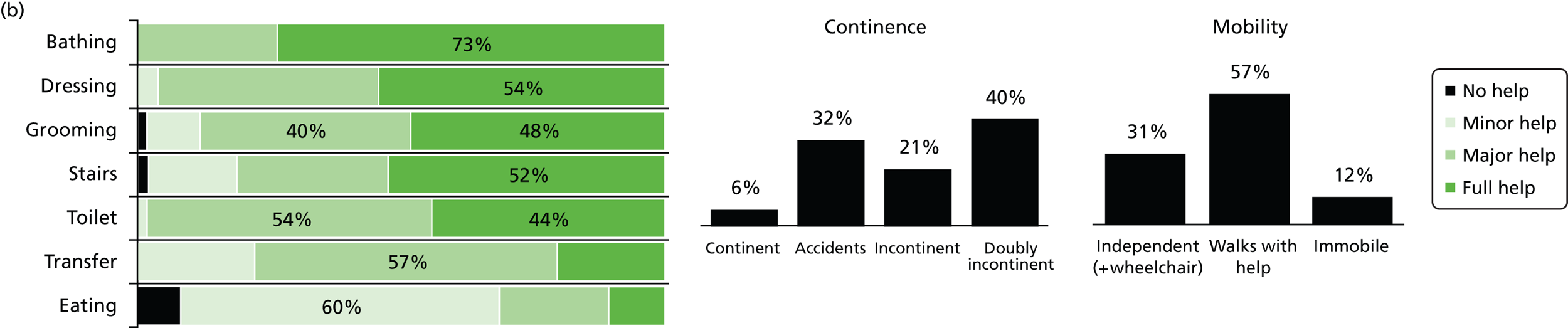
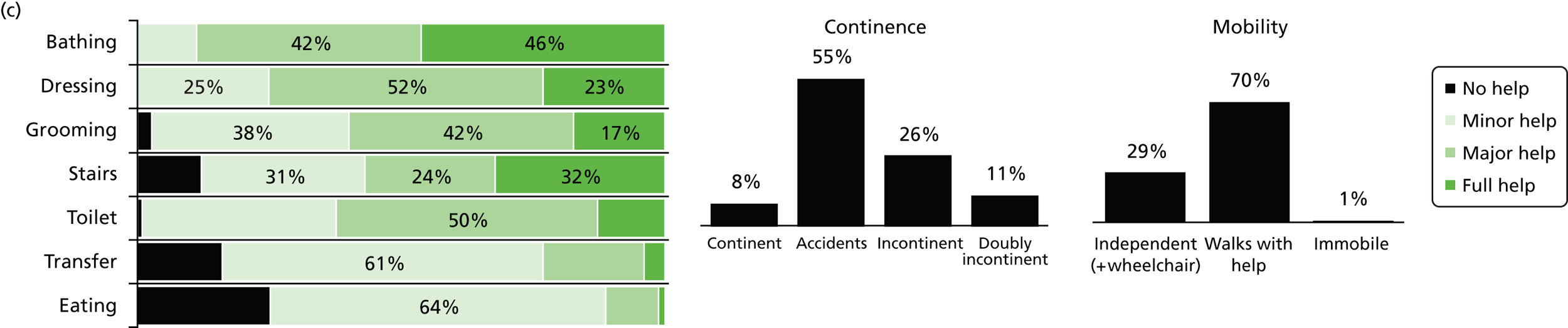
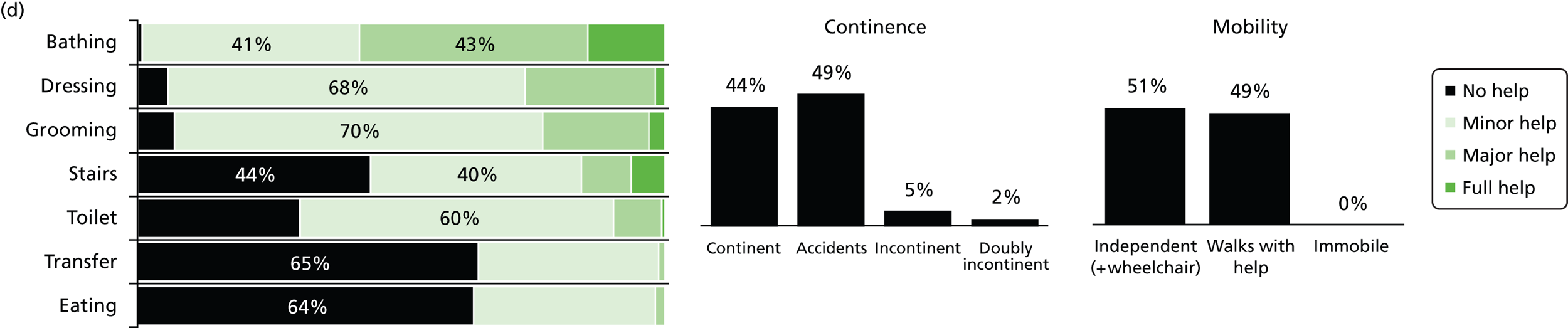
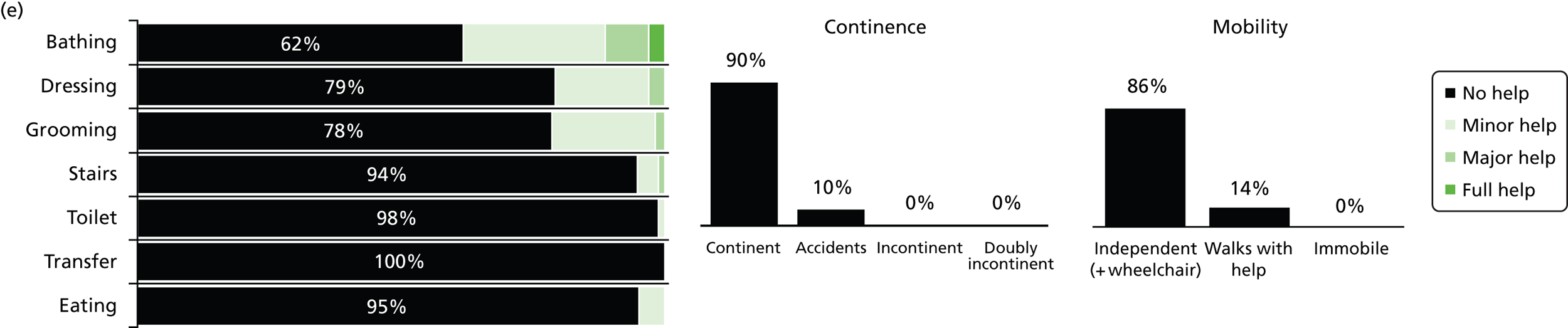
Behaviour scores. (a) High; (b) medium; and (c) low.
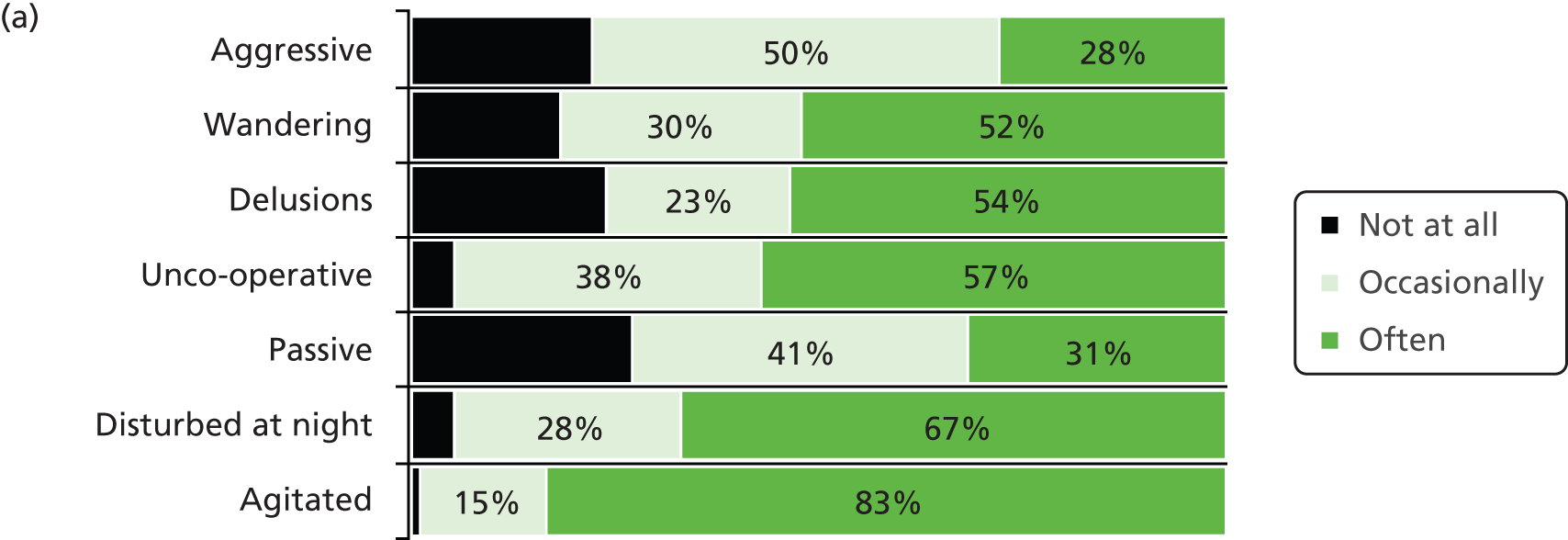
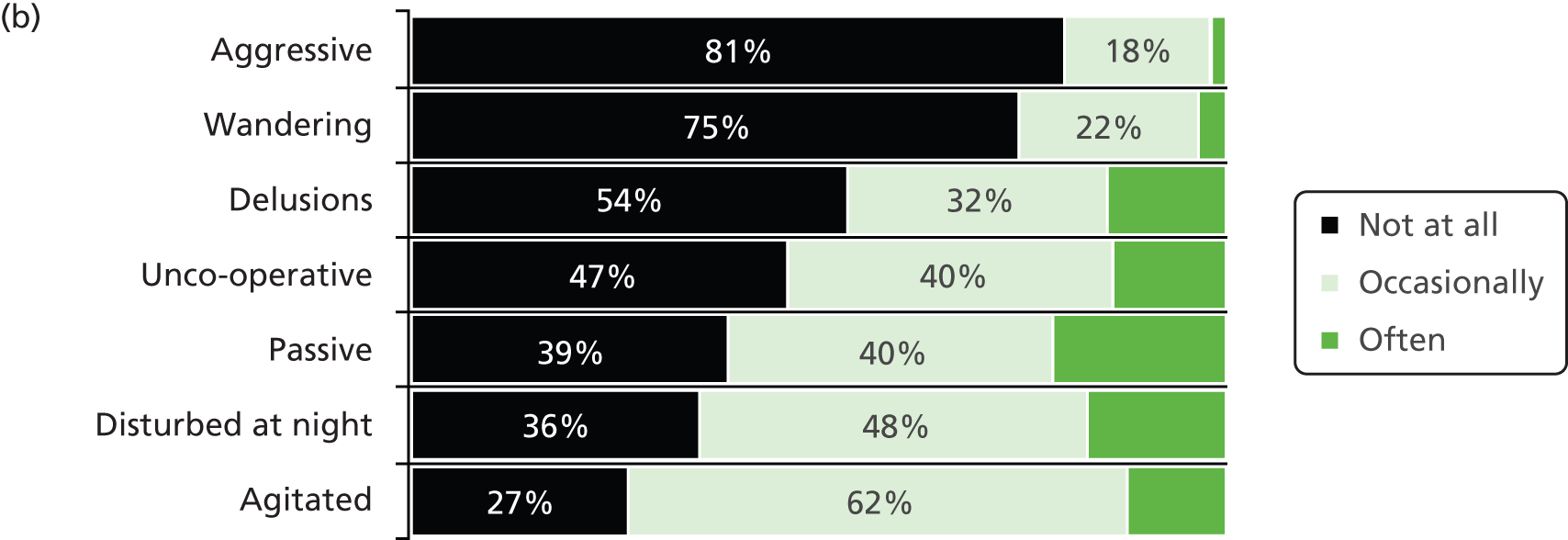
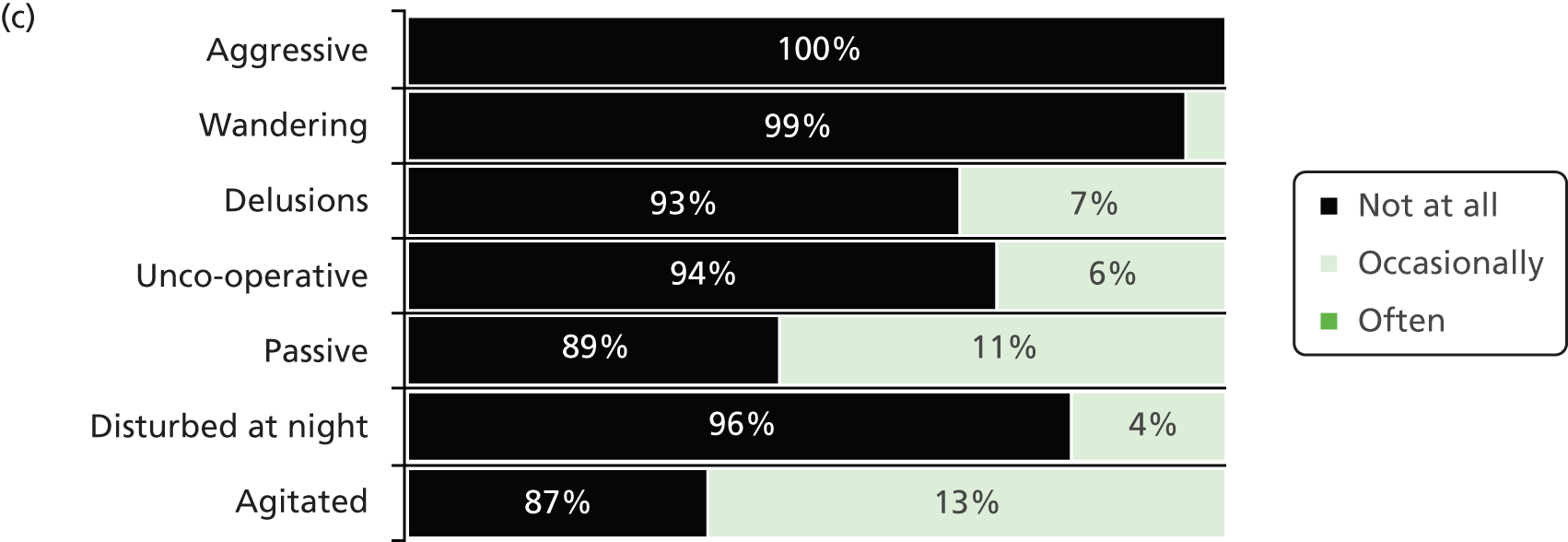
Appendix 11 Examples of care home admission vignettes
The North-West Balance of Care Study: group 17 – Mrs C
Sociodemographic information
Mrs C is a widow in her late 80s who lives alone in a small bungalow.
Information about care needs
-
Activities of daily living: Mrs C walks with a stick and is a little unsteady but can get around within her own home. She is, however, occasionally incontinent of both urine and faeces and needs physical assistance to wash, dress and shower. Although she can feed herself, she needs prompting to eat and drink.
-
Physical health: Mrs C’s physical health is poor. She has been diagnosed with hypertension and osteoarthritis and has a history of transient ischaemic attacks. She also has some difficulty hearing, and rarely remembers to wear her hearing aid.
-
Cognition/mood: Mrs C has vascular dementia and displays marked short-term memory impairment. She is largely disorientated to time and does not always recognise people she knows, including close family. While her speech is quite confused, she is generally able to express her basic needs. There is no indication that she is depressed.
-
Behaviour: Although Mrs C’s behaviour has rarely given cause for alarm, she sometimes appears agitated and has twice been found ‘lost’ not far from her home. If left to her own devices she tends to spend much of the day sleeping in a chair or, indeed, in bed.
Current care
-
Informal support: Mrs C has two daughters who live locally and between them visit each day. They ensure Mrs C has a daily hot meal and undertake all household tasks, as well as providing social support and general supervision.
-
Formal care package: Mrs C is known to the local social services team and has a home care package totalling 10 hours a week, mostly to assist with personal care. She also attends a local day centre 2 days a week. Although Mrs C has no current input from the mental health service, she has been assessed by a consultant psychiatrist in the past.
Assessment issues
-
Risk factors: Mrs C’s daughters are finding it increasingly difficult to support their mother, who now needs prompting and supervision with all activities of daily living. They are also very concerned that she will wander away from home again and may accidentally harm herself.
-
Attitude to future care: Mrs C is not felt to have the capacity to make a decision about her long-term future. Her daughters, however, feel that she should now be in a care home.
The North-West Balance of Care Study: group 23 – Mr J
Sociodemographic information
Mr J is a 69-year-old gentleman who usually lives at home alone but is currently an inpatient in the district general hospital having been admitted further to a fall.
Information about care needs
-
Activities of daily living: Mr J has impaired mobility and needs help to get in and out of bed. He is able to walk a few steps with the help of a zimmer frame, but needs a wheelchair if outside the house and has had three falls within the last 3 months. Although Mr J is usually continent and can feed himself if his food is cut up for him, he needs full help to wash, dress and shower.
-
Physical health: Mr J’s physical health is poor. He has type II diabetes (managed by a combination of medication and diet) and has recently been registered blind (diabetes-related). He also suffers with Parkinson’s disease.
-
Cognition/mood: Mr J has no formal psychiatric diagnosis but at times appears a bit forgetful. Although he has occasional word-finding difficulties, he is generally able to communicate well and can express his needs and preferences. While his physical disabilities tend to get him down, and he has lost interest in some of his previous activities, there is no suggestion that he is clinically depressed.
-
Behaviour: Mr J is generally very grateful for the help he receives. He does on occasion get quite agitated, however, which seems to be related to the experience of visual hallucinations, and can sometimes be unco-operative. Although he mostly sleeps well, he has occasional disturbed nights.
Current care
-
Informal support: Mr J receives a lot of support from his family and friends who until now have provided all his personal care as well as doing his shopping, cleaning and laundry and overseeing his very complicated medication regime. His main carer, his youngest daughter, is shortly to move abroad however, and the current situation is not sustainable.
-
Formal care package: Mr J is known to social services from previous hospital admissions, but has had no recent social care input. He has never had any contact with the mental health service.
Assessment issues
-
Risk factors: Mr J’s physical health is steadily deteriorating and he requires a growing amount of supervision and support to meet his needs and maintain his safety. Since being admitted to hospital he has had two further falls (on one occasion, badly bruising his back), and appears to be experiencing more frequent hallucinations.
-
Attitude to future care: Mr J does not actively wish to move into a care home, but acknowledges that it may not be possible to provide the care he needs at home any longer.
Appendix 12 Examples of inpatient admission vignettes
The North-West Balance of Care Study: group 28a – Mr A
Sociodemographic information
Mr A is a 76-year-old gentleman who lives with his wife.
Past mental health support
Mr A was referred to the mental health service approximately 2 years ago after his wife expressed concern about his increasing forgetfulness and repetition. Further to assessment by a consultant psychiatrist he was diagnosed with a mixed dementia and was seen briefly by the CMHT who provided his wife with information about dementia and local sources of help. Four weeks ago he was re-referred following concerns about his increasingly challenging behaviour and his medication was reviewed. There were also plans to instigate a behaviour management programme, and his wife has been keeping a diary of his presentation.
Presentation immediately prior to/on admission
Activities of daily living: Mr A is very active and has no problems mobilising in or outdoors. He is, however, occasionally incontinent of urine. While he can physically wash, dress and feed himself (and has a good appetite), he needs much encouragement to change his clothes and can rarely be persuaded to have a bath.
Physical health: Mr A has high blood pressure and has previously been treated for prostate cancer. However, his current health is described as fair.
Cognition/mood: As above, Mr A has dementia, now moderate–severe in degree. While he has obvious short-term memory problems and sometimes struggles to express himself, his family can generally understand what he says. There is no indication that he is clinically depressed.
Behaviour: Mr A generally appears restless and agitated and often shouts at the television, seeming to think that the presenters are talking about him. At such times he can become very angry, and it is not uncommon for him to throw things at the television set, while if his wife tries to distract him, he then becomes angry at her. Although he previously slept well, in recent months he appears to have lost all sense of night and day, and is regularly up and about in the night, moving things from place to place. He does not, however, try to leave the house.
Support immediately prior to admission
Mrs A is her husband’s main carer and undertakes all the household tasks as well as providing a high degree of support and reassurance for her husband. Her own physical health is frail, however, and she is clearly very stressed by his recent behaviour.
They do not receive any formal social care.
Reasons for admission
Mr A’s behaviour is causing concern and there are fears that he may, in anger, accidently harm his wife or himself. It is also thought that an inpatient admission would offer the opportunity to review his medication and future care needs.
The North-West Balance of Care Study: group 6 – Mr E
Sociodemographic information
Mr E is a 69-year-old gentleman who usually lives at home with his wife and his beloved spaniel, Oscar.
Past mental health support
Mr E has a long history of bipolar disorder and is well known to the local mental health service. Since he and his wife moved into extra care housing some 9 months ago, he has been relatively well, and his support worker has reduced her visits to once a fortnight. In the past few weeks, however, there have been signs that his mood is deteriorating again, and a medical review was planned. Events overtook this, when, over the course of last weekend he became increasingly confused and agitated and was admitted to the local district general hospital with a possible infection and/or dehydration.
Presentation immediately prior to/on admission
Activities of daily living: Mr E is usually fully self-caring. In the last few weeks, however, he has neglected his personal care, not bothering to shave and needing prompting to change his clothes. He has also lost his appetite and is taking negligible diet. A somewhat frail man to start with, he is rapidly losing weight.
Physical health: Mr E is known to have type II diabetes (medication and diet controlled). Having now been treated for a urinary infection, he no longer needs to be on a medical ward.
Cognition/mood: Although Mr E displays no objective signs of cognitive impairment, he feels his memory is failing and complains of poor concentration. Usually a keen reader and member of the local bowls club, he has recently lost interest in both these activities and at interview appears anxious and preoccupied. While adamant that he would never harm himself because of his wife and dog, he cannot see a future.
Behaviour: The ward notes suggest that Mr E is sleeping poorly and continues to lose weight. There is also mention of some agitation, particularly at night.
Support immediately prior to admission
Mr E’s wife is very supportive and has long been his main emotional support. However, her own health is frail now, and she is much older than her husband, hence the move to extra care housing. The couple both like the warden there, but have no additional support package.
Reasons for admission
Although Mr E has recovered from his urinary infection, he remains frail and low in mood. It is thought that he will continue to neglect himself if he returns home, and that a transfer to the mental health ward for further assessment and treatment would be beneficial.
Appendix 13 Balance of Care Study: unit costs summary
Principles of costing approach
-
Preference has been given to local over national average costs wherever available.
-
Preference has been given to 2010 costs wherever available.
-
National costs for professional input have been adjusted to take account of local staff bandings.
-
Preference has been given to costs for professional input that include indirect as well direct activities undertaken for service users.
-
Preference has been given to costs for professional input that include travel.
-
Preference has been given to costs for professional input that exclude training.
Definitions from Curtis355
-
Per hour of client contact Cost of 1 hour of professional time spent attending to clients. This also allows for the cost of time not spent with clients and allocates the costs of this time to the time spent with clients.
-
Per hour of client-related work Hourly cost of time spent on activities directly related to the client. This is not necessarily time spent in face-to-face contact with the client.
-
Per hour of home visiting Cost of 1 hour spent by a professional undertaking visits to clients at home. This includes the costs of time spent travelling. It also allows for overall time spent on non-clinical activity and allocates this to the total time spent with clients in any setting.
-
Per patient-related work or per patient-related hour Hourly cost of time spent on activities directly related to the patient. This is not necessarily time spent in face-to-face contact with the patient.
| Service | Cost/time frame | Source of costing | Comments |
|---|---|---|---|
| Care home placement: older people, standard residential | £364 per week | Site X 2010–11 costs |
Maximum price ranges between £340 for a single room to £388 for a single room with en-suite including quality premium and no top-up guarantee excellent |
| Care home placement: older people, special registration | £426 per week | Site X 2010–11 costs |
Maximum price ranges between £400 for a single room to £453 for a single room with en-suite including quality premium and no top-up guarantee excellent |
| Care home placement: older people high dependency residential | £426 per week | Site X 2010–11 costs |
Maximum price ranges between £400 for a single room to £453 for a single room with en-suite including quality premium and no top-up guarantee excellent |
| Care home placement: older people, standard nursing, LA costs only | £426 per week | Site X 2010–11 costs |
Maximum price ranges between £400 for a single room to £453 for a single room with en-suite including quality premium and no top-up guarantee excellent. These costs represent the Council’s component for accommodation and personal care only |
| Care home placement: older people, nursing, special registration, LA costs only | £452 per week | Site X 2010–11 costs |
Maximum price ranges between £421 for a single room to £483 for a single room with en-suite including quality premium and no top-up guarantee excellent. These costs represent the Council’s component for accommodation and personal care only |
| Care home placement: older people, standard nursing contribution | £108.70 per week | Age UK, paying for permanent residential care factsheet for 2010/11356 | NHS costs |
| Care home support service | £68 per hour spent on home visits | Curtis355 | Based on the costs of a CMHN unless specified otherwise |
| Carer support group | £23.75 per carer per group | Curtis355 | Based on the costs of a CMHN and support worker. Assumed 2 hours input and eight attendees |
| Case manager | £57 per hour of client contact | Curtis355 (p. 165) | Based on the costs of a specialist nurse, Band 7 |
| CMHN | £68 per hour spent on home visits | Curtis355 (p. 159) | As Curtis’s CMHN figures355 are based on a Band 5, the costs for a community nurse have been used to more closely reflect local salaries |
| Community support worker (mental health) | £27 per hour spent on home visits | Curtis355 (p. 163) | As Curtis’s figures355 are based on a Band 2, these costs have been upgraded by 13% to more closely reflect local salaries |
| Consultant psychiatrist | £275 per hour patient contact | Curtis355 (p. 220) | Curtis’s figures have been downgraded by 3% to reflect local salaries |
| Day care | £30 per day | Site X 2010–11 costs |
There are three bands, depending on dependency level. This is the median |
| Day care: home from home | £39.84 per day | Site X 2010–11 costs |
Based on the costs of 6 hours home care for someone at home (days) assuming two clients attend |
| Day care: specialist | £45 per day | Site X 2010–11 costs |
This is the site X provider model at the higher rate |
| Day hospital: mental health | £200 per day | Curtis355 (p. 73) | Indicative cost based on the costs of NHS day care, assuming will be approximately 50% more |
| Dietician | £50 per hour home visiting plus £2.70 travel per visit | Curtis355 (p. 198) | |
| DN | £24 per 20-minute home visit | Curtis355 (p. 159) | |
| ECH, not specialist | £125 per week | Site X 2010–11 costs |
The costs are made up of a rent, service charge and support charge. Although ECH landlords costs vary, this is the average |
| ECH, specialist dementia/mental health | £213 per week | Hanover Housing (Joanne Goddard, Hanover, 2011, personal communication) 2011 costs |
These are the charges for Hanover Housing’s ECH scheme in site Y (rent £698.44 per month, service charge £200.79 per month, support charge £13.38 per month). Note that the costs given in Curtis355 (p. 58) are very similar |
| Falls clinic | £71.75 per attendance | Curtis355 (pp. 195 and 216) | Costed as a 45-minute assessment (including indirect time) by a medical registrar working 40 hours per week plus an hour’s contact with a hospital physiotherapist |
| General hospital inpatient admission | £271 per night | Furniss et al.;357 Griffiths et al.;358 NICE359 | Based on an average of the costs reported in the literature, uplifted for inflation where necessary |
| GP | £32 per surgery visit lasting 11.7 minutes £106 per home visit lasting 23.4 minutes (includes travel) |
Curtis355 (pp. 166–7) | |
| Home care: private domiciliary help (e.g. cleaning, shopping) | £13.33 per hour | Curtis355 (p. 130) | Extracted from the cost of a community care package for a low-cost client |
| Home care for someone at home (days) | £13.28 per hour £3.32 per 15 minutes £6.64 per 20 or 30 minutes £9.96 per 45 minutes |
Site X 2010–11 costs |
All services are purchased from the private sector at this rate |
| Home care (specialist) for someone at home (days) | £16.23 per hour £4.06 per 15 minutes £8.12 per 20 or 30 minutes £12.18 per 45 minutes |
Challis et al.360 (p. 68) | This is the mean cost of specialist home care for people with dementia as reported in a survey of local commissioners. It is noted that the mean cost of non-specialist home care was almost identical to that in site X at £13.27 per hour |
| Home care for someone in ECH (days) | £12.00 per hour £3.00 per 15 minutes £6.00 per 30 minutes £9.00 per 45 minutes |
Site X 2010–11 costs |
Site X provider care rate |
| Home care for someone living in specialist ECH (days) | £14.64 per hour £3.66 per 15 minutes £7.32 per 30 minutes £10.98 per 45 minutes |
Site X 2010–11 costs |
Figures based on costs of non-specialist home care for people in ECH, increased by the same ratio as for the difference between specialist and non-specialist care for people at home |
| Home care for someone in specialist ECH (nights) waking night | £152.26 per night | Site X 2010–11 costs |
Costed as 8 hours of specialist home care for people in ECH with 1.3 multiplier as suggested in private correspondence with Curtis355 |
| Macmillan nurse | £57 per hour of client contact | Curtis355 (p. 165) | Based on costs for a specialist nurse on Band 7 |
| Meals: delivered meals | £7 per meal | Site X 2010–11 costs |
These costs are part of the block contract with site X’s provider |
| Memory clinic | £208 per attendance | Curtis355 | Cost assuming a 30-minute assessment by a consultant plus the average of a contact with a CMHN or psychologist |
| Mental health inpatient admission | £366 per day for care home calculations (site X only) £311 per day for inpatient calculations (all three sites) |
Curtis242 (p. 119) | For the care home calculations in site X, the national average cost per day has been uplifted by 25% on the basis that local staff salaries are generally higher than those used in Curtis242 and in light of other local information For the inpatient calculations the national average cost per day has been used with the lower and upper quartile figures forming the lower and upper bounds |
| OT (note: not specifically mental health) | £51 per home visit | Curtis355 (p. 152) | Curtis’s355 figures have been upgraded by 22% to more closely reflect local salaries |
| Physiotherapist (note: not specifically mental health) | £41 per home visit | Curtis355 (p. 151) | |
| Psychologist | £92 per hour of client contact plus £1.50 travel per visit | Curtis355 (p. 155) | Curtis’s figures have been upgraded by 14% to more closely reflect local salaries |
| Respite placement | As per a standard week in a care home | Site X 2010–11 costs |
Charge to service user £109.75 (means tested) |
| SW | £158 per hour of face-to-face contact | Curtis355 (p. 172) | The salaries used in Curtis355 are very similar to those reported locally |
| Specialist nurse | £57 per hour of client contact | Curtis355 (p. 165) | |
| Telecare including lifeline, smoke detectors, gas detectors, falls detectors, just checking system | £5.19 per week | Site X 2010–11 costs |
This cost is said to be the same regardless of whether the service user receives one or multiple items |
| Volunteer befriender | £13.28 per hour | Site X 2010–11 costs |
Costed as a home care worker |
| Welfare rights officer | £118.45 per hour of face-to-face contact | Web search plus Curtis355 (p. 174) | Adverts on the web suggest that a council welfare rights officer would be paid in the region of £22,000–29,000 a year. Have taken the mid-point of this and uplifted the cost for an hour of social work assistant contact by 15% to reflect the difference in salaries |
Appendix 14 Balance of Care Study: general approach to costing (care home diversion model)
| Cost component | Care home option | Alternative care option | Cost and source | Comments |
|---|---|---|---|---|
| SSD costs | ||||
| Care home placement | Weekly cost per care home resident | N/A | See Appendix 13 | Based on actual case mix |
| Community care package | N/A | Average weekly cost per person (combined items) | See Appendix 13 | As prescribed by practitioners/RAM Panel. Identical for all service users in a particular case type |
| Social work input | Average weekly cost per care home resident | Average weekly cost per person unless input specified in care plan | £9 per week per care home resident £25 per week in alternative options See Appendix 13 |
There would be at least a minimum level of input for all case types to arrange/review care. Frequency assumed to be every 4 months in a care home; every 6 weeks at home/in ECH (as are active cases) |
| One-off costs | N/A | One-off cost of input (e.g. an OT visit) | See Appendix 13 | As prescribed by practitioners/RAM Panel. Identical for all service users in a particular case type |
| SSD charges | Average weekly charge per person (reduction in SSD costs) | Average weekly charge per person (reduction in SSD costs) | Site X 2010–11 information |
Average percentage recouped from care home clients 39% Average percentage recouped from community care clients 34% |
| NHS costs | ||||
| Registered nursing contribution for people in care homes | Average weekly cost per care home resident | N/A | See Appendix 13 | Based on actual case mix |
| Community mental health service input | Average weekly cost per care home resident (combined items) | Average weekly cost per person (combined items) | £2 per week per care home resident Specified costs in alternative care options See Appendix 13 |
Assume that there is a generic risk of any care home resident receiving mental health services. Assume 10% of residents will have a 1-hour visit from a CMHN per month; 2% will have a 30-minute visit from a consultant every 3 months As prescribed by practitioners/RAM Panel. Identical for all service users in a particular case type |
| General health costs | Average weekly cost per care home resident (combined items) | Average weekly cost per person unless input specified in care plan (combined items) | Community nursing and GP £26.80 per week (Curtis355 p. 50) | In the absence of any evidence to the contrary, general health costs have been based on the care home option and assumed to be the same in the alternative care option |
| General hospital inpatient stay £111 per week (see Appendix 13) | Estimated frequency of general hospital inpatient use 7 nights in every 4 months based on unpublished PSSRU data | |||
| Outpatients £4.50 per week (Curtis355 p. 119) | Estimated frequency of outpatient visits one visit every 8 months based on figures given in Furniss et al.357 | |||
| A&E visits £5.31 per week (Curtis355 p. 119) | Estimated frequency of A&E visits one visit every 4 months based on unpublished PSSRU data | |||
| Emergency ambulance £7.12 per week (Curtis355 p. 119) | Estimated frequency of emergency ambulance use one journey every 8 months based on unpublished PSSRU data | |||
| Routine ambulance £8.20 per week (Curtis355 p. 60) | Estimated frequency of routine ambulance use seven journeys every 8 months based on unpublished PSSRU data | |||
| Medication £12.34 per week (Zermansky et al.361 with inflation uplift) | Mean number of medications assumed to be 6.9 based on figures given in Zermansky et al.361 | |||
| Mental health inpatient services | Average weekly cost per care home resident | Average weekly cost per person | See Appendix 13 | Assume there is a generic risk of any care home resident or community-based service user needing a mental health inpatient admission. Assume 2% will have a 49 inpatient days per year (median LOS for people with an organic disorder in site X) |
| One-off costs | N/A | One-off cost of say a CMHN or consultant visit, or a specified inpatient admission | See Appendix 13 | As prescribed by practitioners/RAM panel. Identical for all service users in a particular case type Inpatient admissions assume 49 days LOS (median LOS for people with an organic disorder in site X) minus cost of community mental health package saved |
| Private costs | ||||
| SSD charges | Average weekly charge per person | Average weekly charge per person | Site X | Average percentage recouped from care home clients, 39%; average percentage recouped from community care clients, 34% |
| Living expenses/housing | Living expenses average weekly costs per person Housing covered by residential placement costs |
Average weekly costs per person | Living expenses for people in care homes £9.80 (Curtis355 p. 50) | |
| Living expenses for people at home £150 (Curtis355 pp. 130–3) | Average weekly living expenses for people at home or in ECH have been adjusted for average household size using the modified Organisation for Economic Co-operation and Development (OECD) equivalised household income scale assuming an average household size of 1.4 in the community and single person occupancy in ECH362 | |||
| Living expenses for people in ECH £175.50 (Curtis355 pp. 130–3) | The living expenses of people living at home or in ECH have been assumed to fall by 50% during short-stay hospital or care home admissions | |||
| Rent for people living at home £70 Dataspring363 | Average weekly rents for people at home have been adjusted for average household size as above. Figures take account of the distribution of different housing types in site X as given in the site X Housing Needs Study364 and use an ‘imputed rent’ for owner occupiers | |||
| Rent for people in ECH as per Appendix 13 | Average weekly rents for people in ECH assume 100% single occupancy. However, as some might not be single occupancy, have given a wider lower bound | |||
| Informal care costs | Average weekly costs per resident (nominal input for ongoing emotional/practical support when in care home) | Average weekly cost per person (input for support that is not provided by care package, including personal, practical and emotional support) | Costed as home care assistant as per Appendix 13 | Care home option: 1, 1.5 or 2 hours a week based on information from baseline data collection. Identical for all service users in a particular case type. Includes travel time Alternative option: Costs are identical for all service users in case type. Based on the representative vignette, taking into account any change in care package from baseline, i.e. informal costs were generally assumed to fall as formal carers took on tasks formerly undertaken by informal carers |
| Benefits | Average weekly attendance allowance per resident | Average weekly attendance allowance per person | £13.13 per week for care home residents (national rates, 2010) | Assumed 25% of residents (i.e. self-funders) received an average of £52.52 a week (based on 80% getting the lower rate, 20% the higher rate) |
| £52.52 per week for people at home and in ECH (national rates, 2010) | Assumed 100% of people received an average of £52.52 per week (based on 80% getting the lower rate, 20% the higher rate) | |||
| Average weekly receipt of housing benefit per person | £7.93 per week housing benefit for people at home365 | Figures were estimated based on the distribution of different housing types in site X given in the site X Housing Needs Study364 and the average award per older person household | ||
| £11.10 per week housing benefit for people in ECH365 | For ECH residents assumed single occupancy, but lowered upper bound as maximum gain to service user could be less | |||
| Average weekly receipt of carer’s allowance/premium per person | £1 per week for people at home and in ECH | In the absence of any statistics on the uptake of these benefits in relation to the care of older people with mental health problems living at home/in ECH, a nominal figure of just £1 has been used Note: Council tax benefit gain has not been counted here as it is assumed to have been covered in living expense costs (i.e. in the reduced outgoings of eligible households) |
||
| Other government costs | ||||
| Benefits | Average weekly attendance allowance per resident | Average weekly attendance allowance per person | £13.13 per week for care home residents (national rates, 2010) £52.52 per week for people at home and in ECH (national rates, 2010) |
|
| Average weekly housing benefit per person | £8 per week housing benefit for people at home365 £11.10 per week housing benefit for people in ECH365 |
Adjusted for average composition of older people’s households as above | ||
| Average weekly council tax benefit per person | £5.12 per week council tax benefit for people in ECH365 £3.66 per week for people at home365 |
Council tax benefits were estimated in same way as housing benefit, except that a simple age-related average allowance could be identified | ||
| Average weekly carer’s allowance/premium per person | £1 per week for people at home and in ECH | |||
| One-off costs | N/A | Welfare rights check | See Appendix 13 | Assumed 1–2 hours input from a welfare rights advisor |
| NGO costs | ||||
| Befriender input | N/A | Average weekly cost per person | See Appendix 13 | |
Appendix 15 The North-West Balance of Care Study: service user interview schedule
Appendix 16 The North-West Balance of Care Study: service user interview part 6 service receipt (community mental health team)
Appendix 17 Community mental health teams for older people literature review: example of search strategy
Community mental health team MEDLINE medical subject heading plus text word 23 September 2008 (final)
Nine hundred and ninety-one references including 8/10 key texts
-
*Mental Health Services/og, hi, ma, st, td, sd, cl, ec, ut, mt, sn (Organization & Administration, History, Manpower, Standards, Trends, Supply & Distribution, Classification, Economics, Utilization, Methods, Statistics & Numerical Data)
-
*Geriatric Psychiatry/st, mt, sn, ec, ut, ma, cl, td, og, hi (Standards, Methods, Statistics & Numerical Data, Economics, Utilization, Manpower, Classification, Trends, Organization & Administration, History)
-
*Community Mental Health Services/sn, ma, og, sd, ec, ut, mt, cl, td, st, hi (Statistics & Numerical Data, Manpower, Organization & Administration, Supply & Distribution, Economics, Utilization, Methods, Classification, Trends, Standards, History)
-
*Psychiatric Nursing/st, mt, sn, ec, ut, td, ma, cl, og, sd, hi (Standards, Methods, Statistics & Numerical Data, Economics, Utilization, Trends, Manpower, Classification, Organization & Administration, Supply & Distribution, History)
-
*Dementia/th, nu (Therapy, Nursing)
-
*Patient Care Team/sn, ma, og, td, ec, mt, cl, ut, st, hi (Statistics & Numerical Data, Manpower, Organization & Administration, Trends, Economics, Methods, Classification, Utilization, Standards, History)
-
"geriatric psychiatry".tw.
-
"old age psychiatr* ".tw.
-
"psychogeriatric* ".tw.
-
"gerontopsychiatry".tw.
-
"mental health service* ".tw.
-
"mental health team* ".tw.
-
"community mental health".tw.
-
"mental health cent* ".tw.
-
"psychiatric nurs* ".tw.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
-
*Health manpower/ or *Health personnel/
-
*Organizations/
-
*"Organization and administration"/ or *patient care management/
-
*Geriatric Assessment/
-
*Interprofessional Relations/
-
*Information Management/
-
*"Delivery of Health Care"/
-
*"Health services needs and demand"/ or *Needs assessment/
-
*Staff development/ or *Workload/
-
*Case management/
-
"model* ".tw.
-
("organi#ation*" or "operation*").tw.
-
("group process*" or "group structure*").tw.
-
("professional relation*" or "multidisciplin*" or "interprofession*" or "interdisciplin*").tw.
-
"role* ".tw.
-
("teamwork" or "integrat*").tw.
-
("refer*" or "access*" or "consult*").tw.
-
"assessment* ".tw.
-
("care manage*" or "care co-ordinat*").tw.
-
("decision making" or " management").tw.
-
"record* ".tw.
-
("training" or "development").tw.
-
17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38
-
*Aged/
-
*"Aged, 80 and over"/
-
*Health Services for the Aged/
-
*Dementia/
-
("old*" or "aged" or "elder*").tw.
-
("geriatric*" or "psychogeriatric*").tw.
-
40 or 41 or 42 or 43 or 44 or 45
-
16 and 39 and 46
-
limit 47 to yr="1969 - 2008"
-
limit 48 to english language
-
Adolescent/ or Child/ or Child, preschool/or infant/
-
49 not 50
-
Residential facilities/ or Assisted living facilities/or Group homes/ or Halfway houses/or Homes for the aged/or Nursing homes/
-
51 not 52
-
Hospital units/ or Hospitals/
-
Hospitalization/ or Institutionalization/
-
54 or 55
-
53 not 56
-
("antidepressant*" or "drug*" or "treatment*" or "prescri*").tw.
-
("therap*" or " psychotherap*").tw.
-
("suicid*" or "survivor*").tw.
-
"spirituality".tw.
-
58 or 59 or 60 or 61
-
57 not 62
-
limit 63 to "all aged (65 and over)"
Appendix 18 Community mental health teams for older people literature review: data extraction form
Appendix 19 Community mental health teams for older people literature review: data items extracted
| Reference | Data items extracted | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Site/setting | Staffing | Management | Supervision | Objectives/policies | Roles | Referral/access | Assessment | Caseload | Service user characteristics | Care co-ordination | Services/interventions | Information sharing | Outreach/training | Carer support | Resources | |
| National/regional publications | ||||||||||||||||
| Abendstern et al. (2006)197 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Audit Commission (2000)46 | 1 | 2 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | |||||
| Audit Commission England (2002)47 | 1 | 2 | 1 | 1 | 1 | 2 | 1 | 1 | ||||||||
| Audit Commission Wales (2002)199 | 2 | 1 | 2 | 2 | ||||||||||||
| Challis et al. (2002)179 | 1 | 1 | 1 | 2 | 2 | 2 | ||||||||||
| Healthcare Commission (2009)50 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| Lingard and Milne (2004)48 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 1 | 2 | 2 | 1 | |||||
| NAO (2007)163 | 2 | 1 | 1 | 1 | 1 | 2 | 1 | 2 | 2 | |||||||
| Tucker et al. (2007)73 | 2 | 1 | 1 | 2 | 1 | |||||||||||
| Tucker et al. (2009)180 | 2 | 1 | 2 | 1 | 1 | 2 | 2 | |||||||||
| Wattis et al. (1999)43 | 1 | 1 | 1 | |||||||||||||
| Local level publications | ||||||||||||||||
| Treloar (1996)220 | 1 | 2 | 2 | |||||||||||||
| O’Connor et al. (1991)216 | 1 | 2 | 1 | 1 | 2 | 1 | 2 | 1 | 1 | |||||||
| Dening (Cambridge) (1992)19 | 2 | 1 | 1 | |||||||||||||
| Bedford et al. (1996)202 | 1 | 2 | 1 | 2 | 1 | 1 | 2 | 1 | 1 | 1 | ||||||
| Melzer et al. (1996)215 | 1 | 1 | 1 | 2 | 1 | 2 | ||||||||||
| Sheard and Cox (Cambridge) (1998)217 | 2 | 2 | 1 | 2 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| Lingard and Milne (Croydon) (2004)48 | 1 | 1 | 1 | 1 | ||||||||||||
| Sheard and Cox (Kingston) (1998)217 | 2 | 1 | 1 | 2 | 1 | 1 | 1 | |||||||||
| Lingard and Milne (Kingston) (2004)48 | 1 | 2 | 1 | 1 | 1 | 2 | 2 | 1 | 1 | 2 | ||||||
| Gupta et al. (1996)207 | 1 | 2 | 1 | 2 | ||||||||||||
| McCrae et al. (2007)213 | 1 | 1 | ||||||||||||||
| McCrae et al. (2008)214 | 1 | 2 | ||||||||||||||
| Coles et al. (1991)203 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | ||||||
| Dening (Lewisham) (1992)19 | 2 | 1 | 1 | 1 | ||||||||||||
| Dening (St Charles) (1992)19 | 1 | |||||||||||||||
| Collighan et al. (1993)190 | 1 | 1 | 2 | 2 | 1 | |||||||||||
| Jenkins and Macdonald (1994)195 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | |||||||||
| Macdonald et al. (1994)191 | 1 | 2 | 1 | 1 | 1 | |||||||||||
| Von Abendorff et al. (1994)25 | 1 | 2 | 1 | 2 | 2 | 1 | ||||||||||
| Banerjee et al. (1996)194 | 1 | 3 | 1 | 2 | 1 | 1 | 1 | |||||||||
| Brown et al. (1996)189 | 1 | 1 | 2 | 1 | 2 | 2 | 3 | |||||||||
| Lindesay et al. (1996)188 | 1 | 2 | 1 | 1 | 1 | 1 | ||||||||||
| Challis et al. (2002)192 | 1 | 1 | 2 | 2 | 1 | 2 | 2 | |||||||||
| MacDonald et al. (2007)193 | 1 | 2 | 1 | 1 | 1 | 1 | ||||||||||
| Philpot et al. (2000)196 | 1 | 1 | 1 | |||||||||||||
| Eastley and Nowers (1997)206 | 2 | 1 | 1 | 1 | 1 | |||||||||||
| Sheard and Cox (Coventry) (1998)217 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | |||||||||
| Baillon et al. (1996)200 | 1 | 1 | 2 | |||||||||||||
| Sheard and Cox (Leicestershire) (1998)217 | 1 | 2 | 1 | 1 | 1 | 2 | ||||||||||
| Arthur et al. (2002)198 | 1 | 1 | 2 | |||||||||||||
| Junaid and Bruce (1994)210 | 2 | 1 | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 2 | ||||||
| Das and Bouman (2008)205 | 2 | 2 | ||||||||||||||
| Jolley et al. (1997)209 | 1 | 1 | 1 | |||||||||||||
| Lawley et al. (2005)211 | 1 | 1 | 1 | 1 | ||||||||||||
| Simpson and De Silva (2002)218 | 1 | 1 | 2 | |||||||||||||
| Mander (2007)212 | 1 | 1 | 1 | 2 | 1 | 1 | ||||||||||
| Dare and Benbow (1997)204 | 1 | 1 | 1 | 1 | ||||||||||||
| Sheard and Cox (Rochdale) (1998)217 | 2 | 1 | 1 | 2 | 2 | 1 | 1 | |||||||||
| Barlow (2006)201 | 1 | |||||||||||||||
| Sheard and Cox (Aberdeenshire) (1998)217 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||
| Sheard and Cox (Fife) (1998)217 | 1 | 1 | 1 | 1 | 2 | |||||||||||
| Stevenson et al. (2006)219 | 1 | 2 | 1 | 1 | 1 | 2 | 1 | 2 | 1 | 1 | ||||||
| Audit Commission (2000)46 | 1 | 1 | 1 | 1 | 1 | 2 | ||||||||||
| Hoskins et al. (2005)208 | 2 | 1 | 1 | 2 | 1 | 1 | 2 | |||||||||
Appendix 20 Community mental health teams for older people literature review: reasons for excluding references
| Reason for exclusion | Objective 1: n excluded | Objective 2: n excluded |
|---|---|---|
| Not UK | 100 | N/A |
| Does not relate to older people | 62 | 75 |
| Not mental health | 15 | 21 |
| Primary care focus | 11 | 15 |
| Team with single professional discipline | 12 | 24 |
| No comparison/outcomes | N/A | 63 |
| Pre-1989 | N/A | 14 |
| Other | 28 | 42 |
Appendix 21 Community mental health teams for older people literature review: centrality rating
The nature of the review, which contains a large descriptive component, means that the standard quality measures and hierarchies of evidence employed in many systematic reviews are inadequate as quality appraisal tools. We thus developed a centrality rating, which took into account:
-
the level of detail provided
-
the role of the publication in contributing to our knowledge and understanding of issues which are central to past or current debates about the organisation and structure of CMHTsOP.
-
Provides a clear picture of the overall functioning of a particular team, or group of teams: the reader comes away with a strong sense of how the team is organised and operates. This will include details/discussion of a number of aspects of team structures and processes, for example staffing and management structures; access and referral arrangements; assessment and care management processes; caseload profiles and service user characteristics; communication and information sharing; services and interventions provided by the team.
Or
-
Provides less information about overall team functioning but focuses in depth on one particular feature or process (e.g. assessment or case finding), providing a clear picture of how this relates to the team(s) and why it is an important issue.
Or
-
Provides detailed comparative information on one or more aspects of team organisation and functioning. The focus here is on the general similarities and variations between teams, rather than how individual teams operate.
Note: In the majority of cases, the focus/setting is the CMHT. However, more broadly focused publications which have detailed sections on CMHT functioning may also be rated high.
Medium-
Contains information about one or more aspects of the structure/processes of a particular team but either (i) these are less detailed because they are secondary to the main focus of the paper, which lies outside the remit of the review (e.g. stress among carers of CMHT service users), or (ii) the exact nature/function of the team remains unclear.
Or
-
Contains detailed comparative information on relevant team functions and processes but the responses do not apply exclusively to CMHTs (e.g. the sample may contain single discipline or non-CMHT MDTs or responses may encompass the activities of non-CMHT staff within the old age psychiatry service).
-
Content and focus means that the publication is of marginal relevance. However, contains some brief details about CMHTs (e.g. staffing arrangements, role of consultant psychiatrist) which contributes to the overall map of CMHT development/variation.
Appendix 22 Community mental health teams for older people literature review: centrality of the literature
| Reference | CMHT or broader focusa | Single issue or generalb | Dementia/depression focusc | Centrality |
|---|---|---|---|---|
| Abendstern et al. (2006)197 | 2 | 3 | 1 | Medium: detailed information on a range of team processes but unclear whether or not all are CMHTs. Evidence of variation between teams in relation to specific thresholds rather than range. No individual team data. Regional |
| Arthur et al. (2002)234 | 1 | 1 | 2 | Medium/high: discusses key targeting/boundary issues. Set in CMHT, though no team characteristics. Study design could not be fulfilled due to cross agency difficulties. Underpowered due to high drop-out rate |
| Audit Commission (2000)46 | 2 | 3 | 4 | High: national data on CMHTs at turn of century. Includes good practice guidance |
| Audit Commission England (2002)47 | 2 | 3 | 4 | High: national data on CMHTs at turn of century, builds on and compares with 2000 data |
| Audit Commission Wales (2002)199 | 2 | 3 | 4 | High: national data on CMHTs at turn of century, builds on and compares with 2000 data |
| Baillon et al. (1996)200 | 1 | 1 | 4 | High: specific issue of care home support/liaison, both attitudes and current practice |
| Banerjee et al. (1996)194 | 1 | 1 | 2 | High: discusses key targeting/boundary issues. Set in CMHT. Challenges existing practice |
| Barlow (2006)201 | 1 | 1 | 4 | Low: raises issue of lack of clarity regarding role of CPN in a CMHT. Relevance reduced due to focus on personal qualities and attributes rather than specific professional roles and functions of CPN |
| Bedford et al. (1996)202 | 1 | 3 | 3 | High: provides good picture of CMHT organisation and functioning and raises important issues about the nature of support given to people with dementia |
| Brown et al. (1996)189 | 1 | 3 | 3 | High: provides detailed information about team processes and caseloads and raises issues about service provision for people with dementia |
| Challis et al. (2002)179 | 1 | 3 | 4 | Medium/high: detailed information of practices and processes within old age psychiatry services but unclear whether they refer to CMHTs exclusively or teams in other settings |
| Challis et al. (2002)192 | 1 | 1 | 1 | High: evaluates two different CMHT models of service |
| Coles et al. (1991)203 | 1 | 3 | 4 | High: detailed description of range of team characteristics, processes and underlying principles. Earliest publication in review |
| Collighan et al. (1993)190 | 1 | 1 | 4 | High: evaluates fundamental issue which distinguishes between two CMHT models |
| Dare and Benbow (1997)204 | 2 | 1 | 4 | Low/medium: broader service focus. Raises important issue (role of COAP in CMHT) but provides only limited data |
| Das and Bouman (2008)205 | 1 | 1 | 4 | High: team focus. Raises important issue (direct access) |
| Dening (1992)19 | 2 | 3 | 4 | High: crucial benchmark of practice at a point in time. Raises important issues and focuses in some detail on team processes |
| Eastley and Nowers (1997)206 | 1 | 3 | 4 | Medium/high: CMHT focus. Provides clear picture of some team processes and rationale for establishing this team |
| George and MacDonald (2005)221 | 1 | 2 | 4 | High: focus on improving access through introduction of new process. Compares duty system with ‘triage’. Detailed description of process given |
| Gupta et al. (1996)207 | 1 | 2/3 | 4 | Medium/high: raises important issues (direct access and home assessment). Information about team organisation and membership; however, exact nature of team unclear |
| Healthcare Commission (2009)50 | 2 | 3 | 4 | Low/medium: broad level data. Unclear how much relates to teams. Provides some information on key issue of integration from six trusts. Reports improved service resulting from integration but evidence to support this is limited |
| Hoskins et al. (2005)208 | 1 | 2 | 1 | Low/medium: main focus not relevant to review questions but provides some contextual data on one team |
| Jenkins and Macdonald (1994)195 | 1 | 2 | 2 | High: discusses key targeting/boundary issues. Set in CMHT. Challenges existing practice |
| Jolley et al. (1997)209 | 1 | 2 | 4 | Low: service rather than team level data. Although minimal reference to CMHT it is an example of the establishment of a team and therefore relevant to the mapping of CMHT development |
| Junaid and Bruce (1994)210 | 1 | 3 | 4 | Medium: good-quality data but only relates to work of CPNs within teams |
| Lawley et al. (2005)211 | 2 | 1 | 4 | Low: limited reference to CMHT although raises issue of role and function of COAP in CMHT. Evidence to support conclusions is anecdotal |
| Lindesay et al. (1996)188 | 1 | 2 | 4 | High: evaluates fundamental issue which distinguishes between two CMHT models |
| Lingard and Milne (2004)48 | 1 | 3 | 4 | High: provides data on a range of integration measures from national survey (32 ‘providers’) and raises issues from wider literature. Descriptions of two teams. Not clear who respondents were |
| MacDonald et al. (1994)191 | 1 | 1 | 3/4 | High: provides detailed information on specific and important issue |
| MacDonald et al. (2007)193 | 1 | 2 | 1/4 | High: provides detailed information on specific and important issue. Rare example of longitudinal data |
| Mander (2007)212 | 2 | 2 | 4 | Medium: broader service focus with some evidence of team processes. In particular this relates to SPA through CMHT with CPNs providing initial screening |
| McCrae et al. (2007)213 | 2 | 1 | 4 | Low: raises issue of management style but broad level data which does not provide information on structures or processes within settings. Minority of data is on CMHT staff |
| McCrae et al. (2008)212 | 1 | 1 | 4 | High: discusses important issue of role clarity and provides detailed case study data |
| Melzer et al. (1996)215 | 1 | 2 | 1 | Medium: raises issue of carer involvement in service development. Provides some information on assessment process for carers by CMHTs |
| NAO (2007)163 | 2 | 2 | 1 | High: national benchmark data. Useful for mapping progress towards integration |
| O’Connor et al. (1991)216 | 1 | 1 | 1 | High: discusses important issue of case finding/targeting and provides detailed team level data |
| Philpot et al. (2000)196 | 1 | 1 | 2 | Low/medium: provides some information on team membership and which professionals work with those discharged from hospital. Other data less relevant to current review |
| Sheard and Cox (1998)217 | 1 | 3 | 1/4 | High: detailed description of range of team characteristics and processes in CMHTs across seven sites |
| Simpson and De Silva (2002)218 | 1 | 1 | 4 | Low/medium: some detailed description on process but evaluation is poorly reported – anecdotal |
| Stevenson et al. (2006)219 | 1 | 1 | 1 | Medium: detailed description of team functioning but only quasi-CMHT (i.e. only provides short-term community assessment and support) |
| Treloar (1996)220 | 1 | 1 | 4 | High: good-quality before/after data on a single process (assessment) but focuses only on what is collected rather than broader assessment issues |
| Tucker et al. (2007)73 | 2 | 3 | 4 | High: good-quality national data on key indicators of integration relating to CMHTs |
| Tucker et al. (2009)180 | 2 | 3 | 4 | High: good-quality national data on key indicators of integration relating to CMHTs |
| Von Abendorff et al. (1994)25 | 1 | 2 | 1/4 | Medium/high: detailed data on staff activities |
| Wattis et al. (1999)43 | 2 | 3 | 4 | Medium: small number of data on CMHTs. Most data relates to role of COAP. Reporting ambiguous in relation to team or service level data |
Appendix 23 Community mental health teams for older people literature review: quality appraisal for five full research articles included in objective 2
| Question no. | Question | Challis et al.192 | Collighan et al.190 | Lindsey et al.188 | MacDonald et al.191 | Treloar220 | Total scores across articles | |
|---|---|---|---|---|---|---|---|---|
| ✓ | N/A | |||||||
| 1 | Was the study population well described? | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 0 |
| 2 | Was the intervention well described (what, how, who, where)? | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 0 |
| 3 | Was the sampling frame or universe of selection for the study population specified? | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 0 |
| 4 | Were the screening criteria for study eligibility specified? | ✓ | ✓ | ✓ | N/A | N/A | 3 | 2 |
| 5 | Was the population that served as the unit of analysis the entire eligible population or a probability sample at the point of observation? | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 0 |
| 6 | Are there any other selection bias issues not otherwise addressed? | ✗ | ✗ | ✗ | ✓ | ✗ | 1 | 0 |
| 7 | Was there an attempt to measure exposure to the intervention? | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 0 |
| 8a | Was the exposure variable valid? | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 0 |
| 8b | Was the exposure variable reliable? | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 0 |
| 9a | Were the outcome and other independent (or predictor) variables valid? | ✓ | ✓ | ✓ | ✗ | ✓ | 4 | 0 |
| 9b | Were the outcome and other independent (or predictor) variables reliable? | ✓ | ✓ | ✓ | ✗ | ✓ | 4 | 0 |
| 10a | Conducting statistical testing (when appropriate)? | ✓ | ✓ | ✓ | N/A | ✓ | 4 | 1 |
| 10b | Reporting which statistical tests were used? | ✓ | ✓ | ✓ | N/A | ✓ | 4 | 1 |
| 10c | Controlling for design effects in the statistical model? | N/A | N/A | N/A | N/A | N/A | 0 | 5 |
| 10d | Controlling for repeated measures in populations that were followed over time? | N/A | N/A | N/A | N/A | N/A | 0 | 5 |
| 10e | Controlling for differential exposure to the intervention? | N/A | N/A | N/A | N/A | N/A | 0 | 5 |
| 10f | Using a model designed to handle multilevel data when they included group-level and individual covariates in the model? | N/A | N/A | N/A | N/A | N/A | 0 | 5 |
| 11 | Are there other problems with the data analysis? | ✗ | ✗ | ✗ | ✗ | ✗ | 0 | 0 |
| 12 | Did at least 80% of enrolled participants complete the study? | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 0 |
| 13a | Did the authors assess whether the units of analyses were comparable prior to exposure to the intervention? | ✓ | N/A | N/A | N/A | ✗ | 1 | 3 |
| 13b | Did the authors correct for controllable variables or institute study procedures to limit bias appropriately (e.g. randomisation, restriction, matching, stratification or statistical adjustment)? | ✓ | N/A | N/A | N/A | ✗ | 1 | 3 |
| Total score per article | 15 | 13 | 13 | 9 | 12 | |||
Appendix 24 Community mental health teams for older people: national survey questionnaire
Appendix 25 Community mental health teams for older people: qualitative interview schedule – team manager
Team manager topic guide
Part 1: scene setting
| Professional background and history within the team | ||
|---|---|---|
| 1 | Can you tell me how you came to join the team? | Probe for: First job as TM? Brief professional history, worked in similar or different settings in past. Did you join the team as the manager? |
Part 2: team focus
| 2 | Interviewer: Refer to pre-interview questions: Is there anything that we want them to expand on (e.g. outreach, specialisation, an example of a typical case and their care pathway)? |
Part 3: membership, management and supervision
| Membership | ||
|---|---|---|
| 3 | Can you briefly describe the roles/functions of each professional/staff group within the team including support workers? | (Check against pre-interview grid) |
| 4 | Are there generic/overlapping roles between the different professional groups? Can you give examples of what these are? | |
| 5 | Are there roles/functions within the team that are specific to particular professions? Can you give examples of what these are? | Probe for: psychologist |
| How the team is managed | ||
| 6 |
|
Probe for: TM responsible for everything/different people responsible for clinical and line management issues |
| 7 | Referring to the grid, are management arrangements different depending on whether someone is a core or extended team member? (If so, how?) | |
| 8 | What is the impact of having a full-time manager/a manager who is also a practitioner? | Probe for: strengths and weaknesses of either practice |
| 9 | How are decisions made about the various aspects of the team’s work?
|
Probe for: team as a whole, seniors, manager only, at meetings SPA – efficient/bottleneck |
| How team members are supervised and supported | ||
| 10 |
|
Probe for: Are these different for different professionals/individuals and if so how and why? Who provides clinical leadership? |
| 11 |
|
|
Part 4: integration
| A: team-level issues | ||
|---|---|---|
| 12 | You have [disciplines] within the team Are there any benefits to this over referring on to separate services outside the team? Does this work well in practice, or are there still restrictions/tensions? |
Probe for: Colocation? IT issues, restrictions on the way that the profession work within the team/who can do what; tensions with other team members because of this? |
| 13 | What professional specialties do you have to refer outside the team for? How does this work in practice? Does it create any difficulties for staff or service users? If so, how have you tried to get around these? |
Probe for: Service level access agreements to other specialties, etc. Particularly ask about SWs, psychological services Is that an age-specific or generic service? |
| 14 | Does each service user have a single care co-ordinator? How does this work in practice? (Ask, for example, our definition: one person who is responsible for co-ordinating all health and social care inputs both within and outside the team?) |
Probe for: What happens if one professional is the care co-ordinator and the service user needs the input of another professional within/outside the team? |
| 15 |
|
|
| 16 | How does the way in which records are completed and accessed/kept and managed impact on the service you deliver? | Probe for: IT issues, electronic vs. hard-copies. Who can access/input? |
| 17 | How has multidisciplinary working within the team changed over time? Can you give examples? (E.g. can be of both increased number of professionals and/or ways of working) |
Probe for: SWs: Ever been in team? (Non-integrated team); How arrived/developed? (Integrated teams) What about OTs/psychologists? |
| B: agency-level issues (particularly with SSD older people’s team) | ||
| 18 |
|
Probe for: Links with named workers; attendance at your/their meetings; joint meetings |
| 19 |
|
Probe for: Description/examples and whether these are more or less effective than formal arrangements Probe for: What is the relationship like between the team and social services older people’s team? |
| 20 |
|
Probe for: Are referrers clear? [GPs/others?] |
| 21 | Can you give an example of the circumstances in which a SW from outside the team would be involved in a CMHT case? | |
| 22 | What happens when nurses or OTs in the team need to access SSD services? | Probe for: Are systems effective/cumbersome? |
| 23 | What is the impact of the way you currently work with social services on service users? | |
| 24 | What do you think are the obstacles to, and facilitators of, joint working/integration with social services? | Probe for: Are there particular flash points (e.g. hospital discharges) or examples of good practice? Would it be different if SWs were in team? |
| 25 | Can you describe the process of referring to the psychologist outside the team? | Probe for: Service level access agreements Age-specific or generic service? |
| 26 | Can you describe the process of referring to the OT outside the team? | How does it work in practice? If there are OTs in the team – what difference does it make? |
| 27 | What is the team’s relationship like with GPs? | |
| 28 | Is there a clear demarcation as who is taken on by the CMHT and who would be supported within primary care? | |
Part 5: the role of the consultant
| 29 | Can you describe the consultant’s clinical role and responsibilities within the team and how these are managed/negotiated? | Probe for: Who takes overall clinical responsibility for cases? Do consultants have any managerial responsibilities? Is there a shared understanding of this role by all team members? Are any people seen by CMHT but not by consultant? |
| 30 | To what extent is the consultant involved with the team on a day-to-day basis? | Probe for: Do they directly manage/supervise anyone in team? |
| 31 | What role do other doctors play in the team? | |
| 32 | How would you describe the nature and degree of the consultant’s influence within the team? | |
| 33 | To what extent are team practices and systems organised around the consultant’s preferred way of working? | Probe for: If more than one in team, do arrangements vary for each? |
| 34 | To what extent do you as TM seek support or guidance from your consultant on non-clinical matters? | Probe for: Are there any examples of where this has not been forthcoming? How has this been resolved? |
| 35 | How has the consultant’s role within the team changed over time? | Probe for: Impact of ‘New Ways of Working’ |
Part 6: the role of the support worker
| 36 | What is the role of the support worker(s) in your team? Is this clear, do you think? What distinguishes their role from others in the team? What is their job title? |
Is there more than one role/title? What about occupational therapy assistant/care management assistant? Are these similar to each other or more akin to the profession they relate to? |
| 37 | What sort of work do they do that is not done by other team members? Do you feel that this is appropriate? | |
| 38 | What are the benefits to the team and service users are having this support worker role? | |
| 39 | Are there other roles undertaken by qualified staff that could be undertaken by support workers? Examples? Do you perceive any problems in extending role of support workers? | Probe: ‘Specialist’ roles, such as dementia home care work |
Part 7: impact of wider resources and service issues
| 40 |
|
Probe/ask for: List including formal and informal/statutory and voluntary |
| 41 |
|
Probe for: Cuts in number of inpatient beds; merging with adult services; position of memory clinic |
Part 8: concluding thoughts
| 42 | Thinking of all the changes that the team has undergone in recent years, have they resulted in an improved quality of service for service users? If so, how? If not, why? |
| 43 | What do you think the impact of integration/lack of integration of your team is on service users? Ask for examples |
| 44 | What do you feel are the best aspects of the way in which your team and their work are organised? |
| 45 | What aspects of the way in which the team and their work are organised would you most like to change? |
| 46 | Is there anything more that you’d like to add/that I have not asked you about (e.g. other changes that have had a impact on the team)? |
Ask if and when appropriate
Do you think the way the team is organised impacts on:
-
The nature of the work undertaken by team members (who does what)?
-
The type of work you are able to do as a team (who you support)?
-
The stability (or lack of stability) of the team (recruitment and retention)?
Appendix 26 Community mental health teams for older people: qualitative interview schedule – consultant
Consultant topic guide
Part 1: scene setting
| Professional background and role in team and service | ||
|---|---|---|
| 1 | Can you briefly describe your professional history and how you came to join the team? | Probe for: Worked in similar or different mental health settings in past? Key player in developing the team? |
| 2 | Can you describe your role and responsibilities within the team and more widely within the service? What proportion of your time is CMHT time? |
Probe for: Nature of input? Daily? Examples of duties outside team? Inpatients (how perceived)? |
| 3 | Are you involved in wider service development? | For example, commissioning advisory groups? |
| 4 | Is there a clear separation between your CMHT work and the other work you do or is this more blurred (e.g. memory clinic)? | |
| 5 | What are the benefits/disadvantages to how you work in relation to inpatients (community/inpatient split or locality based)? | |
| 6 | Do you see yourself as a core member of the CMHT? | |
Part 2: senior clinician and management role
| 7 | To what extent are you involved in managing the team?
|
Officially? Informally? |
| 8 | Do you directly manage/supervise anyone in team? | Doctors? |
| 9 | Do you provide formal/informal supervision to anyone in the team? | |
| 10 | Can you describe how referrals come into the team (direct to you/SPA/other)? | |
| 11 | Who decides who you (and others in the team) see and do not see? How are these decisions made? (Criteria?) |
|
| 12 | If there is a SPA, how does this work – efficient/bottleneck? | |
| 13 | What is your role/involvement in relation to decision making around allocation and closure of cases? | |
| 14 | How would you describe the nature and degree of your influence within the team? | |
| 15 | Can you describe how responsibility for an individual’s care is shared between you and other team members? | Probe for: Who takes overall clinical responsibility for cases? Shared understanding of this approach by all team members? |
| 16 | Do you think everyone in the team understands your role and uses you/your skills effectively/appropriately? | |
| 17 | What is the impact on the team and on patients/service users of the approach you have described? | |
Part 3: integration
| A: team-level issues | ||
|---|---|---|
| 18 | Who undertakes initial assessments within the team? Is this appropriate in your view? |
|
| 19 | If there was the capacity, do you think it would be preferable for all service users/patients to be seen by you/a consultant? | |
| 20 | For integrated teams: You have SWs within the team. What, if any, benefits are there to this over referring to social services outside the team? Does this work well in practice, or are there restrictions/tensions? For non-integrated teams: You do not have SWs within the team. What is the impact of this if a service user/patient needs social work input? How does this work in practice? Are there disadvantages? |
|
| 21 | Is there a single case file that includes your notes or are these kept separately? | |
| 22 | If separate, how do others access your notes and how do you access theirs? | |
| 23 | Do you contribute to shared assessment documents or do you have separate documentation? | |
| B: agency-level issues | ||
| 24 | Is there a clear demarcation between the work of the CMHT and the local social services older people’s team in terms of who should be referred where? If yes: Can you explain what this is? If no: Can you describe how this impacts on the team and on patient/service users? |
|
| 25 | What do you think are the obstacles to, and facilitators of, joint working/integration with social services? | Probe for: Are there particular flash points (e.g. hospital discharges, care home admission, transfer) or examples of good practice? |
Part 4: the role of the support worker
| 26 | What is the role of the support worker(s) in your team? Is this clear, do you think? What is/are their job title/s? |
Is there more than one role/title? What about occupational therapy assistant/care management assistant? Are these similar to each other or more akin to the profession they relate to? |
| 27 | What sort of work do they do that is not done by other team members? Do you feel that this is appropriate? | |
| 28 | What are the benefits to the team and patients/service users of having this support worker role? | |
| 29 | Are there other roles undertaken by qualified staff that could be undertaken by support workers? Examples? Do you perceive any problems in extending role of support workers? | Probe: ‘Specialist’ roles, such as dementia home care work |
Part 5: impact of wider resources and service issues
| 30 | What is the impact of the nature/scope/quality of local services available to older people with mental health problems on the work of the team? | Impact of location of services as well as their nature? What can you refer on to, work with, compliments what you do? |
| 31 | Have there been any recent changes within the trust that have impacted on the team? If yes: Can you describe their impact on the team and the service it provides? |
Probe for: Cuts in number of inpatient beds; merging with adult services; position of memory clinic |
Part 6: concluding thoughts
| 32 | What are the benefits to the patient/service user of the way the work of the team is organised? What are the disadvantages? |
| 33 | Do you think the way the team is organised impacts on:
|
| 34 | Is there anything about your role/involvement that you would like to change? If yes: To what extent would this affect patient/service user outcomes? |
| 35 | Is there anything about how the team operates that you would like to change? If yes: To what extent would this affect patient/service user outcomes? |
| 36 | What causes you most frustration and stress about the role you play in the CMHT/working in a CMHT? |
| 37 | What do you find most rewarding about the role you play in the CMHT/working in a CMHT? |
| 38 | Is there anything more that you’d like to add/that I have not asked you about (e.g. other changes that have had a impact on the team)? |
Appendix 27 Community mental health teams for older people: qualitative interview schedule – support worker
Support worker topic guide
Part 1: background and role in team
| Professional background and history within the team | ||
|---|---|---|
| 1 | Can you tell me how you came to join the team? | Probe for: Brief professional history, worked in similar or different (mental health or other) settings in past |
| Understanding of role by self and others/nature of work | ||
| 2 | What is your job title and what does this mean to you? | |
| 3 | Which profession, if any, do you see yourself as most closely aligned to? | |
| 4 | Can you briefly describe your role? | Main functions/responsibilities? Do you carry a caseload? |
| 5 | Has your role changed during the time you have worked within this CMHT? | |
| 6 | Can you describe how you work with others in the team | |
| 7 | How does your role differ/overlap with others? Both professional and other assistant posts? | Assessment? Caseload size and turnover, amount of face-to-face contact, administration |
| 8 | What if any are the advantages of this overlap (or lack of)? | |
| 9 | Are you clear about what your role involves and where are its boundaries? | |
| 10 | Do you think everyone else in the team understands your role and uses you/your skills effectively/appropriately? | |
| 11 | Are you ever asked to do things that you think are outside your remit? (Too much or too little responsibility?) |
|
| 12 | Do you feel that that your contribution is valued by others in the team? | |
| 13 | What do the activities that you undertake add to the service provided by the team to the service user? | |
| 14 | Does your role have a distinct set of skills and attributes that distinguish it from the work that others in the team do? | |
| Style of work | ||
| 15 | How much flexibility/autonomy do you have about how you work? | Length and intensity of involvement, nature of input? Is this closely monitored/supervised? Are you told what to do or are you able to steer this yourself? Do you make decisions independently? |
| 16 | Do you get the opportunity to be creative? Can you give examples? | |
| 17 | Are you encouraged to take initiative? Can you provide an example? | |
| 18 | Does this arrangement work well for you? Service users? | |
| 19 | How does this compare with how other members of the team work? | |
| Personal development | ||
| 20 | Is there a clear career/role development route for you in this post/as a support worker? Can you describe this? | |
| 21 | If not, what is the impact of this on how you feel about the work you do? | |
| 22 | Do you get opportunities to receive training on various aspect of mental health work? | To the same extent as others? |
Part 2: management, supervision and support
| 23 | Can you tell me who your employer is? Who is your line manager? |
Mental health trust/SSD/other NHS sector? |
| 24 | What are the formal arrangements for clinical supervision? (From whom do you get it?) | Is your line manager also your clinical supervisor? |
| 25 | Do these formal arrangements create any issues around how you are supervised and managed? | Particularly if management and supervision are by different people |
| 26 | Do the formal supervision arrangements meet your needs effectively? If not, what would help? | Enough? Appropriate? |
| 27 | Are the formal arrangements similar to other team members? | More/less/different? |
| 28 | What informal support networks do you use? | Inside and outside the team? |
| 29 | Do you feel you have voice in how the work of the team is organised? (With individuals? Plus broader matters?) | |
| 30 | To what extent are you involved in decisions about:
|
|
Part 3: role of consultant
| 31 | How do you regard the consultants that work in the team? | Equal members? Senior? Manager? |
| 32 | Do you seek advice and support directly from the consultant? | |
| 33 | Do you find the consultant approachable? Readily accessible? Helpful? Remote? | |
Part 4: integration
| 34 | What are the benefits to you of working in a MDT? (What are the problems – if any?) | What difference does it make? |
| 35 | What are the benefits to the service user of working in a MDT? (What are the problems – if any?) | What difference does it make? |
Part 5: concluding thoughts
| 36 | What, if anything, would you most like to change about how the team works? |
| 37 | What is the best thing about how the team works for the service user? |
| 38 | What are the most demanding/stressful/frustrating aspects of your job? |
| 39 | What is the most rewarding part of your work? |
| 40 | Is there anything more that you’d like to add/that I have not asked you about (e.g. other changes that have had a impact on the team)? |
Appendix 28 Community mental health teams for older people: qualitative interview schedule – professional staff member
Staff member topic guide
Part 1: roles and responsibilities
| Professional background and history within the team | ||
|---|---|---|
| 1 | Can you tell me how you came to join the team? | Probe for: Brief professional history, worked in similar or different (mental health or other) settings in past |
| 2 | Can you briefly describe your role? | |
| 3 | How does this differ/overlap with others? | Caseload size and turnover, amount of face-to-face contact, initial assessment |
| 4 | What if any are the advantages of this overlap (or lack of)? | |
| 5 | Are you clear about what your role involves and where are its boundaries? | |
| 6 | Do you feel that this role is clearly linked to your professional identity and skills? If not, in what way? | |
| 7 | Are you asked to do things that are outside your remit? Can you give examples? | (Probe also for tasks with too much/too little responsibility – e.g. initial assessment) |
| 8 | What do the activities that you undertake add to the service provided by the team? | |
| 9 | How much flexibility/autonomy do you have about how you work? | Length and intensity of involvement? Nature of input? Do you make decisions independently? Take initiative, be creative |
| 10 | Do you think everyone in the team understands your role and uses you/your skills effectively/appropriately? | |
| 11 | Do you feel that other team members value the contribution your skills can bring? | |
| 12 | Are you clear about the roles of other team members? Do you feel that other team members’ skills are used effectively? | |
| 13 | If you also have duties outside the team: Can you explain how you work with the team alongside your other duties? | |
Part 2: management, supervision and support
| 14 | Who is your employer? Who is your line manager? |
Mental health trust/SSD/other NHS sector |
| 15 | What are the formal arrangements for clinical supervision (from whom do you get it)? Are there any issues around this (particularly if manager and supervisor are different)? | Probe: Effect if no supervision available from within profession? |
| 16 | Do you have enough contact with your own discipline? Do you identify more strongly with the team or with your own profession? |
Is there adequate peer support? |
| 17 | How do you relate to the others in your profession outside the team? | Networks? Foot in two camps or fully joined up to the CMHT? |
| 18 | What informal support networks do you use? | Inside and outside the team |
| 19 | To what extent are you involved in decisions about:
|
Probe for: Seniors, manager only, democratic process, meetings, etc |
| 20 | Is the role of the TM/leader clear? | What gives them their authority? |
| 21 | Do you think that the professional discipline of the TM makes any difference to the way they can supervise and support staff/the way the team is run/managed? | |
| 22 | If manager carries a caseload: What is the impact of having a manager who is also a practitioner? (Advantages/disadvantages?) | |
Part 3: integration (some of this section might already have been covered in discussion of role)
| A: team-level issues | ||
|---|---|---|
| 23 | What are the advantages/disadvantages of having the particular range of professionals that you have within the team? | Probe for: How well does it work? Communication issues? Any tensions? |
| 24 | What do you think the impact of having/not having SWs in your team is on service users? Ask for examples | |
| 25 | What happens if you are the care co-ordinator and the service user needs the input of another professional within/outside the team? | Example? Differences in integrated/non-integrated teams? |
| 26 | Will you usually be aware of the input to individual service users from other agencies/services? Will they be aware of your input? What is the impact of this for service users? |
Care plans contain all involvement? How does this work (e.g. of good and poor practice)? |
| 27 | For high-integration teams: If a SW from outside the team is involved, does the service user get the same service? Does this occur? What is the difference? | |
| 28 | For low-integration teams: Can you describe the process of referring to social services outside the team? | |
| 29 | How does the way in which records are competed and accessed/kept and managed impact on the service you deliver? | Probe for: IT issues, electronic vs. hard-copies. Who can access/input? Duplication? |
| B: agency-level issues | ||
| Social services | ||
| 30 | What is the working relationship like between the team and generic social services older people’s teams? | Links to named workers? Attendance at meetings? Formal/informal arrangements ? |
| 31 | Is there a clear demarcation between the work of the CMHT and the local social services older people’s team in terms of who should be referred where? If yes: Can you explain what this is? If no: Can you describe how this impacts on the team and on service users? |
|
| 32 | What is the impact of the way you currently work with social services on service users? | |
| 33 | What do you think are the obstacles to, and facilitators of, joint working/integration with social services? | Probe for: Are there particular flash points (e.g. hospital discharges) or examples of good practice? |
| Ask CPNs only | ||
| 34 | Can you describe the process of referring to the psychologist outside the team? | Probe for: Service level access agreements Age-specific or generic service? |
| 35 | Can you describe the process of referring to the OT outside the team? | How does it work in practice? If there are OTs in the team – what difference does it make? |
Part 4: the role of the consultant
| 36 | Can you describe how responsibility for an individual’s care is shared between you and the consultant? What do you think about the way in which this responsibility is shared or not? |
Probe for: Who takes overall clinical responsibility for cases? Do consultants have any managerial responsibilities? Is there a shared understanding of this approach by all team members? |
| 37 | Do you get the appropriate level of support from the consultant/other old age psychiatrist | Accessible/helpful/supportive? What, if anything, would be better? |
| 38 | To what extent is the consultant involved with the team on a day-to-day basis? | Probe for: Do they directly manage/supervise anyone in team? |
| 39 | What role do other doctors play in the team? How do you relate to them? | |
| 40 | How do you regard the consultants that work in your team? | Equal members/different in some way/seniors? |
| 41 | How would you describe the nature and degree of the consultant’s (and other doctors) influence within the team? | |
| 42 | What works well in terms of the way the consultant’s work is organised? | Probe for: Community/inpatient split or locality based? Involvement in meetings, team development, etc.? |
| 43 | What could be better about the way that the consultant’s role operates for:
|
|
| 44 | Based on your own experience in mental health services for older people, how has the consultant’s role within the team changed over time? | |
| 45 | Have changes had any adverse as well as beneficial consequences? | |
Part 5: the role of the support worker
| 46 | What is the role of the support worker(s) in your team? Is this clear, do you think? What is their job title? |
Is there more than one role/title? What about occupational therapy assistant/care management assistant? Are these similar to each other or more akin to the profession they relate to? |
| 47 | What sort of work do they do that is not done by other team members? Do you feel that this is appropriate? | |
| 48 | What are the benefits to the team and service users are having this support worker role? | |
| 49 | Are there other roles undertaken by qualified staff that could be undertaken by support workers? Examples? Do you perceive any problems in extending role of support workers? | Probe: ‘Specialist’ roles, such as dementia home care work |
Part 6: concluding thoughts
| 50 | What are the benefits to the service user (and staff) of the way the work of the team is organised? What are the disadvantages? |
| 51 | Would you like to see further integration and if so – what precisely? |
| 52 | If yes, to what extent would this affect service user outcomes? |
| 53 | What causes you most frustration and stress about the role you play in the CMHT? |
| 54 | What do you find most rewarding about the role you play in the CMHT? |
| 55 | Is there anything more that you’d like to add/that I have not asked you about (e.g. other changes that have had a impact on the team)? |
Appendix 29 Community mental health teams: example of baseline questionnaire
Appendix 30 Community mental health teams: service user interview
Appendix 31 Community mental health teams for older people: follow-up questionnaire
Appendix 32 Community mental health teams: carer questionnaire
Appendix 33 Community mental health teams: staff questionnaire
Appendix 34 Community mental health teams for older people: team similarities and differences
| Team | Structure | Referral and access arrangements | Role responsibilities | Consultant role | Record sharing | Relationship with SSD outside team | |||
|---|---|---|---|---|---|---|---|---|---|
| Management and supervision arrangements | Membership | Initial assessment | Care co-ordination | Organisation of work | Responsibility and influence | ||||
| Network team | |||||||||
| E | Colocation. Separate line management outside team. Peer clinical supervision within disciplines within team. Consultant-led service | Nurses, OTs, support worker Psychiatrist |
No SPA GP referrals direct to CPNs or consultant Consultants also refer to CPNs who then decide on urgency and allocate accordingly within the team |
Nurses, OTs and consultants conduct initial assessments | No single care co-ordinator | Community and inpatient responsibility Separately managed memory clinic |
Multidisciplinary meetings organised around consultant caseload Responsibility for those on her caseload only |
Separate health and social care – no access. Separate nurse and OT | Long-standing informal networks with mental health SWs under threat due to SSD reorganisation Access via central number creates delays. Able to bypass system for urgent cases Fractures in continuity at hospital discharge |
| Non-integrated teams | |||||||||
| H | Single manager Single manager Clinical supervision outside team for some with different discipline to TM |
Nurses, OTs, support worker Psychiatrist |
From GP only SPA to consultant or manager who collate for weekly discussion prior to team meeting No duty system |
Nurses, OT occasionally Consultants involved in some rather than all |
Nurses, OT occasionally (used more for short-term intervention) | Community and inpatient responsibility Memory monitoring within team |
Clinical and team leadership role Ultimate responsibility for all medical decisions on all team cases |
Separate health and social care – no access | Long-standing informal networks with mental health SWs under threat due to SSD reorganisation and loss of colocation Access via central number creates delays. Referring on rather than joint working |
| I | Single manager Clinical supervision outside team for all with different discipline to TM |
Nurses, OTs, support worker Psychiatrist Psychologist Physiotherapist |
From GP only Referrals to consultant. Weekly team meeting used to discuss and allocate cases Daily emergency duty system |
Nurses, OTs Consultants involved in most complex only. Recognises ability of others to collect relevant information |
Nurses, OT | Community only, including separate memory service | Shared responsibility with other team members Has role in monitoring team workload and in promoting changes in practice |
Separate health and social care – no access | Access via central number Flash points at hospital discharge |
| F | Single manager Clinical supervision outside team for all with different discipline to TM |
Nurses, OTs, support worker Psychiatrist Psychologist |
From GP or hospital SPA via duty system. Consultants and TM screen daily and allocate for initial assessment if urgent or hold until weekly team meeting |
Nurses, consultant | Nurses plus OT and psychologist occasionally | Community only (includes memory monitoring within team) | Clinical leadership for all cases Sees around 50%. Formal clinical supervision to non-medical prescribers in team |
Separate health and social care – no access | Refer to individual team. Poor feedback post referral Good safeguarding procedures Recognise their limited understanding of SSD finance |
| G | Single manager Clinical supervision outside team for all with different discipline to TM |
Nurses, OTs, support worker Psychiatrist |
From GP only | Nurses, consultant OT occasionally |
Nurses, OT | ? | Separate health and social care – no access | Regular meetings improve joint working Highlight lack of mental health knowledge of generic social work team |
|
| ‘Semi’-integrated team | |||||||||
| B | Separate health and social care management and supervision. Single manager Clinical supervision outside team for all with different discipline to TM |
Nurses, OTs, support worker Psychiatrist Psychologist SWs |
Separate health and social care access points Informal referral/handover between them if referral is thought to be more appropriate to other side of team Mainly, but not exclusively, from GPs. Social care referrals are open |
Nurses, OT Consultants involved only in most complex |
Nurses and OT | Community and inpatient responsibility (functional mental illness only) Separate memory clinic |
Clinical leadership Influences allocation decisions. Involved in all discharges in health team. Sees less 50% – team members trusted to bring cases to consultant attention when appropriate Partnership with TM in relation to introducing new practices |
Separate health and social care with access | |
| Integrated teams | |||||||||
| C | Single manager Clinical supervision outside team for some with different discipline to TM |
Nurses, OTs, support worker Psychiatrist Psychologist SWs |
Open referrals Trust-wide SPA Manager and consultant discuss all before team Daily duty officer |
Nurses, SWs, consultants involved only in most complex | Nurses, SWs OTs occasionally – used more for short-term intervention |
Community, memory clinic and inpatient responsibility | Ultimate medical responsibility for all team cases Influences allocation and discharge decisions. Recognition of shared responsibility with others based on NWW Partnership with TM regarding workload management and maintaining high standards |
Single shared system | Try to limit this as think it leads to poorer service – less co-ordinated and with less mental health awareness |
| A | Single manager All supervision within team |
Nurses, OTs, support worker Psychiatrist SWs |
Open referrals SPA Manager and consultant do not discuss before team |
Subteam of two nurses do all Consultant not involved |
Nurses, SWs, OTs | Community only Separately managed memory clinic |
Limited role. Responsibility only for those referred to him Concerns from consultant about system of trusting team members to bring cases to consultant attention when appropriate |
Separate health and social care with access | Try to limit this as think it leads to poorer service – less co-ordinated and with less mental health awareness |
| D | Single manager All supervision within team |
Nurses, OTs, support worker Psychiatrist SWs |
From GP only SPA Daily duty officer Manager and consultant discuss some before team |
Nurses, SWs, OT Consultant wants medic involved in all new to team |
Nurses, SWs, OTs | Community, day and inpatient responsibility Delegates some community to senior registrar Separately managed memory clinic |
Ultimate medical responsibility for all team cases Influences allocation and discharge decisions Recognition of shared responsibility with others based on NWW |
New single shared system Previously separate health and social care with access |
Try to limit this as think it leads to poorer service – less co-ordinated and with less mental health awareness |
Appendix 35 Care homes outreach literature review: search criteria
Search criteria
-
Peer-reviewed journal.
-
English language.
-
Published 1989–current.
-
Care home
-
Nursing home
-
Residential home
-
Outreach
-
CMHT
-
Old age psychiatrist
-
Depression
-
Dementia
-
Mental health needs
-
Behavio* problems
-
Medication
-
Anti-psychotic medication
-
CPN
-
Community psychiatric nurse
-
Psychologist
-
Occupational therapist
-
Pharmacist
-
Social worker
-
GP
-
General practitioner
-
Intermediate care
-
Liaison
-
Liaison nurse
-
Crisis resolution
-
Old* people
-
Interdisciplinary
-
Multidisciplinary
-
Multi-disciplinary
-
Alzheimers
-
Mental illness
-
Mental health problems
-
Residential care
-
Training
-
Education
-
Behavio* management
-
1 or 2 or 3 or 32
-
7 or 8 or 9 or 10 or 25 or 29 or 30 or 31
-
4 or 5 or 6 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 26 or 27 or 28 or 33 or 34 or 35
-
36 and 37 and 38
Appendix 36 Care homes outreach literature review: data extraction forms for questions 1 and 2
Appendix 37 Care homes outreach: community mental health team support to care homes survey questionnaire
Appendix 38 Care homes outreach: mental health support to care homes survey questionnaire
Appendix 39 Revised research protocol
Aims and objectives
The programme aims to explore the most effective ways of organising and delivering services for older people with mental health problems, both locally and nationally. The work will address the need for better evidence to inform service delivery at the macro level of planning and strategic development and the mezzo level of the provider unit.
Objectives
-
To refine and apply ‘the balance of care approach’ (a systematic framework for choosing between alternative patterns of support by identifying people whose care needs could be met in more than one setting and comparing their costs and outcomes) to the care of older people with mental health problems.
-
To identify whether, how and at what cost the mix of services provided for this client group might be more optimally developed in a particular locality.
-
To enable other health and social care decision-makers to apply the balance of care framework independently.
-
To identify core features of national variation in the structure, organisation and processes of CMHTsOP.
-
To examine whether or not different CMHT models are associated with different costs and outcomes.
-
To identify core features of national variation in the nature and extent of specialist mental health outreach services for older care home residents.
-
To scope the evidence on the association between different models of outreach and resident outcomes.
-
To disseminate the findings and service development tools from the work to NHS trusts, commissioners, local authorities and national policy-makers.
Research plan
The programme is designed to address key policy and service development issues in old age mental health care11,366,367 and has three core themes:
-
the best combination of inpatient, residential and community services to provide for this population (BoC)
-
the factors that make for effective working of CMHTsOP for older people; and
-
the quality and quantity of mental health support provided to older care home residents (care home outreach).
These reflect the shift of care towards community based provision and the scale of service change required to achieve this; the need to develop explicit coherent models for the delivery of community-based care to support people in their own homes; and the provision of better mental health care for older people in care homes.
The programme contains five interlinked packages of activity and combines national work with detailed research in particular sites. The application for programme funding is designed to permit a focus on the wider picture of the whole system of old age mental health and the interdependency of its component parts. It also enables the creation of a team, critical mass and centre of expertise offering greater value than a series of separate shorter term projects. Appropriate ethical approval will be sought from an NHS Research Ethics Committee and the research governance departments in each study site.
Literature review
The research plan commences with a systematic literature review which will address the three core themes in the study and set these in the wider context. It is planned to complete an initial version of this in the first 6 months of the study. The review will be updated during the programme and a final version produced at the end of the funding in 2012 (objectives 1, 4, 5 and 8).
Balance of care
This package is designed to investigate the overall mix of services needed by older people with mental health problems (objectives 1 and 2). The work focuses on the margins of provision between institutional and community-based care on the one hand, and between health and social care on the other. It investigates whether or not certain groups of people would be better supported in alternative settings or services, and the relative costs and outcomes of any proposed changes.
Design, implementation and analysis
The work will be undertaken within the catchment area of the Manchester Mental Health and Social Care Trust, which is co-terminous with PCT and LA boundaries. There are eight main stages to the method:
-
The collection of detailed local information about the sociodemographic, clinical and service receipt characteristics of six key groups of older people with mental health problems:
-
admissions to acute mental health inpatient beds (a 6-month series of consecutive admissions)
-
admissions to residential and nursing homes (a 3-month series of consecutive admissions with mental health problems identified by the use of mental health indicators contained within a preliminary screen – around 150 cases)
-
very sheltered housing residents (a sample of 30 residents with mental health problems identified by the use of mental health indicators contained within a preliminary screen)
-
people on the community caseloads of CMHT staff (a random sample of 300 active cases)
-
people on the caseloads of graduate primary care mental health staff (a random sample of 50 active cases)
-
people on the caseloads of generic social work staff and not in touch with the specialist mental health services (a sample of 120 clients with mental health problems identified by the use of mental health indicators contained within a preliminary screen).
-
-
The characterisation of each core group into different ‘case types’ by a number of key variables as utilised in previous work. 72,104,118,368 Examples include degree of cognitive impairment, presence or absence of a significant informal carer, and dependency levels.
-
The identification of those case types whose presentation is such that their needs could appropriately be met in more than one way (e.g. by community or institutional care). Groups of professional staff who work with older people with mental health problems (including medical, nursing and social care staff) will consider vignettes representing the most common case types and develop optimal packages of care for each case type. In relation to some core groups, such as nursing home admissions, the critical decisions will relate to whether care home or an alternative is most appropriate. In relation to other care options, such as inpatient episodes, both appropriateness and duration or amount will be evaluated. A separate review of the desirability of service package changes will then be made by groups of older people and their carers, while an external expert reference group of professionals will review the alternative care scenarios. Last, interviews will be conducted with practitioners to identify the factors shaping their decision making processes.
-
An evaluation of the feasibility of providing alternative care. The proposed care plans for the representative case types will then be submitted to an independent expert panel, with considerable experience in the care of older people with mental health services, who will be asked to act as gatekeepers for access to resources and to decide whether or not the proposals could be funded. This process will closely mirror local decision-making procedures.
-
The identification of the outcomes of people with similar needs for care supported in different settings. Wherever possible, this will draw on existing sources (e.g. published studies and/or accessible secondary national data). However, in light of the particular interest in, and paucity of evidence available about, the outcomes of people on the care home/home with specialist mental health support margin, additional primary outcome data will be collected from face-to-face interviews with people in these two settings. This will be designed as a matched cohort study, and will compare the 4-month outcomes of 120 marginal care home cases, represented by a small number of case types, with those of a matched sample of 120 service users who receive CMHT support at home. Older people’s and carers’ experience of these services will be assessed by trained, experienced researchers in people’s own homes or care homes. Variables of interest will include measures of depression (GDS149,150); self-rated health;369 physical functioning and mobility (Barthel Index138,139,147), cognition (MMSE142); QoL (QoL-AD scale152–155); and service utilisation (Client Service Receipt Inventory156).
-
The estimation of the potential cost and outcome consequences of different service provision options for certain groups at individual case and system levels. To adjudge the potential costs and benefits of the current patterns of provision and alternative scenarios, cost comparisons will be made between the different modes of care, adjusted for baseline differences. The focus will be on those marginal cost distributions at the level of the individual which reflect critical differences between different care settings.
-
An evaluation of the desirability of different service outcomes. Key stakeholder perspectives on the different scenarios and their potential cost and feasibility will be evaluated using focus groups and surveys.
-
The production of a workbook which permits the core elements of the methodology to be transferred economically for use elsewhere in NHS and social care organisations.
Outputs
The team will publish papers, a report and an accessible summary based upon the successful PSSRU Research and Policy Updates. This material will be made available on the programme website. A workbook will be produced which will enable other NHS trusts to undertake an evaluation themselves as part of the strategic planning process (objective 3).
Patterns of community mental health services in old age mental health services in England
This programme element aims to provide a baseline picture of the scale, arrangements and patterns of working of CMHTsOP across England (objective 4). It will involve a national survey of CMHT managers focusing on teams’ style, mode of working, range and operational characteristics. The degree of detail on process indicators will complement the work undertaken in the national mental health mapping exercise. 226 This study will provide the context for the subsequent CMHT study, facilitate the classification of typologies and their prevalence, and identify potential sites for detailed study in activity 4.
Outputs
The study will produce published papers, a report and an accessible summary based on the PSSRU Research and Policy Updates both in hard copy and available on the programme website (objective 8).
Different models of community mental health teams for older people
Community mental health teams for older people are a key element of the policy strategy for developing old age mental health services,367 but there is only limited evidence on the processes of care associated with better outcomes. 65 This work is designed to identify and clarify different models of CMHTs and to provide an evaluation of their relative costs and benefits (objective 5).
Design
The study is designed as a natural experiment with economic evaluation of selected, qualitiatively different, models of CMHTsOP. The information from the national survey (activity 3) will be analysed, and a number of key variables (determined a priori from the literature and validated by an expert reference group) will be used to cluster the teams into different service models. From the literature it is expected that at least three distinctively different types of CMHT will be identified. The research team will then undertake a series of validation visits to teams that appear to exemplify each model until robust examples of each model have been identified, i.e. teams that have both ‘model coherence and model fidelity’ ensuring that the sites evaluated reflect deliberately planned and transportable combinations of attributes. Further local data collections of service user, carer and practitioner outcomes will then be undertaken and comparisons will be made to establish whether different team models are associated with different outcomes.
Measures
The primary measure of outcome will be the proportion of clients on CMHTs’ caseloads admitted to acute mental health inpatient care over a 6-month period. Case records and management information systems will be explored to identify a range of process details including length of contact, visit frequency, staff mix and services received.
Older people’s experience of the service will be assessed by trained experienced researchers interviewing in people’s own homes. These interviews will include perceived quality of care; standardised measures of health-related QoL suitable for older people with cognitive impairment;152–155 physical functioning and mobility (Barthel Index138,139,147); depression (GDS143,150); cognition (MMSE142); self-rated health;369 and service utilisation (Client Service Receipt Inventory156). Carer outcomes will include mood status (HADS144) and carer burden (MCSI237).
Community mental health team members will be asked to provide information about staff experience. This will include data about both workload and morale and will incorporate standardised measures of job content and role performance. 243,251 Qualitative interviews will also be undertaken to identify staff perceptions as to the consistency and operational costs and benefits of the different models of team operation.
Sample size
Target sample sizes were based on power calculations, with adjustments to reflect the context of the current study (in particular the capacity of local services). For the primary outcome, a small effect size was cautiously predicted, in the absence of prior evidence of the likely impact of team design on inpatient admissions; the relatively low number of likely admissions over a 6-month period on average; and the importance of including regression-based controls, given a non-experimental design. A total sample size of 960 service users would have 80% power to detect close to a ‘small’ effect size241 in a 2 × 4 contingency table.
Comparison and economic analysis
Comparisons will be made to establish whether different team models are associated with better outcomes for staff and/or clients. In order that the findings are not distorted by differences in substitute and complementary services, and/or the predilections of individual old age psychiatrists, a casemix adjustment, using a measure of the overall characteristics of the CMHT caseloads, will be undertaken in the analysis. Cost comparisons will be made between the different CMHTs, adjusted if necessary for baseline differences. Adjustments will probably also be needed to account for non-normality of data (transformation or non-parametric test). The focus will be on those marginal cost distributions at the level of the individual patient which reflect critical differences between teams. Cost-effectiveness analysis comparisons will be made by combining costs generated from the Client Service Receipt Inventory156 (ranging over primary, secondary and community-based health and social care services) with indicators of service outcome, such as community tenure, and also with measures of well-being.
From the national data on CMHTs collected as part of this package, exploration will be made of the associations between this primary data set and national secondary indicators. This would involve examining the relationship between individual classificatory variables and each service model type and a range of routinely collected information that might be seen as indicative of the quality of care provided such as readmission rates, waiting times and admissions to care homes.
Outputs
The study will produce published papers, a report and an accessible summary. This material will be made available on the programme website (objective 8).
Specialist mental health support for older care home residents: the national picture
Two extensive national surveys will be undertaken in relation to the care homes package of the programme (objective 6). The first will survey all CMHTsOP in England with a view to identifying the range and pattern of approaches to outreach to care homes for older people with mental health problems. This will build on previous approaches which have successfully surveyed professionals in this specialty with high response rates73,179 and, through comparison with the data collected in package 3, will facilitate an analysis of the extent of outreach development during the study period.
The second will survey a sample of care home managers to identify the nature and intensity of current support and to capture perceptions of what would be most valued. A stratified sample of care homes in England will be derived from the Commission for Social Care Inspection (CSCI) or Laing and Buisson databases. The CSCI database lists 9743 care homes providing services for older people in England. It is proposed to undertake a 10% sample of these, stratified by region.
Both surveys will be of intrinsic value in providing a national picture of the nature and extent of specialist mental health support to care homes.
Outputs
The study will produce published papers, a report and an accessible summary both in hard copy and available on the programme website (objective 8).
Main alterations from the original protocol
The protocol was significantly revised in response to the funders’ decision not to support the proposed trial of depression management for older care home residents. The intent to evaluate the cost-effectiveness of different forms of specialist support for older care home residents with depression was thus abandoned.
Other refinements to the protocol included:
-
the decision to focus the first national survey (activity 3) on CMHTsOP in light of further examination of the information available in the national service mapping data set and the desire to ‘add value’
-
the widening of the mapping element of the care home outreach work (activity 5) to incorporate services for older people with mental health problems with dementia and other mental health problems, as well as depression; and
-
the decision to survey CMHT managers (as opposed to consultant psychiatrists) in the revised outreach strand of the study (activity 5), facilitating an analysis of the extent of outreach development during the study period.
Further significant changes to the study protocol prior to commencement of the research
A number of further changes were made to the protocol in the period prior to the study’s commencement in light of the unexpected decision of the LA in the original research area not to participate in the BoC work due to financial retrenchment. This resulted in the recruitment of two further local authorities and an additional mental health trust; necessitated a reduction in the number of settings the study investigated from six to five (there were no graduate primary care services for older people in the new catchment area); and led to the revision of the proposed sample sizes in the first stage of this work.
Appendix 40 Dissemination activity
Published articles
Abendstern M, Harrington V, Brand C, Tucker S, Wilberforce M, Challis D. Variations in structures, processes and outcomes of community mental health teams for older people: a systematic review of the literature. Aging Ment Health 2012;16:861–73. 185
Wilberforce M, Harrington V, Brand C, Tucker S, Abendstern M, Challis D. Towards integrated community mental health teams for older people in England: progress and new insights. Int J Geriatr Psychiatry 2011;26:221–8. 228
Tucker S, Brand C, Wilberforce M, Challis D. The balance of care approach to health and social care planning: Lessons from a systematic literature review. Health Serv Manag Res 2013:26:18–28.
Publications for practitioners and policy-makers
Personal Social Services Research Unit (PSSRU). How Does Your Team Work? A National Survey of Community Mental Health Teams for Older People in England. Research and Policy Update Issue 9. Manchester: PSSRU, University of Manchester; 2010.
Personal Social Services Research Unit (PSSRU). The North-West Balance of Care Study: Caseload Characteristics of Pennine Care (Stockport and Tameside) CMHTs for Older People. Manchester: PSSRU, University of Manchester; 2011.
Personal Social Services Research Unit (PSSRU). The Balance of Care Approach to Health and Social Care Planning: A Systematic Literature Review. Research Focus Issue 4. Spring 2011. URL: www.nursing.manchester.ac.uk/pssru/PSSRUInformation/Issue4.pdf
Personal Social Services Research Unit (PSSRU). Community Mental Health Teams for Older People: A Systematic Literature Review. Research Focus Issue 4. Spring 2011. URL: www.nursing.manchester.ac.uk/pssru/PSSRUInformation/Issue4.pdf
Personal Social Services Research Unit (PSSRU). Community Mental Health Teams for Older People in England. Research and Policy Update Issue 12. Manchester: PSSRU, University of Manchester; 2012.
Tucker S, Wilberforce M, Brand C, Abendstern M, Challis D. All things to all people? The Provision of Outreach by Community Mental Health Teams for Older People in England: Findings From a National Postal Survey. February 2013; DP M271 Personal Social Services Research Unit, University of Manchester; 2013.
Wilberforce M, Tucker S, Abendstern M, Brand C, Giebel C, Challis D. Membership and Management: Structures of Inter-Professional Working in Community Mental Health Teams for Older People in England. Manchester: PSSRU, University of Manchester.
Tucker S, Brand C, Wilberforce M, Challis D. The Balance of Care Approach to Planning Services for Older People with Mental Health Problems: A Handbook for Service Planners, Providers and Commissioners. Manchester: PSSRU, University of Manchester; forthcoming.
Contributions to other studies
Staley K. An Evaluation of Service User Involvement in Studies Adopted by the Mental Health Research Network. London: Mental Health Research Network; 2012.
Our study was selected by the author as an example of patient/public involvement in NIHR-funded research.
Conference and seminar presentations
Programmed for Success. Mental Health Research Network Conference, Bolton, November 2008.
Exploring our Trust’s Research. Manchester Mental Health and Social Care Trust Conference, Manchester, March 2009.
How Does Your Team Work? An Investigation of Joint Working and Integration Within Community Mental Health Teams for Older People. Social Policy Association Annual Conference, Edinburgh, June 2009.
CMHTs for Older People: A Focus on Integration. PSSRU Seminar, Manchester, September 2009.
Celebrating Success in Older Adults Functional Mental Illness and Community Directorate. Sheffield Health and Social Care Trust, April 2010.
Postcards from the Cutting Edge: Driving Service Quality Forwards through Research and Innovations Conference. Surrey and Borders, November 2010.
CMHTs for Older People: The Costs and Outcomes from Different Ways of Working Dementia Seminar. Greater Manchester West, Manchester, May 2011.
Improving the Mix of Services Provided for Older People with Mental Health Problems: The Balance of Care Approach to Health and Social Care Planning. A seminar for professionals, service users and carers on the early findings of the balance of care study. Chancellor’s Conference Centre, Manchester, June 2012.
CMHTs for Older People: Different Ways of Working: Characteristics and Outcomes. Pennine Trust Research Day, Trust HQ, Ashton-under-Lyne, July 2011.
The Balance of Care Study. Pennine Trust Research Day, Trust HQ, Ashton-under-Lyne, July 2011.
Different Perspectives on the Appropriateness of Care Home Entry: Evidence from a Balance of Care Study of Older People with Mental Health Problems. International Long-term Care Policy Network Conference, London School of Economics, September 2012.
Community Mental Health Teams for Older People: The Outcomes and Costs of Different Ways of Working. Health and Social Care Integration in the New Policy Landscape. A joint seminar supported by the Socialist Health Association and the UK Social Policy Association. University of York, York, October 2012.
The North-West Balance of Care Study: Design, Findings and Reflections. PSSRU seminar programme, University of Manchester, Manchester, November 2012.
Workshops
Stockport care home workshop for managers and practitioners, Stockport, October 2011.
Tameside inpatient workshop for managers and practitioners, Manchester, October 2011.
Stockport inpatient workshop for managers and practitioners, Stockport, November 2011.
Manchester inpatient workshop for managers and practitioners, Manchester, November 2011.
Age UK Trafford care home workshop for older people and carers, Manchester, February 2012.
Educate Group Stockport care home workshop for older people with dementia and carers, Stockport, March 2012.
Glossary
- Activities of daily living
- Phrase used to describe everyday activities when measuring levels of dependency in individuals.
- Advocacy service
- A service that supports people to say what they want, represent their interests and obtain the services they need.
- Care co-ordinators
- A health or social care professional with similar functions to a care manager.
- Care homes (formerly residential care homes)
- Care homes registered under Part II of the Care Standards Act 2000 (Great Britain. Care Standards Act 2000. Chapter 14. London: HMSO; 2000), which can be provided by voluntary or private organisations.
- Care homes with nursing (formerly nursing homes)
- Registered care homes (with nursing) are registered under Part II of the Care Standards Act 2000 to provide nursing care.
- Care home support/intervention team
- A multidisciplinary team whose work focuses on providing support to care homes with residents with organic or functional mental ill health.
- Care/case manager
- Usually a social worker who undertakes a range of assessment, monitoring and reviewing functions as well as arranging the input of other services for individuals.
- Care packages
- Social care support for people in the community.
- Care programme approach
- A system, introduced in England in 1991, of delivering community mental health services to individuals which was designed to ensure that different community services are co-ordinated and work together towards an individual’s care. It requires that professionals from the health authority and local authority arrange care collaboratively.
- Carer/informal care
- Usually relatives or friends of service users who provide unpaid informal care.
- Case conference
- Multiagency meeting to discuss individual complex cases.
- Case finding and screening
- Methods of ensuring that services are appropriately targeted.
- Case types
- Division of the population into categories with similar characteristics.
- Client/patient/service user
- Person who uses health and/or social services. Terms are used interchangeably within this report depending on which service and professional group are being described.
- Cognitive–behavioural therapy
- A range of therapies in which the patient works together with a therapist to achieve specific treatment goals including such things as recognising the impact of behavioural and/or thinking patterns on feeling states and encouraging alternative cognitive and/or behavioural coping skills to reduce the severity of symptoms and problems.
- Cohort study
- A form of longitudinal study.
- Community equipment service
- Provides health and social care equipment to promote independent living and enable safe discharge for patients from hospitals.
- Co-morbidity
- Two or more diseases or conditions occurring at the same time, such as depression and anxiety.
- Consultant/Consultant old age psychiatrist
- Terms used interchangeably within this report.
- Council/local authority
- Local government regions in England that are run by local councillors. Terms are used interchangeably within this report.
- Day care
- Either specialist generic day care is provided in centres offering a range of social, leisure and therapeutic activities. A wide range of services can be offered such as personal support, drop-ins, advice and information and programmes of practical, social activities and support for carers.
- Day hospital
- Offers intensive multidisciplinary assessment and treatment for older people with complex mental health needs in order to prevent admission to hospital or to aid recovery following admission.
- Domiciliary assessment
- An assessment that takes place in the home of the person being assessed.
- Dual registered homes
- Care homes registered for both nursing and non-nursing care.
- Extra care housing
- Also known as very sheltered housing, part two and a half, close care, assisted living or retirement villages. Residents have their own flat within a complex designed with the needs of highly dependent people in mind. Support should be available 24 hours a day. Facilities usually include a laundry, restaurant/dining room, domestic support, personal care, enhanced communal facilities and the capacity to offer extra care services, through dedicated care team support.
- Fair Access to Care Services
- A national framework for councils to use when setting eligibility criteria for social care services for adults introduced by the Department of Health in England in 2002.
- Functional mental illness
- Mental illness not caused by brain impairment but by a derangement of the patient’s mind. Also described as mental disorder. Includes depression and anxiety.
- Functionalised model
- Where the work of the consultant psychiatrist is split between hospital and community based patients.
- General practitioner
- A medical practitioner who treats acute and chronic illnesses and provides preventative care for all ages.
- Home care/domiciliary care
- Provides personal and domestic care to older people and their families in their own homes.
- Home treatment team
- See Rapid response team below.
- Individual budget
- Often also called a ‘personal budget’. A sum of money allocated to an individual by his or her local authority based on eligible assessed needs.
- Inpatient care
- The provision of assessment, treatment and rehabilitation within a hospital setting.
- Health/integrated health and social care trust
- An organisation with responsibility for the delivery of a range of health/health and social care services within a geographic region.
- Likert scale
- Traditionally a five-point scale used to measure the strength of a response.
- Link worker
- A member of a community mental health team for older people whose role includes working with one or more specific care homes.
- Memory clinic
- Their aim is to aid the early detection, diagnosis and treatment of dementia via assessments, counselling, the provision of pharmacological treatment, advice and support, follow-up and review.
- Multidisciplinary teams
- Professionals across disciplines or fields of expertise working in the same team.
- Neuroleptics
- Antipsychotic, tranquillising drugs used in the treatment of some mental disorders.
- Observational study
- Where individuals are observed or outcomes measured without any attempt to affect them.
- Open/direct referral system
- Where referrals to the community mental health team for older people can be made directly to them by a range of organisations and by members of the public rather than through the general practitioner.
- Organic mental illness/dementia
- Illnesses such as dementia which stem from brain impairment and result in the deterioration of mental abilities including a decline in cognitive and emotional functioning.
- Outpatient clinics
- Staffed predominantly by doctors, usually in hospital and occasionally in community-based settings. Service users attend for appointments aimed at diagnosis and treatment planning or monitoring.
- Quality of life
- Includes satisfaction within important areas of one’s life, the level of functioning in different areas and the objective circumstances in which one lives. Used to measure change in a person’s condition beyond reduction in symptoms.
- Rapid response team
- Designed to prevent avoidable acute admissions by providing rapid assessment/diagnosis for older people, including rapid access on a 24-hour basis to short-term nursing/therapy support and personal care in the patient’s own home.
- Sectorised model
- Where the work of the consultant psychiatrist covers both hospital and community based patients.
- Single assessment process
- Introduced in 2004 in England, this was an attempt to bring together disparate assessments by a range of professional groups.
- Single point of access
- A system for funnelling referrals to a community mental health team for older people.
- Social Services Department
- The section of a local authority with responsibility for the delivery of social care services.
- Stakeholder
- Anyone with an interest in the organisation or project in question.
- Support workers/support time and recovery workers
- Unqualified health and social care staff who are members of community mental health teams for older people.
- Telecare and ‘just checking’ system
- A range of devices providing remote monitoring to help people live more independently, linked to a 24-hour local community response service. ‘Just checking’ – a wireless monitoring system – is one of a range of devices available.
- 24-hour crisis line
- Personal alarm worn by individual – as a pendant or wrist band – used to alert support services in a crisis; or telephone support service.
List of abbreviations
- A&E
- accident and emergency
- ABC
- antecedent, behaviour, consequences
- ACE-R
- Addenbrooke’s Cognitive Examination-Revised
- ADL
- activities of daily living
- ANOVA
- analysis of variance
- ASSIA
- Applied Social Sciences Index and Abstracts
- BoC
- balance of care
- CCG
- Clinical Commissioning Group
- CHST
- care home support team
- CMHN
- community mental health nurse
- CMHT
- community mental health team
- CMHTOP
- community mental health team for older people
- CPA
- care programme approach
- CPN
- community psychiatric nurse
- CPS
- Cognitive Performance Scale
- CSCI
- Commission for Social Care Inspection
- df
- degree of freedom
- DH
- Department of Health
- DHSS
- Department of Health and Social Security
- DN
- district nurse
- ECH
- extra care housing
- GDS
- Geriatric Depression Scale
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- HMIC
- Health Management Information Consortium
- JDC
- job demand–control
- LA
- local authority
- LOS
- length of stay
- MDT
- multidisciplinary team
- MMSE
- Mini Mental State Examination
- NAO
- National Audit Office
- NICE
- National Institute for Health and Care Excellence
- NoNur/Dem
- without nursing/dementia
- NoNur/NoDem
- without nursing/no dementia
- NSF
- National Service Framework
- NSFOP
- National Service Framework for Older People
- Nur/Dem
- with nursing/dementia
- Nur/NoDem
- with nursing/not dementia
- NVQ
- National Vocational Qualification
- OLS
- ordinary least squares
- ONS
- Office for National Statistics
- OT
- occupational therapist
- PCT
- primary care trust
- PSSRU
- Personal Social Services Research Unit
- QoL
- quality of life
- QoL-AD
- Quality of Life-Alzheimer’s Disease
- RAM
- Resource Allocation Management
- RCT
- randomised controlled trial
- SAP
- single assessment process
- SD
- standard deviation
- SPA
- single point of access
- SSD
- Social Services Department