Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0609-10135. The contractual start date was in March 2011. The final report began editorial review in November 2016 and was accepted for publication in July 2017. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Elizabeth Murray reports grants from the National Institute for Health Research (NIHR) and National School of Primary Care Research during the conduct of the study, and grants from NIHR outside the submitted work. She is also managing director of the not-for-profit HeLP Digital community interest company (CIC), which was established to disseminate the HeLP-Diabetes programme across the NHS. She does not take any remuneration for this work. Kingshuk Pal reports personal fees from HeLP Digital CIC outside the submitted work. Fiona Stevenson reports grants from the NIHR during the conduct of this study. Maria Barnard reports sponsorship for attendance at educational conferences from Novo Nordisk A/S, personal fees from Janssen Pharmaceutica NV and that Janssen-Cilag International NV Sponsor was a sponsor of the multicentre CREDENCE trial (which Whittington Health NHS Health Trust is a site for) outside the submitted work. Lucy Yardley reports grants from NIHR during the conduct of the study; grants from NIHR, the Engineering and Physical Sciences Research Council, Medical Research Council (MRC), medical charities and European Commission outside the submitted work; and membership of the Health Technology Assessment Efficient Study Designs Board and Public Health Research Research Funding Board. Susan Michie reports grants during the conduct of the study from NIHR, the Engineering and Physical Sciences Research Council, MRC, the National Institute for Health and Care Excellence, the Department of Health and Social Care, Public Health England, Cancer Research UK, the British Psychological Society and EC outside the submitted work. David Patterson was one of the founders, and is now Chief Medical Officer, of Helicon Health Ltd, a spin-out company from UCL Business. He does not believe there is any actual conflict of interest between Helicon Health Ltd and this work – other than the fact that his knowledge of information technology and devices was growing during this academic work. Ghadah Alkhaldi reports personal fees from the Saudi Arabian Cultural Bureau, outside the submitted work. Brian Fisher reports that he is the Director of Patient Access to Electronic Record Systems Ltd (now Evergreen Life), which was intended to offer links from the HeLP-Diabetes programme to the patient record outside the submitted work. Orla O’Donnell reports working as the Chief Operating Officer for the HeLP Digital CIC from the end of the programme grant until 1 May 2017. Andrew Farmer reports grants from NIHR and MRC outside the submitted work.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Murray et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Structure and overview of report
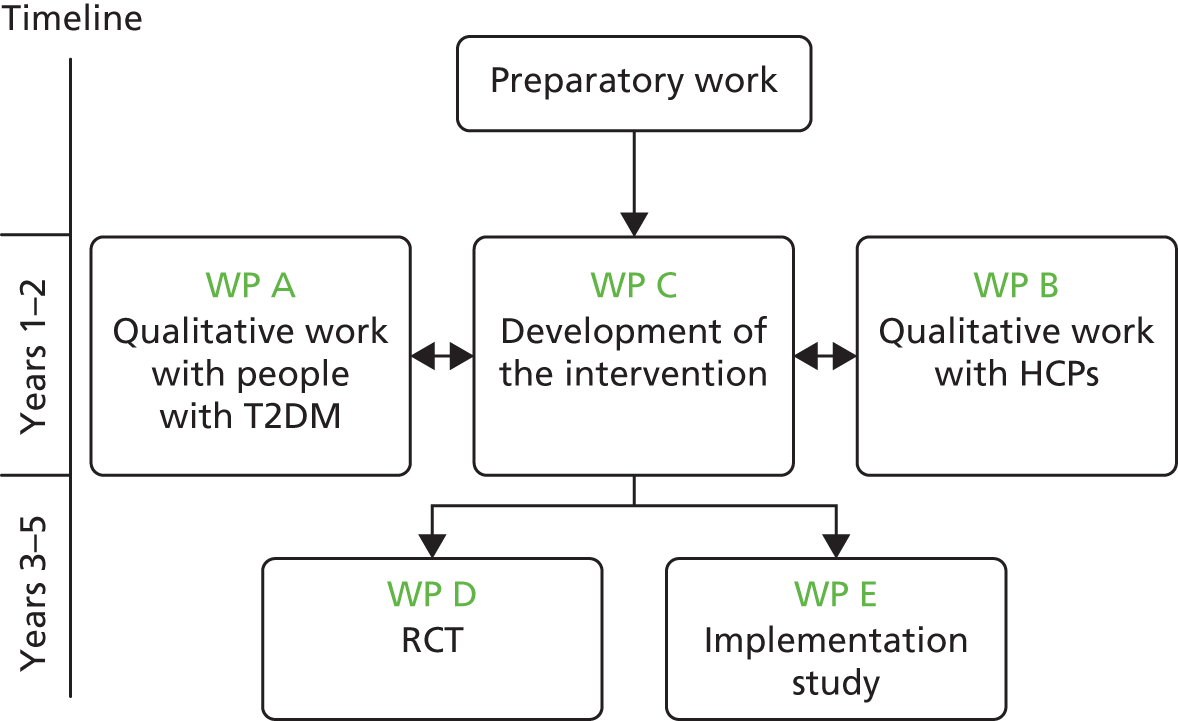
This chapter summarises the contents of the subsequent chapters. The overall structure of the programme of research is presented in Figure 1.
FIGURE 1.
Structure of overall programme with constituent work packages. HCP, health-care professional; RCT, randomised controlled trial; WP, work package.
Summary of Chapter 2: rationale and background
Chapter 2 outlines the rationale for the programme of work, explains why diabetes mellitus is a priority area for the NHS and explores the importance of good self-management in improving health outcomes in people with diabetes mellitus and the problems with current service provision. It suggests reasons why a web-based self-management programme could help address some of these problems and sets out the challenges identified during the planning stage and our approach to these challenges.
As theoretical underpinning is associated with clinical effectiveness in web-based programmes, we had a strong theoretical framework, which is outlined in Chapter 2. Inevitably, there were substantial contextual changes during the 5-year programme of research and these had a considerable impact on the research. These contextual changes are described at the end of this chapter.
Summary of Chapter 3: aims, objectives and additional work undertaken
Chapter 3 describes the aims and objectives of the programme grant and outlines the methods used to address each objective. We were fortunate to be able to undertake a number of studies additional to those originally planned and these are also outlined in this chapter.
Summary of Chapter 4: what do people with type 2 diabetes mellitus want and need from a web-based self-management programme?
Chapter 4 reports on a qualitative study that aimed to determine patient perspectives of the essential and desirable features of a web-based self-management programme for people with type 2 diabetes mellitus (T2DM), including features that would encourage use, such as access to their electronic medical record (EMR) and facilitation by health-care professionals (HCPs).
Summary of Chapter 5: what requirements do health-care professionals have of a web-based self-management programme for people with type 2 diabetes mellitus?
Chapter 5 reports on a qualitative study that aimed to determine the perspectives of HCPs of the essential and desirable features of a web-based self-management programme for people with T2DM and what could be done to encourage uptake and use in the NHS. Additional objectives were to explore HCPs’ views on the type and quantity of facilitation that could be provided in general practice and on patient access to part or all of their EMR.
Summary of Chapter 6: the Healthy Living for People with type 2 Diabetes programme: a web-based self-management programme for people with type 2 diabetes mellitus
Chapter 6 describes the process of developing the Healthy Living for People with type 2 Diabetes (HeLP-Diabetes) programme, including determining and creating the content and functionality. The process was iterative and involved a large multidisciplinary team, with extensive user input through participatory design. We then describe the intervention, procedures for maintaining and updating the intervention and techniques for promoting engagement.
Summary of Chapter 7: randomised controlled trial of the Healthy Living for People with type 2 Diabetes programme
Chapter 7 describes the design and results of a multicentre individually randomised controlled trial in primary care to determine the clinical effectiveness of the HeLP-Diabetes programme.
Summary of Chapter 8: health economic analysis
Chapter 8 presents the within-trial health economic analysis of the HeLP-Diabetes programme.
Summary of Chapter 9: design and evaluation of a plan for implementing the Healthy Living for People with type 2 Diabetes programme into routine NHS care
Chapter 9 describes the design and evaluation of a plan for implementing the HeLP-Diabetes programme into routine care. The aim of this work was to determine how best to integrate an eHealth intervention for patients into routine care, using the HeLP-Diabetes programme as an example.
Specific objectives were to design an implementation plan, evaluate its clinical effectiveness and any reasons for observed variation in implementation and modify the original plan in the light of these emerging data. We were interested in maximising uptake and use by people with T2DM, in exploring ways of overcoming the ‘digital divide’ and the impact that the intervention had on patient outcomes outside a trial.
Summary of Chapter 10: discussion
Chapter 10 summarises the overall findings of the programme of work, considers the strengths and limitations of the work done and the implications for practice, policy and research.
Chapter 2 Rationale and background
Chapter summary
This chapter outlines the rationale for the programme of work, explains why diabetes mellitus is a priority area for the NHS and explores the importance of good self-management in improving health outcomes in people with diabetes mellitus and the problems with current service provision. It suggests reasons why a web-based self-management programme could help address some of these problems and sets out challenges identified during the planning stage and our approach to these challenges.
As theoretical underpinning is associated with effectiveness in web-based programmes, we had a strong theoretical framework, which is outlined here. From its conception, this programme of work was planned and executed with substantial input from people with T2DM, who acted as research partners. This input (also called patient and public involvement; PPI) is summarised in this chapter. Inevitably, there were significant contextual changes during the 5-year programme of research, and these had considerable impact on the research. These contextual changes are described at the end of the chapter.
Diabetes mellitus: a health service priority
In the UK, diabetes mellitus is a NHS priority, affecting around 6% of the population, about 4 million people in the UK,1 of whom around 90% have T2DM. Diabetes mellitus is also a global health priority. Current estimates suggest that there are over 400 million people living with T2DM across the world, with a prevalence of 8.3% in adults aged 20–79 years; numbers are rising and by 2035 there may be 600 million people living with this condition. 2,3
Diabetes mellitus can cause significant morbidity and mortality: complications include cardiovascular disease (leading to heart attack and stroke), peripheral vascular disease (leading to leg ulcers, infection and amputation), nephropathy, retinopathy and neuropathy. People with T2DM are at increased risk of mental health problems, with nearly double the prevalence of depression compared with those without diabetes mellitus (19.1% vs. 10.7%)4 and 25% higher risk of anxiety. 5 There is also a high prevalence of diabetes mellitus-related distress, defined as ‘the concerns and worries about diabetes and its management’. 6 Surveys of populations who have diabetes mellitus have reported rates of diabetes mellitus-related distress of 45%. This matters not only because high levels of distress have an adverse effect on quality of life, but also because high levels of distress are associated with poor diabetes control and increased rates of complications.
Overall, diabetes mellitus has a significant negative impact on life expectancy, reducing it by anything from 3.3. to 18.7 years. 7
There are substantial health-care costs associated with diabetes mellitus, both for health-care systems and for individuals. Around 10% of the NHS budget is estimated to be spent on managing diabetes mellitus and its complications. 8 In 2010, direct costs of diabetes mellitus in the UK were estimated at £13.8B annually. 9 By far the largest proportion of direct health-care costs are as a result of inpatient treatment of complications. 10,11 Overall, health-care costs related to diabetes care are rising because of a combination of increasing prevalence, increased costs of drugs used to treat diabetes mellitus and increased numbers of consultations. 12
Diabetes mellitus self-management education
The Wanless13 report of 2002 argued that two factors were critical to improving health outcomes and containing health-care costs: (1) a population actively engaged in self-care of their health and (2) a responsive health service with high rates of technology uptake. This report reflected and triggered considerable interest in self-management interventions, defined as ‘primarily designed to develop the abilities of patients to undertake management of health conditions through education, training and support to develop patient knowledge, skills or psychological and social resources’. 14
In the field of diabetes mellitus, landmark trials such as the Diabetes Education and Self-Management for Ongoing and Newly Diagnosed (DESMOND) trial15 and the X-PERT programme16 suggested that educating patients about their diabetes mellitus and helping them improve self-management skills could improve glycaemic control, at least in the short term. 17,18 Early studies suggested that the risk of developing complications could be reduced fourfold by appropriate diabetes mellitus self-management education (DSME). 19
Providing people with diabetes mellitus with access to structured DSME at diagnosis, with annual reinforcement thereafter, was thus incorporated into national guidelines. 20 The National Institute for Health and Care Excellence (NICE) included structured education in the clinical guideline for T2DM in 200921 and in the quality standard for diabetes mellitus in adults in 2011. 22 However, uptake remained low, with data from the National Diabetes Audit suggesting that only 7.6% of people with diabetes mellitus reported being offered structured education in 2009–10 and 10.3% in 2010–11,23 with even fewer attending.
Reasons for this low uptake were thought to include provider difficulties in implementing and resourcing high-quality education programmes and patient difficulties in attending the available programmes. 24,25 The dominant model for self-management education is group-based education, usually offered over 1 full day or 2 half-days. Attending groups may be difficult for people who work, have family or caring commitments or simply do not like group-based formats. Moreover, patient needs evolve with time, for example as changes are made to their medication (such as higher doses or additional or different drugs) or as they develop complications. These events are likely to bring new information needs and may be associated with further emotional distress.
Potential benefits of web-based diabetes mellitus self-management education
The web appeared to have considerable potential to improve access to, and uptake of, DSME. Internet access in the UK in 2011 was 73%,26 having increased year-on-year with an expectation of continued growth; indeed, latest estimates suggest that 86% of households had internet access in 2015. 27
Computer and web-based interventions were known to have specific advantages, including convenience (accessible at any time), anonymity (important to people with a stigmatised condition such as T2DM) and easy updating. A particular potential benefit appeared to be the ability to provide the entire range of support needed for a person’s illness journey, since diagnosis to end-stage disease. Good design could ensure that users accessed only the information and services needed at that time but, as needs evolved, they could find resources to match. The processing power and connectivity of desktop, laptop or handheld computers and smartphones allowed for interactive, tailored interventions that could respond to data entered by users with personalised information and advice. Such interventions could provide support for behaviour change,28–31 improve mental health and emotional distress32–35 and offer peer support. 36 There was evidence to support their use in long-term conditions (LTCs),37 including in diabetes mellitus,38 asthma39 and hypertension. 40
Potential pitfalls of web-based diabetes mellitus self-management education
Even at the time that this grant was conceived (i.e. 2009–10), it was clear that the potential benefits of web-based self-management interventions were hard to achieve and that there were a number of pitfalls. Challenges that were particularly evident were:
-
very variable clinical effectiveness between different interventions, with no real understanding of the causes for this43,44
-
significant problems with implementation of digital interventions, with, at that time, almost no examples of their successful integration into routine health care45
-
the digital divide – the divide between those who did and did not use digital technologies. 46
This programme of work was undertaken with these challenges in mind. The process of developing the self-management programme was designed to optimise uptake and use, while maximising the likelihood of clinical effectiveness and future implementation into routine NHS services.
Addressing the challenges
Low uptake and usage
We tackled the problem of low uptake and low usage in several ways. First, we followed the principles of participatory design and heavily involved members of the target user population in the development of the intervention. The aim of participatory design is to ensure that the intervention meets user requirements and is appealing and easy to use.
As the intervention was designed to be used by people with T2DM, in partnership with their HCPs, we defined the target population as people with T2DM and the HCPs with responsibility for them, including general practitioners (GPs), practice nurses, specialist diabetes nurses, consultants in diabetes medicine and dietitians.
This involvement was a three-stage process: (1) we undertook qualitative work with the patients and HCPs to identify the ‘wants and needs’ for such a programme; (2) we recruited patients and professionals to contribute on an ongoing basis to the intervention’s development, including seeking input on decisions for content, look and feel, tone, navigation and functionality; and (3) we undertook user testing of the intervention, asking patients and HCPs to review the programme and identify errors in content, bugs or glitches in functionality and problems with design or navigation. This process is described in detail in Chapters 4–6.
Second, we thought that uptake and use would be enhanced by ensuring that the self-management programme was integrated into people’s routine health care and seen by patients and HCPs as an integral part of the total care package. Previous data have shown that patient-centred clinician communication improves diabetes mellitus self-management behaviours. 47,48 Educational and self-help programmes that are actively supported by clinicians can improve health outcomes for people with LTCs,49 and in people with low health literacy the impact that written material has is increased by verbal recommendations from the HCP. 50 Thus, we conceived of the intervention as a web-based programme together with interactions between HCPs and patients around the programme (Figure 2).
FIGURE 2.
The intervention: not just a computer program.
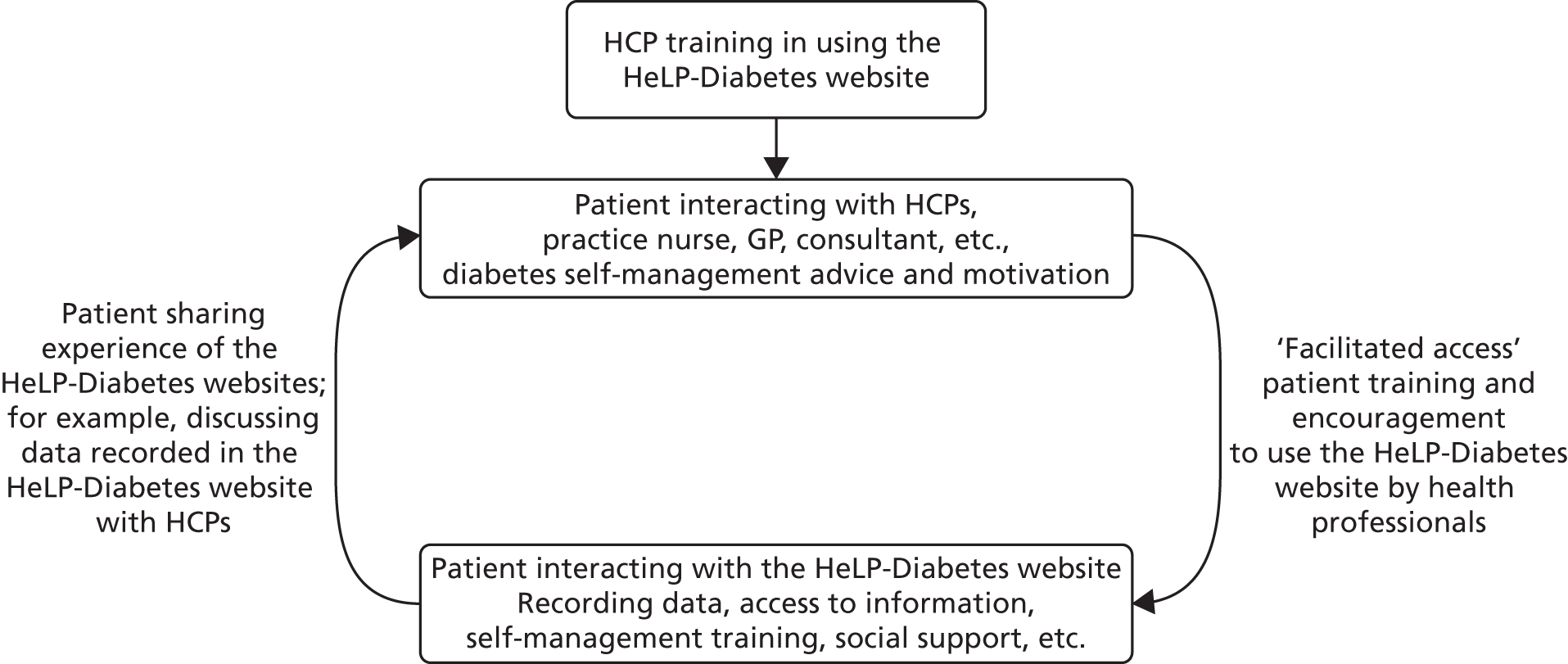
We thought there were at least three ways that HCPs could promote the programme to patients: first, by introducing them to the programme, explaining how it could help them with managing their diabetes mellitus and achieve better health status and quality of life and providing some initial training. Second, we thought that telephone calls would help to encourage the uptake and use of our self-management programme, particularly when patients were new to it and might need a bit of encouragement or help. This was based on experience from the Improving Access to Psychological Therapies programme, which facilitated access to computerised cognitive–behavioural therapy (CBT) through graduate mental health workers who first introduced patients to specific computerised CBT programmes and then telephoned them regularly to encourage adherence to the programme. Third, we hoped that HCPs would refer to our self-management programme in consultations, for example when discussing care plans with patients, or by reviewing any self-monitoring data the patient had entered into the programme.
One inference of this approach of integrating our programme into routine health care was that some linkage between the self-management programme and the patient’s EMR would be useful, and such a linkage formed part of our original grant application.
Variable effectiveness and problems with implementation
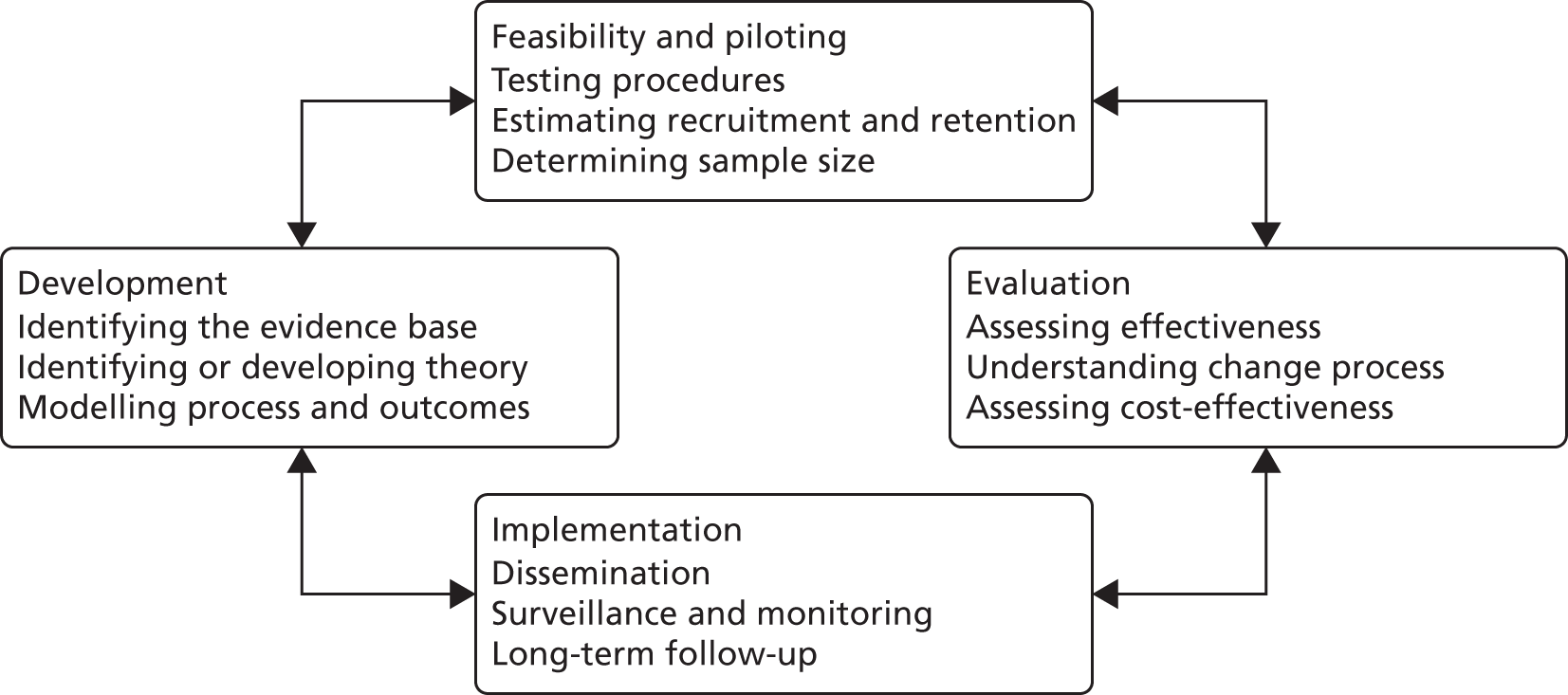
At the time we wrote the grant and developed the intervention, relatively few data existed to explain why some web-based interventions were effective and others were not. 43,44 What few data existed supported the expectation that interventions that were based on theory were more likely to work than those that were not. In the light of this, and following Medical Research Council (MRC)’s guidance for development of complex interventions (Figure 3),51–53 we adopted a strong theoretical framework to guide the development of the intervention. We also followed best practice in using theory to guide us in considering implementation from the outset, aiming to ensure that the intervention was maximally ‘implementable’ and would fit easily into existing NHS structures and workflows.
FIGURE 3.
The MRC framework. 51 Reproduced from Developing and evaluating complex interventions: the new Medical Research Council guidance, Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, Medical Research Council Guidance, 337, a1655,51 Copyright © 2008, with permission from BMJ Publishing Group Limited.
We used three theoretical frameworks or approaches to guide us:
-
Corbin and Strauss’ model54 of the work of managing a LTC
-
Abraham and Michie’s taxonomy of behaviour change techniques (BCTs)55
-
normalisation process theory (NPT). 56
We worked within the paradigm of evidence-based medicine, identifying and applying the best-available evidence for treatment of diabetes mellitus and for any decisions made during development (e.g. around maximising acceptability, uptake, usage and clinical effectiveness).
Corbin and Strauss’ model for managing a long-term condition
In their seminal work Unending Work and Care, published in 1988, Corbin and Strauss54 conceptualised the work of living with a LTC as comprising three tasks: medical management, role management and emotional management. Medical management consists of adopting healthy behaviours (e.g. not smoking, exercising regularly, eating healthy food), working with health professionals (e.g. keeping appointments and following instructions) and taking medicines. Emotional management entails addressing the powerful negative emotions associated with being diagnosed with a LTC, such as anger, guilt, shame and despair. Role management requires coming to terms with the disruption of one’s biographical narrative and sense of self,57 including adjusting to the ‘patient’ role and managing the impact that one’s diagnosis has on relationships with friends, family and colleagues. This conceptualisation was used to create a map of the overall content required in the self-management programme.
Abraham and Michie’s taxonomy of behaviour change techniques
The Corbin and Strauss model and conventional diabetes education curricula both stress the need for behaviour change as part of self-management. For people with T2DM, the key target behaviours are to stop smoking (for smokers), improve their diet, increase physical activity, moderate alcohol consumption and take medicines.
There are a plethora of psychological theories predicting behaviour, many of which include overlapping concepts. 58 Rather than opt for one specific theory, and because we were more interested in changing behaviour than predicting it, we adopted the Abraham and Michie taxonomy of BCT. 55 This taxonomy identified techniques used to change behaviour and there is a growing body of evidence around which techniques are effective. 59–61 One advantage of this taxonomy was that it allowed for those components that were likely to lead to the desired behaviour changes to be implemented elsewhere. 62
Normalisation process theory
The NPT56 is a mid-range sociological theory that explains why interventions do or do not ‘normalise’, that is become integrated into routine practice. It focuses on the work of implementation, integration and embedding new practices, ways of working or other interventions. It has four main constructs: coherence, cognitive participation, collective action and reflexive monitoring (Figure 4).
FIGURE 4.
Normalisation process theory.
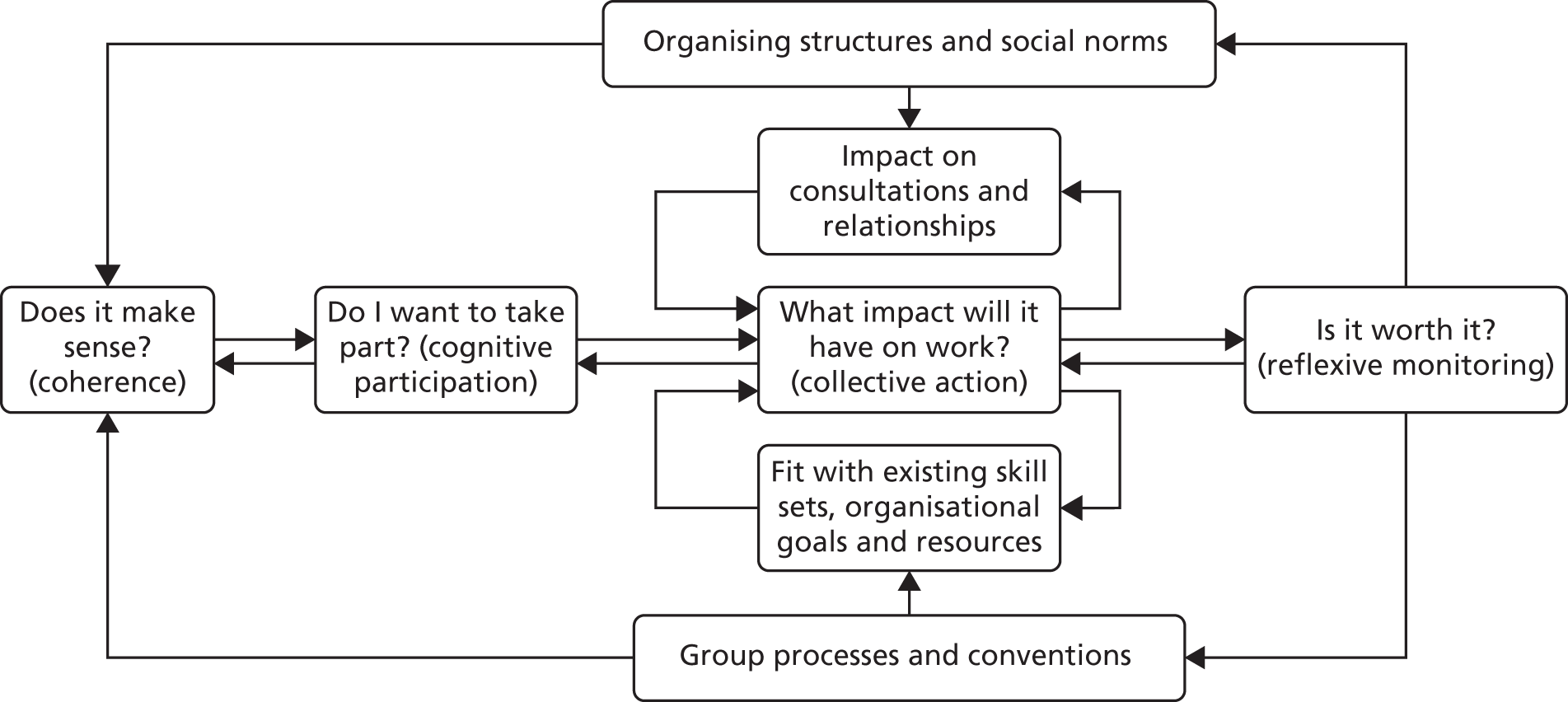
Coherence refers to the ease with which the intervention can be described, understood and distinguished from other interventions or practices. This construct also includes an understanding of the problem that the intervention is designed to address, how the intervention could benefit its target population and what work will be needed for these potential benefits to be realised. Cognitive participation is about the decision whether or not to participate in the intervention. This will include an assessment of the relative benefits of participation (to patients, professionals or the health-care system) weighed against the costs of participation, in particular the expected impact on workload. Collective action is about the impact that the intervention has on the work undertaken by professionals within the organisation and reflexive monitoring is the process of considering whether or not the benefits of the intervention are worth the effort required to implement it. Within this construct is the possibility of altering or adapting the intervention to make it easier to implement in any given setting or organisation.
In turn, collective action has four subsidiary constructs: interactional workability, relational integration, skillset workability and contextual integration. Interactional workability refers to the degree to which the intervention facilitates or impedes the work of professional–patient interactions (consultations). Relational integration is the degree to which the intervention promotes or hinders good communication and relationships between different professional groups, including the degree to which accountability and responsibility are aligned. Skillset workability refers to the degree to which the intervention fits with existing skillsets or roles and the amount of training required to use the intervention. Finally, contextual integration is about the degree to which the intervention fits with existing policies, priorities and practices within the organisation.
The NPT56 predicts that interventions that improve consultations, promote good relationships between professionals, with accountability and responsibility well aligned, that need little training and that fit well with organisational priorities are more likely to normalise than those that do not.
Applying NPT to the development process meant that we were mindful of the following needs for the final self-management programme:
-
it should be easily described, easy to differentiate from other programmes and have clear benefits
-
it should fit with organisational and professional priorities, including enabling people with T2DM to self-manage care, reducing demand on professional time, adhering to NICE guidance and being accessible to a wide range of people
-
it should fit easily into existing working practices and be compatible with existing technology
-
it should make consultations between HCPs and patients easier and more productive and should be very easy to use.
Further details about how we applied NPT to the development of the intervention, and how NPT informed our implementation strategy, can be found in Chapters 5, 6 and 8.
Evidence-based medicine
We applied the paradigm of evidence-based medicine in two ways: first, we ensured that all the information, guidance and advice for patients in the intervention was evidence based and compatible with NICE, or other, national guidelines. Second, we applied the best-available evidence to the whole process of intervention development, drawing on data on best practice from computer science, eHealth, biomedical, health education and health services research.
The digital divide
The term ‘digital divide’ refers to the gap between those who do and do not have access to, or make use of, information and communication technologies. 46 At the time that this grant started (i.e. 2011), there were marked inequalities in internet access, with age, income, educational status and health status all being associated with access. Figures from the 2011 Oxford Internet Institute survey26 showed that, although about 85% of people who were at prime working age (25–55 years) used the internet regularly, only 33% of those aged ≥ 65 years did. Some 99% of households with total annual household income of ≥ £40,000 had internet access, but only 43% of households with an annual income of ≤ £12,500 did. Internet use was around 95% among people with degree-level education, but only 54% in those with a basic or secondary school education. The level of internet use in people with a disability was 41%; however, among people without a disability it was 78%. 26
There was evidence that the digital divide could be overcome with appropriate infrastructure, resources, training and design of interventions. Infrastructure requirements included provision of access to the internet, and the UK has benefited from a policy environment that promoted universal access. For example, most public libraries provide up to 1 hour per day per user of free access to an online computer and many local authorities fund community cluster rooms with associated training opportunities. 63 Provision of appropriate resources and training has been shown to enable diverse disadvantaged populations to make meaningful use of internet resources, including homeless drug users,64 vulnerable elderly people,65 parents of children attending early learning centres66 and people with cardiovascular disease67 or human immunodeficiency virus (HIV) infection or acquired immune deficiency syndrome (AIDS)68 from underserved communities.
We took a multipronged approach to attempting to narrow the digital divide and to ensure that our proposed intervention would be used by people from diverse socioeconomic backgrounds. We thought that people would be more likely to use the programme if it were recommended by trusted HCPs and integrated into routine care. Our previous research had shown that even short training sessions could enable some people who were not used to using computers to be able to use well-designed web-based interventions,69 although some people needed ongoing support. We thought that ongoing engagement would be promoted by HCPs referring to the programme in their consultations with the patient. Finally, we aimed to ensure that the intervention could be easily used by people with low literacy or computer literacy skills, by aiming for intuitive navigation, having liberal use of graphics, using text written for a reading age of 12 years and ensuring that key information was provided in video format, as well as text.
Patient and public involvement
The entire programme of research had very strong PPI input. At the initial development of the grant application, a named PPI co-investigator and two named PPI collaborators were recruited. These PPI members were equal partners in the research team and contributed equally to the decisions made during the programme. All three were members of the overall steering group for the programme. In common with our other co-investigators and collaborators, circumstances changed for some of these key PPI members, leading to their resignation from the programme. In each case, they were replaced. In addition to the overall steering group, each individual work package (WP) had a project management group. Each project management group had at least one, and usually two, PPI members who contributed to the oversight and conduct of the project on an equal footing with the other members of the management group. There was PPI membership of both the trial management group and the trial steering committee. As members of the project and trial management groups and the trial and overall steering committees, PPI members contributed to discussions on recruitment, data collection, data analysis and interpretation of the data and to dissemination. All recruitment and participant-facing materials were designed in collaboration with our PPI members and were revised in accordance with their input. Our PPI collaborators are listed in the Acknowledgements. They were recruited through advertisements and publicity in diabetes networks and interested applicants were sent job descriptions and person specifications. We held interviews with applicants to clarify what was required, select appropriate candidates and match successful applicants to available roles. This process was repeated at various points during the programme, as individual PPI members left or moved on. For the development of the intervention, we recruited a much larger group of PPI. This is described in detail in Chapter 6.
Context changes since grant awarded
Health and Social Care Act 2012
There were a number of significant changes in context between the time that funding for our programme of research was confirmed (in 2010) and its completion (in 2016). By far the biggest of these was the Health and Social Care Act 2012,70 which was described as the ‘biggest single reorganisation’71 and the ‘longest and most complex piece of legislation’ in the history of the NHS. 72
Among its many components was the abolition of primary care trusts (PCTs) and strategic health authorities, which had been responsible for commissioning services. PCTs were replaced by clinical commissioning groups (CCGs), which were intended to control around 60% of the NHS budget, be led by GPs supported by other clinicians and managers and were tasked with meeting the needs of their populations.
This reorganisation resulted in huge workloads for those involved as they struggled to come to terms with new priorities and responsibilities, evolving structures and changes in personnel. This was often accompanied by uncertainty about roles and responsibilities, loss of existing staff with relevant expertise and loss of organisational memory. 73–75
This massive reorganisation occurred at the same time as the NHS entered a period of significant financial austerity. After a period of year-on-year growth in budget, the NHS was charged with making financial savings of £20B over 5 years from 2011–15 while maintaining (or improving) the quality of the service. 76 This required efficiency savings of around 4% per year, compared with maximum previous efficiency savings of around 2% per year. It was recognised that meeting this ‘unprecedented challenge’ would require new ways of working, with an emphasis on reducing hospital admissions for people with LTCs, as well as there being a pay freeze for NHS staff. 76
Not entirely coincidentally, English general practice was, at the same time, entering a period of ‘crisis’,77 with a rapidly rising workload because of increased numbers and complexity of consultations but no concomitant rise in HCP numbers and static or falling incomes. 78,79 As a result, general practices were under enormous pressure. Many were unable to fill vacant clinical posts (both doctors and nurses were hard to recruit), leading to excessive workloads for remaining clinicians. 80 This was reflected in long waiting times for appointments and many GPs reporting low morale, burn out and resistance to change. 80 Although some practices showed considerable resilience, others went into a spiral of decline. 77
This turbulent background had a considerable impact on our research, particularly when it came to implementing the self-management programme into routine care (see Chapter 9).
Closure of the Medical Research Council’s General Practice Research Framework
Our original application included an individually randomised controlled trial of the intervention to be run in primary care. At the time the proposal was submitted, we had a close collaboration with the MRC’s General Practice Research Framework (GPRF) and had designed the trial with the resources and expertise of the GPRF in mind. GPRF practices had trained research nurses available to participate in studies and, therefore, we designed a study that was predicated on unblinded practice nurses undertaking clinical tasks and delivery of the intervention and blinded research nurses undertaking research tasks, including data collection.
However, in 2012, the GPRF was subsumed into the wider National Institute for Health Research (NIHR)’s Primary Care Research Network (PCRN). The PCRN operated a different model of supporting primary care research, with resources focused on promoting recruitment. Most PCRN hubs did not have the resources available to support data collection. This had quite an impact on the feasibility of the trial and, although in the end we were able to recruit sufficient practices and exceed our planned sample size, there were a number of challenges en route that required us to show agility and adaptability (see Chapter 7).
Changes to the Quality and Outcomes Framework
In 2013, the Quality and Outcomes Framework (QOF) was changed to include an incentive for GPs to refer people newly diagnosed with diabetes mellitus to structured education within 9 months of diagnosis. This had an immediate impact on referral rates, which rose from 15% in 2012 to 75% in 2014. Our programme was not designed as ‘structured education’ for newly diagnosed people, but rather as ongoing self-management support for people throughout their illness journey. This mismatch between policy and our intervention affected our research and required us to adapt some of our original ideas. In particular, it led us to develop an additional structured component to our intervention, aimed at newly diagnosed people (see Chapter 3).
Chapter 3 Aims, objectives and additional work undertaken
Chapter summary
This chapter describes the aims and objectives of the programme grant and outlines the methods used to address each objective. We were fortunate to be able to undertake a number of studies that were in addition to those originally planned, and these are also outlined in this chapter.
Aims and objectives
The overall aim of this programme grant was to develop, evaluate and implement a web-based self-management programme for people with T2DM (at any stage of their illness journey), with the goal of improving access to, and uptake of, self-management support and, hence, improve health outcomes in a cost-effective manner. Particular attention was paid to working with users (patients and HCPs) to identify and meet user ‘wants and needs’, overcoming the digital divide and ensuring ‘implementability’.
Specific objectives were grouped under the headings Development, Evaluation and Implementation.
Development
-
Determine patients’ perspectives of the essential and desirable features of the intervention (wants and needs).
-
Determine HCPs’ perspectives of the essential and desirable features of the intervention that would encourage uptake and use in the NHS.
-
Determine the overall content and function of the intervention.
-
Determine the optimal facilitation required to encourage use of the intervention.
-
Determine feasibility, acceptability and short-term effects of facilitated access to the intervention in a naive population.
Evaluation
-
Determine the effect of the intervention on clinical outcomes and health-related quality of life (HRQoL) in people with T2DM.
-
Determine the incremental cost-effectiveness of the intervention compared with usual care from the perspectives of health and personal social services and wider public sector resources.
Implementation
-
Implement the intervention in two PCTs (later redesignated as CCGs).
-
Determine the uptake, use and effects of the intervention in an unselected population in routine care.
-
Determine factors that inhibit or facilitate integration into existing services and use of the intervention.
-
Determine the resources needed for effective implementation.
Methods
The programme grant application described five WPs that together addressed all 11 objectives. Table 1 shows how each WP related to the objectives.
| WP | Objectives | Design | Output |
|---|---|---|---|
| A | 1. Determine patient wants and needs | Qualitative study, using focus groups and individual interviews with a diverse range of people with T2DM | Understanding of patients’ wants and needs from such an intervention, illustrated with examples of good and bad practice |
| 4. Determine optimal facilitation to encourage use of intervention | Information on why, when and how people thought they would use such an intervention, and what would encourage them to use it | ||
| B | 2. Determine HCPs’ perspectives of essential and desirable features | Qualitative study, using focus groups and individual interviews with HCPs who are caring for people with T2DM in primary and secondary care | Understanding of content that HCPs want to see, benefits and problems that they foresee and how they envisaged using it in routine practice |
| 4. Determine optimal facilitation to encourage use of intervention | Information on what degree of facilitation or support that GPs thought would be feasible to offer routinely in primary care | ||
| C | 3. Determine the content and function of intervention | Participatory design, working with the research team, people with T2DM, HCPs, software engineers and web designers to determine and create content, navigation and functionality including usability testing and piloting. All decisions were underpinned by theory and evidence | An acceptable, comprehensive and comprehensible self-management programme called the HeLP-Diabetes programme |
| 5. Determine the feasibility, acceptability and effects of intervention | |||
| D | 6. Determine the effect of the intervention on patients | Individually randomised controlled trial in primary care | Data on the impact of the HeLP-Diabetes programme on diabetes control (as measured using HbA1c levels), diabetes mellitus-related distress (as measured using the PAID scale), QALYs and service use |
| 7. Determine cost-effectiveness | |||
| E | 8. Implement the HeLP-Diabetes programme in two PCTsa | Mixed-methods implementation study | Data on adoption, uptake and use of the HeLP-Diabetes programme by CCGs,a practices and patients |
| 9. Determine uptake | Data on the impact that the HeLP-Diabetes programme has on people with T2DM outside the trial setting | ||
| 10. Determine inhibiting or facilitating factors | Data on the costs and resources required for different models of implementation and associated advantages and disadvantages | ||
| 11. Determine the resources needed for effective implementation |
The first 2 years of the grant (March 2011–February 2013) were dedicated to developing the self-management programme. This work was divided into three WPs: WP A focused on ascertaining patients’ wants and needs for the programme, WP B on identifying HCPs’ wants and needs and WP C on the design and development of the self-management programme itself, which was called the HeLP-Diabetes programme.
The last 3 years of the grant focused on evaluation and implementation, with two WPs running in parallel: WP D was an individually randomised controlled trial in primary care and WP E was an implementation study in two CCGs. Both of these studies started on time in March 2013. WP E was completed on time, but delays in recruitment for the trial (WP D) led to a request for a 6-month no-cost extension. With this extension, we were able to recruit the required sample size, complete the 12-month follow-up, and analyse and disseminate the results.
Additional studies undertaken
Some of the (many) advantages of having a programme grant were the financial stability and duration of funding. This allowed for long-term planning and enabled the core University College London (UCL) team to attract a number of additional students and fellows who worked alongside them, contributing to the main body of work and undertaking additional projects. These additional studies are outlined in the following text and included:
-
the development and formative evaluation of a cardiovascular risk calculator for people with T2DM
-
an evaluation of the impact that the HeLP-Diabetes programme had on the psychological well-being of patients with T2DM: a mixed-methods cohort study
-
a systematic review of technological prompts to improve engagement with digital health interventions
-
two RCTs81 of the use of e-mail and text messages to improve engagement with the HeLP-Diabetes programme
-
a systematic review82 of the implementation of eHealth interventions: an update of a review of reviews
-
the development and formative evaluation of a structured education programme for newly diagnosed patients with T2DM: the HeLP-Diabetes programme – Starting Out
-
the development of a digital T2DM prevention programme: HeLP Stop Diabetes.
In addition, the overall programme of work generated three Doctors of Philosophy (PhDs) and one Doctor in Clinical Psychology. One PhD was undertaken by co-investigator Dr Kingshuk Pal, an academic GP. His PhD focused on the development of the HeLP-Diabetes programme; his thesis was submitted in 2016 and he passed his viva with minor corrections. The second was undertaken by Jamie Ross. Her thesis was based on the implementation study in WP E and she successfully submitted and passed her viva with minor corrections in 2016. The third was undertaken by Ghadah Alkhaldi, whose PhD studentship was funded by the Saudi Arabian Cultural Bureau. Her thesis focused on the promotion of user engagement with digital health interventions, using the HeLP-Diabetes programme as an example. Her thesis was also submitted in 2016 and she too passed her viva with minor corrections. The doctorate in clinical psychology was undertaken by Megan Hoffman and her doctorate was awarded in 2014. The empirical part of the doctorate explored the impact that the HeLP-Diabetes programme had on the emotional well-being in people with T2DM.
The development and formative evaluation of a cardiovascular risk calculator for people with type 2 diabetes mellitus83
Dates: 2012–13.
Lead: Dr Tom Nolan (GP academic registrar).
Collaborators (additional to programme grant co-investigators and UCL team): Professor David Spiegelhalter (Winton Professor of Public Understanding of Risk, Statistical Laboratory, Centre for Mathematical Sciences, University of Cambridge) and Mike Pearson (Statistical Laboratory, Centre for Mathematical Sciences, University of Cambridge).
Additional funding: none.
Background
As part of our overall goal of enabling people with T2DM to understand the risks of diabetes mellitus and the benefits of self-management and medication, we thought it helpful to develop a risk calculator for people with T2DM and explore its effects on their understanding of their personal risk and the impact that this had on their motivation to manage their diabetes mellitus.
The calculator would provide users with an easily understandable presentation of their personal risk, along with estimates of how this risk could be reduced, for example by stopping smoking, losing weight, becoming more active or taking medication. The underlying intention was to motivate users with the thought that it might also help them to prioritise one particular behaviour (e.g. taking prescribed medication or becoming more active).
As Winton Professor of Public Understanding of Risk, David Spiegelhalter had tremendous expertise in presenting risk in a comprehensible format, as well as an interest in exploring the impact that such risk presentation has. Together with Mike Pearson, he had recently developed a cardiovascular risk calculator for people without diabetes mellitus, and was interested in collaborating with us to develop a similar calculator for people with T2DM.
Method
There were three components to this study:
-
Developing the risk estimates, based on the UK Prospective Diabetes Study data. Michael Sweeting, the grant statistician, undertook this, by adapting methods developed by David Spiegelhalter. We worked with T2DM patients to identify which potential risk factors were of most interest to users.
-
Transferring the algorithms and risk estimates into an online risk calculator, which captured data entered by users and used this to provide personalised estimates of risk. The authors followed best practice, according to the literature, in how these risk estimates were presented and worked with users to optimise navigation and usability.
-
Undertaking qualitative evaluation with users to explore understanding and impact of the risk information.
Outcome
Despite following accepted best practice and making every effort to ensure that the information presented was readily comprehensible, our evaluation showed that users struggled to understand their personal risk. Moreover, even when personal risk was understood, user reactions were complex and, overall, were unlikely to lead to desired changes in behaviour. In the light of this, the risk calculator was not included in the final HeLP-Diabetes programme intervention.
An evaluation of the impact that the Healthy Living for People with type 2 Diabetes programme had on the psychological well-being of patients with type 2 diabetes mellitus: a mixed-methods cohort study84
Dates: 2012–14.
Lead: Megan Hoffman (Doctor of Clinical Psychology student). The doctorate was awarded in 2014.
Collaborator (additional to programme grant co-investigators and UCL team): Professor Chris Barker (Professor of Clinical Psychology, Department of Clinical, Educational and Health Psychology, UCL).
Additional funding: none.
Background
Megan Hoffman was a student on the doctoral clinical psychology course at UCL. She was interested in the psychological well-being of people with T2DM and exploring whether or not the HeLP-Diabetes programme could improve well-being.
Method
Megan Hoffman undertook a single-arm mixed-methods study in primary care, recruiting patients with T2DM and facilitating their use of the HeLP-Diabetes programme. She collected quantitative and qualitative data at baseline and after 6 weeks. Quantitative data comprised self-completed validated outcome measures for diabetes mellitus-related distress [as measured using Problem Areas in Diabetes (PAID) scores], depression and anxiety scores [as measured using the Hospital Anxiety and Depression Scale (HADS)] and scores on the Diabetes Management Self-Efficacy Scale (DMSES). Qualitative data comprised semistructured interviews: at baseline participants were asked about their current problems with diabetes mellitus and what help they would like, and at follow-up whether or not the intervention had made any difference and which parts they had found particularly helpful or unhelpful.
Outcomes
The planned sample size (n = 19) was recruited. Participants showed a statistically significant reduction in diabetes mellitus-related distress [baseline: mean PAID score of 26.32 points, standard deviation (SD) 20.88 points; 6 weeks: mean PAID score of 20.94 points, SD 16.53 points; p = 0.04]. Qualitative data showed that, overall, participants found the intervention helpful. Negative impacts reported related to feeling guilty about non-use.
A systematic review of technological prompts to improve engagement with digital health interventions85,86
Dates: 2013–15.
Lead: Ghadah Alkhaldi (PhD student). PhD awarded in 2016.
Collaborator (additional to programme grant co-investigators and UCL team): Dr Fiona Hamilton (NIHR Lecturer in Primary Care, Research Department of Primary Care and Population Health, UCL).
Additional funding: PhD studentship funded by the Saudi Arabian Cultural Bureau.
Background
A well-recognised problem with digital interventions is the lack of engagement. Although this can be overcome by human facilitation, this increases costs and may undermine the economic arguments for digital interventions. Hence, there is an interest in exploring the extent to which automated prompts can improve engagement. Ghadah Alkhaldi joined the UCL team as a PhD student and focused her PhD on the use of automated or technological prompts to increase engagement with the HeLP-Diabetes programme. As part of this, she undertook a systematic review to determine what impact such prompts could have with engagement.
Method
Ghadah Alkhaldi used standard (Cochrane) systematic review methods, with systematic searching, double-screening of abstracts and full papers and independent checking of data extraction.
Outcomes
Technological prompts, such as e-mail and text messages, can have a small positive impact on engagement, but there were insufficient data to determine optimal content, frequency or mode of delivery of such prompts.
Two randomised controlled trials of the use of e-mail and short message services to improve engagement with the Healthy Living for People with type 2 Diabetes programme81
Dates: 2014–16.
Lead: Ghadah Alkhaldi (PhD student). PhD awarded in 2016.
Collaborator (additional to programme grant co-investigators and UCL team): Dr Fiona Hamilton (NIHR Lecturer in Primary Care, Research Department of Primary Care and Population Health, UCL).
Additional funding: PhD studentship funded by the Saudi Arabian Cultural Bureau.
Background
Following her systematic review, Ghadah Alkhaldi explored how best to use e-mail and/or text messages to improve engagement with the HeLP-Diabetes programme.
Methods
Ghadah Alkhaldi employed mixed methods, initially developing e-mail prompts and newsletters in collaboration with our user panel and then using quantitative data to identify which prompts or newsletters were associated with increased numbers of visits to the HeLP-Diabetes programme website. Subsequent ‘think-aloud’ interviews explored which features or prompts were particularly attractive or compelling. Finally, two randomised controlled trials (RCTs) were undertaken to test the hypotheses generated by the qualitative interviews.
Outcomes
Prompts and newsletters had a small positive impact on engagement, but it was not possible to identify the characteristics of effective prompts compared with ineffective ones.
A systematic review of the implementation of eHealth interventions: update of a review of reviews82
Dates: 2014–16.
Lead: Jamie Ross [research associate (RA) and PhD student], supervised by Professor Elizabeth Murray and Dr Fiona Stevenson. PhD awarded in 2016.
Collaborator (additional to programme grant co-investigators and UCL team): Rosa Lau (PhD student).
Additional funding: none.
Background
A systematic review of reviews of factors influencing implementation of eHealth interventions had been completed in 2009. A very large number of studies had since been published, including a large number of additional systematic reviews; however, most focused on specific eHealth topics or types of intervention. Therefore, the authors undertook an update of the original review of reviews.
Methods
Jamie Ross conducted a systematic review of reviews.
Outcomes
The field had moved on very considerably in the intervening years, in terms of both the quality of available reviews and the insights generated. The available data fitted well with the recently developed Consolidated Framework for Implementation Research (CFIR).
The development and formative evaluation of a structured education programme for newly diagnosed patients with type 2 diabetes: The Healthy Living for People with type 2 Diabetes programme – Starting Out (papers not yet published)
Dates: 2014–16.
Lead: Shoba Poduval (academic GP fellow).
Collaborators (additional to programme grant co-investigators and UCL team): Helen Gibson and Rebecca Owen (diabetes specialist nurses).
Additional funding: the National School of Primary Care Research funding round 9.
Background
During the implementation study (WP E), it became clear that, although both people with T2DM and HCPs appreciated the support across the whole of the illness journey provided by the HeLP-Diabetes programme, a slimmer, more structured intervention was needed for newly diagnosed people. GP incentives from the QOF were limited to referral to structured education, and referral to programmes that were accredited by the Quality Institute for Self-Management Education and Training (QISMET) was preferred. QISMET accreditation was available only to programmes with a structured curriculum and clear learning goals. In the light of this, we decided to develop a structured education programme based on the HeLP-Diabetes programme but amended for use by newly diagnosed people and augmented by e-mail and telephone support to improve uptake and completion rates.
Methods
We worked with patients and diabetes nurse educators to develop a structured education programme based on the HeLP-Diabetes programme. The structured education programme’s curriculum addressed the three core tasks identified by Corbin and Strauss54 (medical, emotional and role management) while also meeting NICE and QISMET’s guidance for the content of diabetes mellitus-structured education programmes. This was iteratively user-tested and piloted, with revisions made after each cycle of testing.
Outcomes
HeLP-Diabetes: Starting Out is a structured education programme comprising four mandatory sessions, with an optional fifth and final one. Each session contains three or four modules, with each module taking 10–15 minutes to work through. Users are encouraged to proceed through one session per week, working through as many modules as they choose at each sitting. E-mail and telephone support is provided by specialist diabetes nurse educators to promote engagement. The authors are currently seeking further funding to undertake a feasibility study and then a Phase III RCT.
The development of a digital diabetes prevention programme: HeLP Stop Diabetes (papers not yet published)
Dates: 2016–18.
Lead: Marie-Laure Morelli (academic GP trainee).
Collaborator (additional to programme grant co-investigators): Paulina Bondaronek (PhD student).
Additional funding: the National School of Primary Care Research funding round 11.
Background
With the rapid increase in prevalence of diabetes mellitus, prevention became a national priority. Initial commissioning of T2DM prevention programmes has focused on face-to-face or group-based programmes; however, these are expensive and it is unclear what the uptake will be. A digital T2DM prevention programme could offer a cost-effective alternative to group-based programmes and may improve uptake. In the light of this potential, we are undertaking preliminary work to explore the acceptability, feasibility and desirable content of a digital intervention to prevent diabetes mellitus in high-risk individuals.
Methods
We will conduct qualitative interviews and focus groups to determine user requirements for a digital T2DM prevention programme.
Outcomes
This work has been seriously delayed as a result of the reorganisation of the Health Research Authority, such that it took 10 months to obtain ethics and research governance approvals. Marie-Laure Morelli was then on maternity leave until September 2017; the work restarted on her return and is still underway.
Chapter 4 What do people with type 2 diabetes mellitus want and need from a web-based self-management programme?
Chapter summary
Chapter 4 reports on a qualitative study that aimed to determine patient perspectives of the essential and desirable features of a web-based self-management programme for people with T2DM, including features that would encourage use, such as access to their EMR and facilitation by HCPs.
We undertook focus groups with a maximum variety sample of people with T2DM. Participants in focus groups were shown three existing diabetes mellitus self-management websites, selected to illustrate a range of features, and then asked to consider what they liked or disliked about each programme, as well as what would be included in an ideal programme. A thematic analysis of these data was used to clarify the necessary and desirable content, functionality and approach of our proposed intervention. We subsequently undertook a more deliberative approach, exploring underlying experiences and the meaning ascribed to them by participants.
The four focus groups had a total of 20 participants. A strong shared sense of the overwhelming burden that the diagnosis of diabetes mellitus placed on participants underpinned all of the data generated; it had had severe negative impacts on their emotional well-being, work, social life and physical health. Although participants’ experience of health-care services varied, there was agreement that even the best services were unable to meet all users’ needs and that a web-based self-management support programme could, therefore, be extremely useful in meeting these unmet needs.
Participants had clear views about the features that they would want or need from such a programme, as well as the features that would help generate trust and encourage engagement. They also clearly identified features that would be off-putting and lead to disengagement. These views informed the development of the HeLP-Diabetes programme.
Background
The rationale for focusing on T2DM and for considering a web-based self-management programme has been described in Chapter 2. In this chapter, we describe the rationale for the study objectives and the selected methodology.
Rationale for study objectives
Establishing user requirements for any proposed intervention is a necessary first step. 87 We conceptualised these requirements as ‘wants and needs’, for which ‘wants’ are features that users actively desire and would make them want to use the intervention and ‘needs’ are features that evidence suggested would improve health outcomes.
We postulated that combining wants with needs should combine the attractiveness and appeal of many commercial digital interventions (including games) with the clinical effectiveness of face-to-face interventions. As an example, there was evidence from the literature that forums, where users could interact online, were associated with increased use of an intervention, as people wanted the opportunity to interact with others in similar situations (a ‘want’). 88 However, nothing suggested that this improved health outcomes. 89 In contrast, improving medication adherence is likely to improve health outcomes (a ‘need’), but including such a facility in an intervention is unlikely to promote engagement with, and use of, the intervention. Our goal was to understand both wants and needs with a view to creating an intervention that met both and, hence, was both useful and used.
We were also aware that patients and HCPs used different criteria for assessing web-based self-management interventions90 and that HCPs’ perceptions of patient requirements were often inaccurate. 91 For example, there is evidence that HCPs overestimate patients’ concerns about complications and underestimate their concerns about dietary restrictions. 92 Hence, we were clear that we needed separate, parallel studies to determine patients’ and HCPs’ perceptions of the essential and desirable features of such an intervention.
Previous research by Kerr et al. 90 had established some generic patient requirements for self-management interventions for LTCs. Kerr et al. 90 convened 10 focus groups with 40 patients and carers who generated detailed quality criteria relating to information content, presentation, interactive components and trustworthiness. Participants in that study stated that information needed to be detailed, specific and of practical use. They also advised that long-term use required increasing the depth of information as self-management experience increased, as well as providing new and up-to-date information. Participants wanted information about their condition and the treatments available, practicalities around day-to-day living (holidays, travel and eating out), local services and resources, new research and areas of scientific uncertainty and other people’s experiences and information for family members. They felt that it was important for users to control how much information they accessed at any time and the topic of the information. This was particularly important for ‘bad news’, which they did not want forced on them.
These criteria focused on the need for excellent website design, easy navigation giving intuitive and speedy access to relevant content and an attractive appearance, using colours, graphics, videos, animations, photographs and text broken up into small sections. The tone should be straightforward but not patronising; medical terms and jargon should be explained but not avoided. The criteria for interactive components were that they should be optional, use online assessments to provide tailored advice and monitoring and include an ‘Ask the Expert’ facility and online forum. Finally, trustworthiness was vital and could be established and maintained by information being accurate and regularly updated, the intervention having no commercial links or advertisements and the website being authored or sponsored by a known and trusted organisation, such as the NHS or a local hospital or well-known university or charity. 90
However, technology and website use had changed considerably since the above research was published. Website use had become much more interactive and peer to peer (the so-called Web 2.0). 93 Moreover, although this research had included people with T2DM, it had not specifically focused on diabetes mellitus; rather, it had looked to draw out criteria that were transferable across a range of LTCs. There were no studies in the literature that we could identify that specifically explored the wants and needs of people with T2DM for web-based self-management programmes.
As described in Chapter 2, well-recognised limitations of web-based interventions are non-use and high rates of attrition. 41 In our original grant application, we postulated that engagement with the intervention was likely to be enhanced by HCPs recommending and endorsing both initial and ongoing use. Evidence from internet cognitive–behavioural therapy (ICBT) suggested that facilitated or supported use of ICBT was more effective than unsupported use. 94 However, we also recognised that it is hard to change professional behaviour,95 and that HCP time is a scarce (and expensive) resource. Therefore, we wanted to explore with people the type of facilitation they would find useful and what they thought was realistic.
We were also specifically interested in the possibility of linking the self-management programme with patients’ EMRs. While the work for WP A was being done, there was considerable discussion about the relative advantages and disadvantages of such access. Some pilot studies had suggested that it was feasible, did not lead to excess workload or patient anxiety but did lead to correction of inaccurate data in the record, better-informed patients and more productive consultations. 96–98 However, mainstream opinion, as represented by, for example, the British Medical Association, was unconvinced, citing concerns about privacy, confidentiality, causing unnecessary anxiety among patients and about it resulting in additional workload for doctors. 99 We wanted to explore with patients what they thought about having access to their EMR and, in particular, what information they wanted to see and why. We planned to see whether or not it was possible to find a solution that addressed patients’ wants and needs while respecting clinicians’ concerns.
As an example of the changing context during our research programme, shortly after this study was completed, the Department of Health and Social Care issued new policy, mandating that all patients should have access to their EMR. 100
Rationale for study methods
Two key methodological decisions were to use focus groups for data collection, and, as part of the focus groups, to show participants three existing examples of self-management websites for people with T2DM. These decisions were based on our previous experience with this methodology,90 which had proven feasible and yielded rich data. This work was in turn based on a study by Coulter et al. ,101 which determined quality criteria for traditional paper-based information materials for users.
The use of qualitative methodology allowed participants to explore issues of importance to them, in their own words, generating their own questions and focusing on their own priorities; this was particularly important when exploring self-management and interventions to empower patients. We opted for focus groups, rather than individual interviews, as we wanted participants to explore their underlying reasons for differing perspectives. Group discussions can yield rich data when participants explore and clarify their views through interactions with each other. 102 Group dynamics also involve many different forms of day-to-day communication, such as jokes, anecdotes, teasing and arguing. These natural interactions may allow a more nuanced appreciation of what people know or experience and can reveal ‘shared truths’. 103 A disadvantage of focus groups is that some participants may find it difficult to discuss sensitive or potentially embarrassing topics, such as sexual dysfunction, which can be a common complication of diabetes mellitus. Therefore, we planned to use focus groups as our primary method of data collection, while reserving the option of individual interviews if it appeared that some topics were not being adequately addressed.
The decision to show participants three websites at the start of each focus group was based on the observation that it is much easier to critique existing interventions than to think in the abstract about what one might want. Moreover, the experience of using such interventions allowed users to think about features they looked for, even if they were not present. Our experience from our earlier work had confirmed that participants could review three websites in the time available that, with careful selection, it was possible to ensure that most of the features of interest were included in the websites presented and that there was sufficient difference between the websites to enable participants to compare and contrast them in a fashion that generated useful data. 90
Aims and objectives
The overall aim of the study was to determine patients’ perspectives of the essential and desirable features of a digital self-management intervention for adults with T2DM (i.e. T2DM-specific wants and needs regarding information content, presentation, interactive components and trustworthiness). Additional objectives were to determine the optimal facilitation required to encourage use of the intervention and to explore patient views about integrating the self-management programme with EMRs.
Data from this study contributed to the following objectives of the programme grant:
-
determine patients’ perspectives of the essential and desirable features of the intervention (wants and needs)
-
determine the overall content and function of the intervention
-
determine the optimal facilitation required to encourage use of the intervention
-
determine feasibility and acceptability of facilitated access to the intervention.
Methods
Design
The design was a qualitative study using focus groups for data collection.
Ethics
Ethics approval was provided by the North West London Local Research Ethics Committee on behalf of the National Research Ethics Service (reference number 10/H0722/86).
Setting and participants
As our goal was to develop an intervention that appealed to a wide spectrum of the total population of adults with T2DM, we aimed to recruit a diverse sample that reflected the target population, namely adults with T2DM who could understand spoken or written English. An additional inclusion criterion was the ability to speak English in order for the individual to be able to participate in the focus group. Factors that the literature suggested were likely to influence wants and needs included demographic factors (e.g. age, gender, ethnicity, first language), clinical factors (e.g. duration of diabetes mellitus since diagnosis, current treatment, presence or absence of diabetes mellitus-related complications and previous experience of self-management programmes) and factors related to health and computer literacy (such as educational attainment, previous experience with computers and access to the internet). 46,104–106 Hence, our goal was to recruit a sample that varied across these characteristics.
To achieve this, we adopted a broad recruitment strategy. We placed online advertisements on the Diabetes UK website, a local council website, a black and minority ethnic forum and other diabetes mellitus forums. In addition, we advertised in Balance magazine, which is published bimonthly by Diabetes UK and distributed freely to all Diabetes UK members. We distributed flyers, leaflets and posters through community support groups for people with T2DM, general practices and community diabetes clinics. Most responses were from local support groups and readers of Balance.
Participants who responded to the advertisements were sent an information sheet and consent form and invited to complete a questionnaire to collect the demographic, clinical and literacy factors as described. This information was used to recruit a maximum variation sample. Recruitment and data collection continued until we reached theoretical saturation, that is, until no new data emerged in subsequent focus groups. The research team met after each focus group to discuss the results and consider whether or not there were areas or topics that needed further probing in subsequent groups.
Data collection
Focus groups were run in a community centre with online computer cluster rooms in London, UK. Focus groups lasted 3 hours and were led by at least two facilitators. Each focus group started with round table introductions of the facilitators and participants, as well as a description of the task and the structure of the session. Participants were then asked to move to the personal computers, with each participant having their own computer to use. We asked participants to visit three self-management websites for T2DM. These had been selected by the research team to demonstrate the range of interventions and component parts available. They varied in terms of content, complexity, tone, navigation and presence of interactive features, such as forums, ‘Ask the Expert’ sections or self-monitoring tools.
Participants were asked to spend 20–30 minutes on each site and were given a structured note pad to jot down thoughts as they occurred. Facilitators were on hand to help participants access the three selected sites and to address any problems that arose (e.g. people with little computer experience could find some sites difficult to navigate).
Once participants had explored all three interventions, the group reconvened for some rest and refreshment before starting the group discussion. This discussion was guided by one of the facilitators, with the other observing and noting group dynamics, thinking about the emerging data, occasionally checking or following up on specific themes or ideas that seemed to be emerging and making notes on key points. The lead facilitator followed a topic guide to steer the conversation.
This topic guide reflected the objectives of the study and was informed by our previous work and our theoretical approaches, particularly NPT56 and the Corbin and Strauss model54 of LTC self-management. The topic guide was piloted in an individual interview with one of our PPI representatives and no changes were required. It started by asking participants about their overall impressions of the utility of the three sites and whether or not a self-management website could be useful for people with T2DM. Subsequent areas for discussion included specific likes or dislikes about the three programmes, with the reasons for these reactions, and this led into a discussion on the ‘ideal’ content and form for a new programme.
At this point, participants were encouraged to indulge in ‘blue-sky thinking’ and come up with ideas for features they really wanted, even if they had never seen anything similar. Participants were also asked why and when they might use such a programme, what would encourage them to use it, whether or not they would like to share health-related data with their HCPs and whether or not they would like an HCP to facilitate use and, if so, how.
The focus groups were audio-taped and the tapes transcribed verbatim by a professional transcription company. The transcripts were checked and corrected by the group facilitators, and the notes taken by the second facilitator were included in the data set.
Data analysis
Data analysis was done through iterative cycles. The first cycle of analysis was a rapid review to determine the most important content and design features and the direction of the intervention development. This was done with a multidisciplinary team comprising an experienced medical sociologist, health psychologists and GPs. This team represented a broad range of perspectives, so the coding and analysis was sensitive to the clinical, sociological and psychological context of the data. Transcripts were independently read by each researcher and themes were extracted. This analysis also formed the basis for decisions about data saturation: focus groups continued until no new data emerged regarding design or content.
The second analysis was a more in-depth exploration of people’s experiences of living with T2DM. This work complemented the first cycle of analysis, as it focused on understanding the needs of patients, many of which were not currently well served by existing health or online services. The second cycle of analysis was undertaken by the same multidisciplinary team. Once again, transcripts were independently read by each researcher and important themes were identified. The thematic framework was expanded to describe phenomena beyond a simple description of desirable features and to include the full range of experiences shared by participants to provide a deeper understanding of the needs and wants that were often only implicit in the data. This led to the generation of more interpretive codes that looked at more macro-level phenomena, for example meanings and relationships. 107
The generation of codes was done inductively based on the data. The underlying sociological theory was based on Corbin and Strauss’ work54 on managing chronic illness at home, as discussed in Chapter 2. The main constructs of the model were used to sensitise and encourage a holistic perspective that explored (1) the impact that T2DM had on people’s day-to-day activities, relationships and emotions (life work); (2) the burden of having to take medicines or make lifestyle changes for the medical management of the condition (illness work); and (3) the disruption or changes to the roles that people played within their families and at work (biographical work). This model was not used to define a priori codes or categories but used as a sensitising tool to guide an inductive thematic analysis and to generate codes based on the data. These were used to define the needs of users, and the themes that emerged could all be explained by the types of work described by Corbin and Strauss.
Illustrative extracts of the data are presented in Results, with identification by focus group number and participant number with their age, gender, ethnicity, duration of diabetes mellitus since diagnosis and level of computer experience.
ATLAS.Ti (Scientific Software Development GmbH, Berlin, Germany) was used to manage the transcripts, coding and facilitate the final data analysis.
Results
Participant characteristics
Four focus groups were held with a total of 20 participants. Just over half of the participants were male, with a mean age of 56.8 years (range 36–77 years). Almost half of the participants were retired and over half had degree-level qualifications. Seventy per cent of participants (14/20) were white British, but black, Asian and other (Iranian) ethnicities were also represented. The range of time since diagnosis of diabetes mellitus ranged from 3 months to 36 years. Treatment modalities included diet only, tablets, insulin and other injectable medication. The overwhelming majority of participants had home internet access (19/20) and most had used the internet to look up information about diabetes mellitus (17/20). Sixty per cent of participants (12/20) had been on a diabetes mellitus self-management course (Table 2).
| Characteristic | Number of participants | Percentage of the total |
|---|---|---|
| Gender | ||
| Male | 12 | 60 |
| Female | 8 | 40 |
| Employment status | ||
| Employed | 5 | 25 |
| Not working but looking for work | 2 | 10 |
| Retired | 8 | 40 |
| Retired (semi) | 1 | 5 |
| Not working and not looking for work | 2 | 10 |
| Other – full-time student | 1 | 5 |
| Other – volunteer | 1 | 5 |
| Education | ||
| School leaver | 4 | 20 |
| A level | 5 | 25 |
| Degree | 11 | 55 |
| Ethnicity | ||
| White British | 14 | 70 |
| Black (African, Caribbean and other) | 4 | 20 |
| Asian (Indian) | 1 | 5 |
| Other (Iranian) | 1 | 5 |
| Duration of diabetes mellitus since diagnosis (years) | ||
| < 1 | 2 | 10 |
| 1–5 | 7 | 35 |
| 6–10 | 5 | 25 |
| > 10 | 6 | 30 |
| Diabetes management | ||
| Diet only | 3 | 15 |
| Diet and tablets | 10 | 50 |
| Diet and tablets and liraglutide injection | 1 | 5 |
| Insulin | 6 | 30 |
| Home internet access | ||
| Yes | 19 | 95 |
| No | 1 | 5 |
| Attended diabetes education | ||
| Yes | 12 | 60 |
| No | 8 | 40 |
| Used the internet to look up diabetes mellitus-related information | ||
| Yes | 17 | 85 |
| No | 3 | 15 |
A strong shared sense of the overwhelming burden that the diagnosis of diabetes mellitus placed on participants underpinned all the data generated during the focus groups. The diagnosis had severe negative impacts on their emotional well-being, work, social life and physical health. Although participants’ experiences of health-care services varied, there was agreement that even the best services were unable to meet all users’ needs and that a self-management website could, therefore, be extremely useful in meeting these unmet needs.
Participants had clear views about the features they would want or need from such a programme, as well as features that would help generate trust and encourage engagement. They also clearly identified features that would be off-putting and lead to disengagement.
The burden of diabetes mellitus
Although the topic guide did not directly address the question of what it was like to be diagnosed with diabetes mellitus and the impact that this had on participants’ lives, it was clear that participants were acutely aware of the severe and constant burden that they experienced as a result of the diagnosis. This burden was described most commonly in terms of the emotional impact, but participants also consistently referred to the difficulties their diabetes mellitus caused with their social life, relationships and work. As such, the data resonated strongly with Corbin and Strauss’ model54 of the work of living with a LTC, described in Chapter 2 (Table 3).
| Level | ||
|---|---|---|
| 1 | 2 | 3 |
| Life work and emotional management | Negative emotions associated with living with T2DM | Burn out |
| Denial | ||
| Indifference | ||
| Depression | ||
| Anger | ||
| Frustration | ||
| Self-blame | ||
| Guilt | ||
| Shame | ||
| Triggers for negative emotions | Food | |
| Seeking medical help | ||
| Lack of understanding from family members | ||
| Intrusive comments from family members | ||
| Strategies for keeping a positive outlook | Maintaining optimism | |
| Accept limits on control | ||
| Treat depression | ||
| Sources of support | Caring family members | |
| Peers | ||
| Illness work and medical management | Barriers posed by the health-care system | ‘Tick-box’ consultations |
| Conflicting advice | ||
| Professionals not keeping up to date | ||
| Difficulty getting appointments with GP | ||
| Difficulty accessing DSME | ||
| Poor-quality information (too much, too little, too complicated, not relevant) | ||
| Enablement by the health-care system | Supportive doctors and nurses | |
| Taking time to explain results | ||
| Timely access to DSME | ||
| Low priority of illness work | Lack of time | |
| Features patients want from access to EMR | Access to blood results | |
| Access to a medical summary | ||
| Transparency and ability to correct errors | ||
| Control data sharing | ||
| Biographical work and role management | Self-image | Bereaved – loss of health |
| Deserving punishment | ||
| Feeling like a criminal | ||
| Changes in working roles | Lack of support for making adaptations to work roles | |
| Impact that the changing needs of the patient role has on working role | ||
The following series of exchanges illustrate the data:
[The diagnosis of diabetes mellitus] was like a bereavement . . . It was just before my 50th birthday.
A lot of people say that, because you are, in a sense; you’re grieving for the loss of your . . .?
Liberty. Freedom.
Is that what it is? Right.
Health.
Yes.
Well, it’s more to do with the mortality business, isn’t it? Without wanting to sound grim, but . . .
Patient 5, male, aged 55 years, white British, 5 years since diabetes mellitus diagnosis and Patient 10, male, aged 70 years, white British, 6 months since diabetes mellitus diagnosis (focus group 1)
Many participants described how the demands of an illness that required them to take medication and eat regularly made it impossible for them to carry on with the work they had previously been doing:
I’m a project manager so I work all hours, different hours, and it was very difficult to manage my diabetes because if I’m going to a meeting at 8 o’clock at night, or going to a meeting at 6 o’clock, whatever, or . . . and breaking up . . . it was very difficult to manage it. Employers don’t really care about you’re diabetic, to be honest with you. . . . [Y]ou do forget to eat when you’re busy and you’ve got a meeting at 1 o’clock or 2 o’clock in the afternoon, or 12 o’clock in between your lunch break, and you can’t eat in the meeting because you’ve got about 20 people sitting there, or whatever the case may be. . . . I’ve just given up work about 4 weeks ago, so it’s just really hard to tell you the truth.
Patient 11, female, aged 51 years, black Caribbean, 10 years since diabetes mellitus diagnosis (focus group 2)
They took me off shifts, because I couldn’t remember if I’d taken my pills one week, you know? One week, I’m working early and next week, I’m working lates, and then I’m working nights, and I used to go, I can’t remember if I’ve taken them or not. My manager said, that’s no use, is it? We can’t have you falling over, you know?
Patient 17, male, aged 54 years, white British, 8 years since diabetes mellitus diagnosis (focus group 3)
The impact that dietary changes had on participants’ social and family lives was also difficult to cope with. Some participants found that it was too hard to keep to their planned diet when out with friends or family and would simply try to manage the consequences, whereas others would try to adhere to the changes they’d instituted but reported negative reactions from their families:
My wife was the only person that said anything that was reasonably sensible; she said, we’re going to this person’s house to eat, they need to know you’re a diabetic, otherwise they’re going to give you the same portions that you’ve always had, the same five pints of beer that you always have over lunch.
Patient 16, male, aged 58 years, white British, 4 months since diabetes mellitus diagnosis (focus group 4)
Because we’re talking about food; I mean, I go to my family, and when I say I can’t eat that food, they usually think that’s disrespecting them, so you’ve got all that as well to deal with.
Patient 11, female, aged 51 years, black Caribbean, 10 years since diabetes mellitus diagnosis (focus group 2)
Not surprisingly, given the impact that diabetes mellitus was having on their lives, participants reported strong negative emotions, which they found difficult to manage. Depression, anger, frustration and guilt were commonly felt:
Low, angry, frustrated. Everything. Because, you know, sometimes you’re frustrated because the doctor hasn’t told you what you want to hear. . . . Or you’re angry with the world, and you take it out on your children, your partners, everybody. And then you’ve got the depression that takes you down, because you’re just thinking one thing after another. So there is emotional change.
Patient 11, female, aged 51 years, black Caribbean, 10 years since diabetes mellitus diagnosis (focus group 2)
Stress and depression.
Yes, depression.
And, things related to that, because I know that depression is related to that, which is something, and when you are into that depression, you think very much negative about life and all that, you know? You say that, my sugar levels are not going to get controlled anytime, whatever I do.
Patient 18, male, aged 36 years, Asian Indian, 8 years since diabetes mellitus diagnosis and patient 15, male, aged 54 years, white British, 7 years since diabetes mellitus diagnosis (focus group 3)
Contributing to the difficulties experienced by participants was the perception that other people blamed them for their illness and that the relationship between lifestyle and T2DM led to stigmatisation:
Usually people say, oh, you must have had a bad lifestyle, something or whatever, which may be true sometimes, but it’s not the only reason . . .
Patient 19, female, aged 64 years, white British, 36 years since diabetes mellitus diagnosis (focus group 3)
Problems with existing health services, leading to unmet need
Although some participants were very appreciative of the care they had received from the health service, this was not a universal experience, with many participants reporting difficulties with access to HCPs, lack of interest or expertise among staff and an increasing sense of a ‘tick-box’ culture, in which problems were recorded but not addressed. Even participants who were positive about their care reported a feeling of never having enough time in consultations:
I’ve been very fortunate with my practice in [location] because they’ve given me a huge amount of support actually in terms of information gathering. But I understand that you’ve only got to be a couple of miles down the road and you get nothing at all. And even if you ask the questions, the doctors feel that you’re taking up their time, and in fact that’s true of all doctors, I appreciate that.
Patient 10, male, aged 70 years, white British, 6 months since diabetes mellitus diagnosis (focus group 1)
I found out far more information from those people [a local support group] than through from my local surgery. And it’s still the case now.
Patient 5, male, aged 55 years, white British, 5 years since diabetes mellitus diagnosis (focus group 1)
I’m asked that, once a year, that question, do you feel depressed? Yes. Next question. It’s not like, what are you going to do about it? . . . And when I see the nurse, every 6 months, she just says, are you exercising? And she ticks a little box if I say yes or no. And that’s it.
Patient 6, male, aged 55 years, black African, 10 years since diabetes mellitus diagnosis (focus group 1)
How a web-based self-management programme could meet this need
Participants reacted positively to our endeavour to create a web-based self-management programme for people with T2DM. They were clear that the programme should address all aspects of living with diabetes mellitus, including diet, physical activity, taking medicines, working with HCPs, managing difficult emotions and handling interactions at work, in social occasions and with friends and family.
They wanted information about diabetes mellitus, including how it is caused and how it affects the body; available treatments, including goals of treatment, pros and cons of each treatment and potential side effects; and access to a suite of resources. The participants wanted the programme to be a ‘one-stop shop’ that they could turn to at times of need. There were clear tensions between wanting or needing information and not wanting to be overwhelmed with ‘bad news’. It was vital that the information was presented in a cheerful and upbeat fashion, with an emphasis on what can be done to prevent complications, while acknowledging that diabetes mellitus can be hard to control and avoiding ‘victim blaming’ when things do go wrong:
I suppose I’d want something that was a bit, kind of, an A-to-Z of one’s life.
Patient 20, female, aged 41 years, white British, 5 years since diabetes mellitus diagnosis (pilot interview)
The mainstream medical opinion seems to be all doom and gloom . . . If you just put that diabetes is such-and-such but can be controlled or managed or whatever word you want to use, through very simple means, I think that’s a huge relief to people.
Patient 10, male, aged 70 years, white British, 6 months since diabetes mellitus diagnosis (focus group 1)
I think you’ve always got to look at the positive side of your illness. But yes, you’re always going to have a negative side, and sometimes you’ve got to have a funny side . . .
Patient 8, female, aged 46 years, white British, 16 years since diabetes mellitus diagnosis (focus group 1)
Tables 4 and 5 summarise participants’ views on desirable and undesirable content and presentation.
| Area | Specific topics mentioned |
|---|---|
| Medical information | Medication |
| Side effects | |
| Hypoglycaemia | |
| News and research | |
| Dietary advice | Controlling blood glucose |
| Weight loss | |
| Controlling cholesterol | |
| Understanding food | |
| Recipe ideas | |
| Physical activity | Benefits of exercise |
| Advice about weight loss | |
| Easy-to-do physical activities | |
| Resources for group activities | |
| Alternative medicine | Relaxation therapy and stress reduction |
| Complementary therapies | |
| Peer support | Advice from peers |
| Emotional support | |
| How peers manage, including social norms for key clinical outcomes, such as HbA1c level, blood pressure and weight | |
| Role models | |
| Little enthusiasm for social media | |
| Pregnancya | Safe conception; what to do if pregnant? |
| Practical advice | Travel |
| Work | |
| Driving | |
| Insurance | |
| Financial advice, for example benefits | |
| Information about health services | Services people should have access to |
| Local support groups | |
| Telephone support lines |
| Design feature | Specifications |
|---|---|
| Design and navigation | Easy to use |
| Clear, concise and consistent | |
| Minimal scrolling | |
| Use videos | |
| Pages can be printed in black and white | |
| Interactive features, such as quizzes | |
| Self-monitoring tools | |
| Acts as central hub for all diabetes mellitus-related queries, with links to other resources | |
| Language and tone | Accessible |
| Medical terminology used when needed, but with definitions and explanations | |
| Encouraging and supportive | |
| Not shying away from difficult truths | |
| Sense of humour | |
| Trust | Thorough proofreading |
| No advertising | |
| Working links to/from good websites | |
| Evidence of links with trusted institutions such as the NHS or well-known universities | |
| Avoid irritants | Poor design |
| Not relevant or localised | |
| Out of date | |
| Boring, static |
Views about health-care practitioner facilitation
Participants wanted any self-management support programme to be integrated into their general medical care, rather than as a stand-alone resource. They wanted to work with their health professionals to obtain good health outcomes, although there was a sense that health professionals were not always interested in their efforts:
Yes, I got told off last week for not taking mine [blood glucose diary] in, but part of the reason is, well, you never look at it. What’s the point of me taking it in? . . . It’s like a little token. You know, look, I have been recording, but he doesn’t go, so, what’s happening here?
Patient 15, male, aged 54 years, white British, 7 years since diabetes mellitus diagnosis (focus group 3)
Although, in principle, participants were strongly in favour of HCPs helping patients to register on the programme, showing them how to use it and discussing their use of the programme in diabetes mellitus-related consultations, they were sceptical whether or not this would be possible:
I think it would be a good thing but I can’t see many people doing it. . . . To even ring your GP surgery normally to make an appointment can be very tiresome for a lot of people. You can’t get through.
Patient 8, female, 46 years, white British, 16 years since diabetes mellitus diagnosis (focus group 1)
Access to electronic medical record
In line with their emphasis on the need for self-management to be integrated with HCP management, participants were keen to have access to their GP EMR. Perceived benefits included the ability to correct information in their records and to share correct information with the multiple health-care providers that they encountered, such as opticians, podiatrists, dentists and emergency doctors. Participants were keen to have control over their information, and to decide what to share with whom:
It might be useful to correct things, if you find anything that’s been recorded incorrectly, that at the moment, you’ve got no idea if . . . anything’s wrong or not.
Patient 16, male, aged 58 years, white British, 4 months since diabetes mellitus diagnosis (focus group 4)
It’s not anything to do with diabetes, but the worst thing is, when you go along to A&E [accident and emergency unit], and they say to you . . . ‘Oh, when were you diagnosed?’ You know, and you have to start . . . the whole story from the beginning, and if they’ve got access as well, so, you know . . .
Patient 7, female, aged 65 years, white British, 3 years since diabetes mellitus diagnosis (focus group 4)
Discussion
In this focus group study, it was clear that living with T2DM placed a substantial burden on participants. It negatively affected all aspects of their life, including emotional well-being, work, social life and physical health. This characterisation of the burden of diabetes mellitus resonated well with Corbin and Strauss’ model54 of the work of living with a LTC. Our participants articulated that the ‘work’ of emotional and role management was at least as pertinent to them as that of medical management. Participants felt that health services were unable to address all their needs and, hence, welcomed self-management support, as long as such support adequately reflected their needs. This study confirmed the benefits of our proposed holistic approach to the intervention, as well as providing detailed guidance on how to achieve its objectives.
Our findings fit well with previous literature, building on the previous study by Kerr et al. 90 that generated quality criteria for web-based self-management programmes across a range of LTCs. The burden that such conditions in general,108,109 and T2DM in particular,110 bring has also been well described. Understanding this burden is a prerequisite for developing programmes that genuinely support people with self-management, rather than adding to the burden of treatment without addressing underlying needs.
The strengths of our approach included the use of focus groups and a relatively open topic guide, which allowed participants to raise their own concerns and determine the direction and content of discussions. An additional strength was the use of existing interventions to anchor discussions, which demonstrated what had already been achieved and allowed users to consider how these could be improved, rather than considering the creation of an intervention from scratch.
The main weakness was that our sample, although diverse in its ethnicity, duration of diabetes mellitus since diagnosis and treatment and gender, was highly skewed towards people with an interest in self-management. This was an inevitable result of our recruitment strategy, which advertised for people interested in developing a web-based self-management programme; it is difficult to see how this could have been avoided.
The findings confirmed our decision to use the Corbin and Strauss model54 of medical, emotional and role management to determine overall content, and the guidance provided by participants was relatively easy to put into practice during the development of the HeLP-Diabetes programme, particularly when supported by our participatory design process.
Chapter 5 What requirements do health-care professionals have of a web-based self-management programme for people with type 2 diabetes mellitus?
Chapter summary
This chapter reports on a qualitative study that aimed to determine HCPs’ perspectives of the essential and desirable features of a web-based self-management programme for people with T2DM and what could be done to encourage uptake and use in the NHS. Additional objectives were to explore HCP views on the type and quantity of facilitation that could be provided in general practice and on patient access to part or all of their EMR.
We collected data through seven individual interviews and four focus groups with 18 HCPs who were involved in caring for people with T2DM, including GPs, practice nurses, diabetes specialist nurses, dietitians and consultants in diabetic medicine. Topic and interview guides were semistructured, with participants being encouraged to voice opinions about issues that were important to them, rather than sticking to predefined questions. A multidisciplinary group then analysed the data inductively and mapped themes onto NPT,56 while paying careful attention to identifying any themes that did not map easily. All data mapped easily onto the four main NPT constructs of coherence, cognitive participation, collective action and reflexive monitoring, as described in Chapter 2.
Our proposed web-based self-management programme appeared to be easily understood by participants, who were positive about the benefits of self-management by patients and showed considerable awareness of the challenges faced by people with T2DM, both in terms of the emotional impact of the condition and the overwhelming amount of information they needed to absorb. They were supportive of a web-based approach, deeming that this would help alleviate some of the difficulties with the dominant model of group-based education. These difficulties included long waiting lists, the inconvenience of attending groups at fixed times and the absence of ongoing support once the group had completed.
This understanding of our proposal (coherence) was reflected in a perception that, overall, HCPs would support the implementation of such a programme (cognitive participation), as long as the impact that it had on workload was acceptable (collective action). In particular, our participants said it was important that the proposed programme made consultations more effective, was easy to use, supported current NHS guidelines and enabled GPs to achieve goals related to the QOF. They also had clear views about the types and range of evidence that HCPs would require to continue to engage with the programme once it had been implemented (reflexive monitoring).
In contrast, views about facilitating access to the programme were more nuanced. Although some participants understood what facilitation would require, many were unconvinced of the potential benefits and felt that the impact it would have on workload could not be justified and was not an appropriate use of scarce resources in general practice. Similarly, there was considerable disquiet about patient access to EMRs, with participants being unsure about what information would be accessed and what the benefits might be and having significant concerns about adverse outcomes, including risks to privacy and confidentiality, increased patient anxiety and an increase in workload.
Background
Rationale for study objectives
In Chapter 3, we discussed the need to identify user requirements before developing a web-based self-management intervention. We conceptualised our users as belonging to two groups: (1) people living with T2DM and (2) HCPs who were involved in caring for people with T2DM.
As described in Chapter 2, one of our approaches to improving the uptake and use of the web-based self-management programme was to integrate it into routine health care, so that users perceived it as part of the overall package of care provided by the NHS. We believed that it was important that they were introduced to the self-management programme by a HCP, as this would provide credibility and reassure them that doctors and nurses approved of the programme and wanted them to use it. We considered that ongoing use of the programme would be promoted by doctors and nurses referring to it during consultations, asking patients how they were getting on with it and perhaps jointly reviewing personal goals or self-monitoring data (see Figure 2).
However, we were well aware of the difficulties of achieving such professional behaviour change. 95 Hence, the rationale for the objectives of this study included understanding what HCPs would want from such a programme, what they considered would make them want to use it, what the likely barriers to use would be and what (if anything) could be done to address these barriers. Identifying these factors would allow us to build in motivating features while addressing potential barriers.
Our intention was to develop a programme that would be used in primary care, so our main focus was on HCPs working in that sector. However, people with T2DM are cared for by a wide range of HCPs across primary, community and secondary care. The intervention needed to be acceptable to all of these HCPs, and we believed that it was important that specialists in diabetes medicine approved of the intervention. Hence, our sample included a range of HCPs involved in caring for people with diabetes mellitus.
Factors that the literature predicted would influence HCP views on the potential benefits and pitfalls of self-management interventions and web-delivery included age (with younger people often being more open to technology), gender (with women tending to adopt more patient-centred care supporting self-management) and disciplinary background. 111–115
Data from overseas studies of e-mental health interventions and ICBT demonstrated that facilitation by a HCP led to significantly improved use and greater clinical effectiveness. 94 The disciplinary background of the HCP did not seem to be important, with comparable results obtained by therapists and technicians. 116 Similar findings from the UK were obtained with telephone facilitation of a weight loss intervention. 117 Methods of facilitation that had been shown to be effective included e-mail and telephone support, usually at a frequency of once a week or fortnight. However, facilitation takes time, and time is a scarce resource in general practice. We wanted to explore with HCPs what they thought about facilitation, whether or not they thought it would be a legitimate role for general practice staff and, if so, for what type of staff [practice nurse, receptionist, health-care assistant (HCA) or other] and what level of frequency and intensity would be practicable.
Finally, we wanted to explore HCPs’ perceptions of the advantages and disadvantages of allowing patients access to some parts of EMRs. Early pilot studies suggested that the potential benefits of such access may include more accurate records, more empowered patients and a reduction in duplication of tests and investigations. 96,98 Participants in WP A (see Chapter 4) were keen to have access to at least some of their EMR, stating that it would help them with self-monitoring, managing their medication and understanding their health problems and in communicating with other HCPs. They wanted to be able to share their self-monitoring data with their clinicians. They said that such access would be a powerful motivator for using the self-management programme. In the UK, the public had had the right to see their paper medical record or EMR since November 1991, although relatively few had exercised this right. 118,119 At the time our study was undertaken (2011), there was considerable discussion around forthcoming legislation to mandate patients having online access to their EMR by 2015 (the legislation subsequently passed and people now have this right). 120 Many doctor organisations had expressed strong concerns around privacy and confidentiality. 99,121 Therefore, we thought it important to explore HCP views about providing some linkage between the self-management programme and the patient’s EMR and whether, even if they were opposed to full access to the record, HCPs would consider partial or limited access to EMRs acceptable within strictly defined parameters, such as medication and results of investigations. Given that patients wanted to share self-monitoring data with clinicians, we also wanted to explore this possibility. As our proposed intervention was intended to be used in primary care, and the majority of patients would be cared for in primary care, the possibility of linking with hospital records was not relevant and not pursued.
Rationale for study methods
The main methods considered for this study were focus groups and individual interviews. Focus groups have the advantage that areas of disagreement can be discussed, allowing for illumination and explication of reasons underlying such disagreement and the potential generation of consensual solutions acceptable to all participants. 102 An advantage of individual interviews is the ability to go into specific areas in greater depth, responding to the interviewee’s interests and enthusiasms. Interviews can also be helpful if there are sensitive issues to explore, such as the perceptions of one group of HCPs about the roles, strengths and weaknesses of other groups of HCPs, which participants may be unwilling to share in a less confidential setting. 122 Moreover, focus groups are substantially more difficult than individual interviews to arrange, as they require bringing participants together at a mutually convenient time and location. The challenges of recruiting HCPs to research are well known and were well understood by the research team. 123,124 In view of this, we opted for a combination of individual interviews and focus groups.
As HCP time is at a premium and participants were unable to allocate us more than 30–60 minutes of their time, we did not show them examples of existing self-management programmes as we had the patients. We considered that professionals had sufficient understanding of the type of intervention that we were trying to develop from other digital interventions already in use as part of EMRs or on referral (e.g. ICBT) and that they would know the features that would promote use or act as barriers.
Aims and objectives
The overall aim of the study was to determine HCP perspectives of the essential and desirable features of the intervention that would encourage uptake and use in the NHS. Additional objectives were to explore views about the amount and type of facilitation that patients would need and whether or not and how this could be provided in general practice. Finally, we wanted to explore HCP views about patient access to EMRs.
Data from this study contributed to the following objectives of the programme grant:
-
determine HCP perspectives of the essential and desirable features of the intervention that would encourage uptake and use in the NHS
-
determine the overall content and function of the intervention
-
determine the optimal facilitation required to encourage use of the intervention
-
determine feasibility and acceptability of facilitated access to the intervention.
Methods
Design
Qualitative study using individual interviews and focus groups for data collection.
Ethics
Ethics approval was provided by the North West London Local Research Ethics Committee on behalf of the National Research Ethics Service (reference number 10/H0722/86).
Setting and participants
Our recruitment strategy was designed to reflect our objectives by targeting a range of HCPs who are involved in caring for people with T2DM, with a focus on primary care. Hence, we sought to recruit GPs, practice nurses, diabetes specialist nurses, consultants in diabetes medicine and dietitians. We used a ‘snowball’ method of recruitment, starting with clinicians with whom we had personal contact and following up with contacts of interviewees. This was augmented by advertisements and flyers at primary care conferences and sending e-mails to HCPs delivering structured education in north London. We sought a sample that varied in its age, gender, ethnicity, disciplinary background and seniority and work setting (primary, community or secondary care). Recruitment continued until theoretical saturation was reached and no new data emerged in subsequent interviews or focus groups.
Data collection
A topic guide was designed that reflected our objectives and built on findings from the existing literature. The guide was informed by NPT56 and consisted of open-ended questions designed to encourage participants to think widely around the issues discussed during the interviews and to enable participants to bring up ideas that were important to them, rather than focusing specifically on issues predetermined by the research team.
The topic guide was piloted in an individual interview, and after revisions, repiloted in a focus group. This revised version was used for subsequent focus groups and interviews. The areas covered by the guide included challenges in managing patients with T2DM, potential benefits and pitfalls of using a web-based self-management programme, the impact on consultations and workload, facilitators of and barriers to implementation, strategies to combat attrition and views on patient access to their EMR.
Interviews were held at a time and location convenient for the interviewee, usually their place of work, and often in their lunch hour or after work. Focus groups were held either in participants’ practices or a convenient, quiet meeting room in an academic or NHS venue and were facilitated by a least two researchers. The lead facilitator chaired the discussion, while the second observed, contributing only when needed to clarify points of discussion. The observer kept extensive field notes, including real-time reflections on the data emerging.
Interviews and focus groups were audio-taped and transcribed by a professional transcription company. Transcripts were checked for accuracy by the interviewer or focus group facilitators.
Participants were also asked to complete a brief demographic questionnaire, providing information about age, gender, ethnicity, professional role and level of seniority.
Data collection continued until we reached theoretical saturation with no new data emerging.
Data analysis
A multidisciplinary team, comprising GPs, psychologists, sociologists and health service researchers, analysed the data. Transcripts were read by each member of the research team and then discussed in group meetings or data clinics. Emerging themes were agreed on and transcripts subsequently coded to these themes. 125 Codes and themes were iteratively discussed until agreement was reached by the whole team. Themes were subsequently mapped onto NPT as described in Chapter 2. This two-stage approach had the advantage of maintaining our theoretical perspective, while ensuring that we did not ignore or discard data that did not ‘fit’ with NPT. 126
ATLAS.Ti was used to manage the transcripts, coding and facilitate the final data analysis.
Illustrative extracts of the data are presented in Results, with identification by participant number and professional background.
Results
We held seven individual interviews and four focus groups, with a total of 18 participants. Of the four focus groups, two featured only nurses, one had only doctors and one was multidisciplinary. Eight participants were GPs. Of these, five were currently salaried: two had been partners or principals in the past and three were currently partners or principals. Six participants were nurses, of whom three were diabetes specialists, two were practice nurses and one was a nurse consultant. There were two consultant endocrinologists, one doctor in training and one dietitian. Eleven participants were female and the mean age was 49 years (range 32–64 years, with one participant declining to provide their age). One participant described their ethnicity as Asian and the remainder were white British (Tables 6 and 7).
| Characteristic | Number of participants (N = 18) |
|---|---|
| Profession | |
| Primary care | |
| GP partner | 3 |
| Salaried GP | 5 |
| Practice nurse | 2 |
| GP trainee | 1 |
| Community diabetes team | |
| Diabetes specialist nurse | 3 |
| Dietitian | 1 |
| Secondary care | |
| Endocrinologist | 2 |
| Diabetes nurse consultant | 1 |
| Gender | |
| Male | 7 |
| Female | 11 |
| Age (years) | |
| Mean | 49 |
| Range | 32–64 |
| Group | |
|---|---|
| Number | Composition |
| 1 | Three GPs |
| One diabetes consultant | |
| 2 | One diabetes specialist nurse |
| One diabetes specialist dietitian | |
| One GP | |
| 3 | One diabetes nurse consultant |
| One diabetes specialist nurse | |
| 4 | Two practice nurses |
Main themes
All the data that emerged mapped easily onto the main constructs of NPT. The following subsections are structured by NPT construct: Coherence, Cognitive participation, Collective action and Reflexive monitoring. Each subsection presents data, for the main proposed programme, for facilitated access and then, finally, for access to EMRs.
Coherence
Coherence refers to the ease with which the intervention can be described, understood and distinguished from other interventions or practices. This includes an understanding of how an intervention or practice differs from other interventions and an understanding at the individual and group levels of what the aims and expected benefits of the intervention will be and what individuals will have to do to realise those benefits.
For our participants, the concept of a web-based self-management programme had immediate coherence. Many of our participants were already convinced of the importance of self-management by people with T2DM, stating that patients played a key role in determining health outcomes:
Anything that I as a clinician will do is predicated on the other individual in the relationship actually playing their role, taking part, taking active control of their own lives. And the more information and understanding they have of what is going on, the more they’ll understand why I’m seeking to help them modify their behaviour.
Participant 5, GP partner (individual interview)
Participants were aware that people with T2DM often needed help and support to engage in self-management but that the dominant model of group-based education was not suitable for many:
Well, we don’t have that many people who are in full-time employment in [town] really . . . but they do have other priorities and, you know, their health may not be one of them, sadly. You know, social deprivation, poverty. You know, often we put on education at times that suit us, as health-care professionals, [but] they’ve got children to pick up from school or they’re looking after elderly parents or, you know, they’ve got children with special needs, they’ve got other illnesses themselves.
Participant 12, diabetes nurse consultant (focus group 3)
Other problems with group-based education included long waiting times and the fact that, in most areas, education was available only at the time point after diagnosis, whereas people with T2DM often had an ongoing need for education and support:
We get very, very good feedback about DESMOND, but the wait is just too long for them to go on it, you know. And plus once you’ve had that . . . initial training and education, it doesn’t mean that you’ve not got further training needs, and there’s a massive gap that we encounter for that extra bit of help for patients.
Participant 15, practice nurse (focus group 4)
Participants considered that a web-based programme would have a number of advantages over group-based education, including being available at the time when a patient was ready to engage, being able to be revisited frequently so that users can learn at a speed that suited them and that video and graphics can be used, which would help people with low literacy skills or poor English. Many commented on the volume and complexity of the knowledge required to self-manage effectively:
[It] is quite difficult . . . for the individual, understanding this cruel nature of type 2 diabetes. I think people understand the sort of sugary side of things, but actually understanding the impact on their kidney disease, their heart disease risk, all these other areas where long-term diabetes is important. It’s quite complicated [even] for us. You know, I think for people who perhaps don’t have that kind of medical understanding, it must be really quite daunting to take all that information on at the start.
Participant 6, GP partner (individual interview)
Clinicians were very aware of the emotional burden that diabetes mellitus placed on patients and were keen to see that addressed, recognising that this was a prerequisite before people with T2DM could start the work of taking control of their health:
One is often tempted to say, well it’s the educated people who get the whole thing quickly and they therefore deal with it. But I remember, certainly one patient of mine, a young . . . a very bright young girl, who just did not want to come to terms with her diabetes, and she was all over the place. So it wasn’t to do with her intellect, it was actually the emotional coming to terms with it.
Participant 0, salaried GP (individual interview)
Although the main concept of a web-based self-management programme had good coherence with our participants, there was less agreement about providing some form of facilitation. Although some participants had experience of telephone facilitation for computerised CBT through the Improving Access to Psychological Therapies programme, others were unsure how such facilitation could be offered. Even those who understood the rationale for offering facilitation, in terms of integrating the self-management programme into clinical care and encouraging uptake and use by patients, were uncertain of the benefits:
One of the ways we thought that might help is . . . having someone maybe ring up every so often and say how are you getting on with the program?
I guess that’s possible. I don’t know if that would help, though.
Participant 14, diabetes specialist nurse (individual interview)
Similarly, there were uncertainties about what patient access to their EMR would entail, in terms of the sort of information patients could access, controls over privacy and the impact that this might have on patients and on HCP workload:
I’m not sure about that really . . . I don’t know whether they . . . should see the complete record or whether it, someone should go through it before they have a look, I’m not sure . . . I think if they say perhaps a summary or just maybe the key parts of the past medical history or drug history, which I think is important for a patient to have, then I think patients should have access to that generally, because they present in A&E [accident and emergency unit] or after hours; that is really handy information. So I think that would be a good thing generally. I don’t know how much detail a patient really needs, though, to read; maybe some individual consultations, I’m not quite sure if that would be very helpful.
Participant 11, trainee GP (individual interview)
Cognitive participation
Cognitive participation is about the decision whether or not to participate in an intervention. One of the components of cognitive participation is the concept of ‘legitimation’, or the extent to which the work required by the intervention is a legitimate part of the role of the various HCPs involved.
The HCPs in our study felt that our proposed programme was likely to be widely supported by professionals, who would see its advantages, including recognition of the importance and difficulties of enabling people with T2DM to self-manage and the benefits that accrue when they do self-manage. Ensuring that the programme was trustworthy, by containing up-to-date evidence-based information in formats that were accessible to patients and HCP, would also aid cognitive participation. Trust could be enhanced by the intervention being:
. . . professional, academic, something, you know, not commercially run.
Participant 6, GP partner (individual interview)
Endorsement by relevant bodies, including the Department of Health and Social Care, the Royal College of General Practitioners, the Royal College of Nursing, Diabetes UK and local diabetes consultants or other local opinion leaders would promote uptake and use of the programme by HCPs.
There was also a recognition that patient experience had considerable influence on clinician behaviour: if patients were calling for the intervention to be available, then this was likely to increase HCP buy-in. Similarly, if the programme was used by only a small minority, participants felt that this would lead to HCPs being much less interested in using and promoting it:
You probably want to get the Department of Health [and Social Care] to say that everyone should commission it as part of their care package.
Participant 9, salaried GP (focus group 2)
Getting good feedback from the patients, that’s going to make me recommend it.
Participant 16, practice nurse (focus group 4)
However, the overwhelming factor that would affect use and uptake was considered to be the impact on workload. Any intervention that increased workload was highly unlikely to be adopted:
If it is time-consuming, I think, [that] would be a big barrier, definitely, because as you know, consultations are really time pressured, aren’t they?
Participant 11, trainee GP (individual interview)
Conversely, if the intervention was found to decrease workload and result in more effective consultations, this was likely to promote adoption.
Hence, the prospect of practice staff facilitating access to the programme had low cognitive participation. The HCPs in our study felt that any potential benefits of facilitation were unlikely to justify the increased workload:
Do you think it’s viable to ask practice nurses maybe to ring up patients and say how you getting on with the intervention, are you using it . . .?
No. . . . We’ve got a crisis in practice nursing in London. Expecting . . . partners or clinicians to say ‘Yes, you can . . . my [practice] nurse can take half a day out to ring a whole lot of diabetics and encourage them to use this’, will probably not go down very well.
. . . Receptionists?
Maybe, but again I’d say this is another . . . activity unresourced. Until clinicians see the utility of it and see significant benefit from it for themselves and for their practices and for their patients, I can’t see clinicians spending a lot of resource and time.
Participant 5, GP partner (individual interview)
Just as the issue of patient access to their EMR had low coherence, it also had low cognitive participation. Even participants who could see its potential to empower patients had serious concerns about issues such as privacy and confidentiality, clinical governance and workload:
For this group of people, it’s really important. It’s their information, and they have control of it and understanding of it. So I like the idea, generally, of them owning the information. Pragmatically, I worry about people having dial-in access to our system, being able to hack in and around.
Participant 6, GP partner (individual interview)
Like all of these things, it’s probably fine for most people but there will be a few people who maybe have other problems like anxiety or whatever and then it actually . . . might just make things worse.
Participant 9, salaried GP (focus group 2)
Participants in WP A had discussed the possibility of being able to enter self-monitoring data directly into their clinical record, but this was considered entirely unacceptable by the HCPs in WP B for medicolegal reasons:
And what happens if the individual puts on that their blood sugar is 29 and they’ve got ketones? Am I meant to go and respond and take medical legal responsibility for that?
Participant 6, GP partner (individual interview)
Collective action
Collective action refers to the work of bringing about and maintaining change resulting from a new intervention. In many ways this is the core construct of NPT. There are four constructs within collective action:
-
interactional workability
-
relational integration
-
skillset workability
-
contextual integration.
Interactional workability
Interactional workability refers to the impact that the new intervention has on interactions. NPT posits that an intervention that enhances interactions is more likely to normalise than one that has a negative impact. In terms of our proposed web-based self-management programme, the two relevant interactions were consultations between HCPs and people with T2DM and interactions between users of the programme (whether HCP or patient) and the programme itself – ‘usability’ in human–computer interaction (HCI) terms. Participants in our study were keenly aware of the importance of both these, stating that if the programme helped consultations, making them more constructive and effective, that would be a strong incentive for HCPs to take up and promote use of the programme, whereas anything that interfered with consultations or generated additional work would not be used:
So in the context of my consultation, will it help? I could see that it might: my understanding of what the project is about suggests that actually it will give the patients an opportunity to engage rather more with their condition. And if it’s done right, it will give me and them the opportunity to see fairly quickly, and at a glance, if it’s good enough what they’ve been doing over the past weeks or months, how [good] their physical control is, so if you get some of the physical parameters, and how good, if you like, their overall involvement and engagement with the diabetes issues are.
Participant 0, salaried GP (individual interview)
I would certainly use it in a consultation if it was set up, you know, right, I would certainly use it as part of my consultation. . . . [I]f there was parts on diet, and weight loss, and local services, it would be fantastic to have it all on there on one . . .
Participant 15, practice nurse (focus group 4)
My huge anxiety about these things is being swamped. You know, what I don’t want to is, you know, arrive in my surgery and turn on and get, you know, 300 people who’ve suddenly their most recent blood sugars, you know, it would be unworkable.
Participant 6, GP partner (individual interview)
Equally, participants were clear about the importance of usability, emphasising that the programme should be easy and intuitive to use for both patients and HCPs:
What tends to make people use these kinds of systems is if they work well, if people find them helpful. You know, there are systems that, you know, just run because they’re well designed, they’re thoughtful and they’re helpful, and they make the job work and that’s for the clinicians as well as the patients. There are others which are just clunky and hard work and slow, and you just kind of think, I’m really not going to invest the time in this, so, you know, a well-designed system that . . . added some value . . . would be the biggest incentive to make me use it.
Participant 6, GP partner (individual interview)
Facilitated access was not thought to be a good use of scarce consultation time, whether done face to face or on the telephone and by a clinician or a non-clinician. Participants considering time spent on facilitating access to a programme as time diverted from more important clinical tasks, such as ensuring patients were vaccinated against influenza.
I can only speak as for myself as part of the practice that time constraints, I don’t think people would remember to remind them. We struggle enough with them to ring up for reminding them to come and have their flu jabs and things like that, so realistically I think they wouldn’t.
Participant 15, practice nurse (focus group 4)
Relational integration
Relational integration refers to the extent to which an intervention fits with, or disrupts, existing relationships between different groups, usually professionals. NPT posits that interventions that fit well with existing relationships, and when responsibility and accountability are aligned, are more likely to normalise than disruptive interventions.
Our participants stated that it was important for our proposed programme to be compatible with current NHS guidelines, as problems could arise when patients were led to believe that something could benefit them, but local or national policy meant that this was not available. One example of this was blood glucose testing. In the light of the evidence that regular self-monitoring of blood glucose does not lead to improved diabetes mellitus control, and given the costs associated with self-monitoring, many CCGs were attempting to reduce overall prescribing of blood glucose monitoring sticks. Patients were often confused or annoyed by this:
Well we’ve got a bit of an issue to save money. We’ve recently launched some diabetes monitoring guidelines and basically patients who are on oral hypoglycaemic agents or insulin are, you know, it’s a recommendation that they do blood tests on an ongoing basis but for those who are on diet only or metformin only there’s no provision for them to do that.
Where[as] previously we’d encouraged everyone to test because we felt it was empowerment . . .
From patient data (WP A):
My practice nurse can’t believe that I like to test my own blood sugar. She’s like, oh you don’t need to do that; why do you need to do that? And I find that quite strange.
Patient 13, female, aged 56 years, white British, 16 years since diabetes mellitus diagnosis (focus group 3)
Participants also suggested that one benefit of the proposed programme would be to provide access to information to HCPs, as well as to people with T2DM. This would help with trust between HCPs and patients and also enable the HCP to stay abreast of latest developments:
But I think something that people could see was clinically relevant and was going to help in terms of, I guess, professional learning as well, because people obviously need evidence of that. And that will be good.
Participant 11, trainee GP (individual interview)
No data about facilitated access pertained to relational integration.
Equally, access to EMRs was considered likely to have a negative impact on consultations, with a potential to increase patient anxiety and clinician workload:
You’d probably need to do it prospectively because, you know, a lot of records have been entered historically, not thinking that [patients] could read these . . . At the moment when they request their records, they’ve normally gone through them with a health professional there who will talk them through them and maybe explain them. But actually to just view them on their own at home, they may be misinterpreting what’s been put there, you know. I don’t know. There are definitely pros and cons to that.
Participant 09, salaried GP (focus group 2)
Skillset workability
Skillset workability refers to the fit between a new intervention and existing skillsets. NPT posits that interventions that fit well with existing skillsets, and that are perceived as requiring professionals to undertake tasks that are appropriate for their professional role, are more likely to normalise than those that do not. This construct also highlights the importance of training, to ensure that those who need to use the intervention are able to do so.
Our participants stated that it was important for our proposed intervention to fit with perceived professional roles:
Anything that makes me do things against my professional job, filling in useless forms, taking time, that won’t make [my job] feel enhanced. If it helps me to focus better on the key issues that I think are important, and that I think the patient thinks are important, that will make it valuable; if it distracts me from that conversely it will be unhelpful.
Participant 0, salaried GP (individual interview)
In line with the perception that any benefits of facilitating access were unlikely to justify the additional workload, participants were uncertain as to who, if anyone, would take on this task. However, it was acknowledged that it would have to be a specified role that was clearly allocated:
It would have to be somebody’s specific role to do it, I mean, part . . . considered part of their role.
And don’t ask the poor practice nurse.
No data on access to EMRs pertained to skillset workability.
Contextual integration
Contextual integration refers to the fit between the proposed intervention and the availability of resources. These include not only obvious resources such as staff, time and funds, but also the existence of policies, protocols and priorities.
One major contextual issue for GPs was the QOF, a performance-related pay system that ties performance on key indicators to practice remuneration. GPs were clear that if the proposed programme could help them with the QOF, either by improving performance or by making it easier to record, this would be a major incentive:
Certainly within QOF, and I know there are much more changes to patient-held records, patient information, self-management, and those are the kind of external drives which will probably make something like this work.
Participant 6, GP partner (individual interview)
Participants felt that our proposed self-management programme would fit well with existing local and national policies. This was particularly so in locations that had a history of promoting self-management by patients and were involved in the ‘Year of Care’, a NHS initiative to encourage personalised care planning for people living with LTCs:
We’re doing the Year of Care thing, so actually if we had some sort of system that – rather than sending them a scruffy bit of paper – that we can input it into their system, and alert them to it, or e-mail them to it, so that if they then log in they’ve got their up-to-date information . . . I could see that that would be really useful, you know, having some sort of guide as to . . . whether they’ve improved since last time, or . . .
Participant 16, practice nurse (focus group 4)
It was less clear how facilitated access would help practices achieve clinical priorities or be achieved within existing resources; in other words, facilitated access did not appear likely to have good contextual integration.
Similarly, patient access to EMRs raised questions of resources, particularly the need to ensure that any data entries were seen and acted on. A participant with experience of this suggested that a ‘workflow manager’ would be required to ensure patient safety. Other participants pointed out the resource implications:
Then you’re causing the practice more time, more money.
Participant 1, salaried GP (individual interview)
Reflexive monitoring
Reflexive monitoring refers to the appraisals that people make to assess whether or not a particular intervention is worth continuing. These include assessing whether or not the expected benefits are being realised and whether or not these are worth any additional workload. Our participants could not engage in reflexive monitoring, as the proposed intervention was still hypothetical, but many of them commented on the sort of information that would be likely to be influential.
Participants said that future HCPs would need a range of information to decide whether or not to continue investing time and energy in promoting the use of a web-based self-management programme for people with T2DM. The results of the proposed RCT would be crucial:
I wouldn’t recommend that as someone on the exec unless I knew that there was evidence that it was worthwhile doing.
So what evidence . . . do we need?
Well I don’t . . . I think this is years in advance of where you’re at, when we need to design something that show that it makes a difference or at least have existing evidence that shows that it makes a difference. You know, we need a clear business case for a consortium to be that definite about it.
So we need results of our RCTs showing that it made a difference or not?
Yes, I think so.
Primary outcomes?
With economic data, if possible.
However, they were equally clear that trial data alone would not be enough. They would need information about the numbers of patients using the programme, their demographics (harking back to concerns about the digital divide) and the impact that it would have on these patients. They would be influenced by patient feedback as well as by research evidence. They also wanted to know the impact that it would have on practices and on HCP workload:
Not just how many: who? And how, well, obviously you would feedback about how useful they found it but . . .
Well, ideally, we’d like to have clinical data, did [it] improve the HbA1c [glycated haemoglobin]?
I suppose, you know, . . . the impact it has on workload so, you know, what are the drawbacks? Accessibility to how much downtime there was, how often, you know, it kept on going down.
I think it’s more sort of, you know, what’s the demographic of who accessed it . . . Yes, that’s very important.
I guess if you get good patient feedback from it then you’re more likely to recommend it to other patients.
Participant 11, trainee GP (individual interview)
Given the lack of coherence and cognitive participation and expected problems with collective action for both facilitated access and patient access to EMRs, it is not surprising that there were few data on these that mapped to reflexive monitoring. However, participants did suggest that their views on these, particularly facilitated access, could be changed by appropriate evidence:
You’d need to trial it without and with facilitation and if you show facilitation made a big difference then you’d have to argue that was a case to commission somebody to do, to provide that kind of facilitation, mainly, you know, telephone support.
Participant 9, salaried GP (focus group 2)
Discussion
In this qualitative study, NPT clearly provided a useful and comprehensive lens through which to consider issues that would make a web-based self-management programme attractive to HCPs and, hence, promote its use and uptake. We collected data through semistructured interviews, using open-ended questions, and analysed the findings inductively, that is, the themes emerged from the data and only then were mapped onto NPT. Hence, not all constructs of NPT were reflected in the data, but all the data obtained mapped easily onto NPT constructs, which provides reassurance that this theoretical framework was an appropriate choice for our work.
Overall, the data from this study suggested that HCPs would welcome a web-based self-management programme for people with T2DM. Features that would enhance acceptability, uptake and use included a comprehensive approach to patients’ needs, overtly acknowledging, and helping with, the emotional difficulties faced by patients; a well-designed website that would appeal to a wide range of users and that was user-friendly with intuitive navigation; and high-quality evidence-based information.
Participants were much less positive about general practices providing facilitated access to the intervention and had significant concerns about allowing patients access to EMRs.
Methodological strengths of the study included the use of semistructured topic and interview guides, which gave participants the opportunity to discuss areas that they considered important, rather than being limited to areas raised by the facilitator or interviewer. Equally, the inductive approach to data analysis, undertaken by a multidisciplinary team, was a strength.
However, the study had some weaknesses. The snowball approach to recruitment is likely to have led to a pool of participants who were already interested in the topic and had a bias towards promoting self-management for patients. Thus, although we reached thematic saturation fairly rapidly, a different sampling strategy may have yielded a more diverse participant population and a greater range of views.
Despite this, the findings were extremely useful for informing the development of the web-based self-management programme. They confirmed the importance of considering the work of implementation and use during the design phase and we repeatedly considered how the proposed intervention would fit into routine clinical practice, using a combination of the actual data obtained and predictions based on NPT.
The data suggesting that HCPs felt the potential benefits of facilitating patient access would not justify the additional workload prompted us to consider how to reduce that work, while maintaining the benefits that we believed would accrue. In our view, facilitated access was likely to be necessary to ensure patients viewed the programme as an important part of their overall health care, which in turn would improve uptake and use. We also hypothesised that some degree of HCP facilitation could help overcome the digital divide – a question that was explored in more detail in Chapter 9.
Chapter 6 The Healthy Living for People with type 2 Diabetes programme: a web-based self-management programme for people with type 2 diabetes mellitus
Chapter summary
This chapter describes the development of the HeLP-Diabetes programme website (WP C), including determining and creating its content and functionality, through an iterative process that involved a large multidisciplinary team with extensive user input through participatory design. We then describe the intervention, procedures for its maintenance and updating and techniques for promoting engagement.
Background
Theoretical framework
The rationale for developing a web-based self-management programme for people with T2DM was described in Chapter 2, which also set out the theoretical framework underpinning its development, including:
-
Corbin and Strauss’ model54 of the work of living with a LTC, which we used to define the overall content of the programme
-
NPT,56 used to help us consider issues pertaining to implementation throughout the development process
-
a taxonomy of BCTs, which helped us select appropriate techniques within the programme.
We worked within the paradigm of evidence-based medicine, identifying and applying the best-available evidence for treatment of diabetes mellitus and for any decisions made during development (e.g. around maximising acceptability, uptake, usage and effectiveness).
Users
We identified our potential users as people with T2DM, and HCP involved in their care. The work undertaken to identify users’ ‘wants and needs’ was described in Chapters 4 and 5.
Participatory design
Participatory design is a broad term that covers a range of motivation, methods and levels of user involvement. There are two main rationales for adopting a process of participatory design. The first is pragmatic: interventions developed this way are more likely to be acceptable, have better uptake and be effective. 127 Working together in an iterative fashion, developers and users can learn together and optimise system functionality and service quality. Designers are responsible for pointing out technical options, while users provide information about their practices and how they will use the system. 128 The second rationale is a political or moral imperative: those who will be affected by health information technology (IT) systems should have the opportunity to influence their design and implementation. 129 From this perspective, design of health IT systems can be a way of empowering prospective users. 128 We were motivated by both rationales.
Intervention mapping
Intervention mapping is an explicit six-step process for developing complex interventions,87 which was originally developed in the public health context but since has been shown to be appropriate for a wide range of interventions,130–133 including those online. 134,135 It has been successfully integrated with participatory design136 and enables researchers to incorporate multiple sources of data into a single intervention in a transparent and reproducible fashion. 87 The six steps are:
-
needs assessment
-
detailed mapping of programme objectives and their behavioural and environmental determinants
-
selecting theory-based methods, techniques and strategies to modify the determinants of behaviour and the environment
-
producing intervention components and materials
-
planning for adoption, implementation and sustainability
-
creating evaluation plans and instruments.
Intervention mapping helped us think through the stages of development in an orderly fashion. For each stage, we considered how best to combine the principles generated by our theoretical frameworks, the data from our preliminary qualitative work and the input from our participatory design groups. The process of combining these different inputs was by frequent discussions among the core team followed by periods of drafting text and content, which were then discussed with the software engineers, to ensure appropriate functionality. This was an iterative process, with sections of the intervention being drafted, incorporated into appropriate functionality and reviewed by the participatory design panels. The panels also generated ideas for new content and functionality. Once the main outlines of the content and functionality were broadly agreed, we worked with the designer to ensure an aesthetic experience with intuitive navigation. These components are all described in more detail in Methods.
Methods
The aim of WP C was to develop a theoretically informed evidence-based web-based self-management programme for people with T2DM. Specific objectives (in line with objectives 3 and 5 in Chapter 3) were to:
-
set up and work with participatory design panels that reflect our target populations (people with T2DM and HCPs)
-
recruit and work with software and web design experts to turn our concepts and proposed content into a professional, fully functional, aesthetically pleasing and user-friendly programme
-
determine and develop the content and functionality of the program, ensuring it is accessible to a wide demographic, including those with low literacy skills or for whom English was a second language
-
determine and develop the design and aesthetics of the programme
-
ensure that the programme met appropriate information governance and technical requirements for implementation within the NHS.
Our methods for addressing each of these objectives are described in the following sections.
Recruitment of participatory design panels
As in our preliminary qualitative work (see Chapters 4 and 5), we conceptualised our users as HCPs caring for people with T2DM and people with T2DM. Thus, we recruited two complementary participatory design panels: one of HCPs and one of people with T2DM. Both groups were recruited by advertising, which was supplemented by word of mouth. We advertised for the HCP panel through personal contacts, by contacting participants in WP B and by using e-mail lists to contact local clinicians (e.g. the sessional GP contact list, the local locum contact list and the performers list of local CCGs). For the patient panel, we advertised in GP practices, when we had participant identification centre approval, community centres and Diabetes UK groups and sent direct invitations to participants in WP A. Respondents were sent details of what was required, a person specification and details of remuneration and invited to submit an application and attend an interview (for health professionals) or attend a recruitment day (for patients).
Health-care professional participatory design panel
Twenty-four HCPs expressed interest in being part of the participatory group and 17 completed the necessary application process (10 GPs and seven nurses). Interviews were held in November 2011 and nine HCPs (three GPs, two practice nurses and four diabetes specialist nurses) were appointed. Four half-day sessions were held during the development phase and panel members were remunerated with £200 for each session.
Patient participatory design panels
Twenty-four people with T2DM responded to the advertisements for the patient panel and all were invited to attend a recruitment day in October 2011. The day aimed to appoint people to either a regular or occasional participatory group (Table 8 gives details of the two panels). Our rationale for having two types of panel was that we thought the regular panel would be better at helping us work through ongoing problems and check previously proposed solutions, whereas an occasional panel would help to bring a fresh eye to the design, as participants would be less invested in previous decisions.
| User panel | |
|---|---|
| Regular | Occasional |
| Requires long-term commitment | Requires short-term commitment |
| Minimum of 10 meetings over 12 months (roughly once a month) | Minimum of two meetings over 12 months |
| Provide feedback and check improvements have been made | Provide insight from new user’s point of view |
| Heavily involved in programme development | Less involved in programme development |
The criteria for appointing people to the panel included having:
-
personal experience of T2DM
-
good verbal communication skills, including having the abilities to interact positively with a group, explain thoughts, ideas and experiences clearly and listen to other members
-
the ability to critically evaluate proposed materials
-
the ability to problem solve
-
an interest in self-management
-
commitment to the project and to helping us make the best product possible within the available resources.
In addition, we wanted to recruit a panel that varied in terms of age, gender, ethnicity, duration of diabetes mellitus since diagnosis and level of computer skill.
To help us in these aims, we ran three sessions on the recruitment day, dividing applicants between them to obtain manageable numbers in each session. Each session ran as a mock participatory design panel, to ensure that applicants had a chance to experience the tasks they would subsequently undertake and allow us to assess their performance in these tasks. Hence, within each session, the facilitator (a member of the core research team, Charlotte Dack, Jamie Ross or Kingshuk Pal) explained the purpose of the session, and introduced the tasks. These included providing feedback on template designs, engaging in group discussions, using the internet and commenting on website content.
Twenty-two people attended the recruitment day, of whom eight were appointed to the regular panel and 14 to two occasional panels (seven in each).
The regular panel met eight times between November 2011 and October 2012 and each occasional panel met four times. Participants were paid £75 for each meeting attended.
Recruitment of software engineers and website designers
Our previous experience had underlined the importance of selecting software engineers and web designers with whom it was possible to build a productive and constructive working relationship, including open, respectful communication, mutual responsiveness to issues arising during development and flexibility. We were keen to use an ‘agile’ rather than a ‘waterfall’ approach. Agile development relies on high levels of technical skills, a close working relationship between the software developers and the client, substantial user input and the use of simple designs to deliver working software to users at regular intervals. Agile developers accept and welcome changes to the brief that emerged during the development phase. 137 In addition, we required the software engineers and website designers to have a good understanding (and preferably experience of) the challenges of developing online tools for the use of patients in the NHS. Being mindful of issues of sustainability and long-term use, we were reluctant to be tied into bespoke software that could only be maintained or adapted by one company and, hence, had a preference for a company using open-source software. We approached the process of recruiting suitable partners in the following manner.
Specification and tendering
We developed a detailed specification of our requirements and drew up criteria for selecting a company. We then worked with UCL procurement to develop a tender document, which was widely advertised online and circulated to companies known to the eHealth unit that have a track record of producing high-quality software that met usability, functionality and security specifications. Interested companies were invited to an open day at which we provided additional information and encouraged questions and dialogue. Eighteen companies attended, of which 10 submitted completed applications for the tender.
We established an appointments panel, which included an expert external advisor who has experience of developing software applications for use in the NHS. Applications were ranked against the following criteria:
-
a track record and ability to fulfil the –
-
website development and data collection list of duties and responsibilities
-
technical and security requirements
-
design skills in the list of duties and responsibilities
-
-
having proof of highly efficient project management, communication skills and the ability to adhere to timescales
-
showing consideration of issues around long-term sustainability and maintenance
-
costs, as detailed in the model pricing schedule
-
having enthusiasm for the proposed project.
The four companies with the highest scores were invited to interview; the panel included an external advisor on technical and security considerations. The winning company showed insight and evidence of meeting the following criteria:
-
showing an understanding of, and support for, the project’s aims and requirements
-
using open-source software that could be maintained and adapted by any company or software engineer with the appropriate skills
-
having a flexible and agile approach to development
-
having a user-friendly content management system (CMS)
-
having compatibility with NHS systems
-
undertaking a thorough testing programme prior to release
-
having an understanding of the importance of communication and project management
-
having a reasonable budget and approach to risk-sharing.
Once the basic infrastructure of the intervention had been created, a web designer was recruited to help with the look, feel, navigation and usability of the final website. The software company recommended web designers who it had worked with in the past and a designer was appointed who fitted the selection criteria by having:
-
an understanding of, and support for, the project aims and requirements
-
familiarity with the CMS
-
the ability to work closely with the software company and UCL team
-
skills in usability testing and a portfolio that demonstrated ability to create attractive, interactive and highly usable websites.
Determining and developing content
Using the Corbin and Strauss model of living with a LTC sensitised us to the importance of addressing tasks that are relating to emotional and role management, as well as those pertaining to medical management. We summarised the data on wants and needs from our qualitative work with people with T2DM and HCPs (Table 9).
| Feature | Interview participant | |
|---|---|---|
| People with T2DM (n = 20) | HCPs (n = 18) | |
| Likes/content to include |
|
|
| Dislikes/barriers to use |
|
|
| Presentation |
|
|
| Tone |
|
|
| Engagement |
|
|
We combined these data with the Corbin and Strauss framework to provide an overall list of required content (Table 10), which we mapped against the Corbin and Strauss framework and user data to ensure we had addressed all key areas.
| Key self-management tasks (Corbin and Strauss54) | Content from users | Mapped intervention components |
|---|---|---|
|
Medical management Example tasks to be targeted: |
|
Understanding diabetes
|
Staying healthy
|
||
Treating diabetes
|
||
My health record
|
||
|
Role management Maintaining, changing, and creating new behaviours or life roles. For example: |
|
Living and working with diabetes
|
Forum and help
|
||
|
Emotional management Learning to manage the many emotions commonly experienced by someone with a LTC:Intentions |
|
Managing my feelings
|
Forum and help
|
Medical management and behaviour change
The overall schema in Table 10 includes a set of behaviours that users may need to modify to achieve optimal health, namely dietary intake, physical activity, weight management, smoking, alcohol intake and medicines management. As these behaviours are central to achieving optimal health for everyone, not only people with T2DM, we explored the incorporation of relevant existing behaviour change modules. Our criteria included:
-
that the module was available and the intellectual property (IP) owner had consented to its use
-
that the module had been developed using an appropriate theoretical framework and with user input
-
evidence of its clinical effectiveness
-
that it could be easily incorporated into the HeLP-Diabetes programme.
These criteria led us to select the following behaviour change modules:
-
Down Your Drink – a programme designed to help hazardous and harmful drinkers reduce their alcohol consumption to safer levels. 138 A RCT comparing the Down Your Drink programme with a simple website showed that participants in both groups reduced their alcohol consumption by about half, which was sustained at 12 months. However, there was no difference between groups. 139 The IP was co-owned by chief investigator Elizabeth Murray, so it was a good case study for working through the challenges of incorporating a module into the HeLP-Diabetes programme (including IP, governance, software compatibility and adapting the appearance and aesthetics).
-
Positive Online Weight Reduction (POWeR) – a weight-loss programme developed by co-investigator Lucy Yardley using LifeGuide software (version 1, University of Southampton, Southampton, UK), which adopted a CBT-based approach to weight loss. It had been shown to be effective in a RCT. 140
-
Stop Advisor – a smoking cessation programme that was developed using LifeGuide software and shown to be effective. 141 The IP was co-owned by our co-investigator Susan Michie.
These three modules were shared with our participatory design panels, and it was agreed that they should be incorporated. Ideally, we would have liked to modify these modules to make them explicitly relevant to people with diabetes mellitus but, for technical reasons, the only one that we could modify was the Down Your Drink programme. The LifeGuide software proved impossible to convert to the software used in the HeLP-Diabetes programme; therefore, the POWeR and Stop Advisor programme had to be imported as an inline frame (iFrame) to the website and could not be modified.
We were unable to identify appropriate programmes for eating healthily, being more physically active or managing medicines. Hence, we developed modules addressing these behaviours. To do this, we selected BCTs from the Abraham and Michie taxonomy55 that had been shown to be effective. For example ‘goal-setting (behaviour)’, ‘action-planning’, ‘review behavioural goals’, ‘problem-solving’, ‘prompt self-monitoring’ and ‘provide feedback on performance’ were chosen, as these techniques have been associated with positive outcomes of previous behaviour change interventions59,61,142 and are consistent with self-regulation (control) theory. 143 ‘Prompt self-monitoring’ and ‘provide feedback on performance’ were also the most commonly used techniques in interventions that had an impact on glucose control. 38
From the qualitative work, users identified the following additional BCTs as useful and engaging: ‘information provision’ on a variety of areas (antecedents, consequences, etc.), ‘instructions on how to perform behaviours’ (e.g. exercises, injections), ‘social support’, ‘social comparisons’, ‘self-monitoring’ of behaviour and outcomes, ‘prompts’ and ‘adding objects to the environment’.
Applying these techniques led us to develop a content outline for each behaviour change module comprising the following headings: ‘understand’, ‘decide’, ‘plan’ and ‘staying motivated’. The section titled ‘understand’ aimed to help users understand the rationale for targeting each behaviour and how change could be achieved. Hence, the BCTs used included ‘information provision’ about the expected physical and emotional benefits of the change and ‘instructions on how to perform behaviours’. The aim of the ‘decide’ section was to help users decide whether or not to target that particular behaviour. BCTs included ‘self-assessment’ and ‘feedback’ on current behaviour. The ‘plan’ section aimed to encourage users to commit to making the change and consider how they would do it. Hence, BCTs included ‘action-planning’, ‘goal-setting’ and ‘problem-solving’. Finally, ‘staying motivated’ aimed to help users maintain their planned behaviour change and included the BCTs ‘self-monitoring’, ‘review goals’, ‘provide feedback’, ‘prompt self-rewards’ and ‘prompts/reminders’.
Content and functionality, developed by the team in close collaboration with the software and web designers, were shown iteratively to the participatory groups and wider team in workshops to solicit feedback on any changes needed to improve accuracy, acceptability and usability.
Emotional management
The Corbin and Strauss model emphasises the central importance of managing the strong negative emotions that arise from having a LTC and this had been confirmed by our qualitative work: people with T2DM and HCPs had both stressed the emotional burden of diabetes mellitus. On this basis, we took a three-pronged approach to helping users manage these emotions: (1) all content should be presented in a positive and supportive manner; (2) we would include opportunities to learn about the experiences of other people with T2DM; and (3) we would have specific modules aimed at managing emotions.
As the evidence for the use of computerised CBT for treating depression, anxiety and other mental health problems was strong,32,144–146 we decided to include some CBT-based modules. We searched for existing digital interventions that have been shown to be effective in reducing mild to moderate anxiety and depression. Living Life to the Full was chosen as it was freely available, was UK centric (an important factor for engagement to our users), had been developed with user input and been shown to be clinically effective in reducing depression and anxiety. 147 Living Life to the Full teaches people key skills in tackling and responding to the challenges and demands of everyday living. We worked with its developer, Professor Chris Williams, and our participatory design panel to adapt the Living Life to the Full material to make it more suitable for people with T2DM.
Users had said that hearing other people’s experiences and responses to similar challenges could be beneficial and this view was supported by the research,36 which showed that hearing or reading about other people facing similar problems had the potential to enhance perceived social support and coping mechanisms. Moreover, evidence suggests that people with low literacy or low health literacy are more able to understand experiential information embedded in a patient’s story than abstract information. 148–150 The world leader in provision of such personal stories is healthtalk.org, at the time called HealthTalkOnline (HTO), created by the charity Database of Patient Experiences (DIPEx). 151,152 HTO had created a module of patient experiences of T2DM, with videos of about 40 interviews with people from a range of ethnic and socioeconomic backgrounds. The interviews were carefully curated to present a balanced and comprehensive overview of patient experiences. We approached the academic lead for HTO, Professor Sue Ziebland, and the chief executive officer of DIPEx, Luis Carrasqueiro, for permission to incorporate the HTO module on T2DM and were granted this.
We also decided to include a moderated forum, as users had requested this and the evidence suggested that forums can affect a person’s sense of social support as well as providing experiential knowledge on how to cope with conditions and stressful situations. 153 Providing advice to help others has also been associated with an increase in well-being. 154–156
Role management
The Corbin and Strauss model emphasises the profound sense of ‘biographical disruption’57 caused by a LTC and our qualitative work confirmed that this was important to our users. They were particularly interested in content that would enable them to continue with aspects of daily life that they had previously taken for granted, such as social occasions, holidays, travel, insurance, eating in restaurants, cafes or work canteens and working variable hours, for example shift work.
We could find little evidence for effective interventions addressing these issues and, therefore, were mainly guided by our participatory design panel. The resulting content included acknowledgement that the diagnosis of diabetes mellitus can be life-changing and that some previously routine activities can become challenging and provided information on how to manage these. This information ranged from practical advice about managing medication and diet when working shifts, to resources around employment law, to sections from the HTO videos described in Emotional management and additional videos developed in-house, detailing how other people had felt and their methods of managing these challenges.
We also envisaged the forum as a place where users could exchange information about specific practical challenges. 153
Accessibility: guiding principles for writing content
In parallel with determining content, we considered how the content should be presented. We wanted to ensure that the material was accessible to people with low or moderate literacy skills, or for whom English was a second language. As 85% of the UK population have a reading age of ≥ 12 years,157 we aimed for all our written content to have a reading age of 12 years (similar to that of a tabloid newspaper). In response to requests from the patient participatory panel, we ensured that key information was presented as both as text and by video to suit users with a range of preferred learning styles.
Presenting complex information in simple language is a skill, and one that not all academics have mastered. Hence, we arranged training for the core team in writing for the web, given by a person who was a writer, editor and trainer working in publishing, journalism and public relations. This course covered key skills for presenting information clearly and concisely, targeting a reading age that reflected the national average, styling content and engaging readers. As a result of the training, we developed a style guide to ensure that all contributors wrote in the same style and applied the same principles.
The content to be written was then divided up among the team based on their skills and experience; for example, much of the content on medications was delegated to clinicians, whereas content on emotional management was undertaken by the psychologists. First drafts were then circulated to the rest of the team for internal review. Once agreed, content was added to the website (which was not live at this point) and reviewed by the participatory panels of HCPs and patients. HCPs commented on whether or not the content contained any factual errors, conformed with NICE guidance, was realistic in terms of routine care, was likely to be acceptable to GPs, nurses and other clinicians and whether or not anything was missing or could be improved. Patients commented on the look, feel and tone of the website, whether or not it met their needs and the overall layout and navigation. In some cases, this led to rewriting or reformatting content. Finally, all content was reviewed and edited by a professional editor.
Accessibility: film and video
Early development work indicated that written content should also be displayed in video format to make it accessible to a range of learning styles and preferences. The patient participatory group identified one particular video from the Diabetes UK website that they liked and found informative. We contacted Diabetes UK and sought permission to use this video; they agreed to this, provided we included the acknowledgement ‘Reproduced with the kind permissions of Diabetes UK’. Diabetes UK also provided the details of the film’s producer whom we contacted to discuss amendments to the video (largely around removing content related to type 1 diabetes mellitus and adding some content). The producer was very keen to get involved and subsequently wrote, produced and edited all of the videos.
The participatory design group had identified key areas of information that they wanted presented in video format, which guided our decisions of what videos to create. First, they wanted an explanation of what T2DM is. This content was delivered as animation, ‘Explaining type 2 diabetes’. Second, the group wanted videos that explained important aspects of self-management. Four videos were created that combined animation, health professional interviews and personal accounts of people with T2DM, talking about diet, losing weight, physical activity and taking medications. Finally, the participatory group wanted videos that gave examples of exercises that they could perform. We worked with a personal trainer (identified through the PPI panel), and the director to devise a series of 34 exercise videos that demonstrated exercises that could be performed at home. Three people with T2DM appeared in these videos alongside the personal trainer. Videos demonstrated exercises for beginners and reduced mobility, intermediate fitness levels and more advanced fitness levels. All videos were ‘bite-sized’ and users could create a playlist, with continuous playback so they could follow a circuit at home.
Thus, the final selection of videos included key information about the nature of diabetes mellitus, its treatment and the importance of self-management and the experience of having diabetes mellitus and exercise videos.
Web design
We contracted a web designer to make the intervention attractive, user friendly and easy to navigate and to ensure that it satisfied the Royal National Institute for the Blind guidance for accessibility.
Specific objectives were to restyle the default template to improve attractiveness and readability, design an attractive and simple-to-use home page that provided easy access to all of the functionality of the website, ensure the menu structure and navigation tools were simple and easy to use and to create custom artwork (text boxes, images, animation) for relevant articles.
The web designer was also responsible for sourcing and creating images for the website. These were sourced from Shutterstock (Shutterstock Inc., New York, NY, USA) and Getty Images (Getty Images International, Seattle, WA, USA) or taken by the designer. The web designer adhered to the principles laid out in the style guide and also contributed to this style guide.
One technique used in HCI and web design to improve the usability of a digital intervention is the ‘user journey’. 158 This involves working with either real users or prototypical personae, identifying how they will use the proposed intervention and ensuring that they can find what they are looking for quickly and easily. Together with our web designer, we created seven personae who, between them, represented a diverse spectrum of patient characteristics (based on age, gender, ethnicity, duration of diabetes mellitus since diagnosis, health literacy, computer skills, motivation, diabetes treatment and social circumstances) to help illustrate the range of user needs. These user journeys helped guide the preliminary development of the navigation and site layout, which was then reviewed and refined by our participatory design panels.
Iterative testing and piloting
The HeLP-Diabetes programme was extensively tested and piloted throughout the development process and before going ‘live’. Testing and piloting included the following procedures.
Multidisciplinary reviews
All content and functionality were iteratively tested and reviewed by our patient and HCP participatory design panels. HCP review focused on ensuring that the content was consistent with NICE guidelines, evidence from clinical trials and best clinical practice. Additional checking was undertaken by the multidisciplinary diabetes team at Whittington Health, led by Dr Maria Barnard, co-investigator and a consultant in diabetes mellitus. Our multidisciplinary steering group also reviewed and commented on the intervention during development and before it went live.
Usability testing
We also undertook formal usability testing on the near-final (beta) version of the intervention. Users with little or no previous experience of the intervention were observed carrying out a series of predefined tasks. The sessions were recorded using screen capture and audio-recording software. The data from these tests were reviewed by the web designer to optimise the navigation, look and feel of the intervention and improve the usability of the interactive tools for quizzes, videos and goal-setting.
Bug fixing
We developed multiple systems for reporting technical malfunctions and errors. A tool was installed on the website, visible on all pages, that allowed users of the development site to instantly report a problem to the software developers. The report included details of the page being viewed and the operating system and browser being used to allow the conditions leading to errors to be recreated. The main difficulties were from the Internet Explorer 7 and 8 browsers but, as these were commonly used on NHS IT systems, the browsers were actively supported even though the technology was old and heading for obsolescence.
Early prototypes were subjected to intensive internal testing by the UCL team and problems were reported to the software team. Errors that were picked up by the patient participatory panel at home or during workshops were carefully documented and reported to the software company. Weekly meetings with the software company were used to discuss progress and review results of bug fixing.
Editing
Thorough proofreading and editing were essential for credibility and maintaining users’ trust in the intervention,90 as discussed in Chapter 4. We employed a full-time editor for the last 3 months of the development period to check every page for spelling and grammatical errors and to ensure adherence to the style guide.
Piloting
The final testing was undertaken with two people with T2DM registered at the practice where a co-investigator, Kingshuk Pal, worked as a GP. This piloting aimed to test functionality and sign-up procedures in a real clinical context and identify any serious problems that could have an impact on deployment of the intervention in the RCT and implementation study.
Technical specifications and information governance
As set out under Methods, one important objective was to ensure that the programme met the appropriate information governance and technical requirements for implementation within the NHS. This governed many of our choices for the website software and platform.
The HeLP-Diabetes programme was created using the Joomla! (version 2.5, Open Source Matters, New York, NY, USA) CMS. The criteria for selecting a CMS included that:
-
the interface for the content management be intuitive so that the UCL team could be trained to use it
-
the creation of open-source content in the system was widely supported, to minimise risks – that is, development could be taken over by another software company if needed at the end of the contract or if the contract needed to be terminated early, which also supported the requirement for UCL to own the IP and code created as part of the project rather than simply owning a licence
-
there were high levels of security that would enable the final intervention to meet information security standard International Organization for Standardization (ISO) 270001, as required by the NHS and similar bodies
-
the CMS could be used to create attractive, function-rich and easy-to-use websites; a vibrant and stable development community that ensured the CMS would improve and evolve over time and be regularly updated and patched to deal with new security vulnerabilities or other technical anomalies.
The final intervention was hosted in an ISO 27001-certified environment within England and security audits were done, as required by the NHS Information Governance Toolkit. 159 The intervention was run on a LAMP (Linux, APACHE, MijoSQL and PHP) stack outside the NHS N3 national broadband network. Hosting the intervention within the N3 national broadband network environment would have significantly increased development time and costs, which would not have been feasible within our timelines and budget.
Links with the general practice electronic medical records
Our initial application stated that we would link the patient’s EMR with the HeLP-Diabetes intervention and our qualitative work with people with T2DM confirmed that patients would like to have access to selected parts of their record (see Chapter 4). Clinicians were much more hesitant and voiced concerns about security, privacy and the possibility of patients misunderstanding, or being upset by, information in the EMRs (see Chapter 5).
We worked hard to find a compromise that would be acceptable to both sets of users. The final proposal, agreed by our participatory design panels, was that the summary problem list, medication list and results of investigations (once signed off by the GP) could be exported to the HeLP-Diabetes programme.
We were initially successful (in 2012) in establishing an interface with EMRs for patients who were registered with GPs who used the EMIS Health (formerly Egton Medical Information Systems) medical records system, thanks to our co-investigator, Brian Fisher, who was a director of the Patient Access to Electronic Record Systems (PAERS) company. This was a considerable challenge, both technically and from a clinical governance perspective. The system allowed for registered users of the HeLP-Diabetes programme, with their GP’s permission, to access summary data from the EMIS Health EMR, via the PAERS gateway, and upload it into the My Health Record section of the HeLP-Diabetes programme.
However, EMIS Health subsequently (2012–13) updated its software; this update no longer supported the PAERS gateway, meaning that we could no longer link the HeLP-Diabetes programme with EMRs. We explored alternatives, including the Medical Interoperability Gateway (MIG), provided by Healthcare Gateway, which had been charged by the Department of Health and Social Care with arranging and allowing shared access to GP EMRs. However, the MIG business model was aimed at CCGs and similar large organisations, and its costing structure was based on whole CCGs. As we needed access to individual patient records across different CCGs, this was not appropriate and neither was it affordable. Costs quoted to us, including a discount for academic use, were of the order of £50,000 start-up fees followed by £100,000 per annum.
Therefore, we were unable to provide a link to patient EMRs as part of the HeLP-Diabetes programme.
Maintenance and updating
One key feature of the HeLP-Diabetes programme was that it contained information that was up-to-date and reflected current best practice. Moreover, out-of-date content and broken hyperlinks are known to undermine trust90 (see Chapter 4). In addition, Joomla! and the other software used in the intervention were likely to undergo regular upgrades that would affect performance. Therefore, it was essential to have a system for regular updates and good technical maintenance.
We established a maintenance contract with our software design company to cover bug fixes and upgrades to Joomla!, other software, servers and browsers. This contract also allowed us to update content and, within limits, functionality.
To keep the content up-to-date, we established a system of monthly multidisciplinary meetings, including an information scientist based at the local medical library, clinicians (GPs, diabetes specialist nurses), health service researchers, psychologists and PPI representatives (who had been involved in participatory design). The core academic team and the information scientist scanned the literature for topical stories that would interest our users, such as new research about treatments, new guidance from NICE or reports on diabetes care. These news stories were discussed and the team selected two or three to write it up for the website. The criteria for selection included relevance to patients, underlying positive message (e.g. benefits of a new treatment or behaviour change, rather than ‘bad news’ about, for example, complication risks or survival), and that over a period of time we covered a broad range of relevant topics.
When there was important but negative news or research, we were careful to frame it in a way that encouraged and enabled people to avoid negative outcomes. Articles were written by one member of the team and commented on by the PPI members and the rest of the team to ensure that they were accurate, easily comprehensible, conveyed a clear message and would not depress our users. These articles were sent out to registered users in regular newsletters (see Encouraging engagement for more detail) and added to the main intervention. Each time we added a new article to the intervention, we checked that there was no conflict between the new material and any pre-existing material.
In addition to these monthly updates, we checked every page of the website at least annually to ensure factual accuracy, consistency with latest guidance and full functionality.
Major reviews of the intervention were also required, although it was not clear how often these should be scheduled. The intervention was ‘completed’ in early 2013; in 2015, we undertook a major review. The timing of this review was triggered by the publication of the revised NICE guidance for T2DM. For this review, we set up multidisciplinary working groups of PPIs, clinicians, researchers and administrative support. Each working group took several sections of the intervention and, over a series of workshops, reviewed the content, navigation, design, illustrations and functionality and generated lists of changes that were either required or desired. All of the required changes were undertaken, and as many of the desired changes as feasible within the budget and time available.
This sort of major review is expensive and time-consuming, and the frequency of such reviews will be a significant determinant of the ongoing costs associated with long-term dissemination of the programme.
Results
The final intervention was (and is) a very large website, with over 560 web pages.
Content
The overall content was broken down into eight sections:
-
understanding diabetes (145 web pages; information about the nature and causes of diabetes mellitus and how it affects the body)
-
staying healthy (107 web pages; motivational material about how to maintain optimal physical and emotional health and the importance of self-management; new behaviour change modules and previously validated programmes for diet, weight loss, physical activity, smoking cessation, moderating alcohol intake and taking medicines)
-
treating diabetes (70 web pages; information about medications used in diabetes mellitus, including information about indications, side effects and monitoring; importance of managing cardiovascular risk factors as well as glycaemic levels; importance of regular monitoring to prevent retinopathy, neuropathy and nephropathy; and the types and roles of different HCPs in caring for people with diabetes mellitus)
-
living and working with diabetes mellitus (87 web pages; focus on managing social and work situations, such as shift work, parties or holidays; the impact diabetes mellitus has on relationships, including sexual relationships; and possible impact diabetes mellitus can have on emotions and feelings of self-worth)
-
managing my feelings (61 web pages; self-assessment tools for identifying low mood, CBT modules and mindfulness-based approaches)
-
my health record (45 web pages; opportunity to record appointments with HCPs and results of tests or self-monitoring, with opportunities for graphical displays and feedback)
-
news and research (16 web pages; updates about diabetes treatment, in-depth articles about seminal research papers; and information for HCPs, such as NICE guidelines)
-
forum and help (28 web pages; moderated forum; videos of personal stories about diabetes mellitus used with licence from healthtalk.org; and additional resources, including local resources tailored to the CCG).
Each section combined written information with videos and other graphics. There were interactive and tailored components in each section, apart from news and research. Behaviour change and emotional management sections included opportunities for self-assessment, in the form of validated questionnaires with automated feedback that contained recommendations for action. Users could set the programme to send them automated texts or e-mail reminders and alerts when new entries were posted in the forum. They could opt out of the regular engagement e-mails and newsletters described in Encouraging engagement.
More details of the website’s content, with screenshots, are provided in Appendix 1, with a site map in Appendix 2.
Registration and facilitation
Our grant proposal had emphasised that the intervention would be more than just the web-based programme. We conceptualised it as comprising interactions between people with T2DM and their HCP and the web programme. We thought that it was important that patients were introduced to the programme by a HCP, as we thought this would demonstrate that the programme was part of the overall care offered by the NHS and that their HCP felt that they would benefit from using the programme; HCP input could also help overcome the digital divide.
In our initial application, we described three ways in which HCPs could support use of the intervention: (1) initial registration and introduction to the programme; (2) follow-up phone calls to promote use and address any technical difficulties the user was experiencing; and (3) making reference to the programme within consultations, for example by reviewing progress against personal goals, discussing self-monitoring data or suggesting that a patient could benefit from a particular section.
Our qualitative work described in Chapters 4 and 5 showed that we needed to revise this model. Although people with T2DM welcomed HCP input, both they and HCPs felt that our suggestions were unrealistic. Thus, we refined our model for the trial (see Chapter 7), limiting the facilitation to registration and an initial demonstration of the site (undertaken in one 20-minute appointment). For the implementation study (see Chapter 9), we had to refine the model still further, reducing HCP input to a minimum with a 5-minute registration process; even this proved overly burdensome for some practices, leading to the development of a patient self-registration model.
Encouraging engagement
Further encouragement for people with T2DM to engage with the programme came through regular e-mail or (later) text message prompts. E-mails started in November 2013 and consisted of either a short two- or three-line text with a single message and link to the relevant section of the website; or a longer newsletter (of one A4 page), which summarised recent research or news, explained what this meant for people with T2DM and contained a paragraph or two on a specific health promotion or feature of the programme, all with relevant links.
In October 2014, we added text message prompts. These were very brief, with one clear message and a link to the programme.
Examples of the shorter e-mails included a seasonal reminder of the importance of influenza vaccinations for people with T2DM, with a link to the HeLP-Diabetes programme website explaining how and why they were beneficial and reminding them that GPs offered free influenza vaccinations. We sent around three prompts per month – usually two short e-mails or a text message plus one longer newsletter. Users could opt out of receiving prompts.
The procedure for writing newsletters is described above (under Maintenance and updating). The development of the shorter e-mails and text message followed a similar process, with the multidisciplinary team coming up with ideas that were then prioritised in discussion with PPI members. E-mails or text messages were then drafted by one team member and reviewed by the rest of the team and at least two PPI members.
We undertook some formative evaluation of the engagement e-mails, newsletters and text messages, exploring quantitative data on which e-mails or newsletters were opened and whether or not users who opened these subsequently visited the intervention website. These data suggested a small positive effect on engagement. We also undertook usability testing and qualitative interviews exploring which features of the e-mails or newsletters were perceived as interesting or attractive and what features would promote opening them and subsequently visiting the intervention.
These interviews showed that engagement prompts should be short, easy to understand, contain plenty of links to the main intervention, provide non-directive advice, be personalised and contain news and updates around topics of interest to users. The use of bullet points, pictures and bold colours encouraged users to read the prompts and follow the links to the intervention website. Examples of e-mails and newsletters sent can be found in Appendices 3 and 4.
Discussion
It can be seen from the information in this chapter that developing the HeLP-Diabetes programme was resource-intensive, requiring input from a multidisciplinary team that included substantial user representation, and had a strong theoretical underpinning. The HeLP-Diabetes programme took 2 years to develop and requires significant ongoing investment to maintain. We believe that this careful approach, combining participatory design with theoretical underpinning, academic rigour and an agile approach to software and web design, is a key factor explaining the results of the evaluations reported in the following chapters.
Chapter 7 Randomised controlled trial of the Healthy Living for People with type 2 Diabetes programme
Summary
Previous chapters have described the work leading up to the development of the HeLP-Diabetes programme and given a detailed description of the programme itself. This chapter describes the evaluation of the programme in a multicentre individually randomised controlled trial in primary care. The protocol and the statistical analysis plan for the RCT can be found on the project web page on the NIHR Journals Library website [www.journalslibrary.nihr.ac.uk/programmes/pgfar/RP-PG-0609-10135/#/ (accessed August 2018)].
We recruited adults aged ≥ 18 years who had T2DM and were registered with participating general practices. Consenting participants were randomised to receive either the HeLP-Diabetes programme or a simple, information-only, comparator website. We collected data online, with baseline data being collected prior to randomisation. The joint primary outcomes were diabetes control, as measured by glycated haemoglobin (HbA1c) level, and diabetes mellitus-related distress, as measured by the PAID scale. The secondary outcomes were clinical data, emotional state and satisfaction; the health economic outcomes were quality-adjusted life-years (QALYs) and health service usage. Follow-up was at 3 months and 12 months after randomisation, with 12 months the primary outcome point.
We calculated that a sample size of 350 participants being randomised with 85% retained at follow-up would provide 90% power, at the 5% level of significance, to detect a 0.25% difference in HbA1c levels and a 4.0 difference in PAID scores (reflecting the minimal clinically important differences). The analysis compared groups as randomised (intention to treat) using a linear mixed-effects model, adjusted for baseline data with multiple imputation of missing values.
We recruited 374 participants between September 2013 and December 2014. Of these, 185 were allocated to the intervention group and 189 to the control group. Final (12-month) follow-up data were available for 318 (85%) participants for HbA1c levels and 337 (90%) participants for PAID scores. Of these, 291 (78%) and 321 (86%) responses were recorded within the predefined window of 10–14 months. Participants in the intervention group had lower HbA1c levels than those in the control [mean difference –0.24%; 95% confidence interval (CI) –0.44% to –0.049%; p = 0.014]. There was no significant overall difference between groups in mean PAID score (mean difference –1.5 points; 95% CI –3.9 to 0.9 points; p = 0.21), but prespecified subgroup analysis showed that the intervention had a beneficial impact on participants who had been diagnosed more recently (p = 0.004). The authors conclude that this evidence-based theoretically informed self-management programme may be added to the menu of options available for patients with T2DM in the NHS.
The health economic analysis is described in Chapter 8.
Background
The rationale for developing a web-based self-management programme for people with T2DM has been addressed in Chapter 2. Here, we focus on the rationale for the selected trial methods, including the decisions on the population eligible, individual versus cluster randomisation, the choice of two primary outcomes and web-based data collection. We also comment on the closure of the MRC’s GPRF and the impact this had on the conduct of the trial.
Our specification of the trial population reflected the overall goal of the programme grant, which was to develop a self-management programme that could be used by the great majority of people with T2DM in the UK. Hence, we deliberately kept the inclusion criteria wide and the number of exclusion criteria to a minimum compatible with ethical obligations (e.g. the ability to provide informed consent) and pragmatic considerations (e.g. the physical and mental capacity to use a web-based programme on a computer). There were potential disadvantages to this approach, including a floor effect, in which recruited patients were already so well controlled that there was little or no room for improvement, but we thought this risk was worth taking to maximise the likelihood of the results being generalisable to the relevant population (people with T2DM registered with a GP in the UK).
We debated whether or not the trial should be cluster randomised or individually randomised. Cluster randomisation had the potential to make recruitment easier, as all patients in participating practices could be referred to the allocated intervention; however, we thought it had greater potential to introduce bias, as GPs would know which intervention patients received, which could influence referral patterns, and patients would know which intervention they received, which could influence participation rates. The main risk of bias with individual randomisation was the potential for contamination, in which patients from the same household or social circle were randomised to different interventions and exchanged usernames and passwords. This risk was monitored, by looking for participants with similar names and addresses and by allowing for this in the sensitivity analyses.
The choice of joint primary outcomes was also considered at length. The rationale for two primary outcomes was that these outcomes reflected the twin aims of the intervention: to improve diabetes control and to reduce diabetes mellitus-related distress. Around 40% of people with T2DM have significant levels of distress, which has a severe impact on their quality of life,160 and diabetes mellitus-related distress is an important outcome for patients. 161 Our PPI panel was clear that this should be a primary outcome, and the importance of emotional well-being for people with diabetes mellitus has been described in Chapters 2 and 4. In contrast, a number of HCPs stated categorically that they were only interested in patients’ levels of HbA1c as a measure of diabetes control and that a reduction in distress without an improvement in diabetes control would not be considered a worthwhile outcome and would not lead them to promote or adopt the HeLP-Diabetes programme in their clinical practice. By adopting both as joint primary outcomes, we were able to reflect the priorities of both groups of stakeholders and to ensure that the results of the trial could be compared with alternative self-management programmes and included in meta-analyses, as HbA1c level is almost universally reported in trials of self-management interventions for diabetes mellitus. In line with previous trials in this area,162 we decided to adopt both as co-primary outcomes and to test both at a 5% level of significance. 163
Much of the trial was conducted online. Online trials have several advantages, including reduced costs, as participants enter their self-reported data directly into a web-based form, which is automatically transferred to the trial database, thereby avoiding the need for double data entry. 164 Online data collection also has the potential to reduce the number of missing data, as the questionnaires can be designed to not allow participants to progress until all questions on a page are completed. The main disadvantages with online trials are a difficulty in characterising the population from which the sample was recruited and poor retention. 164
Our selected design aimed to maximise the benefits of online data collection while minimising the disadvantages. By recruiting through general practice, we had a defined population and participants had face-to-face contact with the practice research nurses, thus engendering the feeling of belonging to an important endeavour that has been identified as promoting retention to trials. Furthermore, our design dictated that patients could only be randomised once their baseline data, collected using the web-based form, were complete, thus ensuring a more engaged trial population.
The main disadvantage of working with general practices was the problem of blinding nurses who were involved in data collection. Our original plan had been to run the trial through the MRC’s GPRF. Practices in the GPRF employed additional nurses to act as research nurses. These nurses were trained in research methods and good clinical practice, and understood the importance of obtaining informed consent, remaining blind to intervention allocation and obtaining complete follow-up data. Unfortunately, the GPRF closed between the NIHR decision to fund the overall programme grant and the start of the trial. Its work was subsumed into the PCRN. Practices in the PCRN were often less well-resourced than GPRF practices and many did not have sufficient nursing staff for one nurse to act as a practice nurse (training participants in use of the intervention and providing routine clinical care) and one to act as a research nurse (blind to allocated intervention and collecting follow-up data). In many practices, the decision to participate in research was made by the GPs, but the work was undertaken by nurses. These nurses did not always have any interest in, or understanding of, research methods and, as the research component of their job was often additional to their clinical work, it often took low priority. In some areas the PCRN had employed and trained research nurses but, as the goal of the PCRN was to facilitate recruitment to studies, these nurses were seldom able to help with follow-up.
We addressed these challenges by adopting a flexible approach to working with practices and using funds that had been allocated to the GPRF for data collection and quality control. When practices had two nurses, we reimbursed the practice for the work of data collection and follow-up. Recruitment costs were covered by service support costs. When practices had only one nurse, we negotiated with the local PCRN to identify the best use of available resource. Often this resulted in the PCRN nurse undertaking recruitment and initial training of participants, while the practice nurse undertook follow-up data collection. Occasionally, we directly reimbursed the PCRN nurse for undertaking follow-up. We also communicated closely with the practice nurses in participating practices and tried to find individual solutions for each practice (e.g. offering overtime payments or finding some other incentive that was acceptable to the practice and the nurse).
Aims and objectives
The aims of the trial were to meet the programme’s evaluation objectives (see Chapter 3) to determine the:
-
effect of the HeLP-Diabetes programme on clinical outcomes and HRQoL in people with T2DM
-
incremental cost-effectiveness of the intervention compared with usual care from the perspectives of health and personal social services and wider public sector resources.
The hypothesis was that the use of the intervention would improve diabetes mellitus-related quality of life and health status.
The health economic analysis is reported in Chapter 8.
Methods
Design
The study was a multicentre, two-arm individually randomised controlled trial in primary care.
Setting
The setting was general practices in England.
Participants
Participants were adults, aged ≥ 18 years, with T2DM, registered with participating general practices. In order to maximise the ability to generalise from the results of this pragmatic trial, exclusion criteria were kept to a minimum. We excluded people who were unable to provide informed consent, for example, because of psychosis, dementia or severe learning difficulties; terminally ill patients with < 12 months’ life expectancy; those unable to use a computer as a result of severe mental or physical impairment; those unable to use the intervention because of insufficient mastery of spoken or written English; and those who were currently participating in a trial of an alternative self-management programme. Participants did not need home internet access or prior experience of using the internet to take part. Those with previous or current experience of self-management education were eligible to participate.
Recruitment
Recruitment took place in two stages. First, we recruited practices through research networks, including the PCRN and the North Central London Research Consortium. Second, once a practice had agreed to participate and completed set up procedures, participant recruitment started.
Patient recruitment followed standard opt-in procedures. Each practice had a register of patients with T2DM, as required by the QOF. A nurse or other qualified health professional reviewed the EMR of each patient on this register to screen out those who were ineligible. All of those who were remaining were sent a letter from their GP inviting them to participate in the study. A participant information sheet, consent form, expression of interest and stamped addressed envelope were included. Patients who were interested in participating were asked to return the expression of interest form to the trial manager.
On receipt of expressions of interest, the trial manager contacted the practice research nurse who then offered the patient an appointment at the practice. This provided patients with an opportunity to discuss the pros and cons of participation and, if they wished to proceed, sign the consent form. Baseline clinical data were obtained either at this appointment or a subsequent one. After signing the consent form, patients were asked to complete the self-report baseline data and patients were randomised only once all baseline forms were completed. Randomisation marked the point of study entry.
Randomisation
Randomisation was performed centrally using a web-based randomisation system provided by Sealed EnvelopeTM (London, UK; www.sealedenvelope.com). Randomisation was at the level of the individual participant and conducted using random permuted blocks of sizes 2, 4 and 6, stratified by recruitment centre. The practice nurse was informed which arm the participant had been randomised to so that those in the intervention arm could be offered the training appointment.
Intervention
The intervention consisted of facilitated and supported access to the HeLP-Diabetes programme. There were three components to the supported access: (1) an introductory training session, (2) supportive follow-up telephone calls and (3) ongoing discussion of patient’s self-management goals in routine appointments for diabetes mellitus-related matters.
In the training session, practice nurses registered the patient on either the intervention or the comparator website and gave the patient a booklet containing the unique resource locator (URL) for the programme, the participant’s log-in details and information about the content of the website and how best to use it (a copy of the booklet for the intervention site is available in Appendix 5; a similar booklet was provided for the comparator site). Nurses showed the patient how to access the website and introduced them to the main content areas. The nurse was asked to discuss with the patient what their most pressing needs were and use this to guide them towards certain sections, such as improving diet, being more physically active or managing emotions. Follow-up telephone calls were offered to support the patient in the use of the programme. Nurses and doctors in participating practices were asked to refer to the programme in consultations with participating patients and to integrate information from the programme into management plans.
The HeLP-Diabetes programme was a theoretically informed web-based programme for which the overall goals were to improve health outcomes and reduce diabetes mellitus-related distress. 165 Overall, content was guided by the Corbin and Strauss model of managing a LTC, which posits that patients must undertake medical, emotional and role management. 54 It was developed using participatory design principles, with substantial input from users, defined as people with T2DM and HCPs caring for such patients. All content was evidence based, drew on evidence on management of diabetes mellitus and promoted behaviour change and emotional well-being.
The HeLP-Diabetes website contained information sections on diabetes mellitus, how diabetes mellitus is treated, possible complications of diabetes mellitus, possible impacts that diabetes mellitus can have on relationships at home and at work, dealing with unusual situations such as parties, holidays, travelling or shift work, and what lifestyle modifications will improve health. Further sections addressed skills and behaviour change, including modules on eating healthily, losing weight, being more physically active, smoking cessation, moderating alcohol consumption, managing medicines, glycaemic control and blood pressure control. Users could set the programme to send themselves reminder text messages or e-mails and could specify the content and frequency of such reminders.
The third strand of components focused on emotional well-being, with self-help tools based on CBT and mindfulness. There were multiple personal stories (used with the licence from HTO, now known as healthtalk.org, www.healthtalk.org), and a moderated forum. Participants were free to use the programme as much or as little as they chose. Engagement was promoted through regular newsletters, e-mails and text messages containing updates on latest diabetes mellitus-related research or practice, seasonally relevant advice (e.g. on fasting during Ramadan, benefits of influenza vaccinations), and links to specific relevant parts of the programme. Two or three prompts were sent each month, although users could opt out of receiving them. For more information about the HeLP-Diabetes programme, e-mail and text messages prompts see Chapter 6.
Comparator
From a NHS perspective, the important research question was whether or not the proposed intervention could improve health outcomes when compared with current practice. However, to improve acceptability to participants and help maintain blinding, all participants had access to a website. Participants in the control arm were given access to a simple information website, based on the information available on the Diabetes UK (www.diabetes.org.uk) and NHS Choices (www.nhs.uk) websites. These participants were also given a booklet with a URL and user log-in details, but did not have an introductory session with the nurses, as the site was very limited and the control website did not need an introduction or training for its use.
Outcomes and outcome measures
Parts of this section have been adapted from Murray et al. 166 © 2015 Murray et al. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Primary outcomes
The outcomes to be measured reflected our aims of improving clinical outcomes and HRQoL. We selected two primary outcomes: HbA1c levels and diabetes mellitus-related distress, as measured by the PAID scale. 167,168 The PAID scale has 20 items focusing on areas that cause difficulty for people living with diabetes mellitus, including social situations, food, friends and family, diabetes mellitus treatment, relationships with HCPs and social support. It has been the subject of a number of reviews169–173 comparing available quality-of-life measures for diabetes mellitus. Eigenmann et al. 170 assessed available measures against criteria of reliability – content, face, construct, criterion and convergent validity; responsiveness to change; interpretability; response burden; acceptability and availability – and concluded that the PAID scale was one of three measures that met all criteria. It is sensitive to change and has been widely used to evaluate self-management programmes for people with T2DM, including in the influential DESMOND trial. 15
Secondary outcomes
Secondary outcomes were selected to reflect the proposed pathway of action of our intervention and allow for health economic analysis. They can be categorised as clinical, patient-reported or economic outcomes.
The clinical outcomes were:
-
systolic blood pressure (SBP) and diastolic blood pressure (DBP)
-
body mass index (BMI)
-
total cholesterol and high-density lipoprotein cholesterol (HDL-C) (not fasting)
-
completion of ‘nine essential processes’ (weight, blood pressure, smoking status, measurement of serum creatinine, cholesterol and HbA1c levels, urinary albumin and assessment of eyes and feet) – data were obtained from notes at the 12-month follow-up point for data before randomisation (12 months prior) and after randomisation (12 months after).
The patient-reported outcomes were:
-
depression and anxiety, as measured using HADS13
-
diabetes mellitus-related self-efficacy measured using DMSES174
-
satisfaction with treatment, measures using the status and change versions of the Diabetes Satisfaction with Treatment Questionnaire (DTSQ). 15
The economic outcomes were the EuroQol-5 Dimensions (EQ-5D) and health service use.
In addition, we used automated software to automatically record each participant’s use of the intervention (date and time of log ins and pages visited).
Data collection
Each practice provided information on the number of invitation letters sent out and the age and gender of the patients invited. Baseline data collection covered patient demographic, clinical and other descriptive data. Demographic data consisted of age, gender, highest educational attainment, ethnicity, current employment status, presence or absence of home internet access, level of expertise in computer use and current or previous participation in DSME.
Baseline clinical data obtained from the medical record included:
-
the date of diagnosis of diabetes mellitus
-
HbA1c levels, blood pressure, total cholesterol levels, HDL-C and smoking status at time of diagnosis
-
the presence or absence and date of diagnosis of complications of diabetes mellitus, including ischaemic heart disease, myocardial infarction, congestive cardiac failure, atrial fibrillation, peripheral vascular disease, amputation, cerebrovascular disease, retinopathy, renal failure and neuropathy
-
a list of current medications.
Additional clinical data on height (cm), weight (kg), SBP and DBP, current smoking status and current levels of HbA1c, total cholesterol and HDL-C were obtained during the baseline visit.
Baseline patient-reported outcomes were PAID score, HADS score, DTSQ score, DMSES score and the EuroQol-5 Dimensions, three-level version (EQ-5D-3L) score.
The collection of follow-up data was at 3 and 12 months, with 12 months as the primary outcome point. The window for 3-month data was 60–120 days post randomisation (90 ± 30 days) and for the 12-month data was 305–425 days (365 ± 60 days).
Health service use was recorded for the past 6 months at baseline, the past 3 months at the 3-month follow-up and the past 9 months at the 12-month follow-up. At the 12-month follow-up point, we extracted the data on completion of the nine essential processes for the 12 months before to randomisation and the 12 months after randomisation.
Standard operating procedures (SOPs) covered every aspect of data collection and nurses were trained in these procedures. Adherence to the SOPs was monitored. Participants completed self-reported questionnaires (demographics, the PAID scale, HADS, DMSES, DTSQ and EQ-5D-3L) online, prior to the nurse recording clinical outcomes and taking blood for HbA1c levels and lipids to be tested for. The nurse entered all clinical data directly into the online database and extracted health service use data from clinical records.
Concealment of allocation and protection against bias
After baseline data had been obtained, randomisation was performed centrally. Allocation was not revealed to the participants, who were informed only that the trial would compare two forms of web-based education for diabetes mellitus; in order to maintain blinding of participants, they were not given details of the differences between the two websites. Practice nurses were provided with similar-looking booklets for the comparator and intervention websites. Potential contamination was monitored by recording participants with similar family names and identifying those with the same addresses. When this occurred, it was dealt with in the analysis by reporting the extent and undertaking a sensitivity analysis excluding these individuals.
The risk of bias in the collection of follow-up data was minimised by using standardised data collection instruments, with participants completing self-assessment questionnaires before seeing the nurse to record clinical data. Nurses collecting the clinical data were trained to adhere to detailed SOPs developed in collaboration with UCL’s PRIMENT Clinical Trials Unit. Blood pressure was recorded using automated electronic sphygmomanometers. At the 12-month follow-up point, we extracted the data on completion of the nine essential processes for the 12 months before to randomisation and the 12 months after randomisation to avoid triggering behaviour change among the study nurses. Estimations of HbA1c and blood lipid levels were undertaken by the local hospital laboratory used by each participating practice.
Blinding of staff involved in data collection was maintained by having two nurses at each participating practice. One nurse (usually a practice nurse) was not blinded and was responsible for introducing participants in the intervention group to the intervention website. The other nurse (a different practice nurse or a specialised research nurse) was responsible for data collection at follow-up, with a blinded researcher collecting follow-up data by telephone from persistent non-responders.
Adherence and loss to follow-up
Fidelity of the intervention was promoted and monitored through automatic recording of the use of the intervention and comparator websites. Practice nurses were trained in the procedures for facilitating access and provided with laminated booklets to remind them of each stage of the process.
Every effort was made to promote follow-up, which was co-ordinated by the trial manager centrally. For the 12-month patient-reported data, an automated e-mail was sent to each participant from the trial website containing a hyperlink that took the participant directly through to a questionnaire on the data collection website, with data entered using this link being automatically connected to the participant identification number. This link remained active for 120 days from when first sent. Up to three automated reminders were sent at 15-day intervals if the participant had not completed the questionnaires. Fifteen days after the third automated reminder, persistent non-responders were sent a personal e-mail from the trial manager’s e-mail account. This e-mail also contained the hyperlink that would take participants through to the data collection website, linked to their participant identification number. After a further 7 days, non-responders were sent a letter through the post, referring to the link sent the previous week and also containing a paper copy of the primary outcome measure (the PAID scale), with a letter encouraging online completion of all the measures but, failing that, asking for completion of the paper version of the PAID scale, with a stamped addressed envelope for return to the trial manager. If there was no response after a further 10 days, the trial manager called the participant and obtained the PAID score over the telephone.
The procedures for the patient-reported data at 3 months were similar but less rigorous. Only two automated reminders were sent, followed by a personal e-mail and a letter through the post.
Practice or research nurses, blinded to allocation, were asked to collect the clinical data within the window period, and were reminded to do so by the central trial team.
When a participant withdrew from the trial before the final follow-up, the date of withdrawal and reason for withdrawal were recorded.
Sample size
We hypothesised that use of the intervention would improve both PAID scores and HbA1c levels. The analyses gained power through adjustment for baseline levels, which accounts for the correlation between baseline and follow-up levels. We back-calculated the relevant effective SDs from a previous trial as SD 0.676% for HbA1c level and SD 10.75 points for the PAID score,175 which were substantially lower than the SDs of cross-sectional measures of around 1.4% and 16 points, respectively, because of the correlation between baseline and subsequent measures. We intended to recruit 350 participants; with attrition of up to 15%, we expected to recruit at least 300 participants for the primary analysis, a sample size that would have given us 90% power to detect an average difference in the PAID score of 4.0 points and 90% power to detect a difference of 0.25% in HbA1c level. These are both small effect sizes; therefore, the trial management group decided that, as HbA1c levels and PAID scores are co-primary outcomes measuring very different aspects of the T2DM condition, both should be tested at a 5% significance level.
Analysis
The analysis followed a prespecified analysis plan, based on comparing the groups as randomised (intention to treat). The analysis plan was approved by the trial steering committee before unblinding and uploaded to the trial website. Only HbA1c levels and PAID scores measured within a 10- to 14-month window following randomisation were used in the primary analysis. Missing 12-month outcomes were imputed using multiple imputation and baseline and other outcome data (e.g. 3-month data and final follow-up data collected outside the 10- to 14-month window). Descriptive statistics of the baseline and 3-month outcomes were summarised by randomised group, with a two-sample t-test used to test differences in mean outcomes at 3 months for those individuals in whom the outcome was measured.
A linear mixed-effects model with random centre effects was used to analyse each of the 12-month primary outcomes separately, adjusting for the baseline level of the outcome, age, gender, previous participation in self-management programmes, pre-existing cardiovascular disease and time since diagnosis of diabetes mellitus. Secondary outcome measures were analysed similarly using generalised linear mixed models. Effect modification analysis for the co-primary outcomes was undertaken by baseline glycaemic control (HbA1c level outcome only), baseline PAID score (PAID outcome only) and duration of diabetes mellitus since diagnosis, treating all potential effect modifiers as continuous. The interaction between randomised group and each effect modifier was included in the model separately and assessed using a test of linear trend. The magnitude of effect modification was illustrated by splitting baseline HbA1c level into two subgroups, < 7.5% and ≥ 7.5%, and by splitting baseline PAID score and the duration of diabetes mellitus since diagnosis above and below the median.
Missing data
Multiple imputation using chained equations was used as the primary method to account for missing data in both baseline and follow-up data. 176 A set of imputation models was specified, one for each variable with missing data. Each variable was then regressed on all other variables, including completely recorded baseline and follow-up variables, and stratified by randomised group. Imputations were performed using predictive mean matching, using the five nearest neighbours to the prediction as a set to draw from. The full list of variables considered in the multiple imputation using the chained equations approach is shown in Table 11, together with the number of missing values for each variable and time period.
| Variable | Time point (number of missing values) | ||
|---|---|---|---|
| Baseline | 3 months | 12 months | |
| HbA1c level | 5 | 64 | 56 (83 within 10–14 months)a |
| PAID score | 0 | 54 | 37 (53 within 10–14 months)a |
| SBP | 0 | 57 | 68 |
| DBP | 0 | 57 | 68 |
| BMI | 2 | 58 | 69 |
| Total cholesterol | 2 | 68 | 75 |
| HDL-C | 12 | 73 | 76 |
| Completion of nine essential processes | 69 | – | 69 |
| HADS score | 0 | 74 | 107 |
| DMSES score | 0 | 73 | 109 |
| DTSQ score | 0 | 77 | 109 |
| Age | 0 | – | – |
| Sex | 0 | – | – |
| Duration of diabetes mellitus since diagnosis | 4 | – | – |
| History of cardiovascular disease | 0 | – | – |
| Attending any other self-management class | 0 | – | – |
| Smoking status | 0 | – | – |
| Number of visits to the website | – | – | 0 |
| Number of web pages visited | – | – | 105 |
| Average time per visit | – | – | 105 |
As only measurements within a 10–14 month window were used within the main analyses of HbA1c levels and PAID scores, the following imputation procedure was implemented for these two co-primary outcomes. The 12-month measurements were divided into those measured within 10–14 months (the primary outcome variable) and those that were measured outside 10–14 months (a variable used for imputing only). For HbA1c level, two additional variables were created for use within the imputation model:
-
the time in days from randomisation that the 12-month HbA1c level measurement was actually taken for values inside of the window (and set to 365 days for measurements taken outside the window period)
-
the time in days from randomisation that the 12-month HbA1c level measurement was actually taken for values outside the window period (and set to missing for measurements taken within the window period).
The first of these variables gives the desired time for imputing HbA1c level measurements when they are missing, whereas the second gives information on how far outside the window the actual measurements were taken. Corresponding variables were created for the 12-month PAID score measurement. Finally, two additional variables were created defining the time in days at which HbA1c level and the PAID score were measured at 3 months. All variables were included within the chained equations and imputed when necessary.
Forty imputed data sets were created, the analysis models were fitted to each imputed data set separately and the estimates were pooled using Rubin’s rules.
Causal analyses
The intention-to-treat analysis was supplemented by a complier-average causal effect (CACE) analysis,176,177 in an attempt to investigate how the clinical effectiveness of the intervention was mediated through frequency of website usage. In particular, it was important to understand whether or not prolonged usage of the website modified the efficacy of the intervention. As website usage was measured post randomisation, a naive analysis of correlating usage with outcomes in the intervention group may give biased and misleading results, as there may be unmeasured confounders that are also correlated with the outcomes that distinguish the motivated users who regularly log in from the less motivated ones. Therefore, causal analyses using instrumental variables were used to determine the effect of website usage on outcomes. This approach preserves randomisation (i.e. provides a comparison independent of observed and unobserved confounders). ‘Usage’ was defined as the proportion of follow-up (rescaled as the number of days in a year) that the HeLP-Diabetes website was accessed. Usage of the intervention website in the control group was set to zero.
This main underlying assumption of the causal analysis is that the effect of randomisation to the HeLP-Diabetes intervention on the 12-month outcomes occurs only through use of the website (Figure 5, in which WU is website usage, Y is 12-month outcome, e.g. for HbA1c level or the PAID score, and Z is the randomised intervention). This relies on the ‘exclusion restriction’ assumption that the HeLP-Diabetes intervention has no effect when usage is zero (i.e. for individuals who never log in). Hence, randomisation is assumed to be an instrumental variable.
FIGURE 5.
Causal model for CACE analysis. WU, website usage; Y, 12-month outcome (HbA1c level or the PAID score); Z, the randomised intervention.

Causal model assuming no direct effect of intervention (complete mediation through website usage). In this causal model, randomisation (Z) is the instrumental variable, which acts on the outcome (Y) exclusively through website usage (WU).
Another assumption in the CACE analysis was that the control website was unlikely to be clinically effective and, therefore, usage in the control group was ignored in the model. A structural mean model was fitted using the observed level of compliance and treating randomisation as an instrument (i.e. assuming it is independent of both observed and unobserved confounders and only affects the outcomes through its effect on website usage).
Potential contamination was monitored by recording participants with similar family names and identifying those with the same addresses. When this occurred, it was dealt with in the analysis by reporting the extent and undertaking a sensitivity analysis excluding these individuals.
A number of other sensitivity analyses were performed to assess the robustness of the primary analyses: (1) performing two complete-case analyses disregarding outcomes measured outside 10–14 months and 11–13 months post randomisation; (2) repeating the analysis using multiple imputation of baseline covariates only and (3) fitting linear models excluding centre random effects.
Results
Recruitment took place between September 2013 and December 2014. A total of 6578 invitations were sent out, resulting in 669 expressions of interest. Of these, an initial 421 patients consented to participate, but 47 did not fully complete their baseline questionnaires and, therefore, were not randomised and did not enter the study. A total of 374 participants were randomised, of whom 86% (n = 321) provided data for the PAID scale and 78% (n = 291) had HbA1c levels measured within 10–14 months of randomisation. Additional final outcome data, obtained outside the 10- to 14-month predefined window, were available for a further 27 participants for HbA1c level and 16 participants for PAID score (Figure 6). Data obtained outside the 10- to 14-month window were not used directly in the primary analysis but were entered into the imputation model.
FIGURE 6.
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram. a, Withdrawn from the trial before 60 days; b, defined as a visit 60–120 days after randomisation; c, withdrawn from the trial between 60 and 304 days; and d, defined as a visit 300–420 days after randomisation.
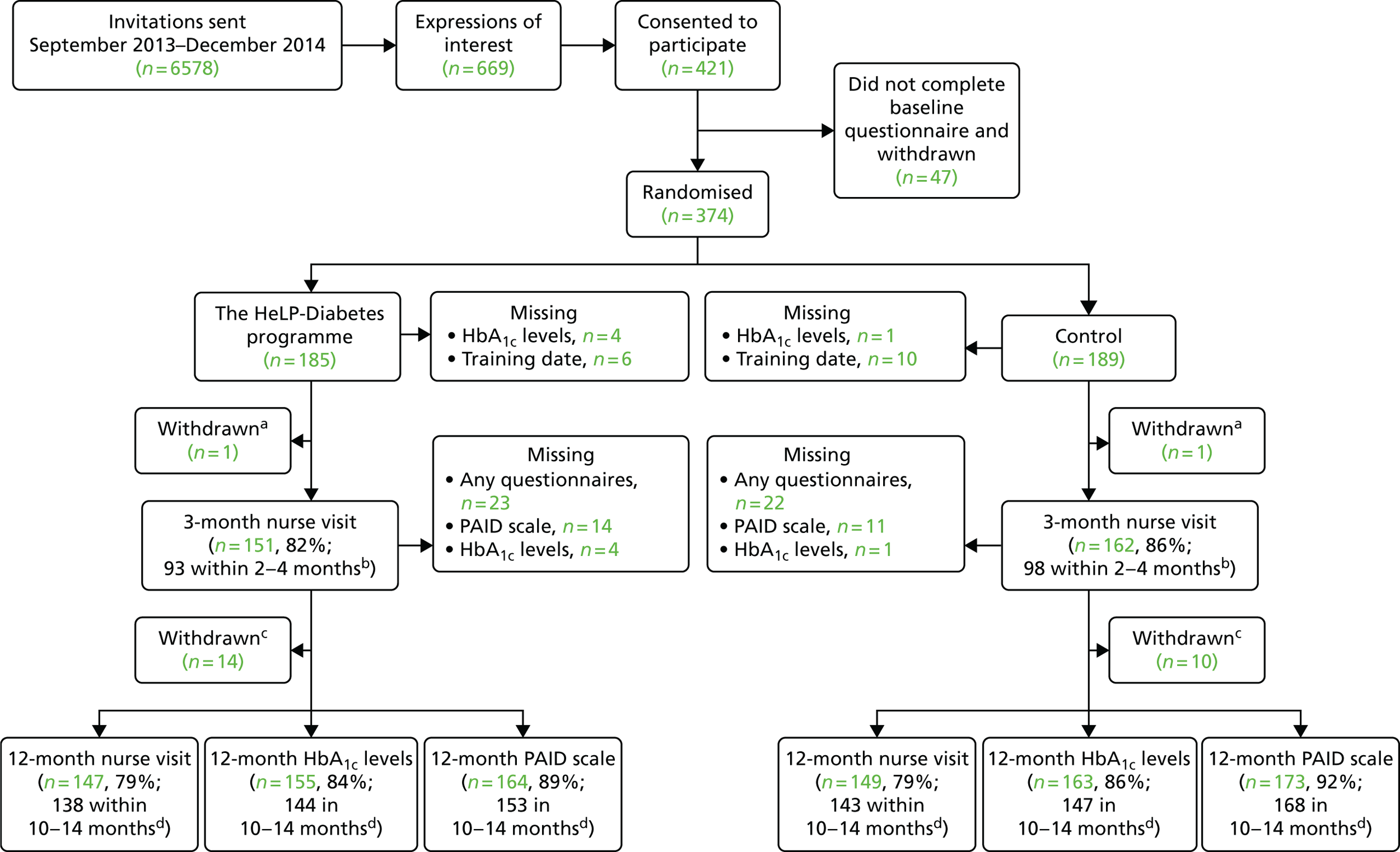
Baseline demographic and clinical characteristics are shown in Table 12. The mean age was nearly 65 years; over two-thirds (n = 258, 69%) of participants were male, and most were white British (n = 300, 80%). Just over half (n = 210, 56%) of the participants rated themselves as experienced computer users. Around one-third (n = 134, 36%) of the participants had been diagnosed for < 5 years, with a further one-third (n = 115, 31%) having been diagnosed between 5 and 9 years ago. Overall, this was a population with well-controlled diabetes mellitus at baseline: mean HbA1c level was 7.3% (56 mmol/mol) and mean SBP and DBP were 135 mmHg and 78 mmHg, respectively. Self-reported levels of distress were low, with a mean PAID score of 19 points.
| Characteristic | Treatment group | Number missing | |
|---|---|---|---|
| Intervention (n = 185) | Control (n = 189) | ||
| Age (years) at randomisation, mean (SD) | 64.9 (9.5) | 64.7 (9.1) | 0 |
| Male gender, n (%) | 127 (69) | 131 (69) | 0 |
| Ethnicity, n (%) | |||
| White English, Welsh, Scottish, Northern Irish, British | 151 (82) | 149 (79) | 1 |
| Indian | 12 (6) | 8 (4) | 0 |
| Other | 21 (11) | 31 (16) | 0 |
| Experience with computers, n (%) | |||
| None | 5 (3) | 4 (2) | 0 |
| Basic | 75 (41) | 80 (42) | 0 |
| Experienced | 105 (57) | 105 (56) | 0 |
| Smoking status, n (%) | |||
| Current smoker | 14 (8) | 14 (7) | 0 |
| Former smoker | 94 (51) | 86 (46) | 0 |
| Never smoker | 77 (42) | 89 (47) | 0 |
| Time since diagnosis (years), n (%) | |||
| 0–4 | 70 (38) | 64 (34) | 4 |
| 5–9 | 55 (30) | 60 (32) | 0 |
| 10–14 | 40 (22) | 40 (21) | 0 |
| ≥ 15 | 18 (10) | 23 (12) | 0 |
| Attending any other self-management class, n (%) | 4 (2) | 4 (2) | 0 |
| Clinical measures, mean (SD) | |||
| SBP (mmHg) | 135 (17) | 135 (17) | 0 |
| DBP (mmHg) | 78 (11) | 77 (10) | 0 |
| Total cholesterol (mmol/l) | 4.11 (1.03) | 4.18 (0.98) | 2 |
| HDL-C (mmol/l) | 1.24 (0.31) | 1.25 (0.36) | 12 |
| Total cholesterol/HDL-C ratio, mean (SD) | 3.43 (1.09) | 3.52 (1.03) | 13 |
| HbA1c level (%) | 7.26 (1.25) | 7.35 (1.37) | 5 |
| HbA1c levels (mmol/mol) | 56 (14) | 57 (15) | 5 |
| BMI score (kg/m2) | 30.1 (5.3) | 29.6 (5.2) | 2 |
| Questionnaires, mean score (points) (SD) | |||
| PAID scale (0–100) | 18.1 (17.1) | 19.9 (19.9) | 0 |
| HADS (0–42) | 9.28 (6.47) | 9.12 (7.52) | 0 |
| Anxiety scale (0–21) | 4.92 (3.70) | 5.21 (4.20) | 0 |
| Depression scale (0–21) | 4.36 (3.48) | 3.91 (3.73) | 0 |
| DMSES (0–150) | 98.6 (33.9) | 103.7 (32.4) | 0 |
| DTSQ (0–48) | 32.1 (7.3) | 32.0 (7.2) | 0 |
| Completion of nine essential processes in the previous 12 months, n (%) | 97 (64) | 96 (62) | 69 |
At 3 months, there were no significant differences in the mean outcomes between groups on any of the outcome measures, among individuals with completed 3-month outcomes (Table 13).
| Clinical measures | Treatment group | p-valuea | Number missing | |||
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| n | Mean (SD) | n | Mean (SD) | |||
| SBP (mmHg) | 152 | 133 (16) | 165 | 134 (17) | 0.423 | 57 |
| DBP (mmHg) | 152 | 76 (10) | 165 | 75 (9) | 0.531 | 57 |
| Total cholesterol (mmol/l) | 149 | 4.17 (0.97) | 157 | 4.16 (1.04) | 0.924 | 68 |
| HDL-C (mmol/l) | 147 | 1.29 (0.37) | 154 | 1.24 (0.37) | 0.304 | 73 |
| Total cholesterol/HDL-C ratio | 147 | 3.48 (1.15) | 152 | 3.52 (1.09) | 0.724 | 74 |
| HbA1c level (%) | 152 | 7.34 (1.48) | 158 | 7.34 (1.24) | 0.968 | 64 |
| BMI (kg/m2) | 151 | 30.0 (5.4) | 165 | 30.0 (5.6) | 0.578 | 58 |
| Questionnaires/scores | ||||||
| PAID scale (0–100) | 154 | 15.2 (15.2) | 166 | 16.7 (17.1) | 0.388 | 54 |
| HADS (0–42) | 147 | 8.84 (6.54) | 153 | 8.86 (7.45) | 0.981 | 74 |
| Anxiety scale (0–21) | 147 | 4.75 (3.88) | 153 | 5.07 (4.24) | 0.500 | 74 |
| Depression scale (0–21) | 147 | 4.10 (3.30) | 153 | 3.80 (3.59) | 0.455 | 74 |
| DMSES (0–150) | 147 | 103.9 (32.2) | 154 | 104.9 (32.7) | 0.788 | 73 |
| DTSQ (0–48) | 145 | 32.8 (6.9) | 152 | 32.9 (6.3) | 0.902 | 77 |
At 12 months, the primary analysis showed a significant difference in change in HbA1c levels between the randomised groups, with participants in the HeLP-Diabetes group having a lower HbA1c level than those in the control group (mean difference –0.24%, 95% CI –0.44% to –0.049%; p = 0.014) (Table 14 and Figure 7). There was no difference in change in PAID scores between the groups at 12 months (mean difference –1.5, 95% CI –3.9 to 0.9; p = 0.209), although both groups showed a decrease in PAID scores over the follow-up of the trial (Figure 8 and see Table 14).
| Outcomes | Treatment group, mean (SE) | Intervention vs. control group | ||||
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| Baseline (n = 185) | Change, baseline to 12 months | Baseline (n = 189) | Change, baseline to 12 months | Mean difference (95% CI) | p-value | |
| Primary outcomes | ||||||
| HbA1c (%) | 7.3 (0.1) | –0.08 (0.07) | 7.3 (0.1) | 0.16 (0.07) | –0.24 (–0.44 to –0.05) | 0.014 |
| HbA1c (mmol/mol) | 56.3 (1.1) | –0.8 (0.8) | 56.8 (1.1) | 1.8 (0.8) | –2.6 (–4.8 to –0.5) | 0.014 |
| PAID score (points) | 18.2 (1.3) | –4.1 (0.9) | 19.8 (1.3) | –2.5 (0.9) | –1.5 (–3.9 to 0.9) | 0.209 |
| Secondary outcomes | ||||||
| SBP (mmHg) | 134.7 (1.5) | –4.2 (1.4) | 134.9 (1.5) | –0.5 (1.4) | –3.8 (–6.6 to –0.9) | 0.010 |
| DBP (mmHg) | 77.8 (1.0) | –2.5 (0.9) | 77.1 (1.0) | –1.9 (0.8) | –0.6 (–2.4 to 1.2) | 0.519 |
| BMI (kg/m2) | 30.1 (0.5) | 0.12 (0.2) | 30.0 (0.5) | –0.04 (0.2) | 0.16 (–0.30 to 0.62) | 0.498 |
| Total cholesterol (mmol/l) | 4.1 (0.1) | –0.08 (0.06) | 4.2 (0.1) | –0.15 (0.06) | 0.07 (–0.09 to 0.2) | 0.370 |
| HDL-C (mmol/l) | 1.25 (0.03) | –0.003 (0.018) | 1.26 (0.03) | 0.004 (0.018) | –0.007 (–0.054 to 0.039) | 0.754 |
| Completed nine essential processes | 65% (3.7%) | –5.1% | 61% (3.8%) | 3.4% | OR 0.78 (0.45 to 1.35) | 0.379 |
| HADS score (points) | 9.3 (0.5) | –1.05 (0.44) | 9.1 (0.5) | –0.60 (0.48) | –0.45 (–1.68 to 0.78) | 0.474 |
| DMSES scorea (points) | 98.8 (2.4) | 2.93 (2.90) | 103.6 (2.3) | 1.38 (2.79) | 1.55 (–5.74 to 8.84) | 0.674 |
| DTSQ score (points) | 32.2 (0.6) | 0.94 (0.57) | 32.2 (0.6) | 0.45 (0.61) | 0.49 (–1.18 to 2.15) | 0.564 |
FIGURE 7.
Mean HbA1c (95% CI) level over the follow-up period by randomised group following multiple imputation. Intervention group, n = 185; control group, n = 189.
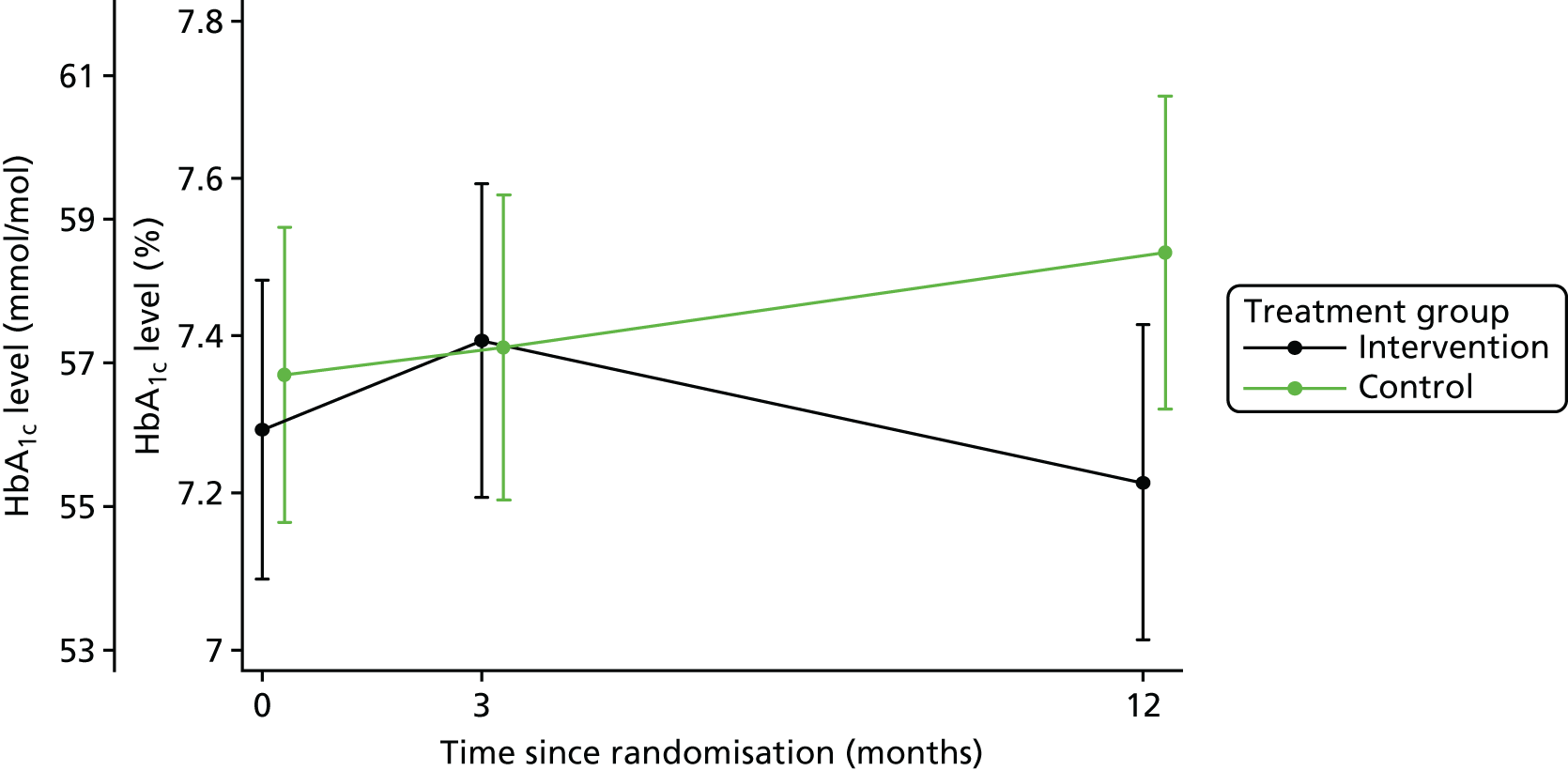
FIGURE 8.
Mean PAID score (95% CI) over the follow-up period by randomised group following multiple imputation. Intervention group, n = 185; control group, n = 189.
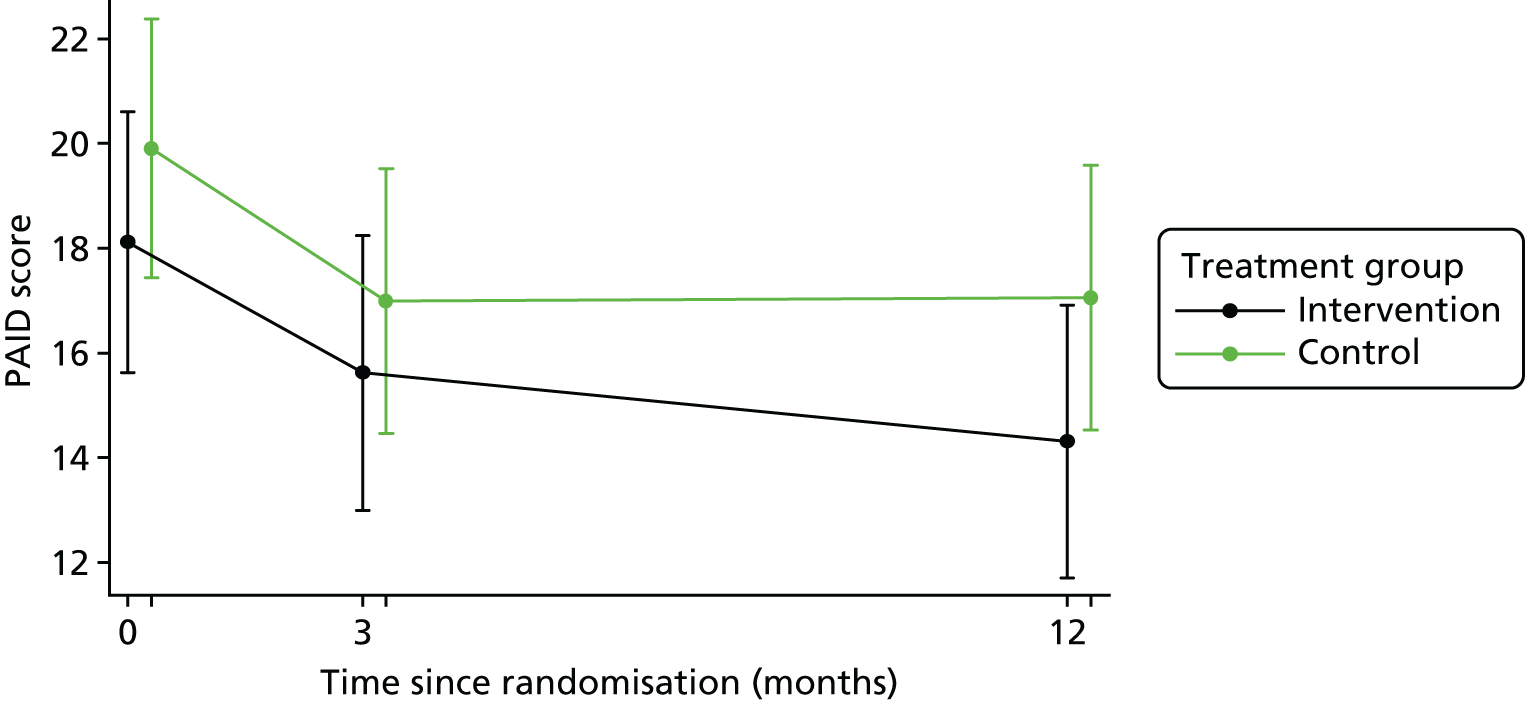
There was no difference in secondary outcomes at 12 months, with the possible exception of SBP, which decreased more in the intervention group than in the control group (p = 0.010) (see Table 14). No adverse effects or events were recorded.
There was a technical error in the software that led to usage data not being collected before 1 January 2014. At this point, 16 participants had been randomised (seven to the intervention and nine to the control). For these 16 participants, the usage data are not based on a full year, but for all other participants data are summarised for the 12 months post randomisation.
The data presented do not include the initial registration visit when participants were introduced to the website by practice nurses. The mean number of log ins was significantly higher in the intervention group than in the control group (18.7 vs. 4.8; p = 0.0001), as was the mean number of pages visited per log in (10.5 vs. 7.7; p < 0.0001) and the mean number of days in which the website was accessed (10.1 vs. 3.3 days; p < 0.0001) (Table 15). The causal analyses estimated that for a ‘high-usage’ population (those with usage ≥ the median of 4 days) the HeLP-Diabetes intervention could, on average, reduce HbA1c levels by –0.44% (95% CI –0.81% to –0.06%) and PAID scores by –2.8 points (95% CI –7.2 to 1.7 points) over 12 months (Figures 9 and 10).
| Usage data | Treatment group | p-valuea | Number missing | |||
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| n | Mean (SD) | n | Mean (SD) | |||
| Number of log ins | 185 | 18.7 (84.0) | 189 | 4.8 (8.0) | 0.0001 | 0 |
| Number of pages visited per log in | 143 | 10.5 (6.7) | 126 | 7.7 (5.0) | < 0.0001 | 105b |
| Time spent per log in (minutes)c | 143 | 12.3 (9.8) | 126 | 8.2 (8.4) | < 0.0001 | 105b |
| Number of days that the website was accessed over follow-up | 185 | 10.1 (22.9) | 189 | 3.3 (5.1) | < 0.0001 | 0 |
FIGURE 9.
Efficacy of the HeLP-Diabetes programme on HbA1c levels at 12 months based on the number of days’ usage, superimposed by distribution of usage observed in the intervention group. Green bars highlight the ‘high-usage’ group that has usage greater than or equal to the median of 4 days.
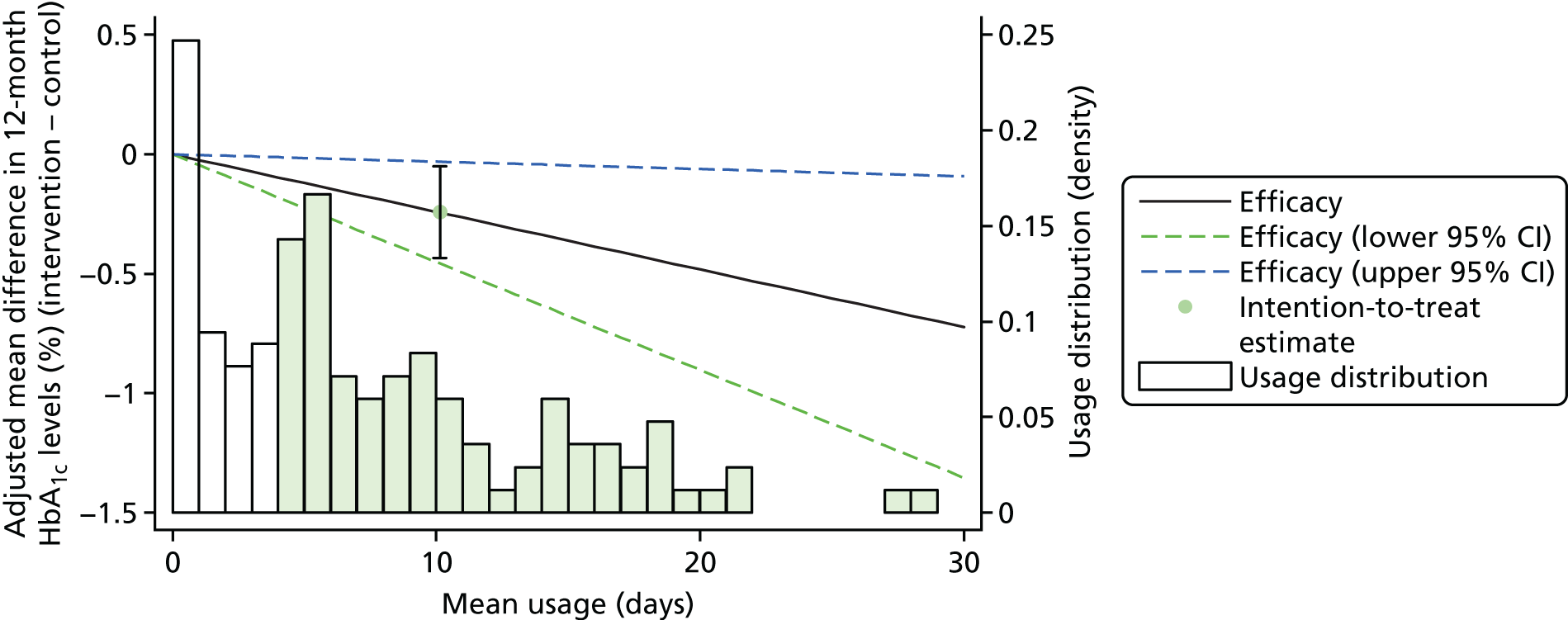
FIGURE 10.
Efficacy of HeLP-Diabetes on PAID score at 12 months based on the number of days’ usage, superimposed by the distribution of usage observed in the intervention group. Green bars highlight the ‘high-usage’ group that has usage greater than or equal to the median of 4 days.
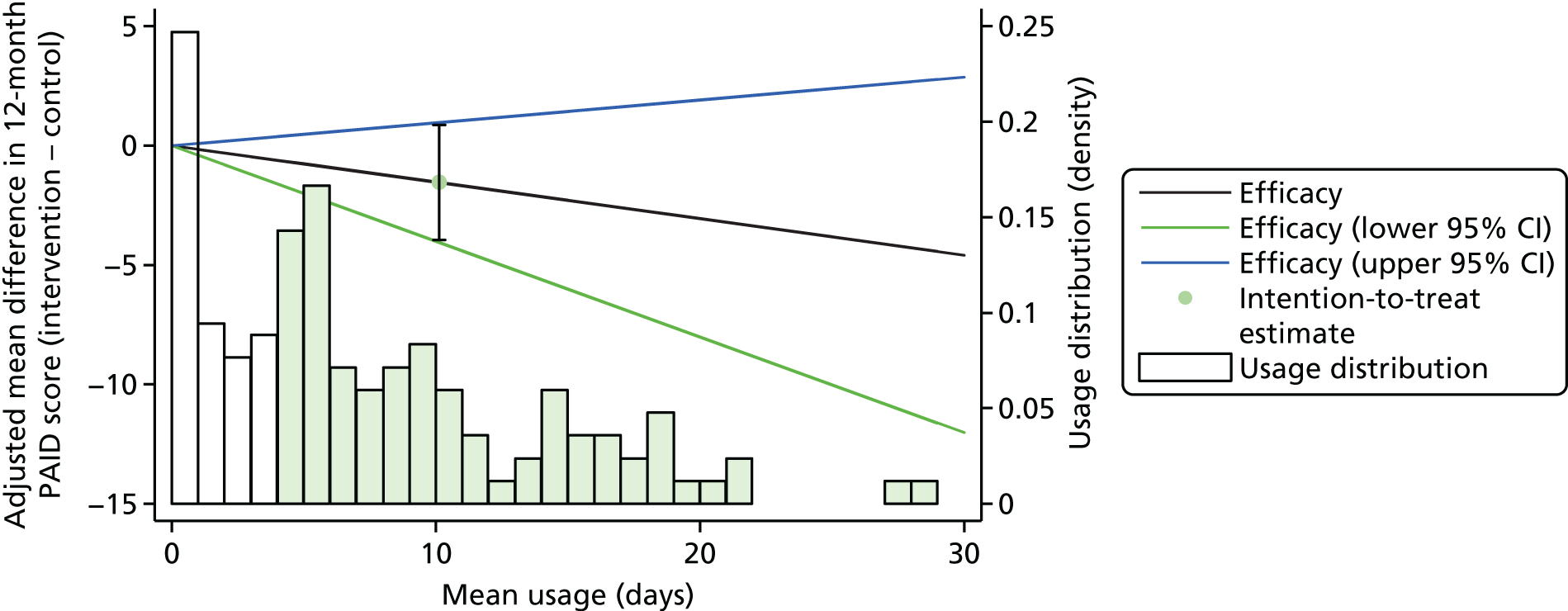
The findings from the sensitivity analyses were similar to the main analysis (Table 16). Participants who were missing 12-month HbA1c levels had a significantly higher mean baseline HbA1c level measure (7.9% vs. 7.1%; p < 0.001), leading to higher imputed HbA1c levels at 12 months in the non-completers group and a greater mean difference between the randomised groups than in the complete-case analyses (Figure 11 and Table 11; see Table 16).
FIGURE 11.
The means and 95% CIs of HbA1c levels over time by randomised group and completers vs. non-completers, after multiple imputation of non-completers group follow-up data.
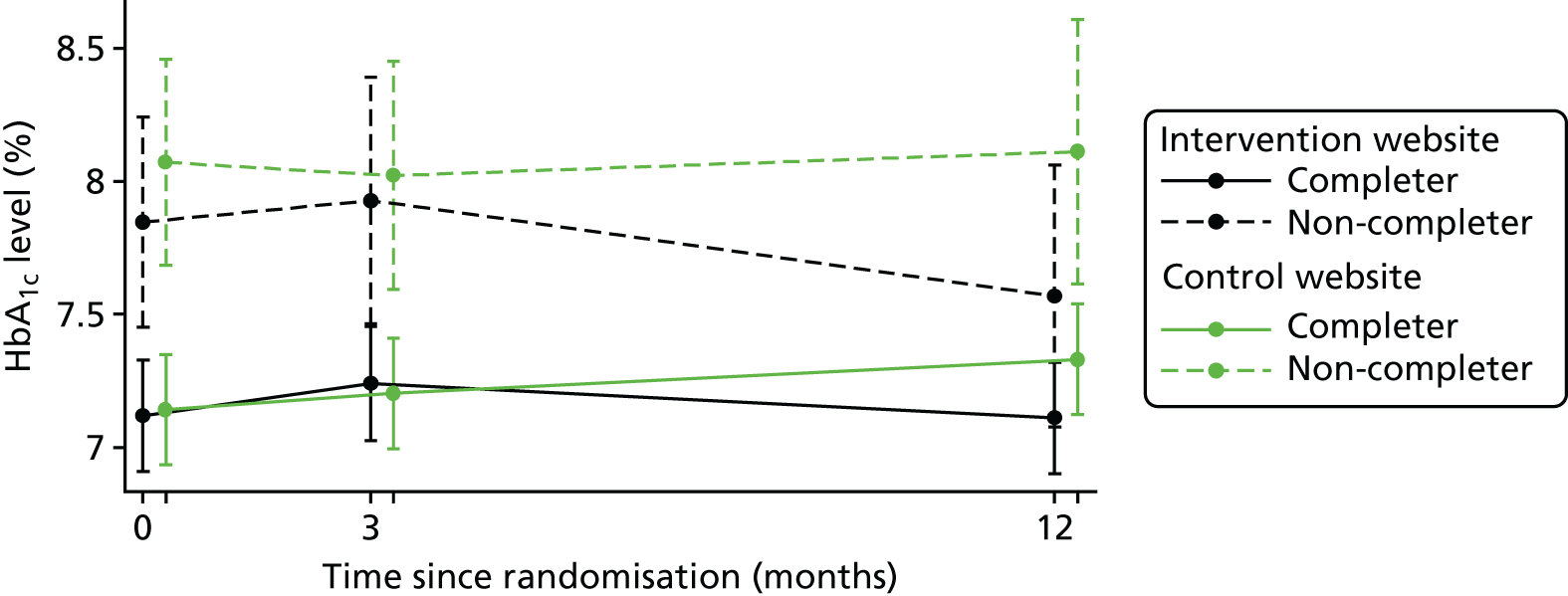
| Analysis | Number of individuals | Mean difference (95% CI) (intervention – control); p-value |
|---|---|---|
| HbA1c levels (%) | ||
| Primary analysis: multiple imputation of baseline and outcomes | 374 | –0.242 (–0.435 to –0.049); p = 0.014 |
| Sensitivity analysis 1: multiple imputation of baseline covariates only | 291 | –0.214 (–0.390 to –0.038); p = 0.017 |
| Sensitivity analysis 2: complete casesa | 284 | –0.207 (–0.385 to –0.028); p = 0.023 |
| Sensitivity analysis 3: complete casesb | 186 | –0.220 (–0.416 to –0.025); p = 0.027 |
| Sensitivity analysis 4: non-contaminated casesc | 370 | –0.225 (–0.418 to –0.032); p = 0.023 |
| Sensitivity analysis 5: linear model excluding centred | 374 | –0.242 (–0.438 to –0.047); p = 0.015 |
| PAID score | ||
| Primary analysis: multiple imputation | 374 | –1.54 (–3.94 to 0.87); p = 0.209 |
| Sensitivity analysis 1: multiple imputation of baseline covariates only | 321 | –1.31 (–3.65 to 1.03); p = 0.274 |
| Sensitivity analysis 2: complete casesa | 317 | –1.29 (–3.66 to 1.08); p = 0.285 |
| Sensitivity analysis 3: complete casesb | 65 | –2.22 (–6.35 to 1.91); p = 0.292 |
| Sensitivity analysis 4: non-contaminated casesc | 370 | –1.57 (–3.99 to 0.85); p = 0.204 |
| Sensitivity analysis 5: linear model excluding centree | 374 | –1.54 (–3.98 to 0.90); p = 0.215 |
There was no evidence of baseline measures of HbA1c level or PAID score being effect modifiers for the mean difference between the groups. There was strong statistical evidence (interaction p = 0.004) to suggest that the duration of diabetes mellitus since diagnosis acted as an effect modifier, with those who had been diagnosed more recently showing more of a reduction in PAID score than those who had been diagnosed for longer periods of time. The duration of diabetes mellitus since diagnosis had no effect on change in HbA1c levels (Table 17).
| Effect modifier | Number of individuals, n/N | Mean difference (intervention – control) (95% CI) | Interaction p-valueb | |
|---|---|---|---|---|
| Complete casesa | Multiple imputation | |||
| HbA1c levels (%) | ||||
| Baseline HbA1c, per % increase | ||||
| < 7.5 | 254/369 | –0.15 (–0.41 to 0.11) | –0.14 (–0.39 to 0.12) | 0.458 |
| ≥ 7.5 | 115/369 | –0.51 (–0.94 to –0.07) | –0.51 (–0.93 to –0.09) | |
| Duration of diabetes mellitus since diagnosis, per year increase | ||||
| < 6.9 | 185/370 | –0.34 (–0.59 to –0.08) | –0.30 (–0.57 to –0.03) | 0.425 |
| ≥ 6.9 | 185/370 | –0.07 (–0.32 to 0.18) | –0.18 (–0.45 to 0.09) | |
| PAID score | ||||
| Baseline PAID score, per unit increase | ||||
| < 12 | 181/374 | –0.3 (–4.6 to 4.1) | –0.1 (–4.2 to 4.1) | 0.066 |
| ≥ 12 | 193/374 | –3.6 (–7.8 to 0.7) | –3.9 (–8.2 to 0.4) | |
| Duration of diabetes mellitus since diagnosis, per year increase | ||||
| < 6.9 | 185/370 | –2.9 (–6.3 to 0.4) | –3.6 (–7.0 to –0.1) | 0.004 |
| ≥ 6.9 | 185/370 | 0.3 (–3.0 to 3.7) | 0.4 (–3.1 to 3.9) | |
Discussion
In this first UK-based trial of a web-based self-management programme for people with T2DM, participants who were randomised to receive the HeLP-Diabetes programme demonstrated improved glycaemic control at 12 months compared with those who were randomised to receive access to a simple information website. This improvement is both clinically and statistically meaningful, appears robust across all prespecified sensitivity analyses and was not dependent on duration of diabetes mellitus since diagnosis, baseline glycaemic levels or levels of diabetes mellitus-related distress. Each 1% reduction in HbA1c level is associated with a risk reduction of 21% for deaths related to diabetes mellitus and a 37% risk reduction for microvascular complications. 178 Given that this web-based intervention could be delivered at low cost and at scale across the UK, the potential for population benefit is considerable. We have no data on whether or not the effects of the HeLP-Diabetes programme attenuate or strengthen with long-term use (> 1 year). However, one of the postulated benefits of the HeLP-Diabetes programme is that the programme is available for people with T2DM to use over the whole of their illness journey, providing access to self-management support at the time of need. This contrasts with the current model of group-based education at the time of diagnosis, for which effects would be expected to attenuate with time and, indeed, have been shown to do so. 17
The programme did not have an overall impact on diabetes mellitus-related distress, but there is some evidence that the HeLP-Diabetes programme appeared to reduce distress in individuals who were diagnosed more recently. However, it is worth noting that baseline PAID scores were exceptionally low in this trial population. In a small pilot study, participants who were offered supported access to the HeLP-Diabetes programme reduced their PAID scores by 6 points (p = 0.04) over 6 weeks. 84
The current ‘gold standard’ for diabetes mellitus self-management support in the UK is the DESMOND trial model of 6 hours of group-based structured education. Comparison of our trial with the DESMOND trial may, therefore, be of interest to readers. The DESMOND trial was cluster randomised, whereas the HeLP-Diabetes trial was individually randomised. The population for the DESMOND trial was substantially larger, involving 207 general practices (102 in the intervention arm) and 824 participants (437 in the intervention arm). 15 The characteristics of the trial participants also differed between the two trials: importantly, the DESMOND trial was for newly diagnosed patients, whereas the HeLP-Diabetes programme was for people at any stage of their illness journey. The DESMOND trial intervention participants had, overall, poorly controlled diabetes at baseline, with a mean HbA1c level of 8.3%, SBP and DBP of 141 and 82 mmHg, respectively, and total cholesterol level of 5.4 mmol/l, compared with the HeLP-Diabetes programme intervention participants who had a mean baseline HbA1c level of 7.3%, SBP and DBP of 135 and 78 mmHg and total cholesterol level of 4.1 mmol/l, implying that DESMOND trial participants had greater opportunity to improve. The HeLP-Diabetes programme participants also differed in their demographic characteristics: 96% of DESMOND trial participants were white, 55% were male and the mean age was 59 years and 80% of HeLP-Diabetes programme participants were white, 69% were male, and the mean age was 65 years. Although both trials used the PAID scale, baseline data from this questionnaire were not reported for DESMOND trial participants. These differences between the participants need to be remembered when considering any differences in trial outcomes.
The main difference in outcomes at 12 months between the two trials is that in the DESMOND trial, HbA1c levels improved in both arms, with no difference between the two arms, whereas in the HeLP-Diabetes programme, HbA1c levels improved in the intervention arm and worsened in the control arm. In terms of secondary outcomes, the DESMOND trial intervention participants showed significantly greater loss in weight (–1.01 kg, 95% CI –1.91 to –0.02 kg) than control participants had, with no difference in any other biomedical outcomes. The HeLP-Diabetes intervention participants showed a decrease in SBP (–3.8 mmHg; 95% CI –6.6 to –0.9 mmHg), with no difference in any other biomedical outcomes. There was no difference between groups in the DESMOND trial for PAID scores at 12 months. The DESMOND team were able to undertake further follow-up at 3 years, by which time there were no differences in biomedical outcomes between groups, although differences in illness beliefs remained.
The trial had many strengths. It was a pragmatic trial that was open to nearly all patients with T2DM in participating practices. There was complete concealment of allocation, as randomisation occurred after baseline data collection. Baseline prognostic factors were well balanced between groups. Every effort was made to achieve blinding, including requiring practices to have two nurses, so that data collection was undertaken by a nurse who was blind to participant allocation. Data for the co-primary outcomes at the primary outcome point were available for 78% and 86% of participants for HbA1c level and PAID score, respectively. All analyses were on an intention-to-treat basis and supplemented by a CACE analysis.
Although response rates for the co-primary outcomes were good, some potential for bias existed. Our primary analysis used multiple imputation methods because evidence shows that the assumptions underpinning this method are more defensible than those assumed using other approaches to missing data. 179 We also undertook sensitivity analyses, including complete cases, non-contaminated cases and a linear model excluding centre; all yielded similar results.
The two co-primary outcomes reflected the twin aims of the intervention: to improve diabetes mellites control and to reduce diabetes mellitus-related distress. Around 40% of patients with diabetes mellitus have significant levels of distress, which has a severe impact on quality of life,160 and this is an important outcome for patients. 161 Our PPI panel was clear that this should be a primary outcome. In contrast, many HCPs were more interested in glycaemic control. In line with previous trials in this area,162 we decided to adopt both as co-primary outcomes and to test each at a 5% level of significance. 163
There are some limitations. Despite maximising the inclusivity of the trial by minimising the exclusion criteria, participants were not representative of the overall population of people with T2DM in England. Compared with the overall population, participants were better educated, more likely to be white British, had better control of their diabetes mellitus and reduced cardiovascular risk factors and were much less distressed. 180 Similar differences between trial and target populations have been reported. 181
Although every effort was made to maintain blinding, it is possible that some participants may have discussed their use of the intervention with research nurses, making it possible to infer which arm they had been allocated to. This could have affected secondary clinical outcomes, such as blood pressure or weight, but could not have affected assessment of HbA1c level, as this assessment was carried out by a laboratory that was blind to allocation. There appeared to be high potential for contamination between two participants who shared the same surname and address, and a further two participants did not receive their allocated intervention because of an error at practice level; excluding these four made no difference to the results.
A further limitation of the trial is that it provides little insight into the mechanism of action of the HeLP-Diabetes programme. This was the result of a deliberate decision to focus on clinically important outcomes and minimise both the response burden and the potential impact the measurement would have on participants.
On the basis of these results, the HeLP-Diabetes programme may be considered as an addition to the current menu of self-management support for people with T2DM and could help increase overall access and uptake. Most commissioned services currently focus on people who are newly diagnosed with T2DM, which leaves a clear unmet need for people who have been diagnosed as having diabetes mellitus for longer but are looking for ways to improve their health. Many patients are not ready to engage in self-management early in their illness journey182 but become motivated to do so later, often as a result of a change in medication or development of a complication. 183
Chapter 8 Health economic analysis of the Healthy Living for People with type 2 Diabetes programme
Chapter summary
This chapter reports on the health economic analysis of the HeLP-Diabetes programme using data collected during the RCT, which is reported in Chapter 7. The analysis was an incremental cost-effectiveness analysis of facilitated access to the HeLP-Diabetes programme compared with usual care for people with T2DM. Following NICE’s guidance, the analysis adopted a NHS and personal social services perspective. The components of the analysis were costs of the active and control interventions, health-care and social services use and health outcomes, including a diabetes mellitus-specific outcome (assessed via the PAID score) and a generic measurement of quality of life (assessed via the EQ-5D-3L questionnaire). Intervention costs were measured directly. The potential impact that the HeLP-Diabetes programme had on diabetes care and complications was measured by the use of NHS and social services. All costs are presented in pounds sterling 2014 prices.
The primary analysis used multiple imputation to estimate missing data. Two additional analyses were performed: a complete-case analysis and a one-way sensitivity analysis assuming increased intervention costs.
Both the primary and the complete-case analysis showed the HeLP-Diabetes programme to be dominant over the control, that is, it was both more effective and less costly. The one-way sensitivity analysis suggested that additional per-patient costs of £511–711 could be incurred for the intervention before it ceased to be cost-effective.
Aims and objectives
The aims of the trial fall under the evaluation objectives set out in Chapter 3:
-
determine the effect of the HeLP-Diabetes programme on clinical outcomes and HRQoL in people with T2DM
-
determine the incremental cost-effectiveness of the intervention compared with usual care from the perspectives of health and personal social services and wider public sector resources.
The previous chapter reported data pertaining to the first trial aim. In this chapter, only the health economic analysis is presented.
Methods
The trial design, setting, participants, recruitment, randomisation and data collection procedures and clinical effectiveness outcomes were reported in Chapter 7. The economic analysis was undertaken from a NHS and personal social services perspective, following NICE guidance. 184 Value-added tax at 20%, salary oncosts and overheads were added, when applicable, to all costs. Whenever possible, we have tried to reflect the true costs of ongoing delivery, rather than the costs incurred during the trial itself. The true costs of ongoing delivery are obtained from the business model and actual costs incurred by the community interest company (CIC) set up to disseminate the HeLP-Diabetes programme across the UK.
Health economic outcomes
The components of the analysis were the costs of the active and control intervention, health-care and social services use and health outcomes, including a diabetes mellitus-specific outcome (diabetes mellitus-related distress) and a generic quality-of-life outcome (EQ-5D-3L).
Intervention cost
The intervention costs had a number of components, including the costs of:
-
developing the intervention
-
delivering, maintaining and updating the intervention
-
facilitated access
-
training NHS staff both in using the intervention and in training patients to use the intervention.
Development costs
The costs of developing the intervention were those incurred in the first 2 years of the programme grant (see Chapter 6). These included the conception and design of the HeLP-Diabetes programme, development of articles and multimedia content for the website, licences or subscriptions for modules used with license from other providers and participatory design panels.
An additional major cost was research staff time. As the development of the intervention and the associated research (e.g. WP A and B) were closely interwoven, it was difficult to separate the costs of development from the costs of research. Research staff kept time sheets that documented their various activities and we intended to use these time sheets to estimate time spent on intervention development but it was often unclear whether or not a specific activity was for research or development of the intervention. Furthermore, the academic staff, including co-investigators, provided significant input to the intervention development. This input was not recorded on time sheets and was intimately entwined with input into the research procedures; therefore, subsequent allocation of academic time as ‘intervention development’ time or ‘research’ time was almost impossible. One reason for the activities being so closely entwined was that the HeLP-Diabetes programme was the first self-management programme developed to take such a wide, inclusive view of the tasks of self-management. Hence, the development team had little guidance from previous literature or experience and spent considerable time thinking about decisions from first principles. This was time-consuming and resource-intensive and future programmes could probably be developed with less resource.
In the light of this uncertainty about the true costs of the intervention development, and given that these costs can be considered as ‘sunk costs’ (i.e. costs that have already been incurred and cannot be recovered), we have not included the development costs in the health economic analysis and report them for information only. This is in line with latest guidance on health economic evaluation of digital health interventions. 185
Delivery and maintenance costs
Activities associated with delivery and maintenance of the HeLP-Diabetes programme are described in detail in Chapter 6. They included ensuring that the content on the HeLP-Diabetes programme was up-to-date and reflected current best evidence and practice, regular reviews of the entire website to check for broken links and consistency of information (i.e. that information updated in one article was also updated in all other relevant articles), moderating the forum, responding to ‘Ask the Expert’ questions and sending e-mails, newsletters and text messages to users to encourage engagement with the intervention. The time taken per task was extracted from staff time sheets. Hourly rates for each member of staff were obtained from either national pay scales, with oncosts and overheads included,186–188 or from invoices when staff involved were not directly employed by UCL.
Additional costs included technical issues, including domain name registration, Secure Sockets Layer (SSL) certification, hosting, adhering to information governance specifications and technical maintenance, such as bug-fixing and updates to software and browsers. To prevent ‘cybersquatting’, in which domain names that are similar to well known or respected sites are used for commercial benefit, we registered the name ‘HeLP-Diabetes’ with all the major domains (e.g. .co.uk, .org and .com). 164
As these activities and costs are essential for the ongoing maintenance and delivery of the HeLP-Diabetes programme, they were included in the economic analysis. When activities had been undertaken in the trial by a high-grade RA, but could reasonably be expected to be undertaken by a lower-grade staff member during ongoing delivery, the costs of the staff required for ongoing delivery were calculated and used in the analysis. All costs were converted to total cost for a 12-month period.
Facilitated access costs
In the trial, facilitated access comprised practice nurses registering patients on the HeLP-Diabetes programme, introducing patients to the wide range of content and encouraging ongoing use. In order for nurses to be able to undertake these tasks, RAs trained one practice nurse in each practice in use of the HeLP-Diabetes programme (including how to register patients) and how to introduce patients to the content and encourage ongoing use. This training took 1 hour. Thus, there were two components to the cost of facilitated access: the 1-hour one-to-one training session for each practice nurse and the time taken by the nurse to register and train each patient. The latter was estimated to take 20 minutes per patient.
The cost of the trainer was estimated as 1 hour of grade 6 time and practice nurse costs were extracted from Unit Costs of Health and Social Care 2014. 187 Outside a trial environment, more than one member of staff may be trained in the use of the HeLP-Diabetes programme. This would increase costs and is reflected in the sensitivity analysis.
Both components of facilitated access were supported by written materials. Practice nurses were provided with laminated booklets summarising the material covered in the training session by the RA. Each practice was also given leaflets to give to people with T2DM, which covered the information practice nurses provided for patients (see Appendix 5). The costs of these printed materials were recorded from invoices.
Thus, the total costs of facilitated access included the time taken to train staff, the time taken by practice staff in supporting patients to use the HeLP-Diabetes programme and the costs of printed materials to support staff and patients in use of the HeLP-Diabetes programme. The costs of the premises and overheads were included in the personnel salary proportional to the time spent.
Comparator costs
Participants in the control group were given access to a simple information website, similar to that provided by NHS Choices or Diabetes UK. As such information websites are freely available, we assumed a zero cost for the comparator.
Costs of health-care and social services
Data on participants’ use of a wide range of health-care and social services were collected at baseline and at 3 months’ and 12 months’ follow-up. Data that were collected at baseline covered the 12 months prior to entering the trial, at 3 months covered months 1–3 of the trial and at 12 months covered months 4–12 of the trial.
Research nurses extracted data from the medical record on consultations with GPs, practice nurses, and podiatrists; attendances at NHS walk-in clinics or out-of-hours services; retinal screening; use of physiotherapy or psychological services; accident and emergency unit (A&E) admissions; clinical tests or investigations; hospital outpatient attendances, day-case attendances and inpatient admissions; and patients’ prescriptions.
Participants’ use of other health-care and social services was collected retrospectively by self-report using a pre-designed questionnaire. These included district nurse consultations, use of the NHS Direct call centre and contact with social workers, occupational therapists or dietitians. As NHS Direct ceased operation in February 2014,189 data on use of this service are reported but not included in the analysis.
Service usage rates were then costed by applying national average unit costs, extracted from Unit Costs of Health and Social Care 2014187 or other sources as appropriate (Table 18). These unit costs include overheads, capital and infrastructure costs, allocated proportionally to the staff time. Data on travel time for home visits were not available; therefore, we adopted the assumed 12 minutes per visit estimate made by Unit Costs of Health and Social Care 2014. 187 No allowance was made for travel expenses.
| Health service use | Unit cost per consultation or episode (£) | Sources |
|---|---|---|
| GP consultation (in surgery) | 38 | Unit Costs of Health and Social Care 2014 187 |
| GP consultation (home visit) | 62 | Unit Costs of Health and Social Care 2014 187 |
| GP consultation (telephone) | 23 | Unit Costs of Health and Social Care 2014 187 |
| Practice nurse consultation (in surgery) | 11 | Unit Costs of Health and Social Care 2014 187 |
| Practice nurse consultation (home visit) | 18 | Unit Costs of Health and Social Care 2014 187 |
| NHS walk-in clinic | 56 | Unit Costs of Health and Social Care 2014 187 |
| Out-of-hours services (telephone advice) | 36 | Out-of-Hours GP Services in England,190 Unit Costs of Health and Social Care 2014187 |
| Out-of-hours services (home visit) | 117 | Out-of-Hours GP Services in England,190 Unit Costs of Health and Social Care 2014187 |
| Out-of-hours services (in surgery) | 86 | Out-of-Hours GP Services in England,190 Unit Costs of Health and Social Care 2014187 |
| A&E admission | 167 | Reference Costs 2013–14 191 |
| Podiatrist | 44 | Reference Costs 2013–14 191 |
| Optometry | 97 | Reference Costs 2013–14 191 |
| Physiotherapy | 46 | Reference Costs 2013–14 191 |
| Counselling (primary care) | 46 | Unit Costs of Health and Social Care 2014 187 |
| Clinical test | 2 | Reference Costs 2013–14 191 |
| Outpatient appointment | 111 | Reference Costs 2013–14 191 |
| Day case | 698 | Reference Costs 2013–14 191 |
| Inpatient admission | 1891 | Reference Costs 2013–14 191 |
| District nurse (home visit) | 46 | Reference Costs 2013–14,191 Unit Costs of Health and Social Care 2014187 |
| District nurse (in surgery/clinic) | 37 | Reference Costs 2013–14 191 |
| Counselling (community) | 138 | Reference Costs 2013–14 191 |
| Social worker | 55 | Unit Costs of Health and Social Care 2014 187 |
| Occupational therapy | 64 | Reference Costs 2013–14 191 |
| Dietitian | 80 | Reference Costs 2013–14 191 |
For the costs of out-of-hours services, we used data from the national audit of out-of-hours service combined with data from Unit Costs of Health and Social Care 2014187 to estimate the required unit costs. The duration of out-of-hours consultations was assumed to be the same as in-hours consultations, and we assumed the same 12 minutes’ travel time for home visits.
The cost per outpatient appointment was the weighted average of both consultant-led and non-consultant-led outpatient attendance. Although the questionnaire was designed initially to separate new and follow-up appointments, confusion occurred during the completion of the questionnaire, rendering it impossible to distinguish between the two. As a result, the unit cost presented in Table 18 was the weighted cost of new and follow-up appointments.
The unit cost of inpatient episodes covered elective inpatients, non-elective inpatients and regular day/night admissions but excluded emergency-led admission, which was accounted for by A&E admission. Although the details of a few clinical tests were collected, the specific unit costs were not found. Therefore, the unit cost of a clinical test was taken as the weighted average of directly accessed pathology services.
Prescription data were also extracted from the medical record by the research nurses at baseline and at 3 months and 12 months. Nurses entered the name of the medication, dose, route and frequency of drugs prescribed at each data collection point. Costs were then calculated by cross-referencing the name, form and strength of the drug with the Prescription Cost Analysis England 2014. 192 When only the trade name was available, an attempt was made to match it to the correct generic name. When the generic name was not successfully identified, the medication was matched by drug name. In the case of missing information on form or strength, the weighted average cost per item was calculated based on the available information.
As most participants were on medication at baseline, we assumed blank entries at follow-up to be missing data, unless the nurse specified that no medication was prescribed. We also assumed that all prescriptions were for long-term use and issued for 1 month at a time. It is probable that some of the medication issued was only for acute use, but we have opted for a conservative approach to avoid underestimating total drug costs. Therefore, it is possible that reported prescription costs are slightly overestimated.
Health outcomes
Two health outcomes were used in the analysis: diabetes mellitus-related distress, as measured by the PAID scale,168 and QALYs, derived from EQ-5D-3L. 193 The PAID scale has 20 items focusing on areas that cause difficulty for people living with diabetes mellitus, including social situations, food, friends and family, diabetes mellitus treatment, relationships with HCPs and social support. The EQ-5D-3L has five domains, each with three levels measuring daily difficulties in that domain. The tariff for each combination of these levels of the UK population was then applied to calculate an index score. 194
Both these self-reported outcome measures were collected at baseline and at 3 months’ and 12 months‘ follow-up. The time difference on QALYs was not accounted for because the assessing period was 12 months.
Analysis
The analysis followed a prespecified plan, based on comparing the groups as randomised (intention to treat). The analysis plan was approved by the trial steering committee before unblinding and was uploaded to the trial website [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/pgfar/RP-PG-0609-10135/#/ (accessed August 2018)]. Only PAID scale scores and EQ-5D-3L data obtained within a 10–14 month period following randomisation were used in the primary analysis. Missing 12-month outcomes were imputed using multiple imputation and baseline and other outcome data (e.g. 3-month data and final follow-up data collected outside the 10- to 14-month window). The EQ-5D-3L index score was presented and then converted to QALYs to enable a cost–utility analysis, as per NICE’s guidance. 184 The QALYs were calculated over the duration of the trial using the area under the curve from the baseline and 3- and 12-month follow-ups. 195
A linear mixed-effects model was fitted with the 12-month outcome as the dependent variable, adjusting for the baseline variables of age, sex, presence of pre-existing cardiovascular disease, duration of diabetes mellitus since diagnosis and smoking status, as well as the corresponding baseline outcome (costs, PAID score and EQ-5D-3L index score, respectively). Centre effects were included as random effects in the analysis. The differences in mean 12-month costs and outcomes were estimated based on the model. As the HeLP-Diabetes programme was dominant over the comparator (being less costly and more effective), the incremental cost per point of PAID score improvement and incremental cost per QALY gained were not calculated.
The non-parametric bootstrap technique was employed to explore the uncertainty of calculated difference in mean 12-month costs and outcomes from multiple-imputed data sets. In total, 5000 bootstrapped data sets were created and the total costs and outcome were estimated for each. The results from bootstrap resampling were used to construct 95% CIs for incremental costs, incremental PAID score and incremental QALYs and to plot the cost-effectiveness plane and cost-effectiveness acceptability curve (CEAC) to show the uncertainty surrounding the conclusion. 196
Missing data
Multiple imputation was used as the primary method to account for missing data in both baseline and follow-up, using the same method as described in Chapter 7. A chained equations model was developed based on the model used in the statistical analysis. Predictive mean matching was used as the imputation method for continuous variables, using the five nearest neighbours to the prediction as a set to draw from. We imputed all missing data separately by trial group.
The electronic format of the questionnaires largely prevented nurses or patients from omitting single items from any questionnaire. Hence, when service use data were missing, it was usually because the research nurse or the patient had not completed any of the service use questionnaire. In the light of this, the imputation was performed at the level of the service use questionnaire rather than at the level of an individual item. Similarly, the HRQoL measures were either completed entirely or missing entirely; therefore, the imputation was performed on overall HRQoL scores.
The imputation technique was applied to:
-
the costs of health services use from data provided by research nurses
-
medication costs from data provided by research nurses
-
costs of health and social services use from data provided by participants
-
PAID score and EQ-5D-3L index score from data provided by participants.
The percentage of missing data was generally low and did not exceed 30% for any individual variable. Therefore, as a rule of thumb, the number of imputations was set to 30. 176
The variables used in the imputation model included age, sex, height, time since diagnosis of T2DM, history of cardiovascular disease and smoking status. These were collected only at baseline. The imputation model also included weight, HbA1c level, SBP and DBP, HDL-C, total cholesterol level, HADS score, DMSES score, DTSQ score and BMI measurement. Along with the costs and HRQoL measures, these were collected at baseline and at 3 months and 12 months. For HbA1c levels, PAID score and EQ-5D-3L, the time since randomisation was also included. BMI measurement was treated as ‘just another variable’ and imputed directly (active imputation), as has been previously recommended. 197
The usage data were dealt with in the same way as described in Chapter 7. The subsequently generated variables (mean time per log-in, number of pages visited per log-in, log-transformed number of unique log-ins) were also included in the imputation model.
Sensitivity analyses
Two sensitivity analyses were undertaken: first, a complete-case analysis to assess the effect of imputing missing data; and, second, a one-way sensitivity analysis examining the uncertainty around the cost of the intervention.
The one-way sensitivity analysis was undertaken to explore the impact that increasing the costs associated with the intervention, (e.g. increasing the amount of facilitation, which would lead to additional cost per user) or by reducing the number of users (which would lead to an increased cost per user, as the costs of delivery and maintenance were largely fixed) would have.
Assuming that the effect on health resources and HRQoL remained the same once the participant took up the intervention, the additional intervention cost per person had a linear relationship with the incremental cost-effectiveness ratio (ICER):
A corresponding ICER was not calculated for the incremental cost-per-unit improvement of PAID score, as there is no national willingness-to-pay (WTP) threshold to compare it with.
Results
Costs
Development costs
Staffing costs accounted for the largest single component of development costs for the intervention. UCL staff employed on the development included one clinical researcher on wage band clinical lecturer grade 9 at 60% full-time equivalent for 2 years, one full-time grade 7 researcher for 2 years and another full-time grade 7 researcher for 18 months. Accounting for oncosts and overheads using the costing method adopted by Unit Costs of Health and Social Care 2014187 and 13.8% employer’s contribution to the national insurance,186 the research staff cost was approximately £430,274 in total.
Not all time was dedicated to intervention development; all three staff were also involved in the associated research (WP A and B, see Chapters 4 and 5), and other academic activities, such as teaching or presenting at conferences. Similarly, other academic staff, including co-investigators and project management staff, were also involved in the development work, but we could not separate activities into ‘research-related’ and ‘intervention development’ activities with any certainty. Therefore, the figure £430,274 represents an estimate based on the best-available information.
Costs of professional IT services were obtained from invoices and receipts. These included software design, web design and work by the PAERS company to link the HeLP-Diabetes programme with EMRs and the total cost was £184,235 (accounting for inflation). Licenses for pre-existing modules (see Chapter 6) and multimedia content came to £75,822. No licence fees were charged for the programmes of Down Your Drink, POWeR or Stop Advisor, and both Living Life To the Full and healthtalk.org kept their charges to the minimum, aiming simply to cover the costs of updating or adapting their material for use in the HeLP-Diabetes programme. Therefore, these costs do not reflect ‘commercial’ costs.
The website infrastructure costs incurred during development (March 2012–March 2014) totalled approximately £4056, including 20% value-added tax. These comprised 10 domain name registrations, SSL certificate fees, website hosting and exclusive internet protocol address. This was an approximate amount for 2 years because each of these services was purchased at a different time and continued for various durations. Some were purchased at a later time or for a longer period and, therefore, continued to operate into the trial period.
The costs of participatory design (the HCP and patient participatory panels) came to £33,116.
Intervention costs
Website delivery and maintenance costs
As detailed in Methods, delivery and maintenance costs of the intervention included staff costs in maintaining website content, and technical costs. Table 19 sets out the staff costs of maintaining the content and engaging users, and the total was an estimated £18,783 for a 1-year period.
| Activities | Intensity | Payment scale/method | Cost (£) | |
|---|---|---|---|---|
| Per hour | Per year | |||
| E-mails, text messages and newsletters | One day/fortnight | Grade 6 staff | 34 | 6675 |
| Librarian review of recent development | One hour/week | Fixed contract | 30 | 1560 |
| PPI feedback on librarian’s review | Thirty minutes/person, two people/fortnight | Cash payment | 18 | 468 |
| Forum monitoring by PPI | Thirty minutes/person, two people/fortnight | Cash payment | 18 | 468 |
| Forum monitoring by staff | One hour/fortnight | Grade 6 staff | 34 | 890 |
| Clinical team website interaction | One hour/time, five times/year | GP | 121 | 605 |
| PPI review feedback from clinical team | Fifteen minutes/person, two persons/time, five times/year | Cash payment | 18 | 45 |
| Content checking, revising and updating by staff | Two hours/fortnight | Grade 6 staff | 34 | 1780 |
| Content checking, revising and updating by clinical team | Two hours/fortnight | GP | 121 | 6292 |
| Total | 18,783 | |||
Web infrastructure costs such as the domain names, hosting, and maintenance contracts were purchased at different times; therefore, for the purposes of this analysis, these costs were estimated for a 1-year period, equivalent to the 12-month trial duration, based on the real charges (Table 20). The total infrastructure cost per year came to £23,013.
| Item | Cost per year (£) |
|---|---|
| Domain namesa | 93 |
| Website hosting | 3600 |
| Maintenance | 19,200 |
| SSL certificate | 120 |
| Total | 23,013 |
Combining the infrastructure and staff activities costs, the total operating cost of the HeLP-Diabetes programme during the trial period was estimated at £41,796. Although the capacity of the server is higher, the number of users who can log onto and actively use the website simultaneously was estimated to be 10,000. Therefore, the average cost per active user was calculated as £4. Once development costs and recurring annual outlays have been met, the marginal cost per user throughout the period up to a capacity of 10,000 is zero.
Facilitated access costs
As detailed in Methods, the facilitated access costs included practice nurse training and associated written training materials. The cost of the training sessions, including trainer and trainee time, was £3785 and the cost of the materials was £78, giving total training costs of £3863 for 1 year. With 185 participants in the intervention group, the average cost per person was £21.
The other component of facilitated access costs was the time spent by nurses in registering participants and teaching them how to use the HeLP-Diabetes programme. Twenty minutes was allocated to this activity per patient, or one-third of a practice nurse’s hourly consultation rate of £44. 187 Each participant in the intervention group also received a training leaflet, which cost £0.95 per leaflet.
Therefore, the total intervention cost was £41 per person and comprised £4 for operating costs; £21 for initial training of practice nurses and £16 for nurse-led facilitation. We deemed there to be no costs for the comparator.
Use of health care and social services
The mean frequency of health-care and social service use per participant in the 12 months prior to randomisation is shown in Table 21. All except one participant had complete data at baseline. This one participant had missing data for the clinical tests taken in the past 12 months. Overall, the use of services was high, although it varied greatly between individuals, with a small number of participants reporting very high levels of service use. For instance, 13 out of 185 participants in the intervention group and 18 out of 189 participants in the control group reported visiting a GP in surgery once a month or more. One participant in each group reported visiting their GP 33 times in the previous 12 months. At baseline, the usage level in the control group appeared to be slightly higher than in the intervention group.
| Service item | Treatment group, mean (SD) | |
|---|---|---|
| Intervention (n = 185) | Control (n = 189) | |
| Services use recorded by nurses | ||
| Primary care | ||
| GP consultation | ||
| In surgery | 4.65 (4.60) | 5.22 (4.54) |
| Home visit | 0.02 (0.18) | 0.05 (0.47) |
| Telephone | 1.01 (1.78) | 1.76 (3.31) |
| Practice nurse consultation | ||
| In surgery | 3.57 (4.51) | 3.43 (4.82) |
| Home visit | 0.02 (0.23) | 0.10 (1.38) |
| Walk-in centre | 0.04 (0.28) | 0.06 (0.30) |
| Out-of-hours service | ||
| Telephone | 0.03 (0.19) | 0.06 (0.32) |
| Home visit | 0.02 (0.16) | 0.02 (0.18) |
| Clinic | 0.06 (0.32) | 0.09 (0.35) |
| Clinical test | 15.59 (28.95)a | 17.30 (32.13) |
| Secondary care | ||
| A&E admission | 0.15 (0.45) | 0.26 (0.68) |
| Outpatient attendance | 2.15 (2.89) | 2.88 (4.16) |
| Day case | 0.16 (0.47) | 0.15 (0.46) |
| Inpatient admission | 0.14 (0.47) | 0.17 (0.72) |
| Community services | ||
| Eye screeningb | 0.91 (0.43) | 0.96 (0.42) |
| Podiatrist attendance | 0.37 (1.19) | 0.35 (1.19) |
| Physiotherapy | 0.32 (1.29) | 0.27 (1.08) |
| Counselling service | 0.18 (1.14) | 0.08 (0.70) |
| Services use reported by participants | ||
| District nurse consultation | ||
| Home visit | 0.11 (0.96) | 0.19 (1.55) |
| Clinic | 0.58 (1.16) | 0.75 (2.07) |
| NHS Direct | 0.20 (0.84) | 0.28 (0.93) |
| Counselling service | 0.12 (0.73) | 0.29 (1.49) |
| Social worker | 0.01 (0.07) | 0.06 (0.53) |
| Occupational therapy | 0.24 (2.06) | 0.11 (0.65) |
| Dietitian attendance | 0.21 (0.77) | 0.41 (1.87) |
At follow-up, the recall period for health-care and social services use was the first 3 months and then the subsequent 9 months of the trial. Table 22 shows the mean usage of individual service items during the two follow-up periods, by group. The number of participants listed above each section is the number of participants who had complete data in that section. Owing to different methods of data collection, the number of responding participants with follow-up data was different for each section. Most participants either completed or missed the entire section. Two participants missed one or two questions in a section. These questions are annotated and are explained under the table.
| Service item | Months, mean (SD) | |||
|---|---|---|---|---|
| 1–3 | 4–12 | |||
| Intervention group | Control group | Intervention group | Control group | |
| Service use recorded by nurses | n = 153 | n = 165 | n = 151 | n = 155 |
| Primary care | ||||
| GP consultation | ||||
| In surgery | 1.39 (1.74) | 1.71 (1.99) | 2.68 (2.78) | 3.10 (2.97) |
| Home visit | 0 | 0.02 (0.13) | 0.01 (0.08) | 0.07 (0.52) |
| Telephone | 0.42 (0.89) | 0.57 (1.05) | 0.91 (1.51) | 1.30 (2.14) |
| Practice nurse consultation | ||||
| Surgery | 1.38 (1.53) | 1.40 (1.96) | 2.50 (3.14) | 2.61 (3.99) |
| Home | 0.18 (1.95) | 0.01 (0.08) | 0 | 0.03 (0.16) |
| Walk-in centre | 0.03 (0.26) | 0.02 (0.15) | 0.08 (0.67) | 0.10 (0.32) |
| Out-of-hours service | ||||
| Telephone | 0.02 (0.18) | 0.02 (0.13) | 0.03 (0.18) | 0.08 (0.34) |
| Home visit | 0 | 0 | 0 | 0.01 (0.16) |
| Clinics | 0.03 (0.02) | 0.02 (0.15) | 0.12 (0.65) | 0.08 (0.41) |
| Clinical test | 3.62 (4.66) | 3.27 (3.36) | 7.42 (5.14) | 7.17 (4.80)a |
| Secondary care | ||||
| A&E admission | 0.07 (0.31) | 0.05 (0.25) | 0.10 (0.36) | 0.15 (0.47) |
| Outpatient attendance | 0.81 (1.33) | 0.79 (1.21) | 1.33 (2.64) | 1.54 (2.10) |
| Day case | 0.03 (0.16) | 0.05 (0.22) | 0.13 (0.47) | 0.12 (0.38) |
| Inpatient admission | 0.05 (0.25) | 0.01 (0.11) | 0.06 (0.26) | 0.10 (0.33) |
| Community services | ||||
| Podiatrist attendance | 0.10 (0.39) | 0.10 (0.34) | 0.30 (0.96) | 0.18 (0.83)a |
| Eye screening | 0.34 (0.48) | 0.32 (0.46) | 0.58 (0.51) | 0.65 (0.48) |
| Physiotherapy | 0.15 (0.62) | 0.16 (0.84) | 0.21 (1.06)a | 0.36 (1.38)a |
| Counselling service | 0.03 (0.27) | 0.02 (0.17) | 0.09 (0.57) | 0.01 (0.11)a |
| Service use reported by participants | n = 143 | n = 152 | n = 129 | n = 135 |
| District nurse consultation | ||||
| Home | 0 | 0.01 (0.08) | 0 | 0.01 (0.09) |
| Clinic | 0.29 (0.61) | 0.36 (0.77) | 0.45 (0.85) | 1.07 (4.35) |
| NHS Direct | 0.06 (0.32) | 0.10 (0.55)b | 0.12 (0.50) | 0.10 (0.39) |
| Counselling service | 0.05 (0.32)a | 0.08 (0.42) | 0.13 (0.76) | 0.19 (0.99) |
| Social worker | 0 | 0 | 0.02 (0.18) | 0 |
| Occupational therapy | 0.01 (0.08) | 0.05 (0.50) | 0.05 (0.33) | 0.07 (0.38)c |
| Dietitian attendance | 0.05 (0.25) | 0.14 (1.25) | 0.15 (0.78) | 0.12 (0.49) |
These data confirm the high level of service use among these participants and the skewed nature of the data, with a small number of participants having very high service use. For example, 24 out of 153 responding participants in the intervention group and 46 out of 165 responding participants in the control group visited their GP in the surgery once a month or more in months 1–3, with one participant reporting 13 GP consultations during this period and eight out of 151 responding participants in the intervention group and 10 out of 155 responding participants in the control group visited their GP in surgery once a month or more in months 4–12.
Costs of health care and social services
The costs for health services collected through different channels were calculated by applying the unit costs detailed in Table 18 to the usage reported in Tables 21 and 22 to give the data presented in Table 23.
| Data sources | Costs covering period | |||||
|---|---|---|---|---|---|---|
| 12 months pre-trial | Months | |||||
| 1–3 | 4–12 | |||||
| Intervention group | Control group | Intervention group | Control group | Intervention group | Control group | |
| Health services use recorded by nurses | ||||||
| n | 184 | 189 | 153 | 164 | 150 | 152 |
| Mean cost (£) (SD) | 1057 (1371) | 1247 (1779) | 358 (621) | 304 (366) | 637 (913) | 772 (928) |
| Health services use reported by participant | ||||||
| n | 185 | 189 | 142 | 152 | 128 | 135 |
| Mean cost (£) (SD) | 75 (199) | 119 (326) | 22 (56) | 40 (125) | 50 (129) | 79 (226) |
The mean cost of health services use recorded by nurses was higher in the control group during the 12 months before the trial and in months 4–12 of the trial, but was lower in months 1–3. For participants’ self-reported use, the mean cost was higher in the control group for all three periods. The large SDs were consistent with the usage pattern reported in Tables 21 and 22.
The mean cost of medication for a 1-month period at baseline was estimated to be £55 in the intervention group and £60 in the control group and there was little change over the trial period (Table 24). Mean costs were accompanied by large SDs and, as for service use, small numbers of participants had high medication costs, whereas only three participants at baseline (two of whom were in the intervention group), three participants at 3 months (only one of them being the same as at baseline) and no participants at 12 months were specified as taking no mediation.
| Time point | Treatment group | |||
|---|---|---|---|---|
| Intervention | Control | |||
| n | Mean cost (£) (SD) | n | Mean cost (£) (SD) | |
| Baseline | 183 | 55 (60) | 187 | 60 (71) |
| 3 months | 144 | 56 (69) | 156 | 60 (73) |
| 12 months | 145 | 58 (68) | 152 | 61 (75) |
The majority of the intervention group had estimated 1-month medication costs of under £30 at baseline and at 3 months and of under £35 at 12 months. The majority of the control group had estimated 1-month medication costs of under £40 at all time points. However, at baseline, 30 participants in the intervention group and 33 in the control group had costs higher than £100. At 3 months, the numbers of participants were 24 (intervention group) and 28 (control group) and at 12 months they were 21 (intervention group) and 25 (control group). The highest costs at baseline (£575) and at 3 months (£551) and 12 months (£567) were all found in the control group.
Health-related quality of life
The Problem Areas in Diabetes score
The PAID score was calculated based on information collected at baseline and at 3 months’ and 12 months’ follow-up (Table 25). The mean score was higher, indicating more distress, in the control group than in the intervention group at all time points. The highest PAID score in the intervention group was 67.5 at baseline, 63.75 at 3 months and 62.5 at 12 months. In contrast, the highest PAID score in the control group was 95 at baseline, 73.75 at 3 months, and 86.25 at 12 months.
| Time point | Treatment group | |||
|---|---|---|---|---|
| Intervention | Control | |||
| n | Mean score (points) (SD) | n | Mean score (points) (SD) | |
| Baseline | 185 | 18.1 (17.1) | 189 | 19.9 (19.9) |
| 3 months | 154 | 15.2 (15.2) | 166 | 16.7 (17.1) |
| 12 months | 153 | 14.1 (14.8) | 168 | 16.5 (18.0) |
The large SDs indicated the diversity of HRQoL in terms of PAID score in both groups. In the intervention group, 28 participants at baseline, 16 participants at 3 months and 12 participants at 12 months scored ≥ 40 points (indicating significant distress). In the control group, 33 participants at baseline, 18 at 3 months, and 25 at 12 months scored ≥ 40 points.
The EuroQol-5 Dimensions, three-level version
The mean EQ-5D-3L index score among the responding participants was higher in the intervention group than in the control group at all three time points (Table 26). Four participants in the intervention group and six in the control group completed the EQ-5D-3L questionnaire at 12 months but not at 3 months, whereas 126 participants in the intervention group and 129 in the control group completed the EQ-5D-3L at all three time points. These 126 and 129 participants showed slightly higher EQ-5D-3L index scores than among the non-responding participants in their group.
| Time point | Treatment group | |||||
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| Mean score (SD) | n | Mean scorea (SD) (n = 126) | Mean score (SD) | n | Mean scorea (SD) (n = 129) | |
| Baseline | 0.793 (0.244) | 185 | 0.807 (0.221) | 0.766 (0.289) | 189 | 0.803 (0.243) |
| 3 months | 0.822 (0.193) | 145 | 0.829 (0.186) | 0.817 (0.250) | 152 | 0.816 (0.252) |
| 12 months | 0.814 (0.229) | 130 | 0.819 (0.222) | 0.796 (0.270) | 134 | 0.800 (0.271) |
Primary outcomes
The outcomes and the incremental costs and effectiveness based on imputed data sets are presented in Tables 27–30. The mean costs of health resources used in months 1–3 were higher in the intervention group than in the control group (£580 vs. £544) (see Table 27). In months 4–12, this position reversed, with the mean costs of health resources used being higher in the control group than in the intervention group (£1231 vs. £1525). Overall, during the 12-month trial period, the costs of health resources used were higher in the control group than in the intervention group. The unadjusted difference in total cost (including intervention cost) was £210, with a lower value in the intervention group. The difference was smaller (£91) when adjusted for baseline health resource costs only, but still higher in the control group. After adjusting for the costs in the 12 months prior to recruitment and baseline variables, the incremental mean cost for the intervention group compared with the control group was –£111.
| Costs | Treatment group, cost (£) | |
|---|---|---|
| Intervention | Control | |
| Intervention cost | 41 | 0 |
| Months, mean cost (SE) | ||
| 1–3 | ||
| Health services use (from nurses) | 385 (56) | 311 (30) |
| Health services use (from participants) | 24 (5) | 50 (11) |
| Medication for 1-month period | 57 (6) | 61 (6) |
| 4–12 | ||
| Health services use (from nurses) | 649 (73) | 825 (90) |
| Health services use (from participants) | 60 (14) | 142 (45) |
| Medication for 1-month period | 58 (5) | 62 (6) |
| Health resources use in the 12-month trial period,a mean (SE) | 1816 (125) | 2067 (144) |
| Total costs in the 12-month trial period,a mean (SE) | 1857 (125) | 2067 (144) |
| Unadjusted incremental cost for intervention group | –210 | n/a |
| Incremental cost for intervention group, adjusted for health resources use cost at baseline only, mean (SE) | –91 (169) | n/a |
| Incremental cost for intervention group, adjusted for health resources use cost at baseline and other baseline variablesb (95% CI) | –111 (–384 to 136) | n/a |
The mean PAID score was higher in the control group than in the intervention group at baseline and at 3 months and 12 months (Table 28). The unadjusted difference in PAID score at 12 months was 3.1 points, with the intervention group scored lower. This difference was reduced to 1.9 points after adjusting for baseline PAID score, which was similar to the score when the adjustment for other baseline variables was also made.
| Time point | Treatment group | |
|---|---|---|
| Intervention | Control | |
| Time point, mean score (points) (SE) | ||
| Baseline | 18.1 (1.3) | 19.9 (1.4) |
| 3 months | 15.7 (1.2) | 17.3 (1.3) |
| 12 months | 14.5 (1.2) | 17.6 (1.4) |
| Unadjusted incremental PAID score (points) at 12 months for intervention group | –3.1 | n/a |
| Incremental PAID score (points) at 12 months for intervention group, adjusted for baseline PAID score only (SE) | –1.9 (1.3) | n/a |
| Incremental PAID score at 12 months for intervention group, adjusted for baseline PAID score and other baseline variablesa (95% CI) | –1.9 (–4.2 to 0.3) | n/a |
The mean EQ-5D-3L index score in both groups increased from baseline to 3 months (see Table 29). At 12 months, the mean index score dropped in both groups, but the reduction was sharper in the control group. QALYs were calculated based on the EQ-5D-3L index score at three time points. The unadjusted value of QALY during the 12 months trial period was 0.802 in the intervention group and 0.764 in the control group, giving a difference of 0.038. The difference was reduced by half after adjusting for baseline EQ-5D-3L index score. After adjusting for EQ-5D-3L index score at baseline and other baseline variables, the incremental QALY was 0.020, comparing the intervention group with the control group.
| EQ-5D-3L and QALYs | Treatment group | |
|---|---|---|
| Intervention | Control | |
| EQ-5D-3L index, mean score (SE) | ||
| Baseline | 0.793 (0.018) | 0.766 (0.021) |
| 3 months | 0.811 (0.016) | 0.786 (0.024) |
| 12 months | 0.793 (0.023) | 0.736 (0.037) |
| QALYs | ||
| QALYs in the 12 months’ trial period, mean (SE) | 0.802 (0.016) | 0.764 (0.023) |
| Unadjusted incremental QALYs for the intervention group | 0.038 | n/a |
| Incremental QALYs for the intervention group, adjusted for baseline EQ-5D-3L index score only (SE) | 0.019 (0.021) | n/a |
| Incremental QALYs for the intervention group, adjusted for baseline EQ-5D-3L index score and other baseline variablesa (95% CI) | 0.020 (–0.000 to 0.044) | n/a |
For both health outcomes, the intervention was less costly and more effective, suggesting dominance by the intervention over the control (Table 30). However, the 95% CIs of all three outcomes included zero, indicating the uncertainty of this conclusion.
| Incremental cost-effectiveness (with control group as comparator) | Mean (95% CI) |
|---|---|
| Incremental cost (£), adjusted for health resources use cost at baseline and other baseline variablesa | –111 (–384 to 136) |
| Incremental PAID score (points) at 12 months, adjusted for baseline PAID score and other baseline variablesa | –1.9 (–4.2 to 0.3) |
| Incremental QALYs, adjusted for baseline EQ-5D-3L index score and other baseline variablesa | 0.020 (–0.000 to 0.044) |
| ΔCost/ΔPAID score | Intervention dominating control, as it is less costly but more effective |
| ΔCost/ΔQALY | Intervention dominating control, as it is less costly but more effective |
Figure 12 shows the cost-effectiveness plane describing the uncertainty surrounding the conclusion of the intervention’s dominance. The dashed lines show the national WTP thresholds of £20,000 and £30,000 per QALY gained. As the WTP threshold increases, the slope of the line will increase. There is considerable uncertainty surrounding the point estimates of the incremental costs and incremental QALYs from the primary analysis, but the majority of the distribution is scattered in the south-east quadrant of the plane, supporting the primary conclusion of the intervention being less costly but more effective. When the distribution falls into the north-east quadrant of the plane (more costly and more effective), most of the data points fall below the WTP thresholds. This indicates that even if the intervention becomes more costly instead of cost-saving, it is still likely to be cost-effective.
FIGURE 12.
The cost-effectiveness plane comparing the intervention group with the control group.
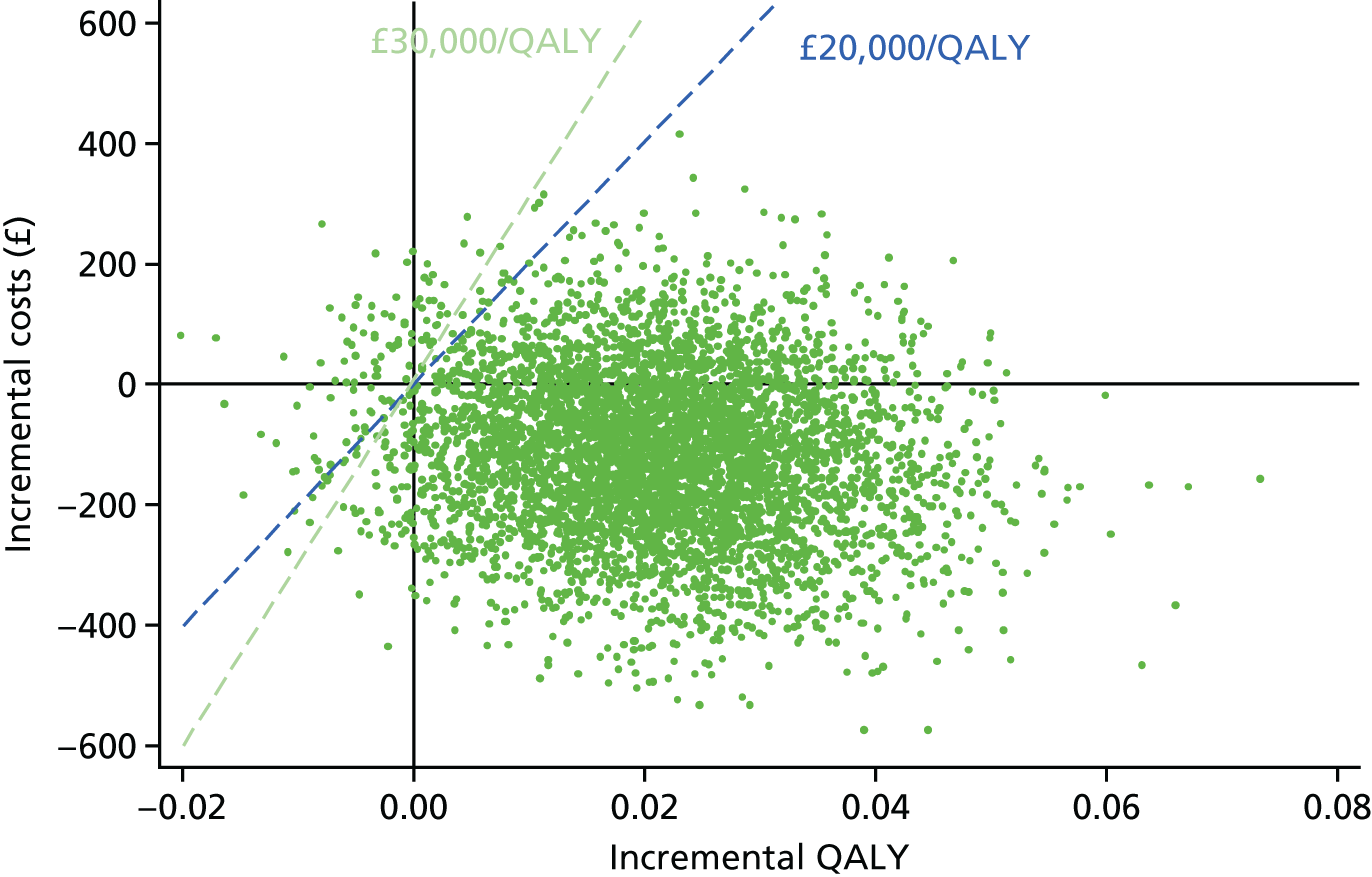
The CEAC constructed using the bootstrapped data shows that the probability of the intervention being cost-effective reaches 95% at a WTP of £6900 (Figure 13). Under the existing WTP threshold of £20,000 to £30,000, the probability of the intervention being cost-effective, compared with the control, was over 97%.
FIGURE 13.
The CEAC for the intervention.
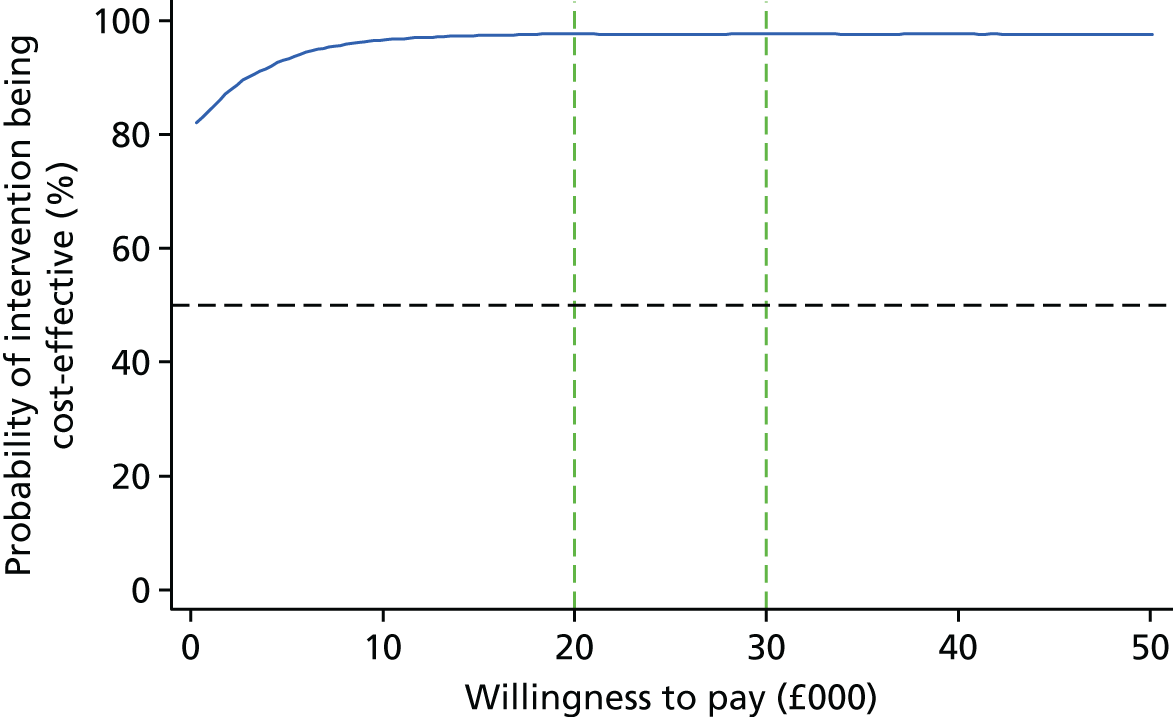
Sensitivity analysis
Complete-case analysis
For the three outcomes used in the primary analysis, the extent of completeness varied (Table 31). The completeness of PAID score at 12 months was the highest among the three. For costs, only the participants who had complete cost data (i.e. heath services use recorded by nurses, health services use reported by participants and medication information) at 3 months and 12 months were considered complete cases, which gave the lowest number of complete cases. In order to calculate QALYs, the EQ-5D-3L must be completed at all three data collecting points to be considered complete.
| Outcomes | Treatment group | |||
|---|---|---|---|---|
| Intervention | Control | |||
| n | Mean (SD) | n | Mean (SD) | |
| Total costs (£) during 12-month trial period | 98 | 1785 (1511) | 103 | 1719 (1525) |
| PAID score (points) at 12 months | 153 | 14.1 (14.8) | 168 | 16.5 (18.0) |
| QALYs | 126 | 0.822 (0.185) | 128 | 0.808 (0.242) |
Taking into account the completeness of the baseline variables required for adjustment, there were 96 participants in the intervention group and 101 participants in the control group who had complete information at all required time points on every required variable. Therefore, the complete-case analysis was performed on these 197 people.
In the complete-case analysis, the mean cost during the 12-month trial period, including intervention and health resource use costs, was £1736 in the intervention group and £1721 in the control group (Table 32). Using the same adjustment methods as in the primary analysis, the intervention group showed a £15 higher mean cost when unadjusted, a £58 lower mean cost when adjusted for baseline health resource use costs and a £37 lower mean cost than the control group after adjusting for all baseline variables.
| Costs | Treatment group, cost (£) | |
|---|---|---|
| Intervention (n = 96) | Control (n = 101) | |
| Intervention cost | 41 | 0 |
| Time point, months, mean cost (SD) | ||
| 1–3 | ||
| Health services use (from nurses) | 332 (503) | 267 (327) |
| Health services use (from participants) | 24 (64) | 27 (68) |
| Medication for 1-month period | 57 (66) | 52 (55) |
| 4–12 | ||
| Health services use (from nurses) | 566 (692) | 693 (963) |
| Health services use (from participants) | 51 (143) | 65 (186) |
| Medication for 1-month period | 61 (73) | 57 (69) |
| Health resources use in the 12-month trial period,a mean (SD) | 1695 (1404) | 1721 (1539) |
| Total costs in the 12-month trial period,a mean (SD) | 1736 (1404) | 1721 (1539) |
| Unadjusted incremental cost for the intervention group | 15 | n/a |
| Incremental cost for the intervention group, adjusted for health resources use cost at baseline only, mean (SD) | –58 (163) | n/a |
| Incremental cost for the intervention group, adjusted for health resources use cost at baseline and other baseline variablesb (95% CI) | –37 (–367 to 282) | n/a |
The mean PAID score at 12 months was 14.6 points in the intervention group and 15.9 points in the control group (Table 33). Although PAID scores continued to reduce in the intervention group, the scores remained the same between 3 and 12 months in the control group. The adjusted difference between groups was 1.6 points at 12 months, with a lower value in the intervention group.
| Time point | Treatment group | |
|---|---|---|
| Intervention (n = 96) | Control (n = 101) | |
| Time point, mean PAID score (points) (SD) | ||
| Baseline | 18.8 (16.8) | 19.0 (16.5) |
| 3 months | 16.9 (16.1) | 15.9 (15.2) |
| 12 months | 14.6 (15.5) | 15.9 (16.7) |
| Unadjusted incremental PAID score (points) at 12 months for the intervention group | –1.3 | n/a |
| Incremental PAID score (points) at 12 months for the intervention group, adjusted for baseline PAID score only, mean (SD) | –1.2 (1.6) | n/a |
| Incremental PAID score (points) at 12 months for the intervention group, adjusted for baseline PAID score and other baseline variablesa (95% CI) | –1.6 (–5.1 to 1.4) | n/a |
The mean QALYs during the 12-month period were 0.816 in the intervention group and 0.833 in the control group (Table 34). The unadjusted difference shows a higher QALY in the control group than in the intervention group. After adjusting for baseline variables, the mean QALYs in the intervention group were 0.010 higher than in the control group.
| EQ-5D-3L and QALYs | Treatment group | |
|---|---|---|
| Intervention (n = 96) | Control (n = 101) | |
| EQ-5D-3L index, mean (SD) | ||
| Baseline | 0.792 (0.232) | 0.829 (0.207) |
| 3 months | 0.824 (0.186) | 0.840 (0.229) |
| 12 months | 0.814 (0.218) | 0.825 (0.250) |
| QALYs | ||
| QALYs in the 12 months’ trial period, mean (SD) | 0.816 (0.183) | 0.833 (0.215) |
| Unadjusted incremental QALYs for the intervention group | –0.017 | n/a |
| Incremental QALYs for the intervention group, adjusted for baseline EQ-5D-3L index score only, mean (SD) | 0.026 (0.015) | n/a |
| Incremental QALYs for the intervention group, adjusted for baseline EQ-5D-3L index score and other baseline variablesa (95% CI) | 0.010 (–0.018 to 0.044) | n/a |
Combining all three outcome measures, among complete cases, the intervention group still showed a lower mean cost and better effectiveness on both PAID score and QALYs (Table 35). Compared with the results from the primary analysis (see Table 30), the complete-case analysis results generally showed a larger SD but a smaller difference between groups.
| Incremental cost-effectiveness | Mean (95% CI) |
|---|---|
| Incremental cost for the intervention group, adjusted for health resources use cost at baseline and other baseline variablesa (95% CI), (£) | –37 (–367 to 282) |
| Incremental PAID score at 12 months for the intervention group, adjusted for baseline PAID score and other baseline variablesa (95% CI) | –1.6 (–5.1 to 1.4) |
| Incremental QALYs for the intervention group, adjusted for baseline EQ-5D-3L index score and other baseline variablesa (95% CI) | 0.010 (–0.018 to 0.044) |
| ΔCost/ΔPAID score | Intervention dominating control, as it is less costly but more effective |
| ΔCost/ΔQALY | Intervention dominating control, as it is less costly but more effective |
Figures 14 and 15 present the cost-effectiveness plane and CEAC plotted using the same technique as in the primary analysis but using data only from the 197 complete cases. From the distribution of the dots on the plane (see Figure 14), it is evident that only about a quarter of them fall in the south-east quadrant, where the intervention would be less costly but more effective. A considerable proportion of dots fall in the left side of the plane, where the intervention would be less effective.
FIGURE 14.
Cost-effectiveness plane comparing the intervention group to the control group (among complete cases).
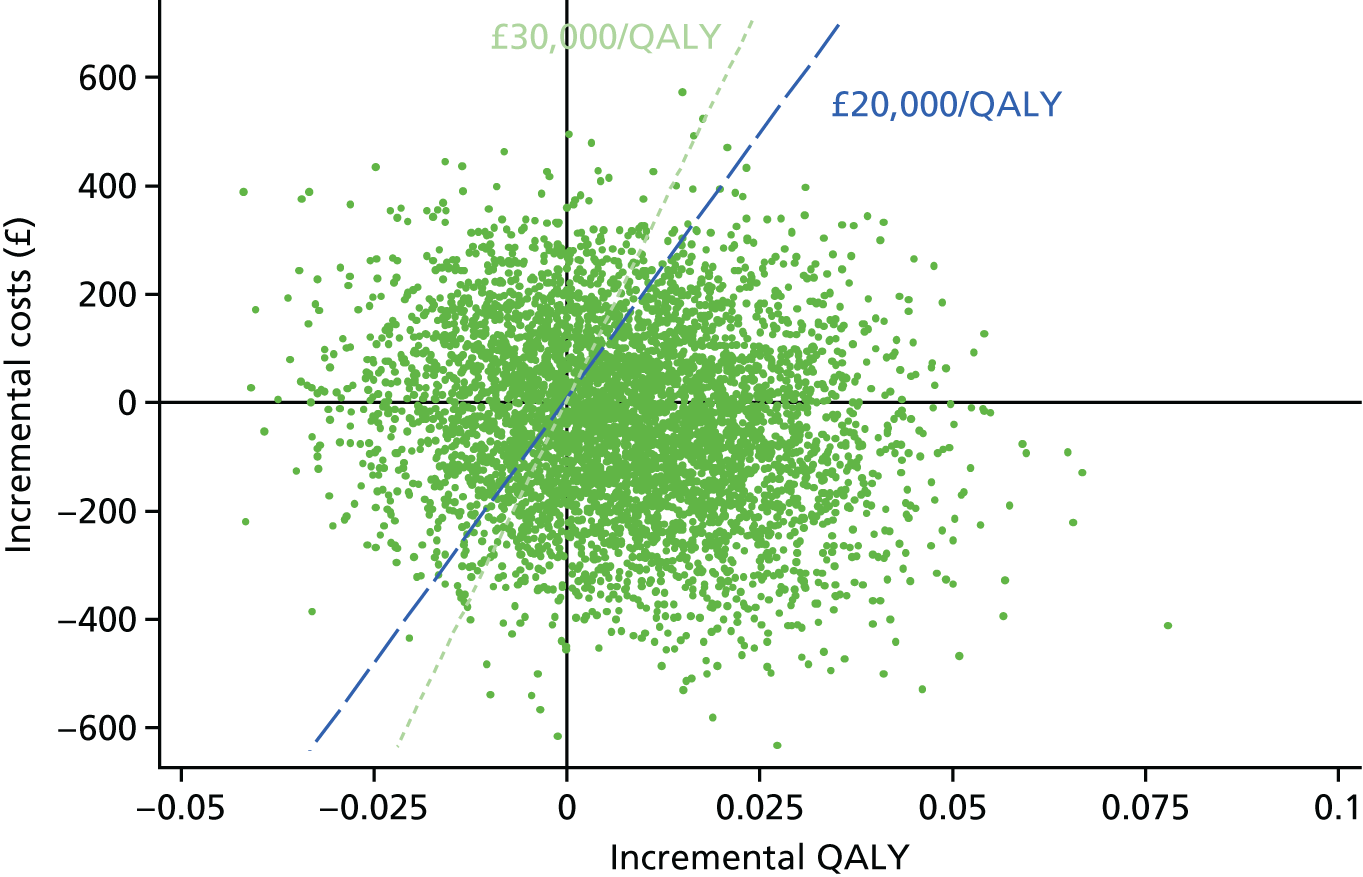
FIGURE 15.
The CEAC for the intervention (among complete cases).
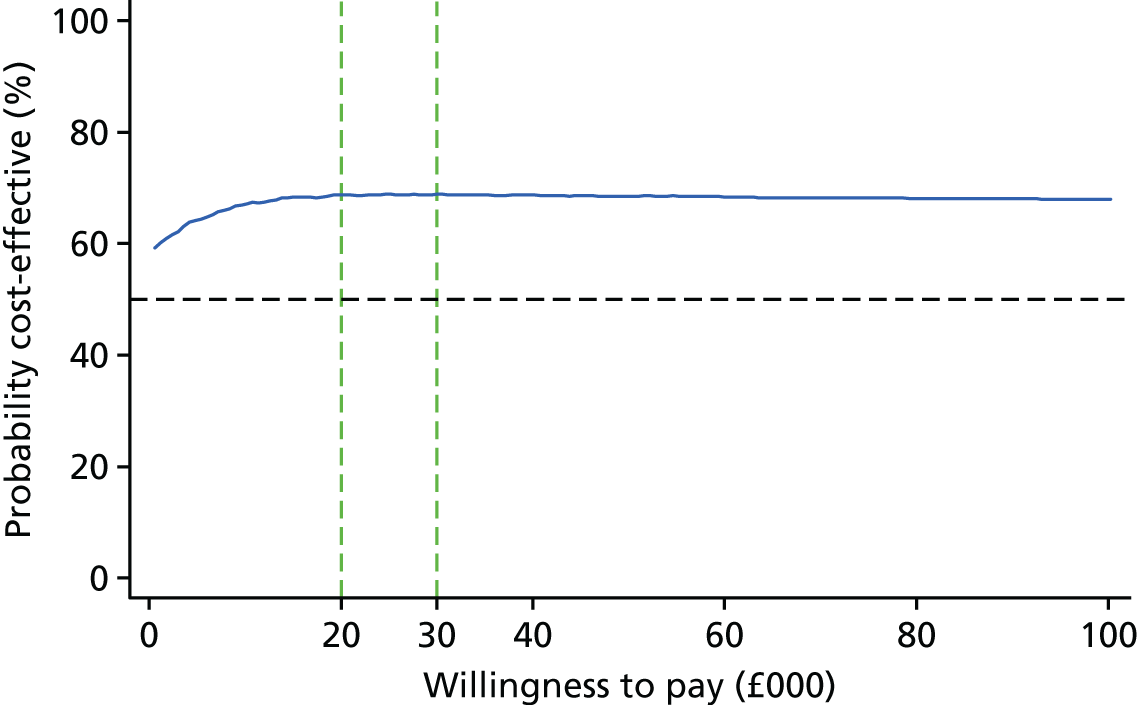
Accordingly, it is not surprising that the probability of the intervention being cost-effective was much lower than estimated from imputed data. In contrast to the high probability (> 97%) of cost-effectiveness in the primary analysis, the complete-case analysis showed a probability of under 70% of the intervention being cost-effective. Between £20,000 and £30,000, the probability only changed 0.2% (from 68.7% to 68.9%). This trend is consistent with the primary analysis. Marginal effects reach near zero quickly. Additional investment in the intervention did not appear to have a big impact.
Comparing the results from the complete-case analysis to the primary analysis, neither showed any apparent change in health resource use costs within groups (Figure 16). The cost of health resources used in the 12 months prior to recruitment in the control group was lower among complete cases than that in the imputed data set, although there was little difference between the two data sets in the intervention group. Given that the baseline data were almost complete, this difference in the control group suggested that the participants who had higher usage of health services were more likely to be lost to follow-up than those with lower usage. The mean costs during the 12-month trial period in both groups were lower in the complete-case data set than in the imputed data set, with the difference in the control group more prominent. This was because the multiple imputation took the higher health resource use cost in the 12 months prior to recruitment as one of the factors for its imputation of missing values. That, in turn, leads to a bigger difference in costs in the imputed data set than in the complete cases (–£111 vs. –£37).
FIGURE 16.
Comparison of the costs of health resources use between imputed data and complete cases.
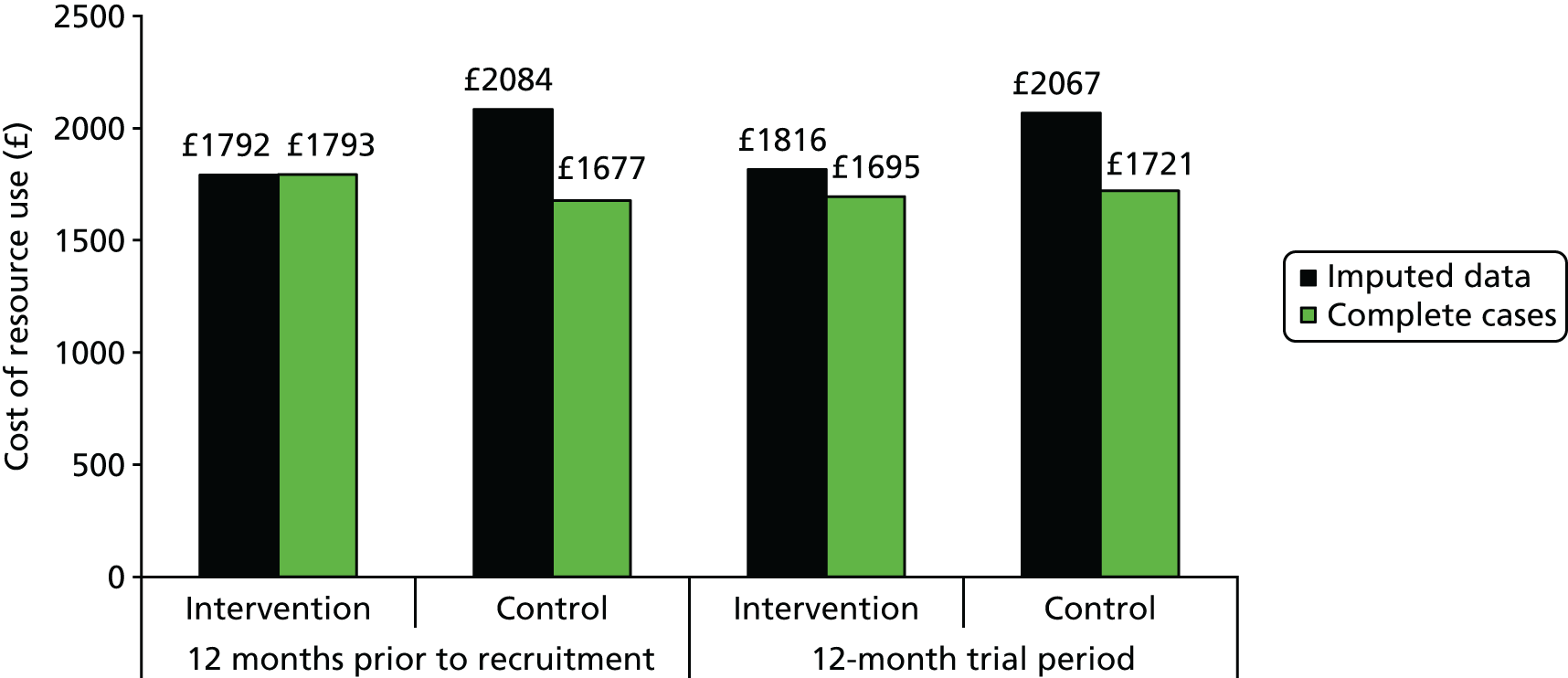
As the imputation was performed on an aggregated level, the individual contribution of the cost of each type of health resource used during the 12-month trial period was not presented in the primary analysis. For complete cases, the biggest drivers in costs were hospital inpatient stays and hospital outpatient appointments (Figure 17), followed by GP consultations in surgery. However, if all forms of GP consultation were aggregated, the costs would approximate to those of hospital outpatient appointments and inpatient stays. It should be noted that Figure 17 does not include medication costs. If our assumption of one prescription item per month was correct, medication costs would be higher than all other costs (£718 in the intervention group and £671 in the control group).
FIGURE 17.
Cost of each health care and social services use during the 12-month trial period among complete cases, by group.
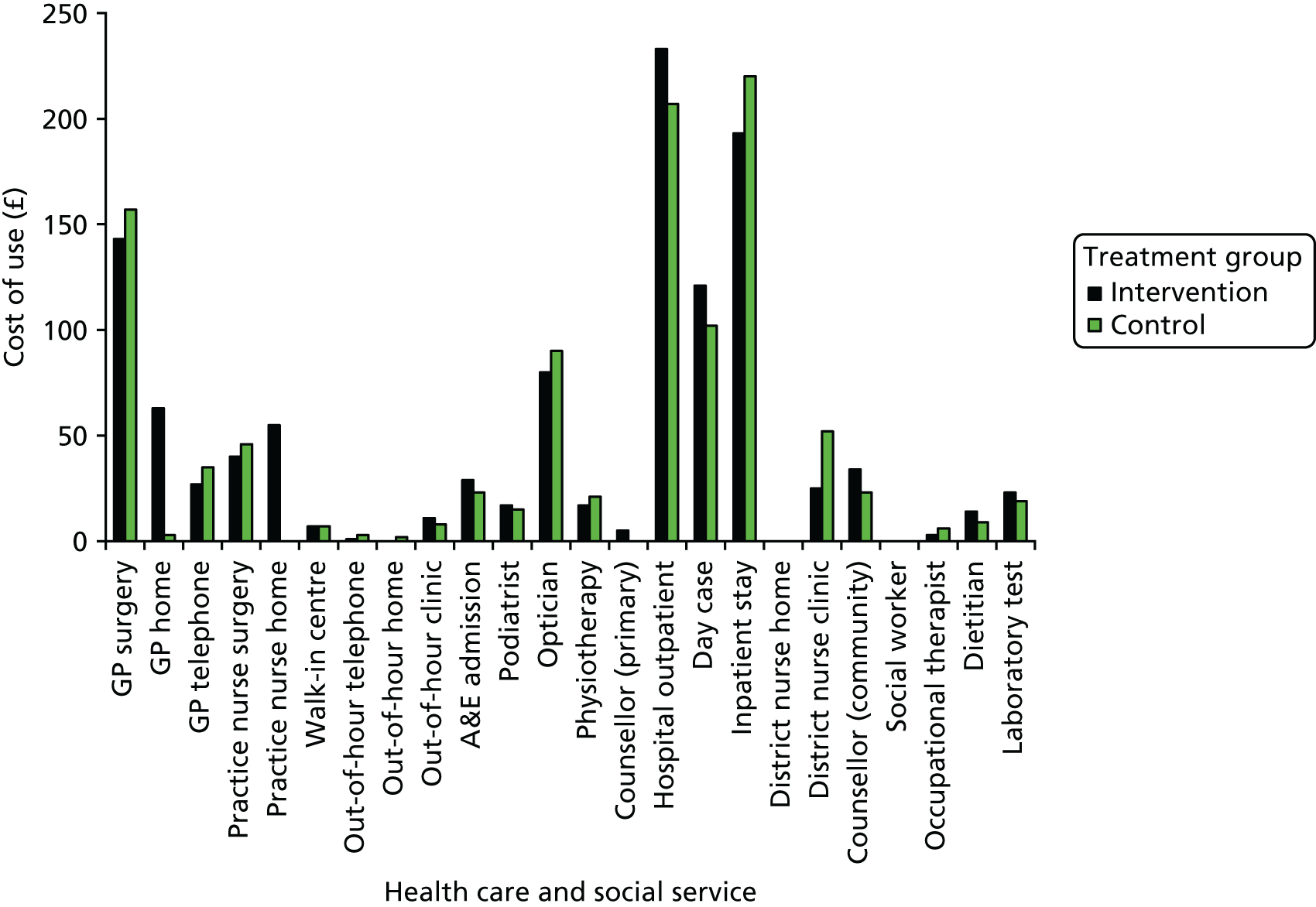
Complete cases showed a similar pattern in change of PAID score in the control group across three time points as in the imputed data set but with lower scores (i.e. less distress) (Figure 18). Meanwhile, the mean PAID score was slightly higher at baseline and at 3 months among complete cases than in the imputed data set, but at 12 months was similar in the complete cases and the imputed data set in the intervention group. This suggested that there were possible opposite missing patterns in the groups. In the intervention group, participants who scored lower on PAID score at baseline were more likely to be lost to follow-up; however, in the control group, those who scored higher were more likely to be lost to follow-up. The difference of PAID score at 12 months was much more prominent in the control group than in the intervention group. After adjusting for baseline PAID score and other variables, this leads to a smaller reduction in PAID score (–1.6 vs. –1.9 points).
FIGURE 18.
Mean PAID score (points) of imputed data set and complete cases at three time points, by group.
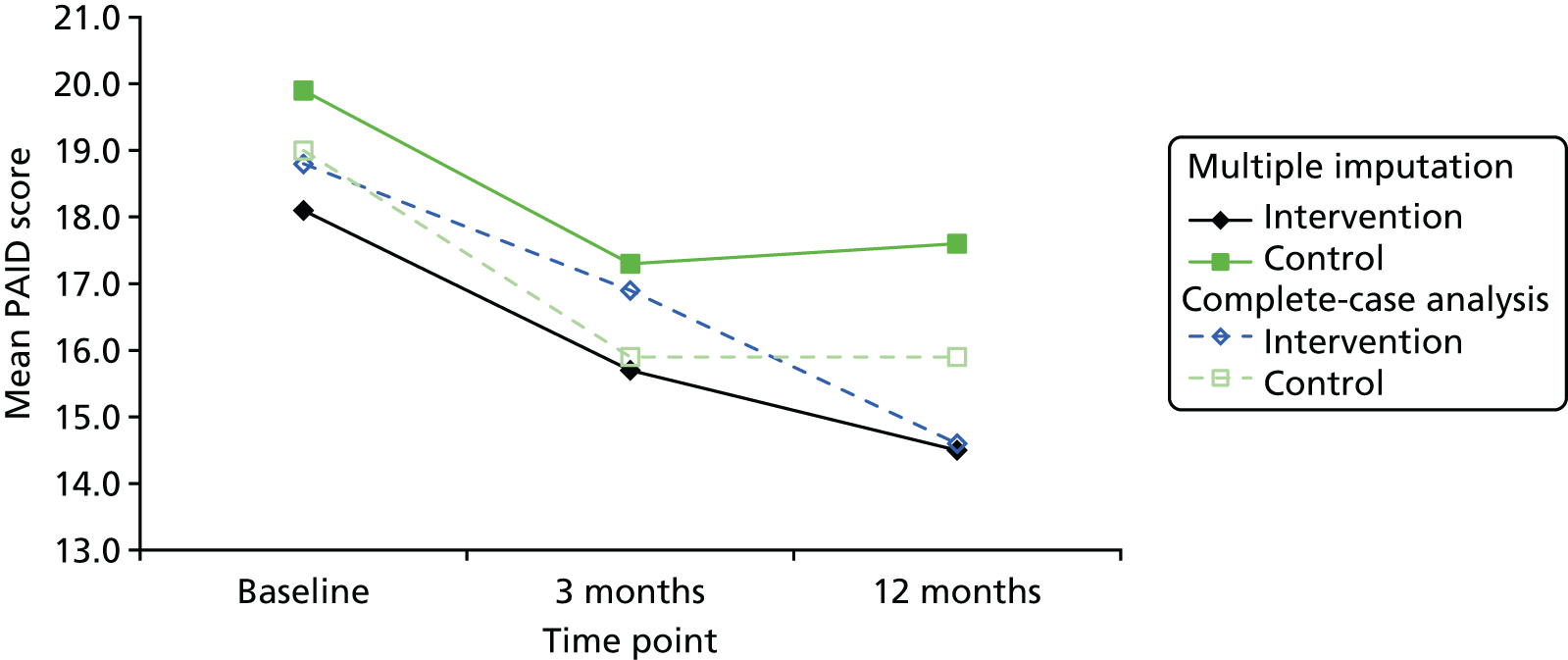
In the complete-case analysis, the general pattern of the mean EQ-5D-3L index score increasing at 3 months and decreasing at 12 months remained, but the mean index scores in the intervention group were higher in the complete cases than in the imputed data set and did not reduce at 12 months as much as in the imputed data set (Figure 19). In the control group, the baseline level of EQ-5D-3L index score was much higher among complete cases than in the imputed data set and remained so at all time points. The mean EQ-5D-3L index scores in the control group increased at 3 months and reduced below the baseline level in both complete cases and imputed data set. The drop of EQ-5D-3L index score level was more gradual and to a lesser extent among the complete cases. Among complete cases, the mean EQ-5D-3L index score in the control group was higher than in the intervention at all time points, opposite to the situation for the imputed data set. This leads to a higher QALYs in the control group when unadjusted. This pattern of change is consistent with the pattern in PAID score where in the control group, participants who had lower EQ-5D-3L index score at baseline were more likely to be lost to follow-up later on. Because the baseline EQ-5D-3L was near complete and taken as a factor in the imputation model, the imputed data set estimated lower values for missing data at 3 and 12 months. After adjusting for all relevant baseline variables, the intervention group still shows a QALYs gain, compared with the control group. This QALYs gain was also smaller than that of the imputed data set (0.010 versus 0.020).
FIGURE 19.
Mean EQ-5D-3L index score of imputed data set and complete cases at three time points, by group.
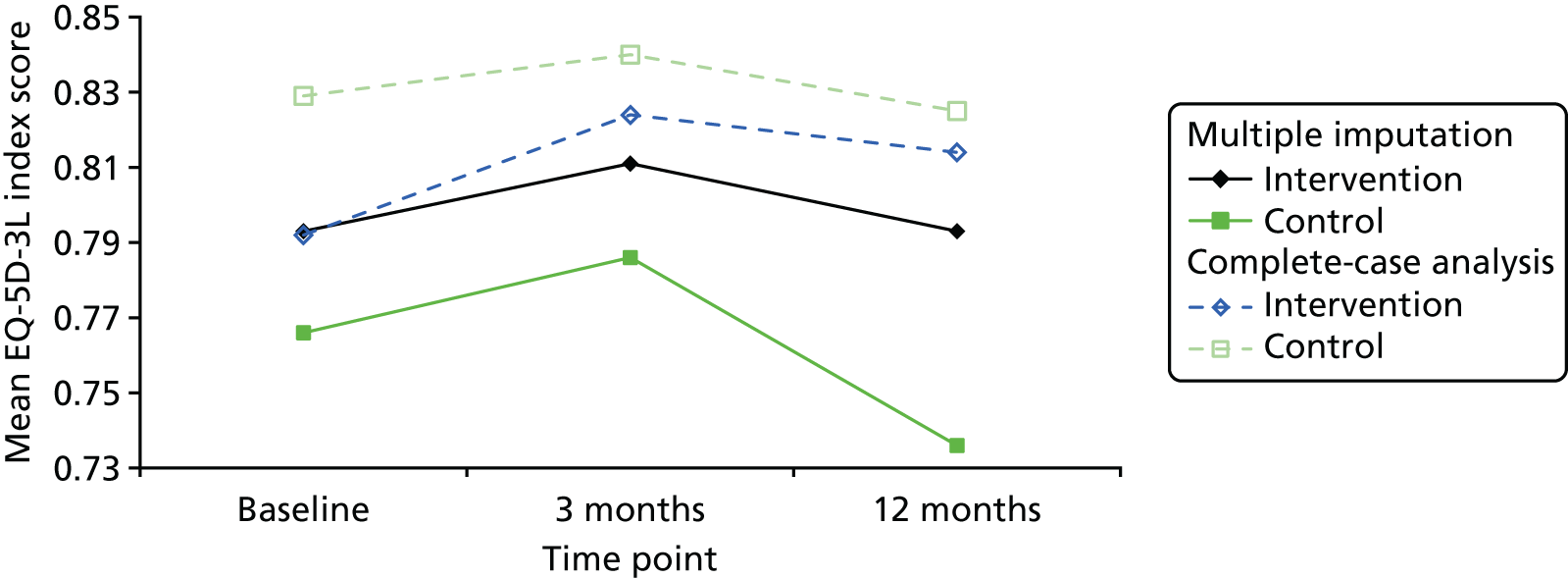
One-way sensitivity analysis for cost of intervention
The intervention cost was estimated at £41 per person for the primary analysis. Using Equation 1, a linear line was drawn, assuming incremental cost per person remained –£111 and incremental QALYs per person remained 0.020 (Figure 20). As the additional intervention cost per person increased, the ICER for the intervention gradually increased. At a £20,000 WTP threshold, the additional intervention cost per person was £511. At a £30,000 WTP threshold, the additional intervention cost per person was £711. That means, on top of what was included in the primary analysis for the intervention, another £511–711 per person could be spent on facilitating activities or running costs of the intervention, and the intervention might still be considered cost-effective.
FIGURE 20.
One-way sensitivity analysis for intervention cost per person, from imputed data set and complete cases. CCA, complete-case analysis; MI, multiple imputation; WTP1, willingness to pay threshold 1 (£20,000); WTP2, willingness to pay threshold 2 (£30,000).
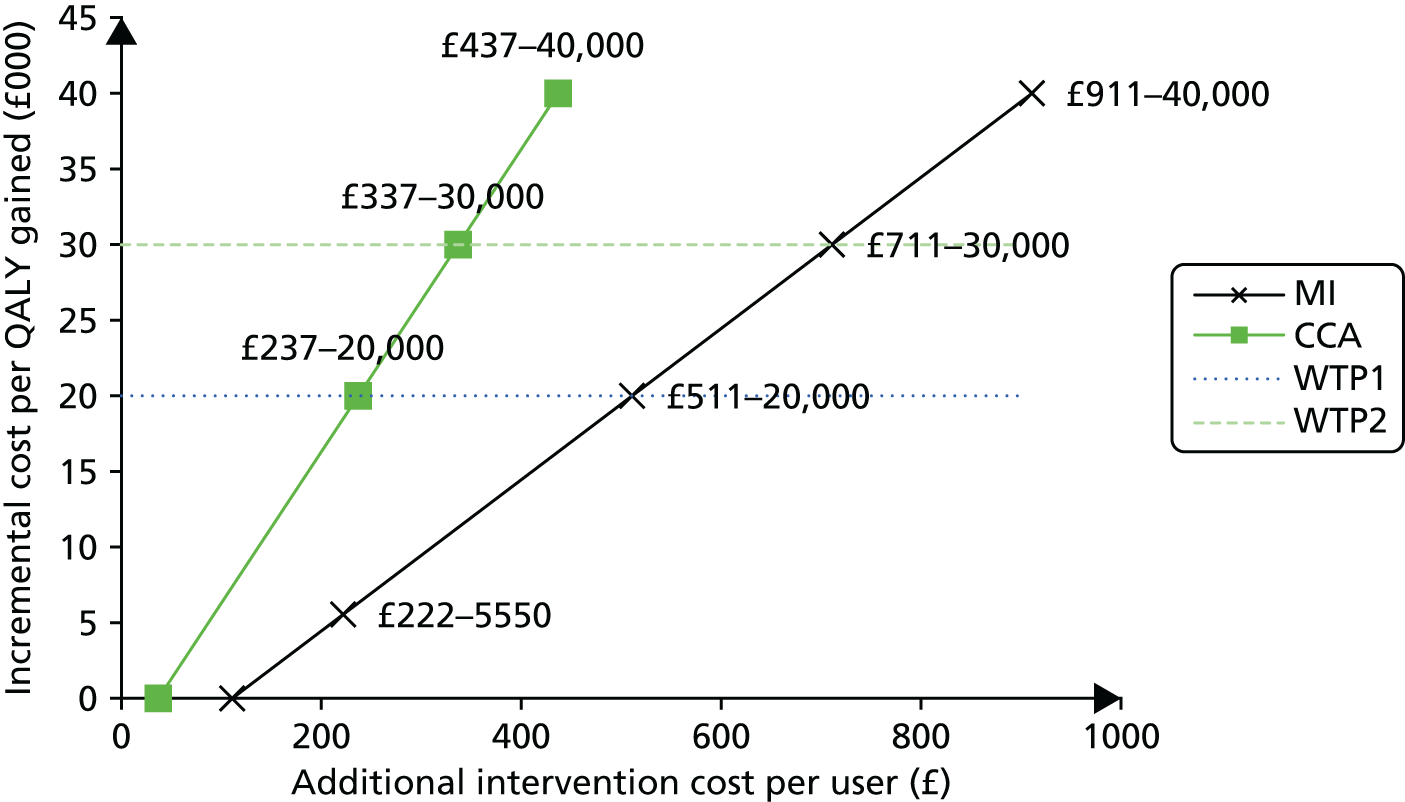
In the analysis, the website operation cost was allocated to 10,000 users, as this was the reported capacity of the server. When it was allocated to the 185 participants in the intervention group, the intervention cost would increase by £222. The ICER, in turn, would be £5550 per QALY gained. Although not less costly any more, the intervention could still be considered cost-effective under the national WTP thresholds, in comparison to the control.
The complete-case analysis demonstrated a more rapid increase in incremental cost per QALY gained than the analysis using imputed data. An increase of £237 in intervention cost per user led to the ICER reaching the lower bound of the current national WTP threshold (£20,000 per QALY). Another £100 additional intervention cost per user led the ICER up to the upper bound of current national WTP threshold (£30,000 per QALY). In other words, in the complete-case analysis, cost-effectiveness was more sensitive to increased costs of the intervention.
Discussion
Main results
In this within-trial health economic analysis, from a NHS and personal and social services perspective, the HeLP-Diabetes programme was found to dominate the comparator, that is, total costs were lower (–£111, 95% CI –£384 to £136) and health outcomes better (incremental QALYs 0.020, 95% CI 0.000 to 0.044 QALYs) in the group allocated to the HeLP-Diabetes programme than in the group allocated to the comparator. The cost-effectiveness plane and CEAC illustrated that, despite considerable uncertainty around the point estimates, this overall conclusion is likely to be robust. The complete-case analysis demonstrates more uncertainty than the primary analysis, which is based on imputed data. Although the total costs were still lower (–£37, 95% CI –£367 to –£282) and health outcomes better (incremental QALYs 0.010, 95% CI –0.018 to 0.044 QALYs) in the HeLP-Diabetes programme group than in the comparator group, the extent of the difference was smaller than in the primary analysis. Consequently, the cost-effectiveness plane showed the cluster of the distribution moving towards centre and widely scattered in all four quadrants. The probability of cost-effectiveness was reduced from 97% in the primary analysis to just under 70% in the complete-case analysis.
This difference in results between the primary and complete-case analyses may be because of the differential retention rates of participants with worse health. People with worse health were more likely to use health-care services, which resulted in higher costs. The comparison of costs and quality of life was consistent with this suggestion, as participants in the complete-case analysis demonstrated better quality of life and lower health resource use than those in the primary analysis. Whether it was the impact of worse health or the burden of completing trial outcome questionnaires on top of their ill health that caused this differential dropout is unclear.
Although both the primary and complete-case analyses suggested that the HeLP-Diabetes programme was highly likely to be dominant over the comparator condition, the uncertainties surrounding both the change in costs and in quality of life, and the fact that these changes were not statistically significant, require this conclusion to be treated with caution. Moreover, as the trial lasted only 12 months, it is possible that some of the drivers of health resource use by participants pre-dated the trial, for example hospital inpatient admissions may have been planned before the start of the trial. Moreover, although it was apparent that the main cost drivers were medications, hospital inpatient stays, hospital outpatient appointments and GP consultations, it was unclear which one in particular or combination of services caused the overall health-care costs to be lower in the intervention group.
As a large proportion of the costs are fixed costs, the average user cost falls and the cost-effectiveness increases as the number of registered users grows. This is particularly important in a highly prevalent condition such as T2DM. Current estimates suggest there are around 4 million people in the UK with T2DM, making the need to identify a cost-effective method of improving health outcomes in these people imperative.
Methodological strengths and weaknesses
The analysis was undertaken following NICE’s guidance. We collected detailed data on health and social service usage. The majority of service use data reported by nurses was extracted from participants’ EMRs, which was a more accurate and reliable method than participants’ self-reported data. Although there may have been under-recording, it is unlikely to have introduced systematic bias. Data on service use obtained directly from participants may have been subject to recall bias and be less reliable but, again, it is hard to see how this could have introduced systematic bias. Prescribed medications were extracted by nurses from participants’ EMRs and, hence, were more likely to be accurate than patient recall. However, it would have been better if we had asked nurses to record defined daily doses, as without these data we relied on the assumption that each prescription item was issued per month (as per national guidelines). Although this added to the uncertainty around total medication costs, it too was unlikely to lead to systematic bias, as it was applied to both groups.
We took the methodological decision to exclude the costs of development of the HeLP-Diabetes programme and include only the costs of maintenance and delivery. The rationale for this decision was that it is these maintenance and delivery costs that the NHS will have to cover if the HeLP-Diabetes programme is implemented nationally and the development costs are true sunk costs, in that they cannot be recovered. However, we have presented estimates of the development costs, for those interested in developing similar interventions for other LTCs.
Owing to the length of the trial (12 months), any future updates were not taken into account in the analysis. With the fast pace of development of technology, it is not certain how frequently major updates would be required or what they would involve or cost.
Our original intention had been to undertake a modelling exercise, using the UK Prospective Diabetes Study model, which simulates the likely occurrence of major complications and costs and quality of life associated with them by four prognostic risk factors: HbA1c level, SBP, the ratio of total cholesterol to HDL-C and smoking status. 198 The main trial analysis reported a significantly better outcome in HbA1c level and SBP in the intervention group than in the control group and no significant difference in the total cholesterol-to-HDL-C ratio or smoking status. Hence, any modelling would be likely to demonstrate reduced complication rates in the intervention group, with associated improved quality of life and reduced health-care costs. We did not wish to overstate our findings and, as modelling would increase the overall uncertainty, we decided not to undertake this modelling.
Fit with existing literature
One of the main drivers for developing digital health interventions is the expectation that they can help health-care systems meet the twin challenges of delivering more and better care at reduced cost. Despite this, there has been a marked lack of formal health economic analyses. Authors of systematic reviews of digital health interventions have repeatedly reported a lack of economic data, preventing them from drawing any conclusions about cost-effectiveness. 29,30,37,199–201 Fortunately, this situation is now improving, particularly in the field of mental health, in which a number of cost-effectiveness studies have been undertaken, enabling a systematic review published in 2015202 to include 16 studies and report the cost-effectiveness of guided internet interventions for depression, anxiety, smoking cessation and alcohol moderation. Recently, there have been a number of reports of health economic analysis of digital health interventions;203–211 overall, these reports confirm that, when effective, digital health interventions, such as the HeLP-Diabetes programme, tend to be cost-effective. However, the current report is the first in which we have been able to identify that a digital health intervention dominates the comparator.
Conclusions
The HeLP-Diabetes programme appears to be a highly cost-effective intervention, which, if adopted nationally, has the potential to be even more cost-effective.
Chapter 9 Design and evaluation of a plan for implementing the Healthy Living for People with type 2 Diabetes programme into routine NHS care
Summary
This chapter describes the design and evaluation of a plan for implementing the HeLP-Diabetes programme into routine care. The aim of this work was to determine how best to integrate an eHealth intervention for patients into routine care, using the HeLP-Diabetes programme as an example.
The specific objectives were to design an implementation plan, evaluate its clinical effectiveness and any reasons for observed variation in implementation and modify the original plan in the light of these emerging data. We were interested in maximising uptake and use by people with T2DM, in exploring ways of overcoming the ‘digital divide’ and the impact that the intervention had on patient outcomes outside a trial.
The study design was iterative: as problems with the implementation plan emerged we made adjustments and then evaluated these. The implementation was planned to take place in two PCTs (which became CCGs shortly before the study commenced). Data collection took place between March 2013 and August 2015. We used a case-study design with mixed methods, combining quantitative data on adoption, uptake and use with qualitative data from semistructured interviews and field notes exploring HCP and patient perceptions of reasons for observed variability in the quantitative data. The qualitative analysis was informed by NPT.
Although both CCGs adopted the HeLP-Diabetes programme, for practical reasons we were only able to study the process in one CCG. In this group, the quantitative data showed high levels of adoption, which was defined as services within the CCG deciding to adopt the HeLP-Diabetes programme and make it available to their patients. Twenty-two out of the 34 practices adopted the HeLP-Diabetes programme, as did the community intermediate service and the local secondary care service. However, the services were less successful at promoting uptake and use of the HeLP-Diabetes programme, with 205 people with T2DM being registered in the study period. These people came from a wide demographic, which reflected the local population: over half (52%) were from black or minority ethnic backgrounds, one-third (36%) had no education after the minimum school-leaving age and over one-third (38%) described their computer skills as ‘basic’. Over half (52%) were male and the age range was 19–81 years. In line with national prevalence figures, 86% reported having home internet access.
A natural experiment arose during the implementation study, in which some practices agreed to our preferred implementation model of having a HCP (receptionist or HCA) registering patients on the HeLP-Diabetes programme and giving them an introduction to the programme, whereas other practices opted for a patient self-sign-up model. By comparing patients who were registered through these two methods, we could determine that the self-sign-up model attracted a cohort of participants who were better educated and had higher levels of computer experience, whereas the facilitated model was associated with a more diverse population. Once registered, no demographic factors (age, gender, ethnicity, educational status, computer expertise, duration of diabetes mellitus since diagnosis or treatment modality) were associated with subsequent use or non-use of the programme.
The qualitative data illuminated these quantitative findings. Qualitative data from HCPs indicated that they valued the programme and could see its benefits. The HCPs were supportive of the idea of promoting self-management by patients, while being aware that patients needed support to be able to self-manage and conscious of the disadvantages of the dominant model of group-based education. The HeLP-Diabetes programme was perceived as a high-quality intervention that could meet unmet need. Its holistic and evidence-based approach was welcomed. There was some resistance to providing facilitation, as, in common with the rest of the country, practices were experiencing significant rises in workload in parallel with falling incomes. However, staff from practices that successfully implemented the HeLP-Diabetes programme, including registering patients, reported finding that the HeLP-Diabetes programme was easy to use for HCPs and patients, that the intervention had the potential to save time and consultations and that HCAs were the most appropriate staff group to help with facilitation.
Data from patients suggested that those who used the HeLP-Diabetes programme found it a helpful and valuable resource that was easy to understand and, for many, a better way of learning than group-based education. For many, it was important that it had been recommended by their doctor or nurse. However, many said they were not ready to engage in self-management for a range of reasons, including that they did not believe they had diabetes mellitus, that they believed that they had only a ‘mild’ form that was unlikely to cause problems, that they were not ready to engage with the diagnosis and were frightened of finding out about the illness, that if the information was important their doctor or nurse would tell them or that they felt that they were already self-managing well and had nothing further to learn.
Background
Rationale for undertaking an implementation study
Implementation research is a relatively new field, concerned with ‘the scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice’. 212 Our reasons for including an implementation study alongside a trial in this programme grant were threefold:
-
Whether or not the HeLP-Diabetes programme itself proved clinically effective in a trial, the policy and financial imperatives for introducing eHealth interventions to help patients improve their health are overwhelming; hence, producing generalisable knowledge about how best to implement such interventions would be useful for the NHS and other health-care systems internationally.
-
Evidence of clinical effectiveness that is derived from RCTs does not always transfer to ‘real-world’ use. By their nature, trials involve tightly controlled procedures and selected participants whose characteristics may differ substantially from non-trial participants. Trial methodology emphasises the importance of fidelity to the intervention and trials of complex interventions will often devote considerable resources to ensuring that the intervention is delivered as intended. However, once the intervention becomes approved for routine use, these resources are often not available and the emphasis often changes from ensuring that there is fidelity to enabling adaptions that will improve local uptake and use. These changes in user population and implementation mean the effects seen in trials may not be replicated in routine use. Therefore, the effects obtained in routine use should be viewed alongside those seen in trials to inform commissioning decisions.
-
One of the overarching aims of the NIHR’s Programme Grants for Applied Health Research programme is for funded work to achieve benefits for the NHS. Hence, it was important to ensure that the programme of research generated all the data required to inform future implementation and use of the HeLP-Diabetes programme throughout the NHS. As part of the planning for this programme grant, we thought about long-term sustainability and maintenance. It was clear that this would require a revenue stream, with NHS commissioning being the most likely source. Commissioners need more information about a service than can be provided from trial data, including information about likely uptake and use and the resources required for effective implementation. This study was designed to address these needs, as well as providing generalisable data of international relevance.
The importance of undertaking implementation research alongside trials is increasingly recognised. 213–215 Broadly speaking, such research addresses two types of question: first, what are the effects of a treatment or intervention in routine use (referred to as Phase IV studies in the MRC framework); and, second, what are the effects of an implementation strategy? Researchers from the US Department of Veterans Affairs (VA) Quality Enhancement Research Initiative (QUERI) have argued for ‘hybrid’ designs that combine both types of research question. 216 They have suggested a taxonomy for such ‘effectiveness-implementation hybrid designs’ in which type 1 hybrid design tests the effect of a clinical intervention on relevant outcomes while observing and gathering information on implementation, type 2 hybrid design tests clinical and implementation interventions and strategies equally and type 3 hybrid design tests an implementation strategy while observing and gathering information on the impact that the clinical intervention has on relevant outcomes. 216 In line with our rationale for undertaking an implementation study, we initially designed the study as a type 3 hybrid design using this taxonomy.
Theoretical underpinning for design of implementation plan
The NPT (see Chapter 2) was used during the development of the HeLP-Diabetes programme to help ensure that the intervention was ‘implementable’ and would fit well with current NHS practice. The NPT emphasises that interventions are more likely to be normalised into routine practice if they are easily understood and described (coherence), target users want to adopt them (cognitive participation) and they fit well with existing workflows (collective action). 56 Areas of particular importance are (1) the impact that the intervention had on consultations between HCPs and patients (interactional workability); (2) the impact the intervention had on relationships between professional groups, including ensuring that accountability and responsibility are aligned (relational integration); (3) ensuring that there was a fit with existing skill sets and role responsibilities (skill set workability); and (4) ensuring that there was a fit with organisational priorities and available infrastructure (contextual integration). Finally, users will engage in a process of reflexive monitoring, in which they consider whether or not the benefits of the intervention are worth the work involved, along with any adaptations or improvements that can be made. This reflection can be based on formal or informal data. These constructs provided an overall framework for us during the development of the implementation plan.
However, although the NPT can be used to sensitise researchers and implementers to challenges and issues that are likely to arise during an implementation process,217 it does not provide a step-by-step guide to developing an implementation plan. Therefore, we augmented our theoretical framework with a model developed by Grol and Wensing218 to assist with the implementation of change in health care. This model provides a step-by-step guide to developing an implementation plan, starting with defining the operational-change objectives and analysing current practice, the target group and the context of the proposed implementation. This then facilitates selection of appropriate implementation strategies, rather than relying on frequently used but potentially inappropriate strategies, such as a generic implementation plan. Crucially, the evaluation of the implementation is included, with a strong emphasis on this happening in parallel with the planned implementation activities, allowing early identification of areas needing attention or strategies that are not working. The importance of an iterative approach whereby implementation and evaluation of the implementation occur in parallel, feeding into each other, has also been stressed by the VA QUERI team. 219,220
Context for the implementation
There are theoretical and empirical grounds for recognising the importance of context in any given implementation. 221–224 In the Consolidated Framework for Implementation Research, Damschroder et al. 221 name two aspects of context: the outer and the inner settings. The outer setting consists of factors such as external (e.g. national) policy and incentives, peer pressure from other organisations and organisational priorities, while the inner setting includes structural characteristics such as the availability of infrastructure, leadership, culture, communication and local or internal incentives and reward structures.
At the time this study commenced (March 2013), the outer setting was dominated by the Health and Social Care Act 2012,70 which was described as the ‘biggest single reorganisation’71 and the ‘longest and most complex piece of legislation’72 in the history of the NHS. Among the many components of the Act were the abolition of PCTs and strategic health authorities, which had been responsible for commissioning services. PCTs were replaced by CCGs, which were intended to control around 60% of the NHS budget, be led by GPs supported by other clinicians and managers and were tasked with meeting the needs of their populations.
This reorganisation resulted in huge workloads for those involved as they struggled to come to terms with new priorities and responsibilities, evolving structures and changes in personnel. This was often accompanied by uncertainties about roles and responsibilities, loss of existing staff with relevant expertise and loss of organisational memory. 74,75
Furthermore, it occurred as the NHS entered a period of significant financial austerity. After a period of year-on-year budget growth, the NHS was charged with making financial savings of £20B over 5 years from 2011–15, while maintaining (or improving) the quality of the service. 76 This required efficiency savings of around 4% per year, compared with maximum previous efficiency savings of around 2% per year. It was recognised that meeting this ‘unprecedented challenge’ would require new ways of working, with an emphasis on reducing hospital admissions for patients with LTCs, as well as a pay freeze for NHS staff. 76
Not entirely coincidentally, at the same time as this reorganisation and economic squeeze, English general practices were entering a period of ‘crisis’,77 with rapidly rising workload as a result of increased numbers and complexity of consultations with no concomitant rise in HCP numbers and static or falling incomes. 78,79 As a result, practices were under enormous pressure. Many were unable to fill vacant clinical posts (both doctors and nurses were hard to recruit), leading to excessive workloads for remaining clinicians. 80 This was reflected in long waiting times for appointments and many GPs reported low morale, burn out and resistance to change. 80 Although some practices showed considerable resilience, others went into a spiral of decline. Over the period of this study, three practices closed in our study CCG.
The inner context for our case study included the features of the two CCGs that we intended to work with. One of the two was a dynamic and largely functional group, with strong clinical leadership and a commitment to innovation. It was one of the first CCGs to be authorised in England,225 going live in April 2013, and had an early goal of ‘cultural change to improve self-management of medical conditions’. 226 Improving prevention and management of LTCs was identified as a key priority, particularly in diabetes mellitus, heart failure and lung disease. PPI was also prioritised, with active patient input to key decision-making committees.
The other CCG also went live in April 2013. Its priorities for its first year were cardiovascular disease, cancer and respiratory disease, with a focus on improving delivery of care through community and primary care services. There was less emphasis on self-management and PPI,227 which are key elements of the HeLP-Diabetes programme.
Aims and objectives
The implementation study was intended in our original grant proposal to fulfil the implementation objectives that were set out in Chapter 3:
-
implement the intervention in two PCTs
-
determine the uptake, use and effects of the intervention in an unselected population in routine care
-
determine factors that inhibit or facilitate integration into existing services and uptake of the intervention by users
-
determine the resources needed for effective implementation.
As we prepared for this study, and in line with the approach by Grol and Wensing outlined in Theoretical underpinning for design of implementation plan,218 it became apparent that the first of these objectives would require developing an implementation plan that would need to be flexible and adaptable in the light of emerging data. Thus, we reconceptualised the aims and objectives to include the development and modification of an implementation plan. As detailed in Chapter 2, we were sensitive to the digital divide and wanted to explore to what extent it was reflected in usage and uptake of the HeLP-Diabetes programme and whether or not this was affected by the mode of implementation. Hence, the revised aims for this WP (WP E) were as follows:
-
to develop an implementation plan
-
to evaluate the implementation plan and apply emerging data to modify it
-
to determine the impact that the HeLP-Diabetes programme had on people with T2DM when implemented into routine care.
For each aim, we developed specific objectives.
-
To develop an implementation plan:
-
apply a theoretical framework (NPT) to development of the plan
-
explore the extent to which models of implementation could overcome the digital divide and enable people who were less used to computer technology to use the intervention
-
describe the resource requirements for effective implementation.
-
-
To evaluate the implementation plan and apply emerging data to modify it:
-
describe the adoption, uptake and use of the HeLP-Diabetes programme by HCPs and patients across participating sites
-
describe the characteristics of patients registering with the HeLP-Diabetes programme
-
describe the impact that the implementation models had on uptake by people with T2DM and the digital divide
-
understand and explain observed variation between sites in adoption, uptake and use by HCPs and patients
-
apply emerging data to revising and improving the original implementation plan
-
describe and assess the final implementation model(s).
-
-
To determine the impact that the HeLP-Diabetes programme had on people with T2DM when implemented in routine care:
-
determine the impact that the HeLP-Diabetes programme had on the trial’s primary outcomes
-
determine the impact that the HeLP-Diabetes programme had on key intermediate or mediator outcomes, to help inform findings of the trial and test the validity of the mechanism of action for the intervention proposed during its development.
-
Methods
Developing an implementation plan
Our original implementation plan was devised to be adaptive and iterative, with evaluation occurring in parallel. It involved a batched roll out, which was started by identifying two or three general practices with a reputation for embracing innovation and successfully managing change. We wanted to work closely with these practices to identify what worked well and what needed further attention, before moving on to further batches of practices.
As described in Chapter 2 and this chapter, the NPT stresses the importance of fitting with existing workflows and work patterns, so the implementation plan was designed to mirror existing systems, thus minimising the behaviour changes required by HCPs. One model of change that GPs were well used to was their local CCG (formerly PCT) commissioning a new service and encouraging practices to use it. We judged that having CCG support for the new service would be important for enhancing credibility and, in NPT terms, likely to promote coherence and cognitive participation.
Selecting clinical commissioning groups
The implementation literature stresses the influence of context on implementation. As described in Context for the implementation, Consolidated Framework for Implementation Research divides context into outer and inner settings and describes both as important. To a great extent, the outer context (national priorities, policies and economic incentives) was outside our control, so it was important to select a CCG in which the inner context was likely to be favourable to our endeavour and in which it would be reasonably easy to study the implementation.
This led to the identification of the following criteria for selecting CCGs to work with:
-
diabetes mellitus should be a local priority
-
there should be interest in promoting self-management by people with T2DM
-
it should be reasonably local, since implementation is promoted by good communication and local ownership
-
the CCG should be interested in working with us.
The research team was based at UCL, which has a long and close relationship with two local CCGs. Both areas had a history of being open to academic initiatives and favouring research in primary care. Moreover, the chief investigator, Elizabeth Murray, was a GP in one CCG, and was already known to, and had good working relationships with, many of the GPs in both CCGs.
At the time we started preparation for the study (October 2012), one CCG was still only a shadow commissioning group, which was due to go live in April 2013, but it had already determined that its priorities would include LTCs, particularly diabetes mellitus, and improving self-management by patients. Therefore, we contacted the group’s clinical vice chairperson to discuss whether or not the CCG would be interested in promoting use of the HeLP-Diabetes programme across its practices. The CCG reacted rapidly and very positively. We were invited to speak at the next meeting of the self-care group in December 2012 and by the time the CCG went live in April 2013, the HeLP-Diabetes programme was part of CCG policy and the CCG mandated the lead commissioner for diabetes mellitus to work closely with us to promote implementation across the group.
In contrast, the other CCG had prioritised other diseases for its first year and was more interested in improving care delivery through community and primary care services, with less emphasis on self-management and PPI. 227 Its main activity in relationship to diabetes mellitus was establishing an integrated practice unit and, although the commissioners and senior managers said they wanted to implement the HeLP-Diabetes programme within the integrated practice unit, their focus was inevitably more on service redesign. Decision-making was also slower in this CCG.
Overall, having such strong support from one of the CCGs was a great benefit. It strengthened the credibility of the intervention, gave us access to inside information about each practice and advice about who to contact, allowed for integration with local IT systems, including EMIS Health templates (version EMIS Web, EMIS Health, Leeds, UK), and Map of Medicine (Map of Medicine, London, UK), and smoothed the various negotiations with other interested bodies, such as the local medical council. However, it did bring one significant challenge, which was that we lost control of the implementation process. The CCG wanted rapid deployment across the whole of the group and would not countenance our batched approach. This had significant implications for our ability to support individual practices with the implementation, as we only had one RA, who was responsible for both promoting the implementation across the CCG and undertaking the associated evaluation study. Therefore, we quickly decided to focus our resources on this CCG and defer implementation in the other CCG until we had more time or resources. Hence, all the research data presented here come from one CCG only.
General practice
There were 37 practices in the CCG at the start of the study (34 by the end), with a total patient list size of 229,457 in 2013–14228 and a prevalence of diabetes mellitus of 4.92% per cent (9447 patients). Practice list sizes ranged from 941 to 15,273 patients, with the number on each practice’s diabetes mellitus register ranging from 74 to 568. 228 As general practice diabetes mellitus registers do not distinguish between type 1 diabetes mellitus and T2DM, we estimated that 90% of patients on the registers would have T2DM, in line with national prevalence.
The initial implementation plan for general practices consisted of an introductory e-mail to either the clinical lead for diabetes mellitus or the practice manager. The e-mail provided a brief description of the HeLP-Diabetes programme and stressed the support of the CCG for the programme and that the HeLP-Diabetes programme would help with achieving the diabetes mellitus locally enhanced service. We offered to visit the practice to demonstrate the programme and offered free staff training if practices decided to adopt it.
The initial practice visit was designed to fit with busy practice routines. Most practices could offer us 15–20 minutes in a lunchtime meeting. We developed a presentation that described the HeLP-Diabetes programme, targeted at the constructs of coherence and cognitive participation and focusing on the key elements of a holistic approach to self-management, covering medical, emotional and role management, the strong evidence base, compatibility with NICE’s guidelines and its accessibility to people with low literacy or poor English. The support of the CCG was also emphasised, along with the fact that this service was being made available free for the duration of the research study (i.e. until February 2016). We then discussed the workload implications for the practice.
Our initial design had included a 40-minute facilitation appointment, in which patients were registered on the HeLP-Diabetes programme and shown how to use it, with demonstrations of key facilities such as goal-setting, action-planning and self-monitoring. The rationale for this appointment was threefold. First, as detailed in Chapter 2, we had always conceived of the total intervention as the web programme plus interactions between HCPs and patients, with HCPs encouraging use of the programme and integrating it into consultations. This approach fitted with the locally enhanced service, which was based around care planning, and goals were agreed between clinicians and patients, as detailed in the Year of Care initiative. 225 Second, we hypothesised that integrating the web programme into routine NHS care would promote trust and help overcome some of the digital divide. The facilitation appointment would encourage and aid people who were not comfortable using computer programs; we had successfully tried a similar approach with a heart disease programme some years earlier. 69 Finally, it was important that the HeLP-Diabetes programme be available only to registered users. This would ensure that there was no contamination of the trial, which was occurring in parallel in a different geographical location, as members of the trial control group would be unable to gain access to the website and we were keen for the HeLP-Diabetes programme to be seen as an NHS resource and not just a free website. Moreover, given the original intention of linking with users’ EMRs, it was essential that the registration process was secure and met NHS governance requirements.
However, it was immediately clear that practices could not countenance dedicating 40 minutes to facilitating use, despite acknowledging that many practice nurses spent at least 40 minutes with newly diagnosed patients, explaining the nature of diabetes mellitus, how to self-care, what to eat and how diabetes mellitus is treated – all topics that are covered in detail by the HeLP-Diabetes programme.
To address this problem, we offered the first practice that we visited researcher time, in which the researcher held weekly sessions in the practice, registering patients who were referred to the HeLP-Diabetes programme and providing the sort of facilitation described previously. The plan was to register all the patients already diagnosed with T2DM, with the hope that the practice nurse would eventually take over the task for newly diagnosed patients.
Given the CCG requirement for mass simultaneous roll out, we could not offer this level of support to each practice, as we calculated it would take several months to register every patient with T2DM. The grant funded only one RA for the implementation study and this researcher was responsible both for achieving implementation and undertaking the evaluation. Hence, we had to urgently reconsider the facilitation model to find one more acceptable to practices.
Practices made it clear that time was of the essence and that the revised model should be as minimal as we could make it. We simplified the registration process so that it could be completed in less than 5 minutes and abolished the requirement for facilitation, although we did ask that, when possible, practice staff at least introduced the patient to some key elements of the programme.
Even this simplified procedure proved to be quite a barrier for some practices. Further analysis revealed two factors at play, both relating to the NPT construct of skill set workability, that is, the degree to which HCPs feel an intervention matches their skills, roles and identity. GPs and practice nurses both felt that nurses were better employed in clinical tasks and not in teaching patients how to use an IT program. Second, some practice nurses were not comfortable using computer technology and found it hard to remember how to register patients.
In the light of these findings, we suggested that practices consider delegating the task of registering patients to HCAs, when in post, or to receptionists. The task seemed particularly well suited to HCAs, who tended to be young, familiar with IT and keen to help patients while being aware that they had little or no clinical knowledge themselves. They reported enjoying using the HeLP-Diabetes programme to learn more about diabetes mellitus themselves and feeling empowered to assist patients by helping them find the answers to their questions on the website rather than having to store them up to ask a nurse or GP. In practices without a HCA, receptionists often took on the task of registering patients. Some practices said that they found it easier to register patients in batches, at a time that was convenient for them, rather than doing it when the patient was present, so we designed a paper form that patients could fill in, which contained all the data needed for registration and which patients could leave with reception for subsequent action.
Our final attempt to overcome the barriers to registering people with T2DM was devised with our PPI representatives, who suggested that trained PPI representatives could go into general practices and promote use of the HeLP-Diabetes programme. Our PPI representatives were very committed to the HeLP-Diabetes programme and extremely keen to maximise uptake. Patient champions and advocates were being used successfully in a neighbouring area to increase patient engagement with education and care (https://knowdiabetes.org.uk/support; accessed 28 June 2017). This suggestion was put to the CCG who agreed it and offered to help with any arising governance issues. Unfortunately, despite repeated offers to general practices of trained patient advocates to help with registering patients on the HeLP-Diabetes programme, no practice took up this offer. It was difficult to establish reasons for this, but informal comments suggested that arranging a room for the patient advocate to work in, referring patients to them or allowing them to hold patient groups in the waiting room all seemed like additional work that the general practice could not undertake. Moreover, there may have been anxieties around confidentiality and governance, despite us providing reassurance about training and CCG support for this move.
Hence, the final implementation model used across most practices was one with a simplified registration process, which could be undertaken by a HCA or receptionist in about 5 minutes, offered in parallel with a self-registration process that patients could undertake themselves. Some practices (n = 6) offered only self-registration.
Allowing patients to self-register required some technical adjustments. We needed to ensure that only patients from the CCG registered (to avoid contaminating the trial) and so we used a system of codes issued to each practice. Practices could either give out hard copies of leaflets, which each contained a single-use code, or they could print out a portable document format (PDF) file from the practice intranet that had a group code on it. Therefore, we could continue to monitor which practices were registering patients and how each patient was registered, which were important data for our evaluation.
Hospital outpatient clinic
The plan detailed in our grant application had focused on implementation through general practice. This decision was based partly on resource and partly on keeping a tight focus on the research question. However, given the contextual issues described in Context for implementation, and with CCG and steering group encouragement, we decided to broaden our implementation focus to include the local hospital outpatient clinic for people with T2DM and the intermediate care service.
The local hospital had strong ownership of the HeLP-Diabetes programme, with the lead consultant for diabetes mellitus being a co-investigator on the programme grant (Maria Barnard) who had contributed very substantially to the development of the intervention.
Patients who attended secondary care for diabetes mellitus tended to be those with complex health problems that their GP did not feel competent to manage, such as diabetes mellitus that was hard to control with standard regimens, frequent hypoglycaemic attacks or complications from their diabetes mellitus. The hospital offered a consultant-led service, with the team including diabetes specialist nurses and junior doctors. Patients were referred from a number of CCGs, including the two CCGs in this study.
The hospital diabetes team agreed to implement the HeLP-Diabetes programme and were trained in the revised, slimmed-down registration procedures. However, the clinic was running on what one staff member described as a ‘skeleton staff’, so nurses had no time to sign patients up. A further significant barrier was the need for nurses to remember to offer the HeLP-Diabetes programme to referrals only from GPs in the two CCGs in this study. The study steering group had decided to restrict registrations in this way for several reasons: the HeLP-Diabetes programme was badged as a CCG service, and in a commissioning model, services that are commissioned by one CCG are not available to patients from a different CCG; we had insufficient resources to cover a third CCG (although we did consider it carefully); and our ethics and research governance approvals did not include patients from outside the two CCGs in this study. By this stage, the invitation to participate in the HeLP-Diabetes programme evaluation study was integrated into the registration procedures (to save staff time) and it would have been too complex to have different registration procedures for patients from different CCGs.
In response to these challenges, we tried two alternative methods of registering people with T2DM. First, the RA went to the outpatient clinic and approached patients in the waiting room, offering to help them sign up. Second, the clinic staff undertook a mass mail out of patient self-sign-up leaflets to all patients from the CCG attending the clinic.
Intermediate care service
The intermediate care service was designed for patients with problems that are too complex to manage in general practice but do not require the level of specialist input available in the hospital (e.g. conversion to insulin). The Diabetes Intermediate Service team consisted of diabetes specialist nurses, dietitians and psychologists, with support from a diabetes consultant, and was based in a primary care centre in the CCG.
Group education and promotion of self-management were key components of the service, which ran the DESMOND trial programme for the area and a 7-week self-management programme (Co-Creating Health), which is designed to help participants build the skills, knowledge and self-belief required to manage their diabetes mellitus effectively.
Once again, CCG support proved extremely useful for gaining access to this service, as it was commissioned by the CCG. The initial response from the service was extremely positive, with the team agreeing in February 2014 to implement the HeLP-Diabetes programme. Unfortunately, very shortly afterwards, the lead diabetes specialist nurse left. It proved difficult to replace them, and there followed a year of rapid turnover and staff shortages, during which the service was unable to implement the HeLP-Diabetes programme.
By February 2015, the Diabetes Intermediate Service team was reconstituted, and another attempt was made to implement the HeLP-Diabetes programme. Once again, the team were enthusiastic about the service but concerned about workload and so agreed to implement the self-sign-up model for patients graduating from the DESMOND trial course.
Evaluating the implementation plan
Design
We used a case-study design, with mixed methods, combining quantitative and qualitative data. The evaluation of the implementation was conducted in parallel with the implementation but kept conceptually separate. Sites (CCG, practices, hospital clinics and intermediate care) and participants (commissioners, HCPs and patients) were offered use of the HeLP-Diabetes programme. Subsequently, whether or not they accepted the offer of the HeLP-Diabetes programme, they were asked if they would like to participate in the research evaluating the implementation. It was made clear at every point that there was no onus on those accepting the service (the HeLP-Diabetes programme) to participate in the evaluation.
Definitions
For the purposes of this study, the following definitions were used:
-
Adoption – a decision by a site (practice, outpatient clinic or service) to make use of the HeLP-Diabetes programme.
-
Use by services – the use made by the service of the HeLP-Diabetes programme, reflected in the number of people registered.
-
Uptake – the uptake of the HeLP-Diabetes programme by people with T2DM, reflected by the number of people signing up to use the programme.
-
Use by patients – the use made by patients, after being registered.
-
Implementation plan – the plan designed by us to implement the HeLP-Diabetes programme into routine care.
-
Innovation or intervention – the HeLP-Diabetes programme.
Ethics and research governance
Ethics and research governance approval for the study design, materials and procedures were obtained from the National Research Ethics Service Committee East Midlands-Leicester, reference number 13/EM/0033, and the local PCTs (later CCGs). Letters of access were issued by the trust for the research to be conducted with primary care staff and patients at practices in their trust.
Setting and participants
The setting was one CCG in north London; participants were health-care commissioners and HCPs who were involved in the implementation of the HeLP-Diabetes programme and people with T2DM who used the HeLP-Diabetes programme. Every attempt was made to obtain data from those who declined to adopt or use the HeLP-Diabetes programme, as well as from those who did use it.
Data collection
Quantitative data
Quantitative data were collected to describe the participating sites and, when available, their populations, rates of adoption, use made of the intervention by each site, uptake and use by people with T2DM, and the characteristics of users. When possible, we obtained these data from existing sources, such as practice and CCG websites, the Health and Social Care Information Centre (now NHS Digital) website, which holds all the information pertaining to the QOF at national, regional, CCG and practice levels, and the Office for National Statistics’ website. When necessary, we supplemented these data with a pro forma completed by the practice manager or other site lead.
The research team collected data on the number and type of services within the CCG that were offered the intervention, the dates and content of all communication with sites, the dates of meetings and staff present, the decisions on adoption made by sites, with reasons when available, the dates of training sessions and staff attending, the type of registration model in use and the number and date of patient registrations.
Automated software, embedded into the intervention, recorded each visit by registered users, including date, time, and the number and URL for each page visited. The requirement for this function was specified at the time of the original tender for developers for the HeLP-Diabetes programme. Initially, the software company argued that Google Analytics would meet our needs; however, when we came to test these data, we discovered it was insufficiently accurate, often failing to record visits made by the research team with the object of testing the data. After lengthy discussions with our software providers, we agreed an alternative, bespoke approach, which used server-side data. Unfortunately, it took some time for the developers to build the requisite software, and so we were only able to collect usage data after 1 January 2014. To avoid overcounting log-ins as a result of, for example, computer time-out, we used the number of days when a log-in occurred as the main measure of use.
All patient users were required to complete a registration form requesting demographic, clinical and contact details. Demographic data included gender, ethnicity, date of birth, highest educational attainment, internet access (home or public) and level of previous computer experience (basic, intermediate or advanced). The first registration form was designed to be completed by an HCP and did not include data on educational attainment. This was added when the form was adapted for completion by patients (5 March 2014). Clinical data were date of diagnosis, duration of diabetes mellitus since diagnosis, current management (lifestyle only; lifestyle and tablets; lifestyle, tablets and insulin or other injectables) and areas that the user would most like help with for their diabetes mellitus. Users could choose as many options as they liked for this last question. Contact details included name, e-mail address, practice where registered and optional mobile or landline numbers, all linked to their username and password so that patients who forgot their password could be sent a reminder.
Qualitative data
There were three main sources of qualitative data:
-
semistructured interviews with HCPs and commissioners
-
semistructured interviews with patients
-
detailed field notes recording researcher observations of meetings, informal conversations, practice visits, telephone calls, e-mails and all other communications with those involved in, or relevant to, the implementation.
Semistructured interviews with commissioners and HCPs were undertaken throughout the study period. We aimed to sample across the range of HCPs involved in the implementation, including GPs, nurses, HCAs, practice managers, administrative and reception staff, consultants and commissioners. We tried to include HCPs from sites that had adopted the intervention and from sites that had either declined the intervention or accepted the adoption but not made any use of it. Sampling continued until the point of data saturation, that is, when no new themes were emerging from subsequent interviews.
Interviews were conducted face to face, generally in the HCP consulting rooms and almost all were individual interviews, with the exception of one focus group of three nurses and a HCA from the same practice, which arose opportunistically from an individual interview arranged with a nurse. Interviews lasted approximately 30 minutes and were recorded using a digital voice recorder.
The topic guide for these interviews was informed by the NPT and it evolved over time in response to emergent themes. It was tailored for each professional group to reflect their different roles in the implementation process. The NPT constructs addressed included coherence (sense-making around self-management for patients with diabetes mellitus in general and the HeLP-Diabetes programme in particular), cognitive participation (reasons for deciding whether or not to adopt the HeLP-Diabetes programme), collective action (impact on workload and workflow) and reflexive monitoring (perceptions of benefits, problems and suggestions for change). Questions covered their own professional role, the nature of the clinical service in which they worked, how the service cared for patients with diabetes mellitus and what they saw as the biggest challenges in providing this care. Participants were asked for their views on self-management and if and how they supported patients in doing this. They were asked about how, in general, the service decides whether or not to adopt a new service and, in particular, why and how they had reached their decision about the HeLP-Diabetes programme. For those working in sites that had adopted the HeLP-Diabetes programme, there were questions about how the intervention had been introduced and used in the site, by whom and with what support and how these decisions had been reached. They were asked to reflect on the success or otherwise of the implementation, asked for their views about barriers to, and facilitators of, this implementation, and for suggestions on how to improve the process.
For ethical reasons, these could only be undertaken with people with T2DM who had agreed to participate in the research process. Nevertheless, we attempted to recruit a sample that varied by age, ethnicity, educational attainment, duration of diabetes mellitus since diagnosis, type of treatment, existence of complications and IT experience. Sampling continued to the point of saturation, when no new themes were emerging from the interviews.
The topic guide for patient interviews was also informed by the NPT. As the NPT focuses on the work of implementing and integrating an intervention into routine practice, it can be hard to see how to apply it to patient interviews. However, NPT has been used to illuminate patient experiences of the ‘work’ of being ill. 229 In accordance with this previous work, the topic guide for people with T2DM focused on their views of the work of managing diabetes mellitus, whether or not and how the HeLP-Diabetes programme helped this work and how the intervention could be improved. Hence, interviews explored issues around what having diabetes mellitus meant to the patient (coherence), their views about their role in their care (cognitive participation for self-management), the work involved in self-management (collective action), including how it affects their relationships with friends and family (interactional workability), support available from the NHS (relational integration), challenges with undertaking the work (skill set workability) and relative priorities within their lives (contextual integration).
The lead researcher on the study (Jamie Ross) kept a detailed research diary. This was used to record data from informal feedback and conversations, telephone calls, the experiences of supporting each practice to implement the intervention, personal reflections, discussions with staff during training sessions, e-mail communications and any other data that could inform the evaluation. Notes were entered into a notebook either during or immediately after interactions with sites and services. These notes were then subsequently transferred to a Microsoft Excel® spreadsheet (Microsoft Corporation, Redmond, WA, USA), with a row for each site and the notes in columns.
Data analysis
Quantitative data
Simple descriptive statistics were used for much of the quantitative data, with the exception of analyses exploring the relationship between user characteristics and intervention use, and impact that mode of registration had on characteristics of registered users, when univariate and multivariate logistic regression analyses were conducted.
Qualitative data
Interviews were digitally recorded and transcribed by a professional transcription service, then checked for accuracy and anonymised by the research team by using a unique identifying code for each interviewee. The analysis was undertaken concurrently with data collection, to allow for rapid adjustments of the implementation plan and to direct future data collection.
Data analysis was initially done thematically, following a data-driven, inductive process. All transcripts were read by the lead researcher (Jamie Ross), the chief investigator (Elizabeth Murray) and another investigator (Fiona Stevenson). They discussed emergent themes, which were then presented to the study steering group. Steering group discussions tended to focus on implications of the data for the implementation plan and how to respond to these. Hence, we also sought additional input into the thematic analysis by holding a data clinic.
Once agreed, main themes from the HCP interviews were mapped onto the constructs of the NPT. This two-stage process has been used by other authors. 126,230,231 Its strength is that it combines the benefits of a theory-driven approach to moving the analysis beyond description, while not forcing data into predetermined categories (although it is acknowledged that the use of the NPT to develop interview guides influenced the emergent themes). We specifically looked for themes that did not map onto any of the NPT constructs, to ensure that they would still be captured and also to form the basis of a critique of the scope and robustness of the NPT in explaining these data. Data from the field notes and research diary were also analysed thematically and used to inform, confirm or refute interpretations of formal interview data.
We attempted to undertake a similar mapping exercise with the patient interview data, but we found that the data did not map well and that the resulting analysis was less informative than the initial thematic analysis. Therefore, we decided against this approach for the patient data.
Illustrative extracts of the data are presented in Results, with identification by participant number with their professional background (for HCPs) or age, gender and level of computer experience (for patients).
Evaluating the impact that the Healthy Living for People with type 2 Diabetes programme had
The planned methodology for determining the impact that the HeLP-Diabetes programme had on both the primary outcomes selected for the trial (HbA1c level and PAID score) and on hypothesised key intermediate outcomes was a series of substudies with a single-arm, pre–post design. Participants who consented to take part in the evaluation would be asked to complete additional questionnaires at baseline and follow-up. We planned to start with a substudy that focused on the impact that the intervention had on diabetes mellitus-related distress, as measured by the PAID scale, to generate data directly comparable to the trial data. Once that had been achieved, we hoped to run repeated substudies exploring outcomes of interest. However, as only 36 out of the 205 patients who registered to use the HeLP-Diabetes programme consented to participate in the associated research, we were unable to pursue this aim.
Results
Developing the implementation plan
The original plan, with modifications, has been described in Developing an implementation plan, General practice.
Evaluating the implementation plan
Objective 2a: describe the adoption, uptake and use of the Healthy Living for People with type 2 Diabetes programme by health-care professionals and patients across participating sites
‘Adoption’ was defined as the service deciding to offer the HeLP-Diabetes programme to their patients, while ‘use by services’ was defined as staff within the service offering the HeLP-Diabetes programme to their patients and registering at least one patient. Adoption rates were high, but usage rates were lower (Table 36).
| Service | Adoption rate (number of sites adopting the programme/number of sites that the programme was offered to; %) | Usage and number of patients registered | Comment |
|---|---|---|---|
| CCGs | 2/2; 100 | 2/2; the first CCG registered 205 patients; and the second CCG registered 12 patientsb | The first CCG was extremely enthusiastic and proactive, so we focused our available resource there |
| General practices | 22/34a; 65 | 18/22 registered at least one patient. The number of patients registered per practice ranged from 1 to 40, with a median of 3 | Of the non-adopters, one site declined because of potential linkage with the EMR, six sites responded positively but we were unable to arrange a practice visit and eight sites never replied to the CCG or research team |
| Intermediate care service | 1/1; 100 | 1/1; registered 1 patient | The service agreed to adoption of the programme but then experienced a year of substantial staff turnover; the new team again agreed to adopt the programme but only shortly before the end of the study |
| Secondary care service | 1/1; 100 | 1/1; registered 30 patients | – |
Uptake and use by patients
‘Uptake by patients’ was defined as the patient registering to use the HeLP-Diabetes programme. A total of 205 people with T2DM registered during the study period (March 2013 to August 2015). Of these, 143 (70%) were registered by a HCP, with the remainder (n = 62; 30%) self-registering. Use by patients was defined as patients using the intervention at least once after the day of registration. Just over half of those registered (n = 104; 51%) used the HeLP-Diabetes programme by this definition.
These users showed a wide range of usage of the intervention. The number of days with a recorded log-in ranged from 1 to 77 days, with a median of 2 days (interquartile range 1–4 days) of use per person. Users appeared to appreciate the availability of the intervention at all times, with page views recorded for every hour of the day. In total, there were 3221 page views, of which just over half (n = 1651; 51.2%) took place outside normal working hours (09.00–17.00) (Figure 21).
FIGURE 21.
Percentage of page views by time of the day.
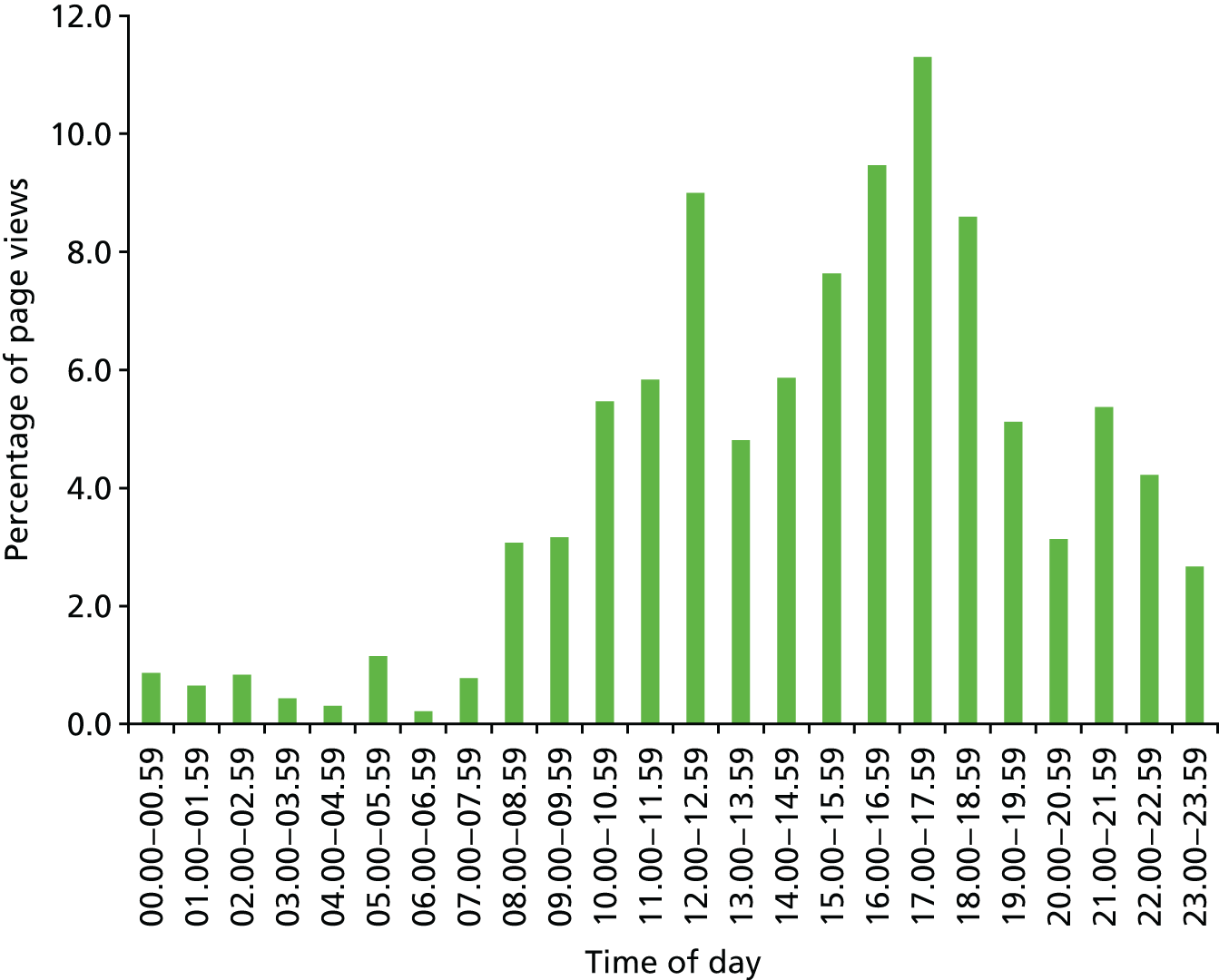
However, less use of the intervention was made at weekends than during the week, with only 20% (n = 88) of visits and 13.7% (n = 443) of page views occurring on a Saturday or Sunday.
Content accessed by users
Users viewed 396 different pages out of the 560 available in the intervention. The most frequently viewed pages are displayed in Table 37: apart from the homepage, pages on food, common diabetes questions, care planning and the forum were accessed most often.
| Title of page accessed | Page views | |
|---|---|---|
| Frequency | Percentage of total views | |
| Home page | 520 | 16.1 |
| Food | 62 | 1.9 |
| Common diabetes questions | 54 | 1.7 |
| My diabetes care plan | 43 | 1.3 |
| Help Diabetes forum | 42 | 1.3 |
| How my body can be affected | 39 | 1.2 |
| My health profile | 39 | 1.2 |
| Eating and drinking | 35 | 1.1 |
| Exercise videos | 32 | 1.0 |
| My test results | 32 | 1.0 |
| Understanding diabetes | 32 | 1.0 |
| Staying healthy | 28 | 0.9 |
| My appointments | 22 | 0.7 |
| Understanding my moods | 22 | 0.7 |
| How is type 2 diabetes treated? | 21 | 0.7 |
| Living and working with diabetes | 20 | 0.6 |
| Physical activity | 20 | 0.6 |
| Looking after yourself | 19 | 0.6 |
| My health record | 19 | 0.6 |
| Snacks and desserts | 19 | 0.6 |
| Forum | 17 | 0.5 |
Objective 2b: describe the characteristics of patients registering with, and using, the Healthy Living for People with type 2 Diabetes programme
Characteristics of patients registered with the Healthy Living for People with type 2 Diabetes programme
A wide range of users registered with the HeLP-Diabetes programme. Over half (n = 107, 52%) of registered users were male and 52% (n = 107) were from ethnicities other than white British, with African, Caribbean, Bangladeshi, Indian and other ethnicities being represented. There was a wide spread of ages (range 19–81 years, mean 56.8 years, SD 11.8 years) and of educational levels. As the question on highest educational qualification was added late, these data were not available for many people. Of the total population of patients registered, 15% (n = 31) had no educational qualifications and a further 16% (n = 33) were school leavers. Of the population of patients registered who provided data on this question, 52% had no educational qualification or were school leavers. Although the majority of those who registered to use the intervention had home internet access (n = 177, 86%), over one-third (n = 79, 39%) described their computer skills as basic. Duration of diabetes mellitus since diagnosis ranged from < 1 year to > 20 years; most patients were treated with lifestyle modification and medication and a few (n = 26, 13%) used insulin (Table 38).
| Characteristics of registered users | Frequency (n = 205) | Percentage of total registered users |
|---|---|---|
| Gender | ||
| Male | 107 | 52.2 |
| Female | 98 | 47.8 |
| Ethnicity | ||
| White British | 98 | 47.8 |
| Non-white British | 107 | 52.2 |
| Education | ||
| None/school leaver | 64 | 31.2 |
| A level or higher | 58 | 28.3 |
| Missing | 83a | 40.5 |
| Duration (years) of diabetes mellitus since diagnosis | ||
| < 1 | 53 | 25.9 |
| 1–5 | 66 | 32.2 |
| 5–10 | 37 | 18.0 |
| > 10 | 44 | 21.5 |
| Missing | 5 | 2.4 |
| Management of diabetes mellitus | ||
| Lifestyle only | 40 | 19.5 |
| Tablets | 128 | 62.4 |
| Insulin | 27 | 13.2 |
| Missing | 10 | 4.9 |
| Internet access | ||
| Home | 177 | 86.3 |
| Public | 9 | 4.4 |
| Missing | 19 | 9.3 |
| Computer skills | ||
| Basic | 79 | 38.5 |
| Intermediate/advanced | 105 | 51.2 |
| Missing | 21 | 10.2 |
| Registration model | ||
| Staff registered | 142 | 69.3 |
| Self-sign up | 63 | 30.7 |
| NHS service type | ||
| GP practice | 175 | 85.4 |
| Hospital | 30 | 14.6 |
| Community clinics | 1 | 0.5 |
| The HeLP-Diabetes programme use | ||
| No use | 101 | 49.3 |
| Low (1–2 days’ use) | 66 | 32.2 |
| High (> 2 days’ use) | 38 | 18.5 |
Predictors of usage of the Healthy Living for People with type 2 Diabetes programme
Just over half of the people (n = 104; 51%) who were registered on the HeLP-Diabetes programme subsequently used the intervention. To determine whether or not there were demographic or clinical predictors of use, we undertook univariable and multivariable binomial logistic regression, comparing non-users with users (Table 39).
| Characteristics associated with some use of the HeLP-Diabetes programme | Regression | ||||||
|---|---|---|---|---|---|---|---|
| Univariable | Multivariable (n = 114) | Multivariable backwards stepwise (n = 184) | |||||
| n | Odds ratio (95% CI) | p-value | Odds ratio (95% CI) | p-value | Odds ratio (95% CI) | p-value | |
| Age (years) | 202 | 1.01 (0.99 to 1.04) | 0.23 | 0.99 (0.95 to 1.04) | 0.74 | ||
| Sex | 205 | 0.30 | 0.54 | ||||
| Male | 1.00 | 1.00 | |||||
| Female | 0.75 (0.43 to 1.29) | 1.34 (0.53 to 3.42) | |||||
| Ethnicity | 205 | 0.08 | 0.28 | ||||
| White British | 1.00 | 1.00 | |||||
| Non-white British | 0.61 (0.35 to 1.06) | 0.61 (0.25 to 1.50) | |||||
| Education | 122 | 0.08 | 0.62 | ||||
| None/school leaver | 1.00 | 1.00 | |||||
| A level or higher | 1.96 (0.93 to 4.12) | 1.30 (0.47 to 3.65) | |||||
| Duration (years) of diabetes mellitus since diagnosis | 200 | 0.17 | 0.73 | ||||
| < 1 | 1.00 | 1.00 | |||||
| 1–5 | 0.62 (0.30 to 1.28) | 0.65 (0.15 to 2.87) | |||||
| 5–10 | 1.17 (0.50 to 2.73) | 1.38 (0.25 to 7.73) | |||||
| > 10 | 1.42 (0.63 to 3.19) | 1.00 (0.15 to 6.65) | |||||
| Management of diabetes mellitus | 195 | 0.31 | 0.59 | ||||
| Lifestyle only | 1.00 | 1.00 | |||||
| Lifestyle and tablets | 1.03 (0.73 to 5.50) | 1.11 (0.23 to 5.45) | |||||
| Lifestyle, tablets, insulin | 2.00 (0.73 to 5.50) | 0.53 (0.05 to 5.04) | |||||
| Computer skills | 184 | 0.0165 | 0.08 | 0.05 | |||
| Basic | 1.00 | 1.00 | 1.00 | ||||
| Intermediate/advanced | 2.07 (1.14 to 3.74) | 2.40 (0.90 to 6.39) | 1.87 (0.99 to 3.55) | ||||
| Registration model | 205 | < 0.0001 | 0.0020 | < 0.0001 | |||
| Staff registered | 1.00 | 1.00 | 1.00 | ||||
| Self-sign up | 5.54 (2.80 to 10.96) | 5.21 (1.83 to 14.82) | 5.91 (2.84 to 12.31) | ||||
It can be seen that there were no demographic predictors of use compared with non-use of the HeLP-Diabetes programme. Those who had self-registered were more likely to use the HeLP-Diabetes programme after registering, presumably reflecting the increased motivation they had demonstrated by signing themselves up.
Objective 2c: describe the impact that the implementation models had on uptake by patients and the digital divide
Although, overall, there was little evidence of the digital divide in registered users, we were concerned that the self-registration model, introduced in response to practice concerns about workload, would favour patients more used to using computers. In the light of this, we undertook multivariable binary logistic regression to explore whether or not there were associations between mode of registration and characteristics of users. This analysis suggested that mode of registration did indeed have an impact on the digital divide, with users who had self-registered being more likely to have higher levels of educational attainment. Educational attainment and computer experience were highly correlated. Age, gender and ethnicity were not associated with mode of registration (Table 40).
| Characteristics associated with some use of the HeLP-Diabetes programme | Regression | ||||||
|---|---|---|---|---|---|---|---|
| Univariable | Multivariable (n = 117) | Multivariable backwards stepwise (n = 118) | |||||
| n | Odds ratio (95% CI) | p-valuea | Odds ratio (95% CI) | p-valuea | Odds ratio (95% CI) | p-valuea | |
| Age (years) | 202 | 1.01 (0.98 to 1.03) | 0.56 | 1.00 (0.97 to 1.03) | 0.95 | ||
| Sex | 205 | 0.12 | 0.42 | ||||
| Male | 1.00 | 1.00 | |||||
| Female | 0.62 (0.34 to 1.14) | 1.43 (0.59 to 3.46) | |||||
| Ethnicity | 205 | 0.57 | 0.27 | ||||
| White British | 1.00 | 1.00 | |||||
| Non-white British | 0.84 (0.46 to 1.52) | 0.62 (0.27 to 1.44) | |||||
| Education | 122 | 0.0001 | 0.0030 | 0.0045 | |||
| None/school leaver | 1.00 | 1.00 | 1.00 | ||||
| A level or higher | 4.52 (2.10 to 9.75) | 3.90 (1.59 to 9.57) | 3.26 (1.44 to 7.38) | ||||
| Computer skills | 184 | 0.10 | 0.10 | 0.08 | |||
| Basic | 1.00 | 1.00 | 1.00 | ||||
| Intermediate/advanced | 1.70 (0.90 to 3.21) | 2.07 (0.87 to 4.94) | 2.08 (0.91 to 4.75) | ||||
Objective 2d: understand and explain observed variation between sites in adoption, uptake and use by health-care professionals and patients
Health-care professional interview data
Twenty-one members of practice and clinic staff took part in 17 interviews and one focus group (with four staff from the same general practice). The majority of staff (18/21) worked in general practices, with a further two based in hospital clinics and one at the CCG headquarters. Unfortunately, no members of staff from community clinics participated. Most interviewees (19/21) worked in services in which the HeLP-Diabetes programme had been adopted and implemented to some extent. The number of patients registered to the HeLP-Diabetes programme from these services ranged from 1 to 40. One participant worked in a practice in which the adoption of the HeLP-Diabetes programme had been declined and another worked in a GP practice in which the HeLP-Diabetes programme had been adopted (adoption agreed) but not used (no patients were registered) (Table 41).
| Identifier | Age range (years) | Gender | Professional role | Service setting | Years in current role | Ethnic background | Internet experience | Practice/clinic implementation status | Number of patients registered |
|---|---|---|---|---|---|---|---|---|---|
| ST1 | 35–44 | Male | GP partner | General practice | 11 | White British | Experienced | Adopted and implemented | 40 |
| ST2 | 55–64 | Female | Diabetes specialist nurse | Hospital | 12 | White British | Experienced | Adopted and implemented | 30 |
| ST3 | 45–54 | Male | Commissioning officer | N/A | 2 | White British | Expert | Adopted | N/A |
| ST4 | 25–34 | Female | Practice nurse | General practice | 2 | White British | Experienced | Adopted and implemented | 28 |
| ST5 | 45–54 | Female | HCA | General practice | 10 | White British | Experienced | Adopted and implemented | 40 |
| ST6 | 35–44 | Male | GP partner | General practice | 3 | Indian | Experienced | Adopted and implemented | 8 |
| ST7 | 35–44 | Female | Receptionist/administrator | General practice | 9 | White British | Experienced | Adopted and implemented | 40 |
| ST8 | 18–24 | Male | Receptionist/administrator | General practice | 1 | White and black Caribbean | Experienced | Adopted and implemented | 11 |
| ST9 | 55–64 | Female | Advanced nurse practitioner | General practice | 4 | White British | Experienced | Adopted and implemented | 3 |
| ST10 | 35–44 | Male | Practice manager | General practice | 7 | White British | Experienced | Not adopted | 0 |
| ST11 | 35–44 | Female | GP partner | General practice | 17 | White British | Experienced | Adopted and implemented | 15 |
| ST12 | 45–54 | Female | Practice nurse | General practice | 4 | White British | Experienced | Adopted and implemented | 11 |
| ST13 | 45–54 | Female | Practice nurse | General practice | 9 | White British | Experienced | Adopted and implemented | 11 |
| ST14 | 35–44 | Female | HCA | General practice | < 1 | Sri Lankan | Experienced | Adopted and implemented | 11 |
| ST15 | 25–34 | Female | Practice nurse | General practice | 8 | White New Zealand/American | Experienced | Adopted and implemented | 11 |
| ST16 | 55–64 | Female | Diabetes specialist nurse | Hospital | 1 | White British | Experienced | Adopted and implemented | 30 |
| ST17 | 45–54 | Female | HCA | General practice | 7 | White British | Expert | Adopted and implemented | 40 |
| ST18 | 25–34 | Female | Receptionist/administrator | General practice | 5 | White British | Experienced | Adopted and implemented | 1 |
| ST19 | 45–54 | Male | Salaried GP | General practice | 1 | White Irish | Experienced | Adopted and implemented | 11 |
| ST20 | 65–74 | Female | Practice nurse | General practice | 17 | White British | Experienced | Adopted, but not implemented | 0 |
| ST21 | 55–64 | Female | Practice nurse | General practice | 20 | White British | Experienced | Adopted and implemented | 3 |
The themes that emerged from the data mapped easily onto the NPT, with no themes that did not map onto any NPT construct. The NPT provided a useful theoretical lens through which to interpret the qualitative data and explain the observed variation in adoption, uptake and use between sites. This variability was reflected in the variation in degree to which the constructs of NPT operated. Hence, the data from the interviews are presented under the main NPT constructs. As in WP B, interviewees distinguished between what they thought of as the main intervention (the HeLP-Diabetes support programme) and the facilitation we asked practices to provide. Overall, the HeLP-Diabetes programme appeared to have reasonably good levels of coherence, cognitive participation and collective action, whereas offering facilitation had poor levels of coherence and cognitive participation and a negative impact on collective action. As a result, overall uptake and use by patients was lower than HCPs had expected, and this led to HCPs perceiving the HeLP-Diabetes programme to be less beneficial than expected (reflexive monitoring). These findings are presented in more detail in the following sections.
Coherence
The HCPs in our study had a clear understanding of the potential benefits of self-management, both intrinsically or philosophically and as a response to lack of capacity in the health-care system to meet all the needs of patients with LTCs, in general, and diabetes mellitus, in particular. Self-management had the potential to improve health outcomes and quality of life for people with T2DM and to reduce health-care costs. They were also aware that patients needed considerable support to self-manage and varied in their capacity and readiness to self-manage and that there were problems with the current dominant model of support, namely group-based structured education shortly after diagnosis (as discussed in Chapters 2 and 5).
Professionals liked the concept of a web-based programme, were impressed by the holistic nature of the HeLP-Diabetes programme (addressing patients’ emotional and role issues as well as more obviously medical concerns), the way it presented information in an accessible format, including videos, and its user-friendly nature. It fitted well with local and national priorities and policies, including promotion of self-management and use of technology. These factors all helped explain the widescale adoption of the HeLP-Diabetes programme:
What HeLP-Diabetes does is it gives people that information that they can access at any time, because it’s on the computer.
ST1, GP partner
People can tailor it or get the information that they want out of it. In terms of timing they can access it whenever they want, rather than having to miss work, which is obviously quite a big issue for these patients.
ST4, practice nurse
In contrast, HCPs had more variable understanding of the need for supporting patients to use the HeLP-Diabetes programme. Although some felt that patients should simply be given the URL and left to it, others could see the value of registering patients and introducing them to the varied content.
Cognitive participation
Most HCPs felt that making the HeLP-Diabetes programme available to their patients was a legitimate part of their role and something that should be supported within the practice. However, for many practices, the structural constraints of workload and staff shortages made it impossible to take on any additional duties, such as registering patients or introducing them to the programme. This was an example of how implementation of even beneficial and legitimate interventions can be compromised by structural inequalities and shortages in resources:
And I think perhaps the fact the partners invited you [researcher] in to come and present about HeLP-Diabetes gave great weight to it as a programme, and because we obviously respect their judgement and they felt this was a good service and something important to promote in the practice.
ST12, practice nurse
It’s a brilliant website that patients can access really good-quality information at home, and take their time over it. Because when they come in to the doctors, sometimes we give information really rapidly and we’re always under time pressure. So, they can actually take their time.
ST13, practice nurse
Collective action
Some practices were able to incorporate the work of implementing the HeLP-Diabetes programme, including setting up systems for registering patients and introducing them to the programme. In these practices, HCPs reported that the HeLP-Diabetes programme had the potential to improve the quality of consultations and save HCP time, by reducing the number of consultations and making them more efficient. These practices found that HCAs were the appropriate professional group to register patients and facilitate access, as this task fitted well with their skill set and professional role. HCAs were often younger, IT-literate and keen to help patients but aware of their lack of clinical knowledge. Hence, HCPs liked being able to answer patient questions by turning to the HeLP-Diabetes programme and searching for the answer together with the patient. It was not a suitable task for general practice nurses, many of whom were not comfortable with IT and who felt their skills should be used on clinical tasks:
Actually, I would argue it shouldn’t be done by the nurse because, you know, it’s quite a low-key IT thing . . . I would rather our practice nurses spend their time, you know, doing the clinical work.
ST1, GP partner
And the barrier was this notion that we’d got to get the receptionist trained to fill in a form and to go online. That all sounded like a bit of a nightmare.
ST11, GP partner
I would register patients as they, as they came . . . It would be 10 minutes out of my day here and there . . . It wouldn’t be a massive, massive burden, no.
ST8, receptionist/administrator
Reflexive monitoring
In practices that managed to develop systems for registering patients on the HeLP-Diabetes programme, staff found that the work was not onerous and was justified by the benefits. In practices that lacked the capacity to incorporate this additional work, relatively few patients were registered, which led to reduced enthusiasm for the programme and even less appetite to take on the work:
I have asked some of them to get back in touch and let me know how they find it . . . because it would be interesting to know, and then I could say to other patients, well, actually patients have found this really helpful, you know.
ST5, HCA
Patient interview data
Interviews were undertaken with 15 patients between April 2014 and February 2015. Of these 15, 11 were male, nine were white British, five had no or only school-leaver qualifications, three had Advanced levels (A levels) or similar and seven had been educated to degree level or higher. Four described their computer skills as basic and a further five as intermediate. The duration of time since their diagnosis of diabetes mellitus ranged from < 1 year to 10–20 years. Treatment modalities included lifestyle only (n = 5) and lifestyle and tablets (n = 10). No interviewees were treated with insulin or other injectables (Table 42).
| Variable | Response options | Sample (n = 15) |
|---|---|---|
| Age (years) | Range | 43–76 |
| Mean (SD) | 59.3 (8.6) | |
| Gender, n | Male | 11 |
| Female | 4 | |
| Ethnic group, n | White (English/Welsh/Scottish/Northern Irish/British) | 9 |
| White (other) | 2 | |
| Black or black British (African) | 1 | |
| Black or black British (Caribbean) | 1 | |
| Mixed (other) | 1 | |
| Other | 1 | |
| Highest educational attainment, n | None | 3 |
| School leaver (e.g. CSE, GCSE, O level, NVQ 1–2) | 2 | |
| A level or vocational equivalent (e.g. NVQ 3) | 3 | |
| Degree or NVQ 4, HND or similar | 5 | |
| Postgraduate degree or NVQ 5 | 2 | |
| Duration of diabetes mellitus since diagnosis (years), n | < 1 | 3 |
| 1–5 | 6 | |
| > 5–10 | 3 | |
| > 10–20 | 3 | |
| How diabetes mellitus managed?, n | Lifestyle only (diet and physical activity) | 5 |
| Lifestyle and tablets | 10 | |
| Internet access, n | Home | 13 |
| Public | 1 | |
| No response | 1 | |
| Computer skills, n | Basic | 4 |
| Intermediate | 6 | |
| Advanced | 5 | |
| Implementation model, n | Patient registered by staff | 11 |
| Patient self-registered | 4 |
The main themes that emerged from the patient interview data related to:
-
the experience of diabetes mellitus
-
perceptions of diabetes mellitus
-
self-management
-
self-management education and support
-
diabetes mellitus information
-
engagement with the HeLP-Diabetes programme
-
use of the HeLP-Diabetes programme.
The inter-relationship between these themes is presented in Figure 22. Perceptions and use of the HeLP-Diabetes programme were contingent on users’ overall experience and perceptions of diabetes mellitus, their views on self-management and the available support and their perceptions of their need for information about diabetes mellitus. These themes did not map easily onto the NPT, and, in our view, use of the NPT as a theoretical lens to interpret these data did not enhance either the robustness or the transferability of the findings. Hence, only the results of the thematic analysis are presented.
FIGURE 22.
Themes identified from the analysis and the connections between them.
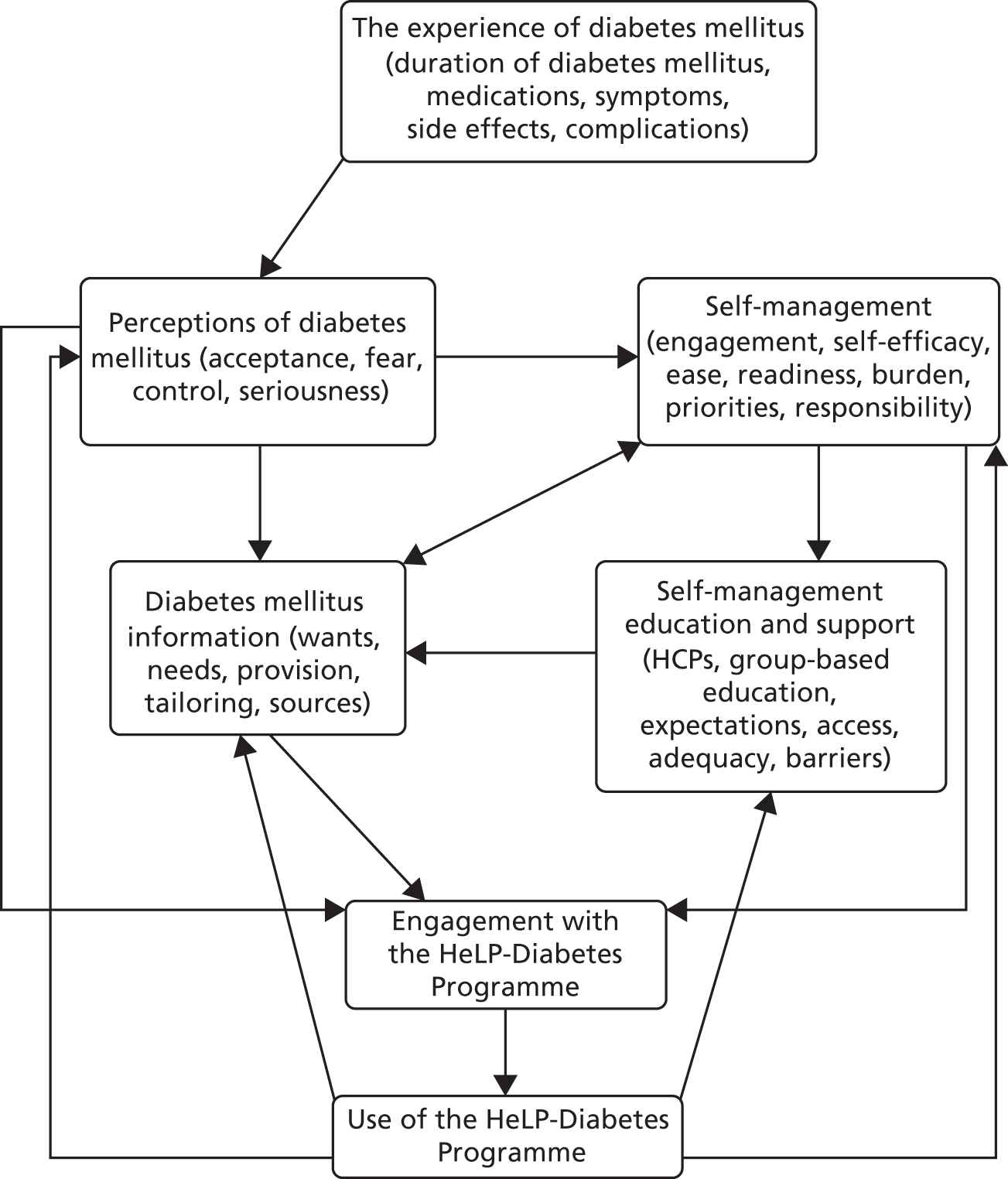
Patients’ experiences and perceptions of diabetes mellitus
This theme influenced all other themes in the data. Many people had difficulty accepting the diagnosis, particularly if they had no symptoms or if their diabetes mellitus was managed with lifestyle modification. Similarly, treatment with lifestyle modification or oral medication, rather than insulin, was often taken to mean that their diabetes mellitus was not ‘serious’:
I do not feel that I’ve got diabetes. I don’t feel, you know . . . I mean, I don’t take no medication. I don’t take nothing at all. I don’t test myself, because I’m not on medication.
PT9, male, aged 66 years, basic computer skills
In contrast, some people experienced symptoms, including fatigue, erectile dysfunction, poor healing and frequent urination, or complications, including neuropathy, peripheral vascular disease or retinopathy. These patients tended to perceive diabetes mellitus as a serious condition and wanted to urge others to take it seriously from the very beginning.
Self-management
Acceptance of their diagnosis of diabetes mellitus and perceptions of its seriousness influenced participants’ reported engagement with self-management, which is in turn important for implementation of the HeLP-Diabetes programme. A fear of disease progression and a desire to prevent future complications and worsening of health was a main priority for many participants engaged in self-management, whereas for others the motivation was a desire to avoid medication or to have a sense of control over their condition and disease trajectory:
Well, I really don’t want to be a diabetic and I certainly don’t want to reach a level where I . . . have to take medication.
PT5, male, aged 76 years, intermediate computer skills
Participants varied greatly in their engagement with self-management and, if engaged, the degree to which they had made lifestyle modifications. Factors included their readiness to engage, relative prioritisation of self-management vis-à-vis the rest of their lives, perceived responsibility for self-management and self-efficacy. Participants who were not ready to accept that they had diabetes mellitus or that it could have serious repercussions were unlikely to want to engage in self-management:
I don’t deal with that sort of thing otherwise I’ll be . . . I mean, I’m a worrier anyway and that would just be another thing just to . . . I’ve kind of put my head in the sand about the long term.
PT11, male, aged 46 years, advanced computer skills
For many, the demands of their lives, including work and family or caring responsibilities, made self-management difficult. Although most participants perceived self-management as their responsibility, some suggested they would prefer more support from professionals. Some found the burden of changing their diets, activity levels or other lifestyle modifications too great, whereas others found them relatively straightforward.
Self-management education and support
For most participants, the main source of HCP input came through primary care services, specifically appointments with GPs and nurses in their surgeries. The general practice also provided access to hospital services for specific diabetes mellitus-related tests and checks, appointments with dietitians and group-based DSME.
There were strong opposing feelings about the care and support participants were getting from their GP surgeries. Some felt their care was excellent, whereas others were dissatisfied, wanting more input, better access, more continuity of care and more practical support:
How would you describe the care that you receive from the NHS?
From my doctor it is absolutely top notch excellent.
PT6, male, aged 58 years, intermediate computer skills
Participants tended to distinguish between tasks that they perceived as the responsibility of HCPs and tasks they thought of as their own responsibility. In general, HCPs were perceived as responsible for providing information, prescribing, adjusting and monitoring medication and performing medical tests and checks, while patients’ responsibilities included being informed, following advice, attending appointments and making changes to diet and exercise.
Not all participants reported having been offered access to group-based structured education, particularly those who had been diagnosed for some years. Those participants who were offered access to group-based structured education reported several barriers to attending, including the fact that they were held during working hours, making it difficult for those in work to attend. Others felt too busy to attend a course that lasted several hours:
I couldn’t attend [group based education] because I had to go to work at the time there, so I couldn’t do it.
PT13, male, aged 52 years, intermediate computer skills
Among those that did attend, perceptions of the value of the course varied widely. Group-based education was particularly suited to those who reported feeling alone with their diabetes mellitus, as it provided an opportunity to connect with others, helped alleviate feelings of isolation and, for some, provided motivation to engage with lifestyle modifications. However, some participants said that the information provided was basic and insufficiently tailored, that the experience had not proved motivating or that they had felt uncomfortable in the group environment. Reasons for discomfort with the group format included difficulties with hearing, difficulties with understanding rapid spoken English and straightforward dislike of group interactions.
Information about diabetes mellitus
Many participants felt that providing information about diabetes mellitus and its treatment was a core responsibility of HCPs. For some, there was the implication that if their HCP did not tell them something, it could not be important and, therefore, there was no need to attend a course. Others were concerned that some HCPs’ knowledge was not up to date, leading to conflicting advice and uncertainty. Although some participants were keen to learn about their condition, others were reluctant, in case they learned something that would cause them anxiety or distress. This led to a range of perceptions about the degree to which patients had unmet informational needs:
PT1: Well, I don’t feel that the GPs – and I’m not blaming . . . my doctor is a very good doctor, but he’s just not up on diabetes. . . . And I just feel that they’re not really in touch.
PT1, male, aged 58 years, advanced computer skills
You say you haven’t really engaged with any information on diabetes because of the way you’re feeling about it?
I would say the bottom line is that . . . there is a kind of fear of confronting it which is sort of holding me back a bit.
PT12, female, aged 52 years, basic computer skills
Engagement with the Healthy Living for People with type 2 Diabetes programme
A range of factors influenced participants’ uptake and use of the HeLP-Diabetes programme, including acceptance of their condition, views about self-management and the burden of illness, satisfaction with their current care and education and a perception of unmet information needs.
Many patients had cogent reasons for not wanting to engage. Those not yet ready to engage with their diabetes mellitus felt that it might make them more aware of their condition, the possible future complications and the importance of self-management; others already felt that they were well informed or believed that they were managing as well as they could and saw no need for the intervention. Some already felt overburdened by the work of living with, and managing, diabetes mellitus, and found the texts, e-mails and newsletters from the HeLP-Diabetes programme an additional burden:
I have signed up to it but I think that would mean everything becomes a bit more real. At the moment, stabbing myself every so often and doing my long-term count . . . I don’t want to look at something knowing that it’s going to be bad.
PT11, male, aged 46 years, advanced computer skills
Well, the reason I don’t use it, as I explained, I feel I’m sort of self-managing it, so I’m not looking at it because I don’t need advice.
PT2, male, aged 63 years, advanced computer skills
Some people with T2DM, however, said they welcomed the HeLP-Diabetes programme, finding it a convenient, discreet (‘private’) and trustworthy source of information. Many reported finding it a useful resource for supplementing, checking and corroborating advice from their HCP:
[Diabetes mellitus] is a very private thing and . . . because you can go on to the website in the privacy of your own space and look things up.
PT7, female, aged 68 years, intermediate computer skills
Trust arose from the programme’s affiliations to the NHS and UCL, bodies that participants said they trusted and respected and that gave the HeLP-Diabetes programme credibility and authority. The fact that the HeLP-Diabetes programme was offered by their GP practice or diabetes clinic further underlined its credibility and trustworthiness. In fact, this endorsement by their HCP was of central importance in participants’ decisions to register and use the HeLP-Diabetes programme. HCP input into the registration process and any introduction to using the programme were warmly welcomed and clearly made a difference to the perceptions of its importance and value:
That was the only reason I signed up, because it was recommended, plus they had a person there to show me what it was like.
PT14, male, aged 56 years, advanced computer skills
Registration and initial introduction seemed particularly important in overcoming the digital divide; participants with only basic computer skills or with English as a second language said that being shown how to use the programme greatly helped build their interest and confidence. Those who had not had this facilitation spontaneously mentioned how such input could have helped them get more out of the programme.
Use of the Healthy Living for People with type 2 Diabetes programme
Almost all participants reported finding the programme easy to use, with straightforward navigation and an attractive appearance. The use of video was much appreciated, and participants reported finding the information clearly presented and easy to understand, even for those with English as a second language or limited literacy:
The two videos I watched about diabetes, anyway, they were very informative and very simple to understand. They weren’t very complicated at all . . . I mean, it presents, I think for me it’s a complicated thing, in a very simple way. You know, everybody can understand, anyway, in any case.
PT13, male, aged 52 years, intermediate computer skills
Many participants used the HeLP-Diabetes programme only for information, either to learn generally about diabetes mellitus and its management or to prepare for consultations with their HCP. Some made use of the interactive components, for example to set goals for behaviour change, to monitor progress or to record clinical data.
Participants reported a range of benefits from use of the HeLP-Diabetes programme. These included improved understanding of the nature of diabetes mellitus, better awareness of the importance of diet and exercise, improved ability to achieve desirable changes in diet and levels of physical activity, a sense of taking control of their health and a realisation that their experiences of diabetes mellitus were widely shared. Participants also reported using the HeLP-Diabetes programme to inform their family and friends about their condition, and thus to enrol family and friends in supporting, rather than hindering, self-management:
And has [the HeLP-Diabetes programme] helped you with any specific aspects of looking after diabetes?
I think the main one was what I should and shouldn’t eat, yes. And sometimes they show in little videos, click on it, it’s exercises and you see, you know, how it can help, yes.
PT4, female, aged 43 years, basic computer skills
Suggestions for improvement
Most respondents had few suggestions for improving the HeLP-Diabetes programme, finding that it met their needs; however, respondents did have suggestions for improving implementation. Participants felt strongly that the HeLP-Diabetes programme should be even more integrated into routine health care. They felt that services should put more effort into registering patients and introducing them to the programme and that people with T2DM should be encouraged to use the programme in routine diabetes appointments. They felt nurses should be trained to routinely ask about use of the programme, and provide encouragement when needed:
It should be part of the initial diagnosis interview. That web address should be given out and the people should be invited to look at it and to ask the relevant questions. And try and encourage them to use it, and then subsequent visits to the diabetic nurse or whatever, perhaps the nurses could be trained to say what have you looked at recently on the website? Are you using it?
PT2, male, aged 63 years, advanced computer skills
Discussion
This mixed-methods case study of the implementation of the HeLP-Diabetes programme in one CCG generated a considerable number of data that can inform a future national roll out of the HeLP-Diabetes programme in particular and use of digital health interventions in general. The main findings were that:
-
the HeLP-Diabetes programme could be implemented in general practice and, when implemented well, is perceived as beneficial to patients and HCPs
-
the use of the NPT in the design phase of the HeLP-Diabetes programme helped sensitise the team to implementation issues and, in turn, led to an intervention that had good potential for implementation; our use of participatory design and the definition of both HCPs and patients as users also aided implementation
-
our hypothesis appears to have been correct that integrating the HeLP-Diabetes programme into routine health care, including providing facilitated access, would promote uptake and use by patients and help overcome the digital divide
-
the data from WP B and predictions by NPT alerted us to the likely difficulties in implementing facilitated access, which enabled us to consider ways to reduce the burden on HCPs and to offer alternative models, including self-registration by people with T2DM
-
the very real resource constraints in general practice at the time of the study prohibited all but the most resilient and well-resourced practices from offering facilitation; however, people with T2DM perceived HCP recommendations and facilitation as essential and, when offered, it was associated with improved uptake and use, and appeared to help overcome the digital divide
-
therefore, we consider HCP support for use of the HeLP-Diabetes programme essential for promoting widespread uptake and use of the programme and, from this, we infer that implementation planning must include adequate resources for this facilitation.
Many of these findings fit with the existing literature on implementation of complex interventions in general, and digital health interventions in particular, and, hence, are likely to transfer to the implementation of other digital health interventions into routine health care.
The drivers for use of digital health interventions in routine health care are overwhelming, as all health-care systems are struggling to provide more and better care with stable or shrinking levels of resource. Thinking about implementation from the very beginning of the development process for an intervention is likely to enhance future ‘implementability’ and should be considered good practice. 214 In common with other researchers who have used the NPT to sensitise developers to implementation issues,232–237 we found that NPT identified the major issues and allowed us to address them during development and we recommend that other researchers consider adopting this approach. The emphasis on participatory design, including both HCPs and patients, helped ensure an intervention that was highly acceptable to users, and this should also be considered good practice in future developments.
The findings that patient perceptions of the value of the intervention were heavily influenced by recommendations from their HCP, and that HCP facilitation promoted uptake and use, are also likely to apply to other digital health interventions. 238 However, this has implications for costs.
Finally, as recognised elsewhere,224,239 the importance of context in implementation cannot be overstated.
Methodologically, this study had many strengths. The use of a case-study design with both quantitative and qualitative data collection allowed us not only to describe what happened but also to consider why it happened. Our flexible, iterative approach enabled us to abandon strategies that were clearly ineffective or unworkable and rapidly develop and deploy alternatives. This, in turn, allowed for a number of ‘natural experiments’, most obviously in terms of comparing the staff registration and patient self-registration models.
Working closely with the CCG was beneficial overall, although it had the immediate effect of causing us to lose control of the implementation process. The use of NPT as a theoretical lens to present the HCP data meant that these data can be compared with other studies using the same lens and helped test the utility of the NPT as a theory to guide implementation.
However, inevitably, there are a number of weaknesses to the study. Some were beyond our control, such as the impact that NHS reorganisation had and the associated workload crisis in general practice. Others could have been pre-empted, for example we should have budgeted more resources for this implementation study. In retrospect, employing two RAs – one to undertake the work of implementation, and one to undertake the research – would have helped considerably with the barrier of providing facilitated access to the HeLP-Diabetes programme.
Although a moderate number of people with T2DM registered to use the HeLP-Diabetes programme, only a tiny number were prepared to participate in the evaluation. Hence, for most users, we had access only to anonymised data and were unable to access their EMR. This prevented us from being able to explore the effects of the HeLP-Diabetes programme on individual users.
Conclusions
The HeLP-Diabetes programme can be successfully implemented in primary care, but successful implementation requires additional resources to enable facilitated access. Providing facilitated access improves uptake and use by patients and appears to help overcome the digital divide. Undertaking an implementation study in parallel with a RCT provided additional data required for subsequent widespread implementation of this intervention and it is a research model that we commend to other researchers.
Chapter 10 Discussion
This chapter summarises the overall findings of the programme of work, considers the strengths and limitations of the work done, lessons learned and the implications for practice, policy and research.
Main results
The overall aim of this programme grant was to develop, evaluate and implement a web-based self-management programme for people with T2DM. This aim was achieved. Within this aim, there were a number of specific objectives, which were also largely achieved.
People with T2DM and the HCPs who work with them clearly articulated features that they considered essential or desirable components of a self-management programme. Initially, we combined user requirements with our theoretical framework and evidence from existing literature. From this we used participatory design to develop a programme that took a holistic approach to self-management, addressing patients’ needs in the areas of medical, emotional and role management. We called it the HeLP-Diabetes programme. Subsequently, the HeLP-Diabetes programme was iteratively user tested for acceptability and functionality before being evaluated for clinical effectiveness and cost-effectiveness.
The clinical effectiveness and cost-effectiveness were determined in an individually randomised controlled trial in primary care. The trial had two co-primary outcomes: diabetes control, as measured by HbA1c level, and diabetes mellitus-related distress, as measured by the PAID scale. At 12 months, the primary analysis showed a significant difference in change in HbA1c levels between the randomised groups, with participants in the HeLP-Diabetes programme group having lower HbA1c levels than those in the control group (mean difference –0.24%, 95% CIs –0.44% to –0.049%; p = 0.014). This difference, although smaller than the 0.25% specified in the original sample size calculation, is clinically meaningful, particularly for a non-pharmacological intervention. Each 1% reduction in HbA1c level is associated with a risk reduction of 21% for deaths related to diabetes mellitus and a 37% risk reduction for microvascular complications. 178 Given that this web-based intervention could be delivered at low cost and at scale across the UK, the potential for population benefit is considerable. There was no difference in PAID scores between the groups at 12 months (mean difference –1.5; 95% CI –3.9 to 0.9; p = 0.21), although prespecified subgroup analysis suggested that the intervention may be effective in reducing distress in people who had been diagnosed more recently (p = 0.004). Both the primary and the complete-case analysis showed the HeLP-Diabetes programme to be dominant over the control, that is, it was both more effective and less costly, following standard NICE procedures for measuring cost-effectiveness per QALY.
The implementation study, conducted in parallel with the trial, identified factors that promoted or inhibited uptake of the HeLP-Diabetes programme into routine care. Promoting factors included a widespread perception that the HeLP-Diabetes programme met an unmet need (ongoing self-management support for people with T2DM) and would be more convenient and acceptable for many patients than the standard model of group-based education and there was appreciation of the holistic, theoretically informed and evidence-based nature of the intervention. However, primary care was experiencing a period of unprecedented turmoil77 and many practices simply did not have capacity to support a new service. Moreover, as predicted by our data from WP B (see Chapter 5) many HCPs did not see the value in facilitating access by patients to the intervention and did not think it was an appropriate use of scarce resources in general practice. Facilitation involved a 5- to 10-minute appointment, with a HCA or receptionist registering patients on the HeLP-Diabetes programme and providing a brief introduction to the programme. Some practices opted not to provide this facilitation and simply gave patients an individual code that enabled the patient to register themselves on the HeLP-Diabetes programme. In sharp contrast, our data suggest that this facilitation was an important factor in overcoming the digital divide. Users who were registered by their HCP reflected the population of people with T2DM in the area, with over half describing themselves as having an ethnicity other than white British, one-third having no formal education after the minimum school-leaving age and one-third describing their computer skills as ‘basic’. Those who registered themselves were more highly educated and had more advanced computer skills.
The long-term nature of the funding for this programme grant allowed us to undertake a number of studies that were additional to those detailed in the original application. These were often undertaken as part of our capacity-building activity, which included three PhDs, one Doctor in Clinical Psychology and several projects for academic GP trainees. These were outlined in Chapter 3 and are also outlined here:
-
development and formative evaluation of a cardiovascular risk calculator for people with T2DM – this study demonstrated that users had complex reactions to personalised risk estimates that were unlikely to promote changes in behaviour that might lead to reduction in risk83
-
a small, single-arm, mixed-methods study examining the impact that the HeLP-Diabetes programme had on psychological well-being in people with T2DM84 – in this study, users demonstrated a significant reduction in diabetes mellitus-related distress, as measured by the PAID scale, over 6 weeks’ use [baseline, mean (SD) scores: 26.32 points (20.88 points); 6 weeks, mean (SD) scores: 20.94 points (16.53 points); p = 0.04]
-
a systematic review of technological prompts to improve engagement with digital health interventions, which demonstrated that such prompts (e.g. e-mails) could have a small beneficial effect85
-
an update of a systematic review of reviews on implementation of eHealth interventions, which emphasised the importance of context for any given implementation82,240
-
development and formative evaluation of a structured education programme for newly diagnosed patients with T2DM – the HeLP-Diabetes programme Starting Out
-
initial work towards the development of a digital T2DM prevention programme (HeLP Stop Diabetes).
There were, however, some objectives that were not achieved. One of our research objectives for the implementation study (WP E) had been to ‘Determine the uptake, use and effects of the intervention in an unselected population in routine care’. Although we were able to determine the uptake and use of the intervention, we were not able to determine its effects in an unselected population in routine care. Our design for this study deliberately separated the offer of the intervention from the research evaluating its implementation and too few patients consented to participate in the research. Thus, we had access only to the routinely available data on uptake and use and were unable to explore the impact.
We were also unable to integrate the EMRs with the intervention. This was not an explicit research objective but had been an element of our funding application and was considered possibly important in contributing to use and uptake, as it would help integrate the intervention into the diabetes mellitus care provided by HCPs. These areas are discussed further under Limitations.
Strengths and limitations
Methodological strengths and limitations of each individual study have been discussed in Chapters 4–9. Here, we focus on the strengths and limitations of the overall programme of work.
Strengths
Theoretical underpinning
The strengths of the programme include a strong emphasis on the theory. The Corbin and Strauss model provided an overall framework for the content of the intervention and the applicability of this model to the work of living with T2DM was confirmed by our early qualitative work. The NPT helped us consider issues to do with implementation from the very beginning of the programme of work and, in our opinion, contributed considerably to the ultimate ‘implementability’ of the intervention.
Patient and public involvement/participatory design
A key strength was our very strong PPI, which had a substantial impact on the design, conduct and reporting of the whole programme of work. This involvement was reflected in having two named PPI co-investigators on the original application, ensuring PPI input into each study through individual WP steering groups and the very substantive PPI input into the development of the intervention. PPI input significantly changed the research design (e.g. ensuring that two co-primary outcomes for the trial reflected patient, as well as HCP, priorities), as well as the intervention design (e.g. the inclusion of exercise videos). It was PPI input that led us to attempt peer-led registration and training for patients in the implementation study (WP E). There was ongoing PPI input into the engagement e-mails and newsletters sent to users, as well as the various updates and revisions we made to the HeLP-Diabetes programme. PPI has also influenced our programme of dissemination and implementation, encouraging the development of a CIC and supporting our work with individual CCGs. Their passionate conviction that what we were doing was worthwhile and would bring benefit to people with T2DM helped us stay motivated and on track throughout the programme of work.
Pragmatic versus explanatory trial
The trial was designed to be pragmatic. The eligibility criteria were deliberately kept broad, to reflect the population of people with T2DM registered in general practice, the setting was the same as the expected setting for routine use (English general practice), the primary outcomes selected were of interest to the participants and the analysis involved all randomised participants following the intention-to-treat principle. However, inevitably, some features verged towards the explanatory end of the continuum: recruitment involved personalised letters to eligible participants, general practices involved in research differ from those that are not, additional resource was made available both for intervention delivery and follow-up and there was considerably less flexibility in the delivery of the intervention in the trial than in the implementation study. 241 Moreover, despite the broad eligibility criteria, the population of patients who participated did not reflect the overall target population, with a preponderance of white British men of retirement age, with considerable experience of computers, a marked absence of diabetes-related distress and good glycaemic control.
Hence, despite the intended pragmatic design, the trial could, in many ways, be considered explanatory. When writing our original grant application, we considered undertaking a cluster randomised trial, as cluster randomisation can enable a more pragmatic design, but decided against this as the risk of bias (as a result of GPs knowing which intervention their patients would get and selecting ‘suitable’ patients) appeared greater than the risk of bias resulting from contamination in an individually randomised trial.
Undertaking an implementation study in parallel with the trial
The decision to undertake an implementation study in parallel with the trial was controversial. A more traditional approach would have been to undertake a process evaluation of the trial, but this would have addressed different questions, such as the reasons for the low participation rate (circa 5%) or patient and nurse experiences of the initial training session on the HeLP-Diabetes programme in which patients were introduced to the programme and shown how to use it. By running an implementation study in parallel, we were able to demonstrate that the low participation rates seen in the trial were at least partly a function of the research rather than the intervention per se. Participation rates in the implementation study (if participation is defined as formally consenting to participate in research) were still only 17.5% (36 out of 205 patients registered), even though the respondent burden was minimal. Moreover, the implementation study demonstrated that even minimal HCP facilitation appeared to have a significant impact on the population of patients registering to use the HeLP-Diabetes programme and helped overcome the digital divide. It would not have been possible to generate this finding from a process evaluation of the trial. Similarly, by exploring the reasons underlying the low overall uptake of the HeLP-Diabetes programme in the implementation study, we were able to add to the overall literature explaining low uptake of structured education for T2DM (the National Diabetes Audit 2013–14 and 2014–15 Report 1: Care Processes and Treatment Targets reports uptake rates of 5.6%). 23
Early assumptions that the delivery mode was the major barrier have not been borne out, and our qualitative data support findings by Winkley et al. ,182,242 showing that patients do not engage for a variety of reasons, including not being ready to come to terms with the diagnosis of diabetes, being concerned that they will learn things they would rather not know (such as the risk of complications), having more urgent priorities in their lives, feeling that their HCP will tell them anything they need to know, and feeling that they already self-manage as well as they can.
Additional findings from the implementation study, which could not have been determined by a process evaluation, include the experience that the offer of a trained patient champion to assist practices with engaging patients in use of the HeLP-Diabetes programme was not taken up by practices, and the overt hostility generated by the potential for linkage with the EMR (discussed in Limitations, Lack of linkage between the Healthy Living for People with type 2 Diabetes programme and general practitioner electronic medical records).
Finally, the implementation study was essential for informing our model for national roll out of the HeLP-Diabetes programme, including the business plan for the CIC, and the advice we offer to CCGs interested in commissioning the HeLP-Diabetes programme for their population.
For all these reasons, we remain convinced that running the trial and implementation study in parallel was a good decision. Given that a core goal of NIHR research funding is for the research to have an impact on patient care, we would recommend that the NIHR consider encouraging such parallel studies in future.
Emphasis on implementation and sustainability
A key feature of this programme of research has been the emphasis on achieving long-term implementation and sustainability. This emphasis started during the preparation for writing the original grant application and was reflected in our use of the NPT to guide development of the intervention, as well as in conducting an implementation study in parallel with the trial. It was also reflected in our choice of collaborators (initially NHS Direct, then, after that closed, NHS Choices). Throughout the 5 years, we were considering how the HeLP-Diabetes programme could be disseminated and implemented across the NHS after the research ended. When it became clear that NHS Choices would not want to take over long-term hosting and maintenance of the HeLP-Diabetes programme, we invested considerable time in meeting a large number of commercial companies to try to find a suitable partner to take on this role. When that search was unsuccessful, we established a not-for-profit CIC, HeLP Digital. A CIC is a form of social enterprise, its aim is to benefit a specific community – in this case, the aim of HeLP Digital is to disseminate and implement digital health interventions similar to the HeLP-Diabetes programme across the NHS.
To date, the CIC has signed contracts with seven CCGs, and we are exploring the possibility of NHS England or Public Health England either commissioning the HeLP-Diabetes programme nationally or taking over responsibility for the programme.
Limitations
Lack of linkage between the Healthy Living for People with type 2 Diabetes programme and general practitioner electronic medical records
In our original application, we argued that the total intervention would consist of the online self-management programme (the HeLP-Diabetes programme) and interactions between patients and their HCP, which would include discussions around patient self-management plans and progress. We expected that linkage with EMRs would promote both patient and HCP engagement with the programme, as patients would find it a convenient way to access information about their medications and test results, and HCPs would find it a quick and efficient way to address progress and problems around the patient’s diabetes. Such discussions would create a virtuous cycle, which encouraged patients to use the HeLP-Diabetes programme and, thus, become more engaged in self-management.
Unfortunately, we were unable to integrate the GP EMRs with the HeLP-Diabetes programme. One of our co-investigators on the grant was Dr Brian Fisher, director of the PAERS company, which we had planned to use to achieve access. PAERS had a functioning link to the EMIS Health EMRs. Unfortunately, it was not possible to reinstate this link after EMIS Health undertook updates to its systems and software. Therefore, our software developers, SoftForge, worked with PAERS to ensure that the HeLP-Diabetes programme was compatible with the PAERS system and, in a sandpit environment, everything worked that could be tested. We subsequently explored alternatives, including the MIG, provided by Healthcare Gateway, which had been charged by the Department of Health and Social Care with arranging and allowing shared access to GP EMRs. However, the MIG business model was aimed at CCGs and similar large organisations and its costing structure was based on a whole CCG. As we needed access to individual patient records across different CCGs, this was neither appropriate nor affordable. (The costs quoted to us, including a discount for academic use, were of the order of £50,000 start-up fees followed by £100,000 per annum.)
Once it became apparent that the delays with EMIS Health were likely to continue, we explored alternatives, including the MIG, provided by Healthcare Gateway, which had been charged by the Department of Health and Social Care with arranging and allowing shared access to GP EMRs. However, the MIG business model was aimed at CCGs and similar large organisations, and its costing structure was based on a whole CCG. As we needed access to individual patient records across different CCGs, this was neither appropriate nor affordable. (The costs quoted to us, including a discount for academic use, were of the order of £50,000 start-up fees followed by £100,000 per annum.)
For these reasons, the final version of the HeLP-Diabetes programme used in the trial and implementation study did not include the potential to provide patient access to their GP EMR.
Although these were technical issues, there were also a number of governance and cultural barriers to an EMR link. HCPs in our preliminary study (WP B) were very reluctant to endorse such access, despite government policy that clearly supported patient access to the EMR. The negotiated agreement, which we considered met patient demand while respecting HCP concerns, was to limit access to the summary list of problems, current medications and values (investigations, blood pressure, weight) once signed off by the general practice. Patients would not have been able to see individual consultation data and would not have been able to upload self-monitoring data into the record. For the implementation study, we negotiated with the CCG that each general practice would have the option of switching this access on (if it became available), and only for selected patients. Even this proved unacceptable to certain GPs, who threatened to use the local medical committee to prevent the entire implementation of the HeLP-Diabetes programme. In the light of this hostility, and given that the technical barriers had yet to be overcome, we made no further efforts to achieve this linkage.
It is difficult to know if and how this affected HCP and patient engagement with the intervention. As and when patient access to EMRs becomes more acceptable to GPs and technically easier, it would be useful to revisit this question.
Lack of data on impact of the Healthy Living for People with type 2 Diabetes programme in routine care
Our second challenge was with obtaining data to assess the impact that using the HeLP-Diabetes programme in routine care had on patients. We considered that the population of patients who participate in trials often differs significantly from those who do not participate (as proved to be the case in our trial), and we also recognised that the resources available in trials to ensure fidelity of intervention are not always available in routine care. These two factors mean that results from a trial might not generalise to routine use.
However, we were unable to gather data from patients in routine care, as insufficient numbers agreed to participate in the implementation research (36 out of the 205 patients registered; 17.5%). Thus, we had access only to demographic and other routinely available data and not to clinical characteristics or self-reported outcomes. A learning point for other implementation studies is to use routinely available data for outcomes (rather than research data requiring individual consent). Further work exploring the impact that the HeLP-Diabetes programme has in routine care is clearly needed.
Lessons learned
A great deal of learning emerged during this programme of work, much of which does not fit easily in the traditional academic modes of dissemination, such as papers and conference presentations. This non-traditional learning is described here.
Developing an effective digital health intervention is a complex process that takes time, resources and an appropriate multidisciplinary team
This may seem an obvious statement, and indeed, when we wrote the grant, we thought we had allowed a considerable amount of time (2 years) and resources (1.75 full-time equivalent RAs, 0.6 of a project manager, 0.6 of a clinical research fellow and 0.3 of a chief investigator, with additional input from co-investigators and funds for commercial collaborators) and had put together an appropriately multidisciplinary team (clinicians, patients, health psychologists, sociologists, health service managers and health service researchers).
However, in retrospect, we would have done better to include an additional year for piloting and refining not only the digital self-management programme (the HeLP-Diabetes programme) but also the surrounding delivery package (facilitated access). Had we done this, we would have been able to trial a sustainable intervention and delivery package that we had shown was feasible and acceptable in general practice. Other researchers in the field of digital health interventions have had similar insights, and this learning has been extensively shared, including in an international workshop on digital health interventions funded by the MRC from the UK and the National Institutes of Health and Robert Wood Johnson Foundation from the USA. This workshop resulted in a panel of publications. 185,243–246
Although our team was very multidisciplinary, with many investigators and collaborators who had considerable experience of undertaking research into digital health interventions, it did not have a computer scientist or HCI specialist. This had been a deliberate decision, as, at the time of writing the grant, we considered the health service research component to be extremely innovative but wanted the technology to be tried and tested, and so had thought that the project would not interest computer scientists who wanted to develop new knowledge in their field. This was the foundation for our decision to tender for commercial software and web-design companies; we also considered that commercial discipline would contribute to delivering on time and in budget. In retrospect, a computer scientist and a HCI specialist on the team would have helped in managing the technical side of the project and the interface with the academic work.
Problems that this might have alleviated included difficulties in communicating with software designers and understanding when we were requesting something that was straightforward to implement compared with something that required a great deal of programming or a new approach. It took us a long time to learn the relevant language and to express our health-related ideas in a form that made sense to the software engineers, despite them being familiar with working with academics and attempting to meet us halfway. Their commitment to the programme and their enjoyment of a challenge meant that, early on, they did not always explain the workload implications of a particular request; alternatively, it would not be clear even to them whether some requested functionality would require 1 or 10 days to program.
In the end, one member of our team who had a natural aptitude towards IT took on the role of ‘translating’ and became the sole communicator with the software team, and we learned to guillotine the amount of time that the engineers could spend on any one request to keep to required timelines.
We had also thought that by using open-source software we would minimise the risk of becoming entirely reliant on one company. In reality, the HeLP-Diabetes programme was such a large and complex programme that only those involved in its development could easily maintain it.
In the light of our experience, we would suggest that similar research programmes include computer science and/or HCI expertise on the team and specifically allow time for piloting the digital health intervention in routine practice to ensure that the surrounding delivery package is feasible and acceptable.
Working with the commercial sector requires careful planning
Before starting this programme of research, we had considerable experience of working with the commercial sector and had developed in-house guidelines for tendering for software and web-design work. This experience was vital in managing the complex process of tendering. We would advise those planning similar work to:
-
ensure that the research team includes an excellent project manager
-
work closely with host university support services (contracts, procurement, business advisors) to ensure that the tender is compliant with UK and European Union legislation
-
think through the specifications in the tender in great detail
-
allow for contingency
-
ensure clear communication channels.
Digital health interventions require ongoing maintenance
Our original grant application was carefully costed and did indeed cover the costs of the development process. What we had not considered sufficiently were the costs of ongoing maintenance, in terms of revising content, improving navigation and design and the need for regular software updates to keep up with the broader technological environment, such as browser updates or new releases of the programs used in our intervention. We advise future researchers to budget for these maintenance costs for the duration of the research, not just for the development period.
Implementation of digital health interventions needs careful planning
Our emphasis on long-term implementation and dissemination has been successful to the extent that we set up a CIC, which obtained contracts with seven CCGs to provide the HeLP-Diabetes programme to their populations. However, the work of marketing and contracting with individual CCGs across England is considerable and in a commercial (albeit not-for-profit) model this work has to be paid for through sales of the product. This increases the cost of the HeLP-Diabetes programme, and it is doubtful whether or not it is a good use of resources in the current financial climate. Central commissioning by either NHS England or Public Health England would be more appropriate for effective digital health interventions, for which the cost per additional user tends to zero with increasing numbers.
Undertaking implementation research in parallel with effectiveness studies
Undertaking implementation research in parallel with clinical effectiveness evaluations has advantages in reducing the overall time taken to generate the data needed to inform policy. Moreover, the use of different research designs in parallel allows for added value in terms of total data generated.
Implications for research and policy
Implications for future research
In our view, our findings highlight a number of areas that need further research:
-
further exploration of the reasons why people with T2DM choose not to engage with self-management support and how they can be encouraged to perceive its value
-
in parallel, more work on how to support HCPs in promoting patient engagement with the HeLP-Diabetes programme or similar programmes – this could include further clarification of underlying reasons that HCPs have for not valuing this work and not seeing it as part of their role, as well as identifying factors that would help them see its value and incorporate it into routine practice
-
as part of this, further work on linking the HeLP-Diabetes programme with the GP EMRs would be useful, exploring how to make this acceptable to GPs and useful to patients and whether or not such linkage does improve uptake of and engagement with the intervention
-
given the importance of overcoming the digital divide, further work on how this can be aided by HCP input would be useful
-
although the trial demonstrated the intervention’s efficacy, we lack data confirming its clinical effectiveness in routine use; this is clearly an area for which further research is needed.
Implications for practice and policy
-
Our findings suggest that widespread deployment of the HeLP-Diabetes programme across the NHS could benefit patients and that it has a very high probability of being cost-effective at standard WTP thresholds.
-
Widespread implementation would be best undertaken centrally, as this would improve the overall cost-effectiveness. The alternative model of implementation by individual CCGs increases costs, particularly in marketing and the costs of agreeing and maintaining contracts.
-
Digital health interventions may have a role in enabling the NHS to deliver more and better care for less resource, but only if there is significant investment in developing acceptable, clinically effective and implementable interventions.
-
Along with this investment in developing and evaluating digital health interventions, there is a need to consider how best to commission, implement and maintain such interventions in a cost-effective manner.
Conclusion
This programme of research has successfully developed, evaluated and implemented a web-based self-management programme for people with T2DM, called the HeLP-Diabetes programme. The evidence from the trial suggests that the HeLP-Diabetes programme enables patients to improve their diabetes control (as measured by HbA1c levels) and reduce their use of health services, leading to an intervention that improves outcomes while reducing costs. The results of a parallel implementation study demonstrate that the HeLP-Diabetes programme can be implemented into routine care and that, if HCPs support the implementation and actively recommend the programme to their patients, it can be used by patients from a wide demographic, effectively crossing the digital divide.
These findings suggest that the HeLP-Diabetes programme could form a useful addition to the current menu of education provision for people with diabetes, which is largely focused on group-based education.
The low uptake of the HeLP-Diabetes programme appears to be related to many people with T2DM not perceiving a need for self-management support. The reasons for this are multifactorial, with some patients not being ready or being frightened to engage with their illness, others feeling they already self-manage as well as they can, and still others thinking that their HCP would tell them anything they really needed to know. This and the role of HCPs in overcoming the digital divide demonstrated in the study suggest that future dissemination and implementation strategies will need to emphasise the importance of HCP involvement and help HCPs appreciate their impact.
Acknowledgements
Contributions of others
The authors wish to thank
Fiona Giles, UCL; Helen Gibson, diabetes specialist nurse; Rebecca Owen, diabetes specialist nurse; Dr Anisoara Jardim, programme manager, NIHR Programme Grants for Applied Research; and Nicolas Barnard, monograph editor.
Additional co-investigators
Dr Stephen Thomas, consultant in diabetes medicine; Charles Gore, PPI and co-investigator; and Mary Jamal, NHS manager, The Whittington Hospital.
Patient representatives
Joni Iniss, PPI and co-investigator; Bindie Wood; Niccy Whitaker; Jonathan Benford; Malcolm Knox; Pamela Ellam; Woolf Van Silver; Charles Prince; Paul Davies; Ros Bacal; Angela Edwards; Caroline Szylit; Robin Healey; Nastir Matabdin; David Forbes; Frank Wood; Andy West; James Munroe; Isidora Walcott; John Mealings (deceased); Tim Saunders; and Trisha Shirt.
The team who worked on the development of the HeLP-Diabetes programme
Joe Palmer, SoftForge; Phil Walton, SoftForge; Christina Lamb, web design; Eleana Papadopoulou, dietitian; Douglas Twenefour, dietitian; Janice Mavroskoufis, dietitian; Adam Cohen, video production; Rupert Charmak, fitness trainer; Angela Nicholas, editing; Julia Bindman, editing; Dr Elsa Gubert, GP academic trainee; and Richard Peacock, information scientist.
The trial steering committee and wider trial team
Professor Frances Mair, University of Glasgow; Professor Peter Hindmarsh, UCL Hospital; Professor Nick Freemantle, UCL; Deborah Haworth, former trial manager; and Kerstin Modrow, data officer, UCL.
The collaborators
Charles Gore, Hepatitis C Trust; Dr John Powell, NHS Choices, editor of the NIHR Journals Library and member of the Health Technology Assessment and Efficacy and Mechanism Evaluation Boards; Professor Irwin Nazareth, UCL Priment; and Dr Tom Aslan, GP, Camden.
Contributions of authors
Professor Elizabeth Murray (UCL: chief investigator) had overall responsibility for the programme, wrote the first and final drafts of the report, with the exception of the first draft of Chapter 8, and supervised all staff and students.
Dr Jamie Ross (UCL: RA and PhD student) contributed to WPs A and B through data collection and analysis, led on PPI for WP C and contributed to development of the HeLP-Diabetes programme, and was the lead researcher on WP E, including developing the implementation plan and methods for evaluating the implementation plan.
Dr Kingshuk Pal (UCL: second investigator and PhD student) was the lead researcher on WPs A and B, contributed to development of the HeLP-Diabetes programme, was the technical lead during development and maintenance of the HeLP-Diabetes programme and was the trial manager for the last 9 months of the trial.
Jinshuo Li (University of York: Research Fellow and Health Economist) in collaboration with Steve Parrott, developed, undertook and wrote up the health economic analysis plan for WP D, was a member of the trial management group and project management group for WP E and wrote the first draft of Chapter 8.
Dr Charlotte Dack [University of Bath (formerly UCL): RA] contributed to design, data collection and data analysis of WPs A and B, contributed to development of the HeLP-Diabetes programme (WP C), was the initial trial manager for WP D, led on refining protocol, obtaining ethics and research governance, recruiting and training practices and participants and data collection procedures and was the co-PPI lead.
Dr Fiona Stevenson (UCL: Reader in Medical Sociology and co-investigator) provided methodological expertise and supervision for WPs A, B and E, including contributing to data collection (A and B) and analysis (A, B and E), supervised Jamie Ross for her PhD and was a member of the project management groups for WPs A, B, C and E and the overall steering group.
Michael Sweeting (University of Cambridge: Statistician, Senior RA and co-investigator) designed the statistical analysis plan for WP D, supervised statistical analyses for WPs D and E and was a member of the trial management group for WP D, the project management group for WP E and the overall steering group.
Steve Parrott (University of York: Reader in Health Economics and co-investigator) supervised Jinshuo Li in designing and undertaking the health economic analyses for WPs D and E and was a member of the trial management group, the project management group for WP E and the overall steering group.
Dr Maria Barnard (The Whittington Hospital, Whittington Health NHS Health Trust: Consultant in Diabetes Medicine and co-investigator) was a member of the project management groups for WPs A, B, C and E, the trial management group for WP D and the overall steering group, contributed to the development of the HeLP-Diabetes programme and advised on all clinical queries arising during the programme grant.
Professor Lucy Yardley (University of Southampton: Professor of Health Psychology and co-investigator) was a member of the project management groups for WPs A, B, C and E, the trial management group for WP D and the overall steering group and advised on digital health intervention development, qualitative research methods, behaviour change, trial design and implementation.
Professor Susan Michie (UCL: Professor of Health Psychology and co-investigator) was a member of the project management groups for WPs A, B, C and E, the trial management group for WP D and the overall steering group, advised on digital health intervention development, qualitative research methods, behaviour change and trial design and co-supervised Kingshuk Pal’s PhD and part of Ghadah Alkhaldi’s PhD.
Professor Carl May (University of Southampton: Professor of Health Care Innovation and co-investigator) was a member of the project management groups for WPs A, B, C and E and the overall steering group and advised on qualitative methods, burden of treatment theory, NPT and implementation science.
Professor David Patterson (The Whittington Hospital, Whittington Health NHS Health Trust: Consultant Clinical Cardiologist and co-investigator) was a member of the project management groups for WPs A, B and E and the overall steering group and advised on clinical issues, development of digital health interventions, long-term implementation and sustainability.
Ghadah Alkhaldi (UCL: PhD student) led on developing and evaluating engagement prompts for the HeLP-Diabetes programme (e-mails and newsletters).
Dr Brian Fisher (PAERS: GP, Director of PAERS and co-investigator) provided advice on integrating digital heath interventions into the NHS (WP B and E) and the integration of GP EMRs with the HeLP-Diabetes programme (WP C) and contributed to developing and reviewing the HeLP-Diabetes programme.
Professor Andrew Farmer (University of Oxford: Professor of Primary Care and co-investigator) was a member of the project management groups for WPs B, C and E, the trial management group and the overall steering group, contributed to developing and reviewing the HeLP-Diabetes programme and advised extensively on trial design and conduct.
Orla O’Donnell (UCL: Project Manager) managed the overall project, including budgets, contracts, ethics and research governance approvals, reporting, timelines, meetings, communication and PPI input, was a member of the project management groups for WPs A, B, C and E, was the chief operating officer for the HeLP Digital CIC and contributed to the development of the HeLP-Diabetes programme.
All authors contributed to writing of the report, commenting on drafts and approving the final version.
Publications
Dack C, Pal K, Gubert E, Stevenson F, Ross J, Murray E. Developing a Computer-Based Self-Management Programme (SMP) for Adults with Type 2 Diabetes: What Did Patients Tell Us? Madingley Society for Academic Primary Care Conference, Cambridge, 2–3 February 2012.
Gubert E, Dack C, Pal K, Ross J, Murray E, Stevenson F. Supporting Clinicians in Promoting Self-Management for People with Type 2 Diabetes. Madingley Society for Academic Primary Care Conference, Cambridge, 2–3 February 2012.
Gubert E, Pal K, Dack C, Murray E. Developing a Computer-Based Self-Management Programme for People with Type 2 Diabetes: User Perspectives. Diabetes UK Annual Professional Conference, Glasgow, March 2012.
Murray E, Pal K, Dack C, Ross J. Developing a Web-Based Self-Management Programme for People with Type 2 Diabetes (HeLP-Diabetes). Eighth Annual Scientific Meeting of the UK Society for Behavioural Medicine, Manchester, December 2012.
Pal K, Dack C, Stevenson F, Murray E. A Qualitative Study Looking at Patient and Professional Views on Internet-Based Self-Management Programmes for Adults with Type 2 Diabetes. Society for Academic Primary Care 41st Annual Conference, Glasgow, October 2012.
Ross J, Dack C, Murray E. Trusting Online Health Information: A Literature Review of Features Which Generate Patient Trust in Health Websites. Madingley Society for Academic Primary Care Conference, Cambridge, 2–3 February 2012.
Dack C, Pal K, Ross J, Stevenson F, Murray E. Developing an Internet Self-Management Intervention for People with Type 2 Diabetes: What Did Patients Tell Us? International Society for Research in Internet Interventions, Chicago, IL, May 2013.
Dack C, Pal K, Stevenson F, Michie S, Ross J, Murray E. Combining Theory and Data to Develop an On Line Self-Management Programme (SMP) for Adults with Type 2 Diabetes. Medicine 2.0, London, September 2013.
Pal K. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. 2013;6:119.
Pal K, Dack C, Ross J, Murray E. Integrating theory, qualitative data and participatory design to develop HeLP-Diabetes: an internet self-management intervention for people with type 2 diabetes. International Society for Research in Internet Interventions, Chicago, IL, May 2013.
Pal K, Dack C, Stevenson F, Murray E. A Qualitative Study of Patient and Professional Preferences for Computer-Based Diabetes Self-Management Interventions. Medicine 2.0, London, September 2013.
Pal K, Eastwood S, Michie S, Farmer A, Barnard M, Peacock R, et al. A Cochrane Systematic Review of Computer-Based Diabetes Self-Management Interventions for Adults with Type 2 Diabetes. International Society for Research in Internet Interventions, Chicago, IL, May 2013.
Pal K, Eastwood S, Michie S, Farmer A, Barnard M, Peacock R, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev 2013;3:CD008776.
Pal K, Murray E. A Cochrane Systematic Review of Computer-Based Self-Management Interventions for Adults with Type 2 Diabetes. Medicine 2.0, London; September 2013.
Pal K, Nolan T, Murray E. Evaluating the Cognitive and Emotional Impact of a Risk Calculator and Support Package for People with Type 2 Diabetes. Medicine 2.0, London, September 2013.
Ross J, Dack C, Pal K, Stevenson F, Murray E. Developing an Internet Self-Management Intervention for People with Type 2 Diabetes: What Did Clinicians Tell Us? International Society for Research in Internet Interventions, Chicago, IL, May 2013.
Pal K. Dialogues and Impact in Digital Health: HeLP-Diabetes – An Online Self-Management Intervention for Adults with Type 2 Diabetes. Digital Health Festival, UCL, London, June 2014.
Pal K, Eastwood S, Michie S, Farmer A, Barnard M, Peacock R, et al. Computer-based interventions to improve self-management in adults with type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 2014;37:1759–66.
Pal K, Murray E. A Cochrane Systematic Review of Computer-Based Diabetes Self-Management Interventions for Adults with Type 2 Diabetes. NIHR School for Primary Care Research Showcase, Oxford, 26 September 2014.
Ross J. Evaluating the Implementation of HeLP-Diabetes within the NHS. Ubi Health Winter School, Puebla, Mexico, January 2014.
Ross J, Stevenson F, Dack C, Pal K, May C, Michie S, et al. Evaluating the implementation of HeLP-Diabetes within NHS services: study protocol. BMC Health Serv Res 2014;14:51.
Alkhaldi G, Hamilton F, Lau R, Webster R, Michie S, Murray E. The effectiveness of technology-based strategies to promote engagement with digital interventions: a systematic review protocol. JMIR Res Protoc 2015;2:2.
Dack C, Ross J, Pal K, Stevenson F, Michie S, Murray E. Developing HeLP-Diabetes: An Internet Self-Management Intervention for People with Type 2 Diabetes. UCL Centre for Behaviour Change Conference, London, February 2015.
Haworth D, Pal K, Ross J, Dack C, Modrow K, Murray E. The HeLP-Diabetes Randomised Controlled Trial: Lessons Learnt from a Pilot Study. Diabetes UK Professional Conference, London, March 2015.
Murray E, Dack C, Barnard M, Farmer A, Li J, Michie S, et al. HeLP-Diabetes: Randomised controlled trial protocol. BMC Health Serv Res 2015;15:578.
Murray E, Pal K, Gibson H, O’Donnell O, Whitaker N, van Silver W. HeLP-Diabetes Dissemination Video. ITN Productions/NHS Alliance; December 2015.
Nolan T, Dack C, Pal K, Stevenson F, Peacock R, Pearson M, et al. Patient reactions to a web-based cardiovascular risk calculator in type 2 diabetes: a qualitative study. Br J Gen Pract March 2015;65:e152–60.
Pal K. Developing HeLP-Diabetes: Integrating Theory and Data to Create an Online Self-Management Programme for Adults with Type 2 Diabetes. Diabetes UK Professional Conference, London, March 2015.
Ross J, Stevenson F, Lau R, Murray E. Exploring the challenges of implementing e-health: a protocol for an update of a systematic review of reviews. BMJ Open 2015;5:e006773.
Ross J, Stevenson F, Pal K, Modrow K, Murray E. Evaluating the implementation of HeLP-Diabetes within the NHS. 5th International Conference on Digital Health, Florence, Italy, May 2015.
Ross J, Stevenson F, Pal K, Modrow K, Murray E. Evaluating the implementation of HeLP-Diabetes within the NHS. The Health Services Research Network Symposium, Nottingham, UK, July 2015.
Alkhaldi G, Hamilton F, Lau R, Webster R, Michie S, Murray E. The effectiveness of prompts to promote engagement with digital interventions: a systematic review. J Med Int Res 2016;18:e6.
Hofman M, Dack C, Barker C, Murray E. The impact of an internet-based self-management intervention (HeLP-Diabetes) on the psychological well-being of adults with type 2 diabetes: a mixed-method cohort study. J Diabet Res 2016;15:1476384.
Murray E. Randomised Controlled Trial of a Web-Based Self-Management Intervention for People with Type 2 Diabetes (HeLP-Diabetes). Society for Academic Primary Care Annual Conference, Dublin, July 2016.
Murray E, Dack C, Alkhaldi G, Ross J, Pal K, Jinshuo Li, et al. Developing, Evaluating and Implementing HeLP-Diabetes. Report from an NIHR Programme Grant for Applied Health Research. HeLP-Diabetes Dissemination Meeting, UCL, London, April 2016.
Orla O’Donnell. HeLP-Diabetes UCL 2034. London, April 2016.
Pal K. Diabetes Self-Care/Shared Care: The spoonful of medicine to help the sugar go down . . . UCL Festival of Digital Health, London, 29 February 2016.
Pal K. Sense and Sensibility: Is Building a Complex Intervention Science or Art? Using Theory and Data to Design HeLP-Diabetes: A New On-Line Self-Management Programme for Adults with Type 2 Diabetes. Madingley Society for Academic Primary Care conference, Cambridge, January 2016.
Pal K, Eastwood S, Michie S, Farmer A, Barnard M, Peacock R, Murray E. A Cochrane Systematic Review of Computer-Based Diabetes Self-Management Interventions. The National School of Primary Care Research Showcase, London, November 2016.
Pal K, Owen R. HeLP-Diabetes – A Recipe for Success. Diabetes UK, Glasgow, 2016.
Ross J. Clinically Effective, Cost Effective and Implemented within the NHS. eResearch Domain Launch, 29 June 2016, London.
Ross J, Stevenson F, Pal K, Modrow K, Murray E. Evaluating the Implementation of an Internet Self-Management Programme for Type 2 Diabetes within the NHS. Madingley Society for Academic Primary Care conference, Cambridge; January 2016.
Murray E. HeLP-Diabetes. A Proven Online Solution for Diabetes Self-Management Support. Quality in Care Diabetes Symposium, Diabetes UK, Manchester, 8–10 March 2017.
Murray E. Should We Undertake Implementation and Effectiveness Research in Parallel or in Sequence? Lessons from an NIHR Programme Grant. Seminars about improvement and implementation, King’s College London, London, April 2017.
Murray E, Sweeting M, Dack C, Pal K, Modrow K, Hudda M, et al. Web-based self-management support for people with type 2 diabetes (HeLP-Diabetes): randomised controlled trial in English primary care. BMJ Open 2017;7:e016009.
Pal K. Digital Diabetes Education: Is IT the Future? Diabetes UK, Manchester, 8–10 March 2017.
Pal K, Owen R. Designing and Delivering an Effective Education Programme in Diabetes. Young Diabetologists and Endocrinologists Workshop, Diabetes UK, Manchester, 8–10 March 2017.
Li J, Parrott S, Sweeting M, Farmer A, Ross J, Dack C, et al. Cost-effectiveness of facilitated access to a self-management website (HeLP-Diabetes) compared to usual care for patients with type 2 diabetes: a randomised-control trial. J Med Int Res 2018;20:e201.
Pal K, Dack C, Ross J, Michie S, May C, Stevenson F, et al. Digital health interventions for adults with type 2 diabetes: qualitative study of patient perspectives on diabetes self-management education and support. J Med Internet Res 2018;20:e40.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health and Social Care.
References
- Diabetes: Facts and Stats. London: Diabetes UK; 2015.
- NCD Risk Factor Collaboration . Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513-30. https://doi.org/10.1016/S0140-6736(16)00618-8.
- Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014;103:137-49. https://doi.org/10.1016/j.diabres.2013.11.002.
- Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord 2012;142:S8-21. https://doi.org/10.1016/S0165-0327(12)70004-6.
- Smith KJ, Béland M, Clyde M, Gariépy G, Pagé V, Badawi G, et al. Association of diabetes with anxiety: a systematic review and meta-analysis. J Psychosom Res 2013;74:89-9. https://doi.org/10.1016/j.jpsychores.2012.11.013.
- Nouwen A. Depression and diabetes distress. Diabet Med 2015;32:1261-3. https://doi.org/10.1111/dme.12863.
- Leung MY, Pollack LM, Colditz GA, Chang SH. Life years lost and lifetime health care expenditures associated with diabetes in the U.S., National Health Interview Survey, 1997-2000. Diabetes Care 2015;38:460-8. https://doi.org/10.2337/dc14-1453.
- Iacobucci G. Diabetes prescribing in England consumes nearly 10% of primary care budget. BMJ 2014;349. https://doi.org/10.1136/bmj.g5143.
- Kanavos P, van den Aardweg S, Schurer W. Diabetes Expenditure, Burden of Disease and Management in 5 EU Countries. London: The London School of Economics and Political Science (LSE) Health and Social Care; 2012.
- Ng CS, Lee JY, Toh MP, Ko Y. Cost-of-illness studies of diabetes mellitus: a systematic review. Diabetes Res Clin Pract 2014;105:151-63. https://doi.org/10.1016/j.diabres.2014.03.020.
- Alva ML, Gray A, Mihaylova B, Leal J, Holman RR. The impact of diabetes-related complications on healthcare costs: new results from the UKPDS (UKPDS 84). Diabet Med 2015;32:459-66. https://doi.org/10.1111/dme.12647.
- Zhuo X, Zhang P, Kahn HS, Bardenheier BH, Li R, Gregg EW. Change in medical spending attributable to diabetes: national data from 1987 to 2011. Diabetes Care 2015;38:581-7. https://doi.org/10.2337/dc14-1687.
- Wanless D. Securing our Future Health: Taking a Long-Term View. London: HM Treasury; 2002.
- Panagioti M, Richardson G, Murray E, Rogers A, Kennedy A, Newman S, et al. Self-management support interventions to reduce health care utilisation without compromising outcomes: a systematic review and meta-analysis. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-356.
- Davies MJ, Heller S, Skinner TC, Campbell MJ, Carey ME, Cradock S, et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ 2008;336:491-5. https://doi.org/10.1136/bmj.39474.922025.BE.
- Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the diabetes X-PERT Programme makes a difference. Diabet Med 2006;23:944-54. https://doi.org/10.1111/j.1464-5491.2006.01906.x.
- Khunti K, Gray LJ, Skinner T, Carey ME, Realf K, Dallosso H, et al. Effectiveness of a diabetes education and self management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus: three year follow-up of a cluster randomised controlled trial in primary care. BMJ 2012;344. https://doi.org/10.1136/bmj.e2333.
- Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159-71. https://doi.org/10.2337/diacare.25.7.1159.
- Nicolucci A, Cavaliere D, Scorpiglione N, Carinci F, Capani F, Tognoni G, et al. A comprehensive assessment of the avoidability of long-term complications of diabetes. A case-control study. SID-AMD Italian Study Group for the Implementation of the St. Vincent Declaration. Diabetes Care 1996;19:927-33. https://doi.org/10.2337/diacare.19.9.927.
- Type 2 Diabetes: National Clinical Guideline for Management in Primary and Secondary Care (Update). London: Royal College of Physicians; 2008.
- Type 2 Diabetes: The Management of Type 2 Diabetes. London: National Institute for Health and Care Excellence; 2009.
- Diabetes in Adults: Quality Standard 6. London: National Institute for Health and Care Excellence; 2011.
- National Diabetes Audit 2013–14 and 2014–15 Report 1: Care Processes and Treatment Targets. Leeds: NHS Digital; 2016.
- Peyrot M, Rubin RR. Access to diabetes self-management education. Diabetes Educ 2008;34:90-7. https://doi.org/10.1177/0145721707312399.
- Peyrot M, Rubin RR, Funnell MM, Siminerio LM. Access to diabetes self-management education: results of national surveys of patients, educators, and physicians. Diabetes Educ 2009;35:246-8. https://doi.org/10.1177/0145721708329546.
- Dutton WH, Blank G. Next Generation Users: The Internet in Britain. Oxford: Oxford Internet Institute, University of Oxford; 2011.
- Internet Access — Households and Individuals: 2015. London: Office for National Statistics; 2015.
- Khadjesari Z, Murray E, Hewitt C, Hartley S, Godfrey C. Can stand-alone computer-based interventions reduce alcohol consumption? A systematic review. Addiction 2011;106:267-82. https://doi.org/10.1111/j.1360-0443.2010.03214.x.
- Bailey JV, Murray E, Rait G, Mercer CH, Morris RW, Peacock R, et al. Interactive computer-based interventions for sexual health promotion. Cochrane Database Syst Rev 2010;9. https://doi.org/10.1002/14651858.CD006483.pub2.
- Harris J, Felix L, Miners A, Murray E, Michie S, Ferguson E, et al. Adaptive e-learning to improve dietary behaviour: a systematic review and cost-effectiveness analysis. Health Technol Assess 2011;15. https://doi.org/10.3310/hta15370.
- Civljak M, Stead LF, Hartmann-Boyce J, Sheikh A, Car J. Internet-based interventions for smoking cessation. Cochrane Database Syst Rev 2013;7. https://doi.org/10.1002/14651858.CD007078.pub4.
- Olthuis JV, Watt MC, Bailey K, Hayden JA, Stewart SH. Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst Rev 2015;3. https://doi.org/10.1002/14651858.CD011565.
- Johansson R, Andersson G. Internet-based psychological treatments for depression. Expert Rev Neurother 2012;12:861-9. https://doi.org/10.1586/ern.12.63.
- Renton T, Tang H, Ennis N, Cusimano MD, Bhalerao S, Schweizer TA, et al. Web-based intervention programs for depression: a scoping review and evaluation. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.3147.
- Hedman E, Ljotsson B, Lindefors N. Cognitive behavior therapy via the Internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev Pharmacoecon Outcomes Res 2012;12:745-64. https://doi.org/10.1586/erp.12.67.
- Ziebland S, Wyke S. Health and illness in a connected world: how might sharing experiences on the internet affect people’s health?. Milbank Q 2012;90:219-49. https://doi.org/10.1111/j.1468-0009.2012.00662.x.
- Murray E, Burns J, See Tai S, Lai R, Nazareth I. Interactive Health Communication Applications for people with chronic disease. Cochrane Database Syst Rev 2005;4. https://doi.org/10.1002/14651858.CD004274.pub4.
- Pal K, Eastwood SV, Michie S, Farmer AJ, Barnard ML, Peacock R, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev 2013;3. https://doi.org/10.1002/14651858.CD008776.pub2.
- Morrison D, Wyke S, Agur K, Cameron EJ, Docking RI, Mackenzie AM, et al. Digital asthma self-management interventions: a systematic review. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.2814.
- McLean G, Band R, Saunderson K, Hanlon P, Murray E, Little P, et al. Digital interventions to promote self-management in adults with hypertension systematic review and meta-analysis. J Hypertens 2016;34:600-12. https://doi.org/10.1097/HJH.0000000000000859.
- Eysenbach G. The law of attrition. J Med Internet Res 2005;7. https://doi.org/10.2196/jmir.7.1.e11.
- Murray E, White IR, Varagunam M, Godfrey C, Khadjesari Z, McCambridge J. Attrition revisited: adherence and retention in a web-based alcohol trial. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2336.
- Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res 2010;12. https://doi.org/10.2196/jmir.1376.
- Portnoy DB, Scott-Sheldon LA, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988–2007. Prev Med 2008;47:3-16. https://doi.org/10.1016/j.ypmed.2008.02.014.
- Mair F, May C, Murray E, Finch T, O’Donnell C, Anderson G, et al. Understanding the implementation and integration of e-Health Services. Report for the NHS Service and Delivery R & D Organisation (NCCSDO). London: NHS Service Delivery and R&D Organisation; 2009.
- van Dijk JAGM. Digital divide research, achievements and shortcomings. Poetics (Amst) 2006;34:221-35. https://doi.org/10.1016/j.poetic.2006.05.004.
- Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med 2002;17:243-52. https://doi.org/10.1046/j.1525-1497.2002.10905.x.
- Heisler M, Cole I, Weir D, Kerr EA, Hayward RA. Does physician communication influence older patients’ diabetes self-management and glycemic control? Results from the Health and Retirement Study (HRS). J Gerontol A Biol Sci Med Sci 2007;62:1435-42. https://doi.org/10.1093/gerona/62.12.1435.
- Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ 2007;335:24-7. https://doi.org/10.1136/bmj.39246.581169.80.
- Coulter A. Patient engagement – what works?. J Ambul Care Manage 2012;35:80-9. https://doi.org/10.1097/JAC.0b013e318249e0fd.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321:694-6. https://doi.org/10.1136/bmj.321.7262.694.
- Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455-9. https://doi.org/10.1136/bmj.39108.379965.BE.
- Corbin JM, Strauss A. Unending Work and Care. San Francisco, CA: Jossey-Bass Inc; 1988.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. https://doi.org/10.1037/0278-6133.27.3.379.
- May C, Finch T. Implementation, embedding, and integration: an outline of Normalization process theory. Sociology 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- Bury M. Chronic illness as biographical disruption. Sociol Health Illn 1982;4:167-82. https://doi.org/10.1111/1467-9566.ep11339939.
- Armitage CJ, Conner M. Social cognition models and health behaviour: a structured review. Psychol Health 2000;15:173-89. https://doi.org/10.1080/08870440008400299.
- Dombrowski SU, Sniehotta FF, Avenell A, Johnston M, MacLennan G, Araújo-Soares V. Identifying active ingredients in complex behavioural interventions for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: a systematic review. Health Psychol Rev 2012;6:7-32. https://doi.org/10.1080/17437199.2010.513298.
- French DP, Olander EK, Chisholm A, Mc Sharry J. Which behaviour change techniques are most effective at increasing older adults’ self-efficacy and physical activity behaviour? A systematic review. Ann Behav Med 2014;48:225-34. https://doi.org/10.1007/s12160-014-9593-z.
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. https://doi.org/10.1037/a0016136.
- Michie S, Abraham C. Advancing the science of behaviour change: a plea for scientific reporting. Addiction 2008;103:1409-10. https://doi.org/10.1111/j.1360-0443.2008.02291.x.
- Milner H. UK Online Centres: Transformational Government for the Citizen. Sheffield; 2009.
- Cashen MS, Sklar BM, Nguyen HH, Just M, Galzagorry G, Bakken S. Implementing a Web-based information resource at an inner-city community church: lessons learned. Comput Inform Nurs 2002;20:244-50. https://doi.org/10.1097/00024665-200211000-00011.
- Billipp SH. The psychosocial impact of interactive computer use within a vulnerable elderly population: a report on a randomized prospective trial in a home health care setting. Public Health Nurs 2001;18:138-45. https://doi.org/10.1046/j.1525-1446.2001.00138.x.
- Salovey P, Williams-Piehota P, Mowad L, Moret ME, Edlund D, Andersen J. Bridging the digital divide by increasing computer and cancer literacy: community technology centers for head-start parents and families. J Health Commun 2009;14:228-45. https://doi.org/10.1080/10810730902805804.
- Masucci MM, Homko C, Santamore WP, Berger P, McConnell TR, Shirk G, et al. Cardiovascular disease prevention for underserved patients using the internet: bridging the digital divide. Telemed J E Health 2006;12:58-65. https://doi.org/10.1089/tmj.2006.12.58.
- Kalichman SC, Weinhardt L, Benotsch E, Cherry C. Closing the digital divide in HIV/AIDS care: development of a theory-based intervention to increase Internet access. AIDS Care 2002;14:523-37. https://doi.org/10.1080/09540120208629670.
- Kerr C, Murray E, Noble L, Morris R, Bottomley C, Stevenson F, et al. The potential of Web-based interventions for heart disease self-management: a mixed methods investigation. J Med Internet Res 2010;12. https://doi.org/10.2196/jmir.1438.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Blight B, Fenn C. NHS Reforms: 100 Voices – Interactive 2012. www.theguardian.com/society/interactive/2012/mar/15/nhs-reforms-100-voices-interactive (accessed 15 March 2012).
- Ham C. What will the Health and Social Care Bill mean for the NHS in England?. BMJ 2012;344. https://doi.org/10.1136/bmj.e2159.
- Checkland K, Coleman A, Segar J, McDermott I, Miller R, Wallace A, et al. Exploring the Early Workings of Emerging Clinical Commissioning Groups: Final Report. London: Policy Research Unit in Commissioning and the Healthcare System; 2012.
- McDermott I, Checkland K, Harrison S, Snow S, Coleman A. Who do we think we are? Analysing the content and form of identity work in the English National Health Service. J Health Organ Manag 2013;27:4-23. https://doi.org/10.1108/14777261311311771.
- Checkland K, Harrison S, Snow S, Coleman A, McDermott I. Understanding the work done by NHS commissioning managers: an exploration of the microprocesses underlying day-to-day sensemaking in UK primary care organisations. J Health Organ Manag 2013;27:149-70. https://doi.org/10.1108/14777261311321752.
- Roberts AM L, Charlesworth A. A Decade of Austerity? The Funding Pressures Facing the NHS from 2010/11 to 2021/22. London: Nuffield Trust; 2012.
- Responsive, Safe and Sustainable: Our Urgent Prescription for General Practice. London: British Medical Association; 2016.
- Roland MB, Barber N, Howe A, Imision C, Rubin G, Storey K. The Future of Primary Care: Creating Teams for Tomorrow. London: Primary Care Workforce Commission; 2015.
- Hobbs FD, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. National Institute for Health Research School for Primary Care Research . Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007-14. Lancet 2016;387:2323-30. https://doi.org/10.1016/S0140-6736(16)00620-6.
- Doran N, Fox F, Rodham K, Taylor G, Harris M. Lost to the NHS: a mixed methods study of why GPs leave practice early in England. Br J Gen Pract 2016;66:e128-35. https://doi.org/10.3399/bjgp16X683425.
- Alkhaldi G, Modrow K, Hamilton F, Pal K, Ross J, Murray E. Promoting engagement with a digital health intervention (HeLP-Diabetes) using email and text message prompts: mixed-methods study. Interact J Med Res 2017;6. https://doi.org/10.2196/ijmr.6952.
- Ross J, Stevenson F, Lau R, Murray E. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0510-7.
- Nolan T, Dack C, Pal K, Ross J, Stevenson FA, Peacock R, et al. Patient reactions to a web-based cardiovascular risk calculator in type 2 diabetes: a qualitative study in primary care. Br J Gen Pract 2015;65:e152-60. https://doi.org/10.3399/bjgp15X683953.
- Hofmann M, Dack C, Barker C, Murray E. The impact of an internet-based self-management intervention (HeLP-Diabetes) on the psychological well-being of adults with type 2 diabetes: a mixed-method cohort study. J Diabetes Res 2016;2016. https://doi.org/10.1155/2016/1476384.
- Alkhaldi G, Hamilton FL, Lau R, Webster R, Michie S, Murray E. The effectiveness of prompts to promote engagement with digital interventions: a systematic review. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.4790.
- Alkhaldi G, Hamilton FL, Lau R, Webster R, Michie S, Murray E. The effectiveness of technology-based strategies to promote engagement with digital interventions: a systematic review protocol. JMIR Res Protoc 2015;4. https://doi.org/10.2196/resprot.3990.
- Bartholomew LK, Parcel GS, Kok G. Intervention mapping: a process for developing theory- and evidence-based health education programs. Health Educ Behav 1998;25:545-63. https://doi.org/10.1177/109019819802500502.
- Gustafson DH, Hawkins R, Boberg E, Pingree S, Serlin RE, Graziano F, et al. Impact of a patient-centered, computer-based health information/support system. Am J Prev Med 1999;16:1-9. https://doi.org/10.1016/S0749-3797(98)00108-1.
- Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A. Health related virtual communities and electronic support groups: systematic review of the effects of online peer to peer interactions. BMJ 2004;328. https://doi.org/10.1136/bmj.328.7449.1166.
- Kerr C, Murray E, Stevenson F, Gore C, Nazareth I. Internet interventions for long-term conditions: patient and caregiver quality criteria. J Med Internet Res 2006;8. https://doi.org/10.2196/jmir.8.3.e13.
- Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, Hofer TP. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make?. J Gen Intern Med 2003;18:893-902. https://doi.org/10.1046/j.1525-1497.2003.21132.x.
- Peel E, Parry O, Douglas M, Lawton J. Diagnosis of type 2 diabetes: a qualitative analysis of patients’ emotional reactions and views about information provision. Patient Educ Couns 2004;53:269-75. https://doi.org/10.1016/j.pec.2003.07.010.
- Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, et al. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2439.
- Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn Behav Ther 2009;38:196-205. https://doi.org/10.1080/16506070903318960.
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003;362:1225-30. https://doi.org/10.1016/S0140-6736(03)14546-1.
- Fisher B, Bhavnani V, Winfield M. How patients use access to their full health records: a qualitative study of patients in general practice. J R Soc Med 2009;102:539-44. https://doi.org/10.1258/jrsm.2009.090328.
- Bhavnani V, Fisher B, Winfield M, Seed P. How patients use access to their electronic GP record – a quantitative study. Fam Pract 2011;28:188-94. https://doi.org/10.1093/fampra/cmq092.
- Fisher B. Patients’ access to their electronic record: offer patients access as soon as you can. Br J Gen Pract 2013;63:e423-5. https://doi.org/10.3399/bjgp13X668384.
- Cross M. BMA warns against letting patients have access to their electronic records. BMJ 2011;342. https://doi.org/10.1136/bmj.d206.
- Webster PC. UK unveils patient-centred electronic health strategy. CMAJ 2012;184:E579-80. https://doi.org/10.1503/cmaj.109-4233.
- Coulter A, Entwistle V, Gilbert D. Informing Patients. An Assessment of the Quality of Patient Information Materials. London: The King’s Fund Publishing; 1998.
- Kitzinger J. Qualitative research. Introducing focus groups. BMJ 1995;311:299-302. https://doi.org/10.1136/bmj.311.7000.299.
- Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. Thousand Oaks, CA: Sage; 2013.
- Dutton WH, Blank G, Groselj D. Cultures of the Internet: The Internet in Britain. Oxford Internet Survey 2013. Oxford: Oxford Internet Institute; 2013.
- Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. J Adv Nurs 2005;49:616-23. https://doi.org/10.1111/j.1365-2648.2004.03331.x.
- Klemm P, Hurst M, Dearholt SL, Trone SR. Gender differences on Internet cancer support groups. Comput Nurs 1999;17:65-72.
- Lofland J, Snow D, Anderson L, Lofland L. Analyzing Social Settings: A Guide to Qualitative Observation and Analysis. Belmont, CA: Wadsworth; 1971.
- Demain S, Gonçalves AC, Areia C, Oliveira R, Marcos AJ, Marques A, et al. Living with, managing and minimising treatment burden in long term conditions: a systematic review of qualitative research. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0125457.
- May CR, Eton DT, Boehmer K, Gallacher K, Hunt K, MacDonald S, et al. Rethinking the patient: using Burden of Treatment Theory to understand the changing dynamics of illness. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-281.
- Bohlen K, Scoville E, Shippee ND, May CR, Montori VM. Overwhelmed patients: a videographic analysis of how patients with type 2 diabetes and clinicians articulate and address treatment burden during clinical encounters. Diabetes Care 2012;35:47-9. https://doi.org/10.2337/dc11-1082.
- Egea JMO, González MVR, Menéndez MR. Profiling European physicians’ usage of eHealth services. Information Research 2011;16.
- Grundstein-Amado R. Ethical decision-making processes used by health care providers. J Adv Nurs 1993;18:1701-9. https://doi.org/10.1046/j.1365-2648.1993.18111701.x.
- Jefferson L, Bloor K, Birks Y, Hewitt C, Bland M. Effect of physicians’ gender on communication and consultation length: a systematic review and meta-analysis. J Health Serv Res Policy 2013;18:242-8. https://doi.org/10.1177/1355819613486465.
- Jones A, Pill R, Adams S. Qualitative study of views of health professionals and patients on guided self management plans for asthma. BMJ 2000;321:1507-10. https://doi.org/10.1136/bmj.321.7275.1507.
- Oberle K, Hughes D. Doctors’ and nurses’ perceptions of ethical problems in end-of-life decisions. J Adv Nurs 2001;33:707-15. https://doi.org/10.1046/j.1365-2648.2001.01710.x.
- Titov N, Andrews G, Davies M, McIntyre K, Robinson E, Solley K. Internet treatment for depression: a randomized controlled trial comparing clinician vs. technician assistance. PLOS ONE 2010;5. https://doi.org/10.1371/journal.pone.0010939.
- Dennison L, Morrison L, Lloyd S, Phillips D, Stuart B, Williams S, et al. Does brief telephone support improve engagement with a web-based weight management intervention? Randomized controlled trial. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.3199.
- Pyper C, Amery J, Watson M, Crook C. Access to electronic health records in primary care-a survey of patients’ views. Med Sci Monit 2004;10:SR17-22.
- Pyper C, Amery J, Watson M, Crook C, Thomas B. Patients’ access to their online electronic health records. J Telemed Telecare 2002;8:103-5. https://doi.org/10.1177/1357633X020080S247.
- de Lusignan S, Mold F, Sheikh A, Majeed A, Wyatt JC, Quinn T, et al. Patients’ online access to their electronic health records and linked online services: a systematic interpretative review. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-006021.
- DAFNE Study Group . Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ 2002;325. https://doi.org/10.1136/bmj.325.7367.746.
- Sim J. Collecting and analysing qualitative data: issues raised by the focus group. J Adv Nurs 1998;28:345-52. https://doi.org/10.1046/j.1365-2648.1998.00692.x.
- Asch S, Connor SE, Hamilton EG, Fox SA. Problems in recruiting community-based physicians for health services research. J Gen Intern Med 2000;15:591-9. https://doi.org/10.1046/j.1525-1497.2000.02329.x.
- Johnston S, Liddy C, Hogg W, Donskov M, Russell G, Gyorfi-Dyke E. Barriers and facilitators to recruitment of physicians and practices for primary care health services research at one centre. BMC Med Res Methodol 2010;10. https://doi.org/10.1186/1471-2288-10-109.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Macfarlane A, O’Reilly-de Brun M. Using a theory-driven conceptual framework in qualitative health research. Qual Health Res 2012;22:607-18. https://doi.org/10.1177/1049732311431898.
- DeSmet A, Thompson D, Baranowski T, Palmeira A, Verloigne M, De Bourdeaudhuij I. Is Participatory Design Associated with the Effectiveness of Serious Digital Games for Healthy Lifestyle Promotion? A Meta-Analysis. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.4444.
- Kushniruk A, Nøhr C. Participatory design, user involvement and health IT evaluation. Stud Health Technol Inform 2016;222:139-51.
- Frauenberger C, Good J, Fitzpatrick G, Iversen OS. In pursuit of rigour and accountability in participatory design. Int J Hum Comput Stud 2015;74:93-106. https://doi.org/10.1016/j.ijhcs.2014.09.004.
- Mann CM, Ward DS, Vaughn A, Benjamin Neelon SE, Long Vidal LJ, Omar S, et al. Application of the Intervention Mapping protocol to develop Keys, a family child care home intervention to prevent early childhood obesity. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2573-9.
- Walters ME, Dijkstra A, de Winter AF, Reijneveld SA. Development of a training programme for home health care workers to promote preventive activities focused on a healthy lifestyle: an intervention mapping approach. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-0936-7.
- Riphagen-Dalhuisen J, Frijstein G, van der Geest-Blankert N, Danhof-Pont M, de Jager H, Bos N, et al. Planning and process evaluation of a multi-faceted influenza vaccination implementation strategy for health care workers in acute health care settings. BMC Infect Dis 2013;13. https://doi.org/10.1186/1471-2334-13-235.
- van Oostrom SH, Anema JR, Terluin B, Venema A, de Vet HC, van Mechelen W. Development of a workplace intervention for sick-listed employees with stress-related mental disorders: intervention mapping as a useful tool. BMC Health Serv Res 2007;7. https://doi.org/10.1186/1472-6963-7-127.
- Zuidema RM, van Gaal BG, van Dulmen S, Repping-Wuts H, Schoonhoven L. An online tailored self-management program for patients with rheumatoid arthritis: a developmental study. JMIR Res Protoc 2015;4. https://doi.org/10.2196/resprot.4571.
- Vonk Noordegraaf A, Huirne JA, Pittens CA, van Mechelen W, Broerse JE, Brolmann HA, et al. eHealth program to empower patients in returning to normal activities and work after gynecological surgery: intervention mapping as a useful method for development. J Med Internet Res 2012;14. https://doi.org/10.2196/jmir.1915.
- Corbie-Smith G, Akers A, Blumenthal C, Council B, Wynn M, Muhammad M, et al. Intervention mapping as a participatory approach to developing an HIV prevention intervention in rural African American communities. AIDS Educ Prev 2010;22:184-202. https://doi.org/10.1521/aeap.2010.22.3.184.
- Dingsøyr T, Nerur S, Balijepally V, Moe NB. A decade of agile methodologies: Towards explaining agile software development. J Syst Softw 2012;85:1213-21. https://doi.org/10.1016/j.jss.2012.02.033.
- Linke S, McCambridge J, Khadjesari Z, Wallace P, Murray E. Development of a psychologically enhanced interactive online intervention for hazardous drinking. Alcohol Alcohol 2008;43:669-74. https://doi.org/10.1093/alcalc/agn066.
- Wallace P, Murray E, McCambridge J, Khadjesari Z, White IR, Thompson SG, et al. On-line Randomized Controlled Trial of an Internet Based Psychologically Enhanced Intervention for People with Hazardous Alcohol Consumption. PLOS ONE 2011;6. https://doi.org/10.1371/journal.pone.0014740.
- Yardley L, Ware LJ, Smith ER, Williams S, Bradbury KJ, Arden-Close EJ, et al. Randomised controlled feasibility trial of a web-based weight management intervention with nurse support for obese patients in primary care. Int J Behav Nutr Phys Act 2014;11. https://doi.org/10.1186/1479-5868-11-67.
- Brown J, Michie S, Geraghty AW, Yardley L, Gardner B, Shahab L, et al. Internet-based intervention for smoking cessation (StopAdvisor) in people with low and high socioeconomic status: a randomised controlled trial. Lancet Respir Med 2014;2:997-1006. https://doi.org/10.1016/S2213-2600(14)70195-X.
- Michie S, Whittington C, Hamoudi Z, Zarnani F, Tober G, West R. Identification of behaviour change techniques to reduce excessive alcohol consumption. Addiction 2012;107:1431-40. https://doi.org/10.1111/j.1360-0443.2012.03845.x.
- Carver CS, Scheier MF. Control theory: a useful conceptual framework for personality-social, clinical, and health psychology. Psychol Bull 1982;92:111-35. https://doi.org/10.1037/0033-2909.92.1.111.
- Kaltenthaler E, Brazier J, De NE, Tumur I, Ferriter M, Beverley C, et al. Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation. Health Technol Assess 2006;10. https://doi.org/10.3310/hta10330.
- Cuijpers P, van SA, Andersson G. Internet-administered cognitive behavior therapy for health problems: a systematic review. J Behav Med 2008;31:169-77. https://doi.org/10.1007/s10865-007-9144-1.
- Farrand P, Woodford J. Effectiveness of cognitive behavioural self-help for the treatment of depression and anxiety in people with long-term physical health conditions: a systematic review and meta-analysis of randomised controlled trials. Ann Behav Med 2015;49:579-93. https://doi.org/10.1007/s12160-015-9689-0.
- Pittaway S, Cupitt C, Palmer D, Arowobusoye N, Milne R, Holttum S, et al. Comparative, clinical feasibility study of three tools for delivery of cognitive behavioural therapy for mild to moderate depression and anxiety provided on a self-help basis. Ment Health Fam Med 2009;6:145-54.
- Bekker HL, Winterbottom AE, Butow P, Dillard AJ, Feldman-Stewart D, Fowler FJ, et al. Do personal stories make patient decision aids more effective? A critical review of theory and evidence. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-S2-S9.
- Jibaja-Weiss ML, Volk RJ, Granchi TS, Neff NE, Robinson EK, Spann SJ, et al. Entertainment education for breast cancer surgery decisions: a randomized trial among patients with low health literacy. Patient Educ Couns 2011;84:41-8. https://doi.org/10.1016/j.pec.2010.06.009.
- Volk RJ, Jibaja-Weiss ML, Hawley ST, Kneuper S, Spann SJ, Miles BJ, et al. Entertainment education for prostate cancer screening: a randomized trial among primary care patients with low health literacy. Patient Educ Couns 2008;73:482-9. https://doi.org/10.1016/j.pec.2008.07.033.
- Herxheimer A, McPherson A, Miller R, Chapple A, Shepperd S, Ziebland S, et al. DIPEx (Database of Individual Patients Experience of illness): a multimedia proposal to share experiences and information about illnesses between patients and health professionals. Aten Primaria 2003;31:386-8. https://doi.org/10.1016/S0212-6567(03)70704-5.
- Herxheimer A, McPherson A, Miller R, Shepperd S, Yaphe J, Ziebland S. Database of patients’ experiences (DIPEx): a multi-media approach to sharing experiences and information. Lancet 2000;355:1540-3. https://doi.org/10.1016/S0140-6736(00)02174-7.
- Kummervold PE, Gammon D, Bergvik S, Johnsen JA, Hasvold T, Rosenvinge JH. Social support in a wired world: use of online mental health forums in Norway. Nord J Psychiatry 2002;56:59-65. https://doi.org/10.1080/08039480252803945.
- Schwartz CE, Sendor M. Helping others helps oneself: response shift effects in peer support. Soc Sci Med 1999;48:1563-75. https://doi.org/10.1016/S0277-9536(99)00049-0.
- Heisler M, Choi H, Piette JD, Rosland A, Langa KM, Brown S. Adults with cardiovascular disease who help others: a prospective study of health outcomes. J Behav Med 2013;36:199-211. https://doi.org/10.1007/s10865-012-9414-4.
- Pagano ME, Post SG, Johnson SM. Alcoholics anonymous-related helping and the helper therapy principle. Alcohol Treat Q 2010;29:23-34. https://doi.org/10.1080/07347324.2011.538320.
- 2011 Skills for Life Survey: Headline findings. London: Department for Business Innovation and Skills; 2011.
- Rogers Y, Sharp H, Preece J. Interaction Design: Beyond Human-Computer Interaction. London: John Wiley & Sons; 2011.
- About The IG Toolkit. London: Department of Health and Social Care; n.d.
- Chew BH, Mohd-Sidik S, Shariff-Ghazali S. Negative effects of diabetes-related distress on health-related quality of life: an evaluation among the adult patients with type 2 diabetes mellitus in three primary healthcare clinics in Malaysia. Health Qual Life Outcomes 2015;13. https://doi.org/10.1186/s12955-015-0384-4.
- Glasgow RE, Peeples M, Skovlund SE. Where is the patient in diabetes performance measures? The case for including patient-centered and self-management measures. Diabetes Care 2008;31:1046-50. https://doi.org/10.2337/dc07-1845.
- Kinmonth AL, Woodcock A, Griffin S, Spiegal N, Campbell MJ. Randomised controlled trial of patient centred care of diabetes in general practice: impact on current wellbeing and future disease risk. The Diabetes Care From Diagnosis Research Team. BMJ 1998;317:1202-8. https://doi.org/10.1136/bmj.317.7167.1202.
- Schulz KF, Grimes DA. Multiplicity in randomised trials I: endpoints and treatments. Lancet 2005;365:1591-5. https://doi.org/10.1016/S0140-6736(05)66461-6.
- Murray E, Khadjesari Z, White IR, Kalaitzaki E, Godfrey C, McCambridge J, et al. Methodological challenges in online trials. J Med Internet Res 2009;11. https://doi.org/10.2196/jmir.1052.
- Pal K, Dack C, Ross J, Murray E. Integrating Theory, Qualitative Data and Participatory Design to Develop HeLP-Diabetes: an Internet Self-management Intervention for People with Type 2 Diabetes. Chicago, IL: International Society for Research on Internet Interventions; 2013.
- Murray E, Dack C, Barnard M, Farmer A, Li J, Michie S, et al. HeLP-Diabetes: randomised controlled trial protocol. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1246-9.
- Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, et al. Assessment of diabetes-related distress. Diabetes Care 1995;18:754-60. https://doi.org/10.2337/diacare.18.6.754.
- Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med 2003;20:69-72. https://doi.org/10.1046/j.1464-5491.2003.00832.x.
- Garratt AM, Schmidt L, Fitzpatrick R. Patient-assessed health outcome measures for diabetes: a structured review. Diabet Med 2002;19:1-11. https://doi.org/10.1046/j.1464-5491.2002.00650.x.
- Eigenmann CA, Colagiuri R, Skinner TC, Trevena L. Are current psychometric tools suitable for measuring outcomes of diabetes education?. Diabet Med 2009;26:425-36. https://doi.org/10.1111/j.1464-5491.2009.02697.x.
- Speight J, Reaney MD, Barnard KD. Not all roads lead to Rome-a review of quality of life measurement in adults with diabetes. Diabet Med 2009;26:315-27. https://doi.org/10.1111/j.1464-5491.2009.02682.x.
- El AY, Nejjari C, Chikri M, Lyoussi B. Disease-specific health-related quality of life instruments among adults diabetic: a systematic review. Diabetes Res Clin Pract 2008;80:171-84. https://doi.org/10.1016/j.diabres.2007.12.020.
- Watkins K, Connell CM. Measurement of health-related QOL in diabetes mellitus. PharmacoEconomics 2004;22:1109-26. https://doi.org/10.2165/00019053-200422170-00002.
- Sturt J, Hearnshaw H, Wakelin M. Validity and reliability of the DMSES UK: a measure of self-efficacy for type 2 diabetes self-management. Prim Health Care Res Dev 2010;11:374-81. https://doi.org/10.1017/S1463423610000101.
- Sturt JA, Whitlock S, Fox C, Hearnshaw H, Farmer AJ, Wakelin M, et al. Effects of the Diabetes Manual 1:1 structured education in primary care. Diabet Med 2008;25:722-31. https://doi.org/10.1111/j.1464-5491.2008.02451.x.
- White IR, Kalaitzaki E, Thompson SG. Allowing for missing outcome data and incomplete uptake of randomised interventions, with application to an Internet-based alcohol trial. Stat Med 2011;30:3192-207. https://doi.org/10.1002/sim.4360.
- Dunn G, Maracy M, Tomenson B. Estimating treatment effects from randomized clinical trials with noncompliance and loss to follow-up: the role of instrumental variable methods. Stat Methods Med Res 2005;14:369-95. https://doi.org/10.1191/0962280205sm403oa.
- Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:405-12. https://doi.org/10.1136/bmj.321.7258.405.
- Molenberghs G, Thijs H, Jansen I, Beunckens C, Kenward MG, Mallinckrodt C, et al. Analyzing incomplete longitudinal clinical trial data. Biostatistics 2004;5:445-64. https://doi.org/10.1093/biostatistics/5.3.445.
- Nicolucci A, Kovacs Burns K, Holt RI, Comaschi M, Hermanns N, Ishii H, et al. Diabetes Attitudes, Wishes and Needs second study (DAWN2): cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet Med 2013;30:767-77. https://doi.org/10.1111/dme.12245.
- Kennedy-Martin T, Curtis S, Faries D, Robinson S, Johnston J. A literature review on the representativeness of randomized controlled trial samples and implications for the external validity of trial results. Trials 2015;16. https://doi.org/10.1186/s13063-015-1023-4.
- Winkley K, Evwierhoma C, Amiel SA, Lempp HK, Ismail K, Forbes A. Patient explanations for non-attendance at structured diabetes education sessions for newly diagnosed type 2 diabetes: a qualitative study. Diabet Med 2015;32:120-8. https://doi.org/10.1111/dme.12556.
- Shirazian S, Crnosija N, Weinger K, Jacobson AM, Park J, Tanenbaum ML, et al. The self-management experience of patients with type 2 diabetes and chronic kidney disease: a qualitative study. Chronic Illn 2016;12:18-2. https://doi.org/10.1177/1742395315614381.
- Guide to the Methods of Technology Appraisal 2013. London: National Institute for Health and Care Excellence; 2013.
- McNamee P, Murray E, Kelly MP, Bojke L, Chilcott J, Fischer A, et al. Designing and undertaking a health economics study of digital health interventions. Am J Prev Med 2016;51:852-60. https://doi.org/10.1016/j.amepre.2016.05.007.
- Non-clinical Grade Structure with Spinal Points — 2013/14. London: University College of London; 2014.
- Curtis L. Unit Costs of Health and Social Care 2014. Canterbury: Personal Social Services Research Unit, University of Kent; 2014.
- HM Revenue & Customs . Rates and Thresholds of Employers 2014 to 2015 HM Revenue &Amp; Customs 2015. www.gov.uk/guidance/rates-and-thresholds-for-employers-2014-to-2015 (accessed 28 June 2017).
- Annual Report and Accounts 2013/14. London: HMSO; 2014.
- Out-of-Hours GP Services in England. London: National Audit Office; 2014.
- Reference Costs 2013–14. London: Department of Health and Social Care; 2014.
- Prescription Cost Analysis England 2014. Leeds: NHS Digital; 2015.
- The EuroQol Group . EuroQol — a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: Centre for Health Economics, University of York; 1999.
- Richardson G, Manca A. Calculation of quality adjusted life years in the published literature: a review of methodology and transparency. Health Econ 2004;13:1203-10. https://doi.org/10.1002/hec.901.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. https://doi.org/10.1002/hec.635.
- Morris TP, White IR, Royston P, Seaman SR, Wood AM. Multiple imputation for an incomplete covariate that is a ratio. Stat Med 2014;33:88-104. https://doi.org/10.1002/sim.5935.
- Clarke PM, Gray AM, Briggs A, Farmer AJ, Fenn P, Stevens RJ, et al. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia 2004;47:1747-59. https://doi.org/10.1007/s00125-004-1527-z.
- Tate DF, Finkelstein EA, Khavjou O, Gustafson A. Cost effectiveness of internet interventions: review and recommendations. Ann Behav Med 2009;38:40-5. https://doi.org/10.1007/s12160-009-9131-6.
- Chen YF, Madan J, Welton N, Yahaya I, Aveyard P, Bauld L, et al. Effectiveness and cost-effectiveness of computer and other electronic aids for smoking cessation: a systematic review and network meta-analysis. Health Technol Assess 2012;16. https://doi.org/10.3310/hta16380.
- Tieman J, Bradley SL. Systematic review of the types of methods and approaches used to assess the effectiveness of healthcare information websites. Aust J Prim Health 2013;19:319-24. https://doi.org/10.1071/PY13030.
- Donker T, Blankers M, Hedman E, Ljótsson B, Petrie K, Christensen H. Economic evaluations of Internet interventions for mental health: a systematic review. Psychol Med 2015;45:3357-76. https://doi.org/10.1017/S0033291715001427.
- Little P, Stuart B, Hobbs FR, Kelly J, Smith ER, Bradbury KJ, et al. An internet-based intervention with brief nurse support to manage obesity in primary care (POWeR+): a pragmatic, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol 2016;4:821-8. https://doi.org/10.1016/S2213-8587(16)30099-7.
- Thiart H, Ebert DD, Lehr D, Nobis S, Buntrock C, Berking M, et al. internet-based cognitive behavioral therapy for insomnia: a health economic evaluation. Sleep 2016;39:1769-78. https://doi.org/10.5665/sleep.6152.
- Aardoom JJ, Dingemans AE, van Ginkel JR, Spinhoven P, Van Furth EF, Van den Akker-van Marle ME. Cost-utility of an internet-based intervention with or without therapist support in comparison with a waiting list for individuals with eating disorder symptoms: a randomized controlled trial. Int J Eat Disord 2016;49:1068-76. https://doi.org/10.1002/eat.22587.
- Kolovos S, Kenter RM, Bosmans JE, Beekman AT, Cuijpers P, Kok RN, et al. Economic evaluation of Internet-based problem-solving guided self-help treatment in comparison with enhanced usual care for depressed outpatients waiting for face-to-face treatment: a randomized controlled trial. J Affect Disord 2016;200:284-92. https://doi.org/10.1016/j.jad.2016.04.025.
- Hedman E, Andersson E, Ljotsson B, Axelsson E, Lekander M. Cost effectiveness of internet-based cognitive behaviour therapy and behavioural stress management for severe health anxiety. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009327.
- Drost RM, Paulus AT, Jander AF, Mercken L, de Vries H, Ruwaard D, et al. A web-based computer-tailored alcohol prevention program for adolescents: cost-effectiveness and intersectoral costs and benefits. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5223.
- Murphy SM, Campbell AN, Ghitza UE, Kyle TL, Bailey GL, Nunes EV, et al. Cost-effectiveness of an internet-delivered treatment for substance abuse: data from a multisite randomized controlled trial. Drug Alcohol Depend 2016;161:119-26. https://doi.org/10.1016/j.drugalcdep.2016.01.021.
- Littlewood E, Duarte A, Hewitt C, Knowles S, Palmer S, Walker S, et al. A randomised controlled trial of computerised cognitive behaviour therapy for the treatment of depression in primary care: the Randomised Evaluation of the Effectiveness and Acceptability of Computerised Therapy (REEACT) trial. Health Technol Assess 2015;19. https://doi.org/10.3310/hta191010.
- Solomon D, Proudfoot J, Clarke J, Christensen H. e-CBT (myCompass), antidepressant medication, and face-to-face psychological treatment for depression in Australia: a cost-effectiveness comparison. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4207.
- Eccles MP, Mittman BS. Welcome to implementation science. Implement Sci 2006;1:1-3. https://doi.org/10.1186/1748-5908-1-1.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2008.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Stetler CB, Mittman BS, Francis J. Overview of the VA Quality Enhancement Research Initiative (QUERI) and QUERI theme articles: QUERI Series. Implement Sci 2008;3. https://doi.org/10.1186/1748-5908-3-8.
- Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care 2012;50:217-26. https://doi.org/10.1097/MLR.0b013e3182408812.
- May C, Rapley T, Mair FS, Treweek S, Murray E, Ballini L, et al. Normalization Process Theory On-Line Users’ Manual, Toolkit and NoMAD Instrument n.d. www.normalizationprocess.org (accessed 28 June 2017).
- Grol R, Wensing M, Grol R, Wensing M, Eccles M, Davis D. Improving Patient Care: The Implementation of Change in Health Care, Second Edition. London: John Wiley & Sons; 2005.
- Curran GM, Mukherjee S, Allee E, Owen RR. A process for developing an implementation intervention: QUERI Series. Implement Sci 2008;3. https://doi.org/10.1186/1748-5908-3-17.
- Stetler CB, Legro MW, Wallace CM, Bowman C, Guihan M, Hagedorn H, et al. The role of formative evaluation in implementation research and the QUERI experience. J Gen Intern Med 2006;21:1-8. https://doi.org/10.1007/s11606-006-0267-9.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing Implement Sci. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Greenhalgh T, Robert G, Bate P, Kyriakidou O, Macfarlane F, Peacock R. How to Spread Good Ideas. A Systematic Review of the Literature on Diffusion, Dissemination and Sustainability of Innovations in Health Service Delivery and Organisation. London: The NHS Service and Delivery Organisation Programme; 2004.
- Pettigrew AM, Woodman RW, Cameron KS. Studying organizational change and development: challenges for future research. Acad Manage J 2001;44:697-713.
- Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q 2010;88:500-59. https://doi.org/10.1111/j.1468-0009.2010.00611.x.
- Islington CCG. About Us London: Islington Clinical Commissioning Group. London: Islington CCG; n.d.
- Islington CCG. Working Together for Better Care. Prospectus 2013–14. London: Islington CCG; 2013.
- Camden CCG. Camden CCG Annual Report and Accounts 2013/14. London: Camden CCG; 2014.
- Quality and Outcomes Framework (QOF) 2013–14. London: Health and Social Care Information Centre; 2014.
- Gallacher K, May CR, Montori VM, Mair FS. Understanding patients’ experiences of treatment burden in chronic heart failure using normalization process theory. Ann Fam Med 2011;9:235-43. https://doi.org/10.1370/afm.1249.
- Mair FS, Hiscock J, Beaton SC. Understanding factors that inhibit or promote the utilization of telecare in chronic lung disease. Chronic Illn 2008;4:110-17. https://doi.org/10.1177/1742395308092482.
- Bamford C, Heaven B, May C, Moynihan P. Implementing nutrition guidelines for older people in residential care homes: a qualitative study using normalization process theory. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-106.
- Dziedzic KS, Healey EL, Porcheret M, Ong BN, Main CJ, Jordan KP, et al. Implementing the NICE osteoarthritis guidelines: a mixed methods study and cluster randomised trial of a model osteoarthritis consultation in primary care – the Management of OsteoArthritis In Consultations (MOSAICS) study protocol. Implement Sci 2014;9:1-15. https://doi.org/10.1186/s13012-014-0095-y.
- Furler JS, Blackberry ID, Walker C, Manski-Nankervis JA, Anderson J, O’Neal D, et al. Stepping up: a nurse-led model of care for insulin initiation for people with type 2 diabetes. Fam Pract 2014;31:349-56. https://doi.org/10.1093/fampra/cmt085.
- Chiang PP, Glance D, Walker J, Walter FM, Emery JD. Implementing a QCancer risk tool into general practice consultations: an exploratory study using simulated consultations with Australian general practitioners. Br J Cancer 2015;112:S77-83. https://doi.org/10.1038/bjc.2015.46.
- Godfrey M, Smith J, Green J, Cheater F, Inouye SK, Young JB. Developing and implementing an integrated delirium prevention system of care: a theory driven, participatory research study. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-341.
- Morden A, Ong BN, Brooks L, Jinks C, Porcheret M, Edwards JJ, et al. Introducing evidence through research ‘push’: using theory and qualitative methods. Qual Health Res 2015;25:1560-75. https://doi.org/10.1177/1049732315570120.
- Finch TL, Bamford C, Deary V, Sabin N, Parry SW. Making sense of a cognitive behavioural therapy intervention for fear of falling: qualitative study of intervention development. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-436.
- Murray E, Linke S, Harwood E, Conroy S, Stevenson F, Godfrey C. Widening access to treatment for alcohol misuse: description and formative evaluation of an innovative web-based service in one primary care trust. Alcohol Alcohol 2012;47:697-701. https://doi.org/10.1093/alcalc/ags096.
- Lau R, Stevenson F, Ong BN, Dziedzic K, Treweek S, Eldridge S, et al. Achieving change in primary care – causes of the evidence to practice gap: systematic reviews of reviews. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0396-4.
- Ross J, Stevenson F, Lau R, Murray E. Exploring the challenges of implementing e-health: a protocol for an update of a systematic review of reviews. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006773.
- Loudon K, Treweek S, Sullivan F, Donnan P, Thorpe KE, Zwarenstein M. The PRECIS-2 tool: designing trials that are fit for purpose. BMJ 2015;350. https://doi.org/10.1136/bmj.h2147.
- Winkley K, Stahl D, Chamley M, Stopford R, Boughdady M, Thomas S, et al. Low attendance at structured education for people with newly diagnosed type 2 diabetes: General practice characteristics and individual patient factors predict uptake. Patient Educ Couns 2016;99:101-7. https://doi.org/10.1016/j.pec.2015.08.015.
- Murray E, Hekler EB, Andersson G, Collins LM, Doherty A, Hollis C, et al. Evaluating digital health interventions: key questions and approaches. Am J Prev Med 2016;51:843-51. https://doi.org/10.1016/j.amepre.2016.06.008.
- Patrick K, Hekler EB, Estrin D, Mohr DC, Riper H, Crane D, et al. The pace of technologic change: implications for digital health behavior intervention research. Am J Prev Med 2016;51:816-24. https://doi.org/10.1016/j.amepre.2016.05.001.
- Yardley L, Spring BJ, Riper H, Morrison LG, Crane DH, Curtis K, et al. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med 2016;51:833-42. https://doi.org/10.1016/j.amepre.2016.06.015.
- Hekler EB, Michie S, Rivera DE, Collins LM, Pavel M, Jimison H, et al. Developing and refining models and theories suitable for digital health interventions. Am J Prev Med 2016;51:825-32. https://doi.org/10.1016/j.amepre.2016.06.013.
Appendix 1 Description of the Healthy Living for People with type 2 Diabetes programme
Content
The overall content was broken down into eight sections developed to improve medical, emotional and role management. The key features in each section are described and shown in the following sections.
Understanding diabetes
This section focused on improving people’s medical management by increasing their knowledge about diabetes, targeting beliefs about diabetes mellitus and encouraging behaviour change. Information was provided to answer a number of common questions about diabetes mellitus (e.g. the nature and causes of diabetes; Figure 23).
FIGURE 23.
Understanding diabetes: an example of the information provided on what causes T2DM.
Information was provided on how diabetes mellitus affects the body including emotional problems, eyes, feet, heart and blood vessels, hyperglycaemia, hypoglycaemia, infections, kidneys, nervous system and sexual problems. For each area, this included an overview, advice on actions that could be taken to prevent complications occurring, checks and tests to expect, associated complications and treatments and links to external organisations (e.g. Society of Chiropodists and Podiatrists; NHS Smokefree). An example for eyes is shown in Figure 24.
FIGURE 24.
Understanding diabetes: an example of the information provided on how diabetes mellitus can affect the eyes that includes an overview, prevention, checks and tests, complications, treatment and links.
There were also a number of structured quick guides that were developed to summarise the most important content across the sections in the intervention on a number of topics. These included ‘About type 2 diabetes’, ‘Understanding medicines’, ‘Eating with type 2 diabetes’, ‘African and Caribbean diets’, ‘Quitting smoking’ and ‘Alcohol’. Each quick guide included the same quiz at the beginning and end to assess any changes in people’s knowledge and to provide feedback. In-between, individuals worked through a number of steps that presented them with written information about the topic and strategies to make behavioural changes (e.g. making plans, setting goals) as well as providing information in a video format. Each guide was designed to take approximately 15 minutes to complete. An example for ‘About type 2 diabetes’ is shown in Figure 25.
FIGURE 25.
Understanding diabetes: an example of a quick guide for people to learn ‘About type 2 diabetes’. The steps to work through include a quiz to assess knowledge and to give feedback, information about diabetes mellitus in written and video formats that include changes people could make to take care of their diabetes mellitus.
Staying healthy
This section contained motivational information about how to maintain optimal physical and emotional health and the importance of lifestyle factors and self-management (Figures 26 and 27).
FIGURE 26.
Staying healthy: an example of information provided on why lifestyle factors are important to self-management.
FIGURE 27.
Staying healthy: an example of information provided on ideas of changes that could improve users’ diabetes mellitus control.
The main focus was on helping people improve their medical management by providing them with BCTs or previously validated behaviour change interventions that had been shown to be effective. The behaviours targeted were eating and drinking, levels of physical activity, alcohol consumption, smoking and taking medicines, as well as weight management. Each behaviour change module consisted of the following headings: ‘Understand’, ‘Decide’, ‘Plan’ and ‘Staying Motivated’. The section titled ‘Understand’ provided people with information on the physical and emotional benefits of changing behaviour and ideas on how a change might be made (Figure 28). Written instructions of how to perform each behaviour or videos showing people performing the behaviour were also provided (Figure 29). In the ‘Decide’ section, people could complete self-assessment quizzes (Figure 30) and receive feedback on whether or not their current behaviour could be improved, which directed users via links to relevant information in the intervention (Figure 31).
FIGURE 28.
Staying healthy: understanding behaviour – an example of the information provided about the physical and emotional benefits of performing a behaviour (e.g. taking medicines).
FIGURE 29.
Staying healthy: understanding behaviour – an example of the videos providing instructions and demonstrations of how to perform a behaviour (e.g. physical activity exercises for beginners).
FIGURE 30.
Staying healthy: making a decision – an example of a self-assessment quiz for taking medicines.
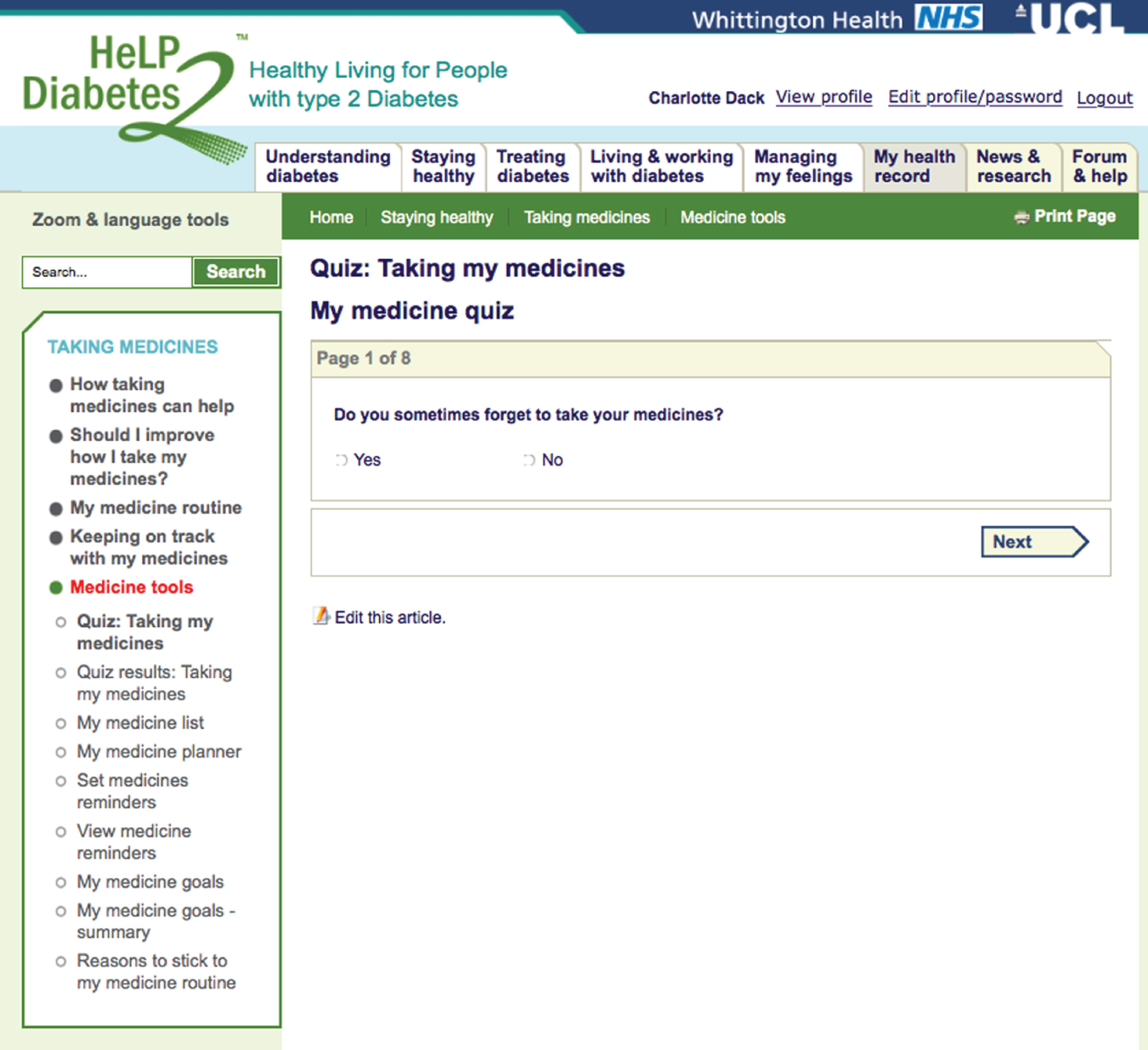
FIGURE 31.
Staying healthy: making a decision – an example of feedback for a user who is finding it difficult to take their medicines (at the top) and for someone who is on the whole taking them as prescribed (bottom).
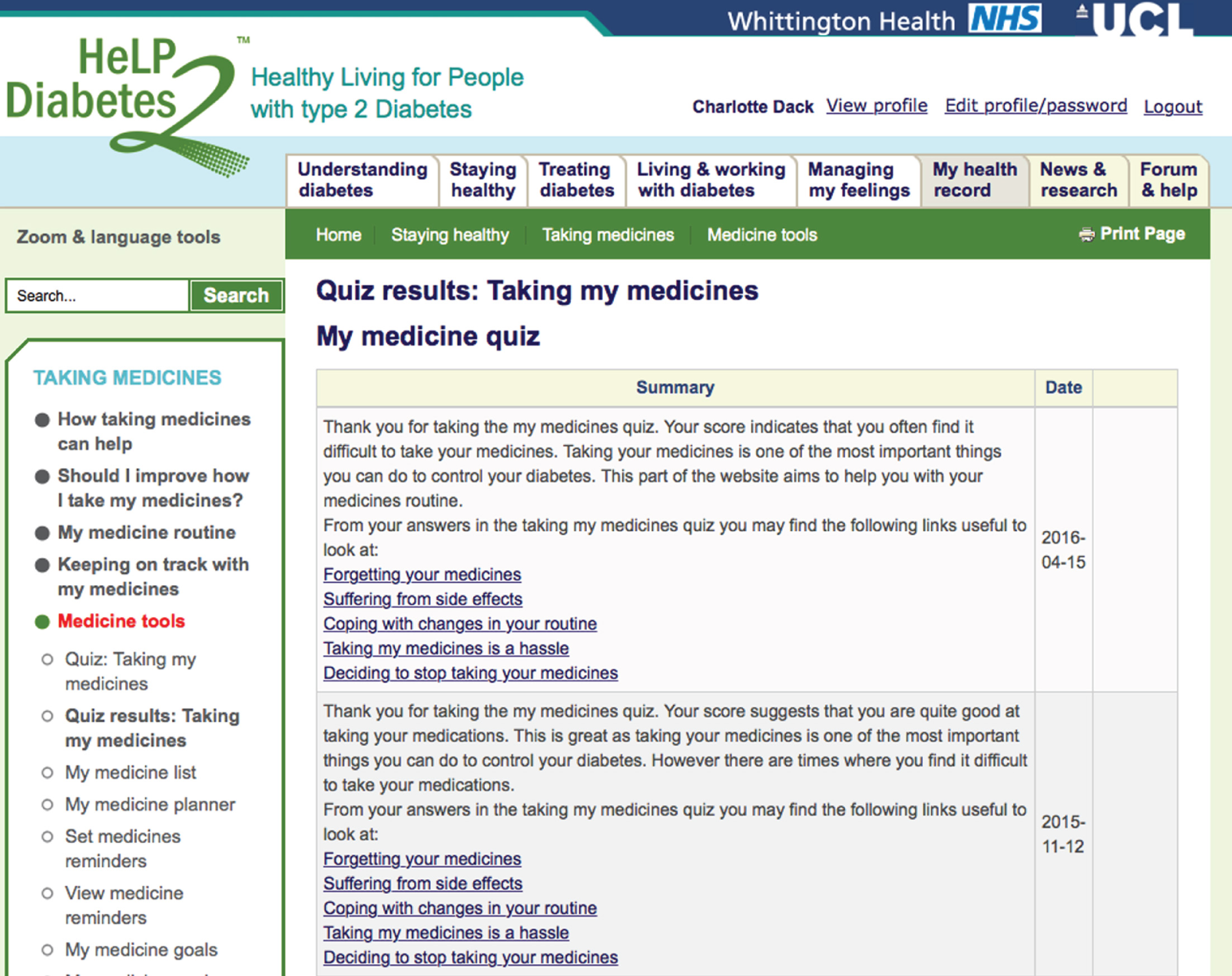
The ‘Plan’ section encouraged users to commit to set a behavioural goal if the feedback from the self-assessment quiz suggested a change might be beneficial in managing their diabetes. They could either choose from a list of popular goals or add their own. To keep users motivated to change, they were asked to think about their reasons for changing and to reflect on whether or not the goal was really important to them (Figure 32). After choosing a goal, users were asked to make an action plan on how they were going to achieve the goal. Users could choose prepopulated plans or they were given information on how to create their own. They were asked to commit to a date to start the plan (Figure 33). Finally, users were asked to review their goal and plan and to think about possible barriers to achieving them and potential solutions to these barriers (Figure 34).
FIGURE 32.
Staying healthy: plan a change – an example of setting a behavioural goal and reasons for change for taking medicines.
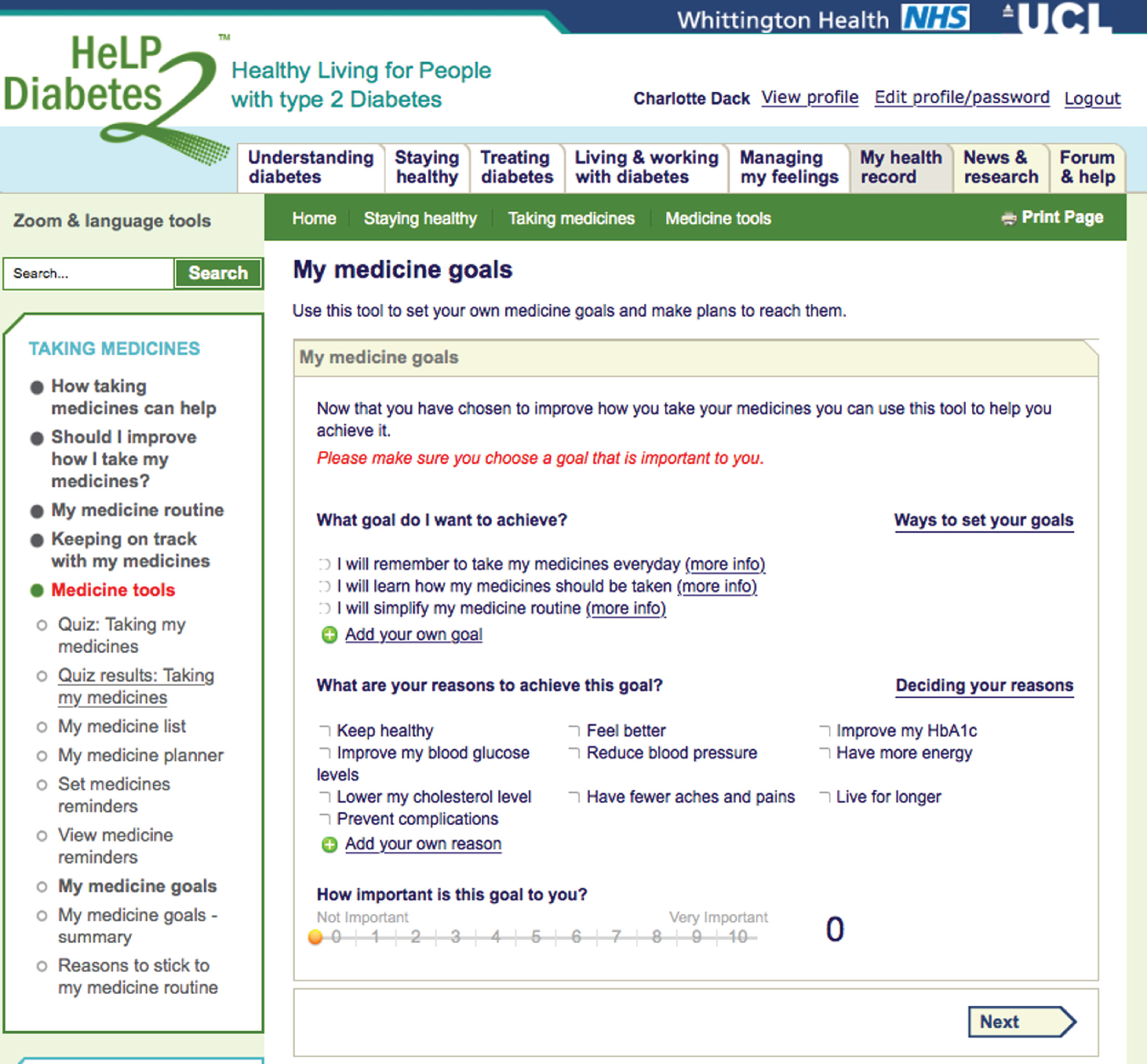
FIGURE 33.
Staying healthy: plan a change – an example of making an action plan and start date for taking medicines.
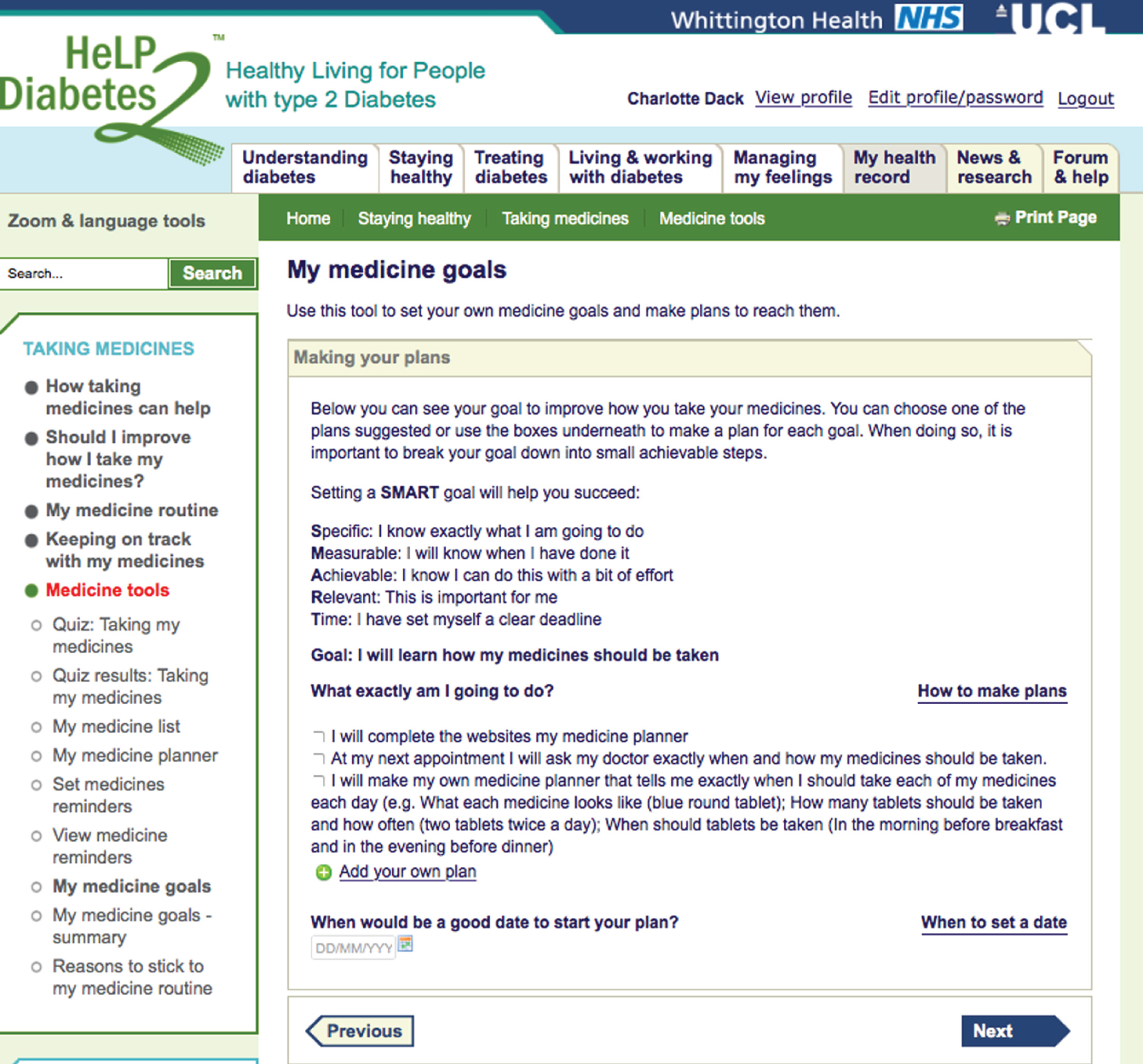
FIGURE 34.
Staying healthy: plan a change – an example of reviewing goals and plans and problem-solving for taking medicines.
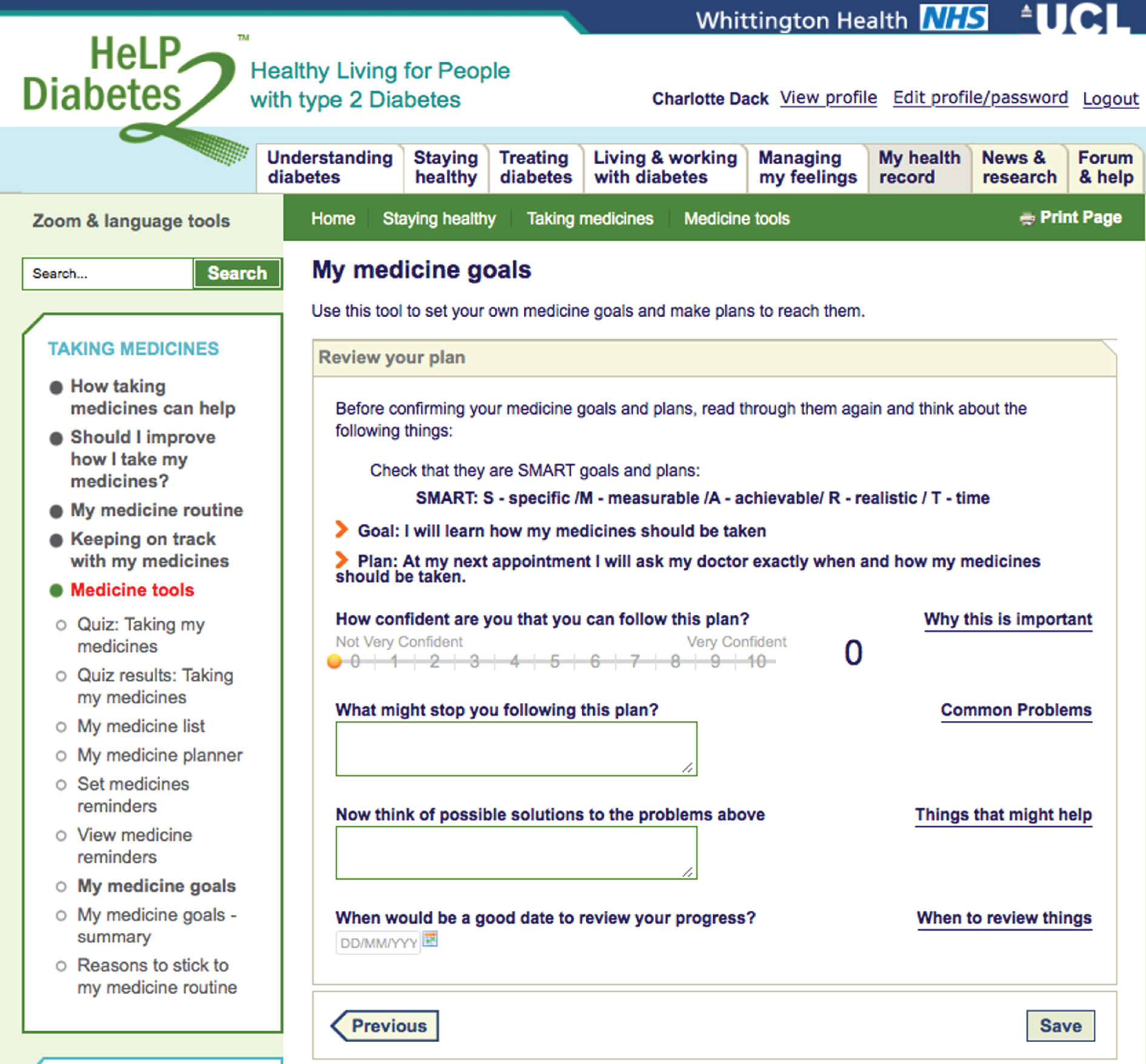
In the ‘Staying Motivated’ section to help people keep to the goals and plans that had been set users were encouraged to reward themselves when successful, to remember the reasons they decided to make a change in the first place, to tell someone about their goal in order to receive support, to monitor their progress using the health tracker feature of the intervention and to aim to make one change at a time (Figure 35). Users were also encouraged to review their goals and plans rating how successful they were at achieving them (Figure 36). The intervention provided motivating messages based on the rating chosen (Figure 37).
FIGURE 35.
Staying healthy: keeping on track – an example of the techniques provided to keep motivated with the goals and plans set for taking medicines.
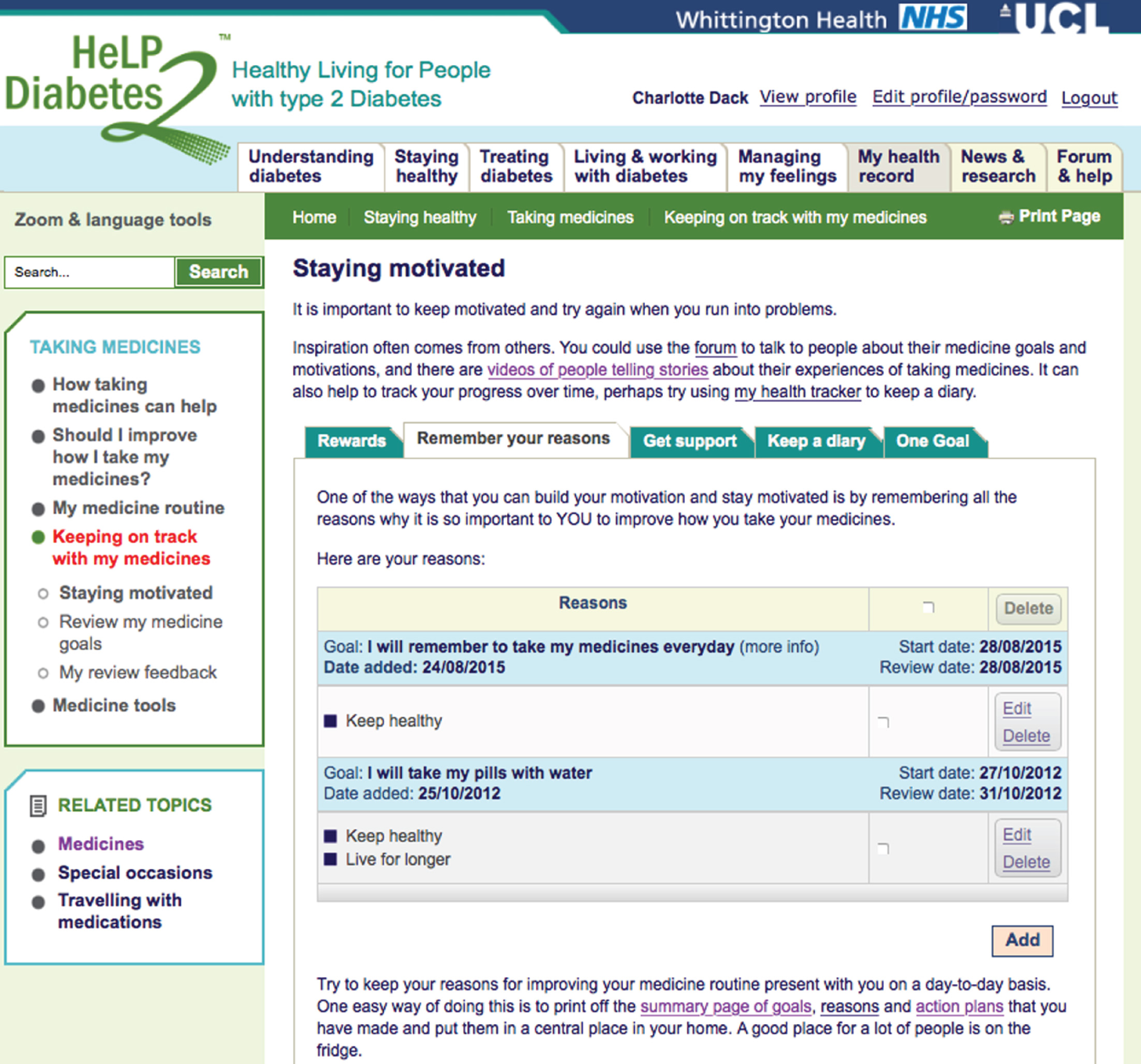
FIGURE 36.
Staying healthy: keeping on track – an example of the tool provided for users to review their process with the goals and plans set.
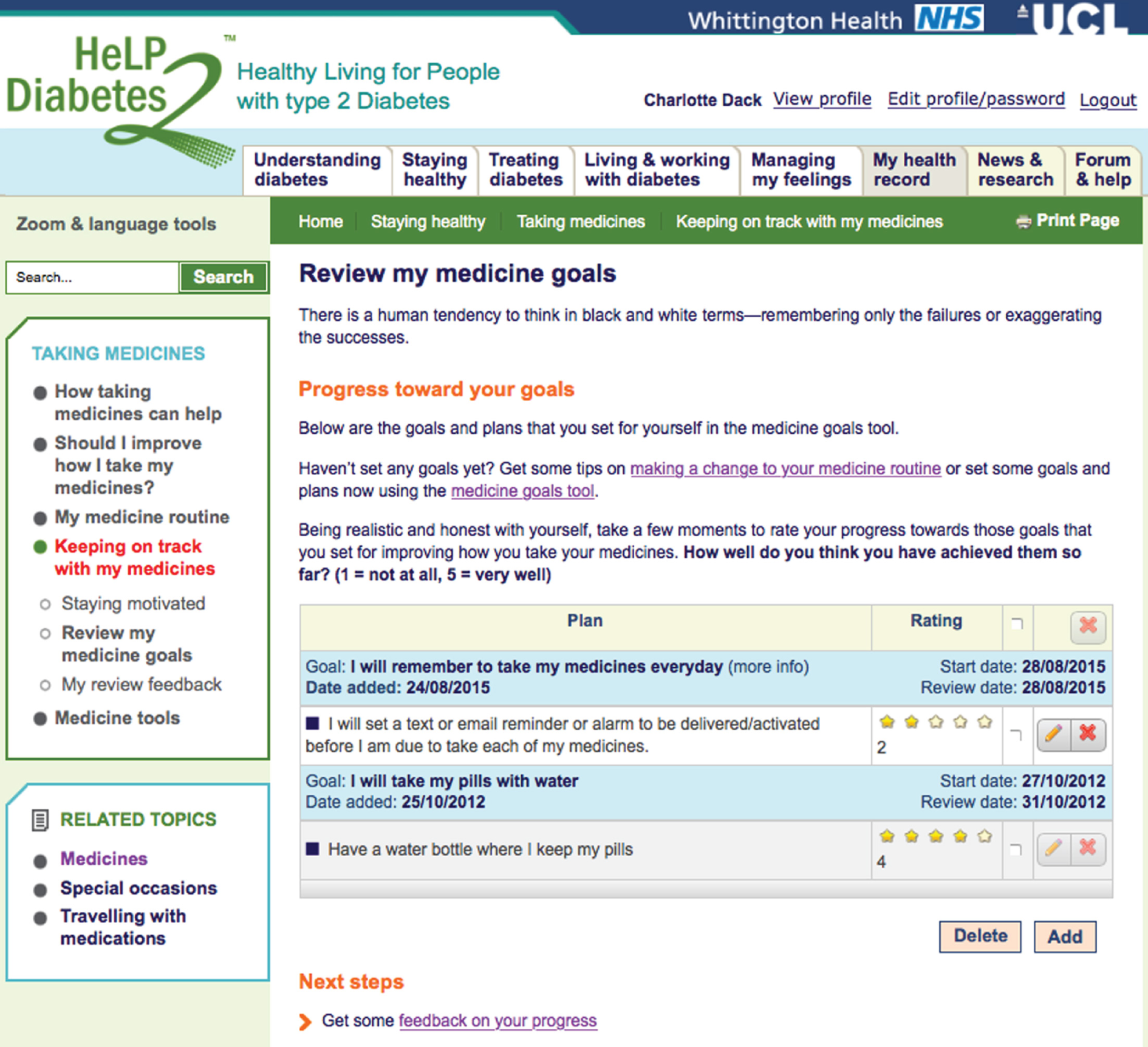
FIGURE 37.
Staying healthy: keeping on track – an example of the motivational feedback given to users based on their progress ratings for their goals and plans.
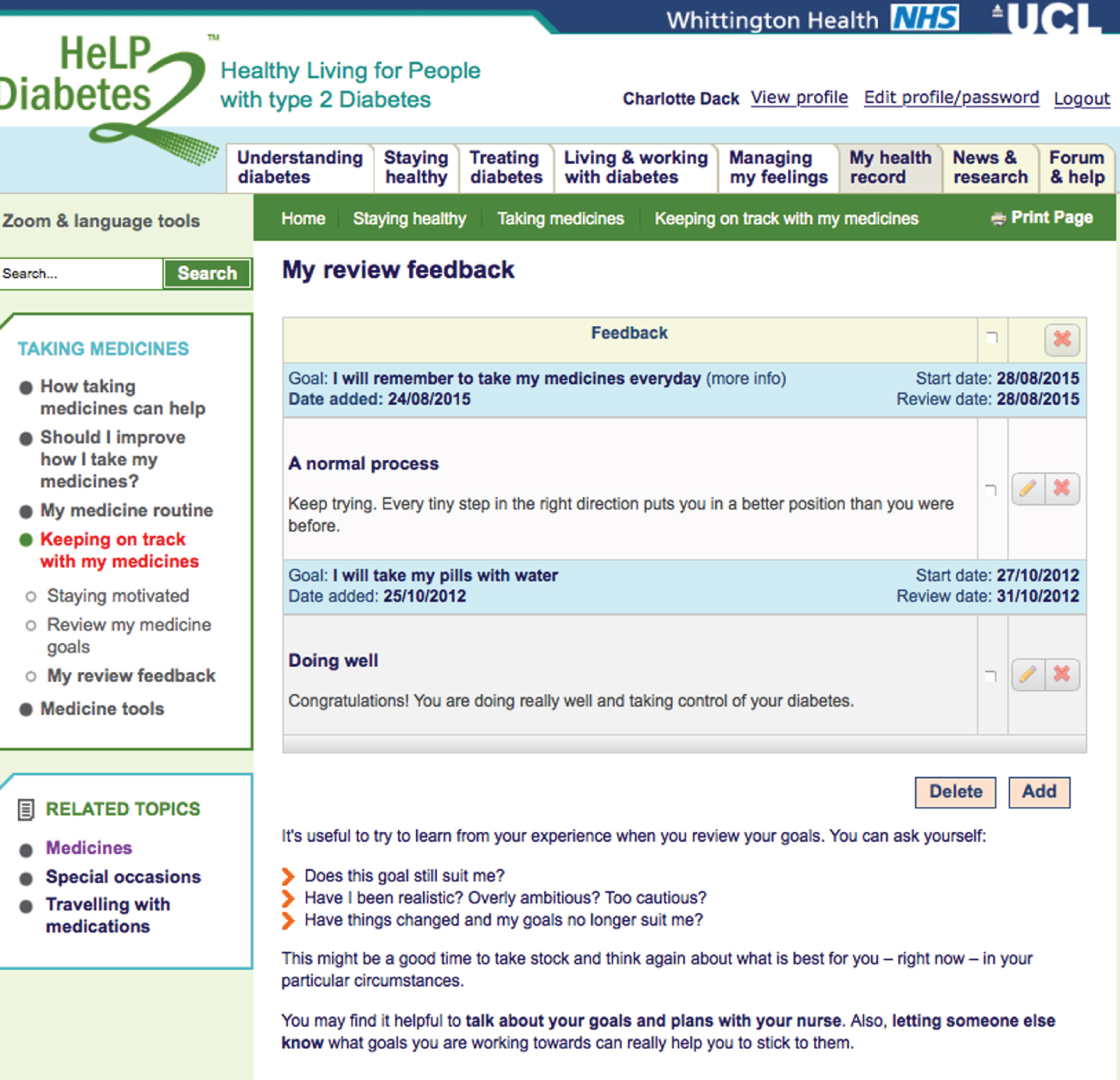
This section also provided users with information about how to work with their diabetes team (Figure 38).
FIGURE 38.
Staying healthy: information on how to interact with people involved in diabetes care.
Treating diabetes
This section provided users with information about how diabetes and its related complications are treated. This included detailed information about a wide range of medicines (including why and how to take it, possible side effects and iteractions with alcohol and information about indications) for blood pressure, cholesterol, glucose control, neuropathy, sexual problems and weight loss. An example for metformin is shown in Figure 39.
FIGURE 39.
Treating diabetes: an example of the information provided for diabetes-related medines using the example of metformin.
Information was provided about the importance of managing cardiovascular risk factors as well as glycaemic levels, on the types of monitoring and tests to expect (blood glucose, HbA1c level, blood pressure, cholesterol level, kidney fuction, weight) and on what the results mean (Figure 40). Information was also provided on potential surgical procedures (e.g. bariatric and vascular), complementary medicine and vaccinations and immunisations. In addition, information about the types and roles of different HCPs involved in caring for people with diabetes mellitus and what to expect from the yearly check up was provided (Figure 41).
FIGURE 40.
Treating diabetes: an example of the information provided on the type of test to expect and what the values of the results mean.
FIGURE 41.
Treating diabetes: an example of the information provided on HCPs and what to expect from the early check up.
Living and working with diabetes mellitus
The aim of this section was to focus on helping people with their role management including managing social situations, such eating in special circumstances (Figure 42), travelling and holidays and driving; managing work situations, such as shift work (Figure 43); and managing relationships, including sexual relationships (Figure 44) and and the possible impact diabetes mellitus can have on emotions and feelings of self-worth.
FIGURE 42.
Living and working with diabetes: information provision on how to manage eating at celebrations.
FIGURE 43.
Living and working with diabetes: information provision on how to manage changes at work.
FIGURE 44.
Living and working with diabetes: information provision on how to manage changes in sexual relationships.
Managing my feelings
The aim of this section was to support people to manage the emotions associated with having diabetes mellitus. Information was provided on how to cope with sadness and depression, fear and anxiety, anger and resentment, denial and guilt. There was also information on actions to take to increase feelings of confidence and happiness. In addition, there were mood tools that included self-assessment quizzes for identifying low mood (Figure 45), eight CBT audio modules with e-books, worksheets, and planner and review sheets (Figure 46) and mindfulness-based approaches.
FIGURE 45.
Managing my feelings: a self-assessment quiz to provide feedback about a user’s current mood.
FIGURE 46.
Managing my feelings: examples of the CBT audio courses and associated materials. Reproduced with permission from Five Areas Ltd. Copyright resources used under license www.fiveareas.com.
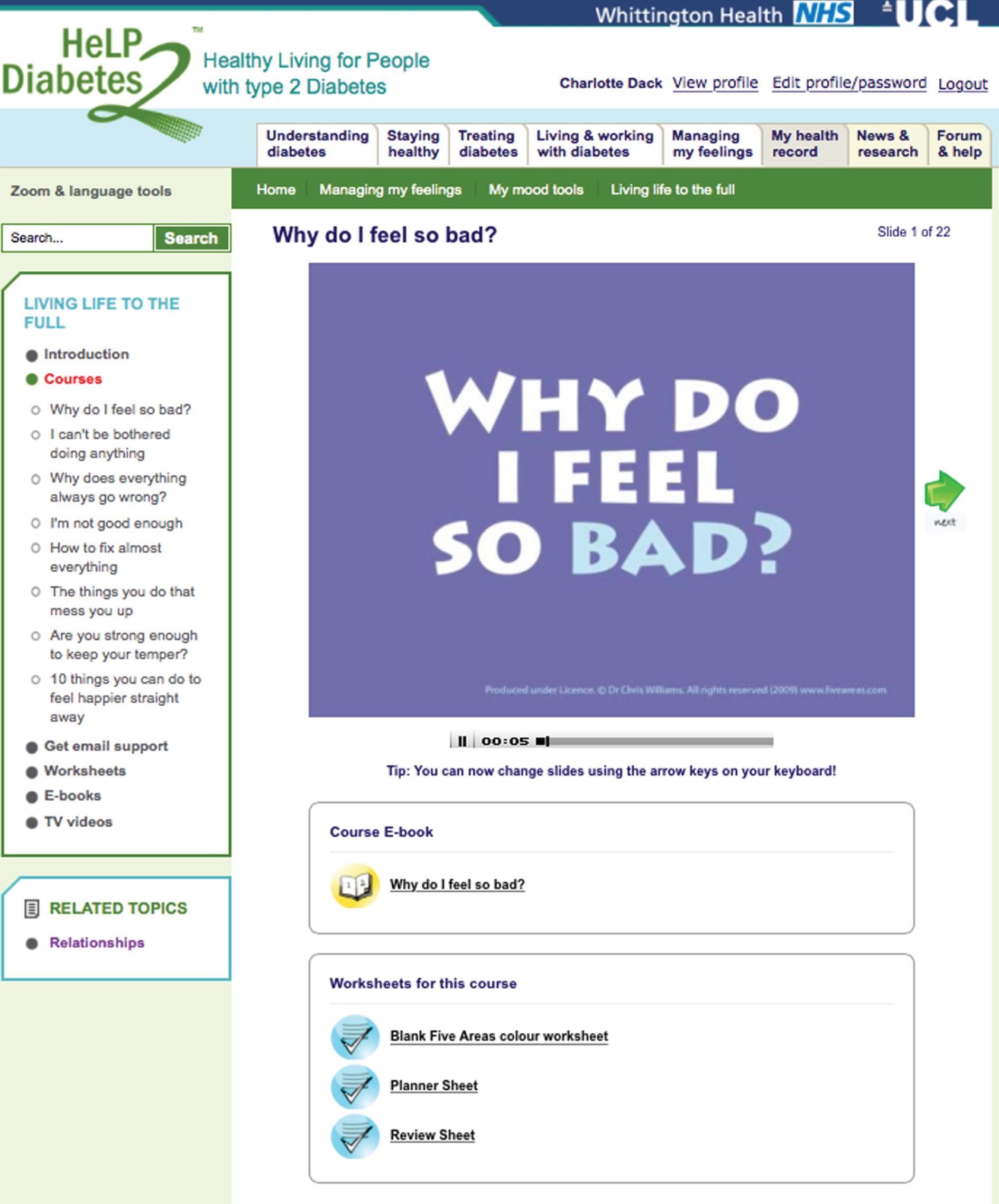
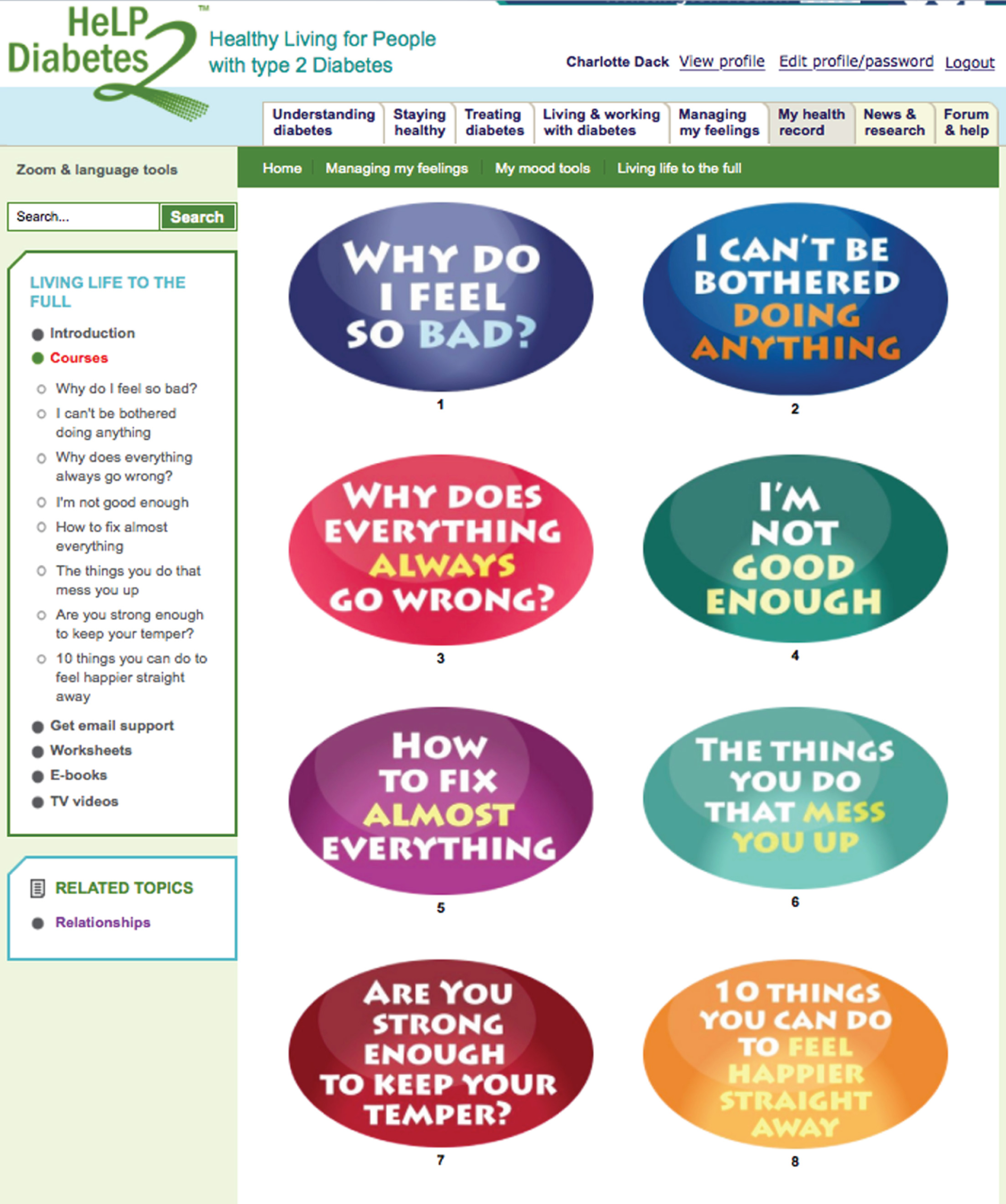
My health record
In this section, users had the opportunity to record and keep track of important appointments with HCPs (Figure 47) and the results of tests used to monitor diabetes (e.g. HbA1c level, blood pressure, cholesterol level, kidney and liver function), with opportunity for graphical displays and feedback (Figure 48).
FIGURE 47.
My health record: an example of the tools available to record appointments with HCPs.
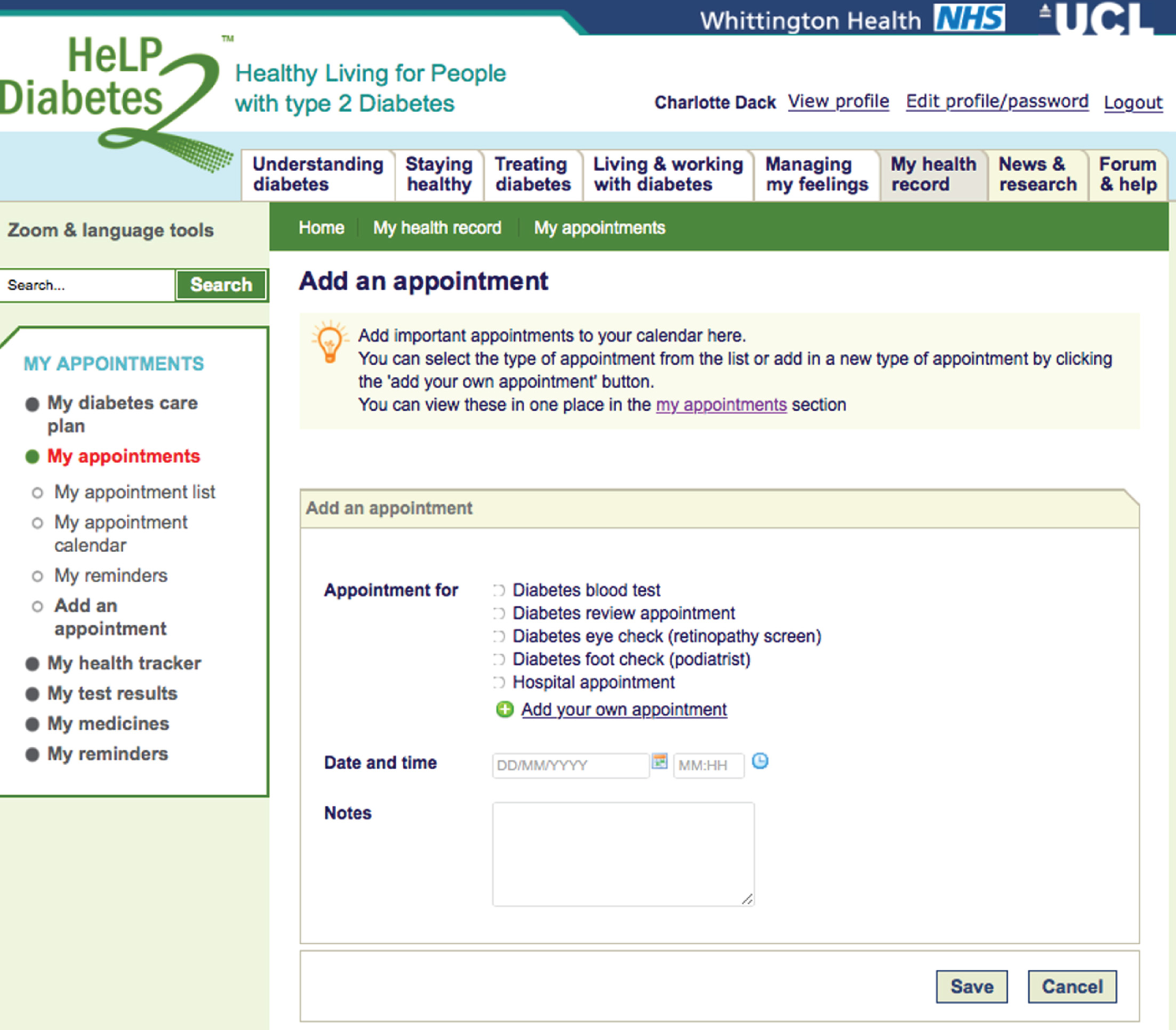
FIGURE 48.
My health record: an example of how users could add their diabetes mellitus test results. These could be displayed graphically with feedback about what the tests meant.
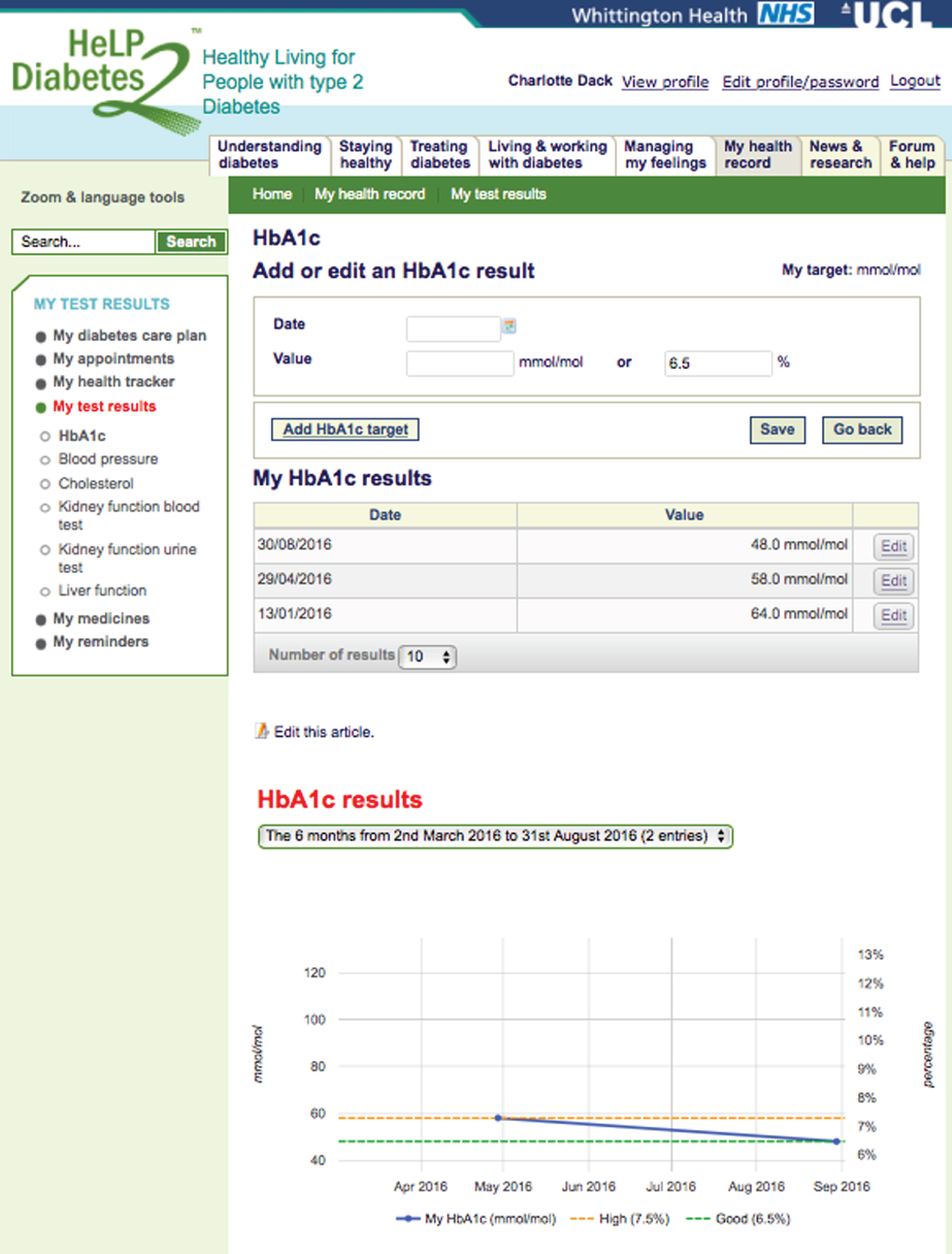
Users could track the results of their own self-monitoring for weight, waist circumference, calorie intake, alcohol consumption and physical activity and blood glucose levels (Figure 49) and keep a list of all their current medicines (Figure 50). Text or e-mail reminders could be added to prompt people about their appointments, to take their medicines or to remind them about any goals or plans set in the Staying Healthy section (Figure 51). All of this information could also be found or added in one place called My Diabetes Care Plan (Figure 52).
FIGURE 49.
My health record: users could add data that might be monitored at home, for example levels of physical activity.
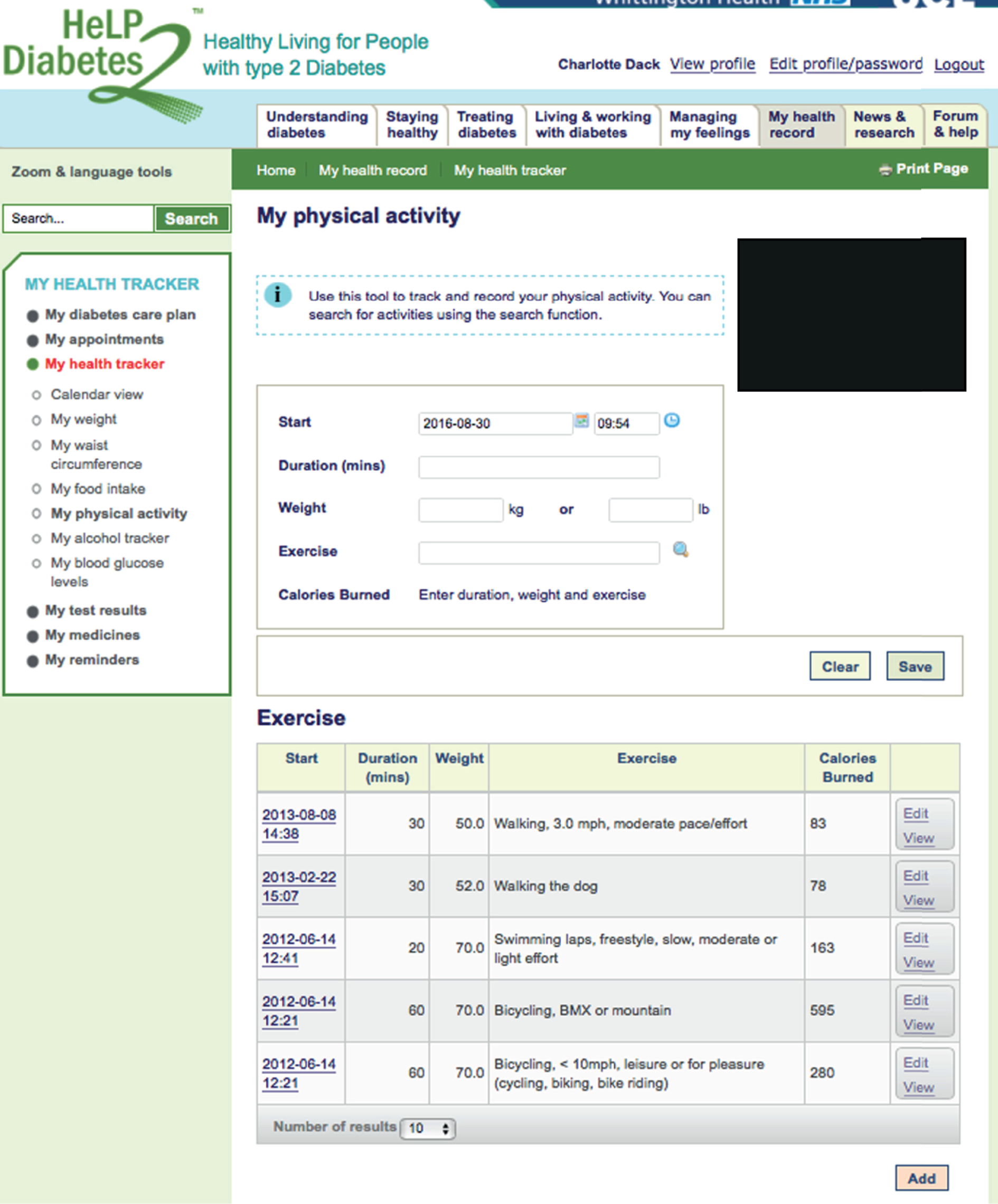
FIGURE 50.
My health record: users could record their current medicine list with an action plan of how to take each one.
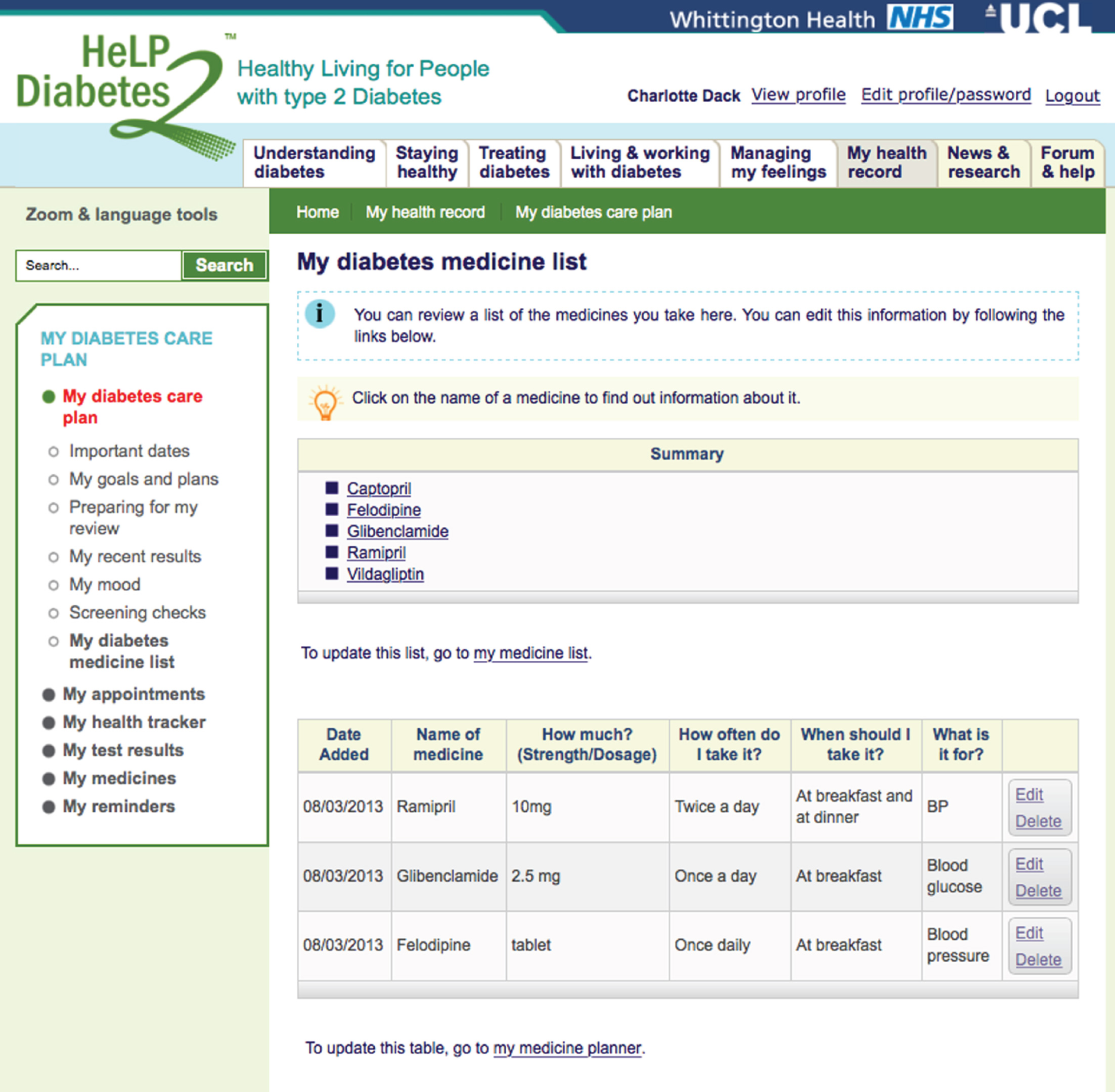
FIGURE 51.
My health record: e-mail or text reminders could be set to prompt users about appointments or to take their medicines, etc.
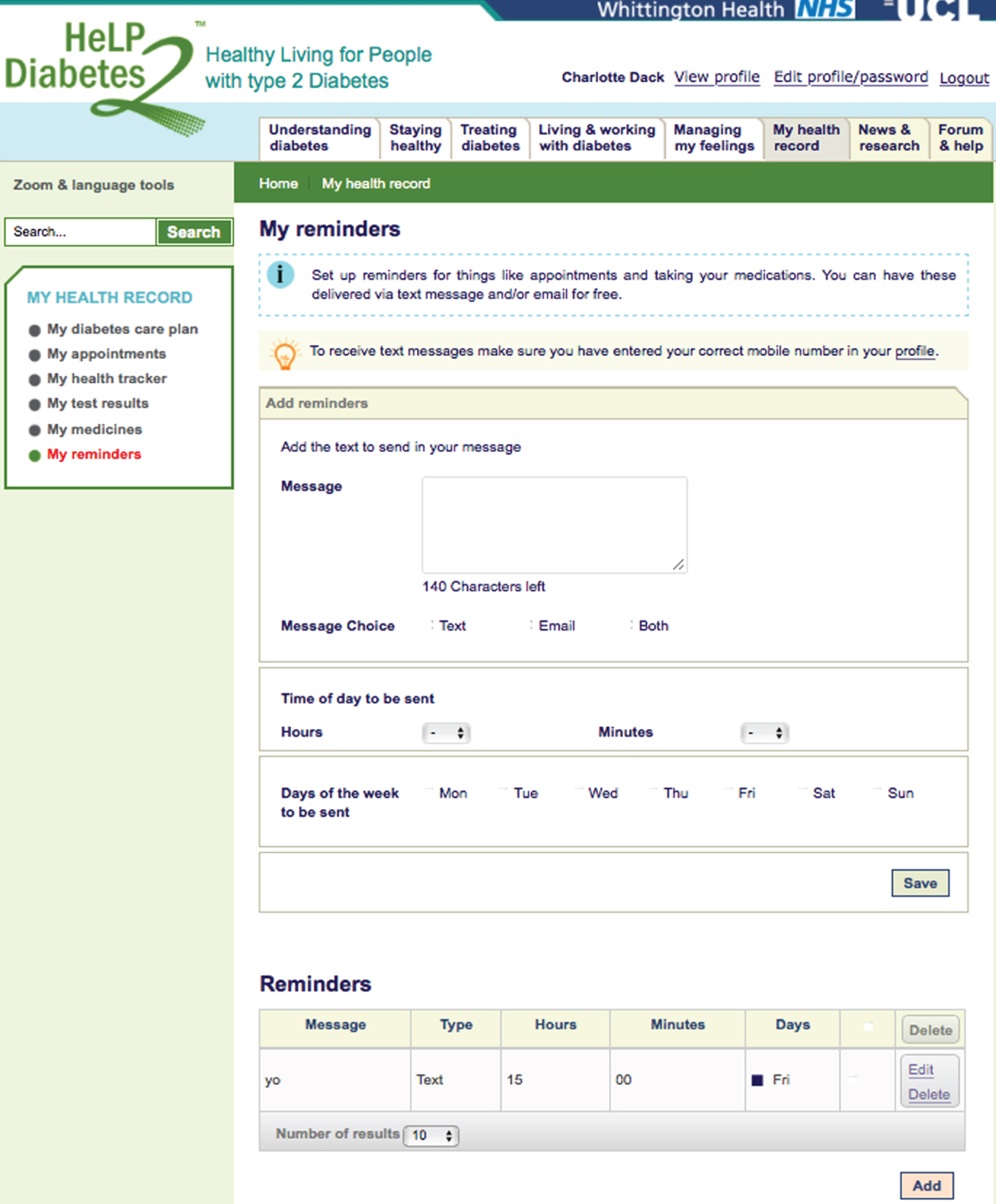
FIGURE 52.
My health record: any information about appointments, test results, medicines and goals and plans set were recorded in a diabetes care plan.
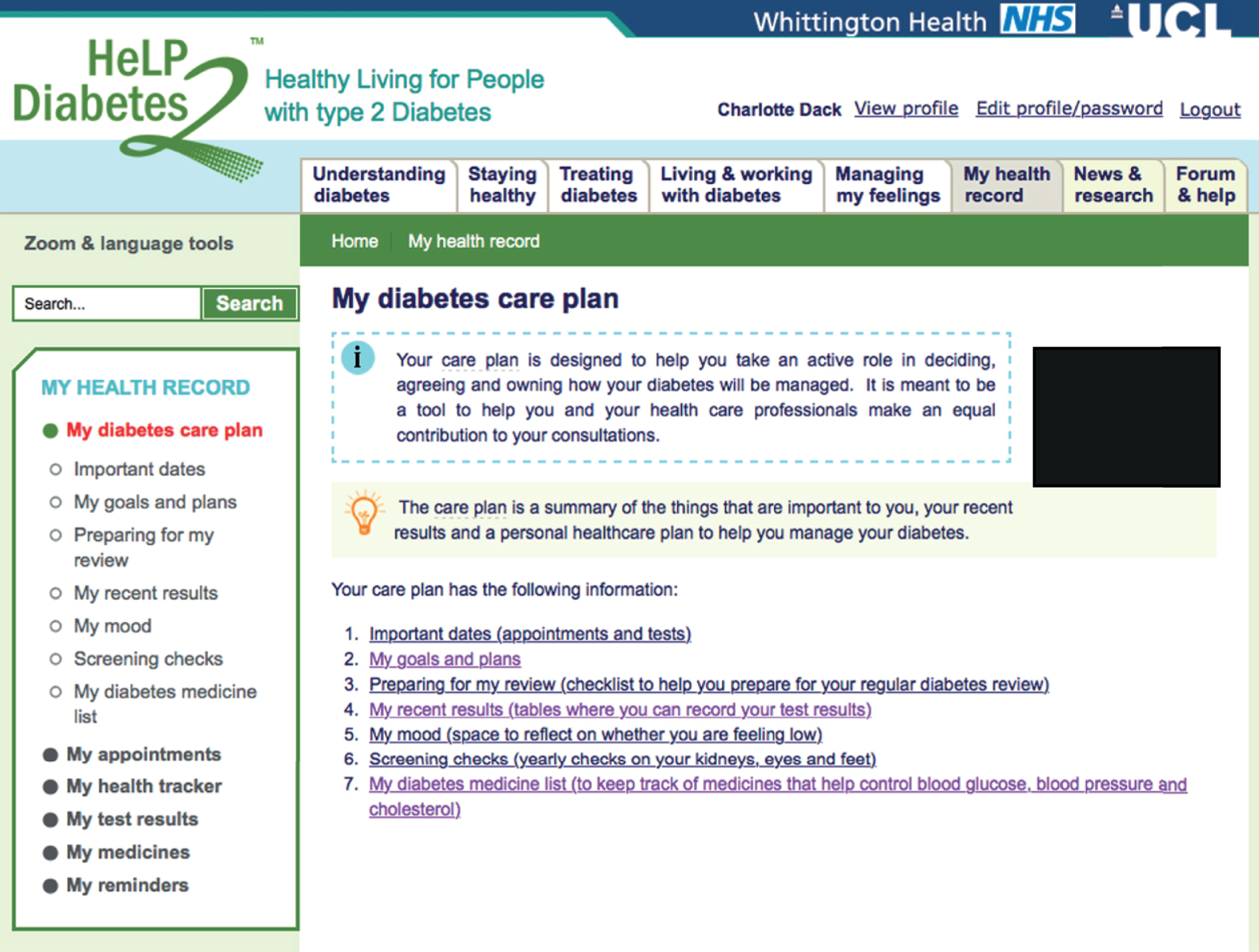
News and research
In this section, there was information about diabetes-related news articles that had appeared in the media (Figure 53), updates about the latest diabetes research (Figure 54) and information about concerns with specific medicines (Figure 55). In-depth information was also provided on articles about seminal research papers.
FIGURE 53.
News and research: an example of the information provided about diabetes-related news articles.
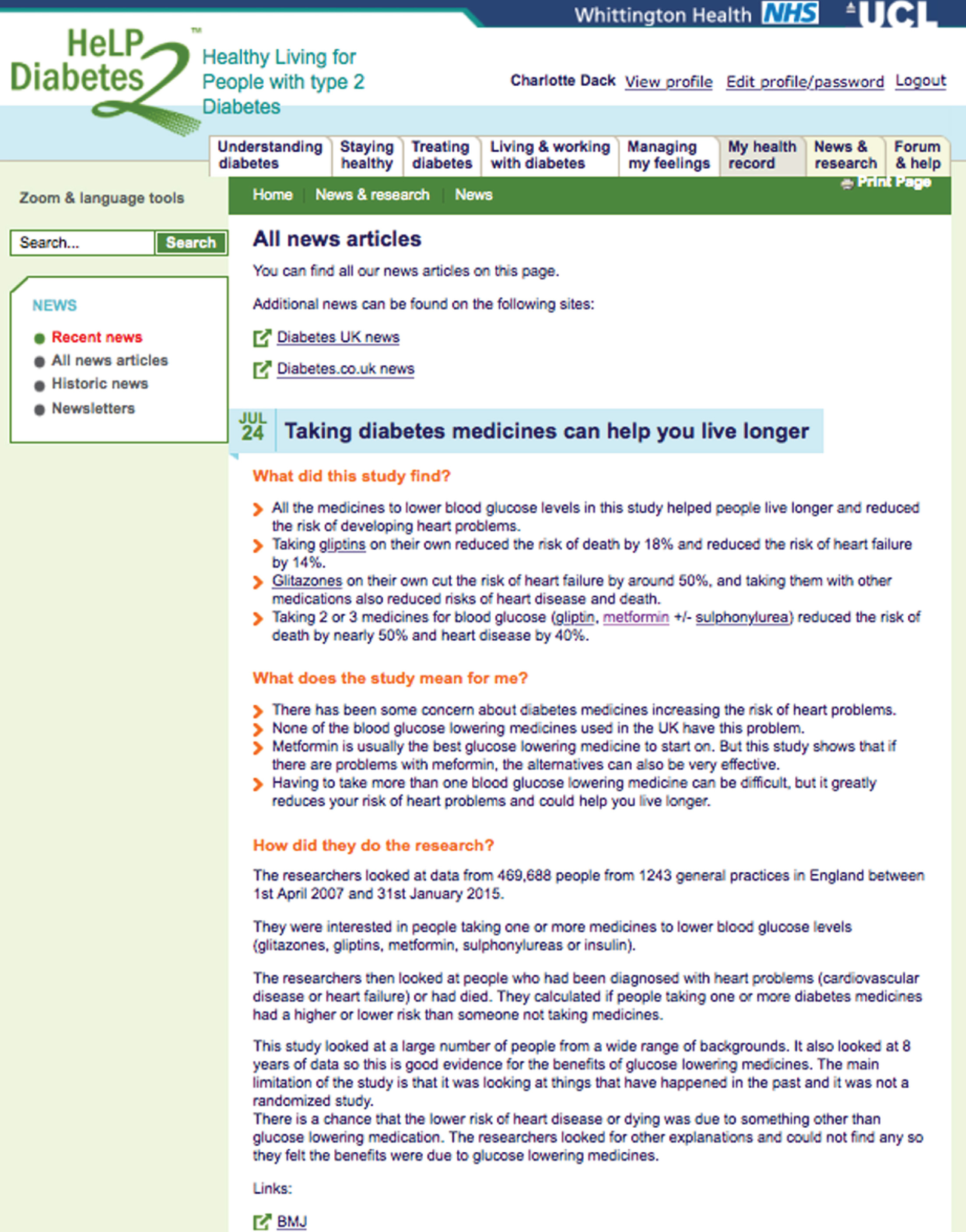
FIGURE 54.
News and research: information provided about diabetes-related research.
FIGURE 55.
News and research: information provided about concerns with diabetes-related medicines.
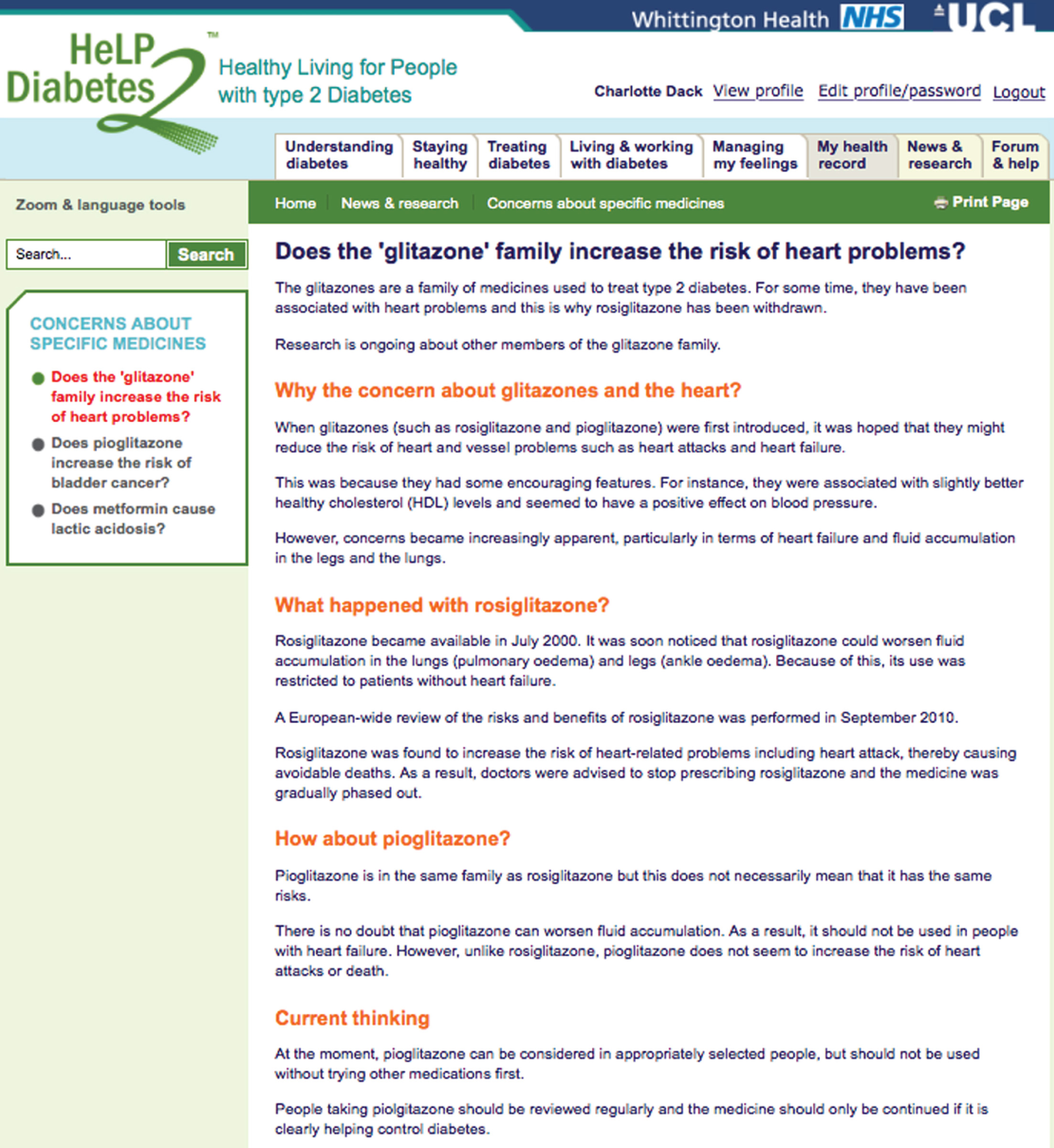
Forum and help
The content in this section was aimed at improving people’s emotional and role management. There was a moderated forum that included an ‘Ask the Expert’ section (Figure 56), videos of personal stories about diabetes mellitus (used with a licence from HTO – Figure 57), useful resources, with local resources tailored according to CCG (Figure 58) and a list of frequently asked questions (Figure 59).
FIGURE 56.
Forum and help: users could interact with other users and ask health professionals questions through a moderated forum.
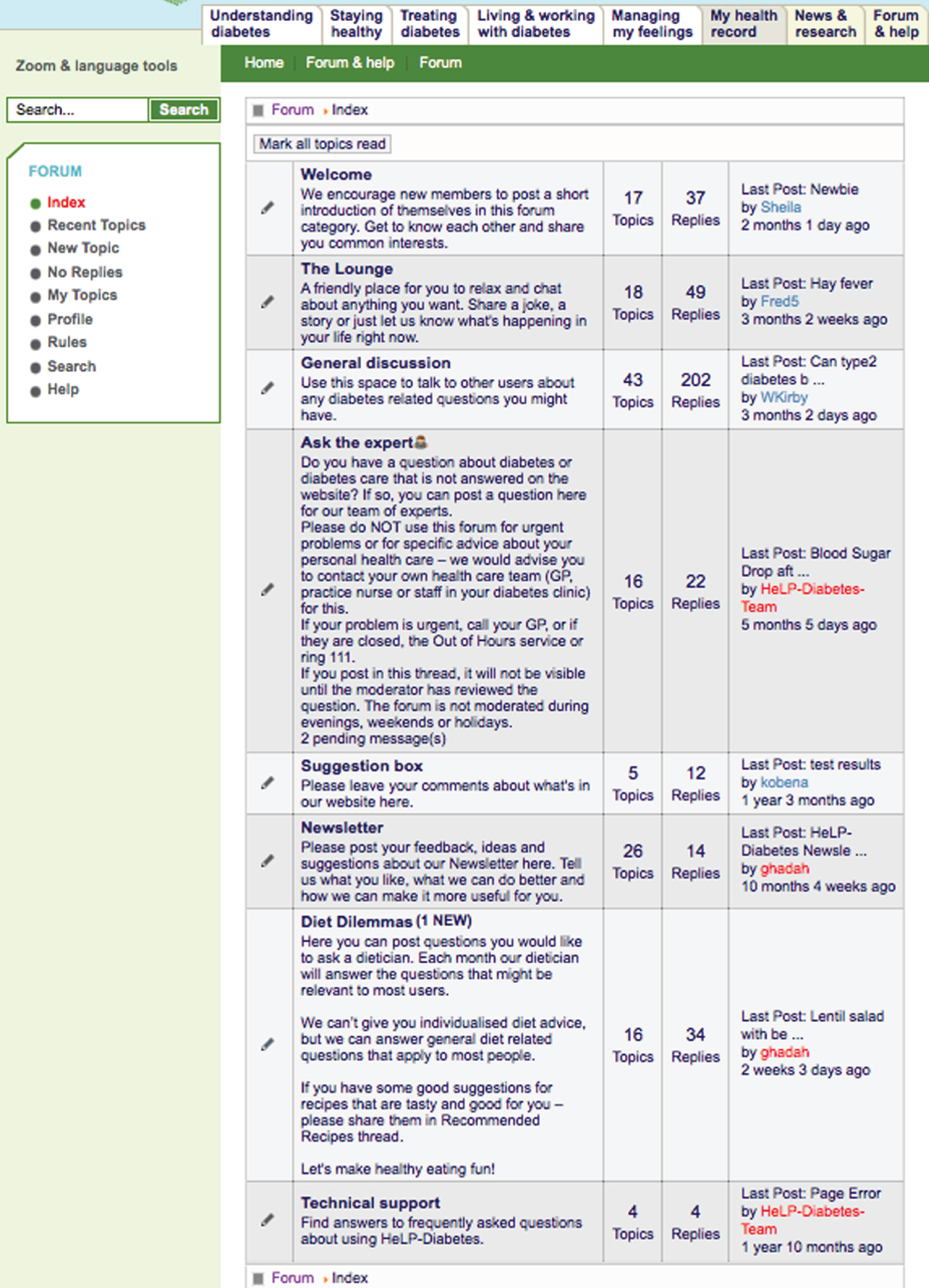
FIGURE 57.
Forum and help: videos, audios and transcripts of people with T2DM discussing their experiences on a range of topics, including the discovery of the diagnosis, controlling diabetes mellitus, possible complications and living and working with diabetes mellitus. Images from HTO used under licence from DIPEx. Copyright © 2012 University of Oxford. All rights reserved.

FIGURE 58.
Forum and help: useful resources (e.g. local groups and facilities such as free internet access) available in each CCG.
FIGURE 59.
Forum and help: users were given the answers to some frequently asked questions about diabetes and using the intervention.
Appendix 2 Site map for the Healthy Living for People with type 2 Diabetes programme
Appendix 3 Example of monthly newsletter sent to the Healthy Living for People with type 2 Diabetes programme users
Appendix 4 Example of fortnightly e-mails sent to the Healthy Living for People with type 2 Diabetes programme users
Appendix 5 Patient information leaflet for the Healthy Living for People with type 2 Diabetes programme
Appendix 6 Topic guides for patient and health-care professional interviews and focus groups
List of abbreviations
- A level
- Advanced level
- A&E
- accident and emergency unit
- BCT
- behaviour change technique
- BMI
- body mass index
- CACE
- complier-average causal effect
- CBT
- cognitive–behavioural therapy
- CCG
- clinical commissioning group
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CIC
- community interest company
- CMS
- content management system
- DBP
- diastolic blood pressure
- DESMOND
- Diabetes Education and Self-Management for Ongoing and Newly Diagnosed
- DIPEx
- Database of Patient Experiences
- DMSES
- Diabetes Management Self-Efficacy Scale
- DSME
- diabetes mellitus self-management education
- DTSQ
- Diabetes Satisfaction with Treatment Questionnaire
- EMR
- electronic medical record
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- GP
- general practitioner
- GPRF
- General Practice Research Framework
- HADS
- Hospital Anxiety and Depression Scale
- HbA1c
- glycated haemoglobin
- HCA
- health-care assistant
- HCI
- human–computer interaction
- HCP
- health-care professional
- HDL-C
- high-density lipoprotein cholesterol
- HeLP-Diabetes
- Healthy Living for People with type 2 Diabetes
- HRQoL
- health-related quality of life
- HTO
- HealthTalkOnline
- ICBT
- internet cognitive–behavioural therapy
- ICER
- incremental cost-effectiveness ratio
- IP
- intellectual property
- ISO
- International Organization for Standardization
- IT
- information technology
- LTC
- long-term condition
- MIG
- Medical Interoperability Gateway
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPT
- normalisation process theory
- PAERS
- Patient Access to Electronic Record Systems
- PAID
- Problem Areas in Diabetes
- PCRN
- Primary Care Research Network
- PCT
- primary care trust
- PhD
- Doctor of Philosophy
- POWeR
- Positive Online Weight Reduction
- PPI
- patient and public involvement
- QALY
- quality-adjusted life-year
- QISMET
- Quality Institute for Self-Management Education and Training
- QOF
- Quality and Outcomes Framework
- QUERI
- Quality Enhancement Research Initiative
- RA
- research associate
- RCT
- randomised controlled trial
- SBP
- systolic blood pressure
- SD
- standard deviation
- SOP
- standard operating procedure
- T2DM
- type 2 diabetes mellitus
- UCL
- University College London
- URL
- unique resource locator
- VA
- US Department of Veterans Affairs
- WP
- work package
- WTP
- willingness to pay
- WU
- website usage
- Y
- 12-month outcome
- Z
- randomised intervention
