Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 16/122/33. The contractual start date was in July 2018. The final report began editorial review in April 2021 and was accepted for publication in December 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Moffatt et al. This work was produced by Moffatt et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Moffatt et al.
Chapter 1 Introduction
Parts of this chapter have been reproduced with permission from Moffatt et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given and any changes made indicated. See: https://creativecommons.org/licenses/by-nc/4.0/.
Introduction
In this chapter, we provide an overview of the background and context of social prescribing in the UK, highlighting the rapidly shifting policy context that has occurred since this evaluation commenced in June 2018. Social prescribing is now firmly embedded within The NHS Long Term Plan2 as a central aspect of the personalisation agenda. Within Primary Care Networks (PCNs) across England, funding to introduce the role of social prescribing link workers into multidisciplinary teams has been available since July 2019. 2,3 In this chapter, we explore how social prescribing is defined and operationalised in the UK. We critically examine the quantitative and qualitative peer-reviewed literature that demonstrates that an evidence base of the effects of social prescribing is derived from a wide range of settings and ‘lags considerably behind practice’. 4 We outline the study design, aims, objectives, study population and intervention, and explain our rationale for the study’s focus on people with type 2 diabetes mellitus (T2DM). We conclude the chapter with a description of the intervention and our approach to patient and public involvement (PPI).
Background and context of social prescribing in the UK
Social prescribing grew from a recognition that patients with complex and long-standing problems require a formal ‘gateway to non-medical management’,5 with estimates that approximately one-fifth of GP consultation time is taken up with non-health matters. 6 Social prescribing-type interventions are not particularly new, especially in the field of mental health. 7 In 2006, the Department of Health and Social Care supported the introduction of social prescribing for people with long-term conditions (LTCs), and there has been increasing interest in social prescribing as a means to address complex health, psychological and social issues presenting in primary care. 8 Social prescribing is highlighted as one of the 10 high-impact actions to reduce workload and increase capacity in general practice9 and is regarded as an intervention with the potential to reduce health inequalities. 2,3
Historically, social prescribing schemes in the UK have been commissioned locally by Clinical Commissioning Groups (CCGs) or local authorities (LAs) and have been delivered by voluntary, community and social enterprise (VCSE) organisations. 10 More recently, however, social prescribing has become part of the NHS personalised care agenda,2 securing national funding through newly formed PCNs. These PCNs bring together neighbouring general practices to expand community multidisciplinary teams, typically covering 30,000–50,000 patients. 2 PCNs can claim reimbursement for the cost of a social prescribing link worker, whom they can employ either directly or via the VCSE organisation. It is projected that, by 2023–24, over 1000 link workers will be funded through PCNs, with 900,000 patients referred. 2 PCNs are being encouraged to work with existing schemes to develop a shared social prescribing plan and expand existing provision. 10 In many regions, local arrangements are still evolving, but uptake of this initiative has been rapid.
How is social prescribing defined and operationalised in the UK?
Despite this rapidly emerging policy context, there remains no agreed single definition of social prescribing within the UK or internationally; however, there is a broad consensus that social prescribing helps patients access non-clinical sources of support, predominantly in the VCSE sector, but also draws on resources supplied by health and local government services. To enable this, front-line health staff, primarily but not solely in primary care, refer patients to a link worker. Once the patient is connected to a link worker, which pre COVID-19 was predominantly face to face, a conversation takes place to identify problems and goals, thereby ‘co-producing a social prescription’ designed to find solutions that will lead to improved health and well-being. 11
Currently within UK practice there is no single model of social prescribing. Rather, social prescribing models cover a spectrum12 that varies according to whether programmes focus on individuals, communities or a combination of both; the level of support offered to patients following referral; and the actual activities offered. Usefully, Husk et al. 4 identified multiple pathways from primary care to activities undertaken and reported that current policy supports link worker-based models. Recognising that patients who are simply given information about a service will not necessarily take it up,13 in most schemes the link worker acts as a ‘facilitator’ and offers personal support, although the level of ongoing support varies considerably. Services into which patients are referred vary and can include clubs offering physical activities, such as gyms, walking groups, gardening clubs and dance clubs, and those offering weight management and healthy eating activities, such as cooking clubs. Addressing wider economic and social issues can involve referral into services that address welfare, debt, housing and employment issues. Support and self-help groups, such as those targeted at people with specific LTCs, for example chronic obstructive pulmonary disease (COPD) or diabetes, may also be accessed via social prescription. 1
The link worker role is central to social prescribing as currently practised in the UK1,14,15 and elsewhere. 16,17 A 2019 survey of UK CCGs reported 75 different terms for this ‘connector’ role,18 and a recent scoping review identified 18 separate terms that described this position. 19 The link worker role is recognised to be ‘complex and demanding’15 and requires a wide range of skills. 20 Executing the link worker role requires time, interpersonal skills and strong community networks and relies on the existence of onward referral services. 15 There is no clear professional pathway into the link worker role, and link workers come from a range of backgrounds, including the social work, teaching, health-care and VCSE sectors,21 which is likely to affect how they perceive and carry out their role. Previous life and work experience are regarded as important;20 link workers employed via the NHS are required to have a National Vocational Qualification (NVQ) at level 3 or above. 13 The relatively limited peer-reviewed literature on the role indicates that link workers can feel inadequately trained to deal with highly vulnerable clients with complex issues that involve time-consuming case management; therefore, link workers can lack capacity to meet the needs of large numbers of referrals and can also face problems related to service cuts or unacceptably long waiting lists for onward referrals. 20,22 There is now a professional membership network for UK link workers23 and, although link working is recognised as a rewarding role,21 lack of clinical supervision and support is commonly reported among link workers based in primary care and is cited as a reason for leaving. 24
Introducing new services into primary care, irrespective of how appropriate they may be, is not straightforward and requires belief in the benefits and ‘buy-in’ from those expected to refer to the service. 14,25,26 Moreover, referrals to PCN link workers can come from hospitals, allied health workers, the police, the fire service, job centres, social services and the VCSE sector, among others. 13 The role of the general practitioner (GP) and other members of the primary care team in relation to social prescribing is not well understood,27 given that overall a relatively small number of GPs have been included in studies about social prescribing26–30 and even fewer studies include other members of the primary care team. 31,32 Enabling linkage between primary care and social prescribing relies on procedures that facilitate appropriate referrals of patients who meet the social prescribing service criteria. This requires co-operation and trust between members of the primary care team and the social prescribing service(s). 32 A recent qualitative study of the barriers to, and facilitators of, social prescribing for patients with mental health problems based on the views of 17 GPs found that most GPs in the study were supportive of social prescribing and reported that it enabled their patients to be better connected to their local VCSE organisations. 27 Link workers were seen to have more time with clients than the GP and, therefore, were able to act as a bridge between the GP and the community. This contrasts with previous findings from interviews with GPs (n = 3) and district nurses (n = 8) in the west of Scotland, who saw their focus as predominantly clinical and expressed concerns about being held accountable for the actions of unknown or unverified organisations that their patients were linked into. 32 In an interesting overlap between the views of GPs,27 link workers33 and the wider VSCE sector,22 capacity, resources and precarity of the VCSE organisation in the context of austerity were seen as significant challenges to social prescribing. 25
Social prescribing has been the topic of a number of editorials in the medical press, with some arguing the case strongly for social prescribing34 and others being more circumspect. 35,36 Concern has also been raised that the use of the term ‘prescribing’ further medicalises problems that require non-medical support. 37,38 Most apparent is unease about the current level of evidence for the effectiveness of social prescribing on health and well-being outcomes and resource use. 35–37,39 It would appear that there is a strong sense of the potential for social prescribing to improve patient well-being and an awareness that conducting robust research on social prescribing is challenging,40 but that obtaining this evidence is necessary for health professionals to more fully engage with social prescribing. 39
What is the evidence for the effectiveness of link worker social prescribing in UK health-care settings?
Quantitative evaluations of the impact of social prescribing
Bickerdike et al. ’s41 systematic review of 15 social prescribing evaluations, published in 2017, included evaluations published between 2000 and January 2016 in which the primary outcome of interest was any measure of health and well-being and/or usage of health services. The authors concluded that there was:
. . . little convincing evidence for either effectiveness or value for money . . . most evaluations are small scale and limited by poor design and reporting . . . common design weaknesses include a lack of comparators, loss to follow-up, short follow-up durations and lack of standardised and validated measuring tools . . . a distinct failure to consider and/or adjust for potential confounding factors, undermining the ability to attribute any reported positive outcomes to the intervention (or indeed interventions) received.
A subsequent evidence synthesis by Public Health England,42 which included eight studies, examined the effectiveness of social prescribing on (1) contact with primary health care and (2) changes in physical and/or mental health. It concluded that there was no clear evidence for effectiveness.
Although the number of peer-reviewed publications on social prescribing has increased considerably since 2017,19 the number of UK peer-reviewed studies using quantitative health-related outcome measures is still relatively small. Focusing on the UK, between the end of Bickerdike et al. ’s41 review period in 2016 and December 2020, we used similar search terms (see Report Supplementary Material 1). We identified 10 peer-reviewed studies that had quantitative outcome measures (five quantitative and five mixed methods) and evaluated the impact of nine UK social prescribing initiatives on clients’ health, well-being or resource use. Our focus was on peer-reviewed studies; however, we did not include a ‘museums on prescription’ intervention43 because this did not involve a link worker-type facilitator and, because of our focus on social prescribing in primary care, we also excluded a social prescribing initiative in secondary care mental health services. 7 The shared characteristic of the social prescribing interventions evaluated (see Appendix 1, Table 36) is that they link primary care and local assets and services via a link worker, connector or facilitator. Thereafter, the similarities end and each study evaluated a different model of social prescribing, funded via different sources and delivered by a different type of ‘facilitator’, including paid staff and a combination of paid staff and volunteers. 44,45 The interventions varied considerably in ‘intensity’, for example six sessions,46 12-week programmes5,45,47,48 or no limits on time with a community links practitioner (CLP). 49 The intervention target populations varied: they were predominantly aimed at adults aged ≥ 18 years, although one intervention was aimed at those aged ≥ 14 years. 46 Most interventions were targeted at people in mid to later life living in areas of high socioeconomic deprivation and experiencing LTCs, multimorbidity, mental health problems, loneliness and social isolation; these people typically have frequent attendance in primary care and polypharmacy.
The specific aims of the evaluated interventions varied. They include supporting people with complex needs and living in deprived inner-city localities;49,50 improving patient well-being, increasing personal self-efficacy, reducing primary care use/health and social care use, addressing polypharmacy;5,44,48 reducing social isolation/loneliness;45,46,51 improving mental health;48,52 and increasing physical activity. 47 A range of study designs and outcome measures were used. Most studies used a before-and-after design. 5,45–48,50–52 Two studies included matched comparison groups: a before-and-after postal questionnaire study design44 and a quasi-experimental cluster-randomised controlled trial (RCT) design. 49 The latter study49 is the most methodologically robust study to date.
Outcome measures included depression and anxiety,44,50 energy expenditure,47 physical activity,49 general/subjective well-being,44,46,48,50,52 loneliness,45 social support,51 social networks46 and health-related quality of life (HRQoL) [as measured using the EuroQol-5 Dimensions, five-level version (EQ-5D-5L)]. 46,49,51 However, in some studies it was not clear what the primary outcome was. Three studies examined changes in primary health-care resource use:5,44,48 one examined self-reported GP usage,46 two studies examined accident and emergency (A&E) use44,48 and one study examined change in repeat medication. 5
The two studies with control groups44,49 found no statistically significant differences in patient-reported outcomes between baseline and 8 months44 or in health-related quality of life (as measured using the EQ-5D-5L) between baseline and 9 months. 49 However, in the latter study,49 some improvements were found in those patients who engaged with the programme as opposed to those simply being referred. 49,53 Outcomes for the uncontrolled studies showed a varying picture, with high rates of attrition and relatively small sample sizes at follow-up being common. In one study,48 statistically significant improvements in measures of health, well-being, patient activation and frailty were identified at the 12-month follow-up (n = 86, constituting 57% of the sample). 48 In another study,52 a statistically significant improvement in subjective well-being was reported from baseline to post intervention. However, this study suffered from high rates of attrition, with 87.8% of patients either lost to follow-up or not engaging with the intervention. 52 Statistically significant improvements in subjective well-being, social networks and EuroQol-5 Dimensions (EQ-5D) overall health rating were reported in another study. 46 However, the number of clients in this study completing the baseline and post-intervention assessments (n = 265) was considerably smaller than the 2250–3750 users reported as being in contact with the service. Furthermore, these results included only individuals who had engaged with the full six sessions. In a national study in which the primary outcome was loneliness,45 over 70% of clients (n = 1634) reported reduced loneliness (p < 0.0001) immediately post intervention; however, 3-month follow-up data from a subsample of users (n = 101) showed that 60% were experiencing increased loneliness. 45 With regard to primary care use and polypharmacy,5 prescribed medication44 and self-reported health-care utilisation,46,49 no differences were found in these measures from baseline to post intervention. However, a statistically significant decrease in the median number of GP consultations was identified,44 although the authors did not rule out regression to the mean. Overall, this body of peer-reviewed research did not robustly demonstrate beneficial effects on quantifiable health outcome measures or health-care resource use, reinforcing Bickerdike et al. ’s41 systematic review conclusions. However, the challenges in identifying which outcomes to measure and in which ways should not be underestimated. 39
Qualitative evaluations of the impact of social prescribing
Qualitative research with patients who accept their referral and engage with services generally indicates positive evaluations of social prescribing services. 1,53,54 In three of the previously mentioned studies with quantitative components,5,44,49 linked qualitative data about the perceived impact of social prescribing by clients indicated positive narratives that were not reflected in the quantitative data. Of these linked studies, the most detailed qualitative analysis identified considerable variation in the perceived impact of the Glasgow ‘Deep-End’ Link Worker Programme, ranging from no change to moderate/major improvement. 53 Twelve adults aged 34–67 years with a combination of social, psychological and physical problems were interviewed. Some saw the CLP as a catalyst for behaviours and activities that improved their well-being. In contrast, others reported that the CLP had provided practical support, which improved psychological well-being but had no effect on health-related behaviours, or that the intervention resulted in no benefits. 53 Feeling understood and developing a supportive relationship with the CLP were identified as important, but not on their own sufficient to facilitate improvements. A further requirement for improvement was the development of ‘wider social relationships and developing competence to engage in the wider community’. 53
A qualitative study of 30 patients aged 40–74 years with LTCs who engaged with a social prescribing intervention identified that most patients experienced multimorbidity combined with mental health problems, low self-confidence and social isolation, and all were adversely affected by their health problems. 1 The social prescribing intervention, with which it was possible to be engaged for up to 3.5 years, engendered feelings of control, self-confidence and reduced social isolation; had a positive effect on health-related behaviours and LTC management; and improved mental health. 1 A qualitative follow-up study54 of 24 individuals, who had been with the social prescribing intervention for between 12 and 24 months, found that participants reported improvements in condition management and health-related behaviours and reduced social isolation. However, setbacks related to multimorbidity, family circumstances and social, economic or cultural factors were also identified, which highlighted the importance of long-term support and link worker continuity. 54 As has been reported elsewhere,25,53,55,56 the availability of a supportive and easily accessible link worker able to deliver a personalised service that reflect individual goal-setting priorities, enable gradual change and deal with issues beyond health was both positively appraised and seen as important to maintaining positive changes. Hanlon et al. 53 and Wildman et al. 54 emphasise the importance of an approach that addresses both individual behavioural change and wider structural barriers in the context of socioeconomic deprivation. Furthermore, as has already been highlighted by GPs and organisations, the availability of suitable onward referral services is an important consideration for social prescribing at a time of severely constrained public spending. 54,55
Qualitative research that has explored challenges in delivering social prescribing services55 and the uptake of and adherence to social prescribing56 further highlights the importance of the link worker–client relationship, the complexity of the link worker role, patient expectations, the availability and cost of onward referral services, fear of stigma about psychosocial problems, short-term programmes and the need for strong community infrastructure. Husk et al. ’s4 recent realist review indicates that patients are more likely to accept a social prescribing referral if the intervention matches their needs and expectations and is presented to them in an acceptable way; patients are more likely to engage if they are supported to connect with accessible activities; and patients are more likely to adhere to the intervention because of skilled facilitators or condition/symptom change.
Quantitative and qualitative research highlights the complex phenomenon that is social prescribing, which is described as a ‘pathway and series of relationships’4 and not a single intervention, making it challenging to evaluate. As yet, it is not possible to make inferences about the efficacy of any particular model over another. 4 Current research into social prescribing indicates the need for longer-term outcome evaluation using robust routine data and mixed-methods design. If quantifiable effects of social prescribing are identified, the important questions are why, how and for whom these effects are seen. If there are no quantifiable effects, questions remain about why this is the case. The literature also highlights many gaps in our understanding of social prescribing, including the link worker role, service user experiences, the role of VCSE, integration into primary care, impacts on secondary services use, cost implications and cost-effectiveness.
Study design, aims and objectives
The study aimed to evaluate the impact and costs of a community-based link worker social prescribing intervention on the health and health-care utilisation of adults aged 40–74 years with T2DM to observe how link workers delivered the intervention and how patients engaged with social prescribing. A further study was undertaken in response to the COVID-19 pandemic that aimed to capture the experiences of patients with LTCs in receipt of social prescribing during and immediately after the first lockdown period.
This multimethods evaluation comprised three work packages (WPs).
Work package 1
Work package 1 (WP1) had the following objectives:
-
to measure the short-term (i.e. 1-year) and long-term (i.e. 2- and 3-year) effects of the social prescribing intervention targeting adults with T2DM on levels of glycated haemoglobin (HbA1c; primary outcome), body mass index (BMI), blood pressure (BP), cholesterol levels, smoking status and health-care utilisation
-
to provide a range of estimated intervention effects based on comparing the intervention group with a number of relevant control groups
-
to examine differential intervention effects in subgroups by gender, age, ethnicity, multimorbidity and deprivation level
-
to measure HRQoL as change in EQ-5D-5L score at the 12-month follow-up in the social prescribing intervention clients.
Work package 2
Work package 2 (WP2) had the following objective:
-
To measure the cost-effectiveness of the social prescribing intervention for health-care utilisation and each of the outcomes. From the perspective of a health service provider, costs and benefits will be compared for individuals in the intervention group and a cohort of individuals who did not receive the intervention. The robustness of the results will be investigated using sensitivity analysis.
Work package 3
Work package 3 (WP3) had the following objectives:
-
to use ethnographic methods to examine –
-
link workers’ experiences of delivering social prescribing
-
patients’ engagement with the social prescribing intervention and whether or not and how social prescribing leads to changes in patients’ lives
-
-
to examine the impact of COVID-19 on people with LTCs and the role of social prescribing during the pandemic.
Study setting
The study setting comprised 10 electoral wards in the inner and outer west of Newcastle upon Tyne in the north-east of East England (with a total population of 100,050; Table 1). Five wards are in the most deprived quintile, four wards are in the fourth-most deprived quintile and one ward is in the third most deprived quintile of the Index of Multiple Deprivation (IMD). 57 All but two of the wards have higher than the English average levels of LTCs or disability that limit day-to-day activities. Seven wards have higher than the English average levels of long-term unemployment and six wards have higher than the English average levels of social renting, a further indication of low income. Just under one-third of the inner-city wards’ population are from black and minority ethnic communities. By contrast, all but one of the outer-city wards are predominantly of white ethnicity.
| 2011 ward | Total population (n) | Gender (%)a | Ethnicity (non-white) (%)a | Day-to-day activities limited by LTC/disability, patients aged 16–64 years (%)a | Social rented households (%)b | Long-term unemployed (%)c | IMD scored | IMD quintiled | |
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | ||||||||
| Benwell and Scotswoode | 12,694 | 48.5 | 51.5 | 9.1 | 48.7 | 40.4 | 3.2 | 43.3 | 5 |
| Blakelaw | 11,507 | 47.7 | 52.3 | 16.0 | 48.1 | 33.6 | 2.3 | 35.8 | 5 |
| Denton | 10,500 | 47.4 | 52.6 | 2.5 | 50.9 | 30.6 | 2.1 | 31.7 | 5 |
| Elswicke | 13,198 | 53.2 | 46.8 | 46.9 | 47.6 | 46.8 | 3.5 | 50.7 | 5 |
| Fenhame | 10,954 | 47.7 | 52.3 | 15.2 | 44.6 | 28.9 | 1.9 | 28.8 | 4 |
| Lemington | 10,228 | 48.2 | 51.8 | 2.3 | 45.2 | 22.1 | 1.9 | 30.4 | 4 |
| Newburn | 9536 | 48.5 | 51.5 | 2.1 | 47.8 | 31.5 | 2.1 | 28.5 | 4 |
| Westerhope | 9196 | 47.9 | 52.1 | 2.3 | 48.5 | 10.2 | 1.0 | 14.8 | 3 |
| Westgatee | 10,059 | 56.0 | 44.0 | 34.9 | 27.3 | 46.1 | 2.5 | 41.1 | 5 |
| Wingrovee | 13,685 | 54.2 | 45.8 | 50.2 | 33.6 | 32.1 | 1.7 | 28.9 | 4 |
| Total (WtW area) | 111,557 | 50 | 50 | 19.8 | 46.8 | 32.9 | 2.3 | – | – |
| England | 53,012,456 | 49.2 | 50.8 | 14.6 | 43.5 | 17.7 | 1.7 | – | – |
Study population
Owing to the large number of people in the social prescribing intervention with a T2DM diagnosis (41%),59 we focused the evaluation on this subsample. The primary outcome was the change in the level of HbA1c, which is a well-recorded objective clinical outcome measure. The study population was identified and selected by North of England Commissioning Support Unit (NECS) and comprised community-dwelling adults aged 40–74 years who had T2DM with or without comorbidity- or disease-related complications or a diagnosis of depression or anxiety.
Diabetes is a major public health issue; some 7% of the UK population live with diabetes, and approximately 1 million people have undiagnosed T2DM. 60 If no changes are made to the way that T2DM is managed and treated, the costs to the NHS are estimated to increase to £17B by 2035, with the associated increases in the wider costs to society estimated to be over £22B. 61,62 Economic analyses show that NHS costs stem mostly from treating diabetes-related complications that are exacerbated by poorly controlled levels of blood glucose. For many people with T2DM, there is scope for improved condition management, resulting in fewer diabetes-related complications and increased cost savings. 63 People with T2DM may have one or more other LTCs64 and T2DM is often associated with mental health conditions, such as anxiety and/or depression, which can negatively affect an individual’s ability to manage their condition. 65 T2DM is socially patterned; the poorest people are 2.5 times more likely to have T2DM66,67 and, once diagnosed, are at increased risk of complications. 68 Although T2DM diagnosis is a criterion for study entry, this does not preclude the co-existence of other physical and mental health conditions. T2DM is also one of the comorbidity risk factors associated with worse COVID-19 outcomes. 69
Intervention
The intervention, detailed in Table 2, is a community-based link worker social prescribing intervention for people aged 40–74 years who have at least one of eight LTCs. 70
| Name | WtW |
|---|---|
| Purpose | WtW social prescribing was based on extensive pilot work and, over an 8-year period (from 2007 to 2015), was co-produced with people with LTCs.72 WtW is a service for people aged 40–74 years in the west of Newcastle upon Tyne who have at least one of eight LTCs (i.e. diabetes type 1 or 2, chronic obstructive pulmonary disease, asthma, coronary heart disease, heart failure, epilepsy or osteoporosis, with or without anxiety and/or depression). The intervention aims to improve health-related outcomes and the quality of life of people with LTCs by increasing their confidence and ability to manage their illness, and to reduce costs and/or improve value to the NHS in their treatment. The intervention has four key objectives:
|
| Resources | Link workers were attached to clusters of primary care practices and employed by not-for-profit organisations. Link workers had experience of working with individuals and were expected to have had experience and knowledge of the community. Provider organisations were contracted by WtW Management Limited (Newcastle upon Tyne, UK), which was funded for 7 years from April 2015 via the Cabinet Office Social Outcomes Fund, Newcastle West Clinical Commissioning Group (now part of Newcastle Gateshead Clinical Commissioning Group), Big Lottery Fund Commissioning Better Outcomes and Social Outcomes Fund and a SIB.73 WtW Limited is a special-purpose vehicle, the role of which is to contract service providers, receive investments and make outcomes payments. Link worker line management was provided by the aforementioned not-for-profit provider organisations with experience in delivery of community programmes, health-care interventions and staff management. Link worker training and development needs were met by both WtW Management Limited (Newcastle upon Tyne, UK) and provider organisations. A bespoke management information system was used by link workers and WtW Management Limited to manage referrals, store and retrieve information relating to patient journeys, and monitor referral and progress targets |
| Procedures |
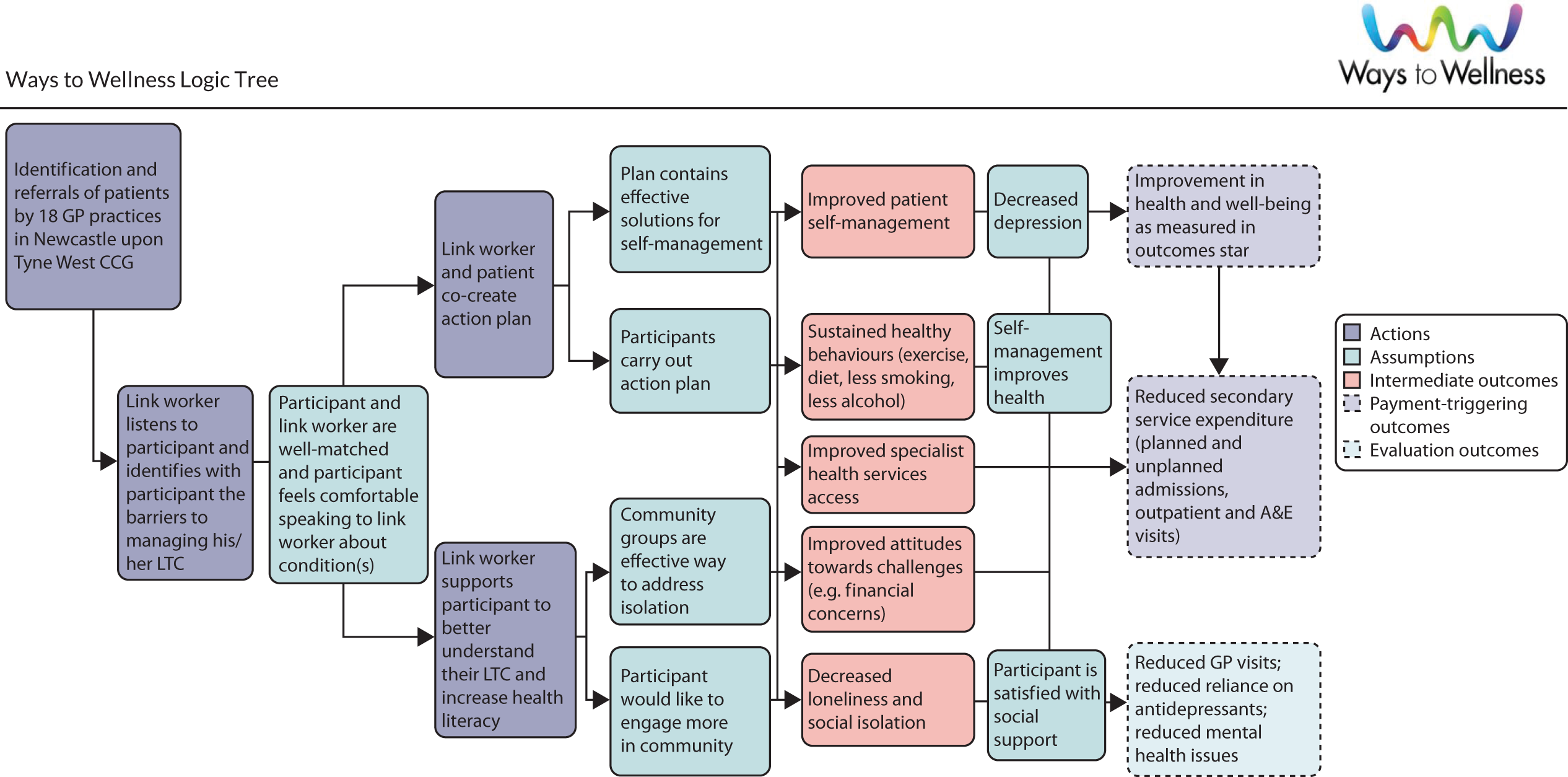
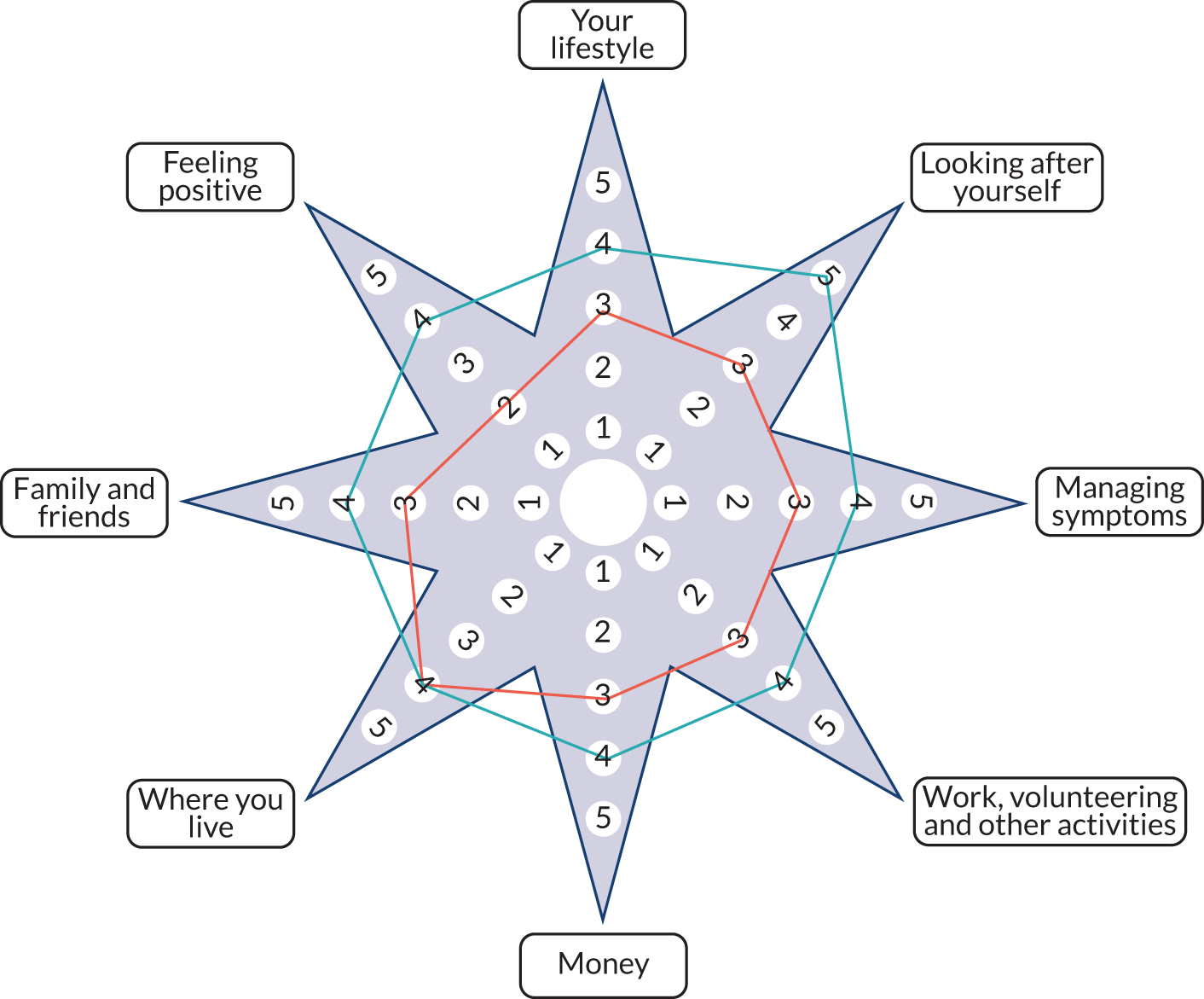
All 18 general practices that were members of the Newcastle West CCG were assigned link workers. Referral to WtW could be made by any primary care professional. Subsequent practice changes reduced practice numbers to 16 in 2018. Practices were encouraged to adapt their clinical computer systems to incorporate and generate a standard referral form to provide an efficient referral mechanism for primary care practitioners. Practices were also encouraged to tag all eligible patients so that in any consultation with HCPs a screen reminder appeared and, if deemed appropriate, a referral to WtW could be offered to the patient with an automated process to decline or accept. If accepted, this triggered a referral to a link worker, via a referral document integrated into the computer system. If the patient declined, a reminder would be flagged on the computing system 6 months later. There was variation in the rate at which practices adapted their computer systems On referral, patients were assigned a link worker who is trained to use the WBS (Triangle Consulting Social Enterprise Ltd, Brighton, UK)74 self-assessment tool (Figure 1). This proprietary tool was conducted approximately every 6 months and aims to help clients to assess their state on a scale of one to five across eight parameters (lifestyle; self-care; symptom management; work, volunteering and activity; money; home environment; personal relationships; and positive feeling). This helps to identify problems and allows the link worker and the patient to co-produce a personalised action plan. The aim is that link workers initiate the intervention by supporting patients to access a range of local community services (e.g. physical activity classes, welfare rights) or, in some cases, by supporting patients to develop self-directed programmes |
| Providers | Link workers come from a range of professional backgrounds, including community work and health care. Over the qualitative study fieldwork period (i.e. October 2018–July 2020), link workers were employed based on pre-existing expertise and experience as there was no recognised qualification. Training in safeguarding, LTCs, the use of the WBS and motivational interviewing was given. Ongoing, in-service training and knowledge exchange events took place regularly |
| How | Initial client contact comprised a one-to-one in-person baseline interview, followed by further contact either face to face or by telephone, text, e-mail or video call. Phases of contact comprised engagement (initial contact and goal-setting), intervention (actively supporting patient to achieve goals), keeping in touch (link worker supports patient to maintain progress and develop new goals if appropriate) followed by discharge. Clients could complete up to seven WBSs, meaning that the maximum length of engagement was approximately 3.5 years |
| Where | Link worker contacts took place in a range of settings, including general practices, provider organisation premises and other community settings. Some home visits could take place. The link worker could accompany patients to support their contact with a community organisation |
| When and how much | Link workers and patients could meet/have contact when they thought necessary. At a minimum, contact was encouraged every 6 months to complete the WBS and this could be either face to face or by telephone |
| Tailoring | The intervention was intended to be personalised to the individual clients’ needs and link workers’ judgements about what help was available |
| Modifications | Although the intervention was not modified during the research, the number of provider organisations fell from four to two. As the intervention was rolled out, recruitment targets and link worker caseload were scheduled to increase within the first year of intervention delivery. Following year 1 of the intervention delivery, the average link worker caseload was 100 (range 80–120) |
| How well | This was a flexible, personalised intervention; fidelity was not assessed |
The intervention began in April 2015 and to the end of our fieldwork period in July 2020 had recruited 5526 patients into the service.
FIGURE 1.
Well-being Star™ (second edition). © Triangle Consulting Social Enterprise Ltd. Authors: Sara Burns and Joy Mackeith. URL: www.outcomesstar.org.uk (accessed 30 May 2020). Reproduced with permission from Triangle Consulting Social Enterprise Ltd (Anna Good, Triangle Consulting Social Enterprise Ltd, 2021, personal communication).
Ethics, governance and sponsor
NHS Research Ethics Committee (REC) approval was obtained for WP1 and WP2 from the Proportionate Review Sub-Committee of the London-Brent REC [REC reference 18/LO/0631; Integrated Research Application System (IRAS) project identification number 238970]. The EQ-5D-5L study was approved by Newcastle University’s Faculty of Medical Sciences REC (reference number 1011), which, via an amendment, approved the COVID-19 study. WP3 was approved by Durham University’s Anthropology Department’s Research and Ethics Data Protection Committee. Newcastle University is the sponsor of the research.
Changes to the protocol
In June 2019, the protocol was amended (version 2) to reflect changes to WP3. The ethnography (WP3) was changed to comprise two separate, but linked, ethnographies: ethnography 1 focused on service user experiences and ethnography 2 focused on link worker roles and practices. In November 2020, the protocol was amended (version 3) to reflect changes to data extraction procedures in WP1 and WP2, to reflect changes to procedures for EQ-5D-5L follow-up data collection measures and to include the additional qualitative fieldwork undertaken as a response to the COVID-19 pandemic. In April 2021, the protocol was amended (version 4) to indicate that a multimethods approach was undertaken for data integration.
Protocol version 4, the final approved version, is available at https://fundingawards.nihr.ac.uk/award/16/122/33 (accessed 19 April 2022).
Independent Study Steering Committee
An independent Study Steering Committee (SSC), which was chaired by Professor Sally Wyke, University of Glasgow, monitored study progress, research standards and conduct. The SSC initially met face to face in June 2019. Two subsequent annual meetings (in March 2020 and January 2021) were held using Zoom (Zoom Video Communications, San Jose, CA, USA) because of the COVID-19 pandemic. See Appendix 2 for SSC membership.
Data Monitoring and Ethics Committee
A Data Monitoring and Ethics Committee was not required because the study did not use a medicinal device and the data for analysis either were anonymised (WP1 and WP2) or were provided with the fully informed consent of the participant (WP3).
Patient and public involvement
The aim of PPI was to involve clients and link workers throughout the study period to optimise the implementation, application and dissemination of the research. Prior to this study taking place, members of the research team had engaged with clients and link workers to execute qualitative interview studies1,15,54 and a quantitative study exploring the feasibility of outcome measurements in impact evaluation. 75 Extensive discussions with link workers in particular, combined with results from our feasibility study, directed us to a design that relied on routine data augmented by EQ-5D-5L data collected by link workers at baseline, rather than relying on self-completion questionnaires. The insights from the qualitative study1 informed the choice of observational/ethnographic methods. As a result of the COVID-19 pandemic, a large-scale planned PPI event scheduled for July 2020 was cancelled. Throughout the period of lockdown and government-imposed restrictions, we were unable to undertake PPI activities. However, below we give an account of the activities that took place, together with our critical reflections.
Patient and public involvement methods
Patients and public
We engaged clients via pre-existing service user groups that had been set up by provider organisations. We accessed members of the public via Newcastle University’s Faculty of Medical Science Public Engagement network.
Link workers
We engaged with link workers at their knowledge exchange events and attended meetings on an ad hoc basis. We sent regular newsletters to link workers and provider organisations informing them about the progress of the study.
Patient and public involvement results
Patients and public
Although initial service user input to recruitment materials was useful, to keep PPI and qualitative/ethnographic fieldwork separate, it was decided not to consult within these fora. Subsequently, these groups became important field sites for ethnography.
Facilitated group discussions with over 100 members of the public about the aims and purpose of social prescribing, as outlined in The NHS Long Term Plan,2 yielded useful information helpful to our interpretation.
Link workers
Link workers were engaged in the research in two main ways. First, link workers were involved in the administration of the baseline EQ-5D-5L questionnaire, which required ongoing communication, including regularly reviewing optimal questionnaire administration, giving monthly feedback about response rates and having ongoing discussions about the best way to increase response rates.
Although the provider organisations were reimbursed for link worker time in baseline questionnaire completion, reimbursement was not the key motivating factor. Concerns about interfering with the development of rapport, client vulnerability and overload, capacity and staff turnover were given as reasons for not facilitating completion of baseline questionnaires. From discussions with link workers, it became clear that researcher-led telephone follow-up would be the most likely method to obtain a good follow-up response rate and would also reduce the burden on hard-pressed link workers.
Second, link workers were involved as research participants, both within focus groups and through participant observation at provider organisations and being ‘shadowed’ by the ethnographer. Link workers, therefore, found themselves both facilitating data collection and being research participants. This did not appear to pose problems for focus group participation, but the less common experience of being observed in their routine practice required time to develop trust with the ethnographer.
Reflections on patient and public involvement
There were aspects of PPI that were helpful to the research endeavour. Our ongoing engagement with link workers enabled us to provide feedback about response rates that acted as regular reminders to link workers about data collection and enhanced the baseline response rate. Equally, we realised that link worker-administered questionnaires would be logistically difficult at follow-up and switched to researcher-administered follow-up, which was likely to have enhanced the follow-up response rate.
The inclusion of two ethnographies meant that we were foregrounding the voices and experiences of those receiving and delivering the intervention. Over the period of the ethnographic fieldwork, we did not feel that it was appropriate to share information derived from the ethnographies with clients or link workers.
On reflection, we experienced some ‘blurred boundaries’ as a result of the involvement of link workers both as participants and in their role administering questionnaires. Furthermore, the constraints imposed by lockdown hampered the planned engagement with broader stakeholders throughout the course of the study. Further stakeholder engagement will take place once the research is fully completed, enabling the research team to include a wide range of perspectives, including study participants, providers, VCSE organisations, primary care, public health and local government, and providing input into the findings, interpretation and implications of the research.
Report structure
This chapter has presented the background to the Social Prescribing in the North East (SPRING_NE) study, its aims and objectives, and has provided an overview of the intervention and study context. Methods and results from the quantitative studies are presented in Chapters 2–4; Chapters 5 and 6 present the results of the ethnographies. Chapter 7 presents data from the additional COVID-19-related study undertaken to explore the impact of the first lockdown on people with LTCs and on the intervention. Chapter 8 draws together the results and discusses their implications. The large-scale adoption of social prescribing within UK primary care creates a timely context for our findings.
Chapter 2 Health outcomes and health-care costs
Parts of this chapter have been reproduced with permission from Moffat et al. 76 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution-Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt and build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given and any changes made indicated. See: https://creativecommons.org/licenses/by-nc/4.0/.
Introduction
In this chapter, we outline the methods and results that enable us to answer the following questions:
-
Does a link worker social prescribing intervention, targeting adults aged 40–74 years with T2DM, result in changes to the levels of HbA1c, BMI, BP, cholesterol levels, smoking status and health-care use and costs?
-
Does the intervention demonstrate greater effectiveness in subgroups (i.e. gender, age, ethnicity, deprivation index) of the eligible population?
In the SPRING_NE study, we exploit the geographical introduction of the intervention as a natural experiment, with treatment and control groups. The intervention was introduced into general practices in the west end of Newcastle upon Tyne (the treatment group) and not into general practices in the east end of Newcastle upon Tyne (the control group). Among the population aged 40–64 years in the intervention-eligible practices, the prevalence of T2DM ranged between 36.00% and 66.67%. Using data from the Quality and Outcomes Framework (QOF), Secondary Uses Service (SUS) and the intervention provider, we were able to estimate a range of difference-in-difference (DiD) models to estimate whether or not the intervention had any impact on a range of clinical outcomes or on secondary care use and costs, and whether or not the results varied by subgroups.
Methods
The intervention was introduced into a geographical area, the west end of Newcastle upon Tyne, allowing us to use DiD methods, a quasi-experimental technique, to estimate treatment effects. Randomisation is normally desirable for estimating treatment effects because it ensures, in theory, that the treatment and control groups are statistically equivalent pre treatment. However, the introduction of the intervention did not allow for randomisation. DiD models recognise that there is no randomisation and that the treatment and control groups may be systematically different from one another. Normally, this raises the issue that individuals self-select into treatment, meaning that the treated and the untreated are not comparable, leading to biased treatment effects. 77 Geographical assignment of treatment rules out, in our case, one element of sample selection, in that general practices cannot self-select into offering the intervention. In our case, even if the general practices in the west end of Newcastle upon Tyne systematically differ from general practices in other parts of the city, then we can still estimate unbiased treatment effects, as long as two further assumptions hold. These two assumptions are the parallel trends assumption, that in the pre treatment, the trends in the outcomes of interest are parallel for the treatment and control groups; and unconfoundedness, that is, that the intervention did not coincide with other treatments that vary by practice and that could influence the outcome measures. Neither of these assumptions can be formally tested and we rely on falsification tests and our modelling strategy to overcome any areas where these assumptions may not hold.
Difference-in-differences models
Linear models for health outcomes
The basic two-period formulation of a DiD model is given in Equation 1:
where yit is the outcome for individual i at time t; Di is a dummy variable that is equal to one if the individual is in the treatment group, and zero otherwise; Tt is a dummy variable that is equal to one if the data are from the post-intervention time period, and zero otherwise; and Di × Tt is an interaction of these two terms. The associated coefficient for the interaction term, τ, is the DiD estimate and is an estimate of the impact of treatment on the outcome, conditional on our assumptions holding. The treatment dummy (Di) controls for the pre-treatment differences between the treatment group and the control group. The time dummy (Tt) controls for common time effects across both groups. The treatment effect is identified on the basis that the two groups are moving along parallel trends and that factors that affect the two groups are identical apart from the allocation of treatment.
Equation 1 can be extended to longitudinal data with multiple time periods. This gives the model that is now commonly referred to as the two-way fixed-effects model:78
In this formulation, we have Xit, a series of observed time-varying controls (in our final models these comprised age and age squared), and Dit, which, as above, is a dummy representing treatment status. However, this treatment status dummy is now time varying and, when the intervention is introduced, shows the change in treatment status from untreated to treated for the treated group. The treatment status dummy is always zero for the control group. We also include individual (λi) and time (γt) fixed effects. These fixed effects are crucial because the individual fixed effects control for all time-invariant unobservable individual heterogeneity, whereas the time fixed effects take account of time-varying factors that may affect both groups. For example, in 2014, the QOF was changed, with the number of targets reduced by 40;79 however, this will have affected all general practices and should be controlled for by the time fixed effects. The individual fixed effects are particularly important because these also absorb GP fixed effects. One risk to model identification is that some general practices may be more engaged with the intervention or make better use of the intervention than other practices. In our data, however, as no individual changes general practice during the duration of our observation period, individual fixed effects absorb the general practice fixed effects, meaning that time-invariant general practice characteristics are also controlled for in our model.
We estimate versions of Equation 2 for all of our health outcomes. We treat the health outcomes as continuous variables because they are, mostly, continuous in the range of values that we are dealing with. For the binary smoking status outcome, we also estimate linear probability models because these models can accommodate the fixed effects in a way that is not possible with standard binary response models, such as the logit. The application of linear probability models is considered appropriate for DiD models because of the estimation of constant marginal effects. 77
As an extension and falsification test, we extend Equation 2 to include leads and lags of treatment. This event-study approach allows us to investigate whether or not there is evidence of parallel trends pre treatment. 80,81 The model that we estimate is:
The parameters of interest are τ1T and τ2T. We normalise effects to zero in 2014/15, the year prior to the introduction of the intervention. Although this is not a formal test of the parallel trends assumption, we have evidence in favour of parallel trends if the τ1T are positive or close to zero and insignificant. Evidence of a treatment effect would come from negative and significant estimates of τ2T.
Treatment and control groups
To apply the DiD model, it is important that we determine the treatment and control groups. With the intervention introduced into geographically determined general practices, there are a number of ways to consider the compositions of the treatment and control groups. Within our data, we have numerous ways to define treatment and control groups, leading to different possible estimates of the treatment effect. Table 3 outlines the possible treatment groups and the different estimates to which they give rise.
| Treatment group | Control group | Estimate | Bias |
|---|---|---|---|
| Study-eligible patients in WtW general practicesa who were in receipt of the intervention at time tb | Study-eligible patients in WtW general practices who were not in receipt of the intervention at time t and who go on to receive the intervention at time t + 1b | τ 1 |
If the intervention is randomly assigned across patients, this should provide a consistent estimate of the short-run effect of the intervention. If individuals in the greatest need are first to receive the intervention, then any significant finding may be an overestimate As t → t + 1, this comparison estimates an intensity of intervention effect – individuals who have been on the programme for over 1 year compared with individuals who have just started the programme |
| Study-eligible patients in WtW general practices who were in receipt of the intervention during the study period | Study-eligible patients in WtW general practices not receiving the intervention during the study period | τ 2 |
If the intervention is randomly assigned this should provide a consistent estimate of the intervention effect If individuals in the greatest need are first to receive the intervention, then any significant finding may be an overestimate. If individuals who may benefit from intervention refuse the intervention, and this is related to our outcomes of interest, then the bias may be in either direction |
| Study-eligible patients in WtW general practices receiving intervention over the study period | Study-eligible patients not in WtW general practices | τ 3 a |
If, pre intervention, the intervention group and the control group have similar trends in their outcomes, and if there are no changes that may affect the control group differentially to the intervention group, this approach should provide the best estimate of the average effect of intervention on the treated. This would give the complier-average causal effect If there are non-social prescribing interventions for the control group that are beneficial, then we would underestimate the benefits of the social prescribing intervention |
| Study-eligible patients in WtW general practices | Study-eligible patients not in WtW general practices | τ 3 b |
If, pre intervention, the intervention group and the control group have similar trends in their outcomes, and if there are no changes that may affect the control group differentially to the intervention group, this approach should provide the best estimate of an intention-to-treat effect. This will be different, and we expect lower, than the average effect of intervention on the treated (τ3b) as our intervention group contains untreated individuals However, it has the benefit of overcoming any problems regarding intervention assignment in social prescribing practices |
Each of the possible comparisons lead to different potential estimations of the treatment effect and the potential ‘bias’ associated with estimated treatment effect. We give most attention to the value τ3b, the intention-to-treat (ITT) estimate of the treatment effect. The ITT estimate overcomes a number of problems associated with the estimation of treatment effects using observational data. First, any treatment is based on a referral process, so that those individuals who are the most ill/most in need, or incurring the highest costs, are those who are referred first. With regression to the mean, it is possible that these individuals see improvements in their health regardless of the intervention and, therefore, the effect of treatment may be overestimated. The ITT analysis mitigates this somewhat by considering all individuals to be treated at the time that treatment becomes available. Second, the ITT analysis accounts for the fact that the intervention will suffer from non-compliance and wide individual heterogeneity in the intervention composition and level of participant engagement. A final advantage of the ITT analysis is that it provides an estimate of the expected effect of the intervention on an individual drawn at random from the treatment practices. However, the ITT estimate cannot distinguish between the effect of the intervention on the individual and the effect of the general practice. It is possible to specify all of the possible combinations of treatment effects, as outlined in Table 3, as ITT analysis. Individuals in the respective treatment groups are deemed to be treated once treatment is available, despite that it may be some time, even years, before individuals actually receive treatment.
As outlined above, there are good reasons for taking an ITT approach. In addition, in recent years it has been noted that the two-way fixed-effects model is potentially biased when treatment assignment varies across time and there is treatment heterogeneity. 78,82 Essentially, the two-way fixed-effects estimator becomes a weighted average of all of the possible two-by-two combinations of treatment and control groups that are available in the data. This leads to the possibility that even when the treatment effect is negative the final estimated treatment effect from two-way fixed effects can be positive. This result depends on the size of effects and the size of the respective groups. To overcome this problem, de Chaisemartin and D’Haultfoeuille78 propose an estimator that is based on the time that treatment occurs, so comparing treatment changes across consecutive time periods with observations whose treatment status did not change. This allows the researcher to investigate the evolution of treatment across time and for the estimation of placebos that are similar to the event-study approaches outlined in Equation 3. Owing to the small number of switchers into treatment, at some of our time points we estimate these models for the main effects only and not for the subgroups. It follows from these recent modelling developments that it is not possible to rank the direction and sign of the potential treatment effects that can be estimated. It is possible that the direction of the estimates is affected by the relative sizes of the groups, the potential treatment heterogeneity and the possibility of heterogeneity in treatment over time. 78
Two-part models for secondary care expenditure outcomes
One of our aims is to estimate the impact of the intervention on health-care expenditure, taking account of usage and cost. Health expenditure is a mixture of distributions because the costs arise from a two-stage procedure. First, there is health-care use and, second, the costs of the health-care usage. As a result, there is considerable density in the distribution at zero because most individuals, including within our data, do not use secondary health-care services in a given year. A further modelling complication arises because, whereas most secondary health service use is of low cost, there are a significant number of individuals who incur very high health-care costs, giving the distribution of the data a long right-hand tail. The consequence of these distributional problems is that the traditional linear model in Equation 2 is not appropriate for investigating expenditure data.
To accommodate the distributional challenges of expenditure data, we follow83 and estimate two-part models (TPMs). The TPM splits the decision into two stages: a use stage and a cost stage. There were four main modelling decisions to be made: first, whether to apply a logit or a probit for the first part of the model (although the consequences of this decision are trivial). We chose a logit model. Second, we had to decide on the link and distribution family for the second-stage generalised linear model (GLM). We made these choices on the basis of the Box–Cox test and the modified Park test. 83 Following this procedure, we chose a log-link function and the gamma distribution. The final decision relates to which variables to include in the linear index. We tried a range of controls to assess their impact on the estimated treatment effect; all models included age and age squared.
The TPM can formally be considered as:83
In this formulation, f0 is the density of yi when yi = 0 and f+ is its conditional density when yi > 0. There has previously been concern that there may not be independence between the two parts of the mode; however, Drukker84 has formally demonstrated that E(yi|xi) can be identified even if there is dependence between the two parts.
The TPM is a non-linear model and, therefore, the derivation of the treatment effect is slightly different from that of a standard two-way fixed-effects model. Following Deb et al. ,83 we can specify a non-linear conditional expectations function for a simple model as:
The control variables (x′i where bold text is used to denote vectors), and the treatment dummy (Di) are a linear function that is transformed by a non-linear function g(*). Now the treatment effect is the difference between two expected values based on the treatment status:
Therefore, in this case, the treatment effect of interest can be obtained from the sample as:
where N is the sample size. Essentially, as shown by Puhani,85 the treatment effect is the difference between the expected value of the outcome in the post-treatment period and the hypothetical expected value in the post-treatment period had the individual not received treatment. In practical terms, the average impact of treatment on the treated can be estimated by taking the average marginal effect from the TPM.
Data
We use data from three different sources: the QOF, SUS and intervention provider. All of these data were provided by NECS.
The QOF is an incentive programme that financially rewards English general practices for quality of patient care and helps to standardise improvements in the delivery of primary care. Under this programme, sets of targets are used to allocate funds, meaning that there can be excellent reporting of a variety of health outcomes for individuals. During the period of our study, there was only one major reform to the QOF targets that may be an issue for our analysis: a reduction in the number of targets by 40 in 2014–15. However, as these changes affected all practices, we would not expect this reform to affect our identification. The QOF provides data on our health outcomes: levels of HbA1c (our primary outcome measure), blood pressure, cholesterol levels, glucose levels, BMI and smoking status. Where individuals had more than one outcome measure per year as a result of repeat visits to their GP, we took the yearly average as the outcome. The level of HbA1c (a measure of glycaemic control) was chosen as our primary outcome measure because it is a key measure of T2DM control. Data on levels of HbA1c are well collected (i.e. there are clear QOF targets for levels of HbA1c) and glycaemic control has a significant effect on long-term health and even small reductions in HbA1c levels can reduce long-term macrovascular and microvascular complications. 86–88
Quality and Outcomes Framework data are populated with measures and Read codes describing the data collected. There are possibilities of errors in routine data collection. For example, HbA1c level measured using International Federation of Clinical Chemistry (IFCC) units can be recorded in the Read codes as DCCT (Diabetes Control and Complications Trial) units. For these reasons, some top coding was required. HbA1c level was top coded at 120 mmol/mol, BMI was top coded at 50 kg/m2 and bottom coded at 20 kg/m2, and cholesterol level was top coded at 10 mmol/l.
The QOF also provides information on patient characteristics, including age, ethnicity (although there are some recording issues with this characteristic leading to inconsistent categorisation and small sample sizes), sex at birth, area of residence and the presence of additional comorbidities. All of the health outcomes and characteristics were extracted by NECS. The QOF was used to identify our sample of patients: individuals within the eligibility age range (40–74 years), registered at a treatment or control GP practice and with a diagnosis of T2DM on 1 April 2015. The data observation period ran from 1 April 2011–12 to 30 March 2018–19. Under our data-sharing agreements, only comorbidities that were part of the eligibility criteria for the intervention were included in our data sample, that is COPD, asthma, heart failure, coronary heart disease, epilepsy and osteoporosis. The area of residence was given as LSOA (lower-layer super output area) and these LSOA markers were linked to the IMD deciles, with 1 being the most deprived decile. Permission to access patients’ QOF register data were given by 13 out of the 16 treatment practices, covering 80% of those referred into the intervention and 11 out of the 15 control practices, providing information on approximately 8300 individuals, with approximately 58% of individuals in treatment practices. The exact number of observations depends on the outcome under consideration, as can be seen in the results.
Secondary uses services data are a record of secondary health-care use in NHS providers. For our study, we used information on the use and cost of outpatient services, inpatient elective services, inpatient non-elective services and A&E services. The costs were measured as the national tariffs that are paid for services at 2019 costs. To prevent extreme values affecting overall results, all costs were capped at the top percentile value.
Finally, we were able to observe who had actually received treatment from the intervention data that provided dates that an individual completed their initial goal-setting meeting with their link worker. We define this date as the point at which an individual started treatment. For the linear health outcome models, we also test the sensitivity of our results by constructing a new treatment group, where the treated are those individuals who have completed at least two goal-setting meetings with their link worker. These meetings typically occur at least 6 months apart.
The three separate data sets were pseudonymised by NECS, using the same key, and linked to form the complete data set. Table 4 shows the variable names and definitions. The pre-treatment summary statistics for the whole sample, and broken down by treatment and control group, are presented in Tables 5 and 6. Summary statistics for the whole time period are given in Appendix 3, Table 37, and Appendix 4, Table 38.
| Variable | Definition |
|---|---|
| HbA1c level | Concentration (IFCC units: mmol/mol) of glycated haemoglobin in the blood |
| BP systolic | SBP (mmHg) |
| BP diastolic | DBP (mmHg) |
| High blood pressureb | Either SBP of > 140 mmHg or diastolic blood pressure of > 90 mmHg |
| Blood glucose level | Concentration (mmol/l) of glucose level in the blood |
| Cholesterol level | Concentration (mmol/l) of total cholesterol in the blood |
| BMI | Body mass index (kg/m2) |
| Smoking status | Currently smoke (1/0) |
| Age | Individual age, years |
| Age start | Age at the start of the data observation period |
| Female | A dummy (0/1) indicating whether an individual’s recorded sex in the QOF is female (1) or male (0) |
| Comorbidities (based on intervention-eligible conditions) | A categorical variable indicating:
|
| Ethnicity, non-white | Based on QOF-reported ethnicity. A dummy (0/1) variable indicating whether an individual is ethnically non-white (1) or white (0) |
| Deprivation decile (IMD deciles) |
The IMD is the official measure of relative deprivation for small areas in England and ranks every LSOA (a LSOA is a geospatial statistical unit containing an average of 1500 residents) from 1 (most deprived) to 32,844 (least deprived). IMD scores are grouped into deciles (e.g. 1 to 3284 represents the 10% most deprived neighbourhoods). Deciles were linked with LSOA data provided by the NECS. Decile 1 represents being in 10% of the most deprived LSOAs; decile 10 represents being in 10% of the least deprived LSOAs The IMD combines information from the seven domains to produce an overall relative measure of deprivation. The domains are combined using the following weights:LSOA location, and so IMD decile, is taken from the QOF and is time invariant |
| Variable | Count (n) | Mean/proportiona | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Control group | |||||
| HbA1c level (mmol/mol) | 2855 | 56.88 | 14.47 | 28.50 | 120.00 |
| BP (mmHg) | |||||
| Systolic | 3170 | 133.54 | 12.27 | 97.33 | 202.75 |
| Diastolic | 3170 | 78.33 | 7.79 | 53.83 | 123.00 |
| High | 3170 | 0.33 | 0.37 | 0 | 1 |
| Blood glucose level (mmol/l) | 1533 | 8.37 | 3.44 | 3.30 | 18.00 |
| Cholesterol level (mmol/l) | 3046 | 4.58 | 1.09 | 2.00 | 9.50 |
| BMI (kg/m2) | 3129 | 33.15 | 6.31 | 20.00 | 50.00 |
| Smoker | 3158 | 0.26 | 0.42 | 0 | 1 |
| Treatment group | |||||
| HbA1c level (mmol/mol) | 3989 | 58.17 | 15.03 | 26.02 | 120.00 |
| BP (mmHg) | |||||
| Systolic | 4506 | 133.53 | 12.38 | 90.00 | 220.00 |
| Diastolic | 4506 | 78.56 | 7.86 | 55.00 | 124.56 |
| High | 4506 | 0.33 | 0.37 | 0 | 1 |
| Blood glucose level (mmol/l) | 2543 | 8.41 | 3.50 | 2.60 | 18.00 |
| Cholesterol level (mmol/l) | 4293 | 4.57 | 1.09 | 1.53 | 10.00 |
| BMI (kg/m2) | 4374 | 32.61 | 6.37 | 20.00 | 50.00 |
| Smoker | 4483 | 0.25 | 0.41 | 0 | 1 |
| Total | |||||
| HbA1c level (mmol/mol) | 6844 | 57.63 | 14.81 | 26.02 | 120.00 |
| BP (mmHg) | |||||
| Systolic | 7676 | 133.53 | 12.33 | 90.00 | 220.00 |
| Diastolic | 7676 | 78.46 | 7.83 | 53.83 | 124.56 |
| High | 7676 | 0.33 | 0.37 | 0 | 1 |
| Blood glucose level (mmol/l) | 4076 | 8.39 | 3.48 | 2.60 | 18.00 |
| Cholesterol level (mmol/l) | 7339 | 4.57 | 21.09 | 1.53 | 10.00 |
| BMI (kg/m2) | 7503 | 32.84 | 6.35 | 20.00 | 50.00 |
| Smoker | 7641 | 0.26 | 0.42 | 0 | 1 |
| Variable | Count (n) | Mean/proportion | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Control group | |||||
| Use any HC | 3455 | 0.62 | 0.41 | 0.00 | 1.00 |
| Total cost | 3455 | 1097.05 | 1958.46 | 0.00 | 14,000.00 |
| A&E use | 3455 | 0.24 | 0.34 | 0.00 | 1.00 |
| A&E cost | 3455 | 41.18 | 74.04 | 0.00 | 500.00 |
| IP elective use | 3455 | 0.18 | 0.30 | 0.00 | 1.00 |
| IP elective cost | 3455 | 367.15 | 918.39 | 0.00 | 7500.00 |
| IP non-elective use | 3455 | 0.11 | 0.24 | 0.00 | 1.00 |
| IP non-elective cost | 3455 | 327.75 | 1100.61 | 0.00 | 1200.00 |
| Outpatients use | 3455 | 0.54 | 0.43 | 0.00 | 1.00 |
| Outpatients costs | 3455 | 318.01 | 456.71 | 0.00 | 2500.00 |
| Treatment group | |||||
| Use any HC | 4941 | 0.60 | 0.41 | 0.00 | 1.00 |
| Total cost | 4941 | 1028.57 | 1862.64 | 0.00 | 14,000.00 |
| A&E use | 4941 | 0.23 | 0.33 | 0.00 | 1.00 |
| A&E cost | 4941 | 39.92 | 73.86 | 0.00 | 500.00 |
| IP elective use | 4941 | 0.17 | 0.30 | 0.00 | 1.00 |
| IP elective cost | 4941 | 365.91 | 937.13 | 0.00 | 7500.00 |
| IP non-elective use | 4941 | 0.10 | 0.24 | 0.00 | 1.00 |
| IP non-elective cost | 4941 | 303.17 | 1036.01 | 0.00 | 12,000.00 |
| Outpatients use | 4941 | 0.52 | 0.43 | 0.00 | 1.00 |
| Outpatients costs | 4941 | 290.01 | 424.12 | 0.00 | 2500.00 |
| Total | |||||
| Use any HC | 8396 | 0.61 | 0.41 | 0.00 | 1.00 |
| Total cost | 8396 | 1056.75 | 1902.84 | 0.00 | 14,000.00 |
| A&E use | 8396 | 0.24 | 0.33 | 0.00 | 1.00 |
| A&E cost | 8396 | 40.44 | 73.93 | 0.00 | 500.00 |
| IP elective use | 8396 | 0.18 | 0.30 | 0.00 | 1.00 |
| IP elective cost | 8396 | 366.42 | 929.41 | 0.00 | 7500.00 |
| IP non-elective use | 8396 | 0.11 | 0.24 | 0.00 | 1.00 |
| IP non-elective cost | 8396 | 313.29 | 1063.07 | 0.00 | 12,000.00 |
| Outpatients use | 8396 | 0.52 | 0.43 | 0.00 | 1.00 |
| Outpatients costs | 8396 | 301.53 | 438.02 | 0.00 | 2500.00 |
The data presented in the tables demonstrate that, in terms of average health outcomes, the treatment and control groups are similar, with the treatment group having, on average, slightly higher levels HbA1c. The tables also indicate that the sample size for blood glucose is much smaller than that for the other outcomes; for this reason, we do not analyse the blood glucose outcome. In terms of health-care costs (and, to some degree, health-care use), the treatment group appears to incur, on average, lower costs (and use) than the control group. Finally, Table 7 shows the characteristics of the sample. Compared with the treatment group, the control group is slightly older, more likely to have an extra multimorbidity and more likely to be male. There are considerable differences in ethnicity, with the treatment group more likely than the control group to be non-white. Large proportions of both the control group (55%) and the treatment group (60%) live in areas in the top quintile of deprivation.
| Variable | Count (n) | Mean/proportion | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Control group | |||||
| Age (years) | 3455 | 58.54 | 8.94 | 39.50 | 73.50 |
| Age (years) at start | 3455 | 55.04 | 8.94 | 36.00 | 70.00 |
| Women | 3455 | 0.42 | 0.49 | 0 | 1 |
| Multimorbidity | 3455 | 0.58 | 0.49 | 0 | 1 |
| Ethnically non-white | 3424 | 0.12 | 0.32 | 0 | 1 |
| Deprived area | 3455 | 0.55 | 0.50 | 0 | 1 |
| Treatment group | |||||
| Age (years) | 4941 | 57.90 | 9.13 | 39.50 | 73.50 |
| Age (years) at start | 4941 | 54.40 | 9.13 | 36.00 | 70.00 |
| Women | 4941 | 0.44 | 0.50 | 0 | 1 |
| Multimorbidity | 4941 | 0.53 | 0.50 | 0 | 1 |
| Ethnically non-white | 4878 | 0.24 | 0.42 | 0 | 1 |
| Deprived area | 4941 | 0.60 | 0.49 | 0 | 1 |
| Total | |||||
| Age (years) | 8396 | 58.16 | 9.06 | 39.50 | 73.50 |
| Age (years) at start | 8396 | 54.66 | 9.06 | 36.00 | 70.00 |
| Women | 8396 | 0.43 | 0.50 | 0 | 1 |
| Multimorbidity | 8396 | 0.55 | 0.50 | 0 | 1 |
| Ethnically non-white | 8302 | 0.19 | 0.39 | 0 | 1 |
| Deprived area | 8396 | 0.58 | 0.49 | 0 | 1 |
Results
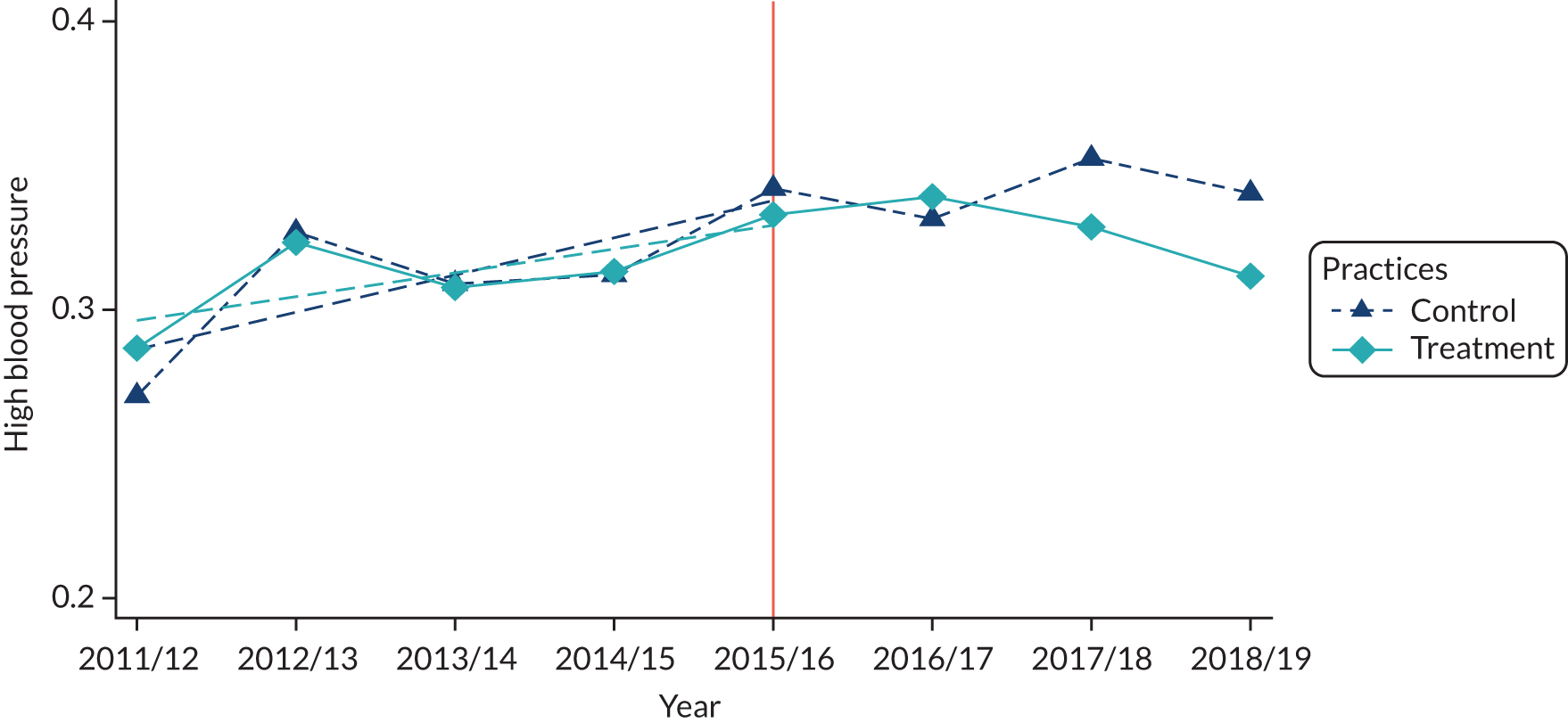
Health outcomes
Figures 2 and 3 and Appendix 5, Figures 11–13, provide the unconditional means for the health outcomes for the treatment and control groups across the whole time period. These are based on the ITT analysis, with individuals classed as being in the treatment group if they are registered with a general practice offering the intervention. We mark the point at which the intervention was available, year 15/16. These graphs help to provide evidence to support our DiD approach. Ideally, the two groups would have similar trends in outcomes in the pre-treatment period. If there is an impact of treatment, we would expect some divergence in outcomes post treatment. However, even if the figures themselves do not demonstrate parallel trends, because these are unconditional trends, it may be that once age, time and individual fixed effects are accounted for the parallel trends assumption holds.
FIGURE 2.
Glycated haemoglobin (HbA1c) level: control vs. treatment by year. Mean outcomes plotted against year for the treatment and control practices, with the orange line indicating the year that the intervention became available.
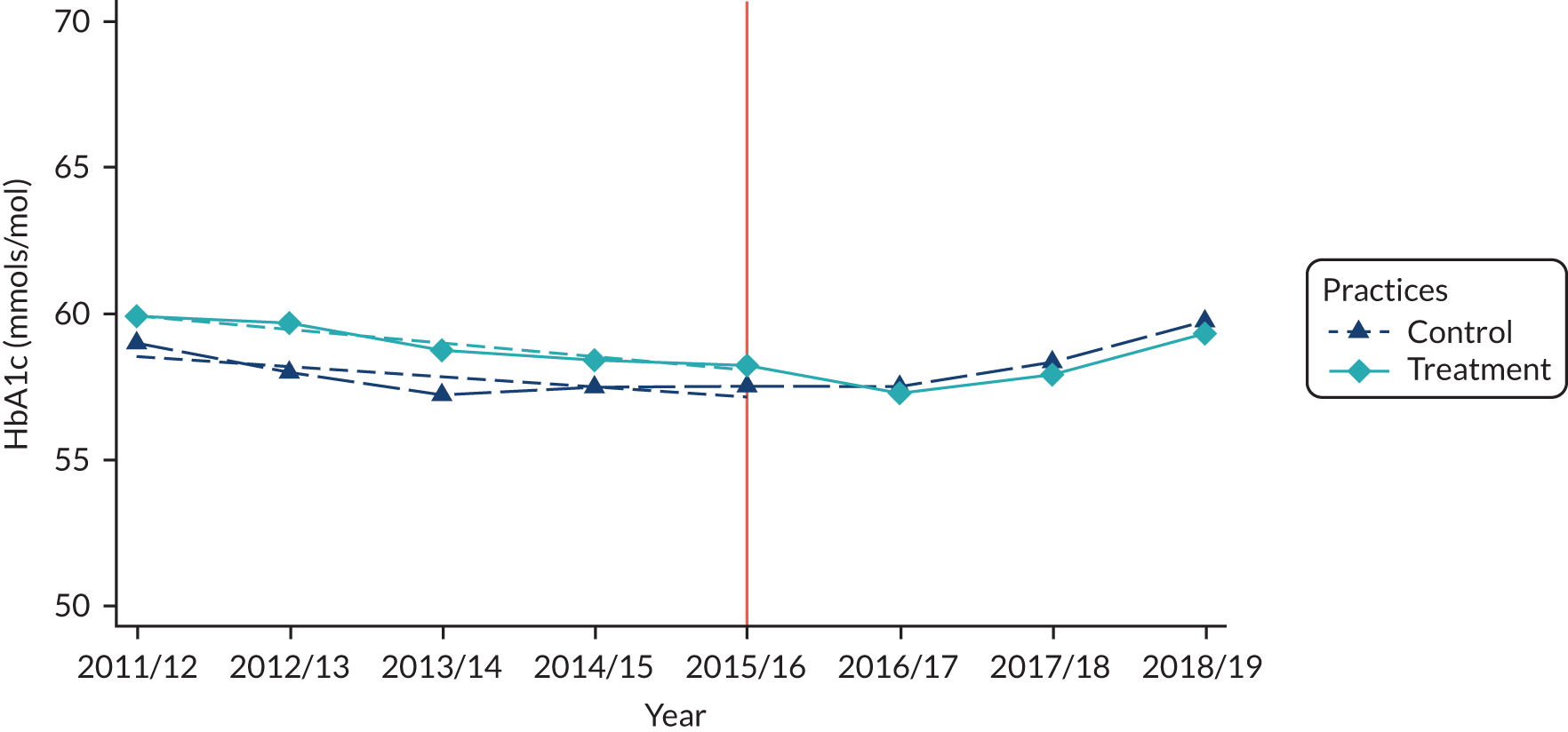
FIGURE 3.
High blood pressure: control vs. treatment by year. Mean outcomes plotted against year for the treatment and control practices, with the orange line indicating the year that the intervention became available.
The trends suggest a mixed picture for the intervention. The average level of HbA1c is lower in the control group than in the treatment group in each year prior to treatment (see Figure 2). The small dashed lines represent the linear trend. Pre treatment, the linear trends are parallel. Following treatment, the average level decreases to below the average for the control group and remains there, suggesting that, on average, the intervention has a role in reducing the levels of HbA1c. However, the range over which levels of HbA1c are changing is very small.
For the probability of having high blood pressure (see Figure 3), we see a similar pattern. Pre treatment, the trends (the small dashed lines) are parallel and the treatment and control groups largely move together. Post treatment, there is a divergence between the treatment group and the control group, with the treated group showing improvements in probability of having high blood pressure. Although, again, this finding is tempered by the fact that the changes are very small in magnitude.
For the other health outcomes, that is BMI, cholesterol level and smoking status (see Appendix 5, Figure 11), there is very little evidence that the intervention had any effect. The trends are largely parallel pre and post treatment. It is, of course, possible that these unconditional averages hide important effects and potential heterogeneity in outcomes. To consider these issues, we need to turn to the regression analysis.
However, before considering the regression analysis, we present the results from the falsification tests. These are event-study approaches, including the leads and lags of the treatment, and provide a test of whether or not there are significant differences in outcome between the treatment group and the control group across the whole time period. The omitted time period is the year prior to treatment. Ideally, pre treatment, the estimated coefficients will be close to zero and insignificant. Post treatment, if treatment is effective, then we would expect to see large estimates that are significantly different from zero.
In Figures 4 and 5 (and Appendix 6, Figure 14), the graphs for levels of HbA1c (see Figure 4) and blood pressure (see Figure 5), and to a lesser extent cholesterol level (see Appendix 6, Figure 14), suggest that we can be confident of the parallel trends assumption and the impact of the intervention. Post treatment, the signs of the estimated coefficients mostly change sign and there is some evidence of significance. For BMI (see Appendix 6, Figure 15) and current smoking status (see Appendix 6, Figure 16), the results are less reassuring. There is no clear evidence of any treatment effect and most of the estimates are insignificant in both the pre-treatment and the post-treatment period.
FIGURE 4.
Health outcomes: falsification results – HbA1C coefficients. Plots of the coefficient [and 95% confidence interval (CI)] estimating the difference in health outcome between the treatment and the control practices for each year, with the orange line indicating the year that the intervention became available.
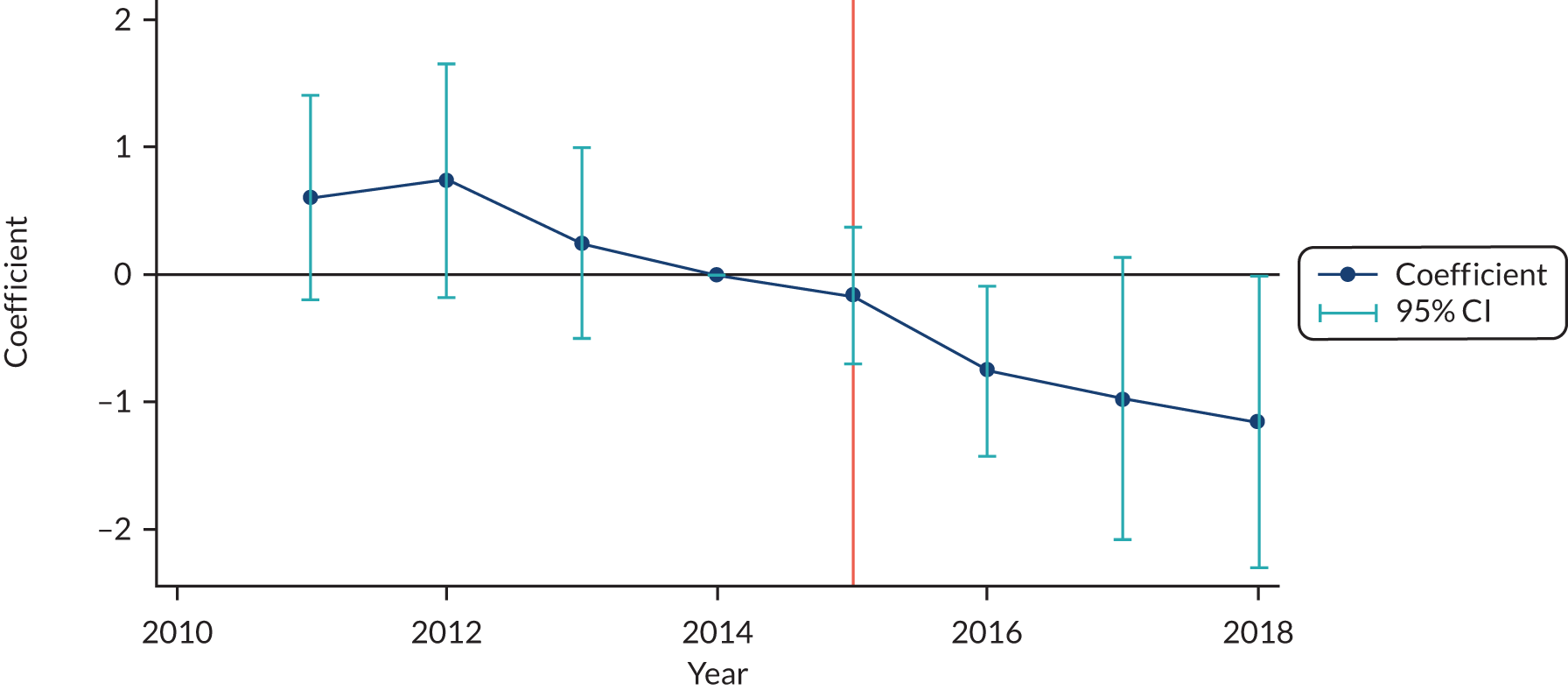
FIGURE 5.
Health outcomes: falsification results – probability of high blood pressure. Plots of the coefficient [and 95% confidence interval (CI)] estimating the difference in health outcome between the treatment and the control practices for each year, with the orange line indicating the year that the intervention became available.
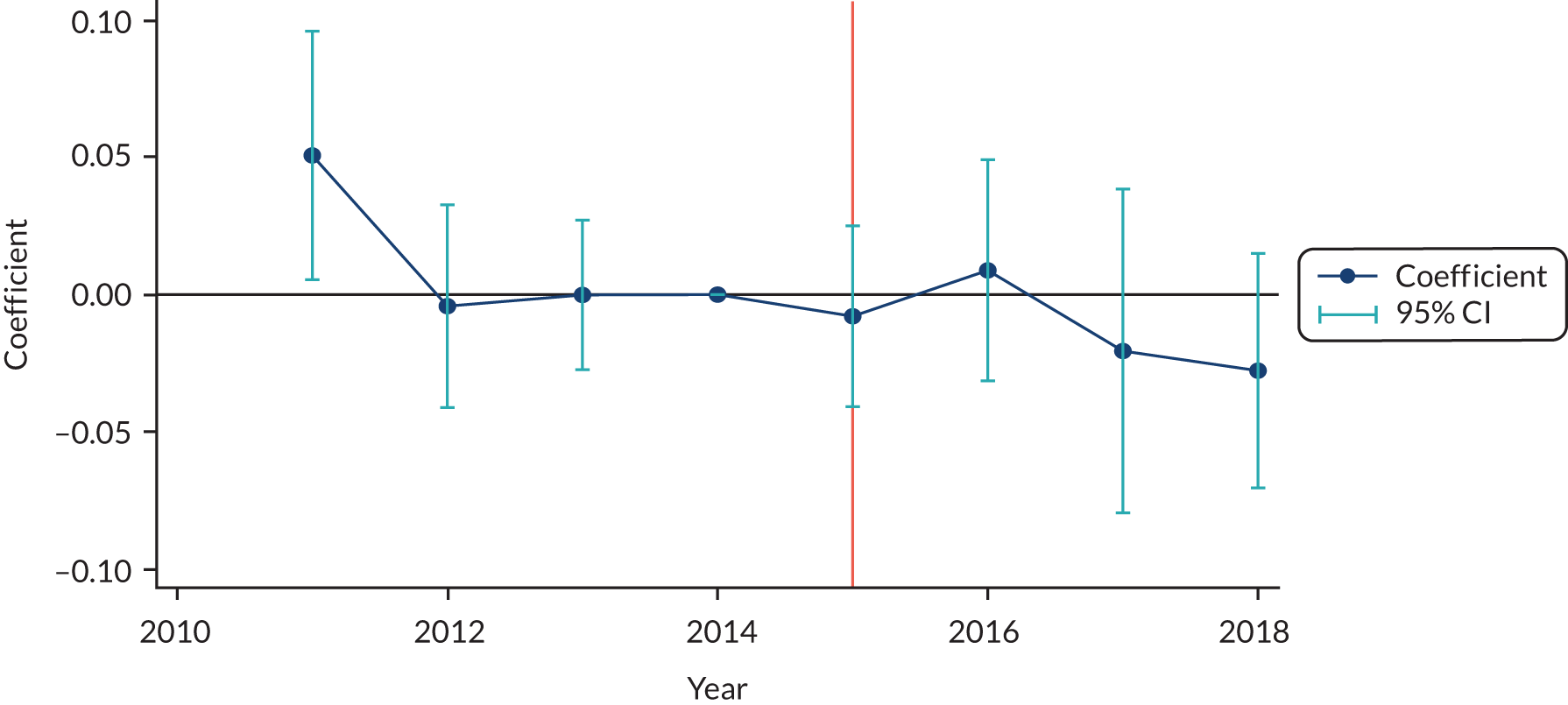
Glycated haemoglobin
The results of the HbA1c ITT analysis are presented in Table 8. These show the overall results and results by subgroup.
| Variable | DID analysis | Subgroup analysis | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall model (1) | By years (2) | Gender | Ethnicity | Age | Comorbidities | BMI | Deprivation decile | ||||||||
| Men (3) | Women (4) | White (5) | Non-white (6) | ≤ 55 years (7) | > 55 years (8) | 0 (9) | 1 (10) | ≥ 2+ (11) | Not obese (12) | Obese (13) | Most deprived (14) | Least deprived (15) | |||
| Treated | |||||||||||||||
| Coefficient | –1.110*** | ||||||||||||||
| 95% CI | –1.878 to –0.342 | ||||||||||||||
| Treated: 2015/16 | |||||||||||||||
| Coefficient | –0.503* | –0.532 | –0.454 | –0.562 | 0.0335 | –0.0514 | –0.901** | –0.720 | –0.683 | 0.239 | –0.971*** | 0.0857 | –0.563 | –0.501 | |
| 95% CI | –1.100 to 0.0932 | –1.395 to 0.332 | –1.408 to 0.500 | –1.260 to 0.135 | –1.037 to 1.104 | –0.938 to 0.836 | –1.759 to –0.044 | –1.713 to 0.274 | –1.517 to 0.151 | –0.764 to 1.243 | –1.606 to –0.335 | –0.883 to 1.054 | –1.660 to 0.534 | –1.248 to 0.246 | |
| Treated: 2016/17 | |||||||||||||||
| Coefficient | –1.093*** | –0.724** | –1.571*** | –1.160*** | –0.428 | –0.938 | –1.228*** | –1.498*** | –1.369*** | 0.173 | –1.255*** | –0.844 | –1.253*** | –1.063*** | |
| 95% CI | –1.682 to –0.504) | –1.403 to –0.0450 | –2.569 to –0.574 | –1.825 to –0.496 | –1.782 to 0.925 | –2.078 to 0.203 | –1.740 to –0.717 | –2.425 to –0.571 | –2.324 to –0.413 | –1.450 to 1.796 | –2.042 to –0.468 | –1.965 to 0.277 | –2.100 to –0.407 | –1.760 to –0.365 | |
| Treated: 2017/18 | |||||||||||||||
| Coefficient | –1.321** | –1.039 | –1.683*** | –1.244* | –1.236 | –1.234 | –1.386*** | –1.906** | –1.451* | –0.0632 | –1.527** | –1.021 | –2.156*** | –0.918 | |
| 95% CI | –2.492 to –0.150 | –2.539 to 0.460 | –2.791 to –0.575 | –2.654 to 0.166 | –2.946 to 0.474 | –3.171 to 0.702 | –2.142 to –0.631 | –3.345 to –0.468 | –3.177 to 0.275 | –2.330 to 2.203 | –2.915 to –0.139 | –2.442 to 0.401 | –3.420 to –0.892 | –2.269 to 0.432 | |
| Treated: 2018/19 | |||||||||||||||
| Coefficient | –1.497** | –1.494** | –1.495** | –1.601** | 0.0857 | –1.558** | –1.445*** | –1.242* | –1.797** | –1.462 | –1.732** | –1.196** | –2.117*** | –1.175* | |
| 95% CI | –2.648 to –0.345 | –2.824 to –0.164 | –2.649 to –0.342 | –2.795 to –0.406 | –1.729 to 1.900 | –3.101 to –0.015 | –2.441 to –0.449 | –2.527 to 0.044 | –3.182 to –0.411 | –3.688 to 0.765 | –3.358 to –0.107 | –2.276 to –0.117 | –3.440 to –0.795 | –2.503 to 0.153 | |
| Constant | 202.5 | 203.8 | 256.5 | –16.25 | 117.2 | 549.0 | 54.40 | 579.5** | 108.0 | 344.7 | 0.243 | 248.4 | 150.9*** | 41.53 | 305.9 |
| 95% CI | –56.19 to 461.2 | –54.93 to 462.6 | –64.56 to 577.7 | –471.4 to 438.9 | –78.24 to 312.7 | –367.5 to 1465.5 | –139.839 to 248.631 | 134.120 to 1024.801 | –212.736 to 428.648 | –152.200 to 841.580 | –38.999 to 39.484 | –231.418 to 728.260 | 64.619 to 237.172 | –211.367 to 294.434 | –94.696 to 706.437 |
| N | 49,752 | 49,752 | 28,399 | 21,353 | 40,299 | 9045 | 23,752 | 26,000 | 21,495 | 17,263 | 10,994 | 28,671 | 20,995 | 16,856 | 32,896 |
| R 2 | 0.649 | 0.649 | 0.626 | 0.680 | 0.639 | 0.692 | 0.653 | 0.623 | 0.649 | 0.653 | 0.646 | 0.643 | 0.659 | 0.668 | 0.640 |
| F-statistic | 19.00 | 12.86 | 3.949 | 20.26 | 8.910 | 4.987 | 3.128 | 11.01 | 4.819 | 10.05 | 16.82 | 20.87 | 9.146 | 4.388 | 7.717 |
Table 8, columns 1 and 2, show the estimates from the ITT DiD analysis. Both columns demonstrate a statistically significant reduction in the level of HbA1c for the treatment group. In column 2 we can also see that the impact of the intervention is increasing over time. This increase probably reflects two factors: first, more individuals are treated over time, and, second, because the treatment addresses the social, as well as the behavioural, determinants of health, it is likely to take time for the impact of the intervention to be felt. However, it is clear that the impact is small in magnitude, even by the fourth year of treatment.
The remaining columns of Table 8 show the estimates by various subgroup analyses. The subgroup analysis largely follows the pattern of the overall results; however, there are three notable results. First, the impact of the intervention seems to differ between white and non-white ethnicities, with a larger estimated treatment effect for those who are ethnically white (see Table 8, columns 5 and 6). Second, individuals with no extra or one extra comorbidity seem to benefit from the intervention to a greater extent than those with two or more extra comorbidities (see Table 9, columns 3, 4 and 5). Finally, individuals living in the most deprived areas seem to benefit from the intervention, but those in less deprived areas do not.
Blood pressure
We consider blood pressure in three different ways: systolic, diastolic and as a binary indicator of whether or not an individual has high blood pressure. The results are presented in Table 9. For brevity, we present results from only the overall post-treatment period. The results for blood pressure are largely insignificant, with small decreases in blood pressure in the post-treatment period. We do, however, observe a significant reduction in the probability of having high blood pressure in the ethnically non-white and those aged ≤ 55 years. In these cases, the probability of having high blood pressure falls by around 4–6 percentage points.
| Variable | Overall model (1) | Subgroup analysis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Ethnicity | Age | Comorbidities | BMI | Deprivation decile | |||||||||
| Men (2) | Women (3) | White (4) | Non-white (5) | ≤ 55 years (6) | > 55 years (7) | 0 (8) | 1 (9) | ≥ 2+ (10) | Not obese (11) | Obese (12) | Most deprived (13) | Least deprived (14) | ||
| Diastolic | ||||||||||||||
| Treatment | ||||||||||||||
| Coefficient | –0.586 | –0.770** | –0.351 | –0.502 | –1.201* | –0.768* | –0.431 | –0.629 | –0.569 | –0.493 | –0.565 | –0.604 | –0.827* | –0.502 |
| t-statistic | –1.592 | –2.213 | –0.792 | –1.422 | –1.992 | –1.743 | –1.228 | –1.367 | –1.488 | –1.191 | –1.501 | –1.428 | –2.024 | –1.257 |
| Constant | ||||||||||||||
| Coefficient | 234.2*** | 251.5*** | 119.0 | 217.9* | 311.1** | 240.5*** | 129.5 | 246.4** | 235.4* | 82.42*** | 218.3*** | 258.0* | 224.7 | 240.0*** |
| t-statistic | 2.960 | 4.372 | 0.458 | 2.052 | 2.783 | 3.843 | 0.740 | 2.668 | 1.797 | 4.811 | 4.637 | 1.853 | 1.507 | 3.027 |
| N | 52,596 | 29,705 | 22,891 | 42,467 | 9694 | 25,749 | 26,847 | 22,732 | 18,145 | 11,719 | 30,350 | 22,142 | 18,218 | 34,378 |
| R 2 | 0.530 | 0.544 | 0.508 | 0.523 | 0.559 | 0.508 | 0.491 | 0.528 | 0.519 | 0.524 | 0.538 | 0.519 | 0.543 | 0.520 |
| F-statistic | 2.613 | 4.180 | 0.795 | 2.063 | 2.929 | 5.510 | 1.996 | 1.668 | 1.863 | 1.586 | 3.613 | 1.824 | 2.142 | 3.653 |
| Systolic | ||||||||||||||
| Treatment | ||||||||||||||
| Coefficient | –0.486 | –0.731 | –0.174 | –0.449 | –1.242 | –0.669 | –0.317 | –0.908 | –0.309 | 0.0836 | –0.463 | –0.440 | –1.007 | –0.283 |
| t-statistic | –0.645 | –1.107 | –0.183 | –0.552 | –1.558 | –0.892 | –0.394 | –1.230 | –0.382 | 0.087 | –0.549 | –0.553 | –1.017 | –0.406 |
| Constant | ||||||||||||||
| Coefficient | 451.9*** | 470.5*** | 348.1*** | 371.4*** | 808.0*** | 361.5*** | 681.1*** | 471.3*** | 452.8*** | 230.7*** | 470.8*** | 433.9*** | 587.4*** | 370.2*** |
| t-statistic | 5.440 | 5.132 | 5.107 | 3.558 | 6.482 | 4.016 | 3.737 | 2.902 | 8.245 | 7.842 | 5.066 | 3.985 | 3.537 | 3.529 |
| N | 52,598 | 29,706 | 22,892 | 42,469 | 9694 | 25,749 | 26,849 | 22,734 | 18,144 | 11,720 | 30,350 | 22,144 | 18,220 | 34,378 |
| R 2 | 0.523 | 0.533 | 0.510 | 0.500 | 0.593 | 0.556 | 0.483 | 0.530 | 0.520 | 0.513 | 0.527 | 0.517 | 0.559 | 0.499 |
| F-statistic | 6.166 | 9.002 | 3.589 | 1.916 | 13.85 | 2.445 | 3.271 | 1.586 | 12.47 | 5.449 | 5.579 | 6.473 | 2.954 | 2.064 |
| High BP | ||||||||||||||
| Treatment | ||||||||||||||
| Coefficient | –0.015 | –0.024 | –0.002 | –0.011 | –0.056** | –0.035* | 0.004 | –0.037 | 0.005 | –0.003 | –0.015 | –0.011 | –0.022 | –0.011 |
| t-statistic | –0.702 | –1.207 | –0.0847 | –0.479 | –2.284 | –1.748 | 0.154 | –1.579 | 0.203 | –0.098 | –0.694 | –0.458 | –0.918 | –0.542 |
| Constant | ||||||||||||||
| Coefficient | 10.15*** | 11.72** | 1.104*** | 9.542* | 12.66*** | 9.910** | 8.017* | 9.161 | 12.87*** | –0.0831 | 9.289** | 11.47** | 9.338** | 10.73 |
| t-statistic | 3.031 | 2.656 | 3.474 | 2.058 | 7.779 | 2.669 | 1.857 | 1.658 | 3.621 | –0.119 | 2.237 | 2.441 | 2.590 | 1.638 |
| N | 52,595 | 29,704 | 22,891 | 42,466 | 9694 | 25,749 | 26,846 | 22,732 | 18,144 | 11,719 | 30,349 | 22,142 | 18,218 | 34,377 |
| R 2 | 0.389 | 0.397 | 0.378 | 0.382 | 0.406 | 0.407 | 0.371 | 0.390 | 0.386 | 0.390 | 0.389 | 0.389 | 0.404 | 0.379 |
| F-statistic | 3.539 | 2.602 | 2.121 | 1.513 | 29.19 | 3.525 | 1.602 | 2.775 | 5.360 | 0.131 | 1.586 | 3.732 | 3.567 | 1.770 |
Body mass index
The results for BMI are presented in Table 10. The estimated treatment effects, both overall and for the subgroups, are close to zero and are insignificant. This suggests that the intervention had no effect on weight changes in the patient group under consideration.
| Variable | Overall model (1) | Subgroup analysis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Ethnicity | Age | Comorbidities | BMI | Deprivation decile | |||||||||
| Men (2) | Women (3) | White (4) | Non-white (5) | ≤ 55 years (6) | > 55 years (7) | 0 (8) | 1 (9) | ≥ 2+ (10) | Not obese (11) | Obese (12) | Most deprived (13) | Least deprived (14) | ||
| Treatment | ||||||||||||||
| Coefficient | –0.0821 | –0.153 | 0.00801 | –0.133 | 0.158 | –0.0351 | –0.122 | –0.0250 | –0.107 | –0.116 | –0.141 | –0.00609 | –0.165 | –0.110 |
| t-statistic | –0.643 | –0.992 | 0.0690 | –0.943 | 1.187 | –0.251 | –0.971 | –0.232 | –0.559 | –0.703 | –0.797 | –0.053 | –0.553 | –0.411 |
| Constant | ||||||||||||||
| Coefficient | 35.50** | 29.89** | 45.98** | 46.48** | –0.524 | 32.50** | 40.63* | 35.78 | 29.29 | 74.33*** | 28.97 | 43.31** | 59.04*** | 19.86 |
| t-statistic | 2.704 | 2.095 | 2.292 | 2.366 | –0.0206 | 2.360 | 1.836 | 1.379 | 1.278 | 25.532 | 1.327 | 2.136 | 3.060 | 0.920 |
| N | 51,873 | 29,427 | 22,446 | 42,189 | 9276 | 25,037 | 26,836 | 22,104 | 18,065 | 11,704 | 29,919 | 21,861 | 17,104 | 34,769 |
| R 2 | 0.888 | 0.881 | 0.891 | 0.878 | 0.922 | 0.894 | 0.879 | 0.892 | 0.888 | 0.882 | 0.888 | 0.885 | 0.800 | 0.836 |
| F-statistic | 10.78 | 7.821 | 4.072 | 7.076 | 3.075 | 0.146 | 6.998 | 1.433 | 4.527 | 74.63 | 10.09 | 5.552 | 2.594 | 16.93 |
Cholesterol levels
The results for cholesterol levels are presented in Table 11. The estimates are largely negative, but are mostly close to zero and statistically insignificant. There is a statistically significant (but small) estimate those aged > 55 years only.
| Variable | Overall model (1) | Subgroup analysis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Ethnicity | Age | Comorbidities | BMI | Deprivation decile | |||||||||
| Men (2) | Women (3) | White (4) | Non-white (5) | ≤ 55 years (6) | > 55 years (7) | 0 (8) | 1 (9) | ≥ 2+ (10) | Not obese (11) | Obese (12) | Most deprived (13) | Least deprived (14) | ||
| Treatment | ||||||||||||||
| Coefficient | –0.0159 | –0.0178 | –0.0119 | –0.0198 | –0.0605 | 0.00679 | –0.0349* | –0.0205 | 0.0120 | –0.0475 | –0.00477 | –0.0279 | –0.0283 | –0.00824 |
| t-statistic | –1.051 | –1.079 | –0.414 | –1.060 | –1.619 | 0.323 | –2.027 | –0.837 | 0.490 | –1.536 | –0.251 | –1.290 | –0.836 | –0.437 |
| Constant | ||||||||||||||
| Coefficient | 16.80* | 17.41 | 17.88*** | 9.502 | 48.61** | 8.604 | 42.00*** | 3.833 | 35.91** | 2.968*** | 14.95 | 19.01** | 14.02** | 18.71 |
| t-statistic | 1.806 | 1.519 | 3.050 | 0.818 | 2.361 | 0.845 | 6.493 | 0.231 | 2.383 | 2.933 | 0.807 | 2.477 | 2.548 | 1.065 |
| N | 47,911 | 27,387 | 20,524 | 38,776 | 8751 | 22,893 | 25,018 | 20,653 | 16,521 | 10,737 | 27,538 | 20,291 | 16,436 | 31,475 |
| R 2 | 0.688 | 0.678 | 0.683 | 0.690 | 0.684 | 0.673 | 0.688 | 0.692 | 0.690 | 0.679 | 0.675 | 0.708 | 0.692 | 0.687 |
| F-statistic | 25.26 | 26.36 | 4.050 | 18.13 | 3.468 | 1.224 | 24.63 | 9.604 | 17.64 | 3.764 | 20.33 | 4.253 | 5.892 | 9.281 |
Smoking status
The results for smoking status are presented in Table 12. Counterintuitively, the results are mostly positive, with some results achieving statistical significance, although, once again, the estimated coefficients are small. These results suggest that the intervention increased the probability of being a current smoker. However, the graphs for the smoking outcome (see Appendix 5, Figures 13 and 16) suggest that the parallel trends assumption is violated for this outcome. The falsification test suggests a clear gradient, with the treatment group increasingly likely to smoke over the observational time period.
| Variable | Overall model (1) | Subgroup analysis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Ethnicity | Age | Comorbidities | BMI | Deprivation decile | |||||||||
| Men (2) | Women (3) | White (4) | Non-white (5) | ≤ 55 years (6) | > 55 years (7) | 0 (8) | 1 (9) | ≥ 2+ (10) | Not obese (11) | Obese (12) | Most deprived (13) | Least deprived (14) | ||
| Treatment | ||||||||||||||
| Coefficient | 0.0113 | 0.0176* | 0.00287 | 0.00862 | 0.0000645 | 0.0157** | 0.00738 | 0.00852 | 0.0232** | –0.00348 | 0.0128 | 0.0109 | 0.0134 | 0.0116 |
| t-statistic | 1.612 | 1.954 | 0.375 | 1.269 | 0.00406 | 2.372 | 0.733 | 1.197 | 2.369 | –0.239 | 1.674 | 1.253 | 0.911 | 1.554 |
| Constant | ||||||||||||||
| Coefficient | 4.369 | 1.481 | 16.81 | 5.278 | –0.0377 | 1.289 | 17.28 | 2.370 | 8.014 | –1.937*** | 2.125* | 7.144 | 7.629 | 2.258 |
| t-statistic | 1.057 | 0.535 | 1.558 | 1.068 | –0.0739 | 0.485 | 1.599 | 1.286 | 0.778 | –4.398 | 1.719 | 0.709 | (1.152 | (0.599 |
| N | 48,698 | 27,696 | 21,002 | 39,641 | 8679 | 23,848 | 24,850 | 20,640 | 16,903 | 11,155 | 28,564 | 20,038 | 16,900 | 31,798 |
| R 2 | 0.787 | 0.778 | 0.799 | 0.780 | 0.819 | 0.799 | 0.764 | 0.793 | 0.791 | 0.767 | 0.790 | 0.773 | 0.796 | 0.782 |
| F-statistic | 4.004 | 2.391 | 0.936 | 4.646 | 0.171 | 2.948 | 8.555 | 0.676 | 7.749 | 8.813 | 6.030 | 0.662 | 0.602 | 4.615 |
Health-care costs
In this section, we present the results from the ITT analysis of health-care costs using TPMs. A priori, we may expect the intervention to reduce A&E and inpatient non-elective use and costs, as individuals become better at managing their conditions with link worker support. For inpatient elective, outpatients and overall costs, the direction of effect could be either positive or negative. More planned use of health care may result from better condition management and link worker support. Although the assumption of parallel trends is more complicated for non-linear models, it can still be of interest to consider the pre-treatment and post-treatment trends. Appendix 7, Figures 17–21, and Appendix 8, Figures 22–26, show the unconditional plots for use, expenditure (see Appendix 7, Figure 17) and for the estimated falsification treatment effects from the TPM (see Appendix 8, Figure 22).
For the regression models, we alter our subgroup analysis slightly because of the reduced sample sizes that arise owing to the low number of individuals using health-care services during the year, which.
Regression results
The TPM ITT results are presented in Table 13. Each column represents the outcome of interest, and the rows represent the average treatment effect on the treated (marginal effects) results from separate regressions (and the associated t-statistics) for models controlling for age, sex at birth and GP fixed effects. The first row shows the overall result, using the whole sample. Subsequent rows give the results from the subgroup analysis. Nearly all of the estimated treatment effects are negative and very few demonstrate statistical significance. However, there are some large estimates with potentially economic significance. For example, individuals with no extra comorbidities (beyond T2DM) see a treatment effect of around –£50, compared with the control groups, for inpatient non-elective costs, and around –£72 for total costs. These represent 16% of the value of the mean inpatient non-elective costs and 7% of the mean total costs. In context, there are approximately 3778 individuals in our total sample with no extra comorbidities. In context, there are approximately 3778 individuals in our total sample with no extra comorbidities, costing approximately £1,183,609 (total £3,992,402) a year, measured at the mean of inpatient non-elective (total) costs. Applying the reduction from treatment would reduce expenditure to £994,710 (total £3,720,386), a saving of approximately £189,000 (total £272,000). Other potentially economically significant results can be seen for the ethnically non-white group and those aged > 55 years. These results suggest that, despite the fact that we have a large sample, there is still a possibility that the study is underpowered for some of the subgroup analyses.
| Variable | Subgroup analysis, treatment costs (£) | Total cost (£) | |||
|---|---|---|---|---|---|
| Inpatient | Outpatient | A&E | |||
| Non-elective | Elective | ||||
| Overall | |||||
| Coefficient | –8.516 | –28.83 | –11.38 | –2.033 | –31.93 |
| t-statistic | –0.280 | –1.245 | –1.339 | –0.950 | –0.801 |
| Gender | |||||
| Men | |||||
| Coefficient | –26.15 | –19.64 | –8.927 | –2.839 | –38.34 |
| t-statistic | –0.579 | –0.745 | –0.765 | –1.344 | –0.722 |
| Women | |||||
| Coefficient | 7.138 | –44.06 | –15.36 | –1.104 | –32.04 |
| t-statistic | 0.135 | –1.382 | –0.974 | –0.336 | –0.497 |
| Deprivation decile | |||||
| Least deprived | |||||
| Coefficient | –23.95 | –31.08 | –0.516 | –2.869 | –7.192 |
| t-statistic | –0.594 | –0.998 | –0.0417 | –0.956 | –0.145 |
| Most deprived | |||||
| Coefficient | –4.190 | –27.32 | –20.69** | –1.710 | –65.90 |
| t-statistic | –0.114 | –0.915 | –1.995 | –0.618 | –1.107 |
| Comorbidities | |||||
| No | |||||
| Coefficient | –50.35 | –13.41 | –16.13 | –5.137 | –72.32 |
| t-statistic | –1.360 | –0.391 | –1.273 | –1.634 | –1.122 |
| Extra | |||||
| Coefficient | 18.22 | –42.69 | –6.869 | –0.143 | –4.005 |
| t-statistic | 0.395 | –1.210 | –0.561 | –0.0529 | –0.0814 |
| Ethnicity | |||||
| White | |||||
| Coefficient | –9.082 | –30.14 | –9.482 | –2.126 | –27.36 |
| t-statistic | –0.242 | –1.096 | –1.197 | –1.096 | –0.630 |
| Non-white | |||||
| Coefficient | –39.94 | –77.24 | –35.62 | –3.997 | –105.1 |
| t-statistic | –0.652 | –1.325 | –0.984 | –0.653 | –0.627 |
| Age | |||||
| ≤ 55 years | |||||
| Coefficient | –11.47 | –21.83 | –17.50 | –0.218 | –37.26 |
| t-statistic | –0.340 | –0.785 | –1.464 | –0.0690 | –0.736 |
| > 55 years | |||||
| Coefficient | –27.81 | –35.53 | –2.151 | –3.945 | –17.59 |
| t-statistic | –0.388 | –0.938 | –0.131 | –1.365 | –0.224 |
Alternative treatment groups
In this section, we repeat the overall analysis using the alternative treatment groups, as outlined in Table 3. Given that this analysis will reduce the sample size further, we restrict our analysis to the overall treatment effect, allowing us to use the largest possible sample for each estimation. By considering as treated only those individuals who receive treatment, we are also able to take into consideration, to an extent, the ‘dose’ of treatment that an individual receives. This ‘dose’ is based on whether or not an individual has attended their second goal-setting meeting with their link worker. These second meetings usually take place around 6–9 months after the first goal-setting meeting and attendance suggests that an individual has stayed engaged, at least to some degree, with the intervention for that period of time. This enables us to form two treatment groups: those who attended their first objective-setting meeting, and so had initial interaction with their link worker, and those who had two or more objective-setting meetings with their link worker.
Tables 14 and 15 show the results for the alternative treatment groups for the health outcomes and cost outcomes. In column (1) we compare the ‘early treated’ with the ‘late treated’, and columns (2) and (3) show the estimates for the treated patients in the treatment practices compared with the non-treated within the same practices. Column (2) shows the results for when treatment is defined as having had the first objective-setting meeting and column (3) shows the results for when treatment is defined as having two or more goal-setting meetings. Columns (4) and (5) show the results, using the same two definitions of treatment, when comparing those treated in treatment practices with those in non-treatment practices. The results vary according to the treatment definitions. For the health outcomes, the estimates are largely similar to the overall results, with estimates that are small in magnitude and mostly insignificant. An exception is the results for level of cholesterol, which were negative and significant, but still small in magnitude.
| Variable | Treatment group | ||||
|---|---|---|---|---|---|
| τ^1 | τ^2 | τ^2(a) | τ^3a | τ^3a(a) | |
| (1) | (2) | (3) | (4) | (5) | |
| HbA1c level (mmol/mol) | |||||
| Coefficient | –0.972 | 0.353 | 0.264 | –0.863* | –0.948 |
| t-statistic | –1.383 | 0.840 | 0.519 | –1.767 | –1.567 |
| N | 5668 | 29,000 | 26,353 | 29,095 | 26,448 |
| High blood pressure (mmHg) | |||||
| Coefficient | –0.011 | –0.026 | –0.033* | –0.034 | –0.040* |
| t-statistic | –0.401 | –1.652 | –1.924 | –1.596 | –1.921 |
| N | 6130 | 31,036 | 28,177 | 30,369 | 27,510 |
| BMI (kg/m2) | |||||
| Coefficient | 0.159 | 0.236 | 0.299* | 0.126 | 0.186 |
| t-statistic | 0.988 | 1.768 | 1.854 | 0.761 | 1.054 |
| N | 6220 | 29,988 | 27,192 | 30,670 | 27,874 |
| Cholesterol level (mmol/l) | |||||
| Coefficient | –0.000394 | –0.0663* | –0.0726* | –0.0620* | –0.0692* |
| t-statistic | –0.0101 | –1.853 | –1.881 | –1.838 | –1.808 |
| N | 5501 | 28,162 | 25,562 | 27,816 | 25,216 |
| Smoking status | |||||
| Coefficient | 0.00432 | –0.00411 | –0.00950 | 0.00890 | 0.00310 |
| t-statistic | 0.498 | –0.587 | –1.588 | 1.196 | 0.411 |
| N | 5625 | 28,679 | 26,045 | 28,201 | 25,567 |
| Variable | Treatment group | ||||
|---|---|---|---|---|---|
| τ^1 | τ^2 | τ^2(a) | τ^3a | τ^3a(a) | |
| (1) | (2) | (3) | (4) | (5) | |
| Inpatient non-elective | |||||
| Coefficient | –61.81 | –30.75 | –53.00 | –33.44 | –50.71 |
| t-statistic | –0.951 | –0.902 | –1.220 | –0.932 | –1.133 |
| N | 1290 | 5492 | 3696 | 5492 | 3696 |
| Inpatient elective | |||||
| Coefficient | 42.91 | 1.942 | 14.49 | –28.02 | –15.41 |
| t-statistic | 0.813 | 0.0572 | 0.402 | –1.063 | –0.517 |
| N | 1290 | 5492 | 3696 | 5492 | 3696 |
| Outpatient | |||||
| Coefficient | 56.54* | 8.061 | 7.848 | –4.295 | –4.358 |
| t-statistic | 1.762 | 0.548 | 0.464 | –0.321 | –0.280 |
| N | 1290 | 5492 | 3696 | 5492 | 3696 |
| A&E | |||||
| Coefficient | 0.700 | –4.736* | –7.309** | –5.127** | –7.543*** |
| t-statistic | 0.202 | –1.935 | –2.543 | –2.113 | –2.777 |
| N | 1290 | 5492 | 3696 | 5492 | 3696 |
| Total | |||||
| Coefficient | 41.79 | –7.570 | –23.95 | –41.01 | –52.66 |
| t-statistic | 0.328 | –0.121 | –0.389 | –0.920 | –1.092 |
| N | 1290 | 5492 | 3696 | 5492 | 3696 |
The results for the expected health-care costs are of more interest. Those who received treatment early experienced increases in their inpatient elective and outpatient care costs following treatment, compared with those who received treatment late. The same results are observed when comparing patients within the treated practices [columns (2) and (3)]. This was hypothesised as a possible outcome as individuals became better at managing their health and used more planned health-care services (rather than emergency services). For non-elective inpatient admissions and for A&E use, the treated saw large and, in the case of A&E services, significant reductions in their health-care costs. The impact was greatest for those individuals who had completed at least two goal-setting meetings.
Time-varying treatment allocation and treatment heterogeneity
As discussed in Methods, Treatment and control groups, the standard two-way fixed-effects model cannot be used to estimate treatment effects when the treatment is allocated at different points in time and there may be treatment heterogeneity. For this reason, thus far we have used ITT-based estimates in which it is assumed that treatment occurs at the same time for all individuals. With linear models, such as those used for the health outcomes, it is possible to estimate models that account for timing of treatment and potential treatment heterogeneity. However, this approach cannot be applied to the TPMs and, therefore, we cannot address this issue for the health-care use and costs elements.
We implemented the de Chaisemartin and D’Haultfoeuille78 estimator to investigate the impact of treatment timing and treatment heterogeneity on the health outcomes. The results are presented in Table 16. The results show treatment effects relative to the time that the treatment first changed, alongside a pre-treatment placebo estimate. There are no estimates for the early compared with the late treated for time period T + 3 because of the small sample size for this comparison. The t-statistics are estimated using a bootstrap procedure with 50 replications.
| Variable | Treatment time | |||||
|---|---|---|---|---|---|---|
| T – 2 | T – 1 | T | T + 1 | T + 2 | T + 3 | |
| HbA1c level | ||||||
| τ^1 | ||||||
| Coefficient | –0.80 | 0 | –1.54*** | –4.05*** | –7.59 | |
| t-statistic | –1.29 | 0 | –2.03 | –2.91 | –1.55 | |
| n | 2155 | 2421 | 1280 | 462 | ||
| τ^2 | ||||||
| Coefficient | –0.98*** | 0 | –0.66 | –1.51*** | –1.87*** | –2.87*** |
| t-statistic | –2.33 | 0 | –1.50 | –2.65 | –2.34 | –2.76 |
| n | 12,290 | 13,436 | 9424 | 5832 | 2721 | |
| τ^3a | ||||||
| Coefficient | –0.72 | 0 | –0.99* | –3.10*** | –4.57*** | –3.69*** |
| t-statistic | –1.26 | 0 | –1.68 | –3.41 | –3.17 | –3.51 |
| n | 12,534 | 13,658 | 9588 | 5978 | 2802 | |
| Probability of having high blood pressure | ||||||
| τ^1 | ||||||
| Coefficient | –0.02 | 0 | –0.03 | 0.01 | 0.03 | |
| t-statistic | –0.47 | 0 | –1.25 | 0.17 | 0.23 | |
| n | 2489 | 2661 | 1426 | 517 | ||
| τ^2 | ||||||
| Coefficient | –0.01 | 0 | –0.01 | –0.04* | –0.03 | –0.11*** |
| t-statistic | –0.39 | 0 | –0.88 | –1.71 | –1.01 | –2.64 |
| n | 13,743 | 14,472 | 10,258 | 6471 | 3065 | |
| τ^3a | ||||||
| Coefficient | –0.01 | 0 | –0.01 | –0.02 | 0.00 | –0.10*** |
| t-statistic | –0.34 | 0 | –0.67 | –0.72 | –0.02 | –2.68 |
| n | 13,943 | 14,684 | 10,426 | 6557 | 3079 | |
| BMI | ||||||
| τ^1 | ||||||
| Coefficient | 0.01 | 0 | 0.27 | 0.59 | 1.03 | |
| t-statistic | 0.07 | 0 | 1.17 | 1.07 | 0.64 | |
| n | 2149 | 2324 | 1246 | 455 | ||
| τ^2 | ||||||
| Coefficient | –0.05 | 0 | 0.20* | –0.03 | –0.19 | 0.24 |
| t-statistic | –0.45 | 0 | 1.67 | –0.14 | –1.06 | 0.96 |
| n | 11,627 | 12,438 | 8814 | 5510 | 2648 | |
| τ^3a | ||||||
| Coefficient | –0.03 | 0 | 0.32* | 0.55 | 0.53 | 0.16 |
| t-statistic | –0.18 | 0 | 1.78 | 1.49 | 0.95 | 0.73 |
| n | 12,374 | 13,124 | 9296 | 5845 | 2810 | |
| Cholesterol level | ||||||
| τ^1 | ||||||
| Coefficient | –0.05 | 0 | –0.04 | –0.12 | –0.02 | |
| t-statistic | –1.25 | 0 | –0.80 | –1.50 | –0.125 | |
| n | 2089 | 2265 | 1207 | 447 | ||
| τ^2 | ||||||
| Coefficient | 0.01 | 0 | –0.06*** | –0.11*** | –0.10** | –0.21*** |
| t-statistic | 0.33 | 0 | –3.00 | –3.67 | –2.00 | –3.00 |
| n | 11,490 | 12,314 | 8736 | 5508 | 2623 | |
| τ^3a | ||||||
| Coefficient | –0.02 | 0 | –0.03 | –0.10** | –0.05 | –0.15*** |
| t-statistic | –0.67 | 0 | –1.00 | –2.00 | –0.625 | –2.14 |
| n | 11,894 | 12,832 | 9121.00 | 5785 | 2768 | |
| Probability of being a current smoker | ||||||
| τ^1 | ||||||
| Coefficient | –0.02** | 0 | –0.01 | 0.04 | 0.05 | |
| t-statistic | –2.00 | 0 | –1.00 | 1.00 | 0.56 | |
| n | 2102.00 | 2247.00 | 1216.00 | 443.00 | ||
| τ^2 | ||||||
| Coefficient | –0.01 | 0 | –0.01 | 0.00 | 0.00 | 0.00 |
| t-statistic | –1.00 | 0 | –1.00 | 0.30 | –0.10 | –0.20 |
| n | 11,573.00 | 12,254.00 | 8737.00 | 5530.00 | 2676.00 | |
| τ^3a | ||||||
| Coefficient | –0.01 | 0 | –0.01 | 0.02 | 0.02 | 0.003 |
| t-statistic | –1.00 | 0 | –0.50 | 0.67 | 0.50 | 0.10 |
| n | 12,176.00 | 12,910.00 | 9158.00 | 5790.00 | 2766.00 | |
The results are qualitatively similar and generally larger than the estimates from the ITT analysis. For example, for levels of HbA1c, the estimated treatment effect can be as high as –7.59 mmol/mol; however, this is not significant, probably because of the small number of observations in this switching period. This is considerably higher than any of the ITT analysis estimates. Where sample sizes are larger, the estimates are still around –1.51 to –4.57 mmol/mol, suggesting that the intervention has made a significant impact on the level of HbA1c. There are similar results for the probability of having high blood pressure, with estimates 3 years after treatment ranging between –0.10 and –0.11, suggesting a 10- to 11-percentage-point reduction in the probability of having high blood pressure. There are some small effects for cholesterol levels, but no clear effects for BMI or smoking status, for which the results are far more mixed.
Discussion
This chapter reports an investigation into the impact of the intervention on a range of health-care and secondary care outcomes. Using a range of regression methods, applied to different definitions of treatment and control groups, we exploited the geographical implementation of the intervention as a quasi-natural experiment. To the best of our knowledge, this has resulted in, to date, the largest and most robust investigation into the impact of social prescribing on selected health outcomes and health-care costs.
The results from this part of the SPRING_NE study are, perhaps unsurprisingly, mixed. Consistent results are seen throughout for levels of HbA1c and blood pressure. Unsurprisingly, the impact of the intervention on these two outcomes depends on which treatment and control groups are specified. The overall estimate for the impact of social prescribing on HbA1c levels using the ITT analysis was –1.11 mmol/mol; accounting for the time-varying nature of treatment on the treated, we saw estimates (that were statistically significant) as high as a –4.57 mmol/mol reduction in levels of HbA1c. At the pre-treatment mean of 57.63 mmol/mol (calculated using the full sample), these results represent a reduction in HbA1c levels of between 2% (not clinically significant) and 8% (clinically significant) compared with the control group. Given that glycaemic control has a significant effect on long-term health and that even small reductions in HbA1c levels can reduce long-term macrovascular and microvascular complications,86–88 these are potentially meaningful results. For the probability of having high blood pressure, similar results were observed. The overall ITT results suggested a (not statistically significant) 1.5-percentage-point decrease in the probability of high blood pressure, compared with the control group, with estimates as high as an 11-percentage-point reduction 3 years post treatment.
For both HbA1c levels and high blood pressure, there were some particularly encouraging results for individuals living in the most deprived areas (estimates as high as –2.1 mmol/mol for reductions in levels of HbA1c and –5.5 percentage points for reductions in high blood pressure) and those individuals who are ethnically non-white (with estimates as high as –5.6 percentage points for high blood pressure). Given the nature of the intervention and the attempt to target inequalities and ethnically diverse groups, these results are promising.
For the other health outcomes, the results are more mixed, with little evidence of the intervention having an effect. This could be the case, first, because the intervention is having no effect on these outcomes or, second, because the intervention takes longer to have an impact on these outcomes. Both of these alternatives seem unlikely. Indeed, it is probably more likely that BMI and smoking behaviour see an immediate response to a social prescribing intervention. A more credible explanation is that levels of HbA1c and blood pressure are well measured by general practices because of the QOF targets, and resulting financial incentives, for these outcomes. Levels of HbA1c and blood pressure are also measured and recorded by a health-care professional (HCP). Smoking status is self-reported. Height and weight data used to calculate BMI are, at least in our data set, poorly recorded. For these reasons, we may be observing results for HbA1c and blood pressure purely because of the more reliable and effective measurement.
Whether or not the changes seen in health outcomes are reflected in changes in health-care use and cost is a difficult question to answer. The evidence from our analysis is mixed; many of the estimates attached to the expected costs analysis are negative, and potentially large, but not statistically significant. The lack of precision in the estimates suggests that the study, even based on a large number of patients, is underpowered to detect changes in secondary care costs. For the overall models, we have estimates for inpatient non-elective care ranging from £18.22 (for individuals with an extra comorbidity) to –£50.35 (for individuals with no extra comorbidity), but neither of these estimates is statistically different from zero, despite the fact that the latter represents approximately 16% of the pre-treatment mean inpatient non-elective costs. That scale of potential effect, although not statistically significant, may be economically significant. Furthermore, there are some large estimates for the ethnically non-white group (but again they are not statistically significant).
Similar issues are observed when we consider the different treatment groups: large, potentially economically significant, estimates are observed for inpatient non-elective care but, again, they are not statistically significant. There is a clear suggestion that, compared with the controls in the same general practice (τ1, τ2 and τ2(a)), there is a shift from unplanned care (i.e. non-elective and A&E admissions) to planned care (i.e. elective and outpatient care). However, once again, power appears to be an issue, with the numbers of treated being only around 1300 to 5500 individuals.
Social prescribing is a heterogeneous intervention aimed at tackling the social as well as behavioural determinants of disease. It is not a medical intervention that is targeting clinical outcomes. In the light of this fact, these results demonstrate some promise for social prescribing. Given the diverse nature of the intervention and the fact that we are relying on routinely collected data, it is unsurprising that the results are often mixed. However, there are some consistent messages that appear, especially in relation to levels of HbA1c, blood pressure and the direction of the health-care cost estimates.
There appears to be heterogeneity in who benefits most from social prescribing, with evidence that the ethnically non-white and those living in the most deprived areas are experiencing benefits, although this depends on the outcome measured. There is also evidence that individuals without extra comorbidities are seeing benefits from the intervention. The benefits are not observed uniformly and there is no clear reason as to why some groups may benefit more than others.
There are some important issues to consider when interpreting these findings. We have already commented on power issues in relation to the health-care use data, but there are other potential limitations. First, the data in the QOF can be sparse and unreliable. Although we may be confident that levels of HbA1c and blood pressure are well recorded, there are still concerns that these records are affected by gaming and exceptions because of the incentives of the QOF targets. 89 Our measure of total cholesterol level is not split into ‘good’ high-density lipoprotein (HDL) and ‘bad’ low-density lipoprotein (LDL) cholesterol, and the other QOF measures are less affected by targets and, therefore, may be poorly recorded overall. Furthermore, the QOF data on the socioeconomic characteristics can also be inconsistent; this is especially true of the self-reported ethnicity data, which do not allow us to split ethnicity into anything more specific than white and non-white. 90 Second, data availability was further hindered by the fact that seven general practices (three providing treatment and four controls) were unwilling to share data with us. Although we covered 80% of all referrals in the time period considered, it would have been preferable for all general practices to share data. As individual patient characteristics were taken from the QOF, the refusal to share data affected the available sample sizes across all data analysis. Furthermore, with no reason given for refusal, we cannot be sure that refusal was unrelated to the intervention and outcomes, although we have no reason to believe it was. Third, we cannot observe the nature or the dose of treatment beyond whether an individual attended one or more goal-setting meetings. This means that we cannot comment on the intensity of link worker involvement or on onward referrals. Fourth, we were able to obtain information about only those comorbidities that determined eligibility for the intervention. As a result, other comorbidities are not reported. This meant that the true extent of comorbidity could not be analysed. Fifth, although we have investigated the robustness of our estimates, it is still possible that there are unobserved factors that could vary over time that introduce bias. For example, although we can control for general practice fixed effects, we cannot control for GP fixed effects and it is possible that some GPs treat some patients’ conditions more aggressively than others. Finally, for the secondary data use we were unable to obtain data for more than 2 years prior to treatment, leading to less precision in our estimates. The original intention was to cover the same time period for which QOF data were available, but, because of organisational issues resulting from the COVID-19 pandemic, it was not possible to obtain the extra data. The COVID-19 problem also applies to our follow-up data: our initial intention had been to follow individuals post treatment until 31 March 2020, but collection of these data was also subsequently affected by the onset of COVID-19.
Chapter 3 Health-related quality of life
Introduction
In this chapter, we present the findings on HRQoL collected via self-report using the EQ-5D-5L,91,92 which consists of the EQ-5D-5L descriptive system and the EQ visual analogue scale (EQ-VAS). The descriptive system comprises five dimensions, each of which has five levels, and the respondent is required to choose one level that best describes their health on that day. The dimensions of mobility, self-care and usual activities use level 1 = no problems, level 2 = slight problems, level 3 = moderate problems, level 4 = severe problems and level 5 = unable; and the dimensions of pain/discomfort and anxiety/depression use level 1 = no, level 2 = slight, level 3 = moderate, level 4 = severe and level 5 = extreme.
An EQ-5D-5L summary health state value, which reflects how good or bad a health state is overall, can be derived by applying a weighting system to an individual’s scores on the five dimensions that have been developed based on country-specific general population preferences for different health states. Health state values for England range from −0.285 (extreme problems on all dimensions) to 1 (no problems in any dimension);93 a higher EQ-5D-5L health state summary value reflects a better health state. We chose to map the EQ-5D-5L to the EQ-5D-5L value set93 rather than to the EQ-5D-3L value set,94 as recommended by NICE (National Institute for Health and Care Excellence), because of the wider range of possible health profiles that the EQ-5D-5L value set can detect. Social prescribing is a heterogeneous intervention and we wanted to use a measure that reflect complex health states and would allow us to characterise the health of individuals using a more sensitive descriptive system. 95
In addition to the EQ-5D-5L descriptive system, the EQ-VAS was used as a judgement of current health on a visual analogue scale from 0 to 100 (i.e. worst health you can imagine to best health you can imagine).
Design and methods
This part of the SPRING_NE study was a within-cohort comparison of individuals referred into the intervention who attended an initial meeting with a link worker within the 12-month period from July 2018 to June 2019. Follow-up occurred at 12 months (from July 2019 to June 2020). Unlike the other WPs, this study included participants with any of the WtW-specified LTCs, not just those with a T2DM diagnosis. Clients were recruited by link workers at their initial (baseline) interview, informed about the study and asked to complete the EQ-5D-5L questionnaire. If necessary, this was carried out with link worker assistance. For those who required a version in a language other than English, a translated information leaflet was provided and a translated EQ-5D-5L version was administered (n = 6). Provider organisations were reimbursed for link worker time in administering the EQ-5D-5L. Anonymised completed questionnaires were securely stored at each provider organisation and collected monthly by a member of the research team. Data were entered into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet, checked and cleaned.
At the 12-month follow-up, an information leaflet and the EQ-5D-5L questionnaire were posted to participants with a stamped addressed envelope for return to the research team. At 12 days, non-responders were telephoned and asked to complete and return the questionnaire, with the option to complete by telephone with the research administrator (Allison Lawson). For participants with a language other than English who wished to complete the questionnaire by telephone, a telephone translation was arranged (n = 5). As a result of national lockdown restrictions imposed because of COVID-19, from April 2020 all follow-up questionnaires were completed by telephone to avoid participants having to leave their homes.
As a result of the potential effects of the pandemic on HRQoL, the data set is separated into two groups: data from those who completed their follow-up questionnaire prior to the pandemic and lockdown (i.e. pre COVID-19: using 28 February 2020 as the cut-off point) and those who completed their follow-up questionnaire between March and June 2020 (i.e. post COVID-19).
Analysis
Descriptive statistics were computed on the demographic variables of the sample at the different assessment points and for the pre-COVID-19 and post-COVID-19 groups. Two-sample t-tests explored differences in demographic variables between the groups. Descriptive statistics on the EQ-5D-5L, EQ-5D-5L health state summary value and EQ-VAS were computed. Paired-sample t-tests were conducted to examine differences between the EQ-5D-5L variables at baseline and the EQ-5D-5L variables at follow-up for the pre-COVID-19 and post-COVID-19 groups separately. Linear regression analyses were conducted to explore whether or not participant characteristics could explain differences in EQ-5D-5L scores from baseline to follow-up.
Finally, to investigate the impact of COVID-19 on the EQ-5D-5L and the EQ-VAS we applied a regression discontinuity design (RDD) to the change in EQ-5D-5L and the change in EQ-VAS scores from baseline to follow-up. Using the change in health status allowed us to control for baseline health. The RDD approach relies on the identification of the treatment effect based on the fact that there is a (potential) discontinuity in the data. The assumption is that individuals who report outcomes just below the point of the discontinuity are similar to individuals who report outcomes just after the point of the discontinuity. In this case, the only factor that should affect a change in responses is the discontinuity itself. 77 In this case, the discontinuity, which we define as March, is provided by the onset of the COVID-19 pandemic and lockdown. Because we do not observe the day that respondents completed their questionnaire, only the month, we are unable to be more precise regarding the advent of COVID-19. We compared changes in health outcomes, between baseline and follow-up, between a treatment group, whose follow-up occurred during the initial COVID-19 lockdown (March–June), and a control group, whose follow-up occurred in the 4 months prior to the initial lockdown (November–February). With only small sample sizes it was not possible to have a narrower bandwidth around the discontinuity. The regression we estimate is:
where Δyit is the change in health status between follow-up and baseline (where a positive result indicates an increase in health status), Post_Covidi is a dummy variable indicating whether the follow-up occurred during the COVID-19 period (March–June) or the pre-COVID-19 period (November–February), Month is a linear time trend and Post_Covidi * Montht is an interaction term. The key parameters here are β1 and β3, which show where there is a significant shift in the level of reported health in the post-COVID-1996 period and whether there is a change in health during the months following the onset of COVID-19.
Sample
Of the 1265 participants who attended an initial meeting with a link worker and for whom demographic data were available, 694 completed a baseline assessment of self-reported HRQoL using the EQ-5D-5L (54.9% response rate). At the 12-month follow-up, 474 participants (68.3% response rate) completed a follow-up EQ-5D-5L.
Table 17 indicates that at baseline the sample was 54.2% female, the sample had a mean age of 59.1 years, just under 14% of the sample were from black and minority ethnic groups and almost 69% of the sample lived in the most deprived two deciles as indicated by IMD score. A similar demographic profile was seen in the follow-up sample in terms of gender and age, but slightly fewer respondents were from black and minority ethnic groups and lived in the two most deprived deciles. Both the baseline and the follow-up samples comprised just over 70% with one WtW referring condition, 22% with two conditions and around 5% with three or more conditions. Comparing the study sample with the sampling frame and to the WtW population, the gender, age and ethnic group profiles were similar. The profile related to the number of referring conditions differed somewhat, with the study sample presenting more WtW referring conditions, indicative of worse health, than the non-responders (those who did not take part in the EQ-5D study) or the WtW population. Deprivation data were not available for the sampling frame or WtW population, as these data were not routinely collected and, therefore, comparisons cannot be drawn.
| Variable | WtW referrals June 2018–May 2019 (n = 1660) | Attended first appointment (sampling frame) (n = 1265) | Baseline sample (n = 694) | Total 12-month follow-up sample (n = 474) | Pre-COVID-19 follow-up group (n = 347) | Post-COVID-19 follow-up group (n = 127) | p-valueb |
|---|---|---|---|---|---|---|---|
| Demographic characteristics | |||||||
| Female (%) | 52.83 | 52.96 | 54.18 | 52.53 | 52.16 | 53.54 | 0.790 |
| Mean age (years) (SD) | 58.95 | 58.9 | 59.07 (9.38) | 60.64 (9.31) | 61.33 (9.02) | 58.76 (9.88) | 0.008 |
| White British/Irish/other (%) | 87.83 | 86.40 | 86.17 | 89.87 | 91.64 | 85.04 | 0.035 |
| Top two IMD deciles (most deprived) (%) | – | – | 68.59 | 64.14 | 62.82 | 67.72 | 0.326 |
| Number of WtW referring conditions (%) | |||||||
| One condition | 78.25 | 75.04 | 71.19 | 72.36 | 71.18 | 75.59 | 0.439 |
| Two conditions | 21.36 | 20.93 | 22.62 | 21.94 | 23.05 | 18.90 | |
| Three or more conditions | 0.38 | 4.03 | 5.19 | 5.70 | 5.76 | 5.51 | |
Table 17 also presents demographic data and tests of difference between the follow-up sample divided according to whether the follow-up questionnaire was completed before or after 28 February 2020, the cut-off point used to disaggregate groups owing to effects of the COVID-19 pandemic. The post-COVID-19 follow-up group were significantly younger and comprised more black and minority ethnic respondents than the pre-COVID-19 follow-up group.
Table 18 presents descriptive statistics of EQ-5D-5L health state value and EQ-VAS at baseline and follow-up for full sample, pre-COVID-19 and post-COVID-19 groups, and by age groups. In addition, the final row of the table presents the UK population norm ratings by equivalent age groups. Overall, the sample in this study reported substantially worse current health at both baseline and follow-up than age-specific population norms. When comparing ratings at baseline with those at follow-up across all age groups, self-reported current health was marginally better at follow-up, with the exception of EQ-5D-5L health state score for those aged 55–64 years, for which a minimal worsening of health was observed. A similar pattern can be seen in the pre-COVID-19 and post-COVID-19 groups, with minimal improvements in the EQ-VAS over time. Within all age groups other than 65–74 years, the EQ-5D-5L health state scores worsened over time in the pre-COVID-19 group, but this pattern was evident only in the 45–54 years age group of the post-COVID-19 group.
| Variable | Age group | All ages | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 40–44 years | 45–54 years | 55–64 years | 65–74 years | |||||||
| EQ-5D value | EQ-VAS | EQ-5D value | EQ-VAS | EQ-5D value | EQ-VAS | EQ-5D value | EQ-VAS | EQ-5D value | EQ-VAS | |
| All, mean score (SD); n | ||||||||||
| Baseline | 0.657 (0.309); 60 | 60.98 (22.33); 60 | 0.637 (0.325); 172 | 54.99 (24.49); 172 | 0.562 (0.327); 221 | 53.56 (24.20); 221 | 0.626 (0.321); 241 | 60.29 (22.77); 241 | 0.611 (0.324); 694 | 56.89 (23.79); 694 |
| Follow-up | 0.664 (0.353); 37 | 63.69 (24.53); 39 | 0.643 (0.336); 85 | 56.57 (26.65); 88 | 0.556 (0.331); 146 | 55.67 (25.43); 148 | 0.654 (0.284); 195 | 65.31 (21.92); 198 | 0.622 (0.317); 463 | 60.53 (24.53); 473 |
| Pre COVID-19, mean score (SD); n | ||||||||||
| Baseline | 0.625 (0.326); 23 | 63.91 (23.60); 23 | 0.681 (0.324); 59 | 56.86 (25.23); 59 | 0.598 (0.319); 112 | 54.57 (24.21); 112 | 0.645 (0.299); 153 | 61.45 (21.13); 153 | 0.635 (0.312); 347 | 58.61 (23.18); 347 |
| Follow-up | 0.541 (0.399); 22 | 63.69 (23.97); 23 | 0.657 (0.344); 59 | 57.78 (26.86); 59 | 0.563 (0.330); 110 | 55.03 (24.56); 112 | 0.661 (0.270); 149 | 64.70 (21.41); 152 | 0.621 (0.315); 340 | 59.95 (23.90); 346 |
| Post COVID-19, mean score (SD); n | ||||||||||
| Baseline | 0.786 (0.241); 16 | 68.44 (21.19); 16 | 0.641 (0.338); 29 | 56.48 (22.66); 29 | 0.502 (0.369); 36 | 54.28 (23.73); 36 | 0.607 (0.353); 46 | 61.30 (26.32); 46 | 0.608 (0.350); 127 | 59.11 (24.34); 127 |
| Follow-up | 0.845 (0.154); 15 | 71.81 (23.72); 16 | 0.613 (0.323); 26 | 54.10 (26.49); 29 | 0.534 (0.336); 36 | 57.67 (28.24); 36 | 0.631 (0.328); 46 | 67.33 (23.66); 46 | 0.625 (0.324); 123 | 62.13 (26.21); 127 |
| UK population,b age range (years) |
35–44:a 0.893 |
35–44:a 86.6 |
0.855 | 82.0 | 0.773 | 81.7 | 0.703 | 77.3 | 0.855 | 82.8 |
Table 19 presents descriptive statistics on the responses to the individual ED-5D-5L dimensions of mobility, self-care, usual activities, pain/discomfort and anxiety/depression at baseline and follow-up for the full sample, and for the pre-COVID-19 and post-COVID-19 groups. The number and percentage of participants reporting some problems shows those who scored 2, 3, 4 or 5 on each dimension, which reflects having slight, moderate, severe or extreme problems, respectively. Overall, the proportion of participants in the full sample reporting having some problems with each dimension of HRQoL is similar at baseline and follow-up. A relatively smaller proportion of participants reported having no problems in relation to pain and discomfort at baseline (19.3%) and follow-up (18.3%) than the other dimensions, for which one-third to half of respondents reported having no problems.
| Group | EQ-5D-5L dimension, n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | ||||||
| Baselinea | Follow-up | Baselinea | Follow-up | Baselinea | Follow-up | Baselinea | Follow-up | Baselinea | Follow-up | |
| Full sample | ||||||||||
| Total number | 694 | 472 | 694 | 471 | 694 | 472 | 694 | 470 | 694 | 472 |
| Reporting no problems | 229 (33.0) | 156 (33.1) | 412 (59.4) | 252 (53.5) | 248 (35.7) | 155 (32.8) | 135 (19.5) | 86 (18.3) | 249 (35.9) | 171 (36.2) |
| Reporting some problems | 465 (67.0) | 316 (66.9) | 282 (40.6) | 219 (46.5) | 446 (64.3) | 317 (67.2) | 559 (80.5) | 384 (81.7) | 445 (64.1) | 301 (63.8) |
| Pre-COVID-19 group | ||||||||||
| Total number | 347 | 345 | 347 | 344 | 347 | 347 | 347 | 345 | 347 | 347 |
| Reporting no problems | 123 (35.4) | 110 (31.9) | 212 (61.1) | 181 (52.6) | 124 (35.7) | 106 (30.5) | 70 (20.2) | 64 (18.6) | 134 (38.6) | 126 (36.3) |
| Reporting some problems | 224 (64.6) | 235 (68.1) | 135 (38.9) | 163 (47.4) | 223 (64.3) | 241 (69.5) | 277 (79.8) | 281 (81.4) | 165 (61.4) | 221 (63.7) |
| Post-COVID-19 group | ||||||||||
| Total number | 127 | 127 | 127 | 127 | 127 | 125 | 127 | 125 | 127 | 125 |
| Reporting no problems | 48 (37.8) | 46 (36.2) | 79 (62.2) | 71 (55.9) | 50 (39.4) | 49 (39.2) | 28 (22.0) | 22 (17.6) | 52 (40.9) | 45 (36.0) |
| Reporting some problems | 79 (62.2) | 81 (63.8) | 48 (37.8) | 56 (44.1) | 77 (60.6) | 76 (60.8) | 99 (78.0) | 103 (82.4) | 75 (59.1) | 80 (64.0) |
In terms of the sample for whom both baseline and follow-up data were available, there is a smaller proportion of respondents reporting no problems at follow-up than baseline for both pre-COVID-19 and post-COVID-19 groups, and a corresponding greater proportion of participants reporting some problems.
Difference in EuroQol-5 Dimension, five level version, scores from baseline to follow-up
For the pre-COVID-19 group, there were no significant differences between baseline and follow-up on the EQ-5D-5L health state value or EQ-VAS score. However, significant decreases from baseline to follow-up were identified for the EQ-5D-5L dimensions of mobility, self-care and usual activities when using the dimension value score (Table 20). Appendix 9, Figures 27 and 28, demonstrate the lack of difference between baseline and follow-up scores for the EQ-5D health state and ED-VAS scores, respectively, at each month across the 8-month study period of the pre-COVID-19 group.
| Variable | Time point, mean (SD) | t-statistic | df | p-value | |
|---|---|---|---|---|---|
| Baseline | Follow-up | ||||
| Health state value | 0.636 (0.310) | 0.621 (0.315) | 1.35 | 339 | 0.178 |
| EQ-VAS | 58.58 (23.21) | 59.95 (23.90) | –1.17 | 345 | 0.244 |
| Mobility | 0.069 (0.072) | 0.076 (0.076) | –2.02 | 344 | 0.044 |
| Self-care | 0.032 (0.049) | 0.038 (0.049) | –2.65 | 343 | 0.008 |
| Usual activities | 0.056 (0.059) | 0.062 (0.059) | –2.00 | 346 | 0.046 |
| Pain/discomfort | 0.118 (0.109) | 0.115 (0.106) | 0.49 | 344 | 0.622 |
| Anxiety/depression | 0.089 (0.997) | 0.089 (0.972) | –0.04 | 339 | 0.969 |
For the post-COVID-19 group, there were no significant differences between baseline and follow-up scores for any of the EQ-5D-5L variables (Table 21).
| Variable | Time point, mean (SD) | t-statistic | df | p-value | |
|---|---|---|---|---|---|
| Baseline | Follow-up | ||||
| Health state value | 0.607 (0.351) | 0.625 (0.324) | –0.85 | 122 | 0.400 |
| EQ-VAS | 59.11 (24.34) | 62.13 (26.21) | –0.42 | 126 | 0.157 |
| Mobility | 0.076 (0.083) | 0.073 (0.078) | 0.61 | 126 | 0.547 |
| Self-care | 0.034 (0.054) | 0.040 (0.055) | –1.32 | 126 | 0.191 |
| Usual activities | 0.031 (0.065) | 0.057 (0.063) | 0.69 | 124 | 0.493 |
| Pain/discomfort | 0.130 (0.120) | 0.121 (0.112) | 0.85 | 124 | 0.395 |
| Anxiety/depression | 0.092 (0.105) | 0.088 (0.095) | 0.40 | 122 | 0.690 |
Difference in EuroQol-5 Dimension, five level version, health state score by participant characteristics
Linear regression analyses showed that for the pre-COVID-19 group the difference in EQ-5D-5L health state scores from baseline to follow-up could not be predicted by age (quartiles from younger to older), ethnicity (being from a black and minority ethnic group or not), gender (male or female) or deprivation (being deprived or not) (p > 0.05). However, comorbidity was associated with the EQ-5D-5L difference score such that people with at least one comorbid WtW referring condition did better than those who had only one WtW referring condition [F(1, 338) = 3.81, p = 0.025]. For the post-COVID-19 group, the difference in EQ-5D-5L index scores from baseline to follow-up could not be predicted by any of the participant characteristics (p > 0.05).
The impact of COVID-19 on the difference in EuroQol-5 Dimension, five-level version, scores
The results of the RDD analysis are presented in Table 22.
| RDD | EQ-5D score difference | VAS score difference | ||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Post_COVID-19 | 0.044 | 0.048 | –0.596 | –1.078 |
| t-statistic | 0.780 | 0.850 | –0.100 | –0.190 |
| Month | < 0.001 | –0.001 | –2.341 | –2.495 |
| t-statistic | < 0.001 | –0.050 | –1.410 | –1.530 |
| Month*Post_COVID-19 | –0.002 | 0.001 | 7.082*** | 8.091*** |
| t-statistic | –0.080 | 0.850 | 2.720 | 3.110 |
| Constant | –0.023 | –0.155 | –3.622 | –13.691 |
| t-statistic | –0.500 | –1.530 | –0.850 | –1.360 |
| Controls | No | Yes | No | Yes |
| N | 291 | 291 | 297 | 297 |
Columns (1) and (3) show the results without including controls for age, gender, deprivation, comorbidities and ethnicity; and columns (2) and (4) show the results including these controls. The results from columns (1) and (2) are also shown graphically in Appendix 10, Figures 29 and 30. None of the estimated results are significant for EQ-5D; in fact, EQ-5D-5L is seen to increase on average (although not significantly) in the post-COVID-19 period. The results for EQ-VAS do suggest an initial, insignificant decrease in reported VAS scores, but during the COVID-19 months EQ-VAS was increasing on a month-by-month basis. As can be seen in Appendix 10, Figure 30, by the end of the period the average increase in the VAS is greater than for any preceding month, suggesting that EQ-VAS score was improving during the COVID-19 period.
Attrition analysis
Table 23 presents differences in the EQ-5D-5L variables and participant characteristics at baseline between the sample of individuals who were subsequently followed up and the individuals who were lost to follow-up. Individuals lost to follow-up reported significantly worse health at baseline in terms of the EQ-5D-5L health state value, EQ-VAS and EQ-5D-5L dimensions of self-care and anxiety/depression. In addition, those individuals in the lost to follow-up sample were significantly younger, and more likely to be from a black and minority ethnic group and be living in more deprived areas.
| Variable | Group | t-statistic | df | p-value | |
|---|---|---|---|---|---|
| Follow-up (n = 463) | Lost to follow-up (n = 231) | ||||
| Health state value, mean (SD) | 0.628 (0.321) | 0.576 (0.327) | –2.01 | 692 | 0.044 |
| EQ-VAS, mean (SD) | 58.70 (23.57) | 53.28 (23.86) | –2.84 | 692 | 0.005 |
| Mobility, mean (SD) | 0.071 (0.075) | 0.078 (0.075) | 1.18 | 692 | 0.237 |
| Self-care, mean (SD) | 0.033 (0.050) | 0.042 (0.055) | 2.18 | 692 | 0.030 |
| Usual activities, mean (SD) | 0.058 (0.061) | 0.063 (0.062) | 1.07 | 692 | 0.286 |
| Pain/discomfort, mean (SD) | 0.120 (0.112) | 0.131 (0.114) | 1.19 | 692 | 0.236 |
| Anxiety/depression, mean (SD) | 0.090 (0.101) | 0.110 (0.105) | 2.45 | 692 | 0.015 |
| Age (years), mean (SD) | 60.68 (9.28) | 55.84 (8.74) | –6.62 | 692 | 0.000 |
| Gender: female (%) | 52.4 | 58.1 | 1.76 | 692 | 0.080 |
| Ethnicity: white (%) | 89.9 | 77.9 | –3.78 | 692 | 0.001 |
| Comorbidity: one condition (%) | 72.3 | 71.9 | –0.04 | 692 | 0.966 |
| Deprivation: most deprived (%) | 64.4 | 77.9 | 3.60 | 692 | 0.001 |
Discussion
Compared with national and age-specific norms, the EQ-5D-5L study sample reported in this chapter reported substantially worse HRQoL in terms of both the EQ-5D-5L health state value and the EQ-VAS measure. Among the sample for whom both baseline and follow-up data were available, proportion of respondents reporting no problems was lower at follow-up than at baseline for in both the pre-COVID-19 and post-COVID-19 groups, with a correspondingly higher proportion of participants reporting some problems at follow-up.
There were no significant differences between baseline and follow-up in either EQ-5D-5L health state value score or EQ-VAS score in either the pre-COVID-19 or post-COVID-19 groups. In terms of findings specific to the pre-COVID-19 group, significant decreases from baseline to follow-up were identified for the EQ-5D-5L dimensions of mobility, self-care and usual activities when using the dimension value score states. In addition, comorbidity was associated with the EQ-5D-5L difference score such that people with at least one WtW referring criteria comorbid condition did better than those people who had only one WtW referring condition.
COVID-19 did not affect the EQ-5D-5L health state difference score. However, the results for the EQ-VAS difference score suggest that self-reported current health measured by the EQ-VAS improved with lockdown.
Respondents who were lost to follow-up and consequently not included in the main analyses presented here had worse health at baseline, were younger, were more likely to be from a black and minority ethnic group and were more likely to be living in more deprived areas.
Mercer et al. ’s49 evaluation of a CLP intervention in Glasgow’s ‘Deep End’ socioeconomically deprived general practices similarly found that a social prescribing intervention had little or no impact on HRQoL in ITT analyses at the 9-month follow-up. Subgroup analyses of patients who saw the CLP on three or more occasions (45% of those referred) showed statistically significant improvements in EQ-5D-5L, although this may have been due to reverse causality. EQ-5D-5L scores among a relatively affluent, ethnically homogeneous group of patients experiencing LTCs who were referred into a social prescribing pathway showed that HRQoL improved between baseline and 4 months, but there was no change at further 6 to 9 months’ follow-up. 51 However, this study experienced severe attrition, with only 9.6% of the baseline sample included in the 6- to 9-month follow-up. Woodall et al. ,46 who evaluated a social prescribing service in a large city in northern England using a before-and-after design, found that VAS scores showed a small but significant improvement between baseline and post stage (actual follow-up period not given). However, data were obtained from a much smaller group than those who received the intervention overall,46 making it difficult to draw conclusions about overall effects on HRQoL.
Our finding, that there is very little effect on overall HRQoL associated with WtW, is in keeping with the limited literature on other social prescribing programmes. 46,49,51 HRQoL was one of a number of outcomes in our study, but was selected because the intervention is generic rather than aimed at a particular problem or condition. It is possible that EQ-5D-5L may lack sensitivity as a measure to detect change over this time frame, but it is also important to point out that the before-and-after design is weak. It is also noted that some participants’ health would have declined owing to increasing age over the course of the study, regardless of their engagement with WtW. Therefore, it is possible that the reason for the absence of any improvement in health state from baseline to follow-up may be that any improvements were masked by age-related decline. Without EQ-5D data for non-responders at follow-up, which are not available, we unfortunately cannot draw further conclusions.
In addition to limitations of our before-and-after study design, the power of our study was reduced by a lower than anticipated baseline response rate and subsequent follow-up response rate, although our response rates and absolute numbers are considerably higher than those of most other published before-and-after evaluations of social prescribing using self-reported methods. 5,44,46,47,51,52 We, therefore, conclude that the robustness of the SPRING_NE study results on HRQoL is limited.
It is also worth highlighting the finding that those in the lost to follow-up sample had worse health at baseline and were more likely to be from a black and minority ethnic group and be living in more deprived areas than those in the follow-up sample. Therefore, it may be the case that those individuals at greatest need and/or with the largest opportunity to benefit from social prescribing were consequently not reflected in our findings. These differences in sample characteristics may reflect less willingness or ability of those in the lost to follow-up sample to maintain longer-term engagement with WtW and/or the EQ-5D-5L study. It may also be the case that the pandemic, and the associated changes to circumstances occurring during the follow-up data collection phase, may have made continuing study involvement less feasible or less of a priority to some individuals with more health and welfare needs.
We found no evidence of any impact of COVID-19 on HRQoL. The numbers in this group were small, the mode of EQ-5D-5L follow-up administration changed and it is likely that the time frame was too short to detect an impact. The qualitative interview study (n = 44) (see Chapter 7) indicated a wide range of impacts from people managing well to some individuals very badly affected as a result of COVID-19. It is possible that the relatively small numbers in the post-COVID-19 sample and the short time frame explain why there appeared to be no impact on HRQoL, or it may be that only those coping well with the pandemic took part. These explanations may also help account for why we did not identify effects in the domain of anxiety and depression, despite larger national samples showing anxiety and depression to be significantly higher during April–June 202, compared with pre COVID levels. 97
Chapter 4 An economic analysis to explore costs and outcomes
Introduction
In this chapter, we outline the methods and results of the economic analysis, which allows us to evaluate the long-term cost-effectiveness of introducing the WtW programme among T2DM patients over the patient lifetime, compared with current practice. Estimates and data from WP1 are used as part of an economic modelling study and the robustness of the results will be investigated using sensitivity analysis.
Methods
To explore the longer-term cost-effectiveness of the intervention among T2DM patients in the SPRING_NE study, an economic modelling study was carried out. A detailed description of the economic model used to estimate the long-term costs and effects of the intervention, compared with current practice, is presented.
Model description
The United Kingdom Prospective Diabetes Study Outcomes Model 2© (UKPDS-OM2) is a well-established simulation model in the area of T2DM, which can be used to estimate life expectancy, quality-adjusted life-years (QALYs), and the cumulative cost of complications among patients with T2DM. 98 The model was developed using patient data from individuals with newly diagnosed T2DM who participated in the UKPDS. Data from 5102 UKPDS patients and 4031 survivors entering a 10-year post-trial period were used to inform model equations forecasting the occurrence of a range of diabetes-related complications and death. The model is capable of predicting event rates for T2DM-related complications [i.e. ischaemic heart disease (IHD), myocardial infarction (MI), heart failure, stroke, amputation, blindness, renal failure, ulcer, death) based on defined demographic characteristics of individual patients, as well as data on relevant risk factors (smoking status, total cholesterol, HDL cholesterol, LDL cholesterol, systolic blood pressure (SBP), levels of HbA1c, peripheral vascular disease (PVD), atrial fibrillation (AF), weight, albuminuria, heart rate, white blood cell (WBC) count, haemoglobin levels, estimated glomerular filtration rate (eGFR)]. Adjustments to risk factor values and, therefore, demographic characteristics, will impact the complication rate for an individual modelled patient, as well as impacting their utility (quality of life).
The UKPDS-OM2 was selected for use in this analysis because its structure and equations are based on a single, large UK-based RCT in the area of T2DM,98 and because its structure is also consistent with T2DM guidelines provided by NICE. 99 The population considered was patients with T2DM aged 40–74 years either undergoing the intervention (link worker social prescribing as part of the WtW programme) or receiving current practice. The key characteristics of the cost-effectiveness analysis are presented in Table 24, while the model structure is shown in Figure 6.
| Variable | Definition |
|---|---|
| Intervention | Link worker social prescribing delivered as part of the WtW programme |
| Comparator | Current patient management |
| Population | Cohort of patients with T2DM; starting age 40–74 years |
| Time frame | Lifetime time horizon; 1-year time cycle |
| Perspective | NHS/Personal Social Services (PSS) |
| Effects | T2DM-related complications, and death |
| Costs | Costs associated with the intervention, patient management and treating patients who have experienced a T2DM-related complication |
| Outcomes | Mortality and QALYs |
| Assessment of costs and effects | Cost per QALY gained associated with the introduction of the intervention |
FIGURE 6.
Flow chart showing the structure of UKPDS-OM2. Reproduced with permission from Hayes et al. 98 Reprinted by permission from Springer Nature Customer Service Centre GmbH: Springer Nature, Diabetologia, ‘UKPDS Outcomes Model 2’. CHD, coronary heart disease.
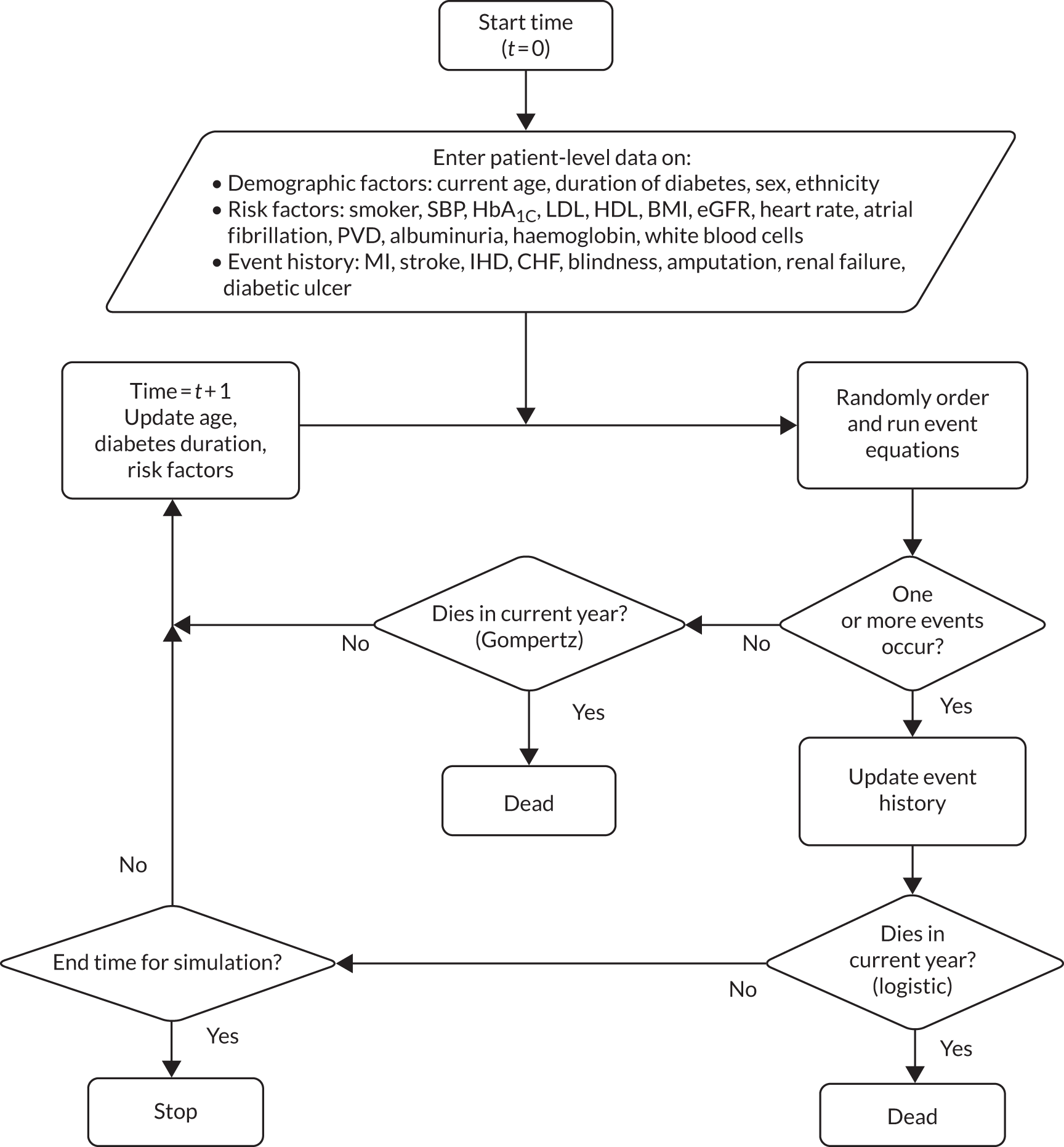
In each cycle, which represents 1 year, individuals face a risk of dying or experiencing complications, where this risk is calculated from the individual characteristics. Each complication that occurs will affect costs and lead to a decrease in utility. To allow for random events, the calculated risk for each is compared, in a random order, with a random number drawn from a [0,1] uniform distribution. If a complication is predicted, it will inform the remaining equations in that cycle. The nature of the complications, if they occur, will affect the underlying risk of death. Each year that an individual survives leads to an appropriate updating of risks, either from existing data sets or from the risk factor time equations. When an individual dies, they exit the simulation and their total costs and QALYs are calculated. Given that a patient-level data set was unavailable for this analysis, the modelled population was sampled based on a combination of baseline data available from the WtW study and from the literature (see Estimation of model parameters).
Estimation of model parameters
Point estimate values for the clinical effectiveness, utility and cost parameters are presented in Appendix 11, Tables 39–41. In addition, uncertainty around the point estimate and a distribution of uncertainty are presented where appropriate and available to allow for a probabilistic analysis to be undertaken.
The model requires the user to define patients’ baseline demographic characteristics and risk factor values (for each risk factor) for individual patients entering the model and on a year-by-year basis. Where these data are unavailable, the model automatically provides two methods to estimate yearly risk factor values for continuous risk factors (HDL cholesterol, LDL cholesterol, SBP, HbA1c, weight, heart rate, WBC count, haemoglobin and eGFR) and two methods for binary risk factors (smoking status, PVD, AF, albuminuria). For continuous risk factors, (1) hold the initial value constant for the simulation period or (2) populate using linear regression (y = mx + c), where y is the result for a given year and x is the value from the previous year or the initial value from the inputs worksheet for the first year. Values for m and c can then be specified by group. For binary risk factors, hold the initial value constant for the simulation period or populate each year with a specified value for each group. 98 For this analysis, binary risk factors were held constant for the simulation period. However, an alternative approach was utilised to populate yearly continuous risk factor values for individual patients based on a distribution of uncertainty surrounding the baseline value. Annual values for each risk factor were sampled from a normal distribution, with a mean value equal to the value of the corresponding risk factor in the previous year and a standard deviation (SD) equal to 10% of that value. All sampled values were then compared with their corresponding range of plausible values, before plugging them into the model.
Clinical effectiveness parameters
Data to sample the baseline characteristics of the modelled population were taken from a range of sources. Data to inform the ethnicity, gender split, average age, height and weight of patients were all derived from QOF data. Data to inform the average duration of diabetes among the patient population were derived from a previous study by Clarke et al. 100 exploring the impact of visual acuity on the quality of life of individuals with T2DM.
Data to inform the baseline risk factor values (see Model description) were primarily derived from published literature, given the unavailability of QOF data in this case. However, the baseline HbA1c and SBP values were available from the QOF data, as well as the baseline percentage of smokers among the population. The baseline percentage of patients with AF and albuminuria, and the baseline values for HDL, LDL, heart rate, WBC, haemoglobin and eGFR, were all taken from the study by Clarke et al. 100 The baseline percentage of patients with PVD was sourced from a study by Hayes et al. 98 These baseline risk factor values and demographic characteristics were used to sample the population entering the economic model. Although the model also allows one to specify the occurrence of pre-existing events (i.e IHD, heart failure, amputation, blindness, renal failure, stroke, MI and ulcer) among the population, information to populate these parameters was unavailable from the QOF data and the literature. Therefore, it was assumed that the patient population had not experienced a previous clinical complication related to T2DM before entering the model.
Where available, QOF data were used to inform the impact of the intervention, that is the decrease or increase on risk factor values. Data on SBP and HbA1c levels were collected directly from study participants and, in this way, the impact of the intervention on risk factor values was incorporated in the analysis. In the base-case analysis, the treatment effect was assumed to last for 4 years (based on the duration of the study period). Following this period, the impacted risk factor value would revert to the value that it would be in the absence of the intervention. It was assumed that it would take affected risk factors 3 years to revert to the values that they would be in the intervention’s absence. The robustness of this assumption was assessed in sensitivity analyses. Additional hypothetical changes in risk factor values that were not captured in the study were considered in sensitivity analysis to explore how longer durations of treatment effect could affect the results. The changes in relevant risk factor values, as well as all other clinical data included in the model, are presented in Appendix 11, Table 39.
Utilities
The initial utility value of T2DM patients was based on the UKPDS patient population and was derived from a study exploring the effect of diabetes complications on HRQoL. 101 Utility decrements associated with experiencing IHD, MI, heart failure, stroke, amputation and blindness in the initial and subsequent years were derived from the same study. 101 In initial and subsequent years, utility decrements associated with renal failure and ulcers were derived from a meta-analysis of quality-of-life studies. 102 The initial utility value, and utility decrements associated with complications in initial and subsequent years, were assumed to be constant regardless of patient age or gender. All utility values included in the model are presented in Appendix 11, Table 40.
Resource use and costs
The cost of the WtW intervention to the NHS was provided by WtW. Costs associated with WtW were assigned to all patients in the intervention arm of the long-term model. A per-patient cost was calculated, utilising data provided by WtW based on the amount of funding received to deliver the programme and the number of T2DM patients utilising the service. This one-off cost was applied to all patients receiving the intervention, from the outset of the model. An annual cost assigned to all patients not experiencing any complications was also included in the model. This cost was based on UKPDS patients and was derived from a related costing paper. 103
Costs of T2DM-related complications were incurred on the occurrence of an adverse event, and in the years following the event. Complication costs associated with IHD, MI, heart failure, stroke, amputation, blindness, renal failure and ulcer were included in the model. Both fatal (where relevant) and non-fatal costs associated with each complication were included, as well as the initial cost of each complication and the associated cost of that complication in subsequent years. Complication costs were assumed to be the same, regardless of patient age or gender. Complication costs for IHD, MI, heart failure, stroke, amputation and blindness were based on estimates derived from UKPDS patients, which were published in a related costing paper. 103 Complication costs for renal failure and ulcer were taken from the NHS Blood and Transplant Programme104 and a UK report on the costs of ulcer and amputation,105 respectively. It was assumed that no specific therapy would be required following complications and, therefore, the costs incurred were only the costs of the complications themselves in initial and subsequent years. All costs included in the model are presented in Great British pounds (£) for a 2020 price year, and, where costs were sourced from previous literature, the costs were inflated to the current year. All costs included in the model are presented in Appendix 11, Table 41.
Assessment of costs and outcomes
The model was run to obtain the expected values for each strategy over a lifetime time horizon. The analysis was designed to generate the incremental cost per QALY gained (per patient) associated with introduction of the intervention. Overall results are presented in the form of an incremental cost-effectiveness ratio (ICER), which is calculated by dividing the difference in cost between strategies by the difference in effectiveness. The ICER can then be assessed by comparing the calculated value with the NICE-recommended willingness-to-pay (WTP) threshold for QALYs (lower threshold of £20,000 used to assess cost-effectiveness). 106 In addition, the cost and QALY difference between strategies, as well as the potential cost savings related to avoidance of complications, are presented based on a cohort of 10,000 patients (5000 in each group) to account for the broader population impact.
Where available, and when appropriate, data were entered into the model as distributions to fully incorporate the uncertainty around parameter values so that a probabilistic sensitivity analysis (PSA) could be undertaken. The PSA was run with 1000 simulations and appropriate probabilistic outputs were produced, that is, cost-effectiveness acceptability curves (CEACs) to show the probability of the intervention being cost-effective across a range of WTP thresholds, as well as cost-effectiveness planes. The combination of 10,000 patients and 1000 simulations were chosen as the numbers where conversion was achieved in test runs. Results of the probabilistic analysis also present the incremental net monetary benefit (NMB) of the intervention. The NMB represents the value of an intervention in monetary terms when a WTP threshold for a QALYs is known, calculated as: (incremental benefit × threshold) – incremental cost. 107 Probabilistic outputs were produced using the heRvis visualisation builder tool in R Shiny (RStudio Inc., Boston, MA, USA). 108 Deterministic sensitivity analyses (see Sensitivity analysis) were also conducted to explore individual and multiple parameter variation and the impact that this would have on the results. All costs and health effects were considered from an NHS and a Personal Social Services (PSS) perspective and were discounted at an annual rate of 3.5%. 109
It should be noted that the base-case analysis considers only the impact of the intervention on two of the baseline risk factor values (SBP and HbA1c level), given the data that are available from the QOF data. However, in all likelihood, the intervention will impact additional parameters that we attempt to explore through sensitivity analyses.
Sensitivity analyses
Sensitivity analysis 1
In this analysis, the duration of the estimated treatment effect was increased from 4 years (base case) to 25 years.
Sensitivity analysis 2
The reduction in SBP and level of HbA1c risk factor values associated with introducing the social prescribing intervention was increased further.
Sensitivity analysis 3
Sensitivity analyses 1 and 2 were combined to account for prolonged treatment effect and reductions in SBP and HbA1c levels.
Sensitivity analysis 4
In this analysis, a scenario was assessed where the treatment effect was again assumed to last for 25 years, with further reductions in SBP, HbA1c levels and eGFR assumed. The reductions assigned to the three risk factor values were all designed to bring these values to optimal levels for this patient cohort. The other risk factors were not varied as the baseline values appear to be within optimal ranges.
Sensitivity analysis 5
In this analysis, a 50% reduction was assigned to the cost of delivering intervention to each patient.
Sensitivity analysis 6
Fixed trajectories were assumed for all risk factors over the time horizon of the model, rather than the base-case assumption of simulated trajectories informed by parameter distributions.
Sensitivity analysis 7
In this analysis, the treatment effect of the intervention (i.e. variation in the impacted risk factor values) was assumed to end immediately following completion of the intervention (rather than having a residual effect for a number of years afterwards, as is assumed in the base-case analysis).
Sensitivity analysis 8
In this analysis, alternative treatment effect values were utilised from the QOF data. Data taken from one of the alternative models used in the econometric analysis indicated that the intervention would result in the following variations over the first 4 years for HbA1c levels and SBP: HbA1c – year 1 = –0.986, year 2 = –3.104, year 3 = –4.569 and year 4 = –3.694; and SBP – year 1 = 0.44, year 2 = –0.28, year 3 = 0.88 and year 4 = –3.05.
Results
Results of the cost-effectiveness analysis are presented. Base-case analyses are presented first (both deterministic and probabilistic), followed by sensitivity analyses.
Base-case results
Deterministic results
The base-case results for the deterministic analysis shown in Table 25 indicate that the redesigned treatment pathway results in a marginal increase in QALYs gained (0.004), but is also more costly overall than the comparator (£1305). However, a cost-saving per patient associated with a reduction in complications is shown (–£23). The ICER of £326,250 indicates that the intervention is unlikely to be cost-effective based on these differences. In this analysis, the highest complication costs are associated with IHD (averaging £2132 per patient in the current practice arm and £2131 in the intervention arm). Stroke is the complication that has the biggest impact on utility, with an average disutility of –0.06 in both the current practice and the intervention arm.
| Strategy | QALY | Cost (£) | ICER (cost per QALYs) (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean of complications | Cost difference | Mean total | QALY difference | ||
| Current practice | 12.1811 | 15,021 | 15,021 | ||||
| Intervention | 12.1848 | 0.004 | 14,998 | –23 | 16,326 | 1305 | 326,250 |
| Difference based on a cohort of 10,000 patients | 40 | –230,000 | 13,050,000 | ||||
In Table 26, the total cost savings associated with the avoidance of individual complications in a cohort of 10,000 T2DM patients are presented. Based on the base-case analysis, the results indicate that the most significant savings occur because of the avoidance of MI and ulcers. These figures can be extrapolated to account for larger patient numbers.
| Type of complication | Cost savings for 10,000 patients (£) |
|---|---|
| IHD | 10,000 |
| MI | 50,000 |
| Heart failure | 30,000 |
| Stroke | 40,000 |
| Amputation | 40,000 |
| Blindness | 10,000 |
| Renal failure | 10,000 |
| Ulcer | 100,000 |
Probabilistic results
The base-case results for the probabilistic analysis are presented in Table 27. These results differ slightly from the results of the deterministic analysis because they take into account the uncertainty associated with individual model parameters and patients. The results indicate that the intervention increases QALYs by 0.004. Costs associated with the intervention arm are higher than those associated with current practice (£1309) (primarily because of the cost of the initial intervention itself – otherwise the intervention would be marginally cost saving). The incremental NMB of the intervention is also presented in Table 27. The results indicate that the NMB of the intervention is negative at both £20,000 and £30,000 WTP thresholds.
| Strategy | QALY (95% CI) | Cost (£) (95% CI) | Incremental net benefit (£) (95% CI) | ICER (cost per QALY) (£) | |||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean total | Difference | £20,000 WTP threshold | £30,000 WTP threshold | ||
| Current practice | 12.091 (9.140 to 14.713) | 15,441 (11,852 to 19,636) | |||||
| Intervention | 12.096 (9.148 to 14.721) | 0.004 (–0.022 to 0.029) | 16,750 (13,181 to 20,935) | 1309 (1192 to 1440) | –1224 (–1874 to –611) | –1182 (–2089 to –314) | 327,250 |
| Difference based on a cohort of 10,000 patients | 40 | 13,090,000 | |||||
Further outputs from the probabilistic analysis are shown in Figures 7 and 8. The cost-effectiveness plane (see Figure 7) shows individual results (points on the scatterplot) from the multiple simulations of the model. All points are above the horizontal line of the plane, indicating that the intervention is likely to be more costly than the comparator. However, there are also more points in the north-east quadrant of the plane, indicating that the intervention is likely to be more effective than the comparator. Results from the CEAC (see Figure 8) indicate that the probability of the intervention being cost-effective increases as the WTP threshold increases, although it is highly unlikely to be cost-effective at existing WTP thresholds. Results from Figures 7 and 8 (as well as from the NMB analysis) suggest that the intervention is likely to be more effective than the comparator, and that as the WTP threshold increases the likelihood of the intervention being cost-effective also increases (because of the additional cost of the intervention in the base-case analysis).
FIGURE 7.
Cost-effectiveness plane base case: results of probabilistic sensitivity analysis.
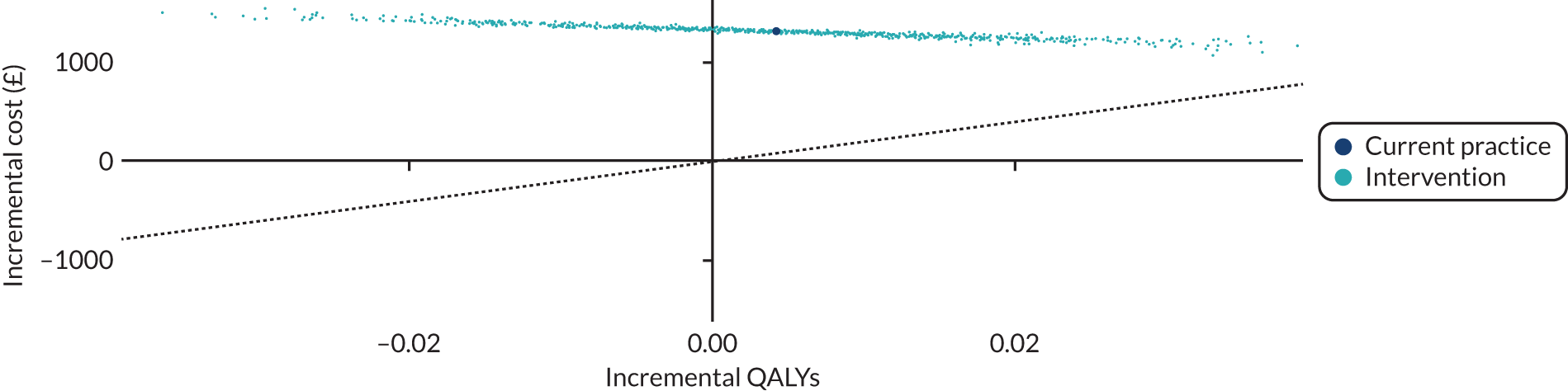
FIGURE 8.
Cost-effectiveness acceptability curve base case: the probability of each preferred intervention being most cost-effective against WTP for each QALY threshold.
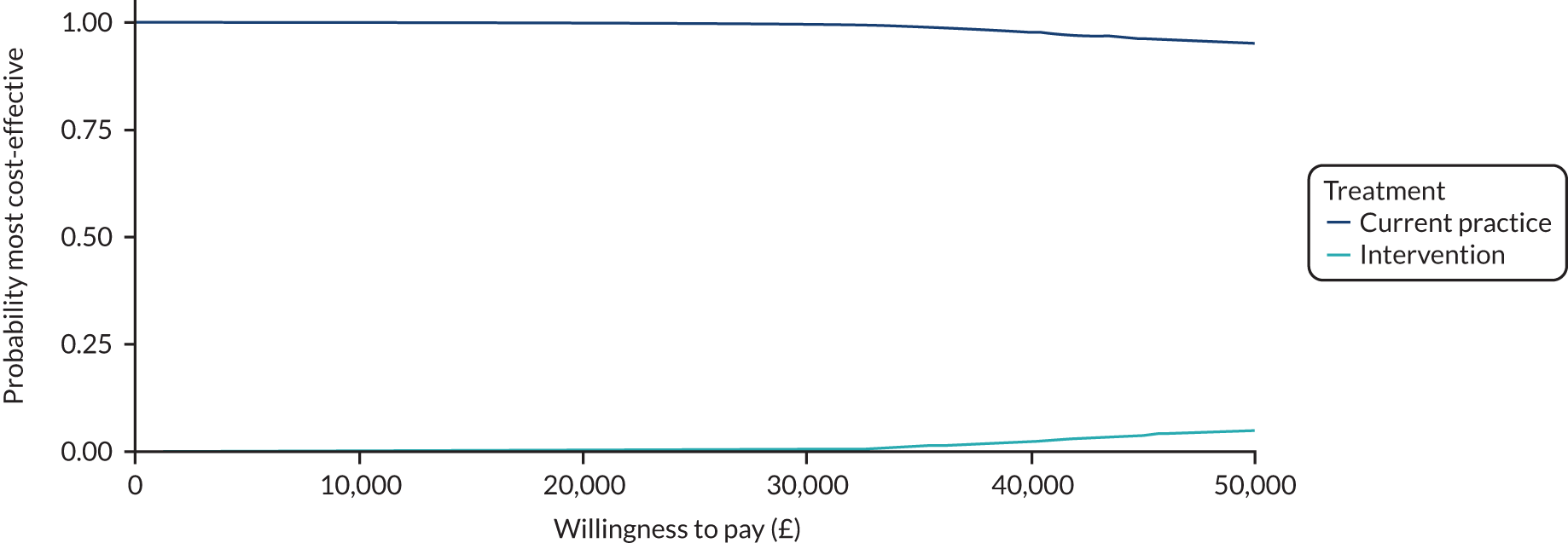
Sensitivity analysis results
Sensitivity analysis 1
In this analysis (Table 28), the treatment effect’s duration was increased from 4 years (base case) to 25 years, with an assumption that no further intervention-related costs would be incurred as a result of the prolonged treatment effect. Compared with the base-case analysis, QALY gains associated with the intervention are increased, and cost savings associated with complications are also increased. However, the ICER is £91,500, indicating that the intervention is unlikely to be cost-effective.
| Strategy | QALY | Cost (£) | ICER (cost per QALY) (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean of complications | Cost difference | Mean total | QALY difference | ||
| Current practice | 12.1811 | 15,021 | 15,021 | ||||
| Intervention | 12.1947 | 0.014 | 14,974 | –46 | 16,302 | 1281 | 91,500 |
| Difference based on a cohort of 10,000 patients | 140 | –460,000 | 12,810,000 | ||||
Sensitivity analysis 2
This analysis (Table 29) assumed that the intervention would reduce baseline SBP and HbA1c values (133.54 mmHg and 57.60 mmol/mol) by 20 mmHg and 21.86 mmol/mol [2 on the Diabetes Control and Complications Trial (DCCT) scale], respectively. Compared with the base-case analysis, QALY gains associated with the intervention are increased (0.09), and cost savings associated with complications are also increased (–£365). The ICER is £10,700 per QALY gained, indicating that the intervention is highly likely to be cost-effective.
| Strategy | QALY | Cost (£) | ICER (cost per QALY) (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean of complications | Cost difference | Mean total | QALY difference | ||
| Current practice | 12.1811 | 15,021 | 15,021 | ||||
| Intervention | 12.2756 | 0.09 | 14,656 | –365 | 15,984 | 963 | 10,700 |
| Difference based on a cohort of 10,000 patients | 900 | –3,650,000 | 9,630,000 | ||||
Sensitivity analysis 3
In this analysis (Table 30), the duration over which the intervention was assumed to have an effect on risk factor values was increased to 25 years, and it was assumed that the intervention would reduce baseline SBP and HbA1c values by 20 mmHg and 21.86 mmol/mol (2 on the DCCT scale), respectively. Compared with the base-case analysis, QALY gains associated with the intervention are increased (0.3) and cost savings associated with complications are also increased (–£946). The ICER is £1273 per QALY gained, indicating that the intervention is highly likely to be cost-effective.
| Strategy | QALY | Cost (£) | ICER (cost per QALY) (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean of complications | Cost difference | Mean total | QALY difference | ||
| Current practice | 12.1811 | 15,021 | 15,021 | ||||
| Intervention | 12.5023 | 0.3 | 14,074 | –946 | 15,402 | 382 | 1273 |
| Difference based on a cohort of 10,000 patients | 3000 | –9,460,000 | 3,820,000 | ||||
Sensitivity analysis 4
In this analysis (Table 31), the duration over which the intervention was assumed to have an effect on risk factor values was increased to 25 years, and it was assumed that the intervention would reduce baseline SBP and HbA1c values by 20 mmHg and 2 mmol/mol, respectively. In addition, it was assumed that the intervention would increase eGFR by 20 ml/minute/1.73 m2. Compared with the base-case analysis, QALY gains associated with the intervention are increased (0.4) and cost savings associated with complications are also increased (–£1344). In this analysis, the intervention is the dominant strategy, meaning that it is more effective, that is it produces more QALYs and is less costly than the comparator.
| Strategy | QALY | Cost (£) | ICER (cost per QALY) (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean of complications | Cost difference | Mean total | QALY difference | ||
| Current practice | 12.1811 | 15,021 | 15,021 | ||||
| Intervention | 12.5442 | 0.4 | 13,678 | –1344 | 15,006 | –15 | Dominant |
| Difference based on a cohort of 10,000 patients | 4000 | –13,440,000 | –150,000 | ||||
Sensitivity analysis 5
In this analysis (Table 32), the cost is £160,250 per QALY gained, indicating that the intervention is unlikely to be cost-effective.
| Strategy | QALY | Cost (£) | ICER (cost per QALY) (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean of complications | Cost difference | Mean total | QALY difference | ||
| Current practice | 12.1811 | 15,021 | 15,021 | ||||
| Intervention | 12.1848 | 0.004 | 14,998 | –23 | 15,662 | 641 | 160,250 |
| Difference based on a cohort of 10,000 patients | 40 | –230,000 | 6,410,000 | ||||
Sensitivity analysis 6
In this analysis (Table 33), it was assumed that the trajectories of all risk factors were fixed over the model’s time horizon. Results are largely consistent with the base-case analysis, with increased QALYs and increased costs associated with the introduction of the intervention. However, the total increase in costs associated with introduction of the intervention (£1280) is not as high as in the base-case analysis and the ICER is lower (£91,429).
| Strategy | QALY | Cost (£) | ICER (cost per QALY) (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean of complications | Cost difference | Mean total | QALY difference | ||
| Current practice | 12.1811 | 15,021 | 15,021 | ||||
| Intervention | 12.1954 | 0.014 | 14,973 | –48 | 16,301 | 1280 | 91,429 |
| Difference based on a cohort of 10,000 patients | 140 | –480,000 | 12,800,000 | ||||
Sensitivity analysis 7
In this analysis (Table 34), it was assumed that the values of those risk factors affected by the intervention revert to the values that they would be in the absence of the intervention immediately following the initial 4-year period (rather than assuming any residual effect of the intervention, as in the base-case analysis). The results indicate that, when this assumption is made, the intervention strategy is marginally less effective, and more costly, than in the base-case analysis.
| Strategy | QALY | Cost (£) | ICER (cost per QALY) (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean of complications | Cost difference | Mean total | QALY difference | ||
| Current practice | 12.1811 | 15,021 | 15,021 | ||||
| Intervention | 12.1843 | 0.003 | 15,000 | –21 | 16,328 | 1307 | 435,667 |
| Difference based on a cohort of 10,000 patients | 30 | –210,000 | 13,070,000 | ||||
Sensitivity analysis 8
In this analysis (Table 35), treatment effect values from an alternative econometric model used in the analysis of patient-level data were utilised. The results indicate that, when this assumption is made, the intervention strategy is more effective than in the base-case analysis. Although cost results are broadly similar to the base-case analysis, the improved effectiveness results in a smaller ICER. However, an ICER of £375,143 would indicate that the intervention is still unlikely to be cost-effective when these values are used.
| Strategy | QALY | Cost (£) | ICER (cost per QALY) (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Difference | Mean of complications | Cost difference | Mean total | QALY difference | ||
| Current practice | 12.1811 | 15,021 | 15,021 | ||||
| Intervention | 12.1846 | 0.0035 | 15,005 | –16 | 16,333 | 1313 | 375,143 |
| Difference based on a cohort of 10,000 patients | 35 | –160,000 | 13,130,000 | ||||
Discussion
An economic analysis was carried out to explore the costs and health outcomes associated with the introduction of the intervention for patients with T2DM. Although clinical data from the SPRING_NE study to use in the cost-effectiveness model were limited, an exploratory analysis was conducted, which considered the key drivers of the model results through multiple sensitivity analyses.
Base-case results from the cost-effectiveness model, which utilised QOF data, indicate that reductions in SBP and HbA1c levels lead to a reduction in clinical complications over the patient lifetime. In addition, the results indicate a reduction in costs associated with clinical complications and an improvement in HRQoL for patients. However, these differences are minor (QALY difference = 0.004, cost difference related to complications = –£23: deterministic model) and, when the cost of the intervention is also considered, the intervention is more costly than the comparator overall (£1305: deterministic model). Probabilistic results from the base-case analysis indicate that the probability of the intervention being cost-effective increases as the WTP threshold increases. Simultaneously, the cost-effectiveness plane presented shows that the intervention is likely to be more costly and more effective than current practice. The results are unsurprising, given that the base-case analysis assumes that only 2 of the 12 modelled risk factors are impacted by the intervention, with all other risk factors assumed to be equivalent in either arm of the model. Despite the minimal impact, the results do seem to indicate that the potential of the social prescribing intervention to reduce SBP and HbA1c risk factor values (even for a finite, and limited, duration of time) has the potential to lead to significant cost savings related to complications, and improvements in quality of life, among this patient cohort.
It is unlikely that the intervention being evaluated has no impact on the other characteristics and parameters that drive the complication rates (and subsequently costs and utilities) in the economic model. Although the model utilises data related to the effect of the intervention on only SBP and HbA1c levels, it is entirely possible that other risk factors for T2DM are also affected. However, these additional impacts were not captured in the study and, therefore, could not be assumed in the base-case analysis. A number of one-way and multiway sensitivity analyses were, therefore, conducted to explore the impact of further clinical and cost parameter variation on the overall cost-effectiveness results. Initially, the duration over which the intervention was assumed to affect risk factors was extended to 25 years, with all other parameter values held constant. This had the effect of improving QALY gains and increasing the cost savings associated with reducing complications; however, overall, the intervention was still not cost-effective when considering the additional cost of the intervention. We then applied arbitrary reduction values to the two risk factor parameters (SBP and HbA1c level) for which we had base-case data. The results indicate that, when these reductions are made, the intervention becomes cost-effective with significant increases in QALY gains and reductions in costs associated with the avoidance of complications. These findings are accentuated further when these variations are made in combination, that is multiway sensitivity analysis.
Further analyses sought to explore the impact of varying risk factor parameters for which we did not have intervention effect data. Therefore, eGFR was varied in addition to SBP and HbA1c level (as well as increasing the duration of treatment effect). This resulted in the intervention producing more QALYs, and a greater overall cost saving, when compared with current practice. Additional analyses explored the impact of varying baseline costs associated with the delivery of the intervention; although we see a reduction in overall costs, the ICER indicates that the intervention is not cost-effective. A further analysis utilised treatment effect data from an alternative econometric model used as part of the cost–consequence analysis, which indicated that the intervention would have a greater impact on HbA1c and SBP than was assumed in the base-case analysis. The results of this analysis indicated that the intervention would be more effective than in the base-case analysis, although the ICER would still be outside acceptable WTP threshold ranges. These results suggest that an extended duration of intervention effect would also need to be assumed for the intervention to be cost-effective, when utilising the improved treatment effect data from the alternative econometric model.
Given the limited number of QOF treatment effect data that we were able to utilise in this established simulation model, it is difficult to make any definitive statements regarding the long-term cost-effectiveness of the intervention. However, based on the data that we do have, the findings are revealing. Even with relatively minor reductions in the baseline levels of SBP and HbA1c (which the intervention has been shown to effect), the cost savings associated with the resulting reduction in clinical complication rates are significant (–£230,000 among a cohort of 10,000 patients). This is also under the assumption that the intervention has a relatively short duration of effect (4 years in the base case). When this duration of effect is extended, and when the impact of the intervention on these two risk factors is assumed to be even more significant, the intervention is likely to be cost-effective overall. Therefore, these complication-related savings increase substantially when further intervention impacts are assumed in sensitivity analysis, including longer duration of intervention effect (–£460,000) and further reductions in impacted risk factor values (–£3,650,000).
There are limitations to the economic evaluation presented. First, as highlighted, data limitations regarding the impact of the social prescribing intervention on relevant risk factors have meant that we have had to undertake an exploratory analysis with significant sensitivity analysis, rather than being able to conduct a robust cost-effectiveness analysis. However, the sensitivity analyses that have been carried out have allowed us to explore this uncertainty to identify the key drivers of the model results. One area that we could not address through sensitivity analysis is that relating to the correlation between patient characteristics. Because we had limited individual-level data on the study participants, we are forced to assume no correlations between patient characteristics. Second, although utilising the established UKPDS-OM2 for this analysis ensured that we were able to appropriately model disease progression and natural history of the disease (given that the model was developed utilising data from a large T2DM patient data set),98 we were not necessarily able to capture all of the benefits that the intervention may have on patient outcomes that go beyond its impact on a defined range of characteristics and risk factors. Social prescribing is not aimed at specific clinical outcomes, which partly drives the issues surrounding the data limitation. For instance, although the model allows one to capture utility decrements associated with clinical complications, we were not able to model any improvements in patient quality of life that may result from their increased assurance in treatment programmes. In addition, we were not able to model confidence because of improved management of the condition that may have been impacted by the intervention. Third, the limited time frame of the study meant that we were able to capture intervention effect over a 4-year period only. However, as highlighted earlier, this particular parameter was explored in sensitivity analysis. The limitations presented would appear to indicate that the results of the base-case analysis probably underestimate the true cost reductions and quality-of-life improvements that may be brought about by such a programme. Finally, a limitation of the UKPDS-OM2 model is the fact that, although it is still the best model of its kind, it is quite old and a number of the relationships in the model may have changed over time. In addition, a key strength of the analysis is that it is the first cost-effectiveness analysis exploring the long-term cost and health outcome implications of a social prescribing intervention among T2DM patients in a UK setting. It may also be used to inform further analyses when additional data become available.
Chapter 5 Link worker ethnography
Introduction
In this chapter, we present the results of an ethnography undertaken with both provider organisations delivering the intervention. The aim was to explore how the intervention was unfolding, with a particular focus on the link worker role. We will describe how a spectrum of social prescribing practices were emerging, shaped by provider organisations, individual link workers and the requirements to meet targets and generate payment. Some detail will also be given about the effect of the pandemic, with further consideration of its impact in Chapter 7.
Methods
In the SPRING_NE study, we explored the experiences of link workers delivering the intervention through participant observation, shadowing, interviews and focus groups, engaging closely with 20 link workers, and also through conducting interviews with managers from provider organisations and staff from the intervention’s umbrella body. Data were collected between August 2019 and June 2020, using in-person methods until February 2020, and then, because of social distancing restrictions associated with the COVID-19 pandemic, using remote methods.
Participant observation
The researcher (Jayne Jeffries) spent 2 days per week over a period of 6 months between August 2019 and February 2020 at the provider organisations in offices shared by link workers, initially gaining a broader understanding of the structure and ethos of each organisation and understanding the professional practice(s) of link workers. This included attendance at meetings, as well as any scheduled training events. All link workers received participant information leaflets and those participating completed informed consent sheets (see Report Supplementary Material 2). Twenty link workers completed a demographic questionnaire (see Report Supplementary Material 2). During this time, the researcher also invited link workers to take part in individual interviews and focus groups to reflect on their experiences of the intervention.
In addition, the researcher spent a more focused period of time between October 2019 and February 2020 shadowing a smaller number of link workers (n = 8) as they went about their daily working routines. This included observing link workers meeting with clients at provider offices, GP surgeries or in the community, and accompanying link workers when they were visiting clients in their homes. Practice staff and patients were informed of the researcher’s (Jayne Jeffries) presence via letters to GP surgeries, GP surgery posters and leaflets (see Report Supplementary Material 2). At opportune times during the working day, short informal interviews were conducted with link workers, during which they were asked to reflect on their practice.
Field notes were recorded after each period of observation in line with standard ethnographic procedures. 110,111 Field notes described scenes and allowed us to explore meaning and reflect on positionality. They supplemented interviews by capturing context and information that was not audio-recorded, such as non-verbal communication.
Interviews and focus groups
During face-to-face fieldwork, interviews were conducted with six link workers using a semistructured interview guide (see Report Supplementary Material 2) and were recorded. Two focus groups were conducted at provider A (n = 7 and n = 3 participants). One focus group was conducted at provider B (n = 6 participants). Topics discussed included link worker roles, referrals, and relationships with GP surgeries, clients and the community sector (see Report Supplementary Material 2). Questions focused on ‘what works’ for clients and how ‘what works’ varies for different clients. Focus groups were audio-recorded with consent.
At the start of the COVID-19 pandemic, face-to-face fieldwork had to cease and the researcher proceeded to undertake a further 13 semistructured interviews with senior link workers, link worker managers, social prescribing stakeholders from both provider organisations and staff from the intervention’s umbrella body. Owing to the differing nature of these roles, topic guides were personalised and focused on professional histories and roles alongside organisational responses to the rapidly changing circumstances. These were conducted by telephone and audio-recorded. These data were also used as part of our exploration of the impact of COVID-19 on the experience of clients during the pandemic (see Chapter 7).
Interview and focus group recordings were transcribed (using intelligent verbatim transcription) and transcripts were checked for accuracy. Transcripts were ‘cleaned up’ during transcription, with dropped consonants and vowels added (e.g. ‘gonna’ to ‘going to’). Some participants often substituted whole words with regional dialect words. These words were not changed during transcription and their meaning is indicated in square brackets. Data were anonymised and pseudonyms applied to preserve anonymity. Data presented are labelled by participant code/pseudonym, provider, source and date as appropriate.
Data analysis
The final qualitative data set comprised interview and focus group transcripts, as well as ethnographic field notes. Thematic content analysis was developed subsequent to data collection and was achieved via coding all data and synthesising codes and categories into emerging themes of understanding. Interview narratives (‘what was said’) were compared with the observations (‘what was done’). Line-by-line coding was conducted using NVivo 12 (QSR International, Warrington, UK) to identify themes in the data, and memos were used to assist in the process of moving from content-based descriptive themes that are relevant to the research questions to more conceptual themes that incorporate differences, similarities, inconsistencies and contradiction in the data. 112 Analysis involved synthesising and theorising the data, and re-contextualising this new knowledge by considering it in the context of other research. Analysis was led by Bethan Griffith, who met regularly with Tessa M Pollard and Suzanne Moffatt to review the coding framework, discuss emerging themes and develop the analysis.
The intervention
At the time of fieldwork, the intervention was delivered by two provider organisations, referred to here as providers A and B, which were contracted by a limited company created as a special-purpose vehicle to manage organisational funding as part of a Social Impact Bond (SIB) arrangement (see Table 2). At the start of the intervention in April 2015, there were four provider organisations, but two had withdrawn by March 2018. This coincided with the cessation of a front-loaded starter payment that allowed providers to recruit link workers who could start engaging GP surgeries to generate referrals. After 2 years, when enough link workers had been recruited, the fixed payment was removed and redistributed to incentivise referrals through a more formal payment by results (PbR) mechanism. The two providers that withdrew had not felt able to generate sufficient referrals. Payments relied on completion of a Well-being Star™ (WBS)74 with clients (see Figure 1). After careful consideration, the WBS had been chosen as the outcome metric that would best reflect improvements for clients. Payments to providers were linked not to changes in this metric, but instead to the number of clients completing it. 73 Payments included a referral payment, a second-stage payment at 6 months and a service continuation payment. Up to seven stars were recorded during a client’s journey. In training sessions, link workers were instructed that when WBS scores were stable clients should be moved into the keeping-in-touch (KIT) phase, before being discharged. In January 2019, the average journey length for a client was reported as 24 months.
Each provider recruited its own link workers using similar but not identical job descriptions. Both mentioned behaviour change, provider B to a lesser degree, focusing more on its commitment to community partnership and building social capital. Around the start of the fieldwork in August 2019, both providers combined employed 18.94 full-time equivalent (FTE) link workers, by July 2020 there were 17.42 FTE link workers in total. Target caseloads per link worker were set by the intervention and varied between 80 and 120. Newly established PCNs employ one link worker per 30,000–50,000 patients, although they can operate alongside existing services. Historical data showed that referral rates had fluctuated. At the start of the ethnography, there had been a slight decline in referrals.
When the COVID-19 pandemic struck, link workers began working remotely by telephone and video calls. In addition to their usual service, the intervention offered general practices a COVID-19 response service, meaning that they could provide link workers with a list of patients they wanted them to contact. These individuals did not have to meet the intervention’s referral criteria and were not considered to be new referrals. However, if they did satisfy eligibility criteria, they could become clients and complete the WBS.
Both providers had historical experience of working in the locality and were simultaneously responsible for delivering other community programmes, including link working. Link worker managers and stakeholders were able to reflect on the history of the intervention, drawing out the complexity of how the intervention developed through extensive stakeholder consultation, including with potential clients, over an 8-year period. Narratives were often embedded in local context and an understanding of the local community. One manager reflected on a high-intensity intervention that her organisation had delivered and the sense that a different kind of intervention, such as that now being delivered, had been required:
Well, [we thought] what about people who need much less support than that, that actually still aren’t thriving because there isn’t services to try and help get people out of the rut, or the lack of hope that they are in about the fact that things could improve?
Annette, B, COVID-19 interview, May 2020
Securing funding to implement the intervention had required collaboration. Despite its complexity, the funding mechanism was perceived to be free of the threats posed by short-term funding cycles experienced by similar initiatives. However, as we will see, this funding structure did appear to shape the intervention at its intersection with the different providers and individual link workers.
Provider approaches
It is worth noting that when the intervention was established social prescribing was not as widespread as it is now. There was little collective understanding and the link worker role was not well defined. Locally, there were historical and contemporary roles that were considered similar, such as community health trainers and primary care navigators. However, by the time of the fieldwork, some managers and stakeholders were also overseeing other link working services. Some of these services operated waiting lists because of high demand, with link workers often having smaller caseloads. Providers had taken different routes through this evolving landscape and arrived at the intervention with their own ethos. One organisation was rooted in community development, whereas the other offered a focus on behaviour change. These differences were best captured in interviews undertaken at the start of the COVID-19 pandemic, when providers paused to reflect on what they were offering clients:
It is important to not become a service that you’re not. We don’t want to become a corona support line, or we don’t [want to] become a Samaritans or befriending. I think it is just trying to stay on track of what we actually are, which is a behaviour change service.
Marianne, A, COVID-19 interviews, June 2020
This sat in contrast to the approach of the second provider:
So, that is kind of very much, I think, the philosophy of the organisation. We want people to thrive. We want people to do well. And well is what feels well to them. Not necessarily to be judged by any other yardstick with that . . . Let’s find out what you are interested in and we will find that close to where you live. And if it doesn’t exist, we will work with you to make it happen. We will find other people who want to do what you want to do and we will help you to run your own group.
Annette, B, COVID-19 interviews, May 2020
The impact of this difference on the day-to-day experience of link workers came to the fore if clients moved from one provider to another:
I know when I took over my caseload, the previous worker had been from a previous provider, and they were what I would think in terms of a support worker. They were doing all this stuff for people, and people were coming in and saying, ‘Where are my benefit forms? My worker was going to do this for me and do that for me’. I’d go, ‘Sorry, it’s not the way I work. I like to give you the skills and let’s work together so that you have the skills to do this with the support from the community’. Really try and empower people to take up ownership. They didn’t like it at the beginning. It was a big shift.
Charlie, A, focus group 1, October 2019
However, these differences were not consistently as stark and, over time, work practices in provider B appeared more aligned with those in provider A:
So we get a lot of pushback from clients saying, ‘Well, you used to take us here’, and, ‘You used to take us there’, so it’s having those conversations with them, to say our service has changed and, actually, the responsibility lies on you to do a lot of these things, especially things around medical assessments. They always wanted us to go and it’s just a time-consuming thing, and you’re having to wait so that’s been a challenge because clients obviously do complain.
Marie, B, interview, December 2019
The suddenly changed environment of the pandemic seemed to reverse this drift somewhat, with the significant disruption to people’s lives requiring a more supportive role, as setting and achieving goals became unrealistic and the acute pressure to provide food, medicines and financial support became dominant:
. . . our main aim is to do the Well-being Stars and to encourage and monitor that healthy behaviour change, but I think at the moment the priorities are leaning a lot more towards corona and checking that people are okay and they’ve got access to food and medicine, that they’re coping with it mentally and they know what they should be doing. So, I think a lot of the phone calls and conversations, we just steer towards that.
Abby, A, COVID-19 interviews, June 2020
Provider ethos shaped link worker practices, but there was also autonomy observed in the way each individual link worker created their role. Personal and professional histories intersected with provider culture, training and the performative pressures of the intervention, generating a spectrum between the extremes of intensive support and the individual behaviour change described here.
Link workers
Link workers drew on a range of previous experiences. Some were recent graduates while others had considerable professional experience of working in the community and voluntary sector, and others of working in the health sector. Most link workers had degrees, some at postgraduate level, and two were non-practising clinicians. Appendix 12, Table 42, summarises the demographic data that were provided by the link workers who completed the questionnaire.
Link workers had varied personal histories. Some had experience of adversity or health problems that had led them into their current role, and, in addition to the relevant qualifications, managers were aware that link workers needed other, less tangible, qualities:
. . . people are either predominately interested in helping somebody else achieve their potential and looking at their life from their eyes. And, over time, I have found that is something that is almost impossible to train, teach somebody. It seems to come from an intrinsic value that they have, and that is very much what we are looking for in an interview.
Annette, B, COVID-19 interviews, May 2019
New starters were expected to undergo an induction programme including mandatory training, such as training in adult safeguarding and health and safety practices. This was delivered by the provider organisations and the intervention:
When asking about the training that is provided in house, and by [WtW], I was told that things like [training name], diabetes and COPD training are organised together with the second provider organisation and each provider provides separate training around the Well-being Star and motivational interviewing.
Field notes, B, September 2019
The cyclical nature of provision saw some new recruits in post for some time before receiving training. Ongoing learning opportunities were also provided by the provider organisation and by the intervention, which included collaborative learning events that brought together link workers from both providers. These formal routes to learning and training were variably received. The agenda at much of the provider training events observed by the researcher was driven by a requirement to meet referral targets and complete the WBS. Some link workers described limited opportunities to guide their own learning.
Less formal routes to learning the role, such as shadowing and sharing tacit knowledge, were seen to be of considerable value. Much of this was facilitated by shared office spaces and opportunities for informal chat that built on individual relationships and unique pieces of knowledge about local services. During the early stages of the pandemic, opportunities for ‘bouncing ideas’ were fewer but, with time, new routes, such as impromptu video calls, were established.
Despite the need for formal training and guidance being recognised by link workers, it was clear that individual approaches were significantly differentiated:
I don’t think you could do the job properly without that training. What you would do, and people who are stubborn and won’t go to training, what they tend to do then is create their own job. That’s when you become a support worker, because you think you know the role and you don’t.
Hilary, A, interview, November 2019
Hilary went on to explain:
I want to be a link worker who links people out, and behavioural change is really important to me, which is coming more into the link worker role now.
This extract illustrates at a link worker level the tension in approaches described earlier between providers, although differences between link workers could not always be categorised by provider, adding a layer of complexity when tracing this variability. Attention is once more drawn to a spectrum of stated approaches, between support work and a focus on behaviour change, differentiated by both provider and link worker, with a sense once more that one approach was favoured over time. For several of the link workers, the role they were performing was not necessarily what they had imagined link working to be:
I thought, when I applied for the job, I’d be doing a lot more of that [support work] than what we’re encouraged to do. So, my impression is that we’re kind of told to shy away from that as much as possible, because we’ve got so many targets for referrals and assessments. But in reality, I think it would be better if we were offering more one-to-one support into going out into the world, going to appointments, going to things.
Abby, B, focus group, September 2019
Another link worker described how she was not aware of the targets when she had applied for the role:
So, it swiftly went from wanting to help people with their day-to-day kind of problems, to, ‘Make sure you get this appointment and make sure you get this referral’. And, although we’re not paid for referrals, it generates the [WBSs]. So, then, again, it’s just payment by results, kind of consistently.
Sara, A, interview, December 2019
To explore these tensions further, we go on to describe in more detail the daily routines undertaken by link workers, drawing out where they emerge in working practices and how they shape delivery of the intervention.
Link working
Work routines
Link workers operated at different sites. Their ‘base’ was at the offices of their provider organisations and in both instances included a shared office space with a kitchen. Each link worker was also allocated a GP surgery at which they had designated ‘surgery time’. They mostly worked with clients from their surgery, but if caseloads were high or staff left, then this could change. Less commonly, link workers visited clients in their homes or in a community setting. It was generally felt that home visits were conducted much less often at the time of fieldwork than at the start of the intervention. One encounter took place in a local library, which was observed, and link workers reported that they could meet clients in cafes, but this was not observed. At one team meeting, it appeared that this could become problematic when clients were unable to afford coffee and provider policy dictated that link workers could not pay from petty cash.
Link workers’ interactions with clients could often begin before formal referral, as they were increasingly responsible for generating referrals, which could include telephoning potential clients to offer the intervention. Following referral from any source, link workers and clients usually met face to face. The first encounter centred on completion of the first WBS and could routinely take upwards of 1 hour. These were seen to take place mostly at GP surgeries but also in clients’ homes and at one of the provider offices. At the end of this interaction, link workers would encourage clients to set goals, often offering onward referral or signposting to relevant organisations to facilitate meeting them. Subsequent contacts were to assess progress, conduct WBSs and set new goals. The expectation was that when WBS scores were stable, or there were no new goals, clients moved to KIT before decisions were made about ending journeys.
During the COVID-19 pandemic, link workers had to adapt their work routines considerably, with all link workers having to work from home. It was, however, apparent that, in addition to supporting existing clients and delivering the supplementary COVID-19 response, they were still being encouraged to meet targets.
The next section presents the four main work routines identified above and explores how these activities were differentiated and shaped within the intervention.
The referral process
As part of the intervention’s original logic, referrals were to be generated by primary care staff, but differential levels of engagement meant low referral rates had to be supplemented by link workers recruiting new clients into the intervention themselves. Meeting referral targets meant that new WBSs could be completed to secure payment.
Some primary care sites allowed link workers access to their patient lists so that they could ‘cold call’ eligible individuals. At other sites, link workers used IT systems to identify eligible patients, then sent a paper request to clinical staff to generate a referral. The process of generating referrals was an unpopular administrative burden and was also felt by many to be an uncomfortable interaction:
Kate [link worker] emphasises the issues regarding list work . . . the unease at ‘cold calling’ NHS patients asking if they need the [intervention]. She says there are issues with staff feeling harassed by their caseload and the volume of work that they have to conduct/balance, by feeling that they are harassing potential clients. ‘There is a lot of pestering’.
Field notes, B, November 2019
Of course, as well as the work of generating the referral, each new client contributed to the link workers’ caseload. Increasing workload was frequently highlighted and attention was drawn to the incongruity of recruiting new clients and not having time to meaningfully engage with them. The following extract from the researcher’s field notes illustrates just how laborious generating referrals could be, potentially obscuring other tasks, such as face-to-face contacts:
It is only in the preceding 10 minutes, chatting away as we travel together that I became aware of the link worker’s role within this [GP] surgery. I already know that [this link worker] is ‘one of our best, he generates loads of referrals . . . and stars’, a comment made by the service manager during a team meeting in November. However, I did not realise that his time at the surgery is strictly for generating referrals; [he] does not see clients face to face at this location.
Sam, B, shadowing, February 2020
After arriving at the surgery, Sam proceeded to a shared office space to call potential clients:
‘My name is . . . , I am calling from [the GP surgery] from [WtW]. Is it possible to speak to [patient]?’. The link worker then goes on to explain the following benefits of the service – GP offers short appointment time, WtW can offer up to an hour, we provide support, information and guidance to patients with LTCs, we can focus on lifestyles, managing your symptoms and social aspects too. Can I send you a letter about our service?
Following the call, Sam had to send a message to a GP to complete the referral:
‘I have spoken to the patient, explained the WtW service, and s/he is happy to have an appointment. Please can you refer this patient?’, The link worker tells me that he has 10 referrals pending in the task list, the time lag is often because he is waiting for the secretaries to action a task, which can take up to 10 days.
Sam, B, shadowing, February 2020
Woven through many of these examples was evidence of the differentiated relationships that link workers had with primary care staff. Engaging primary care to increase awareness of the intervention and secure more referrals was an important part of the link worker’s role and could be challenging:
As the conversation continued, it became clear that link workers had been tasked with shadowing a GP in their surgery/ies, and that a handout was designed to enable link workers to raise questions with staff within the surgery/ies. This was an exercise designed to develop working relationships and to understand the role of different actors within social prescribing, breaking down barriers that might, for example, prevent referrals, by engaging in conversation . . . However, one of the link workers stated that she felt uncomfortable doing this, and it was clear that there were different relations of power and interactions experienced by link workers depending on the surgery they worked in.
Field notes, A, December 2019
During the COVID-19 pandemic, link workers were still encouraged to generate referrals. One link worker, Abby, described how practices had given them lists of vulnerable patients whom they could call as part of the intervention’s COVID-19 response. If they were eligible, they could also offer individuals the intervention.
At the start of the pandemic, there were examples of relationships with primary care being renegotiated and new working practices emerging. The intervention responded rapidly, providing practices with the opportunity to deploy link workers in activities they felt to be the most useful:
There have been opportunities with supporting around the shielded list, and some partners that maybe haven’t necessarily understood our role or utilised the link workers in the past have utilised them.
Janice, A, COVID-19 interviews, June 2020
This experience was not consistent, and link worker managers were able to identify that increasing pressure on primary care teams during the pandemic had occasionally exacerbated existing difficulties with engaging them in the referral process. Nevertheless, it was clear that new possibilities could be negotiated and that strong working relationships with primary care could reshape performative pressures and change existing work routines.
The Well-being Star
Following referral, a face-to-face meeting was arranged between clients and link workers. Following introductions, link workers would usually outline the intervention’s consent and data-sharing procedures. Through repeated observation, it became clear that the remainder of this first meeting was heavily structured around completing the WBS and, although different practices were observed, the sequential movement through all eight domains seemed to permeate all of the encounters. The WBS was popular with link workers as a tool to guide conversations and identify issues that clients may not otherwise mention; however, the need to complete it could, on occasion, be at odds with the natural flow of conversation. Link workers had to navigate this carefully, striking a balance between listening to the client’s concerns and gathering the information for the star.
Between stars, clients ideally worked towards goals, and link workers acted on tasks generated. The aim was to complete stars every 6 months until things were stable, at which point clients were expected to move to KIT:
What do typical journeys look like? The team leader picks up a marker pen turns to the flip chart paper and starts to write, from the point people get referred, people stay in engagement phase until first star, this period of time can be days, weeks or months, we don’t give up on people (stress, bereavements, etc.) – there is no official time limit for the amount of time people can be on the engagement phase it is just what they are classed as being in until the first appointment. Intervention phase begins once client moves between first and second star, typical journey last 18 months – 2 years, over the course of 18 months set goals, supported clients with goals and most goals have been achieved. People are steady, scores have shifted from low to as good as they can get (diabetes under control, exercising, moved house), therefore nothing else needed, so move to KIT (a safety net for the client and a way that link workers can make sure all changes made by clients in 1.5 years are going to be sustained over a long term without the need of a link worker). If we call them in 3 months it gives client the opportunity to say if things are going well, or if things have changed. Hopefully stay in KIT for star five and six, and all scores stay same, have not gone backwards, therefore, we can close them.
Field notes, B, December 2019
This extract charts a linearity, imposed by completing sequential stars, that was often at odds with the routines of link workers and overlooked the complex reality of clients’ lives. This same linearity could also obscure some aspects of practice:
Then you’ve also got the people who have catch-up between their Well-being Stars. I have people that want to be seen every 6 weeks just to keep them on target, they need that space to come and talk through everything that’s going on in their heads. So, I have quite a big handful of people like that. You’ve got them that you’re seeing, then you’ve got your stars every 6 months, then you’ve got your generic catch-ups, which can be anywhere between 2 or 3 months between stars, and then they’re expecting you to get more new ones in as well.
Anna, A, focus group 2, October 2019
During the same focus group, another link worker recounted her experience with a client with whom she had been working:
I did a referral for her for talking therapies. She just turned up at the surgery one day and she wanted to see me, she says, ‘I’ll wait . . . If she’s got people in I’ll wait’. I sometimes work until 6.00 [p.m.], even 6.30 [p.m.] if I have to. I don’t mind, because, to me everybody’s different so it’s that flexibility you give your client. We had a bit of a chat, then I did something else for her and did another referral for her.
Anita, A, focus group 2, October 2019
This incongruity was brought into even clearer focus during the COVID-19 pandemic, when all clients and link workers experienced a significant disruption to their circumstances. The following extract paints a picture that sits in stark contrast to the linear one drawn above:
Life, regardless of whatever interventions, whether it’s us, GPs, or us, it’s waves. It tends to be waves that kind of occur. I guess our job is trying to help try to smooth some of the waves so it’s not as rocky and people don’t get quite as seasick with them, [laughter] for a bit of an analogy. We can’t necessarily . . . We can’t achieve that kind of . . . Right, everybody is okay for the rest of their lives now. That’s not really realistic.
Alice, A, COVID-19 interviews, July 2020
Understanding how the WBS shaped client encounters and imposed a sense of linearity is important because link workers were under a performative pressure to complete them to secure payment, as illustrated by these field notes from a training event led by the team leader at provider B and by a quotation from a link worker from the same provider:
The team leader asks staff for their thoughts on the money associated with WBSs and their awareness of this information. One of the newer link workers states, ‘I find it difficult that we place a monetary value on people. I tend not to think about that side of it’. The team leader states that link workers are in a funny position, ‘at interview we say it is person-centred, it’s holistic, we do it at a client’s pace, that’s why we have the luxury of such a long time working with them’. She also states that link workers have to represent the client-facing caring aspect of the service, without letting them know about the financial implications of the WBS. Getting funding from social investors, that we can pay back, so it is in our interest to do so, but should not let clients know or push them to do stuff.
Field notes, B, December 2019
I know you don’t feel as if you think about the money, but that was one of the first things I was told when I started. So, Jo [link worker] had said to me, ‘We get x-amount for a second star’. And I thought that was commission. That was how it came across and I said, ‘Oh, I didn’t know that it was commission-based’. And she said, ‘It’s not. It’s for the company’. And I was like, ‘Right’.
Abby, B, focus group, September 2019
Once completed, data from the stars had to be put into the IT system; the following extract shows how failing to do this meant that they were of no value:
The team leader moves on to cover the importance of adding a goal for a client, noting that MIS [management information system] order means that if ‘add goal’ is completed first then payment for WBS is missed and therefore MIS will NOT generate a second WBS reminder or show on claims form. The team leader provides instructions about how to reorder the information using ‘input’, stating that all client journeys will stay red until the order is changed.
Field notes, B, December 2019
Once the WBS was completed, link workers were able to move on to the ‘linking’ inherent in their job title.
‘Linking’
Link workers described how they used the WBS to structure goal-setting and offer support to the client. What this meant in practice varied considerably. Goals could be anything from stopping smoking to attending the next appointment. Onward referrals were observed to be lifestyle interventions, such as cookery classes and exercise sessions, with some signposting to more tailored groups, such as fishing clubs and veteran support, although these examples were already known to the clients. Link workers also made referrals to the voluntary sector for welfare advice, wrote letters on behalf of clients, and liaised with GPs and other medical staff to resolve queries about medications. Onward referral and signposting could be difficult, requiring the link worker to align the client’s social world, the requirements of the intervention and local community provision. Pauline, for example, worked with a client who was keen to do more exercise as one of his goals:
The client had previously been referred to the gym, a 10-week session that had now finished. He was waiting for a phone call to move to another class. LW explained that he will still be able to move to another class but that there was a waiting list. The client enjoyed swimming but [his local pool] is currently closed for refurbishment. LW suggested [another pool], but client said it was no good as he would have to use two buses to get there, and two buses to get back.
Pauline, B, shadowing, October 2019
Few direct interactions were observed with VCSE actors. Where they did occur, they involved a link worker contacting an individual they already knew, such as a named contact at the local food bank. It was acknowledged that community sector funding was a key part of social prescribing, with concerns that already precarious funding streams would be further threatened in the post-pandemic landscape. One manager alerted the researcher to concerns about VCSE capacity locally, citing a report that likened the roll-out of NHS link workers to ‘lots of travel agents and no holidays’. 113
In addition to onward referral and signposting, link workers also provided informal and less tangible types of support. For example, one link worker, Lucy, said that she would often text clients in her own time to check on them and remind them of important appointments. Another link worker said that sometimes she just listened:
And you’re just . . . And I’ve had so many clients burst into tears on me at the first meeting going, ‘Finally, somebody’s listening to me. Somebody is going to help me’. I think that’s really important. I think that’s the biggest thing.
Kate, A, focus group 2, October 2019
Variability was apparent between link workers in what they felt the boundary of their role was. Hilary made a clear distinction between support work and behaviour change, citing the following example:
My previous link worker was very much a support worker . . . she did 17 home visits, whereas I brought it down to one. She went to the homes, and once you are in somebody’s home they’ll say, ‘Oh, I can’t do this’. She was very much a, ‘I’ll do it’. Hence the dog washing. This man couldn’t wash his dog. She said, ‘Oh, I’ll do it’. Then it became regular. Then every week she was going round to have coffee, dog washing. I think the problem was is she had lost sight of the role. She was a support worker, not a link worker, and that’s the really big difference for me.
Hilary, A, interview, November 2019
We also touched on a sense that over time link workers were being encouraged more towards a focus on promoting individual behaviour change. Inherent in this was a sense that clients had to be ready for the intervention. For some link workers, this created contradictions between wanting to help clients navigate their complex social reality and acknowledging their reduced capacity to benefit from an intervention that required them to change their behaviour:
Really, I guess, if we really want to be part of social change, then those are the [complex] people that we really want to really try and win over. They’re the people who also DNA [do not attend] for the doctors and nurses, who don’t come and get vaccinations or whatever might help support their health. So, it does make a difference, but those are going to be very miniscule movements. Whereas you get someone further along who’s more motivated and, yes, they’ll go to [exercise classes] or anything that you send them to, and they’ll have a bigger change because you’ve caught them at the right time and they’re ready for it.
Lucy, A, focus group 2, October 2019
We touched on how the proposed linearity of the intervention could be at odds with the complexity of clients’ needs, and here we see how this complexity was poorly aligned with the increasingly dominant narrative of behaviour change.
Ending journeys
Decisions to discharge
The decision to end a client’s journey was not always easy. We saw in the linear account of the intervention given above that clients in KIT who no longer ‘needed’ the link worker’s support were ready to end their journeys. However, the observed reality could deviate from this and appeared to be shaped by the performative pressure of meeting targets. There were examples of link workers being encouraged to end journeys to balance capacity but, equally, discharge could be delayed until after a star was completed to secure payment.
Closure. The link workers refer to their ‘core purpose’, to work with as many people as possible, stating that closure is needed to make room for more. The discussion focused on being able/or not, to free up time to get a new cycle of clients going.
Field notes, A, December 19
Some clients did not feel ready to be moved into a KIT phase or to be discharged. Indeed, one link worker suggested that some clients reported lower scores on their WBS to avoid discharge. It appeared that for some the lived reality of ending a client’s journey could be a complex process, embedded in the therapeutic relationship. In one interaction with her client, Tracy (who we meet again in the next chapter), Lucy introduces the possibility of ending her journey soon:
The link worker states that Tracy has been a WtW client for a while now, and that it won’t be yet but eventually she will have to ‘stand on her own two feet’, she says that Tracy will have more time to focus on herself after all of her appointments subside. Tracy says that she is scared of losing her support networks if she gets too healthy. The link worker recognises her genuine concerns, encouraging her to think about the social benefits of going to the gym, and not to worry about stuff disappearing as ‘you will fill your time with things that are more challenging’.
Lucy, shadowing, February 2020
This echoes earlier narratives about patients not needing the intervention any more and resonated with other accounts where link workers acknowledged that the end point was not to ‘fix’ clients but to help them do things for themselves.
However, primarily because of caseload and regular changes in staff, the process of ending a journey could not always be so carefully negotiated. The start of the pandemic forced many link workers to review client journeys and discharge some clients to balance capacity and workload.
Reflecting on success
When considering what had been successful, link workers often gave nuanced and detailed descriptions of what they had achieved for clients. These were often less tangible than the outcome metrics recorded by the intervention and that generated payment, and were also intertwined with the narratives around ending journeys when clients could ‘stand on their own two feet’:
I think from working and having a caseload, it is seeing people go through the whole process, make big changes in their life and get to that point where they don’t need us and you just think, ‘You’ve done your job properly and you’re in a much better place’, even if it’s just through minor, little changes or really big house moves or whatever it is.
Marie, B, interview, December 2019
You see massive character change, you see confidence change, like, they’re willing to engage change. I’ve got a guy, who when I first started seeing him, was having five or six panic attacks a week, now it’s two or three and he says that’s because of me.
Molly, A, focus group 2, October 2019
In another example, one link worker described how she had worked tirelessly with a cancer patient who was homeless and struggling with her immigration status. She was proud to have arranged accommodation, secured a regular income, worked with the GP to stabilise the client’s medication and had positive correspondence with the Home Office; these are all outcomes that can be traced to the work of ‘linking’ described above.
There are also other examples that could be included, often detailing clients’ complex social circumstances and the wide variety of routes that link workers took to help them. Success was seen variably as an increase in clients’ confidence, making things a bit easier for them, or simply getting clients to attend a follow-up appointment.
Link worker turnover
The intervention had experienced quite a high turnover of link workers, with departures and new appointments both prior to and during fieldwork. This was because of a number of factors. Pressures to achieve targets and an increase in caseload have all been discussed and were occasionally cited:
Kate [link worker] said ‘have you seen the photograph in the office? There are only two link workers remaining from that original photograph’. She continues, ‘our role is defined by stars, no one is happy. It is not fulfilling’. She tells me that ‘they are putting targets on a client’s head, that we keep clients for too long, based on a need for assessment. At the first meeting, I often know they are not going to engage, don’t need our help, but at the following appointment we complete a second star, move them into KIT, then complete a third star 5–6 months later. The assessment moves us away from care. All that matters is stars, we don’t matter’. She tells me that the turnover is ridiculous and that they (the organisation) would replace us (link workers) in a heartbeat.
Field notes, B, November 2019
The other important factor intertwined with this was building relationships. We have identified how building relationships with primary care was a significant part of the link worker routines, with some finding it a particular burden. However, it was also acknowledged that a high staff turnover served only to exacerbate existing difficulties and, perhaps more importantly, compromise client relationships:
That’s also another topic you might want to touch on, [laughter] the building of the relationships and sustaining that. We do have quite a high turnover of staff, and it is something that our clients find difficult.
Lucy, A, focus group 2, October 2019
As Lucy said before, there’s a huge staff turnover and that has an impact on the clients, on the relationship with the clients, and also getting them to come back again . . . I think it was somebody from 2016 that I spoke to, nobody had been in contact with them and they were like, ‘No one’s been in touch, it’s been quite a few years’. And you’re like, ‘I’m really, really sorry. I do apologise, but I’m here now, how can I help you?’. It’s trying to get back on a footing with them as well, try to get their trust again, and building that relationship again.
Anita, A, focus group 2, October 2019
Another reason cited by link workers for staff turnover was concerns about the sustainability of the intervention, not least because there were new PCN-employed link workers beginning to operate locally. Several link workers had left or were due to leave to take up one of these positions.
Discussion
In the SPRING_NE study, we observed a spectrum of approaches to delivering social prescribing within this one intervention, differentiated by both provider and individual link worker and shaped by the need to meet referral targets and complete the WBS. Over time, there appeared to be convergence towards an individual behaviour change approach, although the acute disruption caused by the pandemic appeared to reverse this to some degree. A range of social prescribing models from ‘light touch’ to more intensive and holistic approaches, with the potential to navigate the social determinants of health, have been described previously. 50,54 In 2019, Wildman et al. 15 identified that WtW was targeted at behaviour change while also being conceived of as intensive support addressing the social determinants of health. The authors also outlined barriers to performing the link worker role, including referral practices and pressures to meet targets. Through its engagement with complexity, this ethnography has allowed us to explore these tensions further.
Drawing on the wider literature, we can see how the intervention itself is complex, while also recognising the complexity of the systems into which it is being delivered. 114 In contrast to the linear logic proposed, from referral through to discharge, the intervention had multiple interacting and dynamic parts within a context that was constantly evolving. 115 The intervention emerged as a series of routines, relationships, resources, power structures, ideas and values. 116 Link worker routines were significantly altered by the requirement to generate referrals, a time-consuming task that could leave less time to engage with clients.
The referral process drew out tensions between the intervention and primary care, highlighting how difficult it could be for link workers to become embedded within practice teams, a problem that has been highlighted elsewhere. 49 We observed link workers building relationships within complex structures shaped by institutional histories and power. Individual link workers, and the intervention, were ‘embraced’ or ‘resisted’ to varying degrees within primary care, meaning that link workers had to adjust their practices, with unintended and unpredictable consequences. 117 By viewing primary care as a complex system, we understand that embedded behaviours can be difficult to change118 and see how lack of engagement in the referral process could lead to a disproportionate impact on link worker routines, resulting in less face-to-face contact with clients over time. For community health workers (CHWs) in the USA, the success of their role was contingent on how integrated and supported they were into existing systems. 119 Professional hierarchies structured the role, shaping possibilities and even removing what was seen by some as being most valuable, namely an ‘agenda-less relationship’. 119 Similarly, we saw that a lack of familiarity and clarity around the role of social prescribing within primary care created problems in referral processes that had a major impact on the delivery of the intervention, most importantly reducing time available for clients.
Drawing further on this work, we arrive at another tension: balancing the complex needs of clients with the financial and professional goals of other actors. 119 As a consequence of the funding mechanism for providers, we observed link workers operationalising the intervention’s targets to generate payment in a process that privileged some routines at the expense of others. A SIB was seen as a novel and pragmatic way to fund social prescribing in the absence of existing provision, a recognised benefit of a SIB. 120,121 However, what we observed also speaks to critiques of SIBs in the wider literature. 121,122 The SIB’s focus on output metrics to generate payment seemed to favour certain approaches and, over time, there appeared to be convergence between providers. There was a linearising effect as the requirements of the SIB were conflated with the socially innovative aims of the intervention. Indeed, much of the literature on SIBs focuses on outcome metrics and the challenges of measuring what counts, as opposed to what can be counted. 121
We identified high staff turnover as a threat to this intervention becoming embedded. Link workers cited poor relationships with primary care and targets among other reasons. As link worker numbers increase, the implications of these complexities will be important if they are to become embedded. It will also be important to understand how their work routines are likely to be shaped by the referral pathways, output metrics and targets that they are expected to operationalise.
As a novel service, carving out a space at the intersection of primary care and the VCSE, social prescribing as delivered by link workers has inevitably been shaped by its context, resulting in a heterogeneous, contested and evolving intervention. Our ethnographic methods allowed us to develop an understanding of the social prescribing intervention through the eyes of the link workers who deliver it. Drawing on their accounts through interviews and focus groups, and through developing our understanding of the everyday routines and practices of link workers using participant observation and shadowing, we have been able to provide a rich account of the way in which the intervention has been shaped by these intersections with the provider organisations and the wider VCSE sector, with primary care, and by its funding mechanism. We paint a picture of a heterogeneous intervention through which link workers have offered some clients long-term and responsive support and in other cases have focused on empowering and motivating clients to promote ‘behaviour change’, with evidence of drift towards the latter approach. ‘Link working’ remains a contested role within this intervention, and we link high staff turnover to the challenges of delivering the role. Link working social prescribing will continue to be shaped by the changing environment in which it operates, one that has been dramatically altered by the COVID-19 pandemic, and will evolve further with the roll-out of social prescribing within the NHS.
Chapter 6 Client experiences of the intervention
Introduction
This chapter presents ethnographic data (participant observation and interviews) that examine the impact of the intervention on clients’ social worlds and how their social worlds shaped their responses to the intervention, for example how lifestyle changes were negotiated in local contexts. In Part 1: clients’ experiences of social prescribing, we explore how the intervention was experienced by clients and, in Part 2: social worlds shaping responses to social prescribing, we attend to the relationship between social context and engagement with the intervention.
Methods
In the SPRING_NE study, the researcher (Kate Gibson) engaged with a sample of key participants (i.e. clients) from the beginning to the end of fieldwork to allow us to follow at least part of their ‘social prescribing journey’. We observed participants’ engagement with services and explored practices within their families and social networks. Kate Gibson’s first point of contact with participants was to visit them in their home to conduct a semistructured interview exploring their experiences of health and the intervention (n = 19). Fifteen participants were interviewed again in the final 2 months of fieldwork to follow up their experiences of the intervention. Between the two interviews, opportunities for participant observation were pursued as far as was feasible. For a subsample, particularly those less willing to invite Kate Gibson into their lives for participant observation, photo-elicitation interviews (n = 9) were used to supplement the standard interviews and to generate a more complete picture of the intervention. Kate Gibson also undertook semistructured interviews with family members (n = 7). This equated to over 200 hours spent with participants and/or family members over a period of 20 months (November 2018–July 2020). As necessary, we were flexible and responsive and deployed methods that appeared most productive as we progressed in the light of practical issues, such as the willingness of a diverse range of participants to engage with particular approaches, and the success of different methods in facilitating the collection of rich data.
Participant recruitment
Participants were purposively sampled on the basis of gender, service provider and length of time with the intervention (see Appendix 13, Table 43, for sample demographic data). Based on these specifications, a manager at each provider organisation was asked to select the sample for us to approach. This was to avoid link workers selecting ‘good’ patients, although link workers were asked to use their personal knowledge of clients to advise if any of those selected should not be approached because participating in the study would be likely to cause the client distress (e.g. because of a recent bereavement or a serious mental health problem). During recruitment, the sample was continually monitored for age, area of residence, ethnicity, employment status and household structure to ensure diversity across those demographic categories. As fieldwork proceeded, additional younger and more intensively engaged participants were purposively sampled to populate the younger age range of the sample and to obtain more data about the intervention.
Some participants had been referred into WtW soon after the intervention began when it was delivered by the original four providers (n = 8, referred between September 2015 and May 2017); an additional participant was referred in September 2017, shortly after the number of providers decreased from four to three. The remainder of the sample was referred into WtW under the current arrangement of two providers delivering the intervention (n = 10, referred between January 2018 and March 2019).
We recruited friends and family opportunistically during participant observation with key participants. Family members were approached for interview only with the permission of the relevant key participant.
Participants were provided with an information sheet (see Report Supplementary Material 2) and were asked to provide written informed consent (see Report Supplementary Material 2). Other individuals encountered during the ethnographic observations (but who did not take part in interviews) were offered information sheets (see Report Supplementary Material 2) and asked for verbal consent for the researcher to carry out observations. Informed consent was revisited with participants at regular intervals throughout fieldwork.
Fieldwork and data collection
Interviews
Initial (flexible) interview guides (see Report Supplementary Material 2) asked about participants’ health, their experiences of the intervention and whether or not and how they made changes to their everyday practices as a result of their interactions with link workers. Final interviews were tailored to individual participants and pursued questions and phenomena identified during participant observation, and discussed findings from observations where necessary to avoid misinterpretation. In addition, with participant consent, data documenting client journeys (e.g. notes made by link workers following client meetings) were provided by the intervention (n = 15) (see Report Supplementary Material 2). These records were discussed with key participants at the final interview. Semistructured interviews with family and friends explored health and their perspectives on the intervention (see Report Supplementary Material 2).
Participant observation
Participant observation, or ‘hanging out’, was used to build a ‘thick description’ of participants’ everyday experiences of the intervention. 111 Depending on their individual preferences, participant observation involved spending time in participants’ homes, accompanying participants to appointments with their link worker and accompanying participants to activities and services (e.g. financial advice and volunteering activities), some of which were ‘prescribed’. Further episodes of participant observation were pursued opportunistically and included spending time with friends and family of key participants.
Photo-elicitation interviews
Photo elicitation, that is asking participants to take photographs during their everyday lives and using the photographs to elicit information during a subsequent interview, provided a powerful means of accessing participants’ reflections on mundane and everyday experiences, and aimed to develop insights into how the intervention played out in everyday life. 123,124 Participants interested in taking part were given an information sheet (see Report Supplementary Material 2) that explained the aims of the photo-elicitation interviews, as well as standard ethics procedures for using images in research, particularly the importance of requesting permission when photographing individuals and our assurance that individuals would not be identified in images used in publications. After reading the information sheet and discussing any questions arising, all participants completed an informed consent form (see Report Supplementary Material 2). When Kate Gibson returned to conduct the photo-elicitation interview (see Report Supplementary Material 2), the information sheet and informed consent were revisited and any further questions answered. We lent digital cameras to some participants, while others chose to use their own mobile telephones. Participants were asked to take between 10 and 20 photographs about ‘Ways to Wellness (WtW) in your life’. Most interpreted this instruction to be about health and well-being.
Translation
Some participants did not speak English fluently. Language barriers were overcome by either working alongside paid translators or, at the participant’s request, using a family member. We did not pursue participant observation where language barriers posed problems, as the presence of a translator is unhelpful for this form of data collection. Interviews with non-English-speaking participants were conducted in their first language with Kate Gibson and an experienced translator fluent in the relevant language. Interviews were recorded and simultaneously transcribed and translated into English. The translator participated in discussions about the interpretation of the data to ensure that meanings were correctly understood.
Recording and analysing data
Procedures for recording, transcription and analysis were as described in Chapter 5. Kate Gibson led analysis, and Tessa M Pollard and Suzanne Moffatt contributed through regular meetings to discuss emerging findings. Pseudonyms are used throughout.
Compensation for participants
Key participants received a token of thanks (a £20 shopping voucher) at their first and last interviews, and if they participated in a photo-elicitation interview; family members were also given a £20 voucher for participating in a family interview.
Part 1: clients’ experiences of social prescribing
This section builds on the findings of the previous chapter by connecting a variation in client experiences of WtW with the heterogeneous and changing ways that the intervention has been delivered. Because of the timing of fieldwork, most participants in the KIT stage at first interview were referred into WtW between September 2015 and May 2017 (a time when client numbers were significantly smaller than they were subsequently). The inclusion of these participants has allowed us to gain valuable insight into the early days of the intervention and, consequently, situate participant experiences within the temporalities of the intervention.
Referrals
The WtW logic model (see Appendix 15, Figures 21 and 31) stipulates that general practices identify and refer patients who have ‘expressed willingness/ability to change’. This appears to be the experience of participants who were referred into WtW during its early stages. For instance, despite an extensive period of time passing, Andy clearly recalls a conversation with his GP about his referral into WtW:
It was offered through the doctor. The programme – I don’t know how long it had been going – but they just suggested, ‘Well, we’ve actually got this. Do you want to give it a try?’.
Andy, referred September 2015, first interview, 6 February 2019
A conflicting picture emerges for participants referred into WtW more recently. Although some participants did first hear about WtW from a HCP, as the following quotation demonstrates, they were sometimes slightly reluctant recruits. Patrick recalls with detail a conversation that he had with a health-care assistant:
. . . she [the health-care assistant] went, ‘Mr P, I think you could do by seeing [a link worker]’ . . . And I went, ‘Well, I don’t really know’. She went, ‘Well, let them come and talk to you and see if they can help in any way, with all these problems you’ve got’. But they’re not really problems when I think . . . I don’t class them as problems. And I went, ‘Fair enough’.
Patrick, referred November 2018, first interview, 16 March 2019
Patrick’s conversation with the health-care assistant clearly allowed him to prefigure his referral. However, contrary to following a conversation about ‘readiness to change’ between a patient and a primary HCP, Patrick appears to have been persuaded or ‘recruited’ by the health-care assistant to consider WtW, despite his hesitancy around classifying his ‘problems’ as ‘problems’.
Other accounts of recent referrals suggest a lack of primary HCP involvement in the referral process, and several participants were first alerted to WtW when they received a telephone call from a link worker. For instance, Shirley’s quotation below indicates that she was ‘cold-called’ by a link worker:
She [the link worker] said that my name had been passed on. She’s not at the doctor, but she works in conjunction or something with the doctor.
Shirley, referred September 2018, first interview, 4 February 2019
This experience of being ‘cold-called’ by a link worker confirms the previous chapter’s findings that the introductory stages of clients’ WtW pathways may be shaped by the need to generate referrals, a task often taken in hand by link workers. This temporal ‘drift’, where clients’ different experiences of WtW (in this case, its introduction) relate to the changing trajectory of the intervention as it is operationalised, is something that resurfaces throughout clients’ experience of WtW, as the following sections will elaborate.
Supported linking
Participants in the KIT phase who were in active intervention during the early stages of WtW often reflected on being actively linked into a variety of onward services and activities. These included interventions providing support in seeking employment; advice on benefits; LTC management sessions; small community groups, such as information technology (IT), photography, cookery, gardening, exercise classes and walking groups; social groups; VCSE and NHS-run mental health support; local council fitness programmes; and volunteering opportunities. Moreover, clients received a range of practical support; for instance, link workers often made enquiries or advocated on clients’ behalf, reporting back to the client thereafter (e.g. with GPs, the council and social services). Elsewhere, participants recalled link workers conducting home visits to assist with IT connectivity, supporting clients to navigate housing and benefits system by helping with form filling, sourcing information about grants, and one participant borrowed a link worker’s disabled toilet key while she waited for hers to be issued. Importantly, this was achieved via sustained and continuous interactions with a link worker. For instance, in the following quotation, Brenda recalls an interaction with her link worker following a gym referral. Not only does her link worker follow up on the referral but also the exchange is reciprocal and becomes an opportunity for the link worker to learn more about the gym – an added benefit of their established rapport:
He [LW38] used to ask all about it [the gym], and how it made you feel and what you thought about this, and would you recommend it. Then he used to ask me to ask them questions.
Brenda, referred December 2015, first interview, 5 February 2019
Some participants received telephone reminders concerning impending appointments and activities. As Eddie (referred April 2016) sums up, ‘they would ring me, or send me a text message to remind me that my appointment was getting closer and that kind of thing’. Masood also illustrates this dynamic (referred July 2015); his journey data record detailed activity surrounding several links. After expressing an interest in learning how to ride a bike, Masood was supported to attend a one-to-one bike session. When on the day of the session he indicated he was hesitant to attend, his link worker persisted and accompanied him to the session. Ultimately, Masood was not comfortable with cycling. A few weeks later, Masood was advised by the GP to lose weight and so the link worker put in motion a referral to the local gym and, once again, accompanied him to his first session. For the following weeks thereafter, the link worker called Masood to remind him about his weekly gym sessions. When his attendance dwindled, the link worker liaised with the gym instructor to restart the referral and supported him to attend once more. Alongside this, they continued to send Masood reminders to attend a local IT group.
Masood was not alone in being accompanied to groups. Those in the sample who were in ‘active involvement’ in the early stages of the intervention indicated that they were often accompanied to activities, or at the very least accompaniment was offered. For instance, Zaheer (referred February 2016) was supported by his link worker to apply for Personal Independence Payment (PIP) and his link worker then accompanied him to his appointment:
He [the link worker] ordered the forms, helped me to fill them and then when I got the appointment, he met me at the office where we needed to go, the PIP office. I went in the taxi and I got paid for that. He went with me for the interview. He was a really good support because sometimes you want to say things but you don’t want to say. Where I was, sort of, lacking, he would say something on his own behalf, what he has . . . I mean it wasn’t choreographed or anything. He was there and if he thought I was not saying enough. He would elaborate.
Zaheer, first interview, 9 January 2019
Zaheer’s mention that the link worker ‘was there’ alludes to a form of practical support that resurfaces time and time again in the narratives – and the WtW journey data – of those referred into the intervention in its early stages.
Importantly, the nature and intensity of support appeared to reflect the different needs of clients. Those participants who were enduring more complexities, for example Masood, who was living with multiple LTCs, or Zaheer whose depression and T2DM were exacerbated by redundancy, seemed to have triggered more support from the intervention. Likewise, those with fewer difficulties, for example Geetha (referred August 2016) and Andy, required less support to access activities and, therefore, it is unsurprising that instances of supported linking are relatively absent from their data. As Geetha pointed out, ‘I don’t need support’, and Andy indicated he just needed a ‘point in the right direction’. Furthermore, the WtW journey data show that this group of participants often experienced face-to-face contact with their link worker. The regularity of this face-to-face contact again varied according to clients, but occurred continuously regardless of whether the participant needed support or linking. For instance, even Andy, who just needed a point in the right direction, had face-to-face contact with his link worker every couple of months while in active intervention.
Intervention continuity
Some participants in active intervention during fieldwork experienced a personalised trajectory tailored to their circumstances, similar to participants referred to WtW in its early stages. Particularly important is that these participants reported experiencing regular contact with the same link worker. For example, Patrick had regular contact with his link worker despite saying that he did not really have a need for the intervention (recall he was ‘recruited’ into WtW by the health-care assistant). Nonetheless, he appreciated his link worker ‘checking in’ with him from time to time:
She rang me last week, ‘Are you alright Patrick?’. And all this. I think it’s nice when people . . . You get to know them, and they call you by your first name.
Yes.
It’s nice to know they’re there if they could do anything, if there was anything that I wanted but I don’t really.
Patrick, first interview, 16 March 2019
Throughout fieldwork, Patrick’s link worker ‘checked in’ by telephone or by home visit every couple of months. Patrick’s link worker also got to know his partner well, who said:
He’s got somebody to fall back on because she said, ‘Any time . . . Anything you want’. I suppose that gives you a bit of a boost because you’ve got a bit of safety net.
Patrick’s partner interview, 4 September 2019
Towards the end of the fieldwork, Patrick learnt that his health condition had seriously deteriorated. Because of the relatively frequent contact that he had with his link worker, his change in circumstance was picked up by the intervention soon after his diagnosis; therefore, when Patrick indicated that he required bathroom adaptations, his link worker was on hand to offer support. His link worker got in touch with the appropriate service:
When she came back and said, ‘I’ve been in touch and it’s going to be 18 months or 2 years’. I went, ‘No. I could be dead by then’. . . . I was joking and laughing, and she was. Then she phoned that woman back . . . She said, ‘But I told her you were a lovely man’.
Patrick, exit interview, 7 July 2020
Importantly, the lack of continuity in Patrick’s care did not relate to a lack of contact with his link worker, but was a consequence of inadequately funded public sector services.
Sandeep also experienced regular contact with his link worker. He offered a clear evaluation of his experience at first interview:
I’ve seen him [link worker] probably once. I talk to him quite a few times, just over the phone. He rang me and asked me how I was doing with my daily activities and well-being. I feel like a friend, when he talks. I don’t normally talk to any strangers about how I’m feeling unless it’s a professional that I need to talk to. So, that’s the only time I talk . . . I feel that someone is taking notice and asking me. I feel that if somebody’s helping you once, you try to feel proud of it.
Sandeep, referred January 2018, first interview, 11 March 2019
When Sandeep, who drove for a living, found it increasingly difficult to sit for long periods, he began to reduce his working hours. As with Patrick, because Sandeep was in regular contact with his link worker, his change in circumstance was quickly attended to, and his link worker supported him with an application to PIP and referrals to two other services. Because an established rapport had been fostered with his link worker, Sandeep, who does not ‘normally talk to strangers’, felt comfortable in seeking out the support of his link worker, who felt like ‘a friend’.
Jill also illustrates this dynamic (referred August 2018). At first interview, Jill had no understanding of WtW. She confused the link worker with the diabetes nurse and after several prompts recalled ‘I went to see somebody at the doctor’s surgery’. During fieldwork, and 10 months after their first meeting, Jill received a telephone call from her link worker. Coincidently, the call came soon after Jill’s father passed away, at a time when her mother’s health was deteriorating and her own health issues were in flux. Importantly, the telephone call, to conduct a WBS, acted as a catalyst for activity and triggered a series of four face-to-face meetings over many months. As well as offering emotional support, the focus of these interactions centred on providing practical support for Jill’s mother, such as help with form filling and accessing a disability badge. As Jill’s husband reported:
Sort of practical help that he was offering as well as the just having somebody to talk to as well I think and just reinforce the healthy eating side of things.
Jill’s husband interview, 23 September 2019
Contrary to Jill’s lack of clarity about WtW at first interview, by the final interview her narrative shifted from a complete lack of awareness to a clear evaluation of her link worker:
He offered support, he said . . . ‘Well all these forms we were filling in for my mum’ . . . If we had any problems he would help with them, and he was really – he’s a nice lad. Easy to talk to. But yes, he offered us these walking groups and stuff, but again it’s a group. I didn’t do stuff like that. Yes, I like [link worker].
Jill, exit interview, 3 July 2020
Evidently, although it took 10 months for their relationship to be initiated, the continuity of having the same ‘nice lad’, who was ‘easy to talk to’, together with the relevance of a series of face-to-face interactions to Jill’s context, rendered the intervention memorable for Jill in ways that did not surface in many others, as the following sections will explore.
Unsupported linking
Participants in active intervention at the start of fieldwork reported a tendency to be signposted to services and activities. Interestingly, none of these participants engaged with the signposted activities during the fieldwork period. In addition, participants experienced far less supported linking than previously observed. For instance, at first interview, Shirley discusses an impending gym referral, which her link worker had set in motion following her first WBS some months ago. When Shirley attends her gym induction, she is disappointed to learn that her high blood pressure resulted in the referral being postponed. When she finally commences the gym, it is clear that her link worker had been absent from the referral process bar the initial referral 6 months previously:
I ask if she’s heard from the link worker. She says, ‘Nope, I’ve never heard anything’. Apart from meeting her once in September and chatting on the phone about her gym referral before Christmas, Shirley’s had no contact. She says ‘I’d like to hear from her to find out what happens next’. I say, ‘What do you mean ‘next?’. She replies, ‘What happens after the gym?’.
Shirley, referred September 2018, meeting for coffee, 25 February 2019
At final interview, some 17 months later, Shirley explained, ‘I heard nothing after that’.
Shirley’s referral experience is in sharp contrast to, for example, Zaheer’s and Brenda’s experience of linking, as described above. Their retrospective narratives allude to a depth of support around linking, which is relatively absent from Shirley’s recollection that she ‘heard nothing’ despite her early expectations. This lack of supported linking appears not to relate to client need but to reflect a lack of contact, which in turn means that the intervention often failed to capture changes in circumstances, such as the postponement of Shirley’s referral. Furthermore, during fieldwork, it became apparent that frequency of contact varied according to provider and/or link worker rather than client. For instance, participants with one provider appeared to have less contact overall. Some participants referred to this provider were contacted only to complete a WBS, which was at times conducted late, meaning that there was a considerable gap between contacts. Moreover, a number of these participants had no face-to-face contact with a link worker following their first meeting. The most extreme example of this experience is Bobby, whose referral in July 2018 came just 8 days after his T2DM diagnosis. Following his first face-to-face link worker meeting, Bobby had two further telephone interactions with his link worker, each time to complete a WBS (WBS2, 15 minutes; WBS3, 10 minutes). By the end of fieldwork, some 24 months after his initial referral, he received a total of 1 hour 25 minutes from the intervention.
Labani’s experience also echoed this finding (referred November 2018). In our first interview (19 March 2019), Labani’s daughter, who was helping with translation, after several prompts recalled that they had met ‘someone in the GP’, in turn prompting Labani to recall that the link worker had offered support with her finances: ‘It is cold and we spend a lot and it isn’t enough, so they said they will help us’ [translated from Bengali]. Her daughter added that they had been expecting some information through the post. At the end of the interview, Labani asked Kate Gibson for benefits advice. On learning that they did not know how to contact the link worker, Kate signposted them to the surgery. When Kate returned to conduct the photo-elicitation interview (13 May 2019), Labani again asked for benefits advice. Kate texted Labani the provider’s office number, and Labani called Kate the following week to ask the name of her link worker. When Kate telephoned 1 month later, Labani explained that she had been in touch with the link worker and that she had been sent a ‘benefits pack’: ‘you can come and I will show it to you’ she added. The field notes below describe Kate’s visit the following week:
Labani has been to the GP surgery to meet with the link worker and the link worker had asked about her health and Labani had asked about benefits. I ask if they received help with benefits and she gets out the contents of an envelope for me to look at. I notice a WtW compliments slip which reads, ‘As requested, please find enclosed information . . .’. Labani shows me two A4 printed pages. . . . Her husband is also in the room by this point and on learning that they do not know what to do with the information, I explain to them that ‘Welfare Rights’ refers to benefits advice and that I have brought something similar. I show them the list that I have brought. I point to [two local community resource centres] and ask if they know how to get there? They know both.
Labani, home visit, 24 June 2019
Three months later, neither the link worker nor Labani and her family had followed up on the welfare advice information:
I ask if she still has to go to the doctor’s every couple of weeks for a sick note for benefits. ‘They have stopped the benefits’ she says. I learn that because they were [abroad] for 5 weeks their benefits were stopped and don’t start again until mid-October. ‘How are you managing?’ I ask. ‘We have borrowed some more money from here and there’, she tells me. I ask if they managed to do anything about the debt advice places I gave them last time. Her husband tells me they lost the paper.
Labani, home visit, 24 September 2019
Rather than receiving support to access benefits advice, Labani, like several others, was signposted. However, the conversation that Labani and her family have with Kate around accessing benefits advice suggests that, with continuity and persistence, this link could have come to fruition. Particularly important is the fact that, unlike the examples of Sandeep, Patrick and Jill described above, whose link workers clearly responded to their biographical disruptions, Labani’s link worker was not ‘there’ to know that her benefits had been stopped. This lack of continuity is particularly interesting given that Labani was in touch with the same link worker throughout her journey: a rare experience across the sample. The following section will explore the absence of embedded, continuous and structured link worker–client relationships.
Intervention interruptions
Given that participants sometimes engaged with the intervention for a lengthy period, it is unsurprising that link worker change was a common experience. However, in analysing the impacts of changing link workers, a theme of temporal drift once again emerges.
Many participants did not report having an established rapport with their link worker and, therefore, a change in link worker often had no negative impact on their experience. On the contrary, for some, a change in link worker resulted in a more effective intervention. For example, Steve (referred November 2018), who lives with multiple LTCs and was experiencing housing difficulties, received one telephone call from his link worker shortly after his first meeting. He was then contacted 10 months later by a new link worker, who organised a talking therapies referral:
He went to see a ‘different lass’ a while back. ‘She was quite good actually. She got us a . . .’. He spends several minutes trying to recall the word he was looking for. Eventually it comes to him and he tells me that he’s been seeing a counsellor. The link worker had asked if seeing someone would help him and he told her that he had seen people in the past but that had stopped now. So, she referred him to [service] and within a couple of weeks he was seeing a counsellor.
Steve, telephone call, 18 May 2020
A change of link worker initiated intervention activity for Brenda also. Brenda had previously understood that she was no longer in WtW and was, therefore, surprised to receive a telephone call ‘out of the blue’ from a new link worker. She explains below:
Brenda told her [the new link worker] that the last person she’d seen had said that there was nothing more WtW could do for her so had been discharged. The new link worker explained that she wasn’t sure what happened there because they don’t normally discharge people like that. So they did everything over the phone, including a star [WBS6]. Afterwards the link worker asked if there is anything she’d be interested in doing and Brenda had said ‘Yes, I’d like to join [name of gym] again’. So the new link worker has obviously organised it she tells me as she received a letter inviting her to go to the gym.
Brenda, telephone call, 24 April 2019
Neither Brenda nor Steve position a change of link worker as having a disruptive effect on their WtW journey. For Brenda, who was referred in December 2015, this lack of impact is in contrast to her early experiences of changing link worker, who we note above supported her during her first gym referral:
He [the link worker] was really nice. He was keen, he was interested, and then he just said to us [me], ‘I’ll not see you on your next appointment’, and then he was explaining, and I said, ‘Well, it’s stupid. If you’re here and your clients are happy with you, why are they moving you?’.
Brenda, first interview, 5 February 2019
In fact, many participants referred into WtW in its early stages alluded to a break in continuity triggered by a change in link worker, as the following excerpt demonstrates:
Do you feel like you know your link worker?
The first one and the second one, because I spent quite a bit of time with the first one and the second one. The first one, I spent more time with. I got to know that lady a bit more, and I felt at ease and everything with her. It was the same, as time went on, with the second one, LW17. LW23, it’s like a one-off thing. Sometimes he calls me after 2 months or 3 months or 6 months. It’s not like a progression every week, kind of thing, you know.
Eddie, exit interview, 6 July 2020
Although this account highlights the ways that link worker change resulted in a break in established support, as Eddie indicates, with time and continuity new relationships were built, thus delineating the importance of attending to the link worker–client relationship. Moreover, in addition to underlining the break in continuity that occurred when changing link workers, Eddie’s retrospective narrative further emphasises the extent to which over time link workers have become less embedded in client journeys. It is notable that he alludes to a lack of rapport with his later link worker. To some extent, this is to be expected as these clients gradually move towards the later stages of their journey; however, as we have noted above, a lack of contact also surfaced in the experiences of some participants who had been with the intervention for a shorter time.
Some participants had been with WtW for a long period of time; indeed, six participants were referred into WtW during its first year of operation. For some, this could be attributed to their particular contexts and their long tenure reflected the intensity of their ‘active intervention’ stage. For example, Masood required considerable support to be linked into activities. However, not all participants required such long-term support and, therefore, the long duration of their time with WtW was surprising. For example, following Geetha’s first WBS, she consistently scored 40 out of 40 for the duration of her 3-year journey. Furthermore, for this group of participants, the overall decline in contact was magnified during their later years with the intervention. Rather than a ‘natural decline in frequency of contact’,15 contact became unpredictable and declined sharply. For example, in contrast to their experience of active intervention, Zaheer and Masood, both discharged at WBS7, had not been contacted since completing WBS6 12 months previously. In the extract below, it is clear that Zaheer’s discharge came as a surprise:
I didn’t even know I had to be discharged. It’s just like, you know, when you go to the doctor and you are fine and you have no contact until the next time you go.
Zaheer, exit interview, 3 July 2020
Tracy also illustrates this dynamic. After completing WBS6 (when she scored lower than her previous star), she learnt that she would be discharged in the near future:
She [LW9] phoned to say that they won’t be finishing yet, but they will be finishing soon. Like I said to her, am I getting pushed to the sidelines? Am I not getting any support anymore? . . . I just feel like I’ll go back to square one.
Tracy, referred May 2017, exit interview, 9 July 2020
Particularly striking is that Tracy and Zaheer’s telephone calls were during the first wave of COVID-19. At that time, both Tracy and Zaheer were struggling to manage their LTCs, and their mental health was in decline because of deteriorating domestic relationships and the loss of their limited social connections outside the family home. These narratives about discharge, together with the apparent shift towards contacts driven by WBS completion, further highlight the ways in which the intervention has drifted away from its original provision to deliver holistic, personalised social prescribing tailored to individual circumstances. Furthermore, the finding that many participants were not in regular contact but appeared to be ‘kept open’ until the final possible WBS (WBS7) suggests that their ‘journey’, and especially their exit, was defined by measurable outputs that generated funding for providers (i.e. completed WBSs) rather than their personalised requirements. To conclude this first section, we now turn to focus on ‘the group’ as an alternative means of fostering a continuous experience of WtW.
Onward referrals
On the whole, in contrast to the recalled experiences of participants who had been with the intervention prior to fieldwork, more recently engaged participants were not linked into smaller community groups during fieldwork. Although some participants were signposted to such groups, as we note above, participants were unlikely to engage with signposted activities. Instead, participants were offered formal referrals into larger organisations. These referrals were often time limited and either entailed a one-off appointment, for instance to discuss welfare rights or debt advice, or involved participants participating in another intervention, for instance talking therapies, exercise on referral, and LTC management courses.
Some participants had attended weekly groups that were hosted by each provider: an exercise group and a social support group. These groups were central to these participants’ understanding and experience of WtW. In fact, for these participants, the group was the intervention. As one participant stated, ‘groups like that, WtW, the community needs them. Not wants them, needs them’. In the data presented in the remainder of this section, we have further anonymised participants to break links with their biographies and intervention histories.
One provider had previously hosted exercise groups, which were valued as a means to foster social connections. As one participant summed up:
I like to go to the group. It reduces isolation, when you sit by yourself and then you meet other people.
During fieldwork, Kate Gibson frequently attended two social support groups run by the providers. For one participant, this group was a lifeline:
Before WtW [the group], I didn’t have a life. So, it fits in quite well. Now, I’m introducing, I start to get to know people. I didn’t have anything. I just felt like a recluse.
The social support groups were an important link to further activities and other services. For instance, a local organisation delivered a healthy eating workshop and another local charity delivered a session about welfare benefits. Nevertheless, the interventional focus of behaviour change was highly apparent:
[Facilitator] gets the group started by reading out the welcome statement. She reads ‘Hello my name is . . .’, and then reads the aims of the group: ‘to help each other to help ourselves to take individual responsibility for our health and to motivate each other to make changes and to follow our WtW’.
Support group, A, field notes, 20 May 2019
Participants were encouraged to follow the aims of the group and, apart from initial check-ins, they often took part in various activities. For instance:
[Facilitator] hands out the Balanced Life exercise. She writes her answers down on the board as a starting point and we work separately to add our activities into three columns: self-maintenance, self-development and fun. [Facilitator] has gardening in her fun column – [attendee 1 (A1)] says that he and his wife used to love gardening but people would steal the ornaments, even in the daytime. [A2] says that his wife used to have pots out the front of his house and they were stolen too. [A3] says that she tries to research information about hearts because she doesn’t know anything about them.
Support group, A, field notes, 20 May 2019
Attendees often ‘tinkered’125 with health advice and shared stories, which reinforced, encouraged and sometimes challenged each other. For instance:
A7 says that she was doing ok, but is anxious about the weather turning; last winter she was stuck in the house for 3 weeks. She can’t breathe in the cold air so she is making sure she has tins in. Her sister had gone to the shops for her last winter, but it worries her because she shouldn’t leave the house especially because she’s asthmatic now. A6 asks if she is still worried about choking. A little bit, A7 says. She says following the advice of A5 she had tried lying down and tilting her head back to open her airway and it worked. A5 adds that his brother has emphysema and swears by sticking his head in the fridge before he leaves the house. The rationale being that you inhale the cold air and it’s not such a shock for your lungs when you leave the house. A7 says she’ll definitely try it. She finishes her check-in by adding that she had managed an extra minute on the treadmill last week. Although it’s only a minute she is chuffed with that because it puts her at four minutes now. The rest of the group agree that it was a fantastic achievement.
Support group, B, field notes, 20 November 2018
As a space in which health and sociality were inter-related (sometimes explicit, sometimes not), group members felt listened to and, for this reason, these settings were an important space for peer support. Moreover, they were a space in which peer support and interventional support could come together, as the following field notes detail:
The conversation moves to [name] pool opening and the link worker says ‘I thought of you [A3] because I know you like swimming’. I thought [A3] had nodded off again but she says ‘I used to. I used to have my lifesavers’. ‘What would you need to help you to go?’ the link worker asks. ‘I don’t know’, she says, ‘not right now’. The only other female attendee [A4] says she’d go with A3 and the link worker suggests they call in for a coffee and see what it’s like before they go. A2 interrupts with another story and while he’s talking A4 quietly asks A3 what size swimmers [bathing costume] she is and offers to see if she has anything at home she can dig out for her.
Support group, A, field notes, 29 July 2019
Not only does the quiet and tactful conversation between the only two female attendees about body size illuminate their shared and mutual recognition of the potential discomfort of going to a swimming pool in a large female body, but the supportive role of the link worker is integral to opening up the possibility of swimming in the first place.
These groups enabled the clients who attended them to have regular and embedded contact with a link worker and, consequently, the link worker was continually abreast of participants’ contexts. It is notable that the only participant to be accompanied to an activity during fieldwork was an attendee at a social support group. Echoing the findings thus far, this participant had experienced a gradual drift towards unsupported signposting. For instance, while she recalled ‘feeling safer’ when a link worker accompanied her to a home appointment for debt advice in 2017, she also recalled a recent experience of being signposted to information by a different link worker. As with other participants, the participant did not follow up on the signposts. Nevertheless, through the regular contact that this participant had with a link worker at the social support group, it became apparent that she was keen to attend a local community centre but had never ‘dared’ go in because she was ‘too nervous’. Having fostered a close rapport with the link worker through the social groups, the link worker then accompanied her to the community centre.
Ironically, despite their capacity to both create a synergy with intervention and foster community connectivity, both providers withdrew from these groups. When the exercise group ended, this came as a great disappointment to one participant who had attended regularly:
We were so close to the worker, actually, who did the exercise. Upstairs is the office. They usually go downstairs, do the exercise and go back home. Maybe they haven’t got enough staff as well. I don’t know.
For the social support groups, the link workers handed over the reins to trained volunteers and gradually withdrew. The effects of this differed according to group. One group that had been established for 2 years was well attended by 25 regulars, all of whom had developed close bonds. This group identified the withdrawal of WtW as a positive experience because it left them free of restrictions. Even during the COVID-19 pandemic, members of this group continued to keep in digital contact via WhatsApp (Meta Platforms, Inc., Menlo Park, CA, USA). The other group fared less well. Having been set up only 6 months prior to the provider’s withdrawal, apart from the two volunteer co-ordinators it was attended by just four regulars. There was a genuine concern that the group would ‘fold’, and indeed a lack of social connections established there meant that during lockdown attendees did not remain in contact. There was a feeling that a valuable connection to WtW had been lost. As one participant summed up:
Well, that has stopped, hasn’t it, the WtW? I don’t know why. Since the pullback from the group, there’s not much of the support left there. I feel like they’re forgetting.
Part 1: discussion
The temporal perspective offered by ethnography has allowed us to connect a variation in participants’ experiences to fluctuating link worker–client relationships and a changing intervention over time. From referral through to linking through to discharge, participants’ experiences of WtW in its current provision contrasts with participants’ experiences of the intervention in its early stages.
Participants’ intervention histories suggest that over time WtW has drifted away from a holistic service towards a less intensive form of social prescribing. Participants’ retrospective narratives about WtW during its early days echo Moffatt et al. ’s1 previous research into the experiences of WtW clients that found that ‘participants consistently reported feeling at ease and relaxed with their link worker, which enabled them to develop an open and trusting relationship’. 1 It was rare to find such appraisal during our fieldwork, apart from the narratives of Sandeep, Patrick and Jill recalling their previous experiences. Their experiences resonate with research, which finds that a strong and supportive relationship with a link worker is integral to the workings of social prescribing. 1,4,25,54,56 Through continuous and regular contact they developed a close rapport with their link worker, which, in turn, meant that changes in circumstances could be picked up by the intervention relatively quickly. Similarly, the social support group acted as an avenue to foster regular contact with the intervention, as well as linking clients to further activities and support. However, both providers withdrew resources from these groups despite their value in offering a range of substantive positive impacts.
Although having continued and sustained contact with the same link worker is likely to be beneficial, link worker change is inevitable in lengthy intervention journeys. The experiences of earlier referrals echo Wildman et al. ’s54 research with WtW clients, who reported that changes in the personnel delivering the intervention disrupted the continuum of a previously embedded relationship. Wildman et al. 15 recommend that ‘when continuity with a link worker is not possible, expectation management and careful management of the change is likely to be important for keeping clients engaged in the programme’. 15 For our participants, a change in link worker was often surprising or ‘out of the blue’. This lack of communication surfaced at other points in participants’ journeys: from referral to discharge. In line with previous studies,44,51 many participants were not fully aware of the process or purpose of the intervention.
The value of an effective and supported signposting and referral system that involves link workers regularly communicating with both the onward activity or service provider and the participant is amply demonstrated. However, observations suggest an interventional drift from embedded and continuous support to unsupported signposting and more ad hoc contacts, which evidently follow the temporality of the intervention. As with the wealth of research that posits that signposting to information is unlikely to be effective,4,56,126 the unsupported linking experienced by some participants did not lead to engagement with needed services. This ‘drift’, together with the behavioural change logic underpinning the intervention, allocated responsibility to individuals for navigating their wellness journey irrespective of social context.
The extended period of the fieldwork established that trajectories through the intervention did not always follow a linear pathway to better health; instead, they followed the ‘twists and turns’ of time,125 as the following sections will explore.
Part 2: social worlds shaping responses to social prescribing
In this section, we extend analysis beyond participants’ experiences of the intervention to incorporate wider contexts and everyday settings. We use these contexts as a lens through which to see how sociocultural and individual factors shape participants’ lived experience of WtW. In what follows, we narrate the temporal stories of six participants to explore in detail the contrasting ways in which social prescribing embeds in different contexts. The ideas underpinning these cases arose from the whole data set and reflect how access to resources shapes engagement.
Stable contexts
We first present the stories of Andy, Geetha and Jill, who we suggest engage with their health and WtW from an advantageous social context.
Andy
Andy lives with his wife and their adult son. He owns his home, a semidetached house, which is situated on a quiet, tree-lined street. Andy is higher educated and has worked in the same company for over 20 years. In his first interview, he explains that, when work had taken him to his ‘boiling point’, he was diagnosed with T2DM, took 6 months’ sickness leave and was referred into talking therapies and WtW, which, in turn, referred him to the gym and nutrition classes:
I obviously got a fright because I think of diabetes and think, ‘Blimey, you’re going to lose your feet’, which can happen. So, I got a bit of a fright, and got back into training, got back into well-being, got back to the gym, got back to football, and I’ve been probably the fittest I’ve been for a long time.
First interview, 6 February 2019
Andy takes no medication for his T2DM. His diagnosis and proceeding support provided by the intervention activated and motivated him to re-engage with health-maintaining practices. As we note in Supported linking, Andy needed little encouragement to engage with WtW:
It’s put [me] in the right direction. Obviously, I was going in the wrong direction, lifestyle wise. It gives you the kick-start, reminder wise, and the memory of what you really should be doing, compared to what you are doing. Because you just get a little bit lazy.
Final interview, 14 July 2020
Importantly, the ‘fright’ of a T2DM diagnosis and subsequent link into the gym appeared to be sufficient to ‘kick start’ Andy back into the gym, an experience he later describes as ‘like being back home’. Furthermore, although being at work amplified his mental health issues, when Andy returned to work his employer’s flexibility played a central role in enabling his engagement with the intervention and related referrals. His manager in particular was extremely accommodating:
He would just say, ‘Get yourself away. Half an hour. Just log out. Go and have a little sit, have a good think, and if you want us [me] to come, just ring us [me]’. So, that side of it, they were very, very flexible.
First interview, 6 February 2019
Hence, in addition to Andy’s familiarity with fitness, his present context further worked to enable his engagement in WtW. Not only was his employer flexible, but Andy was able to address his health issues without any financial consequences by taking 6 months’ sickness leave.
Geetha
Geetha is also educated to degree level and owns a semidetached house in a residential area. Originally from the Indian subcontinent, she was referred into WtW shortly after her T2DM diagnosis. Geetha ‘joined’ WtW to discover new activities. She explained that she ‘was really bored’ and wanted to ‘find out what’s happening, what’s going on around the area’. As with Andy, Geetha displays a commitment to investing in her health and well-being. She does this by proactively searching for additional activities. Through WtW, Geetha enjoyed attending exercise classes and, independent of WtW, she regularly attended the gym, a social group and a walking group alongside her close-knit, relatively affluent female network. She wanted to occupy her time following her retirement from working in the VCSE sector, a previous employment that helped shape her understanding of the intervention. For example, Kate Gibson and Geetha bumped into her former work colleague at an activity:
Geetha laughs and says to her friend ‘she asked me who sent me here and I told her I came by myself. I’ve found everything by myself’. Her friend laughs and agrees, saying she used to send people to things like this and now she comes herself. I ask her how she came across the group and she explains that she just searched for local activities on Google [Google Inc., Mountain View, CA, USA] – she’d been to the swimming pool already today. Geetha says that there are lots of ‘interventions’, but not so many for older people. I’m surprised to hear her mention ‘interventions’; I tell them that that’s what I am interested in: interventions.
An activity with Geetha, 22 October 2019
Evidently, Geetha’s autonomy in pursuing these activities is partly enabled by her previous employment, which has equipped her with the knowledge of the VCSE landscape. This, together with her immediate social network and her free time afforded by her recent retirement, creates a social context that facilitates her engagement.
Jill
Jill also owns her own home in a quiet residential area. Jill, who works part time, lives there with her husband. As with Andy and Geetha, Jill was referred into WtW shortly after her T2DM diagnosis and, as outlined in Intervention continuity, WtW was supportive when her mother’s health deteriorated shortly after her father died.
Jill’s diagnosis of T2DM prompted her to exercise more and re-join Slimming World® (Alfreton, UK). She is well supported by her husband, whose use of ‘we’ in the excerpt below emphasises that Jill’s health is a shared family project:
We’re trying to improve her health through exercise, diet. It hasn’t been helped recently by the death of her dad and her mam’s hospitalisation. Hopefully that will get better as time goes on.
Husband, family interview, 23 September 2019
Jill’s journey through dieting and exercise was interrupted by her caring responsibilities for her ageing parents. Her weekly ‘menu’, which she forward planned with Slimming World recipe books, became increasingly difficult to follow when her parents were in hospital. Her father was in hospital at the time of her photo-elicitation interview:
With being at the hospital most days, the menu that we tend to do has gone out of the wall; however, we are cooking tonight what we should be doing. But we had a Chinese on Friday, because it was yon time [late], when we got back. Well, I was in the hospital from half past eight [morning] until about eight o’clock at night, and it was just . . . didn’t want to start cooking then.
Photo-elicitation interview, 29 April 2019
Increasingly, Jill found that she was having ‘bad days’, as indicated by her photograph (Figure 9) and quotation:
That’s quiche and tomatoes. That was probably a bad day. In fact, it was: having quiche. And bread and butter. That would probably be one of my bad days.
FIGURE 9.
Jill’s photograph of quiche and tomatoes.

By her exit interview, when Jill’s mum had settled into a nursing home, Jill had started to make progress with her diet:
I’m still on Slimming World, I’ve lost 11 lb up to now.
Oh brill.
Well yes, but it’s not great considering we’re in lockdown and I should be able to do better.
Exit interview, 3 July 2020
For Jill, prioritising caring for her parents meant that her everyday and routine eating activities were disrupted, which, in turn, affected her diabetes management. It is notable that she no longer had the time (or energy) to plan and cook her healthy ‘menu’ during this unstable time. In spite of her priorities being elsewhere, Jill appears simultaneously to blame herself for individual and moral shortcomings attached to having a ‘bad day’. In addition, it is notable that, although Jill’s self-care practices ‘slip’, once she had established appropriate care for her mum she was able to re-establish her routinised healthy eating practices; despite that she chastised herself for not ‘doing better’. With the support of her husband and the link worker, Jill regained her healthy momentum and returned to prioritising her health. Jill’s experience of the disruption of a well-established routine underlines the importance of stability in managing future health. Not all participants had the privilege of prioritising their self-care most of the time, as the following section will show.
Uncertain contexts
Aisha
Aisha lives with four children and her second husband in a small rented terraced house. Prior to immigrating to England, Aisha attended university. When she arrived in England, she could no longer continue her studies, partly because of language barriers and partly because there was ‘too much violence’ from her first husband. Aisha has had T2DM since 2009 and also has depression. Her current husband also has T2DM.
Aisha has significant caring responsibilities for her children, all of whom have a learning disability and/or a LTC. Importantly, because of her caring responsibilities, Aisha has little time to prioritise self-care:
Sometimes I don’t take medication because I forgot because I’m so concentrated on the kids. My kids need melatonin for sleep. Without melatonin they doesn’t sleep. Imagine the days I forgot to call the GP . . . I need to go ask emergency. And that . . . because it’s 48 hours to wait, there are 2 days the kids don’t sleep and I don’t sleep. And then in the morning the last thing I want is somebody to say, ‘You want to see me?’ or appointment or I need to come to school, you know [laughs]? Even to cook. I look. It’s not like I feel cook in the way I do. I wait until afternoon and I call the pizza, ‘Can you please deliver please?’. I feel really bad because I’m down, down, down, yes.
First interview, 7 March 2019
Aisha was linked into counselling by WtW, which she found helpful; however, she missed a few appointments because of her children’s more pressing medical concerns. During our only interview, she repeatedly returns to her point that she has no time to attend to her own health needs:
I don’t have a rest. Sometimes I eat because I need to eat, not because I’m following, you know, now it’s time to eat. My mind is so concentrating the boys. I try to do different, but sometimes I just want to make sure the kids are alright.
Despite this, Aisha appears reluctant to ask for help:
I start to think I’m going to call these people, start to attend this meeting or sit down, whatever you say. But, you know, I have one fear. I don’t want these people coming to collect my kids from me. I don’t want taking the boys from me.
Aisha’s narrative dwells on being able to function as the primary caregiver to her four children with complex needs in a context of poverty, in which she appears all too aware of the stigma and consequences of being labelled a ‘Troubled Family’ (Shildrick et al. 127 quoting prime minister David Cameron). In the same kind of way that Jill’s family responsibilities caused a short-term disruption, Aisha’s ability to invest in her own health is truncated by the complex health needs of her children. That is, her role as a mother requires her to navigate through a whole host of (gendered) temporal constraints, which intersect with the way that she prioritises her long-term health. In spite of her desire to ‘do different’, Aisha opts for the convenience of pizza delivery because her focus is on the immediacy of her present context. Aisha was not alone in prioritising her present context; also illustrating this dynamic is Eddie.
Eddie
Eddie lives alone in a one-bedroom flat in a social housing complex. He is unemployed, suffers from depression and anxiety, and has had T2DM since 2005. He tries to ‘eat the right foods’, although sometimes ‘it gets on top’ of him because the ‘right foods’ ‘are expensive to buy’. Referred into WtW in 2015, Eddie’s WtW journey has involved a number of activities and referrals. For instance, he was referred to a local gym; however (and despite several text reminders), he never went. He was encouraged to attend a social group, but after a series of cancellations, the link worker concluded that he was ‘uncommitted’. Eddie was then referred for counselling sessions, which he regularly attended.
Eddie’s photograph (Figure 10) and accompanying words emphasise the weighty reality of his everyday life:
FIGURE 10.
Eddie’s photograph of the ground.

Sometimes when I’m out, you see, I don’t like to look ahead. I look down.
Photo-elicitation interview, 7 May 2019
That Eddie ‘doesn’t like to look ahead’ is partly because of the benefits system, which fixes him as powerless, as indicated in the following excerpt:
I can’t do anything at this time until I hear from these people [Department for Work and Pensions]. Like, I’m in limbo, you know, I’m not one thing or the other, so I just have to wait until they come with their decisions on yes or no. So, it’s like they’re controlling my life at the moment.
First interview, 6 March 2019
As fieldwork unfolded, Eddie increasingly struggled to survive on Universal Credit. He contacts the intervention requesting food bank vouchers on an almost weekly basis and, with the threat of eviction, becomes increasingly reliant on food banks. Ultimately, however, the intervention questions the frequency and long-term usage of the vouchers and appears reluctant to issue them so unequivocally. The field notes below detail an occasion when Eddie’s link worker telephoned him after he contacted the intervention requesting a voucher having just collected one the week before:
He looks at the screen, holds up his finger as if to pause our conversation and says it is the link worker. ‘Actually I don’t like going to that one, I usually go to the one up the top . . . OK, see you in a bit’. He tells me with a raised eyebrow that the link worker wants to meet to look over his expenditures with him after the Debt Relief Order (DRO) is sorted – he doesn’t look too pleased. For now though he can go up to the office and get the foodbank voucher.
At the café with Eddie, 14 November 2019
As with Aisha, the ‘present-focused’, reactive nature of Eddie’s everyday practice appears at odds with WtW’s expectation that clients co-produce a future-facing ‘action plan’ to improve their health. Poverty, and its associated lack of stability, interrupts his engagement in ‘sustained healthy behaviour change’ (see Appendix 15, Figures 31 and 32). We next turn to Tracy, who also has limited resources to hand.
Tracy
Tracy is in her early 50s and lives with her partner and her partner’s daughter; they rent a two-bedroom ground-floor flat on a steep terraced street. Tracy has multiple serious LTCs, was diagnosed with T2DM in 2016 and is awaiting major surgery. She takes 16 tablets per day for her LTCs, but her ‘goal is to come off all of them’. Tracy frequently talks of confused interactions with health professionals and often mentions her uncertainty and anxiety around her impending surgery. Tracy’s depression and ensuing health issues were, she says, triggered by the sudden death of her mum. She no longer has any contact with the remainder of her family, who, she feels, blamed her for her mum’s death. She explains:
I was 9 stone until my mum died, and because of what happened with them in [place name], and pushing me out and what have you, I used to eat lots of chocolate. At least 40 bars of chocolate every day . . . Not a meal, just chocolate, until I was sick of it, and it was every day. How I afforded it, I don’t know, but that’s when it went bump, bump, bump, and that’s why I’m like this.
First interview, 12 June 2019
Since being referred into WtW in 2017, Tracy has been linked into several services and activities. In addition, following a heart attack in 2016, Tracy was referred by secondary care into a local health centre at which she enjoys attending the gym and a number of other activities. Below is an extract from a conversation that Kate Gibson had with Tracy about a nutrition class:
I ask her if she thinks she might cook any of the recipes and she tells me she will try the frittata. ‘Will you cook it for [partner or partner’s daughter]?’, I ask. At that suggestion she laughs – ‘all they eat is food from packets and boxes, nothing fresh; I don’t know why, they’ve just always done it’.
At the café with Tracy, 20 November 2019
Significantly, Tracy’s response to the suggestion that she cooked her partner frittata is met with laughter, signifying that her healthy foods are at odds with her household norms. Hence, although Tracy is ‘motivated’ and engages in the intervention, her efforts appear to be without the support of any social networks. Tracy was particularly excited when more recently a link worker accompanied her to a community class; however, her negative experience of attending alone the following week discouraged her from going again. She explained, ‘I haven’t got anyone to go with, and everyone else seems to know someone, so I don’t know what to do with myself’. Tracy then joined a gardening club at a local women’s centre; however, a bout of illness caused her to miss the next few sessions and she never returned, explaining that it was ‘too difficult to go back’. As with Geetha, Tracy talked often of needing to ‘keep busy’; however, she experienced a number of setbacks and her attempts at engagement were thwarted time and time again. In addition to her evident discomfort at various junctures during her social prescribing journey, her multiple LTCs caused several setbacks. For instance, a chest infection caused her to miss several gym sessions, minor surgery triggered a number of further hospital stays and an accident caused her further injury.
Part 2: discussion
These situated accounts in the SPRING_NE study illustrate how different lived experiences shape the responses of clients to WtW. Therefore, we find that social contexts shape individual possibilities for engagement and intervention journeys, as has previously been observed. 128–131 Moreover, like Orton et al. 132 we find that change rarely happens in ‘linear or predictable ways’. 132 To this, we add that access to resources (e.g. employment, employment histories, secure housing, regular incomes and supportive social networks) enabled some participants to better align with WtW’s unidirectional model of behaviour change. Evidently, Andy, Geetha and Jill encounter WtW from social contexts that both enable their engagement and increase the chances of a smooth and straightforward linear trajectory to better health. Furthermore, their social contexts act to minimise the disruptive effects of setbacks on their engagement in ways that appear unavailable to Aisha, Eddie and Tracy. Although Jill’s healthy eating practices are disrupted when her parents are ill, she soon returns to her already-established routines with the support of her husband. Similarly, Andy returns to the familiarity of the gym, thanks to his stable employment affording him the space to engage in his health. As O’Donnell133 has also observed, higher socioeconomic status (SES) participants have more autonomy to ‘remove themselves from the conditions giving rise to their distress and move into a social space where more health-enhancing behaviours were possible’. 133
Tracy’s story is particularly important because, as with Andy, Geetha and Jill, she prioritises engaging in health; however, as with Eddie and Aisha, she encounters WtW from a context of uncertainty. Her WtW journey is interrupted by numerous setbacks, and her attempts at engagement are often ‘thwarted’. 130 More broadly, contexts requiring the prioritisation of immediate social circumstances ultimately act to ‘thwart’ engagement in WtW, for example Aisha’s cancellation of appointments because of her child-care responsibilities and Eddie’s focus on surviving poverty. As in Shildrick et al. ’s127 study of disadvantaged families, Eddie, Aisha, and several other participants living on state welfare benefits were ‘often swamped by the multiplicity of deep troubles they faced’. 127 Indeed, for Aisha, the sheer volume of her responsibilities is almost unspeakable. As an economically and politically marginalised migrant mother, race, gender and poverty intersect to further compound her ‘structural vulnerability.’134
All participants in this study recognised the value of health even when their practices were at odds with this recognition. Although Aisha and Eddie ‘try to do different’, as with many participants, their priorities lay in navigating their ‘living presents, rather than anticipated futures’. 135 Hawe et al. 136 propose that research should consider ‘interventions as events in systems that either leave a lasting footprint or wash out depending on how well the dynamic properties of the system are harnessed’. 136 It is interesting that the retrospective stories of those in the KIT stage, which we detailed in Supported linking, appear to contain more instances of the intervention attending to and embedding in ‘living presents’, and as a consequence, leaving ‘a lasting footprint’. For instance, the continuous nature of link worker presence together with text and telephone call reminders can be interpreted as an interventional acknowledgement that health-related activities may not be at the forefront of every client’s mind. Our findings demonstrate that those living with the greatest disadvantage inevitably have the greatest difficulties engaging with social prescribing.
Chapter 7 Addendum: social prescribing during a pandemic – service provider adaptations and client experiences
Parts of this chapter have been reproduced with permission from Morris et al. 137 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given and any changes made indicated. See: http://creativecommons.org/licenses/by/4.0/.
Introduction
This chapter builds on Chapters 5 and 6 of the SPRING_NE study by highlighting how the intervention adapted to meet clients’ needs in the first wave of the COVID-19 pandemic and how clients experienced these changes. It reports on data collected remotely from clients, link workers and managerial staff regarding experiences of adaptations to service provision in the early months of lockdown and social distancing in response to the COVID-19 pandemic.
Background
During the time of this additional study (April–July 2020), participants were living and providing services under changing government COVID-19 restrictions. On 23 March 2020, the UK government moved into a nationwide ‘lockdown’ as a result of increasing numbers of cases of COVID-19. The ‘stay at home’ restrictions (23 March–12 May) directed people to stay at home throughout this period except for essential purchases, essential work travel (if remote work was not possible), medical needs, one exercise session per day (alone or with household members) and providing care for others. Employees and employers who could work remotely were asked to do so, and others had to cease working. The ‘stay alert’ restrictions (13 May–1 June) stated that anyone who could not work from home was actively encouraged to go back to work, and people were allowed to take ‘unlimited’ outdoor exercise as long as they did not meet with more than one other person from another household. Restrictions were relaxed from 1 June, which included enabling up to six people to meet outside and in private gardens, and clinically extremely vulnerable people to spend time outdoors. ‘Support bubbles’ were allowed from 13 June, with single-adult households able to join with one other household and, for this reason, many of our participants had not experienced a support bubble at the time of interview. 138
Worldwide, COVID-19 is more likely to be experienced severely in older people and those with LTCs, particularly multimorbidities: this is the target group of WtW. 139,140 Consequently, the UK Government’s COVID-19 response included advising people with certain single or multimorbidities (2.2 million clinically extremely vulnerable people) to ‘shield’ in their homes for 12 weeks from 22 March 2020 and to avoid all in-person contact with others, even in their own households. 141 Within this climate, social prescribing has received attention as an intervention that could be remodelled to meet exacerbated public health challenges, including social isolation. 12 For this reason, it was valuable to extend the SPRING_NE study to explore how the intervention functioned during the pandemic, from client, link worker and managerial perspectives.
Aims and objectives
This chapter explores how the intervention changed during the first wave of the COVID-19 pandemic from the service provider perspective and how the intervention was experienced by clients during this period. The objectives are to:
-
describe what changes, challenges and opportunities occurred in delivering the intervention to clients during the first wave of the COVID-19 pandemic
-
explore how clients experienced the intervention during the first wave of the COVID-19 pandemic and what role it played in clients’ overall experience of the pandemic.
Methods
Intervention service providers and other linked services utilising link workers were interviewed remotely between May and June 2020, with one additional interview conducted in September 2020. A qualitative interview study was conducted (11 May–1 July 2020) with a subsample of clients in the before-and-after EQ-5D-5L study (see Chapter 3).
Sampling and recruitment
Client participants included those already in the EQ-5D-5L study who were contacted to complete their 12-month follow-up questionnaire during the lockdown period and who agreed to participate in an additional telephone interview about their experiences during the pandemic (n = 29) and those already in the client ethnography (n = 15) (see Chapter 6). Service provider participants were those already in the link worker ethnography (see Chapter 5), and additional link workers and managerial staff recruited via local connections and snowballing. Participants received information leaflets (see Report Supplementary Material 2) and consent (see Report Supplementary Material 2) was recorded verbally prior to the interview, because of lockdown restrictions.
Data collection
Telephone interviews were recorded with permission. Interviews with clients comprised administering a third iteration of the EQ-5D-5L questionnaire and conducting a semistructured interview. The topic guide (see Report Supplementary Material 2) covered experiences of ill-health; impacts of COVID-19 on interviewees, their LTCs and their household members; support needed or received including social prescribing; and feelings about life during and after lockdown. Demographic data were collected on age, gender, ethnicity, employment, education, household income, housing tenure/type/composition and availability of private outside space (see Report Supplementary Material 2). Service provider interviews followed topic guides that were tailored to each individual but included questions regarding their employing organisation’s philosophy, adaptations to their services since March 2020, and organisational and individual challenges and opportunities. Demographic data were not collected. Data were collected by Stephanie L Morris, Jayne Jeffries, Kate Gibson, Suzanne Moffatt and Tessa M Pollard.
Data analysis
Interview data were transcribed, read and re-read, and an inductive coding framework was developed. Line-by-line coding was used to identify descriptive and conceptual themes, using NVivo to assist with data management. Data were analysed as a ‘snapshot’ in time during the changeable circumstances of the pandemic. Data analysis was led by Stephanie L Morris, in discussion with Josephine M Wildman, Tessa M Pollard, Suzanne Moffatt, Bethan Griffith and Kate Gibson.
Findings
Service providers
The social prescribing service providers interviewed were eight service managerial staff and five link workers or senior link workers and a managerial staff member from the WtW umbrella organisation. The quotations in this section are attributed by anonymous codes using the following template: pseudonym name, provider (A/B), interview date.
The data reported here provide a ‘snapshot’ of the temporary WtW service changes that inevitably altered over time as the pandemic continued. This section builds on Chapter 5 by providing an account of changes, challenges and opportunities, as reported by service providers in semistructured interviews between May and September 2020.
Ways to Wellness adaptations to the COVID-19 crisis: March–June 2020
A few days prior to the UK national lockdown on 23 March 2020, both providers, in agreement with WtW, switched service delivery to a remote working system. This consisted of link workers conducting no face-to-face work with clients, instead conducting their work via telephone appointments while working from home. In addition to maintaining contact with existing clients, link workers began calling people classed as ‘vulnerable’ on GP surgery and city council lists. In the early weeks of the COVID-19 crisis, WtW management reported negotiating with the CCG and the WtW board to temporarily adjust its contract so that they could assist in the period of crisis by working ‘flexibly’ with people outside their original remit on an ‘as-needed basis’ (WtW managerial staff, September 2020). The WtW managerial staff member said:
There’s need. There’s unmet need out there in the community and really vulnerable people. We shouldn’t just be spending all our time working with people we know are okay even if they are, technically, our eligible clients. So very quickly moving to the, ‘Let’s put our resource in the highest value we can’.
To enable WtW to offer its services to work with vulnerable people who did not meet its original eligibility criteria, one of the outcome payments was switched to a ‘block payment’ that acted as a form of ‘engagement payment’ (WtW managerial staff): this payment was not linked to new referrals. This meant that, although WtW primarily continued with the PbR system, a small single-block ‘engagement payment’ resulted in a reduction in financial risk. The WtW staff member explained that WtW was, therefore, able to offer the city council and general practices its services during this period. Link workers and managers reported contacting patients on shielding and vulnerable lists provided by the city council and many GP surgeries.
Referrals to WtW from GP surgeries reduced dramatically during the first wave of the pandemic. Some link workers reported neither receiving nor creating new referrals during this period. WtW tracked its activity with new clients by adjusting its management information system (MIS) to capture the number of people, what types of needs they had, and the number of contacts and time spent with each person. Link workers used such additional options in MIS for items related to COVID-19 so that this work was tracked and payment could be made.
Link workers did not complete WBSs with vulnerable list patients, and instead focused on immediate help and referrals to other services, such as food and medicine deliveries. One link worker reported that approximately 15–20% of vulnerable list patients needed additional support, whereas for most the work required a check-in telephone call only. One link worker summarised this work:
. . . We’ve been given shielding lists by the practices, so the people who are vulnerable, we’re checking on them, but that is not our normal conversations again. That’s just like, ‘Do you have food and medicine?’, if you know the guidelines, stuff like that . . . checking that people are okay and they’ve got access to food and medicine, that they’re coping with it mentally and they know what they should be doing.
Marianne, A, June 2020
If vulnerable list clients required more support, they were recruited into WtW. This was reported as a rare occurrence, but was another means of generating new referrals during the pandemic. It was hoped that following WtW’s rapid adaptation to assisting with vulnerable patients in a time of crisis, general practices would ‘see how important social prescribing is’ and utilise the service more (WtW managerial staff, September 2020).
Chapter 5 explained that link workers continued conducting WBSs with clients meeting the normal eligibility of WtW, and one provider reported an increase in WBSs. However, link workers and managers also reported a change in the intervention generally as conversations with existing clients altered initially in content as they provided advice, information and assistance surrounding COVID-19. Managers explained that this was a priority in the early months of the pandemic, but also suggested that there were attempts to balance this short-term COVID-19 response alongside reframing behaviour change goals (provider A) and supporting people to maintain some of what they had achieved prior to lockdown and not ‘relapse’ with their condition management (provider B):
The type of support that we have been providing has changed slightly as well, in the early days. So people were very worried and concerned, naturally, about COVID and what the likely impact that would potentially have on themselves and their health. They needed information around what they could and what they couldn’t do. So it was just really to help them understand what the government was saying. So a lot of time, initially I think, was supporting people around understanding of what the lockdown restrictions meant for them and finding out what support they needed. Because obviously, a lot of people don’t have family or friends and if they are shielding or isolating, they can’t go to the shops to get their shopping and stuff like that.
Martha, B, June 2020
So if you have improved your condition by getting out a bit more and feeling more hopeful and enlightened by that, and now you have been told you can’t go out, then there will be . . . It is much easier to do something the first time than if you have gained some success and then slipped back. So it is that bit of just trying to help people wherever possible not to lose the ground that they have gained.
Annette, B, May 2020
I think the priorities initially were right, you know, checking in on the people in our current caseloads, making sure they had contact, and whether there was anything that they needed – that sort of immediate support – or they still wanted to engage with ongoing support . . . Whilst obviously it has chucked everything up in the air for everybody, you know, still using our skills and our knowledge to be able to support people to manage this as best they can, and identify if there are goals, although they will be reframed, to still be able to work towards that even in the current climate.
Tina, A, June 2020
It was commonly recognised that the pandemic could have altered existing clients’ lives dramatically and that some who were doing well prior to lockdown may subsequently have been struggling. Some link workers, therefore, reported calling or attempting to call their entire caseload. This was echoed in how the WtW staff member perceived what was happening on the ground in the early months of the crisis and how the practice of ending journeys altered over time:
. . . there was a sense that people were like, ‘Why would I discharge them at a time when everything in their life is up in the air?’. So I think there was a sense that they were, kind of, keeping things open for a little while. I don’t think that’s the case anymore [in September]. I think things feel more stabilised.
WtW managerial staff, September 2020
Despite acknowledgements of how the intervention needed to be attuned to the potentially dramatically altered circumstances of clients in the early months of the crisis, another manager who was interviewed in June explained that link workers in their organisation were encouraged to close some people’s journeys who were not perceived to need further support:
So we also had discussions with them about understanding on the caseload, people that actually probably didn’t need our support. Just to be able to discharge, for want of a better word, people that probably were coming to the end of their intervention with ourselves so we could really focus on those that really did need our support.
Janice, A, June 2020
One link worker from this provider said that they had closed a few journeys during lockdown but another expressed difficulties in doing so:
. . . ideally, if I can close them or put them into KIT, that’s one of the aims . . . But because of the current situation, I haven’t closed them or anything, because of the current situation.
Lucy, A, June 2020
Tension appeared to exist between how the organisations made space on caseloads for new referrals (PbR system required this in order to conduct more WBSs) and what was best for clients during the pandemic. This may have meant keeping some clients in the intervention beyond the threshold number of WBSs or leaving support open in a period of disruption and potential relapses in their health.
Link worker adaptations, innovations and challenges
Some link workers reported having to be more ‘creative’ in how they supported patients during remote delivery (Alice, A, June 2020) and were innovative in adapting their appointments with clients during the initial stages of the pandemic to help them maintain their health. Some said that they were responding to client need, supporting and advocating for clients more. Others explained how they were reproducing in-person support remotely. For example, one link worker (Lucy, A, June 2020) conducted Healthy Lungs activities with patients by telephone as an introduction or re-introduction to such exercises. She said that previously she would have attended the first session with the client. She also had ideas for introducing some clients to meditation by telephone as another means of improving client confidence to join mindfulness online courses or groups.
Link workers reported challenges with engaging clients who were digitally excluded:
If you’re not digitally connected there’s an obvious gap for a lot of our clients.
Lucy, A, June 2020
Some said they found it difficult to refer such individuals to any services in the current climate. In addition, some link workers said that they felt that clients were not interested in online provision:
The people who I have spoken to don’t express an interest in anything like that [online activities]. I mean, a good example would be a client who was attending Slimming World. He mentioned about the Zoom facility that Slimming World have and he said it didn’t work for him. It wasn’t the same as actually going to a group, seeing people and talking to them. This 2D [two-dimensional] representation, if you like, wasn’t the same as having that actual social contact.
Matthew, B, June 2020
Other link workers said that they attempted to adapt their delivery to digitally excluded individuals by posting hard copies of information, which was often personally funded by link workers. However, this adaptation continued to be inaccessible to illiterate clients or those who did not speak or read English:
Some of our clients aren’t particularly tech savvy. Some are on the internet and doing FaceTime [Apple Inc., Cupertino, CA, USA] with grandchildren and all that kind of thing, but I do have . . . Fairly recently . . . I’m finding this a challenge and I’m finding it difficult to know how to overcome really. I do have a couple of clients that are unable to read or write. Ordinarily, where I’d be sending an email with some links to websites or something like that for information during this time or even posting out something, printing something off my own printer, I don’t have that option with these two individuals.
Alice, A, June 2020
In addition to difficulties with communicating information, many said that they were unclear about which services were running remotely and found it difficult to fulfil their role when services that they were signposted or referred to were closed.
Some link workers also reported difficulties with building rapport by telephone if they had not met the client in person previously:
The transition to phone calls has been difficult, because even though we do that anyway, when we first do a Well-being Star with someone, the face to face of that is so important because you’re introducing yourself, what the service is. You need to build that rapport, otherwise people aren’t going to open up to you. So introducing that over the phone has been quite hard . . . you can’t see what people are doing body-language wise, face wise. We’re told to hold silences, but that is very different over the phone.
Marianne, A, June 2020
This link worker found it was challenging to put her conversational and therapeutic skills into practice and observed that from the outset remote delivery had implications for how clients interacted and engaged with the intervention.
Perceptions of client engagement
Remote working brought differences in client interactions and engagement. Link workers often said that they felt that there was an overall increase in anxiety in clients. One manager commented that conducting more WBSs with clients in the lockdown period had provided insights into a decline in clients’ well-being levels (Martha, B, June 2020). Some said that most clients were pleased to have ‘check-in’ telephone calls and that contacting or being contactable to clients was key during lockdown:
The nature of our role is that we are very flexible and we maintain contact. It is very much a contact role and a communication role. I think that is important for people who have been self-isolating and haven’t left their homes. Some people: maybe the furthest they have gone is the garden. It is reassuring to know that you are ringing, they can contact you or if they are having problems with things that you can ask the right questions to the right people and you can feed back information . . . I think that is definitely a strength.
Matthew, B, June 2020
Link workers and managers also reported that using telephone calls during lockdown resulted in many clients being easier to access. However, some clients preferred face-to-face interactions:
Some clients are like, ‘Oh, I prefer face to face because then I can see your facial reactions and your body language and all the rest of it’. It’s the same, I guess, for us, because we can’t really see how things land . . . a lot of the communication cues are visual rather than verbal.
Alice, A, June 2020
Nevertheless, one link worker suggested that some clients were more engaged than they had been previously thanks to remote appointments, and explained how this change made the service more person centred as it was tailored to some clients’ difficulties with accessing their GP surgery:
People who haven’t answered the phone are now answering the phone and they’re wanting to chat. Now that is brilliant, because a lot of people . . . who wouldn’t have wanted to come to the doctor’s surgery [to visit the link worker], or find it difficult . . . they will happily chat on the phone for half an hour, an hour, and they’re really engaging at quite a good level with that, they’re someone who is DNA [did not attend] coming to the doctor’s surgery before. And when I’m now chatting to them, it’s obvious that actually to physically come to the doctor’s surgery is difficult.
Lucy, A, June 2020
The same link worker said that, alongside being more accessible, their clients were more open, inventive and adaptive during lockdown owing to re-evaluating their health and vulnerabilities:
Nearly everyone picks up the phone immediately, and they want to talk to you. They haven’t got other stuff going on. So that’s been amazing. [Laughter] Partly because a little bit of their worries and stuff. They are quite open to ideas to benefit their health, because actually they’re a bit frightened . . . I think the COVID thing has opened up people to a whole load of different new ideas. I kind of sense that a bit, that some people are just thinking, ‘Oh, I’ll give that a go’. It’s like opened up a different intensity about their health almost, that they’re now thinking that there might be other ways of doing things.
Lucy, A, June 2020
Despite this successful engagement in the early months of the restrictions, one manager (Martha, B, June 2020) explained that as restrictions lifted the pattern of successful telephone contact began to dwindle, which she attributed to some clients not being at home as often as they had been previously.
Some managers at provider B talked about WtW as a person-centred intervention: finding out what is important to the person, asking what would make their lives better and considering how they could help clients with the resources available. However, other link workers and managers suggested that WtW was primarily concerned with behaviour change. Some link workers said they felt that lockdown and remote interactions were affecting some clients’ motivation to engage in the intervention and change their behaviour:
We are very social and there is a big social element, I believe, in motivation. For example, if somebody wanted to talk about smoking cessation, we would discuss realistic approaches and, maybe, reduction with a view to them moving on to cessation. I find that that can be quite difficult because people may be motivated to want to change, but not having that contact as well . . . That contact can be reassuring. ‘Oh, I can go and see [link worker] at the GP’. They can book the appointment and come in and see me, have a chat about it and have a real face-to-face conversation as opposed to over the phone.
Matthew, B, June 2020
This link worker suggested that an in-person social interaction could be more helpful for client behaviour change than the remote conversations they were now conducting. Others suggested that clients were not thinking about long-term change in the current climate:
They [clients] don’t really care about behaviour change at the minute . . . I think people just don’t really want the conversation that we want. They’re happy to talk with someone because they’re so bored. I think it is just trying to stay on track of what we actually are, which is a behaviour change service . . . So, even if we’re not doing the conversations like I said, not all focused on behaviour change, we’re still speaking to someone, listening to them and if they do desperately need anything, we can signpost them to that. That is the main job of social prescribing, doing the signposting.
Marianne, A, June 2020
I’m sure there were some that were thinking, ‘Behavioural change, quitting smoking or getting healthier, would be - this is a good time to do it and boost my immunity with COVID’. I think a lot of them were just thinking, ‘I can barely cope. I’m not interested in setting long-term goals. I’m just interested in getting through the week’. It may not have been the best time to work on behaviour change or support people in thinking about the future.
WtW managerial staff, September 2020
Although many managers and link workers said that the aims of WtW continued to be the same, several highlighted a tension between WtW’s shifting priorities to short-term emergency assistance with additional vulnerable clients during the crisis and how this translated into the long-term aims of WtW, which many equated with behaviour change. There were the ‘triage’ conversations link workers had with patients during the pandemic and also pressures to fulfil the overall aims of ‘enabling healthy behaviour change’ (provider A) and ‘working with people to benefit themselves’ (provider A) or their ‘goals’ (provider B). This related to how link workers and managers conceived of the link worker role and social prescribing more broadly (see Chapter 5). The pressures of the pandemic and early lockdown led to an emphasis on supporting individuals with their immediate concerns rather than behaviour change goals.
Clients
The following sections detail how the intervention was experienced by clients and draw attention to some of the overlapping themes across the client and service provider data sets. We begin by describing the sample and providing a contextual description of how COVID-19 restrictions affected the health and well-being of WtW clients, before presenting the key findings regarding the role WtW played in clients’ experiences of the first wave of the pandemic.
Demographics and health status
Appendix 14, Table 44, shows the sociodemographic characteristics of the service users (n = 44), who were mostly over 50 years old, with over one-third being retired and nearly two-thirds owning their own homes. Over half of the sample were claiming some form of benefit, many of which were related to their health status. Nearly one-third were unemployed, often because of ill health, and nearly two-thirds reported annual household incomes less than £20,000. All participants had been with WtW for ≥ 12 months. Nine people reported having a single LTC, which included T1DM, T2DM or COPD. The remaining 35 had multiple conditions, which most commonly comprised T2DM, hypertension, asthma, COPD, fibromyalgia, depression and anxiety. Some had a more complex mix of LTCs, including multiple sclerosis, vascular disease, heart failure, epilepsy and cancer.
Experiences of the COVID-19 pandemic
Some people were coping reasonably well during the pandemic because they had experienced limited disruption in their lives and/or could access and deploy social, digital and financial forms of capital that were beneficial to their well-being and aided self-management of their LTCs. For example, Heather, a retiree who was financially stable during the pandemic, was improving her physical activity routine, which was beneficial for her T2DM, by engaging in six online exercise classes per week through a gym membership (Heather, 19 June 2020). Many utilised local green spaces and gardens for mobility and sociality, which helped them to cope with the situation. Others expressed resilience in that they were used to staying inside or coping with ill health:
Because of my epilepsy, I got so used to being in the house anyway, it really hasn’t bothered me very much.
Eleanor, 14 May 2020
However, over half of the sample experienced struggles and difficulties with their health and well-being during the first wave of the pandemic, and some experienced significant disruptions to their employment and finances. Clients often said that they were anxious and fearful of COVID-19 because of their clinical vulnerability and/or were feeling depressed and frustrated because of limited social connection. Many experienced delays in planned health-care appointments and monitoring check-ups and often reported not knowing how they were managing their T2DM in particular. Many experienced worsening physical ailments (e.g. increased migraines, arthritic pain, asthma, breathing difficulties and sleep problems), which they often understood to be connected to their inability to exercise. For example, William, who had taken early retirement owing to his health conditions, became increasingly anxious about his worsening health and was struggling to exercise in the context of COVID-19:
I have tried to get out for a walk with my mask on but, as I say, I cannot. At the minute . . . my knees, and my breathing at the minute is – especially with one of those masks, I can’t go that far, I find it a bit of a struggle . . . I used to go out on my bike and that, go for walks . . . [but] . . . there are plenty of times when I stand up now and my leg will just give way.
William, 12 June 2020
His ability to self-manage was restricted by his health conditions, which appeared to be worsening in connection with the lack of mobility inflicted by lockdown. William lacked any formal support and was becoming depressed, partly because of a lack of in-person contact with a close but vulnerable family member. Those with complex health problems who were shielding and living alone and/or living in socioeconomically deprived circumstances experienced the greatest difficulties, as many lacked the social or economic capital needed to make life bearable during lockdown. These findings tally with UK survey evidence that shows that older people (aged ≥ 65 years), black and minority ethnic groups and those with lower SES were the least likely to visit green spaces during social distancing restrictions,142 and that clinically vulnerable people, particularly those who were highest risk and shielding, experienced stark reductions in physical activity and increased sitting. 143
Varied contact with link workers
The ways in which social prescribing was received during the first COVID-19 lockdown and subsequent restrictions varied across the sample, suggesting that the aim of the service to contact all clients was patchily achieved. Some recalled regular or irregular contact with their link workers during lockdown. However, most participants had not heard from their link worker during lockdown and some did not recall WtW or a link worker at all. Many were unsure of where they were in their journey with the intervention. All participants had been part of WtW for at least 12 months and, for this reason, many may have already been moved into the KIT phase and, therefore, were receiving less contact before the pandemic. Some were not expecting a call, having understood that they had been ‘signed off’ or because they knew their next scheduled call was at a certain point in the future. However, others were surprised by the lack of contact and some suggested that link workers were currently not working because of the lockdown. For instance, Jude, who was out of work through ill health and had received support with state benefits from WtW prior to lockdown, explained that she had not heard from her link worker for 3–4 months:
No, the last time I heard from her was the beginning of the year, it was either January or February. It was before my tribunal, because she said, ‘I wish you luck’, and that. And then the lockdown happened just after that . . . No. They’ll not be working, will they? . . . I’ve got her phone number, if I need to ring . . . You know, if I need to ring them, I could ring. But I haven’t. Well, like I say, everybody is on lockdown, so . . . There will be a lot of people that aren’t back at work yet, you know. I didn’t expect anything anyway at this time.
Jude, 9 June 2020
When link workers made contact, clients often reported that they valued the support they received, which was, in many cases, well matched with their needs and sometimes better matched during this time of crisis than previously. For example, Jessica, who had received valuable support from her link worker for bereavements prior to lockdown, explained that the link worker had called during lockdown and then sent her valuable resources by e-mail for managing her condition and other issues:
[Name of link worker (LW)] telephoned me and I had a good conversation with LW. And then, as I say, she emailed me some resources and things over, as well, so that was really helpful . . . Just regarding my diabetes and some bereavement information for [daughter] . . . We arranged to speak again . . . we said we’d leave it 6 weeks from our conversation, so it will be June, yes . . . We’ve set a couple of targets, and I thought that gives me time to get my head around it and get going with it. [laughter] . . .
Jessica, 18 May 2020
Jessica, who was very conscious of her health and that of her family, aimed to ensure that all family members were engaging in some form of physical activity during the restrictions and took additional protective strategies to reduce their risk of infection. Although Jessica had anxieties around COVID-19, her family had adapted their working patterns and were living in a stable context (see Stable contexts). Within this context, Jessica appeared future orientated and able to prioritise her health conditions; therefore, WtW was helpful for her condition management.
A few clients who were struggling with more complex lives received useful support from the intervention during the first lockdown. For instance, Eddie, whom we met in Chapter 6, explained that he received unexpected assistance with the delivery of a food parcel and food bank vouchers:
He called, [link worker], a couple of weeks ago I think . . . Ways to Wellness, yes. Just a catch-up thing, and he got this organisation to come down and drop off a little food parcel thing . . . that’s the only time I’ve heard from them . . . He called me out of the blue. I hadn’t heard from him for a little while before that . . . he delivered three of them [food bank vouchers at the start of lockdown] . . . I used two of them. I wasn’t up for going for the next one.
Eddie, 6 July 2020
Although the intervention had previously questioned Eddie’s frequent requests for food bank vouchers (see Uncertain contexts), it seemed that the COVID-19 crisis validated this need. The £20 weekly increase in Eddie’s Universal Credit payment made from the beginning of the pandemic meant that he had more money for food and bills and relied less heavily on food banks than before this benefit uplift.
Another client, Gill, received consistent social and emotional support from WtW over the course of several months prior to and during the pandemic. The link worker–client relationship was central to the success of this support. Gill, who had multiple complex health issues and severe depression in connection with the traumatic death of her partner during lockdown, had a limited social network, lived in retirement accommodation where most people were shielding and reported only one non-local friend for support. She said that she had difficulty trusting new people but when she first met her link worker she found her easy to talk to:
I thought that she was the kind of person that I could actually talk to because I was really, really nervous on the way there because like I have said, I don’t care much for seeing people who I don’t particularly know very well. But I knew I had to go and then I found her manner was just exactly what I needed. She wasn’t condescending or she wasn’t pushing me to do things that I really didn’t want to do at the time, and she has been quite a valuable person to me, ringing up and seeing how I am and things . . .
She explained that during the course of the pandemic, when her partner died, the link worker became even more important in helping her:
Well, it is somebody I can talk to who knows exactly what I have gone through, you know . . . When she rings up, I always feel a lot better after I have been speaking to her . . . But especially at the time where I was going through the devastation of losing Jim and everything, oh, she was just brilliant, you know. She has given me so much encouragement and she tried to get me to see a positive side of things, as well, you know.
Gill, 6 July 2020
Gill had waited many months for counselling and, after this had ceased (after six sessions that were ‘only just touching the surface’ of Gill’s problems), she reported that the link worker was trying to source other counselling for her. At the time of the interview in early July, the link worker and Gill were speaking every other week, and Gill knew when to expect her calls. The continued link worker relationship was key for Gill in a time of traumatic disruption, and the intervention that she received was person centred, holistic and consistent.
‘Just waiting’: social prescribing ‘on hold’
Some clients perceived their journeys with WtW to be ‘on hold’ while they were ‘just waiting’, as they could not physically see their link worker or be linked to the services that they required. For instance, Derrick said that WtW kept in touch with him during lockdown, but that his link worker had changed, and that WtW’s role and his abilities to do anything during this period was limited:
I’ve had a few interviews [with WtW] and stuff and they said they’re going to try and get me into a gymnasium. But with everything closing down and stuff. Swimming and stuff for my legs . . . So yes, I’m just waiting for that now . . . When the virus started, I’ve had a couple of phone calls off a lad, a man, but I don’t know who he is. But he was asking how I was and stuff like that, and how I’m coping. And they’re going to keep in touch . . . But with this virus, there’s not much they can do. Because their hands are tied with what they actually can do. Because I can’t actually go and physically see them one on one . . . if I see them one on one, it’s a lot better, I’ll get my point across a lot more, because I’m actually talking to another person, than being on the phone. Like telling them more, if you know what I mean, like face to face . . . So I hope, once this virus is over, I actually go down there and have a one-on-one interview with them and discuss what I’ve been doing through this virus and how my legs have been and how I’ve coped at work and stuff like that, just see what can be done.
Derrick, 18 June 2020
Derrick viewed WtW as temporarily suspended and limited in how it could help him but appreciated a link worker ‘checking in’. In line with some link workers’ difficulties with building rapport by telephone, Derrick felt that he could communicate better in person. Pre lockdown, Derrick had planned to begin at a gym through a referral that was in process, as well as to gain help from WtW with moving to another rented property. During lockdown, these plans were ‘on hold’, a term used by others in relation to many aspects on their lives and health care, and he described himself as ‘just waiting’. Derrick said that he was lonely, becoming depressed and had been ‘comfort eating’ high-sugar food that he knew he needed to reduce because it would negatively affect his T2DM. However, his living arrangements, which comprised a ‘tiny’ one-bedroom flat in a high-rise block where there was frequent antisocial behaviour and a lack of private outdoor space, as well as a lack of support for errands and social isolation from his partner (who lived elsewhere) hindered positive practices and his ability to act on the ‘good advice’ he said he had received from WtW since lockdown. Derrick explained that he was ‘just coping’ and said, ‘I’ll just take one day at a time, that’s all you can do’. Derrick was thinking long term about his health but his circumstances and being on hold with his WtW journey meant he remained in a present with a ‘short horizon’,135 where it was impossible to act on any long-term health goals.
Some who were also ‘on hold’ in terms of the services accessed said, that they had made significant progress with their health prior to lockdown through WtW linked services and felt ‘back to square one’ because of the temporary closure of these services. Most of these people were also following shielding advice or self-isolating as much as they could. For example, John explained how shielding and, therefore, not moving in his daily working life, and the closure of the referral gym facilities, had affected him:
With the COPD, I had given up smoking, had lost a bit of weight. I was getting better. Since this started [COVID-19], I’ve put the weight [on] . . . There is just no exercise whatsoever.
John also began smoking again because of ‘pure boredom and not being at work’. He explained how useful WtW had been before lockdown and how central his link worker’s skills and personality were to his success:
It was great. The guy I was talking to was brilliant. [Link worker name]. I’ve forgotten his second name. Everything started working. I gave up smoking and I was losing weight and then COVID-19 entered the scene and just ruined everything . . . Just the guy I was talking to was brilliant and that. His opinion and perspective . . . He told me that I’m being too hard on myself. Yes, it was really good . . . He [another link worker] phoned up a few weeks ago just to see how I was doing. He was alright. It’s a different guy. It changed. The last time I was there it got changed. He’s not as good as the first one, but he’s alright . . . Just [spoke about] the same sorts of things. Smoking, putting weight on, state of mind . . .
John, 28 May 2020
The replacement online exercise provision (currently being offered by WtW linked services) was not suited to John:
For me personally, no [not keen on online exercise classes]. I need some motivation. I need to be at the gym with somebody telling me what to do.
For John, the motivation from both his previous link worker and the gym were essential to his successful behaviour change. Without them, WtW did not work and indeed led to reversal in other behaviours that negatively affected his conditions.
Some linked services were attempting to engage those who were less digitally literate. For example, Christine (8 July 2020), who lacked internet access, could not join in with her art class on Zoom. Instead, she was posted art materials, which she said she appreciated. However, she continued to miss the group and also the staff member who often helped her with her benefit forms (she said she needed to complete another form soon). The importance of other in-person groups was further highlighted by Tracy:
I’ve missed it [the social group] because it doesn’t matter what topic of discussion that you’re talking about or whatever. Yes, I’ve missed going there because I felt a sense of, ‘I need it’. You know?
Tracy, 9 July 2020
Losing contact with social prescribing: going ‘back to square one’ and disappearing
Tracy was not digitally connected with the social group that she was part of throughout lockdown and, despite this disruptive sense of loss and feeling of being ‘back to square one’, Tracy found out that her WtW journey was being ended when she felt she still needed support (see Chapters 5 and 6).
Others who had not heard from a link worker or received any other formal support often did not know what kind of support WtW could offer during this time. For example, Reena, who was living alone, shielding and had multiple serious physical LTCs exacerbated by anxiety, had previously made dramatic improvements to her health and well-being with the help of formal activities via WtW. The sudden loss of these activities that she routinely engaged in (swimming, circuit classes, tai chi classes and a walking group) in combination with disruption to other aspects of her daily life had led to severe social isolation:
From being cooped in after my heart attack and frightened to go out, I built up a life for myself, in and out all the time. Now I’m right back to square one again . . . You just get forgotten, don’t you? You just feel like you just disappear. That’s how I feel. I’ve just disappeared.
Reena, 18 May 2020
The cessation of formal in-person groups and gym services, some facilitated through social prescribing, was abrupt and damaging to many, especially those like John, Reena and Tracy, who found themselves ‘back to square one’.
Changes in link workers contributed to a sense of losing contact with social prescribing. Reena further explained that her previous link worker had been ‘really good’ in providing ‘access and information on lots of activities’ when she was referred. However, when that link worker left WtW she said that support ‘dwindled off a bit’ and during the pandemic she had not heard from her new link worker, whom she was nervous about contacting because she did not know her or what formal support she could offer at this time:
I’m not very good at . . . If she’s not expecting me to call, I don’t know. I don’t know her . . . I knew the old one. I knew the old one quite well. I don’t know her.
I don’t know how it can be, because you can’t really do anything or go anywhere. I think this is just how it’s got to be, in a way. You’ve just got to put up with it I think, and get on with it . . . at the moment I don’t know what they [WtW] can do really, apart from just talk to me maybe . . . Occasionally I have thought, ‘Gosh. If I feel like this, I can’t imagine when people’. It is awful. It’s really hard . . . But there are a lot worse off than me . . . That’s what I tell myself . . . For me I hope this isn’t a permanent thing.
Imagining others in more desperate situations than herself may have served to render Reena, in her own eyes, illegitimate for formal support from WtW, which may have contributed to her reluctance to contact her new link worker. Others also (inadvertently) delegitimised themselves from support by suggesting that others needed support more than themselves. Individuals like Reena did not need food or medicines delivered because they were doing online deliveries or had spouse/family support for errands.
Not knowing if or how the intervention could help them during lockdown and having had a change of link worker (which was reported by many of the interviewees) appeared to limit the extent to which the intervention worked for some during the pandemic. Moreover, here our findings echo those of Chapter 6, as we see how a poor client–link worker relationship and lack of contact meant that some clients’ changing circumstances during the pandemic were not identified. It is probable that staff turnover, high caseloads and additional vulnerable list work contributed to some clients, such as Reena, slipping through the net.
Discussion
This chapter has explored how intervention delivery to clients changed during the first wave of the COVID-19 pandemic, including the challenges and opportunities from the service provider perspective and clients’ experiences of the service. We found that the flexing of the PbR system and eligibility criteria enabled WtW to adapt, with the aim of responding to the needs of the vulnerable people in the local area. The content of the intervention changed in the early months of the pandemic as service providers set out to assist with immediate needs (e.g. food parcels, medicine arrangements) and to provide support around COVID-19 guidelines, and anxieties in both the existing client base and other vulnerable individuals in the local area (identified through shielding lists). Service providers experienced better access to clients by telephone in the first months of remote delivery, but some link workers and clients also experienced challenges with engagement owing to digital exclusion. Clients reported a varied experience of the pandemic. Some coped reasonably and others, often those with complex health issues who were shielding or experiencing deprived circumstances, struggled significantly. Clients had varied experiences of the intervention, with some experiencing more in-depth and valued assistance for self-management or social support and others reporting ‘check-in’ calls, but many not hearing from their link workers or being discharged at a time when they felt in need of further support.
Analysis revealed a tension between a conceptualisation prevalent within the service providers (and particularly in one of the service providers) of WtW as primarily focused on behaviour change and the understanding of managers and link workers that during the first months of the pandemic clients had other priorities. Some link workers felt some frustration, feeling that they had to put their normal aims to one side, but they also reported responding sensitively and flexibly to the needs of clients. Some link workers reported innovations regarding how to support people when linked services were unavailable and when clients were unable to self-manage in ways that they had been able to previously. Nevertheless, many clients in our sample experienced no contact with WtW between March and June 2020, including those who were struggling with their health and lacking any formal support. Moreover, some clients who were in contact with WtW said that their journeys were ‘on hold’ or ‘back to square one’ because of the disruption of linked services, such as gyms, walking groups and social groups. This illuminated the vulnerable nature of WtW when community organisation ceases to function: an issue echoed across the board in social prescribing literatures and debates. 55,56
Remote delivery of WtW during the pandemic also raised issues surrounding digital exclusion. Link workers expressed difficulties engaging clients who were digitally excluded or illiterate via remote methods, and some clients reported that services, including online exercise or art classes, were inaccessible or did not work for them. Evidence suggests that digital exclusion has exacerbated social exclusion during the pandemic, particularly in older adults with multimorbidities and functional impairments. 144 The increase in digital inequities in access to health care during the COVID-19 crisis has been raised in debates, and it is suggested that ‘intensive, long-term support networks’ will be needed to address this and help people develop the skills and access needed for digital inclusion. 145 Without additional support, consequences for digitally excluded clients may become greater as time progresses and remote delivery of WtW continues.
For one client, WtW became a central resource for support during a traumatic period made worse by COVID-19, showing how WtW can work successfully in a person-centred way for the most vulnerable clients. However, this success was contingent on the consistent trusting link worker–client relationship that had developed over several months, the capacity that the link worker had, and their skills in dealing with mental health issues, trauma and disruption. A research-in-residence study of the implementation of social prescribing sites in south-west England found that the skills, knowledge and background of link workers affected their confidence and innovation in responding to new challenges. 146 In the case of Gill, the intervention was the link worker–client relationship and the link worker’s skills were essential. Unlike Gill, several clients recalled a change in link worker. Although for some clients (see Chapter 6) this change could be positive, for other clients detailed in this chapter the change had negative consequences, including demotivation (John) and isolation (Reena). Staff turnover, also noted in previous studies,54 that led to changes in link workers for clients played out in a particularly damaging manner for Reena, who appeared to slip through the net. The contrasting cases of Reena and Gill show that link workers’ abilities to detect changes in people’s lives in the pandemic was paramount to the client’s experience of the intervention and, consequently, to their experience of the pandemic.
The social prescribing intervention set out to respond sensitively to the needs of local people during the first few months of the pandemic and delivered much needed support to many. The focus on referrals and completion of WBS that had previously heavily constrained the intervention was relaxed. However, the limitations created by high caseloads and high rates of staff turnover continued, which meant that, although some clients experienced substantial help from their link worker, others did not feel the intervention could support them during these months or did not have any contact with their link worker.
Chapter 8 Discussion
Introduction
This chapter draws together findings from the multiple WPs to deepen our understanding of the impact and lived experience of social prescribing. We examine the findings of the SPRING_NE study in relation to the wider literature, appraise what the quantitative and qualitative data, when considered together, can tell us about the intervention, and follow this with a discussion of the study’s strengths and limitations. We also consider the implications of this research for social prescribing more widely, particularly in relation to health inequalities, and, finally, identify areas for further research.
Health outcomes, health-care usage, health-related quality of life and cost-effectiveness
The intervention was found to impact positively on levels of HbA1c, BP and estimates of health-care costs, although the degree of impact depended on which treatment and control groups were specified. The size of the HbA1c reduction varied from –1.11 mmol/mol (ITT analysis) to –4.57 mmol/mol (time-varying nature of treatment analysis), which represented a 2–8% reduction in HbA1c levels compared with the control group. The probability of high blood pressure fell by between 1.5% (ITT analysis) and 7% (3 years post treatment), compared with the control group, although this reduction was not statistically significant. High blood pressure is the second biggest risk factor for premature death and disability in the UK;147 therefore, this is an important intervention effect. For cholesterol level, BMI and smoking status, there was little evidence of an effect. Subgroup analyses showed that the intervention varied according to ethnicity and had a bigger effect for those living in more deprived areas and for those with fewer intervention-qualifying conditions. A 2015 systematic review of CHW interventions to improve glycaemic control in people with T2DM identified 13 RCTs, nine of which had at least 12 months’ follow-up, and concluded that CHW interventions showed a modest reduction in levels of HbA1c compared with usual care. 148 Two subsequent US RCTs investigating the impact of CHWs on a range of T2DM outcomes found (1) a 0.51-percentage-point reduction in HbA1c levels, reductions in SBP and no differences in cholesterol level at the 12-month follow-up among a Latino population;149 and (2) no significant changes in levels of HbA1c or HRQoL among low-income T2DM patients at 12 months. 150 However, both studies suggested that the intervention may be more beneficial to those with poorer glycaemic control at baseline and emphasised the importance of examining other measures, including access to health care and social determinants of health. Our study, to our knowledge, is the first to date that demonstrates a (small) measurable effect of social prescribing on clinical outcomes for people with T2DM. Taken in conjunction with the literature from the USA on the impacts of CHWs on clinical outcomes for people with T2DM, the findings are promising.
Health-care cost estimates ranged from £12.58 (individuals with one extra comorbidity) to –£46.44 (for individuals with no extra comorbidity), the latter being approximately 16% of the pre-treatment mean inpatient non-elective costs. When considering the different treatment groups, there was a shift from unplanned care (non-elective and A&E admissions) to planned care (elective and outpatient care). Although these are not statistically significant differences, the scale of the potential effect is economically significant. A review of UK evidence on the impact of social prescribing schemes on A&E attendances and other secondary care services151 found that the included studies lacked a control group, making it impossible to attribute any observed effects to the intervention, a shortcoming addressed by this study.
No change was found in HRQoL between baseline and the 12-month follow-up, as found in evaluations of other social prescribing programmes using EQ-5D-5L as an outcome. 46,49,51
Economic analysis found that the intervention, on average, was more costly and more effective than current practice. The reduction in costs associated with clinical complications and improved HRQoL were minor. Results on the basis of a 10,000-patient cohort were estimated to be –£230,000 (QALY difference = 40). Including intervention costs showed it to be more costly than the comparator overall (£13,050,000 per 10,000 patients) (deterministic model). These findings are based on the assumption that the intervention has a 4-year duration of effect. When the duration of effect is extended and the impact of the intervention on level of HbA1c and blood pressure is assumed to be bigger, the intervention may be more cost-effective than current practice. A RCT with economic evaluation of a referrals facilitator between primary care and the voluntary sector targeted at patients with psychosocial problems similarly found clinically important benefits but at a higher cost than usual treatment. 152
Integrating qualitative perspectives on lived experiences of social prescribing
Based on a vision of social prescribing as a novel approach to addressing the social determinants of LTCs, the operational model for the intervention was set out as:
The link worker using motivational skills and knowledge of their local community will be responsible for providing and supporting a personalised action plan which will be all about engaging in activities that build a range of supportive social networks, including peer-to-peer support, to improve the confidence of individuals in self-care.
Drinkwater153
Similarly, the NHS states that social prescribing ‘link workers give people time, focusing on ‘what matters to me’ . . . They connect people to community groups and statutory services for practical and emotional support’ (www.england.nhs.uk/personalisedcare/social-prescribing/; accessed 12 June 2020), and refers to link workers taking a motivational approach to ‘promote independence and resilience’ (www.england.nhs.uk/personalisedcare/upc/comprehensive-model/case-studies/social-prescribing-the-power-of-time-and-connections/; accessed 12 June 2020). Thus, social prescribing is conceived of as offering support and motivating patients to become more confident and independent.
In this section, we draw together the findings from the three qualitative arms of the study to explore how this vision for social prescribing played out in practice in this early implementation of such a service. First, we show how our results demonstrate that social prescribing, as a new service set up at the intersection between primary care and the VCSE sector, was shaped in unanticipated ways by the context in which it was delivered, resulting in a heterogeneous intervention that also changed over time, with a continuing tension between the aims of supporting and the aims of motivating those with LTCs. Building on this understanding of the intervention, we consider what our findings show about the potential for social prescribing to tackle the social determinants of health and reduce health inequalities.
The shaping of a social prescribing intervention
Ways to Wellness was the ‘UK’s first health SIB’ set up to deliver social prescribing. 73 The SIB was considered vital in facilitating the commissioning of the service prior to the UK Government’s commitment to fund social prescribing within the NHS. The Deep Dive Report154 on the SIB, commissioned by the Commissioning Better Outcomes Fund, which aims to encourage the development of SIBs, identified key opportunities and challenges faced by the SIB, including the ‘immense’ challenge of identifying appropriate outcome metrics. Our ethnographic data indicate clearly that the choice of outcome metrics used to allocate payments to the provider organisations had an impact on intervention delivery.
Payments to providers were based on engagement with clients, as measured by the completion of WBSs, so as to avoid incentivising providers to exaggerate the impact of their services and to enable small VCSE organisations to deliver the service by minimising financial risk. 73 As we have seen (see The intervention), the payment mechanism was rebalanced after 2 years, coinciding with the final withdrawal of two of the original provider organisations by March 2018. Over time, the payment structure generated a focus on obtaining referrals into the service and, for clients within the service, on ensuring the completion of WBSs at the cost of other elements of the intervention. The fact that some of the GPs in practices affiliated to the intervention did not directly refer to WtW contributed to an increased emphasis on the generation of referrals by the providers themselves. At the time of the ethnographic fieldwork (November 2018–July 2020), link workers were observed to spend much of their time generating referrals or chasing up WBSs with existing clients, and many link workers expressed concerns about the need to focus on meeting targets for the completion of ‘stars’. For many participants, this focus played out in a feeling of being ‘recruited’, rather than referred, into the intervention. This ‘out of the blue’ contact contrasted with the experiences of participants who had been referred in the early stages of the intervention, who recalled more intensive interactions with their link workers.
It is important to note that more intensive support was by no means absent from the intervention during the period of our study, illustrated by the case of Gill, whose link worker was ‘the kind of person that I could actually talk to’ in the months prior to the COVID-19 pandemic and was particularly vital during the pandemic when Gill’s partner died (see Chapter 7). However, it is also noteworthy that during the pandemic the need for a different set of priorities was recognised. To enable a shift in the service, the payment model was changed to explicitly allow the intervention to respond flexibly to patients’ needs.
We did observe differences between provider organisations in terms of link worker caseload and client contact, and across the period of fieldwork it became apparent that the second provider was increasing its focus on referrals and the completion of ‘stars’, with training days focused on these aspects of their work.
The funding structure was, therefore, fundamentally responsible for a shift over time towards a less intensive, less responsive and more linear intervention, as link worker time was invested in generating referrals and ensuring the completion of WBSs. These findings accord with previous research showing that pressure to generate outcome metrics shapes the operationalisation of SIBs. 155,156 Similarly, our findings resonate with Edmiston and Nicholl’s157 findings that a SIB-funded service will inevitably prioritise achieving its outcome metrics rather than continuity. In this case, the performative pressure emerged from the use of an outcome metric linked mainly to the number of clients recruited into and maintained within the intervention. Although this approach was generated partly by a concern not to impose a singular or narrow measure of success on the providers, the focus on numbers (output) itself distorted the intervention. 122 In essence, this is an example of the unintended consequences of an incentive that diverts providers ‘away from activities that are most needed towards activities that are most measurable’. 156 A focus on measurable outcomes is not unique to SIBs of course and is known to have had unintended consequences more generally in health service provision. 158
The original vision of the social prescribing intervention included an inherent tension between connecting and supporting individuals, tackling (as far as possible) the social determinants of health, and an emphasis on empowering individuals to manage their health and change their ‘lifestyle’. This was partially resolved over time by a drift towards prioritising individual-level behaviour change that aligned with the drift towards a focus on generating WBSs.
From the start, there was a recognition that different providers would bring different perspectives and strengths to the implementation of the intervention and, as described in Chapter 5, the two providers delivering the intervention at the time of our fieldwork each had their own ethos, with one explicitly oriented towards individual-level behaviour change. Link workers employed by this provider were encouraged towards a behaviour change approach and often described their role as motivating and empowering clients to achieve behaviour change. Often this meant focusing on encouraging clients to ‘take control’ of their health by co-creating lifestyle goals and signposting (often what we term ‘unsupported linking’) into local gyms and diet-related services. Other link workers were more oriented to offering wider support to their clients. The tension between these approaches surfaced repeatedly through our fieldwork, for example in the concerns expressed by some link workers about the need to avoid being a ‘support worker’. In responding to those experiencing lockdown in the spring of 2020, the contrast between the two approaches was brought into sharp focus. Working with clients through the threat of COVID-19 and social isolation of lockdown, the intervention’s umbrella organisation and the providers felt that they could be most valuable by aligning with the necessarily ‘present-focused’ concerns of clients (many of whom were already well rehearsed in living in the here and now), but this frustrated some link workers who were committed to the promotion of individual-level behaviour change.
We observed that clients recruited from later periods were less likely to experience the frequent contact and supported linking recalled by those who were recruited in the early years. Observations of link workers in the later years also suggested the dominance of a behaviour change approach. The individual behaviour change model aligned with the ‘lighter touch’ approach to working with clients that the funding model necessitated. Thus, both ethnographies found that the intervention had drifted away from the ‘holistic’ approach that previous qualitative research identified,1,54 towards an approach that shifts responsibility for change on to the individual. Such a drift towards lifestyle-focused approaches has previously been identified within other interventions,31,159,160 and has been observed to be driven partly by the pressures of targets and workload,31 although it is also a reflection of dominant discourses that construct ‘healthy lifestyles’ as the responsibility of individuals. 161 This is not to say that support was absent from the intervention as we observed it, but in general there was limited time available for such work. The average link worker caseload was 100, and an explicit emphasis on setting clients up to independently manage their own health that was narrower than the original vision for the scope of the intervention.
Social prescribing, social determinants of health and health inequalities
Resources shape access to health162–164 and participants with access to resources were more able to engage with the increasingly dominant unidirectional model of individual behaviour change. Warin et al. 135 suggest that people living in circumstances of deprivation are often constrained by ‘short horizons’. We too found that many disadvantaged participants were more inclined to concentrate on the immediacy of their precarious social circumstances, often at the expense of more future-focused health-enhancing practices.
Our findings, therefore, suggest that a drift towards signposting and an emphasis on individual-level behaviour change risks excluding some participants. NHS England states that ‘Active signposting works best for people who are confident and skilled enough to find their own way to services after a brief intervention’. 126 We suggest that this individualised focus ignores the wider context of people’s lives, especially the lives of those living with the greatest disadvantage. The intervention’s emphasis on ‘motivating’ clients to adopt healthy behaviour change and ‘have improved attitudes towards challenges’ (see Appendix 15, Figures 31 and 32) positions local context as an external factor to be addressed only inasmuch as it facilitates or constrains the achievement of the intervention’s objectives. 165 Hence, although we observed a number of referrals made by link workers to lifestyle interventions, such as local gyms and healthy eating programmes, which may have important impacts on individual health and well-being outcomes, they fall far short of addressing structural social determinants of health or impacting on health inequalities. 162
Furthermore, although we do find examples of link workers tailoring the intervention to address individual circumstances and supporting clients to navigate the social determinants of health, the intervention could not remove such structural barriers. Just as significant upstream factors, such as austerity-driven cuts, shaped clients’ priorities to engage with the intervention, so too did they shape what support link workers could offer. In this way, our qualitative findings demonstrate the implausibility of addressing health inequalities via a downstream intervention which emphasises individual lifestyle change. 31
In summary, the ethnographic WPs paint a detailed picture of a social prescribing service that was shaped by the systems in which it was embedded, and of clients whose ability to respond to the intervention was in turn affected by the way it was delivered, and by how it embedded within their own social worlds. Our findings include many examples of link workers providing a service that was greatly valued by clients, but there was also considerable heterogeneity within the intervention, and some clients received a ‘light touch’ version of social prescribing when they required a more intensive form of the intervention. Thus, we suggest that the drift towards a form of social prescribing offering limited time and support to clients and focusing on behaviour change constrained further an already limited opportunity to address the social determinants of health via a downstream intervention.
Considering the quantitative and qualitative data together
The use of multiple methods has enabled the evaluation of the intervention over a period of 5 years (from its inception until July 2020) from a variety of angles. Considering aspects of the quantitative and qualitative data sequentially, with their different logics of enquiry, derived additional insights that would not have otherwise emerged.
The quantitative study found that between 2015–16 and 2018–19 the intervention improved average blood glucose and blood pressure levels and these improvements tended to increase with time spent in the intervention. No interventional effects were observed on BMI, blood cholesterol level and smoking status. The impacts of the intervention were therefore heterogeneous and the benefits were not uniform: unsurprising for such a complex intervention. The qualitative data generated between November 2018 and July 2020 also demonstrated that the intervention was itself heterogeneous. Its heterogeneity lay in the nature of the intervention received as well as in the dose and duration of its delivery. Clients’ experiences spanned a spectrum, which ranged from intensive support encapsulated by supported linking and efforts to address social and material factors that influenced health and well-being to approaches more focused on lifestyle factors and behaviour change and unsupported linking (signposting). The intervention was personalised, although clients’ need, link worker capacity and provider orientation were not always in alignment. It was also clear that there had been changes to the intervention over time. In addition to individual-level behaviour change approaches becoming more dominant, there also appeared to be increased caseloads and less face-to-face client contact, mostly, it seemed, as a result of the financial pressure to ‘recruit’ individuals. The highly varied approaches that encompass a personalised intervention make it impossible to draw conclusions about the merits, or otherwise, of any one specific approach in improving health outcomes. However, the successes observed when clients’ needs, goals and actions aligned with those offered by the link worker point to the value of a personalised approach that is tailored to context.
In the context of heterogeneity within the intervention, and in the light of the fact that the quantitative data were derived from a period mainly preceding our ethnographic fieldwork along with evidence that the delivery of the intervention had changed over time, it is difficult to comment specifically on potential mechanisms responsible for the lower levels of HbA1c in patients of GP practices participating in WtW. Given the time frame of the effect, we suggest that intensive supported linking, that is, link workers offering support to clients and connecting them to local community services and organisations, the model of social prescribing that seemed to have been more dominant in the earlier years of the intervention, may have had a positive impact on glucose control. However, the precise pathways for this effect remain unclear and are themselves likely to be multiple, potentially including changes in diet, increases in physical activity, greater adherence to medication and wider improvements in living circumstances. It is also possible that the effect observed could be the result of GP practices participating in WtW becoming more proactive in supporting patients with diabetes to control their blood glucose, perhaps as a consequence of their engagement with WtW.
The constellation of multiple health problems, lack of adequate resources, and the impact of the underlying social factors shaping health demonstrated by the qualitative data highlights the immensely difficult circumstances of some individuals receiving the intervention. There were examples of link workers helping clients to navigate structural barriers to their health such as accessing additional income, improved housing or more consistent medical care. Equally, there were examples where clients were unable to engage with the intervention because of structural constraints, or where valued services were curtailed.
The finding from the quantitative data that the intervention, in terms of improved blood glucose control, was more effective for individuals in areas of higher socioeconomic deprivation suggests that less advantaged individuals were able to derive clinical benefit from this model of social prescribing. The qualitative data indicate the difficulties that those with fewer resources experience in connecting (and being engaged) with the intervention, but there are clear benefits when this occurs. Had a drift towards more ‘light-touch’ social prescribing not occurred, it is possible that such clinical improvements may have been larger for less advantaged groups. An alternative explanation for this finding is that it reflects heterogeneity within the intervention. The qualitative data clearly demonstrate such heterogeneity, including variation across the remaining two providers, one of which served more deprived areas than the other. It is important to note, however, that, owing to the impact of the COVID-19 pandemic on data availability, our quantitative analyses used data up to March 2019. The qualitative fieldwork began in November 2018, so does not speak directly to the time frame of the quantitative study.
Social prescribing is not a medical intervention targeting clinical outcomes. Yet, identifying a measurable effect is regarded as important to enable HCP ‘buy in’, and justify resource allocation and rollout in primary care. 39,49 The reductions in levels of HbA1c and blood pressure, although small in effect, with their potential to reduce future morbidity and mortality, are therefore extremely favourable outcomes. All health outcomes were selected because of the possibilities afforded by robust analysis of large secondary data sets currently lacking within the social prescribing literature and the opportunities to analyse health-care usage and cost-effectiveness. 41
The qualitative work observed other outcomes that were not measured in this study, many of which would be extremely difficult to capture in a robustly designed evaluation relying on secondary data. Such outcomes included reduced social isolation, increased confidence, increased income (through accessing the benefits system, debt advice, etc.), weight loss, increased physical activity and improved mental health. Even more challenging to evaluation is factoring in the way in which clients and link workers navigated different goals with evolving and ever-changing outcomes as the intervention progressed. Identifying and measuring health outcomes is at the core of debates about quantifying the impact of social prescribing. 39 The question of how to select quantifiable health outcomes that truly reflect the complex, ever-changing and non-linear trajectory of the intervention is extremely problematic. Our qualitative data indicate that an emphasis on finding an appropriate outcome is, perhaps, the wrong focus. Instead, evaluation could focus on how social prescribing becomes embedded and how it responds to the complexities inherent in local contexts, including the strength of the VCSE sector and other onward referral services. 166 This involves a shift away from a linear conceptualisation of the intervention with effects manifest in individual outcomes, to an approach that better reflects the rationale of social prescribing. As a personalised intervention providing tailored support, it is necessary to address ‘what counts’ to individuals instead of, or as well as, ‘what can be counted’. 121
The application of multiple methods has revealed the multifaceted nature and impacts of the intervention and the challenges in the selection and measurement of meaningful outcomes. 167 The health outcomes data have demonstrated an effect, while the qualitative data have provided a deeper appreciation of the context and impact of this social prescribing intervention, highlighting the value of understanding how social prescribing is conceptualised, operationalised, embedded and experienced.
Strengths and limitations
To date, to our knowledge, this is the most comprehensive evaluation of a large-scale social prescribing intervention. The strengths of the study lie in the merits of a multimethod approach drawing on a range of robust and longitudinal quantitative and qualitative methods that allow the intervention to be examined from different perspectives, enabling measurement of health outcomes, health-care usage, assessment of cost-effectiveness and examination of the lived experiences of those delivering and engaging with the intervention. Inevitably, there are limitations within each of the methods, which we outline below. More generally, as 74 years was the upper age limit of the intervention, the study did not include older, frailer multimorbid patients, a moderately large proportion of patients with T2DM in general practice. Furthermore, we did not undertake a comprehensive description and quantification of services that clients were referred on to, and we are therefore unable to quantify any potential wider range of effects, which we acknowledge, in Recommendations for further research, is an area requiring further research.
Work package 1 (health outcomes)
The quasi-experimental ITT design reflects the ‘real-world’ application of this heterogeneous and personalised intervention that measures the impact across the 4-year period for which data were available. The ITT analysis provides an estimate of the expected effect on outcomes for an individual drawn at random from the treatment practices. Taking account of issues associated with the referral process, non-compliance and wide individual heterogeneity, and by considering all individuals to be treated at the time that treatment becomes available, the strength of the ITT approach is that it overcomes a number of problems associated with observational data. The limitations of the study are (1) reduced sample size due to the refusal of seven general practices to share data (three treatment and four controls); (2) the incompleteness and unreliability of some of the QOF data (although levels of HbA1c and blood pressure are well recorded thanks to QOF targets and incentives, this is not the case for BMI, cholesterol, smoking status or ethnicity data); (3) the fact that the only available measurement of treatment intensity was number of completed WBSs, which we know from the qualitative data is not an accurate reflection of the ‘dose’ of interaction with the intervention; and (4) the fact that data about comorbidity were restricted to those who determined intervention eligibility and did not, therefore, indicate the true extent of comorbidity, which we know to be greater. Despite these limitations, this is a robust design that includes large numbers of observations with sufficient power to detect effects.
Work package 1 (health-related quality of life)
The other parts of the evaluation focused only on people with a T2DM diagnosis, and a strength of the HRQoL study was the inclusion of everyone referred into the intervention over a 12-month period, irrespective of their diagnoses. An important finding was the overall poor self-rated health of this subgroup in comparison with national norms. The limitations are the (1) lower than anticipated baseline response rate of just under 55%, which reduced the study power; (2) weakness of a before-and-after design; and (3) requirement to account for the impact of COVID-19 and need to divide the sample into pre- and post-COVID-19 groups, further reducing the power of the study.
Work package 2 (cost-effectiveness)
To our knowledge, this is the first robust cost-effectiveness analysis of a UK social prescribing intervention to date using a well-established T2DM simulation model98 to provide a cost per QALY gained associated with the introduction of the intervention. The limitations are (1) reliance on an exploratory analysis with significant sensitivity analysis due to data limitations on the impact of the intervention on relevant risk factors; (2) the fact that effects were captured over a 4-year period only, rather than over the longer term; and (3) the inability to capture non-clinical outcomes related to social determinants of health.
Work package 3 (qualitative research)
A key strength of ethnography is the use of participant observation (complemented by interviews and focus groups) to gain a holistic understanding of practices within the context in which they take place, over an extended time period (i.e. 20 months for the client ethnography and 10 months for the link worker ethnography). Our use of an ethnographic approach allowed us to ‘see’ the intervention from the perspective of link workers and clients in the settings in which they worked and lived, rather than relying on self-report. 168 The use of two ethnographies focusing on experiences of the intervention from both link worker and client perspectives, in conjunction with interview data during the initial lockdown period, afforded a considerable degree of triangulation and assurance about the reliability of our interpretation of the observational data. A further strength was in the extended time frame that the intervention was observed from the client perspective. The limitations are (1) the reliance on relatively small numbers of research participants; (2) the premature curtailment of face-to-face fieldwork due to COVID-19, particularly impacting on the ‘shadowing’ fieldwork; (3) limited VCSE perspectives; and (4) not including those were eligible for the intervention but who did not participate, along with a lack of data from those involved in the early stages of the intervention but who did not remain engaged, potentially leading to a biased perspective on the early years of the intervention.
Conclusions and implications
During the period of the SPRING_NE study – July 2018–April 2021 – social prescribing became a central element of The NHS Long Term Plan’s personalised care agenda and was asserted to:
. . . strengthen community resilience and personal resilience, and reduce[s] health inequalities by addressing the wider determinants of health, such as debt, poor housing and physical inactivity, by increasing people’s active involvement with their local communities.
NHS England2
As social prescribing is gaining traction within other areas of the NHS, including mental health,169 care of older people with frailty,48 or dementia,170 and children and young people,171 the findings of this evaluation are particularly timely.
The social prescribing intervention evaluated in this study was developed in response to the needs of a diverse urban population living in areas of high socioeconomic deprivation with high levels of LTCs and multimorbidity. We have shown that between 2015 and 2019 the patients of participating practices showed improved glycaemic control, as indicated by a reduction in the levels of HbA1c, indicating a positive impact of WtW within this challenged urban area. We also find that this effect differed across different groups and that the intervention itself was heterogeneous and shaped in unanticipated ways by the context in which it is delivered; therefore, we suggest that the impact of social prescribing varied depending on the personal circumstances of clients. Our findings offer promise for the future, but also suggest that the operationalisation of social prescribing within the UK is explored further using a variety of methods appropriate to the particular intervention and target population.
A particular model of social prescribing, WtW is funded via a SIB and operates with specific targets. Nevertheless, our research provides a number of broader implications for the rapidly developing social prescribing policy and practice landscape. First, our findings indicate the need for a greater consideration of the expectations placed on social prescribing, particularly its role in tackling health inequalities. The rhetorical claims about social prescribing appear to conflate link worker support in the navigation of social determinants of health for individuals with reducing health inequalities. The coalescence of widening levels of income inequality,172 widening health inequalities,173 upstream policies such as state welfare reforms,174 austerity175,176 and the reduction in government funding to local councils that disproportionately impact on areas of higher socioeconomic disadvantage177 is the context within which social prescribing operated pre-COVID. Most recently, cuts to expenditure on social care, public health and health care between 2010–11 and 2014–15 have been linked to the observed slowdown in life expectancy growth in England. 178 The unequal impact of COVID-19 across populations179 and the subsequent impacts of the unequal economic and health effects of the pandemic180 present an even starker environment within which to operate. Enabling access to food bank vouchers, for example, is an important aspect of social prescribing for those who need them, but the ubiquitousness of food banks lays bare the failures of more distal mechanisms that impact on the social determinants of health. Claims that social prescribing can reduce health inequalities, particularly following the fallout of the pandemic,180 are premature at best,181 but there is no doubt that social prescribing can help mitigate upstream pressures. 8 This takes us to our second implication, the need for integration of social prescribing with local community infrastructure; for this to be successful, well-funded public and voluntary sector services are essential. However, pre pandemic, the VCSE sector experienced increased demand from people with increasingly complex needs in the face of austerity-driven public sector cuts113 that have disproportionately fallen on areas serving populations with higher levels of socioeconomic deprivation. 177 Third, supported linking, tailored to client need, requires a considerable allocation of link worker time. Hence, there are cost implications attached to delivering a more holistic intervention tailored to context and, given that the economic analysis identified that in its current form WtW is not cost-effective, this is something that requires careful deliberation, including consideration of the impact beyond health outcomes, including on non-health sectors. Fourth, our study highlights the complexities of outcomes measurement. We show that the identification of a specific outcome metric within the funding model distorted the delivery of the intervention. We also suggest that a focus on specific health outcomes in measuring the success of social prescribing at best obscures the wider impact of social prescribing, and at worst could further distort the intervention itself. Our findings do, however, suggest that health-care usage may be an outcome measure worth further attention. A fifth implication is not to underestimate the intricacies inherent in embedding this complex intervention within primary care, itself a complex system.
In conclusion, holistic social prescribing, fully embedded within primary care, that provides supported linking to navigate social determinants of health and which acknowledges the non-linearity of health improvement is challenging to deliver, but offers opportunities for improvements in health and well-being.
There is no panacea. There never was. But social prescribing offers something to hang on to.
Abbasi182
Recommendations for further research
-
Qualitative research with primary care referrers to explore primary care engagement with social prescribing, which patients are being referred and why and how NHS social prescribing is being operationalised and embedded within PCNs. With very few exceptions, primary care perspectives are largely absent from current UK research on social prescribing.
-
Research into the integration of NHS social prescribing with the VCSE organisations, particularly onward referral mechanisms, capacity and costs. We were unable to examine the implications for social prescribing on the VCSE sector, the success of which is dependent on a well-resourced VCSE sector.
-
Further evaluation of the impact, and mechanisms of impact, of social prescribing on health outcomes, health-care usage and costs, including medication. Such evaluation needs to take into account broader conceptualisations of value.
-
Research on wider, including non-health, effects of social prescribing, acknowledging the wide range of potential effects.
-
Scrutiny of the capacity for social prescribing to address the social determinants of health, in the context of widening inequalities driven by wider societal, political and economic forces.
Acknowledgements
We thank all of the participants, link workers and link worker managers who were involved in this research, without whom this study would not have been possible. We are extremely grateful to Tara Case, Professor Chris Drinkwater, Katie Hopper, Cherry Johnson, Rishi Arora and Mike Bareham from Ways to Wellness, Dr Guy Pilkington from Newcastle Gateshead Clinical Commissioning Group and the participating general practices. We are indebted to Bob Gaffney, Richard McLeod, Ian Davison, Chris Walker and Azim Dinsdale, Billie Moyle, Neil Shutt, Sean Curry, Liane Cotterill and Julie Hynd from North East Commissioning Services for their help with secondary data. We are extremely grateful to Allison Lawson for her administrative support throughout the project and particularly with the EQ-5D-5L data collection. We thank members of the SSC for their advice and guidance. We are also grateful for the continued support of Sue Pargeter at NIHR whose prompt responses, particularly during the COVID-19 period, were extremely helpful for steering the study through such challenging times. Finally, we wish to acknowledge Dr Linda Penn who contributed to the study design and assisted with ethics procedures before her retirement.
Contributions of authors
Suzanne Moffatt (https://orcid.org/0000-0002-8553-249X) (Professor, Social Gerontology) was principal investigator with overall responsibility for the study, conceived the idea, contributed to the study design and methods development, contributed to data interpretation and drafted text.
John Wildman (https://orcid.org/0000-0001-6759-4948) (Professor, Health Economics) contributed to the overall study design, led the design of WP1 and WP2, led the data analysis and interpretation and drafted text.
Tessa M Pollard (https://orcid.org/0000-0002-0544-0158) (Professor, Medical Anthropology) contributed to the study design, co-led the design of WP3 (ethnography), led the data analysis and interpretation and drafted text.
Kate Gibson (https://orcid.org/0000-0002-9812-8269) (Postdoctoral Research Associate, Sociology) undertook ethnographic fieldwork (WP3, client), data analysis, data interpretation and drafted text.
Josephine M Wildman (https://orcid.org/0000-0001-9669-6708) (Postdoctoral Research Associate, Health Services Research) contributed to the study design, oversaw EQ-5D-5L data collection, undertook data analysis for WP1, data interpretation and drafted text.
Nicola O’Brien (https://orcid.org/0000-0002-7773-6871) (Lecturer, Health Psychology) contributed to the study design and methods development, undertook analysis of EQ-5D-5L data, contributed to data interpretation and drafted text.
Bethan Griffith (https://orcid.org/0000-0002-1725-8054) (Research Associate, Primary Care) undertook data analysis for WP3 (link worker ethnography), data interpretation and drafted text.
Stephanie L Morris (https://orcid.org/0000-0002-9005-4680) (Postdoctoral Research Associate, Medical Anthropology) undertook fieldwork for COVID-19 interview study, undertook data analysis, contributed to data interpretation and drafted text.
Eoin Moloney (https://orcid.org/0000-0002-3025-5413) (Postdoctoral Senior Research Associate, Health Economics) undertook data analysis for WP2, interpretation and drafted text.
Jayne Jeffries (https://orcid.org/0000-0002-2814-5880) (Postdoctoral Research Associate, Geography) undertook fieldwork for WP3 (link worker ethnography).
Mark Pearce (https://orcid.org/0000-0002-0583-3779) (Professor, Applied Epidemiology) contributed to the study design and contributed to the data interpretation.
Wael Mohammed (https://orcid.org/0000-0003-0370-4903) (Research Associate, Health Economics) undertook data analysis for WP2 and contributed to data interpretation.
Publications
Journal articles
Wildman J, Wildman JM. Combining health and outcomes beyond health in complex evaluations of complex interventions: suggestions for economic evaluation. Value Health 2019;22:511–17.
Gibson K, Pollard TM, Moffatt S. Social prescribing and classed inequality: a journey of upward health mobility? Soc Sci Med 2021;280:114037.
Wildman J, Wildman JM. Evaluation of a community healthworker social prescribing program among UK patients with type 2 diabetes. JAMA Netw Open 2021;4:e2126236.
Gibson K, Moffatt S, Pollard TM. ‘He called me out of the blue’: an ethnographic exploration of contrasting temporalities in a social prescribing intervention. Sociol Health and Illn 2022, 1–18.
Morris SL, Gibson K, Wildman JM, Griffith B, Moffat S, Pollard TM. Social prescribing during the COVID-19 pandemic: a qualitative study of service providers’ and clients’ experiences. BMC Health Serv Res 2022;22:258.
Wildman JM, Morris S, Pollard T, Gibson K, Moffatt S. ‘I wouldn’t survive it, as simple as that’: syndemic vulnerability among people living with chronic non-communicable disease during the COVID-19 pandemic. Soc Sci Med Qual Res Health 2022;2:10032.
Morris SL, Wildman JM, Gibson K, Moffat S, Pollard TM. Managing disruption at a distance: unequal experiences of people living with long-term conditions during the COVID-19 pandemic. Soc Sci Med 2022;302:114963.
Conference presentations
Gibson K, Pollard T, Moffatt S. Social Prescribing and Classed Inequalities in Health: Exploring a Complex Relationship Using Ethnographic Methods. Presented at Society for Social Medicine & Population Health Virtual Conference, 9–11 September 2020.
Moffatt S. Why is NHS England so Keen on Social Prescribing and How Does it Impact on Health and Wellbeing? Presented at British Geriatrics Society Virtual Annual Conference, 27–28 November 2020.
Gibson K. Social Prescribing and Class: A Journey of Upward Health Mobility? Presented at Chronic Living Virtual Conference, 4–6 March 2021.
Griffith B, Moffatt S, Pollard T. Two Sides of the Same Coin? An Ethnographic Exploration of Primary Care Staff and Link Worker Perspectives on Social Prescribing. Society of Academic Primary Care 49th Annual Scientific Meeting (Living and Dying), 30 June–1 July 2021.
Griffith B, Moffatt S, Pollard T. Link Working at the Intersections: And Ethnographic Explorations of Delivering Social Prescribing in Primary Care. Society for Social Medicine and Population Health 65th Annual Scientific Meeting, 15–17 September 2021.
Morris S, Wildman J, Gibson K, Moffatt S, Pollard T. Managing Disruption at a Distance: Unequal Experiences of People Living with Long-term Conditions During the COVID-19 Pandemic. e-Poster P109 with 3-minute oral presentation. Society for Social Medicine and Population Health 65th Annual Scientific Meeting, 15–17 September 2021.
Data-sharing statement
Quantitative data
Owing to the confidential nature of the quantitative data that were provided for the sole purpose of this study, these data cannot be shared.
Qualitative data
The ethnographic and interview data are not suitable for sharing beyond that contained within the report.
For queries relating to either data set, further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
Appendix 1 Summary of peer-reviewed UK link worker social prescribing evaluations with a quantitative component
| Peer-reviewed UK link worker social prescribing evaluations | Summary |
|---|---|
| What is the value of social prescribing?50 |
Intervention/evaluation period and geographical location 2012–16 – Wellbeing Programme, Bristol, south-west England, UK |
|
Target population and service attributes Target population: patients referred from five GP surgeries Service attributes: two elements –Funded by various, mainly charitable, trusts |
|
|
Study design, outcome measures, number of people referred into service, sample size and response rate Mixed-methods design: |
|
Summary of findings
|
|
|
Author conclusions Social prescribing delivered value, broadly social and for many sectors across society |
|
| Impact of social prescribing on patients in primary care: mixed-methods evaluation44 |
Intervention/evaluation period and geographical location 2014–16 – Hackney, London, UK |
|
Target population and service attributes Target population: frequent attenders and/or socially isolated patients Service attributes: three social prescribing co-ordinators (trained social workers) in 22 GP surgeries Social prescribing co-ordinators provide initial assessment, action plan, referral to community organisations and, if necessary, a volunteer is assigned to help patients achieve goals. Six sessions with social prescribing co-ordinators and unlimited contacts with volunteer Commissioned (i.e. funded) by CCG |
|
|
Study design, outcome measures, number of people referred into service, sample size and response rate Mixed-methods design: |
|
Summary of findings
|
|
|
Author conclusions Quantitative data did not support strong positive narratives identified from the qualitative study. This discrepancy may reflect that standard health outcome measures do not capture the ‘non-health’-related outcomes that reflect patient priorities and their perspective of their own health and well-being |
|
| Impact of social prescribing on general practice workload and polypharmacy5 |
Intervention/evaluation period and geographical location 2015–16 – Derry, Northern Ireland, UK |
|
Target population and service attributes Target population: adults aged 65+ years, with LTCs, polypharmacy and/or frequent attendance Service attributes: 12-week programme linking patients into a range of health and well-being, emotional and practical support, education and self-help activities Funded by the Health and Social Care Trust |
|
|
Study design, outcome measures, number of people referred into service, sample size and response rate Quantitative before-and-after study measuring impact of social prescribing on GP health care use and polypharmacy |
|
Summary of findings
|
|
|
Author conclusions Social prescribing had low rates of uptake, important limitation. The median length of delay of 92 days from referral to starting social prescribing may have contributed. The study was not sufficiently powered to detect difference in outcome measures |
|
| Understanding the effectiveness and mechanisms of social prescribing service46 |
Intervention/evaluation period and geographical location Large city in northern England, UK |
|
Target population and service attributes Target population: aged 14+ years and registered with general practitioner Service attributes: well-being co-ordinators provide individual support and link into local groups and services Referral via GPs, health, social care, other relevant professionals or self-referral Service user needs identified and given signposting or, if needed, provided with a one-to-one assessment. Six sessions given, the mean time with service is 10 weeks. Approximately 1500–2500 service users referred each year |
|
|
Study design, outcome measures, number of people referred into service, sample size and response rate Mixed-methods design:Over 18 months of the research, 2250–3750 service users were in contact with service |
|
Summary of findings
|
|
|
Author conclusions Respondents completing pre–post questionnaires constituted a relatively small proportion of the total number using the service Respondents only included those completing the allotted six sessions. The study lacked a control group. Social prescribing has the potential to address health and social needs of individuals and communities and should be conceptualised as one way to support primary care and tackle unmet needs |
|
| Impact of Luton social prescribing programme on energy expenditure: quantitative before-and-after study;47 impact of Luton social prescribing programme on mental well-being: quantitative before-and-after study52,56 |
Intervention/evaluation period and geographical location 2015–18 – Luton, east England, UK |
|
Target population and service attributes Target population: adults aged 18+ years with high risk of diagnosis for T2DM, COPD, mild/moderate mental health issues, loneliness/social isolation and carers Service attributes: four general practices involved, referral by HCP. ‘Navigator’ initiates initial assessment, onward referral/signpost to non-medical support for up to 12 (free) sessions Intervention funded by the NHS Better Together Care Fund |
|
|
Study design, outcome measures, number of people referred into service, sample size and response rate 2019: |
|
|
Summary of findings 2019: |
|
|
Author conclusions Social prescribing may have the potential to increase physical activity levels of service users and promote uptake of physical activity in inactive patient groups Cannot conclude if the mean difference in SWEMWBS scores is clinically relevant. There was a high rate of loss to follow-up,b possibly due to link worker turnover, but unclear why only 36.2% of patients out of the 448 who were referred completed the SWEMWBS |
|
|
Does a social prescribing ‘holistic’ link worker for older people with complex, multimorbidity improve well-being and frailty and reduce health and social care costs? 12-month before-and-after evaluation48 |
Intervention/evaluation period and geographical location South-west England, UK |
|
Target population and service attributes Target population: older people aged 50+ years with two or more LTCs Service attributes: 12 paid trained (non-health staff) well-being co-ordinators hold initial 30- to 40-minute strengths-based-guided conversations with individuals for up to 12 weeks to enable goal achievement. Service delivered by seven voluntary sector organisations. Referral from statutory and VCSE sectors Commissioned by NHS Foundation Trust |
|
|
Study design, outcome measures, number of people referred into service, sample size and response rate 12-month before-and-after study. Outcome measures: WBS, PAM, WEMWBS and Rockwood Clinical Frailty Scale Service use: A&E, minor injury, inpatient, outpatient, community service, social service, length of stay, GP contacts Cost data: health and community service attendance (National Tariff Payment System); n = 1046 participants, 151 triaged to receive 12-week programme; n = 86 followed up at 12 months, mean age 79.6 years |
|
|
Summary of findings On average, health and well-being, patient activation and frailty showed statistically significant improvement in mean score. The mean activity increased for all services. Thirteen high-cost users account for 59% of the overall cost increase |
|
|
Author conclusions The majority of the target group benefit from holistic social prescribing, irrespective of age, sex and levels of activation and frailty. Larger controlled studies are needed to strengthen claims of causality |
|
|
Effectiveness of CLPs in areas of high socioeconomic deprivation49 |
Intervention/evaluation period and geographical location March–December 2015 – Deep End Practices, Glasgow, Scotland, UK |
|
Target population and service attributes Target population: any patient aged 18+ years with complex needs Service attributes: CLP attached to GP practice – to support patients with complex needs and link to existing community organisations. Contacts were usually one to one and face to face. There were no limits on CLP and patient meetings |
|
|
Study design, outcome measures, number of people referred into service, sample size and response rate Quasi-experimental cluster RCT Adult patients (18+ years) referred to CLPs in seven intervention practices were compared with a random sample of patients from eight comparison practices at baseline and at 9 months Primary outcome: EQ-5D-5L score Secondary outcomes: well-being (ICECAP-A), anxiety, depression (HADS-A/D) and self-reported exercise. Multilevel, multiple regression analyses adjusted for baseline differences |
|
|
Summary of findings Intervention group data were available for 288 and 214 (74.3%) patients at baseline and follow-up, respectively. Comparison group data were available for 612 and 561 (92%) patients in comparison practices. No differences between baseline and comparison groups were found for any outcome in the ITT analysis. Significant improvements in EQ-5D-5L scores, HADS-A/D scores and exercise levels were found in the subgroup analyses of patients who saw a CLP on three or more occasions (45%) of those referred |
|
|
Author conclusions Referrals to primary care-based CLPs in deprived areas was not effective for improving patient outcomes. Overall outcomes might be improved if uptake and engagement were increased. Further research required before wide-scale deployment of this model of social prescribing |
|
|
Impact of social prescribing to address loneliness: mixed-methods evaluation of a national social prescribing programme45 Linked qualitative study 55 |
Intervention/evaluation period and geographical location May 2017–December 2019 – 37 locations in UK |
|
Target population and service attributes Target pop: adults aged 18+ years experiencing or at risk of loneliness Service attributes: Paid link workers alongside volunteers assessing service-user needs, providing person-tailored care for up to 12 weeks Referral routes: statutory services, NHS, LAs, VCSE organisations, self-referral Intervention funded by the British Red Cross |
|
|
Study design, outcome measures, number of people referred into service, sample size and response rate Mixed methods: |
|
Summary of findings
|
|
|
Author conclusions Social prescribing can address loneliness Skilled link workers are a requirement of success Further research required on sustaining improvements and intensity of intervention |
|
| Social prescribing ‘social cure’: longitudinal study of the health benefits of social connectedness with a social prescribing pathway51 |
Intervention/evaluation period and geographical location 2017–19 Nottinghamshire, Midlands, England, UK Relatively affluent, ethnically homogeneous suburb |
|
Target population and service attributes Target population: adults with one or more LTCs (physical or mental) and isolated, lonely or socially isolated Service attributes: NHS-based social prescribing pathway. Patients’ needs assessed by health coach who either recommends self-care management or refers patient to a community-based LW who connects patients to voluntary/community groups. Referral by primary HCPs (90%) and self-referral |
|
|
Study design, outcome measures, number of people referred into service, sample size and response rate Quantitative before-and-after survey Outcomes measured at baseline (T0), 4 months (T1) and 6–9 months (T2) Outcome measures: number of group memberships, community belonging, social support, loneliness (ULS-8), HRQoL (EQ-5D) T0, n = 655; T1, n = 178; T2, n = 63 Response rate: T1 = 27.1% (n = 178); T2 9.6% (n = 63) of T0 |
|
|
Summary of findings Regression analysis: HRQoL improves between T0 and T1, but did not change between T1 and T2 Relationship between increased group memberships and HRQoL was serially mediated by belonging, support and loneliness Group membership declined significantly between T1 and T2 |
|
|
Author conclusions Local community impacts directly on HRQoL. Social prescribing needs to be more explicitly community-health focused with a broader goal of promoting community cohesion and provision The study was limited by the high levels of attrition, particularly at T2 |
Appendix 2 Study Steering Committee members
An independent Study Steering Committee (SSC) supervised the study overall. The independent SSC comprised: Professor Sally Wyke (chairperson), Dean of Research/Deputy Director, Institute of Health and Wellbeing University of Glasgow; Professor Richard Cookson, Professor and NIHR Senior Research Fellow, Centre for Health Economics, York University; Professor Sarah Atkinson, Professor of Geography and Medical Humanities, Durham University; Professor Jane South, Professor of Healthy Communities, Leeds Beckett University; Dr Richard Kimberlee, Senior Research Fellow, University of the West of England; Dr Peter McMeekin, Professor of Health Economics, Northumbria University; Dr Mandy Cheetham, Research Fellow, Northumbria University; Professor Chris Drinkwater, Emeritus Professor of Primary Care, Northumbria University); Professor Suzanne Moffatt (principal investigator), Newcastle University; and Professor John Wildman, Newcastle University.
Project team attendees were Dr Josephine Wildman, Dr Kate Gibson, Dr Eoin Maloney, Dr Bethan Griffiths (Newcastle University), Professor Tessa M Pollard (Durham University), and Dr Nicki O’Brien (Northumbria University).
The SSC met initially face to face during the first year of the project in June 2019. Two subsequent annual meetings (March 2020 and January 2021) were held via Zoom owing to the COVID-19 pandemic. The role of the SSC was to monitor study progress and ensure good conduct and high standards of research.
Appendix 3 Summary statistics: health outcomes
| Variable | Count (n) | Mean/proportion | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Control group | |||||
| HbA1c level (mmol/mol) | 3435 | 57.94 | 13.00 | 33.59 | 120.00 |
| BP (mmHg) | |||||
| Systolic | 3449 | 134.30 | 10.34 | 100.68 | 193.15 |
| Diastolic | 3449 | 78.33 | 6.56 | 58.00 | 119.40 |
| High BP | 3449 | 0.34 | 0.30 | 0 | 1 |
| Blood glucose level (mmol/l) | 1930 | 8.88 | 3.54 | 2.70 | 18.00 |
| Cholesterol level (mmol/l) | 3431 | 4.44 | 0.97 | 2.04 | 8.97 |
| BMI (kg/m2) | 3436 | 32.98 | 6.11 | 20 | 50 |
| Smoker | 3446 | 0.24 | 0.38 | 0 | 1 |
| Treatment group | |||||
| HbA1c level (mmol/mol) | 4922 | 58.22 | 13.41 | 25.87 | 120.00 |
| BP (mmHg) | |||||
| Systolic | 4933 | 133.94 | 10.93 | 94.50 | 200.00 |
| Diastolic | 4933 | 78.16 | 6.65 | 43.00 | 118.00 |
| High BP | 4933 | 0.33 | 0.30 | 0 | 1 |
| Blood glucose level (mmol/l) | 3097 | 8.92 | 3.57 | 2.60 | 18.00 |
| Cholesterol level (mmol/l) | 4912 | 4.42 | 0.95 | 1.80 | 10.00 |
| BMI (kg/m2) | 4903 | 32.39 | 6.18 | 20.00 | 50.00 |
| Smoker | 4929 | 0.23 | 0.38 | 0 | 1 |
| Total | |||||
| HbA1c level (mmol/mol) | 8357 | 58.10 | 13.24 | 25.87 | 120.00 |
| BP (mmHg) | |||||
| Systolic | 8382 | 134.09 | 10.69 | 94.50 | 200.00 |
| Diastolic | 8382 | 78.23 | 6.61 | 43.00 | 119.40 |
| High BP | 8382 | 0.34 | 0.30 | 0 | 1 |
| Blood glucose level (mmol/l) | 5027 | 8.90 | 3.56 | 2.60 | 18.00 |
| Cholesterol level (mmol/l) | 8343 | 4.43 | 0.96 | 1.80 | 10.00 |
| BMI (kg/m2) | 8339 | 32.64 | 6.16 | 20.00 | 50.00 |
| Smoker | 8375 | 0.24 | 0.38 | 0 | 1 |
Appendix 4 Summary statistics: costs and use
| Variable | Count (n) | Mean/proportion | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Control group | |||||
| Use any HC | 3455 | 0.66 | 0.32 | 0.00 | 1.00 |
| Total cost (£) | 3455 | 1244.52 | 1669.78 | 0.00 | 13,432.63 |
| A&E use | 3455 | 0.27 | 0.25 | 0.00 | 1.00 |
| A&E cost (£) | 3455 | 49.19 | 65.73 | 0.00 | 500.00 |
| IP elective use | 3455 | 0.19 | 0.22 | 0.00 | 1.00 |
| IP elective cost (£) | 3455 | 390.90 | 660.52 | 0.00 | 6526.92 |
| IP non-elective use | 3455 | 0.12 | 0.19 | 0.00 | 1.00 |
| IP non-elective cost (£) | 3455 | 413.58 | 973.08 | 0.00 | 9423.44 |
| Outpatients use | 3455 | 0.58 | 0.34 | 0.00 | 1.00 |
| Outpatients costs (£) | 3455 | 351.94 | 401.98 | 0.00 | 2500.00 |
| Treatment group | |||||
| Use any HC | 4941 | 0.63 | 0.33 | 0.00 | 1.00 |
| Total cost (£) | 4941 | 1151.47 | 1562.52 | 0.00 | 13,140.84 |
| A&E use | 4941 | 0.25 | 0.25 | 0.00 | 1.00 |
| A&E cost (£) | 4941 | 46.33 | 64.76 | 0.00 | 500.00 |
| IP elective use | 4941 | 0.18 | 0.22 | 0.00 | 1.00 |
| IP elective cost (£) | 4941 | 372.46 | 662.66 | 0.00 | 7500.00 |
| IP non-elective use | 4941 | 0.12 | 0.19 | 0.00 | 1.00 |
| IP non-elective cost (£) | 4941 | 379.70 | 899.84 | 0.00 | 10,107.50 |
| Outpatients use | 4941 | 0.55 | 0.35 | 0.00 | 1.00 |
| Outpatients costs (£) | 4941 | 314.65 | 369.08 | 0.00 | 2500.00 |
| Total | |||||
| Use any HC | 8396 | 0.64 | 0.32 | 0.00 | 1.00 |
| Total cost (£) | 8396 | 1189.76 | 1608.08 | 0.00 | 13,432.63 |
| A&E use | 8396 | 0.26 | 0.25 | 0.00 | 1.00 |
| A&E cost (£) | 8396 | 47.51 | 65.17 | 0.00 | 500.00 |
| IP elective use | 8396 | 0.18 | 0.22 | 0.00 | 1.00 |
| IP elective cost (£) | 8396 | 380.05 | 661.80 | 0.00 | 7500.00 |
| IP non-elective use | 8396 | 0.12 | 0.19 | 0.00 | 1.00 |
| IP non-elective cost (£) | 8396 | 393.64 | 930.77 | 0.00 | 10,107.50 |
| Outpatients use | 8396 | 0.57 | 0.35 | 0.00 | 1.00 |
| Outpatients costs (£) | 8396 | 329.99 | 383.38 | 0.00 | 2500.00 |
Appendix 5 Yearly trends for health outcomes
FIGURE 11.
Body mass index: control vs. treatment by year. Mean outcomes plotted against year for the treatment and control practices, with the orange line indicating the year that the intervention became available.
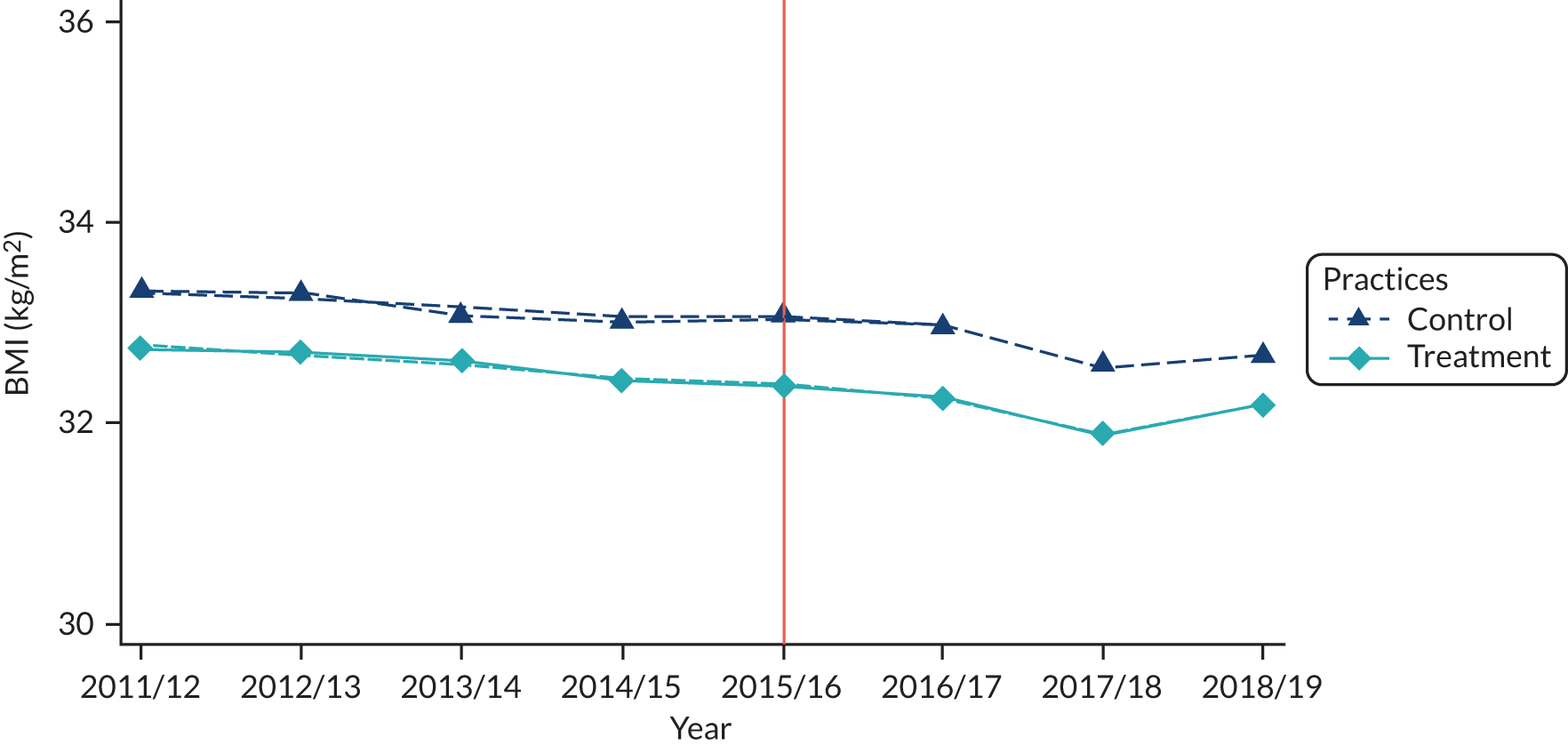
FIGURE 12.
High blood cholesterol levels: control vs. treatment by year. Mean outcomes plotted against year for the treatment and control practices, with the orange line indicating the year that the intervention became available.
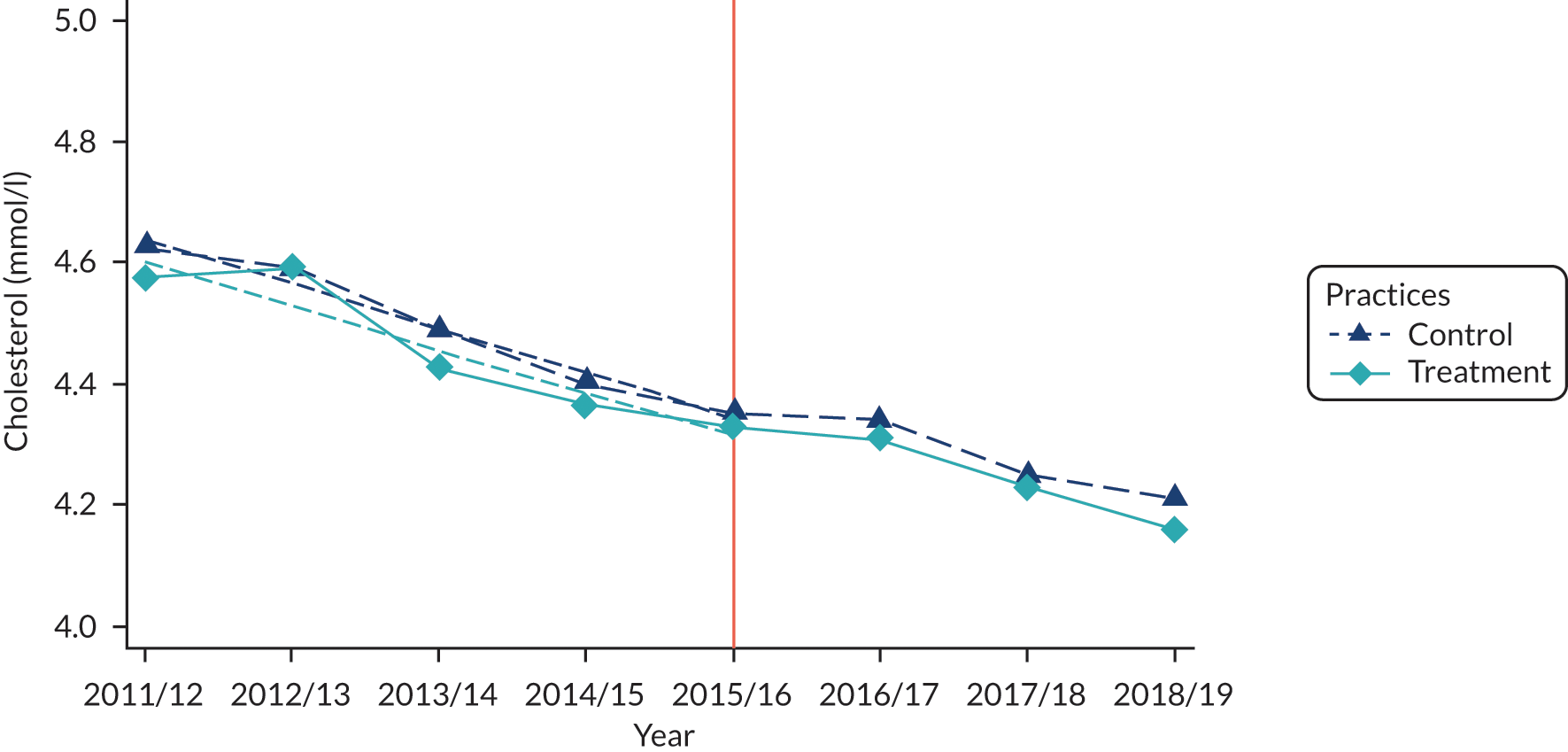
FIGURE 13.
Current smoker: control vs. treatment by year. Mean outcomes plotted against year for the treatment and control practices, with the orange line indicating the year that the intervention became available.
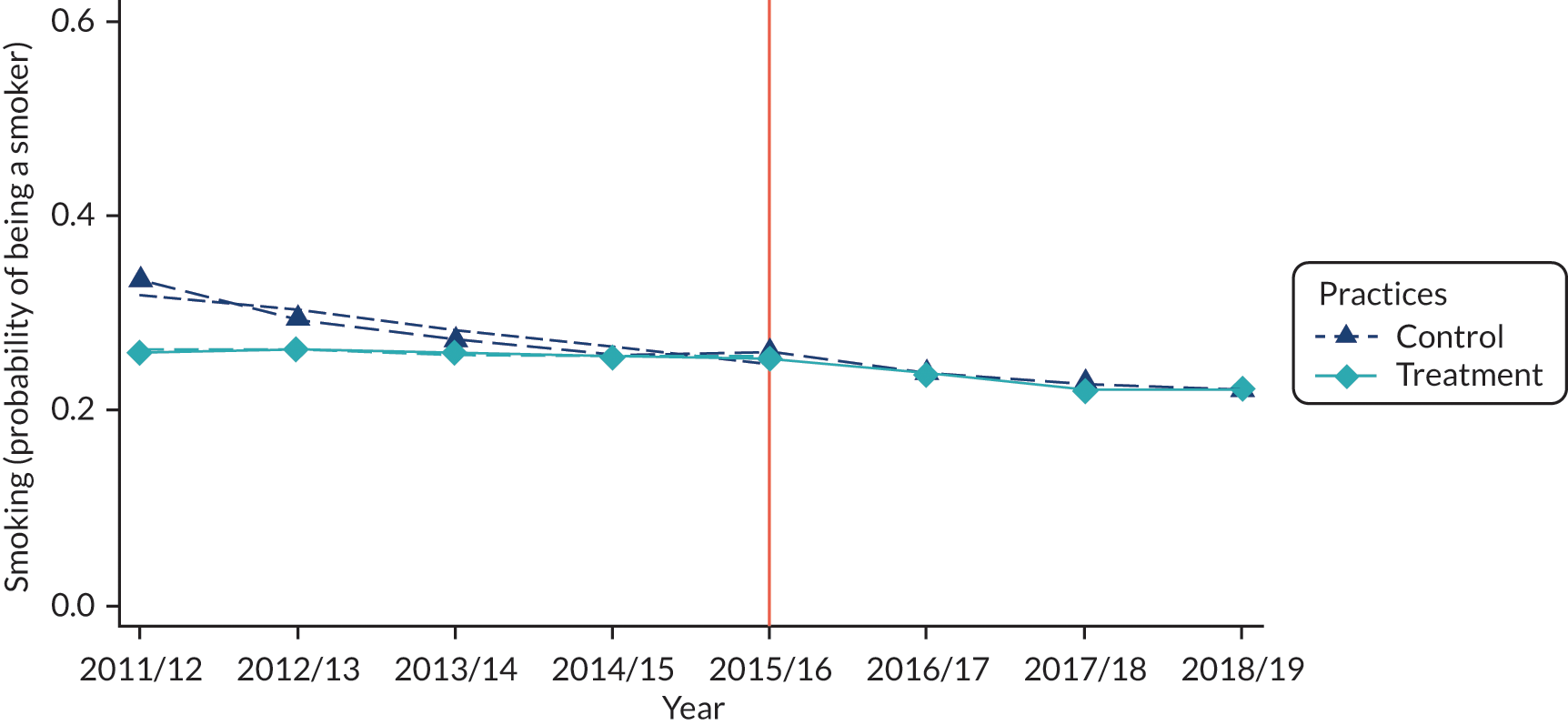
Appendix 6 Health outcomes: falsification results
FIGURE 14.
Falsification results: high blood cholesterol levels. Plots of the coefficient (and 95% CI) estimating the difference in health outcome between the treatment and control practices for each year, with the orange line indicating the year that the intervention became available.
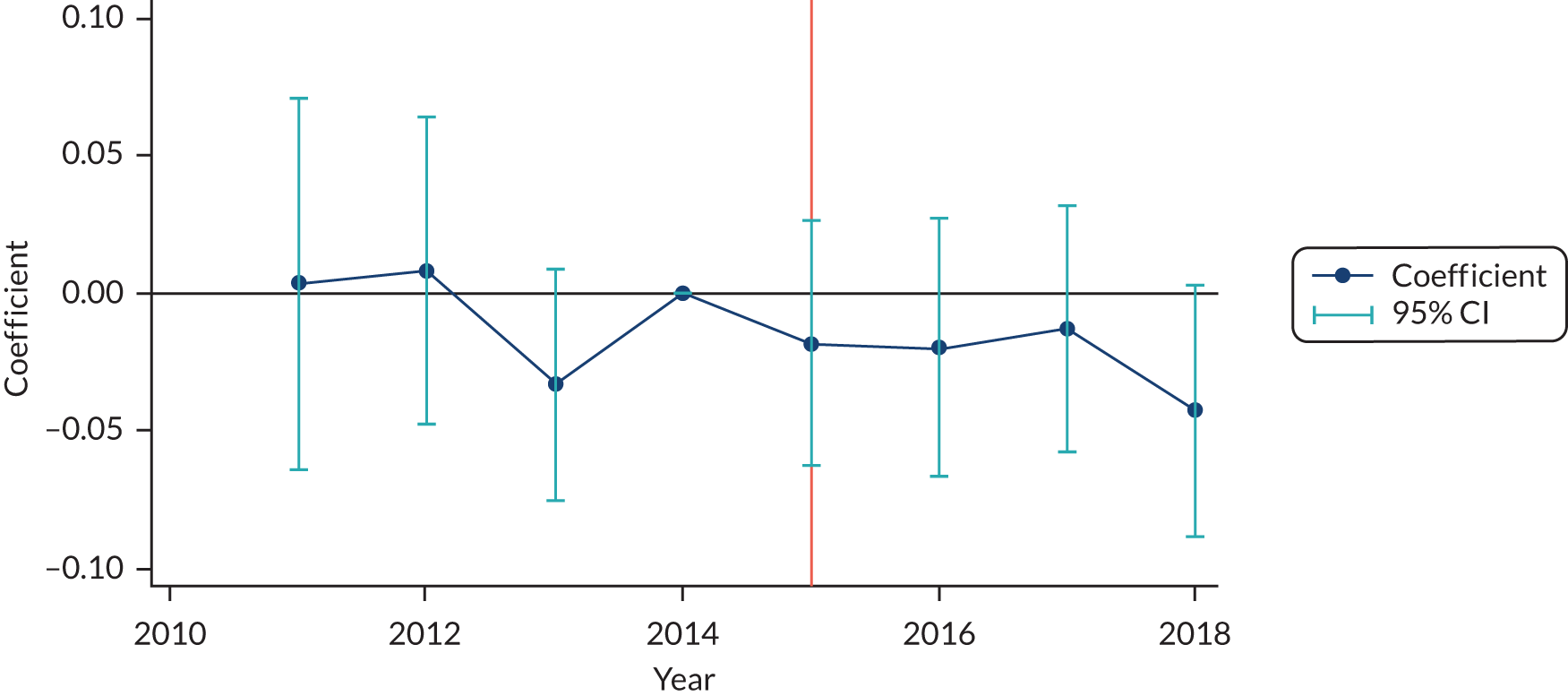
FIGURE 15.
Falsification results: BMI. Plots of the coefficient (and 95% CI) estimating the difference in health outcome between the treatment and control practices for each year, with the orange line indicating the year that the intervention became available.
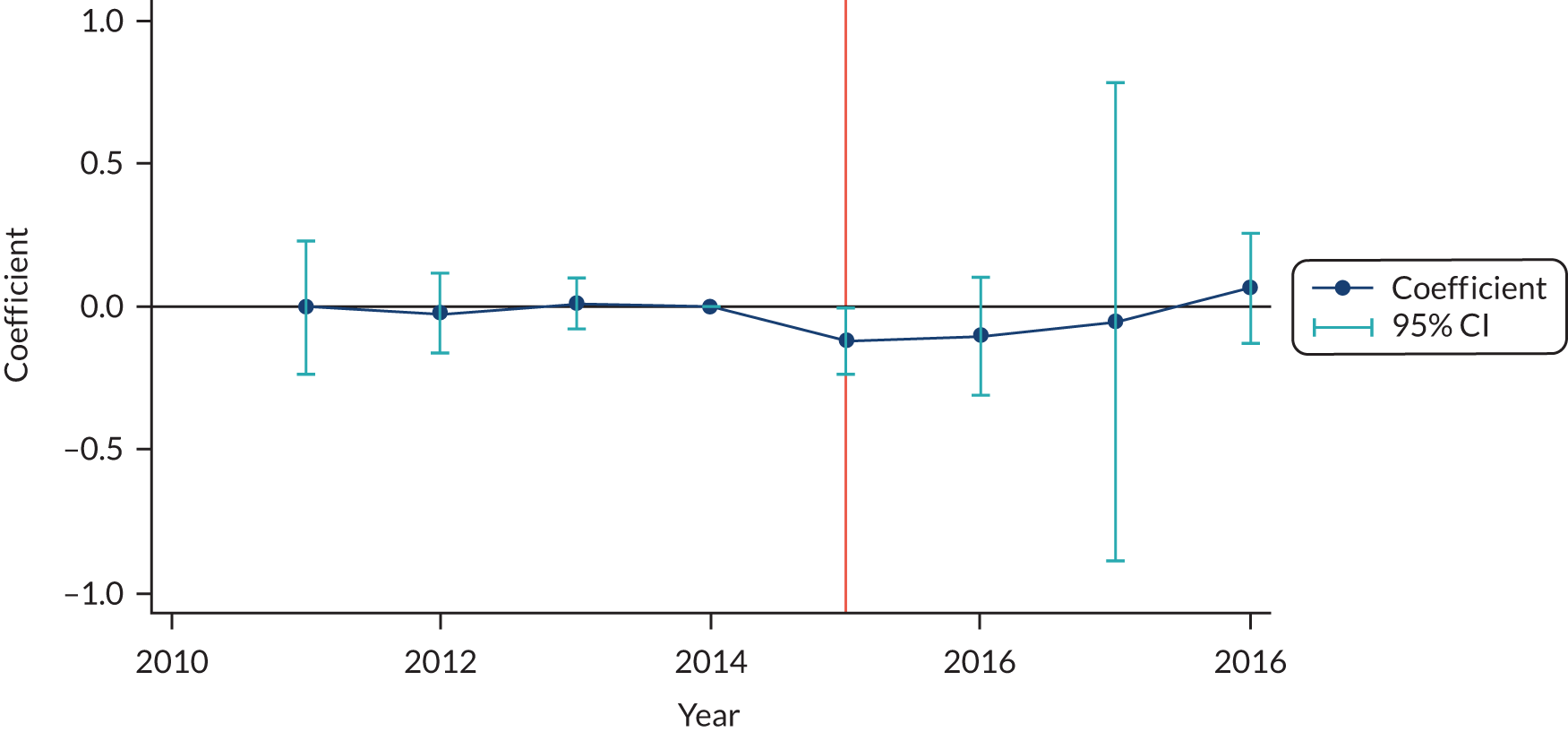
FIGURE 16.
Falsification results: current smoker. Plots of the coefficient (and 95% CI) estimating the difference in health outcome between the treatment and control practices for each year, with the orange line indicating the year that the intervention became available.
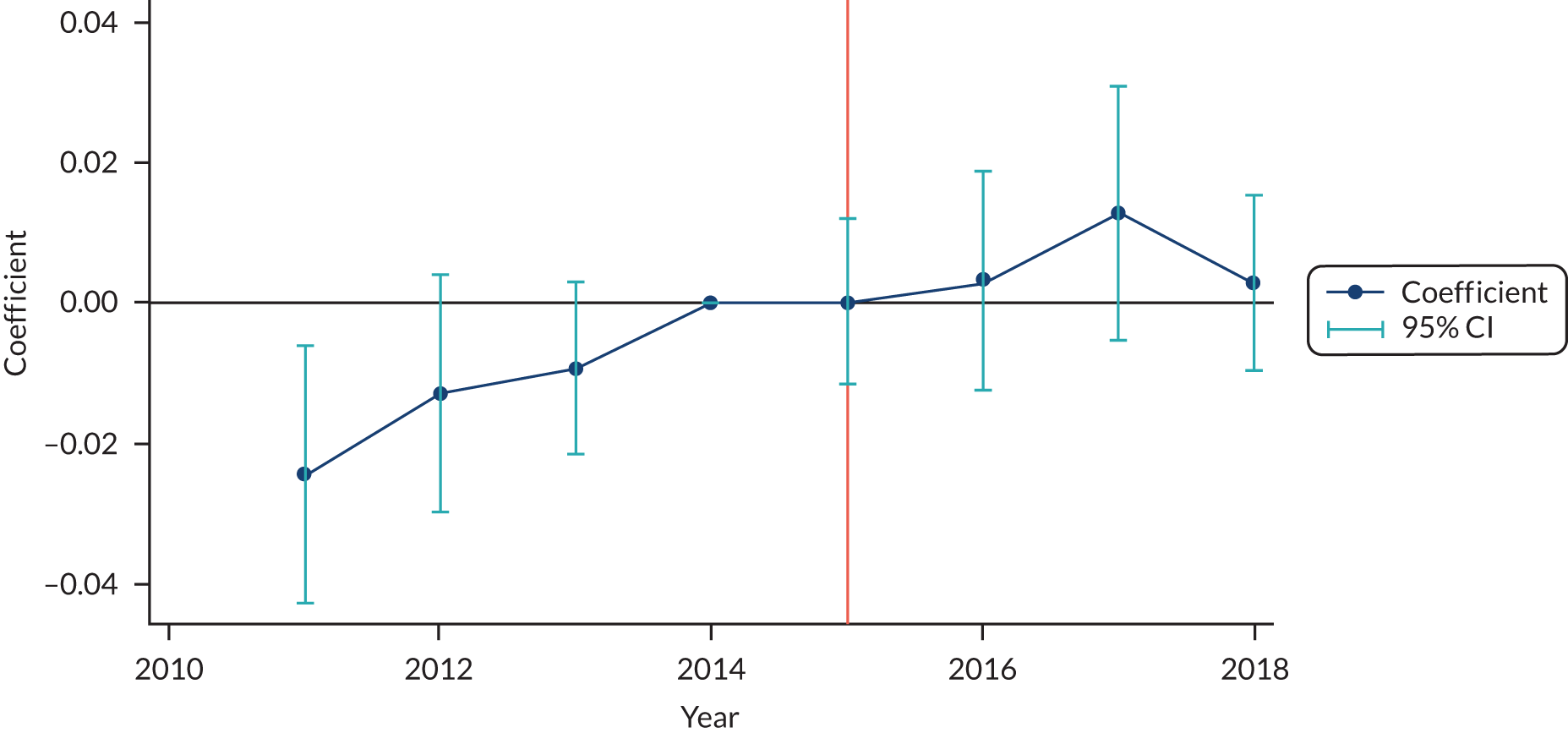
Appendix 7 Secondary care use and costs: treatment versus control
FIGURE 17.
Secondary care use and costs: treatment vs. control – inpatient non-elective. (a) Probability (any use): treatment vs. control by year; and (b) costs: treatment vs. control by year. The left-hand graph shows the proportion of individuals in the treatment and control groups who use secondary health care in each year. The right-hand graph shows the average costs among those individuals who use health care in each year. The orange line at year 3 is 2015/16, the year that the intervention became available.
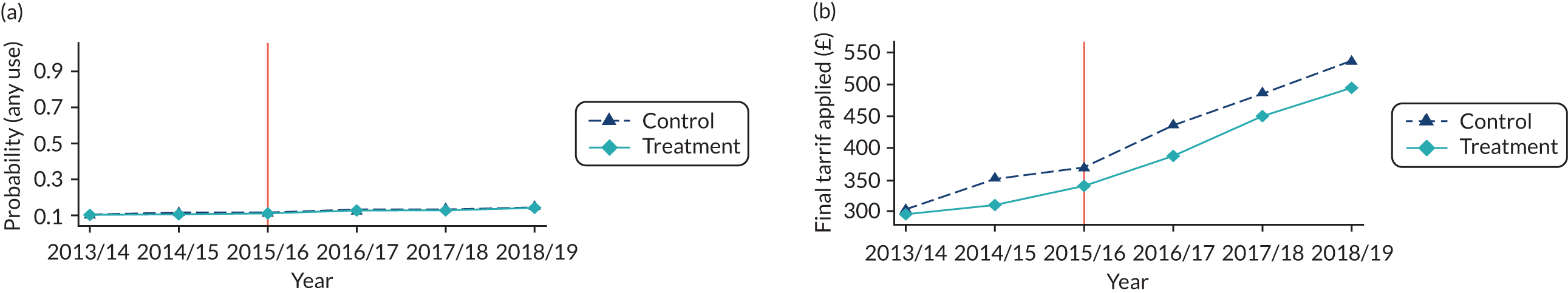
FIGURE 18.
Secondary care use and costs: treatment vs. control – inpatient elective. (a) Probability (any use): treatment vs. control by year; and (b) costs: treatment vs. control by year. The left-hand graph shows the proportion of individuals in the treatment and control groups who use secondary health care in each year. The right-hand graph shows the average costs among those individuals who use health care in each year. The orange line at year 3 is 2015/16, the year that the intervention became available.
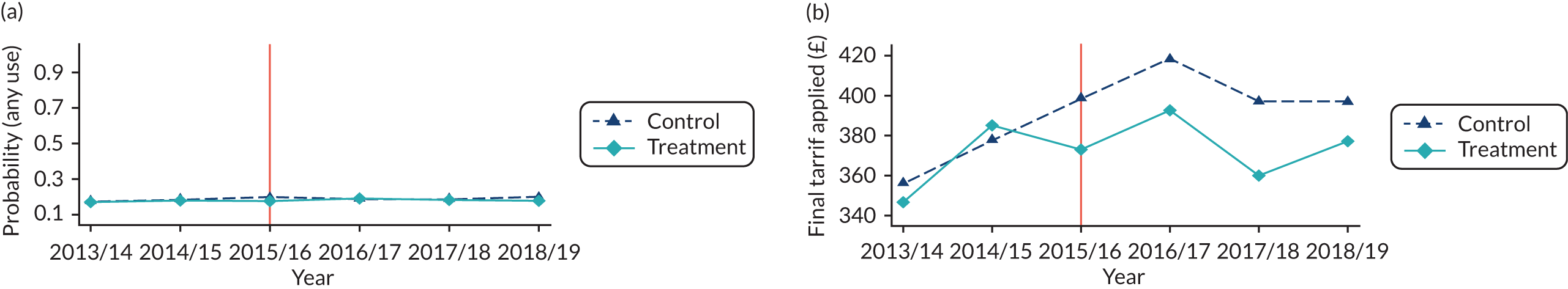
FIGURE 19.
Secondary care use and costs: treatment vs. control – outpatients. (a) Probability (any use): treatment vs. control by year; and (b) costs: treatment vs. control by year. The left-hand graph shows the proportion of individuals in the treatment and control groups who use secondary health care in each year. The right-hand graph shows the average costs among those individuals who use health care in each year. The orange line at year 3 is 2015/16, the year that the intervention became available.
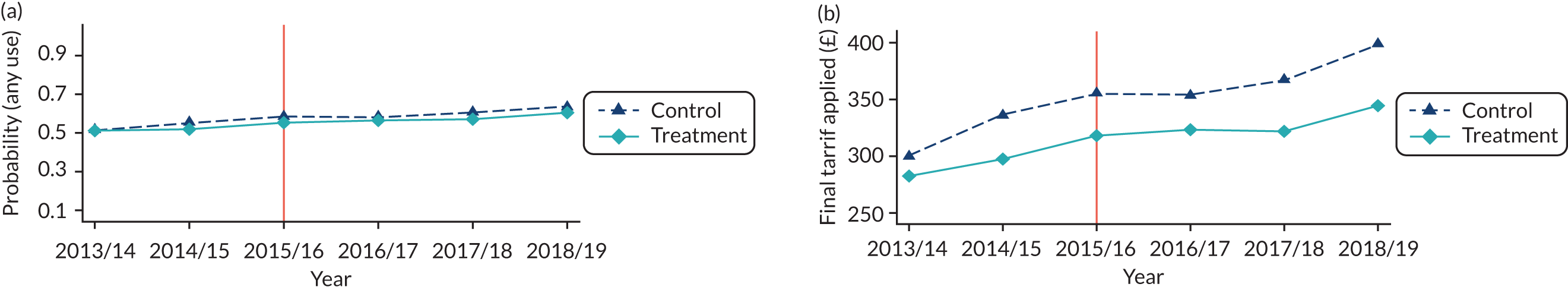
FIGURE 20.
Secondary care use and costs: treatment vs. control – A&E. (a) Probability (any use): treatment vs. control by year; and (b) costs: treatment vs. control by year. The left-hand graph shows the proportion of individuals in the treatment and control groups who use secondary health care in each year. The right-hand graph shows the average costs among those individuals who use health care in each year. The orange line at year 3 is 2015/16, the year that the intervention became available.
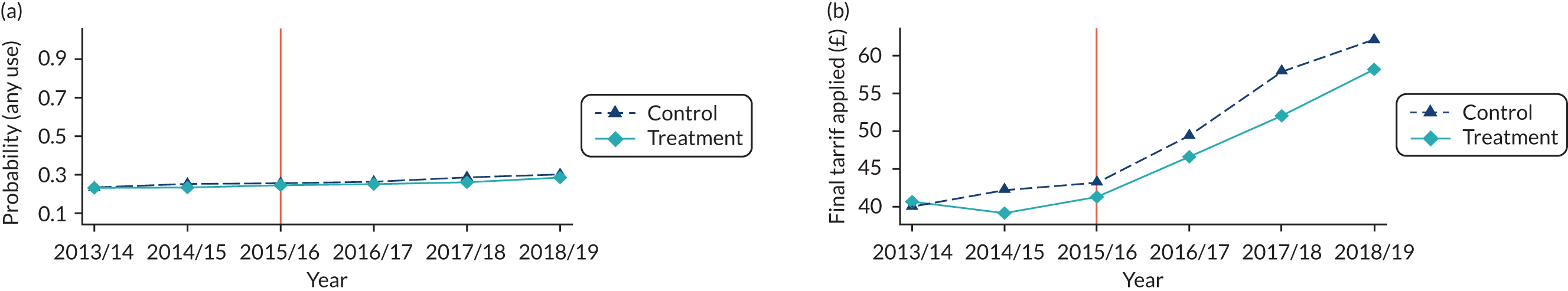
FIGURE 21.
Secondary care use and costs: treatment vs. control – total costs. (a) Probability (any use): treatment vs. control by year; and (b) costs: treatment vs. control by year. The left-hand graph shows the proportion of individuals in the treatment and control groups who use secondary health care in each year. The right-hand graph shows the average costs among those individuals who use health care in each year. The orange line at year 3 is 2015/16, the year that the intervention became available.
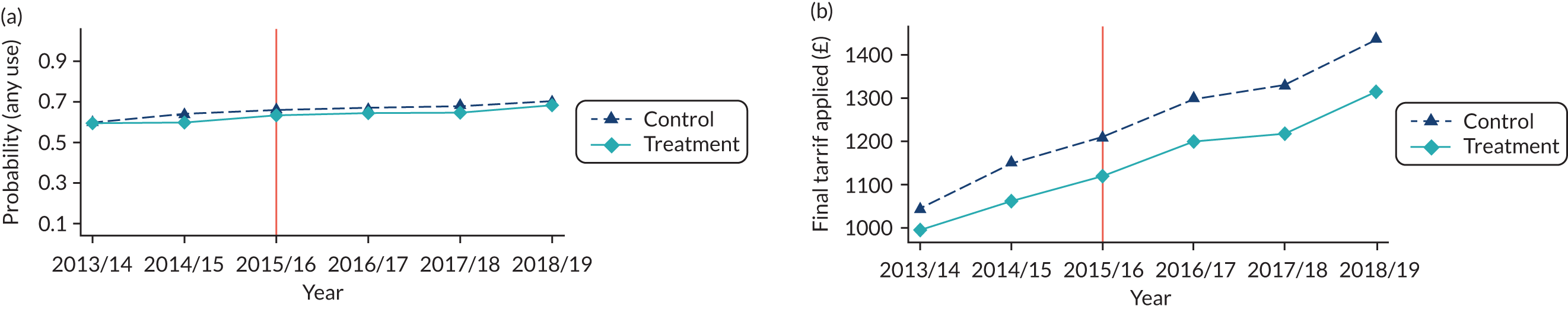
Appendix 8 Secondary care expected costs: falsification results
FIGURE 22.
Secondary care expected costs: falsification results – non-elective. The plots show the difference in the average treatment effect on the treated in each year, and the 95% CI. The orange line at zero shows the time period in which the intervention became available.
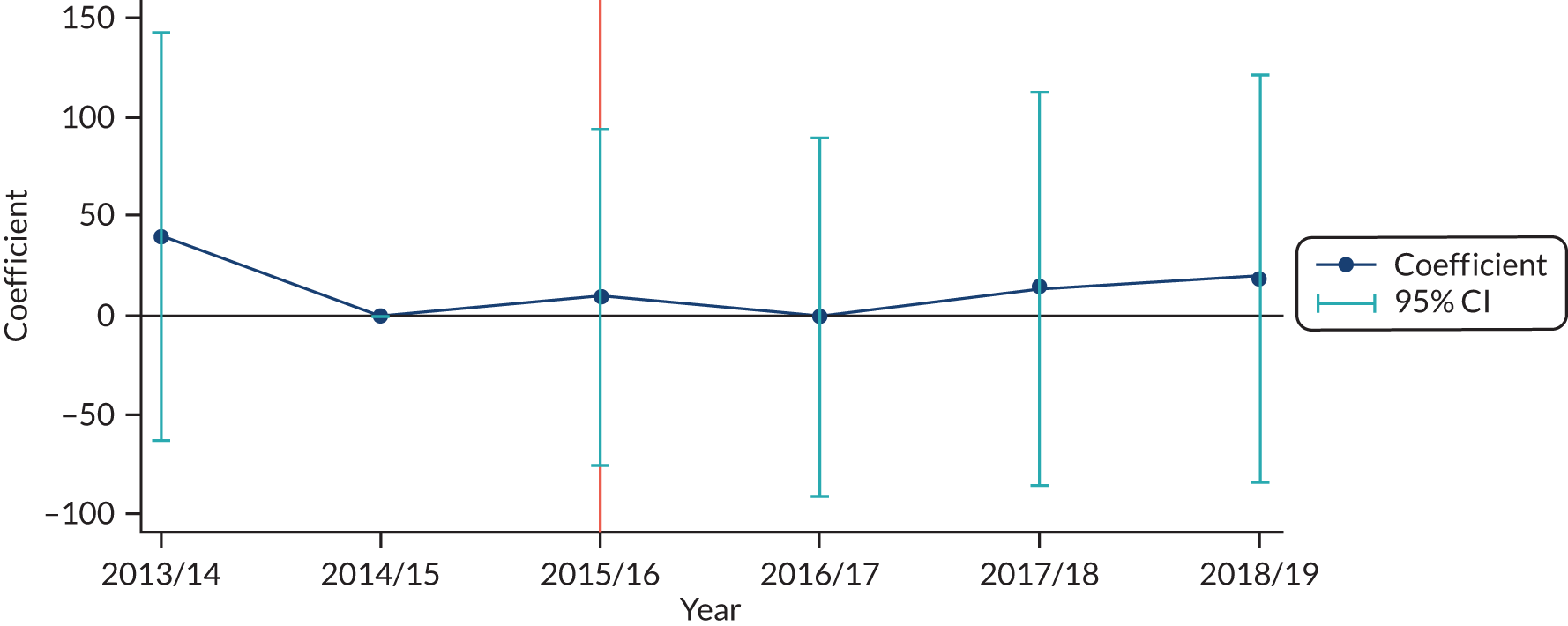
FIGURE 23.
Secondary care expected costs: falsification results – elective. The plots show the difference in the average treatment effect on the treated in each year, and the 95% CI. The orange line at zero shows the time period in which the intervention became available.
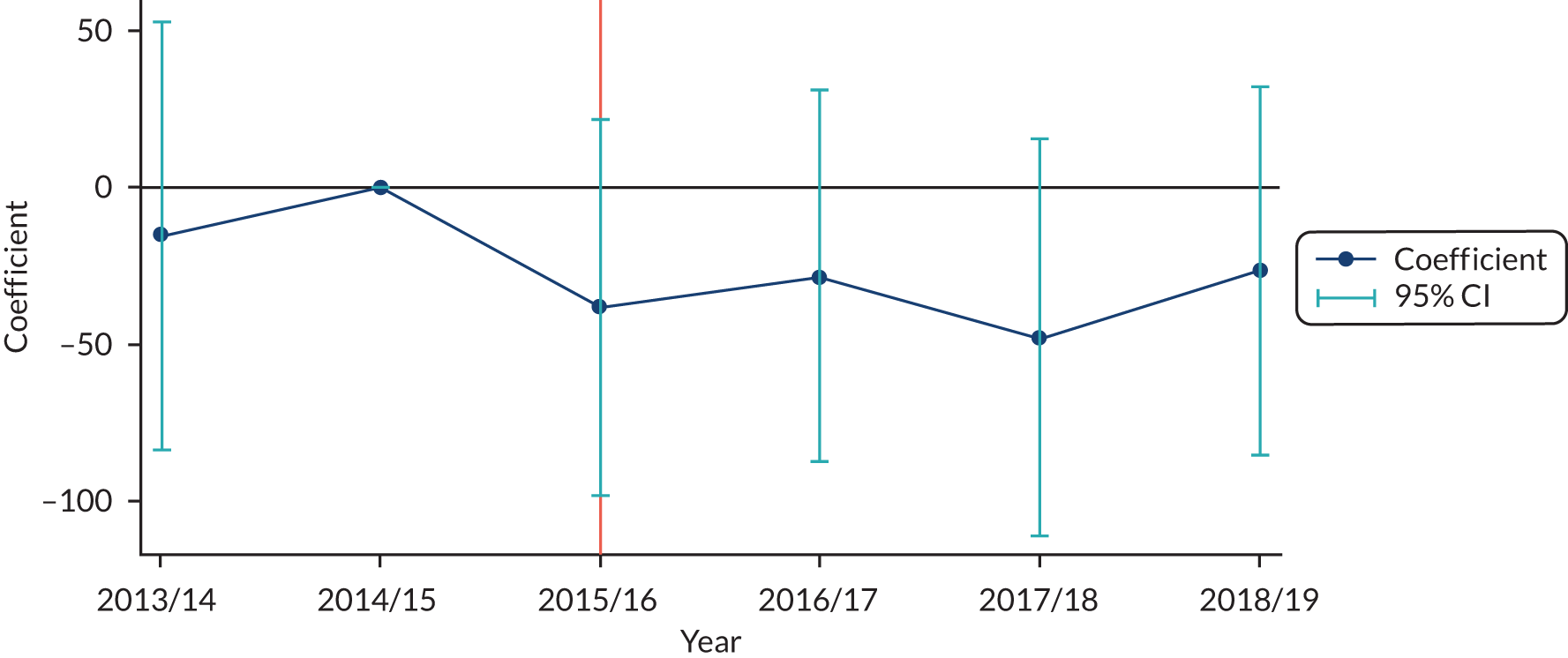
FIGURE 24.
Secondary care expected costs: falsification results – outpatients. The plots show the difference in the average treatment effect on the treated in each year, and the 95% CI. The orange line at zero shows the time period in which the intervention became available.
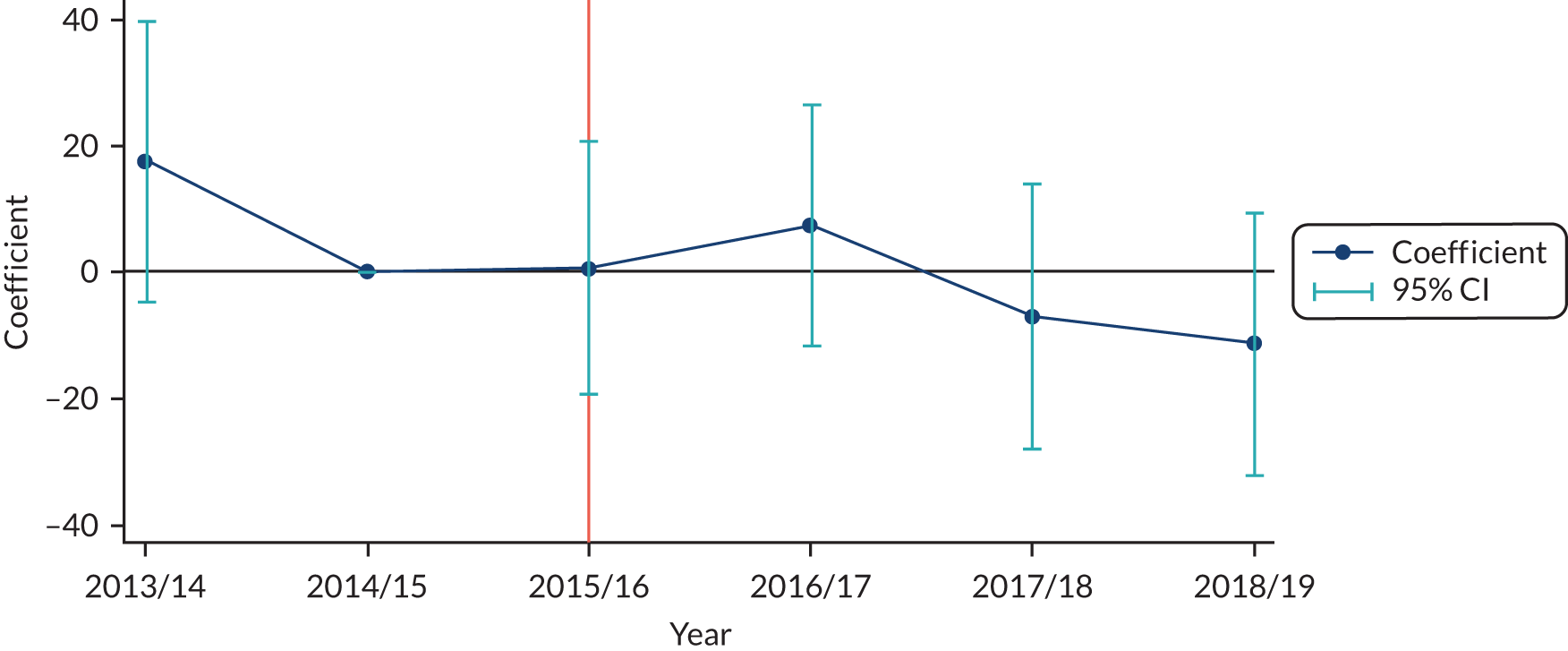
FIGURE 25.
Secondary care expected costs: falsification results – A&E. The plots show the difference in the average treatment effect on the treated in each year, and the 95% CI. The orange line at zero shows the time period in which the intervention became available.
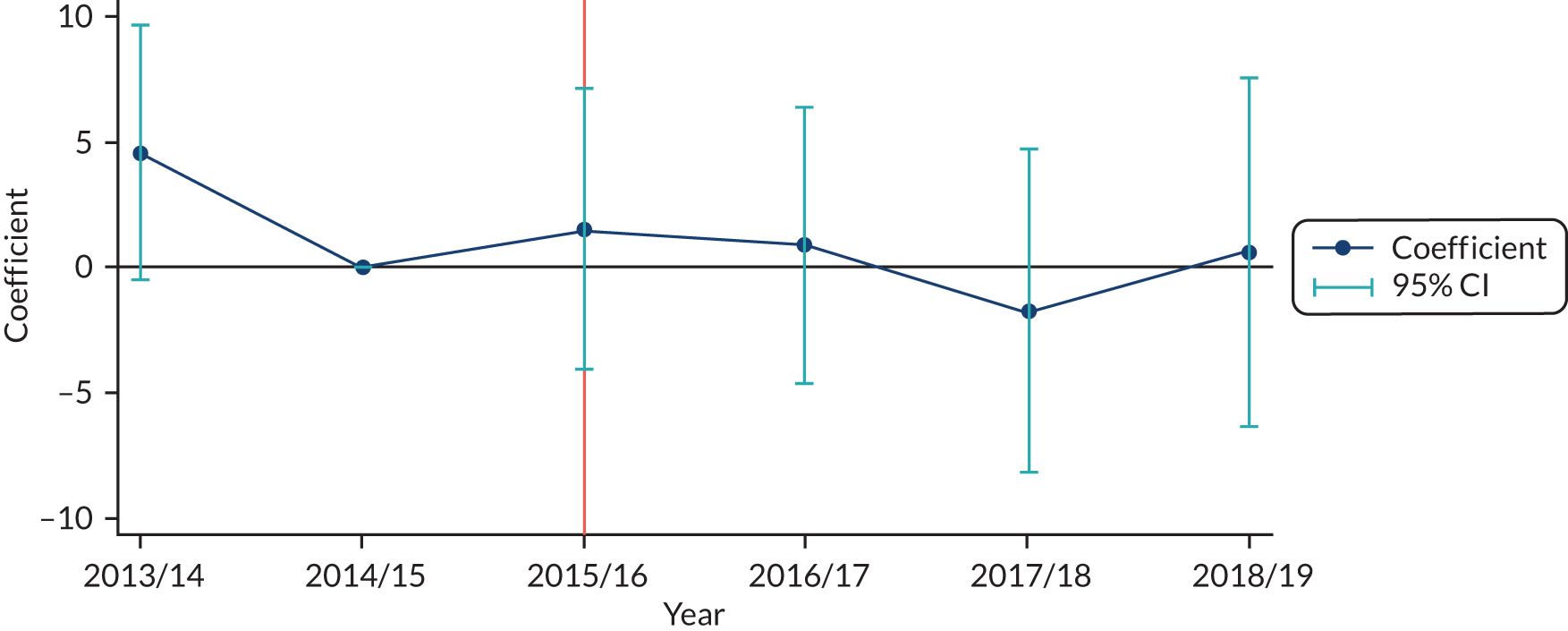
FIGURE 26.
Secondary care expected costs: falsification results – total cost. The plots show the difference in the average treatment effect on the treated in each year, and the 95% CI. The orange line at zero shows the time period in which the intervention became available.
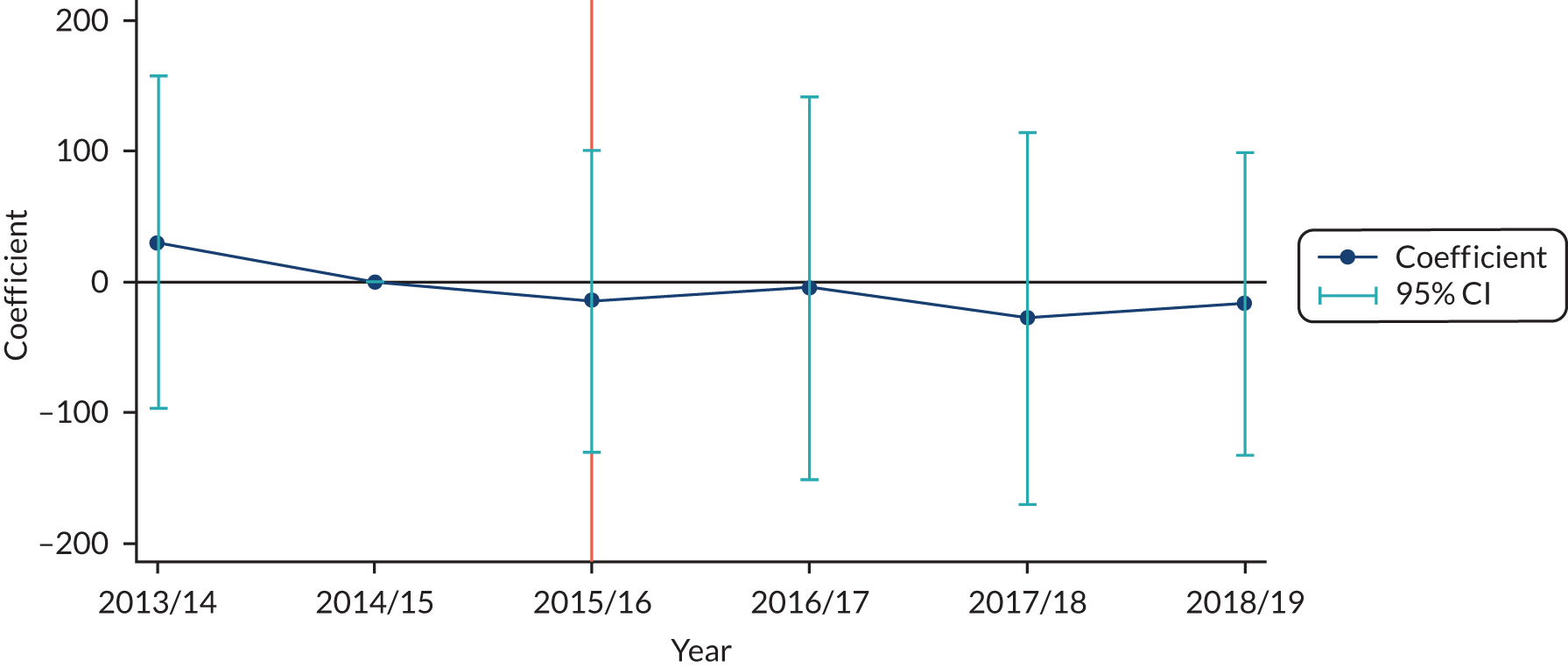
Appendix 9 EuroQol-5 Dimensions and EuroQol-5 visual analogue scale scores at baseline and follow-up
FIGURE 27.
EuroQol-5 Dimensions health state scores at baseline and follow-up across the 8-month study period for the pre-COVID-19 group.
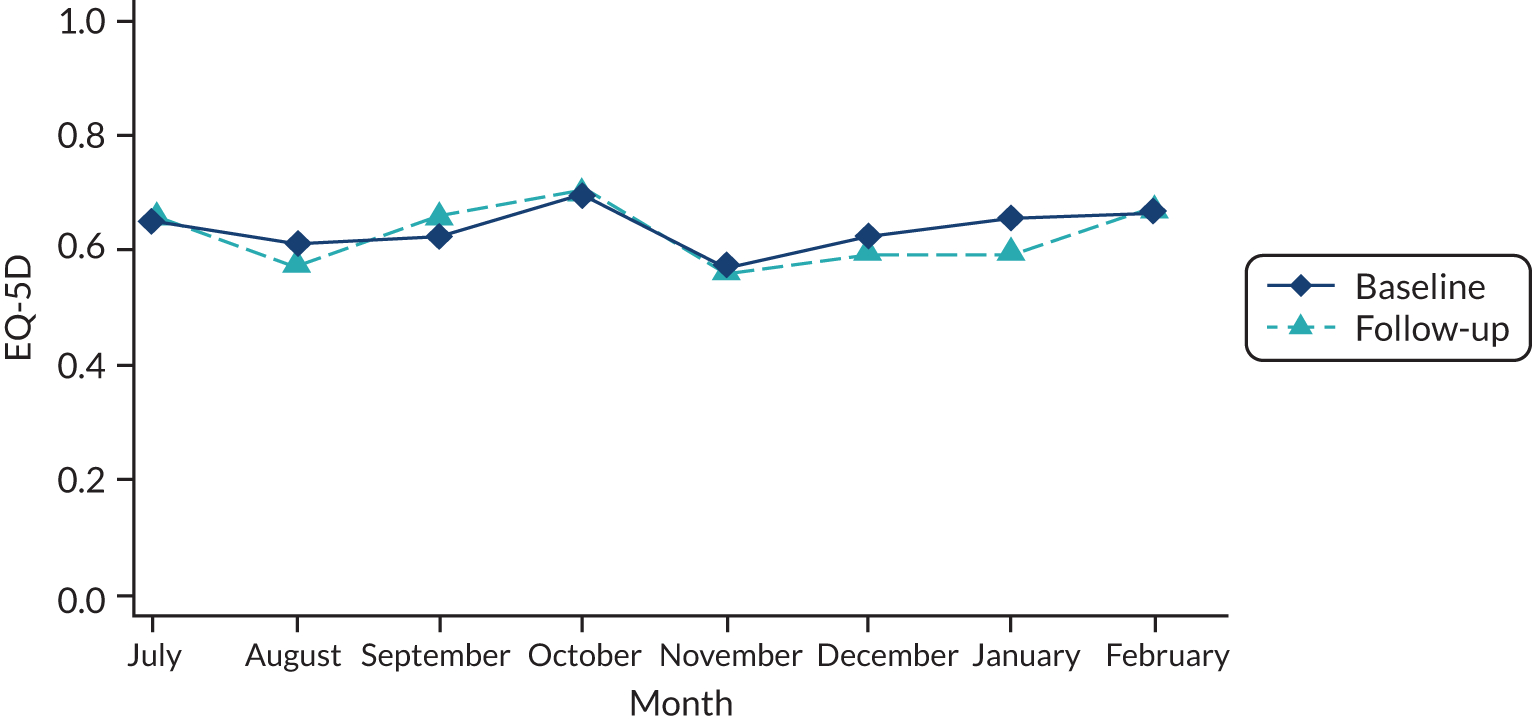
FIGURE 28.
EuroQol-5 visual analogue scale scores at baseline and follow-up across the 8-month study period for the pre-COVID-19 group.
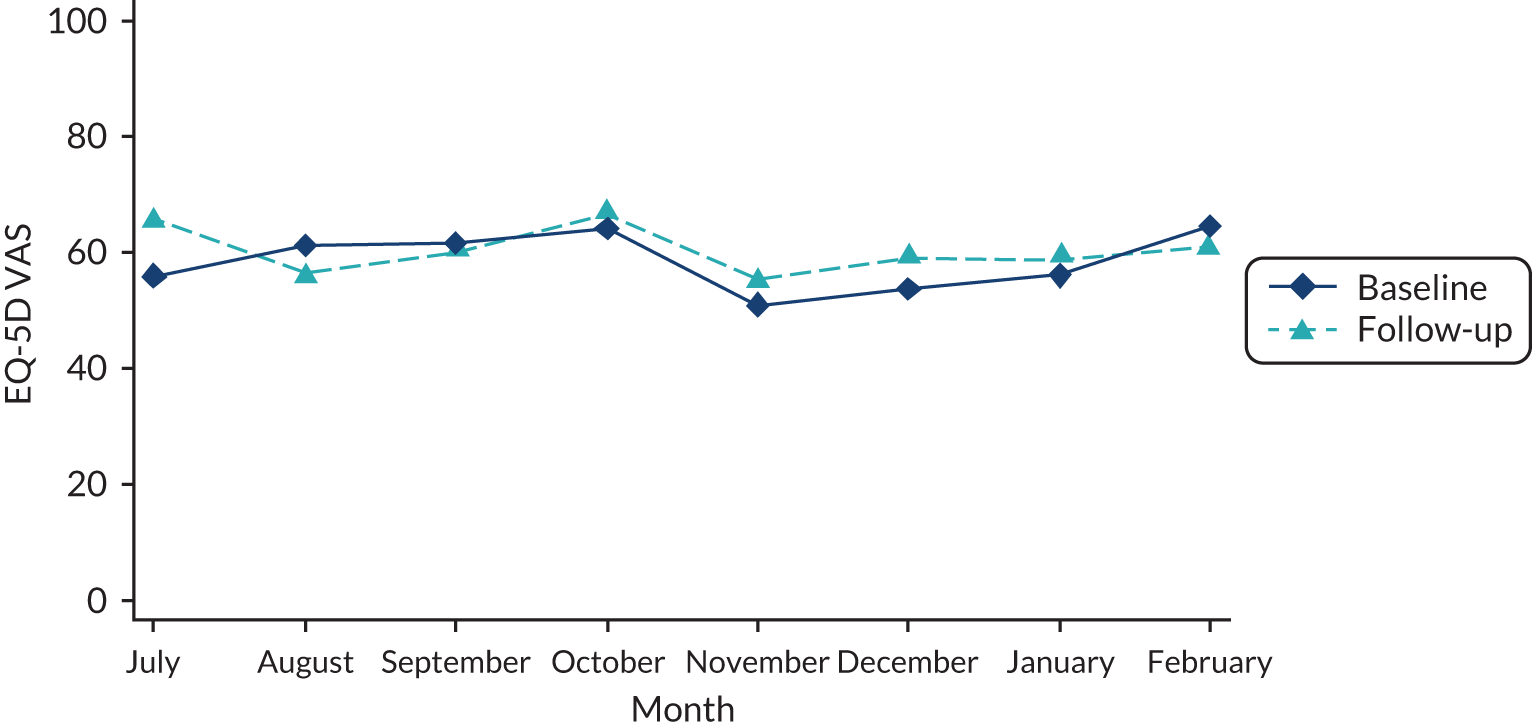
Appendix 10 EuroQol-5 Dimensions and EuroQol-5 visual analogue scale and COVID-19
FIGURE 29.
EuroQol-5 Dimensions health state difference scores collected across the study period with zero showing the timing of COVID-19.
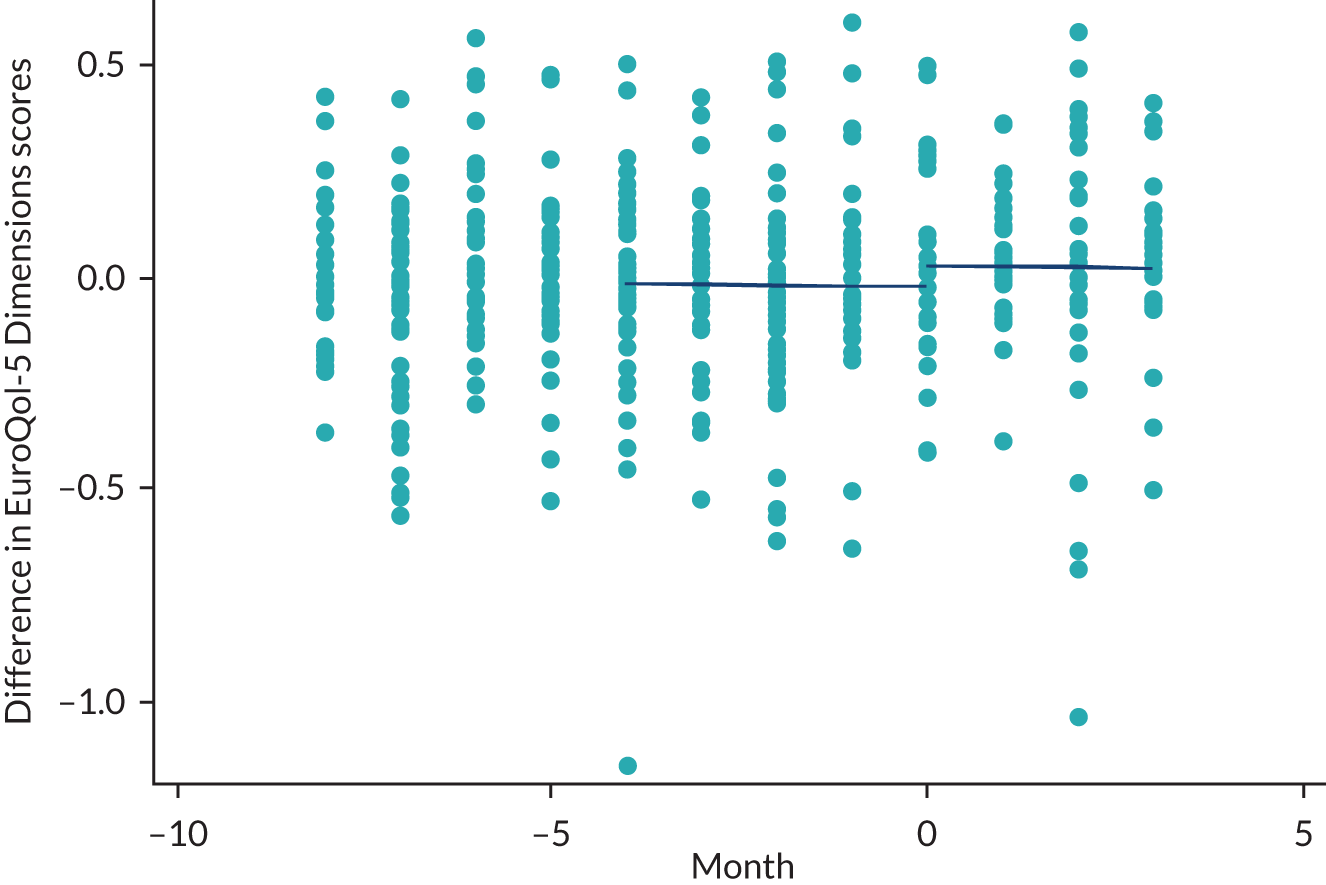
FIGURE 30.
EuroQol-5 visual analogue scale difference scores collected across the study period with zero showing the timing of COVID-19.
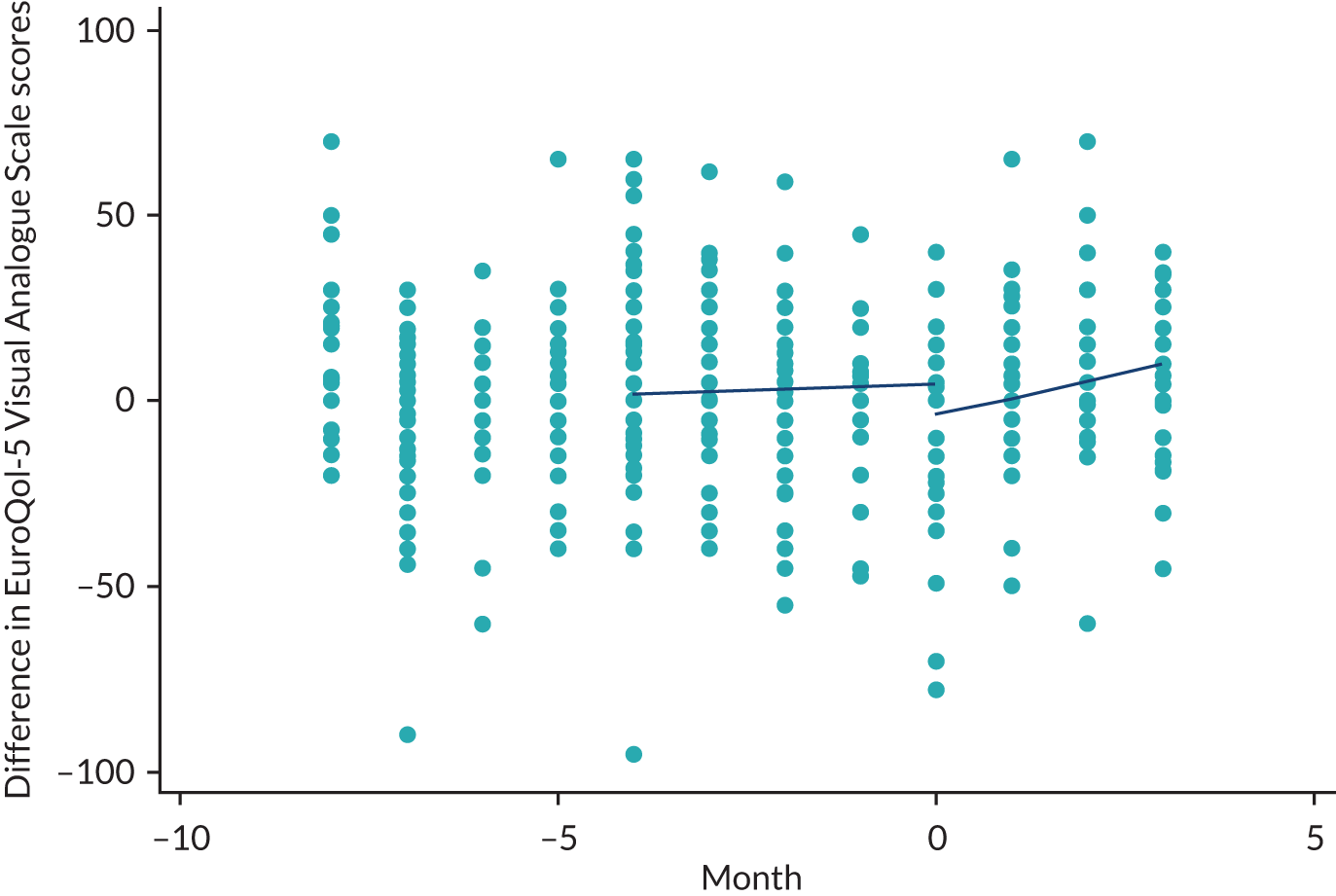
Appendix 11 Parameters included in cost-effective model
| Variables | Value | SD | Distribution | Lower limit | Upper limit | Source |
|---|---|---|---|---|---|---|
| Clinical effectiveness | ||||||
| Baseline demographic characteristics | ||||||
| Ethnicity | ||||||
| White | 81.00% | NA | NA | 0% | 100% | QOF |
| Afro-Caribbean | 3.50% | NA | NA | 0% | 100% | QOF |
| Indian Asian | 16.50% | NA | NA | 0% | 100% | QOF |
| Males | 43.00% | NA | NA | 0% | 100% | QOF |
| Starting age (years) | 54.68 | 9.05 | NA | 46 | 64 | QOF |
| Diabetes duration (years) | 6 | 5.93 | NA | 0 | 12 | Clarke et al.100 |
| Weight (kg) | 93.06 | 21.41 | NA | 72 | 114 | QOF |
| Height (m) | 1.69 | 0.10 | NA | 1.59 | 1.79 | QOF |
| Baseline risk factor values | ||||||
| Percentage of the population with this risk factor (yes/no) | ||||||
| AF | 0.50% | NA | NA | NA | NA | Clarke et al.100 |
| PVD | 2.50% | NA | NA | NA | NA | Hayes et al.98 |
| Smoking | 29.50% | 46.00 | NA | 0 | 75.5 | QOF |
| Albuminuria | 17.70% | NA | NA | NA | NA | Clarke et al.100 |
| HDL (mmol/l) | 1.19 | 0.3 | NA | 0.89 | 1.49 | Clarke et al.100 |
| LDL (mmol/l) | 3 | 0.6 | NA | 2.4 | 3.6 | Clarke et al.100 |
| SBP (mmHg) | 133.54 | 12.34 | NA | 121.20 | 145.88 | QOF |
| HbA1c level (mmol/mol) | 57.94 | 13.00 | NA | 33.59 | 120 | QOF |
| Heart rate (b.p.m.) | 72 | 12 | NA | 60 | 84 | Clarke et al.100 |
| WBC (× 109 per litre) | 6.8 | 1.8 | NA | 5 | 7.6 | Clarke et al.100 |
| Haemoglobin (mmol/mol) | 14.5 | 1.3 | NA | 13.2 | 15.8 | Clarke et al.100 |
| eGFR (ml/minute/1.73 m2) | 77.5 | 15 | NA | 62.5 | 93 | Clarke et al.100 |
| Treatment effect of intervention on risk factor values | ||||||
| AF | NA | NA | NA | NA | NA | NA |
| PVD | NA | NA | NA | NA | NA | NA |
| Smoking status | NA | NA | NA | NA | NA | NA |
| Albuminuria | NA | NA | NA | NA | NA | NA |
| HDL (mmol/l) | NA | NA | NA | NA | NA | NA |
| LDL (mmol/l) | NA | NA | NA | NA | NA | NA |
| SBP (mmHg) | –0.4861 | 0.7532 (standard error) | Normal | –0.9941 (95% CI lower) | 0.0219 (95% CI upper) | QOF |
| HbA1c level (mmol/mol) | –1.11 | 0.393 (standard error) | Normal | –0.188 (95% CI lower) | –0.342 (95% CI upper) | QOF |
| Heart rate (b.p.m.) | NA | NA | NA | NA | NA | NA |
| WBC (× 109 per litre) | NA | NA | NA | NA | NA | NA |
| Haemoglobin (mmol/mol) | NA | NA | NA | NA | NA | NA |
| eGFR (ml/minute/1.73 m2) | NA | NA | NA | NA | NA | NA |
| Variables | Mean | SD | Distribution | Lower limit | Upper limit | Source |
|---|---|---|---|---|---|---|
| Health utility | ||||||
| Initial utility value of T2DM patients | 0.807 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with IHD at time of the event | 0.000 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with MI at time of the event | –0.065 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with heart failure at time of the event | –0.101 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with stroke at time of the event | –0.165 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with amputation at time of the event | –0.172 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with blindness at time of the event | 0.000 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with renal failure at time of the event | –0.330 | NA | NA | NA | NA | Lung et al.102 |
| Utility decrement associated with ulcer at time of the event | –0.210 | NA | NA | NA | NA | Lung et al.102 |
| Utility decrement associated with IHD in subsequent years | 0.000 | NA | NA | NA | NA | Lung et al.102 |
| Utility decrement associated with MI in subsequent years | 0.000 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with heart failure in subsequent years | –0.101 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with stroke in subsequent years | –0.165 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with amputation in subsequent years | –0.172 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with blindness in subsequent years | 0.000 | NA | NA | NA | NA | Alva et al.101 |
| Utility decrement associated with renal failure in subsequent years | –0.330 | NA | NA | NA | NA | Lung et al.102 |
| Utility decrement associated with ulcer in subsequent years | –0.210 | NA | NA | NA | NA | Lung et al.102 |
| Variables | Mean | SD | Distribution | Lower limit | Upper limit | Source |
|---|---|---|---|---|---|---|
| Costs | ||||||
| Per-patient cost of the WtW programme | £1345 | NA | NA | NA | NA | WtW data |
| Annual cost in the absence of complications | £527 | NA | NA | NA | NA | Alva et al.103 |
| Fatal cost of IHD at time of the event | £4327 | NA | NA | NA | NA | Alva et al.103 |
| Non-fatal cost of IHD at time of the event | £11,222 | NA | NA | NA | NA | Alva et al.103 |
| Fatal cost of MI at time of the event | £1748 | NA | NA | NA | NA | Alva et al.103 |
| Non-fatal cost of MI at time of the event | £7329 | NA | NA | NA | NA | Alva et al.103 |
| Fatal cost of heart failure at time of the event | £0 | NA | NA | NA | NA | Alva et al.103 |
| Non-fatal cost of heart failure at time of the event | £3666 | NA | NA | NA | NA | Alva et al.103 |
| Fatal cost of stroke at time of the event | £4543 | NA | NA | NA | NA | Alva et al.103 |
| Non-fatal cost of stroke at time of the event | £7819 | NA | NA | NA | NA | Alva et al.103 |
| Fatal cost of amputation at time of the event | £0 | NA | NA | NA | NA | Alva et al.103 |
| Non-fatal cost of amputation at time of the event | £10,968 | NA | NA | NA | NA | Alva et al.103 |
| Fatal cost of blindness at time of the event | £0 | NA | NA | NA | NA | Alva et al.103 |
| Non-fatal cost of blindness at time of the event | £1557 | NA | NA | NA | NA | Alva et al.103 |
| Fatal cost of renal failure at time of the event | £0 | NA | NA | NA | NA | NHS Blood and Transplant104 |
| Non-fatal cost of renal failure at time of the event | £21,188 | NA | NA | NA | NA | NHS Blood and Transplant104 |
| Fatal cost of ulcer at time of the event | £0 | NA | NA | NA | NA | Kerr et al.105 |
| Non-fatal cost of ulcer at time of the event | £7286 | NA | NA | NA | NA | Kerr et al.105 |
| Cost of IHD in subsequent years | £1396 | NA | NA | NA | NA | Alva et al.103 |
| Cost of MI in subsequent years | £1326 | NA | NA | NA | NA | Alva et al.103 |
| Cost of heart failure in subsequent years | £1692 | NA | NA | NA | NA | Alva et al.103 |
| Cost of stroke in subsequent years | £1293 | NA | NA | NA | NA | Alva et al.103 |
| Cost of amputation in subsequent years | £2059 | NA | NA | NA | NA | Alva et al.103 |
| Cost of blindness in subsequent years | £520 | NA | NA | NA | NA | Alva et al.103 |
| Cost of renal failure in subsequent years | £21,188 | NA | NA | NA | NA | NHS Blood and Transplant104 |
| Cost of ulcer in subsequent years | £7286 | NA | NA | NA | NA | Kerr et al.105 |
Appendix 12 Link worker participant demographic data
| Demographic data | Number of participants |
|---|---|
| Age (years) | |
| 20–30 | 7 |
| 30–40 | 4 |
| 40–50 | 2 |
| 50–60 | 4 |
| No data | 3 |
| Gender | |
| Female | 16 |
| Male | 4 |
| Work | |
| Part-time | 7 |
| Full-time | 11 |
| No data | 2 |
| Ethnicityb | |
| White British | 14 |
| British Asian/Asian | 2 |
| Other | 2 |
| No data | 3 |
| Qualificationsc | |
| RQF Level 3–5 (A Level–HND equivalent) | 3 |
| RQF Level 6 (undergraduate or equivalent) | 9 |
| RQF Level 7 (master’s degree or equivalent) | 4 |
| RQF Level 8 (PhD or equivalent) | 2 |
| No data | 2 |
Appendix 13 Client participant demographic data
| Demographic data | Number of participants (N = 19) |
|---|---|
| Gender | |
| Male | 8 |
| Female | 11 |
| Age (years) | |
| 40–49 | 3 |
| 50–59 | 8 |
| 60–69 | 4 |
| 70+ | 4 |
| Ethnicitya | |
| White British | 14 |
| British Bangladeshi/Pakistani/Indian | 4 |
| Black British | 1 |
| Household income | |
| < £10K | 5 |
| £10–20K | 8 |
| £21–30K | 2 |
| £31–40K | 0 |
| > £40K | 2 |
| Unknown | 2 |
| Employment status | |
| Full-time employment | 3 |
| Part-time employment | 2 |
| Unemployed | 9 |
| Retired | 5 |
| Benefits claimedb | |
| None | 7 |
| Health-related benefits | 9 |
| Means-tested benefits | 3 |
| Number of LTCsc | |
| 1 | 3 |
| 2 or more | 16 |
| Household structure | |
| Lives alone | 5 |
| Lives with partner | 5 |
| Lives with family < 18 years | 2 |
| Lives with family > 18 years | 4 |
| Multigeneration household | 3 |
| Housing status | |
| Owned | 7 |
| Rental (private or social housing) | 11 |
| Other | 1 |
| IMD quintile of home address | |
| 1 (least deprived) | 1 |
| 2 | 1 |
| 3 | 2 |
| 4 | 2 |
| 5 (most deprived) | 13 |
Appendix 14 COVID-19 study participant demographic data
| Demographic data | Number of participants |
|---|---|
| Gender | |
| Male | 19 |
| Female | 25 |
| Age (years) | |
| 40–49 | 6 |
| 50–59 | 11 |
| 60–69 | 17 |
| 70+ | 10 |
| Ethnicitya | |
| White British | 38 |
| British Bangladeshi/Pakistani/Indian | 6 |
| Household income | |
| < £10K | 13 |
| £10–20K | 14 |
| £21–30K | 6 |
| £31–40K | 3 |
| > £40K | 4 |
| Prefer not to say | 4 |
| Employment status | |
| Full-time employment | 4 |
| Part-time employment | 8 |
| Furloughed | 2 |
| Unemployed | 13 |
| Retired | 17 |
| Benefits claimedb | |
| None | 20 |
| Health-related benefits | 18 |
| Means-tested benefits | 6 |
| Number of LTCsc | |
| 1 | 9 |
| 2 or more | 35 |
| Household structure | |
| Lives alone | 12 |
| Lives with partner | 17 |
| Lives with family < 18 years | 10 |
| Lives with family > 18 years | 4 |
| Multigeneration household | 1 |
| Housing status | |
| Owned | 26 |
| Rental (private or social housing) | 17 |
| Other | 1 |
| IMD quintile of home address | |
| 1 (least deprived) | 6 |
| 2 | 4 |
| 3 | 9 |
| 4 | 5 |
| 5 (most deprived) | 20 |
Appendix 15 Ways to Wellness logic model
FIGURE 32.
Ways to Wellness impact logic chain.
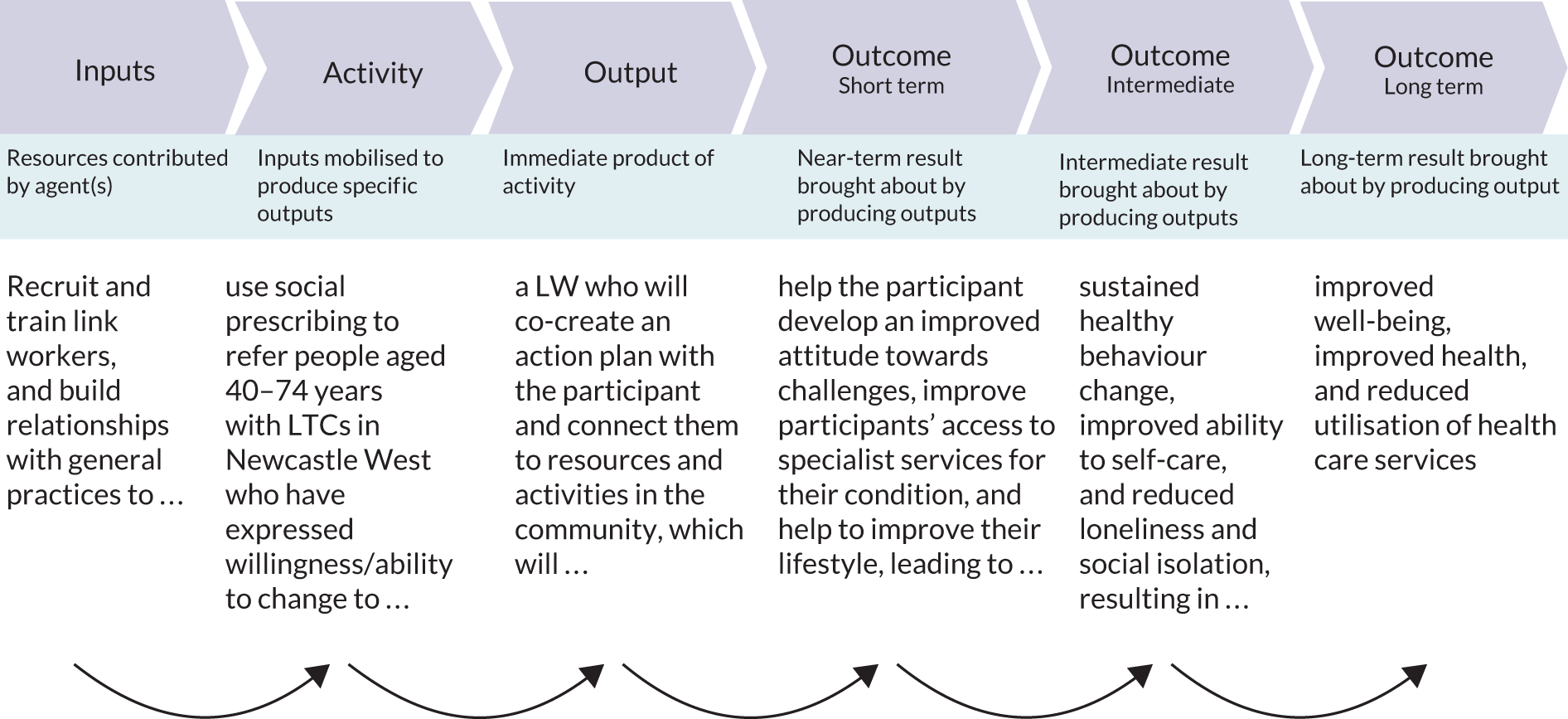
Glossary
- Attendance Allowance
- A non-means-tested benefit available for people of pension age to help with their personal care costs if they have a long-term condition or disability.
- Benefits Review
- A process by which a claimant may appeal a decision by the Department of Work and Pensions about their entitlement to benefits, for instance their entitlement to Personal Independence Payment.
- Body mass index
- A measure used by health professionals that uses your height and weight to assess if your weight is healthy.
- Chronic obstructive pulmonary disease
- A common, treatable (not curable) lung condition causing respiratory symptoms, including breathlessness and cough, and progressive airflow obstruction. Tobacco smoking is a major risk factor for chronic obstructive pulmonary disease.
- Citizens Advice
- A UK-wide charitable service that offers free advice on a range of issues, such as housing, debt, benefits and the law.
- COVID-19
- An infectious disease caused by a new variant of coronavirus. It is a variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
- Debt relief order
- Available for people who have qualifying debts of less than £30,000, can evidence that they have less than £2000 in assets and have less than £75 ‘spare’ each month.
- Department for Work and Pensions
- The UK Government department responsible for welfare and pension policy.
- Disability Living Allowance
- A tax-free benefit for disabled people who need help with mobility or care costs. Since 2013, this benefit has been replaced by Personal Independence Payments for adult claimants.
- EMIS (EMIS Health, Leeds, UK)
- An electronic clinical system used in some general practices.
- Employment and Support Allowance
- A means-tested benefit available for people who are unable to work because of a long-term condition or disability. It is currently being replaced by Universal Credit.
- EuroQol-5 Dimensions, five-level version
- A descriptive system of health-related quality-of-life states comprising five dimensions, each of which can take one of five responses corresponding to five levels of severity.
- Glycated haemoglobin
- A measure of glycaemic control. The level of glycated haemoglobin in the blood is related to the concentration of blood glucose over an approximately 2- to 3-month period. This can be measured by taking a blood sample and analysing the red blood cells.
- Personal Independence Payment
- A non-means-tested benefit available for people aged between 16 years and pension age who can evidence that they require assistance with living costs because of a long-term condition or disability.
- Primary Care Network
- A grouping of general practices, typically covering 30,000–50,000 patients, in which the structure and funding for services is developed locally.
- Type 2 diabetes mellitus
- A common, chronic metabolic condition that causes insulin insufficiency and resistance that results in high levels of blood sugar (glucose).
- Universal Credit
- A means-tested monthly payment introduced to replace several benefits for people of working age who are on a low income. Universal Credit is subject to annual review.
- Universal Credit
- (Limited Capacity for Work) An additional element of Universal Credit for people who have limited capacity to work because of a health condition or disability.
List of abbreviations
- A&E
- accident and emergency
- AF
- atrial fibrillation
- BMI
- body mass index
- BP
- blood pressure
- CCG
- Clinical Commissioning Group
- CEAC
- cost-effectiveness acceptability curve
- CHW
- community health worker
- CLP
- community links practitioner
- COPD
- chronic obstructive pulmonary disease
- DCCT
- Diabetes Control and Complications Trial
- DiD
- difference in difference
- eGFR
- estimated glomerular filtration rate
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQ-VAS
- EuroQol-5 visual analogue scale
- FTE
- full-time equivalent
- GLM
- generalised linear model
- GP
- general practitioner
- HbA1c
- glycated haemoglobin
- HCP
- health-care professional
- HDL
- high-density lipoprotein
- HRQoL
- health-related quality of life
- ICER
- incremental cost-effectiveness ratio
- IFCC
- International Federation of Clinical Chemistry
- IHD
- ischaemic heart disease
- IMD
- Index of Multiple Deprivation
- IT
- information technology
- ITT
- intention to treat
- KIT
- keeping in touch
- LA
- local authority
- LDL
- low-density lipoprotein
- LSOA
- lower-layer super output area
- LTC
- long-term condition
- LW
- link worker
- MI
- myocardial infarction
- MIS
- management information system
- NECS
- North of England Commissioning Support Unit
- NICE
- National Institute for Health and Care Excellence
- NMB
- net monetary benefit
- NVQ
- National Vocational Qualification
- PbR
- payment by results
- PCN
- Primary Care Network
- PIP
- Personal Independence Payment
- PPI
- patient and public involvement
- PSA
- probabilistic sensitivity analysis
- PSS
- Personal Social Services
- PVD
- peripheral vascular disease
- QALY
- quality-adjusted life-year
- QOF
- Quality and Outcomes Framework
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- RDD
- regression discontinuity design
- SBP
- systolic blood pressure
- SD
- standard deviation
- SES
- socioeconomic status
- SIB
- Social Impact Bond
- SPRING_NE
- Social Prescribing in the North East
- SSC
- Study Steering Committee
- SUS
- Secondary Uses Service
- T2DM
- type 2 diabetes mellitus
- TPM
- two-part model
- UKPDS-OM2
- United Kingdom Prospective Diabetes Study Outcomes Model 2©
- VCSE
- voluntary, community and social enterprise
- WBC
- white blood cell
- WBS
- Well-being Star™
- WP
- work package
- WTP
- willingness to pay
- WtW
- Ways to Wellness
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/AQXC8219).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.