Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as award number 15/126/05. The contractual start date was in October 2018. The draft manuscript began editorial review in September 2023 and was accepted for publication in May 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Thompson et al. This work was produced by Thompson et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Thompson et al.
Introduction
This report details the work undertaken to establish the clinical and cost-effectiveness of the Mellow Babies parenting intervention for women experiencing psychosocial stress and their 6- to 18-month-old babies. It arose from a call commissioned by the National Institute for Health and Care Research (NIHR) Public Health Research (PHR) programme ‘15/126 Group-based parenting programmes for improving psychosocial health’. Although the disruption of the COVID-19 pandemic meant the trial was closed before reaching a fully powered sample, there is still significant learning to be gained from the data gathered and the experiences of the research team.
Rationale for research and background
Problems in children’s early social and emotional development are likely to have major long-term consequences for the individual and society;1–6 parental emotional well-being is a major determinant of a child’s social and emotional development. 7,8 Our work with data from the Growing Up in Scotland9,10 and Avon Longitudinal Study of Parents and Children cohorts11–15 demonstrates strong associations between parental mental health, parenting behaviours and children’s psychiatric outcomes. Interventions designed to improve both parental mental health and the parent–child relationship are thus likely to produce substantial benefits in terms of child development and are potentially valuable public health interventions. 16
At the time of instigation this was the first definitive trial of a postnatal group-based parenting programme specifically designed for mothers with psychosocial difficulties who have children aged under 2 years, although we were aware of ongoing Incredible Years for Babies studies (NIHR PHR-13/93/10; ClinicalTrials.gov NCT01931917) and one on Circle of Security (ClinicalTrials.gov NCT02497677), both now completed. A recent (November 2022) topic scoping report commissioned by NIHR highlighted the continued need for randomised controlled trial (RCT)-level evidence for programmes with positive pilot studies, and Mellow Babies was listed as one such programme where more robust evidence was needed. 17
Mellow Babies is a group-based intervention programme with a dual focus on maternal mental well-being and parent–infant interaction. The programme involves attendance on 14 consecutive weeks between roughly 9.30 a.m. and 2.30 p.m. (during school hours) and there is a reunion 1–3 months later. Groups are kept to between 4 and 10 participants, with an ideal group size of 6. Groups can be offered at weekends, and transport, meals and a crèche are provided. Prior to the start of a Mellow Babies group, the group facilitator will visit the mother and child at home on at least one occasion to build rapport and address any anxieties or practical concerns the mother has about attending. During one of these visits, a video of a mealtime will be made for later use in the group, and key interactions in the video will be discussed on a one-to-one basis in preparation for the group. Mellow Babies is always offered as a single-sex group due to the need to create a safe space where participants can relate to each other’s experiences. Many women who have taken part in Mellow interventions will have experience of intrafamilial abuse and post-traumatic stress disorders (PTSDs). While work with fathers is extremely important, it remains true that mothers tend to be the primary caregivers of babies and the typical participant in Mellow interventions.
This research project builds on a large number of before-and-after evaluations of Mellow Babies (Mellow Parenting for children under 18 months) as well as a small-scale waiting list trial. 18 This review by MacBeth et al. (2015) points to some evidence of effectiveness, and subsequent studies have continued to develop this evidence base. 19–21 There nevertheless remains a need for more methodologically robust research trials. The intervention is fully manualised and has been delivered to many thousands of families: it is sufficiently mature to merit a definitive trial.
Objectives
The trial aimed to establish the clinical and cost-effectiveness of delivering Mellow Babies for mothers who are anxious and depressed, along with their 6- to 18-month-old baby. Specifically, it aimed to establish if attending Mellow Babies can improve maternal mental health and child social, emotional and language development at 8 months post randomisation and when the child reaches 30 months of age. Due to the early closure of the trial, prior to the sample being fully recruited, the objectives relating to outcome analysis were removed, and amendments made to the remaining objectives to focus on a series of process-related questions.
The final objectives aimed to maximise learning from implementation of the trial and focused on: (1) the effectiveness of recruitment and retention methods; (2) characterising use of other services during trial participation; (3) sociodemographic characteristics, mental health and participant experience in relation to trial/intervention participation; and (4) the impact of the COVID-19 pandemic on the operation of the trial. We aimed to address the questions below. This report was prepared with reference to the CONSORT and SPIRIT Extension for RCTs Revised in Extenuating Circumstance 2021 statement for reporting completed trials modified due to the COVID pandemic. 22
-
Which eligible mothers agree and which decline to participate in the intervention, and what reasons do they give?
-
Which recruitment methods were most effective and was there any variation in participant characteristics by means of recruitment?
-
How do sociodemographic characteristics and maternal mental health at baseline relate to:
-
level of participation in Mellow Babies?
-
group composition?
-
changes in parenting behaviours?
-
maternal mental state at 8 months post recruitment?
-
child development at 30 months
-
whether recruited pre-pandemic (to March 2020) or post (since Nov 2021)?
-
-
What is the nature of usual care offered to participants?
-
How do participants describe their experience of participating in Mellow Babies, which elements of the intervention are considered most influential, and is participation stigmatising?
-
Are there family characteristics associated with greater adherence to Mellow Babies?
-
Are there family characteristics associated with greater retention of follow-up?
-
How are the features (in terms of process and outcomes of care) of Mellow Babies valued by mothers?
-
What contextual factors facilitate or hinder the delivery of, and engagement with, Mellow Babies?
-
What specific impact did the COVID-19 pandemic have on the ability to run intervention groups and the trial?
The report has been structured around the four areas detailed in the preceding paragraph to provide a smooth structure and to avoid duplication of content. Each of the four areas pertains to an appendix, which provides more detailed methods and findings, and each of the appendices indicates which of the above questions it pertains to.
Methods
This was a single-centre RCT comparing outcomes for mothers and babies offered the Mellow Babies parenting intervention plus usual care with mothers and babies receiving usual care only. Participants were randomised 1 : 1 with minimisation to reduce imbalance between groups in terms of maternal age (< 25 years; ≥ 25 years), deprivation (working household yes/no) and age of child (≤ 12 months; > 12 months).
Eligible participants were women aged ≥ 16 years with primary caregiving responsibility of a child aged 6–18 months at the time of randomisation, who resided in Highland Council area (Scotland) and who scored above a defined threshold (≥ 85th centile) on either the anxiety (≥ 11) or depression (≥ 7) subscales of the Hospital Anxiety and Depression Scale (HADS). 23 Women who were substance dependent (if not stable on recovery programme); were unable to speak or write in English language; who had twins or other multiple births; or who had a baby with significant learning difficulties were excluded from the trial. Women could only take part in the trial once and therefore were excluded from participation for subsequent children. Participants were identified via three core recruitment strategies: health professional referral [e.g. health visitor (HV) or general practitioner (GP)]; self-referral having received a letter of invitation via NHS Patient Identification Centre (PIC) sites; or self-referral through response to advertisements on social media or posters within the local community.
For full details of the trial protocol (v20) see https://fundingawards.nihr.ac.uk/award/15/126/05. Screening and baseline data collection were conducted according to the original protocol. Recruitment was paused, and follow-up data collection commenced in a revised form during 2020 and 2021 due to COVID-19 pandemic restrictions. While the original protocol featured home visits, these data collection appointments had to be conducted remotely. Video conferencing [Zoom (Zoom Video Communications, San Jose, CA, USA) or Teams (Microsoft Corporation, Redmond, WA, USA)] was offered to all participants, but most elected for a phone appointment. All measures for the 8-month post-randomisation assessment could be completed by phone, whereas the 30-month measures were amended because the Bayley Scales required direct interaction with and observation of the child. This was replaced by the Ages and Stages Questionnaire, Third Edition (ASQ-3)24 and the Ages and Stages Questionnaires: Social-Emotional, Second Edition (ASQ-SE2). 25 Although we were able to return to home visits in 2022, the ASQ remained in place as the first 30-month follow-ups for the new cohort took place after we were initially asked to close the trial down and it was thought best to not increase participant burden if outcome analyses would not take place. All follow-up data collection ceased at the end of March 2023 when the final close-down plan was approved by Research Ethics Committee (REC) and the funder. Note, although an add-on study regarding Mellow Babies online had been included in the final protocol, delays in research governance processes, and the subsequent early closure of the trial, meant this work did not take place.
The research team was unable to conduct outcome analysis as was originally planned due to the sample size being too small. No between-group clinical or cost-effectiveness analyses were conducted. Data collected from participants at baseline, 8 months post randomisation and when the child reached 30 months of age were analysed descriptively and subgroup comparisons were conducted based on the revised set of questions above. Note that, due to the small sample size and limited value in comparing subgroups from this sample, no correction for repeated testing nor replacement of missing values has taken place. Any descriptive data are presented at face value as a basis for further discussion. This report provides a synopsis of the findings. Full results are presented in a series of appendices grouped around themes among the research questions.
Process evaluation interviews
Process evaluation interviews were conducted with trial participants and group facilitators. Interviews were conducted by the PhD student (JT) and took place face-to-face, via telephone, or via video call, depending on the preference of the participant. Interviews were audio-recorded, transcribed and analysed using thematic analysis. 26 The number of each type of interview is shown in Table 1.
| Type of interview | Number |
|---|---|
| Pre-group interviews with mothers | 1 |
| Telephone fidelity checks | 9 |
| Mid-group interviews with facilitators | 2 |
| End group interviews with mothers | 14 |
| End group interviews with facilitators | 6 |
| Total | 32 |
Results summary
Trial recruitment and retention
With reference to Appendix 1, we successfully recruited 106 participants for the trial (53 per arm). It took several months to establish the most effective recruitment strategy, but once this strategy was in place the system worked well with high throughput. The most successful method of recruitment was PIC letters which led to the recruitment of 75 women, representing 1.7% of all those approached using this method. HV referrals were comparatively few (26 of those eligible), highlighting the importance of approaching potential participants directly and not relying solely on practitioners as gatekeepers. However, qualitative interviews with women who participated suggested having a PIC letter in tandem with a HV flagging up the trial to a participant seemed to be perceived as particularly effective. The screen positive rate was 78%, indicating that using mainly self-referral did not lead to a disproportionate number of ineligible individuals expressing interest in trial participation.
Descriptive subgroup analyses show little variation across key sociodemographic characteristics or mental health measures for this participant group. It is noteworthy that, although the majority of participants were ‘doing well’ in relation to sociodemographic characteristics such as employment status, socioeconomic deprivation, relationship status, and social support, there were still significant levels of mental ill health. We have demonstrated that it is possible to recruit and retain a good proportion of participants even when they are experiencing mental ill health. Future studies should take care to focus on the specific issues being faced by families rather than using sociodemographic characteristics exclusively as a proxy measure for likely level of need. This analysis also showed little association between any of the sociodemographic characteristics and mental health indicators at baseline and outcomes at either of the follow-up points. While there appears to be a direct relationship between relative affluence and taking part in a wider range of activities more frequently with their child, there are few direct associations on other measures. Together, these findings reflect the views of Goyder and colleagues,17 that it is important to adopt a flexible approach sensitive to families’ individual needs.
Overall, our methods of recruitment and retention in this study were successful, although some trial and error was required to refine these, and they required more time and resources than had been anticipated by the recruitment team. There is a clear need for significant investment in good research infrastructure to allow a flexible and personalised approach to recruitment and study engagement.
Health economic evaluation
With reference to Appendix 2, response rates to the EuroQol measure of overall health and quality of life [EuroQol-5 Dimensions, five-level version (EQ-5D-5L)] and Participant Cost Questionnaire (PCQ) were high, with no missing item data for EuroQol-5 Dimensions (EQ-5D) and very limited missing data for the PCQ. For EQ-5D, 100% of participants completed this questionnaire at baseline and 8-month time points, reducing to 92% at 30 months. For the PCQ, 93% of participants completed this questionnaire at 8-month time point, reducing to 86% at month 30. This suggests that both questionnaires were appropriate for this population and respondent burden was not an issue. In addition, in a future trial, a simplified PCQ may be appropriate given few participants reported accessing NHS or other services during the trial. Further, augmentation with qualitative data would be useful to fully elucidate participants’ experiences of the nature and accessibility of NHS services available to them, especially as these questions focused specifically on maternal mental health and concerns about their child’s development (where services are often difficult to access or simply unavailable). While we did not report EQ-5D data by the arm of the trial, but rather overall summary statistics, on average, these scores increased at the 8-month time point, but they then decreased at the 30-month time point, albeit remaining above baseline scores. Further research is needed to determine the cost-effectiveness of the Mellow Babies intervention.
Intervention participants: characteristics, cohesion and process
With reference to Appendix 3, the characteristics of the five intervention groups which were able to take place (group 3 could not operate due to COVID-19 pandemic restrictions, and group 7 could not due to trial close-down) varied in a number of ways: participant characteristics and group practicalities were different. Only two group sessions took place over the usual full 14 sessions, with the remaining groups having to curtail material for logistical reasons relating to the pandemic (group 2), participant absence (group 5) and facilitator availability (group 6). Most participants took part in at least one session, and the proportion maintaining involvement until intervention completion was good in three of the groups. Participants tended to live in less rural areas of Highland, most likely due to the limited capacity to offer groups in remote areas (i.e. lack of critical mass of participants, lack of appropriate venue and childcare, long travel distances for facilitators). Qualitative interviews with intervention participants and facilitators highlighted a range of important themes around recruitment, delivery, participation and impact of the intervention.
Participants discussed being motivated by a need for a sense of community, connection and support, as well as a desire to contribute to the research. They also discussed barriers to participation, including a sense of stigma (being a ‘bad mum’) and a concern they would know people in their group, as well as concern that they would be taking the place of a ‘more deserving’ participant. Group delivery was facilitated by the practitioners supporting each other, capitalising on their accumulation of experience, and being able to access good supervision to discuss any issues. Managing group dynamics and maintaining professional boundaries were challenges faced by facilitators which may have been improved with enhanced training and increased experience. Other challenges related to the logistics of trying to work part-time as a group facilitator, requiring a lot of non-contact work time, on top of other jobs/work tasks. The flexible and accommodating approach of the intervention (e.g. providing transport and adapting content to meet individuals’ needs) as well as the warm and nurturing approach of the facilitators were highlighted as significant positive factors for participants, and these are key to the ethos of the Mellow Parenting approach. Participants discussed external factors, such as the nature of the venue, and internal factors, such as needing to be in the right frame of mind, as sometimes hindering the intervention. There were anxieties about speaking up in a group which was naturally impacted by group size and the specific dynamics within each group. Group cohesion was also felt to be impacted by participants not attending all sessions and some sessions needing to be cancelled. Finally, a range of positive aspects of the intervention components and outcomes were discussed, including a sense of cohesion through shared vulnerability and the value of a safe, protected time and space. Participants reported feeling better about themselves, having developed a sense of community, having positively altered their perception of health care professionals and having developed new skills in parenting. There were also some negative outcomes discussed, including the impact of PTSD on the experience of group participants, highlighting the need for wrap-around support of mothers and awareness of individual vulnerabilities. Sharing more details about the intervention content and style (e.g. the use of the crèche) with potential participants could also help mothers take part in the intervention feeling more informed.
Impact of the COVID-19 pandemic
With reference to Appendix 4, the COVID-19 pandemic had a significant impact on the trial. Although the trial had been established by February 2020, with the recruitment milestone of 40 participants and 2 established intervention groups met, this activity was forced to cease in March 2020. Recruitment, intervention groups and face-to-face follow-up visits were suspended due to the implementation of lockdown for the COVID-19 pandemic in March 2020. Due to the nature of data collection (within participants’ homes) and of the intervention (requiring face-to-face group interaction), it was not possible to recommence recruitment until restrictions were almost completely lifted. Recruitment recommenced in November 2021 and ran until September 2022, when we were asked to cease recruitment due to the decision not to provide further funding to allow the trial to recruit to completion. We were able to run five intervention groups (with a further two recruited but unable to commence), although one of these had to stop midway through in March 2020. As 14 participants randomised to the intervention then could not receive the full intervention, our Data Monitoring Committee advised we exclude those participants and associated controls from any outcome analysis, reducing our sample size by 28 (leaving us with 78).
There were no differences between the participants recruited pre and post pandemic on any of the key sociodemographic or mental health characteristics measured at baseline. Retention to follow-up was equally good pre and post pandemic. Use of primary care services as measured at follow-up (during pandemic restrictions) was low in general, which is most likely due to the reduced availability of primary care services both during and since restrictions. Trial logistics were severely impacted, with a need for the study team and intervention team effectively to plan from the bottom up in a new, post-COVID context, including changed primary care priorities, different perceptions of potential participants, new intervention venues, new crèche arrangements, new group facilitators, and increased workloads for the [NHS research, development and innovation (RD&I)-based] recruitment staff. The importance of working across agencies and pulling together as a team with a shared goal was important, and we were able to re-establish a viable trial within a relatively short period. Nevertheless, the extra time and funding required to complete the trial to protocol was prohibitive, and the funder decided to close the trial as close to the original end date as possible.
Overall, the COVID-19 pandemic had a devastating effect on what was otherwise a viable trial which would have gone a long way to answering a range of questions, not only about the effectiveness of Mellow Babies for mothers experiencing psychosocial stress, but about the lived experience of this population and how we might better engage them in research in future.
Discussion
This trial was not able to establish the clinical and cost-effectiveness of the Mellow Babies parenting intervention for women experiencing psychosocial stress and their 6- to 18-month-old babies. Due to the close-down of the trial prior to recruiting to the planned sample size, we were unable to conduct any outcome analyses due to insufficient statistical power. There has been some scope for learning, primarily in terms of recruitment and retention strategies, and the rich qualitative data collected through interviews has allowed a thorough exploration of the intervention, including group process.
The recent scoping review by Goyder and colleagues,17 ‘Parenting engagement and support interventions for high risk groups’ provides a useful overview of the current state of the field, and suggests some research questions that could be included in future studies:
-
What are the most effective strategies for identifying and engaging families at increased risk in order to offer parenting interventions?
-
How feasible, acceptable and effective are the assessment tools currently in use to identify those who benefit most from the offer of additional support?
-
What forms of support or content do parents want and need most from parenting programmes; what aspects of current programmes do they value most?
-
What factors make it easier for families to accept or sustain engagement with parenting interventions? What are the reasons that families find it difficult to accept or sustain engagement with parenting interventions?
The present report offers data in relation to each of these questions, although this is limited in the context of an incomplete trial and without having had the time to interview control participants as well as those randomised to the intervention arm.
In terms of recruitment (Q1 above), there is a need to have both direct communication with potential participants (e.g. the PIC letter system) and engagement from practitioners working with families (HVs, GPs and third-sector support staff) to optimise the approach. We are aware that HVs were less engaged with the trial than we had anticipated for a range of reasons, not least the extreme pressure that services were under in terms of reduced resources, reduced staffing capacity and increased needs in the population. We also learnt that the element of randomisation was a significant deterrent to referral by practitioners: they were simply unhappy with suggesting to women in their care that they put themselves forward for a 50 : 50 chance of receiving an intervention they would likely benefit from (in the practitioner’s perception). This aligns with recent findings from Rose et al. 27 that practitioners experience role conflict when asked to recruit to clinical trials, and raises issues around how to manage equipoise when trialling an intervention already popular in practice. One solution to this would be to conduct trials such as this on a regional/service cluster randomisation basis, so that no practitioner is facing this perceived dilemma: the intervention is either available in their area or not. Additionally, feedback from participants indicated that when engaging women, the description around improving bonding with babies may lead to negative feelings about participation, particularly where HVs had made the referral, while reassuring women about how the crèche operates and that babies can come into the group if they do not settle, may reduce anxieties in attending groups. The potentially pivotal role of clinicians/practitioners in recruiting to clinical research studies is clear, and it is important to consider the specific needs/concerns within the context of each given study. 28,29
In relation to the feasibility and acceptability of the assessment tools used in screening for trial eligibility (Q2 above), although we did not gather formal data on this, we received no negative feedback. Prospective participants understood that the trial was aimed at women who were experiencing symptoms of anxiety and/or depression. Some women chose not to go ahead with screening once they had discussed eligibility with the recruiting research nurse and better understood this criterion. There is clearly a balance to be gained where recruitment materials make it clear that the research is aimed at women in psychosocial distress, but does not serve to stigmatise or prevent women from coming forward. Recent work in Highland has shown a strong tendency for women to self-censor their requests for mental health care: there was an expressed sense, especially in a climate of low resource, that women compare themselves to those in more extreme distress and this serves to minimise their own. 30 In the case of The Mellow Babies Trial, recruitment materials were designed with patient and public involvement (PPI) input to ensure language struck an appropriate balance, and the research nurse conducting initial phone calls could then explain more fully the criteria, and use the conversation in the context of her clinical experience to help mothers decide if it was worth going ahead with screening.
In relation to which aspects of the programme were most valued by parents (Q3 above), there was a clear recognition of the need for support, which was often reported to be lacking (or experienced negatively) through established services (e.g. health visiting). The fact that other women within intervention groups were also facing challenges in new parenthood was highlighted as a key strength, with other parent and baby/toddler groups being perceived to be full of parents who were happy and knew what they were doing. The context and ethos of the Mellow Babies group seemed to act to remove the stigma and allow participants to express their challenges and feel a sense of normalisation and validation. Other key positive areas of the intervention highlighted by participants were the sharing of life stories by both participants and facilitators, which reduced barriers within the group, and the provision of the crèche, both of which may be challenging to implement in mainstream services.
We have not been able to fully explore factors that encourage sustained engagement (Q4 above) with the data we have. We did not interview mothers who dropped out of the intervention/research (although simple comments were recorded where possible, such as ‘no time to take part as maternity leave has ended’). Some of the qualitative analysis on group process indicates that group composition, including number of participants, age of children and personal characteristics, were key in the intervention groups becoming cohesive (or not) which was perceived by the participants to have encouraged their sustained participation. As it stands, we had very good retention in the face of significant mental health needs in our sample, possibly due to women having otherwise good support in their lives, as indicated by sociodemographic data. Where women did drop out, it tended to be due to mental well-being concerns or life being too overwhelming and group participation having to be de-prioritised. Outside of a trial setting, and in the context of a sustained intervention programme, there is more likely to be the opportunity for such participants to come back to the intervention (i.e. attend a subsequent group) as strict age and other eligibility criteria would be less likely (e.g. Mellow Parenting tends to be more flexible with its age criterion).
The main challenges to this trial were pragmatic, including difficulty establishing a fruitful recruitment strategy and establishing the infrastructure for intervention delivery in the early months, and the interference of the COVID-19 pandemic once systems were in place and the trial was running successfully. The challenges are outlined in greater detail in Appendix 4 and include a need to redirect our recruitment efforts away from relying solely on HVs and other practitioners towards direct communication with potential participants (PIC letters), difficulties in obtaining critical mass of participants within a reasonable time frame in a low population region, and having to establish an infrastructure for intervention delivery where none previously existed. Nevertheless, the trial was established as viable on two separate occasions (initial start-up and post-pandemic re-start): the final challenge was the need for a longer time period and therefore funds to be able to recruit to power.
There are of course some limitations to consider, which are relevant despite no primary outcome analysis. The sample, although showing significantly poor mental well-being, was otherwise relatively advantaged from a sociodemographic perspective. The applicability of these findings to a wider sociodemographic group is therefore limited. Similarly, this trial focused on mothers for pragmatic reasons (see Publications), so findings cannot be extended to fathers or other adults with parental responsibility. The pragmatic difficulties faced in implementing the intervention raise questions about its viability as a sustained programme within usual services, especially in a region like Highland with a relatively small population size and lack of relevant infrastructure. Specialist practitioner posts are often vulnerable, where there are services essentially offered by lone individuals or very small teams (e.g. infant mental health service). However, this is difficult to assess concretely within the artificial context of a RCT: our findings show, for example, that HVs would have been much more willing to refer mothers had there been the certainty of receiving an intervention. Further qualitative data collection would have been useful to help elucidate the experiences of those who left the intervention early, of those in the control group, and of HVs and other practitioners in the field. Had we been able to interview representatives from each of these groups, our understanding in relation to the secondary questions addressed in this report would have been more comprehensive.
The research team and the intervention team worked extremely hard to engage with key partners and stakeholders in the research to ensure the delivery of intended outcomes. Our connection to NHS Highland and Highland Council was critical: NHS Highland RD&I was the only local organisation able to provide an appropriate infrastructure for recruiting and retaining intervention practitioners, and we relied on the collaboration with the public health department to access the PIC letter system. Health visiting is managed by Highland Council, where key stakeholders were included at the planning stage and as co-investigators in the trial. Their input in overcoming pragmatic barriers was invaluable. Similarly, establishing and maintaining good relationships with these stakeholders allowed a smoother interaction with HVs and other practitioners in participant-facing roles. Although we did connect with colleagues in third-sector services as part of our engagement work, recent Highland-based work, in the post-pandemic, post-Brexit climate, has highlighted how central the role of the third sector is in supporting young families. 30
There are several take-home messages from this research:
-
There is scope to conduct a new trial of Mellow Babies, ideally multisite and including cluster randomisation to facilitate recruitment.
-
It is possible to recruit and retain mothers who are experiencing significant psychosocial stress into trials, provided the infrastructure is realistic and flexibility in approach can be employed.
-
Recruitment needs to be direct, with potential participants being trusted to be their own gatekeepers when putting themselves forward for research. We need to avoid potential paternalism/maternalism in parenting support research.
-
Trials need to be realistically resourced/have a robust infrastructure. Recruitment and group facilitation should ideally be carried out by staff dedicated to these roles – a larger trial would help this.
-
The need for a larger trial with better infrastructure brings the focus back to conducting trials in large urban areas and marginalising those in more remote or rural areas. We need to be more thoughtful about how to ensure all participants meeting clinical eligibility have the chance to participate in an intervention that could realistically and sustainably be delivered to them as part of usual services.
-
Solid engagement with the third sector will be critical for the above.
Patient and public involvement
Both the original Chief Investigator (CI) (PW) and the final CI (LT) had already been investigators on other similar trials [e.g. Trial of Healthy Relationship Initiatives for the Very Early years (THRIVE); Henderson et al. , 201931] which we used to inform our approaches to effective engagement, recruitment, and retention in designing our materials and methodological approach. We recruited a previous THRIVE trial participant to offer PPI input at the start of the trial: she gave feedback on our recruitment posters and methods. We were not able to recruit any further PPI group members before we had to pause study recruitment during the COVID-19 pandemic (March 2020).
We worked closely with the local family nurse partnership (FNP) practitioners who kindly recruited teenage mothers on our behalf in order for the trial manager to meet with them to discuss their thoughts and opinions on various aspects of our recruitment approach. The trial manager met with two teenage mothers identified by FNP in August 2019 to discuss material the team were preparing for Facebook, as well as discussing how best to target their peers for recruitment. The meeting was extremely helpful, and we received insightful comments. They suggested that face-to-face engagement within established community groups would be more effective than social media advertisements, as they did not tend to engage online. They suggested local parent/family groups which the trial manager made contact with/met the facilitator of. There was a need for both virtual and face-to-face approaches. Over time, the research team built a network of third-sector contacts and attended local community groups (run by NHS early years practitioners and third sector) in tandem with social media and other advertisement. Although the families we met in August are not permanent members of the trial’s PPI group, the FNP has assured us they are happy to continue to work with the trial team in order to source young mothers for any future service user meetings.
We successfully recruited four participants from the pre-pandemic period to take part in a discussion about their experiences of participating in the trial and to provide direct feedback on recruitment methods and research procedures in the post-pandemic period. We met with two of them in July 2022 and there were some suggestions for small amendments to our documentation, which could not be implemented as we were asked to stop recruitment soon after. On the whole, the feedback from these participants was positive about their experience as trial participants. The two participants who were unable to attend this session were sent a summary of the discussion via e-mail and given the opportunity to comment (no comments were received).
We plan to generate a brief version of this report to make available (online) to all study participants and any member of the public who might be interested. Although we had planned to have a public-facing dissemination event, there may be little scope for this given the changed research questions and limited resources available. While we are unable to report on the original intended outcome for the trial, there would be merit in discussing the findings in the context of other work happening locally (i.e. the development of perinatal and infant mental health services). LT is working with NHS Highland on the perinatal and infant mental health workstream at present and will liaise with them around effective dissemination.
Equality, diversity and inclusion
Participants: The study was open to any mother meeting the inclusion criteria, including via self-referral. Highland is not an ethnically diverse region, with ˂ 2% of residents not of white European extraction. 32 We considered the main barriers to participation to be stressful lives, mental health, social isolation, literacy/education and living rurally or remotely. There is evidence that parents experiencing these stressors are less likely to engage in parenting interventions. 33–36 Measures to overcome these as much as possible were incorporated into the study design, partly based on the design of the Mellow Babies intervention model. Specifically, home visits were used for obtaining consent and gathering baseline and follow-up data. This meant that all measures, although mostly questionnaires, were conducted in an interview style with the researcher taking time to fit with the participant’s schedule. The participant information sheet was designed to be accessible to those with literacy difficulties, and we sought PPI input into its design. A flexible approach to communication, including the use of whichever means was preferred by the participant and the adoption of a patient approach to reminders (i.e. no ‘three strikes and you’re out’ type rule) allowed us to work around participants’ busy and often stressful lives. Critical to this study, it also allowed mental well-being to be considered: if a participant was having a difficult day and needed to reschedule a visit, we accommodated this. Although living remotely will have been a barrier for some potential participants (i.e. too far to travel to a more populous area with enough critical mass to establish an intervention group), we were careful to target recruitment to areas closer to the urban centres. Where participants did not have access to a car, transport was always provided to allow participation in intervention groups.
We successfully enrolled 106 women with babies 6–18 months old living across the Highland Council region in Scotland. Women enrolled in the trial all scored above the threshold for anxiety and depression, 61% stated they had a diagnosed mental health condition (usually depression or anxiety), and 50% had been prescribed a mental health medication since the birth of their baby. Baseline data showed a high level of education, a high level of paid employment and a high level of home ownership among participants, and most were currently in a relationship with their baby’s father. There were also low levels of stress in terms of life events. This suggests that there is more work to be done to ensure that those experiencing adversity in sociodemographic terms have the opportunity to participate and that barriers to participation need to be better understood. However, while the sample as a whole appeared to be ‘doing well’ on these measures, some participants faced specific challenges. What we do know from those who were screened or recruited is that mothers’ non-attendance when randomised to the intervention arm was linked to life stressors, including moving house, returning to full-time work after maternity leave, not feeling able to commit the time to the group, planned absences during the group, and living too far away from where the group was being delivered. Mothers withdrew from the programme due to life stressors, mental health and child factors. Reasons included experiencing a family bereavement, finding the group made PTSD symptoms worse, and the child not being able to settle in the crèche. Lack of participation in follow-up appointments was also predominantly due to life stressors and participant mental health, including experiencing a recent miscarriage, the birth of a child, time pressures, or not ‘being in a good place’. However, the majority of participants who did not take part in a follow-up did not respond to contact from the research team, so we are unable to determine the reasons for non-participation from these mothers.
Research team: The CI for the majority of the trial was a senior, white, male, medically qualified professor. Once he retired (December 2022), this role was taken over by one of the senior co-investigators, a white female senior research fellow, for the final few months of the trial. The rest of the staff on the trial were female, all of white European ethnicity. Our team included staff from different disciplines (e.g. psychology graduates, medical doctors, nurses) and with a range of experience. The main posts for the running of the trial, the Trial Manager/Research Fellow, Research Assistant, and PhD student, were all young, female, early career researchers. We believe the trial has contributed to developing their careers and capacity within the field. We ensured all staff had the opportunity to contribute to key trial decisions and to train in new areas of skill development. The trial was presented at international conferences by the early career researcher staff members. As well as our PhD student, we had a master’s student (a young female medical student) work on the process evaluation in the first year of the project, and she presented her paper at a conference.
Impact and learning
The main impact of The Mellow Babies Trial has been to demonstrate that complex intervention trials of this nature can be viable in areas lacking a large or diverse population or significant trial infrastructure. It is possible to recruit mothers experiencing psychosocial stress, especially when approaching them directly (i.e. no dependence on a ‘gatekeeper’). It is important to be able to conduct trials away from the main population centres if we are to be confident that our findings are truly applicable to the population more widely. Trials need to be realistically planned, and funded, to be able to allow people from remote and rural areas to participate, or for smaller population centres without the level of trial infrastructure of larger cities to be able to evaluate the effectiveness of interventions in a real-world setting.
Although the participant group was representative of the local population in demographic terms, they showed a relative advantage compared to the target population for the intervention (which is likely to experience a greater disadvantage). 20,21 It is likely more mothers experiencing sociodemographic disadvantage might have been recruited if practitioners working with families had more capacity to recruit to the trial. While the PIC letter has been the most effective means of recruitment, it may be that a formal letter would have been off-putting to some potential participants. A two-pronged approach, involving a letter and direct practitioner contact, would be ideal. It could also have been useful to work more directly with third-sector organisations, who often have more direct contact with families, in recruiting participants. Although we did make contact with as many organisations as possible, in both the pre- and post-pandemic phases of the trial we were just getting to the stage of establishing procedures when we had to stop recruitment.
Regarding trial infrastructure, conducting a trial in Highland meant planning based on tenuous resources. For example, when we submitted the funding application, there was a mobile crèche in operation locally that would have been able to staff the intervention crèche facility. By the time the trial started, this business was no longer in operation and there was no alternative. We worked with local nurseries to develop a preferable alternative (hosting the intervention groups within nurseries where child care could be absorbed), but this could not be reinstated post pandemic partly due to the continued restrictions on adults entering the nursery buildings, but also due to new national legislation increasing early education provision meaning that nurseries no longer had the capacity to host the intervention group or to absorb the child care. Staffing the intervention also presented significant challenges, and ultimately the NHS was the only organisation with the size and infrastructure to accommodate staff in secure posts to allow their sustained involvement in the trial.
The Mellow Babies Trial has been able to demonstrate considerable desire for this type of intervention in the community. Almost 400 mothers expressed interest in the trial. Although only 25% of these ultimately became participants, the artificial barrier created by trial recruitment procedures is almost certainly a significant factor.
We have actively disseminated the learning from this work as much as possible and will continue to do so in the coming months to ensure learning is maximised among key stakeholders. We have presented the protocol and aspects of the development at the following conferences:
-
Thompson L, Buchanan L, Christie H, Wilson P. The Mellow Babies Trial: Early Process Evaluation of a Complex Intervention. Oral presentation at the NHS Highland Research, Development, and Innovation Conference, 2019.
-
Thompson L, Wilson P, The Mellow Babies Trial team. The Mellow Babies Trial Protocol. Poster presentation at the NHS Highland Research, Development, and Innovation Conference, 2019.
-
Tanner J, Wilson P, Thompson L. Group Processes and Interpersonal Change Mechanisms Within a Group-based Intervention for Mothers and Their Infants. Oral presentation at the World Association for Infant Mental Health Congress, 2023.
There are no plans to publish any of the findings contained within this report separately. The interview data have been used in a separate analysis (i.e. different research questions and methods) by Jessica Tanner, a PhD student, as part of her thesis focused on group processes in parenting interventions, successfully examined on 29 April 2024. The paper titles are:
-
Tanner J, Wilson P, Wight D, Thompson L. The importance of group factors in the delivery of group-based parenting programmes: a process evaluation of Mellow Babies. Front Child Adolesc Psychiatry 3:1395365. https://doi.org/10.3389/frcha.2024.1395365
-
Tanner J, Wilson P, Wight D, Thompson L. The Mellow Babies parenting programme: role of group processes and interpersonal change mechanisms. Front Child Adolesc. Psychiatry 2024;3 https://doi.org/10.3389/frcha.2024.1395363
As stated in Patient and public involvement, we plan to generate a brief version of this report to make available (online) to all study participants and any member of the public who might be interested. Although we had planned to have a public-facing dissemination event, there may be little scope for this given the changed research questions and limited resources available. While we are unable to report on the original intended outcome for the trial, there would be merit in discussing the findings in the context of other work happening locally (i.e. the development of perinatal and infant mental health services). LT is working with NHS Highland on the perinatal and infant mental health workstream at present and will liaise with them around effective dissemination to key stakeholders.
Implications for decision-makers
Due to the close-down of the trial prior to recruiting to the planned sample size, we were unable to conduct any outcome analyses due to insufficient statistical power. This limits our capacity to make recommendations for decision-makers. There is, nevertheless, some scope for learning, primarily in terms of recruitment and retention strategies, and the rich qualitative data collected through interviews have allowed a thorough exploration of the intervention, including group process. As articulated in the Discussion section, there is scope to continue to conduct trials of parenting interventions, including of Mellow Babies, taking into account the learning from this trial regarding logistics and the acceptability and effectiveness of our approach to recruitment and retention. Indeed, research evidence regarding the impact of Mellow Babies continues to accumulate,19–21 which provides useful information for decision-makers, but not at the level of a definitive effectiveness trial. Our take-home messages from the Discussion form the basis of implications for decision-makers:
-
There is scope to conduct a new trial of Mellow Babies, ideally multisite and including cluster randomisation to facilitate recruitment.
-
It is possible to recruit and retain mothers who are experiencing significant psychosocial stress into trials, provided the infrastructure is realistic and flexibility in approach can be employed.
-
Recruitment needs to be direct, with potential participants being trusted to be their own gatekeepers when putting themselves forward for research. We need to avoid potential paternalism/maternalism in parenting support research.
-
Trials need to be realistically resourced/have a robust infrastructure. Recruitment and group facilitation should ideally be carried out by staff dedicated to these roles – a larger trial would help this.
-
The need for a larger trial with better infrastructure brings the focus back to conducting trials in large urban areas and marginalising those in more remote or rural areas. We need to be more thoughtful about how to ensure all participants meeting clinical eligibility have the chance to participate in an intervention that could realistically and sustainably be delivered to them as part of usual services.
-
Solid engagement with the third sector will be critical for the above.
In addition to the above specific implications, there is a need to think more generally about the context and infrastructure around trials of complex interventions such as Mellow Babies. The trial was in many ways constrained by resource availability locally. In order to ensure we reach underserved populations there need to be higher-level actions (infrastructure/funding) that take into account the added contextual barriers (e.g. outsourcing of resources at extra cost), in keeping with NIHR INCLUDE guidance37 and the ongoing NIHR Under-served Communities Programme. 38
Although recruitment was successful in this study, it involved considerably more staff time and logistical effort than anticipated. Despite any efforts made, the trial was not able to reach those in the most remote areas, which in part was due to logistics and resources, but also the constraints related to eligibility criteria (age of child) and needing a critical mass for groups within a short time frame. Rurality has been a barrier to implementation of intervention groups outwith the context of a trial in Highland before, so there is a need to learn directly from those experiences to allow appropriate trial design in future.
Those who did not complete the intervention or were lost to follow-up cited mental health and/or life stressors as the underlying reasons. There is scope to explore more thoroughly how best to retain participants in interventions which are designed to be accessible regardless of these stressors. Outwith the rigid constraints of a conventional RCT design, interventions such as Mellow Babies tend to offer as flexible an approach as possible to allow for continued participation. It may be most prudent to ensure that future trials/interventions exist as part of a wider programme where, for example, those unable to maintain participation in a 14-week whole-day programme may still be able to obtain other relevant support (i.e. an online group) that is more accessible. Having trials more embedded with usual care (such as health visits) without compromising scientific validity would seem to be beneficial not only to trial success but also to participant welfare.
Research recommendations
As this trial was unable to recruit to the planned sample size, there is still ample scope for the original question to be addressed: What is the clinical and cost-effectiveness of the Mellow Babies parenting intervention for women experiencing psychosocial stress and their 6- to 18-month-old babies? This is supported by the review by Goyder and colleagues,17 which highlights the need for higher-level evidence for a number of existing programmes, including Mellow Babies. With thoughtful design, a trial could address not only this primary question, but also several secondary questions along the lines of those proposed by Goyder et al. (see Discussion).
Beyond this specific area of enquiry, our recommendations for future research align with those proposed by Goyder et al. Specifically, the example questions posed in their review present an ideal foundation on which to build on the learning from The Mellow Babies Trial (see Discussion).
-
What are the most effective strategies for identifying and engaging families at increased risk in order to offer parenting interventions?
-
How feasible, acceptable and effective are the assessment tools currently in use to identify those who benefit most from the offer of additional support?
-
What forms of support or content do parents want and need most from parenting programmes; what aspects of current programmes do they value most?
-
What factors make it easier for families to accept or sustain engagement with parenting interventions? What are the reasons that families find it difficult to accept or sustain engagement with parenting interventions?
The learning from The Mellow Babies Trial, detailed in previous sections, serves to reinforce the statement made by Goyder et al. , with reference to Hackworth et al. :33 ‘Enabling parents to engage with the offered support requires an understanding of their most immediate support needs and an understanding of the practical, social, economic and cultural barriers that may make it more difficult for parents to accept support or engage with programmes’.
Conclusions
This trial was not able to establish the clinical and cost-effectiveness of the Mellow Babies parenting intervention for women experiencing psychosocial stress and their 6- to 18-month-old babies. Due to the close-down of the trial prior to recruiting to the planned sample size, we were unable to conduct any outcome analyses due to insufficient statistical power. There has been some scope for learning, primarily in terms of recruitment and retention strategies, and the rich qualitative data collected through interviews have allowed a thorough exploration of the intervention, including the group process. Key learning from interviews with intervention participants included the importance of the social cohesion/community the groups offered, having a safe shared space to focus on themselves, as well as the need to be mindful of not only group size but group composition and their potential impact on the intervention experience. Barriers to participation included a sense of stigma, not wanting to deprive those more in need of support, reluctance to use the crèche, and concern about lack of anonymity and speaking out in a small group. Group facilitators need to be carefully selected and trained, as well as provided with ongoing support from each other and professional supervision. Pragmatic issues related to delivering an intervention which is not embedded in services were discussed, including having to work part-time around other commitments and not always being able to be as flexible as the intervention/participants’ needs might require.
There is no doubt that more trials of parenting support interventions are needed, especially where public services are already investing in well-liked programmes lacking a robust evidence base. Any future trial must take on board the recommendations of Goyder et al. ,17 including the need for proper consideration of contextual barriers to participation. This should include consideration of the need to ensure that those in underserved populations, such as those in remote and rural areas, have the chance to meaningfully participate in research.
Additional information
CRediT contribution statement
Lucy Thompson (https://orcid.org/0000-0001-7461-3262): Conceptualisation, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualisation, Writing – original draft, Writing – reviewing and editing.
Jessica Tanner (https://orcid.org/0000-0002-1290-9700): Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualisation, Writing – original draft, Writing – reviewing and editing.
Matthew Breckons (https://orcid.org/0000-0003-3057-6767): Data curation, Formal analysis, Validation, Visualisation, Writing – original draft, Writing – reviewing and editing.
Naomi Young (https://orcid.org/0009-0001-1941-0275): Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualisation, Writing – original draft, Writing – reviewing and editing.
Laura Ternent (https://orcid.org/0000-0001-7056-298X): Conceptualisation, Investigation, Methodology, Supervision, Writing – original draft, Writing – reviewing and editing.
Thenmalar Vadiveloo (https://orcid.org/0000-0001-5531-6289): Data curation, Formal analysis, Validation, Writing – original draft, Writing – reviewing and editing.
Philip Wilson (https://orcid.org/0000-0002-4123-8248): Conceptualisation, Funding acquisition, Investigation, Methodology, Supervision, Writing – original draft, Writing – reviewing and editing.
Danny Wight (https://orcid.org/0000-0002-1234-3110): Conceptualisation, Funding acquisition, Investigation, Methodology, Supervision, Writing – original draft, Writing – reviewing and editing.
Louise Marryat (https://orcid.org//0000-0002-6093-4679): Conceptualisation, Funding acquisition, Investigation, Methodology, Supervision, Writing – original draft, Writing – reviewing and editing.
Iain McGowan (https://orcid.org/0000-0002-7778-8065): Conceptualisation, Funding acquisition, Investigation, Methodology, Supervision, Writing – reviewing and editing.
Graeme MacLennan (https://orcid.org/0000-0002-1039-5646): Data curation, Investigation, Methodology, Supervision, Writing – reviewing and editing.
Angus MacBeth (https://orcid.org/0000-0002-0618-044X): Conceptualisation, Funding acquisition, Investigation, Methodology, Supervision, Writing – reviewing and editing.
James McTaggart (https://orcid.org/0000-0001-7960-148X): Conceptualisation, Funding acquisition, Investigation, Methodology, Writing – reviewing and editing.
Tim Allison (https://orcid.org/0009-0003-0175-6977): Methodology, Resources, Writing – reviewing and editing.
John Norrie (https://orcid.org/0000-0001-9823-9252): Conceptualisation, Funding acquisition, Investigation, Methodology, Writing – reviewing and editing.
Acknowledgements
Philip Wilson was the chief investigator (CI) until December 2022, when he retired. Lucy Thompson worked closely with Phil throughout the trial and took over as CI in January 2023 to manage the trial close-down and prepare the final report.
Other contributions
NHS Highland Research, Development and Innovation team provided study recruitment (Avril Donaldson, Shona MacLeod) and managed the intervention (Frances Hines and her team). Mellow Babies group facilitators were recruited and managed within this team: our thanks to them for their commitment to the trial.
Other members of the University of Aberdeen research team included Dr Hope Christie (Trial Manager 2018–20), Fiona Farrell (Admin support 2019–close), Theresa Hamilton (Admin support 2018–20), Charlotte Murray (research assistant, 2021–3), the late Pam Sherriff (Admin support from bid development to 2019).
Colleagues within the University of Aberdeen Health Services Research Unit/the Centre for Healthcare Randomised Trials (CHaRT) provided invaluable support throughout: Dr Lorna Aucott (Senior Statistician), Dr Seonaidh Cotton (Senior Trial Manager), and Mark Forrest (Senior IT Development Manager).
Previous co-investigators who helped shape the trial: the late Prof James Law, Dr Jing Shen, Clare Simpson, Dr Hugo van Woerden.
Trial Steering Committee: Dr Nick Axford (chair), Matt Forde, Prof Stavros Petrou, Dr Maiken Pontoppidan, and Prof Anna Sarkadi.
Data Monitoring Committee: Prof Jane Barlow (chair), Dr Carole Cummins, and Dr Tim Morris.
Thanks to Mellow Parenting for providing practical advice on intervention implementation.
We would like to acknowledge the contribution of all the practitioners who took the time to learn about the trial, to spread the word and to refer patients.
Finally, we would like to thank all the participants and their babies who took the time to participate in the research.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
The Mellow Babies Trial was reviewed and approved by NHS East Midlands – Nottingham 1 Research Ethics Committee on 13 December 2018, ref 18/EM/0304. All subsequent protocol amendments were reviewed and approved by the same committee. Any modifications made were planned by the chief investigator (PW to December 2022, LT thereafter) with the project management group, co-investigators, Trial Steering Committee and Data Monitoring Committee as required.
Information governance statement
The University of Aberdeen is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, University of Aberdeen is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here (www.abdn.ac.uk/about/privacy/).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/KCVL7125.
Primary conflicts of interest: John Norrie is in receipt of the following NIHR grants to: Long-Term Outcomes of Synthetic Mid-Urethral Slings (Mesh Tapes) in Surgical Treatment of Stress Urinary Incontinence in Women – A Long-term Follow-Up of the SIMS RCT. NIHR133092; Glucocorticoids in Adults With Acute Respiratory Distress Syndrome: Randomised Clinical Trial (GuARDS Trial). NIHR151601; Inpatient GRAduated Compression stocking use as an adjunct to Extended duration pharmacoprophylaxis for venous thromboembolism prevention – the GRACE multicentre randomised controlled trial. NIHR155294; Early Vasopressors in Sepsis (EVIS) trial. NIHR132594 (19/162/02); Thromboprophylaxis in individuals undergoing superficial endoVEnous treatment (THRIVE). NIHR152877; Examining the benefit of graduated compression stockings in the Prevention of vEnous Thromboembolism in low-risk Surgical patients: a multicentre cluster randomised controlled trial (PETS Trial). NIHR133776; ESPriT2: A multi-centre randomised controlled trial to determine the effectiveness of laparoscopic treatment of isolated superficial peritoneal endometriosis for the management of chronic pelvic pain in women. NIHR129801; A randomised Placebo-Controlled Trial of Antenatal Corticosteriods for Planned Birth in Twins: STOPPIT-3. C-10333879 NIHR131352; Duration of External Neck Stabilisation following odontoid fracture in older or frail adults: a randomised controlled trial of early versus late collar removal. NIHR131118; A Placebo Controlled Randomised Trial of Intravenous Lidocaine in Accelerating Gastrointestinal Recovery After Colorectal Surgery. 15/130/95; A parallel group, double-blind, randomised, placebo-controlled trial comparing the effectiveness and cost effectiveness of low-dose oral modified release morphine versus placebo on patient-reported worst breathlessness in people with chronic breathlessness: Morphine and BrEathLessness trial (MABEL). 2019-002479-33; Designing a platform trial to assess the effectiveness of interventions for peripheral arterial disease: The PAEDIS trial Development Project. NIHR155342; Venous leg ulcErs: management and eradIcatioN (VEIN Platform Study). NIHR155477; Alpha 2 Agonists for Sedation to produce Better Outcomes from Critical Illness (A2B TRIAL): A Parallel Group Randomised Controlled Trial Comparing Clonidine, Dexmedetomidine and Current Usual Care. 16/93/01; Diagnostic tools to establish the presence and severity of peripheral arterial disease in people with diabetes. NIHR131855; CHAPS – Compression Hosiery to Avoid Post-Thrombotic Syndrome. 17/147/47; The CATHETER II Study: Randomised Controlled Trial Comparing the Clinical and Cost-Effectiveness of Various Washout Policies Versus No Washout Policy in Preventing Catheter Associated Complications in Adults Living With Long-Term Catheters. 17/30/02; Female Urgency, Trial of Urodynamics as Routine Evaluation (FUTURE). 15/150/05; Feasibility and design of a trial to determine the optimal mode of delivery in women presenting in preterm labour or with planned preterm delivery. 17/22/02 125193; Cervical Ripening at Home or In-Hospital – Prospective Cohort Study and Process Evaluation (CHOICE Study). NIHR127569; NIHR Global Health Research Group on Preterm Birth and Stillbirth at the University of Edinburgh (the DIPLOMATIC Collaboration). 17/63/08; I-Minds: A Digital Intervention to Improve Mental Health and Interpersonal Resilience for Young People Who Have Experienced Online Sexual Abuse – A Non-randomised Feasibility Study With a Mixed-methods Design. NIHR131848; Metformin in Li Fraumeni (MILI) trial: A Phase II randomised open-label cancer prevention study of metformin in adults with Li Fraumeni Syndrome. NIHR131239; Building an international precision medicine platform trial for the acute respiratory distress syndrome (ARDS). NIHR154493; Implementation of Comprehensive Geriatric Assessment based perioperative medicine services to improve clinical outcomes for older patients undergoing elective and emergency surgery with cost effectiveness. [Short title; Perioperative medicine for Older People undergoing Surgery Scale Up (POPS-SUp)]. NIHR157443; NIHR Global Health Research Unit on Respiratory Health (RESPIRE-2). NIHR132826; NIHR Global Health Research Unit on Respiratory Health (RESPIRE) at The University of Edinburgh. 16/136/109; Infant Hypothalamic-pituitary-adrenal Axis Responses Following Antenatal Corticosteroids and Perinatal Outcomes: A Mechanism of Action of Health Intervention Study. NIHR133388; John Norrie has been a member of the following NIHR committees: Chair of MRC/NIHR Efficacy and Mechanism Evaluation Board, 2019–present; EME Funding Committee Sub-Group Remit and Comp Check (August 2019–current); HTA General Committee (1 November 2016–30 November 2019); HTA Post-Funding Committee teleconference (POC members to attend) (1 November 2016–30 November 2019); HTA Funding Committee Policy Group (formerly CSG) (1 November 2016–30 November 2019); COVID-19 Reviewing (1 June 2020–30 September 2020); HTA Commissioning Committee (18 January 2010–28 February 2016); HTA Commissioning Sub-Board (EOI) (1 April 2016–31 March 2017); NIHR CTU Standing Advisory Committee (1 May 2018–1 May 2023; NIHR HTA and EME Editorial Board (1 November 2015–31 March 2019); Pre-Exposure Prophylaxis Impact Review Panel (1 May 2017–1 June 2017); EME Strategy Advisory Committee (2019–present); EME – Funding Committee Members (1 August 2019–1 August 2022). Angus MacBeth is involved with ongoing research collaboration with the organisation Mellow Parenting, for which he receives no direct financial remuneration. No other interests declared.
Publications
This article is the sole publication from the outcome of the trial. We have also presented the study at conferences:
Thompson L, Buchanan L, Christie H, Wilson P. The Mellow Babies Trial: Early Process Evaluation of a Complex Intervention. Oral presentation at the NHS Highland Research, Development, and Innovation Conference, 2019.
Thompson L, Wilson P, The Mellow Babies Trial team. The Mellow Babies Trial Protocol. Poster presentation at the NHS Highland Research, Development, and Innovation Conference, 2019.
Tanner J, Wilson P, Thompson, L. Group Processes and Interpersonal Change Mechanisms Within a Group-based Intervention for Mothers and Their Infants. Oral presentation at the World Association for Infant Mental Health Congress, 2023.
Our PhD student, Jessica Tanner, has published the following papers related to the study:
Tanner J, Wilson P, Wight D, Thompson L. The importance of group factors in the delivery of group-based parenting programmes: a process evaluation of Mellow Babies. Front Child Adolesc Psychiatry 3:1395365. https://doi.org/10.3389/frcha.2024.1395365
Tanner J, Wilson P, Wight D, Thompson L. The Mellow Babies parenting programme: role of group processes and interpersonal change mechanisms. Front Child Adolesc. Psychiatry 2024;3 https://doi.org/10.3389/frcha.2024.1395363
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
List of abbreviations
- ADHD
- attention-deficit/hyperactivity disorder
- ASQ
- Ages and Stages Questionnaire
- ASQ-3
- Ages and Stages Questionnaire, Third Edition
- ASQ-SE2
- Ages and Stages Questionnaires: Social-Emotional, Second Edition
- CI
- chief investigator
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FNP
- family nurse partnership
- FU1
- follow-up 1
- FU2
- follow-up 2
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- HADS-A
- Hospital Anxiety and Depression Scale – Anxiety subscale
- HADS-D
- Hospital Anxiety and Depression Scale – Depression subscale
- HV
- health visitor
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- PCQ
- Participant Cost Questionnaire
- PHR
- Public Health Research
- PIC
- Patient Identification Centre
- PPI
- patient and public involvement
- PTSD
- post-traumatic stress disorder
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RD&I
- research, development and innovation
- REC
- Research Ethics Committee
- SDQ
- Strengths and Difficulties Questionnaire
- SIMD
- Scottish Index of Multiple Deprivation
- SSLM
- Sure Start Language Measure
- THRIVE
- Trial of Healthy Relationship Initiatives for the Very Early years
- VAS
- visual analogue scale
References
- Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Dev Psychopathol 2002;14:179-207.
- Jokela M, Ferrie J, Kivimӓki M. Childhood problem behaviors and death by midlife: the British National Child Development Study. J Am Acad Child Adolesc Psychiatry 2009;48:19-24.
- Wilens TE, Biederman J, Mick E, Faraone SV, Spencer T. Attention deficit hyperactivity disorder (ADHD) is associated with early onset substance use disorders. J Nerv Ment Dis 1997;185:475-82.
- Milberger S, Biederman J, Faraone SV, Chen L, Jones J. ADHD is associated with early initiation of cigarette smoking in children and adolescents. J Am Acad Child Adolesc Psychiatry 1997;36:37-44.
- Miniscalco C, Nygren G, Hagberg B, Kadesjö B, Gillberg C. Neuropsychiatric and neurodevelopmental outcome of children at age 6 and 7 years who screened positive for language problems at 30 months. Dev Med Child Neurol 2006;48:361-6.
- Law J, Plunkett C, Taylor J, Gunning M. Developing policy in the provision of parenting programmes: integrating a review of reviews with the perspectives of both parents and professionals. Child Care Health Dev 2009;35:302-12.
- Eisenberg N, Fabes RA, Shepard SA, Guthrie IK, Murphy BC, Reiser M. Parental reactions to children’s negative emotions: longitudinal relations to quality of children’s social functioning. Child Dev 1999;70:513-34.
- Tough SC, Siever JE, Leew S, Johnston DW, Benzies K, Clark D. Maternal mental health predicts risk of developmental problems at 3 years of age: follow up of a community based trial. BMC Pregnancy Childbirth 2008;8:1-11.
- Wilson P, Bradshaw P, Tipping S, Henderson M, Der G, Minnis H. What predicts persistent early conduct problems? Evidence from the Growing Up in Scotland cohort. J Epidemiol Community Health 2013;67:76-80.
- Scott S, Lewsey J, Thompson L, Wilson P. Early parental physical punishment and emotional and behavioural outcomes in preschool children. Child Care Health Dev 2014;40:337-45. https://doi.org/10.1111/cch.12061.
- Allely CS, Johnson PC, Marwick H, Lidstone E, Kočovská E, Puckering C, et al. Prediction of 7-year psychopathology from mother-infant joint attention behaviours: a nested case-control study. BMC Pediatr 2013;13.
- Marwick H, Doolin O, Allely CS, McConnachie A, Johnson P, Puckering C, et al. Predictors of diagnosis of child psychiatric disorder in adult-infant social-communicative interaction at 12 months. Res Dev Disabil 2013;34:562-72.
- Allely CS, Purves D, McConnachie A, Marwick H, Johnson P, Doolin O, et al. Parent-infant vocalisations at 12 months predict psychopathology at 7 years. Res Dev Disabil 2013;34:985-93.
- Puckering C, Allely CS, Doolin O, Purves D, McConnachie A, Johnson PC, et al. Association between parent-infant interactions in infancy and disruptive behaviour disorders at age seven: a nested, case-control ALSPAC study. BMC Pediatr 2014;14.
- Thomson R, Allely CS, Purves D, Puckering C, McConnachie A, Johnson PC, et al. Predictors of positive and negative parenting behaviours: evidence from the ALSPAC cohort. BMC Pediatr 2014;14.
- Poobalan AS, Aucott LS, Ross L, Smith WC, Helms PJ, Williams JH. Effects of treating postnatal depression on mother-infant interaction and child development: systematic review. Br J Psychiatry 2007;191:378-86.
- Goyder E. Parenting Engagement and Support Interventions for High Risk Groups: Short Report on Topic Scoping by the Public Health Research Review Team. University of Sheffield/NIHR; 2022.
- MacBeth A, Law J, McGowan I, Norrie J, Thompson L, Wilson P. Mellow Parenting: systematic review and meta-analysis of an intervention to promote sensitive parenting. Dev Med Child Neurol 2015;57:1119-28. https://doi.org/10.1111/dmcn.12864.
- Levi D, Ibrahim R, Malcolm R, MacBeth A. Mellow Babies and Mellow Toddlers: effects on maternal mental health of a group-based parenting intervention for at-risk families with young children. J Affect Disord 2019;246:820-7. https://doi.org/10.1016/j.jad.2018.12.120.
- Raouna A, Malcolm R, Ibrahim R, MacBeth A. Promoting sensitive parenting in ‘at-risk’ mothers and fathers: a UK outcome study of Mellow Babies, a group-based early intervention program for parents and their babies. PLOS ONE 2021;16. https://doi.org/10.1371/journal.pone.0245226.
- Davidson C, Raouna A, Malcolm R, Ibrahim R, MacBeth A. ‘There’s more love between us’: the parental experience of attending Mellow Babies, a targeted, early intervention program for parents and their babies. Infant Ment Health J 2023;44:100-16. https://doi.org/10.1002/imhj.22029.
- Orkin AM, Gill PJ, Ghersi D, Campbell L, Sugarman J, Emsley R, et al. CONSERVE Group . Guidelines for reporting trial protocols and completed trials modified due to the COVID-19 pandemic and other extenuating circumstances: the CONSERVE 2021 statement. JAMA 2021;326:257-65. https://doi.org/10.1001/jama.2021.9941.
- Crawford JR, Henry JD, Crombie C, Taylor EP. Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol 2001;40:429-34. https://doi.org/10.1348/014466501163904.
- Squires J, Bricker D. Ages and Stages Questionnaires® (ASQ‐3™): A Parent‐Completed Child Monitoring System. Baltimore, MD: Paul H. Brookes; 2009.
- Squires J, Bricker D, Twombly E. Ages and Stages Questionnaires®: Social-Emotional (ASQ:SE-2™). Baltimore, MD: Paul H. Brookes; 2015.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Rose J, Lynn K, Akister J, Maxton F, Redsell SA. Community midwives’ and health visitors’ experiences of research recruitment: a qualitative exploration using the Theoretical Domains Framework. Prim Health Care Res Dev 2021;22. https://doi.org/10.1017/S1463423621000050.
- Preston NJ, Farquhar MC, Walshe CE, Stevinson C, Ewing G, Calman LA, et al. Strategies designed to help healthcare professionals to recruit participants to research studies. Cochrane Database Syst Rev 2016;2. https://doi.org/10.1002/14651858.MR000036.pub2.
- Rendell JM, Merritt RD, Geddes JR. Incentives and disincentives to participation by clinicians in randomised controlled trials. Cochrane Database Syst Rev 2007;2007. https://doi.org/10.1002/14651858.MR000021.pub3.
- Thompson L. NHS Highland Perinatal and Infant Mental Health Workstream Evaluation. Dublin: World Association of Infant Mental Health Congress; 2023.
- Henderson M, Wittkowski A, McIntosh E, McConnachie A, Buston K, Wilson P, et al. THRIVE Trial Research Team . Trial of healthy relationship initiatives for the very early years (THRIVE), evaluating Enhanced Triple P for Baby and Mellow Bumps additional social and care needs during pregnancy and their infants who are at higher risk of maltreatment: study protocol for a randomised controlled trial. Trials 2019;20. https://doi.org/10.1186/s13063-019-3571-5.
- Scottish Government 2011. www.scotlandscensus.gov.uk/search-the-census#/explore/snapshot (accessed 29 March 2023).
- Hackworth NJ, Matthews J, Westrupp EM, Nguyen C, Phan T, Scicluna A, et al. What influences parental engagement in early intervention? Parent, program and community predictors of enrolment, retention and involvement. Prevent Sci 2018;19:880-93. https://doi.org/10.1007/s11121-018-0897-2.
- Hine RH, Maybery D, Goodyear MJ. Challenges of connectedness in personal recovery for rural mothers with mental illness. Int J Ment Health Nurs 2018;27:672-82. https://doi.org/10.1111/inm.12353.
- Owens JS, Richerson L, Murphy CE, Jagelewski A, Rossi L. The parent perspective: informing the cultural sensitivity of parenting programs in rural communities. Child Youth Care Forum 2007;36:179-94. https://doi.org/10.1007/s10566-007-9041-3.
- Smokowski P, Corona R, Bacallao M, Fortson BL, Marshall KJ, Yaros A. Addressing barriers to recruitment and retention in the implementation of parenting programs: lessons learned for effective program delivery in rural and urban areas. J Child Fam Stud 2018;27:2925-42. https://doi.org/10.1007/s10826-018-1139-8.
- National Institute for Health and Care Research . Improving Inclusion of Under-Served Groups in Clinical Research: Guidance from INCLUDE Project 2020. www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435 (accessed 30 August 2023).
- National Institute for Health and Care Research . Under-Served Communities 2022. www.nihr.ac.uk/about-us/our-key-priorities/under-served-communities.htm (accessed 30 August 2023).
- Scottish Government . Scotland’s Census: Education 2021. www.scotlandscensus.gov.uk/census-results/at-a-glance/education/ (accessed 28 August 2023).
- Brugha T, Bebbington P, Tennant C, Hurry J. The list of threatening experiences: a subset of 12 life event categories with considerable long-term contextual threat. Psychol Med 1985;15:189-94. https://doi.org/10.1017/s003329170002105x.
- Youthinmind . Scoring the Strengths and Difficulties Questionnaire for 2–4 Year Olds 2015. www.sdqinfo.org/py/sdqinfo/c0.py (accessed 4 July 2023).
- Van Hout B, Janssen M, Feng Y, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ 5D 5L: mapping the EQ 5D 5L to EQ 5D 3L value sets. Value Health 2012;15:708-15.
- Hunter RM, Baio G, Butt T, Morris S, Round J, Freemantle N. An educational review of the statistical issues in analysing utility data for cost-utility analysis. PharmacoEconomics 2015;33:355-66.
Appendix 1 Trial recruitment, retention and participant characteristics: full results
This section will include data to address the following questions from the close-down protocol (https://njl-admin.nihr.ac.uk/document/download/2042261; accessed 20 November 2024):
-
Which eligible mothers agree and which decline to participate in the intervention, and what reasons do they give?
-
Which recruitment methods were most effective and was there was any variation in participant characteristics with means of recruitment?
-
======
-
How do sociodemographic characteristics and maternal mental health at baseline relate to:
-
changes in parenting behaviours?
-
maternal mental state at 8 months post recruitment?
-
child development at 30 months, using ASQ rather than Bayley?
-
-
======
-
Are there family characteristics associated with greater adherence to Mellow Babies?
-
Are there family characteristics associated with greater retention to follow-up?
Recruitment
Figure 1 (Consolidated Standards of Reporting Trials diagram) gives details of numbers of participants expressing interest/screened/eligible/recruited to the trial. Of 390 expressions of interest, 179 consented to take part in screening, and 139 of these were eligible for participation. The most common reason for ineligibility was not meeting the HADS threshold criterion (n = 36).
FIGURE 1.
Consolidated Standards of Reporting Trials diagram of recruitment to The Mellow Babies Trial.
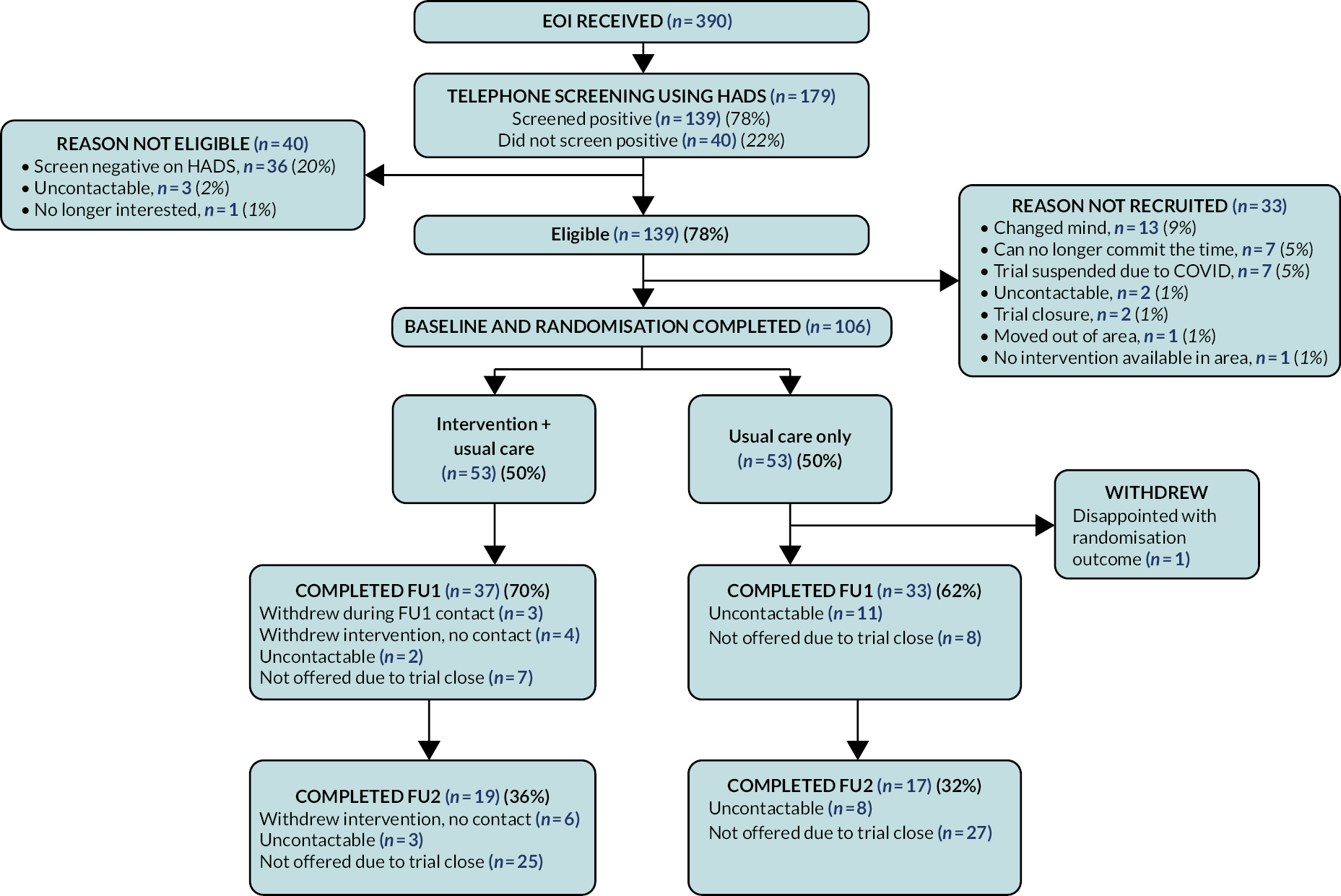
Of those screening negative on the HADS, the median scores were 3 [interquartile range (IQR) 2–5] for Depression and 6 (IQR 3–8) for Anxiety. Scores within this group were fairly evenly spread, with five participants (14%) scoring just below the threshold for Depression and three participants (9%) just below the threshold for Anxiety (Figure 2).
FIGURE 2.
Boxplot of HADS Anxiety and Depression scores among those not meeting screening criteria.
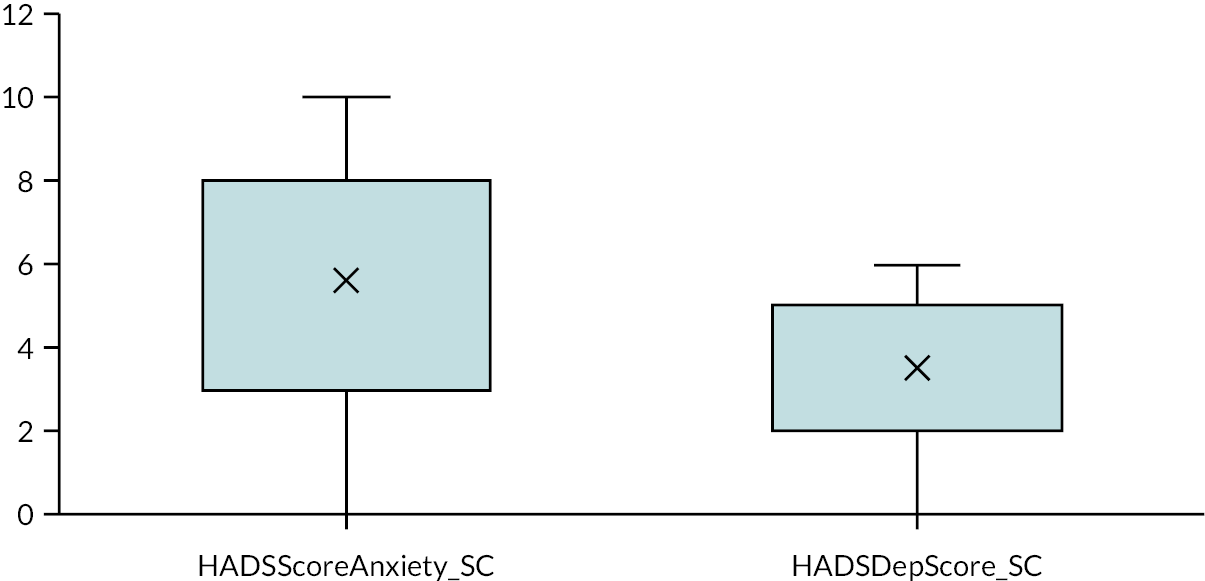
Of those who screened positive, the most effective recruitment strategy by far was PIC letters, resulting in 75 (57%) of eligible participants. While we had anticipated HV referral might be our most successful method, only 26 (20%) of those eligible came from this source. Anecdotally, we understand that HVs were reluctant to refer to a trial where participants had a 50 : 50 chance of receiving an intervention. There were only two referrals from GPs. All other referrals came from social media (n = 19; 14%), the study website (n = 1; 1%) or other forms of self-referral (n = 9; 7%). (Referral source data were not available for 7/139 eligible.) Table 2 shows the proportion eligible per recruitment source and associated median HADS scores. Collapsing the categories and comparing the ‘professional referral’ method (HV or GP) to the others (all ‘self-referral’) made no impact on whether screened as eligible: 90% of ineligible participants were self-referrals versus 79% of those eligible.
| Eligibility criteria met? | HADS anxiety | HADS depression | ||
|---|---|---|---|---|
| Recruitment source | Y, n (%) | N, n (%) | Median (rangea) | Median (rangea) |
| Study website | 1 (33) | 2 (67) | 9 (5–15) | 3 (3–7) |
| Facebook/Instagram | 19 (91) | 2 (9) | 12.3 (6–19) | 9 (1–15) |
| Baby group | 1 (100) | 0 (0) | 11 | 5 |
| Other self-referral | 8 (100) | 0 (0) | 13 (12–20) | 10 (3–16) |
| PIC letter | 75 (70) | 32 (30) | 11 (0–20) | 7 (0–19) |
| HV referral | 27 (87) | 4 (13) | 12 (2–18) | 9 (1–18) |
| GP referral | 2 (100) | 0 (0) | 16 (16–16) | 8.5 (7–10) |
Of those who screened positive but ultimately were not recruited to the trial, the most common reasons were changing their mind (n = 13), no longer being able to commit the time (often due to returning to work after maternity leave) (n = 7), or due to trial recruitment being suspended in March 2020 (n = 7). Only two were uncontactable at this stage, one had left the area, and one chose not to go ahead to baseline visit as there was not going to be an intervention group in her area in the timescale needed. Finally, two participants who had been screened late in 2022 and remained keen to participate ultimately could not due to trial closure.
Demographic characteristics at baseline
Full baseline characteristics for the final sample of 106 are provided in Appendix 5. Key highlights include little ethnic diversity (representative of the region), a high level of education [50 (47%) educated to university level; Scottish national average 26%39], a high level of paid employment (or on maternity leave and planning to return to paid employment) (n = 68, 64%) and a high level of home ownership (n = 55, 52%). Participants ranged from 20 to 46 years of age {mean [standard deviation (SD)] = 32 (5.9)}, and their babies ranged from 5 to 17 months [mean (SD) = 9 (3.7)] at point of screening. About two-thirds of the sample were from relatively affluent areas (i.e. Scottish Index of Multiple Deprivation (SIMD) quintile 3–5), and only 14 (13%) lived in areas classed as remote or very remote rural. See Appendix 5, Table 21 for a full breakdown.
Mental health at baseline
All participants scored above the 85th centile23 on one HADS subscale at screening, and mean scores were 11.7 (SD 4.2) for Hospital Anxiety and Depression Scale – Anxiety subscale (HADS-A) and 7.8 (SD 4.0) for Hospital Anxiety and Depression Scale – Depression subscale (HADS-D). Although 61% stated that they had been diagnosed with a mental illness, much higher proportions (86%/76%/96%) reported experiencing mental ill health before/during/or after pregnancy, respectively. Rates of prescribed medication for mental ill health were 64%/23%/50% before/during/after pregnancy, respectively. The lower rate during pregnancy will likely be due to mothers choosing to cease medication so as not to harm their unborn baby. It is interesting to note that prescription rates did not increase in line with the increased experience of mental ill health postnatally. In a separate question focused on pregnancy, 84% of participants stated they had experienced anxiety or depression during this period (higher than the diagnosed mental illness rate of 61%). See Appendix 5, Table 22 for a full breakdown of responses.
Stressful lives at baseline
Using the Recent Life Events scale,40 with two items added pertaining to child protection (Has a child living in your household been placed on the child protection register or been taken into care?) and homelessness (Have you been homeless?), this sample endorsed relatively few items: the median number of events endorsed was three (IQR = 1–5). Of those who had endorsed life events, most (n = 62, 81%) stated that at least one of these still affected them (median = 2, IQR = 1–4). Regarding the added items, seven participants had been made homeless, with five stating it still affected them; three had experienced a child protection situation within their household, with one stating this still affected them. See Appendix 5, Table 22 for a full breakdown of responses.
Social isolation at baseline
Most participants (84%) were in a relationship at baseline, with all but one stating their partner was the father of their baby. Participants reported good practical and emotional support from partners, although 21 (23%) felt they were less close with their partner since having their baby, and 14 (16%) reporting recent tension, irritability, etc. in their relationship. Reported relationship quality was generally very good, with 81 (91%) stating they enjoyed spending time with their partner. Of some concern was the small number (7) who reported that conflict with their partner had often ‘come close to coming to blows, or worse’, although physical violence was not mentioned in free text comments. With regard to support or advice, family or partner (usually baby’s father) were the most popular sources, with HVs and GPs both being endorsed as an accessible professional source for most. There were very few negative responses to four questions about availability of practical support in the preceding 6 months, with all participants being able to endorse at least one of the four items. See Appendix 5, Table 23 for a full break down of responses.
Retention to follow-up
Of those recruited and randomised (n = 106), the proportions per referral source were similar to the above. Seventy (67%) of those randomised took part in the first follow-up (FU1). One had already withdrawn from the trial prior to FU1 being offered and a further 15 were not offered FU1 due to trial closure. Therefore, of those eligible (n = 90), 78% completed FU1. The reasons for not completing FU1 when eligible are shown in Table 3. Of those completing FU1, there was no significant difference in completion according to whether referred by a clinician or recruited via a self-referral method.
| Reason for non-completion FU1 | N | % |
|---|---|---|
| Uncontactable or aged out | 12 | 67 |
| Withdrew consent for FU1 (but remained in trial) | 3 | 17 |
| Withdrew participation in trial at point of FU1 contact | 3 | 17 |
| Total | 18 | 100 |
Thirty-six (34%) of those randomised took part in the second follow-up (FU2). However, some had withdrawn from the trial prior to FU2 being offered (n = 4, 4%, see Table 3 above) and a further 53 were not offered second follow-up due to the trial closing. Therefore, of those eligible (n = 49), 74% completed FU2. The reasons for not completing FU2 when eligible are shown in Table 4. Of those completing FU2, there was no significant difference in completion according to whether referred by a clinician or recruited via a self-referral method.
| Reason for non-completion FU2 | N | % |
|---|---|---|
| Uncontactable or aged out | 7 | 54 |
| Withdrew consent for FU2 (but remained in trial) | 5 | 38 |
| Withdrew participation in trial at point of FU2 contact | 1 | 8 |
| Total | 13 | 100 |
Full participant characteristics at each stage of follow-up are provided in Appendix 1. Table 5 shows a range of descriptive statistics for those eligible for FU1 or FU2 who did or did not complete that follow-up assessment.
| Completed FU1 | Completed FU2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable at baseline | Yes | No | p | Yes | No | p | ||||
| Study arm n (%) | ||||||||||
| Intervention | 37 | (53) | 16 | (44) | 19 | (54) | 6 | (46) | ||
| Usual care | 33 | (47) | 20 | (56) | 0.41a | 16 | (46) | 7 | (54) | 0.75a |
| Mother’s age, years [mean (SD)] | 32.2 | (5.9) | 31.1 | (5.9) | 0.38b | 31.9 | (5.7) | 32.1 | (4.9) | 0.93b |
| Child’s age, months [mean (SD)] | 9.9 | (3.7) | 8.1 | (3.3) | 0.007b,c | 9.3 | (3.7) | 8.8 | (3.4) | 0.63b |
| SIMD n (%) | ||||||||||
| 1 (most deprived) | 10 | (15) | 8 | (24) | 7 | (21) | 5 | (42) | ||
| 2 | 15 | (22) | 5 | (15) | 6 | (18) | 1 | (8) | ||
| 3 | 11 | (16) | 4 | (12) | 4 | (12) | 2 | (17) | ||
| 4 | 26 | (38) | 15 | (44) | 14 | (41) | 2 | (17) | ||
| 5 (least deprived) | 6 | (9) | 2 | (6) | 0.70a | 3 | (9) | 2 | (17) | 0.38a |
| Rurality n (%) | ||||||||||
| More urban | 48 | (69) | 14 | (78) | 27 | (77) | 10 | (77) | ||
| More rural | 22 | (31) | 4 | (22) | 0.57a | 8 | (23) | 3 | (23) | 0.63a |
| Education n (%) | ||||||||||
| Degree level | 35 | (50) | 7 | (39) | 15 | (43) | 5 | (38) | ||
| Below degree level | 35 | (50) | 11 | (61) | 0.028a | 20 | (57) | 8 | (62) | 0.53a |
| Employment n (%) | ||||||||||
| Currently employed/mat leave | 45 | (64) | 11 | (61) | 22 | (63) | 5 | (38) | ||
| Not employed | 25 | (36) | 7 | (39) | 0.50a | 13 | (37) | 8 | (62) | 0.12a |
| Home ownership n (%) | ||||||||||
| Yes | 37 | (53) | 8 | (44) | 19 | (54) | 4 | (31) | ||
| No | 33 | (47) | 10 | (56) | 0.60a | 16 | (46) | 9 | (69) | 0.13a |
| HADS-A [mean (SD)] | 12.5 | (2.9) | 13.7 | (2.7) | 0.07b | 12.7 | (2.6) | 15.0 | (3.2) | 0.006b,c |
| HADS-D [mean (SD)] | 9.1 | (3.8) | 9.2 | (3.5) | 0.46b | 9.7 | (3.6) | 8.5 | (2.9) | 0.13b |
| Diagnosed mental illness n (%) | ||||||||||
| Yes | 42 | (60) | 15 | (83) | 22 | (63) | 10 | (77) | ||
| No | 28 | (40) | 3 | (17) | 0.05a | 13 | (37) | 3 | (23) | 0.49a |
| Anxiety or depression n (%) | ||||||||||
| Yes | 59 | (84) | 14 | (78) | 31 | (89) | 11 | (85) | ||
| No | 11 | (16) | 4 | (22) | 0.37a | 4 | (11) | 2 | (15) | 0.52a |
| Life events – frequency [mean (SD)] | 3.2 | (2.6) | 3.7 | (2.8) | 0.27b | 3.6 | (2.7) | 3.3 | (3.0) | 0.38b |
| Life events – affect [mean (SD)] | 1.9 | (2.1) | 2.7 | (2.5) | 0.15b | 2.4 | (2.3) | 2.4 | (2.6) | 0.48b |
| Current relationship n (%) | ||||||||||
| Yes | 59 | (84) | 14 | (78) | 29 | (83) | 10 | (77) | ||
| No | 11 | (16) | 4 | (22) | 0.37a | 6 | (17) | 3 | (23) | 0.69a |
| Help in past 6 months n (%) | ||||||||||
| 4 items | 63 | (90) | 11 | (61) | 30 | (86) | 10 | (77) | ||
| 5–7 items | 7 | (10) | 7 | (39) | 0.007a,c | 5 | (14) | 3 | (23) | 0.66a |
There were very few differences in sociodemographic or mental health characteristics at baseline for those who did/did not complete either follow-up assessment. For FU1, the child’s older age at screening and lower level of social support (< 5 items endorsed) were associated with completion. At FU2, only mothers’ higher HADS Anxiety score at screening was associated with non-completion.
Retention in intervention
Thirty-two (60%) of those randomised to the intervention group took part in at least one intervention group session. Six participants were randomised to group 3, but could not participate as the group had to be cancelled due to the COVID-19 pandemic lockdown. Six were randomised to group 7, which did not take place due to trial close-down. A further three stated they could no longer commit the time, due to work or other commitments, one did not want to record a parent–infant interaction video for the intervention, one lived far away and changed her mind, and one changed her mind due to feeling too stressed. For the final three, no reason was recorded.
The groups varied in the specific number of intervention sessions available: only groups 1 and 4 were able to offer the full 14 sessions. Group 2 ended at session 7 due to the onset of the COVID-19 pandemic lockdown restrictions, group 3 could not start for this reason, groups 5 and 6 were curtailed at 10 and 11 sessions, respectively, due to practitioner availability. Group 7 did not take place due to trial close-down. Taking the varying intervention lengths into account, eight participants took part in every intervention session available to them, with 56% attending at least 60% of sessions available to them. Among those who attended any sessions, the mean number of sessions attended was 8 (SD = 3.8), with a wide range of 1–14. Six (19%) left the intervention group prior to week 5, considered a key stage after which few participants tend to drop out.
There were weak associations between attending a lower proportion of available intervention sessions and: higher HADS anxiety at screening (r = −0.39; p = 0.01); older child’s age at screening (r = 0.36; p = 0.02); home ownership (t = 2.2; p = 0.03). There was no systematic association between any other sociodemographic characteristics or mental health variables and retention in the intervention. A more detailed exploration of participant and group characteristics is given in Appendix 3.
Sociodemographic characteristics and maternal mental health at baseline in relation to outcomes at follow-up
Table 6 shows a range of sociodemographic characteristics and mental health measures at baseline according to parenting attitudes and behaviours at each of the three data collection points: baseline, FU1 (8 months post randomisation) and FU2 (child 30 month of age). The PBQ-16 is on the left and activities with child on the right. Looking at the whole sample, mean PBQ-16 scores were low (maximum 80) indicating a good level of post-partum bonding. There was no change from baseline (BL) to FU1 in PBQ-16 scores, and scores increased a little at FU2 (albeit with a smaller and more limited sample). There was no statistically significant change over time. Looking at any differences according to baseline sociodemographic variables, there were few that were statistically significant: mothers who were under 25 at baseline and those who did not own their own home had poorer scores at FU1, and mothers whose babies were over a year old at baseline had poorer scores at FU2.
| PBQ 16, mean (SD) | Activity with child, mean (SD) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BL, n = 103 | FU1, n = 69 | FU2, n = 33 | BL, n = 103 | FU1, n = 68 | FU2, n = 33 | |||||||
| Whole sample | 13.7 | (9.9) | 13.7 | (9.9) | 16.4 | (9.4) | 42.1 | (10.9) | 39.2 | (10.3) | 38.9 | (8.2) |
| Study arm | ||||||||||||
| Intervention | 14.8 | (9.4) | 12.9 | (10.4) | 15.2 | (8.7) | 43.2 | (11.3) | 41.1 | (10.8) | 38.6 | (9.2) |
| Usual care | 12.5 | (10.4) | 14.6 | (11.5) | 17.6 | (10.2) | 40.1 | (10.4) | 37.1 | (9.4) | 39.3 | (7.4) |
| Mother’s age band | ||||||||||||
| < 25 years | 17.9 | (12.5) | 21.9 | (12.6) | 16.8 | (7.0) | 48.0 | (14.9) | 45.7 | (5.5) | 43.6 | (7.7) |
| ≥ 25 years | 13.2 | (9.5) | 12.8 | (9.3)* | 16.3 | (9.8) | 41.4 | (10.2) | 38.5 | (10.5)* | 38.1 | (8.2) |
| Child’s age band | ||||||||||||
| ≤ 365 days | 13.8 | (9.4) | 13.5 | (8.2) | 11.9 | (6.9) | 43.7 | (10.7) | 38.8 | (10.5) | 38.7 | (8.1) |
| > 365 days | 13.5 | (11.3) | 14.0 | (12.5) | 24.2 | (8.0)** | 38.2 | (10.5)* | 39.9 | (10.2) | 39.4 | (8.9) |
| SIMD | ||||||||||||
| 1 (most deprived) | 16.1 | (10.3) | 18.5 | (8.6) | 21.0 | (6.9) | 40.6 | (9.9) | 38.6 | (10.4) | 35.4 | (8.6) |
| 2 | 11.3 | (9.4) | 12.7 | (10.6) | 16.3 | (13.2) | 46.4 | (11.4) | 43.1 | (11.5) | 42.5 | (8.0) |
| 3 | 10.5 | (5.9) | 10.8 | (5.7) | 13.0 | (5.5) | 40.3 | (8.9) | 37.8 | (10.2) | 33.5 | (9.0) |
| 4 | 14.5 | (10.4) | 13.3 | (9.2) | 16.9 | (9.5) | 42.1 | (12.1) | 38.3 | (8.9) | 41.6 | (7.2) |
| 5 (least deprived) | 15.2 | (13.6) | 17.3 | (17.9) | 15.3 | (9.1) | 38.0 | (8.9) | 32.7 | (10.1) | 30.7 | (4.9) |
| Rurality | ||||||||||||
| More urban | 13.3 | (9.8) | 13.7 | (10.8) | 17.0 | (8.4) | 42.3 | (11.5) | 38.3 | (10.6) | 38.5 | (8.0) |
| More rural | 14.6 | (10.3) | 13.8 | (7.9) | 14.7 | (12.0) | 41.5 | (9.5) | 41.3 | (9.4) | 40.1 | (9.2) |
| Education | ||||||||||||
| Degree level | 14.0 | (10.5) | 13.4 | (9.5) | 18.5 | (9.4) | 39.3 | (10.4) | 37.2 | (10.9) | 36.1 | (9.7) |
| Below degree level | 13.4 | (9.5) | 14.0 | (10.4) | 14.6 | (9.3) | 44.5 | (10.8)*** | 41.2 | (9.4) | 41.3 | (6.1)* |
| Employment | ||||||||||||
| Currently employed/mat leave | 14.5 | (10.2) | 12.9 | (9.7) | 14.1 | (6.8) | 40.5 | (10.8) | 37.9 | (9.8) | 36.3 | (8.9) |
| Not employed | 12.4 | (9.4) | 15.1 | (10.3) | 19.9 | (11.8) | 44.7 | (10.7) | 41.5 | (11.0) | 43.0 | (5.2)* |
| Home ownership | ||||||||||||
| Yes | 12.4 | (9.1) | 10.8 | (6.9) | 17.1 | (9.6) | 38.5 | (9.3) | 35.7 | (8.7) | 36.3 | (8.8) |
| No | 15.0 | (10.6) | 17.1 | (11.8)* | 15.6 | (9.3) | 46.2 | (11.2)** | 42.9 | (10.7)*** | 42.1 | (6.4)* |
| Diagnosed mental illness | ||||||||||||
| Yes | 13.9 | (10.3) | 13.0 | (10.6) | 15.1 | (9.0) | 42.8 | (10.8) | 39.0 | (10.0) | 36.6 | (8.3) |
| No | 13.3 | (9.4) | 14.8 | (8.9) | 18.5 | (9.9) | 40.9 | (11.0) | 39.6 | (10.9) | 42.6 | (6.9)* |
| Anxiety or depression | ||||||||||||
| Yes | 14.0 | (10.3) | 13.8 | (10.4) | 15.7 | (8.9) | 43.4 | (10.7) | 40.2 | (10.6) | 39.4 | (8.6) |
| No | 11.9 | (7.5) | 13.5 | (7.5) | 20.4 | (12.2) | 35.4 | (9.6)*** | 33.4 | (6.4)* | 36.4 | (6.3) |
| Current relationship | ||||||||||||
| Yes | 13.0 | (9.1) | 12.7 | (8.1) | 17.0 | (9.3) | 41.6 | (10.7) | 39.1 | (10.6) | 37.5 | (7.7) |
| No | 17.4 | (13.1) | 19.0 | (16.1) | 12.8 | (9.9) | 44.5 | (11.7) | 40.0 | (8.9) | 47.2 | (6.4)* |
| Help in past 6 months | ||||||||||||
| 4 items | 13.0 | (8.7) | 13.0 | (9.6) | 16.7 | (9.3) | 41.2 | (10.4) | 38.7 | (10.5) | 38.6 | (8.6) |
| 5–7 items | 17.9 | (15.1) | 20.0 | (11.7) | 14.3 | (11.0) | 47.1 | (12.8) | 43.6 | (8.3) | 41.3 | (5.7) |
In relation to activities with their child, mean total scores were in the mid-range (maximum 88, with higher scores meaning less activity) and did not seem to change a lot over time, despite the implementation of COVID-19 restrictions for the first 47 in the sample (again, no statistically significant change over time for the whole sample). Significant differences were observed where mothers whose child was over 1 year, those who were educated to degree level or higher, those who owned their own home, and those who did not report previous anxiety or depression at baseline had more activity at that stage of data collection. The association with home ownership remained at both follow-up time points. At FU1 mothers aged 25 or over at baseline and those who did not report previous anxiety or depression reported more activity with their baby/toddler, and at FU2 those educated to degree level or above, those in employment at baseline, those with a diagnosed mental illness at baseline, and those in a relationship at baseline all reported more activity with their baby/toddler.
Mental health at follow-up 1 (8 months post randomisation) in relation to sociodemographic characteristics and mental health at baseline
With reference to Table 7, HADS Anxiety and Depression scores were lower on average at FU1 (9.4 and 6.2, respectively) than at baseline (11.7 and 7.8, respectively), although they were still significantly positively correlated [HADS-A (r = 0.496; p < 0.001) and HADS-D (r = 0.580; p < 0.001)]. Five participants reported a new mental illness since baseline. Although all participants would have scored above the 85th centile on either HADS-A or HADS-D at baseline, only 42% and 39% met these respective thresholds at FU1.
| HADS anxiety | HADS depression | New mental illness (since baseline) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | ≥ 11, n (%) | Mean (SD) | ≥ 7, n (%) | n (%) | ||||||
| Whole sample | 9.4 | (4.2) | 29 | (42) | 6.2 | (4.3) | 27 | (39) | 5 | (7) |
| Study arm | ||||||||||
| Intervention | 9.2 | (4.2) | 15 | (41) | 6.5 | (4.3) | 16 | (43) | 3 | (8) |
| Usual care | 9.8 | (4.2) | 14 | (44) | 5.9 | (4.4) | 11 | (34) | 2 | (6) |
| Mother’s age band | ||||||||||
| < 25 years | 11.6 | (2.2) | 5 | (71) | 10.6 | (4.5) | 5 | (71) | 0 | (0) |
| ≥ 25 years | 9.2 | (4.3) | 24 | (39) | 5.7 | (4.0)* | 22 | (36) | 5 | (8) |
| Child’s age band | ||||||||||
| ≤ 365 days | 9.1 | (4.2) | 17 | (39) | 6.1 | (4.0) | 16 | (36) | 4 | (9) |
| > 365 days | 10.1 | (4.1) | 14 | (48) | 6.4 | (4.9) | 11 | (44) | 1 | (4) |
| SIMD | ||||||||||
| 1 (most deprived) | 10.3 | (3.6) | 5 | (56) | 6.3 | (4.1) | 4 | (44) | 0 | (0) |
| 2 | 9.5 | (4.2) | 5 | (33) | 6.2 | (4.6) | 4 | (27) | 3 | (21) |
| 3 | 8.8 | (5.1) | 4 | (36) | 5.0 | (3.7) | 3 | (27) | 1 | (9) |
| 4 | 9.6 | (3.8) | 12 | (46) | 7.1 | (4.1) | 14 | (54) | 0 | (0) |
| 5 (least deprived) | 7.8 | (5.9) | 2 | (33) | 4.3 | (6.4) | 1 | (17) | 1 | (17) |
| Rurality | ||||||||||
| More urban | 9.5 | (4.3) | 21 | (45) | 6.0 | (4.6) | 18 | (38) | 3 | (6) |
| More rural | 9.4 | (4.0) | 8 | (36) | 6.6 | (3.7) | 9 | (41) | 2 | (9) |
| Education | ||||||||||
| Degree level | 9.03 | 4.041 | 13 | (38) | 5.97 | 3.849 | 13 | (38) | 1 | (3) |
| Below degree level | 9.83 | 4.274 | 16 | (46) | 6.40 | 4.772 | 14 | (40) | 4 | (12) |
| Employment | ||||||||||
| Currently employed/mat leave | 9.2 | (4.3) | 18 | (41) | 6.0 | (4.1) | 16 | (36) | 2 | (7) |
| Not employed | 9.9 | (3.9) | 11 | (44) | 6.6 | (4.7) | 11 | (44) | 2 | (8) |
| Home ownership | ||||||||||
| Yes | 8.4 | (4.0) | 13 | (36) | 5.0 | (3.2) | 11 | (31) | 2 | (6) |
| No | 10.5 | (4.1)** | 16 | (49) | 7.5 | (5.0)** | 16 | (49) | 3 | (9) |
| Current relationship | ||||||||||
| Yes | 9.0 | (4.0) | 22 | (38) | 5.9 | (3.9) | 22 | (38) | 3 | (5) |
| No | 11.6 | (4.6) | 7 | (64) | 7.6 | (6.2) | 5 | (46) | 2 | (18) |
| Help in past 6 months | ||||||||||
| 4 items | 9.32 | 4.246 | 25 | (40) | 6.00 | 4.406 | 23 | (37) | 4 | (7) |
| 5–7 items | 10.43 | 3.259 | 4 | (57) | 7.86 | 3.185 | 4 | (57) | 1 | (14) |
| Diagnosed mental illness (baseline) | ||||||||||
| Yes | 10.6 | (4.0) | 23 | (55) | 5.9 | (4.4) | 16 | (38) | 3 | (8) |
| No | 7.6 | (3.7)* | 6 | (22)* | 6.6 | (4.3) | 11 | (41) | 2 | (7) |
| Anxiety or depression (baseline) | ||||||||||
| Yes | 9.54 | 4.304 | 25 | (42) | 6.25 | 4.393 | 23 | (39) | 5 | (9) |
| No | 8.80 | 3.190 | 4 | (40) | 5.80 | 4.022 | 4 | (40) | 0 | (0) |
There were few associations with sociodemographic characteristics at baseline: for HADS-A those owning their own home had lower scores at FU1 and those without a diagnosed mental illness at baseline had lower scores and were less likely to score above threshold at FU1. For HADS-D, participants aged 25 or older at baseline had lower scores at FU1 as did those owning their own home.
Child development outcomes at follow-up 2 (child reaches 30 months of age) in relation to sociodemographic characteristics and mental health at baseline
Tables 8 and 9 show outcomes on the main developmental measures – the ASQ-3, ASQ-SE2 and Strengths and Difficulties Questionnaire – taken at FU2 (when the child reached 30 months). There were no statistically significant differences between the subgroups on any of these measures, most likely due to the small sample size involved. Of note is that all participants scored above threshold on the ASQ-SE2, indicating that further assessment with a professional may be needed. This is surprising given how few scored above threshold on the ASQ-3, including on the personal-social subscale, and may indicate a specific domain of challenges being faced by this small group.
| ASQ-C | ASQ-GM | ASQ-FM | ASQ-PrSo | ASQ-PeSo | ASQ-SE2 | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean score (SD) | > 22.77, n (%) | Mean score (SD) | > 41.84, n (%) | Mean score (SD) | > 30.16, n (%) | Mean score (SD) | > 24.62, n (%) | Mean score (SD) | > 33.71, n (%) | Mean score (SD) | ‘Refer’a, n (%) | |||||||||||||
| Whole sample | 52.6 | (11.9) | 1 | (3) | 49.6 | (8.9) | 7 | (21) | 44.9 | (14.8) | 6 | (20) | 46.8 | (11.6) | 1 | (3) | 50.0 | (9.0) | 1 | (3) | 131.7 | (24.9) | 33 | (100) |
| Study arm | ||||||||||||||||||||||||
| Intervention | 51.2 | (14.4) | 1 | (6) | 49.7 | (8.9) | 4 | (24) | 46.5 | (14.2) | 3 | (20) | 46.7 | (14.4) | 1 | (7) | 50.9 | (10.3) | 1 | (6) | 132.1 | (22.2) | 17 | (100) |
| Usual care | 54.1 | (8.6) | 0 | (0) | 49.4 | (9.1) | 3 | (19) | 43.3 | (15.8) | 3 | (20) | 46.9 | (8.8) | 0 | (0) | 49.1 | (7.5) | 0 | (0) | 131.3 | (28.3) | 16 | (100) |
| Mother’s age band | ||||||||||||||||||||||||
| < 25 years | 42.0 | (23.1) | 1 | (20) | 51.0 | (8.2) | 0 | (0) | 44.8 | (15.7) | 1 | (20) | 37.4 | (15.8) | 1 | (20) | 47.2 | (8.8) | 0 | (0) | 147.0 | (28.2) | 5 | (100) |
| ≥ 25 years | 54.5 | (8.0) | 0 | (0) | 49.3 | (9.1) | 7 | (25) | 45.0 | (15.0) | 5 | (20) | 48.6 | (10.1) | 0 | (0) | 50.5 | (9.1) | 1 | (4) | 128.9 | (23.8) | 28 | (100) |
| Child’s age band | ||||||||||||||||||||||||
| ≤ 365 days | 52.4 | (14.0) | 1 | (5) | 50.2 | (9.3) | 5 | (24) | 45.4 | (15.1) | 4 | (22) | 47.9 | (12.7) | 1 | (5) | 49.8 | (8.9) | 1 | (5) | 128.1 | (25.9) | 21 | (100) |
| > 365 days | 52.9 | (7.2) | 0 | (0) | 48.3 | (8.3) | 2 | (17) | 44.3 | (15.0) | 2 | (17) | 44.9 | (10.0) | 0 | (0) | 50.5 | (9.5) | 0 | (0) | 137.9 | (22.9) | 12 | (100) |
| SIMD | ||||||||||||||||||||||||
| 1 (most deprived) | 53.0 | (10.4) | 0 | (0) | 44.0 | (2.2) | 1 | (20) | 41.0 | (22.3) | 1 | (25) | 47.5 | (6.5) | 0 | (0) | 49.0 | (5.5) | 0 | (0) | 139.0 | (19.5) | 5 | (100) |
| 2 | 56.7 | (4.1) | 0 | (0) | 53.3 | (5.2) | 0 | (0) | 45.5 | (12.3) | 1 | (17) | 47.0 | (11.9) | 0 | (0) | 48.5 | (10.1) | 0 | (0) | 137.5 | (32.7) | 6 | (100) |
| 3 | 55.0 | (7.1) | 0 | (0) | 53.8 | (12.5) | 1 | (25) | 51.7 | (7.6) | 0 | (0) | 53.8 | (4.8) | 0 | (0) | 50.0 | (10.8) | 0 | (0) | 132.5 | (11.9) | 4 | (100) |
| 4 | 48.2 | (15.9) | 1 | (7) | 48.9 | (9.0) | 4 | (29) | 44.5 | (15.2) | 3 | (23) | 44.4 | (15.1) | 1 | (8) | 50.0 | (10.6) | 1 | (7) | 133.9 | (26.4) | 14 | (100) |
| 5 (least deprived) | 58.3 | (2.9) | 0 | (0) | 55.0 | (5.0) | 0 | (0) | 53.3 | (7.6) | 0 | (0) | 45.3 | (8.1) | 0 | (0) | 51.7 | (2.9) | 0 | (0) | 108.3 | (2.9) | 3 | (100) |
| Rurality | ||||||||||||||||||||||||
| More urban | 51.9 | (13.5) | 1 | (4) | 50.2 | (8.4) | 4 | (17) | 46.7 | (14.2) | 3 | (14) | 44.8 | (12.2) | 1 | (5) | 49.2 | (9.2) | 1 | (4) | 134.6 | (27.0) | 24 | (100) |
| More rural | 54.4 | (5.8) | 0 | (0) | 47.8 | (10.3) | 3 | (33) | 40.9 | (16.3) | 3 | (33) | 51.7 | (9.0) | 0 | (0) | 52.2 | (8.3) | 0 | (0) | 123.9 | (17.3) | 9 | (100) |
| Education | ||||||||||||||||||||||||
| Degree level | 54.7 | (7.2) | 0 | (0) | 46.3 | (8.1) | 5 | (33) | 45.4 | (15.4) | 3 | (21) | 47.0 | (10.5) | 0 | (0) | 51.3 | (6.4) | 0 | (0) | 130.3 | (24.4) | 15 | (100) |
| Below degree level | 50.8 | (14.7) | 1 | (6) | 52.2 | (8.8) | 2 | (11) | 44.5 | (14.8) | 3 | (19) | 46.6 | (12.8) | 1 | (6) | 48.9 | (10.7) | 1 | (4) | 132.8 | (26.0) | 18 | (100) |
| Employment | ||||||||||||||||||||||||
| Currently employed/mat leave | 52.8 | (12.8) | 1 | (5) | 49.3 | (9.1) | 5 | (25) | 46.1 | (13.7) | 3 | (18) | 48.1 | (13.6) | 1 | (6) | 48.8 | (9.2) | 1 | (5) | 131.5 | (24.9) | 20 | (100) |
| Not employed | 52.3 | (10.7) | 0 | (0) | 50.0 | (8.9) | 2 | (15) | 43.4 | (16.6) | 3 | (23) | 44.9 | (8.4) | 0 | (0) | 52.0 | (8.6) | 0 | (0) | 131.9 | (25.9) | 13 | (100) |
| Home ownership | ||||||||||||||||||||||||
| Yes | 55.3 | (6.7) | 0 | (0) | 48.3 | (8.7) | 5 | (28) | 47.8 | (12.4) | 2 | (12) | 48.4 | (10.1) | 0 | (0) | 51.1 | (6.1) | 0 | (0) | 127.8 | (23.9) | 18 | (100) |
| No | 49.3 | (15.7) | 1 | (7) | 51.0 | (9.1) | 2 | (13) | 41.2 | (17.3) | 4 | (31) | 44.8 | (13.3) | 1 | (7) | 48.7 | (11.6) | 1 | (7) | 136.3 | (26.2) | 15 | (100) |
| Current relationship | ||||||||||||||||||||||||
| Yes | 52.3 | (12.2) | 1 | (4) | 49.1 | (8.9) | 6 | (21) | 44.0 | (15.0) | 6 | (22) | 45.9 | (11.8) | 1 | (4) | 51.4 | (6.7) | 0 | (0) | 129.5 | (24.8) | 28 | (100) |
| No | 54.0 | (10.8) | 0 | (0) | 52.0 | (9.1) | 1 | (20) | 53.3 | (11.6) | 0 | (0) | 53.0 | (8.7) | 0 | (0) | 42.2 | (15.9) | 1 | (20) | 144.0 | (24.3) | 5 | (100) |
| Help in past 6 months | ||||||||||||||||||||||||
| 4 items | 54.1 | (8.9) | 0 | (0) | 49.8 | (9.3) | 7 | (24) | 46.3 | (12.9) | 4 | (15) | 48.0 | (9.7) | 0 | (0) | 50.9 | (8.9) | 1 | (3) | 130.0 | (25.0) | 29 | (100) |
| 5–7 items | 41.3 | (23.9) | 1 | (25) | 47.5 | (5.0) | 0 | (0) | 36.0 | (24.7) | 2 | (50) | 38.8 | (21.0) | 1 | (25) | 43.8 | (7.5) | 0 | (0) | 143.8 | (24.3) | 4 | (100) |
| Diagnosed mental illness (baseline) | ||||||||||||||||||||||||
| Yes | 54.3 | (12.2) | 1 | (5) | 48.5 | (9.6) | 5 | (25) | 47.2 | (12.0) | 2 | (11) | 47.0 | (12.9) | 1 | (6) | 49.5 | (10.1) | 1 | (5) | 127.8 | (24.4) | 20 | (100) |
| No | 50.0 | (11.4) | 0 | (0) | 51.2 | (7.7) | 2 | (15) | 41.5 | (18.3) | 4 | (33) | 46.5 | (10.1) | 0 | (0) | 50.9 | (7.1) | 0 | (0) | 137.7 | (25.5) | 13 | (100) |
| Anxiety or depression (baseline) | ||||||||||||||||||||||||
| Yes | 53.2 | (12.3) | 1 | (4) | 49.6 | (8.8) | 5 | (18) | 44.5 | (14.8) | 5 | (20) | 47.3 | (11.9) | 1 | (4) | 50.2 | (9.1) | 1 | (4) | 129.1 | (24.0) | 28 | (100) |
| No | 49.0 | (9.6) | 0 | (0) | 49.0 | (10.2) | 2 | (40) | 47.0 | (16.4) | 1 | (20) | 44.0 | (10.8) | 0 | (0) | 49.0 | (8.9) | 0 | (0) | 146.0 | (27.7) | 5 | (100) |
| SDQ-emotion | SDQ-conduct | SDQ-hyperactivity | SDQ-peer relationships | SDQ-prosocial | SDQ-total difficulties | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean score (SD) | > 2, n (%) | Mean score (SD) | > 3, n (%) | Mean score (SD) | > 5, n (%) | Mean score (SD) | > 2, n (%) | Mean score (SD) | < 7, n (%) | Mean score (SD) | > 12, n (%) | |||||||||||||
| Whole sample | 1.69 | (1.5) | 6 | (17) | 2.8 | (1.6) | 12 | (34) | 4.3 | (2.6) | 10 | (29) | 2.2 | (1.8) | 14 | (40) | 7.3 | (1.8) | 11 | (31) | 11.0 | (5.3) | 14 | (40) |
| Study arm | ||||||||||||||||||||||||
| Intervention | 1.8 | (1.6) | 3 | (17) | 2.7 | (2.0) | 7 | (39) | 4.1 | (2.9) | 5 | (28) | 2.2 | (1.5) | 8 | (44) | 6.9 | (1.9) | 7 | (39) | 10.8 | (6.1) | 8 | (44) |
| Usual care | 1.6 | (1.4) | 3 | (18) | 2.9 | (1.2) | 5 | (29) | 4.5 | (2.2) | 5 | (29) | 2.2 | (2.0) | 6 | (35) | 7.8 | (1.7) | 4 | (24) | 11.2 | (4.5) | 6 | (35) |
| Mother’s age band | ||||||||||||||||||||||||
| < 25 years | 1.8 | (0.8) | 1 | (20) | 3.6 | (1.8) | 2 | (40) | 6.6 | (2.7) | 4 | (80) | 3.2 | (1.9) | 4 | (80) | 6.4 | (2.6) | 3 | (60) | 15.2 | (5.8) | 4 | (80) |
| ≥ 25 years | 1.7 | (1.6) | 5 | (17) | 2.7 | (1.6) | 10 | (33) | 3.9 | (2.4)* | 6 | (20)* | 2.0 | (1.7) | 10 | (33) | 7.5 | (1.7) | 8 | (27) | 10.3 | (4.9) | 10 | (33) |
| Child’s age band | ||||||||||||||||||||||||
| ≤ 365 days | 1.8 | (1.8) | 5 | (22) | 2.7 | (1.8) | 9 | (39) | 4.9 | (2.5) | 8 | (35) | 2.2 | (1.8) | 10 | (44) | 7.2 | (2.0) | 8 | (35) | 11.7 | (5.6) | 10 | (44) |
| > 365 days | 1.4 | (0.9) | 1 | (8) | 2.9 | (1.2) | 3 | (25) | 3.2 | (2.3)* | 2 | (17) | 2.1 | (1.7) | 4 | (33) | 7.6 | (1.4) | 3 | (25) | 9.6 | (4.6) | 4 | (33) |
| SIMD | ||||||||||||||||||||||||
| 1 (most deprived) | 2.3 | (2.4) | 3 | (43) | 2.6 | (1.3) | 1 | (14) | 6.0 | (1.9) | 4 | (57) | 2.4 | (1.6) | 3 | (43) | 8.0 | (1.7) | 1 | (14) | 13.3 | (4.6) | 4 | (57) |
| 2 | 1.2 | (0.8) | 0 | (0) | 2.7 | (1.8) | 3 | (50) | 3.3 | (1.6) | 0 | (0) | 1.8 | (2.2) | 2 | (33) | 8.0 | (1.8) | 1 | (17) | 9.0 | (5.1) | 2 | (33) |
| 3 | 1.0 | (0) | 0 | (0) | 2.0 | (1.0) | 0 | (0) | 4.2 | (2.5) | 1 | (20) | 1.6 | (1.1) | 1 | (20) | 7.6 | (1.5) | 1 | (20) | 8.8 | (2.6) | 1 | (20) |
| 4 | 1.6 | (1.0) | 2 | (14) | 3.1 | (2.0) | 6 | (43) | 4.2 | (3.0) | 5 | (36) | 2.5 | (1.9) | 7 | (50) | 6.7 | (2.0) | 6 | (43) | 11.4 | (6.2) | 6 | (43) |
| 5 (least deprived) | 1.5 | (0.7) | 0 | (0) | 3.5 | (0.7) | 1 | (50) | 2.5 | (3.5) | 0 | (0) | 0.5 | (0.7) | 0 | (0) | 6.0 | (0) | 2 | (100) | 8.0 | (4.3) | 0 | (0) |
| Rurality | ||||||||||||||||||||||||
| More urban | 1.6 | (1.5) | 5 | (19) | 3.0 | (1.6) | 10 | (39) | 4.6 | (2.7) | 9 | (35) | 2.0 | (1.8) | 10 | (39) | 7.4 | (1.8) | 9 | (35) | 11.2 | (5.4) | 11 | (42) |
| More rural | 1.9 | (1.7) | 1 | (11) | 2.1 | (1.5) | 2 | (22) | 3.6 | (2.2) | 1 | (11) | 2.7 | (1.7) | 4 | (44) | 7.3 | (2.0) | 2 | (22) | 10.2 | (5.1) | 3 | (33) |
| Education | ||||||||||||||||||||||||
| Degree level | 2.2 | (1.9) | 3 | (20) | 2.8 | (1.6) | 6 | (40) | 4.5 | (2.6) | 4 | (27) | 2.5 | (1.6) | 6 | (40) | 7.3 | (1.5) | 4 | (27) | 12.1 | (4.8) | 6 | (40) |
| Below degree level | 1.3 | (1.0) | 3 | (15) | 2.8 | (1.7) | 6 | (30) | 4.2 | (2.6) | 6 | (30) | 1.9 | (1.9) | 8 | (40) | 7.4 | (2.1) | 7 | (35) | 10.2 | (5.6) | 8 | (40) |
| Employment | ||||||||||||||||||||||||
| Currently employed/mat leave | 1.6 | (1.6) | 4 | (18) | 2.6 | (1.9) | 8 | (36) | 4.4 | (2.8) | 7 | (32) | 1.9 | (1.6) | 7 | (32) | 7.2 | (2.1) | 8 | (36) | 10.6 | (5.7) | 8 | (36) |
| Not employed | 1.9 | (1.4) | 2 | (15) | 3.1 | (1.0) | 4 | (31) | 4.2 | (2.2) | 3 | (23) | 2.5 | (2.1) | 7 | (54) | 7.5 | (1.3) | 3 | (23) | 11.7 | (4.7) | 6 | (46) |
| Home ownership | ||||||||||||||||||||||||
| Yes | 1.7 | (1.6) | 3 | (16) | 2.3 | (1.6) | 5 | (26) | 3.7 | (2.7) | 4 | (21) | 2.1 | (1.6) | 6 | (32) | 7.2 | (1.8) | 6 | (32) | 9.8 | (5.2) | 5 | (26) |
| No | 1.7 | (1.5) | 3 | (19) | 3.4 | (1.4)* | 7 | (44) | 5.0 | (2.3) | 6 | (38) | 2.3 | (2.0) | 8 | (50) | 7.5 | (1.9) | 5 | (31) | 12.4 | (5.2) | 9 | (56) |
| Current relationship | ||||||||||||||||||||||||
| Yes | 1.8 | (1.5) | 5 | (17) | 2.7 | (1.6) | 10 | (35) | 4.3 | (2.7) | 9 | (31) | 2.5 | (1.7) | 14 | (48) | 7.3 | (1.9) | 9 | (31) | 11.2 | (5.4) | 12 | (41) |
| No | 1.3 | (1.9) | 1 | (17) | 3.5 | (1.8) | 2 | (33) | 4.2 | (1.7) | 1 | (17) | 0.7 | (0.8)** | 0 | (0) | 7.3 | (1.6) | 2 | (33) | 9.7 | (4.9) | 2 | (33) |
| Help in past 6 months | ||||||||||||||||||||||||
| 4 items | 1.7 | (1.5) | 4 | (13) | 2.8 | (1.6) | 11 | (37) | 4.0 | (2.6) | 7 | (23) | 2.1 | (1.7) | 11 | (37) | 7.2 | (1.6) | 10 | (33) | 10.6 | (5.0) | 11 | (37) |
| 5–7 items | 1.4 | (1.5) | 2 | (40) | 2.8 | (1.9) | 1 | (20) | 6.0 | (2.2) | 3 | (60) | 2.8 | (2.2) | 3 | (60) | 8.0 | (2.8) | 1 | (20) | 13.0 | (7.1) | 3 | (60) |
| Diagnosed mental illness (baseline) | ||||||||||||||||||||||||
| Yes | 1.8 | (1.8) | 5 | (23) | 2.8 | (1.8) | 9 | (41) | 4.6 | (2.6) | 7 | (32) | 1.9 | (1.5) | 7 | (32) | 7.5 | (2.1) | 7 | (32) | 11.1 | (5.4) | 9 | (41) |
| No | 1.5 | (0.8) | 1 | (8) | 2.9 | (1.3) | 3 | (23) | 3.8 | (2.6) | 3 | (23) | 2.6 | (2.2) | 7 | (54) | 7.1 | (1.3) | 4 | (31) | 10.8 | (5.2) | 5 | (39) |
| Anxiety or depression (baseline) | ||||||||||||||||||||||||
| Yes | 1.8 | (1.6) | 6 | (20) | 2.8 | (1.7) | 11 | (37) | 4.2 | (2.6) | 8 | (27) | 2.1 | (1.6) | 12 | (40) | 7.4 | (1.8) | 9 | (30) | 10.8 | (5.4) | 12 | (40) |
| No | 1.0 | (0.7) | 0 | (0) | 3.0 | (0.7) | 1 | (20) | 5.0 | (2.8) | 2 | (40) | 2.8 | (2.6) | 2 | (40) | 7.2 | (1.9) | 2 | (40) | 11.8 | (4.8) | 2 | (40) |
Strengths and Difficulties Questionnaire subscale and total mean scores were relatively low, with 40% scoring above threshold (i.e. above the ‘close to average’ category41). There were few significant differences by the various subgroups: children of mothers aged 25 or older at baseline had lower scores on hyperactivity/inattention, and were less likely to score above threshold. Significantly lower hyperactivity/inattention scores were also observed where children were at least a year old at baseline, but they were not less likely to score above threshold. Mothers in a relationship at baseline had children with significantly higher scores on peer relationship problems at FU2. As with the previous section, the lack of significant subgroup differences is most likely due to the small sample size for this data collection point.
Finally, Sure Start Language Measure (SSLM) data are shown in Table 10 and Figure 3. Note that these were based on a smaller range of words than usual: the first 10 words were omitted in error from the data capturing system for those pre COVID; these were captured only for a small subset of participants (those recruited post COVID), so they were omitted from analysis: the highest possible total was 40 words. Not surprisingly, the number of words being spoken by children was much lower at FU1, when children were younger, than at FU2, when all were around 2.5 years old. There were no significant associations between SSLM scores and any of the sociodemographic characteristics or mental health measures featured in the other subgroup descriptive analysis, with the exception of maternal education, suggesting a trend towards those children with mothers having education at degree level or above speaking more words at FU2 [mean (SD) < degree = 28 (13.6); degree + = 34.8 (8.1) (t = 31.8; p = 0.04)]. Most children at FU2 were producing two-word utterances.
| Number of words | Two-word utterances | ||||
|---|---|---|---|---|---|
| Mean (SD) | n (%) | ||||
| FU1 | 9.3 | (10.2) | Often | 16 | (24) |
| Sometimes | 15 | (22) | |||
| Not at all | 37 | (54) | |||
| Missing | 2 | ||||
| FU2 | 31.0 | (11.9) | Often | 32 | (89) |
| Sometimes | 3 | (8) | |||
| Not at all | 1 | (3) | |||
| Missing | 0 | ||||
FIGURE 3.
Boxplot showing distribution of SSLM scores at FU1 and FU2.
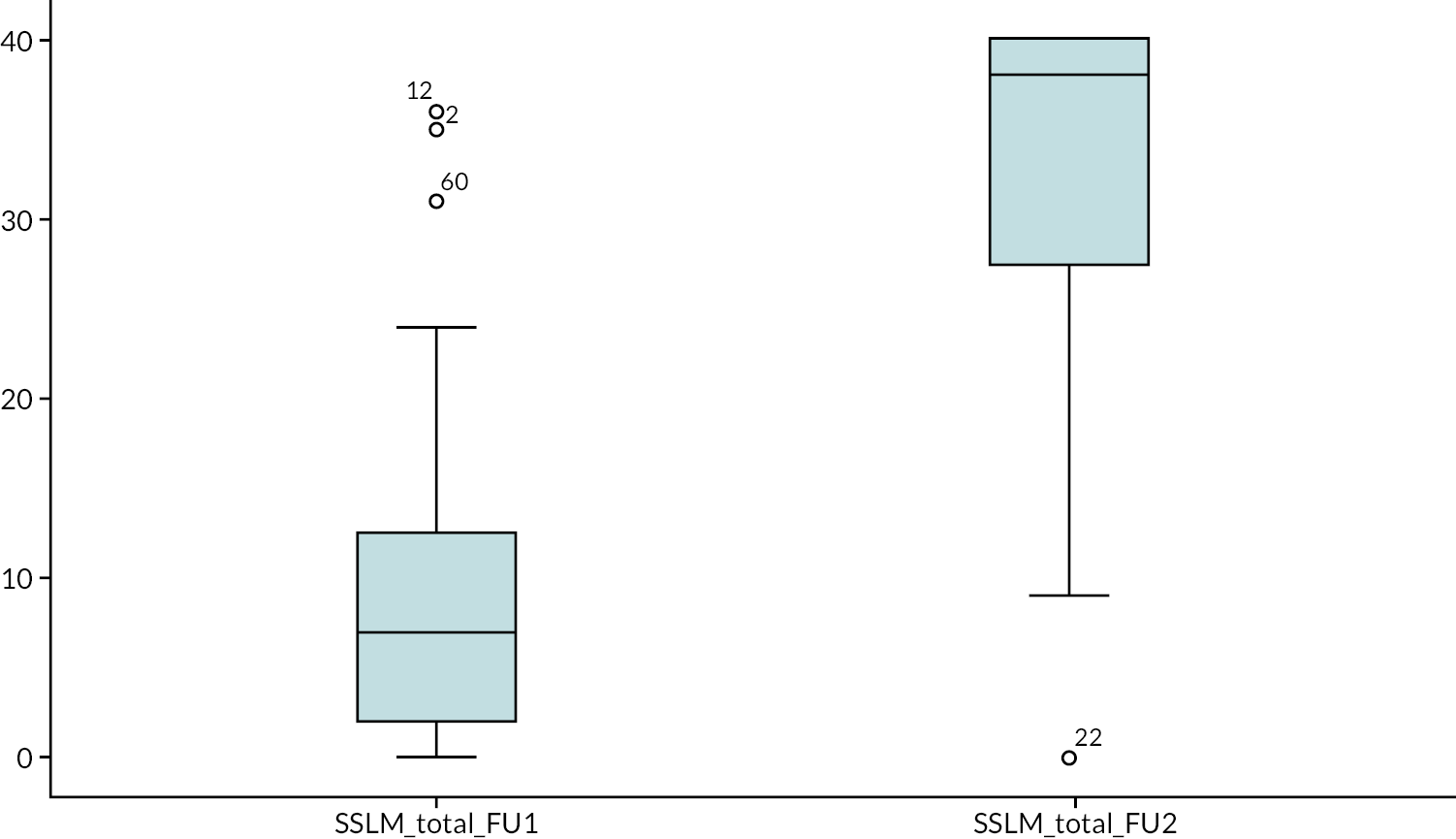
Discussion
Overall, there was a lack of variation across key sociodemographic characteristics or mental health measures for this participant group. It is noteworthy that, although the majority of participants were ‘doing well’ in relation to sociodemographic characteristics such as employment status, socioeconomic deprivation, relationship status and social support, there were still significant levels of mental ill health. Future studies should take care to focus on the specific issues being faced by families rather than exclusively using sociodemographic characteristics as a proxy measure for likely level of need. We have also demonstrated that it is possible to recruit and retain a good proportion of participants even when they are experiencing mental ill health. The reasons for this include the direct approach to participants in tandem with asking practitioners to refer participants/flag up the trial to mothers in their care. Our process evaluation and anecdotal experience of those carrying out liaison with recruiting practitioners suggest that HVs often saw randomisation as a barrier – while they were keen to refer mothers to the interventions, they were often reluctant to do so out of risk that the mother be disappointed/disadvantaged at being randomised to usual care only. Our experience of using the PIC letter system is that mothers were more than willing to put themselves forward and were both understanding and accepting of the randomisation element and what this involved. Many expressed a desire to help with the research, regardless of the individual impact on themselves and their family.
Another factor we would suggest was key in retention of participants was that the trial adopted the ethos of the Mellow Parenting approach – to be nurturing and to meet participants where they are, within the boundaries of the trial methodology. This included being more generous with the number of phone calls or other attempts to contact before deciding a participant was ‘uncontactable’ and that attempts to contact should cease. It was usual to only cease attempts to contact once the child had ‘aged out’ of the eligibility criterion for the study. We also kept an active social media presence (Facebook and Instagram) posting weekly images intended to inspire and show understanding of the challenges being faced by mothers of young children, especially during COVID-19 restrictions. Participants’ children were sent birthday cards and a small gift on their first and second birthdays, which we received positive feedback for. The staff who were responsible for recruitment of participants and those delivering the intervention were carefully selected for their experience and warm manner in working with this participant group.
This analysis also showed little association between any of the sociodemographic characteristics and mental health indicators at baseline and outcomes at either of the follow-up points. While there appears to be a direct relationship between relative affluence and taking part in a wider range of activities more frequently with their child, there are few direct associations on other measures.
Appendix 2 Characterising use of other services during trial participation
This section will include data to address the following questions from the close-down protocol (https://njl-admin.nihr.ac.uk/document/download/2042261; accessed 20 November 2024):
4. What is the nature of usual care offered to participants?
It will also describe baseline and follow-up sample characteristics in terms of quality of life and service use.
Introduction
The Mellow Babies trial closed before reaching its recruitment target of 212 participants. As a result of this closure, the proposed economic analysis, as described in the study protocol, was no longer considered appropriate. In agreement with the funder, the health economic analysis for Mellow Babies comprised:
-
Descriptive statistics for quality-of-life measures at baseline, 8 months, and where available, 30-month time points.
-
Descriptive statistics on completion rates and overall resource use by participants at 8 months and, where available, 30 months. Resource use is presented by service (e.g. primary care, secondary care, mental health services, etc.) and presented as number/type of attendances. Where available, we also describe out of pocket costs reported by participants.
-
We also examined correlations between resource use, quality-of-life measures and other outcomes where data were available.
All data were presented as summary statistics. This includes EQ-5D-5L and EQ-5D-VAS administered at baseline, 8 months post randomisation and 30 months of age as well as participant use of health services at 8 months post randomisation and 30 months of age.
Methods
Health service utilisation
A bespoke PCQ was developed to capture health care resource use over the duration of the trial. This was collected at two time points: 8 months post randomisation and again once the participant’s baby reached 30 months of age. For the 8-month post-randomisation questionnaire, the recall period was 8 months. For the PQC completed when the baby reached 30 months of age, the recall period was bespoke to each participant as the timing of this questionnaire was dictated by the age of the child at study entry. For both PCQs, the participants were asked about the health care services they had accessed during this period specifically in relation to their own anxiety/depression or concerns about their child’s development. This included primary care resource use:
-
number of HV appointments (remote or in person)
-
number of GP appointments (remote or in person)
-
number of nurse appointments (remote or in person)
-
access to early years services
-
number of prescription medications
-
purchase of over-the-counter medication.
Secondary care resource use:
-
number of visits to a paediatrician
-
number of visits to a mental health specialist
-
use of Emergency services.
Mean values and standard deviations for health service use by healthcare practitioner and sector (Primary/Secondary care) were reported for 8- and 30-month time points.
Any additional costs (e.g. out of pocket costs) reported by participants were summarised in tabular form.
Health-related quality of life
Health-related quality of life was measured by the EQ-5D-5L completed at baseline, 8 months post randomisation and when the child reached 30 months of age. The EQ-5D-5L contains the EQ-5D descriptive system and the visual analogue scale (VAS). The descriptive system has five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). In line with current National Institute forsented by service (e.g. primary care, secondary Health and Care Excellence (NICE, 2019) guidelines a crosswalk algorithm was used to map responses onto the EQ-5D-3L value set to generate health state utility values at each time point for each participant using the mapping function recommended by NICE. 42
Quality-adjusted life-years
Quality-adjusted life-years (QALYs) were estimated at 8 months using the area under the curve method. 43 Due to limited sample size and bespoke recall period, QALYs were not estimated using EQ-5D-5L completed when the child was 30 months old.
All data were analysed using Stata version 16 (StataCorp, 2019) (StataCorp LP, College Station, TX, USA).
Treatment of missing data
Where participants did not provide any information about visiting a particular health professional, this was considered to be missing. Where participants had reported that they had visited a health professional but not reported a number of visits, this was also considered missing.
Where participants reported a number of visits but reported not visiting the health professional, or not completing this question, the assumption was made was that the question was incorrectly answered and the number of appointments reported was used in the analysis.
Incorrect reference period on questionnaires
The first 20 participants to reach the 30-month time point received a PCQ which asked about health care utilisation in the previous 30 months or since their baby was born rather than the bespoke period intended.
Correlation between resource use and quality of life
Given the limited data in terms of both sample size and the number of participants accessing health services, this analysis was not undertaken.
Results
Response rates
The response rates for the participant completed health economics questionnaires are shown in Table 11. Response rates for the EQ-5D-5L at base line, 8 months and 30 months were high, with 100% of participants completing baseline and 8-month questionnaires (106 of 106 participants/70 of 70 participants who reached these study time points) and 92% completing at 30 months (33 of 36 participants who reached this time point). PCQs which captured use of health services at 8- and 30-month time points also had high response rates. At 8 months, 93% of participants (65 of 70 participants) completed this questionnaire, reducing to 86% (31 of 36 participants) at 30 months of age.
| Time point | Participants | EQ-5D questionnaires completed (%) | Service Use Questionnaires completed (%) |
|---|---|---|---|
| Baseline | 106 | 106 (100) | (Not given out at baseline) |
| 8 months | 70 | 70 (100) | 65 (93%) |
| 30 months | 36 | 33 (92) | 31 (86%) |
Item non-response
EuroQol-5 Dimensions, five-level version
No data points were missing for EQ-5D-5L at BL, 8- or 30-month time points.
Participant Cost Questionnaire
Table 12 details the item non-response rates for the PCQ. Low levels of missing data are observed across all data points and most categories. Participants were considered to have missing data if they did not fully complete a question; the highest levels of missing data appear in reporting of prescription medication with 21.5% and 35.5% of respondents not completing this question at 8-month post randomisation and 30 months of age time points, respectively. While some participants did not provide any data for specific services, others indicated that they had used a service but did not report level/cost of use. Mean values of service use reported are based on respondents who provided complete data for these questions, that is data were not imputed. However, if participants had reported use of a service but had not indicated a number of visits/uses, these data were included in our summary.
| Item | Participants with missing data at 8 months (n = 65) (%) | Participants with missing data at 30 months (n = 31) (%) |
|---|---|---|
| HV appointments | 2 (3.1) | 1 (3.2) |
| GP appointments | 0 (0) | 5 (16.1) |
| Nurse appointments | 1 (1.5) | 1 (3.2) |
| Paediatrician appointments | 4 (6.2) | 3 (9.7) |
| Use of mental health services | 8 12.3) | 2 (6.4) |
| Use of emergency services | 4 (6.2) | 1 (3.2) |
| Use of early years services | 4 (6.2) | 4 (12.9) |
| Use of prescription medication | 14 (21.5) | 11 (35.5) |
| Use of over-the-counter medication | 4 (6.2) | 3 (9.7) |
EuroQol-5 Dimensions, five-level version scores
EQ-5D-5L utility values and VAS scores at BL, 8 months post randomisation and 30 months of age alongside QALYs at 8 months are shown in Table 13. For EQ-5D-5L, a score of 1 is equivalent to full health and death is scored as 0. At baseline, the mean level of utility was 0.77 across both arms of the trial. At 8 months, the mean level of utility was 0.82 and at 30 months the mean level of utility was 0.79. Corresponding VAS scores, measured on a 0–100 scale, were 69.8, 73.2 and 71.2 at each time point, respectively.
| Time point | Mean EQ-5D index (95% CI) | Mean EQ-5D-5L VAS (95% CI) | Mean QALY (95% CI) |
|---|---|---|---|
| Baseline (n = 106) | 0.77 (0.74 to 0.80) | 69.8 (66.3 to 73.2) | – |
| 8 months (n = 70) | 0.82 (0.78 to 0.86) | 73.2 (68.9 to 77.6) | 0.54 (0.52 to 0.56) |
| 30 months (n = 33) | 0.79 (0.71 to 0.88) | 71.2 (65.4 to 76.9) | – |
Quality-adjusted life-years
Also shown in Table 13 is the mean accumulated QALYs at 8 months. Across both arms of the trial, mean accumulated QALYs at 8 months were 0.54. Given the limited sample size and bespoke recall period, no QALY data are reported at the 30-month time point.
Participant Cost Questionnaire: use of services
Use of primary and secondary healthcare services at 8 months is shown in Tables 14 and 15, respectively. Table 16 describes participants’ use of prescription and over-the-counter medication at 8 months. There were generally low levels of primary care resource use reported. Out of 65 participants who returned this questionnaire, 19 participants in total reported contact with a HV. More participants (26/65) reported contact with their GP either by phone, in person or home consultation. Only four participants reported seeing a nurse, and nine participants reported accessing early years services.
| Healthcare professional | Total number of participants reporting contact with health professional (n) | Number of participants reporting phone consultation (n) | Average number of phone consultations: mean (SD) | Number of participants reporting visiting healthcare professional (n) | Mean visits (SD) | Number of participants reporting home visits (n) | Mean home visits (SD) |
|---|---|---|---|---|---|---|---|
| HV | 19 | N/A | N/A | 2 | 9 (11.3) | 16 | 2.4 (2.2) |
| GP | 26 | 12 | 2.0 (2.0) | 19 | 2.2 (1.4) | 1 | 1 (–) |
| Nurse | 4 | 1 | 2 (–) | 1 | 8 (–) | 2 | 2.5 (2.1) |
| Early years service | 9 | N/A | N/A | 4 | 9.8 (14.9) | 4 | 9.5 (15.0) |
| Health service | Number of participants reporting use | Average visits: mean (SD) |
|---|---|---|
| Paediatrician | 8 | 5.3 (5.9) |
| Mental health specialist | 22 | 7.9 (6.4) |
| Emergency services | 3 | 1 (–) |
| Medication | Number of participants reporting access | Number of times prescribed: mean (SD) | Cost to participant in £: mean (SD) |
|---|---|---|---|
| Prescription medication | 27 | 4.6 (4.14) | N/A |
| Over-the-counter medication | 6 | N/A | 11 (1.4) |
Secondary care resource use was also low at 8 months. Eight participants out of 65 reported seeing a paediatrician over this time period. Mental health specialist services were accessed by 22 participants, with one average 8 visits per participant. Prescription medication use was reported by 27 individuals during this time period.
Tables 17 and 18 show participants’ use of primary and secondary care at 30 months and Table 19 describes medication use at 30 months.
| Healthcare professional | Total number of participants reporting contact with health professional (n) | Number of participants reporting phone consultation (n) | Average number of phone consultations: mean (SD) | Number of participants reporting visiting healthcare professional (n) | Mean visits (SD) | Number of participants reporting home visits (n) | Mean home visits (SD) |
|---|---|---|---|---|---|---|---|
| HV | 10 | N/A | N/A | 0 | – | 9 | 9.1 (11.9) |
| GP | 16 | 5 | 2.8 (1.8) | 8 | 2.5 (0.5) | 1 | 2 (–) |
| Nurse | 2 | 0 | – | 1 | 8 (–) | 0 | – |
| Early years service | 8 | N/A | N/A | 2 | 7 (7.1) | 2 | 14 (15.6) |
| Health service | Number of participants reporting use | Average visits: mean (SD) |
|---|---|---|
| Paediatrician | 5 | 1.5 (0.7) |
| Mental health specialist | 10 | 6.8 (5.8) |
| Emergency services | 1 | 1 (–) |
| Medication | Number of participants reporting access | Number of times prescribed | Cost to participant |
|---|---|---|---|
| Prescription medication | 14 | 1.7 (1.2) | N/A |
| Over-the-counter medication | 4 | N/A | 10 (–) |
At the 30-month time period, 10/31 participants reported contact with a HV. More participants (16/31) reported contact with their GP either by phone, in person or home consultation. Only two participants reported seeing a nurse, and eight participants reported accessing early years services.
Secondary care resource use was also low at 30 months. Five participants reported seeing a paediatrician over this time period. Mental health specialist services were accessed by 10 participants. Prescription medication use was reported by 14 individuals during this time period.
Additional costs
Over the two time points at which the PCQ was administered, six participants reported use of additional services relating to mental health concerns. These included: Samaritans, mother and baby groups, women’s aid services, apps and mental health specialist services. Only one participant reported a cost of £500 for visits to a mental health specialist.
Discussion
Due to the closure of the trial, the data analysis has been limited to the description of response rates and summary statistics. At the request of the funder and due to the limited data, this has been presented across both arms of the trial. No data on either costs or cost-effectiveness of the intervention are presented. There are a number of points worth noting. Firstly, the response rates to the EQ-5D-5L and PCQ were high, with no missing item data for EQ-5D and very limited missing data for the PCQ. This suggests that both questionnaires were appropriate in this population and respondent burden was not an issue. In addition, in a future trial a simplified PCQ may be appropriate given few participants reported accessing NHS or other services during the trial. While we did not report EQ-5D data by arm of the trial, but rather overall summary statistics, on average, these scores increase at the 8-month time point, but then decrease at the 30-month time point although remaining above baseline scores.
Conclusion
Results suggest that data collection tools used in Mellow Babies were appropriate. Further research is needed to determine the cost-effectiveness of the Mellow Babies intervention.
References
-
Position Statement on Use of the EQ-5D-5L Value Set for England (updated October 2019). NICE; 2020. URL: www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l (accessed 10 March 2020).
-
Van Hout B, Janssen M, Feng Y, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ 5D 5L: mapping the EQ 5D 5L to EQ 5D 3L value sets. Value Health 2012;15:708–15.
-
Hunter RM, Baio G, Butt T, Morris S, Round J, Freemantle N. An educational review of the statistical issues in analysing utility data for cost-utility analysis. PharmacoEconomics 2015;33:355–66.
Appendix 3 Intervention participants: characteristics, cohesion and process: full results
This section will include data to address the following questions from the close-down protocol (https://njl-admin.nihr.ac.uk/document/download/2042261; accessed 20 November 2024):
-
3. How do sociodemographic characteristics and maternal mental health at baseline relate to:
-
level of participation in Mellow Babies?
-
group composition?
-
-
=====
-
5. How do participants describe their experience of participating in Mellow Babies, which elements of the intervention are considered most influential, and is participation stigmatising?
-
=====
-
8. How are the features (in terms of process and outcomes of care) of Mellow Babies valued by mothers?
-
9. What contextual factors facilitate or hinder delivery of, and engagement with, Mellow Babies?
Intervention group characteristics
This section is based in qualitative data with reference to quantitative data where appropriate. We have not provided detailed description of the groups of participants assigned to groups 3 and 7, as these were not able to run due to the COVID-19 pandemic and trial close-down, respectively. Table 20 details the sociodemographic characteristics and mental health measures at baseline for those participants assigned to the intervention arm, by group, for each of the five groups that took place.
| Group | 1 | 2 | 4 | 5 | 6 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Date start | 1 November 2019 | 3 February 2020 | 1 March 2022 | 11 June 2022 | 29 August 2022 | |||||
| Number of participants | 10 | 8 | 9 | 4 | 10 | |||||
| Number of sessions available | 14 | 7a | 14 | 10b | 11c | |||||
| Proportion of available sessions attended (median, IQR) | 60.7 | (20–80) | 35.7 | (0–100) | 85.7 | (0–96) | 67.5 | (45–88) | 81.8 | (14–100) |
| Number (%) attending at least one session | 9 | (90) | 5 | (63) | 6 | (67) | 4 | (100) | 8 | (80) |
| Number (%) maintaining enrolment until intervention completion | 7 | (70) | N/Aa | 5 | (56) | 3 | (75) | 7 | (70) | |
| Mother’s age, years [mean (SD)] | 30.6 | (5.9) | 32.4 | (7.3) | 36.9 | (6.4) | 27.5 | (3.7) | 29.5 | (5.8) |
| Child’s age, months [mean (SD)] | 8.4 | (3.2) | 8.9 | (4.5) | 11.0 | (3.8) | 10.3 | (4.6) | 6.9 | (1.3) |
| SIMD n (%) | ||||||||||
| 1 (most deprived) | 3 | (30) | 0 | (0) | 1 | (11) | 1 | (25) | 1 | (10) |
| 2 | 1 | (10) | 2 | (25) | 3 | (33) | 2 | (50) | 1 | (10) |
| 3 | 2 | (20) | 0 | (0) | 1 | (11) | 0 | (0) | 1 | (10) |
| 4 | 3 | (30) | 4 | (50) | 4 | (44) | 1 | (25) | 7 | (70) |
| 5 (least deprived) | 1 | (10) | 2 | (25) | 0 | (0) | 0 | (0) | 0 | (0) |
| Rurality n (%) | ||||||||||
| More urban | 7 | (70) | 6 | (75) | 5 | (56) | 3 | (75) | 6 | (60) |
| More rural | 3 | (30) | 2 | (25) | 4 | (44) | 1 | (25) | 4 | (40) |
| Education n (%) | ||||||||||
| Degree level | 4 | (40) | 3 | (38) | 4 | (44) | 2 | (50) | 5 | (50) |
| Below degree level | 6 | (60) | 5 | (62) | 5 | (56) | 2 | (50) | 5 | (50) |
| Employment n (%) | ||||||||||
| Currently employed/mat leave | 7 | (70) | 4 | (50) | 7 | (78) | 3 | (75) | 7 | (70) |
| Not employed | 3 | (30) | 4 | (50) | 2 | (22) | 1 | (25) | 3 | (30) |
| Home ownership n (%) | ||||||||||
| Yes | 6 | (60) | 2 | (25) | 7 | (78) | 1 | (25) | 4 | (40) |
| No | 4 | (40) | 6 | (75) | 2 | (22) | 3 | (75) | 6 | (60) |
| HADS-A [mean (SD)] | 14.0 | (3.1) | 12.0 | (3.7) | 13.0 | (2.5) | 11.0 | (4.7) | 13.9 | (3.6) |
| HADS-D [mean (SD)] | 11.3 | (3.3) | 8.1 | (3.7) | 10.6 | (4.7) | 9.8 | (4.3) | 8.7 | (3.5) |
| Diagnosed mental illness n (%) | ||||||||||
| Yes | 10 | (100) | 4 | (50) | 6 | (67) | 3 | (75) | 4 | (40) |
| No | 0 | (0) | 4 | (50) | 3 | (33) | 1 | (25) | 6 | (60) |
| Anxiety or depression n (%) | ||||||||||
| Yes | 10 | (100) | 8 | (100) | 8 | (89) | 4 | (100) | 9 | (90) |
| No | 0 | (0) | 0 | (0) | 1 | (11) | 0 | (0) | 1 | (10) |
| Life events – frequency [mean (SD)] | 4.6 | (2.2) | 4.9 | (3.1) | 1.9 | (1.8) | 1.3 | (1.5) | 4.3 | (3.9) |
| Life events – affect [mean (SD)] | 3.0 | (2.0) | 3.1 | (2.5) | 1.0 | (0.9) | 1.0 | (1.0) | 3.0 | (3.4) |
| Current relationship n (%) | ||||||||||
| Yes | 8 | (80) | 6 | (75) | 9 | (100) | 4 | (100) | 8 | (80) |
| No | 2 | (20) | 2 | (25) | 0 | (0) | 0 | (0) | 2 | (20) |
| Help in past 6 months n (%) | ||||||||||
| 4 items | 9 | (90) | 6 | (75) | 8 | (89) | 4 | (100) | 7 | (70) |
| 5–7 items | 1 | (10) | 2 | (25) | 1 | (11) | 0 | (0) | 3 | (30) |
Group 1: Ten participants were recruited to the first Mellow Babies group, with nine attending at least one intervention session. This group was recruited predominantly by HVs, which may account for the high levels of need (highest HADS scores and 100% of mothers having a mental health diagnosis). The group took place in Inverness and was delivered by three practitioners. Follow-up data were gathered remotely during COVID-19 restrictions.
Group 2: Eight participants were allocated to group 2, with five attending at least one session. Group 2 participants had lower levels of need compared to group 1, with a greater number of self-referrals and only 50% having a mental health diagnosis. This group presented as being high in anxiety, despite not having the highest mean HADS-A score at screening. The group took place in Dingwall and was delivered by three practitioners. However, due to COVID-19 social distancing restrictions, the group was suspended after seven sessions and mothers were unable to complete the intervention. Follow-up data were still collected (remotely).
Group 3: Although six participants were recruited to group 3, it was unable to take place due to COVID-19 social distancing restrictions. Babies were too old to take part in the group once the trial resumed following its suspension. Follow-up data for these participants were still collected (remotely).
Group 4: Group 4 was the first group delivered after the trial resumed post COVID-19, with a team of new practitioners. Nine participants were recruited to group 4, although only six attended the intervention. One participant dropped out after the initial session, leaving five mothers who completed the programme. Mothers in group 4 were older in comparison to other groups, with an age range of 31–42, and an average age of 36.9. All mothers in this group were still in relationships with their baby’s father. The group was delivered in Inverness by three practitioners, although one practitioner left unexpectedly midway through delivery.
Group 5: Group 5 was delivered in Tain on a Saturday as participants from the previous group had stated that weekend delivery would have been preferable for them. This also allowed us to use a local child-care establishment which would not have been able to accommodate the group during the week. Four participants enrolled in the group, but one withdrew from the programme after the fourth session. As there were so few participants, multiple sessions were cancelled when there was not a critical mass of at least two mothers available to attend. As a result, the group only received 10 out of 14 sessions. Two practitioners delivered this group. Two of the mothers within this group knew each other prior to commencing the group.
Group 6: Group 6 ran with eight participants, although one participant withdrew from the programme after the first week due to a family bereavement. The group was delivered in Inverness by three practitioners, with one practitioner leaving towards the end of the group when her contract ended. Group 6 mothers had more diversity of ethnicity compared to the other groups, with one mother from the USA and one from Spain. One mother was also of Asian background, whereas the majority of participants within the other four delivered groups were White British. According to the practitioners, mothers in this group had higher levels of anxiety, lower self-esteem and higher isolation compared to other groups. Only 11 out of 14 sessions were delivered for this group due to practitioner availability and being unable to extend practitioner contracts due to trial close-down.
Group 7: Six participants were recruited to group 7. This group was due to be delivered during the close-down period and there were insufficient mothers to form a viable group. We were not able to recruit more mothers and so the group was not delivered.
Findings from process evaluation interviews
Process evaluation interviews explored the facilitators and barriers for recruitment, delivery and participation, along with participants’ perceptions of the benefits of the programme, and the influential components. Four themes and 30 subthemes were identified, depicted in Figure 4.
FIGURE 4.
Themes arising from process evaluation interviews with intervention participants and group facilitators.
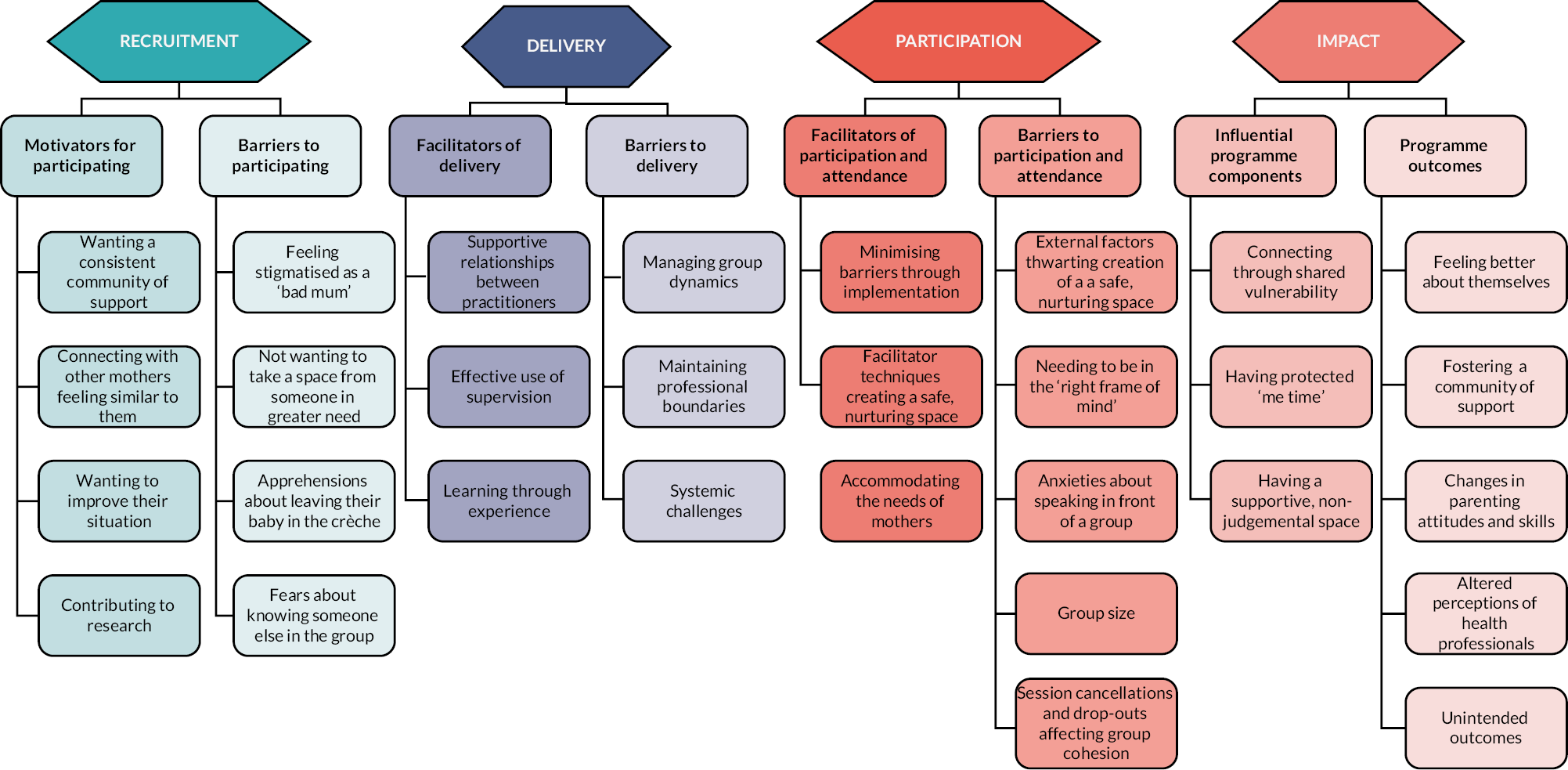
Recruitment
Motivators for participating
Having a ‘consistent community’ of support: ‘The village doesn’t exist anymore’
Mothers expressed their frustrations at the lack of community support, both from formal support services and from informal networks:
The phrase ‘it takes a village to raise a child’ I think is becoming incredibly frustrating to mothers because the villages don’t exist anymore.
MM6, post-group interview
This was especially felt by mothers who did not have family nearby, those who had recently moved to the area, and those confined to the house through a lack of transport and the absence of accessible, local services. Mothers expressed feelings of loneliness and isolation, and a desire to connect with others, for both their own well-being, and to ensure socialisation for their infant. In particular, mothers hoped for a ‘consistent community’, where they were able to develop ongoing, supportive relationships:
I was desperate for community … I just needed a way to get out and people to be around that I could have like consistent community, and I also am very aware that socialising for children is very important, especially at the age that she is now getting to.
MM6, post-group interview
I think it would be nice to see people regularly kind of thing … I’m actually really excited to talk to other mums and get [baby] out of the house.
ML6, pre-group interview
Connecting with other mothers who were feeling similar to them
Although knowing the group was for other mothers who were experiencing challenges with motherhood was also a barrier (see subsequent theme), some reported that the particular appeal of Mellow Babies was knowing that they would be able to connect to others feeling ‘the same way’ as them. Socialising with mothers at other baby groups who seemed to be enjoying motherhood and having little struggles often left participants feeling guilty and dejected about their own experiences. These groups could often feel overwhelming and intimidating, and not a space where mothers felt able to share their honest challenges. Mothers hoped to connect with others who were having more similar experiences of motherhood so they could feel a sense of solidarity, and ‘less alone’ in their feelings:
You go to other groups, and you think everybody is just very happy and content and everything. When this letter came to me, I was like, if I’m going there, I’m going to see mums that are feeling anxious too, or overwhelmed.
MP6, post-group interview
I wouldn’t have liked to go to a group where mums are thriving and they’re getting on really well and I’m just there, and I’m going, ‘But why can’t I do it like that?’ It was really lovely that I could look forward to seeing what those mums’ experiences were like. I thought even if I’m not suffering as much as they are, maybe I can help them out and maybe I can contribute something.
ML6, post-group interview
Wanting help to improve their situation
The primary motivator for most mothers was that they genuinely wanted help to improve either their own mental health or aspects of their parenting or relationship with their baby. Some mothers were in a desperate, low place when they enrolled in the trial, whereas others were coping but recognised that things could be better with the right support:
I was really defeated at the time. Like I was just, as I say just the lowest, I think I’ve ever been. And I just needed, just was hoping to be able to, pick myself up again … I just knew that I needed help and it just seemed like a lifeline at the time.
MK6, post-group interview
I’m someone who cares and loves, and I just hated my life. I was like ‘What have I done to my life?’ and I was sitting there … I just felt low mood, possibly postnatal depression and I had postnatal anxiety going on.
M4C, post-group interview
The desire for help was often exacerbated by dissatisfaction with the level of support from formal services. While some mothers were satisfied with their HV, others relayed frustrations that when they asked for help, requests were either ignored, or the ‘support’ received was unhelpful and left them feeling worse. One mother who had just had her third baby felt she was overlooked, as it was expected that she would be fine and knew what she was doing.
I would say it’s quite poor in general the support you get, if I’m honest, all around. Because your midwife does tend to see you in your first pregnancy, and then in multiples they don’t tend to bother with you really.
MJ5, post-group interview
That lifeline, that person that’s supposed to come and guide me, make sure everything is okay and it just, she kicked me when I was down … And there was another time where I was phoning a different health visitor. Every day for two weeks I phoned her and left her text messages to say ‘Hi, I’m struggling I need help. I can’t do this anymore.’
MK6, post-group interview
Contributing to research
One mother, who was a mental health professional, expressed that her primary motivation for signing up to the trial was to participate in the research study:
I am a believer in helping research, I think just because of my work. I thought, well, if it’s to help research then why not? I’ll do anything to help research.
MI5, post-group interview
For other mothers, this was a secondary motivation: they wanted to participate because they hoped to gain something from being part of the group, but they also recognised the potential of the trial to improve the availability of support for mothers in the Highlands.
One facilitator perceived that the group gelled better when the mothers had the collective goal of improving their situation:
They do genuinely seem to be a bunch of people who want to be there, not to take part in research, but to be there for the Mellow Babies. There is nobody there who thought, ‘well, it’s just a wee time out and it will help with research’. They genuinely want help, which is nice.
FC6, post-group interview
Barriers to recruitment
Feeling stigmatised as ‘a bad mum’
It was not felt that participating in the trial was stigmatising on the grounds of mental health. However, several mothers felt that by enrolling in the trial they were admitting to being a ‘bad mother’. This was exacerbated by some of the wording in the recruitment materials, particularly that the group would help mothers bond with their baby. While wanting to bond with their child was a motivator for some women, for others this felt stigmatising and it initially deterred them from participating in the trial. This was especially the case if mothers had been signposted to the trial through their HV:
I think the issue was I felt I had a good bond with her and the more I read about the lack of bond the more it kind of made me think ‘Oh I’m not a good mother'.
MC4, post-group interview
But equally, I knew that I had a connection with her, so I sort of felt it was a bit like undermining my mental ability.
ME4, post-group interview
Some mothers expressed that it was their separation anxiety that was the main issue they wanted the group to address, and as a result they did not feel the wording in the recruitment materials was applicable to them.
Not wanting to take a space from others in greater need
As the spectrum of poor mental health is so broad, mothers were unsure who the group was being targeted at and what kind of struggles other people would have. Many were concerned that they might be ‘too well’ and would be taking a space from others who were in greater need. A couple of the mothers described themselves as ‘high functioning’ and acknowledged that, although they were struggling, they were able to get through the day, which made them feel less deserving of a place on the programme:
I don’t know what I was expecting but because of the labels associated around this, I was like What am I going to be presented with?
MC4, post-group interview
Am I ill enough? Not ill enough, but do I need it as much as the rest of them?
MD4, post-group interview
For one of the mothers, these feelings intensified after attending the ‘meet-and-greet’ session and hearing the situations of the other mothers:
These are worthier people. I didn’t think I was worthy enough compared to the others, because others had such gigantic things compared to me, that was one of my concerns.
MD4, post-group interview
Reluctance to leave their babies in the crèche
Mothers initially felt overwhelmed by the prospect of leaving their baby in the crèche, as many had never left their child with anyone else before:
I was nervous at first because we had never, we didn’t go to baby groups. We didn’t have family and so I just had not had a lot of opportunity to leave her, so there was just the unknown of how was she going to take this.
MM6, post-group interview
The crèche was a major thing for some of these mums, they’d never left their babies before this. They were quite traumatised by it.
FC6, mid-group interview
Mothers felt that they would have been less apprehensive if they had been given more information about the crèche during the recruitment process, for example, being reassured that they could check on their babies when needed, and that they would be able to take their infants into the session if they would not settle.
Concerns about knowing someone else in the group
Some mothers reported feeling apprehensive about knowing someone else in the group, fearing that it may inhibit them from sharing:
There was obviously the, who’s going to be there? Am I going to know anyone? Because that was one thing that I didn’t really want, I didn’t want to know anyone, that I was going to go and then maybe hold back, sort of thing.
MD4, post-group interview
Practitioners also shared this concern, with worries about how they would manage the group if mothers knew each other, particularly as Inverness is relatively small.
I think in the training they kept talking about getting mums that know each other and how that can be bad. You know when you’re going, ‘Oh my god, in Inverness they’re all going to know each other!’ But none of them did.
FB4, post-group interview
Delivery
Facilitators of delivery
Supportive relationships between practitioners
Due to the emotional demands of group delivery, it was deemed essential for practitioners to have a supportive relationship with each other, where they felt able to share how they were feeling, particularly on days where they felt less able to cope:
We’re really transparent with each other and I’m very lucky that I’ve got somebody that I can work like that with. We have a really good friendship … you can think you’re fine and you can go into a session after a crap weekend and go, ‘Actually, I’m little bit down from the weekend, I can’t handle this so much today.’ Like I said, we’re able to work that out between us, because we’re both so transparent about our feelings and what we’ve been through and stuff.
FB5, post-group interview
Good communication between practitioners was also felt to be essential, particularly sharing information from conversations with mothers that had taken place outside of the immediate group environment. Practitioners did not know each other prior to the trial but completed the Mellow Babies training together.
Having a space to discuss issues in supervision
As the practitioners were new to the delivery of Mellow Babies before the trial, they encountered several issues over the course of the three groups. Practitioners were able to have regular online supervision sessions (usually 2 over the course of a 14-week group) with an experienced consultant from Mellow Parenting, where they were able to talk through their concerns, and get advice and suggestions to improve their practice. These could be individual supervision sessions, or group supervision, depending on the needs and preferences of the practitioners. These supervision sessions were deemed essential to both effective delivery of the group and their development as practitioners, particularly as all practitioners were new to delivering Mellow Babies. Practitioners described several challenges that they faced with group delivery and the solutions that had been implemented based on the advice received during their supervision.
Learning through experience
Practitioners recognised that they were growing in confidence and capabilities with each group they delivered. It was a steep learning curve, and each cohort of women brought different situations and challenges. This equipped them with knowledge and skills that would benefit them for future delivery:
Every time we do learn things, and we know we can make it better.
FB5, post-group interview
Barriers to delivery
Managing group dynamics
One of the key barriers to delivery was being able to hold a nurturing, containing space for the mothers, while still maintaining boundaries so all mothers were able to share their views. Practitioners relayed different situations in each of the groups which required them to step in and remind the mothers of the group agreement:
There was a lot of speaking over and that was the really difficult one because we didn’t want it to be like school, you know?
FA4, post-group interview
Practitioners felt unprepared for some of the situations they encountered and felt like this could have been covered in greater depth during the training, particularly for those who had minimal prior experience delivering groups:
I do think going in as a practitioner, I do think you need to make sure that you’ve got some training of doing groups and stuff
FA4, post-group interview
Maintaining professional boundaries
Delivery of Mellow Babies groups was a marked contrast to practitioners’ previous NHS roles as it involved practitioners sharing their own experiences. This took practitioners a while to get used to, and it felt difficult to navigate the balance between appropriate sharing and maintaining professional boundaries:
Obviously it’s so different from any other NHS post because you don’t share a lot of aspects about your life, whereas at Mellow Babies you must every day!
FB4, post-group interview
It’s not just doing a group and reading off a slide or paperwork, you’re kind of investing a lot of yourself. I think you need to … you know, I don’t know whether ‘skill’ is the right word, but be able to know enough about yourself and your skillset just to know where your limits are within that group.
FA4, post-group interview
Over the course of the groups, two out of the three practitioners experienced situations where their professional boundaries were challenged. One practitioner was known to one of the mothers in a professional capacity, as the mother had worked with both the practitioner and also the practitioner’s husband. The practitioner described her reluctance to share as much as she had in previous groups because of this connection, particularly during the week about sex. They were connected via social media, and the practitioner relayed having to reinforce boundaries that communication relating to the group should take place over professional, not personal, channels.
The second practitioner worked in the maternity unit where many of the women had given birth. Similarly, during the birth stories session, she had to reinforce boundaries that the two roles were separate:
I made it very clear at the start that I work in maternity and stuff, but I make it very clear to them about the boundaries… you know, I won’t go back and share anything with my colleagues or my unit. They don’t know that I’m working with them and vice-versa. I also say to them equally as well, ‘You can share what you want, I don’t have an opinion on these people, I want you to tell me the story of how they made you feel, not to worry that, “Oh my god, she works with her so I can’t say this.”’
FB4, post-group interview
Systemic challenges of delivery
Practitioners described the challenges of delivering the group when they were working part-time, including having extended periods of time when they were unavailable to respond to mothers, particularly if there was a concern, and having insufficient contact time to discuss how sessions should be adapted to meet the groups’ needs. As they were delivering the programme as part of a trial, they did not have the same system of support that would be present for community delivery. They felt their wider team did not fully understand the requirements of delivery, including how emotionally demanding it could be.
Participation
Facilitators of attendance and participation
Implementation minimising barriers to attendance
Implementation strategies removed many of the barriers to attendance. One key barrier was transport to the group, as several mothers were not able to drive, something which prohibited their access to other local mother-baby groups. Having taxis provided allowed these mothers to attend Mellow Babies:
I so appreciated the taxi, like the mobility of it. The fact that I couldn’t get into a local baby group, and I now had a way to get to something was huge for me.
MM6, post-group interview
One mother, who drove to the group, had recently lost her job and separated from her partner. Receiving petrol expenses at the end of the group was important to her as she had some distance to travel and had been using her savings to attend the group:
The financial support at the end was fab because I’m not earning, and I actually lost my job, so I haven’t got any income coming in and so I would have to ask him [ex-partner] for money. I’m just living off my savings and the fact at the end, I’d forgotten the travel expenses, that was a big help to me. I think other mums might have been in a similar position if they’re not earning.
MC4, post-group interview
A second barrier was removed through the crèche. Although mothers initially felt apprehensive about leaving their babies, crèche enabled them to fully engage in Mellow Babies sessions, and have uninterrupted, meaningful conversations with other mothers:
[t]o have a place where I could drop [baby] off and have time to myself with other adults where my brain wasn’t split of watching my child on her chair doing risky play. Yeah, that was just amazing.
MM6, post-group interview
Finally, having the meet-and-greet session at the start of the group provided a forum where mothers could get to know each other on an informal basis before starting sessions. Mothers had already had a visit from the group practitioners by this stage, and found it reassuring to go into this initial meeting knowing a familiar face.
Accommodating the needs of different mothers
The group accommodated mothers with a range of learning needs, including one mother who had attention deficit hyperactivity disorder and one mother who did not have English as her first language. Both these mothers felt the practitioners were supportive and understanding of their specific circumstances, and worked with them in a way to enabled access and participation in session content:
I was very worried at the beginning, but honestly, every time that I was stuck or didn’t know how to say a word or have to write it, I was always like, ‘I’m so sorry, I don’t know how to say this’, I want to explain myself, they were all very, ‘no worries, it’s fine, it’s okay. Just take your time'.
MP6, post-group interview
They let me sit on the floor when I needed to … Both practitioners and the rest of the group, just really accepting of like my needs and things.
MK6, post-group interview
Practitioners were very aware that certain topics may be ‘triggering’ for mothers, and endeavoured to adapt sessions as needed, and check in with mothers:
Different subjects are going to bring up tricky things for different mums, so there were weeks we had to really be aware … you know, thinking ahead, ‘That’s going to be a tricky week for that mum.’ But I think we managed that quite well.
FC6, post-group interview
While mothers appreciated that facilitators checked in with them, the general consensus was that it would help for them to know the next week’s topic in advance, so they were able to emotionally prepare for content they knew they might find challenging.
Facilitator techniques creating a containing, nurturing space
Mothers attributed the success of the group to the facilitation skills of the practitioners. They were able to cultivate a safe, non-judgemental space where people felt comfortable sharing their thoughts and experiences.
I’ve seen it done very well, all three of them to do what they’ve done and to cultivate such a space that we do, I felt as comfortable as we felt.
MA4, post-group interview
Mothers valued how practitioners also participated with the session content, sharing their own challenges, particularly during the Life Stories session. This encouraged mothers to open up and fostered feelings of connectedness with practitioners:
It was really good that they opened up. The life stories. If they hadn’t done their life stories first, I don’t think I would have gone into as much detail, because they did go into detail, and it really helped.
MC4, post-group interview
As women, we tend to feel more comfortable when we’re bonded with somebody or when we share information, so it didn’t feel like a teacher/student situation. I feel like that would really have stopped us from sharing so much.
ME4, post-group interview
Facilitators were also skilled at ‘holding’ the group and maintaining a containing, boundaried space with warmth and compassion:
They’re really, really good because there’s a couple of mums who don’t really pitch in as much, so they’ll give them the space on the floor if they want to speak, but if they don’t want, they allow them to keep their privacy.
MF4, post-group interview
Barriers to attendance and participation
External factors thwarting the creation of a containing, nurturing space
Although, on the whole, all three group venues were received positively by mothers, there were a few factors identified which impacted the experience of the group. Firstly, in one of the venues, there were other people using the room next door and mothers felt self-conscious about sharing in case they were overheard. This was particularly the case during the week where they discussed sex, as there was a group of men in the building.
They had a knitting group next door and like we could hear them so it was really sort of concerning like can they hear what we’re saying too … it was just the fact that when we’re talking about really intimate things and like you’ve got men in the building, now I’m not shy, I’m quite an open person but a lot of the other mums were shy, weren’t open people at all. And it was difficult enough for them to open up with just us and there’s like men floating about the building.
MK6, post-group interview
Facilitators also expressed frustrations that factors outside of their control, including the venue layout and staff, could generate stress for mothers, which they felt impeded their capacity to establish a nurturing space. One group also had a lot of issues with the taxis not turning up, or taxi drivers becoming frustrated if they had to wait for mothers at the end of the session. As a result of this, facilitators adapted session content so that they could ensure they finished the group promptly. These themes were also echoed by mothers in the relevant groups.
That first group [Group 4], the venue staff were quite challenging with getting teas and coffees which shouldn’t have been … [Group 5] were really limited to how we set the room out and the tables were just really long, low tables. So, you couldn’t really make the shape that we would normally have. It felt more like school because we had to really have the us and them, so that really limited us as well. And the amount of complaints we had about the chairs being uncomfortable.
FA5, post-group interview
Some of the taxi drivers are quite rude and don’t like it when people [are late]. We’re rearranging our sessions a bit. So, if there’s a heavier discussion, it’s done earlier and towards the end of it it’s lighter. So that we’re not in that situation to say, ‘well, I’m very sorry you’re crying at the moment, but your taxi is here off you go!’
FA6, mid-group interview
Needing to be ‘in the right frame of mind’
Mothers expressed that there was a need to be ‘in the right frame of mind’ in order to fully participate with course content. Mothers felt it was more difficult to engage if they were currently experiencing significant life stress, or if they were talking about topics that were still raw or unprocessed:
It is quite intense, and you don’t want to be the one not ready to progress and watch everyone else. I think they do have to be in the right frame of mind. Because I definitely wasn’t when I got the first letter.
MF4, post-group interview
I found it quite difficult because I’m going through a lot right now, so we basically all went round the room telling our stories and I was like, ‘I’m not going to be able to do this today,’ just because it’s all very raw what I’m going through right now.
MK6, post-group interview
Anxieties speaking in front of the group
Many mothers had apprehensions about speaking in the group, particularly for sessions such as Life Stories, which required speaking for extended periods of time. This was something they became more comfortable with as the programme progressed, but inhibited their participation within earlier sessions:
I’m not keen on standing up and talking in front of the group. I’m getting better at it, I probably only would do it with that group, I wouldn’t do out of the group but I’m getting better at it. I wasn’t the first couple of weeks, I was a bit, ‘Oh my goodness, you’re going to have to actually speak.’ It was a bit … yes. That’s probably the worst part but it is getting better.
MP1, telephone fidelity check
Mothers felt the safe, non-judgemental space supported them to grow in confidence in sharing their ideas. The group culture, underpinned by the group agreement created at the outset of sessions, was accepting of mothers’ choice to pass if they did not want to participate.
Group size
Mothers and practitioners involved in group 5 (which only had four mothers) all strongly felt that a group of four was too small to be viable group. Having a smaller group affected the quality of group discussions as there were fewer people to share ideas, leading to mothers feeling pressured to participate more than they wanted to. Fewer viewpoints were discussed, which meant sessions could feel ‘slow’, and any strong opinions were less diluted:
I, personally, am finding the sessions quite slow and the material’s quite slow, and they’ve said to me that it’s because we’re such a small group that they don’t necessarily feel like they’ve got sufficient materials to use the full five hours, if that makes sense. They said they’re having to drag things out a bit and it feels quite slow, to me it feels like I leave and I’m a bit like, ‘God, I feel like we haven’t really done anything or covered anything.’
MH5, telephone fidelity check
Three people in a group is not a group really. It’s not in that setting … I feel it’s had a bad effect, I don’t know if that’s comparing it to the previous group but I feel it’s had a bad effect because two of the mums know each other, one of them knows me so the dynamics are already a little bit weird there and then it’s such a small group that if you’re looking for other opinions, you either go, either one or two take over the conversation a little bit or you go the other way that you kind of done, done, done that’s it nobody else wants to discuss.
FA5, post-group interview
Practitioners recognised that this group was less cohesive than other groups, possibly because there were fewer individuals to feel connected to, and therefore they connected less to the group as a collective.
Session cancellations and participant drop-outs disrupting group cohesion
Group cohesion was affected by session cancellations and participant drop-outs, and the mothers found this unsettling. This prevented relationships within the group from solidifying and also impacted on how well the children settled in the crèche:
It was difficult because obviously we had the first week, we were all quite anxious and we got our kids settled in to the nursery and had our first group and got to know each other. And then after that, we only had one other week and then there was a big break, so we were off for like three weeks and because of that, it meant that we had a lot of time where we weren’t together, and the kids were not used to be in the nursery anymore. It felt like starting all over again, I feel we lost the momentum.
MH5, telephone fidelity check
Group 5 got cancelled several times as due to the small size, it was not viable to run if more than one mother was unable to attend. This led to mothers becoming frustrated with both the group, and with each other if sessions were cancelled last minute:
Because it’s such a small group, it meant to begin with if a couple of mums can’t make it, say maybe their kids get ill or they’re not around, it means it gets cancelled for the whole group. I was ready to leave one Saturday.
MI5, telephone fidelity check
Group cohesion was also affected by mothers withdrawing from the programme, and by facilitators leaving midway through. This was intensified in group 5, which went from four to three mothers.
Impact of Mellow Babies
Influential programme components
Connecting through shared vulnerability
Shared vulnerability, particularly through the Life Stories session, was perceived by both mothers and practitioners to be an essential component of the programme. Opening up and hearing about the challenges that other people have experienced, including practitioners, put everyone on ‘a level playing field’ and facilitated connections both between individuals and to the group as a collective.
I think having that, doing the life stories before you get to some of the other stuff is really important because it puts everybody on a level playing field quite early on. And when tricky stuff comes up later, they’re able to speak about it, so yeah, I think that definitely helps. It’s definitely really, really effective, I think it really is. I think that’s the first opportunity we almost actually get to start going a bit deeper, and I think it’s the first opportunity for us as practitioners to go beyond the level as well.
FA5, post-group interview
In a normal baby group you would never get to know these people so well, and I think that was really wonderful because then we actually felt connected and like we knew each other’s stories a bit and I think my favourite session was probably when we learned each other’s stories.
MM6, post-group interview
It also helped break down mothers’ barriers to involvement and gave practitioners a better insight into the group, allowing them to plan future sessions to mothers’ needs.
Having protected ‘me time’ within their week
Mothers relished having a space that was centred on them, and not on their baby. It gave them something to help break up the monotony of their week, which would often otherwise be spent staying at home, and it provided an opportunity to have meaningful conversations with other adults:
It gives me a reason to get up in the morning and take your kids out and get somewhere.
MA1, telephone fidelity check
I think it was the thing I looked forward to every single week, like it’s my day out. It was my socialising and I think it was really good for my mental health … I think sometimes you just need to be able to go somewhere where you can chat with adults and your baby gets looked after or there’s somewhere for them to go, there’s just not enough of that.
MM6, post-group interview
[Other groups are] very much a playgroup for the children and we tag along, whereas Mellow Babies was obviously for us and the babies tagged along at the nursery/crèche.
ME4, post-group interview
Having a safe, non-judgemental, supportive space
Mothers also enjoyed having a non-judgemental space where they were able to offload about their feelings and difficulties. This enabled them to process their thoughts and experiences, and receive support and validation from others:
If I was to pinpoint one, but it was possibly the support aspect for me … They’re a safe place to say because they’re not a friend that knows another friend that you’re gurning about. A safe place to rant to your friends, different perspectives. If I go and say something to my mum, she’s always going to be on my side, or my best friend, she’s always going to be on my side. But they all give you another perspective.
MF4, post-group interview
I think that’s important for them because they’re going to be accepted by those mums, because they know so much about them but still are friends and still there to support them. I think that non-judgemental… someone hearing your story but without being judged is really important for them going forward, because it’s given them a chance to say things out loud that they possibly wouldn’t have said out loud to anybody.
FA6, post-group interview
Programme outcomes
Feeling better about themselves
Mothers reported feeling better about themselves since participating in Mellow Babies, with phrases such as ‘I’m back to me’, ‘uplifted’ and ‘life-saving’ used to describe the group. They felt more confident and content within themselves and their situation as the group helped to normalise the feelings and challenges that they were experiencing. Being able to see themselves through other people’s eyes also facilitated them to see themselves in a more positive light:
It has really changed my attitude to a lot of things. I went in really miserable, really depressed … I know that everything that I’ve been feeling and struggling with as a mum is totally normal.
MK6, post-group interview
I’ve started to feel a bit more like me, but in my own importance as a person. I’m starting to value that I do have a bit more to give, rather than just being one sided [me], I suppose. I felt like I’ve discovered that my brain’s been switched back on, because I’ve been in a fog for an awfully long time.
ME4, post-group interview
Fostering a community of support
Several mothers described how the group had helped combat loneliness and fostered a supportive community with other mothers. Groups 4 and 6 provided ongoing support for each other even after the group had finished, with mothers continuing to chat, offload and offer support and advice via a WhatsApp group:
I think it helped a great deal with the loneliness I was experiencing. And I now have like a mum, at least some mum community even though at this point because the group has ended, I’m not able to go physically see them, but I still have that like the group text, and we still chat about things.
I know I always have people to talk to, whereas before, I didn’t have anyone.
Changes in parenting attitudes and skills
Although some mothers did not feel their parenting or relationship with their child had changed over the course of the group, several stated that this was the biggest impact of Mellow Babies. Mothers reported feeling more confident in their parenting, having a closer bond with their child, and enjoying spending time with them:
I think I was at the point of feeling like everything was a chore before and building up a bit of resentment to everything I had to do all the time. But it just … it was a really simple thing, but it’s made a really big difference to actually sit down and enjoy playing with her.
MB1, telephone fidelity check
I feel like I have a much better relationship and much more confidence with [baby]. That is the biggest, actually the biggest thing and just so much more content with my mothering instincts and looking after her.
MC4, post-group interview
Altered perceptions of healthcare workers
For some mothers, realising that all people have had struggles, including health professionals, was helpful in validating their own lives. Practitioners felt that this would impact on future relationships with healthcare providers, speculating that mothers might feel more trusting and less defensive:
When you see a health professional, you kind of think they’ve got it all together and nothing goes wrong and then when we were listening to [the practitioners] life stories, not everything’s perfect. That really helps.
ME4, post-group interview
One of the mums made a comment that she thought professionals had… I don’t want to swear on this recording! Her phrase was, ‘Professionals have got their shit together.’ One mum said that she really genuinely didn’t realise… she thought professionals were all this, they’ve been to college or uni and they’ve got these lovely lives, they earn money, they’ve got this good academic job, whatever. She didn’t realise that actually they have got the same amount of problems, you just don’t see them because you see them in a professional setting.
FA4, post-group interview
Iatrogenic effects
While the majority of mothers (and all of those in groups 1, 4 and 6) felt they had benefitted from the programme, two mothers in group 5 stated that participating had left them ‘feeling worse’. One of these decided to withdraw from the group as she found that session content was triggering for her PTSD symptoms:
I have PTSD and I find some of the things that we’re talking about are quite triggering for me and I really don’t know how to deal with that. I’ve mentioned to [facilitators] as well that we have some sessions where things will be talked about that I’ll find really challenging, and we leave at the end of the session and there’s no, ‘H ow are you feeling, or do you need any signposting or any extra help?’ It’s like we leave at the end of the sessions, and it’s left to deal with. I’ll go in feeling quite good and then leave feeling quite down.
MH5, post-group interview
Another mother in group 4, despite describing the impact of the group as ‘life-changing’, still described finding the video observation component of the programme challenging and felt it exacerbated some difficult feelings:
I worried about when they were recording me with the feeding. That was really triggering for me because I was so devastated, I was experiencing breastfeeding grief and PTSD around it and like so every time I was feeding her a bottle it was like re-traumatising me. I didn’t want to watch myself feeding.
MC4, post-group interview
Group 4 mothers also expressed that they found their mental health had deteriorated after the group had finished as they had become accustomed to having the space and the regular connections with other mothers. They stated that the ending felt very abrupt after 14 weeks of intense contact, and recommended that future groups ended more gradually, for example, reducing to fortnightly or monthly sessions before terminating. They also felt that check-ins after the group would be helpful:
The only thing that I found not quite for me, not about the topics, but I just found that when we finished, we finished. It was cut … I know it has to come to an end at some point, but it’s been an intense 14 or 15 weeks, if you count the coffee morning, and then nothing. It was kind of like, how do I deal with this now? What do I do with this now?
ME4, post-group interview
With my counselling you don’t just stop, well you can just stop, but like I got to two weekly and now I’ve got to monthly. And I think it would have almost been good to have a phone call or a check in or something like maybe a week or so, not, I’m not saying so much for myself, this is a reflection for the whole, because I’m noticing some of the other mums are like, they’ve gone [downhill].
MC4, post-group interview
Discussion
Overall, this section highlights the heterogeneity not only of intervention participants but also of the groups themselves. Each group varied on a range of characteristics, many of which were logistical and very difficult to mitigate. It also outlines the aspects of the intervention and participation in the trial that intervention participants and practitioners felt strongly about, and provides useful learning both for those delivering this type of intervention in future and for those seeking to conduct further trials into such interventions.
Appendix 4 The impact of the COVID-19 pandemic on The Mellow Babies Trial: full results
This section will include data to address the final question from the close-down protocol (https://njl-admin.nihr.ac.uk/document/download/2042261; accessed 20 November 2024):
-
4. How do sociodemographic characteristics and maternal mental health at baseline relate to:
-
whether recruited pre-pandemic (to March 2020) or post (since November 2021)?
-
-
=====
-
10. What specific impact did the COVID-19 pandemic have on the ability to run intervention groups and the trial?
The COVID-19 pandemic had a significant influence on the trial. When lockdown restrictions were first imposed in March 2020, we had to pause recruitment. We had recently m)et the criteria for the stop/go point (i.e. internal feasibility pilot) of recruiting 40 participants and having 2 intervention groups established. A third intervention group had also been recruited and was due to start in late March. Although we were behind our initial recruitment target, we were aware of the barriers to recruitment, had developed sound strategies to overcome these, and the trial had established momentum. In March 2020 intervention group 2 was interrupted and ultimately could only complete 7/14 sessions. Group 3 could not begin at all. This resulted in 14 participants randomised to the intervention pre pandemic not being able to receive the full intervention. Although we proposed that these participants be offered the online version of Mellow Babies, this was not approved by the funder. Thus, our Data Monitoring Committee advised we exclude those participants and associated controls from any outcome analysis, reducing our sample size by 28 and meaning we would have to over-recruit by that number to be able to meet our target sample size. Trial recruitment re-started in November 2021 and continued until September 2022.
Recruitment pre- and post-COVID-19 restrictions
We recruited and randomised 47 participants prior to mid-March 2020, and a further 59 from November 2021 to August 2022. Recruitment to the trial commenced in January 2019. We found recruitment via practitioners slow to begin with, despite overt buy-in, and so immediately moved to instigate a major amendment which allowed us to use the PIC letter system. We were, however, subject to a 5-month delay from the REC and so could not implement this change until towards the end of 2019. Once we had the PIC system in operation, recruitment proceeded more quickly. We moved our initial stop/go milestone (40 participants and 2 intervention groups established) and were able to meet this by the end of February 2020. Once we were able to recommence recruitment in November 2021, the funder requested that we implement a further stop/go milestone to re-establish trial validity. We committed to recruiting a further 55 participants by the end of July 2022, a target we exceeded (n = 59).
There was a significant difference in source of referral for those randomised: clinician (HV) referral was much more common pre pandemic, with 17/47 (36%) versus 5/59 (9%) being referred from that source [χ2(1) = 12.2; p < 0.001]. PIC letters were much more likely to be a source of referral post pandemic (75% vs. 34%), although these could be employed from the start of recruitment this time, whereas we only had 6 months using these pre pandemic (compared to 11 months post pandemic). There was no significant difference in the proportions screening positive between the two time periods, neither was there any difference in the proportions of those screening positive who went on to be randomised as a trial participant. Post-pandemic intervention participants were equally as likely to not attend the intervention, and this was not impacted by the number for whom the intervention was not available, as both groups 3 and 7 had 6 participants each allocated to them. There was also no difference in the proportion of offered intervention sessions attended by participants.
Despite the considerable stress the pandemic placed on family life, there was no difference in HADS scores at screening or in Recent Life Events scores at baseline. This could mean that the pandemic did not adversely influence the target population as much as might be expected, but it is more likely that those most seriously impacted were unlikely to have expressed interest in participating in the trial.
There was no difference in the proportion of participants retained to FU1 according to whether they were recruited pre or post pandemic. We cannot make a similar comparison for FU2 as most post-pandemic participants were not yet eligible for FU2 at trial close-down.
Trial logistics pre- and post-pandemic
During the pandemic, the Trial Manager left the project, and the PhD student worked as a Research Assistant to assist the senior co-I (now CI) with follow-up data collection. A new Trial Manager and Research Assistant were recruited in August 2021 to allow participant recruitment to recommence in November 2021. They were comparatively less experienced than the previous TM and the PhD student, and so required a greater degree of training and supervision.
Suspension of recruitment lasted for 20 months in total. Although we had established the relevant approvals and had re-staffed to begin recruitment in November 2021, there were changes to the infrastructure surrounding the intervention which meant the need for some pragmatic changes, and therefore a longer set-up period. Pre pandemic, the intervention was being delivered within child-care establishments. This model was developed as the only viable means of providing the intervention in close proximity to child care (there was no mobile crèche service in Highland at that time). Post pandemic, child-care establishments were not permitting any adult visitors to their buildings when the trial first re-started. There had also been a change in Scottish Government policy, whereby all 3-year-old children were now entitled to 30 hours of free pre-school education (previously 16 hours). This meant that none of the establishments we spoke to had any spare capacity either to accommodate intervention groups or to absorb the extra child care. Therefore, it was necessary to revisit a range of possible strategies regarding the logistics of the intervention. With considerable time investment from the intervention team, new venues were identified, and a mobile crèche was now available (albeit geographically distant and therefore more costly). The cost of delivering the intervention in this context was significantly greater than pre pandemic: the efficiency of combining intervention venue and child care into a single cost package had been lost.
It was also necessary to recruit new Mellow Babies practitioners after the pandemic. This also required significant investment of both time and money from the intervention team. A new group of practitioners was trained in October 2021, and the first Mellow Babies intervention group planned to begin early in 2022. Recruitment progress was slower than anticipated at first – there had apparently been a loss of momentum in having the trial paused for so long, and it seemed people were reluctant, in the not-quite-post-pandemic era, to say that their mental health need was any greater than anyone else’s. Anecdotally, there was a sense of feeling quite lucky, relatively speaking, and not feeling that there was a need or a right to ask for extra support given how much worse things had been for families just a few months previously. Having said that, we were able to re-establish the trial and recruit to viable levels. Due to the significant pause in recruitment, and the anticipation that more time and funding would ultimately be required to complete the trial to protocol, a new stop/go criterion was agreed with the funder: to recruit a further 55 participants by the end of July 2022. This was achieved, with 59 recruited (106 in total with the 47 pre pandemic added).
Sadly, a significant further investment of time and money would be required to complete the trial to protocol. We calculated that it would cost the same amount of money and more time than originally planned to reach the intended sample size of 212 participants. Therefore, the funder decided not to continue recruitment to the trial beyond its original end date of November 2022, and rather enter into a close-down period to the end of June 2023. Due to the sample not being sufficiently powered to answer the primary trial outcome question, analysis plans were modified to remove any comparison of outcomes between the trial arms (based on advice from NIHR and our Data Monitoring Committee).
We made a case on moral and ethical grounds to allow those already recruited to take part in at least the first follow-up (FU1) at 8 months post randomisation, and to allow those participants already screened or randomised the opportunity to take part in the intervention. Although these requests were denied, a compromise position allowed us to continue recruiting to the final intervention group (group 7) but without randomisation or follow-up of these participants. The lengthy negotiation period for this compromise (from October to December 2022) meant that, by the time the final group could be arranged, most of those screened or randomised to that group were no longer able to commit the time, or could not attend on the specific day the venue and crèche were available. Ultimately, as only two participants remained interested and available, and as they were aware of the situation and had expressed they would not be negatively affected by the group not taking place, we chose not to run the final intervention. All group 7 participants were referred on to Mellow Parenting, who offered them participation in an online version of the intervention.
Overall, the COVID-19 pandemic had a devastating effect on what was otherwise a viable trial which would have gone a long way to answering a range of questions, not only about the effectiveness of Mellow Babies for mothers experiencing psychosocial stress, but about the lived experience of this population and how we might better engage them in research in future.
Appendix 5 Baseline tables
| Mellow babies | Usual care | ||
|---|---|---|---|
| N = 53 | N = 53 | ||
| Total number of members of the household | Mean (SD) (N) | 3.8 (1.2) (N = 53) | 3.7 (1.0) (N = 53) |
| Median (25th, 75th centile) | 4.0 (3.0, 4.0) | 4.0 (3.0, 4.0) | |
| (Minimum, maximum) | (2.0, 7.0) | (2.0, 6.0) | |
| Ethnic background | White British | 45/53 (84.9) | 47/53 (88.7) |
| White Irish | 1/53 (1.9) | 1/53 (1.9) | |
| Eastern European | 1/53 (1.9) | ||
| Other European | 2/53 (3.8) | 2/53 (3.8) | |
| Other | 1/53 (1.9) | ||
| Asian or Asian British | 2/53 (3.8) | 2/53 (3.8) | |
| White other | 1/53 (1.9) | 1/53 (1.9) | |
| Age when left secondary school | Mean (SD) (N) | 16.9 (1.1) (N = 53) | 16.7 (1.2) (N = 53) |
| Median (25th, 75th centile) | 17.0 (16.0, 18.0) | 17.0 (16.0, 18.0) | |
| (Minimum, maximum) | (14.0, 20.0) | (15.0, 19.0) | |
| Highest educational qualifications | No educational qualifications | 2/53 (3.8) | |
| Standard Grades, Intermediate 1 or 2, O levels, General Certificate of Education (GCS)/General Certificate of Secondary Education (GCSE) | 8/53 (15.1) | 10/53 (18.9) | |
| Higher, Advanced Higher, A levels | 8/53 (15.1) | 1/53 (1.9) | |
| Vocational qualification | 6/53 (11.3) | 7/53 (13.2) | |
| Higher National Certificate (HNC)/Higher National Diploma (HND) | 6/53 (11.3) | 8/53 (15.1) | |
| Undergraduate Degree (e.g. BA/BSc) | 20/53 (37.7) | 16/53 (30.2) | |
| Postgraduate qualification (e.g. MSc, PhD) | 5/53 (9.4) | 9/53 (17.0) | |
| Best description about employment | Currently in paid employment or self-employed | 16/53 (30.2) | 13/53 (24.5) |
| Maternity leave (paid employment) – plan to return to work | 20/53 (37.7) | 19/53 (35.8) | |
| Maternity leave (paid employment) – not plan to return to work | 3/53 (5.7) | 2/53 (3.8) | |
| Not currently working – have been in past paid employment | 14/53 (26.4) | 18/53 (34.0) | |
| Never been in paid employment | 1/53 (1.9) | ||
| Hours of work | Mean (SD) (N) | 22.6 (13.3) (N = 47) | 25.8 (14.6) (N = 39) |
| Median (25th, 75th centile) | 24.0 (15.0, 35.0) | 26.0 (18.0, 35.0) | |
| (Minimum, maximum) | (0.0, 45.0) | (0.0, 60.0) | |
| Current job | Self-employed with NO paid employees | 5/53 (9.4) | 1/53 (1.9) |
| Manager | 4/53 (7.5) | 7/53 (13.2) | |
| Supervisor | 2/53 (3.8) | 5/53 (9.4) | |
| Employee | 42/53 (79.2) | 38/53 (71.7) | |
| Missing | 2/53 (3.8) | ||
| Description what you were doing last week | In paid employment | 14/53 (26.4) | 9/53 (17.0) |
| On maternity leave from paid employment | 23/53 (43.4) | 21/53 (39.6) | |
| Waiting to take up paid work already obtained | 1/53 (1.9) | 1/53 (1.9) | |
| Not working because of temporary sickness or illness | 2/53 (3.8) | 2/53 (3.8) | |
| Permanently unable to work because of long-term sickness or disability | 1/53 (1.9) | 1/53 (1.9) | |
| At college or university full time | 1/53 (1.9) | ||
| Looking after home or family | 11/53 (20.8) | 16/53 (30.2) | |
| Doing something else | 1/53 (1.9) | ||
| Missing | 2/53 (3.8) | ||
| Number of times you moved house in the last year | Mean (SD) (N) | 0.5 (0.9) (N = 53) | 0.3 (0.5) (N = 53) |
| Median (25th, 75th centile) | 0.0 (0.0, 1.0) | 0.0 (0.0, 1.0) | |
| (Minimum, maximum) | (0.0, 4.0) | (0.0, 2.0) | |
| I am currently living | In a house or flat that is owned outright | 6/53 (11.3) | 2/53 (3.8) |
| In a house or flat that is being bought with the help of a mortgage or loan | 23/53 (43.4) | 24/53 (45.3) | |
| In a house or flat rented from a council, local authority, or housing association | 12/53 (22.6) | 13/53 (24.5) | |
| In a house or flat rented from a private landlord | 9/53 (17.0) | 9/53 (17.0) | |
| At home with my parents | 2/53 (3.8) | 2/53 (3.8) | |
| In a hostel, bed and breakfast, homeless shelter, or temporary accommodation | 1/53 (1.9) | ||
| Other | 1/53 (1.9) | 2/53 (3.8) | |
| Number of rooms in your home | 1 | 1/53 (1.9) | |
| 2 | 3/53 (5.7) | 7/53 (13.2) | |
| 3 | 9/53 (17.0) | 13/53 (24.5) | |
| 4 | 21/53 (39.6) | 13/53 (24.5) | |
| 5 | 7/53 (13.2) | 10/53 (18.9) | |
| 6 | 11/53 (20.8) | 3/53 (5.7) | |
| 7 | 1/53 (1.9) | 2/53 (3.8) | |
| 8 | 5/53 (9.4) | ||
| Number of cars and/or vans | Yes | 9/53 (17.0) | 8/53 (15.1) |
| No | 19/53 (35.8) | 23/53 (43.4) | |
| Two | 23/53 (43.4) | 19/53 (35.8) | |
| Three or more | 2/53 (3.8) | 3/53 (5.7) | |
| Had a family holiday | Yes | 20/53 (37.7) | 22/53 (41.5) |
| No | 33/53 (62.3) | 31/53 (58.5) | |
| Age at first pregnancy | Mean (SD) (N) | 27.1 (6.4) (N = 53) | 26.0 (5.7) (N = 53) |
| Median (25th, 75th centile) | 26.0 (22.0, 31.0) | 26.0 (22.0, 29.0) | |
| (Minimum, maximum) | (16.0, 41.0) | (13.0, 39.0) | |
| Had previous pregnancies | 1 | 34/53 (64.2) | 43/53 (81.1) |
| 2 | 19/53 (35.8) | 10/53 (18.9) | |
| Number of pregnancy | 0 | 1/53 (1.9) | |
| 1 | 6/53 (11.3) | 9/53 (17.0) | |
| 2 | 13/53 (24.5) | 21/53 (39.6) | |
| 3 | 6/53 (11.3) | 13/53 (24.5) | |
| 4 | 6/53 (11.3) | 4/53 (7.5) | |
| 5 | 2/53 (3.8) | 2/53 (3.8) | |
| 6 | 4/53 (7.5) | 1/53 (1.9) | |
| 7 | 2/53 (3.8) | 1/53 (1.9) | |
| 10 | 1/53 (1.9) | ||
| Missing | 12/53 (22.6) | 2/53 (3.8) | |
| Scottish Index of Multiple Deprivation | 1 (most deprived) | 8/53 (15.1) | 10/53 (18.9) |
| 2 | 10/53 (18.9) | 10/53 (18.9) | |
| 3 | 6/53 (11.3) | 9/53 (17.0) | |
| 4 | 25/53 (47.2) | 16/53 (30.2) | |
| 5 (least deprived) | 3/53 (5.7) | 5/53 (9.4) | |
| Missing | 1/53 (1.9) | 3/53 (5.7) | |
| Urban/rural classification – eightfold | Other urban areas | 24/53 (45.3) | 33/53 (62.3) |
| Remote small towns | 7/53 (13.2) | 8/53 (15.1) | |
| Very remote small towns | 1/53 (1.9) | 1/53 (1.9) | |
| Accessible rural | 9/53 (17.0) | 9/53 (17.0) | |
| Remote rural | 10/53 (18.9) | 1/53 (1.9) | |
| Very remote rural | 2/53 (3.8) | 1/53 (1.9) | |
| Urban/Rural classification – sixfold | Other urban areas | 24/53 (45.3) | 33/53 (62.3) |
| Remote small towns | 8/53 (15.1) | 9/53 (17.0) | |
| Accessible rural | 9/53 (17.0) | 9/53 (17.0) | |
| Remote rural | 12/53 (22.6) | 2/53 (3.8) |
| Mellow Babies | Usual care | ||
|---|---|---|---|
| N = 53 | N = 53 | ||
| Ever had a social worker | Yes | 5/53 (9.4) | 6/53 (11.3) |
| No | 48/53 (90.6) | 47/53 (88.7) | |
| Details of social worker | Ongoing involvement | 2/5 (40.0) | 3/6 (50.0) |
| Previous involvement | 2/6 (33.3) | ||
| Initial contact for mum and baby, no follow-up | 1/5 (20.0) | 1/6 (16.7) | |
| Parent disability/health | 1/6 (16.7) | ||
| Baby disability/health | 1/6 (16.7) | ||
| Domestic violence | 2/6 (33.3) | ||
| Drug use | 1/6 (16.7) | ||
| Welfare/care of older children | 2/5 (40.0) | 1/6 (16.7) | |
| Currently pregnant | Yes | 1/53 (1.9) | |
| No | 53/53 (100.0) | 51/53 (96.2) | |
| Missing | 1/53 (1.9) | ||
| Smoker (cigarettes/cigars) | Yes | 5/53 (9.4) | 9/53 (17.0) |
| No | 48/53 (90.6) | 44/53 (83.0) | |
| Smokes cannabis | Yes | 1/53 (1.9) | 1/53 (1.9) |
| No | 52/53 (98.1) | 52/53 (98.1) | |
| Uses street drugs | Yes | 1/53 (1.9) | |
| No | 53/53 (100.0) | 52/53 (98.1) | |
| Injects street drugs | No | 53/53 (100.0) | 53/53 (100.0) |
| Takes prescribed opiate substitute | Yes | 1/53 (1.9) | 2/53 (3.8) |
| No | 52/53 (98.1) | 51/53 (96.2) | |
| Receives help for alcohol use | No | 53/53 (100.0) | 53/53 (100.0) |
| Receives help for drug use | Yes | 3/53 (5.7) | |
| No | 53/53 (100.0) | 50/53 (94.3) | |
| Experiences mental ill health before pregnancy | Yes | 46/53 (86.8) | 45/53 (84.9) |
| No | 7/53 (13.2) | 8/53 (15.1) | |
| Experiences mental ill health during pregnancy | Yes | 45/53 (84.9) | 36/53 (67.9) |
| No | 8/53 (15.1) | 16/53 (30.2) | |
| Don’t know | 1/53 (1.9) | ||
| Experiences mental ill health after the baby was born | Yes | 52/53 (98.1) | 50/53 (94.3) |
| No | 3/53 (5.7) | ||
| Don’t know | 1/53 (1.9) | ||
| Has one or more physical disabilities | Yes | 6/53 (11.3) | 6/53 (11.3) |
| No | 47/53 (88.7) | 47/53 (88.7) | |
| Been diagnosed with mental illness | Yes | 35/53 (66.0) | 30/53 (56.6) |
| No | 18/53 (34.0) | 23/53 (43.4) | |
| Details of mental illness | Depression | 22/35 (62.9) | 19/30 (63.3) |
| Anxiety disorder | 20/35 (57.1) | 22/30 (73.3) | |
| Obsessive compulsive disorder (OCD) | 3/35 (8.6) | 2/30 (6.7) | |
| PTSD | 7/35 (20.0) | 4/30 (13.3) | |
| Personality disorder | 4/35 (11.4) | 5/30 (16.7) | |
| Awaiting assessment for ADHD/autism spectrum disorder (ASD) | 2/35 (5.7) | ||
| Previous anxiety and depression | 1/35 (2.9) | 1/30 (3.3) | |
| Takes regular prescribed medications | Yes | 25/53 (47.2) | 35/53 (66.0) |
| No | 25/53 (47.2) | 17/53 (32.1) | |
| Missing | 3/53 (5.7) | 1/53 (1.9) | |
| Details of prescribed medications | SSRI | 13/25 (52.0) | 22/35 (62.9) |
| SNRIs | 1/25 (4.0) | 1/35 (2.9) | |
| Other antidepressant | 2/25 (8.0) | 3/35 (8.6) | |
| Methadone | 2/35 (5.7) | ||
| Anti-psychotic | 1/35 (2.9) | ||
| Benzodiazepine | 1/25 (4.0) | ||
| Betablocker | 1/25 (4.0) | 1/35 (2.9) | |
| Been prescribed medication for mental health problems before pregnancy | Yes | 35/53 (66.0) | 32/53 (60.4) |
| No | 18/53 (34.0) | 20/53 (37.7) | |
| Missing | 1/53 (1.9) | ||
| Been prescribed medication for mental health problems during pregnancy | Yes | 11/53 (20.8) | 13/53 (24.5) |
| No | 42/53 (79.2) | 39/53 (73.6) | |
| Missing | 1/53 (1.9) | ||
| Been prescribed medication for mental health problems after pregnancy | Yes | 23/53 (43.4) | 29/53 (54.7) |
| No | 30/53 (56.6) | 23/53 (43.4) | |
| Missing | 1/53 (1.9) | ||
| Ability to care for or interact with your baby been affected by any health problem or a disability | Yes | 20/53 (37.7) | 18/53 (34.0) |
| No | 33/53 (62.3) | 35/53 (66.0) | |
| How much does your health problem/disability affect your ability to feed your baby? | A lot | 2/53 (3.8) | 1/53 (1.9) |
| A little | 9/53 (17.0) | 4/53 (7.5) | |
| Not at all | 13/53 (24.5) | 20/53 (37.7) | |
| Missing | 29/53 (54.7) | 28/53 (52.8) | |
| How much does your health problem/disability affect your ability to pick up your baby? | A lot | 1/53 (1.9) | 3/53 (5.7) |
| A little | 12/53 (22.6) | 6/53 (11.3) | |
| Not at all | 11/53 (20.8) | 15/53 (28.3) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to change nappies? | A lot | 1/53 (1.9) | 1/53 (1.9) |
| A little | 2/53 (3.8) | 4/53 (7.5) | |
| Not at all | 21/53 (39.6) | 19/53 (35.8) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to dress your baby? | A lot | 1/53 (1.9) | 1/53 (1.9) |
| A little | 9/53 (17.0) | 8/53 (15.1) | |
| Not at all | 14/53 (26.4) | 15/53 (28.3) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to carry your baby? | A lot | 2/53 (3.8) | 3/53 (5.7) |
| A little | 10/53 (18.9) | 5/53 (9.4) | |
| Not at all | 12/53 (22.6) | 16/53 (30.2) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to hold your baby? | A lot | 1/53 (1.9) | 2/53 (3.8) |
| A little | 13/53 (24.5) | 7/53 (13.2) | |
| Not at all | 10/53 (18.9) | 15/53 (28.3) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to cuddle with your baby? | A lot | 2/53 (3.8) | 2/53 (3.8) |
| A little | 12/53 (22.6) | 5/53 (9.4) | |
| Not at all | 10/53 (18.9) | 17/53 (32.1) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to speak to your baby? | A lot | 2/53 (3.8) | 1/53 (1.9) |
| A little | 10/53 (18.9) | 12/53 (22.6) | |
| Not at all | 12/53 (22.6) | 11/53 (20.8) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to read to your baby? | A lot | 3/53 (5.7) | 3/53 (5.7) |
| A little | 9/53 (17.0) | 5/53 (9.4) | |
| Not at all | 12/53 (22.6) | 16/53 (30.2) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to hear/listen to your baby? | A lot | 1/53 (1.9) | |
| A little | 5/53 (9.4) | 7/53 (13.2) | |
| Not at all | 18/53 (34.0) | 16/53 (30.2) | |
| Missing | 30/53 (56.6) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to bath your baby? | A lot | 5/53 (9.4) | 2/53 (3.8) |
| A little | 7/53 (13.2) | 6/53 (11.3) | |
| Not at all | 11/53 (20.8) | 16/53 (30.2) | |
| Missing | 30/53 (56.6) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to play with your baby? | A lot | 4/53 (7.5) | 2/53 (3.8) |
| A little | 13/53 (24.5) | 12/53 (22.6) | |
| Not at all | 7/53 (13.2) | 10/53 (18.9) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to go outside with your baby or take your baby places? | A lot | 12/53 (22.6) | 10/53 (18.9) |
| A little | 10/53 (18.9) | 11/53 (20.8) | |
| Not at all | 2/53 (3.8) | 3/53 (5.7) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your ability to be happy with your baby? | A lot | 4/53 (7.5) | 3/53 (5.7) |
| A little | 16/53 (30.2) | 14/53 (26.4) | |
| Not at all | 4/53 (7.5) | 7/53 (13.2) | |
| Missing | 29/53 (54.7) | 29/53 (54.7) | |
| How much does your health problem/disability affect your other abilities? | A lot | 3/53 (5.7) | 2/53 (3.8) |
| A little | 2/53 (3.8) | ||
| Not at all | 7/53 (13.2) | 10/53 (18.9) | |
| Missing | 43/53 (81.1) | 39/53 (73.6) | |
| Details of other disability | Bonding with your baby (a lot) | 1/53 (1.9) | |
| Going to mum and baby groups (a lot) | 1/53 (1.9) | ||
| Taking baby for vaccinations (a lot) | 1/53 (1.9) | ||
| Require much support from family to look after baby (a lot) | 1/53 (1.9) | ||
| Had a serious illness or been seriously injured | No | 46/53 (86.8) | 48/53 (90.6) |
| Yes, but it does not affect me | 3/53 (5.7) | 3/53 (5.7) | |
| Yes, and it still affects me | 4/53 (7.5) | 2/53 (3.8) | |
| One of your immediate family been seriously ill or injured | No | 38/53 (71.7) | 35/53 (66.0) |
| Yes, but it does not affect me | 5/53 (9.4) | 5/53 (9.4) | |
| Yes, and it still affects me | 10/53 (18.9) | 13/53 (24.5) | |
| Close friends or other close relatives been seriously ill or injured | No | 44/53 (83.0) | 36/53 (67.9) |
| Yes, but it does not affect me | 1/53 (1.9) | 5/53 (9.4) | |
| Yes, and it still affects me | 8/53 (15.1) | 12/53 (22.6) | |
| Had immediate family who died | No | 45/53 (84.9) | 47/53 (88.7) |
| Yes, but it does not affect me | 3/53 (5.7) | 1/53 (1.9) | |
| Yes, and it still affects me | 5/53 (9.4) | 4/53 (7.5) | |
| Missing | 1/53 (1.9) | ||
| Had close friends or other close relatives who died | No | 40/53 (75.5) | 38/53 (71.7) |
| Yes, but it does not affect me | 4/53 (7.5) | 5/53 (9.4) | |
| Yes, and it still affects me | 9/53 (17.0) | 10/53 (18.9) | |
| Have separated from partner (not including death) | No | 47/53 (88.7) | 42/53 (79.2) |
| Yes, but it does not affect me | 1/53 (1.9) | 3/53 (5.7) | |
| Yes, and it still affects me | 5/53 (9.4) | 8/53 (15.1) | |
| Child living in your household been placed on the child protection register or been taken into care | No | 52/53 (98.1) | 51/53 (96.2) |
| Yes, but it does not affect me | 1/53 (1.9) | 1/53 (1.9) | |
| Yes, and it still affects me | 1/53 (1.9) | ||
| Had any serious problem with a close friend, neighbour or relative | No | 42/53 (79.2) | 46/53 (86.8) |
| Yes, but it does not affect me | 4/53 (7.5) | 1/53 (1.9) | |
| Yes, and it still affects me | 7/53 (13.2) | 6/53 (11.3) | |
| You or an immediate family member been subject to serious racial abuse, attack or threats | No | 51/53 (96.2) | 50/53 (94.3) |
| Yes, but it does not affect me | 1/53 (1.9) | 2/53 (3.8) | |
| Yes, and it still affects me | 1/53 (1.9) | 1/53 (1.9) | |
| You or an immediate family member been subject to any abuse, attack, threat – perhaps due to you or someone close to you having a disability of any kind | No | 50/53 (94.3) | 48/53 (90.6) |
| Yes, but it does not affect me | 1/53 (1.9) | 1/53 (1.9) | |
| Yes, and it still affects me | 1/53 (1.9) | 4/53 (7.5) | |
| Missing | 1/53 (1.9) | ||
| You or an immediate family member been subject to any other form of serious abuse, attack or threat | No | 47/53 (88.7) | 49/53 (92.5) |
| Yes, but it does not affect me | 1/53 (1.9) | 2/53 (3.8) | |
| Yes, and it still affects me | 5/53 (9.4) | 2/53 (3.8) | |
| You or your partner been unemployed or seeking work for more than 1 month | No | 42/53 (79.2) | 43/53 (81.1) |
| Yes, but it does not affect me | 5/53 (9.4) | 6/53 (11.3) | |
| Yes, and it still affects me | 6/53 (11.3) | 3/53 (5.7) | |
| Missing | 1/53 (1.9) | ||
| You or your partner been sacked from your job or made redundant | No | 47/53 (88.7) | 51/53 (96.2) |
| Yes, but it does not affect me | 3/53 (5.7) | 1/53 (1.9) | |
| Yes, and it still affects me | 3/53 (5.7) | 1/53 (1.9) | |
| You had any major financial difficulties (e.g. debts, difficulty paying bills) | No | 35/53 (66.0) | 35/53 (66.0) |
| Yes, but it does not affect me | 4/53 (7.5) | 8/53 (15.1) | |
| Yes, and it still affects me | 14/53 (26.4) | 10/53 (18.9) | |
| You or an immediate family member had any police contact or been in a court appearance | No | 47/53 (88.7) | 45/53 (84.9) |
| Yes, but it does not affect me | 5/53 (9.4) | 5/53 (9.4) | |
| Yes, and it still affects me | 1/53 (1.9) | 3/53 (5.7) | |
| You or an immediate family member had been burgled or mugged | No | 53/53 (100.0) | 52/53 (98.1) |
| Yes, but it does not affect me | 1/53 (1.9) | ||
| Another individual who lives with you given birth | No | 53/53 (100.0) | 52/53 (98.1) |
| Yes, but it does not affect me | 1/53 (1.9) | ||
| Another individual who lives with you suffered from a miscarriage or had a stillbirth | No | 53/53 (100.0) | 53/53 (100.0) |
| Moved house (through choice) | No | 37/53 (69.8) | 43/53 (81.1) |
| Yes, but it does not affect me | 10/53 (18.9) | 7/53 (13.2) | |
| Yes, and it still affects me | 6/53 (11.3) | 2/53 (3.8) | |
| Missing | 1/53 (1.9) | ||
| Moved house (not through choice) | No | 48/53 (90.6) | 47/53 (88.7) |
| Yes, but it does not affect me | 2/53 (3.8) | 3/53 (5.7) | |
| Yes, and it still affects me | 3/53 (5.7) | 3/53 (5.7) | |
| Had any housing difficulties | No | 43/53 (81.1) | 39/53 (73.6) |
| Yes, but it does not affect me | 4/53 (7.5) | 6/53 (11.3) | |
| Yes, and it still affects me | 6/53 (11.3) | 7/53 (13.2) | |
| Missing | 1/53 (1.9) | ||
| Been homeless | No | 50/53 (94.3) | 48/53 (90.6) |
| Yes, but it does not affect me | 2/53 (3.8) | ||
| Yes, and it still affects me | 2/53 (3.8) | 3/53 (5.7) | |
| Missing | 1/53 (1.9) | ||
| Had any other significant event happen | No | 30/53 (56.6) | 32/53 (60.4) |
| Yes, but it does not affect me | 2/53 (3.8) | 2/53 (3.8) | |
| Yes, and it still affects me | 18/53 (34.0) | 11/53 (20.8) | |
| Missing | 3/53 (5.7) | 8/53 (15.1) | |
| Details of other significant event | Participant involved in road traffic accident | 1/20 (5.0) | |
| Participant had miscarriage | 1/20 (5.0) | ||
| Participant had difficulties or trauma related to pregnancy or birth experience (current baby) | 7/20 (35.0) | 2/13 (15.4) | |
| Immediate family who does not live in household suffered from a miscarriage | 1/20 (5.0) | 1/13 (7.7) | |
| Immediate/close family member died over 1 year ago, but still affects participant | 2/13 (15.4) | ||
| Participant experienced suicidal crisis, thoughts or behaviours | 1/13 (7.7) | ||
| Participant and/or partner experienced difficulties in workplace (e.g. unfair/toxic environment) | 3/20 (15.0) | ||
| Other illnesses –participant, close family or friends (participant not identified as ‘serious’) | 1/20 (5.0) | ||
| Other stressors or tension – immediate family | 1/20 (5.0) | 2/13 (15.4) | |
| The physical and/or emotional health of my family causes me... | 1 – no concern | 5/53 (9.4) | 4/53 (7.5) |
| 2 | 5/53 (9.4) | 6/53 (11.3) | |
| 3 | 11/53 (20.8) | 10/53 (18.9) | |
| 4 | 11/53 (20.8) | 16/53 (30.2) | |
| 5 – a lot of concern | 21/53 (39.6) | 16/53 (30.2) | |
| Missing | 1/53 (1.9) | ||
| My access to health and other services is... | 1 – good | 23/53 (43.4) | 27/53 (50.9) |
| 2 | 12/53 (22.6) | 13/53 (24.5) | |
| 3 | 16/53 (30.2) | 10/53 (18.9) | |
| 4 | 2/53 (3.8) | 1/53 (1.9) | |
| 5 – poor | 2/53 (3.8) | ||
| The support I have from family and friends is... | 1 – good | 28/53 (52.8) | 27/53 (50.9) |
| 2 | 11/53 (20.8) | 12/53 (22.6) | |
| 3 | 10/53 (18.9) | 7/53 (13.2) | |
| 4 | 2/53 (3.8) | 6/53 (11.3) | |
| 5 – poor | 2/53 (3.8) | 1/53 (1.9) | |
| Employment/unemployment within the family causes me... | 1 – no concern | 24/53 (45.3) | 25/53 (47.2) |
| 2 | 11/53 (20.8) | 7/53 (13.2) | |
| 3 | 9/53 (17.0) | 10/53 (18.9) | |
| 4 | 5/53 (9.4) | ||
| 5 – a lot of concern | 9/53 (17.0) | 6/53 (11.3) | |
| Money causes me... | 1 – no concern | 8/53 (15.1) | 6/53 (11.3) |
| 2 | 11/53 (20.8) | 10/53 (18.9) | |
| 3 | 12/53 (22.6) | 16/53 (30.2) | |
| 4 | 8/53 (15.1) | 11/53 (20.8) | |
| 5 – a lot of concern | 14/53 (26.4) | 10/53 (18.9) | |
| Housing causes me... | 1 – no concern | 34/53 (64.2) | 29/53 (54.7) |
| 2 | 5/53 (9.4) | 11/53 (20.8) | |
| 3 | 6/53 (11.3) | 2/53 (3.8) | |
| 4 | 1/53 (1.9) | 5/53 (9.4) | |
| 5 – a lot of concern | 7/53 (13.2) | 6/53 (11.3) | |
| The use of tobacco, alcohol or other drugs within the household causes me... | 1 – no concern | 47/53 (88.7) | 46/53 (86.8) |
| 2 | 1/53 (1.9) | 2/53 (3.8) | |
| 3 | 3/53 (5.7) | 3/53 (5.7) | |
| 4 | 2/53 (3.8) | ||
| 5 – a lot of concern | 2/53 (3.8) | ||
| Stressful life events, for example childhood experiences, abuse, domestic violence, crime etc., cause me... | 1 - no concern | 15/53 (28.3) | 19/53 (35.8) |
| 2 | 9/53 (17.0) | 7/53 (13.2) | |
| 3 | 12/53 (22.6) | 11/53 (20.8) | |
| 4 | 9/53 (17.0) | 9/53 (17.0) | |
| 5 – a lot of concern | 8/53 (15.1) | 7/53 (13.2) | |
| Being a parent causes me... | 1 – no concern | 3/53 (5.7) | 6/53 (11.3) |
| 2 | 10/53 (18.9) | 10/53 (18.9) | |
| 3 | 18/53 (34.0) | 22/53 (41.5) | |
| 4 | 10/53 (18.9) | 8/53 (15.1) | |
| 5 – a lot of concern | 12/53 (22.6) | 7/53 (13.2) | |
| Details of any other worries | Partner working away from home | 1/53 (1.9) | |
| My mental health | 2/53 (3.8) | 1/53 (1.9) | |
| COVID | 1/53 (1.9) | ||
| Balancing and coping with commitments | 3/53 (5.7) | ||
| Completing regular visa applications | 1/53 (1.9) | ||
| Smoking in wider family (e.g. grandparents) | 1/53 (1.9) |
| Mellow Babies | Usual care | ||
|---|---|---|---|
| N = 53 | N = 53 | ||
| Are you currently in a relationship? | Yes | 46/53 (86.8) | 43/53 (81.1) |
| No | 7/53 (13.2) | 10/53 (18.9) | |
| If no, which of the following best describes you? | I am single/never married | 5/7 (71.4) | 4/10 (40.0) |
| I am divorced | 1/7 (14.3) | ||
| I am separated | 6/10 (60.0) | ||
| Missing | 1/7 (14.3) | ||
| Which statement best describes you? | I am married/in a civil partnership | 23/53 (43.4) | 23/53 (43.4) |
| I live with someone as a couple, but we are not married/in a civil partnership | 21/53 (39.6) | 16/53 (30.2) | |
| I am in a relationship, but we do not live together as a couple | 3/53 (5.7) | 4/53 (7.5) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Partner’s age | Mean (SD) (N) | 34.6 (7.2) (N = 47) | 33.2 (6.5) (N = 44) |
| Partner’s gender | Male | 47/53 (88.7) | 44/53 (83.0) |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| Partner’s ethnic background | White British | 41/53 (77.4) | 41/53 (77.4) |
| White Irish | 1/53 (1.9) | ||
| Eastern European | 1/53 (1.9) | ||
| Other European | 2/53 (3.8) | ||
| Any other background | 5/53 (9.4) | ||
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| How many hours did your partner work last week? | (Minimum, maximum) | (0.0, 70.0) | (0.0, 84.0) |
| Mean (SD) (N) | 38.0 (14.1) (N = 44) | 43.1 (16.3) (N = 40) | |
| Median (25th, 75th centile) | 40.0 (35.0, 40.0) | 40.0 (37.3, 47.5) | |
| Which of these statements best describes your partner’s job status? | They are currently in paid employment or self-employed | 43/53 (81.1) | 40/53 (75.5) |
| They are not currently working but have been in paid employment in the past | 4/53 (7.5) | 4/53 (7.5) | |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| Which of these best describe their current job or your last job if you are not working now? | Self-employed with paid employees | 3/46 (6.5) | 2/43 (4.7) |
| Self-employed with NO paid employees | 3/46 (6.5) | 2/43 (4.7) | |
| Manager | 5/46 (10.9) | 6/43 (14.0) | |
| Supervisor | 7/46 (15.2) | 2/43 (4.7) | |
| Employee | 28/46 (60.9) | 29/43 (67.4) | |
| Missing | 2/43 (4.7) | ||
| Which describes best what your partner was doing last week? | In paid employment | 42/53 (79.2) | 39/53 (73.6) |
| Not working because of temporary sickness or illness | 1/53 (1.9) | ||
| Permanently unable to work because of long-term sickness or disability | 1/53 (1.9) | ||
| Looking after home or family | 2/53 (3.8) | ||
| Providing care for an ill or disabled friend or relative | 1/53 (1.9) | 1/53 (1.9) | |
| Doing something else | 2/53 (3.8) | 2/53 (3.8) | |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| How involved is your partner in your baby’s life? – He/she supports my baby financially | Yes | 47/53 (88.7) | 41/53 (77.4) |
| Maybe | 1/53 (1.9) | ||
| No | 2/53 (3.8) | ||
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| How involved is your partner in your baby’s life? – He/she is emotionally involved in my baby’s life | Yes | 45/53 (84.9) | 42/53 (79.2) |
| Maybe | 2/53 (3.8) | ||
| No | 2/53 (3.8) | ||
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| How involved is your partner in your baby’s life? – He/she sees my baby as often as he/she can | Yes | 45/53 (84.9) | 41/53 (77.4) |
| Maybe | 2/53 (3.8) | 1/53 (1.9) | |
| No | 2/53 (3.8) | ||
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| How involved is your partner in your baby’s life? – He/she is involved in my baby’s upbringing | Yes | 46/53 (86.8) | 40/53 (75.5) |
| Maybe | 1/53 (1.9) | 2/53 (3.8) | |
| No | 2/53 (3.8) | ||
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| Do you feel that having a baby has brought you and your partner – Closer together | Yes | 35/53 (66.0) | 32/53 (60.4) |
| No | 12/53 (22.6) | 12/53 (22.6) | |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| Do you feel that having a baby has brought you and your partner – Made you less close than before | Yes | 12/53 (22.6) | 9/53 (17.0) |
| No | 35/53 (66.0) | 35/53 (66.0) | |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| Do you feel that having a baby has brought you and your partner – Made no difference to our relationship | Yes | 16/53 (30.2) | 12/53 (22.6) |
| No | 31/53 (58.5) | 31/53 (58.5) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Do you feel that having a baby has brought you and your partner – We only started our relationship after baby was born | Yes | 1/53 (1.9) | |
| No | 47/53 (88.7) | 42/53 (79.2) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| I am unable to see or speak to my partner every day because: he/she is currently living or working abroad | Yes | 1/53 (1.9) | |
| No | 47/53 (88.7) | 42/53 (79.2) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| I am unable to see or speak to my partner every day because: he/she is a serving member of the armed forces and deployed overseas | Yes | 1/53 (1.9) | 1/53 (1.9) |
| No | 45/53 (84.9) | 43/53 (81.1) | |
| Missing | 7/53 (13.2) | 9/53 (17.0) | |
| I am unable to see or speak to my partner every day because: we do not live at the same address | Yes | 3/53 (5.7) | 5/53 (9.4) |
| No | 44/53 (83.0) | 39/53 (73.6) | |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| I am unable to see or speak to my partner every day because: I do not want to have contact with him/her | Yes | 1/53 (1.9) | |
| No | 47/53 (88.7) | 43/53 (81.1) | |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| I am unable to see or speak to my partner every day because: my family do not want me having contact with him/her | Yes | 2/53 (3.8) | |
| No | 47/53 (88.7) | 42/53 (79.2) | |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| I am unable to see or speak to my partner every day because: he/she is in prison | Yes | 1/53 (1.9) | |
| No | 47/53 (88.7) | 43/53 (81.1) | |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| I am unable to see or speak to my partner every day because: I have been told by a health or social care professional that if I have contact with him/her I will not be allowed to keep my baby | No | 47/53 (88.7) | 44/53 (83.0) |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| I am unable to see or speak to my partner every day because: he/she was verbally or physically abusive towards me | Yes | 1/53 (1.9) | |
| No | 47/53 (88.7) | 43/53 (81.1) | |
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| I am unable to see or speak to my partner every day because: work rota that requires weeks away from home | Yes | 2/53 (3.8) | |
| No | 53/53 (100.0) | 51/53 (96.2) | |
| I am unable to see or speak to my partner every day because: works long or unsociable hours | Yes | 1/53 (1.9) | |
| No | 52/53 (98.1) | 53/53 (100.0) | |
| I am unable to see or speak to my partner every day because: he/she sometimes chooses not to speak/see us | Yes | 1/53 (1.9) | |
| No | 53/53 (100.0) | 52/53 (98.1) | |
| Has there been tension between you and your partner – irritability, unpleasant silence, etc.? | Never | 2/53 (3.8) | 12/53 (22.6) |
| Rarely | 31/53 (58.5) | 22/53 (41.5) | |
| Often | 11/53 (20.8) | 9/53 (17.0) | |
| Very much | 3/53 (5.7) | ||
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Has your partner tried to share your interests? | Never | 6/53 (11.3) | 3/53 (5.7) |
| Rarely | 10/53 (18.9) | 7/53 (13.2) | |
| Often | 28/53 (52.8) | 26/53 (49.1) | |
| Very much | 3/53 (5.7) | 7/53 (13.2) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Have you felt your partner went out too often without you? | Never | 34/53 (64.2) | 31/53 (58.5) |
| Rarely | 9/53 (17.0) | 8/53 (15.1) | |
| Often | 2/53 (3.8) | 2/53 (3.8) | |
| Very much | 2/53 (3.8) | 1/53 (1.9) | |
| Missing | 6/53 (11.3) | 11/53 (20.8) | |
| Have you been feeling close to your partner since you became pregnant? | Never | 2/53 (3.8) | |
| Rarely | 5/53 (9.4) | 5/53 (9.4) | |
| Often | 19/53 (35.8) | 14/53 (26.4) | |
| Very much | 23/53 (43.4) | 22/53 (41.5) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Does your partner show their approval of you? | Never | 1/53 (1.9) | 1/53 (1.9) |
| Rarely | 6/53 (11.3) | 4/53 (7.5) | |
| Often | 17/53 (32.1) | 15/53 (28.3) | |
| Very much | 23/53 (43.4) | 23/53 (43.4) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Has your partner helped in the running of the house? | Not at all | 3/53 (5.7) | |
| A little | 13/53 (24.5) | 16/53 (30.2) | |
| A lot | 10/53 (18.9) | 7/53 (13.2) | |
| Very much | 24/53 (45.3) | 17/53 (32.1) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Have you felt like putting your arms around your partner and cuddling him/her? | Not at all | 1/53 (1.9) | 1/53 (1.9) |
| A little | 13/53 (24.5) | 8/53 (15.1) | |
| A lot | 10/53 (18.9) | 10/53 (18.9) | |
| Very much | 23/53 (43.4) | 24/53 (45.3) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Do you enjoy spending time with your partner? | Not at all | 1/53 (1.9) | 1/53 (1.9) |
| A little | 5/53 (9.4) | 1/53 (1.9) | |
| A lot | 10/53 (18.9) | 13/53 (24.5) | |
| Very much | 30/53 (56.6) | 28/53 (52.8) | |
| Missing | 7/53 (13.2) | 10/53 (18.9) | |
| Have arguments between you and your partner come close to blows? Or potentially worse? | Never | 34/53 (64.2) | 32/53 (60.4) |
| Rarely | 9/53 (17.0) | 7/53 (13.2) | |
| Often | 4/53 (7.5) | 3/53 (5.7) | |
| Missing | 6/53 (11.3) | 11/53 (20.8) | |
| Have you found it easy to show affection to your partner? | Never | 1/53 (1.9) | |
| Rarely | 10/53 (18.9) | 5/53 (9.4) | |
| Often | 13/53 (24.5) | 18/53 (34.0) | |
| Very often | 23/53 (43.4) | 20/53 (37.7) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Have you felt that your partner was paying you too little attention? | Never | 12/53 (22.6) | 16/53 (30.2) |
| Rarely | 22/53 (41.5) | 19/53 (35.8) | |
| Often | 10/53 (18.9) | 6/53 (11.3) | |
| Very often | 3/53 (5.7) | 2/53 (3.8) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Has your partner seemed to ignore how you were feeling? | Never | 15/53 (28.3) | 15/53 (28.3) |
| Rarely | 20/53 (37.7) | 18/53 (34.0) | |
| Often | 7/53 (13.2) | 8/53 (15.1) | |
| Very often | 5/53 (9.4) | 2/53 (3.8) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Has your partner shown affection to you? | Never | 1/53 (1.9) | |
| Rarely | 8/53 (15.1) | 3/53 (5.7) | |
| Often | 17/53 (32.1) | 16/53 (30.2) | |
| Very often | 22/53 (41.5) | 23/53 (43.4) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Have you wished you could rely more on your partner to look after you? | Never | 22/53 (41.5) | 18/53 (34.0) |
| Rarely | 14/53 (26.4) | 11/53 (20.8) | |
| Often | 7/53 (13.2) | 7/53 (13.2) | |
| Very often | 4/53 (7.5) | 6/53 (11.3) | |
| Missing | 6/53 (11.3) | 11/53 (20.8) | |
| Does your partner talk to you about his/her problems and feelings? | Never | 9/53 (17.0) | 5/53 (9.4) |
| Rarely | 15/53 (28.3) | 13/53 (24.5) | |
| Often | 16/53 (30.2) | 15/53 (28.3) | |
| Very often | 7/53 (13.2) | 10/53 (18.9) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Does your partner smoke cigarettes/cigars? | Yes | 11/53 (20.8) | 9/53 (17.0) |
| No | 36/53 (67.9) | 34/53 (64.2) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Does your partner smoke cannabis? | Yes | 1/53 (1.9) | 4/53 (7.5) |
| No | 46/53 (86.8) | 39/53 (73.6) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Does your partner use street drugs? e.g. heroin, crack/cocaine, valium, ecstasy | No | 47/53 (88.7) | 42/53 (79.2) |
| Don’t know | 1/53 (1.9) | ||
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Does your partner inject street drugs? e.g. heroin, crack/cocaine, temazepam | Yes | 1/53 (1.9) | |
| No | 47/53 (88.7) | 42/53 (79.2) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Does your partner take prescribed opiate substitute drugs? e.g. methadone or buprenorphine (Subutex/Suboxone) | No | 47/53 (88.7) | 43/53 (81.1) |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Does your partner receive help from services for his/her alcohol use? | Yes | 1/53 (1.9) | |
| No | 46/53 (86.8) | 43/53 (81.1) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Does your partner receive help from services for his/her drug use? | Yes | 1/53 (1.9) | 1/53 (1.9) |
| No | 46/53 (86.8) | 42/53 (79.2) | |
| Missing | 6/53 (11.3) | 10/53 (18.9) | |
| Does your baby live with you every day of the week? | Yes | 53/53 (100.0) | 53/53 (100.0) |
| Do any of the following people help you care for your baby? | Nobody, I care for my baby by myself | 9/53 (17.0) | 9/53 (17.0) |
| My husband or partner | 46/53 (86.8) | 39/53 (73.6) | |
| My mum, dad, or in-laws | 18/53 (34.0) | 26/53 (49.1) | |
| Other family member or relative | 4/53 (7.5) | 8/53 (15.1) | |
| A friend | 3/53 (5.7) | 7/53 (13.2) | |
| Religious community (e.g. church, mosque) | 1/53 (1.9) | ||
| Other | 5/53 (9.4) | 3/53 (5.7) | |
| How easy has it been for you to get help or advice from the following people since your baby was born? – My family doctor/GP | Very easy | 15/53 (28.3) | 22/53 (41.5) |
| Easy | 19/53 (35.8) | 19/53 (35.8) | |
| Unsure | 3/53 (5.7) | 4/53 (7.5) | |
| Not easy | 6/53 (11.3) | 5/53 (9.4) | |
| Not easy at all | 10/53 (18.9) | 2/53 (3.8) | |
| I haven’t done this | 1/53 (1.9) | ||
| How easy has it been for you to get help or advice from the following people since your baby was born? – My HV | Very easy | 20/53 (37.7) | 28/53 (52.8) |
| Easy | 22/53 (41.5) | 14/53 (26.4) | |
| Unsure | 8/53 (15.1) | 3/53 (5.7) | |
| Not easy | 2/53 (3.8) | 7/53 (13.2) | |
| Not easy at all | 1/53 (1.9) | ||
| I haven’t done this | 1/53 (1.9) | ||
| How easy has it been for you to get help or advice from the following people since your baby was born? – My social worker | Very easy | 1/53 (1.9) | |
| Easy | 1/53 (1.9) | ||
| Unsure | 1/53 (1.9) | ||
| Not easy at all | 1/53 (1.9) | ||
| I haven’t done this | 51/53 (96.2) | 50/53 (94.3) | |
| Missing | 1/53 (1.9) | ||
| How easy has it been for you to get help or advice from the following people since your baby was born? – Other mothers with small children | Very easy | 13/53 (24.5) | 14/53 (26.4) |
| Easy | 19/53 (35.8) | 14/53 (26.4) | |
| Unsure | 4/53 (7.5) | 9/53 (17.0) | |
| Not easy | 6/53 (11.3) | 1/53 (1.9) | |
| Not easy at all | 1/53 (1.9) | 3/53 (5.7) | |
| I haven’t done this | 10/53 (18.9) | 12/53 (22.6) | |
| How easy has it been for you to get help or advice from the following people since your baby was born? – Drop-in centre for families | Very easy | 1/53 (1.9) | 1/53 (1.9) |
| Easy | 1/53 (1.9) | ||
| Unsure | 1/53 (1.9) | ||
| Not easy | 2/53 (3.8) | ||
| I haven’t done this | 50/53 (94.3) | 49/53 (92.5) | |
| Missing | 1/53 (1.9) | ||
| How easy has it been for you to get help or advice from the following people since your baby was born? – Telephone advice line | Very easy | 10/53 (18.9) | 7/53 (13.2) |
| Easy | 5/53 (9.4) | 5/53 (9.4) | |
| Unsure | 4/53 (7.5) | 1/53 (1.9) | |
| Not easy | 2/53 (3.8) | 2/53 (3.8) | |
| Not easy at all | 2/53 (3.8) | 1/53 (1.9) | |
| I haven’t done this | 30/53 (56.6) | 37/53 (69.8) | |
| How easy has it been for you to get help or advice from the following people since your baby was born? – My family | Very easy | 24/53 (45.3) | 26/53 (49.1) |
| Easy | 18/53 (34.0) | 17/53 (32.1) | |
| Unsure | 1/53 (1.9) | ||
| Not easy | 6/53 (11.3) | 4/53 (7.5) | |
| Not easy at all | 3/53 (5.7) | 4/53 (7.5) | |
| I haven’t done this | 2/53 (3.8) | 1/53 (1.9) | |
| How easy has it been for you to get help or advice from the following people since your baby was born? – The father of my baby | Very easy | 38/53 (71.7) | 30/53 (56.6) |
| Easy | 5/53 (9.4) | 12/53 (22.6) | |
| Not easy | 3/53 (5.7) | 4/53 (7.5) | |
| Not easy at all | 4/53 (7.5) | 5/53 (9.4) | |
| I haven’t done this | 2/53 (3.8) | 2/53 (3.8) | |
| Missing | 1/53 (1.9) | ||
| How easy has it been for you to get help or advice from the following people since your baby was born? – My partner (if different from father of baby) | Very easy | 1/53 (1.9) | 3/53 (5.7) |
| Unsure | 1/53 (1.9) | ||
| Not easy at all | 1/53 (1.9) | ||
| I haven’t done this | 44/53 (83.0) | 44/53 (83.0) | |
| Missing | 7/53 (13.2) | 5/53 (9.4) | |
| During the past 6 months, who would help you if a problem came up? | My husband or partner | 46/53 (86.8) | 42/53 (79.2) |
| My mother, father or in-laws | 47/53 (88.7) | 42/53 (79.2) | |
| Other family member or relative | 22/53 (41.5) | 23/53 (43.4) | |
| A friend | 27/53 (50.9) | 28/53 (52.8) | |
| Religious community | 1/53 (1.9) | 3/53 (5.7) | |
| Someone else | 1/53 (1.9) | 1/53 (1.9) | |
| During the past 6 months, would you have the kinds of help listed below if you needed them? – Someone to loan me £20 | Yes | 51/53 (96.2) | 52/53 (98.1) |
| No | 2/53 (3.8) | 1/53 (1.9) | |
| During the past 6 months, would you have the kinds of help listed below if you needed them? – Someone to help me if I were sick and needed to be in bed | Yes | 49/53 (92.5) | 49/53 (92.5) |
| No | 4/53 (7.5) | 4/53 (7.5) | |
| During the past 6 months, would you have the kinds of help listed below if you needed them? – Someone to take me to the clinic or doctor’s surgery if I needed a lift | Yes | 49/53 (92.5) | 48/53 (90.6) |
| No | 4/53 (7.5) | 5/53 (9.4) | |
| During the past 6 months, would you have the kinds of help listed below if you needed them? – Someone to talk with about my problems | Yes | 52/53 (98.1) | 49/53 (92.5) |
| No | 1/53 (1.9) | 4/53 (7.5) | |
| Is your partner the father of this baby? | Yes | 47/53 (88.7) | 43/53 (81.1) |
| No | 1/53 (1.9) | ||
| Missing | 6/53 (11.3) | 9/53 (17.0) | |
| Do any of the following prevent your baby from having contact with his/her biological father? | We do not live at the same address | 6/53 (11.3) | 10/53 (18.9) |
| I do not want to have contact with him | 5/53 (9.4) | 3/53 (5.7) | |
| My family do not want me having contact with him | 4/53 (7.5) | 2/53 (3.8) | |
| I have been told by a health or social care professional that if I have contact with him I will not be allowed to keep my baby | 1/53 (1.9) | ||
| He was verbally or physically abusive towards me or my baby | 4/53 (7.5) | 3/53 (5.7) | |
| He died | 1/53 (1.9) | 1/53 (1.9) | |
| He does not want to have contact with his baby | 1/53 (1.9) | ||
| He misuses drugs or alcohol | 2/53 (3.8) | ||
| His work rota that requires weeks away from home | 2/53 (3.8) | ||
| How would you describe your relationship with your baby’s biological father? | Very friendly | 27/53 (50.9) | 22/53 (41.5) |
| Friendly | 2/53 (3.8) | 4/53 (7.5) | |
| Neither friendly nor unfriendly | 1/53 (1.9) | 2/53 (3.8) | |
| Unfriendly | 2/53 (3.8) | ||
| Very unfriendly | 1/53 (1.9) | ||
| I do not see or speak to my baby’s biological father | 3/53 (5.7) | 4/53 (7.5) | |
| Missing | 19/53 (35.8) | 19/53 (35.8) |
