Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 17/44/42. The contractual start date was in September 2018. The final report began editorial review in July 2021 and was accepted for publication in March 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Dowrick et al. This work was produced by Dowrick et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Dowrick et al.
Chapter 1 Introduction
Background
Parts of this section have been adapted with permission from Rawlinson et al. 1 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
The prevalence of psychological morbidity, including depression, anxiety, post-traumatic stress disorder (PTSD), and functional impairment among asylum seekers and refugees (AS&Rs) is higher than among other migrant groups and local majority populations. 2–4 Mental health problems are particularly prevalent among war refugees,5 with rates of PTSD up to 10 times higher than in the general population. 6,7 Persistence of mental health problems after resettlement is related to poor socioeconomic conditions, acculturation-related stressors, economic uncertainty and ethnic discrimination. 4,8 As a result, AS&Rs encounter extensive barriers to accessing health care4 and their mental health needs are largely unmet. 9
Making psychological therapies more accessible for AS&Rs is a national research priority. 10 Psychosocial interventions for AS&Rs resettled in high-income countries may provide significant benefits; however, there are few studies of good quality. 11 Evidence of the applicability of psychological interventions by non-specialists in low- and middle-income countries (LMICs) has increased significantly. 12–14 Many countries, including the UK, are seeking to improve health-care delivery by extending the roles of health professionals. 15 Innovations developed in LMICs, including task-sharing,16 have the potential to address current challenges for mental health care in high-income countries. 17
Problem Management Plus (PM+) is a low-intensity, transdiagnostic psychosocial intervention designed to be delivered by lay therapists, who can apply the same treatment principles across common mental health problems without tailoring treatment to a particular diagnosis. 18 PM+ incorporates task-sharing strategies, drawing on evidence of mental health interventions delivered by non-specialists in LMICs12,19,20 and the UK. 21
PM+ aims to help adults experiencing symptoms of common mental health problems, including depression, anxiety, stress and grief, as well as with practical problems, such as unemployment and interpersonal conflict. It therefore offers a potentially appropriate approach for AS&Rs living in high-income settings. PM+ involves five weekly sessions during which psychoeducation is provided and the therapeutic approaches are introduced, with subsequent weeks reinforcing the application to participants’ self-identified problems, and the final session revising learning and identifying future goals and signs of relapse. The PM+ therapeutic approach integrates problem-solving and behavioural treatment principles, including a slow-breathing stress management technique, problem-solving strategies, behavioural activation and strengthening social support. 18
PM+ is a manualised intervention, with separate manuals for the training of trainers and for individual and group PM+ training. It also incorporates the use of lay therapist reference manuals, participant worksheets and group PM+ case study materials. The group and individual PM+ programmes deliver the same content but in different formats: individual PM+ sessions last 90 minutes and involve only the lay therapist and participant, while group PM+ sessions last 2 hours to accommodate group dynamics, and are co-delivered by two lay therapist facilitators. To engage illiterate participants and those whose first language is not English, as well as support disclosure through affiliation with the case study experience, group PM+ adopts a case study format with pictorial materials and an accompanying narrative that follows a person progressing through PM+.
Developed by the World Health Organization (WHO) as part of its Mental Health Gap Action Programme (mhGAP) using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) evidence base,22 PM+ has shown significant benefit in trials in LMICs,18,23–28 and the group version is being tested with Syrian refugees in Jordan. 29 However, at present, there is limited evidence of the effectiveness or cost-effectiveness of interventions such as PM+ offered by lay therapists to AS&Rs in high-income countries. A pilot randomised trial of peer-provided PM+ for 60 Syrian refugees in the Netherlands indicated potential effectiveness in improving mental health outcomes and psychosocial functioning, and potentially cost-effectiveness,30 but further studies are needed with diverse AS&R populations in high-income countries.
Rationale for study
The Red Cross estimates that 65 million people throughout the world have been forced to flee their homes as the number of protracted conflicts has increased. 31 This has created more than 22 million refugees worldwide, of whom an estimated 118,995 live in the UK (2017 figures). 31 The UK received 38,500 asylum applications in 2016. Home Office figures show that in 2012–14, 36% of asylum applications were granted initially, rising to 49% after appeal. 32 Many applications are initially refused because it is difficult for applicants to provide the evidence needed to meet the strict criteria for refugees. The area of England with the largest number of asylum seekers in dispersal accommodation is the north-west (9524 in the first quarter of 2017).
Asylum seekers and refugees experience much higher levels of emotional distress and functional impairment than other migrant groups and local majority populations. 3,6,11 These are related to their reasons for leaving their country of origin and their experiences in transit and on arrival. 4 There may also be inequalities in mental health and well-being between asylum seeker and refugee groups depending on their age, gender, nationality, education, occupational status, length of stay, access to resources and current legal status in the UK. There are particular reasons for concern over the mental health of asylum seekers without leave to remain, who are at risk of destitution as they are neither eligible for state benefits nor allowed to undertake paid employment.
As a result of these factors, AS&Rs commonly have inadequate access to mental health care appropriate to their needs. 4 Their contact with statutory agencies is often crisis driven and mediated through voluntary third-sector organisations, whose staff – although highly motivated – lack knowledge and skills in the management of psychosocial distress. The situation is especially problematic for asylum seekers without leave to remain, who have been required to pay for specialist health care since August 2017. 33
There is, therefore, a need to offer and evaluate an accessible intervention designed to address the mental health and associated practical problems experienced by AS&Rs in the UK.
Aim and objectives
The aim of the PROSPER study was to assess the feasibility of conducting a randomised controlled trial (RCT) in the UK of an evidence-based psychosocial intervention based on PM+, delivered by lay therapists for distressed and functionally impaired AS&Rs.
The objectives of the study were to:
-
adapt the form and content of PM+ to the needs of AS&Rs in the UK
-
assess the feasibility of the proposed training procedures (including the involvement of refugees as lay therapists)
-
assess the feasibility of the proposed procedures for recruiting distressed AS&Rs as study participants
-
assess the feasibility of retaining both lay therapists and study participants through to trial completion
-
assess the fidelity of delivery of the intervention
-
assess the acceptability and utility of the proposed study measures, considering any linguistic and cultural barriers
-
assess how service use data can be measured.
In working towards these objectives, we aimed to specify the parameters of a full RCT to test the effectiveness and cost-effectiveness of PM+ in reducing emotional distress and health inequalities, and improving functional ability and well-being among AS&Rs.
Research design
Following Consolidated Standards of Reporting Trials (CONSORT) extension guidelines,34,35 we undertook a feasibility study of PM+, within which we included a pilot study of the design features of a future definitive RCT.
The feasibility study involved adaptation of PM+, using two parallel and interlinked elements:
-
evidence synthesis to identify the barriers to and facilitators of the uptake of psychosocial interventions delivered by lay therapists to improve the mental health and well-being of asylum seekers and migrants, including how idioms of distress are incorporated into assessments and interventions
-
stakeholder engagement with local stakeholders (migrant service users, care providers and policy-makers) using focus group methodology to ensure that PM+ is adapted for use with AS&R populations in the UK.
We also assessed the feasibility of a two-stage PM+ training procedure, with master trainers providing a training course tailored to the needs of well-being facilitators from a counselling non-governmental organisation (NGO), who in turn provided an 8-day training course and ongoing supervision for lay therapists in NGOs that support AS&Rs.
The pilot trial was designed to assess:
-
Feasibility of recruitment, with procedures based on a partially nested design to adjust for clustering by intervention provider in the test arm, with the client as the unit of randomisation. We assessed the feasibility of recruiting participants through collaborating NGOs and other health and welfare agencies,
-
Feasibility of a randomisation procedure in which participants are randomised using a secure 24-hour web-based randomisation system controlled by Liverpool Clinical Trials Centre (LCTC).
-
Feasibility of the proposed delivery model in relation to three key issues –
-
Retention of lay therapists and study participants through to trial completion. For therapists, this may be an issue, given that refugees recently granted leave to remain may wish to seek paid employment and/or relocate geographically. For study participants, retention may be affected by prioritisation of immediate needs regarding housing and benefits, concerns about the well-being of family members, outcomes of appeals procedures, or official policies on dispersal, resettlement and access to health care.
-
Individual compared with group approaches with regard to relative acceptability, participant preferences, linguistic and cultural issues (e.g. gender and language matching) and hence, retention.
-
Fidelity of intervention delivery – the extent to which lay therapists are able to control risk and stay ‘on message’.
-
-
Relevance and acceptability of the proposed study measures, with reference to –
-
technical aspects of translation
-
how epistemic differences relating to experience of distress are negotiated across language and culture
-
and hence their potential acceptability and suitability for a subsequent definitive trial.
-
Risks and benefits
Asylum seekers and refugees
Risks
For those not granted leave to remain, participation in an officially sponsored trial may raise anxieties about public visibility and heightened risk of deportation. This risk can be mitigated by participants using the contact details of their NGO or primary care team to register. A potential risk for all participants is being offered support from a lay therapist who has a similar linguistic and cultural background but antithetical political or religious views; however, this risk can be mitigated by careful vetting at the therapist–client allocation stage. The risk of stigma associated with mental illness in some cultures, meanwhile, can be mitigated by the focus in PM+ on problems of living rather than on illness. There is also a risk for lay therapists of being overwhelmed by their clients’ distress; however, this can be mitigated by training and supervision, including focussing on boundary issues of who they can and cannot feasibly support; the provision of ongoing support mechanisms; and the development of appropriate care pathways. 36–38
Benefits
This study is intended to offer support to distressed and functionally impaired AS&Rs, who may otherwise have no means of receiving evidence-based psychosocial support. It will offer the lay therapists training and experience in a set of transferable skills. If this study enables a full trial to be implemented, we anticipate benefits in terms of improving the mental health and functioning of AS&Rs and reducing the mental health and well-being inequalities faced by this population. If the effectiveness of PM+ is demonstrated, AS&Rs can expect reduced symptoms of anxiety, depression and post-traumatic stress disorder, as well as improved functioning and subjective well-being. This in turn is likely to enhance their equity of access to existing statutory health and social care services.
Society and NHS
Risks
Given the current level of political controversy over the status of AS&Rs, there is a risk that this study may generate adverse publicity and lead to policy decisions designed to make life in the UK more difficult, especially for asylum seekers who have been refused leave to remain. Given that the participating NGOs are subject to the vagaries of external funding during a period of sustained austerity, and that one or more of those NGOs could reduce or cease their function during the lifetime of the study, there is a risk that their involvement in the management and delivery of PROSPER may compromise our ability to deliver on our objectives. This risk will be mitigated by paying careful attention to NGO funding sources and, if necessary, by advocacy to commissioners and funding agencies. There is also a risk that participants who undertake a psychosocial intervention designed to empower them will make greater use of health and social care services, generating extra demand on these already overburdened services. However, this risk is likely to be mitigated by a reduction in the use of unplanned and emergency care. Beyond the lifespan of the project, there might be an expectation from AS&Rs and organisations supporting them that the intervention can still be accessed, which will not be the case. However, this risk can be mitigated by careful explanation of the time-limited nature of the intervention.
Benefits
The PROSPER study is intended to generate new knowledge of benefit to the NHS and to society. PM+ is recommended by the WHO as an intervention that can be delivered by lay therapists and is an effective intervention for vulnerable populations living in conditions of adversity. It is innovative in that it takes task-sharing strategies that have been used in LMICs and applies them to a high-income country, bringing global mental health to high-income countries. This study is intended to ascertain whether or not lay therapists in NGOs can be trained to deliver PM+ with demonstrable evidence of capacity. It is also intended to provide early indications of whether or not PM+ can lead to demonstrable improvements in mental health and function for distressed AS&Rs in current UK settings. It has the potential to take forward the Increasing Access to Psychological Therapies (IAPT) initiative by identifying prospective new access to care pathways for these vulnerable groups.
We anticipate that this research will provide value for money by establishing the feasibility of conducting a trial of an evidence-based psychosocial intervention delivered by lay therapists for distressed and functionally impaired AS&Rs. There is a lack of evidence on the feasibility of conducting research into psychosocial interventions in these circumstances and this study is intended to address this gap in the evidence base.
Looking further ahead, such a definitive trial has the potential to improve mental health, well-being and functional ability among AS&Rs, and to reduce health inequalities. This may lead to the more equitable and effective use of health care by AS&Rs, with a shift from their receiving emergency care to receiving managed, proactive and preventative care. From a societal perspective, cost-effectiveness and cost–benefit analyses following the definitive trial will indicate the extent to which the intervention confers both direct and indirect benefits.
Patient and public involvement is intended to ensure that the project delivers high-quality, original evidence that has the potential to have a significant impact on the design of the definitive intervention and, subsequently, on policy and practice.
Chapter 2 Feasibility study
Evidence synthesis
We conducted a systematic review of the barriers to and facilitators of the uptake of psychosocial interventions delivered by lay therapists to improve the mental health and well-being of AS&Rs. The systematic review followed the guidance of the Centre for Reviews and Dissemination. It was registered with PROSPERO in 2018 as CRD42018104453.
Definitions
Psychosocial intervention was defined as any type of therapy, education, training or social support aimed at improving mental health symptoms, behaviour and general functioning without the use of psychopharmacological agents.
An asylum seeker was defined as a person who has fled their own country and formally applied to the government of another country for asylum, but whose application is not yet concluded. They remain asylum-seekers while they are awaiting a decision about their application for refugee status. A person moves from asylum seeker status to refugee status when the country in which they have applied for asylum accepts their claim.
A lay health worker was defined as a health worker who performs functions related to health-care delivery and is trained in some way in the context of an intervention, but who has not received a formal professional certificate, paraprofessional certificate, or tertiary education degree. This includes community health workers, village health workers, birth attendants, peer counsellors, nutrition workers and home visitors.
Inclusion criteria
Types of participants
We included studies that focused on the experiences and attitudes of stakeholders about lay health worker programmes in any country. Participants could include lay health workers, refugees, asylum seekers and their families, policy-makers, programme managers, other health workers or any others involved in or affected by the programmes.
Types of interventions
We included studies of programmes that were intended to improve AS&R mental health and well-being, for example sociotherapy, multifamily interventions, PM+, stepped-care approach, peer-to-peer group intervention, Self-Help Plus, and Friendship Bench. Other examples were programmes that had used any type of lay health worker: including community health workers, village health workers, birth attendants, peer counsellors, nutrition workers and home visitors.
Databases
We searched the following electronic databases for literature published between January 2007 and July 2018: MEDLINE (National Library of Medicine, Bethesda, MD, USA), PsycInfo® (American Psychological Association, Washington, DC, USA), CINAHL (Cumulative Index to Nursing and Allied Health Literature), the Cochrane Library (Cochrane Database of Systematic Reviews and Database of Abstracts of Reviews of Effects), the Health Technology Assessment (HTA) database, NHS Economic Evaluation Database (NHS EED), EMBASE® (the Excerpta Medica dataBASE; Elsevier, Amsterdam, the Netherlands), BNI (British Nursing Index), ERIC (Educational Resource Index and Abstracts), SocAbs (Sociological Abstracts), ASSIA (Applied Social Sciences Abstract & Indexes), BiblioMap [the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre) register of health promotion and public health research], Scopus® (Elsevier) and the Social Sciences Citation Index™ (Clarivate™, Philadelphia, PA, USA).
We also searched Evidence Aid (www.evidenceaid.org) for evidence synthesis resources relating to mental health in humanitarian crises. In addition, OpenGrey (GreyNet International, Amsterdam, the Netherlands), Scirus, Social Care Online (Social Care Institute for Excellence, London, UK), the National Research Register, National Institute for Health and Care Research (NIHR) portfolio database, and the Electronic Theses Online Service (EThOS) were searched for grey literature. Trial and research registers were searched for ongoing studies and reviews, including ClinicalTrials.gov, metaRegister of Controlled Trials, the International Standard Randomised Controlled Trial Number (ISRCTN) register, the WHO International Clinical Trials Registry Platform (WHO ICTRP) and the PROSPERO systematic review register.
Data extraction forms were developed and piloted in a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet using a sample of included studies. Data were extracted on study design, population characteristics and outcomes by one reviewer and independently checked for accuracy by a second reviewer, with disagreements resolved through discussion with a third reviewer, where necessary.
Quality assessment
Two review authors independently assessed studies meeting the inclusion criteria for methodological quality using criteria proposed in the Cochrane Handbook for Systematic Reviews or, for qualitative papers, the Critical Appraisal Skills Programme (CASP) quality assessment tool for qualitative studies. We used GRADE as the accepted approach to assessing the certainty of findings of reviews of effectiveness and, for qualitative evidence, the CERQual (confidence in the evidence from reviews of qualitative research) approach, based on the methodological limitations of individual studies contributing to the review finding.
Findings
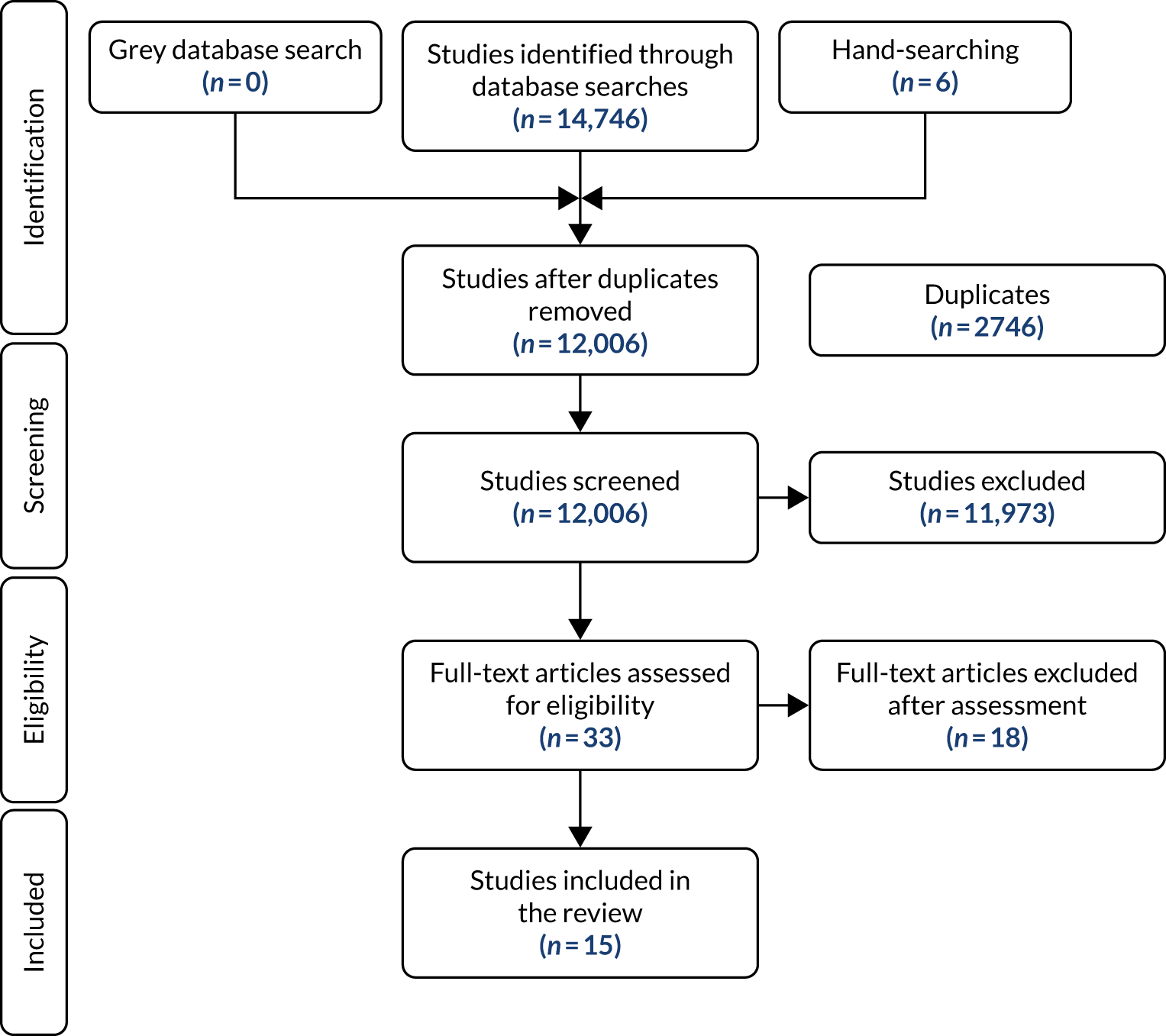
A total of 14,746 titles and abstracts were shortlisted for further assessment, from which 15 papers were identified as suitable for detailed analysis. The pathway from identification to inclusion is shown in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram in Figure 1.
FIGURE 1.
The PRISMA flow diagram for the PROSPER systematic review.
The host countries were Australia, Canada, Jordan, Sweden, Thailand, the UK and the USA. The refugee populations were from China, the Sudan, Burma, Iraq, Bhutan, Liberia, Viet Nam, Cambodia, Somalia, and Bosnia and Herzegovina.
Owing to the heterogeneity of the included studies and the limitations of the available data, statistical analyses were neither possible nor appropriate. The results of the data extraction and quality assessment for each study are, therefore, presented as a narrative summary. This examines the barriers to and facilitators of the uptake of psychosocial interventions, first from the perspectives of AS&Rs and then from the perspectives of lay health workers.
Barriers for asylum seekers and refugees
Beliefs about mental health can be a barrier. Some AS&Rs do not feel that being sad and stressed is a true mental illness and think that it will diminish with prayer and time. 39,40 Others regard trauma symptoms as non-addressable, unlike depressive symptoms. 41
A lack of trust and privacy and not feeling safe are also important barriers. 42 Some AS&Rs are reluctant, or even afraid, to describe their own experiences. They prefer to talk about people they knew and to describe living in a context where such mistreatment is commonplace. 39,43 In some cases, this is exacerbated by political, ethnic, clan and religious divisions within the AS&R communities.
Many are negotiating a sense of loss and isolation, experiencing a conflict between sense of dependence and independence, or experiencing a sense of inferiority in relation to the indigenous population. 44,45
Uncertainty about legal status makes some less willing to seek help, as do a wide variety of stigmatising and discriminatory experiences. 46 Lack of finance or inadequate access to insurance-based care can also be major barriers. 47
A lack of well-trained interpreters, assigned appropriately to AS&Rs in need of assistance can adversely affect the latter group’s ability to find the help they need. 48 In one such instance a man was detained for being suicidal, when in fact he was trying to describe how he would like sleeping pills as he was experiencing worries that were keeping him from sleeping:
Had it been a Karen interpreter the interpreter would interpret that he was not able to sleep because of worries and that would be all. His main concern was to get sleeping pills. [. . .] The interpreter however interpreted that the person wanted to [take their own life].
Power and Pratt49
Facilitators for asylum seekers and refugees
Asylum seekers and refugees are seen as likely to benefit from interventions that are adapted to their local context and are culturally and linguistically appropriate. 50 Uptake is increased by addressing mental health stigma through educational panels and workshops, community gatherings and dialogues, film screenings and cultural shows.
The free-listing of problems is useful,12,51 as is addressing social problems (e.g. income, poor housing, family problems and violence) before mental health. Some favour multiethnic peer support groups, and others emphasise understanding the needs of different groups, especially women. Community advocacy is useful, especially with facilitators who are drawn from AS&R communities. 52
Asylum seekers and refugees are more likely to participate in and benefit from interventions if they feel supported by other asylum seekers, are able to build rapport in a safe setting and have a sense of family comfort with discussing trauma. 53,54 Knowing how others cope with problems encourages AS&Rs to seek help for their own issues. Other important facilitators of AS&R participation in psychosocial interventions include the knowledge that they are not alone in experiencing a specific problem, and an understanding of the connection between mental and physical health.
Barriers for lay health workers
Lay health workers are less likely to engage in or persist with the delivery of psychosocial interventions for AS&Rs if they experience problems with the work itself. Problems include a lack of management direction, conflicts with co-workers, excessive workload, being asked to undertake duties beyond their abilities, and a sense of powerlessness. External barriers include experiencing their own economic and financial problems, travel difficulties, separation from relatives, their own temporary status in the host country and working in a hostile environment. 55
Facilitators for lay health workers
Lay health workers are more likely to engage in or persist with the delivery of psychosocial interventions for AS&Rs if they are invested in outcomes and understand that their main role is to connect and focus on objective, non-judgemental participation. Team cohesion, social support and supervision all mitigate stress in lay health workers.
Lay health workers value being recognised as a resource in their society. Engagement is most effective when people from AS&R communities who have been in the host country for a few years become bridge-builders, co-creating new ways of working and building refugees’ trust in their relationships with staff. In these ways they may become culturally competent paraprofessionals working with their own communities. 56–59
Stakeholder engagement
Stakeholders (including service providers and service users) were recruited from asylum seeker and refugee support organisations across Liverpool City Region in north-west England using purposive sampling via a convenience approach. The research team directly contacted service providers, who comprised social workers, community workers, nurses, psychological therapists, a clergyman, a doctor, a case worker, a health professional, a child psychiatrist and a health service commissioner. Service users were approached during drop-in sessions at the community organisations, and the study was also publicised on a flyer distributed to the four support organisations collaborating in the research project and on social media.
The study received ethics approval from North West – Greater Manchester East Research Ethics Committee (reference 18/NW/0441). All participants provided written informed consent to participate in focus groups and have anonymised quotations reported.
The research is embedded within a social constructionist paradigm. There was emphasis on the meaning-making of people’s perceptions and experiences. Data were collected and analysed following the principles of interpretative phenomenological analysis. 60
We chose to conduct focus groups instead of individual interviews because we wanted to initiate a dialogue between the members of the group. 61 Using focus groups can cause tension when interpretative phenomenological analysis is used to capture individual sense-making. To limit the impact of this tension, careful attention was paid to ensure that data analysis captured the ‘voice’ of the individual rather than being lost at the group level. 62
The interactions that develop from utilising focus groups allow participants to listen, express their views, question others, ask for clarification, encourage others and reflect on what is being verbalised, which in turn can solidify or challenge their own views. 63 Hence, the group context fosters a deeper and reflexive response. 64 This makes the data unique and simultaneously elucidates the research matter:65
Because they involve discussion, and hearing from others, they give participants more opportunity to refine what they have to say.
Ritchie and Lewis61
Twenty-four individuals (16 women and eight men) participated in six focus groups. The participant age ranged between 27 and 76 years. Participants comprised 13 service providers (white, n = 11; Asian, n = 2; African, n = 1) and 11 service users: seven asylum seekers and four refugees. The primary languages spoken by the AS&Rs were Albanian (n = 1), Arabic (n = 3), English (n = 1), Hindi (n = 1), Shona (n = 1) and Urdu (n = 4). Groups comprised three, four or five participants. Three focus groups were conducted with service providers, and three were conducted with service users so that a balanced account of data could be gathered by allowing AS&Rs a safe space in which to express themselves. The focus groups were led by two moderators (NK and CD) using a semistructured guide. All focus groups were moderated and audio-recorded in English. The transcripts were transcribed verbatim.
Data analysis
A thorough group-level analysis was conducted, with the data approached as a whole entity. In brief, Naila Khan began the analysis by reading each transcript several times; this enabled her to become familiar with the transcripts. She then noted preliminary codes followed by interpretations, and later identified emerging themes. The researcher’s preconceptions were managed through the process of bracketing. This involved keeping a reflective journal throughout the analysis and writing up stages of the research.
The next stage involved meticulously highlighting connections, the intention being to develop the master and subordinate themes. This process was iterative, with themes identified in initial transcripts being revised and refined in the light of data in subsequent transcripts. The final step entailed reconsidering the original themes in consultation with Lois Orton and Christopher Dowrick to enhance inter-rater reliability and conduct further analyses to refine, merge and clarify the final themes, and also to establish the superordinate themes and subthemes. Disagreements were resolved and consensus reached through discussion. 60,66 This process of analysis allows researchers to immerse themselves in the findings and in doing so, ascertain an in-depth understanding of how individuals construct knowledge and meaning of their lived experiences. 67. 68
During this process, key quotations were chosen to illustrate the themes identified and preserve the sense-making of the individual. 62 Participants were coded using ‘service provider’ (statutory or voluntary) and ‘refugee/asylum seeker’ identifiers instead of pseudonyms in order to assist the reader in contextualising the narrative.
Researcher reflexivity
Reflexivity forms a significant part of the qualitative researcher’s process. Our identities and professional roles may have had an impact on the data collated. Therefore, we will briefly make our positions as the facilitators clear to enable the reader to understand who the moderators were and how that possibly impacted on the findings. 69 Moreover, ‘to be reflexive we need to be aware of our personal responses and to be able to make choices about how to use them. We also need to be aware of the personal, social and cultural contexts in which we live and work and to understand how these impact on the ways we interpret our world’. 70 Gender, ethnicity, culture, age, socioeconomic status and educational background are all significant facets of one’s identity. 71
All the contributors to this report share knowledge and skills in relation to mental health and a commitment to the welfare of AS&Rs. Our professional backgrounds encompass clinical psychology, counselling, medicine, nursing, politics, public health and sociology. Our authorial team includes people with membership of minority ethnic communities and lived experience of the UK asylum process.
The contributors who facilitated the focus groups (NK and CD) worked to enhance positive relationships and reduce potential power imbalances with participants, ensuring that the groups were arranged to the convenience and comfort of participants, paying careful attention to shared meaning and evolving shared understandings of what was being heard. At times – especially, but not exclusively – in relation to the focus groups with refugees and asylum seekers, this involved empathising with, and later processing, highly distressing narratives of displacement, suffering and loss.
Naila Khan is a British-born second-generation Pakistani woman and the research associate on the project. To counteract the possibility that her gender and ethnicity might have an impact on the research process, she used the process of bracketing. This was the first time she had conducted research in relation to AS&Rs. She had limited awareness of the asylum process, and consciously did not read much literature prior to conducting the focus groups to avoid bias and assumptions.
Christopher Dowrick is an Irish-born, older, white man. Before the focus groups took place he was concerned that these traits, alongside his role as a professor, might prevent participants from freely giving their opinions. However, except for one service provider who directed their remarks to him, his presence did not appear to affect participants. There may indeed have been an opposite effect in that his presence conferred further significance to the focus groups, and participants therefore felt that their views would carry more weight.
Findings
Five superordinate themes were identified: (1) mental health, community and the asylum process; (2) medical and psychological support; (3) religion and culture; (4) the feasibility of PM+; and (5) loss of profession and identity. Here we focus on stakeholder perspectives on the acceptability and feasibility of PM+ (unpublished data).
The content of PM+
Stakeholders generally expressed positive views about PM+ and its usefulness for distressed AS&Rs:
For asylum seekers to know there is something going on they will come, it’s good for everything, I know as an asylum seeker I would go [. . .] If you go the wrong way it’s not good for their future, their future is this place and like you say help those who help themselves.
Service user
I find it empowering to asylum seekers and refugees that when they are able to resolve their problems they are able to put in a position to have high self-esteem and be integrated, be happy.
Service provider
They identified potential advantages over existing service provision, which was often seen as difficult for AS&Rs to access and (for many) available only in crisis:
Used to work in Kensington with a high number of asylum seekers, there would be somebody who kept coming for sleeping tablets, and kept asking for repeat prescriptions and was met strongly with no, can’t give more sleeping tablets but there was nothing to send him to.
Service provider
What we offer with a couple of sessions is good but after that there’s such a long gap on waiting lists and missing out because we don’t have standard processes, so would be beneficial to anyone arriving. They all have some level of anxiety and stress.
Service provider
They saw the delivery of PM+ as beneficial for lay therapists themselves, as well as for their clients:
I think this in being signed up and trained, it’s actually you that benefits first, you get therapy first, and then like anything you want to share with others.
Service provider
The psychoeducation element was considered to be helpful. Stakeholders approved of stress reduction techniques, and the emphasis on managing problems was seen to assist with establishing realistic expectations:
Most people don’t realise they are breathing wrong, you get stressed, you breath shorter and shorter, you think ‘What’s happening to me? Am I going to pass out?’ That’s a very good start. They need to understand the little things.
Service user
I think it’s much, much needed, and the psychoeducation element is often at the bottom of the getting stuck with a GP [general practitioner] because there’s a kind of ‘no I need any pills’ but actually pills won’t make you better, but that bit on psychoeducation can really help that.
Service provider
Some stakeholders raised questions about the scripted nature of PM+ and whether or not this might inhibit the essential therapeutic element of relationship-building:
I’m thinking about the things that seem to help are about establishing relationship, I’m not sure how that happens here [. . .] It seems it has to be quite scripted to be able to pack all of that in, so I just wonder about that kind of wonder about that.
Service provider
Others were concerned about the risks of lay therapists going beyond the limits of PM+, offering bad advice in relation to legal issues and triggering trauma:
I would be cautious about practical help that goes beyond Problem Management Plus. I’m also worried that bad advice in relation to anything legal . . . can be damaging.
Service provider
. . . within trauma therapy one of the things that this seems to sit well within for stabilisation, the initial phase where you’re not moving into reprocessing or triggering traumatic memory as that might be difficult.
Service provider
Still others questioned the therapy orientation of PM+, suggesting that open, friendship-based approaches would be more suitable for their cultural group:
To me it’s just not our thing as Africans to have therapy-type thing, it’s not our thing at all. My opinion what would work for me is a friendship-type thing [. . .] Feels like there is a gap between the person and me, want to develop the common [g]round, good being asylum seeker to asylum seeker, the language as well having walked in my shoes, but not formally, sit there, what have you done.
Service user
Barriers to implementing PM+
There was a common view that the daily lives of AS&Rs were very busy, that regular attendance at sessions could often be problematic for clients, and that PM+ would need to be fitted into other commitments, including child care, education and the asylum system:
It depends on how through the asylum system they are but lots of them have meetings whether signing up at the Home Office or with their solicitor, they’re really good at navigating through things like this so in one way it would fit in very well, in another [it] could be another stressful thing.
Service provider
Stakeholders also noted the ever-present threat of dispersal to another part of the country, which would interfere with clients’ ability to complete a course of PM+ sessions.
There was concern that cultural differences in understandings of mental health or depression may inhibit people from seeking help in this way:
Is the model culturally accessible to all populations living here? We know that mental health models are culturally determined, different countries have really different kind[s] of model so they’re not there’s no such thing as a culturally neutral mental health service, so it’s interesting, it brings out a challenge I completely identify with.
Service provider
First thing is it’s getting to know them, they have their own tradition and culture and have some different things, something they feel may be a threat, how we can get this is with ourselves [. . .] I know people from Albania, I’m the only one involved in and it’s difficult to engage them, there are so few. They don’t get involved because of culture, they are used to a set way of eating they won’t try [anything other than their] own things, it’s very hard to understand.
Service user
It was felt that it was more difficult for women to talk openly about their mental health problems:
It’s a cultural thing they don’t speak openly, and also they think it’s not important to talk about it sometimes, if I’m just depressed and sad they just feel it’s not they are at risk, or [a] state they have, they must do something for their well-being they don’t realise it’s important for them.
Service user
Some noted the possibility of cultural or religious conflicts between therapists and clients, especially for clients who had been forced to flee their home countries following a change in religion:
Other issue will be how to ensure the lay therapists engage and turn up themselves, and sort of the cultural conflict with the therapist and client. Those are the thing[s] you may not know about, you might not ever understand what they are talking about. A lot of people have fled due to changed religion and the sensitivity of it.
Service provider
Confidentiality was raised as an issue when lay therapists and clients came from the same community and also when interpreters were involved in the sessions. Issues raised were not only personal, but also political:
OK, so my only thought is, you’ve got someone that has trained through this to be a lay therapist and is an asylum seeker, we are such a small community and even now, people chat openly, and some people share in houses, if you have a lay therapist in that community, obviously taught about confidentially, people have supported each other with health problems back off from one another.
Service provider
The lady didn’t want face-to-face interpreter, because of her community, the likelihood was it would be someone from her community and therefore she thought she may be poorly viewed in her community with a face-to-face interpreter.
Service provider
The European Kurdish group are absolutely paranoid about meeting other people to begin with, still happening now, for fear they have fled, two of our families are from [city] and they fear that message will get back home that they are here, they are anxious about translators.
Service provider
Facilitators of implementing PM+
Stakeholders recommended that initial contact be by telephone rather than letter, as many AS&Rs associate mail with official communications from the Home Office:
We get a letter and see it on paper, it’s the first sight for every asylum seeker, there are a lot of them to say can you open I don’t want to open it, they are scared, that sends you to anxiety.
Service user
They proposed locating the PM+ sessions in a familiar environment with easy access, such as a voluntary agency with which the client is already in contact. They also emphasised the importance of practical help with childcare and transport (so that clients are not left financially out of pocket as a result of having to attend sessions) and recommended flexibility around appointments to fit in with clients’ busy lives.
Emphasising the confidential nature of the sessions was important in building trust:
Not enough to give them a piece of paper to say it’s confidential. They have to recognise and develop trust.
Service user
Matching the therapist and the client in terms of gender was seen as important, especially for women:
I think for female clients have a female person, will be more open to person of same gender . . .
Service user
Matching language and culture between therapist and client was often, but not always, seen as helpful:
Yes, the idea is lay therapists coming from same or similar cultural background will have more experiences and ability to developing trusting relationships that might make it come through more quickly.
Service provider
You speak their language and are needed at so many levels, but just through speaking Arabic you would work as a social worker just by being from the same language and culture. But sometimes the opposite, they want someone outside their community.
Service provider
Stakeholders felt that, if interpretation services were needed, it would be safer to use a telephone translation service such as LanguageLine (London, UK).
They also offered practical advice on how to publicise the project, including attending community meetings and placing posters in voluntary organisations working with AS&Rs.
Training procedures
Adaptations to the PM+ manuals to fit the lives of AS&R in the UK for the PROSPER study were approved by the WHO. Examples of group PM+ adaptations include creating a male case study and amending the case study narrative and images to reflect the UK context (e.g. replacing reference to help-seeking from a ‘village elder’ with ‘voluntary or statutory organisations’).
PROSPER PM+ training model
PM+ training and supervision broadly followed the cascade apprenticeship model72 outlined in Table 1.
| Components of apprenticeship model in mental health interventions | Application in PROSPER study |
|---|---|
| Selection of apprentices |
|
| Training |
|
| Application of training ‘on the job’ under direct supportive supervision |
|
| Ongoing expansion of training, knowledge and skills under supportive supervision |
|
| Mutual problem-solving |
|
The apprenticeship model foregrounds supportive supervision,73 promoting cycles of experiential learning, doing and reflecting74 as foundations for enhancing lay therapist competency and fidelity while encouraging motivation and job satisfaction. 75 Supportive supervision explicitly values and integrates ‘tacit knowledge’ gained through experiential practice, which is melded with intervention principles to enhance the skills, knowledge and values of those delivering the intervention. 76 Recognising the importance of training and supportive supervision and the need for further evidence on approaches,75 we describe and reflect on our experiences of cascade apprenticeship training and supervision to draw recommendations for others implementing this model, focusing on adjustments when working with lay therapists who are AS&R.
Recruitment
Well-being mentors
The well-being mentors were the PM+ lay therapists’ trainers and supervisors, and they are themselves ‘lay’ professionals in that they are not mental health specialists. For the PROSPER study, no specific qualifications were expected, with the emphasis in the recruitment of well-being mentors being on experience of training and supporting volunteers from diverse communities within health and social care.
The two recruited well-being mentors had counselling qualifications, and between them they also had qualifications in education and youth work and work experience in voluntary mental health settings. They were recruited and employed by the PROSPER intervention partner Person Shaped Support (PSS) in Liverpool, a social enterprise providing mental health and social care services, including to AS&R. The well-being mentors (AM and LB) receive day-to-day support from their PSS team leader (RMcC) and joint monthly supportive supervision from the master trainer (AC) and participated in PROSPER Project Management Group (PMG) meetings. Initially envisaged as part-time, the well-being mentors’ role was extended to a full-time commitment to ensure that they would be available to support lay therapists’ delivery of PM+.
Lay therapists
The recruitment of 12 volunteer lay therapists was conducted by PSS. It began with the distribution of e-mails, posters and information sheets among NGOs supporting AS&Rs in Liverpool. Over 20 AS&Rs attended information sessions at PSS led by the well-being mentors, at which they were introduced to the PM+ intervention and the lay therapist role and criteria (i.e. age > 18 years; knowledge and/or lived experience of migration and/or the asylum process; sufficient ability in speaking, reading and writing English; and residing in Liverpool, UK). Fifteen candidates who met these criteria and expressed an interest in becoming lay therapists attended individual interviews conducted at PSS by the two well-being mentors and their team leader. The interviews commenced by tasking the candidates with producing an origami object, testing their English-language skills and ability to follow instructions; the candidates were then asked five questions about the skills, knowledge, experience and personal qualities that they would bring to the lay therapist role. Following the interviews, 12 candidates were selected to participate in the PM+ lay therapist training (Table 2).
| Gender | Age (years) | Native language | Education level | Employment/voluntary role in UK | Individual or group PM+ | |
|---|---|---|---|---|---|---|
| 1 | Female | 30 | Urdu | Undergraduate | Trainee dental assistant | Individual |
| 2 | Female | 30–40 | Farsi | Graduate | Studying fashion, English, maths | Individual |
| 3 | Male | 30–40 | Arabic | Graduate | Studying English and enrolled in pre-studies for pharmacy | Individual |
| 4 | Male | 30–40 | Urdu | Graduate | Business owner | Group |
| 5 | Female | 30–40 | Arabic | Graduate | Studying English, preparing for master’s studies | Group |
| 6 | Female | 40+ | Turkish | Graduate | Studying English and transferring social work qualifications | Group |
| 7 | Female | 30–40 | Thai | Graduate | Studying English and working in hospitality | Group |
| 8 | Male | 20–30 | Farsi | Not known | Studying | Individual |
| 9 | Male | 20–30 | Farsi | Graduate | Studying pharmacy | Individual |
| 10 | Female | 40+ | English/French | Not known | Working | Individual |
| 11 | Female | 20–30 | Urdu | Not known | Studying | Individual |
| 12 | Male | 40+ | Urdu | Not known | Teaching English in conversation groups | Group |
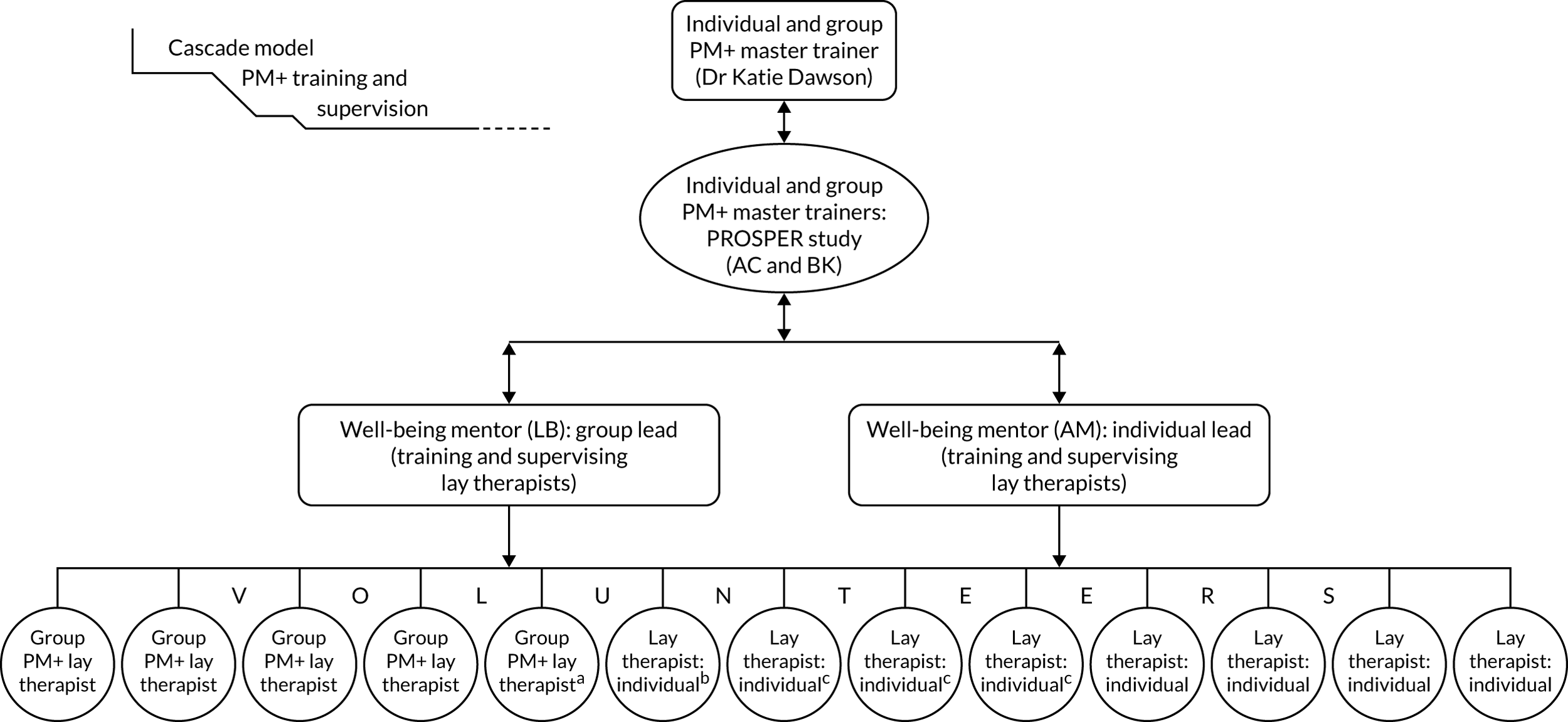
Training
Figure 2 summarises the PM+ cascade training and supervision model.
FIGURE 2.
The PROSPER study PM+ training model. 77 a, Reason for leaving: ill health; b, reason for leaving: moved area; c, reason for leaving: disengaged. Reproduced from Chiumento et al. 77 This article is available under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike License (CC BY-NC-SA), which permits non-commercial use, distribution and reproduction in any medium, provided the original work is properly cited.
Well-being mentor training and practice cases
A 5-day well-being mentor training course was led by two master trainers (including AC) in October 2018. Training followed the PM+ training of trainers programme, which foregrounds basic helping skills, and the PM+ intervention sessions, emphasising the core content and underlying rationale. Training highlighted the different individual and group delivery modalities and skills in training others, such as conducting role-play and providing feedback, and leading supportive supervision. The training situated PM+ in the context of the PROSPER study, exploring the relevance of PM+ to AS&R lives and clarifying the intervention and research relationship. All training was experiential and concluded in role-play with volunteers who had no prior experience of PM+.
Following training, the well-being mentors each completed three individual PM+ practice cases with volunteers (including a medical student with lived experience of migration, social work students, and PSS staff). The practice cases embedded knowledge of and skills in implementing the PM+ intervention, equipping the well-being mentors with experiences of common challenges to PM+ delivery such as participant engagement, responding to difficult disclosure and time management. These experiences were invaluable for the subsequent lay therapist training and supervision.
Following the training and practice cases, the well-being mentors spent time networking with AS&R voluntary organisations. This formed a crucial foundation of the well-being mentors’ role as they became familiar and trusted faces at organisations from which lay therapists (and subsequently, PROSPER research participants) were recruited.
Well-being mentor supportive supervision
Following training, the well-being mentors received monthly supportive supervision from one master trainer and the PSS team leader: this lasted between 1.5 and 2 hours and was complemented with e-mail and telephone discussions where required. Additional PROSPER PMG meetings were conducted bimonthly. These meetings provided a forum for input into the lay therapist team development, and well-being mentors with a space to reflect and learn about PM+ implementation (both in context of the research design and AS&R voluntary organisations and statutory health-care systems). 78
Supervision content was tailored to the project stage,77 moving from an initial focus on embedding PM+ knowledge and skills to planning for the lay therapist PM+ training (including enhancing training skills) and then concentrating on skills for leading supportive supervision with lay therapists. This supportive supervision enhanced the well-being mentors’ knowledgeable application of skills to practice. Specifically, the supportive supervision enabled experiential and reflective learning, supporting the lay therapists to enhance their skills in cascade supervision. 74 Finally, well-being mentor supervision incorporated logistical research planning and additional training (e.g. in good clinical practice, data protection and basic first aid).
Lay therapists’ training and practice cases
The lay therapist training was separated into group PM+ (led by LB) and individual PM+ (led by AM), with six lay therapists trained in each modality. Allocation to each modality was based on availability to attend training on a given day and any expressed preferences of the lay therapist themselves. Training was delivered 1 day per week (10 a.m. to 4 p.m.) over 8 weeks from March to May 2019, with scheduling to accommodate the availability of the AS&R lay therapists around other family, work or education commitments.
The training followed the individual or group PM+ training manuals, covering basic helping skills and experiential learning of PM+ sessions summarised above, and was reinforced through discussions and role-play of the PM+ strategies and sessions for the relevant PM+ modality. The master trainer (AC) visited to observe training and provide feedback to the well-being mentors, to meet the lay therapists and to answer questions about the relationship between the PM+ intervention and PROSPER research. At the end of training, the well-being mentors conducted competency assessments with each lay therapist to ensure that they had the knowledge and skills to deliver PM+ to participants safely. Following this, lay therapists were presented with a certificate attesting to their successful completion of PM+ training.
The training was completed by 11 lay therapists; one person dropped out owing to ill health. These 11 lay therapists then completed one individual or group PM+ practice case with PSS staff and student volunteers.
Lay therapists’ supportive supervision
Lay therapists’ group supportive supervision took place throughout the practice cases and was led by the well-being mentors. In addition to discussing how PM+ sessions were progressing and delivering top-up training in PM+ strategies, the well-being mentors incorporated self-care tasks to equip the lay therapists with techniques to promote their own well-being, which is important in therapeutic interventions. 79 A second lay therapist dropped out during the practice cases owing to their compulsory relocation to another city.
PM+ sessions were delivered by lay therapists at PSS offices, with the well-being mentors available before and after sessions. It became natural for supervision to take place immediately after PM+ sessions, with lay therapists eager to reflect with well-being mentors on their delivery of PM+, including which parts went well, where they encountered challenges, and why they felt they had encountered challenges or had successfully delivered intervention components. The lay therapists sometimes asked the well-being mentors for clarification of a strategy, or checked that they had responded appropriately to participants’ questions or responses to PM+ strategies. This supervision allowed space for the lay therapists to build confidence, gain a focus for the next session and offload before returning to their day-to-day life. This individualised supervision approach immediately after PM+ sessions was found to be highly effective and was complemented by group supervision when logistically feasible (i.e. multiple lay therapists delivering sessions at the same time). This demonstrated flexibility in supervision structures79 and attention to feasibility, as individual supervision avoided the travel time and costs that the lay therapists would have incurred in attending separate group sessions.
Well-being mentors conducted fidelity checks through observation of a random selection of PM+ sessions, assessing lay therapist delivery of PM+ against a structured checklist. These checks provided an important mechanism for the well-being mentor to monitor PM+ quality79 and learn where PM+ knowledge and skills may have been misinterpreted. As above, individual supervision of the lay therapist occurred immediately after the fidelity check, ensuring that experiences of the session were fresh and clear. Before giving fidelity check feedback, self-care activities were completed jointly by the well-being mentor and the lay therapist and this was found to enhance supportive feedback and reflection.
Reflections on PM+ training and supervision
We share some reflections based on our experiences that address themes that emerged in reflective workshops: (1) logistical challenges to working with AS&R lay therapists, (2) strategies employed to encourage lay therapist engagement and (3) team and personal growth (Table 3). We identify examples to illustrate these reflections, focusing on considerations relevant to implementing a task-sharing intervention with AS&R lay therapists.
| Reflection | Specific considerations |
|---|---|
| Logistical challenges | Synchronising schedules with lay therapists’ educational, family and personal responsibilities |
| Mitigating financial hardship | |
| Remaining aware of, and responsive to, the impact of personal asylum journeys | |
| Responding to delays in research timelines | |
| Lay therapist engagement strategies | Collective informal engagement through, for example, shared lunches and joint sightseeing tours |
| Positive recognition of the cultural and linguistic diversity of the PM+ intervention team | |
| Allowing lay therapists to set the level and format of communication with well-being mentors | |
| Team and personal growth | Recognising the unique strengths of each member of the PM+ intervention team |
| Shared learning across the PROSPER research and intervention teams | |
| Active development and implementation of well-being mentor ideas and approaches to lay therapist training and supervision | |
| Skills development of PM+ lay therapists |
Logistical challenges
The lay therapists were enrolled on free and fee-charging English-language, educational and vocational courses as it was important for them to improve their English, and to upskill and adapt their qualifications to UK education and employment systems. Some lay therapists also had families (including school-aged children) to care for, and these factors presented challenges to be worked around when synchronising training schedules. Furthermore, recognising that AS&Rs are provided meagre financial benefits,80 financial hardship was mitigated through the reimbursement of travel expenses and provision of lunch and childcare during training. It is likely that most AS&Rs would have been unable to take on the lay therapist role without financial and childcare support. In addition, many lay therapists were experiencing the uncertainties of personal asylum cases. This could have an impact on their well-being and flexibility, and PROSPER schedules needed to account for this.
Delays in ethics approval meant that PROSPER research timelines were extended and PM+ delivery to participants was delayed, leading to a decrease in project activity, at which point several lay therapists left their roles. To maintain commitment, interactions between the well-being mentors and lay therapists involved supportive supervision to review the PM+ intervention, practise self-care strategies and socialise. The lay therapists also made an information video about PM+ aimed at service providers, offering an opportunity to reinforce their knowledge of PM+ strategies and the research design while ensuring active contributions to the PROSPER study and building their confidence.
The impact of delays reflects broader challenges at the research/service delivery interface. While the research and intervention teams’ relationship has been supportive and provided opportunities such as additional training, it has also led to frustration due to the processes required to adhere to clinical trials regulations, the time for ethics approval, and slow initial recruitment. To navigate this, the well-being mentors have played an important role in balancing the rigid timelines and complex governance processes of a research trial against the expectations of lay therapists keen to commence PM+ delivery.
Lay therapist engagement strategies
Collective informal engagement, such as shared lunches during training (with attention to cultural appropriateness by offering halal meals and respecting fasting during Ramadan) and going on sightseeing tours, helped build intervention team cohesion within and beyond PM+ roles. The linguistic and cultural diversity of the lay therapists added value to the PM+ intervention team and promoted a lively training atmosphere. The lay therapists displayed a comfortable vulnerability when talking about cultural differences and migration experiences, complemented by discussions with the well-being mentors about the local Scouse dialect, which indicated the presence of an open and trusting relationship between lay therapists and well-being mentors. Positively recognising this diversity provided bonding experiences, helping the lay therapists to understand the local culture and the well-being mentors to appreciate the lay therapists’ migration experiences.
During initial stages of PROSPER recruitment, the lay therapists were encouraged to set the level and type of interaction with the well-being mentors; for example, some requested weekly check-in telephone calls or meeting the well-being mentor for coffee, whereas others preferred contact by text message or only when there was a participant for them to deliver PM+ to. Tailoring engagement to each lay therapist has avoided problems of over- or undercommunication, demonstrating the mutual respect that is essential for trusting peer and supervisory relationships. 79,81
Team and personal growth
The PM+ training of trainers programme was intensive and demanding, with a breadth of material to cover and knowledge, skills, and confidence to build. Training delivery was aided, however, by a supportive, open and trusting training atmosphere which facilitated the open acknowledgement of areas of confusion and collective problem-solving. Therefore, although intensive, this training rapidly built relationships, establishing a cohesive intervention team that recognised the strengths of each lay therapist.
During the PM+ training and supportive supervision, the lay therapists benefited from the opportunity to improve their English and communication skills and confidence. Initially, many lay therapists were shy about PM+ role-play but they overcame this through encouragement and support from well-being mentors and their peers, developing confidence in delivering individual or group PM+.
Well-being mentor supportive supervision has facilitated approaches to lay therapist training and supervision that draw on the well-being mentors’ personalities and strengths, such as bringing together individual and group lay therapists to share PM+ delivery skills that both groups could draw on; for example, individual PM+ lay therapists demonstrated effective explanation of key strategies, and group PM+ lay therapists demonstrated facilitation skills such as bounce-back questions. This incorporation of peer- and supervisor-led training in dynamic individual and group supervision formats has proven effective in expanding the knowledge, skills and confidence of lay therapists. 79
Shared learning across the PROSPER intervention and research teams has included taking account of lay therapists’ English literacy levels and familiarity with form-filling, and the logistical co-ordination of delivering PM+ sessions at AS&R voluntary organisations. The PMG meetings have provided a forum to discuss and agree research design, with the well-being mentors and master trainer providing ‘on-the-ground’ insights to ensure that these remained practical for AS&R lay therapists unfamiliar with research procedures. 79
Chapter 3 Pilot trial
Parts of this chapter have been adapted with permission from Rawlinson et al. 1 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
Contextual modifications
As a result of the findings from the feasibility study, we made the following contextual modifications to promote the uptake and relevance of the PROSPER pilot trial:
-
Focusing on English, Arabic, Farsi and Urdu, which were identified as the four languages that are currently most commonly spoken by AS&Rs in Liverpool City region.
-
Excluding new arrivals and those in temporary accommodation on grounds of (1) high probability of dispersal and hence unavailability for intervention and/or follow-up, and (2) low probability of being registered with a GP and hence unable to access trial safeguarding procedures.
-
Altering the text of PM+ manuals to reflect life in Western urban settings rather than South Asian rural settings (e.g. ‘home’ not ‘hut’, ‘reading’ not ‘rearing poultry’, ‘visit job centre’ not ‘speak with village elder’).
-
Adapting the group PM+ case studies to include men.
-
Matching therapists and participants on the bases of gender and language, but not on the bases of religion, politics or culture.
-
Identifying accessible ‘safe spaces’ for research interviews and delivery of PM+ sessions, including availability of childcare.
-
Reimbursing travel expenses for lay therapists and participants.
-
Supervising and supporting lay therapists in the inclusion of boundary issues between therapy and involvement in participants’ lives, as the shared lived experience of the asylum process takes this study beyond the boundaries that have been apparent in other contexts.
On this basis, the PROSPER trial protocol was approved by University Sponsor and Liverpool Research Ethics Committee (reference 19/NW/0345) and subsequently published in Trials. 1
Trial protocol
Aim and objectives
This pilot trial was part of the PROSPER feasibility study, the overall aim of which was to determine whether or not it is possible to conduct a RCT in the UK of the evidence-based PM+ psychosocial intervention delivered by lay therapists, for distressed and functionally impaired AS&Rs.
The primary objective of the PROSPER Pilot was to provide preliminary information on the potential effectiveness of group or individual PM+ compared with standard care for AS&Rs, assessed on the severity of combined anxiety and depressive symptoms at 13 weeks post baseline measured using the Hospital Anxiety and Depression Scale (HADS). 82
The secondary objectives were to provide preliminary information on the potential effectiveness and cost-effectiveness of group or individual PM+ compared with standard care for AS&Rs with regard to:
-
severity of combined anxiety and depressive symptoms at 26 weeks
-
subjective well-being
-
functional impairment
-
progress on problems for which an individual has sought help
-
post-traumatic stress disorder
-
depressive disorder
-
use of services and supports from NHS, social care and voluntary organisations.
Design and setting
The PROSPER Pilot trial was designed as a three-arm, parallel-design pilot RCT with the features of a proposed future definitive RCT. Participants were to be randomised to receive individual PM+, group PM+ or the control (no PM+) in a ratio of 1 : 1 : 1. Appendix 2 lists all protocol amendments.
The pilot trial was conducted in Liverpool City Region. It utilised collaborative working between three universities (University of Liverpool, Liverpool John Moores University and Bangor University) and three NGOs offering advice and support to AS&Rs: PSS, Asylum Link and British Red Cross, local NGOs whose primary function is to provide advice and support to AS&Rs.
Participants
Trial participants were AS&Rs. This included those with pre-asylum status; those who had been offered either discretionary or indefinite leave to remain in the UK; those whose applications for leave to remain were pending or had been refused; those with humanitarian protection; those with refugee status; stateless people; and people in the Vulnerable Persons Resettlement Scheme.
The other inclusion criteria were:
-
aged ≥ 18 years (self-reported)
-
score of ≥ 8 on either the depression or the anxiety subscale of the HADS,82,83 and score of ≥ 17 on the WHO Disability Assessment Schedule 2.0 (WHODAS)84
-
conversational English, as self-assessed by the potential participant
-
registered with a GP in Liverpool City Region
-
willing to provide relevant socioeconomic data
-
provided written informed consent.
The exclusion criteria were:
-
New arrivals to the UK (< 28 days), owing to the high likelihood of dispersal outside the region.
-
In reception centres, usually known as initial accommodation and receiving temporary financial support under section 98 of the Immigration and Asylum Act 199985 for < 28 days: again, because of the high likelihood of dispersal outside the region.
-
Imminent risk of suicide – assessed by researcher using formal protocols, with supervision and arbitration from qualified health-care professionals.
-
Complex mental disorder (bipolar disorder/manic depression or schizophrenia) – assessed by researcher on basis of participant self-reporting a diagnosis and/or participant currently in receipt of antipsychotic medication, defined as medication listed in the British National Formulary, chapter 2 sections 2.3 (bipolar disorder and mania) and 2.6 (psychoses and schizophrenia). If required, further clinical assessment was to occur using standard formal protocols.
-
Cognitive impairment (moderate/severe intellectual disability, any dementia) – assessed by researcher on basis of participant or carer self-report.
-
Substance misuse – assessed by the researcher on basis of participant’s response to the question ‘are you currently having problems with alcohol, cocaine, marijuana or any other drugs?’ If the response was yes or equivocal, then the participant was excluded. If required, further clinical assessment occurred using standard formal protocols.
-
Currently receiving formal psychological therapy, to avoid potential confounding effects.
Outcome measures
Specific outcome measures, which are candidates for inclusion in any future definitive trial of PM+ for AS&Rs, were tested as part of the PROSPER Pilot trial. These measures are summarised in Table 4:
| Objective | Outcome measures | Time point(s) of evaluation |
|---|---|---|
| Efficacy | ||
| Severity of combined anxiety and depressive symptoms | HADS | Baseline, 13-week and 26-week follow-up assessments |
| Functional impairment | WHODAS | |
| Subjective well-being | WHO-586 | |
| Progress with problems for which participant has sought help | PSYCHLOPS87 | |
| PTSD | PCL-588 | |
| Depressive disorder | PHQ-989 | |
| Health economics | ||
| Use of services and supports from NHS, social care and voluntary sectors | Adapted CSRI90 | Baseline, 13-week and 26-week follow-up assessments |
-
HADS is a well-established 14-item scale consisting of two subscales: HADS-A (anxiety; seven items; possible score range 0–21) and HADS-D (depression; seven items; possible score range 0–21). Higher scores indicate more anxiety and/or depression. HADS has been widely used across cultures. It is sensitive to change over time and has good internal consistency, reliability and validity. 83
-
WHO-5 is validated in international studies for both clinical and psychometric properties and is available in many languages.
-
WHODAS is applicable across all health states, including mental disorders. It has good validity in terms of internal consistency, test–retest reliability and agreement with other measures of disability across countries.
-
The Psychological Outcomes Profile (PSYCHLOPS) has internal consistency and convergent validity with measures of emotional distress and is sensitive to change. It covers three domains: problems (two questions), functioning (one question) and well-being (one question).
-
The Post-traumatic Stress Disorder Checklist for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (PCL-5) has good psychometric properties in terms of diagnostic accuracy and internal consistency.
-
The 9-item Patient Health Questionnaire (PHQ-9) is based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) depression diagnostic criteria. The total severity score ranges from 0 to 27, with 10 as conventional cut-off value for diagnosing depressive disorder.
-
The Client Service Receipt Inventory (CSRI) has been adapted for the PROSPER trial to include health, social care and voluntary services with the potential to be used by AS&Rs.
Other elements of PROSPER Pilot trial were assessed and used to inform the feasibility of conducting a full trial, as specified in Table 5.
| Objective | Outcome measure | Time point(s) of evaluation |
|---|---|---|
| To assess the feasibility of the proposed procedures for recruiting distressed AS&Rs as study participants | Number of AS&Rs recruited | Baseline |
| To assess feasibility of randomisation | Successful randomisation of participants | Baseline (randomisation) |
| To assess the feasibility of retaining study participants through to trial completion | Number of study participants in the trial (assessed in individual arms) | 26 weeks |
| To assess the acceptability and utility of specified primary and secondary outcome measures |
Completion of study measures and estimation of between group differences Evaluation of outcome measures |
Baseline, 13 weeks, 26 weeks |
The feasibility of progression to a definitive multicentre RCT was to be informed by the extent to which the criteria below were met using a go–amend–stop system, as specified in Table 6.
| Progression criteria | Go | Amend | Stop |
|---|---|---|---|
| Recruitment of trial participants | ≥ 70% of target | 50–69% of target | < 50% of target |
| Retention of trial participants | ≥ 70% retained | 50–69% retained | < 50% retained |
| Protocol adherence | ≥ 70% of intervention delivered per protocol | 50–69% of intervention delivered per protocol | < 50% of intervention delivered per protocol |
| Completion of outcome measures | ≥ 70% of measures are complete | 50–69% of measures are complete | < 50% of measures are complete |
If criteria met ‘amend’ targets, reasons for this would be investigated with the aim of identifying aspects amenable to change. If criteria met ‘stop’ targets, reasons for this would be analysed through discussion within the project management group and with independent oversight committees. If these rates could be improved then a full trial would not be recommended.
Other progression criteria involving data from the PROSPER Pilot trial that were assessed by the research team are:
-
recruitment of supervisors and lay therapists
-
retention of lay therapists
-
acceptability of outcome measures
-
whether or not clinically important improvement in outcomes are plausible.
Intervention
The PM+ intervention consists of five weekly face-to-face sessions delivered either one to one or in groups. The first session opens with psychoeducation, including information on common reactions to adversity, the rationale for PM+, goal-setting and brief motivational interviewing. Sessions 1–4 each introduce an intervention strategy: (1) managing stress (slow-breathing exercise); (2) managing problems (using problem-solving techniques); (3) get going, keep doing (applying behavioural activation techniques); and (4) strengthening social support. Participants apply these strategies during the intervention session to problems they are facing. Each strategy is reviewed in subsequent sessions, with the application of strategies between sessions encouraged to enhance learning through repetition. The final session involves a revision of learning and education on preventing relapse, and (for group PM+) ends with a culturally appropriate closing ceremony.
To enhance accessibility for groups, the group PM+ intervention is structured around locally relevant and appropriate pictorial materials, and adopts a narrative format to support engagement and individual disclosure of personal difficulties (which can be more difficult in a group format). Specifically, a case example of a woman or a man (depending on the gender of the group participants) experiencing common functioning and emotional problems is shared each week and participants follow their progress through PM+ Group.
All PM+ sessions were to take place at mutually convenient and safe locations where support was available if required. Sessions were to be delivered in organisations that had on-site staff with experience and training in managing emotional distress. No face-to-face sessions would take place in the home of either a participant or a lay therapist. There would be no special criteria for discontinuing or modifying allocated interventions.
Protocol adherence
Consistent with an apprenticeship model,72 protocol adherence was ensured through regular (at least fortnightly) supervision of the lay therapists provided by two well-being mentors. Involving all individual or group lay therapists in a group, supervision lasted up to 3 hours and entailed reviewing the progress of intervention delivery, including case management of participants and additional refresher training on intervention components. The group PM+ lay therapists received the same training as individual PM+ lay therapists in addition to refresher training on group facilitation skills through role-play.
The well-being mentors were in turn supervised by one of the master trainers; supervision was conducted at least monthly during the trial and lasted 2 hours. In addition, well-being mentors had the day-to-day support of their line manager at PSS, who also participated in the 5-day PM+ training with master trainers and participated in the monthly supervision sessions with the master trainer to ensure supervision consistency.
Intervention fidelity was to be monitored through independent observations of 15% of randomly selected sessions of each lay therapist against tailored checklists. These observations were conducted by the well-being mentors. Session logs (per participant) were completed by lay therapists after each PM+ session and captured information regarding the timing, length and content of sessions. The logs were passed to the well-being mentors at weekly supervision meetings. A small number of sessions were to be audio- or video-recorded as an additional assessment of intervention fidelity. Feedback from intervention observations was used in subsequent supervision sessions to improve adherence to intervention protocols.
Intervention compliance by trial participants was measured by assessing adherence to the PM+ protocol with regard to attendance at sessions.
Control arm
Participants randomised to the control arm were not offered any PM+ but were able to access all usual care and support offered by the participating NGOs. To control for the weekly contact that the active arms received, participants randomised to the control arm were invited by the interviewing researcher to attend a local AS&R NGO of their choice. They were to be put in contact with other AS&Rs from similar backgrounds and encouraged to meet with them on a weekly basis for 5 weeks.
Participant identification
Potential participants were identified primarily through NGOs and primary care teams, all designated as participant information agencies (PIAs). PIAs were provided with a short summary of the study, including the main inclusion and exclusion criteria. They were asked to display posters and leaflets and discuss the study opportunistically with AS&Rs who access the services. All participant-facing documentation had the necessary approvals from a Research Ethics Committee.
Potential participants were made known to the research team by one of the following methods:
-
contacting the research team directly by telephone or e-mail
-
agreeing to their details being given to the research team (via a participant recommendation form, completed by the PIA with the AS&R, and returned to the research team by the PIA)
-
attending a researcher-attended drop-in session at collaborating NGOs on a specific date/time, advertised by posters/leaflets/verbally.
Following the identification of a potential participant, a postdoctoral researcher based in the University of Liverpool, who is trained in the PROSPER trial techniques and in discussion about informed consent, arranged a meeting to give more information about the trial.
Informed consent
The researcher contacted the potential participant to arrange an individual face-to-face meeting. This meeting was arranged at the convenience of the AS&R where possible, and could be attended by an interpreter if required. The meeting lasted between 1 and 2 hours. It took place at a convenient location, which could be one of the NGO centres, a community centre, a counselling centre, NHS premises or the University of Liverpool.
Objectives, risks and inconveniences of the trial and the conditions under which it is to be conducted were provided by the researcher. All potential participants were given the opportunity to ask any questions, had the opportunity to discuss the study with others and were given time to consider the information prior to their agreeing to participate. It was made clear to the participant that an eligibility assessment would be conducted once consent was given and that if the participant was found to be ineligible for any reason that they would be unable to participate.
Potential participants were asked to read and review the participant information sheet, which was available in English and the study languages of Farsi, Urdu and Arabic. On the potential participant’s reviewing the document, the researcher explained the research study to them. Both the participant information sheet and discussion with the participant emphasised that participation in the trial was voluntary and that the participant was able to withdraw from the trial at any time, for any reason. Participants were also asked for their permission for the research team to share relevant data with people from the universities taking part in the research or from regulatory authorities, where relevant. This trial did not involve collecting biological specimens for storage. The researcher was aware of the sensitive nature of the research topic and minimised any distress caused to potential participants as a result of the discussions.
If the asylum seeker or refugee decided that they wanted to participate, they then personally signed and dated the informed consent document. The document was then signed and dated by the person obtaining consent and a copy of the informed consent document was given to the potential participant for their records. The original document was maintained by the research team separate from any personal identifiable information collected for any participants. A further copy was sent to LCTC, via secure methods, if the participant was eligible for full trial participation (this was sent separately from any participant data subsequently collected).
If the potential participant required more time to consider involvement in the trial, a further meeting could be arranged at the discretion of the researcher. If the individual did not wish to take part, their reason for not providing consent was recorded on the PROSPER screening log. Once informed consent had been given, the participant could revoke it and withdraw from the trial at any time by revoking their informed consent without being subject to any resulting detriment.
Eligibility and baseline assessments
Once written informed consent had been obtained, the potential participant was assessed for eligibility using the criteria detailed above.
Eligibility assessment followed a staged process. The researcher reviewed responses at the end of each stage and if the potential participant was found to be ineligible, they were informed of this and there was no requirement for completion of the next stage.
First, through discussion with the potential participant, the researcher completed sociodemographic questions. The researcher then assessed the following exclusion criteria: complex mental disorder (bipolar disorder/manic depression, or schizophrenia); cognitive impairment (moderate/severe intellectual disability, any dementia); substance misuse; and currently receiving a formal psychological therapy. If the potential participant remained eligible, they were asked to self-complete the HADS, WHODAS and PHQ-9 in the eligibility questionnaire booklet. All of these questionnaires were available in English, Arabic, Farsi and Urdu. The researcher reviewed the completed PHQ-9 to assess whether or not the potential participant was at imminent risk of suicide. If there were any concerns regarding suicide risk, the researcher followed the procedure outlined in the suicidal ideation guidance document.
If the potential participant was eligible following this process, the researcher conducted the baseline assessments outlined in the following section. This allowed consistency in the completion of outcome measurements and also reduced the need for participants to attend additional meetings. If the researcher had any concerns or uncertainties about the non-clinical eligibility assessment above, they contacted the chief investigator or their nominated deputy to discuss the case.
AS&Rs who were assessed as ineligible could be reconsidered for participation at a later date if circumstances changed (e.g. if they were able to register with a GP). If this occurred more than 2 weeks after consent had been obtained, the consent process was repeated.
Following the completion of the eligibility assessment, the researcher asked the eligible participant to self-complete the baseline questionnaire booklet, which incorporates the remaining baseline assessments: the WHO-5, PSYCHLOPS and PCL-5 questionnaires. The CSRI form, which was adapted for PROSPER, was completed by the researcher in discussion with the participant.
In the case of a potential participant who had completed the eligibility assessment process and was deemed eligible to participate in the PROSPER Pilot trial, but about whom there was concern or uncertainty that necessitated the researcher contacting the chief investigator or nominated deputy, the chief investigator or their nominated deputy reviewed the information provided by the participant to verify their eligibility for trial participation and completed the eligibility and baseline case report form (CRF) before randomisation occurred.
Randomisation
Participants were randomised using a secure web-based randomisation programme. Randomisation lists were generated in a 1 : 1 : 1 ratio, to individual PM+, group PM+ and control, using block randomisation with random variable block sizes to minimise the chance of predictability of allocation.
The randomisation list was generated by a statistician independent of the PROSPER trial. Given the open nature of the trial, it was not possible to blind researchers, trial participants, care providers, outcome assessors or data analysts to the intervention arm to which participants were assigned.
The researcher updated the PROSPER screening log when a participant was randomised and the researcher was responsible for notifying the participant of their allocation. In the event that a participant was randomised to individual or group PM+, the researcher informed the PSS lead. Intervention delivery was co-ordinated by PSS in collaboration with the participant and their lay therapist. The research team notified the participant’s GP by letter of their enrolment into the trial and their intervention allocation.
Assessments and follow-up
All assessments and follow-up were conducted in line with the schedule of assessments, summarised in Table 7.
| Time point (weeks) | Screening and baseline | Randomisation | 13-week follow-up | 26-week follow-up |
|---|---|---|---|---|
| 0 | 0 | 13 ± 2 | 26 ± 2 | |
| Procedures | ||||
| Consent, eligibility screening and confirmation | ||||
| Written and informed consent | ✗ | |||
| Assess eligibility | ✗ | |||
| Confirm eligibility | ✗ | |||
| Randomisation | ✗ | |||
| Confirm consent | ✗ | ✗ | ✗ | |
| Data collection | ||||
| HADS | ✗ | ✗ | ✗ | |
| WHODAS | ✗ | ✗ | ✗ | |
| PHQ-9 | ✗ | ✗ | ✗ | |
| PSYCHLOPS | ✗ | ✗ | ✗ | |
| PCL-5 | ✗ | ✗ | ✗ | |
| WHO-5 | ✗ | ✗ | ✗ | |
| CSRI | ✗ | ✗ | ✗ | |
| Adverse events | ||||
| Assessment of AEs | ✗ | ✗ | ✗ | |
No additional assessments were carried out for participants who discontinued or withdrew from the trial prematurely.
All specified outcomes were measured at 13 (± 2) and 26 (± 2) weeks post baseline; 13 weeks was the primary end point, consistent with previous trials. 24 This allowed time for intervention delivery and often may correspond to the timings of Home Office decisions on leave to remain for asylum seekers.
Follow-up visit 1: 13-week follow-up
We intended for this to be a face-to-face appointment at 13 (± 2) weeks post baseline. During the appointment, various data were acquired and various processes were finalised. These are outlined below:
-
verbal confirmation of continued consent
-
participant completion of the following questionnaires in the follow-up questionnaire booklet: HADS, WHODAS, PHQ-9, WHO-5, PSYCHLOPS, PCL-5
-
the researcher following the steps outlined in the suicidal ideation guidance document if suicidal ideation was disclosed or suspected
-
recording of any adverse event information
-
researcher-led completion of the adapted CSRI
-
completion of follow-up CRF.
Follow-up visit 2: 26-week follow-up
We intended for this to be a face-to-face appointment at 26 (± 2) weeks from baseline following the same process as the follow-up appointment at 13 weeks.
All follow-up appointments were co-ordinated and conducted by the trained researcher. The researcher conducted a preliminary review of the data collected to screen for missing data or responses that might need further follow-up or clinical discussion. Follow-up appointments were expected to take around 1 hour to allow for the completion of all data collection and a review of any adverse events. If a face-to-face appointment could not be arranged during the follow-up window, then the appointment could be conducted by telephone where possible. If the research team were unable to administer the assessments, the option of the participant self-completing the assessments and returning them by post was explored. It was expected that participant responses would be completed during the appropriate appointment window.
Statistical considerations
A detailed statistical analysis plan was developed prior to the first comparative monitoring report to be presented to the Independent Data and Safety Monitoring Committee (IDSMC). The main features of these statistical analyses that refer specifically to the PROSPER Pilot trial are detailed below.
The aim was to recruit 105 participants, and 35 to each of the three arms (individual PM+, group PM+ and control). Individual sessions were to be offered as gender and language specific, that is, the lay therapist and the study participant would be the same gender and would have a language in common. At least four groups were to be offered for the group intervention, each with up to eight or nine participants and each gender-specific, that is, all participants would be the same gender and at least one of the lay therapists would be the same gender as the participants.
The sample size needed to be sufficient to estimate retention levels in a definitive trial. With an expectation of 80% retention, samples of 35 participants for each of the individual, group and control arm would provide an accurate estimate of retention ± 13% (67–93%).
Retention rates were to be assessed in each arm separately, as there may have been systematic differences between them; for example, those randomised to the control arm may have been less likely to remain engaged than those randomised to the individual or group arms, while those randomised to the group arm may have been demotivated if faced with a lengthy wait for their group PM+ session to begin.
No formal interim analysis was planned as this was a pilot study and there were no anticipated problems that would be detrimental to the participant. Monitoring was undertaken by the IDSMC, which provided a recommendation to the Trial Steering Committee (TSC) on the continuation of the trial.
Analysis was by the intention-to-treat principle as far as practically possible. All analyses were to be descriptive, focused on assessing the criteria for deciding whether or not to progress to a full trial. All estimates of proportions are presented with 95% confidence intervals. Rates of recruitment and attrition are presented both for lay therapists and trial participants, along with the proportion of PM+ interventions that were successfully delivered as per protocol. The proportion of missing data in the proposed trial outcome measures was assessed.
Preliminary exploration of estimates of efficacy was intended, involving a groupwise comparison of the primary outcome: severity of combined anxiety and depressive symptoms at 13 weeks post baseline, measured using the HADS.
Sociodemographic data and data on the use of services and supports were captured by the adapted CSRI. 90 These data can be used for a wide range of applications, including estimating the costs of service receipt and societal costs.
We did not intend to carry out formal testing of intervention effect. However, we did intend to present (with 95% confidence intervals) estimates of between-group differences between the test groups and the control in outcome measures to assess whether or not a clinically important improvement in outcome would be plausible in a full trial. We intended to investigate the effect of clustering by intervention provider on outcomes in the two PM+ groups; this would then inform design of a full trial with a partially nested design.
Process evaluation and feasibility assessment
The relevance and acceptability of proposed outcomes were intended to be tested with a view to their incorporation into, or refinement for, a definitive trial. In testing the proposed outcomes, we aimed to determine the:
-
effectiveness of PM+, based on the primary outcome of combined HADS scores
-
cost-effectiveness of PM+ from an NHS perspective, based on the primary outcome of combined HADS scores91,92
-
cost–benefit of PM+ from a societal perspective, given that costs and potential benefits will extend beyond the NHS to local government and voluntary sectors93–95
-
impact of PM+ on health inequalities using the NIHR CLAHRC NWC (Collaboration for Leadership in Applied Health Research and Care North West) Health Inequalities Assessment Toolkit (www.hiat.org.uk), first within AS&R communities in relation to age, gender, nationality, education, prior occupation and asylum status, and second between AS&Rs and national populations, comparing mental health status (anxiety, depression PTSD and well-being) with UK population norms, with reference to published psychiatric morbidity data. 96
The feasibility of the 13- and 26-week time points was assessed, with specific reference to rates of participant attrition.
Researchers undertook a systems-based process evaluation,97 beginning 3 months into the PROSPER Pilot trial, to understand service provider and participant experiences of and perspectives on the acceptability, efficiency, implementation and development of PM+; understand service users’ perceptions and experiences of accessing and participating in PM+; explore how PM+ fits into existing health/social care systems; and understand change process dynamics, including barriers to and facilitators of implementing PM+. An ethnographic method was adopted, including observation of PM+ implementation alongside semistructured interviews and focus group discussions with key stakeholder groups such as lay therapists, well-being mentors, PM+ participants, representatives from NGOs working with AS&R communities, health professionals and commissioners from Liverpool City Region. Heterogeneity within the population was considered alongside whether the intervention’s feasibility and effectiveness might differ by demography or asylum status, and how this might influence the choice of target population for our proposed definitive trial.
Analysis was based on narrative synthesis, combining data tabulation and narrative techniques. This involved iterative review and refinement in order to reach agreement on a set of general propositions in relation to the data. The perspectives of normalisation process theory98,99 were intended to be used to assess the potential for implementing a full RCT, focusing on the progression criteria set out above.
Discontinuation and withdrawal
In consenting to the trial, participants agreed to all trial activities, including the administration of trial intervention and follow-up assessments/visits and data collection. Every effort was made to facilitate the completion of these for every recruited participant. If it was not possible to complete these activities (or if it was deemed inappropriate), the reasons for this were documented.
Participants could discontinue the study intervention for reasons including but not limited to:
-
participant led (i.e. request by the participant)
-
researcher/clinician/lay therapist led –
-
any change in the participant’s condition that justified the discontinuation of the intervention in the researcher/clinician/lay therapist’s opinion
-
reasons for non-adherence to or non-compliance with study intervention or other trial procedures (e.g. unable to complete course of PM+)
-
participant met an exclusion criterion (either newly developed or not previously recognised).
-
Discontinuation from PM+ did not mean discontinuation of the study altogether, and the remaining study procedures – namely the 13- and 26-week follow up visits and data collection, and process evaluation – were completed as indicated in the protocol (unless consent was specifically withdrawn).
Participants were free to withdraw from follow-up at any time without providing a reason, although a reason was recorded if given, and their data collected to that point were included in the analyses. The participant did not contribute further data to the study and LCTC was informed by e-mail to LCTC and via completion of a withdrawal CRF to be returned to LCTC within 24 hours. Death of a participant was recorded on a withdrawal CRF and a death CRF.
For participants moving from the area, every effort was made for the participant to be followed up and to complete their remaining study appointment(s) remotely.
A participant was considered lost to follow-up if she or he failed to return for any scheduled visits and was not contactable by the site research team. If a participant failed to attend/facilitate a required study visit, the following actions were to be taken:
-
The researcher would attempt to contact the participant and reschedule the missed visit (being conscious of acceptable windows for collecting valid data) and advise the participant of the importance of maintaining the assigned visit schedule.
-
Before a participant was deemed to be lost to follow-up, the research team would make reasonable effort to regain contact with the participant.
-
If the participant continued to be unreachable, they would be considered withdrawn from the study with a primary reason of lost to follow-up, and this was to be recorded on the withdrawal CRF.
Confidentiality and access to data
Forms that contained participant identifiers were stored separately from the CRFs. The database was secured with password protection. Participants’ data were not released outside the study without the written permission of the participant documented in the consent form.
The University of Liverpool and Bangor University are registered as data controllers with the Information Commissioner’s Office.
Safety and monitoring
Safety assessments were based on information disclosed by the participant throughout trial duration and by those who have knowledge of their welfare, including GPs, other health professional and NGO members. The chief investigator and other research staff were responsible for monitoring and reporting all adverse events.
Ancillary and post-trial care was the responsibility of the participant’s registered general practitioner.
Data were centrally monitored by LCTC to promote data quality. Monitoring processes are documented in the trial monitoring plan. 1 If necessary, on-site monitoring visits could be triggered and carried out by either LCTC or the sponsor representative.
Safety information and data were independently monitored by the IDSMC. The IDSMC was chaired by an independent senior clinical academic, and included an independent methodological expert and an experienced service user. The IDSMC reported to the TSC and hence to the NIHR Public Health Research Programme Board.
End of trial
The end of the trial was defined as the date on which data for all participants were locked and data entry privileges were withdrawn from the trial database. However, the trial could have been closed prematurely by the TSC on the recommendation of the IDSMC.
Major findings
Recruitment and retention
The trial opened to recruitment on 27 November 2019, with the aim of recruitment being completed in May 2020. However, owing to the COVID-19 pandemic recruitment was stopped in March 2020 with 11 of the planned 105 participants recruited, and was not restarted.
Figure 3 shows the flow of participants through the pilot trial. Twenty potential participants were identified and of those not randomised, three were not approached for consent and six declined to take part. Table 8 shows the numbers recruited per group.
FIGURE 3.
The CONSORT flow diagram: summary of recruitment and follow-up. a, Participants randomised to PM+ who did not receive any intervention are summarised in the ‘control’ group for safety analyses.
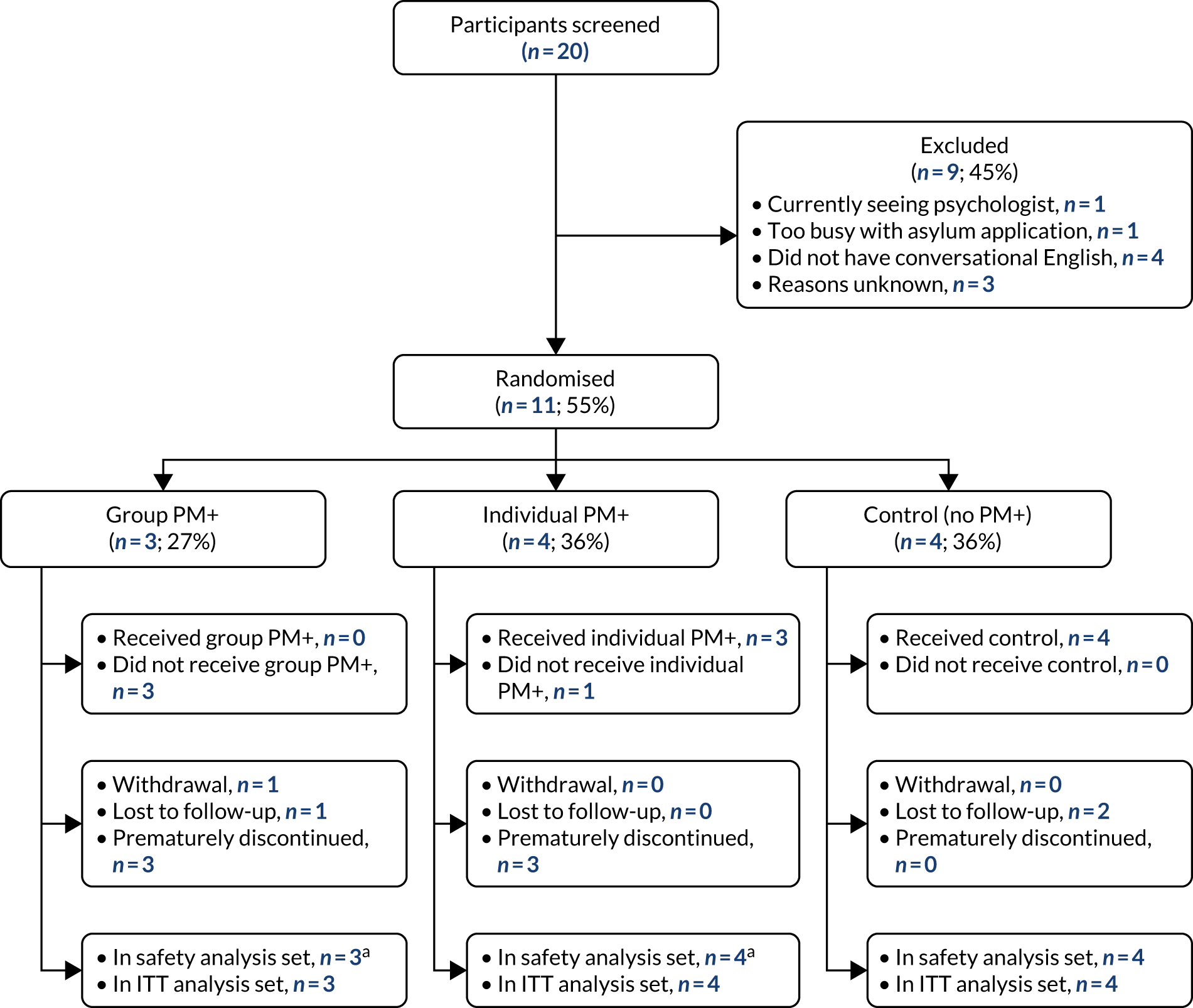
| Allocation | Number recruited/number required | Proportion (95% CI) |
|---|---|---|
| No PM+ | 4/35 | 0.11 (0.03 to 0.27) |
| Group PM+ | 3/35 | 0.09 (0.02 to 0.23) |
| Individual PM+ | 4/35 | 0.11 (0.03 to 0.27) |
| Overall | 11/105 | 0.10 (0.05 to 0.18) |
Progression criterion: recruitment of trial participants
With reference to Table 6, the proportion recruited falls into the ‘stop’ category for this criterion.
Baseline characteristics
Table 9 shows the demographics and baseline characteristics of the participants recruited to the pilot trial. Seven female and four male participants were recruited; they were aged between 23 and 56 years, with a mean age of 35 [standard deviation (SD) 10.5] years. The 11 participants came from eight countries, with the Islamic Republic of Iran being the most common country of origin. Their time in the UK ranged from 37 days to over 10 years. Four participants had leave to remain in the UK.
| Baseline characteristic | Control (no PM+) | Group PM+ | Individual PM+ | Overall |
|---|---|---|---|---|
| Participants randomised, N | 4 | 3 | 4 | 11 |
| Gender, n (%) | ||||
| Female | 2 (50.00) | 1 (33.33) | 4 (100) | 7 (63.64) |
| Male | 2 (50.00) | 2 (66.67) | 0 (0) | 4 (36.36) |
| Age (years) | ||||
| Mean (SD) | 34.50 (7.33) | 40.33 (14.01) | 31.50 (11.82) | 35.00 (10.53) |
| Median (IQR) | 37.00 (29.50–39.50) | 36.00 (29.00–56.00) | 27.00 (25.00–38.00) | 35.00 (27.00–40.00) |
| Minimum, maximum | 24.00, 40.00 | 29.00, 56.00 | 23.00, 49.00 | 23.00, 56.00 |
| Years in education | ||||
| Mean (SD) | 17.00 (2.45) | 17.00 (3.00) | 11.00 (3.16) | 14.82 (3.97) |
| Median (IQR) | 17.00 (15.50–18.50) | 17.00 (14.00–20.00) | 10.50 (8.50–13.50) | 15.00 (12.00–17.00) |
| Minimum, maximum | 14.00, 20.00 | 14.00, 20.00 | 8.00, 15.00 | 8.00, 20.00 |
| Language questionnaires administered in, n (%) | ||||
| English | 4 (100) | 3 (100) | 4 (100) | 11 (100) |
| Country of origin, n (%) | ||||
| Afghanistan | 1 (25.00) | 0 (0) | 0 (0) | 1 (9.09) |
| India | 0 (0) | 0 (0) | 1 (25.00) | 1 (9.09) |
| Islamic Republic of Iran | 2 (50.00) | 1 (33.33) | 1 (25.00) | 4 (36.36) |
| Iraq | 0 (0) | 0 (0) | 1 (25.00) | 1 (9.09) |
| Namibia | 1 (25.00) | 0 (0) | 0 (0) | 1 (9.09) |
| Nigeria | 0 (0) | 1 (33.33) | 0 (0) | 1 (9.09) |
| Pakistan | 0 (0) | 0 (0) | 1 (25.00) | 1 (9.09) |
| Yemen | 0 (0) | 1 (33.33) | 0 (0) | 1 (9.09) |
| Number of days in the UK | ||||
| Mean (SD) | 396.50 (630.44) | 218.00 (64.86) | 1864.75 (2072.77) | 881.73 (1421.92) |
| Median (IQR) | 105.50 (41.00–752.00) | 191.00 (171.00–292.00) | 1746.00 (78.50–3651.00) | 171.00 (65.00–1338.00) |
| Minimum, maximum | 37.00, 1338.00 | 171.00, 292.00 | 65.00, 3902.00 | 37.00, 3902.00 |
| Immigration status, n (%) | ||||
| Pre-asylum | 1 (25.00) | 0 (0) | 0 (0) | 1 (9.09) |
| Asylum seeker pending | 2 (50.00) | 2 (66.67) | 2 (50.00) | 6 (54.55) |
| Leave to remain humanitarian protection | 0 (0) | 1 (33.33) | 0 (0) | 1 (9.09) |
| Leave to remain refugee status | 1 (25.00) | 0 (0) | 2 (50.00) | 3 (27.27) |
Withdrawals and losses to follow-up
There was one formal withdrawal of consent for follow-up from a participant randomised to group PM+. Three participants were recorded as lost to follow-up, two randomised to no PM+ and one to group PM+. Table 10 shows the number of participants remaining in the trial at the 13- and 26-week time points.
| Allocation | Number at 13 weeks/number randomised | Proportion (95% CI) | Number at 26 weeks/number randomised | Proportion (95% CI) |
|---|---|---|---|---|
| No PM+ | 2/4 | 0.50 (0.07 to 0.93) | 2/4 | 0.50 (0.07 to 0.93) |
| Group PM+ | 2/3 | 0.67 (0.09 to 0.99) | 1/3 | 0.33 (0.01 to 0.91) |
| Individual PM+ | 4/4 | 1.00 (0.40 to 1.00) | 4/4 | 1.00 (0.40 to 1.00) |
| Overall | 8/11 | 0.73 (0.39 to 0.94) | 7/11 | 0.64 (0.31 to 0.89) |
Progression criterion: retention of trial participants
With reference to Table 6, the proportion recruited falls into the ‘go’ category for this criterion.
Intervention delivery
The trial was stopped before any group PM+ sessions could take place, so those randomised to group PM+ did not receive any intervention. Of the four participants randomised to individual PM+, one received all five intervention sessions, one received two of the sessions, one received a single session and one did not receive the intervention. The number and proportion of participants who did not receive the full intervention is shown in Table 11.
| Allocation | Number discontinued/number randomised | Proportion (95% CI) |
|---|---|---|
| Group PM+ | 3/3 | 1.00 (0.29 to 1.00) |
| Individual PM+ | 3/4 | 0.75 (0.19 to 0.99) |
| Overall | 6/7 | 0.86 (0.42 to 1.00) |
Progression criterion: protocol adherence
With reference to Table 6, the proportion of interventions delivered per protocol falls into the ‘stop’ category for this criterion.
Completion of outcome assessments
Table 12 shows the number of completed outcome measures. Each participant should have completed six outcome measures at each of three time points.
| Allocation | Number of missed assessments/number of expected assessments | Proportion (95% CI) |
|---|---|---|
| No PM+ | 28/72 | 0.39 (0.28 to 0.51) |
| Group PM+ | 21/54 | 0.39 (0.26 to 0.53) |
| Individual PM+ | 9/72 | 0.13 (0.06 to 0.22) |
| Overall | 58/198 | 0.29 (0.23 to 0.36) |
Progression criterion: completion of outcome assessments
With reference to Table 6, the proportion of outcome measures completed falls into the ‘go’ category for this criterion.
Primary outcome: Hospital Anxiety and Depression Scale
The protocol specified that we would present estimates of between-group differences to assess whether a clinically important improvement in primary outcome would be plausible, and that the effect of clustering by intervention provider would be investigated.
As the trial was stopped early, and because very small numbers were recruited, it was agreed with the trial sponsor that these analyses would not be carried out.
Summary statistics for HADS are presented in Table 13. Individual participant profile plots are shown in Figures 4–6. For full line listings, see Appendix 1, Table 20.
| Variable | Control (no PM+) | Individual PM+ | Group PM+ | Overall |
|---|---|---|---|---|
| Baseline | ||||
| Anxiety subscale | ||||
| na | 4 | 4 | 3 | 11 |
| Mean (SD) | 11.75 (3.50) | 16.00 (2.45) | 9.67 (7.09) | 12.73 (4.80) |
| Median (IQR) | 11.50 (9.00–14.50) | 16.00 (14.50–17.50) | 11.00 (2.00–16.00) | 13.00 (10.00–16.00) |
| Minimum, maximum | 8.00, 16.00 | 13.00, 19.00 | 2.00, 16.00 | 2.00, 19.00 |
| Depression subscale | ||||
| na | 4 | 4 | 3 | 11 |
| Mean (SD) | 12.00 (4.97) | 12.25 (6.08) | 4.67 (3.06) | 10.09 (5.70) |
| Median (IQR) | 12.50 (8.00–16.00) | 12.00 (7.00–17.50) | 4.00 (2.00–8.00) | 8.00 (6.00–17.00) |
| Minimum, maximum | 6.00, 17.00 | 7.00, 18.00 | 2.00, 8.00 | 2.00, 18.00 |
| Total HADS score | ||||
| na | 4 | 4 | 3 | 11 |
| Mean (SD) | 23.75 (5.32) | 28.25 (8.06) | 14.33 (4.04) | 22.82 (8.06) |
| Median (IQR) | 25.50 (20.50–27.00) | 28.00 (21.50–35.00) | 15.00 (10.00–18.00) | 23.00 (16.00–28.00) |
| Minimum, maximum | 16.00, 28.00 | 20.00, 37.00 | 10.00, 18.00 | 10.00, 37.00 |
| Week 13 | ||||
| Anxiety subscale | ||||
| na | 2 | 4 | 2 | 8 |
| Mean (SD) | 7.00 (4.24) | 11.25 (4.99) | 12.50 (3.54) | 10.50 (4.47) |
| Median (IQR) | 7.00 (4.00–10.00) | 10.50 (8.00–14.50) | 12.50 (10.00–15.00) | 10.00 (8.00–13.00) |
| Minimum, maximum | 4.00, 10.00 | 6.00, 18.00 | 10.00, 15.00 | 4.00, 18.00 |
| Depression subscale | ||||
| na | 2 | 4 | 2 | 8 |
| Mean (SD) | 9.50 (2.12) | 9.50 (4.93) | 7.00 (5.66) | 8.88 (4.12) |
| Median (IQR) | 9.50 (8.00–11.00) | 9.50 (5.50–13.50) | 7.00 (3.00–11.00) | 9.50 (5.50–11.50) |
| Minimum, maximum | 8.00, 11.00 | 4.00, 15.00 | 3.00, 11.00 | 3.00, 15.00 |
| Total HADS score | ||||
| na | 2 | 4 | 2 | 8 |
| Mean (SD) | 16.50 (2.12) | 20.75 (9.32) | 19.50 (2.12) | 19.38 (6.48) |
| Median (IQR) | 16.50 (15.00–18.00) | 18.50 (13.50–28.00) | 19.50 (18.00–21.00) | 18.00 (14.50–22.00) |
| Minimum, maximum | 15.00, 18.00 | 13.00, 33.00 | 18.00, 21.00 | 13.00, 33.00 |
| Week 26 | ||||
| Anxiety subscale | ||||
| na | 2 | 4 | 1 | 7 |
| Mean (SD) | 9.00 (2.83) | 12.00 (2.45) | 11.00 (.) | 11.00 (2.52) |
| Median (IQR) | 9.00 (7.00–11.00) | 12.00 (10.50–13.50) | 11.00 (11.00–11.00) | 11.00 (9.00–12.00) |
| Minimum, maximum | 7.00, 11.00 | 9.00, 15.00 | 11.00, 11.00 | 7.00, 15.00 |
| Depression subscale | ||||
| na | 2 | 4 | 1 | 7 |
| Mean (SD) | 10.50 (2.12) | 9.75 (4.79) | 5.00 (0) | 9.29 (3.99) |
| Median (IQR) | 10.50 (9.00–12.00) | 11.00 (6.50–13.00) | 5.00 (5.00–5.00) | 10.00 (5.00–12.00) |
| Minimum, maximum | 9.00, 12.00 | 3.00, 14.00 | 5.00, 5.00 | 3.00, 14.00 |
| Total HADS score | ||||
| na | 2 | 4 | 1 | 7 |
| Mean (SD) | 19.50 (4.95) | 21.75 (4.99) | 16.00 (0) | 20.29 (4.61) |
| Median (IQR) | 19.50 (16.00–23.00) | 22.50 (18.50–25.00) | 16.00 (16.00–16.00) | 22.00 (16.00–23.00) |
| Minimum, maximum | 16.00, 23.00 | 15.00, 27.00 | 16.00, 16.00 | 15.00, 27.00 |
FIGURE 4.
Individual profile plots for HADS anxiety score. a, No PM+; b, group PM+; and c, individual PM+.
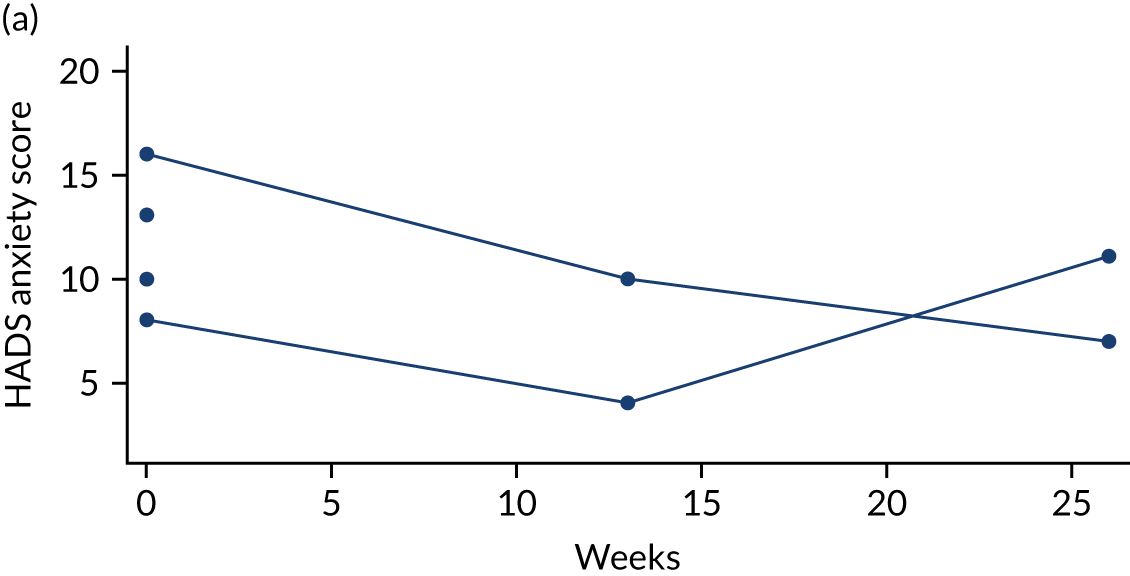
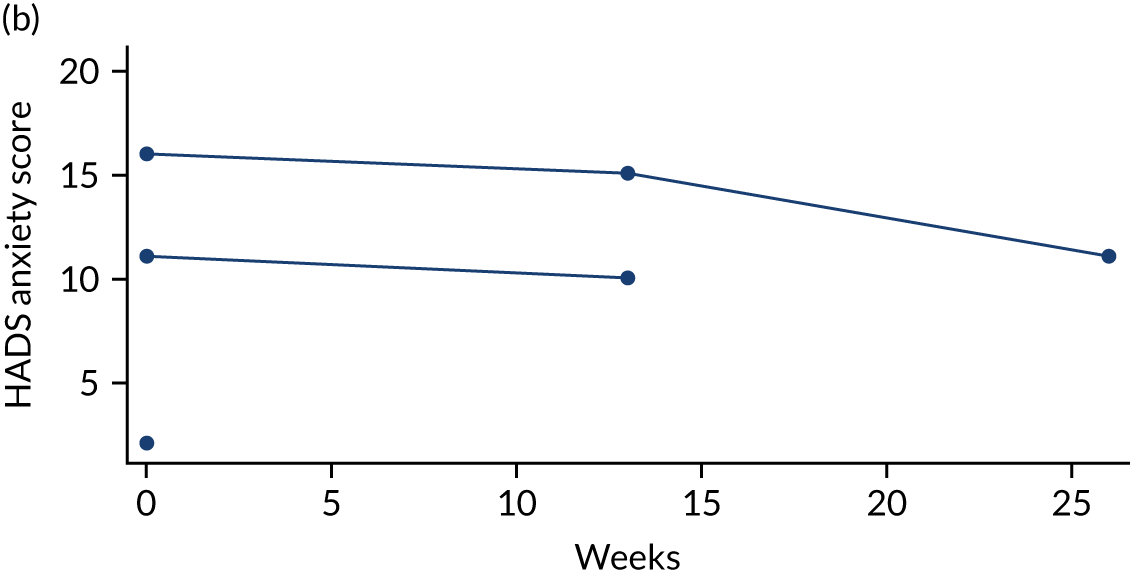
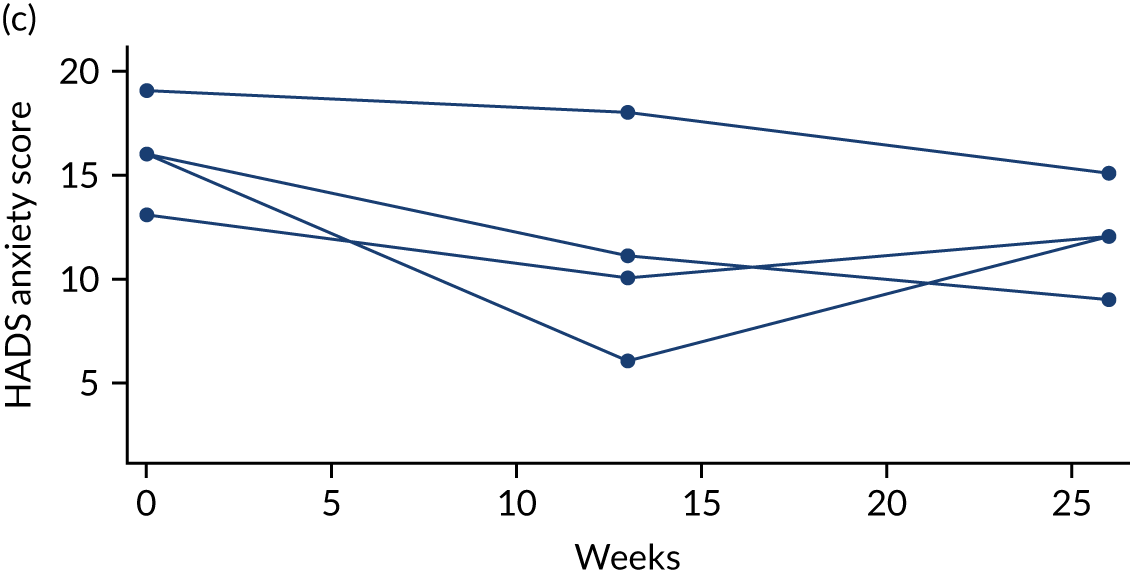
FIGURE 5.
Individual profile plots for HADS depression score. a, No PM+; b, group PM+; and c, individual PM+.
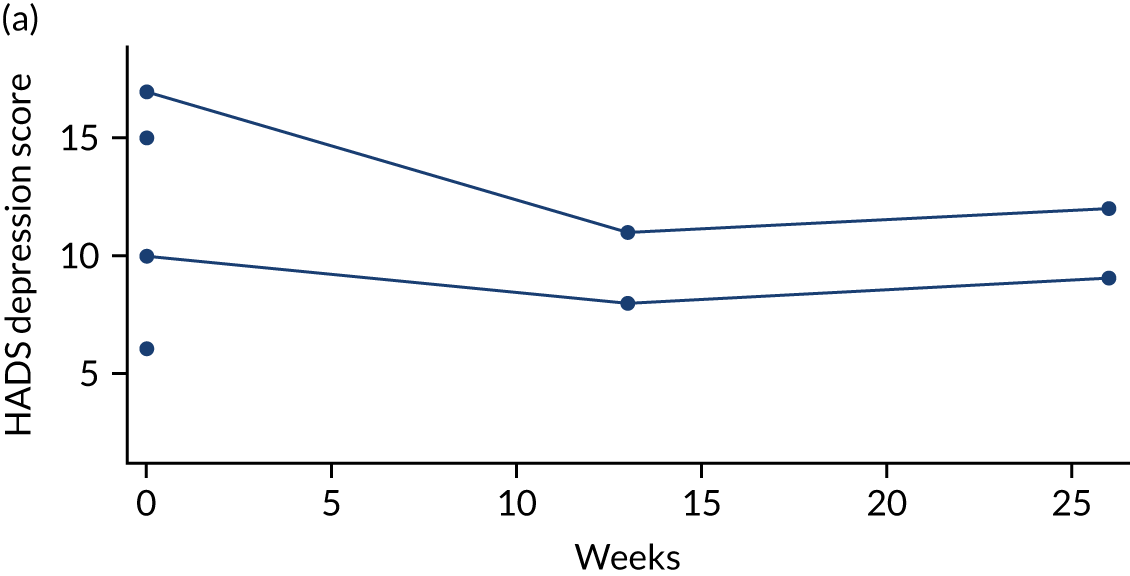
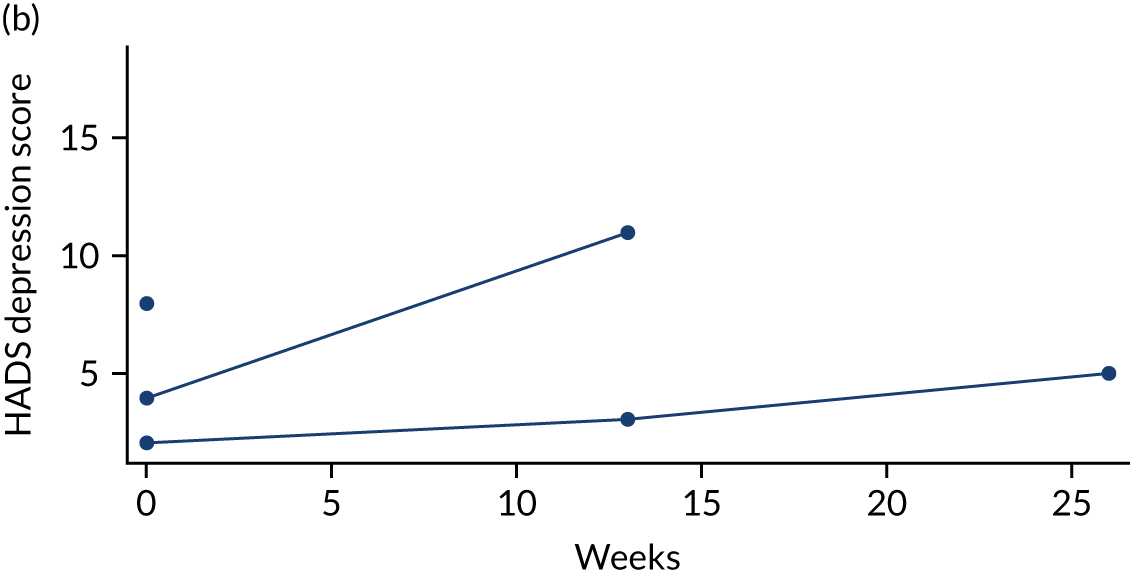
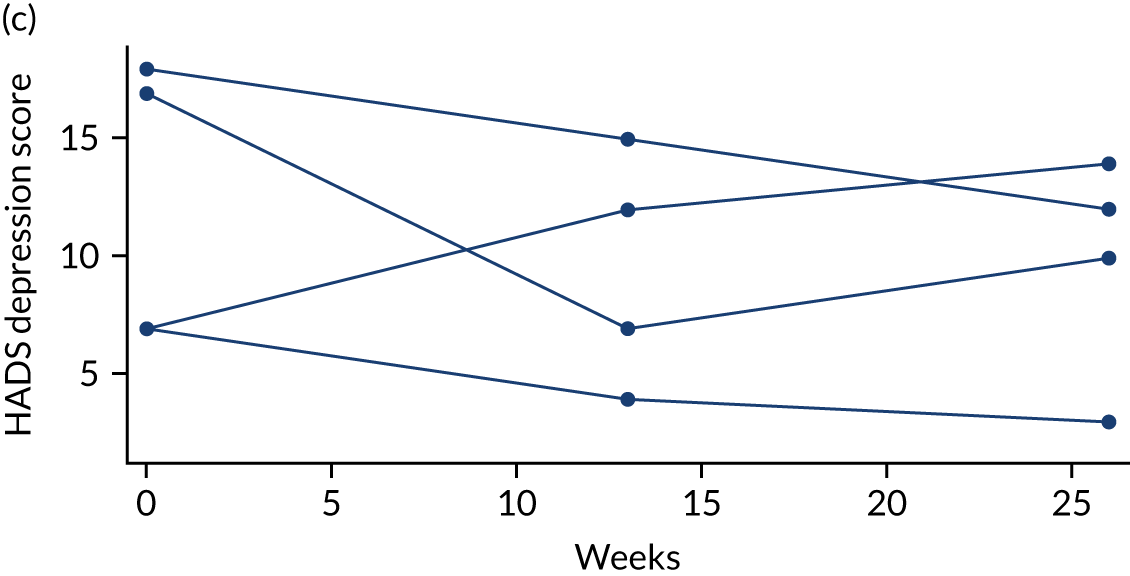
FIGURE 6.
Individual profile plots for HADS total score. a, No PM+; b, group PM+; and c, individual PM+.
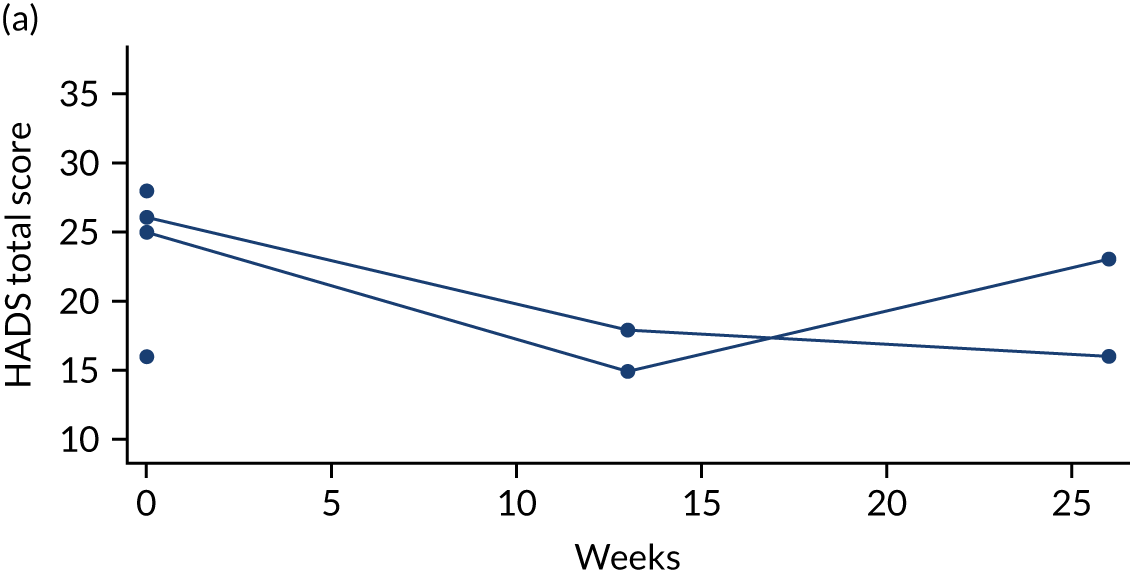
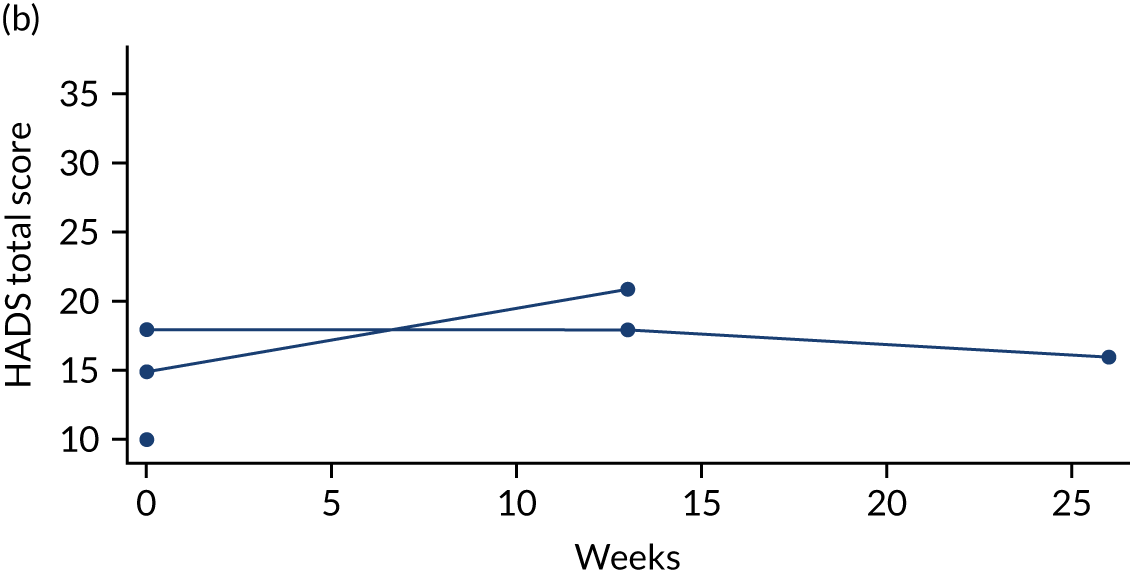
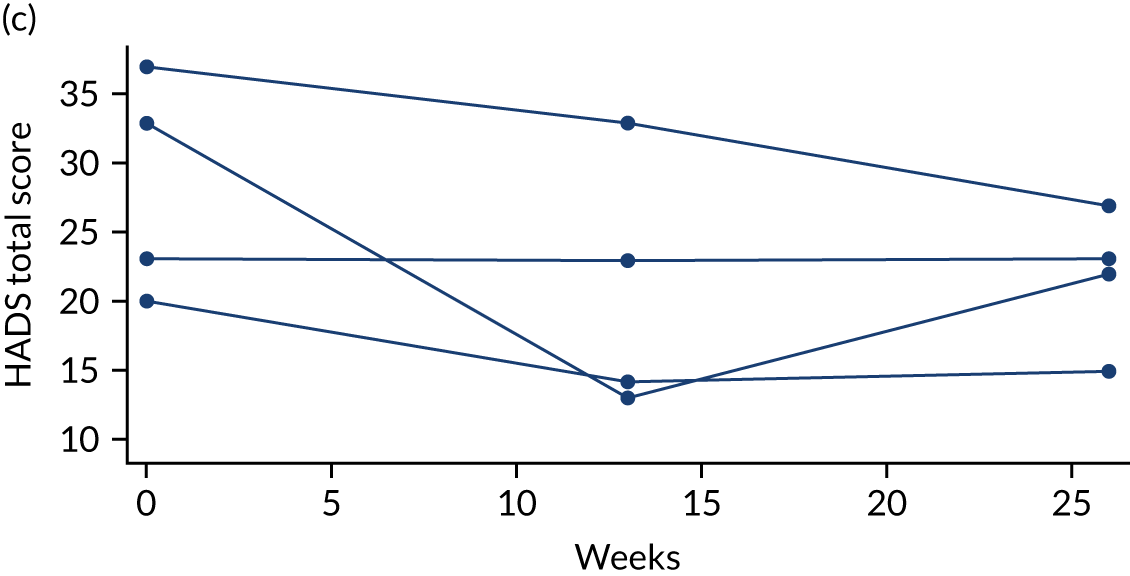
Secondary outcome 1: WHO-5
Summary statistics for the WHO-5 are presented in Table 14. Individual participant profile plots are shown in Figure 7. For full line listings, see Appendix 1, Table 21.
| Time point | Control (no PM+) | Individual PM+ | Group PM+ | Overall |
|---|---|---|---|---|
| Baseline | ||||
| na | 4 | 3 | 3 | 10 |
| Mean (SD) | 18.00 (17.44) | 29.33 (23.44) | 62.67 (10.07) | 34.80 (25.30) |
| Median | 10.00 | 20.00 | 64.00 | 32.00 |
| Minimum, maximum | 8.00, 44.00 | 12.00, 56.00 | 52.00, 72.00 | 8.00, 72.00 |
| Week 13 | ||||
| na | 2 | 4 | 2 | 8 |
| Mean (SD) | 54.00 (14.14) | 41.00 (22.00) | 50.00 (2.83) | 46.50 (16.55) |
| Median | 54.00 | 46.00 | 50.00 | 50.00 |
| Minimum, maximum | 44.00, 64.00 | 12.00, 60.00 | 48.00, 52.00 | 12.00, 64.00 |
| Week 26 | ||||
| na | 2 | 4 | 1 | 7 |
| Mean (SD) | 40.00 (16.97) | 39.00 (15.10) | 56.00 (0) | 41.71 (14.21) |
| Median | 40.00 | 34.00 | 56.00 | 40.00 |
| Minimum, maximum | 28.00, 52.00 | 28.00, 60.00 | 56.00, 56.00 | 28.00, 60.00 |
FIGURE 7.
Individual profile plots for WHO-5. a, No PM+; b, group PM+; and c, individual PM+.
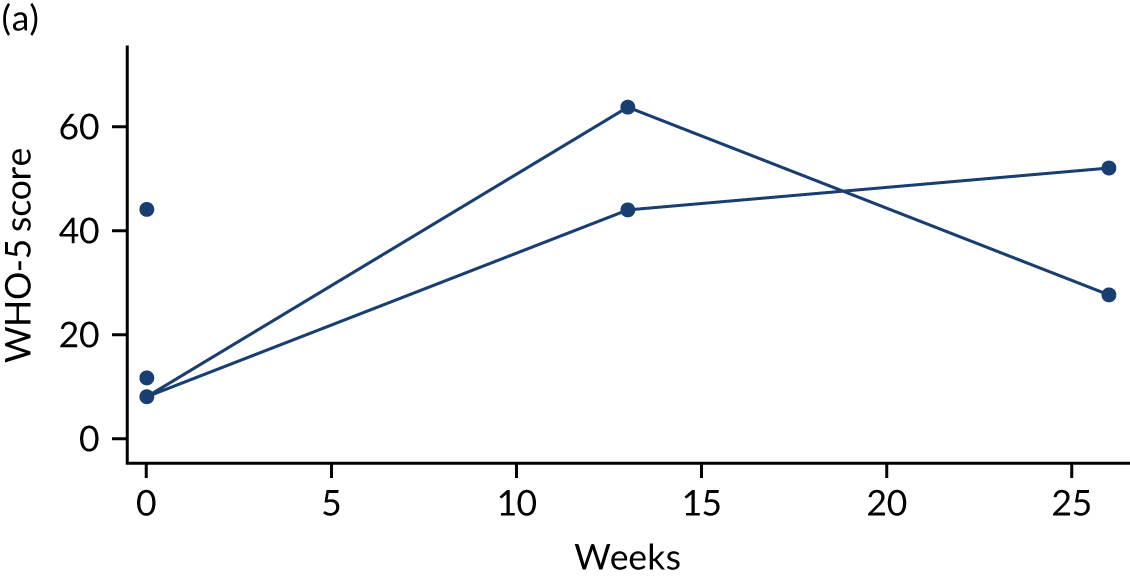
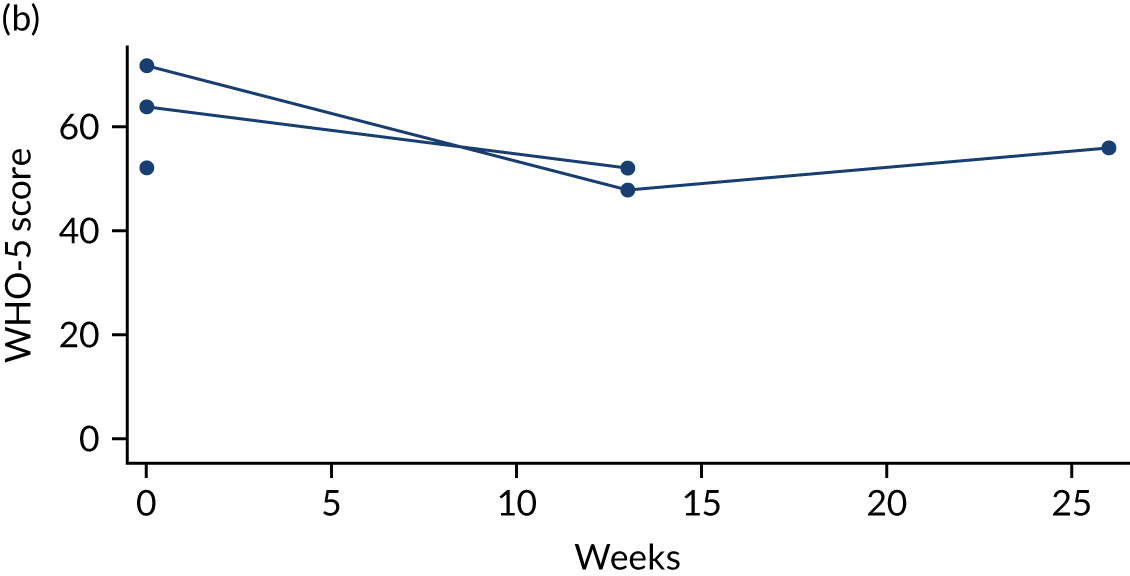
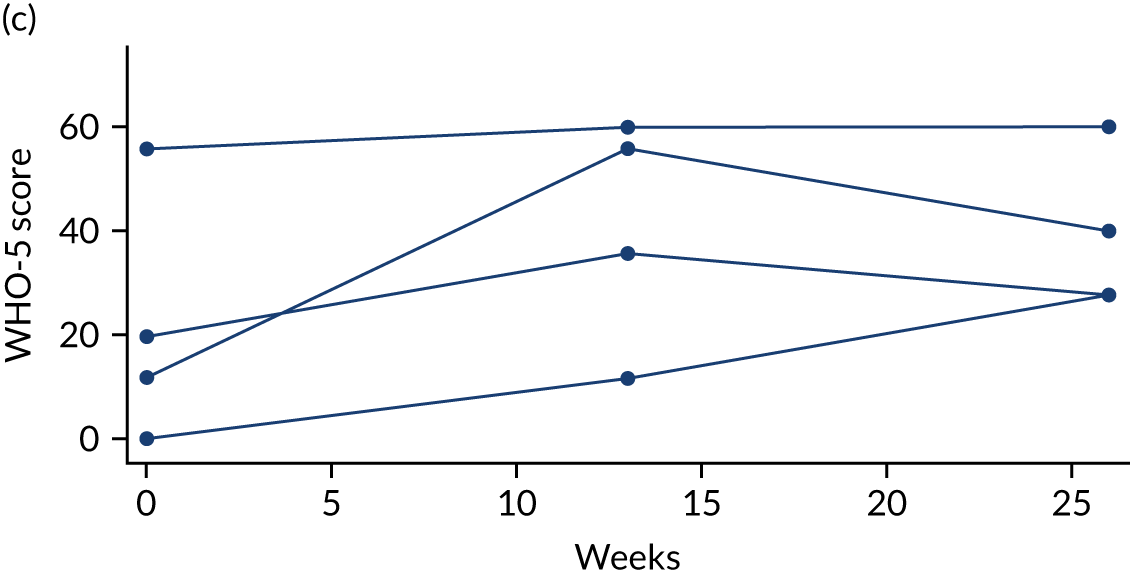
Secondary outcome 2: WHODAS 2.0
Summary statistics for the WHODAS 2.0 are presented in Table 15. Individual participant profile plots are shown in Figure 8. For full line listings, see Appendix 1, Table 21.
| Time point | Control (no PM+) | Individual PM+ | Group PM+ | Overall |
|---|---|---|---|---|
| Baseline | ||||
| na | 4 | 4 | 3 | 11 |
| Mean (SD) | 33.25 (7.85) | 33.75 (8.92) | 22.67 (0.58) | 30.55 (8.25) |
| Median | 29.50 | 30.00 | 23.00 | 29.00 |
| Minimum, maximum | 29.00, 45.00 | 28.00, 47.00 | 22.00, 23.00 | 22.00, 47.00 |
| Week 13 | ||||
| na | 2 | 4 | 2 | 8 |
| Mean (SD) | 21.00 (7.07) | 25.00 (8.91) | 21.50 (2.12) | 23.13 (6.77) |
| Median | 21.00 | 24.00 | 21.50 | 21.50 |
| Minimum, maximum | 16.00, 26.00 | 17.00, 35.00 | 20.00, 23.00 | 16.00, 35.00 |
| Week 26 | ||||
| na | 2 | 4 | 1 | 7 |
| Mean (SD) | 19.50 (4.95) | 27.75 (7.37) | 32.00 (0) | 26.00 (7.30) |
| Median | 19.50 | 28.00 | 32.00 | 23.00 |
| Minimum, maximum | 16.00, 23.00 | 20.00, 35.00 | 32.00, 32.00 | 16.00, 35.00 |
FIGURE 8.
Individual profile plots for WHODAS 2.0. a, No PM+; b, group PM+; and c, individual PM+.
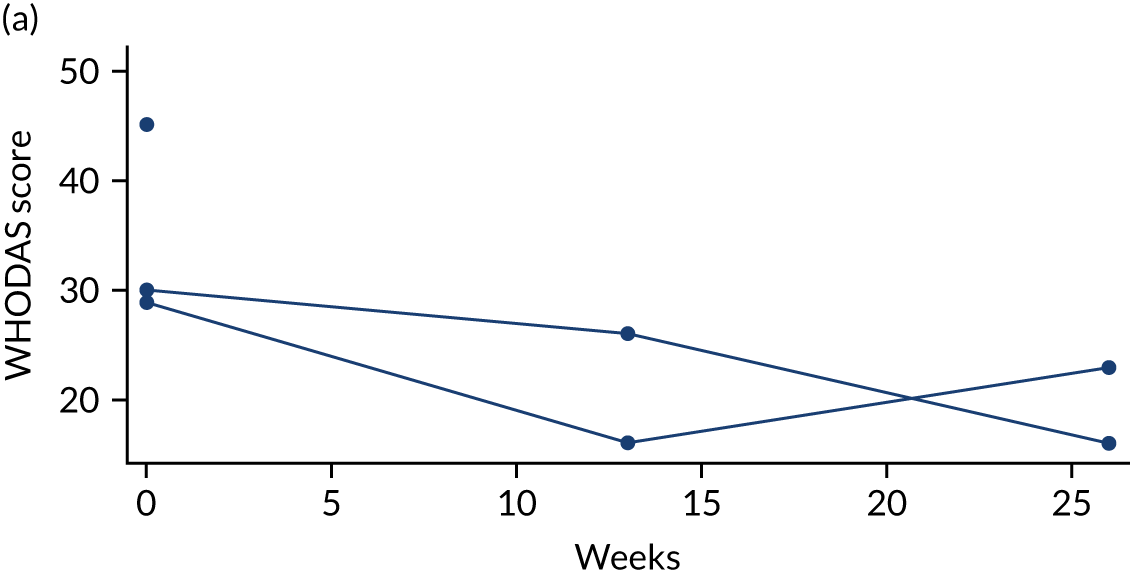
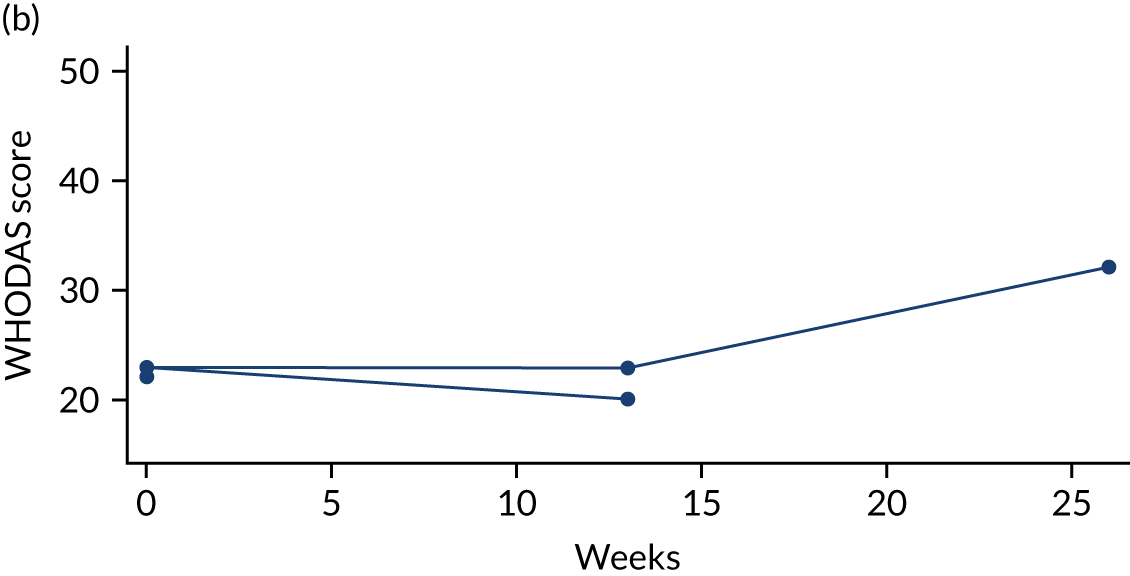
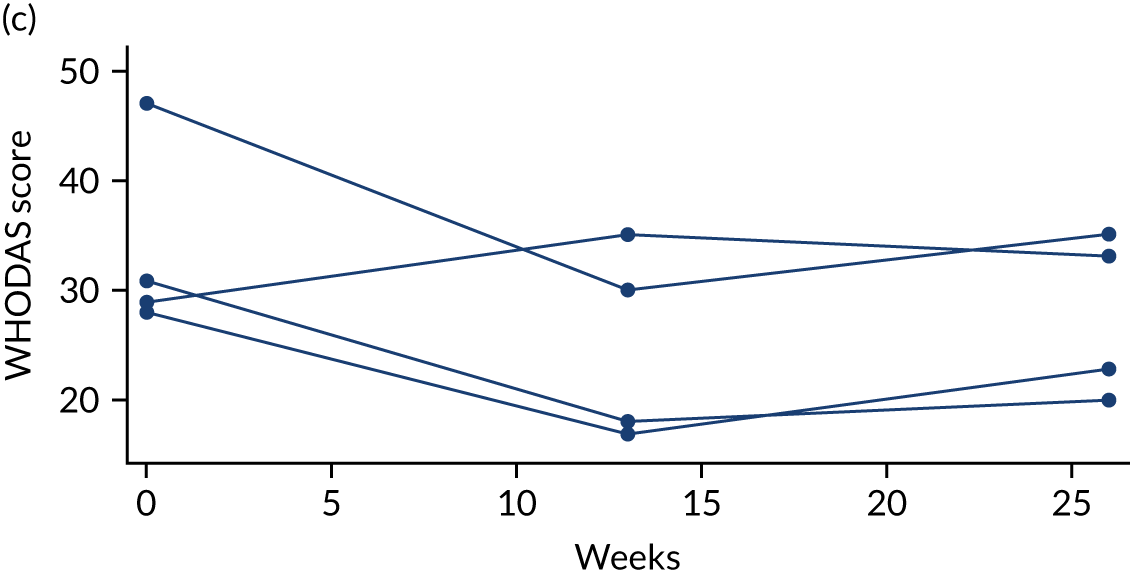
Secondary outcome 3: PSYCHLOPS
Summary statistics for PSYCHLOPS are presented in Table 16.
| Time point | Control (no PM+) | Individual PM+ | Group PM+ | Overall |
|---|---|---|---|---|
| Baseline | ||||
| na | 4 | 4 | 3 | 11 |
| Mean (SD) | 17.25 (1.26) | 17.50 (3.79) | 15.00 (4.00) | 16.73 (3.04) |
| Median | 17.00 | 19.00 | 15.00 | 17.00 |
| Minimum, maximum | 16.00, 19.00 | 12.00, 20.00 | 11.00, 19.00 | 11.00, 20.00 |
This outcome measure was to be collected at the follow-up time points by the PSS team rather than the researcher. It has not been possible to retrieve these data.
Secondary outcome 4: PCL-5
Summary statistics for the PCL-5 are presented in Table 17. Individual participant profile plots are shown in Figure 9. For full line listings, see Appendix 1, Table 21.
| Time point | Control (no PM+) | Individual PM+ | Group PM+ | Overall |
|---|---|---|---|---|
| Baseline | ||||
| na | 4 | 4 | 3 | 11 |
| Mean (SD) | 50.50 (11.12) | 54.50 (16.42) | 25.05 (10.13) | 45.01 (17.50) |
| Median | 53.00 | 55.00 | 23.16 | 51.00 |
| Minimum, maximum | 35.00, 61.00 | 34.00, 74.00 | 16.00, 36.00 | 16.00, 74.00 |
| Week 13 | ||||
| na | 2 | 4 | 2 | 8 |
| Mean (SD) | 36.00 (21.21) | 29.00 (11.17) | 35.00 (9.90) | 32.25 (12.00) |
| Median | 36.00 | 29.50 | 35.00 | 31.50 |
| Minimum, maximum | 21.00, 51.00 | 16.00, 41.00 | 28.00, 42.00 | 16.00, 51.00 |
| Week 26 | ||||
| na | 2 | 4 | 1 | 7 |
| Mean (SD) | 32.50 (23.33) | 39.50 (5.51) | 27.00 (0) | 35.71 (11.47) |
| Median | 32.50 | 40.00 | 27.00 | 37.00 |
| Minimum, maximum | 16.00, 49.00 | 33.00, 45.00 | 27.00, 27.00 | 16.00, 49.00 |
FIGURE 9.
Individual profile plots for PCL-5. a, No PM+; b, group PM+; and c, individual PM+.
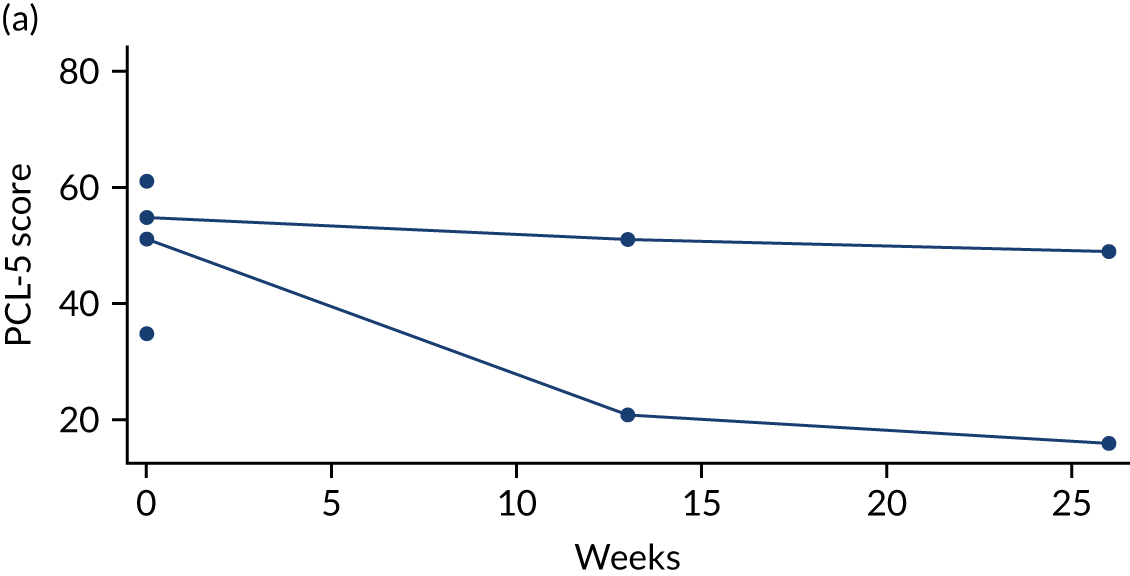
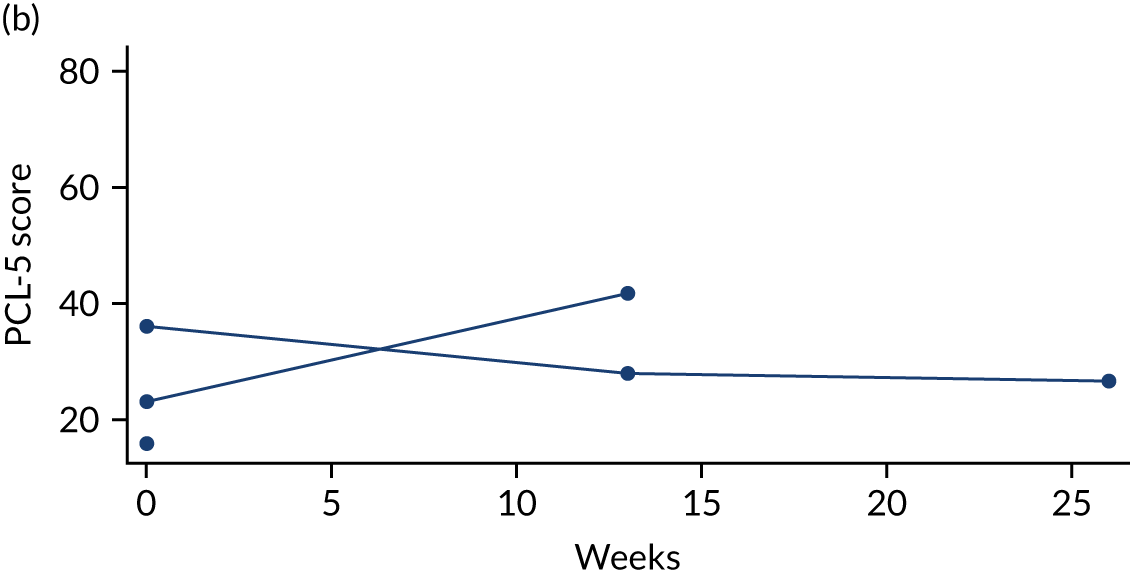
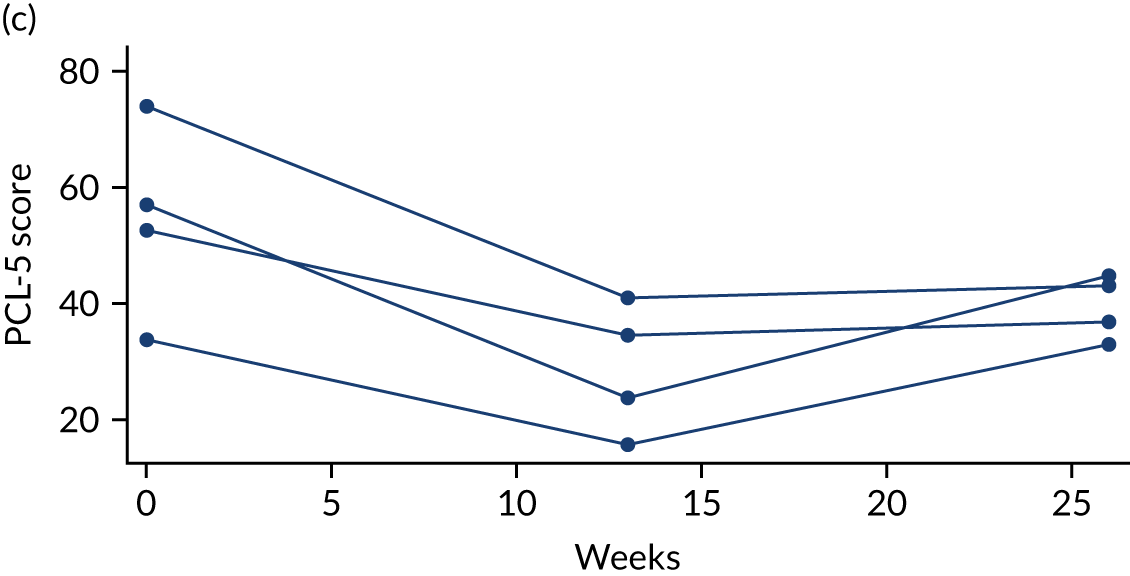
Secondary outcome 4: PHQ-9
Summary statistics for the PHQ-9 are presented in Table 18. Individual participant profile plots are shown in Figure 10. For full line listings, see Appendix 1, Table 21.
| Time point | Control (no PM+) | Individual PM+ | Group PM+ | Overall |
|---|---|---|---|---|
| Baseline | ||||
| na | 4 | 4 | 3 | 11 |
| Mean (SD) | 14.00 (0.82) | 14.50 (7.72) | 9.33 (3.06) | 12.91 (5.03) |
| Median | 14.00 | 14.00 | 10.00 | 13.00 |
| Minimum, maximum | 13.00, 15.00 | 7.00, 23.00 | 6.00, 12.00 | 6.00, 23.00 |
| Week 13 | ||||
| na | 2 | 4 | 2 | 8 |
| Mean (SD) | 6.00 (1.41) | 8.00 (2.16) | 9.56 (0.80) | 7.89 (2.05) |
| Median | 6.00 | 7.50 | 9.56 | 7.50 |
| Minimum, maximum | 5.00, 7.00 | 6.00, 11.00 | 9.00, 10.13 | 5.00, 11.00 |
| Week 26 | ||||
| na | 2 | 4 | 1 | 7 |
| Mean (SD) | 4.00 (1.41) | 11.00 (2.94) | 9.00 (0) | 8.71 (3.95) |
| Median | 4.00 | 10.50 | 9.00 | 9.00 |
| Minimum, maximum | 3.00, 5.00 | 8.00, 15.00 | 9.00, 9.00 | 3.00, 15.00 |
FIGURE 10.
Individual profile plots for PHQ-9. a, No PM+; b, group PM+; and c, individual PM+.
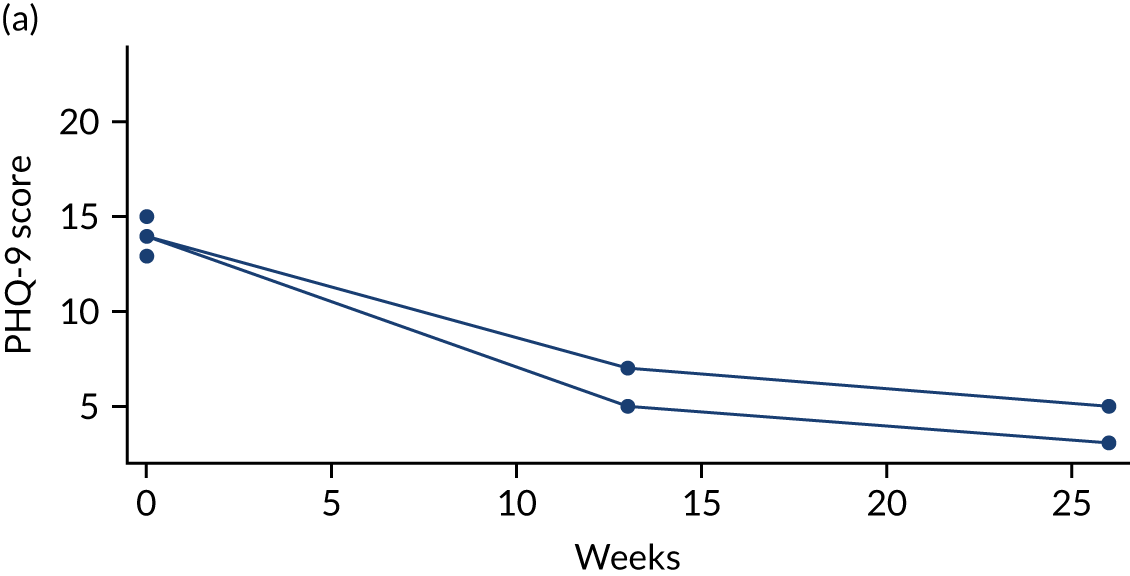
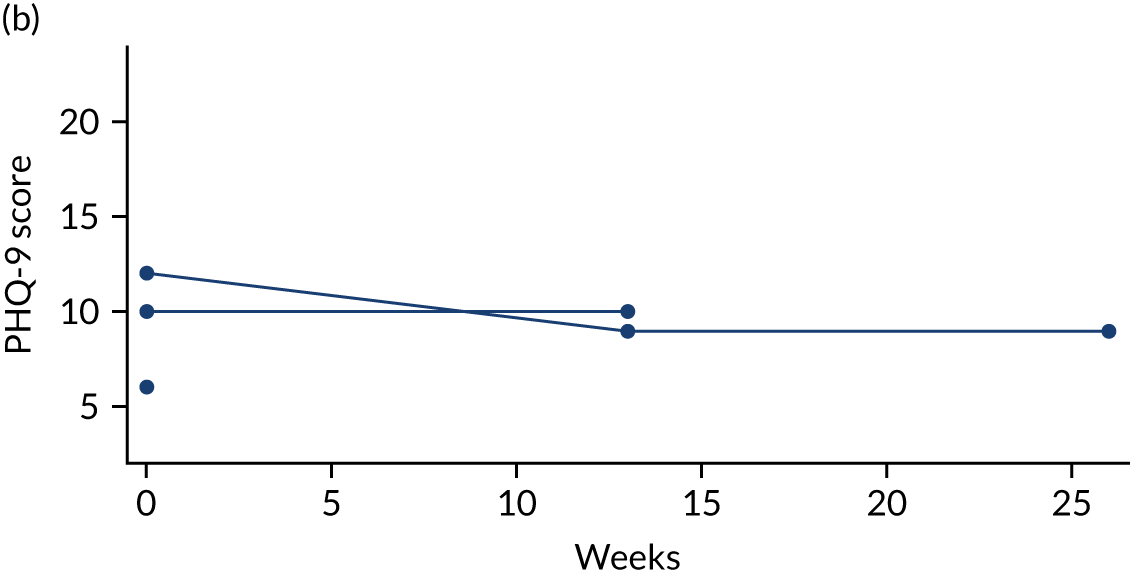
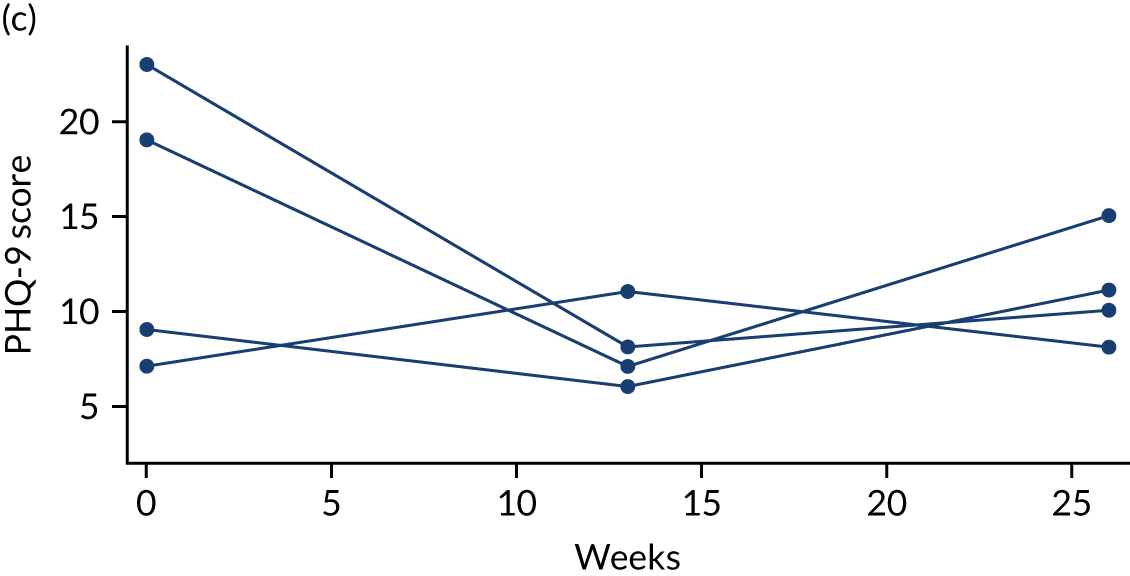
A full listing of outcome variables from the pilot trial is provided in Appendix 1.
Safety
No serious adverse events were reported. One reportable adverse event was observed in a participant who did not receive PM+ (who had a case of suicidal ideation with severity assessed as mild). No reportable adverse events were found in participants who received PM+.
Health economic evaluation
Owing to the interruption of the study by the COVID-19 crisis, we were presented with limited data following the pilot study. We are unable to make any inferences about the burden of cost or general service use of AS&Rs, but we can assess the usefulness and level of completion of the service use data collection tool.
The CSRI has continued to be developed since the 1980s as a way of effectively capturing service use, from prescription medication to GP appointments and hospital stays. Originally, two economic evaluations began the development of the data collection schedule: the evaluation of the North East Thames Regional Health Authority100 and the evaluation of the Department of Health and Social Care-sponsored Care in the Community initiative. 101
The CSRI can be adapted for use across any health and social care study and although it may not be a ‘validated measure’ in the traditional sense of the phrase (questions may not usually be adapted to suit different studies), the CSRI is a much-valued tool in the collection of essential data for health economic evaluations, and it is nevertheless a well-respected measure.
For this study, we were able to devise a CSRI questionnaire adapted for the PROSPER trial to include health, social care and voluntary services, and wider state services (such as the criminal justice system and the welfare system under the Department for Work and Pensions) to be used with AS&Rs. This was developed for inclusion with the main booklet and it was suitable for researchers to complete alongside the participant. We were also able to translate the CSRI to suit the needs of the cohort without having to seek permission from the original devisors and we were able to take advice on what to include or exclude in the very early stages of the project.
Eleven participants were able to complete our CSRI measure at some point during the pilot study. Seven participants did so across all three time points, one participant did so across time points 1 and 2, and three participants completed the CSRI measure across time point 1 only.
We received no negative feedback about the questions included in the CSRI. All domains were filled out appropriately and with the necessary data required across all sections.
The CSRI developed for this pilot study would be of great benefit in conducting a health economics evaluation across a full trial with multiple participants. Health and social care service use would be costed using national unit costs. 102,103
For a full trial, we would also suggest fully costing PM+ to include the training and roll-out of the programme. We would develop a questionnaire for the programme leaders to analyse costs including travel to training and the delivery site, venue hire for any training, and the development and production of materials and hand-outs to be provided during the intervention.
Chapter 4 Impact of the COVID-19 pandemic
Proposed protocol amendments
The COVID-19 pandemic resulted in the pilot trial being stopped in March 2020. Based on national responses to the pandemic (including social distancing), we proposed the following substantial protocol amendments to have the option to continue the trial:
-
Adding options for remote recruitment and follow-up, including consent and baseline assessment. Remote recruitment would include video and telephone contact, with the option of mailing relevant documents to potential participants in advance of planned meetings. Direct contact with potential participants using social media would also increase the potential reach of the trial. Specific additional funding would be needed to allow LCTC to set up remote consent procedures.
-
Expanding recruitment options by (1) removing the exclusion criteria regarding initial accommodation, as remote contact will allow for continued involvement after dispersal; and (2) involving primary care teams as participation identification centres, enabling social prescribing link workers and administrative staff to contact potential participants through searches of practice-based electronic clinical records.
-
Including questions related to COVID at assessment and follow-up. The direct and secondary impact of COVID-19 on AS&Rs is likely to be profound and pervasive; this study provides a valuable opportunity to gather additional primary data to assess this impact directly.
-
Pausing the group intervention. Pausing the group intervention while social distancing measures are in place is necessary. We do not consider it feasible to offer group interventions remotely in this trial as the pace of recruitment makes group formation difficult, and essential processes of trust-building become highly problematic. Such a pause has the advantage of allowing us to amend the language inclusion criteria to include Arabic, Farsi and Urdu (as these were limited only in the group intervention), thus increasing the potential pool of participants. Lay therapists currently trained in the group intervention are currently being retrained in the individual intervention. This pause will not affect the randomisation procedures, which will continue as 2 : 1 intervention : control.
-
Adding an option for the remote delivery of individual intervention. Remote delivery of the individual intervention will not involve changes in content. Lay therapists are currently being trained in this mode of delivery. Safeguards will be in place for clients to ensure that they have safe spaces in which to participate in intervention sessions.
-
Offering follow-up at the primary end point to all participants. All participants will be followed up after the primary end point of 3 months. Those recruited during the first 3 months of the extension could also be followed up at 6 months.
These major amendments were approved by both of the project oversight committees, the sponsor and Liverpool Research Ethics Committee (reference 19/NW/0345, 11 November 2020).
However, it was not possible to obtain sufficient funding to continue the pilot trial, which was therefore not completed as planned.
Process evaluation
A process evaluation was undertaken during and after the COVID-19 lockdown. This explored stakeholder perceptions of the research process and the intervention delivery. In total, 18 stakeholders participated: 11 in an open meeting (including stakeholders from Clinical Commissioning Group, Clinical Research Network, general practice, mental health and voluntary agencies); four lay therapists (three in a focus group, one individual interview); one service user; one service provider; and one researcher (each involved in individual interviews).
Respondents were generally keen for the project to go ahead and highlighted that AS&Rs are a group who are already isolated and may feel this isolation even more during the COVID-19 pandemic.
Views on research process
Respondents noted several barriers to recruiting participants for the pilot trial. The most obvious was the effects of the COVID-19 pandemic:
As soon as it sta[r]ted getting into position we were getting a good few people interested going in the right direction and approval, but then we had to stop due to COVID, feels it’s been one obstacle after another hindering progress.
Researcher
In this regard there were also negative effects of remote working that made it more difficult to establish trust between researchers and participants, particularly when dealing with a subject about which considerable stigma remains, such as mental health:
Trust is a factor in there, not really related to culture or language, maybe if you talk about creating a culture of trust, in general you just look at it and asylum seekers are far more suspicious of things going on, if there is a stigma on mental health in the UK it is far greater for asylum seekers, depending on where they have come from.
Service provider, voluntary agency
There were also concerns about the complicated nature of the pilot trial. It was not easy to explain the nature of the trial to potential participants, and some of the research instruments – for example, the PTSD questionnaire – were not always easy to follow. The processes for patients to contact GPs remotely were also seen as difficult for AS&Rs to understand and negotiate:
The more complicated the message the more time it takes and the less likely it is to work.
Service provider, voluntary agency
There are two things, firstly the asylum seekers themselves, then there’s the teachers and case workers the people that have a wee bit in front of you, some are gatekeepers and I never enjoyed that term but standing in front of somebody and saying this is a study, research, with the university that will lead to a report and possibly new techniques to help people with their mental health, you can see the blank faces looking at you, what’s he saying.
Service provider, voluntary agency
The effect of differences in the dynamics of relationsips when working with different agencies, especially the dynamics between academics and voluntary sector workers, should also not be underestimated:
The dynamics of working with other people and holding yourself differently compared to university main role, you try to be a bit more mellow and fit in a little, holding yourself differently and do your role the best way possible [. . .] when you start there is a lot of momentum but come across all these blocks which can be disheartening.
Researcher
There were concerns about working across cultures; some lay therapists felt that they needed more information and support to translate concepts when working with clients perceived as from different cultural backgrounds, and some were unsure about the relevance of the case studies to different cultures.
There was also discussion of factors facilitating recruitment. Gender matching and language flexibility were valued. Again, trust was key here, especially between lay therapists and potential participants, based on their shared cultural backgrounds:
The thing where the lay therapists were coming in and talking to people and that helps as the language barrier between me and them will be gone . . . if you have someone that’s there and understands what’s being done and has a background in the community, you have natural advocates in the place already . . . never let go of them as they were fired up and keen to do stuff.
Service provider, voluntary agency
Some respondents reported that incentives such as financial vouchers and help with childcare would encourage potential clients to participate. There was also acknowledgement that remote contact had advantages for people on limited incomes (who faced difficulties in arranging time and transport to attend interviews outside their homes) and also for GPs involved in identifying potential participants.
There were suggestions about building links between this type of trial and the increased emphasis on social prescribing, for example by asking social prescribing link workers to take a proactive role in identifying potential participants.
Views on PM+
Service providers emphasised the importance of having face-to-face sessions whenever possible, while ensuring social distancing. When remote sessions were needed, providers noted the need to understand the housing arrangements of potential participants and ensure that they had a space to undertake therapy online without being overheard.
The female service user interviewed (quoted below) was pleased that she had been offered a female therapist and that sessions were given in English. She attended these at PSS and felt that no sacrifices were needed to take part:
It was very good and she was really helpful for me she I could get the message from her [. . .] It was good because I always tried to find someone to speak with and tell them what I have and sometimes I spend another hour with her and tell her my problems and she even gave me an exercise I trying at home which I can get benefit from.
Service user
Lay therapists were generally positive about the effects of their participation in PM+ on their own life and mental health. They reported improvements in their sense of purpose, motivation, enjoyment, connection with others, connection with their old way of life (like being back to their old self) and self-confidence. They could also put the PM+ principles into action in their own lives:
I feel positive to the training and programme as I think it’s useful not only for ourselves as we can apply it to our daily lives if you are bored, and think I’m going to do something, and also good for people around you like your husband and children.
Lay therapist
It has built my confidence as well before I was a little low, when you have been through similar problems you can help others it builds you up [. . .] Every time I do the breathing exercise it helps and I applied it on my own was helpful.
Lay therapist
The lay therapists found it valuable to work as part of a group. They did not report challenges integrating their work on the project with their other roles. They enjoyed working across different cultures and did not note any major concerns:
I found it really helpful for myself as well. I feel I have started working in my old field somehow [lay therapist was formerly a dental hygienist] and I have been through difficulties of asylum process so giving them a helping hand made me feel generous and take them out of that as in the beginning was very isolated and didn’t ask for help and just came from our country to here, it was difficult to adjust with the language barrier when I gave them the support they explored more better and were not alone.
Lay therapist
The lay therapists considered the PM+ manuals generally helpful, albeit sometimes confusing and not always well suited to the UK context:
The case studies are not very good for me, they have some basic needs like no jobs or nothing to eat but they will expect something for their basic needs from us, if we can’t give some concrete things it will not be a good thing for them.
Lay therapist
It was a bit challenging as the tables were in English so took more time to explain to her and translate to English because had to translate and write down.
Lay therapist
There was a sense among lay therapists that individual PM+ was easier to arrange and deliver than group PM+. Lay therapists also appreciated the support they received from their PSS supervisors:
I’m a single parent and have double responsibilities, with my asylum system with my background it was hard, I was pushed to join it and found it quite hard to drop her off to nursery and sort things out, I found it hard to bring her and find things to pay for transport childcare, until the end I thought I wouldn’t be able to do it but staff at PSS made it possible when I got stuck they pulled me up.
Lay therapist
Views on integrating PM+ into existing services
Both policy-makers and lay therapists discussed the benefits of integrating PM+ into existing mental health services for AS&Rs. A Clinical Commissioning Group commissioner stated that it would be good to have volunteers working alongside health-care professionals. A lay therapist recommended embedding PM+ sessions within voluntary organisations:
Have the sessions with partner organisations [such as Asylum Link or Red Cross] so more likely to be lay therapist in those centres so if we were doing in the middle of the centre we can get more clients.
Lay therapist
A lay therapist also proposed a build-up of networks of those who have experienced PM+:
If a woman was helped by the project she could help the other women and involve them all, and establish a kind of network of them maybe buddy or support each other and we can maybe do some activities to bring together people, and support each other. The network can be used for other people and other projects and you can record all the things like address and contact to help use the network for other people later.
Lay therapist
Chapter 5 Discussion
A summary of findings is shown in Table 19.
| Objective | Findings |
|---|---|
| Adapt the form and content of PM+ to the needs of AS&Rs in the UK |
Completed successfully. Key findings from evidence synthesis and stakeholder engagement integrated to provide the following contextual modifications: Focusing on English, Arabic, Farsi and Urdu, identified as the four most common languages currently spoken by AS&Rs in Liverpool City Region Altering the text of PM+ manuals to reflect life in western urban settings rather than south Asian rural settings (e.g. ‘home’ not ‘hut’, ‘reading’ not ‘rearing poultry’, ‘visit job centre’ not ‘speak with village elder’) Adapting the group PM+ case studies to include men Matching therapists and participants on basis of gender and language, where possible, but not on basis of religion, politics or culture Identifying accessible ‘safe spaces’ for research interviews and delivery of PM+ sessions, including availability of childcare Reimbursing travel expenses for lay therapists and participants Supervising and supporting lay therapists in the inclusion of boundary issues between therapy and involvement in participants’ lives, since the shared lived experience of the asylum process takes this study beyond the boundaries that have been apparent in other contexts Further adaptation of PM+ delivery to meet constraints of face-to-face interventions caused by the COVID-19 pandemic |
| Assess the feasibility of the proposed training procedures, including involvement of refugees as lay therapists | Completed successfully. The PM+ training adopted a cascade apprenticeship model, in which master trainers trained and supervised well-being mentors, who subsequently trained and supervise the lay therapists. Twelve people with lived experience of the asylum process were selected for training, 11 of whom successfully completed the training and were deemed competent to offer the trial intervention to study participants |
| Assess the feasibility of the proposed procedures for recruiting distressed AS&Rs as study participants |
Not completed. Intention to recruit 105 participants over 6 months; 11 participants were recruited over 3.5 months Observations: needs considerable investment of time and energy. Most effective recruitment procedures are through involved NGOs |
| Assess the feasibility of retaining both lay therapists and study participants through to trial completion |
Feasibility of retaining lay therapists demonstrated: 10 lay therapists completed training. By August 2020, despite 12 months of delays, 6 lay therapists (5 female and one male) still actively engaged Evidence of feasibility of retaining study participants to follow-up at 3 months (8/11 = 73%) and at 6 months (7/11 = 64%) |
| Assess the fidelity of delivery of the intervention |
Eight completed individual PM+ sessions (conducted by two lay therapists) were reviewed by well-being mentors Comment: ‘Overall the fidelity check and supervision sessions conducted immediately at the end of the PM+ sessions with Lay Therapists indicate good levels of lay therapist fidelity to the PM+ intervention manual, with some areas for further development through ongoing supervision. This is commensurate with what is expected at this stage of the lay therapists’ ‘training’ |
| Assess the acceptability and utility of the proposed study measures, considering any linguistic and cultural barriers |
Complexities of operating across four languages, and with variable levels of competence in English, for both research interviews and PM+ sessions; needs considerable facilitation skill on part of researcher/lay therapists Mental health questionnaires (e.g. regarding PTSD) challenging for participants to complete, especially as many are uncomfortable/unfamiliar with Western mental health concepts Few cultural concerns raised by lay therapists |
| And, hence, to specify the parameters for a full RCT to test the effectiveness and cost-effectiveness of PM+ | Not yet possible |
Strengths and limitations
The strengths of the PROSPER study included substantial patient and public involvement in the design and conduct of the study, with key roles being played by local voluntary agencies, leading to genuine co-creation of study design, co-delivery of interventions and co-analysis of findings. Three local voluntary agencies with expertise in the care and support of AS&Rs – Asylum Link, PSS and the Red Cross – were formally represented on the project management team throughout the lifetime of the study and had active, ongoing involvement with the original study design and its subsequent modifications. One of the academic partners is a former refugee and a survivor of the Rwandan genocide. In terms of project delivery, staff at PSS took responsibility for training and supervision of the lay therapists, while members of Asylum Link and Red Cross were committed to efforts to recruit to the pilot trial. Senior members of all three agencies were involved with analysis and report-writing, and are co-authors of this report.
There was also valuable involvement of policy-makers as local stakeholders through the Clinical Commissioning Group and as members of independent monitoring groups through WHO. There were effective links with other international researchers in the field of low-intensity psychosocial interventions for AS&Rs, via the study team, the master training and the two independent monitoring bodies.
The study provided convincing evidence of the feasibility of recruiting, training and retraining AS&Rs as lay therapists, and reasonable evidence of the feasibility of adapting PM+ to meet the needs of AS&Rs in Liverpool City Region. We proposed modifications to the intervention to overcome the constraints on face-to-face delivery caused by the COVID-19 pandemic, but were unable to test these modifications in practice.
The limitations of the study were, however, substantial. Protracted delays due to governance issues and the COVID-19 pandemic meant that we were unable to complete the pilot trial or to obtain any evidence regarding the feasibility of group PM+. Governance issues were related mainly to the atypical nature of the pilot trial, which involved voluntary (non-NHS) organisations and lay therapists in its delivery. This meant that standard research protocols employed by LCTC were not always fit for purpose and needed to be amended. The atypical nature of the trial was also raised as a matter of concern by the Research Ethics Committee, whose members required additional assurance that the lay therapists would be adequately supported.
Recruitment lasted 3.5 months rather than 6 months. Fewer than 10% (11/105) of the target number of participants were recruited and only 20 people had been screened by March 2020. As noted in the process evaluation, concerns were expressed about the complicated nature of the pilot trial, that some of the research instruments were not always easy to follow, and that processes for patients to contact GPs remotely were difficult to understand and negotiate. Slow recruitment is an indicator that progression to a full trial should not be recommended.
The complexities of working with multiple languages and cultural groups were noted. There were mixed views on how successful this was likely to prove, and we had insufficient evidence to provide a clear conclusion on this.
Relationship with existing evidence
As discussed in the introduction, PM+ and related low-intensity psychosocial interventions delivered by lay health workers have been deployed mainly in LMICs to enhance the mental health and functional capacity of people living with adversity.
PROSPER is not the only study intended to provide evidence of the relevance of PM+ AS&Rs living in a high-income country.
The most relevant comparable study is STRENGTHS, a multicentre study that aims to scale up brief psychological interventions for Syrian refugees in Europe and the Middle East. We note that this study, in contrast to PROSPER, involved refugees with a common language, from a single culture group. Pilot trial data on the effectiveness and cost-effectiveness of individual PM+ for Syrian refugees in the Netherlands have been published as the first stage of this project. 30 Using parameters similar to those proposed for the PROSPER trial, this study found that trial procedures and PM+ delivered by non-specialist peer refugee helpers was acceptable, feasible and safe. Analyses indicate that PM+ may be effective in improving mental health outcomes and psychosocial functioning, and potentially cost-effective. At the 3-month follow-up, total scores on the primary outcome measure (Hopkins Symptom Checklist-25) were significantly lower in the PM+ group (n = 30) than in the care as usual-care group (n = 30) (p = 0.004; d = 0.58). There were also differences in favour of PM+ for several measures used in the PROSPER Pilot trial, including WHODAS psychosocial functioning, PCL-5 symptoms of PTSD and PSYCHLOPS self-identified problems. There were no significant differences in health service costs. The authors conclude that PM+ may potentially be cost-effective and that these results support the development of a definitive RCT.
The WHO has also developed a guided self-help intervention intended for group delivery called Self-Help Plus. Self-Help Plus is a five-session intervention based on Acceptance and Commitment Therapy that can be facilitated by lay therapists following 5 days of basic training. 104 The recently completed RE-DEFINE project (http://re-defineproject.eu/) conducted two RCTs, one in five European Union (EU) countries105 (n = 459) and the other in Türkiye106 (n = 642), to determine the effectiveness of Self-Help Plus intervention for preventing mental disorders among refugees. Adult refugees experiencing psychological distress, but no mental disorder, were randomised to either enhanced treatment as usual or Self-Help Plus. The primary outcome measure was the Mini-International Neuropsychiatric Interview. In the RCT in Türkiye, the risk of Self-Help Plus participants having developed any mental disorder at follow-up after 6 months was half that in the enhanced treatment as usual group (Cramér’s V 0.205, p < 0.001; risk ratio 0.533, 95% confidence interval 0.408 to 0.696), with no differences post intervention. In the EU trial, Self-Help Plus participants had half the risk of mental disorders at post intervention (Cramér’s V 0.13, p = 0.01; risk ratio 0.50, 95% confidence interval 0.29 to 0.87), with no differences at follow-up after 6 months (Cramér’s V 0.007, p = 0.90; risk ratio 0.96, 95% confidence interval 0.52 to 1.78). The proportion of participants lost to follow-up at the 6-month post-randomisation assessment in the EU and Türkiye trials was 34% and 15%, respectively. The findings suggest that Self-Help Plus can be effective in preventing mental disorders among refugees.
Conclusions
Ensuring mental health services are accessible for AS&Rs is of critical importance. Task-sharing psychosocial interventions delivered by those with lived experience of migration or the asylum process embedded within community-based organisations offer one way to achieve this. Evaluations of peer support workers embedded within mental health services identify the benefits of shared lived experiences, and contribute to enhancing practitioners’ understanding of the recovery journey. 81 Our experience with AS&Rs reflects this, highlighting the value of peer support models. There are particular opportunities in high-income settings to explore collaborative care models and integrate telemedicine into lay therapist supervision,107 developing task-sharing models that respond to the situated context in which they are delivered.
Recommendations for practice
We have six recommendations for the future training of lay therapists:77
-
Maintain schedule flexibility to accommodate AS&Rs’ lives, recognising that they are often engaged in multiple educational, vocational and voluntary/employment opportunities, in addition to caring for families and attending to asylum claims.
-
Recognise the need for extensive logistical support given the precarious financial situation of AS&Rs (e.g. reimbursement of expenses, childcare provision and refreshments).
-
Be conscious and supportive of the complexities of AS&Rs’ asylum journeys whilst recognising that this may affect the lay therapists’ own mental well-being (which could necessitate the lay therapist’s suspending or stopping their role).
-
Provide training certifications, building the AS&R lay therapists’ CVs for future education and employment opportunities.
-
Support AS&R lay therapists in the development of supportive professional relationships, and, where appropriate, peer social relationships, strengthening their personal networks.
-
Be responsive to changes in timelines as a result of being embedded within research, and find innovative ways to manage these that ensure lay therapist engagement with and preparation for delivering interventions to participants.
Recommendations regarding a definitive randomised controlled trial
Reviewing the research objectives against predetermined progression criteria for progression to a full RCT of PM+ for AS&Rs, the following conclusions can be drawn:
-
It was possible to recruit and retain sufficient lay therapists.
-
It was not possible to recruit sufficient trial participants.
-
Of those trial participants recruited, it was possible to retain a sufficient proportion at 3 and 6 months’ follow-up.
-
There was evidence of adherence to protocol for delivery of individual PM+ by lay therapists However, no group PM+ sessions were held.
-
There was evidence of satisfactory rates of completion of outcome measures.
We demonstrated that the form and content of PM+ can be adapted to meet the needs of AS&Rs, and that AS&Rs can be successfully trained as lay therapists to deliver this low-intensity psychosocial intervention in local AS&R communities. We were also able to offer guidance on strategies for the recruitment and retention of trial participants and on the acceptability and utility of study measures, which may be of value in future studies of this nature.
Given the early termination of the PROSPER trial, we were unable to provide sufficient evidence either to recommend or to refute the need for a full trial of PM+ delivered by lay therapists to AS&Rs in the UK who are experiencing emotional distress and functional impairment.
Acknowledgements
The authors would like to thank the funders for their support throughout and offer a special thank you to Dawn Jenvey, NIHR Public Health Research Programme Scientific Officer. We would like to thank the sponsor, University of Liverpool and the Research Support Office.
We would like to thank the Trial Steering Committee members (Professor Kate O’Donnell, Dr Alex McConnachie, Mr David McDaid, Professor Maria van den Muijsenbergh, Dr Marit Sijbrandij, Dr Mark van Ommeren, Mr Abdi Ahmed and Ms Collette Venturas) and IDSMC (Dr Melanie Abas, Professor Richard Emsley, Ms Judith Boyles and Professor Anne Macfarlane) for their support and advice throughout.
Contributions of authors
Christopher Dowrick (https://orcid.org/0000-0002-4245-2203) (previous chief investigator/co-investigator) developed the initial study design and contributed to protocol development, was an applicant on the grant, was the chairperson of the PMG, oversaw all aspects of the study and contributed to all parts of the final report.
Anna Rosala-Hallas (https://orcid.org/0000-0001-8012-9995) made a substantial contribution to the analysis of the PROSPER project, contributed to the drafting the final report, and provided approval of the version to be submitted to NIHR.
Rebecca Rawlinson (https://orcid.org/0000-0001-6453-2055) made a substantial contribution to the conception of the PROSPER project, contributed to the drafting the final report, and provided approval of the version to be submitted to NIHR.
Naila Khan (https://orcid.org/0000-0003-3400-7190) made a substantial contribution to the acquisition, analysis and interpretation of data for the work of the PROSPER project, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
Eira Winrow (https://orcid.org/0000-0002-1399-0651) made a substantial contribution to the design of the health economics aspect of the PROSPER project and the subsequent literature reviews, contributed to the drafting of the final report, and provided approval of the version to be submitted to NIHR.
Anna Chiumento (https://orcid.org/0000-0002-0526-0173) made contributions to the design of the PROSPER project, and to the acquisition, analysis and interpretation of data, reviewed and revised the report critically for important intellectual content, and provided approval of the version to be submitted to NIHR.
Girvan Burnside (https://orcid.org/0000-0001-7398-1346) made a substantial contribution to the design, analysis and interpretation of the data from the PROSPER project, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
Rabeea’h Aslam (https://orcid.org/0000-0002-0916-9641) made a substantial contribution to the conception of the PROSPER project, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
Leah Billows (https://orcid.org/0000-0001-6851-8170) made a substantial contribution to the conception of the PROSPER project, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
Malena Eriksson-Lee (https://orcid.org/0000-0003-1323-2567) made a substantial contribution to the design of the PROSPER project, contributed to the drafting of the final report provided approval of the version to be submitted to NIHR.
Daniel Lawrence (https://orcid.org/0000-0002-3651-6135) made a substantial contribution to the conception of the PROSPER project, contributed to the drafting of the final report provided approval of the version to be submitted to NIHR.
Rachel McCluskey (https://orcid.org/0000-0002-0767-3115) made a substantial contribution to the conception of the PROSPER project, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR
Annette Mackinnon (https://orcid.org/0000-0002-0687-7781) made a substantial contribution to the conception of the PROSPER project, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
Tracy Moitt (https://orcid.org/0000-0002-5579-996X) made a contribution to the design of the PROSPER project, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
Lois Orton (https://orcid.org/0000-0002-9641-523X) made a substantial contribution to the conception and design of the PROSPER project, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
Ewan Roberts (https://orcid.org/0000-0002-9510-6363) made a contribution to the conception and design of the PROSPER project, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
Atif Rahman (https://orcid.org/0000-0002-2066-4467) made a substantial contribution to the conception and design of the PROSPER project, provided advice on all aspects of the study during its execution, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
Grahame Smith (https://orcid.org/0000-0003-1859-6036) made a substantial contribution to the design of the PROSPER project, drafting the work or revising it critically for important intellectual content, and provided final approval of the version to be submitted to NIHR.
Rhiannon Tudor Edwards (https://orcid.org/0000-0003-4748-5730) made a substantial contribution to the conception and design of the PROSPER project, contributed to the interpretation of findings, contributed to the drafting of the final report and revising of that report for important intellectual content, and provided approval of the version to be submitted to NIHR.
Philomene Uwamaliya (https://orcid.org/0000-0002-5853-6655) made substantial contributions to the design of the work and revising it critically for important intellectual content, and gave final approval of the version to be submitted to NIHR.
Ross White (https://orcid.org/0000-0003-4026-6439) (chief investigator) made a substantial contribution to the conception and design of the study, the acquisition, analysis and interpretation of data, contributed to the drafting of the final report and provided approval of the version to be submitted to NIHR.
All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Publications
Rawlinson R, Aslam RW, Burnside G, Chiumento A, Eriksson-Lee M, Humphreys A, et al. Lay-therapist-delivered, low-intensity, psychosocial intervention for refugees and asylum seekers (PROSPER): protocol for a pilot randomised controlled trial. Trials 2020;21:367.
Chiumento A, Billows L, Mackinnon A, McCluskey R, White RG, Khan N, et al. Task-sharing psychosocial support with refugees and asylum seekers: reflections and recommendations for practice from the PROSPER study. Intervention 2021;19:67–74.
Data-sharing statement
All requests for data should be sent to the corresponding author. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
- Rawlinson R, Aslam RW, Burnside G, Chiumento A, Eriksson-Lee M, Humphreys A, et al. Lay-therapist-delivered, low-intensity, psychosocial intervention for refugees and asylum seekers (PROSPER): protocol for a pilot randomised controlled trial. Trials 2020;21. https://doi.org/10.1186/s13063-020-04310-5.
- Close C, Kouvonen A, Bosqui T, Patel K, O’Reilly D, Donnelly M. The mental health and well-being of first generation migrants: a systematic-narrative review of reviews. Global Health 2016;12. https://doi.org/10.1186/s12992-016-0187-3.
- Lindert J, Ehrenstein OS, Priebe S, Mielck A, Brahler E. Depression and anxiety in labor migrants and refugees – a systematic review and meta-analysis. Soc Sci Med 2009;69:246-57. https://doi.org/10.1016/j.socscimed.2009.04.032.
- Priebe S, Giacco D, El-Nagib R. Public Health Aspects of Mental Health Among Migrants and Refugees: A Review of the Evidence on Mental Health Care for Refugees, Asylum Seekers and Irregular Migrants in the WHO European Region 2016.
- Bogic M, Njoku A, Priebe S. Long-term mental health of war-refugees: a systematic literature review. BMC Int Health Hum Rights 2015;15. https://doi.org/10.1186/s12914-015-0064-9.
- Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet 2005;365:1309-14. https://doi.org/10.1016/S0140-6736(05)61027-6.
- Slewa-Younan S, Uribe Guajardo MG, Heriseanu A, Hasan T. A systematic review of post-traumatic stress disorder and depression amongst Iraqi refugees located in Western countries. J Immigr Minor Health 2015;17:1231-9. https://doi.org/10.1007/s10903-014-0046-3.
- George U, Thomson MS, Chaze F, Guruge S. Immigrant mental health, a public health issue: looking back and moving forward. Int J Environ Res Public Health 2015;12:13624-48. https://doi.org/10.3390/ijerph121013624.
- Bradby H, Humphris R, Newall D, Phillimore J. Public Health Aspects of Migrant Health: A Review of the Evidence on Health Status for Refugees and Asylum Seekers in the European Region. Copenhagen: WHO Regional Office for Europe; 2015.
- Samele C, Wallcraft J, Nayor C, Keating F, Greatley A. Research Priorities of Service User and Carer-Centred Mental Health Services: Overview Report 2007.
- Nosè M, Ballette F, Bighelli I, Turrini G, Purgato M, Tol W, et al. Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: systematic review and meta-analysis. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0171030.
- Bolton P, Lee C, Haroz EE, Murray L, Dorsey S, Robinson C, et al. A transdiagnostic community-based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLOS Med 2014;11. https://doi.org/10.1371/journal.pmed.1001757.
- Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet 2008;372:902-9. https://doi.org/10.1016/S0140-6736(08)61400-2.
- Wiley-Exley E. Evaluations of community mental health care in low- and middle-income countries: a 10-year review of the literature. Soc Sci Med 2007;64:1231-41. https://doi.org/10.1016/j.socscimed.2006.11.009.
- Delamaire M-L, Lafortune G. Nurses in Advanced Roles: a Description and Evaluation of Experiences in 12 Developed Countries. Paris: Organisation for Economic Co-operation and Development; 2010.
- Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Soc Sci Med 2013;97:82-6. https://doi.org/10.1016/j.socscimed.2013.08.004.
- Sashidharan SP, White R, Mezzina R, Jansen S, Gishoma D. Global mental health in high-income countries. Br J Psychiatry 2016;209:3-5. https://doi.org/10.1192/bjp.bp.115.179556.
- Dawson KS, Bryant RA, Harper M, Kuowei Tay A, Rahman A, Schafer A, et al. Problem Management Plus (PM+): a WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry 2015;14:354-7. https://doi.org/10.1002/wps.20255.
- Murray LK, Dorsey S, Haroz E, Lee C, Alsiary MM, Haydary A, et al. A common elements treatment approach for adult mental health problems in low- and middle-income countries. Cogn Behav Pract 2014;21:111-23. https://doi.org/10.1016/j.cbpra.2013.06.005.
- Sikander S, Ahmad I, Atif N, Zaidi A, Vanobberghen F, Weiss HA, et al. Delivering the Thinking Healthy Programme for perinatal depression through volunteer peers: a cluster randomised controlled trial in Pakistan. Lancet Psychiatry 2019;6:128-39. https://doi.org/10.1016/S2215-0366(18)30467-X.
- Clark DM. Implementing NICE guidelines for the psychological treatment of depression and anxiety disorders: the IAPT experience. Int Rev Psychiatry 2011;23:318-27. https://doi.org/10.3109/09540261.2011.606803.
- Dua T, Barbui C, Clark N, Fleischmann A, Poznyak V, van Ommeren M, et al. Evidence-based guidelines for mental, neurological, and substance use disorders in low- and middle-income countries: summary of WHO recommendations. PLOS Med 2011;8. https://doi.org/10.1371/journal.pmed.1001122.
- Hamdani SU, Huma ZE, Rahman A, Wang D, Chen T, van Ommeren M, et al. Cost-effectiveness of WHO Problem Management Plus for adults with mood and anxiety disorders in a post-conflict area of Pakistan: randomised controlled trial. Br J Psychiatry 2020;217:623-9. https://doi.org/10.1192/bjp.2020.138.
- Rahman A, Hamdani SU, Awan NR, Bryant RA, Dawson KS, Khan MF, et al. Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: a randomized clinical trial. JAMA 2016;316:2609-17. https://doi.org/10.1001/jama.2016.17165.
- Rahman A, Khan MN, Hamdani SU, Chiumento A, Akhtar P, Nazir H, et al. Effectiveness of a brief group psychological intervention for women in a post-conflict setting in Pakistan: a single-blind, cluster, randomised controlled trial. Lancet 2019;393:1733-44. https://doi.org/10.1016/S0140-6736(18)32343-2.
- Rahman A, Riaz N, Dawson KS, Usman Hamdani S, Chiumento A, Sijbrandij M, et al. Problem Management Plus (PM+): pilot trial of a WHO transdiagnostic psychological intervention in conflict-affected Pakistan. World Psychiatry 2016;15:182-3. https://doi.org/10.1002/wps.20312.
- Van’t Hof E, Dawson KS, Schafer A, Chiumento A, Harper Shehadeh M, Sijbrandij M, et al. A qualitative evaluation of a brief multicomponent intervention provided by lay health workers for women affected by adversity in urban Kenya. Glob Ment Health 2018;5. https://doi.org/10.1017/gmh.2017.26.
- Bryant RA, Schafer A, Dawson KS, Anjuri D, Mulili C, Ndogoni L, et al. Effectiveness of a brief behavioural intervention on psychological distress among women with a history of gender-based violence in urban Kenya: a randomised clinical trial. PLOS Med 2017;14. https://doi.org/10.1371/journal.pmed.1002371.
- Akhtar A, Giardinelli L, Bawaneh A, Awwad M, Naser H, Whitney C, et al. Group problem management plus (gPM+) in the treatment of common mental disorders in Syrian refugees in a Jordanian camp: study protocol for a randomized controlled trial. BMC Public Health 2020;20. https://doi.org/10.1186/s12889-020-08463-5.
- de Graaff AM, Cuijpers P, McDaid D, Park A, Woodward A, Bryant RA, et al. Peer-provided Problem Management Plus (PM+) for adult Syrian refugees: a pilot randomised controlled trial on effectiveness and cost-effectiveness. Epidemiol Psychiatr Sci 2020;29:1-24. https://doi.org/10.1017/S2045796020000724.
- Red Cross . Refugee Facts and Figures n.d. www.redcross.org.uk/about-us/what-we-do/how-we-support-refugees/find-out-about-refugees (accessed 19 August 2021).
- Home Office . National Statistics: Asylum 2017 2017. www.gov.uk/government/statistics/immigration-statistics-october-to-december-2016/asylum (accessed 19 August 2021).
- NRPF Network . NHS Charging 2020 n.d. www.nrpfnetwork.org.uk/information-and-resources/policy/nhs-charging (accessed 19 August 2021).
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. PAFS consensus group . CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- Eldridge SM, Lancaster GA, Campbell MJ, Thabane L, Hopewell S, Coleman CL, et al. Defining feasibility and pilot studies in preparation for randomised controlled trials: development of a conceptual framework. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0150205.
- Mendenhall E, De Silva MJ, Hanlon C, Petersen I, Shidhaye R, Jordans M, et al. Acceptability and feasibility of using non-specialist health workers to deliver mental health care: stakeholder perceptions from the PRIME district sites in Ethiopia, India, Nepal, South Africa, and Uganda. Soc Sci Med 2014;118:33-42. https://doi.org/10.1016/j.socscimed.2014.07.057.
- Naeem F, Waheed W, Gobbi M, Ayub M, Kingdon D. Preliminary evaluation of culturally sensitive CBT for depression in Pakistan: findings from Developing Culturally-sensitive CBT Project (DCCP). Behav Cogn Psychother 2011;39:165-73. https://doi.org/10.1017/S1352465810000822.
- Patel V, Chowdhary N, Rahman A, Verdeli H. Improving access to psychological treatments: lessons from developing countries. Behav Res Ther 2011;49:523-8. https://doi.org/10.1016/j.brat.2011.06.012.
- Asgary R, Segar N. Barriers to health care access among refugee asylum seekers. J Health Care Poor Underserved 2011;22:506-22. https://doi.org/10.1353/hpu.2011.0047.
- O’Mahony JM, Donnelly TT, Este D, Bouchal SR. Using critical ethnography to explore issues among immigrant and refugee women seeking help for postpartum depression. Issues Ment Health Nurs 2012;33:735-42. https://doi.org/10.3109/01612840.2012.701707.
- Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: a randomized controlled trial. J Consult Clin Psychol 2008;76:686-94. https://doi.org/10.1037/0022-006X.76.4.686.
- Goodkind JR, Amer S, Christian C, Hess JM, Bybee D, Isakson BL, et al. Challenges and innovations in a community-based participatory randomized controlled trial. Health Educ Behav 2017;44:123-30. https://doi.org/10.1177/1090198116639243.
- Yohani SC, Hagen KT. Refugee women survivors of war related sexualised violence: a multicultural framework for service provision in resettlement countries. Intervention 2010;8:207-22. https://doi.org/10.1097/WTF.0b013e328341665c.
- Bernardes D, Wright J, Edwards C, Tomkins H, Dlfoz D, Livingstone AG. Asylum seekers’ perspectives on their mental health and views on health and social services: contributions for service provision using a mixed-methods approach. Int J Migration Health Soc Care 2010;6:3-19. https://doi.org/10.5042/ijmhsc.2011.0150.
- El-Bialy R, Mulay S. Two sides of the same coin: factors that support and challenge the well-being of refugees resettled in a small urban center. Health Place 2015;35:52-9. https://doi.org/10.1016/j.healthplace.2015.06.009.
- McKell C, Hankir A. Barriers to treatment of mental health problems for Palestinian people in refugee camps in Jordan: a cross-sectional study. Lancet 2018;391. https://doi.org/10.1016/S0140-6736(18)30333-7.
- Shipp MP-L, Francis SA, Fluegge KR, Asfaw SA. Perceived health issues: a perspective from East-African immigrants. Health Culture Soc 2014;6. https://doi.org/10.5195/HCS.2014.113.
- Jewson A, Lamaro G, Crisp BR, Hanna L, Taket A. Service providers’ experiences and needs in working with refugees in the Geelong region: a qualitative study. Aust J Prim Health 2015;21:233-8. https://doi.org/10.1071/PY12132.
- Power DV, Pratt RJ. Karen refugees from Burma: focus group analysis. Int J Migr Health Soc Care 2012;8:156-66. https://doi.org/10.1108/17479891211287058.
- Le Roch K, Pons E, Squire J, Anthoine-Milhomme J, Colliou Y. Two psychosocial assistance approaches for Iraqi urban refugees in Jordan and Lebanon: center-based services compared to community outreach services. J Muslim Ment Health 2010;5:99-119. https://doi.org/10.1080/15564901003613085.
- Bolton P, Tang AM. Using ethnographic methods in the selection of post-disaster, mental health interventions. Prehosp Disaster Med 2004;19:97-101. https://doi.org/10.1017/s1049023x00001540.
- Fish M, Fakoussa O. Towards culturally inclusive mental health: learning from focus groups with those with refugee and asylum seeker status in Plymouth. Int J Migration Health Soc Care 2018;14:361-76. https://doi.org/10.1108/IJMHSC-12-2017-0050.
- Pejic V, Hess RS, Miller GE, Wille A. Family first: community-based supports for refugees. Am J Orthopsychiatry 2016;86:409-14. https://doi.org/10.1037/ort0000189.
- Weine S, Kulauzovic Y, Klebic A, Besic S, Mujagic A, Muzurovic J, et al. Evaluating a multiple-family group access intervention for refugees with PTSD. J Marital Fam Ther 2008;34:149-64. https://doi.org/10.1111/j.1752-0606.2008.00061.x.
- Eriksson CB, Cardozo BL, Ghitis F, Sabin M, Crawford CG, Zhu J, et al. Factors associated with adverse mental health outcomes in locally recruited aid workers assisting Iraqi refugees in Jordan. J Aggress Maltreat Trauma 2013;22:660-80. https://doi.org/10.1080/10926771.2013.803506.
- Kieft B, Jordans MJ, de Jong JT, Kamperman AM. Paraprofessional counselling within asylum seekers’ groups in the Netherlands: transferring an approach for a non-western context to a European setting. Transcult Psychiatry 2008;45:105-20. https://doi.org/10.1177/1363461507088000.
- Nazzal KH, Forghany M, Geevarughese MC, Mahmoodi V, Wong J. An innovative community-oriented approach to prevention and early intervention with refugees in the United States. Psychol Serv 2014;11:477-85. https://doi.org/10.1037/a0037964.
- Nunnery D, Dharod J. Community health worker model: its implementation and importance in reaching refugee populations in the U.S. Int J Migration Health Soc Care 2015;11:169-78. https://doi.org/10.1108/IJMHSC-04-2014-0014.
- Torres S, Spitzer DL, Labonté R, Amaratunga C, Andrew C. Community health workers in Canada: innovative approaches to health promotion outreach and community development among immigrant and refugee populations. J Ambul Care Manage 2013;36:305-18. https://doi.org/10.1097/JAC.0b013e3182a5480f.
- Smith J, Jarman M, Osborn M, Murray M, Chamberlain K. Qualitative Health Psychology: Theories and Methods. London: SAGE Publications Ltd; 1999.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2003.
- Tomkins L, Eatough V. Reflecting on the use of IPA with focus groups: pitfalls and potentials. Qual Res Psychol 2010;7:244-62. https://doi.org/10.1080/14780880903121491.
- Finch H, Lewis J, Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2003.
- Githaiga JN. methodological considerations in utilization of focus groups in an IPA study of bereaved parental cancer caregivers in Nairobi. Qual Res Psychol 2014;11:400-19. https://doi.org/10.1080/14780887.2014.933918.
- Bloor M, Frankland J, Robson K, Thomas M. Focus Groups in Social Research. London: SAGE Publications Ltd; 2001.
- Smith JA, Flowers P, Larkin M. Interpretative Phenomenological Analysis: Theory, Method and Research. London: SAGE Publications Ltd; 2009.
- Bourdieu P, Nice R. Outline of a Theory of Practice. Cambridge: Cambridge University Press; 1977.
- Burr V. Social Constructionism. London: Routledge; 2003.
- McLeod J. Qualitative Research in Counselling and Psychotherapy. London: SAGE Publications Ltd; 2011.
- Etherington K. Becoming a Reflexive Researcher: Using Our Selves in Research. London: Jessica Kingsley Publishers; 2004.
- Modood T, Modood T, Berthoud R, Lakey J, Nazroo J, Smith P, et al. Ethnic Minorities in Britain: Diversity and Disadvantage. London: Policy Studies Institute; 1997.
- Murray LK, Dorsey S, Bolton P, Jordans MJ, Rahman A, Bass J, et al. Building capacity in mental health interventions in low resource countries: an apprenticeship model for training local providers. Int J Ment Health Syst 2011;5. https://doi.org/10.1186/1752-4458-5-30.
- World Health Organization, PEPFAR, UNAIDS . Task Shifting: Rational Redistribution of Tasks Among Health Workforce Teams, Global Recommendations and Guidelines 2007.
- Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Hoboken, NJ: Prentice Hall; 1984.
- Kemp CG, Petersen I, Bhana A, Rao D. Supervision of task-shared mental health care in low-resource settings: a commentary on programmatic experience. Glob Health Sci Pract 2019;7:150-9. https://doi.org/10.9745/GHSP-D-18-00337.
- Welsh I, Lyons CM. Evidence-based care and the case for intuition and tacit knowledge in clinical assessment and decision making in mental health nursing practice: an empirical contribution to the debate. J Psychiatr Ment Health Nurs 2001;8:299-305. https://doi.org/10.1046/j.1365-2850.2001.00386.x.
- Chiumento A, Billows L, Mackinnon A, McCluskey R, White R, Khan N, et al. Task-sharing psychosocial support with refugees and asylum seekers: reflections and recommendations for practice from the PROSPER study. Intervention 2021;19:67-74.
- Ibrahim N, Thompson D, Nixdorf R, Kalha J, Mpango R, Moran G, et al. A systematic review of influences on implementation of peer support work for adults with mental health problems. Soc Psychiatry Psychiatr Epidemiol 2020;55:285-93. https://doi.org/10.1007/s00127-019-01739-1.
- Rothwell C, Kehoe A, Farook S, Illing J. The Characteristics of Effective Clinical and Peer Supervision in the Workplace: A Rapid Evidence Review. Newcastle upon Tyne: Newcastle University; 2019.
- Mayblin L, James P. Asylum and refugee support in the UK: civil society filling the gaps?. J Eth Migrat Stud 2019;45:375-94. https://doi.org/10.1080/1369183X.2018.1466695.
- McLean J, Biggs H, Whitehead I, Pratt R, Maxwell M. Evaluation of the Delivering for Mental Health Peer Support Worker Pilot Scheme. Edinburgh: Scottish Government; 2009.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Al Aseri ZA, Suriya MO, Hassan HA, Hasan M, Sheikh SA, Al Tamimi A, et al. Reliability and validity of the Hospital Anxiety and Depression Scale in an emergency department in Saudi Arabia: a cross-sectional observational study. BMC Emerg Med 2015;15. https://doi.org/10.1186/s12873-015-0051-4.
- Andrews G, Kemp A, Sunderland M, Von Korff M, Ustun TB. Normative data for the 12 item WHO Disability Assessment Schedule 2.0. PLOS ONE 2009;4. https://doi.org/10.1371/journal.pone.0008343.
- Great Britain . Immigration and Asylum Act 1999 1999.
- Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom 2015;84:167-76. https://doi.org/10.1159/000376585.
- Ashworth M, Shepherd M, Christey J, Matthews V, Wright K, Parmentier H, et al. A client-generated psychometric instrument: the development of ‘PSYCHLOPS’. Counsell Psychother Res 2004;4:27-31. https://doi.org/10.1080/14733140412331383913.
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 2015;28:489-98. https://doi.org/10.1002/jts.22059.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Beecham J, Knapp M, Thornicroft G, Brewin CR, Wing J. Measuring Mental Health Needs. London: Gaskell/Royal College of Psychiatrists; 1992.
- Drummond M. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- National Institute for Health and Care Excellence (NICE) . Methods for the Development of NICE Public Health Guidance 2012.
- McIntosh E, Clarke P, Frew E, Louviere JJ. Applied Methods of Cost-Benefit Analysis in Health Care. Oxford: Oxford University Press; 2010.
- Pearce D, Atkinson G, Mourato S. Cost–Benefit Analysis and the Environment. Paris: Organisation for Economic Co-operation and Development; 2006.
- Sugden R, Williams A. The Principles of Practical Cost-Benefit Analysis. Oxford: Oxford University Press; 1978.
- McManus S, Bebbington PE, Jenkins R, Brugha T. Mental Health and Well-being in England: The Adult Psychiatric Morbidity Survey 2014. Leeds: NHS Digital; 2016.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Finch TL, Rapley T, Girling M, Mair FS, Murray E, Treweek S, et al. Improving the normalization of complex interventions: measure development based on normalization process theory (NoMAD): study protocol. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-43.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Beecham J, Hallam A, Knapp Baines B, Fenyo A, Asbury M, Leff J. Care in the Community: Illusion or Reality. Chichester: John Wiley & Sons; 1997.
- Knapp M, Cambridge P, Thomason C, Beecham J, Allen C, Darton R. Care in the Community: Challenge and Demonstration. Aldershot: Ashgate Publishing Ltd; 1992.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: PSSRU, University of Kent; 2015.
- Department of Health and Social Care (DHSC) . Reference Costs 2014–15 2015.
- Epping-Jordan JE, Harris R, Brown FL, Carswell K, Foley C, García-Moreno C, et al. Self-Help Plus (SH+): a new WHO stress management package. World Psychiatry 2016;15:295-6. https://doi.org/10.1002/wps.20355.
- Purgato M, Carswell K, Tedeschi F, Acarturk C, Anttila M, Au T, et al. Effectiveness of Self-Help Plus in preventing mental disorders in refugees and asylum seekers in Western Europe: a multinational randomized controlled trial. Psychother Psychosom 2021;90:403-14. https://doi.org/10.1159/000517504.
- Acarturk C, Uygun E, Ilkkursun Z, Carswel K, Tedeschi F, Batu M, et al. Randomized controlled trial of a WHO psychological intervention to present the development of mental disorders among Syrian refugees in Turkey. World Psychiatry 2022;21:88-95. https://doi.org/10.1002/wps.20939.
- Hoeft TJ, Fortney JC, Patel V, Unützer J. Task-sharing approaches to improve mental health care in rural and other low-resource settings: a systematic review. J Rural Health 2018;34:48-62. https://doi.org/10.1111/jrh.12229.
Appendix 1 Full listings of outcome variables from the pilot trial
| Table ID | Allocation | HADS anxiety score | HADS depression score | HADS total score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Week 13 | Week 26 | Baseline | Week 13 | Week 26 | Baseline | Week 13 | Week 26 | ||
| 1 | No PM+ | 8 | 4 | 11 | 17 | 11 | 12 | 25 | 15 | 23 |
| 2 | No PM+ | 10 | – | – | 6 | – | – | 16 | – | – |
| 3 | No PM+ | 13 | – | – | 15 | – | – | 28 | – | – |
| 4 | No PM+ | 16 | 10 | 7 | 10 | 8 | 9 | 26 | 18 | 16 |
| 5 | Individual PM+ | 19 | 18 | 15 | 18 | 15 | 12 | 37 | 33 | 27 |
| 6 | Individual PM+ | 16 | 6 | 12 | 17 | 7 | 10 | 33 | 13 | 22 |
| 7 | Individual PM+ | 16 | 11 | 9 | 7 | 12 | 14 | 23 | 23 | 23 |
| 8 | Individual PM+ | 13 | 10 | 12 | 7 | 4 | 3 | 20 | 14 | 15 |
| 9 | Group PM+ | 2 | – | – | 8 | – | – | 10 | – | – |
| 10 | Group PM+ | 11 | 10 | – | 4 | 11 | – | 15 | 21 | – |
| 11 | Group PM+ | 16 | 15 | 11 | 2 | 3 | 5 | 18 | 18 | 16 |
| Table ID | Allocation | WHO-5 score | WHODAS score | PSYCHLOPS | PCL-5 score | PHQ-9 score | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Week 13 | Week 26 | Baseline | Week 13 | Week 26 | Baseline | Baseline | Week 13 | Week 26 | Baseline | Week 13 | Week 26 | ||
| 1 | No PM+ | 8 | 64 | 28 | 30 | 26 | 16 | 16 | 55 | 51 | 49 | 14 | 7 | 5 |
| 2 | No PM+ | 44 | – | – | 29 | – | – | 17 | 35 | – | – | 13 | – | – |
| 3 | No PM+ | 12 | – | – | 45 | – | – | 17 | 61 | – | – | 15 | – | – |
| 4 | No PM+ | 8 | 44 | 52 | 29 | 16 | 23 | 19 | 51 | 21 | 16 | 14 | 5 | 3 |
| 5 | Individual PM+ | 0 | 12 | 28 | 47 | 30 | 35 | 11 | 74 | 41 | 43 | 23 | 8 | 10 |
| 6 | Individual PM+ | 12 | 56 | 40 | 28 | 17 | 23 | 19 | 57 | 24 | 45 | 19 | 7 | 15 |
| 7 | Individual PM+ | 20 | 36 | 28 | 29 | 35 | 33 | 15 | 34 | 16 | 33 | 9 | 6 | 11 |
| 8 | Individual PM+ | 56 | 60 | 60 | 31 | 18 | 20 | 20 | 53 | 35 | 37 | 7 | 11 | 8 |
| 9 | Group PM+ | 52 | – | – | 22 | – | – | 18 | 16 | – | – | 6 | – | – |
| 10 | Group PM+ | 64 | 52 | – | 23 | 20 | – | 20 | 23.2 | 42 | – | 10 | 10.1 | – |
| 11 | Group PM+ | 72 | 48 | 56 | 23 | 23 | 32 | 12 | 36 | 28 | 27 | 12 | 9 | 9 |
Appendix 2 Key protocol amendments
| Protocol version and date | Key amendments |
|---|---|
| 3.0 (1 July 2019) | Original approved version |
| 4.0 (7 August 2019) |
Section 3: inclusion criterion changed to have conversational English Section 5: death of a participant will be classed as a withdrawal Section 6: changes to terminology to refer to serious safety event report form rather than serious adverse event form and clarification on how to report and record events |
| 5.0 (11 December 2019) |
Section 5: participant identification: Clarification regarding organisations that may be involved in participant identification Addition of paragraph regarding use of social media in participant recruitment Section 10: correction to indemnity statement |
| 6.0 (19 February 2020) | Section 8: Addition of statement regarding shopping vouchers offered at 13- and 26-week follow-up appointments |
| 7.0 (1 September 2020)a |
Glossary: inclusion of coronavirus disease 2019 (COVID-19) Section 1: Schematic of study design: updated to reflect change to trial design Background: addition of modifications following the COVID-19 pandemic inclusion of the option of remote PM+ sessions Section 2: Changes to the number of intervention arms and randomisation ratio Addition of references to participant identification centres PROSPER Pilot trial outcomes: removal of group PM+ from relevant objectives Section 3: eligibility changes Inclusion criterion added: initially placed within Liverpool City Region Inclusion criterion regarding language changed to good working knowledge of one or more of English, Farsi, Urdu and Arabic Deletion of in Liverpool City region from inclusion criterion registered with a GP Inclusion criterion regarding consent changed to provided written or electronic informed consent Deletion of exclusion criterion in initial accommodation and receiving section 98 support for < 28 days, owing to high likelihood of dispersal outside the region Updates to participant study duration and overall trial duration Section 4: Change to trial design and randomisation ratio Removal of references to group PM+ Addition of remote working Section 5: Inclusion of electronic consent Inclusion of remote methods Other minor typographical errors, corrections and clarifications in order to ensure consistency made throughout |
List of abbreviations
- AS&R
- asylum seeker and refugee
- CRF
- case report form
- CSRI
- Client Service Receipt Inventory
- DSM-5
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- IDSMC
- Independent Data and Safety Monitoring Committee
- LCTC
- Liverpool Clinical Trials Centre
- LMIC
- low- and middle-income country
- NGO
- non-governmental organisation
- NIHR
- National Institute for Health and Care Research
- PCL-5
- Post-traumatic Stress Disorder Checklist for DSM-5
- PHQ-9
- 9-item Patient Health Questionnaire
- PIA
- participant information agency
- PM+
- Problem Management Plus
- PMG
- Project Management Group
- PSS
- Person Shaped Support
- PSYCHLOPS
- Psychological Outcomes Profile
- PTSD
- post-traumatic stress disorder
- RCT
- randomised controlled trial
- SD
- standard deviation
- TSC
- Trial Steering Committee
- WHO
- World Health Organization
- WHO-5
- World Health Organization Five Well-being Index
- WHODAS
- World Health Organization Disability Assessment Schedule
