Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 09/3008/11. The contractual start date was in January 2011. The final report began editorial review in September 2012 and was accepted for publication in February 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2013. This work was produced by O’Mara-Eves et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Community engagement in health care in the UK
Historically, interventions and actions to promote health were driven by professionals with little or no input from the targeted populations. 1 More recently, community engagement has become central to guidance and national strategy for promoting public health (e.g. Department of Health2). Community engagement has been broadly defined as ‘involving communities in decision-making and in the planning, design, governance and delivery of services’ (p. 11). 3 Community engagement activities can take many forms. Examples of some initiatives in the UK include:
-
service user networks
-
health-care forums
-
volunteering
-
courses delivered by trained peers (e.g. Dudley Primary Care Trust’s Expert Patients Programme)
-
interactive websites that enable the submission of views and opinions on various surveys, polls and public consultations.
Community engagement can also mean involvement in the evaluation of services. Community engagement can be provided alone or in combination with other initiatives. In studies in which community engagement is provided as the sole intervention, evidence of effectiveness can be determined because there is a direct link between community engagement and the outcomes being assessed. In contrast, interventions that are multifaceted and include community engagement as one of a number of components have a less direct link with outcomes being assessed. In such cases, an association between the multifaceted initiative and population outcomes may be seen, but it is not possible to discern with confidence how the community engagement aspect of the intervention may have contributed to this effect (pp. 1–2). 4
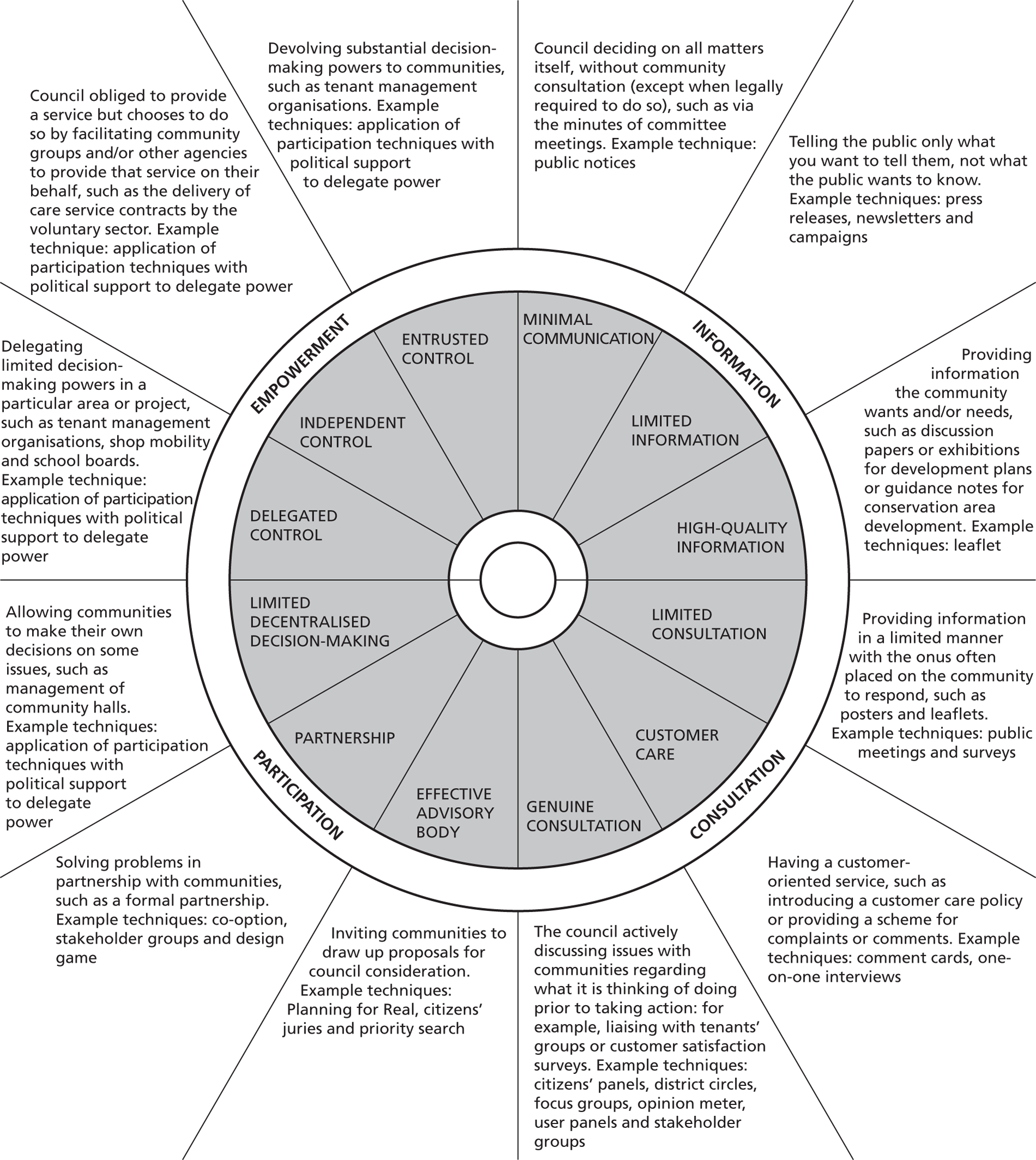
Community engagement can also be seen to operate on different levels, depending on the degree to which community engagement occurs. Wilcox5 describe five levels of increasing community engagement:
-
information-giving, in which people are merely told what is planned
-
consultation, in which people are offered some options and ideas, and organisers listen to feedback, but do not allow new ideas
-
deciding together, in which organisers encourage additional options and ideas, and provide opportunities for joint decision-making
-
acting together, not only to decide together on what is best, but also forming a partnership to carry it out
-
supporting independent community interests, in which local groups or organisations are offered funds, advice or other support to develop their own agendas within guidelines.
A more condensed scale exists for involvement in health research – consultation, collaboration and community control – with information provision not included as a sufficient level of engagement. 6
There is strong policy support for involving people in developing public services and evaluation (e.g. the creation of the Health Inequalities National Support Team7). Various national publications, including Shifting the Balance of Power,8 Commissioning a Patient-led National Health Service,9 the Our Health, Our Care, Our Say White Paper,10A Stronger Local Voice11 and Health Reform in England: Update and Commissioning Framework12 have provided a framework for the engagement of the public in the planning, design and delivery of public health services. Primary care trusts (PCTs) throughout the country have community engagement and public and patient involvement strategies.
Given the increasing policy support for community engagement, it is critical to consider whether such strategies are effective and under what circumstances. The following section outlines the state of research on community engagement in health care.
The evidence base for community engagement
There is some evidence that public involvement in UK health services can be effective. 13 Community engagement is thought to improve health through its impact on the development and delivery of more appropriate and accessible interventions, as well as through its direct positive impact on social cohesion and individual self-esteem and self-efficacy for those who are engaged. 14
Community involvement can be seen as a goal in itself as it encourages public accountability and transparency. 15,16 Through public involvement, communities can have the potential to promote health from the bottom up. 17 Listening to, hearing and acting on the views of the community – particularly those from socially and economically disadvantaged groups – can both empower communities and lead to the co-production and implementation of interventions that are more likely to be feasible, acceptable and ultimately effective in improving health. 4,14 Importantly, community engagement can ‘give a voice to the voiceless’. 18 People with the greatest health needs are often socially excluded and disengaged from services, and their circumstances can make it difficult for organisations to address their needs appropriately. Opportunities to work with their peers through community engagement initiatives may improve the social inclusion of marginalised people.
Although there is a recognised literature recommending community engagement,3,4 there is much uncertainty about how communities might be best engaged; what the results of such engagements are; and how the results should be recorded, analysed and used. 4,19,20 The theory behind recommendations for community engagement is often not linked to empirical evidence.
One of the problems with the current evidence base is a lack of robust synthesis of the research. This makes it difficult to assess the empirical basis for claims about community engagement, as research is scattered across disciplinary and topic-focused boundaries and not pulled together in a coherent way. The few syntheses that have been conducted are helpful, although they have acknowledged limitations, having been completed rapidly from relatively small datasets. 3,4 Limited synthesis in this area also makes it difficult to discern whether community engagement might be an appropriate strategy in any specific situation, as the available evidence is based only on a handful of studies (e.g. Popay et al. ,4 p. 62).
The same lack of high-quality evidence is apparent when looking at the cost-effectiveness of different community engagement strategies, including evidence from the UK. Guidance on community engagement produced by the National Institute for Health and Care Excellence (NICE)21 highlighted a dearth of information in this regard. A review of economic studies on community engagement for health promotion found eight studies, none of which focused specifically on the cost-effectiveness of the community engagement component. 22 A companion systematic review of the economic evidence for community engagement and development strategies to address the wider determinants of health also failed to identify any studies that reported the costs and health benefits of a community engagement approach relative to a comparator;23 some information on the resources required to deliver interventions was, however, reported in 20 studies. A final output of this work for NICE was economic modelling of some community engagement strategies to look at the potential cost-effectiveness of community engagement strategies. 24 However, this was not included in the final guidance because of a lack of robust information on costs and effects; only two vignettes on the role of trained peer educators and community engagement as a way of gaining support for flood defences were included (see also Fischer25).
In summary, the evidence base supporting the effectiveness and cost-effectiveness of community engagement strategies is fragmented and of uncertain quality. This review aims to make good some of these deficiencies with a specific focus on whether community engagement is a useful strategy for improving the health of disadvantaged groups.
The challenge of health inequalities in the UK
The quality of health varies from person to person as a result of biological, environmental, social, economic and lifestyle factors. Factors associated with economic and social circumstances are termed the social determinants of health. 26 These refer to a multitude of factors such as family assets, education, security of employment, relative risks at work, housing, family pressures and retirement provision. 27
These disadvantages tend to concentrate among the same people, and their effects on health accumulate during life. The longer that people live in stressful economic and social circumstances, the greater the physiological wear and tear they suffer, and the less likely they are to enjoy a healthy old age (p. 10). 27
The term ‘health inequalities’ refers to gaps in the quality of health of different groups of people based on differences in social, economic and environmental conditions. 28 Health inequalities are evident where disadvantaged groups (e.g. people with low socioeconomic status, socially excluded people) tend to have poorer health than more affluent members of society. Importantly, the term ‘health inequalities’ refers to differences in modifiable health determinants, such as housing, employment, education, income, access to public services and personal behaviour (e.g. use of tobacco)29 as opposed to fixed determinants such as age, sex and genetics. [However, social inequalities are often associated with fixed determinants (age, sex and genetics) and so these fixed factors might have indirect effects on health status.] The fact that many health determinants are modifiable lies at the very heart of all health inequalities strategies; if they are modifiable, then something can be done to improve them. By improving modifiable determinants of health, it is hoped that health inequalities can be reduced and health outcomes enhanced.
Health outcomes that are typically considered when examining health inequalities include life expectancy/mortality rates, disability-free life expectancy and limiting long-term illness. Other health outcomes and health-related indicators can include (but are not limited to) low birthweight, infant mortality, hospital admissions, teenage pregnancy and uptake of health services. In the UK, taking into account variations between local authorities, the average male in the lowest deprivation decile (i.e. the poorest males) will have a life expectancy that is 6.7 years shorter than that of the average male in the highest deprivation decile (i.e. the most affluent). The poorest females will have a life expectancy that is 4.7 years shorter than that of the most affluent females (figures calculated by Alison O’Mara-Eves using multilevel modelling of data from the London Health Observatory available at www.lho.org.uk/LHO_Topics/national_lead_areas/marmot/marmotindicators.aspx, accessed 15 March 2013). When looking at specific local authorities, some of these differences become even larger. For example, Westminster local authority has the widest within-area inequality gap for males, with a life expectancy for the most affluent males that is almost 17 years longer than that for the poorest males. 30 The widest gap for females is in Halton and Newcastle upon Tyne, at just over 11 years’ difference in life expectancy. The average difference in disability-free life expectancy in England between the most affluent and the least affluent, regardless of area or gender, is 17 years. Clearly the life expectancy and quality of health across the lifespan are much lower, on average, for the most deprived populations.
There is no dispute in the UK that health inequalities exist28 and, as a result, health inequalities have been an increasing focus of policy interest. For instance, in 2004, tackling health inequalities was one of the aims underpinning the 11 standards promoted within the National Service Framework. 31 More recently, the Marmot Review of health inequalities, Fair Society, Healthy Lives,28 has afforded even greater attention to the issue of health inequalities (with a particular focus on England). The review identified the evidence relating to health inequalities in England, developed actionable recommendations for practice, produced guidance on possible objectives and measures of inequalities and developed a starting point for a post-2010 health inequalities strategy. The key recommendations made in the report to address health inequalities fall under the following six broad themes:
-
giving children the best start in life
-
enabling all children, young people and adults to maximise their capabilities
-
creating fair employment and good work for all
-
ensuring a healthy standard of living for all
-
developing healthy and sustainable places and communities
-
strengthening the role and impact of health prevention.
The Marmot Review has received broadly positive responses from both public sector (e.g. NICE) and user and community groups (e.g. Citizens Advice Bureau32). Key to the review, and to the ensuing responses, is the belief that reducing health inequalities is one of the key critical social and political issues of our generation.
Reducing health inequalities is often referred to as ‘narrowing the gap’ or ‘reducing the social gradient’. The social gradient of health suggests that the lower a person’s social position, the worse his or her health, and an emphasis on analysing gradients as opposed to gaps exposes differences in health across the spectrum of advantage and disadvantage and not simply poverty and ill health. 33,34 Understanding whether the gradient has reduced involves examining the gradient over time. Recent analyses released by the Office for National Statistics (ONS)35 suggest that, although the quality of health in the population has improved across all social classes from 1982 to 2006, differences in life expectancy between the least and the most deprived social classes have increased during that period. That is, improvements in life expectancy have risen at a higher rate for more affluent people than the most deprived during that 25-year time frame; this finding was particularly true for men.
Considering the social gradient over time raises questions about how best to reduce inequalities. As the Marmot Review28 emphasised:
It is tempting to focus limited resources on those in most need. But . . . we are all in need – all of us beneath the very best-off. If the focus were on the very bottom and social action were successful in improving the plight of the worst-off, what would happen to those just above the bottom, or at the median, who have worse health than those above them? All must be included in actions to create a fairer society.
p. 16
This leads one to conclude that, to reduce the social gradient of health, we need to improve the plight of the most disadvantaged (through targeted interventions) as well as improve the overall health of the population (through universal interventions). The issue of targeted compared with universal approaches to health has received much consideration from NICE. In 2002, NICE invited 30 members of the public throughout the UK to join a Citizens Council. According to NICE,36 ‘The Citizens Council was established to ensure that the views of those who fund the NHS – the public – are incorporated into the decision-making process’. Still in existence today, the Council meets twice a year for three days at a time and has produced 13 reports to date. NICE then issues a formal response to the recommendations made in the report and any actions that they will take as a consequence. At one meeting in 2006, the Council was asked to discuss how health inequalities should be taken into account when developing national guidance. 37 According to the report of the meeting, they were asked which of the following strategies NICE should follow:
whether to issue guidance that concentrates resources on improving the health of the whole population (which may mean improvement for all groups) even if there is a risk of widening the gap between the socioeconomic groups;
or whether to issue guidance that concentrates resources on trying to improve the health of the most disadvantaged members of our society, thus narrowing the gap between the least and most disadvantaged, even if this has only a modest impact on the health of the population as a whole.
p. 437
The Citizens Council was presented with information from various experts (university academics, service providers, etc.) and they engaged in discussions and participated in practical exercises. On the final day they were asked to vote on which of the two broad strategies seemed more appropriate. They were unable to reach unanimous agreement but concluded that:
Despite our many and varied reservations, a majority of the Citizens Council would look with sympathy on NICE strategies intended not only to improve public health for all, but to do so in a way that offers particular benefit to the most disadvantaged.
p. 537
The Marmot Review28 referred to this approach as ‘proportionate universalism’. Although the NICE Citizens Council is an excellent demonstration of the way in which the public can be engaged in the development of national health guidance, the conclusions of their 2007 report also emphasise the difficulty that policy-makers and service providers face when deciding how to address health inequalities. One possibility for addressing the social gradient, discussed below, is through engaging the community in service design and delivery.
Reducing health inequalities through community engagement initiatives
One of the priority objectives advocated in the Marmot Review28 is to ‘improve community capital and reduce social isolation across the social gradient’ (p. 126). By improving social capital and reducing isolation, the social inequalities that underpin health inequalities could be improved – which would have a flow-on effect on health outcomes. The review summarised evidence which suggested that interventions to reduce social isolation are more effective when communities and individuals are included in their design.
Other researchers have advocated community engagement and participation as a strategy to reduce health inequalities (e.g. Wallerstein and Duran,15 Rifkin et al. 38), yet it is difficult to find empirical evidence to support this. Like the Marmot Review, an international literature review for the World Health Organization (WHO) found that participatory empowerment (a facet of community engagement) has been linked to positive outcomes such as social capital and neighbourhood cohesion for socially excluded groups. 15 However, the author noted that links to health outcomes are more difficult to identify. The few examples identified in the review of the effect of participatory empowerment on health outcomes were mostly in developing countries, which have limited transferability to the UK context.
Similarly, Popay et al.’s rapid review4 found some evidence for improvements in social capital, social cohesion and empowerment as a result of community engagement, but little evidence of improvements for mortality or morbidity/health behaviours or impact on inequalities. The authors concluded that the small number of studies addressing the relationship, plus problems with the designs of the primary studies (e.g. the time to follow-up in the mortality studies was too short to expect any change), were the reasons for not observing a relationship.
Rather than searching for evidence of community engagement effectiveness, Arblaster et al. 39 searched for evaluations of health service interventions designed to reduce health inequalities. They included 94 studies in their systematic review and found that successful interventions often had one or more of the following characteristics:
-
systematic and intensive approaches to delivering effective health care
-
improvement in access and prompts to encourage the use of services
-
strategies employing a combination of interventions and those involving a multidisciplinary approach
-
ensuring that interventions address the expressed or identified needs of the target population
-
the involvement of peers in the delivery of interventions.
The last two recommendations echo the general principles underlying community engagement. Although these characteristics alone were not sufficient for success, it is clear that community engagement may be a promising approach to reducing health inequalities.
In summary, it seems that community engagement is likely to have a positive effect on social inequalities,4,15,28 which might in turn reduce health inequalities,28 although the direct effect on health inequalities is still uncertain. 4,15 The present review will attempt to examine both direct and indirect pathways to reducing health inequalities through community engagement approaches.
Initial conceptual framework for this research
One of the main outputs from this review is a new conceptual framework that encapsulates the way that different types of community engagement might facilitate interventions to impact on health outcomes amongst disadvantaged groups. The conceptual framework that we finished the project with was therefore quite different from the one that we began with, but for reasons of accountability, and to ensure that it is possible for this report to allow the reader to follow the course of the research, we present here the conceptual framework that informed our search strategies and decisions about which studies to include and exclude.
The commissioning brief for this project defined community engagement as ‘approaches to involve communities in decisions that affect them’. Mason et al. 40 have defined community engagement for health promotion as engaging groups of people who share geographies, interests or identities with the aim of improving health and/or reducing health inequalities. The commissioning brief refers to engagement with any organisations that can provide activities for improving public health. Some non-NHS organisations may be directly health-related, such as sports clubs or food retailers. A healthy public policy approach recognises that it would be helpful if organisations with other aims, such as public transport, workplaces or schools, also considered their influence on health.
For the purposes of this systematic review, we have defined community engagement as a direct or indirect process of involving communities in decision-making and/or in the planning, design, governance and delivery of services, using methods of consultation, collaboration and/or community control. Information-giving was not seen as an empowering type of engagement, as this approach does not explicitly facilitate any reflection of users’ perspectives in the identification, design or delivery of an intervention.
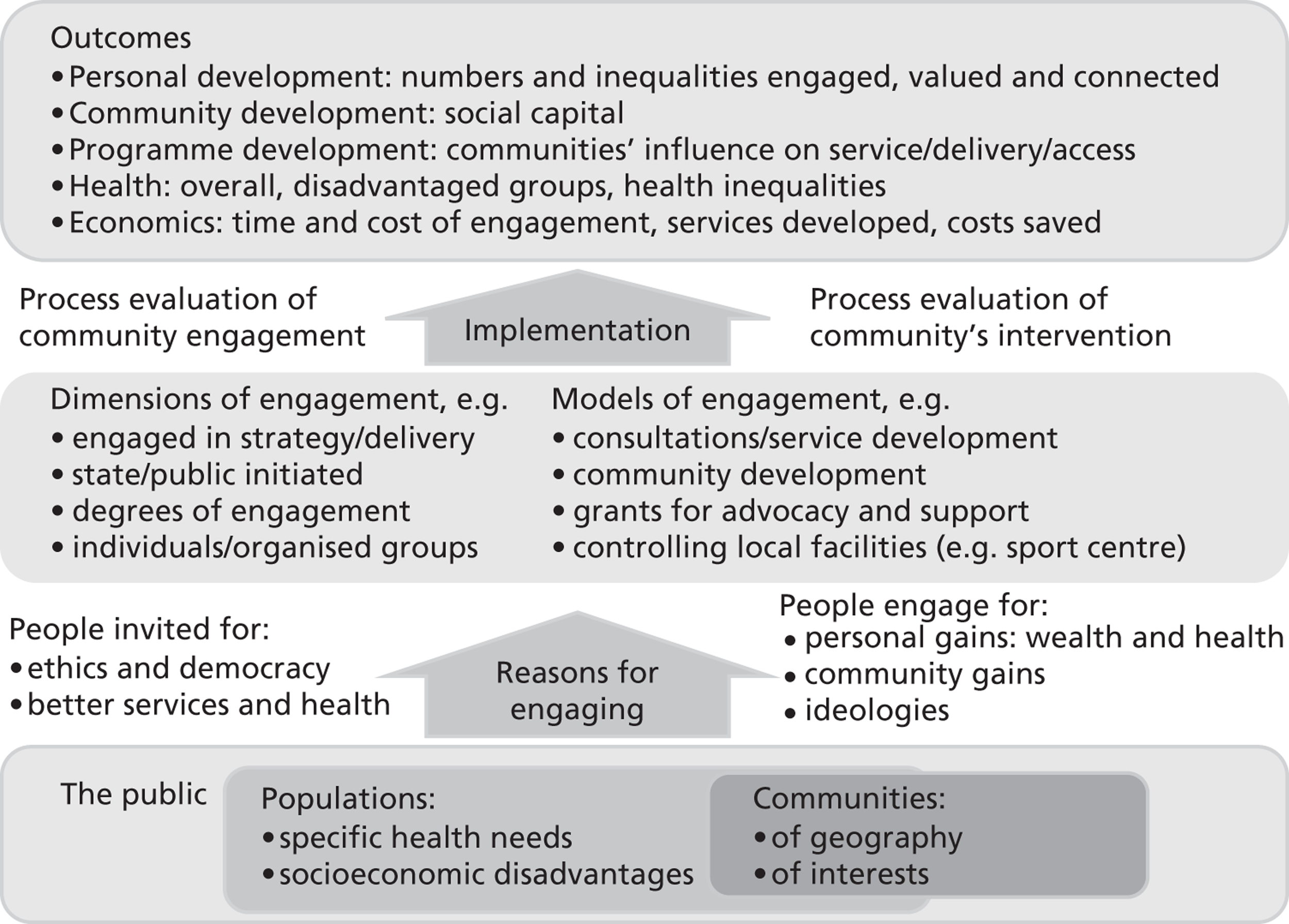
Involving people in decisions that affect them is justified both by ethical and political arguments, and by instrumental arguments asserting that involvement will lead to decisions more relevant to the people being served. Community members are motivated to participate for their own personal material or health benefits, for the gains anticipated for their community or by their own ideologies. 41
There are a broad range of community engagement models for engaging people in developing strategy or implementing services. Key differences in these models include who initiates the engagement (public service organisations or communities); the degree to which people are engaged (consulted, in collaborative partnerships or in control); and whether it is individuals or organised community members who are engaged. 42,43 Communities may be engaged in consultations, group support and advocacy, service development, controlling local facilities and human resources, and community tier government; any such engagement may be supported by education and networking. 42 Success depends on sound implementation of both the community engagement and any interventions resulting from this engagement.
The impact of community engagement can be considered at the level of individuals (personal development), communities (social capital), services (development, delivery, access) and health (population health, health of disadvantaged groups, health inequalities; extended from Slater et al. 44). Ideally, economic analyses would take into account costs incurred by community engagement, subsequent service development and the potential costs that might be incurred/saved as a result of an increased uptake of services that improve health. Data permitting, these are all issues that we proposed to explore in our analyses, and their relationships are summarised in Figure 1.
FIGURE 1.
The original conceptual framework.
Rationale for this review
Previous work has shown that, if communities are ‘signed up’ to the intervention or programme that they are receiving, people are more likely to participate and better outcomes can result. Community engagement is likely to have a positive effect on social inequalities,4,15,28 which might in turn reduce health inequalities,28 although the direct effect on health inequalities is still uncertain. 4,15 However, without a synthesised evidence base, it is not clear whether specific approaches to community engagement help to reduce inequalities in health; or for whom they work, under what circumstances and with what resources. As it would be difficult and expensive to conduct a very large research project that tests multiple approaches to community engagement in different topic areas with different populations, this project synthesised existing evidence and thereby made use of the investment already made in many published research studies.
Systematic reviews pull together all of the available research on a given topic. Through rigorous, structured approaches to identifying, selecting and analysing the evidence, systematic reviews reduce the biases inherent in more traditional reviews of the literature. They are valuable because they enable us to take stock; when based on the entirety of evidence in a given field they are able to tell us what we do, and do not, know. They are efficient because they valorise previous investments in research and, by virtue of the consistent way that they treat included studies, they are able to recast our view of research in a field, challenging existing assumptions and suggesting new areas for investigation. They also facilitate generalisability by looking for knowledge and findings across individual (and possibly atypical) primary studies.
Synthesising research systematically is recognised internationally as being a valuable and necessary activity for helping us to make sense of existing research and ensure that recommendations for policy and practice are based on the best, and most comprehensive, view of the available evidence. However, before this review was conducted, there was a clear gap in evidence synthesis in the case of community engagement in general, and its impact on health inequalities in particular. There was no synthesis of research able to identify specific approaches to community engagement that are able to reduce inequalities in health – and the resource implications of adopting them. Given the current concerns about health inequalities in the UK28 and the policy emphasis on community engagement as a vehicle for facilitating change (e.g. London Mayor45), it is timely to explore what works in engaging the community to reduce health inequalities.
Review aims and objectives
The overarching aims of this project were to identify community engagement approaches that are effective in improving the health of disadvantaged populations and/or reducing inequalities in health; and to describe the approaches in terms of the circumstances in which they work and the costs associated with their implementation. We accomplished these aims by achieving the following objectives:
-
consulting with relevant stakeholders to ensure that our study was informed by their perspectives and experiences
-
identifying a set of primary research studies that evaluate the effectiveness of interventions with a community engagement component in terms of their impacts on the health outcomes of disadvantaged groups
-
making contact with researchers in the field who have investigated the issues relevant to this study to enhance the data set we draw on
-
describing and synthesising the data that we identify
-
drawing conclusions, verifying our findings with stakeholders and writing up and disseminating our results.
Review questions
Our overarching review question is, ‘Can specific approaches to community engagement help to reduce inequalities in health; for whom, under what circumstances and with what resources?’
To answer this question, the following, more focused research questions (RQs) form the basis of our enquiry:
-
RQ1: What is the range of models and approaches underpinning community engagement?
-
RQ2: What are the mechanisms and contexts through which communities are engaged?
-
RQ3: Which approaches to community engagement are associated with improved health outcomes among disadvantaged groups? How do these approaches lead to improved outcomes?
-
RQ4: Which approaches to community engagement are associated with reductions in inequalities in health? How do these approaches lead to reductions in health inequalities?
-
RQ5: Which types of intervention work best when communities are engaged?
-
RQ6: Is community engagement associated with better outcomes for some groups than others? (In particular, does it work better or less well for children and young people?)
-
RQ7: How do targeted and universal interventions compare in terms of community engagement and their impact on inequalities?
-
RQ8: What are the resource implications of effective approaches to community engagement?
-
RQ9: Are better outcomes simply the result of increased resources, or are some approaches to community engagement potentially more cost-effective than others?
RQ1 and RQ2 are addressed through a map of the evidence and a theoretical synthesis of the models and mechanisms reported in the available literature; RQ3–9 through meta-analysis of the effectiveness data and thematic synthesis of the process data; and RQ8 and RQ9 through an economic analysis of costs and resources data.
Chapter 2 Review methods
The protocol for this review is attached in Appendix 11; although there are no checklists for a complex, multimethod review such as this, we have adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance46 and the PRISMA checklist can be found in Appendix 10.
Setting
The systematic review includes studies of interventions conducted in any setting.
Design
The project is a systematic review of known existing research. We start with a map of the evaluation studies (see Chapter 3), which describes the scale and range of community engagement interventions (RQ1 and RQ2). This is followed by syntheses detailed across five chapters:
-
a theoretical synthesis of the literature (see Chapter 4) that describes the models and mechanisms of community engagement interventions (RQ1 and RQ2)
-
an aggregative statistical analysis (i.e. meta-analysis) of a subset of evaluation studies that focus on Marmot policy priority areas (RQ3–7; see Chapter 5)
-
a thematic summary of process evaluations that focus on interventions in Marmot policy priority areas (RQ3–7; see Chapter 6).
-
an economic analysis of costs and resources (RQ8 and RQ9; see Chapter 7)
-
additions to the theoretical synthesis that bring together the learning from the above four components to develop a broad conceptual framework (addressing the broader issues within the RQs; see Chapter 8).
Rather than searching exhaustively for primary studies, which would have meant that most of the project would have been spent searching and screening, we compiled our data set for the analyses from specially selected registers of primary studies and systematic reviews. These registers have been populated using rigorous systematic review search methods.
We considered that a broad range of research was relevant to answering our RQs and thus included three types of research: outcome, economic and process evaluations; we also took account of the existing theoretical literature on community engagement. In the process of identifying the evidence to be synthesised, and before conducting the synthesis itself, we described the evidence with respect to the range of models and approaches underpinning community engagement (RQ1) and the mechanisms and contexts through which communities are engaged (RQ2) in the form of a map of the evidence. We also conducted a theoretical synthesis of the theories evident in the literature, which was the basis of our new conceptual framework.
In the meta-analysis, we analysed many evaluations of community engagement interventions; identified approaches that are most often associated with reductions in inequalities in health; and, to the extent that this was possible over a large number of studies, paid particular attention to the context of the research and the mechanisms by which communities are engaged and the ways this is thought to impact on intervention effectiveness (RQ3–7). The meta-analysis was then complemented with a thematic synthesis of the process evaluations present in the same set of studies. We also analysed the extent to which information on resource use, costs and cost-effectiveness was reported in our data set, as well as identifying data from complementary studies linked to these studies, including the use of modelling approaches to synthesise long-term costs and benefits (RQ8 and RQ9). Following this economic analysis of the literature, the four previous analyses were brought together in a new conceptual framework.
The design and methods were set out in a protocol that was published online on the National Institute for Health Research (NIHR) website (see Appendix 11). Our search strategy was far more successful at identifying studies on community engagement and inequalities than we had anticipated at the outset. (We had expected the number of studies that met that joint requirement to be relatively small, and so developed a particularly sensitive search strategy.) Our funders (the NIHR Public Health Research programme) extended the project to enable us to synthesise this larger quantity of literature. The larger quantity of included studies changed our analysis slightly, making it more aggregative than we expected, and it enabled us to conduct a larger statistical analysis that we had planned (which we had planned to conduct ‘if possible’). The project remained faithful to the protocol and any deviations are specified in Chapter 9.
Information management
All records of research identified by our searches were uploaded to the specialist systematic review software, EPPI-Reviewer 4 [Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), Social Science Research Unit, Institute of Education, University of London, UK], for duplicate stripping and screening. 47 This software recorded the bibliographic details of each study considered by the review, where studies were found and how, reasons for their inclusion or exclusion, descriptive and evaluative codes and text about each included study, and the data used and produced during synthesis. The software enables us to keep track of electronic documents (e.g. PDF files) and take advantage of emerging text mining technologies to help us identify relevant research and efficiently identify commonalities across the studies that we find.
Ethical arrangements
This project was approved by our Faculty Research Ethics board at the Institute of Education (ethics approval reference number FCL 283; copies of the ethics application are available from the report authors). The project complies with the Economic and Social Research Council (ESRC) Research Ethics Framework.
User involvement
The project advisory group provided feedback on the research in the project. The advisory group includes public health policy and practitioner members. We had regular informal contact with members of the group by e-mail and telephone, and a formal face-to-face (with some attending by teleconference) meeting to discuss the review’s conceptual framework and analytical strategies.
In addition, we explored the review’s interim map findings through consultations with young people through the National Children’s Bureau (NCB) Young Research Advisers group48 and a group for looked-after young people in North London that preferred to remain anonymous. The NCB Young Research Advisers is a group of 18 young people aged 10–17 years from all over England that was established by the NCB to engage young people in the research process. Membership of the group is voluntary and the NCB provides expenses, food and appropriate accommodation when required. In recognition of the young person’s time in taking part in meetings, the NCB also gives members gift vouchers.
The young people’s consultations involved one workshop session for each of the two groups at their own venues, and lasted around 2 hours in length. Sessions were timed to fit in as part of the groups’ existing meeting plans. Content included practical exercises to introduce the project and help group members discuss what helps or hinders them to engage with community activities to improve health or reduce inequalities. These discussions were considered when designing the data extraction tools (e.g. the importance of distinguishing peers from non-peer community members was highlighted, and so we ensured that these were coded separately).
We conducted two seminars in late 2012 at which we discussed our findings and conceptual framework. These seminars were both an opportunity for dissemination and an opportunity for us to obtain wider feedback on our new conceptual framework.
Search strategy
Searching across such a broad topic raises particular challenges. Approaches to community engagement cut across many disciplines, topic areas and outcome domains including, for example, housing, transport, social inclusion, accident prevention and substance abuse. 4 Searching broadly requires the location and screening of many reports to identify a much smaller amount of research evidence that is specifically relevant. This can make exhaustive searching costly and time-consuming.
A further challenge relates to identifying different types of evidence. We wanted to find outcome, process and economic evaluations, and the theoretical literature that applied to them. Not only are these often reported in different sources, which broadens the search scope, but also they use diverse terminology that can make recognition of their relevance difficult. The lack of detail about health inequalities in titles and abstracts can also make it difficult to detect studies that include relevant health equity issues.
Given the above challenges, we identified two practical strategies for identifying relevant studies. First, we identified systematic reviews through searching various websites and databases devoted to systematic reviews. The aim of this step was to capitalise on the systematic searches that have already been carried out for other reviews by identifying relevant primary studies included in those. Second, we used a database of studies in health promotion and public health that the EPPI-Centre has built up over many years as a result of carrying out systematic reviews (known as TRoPHI or, the Trials Register of Promoting Health Interventions). The studies in this database are the product of systematic searches and have already been systematically classified; they thus represent a valuable shortcut to evidence. Importantly, the TRoPHI database is updated several times a year, thereby increasing the likelihood that more recent studies not yet included in a review are identified.
Both approaches to searching are detailed below. The syntax that was used in the search process is presented in Appendix 1. Theoretical literature could be identified from the references in the evaluations and through colleague recommendations, and so the strategy described here focuses on the means by which we found the evaluation literature.
Identifying systematic reviews
We searched a range of registers, websites and databases for systematic reviews that discuss how some or all of their included studies contain interventions that utilise community engagement. The reviews were used to identify included primary studies that are relevant to the scope of this project; the systematic reviews themselves were not included in the syntheses in this project (see Study selection and eligibility criteria).
The systematic review registers, websites and databases that we searched were:
-
Database of Promoting Health Effectiveness Reviews (DoPHER). DoPHER is developed and maintained by the EPPI-Centre. It has focused coverage of systematic and non-systematic reviews of effectiveness in health promotion and public health worldwide. It currently contains details of > 2500 reviews of health promotion and public health effectiveness. All reviews are assessed and coded for specific characteristics of health focus, population group and quality (URL: http://eppi.ioe.ac.uk/webdatabases/Intro.aspx?ID=2, accessed 15 March 2013).
-
Cochrane Database of Systematic Reviews (CDSR). CDSR includes all Cochrane Reviews (and protocols) prepared by Cochrane Review Groups in The Cochrane Collaboration. As of Issue 5, 2011, CDSR includes 6641 articles: 4622 reviews and 2019 protocols (URL: www.thecochranelibrary.com/view/0/AboutTheCochraneLibrary.html#CDSR, accessed 15 March 2013).
-
Database of Abstracts of Reviews of Effects (DARE). DARE is developed and maintained by the Centre for Reviews and Dissemination (CRD) and currently contains > 21,000 systematic reviews. It is focused primarily on systematic reviews that evaluate the effects of health-care interventions and the delivery and organisation of health services. The database also includes reviews of the wider determinants of health such as housing, transport and social care when these impact directly on health, or have the potential to impact on health (URL: www.crd.york.ac.uk/CMS2Web/AboutDare.asp, accessed 15 March 2013).
-
The Campbell Library. The Campbell Collaboration’s library of systematic reviews includes reviews and protocols prepared by Campbell review groups under any of the six co-ordinating group themes: crime and justice, education, international development, methods, social welfare and review users (URL: www.campbellcollaboration.org/library.php, accessed 15 March 2013).
-
NIHR Health Technology Assessment (HTA) programme website. The HTA programme produces research about the effectiveness of different health-care treatments and tests for those who use, manage and provide care in the NHS. The HTA website houses all of the reviews published through the HTA programme in the HTA journal series and holds in excess of 550 titles (URL: www.hta.ac.uk/project/htapubs.asp, accessed 15 March 2013).
-
HTA database hosted by the CRD. This database currently holds > 10,000 summaries of completed and ongoing HTAs from around the world. Database content is supplied by the 52 members of the International Network of Agencies for Health Technology Assessment (INAHTA) and 20 other HTA organisations worldwide (URL: www.crd.york.ac.uk/crdweb/AboutHTA.asp, accessed 15 March 2013).
Identifying primary research through the Trials Register of Promoting Health Interventions and NHS Economic Evaluation Database
Searches of the systematic review resources were supplemented by searches of the TRoPHI database and the NHS Economic Evaluation Database (NHS EED).
The TRoPHI database includes focused coverage of trials of interventions in health promotion and public health worldwide. It covers both randomised and non-randomised controlled trials and currently contains details of > 4500 trials and is updated four times a year. This source was searched to ensure that relevant trials published outside of the time frame or scope of the reviews identified in the review databases listed in the previous section are detected.
Part of the TRoPHI data set was used in a comparison of randomised and non-randomised trials49 and we proposed to add additional studies from reviews that were carried out since this study. The approximately 300 studies in this data set were already classified using one of two data collection tools that capture detailed information about their methodology, participants, planning and process measures (if any), intervention and outcomes. [Although many of the studies were potentially relevant, surprisingly few passed both our ‘community engagement’ and ‘inequalities’ filter, and so the vast majority (> 99%) of studies synthesised came from our other searches.]
The NHS EED includes records of economic evaluations of health-care interventions, including cost–benefit, cost–utility and cost-effectiveness analyses; the database currently includes > 11,000 economic evaluations. The database is maintained through weekly literature searches that are conducted by the CRD.
Other search sources
The final component in our search strategy was contact with authors of identified studies. We contacted authors of a small number of key studies that were excluded on methodological grounds to ask them if they had outputs that would meet our inclusion criteria, or if they could provide further information about the study to assess its suitability for inclusion. ‘Key studies’ were large-scale UK-based evaluations, such as the Health Action Zones initiative.
Dates of searches
-
DoPHER: 26 July 2011.
-
TRoPHI: 16 August 2011.
-
The Campbell Library, CDSR, DARE, HTA and NHS EED: 17 August 2011.
-
Supplementary search of HTA journal in Web of Knowledge for papers published 2010–11: 18 August 2011.
Study selection and eligibility criteria
The outcome of the search was a database of references and documents that were screened using the review’s inclusion criteria. The inclusion criteria are a list of statements about what the study should contain to be relevant to the review question; studies must meet all of the criteria to be eligible for inclusion in the review. The criteria were applied twice: first, to identify systematic reviews and, second, to identify relevant primary studies.
The criteria were piloted on a sample of studies before being applied to the larger data set and reviewers discussed screening decisions regularly to ensure consistency in the way that studies were being included and excluded. Five reviewers were involved in screening the evidence [three of the report authors (AO, GB and JK) and two research assistants named in the acknowledgements (KT and JW)]. The other report authors were occasionally consulted when inclusion decisions that might affect the scope of the review were encountered.
Selecting reviews
The purpose of this stage was to identify reviews that might include relevant primary studies. The following criteria were applied to titles and abstracts of reviews:
-
published after 1990 (the date cut-off set by other reviews on which we are building, e.g. Popay et al. 4)
-
a systematic review (i.e. describe search strategies and inclusion criteria used)
-
included outcome, economic, or process evaluation studies
-
described at least one intervention potentially relevant to community engagement
-
included at least one study in the results section
-
written in English
-
measured and reported health or community outcomes.
Studies were limited to the English language because of a lack of resources to translate documents. Each systematic review was assessed against these criteria in a stepwise fashion, such that any review excluded because it failed a criterion later in the list must have passed any preceding criterion. We were deliberately inclusive when considering the concept of community engagement at this stage to avoid missing any reviews that might include studies with community engagement even though it was not mentioned in the review’s abstract; as such, reviews that referred to community-level interventions were typically included except when this conflicted with the inclusion criteria above. Indeed, applying a consistent definition of community engagement across reviews was a challenge. In initial stages we relied on reviewers’ previous experience with the literature and developed written guidance on the definition within EPPI-Reviewer 4 as understandings about the concept emerged through group discussion about the interventions, providers, locations and study aims described across the reviews. It is possible that screening titles and abstracts of reviews may have missed some primary studies that had elements of community engagement. However, because of the reflective method used in consolidating our definition of community engagement early on in the screening process, this is more likely to be because of a lack of detail in the reference information available than because of systematic bias from reviewers.
We then retrieved the full-text copy of all reviews that passed these inclusion criteria. A brief screening of the full-text document was then conducted to check that the review was, in fact, systematic and that it included primary studies of relevance to our review. (Relevance at this stage was judged according to the criteria presented in Selecting trials for the map, although the criteria were not applied stepwise and were not recorded.) Potentially relevant primary studies were then added to the EPPI-Reviewer 4 database for the second stage of screening.
Selecting trials for the map
Once the final set of systematic reviews was obtained, we screened within each review to identify potentially relevant primary studies (trials). This involved scanning the evidence tables and reference lists of the reviews for relevant trials. We then located the abstracts for these trials.
The titles and abstracts of the trials identified during this process, plus those identified through TRoPHI and NHS EED, were then assessed for inclusion in the review. Studies were included if they met all of the following criteria:
-
published after 1990 (the date cut-off set by other reviews on which we are building, e.g. Popay et al. 4)
-
includes primary research, in that data have been collected during that study through interaction with or observation of study participants
-
not a Master’s thesis
-
includes outcome, economic, and/or process evaluations of interventions
-
community engagement is the main approach of the intervention
-
for outcome evaluations, study has a control or comparison group (i.e. it must be a controlled trial, either randomised or non-randomised)
-
published in English.
Once all of the studies had been screened on their titles and abstracts, full reports were obtained for those that appeared to meet the criteria or for which there was insufficient information to be certain. The retrieved articles were then screened based on the full-text article.
Three additional criteria were applied at full-text screening which ensured that sufficient detail was present for critical appraisal to take place and that the study participants were relevant to our focus on inequalities:
-
study characterises study populations or reports differential impacts in terms related to social determinants of health that can be captured by the PROGRESS-Plus framework (this framework, which enables us to characterise different dimensions of potential disadvantage, is described in Chapter 3)
-
study reports health or health-related outcomes for the effectiveness evaluation and/or process data in a process evaluation
-
study was conducted in an Organisation for Economic Co-operation and Development (OECD) country (at the time of screening OECD member countries were Australia, Austria, Belgium, Canada, Chile, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Japan, Korea, Luxembourg, Mexico, Netherlands, New Zealand, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Switzerland, Turkey, UK and the USA).
Those studied that passed the inclusion criteria on the basis of full-text screening were included in the map of engagement models and contributed to the theoretical synthesis.
Selecting trials for in-depth review
With regard to the extraction of outcome data, we carried out a final sift of the studies to determine which would be included in the in-depth review. Some studies were excluded because, on closer inspection, they did not have an adequate (independent) control group or quantitative data from which we could calculate an effect size estimate for the meta-analysis. We also filtered out studies that did not report at least one of the following outcome types:
-
health behaviours (e.g. smoking, food intake, physical activity)
-
community outcomes (e.g. perceived increased access to services in the area)
-
engagee outcomes (e.g. skills acquired by the engagees whilst engaged in the initiative).
Time constraints meant that we had to further narrow the scope of the studies for meta-analysis – it was simply impossible to extract outcome and risk of bias data for all 319 studies included in the map in the time frame available. It was decided, after consultation with the project advisory group, that a sensible way to identify a manageable set of studies was by focusing on health issues that were emphasised in the Marmot Review28 as being particularly problematic in terms of health inequalities in the UK. To achieve this, we identified any health priority areas in the Marmot Review in ‘health inequalities and the social determinants of health’ (see Chapter 2) and ‘policy objectives and recommendations’ (see Chapter 4) that mapped onto the health topics of the studies included in our review. These are presented in Table 1. Only studies categorised under those health topics were included in the in-depth review.
| Broad theme in Marmot Review | Labels used in Marmot Review | Captured under labels used in our data extraction |
|---|---|---|
| Health risks | Smoking | Smoking cessation |
| Smoking/tobacco prevention | ||
| Alcohol | Substance abuse | |
| Obesity | Obesity prevention/weight reduction | |
| Drug use | Substance abuse | |
| Policy Objective A: give every child the best start in life | Increased investment in early years; quality early years education and child care | Antenatal (prenatal) care |
| Breastfeeding | ||
| Childhood immunisation | ||
| Other child (ill) health | ||
| Supporting families to develop children’s skills | Parenting | |
| Policy Objective C: create fair employment and good work for all | Reducing physical and chemical hazards and injuries at work | Worker injury prevention/safety |
| Policy Objective E: create and develop healthy and sustainable places and communities | Integrate planning, transport, housing and health policies | Housing |
| Neighbourhood renewal/regeneration | ||
| Policy Objective F: strengthen the role and impact of ill health prevention | Increased investment in prevention; implement evidence-based ill health preventative interventions | Public health/health promotion/prevention |
| Cancer prevention | ||
| Cardiovascular disease/hypertension prevention | ||
| Healthy eating | ||
| Physical activity |
Data extraction
Data collection (extraction) process
Mapping stage
The mapping stage of the review describes the scale and range of community engagement interventions and contributes to addressing RQ1 and RQ2. Studies that met our inclusion criteria were stored electronically (when possible) and classified according to a standardised data extraction framework that is detailed in Appendix 2. Information was collected on models of community engagement (consultation, collaboration and community control), approach to community engagement (e.g. formation of community coalition, volunteer intervention provider), mechanism of engagement (how the community was recruited/involved), area of health concern (e.g. breastfeeding, smoking cessation), participants’ PROGRESS-plus characteristics and geographical and other contextual details.
Data extraction for the mapping stage was conducted independently by four different reviewers (AO, GB, JK and FJ). The data extraction tool was piloted on a sample of studies by all four reviewers before being applied to the larger data set. The reviewers discussed ambiguities regularly to ensure consistency in the way that studies were being coded.
Analysis stage
Data items
We extracted further data for those studies included in the meta-analysis, synthesis of process evaluations and economic analysis. Additional information was collected on the potential risk of bias in the study (i.e. methodological features related to the evaluation), the outcomes (see Meta-analysis), process issues (e.g. relationships between service provider and engagee), economic issues (e.g. sufficiency of funds) and costs/resources associated with the intervention (e.g. staff costs). The data extraction and risk of bias tool for effectiveness studies is provided in Appendix 3; the tool for extracting process information is provided in Appendix 4; and the tool for extracting information on resources, costs and consequences is provided in Appendix 5. Before being applied to the larger data set, the data extraction tools were piloted on a sample of studies by all reviewers who subsequently used the tools.
Data for the in-depth review were extracted from each study by two members of the team working independently, before meeting to discuss their findings to ensure quality and consistency of interpretation. The reviewers discussed ambiguities regularly to ensure consistency in the way that studies were being coded. Data extraction for the meta-analysis was conducted by AO, GB, JK and FJ. Data extraction for the economic analysis was conducted by DM and TM.
Data extraction for the theoretical synthesis partially took the form of a narrative that describes the models, context and mechanisms of the participants, interventions and approach to community engagement. This was supplemented with a data extraction of the barriers to and facilitators of implementation, which was taken from the process evaluations using a formally developed tool (see Appendix 4). Data extraction for the thematic synthesis of process evaluations was conducted by GB and JK after the tool had been piloted on a sample of studies.
Summary measures
For the meta-analysis, effect sizes were calculated to summarise the impact of the interventions. Because many of the outcomes used different scales and different combinations of continuous and dichotomous data, we used the standardised mean difference50 to enable us to compare and combine results of continuous measures, and odds ratios (ORs) for binary measures. We transformed the ORs to standardised mean difference effect sizes using the methods described in Chinn. 51 The data were screened for outliers and were Winsorised to 2 standard deviations (SDs) from the mean. 52
We also adjusted the standard errors of cluster randomised trials that had a disproportionate weighting. When the intracluster correlation (ICC) was provided, we used the ICC reported by the authors; otherwise, we set the ICC to 0.02. In total, 10 studies were adjusted (two with author-reported ICCs and eight with the imputed ICC).
Following the approach we took in a similar meta-epidemiology,49 outcomes were classified into domains according to a conceptualisation of a pathway to behaviour and health change. The domains, in order of the theory of change, were self-efficacy and social support, health behaviour change, physiological consequences and final health state. In the event, all but one of the studies with outcomes in the final two domains reported only one or the other (i.e. physiological consequences or final health state), so these two domains were combined in the meta-analysis.
We also calculated effect sizes of outcomes for engagees and communities. As such, studies could contribute more than one effect size estimate to the data set under the following conditions:
-
when there were both immediate post-test and delayed follow-up measures, to test the persistence of effects over time and/or
-
when there were outcomes from different points in the pathway to behaviour and health change (i.e. social support, self-efficacy, health behaviours and health consequences) and/or
-
when there were measures of both engagees and public health intervention participants.
For our economic analysis, data on resources used in community engagement strategies to encourage behaviour change and/or uptake of interventions were extracted from studies using a bespoke data extraction sheet, which was incorporated into EPPI-Reviewer. This included categorisation of funded and in-kind resource use, as well as a value placed on the time of volunteers. We documented whether resource use (e.g. units of equipment, hours of paid staff and volunteers) was reported separately from costs. When possible we aimed to distinguish between those elements of resource specifically for community engagement and resources for any actual health-promoting intervention. This would better enable us to make comparisons between different community engagement mechanisms without this being confounded by the total costs of different interventions. 53
We also categorised budgets from which resources are supported. We made use of The Campbell and Cochrane Economic Methods Group – EPPI-Centre Cost Convertor (http://eppi.ioe.ac.uk/costconversion/default.aspx) to ensure that costs were converted to UK pounds sterling and inflated to 2010 prices using purchasing power parity rates from the International Monetary Fund. If a breakdown of cost data for population subgroups was identified this was also recorded. The economic analysis also extracted data on completed economic evaluations, as well as on some issues concerned with the use of financial and other incentives to encourage community engagement, and analysis of the extent to which the financial and organisational sustainability of effective interventions could be maintained.
Quality assessment
The outcome evaluations (controlled trials) were assessed for methodological quality using an adaptation of the Cochrane risk of bias assessment tool. 54 We examined the studies in a range of dimensions including methods of assignment, the comparison group type, the comparability of groups at baseline/methods of adjustment, attrition and selective reporting. In the meta-analysis, we tested to see whether effect size was associated with methodological quality.
The tool we used to assess the quality of the process evaluations was refined in a recent review55 and assesses whether or not steps were taken to minimise bias and error/increase rigour in sampling, data collection and data analysis; findings were grounded in/supported by the data; there was good breadth and/or depth achieved in the findings; and the perspectives of intervention participants were privileged. The findings from process evaluations that did not score well were included but a sensitivity analysis was conducted to assess their impact on the overall analysis, as findings that depend solely on the evidence of poorer quality process evaluations are more provisional than those coming from stronger evaluations.
We had planned to assess the quality of economic evaluation studies using the Consensus on Health Economic Criteria (CHEC) list. 56 In the event, no such evaluations were identified.
Synthesis of results
Once the relevant data were extracted, we mapped the research that we had identified by producing tables and cross-tabulations to show the frequency of different types of engagement and the contexts in which they occur. We also provide a description of the similarities and differences across interventions. The map is focused on trends and gaps in the evidence base rather than detailing each intervention. We then moved on to synthesise the findings of the studies.
As described in the overview, there are four syntheses (theoretical, meta-analysis, thematic synthesis and economic analysis), which build on one another sequentially. The initial theoretical synthesis informed the subsequent syntheses, whereas the later theoretical synthesis (i.e. development of the conceptual framework) extended on the initial theoretical synthesis to incorporate the findings from the other analyses; there are thus five distinct synthesis chapters in this report. This iterative process is summarised in Figure 2. It shows that, although the emerging conceptual framework informed the statistical and economic analyses, it was then itself developed in the light of these syntheses.
FIGURE 2.
The conceptual framework both informed, and was informed by, the statistical and economic analyses.

Theoretical synthesis (see Chapters 4 and 8)
The theoretical synthesis was the first analysis to be completed. This analysis is similar in some respects to Pawson’s57 work on realist synthesis and examines in particular the theories, mechanisms and contexts of community engagement. It does not, however, attempt to engage in causal reasoning, leaving this task to the meta-analysis. The theoretical synthesis has been split into two parts in the report: Chapter 4 (answering RQ1 and RQ2), which presents the range of models of community engagement that have been presented elsewhere and focuses in particular on the theories of change that underpin each model; and Chapter 8, which presents a broad conceptual framework that encapsulates the studies in the statistical and economic analyses as well as the models of engagement in Chapter 4.
The first synthesis in this review aimed to understand the range of models and approaches underpinning community engagement, and the mechanisms and contexts through which communities are engaged. These aims are a way to gain a conceptual understanding of community engagement, rather than a more aggregative systematic review approach of counting the number of studies representing various models, approaches, mechanisms and contexts. 58,59
The theory-building nature of these aims led the research team to use methods of study identification and synthesis more appropriate for conceptual analysis research synthesis. In this type of synthesis, searching aims to build an understanding of a particular phenomenon by gathering a number of articles that present different perspectives on that phenomenon. Once a sufficient range of ideas have been identified, studies that do not add anything new to the topic are put to one side; in effect, a saturation of perspectives has been reached. 60
Using our data set of included studies along with theoretical literature that we identified alongside them, we adopted a purposive search and inclusion strategy more appropriate to gathering concepts, rather than the more traditional approach of exhaustively accumulating all literature on the topic. 61 A set of included studies was created that had been identified by team members as being examples of each of the different community engagement strategies. These studies were then synthesised in two ways.
The team began with the conceptual framework for community engagement (see Figure 1). First, one reviewer read, summarised and extracted data on community engagement aspects from each study and then compared those findings to the team’s conceptual framework to see whether issues in each paper refuted, confirmed or added new information to the model. The conceptual framework was developed as new issues were discovered. This ‘rolling’ or ‘constant comparative’ method of synthesis has been used in previous EPPI-Centre reviews. 62–64 The emerging conceptual framework and the summaries were read and discussed by the research team, to ensure that the framework reflected the combined expertise and individual perspectives of the whole team. A draft of the conceptual framework was presented to the review’s advisory group and the final framework was revised based on their feedback.
Second, all papers identified before in-depth coding in the map (n = 559) were clustered using the Lingo3G text mining algorithm (Carrot Search s.c., Poznan, Poland);65 these clusters were then manually organised according to the area of health concern, type of community engagement, participants’ PROGRESS-Plus characteristics and country/geographical details. This information was then also used to refine the framework. Each study was then manually coded; each time data were extracted from a study, its mechanisms and contexts were compared with our conceptual framework and the framework checked for its adequacy. After the meta-analysis and economic analysis were completed, the framework was again revised to take account of their findings.
Meta-analysis
The meta-analysis (quantitative synthesis) uses various statistical methods to address RQ3–8, by testing whether any observed differences in the results of included studies might be associated with the type of community engagement they employed. This is reported in Chapter 5. Methods used are descriptive statistics, meta-analysis (homogeneity tests), analysis of variance (ANOVA) and meta-regression. 66 For the random-effects model analyses we followed the methods described in Lipsey and Wilson52 and used SPSS (SPSS Inc., Chicago, IL, USA) macros written by Wilson. 67 The risk of bias across studies was assessed as described in Quality assessment.
Analyses were conducted separately for the following outcome types:
-
health behaviours at immediate post-test (e.g. fruit and vegetable intake)
-
health behaviours at delayed follow-up
-
health consequences at immediate post-test (e.g. cholesterol levels)
-
participant self-efficacy related to the health behaviours, at immediate post-test
-
social support related to the health outcomes, at immediate post-test
-
engagee outcomes (e.g. skills, empowerment)
-
community outcomes (e.g. perceived improved access to health services in the local area).
Possible moderating or confounding factors included:
-
the community engagement theory of change
-
whether it was a single or multicomponent intervention, and whether community engagement was evident in all components
-
the Marmot Review28 priority health area
-
characteristics of the intervention (setting, strategy, deliverer, duration)
-
characteristics of the participants (age, PROGRESS-Plus health inequality group)
-
whether the intervention was targeted or universal
-
the potential for risk of bias and characteristics of the evaluation.
Moderators and confounders notwithstanding, we aimed to identify the amount of variance (if any) that is explained by different approaches to community engagement with participants within each review, each topic domain and finally across all studies in the meta-analysis. Specific aspects of the analysis, such as data cleaning (identification and treatment of outliers and skewed data), sensitivity analyses and assessment of publication bias, are reported in the results chapter (see Chapter 5) alongside the relevant results to facilitate understanding of the findings.
We chose to focus our reporting of the results on the trends in pooled effect size estimates, rather than between-group statistical significance – as is usually common in meta-analysis. Typical meta-analyses attempt to infer findings from the sample to a hypothetical population. This is problematic for our review because the issues that we are exploring – community engagement and health inequalities – are so broad and difficult to define that it is impossible to know exactly to what population the results of any inferential statistics would apply. Instead, we emphasise observed trends, to help disentangle some of the differences between the types of evidence we have collected. This can help us to understand what might occur in other similar studies not included in the review, but not in any one specific situation because (and as discussed in Chapter 8) the causal pathways are complex and potentially unique to each study.
Thematic synthesis of process evaluations
The thematic synthesis of process evaluations narratively described emerging themes and factors evident across the process evaluations. Our original plan was to conduct a framework synthesis68,69 of process evaluations using a tool that we had constructed based on an earlier synthesis of community engagement process evaluations. 4 We found, however, that, although the framework ‘worked’ for some aspects of the process evaluations that we were synthesising, it did not cover the range of issues that we were encountering. We therefore moved to a more open structure and applied a process evaluation data extraction tool developed and used in previous EPPI-Centre reviews. 55,70 The complete process evaluation data extraction tool is provided in Appendix 4.
The data extraction tool was used to assess 12 criteria, including data collection method (e.g. interviews, surveys); type of stakeholder who provided the process information; the timing of the process evaluation in relation to the intervention; methods and rigour of sampling, data collection and analysis; assessment of how grounded the data were in authors’ findings; assessment of the breadth and depth of findings; and extent to which the process evaluation privileged the perspectives and experiences of the public. An overall rating (low, medium or high) was given to each study in terms of the study’s methods and the usefulness of each study’s findings in drawing conclusions about what works, why and for whom.
Specific content about processes was coded using the following headings:
-
acceptability of the intervention to the participants or providers
-
accessibility/programme reach
-
consultation/collaboration/partnerships
-
programme content (e.g. use of incentives, fit between content and aims of intervention)
-
costs (e.g. issues of sustainability)
-
implementation (e.g. frequency, duration and amount of adherence to programme content)
-
management/responsibility issues
-
quality of programme materials
-
skills and training of intervention providers
-
other issues.
Within each of the process evaluation data extraction questions, responses from each study were summed and frequencies reported. Ratings of overall reliability and usefulness were determined by reviewing responses to each data extraction question. Findings from each data extraction category were assessed and compared to determine whether:
-
lower rigour/lower usefulness studies came to similar or different conclusions to/from higher rigour/higher usefulness studies
-
findings varied by publication date
-
findings varied by health topic
-
findings varied by the type of community engagement model used.
Economic analysis
The final component of our study, the economic analysis, answers RQ8 and RQ9 and investigates the resource implications of various approaches to community engagement. It also reports on the extent to which they have been evaluated in terms of their potential cost-effectiveness.
The data extracted from the studies were synthesised narratively. Two tools were developed specifically for this project to capture data on economic issues (e.g. sufficiency of funds) and resource utilisation, cost and cost–consequences (e.g. staff costs). These tools were then combined into one data extraction tool (see Appendix 5). Items covered the following domains:
-
resourcing and cost breakdown
-
economic consequences of interventions
-
economic evaluation methods and findings
-
availability or flow of funds
-
sufficiency of funds
-
securing additional funds
-
financial sustainability
-
linking investment in intervention with impact on outcomes
-
sources of funds
-
role of volunteers
-
financial and economic incentives
-
other issues.
The synthesis started with a consideration of trends across the studies in terms of costs, resource use, cost–consequences and economic evaluation methods used. We then explored the findings from individual economic evaluations. Finally, specific issues that we examined in more detail were the value and role of volunteering, the use of financial and other incentive mechanisms to influence rate of community engagement, gains or losses to human and social capital, and funding and sustainability issues.
We also aimed to make use of information extracted from our review of the literature and supplemental information from other studies and community engagement implementers to undertake some limited decision modelling to explore the potential cost–utility and cost-effectiveness of selected different approaches to community engagement.
Chapter 3 Results of the systematic map
About this chapter
This chapter contains information about the results of our systematic search, the studies screened for inclusion, the number of full-text reports retrieved and the final number of studies that met our inclusion criteria.
It then goes on to describe the included studies in terms of the types of intervention that they contain. A more detailed examination of the different models of community engagement found in these studies appears in the following chapter.
Summary
In total, 943 potential systematic reviews elicited a total of 7506 primary study titles and abstracts. Searches of other sources provided an additional 1961 primary study titles and abstracts. Duplicate removal, retrieval and screening of full-text reports resulted in the final inclusion in the map of 361 reports of 319 studies.
Most of the located trials were undertaken in the USA (268 studies, 84%), with only 26 studies (8%) conducted in the UK. Young people were studied most often (180 studies, 56%), followed by adults (168 studies, 53%). The most frequent category of disadvantage under study was ethnicity (120 studies, 38%); 109 of these studies were carried out in the USA. The most frequent category of disadvantage in the UK was socioeconomic position (eight studies), followed by ethnicity (four studies). Participants often suffered from more than one type of disadvantage. Socioeconomic position, education and place of residence join ethnicity as particularly significant types of disadvantage.
Interventions were most often targeted to a specific PROGRESS-Plus group (238 studies, 75%) rather than to a wider population. Interventions to address human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS)/sexually transmitted infection (STI) prevention were most often described (51 studies, 16%), followed by cancer screening/protection (41 studies, 13%) and substance abuse (22 studies, 7%). Interventions took place most often in community settings (141 studies, 44%), using media sources (93 studies, 29%) and in homes (88 studies, 28%). Community members and peers delivered the intervention almost equally across the studies (135 studies, 42%, and 132 studies, 41% respectively). The types of interventions delivered were largely educational (252 studies, 79%) followed by advice (166 studies, 52%) and social support (116 studies, 36%).
Ethnic minority groups were studied in 121 evaluations (38%); these groups were most often targeted for cancer screening and detection (24 studies) followed by HIV/AIDS/STI prevention (16 studies) and diabetes prevention/management and obesity (11 studies each). Low-income groups were studied in 54 evaluations (17%), which focused most often on breastfeeding (nine studies), cancer screening (eight studies) and cardiovascular disease and asthma prevention/treatment (four studies each).
Study selection
Figure 3 describes the flow of literature through the review process. As outlined in the previous chapter, studies were identified for inclusion in the review by searches of specific sources of systematic reviews and of primary research. The flow chart in Figure 3 reflects this two-pronged approach.
FIGURE 3.
Flow of systematic reviews (blue) and primary study reports (green) to the map.
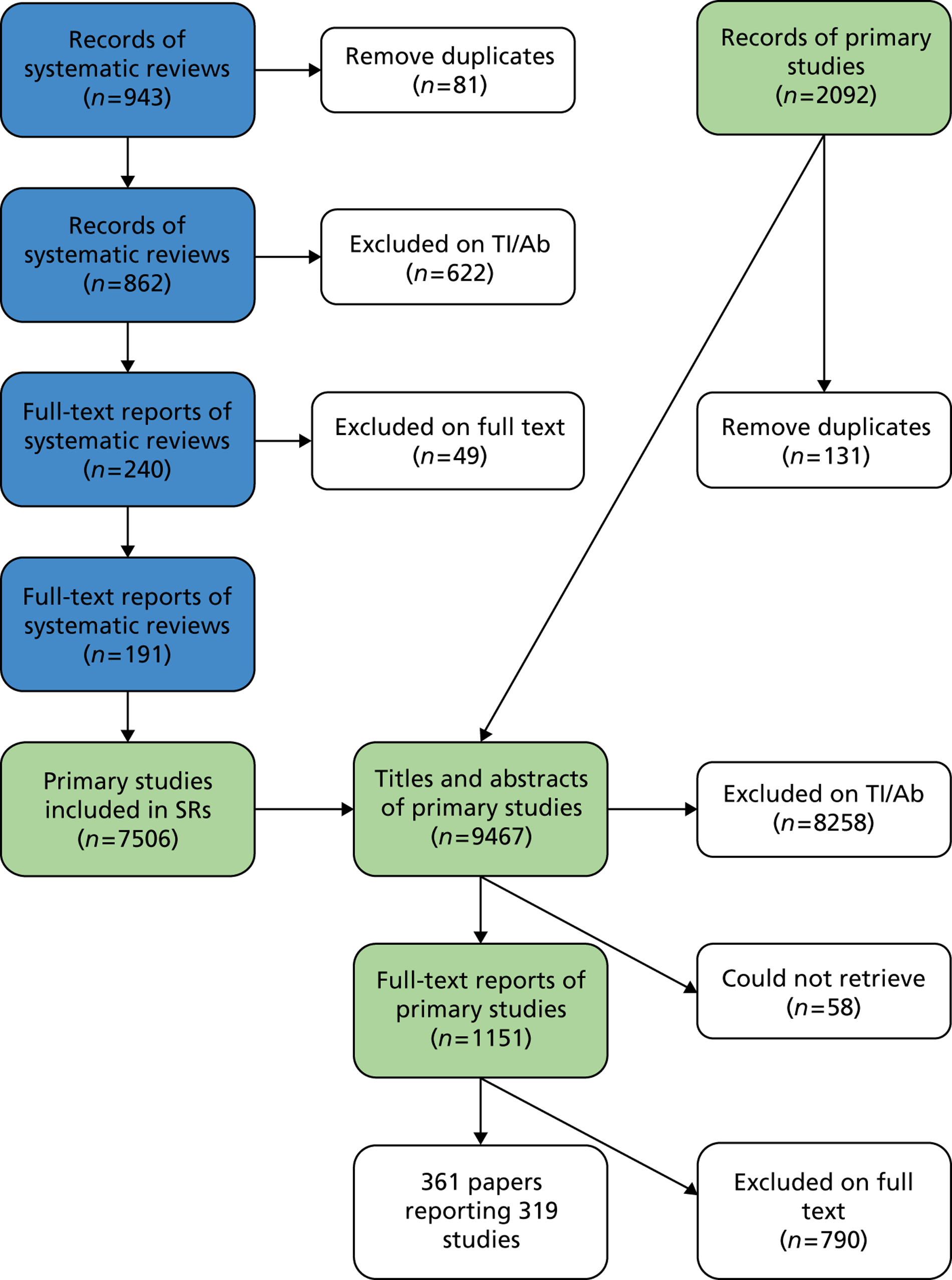
We identified 943 records of potentially relevant systematic reviews, 81 of which were duplicate records. Of the 862 unique records, 622 were excluded on the basis of reading titles and abstracts. The vast majority of records were excluded as not relevant to a study of community engagement (n = 466, 75%). Further reasons for exclusion at this stage were not a systematic review (n = 77, 12%), publication before 1990 (n = 45, 7%), review had no included studies (n = 8, 1%) or health outcomes reported (n = 8, 1%), and not a systematic review of outcome or process evaluations (n = 6, 1%).
Full-text copies of the remaining 240 systematic reviews were obtained and assessed for eligibility. Seven of these subsequently did not meet minimum methodological standards to be regarded as systematic reviews and a further 42 reviews did not include any relevant primary studies. A total of 191 systematic reviews met our inclusion criteria. These reviews included a total of 7506 primary studies, an average of 39 each, with a range of 3–547. The 7506 primary studies included in these eligible reviews were assessed for eligibility using a combination of descriptions and tables of included studies reported in the reviews, and abstracts retrieved online. This process identified 988 eligible studies, all of which were reassessed against inclusion criteria on the basis of a full-text report.
As described in Chapter 2, we also searched databases directly for reports of primary studies, and of course came across other eligible studies before and while working on the review, resulting in 1961 titles and abstracts to screen after duplicate checking. On the basis of their titles and abstracts, the full texts of 163 of these records were retrieved.
In total, this resulted in 1151 reports to screen on full text, of which 361 reports71–431 of 319 studies met our inclusion criteria. Reasons for exclusion were:
-
published before 1990 (n = 7)
-
not primary research (n = 23)
-
not an outcome or process evaluation or economic analysis (n = 53)
-
not community engagement (n = 252)
-
not relevant to PROGRESS-Plus groups (n = 275)
-
no comparison group (effectiveness studies only) (n = 66)
-
no health-related outcomes/process data (n = 26)
-
non-English language (n = 7)
-
not carried out in a country in the OECD (n = 81).
As stated in Chapter 2, after mapping the characteristics of the 319 studies that we had identified, we consulted our advisory group and narrowed the focus of the meta-analysis to those studies that fell into areas which had been identified as being high priority for the UK in the Marmot Review. 28 This is summarised in Figure 4.
FIGURE 4.
Prioritisation and selection of studies for the meta-analysis.
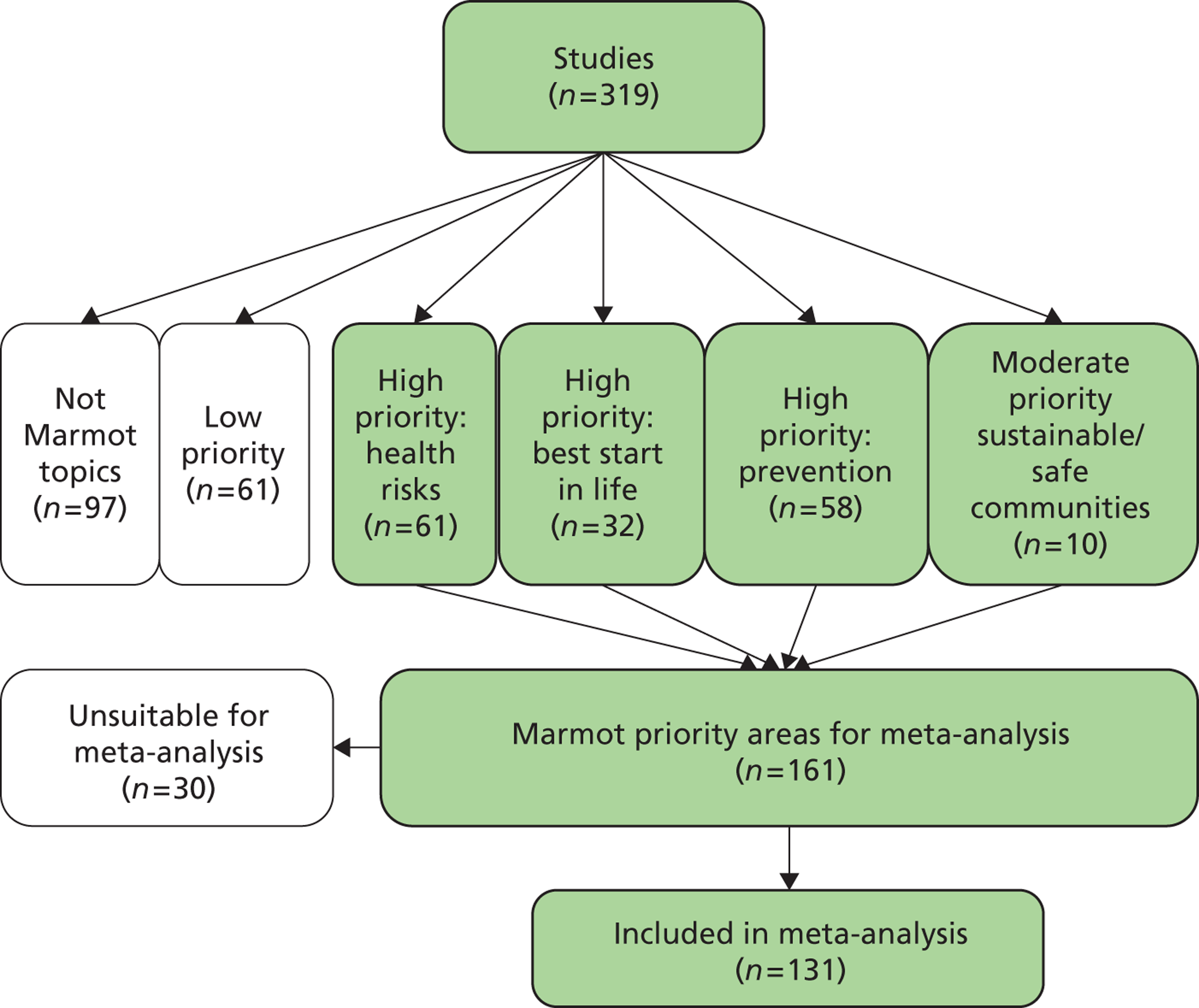
Study characteristics
This section describes the map of research activity as represented by the studies that met our inclusion criteria (319 studies described in 361 reports71–431). The characteristics of all of the studies are provided in Appendix 8, whereas a bibliography of all reports can be found in Appendix 9.
Country
Table 2 details the countries in which the studies were carried out (note that the map was restricted to studies carried out in OECD countries as in the inclusion criteria). As is often the case in systematic reviews of public health research, significantly more studies are carried out in the USA than in any other country, although a reasonable number do hail from the UK.
| Country | No. of studies | % |
|---|---|---|
| UK | 26 | 8.2 |
| USA | 268 | 84.0 |
| Canada | 8 | 2.5 |
| Australia | 3 | 0.9 |
| New Zealand | 2 | 0.6 |
| Other | 13 | 4.1 |
Age groups
Table 3 shows the various age groups targeted by the interventions in the included studies. Proportionately, young people receive the most attention, although the interventions are targeted at all groups.
| Age group of participants | No. of studies | % |
|---|---|---|
| General population based | 51 | 16.0 |
| Children (0–10 years) | 46 | 14.4 |
| Young people (11–21 years) | 180 | 56.4 |
| Adults (22–54 years) | 168 | 52.7 |
| Older adults (55+ years) | 114 | 35.7 |
Sex of participants
Figure 5 depicts the relative numbers of interventions that were targeted at one sex only or at both males and females. The majority of participants were male in < 9% of the studies (n = 2893,157,163,214,227,237,246,260,270,291,292,294,304,305,326,344,361,365,372,383,385,386,394,414,417,428,429,431), whereas the majority were female in 30% of the studies (n = 11072–74,77–79,86,94,95,97,98,102,109,111,120,121,124–126,128–130,132,133,138,140,144,146,147,149–151,155,160–162,168,171,175,177,178,181,183,184,186,187,191,196,198,199,203,205–207,215,223,225,235,239,241,245,249–251,254,261,262,264,265,267,269,272,279,281,283,290,296,297,301,303,308,309,313,318,322,324,334,336,338,340,342,348,350,351,366,373,376,382,387,399,401,402,404,411,413,415,421,424,426,430). Just over half (57%) of the studies included mixed groups of males and females. 71,75,76,80–85,87–92,96,99–101,103–108,110,112–119,122,123,127,131,132,134–137,139,141–143,145,152–154,156,158,159,164–167,169,170,172–174,176,179,180,182,185,188–190,192–195,197,200–202,204,209,210,212,216–220,222,224,226,228,229,232–234,236,238,240,242,243,247,252,258,273–278,284–286,288,289,293,295,298,299,306,307,311,315–317,319,320,323,325,327,328,330,331,335–337,339,341,343,345,346,349,352,353,355,356,358–360,363,364,369–371,374,377–379,384,388,395–398,400,403,405–410,418,420,422,423,425,427
FIGURE 5.
Sex of participants in the studies (n = 319 studies).
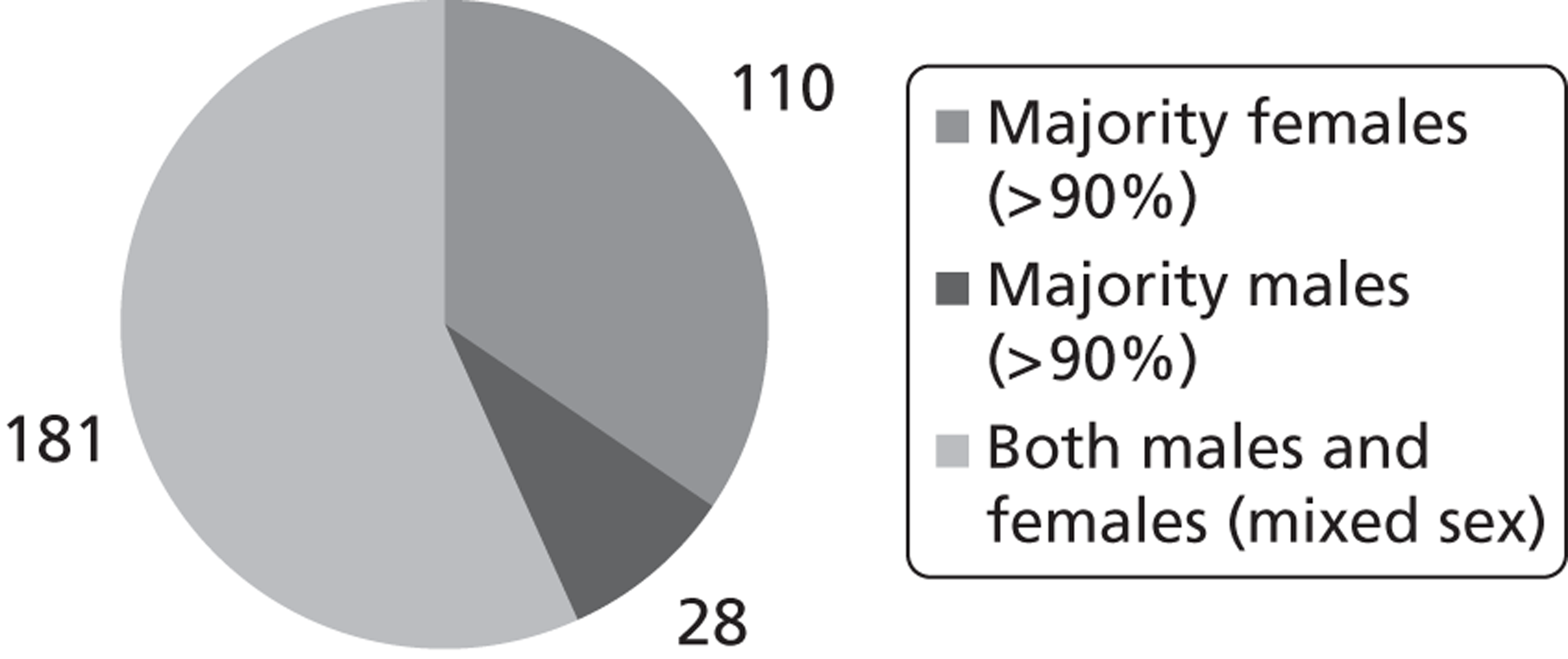
Main PROGRESS-Plus characteristics
In framing the scope of this review we needed to identify, describe and categorise the range of social determinants that, either separately or in combination, influence the health of participants. 432 Given the way that different factors interact in different circumstances, socioeconomic status alone cannot be used to identify potentially vulnerable groups as ‘a person’s socio-economic position is shaped by their position in other structures of inequality’ (p.5). 433 As in previous reviews, socioeconomic position has been captured in terms of (1) broader determinants of health, using the mnemonic of PROGRESS (for Place of residence, Race/ethnicity, Occupation, Gender, Religion, Education, Socioeconomic position and Social capital) developed by Evans and Brown;434 (2) other characteristics that attract discrimination, such as age, disability and sexual orientation, drawing on Krieger’s work;435 and (3) features of relationships such as social exclusion within family or community contexts (e.g. smoking parents, being ‘looked after’ or excluded from school) or time-dependent circumstances (e.g. recovery from illness, or other life transitions) relevant to particular research. Together, these three ways of conceptualising the social determinants of health have been brought together in the PROGRESS-Plus tool. 436
Table 4 contains a breakdown of the main PROGRESS-Plus characteristics of the sample/study population. By some distance, the most frequent category is ethnicity, with 120 studies,71,78–82,85,88,94,96,97,99,103,105–110,112–114,126,127,131,132,140,145,146,150,151,157,161,164–166,173,174,180,182,190,193,194,196,197–199,201,205,210,215,223,224,227,232,236,239,241,243,246,247,249–251,254,258,262,264,265,267,269,275–277,279,283,284,291,292,294,298,299,308,309,311,312,317,318,322,325–327,330,335–337,342,343,348,351,353,359,363,365,366,373,382,386,387,395,400,404,406,409,411,413,422,425,426,428 109 of which were carried out in the USA. The most frequent category of disadvantage in the UK is socioeconomic position (eight studies100,118,149,159,217,240,286,339),followed by ethnicity (four studies157,284,308,355), the reverse of the pattern in the USA. The two studies185,403 in the USA falling into the occupation/employment status category all fell into the worker/employee subcategory rather than blue-collar/manual labourer, with one other study139 focusing on blue-collar workers in Sweden. The three studies338,350,376 in which gender was a cause of potential disadvantage were all focused on females.
| PROGRESS-Plus category | UK | USA | Canada | Australia | New Zealand | Other (specify) | Total |
|---|---|---|---|---|---|---|---|
| Ethnicity: ethnic background | 4 | 109 | 4 | 0 | 1 | 2 | 120 |
| African American/black | 0 | 57 | 0 | 0 | 0 | 0 | 57 |
| American Indian | 0 | 12 | 0 | 0 | 0 | 0 | 12 |
| Asian – Indian, Pakistani, Bangladeshi | 4 | 1 | 0 | 0 | 0 | 0 | 5 |
| Asian – continental (e.g. Chinese, Vietnamese, Filipino) | 0 | 5 | 0 | 0 | 0 | 0 | 5 |
| Hispanic/Latino/Mexican American | 0 | 38 | 0 | 0 | 0 | 0 | 38 |
| Immigrant, refugee, asylum seeker | 0 | 1 | 0 | 0 | 0 | 2 | 3 |
| Other minority ethnic or ‘BME’ | 1 | 6 | 0 | 0 | 0 | 0 | 7 |
| Other indigenous populations | 0 | 2 | 3 | 0 | 1 | 0 | 6 |
| Socioeconomic position | 8 | 39 | 1 | 1 | 1 | 3 | 53 |
| Occupation/employment status | 0 | 3 | 0 | 0 | 0 | 1 | 4 |
| Place of residence | 3 | 16 | 0 | 1 | 0 | 5 | 24a |
| Rural | 0 | 8 | 0 | 1 | 0 | 2 | 11 |
| Urban | 0 | 2 | 0 | 0 | 0 | 0 | 2 |
| Housing characteristics | 0 | 2 | 0 | 0 | 0 | 0 | 2 |
| Other | 3 | 4 | 0 | 0 | 0 | 3 | 9a |
| Sexual orientation | 3 | 8 | 1 | 0 | 0 | 0 | 12 |
| Social capital | 1 | 1 | 0 | 0 | 0 | 0 | 2 |
| Gender | 0 | 3 | 0 | 0 | 0 | 0 | 3 |
| Age | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Disability | 1 | 3 | 0 | 0 | 0 | 0 | 4 |
| Other vulnerable groups | 3 | 29 | 0 | 0 | 0 | 0 | 32 |
| ‘At-risk’ or ‘high-risk’ youths, including homeless/runaways | 0 | 10 | 0 | 0 | 0 | 0 | 10 |
| Substance abuse | 1 | 6 | 0 | 0 | 0 | 0 | 7 |
| Teenage parents/pregnant teens | 0 | 4 | 0 | 0 | 0 | 0 | 4 |
| Other | 2 | 9 | 0 | 0 | 0 | 0 | 11 |
| No main PROGRESS-Plus group | 1 | 31 | 1 | 1 | 0 | 2 | 36 |
| Multiple equally important characteristics | 2 | 30 | 1 | 0 | 0 | 0 | 33 |
The ‘other’ category in the ‘other vulnerable groups’ included at-risk families of newborns, multiethnic, underserved women, parents of children with chronic illnesses, parents of children with juvenile rheumatoid arthritis, pregnant and post-partum women at risk for child placement, pregnant women at risk from partner violence, vulnerable families, low-income mothers and children, phenylketonuric women, migrant farmworkers and male sex workers. These groups were often vulnerable to compounding biological or social influences simultaneously.
Table 5 adds a little more nuance to the picture. It shows, particularly in the US studies, that participants often suffered from more than one type of disadvantage and that socioeconomic position, education and place of residence join ethnicity as particularly significant types of disadvantage.
| Secondary PROGRESS-Plus category | UK | USA | Canada | Australia | New Zealand | Other (specify) |
|---|---|---|---|---|---|---|
| Ethnicity: ethnic background | 1 | 107 | 1 | 2 | 0 | 1 |
| Socioeconomic position | 7 | 123 | 1 | 1 | 0 | 2 |
| Occupation/employment status | 1 | 32 | 1 | 1 | 1 | 5 |
| Education | 0 | 69 | 2 | 1 | 0 | 4 |
| Place of residence | 4 | 67 | 3 | 0 | 0 | 2 |
| Sexual orientation | 0 | 3 | 0 | 0 | 0 | 0 |
| Social capital | 0 | 5 | 0 | 0 | 0 | 0 |
| Gender | 2 | 22 | 1 | 0 | 0 | 2 |
| Religion | 0 | 3 | 0 | 0 | 0 | 0 |
| Age | 2 | 12 | 0 | 0 | 0 | 2 |
| Marital status/family composition | 1 | 37 | 1 | 0 | 1 | 1 |
| Disability | 0 | 1 | 0 | 0 | 0 | 0 |
| Other vulnerable groups | 0 | 26 | 0 | 0 | 0 | 0 |
| No secondary PROGRESS-Plus characteristics | 15 | 60 | 2 | 1 | 1 | 2 |
Addressing health inequalities
In the context of inequalities in health, the manner in which an intervention is delivered is significant. As discussed above, there are multiple and complex determinants of health in different groups, and interventions may therefore need to be carefully targeted; universal programmes risk affecting the population differentially and possibly therefore increase inequalities by benefiting relatively healthy groups disproportionately. Table 6 summarises the approaches taken in the interventions in the map, showing that the majority of interventions are indeed targeted or delivered to a specific PROGRESS-Plus group (237 studies71–75,77–84,86–89,92–96,98–105,107,109,111–113,117,119–126,128–133,137,138,140–142,144–153,155–157,159–172,174–184,186,187,191,193,194,196–199,201,203,205,207,210,214,216,218,219,222–225,227–229,233,237,239,240,242,243,245–247,249,250,254,258,260–262,264–267,270,272–279,281,283–286,288,290–293,296,297,299,301,303–306,308,309,311–313,318–320,322,324,327,328,330,335–338,340–343,345,348,350–354,356,358,359,361,363,366,370,372–374,376–378,382–386,388,394–396,398–404,407–409,413,415,417,418,422–425,427,429–431), rather than being delivered universally (48 studies90,91,108,110,114–116,118,127,134,136,143,154,188,190,192,195,200,204,212,217,220,226,232,238,259,269,289,295,307,314–317,325,326,331,334,339,346,349,364,379,405,410,420,421,426,428). Intervention evaluations could assess the impact on health inequalities in two ways: either by directly targeting a specific PROGRESS-Plus group, for example a minority ethnic group, or by looking at PROGRESS-Plus characteristics within those targeted groups (e.g. assessing differential impact by gender within a minority ethnic group).
| How are health inequalities addressed? | No. of studies (%) |
|---|---|
| Targeted at, or delivered to, specific PROGRESS-Plus group | 237 (74.6) |
| Universal (aimed at the whole group population, not on the basis of individual needs/risks) | 48 (15.0) |
| Targeted and comparison within a PROGRESS-Plus category | 34 (10.7) |
Table 7 expands the above statistics to include the health topics addressed by each method. It shows the wide range of topics addressed by community engagement interventions and also where some of the clearest foci of activity are – and where there may be gaps in our knowledge. For example, within the smoking cessation and prevention literature, it is striking that cessation research is almost exclusively targeted at a PROGRESS-Plus group, but that smoking/tobacco prevention research is universal in nature. A health promotion perspective might suggest that more targeted work on prevention is needed to reduce the need for targeted cessation activity.
| Code | Targeted | Universal | Targeted and comparison | Total |
|---|---|---|---|---|
| Antenatal (prenatal) care | 7 | 0 | 0 | 7 |
| Asthma prevention/treatment/management | 5 | 0 | 0 | 5 |
| Breastfeeding | 12 | 0 | 1 | 13 |
| Cardiovascular disease | 10 | 6 | 2 | 18 |
| Cancer prevention | 7 | 0 | 1 | 8 |
| Cancer screening/detection | 27 | 4 | 10 | 41 |
| Care of older people | 3 | 0 | 1 | 4 |
| Child abuse prevention | 1 | 0 | 1 | 2 |
| Child illness and ill health | 2 | 1 | 1 | 4 |
| Diabetes prevention/management | 12 | 0 | 2 | 14 |
| Disabilities and chronic illness | 6 | 0 | 0 | 6 |
| Healthy eating/nutrition | 3 | 1 | 1 | 5 |
| HIV/AIDS/STI prevention/risk reduction | 43 | 4 | 4 | 51 |
| Hypertension | 3 | 2 | 1 | 6 |
| Immunisation | 4 | 0 | 0 | 4 |
| Injury prevention | 3 | 1 | 1 | 5 |
| Mental health | 3 | 0 | 1 | 4 |
| Neighbourhood renewal/regeneration | 2 | 1 | 1 | 4 |
| Obesity prevention/weight reduction | 14 | 1 | 0 | 15 |
| Parenting | 6 | 0 | 1 | 7 |
| Partner violence | 1 | 0 | 0 | 1 |
| Physical activity | 5 | 1 | 0 | 6 |
| Public health/health promotion/prevention | 11 | 5 | 0 | 16 |
| Reproductive health | 5 | 3 | 1 | 9 |
| Sexual health | 3 | 5 | 0 | 8 |
| Smoking cessation | 13 | 1 | 0 | 14 |
| Smoking/tobacco prevention | 0 | 4 | 0 | 4 |
| Substance abuse | 14 | 6 | 2 | 22 |
| Suicide prevention | 0 | 1 | 0 | 1 |
| Tuberculosis | 4 | 0 | 1 | 5 |
| Violence prevention | 3 | 0 | 2 | 5 |
| Other topics (specify) | 7 | 1 | 0 | 8 |
| Not Marmot topics | 1 | 0 | 0 | 1 |
Table 8 shows where each of the interventions in the 319 studies was delivered. Some of these sites, such as residential care and the WIC (Women, Infants and Children) clinic, suit targeted interventions; others either suit universal interventions or need additional measures to distinguish disadvantaged groups, such as measures of workforce, school enrolment or neighbourhood populations. (The WIC scheme provides federal grants to US states for supplemental foods, health-care referrals and nutrition education for low-income pregnant, breastfeeding and non-breastfeeding post-partum women and to infants and children up to age 5 years who are found to be at nutritional risk. A WIC clinic is a health-care clinic available under this scheme.)
| Intervention site | No. of studies | % |
|---|---|---|
| Community setting | 141 | 44.2 |
| Computer-based, internet-based and virtual interventions | 3 | 0.9 |
| Educational setting (school, college, university) | 73 | 22.9 |
| Home situation (not residential care home) | 88 | 27.6 |
| Mass media – untailored (generic) | 39 | 12.2 |
| Outreach | 33 | 10.3 |
| Primary health care (e.g. GP) | 27 | 8.5 |
| Religious setting (e.g. church) | 28 | 8.8 |
| Residential care (includes nursing homes, sheltered housing) | 7 | 2.2 |
| Secondary health-care unit (e.g. hospital, specialist clinic) | 45 | 14.1 |
| Telephone, print or audio/visual media – tailored | 93 | 29.2 |
| WIC clinic | 10 | 3.1 |
| Workplace site | 13 | 4.1 |
| Unclear/not specified | 18 | 5.6 |
Table 9 details the person or people who delivered the public health intervention.
| Intervener | No. of studies | % |
|---|---|---|
| Community member | 135 | 42.3 |
| Community worker | 52 | 16.3 |
| Computer | 3 | 0.9 |
| Counsellor | 6 | 1.9 |
| Health professional (e.g. GP, dietician, nurse) | 68 | 21.3 |
| Health promotion practitioner | 9 | 2.8 |
| Parent | 8 | 2.5 |
| Peer | 132 | 41.4 |
| Psychologist | 1 | 0.3 |
| Religious leader (e.g. parson, priest) | 6 | 1.9 |
| Researcher | 12 | 3.8 |
| Social worker | 6 | 1.9 |
| Teacher and education professional (e.g. lecturer, principal) | 36 | 11.3 |
| Other | 28 | 8.8 |
| Unclear/not reported | 15 | 4.7 |
The final dimension of interventions captured in the map is intervention type (Table 10). By far the most common type of intervention involved education carried out by either a peer or a community member (10172,73,77,87,93,95,98,100,102,103,118,120,125,133,147,149,153,158,161–164,166,172,176,177,179,181,182,188,192,200,202,209,212,214,219,220,222,233,241,245,247,249,264,270,273,274,284,293,296–299,304,305,308,309,312–318,324,330,337,341,342,345,348,352,354,358,360,361,364,369,373,376,378,379,387,394,396–398,400,401,407,409,410,413,415,422–424,426,429,431 and 11175,79–81,83–85,90–92,94,96,101,103–106,109,112,113,115,117,118,122–124,128,131,132,134,136,137,142,144,145,147,148,150,152,154,158,165,172–174,177,179,182,190,193–195,197–199,201,204,206,207,209,210,212,217,218,222,235,238,243,251,254,262,265,266,272,274,276–279,283,285,288,290–292,298,301,315,316,319,320,322,323,325–327,331,336,338,346,350,354,364,366,377,385,406,407,417,424,430 studies respectively). A cross-tabulation of intervention type by provider is provided in Table 11.
| Code | No. of studies | % |
|---|---|---|
| Education | 252 | 79.0 |
| Advice | 166 | 52.0 |
| Social support | 116 | 36.4 |
| Skill development/training | 112 | 35.1 |
| Activities (e.g. community fairs/fetes) | 95 | 29.8 |
| Service access | 85 | 26.6 |
| Resource access | 68 | 21.3 |
| Role modelling, role playing | 52 | 16.3 |
| Counselling (based on the psychological needs of the individual) | 49 | 15.4 |
| Environmental modification | 46 | 14.4 |
| Incentives | 33 | 10.3 |
| Physical activity, exercise | 32 | 10.0 |
| Screening (medical screening, e.g. breast screening) | 24 | 7.5 |
| Risk assessment (not medical screening) | 22 | 6.9 |
| Other | 12 | 3.8 |
| Clinical treatment | 7 | 2.2 |
| Professional training | 3 | 0.9 |
| Immunisation | 2 | 0.6 |
| Biofeedback | 2 | 0.6 |
In Table 12 we classified the studies according to the policy priorities identified in the Marmot Review,28 as described in Chapter 2. The final table in the map (Table 13) cross-tabulates topic against the main PROGRESS-Plus group in the study. It gives a good indication regarding the distribution of health issue and population group in the map.
| Code | Community member | Community worker | Computer | Counsellor | Health professional (e.g. GP, dietician, nurse) | Health promotion practitioner | Lawyer | Parent | Peer | Psychologist | Religious leader (e.g. parson, priest) | Researcher | Residential worker | Social worker | Teacher and education professional (e.g. lecturer, principal) | Other | Unclear/not reported |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Education | 111 | 42 | 3 | 4 | 60 | 9 | 0 | 7 | 101 | 0 | 6 | 11 | 0 | 5 | 35 | 22 | 12 |
| Advice | 69 | 31 | 2 | 5 | 42 | 2 | 0 | 4 | 71 | 1 | 2 | 5 | 0 | 5 | 7 | 12 | 6 |
| Social support | 56 | 24 | 1 | 4 | 31 | 1 | 0 | 3 | 50 | 0 | 3 | 8 | 0 | 3 | 11 | 5 | 4 |
| Skill development | 43 | 25 | 0 | 3 | 28 | 4 | 0 | 6 | 47 | 0 | 2 | 4 | 0 | 2 | 19 | 8 | 5 |
| Activities (e.g. fairs/fetes) | 53 | 18 | 1 | 2 | 23 | 5 | 0 | 4 | 35 | 0 | 3 | 6 | 0 | 3 | 24 | 12 | 8 |
| Service access | 40 | 19 | 2 | 1 | 25 | 2 | 0 | 1 | 31 | 0 | 1 | 2 | 0 | 3 | 3 | 8 | 4 |
| Resource access | 32 | 17 | 1 | 0 | 11 | 3 | 0 | 1 | 29 | 0 | 1 | 2 | 0 | 1 | 11 | 8 | 5 |
| Role modelling, role playing | 21 | 7 | 1 | 0 | 6 | 0 | 0 | 3 | 28 | 0 | 0 | 3 | 0 | 1 | 13 | 3 | 3 |
| Counselling | 15 | 11 | 1 | 5 | 17 | 1 | 0 | 0 | 19 | 1 | 0 | 3 | 0 | 2 | 4 | 4 | 3 |
| Environmental modification | 26 | 9 | 0 | 0 | 7 | 4 | 0 | 1 | 15 | 0 | 0 | 2 | 0 | 1 | 9 | 7 | 6 |
| Incentives | 13 | 10 | 1 | 1 | 9 | 2 | 0 | 2 | 11 | 0 | 1 | 4 | 0 | 0 | 5 | 4 | 0 |
| Physical activity | 20 | 3 | 0 | 1 | 11 | 4 | 0 | 2 | 8 | 0 | 1 | 3 | 0 | 2 | 6 | 5 | 1 |
| Screening | 11 | 8 | 0 | 0 | 13 | 3 | 0 | 0 | 7 | 0 | 1 | 0 | 0 | 1 | 0 | 2 | 1 |
| Risk assessment | 13 | 6 | 0 | 1 | 5 | 1 | 0 | 0 | 4 | 0 | 2 | 2 | 0 | 1 | 0 | 2 | 2 |
| Other | 5 | 4 | 0 | 1 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 1 |
| Clinical treatment | 0 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| Professional training | 2 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | 1 | 0 |
| Immunisation | 1 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Biofeedback | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Marmot Review category | No. of studies | % |
|---|---|---|
| Health risks | 61 | 19.1 |
| Substance abuse (alcohol and/or drug) | 25 | 7.8 |
| Smoking/tobacco cessation | 16 | 5.0 |
| Obesity prevention/weight reduction | 16 | 5.0 |
| Smoking/tobacco prevention | 4 | 1.3 |
| Best start in life | 32 | 10.0 |
| Breastfeeding | 13 | 4.1 |
| Parenting | 6 | 1.9 |
| Antenatal | 7 | 2.2 |
| Immunisation | 5 | 1.6 |
| Other child (ill) health | 1 | 0.3 |
| Prevention of ill health | 58 | 18.2 |
| Cardiovascular disease/hypertension prevention | 17 | 5.3 |
| Public health/health promotion not captured elsewhere | 17 | 5.3 |
| Physical activity | 9 | 2.8 |
| Cancer prevention | 8 | 2.5 |
| Healthy eating | 7 | 2.2 |
| Sustainable and safe places and communities | 10 | 3.1 |
| Safe community | 5 | 1.6 |
| Neighbourhood renewal/regeneration | 5 | 1.6 |
| Mortality as an outcome | 61 | 19.1 |
| Cancer screening – breast | 22 | 6.9 |
| Cancer screening – breast and cervical | 12 | 3.8 |
| Cardiovascular disease/hypertension management/treatment | 7 | 2.2 |
| Mental health | 6 | 1.9 |
| Violence prevention | 6 | 1.9 |
| Cancer screening – cervical | 4 | 1.3 |
| Cancer screening – other | 4 | 1.3 |
| Code | Ethnicity: ethnic background | Socioeconomic position | No main PROGRESS-Plus group | Multiple equally important characteristics | Place of residence | Sexual orientation | Occupation/employment status | Education | Social capital | Gender | Religion | Age | Marital/family status | Disability | Other vulnerable groups |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total studies with characteristic | 121 | 53 | 35 | 33 | 24 | 12 | 4 | 0 | 2 | 3 | 0 | 1 | 0 | 4 | 34 |
| Antenatal (prenatal) care | 1 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| Asthma prevention/treatment/management | 1 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Breastfeeding | 3 | 9 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cardiovascular disease | 9 | 4 | 2 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cancer prevention | 2 | 2 | 1 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cancer screening/detection | 24 | 8 | 3 | 3 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Care of older people | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Child abuse prevention | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Child illness and ill health | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Diabetes prevention/management | 11 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Disabilities and chronic illness | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 |
| Healthy eating/nutrition | 2 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| HIV/AIDS/STI prevention/risk reduction | 16 | 3 | 5 | 5 | 3 | 10 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 7 |
| Hypertension | 6 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Immunisation | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Injury prevention | 0 | 0 | 1 | 1 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mental health | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Neighbourhood renewal/regeneration | 0 | 1 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Obesity prevention/weight reduction | 11 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Parenting | 0 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Partner violence | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Physical activity | 1 | 1 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Public health/health promotion/prevention | 6 | 3 | 1 | 3 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Reproductive health | 1 | 1 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Sexual health | 2 | 0 | 3 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Smoking cessation | 7 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Smoking/tobacco prevention | 1 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Substance abuse | 6 | 2 | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 |
| Suicide prevention | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Tuberculosis | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Violence prevention | 2 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Other topics | 3 | 3 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Not Marmot topics | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Chapter 4 Synthesis I: theoretical synthesis of models, mechanisms and contexts for community engagement
About this chapter
The previous chapter has presented some of the basic characteristics of the experimental studies in this review that evaluate the impact of community engagement interventions on a range of health outcomes. Before we examine the direction and magnitude of their effects, however, we will examine the theoretical basis for community engagement, recognising that there is no agreed consensus about what it is and how it might work. The theoretical synthesis concludes in Chapter 8 by outlining a logical framework that maps the theories by which different forms of community engagement are thought to result in improved outcomes. The reason for this split is that its development was an iterative process: it began with the review of theories and models presented in this chapter and then continued through the analysis of outcomes, processes and resources; the final presentation of the new framework therefore comes after the other chapters that also contributed to it.
This chapter answers the first two of our RQs:
-
RQ1: What is the range of models and approaches underpinning community engagement?
-
RQ2: What are the mechanisms and contexts through which communities are engaged?
Summary of findings
-
Community – this review has taken a broad definition: ‘a group of people united by at least one but perhaps more than one common characteristic, including geography, ethnicity, shared interests, values, experience or traditions’ (p. 88). 437
-
Engagement – this review uses it as an umbrella term encompassing a continuum of approaches to engaging communities in activities to improve population health and/or reduce health inequalities. 14 These range from more limited amounts of engagement (‘information’ and ‘consultation’) towards ‘development’, ‘participation’ and ‘empowerment’.
-
Empowerment – considered the ideal in models of community engagement, it is rooted in concerns about social justice and movements promoting social and structural change. It is considered socially desirable, equitable and addresses some of the social determinants of ill health, and thus will also result in improved health and reductions in health inequalities. True community empowerment needs to begin within the community; this is at odds with many of the studies in this review, which often start from an academic or health service/systems perspective.
-
Some models of community engagement based on a community empowerment or ideological perspective emphasise the achievement of sociopolitical goals through empowering communities to take control of their own destinies; many interventions take a pragmatic or health systems perspective and seek to involve communities in interventions for utilitarian reasons, because it is thought to make them more effective.
-
Some studies in this review have evaluated the effectiveness of utilising peers or lay people to deliver the intervention. These interventions often do not seek to empower, nor sometimes even to involve communities in intervention design, but achieve a degree of engagement nevertheless; existing models of community engagement often do not encompass this strategy.
Defining ‘community engagement’
Defining ‘community’
The commissioning brief for this project defined community engagement as ‘approaches to involve communities in decisions that affect them’. Mason et al. 40 have defined community engagement for health promotion as engaging groups of people who share geographies, interests or identities; these are the ‘groups with distinct health needs and/or demonstrable health inequalities’ of the commissioning brief. However, there are many different ways of understanding what a community is, and the boundaries between where communities stop and individuals begin can be blurred; other work has thus reviewed both patient and community engagement,438 as the rationale for involving both patients and communities in decisions that affect them can be similar. Indeed, it is possible for the terms ‘patient’, ‘public’ and ‘community’ to be used interchangeably in some contexts, and definitions of what the defining characteristics of a community are vary considerably. 438 Brenner and Manice437 stated: ‘community is a fluid concept; individuals may belong to multiple communities at any one time’ (p. 88). In 1984, Wandersman suggested that there are two broad conceptualisations of community, one being geographical in nature (‘a place’) and the other concerned with ‘a set of relationships and resources’ (cited in Kelly,439 p. 417). This definition is particularly useful – and visionary for its time – when one needs to include virtual communities within an overall understanding of community. Building on these ideas, we have found the following definition helpful in this review: ‘a group of people united by at least one but perhaps more than one common characteristic, including geography, ethnicity, shared interests, values, experience or traditions’ (p. 88). 437
This definition comes closest to encapsulating the range of communities that we have encountered in this review, as a ‘community’ may be no more than a group of people who share a similar characteristic, or it may be a highly organised and integrated group of people pursuing a shared goal.
The above conceptualisation of a community is very much a minimalist viewpoint; it does not require the community to function in any coherent way (as it may have been defined from outside, e.g. by health professionals). More demanding concepts of community have been summarised by the Clinical and Translational Science Awards (CTSA) Community Engagement Key Function Committee Task Force440 and include a systems perspective, which conceptualises different constituents such as individuals, schools and businesses as acting together, like a ‘living creature’; a social perspective, which emphasises the role that social networks play in the operationalisation of the community, and thus the importance of understanding where the network (i.e. community) needs strengthening; a virtual perspective, which focuses on online communities; and the individual perspective, which emphasises individuals’ sense of their community memberships and acknowledges that this may be at odds with researchers’ perspectives, and also the fact that an individual may belong to multiple communities.
Although we have adopted an open definition of community, it is important to note that most community engagement initiatives in this review do involve communities that function (to varying degrees) as integrated systems and that understanding the interplay of the different actors they contain may contribute to developing an appreciation of how they can be mobilised to improve people’s health. Having said this, those in the communities defined by those outside them may well self-identify themselves in quite different ways. The social perspective mentioned above is useful in this regard. Rather than conceptualising communities as being made up of people with shared attributes (e.g. healthy, high income, female), social network theory offers an alternative view which emphasises the relationships and ties that individuals have within their various communities. Some authors suggest that a resource stemming from these relationships is social capital. Although conceived differently by different scholars (see, for example, references 441–443), the general theory suggests that social networks characterised by reciprocity, trust and shared norms can facilitate the achievement of specific shared goals. 444 Social networks, however, can be either health promoting or harming depending on the nature of shared norms. Strong social ties that benefit members of one particular group may also be used to exclude others outside the group from sharing those resources (p. 15). 444 Although this leaves less room for individual agency, it can be a useful way of visualising community structure and identifying the different roles that people within a community might play.
The rationale for examining community engagement in the context of health inequalities needs some consideration at this point (see Chapter 1, The challenge of health inequalities in the UK, for a discussion of health inequalities). Although the use of community engagement to improve the health of disadvantaged groups has been recommended, as they tend to be more disenfranchised than other groups and lack power and control over their lives (e.g. references 15 and 38), individuals may be less able to take advantage of traditional health promotion messages because of this lack of control. Health improvement may thus be less successful in these areas and any universal community engagement intervention (covering both relatively advantaged and disadvantaged groups) risks increasing health inequalities. However, it may be that engaging communities in improving their health achieves the joint objectives of both improving health and making good some of the social gradient in ‘healthy’ community characteristics identified elsewhere. 28 A conceptual framework for reducing inequalities in health through community engagement thus needs to consider some of the challenges to engagement that may exist, along with some possible mechanisms for achieving participation where engagement may be relatively lacking. (We have given here functional definitions of ‘community’ that were operationalisable in this review. The term is of course contested on many levels; see, for example, Finlayson445 and Hillery446 and a recent report by Hamalainen and Jones447 for a critical analysis of the concept that is particularly useful for those working in community engagement.)
Thus, although we recognise that some of the reasons for engaging communities in decisions that affect them may overlap with patients’ involvement in decision-making, in the context of improving inequalities in health we have made an explicit differentiation between the two. The ‘engagement’ (which will be discussed next) needs to be with groups (communities) of individuals and, rather than being concerned with individual’s decision-making, we are concerned with collective decision-making on the part of service users. This has led us to including potential benefits and harms for communities in the range of outcomes that are considered – as well as individuals’ health.
Defining ‘engagement’
‘Engagement’ is a second contested concept that is often associated with terms such as ‘community development’, ‘participation’, ‘empowerment’, ‘competence’, ‘capacity’, ‘cohesiveness’ and ‘social capital’. 448,449 To locate this work within a developing corpus of literature, which is building our understanding of community engagement in the UK, we have employed the same definition as used in an earlier report that laid out a conceptual framework for community engagement. ‘Community engagement’ is therefore ‘an umbrella term encompassing a continuum of approaches to engaging communities of place and/or interest in activities aimed at improving population health and/or reducing health inequalities’ (p. 2). 14
Such a broad definition covers activities that range greatly in scope and impact, from the relatively unengaged exchange of information, through various models of citizen consultation to the delegation of power and control to community organisations, and therefore is particularly useful for investigating a diverse literature.
Other terms overlap conceptually but do not capture the issue of community engagement. These include ‘community participation’, ‘consultation’, ‘information’, ‘development’ and ‘empowerment’. It is important to note that ‘community participation’ and related terms (e.g. ‘community-based participatory research’) sometimes imply both a specific set of research methods or approaches and research that builds relationships with the goals of societal transformation/improved health. Thus, in academic circles, terms can have the joint meaning of being concerned with methods of service design and evaluation as well as being an end in themselves. The term ‘community participation’ is often used interchangeably with ‘engagement’ and, as WHO observes, the quantity of terms and the lack of precision with which they are employed can cause confusion. WHO450 defines ‘community participation’ as:
A process by which people are enabled to become actively and genuinely involved in defining the issues of concern to them, in making decisions about factors that affect their lives, in formulating and implementing policies, in planning, developing and delivering services and in taking action to achieve change.
p. 10
The above definition is considerably narrower than our definition of engagement, and demands a high degree of community involvement – and influence – over local activities. ‘Community engagement’ is, however, a difficult term to define, as it:
Is a rich concept that varies with its application and definition. The way that participation is defined also depends on the context in which it occurs. For some, it is a matter of principle; for others, practice; for still others, an end in itself.
p. 7451
Thus, ‘participation’ does not capture the idea that communities can participate to differing degrees.
Unlike the above, the term ‘community development’ has a clearer definition and a long history of use. It is defined by WHO450 as:
A way of working underpinned by a commitment to equity, social justice and participation that enables people to strengthen networks and to identify common concerns and supports people in taking action related to the networks. It respects community-defined priorities, recognizes community assets as well as problems, gives priority to capacity-building and is a key mechanism for enabling effective community participation and empowerment.
p. 11
Community consultation and information-sharing are perhaps more straightforward concepts. Community consultation suggests that people participate by being consulted or by answering questions. Agents who are external to the community lead in defining the problem and articulating solutions. Such a consultative process does not concede any sharing of decision-making and professionals are typically not obligated to take on board people’s views. 452 Participation through information-sharing on the other hand involves the flow of information between community member(s) and agents. Although often considered a less active form of participation, Cornwall453 argues that ‘transparency over certain kinds of information opens up the possibility of collective action in monitoring the consistency of rhetoric with practice’ (p. 272).
Possibly the most demanding form of community engagement, in terms of the delegation of power and control, is often termed ‘community empowerment’. This concept is discussed at length below and for the purposes of this section we use a definition from Empowerment and Poverty Reduction published by the World Bank:454 ‘Empowerment is the expansion of assets and capabilities of poor people to participate in, negotiate with, influence, control, and hold accountable institutions that affect their lives’ (p. vi).
Empowerment is often portrayed as the ‘ultimate’ form of engagement, as it requires the ceding of power and control to people who traditionally lack such power and control. Feminist perspectives on power and empowerment direct us towards the complexity of the relationship between engagement and empowerment. For example, Yoder and Kahn455 advance a gender-based conceptualisation of power, contrasting a female aim to seek ‘power to’ (i.e. personal empowerment) with a male aim of seeking ‘power over’ (i.e. domination and control). Others have argued that ‘empowerment is a process that changes social and political relationships between individuals and the communities and networks within which social and political power circulate’ (p. 45). 456 Therefore, when engaging communities the directions of these changes are important and considerations of inequalities in gender and ethnicity ought to be considered.
The interaction of these concepts suggest a hierarchical relationship in which each concept is a natural progression from the last. Participation is a clear prerequisite of empowerment and, as community development is a ‘key mechanism’ for both participation and empowerment, it follows that participation and empowerment are subsets of community development. In our ontology of engagement, ‘engagement’ is an umbrella term that encompasses all approaches and activities below it: community development, empowerment, information, consultation and participation.
A visual representation of these related concepts is given in Figure 6, showing that all terms are subsets of the umbrella term ‘engagement’ and that each approach is a necessary condition for its immediate subset.
FIGURE 6.
Set relationships in concepts around engagement.
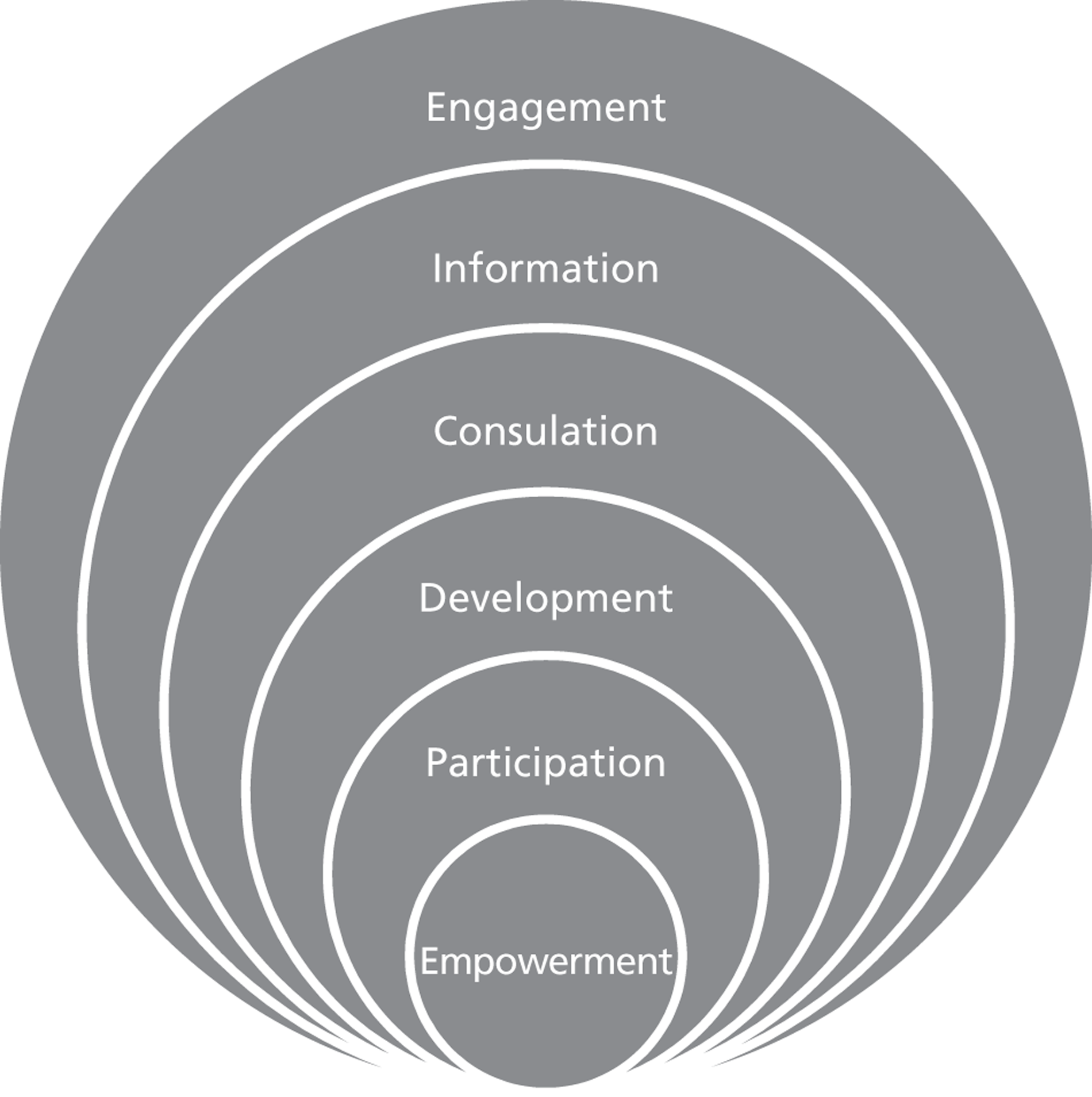
Although the above hierarchy will fit many definitions, it is important to recognise that many people have different conceptualisations of engagement and, as this extended quotation from Stuart Hashagen42 shows, would see ‘engagement’ as involving significant partnership and empowerment:
Engagement suggests a different sort of relationship. It suggests that there is a ‘governance’ system and a ‘community’ system. To build the collaborative relationships on which a complex activity such as community planning would depend, it is necessary for the governance system to fully understand the dynamics of the communities with which it seeks to work, and to be prepared to adapt and develop structures and processes to make them accessible and relevant to those communities. In this way, the term engagement warns us against making assumptions about communities: it asks for a dialogue. It also implies that the development of the relationship itself will need to be a focus for attention: ‘government’ will need to engage with communities as well as asking communities to engage with it.
p. 2
As authors, we have discussed whether the term ‘engagement’ encapsulates the studies that we have been reviewing and whether alternative language, such as ‘participation’, ‘empowerment’ or ‘involvement’, might be better. However, as discussed above, although the language used around community engagement lacks precision, it is possible to identify key relationships and show that each has particular characteristics. Because the extent to which the community is ‘involved’, ‘engaged’ or ‘participating’ varies widely between the studies that we have identified, the umbrella term ‘engagement’ includes all of the ways of interacting with communities contained in the studies found in the review.
This section has been a relatively brief definitional overview to identify relationships between some of the key terms found in the studies that we have reviewed and provide a transparent description of the development of our definition. However, there are a wide range of theoretical models that underpin these different approaches. To develop a conceptual framework that encapsulates this diversity, we now review some of the main models of community engagement.
Models of ‘engagement’
The theoretical foundations of community engagement have developed from broad areas of society including civil rights, public health, medicine, adult learning, youth work and mental health. Although developed from more broad civic-based ideas, these models were soon adopted and modified for use in health services, where managers are charged with its integration whilst simultaneously grappling with costs, effectiveness and ensuring a responsive health-care system. A serious problem for those interested in the impact of community engagement has been the large number of overlapping, competing and contradictory definitions of what community engagement (which is also used interchangeably with other terms such as ‘community participation’, ‘involvement’, ‘mobilisation’ and ‘empowerment’) might be. The multitude of definitions has hindered progress towards assessing the impact of community engagement on health (and other outcomes). 14,457 The reason that the meaning of community engagement is so fuzzy lies in the ways that different people have utilised it to pursue their own ends. In the words of Morgan:449
The proliferation of meanings attached to the phrase ‘community participation in health’ . . . has allowed it to be analyzed as a political symbol capable of being simultaneously employed by a variety of actors to advance conflicting goals, precisely because it means different things to different people.
p. 222
This analysis rings true in light of the many hundreds of studies examined in this review. Although there are some approaches that emphasise the achievement of sociopolitical goals through empowering communities to take control of their own destinies, many interventions take a pragmatic stance and seek to involve communities in interventions for utilitarian reasons, because it is thought to make them more effective (see also Cornwall458 for an examination of democracy and engagement).
Models based on a utilitarian (pragmatic) or health systems perspective
One of the critical points of departure among those advocating community engagement approaches concerns ‘who’ initiates engagement and therefore who is deciding who the community is/are. Community members may engage with issues about their own or their families’ health on an individual basis, but efforts to address inequalities require a collective effort in which a community builds its own identity and engages public institutions, or members of public institutions reach out to the community that they have defined as relevant to the issue. The community may have pre-existing social relationships; or it may be formed to respond to a particular problem. Whether pre-existing or newly evolving, the community may define an issue or need that they wish to change; or others external to the community may identify the issue that requires change, and subsequently define the relevant community, which may consist of individuals or pre-existing groups (‘engagees’). Individuals or groups may thus also come to identify or imagine themselves as a community through the process of engagement. When members of the community define themselves, they may be communities of interest or populations with specific needs. When others define the community, the community could be a socioeconomically disadvantaged population, or ‘communities’ bound by geography for instance. 459 Thus, communities are defined in many different ways, and people living within those communities can identify themselves differently, depending on the context. 459
In the classical patient/consumer involvement model, rationales for health services to engage service users include:
-
involving patients in the decision-making process to choose the most appropriate treatment for complex conditions and improve treatment delivery, patient experiences and patient outcomes
-
involving patients because they have a right to be involved in decisions made about them
-
sharing responsibility to reduce the scope for blame to be attributed on the health service and to provide opportunities for mistakes to be identified. 438
When broadened out to involve communities, many of the aforementioned rationales remain valid, although the model is still one of health (and other) services reaching out to engage particular (actual or potential) service users who they have identified as requiring assistance. In these situations, members of the community who are being engaged may identify themselves as being members of that community, or they may have no more in common with one another than the ‘one common characteristic’437 mentioned above.
The theory of change that accompanies such programmes might resemble that outlined in Figure 7. In this model, the need for intervention is usually identified by expert observation and the appropriate response devised within existing policy, practice and resource frameworks. The utility of involving stakeholders for the reasons given above is becoming widely accepted and people are often involved to differing degrees to improve acceptability and take-up. The key mechanism for improvement here is that the intervention is more effective than it otherwise would have been because of the incorporation of the perspectives of those targeted; the question to be explored later is therefore whether health outcomes increase in proportion to the amount that stakeholders are able to influence (or in some situations to control) the intervention.
FIGURE 7.
Theory of change for patient/consumer involvement.
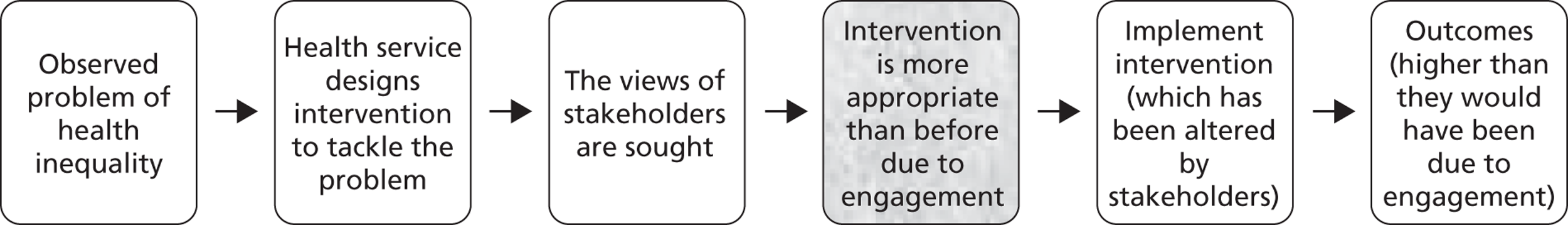
An evaluation by Davis et al. 243 illustrates this model of engagement. The Pathways intervention was developed as a culturally appropriate obesity prevention programme for American Indian school children. In a bid to address nationally high rates of obesity amongst American Indian populations, researchers worked with community members and teachers to develop culturally appropriate curricula, family information packs and family events focused on obesity prevention. This intervention is an example of one that is developed out of a need identified by those outside of the community, in which community members ‘buy in’ to the idea of doing something to tackle an issue, but appear to have very little influence on the initiative’s development, management and evaluation.
A related, but different, model of engagement is the use of peers or lay community members to deliver the intervention. This may be combined with the above health services model, but the particular ‘active ingredient’ in this case is that, rather than being delivered by health professionals, etc., the intervention is delivered by peers/lay people and is more likely to be effective because peers/lay people have more credibility, are able to communicate more effectively and persuasively and are able to respond better to situations ‘on the ground’ than people who are less immersed in the community of interest. 460,461 (There is a veritable industry of peer-delivered health promotion – particularly in North America – which is supported by organisations such as the National Association of Peer Program Professionals; www.peerprogramprofessionals.org/.)
The theory of change that accompanies peer-/lay-delivered interventions is shown in Figure 8. This is a deliberately simplified version which emphasises the main difference from other approaches: the medium of delivery. For example, Anderson et al. 72 describe an evaluation of peer counselling on exclusive breastfeeding in a predominantly Latina low-income community in the USA. Local mothers were trained in breastfeeding counselling skills and provided antenatal, in-hospital and postnatal breastfeeding support and education to women. Initiation and exclusive breastfeeding rates were concurrently assessed. In this model, community members have a high degree of involvement in intervention delivery but do not contribute as partners to that intervention’s design or evaluation. Of course, there are many examples of interventions that have been designed in collaboration with the community of interest which are also delivered by peers, and the theory of change in this case would be a combination of the two. As South et al. 462 conclude, the relationships between peer/lay intervention providers and those that they are working with is complex, and the above theory of change treats the complex range of these interactions as a ‘black box’ within which many different processes take place: ‘social relationships are core to understanding lay health worker programmes and therefore analysis needs to take account of the capacity for community members to move within a spectrum of participation defined by increasing responsibility for others’ (p. 656).
FIGURE 8.
Theory of change for peer-/lay-delivered interventions.
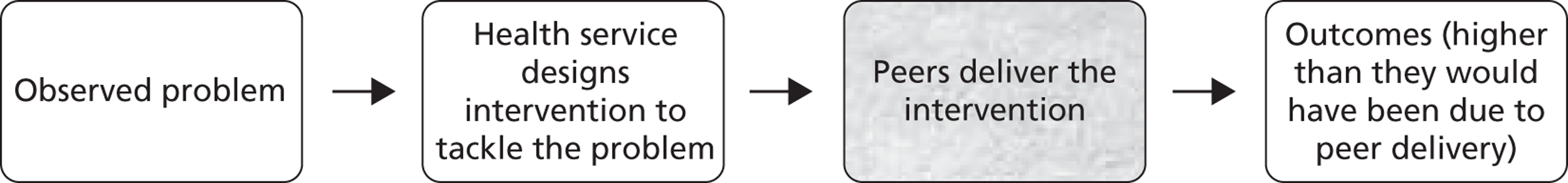
Margaret Whitehead432 considerably extends the above model in her typology of actions to tackle social inequalities in health. Here, rather than a health problem being observed, a health inequality is the focus of attention. Whitehead identifies four categories of policies and interventions to tackle health inequalities: strengthening individuals, strengthening communities, improving living and working conditions and promoting healthy macro-policies. Although the model (outlined in Figure 9) is similar to the model above, in that the identification of the problem and (to differing degrees) its solutions are located outside the community, the typology has a strong emphasis on individual and community empowerment. Individual empowerment is usually framed around a deficit model, in which an individual’s lack of knowledge, skills, self-confidence, etc. is addressed by intervention. More recently, there has been an increasing emphasis on capability models, which recognise individuals’ skills and strengths and seek to remove barriers to their application in healthy lifestyle choices. In strengthening communities, the model addresses social isolation, acknowledging that people’s inability to be fully part of society can have serious impacts on their health. Two models here are put forward: horizontal and vertical. Horizontal interventions aim to strengthen connections within communities, the theory being that well-functioning communities will be able to influence their locality to create healthier conditions. Vertical interventions aim to improve connections between different levels on the social scale to improve inclusiveness and participation, the theory here being that ‘fostering solidarity throughout society produces a less divided society, one with smaller social inequalities and hence more equitable access to the resources for health’ (p. 474). 432
FIGURE 9.
The logic of health inequalities interventions.
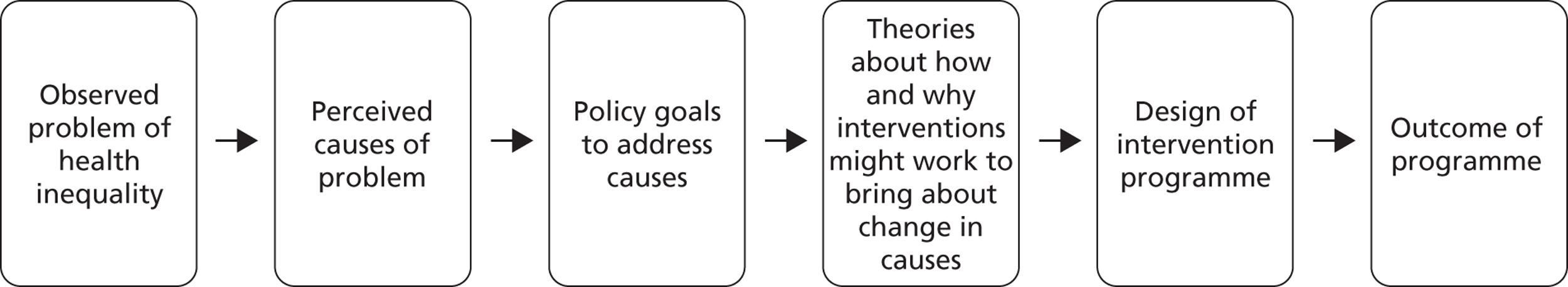
The above comes mostly from a health services perspective, and is the starting point for many interventions (see below). However, models of community engagement also encompass community-led interventions, in which the community drives engagement and specifies the outcomes of interest and the means by which they are to be achieved. This model, often known as community ‘empowerment’, is outlined by Woodall et al. 463 Empowerment as a concept is discussed below, but here it is important to emphasise the genesis of action. Rather than being located within the health service, or as a result of engagement between the health system and the local community, the need for intervention can be identified within the community. This model often begins by outlining the growth from the concerns of an individual, which progress through increasingly large groups through to partnerships, which then result in social and political action (Figure 10). This is therefore speaking to the same issues that Whitehead432 identified in ‘strengthening communities’, the difference being that it is the communities who have mobilised themselves into action.
FIGURE 10.
Community empowerment as a continuum (p. 10464). Reproduced by permission of SAGE Publications, London, Los Angeles, New Delhi and Singapore from Laverack G. Health promotion practice: power and empowerment. London: Sage; 2004. © Laverack, 2004.
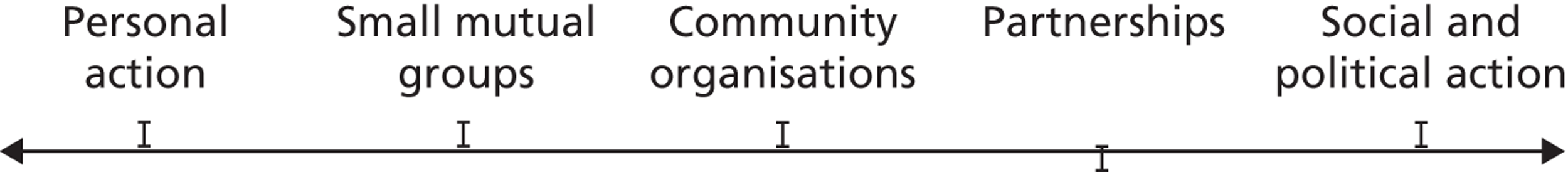
The issue of who identifies the need and who specifies the community goes to the heart of arguments about democracy and accountability that permeate the literature about community engagement (see the following section). They also matter from a theoretical and effectiveness perspective, because many of the arguments advanced in favour of community engagement build on the premise that, if people are ‘signed up’ to the intervention or programme that they are receiving, they are more likely to participate and better outcomes can result (see Chapter 1, The evidence base for community engagement). Understanding how and why people engage in community activity, and why they do not, is therefore a critical component of any coherent conceptual framework, and is also important for this review in terms of being able to identify which models of community engagement are associated with better health outcomes.
Models based on a community empowerment (or ideological) perspective
The previous section has touched on issues of power and empowerment, discussing how some intervention models begin from a health systems perspective, in which people are ‘engaged’ for a range of reasons, whereas in the Whitehead432 taxonomy individuals and communities are empowered to be in a position to impact on their lives and localities. Empowerment is concerned with the movement of control from those who currently are in possession of it to those who currently are not; in this sense it is a zero sum game, with the total amount of power remaining constant. Arnstein’s465 ‘ladder of citizen participation’ (Figure 11) is the oldest, and possibly the most widely known, taxonomy of empowerment. Rooted in a 1960s perspective of citizen involvement in urban planning, it contains eight levels of participation that are grouped into three ranks of citizen control: ‘non-participation’, ‘tokenism’ and ‘citizen power’. It shows how different models of participation are more, or less, empowering than others, beginning with essentially ‘non-participative’ ways in which those with power can reach out to those without, to ‘citizen control’, in which power to direct has been ceded completely. True participation begins only once power is delegated, with the other types of participation being dismissed as ‘tokenism’ and ‘non-participation’.
FIGURE 11.
Arnstein’s465 ‘ladder of citizen participation’. Reproduced by permission of Taylor and Francis Ltd from Arnstein S. A ladder of citizen participation. J Am Inst Plann 1969;35:216– 24. http://dx.doi.org/10.1080/01944366908977225
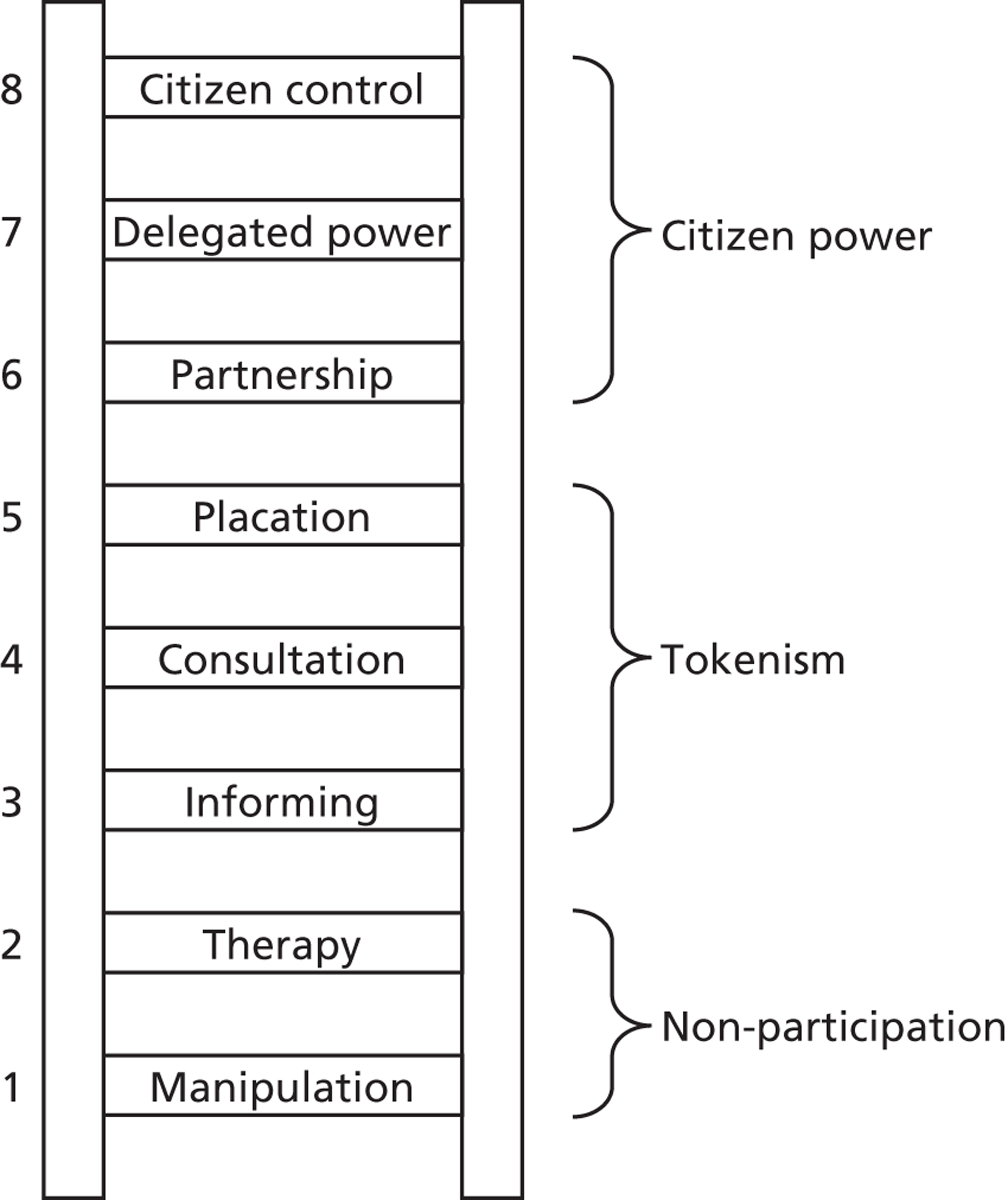
Many other engagement models draw on the ladder metaphor, beginning with minimal ‘interest’ in information-giving and ending with full citizen control. Hart466 differentiated the types of involvement in this framework further when looking at the community participation of children and youth. Wilcox5 drew on both of these theories in developing a theory of public involvement, but suggested that a further process of participation existed: from initiation, preparation and participation to continuation. Further, Wilcox recommended considering issues of control, power and purpose, understanding practitioners’ and stakeholders’ roles, committing to partnerships, generating community-based ideas and developing community confidence and skills. This conceptualisation of community participation has led to the development of specific toolkits that recommend steps to community participation based on underlying principles of what is important in engaging communities. 42,467,468
It is important to recognise the ethical and political dimension of the ladder; as well as representing ‘effective’ ways to involve the public in public policy (and improve the nation’s health), the top of the ladder represents the most democratic and egalitarian approaches towards public service, whereas the lower rungs are associated with authoritarianism and a lack of accountability.
Woodall et al. 463 are concerned with the utility of community empowerment to impact on health outcomes. They define empowerment ‘in its widest and most radical sense’ as being concerned with ‘combating oppression and injustice’ and being ‘a process by which people work together to increase the control they have over events that influence their lives and health’ (p. 9). They relate this to the vision for health promotion set out in the Ottawa Charter469 and related declarations for people to ‘increase control over, and to improve, their health’ (p. 1); that is, that a fundamental aspect of health promotion is people’s empowerment. However, they perceive a disconnection between the aims of health promotion and how it is investigated and practised. 448 They argue that empowerment has become a ‘buzz-word’ that is losing its connection with ‘its original roots as a radical social movement’ (p. 742). Citing Laverack and Wallerstein,470 they argue that a lack of clarity regarding the definition of the term ‘community empowerment’ has resulted in its dilution and its conflation with other terminology such as ‘community competence’, ‘capacity’, ‘cohesiveness’ and ‘social capital’ (p. 744). 448 Although these concepts have their place and their uses, the authors’ concern is that community empowerment is following wider moves in health promotion more broadly ‘toward a reductionist individualistic enterprise focused largely on behaviour change at an individual level, rather than a discipline that focuses on addressing social justice and wider power structures through social and structural change’ (p. 743). 448 Such a view of community empowerment thus fails to appropriately consider existing structural inequalities of economic, social or cultural power that may mediate levels of engagement. According to Laverack and Wallerstein470 then, empowerment is losing its power. Their argument about the term ‘empowerment’ is part of a wider discussion on the past, present and future of health services, in which community participation is seen as being marginalised in the undoubted progress that has been made in other areas of primary health care. 471 Although, to some extent, we have separated conceptually models that are centred on empowerment and those that emphasise other concepts, such as participation, it is clear that the language of empowerment is utilised in different ways and that not all of them adhere to an imperative to ‘combat oppression and injustice’, and argue instead that empowering communities is a sensible way to improve people’s health (a utilitarian perspective – or argument).
The reason that community empowerment is such a key issue is because it is concerned with the wider social determinants of health (and is therefore of critical importance in a review about inequalities in health) and has quite different theoretical foundations from more individualistic approaches. Although individual empowerment can result in individual improvements in health, this can be attained without engagement in any community activities. Interventions that facilitate individual empowerment leave the power structures that gave rise to health inequalities untouched. Interventions that empower communities are to be valued not (only) because they combat oppression, but because they change some of the fundamental dynamics of power that have led to those inequalities in health arising in the first place. The mechanisms of change that underpin these two approaches are quite different, and, although individual empowerment is not unimportant, if empowerment is located only within individuals ‘it overlooks change in the political and social context in which people live’ (p. 743). 448 In contrast, the rationale for empowering communities rather than (or as well as) individuals is that we might expect to see the capacity for communities to improve their own health increased; thus, engagement is to be conceptualised as an outcome in its own right for some interventions, as well as a mediator for improved health across many others.
An example of empowerment is provided in Andrews et al. 73,208 This study used community-based participatory research to develop a culturally sensitive smoking cessation intervention with African American women resident in low-income housing. The community was engaged throughout the project, from identifying a need to tackle tobacco use and approaching researchers for help, to collaborating by way of resource provision; neighbourhood forums to assist with data interpretation and dissemination; an advisory board of residents (60%), housing authority members, pastor, school official, health department, community clinic staff and community agencies; intervention planning and delivery; use of community health workers; and contributions to analysis and interpretation of the pilot study. Among the studies included in our review, almost all community engagement occurred in the interventions’ design or delivery, rather than in its evaluation. Andrews et al. 73,208 is a rare example that we located which also described community engagement in the evaluation of the intervention as well.
Bridging the utilitarian and social justice rationales for empowerment
Notwithstanding the concerns expressed by Woodall et al. 463 about the dilution of empowerment, this chapter will conclude with a new conceptual framework for community engagement that aims to encompass the breadth of perspectives and approaches so far discussed. This will not be the first such framework, however, and it owes much to the work of Jennie Popay in her earlier briefing paper for NICE14 and other consolidating work by WHO (e.g. reference 89).
Popay et al. 4,14,21,472 developed a framework for community involvement in public health, further developing the idea of levels of engagement but within a health services framework. They found that there is considerable complexity in the approaches to community engagement, in the levels of involvement and whether engagement occurs as a reaction to outside pressures or as an internally derived initiative.
Figure 12 outlines the first of two frameworks from this work, which is concerned with understanding different types of community engagement. This framework conceptualises the most powerful type of community engagement as being associated with control being devolved to the community; and the least powerful as lacking in empowerment and being concerned with information provision and exchange. Lying in between the two are consultation and the co-production of knowledge. Although the foundations underpinning each type of engagement lie on this continuum, they cannot be associated with the precise methods used (either singly or in combination), which include ‘citizens panels and juries, rapid appraisal techniques, neighbourhood committees, community forums, participatory evaluation/research and community champions’ (p. 6). 14
FIGURE 12.
A conceptual framework for community engagement.
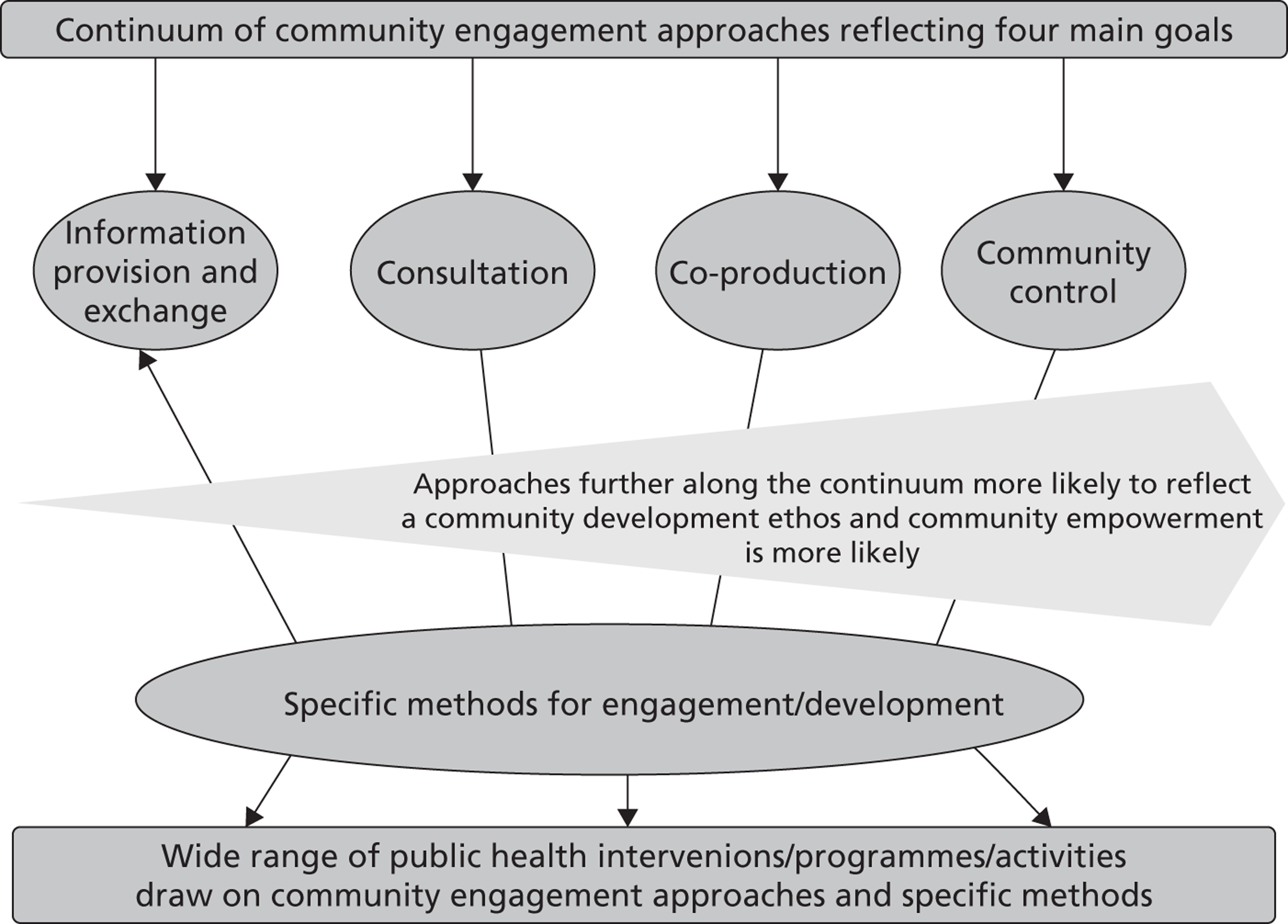
Conceptually, Figure 12 is similar to the community engagement continuum described by the CTSA Community Engagement Key Function Committee Task Force440 and the ‘wheel of participation’ (Figure 13; this figure is outlined in the 2002 WHO paper Community Participation in Local Health and Sustainable Development,450 which is itself developed on the basis of Davidson’s 1998 paper entitled ‘Spinning the Wheel of Empowerment’473). The wheel denotes four cornerstones of participation – information, consultation, participation and empowerment – each with hierarchical levels and examples. Popay et al. 4,14,21,472 observe that it is not possible – or indeed appropriate – always to aim for the ‘top’ of the ladder of empowerment (e.g. the full citizens’ control shown in Figure 11) and that other ‘rungs’ or ‘sectors’ may contain the most suitable approach.
Both Popay and WHO use utilitarian arguments in support of community engagement (or participation), rather than highlighting the social justice and democracy angle as illustrated earlier by Arnstein465 and Woodall et al. 463 WHO makes the point that citizens and communities may argue that they have a right to have a say, but the justification for encouraging participation is made in terms of it being an effective method of increasing democracy, combating social exclusion, enhancing people’s well-being and quality of life through empowerment, mobilising resources, developing holistic and integrated approaches, achieving better decisions and more effective services and ensuring the ownership and sustainability of programmes. The context of the briefing paper by Popay14 was to inform the development of public health programme guidance, so the rationale for engagement is clearly located within a need to improve health and reduce health inequalities.
The final model reviewed here is the ‘pathways from community engagement to health improvement’ diagram in the Popay report (p. 9). 14 This builds on the previous models in that it has the familiar ordinal scale that leads from basic information provision through to community control, but it moves on from this to incorporate a theory of change, and suggests that certain models of community engagement are limited in terms of the extent to which they can impact social and health outcomes. Shown in Figure 14, this model is read from the bottom up, with community participation, empowerment and control increasing until the top level corresponds to full ‘community control’. The theory of change begins with changes to services as a result of the community engagement intervention (‘service outcomes’), through intermediate outcomes (social capital and increased empowerment and improved environment) to final impact on health outcomes. Critically, the model rules out the possibility of the lower levels of community engagement – ‘informing’ and ‘consultation’ – impacting on the intermediate social outcomes, and therefore they are capable of only relatively small improvements in health outcomes. As community participation, empowerment and control increase, so do impacts on the outcomes, with the largest improvements being associated with full community control. Popay14 notes that willing communities and public organisations and workers willing to share power and influence with communities are important (p. 12). She also noted that there are direct benefits and ‘dis-benefits’ to community members who participate;4 and that a lack of training, timing and administrative issues were barriers to successful community engagement. Power misuse by professionals and cultural stereotypes of community members by professionals were also noted to be barriers.
FIGURE 14.
Pathways from community engagement to health improvement.
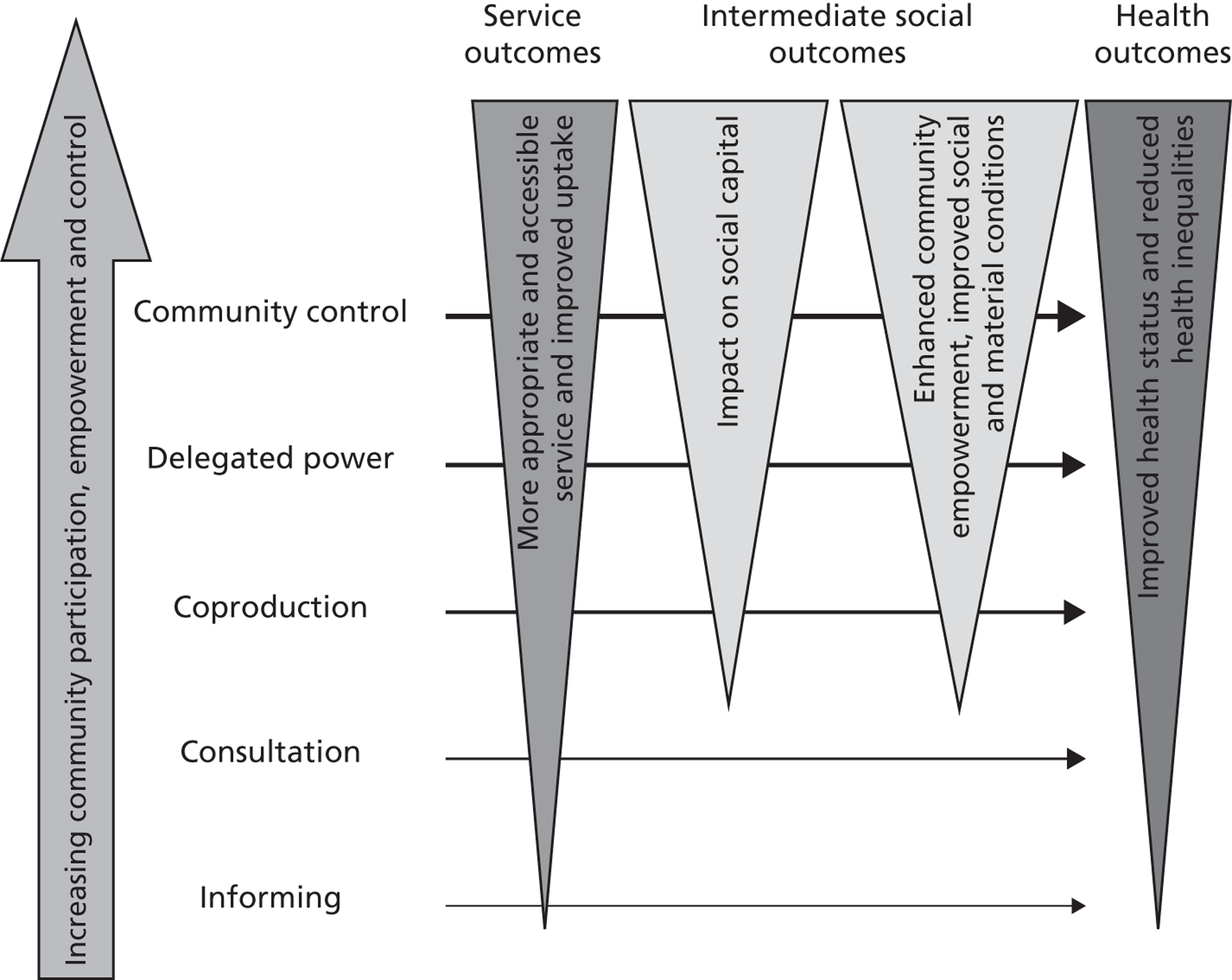
Examples of intervention strategies in line with the above framework include those described in the National Evaluation of Local Strategic Partnerships undertaken through the UK Office of the Deputy Prime Minister. 356 Intended to join up services and community organisations in socioeconomically deprived areas of the UK, multiple locally-developed strategies were developed through partnerships between public sector, private, business, community and voluntary stakeholders. In these types of initiatives, the need for intervention is determined by outside stakeholders; responsibility and authority for addressing the issues are handed to the community members and service providers in that locale.
Chapter summary
This chapter has described the range of theories that underpin community engagement through an examination of the theoretical literature read in the light of the evaluation studies included in this review. This theoretical understanding was then combined with additional learning that came from analysing process evaluations (see Chapter 6) and economic evaluations (see Chapter 7); a synthesis of the three is presented in a new broad conceptual model in Chapter 8, some of which framed a series of hypotheses about the effects of community engagement, which are tested next in Chapter 5. Three overarching conceptualisations of engagement have emerged, which combine aspects of purpose, theory and the way that many interventions occur in practice:
-
Theories of change for patient/consumer involvement. This is engagement with communities or members of communities in strategies for service development, in which empowering individuals enhances their engagement with service professionals to effect sustainable changes in services. It involves community members in the planning or design of an intervention. The need for ongoing investment will depend on the nature of the changes made; ongoing partnership is not necessary for sustaining changes, but can benefit subsequent changes.
-
Theories of change for peer-/lay-delivered interventions. Services engage communities, or individuals within communities, to deliver interventions, thereby empowering them by enhancing their skills. This approach aims to effect sustainable change amongst individuals and their peers. Although the individual behaviour changes sought may be sustainable, the intervention needs ongoing investment from services for subsequent generations.
-
Theories of empowerment to reduce health inequalities. When people are engaged in a programme of community development, an empowered community is the outcome sought by enhancing their mutual support and their collective action to mobilise resources of their own and from elsewhere to make changes within the community. An empowered community can do much to sustain its own efforts.
Chapter 5 Synthesis II: meta-analysis of effectiveness studies
About this chapter
The purpose of this chapter is to consider the overall effectiveness of public health interventions that incorporate community engagement compared with controlled conditions in which no or minimal community engagement is evident. Once the overall effectiveness of such interventions is ascertained, moderators of this effect will be explored. As discussed in Chapter 2, moderators tested include study characteristics (such as the country in which the study was conducted), participant characteristics (such as PROGRESS-Plus group) and features of the evaluations (such as risk of bias). These analyses will help us to answer the following RQs:
-
RQ3: Which approaches to community engagement are associated with improved health outcomes among disadvantaged groups? How do these approaches lead to improved outcomes?
-
RQ4: Which approaches to community engagement are associated with reductions in inequalities in health? How do these approaches lead to reductions in health inequalities?
-
RQ5: Which types of intervention work best when communities are engaged?
-
RQ6: Is community engagement associated with better outcomes for some groups than others? (In particular, does it work better or less well for children and young people?)
-
RQ7: How do targeted and universal interventions compare in terms of community engagement and their impact on inequalities?
Before we synthesise the evidence to answer the RQs, we will give an overview of the theoretical framework underpinning the analyses, including the proposed causal pathway. This will be followed by descriptive information about the participants, interventions, comparators and evaluation characteristics, outcomes and effect size estimates included in the meta-analysis. Finally, we present the sensitivity analyses, risk of bias within studies, results of individual studies, synthesis of the results (including analyses that address the RQs), risk of bias across studies and additional analyses.
Theoretical framework
As described in Chapter 4 (and continued in Chapter 8), we identified a range of dimensions to explore and categorise differences between the community engagement approaches utilised by the interventions in the review. These dimensions formed the basis of a preliminary conceptual framework and included:
-
the extent to which interventions were concerned with community engagement broadly, or health outcomes more narrowly
-
who identified the need for the intervention
-
reasons why people might be motivated to become involved
-
how and where the community was involved in the design and delivery of the intervention
-
the conditions that mediated or moderated engagement
-
the types of actions and resources involved in engagement activities.
We extracted data from each of the primary studies on aspects of these dimensions to enable us to assess whether differences between the community engagement approaches were associated with differing levels of intervention impact.
Across studies, a variety of outcome measures were used to assess impact. We proposed a causal chain in which health behaviours (i.e. actions that people do, such as smoking and physical activity) need to be changed to have an impact on physiological consequences (such as blood pressure, body mass index), which may eventually lead to impacts on final health states (morbidity and mortality associated with relevant diseases). We noted, however, that researchers rarely made a distinction between physiological consequences and health states, and so these were combined in the analyses as ‘health consequence’ outcomes. Psychosocial outcomes – self-efficacy and social support related to the health behaviour – were proposed to be important outcomes in their own right and as mediators of the effect of the intervention on health behaviours. The proposed causal pathway is presented in Figure 15.
FIGURE 15.
Proposed causal pathway from the intervention to health consequences.
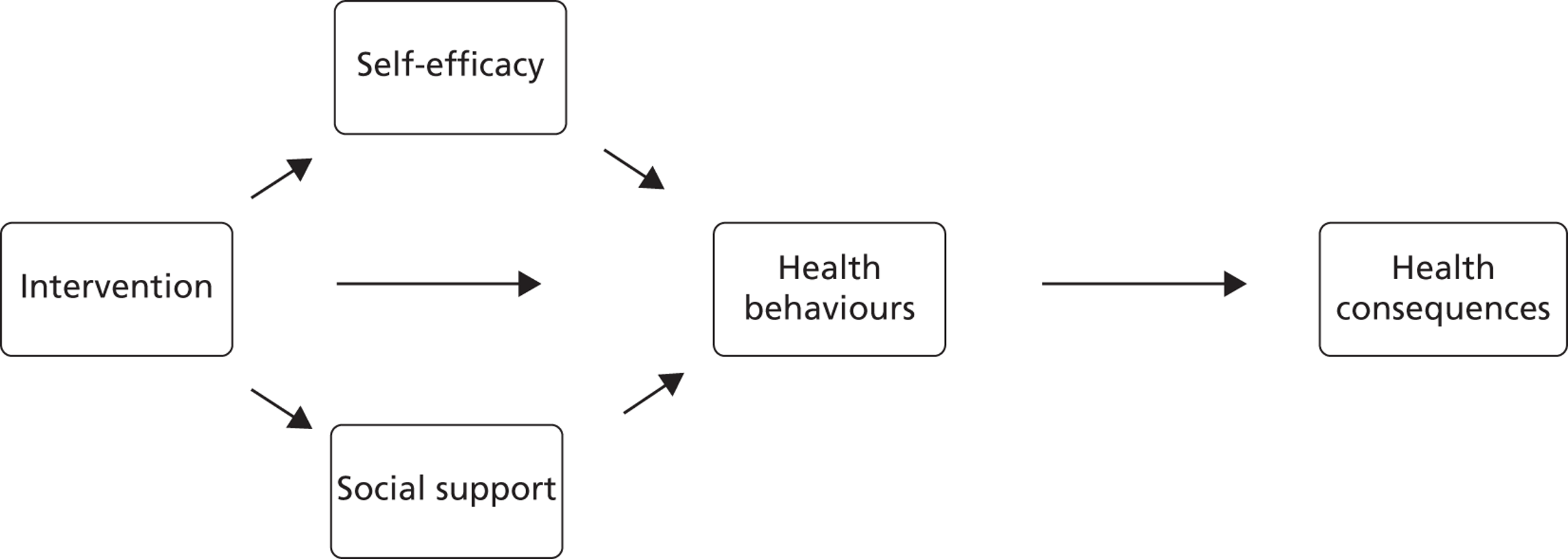
We also extracted, when available, data on community outcomes and outcomes for the engagees. As such, we extracted intervention effectiveness outcomes for the following:
-
health behaviours – outcomes extracted were alcohol abuse, antenatal (prenatal) care, breastfeeding, cardiovascular disease, child illness and ill health, drug abuse, healthy eating, immunisation, injury/safety, parenting, physical activity, smoking cessation, smoking/tobacco prevention and ‘other’ not captured above
-
health consequences (physiological consequences and final health states) – outcomes extracted were cardiovascular disease, child abuse prevention, child illness and ill health, healthy eating, hypertension, injury/safety, mental health, obesity/weight status and ‘other’ not captured above
-
participant self-efficacy pertaining to the health behaviours
-
participant social support in relation to the health outcomes
-
community outcomes (e.g. ‘local area improved in the last 3 years’)
-
engagee outcomes (e.g. physical activity levels or health knowledge of the engagee).
The effectiveness of the interventions was assessed against all of these outcome types, although the main focus is on the primary outcome: health behaviours. There were sufficient data to undertake statistical analyses for all outcomes except community and engagee outcomes, which were synthesised narratively.
Description of the studies included in the meta-analysis
The studies
Of the 131 studies included in the meta-analysis,71–201 five (3.8%) were conducted in the UK,100,119,149,157,159 113 (86.3%) were conducted in the USA,72–99,101,102,104–106,108–118,120,121,123–128,130–133,135,137,138,140–142,144,146–148,150–155,158,160–163,165–181,183–201 five (3.8%) were conducted in Canada71,103,107,145,156 and eight (6.1%) were conducted in other OECD countries. 122,129,134,136,139,143,164,182 In terms of publication date, 63 (48.1%) were published in the 1990s,74,76,78,82,83,88,90,93,94,97,99,102–106,110,111,113,115,118,120,121,124,125,129,130,133,135–137,139–142,144,145,147–151,153,156,157,158,160,166,169–171,174,176,178,179,181,182,186,190–193,198 62 (47.3%) in the 2000s71–73,75,77,81,84–86,89,91,92,95,96,98,100,101,107–109,114,116,117,119,122,123,127,128,132,134,138,143,146,152,154,155,159,161–165,167,168,172,173,175,177,180,183–185,187–189,194–197,199–201 and six (4.6%) in 2010 or later. 79,80,87,112,126,131
The participants
In terms of health inequalities, most studies were classified as being primarily targeted at, or delivered to, ethnic minority groups (n = 56,71,77–82,85,86,88,94,96,97,99,103–110,112–114,126,127,131,132,140,145,146,150,151,155,157,161,164,165,173,174,176,180–182,188,190,191,193–199,201 42.7%), followed by socioeconomic position (n = 34,72,74,75,84,93,98,100,102,115,119,121,125,129,133–135,148,149,153,156,159,160,162,163,169,171,177–179,183–186,192 26.0%). There was also a large group of studies (n = 21,73,76,83,87,89,90,101,111,116,120,128,137,138,152,164,168,170,172,187,189,200 16.0%) that had multiple PROGRESS-Plus categorisations, as clear from the title and abstract; the majority of these represented a combination of ethnic minority group status and low-income and/or inner-city status. Most of the ethnic minority participants were classified as black, African American or Hispanic/Latino.
The database included a spread of participants across all age groups and most of the studies included participants from more than one age group. The majority of the studies included young people (aged 11–21 years; n = 79;72–76,81,82,87–92,95,97–102,104–110,112,113,115,117,118,120,122–125,127,129,130,133–135,138,140–144,146–149,152,153,155,157,158,160–163,167,171,173,175,177–179,181,183,184,186,188,192,194,195,200,201 60.3%) and/or adults (age 22–54 years; n = 65,72–74,77–82,85,90–92,95–98,100–103,105,109,112,113,120,122,125,126,128,129,132–135,137,138,140,143,146–151,155,157,160–164,171,172,175,177,178,181,183,184,186,187,194,196,199 49.6%). In total, 7971,75,76,80–85,87–92,96,99–101,103–108,110,112–119,122,123,127,131,132,134–137,139,141–143,145,148,152–154,156,158,159,164–167,169,170,172–174,176,179,180,182,185,188–190,192–195,197,200,201 (60.3%) studies had mixed sex samples, 4972–74,77–79,86,94,95,97,98,102,109,111,120,121,124–126,128–130,133,138,140,144,146,147,149–151,155,160–162,168,171,175,177,178,181,183,184,186,187,191,196,198,199 (37.4%) had predominantly female samples and three93,157,163 (2.3%) had predominantly male samples.
The interventions
The interventions were conducted over a range of health topics (Table 14). The most commonly targeted health issue was substance abuse (n = 18,75,88,99,107,108,111,118,123,124,127,141,142,158,167,173,179,192,200 13.7%), followed by cardiovascular disease (n = 14,80,82,90,106,126,135,143,154,156,166,170,193,196,199 10.7%).
The interventions were conducted in a range of settings and in many cases across multiple settings within an intervention (Table 15). The most common setting for interventions was in the community (n = 56,73,75,82,85–87,90–92,99,100,102–105,107,113,115,119,122–124,131,134–138,141–143,145,152–154,156,158,159,161,164,167–174,176,177,179,180,190,193,195,201 42.7%). Many interventions also included non-geographic settings, such as media tailored to the participants’ needs (e.g. tailored newsletters or information sheets; n = 53,74–77,79,80,83,85,87,90,91,93–97,101,102,109,110,114,115,117,121,125–128,131,133,135,140,145,146,149,154–156,160,162,163,171,177,178,180,183,184,190,197–201 40.5%) or mass media (n = 21,73,90,100,103,113,115,122,125,127,131,134,136,137,142,145,148,154,156,158,177,180 16.0%); such interventions could be delivered wherever the participant was located.
Most of the interventions included multiple intervention strategies (Table 16). The most common strategy was education provision (n = 105,72,73,75–96,98–115,117,118,120,122–128,131–134,136–139,142–145,147–156,158,159,161–166,172–174,176,177,179,181,182,185,187,188,190–201 80.2%). Advice (n = 71,71,72,74,77–79,82,83,87–89,81–93,95,96,98,99,101,103,107–112,118,121,123,124,128–134,139–144,146,147,149,155,156,160,163,168,171,174,175,177–182,184,186,187,189–191,193,197,198,200,201 54.2%), social support (n = 58,72–74,78,80,84,91–95,98,100,101,103,105–107,109,111,116,118,120,123,124,129,130,141,142,144,147–150,153,155,156,160–163,167,172,175,177,179,181–184,186–190,197,198,201 44.3%) and skill development training (n = 51,72,76,77,79,81,82,84,88,89,92,94,101,102,104,106,107,110,115,118,123,124,126,127,129,138,141,142,145,147,149,152,155,158,161–163,170,171,173,178,179,181,182,192–196,198–200 38.9%) were also common strategies.
The interventions were delivered by a variety of professionals and non-professionals, sometimes in collaboration with each other (Table 17). The most common intervention deliverers were non-peer community members (n = 58,75,79–81,83–85,90–92,94,96,98,103–106,109,112,113,115,116,118,122–124,128,130–132,134,136,137,142,144,145,147,148,150,152,154,157,158,165,167,172–174,177,179,182,190,193–195,198,199,201 44.3%) and peers (n = 49,72–74,77,87,93,95,97,100,102,103,118,120,121,125,129,130,133,135,140,141,146,147,149,152,153,158,160–164,166,168,169,171,175–179,181–184,186,188,192,200 37.4%).
The comparators and evaluation features
A variety of comparators were used in the intervention evaluations. The largest group of evaluations employed usual care comparators (n = 38,71,72,74,76,83,89,97–99,103,108,110,115,120,123,126,127,129,130,135,141,145–147,151,155,157,158,160,162,163,166,169,181,184,192,193,200 29.0%; Table 18). Thirteen (10.0%) of the studies directly compared the effectiveness of community engagement by having a comparison condition that differed from the intervention only in the involvement of community members. 84,88,93,97,98,109,129,157,181,183,184,186,187
Fifty-nine (45.0%) evaluations used randomisation methods to allocate participants to the intervention or comparison condition (Table 19). 71–73,77–80,82,83,85,86,95–98,101,105,106,108,116,117,120,123–129,135,138,141,142,144,146,147,150,153,155,158,161,162,167–169,172,173,175,181,183,184,187,189,190,192,194–197 Twenty-six (19.8%) of the evaluations conducted follow-up testing. 72,75,77–79,87,93,95,98,101,107,114,125,127,129,131,140,144,151,153,173,183,186,191,192,195
| Primary health issue | Frequency | % |
|---|---|---|
| Substance abuse | 18 | 13.7 |
| Cardiovascular disease | 14 | 10.7 |
| Breastfeeding | 13 | 9.9 |
| Obesity prevention/weight reduction | 13 | 9.9 |
| Smoking cessation | 12 | 9.2 |
| Public health/health promotion/prevention | 8 | 6.1 |
| Antenatal (prenatal) care | 7 | 5.3 |
| Cancer prevention | 6 | 4.6 |
| Diabetes prevention/management | 6 | 4.6 |
| Physical activity | 6 | 4.6 |
| Healthy eating/nutrition | 5 | 3.8 |
| Parenting | 5 | 3.8 |
| Immunisation | 4 | 3.1 |
| Injury prevention | 4 | 3.1 |
| Smoking/tobacco prevention | 3 | 2.3 |
| Child illness and ill health | 2 | 1.5 |
| Disabilities and chronic illness | 2 | 1.5 |
| Child abuse prevention | 1 | 0.8 |
| Hypertension | 1 | 0.8 |
| Infant mortality | 1 | 0.8 |
| Intervention setting | Frequency | % |
|---|---|---|
| Community setting | 56 | 42.7 |
| Tailored media | 53 | 40.5 |
| Participant’s home (not care home) | 50 | 38.2 |
| Educational setting | 36 | 27.5 |
| Mass media | 21 | 16.0 |
| Religious setting | 16 | 12.2 |
| Secondary health care | 14 | 10.7 |
| WIC clinic | 9 | 6.9 |
| Workplace | 9 | 6.9 |
| Outreach | 8 | 6.1 |
| Primary health care | 8 | 6.1 |
| Residential care | 1 | 0.8 |
| Computer based | 1 | 0.8 |
| Intervention strategy | Frequency | % |
|---|---|---|
| Education | 105 | 80.2 |
| Advice | 71 | 54.2 |
| Social support | 58 | 44.3 |
| Skill development training | 51 | 38.9 |
| Activities (e.g. community fairs) | 47 | 35.9 |
| Environmental modification | 30 | 22.9 |
| Resource access | 30 | 22.9 |
| Service access | 29 | 22.1 |
| Physical activity | 28 | 21.4 |
| Counselling | 17 | 13.0 |
| Role modelling/role playing | 17 | 13.0 |
| Incentives | 14 | 10.7 |
| Medical screening | 7 | 5.3 |
| Risk assessment (not medical screening) | 6 | 4.6 |
| Professional training | 3 | 2.3 |
| Who delivered the intervention | Frequency | % |
|---|---|---|
| Community member | 58 | 44.3 |
| Peer | 49 | 37.4 |
| Health professional | 24 | 18.3 |
| Community worker | 18 | 13.7 |
| Education professional | 17 | 13.0 |
| Researcher | 7 | 5.3 |
| Health promotion practitioner | 6 | 4.6 |
| Parent | 4 | 3.1 |
| Religious leader | 4 | 3.1 |
| Counsellor | 2 | 1.5 |
| Social worker | 2 | 1.5 |
| Other | 17 | 13.0 |
| Not clear | 10 | 7.6 |
| Comparison group type | Frequency | % |
|---|---|---|
| Usual care | 38 | 29.0 |
| No treatment (inactive) | 31 | 23.7 |
| Alternative/placebo | 27 | 20.6 |
| Wait list/delayed treatment | 15 | 11.5 |
| Matched data from target population | 12 | 9.2 |
| Unclear | 5 | 3.8 |
| Other or combination | 3 | 2.3 |
| Allocation method | Frequency | % |
|---|---|---|
| Randomised | 59 | 45.0 |
| Non-randomised | 56 | 42.7 |
| Partial randomisation | 14 | 10.7 |
| Unclear | 2 | 1.5 |
The effect size estimates
As described in the Chapter 2, studies could contribute more than one effect size estimate to the data set under the following conditions:
-
when there were both immediate post-test and delayed follow-up measures, to test the persistence of effects over time
-
when there were outcomes from different points in the causal pathway (see Figure 15)
-
when there were measures of both engagees and public health intervention participants.
As a result, we calculated multiple effect size estimates for some studies: a total of 212 across the 131 studies. Of the 212 effect size estimates, 191 were calculated from post-test measurements and 21 were from follow-up measurements. The remainder of this section refers only to the 191 post-test effect size estimates. The follow-up measures are explored only in terms of the maintenance of intervention effects (see Maintenance of intervention effects).
Of the post-test effect size estimate, 82 out of 131 studies (62.6%) contributed only one effect size estimate and the mean number of effect size estimates per study was 1.47 (SD = 0.68). 71,72,74,75,83,84,88,89,91–93,95–97,99–109,115,117,118,120,121,123,124,126,128,133,135,137–142,144,146,149,151,152,155,157,159,162,163,169,171,173,174,176,178,180,181,183,184,186,188–193,196–198,200,201,230,259,266,287,335,390,391,403 Figure 16 shows the frequency of studies by number of effect size estimates.
FIGURE 16.
Frequencies of studies with one or more post-test effect size estimates.
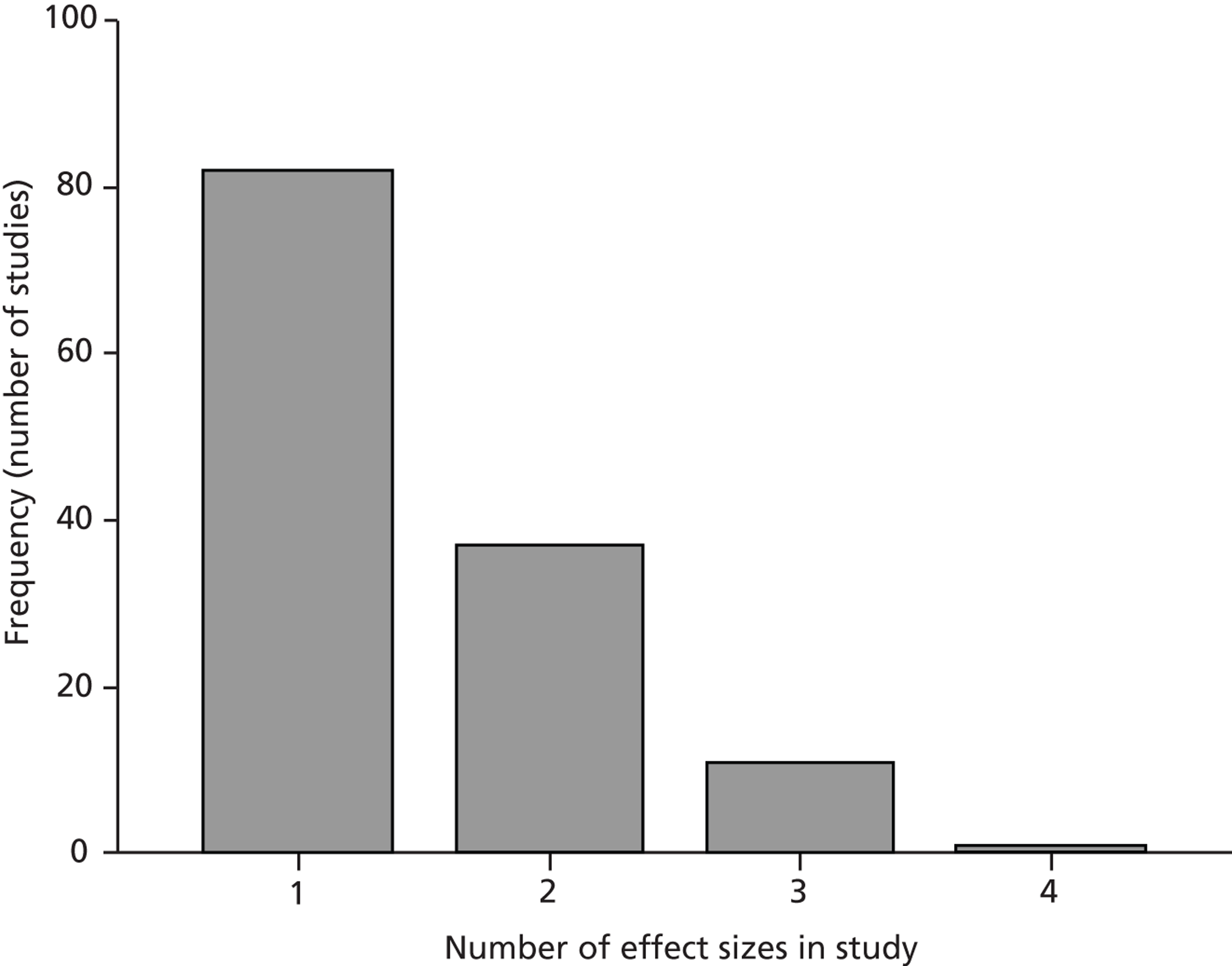
Effect size estimates based on continuous data are represented by d, whereas log-odds ratio (LOR) is used to represent effect size estimates calculated from binary data. The 115 post-test effect size estimates based on continuous data ranged from d = −0.77 to d = 1.43. (The range of values after outliers was Winsorised to 2 SDs above or below the mean and data were reverse coded when necessary such that all positive values indicate that the effect favours the intervention group. Three post-test effect sizes were Winsorised: all three were > 2 SDs above the mean.) A positive d indicates that participants in the treatment group, on average, scored higher than those in the control group. An effect size estimate of d = 1.0 means that participants in the treatment group scored, on average, 1 SD higher than participants in the control group on the particular outcome measure. In total, 12 of the 115 continuous post-test effect size estimates were coded as ‘missing data’ because there was insufficient information to calculate an effect size estimate.
The 76 effect size estimates based on binary data ranged from LOR = −1.05 to LOR = 2.14. (The range of values after outliers was Winsorised to 2 SDs above or below the mean and data were reverse coded when necessary such that all values > 1 indicate that the effect favours the intervention group. Three post-test effect sizes were Winsorised: one low outlier and two high outliers.) A LOR effect size estimate > 0 indicates that participants in the treatment group were more likely to achieve the desired outcome than those in the control group, whereas LOR < 0 indicates that the desired outcome was more likely in the control group. Four of the 76 binary post-test effect size estimates were coded as missing data.
To enable synthesis of the effect size estimates across outcome types (i.e. continuous d effect size estimates and binary LOR effect size estimates), the LOR effect size estimates were converted to d effect size estimates using the procedures discussed in Chapter 2. Figure 17 presents the frequencies of effect size estimates (for health behaviour outcomes only), in which the effect size estimates consist of d-values and LOR-values that have been converted to d-values. This figure indicates the distribution of the effect size estimates and shows that the majority of the effect size estimates were > 0.
FIGURE 17.
Frequencies of effect size estimates for health behaviour outcomes.
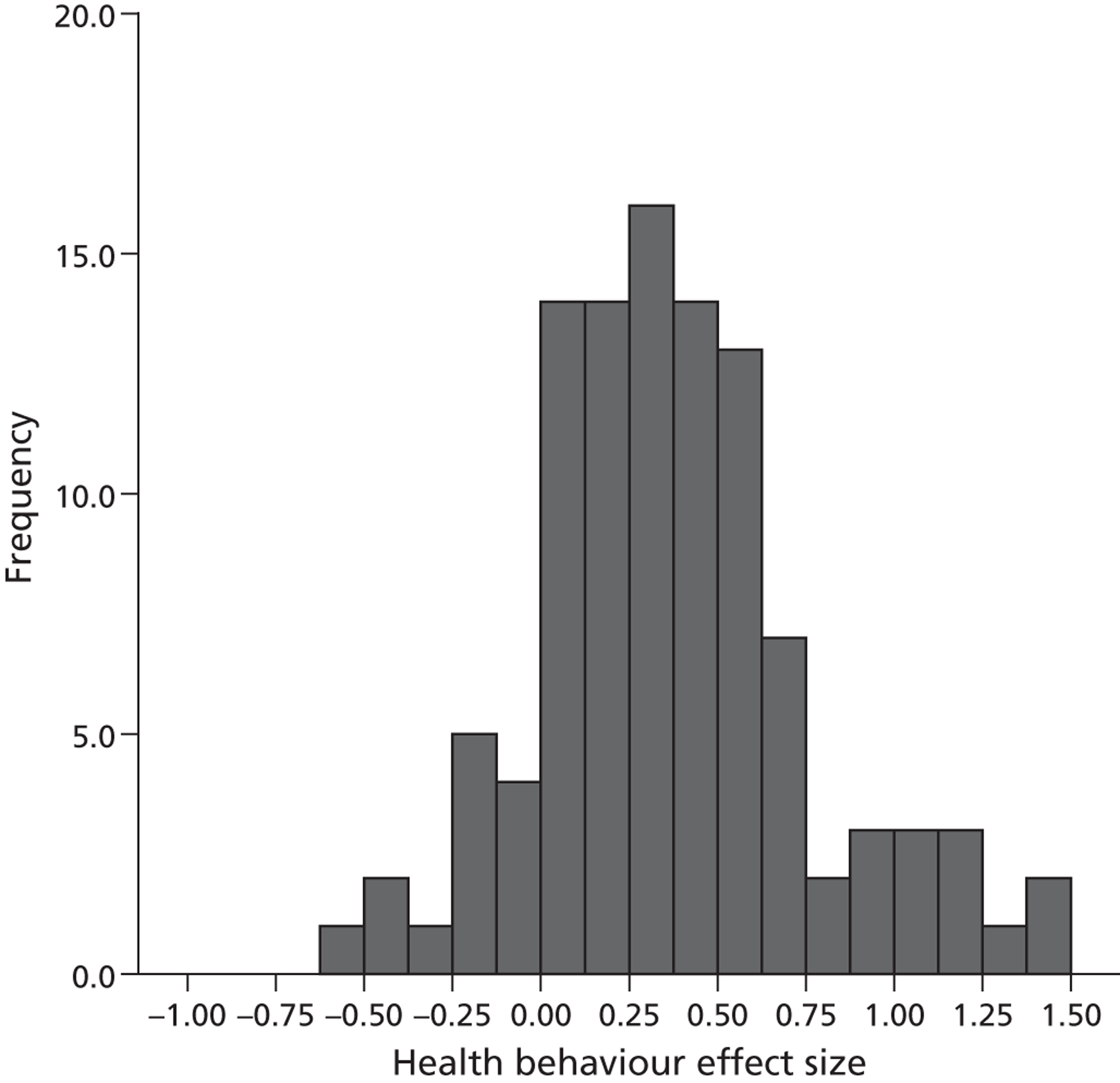
Sensitivity analysis
We conducted a sensitivity analysis to test whether d effect size estimates based on binary data were statistically similar to d effect size estimates based on continuous data. Although pooled binary outcomes tended to be slightly smaller than pooled continuous outcomes, this difference was not statistically different [between-groups heterogeneity QB (1) = 3.03, p = 0.08].
We also tested whether there was a difference between studies that explicitly tested community engagement and those that did not. Most interventions were compared with a comparison condition that differed from the intervention in more ways than just community engagement. For example, the comparison condition might be a completely alternative intervention, or a wait list/delayed treatment control condition. For health behaviour outcomes, there were seven studies346,449,454,458,459,468,474 for which the only difference between the treatment conditions was the presence or absence of community engagement. To illustrate, one such study454 compared peer-led health education with non-peer-led health education using the same healthy eating programme materials. The results of the analysis were not statistically significant (which was unsurprising given the small number of studies with direct comparison evaluation approaches; QB (1) = 0.01, p = 0.93). The group means suggest no trends in either direction: the pooled effect size estimate was 0.34 for studies with a direct comparison and 0.33 for indirect comparisons.
Finally, because the interventions cover a broad range of health topics and health outcomes, which we combine in the analyses under the umbrella of ‘health behaviour outcomes’, we tested the difference between outcome types (Table 20). Two important features are relevant to determining whether it makes sense to combine these outcomes: the between-group heterogeneity statistic and the direction of each subgroup’s pooled effect size estimate. The between-group heterogeneity statistic indicates that the groups are not statistically significantly different from each other [QB (6) = 12.27, p = 0.06]. The pooled effect size estimate for each group is statistically significant from 0 in the positive direction. Although there is some variation in the magnitude of effects, these results do not suggest that we should be concerned about combining these outcomes in the analyses on the basis of statistical differences.
| Outcome | Pooled effect size estimate | 95% CI | n |
|---|---|---|---|
| Breastfeeding | 0.40a | 0.14 to 0.66 | 14 |
| Health service use | 0.33b | 0.11 to 0.55 | 12 |
| Healthy eating | 0.47c | 0.33 to 0.60 | 21 |
| Physical activity | 0.23a | 0.08 to 0.38 | 21 |
| Substance abuse | 0.33a | 0.13 to 0.52 | 12 |
| Tobacco use | 0.18b | 0.03 to 0.34 | 22 |
| Other health behaviours | 0.71a | 0.30 to 1.12 | 3 |
Risk of bias within studies
Appendix 6 presents the risk of bias assessment of the included articles. Soundness was assessed on three criteria: selection bias, attrition bias and selective reporting bias (see Appendix 3 for details of how these biases were operationalised in this review). For a study to be classified as ‘sound’, all three types of bias had to be avoided. On this basis, 69 (52.7%) studies71,73,74,76,77,80,83,85–87,93–95,98–101,106–108,110,111,114,117,118,120,124,126–128,129,131–135,138–142,147,150,153–144,158,162–165,168–170,173–175,180–185,188,190,193,195,197,199 were considered to be sound and 62 (47.3%) studies72,75,78,79,81,82,84,88–92,96,97,102–105,109,112,113,115,116,119,121–123,125,130,136,137,143–146,148,149,151,152,156,157,159–161,166,167,171,172,176–179,186,187,189,191,192,194,196,198,200,201 were considered to be not sound.
Results of individual studies
A series of forest plots (Figures 18–21) show the effect size estimate, confidence interval (CI) and relative weight for each intervention by outcome type (health behaviours, health consequences, participant self-efficacy and participant social support).
FIGURE 18.
Forest plot of effect size estimates and standard errors of all studies reporting health behaviour outcomes.
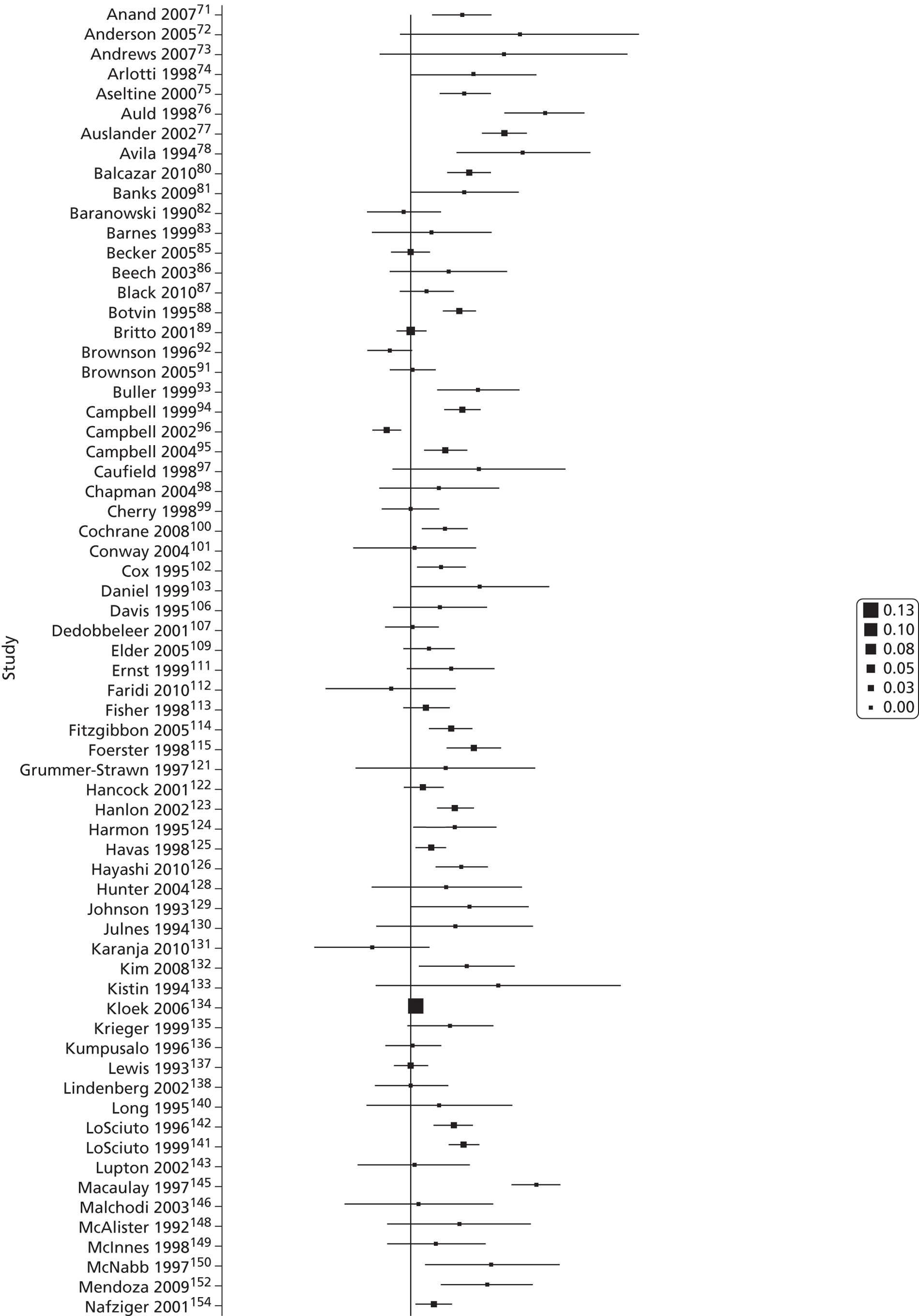
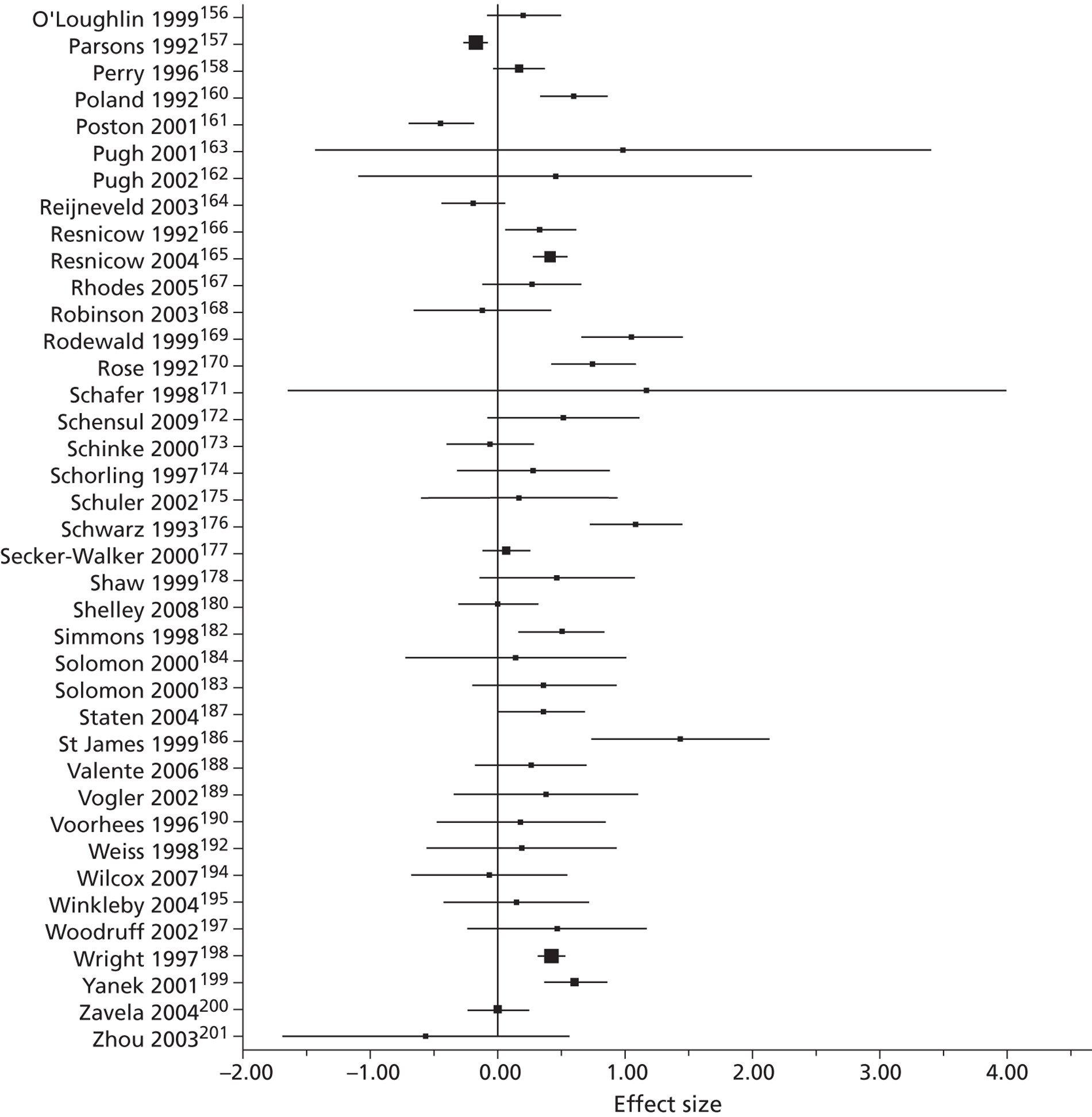
FIGURE 19.
Forest plot of effect sizes estimates and standard errors of all studies reporting health consequences outcomes.
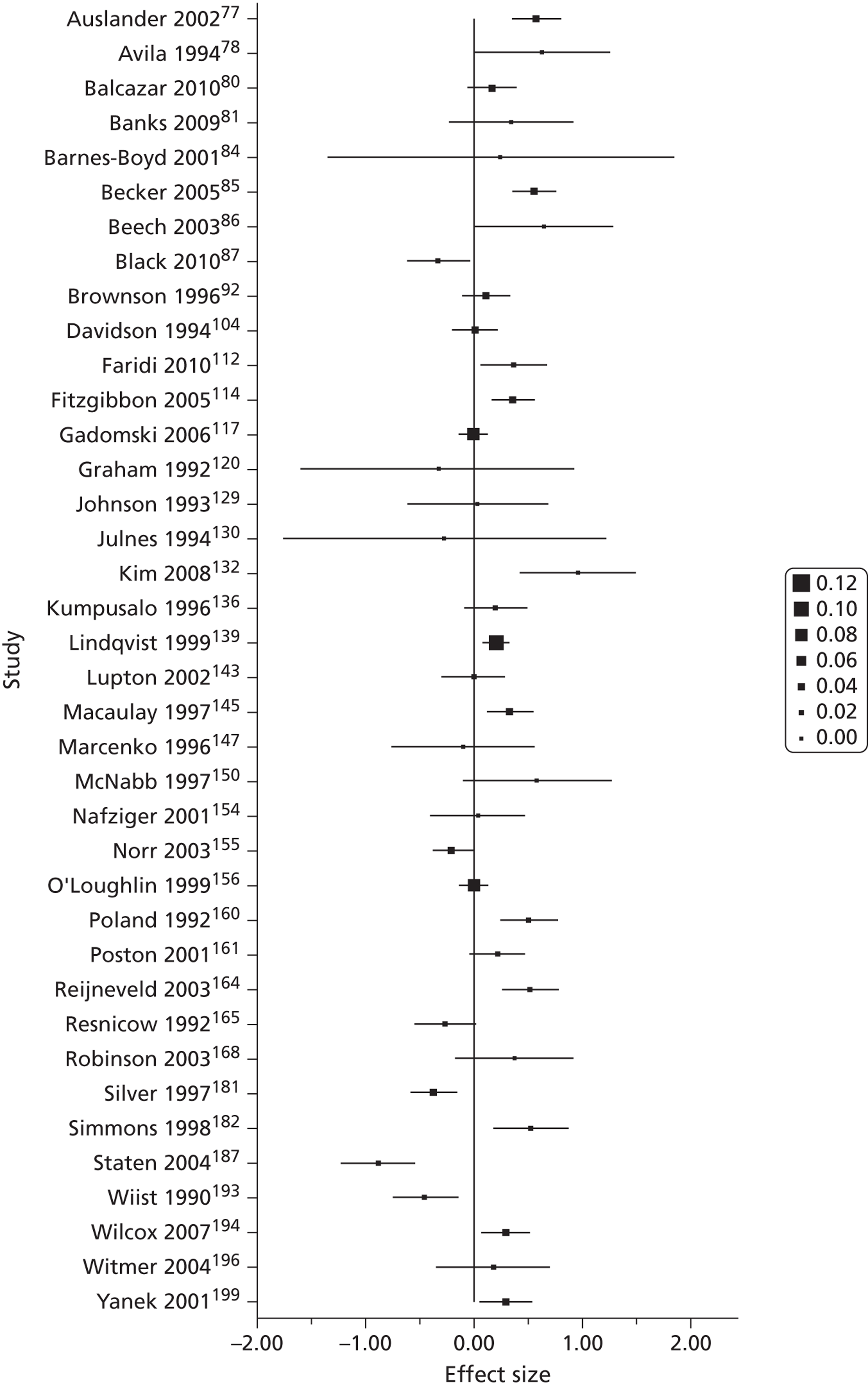
FIGURE 20.
Forest plot of effect size estimates and standard errors of all studies reporting participant self-efficacy outcomes.
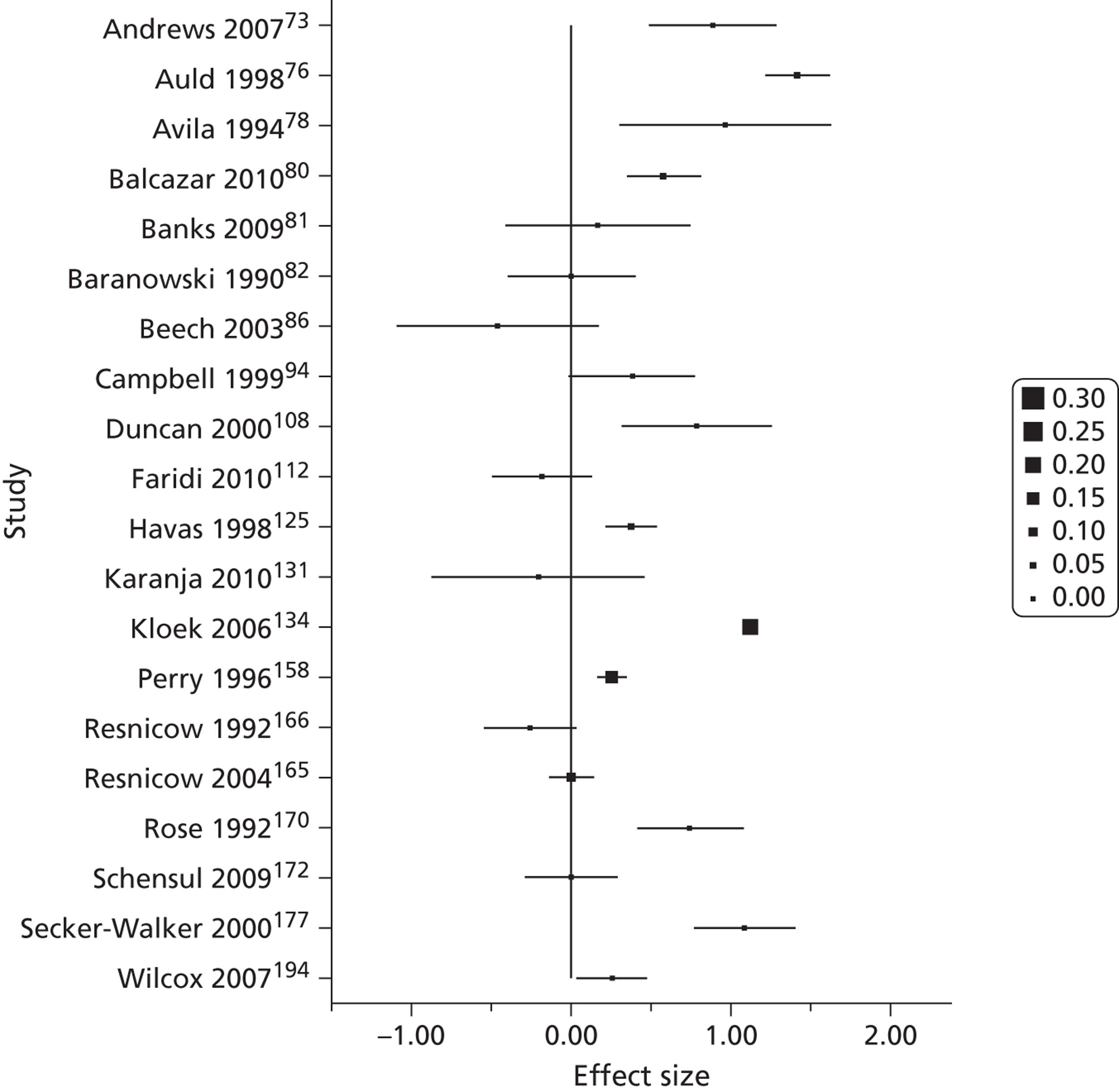
FIGURE 21.
Forest plot of effect size estimates and standard errors of all studies reporting participant social support outcomes.
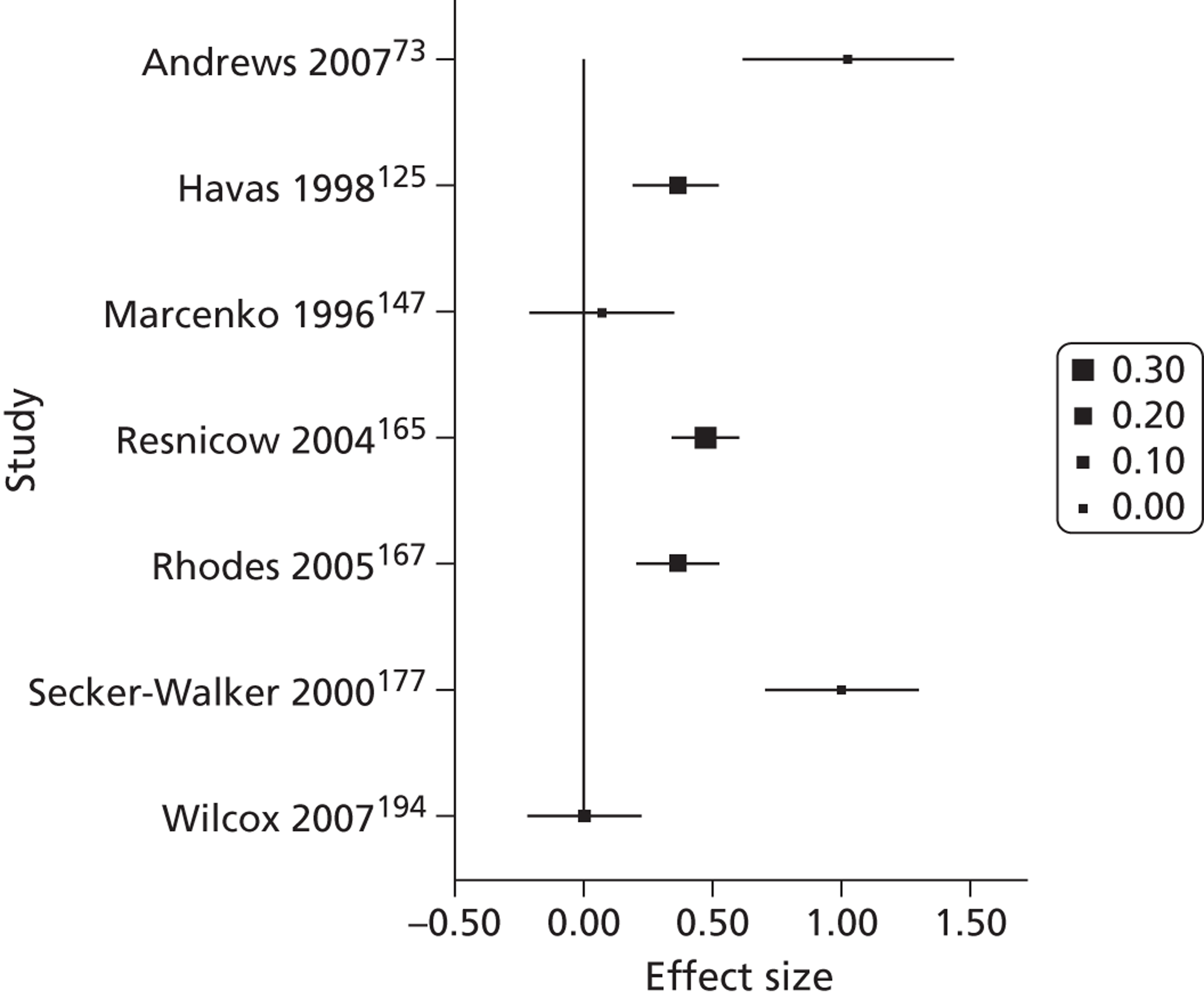
Synthesis of results
In the following sections we report the results of the quantitative synthesis. The sections are organised according to the RQs proposed in Chapter 1. We start by considering whether the interventions were generally effective.
Overall, are community engagement interventions effective?
Across all outcome types, interventions were effective (Tables 21 and 22). There were insufficient effect size estimates for community outcomes and engagee outcomes and so the effect size estimates could not be synthesised statistically; we present these effects in Table 21. It is clear from the available outcome data that there are benefits to the community and engagees; all five outcomes are positive and statistically significantly different from a null effect.
| Study | Outcome type | Outcome description | Effect size estimate | SE |
|---|---|---|---|---|
| Binary data (ORs) | ||||
| Department for Communities and Local Government (2006)119 | Community outcome | Local area improved in the last 3 years | 1.59a | 0.07 |
| Fried (2004)116 | Engagee health | More physical activity at post test | 2.21a | 0.37 |
| Fried (2004)116 | Engagee social support/capital/inclusion | Could have used more emotional support from others in the past year | 6.57a | 0.54 |
| Continuous data (standardised mean differences) | ||||
| Ernst (1999)111 | Community outcome | Connection with health and social services | 0.57b | 0.24 |
| Watkins (1994)191 | Engagee skills | Lay health workers’ knowledge | Missing | Missing |
| Winkleby (2004)195 | Engagee empowerment | Perceptions that advocacy activities would result in changes | 1.43a | 0.14 |
| Outcome | Pooled effect size estimate | 95% CI | n | Heterogeneity | ||
|---|---|---|---|---|---|---|
| τ 2 | Q-statistic | I 2 | ||||
| Health behaviours | 0.33a | 0.26 to 0.40 | 105 | 0.093 | 604.62a | 82.80 |
| Health consequences | 0.16b | 0.06 to 0.27 | 38 | 0.076 | 196.36a | 81.16 |
| Participant self-efficacy | 0.41b | 0.16 to 0.65 | 20 | 0.278 | 480.44a | 96.05 |
| Participant social support | 0.44a | 0.23 to 0.65 | 7 | 0.067 | 42.67a | 85.94 |
Table 22 presents the results for the outcomes: health behaviours, health consequences, participant self-efficacy and participant social support. From Table 22 we can see that the pooled effect size estimate across interventions is positive (indicating that the outcomes measured were in favour of the treatment group) and statistically significant (as indicated by the p-values and 95% CIs) for these four outcomes. The statistical significance of the pooled effect means that the effect size estimate is significantly different from a null effect, in which there are no differences between the intervention group and the comparison group.
There was, however, significant heterogeneity across the four categories of quantitative outcomes observed in Table 22. As such, we conducted moderator analyses to attempt to explain variation in the observed effectiveness of the interventions. These analyses are described in the following sections.
Correlation between outcome types
In Theoretical framework we presented a proposed causal pathway from the intervention to the various outcomes considered in this review (see Figure 15). We were unable to test the direct and indirect pathways to reducing health inequalities because of a lack of data for different outcome types. Modelling this causal pathway was also limited because we did not have longitudinal data to test the proposed causal ordering. We ran correlation analyses to test whether there were any relations between outcomes in the review. The results are presented in Table 23. The only significant correlation is between health behaviours and participant self-efficacy, which was a moderate positive correlation (r = 0.55, p < 0.05). This result indicates that interventions that are more effective in terms of health behaviours are also more effective in terms of self-efficacy.
| Health behaviours | Health consequences | Participant self-efficacy | Participant social support | |
|---|---|---|---|---|
| Health behaviours | 1.000a | 0.216b | 0.553c,d | 0.590e |
| Health consequences | 1.000f | 0.218g | N/A | |
| Participant self-efficacy | 1.000h | 0.811i | ||
| Participant social support | 1.000j |
Maintenance of intervention effects
The maintenance of intervention effects could be synthesised only for health behaviour outcomes because of the lack of follow-up data reported for other outcome types. The pooled effect size estimate at delayed follow-up for the 20 studies that reported health behaviour follow-up outcomes was d = 0.09 [95% CI −0.23 to 0.34]. Significant variation (I2 = 94.43%) indicates that the pooled effect is not a good indicator of long-term effectiveness.
We conducted a meta-regression analysis to attempt to explain the variation. We included post-test effect size estimate as a predictor, so that any variation in the follow-up effect size estimates due to initial intervention effectiveness could be accounted for. We also included the time between the post-test and follow-up measures as a predictor.
The results suggest that post-test effect size estimates do not significantly predict follow-up effect size estimates, although higher post-test effect size estimates tend to be associated with higher follow-up effect size estimates (Table 24). The results also suggest a (just barely non-significant) trend that if the time lapsed after the immediate post-test measure to follow-up measures is < 1 year, the effect size estimate is smaller than follow-up measures taken more than a year later. This could suggest some sort of sleeper effect, in which the benefits of the interventions take more than a year to manifest, or the trend could be due to other factors or random chance. Further longer-term follow-up data are required to clarify this trend.
| Predictor of follow-up effect size estimate | B (SE) |
|---|---|
| Constant | 0.31 (0.19)a |
| Post-test effect size estimate | 0.37 (0.48) |
| < 1 year since post-test measure | −0.66 (0.34) |
Section summary
Overall, public health interventions for disadvantaged groups are effective in improving health behaviours, health consequences, participant self-efficacy and participant perceived social support. Importantly, although few studies have measured such outcomes, interventions did improve outcomes for indirect beneficiaries (the community and engagees) when measured. In combination, these findings suggest that interventions can have benefits beyond the health behaviours and health consequences that are typically targeted by public health interventions.
There was a statistically significant correlation between participant self-efficacy and health behaviour outcomes. Although we were unable to test the causal ordering, this does suggest that improvements in one outcome may facilitate improvements in another.
Further, there is evidence from a small group of studies to suggest that intervention effects are still present long after the intervention has finished, although effects generally are smaller than at post-test. These findings emphasise the importance of well-designed evaluations, to better understand the ‘virtuous circles’ of sustained benefits for both direct and indirect beneficiaries for primary and non-primary outcomes; this issue will be revisited in Chapter 8 (see Conditions).
Research question 3: Which approaches to community engagement are associated with improved health outcomes among disadvantaged groups? How do these approaches lead to improved outcomes?
Introduction and rationale for variables examined
Chapter 4 brought together a range of different models and mechanisms through which members of the community can be engaged in public health interventions. It is clear that people can be engaged in different stages of the process – from identification of the health need to design, delivery and evaluation – and at each stage participants can be involved to differing degrees. There are also variations in the strategies employed (peer health advocacy, community coalitions, etc.), which are driven by implicit or explicit motivations and theories about how involving the community can make interventions more effective. Moreover, community engagement might be only a small part of a larger public health intervention initiative, or it could be the only component of the intervention.
In this section, we aim to explore whether different approaches to community engagement are equally effective by examining trends in the effect size estimates across these various dimensions of involvement. We examined two variables: the theory of change explicitly or implicitly adopted in the community engagement approach, and the extent to which multicomponent interventions incorporated community engagement across all components.
The theory of change was tested because this was the most clear differentiation between community engagement approaches, in terms of both the mechanism through which engagement was proposed to enhance intervention effectiveness and the actual process of engaging the community in different stages of the intervention. Differences between the extent of engagement in multicomponent interventions was tested because we wanted to explore the possibility of the ‘dilution’ of the community engagement aspect of the intervention when other components were included in a public health initiative.
All of the analyses refer to health behaviour outcomes only unless otherwise specified. This is because the other outcome types generally did not have sufficient effect size estimates for subgroup analysis.
Theory of change
Several theories of change were described in Chapter 4. One model proposes that change is facilitated when the health need is identified by the community and those in the community mobilise themselves into action. In a second model, the need for intervention is usually identified by observation from people outside the community, but the views of stakeholders are sought with the belief that the intervention will be more appropriate to the participants’ needs as a result. We identified two main mechanisms by which stakeholder views are sought in the design or planning of the intervention: by collaboration with the community, or by consultation with the community. A third theory of change model does not necessarily involve the community in the design or planning of the intervention; rather, the focus is on community engagement in the delivery of the intervention. In this model, change is believed to be facilitated by the credibility, expertise or empathy that the community member can bring to the delivery of the intervention.
We ran an analysis to compare the effectiveness for health behaviour outcomes of interventions employing these different theories of change. Although there were no overall significant differences between the studies grouped by theory of change, some clear trends emerge (Table 25). Interventions that engaged the community through the delivery of the intervention had the largest pooled effect size estimate, whereas interventions that adopted self-mobilisation, design collaboration or design consultation theories of change (whether implicitly or explicitly) had overall effect size estimates that were similar in magnitude to one another but substantially lower than that of peer-/lay-delivered interventions. Interventions that did not fit into one of the four main theory of change categories had the smallest pooled effect size estimate.
| Theory of change | Pooled effect size estimate | 95% CI | n | Average sample size (SD) |
|---|---|---|---|---|
| Community-identified health need | 0.31a | 0.14 to 0.48 | 17 | 1067.00 (226.30) |
| Collaboration to design more appropriate intervention | 0.32b | 0.13 to 0.51 | 16 | 1924.91 (910.74) |
| Consulted to design more appropriate intervention | 0.25a | 0.12 to 0.38 | 27 | 848.67 (184.53) |
| Lay-delivered to enhance credibility, expertise or empathy | 0.47a | 0.34 to 0.60 | 38 | 309.74 (48.21) |
| Other | 0.17 | −0.07 to 0.42 | 7 | 757.14 (213.08) |
We conducted supplementary analyses to try to explain why the peer-/lay-delivered interventions might be more effective. One explanation that we considered was the size of the studies. We suspected that the peer-/lay-delivered intervention studies tended to be smaller scale and usually more likely to be one-on-one than interventions in which the community was involved in the design of the intervention. From descriptive statistics (see Table 25), we can see that the mean sample size for studies that involved the community only in the delivery of the intervention is much smaller than the mean sample sizes for studies based on alternative theories of change. Post hoc analyses of a one-way ANOVA with sample size as the dependent variable and the different theories of change as the factors indicate that the mean sample size for the peer-/lay-delivered interventions is statistically significantly smaller than the mean sample size for the interventions in which the community identified the health need.
To further interrogate the differences between the theories of change, we cross-tabulated the community engagement strategy with the theory of change (Table 26). Theories of change with a more empowering disposition are more commonly strategies that involve community action, community organisations and community coalition-type models. This broadly fits the model proposed by Popay et al. 4,14,21,472 for community involvement in public health within a health services framework (see Chapter 4, Bridging the utilitarian and social justice rationales for empowerment; Figure 12).
| Community engagement strategy label | Theory of change | ||||
|---|---|---|---|---|---|
| Community-identified health need | Collaboration to design more appropriate intervention | Consulted to design more appropriate intervention | Lay-delivered | Other | |
| Community action | 10 | 8 | 6 | 5 | 2 |
| Community organisations | 5 | 1 | 2 | 1 | 1 |
| Community coalition | 14 | 6 | 5 | 0 | 4 |
| Any peer strategy | 8 | 3 | 10 | 25 | 1 |
| Non-peer health advocacy | 3 | 4 | 9 | 6 | 1 |
| Promotoraa | 0 | 2 | 1 | 5 | 0 |
| Outreach | 0 | 1 | 0 | 4 | 0 |
| Social networks | 1 | 0 | 1 | 2 | 0 |
| Volunteering | 5 | 3 | 5 | 9 | 0 |
| Other community engagement strategy | 1 | 0 | 2 | 2 | 1 |
| No clear community engagement label | 1 | 1 | 0 | 0 | 0 |
| Multiple community engagement labels | 15 | 8 | 11 | 10 | 2 |
Multicomponent interventions
In some studies there were multiple components to an intervention, of which all or only some might have involved community engagement. We categorised the studies into four categories:
-
there is only one component to the public health intervention, which involves community engagement in some way
-
there are multiple components to the public health intervention, all of which involve community engagement in some way (whether through design, delivery or evaluation)
-
there are multiple components to the public health intervention, only some of which involve community engagement in some way (whether through design, delivery or evaluation)
-
unclear.
There were no significant differences between the four categories for health behaviour outcomes, although there was a trend towards single component interventions having higher effect size estimates (Table 27).
| Components in intervention | Pooled effect size estimate | 95% CI | n |
|---|---|---|---|
| Unclear | 0.01 | −0.33 to 0.35 | 4 |
| Only one component | 0.42a | 0.26 to 0.57 | 30 |
| All components involve community engagement | 0.34a | 0.21 to 0.48 | 31 |
| Only some components involve community engagement | 0.31a | 0.20 to 0.43 | 40 |
Research question 3 summary
We tested two dimensions of community engagement in which interventions differed from each other: the theory of change underpinning the engagement, and the extent to which interventions included components that did not involve the community. Interventions that engage community members exclusively in the delivery of the intervention tend to be more effective at improving health behaviours than interventions that empower the community or involve members in the design of the intervention. Whether community members are engaged in all or only some components of a multicomponent intervention does not appear to make a difference.
Research question 4: Which approaches to community engagement are associated with reductions in inequalities in health? How do these approaches lead to reductions in health inequalities?
Introduction and rationale for variables examined
Evidence and theories on reducing health inequalities through community engagement initiatives were discussed in Chapter 1 (see Reducing health inequalities through community engagement initiatives) and have been brought into a new conceptual framework in Chapter 8. An argument was made that community engagement and related concepts (such as participatory empowerment) can have positive outcomes in terms of social capital and cohesion for socially excluded groups,4,15 and, consequently, the social inequalities that underpin health inequalities could be improved. 28 However, there is no clear evidence of the causal pathway between community engagement, improvements in social capital/cohesion and improvements in health outcomes (mortality, morbidity, health behaviours). We therefore attempted to test the causal pathway from intervention to social inequalities to health inequalities (see Figure 15 for the proposed causal pathway).
The second aspect of this RQ relates to how community engagement approaches can reduce health inequalities. The Marmot Review28 indicated that there are some health priorities that are more critical for disadvantaged groups in the UK. As such, we tested whether targeting specific health issues leads to improved outcomes for disadvantaged groups.
Causal pathway from intervention to social inequalities to health inequalities
As discussed in Correlation between outcome types, we were unable to test causal pathways through path modelling. Instead, we sought to explore this issue by examining the correlation between social support (an indicator of social exclusion) and health outcomes. This would provide an indication of whether social inequalities and health inequalities can both be enhanced by community engagement interventions.
The results of the correlation analysis indicate that interventions that are more effective for social support outcomes tend to be more effective for health behaviour outcomes, although this relation was not statistically significant (r = 0.59, p > 0.10). The lack of significance is probably due to the small number of data points: only six studies95,225,311,381,434,475 reported both health behaviour and social support outcomes. Importantly, all six studies reported positive outcomes for both health behaviours and social support.
Health inequality priority areas
In Chapter 2 we described how the selection of studies for inclusion in the quantitative and economic analyses was driven by health priority areas identified in the Marmot Review. 28 Studies were grouped into three broad categories:
-
modifiable health risks (smoking, alcohol abuse, substance abuse and obesity)
-
best start in life (antenatal care, breastfeeding, parenting skills and childhood immunisation)
-
prevention of ill health – topics not captured above (healthy eating, physical activity, general health promotion, injury prevention, cancer prevention and cardiovascular disease/hypertension prevention).
We conducted an analysis to see whether interventions focusing on each of the Marmot Review focus areas were associated with larger effects. We found no significant difference between the three categories for health behaviour outcomes, although there was a trend that impacts were larger for best start in life and ill health prevention interventions than for health risk interventions (Table 28). It is important to emphasise that the pooled effect size estimate for each of the three categories was significantly different from 0 in the positive direction, which indicates that the interventions were generally improving health behaviours, regardless of the health topic.
There were sufficient data to undertake this analysis for health consequence outcomes as well. As with health behaviours, the difference between the three categories was non-significant, although there was a trend in which interventions targeting the best start in life had a smaller pooled effect size estimate than those targeting ill health prevention, which in turn had a smaller pooled effect size estimate than those targeting the modifiable health risks. In contrast to health behaviour outcomes, only the health risks category had a pooled effect size estimate that was significantly different from 0 for health consequence outcomes. In other words, there was no evidence that interventions targeting best start in life or the prevention of ill health had a significant impact on health consequence outcomes.
| Outcome | Marmot Review theme | Pooled effect size estimate | 95% CI | n |
|---|---|---|---|---|
| Health behavioursa | Health risks | 0.24b | 0.11 to 0.37 | 34 |
| Best start in life | 0.38b | 0.19 to 0.56 | 24 | |
| Prevention of ill health and injury | 0.38b | 0.28 to 0.48 | 47 | |
| Health consequencesc | Health risks | 0.23d | 0.06 to 0.40 | 17 |
| Best start in life | 0.05 | −0.29 to 0.39 | 7 | |
| Prevention of ill health and injury | 0.12 | −0.06 to 0.30 | 14 |
Research question 4 summary
We were unable to test the hypothesis that community engagement interventions can reduce health inequalities through their impact on social inequalities, because of insufficient data. There is, however, some evidence to suggest that interventions that improve social inequalities (as measured by social support) also improve health behaviours. In terms of health inequality priority areas identified in the Marmot Review,28 interventions that targeted the prevention of ill health or getting the best start in life were more effective at improving health behaviours than those addressing modifiable health risks. In contrast, interventions targeting modifiable health risks were more effective for improving health consequences.
Research question 5: Which types of intervention work best when communities are engaged?
Introduction and rationale for variables examined
We explored a range of characteristics of the interventions to better understand which types of interventions work best when communities are engaged. The characteristics examined were intervention setting, intervention deliverer, intervention strategies/activities and duration of the intervention. These variables were selected as they cover key features affecting intervention design, implementation and resourcing.
Intervention setting
Interventions were frequently conducted in multiple settings (see Table 15), making this issue difficult to disentangle. Of most interest to this review, we focused on interventions conducted in community settings. We found that interventions delivered (whole or in part) in community settings had a statistically significantly smaller pooled effect size estimate for health behaviour outcomes than interventions that are not conducted in community settings (Table 29).
| Intervention setting | Pooled effect size estimate | 95% CI | n |
|---|---|---|---|
| Community setting | 0.25a | 0.15 to 0.35 | 57 |
| Non-community setting | 0.42a | 0.31 to 0.52 | 48 |
Intervention strategies
We explored the relative effectiveness of different intervention strategies in improving health behaviour outcomes. The variety of intervention strategies observed and their frequencies were presented in Table 16. We focused on five particular intervention strategies that were chosen for their prevalence or substantive interest: education, skill development or training, social support, incentives, or access to health resources or services.
The results did not indicate that the intervention strategy was significantly associated with health behaviour outcomes (Table 30). The results indicate that interventions employing incentives or skill development strategies tend to have higher effect size estimates than other strategies, whereas interventions with education approaches tend to be the least effective.
| Intervention strategy | B (SE) | Mean effect size estimate |
|---|---|---|
| Constant | 0.37 (0.10)a | 0.37 |
| Education | −0.15 (0.10) | 0.22 |
| Skill development or training | 0.12 (0.08) | 0.49 |
| Social support | 0.05 (0.08) | 0.42 |
| Incentives | 0.10 (0.12) | 0.47 |
| Access to resources or services | 0.01 (0.08) | 0.38 |
Intervention deliverer
As with settings, interventions were frequently conducted by multiple intervention deliverers (see Table 17). We focused on four types of intervention deliverer: community members, peers, health professionals and educational professionals. These were the most common intervention deliverers and of the most substantive interest as they reflect a range of lay and professional deliverers.
For health behaviour outcomes, these four types of intervention deliverer did not explain a significant amount of the variation in the effect size estimates (Table 31). However, interventions with health professionals involved in the delivery of the intervention tended to have smaller effect size estimates than interventions with other deliverer types, whereas those involving educational professionals tended to have larger effect size estimates. It is worth noting that this does not mean that interventions delivered by health professionals caused harm to the participants, as the effects were still positive overall.
| Intervention deliverer | B (SE) | Mean effect size estimate |
|---|---|---|
| Constant | 0.34 (0.08)a | 0.34 |
| Community member | −0.03 (0.09) | 0.31 |
| Peer | 0.03 (0.09) | 0.37 |
| Health professional | −0.10 (0.09) | 0.24 |
| Educational professional | 0.08 (0.10) | 0.42 |
By running a reduced model in which we explored only the relative effectiveness of interventions involving community members, peers or other intervention deliverers, we were able to test the effectiveness of the interventions by deliverer type for health consequences and participant self-efficacy (Table 32). For health consequences, we can see a trend towards interventions with community members being more effective than those without community members; however, the results of this model suggest that this is not a significant predictor of effect size estimate.
| Outcome | B (SE) constant | B (SE) community member | B (SE) peer | n | R 2 | Model homogeneity Q-test value (p-value)a |
|---|---|---|---|---|---|---|
| Health consequences | 0.06 (0.11) | 0.17 (0.13) | 0.08 (0.14) | 38 | 0.04 | 1.70 (p = 0.43) |
| Participant self-efficacy | 0.51 (0.21)b | −0.17 (0.23) | 0.00 (0.24) | 20 | 0.03 | 0.58 (p = 0.75) |
The reverse trend is apparent for self-efficacy outcomes: interventions delivered by community members are associated with smaller effect size estimates. Again, intervention deliverer was not a significant predictor of self-efficacy effect size estimates.
Duration of the intervention
We tested whether the duration of the intervention was associated with the effect size estimates for health behaviours, health consequences and self-efficacy outcomes. Because the raw variable was not normally distributed, we used two approaches to testing this variable. For health behaviour outcomes, the data were normalised using a logarithmic transformation. For health consequences and self-efficacy outcomes, the data were still non-normal after log-transformation and so we created a categorical variable of short, medium and long duration interventions.
For health behaviour outcomes, the duration of the intervention is a statistically significant predictor of the effect size estimate: the longer the intervention, the smaller the effect size estimate (Table 33). For health consequences outcomes, the categories were not significantly different from each other in terms of the pooled effect size estimate, although shorter interventions tended to have larger effects (Table 34); this is the same trend observed for health behaviours. For self-efficacy outcomes, there were no trends and the variable was not a significant moderator of effect size estimate (see Table 34).
| Intervention duration | B (SE) |
|---|---|
| Constant | 0.59 (0.14) |
| Duration | −0.07 (0.04)a |
| Outcome | Intervention duration | Pooled effect size estimate | 95% CI | n |
|---|---|---|---|---|
| Health consequencesa | < 6 months | 0.36b | 0.16 to 0.57 | 13 |
| 6–23 months | 0.09 | −0.07 to 0.26 | 16 | |
| ≥ 2 years | 0.06 | −0.16 to 0.28 | 8 | |
| Participant self-efficacyc | < 6 months | 0.41d | 0.01 to 0.81 | 7 |
| 6–23 months | 0.41d | 0.00 to 0.82 | 6 | |
| ≥ 2 years | 0.48d | 0.08 to 0.88 | 6 |
Research question 5 summary
We explored four characteristics for which interventions varied in terms of their implementation. Although interventions were effective overall, we found that the following types of interventions work best when communities are engaged:
-
interventions not conducted in community settings, such as primary and secondary care settings
-
interventions employing skill development or training, or the offering of contingent incentives
-
interventions involving education professionals in delivery of the intervention
-
interventions that are shorter in duration (< 6 months), although this is probably confounded by levels of exposure or intensity of contact with the intervention deliverer.
Research question 6: Is community engagement associated with better outcomes for some groups than others? (In particular, does it work better or less well for children and young people?)
Introduction and rationale for variables examined
This report takes a life course approach to considering inequalities, which focuses on interventions appropriate for each age group; interventions that take into account inequalities that already exist (targeted); and interventions that reduce the development of inequalities in later life. As discussed in Chapter 3, Main PROGRESS-Plus characteristics, investigations of inequalities are often framed in terms of PROGRESS (Place of residence, Race/ethnicity, Occupation, Gender, Religion, Education, Socioeconomic position and Social capital58), the mnemonic for broader determinants of health. We broadened this to include other variables describing ways in which people may be systematically disadvantaged by discrimination, for instance because of their sexual orientation or a disability, by being excluded from social relationships (e.g. teenagers excluded from school) or as a result of challenging life transitions (e.g. teenage pregnancy or parenting). We tested whether community engagement was associated with better outcomes for some PROGRESS-PLUS groups than others.
Targeted age groups
Age group targeted in the intervention was not significantly associated with intervention effectiveness for health behaviour outcomes (Table 35). However, there was a trend such that the effect size estimate for health behaviour outcomes was smaller when the intervention targeted the general population.
| Age group targeted | Pooled effect size estimate | 95% CI | n |
|---|---|---|---|
| General population | 0.22a | 0.11 to 0.34 | 38 |
| Children or young people (0–17 years) | 0.37a | 0.25 to 0.50 | 32 |
| Young people and adults (11–54 years) | 0.36a | 0.17 to 0.56 | 19 |
| Adults (18+ years) | 0.47a | 0.29 to 0.64 | 16 |
Targeted PROGRESS-Plus groups
In our review, groups that were disadvantaged in terms of health included those disadvantaged with regard to socioeconomic status/position and ethnic minority status, ‘at-risk’ or ‘high-risk’ young people experiencing social exclusion or life transitions (including pregnant and parenting adolescents) and those disadvantaged according to place of residence (inner city or rural), in which there was evidence of being medically underserved. There were also many studies with indistinguishable multiple health inequalities (e.g. both low-income and ethnic minority status).
There were no significant trends by PROGRESS-Plus group, although the group of interventions targeted at people who were disadvantaged because of place of residence was the only group that had a pooled effect size estimate that was not significantly different from 0 (Table 36). In other words, there is no clear effect of interventions targeted at people disadvantaged by place of residence. All other groups had pooled effect size estimates that were significantly different from 0, and interventions targeted at people of low socioeconomic position tended to be particularly effective.
| PROGRESS-Plus group | Pooled effect size estimate | 95% CI | n |
|---|---|---|---|
| Socioeconomic status/position | 0.41a | 0.26 to 0.56 | 29 |
| Ethnicity | 0.33a | 0.23 to 0.44 | 44 |
| ‘At-risk’ or ‘high-risk’ young people, including pregnant/parenting teenagers | 0.45b | 0.17 to 0.73 | 6 |
| Place of residence | 0.11 | −0.16 to 0.38 | 6 |
| Multiple health inequalities | 0.28b | 0.12 to 0.45 | 20 |
Research question 6 summary
We found that community engagement is associated with better outcomes for adult populations, although interventions were generally effective across all age groups. We also found that interventions tend to be most effective for participants classified as disadvantaged because of socioeconomic position. Existing interventions targeting participants on the basis of place of residence do not appear to be effective.
Research question 7: How do targeted and universal interventions compare in terms of community engagement and their impact on inequalities?
Introduction and rationale
Bearing in mind the social gradient in ‘healthy’ community characteristics,28 which may mean that more disadvantaged communities benefit less from a community engagement intervention than other, less disadvantaged communities, there is a danger that a universal community engagement intervention may increase inequalities in health by having a proportionately greater impact on more advantaged areas. We therefore tested whether universal interventions were similarly as effective as those targeted to specific PROGRESS-Plus groups.
It is important to note that, as a consequence of our inclusion criteria, the ‘universal interventions’ in this review have been delivered to samples of predominantly people from any of the PROGRESS-Plus categories of inequality (i.e. at least 60% of the sample). The difference between ‘universal’ and ‘targeted’ interventions in this review lies in the explicit focus of the authors of the original studies on targeting a particular PROGRESS-Plus group, compared with delivering an intervention to a sample that just happens to be mostly constituted of people from a PROGRESS-Plus categorisation.
Targeted compared with universal interventions
There were no significant differences between universal and targeted interventions for health behaviour outcomes (Table 37). There was a trend towards larger effect size estimates for universal interventions than targeted interventions.
| Universal or targeted | Pooled effect size estimate | 95% CI | n |
|---|---|---|---|
| Universal | 0.43a | 0.19 to 0.67 | 9 |
| Targeted | 0.32a | 0.24 to 0.40 | 96 |
Research question 7 summary
Universal interventions tended to have larger effect size estimates than targeted interventions, although this trend was not statistically significant. Risk of bias across studies
Risk of bias of included studies
We explored the potential risk of bias by considering three methodological features of studies: the type of comparison group, randomisation of participants to conditions and the soundness of the study. As described in Risk of bias within studies (see also Appendix 3), soundness is a combined measure of the degree of risk of bias on the three subscales of selection bias, attrition bias and selective reporting bias.
For all four outcome types (health behaviours, health consequences, participant self-efficacy and participant social support), the analyses revealed no significant moderators of the effect size estimates. The results are presented in Table 38. As such, we can be reasonably confident that there is no systematic bias in the effect size estimates due to characteristics of the intervention evaluations.
| Outcome | Risk of bias variable | k | Model homogeneity | |
|---|---|---|---|---|
| QBa (p-value) | QWa (p-value) | |||
| Health behaviours | Comparison group type | 7 | 7.71 (p = 0.26) | 97.14 (p = 0.51) |
| Random allocation | 3 | 0.14 (p = 0.93) | 95.60 (p = 0.63) | |
| Soundness | 2 | 1.27 (p = 0.26) | 97.45 (p = 0.64) | |
| Health consequences | Comparison group type | – | Insufficient data | |
| Random allocation | – | Insufficient data | ||
| Soundness | 2 | 0.18 (p = 0.67) | 36.66 (p = 0.44) | |
| Participant self-efficacy | Comparison group type | – | Insufficient data | |
| Random allocation | – | Insufficient data | ||
| Soundness | 2 | 1.68 (p = 0.19) | 20.33 (p = 0.31) | |
| Participant social support | Comparison group type | – | Insufficient data | |
| Random allocation | – | Insufficient data | ||
| Soundness | 2 | 0.04 (p = 0.85) | 7.19 (p = 0.21) | |
Risk of publication bias
Concerns about publication bias have been raised after observations that research evaluations showing beneficial and/or statistically significant findings are more likely to be published than those that have undesirable outcomes or non-significant findings. 54 If this phenomenon does occur, then reviews of a biased evidence base will draw biased conclusions. Unfortunately, it is difficult to assess publication bias because there is no way of knowing the extent of what has not been published.
As a result of these concerns, researchers have developed ways of estimating the extent to which there may be some publication bias in the evidence base. The use of funnel plots (scatter plots in which the effect size estimates from individual studies are plotted against a measure of study precision) is a common method for assessing the possibility of publication bias. Ideally, the spread of effect size estimates should be such that there is more scattering of effect size estimates at the bottom of the plot, where there is less precision, with a narrowing of the scattering towards the top, where there is greater precision.
In Figure 22, the effect size estimates are plotted against their standard errors for continuous and binary outcomes. From the figure, we can see that larger effect size estimates (in terms of magnitude) typically have larger standard errors; that is, larger effects are associated with more variability. This can indicate a potential for publication bias.
We believe, however, that our sampling frame may help protect us from publication bias. By identifying studies primarily through systematic reviews that have taken measures to protect against publication bias (e.g. searching grey literature), our database includes many reports that would not be subject to the presumed publication bias associated with journal articles. We suggest that review methodologists formally evaluate whether this search technique does actually help to avoid publication bias, or whether it compounds the problem by inheriting the search flaws of other reviews.
FIGURE 22.
Plot of effect size estimates against their standard errors for binary and continuous outcomes.
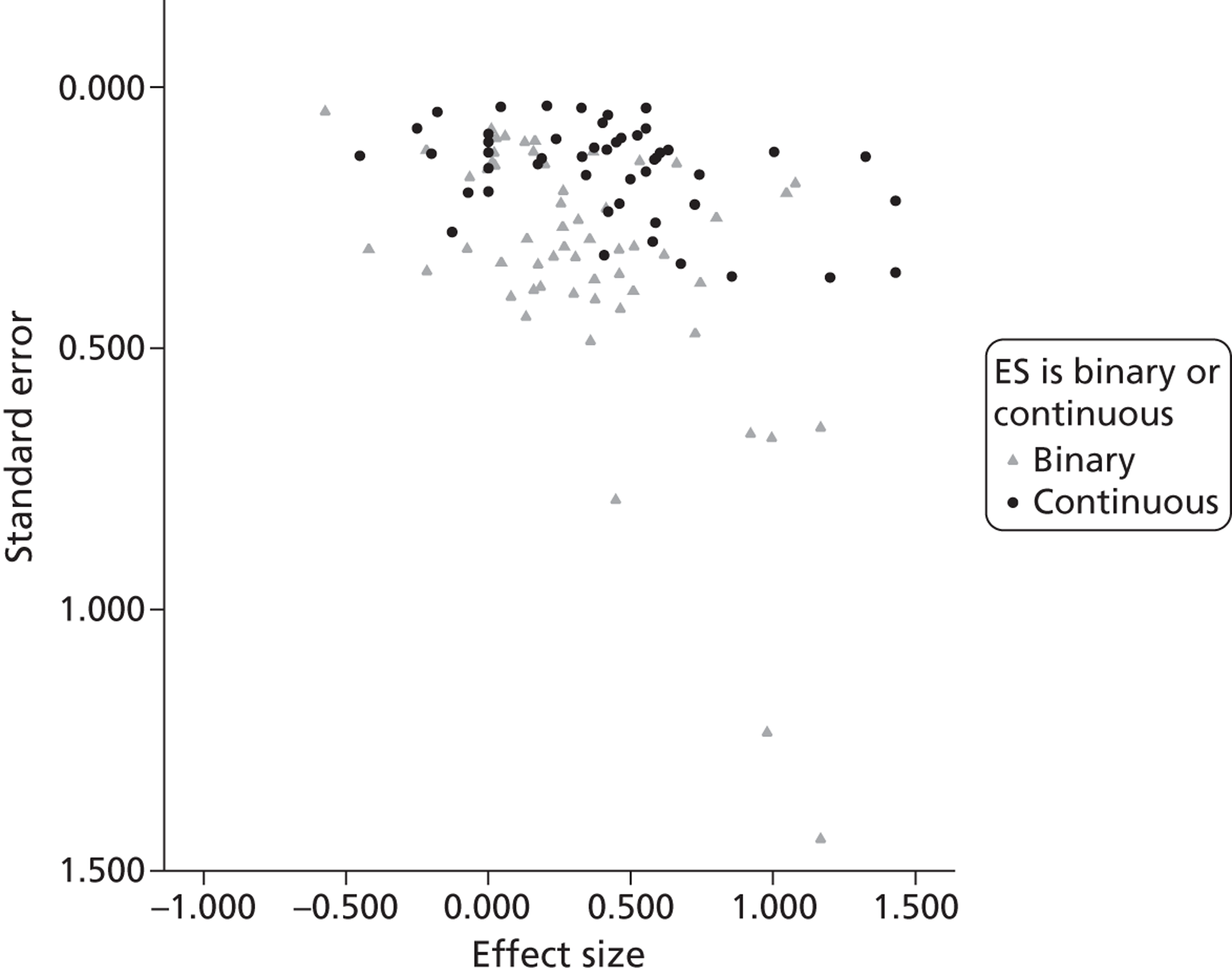
Moreover, current approaches to publication bias assume – but do not test – that missing studies are missing not at random; that is, they do not assess whether these missing studies are likely to be due to random chance or due to systematic factors – the current methods simply assume that sample size (precision) is the systematic factor explaining missing effect sizes. To appropriately test for publication bias, we would need to assess whether the unobserved studies are actually systematically unobserved in relation to the outcome variable, and explore reasons for that systematic difference. Unfortunately, there are currently no adequate techniques for assessing this and it may indeed be impossible.
Additional analyses
Sample size
In Overall, are community engagement interventions effective? (see Table 22), results of a homogeneity test revealed that, for all outcomes, there was significant variability amongst the effect size estimates. Throughout this chapter, we have attempted to explain some of this variability through moderator and predictor variable analyses. Although many trends emerged, we failed to identify variables that could explain the heterogeneity amongst the effect size estimates.
One phenomenon that appeared to be related to the effect size estimates was the size of the study, as indicated by the funnel plot in Figure 22. To explore whether the sample size might explain some of the variation in the effect size estimates, we conducted an unweighted meta-regression. [An unweighted model, in which the weight for all studies was set to 1, was used because including study weights in the model would inflate the observed relationship between sample size (the independent variable) and effect size (the dependent variable). This is because the inverse variance study weights used in meta-analysis are largely a function of sample size.] This model tested whether the log of the sample size of each study predicted the size of the effect for health behaviour outcomes. The results indicated that, although sample size was not a significant predictor of the effect size estimate (unstandardised regression coefficient = –0.10, standard error = 0.08), it did explain about 10% of the variance in the effect size estimates (as indicated by the model R2). As such, it is likely that sample size accounts for some of the heterogeneity observed amongst the effect size estimates.
Summary of findings
-
Overall, public health interventions for disadvantaged groups using community engagement strategies are effective in terms of health behaviours, health consequences, participant self-efficacy and participant perceived social support. These findings appear to be robust and not due to systematic methodological biases.
-
There are also indications from a small number of studies that community engagement interventions can improve outcomes for the community and engagees.
-
Increases in health behaviours are significantly related to increases in self-efficacy.
-
There is evidence from a small group of studies to suggest that intervention effects are still present long after the intervention has finished, although effects generally are smaller than at post test.
-
RQ3: Which approaches to community engagement are associated with improved health outcomes among disadvantaged groups?
-
Interventions that engage community members exclusively in the delivery of the intervention tend to be more effective at improving health behaviours than interventions that empower the community or involve members in the design of the intervention.
-
Single component interventions tend to be more effective than multicomponent interventions for health behaviour outcomes. Whether community members are engaged in all or only some components of a multicomponent intervention does not appear to make a difference to the size of the intervention effect for health behaviour outcomes.
-
-
RQ4: Which approaches to community engagement are associated with reductions in inequalities in health?
-
We were unable to test the hypothesis that community engagements can reduce health inequalities through their impact on social inequalities because of insufficient data. There is some evidence to suggest that interventions that improve social inequalities (as measured by social support) also improve health behaviours.
-
In terms of health inequality priority areas identified in the Marmot Review,28 interventions that targeted the prevention of ill health or getting the best start in life were more effective at improving health behaviours than those addressing modifiable health risks. In contrast, interventions targeting modifiable health risks were more effective for improving health consequences.
-
-
RQ5: Which types of intervention work best when communities are engaged?
-
Interventions conducted in non-community settings tended to be more effective for health behaviour outcomes than those conducted in community settings; this finding was statistically significant.
-
Interventions that employed skill development or training strategies, or which offered contingent incentives, tended to be more effective for health behaviour outcomes than those employing educational strategies.
-
Interventions involving peers, community members or education professionals tended to be more effective for health behaviour outcomes than those involving health professionals.
-
Shorter interventions tended to be more effective than longer interventions for health behaviour outcomes; this finding was statistically significant. However, this is probably confounded by levels of exposure or intensity of contact with the intervention deliverer.
-
-
RQ6: Is community engagement associated with better outcomes for some groups than others? (In particular, does it work better or less well for children and young people?)
-
Interventions tended to be most effective in adult populations and less effective in general populations for health behaviour outcomes.
-
Interventions tended to be most effective for health behaviour outcomes for participants classified as disadvantaged because of socioeconomic position. Interventions targeting participants on the basis of place of residence do not appear to be effective for health behaviour outcomes.
-
-
RQ7: How do targeted and universal interventions compare in terms of community engagement and their impact on inequalities?
-
Universal interventions tended to have (non-significant) higher effect size estimates for health behaviour outcomes than targeted interventions.
-
Chapter summary
Our analyses suggest that public health interventions using community engagement in disadvantaged groups are effective in terms of health behaviours, health consequences, participant self-efficacy and perceived social support. These findings appear to be robust and not due to systematic methodological biases. There are also indications from a small number of studies that interventions can improve outcomes for the community and engagees. This chapter also identified trends in the effectiveness of interventions that can be considered when designing future interventions.
We qualify this overall statement with the observation that there is significant variation in the intervention effectiveness – some interventions were more effective than others, and not all interventions benefited the participants. We tested a set of predetermined variables that we hoped might explain this variance and address the RQs posed. Unfortunately, very few of these variables were statistically significant in explaining differences between interventions.
Supplementary (post hoc) analyses suggested that the number of participants in the intervention accounts for about 10% of the variation in the health behaviour outcomes. We propose that this association is likely to be confounded with different intervention approaches. In Table 25, for example, we noted clear differences in sample sizes between studies employing lay delivery approaches to community engagement and those that adopted empowerment approaches, which is partly attributable to the types of one-to-one, intensive interventions we often see with the peer-/lay-delivered approaches (e.g. home visitation to encourage mothers to breastfeed). For such models, we might expect to see large effects over a narrow range of outcomes, as opposed to empowerment models that might have smaller effects over a broader range of health and social outcomes.
In the next two chapters, we explore some of the process and economic factors that might shed light on the differential effectiveness of community engagement interventions. In particular, issues regarding the evaluation of community engagement interventions might inform our understanding of causal pathways and maintenance of intervention effects.
Chapter 6 Synthesis III: thematic synthesis of integral process evaluations
About this chapter
Process evaluations are a useful way of looking at the delivery and uptake of interventions. In this complex review, they were utilised to draw out information about how interventions work (or do not work), and for whom. As such, they are intended to complement the theoretical synthesis, meta-analysis and economic analysis. Assessment of the process evaluations integrated within outcome evaluations included in the meta-analysis indicates some interesting and complementary findings about the methods of process evaluation and impact of interventions. This chapter briefly describes the included studies in terms of their populations, interventions and outcomes, discusses the quality of efforts to reduce the risk of bias across all nine process evaluations and then draws out information on the different processes that were evaluated.
Studies included in this synthesis
Six of the studies included in the meta-analysis undertook and published results from integral process evaluations; these six studies were included in Synthesis III. A further three outcome evaluations that were excluded from the meta-analysis at a late stage had also published a process evaluation. Because they were late exclusions from the meta-analysis we had already extracted data from the process evaluations and included them in Synthesis III. We decided to retain these three studies in Synthesis III despite the late exclusion of the outcome evaluations from the meta-analysis because there was no apparent bias introduced to the synthesis by their inclusion and they added information about possible process issues. As such, a total of nine process evaluations were included in Synthesis III.
Andrews et al. 73,208 offered a multicomponent smoking cessation intervention to African American women in public housing, offered in part by community health workers. Wilcox et al. 194 utilised church volunteers to provide physical activity interventions to low-income African Americans. Chapman et al. 98,230 provided a breastfeeding programme to urban low-income Latinas using peer counsellors. Wickizer et al. 475 evaluated the benefits of community coalitions for the design and implementation of multicomponent substance abuse prevention programmes for Native American youths. Davis et al. 243 formed a university–community partnership with a Native American community to develop and provide a school-based obesity prevention programme of class curricula and family events. Duggan et al. 476 targeted Hawaiian families at risk of child abuse/neglect by using paraprofessionals to provide early screening and home visiting support. Grant et al. 477 provided paraprofessional postnatal home visits for women at risk of drug abuse to support and guide them in a programme designed in collaboration between university and community members. Quinn et al. 375 designed a church-based weight-loss programme with community leaders, and offered healthy eating and physical activity interventions to urban African American women in churches using volunteers. Finally, Ritchie et al. 381 described a local health department/community partnership to develop and deliver antismoking initiatives such as media events and classes to low-income urban adults in Scotland.
Quality of process evaluation methods
An assessment of the methods undertaken by each process evaluation suggested that, overall, the studies were of low to medium quality in both rigour and usefulness. The quality assessment of each integral process evaluation is summarised in Appendix 7. Five73,98,105,106,208,230,243,244,252,381 of the nine studies used an interview design and four98,230,252,475,477 used documentation review. Three studies105,106,194,243,244,381 undertook surveys and one study each utilised focus groups73,208 or observations. 375 Five of the studies73,105,106,208,230,243,244,252,381 used a combination of two design methods (most often documentation plus one other method).
Process data were gathered most often from study participants and from more than one group of stakeholders. Study participants were questioned in eight73,98,105,106,194,208,230,243,244,252,375,381,477 of the nine process evaluations; three studies105,106,243,244,375,381 focused on intervention providers; two studies73,208,381 focused on advisory group members; and two studies381,476 focused on research staff. Four73,105,106,208,243,244,375,381 of the nine studies conducted process evaluations with more than one type of participant. Seven studies73,98,105,106,208,230,243,244,375,381,475,477 measured processes concurrently with the intervention; one study252 measured processes after the intervention period had ended; and one study194 measured both concurrently and afterward.
Studies were judged on their efforts to ensure methodological rigour and reduced risk of bias in sampling, data collection and analysis. Studies could make a fairly thorough attempt, take several steps or take a few steps, or this was unclear/not described. A total of five studies73,98,105,106,208,230,243,244,375,381 were thorough or took several steps to ensure rigour in sampling, with the remaining four studies194,252,475,477 taking only a few steps or not providing enough information to make a judgement. Only three105,106,243,244,375,381 of the nine studies were equally as rigorous for their methods of data collection and four studies105,106,194,230,243,244,381 were similarly rigorous in their methods of analysis.
Data were grounded fairly well or reasonably well in eight98,105,106,194,230,243,244,252,375,381,475,477 of the nine process evaluations, with authors linking findings back to data either in quotes or statistically. Only three73,194,208,381 studies were deemed to have both breadth (extensive description of process findings) and depth (adequate transformation or synthesis of those findings). The remaining six had limited breadth and depth (n = 3),98,230,252,477 and adequate breadth but limited depth (n = 3). 105,106,243,244,375,475
Of the nine process evaluations, only one study73,208 privileged the perspectives and experiences of the public. Two studies105,106,243,244,381 privileged the public’s experiences somewhat and the remaining six privileged the public’s views either a little (n = 3),194,252,375 or not at all (n = 3). 98,230,475,477
Overall, one study477 was rated low on reliability and low on usefulness, two studies73,208,475 were rated low on reliability with medium usefulness and four studies98,194,230,375,476 were rated of medium reliability and low usefulness. Only one study each was rated of high reliability and medium usefulness243 and high reliability and high usefulness. 381
Analysis of the processes evaluated, resultant size of effects and conclusions made by authors were similar across studies. Authors’ conclusions did not appear to vary by publication date, health topic area or type of community engagement model used.
Evaluated processes
The processes evaluated by the authors are listed in Table 39. Implementation was the most frequently measured type of process, described in eight studies. 73,98,194,208,230,243,375,475–477 The overall quality of programme materials was least often evaluated in this group of process studies. The coded findings from the nine integral process evaluations are described narratively below.
| Study | Process issue | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Acceptability | Accessibility | Consultation/collaboration | Content | Costs | Implementation | Management/responsibility | Quality of programme materials | Provider skills/training | Other | |
| Andrews (2007)73,208 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Chapman (2004)98,230 | ✓ | ✓ | ||||||||
| aDavis (2003)243 | ✓ | ✓ | ✓ | ✓ | ||||||
| bDuggan (1999)476 | ✓ | ✓ | ||||||||
| cGrant (1996)477 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| dQuinn (2001)375 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| eRitchie (2004)381 | ✓ | ✓ | ||||||||
| fWickizer (1998)475 | ✓ | ✓ | ✓ | ✓ | ||||||
| Wilcox (2007)194 | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Total | 4 | 5 | 6 | 2 | 4 | 8 | 2 | 1 | 3 | 2 |
Acceptability
Four studies243,375,381,477 examined issues of acceptability. In each case these studies simply measured participation rates and suggested that higher participation rates implied participant acceptability of the intervention. Three studies discussed different reasons for higher participation rates. Quinn et al. 375 indicated that participation rates may have been influenced by delivery of the interventions by community volunteers in particular. Davis et al. 243 and Grant et al. 477 suggested that participation rates might have been influenced by the way in which the community members (e.g. teachers, volunteers or leaders) approached their involvement in the intervention (i.e. with enthusiasm, supported or feeling confident). Conversely, Ritchie et al. 381 noted that community workers were less likely to address the issue of smoking with low-income community members because of fears of alienating them. Further, the same workers suggested that an approach to smoking cessation in a community must start from a more holistic view of health, raising self-esteem and reducing stress before addressing smoking behaviours.
Accessibility/programme reach
Five studies73,208,194,375,475,476 discussed issues related to the facilitation of accessibility or programme reach for participants, linking these to participation rates. The interaction between community members – study participants and those who supported the intervention in some way – appears to influence how widely a programme reaches. Quinn et al. 375 indicated that participation rates were high because lay health educators were able to recruit extensively from within their church congregations. Wilcox et al. 194 noted that programme awareness was associated with key outcomes. Participants who had spoken with a church member about physical activity during the intervention phase were more likely to be in an action- or maintenance-level stage of change; to be undertaking moderate physical activity; and to have increased fruit and vegetable consumption. When participants reported pastor support for physical activity and healthy eating interventions, a statistically significant higher level of physical activity was reported. Duggan et al. 476 found that assessments by programme staff (rather than hospital staff), conducted in person, may have increased the reach of a programme. In addition, they suggested that, when an index child had considerable identified need, either the family’s recognition of that need or the home visitor’s efforts to encourage that family to take up services influenced the family’s decision to accept an intervention.
The locality of services in facilitating the provision of an intervention also appears to be important to a programme’s accessibility. For example, Andrews et al. 73,208 identified providing locally situated services and concurrent child care to be important.
Finally, one study also suggested a relationship between the types of intervention offered and the overall programme reach. Wickizer et al. 475 noted that medium- or low-intensity interventions such as classes, peer modelling, health fairs or drug-/alcohol-free events achieved higher exposure rates than high-intensity services such as counselling, risk assessment or home repair.
Consultation and collaboration
Issues with consultations and collaborations were described in six studies. 73,194,208,243,381,475,477 The quality of the relationship between partners was discussed by five of these studies. 73,194,208,243,381,475 Andrews et al.,73,208 Wickizer et al. 475 and Davis et al. 243 indicated that successful involvement was important in planning or conducting the intervention, noting that this applied to both culturally similar and culturally diverse partners. Davis et al. 243 emphasised that programme support by all involved partners helped to facilitate positive results. Wilcox et al. 194 stressed the importance of recognising and addressing cultures and values that differ between partners, and noted challenges in keeping partner enthusiasm and support over the course of the programme. They suggested that these had more impact earlier in the project than later. Wilcox et al. 194 also point to the need for a strong and trusting relationship between academic and community partners. This is an issue also echoed by Ritchie et al.,381 who noted that the unequal representation of some partners could leave those partners feeling disempowered.
Issues of power and control were discussed in two studies. Wickizer et al. 475 suggested that coalition members may compromise the partnership to protect their own organisation’s autonomy. They also noted that other priorities within each partner’s organisation or community might supersede those of the programme. Organisational partners and intervention providers in the study by Ritchie et al. 381 voiced the opinion that power imbalances occurred because the more powerful partner was the least amenable to community development and was thus the least able to accommodate flexibly enough for the community project to operate successfully.
Differences between partners regarding the underlying philosophy of the programme may also play a part in its success. Ritchie et al. 381 cite one such example of one partner’s philosophy being concerned with community development, which competed directly with another partner’s philosophy of preventing unhealthy lifestyles. This difference in philosophy may have contributed to a low level of input from community members. Project staff later reflected that this contributed to confusion about whether the health issue being targeted by the programme was truly community defined. Ritchie et al. 381 thus emphasised the importance of clarifying the roles and inputs of agencies involved in partnerships with communities.
Content
Two studies73,208,375 discussed aspects of the content of the intervention that may have influenced the outcomes. Andrews et al.,73,208 in describing a healthy eating intervention targeted to an African American community, suggested that intervention effectiveness was enhanced by having community recommendations on familiar representations in the written materials, incentives, food used and the delivery of the intervention components. Quinn et al. 375 noted that high adherence to programme content (in effect, how completely each session was delivered) influenced the outcomes seen. Thus, community-specific, completely administered programme content appears to be an important process influencing community engagement initiatives.
Costs
Four process evaluations73,98,208,475,477 discussed the implications of costs. Two studies discussed the value of financial recognition of participants and the community members who engage them. Community members advising on an intervention in Andrews et al. 73,208 recommended that participants be paid and receive gifts for taking part, suggesting that this process might have influenced the outcome. Chapman et al. 98 noted that the intervention might have been effective because peer counsellors were paid a wage and full-time counsellors received medical benefits.
Grant et al. 477 noted a cost saving directly attributable to the use of peer advocates. The successful lobbying by one peer advocate on behalf of a client led to that client’s jail sentence being commuted to home confinement – a £35,000 saving.
The ability of programmes to generate funds from sources external to the programme funders was also noted. Wickizer et al. 475 noted that programme partners were able to generate outside funding of at least 25% above initial funding costs. The peer counsellor breastfeeding programme described in Chapman et al. 98 secured funding on a year-by-year basis, suggesting that this contributed to the ongoing success of the programme.
However, it was also suggested that a lack of funds might have limited researchers’ ability to understand why a programme produced particular results. Grant et al.,477 in the study of paraprofessional home visiting advocacy interventions to reduce alcohol and drug use in addicted mothers, reflected that a lack of funding limited the amount of process evaluation that could be undertaken. This limited the extent to which authors could examine why the intervention was not as effective as had been hoped.
Implementation
Eight73,98,194,208,243,375,475–477 of the nine process evaluations measured implementation. Only one study found that implementation was not associated with outcomes. Wilcox et al. 194 measured implementation across church sites, but noted that it did not influence outcomes; however, this finding may have occurred because six church sites failed to implement the programme at all. The remainder of studies found associations or suggested links between process implementation measures and effectiveness.
One study indicated that the timing of intervention delivery could influence outcomes. Andrews et al. 73,208 offered sessions at a variety of times throughout early afternoon and evening hours to accommodate participants’ daily routines.
The intensity of the intervention (i.e. the number of sessions provided) was linked to positive effects in four studies. Chapman et al. 98 examined outcome effectiveness according to the number of visits received and found that women who received both perinatal and postnatal contact with peer counsellors had better outcomes than those who did not receive both. In addition, those women who received early postnatal home visits were more likely to breastfeed than those who did not; and those women who received all three components of the intervention (antenatal, perinatal, post-partum home visits) were more likely to breastfeed for longer than those who did not.
Grant et al. 477 indicated that participants who spent more time with their advocates had better outcomes, although it is not clear whether this refers to frequency or duration of contact. Davis et al. 243 found that longer session duration was related to positive teacher comments, and suggest that positive school staff support may have influenced the intervention’s effectiveness. Quinn et al. 375 described more effective outcomes when the programme content had been more consistently adhered to and delivered.
Paradoxically, one study found that interventions requiring less intensive provider input allowed more of a community to be reached. Wickizer et al. 475 noted that low- and medium-intensity interventions, such as school classes and social events, resulted in a broader exposure across a community than did higher-intensity interventions, including counselling, risk assessment or home repair. ‘Intensity’ in this case appears to refer to the one-to-one nature of the intervention; as such, it is an issue of implementation as well as of accessibility, and is thus discussed in both sections.
Finally, one study476 noted that differences in agency philosophy (i.e. why they interact with at-risk families – for whole family benefit or to intervene on behalf of an at-risk index child) may have influenced how those agencies implemented the intervention with participating families. These authors go on to suggest that this agency philosophy could itself be caused by organisational characteristics such as staff supervision, support worker knowledge and skill, and staff turnover.
Management and responsibility
Only two studies194,477 evaluated the impact of management and responsibility issues on the intervention’s success. One study194 described the challenges of intervention planning and delivery for community members’ own daily time commitments. Wilcox et al. 194 reflected on a need to consider the constraints of volunteers and pastors when developing and delivering church-based interventions, to respect and consider the church hierarchy and to appreciate the challenges relating to the distribution and use of funds within a community, and noted the need for a more detailed process evaluation to more fully explore these issues.
Grant et al. 477 suggested that management strategies to support peers’ involvement (e.g. including ongoing training, caseload management, community recognition, allowing creativity, staff retreats, performance evaluations, salary and benefits, individual advocate supervision and weekly group staff meetings) limited staff turnover, which in turn influenced the success of the intervention. They also provided safety training and staff immunisations to protect advocates who were visiting high-risk households and neighbourhoods. Further, they note the value of utilising a programme evaluator as a staff member to evaluate client progress, communicate with other service and community organisations and foster ongoing programme improvement.
Quality of the programme materials
One study identified the quality of programme materials as being an important process. Andrews et al. 73,208 attributed part of the success of their intervention to programme materials and delivery, which were informed by, and embedded in, the cultural norms and values identified by community members. This included making all programme materials, incentives and food prepared culturally relevant, as well as embedding values of collectivism, storytelling and spirituality throughout the programme.
Skills and training of the intervention providers
Three studies243,375,477 indicated particular aspects of provider skills and training that were important. All three studies noted the importance of training, in particular ongoing training. Davis et al. 243 noted that teachers rated highly the ongoing training that they received each year in the provision of intervention curricula, suggesting that this satisfaction influenced their support of the intervention overall and contributed to its positive outcome. Grant et al. 477 and Quinn et al. 375 also emphasised the need for ongoing training of intervention providers, suggesting a multicomponent formal and informal training programme for project staff, other trained providers and external service provider and community organisations to increase provider knowledge, share experiences and make contact with key external partners in providing care. Additionally, Quinn et al. 375 found that research staff could support lay health educators by providing feedback on their intervention delivery during practice ‘presentations’.
Grant et al. 477 recommended adequate and specific training of providers in the complex behaviours being targeted by interventions. A substantial minimum level of training was also suggested as being helpful: client advocates in Grant et al. 477 were required to undertake 80 hours of formal training and 40 hours of observation with trained providers before accepting a caseload.
Two studies suggested skills and characteristics that may have influenced intervention success. Grant et al. 477 and Quinn et al. 375 made similar suggestions for the specific skills needed in community members who provided interventions: a similar ethnicity and life history; empathy; tenacity; problem-solving skills; a direct, honest, non-judgemental manner; belief in participants’ worth despite their history; and previous experience working with high-risk populations.
Other processes
Finally, two studies194,475 described other processes. Wickizer et al. 475 described the development and submission of a subsequent funding proposal as a result of the community involvement intervention undertaken. Wilcox et al. 194 noted that most programmes were able to generate at least 25% of the total funding outside of the initial grant. Wickizer et al. 475 identified a varying amount of community activation (i.e. the embedding or ownership of a programme by a community) after a programme ended, suggesting that this may have been due to a recognition amongst partners that the coalition had served its purpose and come to a natural end.
Chapter summary
Despite the high number of outcome evaluations located, only nine integral process evaluations (i.e. those conducted alongside outcome evaluations) were identified and assessed for quality and findings. In general, process evaluations were of low to medium quality in their methods and of low to medium usefulness to the review. Authors did not consistently link findings to data, and authors sometimes went beyond findings when drawing conclusions. We found it challenging to capture the complexity of processes because of the varied nature of the interventions and community engagement activities. The differences in epistemologies of community engagement became more evident when using different process evaluation data extraction tools. Several insights were offered into factors affecting process, which included:
-
acceptability: community-designed or -delivered interventions, or culturally relevant programme materials, were linked to acceptability, which authors suggested influenced programme success
-
consultation and collaborations: successful partnerships and efforts to build relationships between partners appear to influence programme outcomes
-
costs: paying community members and participants influences participation
-
costs: some coalitions were able to win external funding, helping the programmes to be sustainable and ‘owned’ by communities beyond initial funding periods
-
implementation: adequate and appropriate intervention timing, frequency, duration and extent of an intervention influence outcomes
-
implementation: intervention types (e.g. media events vs. one-to-one counselling) can affect accessibility or ‘reach’ by enabling exposure to different numbers (and potentially groups) of people
-
implementation: good relationships between engagees and professionals providing an intervention are important for programme implementation
-
management and responsibility: good project management and specific, adequate, ongoing training and support for engagees impacts on implementation.
In the next chapter, we turn our attention to an assessment of the cost and resource implications of studies evaluating community engagement for health inequalities.
Chapter 7 Synthesis IV: economic analysis of costs and resources
About this chapter
It is important to know not only whether community engagement actions are effective, but also how much they cost and their relative cost-effectiveness compared with alternative uses of resources, whether that be for investing in health-related interventions or other uses of resources such as improving housing, tackling crime or improving access to education.
It is insufficient to know whether any community engagement strategies work in any society in which resources are constrained. There is strong policy support for involving people in developing public services and evaluation, but does this investment represent value for money? Is it, for instance, the case that investing in support to encourage peers to promote healthy activities leads to sufficiently greater sustained uptake of those activities and consequent impacts on health outcomes to justify additional expenditure compared with current public health policy?
To date, there have been few attempts to collate information on the costs of community engagement actions and less still on their cost-effectiveness. This reflects challenges in measurement as well as in capacity or the priority given to economic evaluation. Some inputs in particular are difficult to quantify, such as the opportunity costs of volunteers and the inputs of the community as a whole in engagement actions based on empowerment. Guidance on community engagement produced by NICE478 highlighted a dearth of economic information, whereas a review of studies on community engagement for health promotion23 was able to find only potential economic studies, none of which focused specifically on the cost-effectiveness of the community engagement component. A companion systematic review40 of the economic evidence for community engagement and development strategies to address the wider determinants of health also failed to identify any studies that reported the costs and health benefits of a community engagement approach relative to a comparator; some information on the resources required to deliver interventions was, however, reported in 20 studies. Some very limited modelling work on the potential cost-effectiveness of community engagement was undertaken following this review,24 with two vignettes on the role of trained peer educators and community engagement for flood defences prepared. 25
The purpose of this chapter is to look at both what is known about the level of resources required to deliver community engagement interventions and their potential cost-effectiveness. We also included additional complementary economic evaluations and models linked to the effectiveness studies in our review. Two bespoke data extraction questionnaires designed to capture data on economic issues (e.g. sufficiency of funds) and resource utilisation, cost and cost–consequences (e.g. staff costs) were developed. These were then combined into one tool to help identify relevant information from studies (see Appendix 5). This will help us to answer the following review questions:
-
RQ8: What are the resource implications of effective approaches to community engagement?
-
RQ9: Are better outcomes simply the result of increased resources, or are some approaches to community engagement potentially more cost-effective than others?
This chapter also looks at some issues related to the inputs of volunteers to community engagement, the potential role that investing in financial incentives and other mechanisms can play in encouraging participation, and the broader range of benefits beyond health that may strengthen the economic case for investing in community engagement. We also look at some of the challenges associated with cash flow and the long-term sustainability of community engagement actions. These final points build on some of the issues that have been flagged up in the process evaluation in Chapter 6 in respect of effective partnership working and scope for identifying additional sources of funding and/or mainstreaming effective interventions.
Costs, resource use and cost–consequences
Data on the use of resources and costs of interventions were extracted from papers. Comparatively few reported the overall costs of interventions or the resources available for the implementation of the programmes. We also collected some information on individual components of interventions, including the costs of personnel, venues, volunteering and transportation, when this was reported. Although the number of studies reporting costs is limited, as Tables 40 and 41 indicate, some cost data were available for interventions in nearly all of the health topic areas and areas of community engagement.
| Health topic | Costs reported | Costs not reported |
|---|---|---|
| Antenatal care | 1 | 7 |
| Asthma prevention/treatment/management | 1 | 2 |
| Breastfeeding | 5 | 12 |
| Cancer prevention | 2 | 0 |
| Cancer screening/detection | 7 | 5 |
| Cardiovascular disease | 2 | 5 |
| Care of older people | 1 | 0 |
| Child abuse prevention | 6 | 4 |
| Child illness and ill health | 1 | 1 |
| Diabetes prevention/management | 4 | 6 |
| Disabilities and chronic illness | 1 | 1 |
| Healthy eating | 6 | 19 |
| HIV prevention/risk reduction | 3 | 10 |
| Hypertension | 1 | 2 |
| Immunisation | 4 | 3 |
| Injury prevention | 4 | 5 |
| Mental health | 1 | 5 |
| Neighbourhood renewal | 4 | 0 |
| Obesity prevention/weight reduction | 0 | 12 |
| Partner violence | 1 | 2 |
| Physical activity | 4 | 19 |
| Public health/health promotion/prevention | 2 | 11 |
| Reproductive health | 0 | 2 |
| Safe community | 2 | 1 |
| Sexual health | 3 | 9 |
| Smoking cessation | 5 | 11 |
| Smoking prevention | 2 | 1 |
| Substance abuse | 8 | 33 |
| Suicide prevention | 1 | 0 |
| Tuberculosis | 0 | 1 |
| Other topics | 1 | 4 |
| Area of community engagement | Costs reported | Costs not reported |
|---|---|---|
| Community action/support | 1 | 3 |
| Community involvement | 0 | 2 |
| Community mobilisation | 1 | 1 |
| Community partnership | 3 | 2 |
| Community organisations | 2 | 16 |
| Cultural competence | 2 | 0 |
| Health advocacy | 1 | 3 |
| Lay health | 9 | 14 |
| Neighbourhood management | 5 | 10 |
| Neighbourhood Warden Scheme | 1 | 0 |
| Outreach programme | 5 | 7 |
| Participatory research | 1 | 8 |
| Peer counselling | 3 | 5 |
| Peer education | 4 | 12 |
| Peer leaders | 2 | 4 |
| Peer support | 3 | 8 |
| Social networks | 3 | 3 |
| Task force | 1 | 6 |
As these tables indicate, only a small number of papers included in our effectiveness review documented even partial information on the costs of delivering their specific programmes. Few studies disaggregated costs in a detailed manner, so that, even though many studies involved an element of training, no study reported the costs of training per se. For instance, a community-level intervention to reduce the risk of suicide in Japan was shown to be effective and the programme costs were stated; however, these were not disaggregated, nor was there any attempt to include the in-kind contributions of paid staff or volunteers involved in the programme, or to provide any impacts of the time spent by community members in developing prevention plans. 346
This lack of disaggregation meant that in most studies it was difficult to separate out the costs of routine implementation of community engagement initiatives from the costs of evaluation. In terms of the intervention, again it remains difficult to distinguish the resource use and costs associated with mechanisms for community engagement from those aspects of an intervention that would be delivered in any case as part of usual care. Only 12 papers116,142,201,207,239,248,258,311,351,372,393,426 provided distinct information on the costs associated with volunteering and only 18 studies73,79,98,116,140,162,169,178,201,207,208,230,284,329,340,359,372,393 separated out the costs associated with paid staff. Many of the small number of studies that did provide disaggregated cost data also went on to conduct an economic evaluation.
Economic evaluation overview
Economic evaluations compare the costs and outcomes of two or more interventions. Although costs are all measured in monetary terms, outcomes can be measured in different ways, including natural outcome measures, for example life-years gained, changes in cholesterol levels in cost-effectiveness analyses, quality- or disability-adjusted life-years in cost–utility analyses or in monetary terms in cost–benefit analyses. In the UK, the use of incremental cost per quality-adjusted life-year (QALY) gained has been recommended for use in economic studies, although the use of alternative approaches such as cost–consequences analysis has been recognised as helpful in the context of public health. In a UK context, a cost per QALY gained of < £20,000 would be considered to be cost-effective for public health interventions; above this threshold the decision is more debatable. To capture as many studies as possible, we also included cost–consequences analyses that provide multiple effectiveness outcome measures as well as information on costs, but do not synthesise these in the form of a ratio.
Our 21 economic studies can be categorised according to our three models of community engagement: 11140,162,220,226,261,340,365,372,378,479,480 included ‘classical’ or ‘traditional’ peer- or lay-delivered interventions; seven116,164,201,223,224,393,481,482 involved models with varying degrees of collaboration between health and other statutory services and communities; and three136,320,355 were of engagement interventions centred on the concept of empowerment. It is not surprising that most of these evaluations focused on actions with more discrete easy-to-measure outcomes and costs; this again reflects the challenge in evaluating broad community development/empowerment interventions that have multiple actions, outcomes and costs. This is consistent with the findings of a previous review in this area. 40
Table 42 provides an overview of the different methods used. Only three studies372,378,481 took the form of a cost–utility analysis, compared with nine cost–consequences analyses,136,140,162,164,220,223,224,226,261,365,480 five cost-effectiveness studies201,320,355,482 and four cost–benefit analyses. 201,240,372,393,479 Table 43 provides the same breakdown by health topic area.
| Code | Cost-effectiveness analysis | Cost–utility analysis | Cost–benefit analysis | Cost–consequences analysis |
|---|---|---|---|---|
| Community action/support | 0 | 0 | 1 | 0 |
| Community mobilisation | 1 | 0 | 1 | 0 |
| Community organisations | 1 | 0 | 0 | 0 |
| Community partnership | 0 | 0 | 0 | 0 |
| Cultural competence | 0 | 0 | 0 | 2 |
| Health advocacy | 0 | 0 | 0 | 0 |
| Lay health | 0 | 1 | 0 | 1 |
| Neighbourhood management | 0 | 0 | 1 | 0 |
| Neighbourhood Warden Scheme | 0 | 0 | 1 | 0 |
| Outreach programme | 0 | 0 | 0 | 0 |
| Participatory research | 0 | 0 | 0 | 0 |
| Peer counselling | 0 | 0 | 0 | 0 |
| Peer education | 0 | 0 | 0 | 3 |
| Peer leaders | 1 | 1 | 0 | 1 |
| Peer support | 0 | 0 | 0 | 2 |
| Social networks | 1 | 1 | 0 | 0 |
| Task force | 1 | 0 | 0 | 0 |
| Code | Cost-effectiveness analysis | Cost–utility analysis | Cost–benefit analysis | Cost–consequences analysis |
|---|---|---|---|---|
| Antenatal care | 0 | 0 | 0 | 0 |
| Asthma prevention/treatment/management | 1 | 0 | 0 | 0 |
| Breastfeeding | 0 | 0 | 0 | 2 |
| Cancer screening/detection | 1 | 0 | 0 | 2 |
| Cardiovascular disease | 0 | 0 | 0 | 0 |
| Care of older people | 0 | 0 | 0 | 1 |
| Child abuse prevention | 1 | 0 | 0 | 0 |
| Child illness and ill health | 0 | 0 | 0 | 0 |
| Diabetes prevention/management | 0 | 0 | 0 | 2 |
| Disabilities and chronic illness | 0 | 1 | 0 | 0 |
| Healthy eating | 0 | 0 | 0 | 2 |
| HIV prevention/risk reduction | 1 | 1 | 0 | 1 |
| Immunisation | 1 | 0 | 1 | 0 |
| Injury prevention | 0 | 0 | 1 | 0 |
| Mental health | 0 | 0 | 0 | 1 |
| Neighbourhood renewal | 0 | 0 | 1 | 0 |
| Obesity prevention/weight reduction | 0 | 0 | 0 | 0 |
| Partner violence | 0 | 0 | 0 | 0 |
| Physical activity | 0 | 1 | 0 | 1 |
| Public health/health promotion/prevention | 0 | 0 | 0 | 1 |
| Reproductive health | 0 | 0 | 0 | 0 |
| Sexual health | 1 | 1 | 0 | 1 |
| Smoking cessation | 1 | 0 | 0 | 1 |
| Smoking prevention | 0 | 0 | 0 | 0 |
| Substance abuse | 0 | 0 | 0 | 0 |
| Other topics | 0 | 0 | 0 | 0 |
Appendix 8 provides a detailed summary of the characteristics and principal results of these economic evaluations and the methods used. Most of these studies took place outside a UK context and generally report favourable results. They may have a focus not only on health but, in some cases, also on other outcomes when making an economic case. One example of this is an evaluation that focuses on neighbourhood renewal in which the principal outcome considered in the economic analysis was impact on crime. 355 Most of these evaluations focus on the more traditional models of community engagement, involving community peers in delivering a health-related message or action. They particularly concentrate on peer-delivered interventions delivered to minority populations. These types of interventions are relatively easy to measure and cost compared with grassroots more empowerment-oriented actions. Some have used modelling work to build on the results of the empirical studies to extrapolate longer-term costs and benefits or to scale up costs and benefits. 372,481,482 Few complex, multiple-mechanism interventions have included an economic evaluation. Only five studies201,220,320,340,482 in the entire data set considered impacts on productivity or on family informal care, ignoring potential benefits (or costs) of actions.
It is important to note that the low number of economic studies found does not necessarily mean that there is no economics evidence base to support various interventions, particularly those involving the delivery of manualised health promotion programmes, but rather that the evidence on actions involving an additional community engagement approach is more sparse. Parenting programmes provide one example of this: there is now a considerable body of economic and clinical effectiveness literature to support parenting programmes that are delivered predominantly by professional staff. 483
Findings from individual economic evaluations
In this section, we highlight some of the key findings from the economic evaluations that we have identified. In most instances, these studies suggest a favourable economic case for action, but there are many limitations to the strength of effectiveness evidence; moreover, the choice of comparator, study perspective and way that volunteer inputs are valued can distort comparisons. Few take account of uncertainty by performing sensitivity analysis. We discuss findings in terms of our three models of community engagement: peer-/lay-delivered interventions (see Chapter 4, Defining ‘community’); varying degrees of collaboration between health and other statutory services and communities; and interventions centred on the concept of empowerment.
Peer-/lay-delivered interventions
Eleven economic evaluations were of classical or traditional peer-/lay-delivered interventions. 140,162,220,226,261,340,365,372,378,479,480 Many of these studies focused on minority populations for whom language and culture were perceived as barriers to health behaviour change.
The 11 studies identified included an analysis of the role of expert peers in an economic evaluation of the Expert Patient Programme in England, a six-session training programme led by individuals with long-term experience of living with chronic health problems. 378 The comparison was waiting-list control subjects who received treatment as usual. The evaluation reported modest improvements in QALYs gained with reduced costs in terms of health-care services used over a 6-month period, suggesting that the intervention in nearly all circumstances is likely to be cost-effective from a health- and social-care perspective if a £20,000 per QALY gained threshold was used.
Culturally sensitive provision of information to help promote adherence to appropriate follow-up procedures after an abnormal cervical cancer test in a Latino population in the USA was reported to have modest additional costs of just over £245 per woman enrolled compared with no action, with improvements seen in rates of follow-up adherence. 261 No formal attempt to quantify the cost per increase in adherence rate was provided, although this could have been calculated.
A limited cost and consequences analysis in the USA looked at peer support counsellors working alongside community nurses to promote breastfeeding. 162 Although there were only 41 participants in the study, costs were reported to be significantly higher in the intervention group, because of both the costs of the programme (peer counsellors were salaried) and an opportunity cost being assigned to the time that women spend breastfeeding. Average total costs per mother were £3276 in the intervention group compared with £2725 in the control group (p < 0.05). Self-report data from mothers indicated a lower use of health-care resources in the intervention group, with fewer visits to their primary health-care provider, including both check-ups and illness-related visits. The intervention group also had significantly fewer prescriptions and on average 0.1 fewer emergency room visits. However, these impacts on health-care resource use were not costed and no attempt was made to place a value on the benefits of breastfeeding or produce a cost-effectiveness ratio. The authors concluded that the intervention potentially may be cost-effective and feasible, as it changes breastfeeding duration, making it worthy of the attention of policy-makers.
There is also a limited economic analysis put forward of a peer counsellor programme to encourage a minority population in the USA to breastfeed their infants. 140 The costs to the public purse of £990 for employing two part-time counsellors over a 10-month period were more than outweighed by savings of around £9000 by avoiding having to purchase artificial baby milk for mothers, even when allowing for manufacturers’ subsidies. If higher rates of breastfeeding observed at 3 months were maintained then there would also be the potential for improved health outcomes and reduced need for treatment for adverse health problems, but these impacts were not included in the economic analysis.
The cost-effectiveness of training identified popular opinion leaders within gay bars in a town in the USA to communicate HIV risk reduction and safe sex messages to their peers was assessed. 372 It looked at long-term costs and benefits over the life course. An economic model was used to synthesise data on changes in sexual behaviour with retrospective information on the costs of delivering the intervention, as well as the impact on the need for health-care resources. Financial incentives were given to opinion leaders to encourage their participation in the project, which was deemed to be cost saving – reducing overall costs from a health system perspective while gaining additional QALYs.
The costs of a lay health advisor programme to encourage low-income women in North Carolina, USA to make use of mammography were estimated, and the cost per additional mammogram performed was comparable to costs seen with other breast screening uptake initiatives. 365 The authors noted that the costs would be further reduced if unpaid volunteers could be used instead.
The role of such unpaid volunteers was explored in another rural area of the USA in a study comparing volunteer-delivered individual counselling with volunteer community activities and a combination of the two with the aim of raising rates of breast cancer screening. 479 This is one of the most detailed economic evaluations in terms of community engagement that we identified; it has gone to significant lengths to record resource use accurately, including logs for the time of volunteers and women receiving the intervention. Even though volunteers were not paid, unlike most of the studies we identified, the opportunity costs of the time of volunteers were also valued, using the salary cost of a programme assistant or a field research co-ordinator for those who had co-ordination responsibilities. Despite these additional costs, and assuming that the promotion campaign would have a long-lasting impact on behaviour change, the study suggested a cost per life-year saved ratio in 1995 of $56,000 (£50,000 in 2010 prices). This is without including the productivity and quality of life benefits of increased rates of screening.
In England and Wales, an evaluation compared the additional impact of peer counsellors in schools to help prevent the uptake of smoking with usual smoking prevention education. 226 Rates of smoking were significantly lower in the intervention group after 1 year (OR 0.77, 95% CI 0.59 to 0.99] and still lower although not quite significant after 2 years (OR 0.85, 95% CI 0.72 to 1.01). The additional cost per student was £24 but, although the authors considered the intervention to be effective, they did not give an opinion on cost-effectiveness, even though sufficient data had been collected. They noted that involving school students in naming influential students who could be peers appeared to aid the credibility of the peer supporters and increase effectiveness.
However, the use of school-based peer counsellors did not appear to be cost-effective in an Italian study. 220 The use of peer counsellors was compared with teacher-delivered HIV prevention information to 1295 pupils in selected schools in Italy. The study effectively took the form of a cost–consequence analysis, reporting that the peer-delivered programme was almost twice as expensive as the teacher-led programme (£18,571 vs. £9328, or £24.36 per target student involved in the peer-led group vs. £10 in the teacher-led arm). No breakdown in elements of cost was provided and it is not clear whether the opportunity costs to teachers of time spent on training courses have been included in the analysis. No evidence of an impact on sexual behaviour following evaluation was reported for either peer- or teacher-led programmes, suggesting that this intervention is not cost-effective. The peer group did, however, have a small but significantly greater level of improvement (6.7%) in knowledge of HIV prevention.
Although not in our effectiveness review, in looking for economic studies we identified, through citation searching, an additional volunteer-led study providing parenting courses to teenage pregnant women or new teenage mothers in a urban African American community. 480 Volunteers were not paid for home visits to this group but received some funds for their travel expenses. Modest improvements in parenting outcomes were reported, with the costs of the programme not being significantly different from the costs of programmes delivered by professionals. The authors concluded that volunteer-based programmes might be a complement to but not a substitute for professionally delivered programmes.
Varying degrees of collaboration between health/statutory services and communities
Seven economic analyses fell into this broad category of community engagement models. 116,164,201,223,224,393,481,482 They included a study that looked at efforts to engage leaders of the Vietnamese American community to raise hepatitis B awareness, and increase vaccination rates in this population group in Dallas. 201 This was compared with the use of a professional public media campaign targeted at a control population group. Data from the empirical study were used as part of a dynamic simulation model to estimate the lifetime costs and benefits of vaccination. Unusually, the economic analysis placed a value on the time given by volunteers and community leaders involved in developing the community engagement campaign. Although both interventions were considered to be modestly cost-effective against ‘do nothing’, the marginal cost-effectiveness of the public media campaign compared with the community engagement campaign was not calculated (although this would have found the media campaign to dominate), nor was any combination of community engagement and media campaigning considered.
In the Netherlands, a short health education and physical activity programme was adapted to be delivered by a Turkish peer educator to the Turkish migrant community. 164 Although a formal economic evaluation was not conducted, the costs of both the intervention and the comparator, as well as outcomes, were reported. The intervention was associated with improved mental health outcomes but no change in physical activity outcomes. It was delivered at a similar cost as a standard health promotion education programme in a control population, suggesting that it may be a cost-effective action. As the outcomes were measured using the Short Form questionnaire-36 items (SF-36), it would also be possible to subsequently calculate QALY gains associated with the intervention.
The cost-effectiveness of a programme called Breathe Easy for smoking cessation among women in the USA, which included the participation of local community members in planning and implementation, was also assessed. 177,393 Volunteering was one key resource in the programme and over the course of 5 years community coalitions became entirely responsible for smoking cessation plans, with no input from external researchers. Trained volunteer ex-smokers also provided telephone support and support groups to help women quit. The economic analysis was conducted retrospectively both from the perspective of the research funder (including evaluation costs) and from the perspective of implementation costs alone. A partial breakdown of resource use and costs was documented. A simulation modelling approach was used to estimate the lifetime impacts on smoking cessation. A value of between £8 and £20 per hour was placed on the time of volunteers as part of a series of sensitivity analyses for this model. The baseline reported cost-effectiveness of £929 per life-year saved was reported to be attractive compared with that of other smoking cessation programmes. If volunteer costs were included this would rise to as much as £1737 per life-year saved. Although not weighted for quality of life, this is still likely to be considered cost-effective in a USA context.
We looked at a number of studies focused on accidental injury prevention at a community level. Although several studies looked at different ways of mobilising community resources to get across messages and to take actions to improve safety in local communities, only one of these was accompanied by any costing or full economic analysis, the community-based injury prevention programme at Motala in Sweden – a town designated as a WHO Safe Community. 139,329 This involved creating the conditions for a partnership between different members of the community and local political and professional stakeholders to look at ways in which to reduce the risk of accidents and to develop local injury prevention plans. An economic analysis looked at the impact of the programme as a whole, with interventions targeted at children and young people, older people, traffic safety, sports and physical exercise and the workplace. 482 The costs of the programme over 6 years were estimated to be some £0.96M, compared with costs of injuries avoided of £1.81M. The intervention did not include any costs of unpaid community individuals involved in the development of the scheme, nor were all costs of adaptations to homes or use of safety equipment, for example bicycle helmets, covered. It was also suggested that the local budget for road safety may not have been increased during the time period of the programme as a result of the community as a whole prioritising other safety-related actions; moreover, even though resources for road-related actions were not increased, community planning meant that resources were targeted more to accident hot spots.
In respect of interventions for child abuse prevention, we identified one economic evaluation of a programme using home visitors trained to work with parents to improve their interactions with their children. 340 This scheme was found to be cost-effective compared with standard care, albeit measuring outcomes in terms of units of performance in infant co-operativeness, making it difficult to compare with other broader uses of resources. It should also be noted that another evaluation in our analysis, the Hawaii Healthy Starts Programme, a home visiting programme for mothers at risk with newborn babies,477 was to have included an economic evaluation, but this was abandoned according to the study authors because of the lack of effectiveness of the intervention. 474
The importance of perspective in economic analysis of interventions, as well as the use of modelling to look at some of the longer-term impacts of interventions, is also illustrated in the evaluation of the Experience Corp in Baltimore. 116 The scheme hypothesised that the physical, social and mental health of older people would benefit through voluntary participation in activities in schools, working with children up to the age of 8 years, helping them, for instance, with their literacy. Their health status was then followed up over a 4- to 8-month period. An economic model drew on effectiveness data from the trial and extrapolated this to look at the long-term effects on the health of volunteers over a 2-year period, assuming that 25 volunteers in the Corp would operate in each one of 20 schools. 481 In addition to looking at impacts on the health of older people, the long-term economic benefits arising from improved educational performance of children were also estimated. This broader perspective is important as the health gains for older people alone would not generate a cost per QALY gained of < $50,000, a figure generally considered to be cost-effective in a USA context. However, modest improvements in the productivity of children in adulthood as a result of more graduations from high school would mean that the costs of the intervention would be more than outweighed by productivity losses avoided.
Finally, culturally sensitive nurses ran a diabetes self-management course for Mexican Americans living in Texas. A first evaluation looked at a version of the programme involving 24 hours of education and 28 hours of contact time in support groups over a year compared with waiting-list control subjects. 224 Although a formal economic evaluation was not conducted, the costs of the intervention were reported, albeit with an acknowledgement that many additional resources were provided free of charge and thus not included in the cost analysis. Nonetheless, the cost of £309 per person was thought to be modest given the benefits seen in terms of diabetes management. A subsequent analysis specifically looked in more detail at the resource and cost implications of the intervention, finding that a compressed version of the intervention using 16 hours of education and 6 hours of support group time delivered the same level of effect as the previous intervention but with 60% lower costs. It would have the potential to be cost saving if some health-care costs associated with diabetes were avoided. 223
Models of engagement centred on empowerment
Only three economic analyses136,320,355 were linked to models of engagement centred on empowerment. This largely reflects the complexity of evaluation. They include a 1-year study involving community health workers who largely matched the ethnicity of a socioeconomically deprived population in one county in Seattle, USA. 320 These health workers disseminated information to children and their parents on decreasing exposure to indoor asthma triggers. These salaried health workers would work with family members to prepare an action plan following in-house assessment. The resource use and costs of the intervention and its comparator (a low-intensity information programme) were recorded, as were the impacts on health-care resource utilisation and costs. Overall, the intervention was likely to be cost saving, with modest avoidance of costly hospital treatment for asthma attacks and significant improvements in outcomes for children and in quality of life for parents. The study also recorded changes in time off work for parents and time off school for children, although these were not included in the economic analysis. No attempt was made to quantify or value the time that parents invested in working with community health workers.
We have noted that very few studies considered productivity losses and impacts on family members and that few studies looked at the economic value of impacts beyond the health system, despite many of the effectiveness studies identified in our review highlighting non-health outcomes. One of the exceptions is an economic analysis conducted as part of the evaluation of the multicomponent 84 Neighbourhood Warden Schemes in England and Wales. 355 This has empowerment at its heart. This initiative involved the roll out of neighbourhood-level uniformed, semi-official patrols in local communities by individuals living in those communities. The local community was involved in the development of individual schemes, although there was much variety in the way that schemes developed. A formal cost–benefit analysis was undertaken. Total costs over 30 months were estimated to be £34.6M, which included £14.3M from the Neighbourhood Renewal Unit at the Office of the Deputy Prime Minister, and matched funding from local authorities. It was estimated that there was also a further £6M of in-kind contributions from partners, with 83% of schemes managed by councils, 13% by housing associations and 4% by other groups including the police and community organisations. Although a wide range of benefits was identified in resident surveys, including improvements in quality of life, a better environment (e.g. less litter) and reduced antisocial behaviour and fear of crime, the economic analysis focused on crime only. This was because robust data on the value of a reduction in the crime rate were available from the Home Office. Although it was impossible to attribute all reductions in crime to these schemes in local areas, the economic analysis reported that if 10% of the reduction in crime were due to the schemes this would have a value of £37M, outweighing the costs of investing in the programme. This suggests that the scheme has the potential to be highly cost-effective. It was also acknowledged that this economic outcome would become more favourable if other benefits realised were valued, including health-related improvements in quality of life. Again, the resource inputs of community members have not been taken into consideration.
Our third example of an economic analysis of an empowerment model concerns the cost-effectiveness of investing in a health promotion programme delivered through adult education classes compared with no intervention in a number of Finnish villages. 136 Outcomes of interest included changes in diet, physical activity and health status. Ongoing costs of these education classes, as well as the costs of evaluation, were identified. Like nearly all of the studies that we examined, the costing analysis did not attempt to quantify the time and resources involved in developing intersectoral partnerships between village boards, primary health-care centres and local educational establishments. Although no formal cost-effectiveness ratio was provided, costs were modest at £1054 per village per annum. This was thought to represent value for money in a Finnish context given the improvements in cholesterol, vitamin C intake and systolic blood pressure, all of which would decrease the risk of more expensive inpatient medical care. The cost of one referral to the central hospital would have been three times the cost of the programme. The success of the scheme meant that the villages were willing to sustain the approach with their own resources when national grant funding ended.
The value of volunteering
We were also interested in whether studies indicated that volunteers were critical to the success of community engagement schemes, but only 17 studies stated this explicitly or tried to estimate the resource use and opportunity costs of volunteering. 83,112,116,171,172,176,197,204,218,226,248,311,320,346,393,412,426 Although some of the economic evaluations discussed earlier did make detailed efforts to measure and value this time, in most studies that included the costs of the intervention, the time of unpaid volunteers seems to have been treated as a ‘free’ resource. For example, evaluation of a small-scale intervention in which volunteers went on walks with people with dementia looked at impacts on health-care use by patients and their informal carers, but did not seek to look at either the resource use or any costs associated with the volunteer walking programme. 427
Some studies looked at some of the benefits that volunteers might gain from health promotion schemes. A sexual health study indicated that school-based volunteers would gain in personal development from volunteering204 and recognised that there would also be long-term benefits from avoiding teen pregnancies, but did not value this. In another study, volunteers trained to train others in their local community in Nottingham to make use of computers and the internet did receive payment for completing a training course, as well as being promised help in finding other employment opportunities. 218
In making comparisons of the costs of community engagement interventions, it is important therefore to know whether any financial recompense has been included in the costs of delivering a programme. This was not clearly stated in all costing studies. In many instances, volunteers would receive some token payment or gift, or time-limited payments – for instance, to encourage them to complete training courses. In one intervention, looking at the use of lay health volunteers to help encourage colorectal health and screening against cancer, small gifts were given to the volunteers, as well as money for refreshments, but they received no monetary payments and no value was placed on their time. 95
Failure to pay lay health workers/peers/volunteers not only for completing training but also for then engaging with others to implement health-promoting interventions may mean that individuals are reluctant to come forward to participate in schemes. This was noted in a number of studies, for instance in the use of church-recruited lay health workers to promote physical activity and diet to prevent diabetes in the USA. 112 In contrast, payment for both training and subsequent leading of health promotion classes by lay health workers was seen as essential to success in a study focused on the Latino community in Los Angeles. 311 Paying a stipend covering travel and food costs and other costs can also help ensure the participation of volunteers from disadvantaged communities, particularly when they have very low income and/or are retired. 412 In Ireland in the 1990s very small payments of around £3.13 per visit were made to volunteer ‘community mothers’ to encourage them to visit new mothers, an approach that was considered to be a success. 300 Stipends might also help indicate to volunteers that their work is valued. 133
Use of financial and other incentive mechanisms
Financial and other incentive mechanisms may also be used to encourage participation in evaluation, as well as longer-term continued participation of the target population in different health-promoting programmes. In this review, modest incentives were frequently used to encourage individuals to take part in evaluations. For example, free baby rattlers were given to participants in a home-visiting programme aimed at reducing the likelihood of low-birthweight babies. 120 In another study looking at ways to diffuse messages about disaster preparedness in the Latino population in Los Angeles, financial incentives encouraged community members to recruit individuals to the study; these new recruits in turn would be offered the same financial incentive to attract others until a sufficient number of participants was obtained. 258
For training courses involving poor populations, it may be necessary to ensure that food and drink are provided to ensure a good degree of participation. To reach women with young children, it may also be necessary to provide child care. In one study aimed at promoting the health of the Latino community, the volunteer health promoters initially had to use their own resources to provide books and toys for children who were brought by their parents to health promotion classes. 311 The health promoters received a letter of acknowledgement for this work. They also ended up attending the sessions of other health promoters to support them by providing child care. Halfway through the study, it became possible to adjust the budget to pay for child care during these classes. The health promoters also recognised the importance of providing food, especially during evening classes; this would have the added bonus of helping to monitor eating habits. Participants in the health promotion classes also received monetary payments for attendance.
One study looking at training of self-management of chronic health problems in the Bangladeshi community in London, did not find that free transport and the promise of a supermarket voucher after attending five sessions of a Bangladeshi lay-led training course made any difference to attendance rates. 284 This may have implications for the use of incentives to encourage participation in culturally adapted peer-led educational programmes. Other studies also flag up the lack of data on the cost-effectiveness of culturally-specific actions. For example, for an intervention involving peer community link workers for diabetes care in the South Asian community in the English Midlands. 359
In one parenting study, a combination of different incentives was used: cash payments of £173 for completing the entire course and the evaluation materials, and £43 for completing 8 hours of reinforcing workshops; the intervention families received child care in the form of the children’s programme; and a family meal was provided at each session for the intervention families. 153 Some further examples of incentives used are provided in Box 1.
-
One study in the USA reported the costs of training community members; resource mothers were reimbursed for travel and paid a stipend of £85 for the training session and £34 for each visit. 186
-
In a New Zealand study on support for pregnant women, all participants were given a Baby-Beep refrigerator magnet and a wallet-size Baby-Beep business card with the pager number. 225
-
Participants in a family support programme in the USA received a free taxi or the bus fare to make appointments at the health-care centre and at other agencies where services were provided. 144
But what is less clear is the extent to which these incentives form an integral part of the health-promoting intervention. There is little discussion in studies here on the value of financial incentives as mechanisms for behaviour change in their own right or in combination with community engagement actions. Modest financial incentives can, in some instances, help promote behaviour change, especially if the needed behaviour change is short term in nature, that is, turning up at a limited number of community activity sessions. 484,485 How might social marketing techniques be combined with financial incentives to aid community engagement?486
Gains/losses in human and social capital
We were also interested in whether studies documented that either end beneficiaries of health-promoting programmes or those delivering these programmes had improvements (or losses) in their human capital, which could cover, for instance, skills acquired, employment or increased employment opportunities. We also looked at whether studies documented any increase in social capital or related themes such as community cohesiveness. These benefits are often not included in economic evaluations but may strengthen the arguments for investment.
Only a small number of studies looked specifically at skills gained. For example, the case of residents’ consultancy pilot schemes in which ‘consultants’ who themselves were lay individuals who had gained experience on urban regeneration provided advice to other local communities. 354 The acquisition of new skills by both consultants and the communities they worked with in planning and delivering neighbourhood renewal schemes gave some individuals a new confidence to apply for employment opportunities. Another project, looking at community gardening as a catalyst for engaging with political process, included some quotes from participants who felt that their knowledge and skills on how to obtain further sources of funding had improved. 339 A qualitative evaluation of a scheme using members of the community to train others in computing skills noted an increase in confidence in addition to computing skills gained. 218
Marketable skills and new knowledge gained by lay health promoters have been cited, for example, in respect of Latino health promotion in Los Angeles. 311 Community participants in the study were thought to have gained valuable knowledge that can help build community capacity that would be useful for future projects.
Several studies promoting breastfeeding, documented an increase in human capital in a very broad sense, in the recognition of the importance of better health practices. For example, one study reported that the intervention resulted in an increased breastfeeding rate among low-income, minority-population inner-city women in Connecticut. 72 Similarly, in respect of parenting, a US study reported an overall improvement in parenting skills as a result of the intervention. 153 In particular, the authors noted that the evaluation data showed significant, persistent increases in parental self-appraisals and democratic child-rearing practices, with a corresponding decrease in strict discipline. In a study in Ireland, long-term follow-up after 8 years of mothers who had received regular visits from experienced volunteer mothers after the birth of their first child to help enhance their parenting skills, indicated that skills obtained had had beneficial effects for subsequent children, whilst rates of immunisation were also improved. 300
The costs of negative impacts of failed or unsustainable community engagement projects, such as becoming disengaged from the local community, feeling embittered or becoming cynical, have also been noted as important to identify. 4 These do not appear to be highlighted often in studies. This again emphasises the importance of process evaluation to try and identify some of these issues. The next section includes an example of the impact of the loss of funding for a project in Nottingham. 218
Funding and sustainability
Some issues in relation to funding and sustainability have briefly been discussed in the analysis of process evaluations in Chapter 6. Data on these issues have also been examined as part of our economic analysis, as both the effectiveness and cost-effectiveness of community engagement actions may be impacted by funding structures and uncertainty over long-term sustainability. We sought information about the availability of funds for implementation of interventions in a timely way, sufficiency of funds and securing additional funds and ensuring financial sustainability of the programmes. Problems regarding access to funding may weaken the viability of projects; in addition, it is important to recognise that considerable time and effort may need to be invested in building trust in new partnerships and/or in making applications for further sources of public funding. There may also be a need to mainstream a community engagement intervention within statutory services to ensure long-term continuity of service.
Many studies did not discuss these issues or addressed them in only a cursory way,294,312 but a few studies discussed these issues in some depth. For instance, several of the projects concerned with neighbourhood renewal/regeneration in England collected data related to concerns about both the immediate funding of projects and their long-term sustainability. The nature of those projects potentially limits their ability to generate funds through social enterprise-type activities, as in the case of residents’ consultancy pilot schemes in which ‘consultants’ who themselves are lay individuals who have gained experience on urban regeneration, provide advice to other local communities. 354 In the case of one of these schemes, which had an explicit health orientation, the consultant organisation often had to provide free services because of a lack of sources of funding from potential clients. This consultancy help did help identify and secure sources of funding for schemes, but there was a significant degree of uncertainty, which meant that the viability of the health project was endangered at times, and in future it was noted that ‘the sustainability of future activity and the further roll-out of expertise will be reliant however on establishing new income streams’ (p. 22). 354 This scheme did, however, help generate another form of sustainability, as by providing advice and training in different residential communities they in turn would be able to provide this service to others.
The evaluation of the Neighbourhood Warden Scheme in England and Wales also looked in some depth at issues of maintaining funding and sustainability. 355 The schemes always knew that they would have only 3 years of funding and would have to find alternative sources of support for long-term sustainability. This meant that they did expend time and energy on seeking funds, with 73% of schemes securing funding by the time that the evaluation was published. Some schemes were mainstreamed into local authority or housing association services, with others securing funding from a range of UK granting sources as well as the European Regional Development Fund. Scheme expansion has also occurred in a number of areas with substantial increases in numbers of wardens and areas covered. Individual case studies highlighted the perceived success of the schemes as being a catalyst not only for their sustained funding but also for their expansion. For example, in Sedgefield the scheme was replicated in the development of the two new Warden Schemes funded through Communities Against Drugs. It was stated that ‘the value of wardens has also been recognised within the council’s Environmental Enforcement Department and ways of developing their input is being included in discussions surrounding the department’s restructuring’ (p. 53). In Knowsley it was stated that the success of the schemes helped in gaining future funding for replication through the Neighbourhood Renewal Fund. Challenges were also identified as a result of uncertainty over future sustainability, with case studies citing that it was in some case difficult to retain wardens worried about their job security.
In the USA, the Breathe Easy smoking cessation programme177 stands out as being a study in which, during the 5-year lifetime of the project, some efforts to sustain the initiative beyond the period of grant funding were documented. In fact, grant funding did not cover all 5 years of the programme, and to foster sustainability, not-for-profit organisations were created to sustain a legacy from the scheme.
There were also examples of funding support being unexpectedly cut during the lifetime of evaluations, as in the case of a nurse-health advocate visiting programme for new mothers in the USA, in which the end of statutory funding support after 1 year meant a reduction of 50% in staffing, which impacted on planned programme fidelity. 155 Another example concerned the sudden withdrawal of funding for an Ambassador Scheme to enhance computing skills among disadvantaged groups in Nottingham. 218 The failure to decentralise funding meant that the scheme ended abruptly when central sources of support disappeared. The loss of the scheme may have been felt most acutely by those volunteers who had invested the most time in implementation.
Chapter summary
This chapter has summarised the extent to which issues around resource use and cost are routinely reported in evaluations of community engagement interventions. We examined 210 papers that were identified as having some discussion of economic issues,71–75,78–80,83,84,86–89,92,95,97–99,101,104–108,110–114,116–121,123,124,127–136,139–142,144–151,153,155–164,167–169,171–184,186,188–192,195,197,198,201,204,207,208,218,220,221,223–226,228,230–232,239,240,242–245,248,252,253,258,261,266,272,273,279–282,284,286,294,300,302,308,311,312,318–323,329,332,333,335,338–340,343–357,359,361–365,367–369,372,375,377,378,380,381,384–393,397,399,400,404,405,407,410,412,414,416,419,420,426,427,487–492 although in many instances this was limited to a cursory mention of costs or a call for subsequent economic evaluation.
Fifty-eight studies or linked papers included some substantive discussion of costs73,79,92,95,98,101,110,111,116,119,124,129,136,139,140,142,162,164,169,172,176–178,186,201,204,207,208,220,223,224,226,230,239,248,252,253,258,261,284,302,320,329,340,346,351,355–357,359,365,372,378,380,393,405,420,426 and 38 provided some breakdown of the resources needed to implement interventions. 80,95,111,12,116,128,129,136,139,162,164,182,207,220,222,223,231,232,239,261,284,300,302,311,319,320,322,329,340,344,351,361,363,380,384,399,400,404 However, when costs are reported, they are often not disaggregated, meaning that is difficult to disentangle the costs of community engagement elements of an intervention from all other aspects of a health-promoting intervention. Few studies distinguished between the costs of conducting research and the routine costs of delivering a community engagement intervention. Also, most concentrate on costs of training and staff time, with little attention paid to the contribution of unpaid individuals or to in-kind contributions. Tools do exist for this purpose, as highlighted in the study by Andersen et al. ,480 which went to great lengths to value accurately the contribution of volunteers and indeed other in-kind contributions in an initiative to increase the uptake of breast cancer screening. Almost no attention is paid to quantifying the value of contributions of communities as a whole to engagement actions. This is of particular importance when considering empowerment-centred models.
We identified only 21 economic evaluations. 116,136,140,162,164,201,220,223,224,226,261,320,340,355,365,372,378,393,479–482 They are thinly spread across health topic areas and concentrate on traditional peer-/lay-delivered interventions. Only three136,320,355 looked at empowerment-centred models. The majority of these studies were of limited quality. Only eight201,220,340,355,372,378,393,481 included some form of stochastic or sensitivity analysis to address uncertainty around effectiveness and cost estimates. None appeared to undertake any form of subgroup analysis, which can help address inequalities; only five201,220,320,340,482 looked at productivity costs and three140,162,320 considered costs to family members. Positive benefits associated with the acquisition of skills and confidence were noted but not valued in economic studies. Although most of these studies suggest that different community engagement actions can be a cost-effective use of resources, caution must be exercised. The community engagement is not often evaluated as an ‘adjuvant’ to existing interventions.
There is also some literature highlighting the impact that poor cash flow and worries about long-term sustainability can have on the success of different engagement schemes. The impacts of financial incentives on the success of community engagement strategies, as well as the impacts of different levels of payment for peers involved in delivering community engagement interventions, merit further attention.
Chapter 8 Synthesis V: theoretical synthesis to produce a broad conceptual framework for community engagement
About this chapter
We iteratively developed a conceptual model for community engagement in public health interventions to address health inequalities based on an integration of findings from previous theoretical literature (see Chapter 4), outcome evaluations (see Chapter 5), process evaluations (see Chapter 6) and cost/resource evaluation analyses (see Chapter 7). The conceptual model identifies a wide range of dimensions by which community engagement interventions may differ from one another, and gives us a framework within which to understand how different interventions may function.
Introduction to the framework
Chapter 4 outlined some of the sociopolitical arguments advanced in support of community empowerment, and the debate on tackling inequalities in health has an even more overt political dimension. 492,493 Without arguing that the models discussed earlier are deficient in their own terms, they do not cover the breadth of interventions that we identified, nor do they cover the range of issues that we set out to analyse. As mentioned in Chapter 4, they tend to be fairly high-level conceptualisations of how community engagement might or should work; and indeed some may be read as manifestos for reducing inequalities by improving social justice. These models also do not place much emphasis on the reality of resource constraints that may impact on the feasibility of their implementation. We are not arguing that there is anything wrong with such an approach, but here we present a new analytical framework that encapsulates both the social justice mechanisms from existing models as well as the detail of other mechanisms, processes and resources that preceded, and emerged from, our analysis.
Our report has taken a broad understanding of what community engagement is (which must necessarily reflect our political and ethical standpoint, discussed in Chapter 9), and has embraced a range of approaches and perspectives that include, for example, all those depicted in the ‘wheel of participation’ shown in Chapter 4 (see Figure 13). However, coming from an analysis of the evaluative as well as the theoretical literature, we have had to grapple with the fact that interventions often do not fit into neat typologies as they have multiple components, differing types and extents of community participation, and outcomes of interest that can go well beyond health improvement and reducing health inequalities. Where our conceptualisation differs most notably from some of the aforementioned models is in this inclusion of peer-/lay-delivered interventions that may have few other ‘engagement’ characteristics. Peer-/lay-delivered interventions fall within our definition of community engagement, and these are also complex when viewed from an engagement standpoint, as the extent to which the community was able to influence the intervention design varies widely and is not always explicitly stated in reports. The rationale for their inclusion lies in the broad-based way in which we have understood ‘community engagement’; interventions that involve peers in delivery are explicitly recognising their need to be tailored, relevant, credible and appropriately communicated to their target populations. By definition, peers adapt the way that interventions are ‘transmitted’ and implemented in order to suit their target populations and there is therefore engagement and a certain amount of empowerment implicit in this. Thus, not all of the interventions that we have identified would meet the exacting definitions of ‘empowerment’ discussed in Chapter 4, but some do seek to empower people to differing degrees. The use of peers can also help in the diffusion and longer-term sustainability of behaviour change within communities. In addition, and as discussed in the previous chapter, a better understanding of how the availability of appropriate resources helps or hinders intervention delivery is a key part of our understanding of how community engagement interventions might operate.
We therefore identified a range of dimensions that enabled us to explore and categorise differences between the community engagement approaches utilised by the interventions: the extent to which they were concerned with community engagement broadly or health outcomes more narrowly; who identified the need for the intervention; reasons why people might be motivated to become involved; how and where the community was involved in the design and delivery of the intervention; the conditions that mediated or moderated engagement; the types of actions and resources involved in engagement activities; the impacts of the intervention in terms of outcomes and beneficiaries, and their long-term sustainability (e.g. programme continuation or the adaptation of programme ideas through other local infrastructure).
Community engagement and health interventions
Two large triangles, inverted in relation to each other, form the background of the framework shown in Figure 23. One triangle depicts community engagement; the other depicts health interventions. These were represented in this way because the literature has described health interventions that contain varying amounts of community engagement, and the community engagement literature can similarly describe varying amounts of health intervention. The triangles overlap to illustrate the variation, and intermingling, of these two concepts in the literature.
FIGURE 23.
New conceptual framework for representing community engagement in interventions.
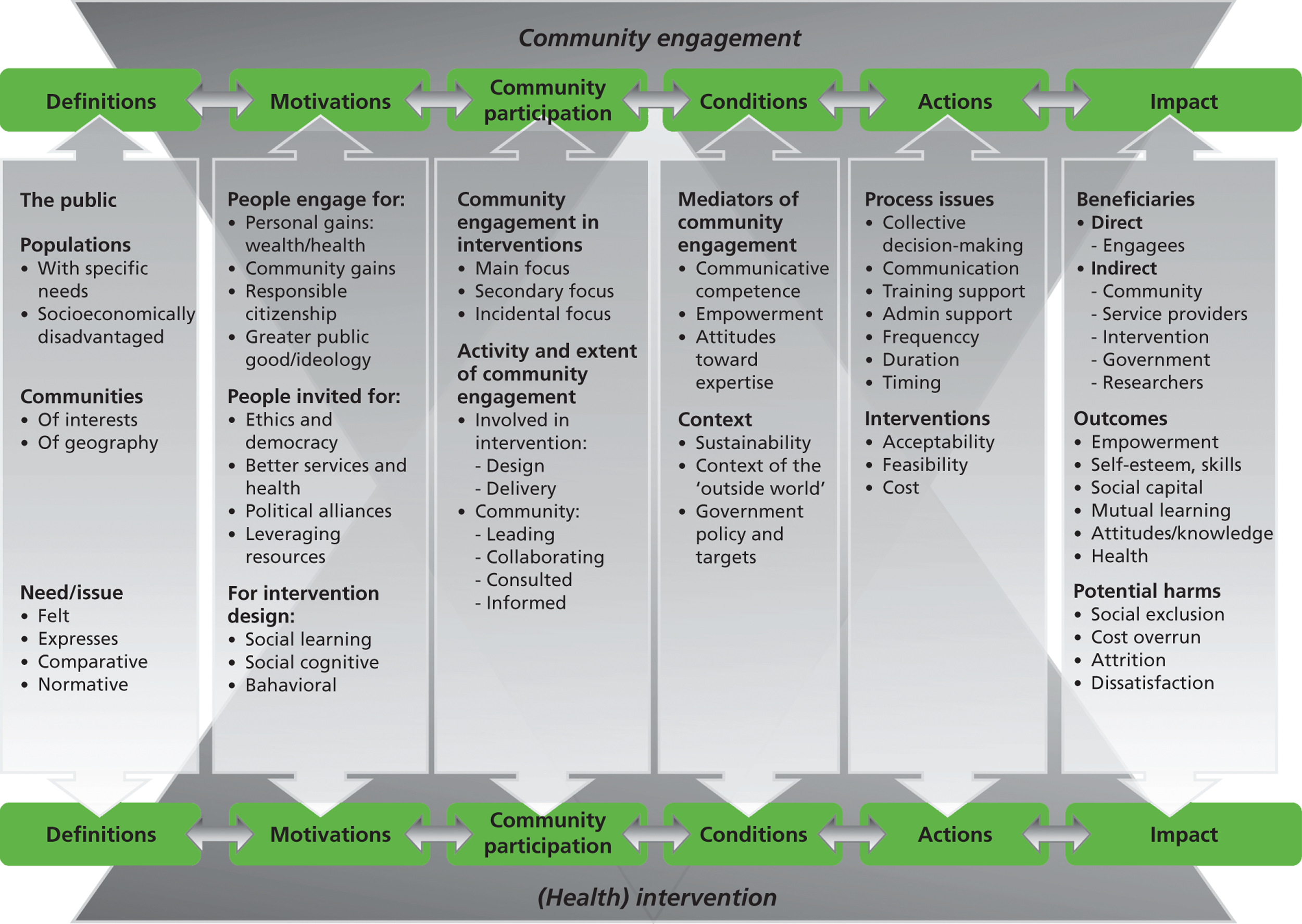
The literature also revealed a series of stages in the process of community engagement and health interventions, shown in green at the top and bottom of the model. The stages have bidirectional arrows between them indicating that each stage is partially dependent on the extent to which key issues in other stages were addressed. The shaded columns under each stage contain the main relevant concepts discussed in the literature.
For simplicity, this model depicts a linear relationship. However, the literature suggests that the processes are much more circular or iterative. For example, changes to key stakeholders during a community engagement process may mean that new relationships need to be established and training and support undertaken anew;495,496 reinforcing feedback loops and ‘virtuous circles’ may be created, whereby the value of a resource may be multiplied (see Conditions). We are therefore looking at a model that can be understood only in terms of it being highly dynamic; that is, the factors located in the model may, in a given situation, operate differently depending on how they interact with one another and the context within which they are located. The idea of ‘complexity’ underpins the model, with the health intervention (bottom of diagram) considered ‘complex’, that is, locally adapted/responsive, and with causality operating through different paths;497 and the community engagement (top triangle) can be also be considered ‘complex’ as the community in which the intervention is introduced has its own dynamic structures. 497–499 With this idea of complexity in mind, the key concepts from the literature highlighted within each stage are discussed below.
Definitions
Community engagement occurs when a need is identified for a particular group of individuals (i.e. a community). The process therefore begins by defining both the community and its health needs or issues.
As discussed in Chapter 4, community can be defined in many different ways, not just by geographical boundaries. Communities might also be defined by social or economic characteristics, interests, values or traditions. Indeed, communities of interest (i.e. groups of people that share an identity, such as the Bangladeshi community, or an experience, such as teenage mothers) were the focus of the majority of the community engagement interventions in this review. A community might be defined by people outside the community and labelled as a population, or a community might define itself as a community. The difference between the terms ‘population’ (externally defined) and ‘community’ (self-identified) in the framework reflects this distinction.
The different ways in which need is identified may be conceptualised as:500
-
a felt need, which is one directly identified by community members themselves
-
an expressed need, which is inferred by observing a community’s use of services
-
a comparative need, derived by comparing service use in a similar community
-
a normative need, derived by comparing measures of living conditions with a society norm or standard, often set by experts.
The above taxonomy of types of need delineates different forms of need, which can be understood as being on a continuum that moves in stages away from expressly community-identified models (felt need) towards expert opinion (normative need). As the descriptive map shows (see Chapter 3), the community was not involved in establishing need for most of the interventions.
Motivations
Depending on the interplay between community engagement and health interventions, there are varying factors that motivate people to participate in community engagement as well as professionals to undertake interventions. People might choose to engage for a range of personal, communal and societal reasons, some of which are peripheral but related to health. These include personal gains, including monetary/wealth, health and the development of new marketable skills and capabilities; benefits to their community; better community neighbourhoods; less crime; improved educational outcomes; or for the ideals of responsible citizenship, altruism and the greater public good. 41,354–356,501–503
When the motivation for action is outside the community, community engagement can occur when those within a specific community are invited to participate by others who have their own motivations for asking. Those who invite community members to participate in an initiative can include, for example, local or state government officials, health-care providers or other members of the community. People can be invited by others to participate for a broad range of reasons, including ethics and democracy; the desire to provide better services and better health; for political alliances or to satisfy a political climate; and to leverage resources and increase the chance of sustainability. 496,504–507 Involving a broad range of stakeholders, including specific communities, can help build public commitment to a health promotion agenda and empower the public to advocate for change. They can also help in determining whether or in what form a health-promoting action is likely to be acceptable for implementation. There may also be a recognition that some local community groups may be more competent in delivering health promotion change or may already be involved in other health-promoting activities. 508 In some contexts there may be legislative or regulatory requirements for a broader group of individuals to participate, for example in situations in which statutory funding is forthcoming only when matched funding in cash or in kind is provided by community partners.
It should also be noted that even in highly engaged communities the motivation to continue to participate in developing and implementing an initiative may diminish over time without sufficient financial and/or other recompense for the opportunity costs of engaging in these activities. As we have seen in Chapter 7, this may be particularly the case in communities that are socioeconomically more deprived or in which there may be other financial constraints on participation, for example the low-income levels of some retired people or the need to find child care.
Community engagement initiatives that focus less on community and more on health interventions are often, but not always, grounded in a specific theory that is used by researchers to understand the ways in which people develop, think or act. Examples of theories underpinning such interventions include social learning theory,509 social cognitive theory,510,511 social ecological theory,512,513 coalition theory,514 diffusion of innovation theory,60 social network theory515 or behavioural theory. 516 It is argued throughout the literature that public health interventions should be based on theory that is relevant to, and appropriate for, the population involved. 226,517–523
Community participation
When community engagement has a health focus, or a health intervention has a community engagement aspect, particular issues can be considered. The extent to which community engagement is ‘embedded’ as a predestined, planned part of a health intervention varies considerably between studies included in this synthesis. In some cases it is the main focus of the intervention, as in local area regeneration programmes. 501 In others it is an important secondary part of the intervention in which the main intervention is supported by, but not dependent on, community engagement. An example of this is a community-informed food labelling system offered as one component of a complex community cardiovascular disease prevention strategy. 522 Additionally, those currently in positions of power may need to be ‘engaged’ in interventions to empower a disadvantaged community and so enable it to improve its own health. 356,524 In other cases the community engagement mechanism occurs as part of the recruitment of those delivering the intervention, such as in the use of peers or lay health advisors to deliver a health message. 271
The definitions of communities and the needs and motivations of those involved underpin how communities participate; specifically, how community engagement is developed and delivered. When community engagement is a key part of the strategy, members of the stakeholder community can take part in the design of an intervention;495,522 when there is less community engagement and more emphasis on a health intervention, members may simply take part in its delivery. 271 The number of people taking part in the community initiative can influence the level of engagement that takes place. 525 The levels of engagement are hierarchical and could include (from least to most engagement) information (giving or receiving), consultation, collaboration and control6 (see Chapter 4 for several examples of this kind of hierarchy). Examples of this are seen across studies included in the synthesis. 459,496,525
Conditions
Some fundamental issues were aired in the included studies regarding the contextual influences or mediators necessary for community engagement initiatives. It was suggested that the presence and strength of these factors impacted on the desired outcomes. These issues included communicative competence;504–506 empowerment and control;286,380,381 and attitudes of community members and providers towards what expertise was important and who held it. 501,526 Again, the extent to which communities can engage may be dependent on the level of financial and other resources available to support their participation. 312,412
Further, the context in which a community engagement initiative or health intervention takes place might influence the extent to which it impacts on health. This would include the degree of stability of funding and support throughout the project,501,526 as well as the level of certainty over future funding or mainstreaming opportunities;355 the social, political, economic and geographical context and its impact on the community engagement or public health intervention;502,528,529 and the influence of externally imposed government policy and targets for achieving health. 217 Another important contextual factor can be the extent to which a community engagement initiative has to compete for resource and visibility with other national/local health promotion initiatives. 355 Changes in the local economic climate may also have an impact on the ability to participate and/or interest in participating in interventions, something that may be captured only if a process evaluation is conducted.
Many of these conditions are thought to create (or fail to create) the environment for virtuous (or vicious) circles to develop, in which some of the above facilitators mutually reinforce one another and help the initiative to become self-sustaining. In contrast, when trust is lacking, or there is no history of previous collaboration, engagement can be difficult to achieve and will have little momentum in terms of sustainability. 356 Such feedback loops are common in complex interventions and may bring disproportionate rewards; for example, at particular critical levels ‘tipping points’ may be reached in which a small increase (or decrease) in resource can bring about a disproportionate change in outcomes. 498
Actions
The way in which a community engagement activity takes place (i.e. the ‘process’) is thought to influence its success in impacting on health outcomes. It is also argued that these processes interact with the interventions in many ways and can thereby alter them. Important process variables were discussed in the literature. These include:
-
clearly defined target groups, objectives, interventions and programme components525,530
-
adequate time for members of community groups and those outside the community to build relationships with one another so that they can negotiate a ‘level playing field’ in terms of language, negotiation and collegial working skills497,503,506,531
-
the development of skills to bid for future sources of funding and acquisition of knowledge on sources of funds354
-
planning for ongoing simple communication between participants and providers286,380,381,519 and between the community engagement group and the wider community286,380,381,517,529
-
adequate training of participants and providers to build skills271,286,497,502,503,517,525
-
the amount and quality of administrative support required to ensure the smooth running of the project286,339,529
-
the timing, duration and frequency of the activity217,519,531,532
-
the stability of cash flow throughout the lifetime of the initiative. 218
Impacts
Understanding and planning for key concepts in the process of community engagement – defining needs and communities, their motivations, the amount and type of community engagement, the conditions in which it takes place and the actions that foster it – is thought to have an impact. The literature suggests that who is affected, and in what ways, can be considerable.
South et al. 533 suggest that a range of people can benefit from community engagement and/or public health interventions. These can be described as ‘direct’ or ‘indirect’ beneficiaries.
Direct beneficiaries are those who take part in the community engagement (the ‘engagees’). In this case, the act of being engaged is the intervention for which outcomes are measured. These can be health outcomes, empowerment, self-esteem, skills development, level of interest and learning activities and gains. 339,529,530
Indirect beneficiaries are the wider community towards which community engagement and/or public health interventions are targeted. They can also be the service providers who engage with the communities;534 they benefit, as do the community members who engage, by mutual learning. Researchers can also be seen as indirect beneficiaries in that further research and interventions can be perpetuated from a community engagement initiative. Government departments benefit from community engagement by showing that their policies made a difference (i.e. targets were met), or that a particular political priority held by that government was successful. 533 The intervention itself can also benefit from the amount and type of community engagement: interventions can be sustained and improve with community engagement. 534 The type of outcomes that are measured for indirect beneficiaries can include health outcomes as well as social capital. When evaluated, community engagement interventions have been shown to have the potential to be cost-effective, taking into account impacts on engagees and the community of interest. This may particularly be the case if multiple health and non-health benefits of an engagement action are taken into account. 355,482
There are also some potential harms that could result from community engagement, especially when communities are less involved: social exclusion, cost overrun, attrition and dissatisfaction and disillusionment. 218,528,534 It has also been suggested that community partners and decision-making organisations should collaborate in a manner that will achieve a balance between ‘soft’ relational outcomes and ‘hard’ policy impacts. 528
Identifying distinct models of community engagement across the dimensions of the new conceptual framework
The above conceptual model identifies a wide range of dimensions by which community engagement interventions may differ from one another, and gives us a framework within which to understand how different interventions may function. Although there are several million ways in which the different dimensions might be arranged, a more limited number of models can be identified.
-
‘Classical’ or ‘traditional’ peer- or lay-delivered interventions (reviewed in Chapter 4, Defining ‘community’). In these interventions, people with specific needs are identified usually by normative or comparative methods, and peers or lay people are recruited so that the intervention can be delivered in the most appropriate way for the population. Communities have no role in the design of the intervention, and the theory of change is around communicative competence rather than empowerment or people’s attitudes towards expertise. Beneficiaries are usually individuals rather than communities, and the people delivering the intervention themselves have often been found to benefit significantly. In some cases these interventions have also been reported to be cost-effective compared with no action and/or professionally delivered services. 164,378,393
-
Varying degrees of collaboration between health and other statutory services and communities. As discussed above, there is a wide range of models that are concerned with engaging the community in intervention design and implementation. Need is usually identified by people outside the community (‘expressed’, ‘comparative’ or ‘normative’), but the theory of change includes explicit engagement with the community of interest to better align the intervention to its needs. The extent to which the community is involved in the intervention can vary considerably, and the framework describes a range of dimensions that capture some of this variability (e.g. whether the community is in a leading role in designing or delivering the intervention, and who the beneficiaries are). The theory depicted in Figure 12 reflects this model and suggests that ‘degree of engagement’ may be a useful analytical approach. ‘The diagram highlights four broad approaches to community engagement differentiated by their engagement goal: the provision and/or exchange of information; consultation; co-production; and community control. These approaches are not readily bounded but rather sit on a continuum of engagement approaches with the focus on community empowerment becoming more explicit and having greater priority to the right of the continuum where community development approaches are located’ (p. 6). 14
-
The final model is centred on the concept of empowerment. Sometimes a subset of the second model above, the need for these interventions may have been identified by the community itself. 243,244 The community will certainly have a lead role in designing the intervention and the underpinning theory of change is around empowering communities to make changes to their social and environmental locales. 104 These initiatives may not be focused exclusively on improving people’s health, as they may be addressing one or more of the multiple causes of disadvantage – of which health is but one outcome. In terms of its contribution to our framework, empowerment is understood both as an outcome and as a ‘mediator’, as empowerment is thought to improve a range of interventions (as per the second model above) as well as being a specific aim of others.
Mapping interventions to the new conceptual framework
The final section of this chapter ‘maps’ the interventions found in the map against the new conceptual framework described in the previous sections. Mapping characteristics in this way helps us to understand the range and specific foci of research activity and helps us to identify gaps in our knowledge. It also tests the applicability of the framework and assesses the extent to which it corresponds with interventions ‘on the ground’. Part of the purpose of the mapping exercise was therefore also to identify areas of the framework that required revision (as per question 19 in the tool shown in Appendix 2).
Need: was the community explicitly involved in identifying the health problem/need?
The community was explicitly involved in identifying the health problem/need in 6183,89,90,98,103–105,119,122,132,134,136,137,139,143,145,149,154,157,159,172,176,179,182,209,210,218,232,243,258,264,272,274,276,283,286,298,304,308,311,319,320,325–327,331,335,337,351,354–356,377,385,387,388,394,395,399,401,420 of the 319 studies. Thus, most of the studies in our map are likely to fall into one of the first two models given in Chapter 4, Models of ‘engagement’ (see Figures 7 and 8) and towards the bottom of the continuum shown in Figure 10.
Multicomponent interventions
One of the challenges of understanding the impact that community engagement may have is ascertaining where a given intervention ‘sits’ on the continuum of engagement. Some health system-led interventions may include an element of participation, but this may be only a small component within a larger multicomponent programme. Table 44 identifies interventions for which this is the case and shows that, of the 319 interventions mapped, 109 were exclusively centred on community engagement within a single-component intervention;72,74,80,81,83,84,86,106,112,120,121,129,130,132,133,135,138,140,144,146,150,155,157,160,164,167,169–171,175,178,181,186,188,192,197,205,218–220,226–228,239–242,247,249,251,258,262,264,273,284,293,295,298,299,301,303,305,314,318–320,323,334,335,337,338,340,342,344,348,349,352,360,361,363,365,366,371,372,374,376–379,382,383,385–387,390,394–396,404–406,408–410,414,415,417,423,426,427,431 83 were similarly focused only on community engagement but the intervention had multiple components;73,77,87,90,93–96,98,101–107,109,111,113,116,117,119,126,145,149,154,156,168,172,174,176,177,179,191,194,195,199,201,207,209,210,215,222,225,232,234,237,243,250,252,254,260,261,266,267,272,274,276,278,281,285,296,304,311,327,339,341,343,345,346,355,356,358,364,369,397,399,400,407,420,422,424,425,430 114 were multicomponent interventions with some aspects of the intervention not involving any engagement;71,75,76,78,79,82,85,88,91,92,97,100,110,114,115,118,122–125,127,128,131,134,136,137,139,141,142,147,148,152,153,158,159,161–163,165,166,173,182–185,187,189,190,193,198,200,202–204,206,212,214,216,217,223,224,229,233,235,236,238,245,246,265,266,269,270,277,279,283,288–292,297,308,309,312,313,315–317,322,324–326,328,330,331,336,350,351,353,354,359,370,373,388,398,401–403,411,413,418,421,428,429 and 13 interventions did not involve the community in delivery or evaluation at all. 89,99,108,143,151,180,196,275,286,294,306,307,384
| Components in intervention | No. of studies |
|---|---|
| Single component (involving community engagement) | 109 |
| Multiple components (all involving community engagement) | 83 |
| Multiple components (only some involving community engagement) | 114 |
| No community involvement in delivery/evaluation | 13 |
Level of community involvement
As discussed earlier, the degree to which the community was involved in the intervention is one of the main ways that community engagement strategies differ from one another. Our framework categorises involvement in terms of involvement in the design and planning of the intervention, its delivery and its evaluation. Within these three areas, involvement has been coded in six ways: leading, collaborating, consulted (including piloting if there was a feedback mechanism), informed, other and not involved (and unclear). As Table 45 shows, communities were more heavily involved in delivering interventions than in planning/designing or evaluating them.
| Extent of engagement | Planning/designing | Delivering | Evaluating |
|---|---|---|---|
| Leading | 17 | 161 | 5 |
| Collaborating | 83 | 122 | 45 |
| Consulted | 74 | 7 | 18 |
| Informed | 5 | 4 | 3 |
| Other | 0 | 2 | 1 |
| Not involved/unclear | 141 | 23 | 248 |
Labels for community engagement strategies
As this chapter has highlighted, there are a multitude of terms by which community engagement programmes are described. Table 46 summarises this range of terms, showing the large number of interventions that utilised peers and lay/community health workers in some form.
| Label | No. of studies |
|---|---|
| Any peer involvement (e.g. peer counselling, peer education, peer leaders, peer leadership, role models, peer support) | 143 |
| Non-peer health advocacy (e.g. lay health workers, community health workers) | 73 |
| Community action/support, community mobilisation/involvement/engagement/participation | 63 |
| Community partnership, community coalitions, community task force | 59 |
| Volunteering/volunteers (explicit use of term) | 50 |
| ‘Outreach’ programme (explicit use of term) | 31 |
| Community organisations – developing new and existing services | 21 |
| Social networks (explicit use of term) | 16 |
| Other community engagement strategy | 16 |
| Promotoraa (explicit use of term) | 14 |
| No clear community engagement label used | 10 |
Training for engagees
Table 47 shows the large number of studies that trained their engagees in some way. Types of training could include class sessions, role playing or rehearsals, and direct observation by ‘shadowing’ already-trained engagees. Little description of training for coalition members could be identified.
| No. of studies | |
|---|---|
| Yes | 224 |
| No | 8 |
| Not stated/unclear | 87 |
Of the 224 studies that provided training to engagees, 45 also measured engagee outcomes. 96,116,129,132,140,161,170,172,186,188,191,194,195,204,207,209,210,217,218,226,247,252,254,270,273,275,306,311,312,315,323,325,340,343,344,353,355,358,360,372,394,404,422,425,431 Similarly, two227,286 of the eight studies that did not provide training for engagees measured their outcomes.
Outcomes measured
Table 48 shows the range of participant or engagee outcomes measured in the 319 studies. Health and process outcomes were most often measured; around one-quarter or less of the studies also examined personal, cost or community capacity outcomes.
| Outcome | No. of studies |
|---|---|
| Health outcomes (e.g. behaviours, knowledge, attitudes) | 297 |
| Process outcomes (e.g. acceptability, appropriateness) | 103 |
| Personal outcomes (e.g. empowerment, self-esteem, efficacy, skills) | 84 |
| Cost or resource use data or cost-effectiveness | 70 |
| Community outcomes (e.g. capacity building, social capital or inclusion) | 26 |
| Other | 9 |
Theories of change relating to different models of engagement
The final section of the map identifies those studies within each of the three main models of community engagement in this review, as outlined in the summary section of Chapter 4.
The first model is centred on the concept of empowerment: the idea that change is facilitated when the health need is identified by the community and community members determine their own courses of action. Although these studies will have been towards the top of Figure 14 and should therefore be capable of impacting on the intermediate social outcomes shown, there will be constraints on community activities that our classification schema does not capture, such as the resources at their disposal and limits to their jurisdiction (as discussed in Chapters 6 and 7). Therefore, the people in the 61 studies83,89,90,98,103–105,119,122,132,134,136,137,139,143,145,149,154,157,159,172,176,179,182,209,210,218,232,243,258,264,272,274,276,283,286,298,304,308,311,319,320,325–327,331,335,337,351,354–356,377,385,387,388,394,395,399,401,420 that fall into this category will have had differing experiences of empowerment. (Empowerment interventions were operationalised in terms of our keywording categories as studies in which the community was explicitly involved in identifying the health problem/need. Community members may or may not have been involved in the design and/or delivery of the intervention.)
In the second model, the need for intervention is usually identified by observation that is external to the community, but the views of stakeholders are sought with the belief that the intervention will be more appropriate to the participants’ needs as a result. We identified two main mechanisms through which stakeholder views are sought in the design or planning of the intervention: through collaboration with the community (47 studies73,78,92,96,106,111,112,127,128,138,152,156,165,171,177,185,199,201,205,207,212,217,238,241,247,249,266,269,289,294,297,307,309,312,314,364,369,374,382,398,405,407,410,411,422,426,430) or through consultation with the community (59 studies71,76,81,82,86,87,94,95,99,100,108,109,113–116,125,131,150,151,158,164,166,168,180,188,189,194,196,198,200,215,223,224,227,235,239,242,245,254,265,267,270,284,317,322,324,330,336,341–343,349,360,373,384,396,408,429). (This second group of interventions was operationalised as studies in which community members collaborated in or were consulted about the design or planning of the intervention but were not involved in identifying the main need. They may or may not have been involved in the delivery of the intervention.)
The final model is concerned with traditional models of peer- or lay-delivered interventions. The theory of change for peer- or lay-delivered interventions is outlined in Figure 8, with the community ‘ingredient’ included through the use of specific people to deliver the intervention; however, beyond informing peers about the intervention, no peer involvement in the intervention’s planning or delivery occurs. There are 136 studies in the map that fall into this category. 72,74,75,77,79,80,84,93,97,101,102,110,117,118,120,121,123,124,126,129,130,133,135,140–142,144,146–148,153,155,160–163,167,169,175,178,181,183,184,186,187,190–192,195,197,202–204,206,214,216,219,220,222,225,226,228,229,233,234,236,237,240,246,250–252,260–262,273,277–279,281,285,288,290–293,295,296,299,301,303,305,313,315,316,318,323,328,334,338–340,344,345,348,350,352,359,361,365,366,370–372,376,378,379,383,386,397,400,402,404,406,409,413–415,417,418,421,423,425,427,428,431 (Traditional models of peer- or lay-delivered interventions were operationalised as studies in which community members led or collaborated in the delivery of the intervention but were not involved in the design of the intervention, nor were they involved in identifying the health need.)
The numbers of studies within each of the three main models are summarised in Table 49.
| Theory of change | No. of studies |
|---|---|
| Empowerment | 61 |
| Views sought in design – collaborative | 47 |
| Views sought in design – consultation | 59 |
| Lay/peer delivered | 136 |
| Other | 16 |
Chapter summary
This chapter has described the final synthesis in this review: a broad conceptual framework that encapsulates the wide range of uses and understandings attached to community engagement. It is a complex model, both in content and meaning, and this chapter has outlined some of the main ways in which community engagement interventions operate. It has also mapped the outcome evaluations against this framework, showing that there are relatively few interventions using the empowerment model and rather more that involve peers or lay people in their delivery.
Chapter 9 Discussion
Summary of evidence
Although there are many ways in which terms relating to community engagement are used, they can all be understood as being situated beneath the ‘engagement’ umbrella, moving from terms that suggest limited amounts of engagement (‘information’ and ‘consultation’) towards ‘development’, ‘participation’ and ‘empowerment’. This final concept, ‘empowerment’, has its roots in concerns about social justice and movements promoting social and structural change, and is held as the ideal in models describing continua of community engagement. Although discussed in relation to community engagement to improve health, those advancing empowerment as a strategy often do so from a wider sociopolitical perspective, in which health is only one aspect of change that people’s empowerment can achieve. Critically, true community empowerment needs to begin within the community; this is at odds with many of the studies in this review, which often start from an academic or health service/systems perspective.
A number of models of community engagement have been advanced, which usually suggest that ‘empowerment’ is the ideal form. This is both because it is considered socially desirable and equitable, and because it addresses some of the social determinants of ill health and thus will also result in improved health and reductions in health inequalities. Taking a different strategy, but still rooted in a concern that interventions should be appropriate, accessible and sensitive to the needs of their target population, some studies in this review have evaluated the effectiveness of utilising peers or lay people to deliver the intervention. These studies often do not seek to empower, nor sometimes even to involve communities in intervention design, but achieve a degree of engagement nevertheless; existing models of community engagement often do not encompass this strategy. We therefore conclude that the following may be a useful heuristic to use when thinking about the range of approaches to community engagement:
-
Theories of change for patient/consumer involvement. This is engagement with communities or members of communities in strategies for service development, in which empowering individuals enhances their engagement with service professionals to effect sustainable changes in services. The need for ongoing investment will depend on the nature of the changes made; ongoing partnership is not necessary for sustaining changes, but can benefit subsequent changes.
-
Theories of change for peer-/lay-delivered interventions. Services engage communities, or individuals within communities, to deliver interventions. The aim of empowering people by enhancing their skills is to effect sustainable change amongst themselves and their peers. Although the individual behaviour changes sought may be sustainable, the intervention needs ongoing investment from services for subsequent generations.
-
Theories of empowerment to reduce health inequalities. When people are engaged in a programme of community development, an empowered community is the outcome sought by enhancing their mutual support and their collective action to mobilise resources of their own and from elsewhere to make changes within the community. An empowered community can do much to sustain its own efforts.
We compared the effectiveness of interventions based on these different theories of change in the meta-analysis of effectiveness data (see Chapter 5, RQ3: Which approaches to community engagement are associated with improved health outcomes among disadvantaged groups? How do these approaches lead to improved outcomes?). The results suggest that peer-/lay-delivered interventions tend to have larger effects than interventions based on empowerment or patient/consumer involvement, although this trend did not significantly explain variation in the effectiveness across studies. We propose that this association is likely to be confounded by other factors such as intervention intensity and exposure (peer-/lay-delivered interventions tend to be more intense, one-on-one or small group interventions than other intervention types). For such models, we might expect to see large effects over a narrow range of outcomes, as opposed to empowerment models that might have smaller effects over a broader range of health and social outcomes. Unfortunately, there were insufficient data to adequately test these relations.
Promisingly, overall, our analyses suggest that community engagement interventions for disadvantaged groups are effective in terms of health behaviours, health consequences, participant self-efficacy and perceived social support. A small number of studies also suggest that interventions can improve outcomes for the community and engagees. Only one subgroup – interventions targeted at participants on the basis of disadvantage according to their place of residence (rural or inner city) – did not have a pooled effect that was statistically significantly different from a null effect. This suggests that community engagement interventions work across a wide range of populations and intervention characteristics.
There is evidence from a small group of studies to suggest that intervention effects are still present long after the intervention has finished, although effects generally are smaller than at post test. Moreover, improvements in health behaviours are significantly related to increases in self-efficacy. These findings suggest that benefits occur across different domains and can be sustained, although more evidence is required to determine whether this is accurate across different conditions and contexts.
The meta-analysis also identified trends in the effectiveness of interventions that can be considered when designing future interventions, such as the intervention setting and duration. We were, however, unable to detect any clear predictors or moderators of intervention effectiveness.
Relatively few outcome evaluations are accompanied with robust process evaluations. The process evaluations that were available to synthesise gave a taste of what might have been available had more studies undertaken this type of evaluation alongside their examinations of effectiveness; and we recognise that there will have been other process evaluations that we did not synthesise, because they did not accompany outcome evaluations. We found that the diversity in conceptualisations, definitions and operationalisations of community engagement made it difficult to identify an appropriate data extraction tool for processes.
We found that community-designed or -delivered interventions, or culturally relevant programme materials, were linked to acceptability, which authors suggested influenced programme success. Successful partnerships and efforts to build relationships between partners appear to influence programme outcomes, and paying community members and participants can influence participation. Some coalitions were able to win external funding, helping the programmes to be sustainable beyond initial funding periods; in some cases, uncertainty over long-term funding had adverse impacts on outcomes. Intervention timing, frequency and duration and extent of an intervention influence outcomes. Intervention type (e.g. media events as opposed to one-to-one counselling) can affect accessibility or ‘reach’. Good project management and specific, adequate, ongoing training and support for engagees impact on implementation, and good relationships between engagees and professionals providing an intervention are important for programme implementation.
We examined 210 papers that were identified as having some discussion of economic issues,71–75,78–80,83,84,86–89,92,95,97–99,101,104–108,110–114,116–121,123,124,127–136,139–142,144–151,153,155–164,167–169,171–184,186,188–192,195,197,198,201,204,207,208,218,220,221,223–226,228,230–232,239,240,242–245,248,252,253,258,261,266,272,273,279–282,284,286,294,300,302,308,311,312,318–323,329,332,333,335,338–340,343–357,359,361–365,367–369,372,375,377,378,380,381,384–393,397,399,400,404,405,407,410,412,414,416,419,420,426,427,488–493 although in many instances this was limited to a cursory mention of costs or a call for subsequent economic evaluation. In total, 58 studies or linked papers included some substantive discussion of costs73,79,92,95,98,101,110,111,116,119,124,129,136,139,140,142,162,164,169,172,176–178,186,201,204,207,208,220,223,224,226,230,239,248,252,253,258,261,284,302,320,329,340,346,351,355–357,359,365,372,378,380,393,405,420,426 and 38 provided some breakdown of the resources needed to implement interventions,80,95,111,12,116,128,129,136,139,162,164,182,207,220,222,223,231,232,239,261,284,300,302,311,319,320,322,329,340,344,351,361,363,380,384,399,400,404 although in many cases this was partial information, often focusing on training and interaction components of community engagement strategies but typically not providing information on the time commitments of personnel, lay health workers and other volunteers. A total of 21 economic evaluations were identified, either as standalone documents in our review database or reported in other papers. 116,136,140,162,164,201,220,223,224,226,261,320,340,355,365,372,378,393,498,499,507,510 Only eight of these studies were identified as being potentially relevant via NHS EED. 136,201,340,372,378,393,498,507
The evaluations are thinly spread across health topic areas and concentrate on traditional peer-/lay-delivered projects, which are considerably easier to evaluate because of their focus on individual interventions. Only three looked at empowerment-centred models. 136,320,355 Some individual studies suggest a good economic case for specific community engagement interventions, for instance the Expert Patient Programme in England for which the cost per QALY gained would fall below £20,000 in nearly all circumstances. 378 Looking at models centred on empowerment, an economic analysis focused not on health outcomes but on a reduction in crime reported strong net benefits from the Neighbourhood Warden Scheme in England. 355
However, the limited number of economic studies identified, in many cases with significant quality concerns, means that it is impossible to reach any general conclusion on the cost-effectiveness of community engagement models per se. Moreover, community engagement is not often evaluated as an ‘adjuvant’ mechanism to usual means of engagement; thus, it is difficult to isolate the costs and effectiveness of a community engagement component as distinct from other aspects of the intervention. Careful thought needs also to be given to the appropriateness of the comparator used, particularly given the dominance of US literature in our review.
The contribution of this study
How this review contributes to knowledge
The ability to compare different models of community engagement and their underlying theories of change is a major contribution of this work. In Chapter 4 we outlined a variety of models that can broadly be classified as having utilitarian (health systems) and social justice (ideological) rationales. To the best of our knowledge, no systematic review has synthesised evidence representing such a broad spectrum of community engagement models that span the utilitarian–social justice divide. This has enabled us to directly compare the effectiveness of different models, consider the implementation and resource implications of different models and ultimately produce a conceptual framework that embraces the diversity of approaches. Importantly, this allows us to consider whether different community engagement approaches might be more effective under different circumstances, rather than constraining our thinking to models that conform to specific underlying theories.
Several process evaluations noted that the quality of the relationship and power sharing between partners influences a programme’s success. Successful partnerships were those that are able to both sustain projects beyond the end of a particular programme and recognise that they had served their purpose and come to a natural end. Swainston and Summerbell3 reviewed the effectiveness of community engagement approaches and methods for health promotion interventions. They described a range of specific approaches suitable for health promotion and, like Popay et al. ,4 noted that power struggles between government, providers and community as well as project devolvement and short-term funding and lack of appropriate space were barriers to community engagement. The authors of these systematic reviews have acknowledged that the strength of their findings is limited because of the small numbers of, and a lack of rigour in, included studies.
In terms of costs, both our review of process evaluations and economic analysis of cost and resource data suggest that financial recognition of participants’ and engagees’ time helps. Other study authors noted that engagees could save government service costs by advocating and intervening with and on behalf of participants. Further, efforts to seek external funding by engagees may have extended programme existence or resulted in their mainstreaming to statutory services. Conversely, a lack of adequate funding identified in some studies limited evaluation efforts.
The effect of implementation varies: the timing, frequency, duration and extent of an intervention are all suggested to influence intervention outcomes. Agency philosophy may influence implementation itself. In other situations, interventions implemented more intensively (i.e. one-to-one vs. many people at once) are effective but have less ‘reach’. The available data allowed only the analysis of the impact of duration on outcome effect sizes in the meta-analysis (see Chapter 5, Duration of intervention).
Good management and support of staff, especially community engagees who train to provide an intervention, impacts on programme success. Specific, comprehensive and ongoing training of community engagees who provide the intervention contributes to programme success, as does engaging similar, empathetic, supportive community members. Further, the accessibility of a programme is influenced by the nature and extent of the interactions between community members (‘engagees’) and participants (i.e. who is interacting, how and where). South et al. 532 undertook a mixed-method evaluation of lay health worker involvement in public health roles. The importance of training issues, support and retention schemes was described, as was the idea that participants could benefit directly from the process, as well as the populations they represent benefiting indirectly. The relationships between lay workers and professionals were highlighted as an important factor in mediating the success of a strategy, as was the relationship between the community participant and the community he or she represents.
Our review of the economic literature adds considerably to previous reviews of economic evaluations in this area. We have been able to collate these evaluations by type of community engagement, which may aid in future analysis of their strengths, weaknesses and potential adaptation to different contexts and settings. However, only 10% of studies included an analysis of both incremental costs and effectiveness. At first glance this may appear surprising, given the growing importance of economic arguments in public health policy, of which there has been a substantive growth in economic literature in recent years. 535 However, this is consistent with many of the reviews commissioned by NICE on the economic evidence for specific public health interventions, which typically identify a modest body of economic literature. A key observation is that low priority appears to be given to collecting resource and cost data as part of evaluations. When looking at actions that may place great weight on unpaid inputs, it is important to assess their opportunity cost, something that still is rarely carried out. This can have a major impact on reported cost-effectiveness ratios. There was little incorporation of equity concerns into economic evaluations, for instance by considering cost-effectiveness from the perspective of population subgroups.
Terminological challenges
As many authors have observed, the concept of ‘community engagement’ suffers from a bewilderingly large number of inconsistent and partially conflicting definitions. 14,448,457 We have not redefined these, nor added a new one to the already extensive catalogue; rather, we have sought to understand the rationales behind some of the more significant definitions and what they mean in practice, and to characterise their differences in terms of their different theories of change. This report will, we hope, complement existing definitions by helping readers to understand what those differences mean in terms of how health outcomes are to be achieved. Our aim is to aid future evaluations and evidence syntheses by suggesting that, rather than focusing on the overarching heterogeneous concept of community engagement, we may be better served by identifying the key characteristics of interventions and how these relate to their underpinning theories of change.
Comparing different models for reducing inequalities in health
The variety of intervention strategies reviewed here speaks to debates about how best to reduce inequalities in health. 4,15 Many interventions have been shown to improve the health of disadvantaged groups. Those with the largest effect size estimates tend to be those that are targeted at a narrow range of health outcomes and which typically employ a peer/lay delivery approach to community engagement. Those interventions that have taken an empowerment approach – and consequently aim to improve a broader range of outcomes, which may include benefits for the engagees and the community – tend to exhibit smaller effect size estimates.
However, we should not then conclude that the simpler, more specific interventions should be recommended over the others. The significant correlation between self-efficacy and behaviour change shown in Chapter 5 (see Correlation between outcome types), plus the positive impacts on other outcomes, including social support, engagee outcomes and community outcomes, identified in the evidence base, are important to understanding different models for reducing health inequalities. This is because these findings support the view that community engagement interventions may be able to impact on a range of outcomes – not just health behaviours and health consequences. If theories on the ‘virtuous circle’ are accurate, then such changes become mutually reinforcing.
To this end, we argue that the impact of an intervention should not be understood as simply being summarised in one or two effect size estimates; rather, the benefits of an intervention should be considered in terms of the combined effects across a range of relevant outcomes. The total effect of an intervention – which considers the effect on direct and indirect beneficiaries, on proximal and distal outcomes and on primary and secondary outcomes – might be useful for comparing different interventions that take different approaches. It is possible that the multiple smaller benefits of empowerment models might be as meaningful as one larger benefit from peer-/lay-delivered models, although this remains to be tested.
Reducing gaps and gradients
The proposed social gradient in community health characteristics28 might mean that more disadvantaged communities benefit less from a community engagement intervention than other, less disadvantaged communities. It is analogous to the old saying that ‘the rich get richer while the poor get poorer’. Following from this, there is arguably a danger that a universal community engagement intervention may increase inequalities in health by having a proportionately greater impact on more advantaged people.
In the meta-analysis (see Chapter 5) we tested whether there was a systematic difference in the effectiveness observed for universal compared with targeted interventions. As a consequence of our inclusion criteria, the ‘universal interventions’ in this review have been delivered to a sample of predominantly people from any of the PROGRESS-Plus categories of inequality (i.e. at least 60% of the sample). The difference between ‘universal’ and ‘targeted’ interventions in this review lies in the explicit focus of the authors of the original studies on targeting a particular PROGRESS-Plus group, compared with delivering an intervention to a sample that just happens to be mostly constituted of people from a PROGRESS-Plus categorisation. This distinction – which was driven by our decision to include only studies with a majority of participants from any PROGRESS-Plus group – means that we are unable to satisfactorily address the issue of targeted compared with universal interventions in its strictest sense. In essence, our analysis in Chapter 5 tested whether interventions with an intended aim of targeting the population are similarly as effective as interventions with a more general aim, regardless of the actual composition of the sample/population. The findings suggest a (statistically non-significant) trend towards interventions with universal aims being more effective than interventions aimed at targeted PROGRESS-Plus groups. This gives us some clues about reducing the social gradient, but it does not address the issue directly.
We are therefore unable to address the dilemma articulated in the Marmot report28 and outlined in Chapter 1:
If the focus were on the very bottom and social action were successful in improving the plight of the worst-off, what would happen to those just above the bottom, or at the median, who have worse health than those above them?
p. 16
This is not to say that the review does not have anything to contribute to the debate about gaps and gradients. As we sought evaluations of interventions that aimed to improve the health of disadvantaged groups, and found ample evidence that it is possible to impact on a wide range of outcomes, it follows that such interventions that are targeted at those with the poorest outcomes will be able to reduce gaps and gradients.
Interventions to achieve universal improvements in health are required, but ideally they should have a disproportionately large impact on those currently with the poorest outcomes. A recent rapid review of reviews on public health interventions (not specifically involving community engagement) found that certain types of interventions show some evidence of increasing inequalities between socioeconomic status groups (e.g. media campaigns, workplace smoking bans) whereas others decreased health inequalities (e.g. structural workplace interventions, provision of resources). Exploring this further with a focus on community engagement public health interventions would help to address the gaps and gradients dilemma. 536
Methodological discussion
This type of meta-epidemiological work is challenging from a methodological perspective. Most systematic reviews aim for a certain amount of homogeneity in order to combine like with like. Such reviews are appropriate to answer specific questions about the balance of benefit and harm attributable to a given intervention, but can answer only fairly narrow questions. In this review, we were asking a very broad question, but one of interest to policy, practice and research. Heterogeneity in its broadest sense is a given – both conceptual and statistical – as the aim is to understand how different approaches to community engagement (itself a heterogeneous concept) work in different situations.
This type of heterogeneity changes the nature of the questions that can be asked (and answered). So instead of asking whether a specific intervention works with a specific population and outcome, we are able to examine the outcomes of different types of strategy of engagement across a range of outcomes (and subject areas). This is a potentially powerful use of research synthesis, although it does have inherent challenges and limitations that are explored below.
The novel search strategy
We adopted an unusual approach to searching that differs from that of other systematic reviews in terms of its emphasis, as we prioritised a different location to identify eligible studies. Searches for relevant studies for inclusion in systematic reviews usually proceed along familiar lines, with sensitive, exhaustive database searches carried out, many thousands of titles and abstracts screened for potential relevance, a few hundred (or sometimes more) papers retrieved for full-text appraisal and the final number of included studies being selected once the full texts of papers have been checked. When other, related systematic reviews are found, they are usually used as a source of primary studies. This process is often supplemented with citation checking, author and expert contact and other searches for ‘grey’ literature (e.g. using Google or specific relevant websites).
We took a different approach in this review because previous experience has shown us that it is often very difficult, if not impossible, to consistently, systematically and reliably identify community engagement approaches and PROGRESS-Plus groups on the basis of study abstracts; therefore, the full text of nearly all citations retrieved through database searching would need to be retrieved to check whether they were suitable for inclusion. This is simply because (as discussed in earlier chapters) both concepts encompass a wide range of terms and, in the case of community engagement, the extent of community involvement may not be clear from the abstract of a paper.
Bearing in mind the above problems of using the titles and abstracts of studies to identify PROGRESS-Plus populations and community engagement approaches, we therefore decided to utilise existing systematic reviews in a way that is unusual, at least in our experience. As systematic reviews usually contain detailed and structured summaries of the studies that they include (often in the form of extensive tables in appendices), we took the view that these summaries would be a useful source of potentially relevant studies, and would often contain more pertinent information for our purposes than is present in many abstracts. As is detailed in Appendix 1, we therefore cast a very wide net for systematic reviews and then retrieved the full text of these and screened their included studies for studies that were potentially relevant to us. We also supplemented this search within reviews with other searches detailed in Chapter 2.
This strategy was far more successful than we had expected. Bearing in mind our somewhat stringent eligibility criteria – that studies needed to have evaluated, using a controlled trial, a community engagement intervention in a PROGRESS-Plus group – we had expected our task to be akin to finding a needle in the proverbial haystack. This assumption was supported by the observation that previous reviews of community engagement initiatives have not found many studies that have a focus on disadvantaged groups and report health or community engagement outcomes3,4,25 (it should be noted that these reviews focused on social determinants of health rather than disadvantaged populations to explore the issue of health inequalities, and so are indicative, rather than directly comparable). In contrast, we found hundreds of relevant studies. The eligibility of many of the studies that we have included could not have been ascertained from their abstracts – and, possibly more importantly, the non-eligibility of most studies could not have been established using this method either. We therefore conclude that we would not have been able to find the range of studies that we did using traditional searching methods [unless we had identified and retrieved many thousands (possibly 10,000+) full-text reports]. This approach has also allowed us methodically to examine studies in a consistent way to identify whether they contain relevant economic data or citations to supplementary economic analyses. One limitation, however, is that we may have missed useful information contained in modelling studies or in individual studies that somehow were not included in a systematic review. By supplementing the search of reviews with a search of the TRoPHI database of trials, we hoped to minimise this risk, but we acknowledge that some studies might have been missed. (As an indication of how difficult it is to construct a standard search for community engagement – without attempting to identify PROGRESS-Plus groups – only eight179,198,235,276,335,349,380,391 of the 361 papers in the map used these terms in their title or abstract: ‘community participation’ or ‘community engagement’ or ‘community empowerment’ or ‘community mobilisation’ or ‘community partnership’. We therefore recommend that future systematic reviews adopt similar search strategies for complex areas such as this.)
Epistemology
This was a challenging project to tackle conceptually, as we had to both aggregate and configure58 concepts and findings from a diverse pool of studies and analyse them across a number of different, and at times competing, dimensions. The development of our conceptual framework was both a finding of and a solution to some of the epistemological challenges posed by our attempts to understand such an uneven field in a coherent way. For example, arguments put forward to promote empowerment begin in a different place from those on the utility of peer-/lay-delivered interventions; and there is a considerable difference between the theory around empowerment and the ways in which this principle is operationalised in practice. To some extent this is inevitable, given the range of studies that we included. Most controlled trials of community engagement interventions are designed by academics who are interested in testing a particular hypothesis; they are usually unable to engage in the sort of community development/empowerment programmes that are called for in the theoretical literature.
Issues in assessing process evaluations
We identified some challenges in our methods of assessing the process evaluations. Although we found using a data extraction tool for community engagement methods by Popay et al. 4 excellent for identifying process issues around power, ownership/responsibility and practices of engagement, it was less able to capture simpler issues relating to, for example, public participation or intervention content. Turning to our own process evaluation data extraction tool that had been previously developed for public health intervention evaluations (see Appendix 4), we found that, although this captured data on methodological rigour, it focused more generally on process issues and did not always capture the complexities of processes. For example, embedding cultural values in an intervention may be partly about acceptability, partly about consultation and collaboration and partly about the quality of the programme materials. We believe that these challenges reflect the wider epistemological tensions in looking at community engagement, which also appear to subsequently influence evaluation methods.
We also noted that very few of the interventions involved the community in evaluation planning, conduct or dissemination. Thus, we are unable to say whether interventions are effective in terms valued by community members.
In general, process evaluations undertaken by study authors were of low to medium quality in terms of their efforts to reduce the risk of bias and their usefulness to this review. A clear link to outcomes was not always seen. For example, authors could report high participation rates but did not clearly link this finding to the programme’s success (or its lack of success). Further, authors appeared to go beyond the findings when drawing conclusions about effectiveness, for example when authors found that staff turnover was low they concluded that this was because of management practices but did not directly measure community engagees’ or participants’ opinions about those specific management practices.
More can be done to examine the impacts of financial incentives on the success of community engagement strategies, as well as the impacts of different levels of payment for peers involved in delivering community engagement interventions. It may also be helpful to use data from process evaluations to look at how cash flow and issues of long-term sustainability may impact on the relative effectiveness of interventions. It may be the case that an effective community engagement mechanism in fact fails because of some of these contextual issues.
Issues in assessing costing, resource and economic evaluations
We have noted that costs, when reported, are often not disaggregated, meaning that is difficult to disentangle the costs of the community engagement elements of an intervention from the costs of all other aspects of the intervention. It was also noticeable that few studies distinguished between the costs of conducting research and the routine costs of delivering a community engagement intervention.
When studies do report costs, most concentrate on costs of training and staff time, with little attention paid to the contribution of unpaid individuals or to in-kind contributions. It is important for both costing analyses and economic evaluations to measure all of the resource use associated with any intervention. Volunteer time is not a free resource, even if individuals are unpaid. The opportunity costs of volunteering should be consistently recognised in all studies so that more meaningful comparisons can be made. One potential way in which to capture some of these data may be through the use of self-report logs for volunteers that record not only time spent engaging with end users but also time spent in empowerment-related actions and/or in deliberations with other stakeholders. Tools do exist for this purpose, as highlighted in the study by Andersen et al. ,479 which went to great lengths to accurately value the contributions of volunteers and other in-kind contributions to an initiative to increase the uptake of breast cancer screening. The same can also be said of measuring the opportunity costs of the time of communities more generally involved in the development and sustainability of actions. This is not an easy issue to deal with but the intensity of a community’s contribution may have a substantial bearing on overall impact and ideally it needs to be recorded and valued.
Few of our included economic studies included any form of modelling, an approach that can be helpful in assessing some of the long-term costs and benefits of actions. This can be of critical importance in public health in which the health consequences of lifestyles and health behaviours may take many years to be seen. Such models could also be used to place a value on some of the long-term benefits that might be realised outside the health sector, for example the benefits to the economy of improved educational performance in children, which were measured in one study of an Experience Corp working with school-age children. 481 It is likely, however, that we have missed some economic analyses that make use of simulation models bringing together data from different effectiveness studies and attaching costs, but we did not identify many such studies within NHS EED.
There is some scope for modelling work retrospectively synthesising cost information with effectiveness data, but again a challenge here is isolating the community engagement element of interventions. Community engagement is not often evaluated as an ‘adjuvant’ to existing interventions. Both the broadness of the definition of community engagement and the need for the synthesis of effectiveness data to focus on general community engagement concepts rather than individual interventions, coupled with the limited amount of costing data we have been able to identify, has meant that we moved away from our initial intention to model the potential cost-effectiveness of specific community engagement mechanisms as part of this review.
Another important issue for future work is to take more account of the implications for equity in economic evaluations of community engagement interventions. Subgroup analysis of the cost-effectiveness of health-promoting interventions has been recommended as a minimum in this respect. 53
One fundamental conclusion from our economic analysis is the need to routinely collect data not only on costs but also on resource use, including those resources required to initiate, develop and potentially sustain funding and support for an effective intervention, as part of any evaluation process. This will allow for economic evaluation to be conducted, even if this is carried out retrospectively. A second fundamental research recommendation therefore is to encourage evaluation funders to build in economic analysis into their terms of reference. This is also fundamental in helping to strengthen the case to policy-makers to invest in any intervention. Modelling can be carried out only on a case-by-case basis rather than for a generic community engagement mechanism.
Issues in interpreting statistical findings
Significant statistical heterogeneity was expected in this review and indeed the exploration of this heterogeneity was part of its design. When operating across such a wide range of topics, populations and intervention approaches, however, there is a disjunction between the conceptual heterogeneity implied by asking broad questions and the methods for analysing statistical variance that are in our ‘toolbox’ for answering them.
First, analysing the variance ‘explained’ by specific subgroups of studies according to our conceptual framework rarely reached accepted standards for statistical significance. This is inevitable, however, because conceptual homogeneity was never achieved through such a subdivision: each type of approach to engagement was observed across populations, topics, outcomes and a wide range of other unknown variables; we would therefore never reach the position of being able to say that the studies within a given subgroup differed only because of sampling error/variance (or that any of our subdivisions was the only way of partitioning the studies present). In other words, potential confounding variables or interactions amongst variables made it difficult to disentangle unique sources of variance across the studies. Second, the use of statistical significance testing in meta-analysis has itself been questioned as lacking a sound statistical basis. 537,538 Although defending the practice, Mark Lipsey539 states that the magnitude of effect size estimates should be given greater weight in meta-analysis than the results of tests for statistical significance (and observes that if such statistical testing is wrong for meta-analysis, then it is almost certainly incorrect for most social scientific research).
In the context of our analysis these debates have a clear relevance, because statistical tests for significance are unlikely to yield statistically significant findings because of complex heterogeneity in the data set. We are therefore left with an interpretive challenge: do we adhere strictly to the p > 0.05 convention before accepting that a given subgroup analysis is meaningful?; or do we place more importance on the magnitude of the differences in effect size estimates between subgroups? In this review, we have attempted to plot a path somewhere between the two extremes. We have tested and reported statistical significance, but have also drawn tentative conclusions from the directions and magnitudes of effects whether or not standard statistical significance had been achieved.
A further issue for the meta-analysis in this review relates to the comparators used in the evaluations. In the vast majority of interventions synthesised in the meta-analysis (118 out of 131, 90%), interventions were compared with a comparison condition that differed from the intervention in more ways than just community engagement. For example, the comparison condition might be a completely different intervention, or a waitlist/delayed treatment control condition. In contrast, a study in which the only difference between the treatment conditions was the presence or absence of community engagement might, for example, compare peer-led with non-peer-led health education using the same programme materials. The lack of a ‘pure’ comparator in most community engagement interventions in this review could cloud our interpretation of the findings. Although we conducted a sensitivity analysis of this issue in Chapter 5 (see Sensitivity analysis) and found no difference between studies with ‘pure’ comparators and studies with contaminated comparators, we are unable to conclude definitively that community engagement is the ingredient necessary for intervention success. More evaluations are required in which community engagement is the only difference between comparison conditions to determine the added value of community engagement.
Publication and evaluation bias
The literature utilised in this systematic review is necessarily partial and contingent on many factors that are outside our control. For example, previous research has shown us that research that has statistically significant ‘positive’ results is:
-
more likely to be published (publication bias)
-
more likely to be published rapidly (time lag bias)
-
more likely to be published in English (language bias)
-
more likely to be published more than once (multiple publication bias)
-
more likely to be cited by others (citation bias). 540
Together, these biases mean that there is a danger that any systematic review gives a distorted view of research carried out because there is a systematic bias in favour of identifying positive findings. For this reason, systematic reviews include ‘grey’ literature and carry out exhaustive searches to find the less well-known research studies (and, by implication, possibly those that have less positive results). Even though this review has benefited from the extensive searches carried out in a large number of other systematic reviews, has conducted its own sensitive searches and has carried out statistical tests for publication bias (see Chapter 5), there is no way of knowing for certain the extent to which it has suffered from publication bias. This is a ‘known unknown’, and we can note only that its existence is possible but unquantifiable.
We know a little more about other biases that may be affecting this review, in particular what we will term evaluation bias. Some of the largest and best-known community engagement evaluations have been discussed in the conceptual framework in Chapter 4, but are absent from the map and subsequent analyses because of the design of their evaluations (which did not meet the inclusion criteria for this review). This is a common problem when reviewing interventions that may be implemented at the community level, as their evaluations sometimes do not have an adequate counterfactual, and so conclusions regarding causality are open to question. Because we wanted to ensure that the statistical analyses that we carried out were defensible, we adhered to standard practice in this regard and included only evaluations with a control group (and our checks for other risks of bias are detailed in Chapter 5). We ensured, however, that the theoretical bases of these interventions were not lost from the review by including them in the development of our conceptual framework.
An additional source of evaluation bias may be the synthesis of process evaluations (see Chapter 5). This was a small subset (< 10%) of the studies in the meta-analysis, the only ones with an integral process evaluation. Although an analysis of processes is a vital and important component in any evaluation, the fact that such a small number included a process evaluation means that there may be other important process measures that were not present in these studies. Further, it is difficult to estimate whether the studies with reported process evaluations are representative of the other studies in the meta-analysis. There is a risk that the interventions covered by these process evaluations are not the most significant, interesting or generalisable, but are simply those that happened to have sufficient resource for, and priority given to, an evaluation of their processes. To some extent we have mitigated any bias by including a discussion of the synthesis of relevant process evaluations carried out elsewhere. 4
Reflections on our position as reviewers
The discussion on empowerment in Chapter 4 leads inexorably to our questioning of our position in this research, as our conceptual framework – and the judgements we make regarding what is within the scope of our review – are inextricably linked to our take on what community engagement is (or should be) and, in a related way, what research is (or should be). If Woodall et al. 463 are correct in their argument that community empowerment risks losing its radical edge through association and elision with its related terms, does our review to some extent contribute to this? Moreover, does our broad understanding of engagement – encompassing empowerment, minimally participatory approaches and peer/lay delivery of interventions – weaken the arguments advanced by those promoting empowerment as the ultimate form of engagement?
Such questions relate to how we see the purpose of research. Some have argued that neutral research does not and cannot exist; and that research should be openly ideological, pursuing political, ethical or aesthetic goals (for a discussion of this see reference 541). Although we may have sympathy with some of these aims, we feel that they seek to redefine what research is: the pursuit of humanly useful knowledge. For example, the issue of inequalities in health did not achieve its current prominence simply through political lobbying; it required a strong evidence base that could not be dismissed as simply being ideologically driven. In the same way, those making decisions to reduce such inequalities need to be informed by an evidence base that helps them to develop policies and implement programmes that stand the best chance of achieving their aims. Thus, rather than advocating for particular community development approaches, or for public health approaches that engage communities in strategy or delivery, we advocate strengthening the evidence, whatever the purpose or approach for engaging communities, with that evidence being framed in terms valued by the communities and people seeking to work with them.
Strengths and limitations of this review
Strengths
To our knowledge this is the only review to have examined systematically the theory, practice, outcomes and economics of using community engagement to improve the health of disadvantaged groups. The studies it includes were identified as the result of a careful, unbiased and systematic search strategy, which gives us confidence that the conclusions we have drawn reflect the state of knowledge in this area accurately.
We were surprised at the consistency of effects we found across topic areas and intervention approaches. Although this made it more difficult than we had expected to draw conclusions about particularly promising approaches, the breadth of our review gives us confidence in drawing conclusions about the relative effects of interventions amongst disadvantaged groups.
Limitations
The evidence base that we drew on
Although based on extensive and rigorous searches, we cannot rule out the possibility that relevant research was missed, either because of deficiencies in our searches or because of publication bias; to some extent this is a weakness inherent in all review work and is a limitation of unknown size or impact. We are also aware that, because we prioritised evaluations that enabled us to ascertain the balance of benefit and harm that might be ascribed to a given intervention, that is, controlled trials, the range of interventions that we could include resulted in some of the largest evaluations being excluded. Again, the impact of this limitation is difficult to ascertain, as without an adequate counterfactual it is hard to identify causal effects (see also Chapter 5, Sensitivity analysis and Risk of bias across studies).
It is also important to note the date and language criteria that we applied when deciding which studies to include. The cut-off date for inclusion was set at 1990. We wanted to ensure the currency of the evidence base (evaluation methods and definitions of health inequalities and engagement have changed much over recent years), and the specific date of 1990 was set to be in line with previous relevant reviews (e.g. Popay et al. 4). It is difficult to assess the extent to which we missed out on relevant evidence because of this date limitation, but we believe that the other topic and methodological limiters are likely to have led to the exclusion of much of the pre-1990 evidence anyway.
Language was set to English only; this was a pragmatic, resource-driven decision. Only four reviews were excluded on the basis of language, and no primary studies were excluded on this basis. Although it is possible that relevant foreign-language evidence was missed, it is unlikely that the small number of missed studies would change the findings of the review; a methodological evaluation of language bias in meta-analysis concluded that, across 303 meta-analyses, ‘excluding trials published in languages other than English has generally little effect on summary treatment effect estimates’ (p. 115). 542 In summary, although date and language limiters should be emphasised when considering the generalisability of the findings, we have no reason to believe that they would systematically affect the evidence base in such a way as to alter the conclusions of the report.
Deviations from the protocol
We deviated from our protocol in five ways. These deviations were due to the surprisingly large number of relevant studies that our search strategy identified. As well as changing some of the points of consultation, this meant that the analytical strategy needed to change slightly.
First, we planned to contact authors of the studies included in the review to gain data on implementation issues. We did not do this for two reasons (although we were in touch with some authors): first, there was not the time available to track down and contact authors from 361 papers, most of whom were based in the USA, and so any effort we did spend on this would have been only partial and would risk not being representative of our data set; and, second, a large number of studies presented process information – some informally – which informed our thinking, and there were sufficient formal process evaluations for us to identify the barriers and facilitators reported in Chapter 6. In addition, we spoke to several people who are actively involved in implementing community engagement interventions (including, but not limited to, members of the project advisory group), and so the practitioner perspective has been consulted and incorporated in this review.
Second, we planned to examine ‘exemplars’ of effective approaches to consider relative resource requirements in the economic analysis. In the event, we examined a far greater number of studies than originally planned. We did this for two reasons. First, it quickly became clear that the range of approaches to community engagement found meant that the number of exemplars would be either too small to represent the data set or too large. Second, and as reported in Chapter 7, the proportion of studies reporting useful resource information was very small; we therefore took the view that it would be better to examine as many studies as possible to make good this deficit.
Although the level of data identified on implementation challenges and resources used for community engagement would have been bolstered through these exemplars, this would not have fundamentally changed our conclusions given the heterogeneity of interventions identified in this review. The review reinforces the importance of prospectively collecting data on resource use and costs alongside analysis of effectiveness. As time passes it becomes ever more difficult to retrospectively obtain accurate information on resource use, particularly for those more ‘hidden’ contributions such as time spent building informal networks and local political/administrative support to implement and sustain an intervention. We aim to conduct follow-up work in which we will collect some information on resource use in both comparable ongoing UK-based projects and those that have been recently completed. There are also potential opportunities, which have arisen out of workshops and meetings with the project advisory group, to liaise with other ongoing initiatives looking at community engagement.
Third, our protocol stated that we would assess the risk of bias in outcome evaluations using a tool developed in previous EPPI-Centre reviews. 55 This tool predated the Cochrane risk of bias assessment54 and, as the two tools assess similar biases, we decided to opt for the more recent Cochrane tool to bring our work in line with current systematic review practice. We also stated that we would exclude studies from the meta-analysis that did not meet a minimum level of quality. In the event, such studies were excluded at the inclusion/exclusion stage of the review (and so were not in the analysis by default); in the meta-analysis, we conducted a sensitivity analysis to see whether differential effects due to methodological characteristics of the studies were detectable.
Finally, the original title has changed from ‘Can specific approaches to community engagement help to reduce inequalities in health; for whom, under what circumstances, and with what resources? A mixed-methods evidence synthesis’ to meet the PRISMA guidance on clearly signposting systematic reviews and meta-analyses.
Small number of studies conducted in the UK
It is important to recall that interventions conducted in the UK were reported in only 26 studies (8%) – most of the located trials were undertaken in the USA (268 studies, 84%). Similar proportions were observed for the subsets of studies included in the meta-analysis and the economic analysis. Given that most of the studies were not conducted in the UK, the applicability of the findings of this review to the UK context needs to be considered.
We employed two methodological decisions to help maximise the relevance of the findings to the UK context. First, we focused on health issues that are more critical for disadvantaged groups in the UK by categorising studies based on the policy objectives and priority areas identified in the Marmot Review. 28 Second, we specifically limited the scope of the review to OECD countries. However, it is clear that OECD countries still differ from each other dramatically in terms of cultural, social, economic and political structures and climates.
A factor that is likely to be particularly relevant to the transferability of findings is the availability of universal health care in the form of the UK’s NHS. Although broadly similar health-care systems funded through taxation or social health insurance are to be found in most OECD countries, this is not the case in all countries, most notably the USA. In the USA, although some groups have de facto access to universal health care, such as the over 65s through Medicare, the state Medicaid systems that provide access to health care for those on low incomes vary enormously in terms of both services provided and levels of entitlement. Individuals whose incomes are not low enough to qualify for Medicaid and who cannot afford to pay for private health-care insurance may find themselves without any adequate health-care coverage. The issue of relatively high costs of health care and gaps in coverage in the USA mean that issues related to some people (particularly those with a low income) seeking or obtaining adequate health care and advice may be very highly prominent in that country, whereas these issues are less evident in the UK for most of the population, other than for undocumented and new migrant groups.
It is also important to be mindful of the differences in funding for community development and engagement projects between the USA and the UK. In the USA, there are sources of funding available specifically for outreach projects for minority communities both from the federal government, for instance through the Office of Minority Health, and at state level. There are also funds available from the Indian Health Service for engagement with the Native American population. It is therefore possible that community engagement interventions designed to make health care available (e.g. by bringing health care to the home, or by providing free health services or resources) might be particularly successful in the USA where the context is very different and a mandate to invest in demonstration projects to reduce disparities in health status is in place.
We suggest that, through community engagement, interventionists should conduct a thorough needs assessment to ensure that any planned intervention will meet the specific needs of the community. This will ensure that interventions are not transplanted to the UK simply because they were successful in the USA, without consideration of local needs and health system structures.
In terms of the content and mechanisms of the interventions, there are no particular reasons to believe that the underlying theories of change should not operate similarly across countries. For example, cultural adaptations in themselves are likely to be transferable, as long as the adaptations are appropriate for the cultural context. Different levels of formal education or literacy between the countries might mean that certain aspects of some interventions might be more or less successful in the different countries – this should be considered in intervention design and is likely to be ameliorated through community engagement.
Regarding the populations included in the review, race/ethnicity clearly differs across countries. The 2011 UK census543 reported that most of the 56.1 million residents of England and Wales belonged to the white ethnic group, with 14% non-white residents. The largest minority ethnic group was Indian (2.5%), followed by Pakistani (2%) and African (1.8%). The 2011 census also highlights growth in ‘other white’ ethnic groups, in particular because of inward migration from Poland, which constituted the second largest group of foreign-born people in the UK in 2011. In contrast, according to the 2010 US census,544 roughly 27.6% of the total population of the USA were from non-white racial groups and 36.3% considered their ethnicity to be non-white. African Americans constituted 12.6% of the US population, and 16.3% of the total population identified themselves as having Hispanic or Latino ethnicity. As such, the ethnic minorities in the UK are quite different from those in the USA. It is, however, unclear whether cultural or biological differences between the ethnic groups that are most prominent in the UK (e.g. Indians, Pakistanis) and those that are most prominent in the USA (e.g. African Americans, Latinos) would influence levels of engagement or impact on the effectiveness of different intervention types.
Despite the differences between the countries in the review, we argue that community engagement interventions are inherently well suited to deal with the issue of transferability. By including members of the community in intervention identification, design and/or delivery, the interventions can be appropriately adapted to meet the differing needs in specific contexts. It is also critical that evaluations of community engagement interventions build in process analysis to help identify specific factors that are needed to deliver an intervention in a specific cultural context and to aid in adaptation to other contexts. We have highlighted a lack of detailed documentation of resource and cost data in most evaluations; this information is also crucial when considering whether it is feasible to implement an intervention in a different setting where the pre-existing infrastructure and human resources may be very different and where different mechanisms for engagement may need to be used.
Chapter 10 Conclusions
About this chapter
In this chapter, we consider the implications for health care and recommendations for research. We present evidence statements that summarise the strength of evidence using the terms ‘solid’, ‘weak’, ‘inconsistent’ and ‘insufficient’. Solid evidence suggests that there were a large number of good-quality studies supporting the statement; weak evidence suggests that there were a small number of studies supporting the statement; inconsistent evidence suggests that some studies support whereas others reject or nullify the statement; and insufficient evidence suggests that there was a lack of available evidence related to the statement.
Implications for health care
The findings presented in this report found public health interventions that employ community engagement approaches to be effective in terms of enhancing health behaviours, health consequences, participant self-efficacy and perceived social support for disadvantaged groups. Albeit from a small number of studies, there also appear to be gains to human and social capital; both the meta-analysis (see Chapter 5, Overall, are community engagement interventions effective?) and the economic analysis (see Chapter 7, Gains/losses in human and social capital) reported evidence of benefits for engagees such as skills and future employment, and the meta-analysis identified significant positive effects on the perceived social support of the intervention participants. The combined evidence suggests that community engagement interventions work across a range of outcomes and beneficiaries.
Furthermore, there is an overall sense that some interventions have the potential to be cost-effective if cost-effectiveness evaluations considered the full range of outcomes and beneficiaries over a substantial period of time. Although the findings were mixed, cost-effective actions were identified for the three main models of community engagement that we identified. However, most of this evidence concentrates on peer-/lay-delivered interventions, which reflects the challenges in evaluating more complex interventions, which potentially could be more cost-effective.
Evidence statement 1: There is solid evidence that community engagement interventions have a positive impact on a range of health and psychosocial outcomes, across various conditions.
Evidence statement 2: There is weak but inconsistent evidence that different types of community engagement interventions can be cost-effective.
We have provided caveats to these overall statements throughout. Particular issues (highlighted in Chapter 9) include the diversity of the intervention characteristics, participants, health issues and evaluation procedures across studies; a lack of a ‘pure’ comparator for disentangling the effects attributable to community engagement; and the major differences in the methods used and reporting of costs and resources considered in the economic models. For example, although volunteering is often presented as a cost-effective approach to public health, it appears that the opportunity costs of the volunteers’ time are usually ignored (see Chapter 7, The value of volunteering).
In terms of understanding the mechanisms through which community engagement approaches reduce health inequalities, or at least improve the health of disadvantaged groups, it appears that there is no clear model that works best across all contexts, populations and health issues. More intensive, controlled, smaller studies (typically those using peer-/lay-delivered approaches) did tend to have larger effect sizes, but this does not take into account whether the outcomes are maintained, nor does it consider the potential impact on indirect beneficiaries (those who did not necessarily receive the intervention directly). Given the trends observed across a variety of subgroup analyses, the evidence suggests that community engagement in public health is more likely to require a ‘fit for purpose’ rather than a ‘one size fits all’ approach.
Synthesis of findings from the process evaluations highlighted several implications for those who plan and deliver community engagement initiatives. First, the majority of process evaluations highlighted the need for ongoing training and support of any community members delivering the intervention. Second, interventions should be designed with careful thought to issues of timing, frequency of contact, duration and extent, to ensure adequate exposure and to create conditions for participant reach. Third, stakeholders should aim to embed good project management and clear lines of responsibility into any intervention programme. Fourth, stakeholders should provide time and opportunities to build good working relationships by discussing issues of power, decision-making authority and responsibility. Finally, the evidence from process evaluations suggested that programmes benefited from interventions provided by similar community members; in contrast, this received limited support in our meta-analysis of effectiveness studies, which demonstrated slightly larger effects for peer- than for non-peer community member delivered interventions (see Chapter 5, Intervention deliverer).
Evidence statement 3: There is insufficient evidence – particularly for long-term outcomes and indirect beneficiaries – to determine whether one particular model of community engagement is likely to be more effective than any other.
Evidence statement 4: There is weak evidence from the effectiveness and process evaluations that certain implementation factors may affect intervention success.
In summary, public health interventions that include community engagement appear to be effective across models of engagement, populations and contexts. Unfortunately, the evidence is less clear about how the intervention and community engagement should be implemented to maximise impact on the desired outcomes for the particular populations and health issues of concern, and whether or not these approaches are cost-effective. In the next section we suggest recommendations for research that will hopefully address these gaps if adopted.
Recommendations for research
We believe that the conceptual framework (presented in Chapter 8) and the theories of change (introduced in Chapter 4 and tested in Chapter 5) are useful for researchers when considering the conflicting definitions of, and approaches to, community engagement with regard to identifying the characteristics of interventions that may be used. We hope that these conceptual tools will be adopted (and adapted where appropriate) by researchers in the community engagement discourse, and in intervention design and evaluation.
We recommend that resources be invested in high-quality evaluations of interventions that utilise the empowerment model of community engagement. Evidence in this area is lacking and, given the strength of theoretical claims for the impact of such approaches, this is a serious research gap (we identified only four studies conducted in the UK that adopted an empowerment approach and measured health behaviour outcomes). Such evaluations need to start imminently in the knowledge that the length of time required for outcomes to become apparent is often very long. Long-term follow-up is essential for detecting the maintenance of intervention effects and any ongoing or unexpected benefits of the intervention as proposed in a ‘virtuous circle’ model.
Key research recommendation 1: There are gaps in the evidence base in terms of long-term outcomes and outcomes for indirect beneficiaries. To assess the potentially diverse impacts of community engagement interventions, researchers need to incorporate a spectrum of outcome measures and plan long-term evaluations.
A particular challenge will be evaluating the benefits of interventions that inherently propose a causal pathway of effects of the intervention on multiple outcomes and beneficiaries (such as multicomponent interventions and those based on community empowerment models), relative to those that propose a direct causal path from the intervention to a narrow range of outcomes, time frames and/or beneficiaries (such as single component interventions or peer-/lay-delivery models). It may be possible to borrow techniques from other research disciplines (e.g. economics) in which complex models are built to create an analysis framework for comparing the relative benefits of different outcomes, but such modelling is very data intensive.
Very few integral process evaluations were located compared with the high number of outcome evaluations. In addition, some process evaluations noted that a lack of funding led to limited evaluation. This limited the ability of outcome evaluations to understand ‘how’ and ‘why’ an intervention worked (or did not). Future research grants could prioritise outcome evaluations that provide integral process evaluations, including analysis of funding and sustainability issues. Furthermore, our assessment of process evaluations identified a gap in the quality of reporting/conducting rigorous sampling, data collection and analysis methods. This suggests a need for future research to attend to the design, conduct and reporting of sampling, data collection and analysis of evaluations. Indeed, we recommend that all evaluations should be accompanied by a rigorous process evaluation, to encourage innovation and improvements in implementation. These evaluations, along with contextual analysis, may flag up important confounding factors that impact on the success or failure of individual community engagement actions. They may also help with issues of transferability and adaptability. This is particularly important given the dominance of US literature, where the context can be very different. Most notably, there are considerable differences in financial barriers to health care.
We further recommend that economic data be reported as a matter of course, that journals insist on this and that future evaluations should include economic and budgetary analyses. Such analyses can make an important contribution to policy and practitioner debates on whether to continue to invest in a particular project or to replicate it elsewhere. This includes separate recording of resource use and costs and valuation of as many opportunity costs as can be reasonably identified and measured. The issue of the comparator in evaluations is also key; if appropriate, evaluations might want to look at community engagement as an adjuvant mechanism as well as an alternative to the status quo. When an economic evaluation was carried out, comparatively little subgroup analysis was conducted. If carried out, this might help in targeting resources to areas in which inequalities in health are of most interest. Quite simply, it is difficult to assess the cost-effectiveness of community engagement interventions adequately given the current lack of cost and resource data reported. It is also important to be able to distinguish between research costs and costs of routine implementation. In sum, committed investment in evaluation is required to further understand what works, for whom and under what circumstances.
Key research recommendation 2: There is little evidence available on the legacy and sustainability of community engagement interventions because of insufficient rigorous process and economic evaluations. Researchers should plan for, and funding agencies could prioritise funding of, evaluations that incorporate process, costing and resource collection and economic evaluation.
Findings from the process evaluations revealed several implications for research design and conduct. The direct experiences and perspectives of participants or community members rarely contributed to the planning, delivery or evaluation of interventions. This limits the ability to make a direct inference between process measures and outcomes. Future research could endeavour to gain a deeper understanding of the perspectives and experiences of all involved community members (i.e. engagees and participants). To this end, qualitative and mixed-methods research should be used to ascertain engagees’ and participants’ experiences of an intervention in conjunction with outcome evaluations; this will help to identify barriers to, and facilitators of, participation, effectiveness and maintenance of effects. It was evident that many UK studies with adequate process evaluations lacked an accompanying outcome evaluation, and most of the identified outcome evaluations conducted in any OECD country lacked a process evaluation or qualitative data. Mixed-methods approaches could also help to identify potential harms resulting from community engagement, especially when communities are less involved, such as those identified in the review: social exclusion, cost overrun, attrition and dissatisfaction and disillusionment. 218,528,534
Also, the process evaluations lacked a direct link between the data collected and an impact on outcomes. This limits the confidence with which process issues can be seen to impact on outcomes. Future research should link measured processes to specific outcomes. Finally, some studies noted that paying community members, whether engagees or participants, influenced participation. Future research grants could prioritise the inclusion of plans for financial remuneration of participants and engagees.
Key research recommendation 3: Mixed-methods research should be conducted to establish intervention effectiveness and the engagees’ and participants’ experiences of an intervention.
For systematic review researchers, we draw attention to the novel search strategy employed here (see Chapter 9, The novel search strategy). Bearing in mind the success of our strategy of examining the evidence tables of large numbers of existing systematic reviews to find eligible studies, we recommend both that this strategy be replicated elsewhere and also that formal evaluations of this method be carried out.
Key research recommendation 4: Systematic reviews of evidence on hard-to-identify topics such as community engagement and health inequalities could replicate the search and identification strategies used in this review. A formal evaluation of this method is recommended.
In conclusion, evaluations of community engagement interventions need to be designed with particular emphasis on long-term assessment, broadening the range of beneficiaries typically measured, rigorous process evaluation and collection of cost and resource data. We anticipate that these additions will help to disentangle the relative effectiveness of different models of community engagement and encourage sustainable initiatives with a lasting health legacy for the community.
Acknowledgements
We would like to thank a number of people who contributed to this work. Katherine Twamley (KT), Carol Vigurs (CV) and Jenny Woodman (JW) all helped with screening and document retrieval. Our advisory group gave us extremely useful advice and guidance, and ongoing contact with some members has been very valuable. The members of the advisory group were Aaron Barbour (Community Links), Patricia Campbell (Glasgow University), David Evans (University of the West of England), Janet Harris (Sheffield University), Jane Kennedy (London Borough of Newham), Jennie Popay (Lancaster University), Ian Shemilt (Cambridge University) and Jane South (Leeds Metropolitan University). We would also like to thank the young people in our two consultative groups for sharing their perspectives on our work. One group wishes to remain anonymous, and we record with thanks the contribution of the NCB Young Research Advisers group.
This report refers to independent research commissioned by the NIHR. Any views and opinions expressed herein are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the Public Health Research programme or the Department of Health.
Contribution of authors
The study was designed by James Thomas (Reader in Social Policy), David McDaid (Senior Research Fellow), Sandy Oliver (Professor of Public Policy), Josephine Kavanagh (Research Officer) and Angela Harden (Professor of Community and Family Health).
The protocol was written by Alison O’Mara-Eves (Research Officer), James Thomas, Josephine Kavanagh, Ginny Brunton (Research Officer), Sandy Oliver, Angela Harden and David McDaid.
Alison O’Mara-Eves, Ginny Brunton, David McDaid, Sandy Oliver, Josephine Kavanagh, Farah Jamal (Research Fellow), Tihana Matosevic (Research Officer), Angela Harden and James Thomas all contributed to determining which research should be included, data extraction and writing of the report.
Main leads on the analyses were James Thomas (Chapter 4), Alison O’Mara-Eves (Chapter 5), Ginny Brunton and James Thomas (Chapters 6 and 7) and David McDaid (Chapter 8).
James Thomas takes responsibility for the integrity of the work as a whole.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Harden A, Oliver S, Oliver S, Peersman G. Using research for effective health promotion. Buckingham: Open University Press; 2001.
- Commissioning and system management – PPE. Real involvement: working with people to improve health services. London: Department of Health; 2008.
- Swainston K, Summerbell C. The effectiveness of community engagement approaches and methods for health promotion interventions. Teeside: University of Teeside; 2008.
- Popay J, Attree P, Hornby D, Milton B, Whitehead M, French B, et al. Community engagement in initiatives addressing the wider social determinants of health: a rapid review of evidence on impact, experience and process. Lancaster: University of Lancaster; 2007.
- Wilcox D. Community participation and empowerment: putting theory into practice. RRA Notes 1994;21:78-82.
- Boote J, Telford R, Cooper C. Consumer involvement in health research: a review and research agenda. Health Policy 2002;61:213-36. http://dx.doi.org/10.1016/S0168-8510(01)00214-7.
- Department of Health . Health Inequalities National Support Team 2011. www.dh.gov.uk/en/Publichealth/NationalSupportTeams/HealthInequalities/index.htm (accessed 16 May 2011).
- Shifting the balance of power: the next steps. London: Department of Health; 2002.
- Commissioning a patient-led National Health Service. London: Department of Health; 2005.
- Our health, our care, our say: a new direction for community services. Norwich: The Stationery Office; 2006.
- A stronger local voice: a framework for creating a stronger local voice in the development of health and social care services. London: Department of Health; 2006.
- Health reform in England: update and commissioning framework. London: Department of Health; 2006.
- Daykin N, Evans D, Petsoulas C, Sayers A. Evaluating the impact of patient and public involvement initiatives on UK health services: a systematic review. Evid Policy 2007;3:47-65. http://dx.doi.org/10.1332/174426407779702201.
- Popay J. Community engagement for health improvement: questions of definition, outcomes and evaluation. A background paper prepared for NICE. London: NICE; 2006.
- Wallerstein N, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract 2006;7:312-23. http://dx.doi.org/10.1177/1524839906289376.
- Nilsen E, Myrhaug H, Johansen M, Oliver S, Oxman A. Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material. Cochrane Database Syst Rev 2006;3. http://dx.doi.org/10.1002/14651858.CD004563.pub2.
- Macdonald G, Davies J, Davies J, Macdonald G. Quality, evidence and effectiveness in health promotion striving for certainties. London: Routledge; 1998.
- Whitehead M, Dahlgren G. Levelling up (part 1): a discussion paper on concepts and principles for tackling social inequities in health. Copenhagen: WHO; 2006.
- Graham P. Whose health, whose care, whose say? Some comments on public involvement in new NHS commissioning arrangements. Crit Publ Health 2009;19:123-32.
- Sheridan K, Tobi P. Towards a community engagement strategy: some practical notes. Br J Healthcare Manag 2010;16:123-8.
- Community engagement to improve health. NICE public health guidance 9. London: NICE; 2008.
- Mason A, Carr-Hill R, Myers L. Rapid review of the economic evidence for community engagement in health promotion: report and evidence tables. York: Centre for Health Economics, University of York; 2006.
- Mason A, Carr-Hill R, Myers L. Rapid review of the economic evidence for community engagement and community development approaches in interventions or initiatives seeking to address wider determinants of health. York: Centre for Health Economics, University of York; 2007.
- Carr-Hill R, Street A. Economic analysis of cost-effectiveness of community engagement to improve health. Discussion Paper 33. York: Centre for Health Economics, University of York; 2008.
- Fischer A. Cost effectiveness vignettes for community engagement. London: NICE; 2007.
- Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. Geneva: WHO; 2008.
- Wilkinson E, Marmot M. Social determinants of health: the solid facts. Geneva: WHO; 2003.
- Fair society, healthy lives: the Marmot review. Strategic review of health inequalities in England post-2010. London: Marmot Review; 2010.
- Great Britain . Greater London Authority Act 2007. www.legislation.gov.uk/ukpga/2007/24 (accessed August 2013).
- London Health Observatory . Health Inequalities: A Challenge for Local Authorities. Marmot Review 1 Year on Press Release 2011. www.lho.org.uk/LHO_Topics/national_lead_areas/marmot/marmotindicators.aspx (accessed 11 May 2011).
- National service framework for children, young people and maternity services. London: Department of Health; 2004.
- Citizens Advice Bureau . Citizens Advice Response to the Marmot Review team’s Report on the Health Impacts of Cold Homes and Fuel Poverty 2011. www.citizensadvice.org.uk/press_20110511 (accessed 13 May 2011).
- Oliver S, Kavanagh J, Caird J, Lorenc T, Oliver K, Harden A, et al. Health promotion, inequalities and young people’s health: a systematic review of research. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2008.
- Kawachi I, Subramanian S, Almedia-Filho N. A glossary for health inequalities. J Epidemiol Community Health 2002;56:647-52. http://dx.doi.org/10.1136/jech.56.9.647.
- Trends in life expectancy by the National Statistics Socio-economic Classification 1982–2006. Newport: ONS; 2011.
- National Institute for Health and Care Excellence . Citizens Council n.d. www.nice.org.uk/aboutnice/howwework/citizenscouncil/citizens_council.jsp (accessed August 2013).
- Report on NICE Citizens Council meeting 8–10 June 2006. London: NICE; 2007.
- Rifkin S, Lewando-Hundt G, Draper A. Participatory approaches in health promotion and health planning: a literature review. London: Health Development Agency; 2000.
- Arblaster L, Lambert M, Entwistle M, Forster M, Fullerton D, Sheldon T, et al. A systematic review of the effectiveness of health service interventions aimed at reducing inequalities in health. J Health Serv Res Policy 1996;1:93-103.
- Mason A, Carr-Hill R, Myers L, Street A. Establishing the economics of engaging communities in health promotion: what is desirable, what is feasible?. Crit Publ Health 2008;18:285-97. http://dx.doi.org/10.1080/09581590802277366.
- Darbas T, Smith T, Hall C. Case studies of community engagement: enhancing community engagement for NRM in the SEQ Western Catchment. Queensland: CSIRO; 2007.
- Hashagen S. Models of community engagement. Glasgow: Scottish Community Development Centre; 2002.
- Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al. Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach. Health Technol Assess 2004;8.
- Slater B, Knowles J, Lyon D. Improvement science meets community development: approaching health inequalities through community engagement. J Integrated Care 2008;16:26-3. http://dx.doi.org/10.1108/14769018200800043.
- The London health inequalities strategy. London: Greater London Authority; 2010.
- Moher D, Liberati A, Tetzlaff J, Altman D. PRISMA group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6. http://dx.doi.org/10.1371/journal.pmed.1000097.
- Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4.0: software for research synthesis. London: EPPI-Centre Software, Social Science Research Unit, Institute of Education, University of London; 2010.
- Public health, education, awareness, research. London: National Children’s Bureau; 2011.
- Oliver S, Bagnall AM, Thomas J, Shepherd J, Sowden A, White I, et al. Randomised controlled trials for policy interventions: a review of reviews and meta-regression. Health Technol Assess 2010;14.
- White I, Thomas J. Standardised mean differences in individually-randomised and cluster-randomised trials, with applications to meta-analysis. Clin Trials 2005;2:141-51.
- Chinn S. A simple method for converting an odds ratio to effects size for use in meta-analysis. Stat Med 2000;19:3127-31. http://dx.doi.org/10.1002/1097-0258(20001130)19:22<3127::AID-SIM784>3.0.CO;2-M.
- Lipsey M, Wilson D. Practical meta-analysis. Thousand Oaks, CA: Sage; 2001.
- McDaid D, Sassi F, Shemilt I, Mugford M, Vale L, Marsh K, et al. Evidence-based decisions and economics: health care, social welfare, education and criminal justice. Chichester: Wiley-Blackwell; 2010.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 n.d. www.cochrane-handbook.org (accessed June 2013).
- Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett-Page E, et al. The effectiveness and cost-effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13 to 19: a systematic review and economic evaluation. Health Technol Assess 2010;14.
- Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: Consensus on Health Economic Criteria. Int J Technol Assess Health Care 2005;21:240-5.
- Pawson R. Evidence-based policy: the promise of realist synthesis. Eval Health Prof 2002;8:340-58. http://dx.doi.org/10.1177/135638902401462448.
- Gough D, Thomas J, Oliver S. Clarifying differences between review designs and methods. Syst Rev 2012;1. http://dx.doi.org/10.1186/2046-4053-1-28.
- Noblitt G, Hare R. Meta-ethnography: synthesizing qualitative studies. London: Sage; 1988.
- Greenhalgh T, Bate P. Diffusion of innovations in health service organisations. London: BMJ Books; 2005.
- Brunton G, Stansfield C, Thomas J, Gough D, Oliver S, Thomas J. An introduction to systematic reviews. London: Sage; 2012.
- Caird J, Rees R, Kavanagh J, Sutcliffe K, Oliver K, Dickson K, et al. The socioeconomic value of nursing and midwifery: a rapid systematic review of reviews. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2010.
- Sutcliffe K, Brunton G, Twamley K, Hinds K, O’Mara-Eves A, Thomas J. Young people’s access to tobacco: a mixed-method systematic review. London: EPPI Centre, Social Science Research Unit, Institute of Education, University of London; 2011.
- Brunton G, Wiggins M, Oakley A. Becoming a mother: a research synthesis of women’s views on the experience of first-time motherhood. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2011.
- Carpineto C, Osinski S, Romano G, Weiss D. A survey of web clustering engines. ACM Comput Surv 2009;47:1-38. http://dx.doi.org/10.1145/1541880.1541884.
- Thompson S, Sharp S. Explaining heterogeneity in meta-analysis: a comparison of methods. Stat Med 1999;18:693-708. http://dx.doi.org/10.1002/(SICI)1097-0258(19991030)18:20<2693::AID-SIM235>3.0.CO;2-V.
- Wilson DB. Meta-Analysis Macros for SAS, SPSS and Stata n.d. http://mason.gmu.edu/∼dwilsonb/ma.html (accessed 15 March 2013).
- Thomas J, Harden A, Newman M, Gough D, Oliver S, Thomas J. An introduction to systematic reviews. London: Sage; 2012.
- Carroll C, Booth A, Cooper K. A worked example of ‘best fit’ framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol 2011;11. http://dx.doi.org/10.1186/1471-2288-11-29.
- Kavanagh J, Trouton A, Oakley A, Powell C. A systematic review of the evidence for incentive schemes to encourage positive health and other social behaviours in young people. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2006.
- Anand SS, Davis AD, Ahmed R, Jacobs R, Xie C, Hill A, et al. A family-based intervention to promote healthy lifestyles in an aboriginal community in Canada. Can J Public Health 2007;98:447-52.
- Anderson AK, Damio G, Young S, Chapman DJ, Perez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Arch Pediatr Adolesc Med 2005;159:836-41. http://dx.doi.org/10.1001/archpedi.159.9.836.
- Andrews JO, Bentley G, Crawford S, Pretlow L, Tingen MS. Using community-based participatory research to develop a culturally sensitive smoking cessation intervention with public housing neighborhoods. Ethn Dis 2007;17:331-7.
- Arlotti JP, Cottrell BH, Lee SH, Curtin JJ. Breastfeeding among low-income women with and without peer support. J Community Health Nurs 1998;15:163-78. http://dx.doi.org/10.1207/s15327655jchn1503_4.
- Aseltine RH, Dupre M, Lamlein P. Mentoring as a drug prevention strategy: an evaluation of ‘across ages’. Adolesc Fam Health 2000;1:11-20.
- Auld GW, Romaniello C, Heimendinger J, Hambidge C, Hambidge M. Outcomes from a school-based nutrition education program using resource teachers and cross-disciplinary models. J Nutr Educ 1998;30:268-80. http://dx.doi.org/10.1016/S0022-3182(98)70336-X.
- Auslander W, Haire JD, Houston C, Rhee CW, Williams JH. A controlled evaluation of staging dietary patterns to reduce the risk of diabetes in African-American women. Diabetes Care 2002;25:809-14. http://dx.doi.org/10.2337/diacare.25.5.809.
- Avila P, Hovell MF. Physical activity training for weight loss in Latinas: a controlled trial. Int J Obes Relat Metab Disord 1994;18:476-82.
- Ayala GX, Elder JP, Campbell NR, Arredondo E, Baquero B, Crespo NC, et al. Longitudinal intervention effects on parenting of the Aventuras para Niños study. Am J Prev Med 2010;38:154-62. http://dx.doi.org/10.1016/j.amepre.2009.09.038.
- Balcazar HG, de Heer H, Rosenthal L, Aguirre M, Flores L, Puentes FA, et al. A promotores de salud intervention to reduce cardiovascular disease risk in a high-risk Hispanic border population, 2005–2008. Prev Chronic Dis 2010;7.
- Banks ER. Being Healthy Counts to H.I.M.: An Examination of Health Behavior Among Participants in a Diabetes Prevention and Health Promotion Program 2009.
- Baranowski T, Simons-Morton B, Hooks P, Henske J, Tiernan K, Dunn JK, et al. A center-based program for exercise change among black-American families. Health Educ Q 1990;17:179-96. http://dx.doi.org/10.1177/109019819001700205.
- Barnes K, Friedman SM, Brickner N, Honig J. Impact of community volunteers on immunization rates of children younger than 2 years. Arch Pediatr Adolesc Med 1999;153:518-24. http://dx.doi.org/10.1001/archpedi.153.5.518.
- Barnes-Boyd C, Fordham N, Nacion KW. Promoting infant health through home visiting by a nurse-managed community worker team. Public Health Nurs 2001;18:225-35. http://dx.doi.org/10.1046/j.1525-1446.2001.00225.x.
- Becker DM, Yanek LR, Johnson WR, Garrett D, Moy TF, Reynolds SS, et al. Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation 2005;111:1298-304. http://dx.doi.org/10.1161/01.CIR.0000157734.97351.B2.
- Beech BM, Klesges RC, Kumanyika SK, Murray DM, Klesges L, McClanahan B, et al. Child- and parent-targeted interventions: the Memphis GEMS pilot study. Ethn Dis 2003;13:S40-53.
- Black MM, Hager ER, Le K, Anliker J, Arteaga SS, Diclemente C, et al. Challenge! Health promotion/obesity prevention mentorship model among urban, black adolescents. Pediatrics 2010;126:280-8. http://dx.doi.org/10.1542/peds.2009-1832.
- Botvin GJ, Schinke SP, Epstein JA, Diaz T, Botvin EM. Effectiveness of culturally focused and generic skills training approaches to alcohol and drug abuse prevention among minority adolescents: two-year follow-up results. Psychol Addict Behav 1995;9:183-94. http://dx.doi.org/10.1037//0893-164X.9.3.183.
- Britto MT, Klostermann BK, Bonny AE, Altum SA, Hornung RW. Impact of a school-based intervention on access to healthcare for underserved youth. J Adolesc Health 2001;29:116-24. http://dx.doi.org/10.1016/S1054-139X(01)00196-3.
- Brownson RC, Baker EA, Boyd RL, Caito NM, Duggan K, Housemann RA, et al. A community-based approach to promoting walking in rural areas. Am J Prev Med 2004;27:28-34. http://dx.doi.org/10.1016/j.amepre.2004.03.015.
- Brownson RC, Hagood L, Lovegreen SL, Britton B, Caito NM, Elliott MB, et al. A multilevel ecological approach to promoting walking in rural communities. Prev Med 2005;41:837-42. http://dx.doi.org/10.1016/j.ypmed.2005.09.004.
- Brownson RC, Smith CA, Pratt M, Mack NE, Jackson-Thompson J, Dean CG, et al. Preventing cardiovascular disease through community-based risk reduction: the Bootheel Heart Health Project. Am J Public Health 1996;86:206-13. http://dx.doi.org/10.2105/AJPH.86.2.206.
- Buller DB, Morrill C, Taren D, Aickin M, Sennott-Miller L, Buller MK, et al. Randomized trial testing the effect of peer education at increasing fruit and vegetable intake. J Natl Canc Inst 1999;91:1491-500. http://dx.doi.org/10.1093/jnci/91.17.1491.
- Campbell MK, Demark-Wahnefried W, Symons M, Kalsbeek WD, Dodds J, Cowan A, et al. Fruit and vegetable consumption and prevention of cancer: the Black Churches United for Better Health project. Am J Public Health 1999;89:1390-6. http://dx.doi.org/10.2105/AJPH.89.9.1390.
- Campbell MK, James A, Hudson MA, Carr C, Jackson E, Oakes V, et al. Improving multiple behaviors for colorectal cancer prevention among African American church members. Health Psychol 2004;23:492-50.
- Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, Belton L, et al. Effects of a tailored health promotion program for female blue-collar workers: health works for women. Prev Med 2002;34:313-23. http://dx.doi.org/10.1006/pmed.2001.0988.
- Caulfield LE, Gross SM, Bentley ME, Bronner Y, Kessler L, Jensen J, et al. WIC-based interventions to promote breastfeeding among African-American women in Baltimore: effects on breastfeeding initiation and continuation. J Hum Lact 1998;14:15-22. http://dx.doi.org/10.1177/089033449801400110.
- Chapman DJ, Damio G, Young S, Perez-Escamilla R. Effectiveness of breastfeeding peer counseling in a low-income, predominantly Latina population: a randomized controlled trial. Arch Pediatr Adolesc Med 2004;158:897-902. http://dx.doi.org/10.1001/archpedi.158.9.897.
- Cherry VR, Belgrave FZ, Jones W, Kennon DK, Gray FS, Phillips F. NTU: an Africentric approach to substance abuse prevention among African American youth. J Prim Prev 1998;18:319-39.
- Cochrane T, Davey RC. Increasing uptake of physical activity: a social ecological approach. J R Soc Health 2008;128:31-40. http://dx.doi.org/10.1177/1466424007085223.
- Conway TL, Woodruff SI, Edwards CC, Hovell MF, Klein J. Intervention to reduce environmental tobacco smoke exposure in Latino children: null effects on hair biomarkers and parent reports. Tob Control 2004;13:90-2. http://dx.doi.org/10.1136/tc.2003.004440.
- Cox RH, Parker GG, Watson AC, Robinson SH, Simonson CJ, Elledge JC, et al. Dietary cancer risk of low-income women and change with intervention. J Am Diet Assoc 1995;95:1031-4. http://dx.doi.org/10.1016/S0002-8223(95)00281-2.
- Daniel M, Green LW, Marion SA, Gamble D, Herbert CP, Hertzman C, et al. Effectiveness of community-directed diabetes prevention and control in a rural Aboriginal population in British Columbia, Canada. Soc Sci Med 1999;48:815-32. http://dx.doi.org/10.1016/S0277-9536(98)00403-1.
- Davidson LL, Durkin MS, Kuhn L, O’Connor P, Barlow B, Heagarty MC. The impact of the Safe Kids/Healthy Neighborhoods Injury Prevention Program in Harlem, 1988 through 1991. Am J Public Health 1994;84:580-6. http://dx.doi.org/10.2105/AJPH.84.4.580.
- Davis S, Gomez Y, Lambert L, Skipper B. Primary prevention of obesity in American Indian children. Ann NY Acad Sci 1993;699:167-80. http://dx.doi.org/10.1111/j.1749-6632.1993.tb18848.x.
- Davis SM, Lambert LC, Gomez Y, Skipper B. Southwest Cardiovascular Curriculum Project: study findings for American Indian elementary students. J Health Educ 1995;26:S72-81.
- Dedobbeleer N, Desjardins S. Outcomes of an ecological and participatory approach to prevent alcohol and other drug ‘abuse’ among multiethnic adolescents. Subst Use Misuse 2001;36:1959-91.
- Duncan TE, Duncan SC, Beauchamp N, Wells J, Ary DV. Development and evaluation of an interactive CD-ROM refusal skills program to prevent youth substance use: ‘refuse to use’. J Behav Med 2000;23:59-72.
- Elder JP, Ayala GX, Campbell NR, Slymen D, Lopez-Madurga ET, Engelberg M, et al. Interpersonal and print nutrition communication for a Spanish-dominant Latino population: Secretos de la Buena Vida. Health Psychol 2005;24:49-57. http://dx.doi.org/10.1037/0278-6133.24.1.49.
- Elder JP, Wildey M, de Moor C, Sallis JF, Eckhardt L, Edwards C, et al. The long-term prevention of tobacco use among junior high school students: classroom and telephone interventions. Am J Public Health 1993;83:1239-44. http://dx.doi.org/10.2105/AJPH.83.9.1239.
- Ernst CC, Grant TM, Streissguth AP, Sampson PD. Intervention with high-risk alcohol and drug-abusing mothers: II. Three-year findings from the Seattle model of paraprofessional advocacy. J Community Psychol 1999;27:19-38. http://dx.doi.org/10.1002/(SICI)1520-6629(199901)27:1<19::AID-JCOP2>3.0.CO;2-K.
- Faridi Z, Shuval K, Njike VY, Katz JA, Jennings G, Williams M, et al. Partners reducing effects of diabetes (PREDICT): a diabetes prevention physical activity and dietary intervention through African-American churches. Health Educ Res 2010;25:306-15. http://dx.doi.org/10.1093/her/cyp005.
- Fisher EB, Auslander WF, Munro JF, Arfken CL, Brownson RC, Owens NW. Neighbors for a smoke free north side: evaluation of a community organization approach to promoting smoking cessation among African Americans. Am J Public Health 1998;88:1658-63. http://dx.doi.org/10.2105/AJPH.88.11.1658.
- Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Two-year follow-up results for Hip-Hop to Health Jr: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr 2005;146:618-25. http://dx.doi.org/10.1016/j.jpeds.2004.12.019.
- Foerster SB, Gregson J, Beall DL, Hudes M, Magnuson H, Livingston S, et al. The California Children’s 5 a Day-Power Play! Campaign: evaluation of a large-scale social marketing initiative. Fam Community Health 1998;21:46-64.
- Fried LP, Carlson MC, Freedman M, Frick KD, Glass TA, Hill J, et al. A social model for health promotion for an aging population: initial evidence on the Experience Corps model. J Urban Health 2004;81:64-78. http://dx.doi.org/10.1093/jurban/jth094.
- Gadomski A, Ackerman S, Burdick P, Jenkins P. Efficacy of the North American guidelines for children’s agricultural tasks in reducing childhood agricultural injuries. Am J Public Health 2006;96:722-7. http://dx.doi.org/10.2105/AJPH.2003.035428.
- Gottfredson DC, Gottfredson GD, Skroban S. A multimodel school-based prevention demonstration. J Adolesc Res 1996;11. http://dx.doi.org/10.1177/0743554896111006.
- Neighbourhood management: an overview of the 2003 and 2006 Round 1 Pathfinder household surveys. London: Department for Communities and Local Government, Neighbourhood Renewal Unit; 2006.
- Graham AV, Frank SH, Zyzanski SJ, Kitson GC, Reeb KG. A clinical trial to reduce the rate of low birth weight in an inner-city black population. Fam Med 1992;24:439-46.
- Grummer-Strawn LM, Rice SP, Dugas K, Clark LD, Benton-Davis S. An evaluation of breastfeeding promotion through peer counseling in Mississippi WIC clinics. Matern Child Health J 1997;1:35-42.
- Hancock L, Sanson-Fisher R, Perkins J, McClintock A, Howley P, Gibberd R. Effect of a community action program on adult quit smoking rates in rural Australian towns: the CART project. Prev Med 2001;32:118-27. http://dx.doi.org/10.1006/pmed.2000.0798.
- Hanlon TE, Bateman RW, Simon BD, O’Grady KE, Carswell SB. An early community-based intervention for the prevention of substance abuse and other delinquent behavior. J Youth Adolesc 2002;31:459-71.
- Harmon MA. Reducing Drug Use Among Pregnant and Parenting Teens: A Program Evaluation and Theoretical Examination 1995.
- Havas S, Anliker J, Damron D, Langenberg P, Ballesteros M, Feldman R. Final results of the Maryland WIC 5-a-Day promotion program. Am J Public Health 1998;88:1161-7. http://dx.doi.org/10.2105/AJPH.88.8.1161.
- Hayashi T, Farrell MA, Chaput LA, Rocha DA, Hernandez M. Lifestyle intervention, behavioral changes, and improvement in cardiovascular risk profiles in the California WISEWOMAN project. J Womens Health 2010;19:1129-38. http://dx.doi.org/10.1089/jwh.2009.1631.
- Hecht ML, Marsiglia FF, Elek E, Wagstaff DA, Kulis S, Dustman P, et al. Culturally grounded substance use prevention: an evaluation of the keepin’ it R.E.A.L. curriculum. Prev Sci 2003;4:233-48.
- Hunter JB, de Zapien JG, Papenfuss M, Fernandez ML, Meister J, Giuliano AR. The impact of a promotora on increasing routine chronic disease prevention among women aged 40 and older at the US–Mexico border. Health Educ Behav 2004;31:18-2.
- Johnson Z, Howell F, Molloy B. Community mothers’ programme: randomised controlled trial of non-professional intervention in parenting. BMJ 1993;306:1449-52. http://dx.doi.org/10.1136/bmj.306.6890.1449.
- Julnes G, Konefal M, Pindur W, Kim P. Community-based perinatal care for disadvantaged adolescents: evaluation of the Resource Mothers Program. J Community Health 1994;19:41-53. http://dx.doi.org/10.1007/BF02260520.
- Karanja N, Lutz T, Ritenbaugh C, Maupome G, Jones J, Becker T, et al. The TOTS community intervention to prevent overweight in American Indian toddlers beginning at birth: a feasibility and efficacy study. J Community Health 2010;35:667-75. http://dx.doi.org/10.1007/s10900-010-9270-5.
- Kim KH, Linnan L, Campbell MK, Brooks C, Koenig HG, Wiesen C. The WORD (wholeness, oneness, righteousness, deliverance): a faith-based weight-loss program utilizing a community-based participatory research approach. Health Educ Behav 2008;35:634-50. http://dx.doi.org/10.1177/1090198106291985.
- Kistin N, Abramson R, Dublin P. Effect of peer counselors on breastfeeding initiation, exclusivity, and duration among low-income urban women. J Hum Lact 1994;10:11-5. http://dx.doi.org/10.1177/089033449401000121.
- Kloek GC, van Lenthe FJ, van Nierop PW, Koelen MA, Mackenbach JP. Impact evaluation of a Dutch community intervention to improve health-related behaviour in deprived neighbourhoods. Health Place 2006;12:665-77. http://dx.doi.org/10.1016/j.healthplace.2005.09.002.
- Krieger J, Collier C, Song L, Martin D. Linking community-based blood pressure measurement to clinical care: a randomized controlled trial of outreach and tracking by community health workers. Am J Public Health 1999;89:856-61. http://dx.doi.org/10.2105/AJPH.89.6.856.
- Kumpusalo E, Neittaanmaki L, Halonen P, Pekkarinen H. Finnish Healthy Village Study: impact and outcomes of a low-cost local health promotion programme. Health Promot Int 1996;11. http://dx.doi.org/10.1093/heapro/11.2.105.
- Lewis CE, Raczynski JM, Heath GW, Levinson R, Hilyer JC, Cutter GR. Promoting physical activity in low-income African-American communities: the PARR project. Ethn Dis 1993;3:106-18.
- Lindenberg CS, Solorzano RM, Bear D, Strickland O, Galvis C, Pittman K. Reducing substance use and risky sexual behavior among young, low-income, Mexican-American women: comparison of two interventions. Appl Nurs Res 2002;15:137-48. http://dx.doi.org/10.1053/apnr.2002.34141.
- Lindqvist K, Timpka T, Schelp L, Ahlgren M. Evaluation of an inter-organizational program for prevention of work-related injuries in a WHO Safe Community. Work 1999;13:89-96.
- Long DG, Funk-Archuleta MA, Geiger CJ, Mozar AJ, Heins JN. Peer counselor program increases breastfeeding rates in Utah Native American WIC population. J Hum Lact 1995;11:279-84. http://dx.doi.org/10.1177/089033449501100414.
- LoSciuto L, Hilbert SM, Fox MM, Porcellini L, Lanphear A. A two-year evaluation of the Wood Rock Youth Development Project. J Early Adolesc 1999;19:488-507. http://dx.doi.org/10.1177/0272431699019004004.
- LoSciuto L, Rajala AK, Townsend TN, Taylor AS. An outcome evaluation of across ages. J Adolesc Res 1996;11:116-29. http://dx.doi.org/10.1177/0743554896111007.
- Lupton BS, Fonnebo V, Sogaard AJ, Langfeldt E. The Finnmark Intervention Study. Better health for the fishery population in an Arctic village in North Norway. Scand J Prim Health Care 2002;20:213-18. http://dx.doi.org/10.1080/028134302321004863.
- Luster T, Perlstadt H, McKinney M, Sims K, Juang L. The effects of a family support program and other factors on the home environments provided by adolescent mothers. Fam Relat 1996;45:255-64. http://dx.doi.org/10.2307/585497.
- Macaulay AC, Paradis G, Potvin L, Cross EJ, Saad-Haddad C, McComber A, et al. The Kahnawake Schools Diabetes Prevention Project: intervention, evaluation, and baseline results of a diabetes primary prevention program with a native community in Canada. Prev Med 1997;26:779-90. http://dx.doi.org/10.1006/pmed.1997.0241.
- Malchodi CS, Oncken C, Dornelas EA, Caramanica L, Gregonis E, Curry SL. The effects of peer counseling on smoking cessation and reduction. Obstet Gynecol 2003;101:504-10. http://dx.doi.org/10.1016/S0029-7844(02)03070-3.
- Marcenko MO, Spence M, Samost L. Outcomes of a home visitation trial for pregnant and postpartum women at-risk for child placement. Children Youth Serv Rev 1996;18:243-59. http://dx.doi.org/10.1016/0190-7409(96)00003-5.
- McAlister AL, Ramirez AG, Amezcua C, Pulley LV, Stern MP, Mercado S. Smoking cessation in Texas–Mexico border communities: a quasi-experimental panel study. Am J Health Promot 1992;6:274-9. http://dx.doi.org/10.4278/0890-1171-6.4.274.
- McInnes RJ. The Glasgow Infant Feeding Action Research Project: An Evaluation of a Community Based Intervention Designed to Increase the Prevalence of Breastfeeding in a Socially Disadvantaged Urban Area 1998.
- McNabb W, Quinn M, Kerver J, Cook S, Karrison T. The PATHWAYS church-based weight loss program for urban African-American women at risk for diabetes. Diabetes Care 1997;20:1518-23. http://dx.doi.org/10.2337/diacare.20.10.1518.
- McNabb WL, Quinn MT, Rosing L. Weight loss program for inner-city black women with non-insulin-dependent diabetes mellitus: PATHWAYS. J Am Diet Assoc 1993;93:75-7. http://dx.doi.org/10.1016/0002-8223(93)92138-N.
- Mendoza J, Levinger D, Johnston B. Pilot evaluation of a walking school bus program in a low-income, urban community. BMC Public Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-122.
- Miller-Heyl J, MacPhee D, Fritz JJ. DARE to be you: a family-support, early prevention program. J Prim Prev 1998;18:257-85.
- Nafziger AN, Erb TA, Jenkins PL, Lewis C, Pearson TA. The Otsego-Schoharie healthy heart program: prevention of cardiovascular disease in the rural US. Scand J Public Health (Suppl) 2001;56:21-32. http://dx.doi.org/10.1080/140349401316898108.
- Norr KF, Crittenden KS, Lehrer EL, Reyes O, Boyd CB, Nacion KW, et al. Maternal and infant outcomes at one year for a nurse-health advocate home visiting program serving African Americans and Mexican Americans. Public Health Nurs 2003;20:190-203. http://dx.doi.org/10.1046/j.0737-1209.2003.20306.x.
- O’Loughlin JL, Paradis G, Gray-Donald K, Renaud L. The impact of a community-based heart disease prevention program in a low-income, inner-city neighborhood. Am J Public Health 1999;89:1819-26. http://dx.doi.org/10.2105/AJPH.89.12.1819.
- Parsons L, Day S. Improving obstetric outcomes in ethnic minorities: an evaluation of health advocacy in Hackney. J Public Health Med 1992;14:183-91.
- Perry CL, Williams CL, Veblen-Mortenson S, Toomey TL, Komro KA, Anstine PS, et al. Project Northland: outcomes of a communitywide alcohol use prevention program during early adolescence. Am J Public Health 1996;86:956-65. http://dx.doi.org/10.2105/AJPH.86.7.956.
- Platt S, Parry O, Ritchie D, Gnich W. Evaluating a community-based anti-smoking programme: lessons for policy, practice and research. Edinburgh RUHBC Research Findings Papers. Edinburgh: Edinburgh Research Unit in Health, Behaviour and Change; 2003.
- Poland ML, Giblin PT, Waller JB, Hankin J. Effects of a home visiting program on prenatal care and birthweight: a case comparison study. J Community Health 1992;17:221-9. http://dx.doi.org/10.1007/BF01321654.
- Poston WS, Haddock CK, Olvera NE, Suminski RR, Reeves RS, Dunn JK, et al. Evaluation of a culturally appropriate intervention to increase physical activity. Am J Health Behav 2001;25:396-40.
- Pugh LC, Milligan RA, Frick KD, Spatz D, Bronner Y. Breastfeeding duration, costs, and benefits of a support program for low-income breastfeeding women. Birth 2002;29:95-100. http://dx.doi.org/10.1046/j.1523-536X.2002.00169.x.
- Pugh LC, Milligan RA, Brown LP. The Breastfeeding Support Team for low-income, predominantly-minority women: a pilot intervention study. Health Care Women Int 2001;22:501-15.
- Reijneveld SA, Westhoff MH, Hopman-Rock M. Promotion of health and physical activity improves the mental health of elderly immigrants: results of a group randomised controlled trial among Turkish immigrants in the Netherlands aged 45 and over. J Epidemiol Community Health 2003;57:405-11. http://dx.doi.org/10.1136/jech.57.6.405.
- Resnicow K, Campbell MK, Carr C, McCarty F, Wang T, Periasamy S, et al. Body and soul. A dietary intervention conducted through African-American churches. Am J Prev Med 2004;27:97-105.
- Resnicow K, Cohn L, Reinhardt J, Cross D, Futterman R, Kirschner E, et al. A three-year evaluation of the know your body program in inner-city schoolchildren. Health Educ Q 1992;19:463-80. http://dx.doi.org/10.1177/109019819201900410.
- Rhodes JE, Reddy R, Grossman JB. The protective influence of mentoring on adolescents’ substance use: direct and indirect pathways. Appl Dev Sci 2005;9:31-47. http://dx.doi.org/10.1207/s1532480xads0901_4.
- Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis 2003;13:S65-77.
- Rodewald LE, Szilagyi PG, Humiston SG, Barth R, Kraus R, Raubertas RF. A randomized study of tracking with outreach and provider prompting to improve immunization coverage and primary care. Pediatrics 1999;103:31-8. http://dx.doi.org/10.1542/peds.103.1.31.
- Rose MA. Evaluation of a peer-education program on heart disease prevention with older adults. Public Health Nurs 1992;9:242-7. http://dx.doi.org/10.1111/j.1525-1446.1992.tb00108.x.
- Schafer E, Vogel MK, Viegas S, Hausafus C. Volunteer peer counselors increase breastfeeding duration among rural low-income women. Birth 1998;25:101-6. http://dx.doi.org/10.1046/j.1523-536x.1998.00101.x.
- Schensul JJ, Radda K, Coman E, Vazquez E. Multi-level intervention to prevent influenza infections in older low income and minority adults. Am J Community Psychol 2009;43:313-29. http://dx.doi.org/10.1007/s10464-009-9235-y.
- Schinke SP, Tepavac L, Cole KC. Preventing substance use among Native American youth: three-year results. Addict Behav 2000;25:387-97.
- Schorling JB, Roach J, Siegel M, Baturka N, Hunt DE, Guterbock TM, et al. A trial of church-based smoking cessation interventions for rural African Americans. Prev Med 1997;26:92-101. http://dx.doi.org/10.1006/pmed.1996.9988.
- Schuler ME, Nair P, Black MM. Ongoing maternal drug use, parenting attitudes, and a home intervention: effects on mother-child interaction at 18 months. J Dev Behav Pediatr 2002;23:87-94. http://dx.doi.org/10.1097/00004703-200204000-00004.
- Schwarz DF, Grisso JA, Miles C, Holmes JH, Sutton RL. An injury prevention program in an urban African-American community. Am J Public Health 1993;83:675-80. http://dx.doi.org/10.2105/AJPH.83.5.675.
- Secker-Walker RH, Flynn BS, Solomon LJ, Skelly JM, Dorwaldt AL, Ashikaga T. Helping women quit smoking: results of a community intervention program. Am J Public Health 2000;90:940-6.
- Shaw E, Kaczorowski J. The effect of a peer counseling program on breastfeeding initiation and longevity in a low-income rural population. J Hum Lact 1999;15:19-25. http://dx.doi.org/10.1177/089033449901500108.
- Shaw RA, Rosati MJ, Salzman P, Coles CR, McGeary C. Effects on adolescent ATOD behaviors and attitudes of a 5-year community partnership. Eval Program Plann 1997;20:307-13. http://dx.doi.org/10.1016/S0149-7189(97)00010-4.
- Shelley D, Fahs M, Yerneni R, Das D, Nguyen N, Hung D, et al. Effectiveness of tobacco control among Chinese Americans: a comparative analysis of policy approaches versus community-based programs. Prev Med 2008;47:530-6. http://dx.doi.org/10.1016/j.ypmed.2008.07.009.
- Silver EJ, Ireys HT, Bauman LJ, Stein REK. Psychological outcomes of a support intervention in mothers of children with ongoing health conditions: the parent to parent network. J Community Psychol 1997;25:249-64. http://dx.doi.org/10.1002/(SICI)1520-6629(199705)25:3<249::AID-JCOP3>3.0.CO;2-R.
- Simmons D, Fleming C, Voyle J, Fou F, Feo S, Gatland B. A pilot urban church-based programme to reduce risk factors for diabetes among Western Samoans in New Zealand. Diabet Med 1998;15:136-42. http://dx.doi.org/10.1002/(SICI)1096-9136(199802)15:2<136::AID-DIA530>3.0.CO;2-P.
- Solomon LJ, Scharoun GM, Flynn BS, Secker-Walker RH, Sepinwall D. Free nicotine patches plus proactive telephone peer support to help low-income women stop smoking. Prev Med 2000;31:68-74. http://dx.doi.org/10.1006/pmed.2000.0683.
- Solomon LJ, Secker-Walker RH, Flynn BS, Skelly JM, Capeless EL. Proactive telephone peer support to help pregnant women stop smoking. Tob Control 2000;9:III72-4. http://dx.doi.org/10.1136/tc.9.suppl_3.iii72.
- Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working-class, multiethnic workers: results of the healthy directions – small business study. Am J Public Health 2005;95:1389-95. http://dx.doi.org/10.2105/AJPH.2004.038745.
- St James PS, Shapiro E, Waisbren SE. The Resource Mothers Program for Maternal Phenylketonuria. Am J Public Health 1999;89:762-4. http://dx.doi.org/10.2105/AJPH.89.5.762.
- Staten LK, Gregory-Mercado KY, Ranger-Moore J, Will JC, Giuliano AR, Ford ES, et al. Provider counseling, health education, and community health workers: the Arizona WISEWOMAN project. J Womens Health 2004;13:547-56. http://dx.doi.org/10.1089/1540999041281133.
- Valente TW, Unger JB, Ritt-Olson A, Cen SY, Anderson J. The interaction of curriculum type and implementation method on 1-year smoking outcomes in a school-based prevention program. Health Educ Res 2006;21:315-24. http://dx.doi.org/10.1093/her/cyl002.
- Vogler SD, Davidson AJ, Crane LA, Steiner JF, Brown JM. Can paraprofessional home visitation enhance early intervention service delivery?. J Dev Behav Pediatr 2002;23:208-16. http://dx.doi.org/10.1097/00004703-200208000-00003.
- Voorhees CC, Stillman FA, Swank RT, Heagerty PJ, Levine DM, Becker DM. Heart, body, and soul: impact of church-based smoking cessation interventions on readiness to quit. Prev Med 1996;25:277-85. http://dx.doi.org/10.1006/pmed.1996.0057.
- Watkins E, Harlan C, Eng E, Gansky S, Gehan D, Larson K. Assessing the effectiveness of lay health advisors with migrant farmworkers. Fam Community Health 1994;16:72-87. http://dx.doi.org/10.1097/00003727-199401000-00010.
- Weiss FL, Nicholson HJ. Friendly PEERsuasionSM against substance use: the Girls IncorporatedSM model and evaluation. Drugs Soc 1998;12:7-22.
- Wiist WH, Flack JM. A church-based cholesterol education program. Public Health Rep 1990;105:381-8.
- Wilcox S, Laken M, Bopp M, Gethers O, Huang P, McClorin L, et al. Increasing physical activity among church members. Community-based participatory research. Am J Prev Med 2007;32:131-8.
- Winkleby MA, Feighery E, Dunn M, Kole S, Ahn D, Killen JD. Effects of an advocacy intervention to reduce smoking among teenagers. Arch Pediatr Adolesc Med 2004;158:269-75. http://dx.doi.org/10.1001/archpedi.158.3.269.
- Witmer JM, Hensel MR, Holck PS, Ammerman AS, Will JC. Heart disease prevention for Alaska Native women: a review of pilot study findings. J Womens Health 2004;13:569-78. http://dx.doi.org/10.1089/1540999041280981.
- Woodruff SI, Talavera GA, Elder JP. Evaluation of a culturally appropriate smoking cessation intervention for Latinos. Tob Control 2002;11:361-7. http://dx.doi.org/10.1136/tc.11.4.361.
- Wright AL, Naylor A, Wester R, Bauer M, Sutcliffe E. Using cultural knowledge in health promotion: breastfeeding among the Navajo. Health Educ Behav 1997;24:625-39. http://dx.doi.org/10.1177/109019819702400509.
- Yanek LR, Becker DM, Moy TF, Gittelsohn J, Koffman DM. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep 2001;116:68-81. http://dx.doi.org/10.1093/phr/116.S1.68.
- Zavela KJ, Battistich V, Gosselink CA, Dean BJ. Say Yes First: follow up of a five-year rural drug prevention program. J Drug Educ 2004;34:73-88. http://dx.doi.org/10.2190/TVU5-FK00-V5MU-K7TR.
- Zhou F, Euler GL, McPhee SJ, Nguyen T, Lam T, Wong C, et al. Economic analysis of promotion of hepatitis B vaccinations among Vietnamese-American children and adolescents in Houston and Dallas. Pediatrics 2003;111:1289-96. http://dx.doi.org/10.1542/peds.111.6.1289.
- Aarons SJ, Jenkins RR, Raine TR, El-Khorazaty MN, Woodward KM, Williams RL, et al. Postponing sexual intercourse among urban junior high school students – a randomized controlled evaluation. J Adolesc Health 2000;27:236-47. http://dx.doi.org/10.1016/S1054-139X(00)00102-6.
- Ahmed NU, Haber G, Semenya KA, Hargreaves MK. Randomized controlled trial of mammography intervention in insured very low-income women. Cancer Epidemiol Biomark Prev 2010;19:1790-8. http://dx.doi.org/10.1158/1055-9965.EPI-10-0141.
- Allen JP, Phillber S, Herrling S, Kupermine GP. Preventing teen pregnancy and academic failure; experimental evaluation of a developmentally based approach. Child Dev 1997;64:729-42. http://dx.doi.org/10.1111/j.1467-8624.1997.tb04233.x.
- Allen P, Thompson JL, Herman CJ, Whyte AN, Wolfe VK, Qualls C, et al. Impact of periodic follow-up testing among urban American Indian women with impaired fasting glucose. Prev Chronic Dis 2008;5.
- Andersen MR, Hagher M, Meischke H, Shaw C, Yasui Y, Urban N. Recruitment, retention, and activity of volunteers promoting mammography use in rural communities. Health Promot Pract 2000;1:341-50.
- Andersen MR, Yasui Y, Meischke H, Kuniyuki A, Etzioni R, Urban N. The effectiveness of mammography promotion by volunteers in rural communities. Am J Prev Med 2000;18:199-207. http://dx.doi.org/10.1016/S0749-3797(99)00161-0.
- Andrews JO, Felton G, Ellen Wewers M, Waller J, Tingen M. The effect of a multi-component smoking cessation intervention in African American women residing in public housing. Res Nurs Health 2007;30:45-60. http://dx.doi.org/10.1002/nur.20174.
- Baker EA, Bouldin N, Durham M, Lowell ME, Gonzalez M, Jodaitis N, et al. The Latino Health Advocacy Program: a collaborative lay health advisor approach. Health Educ Behav 1997;24:495-509. http://dx.doi.org/10.1177/109019819702400408.
- Baker K, Pollack M, Kohn I. Violence prevention through informal socialization: an evaluation of the South Baltimore Youth Center. Stud Crime Crime Prev 1995;4:61-85.
- Baruth M, Wilcox S, Blair S, Hooker S, Hussey J, Saunders R. Psychosocial mediators of a faith-based physical activity intervention: implications and lessons learned from null findings. Health Educ Res 2010;25:645-55. http://dx.doi.org/10.1093/her/cyq007.
- Basen-Engquist K, Coyle KK, Parcel GS, Kirby D, Banspach SW, Carvajal SC, et al. Schoolwide effects of a multicomponent HIV, STD, and pregnancy prevention program for high school students. Health Educ Behav 2001;28:166-85. http://dx.doi.org/10.1177/109019810102800204.
- Batts ML, Gary TL, Huss K, Hill MN, Bone L, Brancati FL. Patient priorities and needs for diabetes care among urban African American adults. Diabetes Educ 2001;27:405-12. http://dx.doi.org/10.1177/014572170102700310.
- Best DL, Davis SW, Vaz RM, Kaiser M. Testicular cancer education: a comparison of teaching methods. Am J Health Behav 1996;20:229-41.
- Bird JA, McPhee SJ, Ha NT, Le B, Davis T, Jenkins CN. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Prev Med 1998;27:821-9. http://dx.doi.org/10.1006/pmed.1998.0365.
- Black MM, Dubowitz H, Hutcheson J, Berenson-Howard J, Starr RH. A randomized clinical trial of home intervention for children with failure to thrive. Pediatrics 1995;95:807-14.
- Blamey A, Ayana M, Lawson L, Mackinnon J, Paterson I, Judge K. Final report: the independent evaluation of Have a Heart Paisley. Glasgow: University of Glasgow; 2004.
- Bolam B, McLean C, Pennington A, Gillies P. Using new media to build social capital for health: a qualitative process evaluation study of participation in the CityNet project. J Health Psychol 2006;11:297-308. http://dx.doi.org/10.1177/1359105306061188.
- Booth RE, Zhang Y, Kwiatkowski CF. The challenge of changing drug and sex risk behaviors of runaway and homeless adolescents. Child Abuse Neglect 1999;23:1295-306. http://dx.doi.org/10.1016/S0145-2134(99)00090-3.
- Borgia P, Marinacci C, Schifano P, Perucci CA. Is peer education the best approach for HIV prevention in schools? Findings from a randomized controlled trial. J Adolesc Health 2005;36:508-16. http://dx.doi.org/10.1016/j.jadohealth.2004.03.005.
- Botvin GJ, Schinke SP, Epstein JA, Diaz T. Effectiveness of culturally focused and generic skills training approaches to alcohol and drug abuse prevention among minority youths. Psychol Addict Behav 1994;8:116-27. http://dx.doi.org/10.1037//0893-164X.8.2.116.
- Broadhead RS, Heckathorn DD, Grund JC, Stern LS, Anthony DL. Drug users versus outreach workers in combating AIDS: preliminary results of a peer-driven intervention. J Drug Issues 1995;25.
- Brown SA, Blozis SA, Kouzekanani K, Garcia AA, Winchell M, Hanis CL. Dosage effects of diabetes self-management education for Mexican Americans: the Starr County Border Health Initiative. Diabetes Care 2005;28:527-32. http://dx.doi.org/10.2337/diacare.28.3.527.
- Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the Starr County border health initiative. Diabetes Care 2002;25:259-68. http://dx.doi.org/10.2337/diacare.25.2.259.
- Bullock LF, Wells JE, Duff GB, Hornblow AR. Telephone support for pregnant women: outcome in late pregnancy. N Z Med J 1995;108:476-8.
- Campbell R, Starkey F, Holliday J, Audrey S, Bloor M, Parry-Langdon N, et al. An informal school-based peer-led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial. Lancet 2008;371:1595-602. http://dx.doi.org/10.1016/S0140-6736(08)60692-3.
- Carballo-Dieguez A, Dolezal C, Leu CS, Nieves L, Diaz F, Decena C, et al. A randomized controlled trial to test an HIV-prevention intervention for Latino gay and bisexual men: lessons learned. AIDS Care 2005;17:314-28. http://dx.doi.org/10.1080/09540120512331314303.
- Carroll DL, Rankin SH. Comparing interventions in older unpartnered adults after myocardial infarction. Eur J Cardiovasc Nurs 2006;5:83-9. http://dx.doi.org/10.1016/j.ejcnurse.2005.09.001.
- Chaisson RE, Barnes GL, Hackman J, Watkinson L, Kimbrough L, Metha S, et al. A randomized, controlled trial of interventions to improve adherence to isoniazid therapy to prevent tuberculosis in injection drug users. Am J Med 2001;110:610-15. http://dx.doi.org/10.1016/S0002-9343(01)00695-7.
- Chapman D, Damio G, Young S, Perez-Escamilla R. Association of degree and timing of exposure to breastfeeding peer counseling services with breastfeeding duration. Adv Exp Med Biol 2004;554:303-6. http://dx.doi.org/10.1007/978-1-4757-4242-8_27.
- Cheadle A, Pearson D, Wagner E, Psaty BM, Diehr P, Koepsell T. A community-based approach to preventing alcohol use among adolescents on an American Indian reservation. Public Health Rep 1995;110:439-47.
- Cheadle A, Wagner E, Walls M, Diehr P, Bell M, Anderman C, et al. The effect of neighborhood-based community organizing: results from the Seattle Minority Youth Health Project. Health Serv Res 2001;36:671-89.
- Chernoff RG, Ireys HT, DeVet KA, Kim YJ. A randomized, controlled trial of a community-based support program for families of children with chronic illness: pediatric outcomes. Arch Pediatr Adolesc Med 2002;156:533-9. http://dx.doi.org/10.1001/archpedi.156.6.533.
- Clarke M, Clarke SJ, Jagger C. Social intervention and the elderly: a randomized controlled trial. Am J Epidemiol 1992;136:1517-23.
- Clover K, Redman S, Forbes J, Sanson-Fisher R, Callaghan T. Two sequential randomized trials of community participation to recruit women for mammographic screening. Prev Med 1996;25:126-34. http://dx.doi.org/10.1006/pmed.1996.0038.
- Corkery E, Palmer C, Foley ME, Schechter CB, Frisher L, Roman SH. Effect of a bicultural community health worker on completion of diabetes education in a Hispanic population. Diabetes Care 1997;20:254-7. http://dx.doi.org/10.2337/diacare.20.3.254.
- Cottler LB, Compton WM, Ben Abdallah A, Cunningham-Williams R, Abram F, Fichtenbaum C, et al. Peer-delivered interventions reduce HIV risk behaviors among out-of-treatment drug abusers. Public Health Rep 1998;113:31-4.
- Coyle K, Basen-Engquist K, Kirby D, Parcel G, Banspach S, Collins J, et al. Safer choices: reducing teen pregnancy, HIV, and STDs. Public Health Rep 2001;116:82-93. http://dx.doi.org/10.1093/phr/116.S1.82.
- Crump SR, Shipp MP, McCray GG, Morris SJ, Okoli JA, Caplan LS, et al. Abnormal mammogram follow-up: do community lay health advocates make a difference?. Health Promot Pract 2008;9:140-8. http://dx.doi.org/10.1177/1524839907312806.
- Curnow MM, Pine CM, Burnside G, Nicholson JA, Chesters RK, Huntington E. A randomised controlled trial of the efficacy of supervised toothbrushing in high-caries-risk children. Caries Res 2002;36:294-300. http://dx.doi.org/10.1159/000063925.
- Davis DT, Bustamante A, Brown CP, Wolde-Tsadik G, Savage EW, Cheng X, et al. The urban church and cancer control: a source of social influence in minority communities. Public Health Rep 1994;109:500-6.
- Davis P, Abou-Saleh MT. Developing an enhanced counseling intervention for the primary prevention of hepatitis C among injecting drug users. Addict Disord Treat 2008;7:65-7. http://dx.doi.org/10.1097/ADT.0b013e3180472098.
- Davis SM, Clay T, Smyth M, Gittelsohn J, Arviso V, Flint WH, et al. Pathways curriculum and family interventions to promote healthful eating and physical activity in American Indian schoolchildren. Prev Med 2003;37:S24-34. http://dx.doi.org/10.1016/j.ypmed.2003.08.011.
- Davis SM, Going SB, Helitzer DL, Teufel NI, Snyder P, Gittelsohn J, et al. Pathways: a culturally appropriate obesity-prevention program for American Indian schoolchildren. Am J Clin Nutr 1999;69:796-802.
- Davis TC, Berkel HJ, Arnold CL, Nandy I, Jackson RH, Murphy PW. Intervention to increase mammography utilization in a public hospital. J Gen Intern Med 1998;13:230-3. http://dx.doi.org/10.1046/j.1525-1497.1998.00072.x.
- Dennison CR, Post WS, Kim MT, Bone LR, Cohen D, Blumenthal RS, et al. Underserved urban African American men: hypertension trial outcomes and mortality during 5 years. Am J Hypertens 2007;20:164-71. http://dx.doi.org/10.1016/j.amjhyper.2006.08.003.
- Dickson-Gomez J, Knowlton A, Latkin C. Hoppers and oldheads: qualitative evaluation of a volunteer AIDS outreach intervention. AIDS Behav 2003;7:303-15.
- Dickson-Gomez J, Weeks M, Martinez M, Convey M. Times and places: process evaluation of a peer-led HIV prevention intervention. Subst Use Misuse 2006;41:669-90. http://dx.doi.org/10.1080/10826080500411403.
- DiClemente RJ, Wingood GM. A randomized controlled trial of an HIV sexual risk-reduction intervention for young African-American women. JAMA 1995;274:1271-6. http://dx.doi.org/10.1001/jama.1995.03530160023028.
- Dignan M, Michielutte R, Blinson K, Wells HB, Case LD, Sharp P, et al. Effectiveness of health education to increase screening for cervical cancer among eastern-band Cherokee Indian women in North Carolina. J Natl Canc Inst 1996;88:1670-6. http://dx.doi.org/10.1093/jnci/88.22.1670.
- Dignan MB, Michielutte R, Wells HB, Sharp P, Blinson K, Case LD, et al. Health education to increase screening for cervical cancer among Lumbee Indian women in North Carolina. Health Educ Res 1998;13:545-56. http://dx.doi.org/10.1093/her/13.4.545.
- Duggan AK, McFarlane EC, Windham AM, Rohde CA, Salkever DS, Fuddy L, et al. Intensive home visitation: a randomized trial, follow up and risk assessment study of Hawaii’s Healthy Start Program. Chicago, IL: National Center on Child Abuse and Neglect; 1996.
- Duggan AK, McFarlane EC, Windham AM, Rohde CA, Salkever DS, Fuddy L, et al. Evaluation of Hawaii’s Healthy Start Program. Future Child 1999;9:66-90. http://dx.doi.org/10.2307/1602722.
- Earp JA, Eng E, O’Malley MS, Altpeter M, Rauscher G, Mayne L, et al. Increasing use of mammography among older, rural African American women: results from a community trial. Am J Public Health 2002;92:646-54. http://dx.doi.org/10.2105/AJPH.92.4.646.
- Earp JA, Flax VL. What lay health advisors do: an evaluation of advisors’ activities. Cancer Pract 1999;7:16-21.
- Earp JA, Viadro CI, Vincus AA, Altpeter M, Flax V, Mayne L, et al. Lay health advisors: a strategy for getting the word out about breast cancer. Health Educ Behav 1997;24:432-51. http://dx.doi.org/10.1177/109019819702400404.
- Earp JL, Altpeter M, Mayne L, Viadro CI, O’Malley MS. The North Carolina Breast Cancer Screening Program: foundations and design of a model for reaching older, minority, rural women. Breast Cancer Res Treat 1995;35:7-22. http://dx.doi.org/10.1007/BF00694740.
- Eisenman DP, Glik D, Gonzalez L, Maranon R, Zhou Q, Tseng CH, et al. Improving Latino disaster preparedness using social networks. Am J Prev Med 2009;37:512-17. http://dx.doi.org/10.1016/j.amepre.2009.07.022.
- Elder JP, Ayala GX, Campbell NR, Arredondo EM, Slymen DJ, Baquero B, et al. Long-term effects of a communication intervention for Spanish-dominant Latinas. Am J Prev Med 2006;31:159-66. http://dx.doi.org/10.1016/j.amepre.2006.04.001.
- Elford J, Bolding G, Sherr L. Peer education has no significant impact on HIV risk behaviours among gay men in London. AIDS 2001;15:535-8. http://dx.doi.org/10.1097/00002030-200103090-00018.
- Ell K, Vourlekis B, Muderspach I, Nissly J, Padgett D, Pineda D, et al. Abnormal cervical screening follow-up among low-income Latinas: Project SAFe. J Womens Health Gend Based Med 2002;11:639-51. http://dx.doi.org/10.1089/152460902760360586.
- Erwin DO, Spatz TS, Stotts RC, Hollenberg JA. Increasing mammography practice by African American women. Cancer Pract 1999;7:78-85. http://dx.doi.org/10.1046/j.1523-5394.1999.07204.x.
- Farrell MA, Hayashi T, Loo RK, Rocha DA, Sanders C, Hernandez M, et al. Clinic-based nutrition and lifestyle counseling for Hispanic women delivered by community health workers: design of the California WISEWOMAN study. J Womens Health 2009;18:733-9. http://dx.doi.org/10.1089/jwh.2008.0871.
- Ferguson SL. Peer counseling in a culturally specific adolescent pregnancy prevention program. J Health Care Poor Underserved 1998;9:322-40. http://dx.doi.org/10.1353/hpu.2010.0291.
- Fernandez-Esquer ME, Espinoza P, Torres I, Ramirez AG, McAlister AL. A su salud: a quasi-experimental study among Mexican American women. Am J Health Behav 2003;27:536-45. http://dx.doi.org/10.5993/AJHB.27.5.5.
- Fisher E, Musick J, Scott C, Miller JP, Gram R, Richardson V, et al. Improving clinic- and neighborhood-based smoking cessation services within federally qualified health centers serving low-income, minority neighborhoods. Nicotine Tob Res 2005;7:S45-56. http://dx.doi.org/10.1080/14622200500078105.
- Flaskerud JH, Nyamathi AM, Uman GC. Longitudinal effects of an HIV testing and counseling programme for low-income Latina women. Ethn Health 1997;2:89-103. http://dx.doi.org/10.1080/13557858.1997.9961818.
- Flax VL, Earp JL. Counseled women’s perspectives on their interactions with lay health advisors: a feasibility study. Health Educ Res 1999;14:15-24. http://dx.doi.org/10.1093/her/14.1.15.
- Fletcher SW, Harris RP, Gonzalez JJ, Degnan D, Lannin DR, Strecher VJ, et al. Increasing mammography utilization: a controlled study. J Natl Canc Inst 1993;85:112-20. http://dx.doi.org/10.1093/jnci/85.2.112.
- Flowers P, Frankis J, Hart G, Watson J, Platt S. Researching health promotion. New York: Routledge; 2000.
- Flowers P, Hart GJ, Williamson LM, Frankis JS, Der GJ. Does bar-based, peer-led sexual health promotion have a community-level effect amongst gay men in Scotland?. Int J STD AIDS 2002;13:102-8. http://dx.doi.org/10.1258/0956462021924721.
- Fogarty LA, Heilig CM, Armstrong K, Cabral R, Galavotti C, Gielen AC, et al. Long-term effectiveness of a peer-based intervention to promote condom and contraceptive use among HIV-positive and at-risk women. Public Health Rep 2001;116:103-19. http://dx.doi.org/10.1093/phr/116.S1.103.
- Fors SW, Jarvis S. Evaluation of a peer-led drug abuse risk reduction project for runaway/homeless youths. J Drug Educ 1995;25:321-33. http://dx.doi.org/10.2190/TU92-LX8W-G7FD-9LEM.
- Fuller CM, Galea S, Caceres W, Blaney S, Sisco S, Vlahov D. Multilevel community-based intervention to increase access to sterile syringes among injection drug users through pharmacy sales in New York City. Am J Public Health 2007;97:117-24. http://dx.doi.org/10.2105/AJPH.2005.069591.
- Gabriel RM, Hopson T, Haskins M, Powell KE. Building relationships and resilience in the prevention of youth violence. Am J Prev Med 1996;12:48-55.
- Galbraith J, Ricardo I, Stanton B, Black M, Feigelman S, Kaljee L. Challenges and rewards of involving community in research: an overview of the ‘Focus on Kids’ HIV Risk Reduction Program. Health Educ Q 1996;23:383-94. http://dx.doi.org/10.1177/109019819602300308.
- Gary TL, Bone LR, Hill MN, Levine DM, McGuire M, Saudek C, et al. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med 2003;37:23-32. http://dx.doi.org/10.1016/S0091-7435(03)00040-9.
- Gibson PG, Shah S, Mamoon HA. Peer-led asthma education for adolescents: impact evaluation. J Adolesc Health 1998;22:66-72. http://dx.doi.org/10.1016/S1054-139X(97)00203-6.
- Gielen AC, Windsor R, Faden RR, O’Campo P, Repke J, Davis M. Evaluation of a smoking cessation intervention for pregnant women in an urban prenatal clinic. Health Educ Res 1997;12:247-54. http://dx.doi.org/10.1093/her/12.2.247.
- Gittelsohn J, Evans M, Helitzer D, Anliker J, Story M, Metcalfe L, et al. Formative research in a school-based obesity prevention program for Native American school children (Pathways). Health Educ Res 1998;13:251-65. http://dx.doi.org/10.1093/her/13.2.251.
- Gokcay G, Bulut A, Neyzi O. Paraprofessional women as health care facilitators in mother and child health. Trop Doct 1993;23:79-81.
- Gosin M, Marsiglia FF, Hecht ML. Keepin’ it REAL: a drug resistance curriculum tailored to the strengths and needs of pre-adolescents of the southwest. J Drug Educ 2003;33:119-42.
- Gotay CC, Banner RO, Matsunaga DS, Hedlund N, Enos R, Issell BF, et al. Impact of a culturally appropriate intervention on breast and cervical screening among native Hawaiian women. Prev Med 2000;31:529-37. http://dx.doi.org/10.1006/pmed.2000.0732.
- Griffiths C, Motlib J, Azad A, Ramsay J, Eldridge S, Feder G, et al. Randomised controlled trial of a lay-led self-management programme for Bangladeshi patients with chronic disease. Br J Gen Pract 2005;55:831-7.
- CDC AIDS Community Demonstration Projects Research Group . Community-level HIV intervention in 5 cities: final outcome data from the CDC AIDS Community Demonstration Projects. Am J Public Health 1999;89:336-45.
- Hamer M, Box V. An evaluation of the development and functioning of the Boscombe Network for Change, a health alliance or partnership for health in Dorset. Health Educ J 2000;59:238-52. http://dx.doi.org/10.1177/001789690005900305.
- Hancock L, Sanson-Fisher R, Perkins J, Girgis A, Howley P, Schofield M. The effect of a community action intervention on adolescent smoking rates in rural Australian towns: the CART project. Cancer Action in Rural Towns. Prev Med 2001;32:332-40.
- Hanson J. Parental self-efficacy and asthma self-management skills. J Pediatr Nurs 1998;3:146-54. http://dx.doi.org/10.1111/j.1744-6155.1998.tb00222.x.
- Helmert U, Shea S, Greiser E, Maschewsky Schneider U. Effects of 3.5 years of community intervention on social class gradients for cardiovascular disease risk factors in the German Cardiovascular Prevention Study. Ann Epidemiol 1993;3.
- Hiatt RA, Pasick RJ, Stewart S, Bloom J, Davis P, Gardiner P, et al. Cancer screening for underserved women: the breast and cervical cancer intervention study. Cancer Epidemiol Biomarkers Prev 2008;17:1945-9. http://dx.doi.org/10.1158/1055-9965.EPI-08-0172.
- Hill MN, Bone LR, Hilton SC, Roary MC, Kelen GD, Levine DM. A clinical trial to improve high blood pressure care in young urban black men: recruitment, follow-up, and outcomes. Am J Hypertens 1999;12:548-54. http://dx.doi.org/10.1016/S0895-7061(99)00007-2.
- Hill MN, Han HR, Dennison CR, Kim MT, Roary MC, Blumenthal RS, et al. Hypertension care and control in underserved urban African American men: behavioral and physiologic outcomes at 36 months. Am J Hypertens 2003;16:906-13. http://dx.doi.org/10.1016/S0895-7061(03)01034-3.
- Howard M, McCabe JB. Helping teenagers postpone sexual involvement. Fam Plann Perspect 1990;22:21-6. http://dx.doi.org/10.2307/2135434.
- Husaini BA, Reece MC, Emerson JS, Scales S, Hull PC, Levine RS. A church-based program on prostate cancer screening for African American men: reducing health disparities. Ethn Dis 2008;18:S2-179.
- Hutcheson JJ, Black MM, Talley M, Dubowitz H, Howard JB, Starr RH, et al. Risk status and home intervention among children with failure-to-thrive: follow-up at age 4. J Pediatr Psychol 1997;22:651-68.
- Ireys HT, Chernoff R, DeVet KA, Kim Y. Maternal outcomes of a randomized controlled trial of a community-based support program for families of children with chronic illnesses. Arch Pediatr Adolesc Med 2001;155:771-7. http://dx.doi.org/10.1001/archpedi.155.7.771.
- Ireys HT, Sills EM, Kolodner KB, Walsh BB. A social support intervention for parents of children with juvenile rheumatoid arthritis: results of a randomized trial. J Pediatr Psychol 1996;21:633-41. http://dx.doi.org/10.1093/jpepsy/21.5.633.
- Jandorf L, Bursac Z, Pulley L, Trevino M, Castillo A, Erwin DO. Breast and cervical cancer screening among Latinas attending culturally specific educational programs. Prog Community Health Partnersh 2008;2:195-204.
- Jemmott JB, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: a randomized controlled trial. JAMA 1998;279:1529-36. http://dx.doi.org/10.1001/jama.279.19.1529.
- Johnson Z, Molloy B, Scallan E, Fitzpatrick P, Rooney B, Keegan T, et al. Community Mothers Programme –seven year follow-up of a randomized controlled trial of non-professional intervention in parenting. J Public Health Med 2000;22:337-42. http://dx.doi.org/10.1093/pubmed/22.3.337.
- Jones ME, Mondy LW. Lessons for prevention and intervention in adolescent pregnancy: a five-year comparison of outcomes of two programs for school-aged pregnant adolescents. J Pediatr Health Care 1994;8:152-9. http://dx.doi.org/10.1016/0891-5245(94)90027-2.
- Kartin D, Grant TM, Streissguth AP, Sampson PD, Ernst CC. Three-year developmental outcomes in children with prenatal alcohol and drug exposure. Pediatr Phys Ther 2002;14:145-53. http://dx.doi.org/10.1097/00001577-200214030-00004.
- Katz ML, Kauffman RM, Tatum CM, Paskett ED. Influence of church attendance and spirituality in a randomized controlled trial to increase mammography use among a low-income, tri-racial, rural community. J Relig Health 2008;47:227-36. http://dx.doi.org/10.1007/s10943-008-9159-0.
- Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: a community-level HIV prevention intervention for young gay men. Am J Public Health 1996;86:1129-36. http://dx.doi.org/10.2105/AJPH.86.8_Pt_1.1129.
- Kelly JA, McAuliffe TL, Sikkema KJ, Murphy DA, Somlai AM, Mulry G, et al. Reduction in risk behavior among adults with severe mental illness who learned to advocate for HIV prevention. Psychiatr Serv 1997;48:1283-8.
- Kelly JA, St Lawrence JS, Stevenson LY, Hauth AC, Kalichman SC, Diaz YE, et al. Community AIDS/HIV risk reduction: the effects of endorsements by popular people in three cities. Am J Public Health 1992;82:1483-9. http://dx.doi.org/10.2105/AJPH.82.11.1483.
- Kennedy MG, Mizuno Y, Hoffman R, Baume C, Strand J. The effect of tailoring a model HIV prevention program for local adolescent target audiences. AIDS Educ Prev 2000;12:225-38.
- Kernohan EE. Evaluation of a pilot study for breast and cervical cancer screening with Bradford’s minority ethnic women; a community development approach, 1991–93. Br J Cancer Suppl 1996;29:S42-6.
- Keyserling TC, Samuel-Hodge CD, Ammerman AS, Ainsworth BE, Henriquez-Roldan CF, Elasy TA, et al. A randomized trial of an intervention to improve self-care behaviors of African-American women with type 2 diabetes: impact on physical activity. Diabetes Care 2002;25:1576-83. http://dx.doi.org/10.2337/diacare.25.9.1576.
- Kiger H. Outreach to multiethnic, multicultural, and multilingual women for breast cancer and cervical cancer education and screening: a model using professional and volunteer staffing. Fam Community Health 2003;26:307-18. http://dx.doi.org/10.1097/00003727-200310000-00007.
- Kim S, Flaskerud JH, Koniak-Griffin D, Dixon EL. Using community-partnered participatory research to address health disparities in a Latino community. J Prof Nurs 2005;21:199-20. http://dx.doi.org/10.1016/j.profnurs.2005.05.005.
- Kim YH, Sarna L. An intervention to increase mammography use by Korean American women. Oncol Nurs Forum 2004;31:105-10. http://dx.doi.org/10.1188/04.ONF.105-110.
- King E, Rimer BK, Benincasa T, Harrop C, Amfoh K, Bonney G, et al. Strategies to encourage mammography use among women in senior citizens’ housing facilities. J Cancer Educ 1998;13:108-15.
- Kirby D, Korpi M, Adivi C, Weissman J. An impact evaluation of project SNAPP: an AIDS and pregnancy prevention middle school program. AIDS Educ Prev 1997;9:44-61.
- Kirby D, Korpi M, Barth R, Cagampang HH. Evaluation of Education Now and Babies Later (ENABL): final report. Berkeley, CA: University of California, School of Social Welfare, Family Welfare Research Group; 1995.
- Kirby D, Korpi M, Barth RP, Cagampang HH. The impact of the Postponing Sexual Involvement curriculum among youths in California. Fam Plann Perspect 1997;29:100-8. http://dx.doi.org/10.2307/2953331.
- Kirby DB, Baumler E, Coyle KK, Basen-Engquist K, Parcel GS, Harrist R, et al. The ‘Safer Choices’ intervention: its impact on the sexual behaviors of different subgroups of high school students. J Adolesc Health 2004;35:442-52.
- Kocken PL, Zwanenburg EJ, de Hoop T. Effects of health education for migrant females with psychosomatic complaints treated by general practitioners. A randomised controlled evaluation study. Patient Educ Counsel 2008;70:25-30.
- Krieger JK, Takaro TK, Allen C, Song L, Weaver M, Chai S, et al. The Seattle-King County healthy homes project: implementation of a comprehensive approach to improving indoor environmental quality for low-income children with asthma. Environ Health Perspect 2002;110:311-22. http://dx.doi.org/10.1289/ehp.02110s2311.
- Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health 2005;95:652-9. http://dx.doi.org/10.2105/AJPH.2004.042994.
- Laraque D, Barlow B, Durkin M, Heagarty M. Injury prevention in an urban setting: challenges and successes. Bull N Y Acad Med 1995;72:16-30.
- Larkey LK, Staten LK, Ritenbaugh C, Hall RA, Buller DB, Bassford T, et al. Recruitment of Hispanic women to the Women’s Health Initiative. The case of Embajadoras in Arizona. Control Clin Trials 2002;23:289-98.
- Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol 2003;22:332-9. http://dx.doi.org/10.1037/0278-6133.22.4.332.
- Lauby JL, Smith PJ, Stark M, Person B, Adams J. A community-level HIV prevention intervention for inner-city women: results of the women and infants demonstration projects. Am J Public Health 2000;90:216-22.
- Levine DM, Becker DM, Bone LR, Stillman FA, Tuggle MB II, Prentice M, et al. A partnership with minority populations: a community model of effectiveness research. Ethn Dis 1992;2:296-305.
- Levine DM, Bone L. The impact of a planned health education approach on the control of hypertension in a high risk population. J Hum Hypertens 1990;4:317-21.
- Levine DM, Bone LR, Hill MN, Stallings R, Gelber AC, Barker A, et al. The effectiveness of a community/academic health center partnership in decreasing the level of blood pressure in an urban African-American population. Ethn Dis 2003;13:354-61.
- Levy JA, Fox SE. The outreach-assisted model of partner notification with IDUs. Public Health Rep 1998;113:160-9.
- Lindqvist K, Timpka T, Schelp L. Evaluation of an inter-organizational prevention program against injuries among the elderly in a WHO Safe Community. Public Health 2001;115:308-16. http://dx.doi.org/10.1038/sj.ph.1900786.
- Lorig KR, Ritter PL, Gonzalez VM. Hispanic chronic disease self-management: a randomized community-based outcome trial. Nurs Res 2003;52:361-9. http://dx.doi.org/10.1097/00006199-200311000-00003.
- Lupton BS, Fonnebo V, Sogaard AJ. The Finnmark Intervention Study: is it possible to change CVD risk factors by community-based intervention in an Arctic village in crisis?. Scand J Public Health 2003;31:178-86. http://dx.doi.org/10.1080/14034940210134077.
- Lupton BS, Fonnebo V, Sogaard AJ, Fylkesnes K. The Finnmark Intervention Study: do community-based intervention programmes threaten self-rated health and well-being? Experiences from Batsfjord, a fishing village in North Norway. Eur J Public Health 2005;15:91-6. http://dx.doi.org/10.1093/eurpub/cki101.
- Marcenko MO, Spence M. Home visitation services for at-risk pregnant and postpartum women: a randomized trial. Am J Orthopsychiatry 1994;64:468-78. http://dx.doi.org/10.1037/h0079547.
- Margolis KL, Lurie N, McGovern PG, Tyrrell M, Slater JS. Increasing breast and cervical cancer screening in low-income women. J Gen Intern Med 1998;13:515-21. http://dx.doi.org/10.1046/j.1525-1497.1998.00161.x.
- May KM, Mendelson C, Ferketich S. Community empowerment in rural health care. Public Health Nurs 1995;12:25-30. http://dx.doi.org/10.1111/j.1525-1446.1995.tb00119.x.
- McAlister AL, Fernandez-Esquer ME, Ramirez AG, Trevino F, Gallion KJ, Villarreal R, et al. Community level cancer control in a Texas barrio: Part II – base-line and preliminary outcome findings. J Natl Canc Inst Monogr 1995:123-6.
- McCue M, Afifi LA. Using peer helpers for tuberculosis prevention. J Am Coll Health 1996;44:173-6. http://dx.doi.org/10.1080/07448481.1996.9937525.
- McFarlane J, Soeken K, Wiist W. An evaluation of interventions to decrease intimate partner violence to pregnant women. Public Health Nurs 2000;17:443-51. http://dx.doi.org/10.1046/j.1525-1446.2000.00443.x.
- McInroy N, MacDonald S. From community garden to Westminster: active citizenship and the role of public space. Manchester: Centre for Local Economic Strategies; 2005.
- McIntosh E, Barlow J, Davis H, Stewart-Brown S. Economic evaluation of an intensive home visiting programme for vulnerable families: a cost-effectiveness analysis of a public health intervention. J Public Health 2009;31:423-33. http://dx.doi.org/10.1093/pubmed/fdp047.
- McNeill LH, Coeling M, Puleo E, Suarez EG, Bennett GG, Emmons KM. Colorectal cancer prevention for low-income, sociodemographically-diverse adults in public housing: baseline findings of a randomized controlled trial. BMC Public Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-353.
- McPhee SJ, Bird JA, Ha NT, Jenkins CN. Pathways to early cancer detection for Vietnamese women: Suc Khoe La Vang (health is gold!). Health Educ Q 1996;23:s60-75.
- McQuiston C, Choi-Hevel S, Clawson M. Protegiendo Nuestra Comunidad: empowerment participatory education for HIV prevention. J Transcult Nurs 2001;12:275-83. http://dx.doi.org/10.1177/104365960101200402.
- Miller RL, Klotz D, Eckholdt HM. HIV prevention with male prostitutes and patrons of hustler bars: replication of an HIV preventive intervention. Am J Community Psychol 1998;26:97-131.
- Morisky DE, Malotte CK, Ebin V, Davidson P, Cabrera D, Trout PT, et al. Behavioral interventions for the control of tuberculosis among adolescents. Public Health Rep 2001;116:568-74. http://dx.doi.org/10.1093/phr/116.6.568.
- Motohashi Y, Kaneko Y, Sasaki H, Yamaji M. A decrease in suicide rates in Japanese rural towns after community-based intervention by the health promotion approach. Suicide Life Threat Behav 2007;37:593-9. http://dx.doi.org/10.1521/suli.2007.37.5.593.
- Nair P, Schuler ME, Black MM, Kettinger L, Harrington D. Cumulative environmental risk in substance abusing women: early intervention, parenting stress, child abuse potential and child development. Child Abuse Neglect 2003;27:997-1017. http://dx.doi.org/10.1016/S0145-2134(03)00169-8.
- Navarro AM, Senn KL, McNicholas LJ, Kaplan RM, Roppe B, Campo MC. Por La Vida model intervention enhances use of cancer screening tests among Latinas. Am J Prev Med 1998;15:32-41. http://dx.doi.org/10.1016/S0749-3797(98)00023-3.
- Neuhauser L, Schwab M, Leonard S, Bieber M. Community participation in health promotion: evaluation of the California Wellness Guide. Health Promot Int 1998;13:211-22. http://dx.doi.org/10.1093/heapro/13.3.211.
- Neumark-Sztainer D, Story M, Hannan PJ, Rex J. New Moves: a school-based obesity prevention program for adolescent girls. Prev Med 2003;37:41-5. http://dx.doi.org/10.1016/S0091-7435(03)00057-4.
- Nguyen TT, Le G, Nguyen T, Le K, Lai K, Gildengorin G, et al. Breast cancer screening among Vietnamese Americans: a randomized controlled trial of lay health worker outreach. Am J Prev Med 2009;37:306-13.
- Nyamathi A, Flaskerud JH, Leake B, Dixon EL, Lu A. Evaluating the impact of peer, nurse case-managed, and standard HIV risk-reduction programs on psychosocial and health-promoting behavioral outcomes among homeless women. Res Nurs Health 2001;24:410-22. http://dx.doi.org/10.1002/nur.1041.
- O’Donnell L, Stueve A, O’Donnell C, Duran R, San D, Wilson RF, et al. Long-term reductions in sexual initiation and sexual activity among urban middle schoolers in the reach for health service learning program. J Adolesc Health 2002;31:93-100. http://dx.doi.org/10.1016/S1054-139X(01)00389-5.
- Evaluation of the residents’ consultancy pilots initiative. London: Office of the Deputy Prime Minister; 2004.
- Neighbourhood Wardens Scheme evaluation. London: Office of the Deputy Prime Minister; 2004.
- National evaluation of local strategic partnerships: formative evaluation and action research programme 2002–2005. London: Office of the Deputy Prime Minister; 2006.
- Neighbourhood management: at the turning point?: programme review 2005–2006. London: Office of the Deputy Prime Minister; 2006.
- O’Hara P, Messick BJ, Fichtner RR, Parris D. A peer-led AIDS prevention program for students in an alternative school. J School Health 1996;66:176-82. http://dx.doi.org/10.1111/j.1746-1561.1996.tb06271.x.
- O’Hare JP, Raymond NT, Mughal S, Dodd L, Hanif W, Ahmad Y, et al. Evaluation of delivery of enhanced diabetes care to patients of South Asian ethnicity: the United Kingdom Asian Diabetes Study (UKADS). Diabetic Med 2004;21:1357-65. http://dx.doi.org/10.1111/j.1464-5491.2004.01373.x.
- Orpinas P, Parcel GS, McAlister A, Frankowski R. Violence prevention in middle schools: a pilot evaluation. J Adolesc Health 1995;17:360-71. http://dx.doi.org/10.1016/1054-139X(95)00194-W.
- Outlaw AY, Naar King S, Parsons JT, Green Jones M, Janisse H, Secord E. Using motivational interviewing in HIV field outreach with young African American men who have sex with men: a randomized clinical trial. Am J Public Health 2010;100:S146-51. http://dx.doi.org/10.2105/AJPH.2009.166991.
- Paradis G, Levesque L, Macaulay AC, Cargo M, McComber A, Kirby R, et al. Impact of a diabetes prevention program on body size, physical activity, and diet among Kanien’keha:ka (Mohawk) children 6 to 11 years old: 8-year results from the Kahnawake Schools Diabetes Prevention Project. Pediatrics 2005;115:333-9. http://dx.doi.org/10.1542/peds.2004-0745.
- Parker EA, Israel BA, Robins TG, Mentz G, Xihong L, Brakefield-Caldwell W, et al. Evaluation of Community Action Against Asthma: a community health worker intervention to improve children’s asthma-related health by reducing household environmental triggers for asthma. Health Educ Behav 2008;35:376-95. http://dx.doi.org/10.1177/1090198106290622.
- Parkin PC, Spence LJ, Hu X, Kranz KE, Shortt LG, Wesson DE. Evaluation of a promotional strategy to increase bicycle helmet use by children. Pediatrics 1993;91:772-7.
- Paskett E, Tatum C, Rushing J, Michielutte R, Bell R, Foley KL, et al. Randomized trial of an intervention to improve mammography utilization among a triracial rural population of women. J Natl Canc Inst 2006;98:1226-37. http://dx.doi.org/10.1093/jnci/djj333.
- Peragallo N, Deforge B, O’Campo P, Lee SM, Kim YJ, Cianelli R, et al. A randomized clinical trial of an HIV-risk-reduction intervention among low-income Latina women. Nurs Res 2005;54:108-18. http://dx.doi.org/10.1097/00006199-200503000-00005.
- Perry CL, Lee S, Stigler MH, Farbakhsh K, Komro KA, Gewirtz AH, et al. The impact of Project Northland on selected MMPI-A problem behavior scales. J Prim Prev 2007;28:449-65. http://dx.doi.org/10.1007/s10935-007-0105-9.
- Perry CL, Williams CL, Komro KA, Veblen-Mortenson S, Forster JL, Bernstein-Lachter R, et al. Project Northland high school interventions: community action to reduce adolescent alcohol use. Health Educ Behav 2000;27:29-4. http://dx.doi.org/10.1177/109019810002700105.
- Philis-Tsimikas A, Walker C, Rivard L, Talavera G, Reimann JO, Salmon M, et al. Improvement in diabetes care of underinsured patients enrolled in Project Dulce: a community-based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care 2004;27:110-15. http://dx.doi.org/10.2337/diacare.27.1.110.
- Philliber S, Allen JP, Miller BC, Card JJ, Paikoff RL, Peterson JL. Preventing adolescent pregnancy: model programs and evaluation. Newbury Park, CA: Sage; 1992.
- Pilote L, Tulsky JP, Zolopa AR, Hahn JA, Schecter GF, Moss AR. Tuberculosis prophylaxis in the homeless. A trial to improve adherence to referral. Arch Intern Med 1996;156:161-5. http://dx.doi.org/10.1001/archinte.156.2.161.
- Pinkerton SD, Holtgrave DR, DiFranceisco WJ, Stevenson LY, Kelly JA. Cost-effectiveness of a community-level HIV risk reduction intervention. Am J Public Health 1998;88:1239-42. http://dx.doi.org/10.2105/AJPH.88.8.1239.
- Powell ME, Carter V, Bonsi E, Johnson G, Williams L, Taylor-Smith L, et al. Increasing mammography screening among African American women in rural areas. J Health Care Poor Underserved 2005;16:11-2. http://dx.doi.org/10.1353/hpu.2005.0071.
- Centers for Disease Control and Prevention . Community-level prevention of human immunodeficiency virus infection among high-risk populations: the AIDS Community Demonstration Projects. MMWR 1996;45:1-24.
- Quinn MT, McNabb WL. Training lay health educators to conduct a church-based weight-loss program for African American women. Diabetes Educ 2001;27:231-8. http://dx.doi.org/10.1177/014572170102700209.
- Quirk ME, Godkin MA, Schwenzfeier E. Evaluation of two AIDS prevention interventions for inner-city adolescent and young adult women. Am J Prev Med 1993;9:21-6.
- Ravesloot CH, Seekins T, Cahill T, Lindgren S, Nary DE, White G. Health promotion for people with disabilities: development and evaluation of the Living Well with a Disability program. Health Educ Res 2007;22:522-31. http://dx.doi.org/10.1093/her/cyl114.
- Richardson G, Kennedy A, Reeves D, Bower P, Lee V, Middleton E, et al. Cost effectiveness of the Expert Patients Programme (EPP) for patients with chronic conditions. J Epidemiol Community Health 2008;62:361-7. http://dx.doi.org/10.1136/jech.2006.057430.
- Rickert VI, Jay MS, Gottlieb A. Effects of a peer-counseled AIDS education program on knowledge, attitudes, and satisfaction of adolescents. J Adolesc Health 1991;12:38-43. http://dx.doi.org/10.1016/0197-0070(91)90039-O.
- Ritchie D. ‘Breathing Space’: reflecting upon the realities of community partnerships and workers’ beliefs about promoting health. Health Educ J 2001;60:73-92. http://dx.doi.org/10.1177/001789690106000108.
- Ritchie D, Parry O, Gnich W, Platt S. Issues of participation, ownership and empowerment in a community development programme: tackling smoking in a low-income area in Scotland. Health Promot Int 2004;19:51-9. http://dx.doi.org/10.1093/heapro/dah107.
- Robinson BB, Uhl G, Miner M, Bockting WO, Scheltema KE, Rosser BR, et al. Evaluation of a sexual health approach to prevent HIV among low income, urban, primarily African American women: results of a randomized controlled trial. AIDS Educ Prev 2002;14:81-96. http://dx.doi.org/10.1521/aeap.14.4.81.23876.
- Roffman RA, Picciano JF, Ryan R, Beadnell B, Fisher D, Downey L, et al. HIV-prevention group counseling delivered by telephone: an efficacy trial with gay and bisexual men. AIDS Behav 1997;1:137-54. http://dx.doi.org/10.1023/B:AIBE.0000002974.64697.32.
- Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: a pilot study. Ann Behav Med 2005;29:225-35. http://dx.doi.org/10.1207/s15324796abm2903_9.
- Rosser BR, Bockting WO, Rugg DL, Robinson BB, Ross MW, Bauer GR, et al. A randomized controlled intervention trial of a sexual health approach to long-term HIV risk reduction for men who have sex with men: effects of the intervention on unsafe sexual behavior. AIDS Educ Prev 2002;14:59-71. http://dx.doi.org/10.1521/aeap.14.4.59.23885.
- Royse D. Mentoring high-risk minority youth: evaluation of the Brothers project. Adolescence 1998;33:145-58.
- Sauaia A, Min SJ, Lack D, Apodaca C, Osuna D, Stowe A, et al. Church-based breast cancer screening education: impact of two approaches on Latinas enrolled in public and private health insurance plans. Prev Chronic Dis 2007;4.
- Saxe L, Reber E, Hallfors D, Kadushin C, Jones D, Rindskopf D, et al. Think globally, act locally: assessing the impact of community-based substance abuse prevention. Eval Prog Plann 1997;20:357-66. http://dx.doi.org/10.1016/S0149-7189(97)00015-3.
- Schuler ME, Nair P, Kettinger L. Drug-exposed infants and developmental outcome: effects of a home intervention and ongoing maternal drug use. Arch Pediatr Adolesc Med 2003;157:133-8. http://dx.doi.org/10.1001/archpedi.157.2.133.
- Schuler ME, Nair P, Black MM, Kettinger L. Mother–infant interaction: effects of a home intervention and ongoing maternal drug use. J Clin Child Psychol 2000;29:424-31. http://dx.doi.org/10.1207/S15374424JCCP2903_13.
- Secker-Walker RH, Dana GS, Solomon LJ, Flynn BS, Geller BM. The role of health professionals in a community-based program to help women quit smoking. Prev Med 2000;30:126-37. http://dx.doi.org/10.1006/pmed.1999.0607.
- Secker-Walker RH, Flynn BS, Solomon LJ, Vacek PM, Dorwaldt AL, Geller BM, et al. Helping women quit smoking: baseline observations for a community health education project. Am J Prev Med 1996;12:367-77.
- Secker-Walker RH, Holland RR, Lloyd CM, Pelkey D, Flynn BS. Cost effectiveness of a community based research project to help women quit smoking. Tob Control 2005;14:37-42. http://dx.doi.org/10.1136/tc.2003.005470.
- Shepherd J, Weare K, Turner G. Peer-led sexual health promotion with young gay and bisexual men: results of the HAPEER Project. Health Educ 1997;97:204-12. http://dx.doi.org/10.1108/09654289710186707.
- Siegel D, DiClemente R, Durbin M, Krasnovsky F, Saliba P. Change in junior high school students’ AIDS-related knowledge, misconceptions, attitudes, and HIV-preventive behaviors: effects of a school-based intervention. AIDS Educ Prev 1995;7:534-43.
- Sieverding J, Boyer CB, Siller J, Gallaread A, Krone M, Chang YJ. Youth United Through Health Education: building capacity through a community collaborative intervention to prevent HIV/STD in adolescents residing in a high STD prevalent neighborhood. AIDS Educ Prev 2005;17:375-85. http://dx.doi.org/10.1521/aeap.2005.17.4.375.
- Sigel DM, Aten MJ, Roghmann KJ, Enaharo M. Early effects of a school-based human immunodeficiency virus infection and sexual risk prevention intervention. Arch Pediatr Adolesc Med 1998;152:961-70. http://dx.doi.org/10.1001/archpedi.152.10.961.
- Sikkema KJ, Anderson ES, Kelly JA, Winett RA, Gore-Felton C, Roffman RA, et al. Outcomes of a randomized, controlled community-level HIV prevention intervention for adolescents in low-income housing developments. AIDS 2005;19:1509-16. http://dx.doi.org/10.1097/01.aids.0000183128.39701.34.
- Sikkema KJ, Kelly JA, Winett RA, Solomon LJ, Cargill VA, Roffman RA, et al. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. Am J Public Health 2000;90:57-63.
- Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomatology in HIV-positive men and women. Health Psychol 2007;26:488-95. http://dx.doi.org/10.1037/0278-6133.26.4.488.
- Skinner CS, Arfken CL, Waterman B. Outcomes of the Learn, Share & Live breast cancer education program for older urban women. Am J Public Health 2000;90:1229-34.
- Slater JS, Ha CN, Malone ME, McGovern P, Madigan SD, Finnegan JR, et al. A randomized community trial to increase mammography utilization among low-income women living in public housing. Prev Med 1998;27:862-70. http://dx.doi.org/10.1006/pmed.1998.0370.
- Sorensen G, Stoddard AM, LaMontagne AD, Emmons K, Hunt MK, Youngstrom R, et al. A comprehensive worksite cancer prevention intervention: behavior change results from a randomized controlled trial (United States). J Public Health Policy 2003;24:5-25. http://dx.doi.org/10.2307/3343174.
- Sox CH, Dietrich AJ, Goldman DC, Provost EM. Improved access to women’s health services for Alaska natives through community health aide training. J Community Health 1999;24:313-23.
- Spoth R, Redmond C, Shin C, Greenberg M, Clair S, Feinberg M. Substance-use outcomes at 18 months past baseline. The PROSPER community–university partnership trial. Am J Prev Med 2007;32:395-402.
- St Lawrence JS, Brasfield TL, Jefferson KW, Alleyne E, O’Bannon RE III, Shirley A. Cognitive-behavioral intervention to reduce African American adolescents’ risk for HIV infection. J Consult Clin Psychol 1995;63:221-37. http://dx.doi.org/10.1037/0022-006X.63.2.221.
- St Pierre Tena L, Mark Melvin M, Kaltreider DL, Campbell B. Boys & girls clubs and school collaborations: a longitudinal study of a multicomponent substance abuse prevention program for high-risk elementary school children. J Community Psychol 2001;29:87-106. http://dx.doi.org/10.1002/1520-6629(200103)29:2<87::AID-JCOP1007>3.0.CO;2-U.
- Stanton B, Harris C, Cottrell L, Li X, Gibson C, Guo J, et al. Trial of an urban adolescent sexual risk-reduction intervention for rural youth: a promising but imperfect fit. J Adolesc Health 2006;38. http://dx.doi.org/10.1016/j.jadohealth.2004.09.023.
- Stanton BF, Li X, Ricardo I, Galbraith J, Feigelman S, Kaljee L. A randomized, controlled effectiveness trial of an AIDS prevention program for low-income African-American youths. Arch Pediatr Adolesc Med 1996;150:363-72. http://dx.doi.org/10.1001/archpedi.1996.02170290029004.
- Stephenson JM, Strange V, Forrest S, Oakley A, Copas A, Allen E, et al. Pupil-led sex education in England (RIPPLE study): cluster-randomised intervention trial. Lancet 2004;364:338-46. http://dx.doi.org/10.1016/S0140-6736(04)16722-6.
- Suarez L, Roche RA, Pulley LV, Weiss NS, Goldman D, Simpson DM. Why a peer intervention program for Mexican-American women failed to modify the secular trend in cancer screening. Am J Prev Med 1997;13:411-17.
- Tan EJ, Xue QL, Li T, Carlson MC, Fried LP. Volunteering: a physical activity intervention for older adults. The Experience Corps program in Baltimore. J Urban Health 2006;83:954-69. http://dx.doi.org/10.1007/s11524-006-9060-7.
- Teti M, Bowleg L, Cole R, Lloyd L, Rubinstein S, Spencer S, et al. A mixed methods evaluation of the effect of the Protect and Respect intervention on the condom use and disclosure practices of women living with HIV/AIDS. AIDS Behav 2010;14:567-79. http://dx.doi.org/10.1007/s10461-009-9562-x.
- Thoits PA, Hohmann AA, Harvey MR, Fletcher B. Similar-other support for men undergoing coronary artery bypass surgery. Health Psychol 2000;19:264-73. http://dx.doi.org/10.1037//0278-6133.19.3.264.
- Thomas JC, Earp JA, Eng E. Evaluation and lessons learned from a lay health advisor programme to prevent sexually transmitted diseases. Int J STD AIDS 2000;11:812-18. http://dx.doi.org/10.1258/0956462001915336.
- Timpka T, Nilsen P, Lindqvist K. The impact of home safety promotion on different social strata in a WHO safe community. Public Health 2006;120:427-33. http://dx.doi.org/10.1016/j.puhe.2005.12.002.
- Tudiver F, Myers T, Kurtz R, Orr K, Rowe C, Jackson E, et al. The talking sex project: results of a randomized controlled trial of small-group AIDS education for 612 gay and bisexual men. Eval Health Prof 1992;83:26-42. http://dx.doi.org/10.1177/016327879201500102.
- Tulsky JP, Pilote L, Hahn JA, Zolopa AJ, Burke M, Chesney M, et al. Adherence to isoniazid prophylaxis in the homeless: a randomized controlled trial. Arch Intern Med 2000;160:697-702. http://dx.doi.org/10.1001/archinte.160.5.697.
- Valente TW, Hoffman BR, Ritt Olson A, Lichtman K, Johnson CA. Effects of a social-network method for group assignment strategies on peer-led tobacco prevention programs in schools. American J Public Health 2003;93:1837-43. http://dx.doi.org/10.2105/AJPH.93.11.1837.
- Wagner EH, Wickizer TM, Cheadle A, Psaty BM, Koepsell TD, Diehr P, et al. The Kaiser Family Foundation Community Health Promotion Grants Program: findings from an outcome evaluation. Health Serv Res 2000;35:561-89.
- Weber BE, Reilly BM. Enhancing mammography use in the inner city. A randomized trial of intensive case management. Arch Intern Med 1997;157:2345-9. http://dx.doi.org/10.1001/archinte.1997.00440410077008.
- Weeks MR, Dickson-Gomez J, Mosack KE, Convey M, Martinez M, Clair S. The risk avoidance partnership: training active drug users as peer health advocates. J Drug Issues 2006;36:541-70. http://dx.doi.org/10.1177/002204260603600303.
- Weinrich SP, Weinrich MC, Stromborg MF, Boyd MD, Weiss HL. Using elderly educators to increase colorectal cancer screening. Gerontologist 1993;33:491-6. http://dx.doi.org/10.1093/geront/33.4.491.
- Welsh AL, Sauaia A, Jacobellis J, Min SJ, Byers T. The effect of two church-based interventions on breast cancer screening rates among Medicaid-insured Latinas. Prev Chronic Dis 2005;2.
- Wiist WH, Jackson RH, Jackson KW. Peer and community leader education to prevent youth violence. Am J Prev Med 1996;12:56-64.
- Wilson Tracey E, Fraser-White M, Feldman J, Homel P, Wright S, King G, et al. Hair salon stylists as breast cancer prevention lay health advisors for African American and Afro-Caribbean women. J Health Care Poor Underserved 2008;19:216-26. http://dx.doi.org/10.1353/hpu.2008.0017.
- Wishart L, Macerollo J, Loney P, King A, Beaumont L, Browne G, et al. ‘Special steps’: an effective visiting/walking program for persons with cognitive impairment. Can J Nurs Res 2000;31:57-71.
- Wohl AR, Garland WH, Valencia R, Squires K, Witt MD, Kovacs A, et al. A randomized trial of directly administered antiretroviral therapy and adherence case management intervention. Clin Infect Dis 2006;42:1619-27. http://dx.doi.org/10.1086/503906.
- Wolitski RJ, Gomez CA, Parsons JT. Effects of a peer-led behavioral intervention to reduce HIV transmission and promote serostatus disclosure among HIV-seropositive gay and bisexual men. AIDS 2005;19:S99-10. http://dx.doi.org/10.1097/01.aids.0000167356.94664.59.
- Zhu K, Hunter S, Bernard LJ, Payne-Wilks K, Roland CL, Elam LC, et al. An intervention study on screening for breast cancer among single African-American women aged 65 and older. Prev Med 2002;34:536-45. http://dx.doi.org/10.1006/pmed.2002.1016.
- Ziersch A, Gaffney J, Tomlinson DR. STI prevention and the male sex industry in London: evaluating a pilot peer education programme. Sex Transm Infect 2000;76:447-53. http://dx.doi.org/10.1136/sti.76.6.447.
- Whitehead M. A typology of actions to tackle social inequalities in health. J Epidemiol Community Health 2007;61:473-8. http://dx.doi.org/10.1136/jech.2005.037242.
- Graham H, Kelly M. Health inequalities: concepts, frameworks and policy. London: Health Development Agency; 2004.
- Evans T, Brown H. Road traffic crashes: operationalizing equity in the context of health sector reform. Inj Contr Saf Promot 2003;10:11-2. http://dx.doi.org/10.1076/icsp.10.1.11.14117.
- Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv 1999;29:295-352. http://dx.doi.org/10.2190/M11W-VWXE-KQM9-G97Q.
- Kavanagh J, Oliver S, Lorenc T, Caird J, Tucker H, Harden A, et al. School-based cognitive-behavioural interventions: a systematic review of effects and inequalities. Health Sociol Rev 2009;18:61-78. http://dx.doi.org/10.5172/hesr.18.1.61.
- Brenner B, Manice M. Community engagement in children’s environmental health research. Mt Sinai J Med 2011;78:85-97. http://dx.doi.org/10.1002/msj.20231.
- Sarrami-Foroushani P, Travaglia J, Eikli M, Braithwaite J. Consumer and community engagement: a review of the literature. Sydney: Centre for Clinical Governance Research, Australian Institute of Health Innovation, Faculty of Medicine, University of New South Wales; 2012.
- Kelly L. Empowering a community: standing up to ‘the powers that be’. J Hum Ecol 2003;14:417-24.
- Principles of community engagement. Atlanta, GA: NIH; 2011.
- Putnam R. Bowling alone: the collapse and revival of American community. New York City: Simon & Schuster; 2000.
- Bourdieau P, Wacquant L. An invitation to reflexive sociology. Chicago: University of Chicago Press; 1992.
- Coleman J. Social capital in the creation of human capital. Am J Sociol 1989;95:95-120. http://dx.doi.org/10.1086/228943.
- Portes A. Social capital: its origins and applications in modern sociology. Ann Rev Sociol 1998;24:1-24. http://dx.doi.org/10.1146/annurev.soc.24.1.1.
- Finlayson A. From beliefs to arguments: interpretive methodology and rhetorical political analysis. Br J Polit Int Relat 2007;9:545-63. http://dx.doi.org/10.1111/j.1467-856X.2007.00269.x.
- Hillery G. Definitions of community: areas of agreement. Rural Sociol 1955;20:111-23.
- Hamalainen L, Jones K. Conceptualising community as a social fix, argument and persuasion in health, housing and local governance. Leicester: De Montfort University; 2012.
- Woodall JR, Warwick-Booth L, Cross R. Has empowerment lost its power?. Health Educ Res 2012;27:742-5. http://dx.doi.org/10.1093/her/cys064.
- Morgan LM. Community participation in health: perpetual allure, persistent challenge. Health Policy Plann 2001;16:221-30. http://dx.doi.org/10.1093/heapol/16.3.221.
- Community participation in local health and sustainable development: approaches and techniques. Copenhagen, Denmark: World Health Organization; 2002.
- Mathbor G. Effective community participation in coastal development. West Long Branch, NJ: Monmouth University; 2008.
- Pretty J. Participatory learning for sustainable agriculture. World Dev 1995;23:1247-63. http://dx.doi.org/10.1016/0305-750X(95)00046-F.
- Cornwall A. Unpacking ‘participation’: models, meanings and practices. Community Dev J 2008;43:269-83. http://dx.doi.org/10.1093/cdj/bsn010.
- Narayan D. Empowerment and poverty reduction: a sourcebook. Washington, DC: World Bank; 2002.
- Yoder J, Kahn A. Toward a feminist understanding of women and power. Psychol Women Q 1992;16:381-8. http://dx.doi.org/10.1111/j.1471-6402.1992.tb00263.x.
- Hicks L. Feminist analysis of empowerment and community in art education. Stud Art Educ 1990;32:36-4. http://dx.doi.org/10.2307/1320398.
- Draper AK, Hewitt G, Rifkin S. Chasing the dragon: developing indicators for the assessment of community participation in health programmes. Soc Sci Med 2010;71:1102-9. http://dx.doi.org/10.1016/j.socscimed.2010.05.016.
- Cornwall A. Democratising engagement. London: Demos; 2008.
- Osborne S, Beattie R, Williamson A. Community involvement in rural regeneration partnerships in the UK: evidence from England, Northern Ireland and Scotland. York: Joseph Rowntree Foundation; 2002.
- Milburn K. A critical review of peer education with young people with special reference to sexual health. Health Educ Res 1995;10:407-20. http://dx.doi.org/10.1093/her/10.4.407.
- Harden A, Weston R, Oakley A. A review of the effectiveness and appropriateness of peer-delivered health promotion interventions for young people. London: EPPI-Centre, Social Science Research Unit, Institute of Education; 1999.
- South J, Kinsella K, Meah A. Lay perspectives on lay health worker roles, boundaries and participation within three UK community-based health promotion projects. Health Educ Res 2012;27:656-70. http://dx.doi.org/10.1093/her/cys006.
- Woodall J, Raine G, South J, Warwick-Booth L. Empowerment and health and well-being – evidence review produced for Altogether Better. Leeds: Leeds Metropolitan University; 2010.
- Laverack G. Health promotion practice: power and empowerment. London: Sage; 2004.
- Arnstein S. A ladder of citizen participation. J Am Inst Plann 1969;35:216-24. http://dx.doi.org/10.1080/01944366908977225.
- Hart R. Children’s participation: from tokenism to citizenship. Florence, Italy: UNICEF; 1992.
- Aslin H, Brown V. A framework and toolkit to work towards whole-of-community engagement. Canberra: Bureau of Rural Sciences; 2005.
- LEAP framework. Glasgow: Scottish Community Development Centre; n.d.
- World Health Organization . Ottawa Charter for health promotion. Health Promot 1986;1:iii-v.
- Laverack G, Wallerstein N. Measuring community empowerment: a fresh look at organizational domains. Health Promot Int 2001;16:179-85. http://dx.doi.org/10.1093/heapro/16.2.179.
- Lawn JE, Rohde J, Rifkin S, Were M, Paul VK, Chopra M. Alma-Ata 30 years on: revolutionary, relevant, and time to revitalise. Lancet 2008;372:917-27. http://dx.doi.org/10.1016/S0140-6736(08)61402-6.
- Milton B, Attree P, French B, Povall S, Whitehead M, Popay J. The impact of community engagement on health and social outcomes: a systematic review. Community Dev J 2012;47:316-34. http://dx.doi.org/10.1093/cdj/bsr043.
- Davidson S. Spinning the wheel of empowerment. Planning 1998;1262:14-5.
- Hornick JP, Bradford B, Bertrand L, Boyes M. Evaluation of Best Start: final process and outcome analysis report. Calgary: Canadian Research Institute for Law and the Family; 2006.
- Wickizer T, Wagner W, Cheadle A, Pearson D, Beery W, Maeser J, et al. Implementation of the Henry J Kaiser Family Foundation’s Community Health Promotion Grant Program: a process evaluation. Milbank Q 1998;76:121-47. http://dx.doi.org/10.1111/1468-0009.00081.
- Duggan A, Windham A, McFarlane E, Fuddy L, Rohde C, Buchbinder S, et al. Hawaii’s healthy start program of home visiting for at-risk families: evaluation of family identification, family engagement, and service delivery. Pediatrics 2000;105:250-9.
- Grant T, Ernst C, Streissguth A. Intervention with high-risk alcohol and drug-abusing mothers I. Administrative strategies of the Seattle model of paraprofessional advocacy. Am J Community Psychol 1999;27:1-18.
- Community engagement to improve health. Public health guidance 9. London: NICE; 2008.
- Andersen MR, Hager M, Su C, Urban N. Analysis of the cost-effectiveness of mammography promotion by volunteers in rural communities. Health Educ Behav 2002;29:755-70. http://dx.doi.org/10.1177/109019802237942.
- Barnet B, Duggan AK, Devoe M, Burrell L. The effect of volunteer home visitation for adolescent mothers on parenting and mental health outcomes: a randomized trial. Arch Pediatr Adolesc Med 2002;156:1216-22. http://dx.doi.org/10.1001/archpedi.156.12.1216.
- Frick KD, Carlson MC, Glass TA, McGill S, Rebok GW, Simpson C, et al. Modeled cost-effectiveness of the Experience Corps Baltimore based on a pilot randomized trial. J Urban Health 2004;81:106-17. http://dx.doi.org/10.1093/jurban/jth097.
- Lindqvist K, Lindholm L. A cost–benefit analysis of the community-based injury prevention programme in Motala, Sweden – a WHO Safe Community. Public Health 2001;115:317-22. http://dx.doi.org/10.1038/sj.ph.1900793.
- McDaid D, Park AL. Investing in mental health and well-being: findings from the DataPrev project. Health Promot Int 2011;26:i108-39. http://dx.doi.org/10.1093/heapro/dar059.
- Loewenstein G, Volpp KG, Asch DA. Incentives in health: different prescriptions for physicians and patients. JAMA 2012;307:1375-6. http://dx.doi.org/10.1097/01.ogx.0000419560.63610.67.
- Long JA, Jahnle EC, Richardson DM, Loewenstein G, Volpp KG. Peer mentoring and financial incentives to improve glucose control in African American veterans: a randomized trial. Ann Intern Med 2012;156:416-24. http://dx.doi.org/10.7326/0003-4819-156-6-201203200-00004.
- Tan EJ, Tanner EK, Seeman TE, Xue QL, Rebok GW, Frick KD, et al. Marketing public health through older adult volunteering: Experience Corps as a social marketing intervention. Am J Public Health 2010;100:727-34. http://dx.doi.org/10.2105/AJPH.2009.169151.
- The COMMIT Research Group . Community Intervention Trial for Smoking Cessation (COMMIT): I. cohort results from a four-year community intervention. Am J Public Health 1995;85:183-92.
- Coutinho SB, de Lira PI, de Carvalho Lima M, Ashworth A. Comparison of the effect of two systems for the promotion of exclusive breastfeeding. Lancet 2005;366:1094-100. http://dx.doi.org/10.1016/S0140-6736(05)67421-1.
- Sahota P, Rudolf MC, Dixey R, Hill AJ, Barth JH, Cade J. Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ 2001;323:1029-32. http://dx.doi.org/10.1136/bmj.323.7320.1029.
- Weiss FL, Nicholson HJ. Friendly PEERsuasionSM against substance use: the Girls IncorporatedSM model and evaluation. Drugs Soc 1998;12:7-22.
- Yancey AK, McCarthy WJ, Harrison GG, Wong WK, Siegel JM, Leslie J. Challenges in improving fitness: results of a community-based, randomized, controlled lifestyle change intervention. J Womens Health (Larchmt) 2006;15:412-29. http://dx.doi.org/10.1089/jwh.2006.15.412.
- Wolfberg AJ, Michels KB, Shields W, O’Campo P, Bronner Y, Bienstock J. Dads as breastfeeding advocates: results from a randomized controlled trial of an educational intervention. Am J Obstet Gynecol 2004;191:708-12. http://dx.doi.org/10.1016/j.ajog.2004.05.019.
- Navarro V. What we mean by social determinants of health. Global Health Promot 2009;16:5-16. http://dx.doi.org/10.1177/1757975908100746.
- Nathanson C, Hopper K. The Marmot review – social revolution by stealth. Soc Sci Med 2010;71:1237-9. http://dx.doi.org/10.1016/j.socscimed.2010.07.007.
- Matthews H. Citizenship, youth councils and young people’s participation. J Youth Stud 2001;4:299-318. http://dx.doi.org/10.1080/13676260120075464.
- Taylor M. Community participation in the real world: opportunities and pitfalls in new governance spaces. Urban Stud 2007;44:297-31. http://dx.doi.org/10.1080/00420980601074987.
- Rogers PJ. Using programme theory to evaluate complicated and complex aspects of interventions. Evaluation 2008;14:29-48. http://dx.doi.org/10.1177/1356389007084674.
- Patton M. Utilization-focused evaluation. Thousand Oaks, CA: Sage; 1997.
- Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. Am J Community Psychol 2009;43:267-76. http://dx.doi.org/10.1007/s10464-009-9229-9.
- Bradshaw J, McLachlan G. Problems and progress in medical care: essays on current research. 7th series. Oxford: Nuffield Provincial Hospital Trust; 1972.
- Anastacio J, Gidley B, Hart L, Keith M, Mayo M, Kowarzik U. Reflecting realities: participants’ perspectives on integrated communities and sustainable development. York: Joseph Rowntree Foundation; 2000.
- Beresford P, Hoban M. Participation in anti-poverty and regeneration work and research: overcoming barriers and creating opportunities. York: Joseph Rowntree Foundation; 2005.
- Birchall J, Simmons R. User power: the participation of users in public services. London: National Consumer Council; 2004.
- Barnes M, Newman J, Knops A, Sullivan H. Constituting ‘the public’ in public participation. Public Admin 2003;81:379-99. http://dx.doi.org/10.1111/1467-9299.00352.
- Barnes M, Sullivan H, Matka E. The development of collaborative capacity in health action zones: a final report from the national evaluation. Birmingham: University of Birmingham; 2003.
- Newman J, Barnes M, Sullivan H, Knops A. Public participation and collaborative governance. J Soc Policy 2004;33:203-23. http://dx.doi.org/10.1017/S0047279403007499.
- Morison J. The government–voluntary sector compacts: governance, governmentality and civil society. J Law Soc 2000;27:98-132. http://dx.doi.org/10.1111/1467-6478.00148.
- Simonsen-Rehn N, Ovretveit J, Laamanen R, Suominen S, Sundell J, Brommels M. Determinants of health promotion action: comparative analysis of local voluntary associations in four municipalities in Finland. Health Promot Int 2006;21:274-83. http://dx.doi.org/10.1093/heapro/dal026.
- Bandura A. Social learning theory. New York: General Learning Press; 1977.
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health 1998;13:623-49. http://dx.doi.org/10.1080/08870449808407422.
- Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004;31:143-64. http://dx.doi.org/10.1177/1090198104263660.
- Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot 1996;10:282-98. http://dx.doi.org/10.4278/0890-1171-10.4.282.
- Hawley A. Human ecology: a theory of community structure. New York: Ronald Press; 1950.
- O’Neill M, Lemieux V, Groleau G, Fortin J-P, Lamarche PA. Coalition theory as a framework for understanding and implementing intersectoral health-related interventions. Health Promot Int 1997;12:79-87. http://dx.doi.org/10.1093/heapro/12.1.79.
- Kawachi I, Kennedy B, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health 1997;87:1491-8. http://dx.doi.org/10.2105/AJPH.87.9.1491.
- Griffiths J, Blair-Stevens C, Thorpe A. Social marketing for health and specialised health promotion: stronger together – weaker apart. London: Royal Society for Public Health and National Social Marketing Centre; 2008.
- Audrey S, Holliday J, Parry-Langdon N, Campbell R. Meeting the challenges of implementing process evaluation within randomized controlled trials: the example of ASSIST (A Stop Smoking in Schools Trial). Health Educ Res 2006;21:366-77. http://dx.doi.org/10.1093/her/cyl029.
- Fisher E, Auslander W, Sussman L, Owens N, Jackson-Thompson J. Community organization and health promotion in minority neighborhoods. Ethn Dis 1992;2:252-72.
- Jemmott LS, Brown EJ, Dodds S. Building community partnerships to improve HIV prevention efforts: implications for nurses. J Assoc Nurses AIDS Care 1998;9:29-40. http://dx.doi.org/10.1016/S1055-3290(98)80018-6.
- Starkey F, Moore L, Campbell R, Sidaway M, Bloor M. ASSIST . Rationale, design and conduct of a comprehensive evaluation of a school-based peer-led anti-smoking intervention in the UK: the ASSIST cluster randomised trial [ISRCTN55572965]. BMC Public Health 2007;7. http://dx.doi.org/10.1186/1471-2458-7-301.
- Treno A, Holder H. Community mobilization: evaluation of an environmental approach to local action. Addiction 1997;92:S173-87. http://dx.doi.org/10.1046/j.1360-0443.92.6s1.2.x.
- Weinehall L, Hellsten G, Boman K, Hallmans G. Prevention of cardiovascular disease in Sweden: the Norsjö community intervention programme – motives, methods and intervention components. Scand J Public Health 2001;29:13-20. http://dx.doi.org/10.1080/140349401316898090.
- Kegler MC, Swan DW. Advancing coalition theory: the effect of coalition factors on community capacity mediated by member engagement. Health Educ Res 2012;27:572-84. http://dx.doi.org/10.1093/her/cyr083.
- Cornish F, Ghosh R. The necessary contradictions of ‘community-led’ health promotion: a case study of HIV prevention in an Indian red light district. Soc Sci Med 2007;64:496-507. http://dx.doi.org/10.1016/j.socscimed.2006.09.009.
- Russell H. National evaluation of local strategic partnerships: issues paper: voluntary and community sector engagement in local strategic partnerships. London: Office of the Deputy Prime Minister; 2005.
- Williams M. Discursive democracy and New Labour: five ways in which decision-makers manage citizen agendas in public participation initiatives. Soc Res Online 2004;9. www.socresonline.org.uk/9/3/williams.html (accessed June 2013).
- Holder HD, Moore RS. Institutionalization of community action projects to reduce alcohol-use related problems: systematic facilitators. Subst Use Misuse 2000;35:75-86. http://dx.doi.org/10.3109/10826080009147687.
- Bickerstaff K, Walker G. Shared visions, unholy alliances: power, governance and deliberative processes in local transport planning. Urban Stud 2005;42:2123-44. http://dx.doi.org/10.1080/00420980500332098.
- Duffy B, Rose J, Butler S, Vince J. Views of New Deal for communities – focus group report. London: MORI; 2005.
- Educe L. Seeking the lessons: Skills and Knowledge Programme evaluation. Research report 19. London: Office of the Deputy Primer Minister; 2005.
- Sridharan S, Gnich W, Moffat V, Bolton J, Harkins C, Hume M, et al. Independent evaluation of Have a Heart Paisley Phase 2. Edinburgh: Research Unit in Health, Behaviour and Change, University of Edinburgh; 2008.
- Goodlad R, Burton P, Croft J. Effectiveness at what? The processes and impact of community involvement in area-based initiatives. Environ Plann C Govern Pol 2005;23:923-38. http://dx.doi.org/10.1068/c45m.
- South J, Meah A, Bagnall A, Kinsella K, Branney P. People in public health: a study of approaches to develop and support people in public health roles. Report for the National Institute for Health Research Service Delivery and Organisation programme. London: Queen’s Printer and Controller of HMSO; 2010.
- Rees R, Oliver S, Gough D, Oliver S, Thomas J. An introduction to systematic reviews. London: Sage; 2012.
- McDaid D, Needle J, Morris Z, Dawson S. The future of health: burdens, challenges, and opportunities. Basingstoke: Palgrave Macmillan; 2009.
- Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health 2013;67:190-93. http://dx.doi.org/10.1136/jech-2012-201257.
- Glass G. Meta-Analysis at 25 2000. www.gvglass.info/papers/meta25.html (accessed 30 May 2013).
- Berk R. Statistical inference and meta-analysis. J Exp Criminol 2007;3:247-70. http://dx.doi.org/10.1007/s11292-007-9036-y.
- Lipsey M. Unjustified inferences about meta-analysis. J Exp Criminol 2007;3:271-9. http://dx.doi.org/10.1007/s11292-007-9037-x.
- Alderson P, Green S. Cochrane Collaboration Open Learning Material for Reviewers 2002. www.cochrane-net.org/openlearning/ (accessed 30 May 2013).
- Hammersley M. Taking sides in social research: essays on partisanship and bias. London: Routledge; 2000.
- Jüni P, Holenstein F, Sterne J, Bartlett C, Egger M. Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol 2002;31:115-23. http://dx.doi.org/10.1093/ije/31.1.115.
- Office for National Statistics . Statistical Bulletin: 2011 Census: Key Statistics for England and Wales, March 2011 2012. www.ons.gov.uk/ons/rel/census/2011-census/key-statistics-for-local-authorities-in-england-and-wales/stb-2011-census-key-statistics-for-england-and-wales.html#tab---Ethnic-group (accessed 4 January 2013).
- US Census Bureau . Overview of Race and Hispanic Origin: 2010 2011. www.census.gov/prod/cen2010/briefs/c2010br-02.pdf (accessed 4 January 2013).
Appendix 1 Search strategies for bibliographic databases
Search strategy: Database of Promoting Health Effectiveness Reviews (searched 26 July 2011)
Keyword search: Health promotion OR inequalities AND (Aims stated AND search stated AND inclusion criteria stated)
Search strategy: Trials Register of Promoting Health Interventions (searched 16 August 2011)
“disadvantage” OR “disparities” OR “disparity” OR “equality” OR “equity” OR “gap” OR “gaps” OR “gradient” OR “gradients” OR “health determinants” OR “health education” OR “health inequalities” OR “health promotion” OR “healthy people programs” OR “inequalities” OR “inequality” OR “inequities” OR “inequity” OR “preventive health service” OR “preventive medicine” OR “primary prevention” OR “public health” OR “social medicine” OR “unequal” OR “variation”
AND
“change agent” OR “citizen” OR “community” OR “champion” OR “collaborator” OR “disadvantaged” OR “lay community” OR “lay people” OR “lay person” OR “member” OR “minority” OR “participant” OR “patient” OR “peer” OR “public” OR “representative” OR “resident” OR “service user” OR “stakeholder” OR “user” OR “volunteer” OR “vulnerable”
AND
“capacity building” OR “coalition” OR “collaboration” OR “committee” OR “compact” OR “control” OR “co-production” OR “councils” OR “delegated power” OR “democratic renewal” OR “development” OR “empowerment” OR “engagement” OR “forum” OR “governance” OR “health promotion” OR “initiative” OR “integrated local development programme” OR “intervention guidance” OR “involvement” OR “juries” OR “local area agreement” OR “local governance” OR “local involvement networks” OR “local strategic partnership” OR “mobilisation” OR “mobilization “ OR “neighbourhood committee” OR “neighbourhood managers” OR “neighbourhood renewal” OR “neighbourhood wardens” OR “networks” OR “organisation” OR “panels” OR “participation” OR “participation compact” OR “participatory action” OR “partnerships” OR “pathways “ OR “priority setting” OR “public engagement” OR “public health” OR “rapid participatory assessment” OR “regeneration” OR “relations” OR “support”
Search strategy: Cochrane databases (searched 17 August 2011)
-
CDSR (Cochrane reviews).
-
DARE (other reviews).
-
HTA database (technology assessments).
-
NHS EED (economic evaluations).
“disadvantage” OR “disparities” OR “disparity” OR “equality” OR “equity” OR “gap” OR “gaps” OR “gradient” OR “gradients” OR “health determinants” OR “health education” OR “health inequalities” OR “health promotion” OR “healthy people programs” OR “inequalities” OR “inequality” OR “inequities” OR “inequity” OR “preventive health service” OR “preventive medicine” OR “primary prevention” OR “public health” OR “social medicine” OR “unequal” OR “variation”
AND
“change agent” OR “citizen” OR “community” OR “champion” OR “collaborator” OR “disadvantaged” OR “lay community” OR “lay people” OR “lay person” OR “member” OR “minority” OR “participant” OR “patient” OR “peer” OR “public” OR “representative” OR “resident” OR “service user” OR “stakeholder” OR “user” OR “volunteer” OR “vulnerable”
AND
“capacity building” OR “coalition” OR “collaboration” OR “committee” OR “compact” OR “control” OR “co-production” OR “councils” OR “delegated power” OR “democratic renewal” OR “development” OR “empowerment” OR “engagement” OR “forum” OR “governance” OR “health promotion” OR “initiative” OR “integrated local development programme” OR “intervention guidance” OR “involvement” OR “juries” OR “local area agreement” OR “local governance” OR “local involvement networks” OR “local strategic partnership” OR “mobilisation” OR “mobilization “ OR “neighbourhood committee” OR “neighbourhood managers” OR “neighbourhood renewal” OR “neighbourhood wardens” OR “networks” OR “organisation” OR “panels” OR “participation” OR “participation compact” OR “participatory action” OR “partnerships” OR “pathways “ OR “priority setting” OR “public engagement” OR “public health” OR “rapid participatory assessment” OR “regeneration” OR “relations” OR “support”
Search strategy: The Campbell Library (searched 17 August 2011)
“disadvantage” OR “disparities” OR “disparity” OR “equality” OR “equity” OR “gap” OR “gaps” OR “gradient” OR “gradients” OR “health determinants” OR “health education” OR “health inequalities” OR “health promotion” OR “healthy people programs” OR “inequalities” OR “inequality” OR “inequities” OR “inequity” OR “preventive health service” OR “preventive medicine” OR “primary prevention” OR “public health” OR “social medicine” OR “unequal” OR “variation”
AND
“change agent” OR “citizen” OR “community” OR “champion” OR “collaborator” OR “disadvantaged” OR “lay community” OR “lay people” OR “lay person” OR “member” OR “minority” OR “participant” OR “patient” OR “peer” OR “public” OR “representative” OR “resident” OR “service user” OR “stakeholder” OR “user” OR “volunteer” OR “vulnerable”
AND
“capacity building” OR “coalition” OR “collaboration” OR “committee” OR “compact” OR “control” OR “co-production” OR “councils” OR “delegated power” OR “democratic renewal” OR “development” OR “empowerment” OR “engagement” OR “forum” OR “governance” OR “health promotion” OR “initiative” OR “integrated local development programme” OR “intervention guidance” OR “involvement” OR “juries” OR “local area agreement” OR “local governance” OR “local involvement networks” OR “local strategic partnership” OR “mobilisation” OR “mobilization “ OR “neighbourhood committee” OR “neighbourhood managers” OR “neighbourhood renewal” OR “neighbourhood wardens” OR “networks” OR “organisation” OR “panels” OR “participation” OR “participation compact” OR “participatory action” OR “partnerships” OR “pathways “ OR “priority setting” OR “public engagement” OR “public health” OR “rapid participatory assessment” OR “regeneration” OR “relations” OR “support”
Appendix 2 Keywording tool
All 319 studies (reported in 361 papers/reports71–431) were keyworded using this tool.
1. In which OECD country does the study take place?
Current OECD member countries: Australia, Austria, Belgium, Canada, Chile, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Japan, Korea, Luxembourg, Mexico, Netherlands, New Zealand, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Switzerland, Turkey, United Kingdom, United States.
-
UK
-
USA
-
Canada
-
Australia
-
New Zealand
-
Other (specify)
2. Name of PH intervention (specify if applicable).
Leave blank (don’t tick box) if no specific name of the programme is provided. Add where a specific programme name is used (e.g. ‘10,000 Steps’ or ‘CATCH’). Include the short name or acronym if commonly used. If the study id on ‘Health Action Zone’, just enter the name of the programme here and stop coding.
3. Age group(s) of participants.
Record the age of the PH intervention participants, not the engagees. Use the categories if age range is specified or labels such as ‘adults’ are used. If the population described in the report fits more than one of the following categories, indicate all relevant categories. If no age range is specified, make an informed choice.
-
General population-based (i.e. there is no information on any specific age categories). Use this if unspecified
-
Children (0–10 years)
-
Young people (11–21 years)
-
Adults (22–54 years)
-
Older people (+55 years)
4. Sex of participants.
-
Majority females (≥ 90%)
-
Majority males (≥ 90%)
-
Both males and females (mixed sex) Use this if unspecified or < 90% of a particular gender
5a. What is the main PROGRESS-Plus characteristic of the sample/population? Select ONE.
Specify the main characteristic of the group that distinguishes them as being disadvantaged (should be mentioned in the title and/or abstract). Only mark one main characteristic. If more than one main characteristic that cannot be distinguished, use the code ‘multiple equally important characteristics’ and specify.
-
Ethnicity: ethnic background
-
African American/black
-
American Indian
-
Asian – Indian, Pakistani, Bangladeshi
-
Asian – continental (e.g. Chinese, Vietnamese, Filipino) Incl. Pacific Islanders
-
Hispanic/Latino/Mexican American
-
immigrant, refugee, asylum seeker
-
other minority ethnic or ‘BME’
-
other indigenous populations
-
-
Socioeconomic position (SEP) Income, means-tested benefits/welfare, affluence measures, deprived area, classification as ‘low’ SEP
-
Occupation/employment status
-
professional
-
skilled
-
unskilled
-
unemployed
-
worker/employee
-
blue collar; manual labourer A blue-collar worker is a member of the working class who performs manual labour. Blue-collar work may involve skilled or unskilled, manufacturing, mining, construction, mechanical, maintenance, technical installation and many other types of physical work. Often something is physically being built or maintained (definition from Wikipedia)
-
-
Education Years in and/or level of education attained, school type. Includes high school dropouts
-
Place of residence
-
rural
-
urban Incl. inner city
-
housing characteristics
-
other
-
-
Sexual orientation Heterosexual, gay, lesbian, bisexual, transgender
-
Social capital Neighbourhood/community/family support
-
Gender
-
male
-
female
-
-
Religion (specify)
-
Age
-
Marital status/family composition
-
Disability Existence of physical or emotional/mental disability
-
Other vulnerable groups (specify) Examples: school non-attendees, looked after YP, YP in criminal justice system, victims of abuse, runaways, teenage parents, mothers as a vulnerable group, substance abusers, sex workers
-
‘at-risk’ or ‘high-risk’ youths, incl. homeless/runaways
-
substance abuse Includes intravenous/injecting drug users and other chronic or hard drug abusers. Does not include minor recreational or experimental drug use
-
teenage parents/pregnant teens
-
other (see specification above)
-
-
No main PROGRESS-Plus group (not mentioned in title and abstract)
-
Multiple equally important characteristics (specify) If there is more than one main characteristics that cannot be distinguished (i.e. are equally focused upon), then use this code and specify
5b. What are any secondary PROGRESS-Plus characteristics of the sample/population?
Select all that apply. Tick any variables that are explicitly mentioned in the body of the paper as characteristics of the MAJORITY of the participants (defined as 60% or more of the sample).
-
Ethnicity: ethnic background
-
African American/black
-
American Indian
-
Asian – continental (e.g. Chinese, Vietnamese, Filipino) Incl. Pacific Islanders
-
Asian – Indian, Pakistani, Bangladeshi
-
Hispanic/Latino/Mexican American
-
immigrant, refugee, asylum seeker
-
other minority ethnic or ‘BME’
-
other indigenous populations
-
Asian (don’t use this code any more; see codes above)
-
-
Socioeconomic position (SEP) Income, means-tested benefits/welfare, affluence measures, deprived area, classification as ‘low’ SEP
-
Occupation/employment status
-
professional
-
skilled
-
unskilled
-
unemployed
-
worker/employee
-
blue collar; manual labourer A blue-collar worker is a member of the working class who performs manual labour. Blue-collar work may involve skilled or unskilled, manufacturing, mining, construction, mechanical, maintenance, technical installation and many other types of physical work. Often something is physically being built or maintained (definition from Wikipedia)
-
-
Education
-
Place of residence
-
rural
-
urban Incl. inner city
-
housing characteristics
-
other
-
-
Sexual orientation
-
Social capital
-
Gender
-
male
-
female
-
-
Religion (specify)
-
Age
-
Marital status/family composition
-
Disability
-
Other vulnerable groups (specify)
-
No secondary PROGRESS-Plus characteristics
6. How are health inequalities addressed?
-
Targeted at or delivered to specific PROGRESS-Plus group Targeted or delivered to a specific PROGRESS-Plus population. Usually, the disadvantaged group will constitute the majority or entire sample of participants
-
Universal (aimed at the whole group population, not on the basis of individual needs/risks) Interventions that target the general public or a whole population group that has not been identified on the basis of individual risk or needs. The PROGRESS-Plus group will usually be identified through subgroup analyses
-
Targeted and comparison within a PROGRESS-Plus category Use if authors report a subgroup analysis, regression or narrative statement about difference between groups (e.g. high or low SES)
7. What was the primary health issue being addressed? Select ONE.
That is, what was the main health issue that the intervention was aiming to improve/prevent (as stated in the title, abstract and aims)?
-
Antenatal (prenatal) care Before birth; during or relating to pregnancy
-
Asthma prevention/treatment/management
-
Breastfeeding
-
Cardiovascular disease Incl. high blood pressure
-
Cancer prevention
-
Cancer screening/detection
-
Care of older people
-
Child abuse prevention
-
Child illness and ill health
-
Diabetes prevention/management
-
Disabilities and chronic illness Incl. chronic diseases and chronic conditions
-
Healthy eating/nutrition
-
HIV/AIDS/STI prevention/risk reduction
-
Housing
-
Hypertension
-
Immunisation
-
Injury prevention
-
Mental health
-
Neighbourhood renewal/regeneration
-
Obesity prevention/weight reduction
-
Parenting Incl. child development training/education
-
Partner violence
-
Physical activity
-
Public health/health promotion/prevention
-
Reproductive health Incl. family planning
-
Safe community
-
Sexual health
-
Smoking cessation
-
Smoking/tobacco prevention
-
Substance abuse
-
Suicide prevention
-
Tuberculosis
-
Violence prevention
-
Other topics (specify)
-
Not Marmot topics
8. What health issues were incorporated into the intervention content/delivery? This can be stated anywhere in the text.
Select all that apply. Must be explicit or very clear. Example: ‘healthy eating’ might be a health issue tackled in an intervention with the aim of ‘cancer prevention’.
-
Antenatal (prenatal) care Before birth; during or relating to pregnancy
-
Asthma prevention/treatment/management
-
Breastfeeding
-
Cardiovascular disease Incl. high blood pressure
-
Cancer prevention
-
Cancer screening/detection
-
Care of older people
-
Child abuse prevention
-
Child illness and ill health
-
Diabetes prevention/management
-
Disabilities and chronic illness
-
Healthy eating/nutrition
-
HIV/AIDS/STI prevention/risk reduction
-
Housing
-
Hypertension
-
Immunisation
-
Injury prevention
-
Mental health
-
Neighbourhood renewal/regeneration
-
Obesity prevention/weight reduction
-
Parenting Incl. child development training/education
-
Partner violence
-
Physical activity
-
Public health/health promotion/prevention
-
Reproductive health Incl. family planning
-
Safe community
-
Sexual health
-
Smoking cessation
-
Smoking/tobacco prevention
-
Substance abuse
-
Suicide prevention
-
Tuberculosis
-
Violence prevention
-
Other topics (specify)
-
Teenage pregnancy
9. To what extent was community engagement integral to the PH intervention? Select ONE.
Completely = all components of intervention delivered through CE; mostly = 50% or more of components of intervention were delivered through CE; little = less than 50% of intervention components were delivered through CE; none = engagees not involved in delivery of intervention
-
Completely community engagement
-
Mostly community engagement
-
Little community engagement
-
No community engagement None = you should have excluded this! Mark ‘Query Exclude’ above and stop coding
10. Was the community explicitly involved in identifying the health problem/need?
-
Yes Includes community-based organisations that involve or ‘listen to’ the community it represents
-
No
11. Intervention site.
Attach as many keywords as appropriate, but only attach a keyword if the report specifically indicates or describes the intervention site(s).
-
Community setting Carried out in an organised community setting, e.g. youth club, night club, community centre. This term should not be used for outreach work or religious settings
-
Religious settings (e.g. churches)
-
Outreach General activities or initiatives organised in the community
-
Educational setting (school, college, university)
-
Home situation (not residential care home)
-
Primary health care (e.g. GP)
-
Secondary health-care unit (e.g. hospital, specialist clinics)
-
WIC clinic
-
Residential care (includes nursing homes, sheltered housing)
-
Correctional institution (e.g. prison, youth detention centre)
-
Workplace site
-
Mass media – untailored (generic) Includes generic/untailored phone call/SMS, television, radio, print media (e.g. newsletters) and other audiovisual media. This includes campaigns using mailing, lobbying
-
Phone, print or audio/visual media – tailored Includes tailored contact via telephone/SMS, letter, print media (e.g. newsletter) and audiovisual media
-
Computer-based, internet-based and virtual interventions
-
Unclear/not specified
12. Person(s) delivering the PH intervention (intervenors).
Here we’re trying to get at who had contact with the PH intervention participants. Use as many keywords as appropriate to include the range of people involved in the delivery of the intervention. Only use a keyword if the report specifically indicates this information.
-
Community member From the community, not employed. Does not include those labelled as ‘peer’
-
Community worker Employed as a worker in a community. Not necessarily from the community
-
Computer
-
Counsellor
-
Health professional (e.g. GP, dietitian, nurse)
-
Health promotion practitioner
-
Lawyer
-
Parent
-
Peer Peers defined as people sharing the same age group (e.g. schools peers) or health behaviour/risk/condition or similar in key aspects (e.g. race/ethnicity, SES, geographic location)
-
Psychologist
-
Religious leader (e.g. parson, priest)
-
Researcher
-
Residential worker
-
Social worker
-
Teacher and education professionals (lecturer, principal, etc.)
-
Other
-
Unclear/not reported
13a. Is this a multicomponent intervention?
-
No – only one component There is only one component to the PH intervention
-
Yes – all components involve CE There are multiple components to the PH intervention, all of which involve community engagement in some way (whether through design, delivery or evaluation)
-
Yes – only some components involve CE There are multiple components to the PH intervention, only some of which involve community engagement in some way (whether through design, delivery or evaluation)
-
Irrelevant – no community engagement in delivery/evaluation
13b. Intervention type.
Select all that apply but only if the report specifically indicates this information.
-
Activities (e.g. community fairs/fetes)
-
Advice One-to-one communication consisting of directional guidance, recommendations or suggestions. Element of tailoring
-
Education Information only, e.g. information leaflets, curriculum
-
Skill development/training Skills are practised or modelled, e.g. condom use, assertiveness skills
-
Counselling (based on the psychological needs of the individual)
-
Social support
-
Environmental modification e.g. improvement in housing conditions, provision of healthier school meals
-
Immunisation
-
Incentives e.g. participants received money, tickets for a prize draw, credits for a course
-
Professional training For interventions targeted at changing professional practice including those involving medical students, etc.
-
Physical activity, exercise
-
Rehabilitation
-
Resource access e.g. condom distribution
-
Risk assessment (not medical screening) e.g. environmental assessment for risk of falling in older people
-
Role modelling, role playing
-
Screening. For medical screening, e.g. breast screening
-
Service access e.g. establishing a drop-in centre, extended opening times of a family planning clinic, referral to a service
-
Clinical treatment
-
Biofeedback e.g. feedback on a personal basis of increased levels of carbon monoxide in one’s breath as a prevention strategy for smoking
-
Other
14. For each aspect of an initiative (design, delivery, evaluation), what was the level of community engagement?
-
Design/planning
-
Leading Responsibility and decision-making authority reside with the community members
-
Collaborating Community members have shared responsibility and authority for design with others
-
Consulted (piloting of intervention is included here if there is a feedback mechanism) Community members are asked about design/planning, but authority and responsibility lie outside the community. Includes focus groups
-
Informed Community members told what’s going to happen to them
-
Other
-
Not involved/unclear
-
-
Delivery
-
Leading The community member has autonomy (doing it on their own). They make decisions about when and how things are done during the delivery
-
Collaborating Delivery is done by community member as part of a team
-
Consulted (piloting of intervention delivery is included here if there is a feedback mechanism)
-
Informed
-
Other
-
Not involved/unclear
-
-
Evaluation
-
Leading Responsibility and authority for measurement tools and data collection held solely by community members (but not necessarily analysis though)
-
Collaborating Shared responsibility and authority for measurement tools and data collection by community members and others
-
Consulted Views and opinions of community members about tools and data collection methods are sought; piloting of an evaluation tool, e.g. survey, is included here – responsibility and authority for tools and collection held by others outside the community
-
Informed Community members told what the evaluation will look like
-
Other
-
Not involved/unclear
-
15. Label/s for community engagement strategy
-
Community action/support; community mobilisation/involvement/engagement/participation
-
Community organisations – developing new and existing services
-
Community partnership; community coalitions; community task force Also includes forum; committee; advisory group
-
Any peer involvement, e.g. peer counselling, peer education, peer leaders, peer leadership, role models, peer support Peers defined as people sharing the same age group (e.g. schools peers) or health behaviour/risk/condition or similar in key aspects (e.g. race/ethnicity). NOT promotoras
-
Non-peer health advocacy (e.g. lay health, community health workers) For members of the community that are NOT peers of the target participants, where ‘peer’ is defined as sharing the same age group or health risk/condition or similar in key aspects (e.g. race/ethnicity). NOT promotoras
-
Promotora (explicit use of term) Must use specific ‘promotora’ label
-
‘Outreach’ programme (explicit use of term)
-
Social networks (explicit use of term)
-
Volunteering/volunteers (explicit use of term)
-
Other community engagement strategy
-
No clear community engagement label used (explain)
16. Was training provided to the engagees?
-
Yes
-
No
-
Not stated/unclear
17. Were outcomes measured for the engagees (people participating in community engagement)?
-
Yes
-
No
18. What categories of outcomes were reported? (specific outcomes will be captured elsewhere)
Select all that apply
-
Health outcomes, e.g. behaviours, knowledge, attitudes. Can include health service use outcomes such as number of visits to a clinic
-
Personal outcomes, e.g. empowerment, self-esteem, efficacy, skills
-
Community outcomes, e.g. capacity building, social capital or inclusion
-
Process outcomes, e.g. acceptability, appropriateness
-
Costs or resource use data, or cost-effectiveness Select this if any mention of costs
-
Not stated/unclear
-
Other
19. Is there anything within this study that is not reflected in our conceptual framework?
-
No
-
Yes (explain)
Appendix 3 Data extraction and risk of bias tool for effectiveness studies
1. What was the duration of the intervention?
In weeks; assume 4.5 weeks per month when converting
-
Enter value in weeks (add details)
-
Duration unclear/not reported
2. What was the length of time between evaluation measures in weeks?
-
Time between pre-test and post-test In weeks. If less than one week (e.g. a one-off session, or on two days), then use weeks = 1. Pre-test is defined as the baseline or time between start of intervention and post-test (first measurement after intervention ceases/prior to first follow-up)
-
Time between post-test and first follow-up (use if > 1 follow-up) In weeks
-
Time between post-test and only/final follow-up In weeks
-
Measurement time unclear/not reported
3. Type of control group (select 1 only).
If more than two groups, only mark the comparison group used in effect size calculation
-
Waitlist/delayed treatment
-
Inactive control E.g. ‘Participants in the control group did not receive any intervention during the treatment or follow-up phases’
-
Matched data from target population, without assignment The control group does not know it is a control group. Not applicable to randomised studies. E.g. comparison with area or population level statistics; comparison with prior programme participants; historical records
-
Usual treatment/care, with assignment
-
Alternative/placebo intervention Use if the comparison group receives a different intervention to the treatment group that is not the same as usual care and which has different aims or deliverer to the main intervention
-
Other (add details)
-
Comparator unclear/not reported
4. How were participants/clusters allocated to intervention and control/comparison groups?
Participants were allocated using an acceptable method of randomisation. NB: If method of randomisation is not stated, tick ‘yes’ but indicate this in your comments. If you have suspicions about whether methods of allocation were randomised by an acceptable method, please also indicate these here.
-
Random E.g. table of random numbers, computer-generated random sequences
-
Partial randomisation
-
Non-random E.g. date of birth, order in which participants were recruited to the study, self-selection, needs-based, matched controls
-
Allocation unclear/not reported
5. Selection bias: were participants in the two groups equivalent or adjusted in the analyses to be equivalent?
NB (1): Major prognostic factors are balanced between groups if the groups are drawn from similar populations and have similar sociodemographic variables and baseline values of all outcome measures. Record the extent to which your decision is supported by presented data on outcomes and/or by other information in the report (e.g. statements in text). (i) Study can ‘pass’ if participants were allocated using an acceptable method of randomisation OR (ii) studies can ‘pass’ if (1) baseline values of major prognostic factors are reported for each group for virtually all participants as allocated AND if baseline values of major prognostic factors are balanced between groups in the trial OR imbalances were adjusted for in analysis.
-
Yes – participants were allocated using acceptable method of randomisation AND groups equivalent or unimportant differences
-
Yes – baseline characteristics reported for virtually all of each group as allocated AND groups were equivalent
-
Yes – baseline characteristics reported for virtually all of each group as allocated AND imbalances between groups adjusted for in analysis
-
No – SB not avoided
-
SB unclear/not reported
6. Was attrition bias avoided? (Add details)
Study can pass this component if (1) the attrition rate is reported separately according to allocation group AND if (2) the attrition rate differs across groups by < 10% and is < 30% overall OR baseline values of major prognostic factors were balanced between groups for all those remaining in the study for analysis. NB: For studies which are not trials, this question should simply read ‘Is the attrition rate < 30% of the original participants?’
-
Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% Attrition rate is reported separately according to allocation group AND attrition rate differs across groups by < 10% AND is < 30% overall
-
Yes – ALL baseline values of prognostic factors were balanced between groups Attrition rate is reported separately according to allocation group AND baseline values of prognostic factors were balanced between groups for all those remaining in the study for analysis
-
Yes – unimportant differences between groups in terms of differences between baseline values of participants and dropouts (specify) Attrition rate is reported separately according to allocation group AND baseline values of major prognostic factors were balanced between groups for all those remaining in the study for analysis
-
Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis
-
No – AB not avoided
-
AB unclear/not reported
7. Was selective reporting bias avoided?
Studies can pass this component if authors report on all outcomes they intended to measure as described in the aims of the study.
-
Yes – SRB avoided Authors report on all outcomes they intended to measure as described in the aims of the study
-
No – SRB not avoided
8. Was the study sound?
To be sound, a study has to avoid all three of the specified types of bias in Q5–7 (selection bias, attrition bias and selective reporting bias)
-
Sound Study avoids all three of the specified types of bias (selection bias, follow-up bias and selective reporting bias)
-
Not sound
9. Multiple treatment or comparison arms?
Does the study have more than two groups?
-
Yes – multiple treatment or comparison arms
-
No – only one intervention and one comparison group
10. Outcomes
-
Health outcomes Only extract health status outcomes if a health behaviour has also been measured
-
alcohol abuse
-
antenatal (prenatal) care
-
breastfeeding
-
cancer screening
-
cardiovascular disease
-
child abuse prevention
-
child illness and ill health This also includes birth outcomes (e.g. low birthweight LBW)
-
drug abuse
-
healthy eating
-
hypertension
-
immunisation
-
injury/safety
-
mental health
-
neighbourhood renewal/regeneration
-
obesity/weight status
-
parenting Includes child development training/education
-
physical activity
-
sexual health related to teenage pregnancy Outcomes incl. pregnancy, contraceptive use/safe sex practices, abstinence etc.
-
smoking cessation
-
smoking/tobacco prevention
-
other not captured above
-
-
Community outcomes
-
community outcome
-
-
Engagee personal outcomes
-
engagee empowerment
-
engagee self-esteem
-
engagee skills
-
engagee social support/capital/inclusion
-
engagee health
-
-
PH participant personal outcomes
-
PH participant self-efficacy
-
PH participant social support/capital
-
-
Outcome classification codes
-
immediate post-test (required) Mark if the data were measured at immediate post-test (i.e. the first measure taken after the intervention is completed). Effect sizes must be coded as either ‘Immediate post-test’ or ‘Final follow-up’.
-
first follow-up (if more than one) (1FU)
-
ONLY/final follow-up (O/FFU) Mark if the data were measured at follow-up (also called delayed post-test). This should be the final measure taken after the intervention is completed, regardless of amount of time lapsed or number of other measurements taken between completion and final measurement. Effect sizes must be coded as either ‘Immediate post-test’ or ‘Final follow-up’.
-
effect 1: favours intervention (required) Effect sizes must be coded as either ‘favours intervention’ or ‘favours control’
-
effect 2: favours control (required) Effect sizes must be coded as either ‘favours intervention’ or ‘favours control’
-
health behaviour: actions Mark if the outcome is an observable behaviour (i.e. things people do), such as drinking, smoking, cooking, physical activity or a measure of intake such as amount of fruit consumed or cigarettes smoked
-
status 1: physiological consequences Only extract if health behaviours are also extracted – unless measure of teenage pregnancy. These are not something that you do, they are the consequences of your behaviours. Consequences of behaviours (metabolic and physiological risk factors and related biomarkers), such as pregnancy, blood pressure, cotinine levels, cholesterol, BMI
-
status 2: final health outcomes Only extract if health behaviours are also extracted. Final health outcomes: diagnosis, morbidity and mortality associated with relevant diseases. Incl. clinical diagnoses such as obesity, CVD, diabetes, cancer
-
calculation required imputation Mark if not all of the necessary data were explicitly reported and some imputation was required (e.g. assuming equal numbers in treatment and control groups if exact n not stated; imputing values from ‘p <’)
-
measure is self-report Mark if the effect size is calculated from data that was measured using self-report.
-
subgroup analysis
-
-
Subsample health inequality This refers to the PROGRESS-Plus group of the subsample for which the effect size is calculated.
-
ethnicity
-
socioeconomic status/position Income, means-tested benefits/welfare, affluence measures, deprived area, classification as ‘low’ SEP
-
occupation/employment status
-
education Years in and/or level of education attained, school type. Includes high school dropouts
-
place of residence
-
sexual orientation
-
social capital
-
gender
-
religion
-
age
-
marital status/family composition
-
disability
-
‘at-risk’ or ‘high-risk’ youths, incl. homeless/runaways
-
substance abuse (e.g. injecting drug users) Includes intravenous/injecting drug users and other chronic or hard drug abusers. Does not include minor recreational or experimental drug use
-
teenage parents/pregnant teens
-
multiple health inequalities
-
other vulnerable groups
-
Appendix 4 Tool for extracting process information
From Shepherd et al. 55 and Kavanagh et al. 70
1. Screening
1A. Is this a Marmot topic?
Guidance: Marmot topics:
-
health risks (e.g. smoking, obesity, drug/alcohol use, healthy eating, physical activity)
-
mortality risks (e.g. cardiovascular disease, cancer prevention)
-
best start in life (e.g. antenatal care, parenting, immunisation, teenage pregnancy)
-
employee health/safety (e.g. injury prevention)
-
illness prevention (general health promotion)
-
Yes
-
No
-
If no, stop coding.
1B. Is this a process evaluation?
-
Yes
-
No
If no, stop coding.
2. Which processes were evaluated?
Guidance: Tick as many as appropriate. Specify further where possible
-
Perceptions, understanding or acceptability of an intervention
-
Accessibility of the intervention/programme reach
-
Consultation or collaboration
-
Content of the intervention
-
Implementation of the intervention
-
Costs associated with the intervention
-
Management and responsibility
-
Quality of the programme materials
-
Skills and training of the intervention providers
-
Other (please add details)
3. About which processes do authors offer conclusions?
Guidance: Tick as many as appropriate. Specify further where possible
-
Perceptions, understanding or acceptability of an intervention
-
Accessibility of the intervention/programme reach
-
Consultation or collaboration
-
Content of the intervention
-
Implementation of the intervention
-
Costs associated with the intervention
-
Management and responsibility
-
Quality of the programme materials
-
Skills and training of the intervention providers
-
Other (please add details)
4. What methods were used to collect data on the processes involved?
Guidance: Tick as many as appropriate. Specify further where possible
-
Not stated/unclear
-
Documentation
-
Focus group
-
Interview
-
Observation
-
Self-completion report/diary/questionnaire
-
Other (specify)
5. Who were data collected from?
-
Not stated/unclear
-
Intervention provider – write in numbers
-
A sample of the study population – write in numbers
6. When did the evaluation take place in relation to the intervention?
Tick as many as appropriate. Specify further where possible
-
Not stated/unclear
-
Afterwards – please specify
-
Concurrently
-
For a limited period during the intervention – please specify when
-
Other (please specify)
7. Were steps taken to increase rigour/minimise bias and error in the sampling for the process evaluation?
Guidance: Consider whether:
-
the sampling strategy was appropriate to the questions posed in the process evaluation (e.g. was the strategy well reasoned and justified?)
-
attempts were made to include all relevant stakeholders and/or obtain a diverse sample (think about who might have been excluded who may have had a different perspective to offer)
-
characteristics of the sample critical to the understanding of the study context and findings were presented (i.e. do we know who the participants are in terms of, for example, role in the intervention/evaluation, basic sociodemographics, etc.)
-
Yes, fairly thorough attempt made – please specify
-
Yes, several steps taken – please specify
-
Yes, a few steps taken – please specify
-
Unclear/can’t tell/not stated – please specify
-
No, not at all
-
8. Were steps taken to increase rigour/minimise bias and error in the data collected for the process evaluation?
Guidance: Consider whether:
-
data collection tools were piloted/validated (if quantitative)
-
data collection was comprehensive, flexible and/or sensitive enough to provide a complete and/or vivid and rich description/evaluation of the processes involved in the intervention [e.g. Did the researchers spend sufficient time at the site/with participants? Did they keep ‘following up’? Were steps taken to ensure that all participants were able and willing to contribute? (e.g. confidentiality, language barriers, power relations between adults and young people) Was more than one method of data collection used? Was there a balance between closed and open-ended data collection methods?]
-
Yes, fairly thorough attempt made – please specify
-
Yes, several steps taken – please specify
-
Yes, a few steps taken – please specify
-
Unclear/can’t tell/not stated – please specify
-
No, not at all – please specify
-
9. Were steps taken to increase rigour/minimise bias and error in the analysis of the process data?
Guidance: Consider whether:
-
data analysis methods were systematic (e.g. was a method described/can a method be discerned?)
-
diversity in perspective was explored
-
the analysis was balanced in the extent to which it was guided by preconceptions or by the data (i.e. participants’ views, researcher observations, etc.)
-
the analysis sought to rule out alternative explanations for findings (in qualitative research this could be done by, for example, searching for negative cases/exceptions, feeding back preliminary results to participants, asking a colleague to review the data, or reflexivity; in quantitative research this may be done by, for example, significance testing)
-
Yes, fairly thorough attempt made – please specify
-
Yes, several steps taken – please specify
-
Yes, a few steps taken – please specify
-
Unclear/can’t tell/Not stated – please specify
-
No, not at all – please specify
-
10. Were the findings of the process evaluation grounded in/supported by the data?
Guidance: Consider whether:
-
enough data are presented to show how the authors arrived at their findings
-
the data presented fit the interpretation/support claims about patterns in data
-
the data presented illuminate/illustrate the findings
-
(for qualitative studies) quotes are numbered or otherwise identified so that the reader can see that they don’t just come from one or two people
-
Reasonably well grounded/supported – please specify
-
Fairly well grounded/supported – please specify
-
Limited grounding/support – please specify
-
11. Please rate the findings of the process evaluation in terms of their breadth and depth
Guidance: Consider whether:
(NB: it may be helpful to consider ‘breadth’ as the extent of description and ‘depth’ as the extent to which data have been transformed/analysed)
-
a range of processes/issues were covered in the evaluation
-
the perspectives of participants are fully explored in terms of breadth (contrast of two or more perspectives) and depth (insight into a single perspective)
-
both the strengths and weaknesses of the intervention are described/explored
-
the context of the intervention has been fully described/explored
-
richness and complexity has been portrayed (e.g. variation explained, meanings illuminated)
-
there has been theoretical/conceptual development
-
Limited breadth or depth
-
Good/fair breadth but very little depth
-
Good/fair depth but very little breadth
-
Good/fair breadth and depth
-
12. To what extent does the process evaluation privilege the perspectives and experiences of the public?
Guidance: Consider whether:
-
the public are included in the process evaluation
-
there was a balance between open-ended and fixed-response options
-
whether the community were involved in designing the research
-
there was a balance between the use of an a priori coding framework and induction in the analysis
-
the position of the researchers (did they consider it important to listen to the perspectives of the community?)
-
steps were taken to assure confidentiality and put people at their ease
-
Not at all – please specify
-
A little – please specify
-
Somewhat – please specify
-
A lot – please specify
-
13. Overall, what weight would you assign to this process evaluation in terms of the reliability of its findings?
Guidance: Think (mainly) about the answers you have given to questions 7–10 above.
-
Low reliability
-
Medium reliability
-
High reliability
14. What weight would you assign to this process evaluation in terms of the usefulness of its findings?
Guidance: Think (mainly) about the answers you have given to questions 10–12 above and consider:
-
how well intervention processes are described (e.g. does it provide useful information on barriers and facilitators to implementation – factors that others implementing the intervention would need to consider?)
-
whether the findings can help us to explain the relationship between intervention process and outcome (e.g. why the intervention worked or did not work; factors influencing effectiveness; how the intervention achieved its effects)
-
Low usefulness
-
Medium usefulness
-
High usefulness
-
Appendix 5 Tool for extracting information on resources, costs and consequences
-
Overview
-
Are the costs of the intervention reported?
-
Yes If costs are reported please state price year used, currency, and if more than one year in duration, whether costs have been discounted and at what rate.
-
No
-
-
Is resource use separately reported from cost? If there is no breakdown of total cost please provide information on summary costs, for instance stating duration of time period that costs cover, distinguishing between costs per participant and total cost for the population group.
-
Yes
-
No
-
-
Are there significant differences in total costs between intervention and comparator?
-
Yes
-
No
-
-
-
Resourcing and cost breakdown It is difficult to anticipate exactly how resource data and costs will be broken down and reported in different studies. The level of data will vary enormously. This makes it difficult to standardise a way of extracting and recording these data. The data below are for general guidance. In many cases papers will provide one or more tables containing most of the resource and cost data (and uncertainty around this data) can be extracted. Costs of intervention may be compared with costs of a counterfactual. We provide some notes in respect of different types of resource use and cost to be aware of. The first section is concerned with some of the principal types of human resources; we then look at other resources used. Human resources community engagement interventions will rely heavily on human resource inputs, many of which may come from unpaid volunteers. Specialist staff such as trainers might be employed; there could be a range of other paid staff.
-
Trainers If possible please extract data on resource use and costs for trainers that are reported, for instance the number of staff involved, the unit cost of staff time, e.g. per hour, day, month, etc. as appropriate, time inputs and total cost. If confidence intervals or standard deviations are reported please include.
-
Is resource use information on trainers reported?
-
Yes
-
No
-
-
Are costs of trainers reported?
-
Yes
-
No
-
-
-
Paid staff If possible please extract available resource and cost information for different staff types reported, e.g. the number of staff involved, the unit cost of staff time, e.g. per hour, day, month, etc., total time inputs and total cost. If confidence intervals or standard deviations are reported please include.
-
Is resource use information on paid staff reported?
-
No
-
Yes
-
-
Are the costs of paid staff reported?
-
Yes
-
No
-
-
-
Volunteers If possible please extract available resource and cost information related to volunteers for different staff types reported, e.g. the number of volunteers involved; time spent volunteering; and total costs. Please list the following information where available: all staff types reported; the number of staff involved; the unit cost of staff time, e.g. per hour, day, month, etc. and total cost.
-
Is resource use information for volunteers reported?
-
Yes
-
No
-
-
Are any costs associated with volunteers, e.g. expenses and allowances, reported?
-
Yes
-
No
-
-
-
Premises/venues Please extract available information on premises/venues given, including those that are provided free of charge. For instance, this might include frequency of use; actual amount of space in metres; unit costs if provided, e.g. hire cost per day; total costs
-
Is resource use information for premises/venues reported?
-
Yes
-
No
-
-
Are any premises/venues reported to be provided free of charge?
-
Yes
-
No
-
-
Are the costs of premises/venues reported?
-
Yes (please describe)
-
No
-
-
-
Transportation Please extract information provided in the paper on any transport resources and costs incurred by the programme. For instance, this might include information on frequency and duration of use, unit costs and total costs. Please include resource use for any transport services provided in kind.
-
Are resource use information for transportation reported?
-
Yes
-
No
-
-
Is any transportation reported to be provided free of charge?
-
Yes
-
No
-
-
Are the costs of premises/venues reported?
-
Yes (please describe)
-
No
-
-
-
Sundry resource use Please extract information on the resources and their costs. This might include a range of diverse items such as printing and material costs for posters. For each type if possible provide information on frequency and duration of use, amount of resources used, unit cost and total costs. Please include any services that are provided free of charge if these are reported.
-
Are any other sundry resources use reported?
-
Yes (please describe)
-
No
-
-
Are any other sundry resources use costs reported to be provided free of charge?
-
Yes (please describe)
-
No
-
-
Are the costs of sundry resource use reported?
-
Yes (please describe)
-
No
-
-
-
-
Economic consequences of interventions Papers may also report the economic impacts of interventions, such as impact on time out of work by participants in community engagement projects. There may also be impacts on the productivity of other family members who have to provide informal care and support.
-
Productivity impacts If reported please extract information available. If possible try and distinguish between average impact per participant, which may be measured using some measure of time such as days out of work or on sick leave, cost per day and total cost per participant, and for the population as a whole.
-
Are any impacts on the productivity of participants reported?
-
Yes (please describe)
-
No
-
-
-
Family members/unpaid carers If reported please extract information available. If possible try and distinguish between average impact per family member/unpaid carer, which may be measured using some measure of time such as days out of work or on sick leave, cost per day and total cost per participant, and for the population as a whole.
-
Are any impacts on the productivity of family members/unpaid carers reported?
-
Yes
-
No
-
-
-
Impacts of use of health/other services Papers may also report whether there is any change in the use of resources as a consequence of the community engagement programme. There might, for example, be consequences for the number of contacts and cost of primary care consultations. There may also be impacts for other public services such as social care, education, criminal justice, etc. Please extract any data that are provided on consequential change in the use of public services, again where possible distinguishing between changes in resource use and change in costs.
-
Are any other resource impacts on the use of health services reported?
-
Yes
-
No
-
-
Are the monetary impacts of changes in the use of health service resources reported?
-
Yes
-
No
-
-
Are any other resource impacts on the use of other publicly funded services (e.g. education, housing, social welfare, social care, criminal justice system) reported?
-
Yes
-
No
-
-
Are the monetary impacts of changes in the use of other public funded service resources reported?
-
Yes
-
No
-
-
-
-
Economic evaluation
-
Compared with a counterfactual, e.g. treatment as usual or ‘do nothing’, have incremental costs of the intervention synthesised alongside incremental changes in outcomes been reported?
-
Yes
-
No
-
-
What type of economic evaluation method was used? Please report summary findings, e.g. incremental cost per benefit gained.
-
Cost-effectiveness analysis (CEA)
-
Cost–utility analysis (CUA)
-
Cost–benefit analysis (CBA)
-
Cost–consequences analysis (CCA)
-
Other (please describe)
-
-
Was any sensitivity analysis of the robustness of economic findings reported?
-
Yes (please describe) If so please briefly indicate whether findings are robust or sensitive to some factor.
-
No
-
-
Do authors indicate whether they consider intervention to be cost-effective? Please state briefly point made – (may be possible to cut/paste any summary statement referring to this).
-
Yes (please describe)
-
No
-
-
-
Availability/flow of funds
-
Were funds available for implementation of initiatives in a timely way (i.e. when needed)?
-
Yes – timely
-
Yes – blocked, sporadic or difficulty accessing
-
No/not described
-
Yes – blocked, sporadic or difficulty accessing
-
-
-
Sufficiency of funds
-
Explicit discussion/acknowledgement of funding sufficiency/insufficiency? Blockages in access to funds/cash can potentially hamper implementation of initiatives. Is there any explicit discussion or acknowledgement of this issue or conversely of the positive benefits of a good flow of funds?
-
Lack of funds hampered
-
Ample sufficient funds helped
-
Not discussed
-
-
-
Securing additional funds
-
Does the paper document any additional funds secured during lifetime of the initiative?
-
Yes
-
No/not discussed
-
-
-
Financial sustainability
-
Is there any explicit discussion on time/resources invested in actions to ensure sustainability/mainstreaming of initiative funding?
-
Yes
-
No/not discussed
-
-
-
Linking investment in intervention and outcome
-
Do authors make an explicit link between investment of time/resources in ensuring sustainability and initiative outcome?
-
Yes – facilitated positive outcome
-
Yes – contributed to poor outcome
-
No/not discussed
-
-
-
Sources of funds
-
Does the paper document the sources of funds for the initiative? (please describe)
-
Charitable institutions
-
User charges/contributions
-
Research grants (includes universities unless otherwise stated)
-
Statutory funding
-
Private sector
-
Other (please describe)
-
Not reported
-
-
-
Role of volunteers
-
Explicit comment/indication that initiative dependent on contribution of unpaid volunteers?
-
Yes, described
-
No/not described
-
-
-
Financial and economic incentives
-
Does the intervention include any use of financial incentives?
-
Cash payments
-
Vouchers
-
Prizes
-
Gym membership
-
Public transportation
-
Child care
-
Other (please describe)
-
Not reported
-
-
Impact on human capital
-
Do authors document an increase in human capital for participants/volunteers in the initiative?
-
Employability
-
Skills
-
Social capital
-
Other (please describe)
-
No/not described
-
-
-
-
Other issues (please describe)
Appendix 6 Results of risk of bias assessment
| Study | Type of control group | Was selection bias avoided? | Allocation method | Was attrition bias avoided? | Was selective reporting bias avoided? | Was the study sound overall? |
|---|---|---|---|---|---|---|
| Anand (2007)71 | Usual treatment/care, with assignment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Anderson (2005)72 | Usual treatment/care, with assignment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | No | Not sound |
| Andrews (2007)73 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Arlotti (1998)74 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – unimportant differences between groups in terms of differences between baseline values of participants and dropouts | Yes | Sound |
| Aseltine (2000)75 | Inactive control | Selection bias unclear/not reported | Partial randomisation | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Not sound |
| Auld (1998)76 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – unimportant differences between groups in terms of differences between baseline values of participants and dropouts | Yes | Sound |
| Auslander (2002)77 | Inactive control | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – unimportant differences between groups in terms of differences between baseline values of participants and dropouts | Yes | Sound |
| Avila (1994)78 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | No – attrition bias not avoided | Yes | Not sound |
| Ayala (2010)79 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | No | Not sound |
| Balcazar (2010)80 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Banks (2009)81 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias not avoided | No | Not sound |
| Baranowski (1990)82 | Inactive control | No – selection bias was not avoided | Random | No – attrition bias was not avoided | Yes | Not sound |
| Barnes (1999)83 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Barnes-Boyd (2001)84 | Matched data from target population, without assignment | No – selection bias was not avoided | Non-random | No – attrition bias was not avoided | No | Not sound |
| Becker (2005)85 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Beech (2003)86 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Black (2010)87 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Partial randomisation | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Botvin (1995)88 | Alternative/placebo intervention | No – selection bias was not avoided | Non-random | Yes – all baseline values of prognostic factors were balanced between groups | Yes | Not sound |
| Britto (2001)89 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Brownson (1996)92 | Matched data from target population, without assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Brownson (2004)90 | Comparator unclear/not reported | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Brownson (2005)91 | Comparator unclear/not reported | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Buller (1999)93 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Partial randomisation | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Campbell (1999)94 | Waitlist/delayed treatment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Partial randomisation | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Campbell (2002)96 | Waitlist/delayed treatment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Attrition bias unclear/not reported | Yes | Not sound |
| Campbell (2004)95 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Caulfield (1998)97 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | No – attrition bias was not avoided | No | Not sound |
| Chapman (2004)98 | Usual treatment/care, with assignment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Cherry (1998)99 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Cochrane (2008)100 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Conway (2004)101 | Inactive control | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Cox (1995)102 | Alternative/placebo intervention | Selection bias unclear/not reported | Allocation unclear/not reported | Attrition bias unclear/not reported | Yes | Not sound |
| Daniel (1999)103 | Usual treatment/care, with assignment | No – selection bias was not avoided | Non-random | Attrition bias unclear/not reported | No | Not sound |
| Davidson (1994)104 | Matched data from target population, without assignment | No – selection bias was not avoided | Non-random | Attrition bias unclear/not reported | Yes | Not sound |
| Davis (1993)105 | Waitlist/delayed treatment | Selection bias unclear/not reported | Random | Attrition bias unclear/not reported | No | Not sound |
| Davis (1995)106 | Waitlist/delayed treatment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Dedobbeleer (2001)107 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Duncan (2000)108 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Elder (1993)110 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Partial randomisation | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Elder (2005)109 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Partial randomisation | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | No | Not sound |
| Ernst (1999)111 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Partial randomisation | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Faridi (2010)112 | Waitlist/delayed treatment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Fisher (1998)113 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Attrition bias unclear/not reported | No | Not sound |
| Fitzgibbon (2005)114 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Partial randomisation | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Foerster (1998)115 | Usual treatment/care, with assignment | No – selection bias was not avoided | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Fried (2004)116 | Waitlist/delayed treatment | No – selection bias was not avoided | Random | No – attrition bias was not avoided | Yes | Not sound |
| Gadomski (2006)117 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Gottfredson (1996)118 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Department for Communities and Local Government (2006)119 | Inactive control | No – selection bias was not avoided | Non-random | No – attrition bias was not avoided | No | Not sound |
| Graham (1992)120 | Usual treatment/care, with assignment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Grummer-Strawn (1997)121 | Matched data from target population, without assignment | Selection bias unclear/not reported | Non-random | Attrition bias unclear/not reported | Yes | Not sound |
| Hancock (2001)122 | Comparator unclear/not reported | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Partial randomisation | Attrition bias unclear/not reported | No | Not sound |
| Hanlon (2002)123 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Attrition bias unclear/not reported | Yes | Not sound |
| Harmon (1995)124 | Waitlist/delayed treatment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Havas (1998)125 | Other | No – selection bias was not avoided | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Not sound |
| Hayashi (2010)126 | Usual treatment/care, with assignment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Hecht (2003)127 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Hunter (2004)128 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Johnson (1993)129 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Julnes (1994)130 | Usual treatment/care, with assignment | No – selection bias was not avoided | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Not sound |
| Karanja (2010)131 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Kim (2008)132 | Waitlist/delayed treatment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Kistin (1994)133 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Kloek (2006)134 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – all baseline values of prognostic factors were balanced between groups | Yes | Sound |
| Krieger (1999)135 | Usual treatment/care, with assignment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Kumpusalo (1996)136 | Alternative/placebo intervention | Selection bias unclear/not reported | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Lewis (1993)137 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Lindenberg (2002)138 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Lindqvist (1999)139 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – all baseline values of prognostic factors were balanced between groups | Yes | Sound |
| Long (1995)140 | Matched data from target population, without assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| LoSciuto (1996)142 | Inactive control | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| LoSciuto (1999)141 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Lupton (2002)143 | Matched data from target population, without assignment | No – selection bias was not avoided | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Not sound |
| Luster (1996)144 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | No – attrition bias was not avoided | Yes | Not sound |
| Macaulay (1997)145 | Usual treatment/care, with assignment | No – selection bias was not avoided | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Malchodi (2003)146 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | No – attrition bias was not avoided | Yes | Not sound |
| Marcenko (1996)147 | Usual treatment/care, with assignment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| McAlister (1992)148 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| McInnes (1998)149 | Inactive control | No – selection bias was not avoided | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Not sound |
| McNabb (1993)151 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| McNabb (1997)150 | Waitlist/delayed treatment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | No – attrition bias was not avoided | Yes | Not sound |
| Mendoza (2009)152 | Waitlist/delayed treatment | No – selection bias was not avoided | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Miller-Heyl (1998)153 | Inactive control | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Nafziger (2001)154 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – unimportant differences between groups in terms of differences between baseline values of participants and dropouts | Yes | Sound |
| Norr (2003)155 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| O’Loughlin (1999)156 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Parsons (1992)157 | Usual treatment/care, with assignment | No – selection bias was not avoided | Non-random | No – attrition bias was not avoided | No | Not sound |
| Perry (1996)158 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Platt (2003)159 | Matched data from target population, without assignment | No – selection bias was not avoided | Non-random | Attrition bias unclear/not reported | No | Not sound |
| Poland (1992)160 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Poston (2001)161 | Waitlist/delayed treatment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | No – attrition bias was not avoided | Yes | Not sound |
| Pugh (2001)163 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Pugh (2002)162 | Usual treatment/care, with assignment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Reijneveld (2003)164 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Partial randomisation | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Resnicow (1992)166 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Resnicow (2004)165 | Comparator unclear/not reported | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Partial randomisation | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Rhodes (2005)167 | Waitlist/delayed treatment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | No | Not sound |
| Robinson (2003)168 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Rodewald (1999)169 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Rose (1992)170 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Schafer (1998)171 | Inactive control | No – selection bias was not avoided | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Schensul (2009)172 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | No – attrition bias was not avoided | Yes | Not sound |
| Schinke (2000)173 | Inactive control | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Schorling (1997)174 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Schuler (2002)175 | Inactive control | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Schwarz (1993)176 | Inactive control | No – selection bias was not avoided | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Not sound |
| Secker-Walker (2000)177 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Shaw (1997)179 | Matched data from target population, without assignment | Selection bias unclear/not reported | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Not sound |
| Shaw (1999)178 | Other | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | No – attrition bias was not avoided | Yes | Not sound |
| Shelley (2008)180 | Inactive control | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Silver (1997)181 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Simmons (1998)182 | Waitlist/delayed treatment | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Solomon (2000)184 | Usual treatment/care, with assignment | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Solomon (2000)183 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Sorensen (2005)185 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Partial randomisation | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Staten (2004)187 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | No – attrition bias was not avoided | Yes | Not sound |
| St James (1999)186 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Attrition bias unclear/not reported | No | Not sound |
| Valente (2006)188 | Alternative/placebo intervention | Selection bias unclear/not reported | Partial randomisation | Yes – all baseline values of prognostic factors were balanced between groups | Yes | Sound |
| Vogler (2002)189 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Attrition bias unclear/not reported | Yes | Not sound |
| Voorhees (1996)190 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Watkins (1994)191 | Other | Selection bias unclear/not reported | Allocation unclear/not reported | No – attrition bias was not avoided | Yes | Not sound |
| Weiss (1998)192 | Waitlist/delayed treatment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Random | Attrition bias unclear/not reported | Yes | Not sound |
| Wiist (1990)193 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Wilcox (2007)194 | Waitlist/delayed treatment | Selection bias unclear/not reported | Random | No – attrition bias was not avoided | Yes | Not sound |
| Winkleby (2004)195 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | Yes | Sound |
| Witmer (2004)196 | Waitlist/delayed treatment | Selection bias unclear/not reported | Random | Attrition bias unclear/not reported | Yes | Not sound |
| Woodruff (2002)197 | Alternative/placebo intervention | Yes – participants were allocated using acceptable method of randomisation and groups equivalent or unimportant differences | Random | Yes – all baseline values of prognostic factors were balanced between groups | Yes | Sound |
| Wright (1997)198 | Matched data from target population, without assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and groups were equivalent | Non-random | Attrition bias unclear/not reported | No | Not sound |
| Yanek (2001)199 | Alternative/placebo intervention | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Partial randomisation | Yes – ITT approach or imbalances in attrition between groups adjusted for in analysis | Yes | Sound |
| Zavela (2004)200 | Usual treatment/care, with assignment | Yes – baseline characteristics reported for virtually all members of each group as allocated and imbalances between groups adjusted for in analysis | Non-random | Attrition bias unclear/not reported | Yes | Not sound |
| Zhou (2003)201 | Matched data from target population, without assignment | Selection bias unclear/not reported | Non-random | Yes – the difference in attrition rates between the groups is < 10% and the total sample attrition rate is < 30% | No | Not sound |
Appendix 7 Results of methodological assessment of process evaluations
| Study | Methods of data collection | PE participants | PE timing with respect to intervention | PE sampling methods | PE data collection methods | PE analysis methods | Findings supported by data | Breadth and depth of findings | Extent PE privileges views | Reliability of findings | Usefulness of findings |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Andrews (2007)73 | Focus group (p. 333, Table 1); interview (p. 333, Table 1); other (specify) – analysis and interpretation of pilot study (p. 333, Table 1) | A sample of the study population (p. 333) – study participants and advisory board members, unknown numbers | Concurrent (pp. 333–4, Tables 1 and 2) | Yes, several steps taken (p. 333) –reasonable multimethod PE with two different types of community members – but could have asked community health workers | Yes, a few steps taken (p. 333) – two different types of data collection methods given –but no further detail on tool development or testing provided | Unclear/can’t tell/not stated – none given | Limited grounding/support – no quotes | Good/fair breadth and depth – surface and deep structures described – their application to intervention development described = transformation | A lot – intervention obviously built on interviewees feedback | Low reliability | Medium usefulness |
| Chapman (2004)98 | Documents (p. 900); interviews (p. 900) | A sample of the study population (p. 899, Figure 1) – 77 intervention, 67 control – those included in analyses only | Concurrently (p. 899, Figure 1) | Yes – fairly thorough attempt made (p. 900, Table 1) | Yes, a few steps taken (p. 899) –several interviews during intervention and record review | Yes – several steps taken (p. 900, Figure 2) – relative risks, 95% CIs | Reasonably well grounded/supported –dosage being evaluated, appropriately done | Limited breadth or depth – dosage only | Not at all – views not sought, just frequency of contact and breastfeeding Y/N | Medium reliability | Low usefulness |
| Davis (1999)243,244 | Interviews –teachers; other (specify) – surveys | Intervention provider – teachers (n = 235); a sample of the study population – students (n = 585),families (unknown n) | Concurrently –each year | Yes – fairly thorough attempt made –whole sample evaluated | Yes, several steps taken – mixed-methods tool, previously developed, repeatedly administered | Yes – several steps taken –descriptive and inferential methods described, regression modelling – but qualitative methods of analysis not described | Reasonably well grounded/supported –statistics and quotes provided | Good/fair breadth but very little depth –’reach’, extent and fidelity measured –reach is meaningless as all students had to do intervention; amount of implementation presented, but little further analysis of this; qualitative component might have added to this but findings do not appear to have been presented | Somewhat – open-ended-questions; community engagement in formative part of design; but no mention of confidentiality, researcher perspective or qualitative synthesis methods | High reliability | Medium usefulness |
| Duggan (1999)476 | Documents; interviews – ’structured maternal interviews’ | A sample of the study population (n = 5810) – records reviewed, unknown number of maternal interviews (possibly 353) | Afterwards – at 1 year | Yes, a few steps taken – clear description of results of documentation data collection but not maternal interviews | Yes, a few steps taken – clear description of results of documentation data collection but not maternal interviews | Yes – a few steps taken –ANOVA and chi-square described – no mention of interview data analysis methods | Fairly well grounded/supported – for quantitative data, but not for qualitative data! | Limited breadth or depth – very little information on accessibility or implementation – from documentation sources only | A little – maternal interviews listed in methods section but no further detail on sample, methods or results provided | Medium reliability – large sample size for quantitative analysis, reasonable methods of analysis described, findings grounded in data but missing qualitative data! | Low usefulness |
| Grant (1999)477 | Documents (Grant p. 14) | A sample of the study population – unknown numbers | Concurrently (Grant, p. 13) | Unclear/can’t tell/not stated – not described | Unclear/can’t tell/not stated –not described | Yes – a few steps taken –appropriate statistics but strange categories for participation as authors combined two quartile ranges into one so that there were three categories describing amount of provider contact: 32–36 months, 9–31 months and < 8 months | Fairly well grounded/supported) – but 50th and 75th quartiles combined | Limited breadth or depth – because of quartile grouping – only contact/exposure measured | Not at all | Low reliability | Low usefulness |
| Quinn (2001)375 | Observation (p. 235) | Intervention provider (p. 235) – all providers and participants were included in the process evaluation | Concurrently (p. 235) | Yes – fairly thorough attempt made (p. 235) – all participants, providers; all sessions | Yes, several steps taken (p. 235) – structured observation, multiple ways of assessing content delivery, but no pretesting or inter-rater reliability described | Unclear/can’t tell/not stated | Reasonably well grounded/supported (p. 235) –participation rates | Good/fair breadth but very little depth –participation rates reported, no further analysis | A little – community engagement in design of study but not in PE | Medium reliability | Low usefulness |
| Ritchie (2004)381 | Interviews (p. 53); other (specify) (p. 53) – before/after surveys | Intervention provider (p. 53) – intervention team members, community workers; a sample of the study population (p. 53) –possibly community members in ‘subgroup’; other (p. 53) –managers, project co-ordinators | Concurrently (p. 53) | Yes, several steps taken (p. 53) – different participant stakeholders but not participants themselves | Yes – fairly thorough attempt made (p. 53) –mixed-methods data collection, tool development described and adequate, recorded interviews | Yes – fairly thorough attempt made (p. 53) – three researchers involved, transcribed and thematically analysed, congruence of coding tested, descriptive frequencies for quantitative data | Reasonably well grounded/supported (pp. 54–5) – quotes used | Good/fair breadth and depth (pp. 54–5) | Somewhat – lots of organisation members and service providers, community members possibly represented in ‘subgroup’ interviews but not clear | High reliability | High usefulness |
| Wickizer (1998)475 | Documents (p. 125) | Not stated/unclear (p. 125) – likely researchers | Concurrently (p. 125) | Yes, a few steps taken – grant holders but not community members | Yes, a few steps taken – ongoing data collection but that’s all | Unclear/can’t tell/not stated – not described | Fairly well grounded/supported – data presented in tables support text | Good/fair breadth/depth – several processes described | Not at all –researchers’ views not public’s! | Low reliability | Medium usefulness –because lots of processes |
| Wilcox (2007)194 | Other (specify) (p. 132) – telephone survey | A sample of the study population – unknown numbers | Afterwards (p. 133) –programme implementation; concurrent (p. 132) –programme awareness | Unclear/can’t tell/not stated (p. 132) – ’church members’ but unclear whether participants/engagees | Yes, a few steps taken (p. 133) –ongoing surveys, no mention of tool pretesting, development; also only one type of data collection method used | Yes – fairly thorough attempt made (p. 133) – generalised estimating equation modelling | Reasonably well grounded/supported (pp. 134–5) – results reported according to survey responses – %s, ORs, CIs | Good/fair breadth and depth – given that they assessed limited processes | A little – participants were asked about pastor support, programme awareness and participation, but very little information beyond this | Medium reliability | Low usefulness |
Appendix 8 Characteristics of included studies
Characteristics of studies included in the map
| Study | Population characteristics | Intervention | Community engagement | Outcomes |
|---|---|---|---|---|
| Aarons (2000)202 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-Plus characteristic: gender Secondary PROGRESS-Plus characteristics: ethnicity: ethnic background, socioeconomic position, education, social capital, gender Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: reproductive health Other health issues: reproductive health, sexual health, teenage pregnancy Site: educational setting (school, college, university) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, risk assessment (not medical screening), screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: consulted Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Ahmed (2010)203 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-Plus characteristic: socioeconomic position Secondary PROGRESS-Plus characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: outreach; phone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Intervention type: education, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
Health outcomes: cancer screening |
| Allen (1997)204 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-Plus characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-Plus characteristics: ethnicity: ethnic background, gender Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: reproductive health Other health issues: HIV/AIDS/STI prevention/risk reduction, mental health, sexual health, teenage pregnancy Site: community setting, outreach, educational setting (school, college, university) Person(s) delivering the intervention: community member, community worker, teacher and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, other Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
|
| Allen (2008)205 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-Plus characteristic: ethnicity: ethnic background Secondary PROGRESS-Plus characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: other topics (specify) Other health issues: diabetes prevention/management, healthy eating/nutrition, physical activity Site: unclear/not specified Person(s) delivering the intervention: researcher Is this a multicomponent intervention? No – only one component Intervention type: education, social support Was training provided to the engagees? No Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: other community engagement strategy |
|
| Anand (2007)71 | Country: Canada Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-Plus characteristic: ethnicity: ethnic background Secondary PROGRESS-Plus characteristics: occupation/employment status, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, physical activity Site: home situation (not residential care home) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, counselling (based on the psychological needs of the individual), resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: healthy eating, physical activity |
| Andersen (2000)206 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: Place of Residence Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, religious settings (e.g. churches), home situation (not residential care home), residential care (includes nursing homes, sheltered housing), mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term), volunteering/volunteers (explicit use of term) |
|
| Andersen (2000)207 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, education, marital status/family composition Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, primary health care (e.g. GP), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Intervention type: activities (e.g. community fairs/fetes), advice, education, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
|
| Anderson (2005)72 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: breastfeeding Site: home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinics) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, counselling (based on the psychological needs of the individual), social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Andrews (2007)73 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: community setting, home situation (not residential care home), mass media – untailored (generic) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, counselling (based on the psychological needs of the individual), social support, incentives, resource access, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community partnership, community coalitions, community task force; any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: smoking cessation Public health participant personal outcomes: public health participant self-efficacy, public health participant social support/capital |
| Arlotti (1998)74 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: social capital Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: breastfeeding Site: WIC clinic; telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, counselling (based on the psychological needs of the individual), social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Aseltine (2000)75 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: public health/health promotion/prevention, substance abuse Site: community setting, educational setting (school, college, university), residential care (includes nursing homes, sheltered housing), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, teacher and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: inactive control Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: other community engagement strategy |
Health outcomes: alcohol abuse, drug abuse |
| Auld (1998)76 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, gender Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: healthy eating/nutrition Other health issues: healthy eating/nutrition Site: educational setting (school, college, university), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: teachers and education professionals (lecturer, principal, etc.), other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, skill development/training, professional training Was training provided to the engagees? No Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks): measurement time unclear/not reported Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: no community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: other community engagement strategy |
Health outcomes: healthy eating Public health participant personal outcomes: public health participant self-efficacy |
| Auslander (2002)77 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: healthy eating/nutrition Site: telephone, print or audio/visual media – tailored, unclear/not specified Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: healthy eating |
| Avila (1994)78 | Country: USA Age group: adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, physical activity Site: unclear/not specified Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, social support, physical activity, exercise Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: healthy eating, obesity/weight status, other not captured above Public health participant personal outcomes: public health participant self-efficacy |
| Ayala (2010)79 | Country: USA Age group: adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, parenting, physical activity Site: outreach, educational setting (school, college, university), home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, environmental modification Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Time between post-test and only/final follow-up Type of control group: inactive control Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term) |
Health outcomes: parenting Public health participant personal outcomes: public health participant self-efficacy |
| Baker (1995)209 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, gender, other vulnerable groups (specify) Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: violence prevention Other health issues: mental health, safe community, substance abuse, violence prevention Site: community setting, outreach Person(s) delivering the intervention: community member, community worker, peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, social support, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term) |
|
| Baker (1997)210 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: public health/health promotion/prevention Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community organisations – developing new and existing services, community partnership, community coalitions, community task force, non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
|
| Balcazar (2010)80 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: cardiovascular disease, healthy eating/nutrition, hypertension, physical activity Site: secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: education, social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term) |
Health outcomes: obesity/weight status Public health participant personal outcomes: public health participant self-efficacy |
| Banks (2009)81 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: diabetes prevention/management, healthy eating/nutrition, physical activity, public health/health promotion/prevention Site: religious settings (e.g. churches) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, physical activity, exercise Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), volunteering/volunteers (explicit use of term) |
Health outcomes: physical activity, other not captured above Public health participant personal outcomes: public health participant self-efficacy |
| Baranowski (1990)82 | Country: USA Age group: children (0–10 years), young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, education, gender, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, physical activity Site: community setting Person(s) delivering the intervention: counsellor Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, incentives, physical activity, exercise Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: consulted (piloting of intervention delivery is included here if there is a feedback mechanism) Community involvement in evaluation: not involved/unclear Community engagement strategy: other community engagement strategy |
Health outcomes: physical activity Public health participant personal outcomes: public health participant self-efficacy |
| Barnes (1999)83 | Country: USA Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: immunisation Other health issues: immunisation Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: volunteering/volunteers (explicit use of term) |
Health outcomes: immunisation |
| Barnes-Boyd (2001)84 | Country: USA Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: other topics (specify) Other health issues: breastfeeding, child illness and ill health, healthy eating/nutrition, parenting Site: home situation (not residential care home) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: child illness and ill health |
| Basen-Engquist (2001)212 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: sexual health Other health issues: HIV/AIDS/STI prevention/risk reduction, reproductive health, sexual health, teenage pregnancy Site: community setting, educational setting (school, college, university), mass media – untailored (generic) Person(s) delivering the intervention: community member, peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, resource access, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Becker (2005)85 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: education, gender, marital status/family composition Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: hypertension Other health issues: healthy eating/nutrition, hypertension, physical activity, smoking cessation Site: community setting, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, counselling (based on the psychological needs of the individual), physical activity, exercise, resource access, risk assessment (not medical screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: leading Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: cardiovascular disease, healthy eating |
| Beech (2003)86 | Country: USA Age group: children (0–10 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, gender Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, physical activity Site: community setting Person(s) delivering the intervention: other Is this a multicomponent intervention? No – only one component Intervention type: activities (e.g. community fairs/fetes), education, physical activity, exercise Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: obesity/weight status, physical activity Public health participant personal outcomes: public health participant self-efficacy |
| Best (1996)214 | Country: USA Age group: young people (11–21 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer prevention Other health issues: cancer prevention Site: educational setting (school, college, university) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: cancer screening |
| Bird (1998)215 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education, marital status/family composition, other vulnerable groups (specify) Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: unclear/not specified Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, incentives Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Black (1995)216 | Country: USA Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: child illness and ill health Other health issues: healthy eating/nutrition, parenting, other topics (specify) Site: home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, counselling (based on the psychological needs of the individual), risk assessment (not medical screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Black (2010)87 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, physical activity Site: community setting, home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, physical activity, exercise, resource access, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: obesity/weight status, physical activity |
| Blamey (2004)217 | Country: UK Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, physical activity, smoking/tobacco prevention Site: community setting, primary health care (e.g. GP) Person(s) delivering the intervention: community member, other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, physical activity, exercise, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services, volunteering/volunteers (explicit use of term) |
|
| Bolam (2006)218 | Country: UK Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: mental health, public health/health promotion/prevention Site: computer based, internet based and virtual interventions Person(s) delivering the intervention: community member, computer, other Is this a multicomponent intervention? No – only one component Intervention type: advice, education, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), social networks (explicit use of term) |
|
| Booth (1999)219 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health, substance abuse Site: unclear/not specified Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Borgia (2005)220 | Country: other (specify) Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health Site: educational setting (school, college, university) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Botvin (1995)88 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: substance abuse Site: educational setting (school, college, university) Person(s) delivering the intervention: other, unclear/not reported Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: informed Community involvement in evaluation: not involved/unclear Community engagement strategy: other community engagement strategy |
Health outcomes: alcohol abuse, drug abuse Public health participant personal outcomes: public health participant self-efficacy |
| Britto (2001)89 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: socioeconomic position, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: child abuse prevention, sexual health, substance abuse, other topics (specify) Site: educational setting (school, college, university) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), unclear/not reported Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: advice, education, skill development/training, counselling (based on the psychological needs of the individual), service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: no clear community engagement label used (explain) |
Health outcomes: other not captured above |
| Broadhead (1995)222 | Country: USA Age group: adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, gender Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, substance abuse Site: community setting Person(s) delivering the intervention: community member, peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, incentives, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term) |
|
| Brown (2002)223 | Country: USA Age group: general population based Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: healthy eating/nutrition, physical activity, other topics (specify) Site: community setting, religious settings (e.g. churches), educational setting (school, college, university), primary health care (e.g. GP) Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, skill development/training, social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: other not captured above Public health participant personal outcomes: public health participant social support/capital |
| Brown (2005)224 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: healthy eating/nutrition, physical activity, other topics (specify) Site: community setting, religious settings (e.g. churches), educational setting (school, college, university), primary health care (e.g. GP) Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, skill development/training, social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Brownson (1996)90 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: education, place of residence, other vulnerable groups (specify) Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, physical activity Site: community setting, religious settings (e.g. churches), mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, other Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification, physical activity, exercise, screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force |
Health outcomes: obesity/weight status, physical activity |
| Brownson (2004)91 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education, place of residence Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: physical activity Other health issues: healthy eating/nutrition, physical activity, smoking/tobacco prevention Site: community setting, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health promotion practitioner, researcher Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, social support, environmental modification, incentives, resource access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: duration unclear/not reported Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: comparator unclear/not reported Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community organisations – developing new and existing services; community partnership, community coalitions, community task force |
Health outcomes: physical activity |
| Brownson (2005)92 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education, gender Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: physical activity Other health issues: diabetes prevention/management, healthy eating/nutrition, physical activity, public health/health promotion/prevention Site: community setting, primary health care (e.g. GP) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, social support, environmental modification, incentives, physical activity, exercise Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: comparator unclear/not reported Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services |
Health outcomes: physical activity |
| Buller (1999)93 | Country: USA Age group: general population based Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: healthy eating/nutrition Other health issues: healthy eating/nutrition Site: workplace site, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: healthy eating |
| Bullock (1995)225 | Country: New Zealand Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics, occupation/employment status, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: parenting, other topics (specify) Other health issues: breastfeeding, healthy eating/nutrition, mental health, parenting, smoking cessation, substance abuse Site: telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: counselling (based on the psychological needs of the individual), social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
|
| Campbell (1999)94 | Country: USA Age group: general population based Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer prevention Other health issues: healthy eating/nutrition Site: Religious settings (e.g. churches etc.), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Religious leader (e.g. parson, priest) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, social support, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership; community coalitions; community task force Non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: healthy eating Public health participant personal outcomes: public health participant self-efficacy |
| Campbell (2002)95 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: occupation/employment status Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, gender, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: cancer screening/detection, healthy eating/nutrition, physical activity, smoking cessation Site: workplace site, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, social support, environmental modification Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: healthy eating, smoking cessation |
| Campbell (2004)96 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer prevention Other health issues: cancer screening/detection, healthy eating/nutrition, physical activity Site: religious settings (e.g. churches), outreach, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: healthy eating |
| Campbell (2008)226 | Country: UK Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence, gender Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: smoking/tobacco prevention Other health issues: smoking/tobacco prevention Site: educational setting (school, college, university) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) time between post-test and only/final follow-up Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), social networks (explicit use of term) |
Health outcomes: smoking/tobacco prevention |
| Carballo-Dieguez (2005)227 | Country: USA Age group: general population based Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: sexual orientation Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: unclear/not specified Person(s) delivering the intervention: teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? No – only one component Intervention type: education, counselling (based on the psychological needs of the individual), social support, incentives Was training provided to the engagees? No Were outcomes measured for the engagees? Yes |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: no clear community engagement label used (explain) |
|
| Carroll (2006)228 | Country: USA Age group: older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: social capital Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: care of older people Other health issues: cardiovascular disease, care of older people Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Caulfield (1998)97 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, education, marital status/family composition Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: breastfeeding Other health issues: breastfeeding Site: home situation (not residential care home), WIC clinic, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| CDC AIDS Community Demonstration Projects Research Group (1999)285 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: outreach, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, resource access, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
|
| Centers for Disease Control and Prevention (1996)374 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: place of residence, sexual orientation Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: community setting, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker Is this a multicomponent intervention? No – only one component Intervention type: advice, skill development/training, environmental modification, incentives, risk assessment (not medical screening), role modelling and role playing, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
|
| Chaisson (2001)229 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, occupation/employment status Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: tuberculosis Other health issues: HIV/AIDS/STI prevention/risk reduction, public health/health promotion/prevention, substance abuse, tuberculosis Site: secondary health-care unit (e.g. hospital; specialist clinics) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer, other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: counselling (based on the psychological needs of the individual), social support, incentives, clinical treatment Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Chapman (2004)230 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: antenatal (prenatal) care, breastfeeding Site: home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, social support, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Cheadle (2001)232 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: public health/health promotion/prevention Other health issues: HIV/AIDS/STI prevention/risk reduction, reproductive health, substance abuse, violence prevention, teenage pregnancy Site: community setting Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force |
Community outcomes |
| Chernoff (2002)233 | Country: USA Age group: children (0–10 years), young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: disability Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: disabilities and chronic illness Other health issues: mental health, parenting Site: community setting, home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Cherry (1998)99 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, social capital, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: parenting, smoking cessation, smoking/tobacco prevention, substance abuse Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: other, unclear/not reported Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: activities (e.g. community fairs/fetes), advice, education, counselling (based on the psychological needs of the individual), resource access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks): measurement time unclear/not reported Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community organisations – developing new and existing services; community partnership, community coalitions, community task force |
Health outcomes: drug abuse |
| Clarke (1992)234 | Country: UK Age group: older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: social capital Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group; targeted and comparison within a PROGRESS-Plus category |
Primary health issue: care of older people Other health issues: care of older people Site: home situation (not residential care home) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Clover (1996)235 | Country: Australia Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, screening. For medical screening, e.g. breast screening, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services |
|
| Cochrane (2008)100 | Country: UK Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: physical activity Other health issues: physical activity Site: community setting, primary health care (e.g. GP), mass media – untailored (generic) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, social support, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: physical activity |
| Conway (2004)101 | Country: USA Age group: children (0–10 years), young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: child illness and ill health Other health issues: smoking cessation, smoking/tobacco prevention Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, skill development/training, social support, biofeedback Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Time between post-test and only/final follow-up Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term) |
Health outcomes: child illness and ill health |
| Corkery (1997)236 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education, place of residence, social capital Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: diabetes prevention/management Other health issues: diabetes prevention/management Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
|
| Cottler (1998)237 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: mental health, sexual health, substance abuse, other topics (specify) Site: secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, resource access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: ‘outreach’ programme (explicit use of term) |
|
| Cox (1995)102 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer prevention Other health issues: healthy eating/nutrition Site: community setting, home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: healthy eating |
| Coyle (2001)238 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: sexual health Other health issues: HIV/AIDS/STI prevention/risk reduction, reproductive health, sexual health, teenage pregnancy Site: community setting, outreach, educational setting (school, college, university), home situation (not residential care home) Person(s) delivering the intervention: community member, researcher, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, counselling (based on the psychological needs of the individual), social support, resource access, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), non-peer health advocacy (e.g. lay health, community health workers) |
|
| Crump (2008)239 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker Is this a multicomponent intervention? No – only one component Intervention type: advice, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Curnow (2002)240 | Country: UK Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: other topics (specify) Other health issues: other topics (specify) Site: educational setting (school, college, university) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: skill development/training, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
|
| Daniel (1999)103 | Country: Canada Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: education, gender, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: healthy eating/nutrition, physical activity, smoking cessation Site: community setting, mass media – untailored (generic) Person(s) delivering the intervention: community member, community worker, health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, social support, incentives, physical activity, exercise, screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services; community partnership, community coalitions, community task force; any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: physical activity |
| Davidson (1994)104 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: injury prevention Other health issues: safe community, violence prevention Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, environmental modification, physical activity, exercise, resource access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force |
Health outcomes: injury/safety |
| Davis (1993)105 | Country: USA Age group: children (0–10 years), young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: cardiovascular disease, healthy eating/nutrition, physical activity, smoking/tobacco prevention Site: community setting, educational setting (school, college, university), home situation (not residential care home) Person(s) delivering the intervention: community member, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks): measurement time unclear/not reported Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: obesity/weight status |
| Davis (1994)241 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: religious settings (e.g. churches) Person(s) delivering the intervention: health promotion practitioner, peer Is this a multicomponent intervention? No – only one component Intervention type: education, screening (for medical screening, e.g. breast screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), social networks (explicit use of term) |
|
| Davis (1995)106 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: gender Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cardiovascular disease Other health issues: cardiovascular disease, healthy eating/nutrition, physical activity, smoking cessation, smoking/tobacco prevention Site: educational setting (school, college, university) Person(s) delivering the intervention: community member, community worker, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, skill development/training, social support, environmental modification, professional training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: consulted Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
Health outcomes: smoking cessation |
| Davis (1998)245 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Davis (2003)243 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, physical activity Site: community setting, educational setting (school, college, university), residential care (includes nursing homes, sheltered housing) Person(s) delivering the intervention: community member, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: comparator unclear/not reported Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation Any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
Health outcomes: healthy eating |
| Davis (2008)242 | Country: UK Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: substance abuse Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? No – only one component Intervention type: advice, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
|
| Dedobbeleer (2001)107 | Country: Canada Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: physical activity Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse), social worker, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, counselling (based on the psychological needs of the individual), social support, physical activity, exercise, resource access, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services; community partnership, community coalitions, community task force |
Health outcomes: alcohol abuse |
| Dennison (2007)246 | Country: USA Age group: adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background, multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: hypertension Other health issues: hypertension Site: community setting, home situation (not residential care home), primary health care (e.g. GP), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, counselling (based on the psychological needs of the individual), social support, clinical treatment Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Department for Communities and Local Government (2006)119 | Country: UK Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: housing Site: community setting Person(s) delivering the intervention: community worker, other Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: other Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
Community outcomes |
| Dickson-Gomez (2006)248 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health, substance abuse Site: community setting, outreach Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| DiClemente (1995)249 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction, not Marmot topics Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Dignan (1996)250 | Country: USA Age group: general population based Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Dignan (1998)251 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education, marital status/family composition Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: home situation (not residential care home) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Duggan (1996)252 | Country: USA Age group: children (0–10 years), young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: child abuse prevention, parenting Other health issues: child abuse prevention, child illness and ill health, healthy eating/nutrition, housing, injury prevention, parenting, partner violence, substance abuse Site: home situation (not residential care home) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, skill development/training, social support, role modelling and role playing, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community organisations – developing new and existing services |
|
| Duncan (2000)108 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: substance abuse Other health issues: substance abuse Site: educational setting (school, college, university), computer-based, internet-based and virtual interventions Person(s) delivering the intervention: computer Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: advice, education, incentives, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: no clear community engagement label used (explain) |
Public health participant personal outcomes: public health participant self-efficacy |
| Earp (2002)254 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: outreach, primary health care (e.g. GP), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, community worker, other Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, social support, incentives, resource access, screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
|
| Eisenman (2009)258 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: other topics (specify) Other health issues: other topics (specify) Site: unclear/not specified Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term), social networks (explicit use of term) |
|
| Elder (1993)110 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: smoking/tobacco prevention Other health issues: smoking/tobacco prevention Site: educational setting (school, college, university), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, non-peer health advocacy (e.g. lay health, community health workers), volunteering/volunteers (explicit use of term) |
Health outcomes: smoking/tobacco prevention |
| Elder (2005)109 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: healthy eating/nutrition Other health issues: healthy eating/nutrition Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term) |
Health outcomes: healthy eating |
| Elford (2001)260 | Country: UK Age group: general population based Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction Site: outreach Person(s) delivering the intervention: peer Intervention type: advice Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Ell (2002)261 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer prevention Site: secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, counselling (based on the psychological needs of the individual), screening (for medical screening, e.g. breast screening), service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Ernst (1999)111 | Country: USA Age group: general population based Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: child illness and ill health, mental health, public health/health promotion/prevention, reproductive health, other topics (specify) Site: home situation (not residential care home) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, social support, risk assessment (not medical screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: drug abuse Community outcomes |
| Erwin (1999)262 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer prevention Site: religious settings (e.g. churches) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: leading Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Faridi (2010)112 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: healthy eating/nutrition, physical activity Site: Religious settings (e.g. churches etc.) Outreach Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term) |
Health outcomes: obesity/weight status, physical activity Public health participant personal outcomes: public health participant self-efficacy |
| Ferguson (1998)264 | Country: USA Age group: young people (11–21 years) Sex: majority females (≥90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: Reproductive health Other health issues: sexual health Teenage pregnancy Site: unclear/not specified Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Fernandez-Esquer (2003)265 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting Mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
|
| Fisher (1998)113 | Country: USA Age group: children (0–10 years), young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Smoking/tobacco prevention Site: community setting Religious settings (e.g. churches etc.) Outreach Home situation (not residential care home) Mass media – untailored (generic) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
Health outcomes: smoking cessation |
| Fisher (2005)266 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: community setting, outreach, primary health care (e.g. GP), mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, social support, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force, ‘outreach’ programme (explicit use of term) |
Community outcomes |
| Fitzgibbon (2005)114 | Country: USA Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, physical activity Site: educational setting (school, college, university), home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: parent, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, incentives, physical activity, exercise Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Time between post-test and only/final follow-up Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: obesity/weight status |
| Flaskerud (1997)267 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: reproductive health Site: WIC clinic, unclear/not specified Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, skill development/training, counselling (based on the psychological needs of the individual), incentives, resource access, screening (for medical screening, e.g. breast screening), other Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Fletcher (1993)269 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education, place of residence, age Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, primary health care (e.g. GP), secondary health-care unit (e.g. hospital, specialist clinic), mass media – untailored (generic) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, screening. For medical screening, e.g. breast screening, service access Was training provided to the engagees? No Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force |
|
| Flowers (2002)270 | Country: UK Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: sexual health Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health Site: community setting, secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer, other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation, other Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Foerster (1998)115 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: healthy eating/nutrition Other health issues: healthy eating/nutrition Site: community setting, educational setting (school, college, university), home situation (not residential care home), mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, community worker, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, environmental modification, incentives, resource access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks): measurement time unclear/not reported Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force, volunteering/volunteers (explicit use of term) |
Health outcomes: healthy eating |
| Fogarty (2001)272 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: public health/health promotion/prevention, sexual health Site: community setting, mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, community worker, other Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, skill development/training, social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
|
| Fors (1995)273 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: substance abuse Site: residential care (includes nursing homes, sheltered housing) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Fried (2004)116 | Country: USA Age group: older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: public health/health promotion/prevention Other health issues: care of older people, mental health, physical activity Site: educational setting (school, college, university) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: social support, physical activity, exercise, other Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
Health outcomes: physical activity Engagee personal outcomes: engagee social support/capital/inclusion, engagee health Public health participant personal outcomes: public health participant social support/capital |
| Fuller (2007)274 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, substance abuse Site: community setting, telephone, print or audio/visual media – tailored, computer-based, internet-based, and virtual interventions Person(s) delivering the intervention: community member, community worker, computer, peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, counselling (based on the psychological needs of the individual), resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Gabriel (1996)275 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: violence prevention Other health issues: violence prevention Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: activities (e.g. community fairs/fetes), education, role modelling and role playing, other Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
|
| Gadomski (2006)117 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: injury prevention Other health issues: injury prevention Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Time between post-test and only/final follow-up Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: injury/safety |
| Galbraith (1996)276 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health, substance abuse Site: community setting, home situation (not residential care home) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
|
| Gary (2003)277 | Country: USA Age group: adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: diabetes prevention/management, healthy eating/nutrition, physical activity, smoking cessation Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, social support, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Gibson (1998)278 | Country: Australia Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, occupation/employment status Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: asthma prevention/treatment/management Other health issues: asthma prevention/treatment/management Site: educational setting (school, college, university) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Gielen (1997)279 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: antenatal (prenatal) care, smoking/tobacco prevention Site: primary health care (e.g. GP), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, counselling (based on the psychological needs of the individual), risk assessment (not medical screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Time between post-test and only/final follow-up Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: smoking cessation |
| Gokcay (1993)281 | Country: other (specify) Age group: general population based Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: reproductive health Other health issues: antenatal (prenatal) care, immunisation, parenting, reproductive health Site: home situation (not residential care home), primary health care (e.g. GP) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Gotay (2000)283 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored, unclear/not specified Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, social support, incentives, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Gottfredson (1996)118 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: substance abuse Other health issues: HIV/AIDS/STI prevention/risk reduction, smoking cessation, smoking/tobacco prevention Site: educational setting (school, college, university) Person(s) delivering the intervention: community member, peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, social support, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
Health outcomes: drug abuse Public health participant personal outcomes: public health participant self-efficacy |
| Graham (1992)120 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: antenatal (prenatal) care Other health issues: antenatal (prenatal) care, healthy eating/nutrition Site: home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education, counselling (based on the psychological needs of the individual), social support, role modelling and role playing, screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks): measurement time unclear/not reported Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: no clear community engagement label used (explain) |
Health outcomes: child illness and ill health |
| Griffiths (2005)284 | Country: UK Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: occupation/employment status Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: disabilities and chronic illness Other health issues: disabilities and chronic illness, physical activity Site: community setting, primary health care (e.g. GP) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, counselling (based on the psychological needs of the individual), role modelling and role playing, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Grummer-Strawn (1997)121 | Country: USA Age group: general population based Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: antenatal (prenatal) care, breastfeeding Site: WIC clinic, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? No – only one component Intervention type: advice Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: duration unclear/not reported Length of time between evaluation measures (weeks): measurement time unclear/not reported Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Hamer (2000)286 | Country: UK Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: public health/health promotion/prevention Site: unclear/not specified Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: other Was training provided to the engagees? No Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: collaborating Community engagement strategy: community partnership; community coalitions; community task force |
|
| Hancock (2001)122 | Country: Australia Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer prevention Other health issues: smoking cessation, smoking/tobacco prevention Site: community setting, workplace site, mass media – untailored (generic) Person(s) delivering the intervention: community member, health promotion practitioner, other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification, incentives, resource access, risk assessment (not medical screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: comparator unclear/not reported Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force |
Health outcomes: smoking cessation |
| Hanlon (2002)123 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: HIV/AIDS/STI prevention/risk reduction, smoking/tobacco prevention, substance abuse, violence prevention, other topics (specify) Site: community setting Person(s) delivering the intervention: community member, community worker Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, social support, resource access, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), volunteering/volunteers (explicit use of term) |
Health outcomes: alcohol abuse, drug abuse |
| Hanson (1998)288 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: asthma prevention/treatment/management Other health issues: asthma prevention/treatment/management Site: outreach, secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Intervention type: advice, education, skill development/training, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Harmon (1995)124 | Country: USA Age group: young people (11–21 years) Sex: majority females (≥90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics, occupation/employment status, education, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: Parenting Partner violence Sexual health Smoking cessation Smoking/tobacco prevention, substance abuse Suicide prevention Site: community setting Person(s) delivering the intervention: community member Community worker Counsellor Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training Counselling (based on the psychological needs of the individual), social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
Health outcomes: alcohol abuse, drug abuse Smoking cessation |
| Havas (1998)125 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer prevention Other health issues: healthy eating/nutrition Site: WIC clinic, mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: other (add details) Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: healthy eating Public health participant personal outcomes: public health participant self-efficacy, public health participant social support/capital |
| Hayashi (2010)126 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, physical activity, smoking/tobacco prevention Site: secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, skill development/training, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term) |
Health outcomes: healthy eating |
| Hecht (2003)127 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: substance abuse Other health issues: substance abuse Site: educational setting (school, college, university), mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, skill development/training, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: consulted (piloting of intervention delivery is included here if there is a feedback mechanism) Community involvement in evaluation: not involved/unclear Community engagement strategy: no clear community engagement label used (explain) |
Health outcomes: alcohol abuse, drug abuse, smoking cessation Public health participant personal outcomes: public health participant self-efficacy |
| Helmert (1993)289 | Country, other (specify) Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, obesity prevention/weight reduction, physical activity, public health/health promotion/prevention, smoking cessation, smoking/tobacco prevention Site: community setting, unclear/not specified Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force |
Health outcomes: hypertension, smoking cessation |
| Hiatt (2008)290 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education, marital status/family composition, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, outreach, primary health care (e.g. GP) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, screening (for medical screening, e.g. breast screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Hill (1999)291 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: hypertension Other health issues: hypertension Site: home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Hill (2003)292 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, place of residence, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: cardiovascular disease Site: home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, social support, service access, other Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Howard (1990)293 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: reproductive health Other health issues: reproductive health, teenage pregnancy Site: educational setting (school, college, university) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Hunter (2004)128 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education, place of residence, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: other topics (specify) Other health issues: cardiovascular disease, cancer screening/detection, diabetes prevention/management Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), promotora (explicit use of term) |
Health outcomes: other not captured above |
| Husaini (2008)294 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, education, marital status/family composition Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: religious settings (e.g. churches), mass media – untailored (generic) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: education Was training provided to the engagees? No Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: other Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), other community engagement strategy |
Health outcomes: cancer screening |
| Hutcheson (1997)295 | Country: USA Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, marital status/family composition Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: child illness and ill health Other health issues: child illness and ill health, parenting Site: home situation (not residential care home) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, social support, resource access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Ireys (1996)296 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: mental health Other health issues: mental health, parenting Site: community setting, home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, counselling (based on the psychological needs of the individual), social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), social networks (explicit use of term) |
|
| Ireys (2001)297 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: mental health Other health issues: mental health, parenting Site: community setting, home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, counselling (based on the psychological needs of the individual), social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), social networks (explicit use of term) |
|
| Jandorf (2008)298 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, marital status/family composition Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, religious settings (e.g. churches), educational setting (school, college, university), home situation (not residential care home) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), peer, researcher Is this a multicomponent intervention? No – only one component Intervention type: education, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), non-peer health advocacy (e.g. lay health, community health workers), volunteering/volunteers (explicit use of term) |
|
| Jemmott (1998)299 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health Site: educational setting (school, college, university) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Johnson (1993)129 | Country: other (specify) Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics, occupation/employment status, place of residence, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: parenting Other health issues: child illness and ill health, healthy eating/nutrition, immunisation, parenting, public health/health promotion/prevention, other topics (specify) Site: home situation (not residential care home) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? No – only one component Intervention type: advice, skill development/training, social support, immunisation Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: child illness and ill health, immunisation |
| Jones (1994)301 | Country: USA Age group: young people (11–21 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, age, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: reproductive health Other health issues: antenatal (prenatal) care, reproductive health, teenage pregnancy Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: education, risk assessment (not medical screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
|
| Julnes (1994)130 | Country: USA Age group: young people (11–21 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: antenatal (prenatal) care Other health issues: antenatal (prenatal) care, parenting Site: home situation (not residential care home) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: duration unclear/not reported Length of time between evaluation measures (weeks): measurement time unclear/not reported Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
Health outcomes: antenatal (prenatal) care, child illness and ill health |
| Karanja (2010)131 | Country: USA Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: breastfeeding, healthy eating/nutrition, other topics (specify) Site: community setting, home situation (not residential care home), mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, environmental modification Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Time between post-test and only/final follow-up Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: breastfeeding, obesity/weight status Public health participant personal outcomes: public health participant self-efficacy |
| Katz (2008)303 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education, place of residence, age Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Kegeles (1996)304 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health Site: community setting, educational setting (school, college, university), mass media – untailored (generic) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term), social networks (explicit use of term), volunteering/volunteers (explicit use of term) |
|
| Kelly (1992)305 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health Site: community setting, outreach Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), other community engagement strategy |
|
| Kelly (1997)306 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: disability Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: advice, education, skill development/training, other Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: informed Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Kennedy (2000)307 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health Site: community setting, outreach, mass media – untailored (generic) Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: education, resource access, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: other Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force |
|
| Kernohan (1996)308 | Country: UK Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, educational setting (school, college, university), primary health care (e.g. GP), secondary health-care unit (e.g. hospital, specialist clinic), workplace site, mass media – untailored (generic) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), non-peer health advocacy (e.g. lay health, community health workers) |
|
| Keyserling (2002)309 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: occupation/employment status, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: diabetes prevention/management, healthy eating/nutrition, physical activity Site: secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: counsellor, health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, counselling (based on the psychological needs of the individual), social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Kim (2004)312 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: religious settings (e.g. churches) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer, religious leader (e.g. parson, priest) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community partnership, community coalitions, community task force Any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Kim (2005)311 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: healthy eating/nutrition, physical activity, smoking cessation, smoking/tobacco prevention Site: community setting, outreach Person(s) delivering the intervention: community member Intervention type: advice Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), promotora (explicit use of term), ‘outreach’ programme (explicit use of term), social networks (explicit use of term) |
|
| Kim (2008)132 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, obesity prevention/weight reduction, physical activity Site: religious settings (e.g. churches) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education, physical activity, exercise Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: community organisations – developing new and existing services; community partnership, community coalitions, community task force; non-peer health advocacy (e.g. lay health, community health workers), social networks (explicit use of term) |
Health outcomes: obesity/weight status, physical activity |
| King (1998)313 | Country: USA Age group: older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: socioeconomic position, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: residential care (includes nursing homes, sheltered housing) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, screening (for medical screening, e.g. breast screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Kirby (1995)315 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, other vulnerable groups (specify) Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: reproductive health Other health issues: reproductive health, teenage pregnancy Site: community setting, educational setting (school, college, university), mass media – untailored (generic) Person(s) delivering the intervention: community member, peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
|
| Kirby (1997)314 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: sexual health Other health issues: reproductive health, sexual health, teenage pregnancy Site: educational setting (school, college, university) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Kirby (1997)316 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: reproductive health Other health issues: reproductive health, sexual health, teenage pregnancy Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: community member, peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Kirby (2004)317 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: sexual health Other health issues: HIV/AIDS/STI prevention/risk reduction, reproductive health, sexual health, teenage pregnancy Site: educational setting (school, college, university), mass media – untailored (generic) Person(s) delivering the intervention: peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Kistin (1994)133 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: breastfeeding, healthy eating/nutrition, parenting Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Kloek (2006)134 | Country: other (specify) Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: education Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: public health/health promotion/prevention Other health issues: healthy eating/nutrition, physical activity, public health/health promotion/prevention, smoking cessation, smoking/tobacco prevention, substance abuse Site: community setting, outreach, educational setting (school, college, university), mass media – untailored (generic) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), researcher, social worker, other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, environmental modification, physical activity, exercise Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, volunteering/volunteers (explicit use of term) |
Health outcomes: healthy eating Public health participant personal outcomes: public health participant self-efficacy |
| Kocken (2008)318 | Country: other (specify) Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: occupation/employment status, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: mental health Other health issues: mental health Site: primary health care (e.g. GP) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, counselling (based on the psychological needs of the individual), social support, role modelling and role playing, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Krieger (1999)135 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cardiovascular disease Other health issues: cardiovascular disease, other topics (specify) Site: community setting, home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
Health outcomes: other not captured above |
| Krieger (2002)319 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: asthma prevention/treatment/management Other health issues: asthma prevention/treatment/management Site: home situation (not residential care home) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, counselling (based on the psychological needs of the individual), social support, environmental modification, risk assessment (not medical screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
|
| Krieger (2005)320 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education, place of residence, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: asthma prevention/treatment/management Other health issues: asthma prevention/treatment/management Site: home situation (not residential care home) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, counselling (based on the psychological needs of the individual), social support, environmental modification, risk assessment (not medical screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
|
| Kumpusalo (1996)136 | Country: other (specify) Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: public health/health promotion/prevention Other health issues: healthy eating/nutrition, physical activity, public health/health promotion/prevention Site: community setting, educational setting (school, college, university), mass media – untailored (generic) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, physical activity, exercise Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force |
Health outcomes: obesity/weight status, physical activity |
| Larkey (2002)322 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: cardiovascular disease, cancer prevention, cancer screening/detection, other topics (specify) Site: unclear/not specified Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), other community engagement strategy |
|
| Latkin (2003)324 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, place of residence, other vulnerable groups (specify) Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health, substance abuse Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, social support, resource access, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term) |
|
| Lauby (2000)324 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, place of residence, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health Site: community setting, outreach, mass media – untailored (generic) Person(s) delivering the intervention: peer, other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, resource access, role modelling and role playing, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term), volunteering/volunteers (explicit use of term) |
|
| Levine (1990)326 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: hypertension Other health issues: hypertension Site: secondary health-care unit (e.g. hospital, specialist clinic), unclear/not specified Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, screening (for medical screening, e.g. breast screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
|
| Levine (1992)325 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: hypertension Other health issues: healthy eating/nutrition, hypertension, physical activity Site: secondary health-care unit (e.g. hospital, specialist clinic), unclear/not specified Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), social worker Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, screening (for medical screening, e.g. breast screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, non-peer health advocacy (e.g. lay health, community health workers) |
|
| Levine (2003)327 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, education, place of residence, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: hypertension Other health issues: healthy eating/nutrition, hypertension, physical activity Site: outreach, home situation (not residential care home) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, counselling (based on the psychological needs of the individual), social support, screening (or medical screening, e.g. breast screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
|
| Levy (1998)328 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction Site: community setting, outreach Person(s) delivering the intervention: counsellor, peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, counselling (based on the psychological needs of the individual), social support, other Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: ‘outreach’ programme (explicit use of term) |
|
| Lewis (1993)137 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: physical activity Other health issues: physical activity Site: community setting, mass media – untailored (generic) Person(s) delivering the intervention: community member, researcher Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, physical activity, exercise, risk assessment (not medical screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community organisations – developing new and existing services, community partnership, community coalitions, community task force |
Health outcomes: physical activity |
| Lindenberg (2002)138 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health, substance abuse Site: community setting Person(s) delivering the intervention: other Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, role modelling and role playing Was training provided to the engagees? No Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: consulted Community engagement strategy: community partnership, community coalitions, community task force |
Health outcomes: alcohol abuse |
| Lindqvist (1999)139 | Country: other (specify) Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: occupation/employment status Secondary PROGRESS-PLUS characteristics: education, gender, age Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: injury prevention Other health issues: injury prevention, safe community Site: secondary health-care unit (e.g. hospital, specialist clinic), workplace site Person(s) delivering the intervention: other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, environmental modification, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services; community partnership, community coalitions, community task force |
Health outcomes: injury/safety |
| Long (1995)140 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: antenatal (prenatal) care, breastfeeding Site: home situation (not residential care home), WIC clinic, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Time between post-test and only/final follow-up Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Lorig (2003)330 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: Disabilities & chronic illness Other health issues: Disabilities & chronic illness, healthy eating/nutrition, physical activity Site: community setting Religious settings (e.g. churches etc.) Secondary health care unit (e.g. hospital; specialist clinics) Mass media – untailored (generic) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training Counselling (based on the psychological needs of the individual), physical activity, exercise Service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| LoSciuto (1996)142 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: public health/health promotion/prevention, substance abuse Site: community setting, educational setting (school, college, university), home situation (not residential care home), mass media – untailored (generic) Person(s) delivering the intervention: community member, researcher, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, counselling (based on the psychological needs of the individual), social support, incentives, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: other community engagement strategy |
Health outcomes: alcohol abuse, drug abuse |
| LoSciuto (1999)141 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: smoking cessation, smoking/tobacco prevention, substance abuse, violence prevention Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: peer, researcher, other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, skill development/training, social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term), volunteering/volunteers (explicit use of term) |
Health outcomes: alcohol abuse, drug abuse, smoking cessation |
| Lupton (2002)143 | Country: other (specify) Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristic: occupation/employment status Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cardiovascular disease Other health issues: cardiovascular disease, healthy eating/nutrition, injury prevention, physical activity, smoking cessation Site: community setting, educational setting (school, college, university), primary health care (e.g. GP), workplace site Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), other Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: advice, education, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: consulted (piloting of intervention delivery is included here if there is a feedback mechanism) Community involvement in evaluation: informed Community engagement strategy: other community engagement strategy |
Health outcomes: hypertension, smoking cessation |
| Lupton (2003)331 | Country: other (specify) Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristic: occupation/employment status Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cardiovascular disease Other health issues: cardiovascular disease, healthy eating/nutrition, injury prevention, physical activity, public health/health promotion/prevention, smoking cessation Site: community setting, educational setting (school, college, university), primary health care (e.g. GP), workplace site, mass media – untailored (generic) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, environmental modification Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: social networks (explicit use of term), other community engagement strategy |
Health outcomes: smoking cessation |
| Lustre (1996)144 | Country: USA Age group: young people (11–21 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: antenatal (prenatal) care Other health issues: antenatal (prenatal) care, parenting Site: home situation (not residential care home) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: parenting |
| Macaulay (1997)145 | Country: Canada Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: healthy eating/nutrition, obesity prevention/weight reduction, physical activity Site: community setting, educational setting (school, college, university), home situation (not residential care home), mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, environmental modification, incentives, physical activity, exercise, resource access, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: consulted Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services; community partnership, community coalitions, community task force, volunteering/volunteers (explicit use of term) |
Health outcomes: obesity/weight status, physical activity |
| Malchodi (2003)146 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, occupation/employment status, education, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: smoking cessation |
| Marcenko (1996)147 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify), multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education, place of residence, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: child abuse prevention Other health issues: healthy eating/nutrition, mental health, parenting, substance abuse, violence prevention Site: home situation (not residential care home) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), peer, social worker Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: child abuse prevention, mental health Public health participant personal outcomes: public health participant social support/capital |
| Margolis (1998)334 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? No – only one component Intervention type: screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| May (1995)335 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: cardiovascular disease, cancer screening/detection, diabetes prevention/management, hypertension Site: community setting Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? No – only one component Intervention type: activities (e.g. community fairs/fetes), screening. For medical screening, e.g. breast screening Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating, consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, promotora (explicit use of term) |
|
| McAlister (1992)148 | Country: USA, other (specify) Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: outreach, mass media – untailored (generic) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, social networks (explicit use of term) |
Health outcomes: smoking cessation |
| McAlister (1995)336 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, outreach, mass media – untailored (generic) Person(s) delivering the intervention: community member, researcher Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: informed Community engagement strategy: community organisations – developing new and existing services, ‘outreach’ programme (explicit use of term), social networks (explicit use of term), volunteering/volunteers (explicit use of term) |
|
| McCue (1996)337 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: tuberculosis Other health issues: tuberculosis Site: educational setting (school, college, university) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
|
| McFarlane (2000)338 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education, age, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: partner violence Other health issues: partner violence, violence prevention Site: home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, counsellor Is this a multicomponent intervention? No – only one component Intervention type: education, counselling (based on the psychological needs of the individual), social support, risk assessment (not medical screening), service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term) |
|
| McInnes (1998)149 | Country: UK Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: socioeconomic position, age, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: breastfeeding Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, skill development/training, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| McInroy (2005)339 | Country: UK Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: neighbourhood renewal/regeneration Other health issues: neighbourhood renewal/regeneration Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: environmental modification Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
|
| McIntosh (2009)340 | Country: UK Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: violence prevention Other health issues: parenting Site: home situation (not residential care home) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, social support, environmental modification Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| McNabb (1993)151 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: diabetes prevention/management, healthy eating/nutrition, physical activity Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: education Was training provided to the engagees? No Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: no community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: other community engagement strategy |
Health outcomes: obesity/weight status |
| McNabb (1997)150 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: diabetes prevention/management, healthy eating/nutrition, physical activity Site: religious settings (e.g. churches) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: education, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), volunteering/volunteers (explicit use of term) |
Health outcomes: obesity/weight status |
| McNeill (2009)341 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, occupation/employment status, education, place of residence, age, marital status/family composition, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: healthy eating/nutrition, physical activity, smoking cessation Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| McPhee (1996)342 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: diabetes prevention/management, HIV/AIDS/STI prevention/risk reduction, reproductive health Site: home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: activities (e.g. community fairs/fetes), advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), social networks (explicit use of term) |
|
| McQuiston (2001)343 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: gender Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: community setting Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, social support, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Mendoza (2009)152 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: physical activity Other health issues: injury prevention, physical activity Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: community member, health promotion practitioner, parent, other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, physical activity, exercise Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: informed Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, volunteering/volunteers (explicit use of term) |
Health outcomes: physical activity |
| Miller (1998)344 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, place of residence, age, other vulnerable groups (specify) Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Miller-Heyl (1998)153 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: parenting Other health issues: substance abuse Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Time between post-test and only/final follow-up Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
Health outcomes: parenting Public health participant personal outcomes: public health participant self-efficacy |
| Morisky (2001)345 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: age Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, place of residence, gender, age Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: tuberculosis Other health issues: tuberculosis Site: community setting, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: parent, peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, incentives Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Motohashi (2007)346 | Country, other (specify) Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristic: age Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: suicide prevention Other health issues: care of older people, mental health Site: community setting, home situation (not residential care home) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), religious leader (e.g. parson, priest), social worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, social support, risk assessment (not medical screening), service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: informed Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services, volunteering/volunteers (explicit use of term) |
|
| Nafziger (2001)154 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: occupation/employment status, education, marital status/family composition Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, physical activity, public health/health promotion/prevention, smoking cessation, smoking/tobacco prevention Site: community setting, educational setting (school, college, university), home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinic), workplace site, mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, community worker, health professional (e.g. GP, dietitian, nurse), health promotion practitioner Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification, physical activity, exercise, screening (for medical screening, e.g. breast screening), service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force, non-peer health advocacy (e.g. lay health, community health workers), volunteering/volunteers (explicit use of term) |
Health outcomes: cardiovascular disease, hypertension |
| Navarro (1998)348 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: leading Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Neuhauser (1998)349 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: socioeconomic position, gender Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: public health/health promotion/prevention Other health issues: antenatal (prenatal) care, breastfeeding, cardiovascular disease, cancer prevention, healthy eating/nutrition, injury prevention, mental health, obesity prevention/weight reduction, parenting, partner violence, physical activity, smoking cessation, smoking/tobacco prevention, substance abuse, violence prevention Site: mass media – untailored (generic) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? No – only one component Intervention type: education, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community organisations – developing new and existing services |
|
| Neumark-Sztainer (2003)350 | Country: USA Age group: young people (11–21 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: gender Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, mental health, physical activity Site: educational setting (school, college, university) Person(s) delivering the intervention: community member, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, physical activity, exercise, resource access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
Health outcomes: physical activity Public health participant personal outcomes: public health participant self-efficacy, public health participant social support/capital |
| Nguyen (2009)351 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, skill development/training, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Norr (2003)155 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, occupation/employment status, education, place of residence, social capital Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: parenting Other health issues: child abuse prevention, healthy eating/nutrition, immunisation, mental health, reproductive health Site: home situation (not residential care home), WIC clinic, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, social support, environmental modification, incentives, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: child illness and ill health, immunisation |
| Nyamathi (2001)352 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: residential care (includes nursing homes, sheltered housing) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| O’Donnell (2002)353 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: sexual health Other health issues: HIV/AIDS/STI prevention/risk reduction, reproductive health, teenage pregnancy Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: community member, teacher and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes) Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: informed Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, volunteering/volunteers (explicit use of term) |
|
| Office of the Deputy Prime Minister (2004)355 | Country: UK Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: neighbourhood renewal/regeneration Other health issues: housing, violence prevention Site: community setting Person(s) delivering the intervention: community member, community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), environmental modification, resource access, risk assessment (not medical screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: leading, consulted Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
|
| Office of the Deputy Prime Minister (2004)354 | Country: UK Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: neighbourhood renewal/regeneration Other health issues: housing, violence prevention Site: community setting Person(s) delivering the intervention: community member, community worker, peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, environmental modification, resource access, risk assessment (not medical screening), service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community partnership, community coalitions; community task force |
|
| Office of the Deputy Prime Minister (2006)356 | Country: UK Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: neighbourhood renewal/regeneration Other health issues: housing, safe community, violence prevention Site: community setting Person(s) delivering the intervention: community member, other Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), environmental modification, resource access, risk assessment (not medical screening), service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force, volunteering/volunteers (explicit use of term) |
|
| O’Hara (1996)358 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: public health/health promotion/prevention, sexual health Site: educational setting (school, college, university) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| O’Hare (2004)359 | Country: UK Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: age Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: cardiovascular disease Site: primary health care (e.g. GP) Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, resource access, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| O’Loughlin (1999)156 | Country: Canada Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, obesity prevention/weight reduction, physical activity, smoking cessation Site: community setting, educational setting (school, college, university), home situation (not residential care home), primary health care (e.g. GP), mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, social support, environmental modification, physical activity, exercise, resource access, screening (for medical screening, e.g. breast screening), service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
Health outcomes: obesity/weight status, smoking cessation |
| Orpinas (1995)360 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: violence prevention Other health issues: mental health Site: educational setting (school, college, university) Person(s) delivering the intervention: peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Outlaw (2010)361 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: ‘outreach’ programme (explicit use of term) |
|
| Parker (2008)363 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: asthma prevention/treatment/management Other health issues: public health/health promotion/prevention, smoking cessation Site: home situation (not residential care home) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, environmental modification, incentives, resource access, risk assessment (not medical screening), service access, biofeedback Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: leading Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force |
|
| Parkin (1993)364 | Country: Canada Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: injury prevention Other health issues: injury prevention Site: educational setting (school, college, university), home situation (not residential care home) Person(s) delivering the intervention: community member, peer, teachers and education professionals (lecturer, principal, etc.), other Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification, resource access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
Health outcomes: injury/safety |
| Parsons (1992)157 | Country: UK Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: antenatal (prenatal) care Other health issues: antenatal (prenatal) care Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: antenatal (prenatal) care |
| Paskett (2006)365 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, home situation (not residential care home), primary health care (e.g. GP) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Peragallo (2005)366 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: partner violence, substance abuse Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, role modelling and role playing, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Perry (1996)158 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: substance abuse Other health issues: parenting Site: community setting, educational setting (school, college, university), mass media – untailored (generic) Person(s) delivering the intervention: community member, peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, environmental modification, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community organisations – developing new and existing services; community partnership, community coalitions, community task force; any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: alcohol abuse, drug abuse, smoking cessation Public health participant personal outcomes: public health participant self-efficacy |
| Philis-Tsimikas (2004)369 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: diabetes prevention/management Other health issues: healthy eating/nutrition Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, skill development/training, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term), no clear community engagement label used (explain) |
|
| Philliber (1992)370 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristic: gender Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: reproductive health Other health issues: other topics (specify), teenage pregnancy Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: other Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: volunteering/volunteers (explicit use of term) |
|
| Pilote (1996)371 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: socioeconomic position, gender, other vulnerable groups (specify) Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: tuberculosis Other health issues: tuberculosis Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: incentives, service access, clinical treatment Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Pinkerton (1998)372 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Platt (2003)159 | Country: UK Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation, smoking/tobacco prevention Site: community setting Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification, resource access, service access, clinical treatment Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? Yes Duration: duration unclear/not reported Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force |
Health outcomes: smoking cessation |
| Poland (1992)160 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: antenatal (prenatal) care Other health issues: breastfeeding, child abuse prevention, housing, injury prevention, mental health, parenting Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, social support, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks): measurement time unclear/not reported Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: antenatal (prenatal) care, child illness and ill health |
| Poston (2001)161 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: healthy eating/nutrition, physical activity Site: community setting Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, skill development/training, social support, physical activity, exercise Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), social networks (explicit use of term) |
Health outcomes: obesity/weight status, physical activity |
| Powell (2005)373 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Pugh (2001)163 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: breastfeeding Site: home situation (not residential care home), secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Pugh (2002)162 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: breastfeeding Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, skill development/training, social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Quirk (1993)376 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: gender Secondary PROGRESS-PLUS characteristics: socioeconomic position, age, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health, substance abuse Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Ravesloot (2007)377 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: disability Secondary PROGRESS-PLUS characteristic: marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: disabilities and chronic illness Other health issues: healthy eating/nutrition, mental health, physical activity Site: residential care (includes nursing homes, sheltered housing) Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Reijneveld (2003)164 | Country, other (specify) Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: education, gender Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: public health/health promotion/prevention Other health issues: healthy eating/nutrition, mental health, physical activity Site: community setting Person(s) delivering the intervention: health promotion practitioner, peer Is this a multicomponent intervention? No – only one component Intervention type: education, physical activity, exercise Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: mental health, physical activity |
| Resnicow (1992)166 | Country: USA Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristics: ethnicity: ethnic background, place of residence Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, physical activity Site: educational setting (school, college, university) Person(s) delivering the intervention: peer, teacher and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification, physical activity, exercise Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: cardiovascular disease, healthy eating Public health participant personal outcomes: public health participant self-efficacy |
| Resnicow (2004)165 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: religion (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: healthy eating/nutrition Other health issues: healthy eating/nutrition Site: religious settings (e.g. churches) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: duration unclear/not reported Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: comparator unclear/not reported Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation; community partnership, community coalitions, community task force, volunteering/volunteers (explicit use of term) |
Health outcomes: healthy eating Public health participant personal outcomes: public health participant self-efficacy, public health participant social support/capital |
| Rhodes (2005)167 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, gender, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: substance abuse Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
Health outcomes: alcohol abuse, drug abuse Public health participant personal outcomes: public health participant social support/capital |
| Richardson (2008)378 | Country: UK Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: disability Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: disabilities and chronic illness Other health issues: healthy eating/nutrition, physical activity Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Rickert (1991)379 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Robinson (2002)382 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, gender Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: community setting Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, social support, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: consulted Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Robinson (2003)168 | Country: USA Age group: children (0–10 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: obesity prevention/weight reduction Other health issues: physical activity Site: community setting, home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, environmental modification, physical activity, exercise Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: no community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation Any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: obesity/weight status, physical activity |
| Rodewald (1999)169 | Country: USA Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: immunisation Other health issues: immunisation Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), ‘outreach’ programme (explicit use of term) |
Health outcomes: immunisation |
| Roffman (1997)383 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, counsellor, psychologist, social worker Is this a multicomponent intervention? No – only one component Intervention type: advice, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Rosal (2005)384 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristic: education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: healthy eating/nutrition, mental health, physical activity Site: community setting, outreach, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, incentives Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: ‘outreach’ programme (explicit use of term), no clear community engagement label used (explain) |
|
| Rose (1992)170 | Country: USA Age group: older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, education, place of residence, gender, age Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, mental health, physical activity, smoking cessation Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: informed Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: cardiovascular disease Public health participant personal outcomes: public health participant self-efficacy |
| Rosser (2002)385 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: sexual health Other health issues: HIV/AIDS/STI prevention/risk reduction Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: leading Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Royse (1998)386 | Country: USA Age group: young people (11–21 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: other topics (specify) Other health issues: mental health, substance abuse, violence prevention Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: social support Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Sauaia (2007)387 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, religion (specify), age Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: religious settings (e.g. churches), home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term) |
|
| Saxe (1997)388 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: substance abuse Site: community setting Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, counselling (based on the psychological needs of the individual), social support, environmental modification, risk assessment (not medical screening), service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force |
|
| Schafer (1998)171 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: healthy eating/nutrition, parenting Site: community setting, home situation (not residential care home), WIC clinic, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, skill development/training, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: duration unclear/not reported Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Schensul (2009)172 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence, disability Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: immunisation Other health issues: care of older people, public health/health promotion/prevention Site: community setting, home situation (not residential care home) Person(s) delivering the intervention: community member, peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, social support, environmental modification, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: immunisation Public health participant personal outcomes: public health participant self-efficacy |
| Schinke (2000)173 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: gender Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: substance abuse Other health issues: smoking/tobacco prevention Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: community member, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: inactive control Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: informed Community involvement in intervention delivery: informed Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
Health outcomes: alcohol abuse, drug abuse, smoking cessation |
| Schorling (1997)174 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: place of residence, religion (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: community setting, religious settings (e.g. churches) Person(s) delivering the intervention: community member, religious leader (e.g. parson, priest) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force |
Health outcomes: smoking cessation |
| Schuler (2002)175 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: parenting Other health issues: housing, mental health, partner violence, public health/health promotion/prevention, substance abuse Site: home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, social support, environmental modification, resource access, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: alcohol abuse, drug abuse |
| Schwarz (1993)176 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: injury prevention Other health issues: violence prevention Site: community setting, home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification, risk assessment (not medical screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community partnership, community coalitions, community task force, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: injury/safety |
| Secker-Walker (2000)177 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: community setting, educational setting (school, college, university), home situation (not residential care home), primary health care (e.g. GP), secondary health-care unit (e.g. hospital, specialist clinic), WIC clinic, workplace site, mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, social support, environmental modification, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation; community partnership, community coalitions, community task force; any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
Health outcomes: smoking cessation Public health participant personal outcomes: public health participant self-efficacy, public health participant social support/capital |
| Shaw (1997)179 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: parenting, smoking cessation Site: community setting, educational setting (school, college, university), workplace site Person(s) delivering the intervention: community member, parent, peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, social support, environmental modification Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: collaborating Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation; community partnership, community coalitions, community task force; any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: alcohol abuse, drug abuse, smoking cessation |
| Shaw (1999)178 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: breastfeeding Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: other (add details) Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: breastfeeding |
| Shelley (2008)180 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: community setting, primary health care (e.g. GP), secondary health-care unit (e.g. hospital, specialist clinic), mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: activities (e.g. community fairs/fetes), advice, environmental modification, resource access, clinical treatment Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: inactive control Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: no community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force |
Health outcomes: smoking cessation |
| Shepherd (1997)394 | Country: UK Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: community setting, outreach, home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term) |
|
| Siegel (1995)395 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health, substance abuse, other topics (specify) Site: educational setting (school, college, university) Person(s) delivering the intervention: teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, resource access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: consulted (piloting of intervention delivery is included here if there is a feedback mechanism) Community involvement in evaluation: not involved/unclear Community engagement strategy: no clear community engagement label used (explain) |
|
| Sieverding (2005)396 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STIs Prevention/risk reduction Other health issues: sexual health Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term) |
|
| Sigel (1998)397 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: gender Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction, sexual health, substance abuse Site: educational setting (school, college, university) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, skill development/training, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: consulted Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Sikkema (2000)399 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: Place of residence Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: reproductive health, sexual health Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, skill development/training Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation; community partnership, community coalitions, community task force; any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Sikkema (2005)398 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: community setting Person(s) delivering the intervention: health promotion practitioner, peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, environmental modification, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Silver (1997)181 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: parenting Other health issues: child illness and ill health, disabilities and chronic illness Site: home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, skill development/training, social support, environmental modification, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: mental health |
| Simmons (1998)182 | Country: New Zealand Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: diabetes prevention/management Other health issues: healthy eating/nutrition, obesity prevention/weight reduction, physical activity Site: religious settings (e.g. churches) Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, social support, physical activity, exercise, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation; community partnership, community coalitions, community task force; any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
Health outcomes: obesity/weight status, physical activity |
| Simoni (2007)400 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: mental health, sexual health, substance abuse Site: secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, skill development/training, social support, incentives Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Skinner (2000)401 | Country: USA Age group: older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education, marital status/family composition Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer prevention, care of older people Site: community setting Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: consulted (piloting of intervention delivery is included here if there is a feedback mechanism) Community involvement in evaluation: consulted Community engagement strategy: community partnership, community coalitions, community task force, social networks (explicit use of term) |
|
| Slater (1998)402 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term) |
|
| Solomon (2000)184 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: socioeconomic position, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: smoking cessation |
| Solomon (2000)183 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: social support, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: smoking cessation |
| Sorensen (2003)403 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: occupation/employment status Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer prevention Other health issues: healthy eating/nutrition, public health/health promotion/prevention, smoking cessation Site: workplace site Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), environmental modification, risk assessment (not medical screening) Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: leading Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force |
|
| Sorensen (2005)185 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: occupation/employment status Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, education Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer prevention Other health issues: healthy eating/nutrition, physical activity Site: workplace site Person(s) delivering the intervention: unclear/not reported Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, environmental modification Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks): measurement time unclear/not reported Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: consulted (piloting of intervention delivery is included here if there is a feedback mechanism) Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, community partnership, community coalitions, community task force |
Health outcomes: healthy eating |
| Sox (1999)404 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: HIV/AIDS/STI prevention/risk reduction Site: primary health care (e.g. GP) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? No – only one component Intervention type: screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Spoth (2007)405 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: substance abuse Other health issues: smoking cessation Site: educational setting (school, college, university), home situation (not residential care home) Person(s) delivering the intervention: parent, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: consulted (piloting of intervention delivery is included here if there is a feedback mechanism) Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force |
Health outcomes: alcohol abuse, drug abuse, smoking cessation |
| St James (1999)186 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position, other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: antenatal (prenatal) care Other health issues: breastfeeding, healthy eating/nutrition, parenting Site: home situation (not residential care home) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, social support, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: duration unclear/not reported Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: healthy eating |
| St Lawrence (1995)406 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: gender Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: reproductive health, sexual health Site: educational setting (school, college, university) Person(s) delivering the intervention: community member, unclear/not reported Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, social support, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| St Pierre Tena (2001)407 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: substance abuse Other health issues: smoking/tobacco prevention, substance abuse Site: community setting, educational setting (school, college, university), home situation (not residential care home) Person(s) delivering the intervention: community member, parent, peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community organisations – developing new and existing services, volunteering/volunteers (explicit use of term) |
|
| Stanton (1996)409 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, place of residence Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: reproductive health, sexual health Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, incentives, resource access, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Stanton (2006)408 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction Site: educational setting (school, college, university) Person(s) delivering the intervention: teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? No – only one component Intervention type: activities (e.g. community fairs/fetes), education, skill development/training Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: other community engagement strategy |
|
| Staten (2004)187 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status, education, age Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: disabilities and chronic illness Other health issues: cardiovascular disease, cancer prevention, healthy eating/nutrition, obesity prevention/weight reduction, physical activity Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: obesity/weight status, physical activity |
| Stephenson (2004)410 | Country: UK Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristic: gender Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: sexual health Other health issues: HIV/AIDS/STI prevention/risk reduction, teenage pregnancy Site: educational setting (school, college, university) Person(s) delivering the intervention: peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? No – only one component Intervention type: activities (e.g. community fairs/fetes), education, skill development/training, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Suarez (1997)411 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education, other vulnerable groups (specify) Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, religious settings (e.g. churches), outreach, mass media – untailored (generic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health professional (e.g. GP, dietitian, nurse), peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: role modelling and role playing, screening (or medical screening, e.g. breast screening) Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), ‘outreach’ programme (explicit use of term), volunteering/volunteers (explicit use of term) |
|
| Teti (2010)413 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction Site: secondary health-care unit (e.g. hospital, specialist clinic) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), peer, researcher Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: education, skill development/training, counselling (based on the psychological needs of the individual), social support, incentives, risk assessment (not medical screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Thoits (2000)414 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: socioeconomic position, occupation/employment status Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: mental health Other health issues: mental health, public health/health promotion/prevention Site: secondary health-care unit (e.g. hospital; specialist clinics) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), volunteering/volunteers (explicit use of term) |
|
| Thomas (2000)415 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: sexual health Site: outreach Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Tudiver (1992)417 | Country: Canada Age group: general population based Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction Site: home situation (not residential care home) Person(s) delivering the intervention: community member, community worker Is this a multicomponent intervention? No – only one component Intervention type: advice, education, social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term), other community engagement strategy |
|
| Tulsky (2000)418 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: tuberculosis Other health issues: tuberculosis Site: outreach, secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: incentives, clinical treatment Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Valente (2006)188 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: smoking/tobacco prevention Other health issues: smoking/tobacco prevention Site: educational setting (school, college, university) Person(s) delivering the intervention: peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? No – only one component Intervention type: activities (e.g. community fairs/fetes), education, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support), social networks (explicit use of term) |
Health outcomes: smoking/tobacco prevention |
| Vogler (2002)189 | Country: USA Age group: children (0–10 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position, other vulnerable groups (specify) Method of addressing health inequalities: targeted and comparison within a PROGRESS-Plus category |
Primary health issue: child illness and ill health Other health issues: child illness and ill health, healthy eating/nutrition, injury prevention, parenting Site: home situation (not residential care home) Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, social support, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
Health outcomes: child illness and ill health |
| Voorhees (1996)190 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: smoking cessation Other health issues: cardiovascular disease Site: community setting, religious settings (e.g. churches), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, religious leader (e.g. parson, priest) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, social support, risk assessment (not medical screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
Health outcomes: smoking cessation |
| Wagner (2000)420 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, place of residence Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: other topics (specify) Other health issues: other topics (specify) Site: outreach Person(s) delivering the intervention: other Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: other Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and first follow-up (use if >1 follow-up) Type of control group: comparator unclear/not reported |
Extent of community engagement: completely community engagement Health problem/need identified by the community? Yes Community involvement in intervention design/planning: leading Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: no clear community engagement label used (explain) |
|
| Watkins (1994)191 | Country: USA Age group: general population based Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: antenatal (prenatal) care Other health issues: antenatal (prenatal) care Site: unclear/not specified Person(s) delivering the intervention: community worker Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, education, incentives, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: other (add details) Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), other community engagement strategy |
Engagee personal outcomes: engagee skills |
| Weber (1997)421 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, primary health care (e.g. GP) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, incentives, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Weeks (2006)422 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: place of residence, other vulnerable groups (specify) Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: substance abuse Site: outreach, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, social support, resource access, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Weinrich (1993)423 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: age Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: peer, other Is this a multicomponent intervention? No – only one component Intervention type: education Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Weiss (1998)192 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: socioeconomic position Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: substance abuse Other health issues: substance abuse Site: educational setting (school, college, university) Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education, skill development/training, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: alcohol abuse, drug abuse, smoking cessation |
| Welsh (2005)424 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: religious settings (e.g. churches) Person(s) delivering the intervention: peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, social support Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: informed Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term) |
|
| Wiist (1990)193 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition Site: community setting, religious settings (e.g. churches) Person(s) delivering the intervention: community member Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: informed Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers), volunteering/volunteers (explicit use of term) |
Health outcomes: cardiovascular disease |
| Wiist (1996)425 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: violence prevention Other health issues: violence prevention Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: community member, parent, peer Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: advice, skill development/training, social support, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Wilcox (2007)194 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: physical activity Other health issues: healthy eating/nutrition Site: religious settings (e.g. churches) Person(s) delivering the intervention: community member, religious leader (e.g. parson, priest), researcher Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, skill development/training, incentives, physical activity, exercise Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: consulted Community engagement strategy: volunteering/volunteers (explicit use of term) |
Health outcomes: obesity/weight status, physical activity Public health participant personal outcomes: public health participant self-efficacy, public health participant social support/capital |
| Wilson (2008)426 | Country: USA Age group: general population based Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: socioeconomic position Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: community setting Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: education, counselling (based on the psychological needs of the individual) Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: collaborating Community engagement strategy: other community engagement strategy |
|
| Winkleby (2004)195 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: no main PROGRESS-Plus group (not mentioned in TITLE AND ABSTRACT) Secondary PROGRESS-PLUS characteristic: ethnicity: ethnic background Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: smoking/tobacco prevention Other health issues: smoking cessation, smoking/tobacco prevention Site: community setting, educational setting (school, college, university) Person(s) delivering the intervention: community member, other Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, skill development/training, environmental modification Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Time between post-test and only/final follow-up Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: completely community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation, volunteering/volunteers (explicit use of term) |
Health outcomes: smoking/tobacco prevention Engagee personal outcomes: engagee empowerment |
| Wishart (2000)427 | Country: Canada Age group: older people (55+ years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: care of older people Other health issues: physical activity Site: community setting Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: social support, physical activity, exercise Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: volunteering/volunteers (explicit use of term) |
|
| Witmer (2004)196 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, mental health, physical activity, smoking/tobacco prevention Site: primary health care (e.g. GP) Person(s) delivering the intervention: health professional (e.g. GP, dietitian, nurse), health promotion practitioner Is this a multicomponent intervention? Irrelevant – no community engagement in delivery/evaluation Intervention type: education, skill development/training, counselling (based on the psychological needs of the individual), screening (for medical screening, e.g. breast screening) Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: waitlist/delayed treatment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: not involved/unclear Community involvement in evaluation: not involved/unclear Community engagement strategy: no clear community engagement label used (explain) |
Health outcomes: cardiovascular disease |
| Wohl (2006)428 | Country: USA Age group: young people (11–21 years), adults (22–54 years), older people (55+ years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristic: occupation/employment status Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: HIV/AIDS/STI prevention/risk reduction Site: secondary health-care unit (e.g. hospital, specialist clinic), unclear/not specified Person(s) delivering the intervention: community worker, other Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: counselling (based on the psychological needs of the individual), service access, clinical treatment Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No |
Extent of community engagement: little community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Wolitski (2005)429 | Country: USA Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥ 90%) Main PROGRESS-PLUS characteristic: sexual orientation Secondary PROGRESS-PLUS characteristic: sexual orientation Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STI prevention/risk reduction Other health issues: mental health, sexual health, substance abuse Site: telephone, print or audio/visual media – tailored, unclear/not specified Person(s) delivering the intervention: peer, other Intervention type: education, incentives, resource access, service access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
|
| Woodruff (2002)197 | Country: USA Age group: general population based Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: smoking cessation Other health issues: smoking cessation Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Is this a multicomponent intervention? No – only one component Intervention type: advice, education, social support, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: promotora (explicit use of term) |
Health outcomes: smoking cessation |
| Wright (1997)198 | Country: USA Age group: general population based Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: breastfeeding Other health issues: breastfeeding Site: secondary health-care unit (e.g. hospital, specialist clinic), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, community worker, health professional (e.g. GP, dietitian, nurse) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: advice, education, skill development/training, social support, resource access, role modelling and role playing Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
Health outcomes: breastfeeding |
| Yanek (2001)199 | Country: USA Age group: adults (22–54 years), older people (55+ years) Sex: majority females (≥ 90%) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cardiovascular disease Other health issues: healthy eating/nutrition, physical activity, smoking/tobacco prevention Site: religious settings (e.g. churches), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, health promotion practitioner Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: education, skill development/training, physical activity, exercise, other Was training provided to the engagees? Yes Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: alternative/placebo intervention Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community action/support, community mobilisation/involvement/engagement/participation |
Health outcomes: cardiovascular disease, healthy eating |
| Zavela (2004)200 | Country: USA Age group: young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: place of residence Secondary PROGRESS-PLUS characteristics: ethnicity: ethnic background, socioeconomic position Method of addressing health inequalities: universal (aimed at the whole group population, not on the basis of individual needs/risks) |
Primary health issue: substance abuse Other health issues: other topics (specify) Site: outreach, educational setting (school, college, university), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: parent, peer, teachers and education professionals (lecturer, principal, etc.) Is this a multicomponent intervention? Yes – only some components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, skill development/training, resource access, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? Yes Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: usual treatment/care, with assignment Multiple treatment or comparison arms? No – only one intervention and one comparison group |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: consulted (piloting of intervention is included here if there is a feedback mechanism) Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Health outcomes: alcohol abuse, drug abuse, smoking cessation, smoking/tobacco prevention |
| Zhou (2003)201 | Country: USA Age group: children (0–10 years), young people (11–21 years) Sex: both males and females (mixed sex) Main PROGRESS-PLUS characteristic: ethnicity: ethnic background Secondary PROGRESS-PLUS characteristics: socioeconomic position, education Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: immunisation Other health issues: immunisation Site: community setting, religious settings (e.g. churches), outreach, educational setting (school, college, university), home situation (not residential care home), primary health care (e.g. GP), WIC clinic, telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member, community worker, health professional (e.g. GP, dietitian, nurse), researcher Is this a multicomponent intervention? Yes – all components involve community engagement Intervention type: activities (e.g. community fairs/fetes), advice, education, social support, immunisation, professional training, service access Was training provided to the engagees? Not stated/unclear Were outcomes measured for the engagees? No Duration: enter value in weeks (add details) Length of time between evaluation measures (weeks) Time between pre-test and post-test Type of control group: matched data from target population, without assignment Multiple treatment or comparison arms? Yes – multiple treatment or comparison arms |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: collaborating Community involvement in evaluation: not involved/unclear Community engagement strategy: community partnership, community coalitions, community task force, ‘outreach’ programme (explicit use of term) |
Health outcomes: immunisation |
| Zhu (2002)430 | Country: USA Age group: older people (55+ years) Sex: majority females (≥90%) Main PROGRESS-PLUS characteristic: multiple equally important characteristics (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: cancer screening/detection Other health issues: cancer screening/detection Site: home situation (not residential care home), telephone, print or audio/visual media – tailored Person(s) delivering the intervention: community member Intervention type: education, incentives, resource access, role modelling and role playing Was training provided to the engagees? Yes Were outcomes measured for the engagees? No |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: collaborating Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: non-peer health advocacy (e.g. lay health, community health workers) |
|
| Ziersch (2000)431 | Country: UK Age group: young people (11–21 years), adults (22–54 years) Sex: majority males (≥90%) Main PROGRESS-PLUS characteristic: other vulnerable groups (specify) Secondary PROGRESS-PLUS characteristics: no secondary PROGRESS-Plus characteristics Method of addressing health inequalities: targeted at or delivered to specific PROGRESS-Plus group |
Primary health issue: HIV/AIDS/STIs Prevention/risk reduction Other health issues: HIV/AIDS/STIs Prevention/risk reduction Sexual health Site: Workplace site Person(s) delivering the intervention: peer Is this a multicomponent intervention? No – only one component Intervention type: advice, education, resource access Was training provided to the engagees? Yes Were outcomes measured for the engagees? Yes |
Extent of community engagement: mostly community engagement Health problem/need identified by the community? No Community involvement in intervention design/planning: not involved/unclear Community involvement in intervention delivery: leading Community involvement in evaluation: not involved/unclear Community engagement strategy: any peer involvement (e.g. peer counselling, peer education, peer leaders; peer leadership; role models, peer support) |
Characteristics of studies analysed in Chapter 7
| Study | Sample size | Time horizon (T), type of community engagement (CE), type of economic evaluation (EE) | Intervention (I) and comparator (C) | Outcome measure(s) used in economic analysis | Resources separately reported from costs (R), sensitivity analysis performed (S), study perspective (P) | Main results |
|---|---|---|---|---|---|---|
| Andersen (2002),479 USA | 40 rural communities; hypothetical cohorts of 1000 women in each community | T: lifetime CE: peer/lay delivered EE: CEA |
I: individual counselling (IC) or community activities (CA) or combination of the two (IC-CA) C: no intervention |
Mammography rates and life-years saved 1995 US$ |
R: yes S: no P: public services plus volunteers |
The cost of each additional mammography per user was US$1953 (95% CI US$578 to infinite) for the CA intervention; this dominated results in the other groups. The cost per additional life-year saved was US$56,000, just above the level that is generally considered to be cost-effective. However, the lifetime benefits from early screening and treatment are not included in the analysis |
| Barnet (2002),480 Baltimore, USA | Urban African American adolescent mothers I: 118, C: 114 |
T: 15 months CE: peer/lay delivered EE: CCA |
I: peer volunteers delivering a weekly parenting curriculum plus usual care C: usual care |
Parent–child interaction and parenting behaviour | R: no S: no P: social services |
Significantly improved parent–child interaction (p = 0.05) and favourable trends but not significant for parenting behaviour and mental health. Costs per teenager supported between US$3704 and US$5245 in both programmes. The costs of a volunteer support programme were not substantially less than those for professionally delivered programmes elsewhere. The authors concluded that volunteer-based programmes might be a complement to but not a substitute for professionally delivered programmes |
| Borgia (2005),220 Rome, Italy | Students in 18 high schools I: 682, C: 613 |
T: 5 months CE: peer/lay delivered EE: CCA |
I: peer-led HIV prevention programme C: teacher-led HIV prevention programme |
Changes in sexual behaviour 2004 € |
R: no S: yes P: societal |
Peer-delivered programme was almost twice as expensive as teacher-led programme (€21,500 vs. €10,800 or €28.2 per target student involved in the peer-led group vs. €11.6 in the teacher-led arm). No changes were observed in sexual behaviour for either group, although knowledge of HIV improved by 6.7% in peer group |
| Brown (2002),224 Texas, USA | Mexican Americans living near border with type 2 diabetes I: 126, C: 126 |
T: 12 months CE: collaboration between health/statutory services and communities EE: CCA |
I: culturally sensitive nurses running diabetes self-management training courses C: waiting-list control subjects |
HbA1c and fasting blood glucose and diabetes knowledge scores 2002 US$ |
R: no S: no P: health system |
Experimental groups showed significantly lower levels of HbA1c and fasting blood glucose at 6 and 12 months and higher diabetes knowledge scores. Although a formal economic evaluation was not conducted, cost of US$384 per person thought to be modest given the benefits in terms of diabetes management seen. Many in-kind resources also provided but not included in cost analysis |
| Brown (2005),223 Texas, USA | Mexican Americans living near border with type 2 diabetes I: 114, C:102 |
T: 12 months CE: collaboration between health/statutory services and communities EE: CCA |
I: culturally sensitive nurses running compressed diabetes self-management training courses C: culturally sensitive nurses running standard-length diabetes self-management training courses |
HbA1c and fasting blood glucose and diabetes knowledge scores | R: yes S: no P: health system |
A compressed version of the intervention in Brown et al.224 using 16 hours of education and 6 hours of support group time delivered the same level of effect with 60% lower costs. It would have the potential to be cost saving if some health-care costs associated with diabetes were avoided |
| Campbell (2008),226 England and Wales | 12- to 13-year-old students in 59 schools I: 5358, C: 5372 |
T: 24 months CE: peer/lay delivered EE: CCA |
I: peer-led intervention for smoking prevention C: usual smoking prevention education |
Smoking rates 2008 UK£ |
R: yes S: no P: public purse |
The OR of being a smoker in the intervention group compared with the control group was significantly lower at 1 year, but, although still lower, was not significantly lower at the end of year 2. The average cost of the intervention was £27 (95% CI £19 to £48) per student and £4700 (95% CI £2408 to £6786) per school. The average cost excluding travel was £23 (95% CI £16 to £43) per student and £3937 (95% CI £2221 to £5511) per school. Overall, considered to be effective but no opinion given on cost-effectiveness |
| Ell (2002),261 California, USA | Mostly Latino low-income women I: 196 women, C: 369 women |
T: 12 months CE: peer/lay delivered EE: CCA |
I: peer counsellor and professional social worker information, risk assessment and support C: no intervention |
Adherence rates to recommended follow-up to Pap tests for cervical cancer 2001 US$ |
R: no S: no P: health care |
Improvements in adherence observed at a cost of US$319 per woman in the intervention group. Better rates of adherence to at least one follow-up appointment among enrolled women (low-grade lesions 83% vs. 58%, OR 3.4, 95% CI 1.5 to 7.7, p = 0.002; high-grade lesions 93% vs. 67%, OR 6.5, 95% CI 2.5 to 16.9, p = 0.001). Adherence to follow-up appointments over 1 year was also significantly associated with enrollment, with higher rates of non-adherence among non-enrollees (p = 0.003) |
| Frick (2004),481 Baltimore, USA | Volunteers aged 60+ years I: hypothetical cohort of 500 volunteers working at 20 schools C: 500 older people |
T: 2 years for peers; lifetime for children at school CE: peer/lay delivered EE: CUA |
I: peer volunteers supporting children in schools C: no programme |
QALYs gained by peer volunteers, graduation rates of children 2003 US$ |
R: no S: yes P: health care |
The average cost per QALY gained, once the cost of the programme and medical expenditure savings were combined, was US$205,000 when the Experience Corps programme was compared with no programme. If an additional 12 students graduate, the ratio would be < US$50,000 per QALY. With a further three students the programme would be cost saving. Experience Corps Baltimore is not cost-effective if focused only on health improvements in older adults, but required only long-term educational benefits for children to make the programme cost-effective or cost saving |
| Krieger (2005),320 Seattle, USA | Low-income households containing a child aged 4–12 years who had asthma I: 138, C: 136 |
T: 12 months CE: empowerment EE: CBA |
I: high-intensity community health worker/family intervention to reduce risk of asthma attacks C: low-intensity intervention – only one community health worker visit, assessment, action plan |
Caregiver quality of life, asthma attacks requiring hospitalisation, activity limitations | R: yes S: no P: health system plus parental/child productivity losses |
The high-intensity group improved significantly more than the low-intensity group in its paediatric asthma caregiver quality of life score (p = 0.005) and asthma-related urgent health services use (p = 0.026). Overall, the intervention was likely to be cost saving, with modest avoidance of costly hospital treatment for asthma attacks and significant improvements in outcomes for children and in quality of life for parents. The study also recorded changes in time off work for parents and time off school for children, although these were not included in the economic analysis |
| Kumpusalo (1996),136 Finland | Six rural village communities I: 4 villages, C: 2 villages |
T: 36 months CE: empowerment EE: CCA |
I: community diagnosis technology for primary care and community-oriented strategy for health promotion C: no intervention |
Changes in cholesterol, vitamin C intake and systolic blood pressure 1996 prices |
R: no S: no P: health system |
Although no formal cost-effectiveness ratio was provided, costs were modest at £750 per village per annum. This was thought to represent value for money in a Finnish context given the improvements in cholesterol, vitamin C intake and systolic blood pressure, all of which would decrease the risk of more expensive inpatient medical care. The cost of one referral to the central hospital would have been three times the cost of the programme |
| Lindqvist (2001),482 Sweden | I: municipality of 41,000 C: historic data from municipality |
T: 72 months CE: collaboration between health/statutory services and communities EE: CBA |
I: community-developed injury prevention programmes C: no intervention |
Impact on rate and severity of injuries in community 1995 Swedish kroner (SEK) |
R: yes S: no P: societal |
Intervention has positive net benefits. The costs of injuries decreased from 116 million SEK to 96 million SEK, and the cost of the intervention was approx. 10 million SEK |
| Long (1995),140 Salt Lake City, USA | Native American women, infants and children I: 63, C: 78 |
T: 10 months CE: peer/lay delivered EE: CCA |
I: breastfeeding peer counsellor programme C: historic control subjects with usual care |
Rates of breastfeeding 1991 US$ |
R: no S: no P: Utah Women, Infants and Children Program |
Costs of employing two part-time counsellors over a 10-month period of US$1000 were outweighed by savings of US$9000 by avoiding purchasing artificial baby milk for mothers. If higher rates of breastfeeding observed at 3 months were maintained then potential for improved health outcomes and reduced need for treatment, but these impacts were not included in the economic analysis |
| McIntosh (2009),240 England | New mothers I: 67, C:64 |
T: 18 months CE: peer/lay delivered EE: CEA |
I: an intensive weekly programme of visits by home visitor trained in working in partnership and in promoting parent–infant interaction C: standard service |
Infant co-operativeness and maternal sensitivity 2004 UK£ |
R: yes S: yes P: societal |
The mean societal cost was £7120 for home intervention vs. £3874 for standard care. There were significant differences in maternal sensitivity and infant co-operativeness favouring the intervention. Incremental cost-effectiveness ratio per unit improvement in maternal sensitivity was £2723 and per unit improvement in infant co-operativeness was £2033. There was a 95% chance of the intervention being cost-effective if the willingness to pay for a unit increase in maternal sensitivity was £16,100 and the willingness to pay for a unit improvement in infant co-operativeness was £4000. Authors concluded cost-effectiveness a matter of judgement |
| Office of the Deputy Prime Minister (2004),355 England and Wales | Deprived urban communities I: 84 schemes, C: scheme areas before action |
T: 30 months CE: empowerment EE: CBA |
I: community-based Neighbourhood Warden Schemes C: no intervention |
Impact on crime only, although health and other impacts also recorded 2003 UK£ |
R: no S: yes P: public purse including criminal justice |
Total costs were estimated to be more than £29M, including £5M of in-kind contributions from partners. The economic analysis focused on crime only. If 10% of the reduction in crime were due to schemes this would have a value of £31M, outweighing the costs of investing in the programme. Scheme has the potential to be highly cost-effective. Economic case would become more favourable if other benefits realised were valued, including health-related improvements in quality of life |
| Paskett (2006),365 North Carolina, USA | Rural, low-income women I: 453, C: 444 |
T: 14 months CE: peer/lay delivered EE: CCA |
I: peer health advisors C: usual care |
Changes in mammography rates | R: no S: no P: health system |
Intervention group had higher mammography rates at follow-up (42.5% vs. 27.3%) (significance not reported). This effect was found for all three racial groups (white, Native American and African American). Incremental cost per additional mammogram received was US$4986, comparable to other interventions. Using volunteers might reduce costs further |
| Pinkerton (1998),372 Milwaukee USA | Men frequenting gay bars I: 330, C: 330 |
T: lifetime CE: peer/lay delivered EE: CEA and CUA |
I: community-level HIV prevention intervention using peer leaders to support risk-reducing behaviour amongst gay men C: no intervention |
HIV cases averted, QALYs gained 1996 US$ |
R: no S: yes P: health care |
The intervention prevented 0.262 HIV infections and saved just under 3 QALYs (discounted at 3%) on the basis of the intervention being effective at altering behaviour for 2 months. Costs were US$65,458 per case of HIV averted. The lifetime costs of care associated with HIV are $87,045 per case (discounted at 3%). The intervention was cost saving (approx. $21,587 per case). Costs and benefits were not synthesised as the intervention was associated with lower cost and better outcomes for the patient. Sensitivity analysis indicated that intervention remained cost saving |
| Pugh (2002),162 Mid-Atlantic USA | Low-income breastfeeding women I: 21, C: 20 |
T: 6 months CE: peer/lay delivered EE: CCA |
I: usual care plus additional visits from nurse/peer counsellor team and peer counsellor telephone support C: usual care |
Change in time spent breastfeeding 1999 US$ |
R: yes – but not shown S: no P: health care; local authority and impacts on parents |
Total costs were significantly higher in the intervention group (US$3840 vs. US$3194, p < 0.05). Consistently higher rates of breastfeeding in the intervention group (p = 0.09–0.12). The intervention group had significantly fewer prescriptions and visits to the emergency room (p < 0.05). These resource savings were not included in an economic analysis |
| Reijneveld (2003),164 Netherlands | Turkish immigrants aged 45+ years I: 74, C: 52 |
T: 10 weeks CE: collaboration between health/statutory services and communities EE: CCA |
I: Turkish peer educator-supported health promotion programme C: standard health promotion programme |
Physical and mental health and well-being components SF-12/SF-36 2001 € |
R: no S: no P: health system |
Participants in the intervention group showed an improvement in mental health (effect size 0.38 SD, p = 0.03); the oldest subgroup also in mental well-being (effect size 0.75 SD, p = 0.01). No improvements were seen in physical well-being and activity, nor in knowledge. No difference in costs reported, at €1400 per programme |
| Richardson (2008),378 England | I: 247 adults in Expert Patients Programme (EPP) group, C: 243 in control group | T: 6 months CE: peer/lay delivered EE: CUA |
I: EPP – lay-led, six 2.5-hour group sessions held weekly C: usual care |
QALYs gained 2004 UK£ |
R: yes S: yes P: health and social care |
Difference in mean QALYs gained 0.020 (95% CI 0.007 to 0.034). Mean costs per patient in the EPP group £1912 vs. £1939 in the control group (95% CI –£368 to £422). Intervention dominant (lower costs and more effective). At a willingness-to-pay threshold of £20,000 per QALY gained, EPP had a 94% probability of being cost-effective |
| Secker-Walker (2005),393 Vermont, USA | Women aged 18–64 years | T: lifetime CE: peer/lay delivered EE: CEA |
I: delivery of smoking cessation services through support systems, health professionals, educators, work sites and the media C: usual care |
Life-years saved 2002 US$ |
R: no S: yes P: granting agency |
The incremental cost per life-year saved in the intervention group was US$1922 (90% CI US$1024 to US$15,647) with discounting at 5%. This was considered to be cost-effective by the authors. Costs of the evaluation were excluded from the costs of the intervention |
| Zhou (2003),201 Houston and Dallas, USA | Vietnamese American children and adolescents I: 5657, C: 8692 (media intervention) |
T: lifetime CE: collaboration between health/statutory services and communities EE: CEA and CBA |
I: community mobilisation for health promotion C: media-led information and education campaign C: no action |
Years of life saved 2000 US$ |
R: no S: yes P: societal |
The media intervention was found to be more cost-effective than the community mobilisation intervention. No ratio was reported as both interventions saved lives and have cost savings. No incremental analysis between the two was performed. Total intervention and vaccination costs were US$313,904 for the media group and US$169,561 for the community group. Net savings, accounting for costs of illness averted, were US$1,336,667 for the media intervention and US$588,184 for the community mobilisation group |
Appendix 9 Bibliography of included studies
This appendix contains a bibliography of the 361 references for the 319 studies that appear in the map (see Chapters 3 and 8) and meta-analysis (see Chapter 5), all of which were classified using the keywording tool (see Appendix 2). They are separated into the 131 studies that were in the meta-analysis and the map and the remaining 230 studies that are in the map only. Please see Chapter 3 for an account of study selection.
References in both the map and the meta-analysis (n = 131)
- Anand SS, Davis AD, Ahmed R, Jacobs R, Xie C, Hill A, et al. A family-based intervention to promote healthy lifestyles in an aboriginal community in Canada. Can J Public Health 2007;98:447-52.
- Anderson AK, Damio G, Young S, Chapman DJ, Perez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Arch Pediatr Adolesc Med 2005;159:836-41.
- Andrews JO, Bentley G, Crawford S, Pretlow L, Tingen MS. Using community-based participatory research to develop a culturally sensitive smoking cessation intervention with public housing neighborhoods. Ethn Dis 2007;17:331-7.
- Arlotti JP, Cottrell BH, Lee SH, Curtin JJ. Breastfeeding among low-income women with and without peer support. J Community Health Nurs 1998;15:163-78.
- Aseltine RH, Dupre M, Lamlein P. Mentoring as a drug prevention strategy: an evaluation of ‘across ages’. Adolesc Fam Health 2000;1:11-20.
- Auld GW, Romaniello C, Heimendinger J, Hambidge C, Hambidge M. Outcomes from a school-based nutrition education program using resource teachers and cross-disciplinary models. J Nutr Educ 1998;30:268-80.
- Auslander W, Haire JD, Houston C, Rhee CW, Williams JH. A controlled evaluation of staging dietary patterns to reduce the risk of diabetes in African-American women. Diabetes Care 2002;25:809-14.
- Avila P, Hovell MF. Physical activity training for weight loss in Latinas: a controlled trial. Int J Obes Relat Metab Disord 1994;18:476-82.
- Ayala GX, Elder JP, Campbell NR, Arredondo E, Baquero B, Crespo NC, et al. Longitudinal intervention effects on parenting of the Aventuras para Niños study. Am J Prev Med 2010;38:154-62.
- Balcazar HG, de Heer H, Rosenthal L, Aguirre M, Flores L, Puentes FA, et al. A promotores de salud intervention to reduce cardiovascular disease risk in a high-risk Hispanic border population, 2005–2008. Prev Chronic Dis 2010;7.
- Banks ER. Being Healthy Counts to H.I.M.: An Examination of Health Behavior Among Participants in a Diabetes Prevention and Health Promotion Program 2009.
- Baranowski T, Simons-Morton B, Hooks P, Henske J, Tiernan K, Dunn JK, et al. A center-based program for exercise change among black-American families. Health Educ Q 1990;17:179-96.
- Barnes K, Friedman SM, Brickner N, Honig J. Impact of community volunteers on immunization rates of children younger than 2 years. Arch Pediatr Adolesc Med 1999;153:518-24.
- Barnes-Boyd C, Fordham N, Nacion KW. Promoting infant health through home visiting by a nurse-managed community worker team. Public Health Nurs 2001;18:225-35.
- Becker DM, Yanek LR, Johnson WR, Garrett D, Moy TF, Reynolds SS, et al. Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation 2005;111:1298-304.
- Beech BM, Klesges RC, Kumanyika SK, Murray DM, Klesges L, McClanahan B, et al. Child- and parent-targeted interventions: the Memphis GEMS pilot study. Ethn Dis 2003;13:S40-53.
- Black MM, Hager ER, Le K, Anliker J, Arteaga SS, Diclemente C, et al. Challenge! Health promotion/obesity prevention mentorship model among urban, black adolescents. Pediatrics 2010;126:280-8.
- Botvin GJ, Schinke SP, Epstein JA, Diaz T, Botvin EM. Effectiveness of culturally focused and generic skills training approaches to alcohol and drug abuse prevention among minority adolescents: two-year follow-up results. Psychol Addict Behav 1995;9:183-94.
- Britto MT, Klostermann BK, Bonny AE, Altum SA, Hornung RW. Impact of a school-based intervention on access to healthcare for underserved youth. J Adolesc Health 2001;29:116-24.
- Brownson RC, Smith CA, Pratt M, Mack NE, Jackson-Thompson J, Dean CG, et al. Preventing cardiovascular disease through community-based risk reduction: the Bootheel Heart Health Project. Am J Public Health 1996;86:206-13.
- Brownson RC, Baker EA, Boyd RL, Caito NM, Duggan K, Housemann RA, et al. A community-based approach to promoting walking in rural areas. Am J Prev Med 2004;27:28-34.
- Brownson RC, Hagood L, Lovegreen SL, Britton B, Caito NM, Elliott MB, et al. A multilevel ecological approach to promoting walking in rural communities. Prev Med 2005;41:837-42.
- Buller DB, Morrill C, Taren D, Aickin M, Sennott-Miller L, Buller MK, et al. Randomized trial testing the effect of peer education at increasing fruit and vegetable intake. J Natl Canc Inst 1999;91:1491-500.
- Campbell MK, Demark-Wahnefried W, Symons M, Kalsbeek WD, Dodds J, Cowan A, et al. Fruit and vegetable consumption and prevention of cancer: the Black Churches United for Better Health project. Am J Public Health 1999;89:1390-6.
- Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, Belton L, et al. Effects of a tailored health promotion program for female blue-collar workers: health works for women. Prev Med 2002;34:313-23.
- Campbell MK, James A, Hudson MA, Carr C, Jackson E, Oakes V, et al. Improving multiple behaviors for colorectal cancer prevention among African American church members. Health Psychol 2004;23:492-50.
- Caulfield LE, Gross SM, Bentley ME, Bronner Y, Kessler L, Jensen J, et al. WIC-based interventions to promote breastfeeding among African-American women in Baltimore: effects on breastfeeding initiation and continuation. J Hum Lact 1998;14:15-22.
- Chapman DJ, Damio G, Young S, Perez-Escamilla R. Effectiveness of breastfeeding peer counseling in a low-income, predominantly Latina population: a randomized controlled trial. Arch Pediatr Adolesc Med 2004;158:897-902.
- Cherry VR, Belgrave FZ, Jones W, Kennon DK, Gray FS, Phillips F. NTU: an Africentric approach to substance abuse prevention among African American youth. J Prim Prev 1998;18:319-39.
- Cochrane T, Davey RC. Increasing uptake of physical activity: a social ecological approach. J R Soc Health 2008;128:31-40.
- Conway TL, Woodruff SI, Edwards CC, Hovell MF, Klein J. Intervention to reduce environmental tobacco smoke exposure in Latino children: null effects on hair biomarkers and parent reports. Tob Control 2004;13:90-2.
- Cox RH, Parker GG, Watson AC, Robinson SH, Simonson CJ, Elledge JC, et al. Dietary cancer risk of low-income women and change with intervention. J Am Diet Assoc 1995;95:1031-4.
- Daniel M, Green LW, Marion SA, Gamble D, Herbert CP, Hertzman C, et al. Effectiveness of community-directed diabetes prevention and control in a rural Aboriginal population in British Columbia, Canada. Soc Sci Med 1999;48:815-32.
- Davidson LL, Durkin MS, Kuhn L, O’Connor P, Barlow B, Heagarty MC. The impact of the Safe Kids/Healthy Neighborhoods Injury Prevention Program in Harlem, 1988 through 1991. Am J Public Health 1994;84:580-6.
- Davis S, Gomez Y, Lambert L, Skipper B. Primary prevention of obesity in American Indian children. Ann NY Acad Sci 1993;699:167-80.
- Davis SM, Lambert LC, Gomez Y, Skipper B. Southwest Cardiovascular Curriculum Project: study findings for American Indian elementary students. J Health Educ 1995;26:S72-81.
- Dedobbeleer N, Desjardins S. Outcomes of an ecological and participatory approach to prevent alcohol and other drug ‘abuse’ among multiethnic adolescents. Subst Use Misuse 2001;36:1959-91.
- Neighbourhood management: an overview of the 2003 and 2006 Round 1 Pathfinder household surveys. London: Department for Communities and Local Government, Neighbourhood Renewal Unit; 2006.
- Duncan TE, Duncan SC, Beauchamp N, Wells J, Ary DV. Development and evaluation of an interactive CD-ROM refusal skills program to prevent youth substance use: ‘refuse to use’. J Behav Med 2000;23:59-72.
- Elder JP, Wildey M, de Moor C, Sallis JF, Eckhardt L, Edwards C, et al. The long-term prevention of tobacco use among junior high school students: classroom and telephone interventions. Am J Public Health 1993;83:1239-44.
- Elder JP, Ayala GX, Campbell NR, Slymen D, Lopez-Madurga ET, Engelberg M, et al. Interpersonal and print nutrition communication for a Spanish-dominant Latino population: Secretos de la Buena Vida. Health Psychol 2005;24:49-57.
- Ernst CC, Grant TM, Streissguth AP, Sampson PD. Intervention with high-risk alcohol and drug-abusing mothers: II. Three-year findings from the Seattle model of paraprofessional advocacy. J Community Psychol 1999;27:19-38.
- Faridi Z, Shuval K, Njike VY, Katz JA, Jennings G, Williams M, et al. Partners reducing effects of diabetes (PREDICT): a diabetes prevention physical activity and dietary intervention through African-American churches. Health Educ Res 2010;25:306-15.
- Fisher EB, Auslander WF, Munro JF, Arfken CL, Brownson RC, Owens NW. Neighbors for a smoke free north side: evaluation of a community organization approach to promoting smoking cessation among African Americans. Am J Public Health 1998;88:1658-63.
- Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Two-year follow-up results for Hip-Hop to Health Jr: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr 2005;146:618-25.
- Foerster SB, Gregson J, Beall DL, Hudes M, Magnuson H, Livingston S, et al. The California Children’s 5 a Day-Power Play! Campaign: evaluation of a large-scale social marketing initiative. Fam Community Health 1998;21:46-64.
- Fried LP, Carlson MC, Freedman M, Frick KD, Glass TA, Hill J, et al. A social model for health promotion for an aging population: initial evidence on the Experience Corps model. J Urban Health 2004;81:64-78.
- Gadomski A, Ackerman S, Burdick P, Jenkins P. Efficacy of the North American guidelines for children’s agricultural tasks in reducing childhood agricultural injuries. Am J Public Health 2006;96:722-7.
- Gottfredson DC, Gottfredson GD, Skroban S. A multimodel school-based prevention demonstration. J Adolesc Res 1996;11.
- Graham AV, Frank SH, Zyzanski SJ, Kitson GC, Reeb KG. A clinical trial to reduce the rate of low birth weight in an inner-city black population. Fam Med 1992;24:439-46.
- Grummer-Strawn LM, Rice SP, Dugas K, Clark LD, Benton-Davis S. An evaluation of breastfeeding promotion through peer counseling in Mississippi WIC clinics. Matern Child Health J 1997;1:35-42.
- Hancock L, Sanson-Fisher R, Perkins J, McClintock A, Howley P, Gibberd R. Effect of a community action program on adult quit smoking rates in rural Australian towns: the CART project. Prev Med 2001;32:118-27.
- Hanlon TE, Bateman RW, Simon BD, O’Grady KE, Carswell SB. An early community-based intervention for the prevention of substance abuse and other delinquent behavior. J Youth Adolesc 2002;31:459-71.
- Harmon MA. Reducing Drug Use Among Pregnant and Parenting Teens: A Program Evaluation and Theoretical Examination 1995.
- Havas S, Anliker J, Damron D, Langenberg P, Ballesteros M, Feldman R. Final results of the Maryland WIC 5-a-Day promotion program. Am J Public Health 1998;88:1161-7.
- Hayashi T, Farrell MA, Chaput LA, Rocha DA, Hernandez M. Lifestyle intervention, behavioral changes, and improvement in cardiovascular risk profiles in the California WISEWOMAN project. J Womens Health 2010;19:1129-38.
- Hecht ML, Marsiglia FF, Elek E, Wagstaff DA, Kulis S, Dustman P, et al. Culturally grounded substance use prevention: an evaluation of the keepin’ it R.E.A.L. curriculum. Prev Sci 2003;4:233-48.
- Hunter JB, de Zapien JG, Papenfuss M, Fernandez ML, Meister J, Giuliano AR. The impact of a promotora on increasing routine chronic disease prevention among women aged 40 and older at the US–Mexico border. Health Educ Behav 2004;31:18-2.
- Johnson Z, Howell F, Molloy B. Community mothers’ programme: randomised controlled trial of non-professional intervention in parenting. BMJ 1993;306:1449-52.
- Julnes G, Konefal M, Pindur W, Kim P. Community-based perinatal care for disadvantaged adolescents: evaluation of the Resource Mothers Program. J Community Health 1994;19:41-53.
- Karanja N, Lutz T, Ritenbaugh C, Maupome G, Jones J, Becker T, et al. The TOTS community intervention to prevent overweight in American Indian toddlers beginning at birth: a feasibility and efficacy study. J Community Health 2010;35:667-75.
- Kim KH, Linnan L, Campbell MK, Brooks C, Koenig HG, Wiesen C. The WORD (wholeness, oneness, righteousness, deliverance): a faith-based weight-loss program utilizing a community-based participatory research approach. Health Educ Behav 2008;35:634-50.
- Kistin N, Abramson R, Dublin PEop. Effect of peer counselors on breastfeeding initiation, exclusivity, and duration among low-income urban women. J Hum Lact 1994;10:11-5.
- Kloek GC, van Lenthe FJ, van Nierop PW, Koelen MA, Mackenbach JP. Impact evaluation of a Dutch community intervention to improve health-related behaviour in deprived neighbourhoods. Health Place 2006;12:665-77.
- Krieger J, Collier C, Song L, Martin D. Linking community-based blood pressure measurement to clinical care: a randomized controlled trial of outreach and tracking by community health workers. Am J Public Health 1999;89:856-61.
- Kumpusalo E, Neittaanmaki L, Halonen P, Pekkarinen H. Finnish Healthy Village Study: impact and outcomes of a low-cost local health promotion programme. Health Promot Int 1996;11.
- Lewis CE, Raczynski JM, Heath GW, Levinson R, Hilyer JC, Cutter GR. Promoting physical activity in low-income African-American communities: the PARR project. Ethn Dis 1993;3:106-18.
- Lindenberg CS, Solorzano RM, Bear D, Strickland O, Galvis C, Pittman K. Reducing substance use and risky sexual behavior among young, low-income, Mexican-American women: comparison of two interventions. Appl Nurs Res 2002;15:137-48.
- Lindqvist K, Timpka T, Schelp L, Ahlgren M. Evaluation of an inter-organizational program for prevention of work-related injuries in a WHO Safe Community. Work 1999;13:89-96.
- Long DG, Funk-Archuleta MA, Geiger CJ, Mozar AJ, Heins JN. Peer counselor program increases breastfeeding rates in Utah Native American WIC population. J Hum Lact 1995;11:279-84.
- LoSciuto L, Rajala AK, Townsend TN, Taylor AS. An outcome evaluation of across ages. J Adolesc Res 1996;11:116-29.
- LoSciuto L, Hilbert SM, Fox MM, Porcellini L, Lanphear A. A two-year evaluation of the Wood Rock Youth Development Project. J Early Adolesc 1999;19:488-507.
- Lupton BS, Fonnebo V, Sogaard AJ, Langfeldt E. The Finnmark Intervention Study. Better health for the fishery population in an Arctic village in North Norway. Scand J Prim Health Care 2002;20:213-18.
- Luster T, Perlstadt H, McKinney M, Sims K, Juang L. The effects of a family support program and other factors on the home environments provided by adolescent mothers. Fam Relat 1996;45:255-64.
- Macaulay AC, Paradis G, Potvin L, Cross EJ, Saad-Haddad C, McComber A, et al. The Kahnawake Schools Diabetes Prevention Project: intervention, evaluation, and baseline results of a diabetes primary prevention program with a native community in Canada. Prev Med 1997;26:779-90.
- Malchodi CS, Oncken C, Dornelas EA, Caramanica L, Gregonis E, Curry SL. The effects of peer counseling on smoking cessation and reduction. Obstet Gynecol 2003;101:504-10.
- Marcenko MO, Spence M, Samost L. Outcomes of a home visitation trial for pregnant and postpartum women at-risk for child placement. Children Youth Serv Rev 1996;18:243-59.
- McAlister AL, Ramirez AG, Amezcua C, Pulley LV, Stern MP, Mercado S. Smoking cessation in Texas–Mexico border communities: a quasi-experimental panel study. Am J Health Promot 1992;6:274-9.
- McInnes RJ. The Glasgow Infant Feeding Action Research Project: An Evaluation of a Community Based Intervention Designed to Increase the Prevalence of Breastfeeding in a Socially Disadvantaged Urban Area 1998.
- McNabb W, Quinn M, Kerver J, Cook S, Karrison T. The PATHWAYS church-based weight loss program for urban African-American women at risk for diabetes. Diabetes Care 1997;20:1518-23.
- McNabb WL, Quinn MT, Rosing L. Weight loss program for inner-city black women with non-insulin-dependent diabetes mellitus: PATHWAYS. J Am Diet Assoc 1993;93:75-7.
- Mendoza J, Levinger D, Johnston B. Pilot evaluation of a walking school bus program in a low-income, urban community. BMC Public Health 2009;9.
- Miller-Heyl J, MacPhee D, Fritz JJ. DARE to be you: a family-support, early prevention program. J Prim Prev 1998;18:257-85.
- Nafziger AN, Erb TA, Jenkins PL, Lewis C, Pearson TA. The Otsego-Schoharie healthy heart program: prevention of cardiovascular disease in the rural US. Scand J Public Health (Suppl) 2001;56:21-32.
- Norr KF, Crittenden KS, Lehrer EL, Reyes O, Boyd CB, Nacion KW, et al. Maternal and infant outcomes at one year for a nurse-health advocate home visiting program serving African Americans and Mexican Americans. Public Health Nurs 2003;20:190-203.
- O’Loughlin JL, Paradis G, Gray-Donald K, Renaud L. The impact of a community-based heart disease prevention program in a low-income, inner-city neighborhood. Am J Public Health 1999;89:1819-26.
- Parsons L, Day S. Improving obstetric outcomes in ethnic minorities: an evaluation of health advocacy in Hackney. J Public Health Med 1992;14:183-91.
- Perry CL, Williams CL, Veblen-Mortenson S, Toomey TL, Komro KA, Anstine PS, et al. Project Northland: outcomes of a communitywide alcohol use prevention program during early adolescence. Am J Public Health 1996;86:956-65.
- Platt S, Parry O, Ritchie D, Gnich W. Evaluating a community-based anti-smoking programme: lessons for policy, practice and research. Edinburgh: Edinburgh Research Unit in Health, Behaviour and Change; 2003.
- Poland ML, Giblin PT, Waller JB, Hankin J. Effects of a home visiting program on prenatal care and birthweight: a case comparison study. J Community Health 1992;17:221-9.
- Poston WS, Haddock CK, Olvera NE, Suminski RR, Reeves RS, Dunn JK, et al. Evaluation of a culturally appropriate intervention to increase physical activity. Am J Health Behav 2001;25:396-40.
- Pugh LC, Milligan RA, Brown LP. The Breastfeeding Support Team for low-income, predominantly-minority women: a pilot intervention study. Health Care Women Int 2001;22:501-15.
- Pugh LC, Milligan RA, Frick KD, Spatz D, Bronner Y. Breastfeeding duration, costs, and benefits of a support program for low-income breastfeeding women. Birth 2002;29:95-100.
- Reijneveld SA, Westhoff MH, Hopman-Rock M. Promotion of health and physical activity improves the mental health of elderly immigrants: results of a group randomised controlled trial among Turkish immigrants in the Netherlands aged 45 and over. J Epidemiol Community Health 2003;57:405-11.
- Resnicow K, Cohn L, Reinhardt J, Cross D, Futterman R, Kirschner E, et al. A three-year evaluation of the know your body program in inner-city schoolchildren. Health Educ Q 1992;19:463-80.
- Resnicow K, Campbell MK, Carr C, McCarty F, Wang T, Periasamy S, et al. Body and soul. A dietary intervention conducted through African-American churches. Am J Prev Med 2004;27:97-105.
- Rhodes JE, Reddy R, Grossman JB. The protective influence of mentoring on adolescents’ substance use: direct and indirect pathways. Appl Dev Sci 2005;9:31-47.
- Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis 2003;13:S65-77.
- Rodewald LE, Szilagyi PG, Humiston SG, Barth R, Kraus R, Raubertas RF. A randomized study of tracking with outreach and provider prompting to improve immunization coverage and primary care. Pediatrics 1999;103:31-8.
- Rose MA. Evaluation of a peer-education program on heart disease prevention with older adults. Public Health Nurs 1992;9:242-7.
- Schafer E, Vogel MK, Viegas S, Hausafus C. Volunteer peer counselors increase breastfeeding duration among rural low-income women. Birth 1998;25:101-6.
- Schensul JJ, Radda K, Coman E, Vazquez E. Multi-level intervention to prevent influenza infections in older low income and minority adults. Am J Community Psychol 2009;43:313-29.
- Schinke SP, Tepavac L, Cole KC. Preventing substance use among Native American youth: three-year results. Addict Behav 2000;25:387-97.
- Schorling JB, Roach J, Siegel M, Baturka N, Hunt DE, Guterbock TM, et al. A trial of church-based smoking cessation interventions for rural African Americans. Prev Med 1997;26:92-101.
- Schuler ME, Nair P, Black MM. Ongoing maternal drug use, parenting attitudes, and a home intervention: effects on mother-child interaction at 18 months. J Dev Behav Pediatr 2002;23:87-94.
- Schwarz DF, Grisso JA, Miles C, Holmes JH, Sutton RL. An injury prevention program in an urban African-American community. Am J Public Health 1993;83:675-80.
- Secker-Walker RH, Flynn BS, Solomon LJ, Skelly JM, Dorwaldt AL, Ashikaga T. Helping women quit smoking: results of a community intervention program. Am J Public Health 2000;90:940-6.
- Shaw E, Kaczorowski J. The effect of a peer counseling program on breastfeeding initiation and longevity in a low-income rural population. J Hum Lact 1999;15:19-25.
- Shaw RA, Rosati MJ, Salzman P, Coles CR, McGeary C. Effects on adolescent ATOD behaviors and attitudes of a 5-year community partnership. Eval Program Plann 1997;20:307-13.
- Shelley D, Fahs M, Yerneni R, Das D, Nguyen N, Hung D, et al. Effectiveness of tobacco control among Chinese Americans: a comparative analysis of policy approaches versus community-based programs. Prev Med 2008;47:530-6.
- Silver EJ, Ireys HT, Bauman LJ, Stein REK. Psychological outcomes of a support intervention in mothers of children with ongoing health conditions: the parent to parent network. J Community Psychol 1997;25:249-64.
- Simmons D, Fleming C, Voyle J, Fou F, Feo S, Gatland B. A pilot urban church-based programme to reduce risk factors for diabetes among Western Samoans in New Zealand. Diabet Med 1998;15:136-42.
- Solomon LJ, Scharoun GM, Flynn BS, Secker-Walker RH, Sepinwall D. Free nicotine patches plus proactive telephone peer support to help low-income women stop smoking. Prev Med 2000;31:68-74.
- Solomon LJ, Secker-Walker RH, Flynn BS, Skelly JM, Capeless EL. Proactive telephone peer support to help pregnant women stop smoking. Tob Control 2000;9:III72-4.
- Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working-class, multiethnic workers: results of the healthy directions – small business study. Am J Public Health 2005;95:1389-95.
- Staten LK, Gregory-Mercado KY, Ranger-Moore J, Will JC, Giuliano AR, Ford ES, et al. Provider counseling, health education, and community health workers: the Arizona WISEWOMAN project. J Womens Health 2004;13:547-56.
- St James PS, Shapiro E, Waisbren SE. The Resource Mothers Program for Maternal Phenylketonuria. Am J Public Health 1999;89:762-4.
- Valente TW, Unger JB, Ritt-Olson A, Cen SY, Anderson J. The interaction of curriculum type and implementation method on 1-year smoking outcomes in a school-based prevention program. Health Educ Res 2006;21:315-24.
- Vogler SD, Davidson AJ, Crane LA, Steiner JF, Brown JM. Can paraprofessional home visitation enhance early intervention service delivery?. J Dev Behav Pediatr 2002;23:208-16.
- Voorhees CC, Stillman FA, Swank RT, Heagerty PJ, Levine DM, Becker DM. Heart, body, and soul: impact of church-based smoking cessation interventions on readiness to quit. Prev Med 1996;25:277-85.
- Watkins E, Harlan C, Eng E, Gansky S, Gehan D, Larson K. Assessing the effectiveness of lay health advisors with migrant farmworkers. Fam Community Health 1994;16:72-87.
- Weiss FL, Nicholson HJ. Friendly PEERsuasionSM against substance use: the Girls IncorporatedSM model and evaluation. Drugs Soc 1998;12:7-22.
- Wiist WH, Flack JM. A church-based cholesterol education program. Public Health Rep 1990;105:381-8.
- Wilcox S, Laken M, Bopp M, Gethers O, Huang P, McClorin L, et al. Increasing physical activity among church members. Community-based participatory research. Am J Prev Med 2007;32:131-8.
- Winkleby MA, Feighery E, Dunn M, Kole S, Ahn D, Killen JD. Effects of an advocacy intervention to reduce smoking among teenagers. Arch Pediatr Adolesc Med 2004;158:269-75.
- Witmer JM, Hensel MR, Holck PS, Ammerman AS, Will JC. Heart disease prevention for Alaska Native women: a review of pilot study findings. J Womens Health 2004;13:569-78.
- Woodruff SI, Talavera GA, Elder JP. Evaluation of a culturally appropriate smoking cessation intervention for Latinos. Tob Control 2002;11:361-7.
- Wright AL, Naylor A, Wester R, Bauer M, Sutcliffe E. Using cultural knowledge in health promotion: breastfeeding among the Navajo. Health Educ Behav 1997;24:625-39.
- Yanek LR, Becker DM, Moy TF, Gittelsohn J, Koffman DM. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep 2001;116:68-81.
- Zavela KJ, Battistich V, Gosselink CA, Dean BJ. Say Yes First: follow up of a five-year rural drug prevention program. J Drug Educ 2004;34:73-88.
- Zhou F, Euler GL, McPhee SJ, Nguyen T, Lam T, Wong C, et al. Economic analysis of promotion of hepatitis B vaccinations among Vietnamese-American children and adolescents in Houston and Dallas. Pediatrics 2003;111:1289-96.
References in the map that are not also in the meta-analysis (n = 230)
- Aarons SJ, Jenkins RR, Raine TR, El-Khorazaty MN, Woodward KM, Williams RL, et al. Postponing sexual intercourse among urban junior high school students – a randomized controlled evaluation. J Adolesc Health 2000;27:236-47.
- Ahmed NU, Haber G, Semenya KA, Hargreaves MK. Randomized controlled trial of mammography intervention in insured very low-income women. Cancer Epidemiol Biomark Prev 2010;19:1790-8.
- Allen JP, Phillber S, Herrling S, Kupermine GP. Preventing teen pregnancy and academic failure; experimental evaluation of a developmentally based approach. Child Dev 1997;64:729-42.
- Allen P, Thompson JL, Herman CJ, Whyte AN, Wolfe VK, Qualls C, et al. Impact of periodic follow-up testing among urban American Indian women with impaired fasting glucose. Prev Chronic Dis 2008;5.
- Andersen MR, Hagher M, Meischke H, Shaw C, Yasui Y, Urban N. Recruitment, retention, and activity of volunteers promoting mammography use in rural communities. Health Promot Pract 2000;1:341-50.
- Andersen MR, Yasui Y, Meischke H, Kuniyuki A, Etzioni R, Urban N. The effectiveness of mammography promotion by volunteers in rural communities. Am J Prev Med 2000;18:199-207.
- Andrews JO, Felton G, Ellen Wewers M, Waller J, Tingen M. The effect of a multi-component smoking cessation intervention in African American women residing in public housing. Res Nurs Health n.d.;30:45-60.
- Baker EA, Bouldin N, Durham M, Lowell ME, Gonzalez M, Jodaitis N, et al. The Latino Health Advocacy Program: a collaborative lay health advisor approach. Health Educ Behav 1997;24:495-509.
- Baker K, Pollack M, Kohn I. Violence prevention through informal socialization: an evaluation of the South Baltimore Youth Center. Stud Crime Crime Prev 1995;4:61-85.
- Baruth M, Wilcox S, Blair S, Hooker S, Hussey J, Saunders R. Psychosocial mediators of a faith-based physical activity intervention: implications and lessons learned from null findings. Health Educ Res 2010;25:645-55.
- Basen-Engquist K, Coyle KK, Parcel GS, Kirby D, Banspach SW, Carvajal SC, et al. Schoolwide effects of a multicomponent HIV, STD, and pregnancy prevention program for high school students. Health Educ Behav 2001;28:166-85.
- Batts ML, Gary TL, Huss K, Hill MN, Bone L, Brancati FL. Patient priorities and needs for diabetes care among urban African American adults. Diabetes Educ 2001;27:405-12.
- Best DL, Davis SW, Vaz RM, Kaiser M. Testicular cancer education: a comparison of teaching methods. Am J Health Behav 1996;20:229-41.
- Bird JA, McPhee SJ, Ha NT, Le B, Davis T, Jenkins CN. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Prev Med 1998;27:821-9.
- Black MM, Dubowitz H, Hutcheson J, Berenson-Howard J, Starr RH. A randomized clinical trial of home intervention for children with failure to thrive. Pediatrics 1995;95:807-14.
- Blamey A, Ayana M, Lawson L, Mackinnon J, Paterson I, Judge K. Final report: the independent evaluation of Have a Heart Paisley. Glasgow: University of Glasgow; 2004.
- Bolam B, McLean C, Pennington A, Gillies P. Using new media to build social capital for health: a qualitative process evaluation study of participation in the CityNet project. J Health Psychol 2006;11:297-308.
- Booth RE, Zhang Y, Kwiatkowski CF. The challenge of changing drug and sex risk behaviors of runaway and homeless adolescents. Child Abuse Neglect 1999;23:1295-306.
- Borgia P, Marinacci C, Schifano P, Perucci CA. Is peer education the best approach for HIV prevention in schools? Findings from a randomized controlled trial. J Adolesc Health 2005;36:508-16.
- Botvin GJ, Schinke SP, Epstein JA, Diaz T. Effectiveness of culturally focused and generic skills training approaches to alcohol and drug abuse prevention among minority youths. Psychol Addict Behav 1994;8:116-27.
- Broadhead RS, Heckathorn DD, Grund JC, Stern LS, Anthony DL. Drug users versus outreach workers in combating AIDS: preliminary results of a peer-driven intervention. J Drug Issues 1995;25.
- Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the Starr County border health initiative. Diabetes Care 2002;25:259-68.
- Brown SA, Blozis SA, Kouzekanani K, Garcia AA, Winchell M, Hanis CL. Dosage effects of diabetes self-management education for Mexican Americans: the Starr County Border Health Initiative. Diabetes Care 2005;28:527-32.
- Bullock LF, Wells JE, Duff GB, Hornblow AR. Telephone support for pregnant women: outcome in late pregnancy. N Z Med J 1995;108:476-8.
- Campbell R, Starkey F, Holliday J, Audrey S, Bloor M, Parry-Langdon N, et al. An informal school-based peer-led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial. Lancet 2008;371:1595-602.
- Carballo-Dieguez A, Dolezal C, Leu CS, Nieves L, Diaz F, Decena C, et al. A randomized controlled trial to test an HIV-prevention intervention for Latino gay and bisexual men: lessons learned. AIDS Care 2005;17:314-28.
- Carroll DL, Rankin SH. Comparing interventions in older unpartnered adults after myocardial infarction. Eur J Cardiovasc Nurs 2006;5:83-9.
- CDC AIDS Community Demonstration Projects Research Group . Community-level HIV intervention in 5 cities: final outcome data from the CDC AIDS Community Demonstration Projects. Am J Public Health 1999;89:336-45.
- Centers for Disease Control and Prevention . Community-level prevention of human immunodeficiency virus infection among high-risk populations: the AIDS Community Demonstration Projects. MMWR 1996;45:1-24.
- Chaisson RE, Barnes GL, Hackman J, Watkinson L, Kimbrough L, Metha S, et al. A randomized, controlled trial of interventions to improve adherence to isoniazid therapy to prevent tuberculosis in injection drug users. Am J Med 2001;110:610-15.
- Chapman D, Damio G, Young S, Perez-Escamilla R. Association of degree and timing of exposure to breastfeeding peer counseling services with breastfeeding duration. Adv Exp Med Biol 2004;554:303-6.
- Cheadle A, Pearson D, Wagner E, Psaty BM, Diehr P, Koepsell T. A community-based approach to preventing alcohol use among adolescents on an American Indian reservation. Public Health Rep 1995;110:439-47.
- Cheadle A, Wagner E, Walls M, Diehr P, Bell M, Anderman C, et al. The effect of neighborhood-based community organizing: results from the Seattle Minority Youth Health Project. Health Serv Res 2001;36:671-89.
- Chernoff RG, Ireys HT, DeVet KA, Kim YJ. A randomized, controlled trial of a community-based support program for families of children with chronic illness: pediatric outcomes. Arch Pediatr Adolesc Med 2002;156:533-9.
- Clarke M, Clarke SJ, Jagger C. Social intervention and the elderly: a randomized controlled trial. Am J Epidemiol 1992;136:1517-23.
- Clover K, Redman S, Forbes J, Sanson-Fisher R, Callaghan T. Two sequential randomized trials of community participation to recruit women for mammographic screening. Prev Med 1996;25:126-34.
- Corkery E, Palmer C, Foley ME, Schechter CB, Frisher L, Roman SH. Effect of a bicultural community health worker on completion of diabetes education in a Hispanic population. Diabetes Care 1997;20:254-7.
- Cottler LB, Compton WM, Ben Abdallah A, Cunningham-Williams R, Abram F, Fichtenbaum C, et al. Peer-delivered interventions reduce HIV risk behaviors among out-of-treatment drug abusers. Public Health Rep 1998;113:31-4.
- Coyle K, Basen-Engquist K, Kirby D, Parcel G, Banspach S, Collins J, et al. Safer choices: reducing teen pregnancy, HIV, and STDs. Public Health Rep 2001;116:82-93.
- Crump SR, Shipp MP, McCray GG, Morris SJ, Okoli JA, Caplan LS, et al. Abnormal mammogram follow-up: do community lay health advocates make a difference?. Health Promot Pract 2008;9:140-8.
- Curnow MM, Pine CM, Burnside G, Nicholson JA, Chesters RK, Huntington E. A randomised controlled trial of the efficacy of supervised toothbrushing in high-caries-risk children. Caries Res 2002;36:294-300.
- Davis DT, Bustamante A, Brown CP, Wolde-Tsadik G, Savage EW, Cheng X, et al. The urban church and cancer control: a source of social influence in minority communities. Public Health Rep 1994;109:500-6.
- Davis P, Abou-Saleh MT. Developing an enhanced counseling intervention for the primary prevention of hepatitis C among injecting drug users. Addict Disord Treat 2008;7:65-7.
- Davis SM, Going SB, Helitzer DL, Teufel NI, Snyder P, Gittelsohn J, et al. Pathways: a culturally appropriate obesity-prevention program for American Indian schoolchildren. Am J Clin Nutr 1999;69:796-802S.
- Davis SM, Clay T, Smyth M, Gittelsohn J, Arviso V, Flint WH, et al. Pathways curriculum and family interventions to promote healthful eating and physical activity in American Indian schoolchildren. Prev Med 2003;37:S24-34.
- Davis TC, Berkel HJ, Arnold CL, Nandy I, Jackson RH, Murphy PW. Intervention to increase mammography utilization in a public hospital. J Gen Intern Med 1998;13:230-3.
- Dennison CR, Post WS, Kim MT, Bone LR, Cohen D, Blumenthal RS, et al. Underserved urban African American men: hypertension trial outcomes and mortality during 5 years. Am J Hypertens 2007;20:164-71.
- Dickson-Gomez J, Knowlton A, Latkin C. Hoppers and oldheads: qualitative evaluation of a volunteer AIDS outreach intervention. AIDS Behav 2003;7:303-15.
- Dickson-Gomez J, Weeks M, Martinez M, Convey M. Times and places: process evaluation of a peer-led HIV prevention intervention. Subst Use Misuse 2006;41:669-90.
- DiClemente RJ, Wingood GM. A randomized controlled trial of an HIV sexual risk-reduction intervention for young African-American women. JAMA 1995;274:1271-6.
- Dignan M, Michielutte R, Blinson K, Wells HB, Case LD, Sharp P, et al. Effectiveness of health education to increase screening for cervical cancer among eastern-band Cherokee Indian women in North Carolina. J Natl Canc Inst 1996;88:1670-6.
- Dignan MB, Michielutte R, Wells HB, Sharp P, Blinson K, Case LD, et al. Health education to increase screening for cervical cancer among Lumbee Indian women in North Carolina. Health Educ Res 1998;13:545-56.
- Duggan AK, McFarlane EC, Windham AM, Rohde CA, Salkever DS, Fuddy L, et al. Intensive home visitation: a randomized trial, follow up and risk assessment study of Hawaii’s Healthy Start Program. Chicago, IL: National Center on Child Abuse and Neglect; 1996.
- Duggan AK, McFarlane EC, Windham AM, Rohde CA, Salkever DS, Fuddy L, et al. Evaluation of Hawaii’s Healthy Start Program. Future Child 1999;9:66-90.
- Earp JA, Flax VL. What lay health advisors do: an evaluation of advisors’ activities. Cancer Pract 1999;7:16-21.
- Earp JL, Altpeter M, Mayne L, Viadro CI, O’Malley MS. The North Carolina Breast Cancer Screening Program: foundations and design of a model for reaching older, minority, rural women. Breast Cancer Res Treat 1995;35:7-22.
- Earp JA, Viadro CI, Vincus AA, Altpeter M, Flax V, Mayne L, et al. Lay health advisors: a strategy for getting the word out about breast cancer. Health Educ Behav 1997;24:432-51.
- Earp JA, Eng E, O’Malley MS, Altpeter M, Rauscher G, Mayne L, et al. Increasing use of mammography among older, rural African American women: results from a community trial. Am J Public Health 2002;92:646-54.
- Eisenman DP, Glik D, Gonzalez L, Maranon R, Zhou Q, Tseng CH, et al. Improving Latino disaster preparedness using social networks. Am J Prev Med 2009;37:512-17.
- Elder JP, Ayala GX, Campbell NR, Arredondo EM, Slymen DJ, Baquero B, et al. Long-term effects of a communication intervention for Spanish-dominant Latinas. Am J Prev Med 2006;31:159-66.
- Elford J, Bolding G, Sherr L. Peer education has no significant impact on HIV risk behaviours among gay men in London. AIDS 2001;15:535-8.
- Ell K, Vourlekis B, Muderspach I, Nissly J, Padgett D, Pineda D, et al. Abnormal cervical screening follow-up among low-income Latinas: Project SAFe. J Womens Health Gend Based Med 2002;11:639-51.
- Erwin DO, Spatz TS, Stotts RC, Hollenberg JA. Increasing mammography practice by African American women. Cancer Pract 1999;7:78-85.
- Farrell MA, Hayashi T, Loo RK, Rocha DA, Sanders C, Hernandez M, et al. Clinic-based nutrition and lifestyle counseling for Hispanic women delivered by community health workers: design of the California WISEWOMAN study. J Womens Health 2009;18:733-9.
- Ferguson SL. Peer counseling in a culturally specific adolescent pregnancy prevention program. J Health Care Poor Underserved 1998;9:322-40.
- Fernandez-Esquer ME, Espinoza P, Torres I, Ramirez AG, McAlister AL. A su salud: a quasi-experimental study among Mexican American women. Am J Health Behav 2003;27:536-45.
- Fisher E, Musick J, Scott C, Miller JP, Gram R, Richardson V, et al. Improving clinic- and neighborhood-based smoking cessation services within federally qualified health centers serving low-income, minority neighborhoods. Nicotine Tob Res 2005;7:S45-56.
- Flaskerud JH, Nyamathi AM, Uman GC. Longitudinal effects of an HIV testing and counseling programme for low-income Latina women. Ethn Health 1997;2:89-103.
- Flax VL, Earp JL. Counseled women’s perspectives on their interactions with lay health advisors: a feasibility study. Health Educ Res 1999;14:15-24.
- Fletcher SW, Harris RP, Gonzalez JJ, Degnan D, Lannin DR, Strecher VJ, et al. Increasing mammography utilization: a controlled study. J Natl Canc Inst 1993;85:112-20.
- Flowers P, Frankis J, Hart G, Watson J, Platt S. Researching health promotion. New York: Routledge; 2000.
- Flowers P, Hart GJ, Williamson LM, Frankis JS, Der GJ. Does bar-based, peer-led sexual health promotion have a community-level effect amongst gay men in Scotland?. Int J STD AIDS 2002;13:102-8.
- Fogarty LA, Heilig CM, Armstrong K, Cabral R, Galavotti C, Gielen AC, et al. Long-term effectiveness of a peer-based intervention to promote condom and contraceptive use among HIV-positive and at-risk women. Public Health Rep 2001;116:103-19.
- Fors SW, Jarvis S. Evaluation of a peer-led drug abuse risk reduction project for runaway/homeless youths. J Drug Educ 1995;25:321-33.
- Fuller CM, Galea S, Caceres W, Blaney S, Sisco S, Vlahov D. Multilevel community-based intervention to increase access to sterile syringes among injection drug users through pharmacy sales in New York City. Am J Public Health 2007;97:117-24.
- Gabriel RM, Hopson T, Haskins M, Powell KE. Building relationships and resilience in the prevention of youth violence. Am J Prev Med 1996;12:48-55.
- Galbraith J, Ricardo I, Stanton B, Black M, Feigelman S, Kaljee L. Challenges and rewards of involving community in research: an overview of the ‘Focus on Kids’ HIV Risk Reduction Program. Health Educ Q 1996;23:383-94.
- Gary TL, Bone LR, Hill MN, Levine DM, McGuire M, Saudek C, et al. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med 2003;37:23-32.
- Gibson PG, Shah S, Mamoon HA. Peer-led asthma education for adolescents: impact evaluation. J Adolesc Health 1998;22:66-72.
- Gielen AC, Windsor R, Faden RR, O’Campo P, Repke J, Davis M. Evaluation of a smoking cessation intervention for pregnant women in an urban prenatal clinic. Health Educ Res 1997;12:247-54.
- Gittelsohn J, Evans M, Helitzer D, Anliker J, Story M, Metcalfe L, et al. Formative research in a school-based obesity prevention program for Native American school children (Pathways). Health Educ Res 1998;13:251-65.
- Gokcay G, Bulut A, Neyzi O. Paraprofessional women as health care facilitators in mother and child health. Trop Doct 1993;23:79-81.
- Gosin M, Marsiglia FF, Hecht ML. Keepin’it REAL: a drug resistance curriculum tailored to the strengths and needs of pre-adolescents of the southwest. J Drug Educ 2003;33:119-42.
- Gotay CC, Banner RO, Matsunaga DS, Hedlund N, Enos R, Issell BF, et al. Impact of a culturally appropriate intervention on breast and cervical screening among native Hawaiian women. Prev Med 2000;31:529-37.
- Griffiths C, Motlib J, Azad A, Ramsay J, Eldridge S, Feder G, et al. Randomised controlled trial of a lay-led self-management programme for Bangladeshi patients with chronic disease. Br J Gen Pract 2005;55:831-7.
- Hamer M, Box V. An evaluation of the development and functioning of the Boscombe Network for Change, a health alliance or partnership for health in Dorset. Health Educ J 2000;59:238-52.
- Hancock L, Sanson-Fisher R, Perkins J, Girgis A, Howley P, Schofield M. The effect of a community action intervention on adolescent smoking rates in rural Australian towns: the CART project. Cancer Action in Rural Towns. Prev Med 2001;32:332-40.
- Hanson J. Parental self-efficacy and asthma self-management skills. J Pediatr Nurs 1998;3:146-54.
- Helmert U, Shea S, Greiser E, Maschewsky Schneider U. Effects of 3.5 years of community intervention on social class gradients for cardiovascular disease risk factors in the German Cardiovascular Prevention Study. Ann Epidemiol 1993;3.
- Hiatt RA, Pasick RJ, Stewart S, Bloom J, Davis P, Gardiner P, et al. Cancer screening for underserved women: the breast and cervical cancer intervention study. Cancer Epidemiol Biomarkers Prev 2008;17:1945-9.
- Hill MN, Bone LR, Hilton SC, Roary MC, Kelen GD, Levine DM. A clinical trial to improve high blood pressure care in young urban black men: recruitment, follow-up, and outcomes. Am J Hypertens 1999;12:548-54.
- Hill MN, Han HR, Dennison CR, Kim MT, Roary MC, Blumenthal RS, et al. Hypertension care and control in underserved urban African American men: behavioral and physiologic outcomes at 36 months. Am J Hypertens 2003;16:906-13.
- Howard M, McCabe JB. Helping teenagers postpone sexual involvement. Fam Plann Perspect 1990;22:21-6.
- Husaini BA, Reece MC, Emerson JS, Scales S, Hull PC, Levine RS. A church-based program on prostate cancer screening for African American men: reducing health disparities. Ethn Dis 2008;18:S2-179.
- Hutcheson JJ, Black MM, Talley M, Dubowitz H, Howard JB, Starr RH, et al. Risk status and home intervention among children with failure-to-thrive: follow-up at age 4. J Pediatr Psychol 1997;22:651-68.
- Ireys HT, Sills EM, Kolodner KB, Walsh BB. A social support intervention for parents of children with juvenile rheumatoid arthritis: results of a randomized trial. J Pediatr Psychol 1996;21:633-41.
- Ireys HT, Chernoff R, DeVet KA, Kim Y. Maternal outcomes of a randomized controlled trial of a community-based support program for families of children with chronic illnesses. Arch Pediatr Adolesc Med 2001;155:771-7.
- Jandorf L, Bursac Z, Pulley L, Trevino M, Castillo A, Erwin DO. Breast and cervical cancer screening among Latinas attending culturally specific educational programs. Prog Community Health Partnersh 2008;2:195-204.
- Jemmott JB, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: a randomized controlled trial. JAMA 1998;279:1529-36.
- Johnson Z, Molloy B, Scallan E, Fitzpatrick P, Rooney B, Keegan T, et al. Community Mothers Programme –seven year follow-up of a randomized controlled trial of non-professional intervention in parenting. J Public Health Med 2000;22:337-42.
- Jones ME, Mondy LW. Lessons for prevention and intervention in adolescent pregnancy: a five-year comparison of outcomes of two programs for school-aged pregnant adolescents. J Pediatr Health Care 1994;8:152-9.
- Kartin D, Grant TM, Streissguth AP, Sampson PD, Ernst CC. Three-year developmental outcomes in children with prenatal alcohol and drug exposure. Pediatr Phys Ther 2002;14:145-53.
- Katz ML, Kauffman RM, Tatum CM, Paskett ED. Influence of church attendance and spirituality in a randomized controlled trial to increase mammography use among a low-income, tri-racial, rural community. J Relig Health 2008;47:227-36.
- Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: a community-level HIV prevention intervention for young gay men. Am J Public Health 1996;86:1129-36.
- Kelly JA, St Lawrence JS, Stevenson LY, Hauth AC, Kalichman SC, Diaz YE, et al. Community AIDS/HIV risk reduction: the effects of endorsements by popular people in three cities. Am J Public Health 1992;82:1483-9.
- Kelly JA, McAuliffe TL, Sikkema KJ, Murphy DA, Somlai AM, Mulry G, et al. Reduction in risk behavior among adults with severe mental illness who learned to advocate for HIV prevention. Psychiatr Serv 1997;48:1283-8.
- Kennedy MG, Mizuno Y, Hoffman R, Baume C, Strand J. The effect of tailoring a model HIV prevention program for local adolescent target audiences. AIDS Educ Prev 2000;12:225-38.
- Kernohan EE. Evaluation of a pilot study for breast and cervical cancer screening with Bradford’s minority ethnic women; a community development approach, 1991–93. Br J Cancer Suppl 1996;29:S42-6.
- Keyserling TC, Samuel-Hodge CD, Ammerman AS, Ainsworth BE, Henriquez-Roldan CF, Elasy TA, et al. A randomized trial of an intervention to improve self-care behaviors of African-American women with type 2 diabetes: impact on physical activity. Diabetes Care 2002;25:1576-83.
- Kiger H. Outreach to multiethnic, multicultural, and multilingual women for breast cancer and cervical cancer education and screening: a model using professional and volunteer staffing. Fam Community Health 2003;26:307-18.
- Kim S, Flaskerud JH, Koniak-Griffin D, Dixon EL. Using community-partnered participatory research to address health disparities in a Latino community. J Prof Nurs 2005;21:199-20.
- Kim YH, Sarna L. An intervention to increase mammography use by Korean American women. Oncol Nurs Forum 2004;31:105-10.
- King E, Rimer BK, Benincasa T, Harrop C, Amfoh K, Bonney G, et al. Strategies to encourage mammography use among women in senior citizens’ housing facilities. J Cancer Educ 1998;13:108-15.
- Kirby D, Korpi M, Barth R, Cagampang HH. Evaluation of Education Now and Babies Later (ENABL): final report. Berkeley, CA: University of California, School of Social Welfare, Family Welfare Research Group; 1995.
- Kirby D, Korpi M, Adivi C, Weissman J. An impact evaluation of project SNAPP: an AIDS and pregnancy prevention middle school program. AIDS Educ Prev 1997;9:44-61.
- Kirby D, Korpi M, Barth RP, Cagampang HH. The impact of the Postponing Sexual Involvement curriculum among youths in California. Fam Plann Perspect 1997;29:100-8.
- Kirby DB, Baumler E, Coyle KK, Basen-Engquist K, Parcel GS, Harrist R, et al. The ‘Safer Choices’ intervention: its impact on the sexual behaviors of different subgroups of high school students. J Adolesc Health 2004;35:442-52.
- Kocken PL, Zwanenburg EJ, de Hoop T. Effects of health education for migrant females with psychosomatic complaints treated by general practitioners. A randomised controlled evaluation study. Patient Educ Counsel 2008;70:25-30.
- Krieger JK, Takaro TK, Allen C, Song L, Weaver M, Chai S, et al. The Seattle-King County healthy homes project: implementation of a comprehensive approach to improving indoor environmental quality for low-income children with asthma. Environ Health Perspect 2002;110:311-22.
- Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health 2005;95:652-9.
- Laraque D, Barlow B, Durkin M, Heagarty M. Injury prevention in an urban setting: challenges and successes. Bull N Y Acad Med 1995;72:16-30.
- Larkey LK, Staten LK, Ritenbaugh C, Hall RA, Buller DB, Bassford T, et al. Recruitment of Hispanic women to the Women’s Health Initiative. The case of Embajadoras in Arizona. Control Clin Trials 2002;23:289-98.
- Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol 2003;22:332-9.
- Lauby JL, Smith PJ, Stark M, Person B, Adams J. A community-level HIV prevention intervention for inner-city women: results of the women and infants demonstration projects. Am J Public Health 2000;90:216-22.
- Levine DM, Bone L. The impact of a planned health education approach on the control of hypertension in a high risk population. J Hum Hypertens 1990;4:317-21.
- Levine DM, Becker DM, Bone LR, Stillman FA, Tuggle MB II, Prentice M, et al. A partnership with minority populations: a community model of effectiveness research. Ethn Dis 1992;2:296-305.
- Levine DM, Bone LR, Hill MN, Stallings R, Gelber AC, Barker A, et al. The effectiveness of a community/academic health center partnership in decreasing the level of blood pressure in an urban African-American population. Ethn Dis 2003;13:354-61.
- Levy JA, Fox SE. The outreach-assisted model of partner notification with IDUs. Public Health Rep 1998;113:160-9.
- Lindqvist K, Timpka T, Schelp L. Evaluation of an inter-organizational prevention program against injuries among the elderly in a WHO Safe Community. Public Health 2001;115:308-16.
- Lorig KR, Ritter PL, Gonzalez VM. Hispanic chronic disease self-management: a randomized community-based outcome trial. Nurs Res 2003;52:361-9.
- Lupton BS, Fonnebo V, Sogaard AJ. The Finnmark Intervention Study: is it possible to change CVD risk factors by community-based intervention in an Arctic village in crisis?. Scand J Public Health 2003;31:178-86.
- Lupton BS, Fonnebo V, Sogaard AJ, Fylkesnes K. The Finnmark Intervention Study: do community-based intervention programmes threaten self-rated health and well-being? Experiences from Batsfjord, a fishing village in North Norway. Eur J Public Health 2005;15:91-6.
- Marcenko MO, Spence M. Home visitation services for at-risk pregnant and postpartum women: a randomized trial. Am J Orthopsychiatry 1994;64:468-78.
- Margolis KL, Lurie N, McGovern PG, Tyrrell M, Slater JS. Increasing breast and cervical cancer screening in low-income women. J Gen Intern Med 1998;13:515-21.
- May KM, Mendelson C, Ferketich S. Community empowerment in rural health care. Public Health Nurs 1995;12:25-30.
- McAlister AL, Fernandez-Esquer ME, Ramirez AG, Trevino F, Gallion KJ, Villarreal R, et al. Community level cancer control in a Texas barrio: Part II – base-line and preliminary outcome findings. J Natl Canc Inst Monogr 1995:123-6.
- McCue M, Afifi LA. Using peer helpers for tuberculosis prevention. J Am Coll Health 1996;44:173-6.
- McFarlane J, Soeken K, Wiist W. An evaluation of interventions to decrease intimate partner violence to pregnant women. Public Health Nurs 2000;17:443-51.
- McInroy N, MacDonald S. From community garden to Westminster: active citizenship and the role of public space. Manchester: Centre for Local Economic Strategies; 2005.
- McIntosh E, Barlow J, Davis H, Stewart-Brown S. Economic evaluation of an intensive home visiting programme for vulnerable families: a cost-effectiveness analysis of a public health intervention. J Public Health 2009;31:423-33.
- McNeill LH, Coeling M, Puleo E, Suarez EG, Bennett GG, Emmons KM. Colorectal cancer prevention for low-income, sociodemographically-diverse adults in public housing: baseline findings of a randomized controlled trial. BMC Public Health 2009;9.
- McPhee SJ, Bird JA, Ha NT, Jenkins CN. Pathways to early cancer detection for Vietnamese women: Suc Khoe La Vang (health is gold!). Health Educ Q 1996;23:s60-75.
- McQuiston C, Choi-Hevel S, Clawson M. Protegiendo Nuestra Comunidad: empowerment participatory education for HIV prevention. J Transcult Nurs 2001;12:275-83.
- Miller RL, Klotz D, Eckholdt HM. HIV prevention with male prostitutes and patrons of hustler bars: replication of an HIV preventive intervention. Am J Community Psychol 1998;26:97-131.
- Morisky DE, Malotte CK, Ebin V, Davidson P, Cabrera D, Trout PT, et al. Behavioral interventions for the control of tuberculosis among adolescents. Public Health Rep 2001;116:568-74.
- Motohashi Y, Kaneko Y, Sasaki H, Yamaji M. A decrease in suicide rates in Japanese rural towns after community-based intervention by the health promotion approach. Suicide Life Threat Behav 2007;37:593-9.
- Nair P, Schuler ME, Black MM, Kettinger L, Harrington D. Cumulative environmental risk in substance abusing women: early intervention, parenting stress, child abuse potential and child development. Child Abuse Neglect 2003;27:997-1017.
- Navarro AM, Senn KL, McNicholas LJ, Kaplan RM, Roppe B, Campo MC. Por La Vida model intervention enhances use of cancer screening tests among Latinas. Am J Prev Med 1998;15:32-41.
- Neuhauser L, Schwab M, Leonard S, Bieber M. Community participation in health promotion: evaluation of the California Wellness Guide. Health Promot Int 1998;13:211-22.
- Neumark-Sztainer D, Story M, Hannan PJ, Rex J. New Moves: a school-based obesity prevention program for adolescent girls. Prev Med 2003;37:41-5.
- Nguyen TT, Le G, Nguyen T, Le K, Lai K, Gildengorin G, et al. Breast cancer screening among Vietnamese Americans: a randomized controlled trial of lay health worker outreach. Am J Prev Med 2009;37:306-13.
- Nyamathi A, Flaskerud JH, Leake B, Dixon EL, Lu A. Evaluating the impact of peer, nurse case-managed, and standard HIV risk-reduction programs on psychosocial and health-promoting behavioral outcomes among homeless women. Res Nurs Health 2001;24:410-22.
- O’Donnell L, Stueve A, O’Donnell C, Duran R, San D, Wilson RF, et al. Long-term reductions in sexual initiation and sexual activity among urban middle schoolers in the reach for health service learning program. J Adolesc Health 2002;31:93-100.
- Evaluation of the residents’ consultancy pilots initiative. London: Office of the Deputy Prime Minister; 2004.
- Neighbourhood Wardens Scheme evaluation. London: Office of the Deputy Prime Minister; 2004.
- National evaluation of local strategic partnerships: formative evaluation and action research programme 2002–2005. London: Office of the Deputy Prime Minister; 2006.
- Neighbourhood management: at the turning point?: programme review 2005–2006. London: Office of the Deputy Prime Minister; 2006.
- O’Hara P, Messick BJ, Fichtner RR, Parris D. A peer-led AIDS prevention program for students in an alternative school. J School Health 1996;66:176-82.
- O’Hare JP, Raymond NT, Mughal S, Dodd L, Hanif W, Ahmad Y, et al. Evaluation of delivery of enhanced diabetes care to patients of South Asian ethnicity: the United Kingdom Asian Diabetes Study (UKADS). Diabetic Med 2004;21:1357-65.
- Orpinas P, Parcel GS, McAlister A, Frankowski R. Violence prevention in middle schools: a pilot evaluation. J Adolesc Health 1995;17:360-71.
- Outlaw AY, Naar King S, Parsons JT, Green Jones M, Janisse H, Secord E. Using motivational interviewing in HIV field outreach with young African American men who have sex with men: a randomized clinical trial. Am J Public Health 2010;100:S146-51.
- Paradis G, Levesque L, Macaulay AC, Cargo M, McComber A, Kirby R, et al. Impact of a diabetes prevention program on body size, physical activity, and diet among Kanien’keha:ka (Mohawk) children 6 to 11 years old: 8-year results from the Kahnawake Schools Diabetes Prevention Project. Pediatrics 2005;115:333-9.
- Parker EA, Israel BA, Robins TG, Mentz G, Xihong L, Brakefield-Caldwell W, et al. Evaluation of Community Action Against Asthma: a community health worker intervention to improve children’s asthma-related health by reducing household environmental triggers for asthma. Health Educ Behav 2008;35:376-95.
- Parkin PC, Spence LJ, Hu X, Kranz KE, Shortt LG, Wesson DE. Evaluation of a promotional strategy to increase bicycle helmet use by children. Pediatrics 1993;91:772-7.
- Paskett E, Tatum C, Rushing J, Michielutte R, Bell R, Foley KL, et al. Randomized trial of an intervention to improve mammography utilization among a triracial rural population of women. J Natl Canc Inst 2006;98:1226-37.
- Peragallo N, Deforge B, O’Campo P, Lee SM, Kim YJ, Cianelli R, et al. A randomized clinical trial of an HIV-risk-reduction intervention among low-income Latina women. Nurs Res 2005;54:108-18.
- Perry CL, Williams CL, Komro KA, Veblen-Mortenson S, Forster JL, Bernstein-Lachter R, et al. Project Northland high school interventions: community action to reduce adolescent alcohol use. Health Educ Behav 2000;27:29-4.
- Perry CL, Lee S, Stigler MH, Farbakhsh K, Komro KA, Gewirtz AH, et al. The impact of Project Northland on selected MMPI-A problem behavior scales. J Prim Prev 2007;28:449-65.
- Philis-Tsimikas A, Walker C, Rivard L, Talavera G, Reimann JO, Salmon M, et al. Improvement in diabetes care of underinsured patients enrolled in Project Dulce: a community-based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care 2004;27:110-15.
- Philliber S, Allen JP, Miller BC, Card JJ, Paikoff RL, Peterson JL. Preventing adolescent pregnancy: model programs and evaluation. Newbury Park, CA: Sage; 1992.
- Pilote L, Tulsky JP, Zolopa AR, Hahn JA, Schecter GF, Moss AR. Tuberculosis prophylaxis in the homeless. A trial to improve adherence to referral. Arch Intern Med 1996;156:161-5.
- Pinkerton SD, Holtgrave DR, DiFranceisco WJ, Stevenson LY, Kelly JA. Cost-effectiveness of a community-level HIV risk reduction intervention. Am J Public Health 1998;88:1239-42.
- Powell ME, Carter V, Bonsi E, Johnson G, Williams L, Taylor-Smith L, et al. Increasing mammography screening among African American women in rural areas. J Health Care Poor Underserved 2005;16:11-2.
- Quinn MT, McNabb WL. Training lay health educators to conduct a church-based weight-loss program for African American women. Diabetes Educ 2001;27:231-8.
- Quirk ME, Godkin MA, Schwenzfeier E. Evaluation of two AIDS prevention interventions for inner-city adolescent and young adult women. Am J Prev Med 1993;9:21-6.
- Ravesloot CH, Seekins T, Cahill T, Lindgren S, Nary DE, White G. Health promotion for people with disabilities: development and evaluation of the Living Well with a Disability program. Health Educ Res 2007;22:522-31.
- Richardson G, Kennedy A, Reeves D, Bower P, Lee V, Middleton E, et al. Cost effectiveness of the Expert Patients Programme (EPP) for patients with chronic conditions. J Epidemiol Community Health 2008;62:361-7.
- Rickert VI, Jay MS, Gottlieb A. Effects of a peer-counseled AIDS education program on knowledge, attitudes, and satisfaction of adolescents. J Adolesc Health 1991;12:38-43.
- Ritchie D. ‘Breathing Space’: reflecting upon the realities of community partnerships and workers’ beliefs about promoting health. Health Educ J 2001;60:73-92.
- Ritchie D, Parry O, Gnich W, Platt S. Issues of participation, ownership and empowerment in a community development programme: tackling smoking in a low-income area in Scotland. Health Promot Int 2004;19:51-9.
- Robinson BB, Uhl G, Miner M, Bockting WO, Scheltema KE, Rosser BR, et al. Evaluation of a sexual health approach to prevent HIV among low income, urban, primarily African American women: results of a randomized controlled trial. AIDS Educ Prev 2002;14:81-96.
- Roffman RA, Picciano JF, Ryan R, Beadnell B, Fisher D, Downey L, et al. HIV-prevention group counseling delivered by telephone: an efficacy trial with gay and bisexual men. AIDS Behav 1997;1:137-54.
- Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: a pilot study. Ann Behav Med 2005;29:225-35.
- Rosser BR, Bockting WO, Rugg DL, Robinson BB, Ross MW, Bauer GR, et al. A randomized controlled intervention trial of a sexual health approach to long-term HIV risk reduction for men who have sex with men: effects of the intervention on unsafe sexual behavior. AIDS Educ Prev 2002;14:59-71.
- Royse D. Mentoring high-risk minority youth: evaluation of the Brothers project. Adolescence 1998;33:145-58.
- Sauaia A, Min SJ, Lack D, Apodaca C, Osuna D, Stowe A, et al. Church-based breast cancer screening education: impact of two approaches on Latinas enrolled in public and private health insurance plans. Prev Chronic Dis 2007;4.
- Saxe L, Reber E, Hallfors D, Kadushin C, Jones D, Rindskopf D, et al. Think globally, act locally: assessing the impact of community-based substance abuse prevention. Eval Prog Plann 1997;20:357-66.
- Schuler ME, Nair P, Black MM, Kettinger L. Mother–infant interaction: effects of a home intervention and ongoing maternal drug use. J Clin Child Psychol 2000;29:424-31.
- Schuler ME, Nair P, Kettinger L. Drug-exposed infants and developmental outcome: effects of a home intervention and ongoing maternal drug use. Arch Pediatr Adolesc Med 2003;157:133-8.
- Secker-Walker RH, Flynn BS, Solomon LJ, Vacek PM, Dorwaldt AL, Geller BM, et al. Helping women quit smoking: baseline observations for a community health education project. Am J Prev Med 1996;12:367-77.
- Secker-Walker RH, Dana GS, Solomon LJ, Flynn BS, Geller BM. The role of health professionals in a community-based program to help women quit smoking. Prev Med 2000;30:126-37.
- Secker-Walker RH, Holland RR, Lloyd CM, Pelkey D, Flynn BS. Cost effectiveness of a community based research project to help women quit smoking. Tob Control 2005;14:37-42.
- Shepherd J, Weare K, Turner G. Peer-led sexual health promotion with young gay and bisexual men: results of the HAPEER Project. Health Educ 1997;97:204-12.
- Siegel D, DiClemente R, Durbin M, Krasnovsky F, Saliba P. Change in junior high school students’ AIDS-related knowledge, misconceptions, attitudes, and HIV-preventive behaviors: effects of a school-based intervention. AIDS Educ Prev 1995;7:534-43.
- Sieverding J, Boyer CB, Siller J, Gallaread A, Krone M, Chang YJ. Youth United Through Health Education: building capacity through a community collaborative intervention to prevent HIV/STD in adolescents residing in a high STD prevalent neighborhood. AIDS Educ Prev 2005;17:375-85.
- Sigel DM, Aten MJ, Roghmann KJ, Enaharo M. Early effects of a school-based human immunodeficiency virus infection and sexual risk prevention intervention. Arch Pediatr Adolesc Med 1998;152:961-70.
- Sikkema KJ, Kelly JA, Winett RA, Solomon LJ, Cargill VA, Roffman RA, et al. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. Am J Public Health 2000;90:57-63.
- Sikkema KJ, Anderson ES, Kelly JA, Winett RA, Gore-Felton C, Roffman RA, et al. Outcomes of a randomized, controlled community-level HIV prevention intervention for adolescents in low-income housing developments. AIDS 2005;19:1509-16.
- Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomatology in HIV-positive men and women. Health Psychol 2007;26:488-95.
- Skinner CS, Arfken CL, Waterman B. Outcomes of the Learn, Share & Live breast cancer education program for older urban women. Am J Public Health 2000;90:1229-34.
- Slater JS, Ha CN, Malone ME, McGovern P, Madigan SD, Finnegan JR, et al. A randomized community trial to increase mammography utilization among low-income women living in public housing. Prev Med 1998;27:862-70.
- Sorensen G, Stoddard AM, LaMontagne AD, Emmons K, Hunt MK, Youngstrom R, et al. A comprehensive worksite cancer prevention intervention: behavior change results from a randomized controlled trial (United States). J Public Health Policy 2003;24:5-25.
- Sox CH, Dietrich AJ, Goldman DC, Provost EM. Improved access to women’s health services for Alaska natives through community health aide training. J Community Health 1999;24:313-23.
- Spoth R, Redmond C, Shin C, Greenberg M, Clair S, Feinberg M. Substance-use outcomes at 18 months past baseline. The PROSPER community–university partnership trial. Am J Prev Med 2007;32:395-402.
- Stanton B, Harris C, Cottrell L, Li X, Gibson C, Guo J, et al. Trial of an urban adolescent sexual risk-reduction intervention for rural youth: a promising but imperfect fit. J Adolesc Health 2006;38.
- Stanton BF, Li X, Ricardo I, Galbraith J, Feigelman S, Kaljee L. A randomized, controlled effectiveness trial of an AIDS prevention program for low-income African-American youths. Arch Pediatr Adolesc Med 1996;150:363-72.
- Stephenson JM, Strange V, Forrest S, Oakley A, Copas A, Allen E, et al. Pupil-led sex education in England (RIPPLE study): cluster-randomised intervention trial. Lancet 2004;364:338-46.
- St Lawrence JS, Brasfield TL, Jefferson KW, Alleyne E, O’Bannon RE III, Shirley A. Cognitive-behavioral intervention to reduce African American adolescents’ risk for HIV infection. J Consult Clin Psychol 1995;63:221-37.
- St Pierre Tena L, Mark Melvin M, Kaltreider DL, Campbell B. Boys & girls clubs and school collaborations: a longitudinal study of a multicomponent substance abuse prevention program for high-risk elementary school children. J Community Psychol 2001;29:87-106.
- Suarez L, Roche RA, Pulley LV, Weiss NS, Goldman D, Simpson DM. Why a peer intervention program for Mexican-American women failed to modify the secular trend in cancer screening. Am J Prev Med 1997;13:411-17.
- Tan EJ, Xue QL, Li T, Carlson MC, Fried LP. Volunteering: a physical activity intervention for older adults. The Experience Corps program in Baltimore. J Urban Health 2006;83:954-69.
- Teti M, Bowleg L, Cole R, Lloyd L, Rubinstein S, Spencer S, et al. A mixed methods evaluation of the effect of the Protect and Respect intervention on the condom use and disclosure practices of women living with HIV/AIDS. AIDS Behav 2010;14:567-79.
- Thoits PA, Hohmann AA, Harvey MR, Fletcher B. Similar-other support for men undergoing coronary artery bypass surgery. Health Psychol 2000;19:264-73.
- Thomas JC, Earp JA, Eng E. Evaluation and lessons learned from a lay health advisor programme to prevent sexually transmitted diseases. Int J STD AIDS 2000;11:812-18.
- Timpka T, Nilsen P, Lindqvist K. The impact of home safety promotion on different social strata in a WHO safe community. Public Health 2006;120:427-33.
- Tudiver F, Myers T, Kurtz R, Orr K, Rowe C, Jackson E, et al. The talking sex project: results of a randomized controlled trial of small-group AIDS education for 612 gay and bisexual men. Eval Health Prof 1992;83:26-42.
- Tulsky JP, Pilote L, Hahn JA, Zolopa AJ, Burke M, Chesney M, et al. Adherence to isoniazid prophylaxis in the homeless: a randomized controlled trial. Arch Intern Med 2000;160:697-702.
- Valente TW, Hoffman BR, Ritt Olson A, Lichtman K, Johnson CA. Effects of a social-network method for group assignment strategies on peer-led tobacco prevention programs in schools. American J Public Health 2003;93:1837-43.
- Wagner EH, Wickizer TM, Cheadle A, Psaty BM, Koepsell TD, Diehr P, et al. The Kaiser Family Foundation Community Health Promotion Grants Program: findings from an outcome evaluation. Health Serv Res 2000;35:561-89.
- Weber BE, Reilly BM. Enhancing mammography use in the inner city. A randomized trial of intensive case management. Arch Intern Med 1997;157:2345-9.
- Weeks MR, Dickson-Gomez J, Mosack KE, Convey M, Martinez M, Clair S. The risk avoidance partnership: training active drug users as peer health advocates. J Drug Issues 2006;36:541-70.
- Weinrich SP, Weinrich MC, Stromborg MF, Boyd MD, Weiss HL. Using elderly educators to increase colorectal cancer screening. Gerontologist 1993;33:491-6.
- Welsh AL, Sauaia A, Jacobellis J, Min SJ, Byers T. The effect of two church-based interventions on breast cancer screening rates among Medicaid-insured Latinas. Prev Chronic Dis 2005;2.
- Wiist WH, Jackson RH, Jackson KW. Peer and community leader education to prevent youth violence. Am J Prev Med 1996;12:56-64.
- Wilson Tracey E, Fraser-White M, Feldman J, Homel P, Wright S, King G, et al. Hair salon stylists as breast cancer prevention lay health advisors for African American and Afro-Caribbean women. J Health Care Poor Underserved 2008;19:216-26.
- Wishart L, Macerollo J, Loney P, King A, Beaumont L, Browne G, et al. ‘Special steps’: an effective visiting/walking program for persons with cognitive impairment. Can J Nurs Res 2000;31:57-71.
- Wohl AR, Garland WH, Valencia R, Squires K, Witt MD, Kovacs A, et al. A randomized trial of directly administered antiretroviral therapy and adherence case management intervention. Clin Infect Dis 2006;42:1619-27.
- Wolitski RJ, Gomez CA, Parsons JT. Effects of a peer-led behavioral intervention to reduce HIV transmission and promote serostatus disclosure among HIV-seropositive gay and bisexual men. AIDS 2005;19:S99-10.
- Zhu K, Hunter S, Bernard LJ, Payne-Wilks K, Roland CL, Elam LC, et al. An intervention study on screening for breast cancer among single African-American women aged 65 and older. Prev Med 2002;34:536-45.
- Ziersch A, Gaffney J, Tomlinson DR. STI prevention and the male sex industry in London: evaluating a pilot peer education programme. Sex Transm Infect 2000;76:447-53.
Appendix 10 PRISMA checklist
| Section/topic | Checklist item | Reported | |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis or both | p. i |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number | p. v–vi |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known | Chapter 1, Rationale for this review |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes and study design (PICOS) | Chapter 1, Review aims and objectives and Review questions |
| Methods | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g. web address) and, if available, provide registration information including registration number | Appendix 11 |
| Eligibility criteria | 6 | Specify study characteristics (e.g. PICOS, length of follow-up) and report characteristics (e.g. years considered, language, publication status) used as criteria for eligibility, giving rationale | Chapter 2, Study selection and eligibility criteria |
| Information sources | 7 | Describe all information sources (e.g. databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched | Chapter 2, Search strategy |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated | Appendix 1 |
| Study selection | 9 | State the process for selecting studies (i.e. screening, eligibility, included in systematic review and, if applicable, included in the meta-analysis) | Chapter 2, Study selection and eligibility criteria |
| Data collection process | 10 | Describe method of data extraction from reports (e.g. piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators | Chapter 2, Data extraction |
| Data items | 11 | List and define all variables for which data were sought (e.g. PICOS, funding sources) and any assumptions and simplifications made | Chapter 2, Analysis stage |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis | Chapter 2, Quality assessment |
| Summary measures | 13 | State the principal summary measures (e.g. risk ratio, difference in means) | Chapter 2, Summary measures |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g. I2) for each meta-analysis | Chapter 2, Synthesis of results |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g. publication bias, selective reporting within studies) | Chapter 2, Quality assessment, and Chapter 5, Risk of bias across studies |
| Additional analyses | 16 | Describe methods of additional analyses (e.g. sensitivity or subgroup analyses, meta-regression), if done, indicating which were prespecified | Chapter 2, Meta-analysis |
| Results | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram | Chapter 3, Study selection |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g. study size, PICOS, follow-up period) and provide the citations | Chapter 3, Study characteristics, and Appendix 8 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12) | Chapter 5, Risk of bias within studies, and Chapter 6, Quality of process evaluation methods |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group, (b) effect estimates and confidence intervals, ideally with a forest plot | Chapter 5, Synthesis of results |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency | Chapter 5, Synthesis of results |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15) | Chapter 5, Risk of bias across studies |
| Additional analysis | 23 | Give results of additional analyses, if done [e.g. sensitivity or subgroup analyses, meta-regression (see Item 16)] | Chapter 5, Additional analyses |
| Discussion | |||
| Summary of evidence | 24 | Summarise the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g. health-care providers, users and policy-makers) | Chapter 9, Summary of evidence |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g. risk of bias) and at review level (e.g. incomplete retrieval of identified research, reporting bias) | Chapter 9, Limitations |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research | Chapter 10 |
| Funding | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g. supply of data); role of funders for the systematic review | Acknowledgements |
Appendix 11 Protocol
PHR Protocol – project ref: 09/3008/11
Version: 1
Date: 3 October 2011
Community engagement to reduce inequalities in health: protocol for a systematic review
1. Aims/Objectives:
The overarching aim of this project is to identify community engagement approaches that are effective in reducing inequalities in health, and to describe the approaches in terms of the circumstances in which they ‘work’ and the costs associated with their implementation. We will do this by achieving the following objectives:
-
Consulting with relevant stakeholders in order to ensure that our study is based on their perspectives and experiences.
-
Identifying a set of primary research studies that evaluate the effectiveness of interventions with a community engagement component in terms of their impacts on inequalities in health.
-
Making contact with researchers in the field who have investigated the issues relevant to this study in order to enhance the dataset we draw upon.
-
Describing and synthesising the data we identify.
-
Drawing conclusions, verifying our findings with stakeholders, and writing up and disseminating our results.
Review questions
Our overarching review question is: Can specific approaches to community engagement help to reduce inequalities in health; for whom, under what circumstances, and with what resources?
In order to answer this question, the following, more focused research questions (RQ) will form the basis of our enquiry:
-
What is the range of models and approaches underpinning community engagement?
-
What are the mechanisms and contexts through which communities are engaged?
-
Which approaches to community engagement are associated with improved health outcomes among disadvantaged groups? How do these approaches lead to improved outcomes?
-
Which approaches to community engagement are associated with reductions in inequalities in health? How do these approaches lead to reductions in health inequalities?
-
Which types of intervention work best when communities are engaged?
-
Is community engagement associated with better outcomes for some groups when compared to others? (In particular, does it work better or less well for children and young people?)
-
How do targeted and universal interventions compare in terms of community engagement and their impact on inequalities?
-
What are the resource implications of effective approaches to community engagement?
-
Are better outcomes simply the result of increased resources, or are some approaches to community engagement potentially more cost effective than others?
RQ1 and RQ2 will be addressed through a narrative synthesis of the models and mechanisms reported in the available literature, RQ3 to RQ9 will be addressed through narrative and quantitative (where appropriate) syntheses of the evidence, and RQ8 and RQ9 will be further explored through cost-effectiveness analyses.
2. Background:
Community engagement in health care in the UK
Historically, interventions and actions to promote health were driven by professionals with little or no input from the targeted populations (Harden & Oliver, 2001). More recently, ‘community engagement’ has become central to guidance and national strategy for promoting public health (e.g., Department of Health, 2008). Community engagement has been broadly defined as ‘Involving communities in decision-making and in the planning, design, governance and delivery of services’ (Swainston & Summerbell, 2008, p. 11). Community engagement activities can take many forms; examples of some initiatives in the UK include [Examples from Dudley Primary Care Trust. Dudley PCT website http://www.nhsdudley.nhs.uk/sites/your-nhs-community-engagement/index.asp?id=9070 (accessed 18 May 2011)]:
-
service user networks,
-
healthcare forums,
-
volunteering,
-
courses delivered by trained peers (e.g., Dudley Primary Care Trust’s ‘Expert Patient Programme’), and
-
interactive websites that enable the submission of views and opinions on various surveys, polls and public consultations.
Community engagement can be provided alone or in combination with other initiatives. In studies where community engagement is provided as the sole intervention, evidence of effectiveness can be determined because there is a direct link between community engagement and the outcomes being measured. In contrast, indirect community engagement initiatives are multi-faceted, including community engagement as one of a number of intervention features. In such cases, an association between the multi-faceted initiative and population outcomes may be seen, but it is not possible to discern with confidence how the community engagement aspect of the intervention may have contributed to this effect (Popayet al. , 2007: p. 1–2).
Community engagement can also be seen to operate on different levels, depending on the degree to which community engagement occurs. Wilcox et al. (1999) describe five levels of increasing community engagement:
-
information-giving, in which people are merely told what is planned;
-
consultation, where people are offered some options and ideas, and organizers listen to feedback, but do not allow new ideas;
-
deciding together, in which organizers encourage additional options and ideas, and provide opportunities for joint decision-making;
-
acting together, to not only decide together on what is best, but forming a partnership to carry it out; and
-
supporting independent community interests, where local groups or organizations are offered funds, advice or other support to develop their own agendas within guidelines.
A more condensed scale exists for involvement in health research: consultation, collaboration, and community control, with information provision not included as a sufficient level of engagement (Booteet al. 2002).
There is strong policy support for involving people in developing public services and evaluation (e.g., the creation of the Health Inequalities National Support Team, Department of Health, 2011). Various national publications, including Shifting the Balance of Power (Department of Health, 2002); Commissioning a Patient-led National Health Service (Department of Health, 2005); the Our Health, Our Care, Our Say White Paper (Department of Health January 2006); A Stronger Local Voice (Department of Health July 2006); and Health reform in England: update and commissioning framework (Department of Health July 2006) have provided a framework for the engagement of the public in the planning, design, and delivery of public health services. Primary care trusts (PCTs) throughout the country have community engagement and public and patient involvement strategies.
Given the increasing policy support for community engagement, it is critical to consider whether such strategies are effective and under what circumstances. The following section outlines the state of research on community engagement in health care.
The evidence base for community engagement
There is some evidence that public involvement in UK health services can be effective (Daykinet al. , 2007). Community engagement is thought to improve health via its impact on the development and delivery of more appropriate and accessible interventions, as well as a direct positive impact on social cohesion and individual self-esteem and self-efficacy for those who are engaged (Popay, 2006).
Community involvement can be seen as a goal in itself as it encourages public accountability and transparency (Nilsenet al. , 2006; Wallerstein, 2006). Through public involvement, communities can have the potential to promote health from the bottom up (MacDonald & Davies, 1998). Listening to, hearing, and acting upon the views of the community – particularly those from socially and economically disadvantaged groups – can both empower communities and lead to the co-production and implementation of interventions that are more likely to be feasible, acceptable and ultimately effective in improving health (Popayet al. , 1996, 2007). Importantly, community engagement can ‘give a voice to the voiceless’ (Whitehead & Dahlgren 2006). People with the greatest health needs are often socially excluded and disengaged from services, and their circumstances can make it difficult for organisations to address their needs appropriately. Opportunities to work with their peers via community engagement initiatives may improve the social inclusion of marginalised people.
While there is a recognised literature recommending community engagement (Popayet al. , 2007; Swainston & Summerbell, 2008), there is much uncertainty about how communities might be best engaged; what the results of such engagements are; and how the results should be recorded, analysed, and used (Graham, 2009; Popayet al. , 2007; Sheridanet al. , 2010). The theory behind recommendations for community engagement is often not linked to empirical evidence.
One of the problems with the current evidence base is a lack of robust synthesis of the research. This makes it difficult to assess the empirical basis for claims about community engagement, as research is scattered across disciplinary and topic-focused boundaries and not pulled together in a coherent way. The few syntheses that have been conducted are helpful, though have acknowledged limitations, having been completed rapidly from relatively small datasets (Popayet al. , 2007; Swainston & Summerbell, 2008). Limited synthesis in this area also makes it difficult to discern whether community engagement might be an appropriate strategy in any specific situation, as the available evidence is based only on a handful of studies (e.g., Popayet al. , 2007, p. 62).
The same lack of high quality evidence is apparent when looking at the cost effectiveness of different community engagement strategies, particularly with respect to the UK context. Guidance on community engagement produced by NICE (2008) highlighted a dearth of information in this regard. A review of economic studies on community engagement for health promotion found eight studies, none of which focused specifically on the cost effectiveness of the community engagement component (Mason et al. , 2006). A companion systematic review of the economic evidence for community engagement and development strategies to address the wider determinants of health also failed to identify any studies that reported the costs and health benefits of a community engagement approach relative to a comparator (Masonet al. , 2007); some information on the resources required to deliver interventions was, however, reported in twenty studies. A final output of this work for NICE was economic modelling of some community engagement strategies to look at the potential cost effectiveness of community engagement strategies (Carr-Hill & Street, 2008). However, this was not included in the final guidance because of a lack of robust information on costs and effects; only two vignettes on the role of trained peer educators and community engagement as a way of gaining support for flood defences were included (see also Fischer, 2007).
In summary, the evidence base supporting the effectiveness and cost-effectiveness of community engagement strategies is fragmented and of uncertain quality. The review described in this protocol aims to make sense of the research literature through a map of the available research and analyses of the relevant evidence.
A particular focus of the review will be placed on the ways in which community engagement can help to reduce health inequalities. The rationale for focusing on health inequalities is presented in the following section.
The challenge of health inequalities in the UK
The quality of health varies from person to person as a result of biological, environmental, social, economic, and lifestyle factors. The term ‘health inequalities’ refers to gaps in the quality of the health of different groups of people based on differences in social, economic, and environmental conditions (Marmot, 2010). Health inequalities are evident where disadvantaged groups (e.g., people with low socioeconomic status, socially excluded people) tend to have poorer health than more affluent members of society. Importantly, health inequalities refer to differences in modifiable health determinants, such as housing, employment, education, income, access to public services, and personal behaviour (e.g., use of tobacco) (Greater London Authority Act, 2007), as opposed to fixed determinants such as age, sex, and genetics. [However, social inequalities are often associated with fixed determinants (age, sex, and genetics), and so these fixed factors might have indirect effects on health status.] The fact that many health determinants are modifiable lies at the very heart of all health inequalities strategies – if they are modifiable, then something can be done to improve them. By improving modifiable determinants of health, it is hoped that health inequalities can be reduced and health outcomes enhanced.
Health outcomes that are typically considered when examining health inequalities include life expectancy/mortality rates, disability-free life expectancy, and limiting long-term illness. Other health outcomes and health-related indicators can include (but are not limited to) low birth weight, infant mortality, hospital admissions, teenage pregnancy, and uptake of health services. In the UK, taking into account variations between local authorities, the average male in the lowest deprivation decile (i.e., the poorest males) will have a life expectancy that is 6.7 years shorter than the average male in the highest deprivation decile (i.e., the most affluent; Figures calculated by Alison O’Mara-Eves using multilevel modelling of data from the London Health Observatory available at http://www.lho.org.uk/LHO_Topics/national_lead_areas/marmot/marmotindicators.aspx.). The poorest females will have a life expectancy that is 4.7 years shorter than the most affluent females. When looking at specific local authorities, some of these differences become even larger. For example, Westminster local authority has the widest within-area inequality gap for males, with almost 17 years longer life expectancy for the most affluent males compared to the poorest (London Health Observatory, 2011). The widest gap for females is in Halton and Newcastle upon Tyne at just over 11 years difference in life expectancy (LHO, 2011). The average difference in disability-free life expectancy in England – regardless of area or gender, is 17 years. Clearly the life expectancy and quality of health across the lifespan are much lower, on average, for the most deprived than the most affluent.
There is no dispute in the UK that health inequalities exist (Marmot, 2010), and as a result, health inequalities have been an increasing focus of policy interest. For instance, in 2004, tackling health inequalities was one of the aims underpinning the eleven standards promoted within the National Service Framework (NSF) (Department of Health 2004). More recently, the Marmot Review of health inequalities, ‘Fair Society, Healthy Lives’, has afforded even greater attention to the issue of health inequalities (with a particular focus on England). The Review identified the evidence relating to health inequalities in England; developed actionable recommendations for practice; produced guidance on possible objectives and measures of inequalities; and developed a starting point for a post-2010 health inequalities strategy. The key recommendations made in the report to address health inequalities fall under the following six broad themes:
-
giving children the best start in life,
-
enabling all children, young people and adults to maximise their capabilities,
-
creating fair employment and good work for all,
-
ensuring a healthy standard of living for all,
-
developing healthy and sustainable places and communities, and
-
strengthening the role and impact of health prevention.
The Review has received broadly positive responses from both public sector (e.g., NICE) and user and community groups (e.g., Citizens Advice Bureau). Key to the Review, and to the ensuing responses, is the belief that reducing health inequalities is a critical social and political issue of our generation.
Reducing health inequalities is often referred to as ‘narrowing the gap’ or ‘reducing the social gradient’. The social gradient of health suggests that the lower a person’s social position, the worse his or her health. Understanding whether the gradient has reduced involves analysing the gradient over time. Recent analyses released by the Office of National Statistics (ONS, 2011) suggest that, although the quality of health in the population has improved across all social classes from 1982 to 2006, differences in life expectancy between the least and most deprived social classes has increased during that period. That is, improvements in life expectancy have risen at a higher rate for more affluent people than the most deprived during that 25 year timeframe – this finding was particularly true for males.
Considering the social gradient over time raises questions about how best to reduce inequalities. As the Marmot Review emphasised,
It is tempting to focus limited resources on those in most need. But . . . we are all in need – all of us beneath the very best-off. If the focus were on the very bottom and social action were successful in improving the plight of the worst-off, what would happen to those just above the bottom, or at the median, who have worse health than those above them? All must be included in actions to create a fairer society
Marmot Review, 2010, p. 16
This leads one to conclude that, to reduce the social gradient of health, we need to improve the plight of the most disadvantaged (through targeted interventions) as well as improve the overall health of the population (through universal interventions). The issue of targeted versus universal approaches to health has received much consideration from the National Institute for Health and Clinical Excellence (NICE). In 2002, NICE invited 30 members of the public throughout the UK to join a ‘Citizens Council’. According to NICE (2011), ‘The Citizens Council was established to ensure that the views of those who fund the NHS – the public – are incorporated into the decision-making process’. Still in existence today, the Council meets twice a year for three days at a time, and has produced 13 reports to date. NICE then issues a formal response to the recommendations made in the report and any actions that they will take as a consequence. At one meeting in 2006, the Council was asked to discuss how health inequalities should be taken into account when developing national guidance (NICE Citizens Council, 2007). According to the report of the meeting, they were asked which of the following strategies NICE should follow:
whether to issue guidance that concentrates resources on improving the health of the whole population (which may mean improvement for all groups) even if there is a risk of widening the gap between the socio-economic groups;
or whether or to issue guidance that concentrates resources on trying to improve the health of the most disadvantaged members of our society, thus narrowing the gap between the least and most disadvantaged, even if this has only a modest impact on the health of the population as a whole.
The Citizens Council was presented with information from various experts (university academics, service providers, etc.), they engaged in discussions, and they participated in practical exercises. On the final day, they were asked to vote on which of the two broad strategies seemed more appropriate. They were unable to reach unanimous agreement but concluded that
Despite our many and varied reservations, a majority of the Citizens Council would look with sympathy on NICE strategies intended not only to improve public health for all, but to do so in a way that offers particular benefit to the most disadvantaged.
The Marmot Review (2010) referred to this approach as ‘proportionate universalism’. Whilst the NICE Citizens Council is an excellent demonstration of the way in which the public can be engaged in the development of national health guidance, the conclusions of their 2007 report also emphasises the difficulty that policymakers and service providers face when deciding how to address health inequalities. One possibility for addressing the social gradient, discussed below, is through engaging the community in service design and delivery.
Reducing health inequalities through community engagement initiatives
One of the priority objectives advocated in the Marmot Review (2010) is to ‘Improve community capital and reduce social isolation across the social gradient’ (p. 126). By improving social capital and reducing isolation, the social inequalities that underpin health inequalities could be improved – which would have a flow-on effect to health outcomes. The Review summarised evidence that suggested that interventions to reduce social isolation are more effective when communities and individuals are included in the design of the intervention.
Other researchers have advocated community engagement and participation as a strategy to reduce health inequalities (e.g., Rifkinet al. , 2000; Wallerstein, 2006), yet it is difficult to find empirical evidence to support this. Like the Marmot Review, an international literature review for the World Health Organisation found that participatory empowerment (a facet of community engagement) has been linked to positive outcomes such as social capital and neighbourhood cohesion for socially excluded groups (Wallerstein, 2006). However, the author noted that links to health outcomes are more difficult to identify. The few examples of the effect of participatory empowerment on health outcomes identified in the review were mostly in developing countries, which have limited transferability to the UK context.
Similarly, Popayet al. ’s (2007) rapid review found some evidence for improvements in social capital, social cohesion, and empowerment as a result of community engagement, but little evidence of improvements for mortality, morbidity/health behaviours, or impact on inequalities. The authors noted that the small number of studies addressing the relationship, plus problems with the designs of the primary studies (e.g., the time to follow-up in the mortality studies was too short to expect any change), were the reasons for not observing a relationship.
Rather than searching for evidence of community engagement effectiveness, Arblasteret al. (1996) searched for evaluations of health service interventions designed to reduce health inequalities. They included 94 studies in their systematic review, and found that successful interventions often had one or more of the following characteristics:
-
systematic and intensive approaches to delivering effective health care;
-
improvement in access and prompts to encourage the use of services;
-
strategies employing a combination of interventions and those involving a multi-disciplinary approach;
-
ensuring interventions address the expressed or identified needs of the target population; and
-
the involvement of peers in the delivery of interventions.
The last two recommendations echo the general principles underlying community engagement. Although these characteristics alone were not sufficient for success, it is clear that community engagement is a promising approach to reducing health inequalities.
In summary, it seems that community engagement is likely to have a positive effect on social inequalities (Marmot, 2010; Popayet al., 2007; Wallerstein, 2006), which might in turn reduce health inequalities (Marmot, 2010), although the direct effect on health inequalities is still uncertain (Popayet al., 2007; Wallerstein, 2006). The present review will attempt to examine both direct and indirect pathways to reducing health inequalities through community engagement approaches.
Conceptual framework for this research
The commissioning brief for this project defined community engagement as ‘approaches to involve communities in decisions that affect them’. Masonet al. (2008) have defined community engagement for health promotion as engaging groups of people who share geographies, interests or identities with the aim of improving health and/or reducing health inequalities; these are the ‘groups with distinct health needs and/or demonstrable health inequalities’ of the commissioning brief. The commissioning brief refers to engagement with any organisations that can provide activities for improving public health. Some non-NHS organisations may be directly health-related, such as sports clubs or food retailers. A Healthy Public Policy approach recognises that organisations with other aims, such as public transport, workplaces or schools, may also consider their influence on health. For the purposes of this systematic review, we will define community engagement as a direct or indirect process of involving communities in decision-making and/or in the planning, design, governance and delivery of services, using methods of consultation, collaboration, and/or community control. Information-giving was not seen as an empowering type of engagement.
Involving people in decisions that affect them is justified both by ethical and political arguments and by instrumental arguments asserting that involvement will lead to decisions more relevant to the people being served. Community members are motivated to participate for their own personal material or health benefits, for the gains anticipated for their community, or by their own ideologies (Darbaset al. , 2007).
There are a broad range of community engagement models for engaging people in developing strategy or implementing services. Key differences in these models include who initiates the engagement (public service organisations or communities); the degree to which people are engaged (consulted, in collaborative partnerships, or in control); and whether it is individuals or organised community members who are engaged (Hashagen, 2002; Oliveret al. , 2004). Communities may be engaged in consultations, group support and advocacy, service development, controlling local facilities and human resources, and community tier government; any such engagement may be supported by education and networking (Hashagen, 2002). Success depends on sound implementation of both the community engagement and any interventions resulting from this engagement.
The impact of community engagement can be considered at the level of individuals (personal development), communities (social capital), services (development, delivery, access) and health (population health, health of disadvantaged groups, health inequalities (extended from Slateret al2008). Ideally economic analyses would take into account costs incurred by community engagement, subsequent service development, and the potential costs that might be incurred/costs saved as a result of an increased uptake of services that improve health. These are all issues we propose to explore in our analyses, and their relationships are summarised in Figure 1.
FIGURE 1.
Conceptual framework.
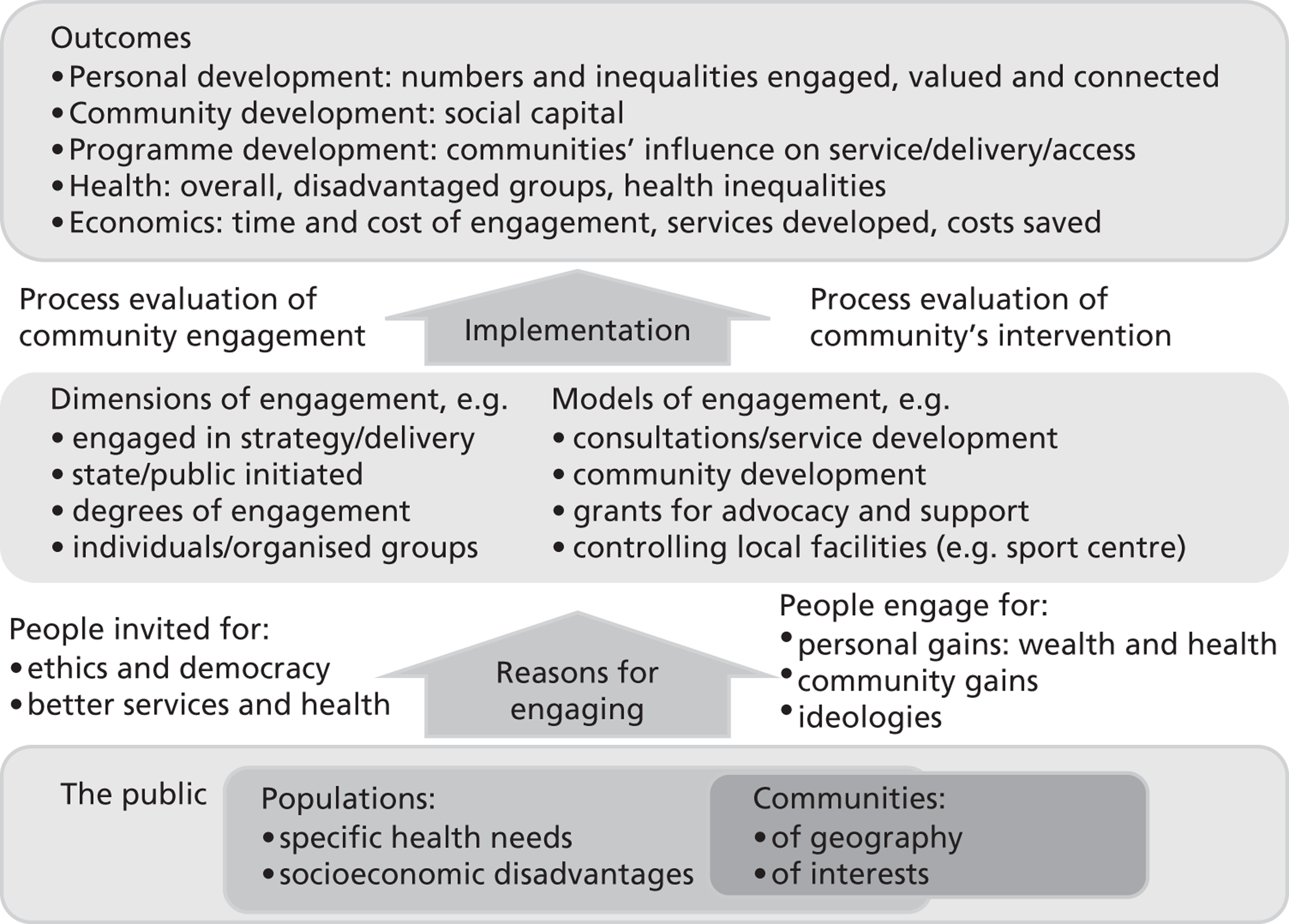
3. Need
Previous work has shown that if communities are ‘signed up’ to an intervention or programme that they are receiving, people are more likely to participate and that better outcomes can result. Community engagement is likely to have a positive effect on social inequalities (Marmot, 2010; Popayet al. , 2007; Wallerstein, 2006), which might in turn reduce health inequalities (Marmot, 2010), although the direct effect on health inequalities is still uncertain (Popayet al. , 2007; Wallerstein, 2006). However, without a synthesised evidence base, it is not clear whether specific approaches to community engagement help to reduce inequalities in health; for whom, under what circumstances, and with what resources. As it would be difficult and expensive to conduct a very large research project that tests multiple approaches to community engagement in different topic areas with different populations, we propose to conduct a synthesis of existing evidence and thereby make use of the investment already made in many published research studies.
Systematic reviews pull together all the available research on a given topic. Through rigorous, structured approaches to identifying, selecting, and analysing the evidence, systematic reviews reduce the biases inherent in more traditional reviews of the literature. They are valuable because they enable us to ‘take stock’; when based on the entirety of evidence in a given field they are able to tell us what we do, and do not, know. They are efficient, because they valorise previous investments in research and, by virtue of the consistent way they treat included studies, they are able to ‘recast’ our view of research in a field, challenging existing assumptions and suggesting new areas for investigation. They also facilitate generalisability by looking for knowledge and findings across individual (and possibly atypical) primary studies.
Synthesising research systematically is recognised internationally as being a valuable and necessary activity for helping us to make sense of existing research and ensure that recommendations for policy and practice are based on the best, and most comprehensive view, of the available evidence. However, there is a clear gap in evidence synthesis in the case of community engagement in general, and its impact on health inequalities in particular. There is currently no synthesis of research that is able to identify specific approaches to community engagement that are able to reduce inequalities in health – and what are the resource implications of adopting them. Given the current concerns about health inequalities in the UK (Marmot, 2010) and the policy emphasis on community engagement as a vehicle for facilitating change (e.g., Mayor of London, 2010), it is timely to explore what works in engaging the community to reduce health inequalities.
4. Methods
a. Setting
The systematic review will include studies of interventions conducted in community settings.
a. Design
The project is a systematic review of known existing research. There are two components to the review:
-
A map of the literature that will describe the scale and range of CE interventions. This will serve to address RQs 1 and 2.
-
Analyses of a final selection of studies that will be determined by our advisory groups. The analyses will address RQs 3–9.
In order to focus our activities on our analyses, rather than searching exhaustively for primary studies, we will compile our data set for analysis from specially-selected registers of primary studies and systematic reviews. These registers have been populated using rigorous systematic review search methods. In order to compile a data set rich in contextual detail, we will also contact authors and intervention implementers to supplement the information available in published form.
We anticipate that a broad range of research will be relevant to answering our review questions and thus propose to include two types of research: outcome and process evaluations. In the process of identifying the evidence to be synthesised, and prior to conducting the synthesis itself, we will describe the evidence with respect to the range of models and approaches underpinning community engagement (RQ1) and the mechanisms and contexts through which communities are engaged (RQ2). This is the mapping component of the review.
In the analysis component (RQs 3–7), we aim to analyse many evaluations of community engagement interventions; identify approaches that are most often associated with reductions in inequalities in health; and pay particular attention to the context of the research and the mechanisms by which communities are engaged and the ways this is thought to impact on intervention effectiveness. After we have identified a range of effective approaches, we will consider their relative resource requirements in order to draw conclusions as to their potential cost implications for different stakeholders (RQs 8 and 9). The methods selected for analysis are driven by our review questions and comprise:
-
theoretical narrative synthesis;
-
quantitative synthesis (if data permit); and
-
economic analysis.
b. Data collection
Searching such a broad topic raises particular challenges. Approaches to community engagement cut across many disciplines, topic areas and outcome domains including, for example, housing, transport, social inclusion, accident prevention and substance abuse (Popayet al. , 2007). Additionally, searching broadly requires the location and screening of many reports in order to identify a much smaller amount of research evidence that is specifically relevant. This can make exhaustive searching costly and time-consuming. Given these challenges, we have identified two practical strategies for identifying relevant studies. First, we will make use of systematic searches that have already been carried out for other reviews, using the studies identified by existing systematic reviews. These reviews will be identified through searching various websites and databases that devoted to systematic reviews. Second, we will use a database of studies in health promotion and public health that the EPPI-Centre has built up over many years as a result of carrying out systematic reviews (known as TRoPHI). The studies in this database are the product of systematic searches and have already been systematically classified and outcome data calculated; they thus represent a valuable ‘short cut’ to evidence. Both approaches to searching are detailed below. The search syntax that will be used in the search process is presented in the Appendix.
Identifying systematic reviews
We will search a range of registers, websites, and databases for systematic reviews that discuss how some or all of their included studies contain interventions which utilise community engagement. The reviews will be used to identify included primary studies that are relevant to the scope of this project; the systematic reviews themselves will not be included in the synthesis in this project (see section on ‘Evidence selection’).
The systematic review registers, websites, and databases that we will search are:
-
Database of promoting health effectiveness reviews (DoPHER). DoPHER is developed and maintained by the EPPI-Centre. It has focussed coverage of systematic and non-systematic reviews of effectiveness in health promotion and public health worldwide. It currently contains details of over 2,500 reviews of health promotion and public health effectiveness. All reviews are assessed and coded for specific characteristics of health focus, population group and quality (http://eppi.ioe.ac.uk/webdatabases/Intro.aspx?ID=2).
-
Cochrane database of systematic reviews (CDSR). The CDSR includes all Cochrane Reviews (and protocols) prepared by Cochrane Review Groups in The Cochrane Collaboration. As of Issue 5, 2011, the CDSR includes 6641 articles: 4622 reviews; and 2019 protocols (http://www.thecochranelibrary.com/view/0/AboutTheCochraneLibrary.html#CDSR).
-
Database of abstracts of reviews of effects (DARE). DARE is developed and maintained by the Centre for Reviews and Dissemination (CRD), and currently contains over 21,000 systematic reviews. It is focused primarily on systematic reviews that evaluate the effects of health care interventions and the delivery and organisation of health services. The database also includes reviews of the wider determinants of health such as housing, transport, and social care where these impact directly on health, or have the potential to impact on health (http://www.crd.york.ac.uk/CMS2Web/AboutDare.asp).
-
Campbell Library. The Campbell Collaboration’s library of systematic reviews includes reviews and protocols prepared by Campbell review groups under any of the six coordinating group themes: crime and justice, education, international development, methods, social welfare, and review users (http://www.campbellcollaboration.org/library.php).
-
NIHR Health Technology Assessment (HTA) programme website. The HTA programme produces research about the effectiveness of different healthcare treatments and tests for those who use, manage and provide care in the NHS. The HTA website houses all the reviews published through the HTA programme in the HTA journal series and holds in excess of 550 titles (http://www.hta.ac.uk/project/htapubs.asp).
-
Health Technology Assessment (HTA) database hosted by CRD. This database currently holds over 10,000 summaries of completed and ongoing health technology assessments from around the world. Database content is supplied by the 52 members of the International Network of Agencies for Health Technology Assessment (INAHTA) and 20 other HTA organisations worldwide (http://www.crd.york.ac.uk/crdweb/AboutHTA.asp).
Identifying primary research through TRoPHI and NHS EED
Searches of the systematic reviews resources will be supplemented by searches of the Trials Register of Promoting Health Interventions (TRoPHI) database and the NHS Economic Evaluation Database (NHS EED).
TRoPHI has focussed coverage of trials of interventions in health promotion and public health worldwide. It covers both randomised and non-randomised controlled trials and currently contains details of over 4,500 trials and is updated four times a year (http://eppi.ioe.ac.uk/webdatabases/Intro.aspx?ID=5). This source will be searched to ensure that relevant trials published outside of the timeframe or scope of the reviews identified in the review databases listed above are detected. All the studies were in systematic reviews carried out by the EPPI-Centre and other collaborators including the Cochrane Collaboration between (1996 and 2009) in the following areas: sexual health, workplace health promotion, peer delivered health promotion, incentive-based interventions, young people, pregnancy and social exclusion, smoking cessation in pregnancy, and the promotion of mental health, physical activity and healthy eating.
Part of the TRoPHI dataset was used in a comparison of randomised and non-randomised trials (Oliveret al2010), though we propose to add additional studies from reviews that were carried out since this study. The approximately 300 studies in this dataset have already been classified using one of two data collection tools that capture detailed information about their methodology, participants, planning and process measures (if any), intervention and outcomes. We will need to code for their strategies of community engagement (where present) in addition to this, but the presence of this database means that we are able to accomplish far more with the resources requested than would otherwise be possible.
NHS EED includes records of economic evaluations of health care interventions, including cost–benefit analyses, cost-utility analyses, and cost-effectiveness analyses. the database currently includes over 11,000 economic evaluations (http://www.crd.york.ac.uk/crdweb/). The database is maintained through weekly literature searches that are conducted by CRD.
Other search sources
To further ensure wide coverage of the evidence base, we will check the bibliographies of the rapid evidence assessments conducted to support the National Institute for Health and Clinical Excellence’s 2008 Public Health Guidance ‘Community Engagement to Improve Health’ (NICE, 2008).
The final component in our search strategy is contact with authors and intervention implementers. We will contact authors of key included studies to ask them if they know of any other studies of interventions utilising community engagement (preferably including an analysis which examines inequalities in some way). As part of this process, we will also ask whether they would be willing to supply additional information about the study which we have included. In particular, we anticipate that we may need further information concerning resource use and costs of community engagement actions. A questionnaire will be developed on resource use and costs incurred in the implementation of community engagement strategies. This questionnaire would also provide an opportunity to explore additional resources required to adapt interventions to different contexts from those where they originally implemented.
At the end of the above process, summarised in Figure 2, we will have a dataset of primary studies which we are able to classify and interrogate according to the structure set out in our conceptual framework: i.e. who is engaging, how, why, the dimension(s) of engagement, and the outcomes assessed.
FIGURE 2.
Search strategy.
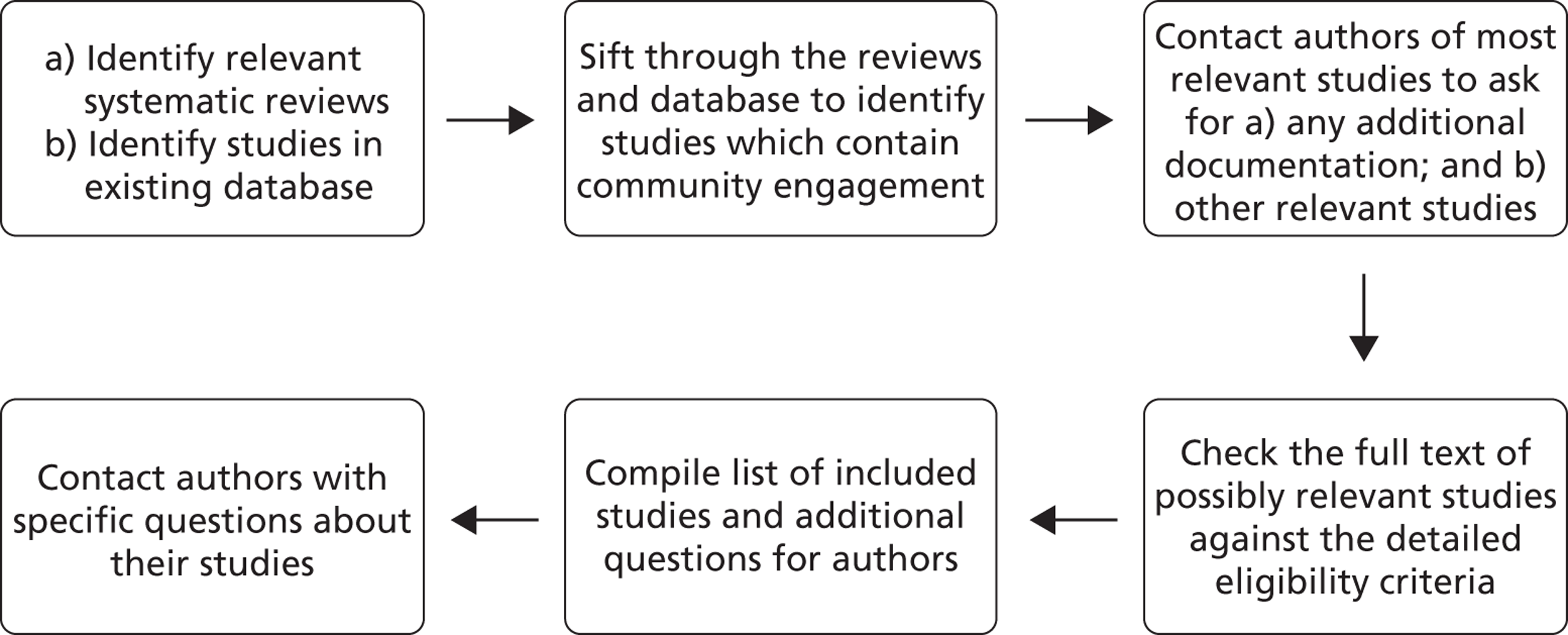
Evidence selection (inclusion criteria)
The outcome of the search will be a database of references and documents which will be screened using the review’s inclusion criteria. The inclusion criteria are a list of statements about what the study should contain to be relevant to the review question; studies must meet all of the criteria to be eligible for inclusion in the review. The criteria will be applied twice; first, to identify systematic reviews; and second, to identify relevant primary studies.
The criteria will be piloted on a sample of studies before being applied. An early sample of screening will be double checked by the lead reviewer. The reviewers will regularly discuss screening to ensure consistency in the way that studies are being included and excluded.
Identifying reviews
The following criteria will be applied to titles and abstracts of reviews, which will be included if they:
-
Are published after 1990;
-
Are a systematic review (i.e. describe search strategies and inclusion criteria used);
-
Include outcome or process evaluation studies;
-
Describe at least one intervention potentially relevant to community engagement;
-
Include at least one study in the results section;
-
Are written in English; and
-
Measure and report health outcomes.
Each systematic review will be assessed against these criteria in a stepwise fashion, such that any review excluded because it failed a criterion later in the list must have passed any preceding criteria. We will retrieve the full-text copy of all reviews that pass these inclusion criteria. Then, a brief screening of the full-text document will be conducted to check that the review is, in fact, systematic, and that the review includes some primary studies of relevance to our review (Relevance at this stage will be judged according to the criteria presented in the section ‘Identifying trials’, although the criteria will not be applied stepwise and will not be recorded.)
Identifying trials
Once the final set of systematic reviews is obtained, we will screen within each review to identify relevant-sounding primary studies (trials). This will involve scanning the evidence tables and reference lists of the reviews for relevant trials. We will then locate the abstracts for these trials.
The titles and abstracts of the trials identified during this process will then be assessed for inclusion in the review. Studies will be included if they meet all of the following criteria:
-
Study is published after 1990 (the date of the other reviews on which we are building, e.g., Popayet al. 2007);
-
The study is primary research, in that data have been collected during that study through interaction with or observation of study participants, but is not a Masters thesis;
-
Study includes outcome and/or process evaluations of interventions;
-
Community engagement is the main focus of the study;
-
Study is published in English;
-
For outcome evaluations: study has a control or comparison group (i.e., it must be a controlled trial, either randomised or non-randomised);
Once all studies have been screened on title and abstract, full reports will be obtained for those studies that appear to meet the criteria or where there is insufficient information to be certain. The retrieved articles will then be screened based on the full-text article.
Two additional criteria will be applied at full-text screening that will allow critical appraisal and ensure that the documents are relevant to the issue of inequalities. Investigations of inequalities are often framed in terms of PROGRESS (Place of residence, Race/ethnicity, Occupation, Gender, Religion, Education, Socio-economic position and Social capital (Evans & Brown, 2003), the mnemonic for broader determinants of health. Kreiger (1999) has drawn attention to other characteristics that attract discrimination (e.g., age, disability, sexual orientation). These concepts have been combined with other determinants of health or sources of social exclusion within family or community contexts relevant to particular research (e.g., smoking parents, being ‘looked after’ or excluded from school) to extend PROGRESS-Plus (Kavanaghet al. , 2009). Thus PROGRESS-Plus provides a useful framework to scope the review and analyse the included studies.
The additional criteria to be applied at full-text are:
-
Study reports their methods in sufficient detail to allow critical appraisal (i.e., must clearly report both data collection and methods of analysis); and
-
Reports characterise study populations or report differential impacts in terms related to social determinants of health that can be captured by the PROGRESS-PLUS framework.
Those that pass the inclusion criteria on the basis of full-text screening will be included in the description of engagement models and synthesis. The methods for the mapping and analysis components of the review follow.
c. Data analysis
Mapping stage
The mapping stage of the review aims to describe the scale and range of community engagement interventions and will address RQs 1 and 2. Studies that meet our inclusion criteria will be stored electronically and classified according to a standardised data extraction framework. Information will be collected on: models of community engagement (consultation, collaboration, and community control); approach to community engagement (e.g., formation of community coalition, volunteer intervention provider); mechanism of engagement (how the community were recruited/involved); area of health concern (e.g., breastfeeding, smoking cessation); participants’ PROGRESS-plus characteristics; and geographical and other contextual details.
After the relevant data have been extracted, we will produce tables and cross-tabulations to show the frequency of different types of engagement and the contexts in which they occur. We will also provide a description of the similarities and differences across interventions. We will focus on trends and gaps in the evidence base, rather than detailing each intervention.
Analysis stage
The map will provide a broad picture of the types of community engagement covered in the research literature and will complement the development of the theoretical framework. However, we also want to gain a more detailed understanding of what works and does not work, for whom, and under what circumstances. For this, we will conduct a series of analyses addressing RQs 3–9. In the event that the studies identified throughout the search and screening process are either too numerous or too heterogeneous to allow sensible analysis, we will select a subsample of studies on which to focus the analyses. The refinement of the inclusion criteria for the analyses will be determined in consultation with our advisory groups.
We will extract further data for those studies included in the analysis component of the review. Additional information will be collected on: the intervention, study participants, the dimensions, models, context and outcomes of community engagement, and health outcomes.
Data extraction for the theoretical synthesis will take the form of a narrative that describes the context and mechanisms of the participants, interventions and approach to community engagement. Synthesis and data extraction for this part of our analysis will run in parallel: each time data are extracted from a study, its mechanisms and contexts will be compared with our initial conceptual framework and data already extracted from other studies. In this way, we plan to build up an iterative framework of mechanisms of community engagement which can be applied to subsequent studies with increasing efficiency.
For the quantitative synthesis (meta-regression), effect sizes will be calculated to summarise the impact of the intervention. Since we expect that many of the outcomes will have used different scales and different combinations of continuous and dichotomous data, we will use the standardised mean difference (White & Thomas, 2005) to enable us to compare and combine results. EPPI-Reviewer software will be used to calculate effect sizes from a variety of data types (means and standard deviations, t-values, etc.).
Following the approach we took in a similar analysis (Oliveret al. , 2010), outcomes will be classified as being in either ‘engagement outcome’ domains (personal development, community development, programme development) or ‘health outcome’ domains (knowledge, attitudes, behaviour and health state). For studies which report more than one outcome per domain, we will include in our analysis only the outcome which was most commonly reported across all studies in the review in which the study was identified. Thus each study can have up to seven outcomes calculated, though many will not report outcomes in all our domains.
To help inform the economic analysis, data on resources used in community engagement strategies to encourage behaviour change and/or uptake of interventions will be extracted from studies. This will include categorisation of funded and in-kind resource use, as well as the time of volunteers. Where possible, resource use (e.g. units of equipment, hours of paid staff and volunteers) will be reported separately from costs. We will also categorise the budgets from which resources are supported if data are available. Cost data will be reported in one base price year; where necessary costs will be converted to Pounds sterling (£) using international purchasing power parity rates. If a breakdown of cost data for population sub-groups can be identified this will also be recorded.
Data will be extracted by two members of the team working independently before meeting to discuss their findings in order to ensure quality, and consistency of interpretation.
Quality assessment
As specified in the eligibility criteria, we plan to include two types of study in this review (which are frequently combined within the same research project): outcome and process evaluations.
The outcome evaluations (controlled trials) will be assessed for methodological quality using an instrument that has been used in many reviews by the EPPI-Centre and others (most recently in Shepherdet al. , 2010). Like the Cochrane risk of bias assessment (Higgins and Green, 2009), this tool examines the studies in a range of dimensions including: methods of assignment; the comparability of groups at baseline; attrition; selective reporting; validity of assessment tools; length of follow up; and unit of data analysis.
The tool we will use to assess the quality of the process evaluations was refined in a recent review (Shepherdet al. , 2010) and assesses whether or not: steps were taken to minimise bias and error/increase rigour in sampling, data collection and data analysis; findings were grounded in/supported by the data; there was good breadth and/or depth achieved in the findings; the perspectives of intervention participants were privileged.
Outcome evaluations which do not meet a minimum level of quality will not be included in the meta-regression. The findings from process evaluations which do not score well will still be included, but a sensitivity analysis will be conducted to assess their impact on the overall analysis; findings which depend solely on the evidence of poorer quality process evaluations will be more provisional than those coming from stronger evaluations.
In addition to analysis of outcomes and process evaluations, we may also identify economic evaluations through our review. The quality of these studies will be assessed using the Consensus on Health Economic Criteria (CHEC) criteria list for assessment of methodological quality of economic evaluations (Everset al. , 2005).
Synthesis
As described in the overview above, there will be three syntheses (theoretical, quantitative, and economic), which build upon one another sequentially.
The theoretical synthesis will be the first analysis to be completed. This analysis builds on Pawson’s work on ‘realist synthesis’ (Pawson, 2002) and will examine in particular the mechanisms and contexts of community engagement in each study in two dimensions: how the particular strategy of engagement is purported to engage the community in question; and how the particular strategy of engagement will result in better intervention outcomes. Thus, while community engagement interventions might ‘look’ quite different in different contexts, there may be a common theoretical thread running through them that it will be useful to identify and take forward in the meta-regression.
The quantitative synthesis, or meta-regression (Thompsonet al. , 1999), will address review questions 3–8 statistically, by testing whether any observed differences in the results of included studies might be associated with the type of community engagement they employed, by comparing different types and levels of community engagement between different communities. Possible moderating or confounding factors will include the topic or review that a study was found from; the design of the study; the intervention in question; the outcome assessment tool etc. Moderators and confounders notwithstanding, we will be able to identify the amount of variance (if any) that is explained by different approaches to community engagement with participants within each review, each topic domain, and finally across all studies in the analysis.
The outcome of the first two analyses will be strategies for community engagement with particular groups of people that have been shown to be particularly effective. In the final component of our study, the economic analysis, we will answer research questions 7 and 8, and investigate resource implications of these approaches to community engagement and consider the extent to which they may be considered cost effective. Crucially, and where possible, we aim to estimate only the resource use, including volunteer and in-kind contributions, involved in that aspect of any intervention that is devoted to community engagement, rather than resources for any actual health promoting intervention. This will enable us to compare the relative costs of approaches, without this being confounded by the total costs of different interventions (McDaid & Sassi, 2010).
To address review question 8 we will, using information extracted from our review of the literature and supplemental information from study authors and community engagement implementers, undertake some limited decision modelling to explore the potential cost utility and cost effectiveness of investing in selected different approaches to community engagement to increase uptake of health promoting interventions in several settings and contexts. We will use Treeage Pro software to build these decision models. This will include a range of sensitivity analysis to account for uncertainty in our estimates of resources, cost and effectiveness, as well as threshold analysis to identify the minimum level of effectiveness/maximum level of cost at which engagement approach would be considered cost effective.
5. Contribution of existing research
The work will: build on the evidence that underpins the current NICE guidance on Community Engagement; draw on new and existing data sets of effectiveness in aspects of health demonstrating inequalities; incorporate measures of inequalities, engagement, cost and health; identify effective strategies for improving health and reducing inequalities.
The findings will be disseminated through open access academic publication, relevant practitioner journals and conferences, and published on the websites of each partner institution (including non-technical brief summaries of findings). We will also seek to produce a policy brief as part of the WHO Health Evidence Network policy brief and host a seminar for public health practitioners, policy makers and researchers. A database of the studies we identify will be placed online for others to use.
6. Plan of Investigation
The project will take 12 months. Key milestones of the project are presented in the table below.
| Activity | Milestones | Expected completion |
|---|---|---|
| Project initiation; protocol | Set advisory group meetings | November 2011 |
| Obtain ethics approval from faculty panel | May 2011 | |
| Write protocol | October 2011 | |
| Searching & identification of studies; advisory group meetings | Identify relevant studies on database | August 2011 |
| Screen relevant reviews | August 2011 | |
| Identify relevant studies | October 2011 | |
| Contact authors | November 2011 | |
| Finalise list of included studies | November 2011 | |
| Meet advisory groups (professionals and young people) | November 2011 | |
| Data extraction/collection | Finalise extraction tools | December 2011 |
| Complete data extraction & quality assessment and independent checks for quality and consistency | January 2012 | |
| Data analysis | Complete analyses | February 2012 |
| Dissemination | Complete technical report, summaries and briefing notes | November 2011 |
| Meet advisory groups (professionals and young people) | March 2012 | |
| Submit final report | April 2012 | |
| Hold seminar(s) | After submission, 2012 |
7. Project Management
This project is a collaboration between a multidisciplinary team from the Institute of Education, University of London; University of East London; and London School of Economics. The team has collective experience in evidence synthesis and primary research across a range of disciplines. The project is based at the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre) is part of the Social Science Research Unit at the Institute of Education, University of London, under the supervision of the Principal Investigator, Dr James Thomas.
The co-investigators are:
-
Mr David McDaid, London School of Economics and Political Science
-
Professor Sandy Oliver, Institute of Education, University of London
-
Dr Adam Oliver, London School of Economics
-
Ms Josephine Kavanagh, Institute of Education, University of London
-
Professor Angela Harden, University of East London, Barts Health NHS Trust.
The co-investigators will have strategic input into all aspects of the project and participate directly in some project tasks.
The research team also comprises:
-
Dr Alison O’Mara-Eves, Institute of Education, University of London
-
Mrs Ginny Brunton, Institute of Education, University of London
-
Dr Katherine Twamley, Institute of Education, University of London
-
Other researchers as required.
The research team will be involved in strategic planning of aspects of the project and systematic review activities (including screening, data extraction, and data synthesis).
The full project team will meet at least three times in person to discuss progress, upcoming milestones, strategic directions of the project, and assign tasks. An advisory group will meet twice to provide feedback on the progress and direction of the review.
Information management
All records of research identified by searches will be uploaded to the specialist systematic review software, EPPI-Reviewer 4, for duplicate stripping and screening (Thomaset al. 2010). This software will record the bibliographic details of each study considered by the review, where studies were found and how, reasons for their inclusion or exclusion, descriptive and evaluative codes and text about each included study, and the data used and produced during synthesis. The software enables us to keep track of electronic documents (e.g., pdf files) and take advantage of emerging ‘text mining’ technologies to help us identify relevant research and identify commonalities within the studies we find efficiently. The data from the existing reviews that we plan to use are already in this software.
Ethical arrangements
This project has been approved by the Faculty Research Ethics board at the Institute of Education (ethics approval reference number FCL 283; copies of the ethics application are available from the report authors). The project complies with the ESRC Research Ethics Framework.
8. Service users/public involvement
The Public Health Research steering group will provide feedback on the research throughout the project. The steering group includes public health policy and practitioner members. We will have regular contact via email, phone, and face-to-face meetings with the steering group to ensure that the research is meeting the stated needs of the research consumers.
In addition, young people, practitioners, and local authority representatives will be involved in consultations about interim findings to improve the review’s validity and enable us to frame the review in a way that is accessible to the target audience. This will entail:
-
Exploring the review’s interim findings through consultations with young people via the National Children’s Bureau’s Young Research Advisers group (NCB, 2011) and the Islington Borough Council’s Children’s Active Involvement Service (CAIS) (Islington Borough Council, 2011).
-
Convening an advisory group of professionals (practitioners and local authority representatives) that will meet twice to discuss shaping the project and interpreting the emerging findings.
The people we will approach for consultation, and the nature of the consultations, are described below.
The young people’s consultations with NCB Young Research Advisers and CAIS members will involve one workshop session for each of the two groups, likely to be two hours total in length. We shall visit the groups at their own venues. Sessions will be timed, in consultation with the groups’ convenors, to fit in as part of the two groups’ existing meeting plans. Sessions will include practical exercises to introduce the project and help group members discuss what helps or hinders them engage with community activities to improve health or reduce inequalities. There may also be small-group discussion of the research team’s preliminary findings and use of post-it notes and stickers to record preferences/interpretations. Group activities will be audio recorded if participants give their consent.
-
NCB Young Research Advisers is a group of 18 young people from all over England aged 10 to 17 years that was established by the NCB to engage young people in the research process. Membership of the group is voluntary and the NCB provide expenses, food and appropriate accommodation where required. In recognition of the young person’s time in taking part in meetings, the NCB also gives members gift vouchers.
-
CAIS is a service offered to looked-after children, disabled children, and young people receiving services from Islington Borough Council. It is designed for young people experiencing social disadvantage to participate in civic activities. The service offers a range of activities including a newsletter, helping to select and train staff, giving presentations to senior staff and councillors, and events such as drama and dance. CAIS also offers support and advocacy service if the child is unhappy with any aspect of their placement, carer, or social worker. Children can refer themselves and the application or procedure is via telephone, text, or email.
The advisory group of professionals – consisting of both practitioners and local authority representatives – will meet twice to discuss shaping the project (meeting one) and interpreting the emerging findings (meeting two).
-
The local authority organisations to be invited to the advisory group of professionals include:
-
the Local Government Association, which provides a voice in the national arena about policy, legislation and funding on behalf of our member councils and the people and communities they serve;
-
Local Authorities Research Consortium, a collaboration between 30 local authorities;
-
the National Foundation of Education Research, which aims to improve education nationally and internationally by undertaking research and dissemination activities;
-
Research in Practice, which aims to build the capacity for evidence-informed practice in children’s services; and
-
Local Government Improvement and Development, which supports improvement and innovation in local government by working with local authorities and their partners to develop and share good practice.
-
-
The practitioners to be invited to the advisory group of professionals will be contacted through the London Civic Forum’s Community Development Network, which is the evolving informal network for peer support, policy discussion and campaigning by and for community development practitioners in London.
9. References
- Arblaster L, Lambert M, Entwistle M, Forster M, Fullerton D, Sheldon T, et al. A systematic review of the effectiveness of health service interventions aimed at reducing inequalities in health. J Health Serv Res Policy 1996;1:93-103.
- Boote J, Telford R, Cooper C. Consumer involvement in health research: a review and research agenda. Health Policy 2002;61:213-36.
- Carr-Hill R, Street A. Economic Analysis of Cost-Effectiveness of Community Engagement to Improve Health. Discussion Paper 33 2008.
- Citizens Advice Bureau . Citizens Advice Response to the Marmot Review team’s Report on the Health Impacts of Cold Homes and Fuel Poverty n.d. URL: http://www.citizensadvice.org.uk/press_20110511 (accessed 13 May 2011).
- Darbas T, Smith T, Hall C. Case Studies of Community Engagement: Enhancing Community Engagement for NRM in the SEQ Western Catchment. Report Prepared As Part of the AG-SIP 18 Project: Effective Engagement for NRM in the SEQ Western Catchments 2007.
- Daykin N, Evans D, Petsoulas C, Sayers A. Evaluating the impact of patient and public involvement initiatives on UK health services: a systematic review. Evidence &Amp; Policy: A Journal of Research, Debate and Practice 2007;3:47-65.
- Shifting the Balance of Power: The Next Steps. London: Department of Health; 2002.
- National Service Framework for Children, Young People and Maternity Services. London: Department of Health; 2004.
- Commissioning a Patient-led National Health Service. London: Department of Health; 2005.
- A Stronger Local Voice: A framework for creating a stronger local voice in the development of health and social care services. London: Department of Health; 2006.
- Health reform in England: update and commissioning framework. London: Department of Health; 2006.
- Real involvement: Working with people to improve health services. London: Department of Health; 2008.
- Department of Health [website] . Health Inequalities National Support Team n.d. URL: http://www.dh.gov.uk/en/Publichealth/NationalSupportTeams/HealthInequalities/index.htm (accessed 16 May 2011).
- Our Health, Our Care, Our Say: A New Direction for Community Services (White Paper). Norwich: The Stationery Office; 2006.
- Evans T, Brown H. Road traffic crashes: Operationalizing equity in the context of health sector reform. Injury Control and Safety Promotion 2003;10:11-2.
- Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: Consensus on Health Economic Criteria. International Journal of Technology Assessment in Health Care 2005;21:240-5.
- Fischer A. Cost effectiveness vignettes for community engagement. London: NICE; 2007.
- Graham P. Whose health, whose care, whose say? Some comments on public involvement in new NHS commissioning arrangements. Critical Public Health 2009;19:123-32.
- Greater London Authority Act, Chapter 24 2007.
- Harden A, Oliver S, Oliver S, Peersman G. Using Research for Effective Health Promotion. Buckingham: Open University Press; 2001.
- Hashagen S. Models of community engagement. Scottish Community Development Centre; 2002.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2. The Cochrane Collaboration; 2009.
- Islington Borough Council . Children’s Active Involvement Service, CAIS n.d. URL: http://www.islington.gov.uk/directories/page.aspx?dir=LTCDP&dir_name=LTCDP&docid=0901336c803ceb9e (accessed 7 April 2011).
- Kavanagh J, Oliver S, Lorenc T, Caird J, Tucker H, Harden A, et al. School-based cognitive-behavioural interventions: a systematic review of effects and inequalities. Health Sociology Review 2009:61-78.
- Krieger N. Embodying inequality: a review of concepts, Measures, and methods for studying health consequences of discrimination. International Journal of Health Services 1999;29:295-352.
- London Health Observatory . Health inequalities: a challenge for local authorities. Marmot Review 1 Year on Press Release n.d. URL: http://www.lho.org.uk/LHO_Topics/national_lead_areas/marmot/marmotindicators.aspx (accessed 11 May 2011).
- Macdonald G., Davies J., Davies J., Macdonald G. Quality, Evidence and Effectiveness in Health Promotion. Striving for Certainties. London: Routledge; 1998.
- Fair society, healthy lives: the Marmot Review. Strategic review of health inequalities in England post-2010. London: Marmot Review; 2010.
- Mason A, Carr-Hill R, Myers L. Rapid review of the economic evidence for community engagement and community development approaches in interventions or initiatives seeking to address wider determinants of health. York: Centre for Health Economics, University of York; 2007.
- Mason AR, Carr-Hill R, Myers LA, Street AD. Establishing the economics of engaging communities in health promotion: what is desirable, what is feasible?. Critical Public Health 2008;18:285-97.
- The London Health Inequalities Strategy. London: Greater London Authority; 2010.
- McDaid D, Sassi F, Shemilt I, Mugford M, Vale L, Marsh K, et al. Evidence-based decisions and economics: health care, social welfare, education and criminal justice. Wiley, BMJ Books; 2010.
- National Institute for Health and Clinical Excellence Citizens Council . Report on NICE Citizens Council Meeting 8–10 June 2006 Inequalities in Health 2007.
- NICE public health guidance 9: Community engagement to improve health. London: NICE; 2008.
- National Institute for Health and Clinical Excellence . Citizens Council n.d. URL: http://www.nice.org.uk/aboutnice/howwework/citizenscouncil/citizens_council.jsp (accessed 13 May 2011).
- NCB . Public Health, Education, Awareness, Research n.d. URL: http://www.youngncb.org.uk/pdf/Role%20description12.7.10.pdf (accessed 7 April 2011).
- Nilsen ES, Myrhaug HT, Johansen M, Oliver S, Oxman AD. Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material. Cochrane Database Syst Rev 2006;3.
- Trends in life expectancy by the National Statistics Socio-economic Classification 1982–2006. Newport: ONS; 2011.
- Oliver S, Bagnall AM, Thomas J, Shepherd J, Sowden A, White I, et al. Randomised controlled trials for policy interventions: a review of reviews and meta-regression. Health Technology Assessment 2010;14.
- Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al. Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach. Health Technology Assessment 2004;8:1-148.
- Pawson R. ‘Evidence-based policy: the promise of realist synthesis’. Evaluation 2002;8:340-58.
- Popay J, Williams G. Public Health Research and Lay Knowledge. Social Science and Medicine 1996;42:759-68.
- Popay J. Community Engagement for Health Improvement: Questions of Definition, Outcomes and Evaluation 2006.
- Popay J, Attree P, Hornby D, Milton B, Whitehead M, French B, et al. Community Engagement in Initiatives Addressing the Wider Social Determinants of Health: A rapid review of evidence on impact, experience and process. Lancaster: University of Lancaster; 2007.
- Rifkin SB, Lewando-Hundt G, Draper AK. Participatory approaches in health promotion and health planning a literature review. London: Health Development Agency; 2000.
- Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett-Page E, et al. The effectiveness and cost-effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13 to 19: a systematic review and economic evaluation. Health Technology Assessment 2010;14:1-206.
- Sheridan K, Tobi P. Towards a community engagement strategy: some practical notes. British Journal of Healthcare Management 2010;16:123-8.
- Slater B, Knowles J, Lyon D. Improvement Science meets Community Development: Approaching Health Inequalities through Community Engagement. Journal of Integrated Care 2008;16:26-3.
- Swainston K, Summerbell C. The effectiveness of community engagement approaches and methods for health promotion interventions. Teeside: University of Teeside; 2008.
- Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4.0: software for research synthesis. London: Social Science Research Unit, Institute of Education; 2010.
- Thompson SG, Sharp SG. Explaining heterogeneity in meta-analysis: A comparison of methods. Statistics in Medicine 1999;18:2693-708.
- Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract 2006;7:312-23.
- White IR, Thomas J. Standardised mean differences in individually-randomised and cluster-randomised trials, with applications to meta-analysis. Clinical Trials 2005;2:141-51.
- Whitehead M, Dahlgren G. Levelling up (part 1): A discussion paper on concepts and principles for tackling social inequities in health. Copenhagen: WHO; 2006.
Appendix: Search strategy for bibliographic databases
Search Strategy: DoPHER
Keyword search:
Health promotion OR inequalities AND (Aims stated AND search stated AND inclusion criteria stated)
Search Strategy: TRoPHI
“disadvantage” OR “disparities” OR “disparity” OR “equality” OR “equity” OR “gap” OR “gaps” OR “gradient” OR “gradients” OR “health determinants” OR “health education” OR “health inequalities” OR “health promotion” OR “healthy people programs” OR “inequalities” OR “inequality” OR “inequities” OR “inequity” OR “preventive health service” OR “preventive medicine” OR “primary prevention” OR “public health” OR “social medicine” OR “unequal” OR “variation”
AND
“change agent” OR “citizen” OR “community” OR “champion” OR “collaborator” OR “disadvantaged” OR “lay community” OR “lay people” OR “lay person” OR “member” OR “minority” OR “participant” OR “patient” OR “peer” OR “public” OR “representative” OR “resident” OR “service user” OR “stakeholder” OR “user” OR “volunteer” OR “vulnerable”
AND
“capacity building” OR “coalition” OR “collaboration” OR “committee” OR “compact” OR “control” OR “co-production” OR “councils” OR “delegated power” OR “democratic renewal” OR “development” OR “empowerment” OR “engagement” OR “forum” OR “governance” OR “health promotion” OR “initiative” OR “integrated local development programme” OR “intervention guidance” OR “involvement” OR “juries” OR “local area agreement” OR “local governance” OR “local involvement networks” OR “local strategic partnership” OR “mobilisation” OR “mobilization “ OR “neighbourhood committee” OR “neighbourhood managers” OR “neighbourhood renewal” OR “neighbourhood wardens” OR “networks” OR “organisation” OR “panels” OR “participation” OR “participation compact” OR “participatory action” OR “partnerships” OR “pathways “ OR “priority setting” OR “public engagement” OR “public health” OR “rapid participatory assessment” OR “regeneration” OR “relations” OR “support”
Search Strategy: Cochrane Databases
-
Cochrane Database of Systematic Reviews (Cochrane Reviews)
-
Database of Abstracts of Reviews of Effects (Other Reviews)
-
Health Technology Assessment Database (Technology Assessments)
-
NHS Economic Evaluation Database (Economic Evaluations)
“disadvantage” OR “disparities” OR “disparity” OR “equality” OR “equity” OR “gap” OR “gaps” OR “gradient” OR “gradients” OR “health determinants” OR “health education” OR “health inequalities” OR “health promotion” OR “healthy people programs” OR “inequalities” OR “inequality” OR “inequities” OR “inequity” OR “preventive health service” OR “preventive medicine” OR “primary prevention” OR “public health” OR “social medicine” OR “unequal” OR “variation”
AND
“change agent” OR “citizen” OR “community” OR “champion” OR “collaborator” OR “disadvantaged” OR “lay community” OR “lay people” OR “lay person” OR “member” OR “minority” OR “participant” OR “patient” OR “peer” OR “public” OR “representative” OR “resident” OR “service user” OR “stakeholder” OR “user” OR “volunteer” OR “vulnerable”
AND
“capacity building” OR “coalition” OR “collaboration” OR “committee” OR “compact” OR “control” OR “co-production” OR “councils” OR “delegated power” OR “democratic renewal” OR “development” OR “empowerment” OR “engagement” OR “forum” OR “governance” OR “health promotion” OR “initiative” OR “integrated local development programme” OR “intervention guidance” OR “involvement” OR “juries” OR “local area agreement” OR “local governance” OR “local involvement networks” OR “local strategic partnership” OR “mobilisation” OR “mobilization “ OR “neighbourhood committee” OR “neighbourhood managers” OR “neighbourhood renewal” OR “neighbourhood wardens” OR “networks” OR “organisation” OR “panels” OR “participation” OR “participation compact” OR “participatory action” OR “partnerships” OR “pathways “ OR “priority setting” OR “public engagement” OR “public health” OR “rapid participatory assessment” OR “regeneration” OR “relations” OR “support”
Search Strategy: Campbell Library
“disadvantage” OR “disparities” OR “disparity” OR “equality” OR “equity” OR “gap” OR “gaps” OR “gradient” OR “gradients” OR “health determinants” OR “health education” OR “health inequalities” OR “health promotion” OR “healthy people programs” OR “inequalities” OR “inequality” OR “inequities” OR “inequity” OR “preventive health service” OR “preventive medicine” OR “primary prevention” OR “public health” OR “social medicine” OR “unequal” OR “variation”
AND
“change agent” OR “citizen” OR “community” OR “champion” OR “collaborator” OR “disadvantaged” OR “lay community” OR “lay people” OR “lay person” OR “member” OR “minority” OR “participant” OR “patient” OR “peer” OR “public” OR “representative” OR “resident” OR “service user” OR “stakeholder” OR “user” OR “volunteer” OR “vulnerable”
AND
“capacity building” OR “coalition” OR “collaboration” OR “committee” OR “compact” OR “control” OR “co-production” OR “councils” OR “delegated power” OR “democratic renewal” OR “development” OR “empowerment” OR “engagement” OR “forum” OR “governance” OR “health promotion” OR “initiative” OR “integrated local development programme” OR “intervention guidance” OR “involvement” OR “juries” OR “local area agreement” OR “local governance” OR “local involvement networks” OR “local strategic partnership” OR “mobilisation” OR “mobilization “ OR “neighbourhood committee” OR “neighbourhood managers” OR “neighbourhood renewal” OR “neighbourhood wardens” OR “networks” OR “organisation” OR “panels” OR “participation” OR “participation compact” OR “participatory action” OR “partnerships” OR “pathways “ OR “priority setting” OR “public engagement” OR “public health” OR “rapid participatory assessment” OR “regeneration” OR “relations” OR “support”
List of abbreviations
- AIDS
- acquired immunodeficiency syndrome
- ANOVA
- analysis of variance
- CDSR
- Cochrane Database of Systematic Reviews
- CI
- confidence interval
- CRD
- Centre for Reviews and Dissemination
- CTSA
- Clinical and Translational Science Awards
- DARE
- Database of Abstracts of Reviews of Effects
- DoPHER
- Database of Promoting Health Effectiveness Reviews
- EPPI-Centre
- Evidence for Policy and Practice Information and Co-ordinating Centre
- HIV
- human immunodeficiency virus
- HTA
- Health Technology Assessment
- ICC
- intracluster correlation
- LOR
- log-odds ratio
- NCB
- National Children’s Bureau
- NHS EED
- National Health Service Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OECD
- Organisation for Economic Co-operation and Development
- ONS
- Office for National Statistics
- OR
- odds ratio
- PCT
- primary care trust
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROGRESS-Plus
- Place of residence, Race/ethnicity, Occupation, Gender, Religion, Education, Socioeconomic position, Social capital, plus other characteristics that attract discrimination such as age, disability and sexual orientation
- QALY
- quality-adjusted life-year
- RQ
- research question
- SD
- standard deviation
- STI
- sexually transmitted infection
- TRoPHI
- Trials Register of Promoting Health Interventions
- WHO
- World Health Organization
- WIC
- Women, Infants and Children clinic