Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 09/3004/01. The contractual start date was in October 2011. The final report began editorial review in July 2013 and was accepted for publication in July 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
The Universities of Sheffield, Bangor, Southampton and Northumbria, Community Network and Age UK received grant funding from the National Institute for Health Research Public Health Research programme for this study. The University of Sheffield also received grant funding from Age UK to pay subcontractors for delivering the intervention. Community Network is a national charity and social enterprise that runs telephone friendship groups and a commercial teleconferencing service for the third sector, which could be perceived as having influenced contributions to the report. As an employee of Community Network, Angela Cairns acknowledges a financial relationship with a commercial entity that might have an interest in the submitted work.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Hind et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Scientific background
There is increasing evidence of a direct association between loneliness and ill health. Loneliness is a strong risk factor for depression and increases mortality rates significantly in older people with depression. 1 Research has shown that loneliness predicts all-cause mortality in older people. 2 Loneliness is associated with poor self-rated health,3 increased blood pressure,4 higher levels of some vascular biomarkers,5 poor sleep quality6 and greater likelihood of health risk behaviours. 7 Greater cognitive decline and an increased risk of Alzheimer’s disease are also associated with loneliness. 1,2 Although previous reviews have considered the effectiveness of loneliness interventions in alleviating loneliness, they have not considered the link between loneliness and the wider public health factors associated with loneliness and ill health, for example health inequalities. With such major impacts on health, an understanding of what, how and why public health interventions prevent or alleviate loneliness in older people is critical. Overall, health and life expectancy are linked to social circumstances. Older people are socially excluded when they experience economic and material deprivation and/or lack access to social networks, services and activities. 7 Therefore, social exclusion can impact on loneliness, which in turn can impact on mental and physical health. Thus, loneliness may mediate the pathway between social inequalities and health inequalities.
The number of older people is increasing globally. In the UK, > 17% of the population is aged ≥ 65 years and this is predicted to rise to 20% by 2024. Life expectancy is also increasing and now stands at 78.1 years for men and 82.1 years for women. The number of older people living alone is currently rising. Among women aged ≥ 75 years, 60% live alone. 8 One of the risk factors for loneliness is living alone, although this may be linked to the time spent alone and the size of an individual’s social network. 9 Loneliness is frequently reported by people living in rented accommodation and in single dwellings, particularly if they have been forced into the situation as a result of widowhood or divorce. 10 Social breakdown, inadequate systems to support older people and lack of infrastructure to maintain social networks can lead to loneliness and social exclusion. 11 Older people are at greater risk of enduring loneliness, because of a reduction in personal and external resources available to them. Between 30% and 40% of older people are sometimes or often lonely,12 and this figure has remained fairly constant for the past 40 years. With the increase in the number of older people, the actual number experiencing loneliness is therefore increasing. Loneliness can occur as a result of one or more event or it can be chronic and made worse by transition into old age. Events that can cause loneliness include loss and bereavement, widowhood, migration and perceived and actual poor health, whereas other risk factors for loneliness include lack of resources, living alone and time spent alone. 12 Physical limitation through loss of mobility and/or sensory impairment is the largest single predictor of loneliness. 13 The prevalence of visual impairment increases exponentially with age, with > 50% of visually impaired older people feeling lonely. 14 With such overwhelming evidence of the societal costs of loneliness, a wide range of interventions has been developed to prevent and/or alleviate loneliness in later life.
Social isolation and loneliness have long been identified as being problems associated with later life. According to Age Concern England,15 many of Britain’s older people are living in isolation, with those aged > 65 years being twice as likely as other age groups to spend > 21 hours of the day alone. Mental illness, low morale, poor rehabilitation and admission to residential care have all been found to be correlated with either social isolation or loneliness or both. 16 Six independent vulnerability factors for loneliness have been identified: marital status, increases in loneliness and time alone over the previous decade, elevated mental morbidity, poor current health and poorer health in old age than expected. 17 In response to research gaps highlighted in National Institute for Health and Care Excellence (NICE) guidance on interventions to promote mental well-being in older people,18 this study was funded to provide evidence of population benefit of one home-based intervention that aims to improve the mental well-being of community-living older people who may be vulnerable.
Over the last decade there has been a continued focus on the value of providing health-promoting interventions to older people with the aim of compressing morbidity in the later stages of the life course and promoting quality of life. 7,15,18–21 This is supported by robust evidence that has demonstrated the relationship between extent of social activity and morbidity and mortality. 22 The NICE guidance on interventions to promote mental well-being18 was underpinned by a systematic review of the evidence of effectiveness and cost-effectiveness of interventions. 21 However, the evidence to support the introduction of many interventions in practice, and particularly those that aim to promote socialisation and alleviate loneliness, is lacking. 8,10 A systematic review23 of research into interventions that aim to promote socialisation identified 11 studies with sufficiently robust findings out of 30 that met the review inclusion criteria, with the majority of studies originating from North America. Despite the methodological challenges that this review posed, the review was able to identify that the most effective interventions were those conducted in a group with educational and/or supportive input. Only one study showed that benefit could be derived from one-to-one interventions. Further to this, Cattan et al. 24,25 conducted an evaluation of eight schemes that participated in the Call in Time initiative, promoted through Help the Aged (later to merge with Age Concern to become Age UK), a national charity, and Zurich Community Trust. The results of the evaluation found that telephone befriending can provide a vital lifeline in helping older people who spend a lot of time in their home to regain confidence and increase their levels of engagement and participation. However, older people in the study also emphasised a desire for choice in the types of support services on offer, including face-to-face contact and peer support. A recommendation from the study was therefore for a model that, in addition to one-to-one telephone support, included scope for developing peer support through telephone clubs. This recommendation echoes that given in earlier work conducted in North America. 26 The Foresight report27 also notes that there is a strong case for giving priority to research that assesses the potential use of technologies through the life course, and their impact on individuals; an example cited is social networking for older adults (p. 248).
Rationale
The Putting Life in Years (PLINY) trial was designed to evaluate the effectiveness and cost-effectiveness of a 12-week, telephone-delivered, group intervention based on de Jong Gierveld’s loneliness model28 and Bandura’s theory of self-efficacy,29 and delivered by the voluntary sector. The intervention was designed to include a number of short one-to-one telephone calls with a trained volunteer with the purpose of introducing participants to the concept of group telephone calls. Participants received all calls in their own home using their existing equipment and were connected to their volunteer and group participants via the Community Network’s teleconferencing system. The intervention was based on recommendations in the work by Cattan et al. 24,25 All interventions were delivered by trained volunteer facilitators whose competence was assessed using a treatment fidelity framework to evaluate whether delivery was consistent. 17
Funding for intervention delivery was provided by Age UK (national), the national charity formed from Age Concern and Help the Aged in 2009. There is a network of independent Age UK and Age Concern branches across England. One of these, hereafter the service provider, agreed to recruit and manage the volunteers necessary to deliver the intervention. Community Network provided the infrastructure to enable participants and their volunteer to be joined together by telephone. Community Network is a national charity working with local, regional and other national charities to help connect people who may experience social isolation.
Chapter 2 Methods
Methods for the implementation of the intervention
To understand the course of this study and its outcomes it is necessary for the reader to have a clear sense of how the intervention was implemented. For this reason, before presenting the main trial results (see Chapter 3), we provide a narrative summary of the barriers to intervention implementation. Statements are supported, when possible, by e-mail communication, trial management group (TMG) meeting minutes and field notes.
Methods for the main trial
This report is concordant with the extension of the Consolidated Standards of Reporting Trials (CONSORT) statement to improve the reporting of pragmatic trials. 30 This is a pragmatic two-arm parallel-group randomised controlled trial (RCT) with a feasibility phase. Formal stop–go criteria were established to assess the feasibility of the trial: (1) sufficient participants willing to enter the trial and (2) retention of sufficient participants to assess the primary outcome measure. The final study protocol can be found in Appendix 1, along with a table of changes made to the protocol over the course of the project, which were approved by South Yorkshire Research Ethics Committee (REC).
Participants
Two main methods were used to identify potentially eligible study candidates. We worked with an existing research cohort that is following the lives of 20,000 adults in the area over a period of 10 years and includes individuals who have signalled a willingness to be contacted about further research. Between June 2011 and July 2011 we sent letters with a postage-paid response card and a candidate leaflet to 528 participants in the cohort aged ≥ 75 years. We also invited general practices to help identify potentially eligible study candidates. Between June 2011 and December 2012, 18 general practices sent letters to 9051 patients. The letters included the same candidate leaflet and an invitation to complete a postage-paid response card to express an interest in the study. Response cards were returned to the recruiting site (University of Sheffield, Sheffield, UK).
A pack containing the same candidate leaflet and postage-paid response card was also given to workers in services across the city that were likely to come into contact with older people with the aim of asking them to identify potential participants. In many instances, researchers personally delivered packs and spent time with workers explaining the aims of the study and what it entailed. The Community Intermediate Care Service (NHS) was provided with 500 packs, the city council’s main library received 50 packs and the mobile library service received 200 packs. In addition, two A3 and 30 A4 posters were provided for display. The Community Access and Reablement Service (CARS) was given 100 packs and the local Meals on Wheels service received 120 packs. In addition, 200 packs were given to an extra care scheme (housing with care services available if or when required), a local housing association and the local churches council for community care. Research assistants distributed 200 packs at community events in the locality including a Lifewise event, Regenerate RISE (Reaching the ISolated Elderly) and a local well-being festival (150 packs). Two referrer information sheets and 100 packs were sent to the Allied Healthcare Group; one referrer information sheet and a study leaflet were sent to the Older People’s Partnership Board and distributed to its network (22 May 2012); and five packs each were given to nine Healthy Living Pharmacies.
An unknown number of packs was also sent to relevant public and voluntary sector outlets: the local Expert Elders Network, the local Pensioners Action Group, the local Wellbeing Consortium, Age Well, a victim support group, an older adults community mental health team and a black and minority ethnic community mental health development worker.
Information about the study was circulated to local community and media outlets including the city council’s Help Yourself web page and the local newspaper.
Research assistants telephoned all potential candidates who had returned a response card. A number of candidates telephoned the research team directly. Research assistants checked initial eligibility during the telephone call, for example age and living situation. Research assistants arranged to visit those who were identified as being potentially eligible and interested in finding out more about the study. Appointments were arranged approximately 5 days after the telephone call to allow sufficient time for the candidates to receive and read the Participant Information Sheet, which was posted out (or e-mailed on request) by the research assistants. The Participant Information Sheet was reviewed by the lay representative on the TMG as part of the submission of essential documents to the REC. Research assistants visited potentially eligible candidates in their own home to conduct a screening visit. Those eligible to join the study were aged ≥ 75 years; had good cognitive function, defined as having a six-item Cognitive Impairment Test (6CIT) score of ≤ 7; were living independently (including those who were co-resident with others) or in sheltered extra care housing; and were able to understand and converse in English. The exclusion criteria were (1) the inability to use a telephone effectively with appropriate assistive technology; (2) living in a residential/nursing care home; and (3) already receiving a telephone intervention.
Written informed consent was obtained by research assistants either at the screening visit or at a separate visit if additional time was required to make a decision whether or not to participate. Research assistants administered the 6CIT and calculated the score during the visit. Candidates who were ineligible because of a 6CIT score > 7 were subsequently contacted by a clinically qualified member of the research team and told that they were not eligible to be involved and advised to contact their doctor. A letter containing the score was sent to the candidate. For candidates who were eligible, the research assistant taking consent and administering the baseline questionnaires informed another member of the research team (research assistant or trial manager) of the screening identifier so that they could randomise and inform participants of their allocation. On allocation, and before they were contacted by a volunteer, participants allocated to receive telephone friendship (TF) were sent a ‘question and answer’ document about TF groups by the research team (see Appendix 2) and were advised that the service provider’s volunteer would contact them. The research assistants or the study manager informed the service provider of intervention participants by letter. Initially, this was carried out each time a participant was allocated to receive TF. However, the research team and the service provider subsequently agreed to wait until six participants (sufficient to make a group) had been allocated before forwarding details to the service provider.
Participants were able to withdraw from active participation in the study on request. Individuals who withdrew from the intervention were not replaced. Written consent was obtained to share information with the NHS Health and Social Care Information Centre and other central UK NHS bodies to check participants’ health status and help minimise the risk of telephoning or writing to participants who died before follow-up. Both study arms received postal updates on the study at 2 and 4 months after randomisation.
Interventions
The intervention design is detailed in Appendix 3.
Candidates were screened as described in the previous section. Those who consented were randomly allocated to one of two groups (see Randomisaton and blinding):
-
TF group calls provided through the voluntary (charitable) sector
-
a control group who received usual health and social care following randomisation.
The aim of the intervention was to increase contact between individuals with the intention of forming new acquaintances and friendships. By improving perceptions of companionship and support the aim was to reduce perceived isolation and improve participants’ sense of confidence and mental well-being. The intervention was designed by MC and built on the findings of a previous study which suggested that group calls, following one-to-one befriending, may help older adults to share interests. 24,25
The interventions were delivered by trained volunteer facilitators. Volunteers were recruited by the service provider. Volunteers had no previous experience of protocolised befriending or facilitating conversations, either face to face or by telephone.
The one-to-one individual intervention consisted of up to six calls between each participant and a volunteer befriender. The purpose of the one-to-one calls was to support the participant and prepare him or her for the group conversations. One-to-one calls were brief (10–20 minute) friendly conversations that were held each week for a duration of 6 weeks, beginning with familiarisation and everyday conversation and moving towards a focus on the group calls including topics of interest and supporting the participants with concerns about starting group sessions. Volunteer befrienders telephoned participants using the Community Network’s teleconferencing system. Although not designed for one-to-one calls, the use of the system enabled cost-free calls for participants and volunteers. A detailed description of the training is provided in Appendix 4.
Roles and remit of the service provider and Community Network
Implementation meetings of between 1 and 2 hours were held with the service provider or its delegates (the volunteer co-ordinators) every 2–4 weeks between 20 October 2011 and 16 January 2013. The same individuals from the service provider and representatives of Community Network also attended the monthly TMG meetings, at which the perspectives of members of the public about process and documentation were also elicited. At implementation meetings the trial manager provided advice, guidance and additional documentation as required to the volunteer co-ordinators. E-mail and telephone communication was also frequent, including reminders about training date cut-offs and suggestions for promoting the volunteer opportunity to charities and community groups in the city and within the university. The trial manager attended all but one volunteer induction session and all one-to-one training sessions. The chief investigator initiated the meetings with the service provider and attended implementation meetings on request.
A worker from the service provider was responsible for recruiting all volunteers and provided an induction to the organisation, including the provision of information on issues facing older people and shadowing paid workers in day centres. Those who were deemed to be appropriate for the telephone befriending role were then trained by the same member of staff to make the one-to-one calls in accordance with the training manual (see Appendix 4) before progressing to the group training. Volunteers received group facilitation skills training by telephone. The training lasted 4 hours in total and was delivered in 1-hour sessions over the telephone by a professional trainer who delivers training on behalf of Community Network. Training groups were designed to consist of a maximum of five trainee facilitators and the trainer. However, this was difficult to fulfil for this study (see Chapter 3, The contract with the service provider). Group training included how to run groups in a style conducive to creating group cohesion and promoting a safe environment for participants. Volunteers were told that assisting the group to be self-sustaining if possible was an important goal. The trainer from the service provider also committed to offer volunteers ongoing mentoring. The contract with the service provider subsequently included an agreement for volunteer mentoring but did not specify its type and frequency.
Table 1 summarises the facilitation skills training content. Detailed information is provided in Appendix 4.
| Session 1 | Session 2 | Session 3 | Session 4 |
|---|---|---|---|
|
|
|
|
The group intervention consisted of 12 weekly telephone calls facilitated by the trained volunteer at a prearranged time each week, as agreed between members and the volunteer facilitator. Community Network provided the teleconferencing facility, which involved the volunteer facilitator booking the time/date of group calls in advance. The operator called the volunteer facilitator first and then each participant in turn at the prearranged time. TF groups ideally involved six participants and one volunteer facilitator. Group telephone discussions were designed to last about 1 hour to allow sufficient time for sharing experiences and interests and talking about everyday life. Participants were able to contact Community Network and/or the TF group service provider if they would not be taking part in a call. The purpose of the group discussions on the telephone was to increase social contact and reduce perceived isolation. The intervention was not designed to actively instil major behaviour change. Technical and procedural strategies covered by the facilitation skills training were based on psychological models for how groups develop and how facilitators should run groups in a style conducive to creating group cohesion that provides a safe environment for achieving underlying quality of life goals of the intervention, such as to ‘review life experiences’. 31 Volunteer facilitators were instructed about circumstances in which they should intervene to retain a safe environment, for instance if there was conflict or if the ground rules of the group were broken. Volunteer facilitators were present to make the work of the group ‘easy’ and to allow the group to be self-sustaining if possible.
Participants randomised to the control arm did not receive any study intervention. However, they did participate in the baseline and outcome measurements and the extent of their health and social care service usage was assessed (as for all participants).
Objectives
The primary objective of the main study, a parallel-group RCT, was to determine whether mental well-being, as measured by the Short Form questionnaire-36 items (SF-36) (mental health dimension) 6 months after randomisation, is significantly increased in participants allocated to receive the TF group intervention compared with participants allocated to a control group (receiving only contact by card/letter at months 2, 4, 8 and 10 with no further contact other than follow-up assessment).
Secondary objectives were to:
-
Identify, using qualitative methods, the psychosocial and environmental factors, as well as implementation issues, that may mediate or modify the effectiveness of the intervention, specifically voluntary sector readiness to take forward new forms of services, the best modes of delivery of telephone support/friendship, how volunteers (facilitators) can be supported and retained, and the extent to which fidelity of the intervention is maintained within and across the participating organisations.
-
To determine any lasting impact on mental well-being by repeat measurement with all participants 12 months after baseline assessment.
-
To examine whether there is any significant improvement in the intervention arm compared with the standard care arm in the physical dimension of the SF-36 at 6 months and 12 months following baseline assessment.
-
To measure the extent of use of health and social care and community facilities by participants over time to determine whether the intervention is cost-effective compared with standard care.
Outcomes
Table 2 shows the timing of the assessments and interventions. All baseline assessments and interventions were carried out in participants’ homes using the case report form (see Appendix 5). Follow-up assessment at 6 months post randomisation was carried out by telephone (unless a home visit was indicated). The primary end point was the level of mental well-being at 6 months post randomisation using the SF-36 mental health dimension. Secondary end points were:
-
other dimensions of the SF-36 to measure all aspects of health including physical health32
-
the Patient Health Questionnaire – nine questions (PHQ-9)33
-
the European Quality of Life-5 Dimensions (EQ-5D) score (for health economic analysis)34
-
the General Perceived Self-Efficacy Scale (GSE) score35
-
the de Jong Gierveld Loneliness Scale score36
-
Office for National Statistics (ONS) well-being measure37
-
a health and social care resource use questionnaire to collect participants’ use of health, social care and community services (for health economic analysis). 38
| Assessment/intervention | ≈Minus 2 weeks | ≈Minus 1 week | Baseline | 2 months | 4 months | 6 months | 8 months | 10 months | 12 months |
|---|---|---|---|---|---|---|---|---|---|
| Study promotion text/referrer information sheet | ✓ | ||||||||
| Invitation letter | ✓ | ||||||||
| Response card/first contact form | ✓ | ||||||||
| Initial screening | ✓ | ||||||||
| Participant information sheet | ✓ | ||||||||
| Screening visit | ✓ | ||||||||
| Cognitive impairment test (6CIT) | ✓ | ||||||||
| Consent form | ✓ | ||||||||
| Baseline questionnaires | ✓ | ||||||||
| Randomisation | ✓ | ||||||||
| TF group questions and answers (intervention) | ✓ | ||||||||
| Contact card/letter | ✓ | ✓ | ✓ | ✓ | |||||
| Follow-up questionnaires | ✓ | ✓ |
All primary and secondary outcomes were measured at 6 months post randomisation.
Sample size
For the purposes of sample size estimation the primary outcome was the mean SF-36 mental health dimension score at 6 months post randomisation. The SF-36 mental health dimension is scored on a scale from 0 (poor) to 100 (good health). A previous general population survey of residents demonstrated that the SF-36 can successfully be used as an outcome measure for community-dwelling residents aged ≥ 75 years, with a response rate of 82% being achieved. 39 From this general population survey of 3084 community residents, the mean SF-36 mental health score was 68.3, with a standard deviation (SD) of 19.9. 39
The developers of the SF-36 have suggested that differences between treatment groups of between 5 and 10 points on the 100-point scale can be regarded as ‘clinically and socially relevant’. 40 We assumed a SD of 20 points for the SF-36 mental health dimension at 6 months post randomisation and that a mean difference in mental health score of ≥ 8 points between the intervention group and the control group is the smallest difference that can be regarded as clinically and practically important.
Assuming that a mean difference of ≥ 8 points on the SF-36 mental health dimension between the intervention group and the control group is the smallest difference of clinical and practical importance that is worth detecting, then with 248 subjects (124 intervention, 124 control) the trial was originally determined to have 90% power to detect this mean difference or greater as statistically significant at the 5% (two-sided) significance level using a two independent samples t-test. We assumed a correlation of 0.50 between the baseline and the 6-month SF-36 mental health scores. However, the telephone befriending intervention is a group or facilitator-led intervention. Therefore, the success of the intervention may depend on the volunteer facilitator delivering it so that the outcomes of the participants in the same group with the same volunteer facilitator may be clustered. We therefore assumed an average cluster size of six participants per telephone befriending group and an intracluster correlation (ICC) of 0.04 so the design effect is 1.28. With these assumptions and 99 participants per group, the power of the analysis was reduced to 80% to detect a mean difference of ≥ 8 points in the 6-month SF-36 mental health score. If 20% of the participants drop out and are lost to follow-up then we would have needed to recruit and randomise 124 participants per arm (248 in total).
Randomisation and blinding
Eligible participants were randomised to one of the two arms by the trial manager or a research assistant through a centralised web-based randomisation service provided through the Clinical Trials Research Unit (CTRU). The randomisation sequence was generated in advance by a CTRU statistician, not by the trial team. There were no stratification factors in the randomisation sequence. A sequence of treatment/intervention assignments was randomly permuted in blocks of varying size to ensure that enough participants were allocated evenly to each arm of the trial. Participants, outcome assessors and the trial manager were not blind to treatment allocation because of the practical nature of the intervention. All outcomes were self-reported using validated questionnaires (except for sociodemographics and health and social care resource use, which were assessed using bespoke instruments). Trial statisticians and the principal investigator were blinded to the treatment allocation codes until after the final analysis. Data presented to the trial steering committee (TSC) and the TMG did not identify treatment allocations.
Statistical methods
Analysis population
The intention-to-treat (ITT) data set included all participants who were randomised during the time period when participants were able to receive the intervention (ignoring any occurrences post randomisation such as protocol or treatment non-compliance and withdrawals). This included participants randomised on or before 30 September 2012, plus one participant (R1/081) randomised after this date (who received the intervention because another participant dropped out before receiving the intervention), and followed up for 6 months. Participants randomised to the intervention from October 2012 onwards (with the exception of R1/081) did not receive the intervention because there were not enough volunteers to deliver it. No attempt was made to follow up participants recruited in this time period and they did not form part of the outcome analyses.
The SF-36 mental health dimension data were defined as complete if at least half of the items that make up the mental health dimension score were available. The mental health dimension is made up of five items/questions from the SF-36 questionnaire; if at least three of these items were available then the participant was defined as having complete SF-36 mental health dimension data (see the following section for a description of missing data).
A per-protocol data set was defined as all participants in the control group and participants in the intervention group who completed ≥ 75% of the group telephone calls over the 12 weeks of the group intervention (the one-to-one telephone calls with a volunteer were not included in the definition of ‘per protocol’). This means that, if a TF group completed 12 group telephone calls, individuals were part of the per-protocol data set if they were present for the duration of nine or more of the calls. Sensitivity analysis on the per-protocol data set was performed.
As a pilot study the main trial analysis was largely descriptive and focused on confidence interval (CI) estimation and not formal hypothesis testing. Rates of consent, recruitment, adherence and follow-up by randomised group are reported. Outcome measures are summarised by randomisation group. Data from the pilot study are used to estimate the variability of the continuous outcome (SF-36) in the trial population. As the intervention is volunteer led we also used the data to estimate the ICC. As part of the pilot analysis we estimated the effect size for the 6-month SF-36 mental health outcome with CIs to check whether or not the likely effect was within a clinically relevant range.
Handling incomplete telephone call data or missing measurements
Missing items in the SF-36 mental health dimension were imputed with the mean of the complete items in that dimension, given that at least half of the items in the mental health dimension are completed. If half or more of the items were missing (i.e. three or more) then the mental health dimension score was not calculated. For sensitivity analysis, imputation was used to obtain complete 6-month SF-36 mental health dimension data. Missing data were imputed using three methods: last observation carried forward (LOCF), regression and multiple imputation. The primary analysis was repeated for these imputed data sets and displayed alongside the ITT analysis results.
Statistical analysis
Baseline characteristics
The baseline and sociodemographic characteristics and person-reported outcome data (SF-36, PHQ-9, EQ-5D, GSE, de Jong Gierveld Loneliness Scale, 6CIT) were summarised and assessed for comparability between the TF group and the control group. 41–43 Age and SF-36, PHQ-9, EQ-5D, GSE, de Jong Loneliness Scale and 6CIT scores were presented on a continuous scale. For these continuous variables, summary statistics such as the minimum, maximum, mean, SD, median and interquartile range (IQR) were presented depending on the distribution of the data. Numbers of observations and number and percentage in each category are presented for categorical variables (e.g. sex and ethnicity). All of these summaries are presented by treatment group and overall and are assessed for comparability. No statistical significance testing has been carried out to test baseline imbalances between the arms but any noted differences are reported descriptively. 44,45
Data completeness
Data completeness is summarised in a CONSORT flow chart, from participants’ enrolment, during follow-up and at the close of the trial. Data completeness is based on the primary outcome (SF-36 mental health dimension score) and having a valid measurement at 6 months post randomisation.
Effectiveness analyses
The mean SF-36 mental health dimension score was compared between participants allocated to receive the TF group intervention and participants allocated to the control group using a marginal general linear model (GLM) with robust standard errors, and an exchangeable correlation. 46 The marginal model used generalised estimating equations (GEEs) to estimate the regression coefficients. The intervention is a group-based intervention with each group led by a single volunteer facilitator. The statistical analysis allows for the possibility that there may be clustering or correlation of the participants’ outcomes within the same telephone befriending group. Participants in each telephone befriending group were regarded as a cluster in the analysis. Participants in the control group were treated as a cluster of size one in the analysis. The exchangeable correlation assumes that individual outcomes in the same cluster (TF group) have the same correlation. A 95% CI for the difference in SF-36 mental health dimension scores between the intervention group and the control group is also reported. An adjusted analysis was performed alongside this unadjusted analysis, which included the potential baseline prognostic covariates of age, sex and baseline SF-36 mental health dimension score in the marginal GLM. The inclusion of baseline covariates was informed by the investigation of baseline imbalance and previous research, which suggested that health-related quality of life varies by age and sex. 39 The mean (SD) SF-36 mental health dimension scores for the treatment and control groups and the number in each group were displayed. This was accompanied by the adjusted and unadjusted mean difference between the intervention group and the control group with the associated CIs (see Table 2).
Analysis of secondary outcomes
The remaining SF-36 dimensions (physical functioning, role – physical, bodily pain, general health, vitality, social functioning and role – emotional) were computed and rescaled in the same manner as the mental health scale described in the previous section. The two component scores (physical component summary and mental component summary) were also computed and normalised using data from US norms. 32 The PHQ-9 is calculated as the total score of the nine questions; each is scored from 0 to 3, giving a total score in the range 0–27. The total was calculated only if all nine questions were answered. Two measures for the EQ-5D were analysed:
-
The EQ-5D tariff, derived from five three-level questions using UK norms. 34 The tariff was calculated only if all five questions were answered.
-
The single-item EQ-5D ‘thermometer’ scale.
Three measures from the de Jong Gierveld Loneliness Scale were analysed:
-
Emotional loneliness: this is calculated from questions 2, 3, 5, 6, 9 and 10 and is the number of items scored ‘yes’ or ‘more or less’. It is scored from 0 to 6 and is defined only when all six questions are answered.
-
Social loneliness: this is calculated from questions 1, 4, 7, 8 and 11 and is the number of items scored ‘no’ or ‘more or less’. It is scored from 0 to 5 and is defined only when all five questions are answered.
-
Overall loneliness: this is the sum of the emotional and social loneliness scores. It is defined when 10 or 11 of the questions are answered.
The GSE is the sum of 10 questions, each of which is scored from 1 to 5, giving a total score in the range 10–50. It is defined when at least seven of the 10 questions are answered; if < 10 are answered, the revised total is given by GSE = total × (10/number of questions answered).
Secondary outcomes (other dimensions of the SF-36, PHQ-9, EQ-5D, de Jong Gierveld Loneliness Scale, GSE) at 6 month post randomisation were compared between the intervention group and the control group using a marginal GLM with robust standard errors and exchangeable correlation with and without adjustment for baseline covariates. The means and SDs (and numbers used for each calculation) for the treatment and control groups with adjusted and unadjusted mean differences and associated CIs are reported.
Estimates of the critical parameters that would be used for a sample size calculation (SD, correlation between baseline and 6-month outcomes and the ICC) are also reported.
Economic analysis
The case report form (see Appendix 5) included questions about the use of primary and secondary care health services, social care services and voluntary and private sector services.
The following elements were planned for the health economics analysis:
-
Costing of the TF service.
-
Costing of participants’ health, social care and voluntary service use during the trial.
-
Cost-effectiveness analysis using a range of outcome measures and a cost–utility analysis using the EQ-5D. The resulting cost per quality-adjusted life-year (QALY) would be compared with the NICE threshold of £20,000–30,000 per QALY gained.
-
An exploratory analysis of participants’ willingness to pay for a TF scheme.
Because of the early closure of the trial for reasons outlined in Chapter 4 (see Assessment of study feasibility), a high proportion of participants allocated to the intervention arm did not receive the intervention and it was therefore not appropriate to conduct the planned health economics analysis. Frequency tables for participants’ service use are presented in Chapter 4 (see Health and social care resource use); differences between the intervention group and the control group at follow-up should be interpreted with caution.
Methods for the qualitative research
Background
This report is concordant with Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines for reporting qualitative research. 47 The purpose of the qualitative research was to evaluate the impact of TF groups on older people as well as their perceived advantages and disadvantages in terms of well-being. The objective was an assessment of the acceptability and appropriateness of the intervention for preventing loneliness and maintaining good mental health. Some aspects of the fidelity assessment (e.g. views on the receipt and enactment of the intervention) were also informed by the qualitative research (see Methods for the fidelity assessment).
Methods for the participant interviews
The aim of the qualitative research was to explore to what extent older people considered TF groups to have made an impact on their well-being. A topic guide (see Appendix 6) was used to undertake semistructured interviews. This was based on a previous study25 and was tailored by MC and RG-W in line with the secondary end points for the trial. The topic guide was not piloted but was reviewed by the lay representative on the TMG as part of the review of essential documents submitted for ethical approval.
The topic guide covered questions regarding participants’ needs and expectations of telephone befriending, its impact on their health and well-being and accessibility and acceptability of the telephone discussion. It also inquired after participants’ experiences of the volunteer facilitator and whether they felt that the telephone discussions were or were not a good way to give them the support that they needed.
All participants allocated to the telephone befriending intervention and provided with a volunteer facilitator were invited (by telephone) to participate in a semistructured interview (24 individuals). We interviewed all 19 participants who volunteered to take part. Reasons for declining a research interview were not elicited but were recorded if volunteered by the participant. One female research associate (RG-W) and one female research assistant (RD) performed the interviews in April 2013. RG-W had studied qualitative research techniques as part of her MA in Research Methods and had experience of in-depth and semistructured interviews. RD had experience of qualitative interviews but was a novice in terms of qualitative analysis. Neither of the interviewers delivered the intervention to the interviewees. RD visited some interviewees to collect baseline data and/or collected 6-month follow-up data by telephone for the main trial. Interviewees would have known that the interviewers were on the research team and were from the University of Sheffield and may have associated them with the volunteers delivering the intervention and/or with delivery of the intervention. The interviewers were asked to withhold their own opinions, personal goals and characteristics and to reiterate the purpose of the research and that this interview was separate from the intervention. No repeat interviews were undertaken or field notes taken.
The interviews lasted between 14 and 63 minutes (median 29 minutes) and were conducted face to face in a place selected by the participants. All were conducted in participants’ homes. Written consent for audio recording was obtained when participants entered the study. For all but three interviews no one was present except for the participant and the researcher. Three interviews were interrupted by (1) a participant’s daughter (bringing a drink), (2) a participant’s cleaner and (3) a visitor. Sociodemographic data were collected from participants as part of the main trial and are reported in Chapter 4. Interviews were digitally recorded and transcribed verbatim. Transcripts were not returned to the participants for comment or correction.
Data analysis commenced during the data collection period using a constant comparative method to identify themes and where interviews and analysis each informed the other. Data analysis of the transcripts was conducted using NVivo 9 (QSR International, Warrington, UK). We used a ‘framework’ approach to analysis in which a priori and emergent themes were identified using the following stages: familiarisation, identifying a thematic framework, indexing, mapping and interpretation (charting was not undertaken). 48 A priori themes of interest were acceptability and accessibility of the group telephone discussion; subthemes were derived inductively through familiarisation with the transcripts. 48,49 Results were used to explore factors that may have mediated and moderated the intervention and contributed towards the findings of the trial and to identify any other emerging issues or factors that may have influenced the uptake of the intervention and which had not previously been documented. 50 It is unlikely that data saturation was achieved. 51 Participants were not asked to provide feedback on the identified themes.
Initially, we indexed transcripts using our own thematic framework (see Appendix 7); this was later supplemented with codes based on concepts from the group dynamics literature, relating to characteristics of functioning groups, specifically group cohesion and disclosure. 31
Methods for the volunteer interviews
The aim of the qualitative research was also to explore the experiences of volunteer facilitators in delivering the intervention. A semistructured topic guide was used with themes including the accessibility and acceptability of delivering befriending by telephone and the motivations of volunteers to take part and their experiences of facilitating group discussions, including their perceptions of participant benefit. All volunteers who remained in contact with the service provider were invited to take part in a semistructured interview. This included volunteers who dropped out before, mid and post completion of facilitator training, resulting in a sample of three. Two had completed the one-to-one and group telephone call phases of the intervention and one dropped out during the group facilitator training. We did not elicit reasons for declining an interview. RG-W performed the interviews in April 2013 and had a previous relationship with all volunteers having attended volunteer induction and one-to-one training sessions to support the service provider (by request). Interviewed volunteers knew that the interviewer was on the research team and from the University of Sheffield and not from the service provider. The interviewer was asked to withhold her own opinions and to reiterate the purpose of the research and that the interview was separate from the intervention and the service provider. No repeat interviews were undertaken or field notes taken.
The interviews lasted between 18 and 59 minutes (median 43 minutes) and were conducted face to face in a place selected by participants. Two interviews were conducted at the home of the volunteers and one was conducted at the University of Sheffield. For all interviews no one was present except for the participant and the researcher. Sociodemographic data were not collected for volunteers. A topic guide (see Appendix 6) was used. This was based on the secondary end points of the study and was informed by some elements of the fidelity framework, for instance whether the group experienced conflict or followed ground rules (see Methods for the fidelity assessment). The topic guide was not piloted.
Interviews were digitally recorded and transcribed verbatim. Transcripts were not returned to the participants for comment or correction. Data analysis of transcripts was conducted by RG-W by hand using a constant comparative method to identify themes. Analysis and interpretation followed relevant themes from the qualitative research framework developed from the participant interviews (see Chapter 5, Results of the participant interviews). Results were used to explore potential explanations for the quantitative findings and identify other emerging issues or factors influencing volunteer-led interventions. The final outcome was a synthesis of coded data and subthemes including those relevant to the fidelity assessment.
Methods for the fidelity assessment
The importance of describing complex interventions and actual content delivered is well established. 52,53 The fidelity substudy assessed how well the TF intervention was delivered according to the intervention protocol. An intervention fidelity framework based on that identified by the Behaviour Change Consortium54 was developed (see Appendix 1). The framework sets out the parameters by which quality and fidelity would be measured, under the headings of study design, training, delivery, receipt and enactment.
Telephone befriending design
To assess comparable ‘treatment dose’, the number, frequency and duration of one-to-one and group telephone contacts were established. The minimum number of one-to-one contacts was recommended as three on the basis that some participants would need more one-to-one contacts to be sufficiently confident to join the group discussions. A maximum of six one-to-one contacts was set. A maximum of 12 group telephone contacts was established and a minimum (in terms of treatment dose) was set at nine (of 12) group calls. The frequency of all telephone contact was weekly.
Telephone befriending training content assessment and methods
Volunteers were trained by Community Network’s group facilitation skills trainer. Attendance at training sessions was monitored by register taken by the single trainer who trained all volunteer facilitators. The training was delivered over the telephone to a number of trainees (maximum five) over four 1-hour sessions. The session content focused on providing skills and techniques to enable the facilitator to support the group to work well as a group and fulfil its purpose (see Methods for the main trial, Interventions).
The trial manager (RG-W) developed a fidelity checklist based on the standard training delivered to all volunteers who facilitate telephone discussion via the Community Networks’ teleconferencing system. This was reviewed by the content expert (MC) and the Community Network trainer to ensure that core components were included and that materials and practice delivered by the trainer could be assessed for consistency across groups. The checklist also included components to assess volunteer facilitator skill acquisition. The checklist was piloted by RG-W and MC using a sample of audio recordings, with modifications made where necessary (see Appendix 8, Training content checklist).
A purposive sample of training sessions was audio recorded across and within the training groups. RG-W and a research assistant (LN) used the training content checklist to assess the content and delivery techniques conveyed to trainee (volunteer) facilitators and facilitator skill acquisition. Checklists were completed and scored separately by the two coders and scores were compared. All scores were reviewed to ensure consistency in interpretation of the checklist items, with areas of dispute discussed and agreement reached by consensus. When agreement could not be reached the original observations, and therefore scores, remained the same. Median scores were calculated to provide an overall fidelity score for each training group and show the degree of consistency in the content delivered to trainee facilitators.
Treatment fidelity assessment and methods
To ensure that the criteria for treatment fidelity were met, those delivering the group befriending intervention (volunteer facilitators) were assessed for adherence to the intervention protocol across the 12 weeks. The assessment of treatment fidelity by volunteer facilitators used an intervention delivery checklist developed by RG-W based on the techniques delivered in the facilitator skills training and on a one-to-one training manual provided to volunteers (see Appendix 4). The training fidelity checklist was reviewed by MC and the Community Network trainer with modifications made where appropriate (see Appendix 8, Intervention delivery checklist).
According to the facilitation skills training, as groups develop, the level of input required from the volunteer facilitator should diminish over time. Therefore, the sample of audio recordings included three time points (weeks 1, 6 and 12) to assess the degree to which volunteers used their acquired skills and adhered to the intervention protocol during delivery. The checklists were designed to take into account variation in the content of sessions and the fact that, if some scenarios did not arise, volunteer facilitators could not be expected to demonstrate the appropriate response.
Telephone befriending delivery
Attendance at all planned sessions was recorded through call registers completed by volunteer facilitators at every session during both the one-to-one phase and the group phase. Volunteer facilitators recorded any difficulties with the delivery of the intervention protocol on the call registers. Issues arising during delivery of the intervention were noted by the service provider and forwarded to the research team. The challenges of implementation and barriers to uptake were examined with a convenience sample of volunteer facilitators (see Methods for the qualitative research and Chapter 5, Results of the volunteer interviews).
A purposive sample of audio recordings of group sessions was used to assess the match with the intervention protocol in terms of the content and techniques delivered and the extent to which volunteer facilitators enabled choice and decision-making. Note that the protocol (see Appendix 1) also incorrectly refers to the concept of intervention ‘drift’, which implies a trend away from intervention fidelity known to exist at baseline, something not established in this study. Samples were taken at three time points – weeks 1, 6 and 12 – to examine intervention delivery and volunteer facilitator skills and receipt of the intervention and enactment by participants. Checklists were completed and scored separately by the two observers and scores were compared. Coders reviewed scores to ensure consistency in interpretation of checklist items, with areas of dispute discussed and agreement reached by consensus. When agreement could not be reached the original observations, and therefore scores, remained the same. Median scores were calculated to provide an overall percentage score for each facilitated group.
Telephone befriending receipt and enactment
Unlike formal behaviour change interventions, such as cognitive–behavioural therapy or motivational interviewing, the PLINY intervention does not attempt to tightly regulate behaviour outside the delivery setting. The intervention attempts to reduce the discrepancy or (mis-)match between the quality and quantity of existing relationships and relationship expectations. 55 The intervention, through facilitated dialogue between participants, is intended to create a safe environment in which social contact can improve perceptions of available companionship and support (see Appendix 3). It follows that, if the volunteer facilitators are delivering the intervention per protocol, then the group is ‘working’ well and participants should not be exhibiting problem behaviours known to inhibit successful group experiences. For this reason, we limit our assessment of participant receipt and enactment to evidence of their performance as part of a friendship group. To try and identify whether participants found the group intervention to be appropriate, acceptable and beneficial (see Methods for the qualitative research and Chapter 5, Results of the participant interviews), we specifically reviewed interview transcripts with participants and volunteer facilitators for evidence of characteristics which indicated that the groups were in a transitional phase, towards functioning well as a group:31
-
defensiveness and resistance
-
conflict
-
confrontation.
Other characteristics – anxiety, the struggle for control, challenges to the group leader and the leader’s reactions to resistance – were not seen as relevant in this intervention, as the level of disclosure, anxiety and resistance within befriending groups was anticipated to be lower than in a therapeutic group.
Interview transcripts and audio recordings were also reviewed for the following problem behaviours that are counterproductive to group functioning:31
-
silence and lack of participation
-
monopolistic behaviour
-
hostile behaviour
-
dependency
-
acting superior
-
socialising (before the end of the programme)
-
‘band-aiding’ (e.g. try to sooth/lessen pain when someone is upset).
Other behaviours – storytelling, questioning, giving advice, intellectualising, emotionalising (dwelling on getting in touch with their feelings) – were not seen as problematic in this intervention.
Chapter 3 Results of the implementation of the intervention
Interaction with the service funder and service provider
Conditional funding
It was originally intended to use multiple service providers to deliver the intervention. This was not possible for the following reasons. We considered it likely that the delivery at scale of a manualised intervention by volunteers would need the stable base offered by formal training and monitoring by experienced volunteer co-ordinators. For this, it was essential to secure funding. The funding was secured from a national charity on condition that we would use the money to deliver the intervention through one or more of its local branches only; we were unable to use other organisations to deliver the intervention. We looked at the viability of recruiting other branches of the charity to deliver the intervention. Other branches did express an interest but were unable to provide the intervention to participants recruited in the urban centre where the study was ongoing. Each branch of the charity was restricted through its constitution to serve the needs of its (bounded) local population. No branch could provide volunteers to work outside its geographical area. The research team was not adequately resourced to work in other geographical areas, which, in participant recruitment terms, was unnecessary in a conurbation with an estimated population of over half a million people.
An overview of the funding made available by the national charity is provided in Table 3. Detailed breakdowns follow of the resource for (1) the service provider, the local branch of the national charity, to recruit, train and mentor volunteer befriending facilitators (Table 4) and (2) a specialist trainer in group facilitation to support the manualisation of the intervention, provide advice on assessing its fidelity and train the volunteer facilitators (Table 5).
| Item | Cost (£) | Assumptions/notes |
|---|---|---|
| Service provider costs | ||
| Staffing and resources (three recruitment waves) | 6078.60 | See Table 4 |
| Overheads | 1215.72 | |
| Subtotal | 7294.32 | Excluding VAT (service provider confirmed that it would not charge VAT) |
| Group facilitation trainer costs | ||
| Training content | 3300.00 | Assume 5.5 days’ work @ £600 per day |
| Volunteer training | 4200.00 | Based on 30 volunteers retained by the service provider for facilitator training. Training provider – four 1-hour sessions for five people at £700 |
| Manuals/materials | 117.60 | See Table 5 |
| Participant – facilitator training | 700.00 | Assume that five participants will start their own group |
| Fidelity advice | 1200.00 | Advice to content expert and study manager on fidelity – approximately 2 days at £600 per day |
| Subtotal | 9517.60 | |
| VAT @ 20% | 1903.52 | |
| Total | 11,421.12 | |
| Item | Unit | Number of units | Cost per unit (£) | Total cost (£) | Notes/assumptions |
|---|---|---|---|---|---|
| Advertising | |||||
| Website | Updates | 1 | 30 | 30.00 | External costs incurred for website support |
| Mail-outs | Mail-outs | 100 | 0.85 | 85.00 | Second-class post and stationary plus return envelopes |
| E-mail-outs | Hours | 2 | 12 | 24.00 | Internal staff time – BDA (includes staff time for postal mail-outs) |
| Window advertisement | Posters | 0 | 0.00 | Internal printing only | |
| VAS | 0 | 0.00 | Assumes no charge for VAS | ||
| Press advertising | Press adverts | 2 | 300 | 600.00 | Estimated costs of local ‘freebies’ |
| Radio | 0.00 | ||||
| Subtotal | 739.00 | ||||
| Initial day course orientation to working with older people and training in one-to-one befriending (assumes 15 volunteers per day) | |||||
| Preparatory work | Hours | 4 | 0 | 0.00 | Induction to working with older people plus summary of the trial |
| Introductory day | Days | 2 | 150 | 300.00 | Assumes 10 volunteers per day can be accommodated in the venue |
| Venue | Days | 2 | 50 | 100.00 | |
| Refreshments | Volunteers | 20 | 3.5 | 70.00 | Includes lunch, tea/coffee/water, biscuits |
| Equipment | 0.00 | Own equipment used | |||
| Handouts | 20 | 2.5 | 50.00 | Handouts printed internally | |
| Subtotal | 520.00 | ||||
| Administration | |||||
| Collate applications | Hours | 3 | 12 | 36.00 | Internal staff time – BDA |
| Invitations to applicants | Invitations | 20 | 0.46 | 9.20 | Second-class post and stationary |
| CRB checks | Volunteers | 10 | 0 | 0.00 | External costs to process – no charge for volunteers |
| CRB checks administration | Hours | 5 | 12 | 60.00 | Internal staff time – BDA |
| Vetting administration | Hours | 5 | 12 | 60.00 | Internal staff time – BDA |
| Subtotal | 165.20 | ||||
| Interim – mentoring and review per wave | |||||
| Mentor and review sessions | Half-days | 4 | 75 | 300.00 | Assumes five volunteers per half-day |
| Venue | Half-days | 4 | 30 | 120.00 | |
| Refreshments | Volunteers × half-days | 20 | 1.5 | 30.00 | Includes tea/coffee/water, biscuits |
| Equipment | 0.00 | Own equipment used | |||
| Handouts | Handouts × sessions | 20 | 1 | 20.00 | Handouts printed internally |
| Follow-up | Hours | 6 | 22 | 132.00 | Internal staff time – CEM |
| Subtotal | 602.00 | ||||
| Total per wave of 20 inducted, 10 retained (excluding overheads) | 2026.20 | ||||
| Overheads | |||||
| Contribution to service provider overheads (20%) | 405.24 | ||||
| Total per wave of 20 inducted, 10 retained (including overheads) | 2431.44 | ||||
| Total across three waves (including overheads) | 7294.32 | ||||
| Item | Cost (£) | Notes/assumptions |
|---|---|---|
| Training content development | 3300 | Assumed 5.5 days’ work @ £600 per day |
| Training | ||
| Four × 1-hour course | 4200 | Based on £700 per four volunteers (n = 30) |
| Subtotal | 7500 | |
| Manual and materials (estimate) | ||
| Cover letter (n = 30) | 3 | |
| Confidentiality sheet (n = 30) | 3 | |
| Facilitator handbook (25 pages; n = 30) | 75 | |
| Facilitator recording sheet (n = 252) | 3 | |
| Certificates (n = 30) | 3 | |
| Content/session sheets (n = 252) | 3 | |
| Postage (n = 30) | 28 | |
| Subtotal | 118 | |
| Fidelity advice | ||
| Advice to content expert on fidelity | 1200 | e.g. Facilitator adherence to intervention protocol |
| Subtotal | 1200 | |
| Volunteer facilitator training | ||
| Train four volunteers as facilitators | 700 | |
| Subtotal | 700 | |
| Total | 9518 | |
The contract with the service provider
Contractual negotiations with the service provider ran between 20 October 2011 and 14 June 2012 when the contract was signed. The service provider was contracted to:
-
Identify and recruit suitable volunteers for the role of volunteer/facilitator for the delivery of the PLINY research intervention, including carrying out Criminal Records Bureau (CRB) checks.
-
Ensure that volunteers are oriented to working with older people and willing to deliver telephone befriending, are trained to carry out one-to-one calls in line with the PLINY research intervention and are ready to receive training in telephone befriending facilitation (to be delivered by a third party) in the numbers and by the dates shown in Table 6.
-
Ensure that volunteers take responsibility for scheduling and (subject to participant adherence) delivery of up to six one-to-one and 12 group telephone sessions for each person recruited to the PLINY research study and randomised to the TF group.
-
Ensure that there are sufficient volunteers to provide cover in the event of volunteer facilitator absence or discontinuation.
-
Provide ongoing ‘mentoring’ to volunteers, in line with the service provider’s policies and procedures and the PLINY research intervention, to ensure a point of contact and support.
-
Provide regular (at least monthly) updates to the research team on levels of volunteer recruitment and retention and feed back information, including the one-to-one and group call registers, to inform the research.
-
Alert the research team at the earliest opportunity if a participant wishes to withdraw or is unable to participate in the intervention (TF groups), with reasons recorded (if provided by the participant).
| Deadline | Recommended number of volunteers recruited and trained | Minimum number of volunteers recruited and trained |
|---|---|---|
| 1 May 2012 | 20 | 10 |
| 1 September 2012 | 20 | 10 |
| 1 January 2013 | 20 | 10 |
Item (3), the delegation of first contact and scheduling of calls, might not be considered best practice for sustaining a volunteer befriending service. For instance, a Delphi survey of volunteer co-ordinators managing befriending services found general agreement that they should be managed either by a full-time or a part-time project co-ordinator. 25 The volunteer co-ordinators also agreed that it was essential to have a monitoring system in place (p. 51). 24 We were unable to broker such an arrangement within the available finances.
Recruitment and retention of volunteers
Recruitment and retention of volunteers was an important criterion for the feasibility of the study (see Chapter 4, Assessment of study feasibility) and for the continuity of the service for individual participants and their groups. Matching service demand (participant recruitment) with the capacity of the service provider was part of the study design. Participant recruitment was intended to be conducted over three waves. It was estimated that a minimum of 10 and a maximum of 20 volunteers would be required in each wave. Therefore, a minimum of 30 (maximum of 60) volunteers was agreed with the service provider as being necessary to facilitate approximately 20 friendship groups over the life of the study. This would ensure capacity to continue the service in the event of dropout or planned and unplanned absences.
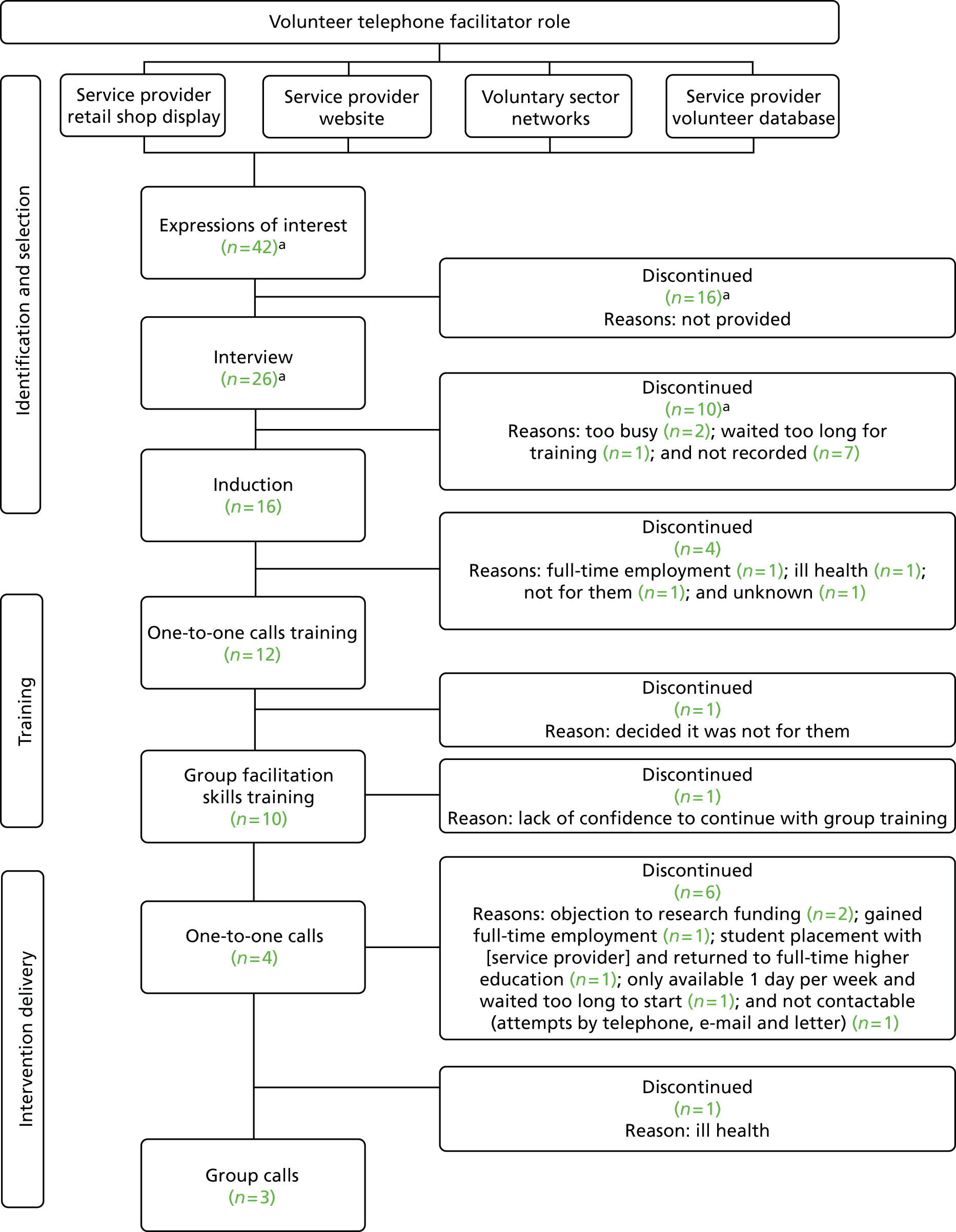
The service provider experienced difficulties with recruiting and retaining a sufficient number of volunteers. These difficulties were explored within the four categories of marketing, training, monitoring and boundaries. Figure 1 shows the flow of volunteers throughout the study. Ten (24%) out of 42 volunteers who expressed an interest in the study completed the training of whom three (33%) delivered the intervention. Reasons for dropping out were captured when possible to provide an indication of the acceptability and accessibility of the volunteer role to those expressing an interest in the role.
FIGURE 1.
Flow of service provider’s volunteers. a, Information supplied by the service provider (field note, 13 November 2012). Detailed information was not captured for all expressions of interest/referrals to the service provider (including agencies, e.g. Jobcentre Plus). The service provider reported that all candidates were screened for suitability for a number of volunteer opportunities, including the telephone group facilitator role.
Marketing
Activity by the service provider to promote the volunteer opportunity included its website (news archive, 25 September 2012; accessed 10 May 2013), the Northern Community Assembly website (field note, 21 November 2012), the local Wellbeing Consortium (field note, 20 November 2012), a local newspaper and a range of community and voluntary networks and organisations available in the locality, which we have not named to preserve the anonymity of the service provider (field note, 14 June 2012; TMG, 15 November 2013). The service provider reported that potential volunteers referred to them by other agencies (e.g. Jobcentre Plus) were often not suitable for the facilitator role (TMG, 19 September 2012).
Suggestions for additional strategies to promote the volunteer role in the locality were made by the study team (e.g. TMG, 15 November 2013).
Training
Training sessions for the group intervention required a minimum of four volunteers for the training group to be feasible. The service provider identified an initial group of six volunteers early in the project (TMG, 20 February 2012) and scheduled one-to-one training for them in March 2012. The charity reported a number of implementation issues including matching the availability of volunteers to training dates (TMG, 20 February 2012). They also found that retaining volunteers between recruitment and training was difficult and required more resources than anticipated (TMG, 20 August 2012). It should be noted that the first group of volunteers (n = 4 in two groups) received induction and one-to-one calls training from the service provider in March 2012, 2 months before the scheduled start of participant recruitment. In fact, participant recruitment did not commence until June 2012, 1 month late, because of delays in contracting. A lower than anticipated response to the initial recruitment strategy (direct mail out to participants of a population cohort) meant a further delay before the research team had recruited and randomised the six intervention-arm participants needed for a group. According to the service provider, this delay caused the attrition of several existing volunteers (see Figure 1). At a time when the rate of participant recruitment was starting to increase, the service provider advised the study team that it was not actively recruiting volunteers (TMG, 19 September 2012) because there was an insufficient number of randomised participants. Instead, the service provider was waiting for candidate volunteers to approach them in response to advertisements.
Once the research team had managed to increase the rate of participant recruitment through general practice mail-outs, the service provider experienced repeated difficulties identifying volunteers to fill facilitator training groups. As a result, the first two training sessions (May 2012) contained only two genuine volunteers; to make the training viable, the service provider’s staff and members of the study team – who did not intend to deliver the intervention – made up the places to make the training viable. A finite training budget meant that running sessions with insufficient numbers of genuine volunteers was not sustainable. As a result, we agreed that the four (ideally five) places on training sessions scheduled for some time in the future had to be filled by a certain date – the ‘book by’ date – or they would be cancelled. ‘Book by’ dates were arranged with the group facilitator trainer to assist the service provider as it reported (TMG, 14 June 2012) practical difficulties in co-ordinating volunteers at the times and pace required by (1) the trial, which had a window of 1 year to recruit 248 participants to test the effectiveness of a public health intervention, which had to be rolled out at scale, and (2) the group training (four 1-hour telephone sessions on different days). The service provider did not always confirm whether sufficient volunteers had been identified by the ‘book by’ date despite reminders from the trainer/study manager (e-mail and telephone, 16 November 2012).
The total number of volunteers group trained between 17 May 2012 and 22 October 2012 was 11, instead of the 20 who should have been trained. Two trained volunteers were not available to take on a group; one was on a student placement with the service provider and needed to return to full-time education and one was available for only 1 day per week, having assumed that they could make befriending calls in the evening. Three training sessions (during which 15 more volunteers should have been trained) were cancelled between August 2012 and January 2013 because of a lack of take-up. Three volunteers facilitated four groups (n = 24) to completion between September 2012 and May 2013 (with up to 6 weeks one-to-one befriending beforehand). One group received one-to-one befriending from a fourth volunteer facilitator who dropped out before the group stage. An existing volunteer took over for the group calls stage (see Monitoring volunteers). The number of days that volunteers ‘survived’ in the project (from completing group training to the day that they dropped out) ranged from 12 to 118 (mean 62 days).
Monitoring volunteers
Feedback from volunteers was collected by the service provider and reported to the TMG and, when relevant, to other volunteers delivering the service. The study team also captured implantation issues during set-up and recruitment in field notes.
The service provider was responsible for providing ongoing ‘mentoring’ to volunteers, in line with its existing policies and procedures relating to volunteers and the intervention protocol, to ensure a point of contact and support for the volunteers whilst they were delivering the TF service. The charity provided a summary of the project in its induction pack together with copies of the one-to-one training manual (field notes, 20 March 2012, 15 June 2012, 9 October 2012). Volunteers often contacted the study team with enquiries about what to do in certain circumstances, for instance if participants missed calls and the facilitator had been only able to contact one (of six) participants in the first week (field note, 30 October 2012), they were going on holiday (field note, 17 September 2012) or if they experienced technical difficulties with audio recording calls (field note, 29 September 12) (see also Boundaries between research and service delivery). The reasons why volunteers contacted the study team rather than the service provider are considered in Boundaries between research and service delivery and Chapter 5 (see Results of the volunteer interviews).
Volunteers reported difficulties in contacting participants to arrange the initial and subsequent one-to-one telephone calls (see Chapter 5, Results of the volunteer interviews). Volunteers reported that it would be better to make calls in the early evening and that some participants had also reported this. however, to safeguard participants using the service the provider did not permit volunteers to make calls before 0900 or after 1700 from Monday to Friday. This resulted in one volunteer dropping out (see Figure 1).
In reviewing volunteer identification and recruitment (field note, 5 December 2012), the service provider identified three issues that it felt were impacting on the recruitment and retention of volunteers: (1) existing volunteers found it difficult to contact participants for the one-to-one calls as they were ‘socially active’, resulting in the volunteers being reluctant to take on another group; (2) there was a time delay between volunteers being trained and actually delivering the service; and (3) there was a lack of introductions by the service provider between the volunteers and the ‘participants’. The service provider decided that volunteers would introduce themselves to study participants at the first contact (one-to-one call) and be responsible for scheduling one-to-one and group calls (field note, 22 March 2012). One of the volunteer co-ordinators stated that, for their face-to-face visiting service, volunteers often want to be introduced to clients by the service provider staff and felt that this may have contributed to the difficulty in recruiting or retaining volunteers (field note, 2 January 2012).
One volunteer (out of 10) who completed all training dropped out during intervention delivery (between completion of the one-to-one calls and the start of the group calls) because of ill-health. Attempts by the service provider to contact two trained volunteers failed and, because of the already limited pool of volunteers, the only facilitators available were those already running a friendship group. The service provider reported contacting participants of the group to let them know and asked the existing volunteers (n = 2) if they would be willing to take on the group (field note, 5 December 2012). One volunteer agreed but did not run the groups concurrently, which resulted in a delay in the group calls starting. Some participants were difficult to contact (field note, 14 February 2012) and at least one member of the group was not contacted (see Chapter 5, Results of volunteer interviews).
In accordance with the intervention design, the service provider asked volunteer facilitators to discuss with participants in their groups whether they would like to volunteer to run their own group when they had finished their own involvement, thereby contributing to the notion of older people helping other older people. Feedback on responses was not provided.
Boundaries between research and service delivery
Boundaries between the research and the service being investigated were blurred in some instances. Participants called the study team to advise that they would miss the week’s call; volunteers called the study team directly if they were unsure about what to do (see Monitoring volunteers). For instance, one volunteer enquired about what information participants had received about ‘how it all works’ (field note, 26 September 2012). Another enquired about how the group could exchange contact details so that members could meet up (field note, 25 March 2013). The service provider also referred volunteers to the study team for information, for example one volunteer enquired about the Christmas period (VF03, female, field note, 3 December 2012) and one volunteer (not interviewed, female) contacted the team because she lacked confidence in making the calls via the Community Network system (field note, 2 November 2013). Additional training was provided to this volunteer by the study team (field note, 8 November 2012).
Chapter 4 Results of the main trial
Assessment of study feasibility
The criteria used to assess the feasibility of the trial as part of the internal pilot were (1) sufficient participants willing to enter the trial; (2) retention of sufficient participants to assess the primary outcome measure; and (3) recruitment and retention of adequate volunteers to deliver TF to trial participants. Criteria (1) and (2) formed the basis of formal stop–go criteria agreed with the funders for the primary outcome assessment time point of 6 months.
Assessment of feasibility was made at 6 months from the start of participant recruitment. The review found that two criteria were satisfactorily met, with participant recruitment and retention by the trial team being feasible. However, the recruitment and retention of volunteer facilitators by the service provider was not adequate to deliver the intervention to the participants randomly allocated to receive the TF intervention. Training courses were not filled to capacity and, although implementation issues were reported by the service provider and addressed when possible, recruitment and retention were not adequate (see Chapter 3, Recruitment and retention of volunteers).
Participant recruitment was stopped, with the last participant randomised on 11 January 2013. The main consideration contemplated by the TMG at the point of suspension was that 50 out of the 78 participants allocated to the research arm had not been allocated a volunteer facilitator, that is, had not been treated per protocol.
Attempts were made to identify an alternative service provider. This included potential service providers in neighbouring districts; however, they were restricted by charitable aims preventing service delivery to a population outside their geographical area. After clarifying that no other service provider was capable of recruiting and retaining volunteer facilitators in the numbers required, the TMG took the decision on 17 January 2013 to close the trial early. The TSC and Public Health Research programme were advised of the TMG’s decision and recommended action. This included ensuring that participants were informed about how the decision would impact on them. Following approval from the NHS REC, participants still receiving the intervention were advised that they would continue to receive calls for 12 weeks. Participants in the intervention arm were advised whether or not they would be invited to take part in an interview about their experiences in the groups. Participants in both arms were also informed whether they would be followed up at the 6-month primary outcome assessment time point (by the end of March).
Recruitment of trial participants
Main results
Figure 2 shows the participant flow diagram; 157 participants were consented and randomised to the intervention group (n = 78) or the control group (n = 79).
FIGURE 2.
Participant flow diagram. SYC, South Yorkshire cohort. a, Three were ineligible, 21 were not interested in the intervention, 11 did not have enough time to participate, two were not willing to complete the questionnaires, two needed more information, one was not willing to take part if they did not receive the intervention, one preferred not to give a reason and 47 stated other reasons. b, 17 failed the 6CIT, one was already receiving telephone services and one was unable to use the telephone. c, One did not want to take part and one wanted to discuss the study with a family member. d, One was withdrawn by the chief investigator because of a protocol violation relating to eligibility, two withdrew consent shortly after allocation [one was unhappy with the involvement of (service provider) and one did not feel the study was for them], five withdrew consent at the point of arranging the 6-month follow-up (one because of ill-health, one was no longer unhappy and so did not want to take part, one was unhappy with the intervention – at this point they had not received any calls, one was unhappy with being left uninformed about the lack of intervention and one withdrew because of personal or family issues) and one was not contactable (at least six attempts were made by telephone and a reminder letter was sent). e, One withdrew consent at the point of arranging the 6-month follow-up (unhappy with allocation to the study arm), one was not contactable (no dial tone; letter and e-mail reminders sent), one was on holiday for 4 weeks and two refused (one did not want to answer the same questions as they did not feel any different and one felt too ill to answer any questions). f, Two no longer wanted the intervention (one was too busy and one thought that the intervention was not for them) and one did not give any reason for withdrawal from the intervention. g, Assigned to TF group 5 but the intervention was not delivered because the volunteer facilitator dropped out.
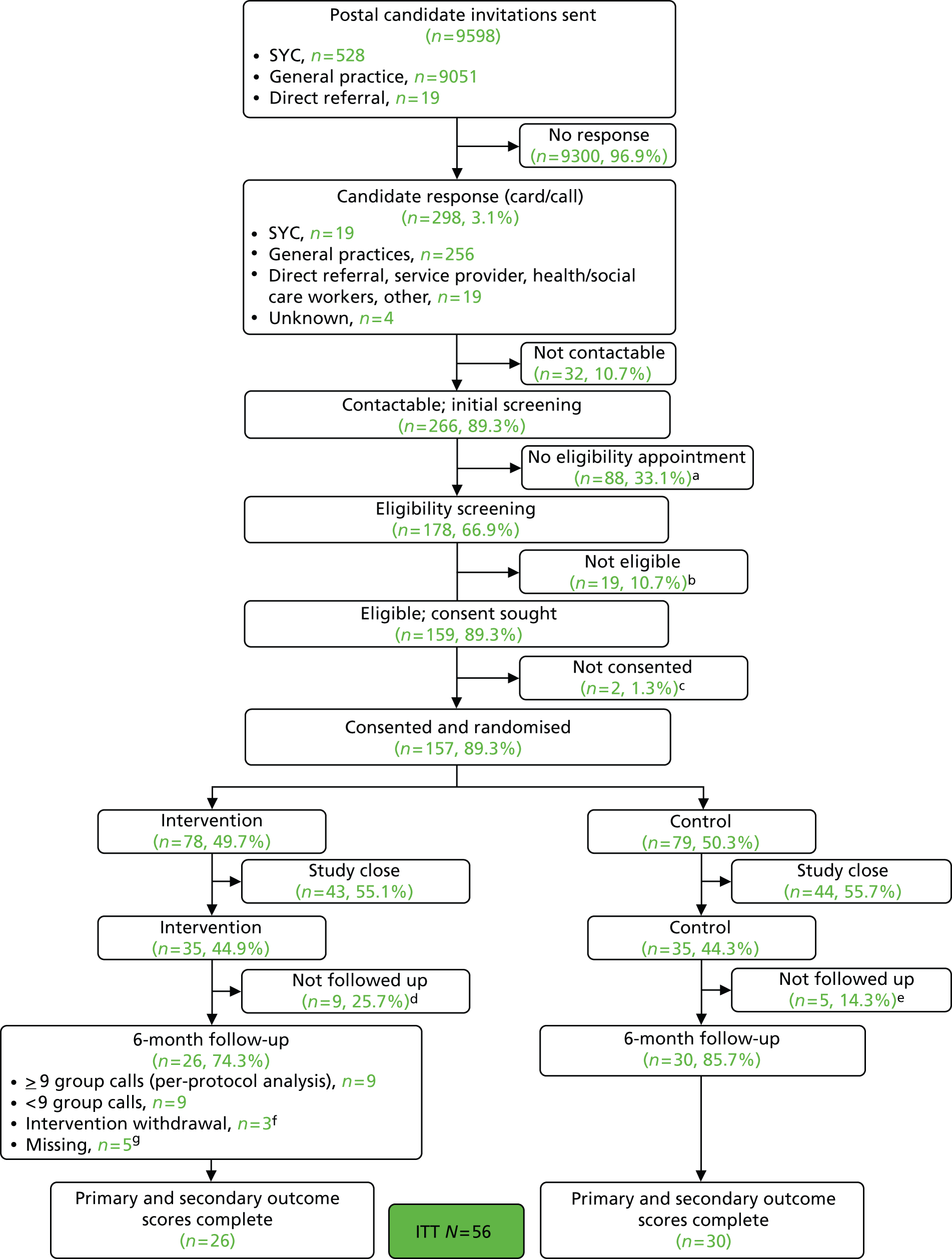
Table 7 shows the baseline characteristics of the 157 randomised participants. Overall, the two randomised groups were well matched with respect to baseline demographic characteristics. Tables 8 and 9 show the baseline participant-reported outcome scores for the SF-36, EQ-5D, PHQ-9, de Jong Gierveld Loneliness Scale, ONS well-being outcome and the GSE. Again, the two randomised groups were well matched with respect to baseline quality of life scores.
| Variable | Scoring | Control (n = 79) | Intervention (n = 78) | Total (n = 157) |
|---|---|---|---|---|
| Sex, n (%) | Female | 51 (65) | 54 (69) | 105 (67) |
| Male | 28 (35) | 24 (31) | 52 (33) | |
| Age (years) | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 80.3 (4.3) | 81.4 (4.9) | 80.8 (4.6) | |
| Median (IQR) | 79 (77–83) | 81 (78–84) | 80 (77–84) | |
| Min. to max. | 75 to 91 | 75 to 95 | 75 to 95 | |
| Ethnicity, n (%) | English/Welsh/Scottish/Northern Irish/British | 74 (94) | 74 (95) | 148 (94) |
| Any other white background | 4 (5) | 1 (1) | 5 (3) | |
| Caribbean | 0 (0) | 1 (1) | 1 (1) | |
| Indian | 1 (1) | 0 (0) | 1 (1) | |
| Irish | 0 (0) | 1 (1) | 1 (1) | |
| Prefer not to say | 0 (0) | 1 (1) | 1 (1) | |
| Live with anyone?, n (%) | Yes | 23 (29) | 22 (28) | 45 (29) |
| No | 56 (71) | 56 (72) | 112 (71) | |
| Live with spouse/partner, n (%) | Ticked | 20 (25) | 19 (24) | 39 (25) |
| Live with children, n (%) | Ticked | 3 (4) | 3 (4) | 6 (4) |
| Live with others, n (%) | Ticked | 0 (0) | 1 (1) | 1 (1) |
| Education, n (%) | ||||
| One to four O levels/GCSEs/CSEs | Ticked | 4 (5) | 3 (4) | 7 (4) |
| Five or more O levels/GCSEs/CSEs | Ticked | 8 (10) | 11 (14) | 19 (12) |
| One A level/two to three AS levels | Ticked | 1 (1) | 1 (1) | 2 (1) |
| Two or more A levels/four or more AS levels | Ticked | 5 (6) | 1 (1) | 6 (4) |
| Degree | Ticked | 5 (6) | 14 (18) | 19 (12) |
| Higher degree | Ticked | 3 (4) | 3 (4) | 6 (4) |
| Professional | Ticked | 6 (8) | 9 (12) | 15 (10) |
| NVQ4 | Ticked | 0 (0) | 1 (1) | 1 (1) |
| Apprenticeship | Ticked | 3 (4) | 2 (3) | 5 (3) |
| Other | Ticked | 14 (18) | 5 (6) | 19 (12) |
| Occupation, n (%) | Employed or self-employed | 1 (1) | 0 (0) | 1 (1) |
| Looking after home/family | 0 (0) | 3 (4) | 3 (2) | |
| Retired | 78 (99) | 75 (96) | 153 (97) | |
| Variable | Scoring | Control (n = 79) | Intervention (n = 78) | Total (n = 157) |
|---|---|---|---|---|
| Mental health (baseline) | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 77.5 (17.9) | 78.1 (14.4) | 77.8 (16.2) | |
| Median (IQR) | 80 (70–90) | 80 (70–90) | 80 (70–90) | |
| Min. to max. | 5 to 100 | 15 to 100 | 5 to 100 | |
| Physical function (baseline) | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 61.4 (28.7) | 63.6 (26.2) | 62.5 (27.4) | |
| Median (IQR) | 65 (40–90) | 70 (50–85) | 70 (40–85) | |
| Min. to max. | 5 to 100 | 0 to 100 | 0 to 100 | |
| Role – physical (baseline) | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 66.7 (29.8) | 65.6 (27.9) | 66.2 (28.8) | |
| Median (IQR) | 68.8 (43.8–93.8) | 65.6 (43.8–100) | 68.8 (43.8–93.8) | |
| Min. to max. | 0 to 100 | 0 to 100 | 0 to 100 | |
| Bodily pain (baseline) | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 58.4 (27.2) | 61.5 (27.2) | 59.9 (27.1) | |
| Median (IQR) | 52 (41–74) | 62 (41–84) | 61 (41–80) | |
| Min. to max. | 0 to 100 | 0 to 100 | 0 to 100 | |
| General health (baseline) | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 57.8 (22.7) | 61.7 (23.4) | 59.7 (23.1) | |
| Median (IQR) | 57 (42–77) | 67 (45–77) | 62 (45–77) | |
| Min. to max. | 5 to 100 | 0 to 100 | 0 to 100 | |
| Vitality (baseline) | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 54.7 (21.4) | 58.5 (21.6) | 56.6 (21.5) | |
| Median (IQR) | 56.3 (43.8–68.8) | 62.5 (43.8–68.8) | 56.3 (43.8–68.8) | |
| Min. to max. | 0 to 100 | 0 to 100 | 0 to 100 | |
| Social function (baseline) | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 79.9 (26.8) | 79.3 (26.6) | 79.6 (26.6) | |
| Median (IQR) | 100 (62.5–100) | 87.5 (62.5–100) | 100 (62.5–100) | |
| Min. to max. | 12.5 to 100 | 12.5 to 100 | 12.5 to 100 | |
| Role – emotional (baseline) | n (%) | 79 (100) | 77 (98.7) | 156 (99.4) |
| Mean (SD) | 86.7 (24.6) | 86.9 (21.6) | 86.8 (23.1) | |
| Median (IQR) | 100 (83.3–100) | 100 (83.3–100) | 100 (83.3–100) | |
| Min. to max. | 0 to 100 | 0 to 100 | 0 to 100 | |
| Physical component score (baseline) | n (%) | 79 (100) | 77 (98.7) | 156 (99.4) |
| Mean (SD) | 40.3 (12.1) | 41.5 (11.5) | 40.9 (11.8) | |
| Median (IQR) | 41.9 (29.8–49.6) | 43.1 (32.7–50.5) | 42.8 (30.8–50.5) | |
| Min. to max. | 11.9 to 70.7 | 10.9 to 61.7 | 10.9 to 70.7 | |
| Mental component score (baseline) | n (%) | 79 (100) | 77 (98.7) | 156 (99.4) |
| Mean (SD) | 53.1 (10.8) | 53.5 (8.1) | 53.3 (9.5) | |
| Median (IQR) | 56.8 (49.5–59.5) | 55.2 (49.0–58.8) | 56.4 (49.2–59.5) | |
| Min. to max. | 16.5 to 69.9 | 24.3 to 68.1 | 16.5 to 69.9 |
| Variable | Scoring | Control (n = 79) | Intervention (n = 78) | Total (n = 157) |
|---|---|---|---|---|
| EQ-5D (baseline)a | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 0.7 (0.25) | 0.72 (0.27) | 0.71 (0.26) | |
| Median (IQR) | 0.73 (0.62–0.85) | 0.76 (0.66–0.85) | 0.73 (0.66–0.85) | |
| Min. to max. | –0.07 to 1 | –0.37 to 1 | –0.37 to 1 | |
| EQ-5D VAS (baseline)b | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 70.7 (19.2) | 72.8 (17) | 71.7 (18.1) | |
| Median (IQR) | 75 (59–85) | 77.5 (62–85) | 75 (60–85) | |
| Min. to max. | 18 to 100 | 15 to 100 | 15 to 100 | |
| de Jong Gierveld emotional loneliness (baseline)c | n (%) | 79 (100) | 77 (98.7) | 156 (99.4) |
| Mean (SD) | 2.1 (1.9) | 2.1 (1.9) | 2.1 (1.9) | |
| Median (IQR) | 2 (0–4) | 2 (0–3) | 2 (0–4) | |
| Min. to max. | 0 to 6 | 0 to 6 | 0 to 6 | |
| de Jong Gierveld social loneliness (baseline)d | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 1.5 (1.7) | 1.5 (1.7) | 1.5 (1.7) | |
| Median (IQR) | 1 (0–2) | 1 (0–3) | 1 (0–3) | |
| Min. to max. | 0 to 5 | 0 to 5 | 0 to 5 | |
| de Jong Gierveld overall loneliness (baseline)e | n (%) | 79 (100) | 77 (98.7) | 156 (99.4) |
| Mean (SD) | 3.5 (3.2) | 3.6 (3.2) | 3.6 (3.2) | |
| Median (IQR) | 2 (1–5) | 3 (1–6) | 3 (1–5) | |
| Min. to max. | 0 to 11 | 0 to 11 | 0 to 11 | |
| PHQ-9 (baseline)f | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 3.2 (4) | 3.1 (3.8) | 3.1 (3.9) | |
| Median (IQR) | 2 (0–5) | 2 (0–4) | 2 (0–4) | |
| Min. to max. | 0 to 22 | 0 to 17 | 0 to 22 | |
| ONS well-being (baseline)g | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 7.6 (2.1) | 7.8 (1.8) | 7.7 (2) | |
| Median (IQR) | 8 (7–9) | 8 (7–9) | 8 (7–9) | |
| Min. to max. | 0 to 10 | 0 to 10 | 0 to 10 | |
| GSE (baseline)h | n (%) | 79 (100) | 78 (100) | 157 (100) |
| Mean (SD) | 32.1 (5.5) | 33.6 (4.7) | 32.9 (5.1) | |
| Median (IQR) | 32 (28–36) | 34.5 (30–38) | 34 (29–37) | |
| Min. to max. | 10 to 40 | 22 to 40 | 10 to 40 |
Only 70 out of the 157 randomised participants were followed up for 6 months post randomisation. These participants were part of the initial internal pilot study to assess the feasibility of the full RCT. Table 10 shows the baseline demographic characteristics of these 70 randomised participants. The two groups were reasonably well matched with respect to baseline demographic characteristics, although there is some evidence that slightly more women were randomised to receive the intervention. Tables 11 and 12 show the mean baseline participant-reported outcome scores for these 70 participants. The mean participant-reported outcome scores were broadly similar for both groups, although there is some evidence that the intervention group had a slightly better quality of life at baseline, as measured by the SF-36 mental health, general health and vitality dimensions.
| Variable | Scoring | Control (n = 35) | Intervention (n = 35) | Total (n = 70) |
|---|---|---|---|---|
| Sex, n (%) | Female | 18 (51) | 23 (66) | 41 (59) |
| Male | 17 (49) | 12 (34) | 29 (41) | |
| Age (years) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 80.1 (3.7) | 81.8 (5.8) | 80.9 (4.9) | |
| Median (IQR) | 80 (76–82) | 80 (78–85) | 80 (77–84) | |
| Min. to max. | 75 to 90 | 75 to 95 | 75 to 95 | |
| Ethnicity, n (%) | English/Welsh/Scottish/Northern Irish/British | 33 (94) | 34 (97) | 67 (96) |
| Any other white background | 2 (6) | 1 (3) | 3 (4) | |
| Live with anyone?, n (%) | Yes | 8 (23) | 10 (29) | 18 (26) |
| No | 27 (77) | 25 (71) | 52 (74) | |
| Live with spouse/partner, n (%) | Ticked | 6 (17) | 8 (23) | 14 (20) |
| Live with children, n (%) | Ticked | 2 (6) | 1 (3) | 3 (4) |
| Live with others, n (%) | Ticked | 0 (0) | 1 (3) | 1 (1) |
| Education, n (%) | ||||
| One to four O levels/GCSEs/CSEs | Ticked | 2 (6) | 2 (6) | 4 (6) |
| Five or more O levels/GCSEs/CSEs | Ticked | 3 (9) | 3 (9) | 6 (9) |
| Two or more A levels/four or more AS levels | Ticked | 1 (3) | 0 (0) | 1 (1) |
| Degree | Ticked | 1 (3) | 5 (14) | 6 (9) |
| Higher degree | Ticked | 1 (3) | 1 (3) | 2 (3) |
| Professional | Ticked | 4 (11) | 7 (20) | 11 (16) |
| Apprenticeship | Ticked | 1 (3) | 0 (0) | 1 (1) |
| Other | Ticked | 6 (17) | 2 (6) | 8 (11) |
| Occupation, n (%) | Looking after home/family | 0 (0) | 1 (3) | 1 (1) |
| Retired | 35 (100) | 34 (97) | 69 (99) | |
| Variable | Scoring | Control (n = 35) | Intervention (n = 35) | Total (n = 70) |
|---|---|---|---|---|
| Mental health (baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 74.7 (21.6) | 77.9 (17.5) | 76.3 (19.6) | |
| Median (IQR) | 80 (65–90) | 80 (70–90) | 80 (70–90) | |
| Min. to max. | 5 to 100 | 15 to 100 | 5 to 100 | |
| Physical function (Baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 67 (27.3) | 65.6 (27.4) | 66.3 (27.2) | |
| Median (IQR) | 75 (40–90) | 70 (55–90) | 72.5 (45–90) | |
| Min. to max. | 15 to 100 | 0 to 100 | 0 to 100 | |
| Role – physical (baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 73.6 (25.3) | 71.3 (25.2) | 72.4 (25.1) | |
| Median (IQR) | 81.3 (56.3–100) | 75 (50.0–100) | 75 (50.0–100) | |
| Min. to max. | 12.5 to 100 | 25 to 100 | 12.5 to 100 | |
| Bodily pain (baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 64 (26) | 64.4 (29) | 64.2 (27.4) | |
| Median (IQR) | 62 (51–84) | 72 (41–100) | 62 (41–84) | |
| Min. to max. | 12 to 100 | 0 to 100 | 0 to 100 | |
| General health (baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 60 (19.4) | 69.2 (21.4) | 64.6 (20.8) | |
| Median (IQR) | 57 (45–77) | 72 (57–82) | 66 (47–82) | |
| Min. to max. | 20 to 100 | 25 to 100 | 20 to 100 | |
| Vitality (baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 54.3 (21.4) | 62.3 (20.3) | 58.3 (21.1) | |
| Median (IQR) | 56.3 (37.5–68.8) | 68.8 (50.0–75.0) | 62.5 (43.8–75.0) | |
| Min. to max. | 0 to 93.8 | 6.3 to 100 | 0 to 100 | |
| Social function (baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 81.4 (26) | 85 (22.6) | 83.2 (24.3) | |
| Median (IQR) | 100 (75–100) | 100 (75–100) | 100 (75–100) | |
| Min. to max. | 12.5 to 100 | 25 to 100 | 12.5 to 100 | |
| Role – emotional (baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 86.4 (24) | 88.6 (19.2) | 87.5 (21.6) | |
| Median (IQR) | 100 (66.7–100) | 100 (83.3–100) | 100 (83.3–100) | |
| Min. to max. | 0 to 100 | 25 to 100 | 0 to 100 | |
| Physical component score (baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 43.7 (11) | 43.8 (10.5) | 43.7 (10.6) | |
| Median (IQR) | 45.2 (36.9–52.8) | 44.2 (34.0–53.7) | 44.7 (35.6–53.0) | |
| Min. to max. | 22.7 to 70.7 | 22.7 to 61.2 | 22.7 to 70.7 | |
| Mental component score (baseline) | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 51.3 (12.5) | 54.1 (9.1) | 52.7 (11) | |
| Median (IQR) | 55.7 (49.5–59.8) | 56.2 (50.9–59.3) | 56.1 (49.5–59.3) | |
| Min. to max. | 16.5 to 67.7 | 24.3 to 68.1 | 16.5 to 68.1 |
| Variable | Scoring | Control (n = 35) | Intervention (n = 35) | Total (n = 70) |
|---|---|---|---|---|
| EQ-5D (baseline)a | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 0.73 (0.24) | 0.73 (0.29) | 0.73 (0.27) | |
| Median (IQR) | 0.73 (0.62–1) | 0.8 (0.62–1) | 0.76 (0.62–1) | |
| Min. to max. | 0.08 to 1 | –0.37 to 1 | –0.37 to 1 | |
| EQ-5D VAS (baseline)b | n (%) | 35 (100%) | 35 (100%) | 70 (100%) |
| Mean (SD) | 72.5 (18.8) | 75.1 (18.6) | 73.8 (18.6) | |
| Median (IQR) | 75 (62–87) | 80 (61–90) | 79 (62–90) | |
| Min. to max. | 18 to 100 | 26 to 100 | 18 to 100 | |
| de Jong Gierveld emotional loneliness (baseline)c | n (%) | 35 (100) | 34 (97.1) | 69 (98.6) |
| Mean (SD) | 2.3 (2) | 1.9 (1.8) | 2.1 (1.9) | |
| Median (IQR) | 2 (0–4) | 1 (0–3) | 2 (0–3) | |
| Min. to max. | 0 to 6 | 0 to 6 | 0 to 6 | |
| de Jong Gierveld social loneliness (baseline)d | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 1.7 (1.8) | 1.4 (1.7) | 1.5 (1.8) | |
| Median (IQR) | 1 (0–3) | 1 (0–3) | 1 (0–3) | |
| Min. to max. | 0 to 5 | 0 to 5 | 0 to 5 | |
| de Jong Gierveld overall loneliness (baseline)e | n (%) | 35 (100) | 34 (97.1) | 69 (98.6) |
| Mean (SD) | 4 (3.5) | 3.3 (3.1) | 3.7 (3.3) | |
| Median (IQR) | 3 (1–6) | 2 (1–6) | 3 (1–6) | |
| Min. to max. | 0 to 11 | 0 to 11 | 0 to 11 | |
| PHQ-9 (baseline)f | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 3.3 (4.8) | 2.9 (3.6) | 3.1 (4.2) | |
| Median (IQR) | 2 (0–5) | 2 (0–4) | 2 (0–4) | |
| Min. to max. | 0 to 22 | 0 to 16 | 0 to 22 | |
| ONS well-being (baseline)g | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 7.5 (2.5) | 7.8 (2.4) | 7.7 (2.5) | |
| Median (IQR) | 8 (7–9) | 8 (7–9) | 8 (7–9) | |
| Min. to max. | 0 to 10 | 0 to 10 | 0 to 10 | |
| GSE (baseline)h | n (%) | 35 (100) | 35 (100) | 70 (100) |
| Mean (SD) | 31.3 (5.5) | 33.7 (4.5) | 32.5 (5.2) | |
| Median (IQR) | 31 (28–35) | 35 (29–38) | 33 (29–37) | |
| Min. to max. | 10 to 39 | 24 to 40 | 10 to 40 |
By 6 months post randomisation, 56 participants had valid primary outcome data (SF-36 mental health dimension). There were 30 responders and five non-responders at 6 months in the control group and 26 responders and nine non-responders in the intervention group. Tables 13 and 14 show the baseline demographic and quality of life characteristics of these four groups of participants respectively.
| Variable | Scoring | Control 6-month responder (n = 30) | Control 6-month non-responder (n = 5) | Intervention 6-month responder (n = 26) | Intervention 6-month non-responder (n = 9) |
|---|---|---|---|---|---|
| Sex, n (%) | Female | 16 (53) | 2 (40) | 18 (69) | 5 (56) |
| Male | 14 (47) | 3 (60) | 8 (31) | 4 (44) | |
| Total | 30 (100) | 5 (100) | 26 (100) | 9 (100) | |
| Ethnicity, n (%) | English/Welsh/Scottish/Northern Irish/British | 28 (93) | 5 (100) | 25 (96) | 9 (100) |
| Any other white background | 2 (7) | 0 (0) | 1 (4) | 0 (0) | |
| Total | 30 (100) | 5 (100) | 26 (100) | 9 (100) | |
| Live with others?, n (%) | No | 22 (73) | 5 (100) | 21 (81) | 4 (44) |
| Yes | 8 (27) | 0 (0) | 5 (19) | 5 (56) | |
| Total | 30 (100) | 5 (100) | 26 (100) | 9 (100) | |
| Main activity, n (%) | Retired | 30 (100) | 5 (100) | 25 (96) | 9 (100) |
| Looking after home/family | 0 (0) | 0 (0) | 1 (4) | 0 (0) | |
| Total | 30 (100) | 5 (100) | 26 (100) | 9 (100) | |
| Occupation type, n (%) | Professional | 8 (27) | 0 (0) | 10 (40) | 3 (33) |
| Managerial/technical | 8 (27) | 2 (40) | 7 (28) | 3 (33) | |
| Skilled (non-manual) | 6 (20) | 0 (0) | 1 (4) | 0 (0) | |
| Skilled (manual) | 3 (10) | 0 (0) | 3 (12) | 0 (0) | |
| Partly skilled | 2 (7) | 2 (40) | 2 (8) | 1 (11) | |
| Unskilled | 3 (10) | 1 (20) | 2 (8) | 2 (22) | |
| Total | 30 (100) | 5 (100) | 25 (100) | 9 (100) |
| Baseline variable | Control 6-month responder (n = 30) | Control 6-month non-responder (n = 5) | Intervention 6-month responder (n = 26) | Intervention 6-month non-responder (n = 9) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | |
| Age (years) | 30 | 80.2 | 3.8 | 5 | 79.2 | 3.7 | 26 | 83.2 | 6 | 9 | 77.7 | 2.4 |
| SF-36a | ||||||||||||
| Physical function | 30 | 65.8 | 27.7 | 5 | 74 | 26.1 | 26 | 64.3 | 27.2 | 9 | 69.4 | 29.5 |
| Role – physical | 30 | 72.9 | 26.2 | 5 | 77.5 | 21 | 26 | 68.3 | 25.8 | 9 | 79.9 | 22.7 |
| Bodily pain | 30 | 63.7 | 27.8 | 5 | 66.2 | 12.2 | 26 | 64.5 | 30 | 9 | 64.1 | 27.7 |
| General health | 30 | 60.6 | 18 | 5 | 56.2 | 28.8 | 26 | 70.1 | 20.2 | 9 | 66.6 | 25.8 |
| Vitality | 30 | 53.5 | 21.4 | 5 | 58.8 | 23.6 | 26 | 63 | 21.6 | 9 | 60.4 | 17.1 |
| Social function | 30 | 82.1 | 25.1 | 5 | 77.5 | 33.5 | 26 | 82.2 | 24.8 | 9 | 93.1 | 12.7 |
| Role – emotional | 30 | 87.5 | 24.2 | 5 | 80 | 24 | 26 | 87.5 | 21 | 9 | 91.7 | 13.2 |
| Mental health | 30 | 76.7 | 19.7 | 5 | 63 | 31.1 | 26 | 77.3 | 19.5 | 9 | 79.4 | 10.4 |
| Physical component score | 30 | 43 | 11.5 | 5 | 47.4 | 6.1 | 26 | 43.4 | 10.3 | 9 | 44.8 | 11.6 |
| Mental component score | 30 | 52.2 | 11.5 | 5 | 45.9 | 18.3 | 26 | 53.8 | 10.1 | 9 | 55.2 | 5.6 |
| EQ-5Db | 30 | 0.75 | 0.22 | 5 | 0.62 | 0.34 | 26 | 0.73 | 0.31 | 9 | 0.72 | 0.25 |
| EQ-5D VASc | 30 | 73.1 | 17.1 | 5 | 68.8 | 29.2 | 26 | 75.1 | 17.7 | 9 | 75 | 22.4 |
| de Jong Gierveld emotional lonelinessd | 30 | 2.2 | 2 | 5 | 3 | 2.4 | 25 | 2.1 | 1.8 | 9 | 1.2 | 1.6 |
| de Jong Gierveld social lonelinesse | 30 | 1.6 | 1.8 | 5 | 2 | 2 | 26 | 1.3 | 1.6 | 9 | 1.7 | 2.1 |
| de Jong Gierveld overall lonelinessf | 30 | 3.8 | 3.4 | 5 | 5 | 3.9 | 25 | 3.4 | 3.1 | 9 | 2.9 | 3.3 |
| PHQ-9g | 30 | 2.6 | 3.4 | 5 | 7.4 | 9 | 26 | 3.2 | 4 | 9 | 2.1 | 2.1 |
| ONS well-beingh | 30 | 7.7 | 2.4 | 5 | 6.6 | 3.6 | 26 | 7.5 | 2.7 | 9 | 8.4 | 1.1 |
| GSE (baseline)i | 30 | 31.1 | 5.7 | 5 | 32.6 | 4 | 26 | 33 | 4.8 | 9 | 35.5 | 3.1 |
At 6 months post randomisation, the SF-36 mental health mean (SD) scores were 77.5 (18.4) in the intervention group and 70.7 (21.2) in the control group, a mean difference of 6.5 (95% CI –3.0 to 16.0); after adjusting for age, sex and baseline score the mean difference was 9.5 (95% CI 4.5 to 14.5) (Table 15). The estimated ICC from the marginal model for the primary outcome was –0.06, indicating little if any clustering by facilitator; the correlation between baseline and 6-month mental health scores was 0.78.
| Outcome | Intervention | Control | Unadjusteda | Adjustedb | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Mean difference | 95% CI | Mean difference | 95% CI | |
| SF-36c | ||||||||||
| Mental health | 26 | 77.5 | 18.4 | 30 | 70.7 | 21.2 | 6.5 | –3.0 to 16.0 | 9.5 | 4.5 to 14.5 |
| Physical function | 26 | 60.3 | 29.9 | 30 | 56 | 29.9 | 3.4 | –10.8 to 17.5 | 5 | –0.9 to 10.9 |
| Role – physical | 26 | 72.6 | 24.7 | 30 | 55.4 | 27.6 | 15.6 | 3.8 to 27.4 | 20.2 | 9.9 to 30.6 |
| Bodily pain | 26 | 71 | 26 | 30 | 53.9 | 29.8 | 17.1 | 2.5 to 31.7 | 16.6 | 8 to 25.3 |
| General health | 26 | 66.2 | 24.2 | 30 | 56.1 | 22.9 | 10.3 | –1.2 to 21.9 | 2.5 | –6.4 to 11.4 |
| Vitality | 26 | 59.4 | 19.8 | 30 | 49.6 | 25.5 | 9.8 | –2.0 to 21.7 | 3.1 | –2.8 to 9 |
| Social function | 26 | 84.1 | 22.8 | 30 | 70 | 31.1 | 13.4 | 1.4 to 25.4 | 18.1 | 7.9 to 28.3 |
| Role – emotional | 26 | 89.1 | 19.4 | 30 | 81.7 | 23.9 | 7.4 | –3.1 to 17.9 | 8.6 | –0.8 to 18 |
| Physical component score | 26 | 43.5 | 10.9 | 30 | 38.3 | 11.5 | 5.1 | –0.4 to 10.7 | 4.5 | 1.4 to 7.5 |
| Mental component score | 26 | 53.9 | 9.8 | 30 | 49.7 | 11.5 | 4.1 | –0.5 to 8.7 | 4.7 | 2 to 7.5 |
| EQ-5Dd | 26 | 0.73 | 0.35 | 29 | 0.71 | 0.27 | –0.04 | –0.17 to 0.10 | 0.02 | –0.05 to 0.09 |
| EQ-5D VASe | 26 | 75.5 | 19.5 | 30 | 70.5 | 21.8 | 4.7 | –4.6 to 14.0 | 5.1 | –4.9 to 15.2 |
| de Jong Gierveld emotional lonelinessf | 26 | 2.2 | 2 | 30 | 2.2 | 1.9 | 0.2 | –0.5 to 0.9 | 0 | –0.6 to 0.6 |
| de Jong Gierveld social lonelinessg | 25 | 1.3 | 1.9 | 30 | 1.2 | 1.5 | –0.1 | –0.7 to 0.5 | 0.3 | –0.2 to 0.8 |
| de Jong Gierveld overall lonelinessh | 26 | 3.5 | 3.4 | 30 | 3.3 | 2.9 | 0.0 | –1.0 to 1.0 | 0.6 | –0.4 to 1.6 |
| PHQ-9i | 26 | 3.1 | 4 | 30 | 3.6 | 4.6 | –0.4 | –2.2 to 1.3 | –1.3 | –2.6 to 0.0 |
| ONS well-beingj | 26 | 8 | 1.5 | 30 | 7.6 | 1.8 | 0.5 | –0.2 to 1.2 | 0.8 | 0.2 to 1.4 |
| GSEk | 26 | 32.9 | 4.7 | 30 | 32.1 | 3.8 | 0.8 | –1.5 to 3.2 | 1.2 | –0.7 to 3.1 |
The developers of the SF-36 have suggested that differences between treatment groups of between 5 and 10 points on the 100-point scale can be regarded as ‘clinically and socially relevant’. 40 For the original sample size calculation we assumed that a mean difference in SF-36 mental health dimension scores of ≥ 8 points at 6 months post randomisation between the intervention group and the control group is the smallest difference that can be regarded as clinically and practically important. The point estimates for the primary outcome and their associated CIs suggest that the likely effect of the telephone befriending intervention is within a clinically relevant range. However, Figure 3 shows how the SF-36 mental health scores change over time in the two randomised groups; over the 6 month follow-up period there is no change in scores in the intervention group but there is a decline or deterioration in scores in the control group.
FIGURE 3.
Mean SF-36 mental health dimension scores over time by randomised group.
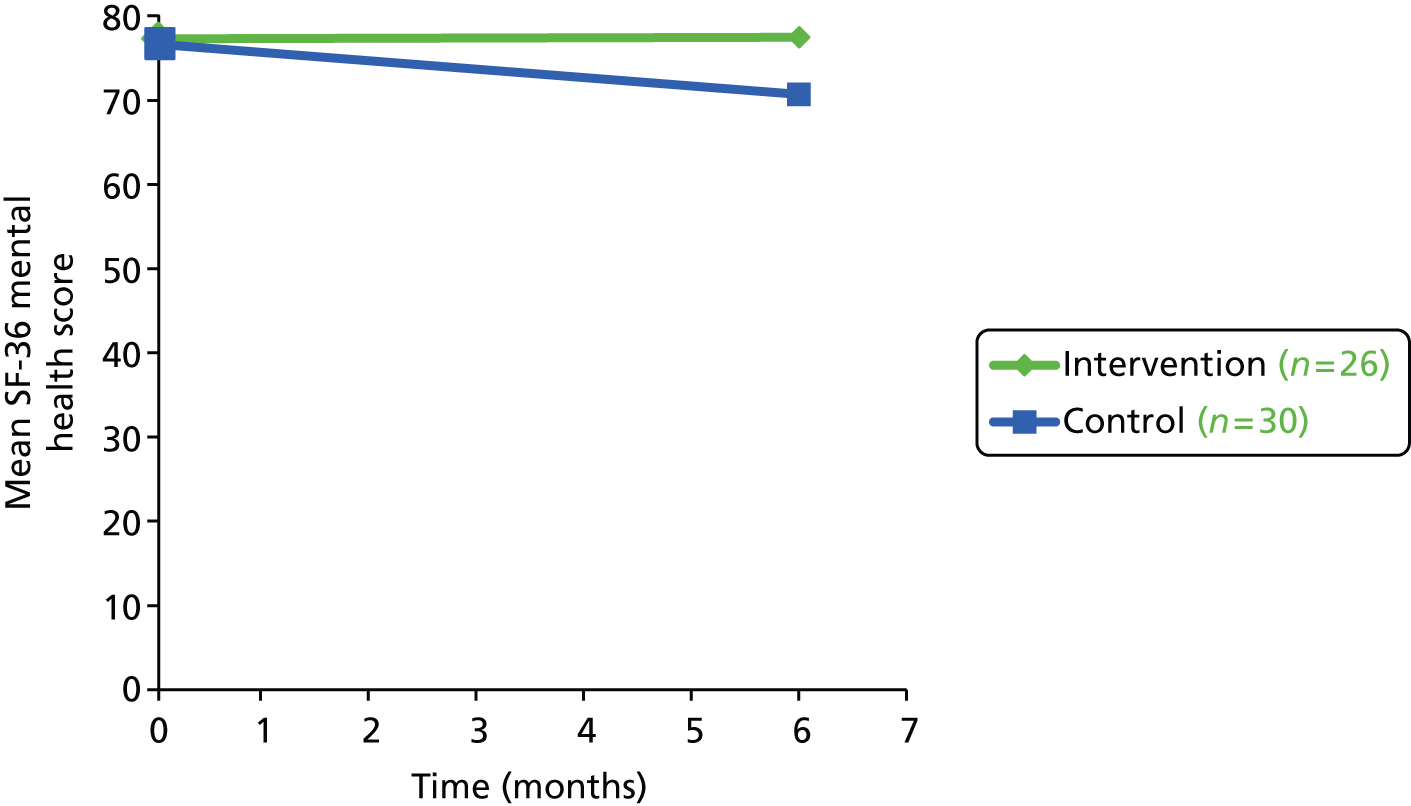
Table 15 also shows that for the secondary participant-reported outcomes, such as the other dimensions of the SF-36, the differences in quality of life favoured the intervention group. For five dimensions of the SF-36 (role – physical, bodily pain, social functioning, physical component score and mental component score), after adjustment for baseline score, age and sex, the CI excluded zero, suggesting a non-zero effect (Figure 4).
FIGURE 4.
Forest plot of mean differences in 6-month post-randomisation SF-36 outcomes between groups, adjusted for age, sex and baseline score (n = 56).
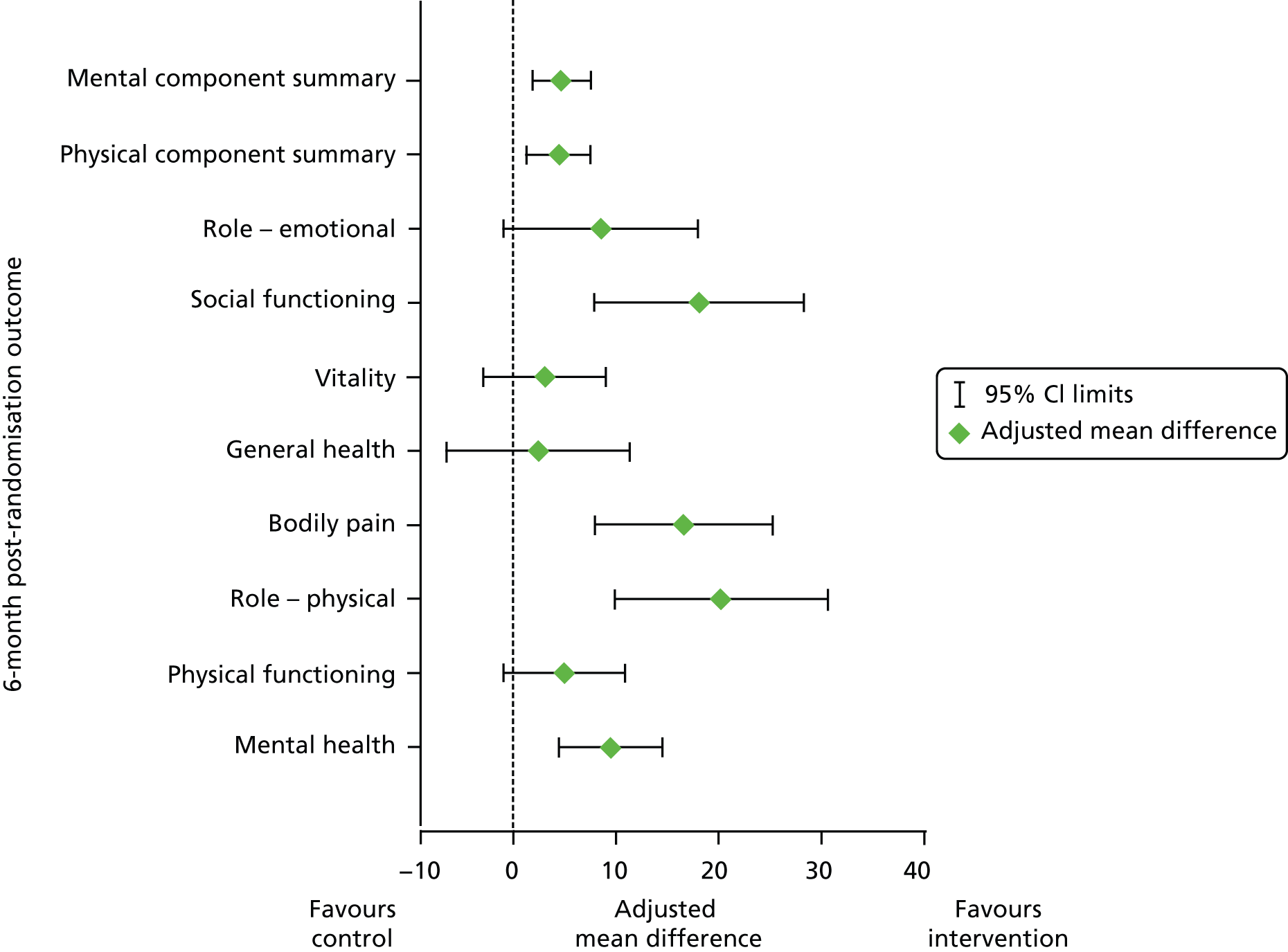
There were no differences in mean scores between the intervention group and the control group for the other participant-reported outcomes, except for the ONS well-being total score.
The attrition rate at 6 months was 20%, with only 80% (56/70) of participants having valid primary outcome data; however, the results for the primary outcome were robust to missing data. Table 16 shows the results of a sensitivity analysis of the primary outcome, the mean 6-month post-randomisation SF-36 mental health dimension score, using a variety of methods to impute missing primary outcome data. All imputation methods produced similar results (Figures 5 and 6). Figure 5 shows the sensitivity analysis with adjustment for covariates (baseline score, age and sex) and Figure 6 shows the results without adjustment for any covariates. The estimated treatment effects from the various sensitivity analyses performed produced broadly similar results, suggesting that the results are fairly robust.
| Outcome | Intervention | Control | Unadjusted | Adjustedb | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SDc | n | Mean | SDc | Mean difference | 95% CI | Mean difference | 95% CI | |
| Observed data (n = 56) | 26 | 77.5 | 18.4 | 30 | 70.7 | 21.2 | 6.5 | –3.0 to 16.0 | 9.5 | 4.5 to 14.5 |
| LOCF imputed data (n = 70) | 35 | 78 | 16.6 | 35 | 69.6 | 22.5 | 8.3 | –0.5 to 17.2 | 7.7 | 3.7 to 11.8 |
| Regression imputed data (n = 70)d | 35 | 77.8 | 16.2 | 35 | 69.8 | 21.4 | 7.8 | –0.6 to 16.2 | 7.6 | 3.6 to 11.6 |
| Multiple imputation PMM (n = 70)e | 35 | 78.9 | 3.7 | 35 | 70.6 | 3.7 | 8.3 | –0.6 to 17.2 | 8.0 | 2.8 to 13.3 |
| Multiple imputation regression (n = 70)e | 35 | 77.3 | 3.2 | 35 | 69.7 | 3.9 | 7.6 | –1.8 to 16.9 | 7.4 | 1.8 to 13.0 |
| Per-protocol data (n = 39) | 9 | 73.9 | 17.5 | 30 | 70.7 | 21.2 | 3.2 | –5.2 to 11.6 | 8.0 | 3.3 to 12.7 |
FIGURE 5.
Forest plot of sensitivity analysis of mean difference in 6-month post-randomisation SF-36 mental health dimension scores between groups, adjusted for age, sex and baseline score. PMM, predictive mean matching.
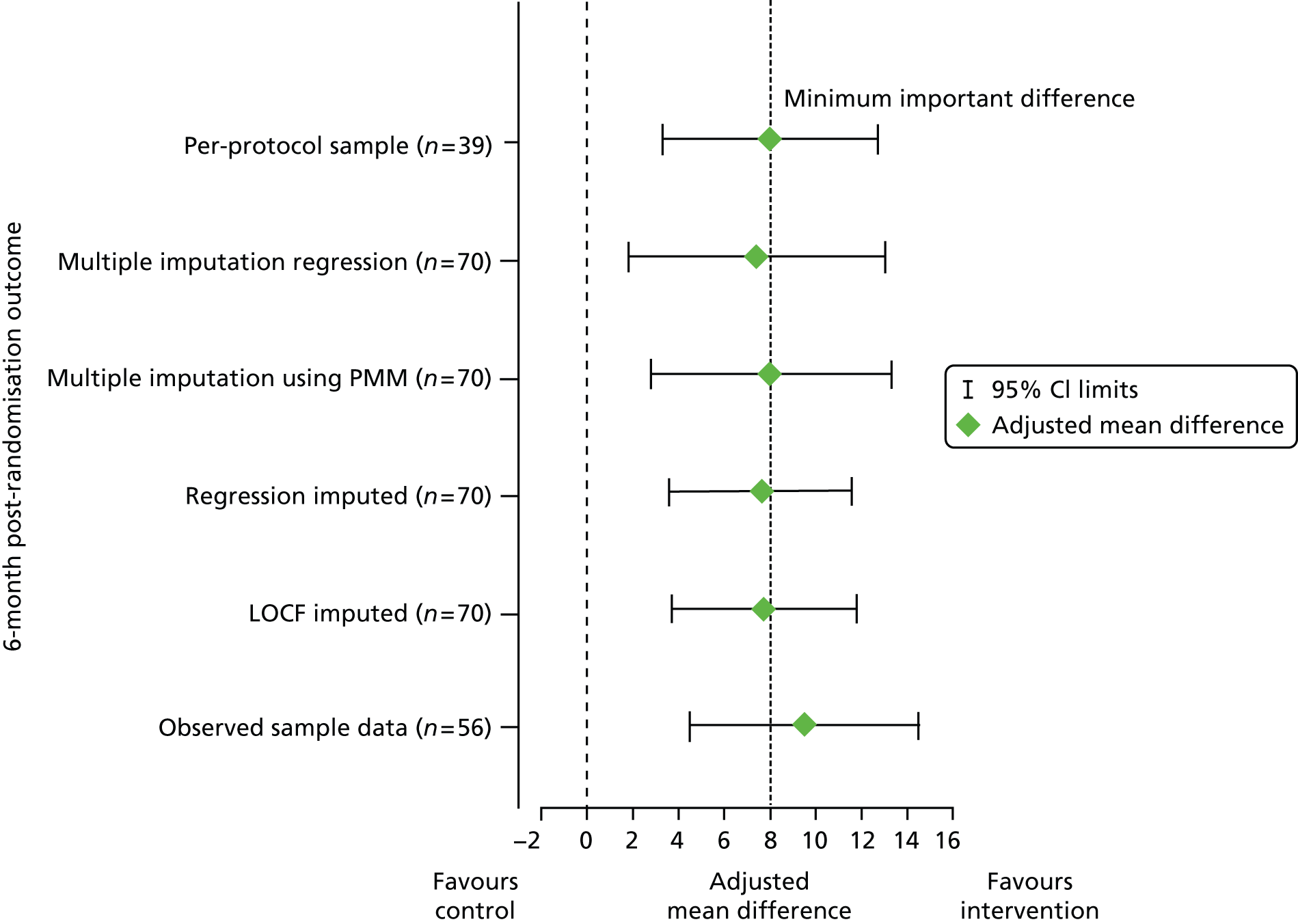
FIGURE 6.
Forest plot of sensitivity analysis of mean difference in 6-month post-randomisation SF-36 mental health dimension scores between groups. PMM, predictive mean matching.
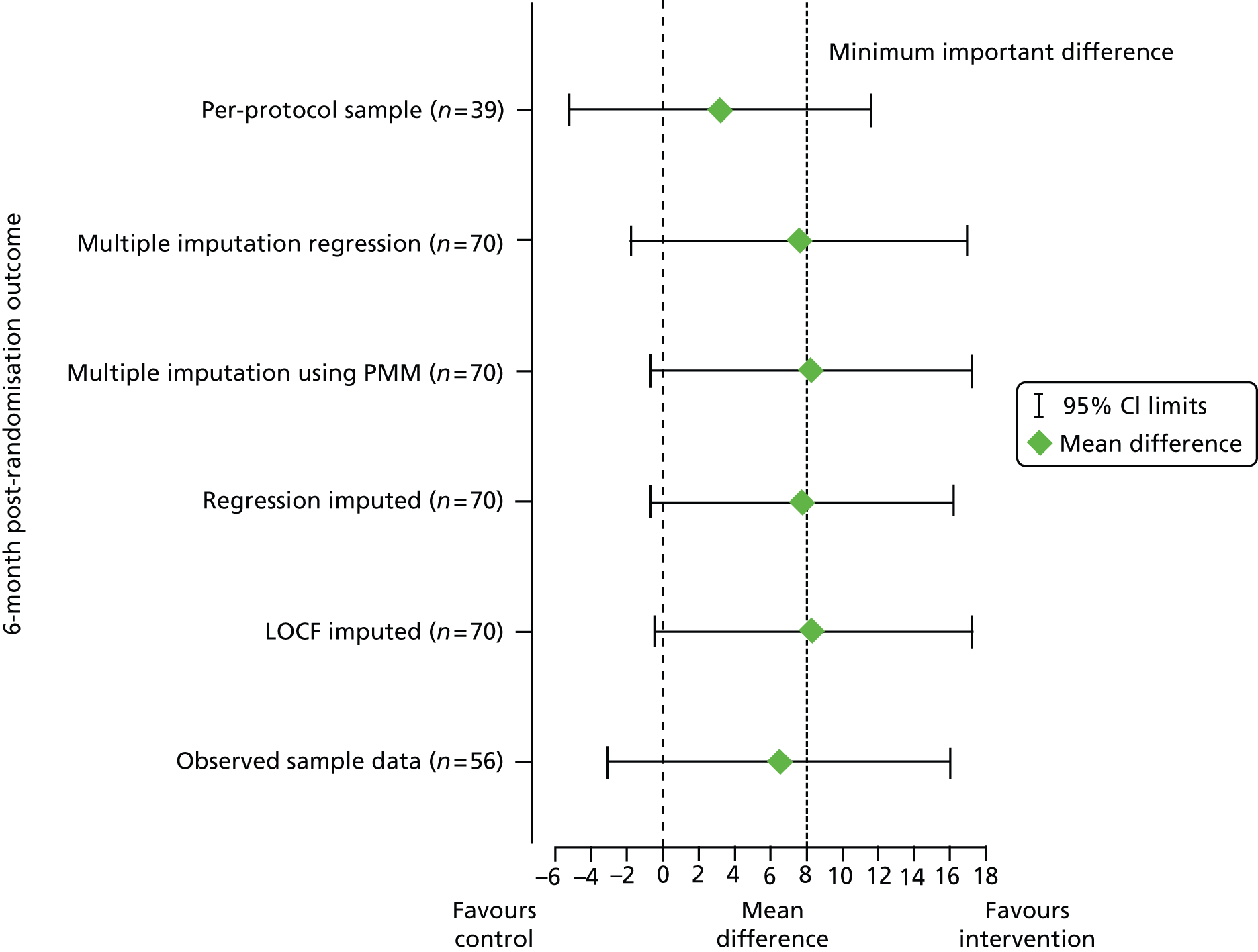
A per-protocol data set was defined as all participants in the control group and participants in the intervention group who completed ≥ 75% of the group telephone calls over the 12 weeks of the group intervention (the one-to-one telephone calls with a volunteer were not included in the definition of ‘per protocol’). This means that if a TF group completed 12 group telephone calls, individuals were part of the per-protocol data set if they were present for the duration of nine or more of the calls. Only 35% (9/26) of the participants in the intervention group who had valid 6-month outcome data had completed ≥ 75% of the group telephone calls over the 12 weeks of the group intervention. Table 16 and Figure 7 show the results for the per-protocol sample for the primary outcome only. At 6 months post randomisation, the mean (SD) SF-36 mental health dimension scores were 73.9 (17.5) for the nine participants in the intervention group and 70.7 (21.2) for the control group, a mean difference of 3.2 (95% CI –5.2 to 11.6); after adjusting for age, sex and baseline score, the mean difference was 8.0 (95% CI 3.3 to 12.7). The full results for the per-protocol population are reported in Appendix 9.
FIGURE 7.
Mean SF-36 mental health dimension scores over time for the ITT and per-protocol samples.
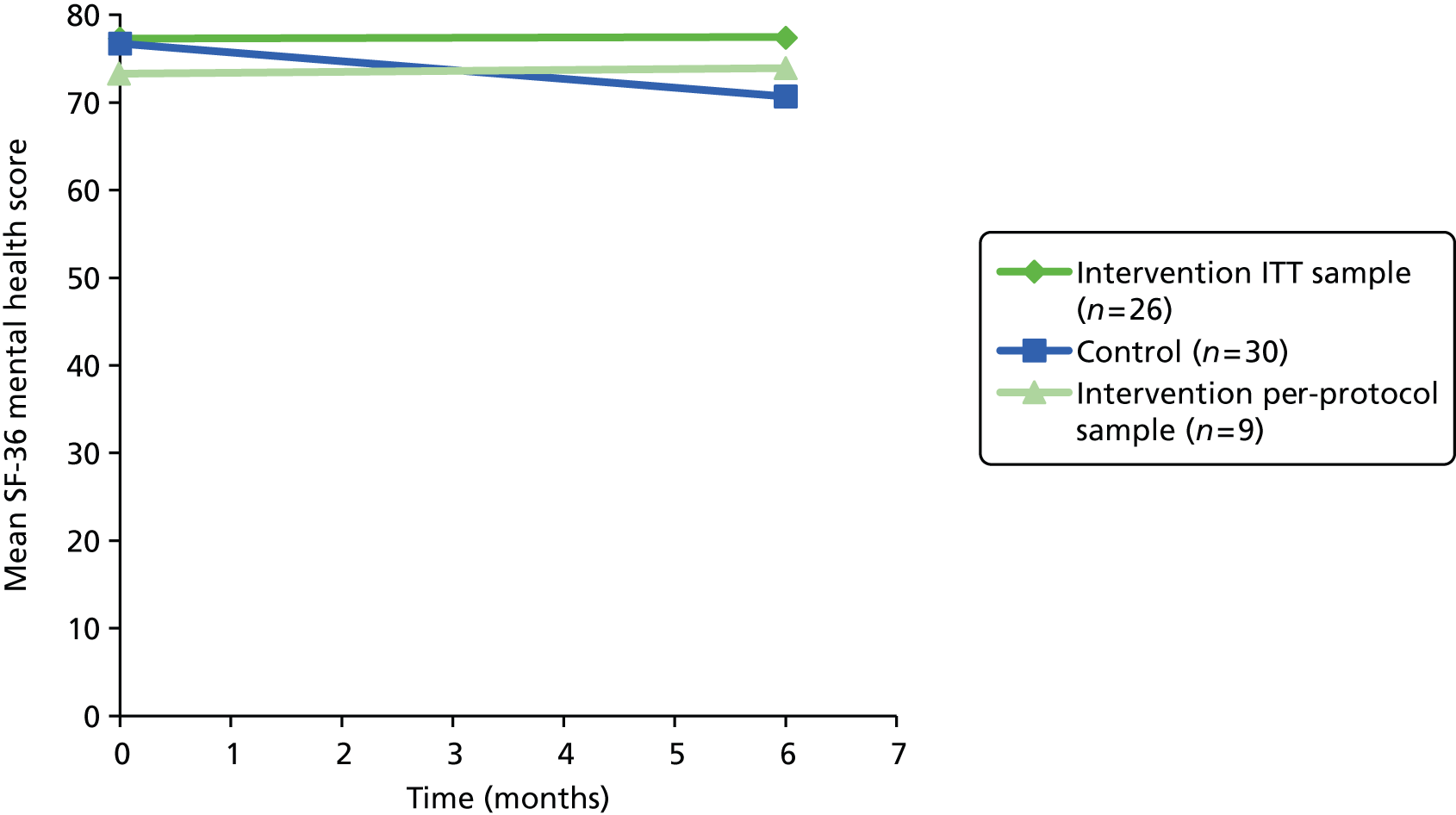
Health and social care resource use
The health and social care resources recorded are presented for hospital use (Tables 17–19), medication (Tables 20–22), day services (Tables 23–25) and community services (Tables 26–28).
Hospital use
| Resource | Intervention (n = 78), mean (SD), min. to max., n (%) | Control (n = 79), mean (SD), min. to max., n (%) |
|---|---|---|
| Outpatient appointment | 1.37 (2.06), 0 to 10, 39 (50) | 1.44 (2.92), 0 to 16, 40 (51) |
| A&E attendance | 0.14 (0.35), 0 to 1, 11 (14) | 0.05 (0.22), 0 to 1, 4 (5) |
| Hospital attendance – other | 0.04 (0.19), 0 to 1, 3 (4) | 0.04 (0.25), 0 to 2, 2 (3) |
| Medical inpatient nights | 0.10 (0.69), 0 to 6, 3 (4) | 0.08 (0.42), 0 to 3, 3 (4) |
| Assessment/rehabilitation inpatient nights | 0.01 (0.11), 0 to 1, 1 (1) | 0 |
| Other inpatient nights | 0.01 (0.11), 0 to 1, 1 (1) | 0.03 (0.23), 0 to 2, 1 (1) |
| Resource | Intervention (n = 35), mean (SD), min. to max., n (%) | Control (n = 35), mean (SD), min. to max., n (%) |
|---|---|---|
| Outpatient appointment | 1.49 (2.33), 0 to 10, 19 (54) | 1.71 (3.38), 0 to 16, 17 (49) |
| A&E attendance | 0.17 (0.38), 0 to 1, 6 (17) | 0.06 (0.24), 0 to 1, 2 (6) |
| Hospital attendance – other | 0.03 (0.17), 0 to 1, 1 (3) | 0 |
| Medical inpatient nights | 0.17 (1.01), 0 to 6, 1 (3) | 0.14 (0.60), 0 to 3, 2 (6) |
| Assessment/rehabilitation inpatient nights | 0.03 (0.17), 0 to 1, 1 (3) | 0 |
| Other inpatient nights | 0 | 0 |
| Resource | Intervention (n = 27), mean (SD), min. to max., n (%) | Control (n = 34), mean (SD), min. to max., n (%) |
|---|---|---|
| Outpatient appointment | 1.12 (1.53), 0 to 6, 15 (57) | 1.57 (2.03), 0 to 7, 16 (53) |
| A&E attendance | 0.12 (0.59), 0 to 3, 1 (4) | 0.17 (0.38), 0 to 1, 5 (17) |
| Hospital attendance – other | 0.04 (0.20), 0 to 1, 1 (4) | 0 |
| Medical inpatient nights | 0 | 0.30 (1.29), 0 to 7, 3 (10) |
| Assessment/rehabilitation inpatient nights | 0.04 (0.20), 0 to 1, 1 (4) | 0.03 (0.18), 0 to 1, 1 (3) |
| Other inpatient nights | 0 | 0 |
Medication
| Resource | Intervention (n = 78), meana (SD), min. to max., n (%) | Control (n = 79), meana (SD), min. to max., n (%) |
|---|---|---|
| Sleeping medication | 0.12 (0.36), 0 to 2, 8 (10) | 0.06 (0.29), 0 to 2, 4 (5) |
| Depression/anxiety/mood medication | 0.13 (0.34), 0 to 1, 10 (13) | 0.08 (0.27), 0 to 1, 6 (8) |
| Total | 0.12 (0.35), 0 to 2, 17 (22) | 0.07 (0.28), 0 to 3, 9 (11) |
| Resource | Intervention (n = 35), meana (SD), min. to max., n (%) | Control (n = 35), meana (SD), min. to max., n (%) |
|---|---|---|
| Sleeping medication | 0.20 (0.47), 0 to 2, 6 (17) | 0.09 (0.37), 0 to 1, 5 (14) |
| Depression/anxiety/mood medication | 0.14 (0.36), 0 to 2, 2 (6) | 0.09 (0.28), 0 to 1, 3 (9) |
| Total | 0.17 (0.42), 0 to 2, 10 (29) | 0.09 (0.33), 0 to 3, 4 (11) |
| Resource | Intervention (n = 27), meanb (SD), min. to max., n (%) | Control (n = 34), meanb (SD), min. to max., n (%) |
|---|---|---|
| Sleeping medication | 0.15 (0.37), 0 to 1, 4 (15) | 0 |
| Depression/anxiety/mood medication | 0.15 (0.37), 0 to 1, 4 (15) | 0.07 (0.25), 0 to 1, 2 (7) |
| Total | 0.15 (0.36), 0 to 1, 8 (31) | 0.03 (0.18), 0 to 1, 2 (7) |
Day service use
| Resource | Intervention (n = 78), mean (SD), min. to max., n (%) | Control (n = 79), mean (SD), min. to max., n (%) |
|---|---|---|
| Lunch club | 1.26 (3.50), 0 to 15, 12 (15) | 0.62 (3.20), 0 to 24, 4 (5) |
| Social club | 0.81 (3.54), 0 to 3, 1 (1) | 0.89 (3.40), 0 to 3, 1 (1) |
| Other | 0.73 (3.44), 0 to 25, 6 (8) | 2.95 (10.70), 0 to 72, 9 (11) |
| Total | 0.93 (3.49), 0 to 28, 18 (23) | 1.49 (6.79), 0 to 78, 16 (20) |
| Resource | Intervention (n = 35), mean (SD), min. to max., n (%) | Control (n = 35), mean (SD), min. to max., n (%) |
|---|---|---|
| Lunch club | 0.66 (2.71), 0 to 12, 2 (6) | 0 |
| Social club | 0 | 0.17 (1.01), 0 to 6, 1 (3) |
| Other | 0 | 0 |
| Total | 0.22 (1.58), 0 to 12, 2 (6) | 0.06 (0.59), 0 to 6, 1 (3) |
| Resource | Intervention (n = 27), mean (SD), min. to max., n (%) | Control (n = 34), mean (SD), min. to max., n (%) |
|---|---|---|
| Lunch club | 1.08 (3.27), 0 to 12, 4 (15) | 1.10 (3.90), 0 to 18, 3 (10) |
| Social club | 2.35 (6.83), 0 to 30, 4 (15) | 0.90 (2.76), 0 to 12, 4 (13) |
| Other | 4.65 (11.20), 0 to 42, 5 (19) | 0.50 (1.94), 0 to 9, 2 (7) |
| Total | 2.69 (7.84), 0 to 42, 10 (37) | 0.83 (2.95), 0 to 18, 9 (30) |
Community service use
| Resource | Intervention (n = 78), mean (SD), min. to max., n (%) | Control (n = 79), mean (SD), min. to max., n (%) |
|---|---|---|
| GP | 1.51 (1.42), 0 to 8, 59 (76) | 1.28 (1.61), 0 to 6, 44 (56) |
| Practice nurse | 1.08 (1.84), 0 to 13, 39 (50) | 1.28 (2.23), 0 to 12, 38 (48) |
| District nurse | 0.24 (1.43), 0 to 12, 4 (5) | 0.70 (3.42), 0 to 25, 6 (8) |
| Chiropodist | 0.32 (0.67), 0 to 2, 16 (21) | 0.28 (0.68), 0 to 3, 14 (18) |
| Counsellor | 0 | 0.05 (0.45), 0 to 4, 1 (1) |
| Dietitian | 0.01 (0.11), 0 to 1, 1 (1) | 0 |
| Health visitor | 0.04 (0.34), 0 to 3, 1 (1) | 0 |
| Home care worker | 0.63 (5.55), 0 to 49, 1 (1) | 3.39 (22.65), 0 to 84, 2 (3) |
| Home care assistant | 11.14 (53.20), 0 to 357, 4 (5) | 5.01 (44.55), 0 to 396, 1 (1) |
| Home care attendant | 1.18 (10.42), 0 to 92, 1 (1) | 0 |
| Care manager | 0.01 (0.11), 0 to 1, 1 (1) | 0.01 (0.11), 0 to 1, 1 (1) |
| Occupational therapist | 0.03 (0.23), 0 to 2, 1 (1) | 0.08 (0.68), 0 to 6, 1 (1) |
| Physiotherapist | 0.59 (1.98), 0 to 12, 9 (12) | 0.41 (2.29), 0 to 19, 5 (6) |
| Social worker | 0.01 (0.11), 0 to 1, 1 (1) | 0 |
| Other | 0.27 (1.41), 0 to 12, 7 (9) | 0.22 (1.39), 0 to 12, 4 (5) |
| Total | 1.14 (14.28), 0 to 360, 70 (90) | 0.85 (12.98), 0 to 396, 65 (82) |
| Resource | Intervention (n = 35), mean (SD), min. to max., n (%) | Control (n = 35), mean (SD), min. to max., n (%) |
|---|---|---|
| GP | 1.57 (1.29), 0 to 4, 27 (77) | 1.31 (1.68), 0 to 6, 18 (51) |
| Practice nurse | 0.97 (2.32), 0 to 13, 12 (34) | 1.11 (2.03), 0 to 10, 16 (46) |
| District nurse | 0.09 (0.51), 0 to 3, 1 (3) | 0.03 (0.17), 0 to 1, 1 (3) |
| Chiropodist | 0.29 (0.62), 0 to 2, 7 (20) | 0.20 (0.53), 0 to 2, 5 (14) |
| Counsellor | 0 | 0.11 (0.68), 0 to 4, 1 (3) |
| Dietitian | 0.03 (0.17), 0 to 1, 1 (3) | 0 |
| Health visitor | 0.09 (0.51), 0 to 3, 1 (3) | 0 |
| Home care worker | 1.40 (8.28), 0 to 49, 1 (3) | 0 |
| Home care assistant | 20.03 (73.84), 0 to 357, 3 (9) | 0 |
| Home care attendant | 2.63 (15.55), 0 to 92, 1 (3) | 0 |
| Care manager | 0.03 (0.17), 0 to 1, 1 (3) | 0 |
| Occupational therapist | 0.06 (0.34), 0 to 2, 1 (3) | 0 |
| Physiotherapist | 0.89 (2.62), 0 to 12, 5 (14) | 0.11 (0.47), 0 to 2, 2 (6) |
| Social worker | 0.03 (0.17), 0 to 1, 1 (3) | 0 |
| Other | 0.14 (0.49), 0 to 2, 3 (9) | 0.09 (0.51), 0 to 3, 1 (3) |
| Total | 1.88 (19.98), 0 to 360, 30 (86) | 0.20 (0.83), 0 to 17, 27 (77) |
| Resource | Intervention (n = 27), mean (SD), min. to max., n (%) | Control (n = 34), mean (SD), min. to max., n (%) |
|---|---|---|
| GP | 1.08 (1.57), 0 to 6, 13 (50) | 1.43 (1.87), 0 to 7, 19 (63) |
| Practice nurse | 0.42 (0.76), 0 to 3, 8 (31) | 1.17 (2.05), 0 to 10, 14 (47) |
| District nurse | 0.04 (0.20), 0 to 1, 1 (4) | 0.07 (0.37), 0 to 2, 1 (3) |
| Chiropodist | 0.58 (0.95), 0 to 3, 9 (35) | 0.27 (0.64), 0 to 2, 5 (17) |
| Counsellor | 0 | 0 |
| Dietitian | 0 | 0 |
| Health visitor | 0 | 0 |
| Home care worker | 0.15 (0.78), 0 to 4, 1 (4) | 0 |
| Home care assistant | 14.19 (72.16), 0 to 368, 2 (8) | 0 |
| Home care attendant | 3.54 (18.04), 0 to 92, 1 (4) | 0 |
| Care manager | 0.12 (0.59), 0 to 3, 1 (4) | 0 |
| Occupational therapist | 0 | 0 |
| Physiotherapist | 0 | 0.30 (1.21), 0 to 4, 2 (7) |
| Social worker | 0 | 0 |
| Other | 10.77 (54.91), 0 to 280, 1 (4) | 0.27 (0.24), 0 to 3, 4 (13) |
| Total | 2.06 (23.82), 0 to 369, 21 (81%) | 0.23 (0.92), 0 to 11, 23 (77%) |
Chapter 5 Results of the qualitative research
Results of the participant interviews
The sample
Twenty-four participants out of 78 (pilot study n = 35) randomly allocated to the research intervention arm were allocated to a volunteer over the course of the study. We attempted to interview all 24. One participant was withdrawn from the study (because of protocol non-compliance) before being invited to an interview. Of the remaining 23 participants, two did not consent to an interview (one had withdrawn after the first one-to-one call and one had withdrawn before the calls started), one could not be contacted (no dial tone, e-mail sent) and one declined to take part in an interview (no reason given). Those participants allocated to the intervention but who were not allocated a volunteer facilitator and were not followed up were not invited to take part in an interview.
Nineteen (83% of the target) participants in the intervention arm participated in semistructured interviews between March 2013 and April 2013. The baseline characteristics of the interview population compared well with the baseline characteristics of the trial participants who did not take part in interviews. Those interviewed were slightly older than those not interviewed, were more likely to live alone (79% vs. 63%) and scored slightly higher for mental health function at baseline. Conversely, those interviewed scored slightly lower for physical function at baseline (see Appendix 10).
Prior states
Reasons for taking part
Altruism
Participants reported wanting to help with what they felt was useful research. Some were recognisable as serial ‘joiners’, with one describing herself as ‘always willing to be a guinea pig’ (037, female). Six participants explicitly asserted that they were helping others by participating and did not need help themselves (see also Value).
I joined the group because I wanted to help this research, not because I desperately needed to talk to somebody.
006, female
Curiosity
Some participants said that they were motivated to participate by general interest in the research or in what other participants might have to say or that they were novelty-seeking. One person was specifically interested in how the group calls worked in case his church ever thought of having a telephone group.
External influence
One participant felt that he should participate as the invitation letter came from his general practitioner (GP):
I thought probably he’d [GP] referred me because . . . knowing that I’m on my own and that I do smoke . . . I thought it was probably an anti-smoking group or something like that.
019, male
Expectations of telephone friendship groups
Prior expectations of the TF groups generally overlapped considerably with the altruistic reasons for participating in the project. An exception was when participants recalled having concerns about the practicalities of talking over the telephone with a group of people, including how conversations would be facilitated (see Acceptability):
I thought we might, I must confess, I thought we might find ourselves talking over one another or horrible pauses, not knowing where to come in and so on.
058, male
Perceived needs
Again, most participants expected that they would be helping those in need rather than benefiting themselves by participating (see Altruism). They characterised themselves as self-sufficient, socially active or happy in their own company, but felt that the telephone groups would be helpful for those who are housebound or who have less contact:
I don’t feel the need quite as much as I can understand some people, you know, who have interests but a limited access to various things.
055, female
Only a small minority of participants referred to their own needs and then often still with reference to an imagined, more generalised need:
I mean I’ve been feeling very sorry for myself after my husband died . . . I was still in a fog . . . yeah I can see why people would go into the homes and if they’d lost somebody they could . . . sort of shut themselves off if you like.
081, female
Acceptability
Twelve participants described TF in positive terms such as ‘enjoyable’, ‘pleasant’ or ‘quite good’. Nine participants described the process as being easy. A further three participants described their experience as ‘interesting’. Some of these participants found the group to be an acceptable vehicle for sharing life experiences:
It was interesting, it was good to meet other people [er] and find out about them and how they ticked and how they, you know, had a life before, it was good, I enjoyed it.
006, female
Conversely, some participants felt that the one-to-one volunteer befriending was acceptable but that the group was not for them:
You don’t know what to talk about when you don’t know people and you don’t know what they want to talk about.
015, female
Some participants described a level of initial apprehension, which diminished over time as they began to recognise the voice that was speaking and found that they had enough in common with other group members. A minority of participants found friendships based solely on telephone conversation inferior to those outside the group that also involved face-to-face communication:
Well it’s an unusual sort of, I mean if I want to telephone friends I do, you know, of course talking to people who you don’t know and you haven’t seen, that’s different.
038, female
the thing I found difficult first was that you were talking to people you’d never seen, I think visual things are so important, and therefore when you are talking in a group, you’re listening politely to what they say, and you don’t know really when to come in.
065, male
it was strange . . . you listen to one person and then you listen to another person and then another, I just found it difficult.
015, female
Technical concerns
The majority of those interviewed found the timing, duration and frequency of the TF group meetings acceptable and accessible. Three participants felt that the group calls could have been made at a more convenient time and noted that the time was a compromise for the group. One reported feeling ‘tied down’ by the booking. Participants in two different groups found their groups too small after members dropped out. They reflected on how this restricted the range of topics and discussion and that the length of calls was reduced to 30–45 minutes (see also Group dynamics). A minority of interviewees reported having difficulty hearing some members in their group and one reported having difficulties with the telephone line.
Closure of time-limited groups
How individual participants characterised the experiences of their group ending was influenced by the group that they were in (see Assessment of group intervention delivery by volunteer facilitators). In general, most accepted that the groups were time-limited. Some felt that it was a pity that the calls were ending and wanted the groups to continue and to stay in touch with members of the group (see Value). Nine participants described feeling sad, disappointed or sorry that the group calls ended:
Awful because I’d nothing to look forward to . . . And that was quite, quite . . . yeah I missed talking to them.
008, female
I would like to get to meet these people . . . seeing them is better than a voice . . . so I thought, sort of form a friendship . . . that’s what I thought it would lead to and that’s not been the case.
027, male
Well, I enjoyed doing it but as I say, I was so upset when they came to a full stop.
019, female
Some participants criticised the way in which the facilitators ended the 12-week group call programme (see the following section). Several talked about the end of the programme being like a ‘full stop’ or being ‘cut off’. Some reported having discussions in their group about staying in touch after closure. There was a general feeling that this aspect was not well managed by the facilitators, resulting in some reported disappointment. Six participants reported acceptance that the groups were time-limited or relief that a perceived obligation had been lifted.
Implementation and facilitator performance
Participants who found the befriending groups acceptable generally described their volunteer facilitator in favourable terms, such as ‘good’ or ‘unobtrusive’ or as a ‘co-ordinator’ or a ‘leader’. Participants who were less satisfied focused on facilitators changing the topic of discussion (e.g. when it had strayed onto politics) or intervening when it was not necessary. Some participants in larger groups experienced problems starting conversations, with everyone trying to talk at the same time:
[the volunteer] butted in from time to time, diverted us to get onto things, that did a little bit and then tended to sort of fizzle out and I didn’t want to sort of chip in and, and dominate things so, you know, I waited to have a little sort of, little sort of lead from the other two but it rarely materialised.
037, female
Volunteer facilitators were trained to establish minimum ground rules for participants, including saying your name before speaking, but one participant described this not being implemented:
At first we didn’t recognise each other’s voice until someone said, ‘hello, this is . . .’ . . . and I have a very bad memory and I couldn’t remember the names and I felt quite bad that I couldn’t remember . . . and I wrote them down but I still couldn’t remember who was talking.
005, male
Participants who talked about the one-to-one calls that they received from the volunteer before joining the group, generally felt that they were a good idea, with three participants stating that they preferred them to the group calls. There were some complaints about continuity of care. Volunteer attrition meant that some individuals received a different volunteer in the one-to-one and group calls, but some reported that they were not warned of this or told why (see also Chapter 3, Monitoring volunteers).
Maintaining contact with other participants after closure of the time-limited groups was of concern to many participants, but they often felt that closure of the groups was not dealt with well. Volunteer facilitators had been advised by the host charity to inform the charity if participants wanted to share contact details. One volunteer facilitator failed to refer such a request back. Another arranged a face-to-face meeting but some participants were not given or were not able to follow the instructions, resulting in failure of the meeting and some dissatisfaction.
Group dynamics
The dynamics of each group were in part influenced by the volunteer facilitator; coded content was often also coded under the heading ‘acceptability’. Three key subthemes were identified within group dynamics: cohesiveness, disclosure and peers.
Cohesiveness
Both within and across the groups participants varied in the extent to which they felt part of the group. The degree to which the groups ‘bonded’ is likely to be linked to ‘facilitator performance’ (see Group dynamics and Results of the fidelity assessment) and the ‘needs’ and expectations of the members of the groups. The size of the groups varied from three to six participants across the 12 weeks because of participants withdrawing from or missing group calls. One group that experienced no withdrawals seemed relatively cohesive to participants, four of whom had a health-care career in common:
We gelled, we waited for each other, we were patient with each other, we wanted to know, we were interested.
006, female
Not everyone within the larger groups identified as much with the other members of the group, with some individuals feeling excluded from topics of conversation at times, despite the efforts of facilitators to involve them. A number of participants in the two smaller groups noted that having more members might have enriched the groups’ conversations, although another participant suggested that those who were left in the group were more interested in taking part:
And how many did that go down to?
Oh, it went down to about three or four at the end of it.
Did that make any difference to the discussions?
Not really because [er] the people who were interested and involved kept on with the course.
019, male
Across the groups none of the participants identified a clear goal of or purpose to the group. A number of the interviewees discussed the need to have a mix of people in the group, with different needs and interests, to keep it stimulating:
I still feel you’ve got to have some interesting people to keep the group active.
055, female
I feel it’s more beneficial to people who are actually housebound because it’s a contact with the outside world. Whereas, as you can see, I’m pretty active and, you know, and [erm] and busy, but I can see the reason why you need the mixture because if they’re all not getting out there’s going to be no conversation, so I see a benefit both ways.
055, female
Disclosure
No direct conflicts were reported to have occurred in any of the groups. The majority of members described the discussions as being about everyday occurrences. Some participants wanted the discussions to be about superficial events and to keep the conversations light and not to go too deep:
were nothing very deep or, you know, political . . . it’s got to be avoided things like that, so you know then we, we’ve kept it very smooth and easy.
038, female
if you go into somethin’ too deep with people who you don’t know, you fall out . . . nobody wanted to fall out you know . . . so we skipped over things like that.
003, female
Conversely, other participants felt that the conversations were too light and that they wanted more meaningful conversation or to explore specific topics:
but it was just chat . . . nothing too interesting.
027, male
Value
Perceived benefit
Participants did not identify direct changes to their health or their ability to carry out tasks as a result of being part of a group. One participant felt that the group had made her more inclined to socialise and another felt that the group had enabled her to meet people without inconveniencing others:
Well I have always liked socialising, I always have, but the thing is, to get anywhere I have to be taken and that interferes with other people’s lives . . . I enjoyed it ‘cos you were meeting people without physically meeting them.
003, female
The majority of participants who remained in their groups talked in positive terms about hearing other people’s perspectives, opinions and views on the world. Some felt that they had developed or found comfort in the groups:
all in all I think it’s made me more observant, not only of the natural world, but people around me.
081, female
It helps me, it helps me to think that there are other people in [locality] to whom I’ve been talking and they are getting on with their lives and so you get on with yours.
006, female
Yeah it was nice . . . it filled . . . the winter days . . . And I looked forward to it, yes.
002, female
Four participants talked about the moral support that they received from being in the group, that it inspired them to try new things and that they gained confidence in their voice:
Well, when you’re talking on the phone it’s, it’s a sort of moral support you get . . . you’re just talking to people, you’ve never met them . . . and you just have to sort of grasp, you know, who they are and what they do, or what they’ve done. [Er] You know, to give you an insight on [er], you know, on [er] on things.
003, female
Several participants reported that it had been nice but that it had no direct benefits or that they did not learn anything:
Personally I don’t know that it brought any great benefit . . . I don’t know that it, it’s changed my life or not or made me think of anything wildly different or anything of that kind.
058, male
I wouldn’t say they were important, they were interesting . . . you know, and enlivened the day and there are masses of days when you didn’t see or hear . . . from anybody . . . ‘cos I’m a voracious reader and enjoy listening to music . . . I’ve learnt to occupy myself.
037, female
One of the reasons that participants gave for joining the study was the perceived needs of ‘others’ (see Prior states). Many participants expressed hope that, although the group was not benefiting them directly, it was helping other people. However, one participant who started her participation in the group with this belief felt that in the end the group had helped her because she was unable to go out as she was recovering from a lengthy stay in hospital:
whereas like, you’d go out with your friends and go for a coffee . . . or go for a meal. Well I couldn’t do that at that time. So I suppose, yeah, I suppose it did help really.
002, female
Preferred alternatives
Fifteen participants talked about alternatives to telephone-based discussions. The alternatives suggested were meeting facet to face as a group; taking part in an activity group; including people of similar or different ages in the group; and having one-to-one telephone conversations rather than group telephone calls. A number of participants also suggested that the telephone group could be improved by being able to see the other people in the group, for example through the use of video conferencing.
this thing of getting us all together to talk, I thought was wonderful [er] it’s marvellous what they can do now, you know, all we need now is as Skype.
065, male
Six participants indicated that it was difficult to form new relationships without face-to-face contact (see also Group dynamics).
You can’t see people’s gestures, you can’t see people visually, and you can’t see . . . those facial expressions, I haven’t felt anything like that from the conversations, but I’d like to have seen more.
065, male
I would like to get to meet these people . . . seeing them is better than a voice . . . sort of form a friendship . . . That’s what I thought it would lead to . . . Well, like I say it was just a voice.
027, male
I think there’s only so long you can speak to people in that way, you know, it’s not like having close friends.
055, female
Participants often talked about other members of the group not being there, either dropping out or missing calls (see also Group dynamics). Reasons for missing calls included planned events such as going on holiday, attending hospital appointments or having visitors. Several participants commented that they had to leave calls part-way through because of the arrival of carers, family or friends.
Willingness to pay
Six participants said that they would pay for the service; however, the majority of the participants were not willing to pay for the service for a variety of reasons, including feeling that they did not need the group, that there was a better alternative that they could spend their money on or that they should not have to pay. Some participants were willing to pay if they felt that they needed it but thought that it was not for them at this point in time.
Results of the volunteer interviews
The sample
We attempted to interview all volunteers who remained in contact with the service provider (n = 8) about their experiences. This included volunteers who dropped out before, midway through and post completion of the group facilitation skills training. Three volunteers consented to an interview: two had completed delivery of the intervention and one had dropped out during the group facilitator training.
The volunteers participated in semistructured interviews between February 2013 and April 2013. Sociodemographic data were not collected for volunteers; however, those who were inducted by the service provider were aged from their 20s to their 70s. The sample included one volunteer of working age (working part-time) and two who were retired.
We used the same macrolevel themes for the volunteer interviews as for the participant interviews and most material could be categorised under the ‘prior states’ and ‘technical’ headings. The results of the volunteer interviews are presented first and the analysis of intervention fidelity is presented in Results of the fidelity assessment.
Prior states and expectations
All facilitators said that they had volunteered because of a desire to help others and because the telephone facilitator role sounded interesting. Two volunteers said that they wanted to get something out of volunteering themselves (VF01, VF03). One volunteer expected the role to involve more face-to-face interaction with participants (VF02). Having dropped out, they also reflected on the type of role that they would have preferred, such as working in a day centre where they would meet people. Another volunteer described being apprehensive about making group calls and being especially worried about conflict arising in the group (VF03). Volunteers expected TF groups to consist of participants who were isolated, lonely and housebound but found that there was more variation (see Chapter 3, Monitoring volunteers).
Technical
Acceptability and accessibility of telephone friendship groups
Generally, both volunteers who had delivered the intervention described their experience as good and felt that they had benefited from taking part. One noted that the one-to-one calls were very easy, that the 12 weeks of group calls went quicker than she anticipated and that it was so enjoyable that she had since found two other volunteer roles (VF03). The other talked about the calls broadening his knowledge of the locality and challenging his assumptions about people (VF01).
There were perceived problems for the facilitators. One volunteer described wanting more direct contact with ‘participants’ (VF03). Both volunteers felt that the time commitment associated with facilitation was significant. One reported that the combination of the calls and the paperwork meant that involvement with the programme took longer than an hour a week (VF03). The other found it difficult to catch individual participants at home for one-to-one calls and to schedule a convenient day and time for the group calls (VF01). This volunteer reported that using the Community Network system for one-to-one calls was time-consuming, especially as participants often put off a prearranged call for other priorities, such as going out or having their tea. He felt that the majority of participants did not need the one-to-one calls before participating in the group calls (see Prior states) and that the number of one-to-one calls could be reduced from six to three or four. This volunteer facilitator also suggested that the availability of participants should be ascertained before recruiting them for the service, although he did not suggest who might carry out this work (see also Monitoring volunteers).
One volunteer commented that there had been good communication with the Community Network operators, which helped her keep track of group member cancellations (VF03). The other volunteer felt that it would have been desirable to be able to make calls after 1700 as participants were more available after this time; however, this facility was not available (VF01).
Volunteer training
Volunteers talked about the one-to-one and group facilitation skills training. All volunteers said that they found the information provided by the service provider about the telephone facilitator role clear. Volunteers discussed how prepared they were for the role. Generally, volunteers felt that the one-to-one training was good. Volunteers’ views of the group training varied. One felt overfaced by the amount of material and selected what they felt was most useful from the group training (VF01). The other volunteer who went on to facilitate a group felt that the group training was good but that it did not prepare her for actually carrying out the role (VF03). This volunteer also commented that the interval between the facilitation skills training and facilitating a group could have been shortened, suggesting that 2–3 weeks would be desirable. The other volunteer discontinued training because of a lack of confidence and because of finding the group training intimidating (VF02).
Volunteer monitoring and support from the service provider
Only one volunteer who facilitated a telephone group described having any mentoring contact with the service provider’s volunteer co-ordinator (VF01). He had been contacted by the service provider in the early stages of the group work. The same volunteer went on to say that there were times when he was unsure about how to deal with certain situations, for instance when participants missed calls, and had resorted to contacting the study team and Community Network rather than the service provider.
Facilitator performance
Volunteers demonstrated variable understanding of the training provided and their role in issues such as maintaining confidentiality. One volunteer (VF03) showed awareness of a procedure, if not the precise details, for allowing participants to stay in touch with each other after the termination of the facilitated group (see Chapter 2, Methods for the fidelity assessment, and Appendix 4). The same volunteer also prepared the group for the end of the 1-hour discussion and allowed space for the group to choose topics for the following week (see Chapter 2, Methods for the fidelity assessment, and Appendix 4). However, contrary to the facilitation skills training, the volunteer also found it difficult not to ‘participate’ in the group discussions and felt that she needed to join in to help the conversation flow. She described the role of the volunteer facilitator as different from her approach, acknowledging that she was more comfortable joining in. The other volunteer (VF01) described his approach to facilitating the discussion as ‘laissez-faire’, when he should have been facilitating the group members to agree topics for discussion. This is echoed by the participants, who felt that the groups could have been more focused on ‘topics’ of conversation rather than just ‘chat’ (see Group dynamics). One volunteer (VF03) described the training materials as ‘guidelines’ and useful for instructions on technical issues, but did not refer to instructions on her role in facilitating the group (see Chapter 3, Training). The two volunteer facilitators (VF01, VF03) discussed the group calls coming to an end with their groups. Both volunteers introduced the idea of group members staying in touch and/or meeting face to face. One volunteer facilitator said that participants had ‘hinted at it’ before the end and had prepared in advance by checking the handbook for instructions (VF03).
Perceived benefit to participants
The volunteers did not feel that the group had benefited participants greatly because many participants were physically or socially active. However, they still perceived a level of enjoyment from the telephone calls by members of the group. They went on to say that the participants felt that the service would have benefited people who they knew who were very lonely and isolated. Both volunteer facilitators noted that participants seemed to share more in the group discussions than during one-to-one calls, describing group members as ‘more forthcoming’ (VF01) and the group calls as more ‘dynamic’ than the one-to-one calls (VF03).
Results of the fidelity assessment
The fidelity assessment aimed to examine the extent to which volunteers facilitated the group telephone calls as intended. A number of strategies were employed across the study to aid this assessment. The strategies were based on the framework set out by the Behaviour Change Consortium:54 study design, training, delivery, receipt and enactment. Volunteer facilitators’ assessment of their own performance (see Results of the volunteer interviews, Technical) and participants’ engagement in the intervention, when relevant, are brought together with reference to this framework.
Study design
A minimum and maximum number, duration and frequency of telephone contacts were established as part of the intervention design (see Chapter 2, Interventions and Telephone befriending design). Nine participants received the per-protocol minimum number of calls of nine (out of 12). Table 29 summarises the number of group calls made by the volunteer facilitators and shows the time period over which calls took place. Two volunteer facilitators conducted 12 discussions with each taking place 1 week apart for 12 weeks. The two other groups, facilitated by the same volunteer (consecutively), completed 12 calls over a longer period of time.
| Group | Completed 12 calls | Duration (weeks) | Description (occasions) |
|---|---|---|---|
| 1 | Yes | 12 | |
| 2a | Yes | 18 | Break after week 1 (4 weeks), reason unknown; break for Christmas (2 weeks) |
| 3 | Yes | 12 | |
| 4a | Yesb | 14 | Facilitator absence (n = 1); availability of participants (n = 1) |
Assessment of volunteer experience and competence (training)
A set of qualities and skills required of volunteers to enable them to carry out the volunteer befriender/facilitator role were agreed prior to the service provider promoting the opportunity in the locality. Volunteers were screened by the service provider, which included a criminal records check with the UK Disclosure and Barring Service to assess their suitability for the role. All volunteers had some experience of communicating either face to face or by telephone in their current or previous employment. The majority of the volunteers had some experience of volunteering although none had done so by telephone.
One-to-one calls training
Induction sessions were led by the service provider’s customer engagement manager. Generally, volunteers were inducted and trained in making one-to-one calls in groups of between two and seven, depending on the number of volunteers expressing an interest in the role at the time. Induction sessions lasted between 1 and 2.5 hours, depending on the size of the group. The induction consisted of an ice-breaker and provided information on issues facing older people (training video), information on confidentiality and equality and an introduction to the TF groups service. The induction also included information about the research study and training in making one-to-one calls. On occasion, the content was delivered over two sessions, with ‘new’ (potential) volunteers being invited to join meetings with volunteers who had already agreed to take on the role. The service provider held regular meetings with volunteers between the initial contact and the start of intervention delivery. The customer engagement manager contacted volunteers periodically during the group call part of the intervention; the frequency of contact was not recorded (see Results of the volunteer interviews, Technical, and Chapter 3, Monitoring volunteers).
Group facilitator training
Volunteers received four 1-hour training sessions in group facilitation skills. Training was delivered over the telephone using Community Network’s teleconferencing system and training groups included up to a maximum of five trainees. All volunteers were trained by the same trainer and received the standardised content that is delivered to all volunteer facilitators running TF groups using Community Network’s system. The training modelled the scenarios that volunteers could expect when facilitating their own groups, including facilitating a 5- to 10-minute group discussion. The training was supported by a written manual that was adapted to align it with the intervention design (e.g. references to one-to-one calls). Community Network’s existing policies regarding confidentiality and sharing information relating to participants were adopted for the study. The service provider also worked with its existing volunteer policies in terms of confidentiality and safeguarding ‘participants’ (see Chapter 3, The contract with the service provider).
Assessment of training content delivered by the trainer
The sample
Facilitator training was delivered in four 1-hour sessions. Nine (56%) of these 1-hour sessions were audio recorded. Training content could vary across the four sessions depending on the understanding of each trainee in a group; therefore, at least two samples of each of the four sessions were recorded. The sample of recordings was assessed by two observers using the training content checklist (see Appendix 8). The checklist was designed to ensure consistency in the content delivered to volunteers and to make sure that the trainer tailored the content to ensure provider (volunteer) skill acquisition. The checklist accounted for content anticipated but not covered in the sampled session, for instance if the trainer had to spend longer on one component and moved other content to the next session.
Training content fidelity scores
Table 30 shows the percentage fidelity scores of the training content delivered to volunteers by the trainer. The median was used to calculate the overall percentage fidelity score for each group. The trainer scored > 91.0% based on the median scores taken from the observers. For groups 1 and 2, the percentage fidelity score was > 95.0%. Observers noted that groups 1 and 2 seemed different from group 4 in terms of the flow of discussion and a greater degree of input from the trainees, although this was not formally measured.
| Group 1 | Group 2 | Group 4 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Observer 1 | Observer 2 | Median | Observer 1 | Observer 2 | Median | Observer 1 | Observer 2 | Median | |
| Score | 35/36 | 34/36 | 34.5 | 39/42 | 38/39 | 38.5 | 33/36 | 35/38 | 34.0 |
| Percentage fidelityb | 97.2 | 94.4 | 95.8 | 92.9 | 97.6 | 95.1 | 91.7 | 92.7 | 91.9 |
The checklist also assessed provider (volunteer) skill acquisition using three items: reflection on own style of communication, impact of their style on the group and reflects on skills learned. Observers scored trainees in all groups as 100% for overall fidelity against these criteria. Volunteers’ perceptions of the facilitation skills training are detailed in Results of the volunteer interviews, Technical.
Assessment of group intervention delivery by volunteer facilitators
The sample
A sample of facilitated telephone discussions was audio recorded by Community Network, both within and across groups. We assumed that overall facilitator performance may not always adhere to that prescribed by the training content delivered and that the groups would require less input from volunteer facilitators as they developed over time (see Appendix 4). The sample therefore consisted of recordings of the same group at different time points throughout intervention delivery to enable facilitator performance to be assessed. A total of 11 (22.1%) audio recordings were made from four groups at three time points: weeks 1, 6 and 12. At least three samples at each time point were audio recorded. The sample was assessed by two observers using the intervention delivery checklist (see Appendix 8). The checklist included core skills and practices that are important to help the groups fulfil their purpose. The checklist was designed to examine whether the intervention’s core components were implemented. 56 The checklist accounted for content that was not applicable to individual sessions sampled. The minimum duration of the group telephone discussions sampled was 23 minutes and the maximum was 69 minutes, with a median of 55 minutes.
A narrative summary of observations made during completion of the checklist is presented alongside the fidelity scores.
Intervention delivery fidelity scores
Table 31 shows the percentage fidelity score for each group volunteer facilitator at the three time points sampled. The median from the observed scores was used to calculate the overall percentage fidelity for each group. The volunteer facilitators scored between 30.2% (group 2) and 52.1% (group 4) based on the median score taken from the observers.
| Group 1 | Group 2 | Group 3a | Group 4 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Observer 1 | Observer 2 | Median | %b | Observer 1 | Observer 2 | Median | %b | Observer 1 | Observer 2 | Median | %b | Observer 1 | Observer 2 | Median | %b | |
| Week 1 | 18 | 21 | 20 | 47.6 | 12 | 14 | 13 | 32.5 | 19 | 18 | 19 | 55.2 | 27 | 27 | 27 | 70.1 |
| Week 6 | 13 | 14 | 14 | 45.8 | 7 | 6 | 7 | 20.6 | 17 | 12 | 15 | 46.0 | 13 | 15 | 14 | 38.9 |
| Week 12 | 10 | 9 | 10 | 33.3 | 13 | 12 | 13 | 35.7 | – | – | – | – | 15 | 13 | 14 | 45.2 |
| Percentage fidelityc | 41 | 44 | 43 | 42.9 | 32 | 32 | 32 | 30.2 | 36 | 30 | 33 | 50.7 | 55 | 55 | 55 | 52.1 |
Overall, the fidelity scores for all volunteer facilitators were low. The highest score was just over 50%. This indicates that volunteers did not facilitate the group discussions in line with the training content delivered.
Two groups show a decline in fidelity score over the time points sampled. The volunteer facilitator of group 4 scored the highest (70.1%) weekly score overall. The lowest weekly score of 20.6% was observed in group 2. The percentage fidelity score overall for this group was also the lowest across all of the groups. It is worth noting that the number of items observed as ‘not applicable’ reduced over time in all groups. These were items that did not arise during the conversations sampled (e.g. encourages a quieter participant to join in).
The extent to which the volunteer facilitators discussed and agreed ground rules with their group varied. Establishing norms within the group is important57 and agreeing ground rules is one technique for establishing norms. The facilitator training material recommends setting minimum ground rules, of which confidentiality and respect are key (see Appendix 8). Volunteer facilitators are trained to establish ground rules with the group, inviting discussion and agreement. This creates an environment in which the group can develop into a ‘group’, perform well and fulfil its purpose. 57 One volunteer facilitator mentioned confidentiality; however, not all members of the group had joined the call at this point (group 2, week 1). This volunteer facilitator went on to tell all participants to use only first names and not to share contact details and also stated the purpose of the group (to share interests and experiences). However, this volunteer facilitator then addressed one member of the group and informed her that he had met someone recently who knew her (group 2, week 1). The context of the discussion between the volunteer facilitator and the acquaintance is unknown; however, volunteer facilitators were trained by the service provider not to discuss participants outside the group. In addition, disclosing this information to the group may have impacted on the participants (see Results of the participant interviews, Group dynamics).
One volunteer facilitator mentioned that members of the group should say their name before speaking but did not discuss ground rules (group 1, week 1). The volunteer facilitator of group 4 demonstrated a good understanding of the process of establishing ground rules. They talked briefly about her role and stated that participants did not have to talk, that sessions are time limited and that participants should stop talking when asked. Although she did not specifically mention confidentiality, she did talk about respecting others in the group, providing examples. This volunteer facilitator also invited the group to think of any additional ground rules (group 4, week 1).
The facilitator role is to make the group conversations ‘easy’. 58 The facilitator training informed volunteers that a ‘high-performing’ group is one in which little intervention is needed from the volunteer facilitator. Observers noted that on several occasions checklist items were performed by group participants (e.g. group 1, weeks 6 and 12; group 4, weeks 1 and 6), which suggests that less input was required from the volunteer facilitator and provides an indication that some groups were working well (see Chapter 2, Interventions and Telephone befriending design). Conversely, observers noted in all groups that the extent to which volunteer facilitators intervened in (or ‘directed’) group discussions was greater than necessary. This theme emerged in a number of participant interviews and in one volunteer facilitator interview (see Results of the volunteer interviews, Technical, Facilitator performance, and Results of the qualitative research, Acceptability, Implementation and facilitator performance). The type and degree of ‘direction’ by volunteer facilitators varied between groups. For instance, the volunteer facilitator of group 2 often directed closed questions to specific members of the group. They responded to their own question rather than leaving space for others to join in and the facilitator then asked a different question to another participant. Little space (‘silences’) was left to allow quieter group members to join in or respond to discussion. The degree of direction did not lessen over time as this was also observed in weeks 6 and 12. Observers noted that this ‘style’ resulted in the group calls ending abruptly, with one participant (who was talking about needing to leave) and the volunteer facilitator saying goodbye. The volunteer facilitator did not invite final thoughts or a group ‘goodbye’ (group 2, weeks 1 and 6). The other groups diverged from this style and conversation seemed more inclusive and steered by the group rather than by the volunteer facilitator. The volunteer facilitators of groups 1 and 4 asked questions but these were more often addressed to the group and were open rather than closed. The facilitator of group 1 had less input to the conversations and allowed space for the group to talk. Observers noted examples of ‘monitoring’, for instance noticing an issue with background noise (group 1, week 1) and bringing participants in who others were talking over (group 1, week 12). However, in group 1 participants were observed talking over each other and the volunteer facilitator did not intervene (week 6). At this point one intervention by the volunteer facilitator might be to remind the group about the ground rules; however, this volunteer facilitator had not agreed any ground rules with the group.
All volunteer facilitators contributed to the discussion in a number of ways including giving advice, offering opinions and talking about their interests and experiences. Volunteer facilitators are trained to give responsibility to the group whenever possible and to ask the group before giving advice. No occasions were observed when the volunteer facilitator asked the group before offering advice or opinions. Some examples included giving advice about falls (group 1, week 1), offering opinions on taxation (group 1, week 6) and social networking and privacy (group 4, week 6), recalling historical events and offering opinions on nuclear power (group 4, week 12), asking a leading question on corporal punishment and offering their own view (group 1, week 1) and sharing local knowledge (group 2, week 12).
It was the role of the volunteer facilitator to discuss with the group their choice of topics. Specific intervention by volunteers in terms of giving responsibility to the group to discuss and agree topics was limited in the observed sample. This was echoed by some participants who reported being unsure of what to talk about in the group (see Prior states). Volunteer facilitators of groups 1 and 4 were observed changing the topics being discussed by the group. The reasons for this were sometimes obvious and demonstrated an understanding of their role as a facilitator. For instance, one discussion resulted in a participant’s perspective isolating them from the rest of the group (group 4, week 6). One volunteer facilitator changed the topic because the same topic had been discussed for 30 minutes without a clear perceived need expressed by the participants or identified by the observers (group 2, week 6).
Observers noted instances of volunteer facilitators diverging from the training, including introducing information discussed with an individual (in the one-to-one calls) by asking direct questions to that member of the group. Furthermore, one volunteer facilitator (group 2) said that he would call a participant who the operator had said was not answering the telephone (group 2, week 12). The service provider’s policy was for volunteers to contact the service provider if a participant did not answer a prearranged call.
Observers noted occasions when volunteer facilitators appropriately and proportionately balanced the needs of the individual with those of the group. One volunteer facilitator allowed a participant to talk about an upsetting experience and then moved the conversation on when another member of the group tried to change the subject (group 4, week 1).
The volunteer facilitator of group 1 shared his telephone number with group members during the 12-week group phase; this was not prohibited but the intervention protocol did state that contact was supposed to be through Community Network’s telephone services, to protect personal information (participant telephone numbers). The same volunteer also arranged for the group to meet face to face (group 1, week 12) without referring this activity through the service provider as per protocol; a member of the group was inappropriately excluded from this meeting because of restricted mobility. An individual participant was saddened by this experience (see Results of the participant interviews, Value).
In summary, intervention fidelity scores achieved by volunteer facilitators were low, indicating that the volunteers did not facilitate the group discussions in line with the training content provided. Group 4 also demonstrated a decline in fidelity score over the time points sampled, from an initially satisfactory score. Volunteer facilitators were inconsistent in how they set ground rules, maintained participant confidentiality and satisfactorily and sensitively brought the 12-week group programmes to an end.
Participant engagement in group calls (receipt)
Interview transcripts from the qualitative interviews and audio recordings of observed group discussions were reviewed for problem behaviours associated with group cohesion. 31 One volunteer facilitator mentioned an incidence of monopolistic behaviour in her group (VF03). One incidence of silence and lack of participation was self-reported by a participant (R002). There was no evidence of band-aiding, acting superior, hostile behaviour, dependency or socialising outside of group calls before the end of the programme.
The intervention delivery checklist included four fidelity items that assessed group members’ participation in calls: observing ground rules, introducing topics, showing support and commitment (see Appendix 8, Intervention delivery checklist). The role of the facilitator was to make it easy for participants to join together as a group to discuss whatever they liked. The volunteers were asked to use their skills to facilitate discussion, monitor development of the group and allow the group to ‘perform’ as a group. The extent to which participants were able to ‘perform’ in the group is closely related to volunteer facilitator performance, for instance if the volunteer facilitator did not discuss and agree ground rules then the participants could not be expected to comply with them. This was accounted for in the scoring of the checklist.
Table 32 shows participant fidelity scores for each time point by group and overall percentage fidelity based on median observed scores.
| Group 1 | Group 2 | Group 3 | Group 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Observer 1 | Observer 2 | Median | Observer 1 | Observer 2 | Median | Observer 1 | Observer 2 | Median | Observer 1 | Observer 2 | Median | |
| Week 1 | 7/12 | 8/12 | 8 | 6/12 | 4/12 | 5 | 6/12 | 6/12 | 6 | 11/12 | 9/12 | 10 |
| Week 6 | 7/12 | 9/12 | 8 | 5/12 | 5/12 | 5 | 9/12 | 8/12 | 9 | 8/12 | 7/12 | 8 |
| Week 12 | 6/12 | 8/12 | 7 | 8/12 | 7/12 | 8 | – | – | – | 9/12 | 8/12 | 9 |
| Percentage fidelity | 20/36 | 25/36 | 62.5% | 19/36 | 16/36 | 48.6% | 15/24 | 14/24 | 60.4% | 28/36 | 24/36 | 70.8% |
The small sample of observed groups prevents the use of formal statistical tests to investigate the association between low facilitator fidelity and low participant fidelity, but some observations on apparent association may be worthwhile. Participants in group 2 were observed as having the lowest overall percentage fidelity; the volunteer facilitator score for this group was also the lowest across the groups sampled. Similarly, the highest volunteer facilitator and participant fidelity scores observed across groups were both in group 4.
Interview transcripts and audio recordings were also reviewed for relevant characteristics associated with the transitional phase, which the group must recognise and deal with to progress to the working stage (see Chapter 2, Methods for the fidelity assessment, Telephone befriending receipt and enactment). 32 One incidence of confrontation was reported (see Results of the volunteer interviews, Technical, Facilitator performance) and one incidence of conflict was observed (group 4, week 1). There was no evidence of defensiveness and resistance.
In summary, the assessment of participant fidelity indicated little evidence of groups moving through the behaviours expected in the transitional phase of group formation, which group dynamics theorists think of as necessary in the early stages for a group to become high functioning. In lay terms, the group members are acting in ways that could be characterised as reserved and tentative rather than open and expressive. These findings almost certainly relate to both the generally poor intervention fidelity of the volunteer facilitators and the fact that the groups were time-limited, discouraging emotional investment.
Chapter 6 Discussion
Summary of findings
The internal pilot study assessed the feasibility of the main trial against three success criteria. Two objectively defined success criteria were whether the trial team could, first, recruit ≥ 68 participants in 95 days and, second, follow up 80% of those recruited, 6 months after randomisation. The third success criterion was to determine whether the service provider could recruit and retain a sufficient number of volunteers to deliver the intervention. Although this criterion was not defined quantitatively, targets for the recruitment and training of volunteers were agreed and built into the subcontract between the University of Sheffield and the service provider.
The first two criteria were met: 70 participants were consented and randomised in the first 95 days of recruitment, of whom 56 (80%) provided valid primary outcome data 6 months later, demonstrating that the main trial was feasible. However, the service provider was unable to match the supply of volunteers to the demand from participants randomised to the intervention arm of the trial. As a consequence, participant recruitment closed on 11 January 2013 at which time 50 out of 78 participants allocated to the research arm had not been allocated a volunteer facilitator, that is, had not been treated per protocol. After clarifying that the service provider could not recruit the required number of volunteers and that it would not be viable for another agency to take over this role, the decision to close the trial early was made on 17 January 2013.
Strengths and limitations
Strengths and limitations of the randomised controlled trial
This report presents the results of a pilot trial phase of a discontinued study. As such, it would be inadvisable to use the results as a guide to the potential mental health benefits achievable through befriending programmes; any estimates of beneficial effect presented in the results may be unrealistic because of the limited sample size. The report does, however, demonstrate that recruitment to, and retention in, such a trial is possible.
Recruitment to trials evaluating preventative interventions is known to be problematic, with typically 1–5% of those screened being randomised compared with 20–26% in trials evaluating therapeutic interventions according to one overview. 59 Our consent rate was 1.6% with 147 participants recruited from targeted mail-outs and 10 from referral by health and social care professionals, the voluntary sector or advertisements. These figures are consistent with other trials of health promotion interventions using mass mail-outs for participant recruitment in the same geographical region; these studies also show recruitment through health and social care referral to be wholly inadequate for timely participant accrual. 60,61 It follows that the low take-up rate need not indicate poor acceptability of either the study procedures or the intervention, although it may raise questions whether telephone befriending can be understood as a public health intervention. 62 Similarly, attrition in RCTs evaluating preventative measures in community-dwelling older people is frequently between 20% and 30% because of comorbidity, exhaustion and respondent burden. 63 Our study performed well in limiting attrition to 20%.
At least one RCT evaluating professionally led befriending groups for older people has been published. 64 To our knowledge, this is the first RCT that has sought to evaluate a volunteer-led group intervention co-ordinated by the voluntary sector, or one mediated by telephone rather than face to face. However, there are three aspects of the trial’s external validity of which readers should be aware before attempting to generalise from our results. These are the unique use of a hybrid (one-to-one followed by group) intervention (see Other studies evaluating interventions to address loneliness); intervention delivery by a local franchise of a charity with a federal structure (see Other studies involving volunteer provision); and the character of the randomised population, which we consider now.
Trial participants who were interviewed for the qualitative substudy did not generally identify a need to take part in a telephone group, instead expressing a wish to help with the research or to help other older people who were genuinely lonely or isolated (see Chapter 5, Results of the participant interviews, Prior states). There are a variety of ways in which we can interpret this finding. First, it is possible that the study was subject to a severe form of ‘volunteer bias’ or ‘self-selection bias’, defined as systematic error deriving from the sample containing only those people who are willing to participate in the research study and not those who would otherwise have sought help from the service. 65 This hypothesis is given weight by the distribution of scores for the de Jong Gierveld Loneliness Scale and the GSE. The mean (SD) de Jong Gierveld Loneliness Scale score for intervention participants in our study was 3.6 (3.2), on a scale in which a score of ≥ 3 indicates loneliness and a score of ≥ 9 indicates severe loneliness. 66 de Jong Gierveld reports the Dutch population norm for this scale as 4.9, somewhat higher than the mean in our study. GSE mean (SD) scores for intervention participants at baseline [32.9 (5.1)] are also higher than the population mean reported in a multinational psychometric study [29.5 (5.32)]. 67 It is relatively well documented that ‘joiners’ – those with a propensity to establish and sustain group membership – are psychologically healthier than those who are not ‘joiners’. 68 There were indications through intervention delivery and reiterated during interviews that some participants were well supported and socially engaged (see Chapter 5, Results of volunteer interviews, Technical). However, we must allow for the possibility that a number of participants were genuinely help-seeking but unwilling to define themselves as such, anticipating that they would be viewed negatively by the interviewer (social desirability bias69 or unacceptable disease bias65). Similar claims, that participation in research is altruistic and not help-seeking, have been noted in other studies in which the medical condition (e.g. depression) or risk factor (e.g. loneliness) is in some way stigmatised. 70,71 Although this may appear to have serious consequences for the external validity of the research, there is some evidence that this dynamic does characterise routine clinical practice too. For instance, a strength of group psychotherapy is that people gain a sense of self-worth by being part of the group and from feeling of benefit to others rather than being a burden. 57 For these reasons we might understand the expression of altruism and denial of need as not only inevitable in research but also a likely response to service receipt.
Sustained attempts were made between September 2011 and March 2012 to engage members of the public in the development and implementation of the intervention, beyond the support offered by lay representatives on the TMG and TSC. These attempts were unsuccessful and may have adversely affected the quality of the project outputs. That said, the intervention was based on the findings of consultations with those who had delivered and received telephone befriending based in other settings and so the design and implementation of the intervention were not without lay perspectives.
Strengths and limitations of the qualitative research
A qualitative research component was integrated into the study to better understand the success or failure of the delivery of the intervention. 72,73 The design and conduct of the qualitative research met the recommended standards for conduct and reporting, with qualitative researchers, independent from the interventionists, contributing throughout with clearly stated aims. 74 Although we made every effort to interview as many as possible of those who received the intervention, the small numbers available mean that it is unlikely that descriptive or theoretical saturation was achieved. Many of the reported themes identified echo findings from existing related literature, but we cannot overlook the possibility that new descriptive codes, categories or themes might have emerged with the analysis of further data.
Strengths and limitations of the fidelity assessment
A major strength of this study is the detail presented on the development of the intervention and its adaptation for delivery through a particular teleconference provider under the co-ordination of a host charity in one locality. The content of and adherence to the volunteer training programme and the intervention delivered to participants are described in detail. Standardised manuals, guidelines and training were all provided to ensure that each volunteer received the same support to deliver the intervention. This level of description of the complexity of the intervention is in line with the Medical Research Council framework75 and is beyond that available for most interventions intended to ameliorate social isolation or loneliness. 53
Although the service provider initially agreed to give volunteers ongoing support after training, in the end they had a ‘hands-off’ approach to co-ordination, without any monitoring of volunteer facilitators or feeding back to volunteer facilitators on the quality of their intervention delivery. Given the resource and knowledge constraints under which devolved charities operate, this model is likely to be generalisable for third-sector organisations that operate as small independent ‘franchise’ organisations. Charities that operate a command and control model may be better resourced to undertake the ongoing support and continuous quality improvement work necessary to facilitate intervention adherence and prevent intervention ‘drift’, a decline over time in the fidelity with which the intervention is delivered, when initial competence is established. 54
The fidelity substudy, embedded within the trial, used a framework based on that developed by the Behaviour Change Consortium. 54 Although this system worked well for evaluating training and delivery, it proved problematic for assessing the receipt and enactment of the intervention, the mechanics of which were aimed at the management of group dynamics within 1-hour group sessions (see Chapter 2, Treatment fidelity assessment and methods) rather than at changing individual clinical outcomes over the long term. Enactment is one facet of a more general concept of responsiveness, which our qualitative research tried to assess in terms of which participants viewed the intervention as being of relevance to them. The results suggested that some participants were not fully engaged in the group discussions. In part, this response may be an effect of the nesting of the intervention within a research study (see Chapter 3, Boundaries between research and service delivery). The denial of need by many participants (see Chapter 5, Results of the participant interviews, Prior states) as well as the occasional claims that group cohesiveness could be low (see Chapter 5, Results of the participant interviews, Group dynamics) may suggest that the participants were unresponsive to the intervention, regardless of intervention fidelity achieved by the volunteers. These findings provide an important frame through which the positive but uncertain quantitative results should be viewed.
A shortcoming of the fidelity substudy was that limited data were collected on the content delivered by volunteers during the one-to-one calls. The study used Community Network’s system to record a sample of one-to-one and group conversations. One volunteer reported to the study manager having technical difficulties recording one-to-one calls, and Community Network reported difficulties in extracting the recordings from the system as volunteers were able to arrange calls at any time rather than them being set up through an operator (Community Network)-managed call. The group intervention delivery checklists will not have captured some volunteer behaviour during one-to-one calls that may have contravened the protocol and/or impacted on outcomes. For example, we would not be aware if, during these one-to-one discussions, volunteer facilitators had introduced participants to group ground rules, which are supposed to be agreed by all participants at the outset but were not evidenced through the recorded group calls in most cases.
Perspectives on the intervention from the group therapy intervention literature
We have already identified that a strength of the research intervention was that it required a protocolised training programme for its volunteer facilitators, which informed them about how to manage group dynamics and the practice of group facilitation. The format of the training itself enabled trainee facilitators to receive a group experience as a participant. Because of resource constraints, the training programme was relatively limited compared with that provided for trainee psychotherapists, who would typically be able to observe experienced group therapists at work and receive close supervision when facilitating their maiden group. 57 The practice of psychotherapy is not necessarily a good analogue for what is achievable or desirable in interventions to enhance social support or increase opportunities for social interaction (see Other studies evaluating interventions to address loneliness). Nonetheless, our sense is that, without ongoing training and monitoring, 4 hours of training was insufficient, given the fidelity scores (see Perspectives on the intervention from the group therapy intervention literature and Other befriending intervention studies). In the face of public health challenges there is a temptation to think that any service is better than none. 76,77 Although group interventions have the power to transform the health and potential of individuals, it is well documented that groups that are hastily thrown together or led by someone without proper training may be ‘more damaging than beneficial’ (p. 5). 31 Although a small number of participants were dissatisfied with the intervention and others expressed disappointment at how the groups ended, the study did not find any evidence of harm. Nonetheless, the ongoing monitoring of group characteristics and processes throughout an intervention is the sine qua non of a successful group intervention and our research casts doubt that volunteers with 4 hours of training in group facilitation are properly prepared for the task. 31,57,58
Good mental health or well-being outcomes and participant adherence are typically associated with good group cohesion, which in turn is made possible through the promotion of group bonding during early sessions. 31,57 Group cohesion is linked to an individual’s motivations and feelings about the group, the extent to which the members of the group feel similar to one another and whether the group has a goal or objective. 78 The early closure of the trial means that there are too few data to make any definitive remarks about the success of the intervention in promoting group cohesiveness. However, participant interviews indicated that one group, which expressed high levels of mutual interest and reported flowing conversation, maintained all six group members throughout the programme and seemed to be the most cohesive of the four groups. Participants from the smaller groups discussed members leaving the group and missing calls, leaving the group with less to talk about (see Chapter 5, Results of the participant interviews, Group dynamics). Although optimal group size is a function of session and programme duration, there seems to be some agreement in the literature that the group size for adults should not drop below five or six participants with one facilitator. 31,57,79 The opportunities to engage with others are reduced as the group size diminishes, with passive behaviour and negative group image being frequent consequences. For these reasons, some theorists advocate replacing group members or combining small groups in preference to persisting with insufficient membership. 57 These techniques were deliberately eschewed in the design of the PLINY intervention as the introduction of new members can adversely affect the promotion of group cohesion. 31 Face-to-face group therapists can address this issue by setting the group size at nine or ten, the level at which a group can withstand likely attrition, especially if closed to new participants and time limited. 57 However, we are uncertain whether a group of this size can be sustained with a group telephone intervention.
Elsewhere in the literature, group cohesiveness is associated with high self-disclosure. 57 No participant from any group expressed high levels of self-disclosure in our study, with some participants indicating the difficulties in developing real friendships without face-to-face contact (see Results of the participant interviews, Value). This finding is confirmed in other qualitative research that has explicitly compared telephone with face-to-face befriending for older people in the sighted population. 80 However, it is worth noting that a recently completed study found that older people with visual impairment often prefer technology-based communication (social media, e-mail, telephone). The lack of visual cues did not give them additional communication difficulties but, rather, made them feel equal with those with whom they were communicating through electronic media (Patrick Okonji, Northumbria University, 2013, personal communication).
The intervention was designed so that, when possible, participants with ‘similar interests’ would be placed in the same group. This was not possible in practice because of resource constraints but also because of restrictions imposed by the design of the intervention itself. More specifically, one-to-one calls had to be initiated by a volunteer facilitator before interests could be established. It was felt that continuity of volunteer contact between the one-to-one and the group phases was more important than the matching of interests, which would have necessitated passing participants between volunteers to form a group with specific shared interests. The service provider decided to allocate six participants sequentially to each group, delegating first contact with this group of participants to the next available volunteer. Participants would have waited longer for a group to start if they were to be matched to others with similar interests. ‘Matching’ participants on the basis of similar interests is, in general, less critical to successful group composition in personal growth interventions. 31 Some research suggests that older people tend to place a higher value on social skills and a friendly disposition than on shared interests. 80
Group cohesion can be increased or challenged by members socialising outside scheduled sessions. 31 The original intention was that our research intervention should encourage contact among participants in the hope that they would establish acquaintances and friendships that could extend beyond the 12-week group programme, which would include the initiation of independent calls during the 12 weeks of facilitated calls. However, the policy of the teleconference provider, Community Network, discouraged contact outside friendship group calls, to maintain confidentiality and ensure that participants do not share personal information. Volunteer facilitators were therefore trained to discourage contact and were advised to introduce confidentiality as a ‘minimum’ ground rule. The facilitator training also highlighted the potential impact of such contact on the dynamics of the groups, for instance cliques may form or some participants may become isolated within the group. Community Network advises host organisations to decide whether to permit sharing of information among users of the service and to manage this process, recommending that written permission for sharing telephone numbers is obtained ideally at the end of group calls to limit adverse impacts on the group. From what we are able to ascertain from the interviews with the volunteer facilitators and participants and observations recorded in field notes, adherence with Community Network policy was uneven. On the one hand, information seems to have been shared between participants and/or the volunteer facilitator without express permission, against the intervention protocol (see Chapter 5, Results of the fidelity assessment, Assessment of group intervention delivery by volunteer facilitators). On the other hand, some participants who wanted to continue with contact after the group ended were left disappointed (see Chapter 5, Results of the participant interviews, Acceptability).
Strengths/limitations of the research compared with those of other studies
Other befriending intervention studies
One recent non-systematic review has highlighted the absence of, and need for more, RCTs that, like our own, incorporate standardised quality of life measures. 53 We are aware of one systematic review of RCTs of interventions focused on community befriending, the searches for which were updated in April 2008. 81 Compared with usual care or no treatment, befriending demonstrated a small but statistically significant effect on self-reported symptoms of depression in nine studies with follow-ups of < 12 months [standardised mean difference (SMD) 0.27, 95% CI 0.48 to 0.06, from nine studies) and > 12 months (SMD 0.18, 95% CI 0.05 to 0.32, from five studies). These results should be interpreted with caution for at least two reasons. First, the researchers used a funnel plot, a graph developed to assess the risk of publication bias, to show that studies with negative results may remain unpublished. Second, only half of the studies in the systematic review involved befriending by lay volunteers, as in our study, with the remainder evaluating provision by various professionals. The content, duration, frequency and intensity of the befriending programmes are not explicit in the data abstraction tables but, based on the findings of the other review,53 interventions are unlikely to be well described in the original articles.
One well-described UK RCT, the Befriending and Cost of Caring (BECCA) study, evaluated the effectiveness of volunteer-led befriending for carers of people with dementia, successfully recruiting 236 participants to the trial. 82 As with our study the befriending schemes were established for the purposes of the trial and were nested within charitable organisations with experience of supporting volunteers undertaking befriending. Like the PLINY trial, the BECCA project worked with a national charity to set up local networks of volunteer befrienders. Unlike the PLINY trial, the BECCA team partnered with organisations other than local branches of the partner national charity. The BECCA team also found the resource to employ dedicated volunteer co-ordinators in each locale, jointly managed by the operations manager from the ‘host’ organisations and the research team. In contrast, the part-time volunteer co-ordinator in the PLINY project was an existing member of staff at the host organisation, with existing commitments and responsibilities. BECCA volunteers received 12 hours of training and were supported by the organisations throughout. Volunteers and carers were matched and introduced by the befriender co-ordinator. Training content was similar to that received by volunteers in the PLINY trial; however, PLINY volunteers made their own introductions to participants during the first one-to-one call. The boundaries for volunteers – for instance signposting, rather than giving advice – although slightly different from those of the PLINY trial, were clearly set out in the training. The BECCA trial reported that 60 out of 124 (48%) volunteers who expressed an interest completed training and that 49 out of these 60 (82% of those trained) delivered the intervention; this compared with 10 out of 42 (24%) and three out of 10 (30%), respectively, in our study.
Other studies involving volunteer provision
Our study shows that the ability of a local franchise of a national charity to recruit and retain volunteers (interventionists) will not always be adequate for the rapid roll-out of a public health intervention at scale during a trial. The literature on volunteering is dominated by correlates studies, proposing psychometric or demographic factors that characterise those who volunteer and who adhere to volunteer roles, with comparatively few articles describing the frequency and duration of volunteer involvement in the population, recruitment techniques or organisational factors that improve volunteer recruitment and retention. 83
As we have demonstrated, volunteer recruitment represents a significant management challenge, particularly for smaller organisations, even when a part-time paid volunteer co-ordinator exists, unless that post is dedicated to the intervention. The limited evidence on best practice, summarised by an up-to-date systematic review,84 indicates that direct contact by representatives of the organisation and word of mouth are the most common and probably the most effective methods of recruiting volunteers, with advertising providing a supporting role. 85 From this, as well as from personal communications with representatives of Age UK National, we might conclude that the right methods of recruitment were used but that the task of recruitment that was set for the service provider was too onerous, given the rates of volunteer recruitment required for the success of our study.
The literature divides the variables that affect the retention of volunteers once recruited into categories of personal and organisational factors. 84,86 There is only weak or contradictory evidence for an association between volunteer retention and demographic or psychometric variables. Personal factors that do appear to predict adherence to volunteer programmes include higher levels of education, previous experience as a volunteer and ‘stability or continuity in the life course’, including a volunteer’s changing relationships with the geographical locality, higher education, their family and the labour market. The requirement by the UK government for those receiving state benefits to be available for paid work, along with the increasingly tough sanctions for those perceived as ‘work-shy’, are thought to be making volunteering increasingly difficult for many who were previously in a position to do so. 87 In our study, two volunteers dropped out, one before and one after training, because of finding full-time work or additional part-time work. The service provider also reported having to take on volunteers referred by Jobcentre Plus, an executive agency of the UK Department for Work and Pensions, but that these volunteers were unsuitable for delivery of the study intervention, being extrinsically motivated.
This is not the only area of interaction between the state and the voluntary sector that might make recruitment and retention of volunteers difficult. Two trained volunteers cited discomfort with the programme itself as a reason for them discontinuing their involvement. One expressed a belief that funding for the research was inappropriately taking funds away from health services. The other felt that the research was trying to prove that services that might otherwise be delivered by health and social care professionals could be delivered ‘on the cheap’ by using volunteers. By the time the PLINY intervention was being delivered it had become difficult to talk about voluntary work in the UK without reference to the 2010 government’s Big Society policy, a stated objective of which is ‘a society where people come together to solve problems and improve life for themselves and their communities’. 88 This policy has had its detractors in the academic literature with some seeing it as ineffective89–94 and others going further, accusing it of providing rhetorical cover for an agenda of spending cuts, privatisation and regressive taxation that will increase inequality,95–98 not least because small-scale voluntary sector organisations are thought to have been most seriously compromised by the deficit reduction programme. 99 Our study provides limited evidence that some individuals who might previously have volunteered are deterred by an association with a political agenda that they eschew, which adds to an ongoing debate about whether such policies are eroding confidence in the third sector. 100,101 More generally, voluntary sector organisations committed to delivering a service using volunteers should seek to establish congruence between the goals and ideals of the volunteers and those of the organisation. 86
A number of organisational factors thought to influence volunteer retention are more in the control of voluntary sector organisations. Negative experiences related to organisational factors are commonly cited reasons for volunteer attrition. 86,102–104 Field notes from our study recorded instances when volunteers reported frustration at being unable to reach the volunteer co-ordinator at the service provider, which was reflected in an over-reliance on the study team to answer queries or solve problems associated with intervention delivery (see Chapter 3, Boundaries between research and service delivery). Commitment is known to be positively related to the reception of sufficient support to ensure that volunteers are comfortable with their role and its procedures. 85,86,104–106 A related factor that is known to be a key motivator in retaining volunteers is the availability of ongoing training. Volunteers often cite the availability of ongoing training whilst they are delivering an intervention as a motivation for adherence to a programme. 85,86,105,107 We have already commented on the lack of ongoing training to increase the confidence of volunteers and to maintain intervention adherence; this is a consequence of constrained costs and is a clear weakness of the intervention evaluated in our study (see Perspectives on the intervention from the group therapy intervention literature). When resources allow and volunteers are enthusiastic, volunteer befriending programmes should conduct training booster sessions, conduct in vivo observations or record and review sessions, conduct weekly supervision and hold periodic meetings with, or allow easy access for questions to, trainers for the sake of both intervention fidelity and volunteer retention. 54,57
Participant recruitment rates to primary prevention trials are known to be low compared with those in therapy trials59 and it seems likely that the slow start to participant recruitment in the PLINY trial had an impact on volunteer retention (see Chapter 3, Recruitment and retention of volunteers). Rapid allocation of volunteers to participants on a large scale is possible in established, centrally organised national services such as Talk and Support, the telephone befriending scheme run by the Royal National Institute for the Blind (RNIB), which aims to match a client with a TF group within 4 weeks. 108 Our study suggests that the capacity and degree of flexibility within a local franchise of a national charity to respond to variations in client demand for a newly established service is apparently limited. Talk and Support facilitators usually start facilitating a group within 2 weeks of completing training (Mark Berkeley, RNIB, 24 June 2013, personal communication). Our study suggests that volunteers may be unwilling to wait a period of weeks following training for their role to start (in this case, for there to be sufficient clients to form a friendship group). This indicates a key threat to the successful implementation of volunteer-led interventions co-ordinated by the voluntary sector and to their evaluation in RCTs, which will be met only by more committed and supportive management by volunteer co-ordinators and by the availability of ongoing training.
Other studies evaluating interventions to address loneliness
One of the key aims of the study was to examine the benefits of an intervention that may allay loneliness. Since the start of our study, two systematic reviews of RCTS evaluating interventions to reduce social isolation have been conducted. The first, by Dickens et al. ,109 aimed to evaluate interventions designed to reduce social isolation and loneliness in older people. The review included studies of group and one-to-one interventions, with 79% and 55%, respectively, reporting at least one improved participant outcome. The review found two studies that involved telephone interventions. A quasi-experimental study that examined 1-hour group telephone support for blind community-dwelling older people in the USA reported reduced loneliness and an increased number of social activities at 8 weeks. 110 The intervention is described as ‘short-term problem-solving and discussion of coping methods’. The second study reported that one-to-one telephone support for low-income housing residents in the USA did not result in a reduction in the level of self-reported loneliness compared with no intervention. 26 Only one study included in this review combined one-to-one approaches with group approaches to combat social isolation; this was in caregivers to people with Alzheimer’s disease in the USA. 111 The reviewers concluded that the evidence base needs to be improved by carrying out well-conducted studies. They did indicate that ‘common characteristics of effective interventions may include having a theoretical basis, and offering social activity and/or support within a group format’. The reviewers also noted that interventions that include older people as ‘active participants also appeared more likely to be effective’ (p. 20). 109 These primary research studies, all of which were classified by the reviewers as at high risk of bias,109 confirm that the combination approach to intervention (one-to-one plus group befriending) was relatively novel and that our study is one of the better designed and conducted of its type.
The second systematic review, by Masi et al. ,112 evaluated four primary intervention strategies. Four trials evaluating social cognitive training interventions showed greater effect sizes than 12 trials of interventions to enhance social support, two trials of interventions to improve social skills and two trials of interventions to increase opportunities for social interaction. Potential modifiers of effect, such as group-based format or the use of technology, were not found to be statistically significant. The reviewers concluded that ‘simply bringing lonely people together may not result in new friendships because the thoughts and behaviours of lonely individuals make them less attractive to one another as relationship partners’ (p. 257). 113 On the other hand, ‘correcting maladaptive social cognition (for instance through CBT [cognitive–behavioural therapy]-style interventions) offers the best chance for reducing loneliness’ (p. 259). 113 This review, then, provides a question mark over the value of befriending interventions that do not involve an active psychological component intended to induce behaviour change. This said, it is far from clear that cognitive–behavioural approaches can address precursors of loneliness such as bereavement,113 and our research team shares the concerns of those who counsel against the medicalisation of commonplace experiences such as loneliness. 114,115 Even if one accepts the research findings of Masi et al. ,112 financial constraints and policy decisions by state health providers mean that access to trained cognitive–behavioural therapists is limited and available only within stepped-care models for those with more serious mental health problems. 116 Given the ability of volunteers to faithfully deliver quite basic group facilitation, when trained within typical voluntary sector financial constraints, it seems unlikely that widespread and systematic access to more psychologically sophisticated behaviour change interventions is feasible for the alleviation of loneliness, even if they do have an impact.
Previous studies evaluating interventions to prevent loneliness and social isolation have been criticised for failing to publish data on organisational set-up and implementation costs. 53,109 Although we were unable to conduct a full cost-effectiveness analysis as part of our study, a strength of our report is that it does include cost impact data.
Implications for providers and policy-makers
Our research does not provide definitive evidence that telephone befriending is an effective way to alleviate loneliness in community-dwelling older people. The key implications for those considering commissioning a befriending intervention relate to three challenges: the recruitment and retention of volunteers; the buy-in of local providers for the management and support of volunteers; and the ability of providers to match clients with similar interests and identities in groups.
The recruitment of large numbers of volunteers from a given locality in a short space of time is a challenging prospect for volunteer co-ordinators of small or local franchises of voluntary sector organisations. For an intervention such as telephone befriending, in which face-to-face contact is not necessary, one solution may be to outsource to a provider who is experienced in and resourced for the recruitment and retention of volunteers and able to provide the training, support and oversight that the intervention entails (see Other studies involving volunteer provision). Community Network recruit and retain volunteers to befriend people with a view to preventing loneliness. In 2012–13, Community Network trained 126 volunteer facilitators for its funded projects, working in partnership with other organisations, and ran 38 telephone befriending groups across different projects. It provided a teleconferencing infrastructure with or without support training according to resources. Some host charities already use volunteers as well as infrastructure sourced through Community Network (Angela Cairns, Community Network, 1 July 2013, personal communication).
The difficulties experienced by the service provider and volunteers in delivering the intervention per protocol, or in being responsive to the declared wishes of the participants (see Perspectives on the intervention from the group therapy intervention literature), reflect both organisational and individual capacities and capabilities. In signing the contract the service provider seems to have overestimated its ability to recruit and retain sufficient numbers to a timetable that was contingent on the availability of a professional group facilitation trainer (see Chapter 3, The contract with the service provider, item 2) or to provide cover for groups (see Chapter 3, The contract with the service provider, item 4). The service provider did not feel equipped to co-ordinate the intervention, specifying that volunteers would be responsible for scheduling calls with clients (see Chapter 3, The contract with the service provider, item 3). Certain aspects of the contract between the University of Sheffield and the service provider could have been more specific, for example the contract included a requirement that the service provider ‘provide ongoing “mentoring” to volunteers’, but the minimum frequency, duration or content of mentoring could have been better described (see Chapter 3, The contract with the service provider, item 5). The needs of volunteers were sometimes wide-ranging; those who were interviewed reported not knowing whom to contact with queries about client management, and appeals of this nature were directed to the study team.
The problems that the service provider had with accepting ownership of the intervention may have resulted in part from the unusual nature of how it was established within the service, as part of a robust, university-led research study. This undoubtedly led to unrealistic promises being made by the service provider and may have caused some uncertainty and anxiety among those then charged with delivering what had been agreed. Our study aimed to recruit 30 volunteers to deliver telephone befriending to 20 groups of six people over 1 year in one urban centre. By comparison, the RNIB, a charity with a national command and control structure, maintains 90 volunteers, running 100 groups of six people UK wide. 108 It has been able to build this capacity up over a period of > 10 years, using a strict, centrally agreed and disseminated intervention protocol, in a way that is likely to be beyond small, locally based, independently constituted voluntary sector organisations. Also, such organisations that have existing successful telephone befriending services have committed to the intervention as part of their portfolio of activity and properly resourced it. It follows that researchers and policy-makers wishing to roll out evidence-based interventions for older people should form partnerships with large-scale organisations in which volunteer co-ordinators are empowered and sufficiently resourced and take responsibility for bridging ‘the gap between organisational bureaucracy and communities’ (p. 237). 117 It is also important to consider the role of researchers as intervention innovators – is this appropriate or is it more acceptable and feasible to evaluate services that are already well established outside of research?
Successful group interventions require participants to identify with a common purpose. 31,57 In the absence of an active psychological component, some may feel that there is a need to match clients based on shared values, needs or experiences. This is also true for successful, large-scale telephone befriending services, for example the RNIB aims to match adults with sight loss with others with similar interests108 and Community Network aims to bring retired seafarers together. 118 Both the RNIB and Community Network use paid staff to match participants to groups as it is a skilled and time-consuming activity. Arguably, this matching of interests becomes even more difficult in programmes supporting essentially healthy populations, such as older people at risk of loneliness, with no obvious pre-existing work-related or social connections. With no geographical limits on telephone befriending, the identification and interest matching of participants might be more easily achieved through a national approach, with members of any friendship group drawn from diverse areas of the country, if this was acceptable to participants.
Implications for researchers and funders
The scope of this research was identified, prioritised and commissioned by the National Institute for Health Research Public Health Research programme. In common with the design of a number of other contemporary psychosocial studies, the research involved modelling a new complex intervention and embedding it into a service with accompanying rigorous evaluation.
Considerations for future service evaluation and research are summarised in the following sections.
Service development and implementation
In common with the findings from previous research,53,117 we found that the successful implementation of a service that aims to reduce loneliness requires strong partnership arrangements with commissioners and other providers. The scale of operation of individual third-sector organisations, such as the local provider involved in this study, means that, for any intervention to be delivered to more than a small number of individuals, partnership and cross-agency working is essential.
To demonstrate future sustainability, funding to deliver the intervention had to be identified from organisations that might feasibly provide such a service. Identifying funding for an intervention to meet needs that currently fall outside the remit of existing statutory service provision proved challenging, with third-sector organisations being the only avenue available. This provides some indication of the extent of change that is necessary within both statutory and non-statutory services to meet the current and future needs of an ageing population. The difficulty of identifying people who are lonely and isolated was a factor in recruitment to this study but is also an important consideration for services that aim to meet their needs.
Our findings supports those of a previous Delphi survey which indicated that the sustainability and scalability of telephone befriending services is predicated on sufficient time and resources being dedicated to administer the service. 24 The results of this research demonstrate the deleterious impact of insufficient resources being allocated to volunteer recruitment and ongoing support. After the study closed it emerged that the number of volunteers required for this study equated to the existing total volunteer workforce of the service provider. Therefore, capacity to support the volunteers would have had to double to take into account the needs of the study. The problems resulting from over-reliance on the good will of one or two individuals to scale up services was evident.
The intervention delivered through this study necessitated volunteer participation in mandatory training to prepare them to deliver specific skills. This level of demand can negatively impact on volunteer turnover, with retention then demanding a higher level of resources from the host organisation. 119 Additionally, delivering services that are evidence based is arguably more likely to involve structured and possibly specialised training. This offers greater opportunities for a volunteer workforce who may be looking to improve skills and gain valuable experience for paid work but also places greater resource demands on the host, particularly when a high turnover of volunteers exists. Therefore, the sustainability of such a workforce and what it might deliver can be fragile, emphasising the need to determine the true resource implications of using volunteers to deliver services.
Research
The intervention designed, implemented and evaluated in this study was intended for lonely and isolated older people, particularly the housebound. The process of recruitment confirmed the difficulty of reaching out to these individuals. Substantial efforts were made to involve relevant health and social care professionals in the process of recruitment. However, this was unsuccessful and few people were identified through this route for potential participation. The reasons for lack of recruitment through front-line professionals can be postulated, even though we were not able to pursue this, for example negative connotations of randomisation, lack of time to explain the study, low on list of priorities. In ideal circumstances the study timeline would provide scope to be able to ameliorate such barriers, and resources would be available to be able to recruit through communities, which can be a successful strategy. Nevertheless, in this instance it proved necessary to use mass mail-outs to potential recruits through GP surgeries to meet the target numbers in the available time. Questions remain regarding how to effectively reach those in need of such an intervention. This is important given the indications of benefit that this research identified.
The need to take time to embed such an intervention into day-to-day practice before subjecting it to rigorous evaluation has been illustrated. Other studies that comprise the development and evaluation of a complex intervention can involve further pilot work or a multistage programme with clear interim progression criteria. This is beneficial when there are a large number of factors involved in both service delivery and the associated research. Quite early in this study it became clear that the demands of the research eroded the already limited capacity of the service provider to organise intervention delivery. Also, study requirements involved protocolisation and randomisation, which is counter to the philosophy of reduced bureaucracy and creating community capital that can exist within charitable organisations. 117 Conversely, it was evident that the idiosyncrasies of the delivery site challenged study progression.
This research demonstrated that a definitive RCT comparing telephone befriending with no telephone befriending is feasible. However, overall success was dependent on two recruitment targets, the first being for older people as participants and the second being for volunteers who were suitable to be trained and supported in a facilitation role. Future research involving volunteers needs to take account of this dual recruitment target. A number of other issues with the implementation of such a trial are worthy of mention to inform the design of future studies.
Was it realistic to expect a franchised third-sector provider to introduce a new intervention and support individuals to deliver it at scale in the manner attempted through this study? Our results would indicate not in the short to medium term. Two other UK voluntary sector organisations are successful in achieving larger-scale delivery of telephone befriending but they have been able to build this capacity over many years and both have paid staff dedicated to running the service and supporting the volunteer workforce. The findings of this study suggest that reduced ambition is necessary to match the capabilities of the programmes under evaluation and there might be benefit in including research to determine the service models that can lead to successful delivery of community-based interventions within constrained finances. However, if funders and researchers deem a full-scale pragmatic trial an appropriate step, then it should be multicentre and, to minimise the risk of intervention failure, use established services already operating at scale, when intervention funding allows. Additionally, there are issues regarding the extent to which intervention components should be standardised and the degree of local adaptation that is acceptable to meet the real-world challenges of delivery.
Research recommendations
As already stated, if funders and researchers deem a full-scale pragmatic trial an appropriate next step, then it should be multicentre and, to minimise the risk of intervention failure, use established services already operating at scale, when intervention funding allows.
If funders and researchers deem further feasibility/pilot work appropriate we recommend that methodological research should be undertaken to inform future trials evaluating specially commissioned volunteer-led services. Mixed-methods research, combining literature review, a time-and-motion study and qualitative research, should be commissioned to record how, and over what period of time, it is possible to develop and sustain large-scale, volunteer-led befriending programmes. Observation of pre-existing, successful, scaled-up and routinely delivered voluntary sector services could help commissioners, policy-makers and researchers understand how the training and management of volunteers can be optimised as well as establish realistic expectations for intervention delivery and fidelity.
Chapter 7 Conclusions
The quantitative findings of this study suggest that, compared with no intervention, TF groups might sustain mental health in community-dwelling older people within a clinically relevant range. However, we were not able to deliver the intervention as specified in the protocol to the majority of participants, which led to early termination of the study. Participant recruitment, retention and safety and intervention acceptability do not present barriers to the definitive RCT needed to replicate these results. Questions remain regarding how to maintain a sufficient number of volunteers to deliver such an intervention and how to resource its management, as well as what techniques and procedures it is reasonable to expect volunteers to learn and deliver.
Before progressing to a full trial evaluating this or a similar intervention, further research may be required to optimise the recruitment and retention of volunteers for the delivery of interventions to address social isolation. In particular, the rates of recruitment and retention of volunteers achieved by different organisational models should be compared to allow realistic planning of future RCTs to evaluate health and social care interventions by the voluntary sector.
Acknowledgements
We gratefully acknowledge support and advice from the following: Professor Jon Nicoll, University of Sheffield, as sponsor representative; James Goodwin, Age UK; Julie Howe, Expert Elders Network; the service provider and volunteers for intervention delivery; Mike Bradburn, Tim Chater, Amanda Loban, Karen Beck and Lauren O’Hara, Sheffield CTRU, for support and advice on statistical, data management and administrative concerns; Mark Berkeley, RNIB, for information concerning the Talk and Support telebefriending scheme; and Pat Linck, University of Bangor, for advice on administering the REMCARE health and social care resource use questionnaire.
We offer special thanks to the members of our two oversight committees, the TSC and the Data Monitoring and Ethics Committee (DMEC): Yvonne Birks (Chair of the TSC), Professor of Health and Social Care, University of York; Louise Robinson, Professor of Primary Care and Ageing, University of Newcastle; Chris Armitage, Professor of Health Psychology, University of Manchester; Joan Hubbard, Expert Elders Network; Catherine Hewitt (Chair of the DMEC), Senior Statistician, University of York; Georgina Charlesworth, Lecturer, University College London; Karen Spilsbury, Chair in Nursing, University of York; and Kim Cocks, Acting Chair and Senior Statistician, University of York.
Contribution of authors
Daniel Hind (Assistant Director, CTRU) contributed to the concept and design of the trial and qualitative substudies, contributed to the qualitative research analysis and prepared results for publication.
Gail Mountain (Professor of Health Services Research – Assistive Technology) contributed to the concept and design of the trial, took day-to-day responsibility for its management, chaired the trial management group and took part in preparing the report for publication.
Rebecca Gossage-Worrall (Trial Co-ordinator/Research Associate) contributed to the concept and design of the fidelity assessment, conducted data collection and analysis of qualitative participant and volunteer interviews and fidelity assessment and prepared results for publication.
Stephen J Walters (Professor of Medical Statistics and Clinical Trials) contributed to the concept and design of the trial, conducted the statistical analysis and prepared results for publication.
Rosie Duncan (Research Assistant) conducted candidate screening, participant recruitment and data collection for the RCT and participant interviews, contributed to the qualitative analysis and took part in preparing the report for publication.
Louise Newbould (Research Assistant) conducted candidate screening, participant recruitment and data collection for the RCT and fidelity assessment.
Saleema Rex (Data Manager) contributed to the statistical analysis of the main trial results.
Carys Jones (Health Economist) conducted the review of health economic data.
Ann Bowling (Professor of Health Sciences) contributed to the concept and design of the main trial and took part in preparing the report for publication.
Mima Cattan (Professor in Public Health – Knowledge Translation) contributed to the concept and design of the main trial and qualitative substudies and took part in preparing the report for publication.
Angela Cairns (Chief Executive Officer) contributed to the preparation of the report for publication.
Cindy Cooper (Director of CTRU) contributed to the concept and design of the trial and took part in preparing the report for publication.
Elizabeth Goyder (Professor of Public Health) contributed to the concept and design of the trial and prepared the report for publication.
Rhiannon Tudor Edwards (Professor of Health Economics) contributed to the concept and design of the cost-effectiveness element of the main trial and the review of the health economic analysis, and took part in preparing the report for publication.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
Publications
Mountain GA, Hind D, Gossage-Worrall R, Walters SJ, Duncan R, Newbould L, et al. ‘Putting Life in Years’ (PLINY) telephone friendship groups research study: pilot randomised controlled trial. Trials 2014;15:141.
References
- Luanaigh CO, Lawlor BA. Loneliness and the health of older people. Int J Geriatr Psychiatry 2008;23:1213-21. http://dx.doi.org/10.1002/gps.2054.
- Hawkley L, Cacioppo J. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med 2010;40:218-27. http://dx.doi.org/10.1007/s12160-010-9210-8.
- Nummela O, Seppänen M, Uutela A. The effect of loneliness and change in loneliness on self-rated health (SRH): a longitudinal study among aging people. Arch Gerontol Geriatr 2011;53:163-7. http://dx.doi.org/10.1016/j.archger.2010.10.023.
- Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging 2010;25:132-41. http://dx.doi.org/10.1037/a0017805.
- O’Luanaigh C, O’Connell H, Chin AV, Hamilton F, Coen R, Walsh C, et al. Loneliness and vascular biomarkers: the Dublin Healthy Ageing Study. Int J Geriatr Psychiatry 2012;27:83-8. http://dx.doi.org/10.1002/gps.2695.
- Smith SS, Kozak N, Sullivan KA. An investigation of the relationship between subjective sleep quality, loneliness and mood in an Australian sample: can daily routine explain the links?. Int J Soc Psychiatry 2012;58:166-71. http://dx.doi.org/10.1177/0020764010387551.
- A Sure Start to Later Life; Ending Inequalities for Older People. London: Office of the Deputy Prime Minister; 2006.
- Older People’s Day 2011. London: Office for National Statistics; 2011.
- Greenfield EA, Russell D. Identifying living arrangements that heighten risk for loneliness in later life: evidence from the US National Social Life, Health, and Aging Project. J Appl Gerontol 2011;30:524-34. http://dx.doi.org/10.1177/0733464810364985.
- Franklin A, Tranter B. Housing, Loneliness and Health. Melbourne: Australian Housing and Urban Research Institute; 2011.
- The Forgotten Age: Understanding Poverty and Social Exclusion in Later Life. London: Centre for Social Justice; 2010.
- Victor C, Scrambler S, Bond J. The Social World of Older People: Understanding Loneliness and Social Isolation in Later Life. Maidenhead: Open University Press/McGraw-Hill; 2009.
- Cann P. Safeguarding the Convoy. Oxford: Campaign to End Loneliness/Age UK; 2011.
- Alma MA, Van der Mei SF, Feitsma WN, Groothoff JW, Van Tilburg TG, Suurmeijer TPBM. Loneliness and self-management abilities in the visually impaired elderly. J Aging Health 2011;23:843-61. http://dx.doi.org/10.1177/0898264311399758.
- Promoting Mental Health and Wellbeing in Later Life: a First Report into the UK Enquiry into Mental Health and Wellbeing in Later Life. London: Age Concern and Mental Health Foundation; 2006.
- Wenger GC, Davies R, Shahtahmasebi S, Scott A. Social isolation and loneliness in old age: review and model refinement. Ageing Soc 1996;16:333-58. http://dx.doi.org/10.1017/S0144686X00003457.
- Victor CR, Scambler SJ, Bowling A. The prevalence of, and risk factors for, loneliness in later life: a survey of older people in Great Britain. Ageing Soc 2005;25:357-75. http://dx.doi.org/10.1017/S0144686X04003332.
- Guidance on Occupational Therapy and Physical Activity Interventions that Promote Good Health and Wellbeing in Older People. London: NICE; 2008.
- Active Ageing: a Policy Framework. Geneva: World Health Organization; 2002.
- Godfrey M, Townsend J, Denby T. Building a Good Life for Older People in Local Communities. York: Joseph Rowntree Foundation; 2004.
- Windle G, Hughes D, Linck P, Morgan R, Burholt V, Edwards RT, et al. Public Health Interventions to Promote Mental Well-being in People Aged 65 and Over: Systematic Review of Effectiveness and Cost-Effectiveness. Bangor: University of Wales; 2007.
- Glass TA, De Leon CM, Marottoli RA, Berkman LF. Population based study of social and productive activities as predictors of survival among elderly Americans. BMJ 1999;319:478-83. http://dx.doi.org/10.1136/bmj.319.7208.478.
- Cattan M, White M, Bond J, Learmouth A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing Soc 2005;25:41-67. http://dx.doi.org/10.1017/S0144686X04002594.
- Cattan M, Kime N, Bagnall AM. Low-Level Support for Socially Isolated Older People: an Evaluation of Telephone Befriending. Leeds: Leeds Metropolitan University; 2008.
- Cattan M, Kime N, Bagnall AM. The use of telephone befriending in low level support for socially isolated older people – an evaluation. Health Soc Care Community 2011;19:198-206.
- Heller K, Thompson MG, Trueba PE, Hogg JR, Vlachos-Weber I. Peer support telephone dyads for elderly women: was this the wrong intervention?. Am J Community Psychol 1991;19:53-74. http://dx.doi.org/10.1007/BF00942253.
- Foresight Mental Capital and Wellbeing Project: Final Project Report. London: Government Office for Science; 2008.
- de Jong-Gierveld J. Personal relationships, social support, and loneliness. J Soc Pers Relat 1989;6:197-221. http://dx.doi.org/10.1177/026540758900600204.
- Bandura A. Self-Efficacy: the Exercise of Control. New York, NY: Freeman; 1997.
- Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B, et al. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a2390.
- Corey MS, Corey G. Groups: Process and Practice. Pacific Grove, CA: Brooks/Cole; 1997.
- Maruish ME. User’s Manual for the SF-36v2 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2011.
- Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JB, deGruy FV, et al. Health-related quality of life in primary care patients with mental disorders. JAMA 1995;274:1511-17. http://dx.doi.org/10.1001/jama.1995.03530190025030.
- Brazier J, Ratcliffe J, Salomon JA, Tsuchiya A. Measuring and Valuing Health Benefits for Economic Evaluation. Oxford: Oxford University Press; 2007.
- Schwarzer R, Jerusalem M, Weinman J, Wright S, Johnston M. Measures in Health Psychology: a User’s Portfolio. Causal and Control Beliefs. Windsor, UK: NFER-Nelson; 1995.
- de Jong-Gierveld J, Kamphuls F. The development of a Rasch-type loneliness scale. Appl Psychol Meas 1985;9:289-99. http://dx.doi.org/10.1177/014662168500900307.
- Tinkler L, Hicks S. Measuring Subjective Well-being. London: ONS; 2011.
- Woods RT, Bruce E, Edwards RT, Elvish R, Hoare Z, Hounsome B, et al. REMCARE: reminiscence groups for people with dementia and their family caregivers – effectiveness and cost-effectiveness pragmatic multicentre randomised trial. Health Technol Assess 2012;16. http://dx.doi.org/10.3310/hta16480.
- Walters SJ, Munro JF, Brazier JE. Using the SF-36 with older adults: a cross-sectional community-based survey. Age Ageing 2001;30:337-43. http://dx.doi.org/10.1093/ageing/30.4.337.
- Ware JEJ, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston, MA: Health Institute, New England Medical Centre; 1993.
- Structure and Content of Clinical Study Reports. Geneva: ICH E3; 2010.
- Burgess DC, Gebski VJ, Keech AC. Baseline data in clinical trials. Med J Aust 2003;179:105-7.
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Clin Oral Investig 2003;7:2-7.
- Pocock SJ, Assmann SE, Enos LE, Kasten LE. Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practice and problems. Stat Med 2002;21:2917-30. http://dx.doi.org/10.1002/sim.1296.
- Senn S. Testing for baseline balance in clinical trials. Stat Med 1994;13:1715-26. http://dx.doi.org/10.1002/sim.4780131703.
- Walters SJ. Quality of Life Outcomes in Clinical Trials and Health-Care Evaluation: a Practical Guide to Analysis and Interpretation. Chichester: Wiley; 2009.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57.
- Ritchie J, Spencer L, O’Connor W, Ritchie J, Lewis J. Qualitative Research Practice: a Guide for Social Science Students and Researchers. London: Sage; 2003.
- Pope N, Zeibland S, Mays N, Pope C, Mays N. Qualitative Research in Health Care. Oxford: Blackwell; 2006.
- O’Cathain A, Thomas K, Pope C, Mays N. Qualitative Research in Health Care. Oxford: Blackwell; 2006.
- Glaser BG, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine; 1967.
- A Framework for Development and Evaluation of RCTs for Complex Interventions to Improve Health. London: Medical Research Council; 2008.
- Windle K, Francis J, Coomber C. Preventing Loneliness and Social Isolation: Interventions and Outcomes. London: Social Care Institute for Excellence; 2011.
- Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 2004;23:443-51. http://dx.doi.org/10.1037/0278-6133.23.5.443.
- De Jong Gierveld J, Tilburg T. The De Jong Gierveld short scales for emotional and social loneliness: tested on data from 7 countries in the UN generations and gender surveys. Eur J Ageing 2010;7:121-30. http://dx.doi.org/10.1007/s10433-010-0144-6.
- Nelson MC, Cordray DS, Hulleman CS, Darrow CL, Sommer EC. A procedure for assessing intervention fidelity in experiments testing educational and behavioral interventions. J Behav Health Serv Res 2012;39:374-96. http://dx.doi.org/10.1007/s11414-012-9295-x.
- Yalom ID, Leszcz M. The Theory and Practice of Group Psychotherapy. New York, NY: Basic Books; 2005.
- de Lichtenberg J, London M. Evaluating group interventions: a framework for diagnosing, implementing, and evaluating group interventions. Group Facil 2008;9:37-48.
- Spilker B, Cramer JA. Patient Recruitment in Clinical Trials. New York, NY: Raven; 1991.
- Forster SE, Jones L, Saxton JM, Flower DJ, Foulds G, Powers HJ, et al. Recruiting older people to a randomised controlled dietary intervention trial – how hard can it be?. BMC Med Res Methodol 2010;10. http://dx.doi.org/10.1186/1471-2288-10-17.
- Scott E, Dimairo M, Hind D, Goyder E, Copeland R, Breckon J, et al. ‘Booster’ interventions to sustain increases in physical activity in middle-aged adults in deprived urban neighbourhoods: internal pilot and feasibility study. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-129.
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322-7. http://dx.doi.org/10.2105/AJPH.89.9.1322.
- Ferrucci L, Guralnik JM, Studenski S, Fried LP, Cutler GB, Walston JD, et al. Designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons: a consensus report. J Am Geriatr Soc 2004;52:625-34. http://dx.doi.org/10.1111/j.1532-5415.2004.52174.x.
- Pitkala KH, Routasalo P, Kautiainen H, Tilvis RS. Effects of psychosocial group rehabilitation on health, use of health care services, and mortality of older persons suffering from loneliness: a randomized, controlled trial. J Gerontol A Biol Sci Med Sci 2009;64A:792-800. http://dx.doi.org/10.1093/gerona/glp011.
- Sackett DL. Bias in analytic research. J Chronic Dis 1979;32:51-63. http://dx.doi.org/10.1016/0021-9681(79)90012-2.
- de Jong-Gierveld J, Tilburg TV. Manual of the Loneliness Scale. Amsterdam: VU University, Faculty of Social Sciences, Department of Sociology; 1999.
- Scholz U, Doña, BG, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur J Psychol Assess 2002;18:242-51. http://dx.doi.org/10.1027//1015-5759.18.3.242.
- Wann DL, Ensor CL. The psychological health of ‘joiners’. Psychol Rep 2001;89. http://dx.doi.org/10.2466/pr0.2001.89.1.122.
- Nederhof AJ. Methods of coping with social desirability bias: a review. Eur J Soc Psychol 1985;15:263-80. http://dx.doi.org/10.1002/ejsp.2420150303.
- Hind D, O’Cathain A, Cooper CL, Parry GD, Isaac CL, Rose A, et al. The acceptability of computerised cognitive behavioural therapy for the treatment of depression in people with chronic physical disease: a qualitative study of people with multiple sclerosis. Psychol Health 2009;25:699-712. http://dx.doi.org/10.1080/08870440902842739.
- Fox KR, Stathi A, McKenna J, Davis MG. Physical activity and mental well-being in older people participating in the Better Ageing Project. Eur J Appl Physiol 2007;100:591-602. http://dx.doi.org/10.1007/s00421-007-0392-0.
- O’Cathain A, Murphy E, Nicholl J. Multidisciplinary, interdisciplinary, or dysfunctional? Team working in mixed-methods research. Qual Health Res 2008;18:1574-85. http://dx.doi.org/10.1177/1049732308325535.
- Craig C, Mountain G. Lifesyle Matters: an Occupational Approach to Healthy Ageing. Bicester: Speechmark; 2007.
- Rapport F, Storey M, Porter A, Snooks H, Jones K, Peconi J, et al. Qualitative research within trials: developing a standard operating procedure for a clinical trials unit. Trials 2013;14. http://dx.doi.org/10.1186/1745-6215-14-54.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud 2013;50:587-92. http://dx.doi.org/10.1016/j.ijnurstu.2012.09.010.
- Petty TL. Don’t just do something and stand there!. Arch Intern Med 1979;139:920-1. http://dx.doi.org/10.1001/archinte.1979.03630450062020.
- Doust J, Del Mar C. Why do doctors use treatments that do not work?. BMJ 2004;328:474-5. http://dx.doi.org/10.1136/bmj.328.7438.474.
- Carron AV, Brawley LR. Cohesion: conceptual and measurement issues. Small Group Res 2012;43:726-43. http://dx.doi.org/10.1177/1046496412468072.
- Latané B. The psychology of social impact. Am Psychol 1981;36:343-56. http://dx.doi.org/10.1037/0003-066X.36.4.343.
- Lester H, Mead N, Graham CC, Gask L, Reilly S. An exploration of the value and mechanisms of befriending for older adults in England. Ageing Soc 2012;32:307-28. http://dx.doi.org/10.1017/S0144686X11000353.
- Mead N, Lester H, Chew-Graham C, Gask L, Bower P. Effects of befriending on depressive symptoms and distress: systematic review and meta-analysis. Br J Psychiatry 2010;196:96-101. http://dx.doi.org/10.1192/bjp.bp.109.064089.
- Charlesworth G, Shepstone L, Wilson E, Reynolds S, Mugford M, Price D, et al. Befriending carers of people with dementia: randomised controlled trial. BMJ 2008;336:1295-7. http://dx.doi.org/10.1136/bmj.39549.548831.AE.
- Wilson J. Volunteering. Annu Rev Sociol 2000;26:215-40. http://dx.doi.org/10.1146/annurev.soc.26.1.215.
- Smith K, Cordery CJ. What Works? A Systematic Review of Research and Evaluation Literature on Encouragement and Support of Volunteering 2011. www.communitymatters.govt.nz/vwluResources/publications-lottery-WhatWorksVolunteering/$file/publications-lottery-WhatWorksVolunteering.pdf (accessed 31 May 2013).
- Bussell H, Forbes DL. The volunteer life cycle: a marketing model for volunteering. Voluntary Action 2003;5:61-79.
- Locke M, Ellis A, Smith JD. Hold on to what you’ve got: the volunteer retention literature. J Soc Serv Res 2003;20:73-97.
- Lister R. The dilemmas of pendulum politics: balancing paid work, care and citizenship. Econ Soc 2002;31:520-32. http://dx.doi.org/10.1080/0308514022000020661.
- Conservative Party . Invitation to Join the Government of Britain: The Conservative Manifesto 2010 n.d. www.conservatives.com/∼/media/files/activist%20centre/press%20and%20policy/manifestos/manifesto20102010 (accessed 1 June 2013).
- Davies JS, Pill M. Empowerment or abandonment? Prospects for neighbourhood revitalization under the big society. Public Money Manag 2012;32:193-200. http://dx.doi.org/10.1080/09540962.2012.676276.
- Evans D. The Big Society needs robust public health evaluation. J Public Health 2011;33:11-2. http://dx.doi.org/10.1093/pubmed/fdr007.
- Heath I. Life and death. How far is it from no society to Big Society and back again?. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d303.
- Hunter DJ. Is the Big Society a Big Con?. J Public Health 2011;33:13-4. http://dx.doi.org/10.1093/pubmed/fdr009.
- Kisby B. The Big Society: power to the people?. Polit Q 2010;81:484-91. http://dx.doi.org/10.1111/j.1467-923X.2010.02133.x.
- Ransome P. ‘The Big Society’ fact or fiction? – a sociological critique. Sociol Res Online 2011;16. http://dx.doi.org/10.5153/sro.2383.
- Bone JD. The neoliberal phoenix: the Big Society or business as usual. Sociol Res Online 2012;17. http://dx.doi.org/10.5153/sro.2687.
- Corbett S, Walker A. The Big Society: back to the future. Polit Q 2012;83:487-93. http://dx.doi.org/10.1111/j.1467-923X.2012.02338.x.
- Levitas R. The just’s umbrella: austerity and the Big Society in coalition policy and beyond. Crit Soc Policy 2012;32:320-42. http://dx.doi.org/10.1177/0261018312444408.
- Sullivan H. Debate: a Big Society needs an active state. Policy Polit 2012;40:145-8. http://dx.doi.org/10.1332/147084411X581925.
- Kane D, Allen J. Counting the Cuts. London: National Council for Voluntary Organisations; 2011.
- Milbourne L, Cushman M. From the third sector to the big society: how changing UK government policies have eroded third sector trust. Voluntas 2013;24:485-508. http://dx.doi.org/10.1007/s11266-012-9302-0.
- Pattie C, Johnston R. How big is the Big Society?. Parliam Aff 2011;64:403-24. http://dx.doi.org/10.1093/pa/gsr013.
- Alexander J. An Investigation into the Premature Wastage of Special Constables. London: HMSO; 2000.
- Gaston K, Alexander J. Effective organisation and management of public sector volunteer workers: police special constables. Int J Public Sect Manage 2001;14:59-74. http://dx.doi.org/10.1108/09513550110387075.
- Hidalgo MC, Moreno P. Organizational socialization of volunteers: the effect on their intention to remain. J Community Psychol 2009;37:594-601. http://dx.doi.org/10.1002/jcop.20317.
- Dennis CL. Breastfeeding peer support: maternal and volunteer perceptions from a randomized controlled trial. Birth 2002;29:169-76. http://dx.doi.org/10.1046/j.1523-536X.2002.00184.x.
- Stirling C, Kilpatrick S, Orpin P. A psychological contract perspective to the link between non-profit organizations’ management practices and volunteer sustainability. Hum Resource Dev Int 2011;14:321-36. http://dx.doi.org/10.1080/13678868.2011.585066.
- Fahey C. Training can be a recruitment and retention tool for emergency service volunteers. Aust J Emerg Manage 2002;17:3-7.
- Royal National Institute for the Blind . RNIB Telebefriending Service n.d. www.rnib.org.uk/services-we-offer-advice-and-support-services-talk-and-support/rnib-telebefriending-service (accessed 27 June 2013).
- Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: a systematic review. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-647.
- Evans RL, Jaureguy BM. Phone therapy outreach for blind elderly. Gerontologist 1982;22:32-5. http://dx.doi.org/10.1093/geront/22.1.32.
- Drentea P, Clay OJ, Roth DL, Mittelman MS. Predictors of improvement in social support: five-year effects of a structured intervention for caregivers of spouses with Alzheimer’s disease. Soc Sci Med 2006;63:957-67. http://dx.doi.org/10.1016/j.socscimed.2006.02.020.
- Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev 2011;15:219-66. http://dx.doi.org/10.1177/1088868310377394.
- Currier JM, Holland JM, Neimeyer RA. Do CBT-based interventions alleviate distress following bereavement? A review of the current evidence. Int J Cogn Ther 2010;3:77-93. http://dx.doi.org/10.1521/ijct.2010.3.1.77.
- Murray J, Banerjee S, Byng R, Tylee A, Bhugra D, Macdonald A. Primary care professionals’ perceptions of depression in older people: a qualitative study. Soc Sci Med 2006;63:1363-73. http://dx.doi.org/10.1016/j.socscimed.2006.03.037.
- Crawford R. Healthism and the medicalization of everyday life. Int J Health Serv 1980;10:365-88. http://dx.doi.org/10.2190/3H2H-3XJN-3KAY-G9NY.
- Depression: Management of Depression in Primary and Secondary Care. London: NICE; 2008.
- Kime N, Cattan M, Bagnall AM. The delivery and management of telephone befriending services – whose needs are being met?. Qual Ageing Older Adults 2012;13:231-40. http://dx.doi.org/10.1108/14717791211264278.
- Community Network . Seafarers 2013. http://communitynetworkprojects.org/our-projects/seafarers/ (accessed 24 June 2013).
- Tang F, Morrow-Howell N, Choi E. Why do older adult volunteers stop volunteering?. Ageing Soc 2010;30:859-78. http://dx.doi.org/10.1017/S0144686X10000140.
- Mountain G, Mozley C, Craig C, Ball L. Occupational therapy led health promotion for older people: feasibility of the Lifestyle Matters programme. Br J Occup Ther 2008;71:406-13.
- Jackson J, Mandel D, Blanchard J, Carlson M, Cherry B, Azen S, et al. Confronting challenges in intervention research with ethnically diverse older adults: the USC Well Elderly II Trial. Clin Trials 2009;6:90-101. http://dx.doi.org/10.1177/1740774508101191.
- Brooke P, Bullock R. Validation of a 6 item cognitive impairment test with a view to primary care usage. Int J Geriatr Psychiatry 1999;14:936-40. http://dx.doi.org/10.1002/(SICI)1099-1166(199911)14:11<936::AID-GPS39>3.0.CO;2-1.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 2010;152:726-32. http://dx.doi.org/10.7326/0003-4819-152-11-201006010-00232.
- Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, et al. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy 2009;93:85-92. http://dx.doi.org/10.1016/j.healthpol.2009.07.012.
- Edwards RT, Hounsome B, Linck P, Russell IT. Economic evaluation alongside pragmatic randomised trials: developing a standard operating procedure for clinical trials units. Trials 2008;9. http://dx.doi.org/10.1186/1745-6215-9-64.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials (Handbook for Health Economic Evaluation). Oxford: Oxford University Press; 2007.
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves – facts, fallacies and frequently asked questions. Health Econ 2004;13:405-15. http://dx.doi.org/10.1002/hec.903.
- Ritchie J, Lewis J. Qualitative Research Practice: a Guide for Social Science Students and Researchers. London: Sage; 2003.
- Silverman D. Interpreting Qualitative Data. Methods for Analysing Talk, Text and Interaction. London: Sage; 1997.
- Bandura A. Perceived self-efficacy in cognitive development and functioning. Educ Psychol 1993;28:117-48. http://dx.doi.org/10.1207/s15326985ep2802_3.
- Stewart M, Mann K, Jackson S, Downe-Wamboldt B, Bayers L, Slater M, et al. Telephone support groups for seniors with disabilities. Can J Aging 2001;20:47-72. http://dx.doi.org/10.1017/S0714980800012137.
Appendix 1 Protocol and changes to protocol
| Change to protocol | Progress report | Date | Approved by |
|---|---|---|---|
| Protocol version 2.0 (7 February 2012) approved following request by the REC to complete 6 and 12 month follow-up by telephone (rather than post). Version 1.0 was therefore never approved by the REC | 1 | 17 February 2012 | South Yorkshire REC |
| Protocol version 3.0 (10 April 2012) added an additional document, ‘Telephone Friendship Group Questions and Answers’, for participants allocated to the intervention arm; added an additional procedure to send letters to candidates not eligible due to cognitive impairment; removed partner logos and changed to funder’s template; ISRCTN reference and DMC members added following registration; telephone version of EQ-5D-3L; clarification that 6CIT and screening checklist formed the ‘Eligibility form’ (approved by the REC); and Appendix 2: SAE Checklist (and page 21) changed to ‘. . . last 6 months’. Minor changes to First Contact Form, Response card, General Self–efficacy scale and resource use questionnaires were also included | 2 | 19 April 2012 | South Yorkshire REC |
| Protocol version 4.0 (30 October 2012) added a procedure for sending a letter/e-mail to candidates returning a response card without a telephone number. Use of e-mail for sending Participant Information Sheet and Q&A document and/or making initial contact when no telephone number provided. Added a ‘Contact Card’ for use at end of recruitment; and a minimum of three messages (six calls when no answerphone service is available) and a reminder letter in order to attempt the 6/12 month follow-up. Minor spelling and typographical errors corrected | Not reported (report no. 3 not required) | 21 November 2012 | South Yorkshire REC |
Appendix 2 Participant telephone friendship group: questions and answers
Appendix 3 Putting Life in Years intervention design
Theoretical underpinning
Social isolation and loneliness
The intervention draws on de Jong Gierveld’s loneliness model,28 which is based on a cognitive theoretical approach to loneliness. Characteristic of this approach to loneliness is the emphasis on the discrepancy between what one wants in terms of interpersonal affection and intimacy and what one has; the greater the discrepancy, the greater the loneliness. Importantly, it differentiates between social loneliness and emotional loneliness. Social loneliness refers to the absence of a broader engaging social network of friends and acquaintances, whereas emotional loneliness relates to the absence of an intimate companion.
See http://home.fsw.vu.nl/TG.van.Tilburg/manual_loneliness_scale_1999.htm (accessed 20 June 2013).
Some recent literature distinguishes two aspects of isolation: ‘social disconnectedness’ – a lack of contacts with others and indicated by situational factors, for example small network sizes – and ‘perceived isolation’ – the subjective experience of a shortfall in one’s social resources, for example companionship and support.
The intervention will impact on social and emotional loneliness by reducing the discrepancy between the older person’s relationship expectations (or standards) and his or her cognitive evaluation of the (mis)match between the quality and quantity of existing relationships. 55 The intervention will reduce perceived isolation by improving perceptions of companionship and support.
Self-efficacy refers to the ability to gain and maintain a belief in personal competence or control in achieving various aspects of well-being. The higher a person’s self-efficacy is with respect to obtaining external resources, the more likely it is that the person will undertake those activities and apply the effort needed to do so. 14 A low sense of self-efficacy has been shown to indicate low self-esteem and the potential for depression and feelings of anxiety and helplessness, whereas high levels of self-efficacy will encourage more investment in terms of individual effort and persistence and, ultimately, generate improvements in quality of life.
A declining sense of self-efficacy may often stem more from disuse and negative cultural expectations than from biological ageing and can set in motion self-perpetuating processes that result in lower cognitive and behavioural functioning. Monotonous environments that require little independent thought or judgement diminish the quality of functioning, whereas intellectually challenging ones enhance it (Bandura, 1993). 131 Research suggests that there is a strong association between high self-efficacy and less feelings of loneliness. 14
Bandura’s theory of self efficacy29 describes individuals’ self-belief in coping with adversity in various domains of functioning, such as persistence in the face of barriers and recovery from setbacks, and involves four main approaches: mastery, vicarious (observed) experience, verbal persuasion and perception of affective and physiological states.
Social learning theory states that people’s perceptions of their capabilities (i.e. self-efficacy) affect their behaviour, thinking and emotional reactions in stressful situations. It has been suggested that social learning theory can inform interpretations of behaviour and cognitive change in support/self-help groups. Other people, viewed as role models, can elicit and enhance experiential knowledge based on first-hand experience (p. 51). 132 Social learning theory suggests that there are four requirements for people to learn and adapt behaviour: attention, retention (remembering what one observed), reproduction (ability to reproduce the behaviour) and motivation (good reason) to want to adopt the behaviour. Although the aim of the intervention is to reduce feelings of loneliness, which may be linked to self-efficacy, it is unlikely that we will be able to measure sustainable changes in self-efficacy over the study period. We should also be clear that the purpose of the group discussions on the telephone is not about setting and achieving goals or major behaviour change but about reducing loneliness and social isolation and improving participants’ sense of confidence and mental well-being (in some cases reducing depression).
Intervention components
Before the conversations start
The outline of the six weekly conversations (the intervention) will be described to the potential participants and they will be offered the opportunity to ask questions, raise concerns and make comments. Older people who may benefit from this intervention are recruited through GP practices in ▪. As far as possible, volunteers (befrienders) will be matched to the participants on the basis of common interests and any particular wishes made by the participants. However, befrienders are trained to facilitate conversations such that the older person’s interests are always prioritised. This will avoid any delay in establishing the one-to-one intervention.
The first stage: detail
The first stage, six one-to-one telephone conversations, will take the format of brief (10–20 minutes) friendly conversations about regular everyday events. Three stages are suggested, which will support the older person and also prepare them for the group conversations. The three stages are (1) familiarisation – getting to know each other’s interests and the older person’s expectations; (2) everyday conversation – recent events, sharing experiences, focusing on the positives, but also allowing space for ‘chat’ about the older person’s health, feelings, worries, etc.; and (3) everyday conversation continues with added focus on developing specific conversation topics, such as resources and accessing services, current affairs, television programmes, grandparenting, special interests (gardening, music, etc.). The older person will be encouraged to raise these topics in the ensuing group sessions.
The one-to-one sessions are not intended as professional counselling sessions. Should this need become apparent (expressed by the older person), the volunteer will, without breaking confidentiality, raise it with the volunteer co-ordinator and an individualised solution will be proposed (referring him or her back to the recruiting charity, providing him or her with a named contact for support).
It is important that the older person who is the recipient of the telephone call is in control of the topics discussed. However, the befriending volunteer will guide the conversations through the three stages, which may not always happen neatly in this sequence but are likely to be covered over the six sessions.
At the end of each conversation, the volunteer and the older person agree the time and date when the next conversation will take place.
Should an individual not wish to move on to participate in group conversations, the host charity will be asked if it has the capacity to continue providing a one-to-one befriending service for the individual. This option will not be offered at the start of the programme as an alternative to the group conversation. It will be considered only in those situations in which an individual expressly states that he or she does not wish to continue in a group.
Week 1
The volunteer introduces her/himself and the participant also introduces her/himself.
The volunteer ensures that the older person understands the purpose of the telephone conversation and asks about his or her expectations. Ground rules, for example confidentiality, boundaries about what is/is not discussed, what happens if the need for professional help is expressed, and the right to withdraw from the study are agreed. The time scale of the conversations and the ensuing group conversations is explained.
The volunteer facilitates an open conversation to ‘get to know each other’ (this could be talking about memories) and to find common interests. The befriender may encourage the older person to talk about his or her aspirations for this intervention and what he or she is hoping to get out of it. The befriender may also explore any concerns or fears that the older person may have and discuss how these might be overcome.
The conversation is concluded by the volunteer preparing the older person for the ‘finish’ and reminding him or her of the next ‘date’.
Week 2
Following greetings the volunteer enquires about the participant’s health and any events during the past week.
The volunteer encourages the older person to talk further about interests, memories, worries (could be health, family, neighbourhood, etc.) and also shares some of his or her memories, interests, etc. Encouragement and support is given to achievements (from the older person’s perspective) since the last conversation.
The volunteer reminds the participant that topics discussed are confidential (especially if asking questions about health) and offers reassurance that it is okay to have boundaries for what they do/do not discuss.
Weeks 3 and 4: everyday conversations
Following greetings, the volunteer opens up the conversation to discussion about recent events, health, family and feelings. The volunteer should facilitate the conversations in such a way that the older person feels and is in control of what is talked about and develops a stronger sense of confidence in him- or herself.
The volunteer can refer to issues/topics from week 2 (and/or week 3) if appropriate.
Week 5
The conversation follows a similar pattern to weeks 3 and 4. When possible the volunteer places greater emphasis on developing specific conversation topics. This may be about hobbies, current affairs, family or television programmes. The older person will, however, continue to be in control of the conversation so that, if, for example, he or she has had ‘a bad night’ and wishes to talk about his or her worries, he or she should be able to do so.
The volunteer reminds the older person that the following week is the final week of one-to-one conversations, which will be followed by group discussions. The volunteer also suggests that the older person might want to think about what he or she would like to talk about in the group and what he or she hopes to get out of it.
Week 6
Following greetings the volunteer will start by reminding the older person that this is the last week of their conversations. The conversation then follows a similar pattern to that of week 5. Towards the end of the conversation the volunteer will discuss the ensuing group conversations with the participant and encourage him or her to raise topics and interests in the group. At this stage, if the older person expresses a reluctance to participate in a group, other options will have to be explored.
If an older person expresses concern about joining a group, the volunteer could explore these concerns and barriers with him or her, which would link into mastery and planning for how to cope with barriers.
Stage 2
The second stage consists of one group conversation per week over 12 weeks. Older people who have taken part in six one-to-one conversations are ideally allocated to groups in which, on the basis of the previous conversations, they are most likely to have common interests. The size of the groups will range from six to eight individuals and the sessions will last between 30 and 60 minutes.
The trained facilitator will be provided with a handbook on group facilitation. The role of the facilitator will be to make it easy for the group to achieve its purpose. He or she will do this by:
-
creating and maintaining a safe and stimulating space for discussion
-
enabling the group to listen and respond to other members of the group
-
ensuring the interests of one or two individuals do not dominate the group
-
ensuring that all participants have an opportunity to contribute
-
ensuring that the discussions are not ‘destructive’ or damaging to individuals in the group and
-
constantly monitoring and fostering the purpose of the group as well as the relationships and individuals within it.
Before the meetings start, the facilitator will communicate with the participants to determine a mutually agreeable time for the meetings. Conversations should ideally take place on the same day of the week and at the same time. Participants will receive written information about teleconferencing and:
-
what to do if they are unable to participate in one conversation
-
what happens if they do not answer when the facilitator phones
-
the acceptability of initiating between-call contact with other participants
-
the confidentiality of what is discussed in the group
-
boundaries between what is/is not discussed
-
what happens if a group member expresses the need for help with regard to his or her health
-
how the facilitator will manage disagreements during the conversations
-
what happens if there are technical problems, such as how to reconnect if they are accidentally disconnected or have to leave for part of the meeting
-
key contacts
-
the right to withdraw from the study.
These points will be discussed with the group during the first meeting. Depending on the composition of the group, the conversation session structure may develop in one of two ways:
-
as a subject interest group (e.g. current affairs, local history, music), who will discuss the same subject matter each time or
-
a friendship support group, in which members agree the topic to be discussed at each session.
Cattan et al. ’s23 systematic review suggests that both types of group (subject interest and friendship support) may be effective. The review also highlighted that improving self-esteem and internal locus of control (elements of self-efficacy) could enhance the effectiveness of an intervention to reduce feelings of loneliness.
Week 1
The trained volunteer facilitator will facilitate the introduction of group members to each other, draw attention to the purpose of the conversations and discuss the ground rules of teleconferencing with the participants (as in the written information). Participants will be given time to raise any technical/practical/safeguarding problems that require attention by the research team.
In the first meeting, the facilitator will encourage participants to introduce topics and interests to the group to be discussed over the 12 weeks. The facilitation of this first step will depend on the composition of the group and the methods used to select participants for the group.
Towards the end of the allocated/agreed time, the facilitator will draw the discussion to an end and remind members of the day/date and time of the next group discussion.
Weeks 2–10
The facilitator calls the participants. Participants introduce themselves and are reminded of basic ground rules.
The facilitator encourages the group to recap on the previous conversation and invites participants to comment on the week that has passed (have they initiated calls outside the group conversation, taken part in some external activity, requested information about, for example, becoming a volunteer, etc.).
Participants are encouraged to make suggestions for that day’s and the following weeks’ discussions, to share information and to contribute to the discussion.
Towards the end of the allocated/agreed time, the facilitator will draw the discussion to an end and remind members of the day/date and time of the next group discussion.
Week 11
The group call in week 11 follows the same format as in weeks 2–10. In addition, the facilitator reminds participants that the following week is the last conversation that they have signed up for. Participants are asked to think about what they plan to do following the end of these conversations.
Week 12
The group call in week 12 follows the same format as in weeks 2–10. However, more emphasis is put on participants discussing their plans following the end of the group conversations. The facilitator concludes the discussion, giving everyone a chance to say goodbye.
The changes in self-efficacy are likely to be small. The most likely improvements are an increase in self-confidence and increased feelings of competence and self-control. These improvements may be observed through increased information exchange, participants wanting to initiate/or initiating calls outside the group, participants feeling able to suggest a particular topic for discussion and participants wanting to become/or becoming volunteers.
Intervention development
In May 2005, Help the Aged and Zurich Community Trust launched a 2-year national programme called A Call in Time, intended to provide low-level support and telephone befriending services to older people who are lonely, isolated or vulnerable. Eight projects were funded across the UK. A service mapping exercise described the content of these projects. 24 A Delphi survey was conducted with the project co-ordinators of all eight projects to reach a consensus view about a ‘model of best practice’. 24 The consensus was for ‘a telephone befriending model to be based on a combination of telephone calls and peer-to-peer support, where all members are encouraged to make telephone calls as well as receive them, thereby developing “telephone clubs” ‘ (p. 50). 24 Concurrent qualitative research with older people who received telephone befriending services, including those involved in telephone clubs, confirmed the value of this model. 24,25
Between October 2011 and January 2012, following the commission of the PLINY project by the National Institute for Health Research, the manual for the one-to-one calls was drawn up by Mima Cattan and Rebecca Gossage-Worrall, with input from the PLINY service provider and the TMG public representative. The manual for the group calls was based on the standard Community Network manual and was drawn up by the same individuals with additional input from a professional group facilitation trainer. The content of both the one-to-one manual and the group manuals drew on material from manuals reviewed by Mima Cattan as part of her service mapping exercise24 and was reviewed by the first wave of volunteer facilitators in March 2011. These volunteers requested clarification on many issues in the one-to-one and group manuals and this consultation resulted in changes to the manuals and the insertion of the ‘Questions and Answers for Participants’ section.
Appendix 4 Training materials
Community Network facilitator's hanbook (PDF download)
Community Network 2012 © All rights reserved
Appendix 5 Questionnaire booklet for participants at baseline
Appendix 6 Interview topic guides
Appendix 7 Qualitative research framework
| Theme | Subtheme | Description |
|---|---|---|
| Prior statesa | 1.1 Reason for participation | Motivations and factors associated with taking part |
| 1.2 Prior expectations | Expectations of the intervention prior to receiving one-to-one/group calls | |
| 1.3 Needs | Needs of participants prior to receiving the intervention, with a particular emphasis on health and well-being | |
| Technicala | 2.1 Accessibility | Extent to which the calls were accessible; factors that lessened or enhanced accessibility |
| 2.2 Acceptability | Factors that impacted on the level of acceptability to participants | |
| 2.3 Facilitator performance | Participants’ perceptions of their volunteer facilitator | |
| Group dynamics | 3.1.1 Cohesiveness | Extent to which groups ‘gelled’ |
| 3.1.2 Disclosure | Extent (and level) to which participants engaged in discussions | |
| 3.1.3 Peers | Influence of peers within the group and the impact on participants’ experiences | |
| Value | 4.1 Perceived benefits | Extent to which the intervention met the needs of participants |
| 4.2 Preferred alternatives | The alternative forms of ‘friendship’ and differing priorities from those in the delivered intervention | |
| 4.3 Willingness to pay | Willingness (in theory) to pay for calls to take part in TF groups |
Appendix 8 Fidelity checklists
Appendix 9 Main trial results
| Outcome | Intervention | Control | Unadjusteda | Adjustedb | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (SE) | n | Mean (SE) | Mean difference (95% CI) | p-value | Mean difference (95% CI) | p-value | |
| SF-36 | ||||||||
| Mental health | 9 | 73.9 (5.8) | 30 | 70.7 (3.9) | 3.2 (–5.2 to 11.6) | 0.452 | 8.0 (3.3 to 12.7) | < 0.001 |
| Physical functioning | 9 | 51.5 (11.4) | 30 | 56.0 (5.5) | –4.5 (–18.0 to 9.1) | 0.519 | 1.3 (–23.0 to 25.7) | 0.914 |
| Role – physical | 9 | 57.6 (8.3) | 30 | 55.4 (5.0) | 2.2 (–7.7 to 12.2) | 0.662 | 11.3 (–2.3 to 24.9) | 0.104 |
| Bodily pain | 9 | 59.7 (10.7) | 30 | 53.9 (5.4) | 5.8 (–14.9 to 26.5) | 0.583 | 12.1 (–2.5 to 26.7) | 0.105 |
| General health | 9 | 59.8 (9.4) | 30 | 56.1 (4.2) | 3.6 (–11.6 to 18.9) | 0.639 | 0.6 (–8.4 to 9.7) | 0.888 |
| Vitality | 9 | 55.6 (6.9) | 30 | 49.6 (4.7) | 6.0 (–9.2 to 21.1) | 0.440 | 1.7 (–6.0 to 9.5) | 0.661 |
| Social functioning | 9 | 72.2 (9.7) | 30 | 70.0 (5.7) | 2.2 (–13.8 to 18.3) | 0.786 | 8.2 (–8.6 to 25.0) | 0.336 |
| Role – emotional | 9 | 78.7 (9.2) | 30 | 81.7 (4.4) | –3.0 (–22.9 to 16.9) | 0.770 | –8.9 (–59.8 to 42.0) | 0.731 |
| Physical component summary | 9 | 38.9 (4.8) | 30 | 38.3 (2.1) | 0.7 (–7.5 to 8.8) | 0.873 | 1.9 (–2.7 to 6.4) | 0.416 |
| Mental component summary | 9 | 51.0 (3.9) | 30 | 49.7 (2.1) | 1.3 (–5.4 to 8.0) | 0.704 | 6.7 (4.3 to 9.2) | < 0.001 |
| PHQ-9 | ||||||||
| Overall score | 9 | 4.4 (1.5) | 30 | 3.6 (0.8) | 0.9 (–1.8 to 3.6) | 0.526 | –1.4 (–2.6 to –0.2) | 0.021 |
| EQ-5D | ||||||||
| Tariff | 9 | 0.64 (0.14) | 29 | 0.71 (0.05) | –0.08 (–0.24 to 0.09) | 0.372 | –0.01 (–0.15 to 0.12) | 0.880 |
| Thermometer | 9 | 69.4 (8.8) | 30 | 70.5 (4.0) | –1.0 (–13.2 to 11.1) | 0.869 | –9.0 (–18.3 to 0.2) | 0.054 |
| de Jong Gierveld | ||||||||
| Emotional loneliness score | 9 | 3.1 (0.7) | 30 | 2.2 (0.3) | 0.9 (–0.0 to 1.9) | 0.056 | 0.6 (–0.1 to 1.3) | 0.093 |
| Social loneliness score | 9 | 1.6 (0.7) | 30 | 1.2 (0.3) | 0.4 (–0.4 to 1.2) | 0.354 | –0.2 (–0.5 to 0.1) | 0.235 |
| Overall loneliness score | 9 | 4.7 (1.2) | 30 | 3.3 (0.5) | 1.3 (–0.4 to 3.0) | 0.122 | –0.3 (–0.8 to 0.2) | 0.255 |
| GSE | ||||||||
| Total score | 9 | 32.3 (2.2) | 30 | 32.1 (0.7) | 0.2 (–3.7 to 4.2) | 0.905 | 1.1 (–0.9 to 3.0) | 0.275 |
| ONS well-being | ||||||||
| Total score | 9 | 7.2 (0.6) | 30 | 7.6 (0.3) | –0.3 (–1.3 to 0.7) | 0.499 | 0.1 (–0.4 to 0.6) | 0.637 |
Appendix 10 Qualitative research results
| Variable | Scoring | Interviewed (n = 19) | Not interviewed (n = 16) | Total (n = 35) |
|---|---|---|---|---|
| Sex, n (%) | Female | 13 (68) | 10 (63) | 23 (66) |
| Male | 6 (32) | 6 (38) | 12 (34) | |
| Age (years) | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 83.3 (6.3) | 79.9 (4.8) | 81.8 (5.8) | |
| Median (IQR) | 81 (78–88) | 78 (76–83) | 80 (78–85) | |
| Min. to max. | 75 to 95 | 75 to 91 | 75 to 95 | |
| Ethnicity, n (%) | English/Welsh/Scottish/Northern Irish/British | 19 (100) | 15 (94) | 34 (97) |
| Any other white background | 0 (0) | 1 (6) | 1 (3) | |
| Live with anyone?, n (%)a | Yes | 4 (21) | 6 (38) | 10 (29) |
| No | 15 (79) | 10 (63) | 25 (71) | |
| Live with spouse/partner, n (%) | Ticked | 2 (11) | 6 (38) | 8 (23) |
| Live with children, n (%) | Ticked | 0 (0) | 1 (6) | 1 (3) |
| Live with others, n (%) | Ticked | 1 (5) | 0 (0) | 1 (3) |
| Education, n (%) | ||||
| One to four O levels/GCSEs/CSEs | Ticked | 0 (0) | 2 (13) | 2 (6) |
| Five or more O levels/GCSEs/CSEs | Ticked | 1 (5) | 2 (13) | 3 (9) |
| Degree | Ticked | 2 (11) | 3 (19) | 5 (14) |
| Higher degree | Ticked | 1 (5) | 0 (0) | 1 (3) |
| Professional | Ticked | 5 (26) | 2 (13) | 7 (20) |
| Other | Ticked | 2 (11) | 0 (0) | 2 (6) |
| Occupation | Looking after home/family | 1 (5) | 0 (0) | 1 (3) |
| Retired | 18 (95) | 16 (100) | 34 (97) | |
| Variable | Scoring | Interviewed (n = 19) | Not interviewed (n = 16) | Total (n = 35) |
|---|---|---|---|---|
| Mental health | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 79.2 (15.1) | 76.3 (20.4) | 77.9 (17.5) | |
| Median (IQR) | 80 (70–90) | 80 (67.5–90) | 80 (70–90) | |
| Min. to max. | 40 to 100 | 15 to 100 | 15 to 100 | |
| Physical function | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 64.3 (29.8) | 67.2 (25.2) | 65.6 (27.4) | |
| Median (IQR) | 75 (35–90) | 67.5 (58–88) | 70 (55–90) | |
| Min. to max. | 0 to 100 | 10 to 100 | 0 to 100 | |
| Role – physical | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 68.4 (26.1) | 74.6 (24.5) | 71.3 (25.2) | |
| Median (IQR) | 56.3 (50.0–100) | 78.1 (59.4–100) | 75 (50.0–100) | |
| Min. to max. | 25 to 100 | 25 to 100 | 25 to 100 | |
| Bodily pain | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 62.2 (32.9) | 66.9 (24.4) | 64.4 (29) | |
| Median (IQR) | 72 (31–100) | 67 (41–92) | 72 (41–100) | |
| Min. to max. | 0 to 100 | 32 to 100 | 0 to 100 | |
| General health | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 71.7 (20.9) | 66.2 (22.4) | 69.2 (21.4) | |
| Median (IQR) | 77 (57–87) | 72 (54–79) | 72 (57–82) | |
| Min. to max. | 30 to 100 | 25 to 97 | 25 to 100 | |
| Vitality | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 65.8 (22.8) | 58.2 (16.7) | 62.3 (20.3) | |
| Median (IQR) | 68.8 (43.8–81.3) | 59.4 (50.0–71.9) | 68.8 (50.0–75.0) | |
| Min. to max. | 6.3 to 100 | 25 to 81.3 | 6.3 to 100 | |
| Social function | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 82.2 (26.5) | 88.3 (17.4) | 85 (22.6) | |
| Median (IQR) | 100 (75.0–100) | 93.8 (87.5–100) | 100 (75.0–100) | |
| Min. to max. | 25 to 100 | 37.5 to 100 | 25 to 100 | |
| Role – emotional | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 83.8 (23.3) | 94.3 (10.9) | 88.6 (19.2) | |
| Median (IQR) | 100 (66.7–100) | 100 (91.7–100) | 100 (83.3–100) | |
| Min. to max. | 25 to 100 | 66.7 to 100 | 25 to 100 | |
| Physical component | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 43.5 (11.4) | 44.1 (9.6) | 43.8 (10.5) | |
| Median (IQR) | 45.4 (33.4–55.0) | 43.8 (35.7–52.1) | 44.2 (34.0–53.7) | |
| Min. to max. | 22.7 to 57.2 | 29.6 to 61.2 | 22.7 to 61.2 | |
| Mental component | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 53.9 (8.8) | 54.3 (9.7) | 54.1 (9.1) | |
| Median (IQR) | 56.1 (49.2–59.3) | 56.7 (51.0–60.1) | 56.2 (50.9–59.3) | |
| Min. to max. | 25.3 to 63.6 | 24.3 to 68.1 | 24.3 to 68.1 |
| Variable | Scoring | Interviewed (n = 19) | Not interviewed (n = 16) | Total (n = 35) |
|---|---|---|---|---|
| EQ-5Da | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 0.71 (0.36) | 0.75 (0.2) | 0.73 (0.29) | |
| Median (IQR) | 0.85 (0.62–1) | 0.8 (0.67–0.83) | 0.8 (0.62–1) | |
| Min. to max. | –0.37 to 1 | 0.2 to 1 | –0.37 to 1 | |
| EQ-5D VASb | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 77.3 (17.8) | 72.4 (19.8) | 75.1 (18.6) | |
| Median (IQR) | 80 (67–90) | 80 (50–90) | 80 (61–90) | |
| Min. to max. | 26 to 96 | 40 to 100 | 26 to 100 | |
| de Jong Gierveld emotional loneliness scorec | n (%) | 18 (94.7) | 16 (100) | 34 (97.1) |
| Mean (SD) | 2.3 (2) | 1.4 (1.4) | 1.9 (1.8) | |
| Median (IQR) | 3 (0–4) | 1 (0–3) | 1 (0–3) | |
| Min. to max. | 0 to 6 | 0 to 4 | 0 to 6 | |
| de Jong Gierveld social loneliness scored | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 1.5 (1.7) | 1.3 (1.8) | 1.4 (1.7) | |
| Median (IQR) | 1 (0–3) | 0 (0–2.5) | 1 (0–3) | |
| Min. to max. | 0 to 5 | 0 to 5 | 0 to 5 | |
| de Jong Gierveld overall loneliness scoree | n (%) | 18 (94.7) | 16 (100) | 34 (97.1) |
| Mean (SD) | 3.9 (3.3) | 2.6 (2.8) | 3.3 (3.1) | |
| Median (IQR) | 3 (1–6) | 1 (1–5) | 2 (1–6) | |
| Min. to max. | 0 to 11 | 0 to 9 | 0 to 11 | |
| PHQ-9f | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 2.7 (3.6) | 3.2 (3.8) | 2.9 (3.6) | |
| Median (IQR) | 1 (0–4) | 2.5 (2–4) | 2 (0–4) | |
| Min. to max. | 0 to 13 | 0 to 16 | 0 to 16 | |
| ONS well-beingg | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 7.3 (3) | 8.4 (1.3) | 7.8 (2.4) | |
| Median (IQR) | 8 (7–9) | 8 (8–10) | 8 (7–9) | |
| Min. to max. | 0 to 10 | 6 to 10 | 0 to 10 | |
| GSEh | n (%) | 19 (100) | 16 (100) | 35 (100) |
| Mean (SD) | 33.1 (5) | 34.3 (4) | 33.7 (4.5) | |
| Median (IQR) | 34 (29–38) | 35.5 (30–37) | 35 (29–38) | |
| Min. to max. | 24 to 40 | 27 to 39 | 24 to 40 |
Glossary
- de Jong Gierveld Loneliness Scale
- This multidimensional scale uses self-reported characteristics such as social networks and levels of social contact to assess loneliness and is based on the assumption that feelings of loneliness result when there is a discrepancy between what an individual wants from interpersonal relationships and what they actually have.
- Intervention fidelity
- An examination of whether the intervention was delivered as intended. In this study, this included examining whether the trainer delivered training to volunteers as stated and whether volunteers followed the training provided to them when they facilitated group calls.
- Research assistant
- In this study, research assistants were employed to conduct research activities (screening candidates for study eligibility and collecting baseline and follow-up data).
- Self-efficacy theory
- Defined by Albert Bandura as an individual’s belief in his or her own capabilities to carry out actions that are required to manage future situations.
List of abbreviations
- 6CIT
- six-item Cognitive Impairment Test
- BECCA
- Befriending and Cost of Caring
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CTRU
- Clinical Trials Research Unit
- DMEC
- Data Monitoring and Ethics Committee
- EQ-5D
- European Quality of Life-5 Dimensions
- GEE
- generalised estimating equation
- GLM
- general linear model
- GP
- general practitioner
- GSE
- General Perceived Self-Efficacy Scale
- ICC
- intracluster correlation
- IQR
- interquartile range
- ITT
- intention to treat
- LOCF
- last observation carried forward
- NICE
- National Institute for Health and Care Excellence
- ONS
- Office for National Statistics
- PHQ-9
- Patient Health Questionnaire – nine questions
- PLINY
- Putting Life in Years
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- RNIB
- Royal National Institute for the Blind
- SD
- standard deviation
- SF-36
- Short Form questionnaire-36 items
- SMD
- standardised mean difference
- TF
- telephone friendship
- TMG
- trial management group
- TSC
- trial steering committee